Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/110/01. The contractual start date was in February 2013. The draft report began editorial review in February 2015 and was accepted for publication in July 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Macdonald et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background, aims and objectives
Child maltreatment is a serious public health issue and a major cause of health inequality. 1 Children who experience serious or persistent maltreatment are at risk of a range of social, emotional, behavioural and economic adversities, alongside the impact of maltreatment on their physical and mental health. The major focus of UK policy has been on preventing serious abuse and neglect, triggered and sustained by periodic reports of the circumstances surrounding child deaths. 2–4 Little attention has been given to how best to address the consequences of maltreatment for those who have experienced it or been adversely affected by it. While prevention is preferable to dealing with the consequences of maltreatment, the reality is that in 2014 almost 50,000 children in England were subject to a child protection plan because of maltreatment or risk of significant harm. Behind those 50,000 children are many more who also experience maltreatment, but who either do not come to the attention of social services or whose maltreatment falls below the undoubtedly high thresholds of harm currently operated by Children’s Services Departments. In 2012, the Health Technology Assessment (HTA) programme commissioned two evidence syntheses that were relevant to the needs of maltreated children. One was a review of interventions aimed at improving outcomes for children exposed to domestic violence (PHR 11/3007/01). 5 The second was an evidence synthesis of psychosocial interventions aimed at improving outcomes for children who experienced maltreatment, and this is the focus of this report.
Categories of maltreatment
Child maltreatment has been defined as any act or series of acts of commission (physical abuse, sexual abuse, emotional/psychological abuse) or omission (neglect) by a parent, caregiver or other person, which leads to harm, the potential for harm, or threat of harm to a child (someone under 18 years). Most child maltreatment takes place within the family home, but it can also occur in an institutional or a community setting. The perpetrators of maltreatment are usually known to the children concerned, but more rarely they may be strangers. Although most maltreatment is attributable to adults, child-to-child maltreatment is also a concern. Some forms of maltreatment can take place on the internet.
Detailed definitions can be found in a number of guidelines. 6–9
Briefly:
-
Physical abuse may involve hitting, shaking, throwing, poisoning, burning or scalding, drowning, suffocating or otherwise causing physical harm to a child. Physical harm may also be caused when a parent or carer fabricates the symptoms of, or deliberately induces, illness in a child.
-
Emotional/psychological abuse is the persistent emotional abuse of a child such as to cause severe and persistent adverse effects on the child’s emotional development. Emotional maltreatment may take the form of age or developmentally inappropriate expectations on children. It may involve conveying to children that they are worthless or unloved; not giving them opportunities to express their views or ‘making fun’ of what they say or how they communicate; seeing or hearing the ill-treatment of another; being seriously bullied (including cyberbullying), or exploited or corrupted. Emotional abuse is involved in all types of maltreatment, although it may occur alone. Children who are the subject of fabricated illness are also subject to emotional abuse, either as a result of being brought up in a fabricated sick role, or because of an abnormal relationship with their carer, or disturbed family relationships. 10–15 More recently, domestic violence has been recognised as maltreatment, and is a common cause of emotional or psychological harm to children.
-
Sexual abuse involves forcing or enticing a child or young person to take part in sexual activities, not necessarily involving a high level of violence, whether or not the child is aware of what is happening. Activities may involve physical contact, including assault by penetration or non-penetrative acts and non-contact activities, such as involving children in watching sexual activities, encouraging them to behave in sexually inappropriate ways, or grooming them in preparation for abuse (including via the internet). Sexual abuse is perpetrated by men and women, although the majority of sexual abuse of children is by male perpetrators against female children, typically someone known to them (i.e. a family member or family friend). Abuse by a stranger is less common. Sexual abuse can occur between children.
-
Neglect is the persistent failure to meet a child’s basic physical and/or psychological needs, likely to result in the serious impairment of his or her health or development. Neglect may occur during pregnancy as a result of maternal substance abuse. Once a child is born, neglect may involve a parent or carer failing to provide a child with adequate food, clothing and shelter (including exclusion from home or abandonment); failing to protect him or her from physical and emotional harm or danger; or failing to ensure access to appropriate medical care or treatment. It may include neglect of, or unresponsiveness to, a child’s basic emotional needs.
Most children experience more than one form of maltreatment, and there is growing recognition of the need to better take into account children’s profiles of maltreatment in order to improve policy and practice. 16–18 Although maltreatment can result in death, serious injury or impairment (see below), it is not itself a disorder but an event or exposure; not all maltreated children experience impairment.
Prevalence, aetiology, contributory factors
Child maltreatment poses significant threats to children’s health, development and well-being. It is recognised that statistics on the number of referrals to child protection services, and the numbers of children for whom there is a child protection plan, let alone the number of criminal offences against children, are an underestimate of the scale of the problem within the UK. The term ‘registration’ is used here to describe children for whom there is a child protection plan (England) or whose names are on child protection registers (Wales, Scotland and Northern Ireland). As at March 2009, registrations in the UK were England, 34,100; Wales, 2512; Northern Ireland, 2488; and Scotland, 2682. It is important to note that these data may not be measuring precisely the same thing in each jurisdiction. Data on trends in child maltreatment are difficult to interpret,19 but, overall, the numbers of children registered in each jurisdiction has increased steadily since 2002, although there is some evidence of a fall in the numbers of violent child deaths in infancy and middle childhood within the UK. 20 The 2014 figure for children subject to a child protection plan in England as at 31 March was 48,300 (excluding unborn children), an increase of 12.1% on the numbers at the same time in 2013. This represents an increase of 23.4% since 31 March 2010. In 2011 the National Society for the Prevention of Cruelty to Children (NSPCC) published a cross-sectional, self-report survey of 2275 children aged 11–17 years and adults aged 18–24 years. Their findings indicated that 18.6% of the 11- to 17-year-olds ‘had been physically attacked by an adult, sexually abused, or severely neglected’ and 25.3% of the 18- to 24-year-olds reported severe maltreatment during childhood. 21
Consequences of maltreatment
A growing body of evidence suggests that being exposed to maltreatment may result in structural and functional changes to the developing brain,22–24 as well as long-lasting changes in the way genes are expressed in the brain. 25–27 The adverse effects of maltreatment can be found across multiple domains of functioning, including physical and mental health and well-being, security of attachment, cognitive and emotional development, aggression, violence and criminality, and socioeconomic attainment. 28–33 Maltreatment is a non-specific risk factor for a wide range of adverse long-term health and social care outcomes, and children who experience multiple forms of maltreatment are at increased risk. 34–36 There is also some evidence of maltreatment type-specific risks, although generally this is stronger for sexual abuse than other forms of child maltreatment. Widom et al. 37 found that both child physical abuse and neglect, but not sexual abuse, were associated with an increased risk for lifetime major depressive disorder in young adulthood, with children exposed both to physical abuse and neglect being most at risk. A longitudinal study by Kotch et al. 38 concluded that neglect within the first 2 years of life, in the absence of other forms of maltreatment, predicted levels of aggression at ages 4, 6 and 8 years. Preschool children exposed to severe physical neglect have been found to evidence increased rates of internalising symptomatology and withdrawn behaviour compared with other maltreated children. 39 Generally though, the fact that few children experience only one form of maltreatment makes it difficult to link particular forms of maltreatment with specific risks or adverse outcomes.
The impact of maltreatment may depend on the interaction of a number of factors, including the child’s genetic endowment, age, gender, type(s) of abuse, severity, frequency and duration of maltreatment, and the availability of protective factors that function to enhance a child’s resilience. 40–45 Children who appear to be ‘asymptomatic’ following maltreatment may, nonetheless, be at risk for the development of later psychosocial problems, triggered by subsequent stressors and the need to negotiate key developmental tasks, for example forming intimate relationships, managing interpersonal conflict, becoming a parent and so on.
For the child who is removed from their birth parents or other primary carers under relevant legislation, the adverse effects of maltreatment may be compounded by delays arising from lengthy care proceedings and instability of placements. For infants and young children, these factors may exacerbate attachment difficulties or disorders. In developing effective interventions, it is therefore important to understand how and why maltreatment impacts throughout the life course, and the variables that either mediate or moderate adverse sequelae.
Economic consequences of maltreatment
The economic costs of maltreatment, both to individuals46–50 and to society,51–55 are well documented. Costs to individuals include adverse effects on physical and mental health; social and emotional development; cognitive development and levels of educational attainment; and employment status and earnings. Societal costs include the health and social care costs of illness or injury; the intergenerational costs of teenage pregnancy and poor parenting; criminal justice system costs; and losses in productivity.
Psychosocial interventions
There is a wide range of psychosocial interventions currently available to children and young people who have experienced maltreatment, although availability varies enormously. 56–58 These are based on a variety of theoretical underpinnings and include:
-
interventions based on cognitive theories, including cognitive–behavioural therapy (CBT), trauma-focused CBT (TF-CBT) and abuse-focused CBT
-
eye movement desensitisation and reprocessing (EMDR)
-
interventions based primarily on forms of expression and communication drawn from the arts, including art therapy, drama therapy, music therapy, play therapy and narrative group therapy
-
attachment-based interventions
-
interventions based on psychoanalytic theories, offered to the child or parent–child dyad.
-
family/systemic interventions.
-
multisystemic therapy (MST)
-
peer mentoring.
-
enhanced foster care, including treatment foster care
-
residential care, including models of therapeutic residential care, such as CARE® (Cornell University, Ithaca, NY, USA) and Sanctuary® (Sanctuary Institute, Philadelphia, PA, USA).
Interventions may be delivered in one or more of a range of contexts, for example clinic, school, community. Interventions may be individual or group based, or a combination, and may involve only the child or the child and his or her primary carer(s). Some entail a change of caregiver, as in adoption, kinship care, foster care or residential care. Most are commissioned, or provided by, the UK NHS. Some are available from a range of voluntary and private sector providers, and some are primarily social care or education based.
Timing of, and pathways to, treatment
For some forms of maltreatment, treatment can be offered appropriately only after the child is protected from further abuse. This applies to sexual abuse and serious physical injury, and here protection can be ensured only when the contact between the child and the abuser is constantly supervised or halted. In the more persistent or chronic forms of maltreatment – emotional abuse and neglect – treatment may be offered to the child and caregivers simultaneously to deal both with the effects of the maltreatment and with the harmful parent–child interactions.
Maltreatment per se may be the trigger for some referrals to Child and Adolescent Mental Health Services (CAMHS). For example, a child may be referred following recognition of a specific form of maltreatment, most commonly sexual abuse. Sometimes children are referred as a result of maltreatment although the precise nature of that maltreatment may not be known. Other children may be referred because they have experienced several forms of maltreatment. Emotional maltreatment is often seen as integral to other forms of abuse or neglect.
Some children will be referred for help with specific symptoms, for example post-traumatic stress disorder (PTSD), depression or anxiety. In some cases this will be clearly identified as the results of exposure to maltreatment, such as physical or sexual abuse or intimate partner violence (IPV). Others will be referred when there is no mention or initial awareness of the existence or relevance of previous maltreatment, but where a causal link is subsequently found. This review focuses on those children whose pathways to referral are clearly linked with maltreatment.
Treatment acceptability and engagement
Children who have experienced abuse and neglect can be difficult to engage, not least because of the adverse impact of maltreatment on their ability and willingness to engage with, or trust, adults. Evidence from a NSPCC survey21 indicated that some 80% of young adult women who reported abuse by a caregiver said they had talked to a professional following the abuse taking place, compared with just 18% of boys. However, those who sought help from a professional did not always think that it had brought about a better outcome. Carers too can feel excluded from some therapeutic approaches, when their involvement may be critical.
But many children do not have the opportunity of help. Historically, child maltreatment has been seen as a problem for social care, rather than CAMHS,59 and effective interagency working between CAMHS and social services continues to be elusive. Referral pathways to CAMHS are long and complex,60,61 and, for those referred, acceptance thresholds are high and waiting lists are often extremely long. Little, if anything, is known about what maltreated children want from health-care professionals or what kinds of intervention or service arrangements they find acceptable, and possible to engage with, or unacceptable.
Importance of this evidence synthesis
Reviews in this area suffer from a number of weaknesses. 62 These include (1) searches that are out of date, have restricted search dates or language restrictions; (2) the predominance of research conducted in North America, with little or no consideration of the generalisability of evidence to other policy contexts; (3) a lack of adequate consideration of the maltreatment profiles of study participants; (4) a lack of consideration of the logic models underpinning included interventions; (5) inadequate, and sometimes no, consideration of the risk of bias of included studies; (6) heterogeneity of outcomes and measures used; and (7) a lack of consideration of issues of acceptability or accessibility of interventions for children and their families.
Most reviews, for good methodological reasons, restrict their inclusion criteria to randomised or quasi-randomised trials. Although it is arguably unethical to expose maltreated children to interventions of unknown effectiveness, the technical challenges of implementing randomised trials of maltreatment interventions are considerable, sometimes resulting in studies with high risk of bias63,64 or little useful information. Other types of study may provide valuable information about interventions not yet subjected to more rigorous evaluation, and may provide a picture of the evidence gaps when compared with the profile of available services.
As with studies and reviews of interventions, most studies of the cost-effectiveness of interventions appear to have focused on primary prevention rather than secondary and tertiary prevention, or the treatment of children who have experienced maltreatment. 65–67 A review by Goldhaber-Fiebert et al. 68 identified 19 reviews and 30 original papers reporting research on the costs and effectiveness of interventions for children at risk of (the majority), or already involved in, child welfare (protection) services. They observe that existing model-based evaluations of secondary prevention have, so far, used ‘relatively simple multiplicative decision trees’ that do not reflect the variety of pathways that children follow, how these may impact on the effectiveness of subsequent interventions or adequately address factors such as the child’s age (p. 737). They concluded that current epidemiological data, combined with evidence from well-conducted outcome studies and improved modelling techniques, make it timely to revisit the cost-effectiveness of interventions for maltreated children.
Research aims and objectives
This review aimed to bring high standards of evidence synthesis to bear in this important but challenging area of public health. It provides an up-to-date overview of research on interventions aimed at addressing the adverse consequences of child maltreatment, and a synthesis of what we know about their effectiveness and cost-effectiveness. The objectives of the research were to answer the following questions:
-
Which interventions are effective, for which children, with what maltreatment profiles, in what circumstances?
-
When two or more interventions might be appropriate, which is most likely to be effective?
-
Which interventions are of no benefit or may result in harm?
-
Which interventions are most accessible and acceptable to carers, children and young people?
-
What do we know about the economic benefits of interventions, and the potential value of undertaking future research?
Chapter 2 Review methods
Focus of the review
In line with the HTA brief, this review sought to include effectiveness studies of any psychosocial intervention provided to maltreated infants, children or adolescents in any setting (e.g. family, community, residential) specifically to address the consequences of maltreatment. We included studies of any intervention aimed at addressing the consequences of any type of maltreatment, irrespective of service provider or setting (e.g. family, institution, school), whether or not provided to children individually or in a group format, and whether or not the treatment involved parents or other carers. We included studies in which the intervention was delivered to a child by, or through, a parent or other carer, as long as this was concerned with addressing the consequences for the child of his or her experiences of maltreatment.
This meant excluding two groups of studies that are also relevant to improving outcomes for children experiencing maltreatment or who are at risk of maltreatment, namely:
-
Studies aimed at the secondary prevention of maltreatment. These are studies of interventions aimed primarily at improving quality of parenting in families in which there are concerns about maltreatment. Arguably, by improving parenting in ways that prevent future maltreatment and enhance the quality of parenting and family relationships, such interventions make an important contribution towards addressing the adverse consequences caused by maltreatment to children within these families. There are a number of parenting programmes that specifically target these vulnerable families, but their focus is primarily the parents and their parenting, rather than the children. Only if the programme combined an intervention aimed specifically at the child, as well as the parents, were such studies included in this review.
-
Studies concerned with evaluating interventions that addressed problems known to be associated with maltreatment (such as depression or PTSD) but for which the target population was any child experiencing the health problem. In other words, these studies did not set out to recruit children who, because of maltreatment, were experiencing depression, anxiety, behaviour problems and so on. Our searches identified many studies of this kind, in which the study sample included participants (typically adolescents or young adults) who might have experienced maltreatment, but whose maltreatment was not the reason for their recruitment.
Project oversight
The research team were experienced in systematic review methodology and provided topic expertise in this field. Alongside the research team, a Steering Group was established to guide the overall direction of the project, and to ensure that a range of expertise and perspectives, particularly those of guideline developers, were properly considered in decisions taken during the course of the review. The research team and Steering Group members are listed in Appendix 1.
Professional Advisory Group
To enhance the clinical and professional representation in the project, a Professional Advisory Group (PAG) was established to help shape the work, interpret the evidence and draw conclusions from the data. Approximately 50 professionals were invited to participate. They represented a range of disciplines (including mental health nursing, general practice, psychology, psychiatry, social work, teaching and foster care) from different settings (tertiary care, CAMHS, residential care, community, etc.) and different providers (NHS, private and voluntary sectors). The objective of the PAG consultations was to help ensure relevance to health and social care provision in the UK. In particular, these consultations helped with the identification of potential barriers and facilitators to implementation from the perspective of those (1) involved in identifying children who need psychosocial interventions as a result of maltreatment; (2) responsible for referring them to appropriate services; and (3) delivering services. Information was shared with the PAG throughout the project and two face-to-face meetings were convened in London. The first meeting, involving around 40 participants, took place near the start of the project on 1 May 2013, and was designed to help identify and prioritise key issues. The second meeting, involving around 20 participants, took place on 27 November 2014 once the initial findings were available, and was intended to take the form of a consensus meeting. The names of PAG participants are provided in Appendix 2.
Young Persons’ Advisory Groups
Several Young Persons’ Advisory Groups were convened to provide advice on general issues relevant to the project. In particular, the groups were established to help us understand the experience of receiving treatment from professionals concerned with maltreated children, the factors that enhance acceptability of treatment, and what outcomes matter most to children and adolescents. One group in Belfast, Voice of Young People in Care (VOYPIC) and one Cardiff-based group, Voices from Care, were approached and invited to participate in the project. At the beginning of the project, an initial meeting of seven young people aged between 16 and 24 years from the VOYPIC group was convened in Belfast on 27 March 2013. A subsequent meeting of seven young people aged ≥ 18 years from the Voices from Care group was convened in Cardiff on 9 April 2013. Both meetings were coconvened by dedicated facilitators from their respective organisations, who were experienced in consulting with young people in care or previously in care, as well as one member of the research team (either NL or JH). Towards the end of the project, a group of six young people aged between 15 and 19 years contributed to the interpretation of the project’s findings during a NSPCC participation event held on 27 October 2014.
Early planning with advisory groups
A plan for undertaking consultations was agreed with the project Steering Group. The early advisory groups were intended to help shape the plan of the review. The key questions and methods used for these initial advisory group meetings were broadly similar. Both professionals and Young Persons’ Advisory Groups were consulted on relevant outcomes following psychosocial interventions for maltreated young people, factors that would facilitate their getting the help they needed, and factors that would act as barriers to their getting that help. The Young Persons’ Advisory Groups were asked to consider three additional questions:
-
What difference would ‘helpful help’ make for a child or young person who had been treated badly?
-
What would make it easier to ask for help or get help?
-
What would make it harder to ask for help or get help?
In both the PAG and the Young Persons’ Advisory Groups, a sorting and ranking exercise called the Q-sort was used to elicit individual views and help develop some consensus views. On the basis of their knowledge of the field, the research team and the Steering Group agreed an initial set of potential outcomes, facilitators for getting help, and barriers to getting the help they needed. Group members were presented with a group of cards, each of which had a different possible outcome, facilitator or barrier. Group members were first asked to review the cards individually and consider their own opinions on where each card should be placed on the large Q-sort pyramidal grid. They were then asked to discuss their opinions in the group, and to work together to create one single agreed Q-sort pyramid. Cards placed to the right of the grid would be those that were the most important outcomes/facilitators/barriers and the least important to the left. Group members were informed that they could amend the cards if necessary. They were also welcome to add new cards if they felt that any potential factors were missing and to remove any cards that they felt were irrelevant.
The Q-sort process proved to be quite effective at engaging the young people and serving as a basis for discussion. Based on the experience of the first group, the process was slightly modified for the following sessions, so that the sequence of issues was revised and part of the session was spent in smaller subgroup discussions.
In view of the large size of the PAG, to enable meaningful discussion the Steering Group decided to establish smaller groups based on professional discipline for the Q-sort task. This allowed all groups to contribute, but also highlighted areas of agreement and differences between the groups, so that potential reasons could be discussed. Each small group was facilitated by a member of the research team/Steering Group.
Final Professional Advisory Group meeting
A detailed and technical presentation of the review findings was provided for this PAG. The smaller number of participants at this meeting enabled whole-group discussion.
Participants were first asked to consider a series of questions about the findings of the review, including whether or not there were any important studies missing, any surprises about the coverage of maltreatment types or the profile of evidence across different types of intervention, and whether or not any of the findings were puzzling/unexpected. Participants were also asked the extent to which the review findings matched their experience of what is offered through health and social care services and, if different, what might account for this (e.g. training, therapeutic context, therapeutic preferences, resource constraints or other explanations).
They were then asked to consider how clinicians were likely to react to the messages about the weight of evidence in favour of CBT interventions, whether or not there were likely to be any barriers to implementing the findings and how these issues might be considered in the final report.
Finally, in light of existing evidence, participants were asked to identify any priorities for future research.
Final Young Persons’ Advisory Group meeting
The young persons’ group was cofacilitated by members of the research team and Steering Group, without an adult present whom the young people knew well. This session was part of a broader participation event, for which known and trusted adults were available to support the young people should they become distressed. We explained to them that during the session they would hear quite powerful quotations from young people, which they might find unsettling. In such an event we told them that they could let us know if they wanted a break or simply take themselves off to the agreed point to find their identified adult supporter.
In the first part of the session, members of the research team provided an overview of the key intervention types that were identified through the review: CBT; counselling or psychotherapy; family intervention; attachment therapy; activity-based interventions; and therapeutic residential care. In addition to talking about these, pictures were provided on large laminated sheets to help illustrate key features of these approaches. The main part of the session was focused around three sets of questions/statements:
-
Prioritising between interventions:
-
Which of these intervention types would young people want more?
-
Some therapies have a lot of evidence showing that they work, but others do not. If you were the government, to which ones would you give the money?
-
-
Responses to ‘acceptability’ statements:
-
‘Therapy doesn’t help people to forget about abuse, they just make them talk about it over and over again.’
-
‘In some situations where the child starts therapy, they can get upset, and the parent then doesn’t want them to go. What advice would you give a parent if their child was upset for the first time?’
-
‘It’s not just the child that needs help, parents do too.’
-
‘Do other people need to know what the therapist and child talk about?’
-
‘Does a young person have to like their therapist for treatment to help?’
-
-
Disseminating research evidence and findings to young people: suggestions for how to do this most effectively.
The group was given a range of tools to help the discussion. For example, they were given a pile of fake bank notes to help them allocate the funds to different intervention types. The visual component to this was important and the young people ensured that they distributed the money carefully, to reflect their priorities. They were also given voting cards with which to respond to the acceptability statements, with different colours representing different options.
Protocol
The evidence synthesis work was planned in accordance with guidance provided by the NHS Centre for Reviews and Dissemination69 and the Cochrane Collaboration. 70 The nature of the research objectives required evidence syntheses of (1) studies of the effectiveness of psychosocial interventions provided for children and adolescents who have suffered maltreatment; (2) studies of their acceptability to children, adolescents and their carers; and (3) the cost-effectiveness of these interventions.
A protocol for the review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria71 was developed and agreed with the Steering Group. The review protocol, which details the objectives, types of study design, participants, interventions and outcomes considered, is registered with PROSPERO (PROSPERO 2013: CRD42013003889). A copy of the review protocol is available at www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42013003889.
Inclusion and exclusion criteria
As this review was designed to address questions of effectiveness, acceptability and economic benefits, it was necessary to consider different study types. The inclusion criteria were tailored accordingly and our inclusion criteria and associated searches were kept deliberately broad to identify studies relevant to the aims set out in Chapter 1. The review considered both published and unpublished literature.
Types of study
Synthesis of evidence of effectiveness
Any controlled study (CS) in which psychosocial interventions were evaluated for this population was considered, including randomised and quasi-randomised trials, quasi-experimental (QEx) controlled studies and controlled observational studies (COSs). We used the following definitions.
Randomised controlled trial (RCT) Individuals followed in the trial are actively assigned to one of two (or more) alternative forms of intervention or health care, using an entirely random method of allocation (such as computer random number generation).
Quasi-randomised trial Individuals followed in the trial are actively assigned to one of two (or more) alternative forms of intervention or health care, using a quasi-random method of allocation (such as alternation, date of birth or case record number).
Quasi-experimental study Individuals followed in the study are actively assigned to one of two (or more) alternative forms of intervention or health care, using a non-random method of allocation (such as assignment based on experimenter’s choice).
Controlled observational study Individuals followed in the study are receiving one of two (or more) alternative forms of intervention or health care. However, they are not actively assigned to the alternative forms of intervention or health care. The control group is likely to comprise those who were not offered the intervention or who refused to participate in the intervention.
Uncontrolled study All individuals followed in the study are given the same treatment or health care, and simply followed for a period of time to see if they improve, with no comparison against another group (control group) that is either taking another treatment or no treatment at all.
Where no controlled effectiveness studies were identified, other study designs were considered, but purely for the purposes of informing the development of future research.
Case studies, descriptive studies, editorials, opinion papers and evaluations of pharmacological or physical interventions without an adjunctive psychosocial component were excluded from the synthesis of effectiveness studies.
Synthesis of acceptability studies
For this part of the review, studies that asked participants for their views were included, irrespective of study design or data type.
Any studies that provided quantitative data on non-participation, withdrawal and adherence rates were included as part of the effectiveness synthesis. We imposed no restrictions on design for this synthesis, as long as the study was about psychosocial interventions for treating the consequences of child maltreatment.
Economic evaluation
For this part of the review, we included economic evaluations that were carried out alongside trials and decision-analytic models, and uncontrolled study designs – such as uncontrolled costing studies – were considered, in addition to the study designs included in the synthesis of evidence of effectiveness. For the purposes of the synthesis of economic studies, whether trial based or decision model, economic evaluations based on data from RCTs were prioritised, although QEx controlled studies and COSs (cohort studies and case–control studies) were also considered. Uncontrolled study designs and descriptive costing studies were also considered, in addition to the study designs included in the synthesis of evidence of effectiveness, for the purposes of populating a decision model.
Types of populations/patients
Studies were eligible if recruitment was targeted at maltreated. Because young people in care remain entitled to support up until the age of 25 years, and because the effects of maltreatment are not always immediate, we included studies in which maltreatment took place before 17 years 11 months, but where the participants were aged up to 24 years 11 months. This also enabled us to minimize the loss of potentially relevant data. If the age range of participants was broader (e.g. 10–30 years) but the study met all other criteria, authors were contacted for further information, as appropriate.
Studies of interventions for a wide range of maltreatment types, including physical abuse, emotional and psychological abuse (including those witnessing domestic violence), sexual abuse and neglect were included. Studies were included if they involved maltreated participants as well as children and young people who had suffered other kinds of trauma (e.g. violent assault by a stranger) only if the participants were randomised and data for analyses were presented separately (or were obtainable). Studies that described children as ‘at risk’ because they had already experienced maltreatment were included. Studies involving children in care were included only if there was evidence that the participants were maltreated and the focus of the intervention was designed to address the sequelae of maltreatment. Studies were included whether or not the children involved were displaying any symptoms.
We excluded studies that were designed to evaluate interventions for other kinds of trauma, including teenage dating violence, those with children who had experienced violent physical assault by a stranger, and those where maltreatment had occurred during a conflict/war situation. We excluded studies that may have involved, but did not specifically target, maltreated children (e.g. studies of psychosocial interventions for depression in children and adolescents) and studies in which children were described as ‘at risk’ of maltreatment but which provided no evidence that they had already experienced maltreatment.
Types of interventions
Any psychosocial intervention provided to maltreated infants, children or adolescents in any setting (e.g. family, community, residential, school), and by any provider, aiming specifically to address the consequences of any form of maltreatment, with or without the involvement of a carer or carers.
Examples of eligible psychosocial interventions are listed in Chapter 1. We included any intervention based on cognitive theories (e.g. CBT, TF-CBT and abuse-focused CBT); EMDR; interventions based primarily on forms of expression and communication drawn from the arts (e.g. art therapy, drama therapy, music therapy, play therapy and narrative group therapy); attachment-based interventions; interventions based on psychoanalytic theories, offered to the child or parent–child dyads; family/systemic interventions; MST; peer mentoring; enhanced foster care, including treatment foster care; and residential care, including models of therapeutic residential care, such as CARE® and Sanctuary®. Further details about included interventions are provided in Appendix 5.
We included studies in which interventions were targeted at those responsible for the child (e.g. parents or services) and included outcomes for the children studied. Studies in which psychotropic medication was provided alongside psychosocial interventions were included.
As the review was focused on interventions addressing the consequences of maltreatment, we excluded studies that were aimed at the prevention, identification and cessation of maltreatment. We also excluded any study that assessed outcomes of those in standard foster care or standard residential care, for which no specific therapeutic aspect was being evaluated.
Types of comparisons
Studies comparing psychosocial interventions with no-treatment arms, wait-list control groups, ‘treatment as usual’ (TAU) and ‘other active treatment controls’ were included.
Types of outcomes
As described above, consultations were undertaken with key stakeholders in order to ensure appropriate primary and secondary outcomes were considered and at meaningful time points. We were interested in the following broad core outcome domains.
Primary outcomes of interest for children included the following domains: (1) psychological distress/mental health (particularly PTSD, depression and anxiety and self-harm); (2) behaviour (particularly internalising and externalising behaviours); (3) social functioning, including attachment and relationships with family and others; (4) cognitive/academic attainment; and (5) quality of life.
Secondary outcomes included (1) substance misuse; (2) delinquency; (3) resilience; and (4) acceptability.
We were also interested in recording any outcome related to carer distress, carer efficacy (the degree to which they feel empowered to care for the child appropriately and safely) and, where appropriate, placement stability. Outcomes themselves were not used as inclusion/exclusion criteria.
Search methods
One overarching search strategy was developed to ensure coverage across all elements of the review. Research, professional, policy and grey literature was searched using systematic and comprehensive search strategies of appropriate bibliographic databases and relevant websites.
Search term generation
Search terms relating to the key concepts of the review were initially identified through discussion between the research team and information scientists working for the Cochrane Developmental, Psychosocial and Learning Problems Review Group and the Cochrane Depression, Anxiety and Neurosis Group. Background literature and controlled vocabulary lists of relevant databases (e.g. medical subject heading terms in MEDLINE) were also scanned. Initial pilot search strategies were developed and discussed by the research team and Steering Group, and the electronic search strategy was modified and refined several times before implementation. No language limits or study design filters were applied. Examples of final electronic search strategies for several different databases [via MEDLINE Ovid; Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews (CDSR) and Database of Abstracts of Reviews of Effects (DARE) (via The Cochrane Library); ProQuest; EBSCOhost; eppi.ioe.ac.uk/webdatabases] are provided in Appendix 3.
Electronic searches
The following databases were first searched from the date of their inception between 28 February and 5 March 2013. Updating searches of the main databases were undertaken between 29 May 2014 and 2 June 2014. A full list of databases searched, with exact dates, is provided in Appendix 6.
-
Health and allied health literature [Ovid MEDLINE, CINAHL PsycINFO, EMBASE, CENTRAL, CDSR, DARE, Science Citation Index Expanded (SCIE), Health Management Information Consortium (HMIC)].
-
Social sciences and social welfare literature [Social Services Abstracts, Social Care Online, Social Science Citation Index (SSCI), Campbell Library of Systematic Reviews].
-
Education literature [Education Resources Information Center (ERIC), Australian Education Index, British Education Index].
-
Other evidence-based research repositories [Database of Promoting Health Effectiveness Reviews (DoPHER), Trials Register of Promoting Health Interventions (TRoPHI).
-
Economic databases [NHS Economic Evaluation Database (NHS EED), Paediatric Economic Database Evaluation (PEDE), Health Economic Evaluations Database (HEED), EconLit and the IDEAS economics database.
Updating searches planned prior to publication included trials registers [International Clinical Trials Registry Platform (ICTRP) and ClinicalTrials.gov; UK Clinical Research Network (UKCRN) Study Portfolio].
Grey literature and other resource searches
Material generated by user-led or voluntary sector enquiry was identified via OpenGrey, searching the internet (using Google and Google Scholar) and browsing the websites of relevant UK government departments and charities (Mental Health Foundation, Barnardo’s, Carers UK, ChildLine, Children’s Society, Depression Alliance, MIND, Anxiety UK, NSPCC, Princess Royal Trust for Carers, SANE, The Site, Turning Point, Young Minds and the National Child Traumatic Stress Network). These sites were systematically searched by members of the research team or members of the wider Steering Group using a selection and combination of search terms as appropriate. The process is described in detail in Appendix 7. Grey literature searches were up to date as of 25 June 2014. Requests were also sent to members of the Steering Group for additional studies.
Reference lists
We checked references in studies that met the inclusion criteria, in previous reviews and other studies.
Targeted author searches
We conducted targeted author searchers following the identification of key researchers in the field and looked for follow-up studies using Google Scholar. Authors of ongoing and recently completed research projects were also contacted directly as required to establish whether or not any results were available.
Data collection and analysis
Screening of citations and study selection
The original search was completed on 26 June 2013 and an updated search was undertaken on 4 June 2014. Search results were either imported into EndNote version 4 (Thomson Reuters, CA, USA) or saved as text files. After removing obvious duplicates and irrelevant records, remaining records were imported into EPPI-Reviewer 4.7172 (Evidence for Policy and Practice Information and Co-ordinating Centre, University of London, London, UK), through which further duplicates were removed. Duplicates were removed by two reviewers (NL and JH). Citations were then stored for sifting and management using EPPI-Reviewer.
Owing to the volume of citations identified, it was not possible to double-code the screening of all citations. To ensure that reviewers were consistent in their decisions, five reviewers (JH, NL, CMcC, MC, GM) initially coded the same 300 citations. Decisions were discussed, and selection criteria refined and clarified. Once this process was complete and reviewers were satisfied that selection criteria were being understood and applied consistently, each reviewer was assigned citations in batches of 1000 citations at a time. To ensure that reviewers decisions remained consistent, 10% of citations were double-coded and disagreements were resolved by discussion before moving on to the next batch of citations. Wherever a reviewer was uncertain about which code should be applied a second opinion was sought from another member of the research team.
When both reviewers agreed on inclusion, or whenever there was disagreement or uncertainty about inclusion, the full-text article was obtained. When potentially relevant studies were published as abstracts, or when there was insufficient information to assess eligibility or extract the relevant data, authors were contacted directly. To ensure consistency in the application of inclusion criteria for full-text articles, the same checking procedures were used. Each reviewer was assigned full-text articles in batches of 500 articles. Although 10% of full-text articles were initially cross-checked, second opinions were required on almost every article. Therefore, two reviewers read full reports and determined eligibility for all studies.
Any unresolved disagreements were discussed with the research team and, where necessary, eligibility criteria were further operationalised through discussion with input from the Steering Group. When maltreatment was not confirmed in the population but was considered likely to have occurred (e.g. concern from referring person that neglect was occurring), authors were contacted for further information. Principal reasons for the exclusion of studies were recorded.
Data extraction and management
Data extraction forms tailored to review objectives were developed for both the effectiveness and acceptability studies. These were piloted and refined using the first 10 papers marked for inclusion. For each included study, two review authors independently extracted and recorded the following data using a data collection form: study design and methods, sample characteristics, intervention characteristics (including theoretical underpinning of services, delivery, duration, outcomes and within-intervention variability), outcome measures and assessment time points. Where necessary, study investigators were contacted for clarification about study characteristics and data. Any differences that could not be resolved were noted.
As expected, the studies that met our inclusion criteria covered a heterogeneous group of psychosocial interventions designed to address the adverse consequences of child maltreatment. For the purposes of this review, we sought to group these according to common factors in their underlying theories of change. We recognise that there is much debate about the theoretical underpinnings and classification of different types of therapy, and that some may disagree about the decisions we have made.
We summarised therapies according to the groupings below. Further details and descriptions of the therapeutic approaches can be found in Appendix 5.
-
Cognitive–behavioural therapies:
-
CBT
-
behavioural therapies
-
modelling and skills training
-
TF-CBT
-
EMDR.
-
-
Relationship-based interventions (RBIs):
-
attachment-orientated interventions
-
Attachment and Biobehavioral Catch-up (ABC)
-
parent–child interaction therapy (PCIT)
-
parenting interventions
-
dyadic developmental psychotherapy (DDP).
-
-
Systemic interventions:
-
systemic family therapy (FT)
-
transtheoretical intervention
-
MST
-
multigroup FT
-
family-based programme.
-
-
Psychoeducation
-
Group work with children
-
Psychotherapy (unspecified)
-
Counselling
-
Peer mentoring
-
Intensive service models:
-
treatment foster care
-
therapeutic residential/day care
-
co-ordinated care.
-
-
Activity-based therapies:
-
arts therapy
-
play/activity interventions
-
animal therapy.
-
Assessment of risk of bias/study quality
Risk of bias in RCTs was assessed using the Cochrane Risk of Bias Tool. 73 We searched ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform to identify prospectively registered trial.
For non-randomised studies, the Downs and Black Checklist74 for non-randomised studies was used. The quality of acceptability studies was assessed against the relevant Critical Appraisal Skills Programme tool75 and the principles of good practice for conducting social research with children. The quality/risk of bias of all eligible studies was assessed, but no study was excluded from the acceptability phase of the review on the basis of its strength of evidence. The quality of data included within the economic evaluation was assessed using the critical appraisal criteria proposed by Drummond et al. 76 (see Appendix 8). The aim of the checklist is to assist users of economic evaluations to assess the validity of the results by attempting to determine if the methodology used in the study is appropriate. The checklist asks 10 questions, as reproduced in Appendix 7.
Data synthesis: effectiveness studies
We first mapped all of the studies of interventions against type of maltreatment (specific or multiple) and goals of treatment (outcome domains and measures). Interventions were grouped according to a simple classification system (e.g. whether or not the intervention had a given component, i.e. psychodynamic, cognitive). Priority was given to randomised and quasi-randomised trials, followed by non-randomised studies with comparison groups, although only data from RCTs were included in any meta-analyses, largely due to concerns about the quality of the data.
Measures of treatment effect
Dichotomous outcomes For dichotomous outcomes (e.g. attachment behaviours), we calculated effect sizes as odds ratios (ORs) with 95% confidence intervals (CIs). We converted continuous outcome data (e.g. post-intervention depression) into standardised mean differences (SMDs) and presented data with 95% CIs.
Continuous data Unadjusted data were extracted where possible, both for consistency of interpretation across studies and because we anticipated that this data source would be less susceptible to selective reporting bias (in particular, the strategy prevents the possibility of biased selection of covariates for inclusion in the model). Ideally we would use ‘change from baseline’ measures in the meta-analyses because these reflect the correlations between measures at baseline and follow-up within individuals, and also avoids biases that can be introduced if there is an imbalance in baseline measures across arms (The Cochrane Handbook). However, ‘change from baseline’ measures were only rarely reported. We instead use follow-up measures in the meta-analyses; however note that these measures can be biased, especially if there is an imbalance in baseline measures between arms (which may occur because of flaws in randomisation process or simply due to small numbers). We compared baseline characteristics between arms and across studies, and for outcomes where there was an indication of intervention efficacy, we checked the robustness of these results by performing a sensitivity analysis to using ‘change from baseline measures’ with assumed values for correlation (see Sensitivity analyses).
Data synthesis
Where appropriate data were available, data synthesis was performed to pool the results. As clinical and trial heterogeneity were expected (even similar interventions are provided under different circumstances, by different providers, to different groups), we used a random-effects model. 77
Assessment of heterogeneity
We explored the extent to which age (< 10 years old vs. > 10 years old), gender, ethnicity, type of maltreatment (sexual vs. physical), intervention type and parent involvement (child-only intervention vs. parent-and-child intervention) might moderate the effects of psychosocial interventions.
Sensitivity analyses
Publication bias and small study effects were investigated using standards methods (e.g. funnel plots) and also within the synthesis models. 78 When the data did not support such methods, the likelihood of publication bias was summarised narratively.
We examined the impact of trial/study factors, including risks of bias domains and cointerventions.
For outcomes where there was an indication of intervention efficacy, we checked the robustness of results to using a ‘change from baseline’ measure, rather than ‘follow-up’ measure. In the sensitivity analysis, we derived ‘change from baseline’ measures by assuming values for the correlation between baseline and follow-up measures: p = 0, 0.25, 0.5, 0.75, 1. The standard deviation (SD) of the mean change from baseline, sdchange, can then be estimated from the SD at baseline, sd0, and the SD at follow-up, sd1, using the formula:
Data synthesis: acceptability studies
A synthesis of acceptability data was undertaken, using a narrative approach to synthesis. 79 Studies were grouped into theoretically distinct subgroups. Using these intervention subgroupings, each study was described, and data synthesis was conducted and reported using the following categories: children’s views of the intervention, caregiver views, clinician views and attrition/engagement metrics. The structure of this narrative was informed and framed by the content and methodological expertise available within the research team and consultation with Young Persons’ Advisory Groups. Thematic analysis was also carried out to identify common issues and barriers relating to acceptability.
Data synthesis: economic evidence
The economic component of the project aimed to (1) systematically review all full economic evaluations of interventions that were designed to improve outcomes for maltreated children, using a narrative approach, where full economic evaluation is defined as the analysis of both the costs and effects of one intervention compared with another (including cost-effectiveness, cost–utility, cost–benefit or cost–consequences analysis); (2) produce a decision-analytic model to quantitatively explore the relative cost-effectiveness of interventions found to show promising levels of effectiveness in the effectiveness review and meta-analyses; and (3) perform a value of information analysis to quantify the extent to which further primary research to reduce uncertainty is warranted and where additional research may be most valuable. However, lack of relevant economic evidence precluded both decision-analytic modelling and value-of-information analyses.
Instead, we conducted cost-effectiveness analyses for the most promising intervention using SMDs from meta-analyses as the measure of outcome, and, additionally, using the results of a meta-analysis of a subgroup of studies that reported outcomes in terms of a single clinical measure – the Children’s Depression Inventory (CDI). 80 Although the first analysis allowed us to utilise all the available evidence, the second analysis provides evidence that is easier to interpret, focusing on the additional cost per unit improvement in CDI score, rather than per unit improvement in SMD.
Intervention costs were calculated from data included in each paper on the nature of the intervention under evaluation, including the number and duration of sessions and the format of delivery (group or individual). Unit costs were estimated using nationally applicable UK unit costs per hour of face-to-face contact for relevant professionals81 (www.pssru.ac.uk/project-pages/unit-costs/2014/). It was not always clear from the papers which professionals had delivered the interventions and thus we estimated costs for three categories of professional: clinical psychologist, psychologist and counsellor. We applied an average cost of the three categories of professionals, weighted to take into consideration the number of group-based interventions compared with individual interventions. Data on the use of broader health and social care services were not available from the literature, so these costs were excluded.
Cost-effectiveness was explored initially through the calculation of incremental cost-effectiveness ratios (ICERs), defined as the difference in mean costs divided by the difference in mean effects between the two groups. 82 We report the ICERs for SMD and CDI80 post treatment (for which the greatest number of studies were available) and 12-month follow-up (to capture the longer-term implications).
Uncertainty was explored using probabilistic sensitivity analysis, a form of analysis that involves assigning probability distributions to parameters (costs and effects) and sampling at random from the distributions to generate an empirical distribution for each parameter. 83 To represent uncertainty in costs, we fitted a gamma distribution constrained between 0 and positive infinity, to reflect the fact that cost data are commonly skewed in nature. For SMD and CDI,80 we assigned a normal distribution. Cost-effectiveness acceptability curves (CEACs) are presented, which are derived from the joint density of incremental costs and incremental effects and represent the probability of one intervention being more cost-effective than the comparison as a function of the willingness to pay for a unit improvement in outcome. 84 As willingness to pay for an improvement in SMD and CDI80 are not known, a range of possible values of willingness to pay are plotted.
Changes from the original protocol
During the course of the review, we had cause to agree several minor departures from the original published protocol, as described below.
Inclusion of unpublished dissertations We had originally intended to include unpublished dissertations. The search strategy identified a much larger than anticipated number of citations, including 290 unpublished dissertations, many of which proved very difficult to access (most were from American universities). Owing to resources constraints, we took a pragmatic decision to exclude these from the review. To minimise the loss of relevant studies, two reviewers (JH, NL) independently reviewed the title and abstract of all 290 dissertations a second time, to identify any that were clearly evaluations of relevant interventions. We then searched for published papers associated with the 36 dissertations so identified, all of which had already been found in the original search.
Population A clarification is necessary regarding eligible study participants. As per protocol, we included only papers that aimed to address the sequelae of maltreatment. We had also originally aimed to include studies in which recruitment was ‘biased towards’ maltreated children. During the course of the review, we identified studies in which recruitment may have favoured maltreated children (e.g. foster children) but which did not actually address a sequelae of maltreatment. These studies were therefore excluded.
Outcomes We originally intended to map treatment goals and measures used as part of an examination of the underpinning ‘logic model’ of interventions and to inform future research priorities. The studies identified rarely provided sufficient information to be of any value in making such an assessment. Instead, for descriptive purposes, where available, we recorded the aim of the intervention and the outcome measures reported for all included papers. This information is presented in Chapter 3 (see Tables 3 and 4).
Searches We had planned to hand-search relevant journals. In view of the considerable number of potentially relevant studies that were identified through other search strategies, the research group agreed that additional hand searches were no longer necessary. We had also planned to search Health Searches Research Projects in Progress, but this database retrieves many hundreds of records of funded projects without publication details or links to reports. It was decided that the resources required to properly search this resource could not be justified.
Study screening and selection We used EPPI-Reviewer version 4 (Evidence for Policy and Practice Information and Co-ordinating Centre, University of London, London, UK) rather than a project website for the submission and addition of new references so that the team could screen and discuss them. Owing to the complexity of the topic, we chose not to check inter-rater reliability for judgements on study screening and selection, instead favouring detailed discussion and consensus about studies of uncertain eligibility.
Data synthesis – effectiveness studies We originally planned to contact study authors about any missing information so that we could consider the extent to which this might alter the conclusions of the syntheses. The considerable volume of eligible studies and the poor quality of the available data meant this was not an appropriate use of resources. If the data had allowed, we had planned to extend our meta-analysis by fitting network meta-analysis models to explore in more detail the effectiveness of different types and different components of interventions. 85,86 The quantity and quality of the data did not allow for this technique to be used.
Subgroup analyses If the available data had allowed, we had planned to explore the extent to which a variety of study characteristics moderated the effects of treatment. We did not have sufficient data to support these analyses and therefore present data descriptively where available, including: impact of current symptoms; ethnicity; maltreatment history (including whether intra- or extra-familial); time since maltreatment; care setting (family/out-of-home care including foster care/residential); care history; characteristics of intervention (setting, provider, duration); and the adjunctive treatments.
We had planned to perform sensitivity analyses based on the inclusion of the QEx-randomised and non-randomised studies but, owing to concerns about the quality of the data, we pooled data only from RCTs in any of the meta-analyses.
Economic synthesis We had planned to undertake decision-analytic modelling of the relative cost-effectiveness of interventions found to show promising levels of effectiveness in the effectiveness review and meta-analyses, and to use the decision model developed to perform a value-of-information analysis to quantify the extent to which further primary research to reduce uncertainty is warranted. However, lack of relevant economic evidence precluded decision modelling and thus the value-of-information analyses, as described above.
Overview of the evidence base
The search and sifting process is summarised in the PRISMA flow chart in Figure 1. A total of 39,541 citations were identified in the search, which were either imported into EndNote or saved as text files. After removing obvious duplicates and irrelevant records, a total of 39,303 records were imported into EPPI-Reviewer, and a further 12,799 duplicates were removed, leaving 26,504 citations to be sifted by title and abstract. Reviewers excluded 21,953 citations based on title and abstract. Reasons for exclusion included:
FIGURE 1.
Maltreatment review: flow chart. Original search date 26 June 2013, search update 4 June 2014. Numbers reflect the number of records, not the included studies for which there may be multiple citations. Sifting decisions are up to date as of 30 January 2014. Green numbers refer to records and black numbers refer to studies.

-
duplicate citation (819)
-
clearly irrelevant (4634)
-
adult participants (661)
-
not a maltreated sample (1515)
-
form of maltreatment not included in the review, for example peer bullying, trauma due to war (445)
-
participants were maltreated children but study not an evaluation study (7083)
-
a relevant intervention was described but not evaluated (2348)
-
evaluation of an intervention that was not relevant, for example abuse prevention programmes or drug interventions (999)
-
evaluation used a study design excluded from the review, for example case study (2093)
-
paper contained relevant background information but not an evaluation of a relevant intervention (299)
-
paper was a review paper not primary research (1057).
The remaining 4551 were initially brought forward to be sifted by full text. However, two published papers87,88 could not be accessed despite searches via a number of university libraries, interlibrary loans and attempts to contact the authors and 36 dissertations were not accessed. An additional seven papers were identified through searches of the reference list of included studies. Of those articles reviewed at the full-text stage, 4196 were excluded (of which 81 were duplicates), leaving 324 citations brought forward for data extraction. Of these citations, 230 were potentially relevant for effectiveness, 17 cost-effectiveness, 54 acceptability, four relevant to both effectiveness and cost-effectiveness, 18 relevant to both effectiveness and acceptability, and one relevant to all three.
A number of these citations were subsequently excluded after discussions within the review team (34 effectiveness, 16 cost-effectiveness – see Chapter 3, Table 7). This left 219 effectiveness citations, six economic citations and 73 acceptability papers.
Chapter 3 Description of studies
Effectiveness studies
Included studies
In total, we identified 198 studies (217 citations) assessing the effectiveness of relevant psychosocial interventions for maltreated children. Of these, 62 studies followed a randomised (n = 61) or quasi-randomised (n = 1) design. QEx designs were identified in eight studies, with a further 26 COSs and 101 uncontrolled studies. Table 1 provides an overview of evaluations of interventions by study design. Table 2 provides an overview of the distribution of evaluations across intervention category and maltreatment types, by study design (controlled, uncontrolled).
| Intervention category | Study design | Total | |||||
|---|---|---|---|---|---|---|---|
| RCT | Q-RCT | QEx | COS | UCS | |||
| CBT | CBT for sexual abuse | 11 | 1 | 30 | 56 | ||
| CBT for physical abuse | 3 | ||||||
| CBT for multiple abuse | 7 | ||||||
| EMDR | 2 | ||||||
| RBIs | Attachment-oriented interventions | 9 | 1 | 10 | 24 | ||
| PCIT | 3 | ||||||
| Parenting interventions | 2 | ||||||
| Systemic interventions | Systemic FT | 1 | 14 | 22 | |||
| Trans-theoretical intervention | 1 | ||||||
| Multisystemic FT | 3 | 1 | |||||
| Multigroup FT | 1 | ||||||
| Family-based programme | 1 | ||||||
| Psychoeducation | Psychoeducation | 7 | 3 | 7 | 11 | 28 | |
| Group work with children | Group work with children | 1 | 4 | 3 | 8 | ||
| Psychotherapy/counselling | Psychotherapy/counselling | 3 | 1 | 3 | 4 | 11 | |
| Peer mentoring | Peer mentoring | 2 | 0 | 2 | |||
| Intensive service models | Treatment foster care | 4a | 2 | 15 | 24 | ||
| Therapeutic residential/day care | 1 | 2 | |||||
| Co-ordinated care | 1 | ||||||
| Activity-based therapies | Arts therapy | 2 | 14 | 21 | |||
| Play/activity interventions | 1 | 1 | 1 | ||||
| Animal therapy | 2 | ||||||
| Totalsb | 61 | 1 | 8 | 26 | 101 | 198 | |
| Intervention category | Types of abuse (controlled, uncontrolled) | |||||
|---|---|---|---|---|---|---|
| Physical | Emotional | Sexual | Neglect | Multiple | Other | |
| CBT | 21 (11, 10) | 8 (4, 4) | 45 (20, 25) | 6 (3, 3) | 11 (3, 8) | 10 (6, 4) |
| Relationship-based interventions | 13 (7, 6) | 6 (5, 1) | 7 (3, 4) | 14 (7, 6) | 7 (5, 2) | 14 (9, 5) |
| Systemic interventions | 11 (6, 5) | 5 (2, 3) | 12 (4, 8) | 5 (3, 2) | 3 (1, 2) | 4 (0, 4) |
| Psychoeducation | 9 (7, 2) | 5 (7, 1) | 21 (12, 9) | 5 (3, 2) | 4 (2, 2) | 8 (6, 2) |
| Group work with children | 0 (0, 0) | 0 (0, 0) | 8 (5, 3) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Psychotherapy (unspecified) | 4 (3, 1) | 1 (1, 0) | 10 (6, 4) | 3 (3, 0) | 2 (2, 0) | 0 (0, 0) |
| Peer mentoring | 2 (2, 0) | 0 (0, 0) | 0 (0, 0) | 2 (2, 0) | 1 (1, 0) | 0 (0, 0) |
| Intensive service models | 16 (7, 9) | 5 (4, 1) | 14 (5, 9) | 11 (6, 5) | 8 (6, 2) | 7 (1, 6) |
| Activity-based therapies | 8 (3, 6) | 1 (0, 1) | 16 (5, 11) | 4 (1, 3) | 2 (0, 2) | 6 (2, 4) |
| Totals | 84 (45, 39) | 30 (19, 11) | 134 (60, 72) | 49 (28, 21) | 38 (20, 18) | 49 (24, 25) |
The interventions and comparisons evaluated are summarised below and described in detail in Chapter 4. All controlled studies are summarised in Table 3 (participant characteristics), Table 4 (intervention characteristics and comparators) and Table 5 (outcomes domains and outcome measures used). The uncontrolled studies identified are summarised in Table 6. In the protocol, we specified that these studies would be included only if no other controlled studies were identified for the intervention evaluated. This was the case only for ‘systemic interventions’ for ‘other’ types of abuse (e.g. witnessing domestic violence, Munchausen’s syndrome by proxy) and ‘activity-based interventions’ for ‘emotional’ forms of abuse. We therefore consider these only in Chapter 6, in the context of highlighting important gaps in the evidence base.
| Intervention category | Design | Study/record | Country | n | Mean age (SD), range | % Female | P | E | S | N | M | O |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT for sexual abuse | RCT | Berliner 199689 | USA | 154 | 8 years | 89 | ✗ | |||||
| RCT | Celano 199690 | USA | 47 | 10.5, 8–13 years | 100 | ✗ | ||||||
| RCT | Cohen 199691,92 | USA | 86 | 4.68, 2.11–7.1 years | 58 | ✗ | ||||||
| RCT | Cohen 199893,94 | USA | 82 | 11, 7.2–15.3 years | 68 | ✗ | ||||||
| RCT | Cohen 200495,96 | USA | 229 | 10.76, 8–14.9 years | 79 | ✗ | ||||||
| RCT | Deblinger 199697,98 | USA | 100 | 9.89 (2) 7–13 years | 83 | ✗ | ||||||
| RCT | Deblinger 200199 | USA | 63 | 5.45 (1.47), 2–8 years | 61 | ✗ | ||||||
| RCT | Deblinger 2011100 | USA | 210 | 7.6 (2.07), 4–11 years | 62 | ✗ | ||||||
| RCT | Foa 2013101 | USA | 61 | Intervention: 15.4, 14.9–15.8 years Control: 15.3, 14.7–15.9 years |
100 | ✗ | ||||||
| RCT | Jaberghaderi 2004102 | Iran | 14 | 12–13 years | 100 | ✗ | ||||||
| RCT | King 2000103 | Australia | 36 | 11.4, 5.2–17.4 years | 69 | ✗ | ||||||
| COS | Paquette 2011104,105 | Canada | 35 | 14.3 (1.5) years | 100 | ✗ | ||||||
| CBT for physical abuse | RCT | LeSure-Lester 2002106 | USA | 12 | 13.16, 12–16 years | 0 | ✗ | |||||
| RCT | aKolko 1996107,108 | USA | 55 | 8.6 (2.2) years (no information on control group) | 28 | ✗ | ||||||
| RCT | Runyon 2010109 | USA | 75 | 9.88 (2.02), 7–13 years | 47 | ✗ | ||||||
| CBT for multiple abuse | RCT | Champion 2012110 | USA | 559 | 16.46 (1.34) 14–18 years | 100 | ✗ | ✗ | ✗ | |||
| RCT | Church 2012111 | Peru | 16 | 13.9, 12–17 years | 0 | ✗ | ||||||
| RCT | Jensen 2014112,113 | Norway | 156 | 15.1 (2.2), 10–18 years | 80 | ✗ | ✗ | ✗ | ||||
| RCT | Linares 2006114 | USA | 128 | 6.2 (2.3), 3–10 years | No info | ✗ | ✗ | ✗ | ||||
| RCT | Linares 2012115 | USA | 94 | 6.7 (1.1) 5–8 years | 51 | ✗ | ✗ | ✗ | ||||
| RCT | Rushton 2010116 | UK | 38 | 67 (18), 36–102 months | 55 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| RCT | Shirk 2014117 | USA | 43 | Intervention: 15.25 (1.52) years Control: 15.69 (1.55), 13–17 years |
84 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| COS | Kolko 2011118 | USA | 52 | 9.1 (3.7), 3–17 years | 48 | ✗ | ✗ | ✗ | ||||
| COS | Rondeau 1983119 | USA | 17 | 7.6 years (median) | 24 | ✗ | ||||||
| EMDR | RCT | Farkas 2008120 | Canada | 65 | Intervention: 14.3 (1.4) years Control: 14.9 (1.3) years |
63 | ✗ | |||||
| RCT | Scheck 1998121 | USA | 85 | 20.93, 16–25 years | 100 | ✗ | ✗ | ✗ | ||||
| Attachment-orientated interventions | RCT | Bernard 2012122 | USA | 120 | Intervention: 19.2 (5.2), 1.7–21.4 months Control: 19.2 (5.8), 1.7–21.4 months |
43 | ✗ | ✗ | ||||
| RCT | Cicchetti 2006123 | USA | 189 | 13.31 (0.81) months | 53 | ✗ | ✗ | ✗ | ✗ | |||
| RCT | Cicchetti 2011124 | USA | 137 | Intervention 1: 13.36 (0.87) months Control 1: 13.32 (0.87) months Intervention 2: 13.36 (0.82) months Control 2: 13.32 (0.71) months |
51 | ✗ | ✗ | ✗ | ✗ | |||
| RCT | Dozier 2006125,126 | USA | 60 | Intervention: 19.01 (9.64) 3.9–39.4 months Control: 16.3 (7.42) 3.6–33.6 months |
50 | ✗ | ||||||
| RCT | Lieberman 2005127–129 | USA | 75 | 4.06 (0.82) 3–5 years | 52 | ✗ | ||||||
| RCT | Moss 2011130 | Canada | 79 | Intervention: 3.29 (1.44) years Control: 3.42 (1.34) years |
39 | ✗ | ✗ | ✗ | ✗ | |||
| RCT | Spieker 2012131 | USA | 210 | Intervention: 18.29 (5.32) months Control: 18.15 (4.79) months |
44 | ✗ | ||||||
| RCT | Sprang 2009132 | USA | 58 | 42.5 (18.6) months | 49 | ✗ | ||||||
| RCT | Toth 2002133 | USA | 155 | Intervention 1: 48 (7.71) months Control 1: 49.16 (7.54) months Intervention 2: 47.86 (6.07) months Control 2: 47.77 (6.66) months |
45 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| COS | Becker-Weidman 2006134,135 | USA | 69 | Intervention: 9.4 (2.6) 6.0–15.2 years Control: 11.7 (4.0) 5.3–16.2 years |
41 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| PCIT | RCT | Chaffin 2004136 | USA | 110 | 4–12 years | No info | ✗ | ✗ | ||||
| RCT | Thomas 2011137 | Australia | 150 | 5 (1.6) years | 30 | ✗ | ✗ | ✗ | ||||
| RCT | Thomas 2012138 | Australia | 151 | 4.75 (1.3) years | 29 | ✗ | ✗ | ✗ | ||||
| Parenting interventions | RCT | Hughes 2004139 | Canada | 28 | Intervention: 65 (19.09) 42–100 months Control: 61 (17.63) 36–93 months |
38 | ✗ | |||||
| RCT | Valentino 2013140 | USA | 44 | Intervention: 5.44 (0.23) years Control: 5.59 (0.22) years |
55 | ✗ | ||||||
| Systemic FT | RCT | aKolko 1996107,108 | USA | 55 | 8.6 (2.2) years (no info on control group) | 28 | ✗ | |||||
| Transtheoretical intervention | RCT | Linares 2015141 | USA | 22 | Average age of sibling pairs 7.2 – 9.7 years | 55 | ✗ | ✗ | ||||
| Multisystemic FT | RCT | Brunk 1987142 | USA | 43 | 8.3 years | 45 | ✗ | ✗ | ||||
| RCT | Danielson 2012143 | USA | 30 | 14.8 (1.5) 13–17 years | 88 | ✗ | ||||||
| RCT | Swenson 2010144 | USA | 90 | Intervention: 13.81 (2.22) years Control: 13.95 (1.91) years |
56 | ✗ | ||||||
| RCT | Biehal 2012145,146 | UK | 34 | 12.7 years | ✗ | |||||||
| COS | Schaeffer 2013147 | USA | 44 | Intervention: 12.8 years Control: 10.8 years |
44 | ✗ | ✗ | ✗ | ||||
| Multigroup FT | RCT | Meezan 1998148,149 | USA | 81 | 2–11 years | No info | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Family-based programme | QEx | Bagley 2000150 | Canada | 93 | Intervention: 11.2 years Control: 11.8 years |
100 | ✗ | |||||
| Psychoeducation | RCT | Graham-Berman 2007151 | USA | 181 | 8.49 (2.16) 6–12 years | 50 | ✗ | ✗ | ||||
| RCT | Howell 2013152 | USA | 113 | 4.95 (0.86) 4–6 years | 47 | ✗ | ||||||
| RCT | Overbeek 2013153 | Netherlands | 164 | Intervention: 9.35 (1.55) years Control: 8.99 (1.43) years |
45 | ✗ | ||||||
| RCT | Sullivan 2002154 | USA | 80 | 8.3, 6.5–11 years | 55 | ✗ | ✗ | ✗ | ||||
| RCT | Trowell 2002155 | UK | 71 | 10 (2.2) 6–14 | 100 | ✗ | ||||||
| RCT | Wagar 1995156 | Canada | 42 | Intervention: 10.2 (1.74) years Control: 10.57 (1.93) years |
29 | ✗ | ||||||
| RCT | Wolfe 2003157 | Canada | 191 | Intervention: 15.1 (1.1) years Control: 15.2 (1.1) years |
52 | ✗ | ✗ | ✗ | ✗ | |||
| QEx | Noether 2007158 | USA | 253 | 7.28 years | 90 | ✗ | ✗ | ✗ | ||||
| QEx | Simoneau 2008159 | Canada | 57 | 9.19 (2.0) 6–13 | 78.9 | ✗ | ||||||
| QEx | Tourigny 2007160 | Canada | 55 | Intervention 1: 14.4 years Control 1: 14.8 years Intervention 2: 15.2 years |
100 | ✗ | ||||||
| COS | Barth 1994161 | USA | 27 | Intervention: 8.2 years Control: 9.6 years |
83 | ✗ | ||||||
| COS | Duffany 2009162 | USA | 834 | 6.8 (2.6) 3–12 years | 51 | ✗ | ||||||
| COS | Hébert 2010163 | Canada | 107 | Intervention: 8.67 (2.00) years Control: 8.64 (1.78) years |
80 | ✗ | ||||||
| COS | Holland 2004164 | Canada | 66 | 13 (median), 5–19 years | 70 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| COS | Santibáñez 2000165 | Spain | 30 | 14.35 (1.65) 11–16 years | 37 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| COS | Tourigny 2005166,167 | Canada | 42 | Intervention: 14.8 years Control: 14.3 years |
100 | ✗ | ||||||
| COS | Tourigny 2008168 | Canada | 53 | Intervention: 15.5 years Control: 14.6 years |
no info | ✗ | ||||||
| Group work with children | Q-RCT | Monck 1996169 | UK | 47 | 4–13 years | 85 | ✗ | |||||
| COS | De Luca 1995170 | Canada | 70 | 7–12 years | 100 | ✗ | ||||||
| COS | Grayston 1995171 | Canada | 12 | 7–10 years | 0 | ✗ | ||||||
| COS | McGain 1995172 | USA | 30 | 10.5 (1.21), 9–12 years | 100 | ✗ | ||||||
| COS | Verleur 1986173 | USA | 30 | 13–17 years | 100 | ✗ | ||||||
| Psychotherapy/counselling | RCT | Thun 2002174 | USA | 13 | 16–18 years | 100 | ✗ | |||||
| RCT | Haight 2010175 | USA | 22 | 9.6, 7–14.6 years | 40 | ✗ | ✗ | ✗ | ✗ | |||
| RCT | Reddy 2013176 | USA | 70 | 14.7 (1.14) years | 56 | ✗ | ✗ | ✗ | ✗ | |||
| RCT | Trowell 2002155 | UK | 71 | 11.5; 11.4 [I;C] (2.2) 6–14 | 100 | ✗ | ||||||
| QEx | Cadol 1975177 | USA | 140 | Intervention 1: 17.2 months Control 1: 15.8 months Intervention 2: 14.0 months Control 2: 17.7 months |
34 | ✗ | ✗ | ✗ | ||||
| COS | Nolan 2002178 | Ireland | 38 | Intervention 1: 12.6 (2.3) 6–17 years Intervention 2: 12.7 (2.2) 6–17 years |
93 | ✗ | ||||||
| COS | Sullivan 1992179 | USA | 72 | 12–16 years | 29 | ✗ | ||||||
| COS | Downing 1988180 | USA | 22 | 6–12 years | 59 | ✗ | ||||||
| Peer mentoring | RCT | Fantuzzo 1988181 | USA | 36 | 4.3, 3.1–5.3 years | 22 | ✗ | ✗ | ||||
| RCT | Fantuzzo 1996182 | USA | 46 | Intervention: 4.53 (0.21) years Control: 4.34 (0.30) years |
60 | ✗ | ✗ | ✗ | ||||
| Treatment foster care | RCT | Fisher 2005183–188 | USA | 177 | 4.4 (0.79–0.86), 3–6 years | 47 | ✗ | ✗ | ✗ | ✗ | ✗ | |
| RCT | Smith 2011189 | USA | 100 | 11.54 (0.48) years | 100 | ✗ | ✗ | |||||
| RCT | Taussig 2010190,191 | USA | 156 | 10.4 (0.9), 9–11 years | 49 | ✗ | ✗ | ✗ | ✗ | |||
| COS | Fisher 2000192 | USA | 30 | Intervention: 5.35 years Control 1: 4.40 years Control 2: 4.48 years |
30 | ✗ | ||||||
| COS | Graham 2012193 | USA | 37 | 73.26 (10.9), 59.89–106.09 months | 49 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Therapeutic residential and day care | RCT | Moore 1998194 | USA | 61 | Intervention: 0.92 (0.6) years Control: 1.1 (0.7) years |
54 | ✗ | |||||
| COS | Culp 1987195,196 | USA | 70 | 2.4, 0.1–6.2 years | 44 | ✗ | ✗ | |||||
| COS | Culp 1991197 | USA | 34 | 4.8, 3.9–5.9 years | 44 | ✗ | ✗ | |||||
| Co-ordinated care | RCT | Swenson 2000198 | USA | 66 | 8, 0–16 years | 53 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Arts therapy | QEx | Brillantes-Evangelista 2013199 | Philippines | 33 | 13–18 years | 64 | ✗ | ✗ | ||||
| QEx | Pretorius 2010200 | South Africa | 12 | 8–11 years | 100 | ✗ | ||||||
| Play/activity | COS | D’Andrea 2013201 | USA | 88 | 12–21 years | 100 | ✗ | ✗ | ✗ | |||
| RCT | McDonald 1989202 | USA | 38 | 8–17 years | 50 | ✗ | ||||||
| QEx | Udwin 1983203 | UK | 34 | Intervention: 58.3 (9.45) months Control: 55.82 (12.29) months |
41 | ✗ | ||||||
| Animal therapy | COS | Dietz 2012204 | USA | 153 | Intervention 1: 11.57 (2.85) years Intervention 2: 10.97 (2.63) years Control: 11.63 (2.46) years |
95 | ✗ | |||||
| – | Hamama 2011205 | Israel | 18 | Intervention: 15.33 (1.12) years Control: 14.56 (1.88) years |
100 | ✗ | ✗ | |||||
| Cognitive-behavioural | Relationship based | Systemic | Psychoeducation | |||||||||
| Psychotherapy/counselling | Peer mentoring | Intensive service models | Activity based | |||||||||
| Group work with children | ||||||||||||
| Intervention category | Study | Design | Setting | Name, aim, theory | Comparators |
|---|---|---|---|---|---|
| CBT for sexual abuse | Berliner 199689 | RCT | Health service/hospital | Name: Enhanced group treatment approach Aim: To reduce fear and anxiety in sexually abused children Theory: Designed to be a structured equivalent of conventional sexual abuse-specific group therapy treatment – included elements of GE treatment procedures and SIT |
Comparison treatment included common elements of conventional sexual abuse treatment, but it did not include SIT |
| Celano 199690 | RCT | Health service/hospital | Name: RAP Aim: To address children’s maladaptive beliefs, affects, and behaviour along four dimensions, (self-blame/stigmatisation, betrayal, traumatic sexualisation, powerlessness) Theory: Finkelhor’s and Browne’s (1985206) theoretical model of the four traumagenic dynamics intrinsic to sexual abuse |
TAU | |
| Cohen 199691,92 | RCT | Health service/hospital | Name: CBT for sexually abused preschoolers Aim: Treatment of the sequelae of sexual abuse in preschool children and their parents Theory: CBT |
Non-directive supportive therapy | |
| Cohen 199893,94 | RCT | Health service/hospital | Name: SAS-CBT and behavioural difficulties related to sexual abuse Theory: Finkelhor (1987)207 – theoretical model of the impact of sexual abuse on children |
Non-directive supportive therapy | |
| Cohen 200495,96 | RCT | Health service/hospital | Name: TF-CBT Aim: Treatment of the sequelae of sexual abuse Theory: Cognitive and learning theories about PTSD in children |
CCT | |
| Deblinger 199697,98 | RCT | Community | Name: CBT for PTSD for sexually abused children Aim: To target sexually abused children’s PTSD symptoms, as well as other behavioural and emotional problems Theory: CBT |
Standard community care | |
| Deblinger 200199 | RCT | Not reported | Name: Cognitive Behavioural Group Aim: (1) Help child communicate about their feelings; (2) identify ‘OK’ and ‘Not OK’ touches; and (3) learn abuse response skills Theory: No specific but CBT theoretical framework is well known. Supportive therapy: unclear |
Supportive counselling | |
| Deblinger 2011100 | RCT | Not reported | Name: TF-CBT Aim: Assess effects of treatment on severity of the PTSD, internalising, externalising, depressive and anxiety symptoms of the children, along with their levels of sexualised behaviours, fear, shame and body safety skills Theory: CBT |
No non-CBT comparison – study compared TF-CBT with and without TN | |
| Foa 2013101 | RCT | Health service/hospital | Name: Prolonged exposure programme modified for adolescent girls with sexual abuse-related PTSD Aim: To reduce PTSD severity, rate of PTSD diagnosis, self-reported PTSD severity and depression, and improve general functioning Theory: Prolonged exposure therapy |
Supportive counselling | |
| Jaberghaderi 2004102 | RCT | Health service/hospital – university clinic | Name: (1) EMDR and (2) CBT Aim: Overall aim of both – to address the sequelae of sexual abuse Theory: Not specified |
No non-CBT comparisons – study compared CBT with EMDR | |
| King 2000103 | RCT | Not reported | Name: Child CBT Intervention Aim: To help the child overcome his or her post-abuse distress and PTSD symptoms Theory: Deblinger’s work20,208 on the CBT of sexually abused children exhibiting PTSD was particularly influential in the development and refinement of the treatment protocol |
Wait-list control | |
| Paquette 2011104,105 | COS | Community | Name: Group therapy programme Aim: To ‘reduce the after effects associated with sexual abuse, increase social support seeking and prevent revictimisation’ Theory: An ‘eclectic viewpoint (cognitive–behavioural, cognitive and humanistic) was adopted while various technical approaches were used (e.g. modelling, social support, cognitive reframing)’ |
No treatment comparison group | |
| CBT for physical abuse | LeSure-Lester 2002106 | RCT | Care setting | Name: Cognitive behaviour therapeutic approach Aim: To ‘teach the adolescent alternative ways of thinking about, responding to, and feeling about, stressful situations typical to the adolescents social encounters’ Theory: Cognitive–behavioural therapeutic approach |
Active listening |
| Kolko 1996107,108 | RCT | Home based/health service/hospital | Name: Individual child–parent CBT Aim: Designed to alter participants’ cognitive, affective and behavioural–social repertoires Theory: Social learning principles |
Routine community services | |
| Runyon 2010109 | RCT | Health service/hospital | Name: Combined parent–child cognitive–behavioural group therapy for families Aim: (1) Decrease the risk of recurrence of physically abusive episodes; (2) assist parents in correcting unrealistic expectations and misinterpretations of children’s behaviours; (3) increase parents’ ability to manage their anger and utilise non-violent child management skills; (4) increase positive parent–child interactions; and (5) improve children’s overall emotional adjustment Theory: CPC-CBT is based on cognitive–behavioural principles and includes some of the CBT techniques that have been included in pre-existing empirically validated models, such as TF-CBT (Deblinger and Heflin 1996208) |
No non-CBT comparison – study compared CPC-CBT with parent-only CBT | |
| CBT for multiple abuse | Champion 2012110 | RCT | Health service/hospital | Name: PI intervention Aim: Counselling for abused ethnic minority adolescent women on infection with STI Theory: Theory-based ARRM; (Catania et al. 1990209) cognitive–behavioural intervention model vs. enhanced counselling |
Enhanced clinical counselling |
| Church 2012111 | RCT | Care setting | Name: EFT Aim: Treatment for traumatic stress Theory: ‘EFT employs brief forms of certain components of therapies that have demonstrated efficacy, such as cognitive restructuring and exposure. To these it adds a somatic component, having therapists or subjects tap with their fingers on prescribed acupuncture points while cognitive statements are made’ |
Wait-list control | |
| Jensen 2014112,113 | RCT | Health service/hospital | Name: TF-CBT Aim: To treat children and youth exposed to traumatising events Theory: CBT |
TAU | |
| Linares 2006114 | RCT | Not reported | Name: Parenting course (Incredible Years210) Aim: The proximal outcomes are positive discipline practices and collaborative coparenting, whereas the distal goal is the reduction of child externalising problems over time Theory: Coparenting strategy, whereby caregivers acknowledge the inequality in their roles, learn to communicate and resolve conflict directly and work to promote the emotional adjustment of children in foster care |
Standard UC condition | |
| Linares 2012115 | RCT | A classroom-like setting at each study site | Name: Child training – using 12 out of 18 lessons from Incredible Years Dina Program for Young Children211 Aim: Reducing conduct problems at home and school and improving conflict management strategies with peers Theory: Incredible Years Dina Program for Young Children211 |
Standard UC condition | |
| Rushton 2010116 | RCT | Home based | Name: Cognitive–behavioural intervention Aim: To improve the adopters’ understanding of the meaning of the children’s current behaviour and increase their ability to manage the behaviour Theory: ‘The cognitive–behavioural approach. The most direct influence in writing the manual for this approach has been the work of Webster-Stratton (Webster-Stratton 2003;212 Webster-Stratton and Hancock 1998213)’ |
Wait-list control | |
| Shirk 2014117 | RCT | Health service/hospital | Name: m-CBT Aim: Focus on addressing cognitive deficits and distortions to treat depression in traumatised adolescents Theory: CBT with focus on mindfulness techniques |
TAU | |
| Kolko 2011118 | COS | Community | Name: Alternatives for Families Aim: AF-CBT is an EBT for child physical abuse and family aggression/conflict Theory: Social learning/behavioural theory; family-systems theory; cognitive therapy; developmental victimology |
No non-CBT comparison – study compared AF-CBT with combination of other EBTs, including TF-CBT, PCIT, CPP, cognitive behavioural intervention for trauma in schools | |
| Rondeau 1983119 | COS | Care setting | Name: Art therapy, with or without token reward system Aim: Increase co-operative behaviour and art production Theory: Operant conditioning social exchange theory |
Art therapy without token reward system | |
| EMDR | Farkas 2008120 | RCT | Not reported | Name: MASTR/EMDR Aim: To reduce trauma symptoms and behavioural problems Theory: MASTR and EMDR |
Wait-list controls receiving routine care |
| Scheck 1998121 | RCT | Therapist setting | Name: EMDR Aim: ‘Using a series of manualised steps, the client reactivates the troubling memory while the practitioner intervenes at a variety of choice points to resolve distress (Shapiro 1995214)’ Theory: ‘EMDR is a specific desensitising treatment designed around a complex method’ |
Active listening | |
| Attachment-orientated interventions | Bernard 2012122 | RCT | Home based | Name: ABC Aim: ‘Targets nurturing, sensitive care among the parents identified as being at risk for neglecting their young children, with the aim of decreasing disorganised attachment’ Theory: Attachment theory |
DEF |
| Cicchetti 2006123 | RCT | Home based | Name: (1) IPP (2) PPI Aim: To foster secure attachment in infants in maltreating families Theory: IPP is derived from the work of Fraiberg et al. (1975215); PPI is derived from the work of Olds et al. (Olds et al. 1997,216 1998;217 Olds and Kitzman 1990218) |
Community standard group – received services as usual | |
| Cicchetti 2011124 | RCT | Home based | Name: CPP PPI Aim: CPP ‘encourages sensitive interactions between caregivers and their children by helping parents form positive representations of themselves and the caregiver–child relationship;’ PPI ‘teaches parenting skills, relaxation techniques, and behaviours that promote social support’ Theory: CPP is attachment based; PPI is a behavioural/education-based intervention |
Community Standard group – received services as usual | |
| Dozier 2006125,129 | RCT | Home based | Name: ABC Aim: Designed to help children develop regulatory control by helping foster carers to reinterpret children’s difficult behavior, overcome personal issues that interfere with their ability to provide nurturing care, and provide an environment that facilitates the development of self-regulation in children Theory: The intervention draws on strategies known to be associated with children’s ability to self-regulate, for example, following the child’s lead, recognizing the importance of value of touch, and creating the conditions under which children can express their emotions, and learn to recognize and understand them |
DEF | |
| Lieberman 2005127–129 | RCT | Not reported | Name: CPP Aim: To alleviate children’s traumatic stress symptoms and behaviour problems Theory: Attachment theory; developmental psychopathology models |
Case management plus individual psychotherapy | |
| Moss 2011130 | RCT | Home based | Name: Short-term attachment-based home-visiting intervention Aim: ‘Enhancing maternal sensitivity to child emotional and behavioural signals in order to promote greater child security’ Theory: Based on the work of Bakermans-Kranenburg et al. (1998219), Dozier et al. (2006125) and Moran et al. (2005220) |
Standard agency services | |
| Spieker 2012131 | RCT | Home based | Name: PFR Aim: To ‘increase caregiver awareness of children’s behavioural cues and miscues for nurturance’ Theory: ‘PFR includes many of the effective elements of brief attachment-based interventions summarised by Bakermans-Kranenburg et al.219’ |
EES | |
| Sprang 2009132 | RCT | Home based | Name: ABC Aim: To promote self-regulation among children in foster care by means of optimizing the parenting skills of foster parents Theory: Maltreated children often engage in resistant-avoidant behaviour, which can result in their carers withdrawing from them (Stovall-McClough and Dozier 2004221). By helping foster carers provide them with optimally sensitive parenting, children learn to depend on their assistance to manage their emotions, thereby develop their own emotional self-regulation skills |
Wait-list controls attended a biweekly support group | |
| Toth 2002133 | RCT | Home based/health service/hospital | Name: PPP, PHV Aim: The PPP model highlights the importance of parent–child attachment in fostering positive child development, improved parent–child interaction and decreases in child maltreatment. PHV focuses on parenting skill improvement and child adaptive competencies Theory: PPP based on attachment theory; PHV integration of ecological–transactional development model with psychoeducational and behavioural techniques |
Community Standard group | |
| Becker-Weidman 2006134,135 | COS | Health service/hospital | Name: DDP Aim: To reduce symptoms of attachment disorder, to increase capacity to use the caregiver as a secure base for comfort and security, to resolve grief and loss issues, to improve ability to form social relationships, to improve cause–effect thinking, to reduce aggression, to reduce delinquent behaviour Theory: An attachment-based treatment approach ‘Developmental Psychotherapy has as its core, or central therapeutic mechanism and as essential for treatment success, the maintenance of a contingent collaborative and affectively attuned relationship between therapist and child, between caregiver and child, and between therapist and caregiver’ |
UC from other providers at other clinics | |
| PCIT | Chaffin 2004136 | RCT | Health service/hospital | Name: PCIT Aim: Disrupting escalating coercive cycles and improving the quality of parent–child interactions Theory: Social learning theory based |
Standard community group |
| Thomas 2011137 | RCT | No information | Name: PCIT Aim: To address risk factors associated child maltreatment Theory: ‘PCIT was developed to improve parenting skills and parent–child interactions among families struggling with their children’s (ages 3–7 years) behaviour problems (e.g. ODD; Eyberg 1988;222 Hembree-Kigin and Neil 1995223)’ |
Wait-list control | |
| Thomas 2012138 | RCT | Tertiary referral service/research programme | Name: PCIT Aim: To compare the effectiveness of standard PCIT with PCIT that only moves from child-directed interaction to parent-directed interaction when mastery criteria for child-directed interaction have been reached Theory: As Thomas 2011137 |
Wait-list control | |
| Parenting Interventions | Hughes 2004139 | RCT | Community | Name: The Webster-Stratton parent programme Aim: To assist parents in improving their parenting ‘by helping they learn how to (a) play with and assist children to learn; (b) use praise and give reinforcement; (c) set age-appropriate limits; and (d) handle misbehaviour’ Theory: Intervention based on Social Learning Theory (Bandura 1977224) |
Wait-list control |
| Valentino 2013140 | RCT | Home based | Name: RET Aim: To help maltreating parents improve their communication skills and relationships with their children Theory: Parent–child reminiscing |
Wait-list control | |
| Systemic FT | Kolko 1996107,108 | RCT | Home based/health service/hospital | Name: FT Aim: To enhance family functioning and relationships Theory: ‘FT was designed to enhance family functioning and relationships (Alexanders and Parsons 1982;225 Robin and Foster 1989226), in accord with the interactional or ecological model approach to child maltreatment (Belsky 1993227)’ |
Routine community services |
| Transtheoretical intervention | Linares 2015141 | RCT | Community | Name: PSB Aim: To increase positive interaction between siblings, reduce conflict during play and promote conflict mediation strategies Theory: ‘Transtheoretical intervention model, which integrates principles of family systems, emotional regulation, social learning and parent mediation’ |
TAU |
| Multisystemic FT | Brunk 1987142 | RCT | Home based/care setting | Name: MST Aim: To effect ‘change in parental control strategies, including parental responsibility and effectiveness and child compliance’ Theory: Behaviour problems are assumed to be multidetermined and multidimensional; they therefore require interventions that can target one or more systems or combinations of systems |
Standard outpatient plus parent training |
| Danielson 2012143 | RCT | Health service/hospital | Name: RRFT Aim: To reduce risk of substance use and other high-risk behaviours and trauma-related psychopathology in adolescents who have experienced CSA Theory: Ecological Theory, Mowrer’s Two-Factor Theory (Mowrer 1960228) and Negative Reinforcement Theory (Baker et al. 2004229) |
TAU | |
| Swenson 2010144 | RCT | Home based/school/other convenient locations | Name: MST-CAN Aim: To ‘improve youth and parent functioning, reduce abusive parenting behaviour, and decrease reabuse and placement to a greater degree than an enhanced version of the standard outpatient treatment for child physical abuse provided at that agency (i.e. EOT)’ Theory: The core components of standard MST (Henggeler et al. 2009230) adapted for use with maltreated youth and their families |
EOT: Included the standard services the centre provided for physically abused youths and their parents, as well as enhanced engagement and parent training interventions | |
| Schaeffer 2013147 | COS | Home based | Name: MST-BSF Aim: To address ‘the co-occurring problem of parental substance abuse and child maltreatment among families involved in the child welfare system’ Theory: Ecological theory, systems and social learning theory |
Comprehensive community treatment | |
| Multigroup FT | Meezan 1998148,149 | RCT | Community | Name: MFGT Aim: To prevent and treat child abuse and neglect, to reduce abusive and neglectful carer behaviours, and to reduce the effects of maltreatment on the child Theory: Components of the intervention were drawn from family systems theory, structural FT, group therapy, CBT, reality therapy, parent education and crisis intervention |
Traditional FT (several theoretical frameworks including structural FT, behaviour modification and CBT strategies; also some case management) |
| Family-based program | Bagley 2000150 | QEx | Not reported | Name: CSATP Aim: Treatment of children subject to sexual abuse Theory: Maslow’s self-actualisation Theory, ‘A person’s strongest drive is to feel contented about himself or herself, and about others, ‘described as a humanistic model of intervention’ |
No treatment comparison group |
| Psychoeducation | Graham-Berman 2007151 | RCT | Community | Name: Kids’ Club Aim: To educate children about family violence and influence their attitudes and beliefs about families and family violence; to facilitate their emotional adjustment and promote their social competence Theory: ‘Relies on the theoretical assumptions that children may be distressed or made anxious by exposure to IPV as well as learn deleterious patterns of behaviour, attitudes, and beliefs as a result of observing violence (e.g. engage in aggressive behaviour with others; believe that violence is acceptable)’ |
Wait-list control |
| Howell 2013152 | RCT | Community | Name: The Preschool Kids’ Club intervention Aim: To promote the social competence of preschool children who have witnessed domestic violence Theory: as for Graham-Berman 2007151 |
No treatment comparison group | |
| Overbeek 2013153 | RCT | Not reported | Name: ‘Ennuik . . . !’ (‘It’s my turn now!’) Aim: ‘(a) To process the interparental violence experiences; (b) to learn how to differentiate and express emotions; and (c) to learn how to cope with feelings and problems in a different (non-violent) way’ Theory: Trauma theory (Perry 1993231) |
Control programme ‘Jij hoort erbij’ (‘You belong’) The control programme was based on an analysis of non-specific factors used in the specific factors intervention programme |
|
| Sullivan 2002154 | RCT | Community | Name: Community-based programme for battered women and their children Aim: Therapy aimed to: alleviate children’s guilt, treat their depression, help them learn to express anger, provide them with basic information about normal sexuality, help them deal with sexual preference and maltreatment issues, teach them self-protection techniques and equip them with an affective vocabulary to label emotions and feelings, promote emotional independence, and help them to establish a meaningful and stable identity, a personal value system and a capacity for lasting relationships Theory: The role of domestic violence support and education groups in helping children; the effect of mothers’ well-being on children’s well-being |
Services as usual | |
| Trowell 2002155 | RCT | Home based/health service/hospital | Name: Psychoeducational group therapy Aim: Reduction in psychiatric disorders and traumatogenic response; reduced frequency of sexualised and eroticised behaviour; and emotional development Theory: No explicit theory. Described as group psychotherapy with a psychoeducational component |
Brief focused individual psychotherapy | |
| Wagar 1995156 | RCT | Not reported | Name: Group treatment programme Aim: To ‘help children modify their responses and adopt new responses to past experiences of witnessing violence, to develop new problem-solving skills for future encounters, to address interpersonal responsibilities and attitudes regarding behaviours, and to examine present modes of conflict resolution and to foster self-esteem’ Theory: Programme developed by Jaffe et al. 1986232 |
No treatment comparison group | |
| Wolfe 2003157 | RCT | Community | Name: YRP Aim: To enable teenagers to make informed choices and learn non-violent means of communicating with their current and future partners Theory: Based on learning and feminist theories (Dobash and Dobash 1992233) |
Standard CPS | |
| Noether 2007158 | QEx | Health service/hospital | Name: Skills-based approach to promoting resilience Aim: To promote resilience Theory: Psychoeducation enhances the emotional and behavioural strengths of children |
Children in the comparison group received individual, group and family services | |
| Simoneau 2008159 | QEx | Community | Name: Group psychotherapy Aim: To reduce the sequelae associated with sexual abuse Specific objectives: Reduce social isolation; improve self-esteem; reduce behaviour problems; reduce guilt Theory: Describes evidence base for group therapy (as opposed to individual psychotherapy) |
Service as usual | |
| Tourigny 2007160 | QEx | Community | Name: Group treatment Aim: To reduce the negative and traumatic consequences of sexual abuse; to ensure survivors may attain normal development; to reduce social isolation and to reduce shame and culpability; and to help rely on personal resources and develop skills Theory: The psychoeducational approach |
No non-experimental comparison – study compared open-group format to closed-group format | |
| Barth 1994161 | COS | Not reported | Name: Psychoeducational group for foster parents Aim: To provide specialised training for foster parents caring for sexually abused children Theory: Providing foster parents with an understanding of the impact of sexual abuse on children’s behaviour will help them to be more empathetic and enable them to help their foster children to express their fears and concerns, instead of acting them out |
No treatment comparison group | |
| Duffany 2009162 | COS | Community | Name: CTP Aim: To prevent children who have been sexually abused from being reabused Theory: Group therapy may reduce feelings of stigmatization, isolation and shame. Groups provide ‘corrective’ experiences of their perceptions of self, and enable them to explore their experience of abuse and its consequences, and develop coping strategies |
No treatment comparison group | |
| Hébert 2010163 | COS | Health service/hospital | Name: Psychoeducational Group Intervention Aim: To ‘(a) reduce the negative consequences associated with CSA; (b) foster positive self-esteem; (c) help children recognise and express their feelings; (d) help children identify their personal coping resources to manage the aftermaths of CSA; (e) reduce sense of social isolation and shame; (f) foster positive parent–child relationship; and (g) prevent revictimisation’ Theory: Groups enable children to share experiences with other abused children, providing an opportunity to reduce any sense of isolation or stigmatisation. Groups provide a supportive social network and an opportunity for peer-to-peer learning, and building a sense of empowerment and self-esteem. They also provide an important forum for developing the skills associated with therapeutic objectives, e.g. social skills, expressing and communicating emotions about the traumatic event |
UC services | |
| Holland 2004164 | COS | Health service/hospital | Name: Sexual Abuse Intervention Program Aim: The client-centred, life space intervention methods used are individual counselling, family support, and group work (psychoeducational and social skills training, closed, 16 weeks) within a case management model Theory: Eclectic practice framework seems based on elements of generalist, problem-solving, ecological systems, and some feminist theories |
No treatment comparison group | |
| Santibáñez 2000165 | COS | Care setting | Name: Self-management programme Aim: To improve the educational intervention self-control and moral development of children living in homes dependent on the public network of group homes Theory: Draws various theories and experts, including Kanfer (1975234), Karoly (1977235) and Bandura (1969236) |
No treatment comparison group | |
| Tourigny 2005166,167 | COS | Community | Name: Psychoeducational group Aim: Reduce negative consequences of sexual abuse, social isolation, shame and culpability, and enhance coping skills development Theory: Psychoeducational approach – group discussions, personal testimonies, exercises and lectures |
Wait-list control | |
| Tourigny 2008168 | COS | Health service/hospital | Name: Brief group therapy Aim: To support victims of sexual abuse and to reduce sequelae associated with aggression; to reduce symptoms associated with sexual abuse (anxiety, depression, low self-esteem, behavioural problems, aggression, post-traumatic stress, school difficulties); to improve functioning, reduce isolation, reduce guilt, to help them use their internal resources to develop coping strategies; and to improve sense of control Theory: Describes group-based efficacy (cost-effectiveness, peer support); psychoeducational approach includes group discussions, storytelling, relaxation and visualisation/main themes covered but open to influence by participants |
No treatment comparison group | |
| Group Work with Children | Monck 1996169 | Q-RCT | Health service/hospital | Name: Family network treatment programme with or without group treatment Aim: To reduce effects of sexual abuse Theory: Intervention makes use of psychoeducation and narrative therapeutic activities (e.g. storytelling). Study refers to group work approach by Giaretto (1980237) and the family systems approach by Furniss (1983238) |
Family network treatment programme without group treatment |
| De Luca 1995170 | COS | Not reported | Name: Group therapy programme at the University of Manitoba Aim: To address issues and themes regarded as central in the treatment of sexual abuse (e.g. feelings about the offender, body image and self-esteem enhancement, social skills, sex education, prevention of abuse) Theory: Groups may reduce social isolation, as they provide sexually abused children with an opportunity to can meet others who have had similar experience. Groups provide opportunities for children to expand their social support networks and provide a number of educational opportunities, e.g. to develop their coping and social skills, and learn about healthy relationships. They are also cost-effective |
No treatment comparison group | |
| Grayston 1995171 | COS | Health service/hospital | Name: Group therapy programme Aim: Unclear: treating sexually abused boys, reducing internalising, externalising and sexual behaviour problems Theory: Unclear |
Wait-list control | |
| McGain 1995172 | COS | Community | Name: Group treatment Aim: To provide a safe environment in which children can discuss their experiences of abuse, and which can enhance their self-worth. To prevent remolestation. To avoid long-term psychological damage to children, and provide appropriate, non-exploitative adult role models. To provide support for children during court proceedings, and teach them practical steps to help them to protect themselves. The intervention also aims to help children talk about the dynamics of abuse, and to provide them with sustained peer support. Finally, the intervention aims to secure approval for treatment of the child’s family. Achieving these aims is thought to secure a decrease in distress and symptomatology Such a programme ought to (11) provide a decrease in distress and symptomology Theory: Social Learning Theory |
Wait-list control | |
| Verleur 1986173 | COS | Care setting | Name: Group therapy for female incest victims Aim: To increase self-esteem and knowledge of human sexuality, birth control and venereal disease Theory: Poor self-esteem is targeted as this appears to be a problem with the majority of incest victims |
No treatment comparison group | |
| Psychotherapy/counselling | Thun 2002174 | RCT | Not reported | Name: Group therapy Aim: To improve the self-image of adolescent survivors of sexual abuse Theory: A multidimensional model incorporating skills, psychotherapeutic and educational components |
No treatment comparison group |
| Haight 2010175 | RCT | Care setting | Name: LSI Aim: To establish an emotionally supportive relationship with the children, to help children interpret and gain a feeling of control and continuity in their lives, rethink views of themselves and others, and begin to alter problematic beliefs Theory: Theoretical perspective and methods of cultural developmental science (e.g. Rogoff 2003;239 Shweder et al. 2006240) |
No non-experimental comparison – study compared IT to IGT | |
| Trowell 2002155 | RCT | Home based/health service/hospital | Name: Focused individual psychotherapy vs. psychoeducational group therapy Aim: Reduction in psychiatric disorders and traumatogenic response, reduced frequency of sexualised and eroticised behaviour and emotional development Theory: Describes itself as individual psychoanalytic psychotherapy and the group as psychotherapeutic with a psychoeducational component |
Other treatment control | |
| Reddy 2013176 | RCT | Not reported | Name: CBCT Aim: Developing acceptance and understanding of others (Salzberg 2002241), stress management and coping techniques, additional health-relevant benefits Theory: Mindfulness meditation modified for children |
No treatment comparison group | |
| Cadol 1975177 | QEx | Health service/hospital | Name: Counselling Aim: ‘Feeling secure in social situations and community; managing crisis situations; assertiveness; personal awareness; educational counselling; child-care techniques; language improvement based on developmental delay of each child; appropriate expectations of children; recognising and rewarding positive behaviours’ Theory: No information |
Wait-list control group | |
| Nolan 2002178 | COS | Health service/hospital | Name: IT vs. combined IGT Aim: Treatment of the psychological sequelae of CSA Theory: ‘Therapy was predominantly integrative and based on principles drawn from IGT practices within the broad traditions of psychodynamic psychotherapy, client-centred therapy and CBT’ |
Wait-list control group | |
| Sullivan 1992179 | COS | Care setting | Name: Psychotherapy Aim: Alleviation of guilt, treatment of depression, learning to express anger, providing basic information about normal human sexuality, dealing with sexual preference, dealing with maltreatment issues, teaching the children self-protection techniques, development of an affective vocabulary to label emotions and feelings, attainment of emotional independence in the children, assistance in the establishment of a meaningful and stable identity, development of a personal value system; and development of a capacity for lasting relationships Theory: The psychological and behavioural impact on children of witnessing domestic violence is influenced by the availability of support and education groups, and their mother’s psychological well-being |
No treatment comparison group | |
| Downing 1988180 | COS | School | Name: Psychodynamic group counseling Aim: ‘to help families build support within their family unit: help families explain ideas, feelings and the nature of abusive events. Focus of treatment was (a) relief of guilt and (b) building positive self-concepts. Reinforcement orientation aimed to help parents provide the best possible child-rearing atmosphere’ Theory: Psychodynamic and reinforcement theories |
No non-experimental comparison group – study compared psychodynamic orientation group to reinforcement orientation | |
| Peer mentoring | Fantuzzo 1988181 | RCT | Community | Name: (1) Peer social initiation and (2) adult social initiation Aim: To increase positive social behaviour Theory: Social initiation procedures |
In control-group dyads peers or teacher’s aide were instructed to respond positively to social initiations but not to initiate social interactions |
| Fantuzzo 1996182 | RCT | School | Name: RPT Aim: ‘To promote the development of social competencies for preschool children in the context of classroom play mediated by a resourceful peer’ Theory: RPT |
Comparison children were each paired with a classmate of average interactive play ability | |
| Treatment foster care | Fisher 2005183–188 | RCT | Home based/care setting | Name: MTFC-P Aim: To facilitate attachment with caregivers, reduce insecure behaviour, decrease resistant and avoidant behaviours, and decrease permanent placement failure rate Theory: Attachment theory, social learning theory, systems theory |
Foster care services as usual |
| Biehal 2012145,146 | RCT | Home based/care setting | Name: MTFC-A Aim: To reduce problem behaviour, promote pro-social behaviour and enhance placement stability Theory: Social learning theory, systems theory |
RFC | |
| Smith 2011189 | RCT | Home based/care setting | Name: Preventive intervention for girls in foster care Aim: To prevent ‘internalising and externalising problems during the transition to middle school to help prevent more serious, longer-term outcomes, such as delinquency, substance use, and high-risk sexual behaviour in later middle school’ Theory: Aims could be achieved by helping participants set personal goals, establish and maintain positive relationships with peers and adults, develop effective decision-making and problem-solving strategies, develop support systems for reaching goals and modelling, practising and reinforcing adaptive behaviours |
Foster care services as usual | |
| Taussig 2010190,191 | RCT | Not reported | Name: FHF preventive intervention Aim: Skills groups were designed to bring children in foster care together in order to reduce stigma and provide opportunities for them to learn skills in a supportive environment Mentoring was designed to provide children in foster care with an additional supportive adult who could serve as a role model and advocate Theory: No information |
No treatment comparison group | |
| Fisher 2000192 | COS | Home based/school | Name: EIFC, RFC, Community Comparison of Non-maltreated Children Aim: To meet the developmental needs of foster children. ‘It uses the foster care setting as the milieu for therapeutic intervention and actively engages foster parents as therapeutic agents’ Theory: Aims can be achieved by (1) consistent, non-abusive discipline; (2) high levels of positive reinforcement; and (3) close monitoring and supervision of the child’ |
Foster care services as usual | |
| Graham 2012193 | COS | Home based/community | Name: MTFC-P Aim: To facilitate attachment with caregivers, reduce insecure behaviour, decrease resistant and avoidant behaviours, and decrease permanent placement failure rate Theory: Attachment theory |
Foster care services as usual | |
| Therapeutic residential and day care | Moore 1998194 | RCT | Community | Name: Childhaven Aim: Therapeutic early intervention for maltreated children Theory: Study cited the theories of Gogerty and Durkan 1981;242 Miller and Whittaker 1988;243 DePanfilis 1996;244 and Durkin 1986245 |
CPS services as usual |
| Culp 1987195,196 | COS | School | Name: Therapeutic day-treatment programme Aim: To develop strong teacher–child relationships, facilitate self-esteem, develop caring peer relationships, and help children to recognise and deal with their own feelings Theory: Cognitive–developmental model |
No treatment comparison group | |
| Culp 1991197 | COS | Community | Name: Therapeutic day-treatment programme Aim: To improve ‘children’s psychological health, their ability to interact with peers and adults, and their developmental level’ Theory: No information provided |
Wait-list control | |
| Coordinated care | Swenson 2000198 | RCT | Home based/care setting | Name: Charleston Collaborative Project Aim: Reduce risk factors to promote child safety, child functioning and caregiver functioning; provide cost savings; improve service system efficiency Theory: Family-based intervention based on the manual by Ralston and Swenson 1998246 |
TAU following state guidelines |
| Arts therapy | Brillantes-Evangelista 2013199 | QEx | Health service/hospital | Name: (1) Visual arts group or (2) poetry group Aim: To alleviate depression and PTSD Theory: Narrative/constructivist approach, Gestalt approach, response and arousal, psychoanalytic approach, Jung’s active imagination and archetypes, mindfulness and spiritual encounter |
No treatment comparison group |
| Pretorius 2010200 | QEx | Not reported | Name: Structured group art therapy programme Aim: To reduce depression, anxiety, sexual trauma and low self-esteem Theory: ‘Based on the existential–humanistic perspective, and incorporated principles from Gestalt therapy (Naranjo 2000;247 Perls 1990248), the client-centred approach (Rogers 1967;249 Du Toit et al. 1998250) and the abuse-focused approach (Briere 1992251)’ |
No treatment comparison group | |
| Play/activity Interventions | D’Andrea 2013201 | COS | Care Setting | Name: DtG sports-based intervention Aim: Treating maltreated children Theory: Intervention designed using trauma-informed treatment principles |
TAU |
| McDonald 1989202 | RCT | Care setting | Name: Challenge/initiative programme Aim: To enhance self-concept, using ‘new’ cooperative and adventure games, in an existing recreation setting (as opposed to the typical wilderness/outdoor settings) Theory: Low-income families tend to have least access to open space. Previously challenge/initiative programmes have been shown to be effective but usually in a ‘wilderness/adventure’ programme. This is testing a lower-cost alternative |
Played other games with the same researcher (such as kickball, volleyball, etc.) with no debriefing | |
| Udwin 1983203 | QEx | Not reported | Name: Imaginative play training Aim: To improve imaginative play, levels of concentration, positive affect and social interaction, and aggression Theory: Not stipulated. Previous research suggests that imaginative play training can under controlled conditions, enhance both the scope and frequency of imaginative play amongst lower class children (e.g. Feitelson and Ross 1973;252 Freyberg 1973253). Gains have also been demonstrated in relation to children’s affect, cognition and social competence |
Control group exposed to 10 play sessions, but with no active training in make-believe | |
| Animal therapy | Dietz 2012204 | COS | Not reported | Name: AAT in group treatment for CSA Aim: To address trauma symptoms including anxiety, depression, anger, PTSD, dissociation, and sexual concerns Theory: AAT is a goal-directed intervention in which an animal that meets specific criteria is an integral part of the treatment process. ‘AAT is directed and/or delivered by a health/human service professional with specialised expertise, and within the scope of practice of his or her profession’ (Delta Society, 2012254) |
No treatment comparison group |
| Hamama 2011205 | COS | High school | Name: Canine-assisted therapy Aim: To improve psychological stress (depression and PTSD symptoms) among traumatised teenage girls (sexual or physical abuse) Theory: The presence of an animal can lower anxiety and facilitate trust building between therapist and client. Talking to the animal while the therapist listens is easier than talking to the therapist, and can help clients focus on an issue while they interact with the animal. Engagement with the animal can help clients engage with their feelings and share these. Animals offer an opportunity for unconditional acceptance and interaction |
No treatment comparison group |
| Intervention category | Abuse type | Design | Study/record | Outcome domain | Outcome measures |
|---|---|---|---|---|---|
| CBT for sexual abuse | Sexual | RCT | Berliner 199689 | Primary: | |
|
|
||||
| Sexual | RCT | Celano 199690 | Primary: | ||
|
|||||
| Other: | |||||
|
|||||
| Sexual | RCT | Cohen91,92 | Primary: | ||
|
|||||
| Sexual | RCT | Cohen 199893,94 | Primary: | ||
|
|||||
| Sexual | RCT | Cohen 200495,96,267 | Primary: | ||
|
|
||||
| Secondary: | |||||
|
|||||
| Sexual | RCT | Deblinger 199697,98 | Primary: | ||
|
|||||
| Other: | |||||
|
|
||||
| Sexual | RCT | Deblinger 200199 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|
||||
| Other: | |||||
|
|
||||
| Sexual | RCT | Deblinger 2011100 | Primary: | ||
|
|
||||
| Other: | |||||
|
|||||
| Sexual | RCT | Foa 2013101 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|
||||
| Sexual | RCT | Jaberghaderi 2004102 | Primary: | ||
|
|||||
| Sexual | RCT | King 2000103 | Primary: | ||
|
|
||||
| Sexual | COS | Paquette 2011104,105 | Primary: | ||
|
|||||
| CBT for physical abuse | Physical | RCT | LeSure-Lester 2002106 | Primary: | |
|
|
||||
| Physical | RCT | Kolko 1996107,108 | Primary: | ||
|
|
||||
| Secondary: | |||||
| Physical | RCT | Runyon 2010109 | Primary: | ||
|
|||||
| Other: | |||||
|
|
||||
| CBT for multiple abuse | Physical, emotional, sexual | RCT | Champion 2012110 | Other: | |
|
|
||||
| Other | RCT | Church 2012111 | Primary: | ||
|
|||||
| Physical, sexual, multiple | RCT | Jensen 2014112,113 | Primary: | ||
|
|
||||
| Physical, neglect, other | RCT | Linares 2006114 | Primary: | ||
|
|||||
| Other: | |||||
|
|||||
| Physical, sexual, neglect | RCT | Linares 2012115 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|
||||
| Physical, emotional, sexual, neglect, multiple, other | RCT | Rushton 2010116 | Primary: | ||
|
|
||||
| Secondary: | |||||
|
|
||||
| Other: | |||||
|
|||||
| Physical, emotional, sexual, multiple, other | RCT | Shirk 2014117 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|||||
| Physical, sexual, other | COS | Kolko 2011118 | Primary: | ||
|
|
||||
| Other | COS | Rondeau 1983119 | Primary: | ||
|
|
||||
| EMDR | Sexual | RCT | Farkas 2008120 | Primary: | |
|
|||||
| Physical, emotional, sexual | RCT | Scheck 1998121 | Primary: | ||
|
|
||||
| Attachment-orientated interventions | Neglect, other | RCT | Bernard 2012122 | Primary: | |
|
|
||||
| Physical, emotional, neglect, multiple | RCT | Cicchetti 2006123 | Other: | ||
|
|
||||
| Physical, emotional, neglect, multiple | RCT | Cicchetti 2011124 | Primary: | ||
|
|
||||
| Other | RCT | Dozier 2006125,126 | Primary: | ||
|
|
||||
| Other | RCT | Lieberman 2005127–129 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|||||
| Physical, sexual, neglect, multiple | RCT | Moss 2011130 | Primary: | ||
|
|||||
| Other: | |||||
|
|
||||
| Other | RCT | Spieker 2012131 | Primary: | ||
|
|
||||
| Other: | |||||
|
|
||||
| Other | RCT | Sprang 2009132 | Primary: | ||
|
|||||
| Other: | |||||
|
|||||
| Physical, emotional, sexual, neglect, multiple | RCT | Toth 2002133 | Primary: | ||
|
|
||||
| Physical, emotional, sexual, neglect, multiple, other | COS | Becker-Weidman 2006134,135 | Primary: | ||
|
|||||
| PCIT | Physical, neglect | RCT | Chaffin 2004136 | Primary: | |
|
|
||||
| Other: | |||||
|
|
||||
| Physical, neglect | RCT | Thomas 2012138 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|
||||
| Physical, neglect | RCT | Thomas 2011137 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|
||||
| Parenting interventions | Other | RCT | Hughes 2004139 | Primary: | |
|
|
||||
| Other: | |||||
|
|
||||
| Other | RCT | Valentino 2013140 | Primary: | ||
|
|
||||
| Systemic FT | Physical | RCT | Kolko 1996107,108 | Primary: | |
|
|
||||
| Secondary: | |||||
| Transtheoretical intervention | Physical, neglect | RCT | Linares 2015141 | Primary: | |
|
|
||||
| Other: | |||||
|
|
||||
| Multisystemic FT | Physical, neglect | RCT | Brunk 1987142 | Primary: | |
|
|
||||
| Sexual | RCT | Danielson 2012143 | Primary: | ||
|
|
||||
| Physical | RCT | Swenson 2010144 | Primary: | ||
|
|||||
| Other: | |||||
|
|||||
| Multiple | RCT | Biehal 2012145,146 | Primary: | ||
|
|
||||
| Secondary: | |||||
|
|
||||
| Other: | |||||
|
|
||||
| Physical, emotional, sexual | COS | Schaeffer 2013147 | Primary: | ||
|
|
||||
| Other: | |||||
|
|||||
| Multigroup FT | Physical, emotional, sexual, neglect, multiple | RCT | Meezan 1998148,149 | Primary: | |
|
|||||
| Other: | |||||
|
|
||||
| Family-based programme | Sexual | QEx | Bagley 2000150 | Primary: | |
|
|||||
| Secondary: | |||||
|
|||||
| Psychoeducation | Physical, other | RCT | Graham-Berman 2007151 | Primary: | |
|
|||||
| Other: | |||||
|
|||||
| Other | RCT | Howell 2013152 | Primary: | ||
|
|
||||
| Other: | |||||
|
|||||
| Other | RCT | Overbeek 2013153 | Primary: | ||
|
|
||||
| Other: | |||||
|
|
||||
| Physical, emotional, other | RCT | Sullivan 2002154 | Primary: | ||
|
|
||||
| Other: | |||||
|
|||||
| Sexual | RCT | Trowell 2002155 | Primary: | ||
|
|||||
| Other | RCT | Wagar 1995156 | Primary: | ||
|
|
||||
| Physical, emotional, sexual, neglect | RCT | Wolfe 2003157 | Primary: | ||
|
|||||
| Physical, sexual, other | QEx | Noether 2007158 | Primary: | ||
|
|
||||
| Secondary: | |||||
|
|||||
| Sexual | QEx | Simoneau 2008159 | Primary: | ||
|
|
||||
| Sexual | QEx | Tourigny 2007160 | Primary: | ||
|
|
||||
| Secondary: | |||||
|
|||||
| Sexual | COS | Barth 1994161 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|
||||
| Sexual | COS | Duffany 2009162 | Primary: | ||
|
|
||||
| Secondary: | |||||
|
|
||||
| Sexual | COS | Hébert 2010163 | Primary: | ||
|
|
||||
| Physical, emotional, sexual, neglect, multiple | COS | Holland 2004164 | Primary: | ||
|
|
||||
| Secondary: | |||||
|
|
||||
| Physical, emotional, sexual, neglect, multiple | COS | Santibáñez 2000165 | Primary: | ||
|
|||||
| Sexual | COS | Tourigny 2005166,167 | Primary: | ||
|
|
||||
| Sexual | COS | Tourigny 2008168 | Primary: | ||
|
|
||||
| Group work with children | Sexual | Q-RCT | Monck 1996169 | Primary: | |
|
|||||
| Other: | |||||
|
|||||
| Sexual | COS | De Luca 1995170 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|
||||
| Sexual | COS | Grayston 1995171 | Primary: | ||
|
|||||
| Sexual | COS | McGain 1995172 | Primary: | ||
|
|||||
| Sexual | COS | Verleur 1986173 | Primary: | ||
|
|
||||
| Psychotherapy/counselling | Sexual | RCT | Thun 2002174 | Primary: | |
|
|
||||
| Physical, sexual, neglect, multiple | RCT | Haight 2010175 | Primary: | ||
|
|||||
| Secondary: | |||||
|
|
||||
| Physical, emotional, sexual, neglect | RCT | Reddy 2013176 | Primary: | ||
|
|
||||
| Sexual | RCT | Trowell 2002155 | Primary: | ||
|
|||||
| Physical, neglect, multiple | QEx | Cadol 1975177 | Primary: | ||
|
|
||||
| Other: | |||||
|
|
||||
| Sexual | COS | Nolan 2002178 | Primary: | ||
|
|||||
| Sexual | COS | Sullivan 1992179 | Primary: | ||
|
|
||||
| Sexual | COS | Downing 1988180 | Primary: | ||
|
|
||||
| Peer mentoring | Physical, neglect | RCT | Fantuzzo 1988181 | Primary: | |
|
|||||
| Physical, neglect, multiple | RCT | Fantuzzo 1996182 | Primary: | ||
|
|||||
| Treatment foster care | Physical, emotional, sexual, neglect, multiple | RCT | Fisher 2005183–188 | Primary: | |
|
|
||||
| Other: | |||||
|
|
||||
| Physical, sexual | RCT | Smith 2011189 | Primary: | ||
|
|
||||
| Physical, emotional, sexual, neglect | RCT | Taussig 2010190,191 | Primary: | ||
|
|
||||
| Other: | |||||
|
|
||||
| Economic: | |||||
|
|
||||
| Multiple | COS | Fisher 2000192 | Primary: | ||
|
|||||
| Physical, emotional, sexual, neglect, multiple | COS | Graham 2012193 | Other: | ||
|
|||||
| Therapeutic residential and day care | Multiple | RCT | Moore 1998194 | Primary: | |
|
|||||
| Secondary: | |||||
|
|
||||
| Physical, neglect | COS | Culp 1987195,196 | Primary: | ||
|
|||||
| Physical, neglect | COS | Culp 1991197 | Primary: | ||
|
|||||
| Coordinated Care | Physical, emotional, sexual, neglect, multiple, other | RCT | Swenson 2000198 | Primary: | |
|
|||||
| Secondary: | |||||
|
|||||
| Other: | |||||
|
|
||||
| Economic: | |||||
|
|
||||
| Arts therapy | Physical, sexual | QEx | Brillantes-Evangelista 2013199 | Primary: | |
|
|||||
| Sexual | QEx | Pretorius 2010200 | Primary: | ||
|
|||||
| Play/activity | Physical, sexual, neglect | COS | D’Andrea 2013201 | Primary: | |
|
|
||||
| Other | RCT | McDonald 1989202 | Primary: | ||
|
|
||||
| Other | QEx | Udwin 1983203 | Primary: | ||
|
|||||
| Animal therapy | Sexual | COS | Dietz 2012204 | Primary: | |
|
|
||||
| Physical, sexual | COS | Hamama 2011205 | Primary: | ||
|
|
||||
| Secondary: | |||||
|
|||||
| Intervention | Study/record | Country | n | Mean (SD), range | % female | P | E | S | N | M | O |
|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT | Arnold 2003480 | USA | 45 | 12–17 years | 100 | ✗ | |||||
| Barker 2005481 | UK | 67 | 9.2, 4–18 years | 60 | ✗ | ✗ | ✗ | ✗ | |||
| Chasson 2008482 | USA | 99 | 10.88 (3.48), 5–19 years | 68 | ✗ | ||||||
| Clarke 1994483 | UK | 3 | 22.33, 19–24 years | 100 | ✗ | ||||||
| Cohen 2007484 | USA | 12 | 10–17 years | 100 | ✗ | ||||||
| Deblinger 1990485 | USA | 19 | 7.79, 3–16 years | 100 | ✗ | ||||||
| Feather 2006486 | New Zealand | 4 | 10.75 (2.06), 9–13 years | 50 | ✗ | ||||||
| Feather 2009487 | Canada | 8 | 11.63 (1.3), 9–13 years | 50 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Habib 2013488 | USA | 24 | 14–21 years | 75 | ✗ | ||||||
| Habigzang 2008489 | Brazil | 10 | 9–13 years | 100 | ✗ | ✗ | |||||
| Habigzang 2009490 | Brazil | 40 | 9–16 years | 100 | ✗ | ||||||
| Habigzang 2013491 | Brazil | 49 | 11.43 (1.81), 9–16 years | 100 | ✗ | ||||||
| Hubel 2014492 | USA | 97 | 10 (1.63), 6.97–12.83 years | 77 | ✗ | ||||||
| Jarero 2013493 | Mexico | 34 | 9–14 years | 47 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Kirsch 2011494 | Germany | 15 | 10.5 (1.8) years | 40 | ✗ | ✗ | ✗ | ✗ | |||
| Kjellgren 2013495 | Sweden | 25 | 9.2 (1.8), 6–14 years | 40 | ✗ | ||||||
| Kruczek 1999496 | USA | 41 | 14.21, 13–17 years | 100 | ✗ | ||||||
| Lange 2010497 | The Netherlands | 24 | 20 (3.5), 14–25 years | No information | ✗ | ||||||
| Lanktree 1995498 | USA | 105 | 11.6, 8–15 years | 85 | ✗ | ||||||
| Matulis 2014499 | Germany | 12 | 18.08 (1.67), 15–21 years | 83 | ✗ | ✗ | ✗ | ||||
| Misurell 2011500 | USA | 123 | 7.93 (1.5), years | 63 | ✗ | ||||||
| Misurell 2014501 | USA | 45 | 10 (median) (3.44) years | 74 | ✗ | ||||||
| Rosenberg 2011502 | USA | 9 | 16, 14–18 years | 75 | ✗ | ✗ | ✗ | ||||
| Runyon 2009503 | USA | 33 | 8.1 (2.65), 4–14 years | 39 | ✗ | ✗ | ✗ | ||||
| Salloum 2014504 | USA | 6 | 4.7 (0.87) years | 22 | ✗ | ✗ | ✗ | ||||
| Silovsky 2007505 | USA | 85 | 4.9 (1.1) years | 58 | ✗ | ||||||
| Smith 2008506 | Australia | 6 | 14, 11–16 years | 33 | ✗ | ||||||
| Stauffer 1996507 | USA | 19 | 4.21 (1.08), 2–6 years | 67 | ✗ | ||||||
| Sullivan 2004508 | USA | 79 | No information | ✗ | |||||||
| Timmons-Mitchell 1986509 | USA | 16 | 44 | ✗ | ✗ | ||||||
| RBIs | Ducharme 2000510 | USA | 15 | 3–10 years | No information | ✗ | ✗ | ||||
| Golding 2004511 | UK | 57 | 5–15 years | 37 | ✗ | ✗ | |||||
| Jackson 2009512 | Australia | 56 | 10.87, 0.6–17 years | 40 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Lanier 2011513,514 | USA | 120 | 6.6 (2.8), 2–13 years | 36 | ✗ | ✗ | ✗ | ||||
| Osofsky 2007515 | USA | 57 | 20.19 (10.91), 2–52 months | 35 | ✗ | ||||||
| Puckering 2011516 | Scotland/UK | 12 | 6–9 years | 25 | ✗ | ✗ | |||||
| Timmer 2005517 | USA | 307 | 4.58, 2–8 years | 33 | ✗ | ✗ | ✗ | ||||
| Timmer 2006518 | USA | 4.46 years | ✗ | ||||||||
| Timmer 2010519 | USA | 129 | 4.6 (1.5), 2–8 years | 33 | ✗ | ✗ | ✗ | ||||
| Winton 1990520 | USA | 23 | 4.63 (2.37) years | 78 | ✗ | ||||||
| Systemic interventions | Arabgol 2014521 | Iran | 73 | 4 (3.12) years | 41 | ✗ | ✗ | ||||
| Bentovim 1987522 | UK | 274 | 77 | ✗ | |||||||
| Berg 1999523 | UK | 13 | 24 (23), 1–78 months | 46 | ✗ | ||||||
| Coren 2013524 | UK | 42 | 12.75 (3.28), 4–18 years | 69 | ✗ | ||||||
| Crusto 2008525 | USA | 82 | 3.3, 0–6 years | 56 | ✗ | ✗ | |||||
| Danielson 2010526 | USA | 10 | 15 (1.7), 13–17 years | 100 | ✗ | ||||||
| De Paul 2003527 | Spain | 289 | 0–18 years | ✗ | ✗ | ✗ | ✗ | ||||
| Donohue 1999528 | USA | 47 | 9 (5), 0–17 years | 57 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Forbes 2003529 | UK | 31 | 9 (2.92), 4–14 years | 74 | ✗ | ||||||
| Huang-Storms 200625 | USA | 20 | 10.43 (2.66), 6–15.5 years | 45 | ✗ | ||||||
| McClure 2005530 | USA | 6 | 14.67 (1.21), 13–16 years | No information | ✗ | ✗ | |||||
| Staff 1995531 | USA | 244 | 9 (median), 2–16 years | > 50 | ✗ | ||||||
| Tourigny 1998532 | Canada | 41 | 11.6 years | 73 | ✗ | ||||||
| Woodworth 1991533 | USA | 22 | 13.3 years | > 50 | ✗ | ||||||
| Psychoeducation | De Luca 1995170 | Canada | 6 | 10–11 years | 100 | ✗ | |||||
| Grosz 2000534 | USA | 246 | 2–14 years | 58 | ✗ | ||||||
| Hack 1994535 | Canada | 6 | 8–11 years | 0 | ✗ | ||||||
| Harbeck 1992536 | USA | 20 | 10.05, 4–16 years | 80 | ✗ | ||||||
| Hiebert-Murphy 1992537 | Canada | 6 | 100 | ✗ | |||||||
| Hyde 1995538 | UK | 47 | 4–16 years | 85 | ✗ | ||||||
| Lee 2012539 | USA | 27 | 8.41, 6–11 years | 59 | ✗ | ||||||
| Macmillan 2003540 | Canada | 47 | 9.02 (1.91) years | 49 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Merrick 1994541 | USA | 47 | 12.57, 4–17 years | 79 | ✗ | ✗ | ✗ | ✗ | |||
| Mukaddes 2000542 | Turkey | 15 | 31.4, 21–45 months | 44 | ✗ | ||||||
| Nelki 1989543 | UK | 6 | 4–8 years | 100 | ✗ | ||||||
| Group work with children | Lindon 1994544 | UK | 6 | 13–17 years | 100 | ✗ | |||||
| Reeker 1998545 | USA | 19 | 6.32 (0.95), 4–8 years | 47 | ✗ | ||||||
| Sinclair 1995546 | USA | 43 | 12–18 years | 100 | ✗ | ||||||
| Psychotherapy | Friedrich 1992547 | USA | 42 | 4–16 years | 0 | ✗ | |||||
| Rust 1991548 | USA | 25 | 12.5, 9–18 years | 100 | ✗ | ||||||
| Counselling | Jarvis 2006549 | USA | 62 | 9.9, 4–18 years | 44 | ✗ | ✗ | ||||
| Wagner 1993550 | USA | 36 | 12.19 years | 100 | ✗ | ||||||
| Intensive service models | Brown 2013551 | USA | 70 | 0 | ✗ | ✗ | ✗ | ✗ | |||
| Cross 2004552 | USA | 384 | 6+ years | 47 | ✗ | ✗ | |||||
| Culp 1987195,196 | USA | 109 | 2.4 (0.1–6.2) years | 44 | ✗ | ✗ | |||||
| Gallagher 2013553 | UK | 16 | 18.8, 16–24 years | 63 | ✗ | ✗ | ✗ | ✗ | |||
| Grey 2000554 | USA | 27 | 6–11 years | 59 | ✗ | ✗ | ✗ | ✗ | |||
| Heede 2009555 | Denmark | 24 | 6–16 years | ✗ | |||||||
| Hussey 2005556 | USA | 119 | 9.7 (4.03), 5–18 years | 60 | ✗ | ✗ | ✗ | ✗ | |||
| Jones 2010557 | USA | 58 | 12.3 (1.9), 9–18 years | 22 | ✗ | ✗ | ✗ | ||||
| Oates 1995558 | USA | 24 | 3 years | 54 | ✗ | ✗ | |||||
| Parish 1985559 | USA | 53 | 30–60 months | 45 | ✗ | ||||||
| Pugh 1987560 | USA | 246 | 6.94 years | 35 | ✗ | ||||||
| Ray 1995561 | USA | 15 | 10.5, 7–15 years | 27 | ✗ | ||||||
| Schram 1991562 | USA | 24 | 17.8 (median), years | 100 | ✗ | ✗ | ✗ | ||||
| Stubenbort 2010563 | USA | 53 | 47 months | 51 | ✗ | ||||||
| Vernberg 2004564 | USA | 50 | 9.64 (2.05) years | 16 | ✗ | ||||||
| Activity-based therapies | Coulter 2000565 | USA | 9 | 9–17 years | 44 | ✗ | ✗ | ✗ | |||
| Ernst 2007566 | USA | 58 | 8.5 (3.5), 3–17 years | 51 | ✗ | ||||||
| Hall-Marley 1993567 | USA | 13 | 4–7 years | 54 | ✗ | ||||||
| Kemp 2013568 | Australia | 30 | 12.65, 8–17 years | 80 | ✗ | ||||||
| Mackay 1987569 | Canada | 5 | 12–18 years | 100 | ✗ | ✗ | ✗ | ||||
| Clausen 2012570 | USA | 20 | 5–10.7 years | 30 | ✗ | ||||||
| Nilsson 2010571 | Sweden | 15 | 15.6 (2), 13–18 years | 87 | ✗ | ✗ | |||||
| Pifalo 2002572 | USA | 13 | 8–17 years | 100 | ✗ | ||||||
| Pifalo 2006573 | USA | 13 | 8–17 years | 100 | ✗ | ||||||
| Purvis 2006574 | USA | 12 | 7.84 years | 17 | ✗ | ✗ | |||||
| Purvis 2007575 | USA | 19 | 8.2, 3–14 years | 53 | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Reyes 2005576 | USA | 18 | 11.1, 7.3–16.6 years | 72 | ✗ | ||||||
| Schultz 2007577 | USA | 63 | 10.8, 4–16 years | 41 | ✗ | ✗ | ✗ | ||||
| Scott 2003578 | USA | 26 | 5.6 years | 73 | ✗ |
Summary of study characteristics
Sample size
Sample sizes in identified studies varied considerably with samples ranging ranged from just 3 to 834 participants. The majority of studies (107) had < 50 participants, with just 14 having > 200 participants.
Location
The overwhelming majority of studies were conducted in the USA (130 out of 196). The remaining studies took place in Canada (22), the UK (17) or other European countries (11), Australia (6) or New Zealand (1), North America (1), South America (4), Iran (2), Israel (1), South Africa (1), Turkey (1) and the Philippines (1).
Age
Participants in identified studies ranged in age from 0 to 25 years old. The median age across all studies was approximately 10 years old. There appeared to be differences in the age groups targeted by different interventions. Cognitive–behavioural approaches included participants from 4 to 24 years old with a mean age of approximately 13 years old. Attachment-orientated interventions tended to target younger children, with most aged between 1 and 4 years old. Systemic interventions appeared to be targeted towards children between 2 and 17 years old with a mean age of approximately 8 years old. For psychotherapy/counselling mean age was often not reported but participants ranged from 3 to 19 years old. Finally, Intensive service models mainly included young participants from birth to age 16 years, with a mean age of approximately 5 years.
Gender
The victims of abuse in the identified studies were typically female (61% female, 39% male). In studies that were specifically addressing the consequences of sexual abuse, 80% of participants were female, with many interventions targeting only female survivors of child sexual abuse (CSA). A total of 31 of these studies (see Table 3) included only female participants compared it with just three studies including only male participants. By contrast, in studies specifically addressing physical abuse, participants were more likely to be male (60% male, 40% female).
Abuse type
The majority of studies included children who had suffered from multiple types of abuse. A total of 135 studies (see Table 3) included participants who had experienced sexual abuse. Participants who had experienced physical abuse were included in 85 of the included studies. Participants who had experienced neglect were included in 50 studies. Participants who had experienced emotional abuse were included in 31 studies. A total of 37 studies specified that their participants had experienced ‘multiple’ forms of abuse. Finally, 49 studies included participants who had experienced ‘other’ forms of abuse (e.g. witnessing domestic violence, Munchausen’s syndrome by proxy, etc.).
Outcomes
We were interested in five primary outcome domains [(1) psychological distress/mental health, particularly PTSD, depression and anxiety, self-harm; (2) behaviour, particularly internalising and externalising behaviours; (3) social functioning, including attachment and relationships with family and others; (4) cognitive/academic attainment; and (5) quality of life]. We also wanted to record the reporting of other outcomes, including substance misuse, delinquency, resilience and treatment acceptability, outcomes related to parent/carer distress, parent/carer efficacy (the degree to which they feel empowered to care for the child appropriately and safely) and, where appropriate, placement stability.
A wide variety of types and forms of measures have been used to evaluate outcomes in this field. A good many that are used routinely are well accepted and appear with citations demonstrating some aspect of validity and reliability. Some have been developed around the evaluation of formal diagnostic criteria [e.g. the Kiddie Schedule for Schizophrenia and Affective Disorders (KSADS);268] problem behaviour [e.g. the Child Behavior Checklist (CBCL)260] or in relation to specific therapeutic approaches [e.g. Beck Depression Inventory (BDI)272]. Others have been developed by study investigators for the evaluation of specific outcomes which, although potentially strong in terms of face validity, are generally without supporting evidence. Outcome measures routinely used in this field most often take the form of rating scales and questionnaires, and can be administered by an assessor or completed self-report.
We identified a considerable number of measures intended to evaluate the different outcome domains, either partially or fully (see Table 5). The measurement of psychological distress alone was undertaken using over 60 different measures or adaptations of measures across these studies. A list of the outcome domains, and judgements about the main measures used to assess them, is provided in Appendix 9. A sizeable proportion of these studies reported multiple measures ostensibly assessing the same outcome domains, or a mix of overlapping global and specific measures. The choice of outcome measure was often appropriately influenced by the nature of the intervention and/or the target group, although in view of the consequences and longer-term sequelae of maltreatment, the range of outcome domains considered by many studies was frequently quite limited.
Cognitive–behavioural therapy interventions
Of the 12 studies89–105 examining the effects of CBT for sexual abuse, all measured psychological distress, 11 recorded behaviour outcomes,89–100,102–105 seven measured some form of social functioning90,95–101,104,105 and three measured acceptability. 99,101 Five studies90,95–100 also looked at parent/carer outcomes.
Of the three studies106–109 using CBT to specifically target physical abuse, all three measured some form of behavioural outcomes, two studies107–109 measured psychological distress, two studies107–109 measured cognitive function/academic attainment and one study107,108 measured social functioning. One study109 also looked at parent/carer outcomes.
Five111,112,116–118 of the nine studies that looked at CBT for multiple abuse measured psychological distress, six studies114–119 measured behaviours, four studies115,117–119 measured social functioning, four studies115–119 looked at cognitive function/academic attainment,114,115,117,118 three studies115–117 looked at acceptability and four studies115,117–119 looked at parent/carer outcomes.
Of the two studies120,121 that used EMDR, both looked at psychological distress, and one study120 also measured behaviour outcomes.
Relationship-based interventions
Of the 15 studies122–140 that looked at attachment-orientated and parenting interventions, nine studies evaluated psychological distress, 10 studies measured behavioural outcomes, three studies looked at social functioning and six studies measured cognitive function. Six of these studies looked at parent/carer outcomes.
Systematic interventions
Eight107,108,142–150 of the nine studies107,108,141–150 looking at systemic and family-focused interventions measured outcomes related to psychological distress and behaviour. Six studies looked at social functioning;107,108,141–144,148,149 two included measures related to cognitive functioning. 107,108,148,149 One UK study145,146 examined the impact of intervention on education and two UK studies reported delinquency as an outcome. 145,146,150 Carer efficacy and/or distress were measured in three studies141,144,148,149 and placement stability in two studies. 145,146,148,149
Psychoeducation
Of the 17151–153,155–168 psychoeducation intervention studies, 15 studies150,152,153,155,157–160,163–168 measured a psychological distress outcome, 12 studies looked at behaviour outcomes,151–153,158–161,163–168 10 studies152,155,157–160,163–168 looked at social functioning and eight studies153,159–161,163,165–168 looked at some measure of cognitive functioning/academic attainment. One study157 measured substance misuse, two studies162,164 looked at delinquency, three studies160,166–168 measured resilience and one study161 looked at acceptability. Two studies150,152 also looked at parent/carer outcomes.
Group work
Of the five studies169–173 looking at group work with children, three studies169,170,173 looked at psychological distress outcomes, four studies169–172 measured behaviour and four studies169–171,173 measured cognitive functioning. One study170 also looked at acceptability and one study169–171 recorded parent/carer outcomes.
Psychotherapy/counselling
Of the seven studies174–180 evaluating psychotherapy/counselling, five studies174–178 measured psychological distress outcomes, all but one174 measured behaviour outcomes, five studies175–178 looked at cognitive outcomes, and one study177 looked at placement stability. One study175 reported on the intervention’s acceptability.
Peer mentoring
The two peer-mentoring studies181,182 both reported behaviour and social functioning outcomes.
Intensive service models
Nine studies183–198 examined the effects of these models of care. Five studies183–188,190,191,194,198 measured psychological distress, five studies189,192,194,197,198 looked at behavioural outcomes, four studies190,191,194,195,197 explored social functioning, three studies190,191,197 measured cognitive performance, two studies194,198 examined addiction behaviour, one study190,191 examined resilience and two studies190,191 looked at placement stability.
Excluded studies
A total of 34 records280,579–611 were excluded from this review (Table 7). Of these records, five586,592,598–600 were excluded because the focus of the study was on preventing abuse, not treating the sequelae of abuse. Five records581,584,596,608,609 were excluded because they focused on the family preservation services, rather than treating the child. Three records580,591,611 were excluded because the focused was on parenting stress and parenting outcomes, rather than child-focused outcomes. Seven records579,582,589,593,597,606,607 were excluded because participants were not recruited or selected on the basis of their maltreatment; instead they were recruited on the basis of problems including depression, PTSD, substance abuse and delinquency. Three records585,587,603 were excluded because they focused on general services, such as general foster care and child protection service, and did not focus on a therapeutic intervention for maltreatment. Five studies280,601,604,605,610 were excluded because they did not include a relevant evaluation of the intervention of interest. The remaining six studies583,588,590,594,595,602 were excluded because there was either no specific focus on child outcomes (n = 3583,590,602) or no specific focus on maltreatment (n = 3588,594,595).
| Study ID | Reason for exclusion | Design | Intervention category |
|---|---|---|---|
| Amaya-Jackson 2003579 | Intervention focus is not maltreatment but PTSD | UCS | CBT |
| Barton 1994580 | Focus is family stress reduction through intensive support; the intervention does not focus on the child | CS | Systemic interventions |
| Barton 1994581 | Family preservation services – not focused on treating the child | QEx | Systemic interventions |
| Brook 2007582 | Focus on substance abuse intervention | CS | Systemic interventions |
| Cohen 1998280 | Focus of the study on mediating factors, now effectiveness | RCT | CBT |
| Cohen 2000583 | No outcome data presented | RCT | CBT |
| Coleman 2000584 | Family preservation services – not focused on treating the child | UCS | Systemic interventions |
| Collado 2007585 | Foster care, not an evaluation of a specific intervention | UCS | Intensive service models |
| Currier 1996586 | Focus was on preventing abuse, not treating the sequelae of abuse | UCS | Systemic interventions |
| DeSena 2005587 | Intervention to improve the working of child protection/welfare – not a therapeutic intervention for maltreatment | CS | Intensive service models |
| Edinburgh 2009588 | Focus was on sexual exploitation | UCS | Systemic interventions |
| Friman 1997589 | No focus on maltreatment | UCS | Intensive service models |
| Graham-Berman 2013590 | No child outcomes reported for the children’s group | RCT | Group work with children |
| Hakman 2009591 | Focus on the parents, to prevent abuse recidivism and not treat the child | RCT | Systemic interventions |
| Harder 2005592 | Intervention targeted at parents with the aim of preventing further abuse | CS | Systemic interventions |
| Harold 2013593 | Focus on delinquency, not maltreatment | RCT | Intensive service models |
| Howes 1998594 | Therapeutic preschool programme, but no maltreatment | UCS | Intensive service models |
| Iwaniec 1997611 | Focus was on parent intervention and parent outcomes | CS | Systemic interventions |
| Iwaniec 2003595 | Not clearly maltreated and intervention is not clear | UCS | Intensive service models |
| Kirk 2004596 | Focus was on family preservation | CS | Intensive service models |
| Lewis 2010597 | Focus was on participants with depression, not abuse | RCT | CBT |
| Lorber 1984598 | Abuse prevention only | UCS | Systemic interventions |
| MacMillan 2005599 | Abuse prevention only | RCT | Systemic interventions |
| Mersky 2011600 | Abuse prevention only | QEx | Systemic interventions |
| Overbeek 2014601 | Not evaluating the intervention – assessing risk factors as moderators of recovery across both interventions (i.e. two interventions combined as one) | RCT | Systemic interventions |
| Pereira 2013602 | No child outcomes | UCS | RBI |
| Rivara 1985603 | Not child focused | UCS | Psychotherapy |
| Sagatun 1988604 | No evaluation | UCS | Intensive service models |
| Sullivan 1990605 | No data presented and no specific information about the intervention aside from general descriptions of the techniques used in the facility | CS | Psychotherapy |
| Swart 2014606 | Participants were not recruited/selected on the basis of their maltreatment | RCT | CBT |
| Swart 2014607 | Participants were not recruited/selected on the basis of their maltreatment | RCT | CBT |
| Szykula 1985608 | Focus on family preservation | CS | Intensive service models |
| Vitulano 1990609 | Family preservation; the only results presented are about placement and removal from home | CS | Intensive service models |
| Waxman 2009610 | Child advocate programme, not a therapeutic intervention | CS | Intensive service models |
Economic studies
Included studies
In total we identified six studies198,612–616 assessing the cost-effectiveness of relevant psychosocial interventions for maltreated children: five studies198,613–616 were carried out using data from a trial and one study612 used a decision-analytic model. Of the five trial-based studies,198,613–616 data were from four RCTs198,613–615 and one cohort study. 616 All six studies198,612–616 were published in English and were carried out in the USA198,615,616 (n = 3), the UK613,614 (n = 2) and Australia612 (n = 1). The basic characteristics of the six included studies198,612–616 are presented in Table 8, and more detailed descriptions are presented in Chapter 4.
| Intervention category | Design | Study record | Country | Intervention | Comparator | Type of abuse | Method of economic evaluation | Measure of outcome | Costs included | Time horizon |
|---|---|---|---|---|---|---|---|---|---|---|
| CBT | Decision model | Gospodarevskaya 2012612 | Australia | TF-CBT and TF-CBT plus SSRI | Non-directive counselling and no treatment | Sexual abuse | Cost–utility | QALYs | Cost of intervention only | 1 year and 30 years |
| RCT | Sharac 2011613 | UK | Parenting programmes | Services as usual | Not specified | Cost-effectiveness | Strengths and difficulties and parent satisfaction | Health, social care and education | 6 months | |
| Psychoeducation | RCT | McCrone 2005614 | UK | Individual psychotherapy | Group-based psychoeducational therapy | Sexual abuse | Cost–consequences | Various symptom and functioning | Cost of intervention only | 2 years |
| Intensive service models | RCT | Lynch 2014615 | USA | MTFC | RFC | Not specified | Cost-effectiveness | Placement permanency | Health, social care and education | 2 years |
| Cohort | Wood 1988616 | USA | Families First child abuse prevention service | Services as usual | Abuse or neglect | Cost–consequences | Family functioning and out-of-home placements | Cost of intervention and out-of-home placements | 1 year | |
| Co-ordinated care | RCT | Swenson 2000198 | USA | Charleston Collaborative Project for maltreated children | Services as usual | Abuse or neglect | Cost–consequences | Caregiver and child psychosocial functioning | Programme costs, youth service and out-of-home placements | 3 months |
Summary of study characteristics
Participants
Age In the RCT-based evaluations, one study615 included preschool children in foster care aged between 3 and 5 years, one study615 included children who had been adopted between the ages of 3 and 8 years,613 and two studies198,614 included a broader age range: the first study198 involved maltreated children between 1 and 16 years and the second study614 used a sexual abuse sample of children aged between 6 and 14 years. In the cohort study,616 no age range was reported, just the mean of the groups, which was 8.9 years in one group and 5.4 years in the other. The decision model612 focused on a hypothetical cohort of 10-year old children.
Gender Four198,613,615,616 of the five trial-based studies included both girls and boys, with an average of 49% being girls (range 43–54%). The exception focused on an intervention that was specifically for girls who had been victims of sexual abuse. 614
Abuse type Two studies612,614 evaluated interventions for sexual abuse, two studies198,616 described the maltreatment type as abuse and neglect, and the remaining two were unspecified,613,615 focusing on adopted or foster care populations.
Interventions
The interventions evaluated in these economic evaluations were heterogeneous, including treatment-focused CBT compared with non-directive counselling and a no-treatment arm for sexual abuse, parenting programmes compared with services as usual for adoptive parents, individual psychotherapy compared with group-based psychoeducation therapy for sexual abuse, multidimensional treatment foster care (MTFC) compared with regular foster care (RFC) for preschool children with emotional and behavioural problems, a child abuse prevention service compared with services as usual, and a collaborative care intervention for maltreated children compared with services as usual.
Economic study type and quality
The method of economic evaluation was a cost-effectiveness analysis in two studies613,615 (effects measured on disease-specific scales), a cost–utility analysis in a third study612 [effects measured using a generic quality-of-life scale capable of generating quality-adjusted life-years (QALYs)] and the remaining three studies198,614,616 are most accurately described as cost–consequences analyses (costs and outcomes presented separately and not formally combined).
The performance of each study on the economic evaluation critical appraisal checklist76 is summarised in Table 9. Sample sizes were small in all of the trial-based studies,198,613–616 ranging from a total of 37 participants (two groups of 19 and 18) to a maximum of 117 participants (two groups of 57 and 60). Perspectives were commonly narrow, with two studies612,614 including only the cost of the interventions under evaluation and two studies198,616 additionally including the cost of out-of-home placements. The remaining two studies613,615 took a broader perspective, covering health, social care and education. Incremental analyses were reported in three612,613,615 of the six studies and uncertainty was explored in only one study. 612 Discounting of costs and effects was not applied in two614,615 of the three studies with a follow-up duration of > 1 year. Quality varied greatly, with the decision model,612 published in 2012, meeting a relatively high number of the critical appraisal criteria and the cohort study,616 published in 1988, meeting relatively few.
| Critical appraisal checklist criteria | Gospodarevskaya 2012612 | Sharac 2011613 | McCrone 2005280 | Lynch 2014615 | Wood 1988616 | Swenson 2000198 |
|---|---|---|---|---|---|---|
| 1. Was a well-defined question posed? | Yes | Yes | Yes | Yes | Yes | Yes |
| 2. Comprehensive description of competing alternatives? | Yes | Yes | Yes | Yes | Yes | Yes |
| 3. Was the effectiveness established? | Yes | Yes | Yes | Yes | Yes | Yes |
| 4. Were all costs and outcomes identified? | No | Yes | No | Yes | No | Yes |
| 5. Were costs and outcomes measured accurately? | Yes | Yes | Yes | Yes | Yes | Yes |
| 6. Were costs and outcomes valued credibly? | Yes | Yes | Yes | Yes | No | Yes |
| 7. Were costs and outcomes adjusted for differential timing? | Yes | N/A | No | No | N/A | N/A |
| 8. Was an incremental analysis performed? | Yes | Yes | No | Yes | No | No |
| 9. Was allowance made for uncertainty? | Yes | No | No | No | No | No |
| 10. Were all issues of concern to users included? | Yes | No | Yes | No | No | No |
Excluded economic studies
A total of 16 papers116,504,587,588,617–628 were excluded from the review of economic evidence and these are reported in Table 10. Six papers619–621,623,626,628 were excluded because they did not involve an intervention and four papers587,618,624,625 because the intervention in question did not meet criteria for inclusion, focusing on prevention rather than treatment. Two records622,627 did not have a specific focus on maltreatment, three records116,504,588 did not meet criteria for a full economic evaluation and one record617 was a conference abstract.
| Report ID | Reason for exclusion | Design | Intervention category |
|---|---|---|---|
| Blazey 2011618 | Not an included intervention | UCS | Intensive service models |
| Clark 2011619 | No intervention | UCS | N/A |
| Cohen 1998620 | No intervention | UCS | N/A |
| Conrad 2006621 | No intervention | UCS | N/A |
| DePanfilis 2008622 | No maltreatment | RCT | Systemic interventions |
| DeSena 2005587 | Not an included intervention | CS | Intensive service models |
| Edinburgh 2009588 | Not a full economic evaluation | UCS | Systemic interventions |
| Florence 2013623 | No intervention | N/A | N/A |
| Foster 2008624 | Not an included intervention | UCS | Multiservice |
| Lynch 2011617 | Conference abstract | N/A | Intensive service models |
| Maher 2012625 | Not an included intervention | UCS | Systemic interventions |
| New 2000626 | No intervention | UCS | N/A |
| Reynolds 2002627 | No maltreatment | CS | Systemic interventions |
| Rovi 2014628 | No intervention | UCS | N/A |
| Rushton 2010116 | Not a full economic evaluation | RCT | CBT |
| Salloum 2014504 | Not a full economic evaluation | UCS | CBT |
Acceptability studies
Description of included acceptability studies
Of the 73 included acceptability studies, the majority were set in the USA (42 studies107,108,161,175,176,482,492,504,505,510,515,526,533,621,629–657). The remainder were in Canada (four studies170,658–661), the UK (14 studies145,169,481,511,538,662–670) and elsewhere in Europe: the Netherlands (three studies497,671,672), Norway (three studies673–675) and Sweden (one study676), with one multisite review of services145,146,640,665–670 across Italy, the Netherlands and the UK. A small number of studies were based outside North America and Europe: Australia (two studies506,677), Brazil (one study678), India (one study679) and the Philippines (one study680).
Most studies were uncontrolled, with only one RCT. 107,108,145 Sample sizes varied greatly from single case studies (two studies621,629) to a large national sample of n = 1085. 634 The majority of sample sizes were < 50 cases (40 studies169,175,497,504,506,510,511,526,533,538,621,629,636–639,641–643,645,646,648,651,652,658,661–663,665,666,668–670,675,677,678,680), between 50 and 100 cases (15 studies107,170,176,481,482,492,505,644,647,650,660,664,671,673,674) and 18 studies145,515,630–634,640,649,653–658,667,672,679 had sample sizes of > 100 cases.
Sexual abuse was the most commonly cited type of abuse across the acceptability studies (33 studies161,169–171,189,492,497,505,506,526,533,538,621,633,636–638,640–643,645,647,648,653,657,660,662,664,668,673,677–680) and some intervention categories reported data for only this population group [systemic interventions,526,533,621,673,678 psychoeducational interventions,161,538,647,664 peer mentoring660 (note: there was only one study in this category)]. Three studies510,639,652 also reported on a physical abuse sample that had also witnessed domestic violence. Considering the large number of studies reporting a sexual abuse sample and targeted intervention, a large proportion of studies had a 100% or majority female population, and fewer than half of the studies had a majority male population, with only two studies170,171 that had 100% male population. The age range of included studies was 1–22 years.
Chapter 4 Results
In this chapter we present evidence for the clinical effectiveness and cost-effectiveness of treatment modalities as described in the previous chapters, drawing solely on the evidence of controlled trials or, in the case of economic evidence, decision models. The evidence is organised around intervention groups.
The breadth of this evidence synthesis meant that it was not possible, a priori, to establish a limited number of primary and secondary outcomes. In Chapter 3, we presented descriptively the broad outcome domains that studies reported having measured, whether or not data were presented. In this chapter, and based on what we know about the proximal adverse effects of maltreatment on children’s emotional and psychological well-being, we examine the evidence for the impact of interventions on mental health outcomes, such as post-traumatic effects, depression and anxiety. We then assess the evidence for the effectiveness of interventions on those outcomes that the study authors stated were their intended outcomes; however, we recognise that, in doing so, we may be underestimating biases that are associated with selective outcome reporting, as well as publication bias more generally. Finally, we report any evidence of cost-effectiveness located in the systematic review.
Cognitive–behavioural therapy
We identified 26 controlled studies90–103,106–112,114–117,121,176,268 of cognitive–behavioural interventions (CBT), of which 23 were randomised trials. There were sufficient randomised trials to attempt to explore the differential effect on different maltreatment histories, broadly defined, and so this section is organised into the following three groupings, and does not include the three COSs of CBT interventions.
-
CBT interventions for children who have been sexually abused89–103
-
CBT for children with maltreatment histories, including those with experience of multiple forms of maltreatment and those that recruit children irrespective of type of maltreatment history. 110–112,114–117,121,176
Description of studies
Of the 11 studies89–103 of CBT interventions for children who have been sexually abused, two89,90 were studies of group-based treatments and nine91–103 were studies of treatments provided to children individually, sometimes in parallel with treatment for the non-offending parent or carer.
Six89–99 of the 11 studies were conducted by a team of clinical researchers who had developed a particular approach to treating children traumatised by sexual abuse, known sometimes as TF-CBT. Although among the most rigorous and well-conducted studies, studies of this particular intervention (and others) are compromised by the lack of independent evaluation.
Location of studies
All studies were conducted in the USA, with the exception of the study by Jaberghaderi et al. ,102 which was conducted in Iran, and King et al. ,103 which was undertaken in Australia.
Study size
Five studies90,99,101–103 had small samples sizes ranging from 18 to 63 participants. A multisite trial by Cohen 2004,95,96 had a sample of 229 participants. The remainder ranged from 82 to 210 participants. 91–94,97,98,100 As a result, the meta-analyses we conducted were not sufficiently powered to detect small, but potentially important, effects. Baseline differences in these studies also proved problematic in drawing any conclusions based on end-point data, as it did for almost all included studies.
Participants
Gender
Three studies90,101,102 focused solely on girls who had been sexually abused. The remaining studies included both boys and girls, with the percentage of boys ranging from 11%89 to 42%. 91,92
Age
One study91,92 was concerned with preschoolers (boys and girls aged 3–6 years). Five studies90,95–98 set inclusion criteria for similar age groups: 7–13 years,90,97,98 8– 14 years,95,96 12–13 years102 and 13–18 years. 101 Inclusion criteria for the other five studies89,93,94,99,103 ranged from children aged 2–8 years99 to children aged 4–13 years,89 5–17 years103 and 7–15 years. 93,94
Maltreatment
The range of abuse experienced by participants was broad, and differently reported, but the following picture of participants emerged. Most were abused by men known to them. The majority of perpetrators were family members. In three studies,89,90,93,94 approximately half of the children and young people had experienced oral, vaginal or anal penetration. In the study91,92 dealing with the youngest participants, the percentage that had experienced vaginal or anal intercourse was 26%. 91,92 In the study of children aged 2–8 years,99 the number reported to have experienced penile penetration was 16%. Participants in all studies ranged from those who had experienced one incident of abuse to those who had experienced multiple incidents, sometimes over many years. Many participants also reported the use of force, or threat of force. Not all studies reported detailed abuse data, for example Deblinger 200199 or Jaberghaderi 2004. 102 See Table 3 for a profile of participants in each study.
Inclusion criteria
All studies had inclusion criteria that specified contact sexual abuse. All but two trials101,102 made the independent substantiation of sexual abuse an inclusion criterion. Most set cut-off points on the time of last episode of abuse as an inclusion criterion, ranging from 3 months101 through 6 months91–94 to 2 or 3 years. 103 Although Deblinger et al. 99 did not set a time limit, the authors report that the mean age of the children was 5.45 years (SD 1.47 years) and the mean age of first experience of sexual abuse was 4.5 years (SD 1.47 years), based on mothers’ estimates. The report by Berliner and Saunders89 did not specify inclusion or exclusion criteria, but all participants were said to have provided statements, substantiated by independent assessment, that they had been sexually abused. The Jaberghaderi et al. study102 required that girls had experienced sexual abuse at ≥ 6 months prior to the study.
The presence and severity of symptoms as inclusion criteria were highly variable. Six studies91,92,95–98,101–103 reported the presence of particular symptomatology thresholds as an inclusion criterion. Cohen et al. 91,92 required a minimal level of symptomatology defined as a Weekly Behavior Report total behaviour score of > 7 or any sexually inappropriate behaviour reported on the Child Sexual Behavior Inventory (CSBI). 259 Cohen et al. 95,96 stipulated that participants had to meet five criteria for sexual abuse-related Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV)-defined PTSD, including at least one in each of the three clusters (re-experiencing, avoidance or numbing and hyperarousal). Deblinger et al. 97,98 required the presence of three PTSD symptoms, including at least one symptom of avoidance or re-experiencing the phenomenon. Investigators decided to take both children who met full Diagnostic and Statistical Manual of Mental Disorders-Third Edition, Revised criteria for PTSD and those with partial PTSD symptoms because of the possibility of delayed onset of episodic course. King et al. 103 required that the children met diagnostic criteria for PTSD or provided evidence of high risk of developing the disorder. Foa et al. 101 required a primary diagnosis (DSM-IV, Text Revision) of chronic or subthreshold PSTD. Jaberghaderi et al. 102 recruited girls whose scores on the Child Report of Post-traumatic Symptoms (CROPS)229 indicated a clinically significant level of post-traumatic symptoms.
Interventions and comparison
Two studies99,268 provided a group-based intervention, and the remainder provided individual therapy (IT).
Group treatments
Interventions
In Berliner and Saunders 199689 both groups received a therapy described as a ‘structured equivalent of sexual abuse-specific group therapy’. In the experimental arm, a focus was added on explaining fear (in the session on feelings), stress inoculation therapy (SIT) was substituted for one of the two ‘family and friends’ sessions, two sessions were devoted to GE and SIT principles were applied to sessions on disclosure impact and self-esteem. Children were taught about the automatic nature of fear as a response to danger and how to manage this through progressive relaxation and coping strategies (quieting reflex and thought-stopping). Children were encouraged to practice these skills between group sessions (pp. 299–30).
Deblinger et al. 200199 provided group-based CBT to children and their mothers in separate groups. The parents’ groups covered a range of topics that varied somewhat according to the specific needs of each group but commonly followed the following order and number of sessions: education/coping (three sessions), communication, modelling, GE (two sessions) and behaviour management (six sessions). The children’s group took the form of an interactional behavioural therapy, facilitated by an interactive workbook,507 and which incorporated a range of cognitive–behavioural methods, including GE, modelling, education, coping and body safety training. In addition, members of the CBT group met for an additional 15 minutes each week for a joint parent and child activity session.
Comparisons
The comparison groups in Berliner and Saunders 199689 received conventional sexual abuse-specific group therapy with or without SIT and the specific CBT focus on fear and anxiety. The sessions covered: getting acquainted and establishing ground rules; feelings; family and friends (two sessions); disclosure impact, self-esteem and sexual abuse; body awareness and sexuality (two sessions) and prevention and termination.
Deblinger et al. 200199 compared the effectiveness of group CBT for parents and children with supportive group therapy (for parents) paired with a more didactic, information-based approach for children.
Individual treatments
Those studies headed by Cohen and Deblinger95,96 are essentially evaluations of a manualised programme first developed by the authors in the early nineties. 283
Cohen 199591,92 evaluated a manualised, short-term treatment model designed for sexually abused children and their parents, named Cognitive–Behavioural Therapy-Sexually Abused Preschool Children. Children receive safety education and assertiveness training, are helped to identify appropriate compared with inappropriate touching, and to deal with attributions regarding the abuse, ambivalent feelings towards the perpetrator, regressive and inappropriate behaviours, and fear and anxiety. Specific issues for parents include ambivalence in their belief in the child’s account, ambivalent feelings towards the perpetrator, attributions regarding the abuse, concerns that the child is ‘damaged’, how to provide appropriate emotional support for the child and manage inappropriate child behaviours, fear and anxiety. Interventions include the use of cognitive reframing, thought-stopping, positive imagery, contingency reinforcement programmes, parent management training and problem-solving. Psychoeducation and support are embedded in the programme.
Cohen 199893,94 evaluated a programme entitled Sexual Abuse-Specific Cognitive–Behavioural Therapy (SAS-CBT). The programme is not described in detail, but it was designed specifically to address depression, anxiety and behavioural difficulties. SAS-CBT addressed feelings of helplessness (including not being believed), distorted attributions (self-blame) about the abuse and other negative events, feeling damaged/different, and consequent low self-esteem. It incorporated anxiety reduction techniques, such as thought replacement, positive imagery/relaxation, enhancement of safety and management of intrusive thoughts. It helped children to address behavioural problems by teaching them about the connections between thoughts, feelings and behaviour, management techniques and problem-solving skills. The focus in the parents’ groups was on reducing their emotional distress (again, including addressing distorted attributions, anxiety and anger), enhancing their ability to support their child and behaviour management.
Deblinger 199697,98 explored variations of a programme described as similar to that of Cohen and Mannarino. 91,92 Participants were assigned to one of three experimental conditions: child only, parent only or combined child and parent. Children in all of the experimental arms received an intervention that included GE, modelling, education, coping and body safety skills. GE was described as the cornerstone of the intervention aimed at helping the children to disconnect the associations frequently made between highly negative emotions and abuse-related thoughts, discussion and other reminders. Parents in the experimental arms were taught how to respond therapeutically to their children’s behaviours and needs, that is, how to reduce their fears and avoidance behaviours (through the use of modelling, GE and processing exercises); how to analyse their own interactions with their children behaviourally, thus identifying those situations when they might inadvertently have reinforced problem behaviours and the maintenance of PTSD symptoms; and child management skills.
Cohen 200495,96 delivered the same manualised TF-CBT intervention used in earlier studies by this team, but in a more representative sample of children across two sites. This manualised intervention also forms the basis of the study conducted by Deblinger et al. 100 in 2011. In this paper100 the authors describe the TF-CBT intervention evaluated in this study as including components ‘that spell out the acronym PRACTICE:
-
Psychoeducation and parenting
-
Relaxation
-
Affective modulation
-
Cognitive coping
-
Trauma narrative (TN)
-
In vivo exposure
-
Conjoint parent–child sessions, and
-
Enhancing safety and future development’ (p. 69; © 2010 Wiley-Liss, Inc. Reproduced with permission).
In this study,100 the authors were concerned to investigate the importance of the TN to effective treatment of children with PTSD. This four-arm trial compared two versions of TF-CBT (as described for Deblinger 200199), one with, and one without, the inclusion of the TN component and at the same time manipulated the length of treatment and degree of time given to the TN. The authors report that in all conditions both children and parents received psychoeducation about CSA and skill-building (e.g. relaxation, affective modulation, cognitive coping and body safety training), as well as parenting skills training. However, only those children assigned to the two TN groups ‘were actively encouraged to develop a detailed narrative about the sexual abuse and related experiences, which they processed and reviewed with the therapist as well as their non-offending parent’ (p. 69). 100 Children in the eight-session TN condition spent three to four sessions on the TN component; this was at least doubled in the 16-session condition.
King et al. 103 evaluated the effectiveness of two CBT interventions, both of which the authors say were particularly influenced by the work of Deblinger et al. 208,485 The first was a child-only intervention. This began with a session that specified the problem areas, presented the rationale for the programme and set goals. The following three sessions focused on teaching coping skills to enable children to deal with disturbing memories of abuse and their feelings of anxiety and guilt (relaxation training, behaviour rehearsal and cognitive therapy). Sessions 5 through to 18 focused on graded exposure, and sessions 19–20 on relapse prevention and education, including personal safety skills. The second intervention was family CBT, in which the child received the programme outlined above, and non-offending mothers also received a CBT intervention. The parent intervention began with the rationale of the programme and issues relating to CSA, followed by nine sessions ‘on the development of parent–child communication skills in order to facilitate listening and problem sharing and to overcome avoidance of abuse-related discussion within the family’ (p. 1350). 103 The remaining 10 sessions focused on child behaviour management, including antecedent stimulus control and contingency management. Parents were encouraged to monitor their own emotional responses in order to provide an appropriate coping model for the child.
Celano et al. 90 evaluated the impact of the Recovering from Abuse Program, an eight-session group that focused on children’s maladaptive beliefs, affects and behaviour along four dimensions: self-blame/stigmatisation; betrayal; traumatic sexualisation and powerlessness.
Jaberghaderi 2004102 compared individual CBT with EMDR, and Foa 2013101 compared exposure therapy with supportive counselling.
Foa 2013101 evaluated the effectiveness of prolonged exposure therapy, delivered in eight modules, comprising (1) explaining the treatment rationale; (2) establishing an index of trauma and teaching participants breathing control; (3) presenting common reactions to trauma; (4) explaining the rationale for in vivo exposure, establishing an in vivo hierarchy and arranging homework for the participant; (5) two to five sessions of imaginal exposure lasting between 15 and 45 minutes, combined with reprocessing of the experiences; (6) four to seven further sessions of imaginal exposure centred on the most extreme periods of trauma; (7) generalisation of newly acquired skills and relapse prevention; and (8) a final project, ‘such as making booklets about the trauma and the gains made in treatment’ (Foa 2013101 p. 2652).
Comparisons
Four studies91–94,101 compared CBT for children and parents with non-directive supportive therapies:
Cohen 200495,96 compared TF-CBT with child-centred therapy (CCT), described as ‘child/parent[-]centred treatment model focused on establishing a trusting therapeutic relationship that is self-affirming, empowering, and validating for the parent and child . . . Therapists provided active listening, reflection, accurate empathy, encouragement to talk about feelings, and belief in the child’s and parent’s ability to develop positive coping strategies for abuse-related difficulties . . . Although sessions were generally client directed, written psychoeducational information about CSA was provided, and children, specifically, were prompted to share their feelings about sexual abuse during two therapy sessions if they did not do so spontaneously’95 (p. 398; reproduced with permission).
Deblinger 199697,98 and King et al. 103 included a community control and wait-list group, respectively.
Celano et al. 90 compared the efficacy of CBT provided to children and their mothers with supportive, unstructured psychotherapy, also to children and their mothers.
Jaberghaderi 2004102 compared individual CBT with EMDR.
Deblinger 2011100 explored the differential effectiveness of eight sessions compared with 16 sessions of TF-CBT, with or without a TN component, that is, a four-arm trial.
Number and duration of sessions
Group treatments
The group-based therapies were provided over 10 and 11 sessions, respectively. 89,99 For the experimental group, Berliner 199689 augmented the conventional sexual abuse specific group therapy provided to the control group with sessions specifically explaining the nature of fear, the principles of SIT and their application to disclosure impact and self-esteem. In the Deblinger 200199 study, parents and children met for a joint group session of 15 minutes each week.
Individual treatments
The individual therapies were provided for between 8 and 20 sessions. Participants in the Celano et al. 90 study had eight sessions of 1 hour each. In all but two or three sessions, the therapist spent half of the time with the mother and half with the child. The remaining sessions were conducted conjointly.
Three studies91–93,95,96 provided around 1.5 hours per week, divided between parents and child over 8 and 12 weeks, respectively.
Deblinger 199697,98 provided therapy in 12 × 45-minute sessions to participants in the parent-only and child-only arms. In the parent-and-child arm, therapy also entailed 12 sessions, but this time of up to 90 minutes. In King 2006,103 all participants each received 20 × 50-minute sessions. This means that, in the parent-and-child arm, 40 × 50-minute sessions were provided.
Adolescent girls in Foa 2013101 received up to 14 sessions of between 60 and 90 minutes, and in the Jaberghaderi et al. 102 study they received up to 12 sessions of 45 minutes in the experimental group and 30 in the EMDR comparison group.
Participants in Deblinger 2011100 were allocated to one of four TF-CBT treatment conditions: eight sessions with a TN component; eight sessions without a TN component; 16 sessions with a TN component; 16 sessions without a TN component. Sessions were each 90 minutes, usually divided into two 45-minute individual sessions for the child and caregiver, respectively. Some sessions included 30 minutes of conjoint parent–child time.
Outcomes and measures used in studies of cognitive–behavioural therapy for sexually abused children
Outcomes assessed using the same measure
When the impact of intervention on parenting practices was assessed, the measure used was the Parenting Practices Questionnaire (PPQ). 274
In each study that examined child depression, child sexual behaviour and child behaviour, the same measures were used, namely the CDI,80 the CSBI259 and the CBCL,260 respectively, although different authors may cite different sources for the same measure.
Outcomes assessed using different measures
Post-traumatic stress disorder
Six studies90,93–99,103 assessed the impact of CBT on symptoms of post-traumatic stress using six different measures.
In addition, Celano 199690 and King 2000103 used both the PTSD subscale of the CBCL,260 completed by the child’s parent, and one other measure of PTSD.
Celano 199690 used a child report measure [Children’s Impact of Traumatic Events Scale-Revised (CITES-R); Wolfe and Gentile, Department of Psychology, London Health Sciences Centre, London, 1991, unpublished] and King et al. 103 used a measure administered by a research assistant (the child version of the Anxiety Disorders Interview Schedule for DSM-IV290).
Two studies97–99 used the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic Version administered to parents;275 two studies95,96,100 used the Kiddie Schedule for Schizophrenia and Affective Disorders, Present and Lifetime Version (KSADS-PL). 268
Cohen 199693,94 used the Trauma Symptom Checklist for Children (TSCC325). Jaberghaderi 2004102 used two measures of post-traumatic symptomatology, the Parent Report of Post-traumatic Symptoms (PROPS) and CROPS. 288
Foa 2013101 assessed PTSD with the Child PTSD Symptom Scale-Interview286,287 and (as a secondary outcome measure) a self-report version of the same measure.
Anxiety
Of the studies using the Stait-Trait Anxiety Inventory for Children (STAI-C), we used data on STAI-C State subscale (as opposed to STAI-C Trait subscale), as this measures present state anxiety. 93–97 Other measures used to assess the impact of interventions on anxiety, included the Revised Children’s Manifest Anxiety Scale (RCMAS)681 and the STAI-C. 682
Fear
Three measures of fear were used in four of the included studies. Berliner and Saunders89 used the Fear Survey Schedule for Children-Revised255 and the Sexual Abuse Fear Evaluation Scales (SAFE). 306 King et al. 103 used the Fear Thermometer for Sexually Abused Children. 291
Study authors typically reported data for study completers rather than for those recruited to the study, for example Cohen and Mannarino. 91,92
Risk of bias: randomised controlled trials of cognitive–behavioural therapy for sexually abused children
Quality aspects were generally not well reported. Of the CBT studies, this is probably the strongest group in terms of risk of bias, although the amount of missing information makes this judgement somewhat speculative.
The difficulties of blinding participants and personnel in studies of psychosocial interventions means that this risk-of-bias domain has largely been assessed as high risk of bias, and, unless there are reasons to believe that the lack of blinding has not resulted in a high risk of bias, we do not comment on this in the following text.
The reliance in many studies on self-report measures, in the absence of other ‘masked’ data collection, also contributes to judgements of high risk of bias in relation to detection bias. On the other hand, we recognise that self-report measures may be a more valid approach to the assessment of some outcomes.
Full details of our assessments of these studies (and all others in this chapter) can be found in Appendix 10. Figure 24 provides an overview of the risk of bias in the body of evidence as a whole for CBT interventions for children who have experienced sexual abuse.
Sequence generation
Sequence allocation was deemed sufficiently robust to be judged low risk of bias in four studies. 89,91–94,99 The Jabergadheri et al. 102 study was judged as being of ‘unclear’ risk of bias because the authors write ‘Participants were randomly assigned to treatment condition, with some adjustments to promote equivalence between groups’ but then go on to describe a blocked randomisation approach (p. 361). The remaining studies were also judged ‘unclear’, as the authors simply report that participants were randomly assigned. 90,95–98,100–103
Allocation concealment
Only two studies89,101 described steps taken to conceal allocation or stated clearly that allocation had been concealed. The Berliner and Saunders89 study reported that ‘Assigned therapists and other staff were blind to the random assignment schedule’ (p. 299) and the Foa et al. 101 study reported that ‘On completing the preparatory phase but prior to the patient beginning treatment, a research assistant consulted the randomisation table and notified the therapist of the patient’s treatment condition’ (p. 2651).
No information was provided in the remaining studies. The Jabergadheri et al. 102 study was assessed as ‘unclear’ on this basis.
Blinding of outcome assessors
Four trials90,93,94,101,102 were judged as ‘low risk of bias’ for outcome assessment. Foa et al. 101 state that ‘assessment was conducted by two psychologists, blind to assignment’ (p. 2651), and Cohen 199893,94 say that ‘The evaluator conducting the initial and follow-up assessments was blind to treatment condition or assignment’ (p. 139); Jaberghaderi et al. 102 says that assessment was conducted ‘by two psychologists, blind to assignment’ (p. 362). Celano et al. 90 reported that ‘standardised measures were administered by a clinician not involved in the child’s treatment. Additionally, a psychiatrist or psychologist blind to treatment condition rated the child’s overall psychosocial functioning based on child and caretaker interviews’.
The remaining studies91,92,95,96,99,100,103 were deemed as ‘high risk of bias’, as they relied wholly on self-report or parent-report measures.
Incomplete outcome data
Four studies93–96,100,101 were assessed as ‘low risk of bias’ for incomplete outcome data. All four analysed data on an intention-to-treat (ITT) basis, although Cohen 200495,96 used SAS multiple imputation for missing data [release 8.2 (2001); SAS Institute Inc., Cary, NC, USA].
Berliner and Saunders89 experienced high levels of attrition and reported on around only 50% of those children who completed at least eight sessions and provided data at one of the follow-up assessment points. The statistical checks undertaken by the authors do not attenuate the likelihood of bias. The levels and approach to attrition was also an issue for Cohen 1996,91,92 King et al. 103 and Jabergadheri et al. 102 The impact of missing data was less clear in the studies by Celano et al. ,90 Deblinger et al. 97,98 and Deblinger et al. ,99 and these were judged to be ‘unclear’.
Selective outcome reporting
Both Foa et al. 101 and Cohen 200495 registered their trials. Foa et al. 101 reported findings for the primary outcome listed; there were no secondary outcomes identified on the trial registration (ClinicalTrials.gov identifier NCT02148484). In addition to all outcome measures listed in the trial registration, Cohen et al. 95 also report post hoc on changes in child behaviour, but overall we judged this trial to be ‘low risk of bias’ on this domain (ClinicalTrials.gov identifier NCT00000383).
In the absence of study protocols it is extremely difficult to assess the risk of selective outcome reporting. In general, most other studies appeared to indicate that they were reporting on all predetermined outcomes. In that respect, almost all were assessed as ‘low risk of bias’. However, Cohen 199893,94 did not report the results for one measure in their report of initial outcomes, but did report outcomes for all time points at 1-year follow-up. Deblinger 2011100 report only the results of analysis of covariance (ANCOVA) for complete sets of data. These two studies93,94,100 were therefore judged to be of ‘high risk of bias’.
Other sources of bias
No other potential sources of bias were identified in these studies. In Jaberghaderi et al. 102 the therapists delivering the CBT and EMDR were both authors on the paper, but, as each was delivering the therapy in both arms of the trial, we judged this to be of ‘low risk of bias’.
Results: cognitive–behavioural therapy for sexually abused children
We were able to combine data from different studies for eight outcomes, at up to three time points: immediately post intervention, 3–6 months later and at least 1 year later. When studies had more than one treatment group, these were combined for the purposes of meta-analysis.
The results presented here involve only participants included by the study authors in their analyses, many of which excluded participants due to dropout, uncollected data or for reasons they do not report. Each result reported is the post-test score in the intervention group compared with the control group.
Post-traumatic stress disorder
Six studies90,93–99,103 examined the impact of CBT on post-traumatic stress using a variety of scales (see Table 5). These studies90,93–99,103 yielded an average reduction of 0.44 SDs based on various child PTSD scales (95% CI 4.43 to 1.53; I2 = 46%; p-value for heterogeneity 0.10; τ2 = 0.05) immediately after treatment, and three of these93–98 suggested a reduction of 0.38 SDs (95% CI 0.65 to 0.11; I2 = 4%; p-value for heterogeneity 0.35; τ2 = 0.00) after at least 1 year (Figure 2).
FIGURE 2.
Cognitive–behavioural therapy vs. no CBT for PTSD. df, degrees of freedom; IV, instrumental variable.
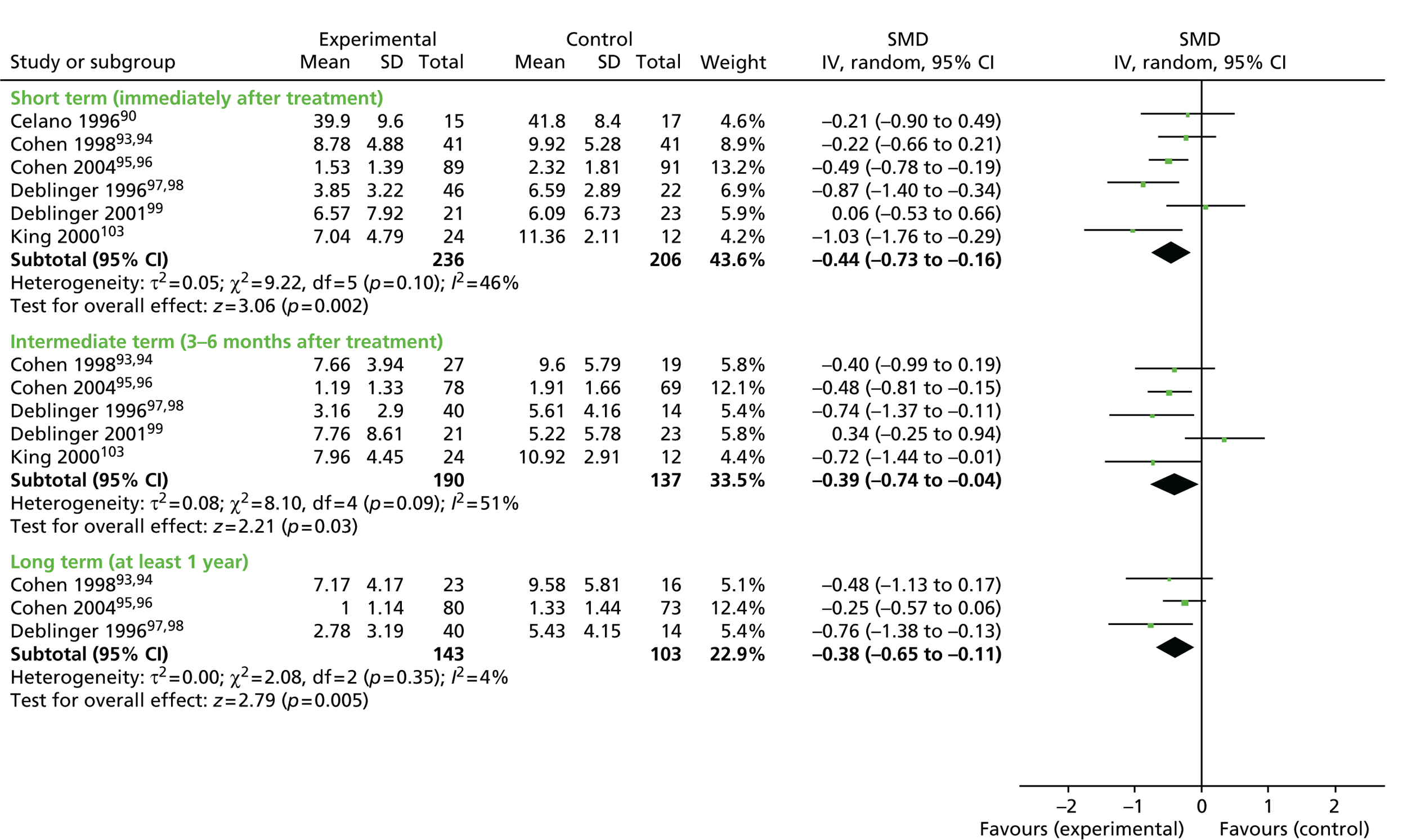
In our sensitivity analysis we found that over the range of correlations assumed (ρ= 0, 0.25, 0.5, 0.75, 1), results for PTSD are robust to whether follow-up measures or change score measures are used. This was the case for both post-test outcomes and 1-year outcomes.
Depression
Five studies90,93–98,103 looked at the impact of CBT on depression in children using the CDI. When combined in a meta-analysis, these five studies yielded an average reduction of 2.83 points on the CDI immediately after intervention (95% CI –4.53 to 1.13; I2 = 22%; p-value for heterogeneity 0.27; τ2 = 0.84) (Figure 3).
FIGURE 3.
Cognitive–behavioural therapy vs. no CBT for depression. df, degrees of freedom; IV, instrumental variable.

Four of these studies89,93–98 sustained an average decrease of 1.42 points (95% CI –2.91 to 0.06; I2 = 0%; p = 0.06; τ2 = 0.0) after at least 1 year (see Figure 3). A decrease of 2.9 on the CDI represents something in excess of a modest change in a scale that previous studies683,684 indicate has a SD of approximately 7. This represents a small to moderate effect size, broadly equivalent to that seen on the anxiety scales in meta-analyses in this review.
In our sensitivity analysis, we found that for both post-test measures and 1-year follow-up measures, the results were closer to ‘no effect’ when using change scores rather than follow-up scores. CIs became wider as the assumed correlation reduced, but even when the correlation is assumed to be 1, the estimated mean difference (MD) is –1.98 for post-test scores with a 95% CI of –4.59 to 0.63, and –0.51 for 1-year follow-up scores with a 95% CI of –3.0 to 2.0.
Anxiety
Five studies89,93–98,103 examined the impact of CBT on anxiety. These yielded an average decrease of 0.23 SDs on various child anxiety scales (95% CI 0.03 to 0.42; I2 = 0%; p-value for heterogeneity 0.84; τ2 = 0.0) immediately after treatment, and four of these89,93–98 reported a sustained decrease of 0.28 SDs (95% CI –0.52 to –0.04; I2 = 0%; p-value for heterogeneity = 0.62; τ2 = 0.0) after at least 1 year (Figure 4).
FIGURE 4.
Cognitive–behavioural therapy vs. no CBT for anxiety. df, degrees of freedom; IV, instrumental variable.
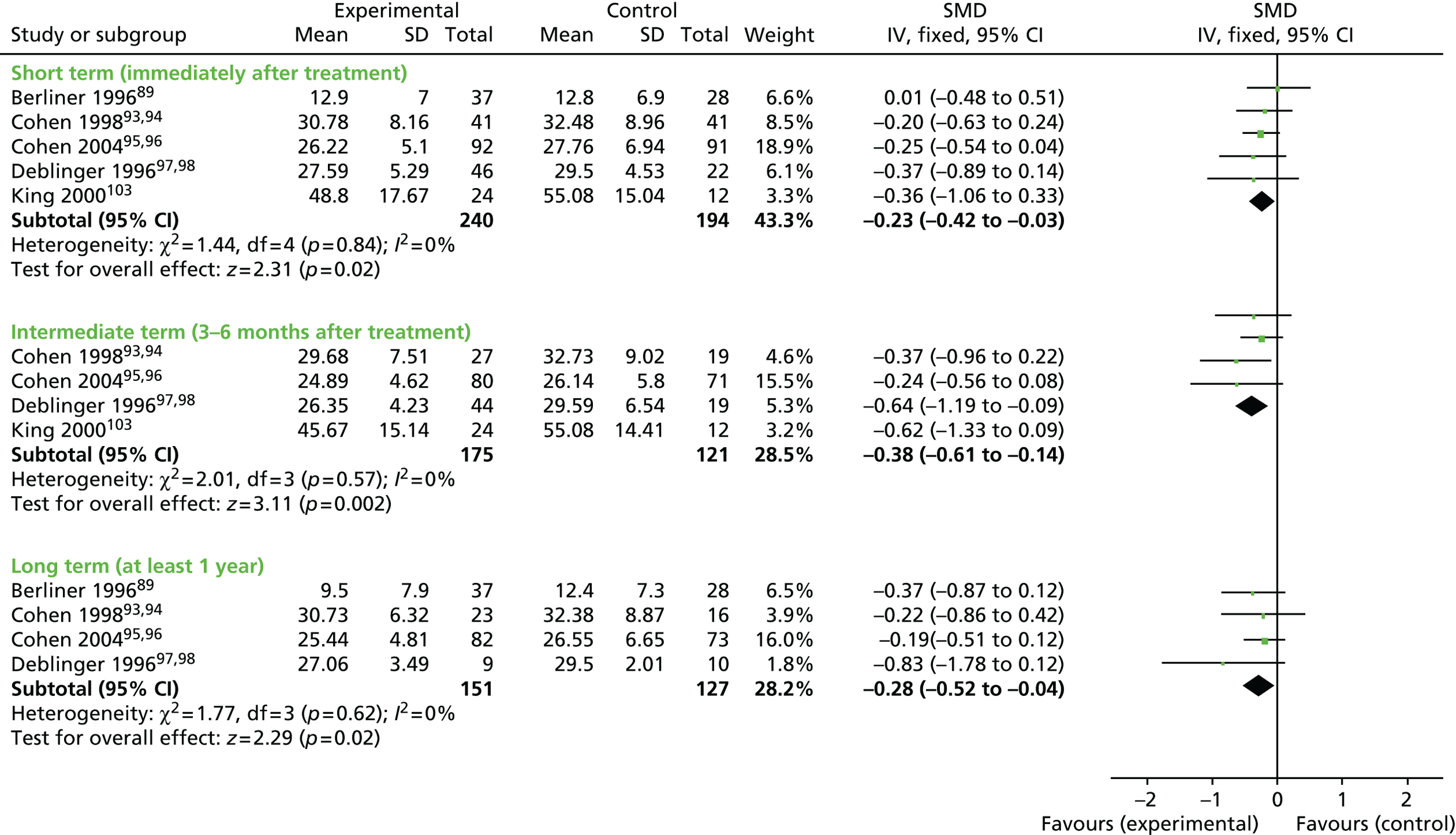
In our sensitivity analysis, we found that for post-test measures, the results were closer to ‘no effect’ when using change scores rather than follow-up scores. CIs increased as the assumed correlation reduced, but, even when the correlation is assumed to be 1, the estimated SMD is –0.19 with a 95% CI of –0.51 to 0.12. For 1-year follow-up measures, results were robust with similar results using change scores as with follow-up scores, showing no evidence of effect.
Sexualised behaviour
Five studies89,91–96,99 provided conflicting evidence on the effectiveness of CBT in the domain of child behaviour problems, assessed using the CSBI (I2 = 67%, p-value for heterogeneity 0.02; τ2 = 6.81). Two studies89,99 observed increases of 4.7 and 1.7 points and three studies91–96 observed decreases, one91,92 of which was statistically significant. In a meta-analysis, there was no evidence of an effect on average (mean decrease of –0.65 points, 95% CI –3.53 to 2.24 points).
Four studies89,91–96 provided longer-term data. The first of these observed a much smaller increase than the same study in the short term. Overall, the average effect found at the 3- to 6-month assessment point was similar to that immediately after treatment but was not statistically significant (–0.46 points, 95% CI –5.68 to 4.76 points; Figure 5). Note that Cohen 200495,96 did not report data for this outcome because it was not statistically significant. Although we have not been able to retrieve these data, their inclusion is highly unlikely to change the overall conclusion for this outcome.
FIGURE 5.
Cognitive–behavioural therapy vs. no CBT for sexualised behaviour. df, degrees of freedom; IV, instrumental variable.
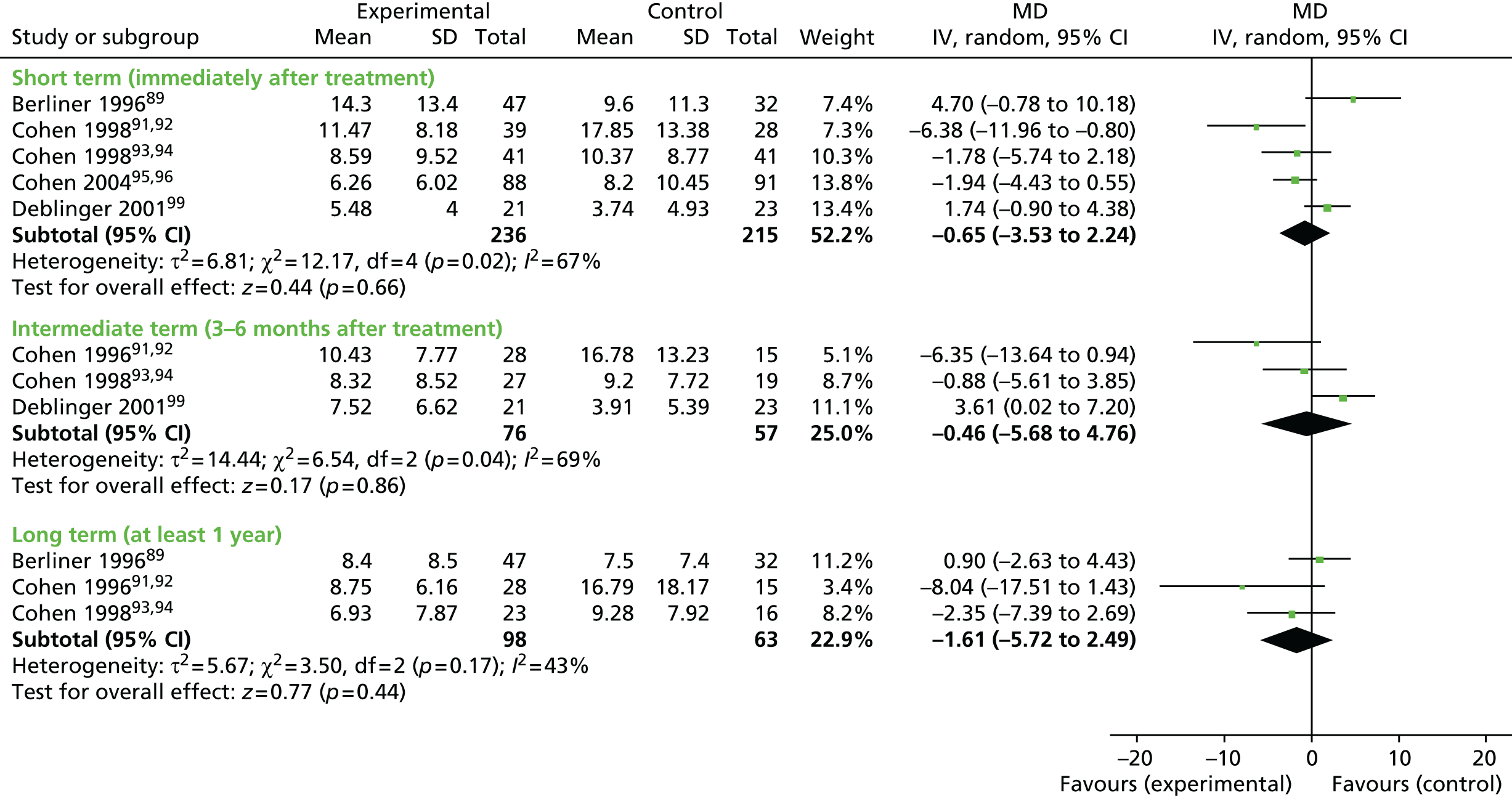
Externalising behaviour (e.g. aggression, ‘acting out’)
Seven studies89–98,103 provided data on the CBCL, using the externalising behaviour scale. A meta-analysis of standardised differences in means (owing different scoring systems being used for the scale) did not provide evidence of a beneficial effect on average (decrease of 0.12 SDs, 95% CI –0.40 to 0.17). However, the results were inconsistent (I2 = 58%; p-value for heterogeneity 0.03; τ2 = 0.08), with one study89 observing a statistically significant increase and one study observing a statistically significant decrease. 97,98
Only five studies90–98 provided longer-term data from which no clear picture merged of either benefit or harm (Figure 6).
FIGURE 6.
Cognitive–behavioural therapy vs. no CBT for child externalising behaviour. df, degrees of freedom; IV, instrumental variable.

Behaviour management skills of parents
Data from three studies95–99 provide information on the effects of involving parents in CBT interventions with their children on their ability to manage their children’s behaviour. All three studies used the PPQ to assess change. Only two95,96,99 of these studies reported follow-up data for 1 year post treatment. A meta-analysis of outcome data from these two studies indicates a decrease in mean scores of –0.89 1 year after treatment (95% CI –4.89 to 3.11). The long-term effects were not statistically significant but raise doubt about the maintenance of change shown in the post-treatment results, which favoured CBT (Figure 7).
FIGURE 7.
Cognitive–behavioural therapy vs. no CBT for behaviour management skills of parents. df, degrees of freedom; IV, instrumental variable.
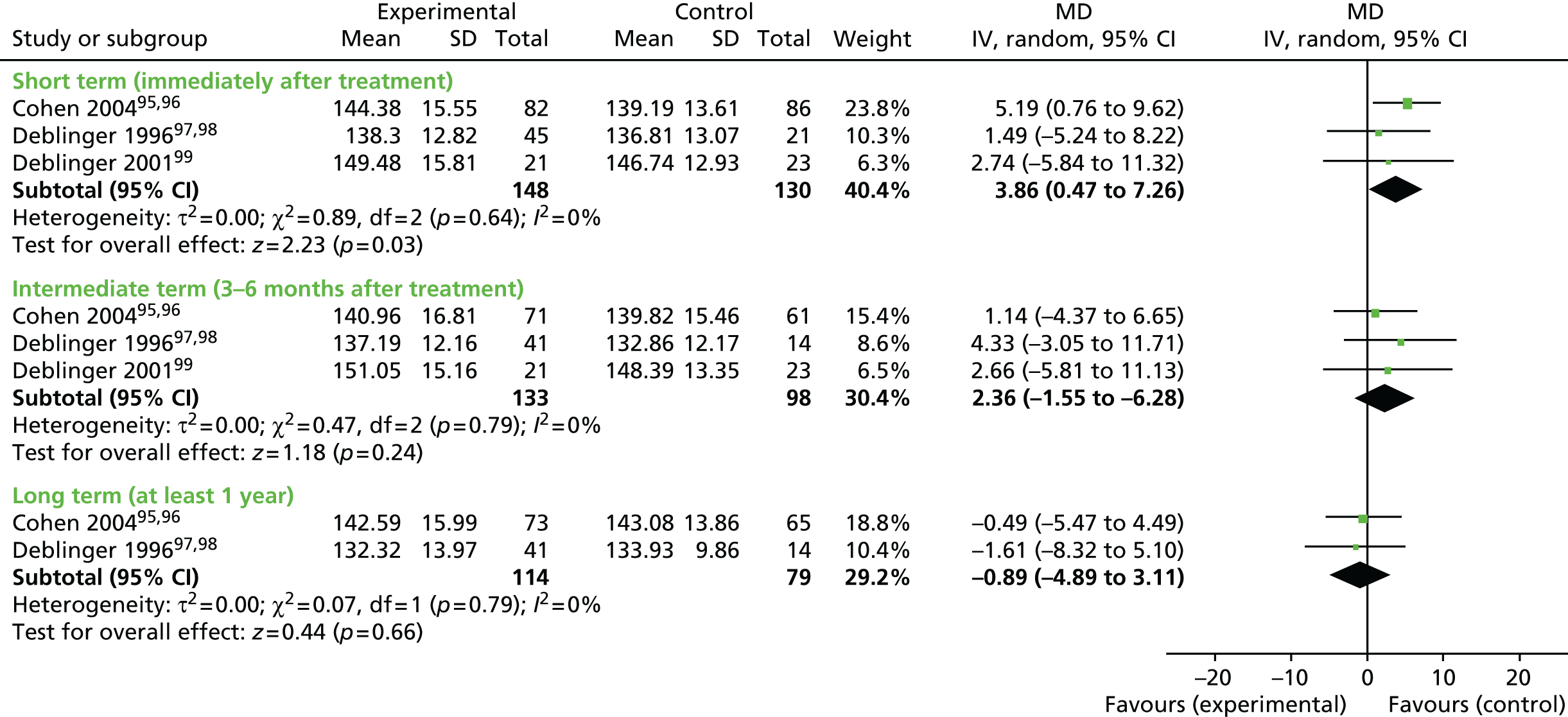
Two studies90,95,96 used, respectively, the Parental Reaction to Incest Disclosure Scale and the Parental Support Questionnaire to measure parental belief of their children and support for them. A meta-analysis of standardised differences in means gave a statistically significant increase of 0.3 SDs in favour of CBT (95% CI 0.03 to 0.57) (Figure 8).
FIGURE 8.
Cognitive–behavioural therapy vs. no CBT for parental support to child. df, degrees of freedom; IV, instrumental variable.

Only one study90 examined parental attributions. In this study,90 the author reported small, statistically non-significant improvements on four aspects of parental attributions, using the Parental Attribution Scale. Parents who had been involved in the CBT arm of this study90 were less likely to blame themselves or their child for what had happened, were slightly more optimistic about their child’s future than those in the TAU group and more likely to hold the perpetrator responsible. However, the CIs were very wide, crossing the line of no effect.
The Parent Emotional Reaction Questionnaire (PERQ) is designed to assess stressful parental emotional reactions to the sexual abuse of their children. Parents are asked to endorse the frequency of specific reactions including fear, sadness, guilt, anger, embarrassment, shame and emotional preoccupation. No psychometric data are currently available for this measure. In the two studies95,96,99 that used the PERQ we found a decrease of seven points in parents’ negative reactions (95% CI 3.8 to 10.1). Cohen 200495,96 measured outcomes longer term, and observed a smaller but still statistically significant, decrease of 4.6 points at 1 year.
Additional results: studies of cognitive–behavioural therapy for sexually abused children
The above meta-analyses incorporate most of the data available from the randomised trials of CBT for children who have been sexually abused. Some studies reported on outcomes that are not covered above, or presented data in ways that could not be incorporated. These are briefly summarised here.
King et al. 103 assessed the effectiveness of CBT for improving children’s self-efficacy as measured by the (self-report) Coping Questionnaire for Sexually Abused Children (developed by the author) but reported no significant differences between the group receiving CBT and a wait-list control group.
Deblinger 200199 reported a significant difference in favour of CBT for the total score on the CBCL [repeated-measures multivariate analysis of variance (MANOVA), time/time × group)]. They commented that children in neither group were encouraged to talk in detail about their abusive experiences, owing to their young age, which might account for the smaller reductions in PTSD among the CBT group compared with the control group.
Jaberghaderi et al. 102 compared the effectiveness of CBT with EMDR, using two outcome measures. The first was a broad-spectrum, self-report questionnaire-based measure of post-traumatic symptoms (rather than PTSD), CROPS and PROPS. 288 The second was a teacher report scale of potential mental disturbance: the Rutter Teacher Scale. 289 For post-traumatic symptoms the authors reported large effect sizes (pre- to post-treatment) for both CBT and EMDR and a moderate effect size for the behavioural measure (the Rutter Scale). No significant differences were found between the two treatments. This was a small study102 (n = 14) with no follow-up and was one of the few studies conducted outside the USA.
Foa et al. 101 assessed the impact of prolonged exposure therapy using piecewise linear mixed models (LMMs) for continuous data and generalised LMMs for dichotomous data. The authors reported that those treated with prolonged exposure derived greater benefit than those who received supportive counselling, even when delivered by counsellors who typically delivered that form of therapy. Those who received prolonged exposure demonstrated greater improvements on the PTSD symptom severity scale (primary outcome) and on all secondary outcomes, namely self-reported PTSD severity, depression and global functioning. Treatment differences were maintained at 1-year follow-up.
Effectiveness of cognitive–behavioural therapy for children who have been sexually abused
Summary
We identified 11 studies of CBT interventions for children and young people who have been sexually abused. Six studies90–96,99,101 compared CBT with supportive, non-directive therapy and two studies97,98,103 compared CBT with no-treatment controls (community and wait-list). One study102 compared CBT with another treatment (EMDR) and two studies89,90 compared variations of CBT treatments, that is CBT with and without a focus on SIT and a focus on fear and anxiety,89 or different exposures of CBT with or without a TN component. 100
For children who have been sexually abused, various adaptations of CBT, some offered individually, some in groups and some including work with parents proved of some benefit in reductions in PTSD, depression and anxiety, which were sustained at 1 year post treatment. One102 small study reported equal benefit for CBT and EMDR in reducing PTSD symptoms. There was no evidence of benefit of CBT in reducing sexualised and externalising behaviours. Regarding changes in parents, there was evidence of some improvement in parents’ management of children’s behaviour and support for children, and some change in parents’ attributions regarding the abuse. No harms were reported in any study, but no study set out specifically to examine harms.
This evidence is in line with the conclusions of earlier reviews (e.g. Macdonald et al. ,685 Harvey and Taylor686 and de Medeiros Passarela et al. 687), suggesting that these approaches may be beneficial compared with non-directive, supportive therapies, but the evidence base remains limited.
Completeness and applicability
None of these studies was conducted in the UK, with most undertaken within the USA. However, the profile of participants is clinically comparable to the population of children who might benefit from child and mental health services in the UK, and the therapies evaluated are recognised, and available, in the UK.
Quality of the evidence
Studies of CBT for children who have been sexually abused could be improved, and would benefit from careful and explicit reporting against Consolidated Standards of Reporting Trials (CONSORT) guidelines. Of some concern is that the field is somewhat dominated by a small team of US researchers who evaluate a version of CBT that they themselves developed.
Economic evidence
One612 economic evaluation, carried out in Australia, explored the cost-effectiveness of CBT for children who have been sexually abused. The study612 used a decision-analytic design to establish the cost–utility of three different treatment strategies for PTSD secondary to childhood sexual abuse, compared with a no-treatment comparator: individual TF-CBT, combined individual TF-CBT plus pharmacotherapy [selective serotonin reuptake inhibitor (SSRI)], and non-directive counselling. Costs and outcomes were modelled for a hypothetical cohort of 10-year-old children diagnosed with PTSD or PTSD plus depression, subsequent to sexual abuse.
The decision model included a decision tree that modelled the costs and benefits of each treatment during the post-treatment and 12-month follow-up period observed in clinical trials, and a subsequent Markov model that estimated the long-term costs and consequences of the alternative treatments over a 30-year period. The economic evaluation was conducted from the perspective of the Australian mental health care system, and costs and benefits were expressed in 2010–11 Australian dollars (A$) and discounted at a rate of 5% per year.
The model was populated with data obtained from a number of clinical trials and the 2007 Australian Mental Health Survey. 402 Resources included in the model were the cost of therapists’ time and the costs of SSRI medication for the combined treatment group. The impact of intervention on the use of other health and social care services (‘knock-on’ effects) was not included. Resources were valued using national published sources for unit costs. Outcomes were reported in terms of QALYs calculated from the Analysis of Quality of Life (AQoL-4D), a generic preference-based instrument included in the 2007 Australian Mental Health Survey. Data from the survey were selected for children and adolescents with a history of childhood sexual abuse, who also met the criteria for PTSD, depression or PTSD and depression.
The results suggest that all treatments would be considered good value for money compared with no treatment from the perspective of the Australian mental health system (all ICERs < A$7000 per QALY gained, compared with a stated threshold of A$50,000 per QALY gained). Non-directive counselling was dominated by TF-CBT (more expensive and less effective) and TF-CBT plus SSRI appears more cost-effective than TF-CBT alone. However, results were sensitive to variation in the clinical effectiveness parameters, and the analysis was limited, particularly by the narrow cost perspective.
Cognitive–behavioural therapy: children who have been physically abused
Three studies106–109 examined the effectiveness of CBT specifically with children who had experienced physical abuse.
Description of studies
Participants
Age
The mean ages of children in the studies by Kolko107,108 and Runyon et al. 109 were 8.6 years and 9.88 years, respectively. Adolescents in the LeSure-Lester106 study were aged 12–16 years.
Gender and ethnicity
The 12 participants in LeSure-Lester106 study were African American males, 28 of 36 completers in the Kolko107,108 study were boys, and, of those who completed at least three sessions of therapy in the Runyon et al. 109 study, 28 of 44 were girls.
Recruitment
In the Runyon et al. study109 all but five of the families in the final sample were referred by child protection service agencies. Those in the Kolko107,108 study were referred by Child Protective Services (CPS) caseworkers. In the LeSure-Lester study,106 participants were recruited from a group home where they had been placed by CPS.
Maltreatment
Participants in all three106–109 studies had experienced physical abuse or (four cases in the Kolko107,108) study severe or frequent forms of physical discipline with a risk of injury.
Interventions and comparison
Kolko107,108 evaluated the impact of two interventions: a manualised FT treatment for physically abused children and a manualised CBT intervention for individual children and their parent(s). In the CBT arm, children and parents received therapy from separate therapists, who implemented parallel protocols based on social learning principles that were designed to address cognitive, affective and behavioural problems. Treatment for the children addressed their perceptions of family stress and their environments; training to develop coping and self-control skills; and interpersonal effectiveness. The intervention for parents focused on their views on violence and physical punishment, their attribution style and expectations, self-control and contingency management. There was throughout an emphasis on teaching intrapersonal and interpersonal skills. The FT was based on Belsky’s227 interactional or ecological model approach to child maltreatment. It sought to ‘enhance the cooperation and motivation of family members by promoting understanding of coercive behaviour and by teaching the family positive communication skills and how to solve problems together’ (p. 326). 227
The control group received routine community services from providers not associated with the project, as mandated by family service workers. Services were based on an extensive risk assessment and included ‘home visits to provide support and information, family skills specialists who taught homemaking and related skills, and parenting information and support groups’108 plus regular telephone contact from the caseworker (p. 326).
Runyon et al. 109 assessed the added value of providing treatment to children [combined parent–child cognitive–behavioural therapy (CPC-CBT)], as well as parents (parent-only CBT). Children in the CPC-CBT arm received an intervention covering psychoeducation; affect regulation; coping skills; cognitive coping; assertiveness skills and anger management; general safety skills; application of skills; development of a personal safety plan; role perspective-taking skills; problem-solving skills; preparing a letter of praise; developing a TN; and agreeing and sharing a joint TN (with parents). In addition to the usual parents’ programme (see Comparisons), parents in the experimental arm received input on parent training with the child; refinement and rehearsal of personal safety plans with the child; attention to abuse clarification and the development of the joint TN plus coaching in parent–child interactions; behaviour rehearsal of coping skills; parenting skills and safety plan; sharing of TN; and abuse clarification.
The parent-only CBT control arm received an intervention that comprised disclosure of the referral incident, engagement and assessing parents’ goals, motivational interviewing and commitment to no violence (two sessions), followed by psychoeducation and an introduction to anger management skills (two sessions), continuation of coping skills (three sessions), review and applications of skills, including ABCs of parent–child interactions, development of personal safety plans (three sessions); review of ABCs of parent–child interactions and integration/generalisation of skills (four sessions) and parent training (parent only, two sessions).
LeSure-Lester106 provided CBT to groups of two to three participants. The intervention was designed to teach participants the feelings associated with anger and aggression, relaxation and self-talk, and alternative ways of coping. It comprised a three-stage education and training module, beginning with education relaxation techniques. This was followed by education and GE and then education and anger control. The therapist used vignettes (as the basis for discussions) that reflected the participants’ natural environments, that is, the residential setting. Participants in the control arm received ‘traditional indirect therapy’ consisting of open-ended discussions and communications of the participants’ self-reports of activities and current events in their daily lives. The therapists were said to have exercised warmth, empathy and genuineness – no specific coping skills were taught.
Number and duration of sessions
Each intervention in the Kolko107,108 study entailed at least 12 1-hour weekly clinic sessions over a 16-week period, for a total of about 18 hours of service. Those in the routine community services (control) arm received variable amounts of help, ranging from services delivered on a once or twice per week basis for an indefinite period of time, to treatment plans comprising up to 20 hours of home-based service per week for up to 3 months.
In the Runyon et al. 109 study, parents in the ‘combined intervention’ attended 16 2-hour group sessions over a 16- to 20-week period. Groups were initially conducted concurrently for the first hour and 45 minutes, with the last 15 minutes involving joint parent–child sessions based on families’ needs. The balance between concurrent and joint time shifted over the course of the intervention so that in sessions 12–16 the joint sessions lasted 60–75 minutes. Parents in the ‘Parent only’ condition received a similar CBT parenting intervention, but spent more time discussing the implementation of behaviour management strategies. Parents in the ‘Combined’ arm spent less time on parent skills training and more time preparing their ‘clarification letter’ (a letter that demonstrated that they took full responsibility for their abuse behaviour) and preparing for, and interacting with, their children in joint sessions. This was one of only a few interventions that included the non-offending parent.
In the LeSure-Lester106 study, participants in both arms received 26 weeks of traditional indirect therapy, and were then randomised to continue with that therapy or to receive 26 weeks of CBT. Both therapies were delivered for 1 hour, twice per month.
Outcomes and measures used in studies of cognitive–behavioural therapy for physically abused children
Post-traumatic stress disorder
Only Runyon et al. 109 assessed the impact of intervention on PTSD, using the KSADS-PL268 (see Post-traumatic stress disorder). This was the primary outcome in this study. 109
Behaviour
Runyon et al. 109 and Kolko107,108 both used the CBCL260 to assess change in child behaviour, along with the Child Conflict Index (CCI). 688
LeSure-Lester106 used a rating system of behavioural appropriateness developed within the residential setting, and comprising aggression towards peers, towards staff and compliance with house rules (all scored low or high).
Risk of bias: randomised controlled trials of cognitive–behavioural therapy for physically abused children
Sequence generation
Kolko107,108 used a computer-generated procedure based on Efron’s biased coin toss and was assessed as low risk of bias. Runyon et al. 109 used a computer program to randomly determine the treatment type for each group, and on that basis was deemed low risk of bias. No information was provided by LeSure-Lester106 and so this study was judged unclear.
Allocation concealment
The LeSure-Lester study106 was judged as ‘high risk’, as the author was both the provider of the intervention and the researcher. The project co-ordinator in the Runyon et al. 109 study was blind at pre-treatment so we concluded that allocation was concealed at this point (low risk of bias). Kolko107,108 provided no information and so was judged unclear risk of bias.
Blinding of participants and personnel
High risk: participants and personnel were not blinded in any of the three trials. 106–109
Blinding of outcome assessors
Runyon et al. 109 stated that the project co-ordinator (who conducted all assessments) ‘remained blind, to the extent possible, to condition assignment’ but it is not clear to what extent this was achieved. The determination of unclear risk of bias was made. Risk of bias was high in the study by LeSure-Lester106 as outcome data were provided by staff in the residential care home. Kolko108 reported that ‘[P]roject staff administering the assessment protocol were unaware of the treatment conditions to which participants were assigned’ and was judged low risk of bias, although the same data were self-reported.
Incomplete outcome data
Attrition in the Kolko107,108 study was around 6% (one case) in the FT arm, 20% (five cases) in the CBT arm and 17% (two cases) in the routine community services groups. Although these cases did not appear to be different in characteristics, the differential attrition between the two active treatment arms resulted in a judgement of high risk of bias (the reasons for dropout might be related to the intervention). No attrition occurred in the LeSure-Lester106 study, so this was judged as ‘low risk’. The Runyon et al. 109 study was judged as ‘high risk of bias’: 25% children who completed 3 weeks’ therapy did not provide data post test, and their pre-test scores were carried forward. Attrition increased at follow-up and the authors present no means or SDs at this assessment point.
Selective outcome reporting
The LeSure-Lester106 study was assessed as low risk for selective outcome reporting. This study106 is small, modest in design and implementation, and data are given on those outcomes that the intervention was seeking to address (using ‘home-made’ measures). Kolko107,108 and Runyon et al. 109 appear to have reported on all outcomes covered in the methods section, but, in the absence of a published protocol for either study106 both were assessed as unclear for this domain.
Other sources of bias
LeSure-Lester’s106 study was compromised by the conflation of roles held by the author, that is, researcher and therapist.
Results: cognitive–behavioural therapy for physically abused children
Meta-analysis was not possible across these studies,106–109 which are summarised narratively.
Post-traumatic stress disorder
The Runyon et al. 109 study reported significant pre- to post-improvement on the total number of PTSD symptoms among all children, with the adjusted mean post-test scores for those in the combined CBT parent and CBT child group being significantly lower than those for the parent-only CBT group.
Child depression
In the Kolko107,108 study, children’s reports on the CDI80 indicated a significant reduction in severity of depressive symptoms over time [χ2 = 16.01(3); p < 0.001], but reports were said to be ‘generally low and similar across time, indicating no significant group differences’108 (p. 333).
Child behaviour
As measured by the Youth Self-Report (YSR) of the CBCL, children in all three groups in the Kolko107,108 study (CBT, FT and routine services) reported a significant reduction over time in both internalising symptoms [χ2 = 33.54(3); p < 0.0001] and externalising symptoms [χ2 = 12.26 (3); p < 0.002], with both CBT and FT showing most change on these measures. No effect was found for social competence.
Parent report on the CBCL indicated lower ratings of serious internalising behaviours over time (p < 0.07), particularly for the two treatment arms. Parents reported a significant reduction in externalising behaviour over time [χ2 = 9.53(3); p < 0.02]. Based on an inspection of the means over time, CBT appeared to show the greatest initial change and FT the greatest change at follow-up (1 year) compared with routine community services, which showed minimal change during that period.
A significant interaction was reported on the CCI [χ2 = 13.12(3); p < 0.04], reflecting the greatest decrease in scores for CBT. This measure (scored by telephone interview with the parent) estimates the presence or absence of common individual behavioural or emotional problems commonly displayed in boys or girls within the previous 24 hours.
Runyon et al. 109 reported significant pre- to post-improvement in internalising and externalising scores (CBCL) for the CBT parent-only condition.
LeSure-Lester106 reported greater rates of behaviour change from pre-test to post-test for the six adolescents who received CBT. Using the rating system used by staff within the home, these six adolescents demonstrated greater rates of behaviour compliance (t = –5.64; p < 0.001) and less aggression towards staff (t = –4.56; p < 0.001) and other residents (t = –5.64; p < 0.001).
The effectiveness of cognitive–behavioural therapy for children who have been physically abused
Summary
We identified only three studies106–109 of CBT interventions for children and young people who have been physically abused. Each focused on children of somewhat different ages, from middle childhood to adolescence. One study107,108 compared a CBT intervention for children and their parents with systemic FT; one study109 compared a CBT intervention for parents with one that included a parallel intervention for children, and the third study106 compared a small group version of a CBT provided to African American adolescents living in a group home as a direct result of their maltreatment, compared with non-directive group discussions.
Although very different, the three CBT interventions106–109 shared some common characteristics, namely a focus on children’s thoughts, feelings and behaviour. There was a marked psychoeducational component in both the Runyon et al. 109 and the LeSure-Lester106 study, aimed at helping children to recognise and understand the consequences of abuse, and develop appropriate coping and problem-solving skills, including the development of skills to minimise risk of abuse107,108 or personal safety plans. 109
The three106–109 studies are all extremely small and the overall quality is, at best, moderate in relation to risk of bias. Together with the fact that we can summarise the evidence only narratively, considerable caution is required in interpreting the data. All three106–109 studies report improvement in children’s internalising and externalising behaviour problems (common sequelae of physical abuse), but one109 of the studies found an improvement in externalising behaviour in the parent treatment group only.
The one109 study examining PTSD reported a reduction in symptoms in all children, with the most significant reduction occurring for those where both parents and children received CBT. Depression, examined in one109 study, reduced over time in both the experimental and comparison groups.
Both CBT and FT generally outperformed routine community services, resulting in greater reductions in children’s externalising behaviour and on child-reported parent-to-child violence and parent-reported child-to-parent violence.
Completeness and applicability
All three106–109 studies were conducted in the USA. Two107–109 studies were concerned with families who had come to the attention of services because of maltreatment, but where the child remained in the home. They aimed to minimise the risk of further physical abuse and to address the adverse consequences of past abuse and current maladaptive parenting. In Kolko107,108 maltreatment was judged as ‘mild/moderate’ in 87% cases, although almost half the families had children that had been hit with an object, and 50% had children who had been smacked with an open hand. In the Runyon et al. 109 study, 53% families had a substantiated allegation of physical abuse or had acknowledged the use of excessive physical punishment (e.g. 65% had hit their children with an object). Many of the children in these three studies would be subject to a child protection plan in the UK, and in the Runyon et al. 109 study (although not in the Kolko107,108 study) the inclusion criteria required children to have either four PTSD symptoms or an elevated score (T score of ≥ 65) on at least one externalising behaviour subscale on the CBCL. 260 In this study, siblings were included in the treatment as long as they too could meet these criteria and were a focus of child protection workers’ concerns. These studies106–109 therefore have relevance to the UK context, although they are limited in their scope and the evidence base is sparse.
LeSure-Lester106 evaluated an intervention that was designed specifically to address the aggressive behaviours of boys who had been removed from the family home as a result of maltreatment. Although the focus on addressing maltreatment-related aggression is highly relevant to the UK context, the study106 says little about the intervention, and the outcome measures focus on resident–staff interaction (with an emphasis on compliance) and peer–peer violence within the home. Although the intervention is reported to have made a significant impact, the size of the study,106 plus the absence of measures or time periods to indicate the generalisability or likely maintenance of reported behaviour change, mean that its applicability is limited.
Quality of the evidence
Studies of CBT for children who have been physically abused are few in number, poorly reported, and overall of limited quality, although poor reporting may account for many of the identified risks of bias.
Economic evidence
No economic evaluations of CBT were located for children who have been physically abused.
Cognitive–behavioural therapy: children who have experienced different types of maltreatment
Nine randomised trials of CBT or enhanced CBT interventions were identified110–112,114–117,120,121 that were designed to address the consequence of maltreatment, irrespective of maltreatment type. The studies were themselves heterogeneous, and fall into four broad categories:
-
interventions to enhance the parenting skills of foster parents and adopters, in order to help them address the particular challenges of parenting children with maltreatment histories112,114–116
-
interventions addressing PTSD and associated symptoms in maltreated young people111,117
-
risk reduction interventions to reduce human immunodeficiency virus (HIV) and sexually transmitted infections (STIs) among abused and neglected young people110
Description of studies
Location
All but four111,112,116,120 studies were conducted in the USA. The Rushton et al. 116 study was conducted in the UK, the Farkas et al. 120 study in Quebec, Canada, the Church et al. 111 study in Peru and the Jensen et al. 112,113 study in Norway.
Sample size
Five110,111,117,120,121 studies recruited and randomised individual participants who had been maltreated. The Church et al. 111 study recruited just 16 participants, whereas the studies by Farkas et al. 120 and Scheck et al. 121 recruited, respectively, 40 and 60 participants to their studies of EMDR and the Shirk et al. 117 study randomised 43 adolescents. Champion and Collins110 randomised 559 adolescent women.
The Jensen et al. 112,113 study randomised 156 parents. (Only 135 parents participated in the study.)
The remaining three studies recruited participant pairs. Rushton et al. 116 recruited 38 adoptive families. One study by Linares et al. 115 enrolled 94 children, with the intervention targeted at foster parent/biological parent pairs, whereas the other Linares et al. 114 study recruited 63 biological/foster parent pairs.
Participants
Age
Three114–116 studies focused on children aged < 10 years. Children in the Rushton et al. 116 study were between 3 years and 7 years 11 months at recruitment; the Linares et al. 115 study recruited foster parents caring for children aged 5–8 years, and children in the Linares et al. 114 study were aged 3–10 years.
Five110,111,117,120,121 studies recruited adolescents. The studies by Champion and Collins110 and Church et al. 111 recruited adolescent women aged 14–18 years and 12–17 years, respectively. Shirk et al. 117 recruited adolescents aged 13–17 years. The two120,121 EMDR studies recruited adolescents aged 13–17 years120 and 16–25 years. 121
Jensen et al. 112,113 recruited the caretakers of children and young people aged 10–18 years.
Gender
Six112,114–117,120 of these studies recruited both male and female children or their carers. Some had a preponderance of one gender, for example the samples in the studies by Shirk et al. 117 and Farkas et al. 120 were largely female (85% and 74%, respectively). Participants in the Church et al. 111 study were all male, whereas in the studies by Champion and Collins110 and Scheck et al. 121 the participants were all female.
Referrals
The Rushton et al. 116 study recruited adoptive parents referred from English local authorities that had high rates of adoption. Adoptors were eligible if at least one of their adopted children scored above a certain threshold on the Strengths and Difficulties Questionnaire (SDQ), completed by either the adoptor or the child’s social worker, or both. The Champion and Collins110 study recruited participants from women seeking health care at a district health clinic.
Participants in the Linares et al. 115 study were drawn from community-based mental health services, but it is not clear how they were recruited. Linares et al. 114 recruited foster parents from one child welfare agency.
Church et al. 111 recruited young men who were resident in a residential treatment refuge (Peru). Adolescents in the Shirk et al. 117 study had been referred to an outpatient department in a large, urban mental health centre, and those in Jensen et al. 112,113 were children referred to one of eight community clinics via normal referral routes [general practitioner (GP), Child Protection Services] who had experienced a traumatic event and who scored ≥ 15 on the Child PTSD Sympton Scale (CPSS). 286
One121 of the EMDR studies recruited volunteers from adverts in a range of agencies,121 whereas the other120 took referrals only from youth protective services.
Maltreatment type
In Linares 2006,114 children had experienced physical abuse or neglect, but (by chance) only neglected children were allocated to the control condition, compared with 71% in the intervention group.
In the Linares 2012,115 children had officially substantiated histories of child maltreatment: 77% were neglected and 23% were abused either physically (18%) or sexually (5%). Some children experienced more than one form of maltreatment.
Children in the Church et al. 111 study had a history of physical, psychological or sexual abuse or neglect/parental abandonment. The majority of participants in the Champion and Collins110 study (76%) had histories of sexual, physical and emotional abuse. This study110 recruited women with abuse histories or histories of STIs (because of the over-representation of maltreatment in the histories of adolescents) and was designed to ‘provide a study sample of adolescents with both a history of STI and abuse’110 (p. 142).
Participants in both EMDR studies120,121 had histories of maltreatment. Most of those in the Farkas et al. 120 study had been referred to Youth Protective Services for a variety of forms of parental neglect or abuse, although some were referred for reasons of serious behaviour problems. Most participants had been referred for, or had experienced more than one form of, maltreatment; it was not possible to identify the proportion of participants who had not been maltreated. A total of 90% of participants in the Scheck et al. 121 study reported being victims of physical or emotional abuse as a child, and over half of the traumas reported related to traumatic sexual experiences, such as rape or child molestation.
Adolescents in Jensen et al. 112,113 had been exposed to a range of traumas, including physical and sexual abuse, and witnessing violence.
Interventions and comparisons
The interventions in the studies by Rushton et al. 116 and Linares et al. 114,115 were modified versions of Webster-Stratton’s Incredible Years Program (IY). 212
Linares et al. 114 used the manualised, group-based Parents and Children Basic Series Program (IY, Webster-Stratton et al. 210) plus a coparenting intervention delivered on individually to biological and foster parent pair and target child, and which focused on learning about each other, practising open communication and negotiating interparental conflict. Therapists used family systems strategies, such as joining, didactic lesson, re-enactment and restructuring.
Linares 2012115 used a subset of the 18 IY manualised lessons contained in the Dina Program for Young Children. Modules were Understanding and Detecting Feelings; Detective Wally Teaches Problem-Solving Steps; and Tiny Turtle Teaches Anger Management, plus a lesson developed for the project and designed to promote a sense of belonging to this foster home – My Homes, My Families.
In both114,115 of these studies, foster carers in the control group received ‘usual services’.
Rushton et al. 116 used the IY programme as a basis for a cognitive–behavioural programme tailored to the needs of adoptive parents, placing an emphasis on the need to conduct daily play sessions with the child and to help adopters when their child rejects their praise or their rewards. First and last sessions were focused, respectively, on getting to know the parents and introducing the programme, and reviewing progress and ending. Other sessions focused on using positive attention to change behaviour; the value of play for establishing positive relationships; using verbal praise; rewards; learning clear commands and boundaries; using ‘ignoring’ to reduce inappropriate behaviour; defining for the child the consequences of undesirable behaviour; ‘time out’ and problem-solving. Adoptive parents in the control group received an educational approach designed by an adoption adviser ‘to improve adopters’ understanding of the meaning of the children’s current behaviour and help them see how past and present might be connected’116 (p. 532), thereby helping adopters to respond more appropriately to challenges.
Church et al. 111 provided a brief, single-session exposure therapy entitled emotional freedom techniques (EFT), comprising certain components of CBT and exposure therapy combined with a somatic component, having therapists or participants tap their fingers on prescribed acupuncture points. Those in the control group received no treatment.
Champion and Collins110 provided a theory-based [AIDS Risk Reduction Model (ARRM)209] CBT intervention designed to reduce risk-taking behaviour – Project Image (PI). PI is described as ‘grounded in knowledge of the target population’s behaviour and culture . . . Emphasis is placed upon understanding and dealing with male-female power relationships in African-and Mexican American culture’110 (p. 144). The intervention began with a physical examination (for STIs, etc.) followed by an enhanced counselling session (addressing adherence to medication, other treatments, sexual activity, etc.). Intervention participants were then offered two workshop sessions, 1 week apart, followed by group work and further individual counselling. The workshops and group work described have a strong psychoeducational component and a tailored skills component. Control group participants received the physical examination, abuse and enhanced clinical counselling at baseline, plus a follow-up physical examination at the end of the intervention.
Shirk et al. 117 evaluated a modified CBT intervention (m-CBT) that combined CBT elements (mood monitoring, cognitive restructuring, relaxation training, activity scheduling and interpersonal problem-solving), with mindfulness-based strategies, such as taking a non-judgemental stance of observing, describing and tolerating trauma-related emotions and cognitions (Linehan et al. 689). The effectiveness of m-CBT was assessed in relation to usual care (UC), in which therapists agreed to use, with control group participants, the treatment strategies and procedures that they regularly used and believed to be effective in their clinical practice).
The EMDR intervention in the Scheck et al. 121 study consisted of two treatment sessions of 1 hour, 1 week apart. EMDR followed the standard protocol devised by Shapiro. 690 In this study,121 EMDR was compared with an active listening intervention.
In Farkas et al. 120 study, EMDR was combined with motivation–adaptive skills–trauma resolution (MASTR), aimed at addressing conduct problems (Greenwald691), motivational interviewing and a range of cognitive–behavioural training and coping skills development. MASTR is a trauma-focused treatment package that was developed for use with adolescents with conduct problems, which ‘addresses treatment obstacles by establishing sense of safety within therapy, encouraging clients to be the agents of their change, improving motivation and guiding them towards progressive successes to their goals’120 (p. 128). Participants received 12 weekly sessions of 1.5 hours of MASTR/EMDR therapy. They also continued with other forms of individual (14%), family (14%) and group therapy (29%). In this study of EMDR, Farkas et al. 120 used a ‘routine care’ control group in which participants were exposed to a variety of alternative therapies.
Jensen et al. 112 described the TF-CBT programme that they use as a ‘trauma specific treatment consisting of psychoeducation, learning relaxation skills, affective modulation skills, cognitive coping skills, working through the TN, cognitive processing, in vivo mastery of trauma reminders, and enhancing safety and future developments, coupled with the parental component’112 (p. 6). The parental component looked to improve parenting skills and was also used to demonstrate for the parent each treatment component that was provided to the child. Those in the control group received ‘the treatment they (TAU Therapists) considered most suitable in each individual case’112 (p. 6). Almost half of the TAU therapists described their theoretical orientation as psychodynamic, 30% as cognitive behavioural, and around 25% as family/systemic (percentages rounded up). In 35 of the 52 completed TAU cases, parents were involved in some way in more than three sessions of the child’s therapy.
Comparisons
Number and duration of treatments
The IY or IY-based interventions used in the studies by Rushton et al. 116 and Linares et al. 114,115 were delivered in 12 weekly sessions of 2 hours.
Church et al. 111 provided one, 2-hour, single session of brief EFT.
The intervention described by Champion et al. 110 comprised one ‘extensive’ individual session for physical examination and a semistructured, one-on-one interview/enhanced counselling at the outset (1.5–2 hours), followed by two workshop sessions of between 3 and 4 hours, a follow-up visit (for screening, pregnancy testing and STI treatment, if necessary) and three to five sessions of support group work followed by two or more individual sessions.
The intervention evaluated by Shirk et al. 117 was designed to provide 12 weekly sessions to be delivered over a 16-week period but adolescents could continue with treatment beyond the 16-week study assessment. The same was true for the TAU group.
The TF-CBT intervention in Jensen et al. 112,113 comprised 12–15 individual sessions.
In Scheck et al. ,121 EMDR was delivered in two sessions, 1 week apart, and in the Farkas et al. 120 study it was provided in 12 weekly sessions (duration unspecified).
Where relevant, the number and duration of comparison treatments was similar to those of the experimental intervention.
Outcomes and measures used in studies of cognitive–behavioural therapy for children who have experienced different types of maltreatment
Post-traumatic stress disorder
Jensen et al. 112,113 used two measures of PTSD. The first was the CPSS,286 a self-report questionnaire developed for children aged 10–18 years, which examines post-traumatic stress symptomatology described in the DSM-IV (criterion B, re-experience; criterion C, avoidance; and criterion D, hyperarousal). 692 The second was the Clinician-Administered PTSD Scale for Children and Adolescents, a structured clinical interview that assesses the frequency and intensity of the 17 DSM-IV-defined PTSD symptoms. 304,305
Scheck et al. 121 and Church et al. 111 assessed the impact of intervention using the Impact of Events Scale (IES279). Both used the total score; Church et al. 111 also report outcomes for the memories and avoidance subscales.
Farkas et al. 120 used two measures of PTSD. First, the relevant module of the Diagnostic Interview Schedule for Children (DISC693) and, second, the TSCC,325,328 to assess trauma-related difficulties.
Scheck et al. 121 also used the Penn Inventory for Posttraumatic Stress Disorder (PENN334), a self-report scale that measures symptom severity.
Depression
Jensen et al. 112,113 used the Mood and Feelings Questionnaire694 to assess depressive symptoms, as this measures the full range of DSM-IV diagnostic criteria for depressive disorders, and includes items ‘reflecting common affective, cognitive, somatic features of childhood depression’ (p. 361).
Shirk et al. 117 and Scheck et al. 121 used, respectively, the Beck Depression Inventory-Second Edition (BDI-II320) and the BDI332 to assess the impact of EMDR on depression.
Anxiety
Scheck et al. 121 used the state subscale of the State-Trait Anxiety Inventory (STAI333) to measure the impact of EMDR on anxiety.
Jensen et al. 112,113 used the Screen for Child Anxiety Related Disorders (SCARED)307 to measure anxiety symptoms. SCARED is a self-report questionnaire with 41 items covering five specific anxiety disorders: panic disorder or significant somatic symptoms, generalised anxiety disorder, separation anxiety disorder, social anxiety disorder and school avoidance.
Behaviour
Rushton et al. 116 and Jensen et al. 112,113 used the SDQ. 308 Jensen et al. 112,113 also used visual analogue scales to assess how far an individual child progressed on emotional distress, misbehaviour and attachment. Rushton et al. 116 relied on adopter report, whereas Jensen et al. 112,113 used YSR.
In Linares 2012,115 foster parents completed a six-item measure compiled from the CBCL 5-18 aggression subscale,294 and classroom teachers completed a seven-item measure compiled from the 38-item Sutter–Eyberg Student Behaviour Inventory-Revised (SESBI-R311).
The intervention evaluated in Linares 2006114 was designed to reduce externalising behaviour, and its effectiveness was assessed using three measures, and drawing on foster parent-report and biological parent-report; the CBCL;294,309 the Eyberg Child Behavior Inventory-Revised310 and the SESBI-R. 311
Farkas et al. 120 used the parent version of the CBCL,269,294 alongside modules of the DISC to measure conduct disorder (CD) and oppositional defiant disorder.
Risky behaviour
In line with the aim of the intervention, Champion and Collins110 assessed new incidents of STI as a dichotomous variable (yes, no) at off-site, problem or scheduled follow-up visit at 6 and 21 months.
Self-control
Linares 2012115 used a 51-item measure of self-control, developed for this study and administered to foster parent and teacher using parallel versions.
Risk of bias: randomised controlled trials of cognitive–behavioural therapy for children who have experienced different types of maltreatment
Sequence generation
We judged three112,116,121 studies to be at low risk of bias. In the Rushton et al. ,116 study adoptive parents were randomised independently by the clinical trials unit using permuted block randomisation. Jensen et al. 112,113 state that a computer-generated randomised block procedure was used, and Scheck et al. 121 used envelopes filled with papers labelled either EMDR or active listening (AL). These were then shuffled before being numbered 1 through 100. Envelopes were opened (consecutively) during interviews with participants, which took place after the collection of baseline data, thereby identifying to which therapy the participant was allocated.
Linares 2012115 state that children were consecutively identified, assessed and randomly assigned within agencies, but no further information was provided on sequence generation or allocation concealment.
The studies by Champion and Collins,110 Church et al.,111 Linares 2006,114 Farkas et al. 120 and Shirk et al. 117 provide no information on sequence generation and were judged to be of unclear risk of bias.
Allocation concealment
None of the RCTs included provided adequate information on allocation concealment, although Rushton et al. 116 used a clinical trials unit to randomise participants, so all were judged as being of unclear risk of bias. The remaining eight110–112,114,115,117,120,121 studies provide no information on allocation concealment and were therefore judged unclear risk of bias.
Blinding of participants and personnel
We judged all studies110–112,115–117,120,121 as being of high risk of bias because no participant or personnel were blinded.
Blinding of outcome assessors
Rushton et al. 116 make clear that blinding at follow-up interviews was not possible because involvement in the treatment was the focus of questions. It was therefore assessed as high risk.
Five110–112,114,115 studies were assessed as low risk. In both studies by Linares et al. ,114,115 the authors state that intervention and assessment teams were assembled to keep interviewers blind to group assignment. Church et al. 111 state that data were scored off-site and blind to the statistician. Champion and Collins110 state that group status was revealed only at the end of follow-up interviews.
Jensen et al. 112,113 state that the assessments were computer assisted and conducted by an independent clinician who was blinded to the treatment conditions.
Shirk et al. 117 state that post-treatment assessments were made by an independent evaluator, but the depression measure used (BDI) relies on self-completion, and so the study was assessed as being of unclear risk of bias.
In both of the EMDR studies120,121 the authors state that assessors were blind, but the measures used were largely self- and parent-report, so we judged this as being of high risk of bias.
Incomplete outcome data
There were no missing data in the studies by Church et al.,111 Rushton et al. 116 or Linares 2012,115 which were therefore judged to be of low risk of bias. Linares 2006114 suffered attrition but reasons for attrition were largely the same (moved, discharged), although more parents in the intervention group refused to provide data post treatment and at follow-up than in the usual services group (eight vs. one). The authors also analysed the data on ITT principles and, overall, we judged the study114 to be of low risk of bias. Attrition in the Jensen et al. 112,113 study was similar across the two arms, and there were no significant differences between the retention group and the attrition group, other than that the attrition group was significantly older than the retention group and the attrition group reported being exposed to significantly higher numbers of different traumatic events. The authors explore reasons for attrition and they are methodical in their analyses, undertaking both ITT analyses and per-protocol analyses, and completed case analyses (defined as those participants who completed at least six sessions). Overall we judged the Jensen et al. 112,113 study to be of low risk of bias.
In the Champion et al. 110 study, data are presented for only for 318 out of 409 women at 6-month follow-up (78% unadjusted) and 333 women at 12-month follow-up (81% unadjusted). Given the intervention and the participants, this level of attrition is impressively low, but it was deemed sufficiently large to warrant a judgement of high risk of bias.
Farkas et al. 120 was also judged high risk of bias, primarily on the grounds of significant attrition. Of 65 adolescents randomised in this study, 15 dropped out by post treatment and a further eight by the 3 months’ follow-up. More young people dropped out of the experimental group than control group during treatment (10/33 vs. 5/32); of these, 2 of the 10 dropped out for reasons related to the treatment (refused to discuss their traumas) and two because they ceased to be in the custody of YPS and their families stopped their participation. All but one of the remaining participants dropped out because they ‘changed their minds’.
In the Scheck et al. 121 study there was considerable attrition post treatment that was not accounted for in the results. We judged this to be high.
Data for 7 out of 43 randomised participants were missing at follow-up in the Shirk et al. 117 study [four in m-CBT and three in UC]. Investigation led the authors to conclude that no systematic bias had occurred in attrition, and they conducted their analyses on ITT principles. We therefore assessed this study as low risk of bias.
Selective outcome reporting
Three110,112,116 studies were registered with ClinicalTrials.gov: Champion and Collins110 (NCT01387646); Rushton et al. 116 (NCT04448012) and Jensen et al. 112,113 (NCT00635752).
Champion and Collins110 report findings for the primary outcome (STIs at 12 months) but, in the paper identified for this review, have not yet reported on secondary outcomes (substance use, experience of abuse and frequency of unintended pregnancies). Overall, we judged this as ‘unclear’ risk of bias. The studies by Rushton et al. 116 and Jensen et al. 112,113 report on all primary and secondary outcomes and were therefore judged as ‘low’ risk of bias.
In general, the remaining studies appeared to indicate that they were reporting on all predetermined outcomes. However, in the absence of study protocols it is difficult to assess the risk of selective outcome reporting. Therefore, all studies were assessed as ‘unclear’ risk of bias.
Other sources of bias
None were identified.
Results: cognitive–behavioural therapy for children who have experienced different types of maltreatment
No meta-analyses were possible for data from these studies,110–112,114–117,120,121 the results of which are therefore reported in narrative form.
Post-traumatic stress disorder
Jensen et al. 112,113 report a mean effect (ITT analyses) of treatment condition on child PTSD (measured by the CPSS) at time 3 (T3), some 7.5 months after treatment began: children in the TF-CBT group scored significantly lower at T3 [mean (M) = 11.34, SD 10.52] than participants in the comparison group [M = 16.87, SD 11.49; d = 0.51, t(154) = 3.30; p = 0.001; with Holm adjustment p = 0.006]. The authors also report a significant time by group interaction effect (F(2) = 5.01; p = 0.007; with Holm adjustment p = 0.037). Both groups showed reductions in PTSD from pre- to post-therapy assessments, and a main effect of treatment condition on functional impairment such that trauma influenced daily functions significantly less (indicated by higher scores) in the TF-CBT group (M = 10.33, SD 1.99) than in the TAU group (M = 9.22, SD 2.09) at the end of therapy [d = –0.55, t(154) = –3.32; p = 0.001; with Holm adjustment p = 0.006]. They also report a main effect of treatment on time in both groups. Analyses of completed cases yielded similar results.
Statistically significant between-group differences were found by Church et al. 111 in favour of the intervention (EFT). One month after pre-test, participants who had received the intervention demonstrated a statistically significant decrease on both the total score for the IES279 and the two subscales (memories and avoidance). All participants had scored in the clinical range at baseline, and control participants remained in the ‘moderate clinical’ range post test, in contrast to those in the intervention group, none of whom was in the clinical range post test.
Analyses of PENN post-test scores in the Scheck et al. 121 study indicated a significant difference in favour of the EMDR group [F(1,55) = 6.03; p = 0.02]. A similar result was found for the IES [F(1,57) = 9.93; p = 0.002].
Post treatment, Farkas et al. 120 reported significant improvements in the experimental group (MASTR/EMDR) compared with control group participants for PTSD symptoms as measured by DISC [F(1,40) = 6.05; p = 0.05]. Significant improvements were also reported for the TSCC325 (trauma-related difficulties) on each of six subscales: stress, anger, depression, dissociation, anxiety and sexual concerns. 120
Depression
Jensen et al. 112,113 found a main effect of treatment condition on children’s depressive symptoms, with participants in the TF-CBT group (M = 14.40, SD 13.67) scoring significantly lower than those in the TAU condition (M = 22.67, SD 16.24) at T3 [d = 0.54, t(154) = 2.79; p = 0.006; with Holm adjustment p = 0.018].
Scheck et al. 121 reported a significant effect for EMDR on depression [F(1,58) = 5.39; p = 0.024].
Shirk et al. 117 reported significant reductions over time in BDI depression scores but no between-group differences.
Anxiety
Jensen et al. 112,113 found no main effect of treatment condition on children’s anxiety symptoms. Participants in the TF-CBT group [d = 0.30, t(150) = 1.47; p = 0.114; with Holm correction p = 0.114]. Analyses of the SCARED subscales found a main effect only for generalised anxiety disorder. Completer analyses produced similar results.
Scheck et al. 121 reported a significant effect for EMDR on STATE anxiety [F(1,57) = 4.89; p = 0.031].
Behaviour
Rushton et al. 116 found no significant differences in child problems between the two groups at 6 months’ follow-up, although a significant difference (p < 0.007) was found for ‘satisfaction with parenting’ in favour of the intervention group (effect size d = 0.7).
Jensen et al. 112,113 found a main effect of treatment condition on the SDQ (interpreted as general mental health problems). Participants in the TF-CBT group had significantly lower scores (M = 11.95, SD 6.51) than those in the TAU group (M = 14.54, SD 6.12) at the end of therapy [d = 0.45, t(152) = 2.46; p = 0.015; with Holm adjustment p = 0.030]. Completer analyses produced similar results.
In Linares 2012,115 the authors report that physical aggression decreased over time for both groups (IY, UC) but there were no between-group differences. After adjusting for gender, ethnicity, initial diagnosis of attention deficit hyperactivity disorder and study site, children in the UC group showed more improvement than those in the IY training group on foster parent reports of physical aggression. Rates of improvement were highest among children in the UC condition. Teachers reported no differences.
In Linares 2006,114 intervention children were reported as having lower CBC externalising T scores [F(1,97) = 2.71; p = 0.10] and Eyberg Child Behavior Inventory (ECBI) total T score [F(1,94) = 2.30; p = 0.13] at follow-up but these were not statistically significant.
Farkas et al. 120 reported significant differences on the CBCL260 in favour of MASTR/EMDR for externalising behaviour [F(1,40) = 9.77; p = 0.05], but not for internalising behaviour.
Risky behaviour
Champion 2012110 reported a significant impact of the intervention, with those who had received the theory-based (ARRM209) CBT intervention experiencing fewer infections at intervals of 0–6 months (0% vs. 6.6%; p = 0.001), 6–12 months (3.6% vs. 7.8%; p = 0.005, 95% CI 0.001 to 0.386) and 0–12 months (4.8% vs. 13.2%; p = 0.002, 95% CI 0.002 to 0.531).
Self-control
Linares 2012115 report a main effect in relation to foster care reports of higher levels, and steeper rates of improvement in relation to self-control, in favour of the control group (UC).
Self-esteem
Scheck et al. 121 reported a significant effect of EMDR for the TSCC335 [F(1,57) = 4.573; p = 0.04].
Parent–child relationships
Emotional Freedom Questionnaire (EFQ) scores among control children in the Rushton et al. study116 remained unchanged, whereas they were more positive at all time points for the intervention group; however, these were not significant when controlling for baseline scores.
Although not directly relevant, Linares et al. 114 reported a significant difference between the intervention and UC group on coparenting flexibility [F(1,104) = 4.14; p < 0.05], coparenting problem-solving [F(1,102) = 6.38, p < 0.01] and coparenting total [F(1,97) = 5.13; p < 0.05]. This was a key aim of the study114 and was likely to have a positive impact on the experience of children in foster care.
Effectiveness of cognitive–behavioural therapy for children who have experienced different types of maltreatment
Summary
Four112,114–116 of the nine studies that we identified focused on helping caregivers (including birth parents, adoptive or foster parents) to address the consequences of maltreatment, by enhancing their knowledge and skills and providing support. Unsurprisingly, most of these studies provided services to carers of children aged < 10 years, but one112 study recruited those caring for older children. The studies compared modifications of the IY parenting programme with either TAU114 or, in the only UK study,116 with an educational approach.
The other five110,111,117,120,121 studies provided services directly to maltreated young people aged > 12 years. They included two120,121 studies that compared EMDR with alternative treatments (as usual), and three110,111,117 studies comparing modified forms of CBT or CBT ‘plus’ with either no treatment, UC or a modified form of UC.
Overall, within the range of different studies included in this section, there was some reduction in symptoms PTSD and depression with treatment. Results regarding improvement in children’s behaviour vary between the studies. One115 study targeted physical aggression and self-control in foster children, and found no differences between children whose foster parents had participated in the IY programme and those who had received UC. Indeed, when appropriate adjustments were made, those in the control group did rather better than those in the experimental group. No differences were found between the behaviour of children whose adoptive parents received a CBT parenting programme based on IY, although these parents were significantly more satisfied with parenting and were less likely to use negative parenting approaches than those in the control group. 116
Conflicts between foster parents and biological parents contribute to placement instability, and work against reunification. One114 study examined an intervention designed to improve relationships between parents, foster parents and children, and enhance the consistency of parenting across the two homes. The results of this study were very positive, and have relevance to the UK context.
One110 study, focusing specifically on risky behaviour by girls, showed reduction in rates of STIs.
It is difficult to draw conclusions about EMDR, as in one120 study this was a very different intervention to the standard protocol, and it was compared with another treatment arm that was quite intensive. 120
Completeness and applicability
Only one study was conducted in the UK,116 and one study was conducted in Norway. 112 Both studies112,116 focused on children in a family context, and aimed to improve outcomes for children who had experienced very serious maltreatment. In the UK study, participants were recruited from social welfare agencies that were responsible for supporting adoptive parents. In Norway, the settings were trauma clinics, that is, routine community settings.
Webster-Stratton’s IY programme has been endorsed as an evidence-based parenting programme in the UK, and the applications evaluated in three114–116 of these studies have relevance to the needs of children in foster and adoptive care in the UK. The application of this programme to some of the challenges of fostering maltreated children is highly relevant, but the findings are mixed and the evidence base is limited.
Quality of the evidence
Most studies are small and there are few of them. Their heterogeneity (in terms of interventions, participants and outcome measures) prevented us from combining data in meta-analyses, and therefore the results from this part of the review should be treated with caution.
Overall, the quality of the evidence relating to studies of CBT for children who have experienced a range of forms of maltreatment is moderate, largely because of the impact of lack of information, which, if available, might demonstrate enhanced quality – or the reverse.
Economic evidence
One economic evaluation,613 carried out in the UK, explored the cost-effectiveness of two parenting programmes, including a cognitive–behavioural approach, for adoptive parents. The study613 used data from the Rushton et al. 116 RCT, described above, and compared the two parenting programmes (a cognitive–behavioural approach and an educational approach), which were combined due to small sample sizes (n = 19) to services as usual (n = 18). The intervention was delivered to adoptive parents of children who were adopted at between the ages of 3 and 8 years, who were screened for serious behavioural problems early in the placement.
Cost-effectiveness was explored in terms of the primary outcome measure of the study, the SDQ, and, additionally, in terms of parent satisfaction, shown to be more effective in the parenting programmes than service as usual. Resource use included health, social care and specialist educational services, as well as the use of the parenting programmes, which were costed using nationally applicable unit costs. Costs were expressed in 2006–7 pounds sterling (£). No discounting was applied to costs and effects because of the short time horizon of the study, with follow-ups carried out post treatment (approximately 12 weeks after study entry) and 6 months post treatment (approximately 9 months after study entry).
At the 6-month post-treatment follow-up, costs were significantly higher for the parenting programmes and there was no significant difference between the two groups on the SDQ. However, parental satisfaction was significantly higher for the combined parenting programme group. Thus, in terms of the primary clinical outcome, service as usual was found to dominate the parenting programmes (less expensive and no difference in outcomes), whereas for parental satisfaction, the authors report an ICER of £337 per unit improvement in satisfaction. The authors conclude that the parenting programmes may be cost-effective in enhancing parental satisfaction. However, the study613 was severely limited in a number of important ways, which would caution against such a conclusion. In particular, sample sizes were extremely small and thus the results are unlikely to be adequately powered. In addition, the significant results were based on the only secondary outcome measure to show a significant difference in favour of the intervention, suggestive of a post hoc analysis, and no exploration of uncertainty was undertaken.
Economic analysis: cognitive–behavioural therapy
Given the effectiveness evidence presented showing promising benefits of CBT for sexually abused children, it was thought appropriate for consideration to be given to the development of a decision-analytic model to more fully explore the cost-effectiveness of CBT in this population. As described above, however, only one relevant economic evaluation of CBT for sexually abused children was located, a decision model based on Australian data with cost data limited to the cost of CBT only, showing cost-effectiveness advantages for CBT. One further economic evaluation of CBT, focusing on children who have experienced different types of maltreatment, was located, but this trial-based study was limited by small sample sizes and showed no economic advantage for CBT in terms of the primary clinical outcome. In the absence of any other better quality UK-based data, a decision model was ruled out.
Instead, we conducted cost-effectiveness analyses of CBT for sexually abused children using PTSD, anxiety and depression outcomes combined with intervention costs, calculated as described in Chapter 2. For PTSD and anxiety, we used SMDs. For depression we used CDI scores,80 reported in five studies. Given the sensitivity of the effectiveness results for some outcomes to the use of change scores, suggesting baseline imbalance, outcome data were calculated using random-effects meta-analyses for mean change from baseline and assuming a correlation between baseline and follow-up of 0.5. Correlation was varied between 0 and 1 in sensitivity analysis but this did not alter the results, so only the results for a correlation of 0.5 are reported. All results are reported for outcomes post treatment (the time point with the greatest amount of data) and at 12-month follow-up (the time point at which the advantage for CBT is the smallest, thus a more conservative approach). Analyses were repeated for all maltreatment types, but this did not alter the results so they are not reported here.
Results
Table 11 reports the cost and outcome parameters and the deterministic and probabilistic ICERs for SMD and CDI outcomes. ICERs are the additional cost per unit change in SMD, for PTSD and anxiety, and the additional cost per unit change in CDI score, for depression. In all analyses, the CBT group are associated with higher costs and better effects than the control group. In addition, effectiveness advantages for CBT compared with the control group are always greater post treatment than at 12-month follow-up, resulting in larger ICERs at 12-month follow-up (larger expenditure needed to generate a unit improvement in outcome).
| Cost and outcome parameters | Meana (SD) | ICER (£) | ||
|---|---|---|---|---|
| Deterministic | Probabilistic | |||
| Weighted average cost of CBT (£) | 1433 (320) | |||
| SMD for anxiety outcomes | Post treatment | –0.188 (0.180) | 7623 | 3816 |
| 12-month follow-up | –0.180 (0.560) | 7961 | 4327 | |
| SMD for PTSD outcomes | Post treatment | –0.508 (0.263) | 2821 | 752 |
| 12-month follow-up | –0.310 (0.560) | 4623 | 3981 | |
| CDI change score differences | Post treatmenta | –1.844 (1.285) | 777 | 795 |
| 12-month follow-upa | –0.208 (1.342) | 6890 | 6329 | |
For the SMD outcomes, Figures 9 and 10 show the cost-effectiveness plane for both PTSD and anxiety outcomes, post treatment and at 12-month follow-up, respectively. The cost-effectiveness plane is used to illustrate differences in costs and effects between different strategies, in this case CBT and the control. It consists of four quadrants, for which the x-axis represents the additional level of effectiveness generated by one intervention compared with another and the y-axis represents the additional cost of one intervention compared with another. The scatter points on the cost-effectiveness plane represent multiple cost and effectiveness pairs generated by the probabilistic sensitivity analysis, but for ease of interpretation, can be viewed as pairs of individuals, one receiving CBT and the other in the control group. Points that fall in the north-west quadrant represent the situation in which CBT is more expensive and less effective and thus dominated by the control group. For those in the south-east quadrant, CBT is more effective and less expensive and thus dominates the control. For those in the north-east quadrant, CBT is more effective but also more expensive, and, for the south-west, CBT is less effective but also less expensive; both of these quadrants involve a trade-off between costs and effects.
FIGURE 9.
Cost-effectiveness plane for PTSD and anxiety outcomes post treatment.

FIGURE 10.
Cost-effectiveness plane for PTSD and anxiety outcomes at 12-month follow-up.

As only the cost of CBT was considered in the current analysis, all points fall above the x-axis (costs higher for the CBT group than the control group). In terms of effects, although the SMD results from the meta-analyses suggest advantages for CBT rather than the comparison, this advantage is no longer evident in the probabilistic analysis (involving assigning probability distributions to costs and effects, as outlined in Chapter 2). Instead, differences in effect are relatively equally distributed to both the right of the y-axis (effects better for CBT) and the left (effects better for control).
Associated uncertainty is displayed in the CEACs in Figures 11 and 12, which illustrates the probability that CBT is more cost-effective than the control, for different levels of willingness to pay for additional benefits. The CEACs suggest that the probability of CBT being more cost-effective than the control post treatment does not rise much above 50% for PTSD outcomes and remains below 50% for anxiety outcomes post treatment (see Figure 11). The results are similar at 12-month follow-up (see Figure 12).
FIGURE 11.
Cost-effectiveness acceptability curves for PTSD and anxiety outcomes post treatment.

FIGURE 12.
Cost-effectiveness acceptability curves for PTSD and anxiety outcomes at 12-month follow-up.

Figures 13 and 14 show the cost-effectiveness plane for CDI outcomes post treatment and 12-month follow-up, respectively. Again, as only the cost of CBT was considered in the analysis, all points fall above the x-axis (incremental costs higher for the CBT group than the control group). In terms of effects, the results are similar at 12-month follow-up to those for SMD outcomes, showing no clear advantage for CBT compared with the control. The post-treatment results, however, suggest some effectiveness advantage for CBT, with a larger proportion of points falling to the right of the y-axis (effects better for CBT) than the left (effects better for control).
FIGURE 13.
Cost-effectiveness plane for CDI outcomes post treatment.

FIGURE 14.
Cost-effectiveness plane for CDI outcomes at 12-month follow-up.
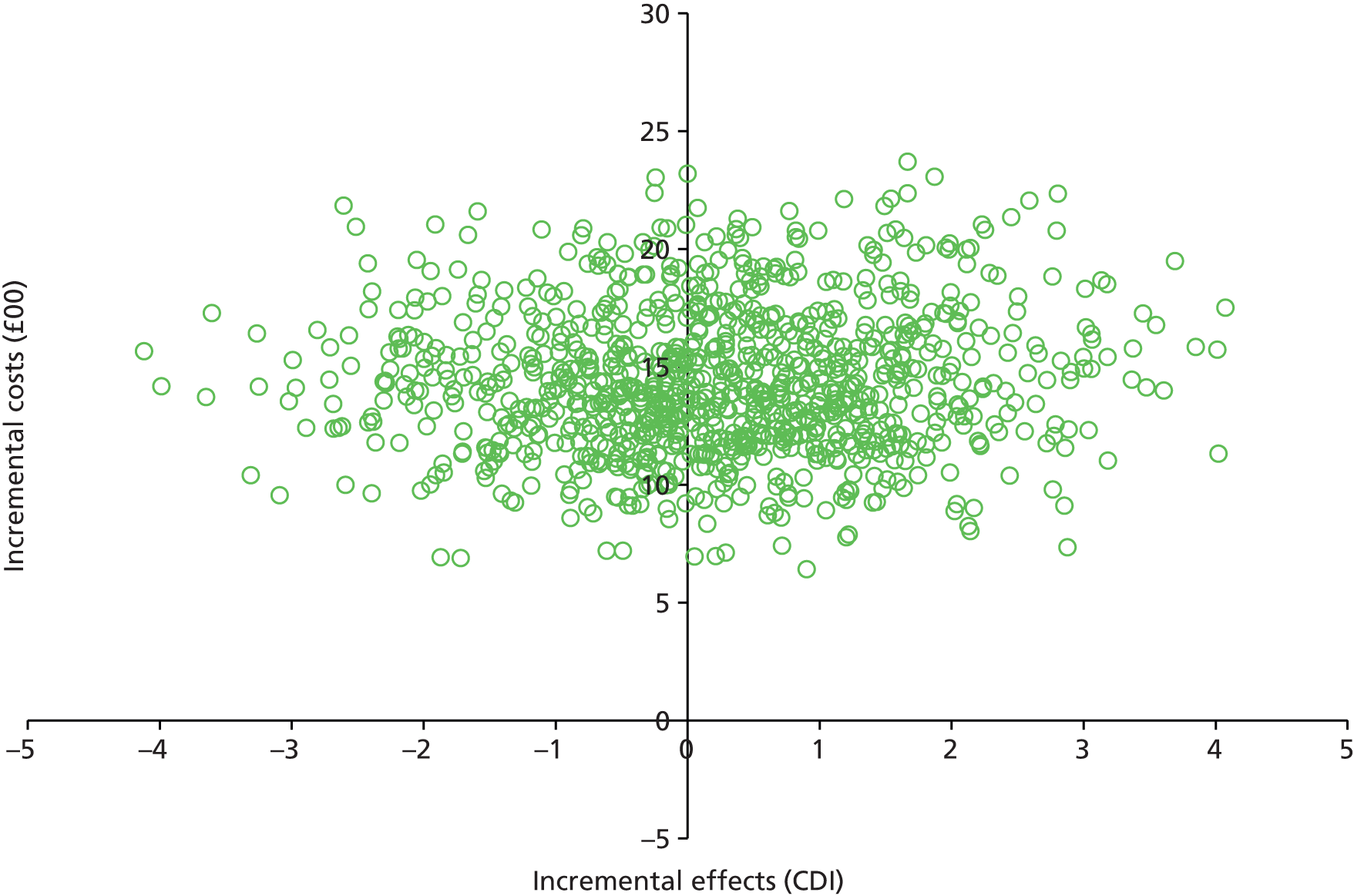
Uncertainty is illustrated by the CEACs reported in Figures 15 and 16 for post-treatment and follow-up outcomes, respectively. The post-treatment results suggest that the probability of CBT being more cost-effective than the control reaches approximately 90% for willingness-to-pay values of around ≥ £5000. Using the 12-month follow-up data, however, the results are similar to those for SMD outcomes and do not rise much above 50%.
FIGURE 15.
Cost-effectiveness acceptability curve for CDI outcomes post treatment.

FIGURE 16.
Cost-effectiveness acceptability curves for CDI outcomes at 12-month follow-up.

Relationship-based interventions
Studies covered in this section focus on interventions that seek to improve relationships between children and their parents (RBIs). They include those designed to promote secure child attachment and the positive outcomes associated with that, and parenting interventions designed to improve the quality of parenting of maltreating parents, thereby bringing about positive benefits to children who have already experienced maltreatment.
In total, we identified 15 controlled studies122–140 that assessed the effectiveness of RBIs. The studies are grouped as follows:
Because of the imbalance of numbers, we are not dealing with each subset of interventions entirely separately, but, where appropriate, we group them for descriptive and reporting purposes. We do not comment on gender in this section, as, by definition, all RBIs address the relationship between parents and their children, irrespective of gender. Details of child gender, where reported, are available in Chapter 3.
Description of studies
Study designs
The Becker-Weidman134,135 study was a COS. The remaining studies122–133,136–140 were randomised trials.
Location
All studies were conducted in the USA123–129,131–136,140 except for Moss et al. 130 (Quebec, Canada), Hughes and Gottlieb139 (Eastern Canada) and Thomas and Zimmer-Gembeck137,138 (Australia).
Sample sizes
Controlled studies ranged from small to a moderately large sample size; the smallest sample size was 60 (with only 46 ultimately included in the analyses)125,126 and the largest were 151137,138 and 210. 131 See Chapter 3 for further information.
Participants
Attachment-orientated interventions
Five of the attachment-orientated studies focused on infants up to 24 months of age. Infants in the Bernard et al. 122 study were aged between 1.7 and 21.4 months at enrolment (mean 10.1 months), and those in Dozier et al. 125,126 were aged 3.6–39.4 months [note: two papers report the results of this study: one125 deals with the ‘first 60 children who completed the experimental or control intervention’ (p. 773) and reports on cortisol levels and behaviour problems; the second study126 reports on ‘the first 46 children who completed the experimental or control intervention’ (p. 5) and reports on attachment behaviours]. In both Cicchetti trials,123,124 infants had a mean age of just over 13 months. Spieker et al. 131 recruited mother–infant dyads, for which the infants were aged 10–24 months.
Four studies recruited older children. 127–130,132,133 Preschoolers in the Toth et al. 133 study had a mean age of 48.2 months (SD 6.88); in the Sprang132 study the mean age was 42.5 months (SD 18.6 months); children in Lieberman 2005127–129 were aged 3–5 years, and in the Moss et al. 130 study they were between 12 and 71 months.
In the Becker-Weidman134,135 study, children’s ages ranged from 5 to 16 years.
In the Dozier et al. 125,126 study, foster parents were referred at the time of initial infant placement (presumably by child welfare staff). Consent from both birth parents and foster parents was required. In the Bernard et al. 122 study parents were referred by agencies working with Child Protection Services. In the Sprang132 study parents were referred for a relational intervention following a university-based assessment.
In Cicchetti 2006,123 a recruitment liaison officer was retained in the Department of Human Services to identify all infants who were known to have been maltreated or who were living in maltreating families with their biological mothers. The same method was used in Cicchetti 2011,124 Spieker et al. 131 and Toth et al. 133 Spieker et al. 131 used a liaison officer to identify infants of ‘an appropriate age who had experienced a court-ordered placement that resulted in a change of primary caregiver with the prior seven weeks’ (p. 5). Toth et al. 133 used a liaison officer to identify families with a preschool-aged child with a documented history of maltreatment.
Participants in the Lieberman et al. 127–129 study were referred to the study by paediatric providers, family resource programmes, child-care providers and child protection workers when there were clinical concerns about the child’s behaviour. Those in the Moss et al. 130 study were referred by welfare or community services.
Becker-Weidman134,135 used data from cases closed in 2001 or 2002 in which children had received a diagnosis of reactive attachment disorder and there was a significant history of physical abuse, emotional abuse or neglect, sexual abuse or institutional care. One group comprised 34 children who had received DDP and another group of 30 children who received UC.
Parent–child interaction therapy interventions
Children in the PCIT studies were aged 4–12 years in the study by Chaffin et al. 136 In the studies conducted by Thomas and Zimmer-Gembeck, all but three of the children in the 2011137 study were age between 2.5 and 7 years, and in the 2012138 study the authors report a mean age of 4.57 (SD 1.3) years.
In the PCIT trials, referrals came from welfare workers in the Chaffin et al. 136 study and from a variety of sources, including self-referral in the Thomas and Zimmer-Gembeck137,138 studies. Eligibility in the Thomas and Zimmer-Gembeck137,138 studies depended on being assessed as at high risk for child maltreatment, using a semistructured interview designed to identify proximal risk factors such as high levels of parental distress, aggressive patterns of communication and use of inappropriate discipline strategies.
Parent-focused interventions
Eligible families were identified by child protection agency staff as in need of parent training in the Hughes and Gottlieb139 study. Cases were not necessarily on the Child Abuse Registry. In the study by Valentino et al.,140 families were recruited from the Department of Child Services, which provided families with information from flyers and from individual case workers.
Maltreatment
Attachment-orientated interventions
In each of the attachment-focused studies, the intervention was directed at a mother–infant dyad. Five123,125,126,131,132 studies focused on children in out-of-home placements as a result of maltreatment. The remaining five122,124,127–130,133 studies focused on children living with their biological parents.
Dozier et al. 125,126 included young children newly placed in foster care. Apart from children placed at birth, these children would have experienced neglect or abuse prior to placement. In Sprang132 the children were in foster care, having experienced ‘severe maltreatment’ (p. 82) with an attachment disorder that threatened to disrupt the placement. Children in the study by Cicchetti 2006123 were also in foster care as a result of maltreatment, with disorganised attachment. Spieker et al. 131 recruited toddlers who had experienced a recent, court-ordered placement and their caregivers. Children in foster care were participants in the COS. 134,135
In Cicchetti 2011,124 infants who were known to have been maltreated or who were living in maltreating families with their biological mothers were identified for recruitment. All forms of maltreatment were included. In the recruited sample, almost 72% of infants had directly experienced abuse and/or neglect during the first year of life: 83% of infants had been neglected and 69% had been emotionally maltreated. None of the infants had been sexually abused. Over half of the infants had experienced more than one type of maltreatment.
In Bernard et al. 122 the infants in were in families where there was a risk of out-of-home placement for a variety of reasons, including domestic violence, parental substance use, homelessness and child neglect.
In Moss et al. 130 the majority of primary caregivers (72%) had been reported for child neglect: 7% of primary caregivers were reported for physical abuse and 3% of primary caregivers for sexual abuse; 16% of children had been both physically abused and neglected, and 2% of children were both neglected and sexually abused.
Toth et al. 133 recruited families with a preschool aged child with a documented history of maltreatment. Almost 60% of the children had experienced more than one form of maltreatment; 21% had experienced neglect; and 14% had experienced emotional maltreatment. Two children had been sexually abused.
Lieberman et al. 127–129 recruited child–mother dyads where the child had been exposed to marital violence (confirmed by mother’s report on the Revised Conflict Tactics Scale398), when the father figure perpetrating the violence was no longer in the home and there were concerns about the child’s behaviour or mother’s parenting.
Parent–child interaction therapy
In the Chaffin et al. 136 study, children were referred for concerns about physical abuse. In both studies by Thomas and Zimmer-Gembeck,137,138 families were referred for physical and emotional maltreatment or neglect. Children with a history of sexual abuse were excluded, as PCIT is contraindicated for this form of maltreatment. Parents could self-refer and were accepted if the pre-assessment interview revelaed previous experience of a parenting intervention, a high risk of child maltreatment and high levels of child behaviour problems.
Interventions and comparisons
Attachment-orientated interventions
The included studies122,125,126,130,132 covered four interventions.
Dozier et al. ,125,126 Sprang132 and Bernard et al. 122 assessed the effectiveness of ABC (see Appendix 5). In the Dozier et al. 125,126 study, parent trainers were professional social workers or psychologists with at least 5 years’ experience; in the Sprang132 study, they were social workers, psychiatrists or psychiatric nurse practitioners. Bernard et al. 122 used parent trainers who had experience of children and strong interpersonal skills.
Dozier et al. 125,126 and Bernard et al. 122 compared ABC with an educational intervention borrowed partly from the home visitation component of the early intervention programme developed by Ramey et al. ,695,696 which was designed to enhance cognitive and, especially, linguistic development. Components that involved parental sensitivity to child cues were excluded specifically to keep the interventions distinct.
In Sprang,132 ABC was compared with a wait-list control in which participants accessed the bi-weekly support group for parents that was also accessed (separately) by the intervention group.
Moss et al. 130 assessed the effectiveness of an unnamed short-term attachment intervention designed to promote maternal sensitivity and child attachment. Mothers in both arms of the trial received services as usual (comprising a monthly visit by a child welfare caseworker), but only mothers in the experimental group received the attachment intervention. Bernard et al. 122 describe the intervention provided by Moss et al. 130 as one based on their own ABC intervention combined with interventions developed by Backermans-Kranenburg et al. 219 and Moran et al. 220 The intervention was provided in home, using video feedback, by experienced clinicians with at least a bachelor’s degree in psychology, who received training from attachment experts.
In three studies, Cicchetti et al. 123,124,133 evaluated the effectiveness of each age-related version of this therapy with another manualised home-based intervention. Lieberman et al. 127–129 also assessed CPP.
Toth et al. ,133 Cicchetti 2006123 and Cicchetti 2011123 compared CPP with a psychoeducational parenting intervention (PPI), and referred to as psychoeducational home visiting in Toth et al. 133 and a management-as-usual group, in which families received services typically available to maltreating families in the community. PPI/psychoeducational home visitation (PHV) was based on the home visiting programme developed by Olds et al.,216–218 augmented by ‘a variety of cognitive and behavioural techniques in order to address parenting skill deficits and social-ecological factors, such as limited personal resources, poor social support, and stresses in the home associated with maltreatment’ (p. 794). The interventions were provided by trained, master’s level therapists, on a weekly basis over the course of 1 year.
Lieberman et al. 127–129 compared CPP with individual psychotherapy plus case management.
Spieker et al. 131 evaluated PFR, a manualised, infant mental health training programme, aimed at early years’ professionals. This formed the basis of an intervention programme tailored to the needs of children in care who had experienced disrupted placements. PFR was compared with early education support, a home visiting intervention aimed at connecting families to community resources and suggested activities to promote development.
Becker-Weidman134,135 compared DDP with TAU – essentially assessment and, for just over half, another form of treatment.
Parent–child interaction therapy
In Chaffin et al. ,136 a variety of therapists (including basic trainees, experienced trainees and experts) delivered PCIT (see Appendix 5) alone or in enhanced form (i.e. with the addition of services targeting family-specific problems, such as domestic violence, substance abuse or parental depression). Participants in the control group took part in a standard community-based parenting group.
Thomas and Zimmer-Gembeck 2011137 compared time-variable PCIT (TV/PCIT) with an attention only wait-list control in which parents were contacted weekly for brief conversations regarding family or other concerns for 12 weeks. In TV/PCIT parents are coached during the Child Directed Interaction phase (CDirI; see Appendix 5) until mastery criteria were achieved for two consecutive sessions, before moving onto parent-directed interaction (PDI) phase.
Thomas and Zimmer-Gembeck 2012138 compared standard PCIT (S/PCIT), in which participants received only 12 coaching sessions, regardless of proficiency, with an attention wait-list control. In this study the authors also used their data to compare the effectiveness of S/PCIT with TV/PCIT by drawing on the data available from their earlier trial.
Parent-focused interventions
The intervention in Valentino et al. 140 (reminiscing and emotion training, RET) focused on encouraging parents to engage in elaborative and emotionally supportive reminiscing about positive and negative everyday past events as a means of increasing parental sensitivity and addressing multiple developmental sequelae of maltreatment. Sessions were led by bachelor-level family coaches, and included the use of video feedback and daily homework. In Hughes and Gottlieb,139 the intervention was the Webster-Stratton IY parenting programme, a standardised, video-based, modelling intervention based on social learning theory and tailored to the developmental needs of families with young children. The group facilitator was the first author of the study. Both Hughes and Gottlieb139 and Valentino et al. 140 compared the experimental intervention to a wait-list control.
Number and duration of sessions
Attachment-orientated interventions
In the studies by Dozier et al. ,125,126 Bernard et al. 122 and Sprang,132 both interventions (experimental and control) were provided in 10 weekly, hour-long sessions, based on a structured training manual.
Parents receiving both IPP and CPP (see above) in the Cicchetti 2006123 study received weekly home visits over a 12-month period, with an average of 21 sessions conducted in the IPP group and 25 sessions conducted in the IPP group. In the Cicchetti 2011124 study, participants in the CPP and IPP arms also received weekly home visits over a 12-month period, with the average number of visits being approximately 46 for the CPP group and 49 for the IPP group.
The CPP intervention in Lieberman et al. 127–129 was delivered weekly for 50 weeks, with each session lasting approximately 60 minutes. Most dyads attended a mean of 32 CPP sessions; those receiving individual psychotherapy had, minimally, monthly phone calls from a case manager (who they could also contact if needed) plus information and referral to mental health clinics of their choice. Face-to-face meetings were scheduled when clinically indicated. Most mothers received individual treatment (77%) and 55% of children also received individual treatment.
Recipients of PPP were seen for weekly 60-minute dyadic sessions over a 12-month period. Those receiving PHV received a similar ‘dose’.
In the Moss et al. 130 study, the manualised intervention consisted of eight home visits, of approximately 90 minutes, once a week.
PFR was delivered in 10 weekly sessions of 60–75 minutes in the home. 131 Those receiving early educational services received 3-monthly 90-minute, in-home sessions delivered by an early education specialist.
Parent–child interaction therapy
As indicated above, in the 2011 Thomas and Zimmer-Gembeck study137 parents receiving TV/PCIT received as many sessions of CDInt as was necessary to achieve the prescribed mastery criteria, before proceeding to PDI. On average, PCIT participants who completed treatment engaged in a total of 11.8 sessions and five PDI coaching sessions. In Thomas and Zimmer-Gembeck 2012,138 parents in receipt of S/PCIT received 12 sessions of coaching only, irrespective of whether or not they had reached the mastery threshold for progression from CDInt to PDI.
Outcomes and measures used in studies of relationship-based interventions
Attachment
Three122,123,130 studies assessed the impact of the intervention on attachment using the Ainsworth Strange Situation Procedure. 336
Dozier et al. 125,126 asked foster parents to record infants’ behaviour when distressed and in the presence of their primary caregiver using the Parent Attachment Diary (PAD697). Spieker et al. 131 used the Toddler Attachment Sort-45,350 a modified version of the Attachment Q-sort698 to assess children’s attachment security, and Becker-Weidman134,135 used the Randolph Attachment Disorder Questionnaire. 364
Internal working models
Toth et al. 133 specifically explored the effectiveness of two developmentally informed preventative interventions on children’s internal representations of self, and of self in relation to other, using a narrative story stem task from the MacArthur Story Stem Battery (Bretherton I, Oppenheim D, Buchsbaum H, Emde RN & the MacArthur Narrative Group, University of Wisconsin-Madison, 1990, unpublished).
Child behaviour
Six130–132,134,135,137,138 studies examined the impact of attachment-based interventions on child behaviour, using the CBCL. 260
In addition to the CBCL,260 Thomas and Zimmer-Gembeck 2011137 and 2012138 assessed the impact of PCIT on child behaviour using the ECBI (parent report),310 and Spieker et al. 131 did so using the Brief Infant Toddler Social and Emotional Assessment (BITSEA352) and selected items from the Bayley III Screening Test. 355 Chaffin et al. 136 used the Behavior Assessment System for Children. 365
Hughes and Gottlieb139 used the Child Autonomy Observational Scale to assess child autonomy. Again, this tool was developed for the study, based on the theoretical underpinnings of Deci and Ryan. 699,700
Dozier et al. 125,126 assessed the impact of the intervention on children’s behaviour using the Parent Daily Report (adapted from Chamberlain and Reid458).
Child stress
Dozier et al. 125,126 and Cicchetti et al. 124 used analyses of cortisol to assess levels of stress in infant participants.
Parent behaviour
The Dyadic Parent–Child Interaction Coding System (DPICS)701,702 was used by all three PCIT studies,136–138 although Chaffin et al. 136 used the DPICS-II702 and Thomas and Zimmer-Gembeck137,138 used the DPICS-III. 701
Sprang132 and Thomas and Zimmer-Gembeck137,138 examined the effect of the intervention on parents’ abuse potential using the Child Abuse Potential Inventory (CAPI366).
Parental stress
Spiekar et al. ,131 Sprang132 and Thomas and Zimmer-Gembeck137,138 assessed the impact of the intervention on parenting stress, using the Parenting Stress Index-Short Form. 342
Maternal sensitivity
The primary caregiver outcome in the Spieker et al. 131 study was maternal sensitivity, assessed using a modified score of the Nursing Assessment Teaching Scale,358 the secondary outcomes being a measure of parenting support for the child, using the Indicator of Parent–Child Interaction351 and commitment to the child, assessed by answer to interview questions from This Is My Baby. 359 Moss et al. 130 measured maternal sensitivity using the Maternal Sensitivity: Maternal Behaviour Q-Set. 339
Parenting behaviour
In the Hughes and Gottlieb139 study, a scale was developed that reflected the theoretical underpinnings of the study, namely the Parenting Skills Observation Scale (developed by the authors for this study).
Risk of bias: randomised controlled trials of relationship-based interventions
Sequence generation
All studies, except for Spieker et al. 131 and Hughes and Gottlieb,139 were judged to be ‘unclear’ risk of bias for sequence generation because no information was provided on how the randomisation sequence was generated. Spieker et al. 131 and Hughes and Gottlieb139 were assessed as ‘low’ risk. Spieker131 stated that they used a computer-generated sequence, blocked by caregiver type. Hughes and Gottlieb139 referred to a random numbers chart.
Allocation
All studies122–140 were judged unclear risk of bias on allocation concealment because of a lack of information.
Blinding of personnel and participants
All but two123,125,126 studies were assessed as unclear risk of bias for blinding of participants, predominantly due to lack of information. Dozier et al. 125,126 stated that ‘foster parents and birth parents were blind to condition’ and was therefore judged low risk of bias. Cicchetti 2006123 did not blind participants but this was deemed unlikely to influence outcomes of this study because all participants in this study were infants aged, on average, 13–31 months.
Blinding of outcome assessors
All studies, except for Sprang,132 were judged as ‘low risk of bias’ for blinding of outcome assessors because assessors were blinded to the hypotheses, the assignment of participants and/or to the collected data. Thomas and Zimmer-Gembeck 2011137 did not state that their outcome assessors were blinded, but this trial used the same procedures and outcomes measures as the 2012138 trial to which it was linked, and in the 2012 study the outcome assessors are said to be ‘blind to treatment condition’. Sprang132 was assessed as high risk as the authors relied solely on self-completed measures collected by the treatment staff at post test.
Incomplete outcome data
With the exception of Toth et al. ,133 all studies were deemed to be at low risk of bias. Some studies122,136–138 had no missing data, some studies127–129,131,132 used a supplementary ITT analysis and the remaining studies123–126,130,133–135,139,140 conducted analyses of those who dropped out and those who completed treatment, and concluded that they did not differ. The Toth et al. 133 study was assessed as ‘unclear’ risk of bias as missing data were not reported and analyses included only participants who completed treatment.
Selective outcome reporting
Cicchetti 2006123 was judged as ‘unclear’ risk of bias because, despite prospective registration and a (broad-brush) description of measures relevant to the domains outlined in that protocol, the paper reports only on attachment classifications. Cicchetti 2011124 was judged as ‘unclear’ risk of selective outcome reporting bias because no means or SDs were presented and only latent growth curve data.
Spieker et al. 131 and Lieberman et al. 127–129 also registered their trials (ClinicalTrials.gov identifiers NCT00339365 and NCT00187772, respectively). Spieker et al. 131 reports on those outcomes listed in the trial registration and was judged as ‘low’ risk of bias on this domain. Lieberman et al. 127–129 reports on all primary outcomes and one of two secondary outcomes. Overall we judged this study to be ‘low risk’ of bias on this domain. The secondary outcome not reported on by Lieberman et al. 127–129 is child’s cognitive functioning.
All but one125,126 of the remaining studies were deemed unclear risk of bias, as although they appeared to report on all of those outcomes expected, without access to the original study protocols, we cannot be certain. Dozier et al. 125,126 was assessed as ‘high risk of bias’ in light of the fact that two papers reporting the results of this study use different samples and report different outcomes without complete cross-referencing to a statement of all per-protocol outcomes.
Other sources of bias
No other potential sources of bias were identified in most of the studies. However, Sprang132 had an unclear risk-of-bias assessment because the authors reported that expectancy effects and trust in instructors may have played a role in the findings. Furthermore, Bernard et al. 122 and Dozier et al. 125,126 had an additional high risk of bias because the Ainsworth Strange Situation Procedure was used as a measure for participants aged > 24 months, which extends beyond the age range for which it has been validated.
Summary details of the risk-of-bias assessments of these trials can be found in Appendix 10.
Risk of bias: controlled observational studies of relationship-based interventions
The quality of the COS of Becker-Weidman134,135 was variable. No attempt (or no information on any attempt) was made to blind participants or outcome assessors in this study. This study134,135 provided a clear description of its objectives, the main outcomes to be measured, the characteristics of patients included, the intervention of interest and the potential confounders. Although the main findings were adequately described, the relevant adverse events were not adequately addressed. Characteristics of participants lost to follow-up were adequately described and accounted for. It was not possible to determine whether or not the participants and treatment received were representative of the population of interest. Becker-Weidman134,135 used appropriate statistical tests and accounted for confounding variables in their analysis.
Results: relationship-based interventions
Given the heterogeneity of the interventions, we report the results as they relate to the three groupings set out above, starting with meta-analyses where available.
Attachment-focused interventions
Secure attachment
Bernard et al. ,122 Cicchetti 2006123 and Moss et al. 130 assessed the impact of attachment-based interventions on the security of a child’s attachment as measured by Ainsworth Strange Situation Procedure. The pooled estimate using a random-effects model was 0.14 (SMD) (95% CI 0.03 to 0.70) (Figure 17).
The I2-statistic indicates that 82% of the variation in the point estimates is due to heterogeneity (p-value for heterogeneity = 0.004; τ2 = 1.52).
FIGURE 17.
Secure attachment. df, degrees of freedom; M–H, Mantel–Haenszel.

Disorganised attachment
Bernard et al. ,122 Cicchetti 2006123 and Moss et al. 130 assessed the impact of attachment-based interventions on a reduction of a child’s disorganised attachment style, as measured by Ainsworth Strange Situation Procedure. The pooled estimate using a random-effects model was 0.23 (SMD) (95% CI 0.13 to 0.42; p = 0.00001) (Figure 18). The I2-statistic indicates 17% of the variation in the point estimates is due to heterogeneity (p-value for heterogeneity = 0.030; τ2 = 0.05).
FIGURE 18.
Disorganised attachment. df, degrees of freedom; M–H, Mantel–Haenszel.

Avoidant attachment
Both Cicchetti 2006123 and Moss et al. 130 assessed the impact of attachment-based interventions on a child’s avoidant attachment style, as measured by Ainsworth Strange Situation Procedure. The pooled estimate using a random-effects model was 0.90 (SMD) (95% CI 0.13 to 6.37; p = 0.09) (Figure 19).
FIGURE 19.
Avoidant attachment. df, degrees of freedom; M–H, Mantel–Haenszel.

The I2-statistic indicates 64% of the variation in the point estimates is due to heterogeneity (p-value for heterogeneity= 0.09; τ2 = 1.29).
Other attachment measures
Using an ANCOVA, Spieker et al. 131 found no significant differences between intervention and control groups for security of attachment at either post-test or 6-month follow-up (post-test F = 0.68, d = 0.16; p = 0.410; follow-up F = 0.12, d = –0.13; p = 0.746).
Dozier et al. 125,126 used an ANCOVA (intervention group by time) and found that children in the treatment group had less attachment avoidance than those in the control group over time [F(1,44) = 5.02; p < 0.05]. There was no difference for attachment security (p > 0.10).
Stress
Cicchetti et al. 124 used latent growth curve analysis to examine trajectories of cortisol regulation over time, in an analysis combining data from the experimental and ‘other treatment control’ groups (i.e. CPP and PPI). The authors found divergences emerging between the three groups (maltreated intervention, maltreated community control and poor, but non-maltreated, comparison), starting half way through the intervention. Contrary to expectation, no differences were found between those maltreated infants in the intervention groups and those in the control group at baseline. Whereas infants in the maltreated group showed a steady decline in morning cortisol levels (which is elevated in normal samples) over the 2-year study period this did not occur for infants in the maltreated intervention group, for whom cortisol levels were normalised (i.e. no different from infants in the non-maltreated comparison group) and remained so at 1-year post-intervention follow-up. A similar change in cortisol secretion was also found by the Dozier et al. 125,126 study, for which an ANCOVA (intervention group by time) found that children in the intervention group showed significantly lower overall cortisol levels than the control group over time [F(1,46) = 4.55; p = 0.04].
Additional results
In the Spieker et al. 131 study, child competency improved post test but this was no longer significant at follow-up (post-test: F = 4.77, d = 0.42, p = 0.03; follow-up: F = 0.63, d = –0.16, p = 0.429). Child sleep problems were different between groups at follow-up but with a small effect size (d = –0.13; p = 0.09).
Toth et al. 133 used a general linear model and found that, looking at the interaction of study conditions by time, and three out of six narrative variables showed improvement. The improvement was for maladaptive maternal representations [F(3,118) = 3.13; p < 0.05], negative self-representation [F(3,118) = 4.93, p < 0.01] and mother–child relationship expectations [F(3,118) = 2.72; p < 0.05].
Becker-Weidman134,135 found that at 4-year follow-up the treatment group had a statistically significantly improvement compared with the control group for security of attachment (t = –12.23; p < 0.001), withdrawal (t = –4.352; p < 0.001), social problems (t = –2.654; p < 0.05), thought problems (t = –3.505; p < 0.01), attention problems (t = –4.239; p < 0.001), rule-breaking behaviour (t = –6.733, p < 0.001) and aggressive behaviour (t = –7.104; p < 0.001), but not for anxiety/depression (t = –1.091; p = 0.28).
Parent–child interaction therapy
Child behaviour (externalising)
Both Chaffin et al. 136 and Thomas and Zimmer-Gembeck 2011137 and 2012138 assessed the impact of PCIT on child externalising behaviours (as measured by various scales). Thomas and Zimmer-Gembeck 2012138 used a control group that overlapped with their 2011 study,137 and the extent of the overlap was unclear, so we decided only to include the data from their 2011 report of TV/PCIT in the meta-analysis to avoid the problem of double counting.
The pooled estimate, using a random-effects model, was 0.03 (SMD) (95% CI –0.38 to 0.43) (Figure 20). The I2-statistic indicates that 44% of the variation in point estimates between the two studies is due to heterogeneity, making it difficult to draw conclusions about the effect of PCIT on externalising behaviours/symptoms in maltreated children from these two studies. It is perhaps worth noting that Thomas and Zimmer-Gembeck 2012138 also report significant improvements in the behavior of children whose parents participated in S/PCIT and, in both studies,137,138 gains were said to be greater for those who completed PCIT.
FIGURE 20.
Child externalising behaviour. df, degrees of freedom; IV, instrumental variable.

It is also worth noting that Thomas and Zimmer-Gembeck 2012138 report a greater improvement in externalising behaviours/symptoms (p < 0.001) after treatment with S/PCIT than with wait-list controls. This study also found a greater improvement in externalising behaviours/symptoms (p = 0.002) after treatment with S/PCIT than with TV/PCIT.
Thomas and Zimmer-Gembeck 2011137 and 2012138 also measured the intensity of behaviour problems using the ECBI.
Thomas 2011137 found a greater reduction in child behaviour problems (p < 0.001) and intensity (p < 0.001) after treatment with TV/PCIT than with wait-list controls.
Thomas 2012138 found a greater reduction in child behaviour problems (p < 0.000) and intensity (p = 0.019) after treatment with S/PCIT than with wait-list controls.
Thomas 2012138 also found a greater reduction in child behaviour problems (p = 0.001) after treatment with S/PCIT than with TV/PCIT. However, there was no difference between S/PCIT and TV/PCIT for child behavior intensity (p = 0.096).
Parenting interventions
In the study by Valentino et al. ,140 children in the intervention group had richer memory recall (p < 0.01, d = 0.71) and made more emotion references (p < 0.001, d = 1.35) than control children during conversation with parents but not with experimenters.
Contrary to expectation, there was no effect of the Webster-Stratton IY parent programme on child autonomy in the Hughes and Gottlieb study. 139
Effectiveness of relationship-based interventions for maltreated children
Summary
We identified three groups of RBIs.
The first group of 10122–135 studies addressed the problems of insecure or disorganised attachments among maltreated children. Of these, four122,125,126,132 studies evaluated the effectiveness of the short intervention ABC or based on ABC, and four123,124,127–129,133 studies evaluated an attachment theory informed intervention known as IPP. All were short-term, manualised programmes, and they focused on promoting sensitive and responsive care to children adversely affected by maltreatment, with the focus on the carer–child relationship and patterns of interaction. In only one134,135 study were children and young people seen by a therapist. In this study,134,135 the therapy, DDP, is described as a FT treatment based on attachment theory, in which the relationship between therapist and child, caregiver and child, and therapist and caregiver provide the context for treatment. The last131 study evaluated the impact of training early years professionals.
The body of evidence relating to attachment informed interventions is promising, particularly in relation to ABC and IPP interventions. Meta-analyses of data from three122,123,130 studies (two ABC, one IPP) indicate significant increases in attachment security and decreases in disorganised attachment. These results are consistent with those reported in studies, the data for which we were unable to combine in these meta-analyses, with some indication that children in the control group evidenced deterioration, that is, more developed disorganised attachment. This suggests that timely interventions may be able to prevent cumulative consequences of maltreatment.
Findings in relation to children’s behaviour were mixed, and generally did not reach the level of statistical significance. One130 study that recruited children with a wide age range (1–5 years) explored the moderating impact of age and found that reductions in child externalising and internalising problems was associated with increasing age in the intervention group, whereas a marginal increase in behaviour problems was found with age for the control group. Such analyses can only be hypothesis generating and, given the size of the study,130 probably highly speculative. However, the authors note that the maladaptive trajectories for maltreated children increasingly diverge from their non-maltreated peers over time, with the transition to school often being particularly difficult for maltreated children who maintain increasingly socially dysfunctional patterns of aggression and social withdrawal. Therefore, an intervention that has the potential to reduce behaviour problems in preschool children may well be particularly helpful. A similar pattern was noted by Dozier et al. 125,126
Children’s stress levels, as measured by cortisol secretion patterns, also improved with attachment-based interventions.
We identified three randomised trials of PCIT. All were concerned with addressing behaviour problems resulting from physical abuse by helping parents change the way they interacted with their children. A meta-analysis of data from measures of child externalising behaviour indicated no effect of PCIT. Chaffin et al. 136 say in the discussion that this may be because, in this study, PCIT was evaluated as a parent treatment; the study included children older than those customarily included in PCIT for child behaviour problems. Given the relational context of maltreatment, and the emphasis placed by these authors on the importance of the escalating coercive interactions, this account reads as a ‘post hoc’ explanation of an unexpected finding. There is some uncertain evidence regarding the potential reduction in child externalising behaviour problems following PCIT. Thomas and Zimmer-Gembeck137 report a decrease in the severity of behaviour problems of children receiving PCIT, as perceived by parents, but these children evidence no diminution in externalising behaviour as assessed by the CBCL260 (parent report).
As intended, the RET intervention improved children’s memory recall and emotion referencing, with their parents.
Completeness and applicability
None of these studies was conducted in the UK, but all are concerned with relationship problems that are familiar to mental health professionals and social workers. It is difficult to overstate the importance of secure attachment as a public health issue, and the attachment difficulties that so often result from maltreatment present a cumulative threat to children who experience abuse and neglect. The attachment interventions evaluated are relatively brief, manualised interventions that include techniques and strategies currently in use by many health professionals in the UK, for example video interactive guidance. Given the findings reported, well-conducted trials of these interventions in the UK would be appropriate prior to recommending their widespread adoption.
There is currently no strong evidence to support the use of either PCIT or Webster-Stratton’s IY Program as an intervention to address the emotional or behavioural problems of maltreated children, and their impact on improving parenting is clinically questionable.
Quality of the evidence
Only three122,125,126,132 of these studies were judged to be of high risk of bias in any of the seven domains assessed, but most were so poorly reported that judgements of unclear risk of bias outnumbered those of low risk. Overall, these studies do better in terms of detection bias (the blinding of outcome assessors) and attrition bias (incomplete outcome data). Six122–128,132 of these studies were conducted by two American teams, and essentially replicate one another, with variations in the profile of participants. Each team is evaluating an intervention that they have helped to develop. Additional, independent evaluations of both interventions (ABC and IPP) would be helpful, together with better reporting.
Economic evidence
No economic evaluations of RBIs for children who have been maltreated were located.
Systemic interventions
This category includes interventions that aim to benefit the child by bringing about change within the family and other systems in which the child’s life is embedded. Altogether, we identified eight controlled studies (19 citations) that assessed the effectiveness of systemic interventions. We organised these into the following five subcategories:
-
a transtheoretical intervention that integrated family systems, social learning theory and a conflict mediation perspective141
-
a family-based programme for the treatment of CSA. 150
In what follows, we provide descriptive data on the entire group of eight studies,107,108,141–144,147–149 separating them out only when we describe the types of intervention and the results.
Description of studies
Study design
Of the eight107,108,141–144,147–150 controlled studies, six107,108,141–144,148,149 were randomised trials. One was the QEx Bagley and LaChance study150 and one was a COS. 147
Location
One150 study was conducted in in Canada. The remainder of the studies107,108,141–144,148,149 were carried out in the USA.
Sample sizes
Sample sizes were generally small. Linares 2015141 randomised 22 sibling pairs. Meezan and O’Keefe148,149 and Swenson et al. 144 had samples of 81 and 90, respectively, and the remaining RCTs had sample sizes of 30143, 43142 and 55107,108, respectively. Bagley and LaChance150 had a sample size of just 65 (after attrition and exclusions) and Schaeffer et al. 147 had a sample size of 25 youth–mother dyads.
Participants
Systemic family therapy
Multisystemic therapy
Brunk et al. 142 give the mean ages of children in each arm of the study (9.8 years MST, 6.8 years control) but no overall mean age or age range. Schaeffer et al. 147 recruited families with children aged 6–17 years. Swenson et al. 144 and Danielson et al. 143 reported that the mean age of children was around 14 years.
Multigroup family therapy
Transtheoretical
Sibling pairs in the Linares 2015141 study were between 7.2 and 9.7 years of age, and the authors report no significant between-group differences in sibling configuration, with 26% being both males, 37% both females and 37% mixed gender.
Family-based intervention for child sexual abuse
Bagley and LaChance150 targeted only female victims of sexual abuse, with mean ages of 11.2 years and 11.8 years in the experimental and control groups, respectively.
Referrals: all systemic interventions
Linares et al. 141 recruited eligible children and foster carers from three participating fostering agencies. Families in the other seven107,108,142–144,147–150 systemic intervention studies were recruited from CPS or similar governmental agencies. In the study by Danielson et al. ,143 families were also referred or recruited from clinics/treatment providers.
Maltreatment type
Systemic family therapy
Kolko107,108 recruited families in which children had been physically abused.
Multisystemic therapy
Participants in the Danielson et al. 143 study were sexually assaulted adolescents. Brunk et al. 142 and Swenson et al. 144 recruited families with problems of physical abuse and neglect (excluding children who had been sexually abused). Schaeffer et al. 147 recruited families in which children had been exposed to abuse or neglect (within the previous 180 days) and in which parental substance misuse was confirmed or suspected by CPS.
Multigroup family therapy
Meezan and O’Keefe148,149 recruited families where there was abuse or neglect, and where sexual abuse was not the primary allegation, as this was deemed to constitute a substantially different dynamic. Two-thirds were referred for physical abuse, 29% experienced severe neglect and in 24% of cases emotional abuse was also alleged. Ten per cent of participants in this study also suffered sexual abuse.
Transtheoretical
Ninety per cent of the children in the Linares et al. 141 study were in foster care because of neglect (the other 10% were missing this information on their files).
Family based
Bagley and LaChance150 recruited families in which female children had been subject to intrafamilial sexual abuse.
Sources of maltreatment
Where specified, the source of maltreatment was within the family, including biological parents, step-parents, or a parent’s cohabiting partner. In Danielson et al. 143 the source of maltreatment was not reported.
Interventions and comparisons
Systemic family therapy
Kolko107,108 compared a manualised FT treatment for physically abused children to individual child and parent CBT and a control group comprising usual services. The FT was based on Belsky’s227 interactional or ecological model approach to child maltreatment.
Multisystemic therapy
Please see description of MST in Appendix 5.
In the Brunk et al. 142 study, MST was compared with parent training groups. Families in the control group in the study by Danielson et al. 143 received TAU in a specialist clinic utilising evidence-based interventions. Participants who received Multisystematic Therapy for Child Abuse and Neglect (MST-CAN) in Swenson et al. 144 were compared with a group who received Enhanced Outpatient Treatment (EOT). EOT comprised the services usually provided by the treatment centre for physically abused young people and their parents (including individual and FT, and referral for other services, including medication); enhanced engagement (including telephone reminders, rescheduling of missed appointments, costs of transport to the Centre); and the parenting programme ‘Systematic Training for Effective Parenting of Teens (STEP-TEEN)’ – a structured, group-based programme of seven lessons that combines didactic instruction, role-play, videotapes and group discussion to equip parents with the skills needed to understand and communicate with teenagers, to problem-solve, helping parents to accept responsibility for the abuse and encourage co-operation.
Multigroup family therapy
Meezan and O’Keefe148,149 compared multifamily group therapy (MFGT) with traditional FT. MFGT included elements of family systems theory, structural FT, group therapy, behaviour modification, CBT, reality therapy, parent education, and crisis intervention. The traditional FT was described as drawing on several theoretical frameworks, including structural FT, behaviour modification and cognitive–behavioural strategies.
Transtheoretical systemic
This is the description used by Linares et al. 141 to describe a family-focused programme with three components: sibling pair; foster parent; and joint sibling/foster parent. The programme is delivered by two master’s level clinicians (one working with the sibling pair, whereas the other delivers the parent sessions to the foster carers); joint sessions taking place at the beginning and end of every session. The content of sibling and parent sessions was largely skills based, with behaviour rehearsal and reinforcement. Homework and between-sessions practice were integral components. In this study141 the control group received ‘usual services’ (unspecified).
Family-based intervention for child sexual abuse
The Child Sexual Abuse Treatment Program (CSATP704) drew on Maslow’s self-actualisation theory and included IT, dyadic therapy (victim–mother, victim–sibling), group therapy (victims), and FT (victim, mother, father and available siblings). The control group consisted of those eligible for treatment but ultimately not referred by CPS, as it was thought the child was less severely affected by the abuse.
Number and duration of sessions
Systemic family therapy
Both the FT and CBT interventions in the Kolko107,108 study were provided for at least 12 sessions, of 1 hour, over 16 weeks.
Multisystemic therapy
In the Brunk et al. 142 study, MST was delivered in eight, weekly, 1.5-hour sessions. In the Danielson et al. 143 study, Risk Reduction through Family Therapy (RRFT) was delivered in 1- to 1.5-hour-long sessions over an average of 34 weeks.
Treatment duration in the studies by Schaeffer et al. 147 and Swenson et al. 144 was based on family need. In the Swenson et al. 144 study, the number and duration of sessions ranged from daily sessions to one or two per week, with an additional ‘on-call’ 24-hour service for dealing with crises. On average, families availed of 88 hours over 7.6 months (range 2–12 months). In the Schaeffer et al. 147 study, participants remained in treatment for an average of 285 days (range 144–365 days) with 92% being judged as having completed treatment.
Multigroup family therapy
Families receiving MGFT met with a four-person clinical team (in groups of three to four families) for a total of around 80 hours over a 34-week period. On average, most families received 20 family-to-family sessions lasting around 2.5 hours each, although this varied considerable across families. No information was available on the amount of traditional FT provided to control participants.
Transtheoretical systemic
The foster family-focused programme in the Linares 2015141 study was delivered in eight, 90-minute, weekly sessions by two master’s level clinicians (one working with the sibling pair, the other delivering the parent sessions to the foster carers), with joint sessions taking place at the beginning and end of every session. No information was available on the quantum of ‘usual service’ provided to the comparison group.
Family-based intervention for child sexual abuse
The CSATP150 included an average of 78 hours of IT, 37 hours of dyadic therapy (victim–mother, victim–sibling), 32 hours of group therapy (victims) and 14 hours of FT. No information is available on the usual services provided to the control group.
Outcomes and outcome measures: systemic interventions
Outcomes varied by intervention type and included outcomes related to child functioning and adjustment; externalising behaviours; risky sexual behaviour; substance use; internalising behaviours; and mental health, including anxiety, depression and PTSD.
Post-traumatic stress disorder
Swenson et al. 144 and Schaeffer et al. 147 both used the TSCC. 378,383 Danielson et al. 705 used the University of California Los Angeles PTSD Index for DSM-IV (Adolescent version) (UCLA-A) and Caregiver version. 374
Depression
Danielson et al. 143 and Kolko107,108 both assessed the impact of intervention on depression using the CDI. 299
Bagley and LaChance150 used the Center for Epidemiologic Studies Depression Scale (CES-D369).
Behaviour problems
Kolko 1996,107,108 Swenson et al. 144 and Meezan and O’Keefe148,149 assessed changes in problematic behaviour using various reporting forms and versions of the CBCL YSR. 198,269,706,707 Danielson et al. 143 used the Behavior Assessment System for Children-Second Edition365 and Bagley and LaChance150 relied on parent, social worker and self-report of problem/delinquent behaviours. Brunk et al. 142 used the Behavior Problem Checklist (BPC; Quay and Peterson, University of Miami, Coral Gables, FL, 1975, unpublished).
Kolko107,108 also assessed child conflict with the CCI688 and hostility using the Children’s Hostility Inventory. 301
Self-esteem
Bagley and LaChance150 used the Rosenberg Self-Esteem Scale (RSES no reference provided by the authors).
Child functioning
Kolko 1996107,108 assessed overall child functioning with the Kiddie Global Assessment Scale (KGAS) (no reference provided by the author) and assessed peer relationships using The Friendship Questionnaire. 300 Meezan and O’Keefe148,149 used the Children’s Action Tendency Scale CAS385 and the Index of Peer Relations386.
Substance use
Danielson et al. 143 used the Time Line Follow Back Interview376 and urine drug screens to assess the impact of intervention on substance use and risky behaviour.
Other outcomes measured by studies of systemic interventions
Maltreatment
Repeat abuse or high-risk parental behaviours were measured by Kolko,107,108 Swenson et al. ,144 and Schaeffer et al. 147 Child abuse potential was assessed with the CAPI366 by Kolko107,108 (CAPI366) and Meezan and O’Keefe148,149 (CAPI361,708). Schaeffer et al. 147 also reported out-of home placements.
Parental functioning
A number of studies assessed the impact of interventions on parental functioning.
Swenson et al. 144 report on the impact of MST on parental psychiatric distress using the Brief Symptom Inventory (BSI; Derogatis 1975380).
Schaeffer et al. 147 used a number of measures to assess the impact of the intervention on ‘key risk factors and indices of child maltreatment and maternal substance use147 (p. 599). These included the Addiction Severity Index-Fifth Edition,384 the Beck Depression Inventory-Second Edition (BDI-II272) and the Conflict Tactics Scale (CTS302). Linares 2015141 used a modified version of the Child Conflixt Index370 to assess the conflict resolution skills in their study with foster parents.
Meezan and O’Keefe148,149 incorporated measures of social support (Social Support Index387) parental problem solving (Problem-Solving Inventory388), attitudes towards child rearing (Adult-Adolescent Parenting Inventory709), and knowledge of child development (using a 30-item measure designed for the study).
Brunk et al. 142 used the BSI371 to assess parental functioning.
Family functioning an adjustment
Kolko,107,108 Brunk et al. 142 and Danielson et al. 143 each used the FES (respectively citing372,375,710).
Kolko107,108 also used two additional measures: the FAD711 and the Conflict Behavior Questionnaire. 226 Meezan and O’Keefe148,149 used the Family Assessment Form (FAF). 390
Risk of bias: randomised controlled trials of systemic interventions
Figures 31–32 and Appendix 10 provide a summary of the risk of bias of studies of systemic interventions.
Sequence generation
Risk of bias in sequence generation was judged low in three trials: Kolko107,108 used a computer-generated procedure based on Efron’s biased coin toss; Swenson et al. 144 used a computer-generated table of random numbers; and Danielson et al. 143 randomised participants using computerised blocked randomisation.
The remaining RCTs141,142,148,149 were judged to be ‘unclear’, as the only information available was that participants were ‘randomised’.
Allocation concealment
None of the RCTs included provided adequate information on allocation concealment and so all were judged as being of unclear risk of bias.
Blinding of participants and personnel
With the exception of Swenson et al.,144 who stated clearly that participants were not blinded, no study referred to the blinding of participants or personnel. Given the nature of the intervention, it is unlikely that blinding was possible in any of the studies, so we judged these to be high risk of bias.
Blinding of outcome assessors
Blinding of outcome assessors was carried out in the studies by Brunk et al. 142 and Linares et al. ,141 so these studies were classed as being of low risk of bias. The use of self- and parent-report measures in the studies by Danielson et al. ,143 Meezan 1998148,149 and Swenson et al. 144 resulted in a judgement of ‘high risk of bias’, and also in Kolko 1996107,108 in which self-report measures undertaken at the beginning of the FT sessions with the family all present as a potential source of bias.
Incomplete outcome data
We judged the risk of bias as a result of missing data to be low in three trials. 141,143,144 These trials minimised potential bias by maintaining a high retention rate and clear reporting144 or using ITT analysis. 141,143 Attrition in Kolko107,108 was around 6% (one case) in the FT arm, 20% (five cases) in the CBT arm and 17% (two cases) in the routine community services groups. The differential attrition between the two arms resulted in a judgement of high risk of bias (reasons for dropout might be related to the intervention). Brunk et al. 142 and Meezan and O’Keefe148,149 were also judged to be of high risk of bias. Meezan and O’Keefe148,149 took no account of attrition and analyses were based on available case data, resulting in a judgement of high risk of bias. Dropouts in Brunk et al. 142 were evenly distributed across the two arms of the trial, but reasons for drop out are not given, and the authors do not report main effects. We therefore deemed this trial high risk of bias.
Selective outcome reporting
Three142,144,148,149 studies were assessed as being of high risk of bias: Swenson et al. 144 did not report means and SDs for pre and post measures at each time point, and effect sizes were missing for some measures, leading to high risk of bias; Brunk et al. 142 do not report data on main effects or provide post-treatment means, with insufficient data for effect size calculations, and, although stating that they measured child behaviour problems using the BPC (Quay and Peterson, 1975, unpublished), they present no results for this measure. Meezan and O’Keefe148,149 did not report data for ‘non-significant’ results, leading to high risk of bias.
Linares 2015141 was assessed as unclear, as, although there is no evidence that other outcomes were planned and then not reported, there is no published protocol for this study.
The study by Danielson et al. 143 was judged to be of ‘low risk of bias’: the authors report on the primary outcome measure specified in the trial registration (ClinicalTrials.gov NCT00998153) and two of the three secondary measures of PTSD and family environment, but not on risk behaviours as measure by the Youth Risk Behavior Survey.
Other sources of bias
No other source of bias were identified.
Summary details of the risk-of-bias assessments of these trials can be found in Appendix 10.
Risk of bias: quasi-experimental and controlled observational studies of systemic interventions
The quality of the QEx study150 and the COS147 was variable; overall, the quality of the Schaeffer et al. 147 study was good and that of the Bagley and LaChance study150 was adequate. No attempt (or no information on any attempt) was made to blind participants or outcome assessors in either study. Both studies147,150 provided a clear description of the objectives of the study, the main outcomes to be measured, the characteristics of included participants and the intervention. Distribution of potential confounders was adequately described in the Schaeffer et al. 147 study and not described in the Bagley and LaChance150 study. Both clearly described the main findings and relevant adverse events. Characteristics of patients lost to follow-up were adequately described and accounted for in the analysis in both studies. 147,150 The participants and treatment received in the Schaeffer et al. study147 was representative of the population of interest. Bagley and LaChance150 appeared to include those children who were more severely affected by the abuse in the treatment group.
In terms of the analysis, Schaeffer et al. 147 and Bagley and LaChance150 used appropriate statistical tests and accounted for confounding variables in their analyses.
Results: systemic interventions
Meta-analysis was not possible across these studies, which are summarised narratively. Given the heterogeneity across studies, we report the results in the three groupings used above: FT, MST and ‘other systemic’.
Family therapy: results
The following results are these reported by Kolko. 107,108
Child depression
Children’s reports on the CDI indicated a significant reduction in severity of depressive symptoms over time [χ2 = 16.01(3); p < 0.001], but there were no significant between-group differences.
Child behaviour
As measured by the YSR of the CBCL, children in all three groups (CBT, FT and routine services) reported a significant reduction over time in both internalising [(χ2 = 33.54(3); p < 0.0001) and externalising symptoms [χ2 = 12.26(3); p < 0.002], with both CBT and FT showing most change on these measures. No effect was found for social competence.
Parent report on the CBCL indicated lower ratings of serious internalising behaviours over time (p < 0.07) particularly for the two treatment arms. Parents reported a significant reduction in externalising behaviour over time [χ2 = 9.53(3); p < 0.02]. Based on an inspection of the means over time, CBT appeared to show the greatest initial change and FT the greatest change at follow-up (1 year) compared with routine community services, which showed minimal change during that period.
A significant interaction was reported on the CCI [χ2 = 13.12(3); p < 0.04] reflecting the greatest decrease in scores for CBT. This measure (scored by telephone interview with the parent) estimates the presence or absence of common individual behavioural or emotional problems displayed in boys or girls within the previous 24 hours.
The authors did not report statistical tests for children’s hostility but the presented means and SD indicate that participants receiving FT reported a small decrease in hostility scores over time.
Child global functioning
Kolko107,108 reported a significant increase in K-GAS (Global Assessment Scale for Children: Kiddie-GAS) scores over time for all children in the study, with no group differences. There was no difference between the CBT, FT and control groups in reduction over time on fears related to abuse.
Family functioning
The results of subscales for the FES and the FAD indicate more improvement over time among children and parents in the CBT and FT arms than those in routine services.
Multisystemic therapy: results
No meta-analysis was possible for MST because of the limited number of studies reporting appropriate data. For these interventions, we report the results for those outcomes that were directly related to children and young people, and not those related to parents, which includes measures of parental substance abuse,147 parenting stress,142 parental mental health,142,144,147 parenting behaviour,144,147 social support144 and re-abuse. 144
Post-traumatic stress disorder
Danielson et al. 143 report that a mixed-effect regression model indicated that MST youth demonstrated a decrease in parent-reported PTSD from baseline to 6-month follow-up. This was significant (p < 0.001) and the decrease was greater than that reported by those in the ‘TAU’ control group (for the difference; p = 0.004). The between-group difference for adolescent-reported PTSD was non-significant, although both groups reported improvement. In this small study,143 there was considerable baseline inequality and results of this pilot study need to be treated very cautiously.
Swenson et al. 144 found a significantly greater improvement in PTSD symptoms in the MST-CAN group, with the number of youth scoring in the clinical range reducing by half (17.8% at baseline to 8.9% 16 months later) compared with enhanced outpatient treatment groups (19% at baseline and 21.4% at 16 months).
Schaeffer et al. 147 did not find any change in PTSD or dissociation following treatment with Multisystemic Therapy-Building Stronger Families, but report data for only the treatment group.
Depression
Danielson et al. 143 report that a mixed-effect regression model indicated that intervention youth demonstrated a decrease in CDI scores from baseline to 6-month follow-up. This was significant (p < 0.001) and the decrease was greater than that reported by those in the ‘TAU’ control group (for the difference; p = 0.008). Baseline inequality augurs caution in interpreting these results. No change was reported by Schaeffer et al. 147 for youth depression.
Anxiety
Schaeffer et al. 147 reported that youths whose families received the intervention experienced a significant decrease in symptoms of anxiety (medium effect size), as measured by the TSCC. Unfortunately, this study147 presents data only on pre–post intervention and does not compare this reduction with outcomes for the control group.
Child behaviour
Danielson et al. ,143 based on their mixed-effects regression model, report improvements from baseline to 6 months’ follow-up for internalising behaviour in both intervention and TAU groups, but the experimental group did significantly better (p = 0.008). No between-group differences were found for externalising behaviour (improvement occurred in both groups over time).
Swenson et al. 144 found statistically significant improvement in parent-reported internalising behaviour in the intervention (MST-CAN) group with no improvement evident in those receiving enhanced outpatient treatment. No differences were found between enhanced outpatient treatment and MST in externalising behaviours (measured by CBCL).
Brunk et al. 142 reported measuring child behaviour problems using the BPC (Quay and Peterson, 1975, unpublished), but no results are provided for this measure.
Substance use and risky behaviour
Danielson et al. 143 specifically targeted the risk of substance use and mental health problems of sexually assaulted adolescents. The authors conducted a Poisson mixed-effects regression model, which indicated greater reductions in substance use (number of days’ use from baseline to 6 months) among experimental youth than in those in the TAU control. No between-group differences were found for risky sexual behaviour (assessed by numbers of sexual partners and/diagnoses of STIs in previous 3 months).
Family functioning
Danielson et al. 143 reported improvements in adolescent and parent reports of family cohesion (FES Cohesion scale) and reductions in family conflict (FES Conflict scale).
Family-based systemic interventions (including transtheoretical): results
Depression and self-esteem
Bagley and LaChance150 used measures of depression (the CES-D369) and self-esteem (RSES404) because the authors regarded them as ‘valid and reliable measures of psychological vulnerability’ (p. 208). Statistically significant gains are reported for adolescents in the intervention compared with those who did not receive the family-based programme.
Behaviour
Bagley and LaChance150 reported a reduction in problem behaviours among the sexually abused adolescent girls in this study, assessed from parent and social worker reports of at least one incident of delinquency, marked aggression in school, school dropout, suicidal behaviours, running away from home or problem sexual behaviour. Adolescents exhibiting at least one of these behaviours in the treatment group reduced from 48% to 7%. By contrast, a small increase from 33% to 40% was reported for those in the control group. The difference between groups was statistically significant (p < 0.05).
Meezan and O’Keefe148,149 reported improvements for child externalising behaviour, both for those in the intervention group (MFGT) and those in the comparison group (who received FT). The measure used was the CBCL and the difference was not statistically significant.
Physical aggression from older towards younger siblings in the Linares 2015141 study was reduced in the intervention group (p < 0.05) but no between-group differences were found for verbal aggression from older to younger siblings, or verbal and physical aggression from younger to older siblings.
Family functioning
Meezan and O’Keefe148,149 assessed the impact of intervention on family functioning using a modified version of the FAF (interview). The authors report significant improvements in the experimental group in relation to the amount of support available to them, their parent–child interactions, and the amount of stimulation available to their children. In contrast, the control group showed significant change only in relation to the support available to them. The reports give the reader the impression that the authors are interpreting the data in the most favourable ways possible.
Effectiveness of systemic interventions for maltreated children
Summary
We identified eight107,108,141–144,147–150 studies that evaluated a heterogeneous group of interventions informed by systems theory and offered to different participants. Four studies evaluated various forms of MST, comparing this with CBT,142 TAU,143 enhanced outpatient treatment,144 and Comprehensive Community Treatment. 147
Of the remaining four studies, one compared systemic FT with CBT;107,108 one worked systemically with families in which a young person had been the subject of incestuous abuse;150 a third used MFGT;148,149 and the final study141 described itself as a transtheoretical intervention that focuses on three family subsystems: sibling pairs in foster care, the foster parent, and foster parent/sibling pairs.
All of these interventions included cognitive–behavioural strategies and psychoeducation, but their underlying theories of change were primarily systemic.
The four142–144,147 MST studies are heterogeneous and the results are variable. Only one144 study of the three143,144,147 MST studies assessing the impact of the intervention on PTSD reported a significant benefit in favour of MST. This rather larger study144 (n = 90) halved the percentage of youth scoring in the clinical range for self-reported PTSD symptoms from 18% at baseline to 9% at 16 months post baseline, in contrast with the group receiving enhanced outpatient services, for which the percentage increased from 19% to 21%. Retention in both the treatment and the study144 was high, and the intervention appears to have been successful at not only addressing the mental health symptoms of participating youth, but also addressing those aspects of parenting associated with maltreatment from both youth and parent perspectives, in particular reducing parental neglect and assault. The other two studies143,147 found no significant between-group differences in depression or PTSD. Schaeffer et al. 147 observe that these young people reported subclinical levels of concern at baseline. Danielson et al. 143 (who studied sexually abused children) hypothesise that the absence of effect is, in part, because of the small size of the study and considerable baseline inequality. In this study143 the primary outcome was substance use risk and mental health problems, and the authors report a significant reduction in substance use and associated risk factors among MST youth compared with TAU.
As indicated earlier, both CBT and FT outperformed routine community services. This early comparative study107,108 was one of the first to submit FT to rigorous evaluation and the authors note that FT has been less frequently used in the context of child maltreatment than CBT; they recommend further development, including the incorporation of a structured approach to address the parent–child relationship. At the same time, they highlight the need for CBT to give attention to how best to discuss children’s attributions of their victimisation.
There is no strong evidence of benefit to children from multigroup FT with abusive and neglectful families. 148,149 Linares et al. 141 report promising, but mixed results of an intervention designed to reduce sibling aggression in foster care, and this small study141 requires replication before any conclusions can be drawn. However, there is some indication that foster parents can learn strategies to minimise sibling aggression and its adverse effects on psychological child well-being. 712
Completeness and applicability
All of these generally very small studies were conducted in North America. MST enjoys a strong evidence base in relation to vulnerable groups such as young offenders, and the extension to abusive and neglectful families suggests that MST-CAN has potential as an effective intervention for families whose behaviour places their children at risk of significant harm. Results of the other MST studies are less persuasive than those of Swenson et al. 144 but of particular interest is the QEx study by Schaeffer et al. 147 This study147 examined the impact of an MST intervention for maltreating families in which parental substance abuse was a major issue. Although this study147 showed a reduction only in child anxiety, given the numbers of children with child protection plans for whom parental substance misuse is a key factor, this intervention is potentially highly relevant, and the authors report an ongoing, large-scale longitudinal randomised trial that will allow the investigation of the programme’s effectiveness with different subgroups, that is, different substance misuse and maltreatment characteristics. MST is a costly intervention, but may be cost advantageous.
Quality of the evidence
Six107,108,141–144,148-149 of the included controlled studies were randomised trials, but the majority of risk-of-bias judgements made were ‘unclear’ as a result of poor reporting. The QEx study147 was judged good overall (but it was a small study), and the COS147 was judged adequate. Overall, the quality and extent of the evidence for systemic interventions to address the effects of child maltreatment are parsimonious.
Economic evidence
No economic evaluations of systemic interventions were located for children who have been maltreated.
Psychoeducation
Psychoeducation forms an important component in a range of different interventions, but those coded as psychoeducational interventions use it as their main focus. They draw heavily on social learning and cognitive theory to conceptualise and address maladaptive patterns of behaviour and beliefs that have developed as the result of exposure to abuse or neglect.
We identified 17151–168 studies that assessed the effectiveness of psychoeducational interventions.
Description of studies
Study design
Seven151–157 of the psychoeducational intervention studies were randomised trials. Trowell et al. 155 was designed as an other-treatment control study, comparing a psychoeducational group with IT.
Three158–160 studies used a QEx design and the remaining seven161–168 studies were COSs.
Location
All151,152,154,156,157 but four155,158,159,165 of the psychoeducational intervention studies were conducted in North America.
One155 RCT was conducted in the UK. The remaining six151,152,154,156,157 randomised trials took place in the USA151–154 and Canada. 156,157
Two159,160 of the three QEx studies were carried out in Canada and the third158 was conducted in the Netherlands.
The remaining COSs took place in the USA161,162 Canada163,164,166–168 and Spain. 165
Sample sizes
All of the randomised trials made use of small to moderate sample sizes, ranging from a total of 42 participants (with only 38 participants completing post-treatment interviews)156 to 181 participants (with 174 participants completing the follow-up interview). 151
Of the QEx studies, Noether et al. 158 had a large sample size of 253 participants (with 210 participants completing the 12-month follow-up interview); Simoneau et al. 159 and Tourigny 2007160 recruited 49 and 55 participants, respectively.
Sample size in four of the COSs was small, ranging from 27 participants161 to 42. 166,167 Holland et al. 164 and Hébert et al. 163 had samples of 66 and 90, respectively, although data were presented for only 88 participants in the Hébert and Tourigny163 study, and Duffany and Panos162 recruited a sample of 617.
Participants
Age
Across all studies, the mean age of child participants ranged from 4.95 years152 to 14.8 years. 166,167 Barth et al. 161 recruited the foster parents of children aged 9 years on average.
Gender
Four studies focused exclusively on females. 155,160,166–168 Of those with mixed samples, nine151,154,157,159,161–164 had a sample that was at least 50% female. Five152,153,156,158,165 studies had a sample that was at least 50% male.
Recruitment
Participants from all 17151–168 studies were recruited from a wide range of mainly government agencies, including child protection agencies,157,160,166–168 Family Services,153,164 Family Sexual Abuse Action Centre,163 Children’s Justice Centre,162 social services agencies,151,154,156 local residential homes,165 the authors’ own clinics and local agencies155 and community and shelter outreach centres. 152 Noether et al. recruited participants from mothers who participated in a national, ‘longitudinal study of women with histories of violence and co-occurring substance use and mental health disorders’158 (p. 827). We have no information on the recruitment sources for Barth et al. 161
Maltreatment
Five151–154,156 of the seven RCTs focused on children who had witnessed or been exposed to IPV. Graham-Bermann et al. 151 reported that 30% of the children in this study had also experienced physical harm.
In Noether et al. 158 (quasi-experiment), the sample was drawn from a longitudinal study of women with a history of violence, and co-occurring substance use and mental health disorders.
One155 randomised trial and two quasi-experiments159,160 focused on sexual abuse, as did five161–164,166,167 of the COSs.
One157 randomised trial and two COSs165,168 focused on children who had experienced physical abuse, emotional abuse, sexual abuse and neglect.
Interventions and comparisons
All 17151–168 studies used a group-based format of psychoeducation. Although the interventions were predominantly child focused, one intervention provided training for foster carers. 161 Control group participants in all but two of the psychoeducational studies received either no intervention or management as usual. Overbeek et al. 153 made use of a control programme ‘Jij hoort erbij’ (‘You belong’), based on an analysis of non-specific factors used in the specific factors intervention programme. Trowell et al. 155 compared group psychoeducation with brief, focused, individual psychoanalytic psychotherapy.
Psychoeducation for children exposed to intimate partner violence
Graham-Bermann et al. 151 described two psychoeducational interventions: one focused solely on children, and one combining a programme for children with a programme for their mothers. The programme is known as Kids Club. 713 The child intervention sought to improve children’s knowledge about family violence, influence their attitudes and beliefs about families and family violence; and improve their emotional adjustment and social skills. The intervention for parents aimed at improving their repertoire of parenting and disciplinary skills, enhancing their social and emotional adjustment, thereby reducing the children’s behavioural and adjustment difficulties. Howell et al. 152 evaluated a preschool version of the combined parent-and-child intervention described by Graham-Bermann et al. 151 In this version the children’s intervention was designed to promote social competence and the mothers’ programme to improve their social and emotional adjustment. In both studies, children were from families through which they had been exposed to IPV.
Overbeek et al. 153 developed a child’s psychoeducational intervention based on Graham-Bermann’s Kids’ Club713 but with some topics amended (e.g. more time spent on identifying, differentiating and dealing with emotions) and added (e.g. secrets, contact with the violent parent, and the future). Traumatic experiences are directly addressed in order to prevent avoidance of the topic and provide children with a sense of mastery. The intervention covered affective modulation, emotion regulation skills, coping and processing, social skills and enhancing future safety and development. Overbeek et al. 153 developed parallel parent sessions independently from Kids’ Club,713 for which the focus was on psychoeducation, improving parenting and disciplinary skills, and helping parents accurately interpret children’s feelings and behaviour, providing them with emotional support.
In the Sullivan et al. 154 study, children attended a psychoeducation group (The Learning Club) in which they learned about safety, feelings and respect for themselves and others. In addition, the mothers and children also had the services of an advocate who helped them to access community resources.
Wagar and Rodway156 describe the programme as aiming at helping children to modify their responses to past experiences of witnessing violence, to develop problem-solving skills for future encounters, to address interpersonal responsibilities and attitudes regarding behaviours and foster self-esteem.
Psychoeducation for children who experienced sexual abuse
Trowell et al. 155 describe psychoeducational group therapy for girls in which sessions were topic based, with information and suggestions given and explained in the group. The relationship between girls and the cotherapist leading the groups was also a focus, being linked with past and current relationships, losses and disruptions. In this intervention, carers also received group-based support.
Hébert and Tourigny163 evaluated a closed group led by two trained practitioners. The psychoeducational approach used combined a variety of therapeutic activities (e.g. group discussions, personal testimonies and stories, exercises and lectures). Some of the exercises targeted emotional regulation skills and cognitive coping strategies. Sessions included sex education and abuse prevention skills, and practice in social interactions with peers. Parents were invited to accompany the child for the first four sessions, which were used to promote positive child–caregiver interactions, improve communication and reinforce secure relationship. The intervention in Tourigny 2005166,167 and Tourigny 2007160 was also a closed group that used broadly the same approach, but without parental involvement. Each session used a similar format and was centred on a specific theme, such as disclosure of the abuse, the cycle of the abuse, consequences of abuse, relationship to the perpetrator, and so on.
Barth et al. 161 provided psychoeducational groups for foster parents (both kin and non-kin), designed to provide an understanding of the types of behaviours presented by children who had been sexually abused and how these might best be managed.
The Children’s Treatment Program, evaluated by Duffany and Panos,162 comprised 12 lessons on important topics to the participating children and families, including My Body, Assertiveness, Touches, Who Can You Tell, Fears and Nightmares, and Inner Strength. The groups were open to avoid families having to wait, and siblings were also allowed to attend.
The study by Holland et al. 164 evaluated a multimethod intervention for Aboriginal children in the Stól:lō Nation in British Columbia, Canada, who had been sexually abused. The intervention included group work that comprised psychoeducation and social skills training in a closed group format. No other information is provided other information.
The intervention in the study by Simoneau et al. 159 was group work, with boys and girls organised by age (6–8 years, 9–13 years). They were accompanied by parents for the first five sessions. Children who missed more than two sessions, were offered entry into the next group. Focus of the groups was to (1) reduce sense of social isolation; (2) improve self-perception; (3) reduce behavioural difficulties; (4) improve the closeness with the caregiver; and (5) reduce or cease feelings of guilt linked to the abuse.
The intervention in the study by Santibáñez165 is also a multimethod programme that incorporates individual and group work-element focused, plus ‘unstructured daily life interventions’. Staff meet weekly to determine which interventions are to be used for the young people both in individual and group sessions, and daily life activities are prepared to encourage wider learning. Specifically, there are weekly activities with the young people tackling self-control and moral development. The self-control sessions are individual and each young person chooses an area to change (e.g. to reduce hitting, increase studying, participate more). Each young person is taught self-control step by step: contingency contract, learning how to self-control, choosing the problem to tackle, defining the behaviour to control or accept, behavioural self-observation, multimodal self-observation, self-evaluation and conclusions about the extent of the problem, questioning oneself about how to proceed, proposing realistic goals for change, learning at least one technique of self-control and how to apply it to another problem. For moral development, weekly group work sessions are held, at which there is discussion about questions that are of importance to each of the young people; friendship, characteristics of good friends, helping others, rules of the home, personal responsibility and losing control.
Number and duration of interventions
Duration of sessions ranged from 1 to 2 hours each, with sessions lasting 9–20 weeks (most are between 10 and 12 weeks), with the exception of Santibáñez,165 in which the programme lasted 4 months, and appears to have comprised weekly group and individual sessions plus everyday activities in the residential homes to promote generalisation of learning.
Outcomes: studies of psychoeducation
Post-traumatic stress disorder
Four measures of children’s post-traumatic stress symptoms were used across the seven153,155,160,163,166–168 studies assessing this outcome. Four153,160,166–168 studies used the Trauma Symptom Checklist (TSC). Overbeek et al. 153 also used the Trauma Symptom Checklist for Young Children (TSCYC), Hébert and Tourigny163 used the Children’s Impact of Traumatic Events Scale-II (Wolfe, unpublished assessment instrument – available from VV Wolfe, Child and Adolescent Centre, London Health Sciences Centre, London, ON, Canada) and Trowell et al. 155 used the 1989 version of Orvaschel’s PTSD scale406 – an extension of the KSADS instrument. 268 The Trauma Symptom Checklist-40 (TSC-40408) was used by Wolfe et al. 157 to assess symptoms of emotional distress.
Depression
Hébert and Tourigny163 assessed the impact of psychoeducation on childhood depression using the CDI. 80 Trowell et al. 155 used a shortened version of the KSADS. 268
Self-harm
Self-harm was assessed in all three Tourigny studies160,166–168 using the Self-Injurious Behavior Questionnaire (Sadvosky, unpublished). Holland et al. 164 also examined this outcome using administrative data.
Anxiety
Hébert and Tourigny et al. 163 assessed anxiety as an outcome, using the RCMAS. 256 This study also assessed symptoms of dissociation using the Child Dissociative Checklist. 426
Behaviour problems
The effect of psychoeducation on children’s problem behaviour was examined by seven studies using various versions of the CBCL. The studies by Graham-Bermann et al. ,151 Overbeek et al. ,153 Hébert and Tourigny163 and Barth et al. 161 used the Parent Report Form, and both studies by Tourigny et al. 160,166–168 used the YSR Form.
Two studies assessed delinquency: Tourigny 2005166,167 used the Criminal and Delinquent Behaviours Questionnaire714 and Holland et al. 164 used administrative data.
Antisocial and criminal behaviour was assessed using the Antisocial and Criminal Behavior Questionnaire715 in the study conducted by Santibáñez,165 who also investigated cognitive mediators of aggression using a 20-item Likert-type scale. 427
Noether et al. 158 used mother/carer ratings of the Behavioral and Emotional Rating Scale (BERS410) as the measure of the primary outcome measure.
The primary outcome in Duffany and Panos162 was recidivism (being re-abused or becoming abusers), assessed using the Youth Outcome Questionnaire. 424
Self-control
Self-control was assessed in Santibáñez165 using the Shapiro Control Inventory428 in its Spanish version.
Social competence
In the Howell et al. 152 study the primary outcome was enhancing social competence in children who had witnessed IPV which they measured using the Social Competence Scale (Conduct Problems Prevention Research Group395).
Self-concept and self-adequacy
Sullivan et al. 154 measured changes in the well-being of children who had been exposed to domestic violence using Harter’s Self-Perception Profile for Children (SPPC; 8- to 12-year-old version431). Hébert and Tourigny163 used the same measure as part of his larger battery of outcome measures for a group of sexually abused children.
All three Tourigny et al. 160,166–168 studies assessed the impact of intervention on coping strategies using a French version of the Ways of Coping Questionnaire. 419 They also deployed four of the five dimensions that make up the Empowerment Scale,421 namely optimism, self-efficacy, helplessness and justified anger plus the French version of the Children’s Attributions and Perceptions Scale. 270
Sexual behaviour
Barth et al. 161 and Holland et al. 164 examined the impact of intervention on children’s sexual behaviours using the CSBI. 423 Holland et al. 164 also used administrative data.
Relationships
Healthy relationship skills were assessed in the study by Wolfe et al. 157 using the Adolescent Interpersonal Competence Questionnaire. 409
Two studies151,156 focused on children’s attitudes and beliefs about the acceptability of family violence. Graham-Bermann et al. 151 assessed change in this outcome using the Attitudes About Family Violence scale,394 whereas Wagar and Rodway156 used a Child Witness to Violence Questionnaire (no reference provided) to assess children’s knowledge of wife abuse, who children feel are responsible, and their responses and attitudes to anger, their problem-solving abilities related to safety skills.
Risk of bias: randomised controlled trials of psychoeducation
Sequence generation and allocation concealment
It was not possible to judge whether sequence generation was adequately conducted, as five153–157 of the seven trials provided no other information other than participants were ‘randomly assigned’. These studies were therefore assessed as ‘unclear’ risk of bias for both sequence generation and allocation concealment.
Graham-Bermann et al. 151 and Howell et al. 152 both describe a modified, sequential random assignment procedure. In the study by Graham-Bermann et al. ,151 the first seven children were assigned to the ‘child-only intervention’, the next seven children to the ‘child plus mother intervention’ and the next seven children to the wait-list control. In the Howell et al. 152 study, the first five families were allocated to the experimental arm and the next five to the control arm, but the paper said nothing about allocation concealment. Both studies were assessed as ‘low risk of bias’ for sequence generation and unclear for allocation concealment.
Blinding of participants and personnel
Trowell et al. 155 stated that it was not possible to blind participants. None of the other studies makes any reference to procedures to blind the participants or personnel, and neither is likely to have been undertaken, given the nature of the intervention. All studies were therefore assessed as ‘high risk of bias’ for this bias domain.
Blinding of outcome assessors
Outcome assessors were blinded in Overbeek et al. 153 Graham Bermann et al. 151 state that baseline interviews were conducted by researchers blind to group assignment and separate from those who provided the intervention; however, with the exception of child attitudes, the study151 relied solely on mother self-report and we judged this study151 overall to be of high risk of bias on this domain.
Wagar and Rodway156 state that group leaders conducted the pre-group interviews and administered the measurement tools, as well as facilitating the groups, and so this study was judged to be of high risk of bias for outcome assessment. Trowell et al. 155 state that blinding of assessors was probably compromised because the children and their mothers often mentioned the specific therapy during assessment.
The absence of information on blinding of outcome assessors, together with the use of use of self-report and parent-reported measures in the studies by Howell et al. ,152 Sullivan et al. 154 and Wolfe et al. ,157 suggest that outcome assessors were not masked in these studies, leading to a judgement of high risk of bias.
Incomplete outcome data
Three153–155 of the seven trials sought to minimise potential attrition bias by analysing participants based on ‘assigned treatment’ rather than ‘treatment completed’ and so were judged low risk of bias. Graham-Bermann et al. 151 identify differential attrition as a cause of concern and this study was accordingly judged high risk of bias, as were the studies by Wagar and Rodway156 (which lost around 10% of children, all four from the experimental arm) and Wolfe et al. 157 (which reported differential attrition of 21% experimental and 11% control and undertook completer-only analyses). Howell et al. 152 was also deemed high risk of bias because 21 of the 113 children recruited to the study were missing from the final analyses (seven dropouts in the experimental group and 14 in the control group).
Selective outcome reporting
Although the studies all differed somewhat in their choice of outcomes, there appears to be no evidence that other outcomes were planned and then omitted from the results. In the absence of study protocols it is extremely difficult to assess the risk of selective outcome reporting. In that respect, almost all were assessed as unclear risk of bias. However, two156,157 of the included studies failed to report specific means and SDs for their post-intervention results and were therefore judged to be of high risk of bias.
Other sources of bias
Some other potential sources of bias were noted in two151,154 of the studies, including a suggestion that the sample was nationally unrepresentative151 and potential bias associated with paying participants for their continued involvement in the study. 154
Full details of risk-of-bias assessments for each study can be found in Figures 33 and 34 in Appendix 10.
Quality assessment of quasi-experimental and controlled observational studies of psychoeducation
The quality of the three158–160 QEx studies and seven161–168 COSs was variable.
All studies158–168 provided a clear description of the study objectives, and, except for Holland et al. ,164 all gave a clear description of the outcome and adequate descriptions of their participants.
Five159,162,164,166–168 of the included studies did not give an adequate description of the theoretical basis of their intervention. All of the studies158–168 at least partially addressed potential confounders in their research, and all provided a clear description of their findings; however, only two studies165,168 addressed potential adverse effects. Only two166–168 of the 10158–168 studies described the characteristics of patients lost to follow-up. Four158,160,162,163 of the 10 studies reported probability values for the main outcomes.
It was not possible to determine, for any of the studies, whether or not those who participated, and the staff involved in the study, were representative of the entire population from which they were recruited.
Blinding of participants or outcome assessors was not attempted in five161,162,164–167 of the studies, and, although it was unclear whether or not it was attempted in the remaining four158–160,163,168 studies, it seems unlikely that it would have been feasible because of the psychosocial nature of the intervention. Three of the studies164,166–168 did not recruit patients for intervention groups and controls from the same population.
Results: psychoeducation
Post-traumatic stress
Both Wolfe et al. 157 and Overbeek et al. 153 assessed the impact of the psychoeducational intervention on children’s post-traumatic stress, albeit with two measures (as measured by the TSC-40408 and the TSCYC,399 respectively). We were unable to combine these data in a meta-analysis. Based on ITT and completer analyses, Overbeek et al. 153 found no differences between children in the experimental and control group; children in both groups improved.
Working with teenagers with histories of child maltreatment, Wolfe et al. 157 reported improvements in symptoms of trauma.
Children’s PTSD was also assessed by Trowell et al. 155 However, unlike the studies by Overbeek et al. 153 and Wolfe et al. ,157 this study155 compared two active treatments. In Trowell et al. ,155 univariate analyses failed to identify a difference between those receiving group or IT on the PTSD dimension of ‘persistent symptoms of increased arousal’ used in the study. 405 Following Cohen,716 the authors used an effect size of 0.5 as a threshold of moderate effect, and undertook no further analyses relating to PTSD symptoms.
Controlling for the impairment score on the KGAS405 in a multivariate analysis, the authors report a significant effect of IT for ‘the re-experiencing of trauma’ dimension of PTSD (baseline to 1- and 2-year follow-up, and baseline to exit), and – for the ‘persistence/avoidance of stimuli’ dimension – at baseline to first-year follow-up. When KGAS is replaced by the baseline score on the same dimensions, the significance of the effects is attenuated.
Children’s PTSD symptoms were also assessed in three COSs163,166–168 and one QEx study. 160 Owing to the high risk of bias in all four of these studies,160,163,166–168 results were not incorporated into the meta-analyses and are instead presented narratively. Their results indicate that adolescents who were part of the psychoeducational intervention group improved significantly compared with controls on post-traumatic stress scores at both post test160,163,166,167 and 6-month follow-up. 166,167 A fourth study168 found no statistically significant differences, although clinical measures suggested improvement for the treatment group compared with the control group.
Depression
In the trial conducted by Trowell et al. ,155 the between-group differences on the KGAS failed to reach the threshold effect size adopted by the authors of 0.5 (following Cohen716). In the one CS163 that assessed childhood depression, participants in the intervention group demonstrated only marginally fewer symptoms of depression following the intervention.
Behavioural problems
Graham-Bermann et al. 151 and Overbeek et al. 153 assessed the impact of the psychoeducational intervention on child externalising and child internalising behaviours (as measured by the CBCL).
Externalising behaviours The pooled estimate using a random-effects model was –0.19 (SMD) (95% CI –0.45 to 0.06) (Figure 21). The I2-statistic indicates 0% of the variation in the point estimates is due to heterogeneity.
FIGURE 21.
Externalising behaviours. df, degrees of freedom; IV, instrumental variable.

Internalising behaviours The pooled estimate using a random-effects model was –0.00 (SMD) (95% CI –0.25 to 0.25; p = 0.84) (Figure 22). The I2-statistic indicates 0% of the variation in the point estimates is due to heterogeneity.
FIGURE 22.
Internalising behaviours. df, degrees of freedom; IV, instrumental variable.
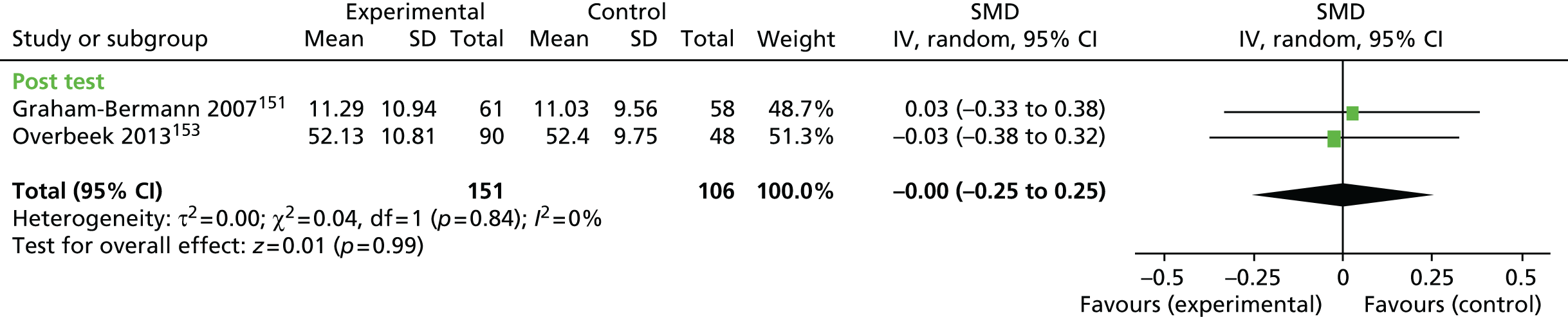
Children’s behavioural problems were also assessed in three161,163,166–168 COSs and two158,160 QEx studies.
Four158,163,164,166,167 of the included studies found that post-test scores on behavioural measures were significantly lower for children who had received a psychoeducational intervention.
One study160 found that although intervention group participants (all girls) showed a significant decrease in internalising behaviours and social problems, change scores on externalising behaviours problems were not significant. One study168 found no statistically significant differences for internalising or externalising behaviours. Another study162 found that approximately one-third (15/47) of the children showed no change, or an insignificant worsening of behavioural and/or emotional symptoms following the intervention, and the last study161 reported that behaviour in both intervention and control groups worsened in equal measure from the pre-test to the follow-up.
Other outcomes
Self-injurious behaviours
Self-injurious behaviours were assessed in three164,166–168 COSs and one160 QEx study. Three160,166–168 of the studies demonstrated that children who were part of the intervention group improved significantly compared with control group participants. The fourth study164 indicated that there was no significant difference between groups for attempted/threatened suicide.
Anxiety and symptoms of dissociation
The same COS163 reported that participants in the intervention group demonstrated significantly less anxiety following the intervention and marginally fewer symptoms of dissociation.
Children’s sexual behaviours
Two161,164 COSs assessed children’s sexual behaviours. Holland et al. 164 found no significant effects. Barth et al. 161 reported a statistically significant treatment group effect (improvements) for two out of 36 items on the Coping Scales Inventory (CSI): ‘looks at people when nude’ and ‘shy about undressing’.
Delinquency
Three165–167 COSs assessed delinquency and antisocial behaviour. Tourigny 2005166,167 reported that children in the intervention group had a greater reduction in delinquent behaviours than children in the control group at the 6-month follow-up interview. Holland et al. 164 and Santibáñez165 found no significant differences.
Self-control
The one165 study that assessed children’s self-control following the intervention found no significant difference between the intervention group and control group – despite finding some significant improvements – compared with control group participants – in levels of moral reasons and some of the factors believed to mediate aggression.
Coping strategies
Coping strategies were assessed in two166–168 COSs and one160 QEx study. All three160,166–168 studies demonstrated that children who were part of the intervention group improved significantly compared with control group participants in abuse-related attributions.
Self-competence
Children’s self-competence was assessed in one COS163 and one randomised CS. 154 The RCT154 found that children who received the psychoeducational intervention demonstrated increased self-competence in their 4-month follow-up interview, whereas the self-competence of children in the control group remained relatively unchanged overall. Hébert and Tourigny163 found no significant difference in adjusted post-test scores for self-competence.
Sense of empowerment
Children’s sense of empowerment was assessed in two COSs166–168 and one QEx study. 160 In all three studies,160,166–168 children who were part of the intervention group improved significantly compared with control group participants in abuse-related attributions.
Social competence
One RCT152 assessed participant’s prosocial skills, finding a significant improvement among children who received the intervention.
Relationships
In Wolfe et al. 157 (RCT) intervention youths did not show the expected growth in healthy relationships skills over time.
Children’s attitudes and beliefs about the acceptability of family violence were measured in two randomised trials,151,156 using different measures (see Outcomes: studies of psychoeducation). Graham-Bermann et al. 151 found that children who were part of the child and mother intervention made most improvement over time in attitudes about violence compared with those in the child-only and control groups. An ANCOVA of the pre-/post-treatment data by Wagar and Rodway. 156 indicated significant differences in children’s ‘attitudes and responses to anger’ and ‘sense of responsibility for the parents & for the violence’. There were no significant differences between groups for ‘knowledge of safety & support skills’.
Effectiveness of psychoeducational interventions for maltreated children
Summary
We identified a large number of studies of psychoeducational interventions including seven151–157 randomised trials, three158–160 QEx studies and seven161–168 COSs. All included or comprised a group-based format, and although the groups used a variety of formats (activities, discussion, etc.) they generally included an educative component (focused on the nature of maltreatment suffered by the children), affect modulation, emotion regulation skills, coping and processing, social skills and addressing future safety.
Although the findings of this heterogeneous body of evidence vary somewhat, there is evidence of effectiveness in relation to symptoms of PTSD.
The evidence for improving children’s behaviour is more mixed. On the basis of ‘vote counting’ most report a positive impact on externalising, internalising, delinquency and antisocial behaviour and self-injurious behaviour. A minority report ‘no difference’ and Barth et al. 161 report a worsening in children’s behaviour. Participants in the Barth et al. 161 study were foster parents caring for sexually abused children, who rarely implemented the homework tasks required of them during this short intervention but who appreciated the intervention.
Where examined, similar results in favour of psychoeducation were reported for positive changes, such as improvements in coping, enhanced self-competence, social competence and sense of empowerment. Generally, the involvement of parents (often in parallel groups) was found to be helpful.
Completeness and applicability
All but four of the studies were conducted in North America. Two153,158 studies were conducted in the Netherlands, one165 study in Spain and one155 study in the UK.
Nine155,159–164,166–168 of the seventeen studies focused on sexually abused children, including the one UK study,155 which compared the effects of two manualised therapies: an individual psychotherapy and a group therapy that included psychoeducation. Six151–154,156,158 studies addressed the consequence of witnessing IPV, and two157,165 studies recruited children who had experienced other forms of maltreatment, including multiple abuse. The studies are broadly relevant to the UK, in terms of participants, settings and transferability of the interventions, but are sometimes limited by the cultural specificity of some interventions (e.g. Holland et al. 164). There is clearly a bias towards evaluating interventions aimed at children who have been sexually abused or exposed to domestic violence, and less evidence about the usefulness of psychoeducational interventions to other groups of maltreated children.
Quality of the evidence
The seven151–157 trials of psychoeducation are generally of very poor quality, particularly in relation to detection bias and attrition bias (where only the study by Overbeek et al. 153 was judged low risk of bias), and the quality of the quasi-experiments and COSs is variable. All in all, although the trends generally favour psychoeducation, there is a need for well-designed studies of psychoeducational interventions that are carefully designed in respect of their theories of change, carefully implemented, rigorously evaluated against agreed outcomes and outcome measures, and fully reported.
Economic evidence
One614 economic study, carried out in the UK, evaluated a group-based psychoeducation intervention for girls who had been sexually abused. The study614 used data from the Trowell et al. 155 RCT, described above, and compared the psychoeducation intervention (n = 36) to individual psychotherapy (n = 35) for girls aged between 6 and 14 years.
Although described by the authors as a cost-effectiveness study,614 the economic evaluation should more accurately be classified as cost–consequences analyses, presenting costs and a range of disease-specific outcome measures separately. The study614 was carried out after the end of the Trowell et al. 155 clinical trial, which precluded the prospective collection of resource-use data. As a result, the study614 was limited to a narrow economic perspective, including only the two interventions that were costed using nationally applicable unit costs and expressed in 1998–9 pounds sterling (£). No discounting was applied, despite a 2-year time horizon. Outcomes measured included psychiatric symptoms, global functioning, measures of PTSD and the experiences of carers.
Outcomes between the two groups were similar for the range of measures of effectiveness and costs were significantly higher for IT than the psychoeducation group therapy. The authors conclude that, with similar outcomes and higher costs, IT is less cost-effective than group therapy. However, they note that the logistics of setting up groups may mean children having to wait until there are sufficient numbers of a similar age before a group can start, resulting in a trade-off between potential savings to be gained from a group format and potential delays to treatment start for traumatised children. In addition, the study614 was limited in a number of important ways, including the narrow perspective, the lack of a TAU option or other control group, and the failure to formally combine costs and effects or explore uncertainty.
Group work with children
Five169–173 studies assessed the effectiveness of therapies that used the group format as an important therapeutic mechanism of change, but which are not described as psychoeducational.
Description of studies
Location of studies
Only one169 study took place in the UK. Of the COSs, two studies170,171 took place in Canada and two172,173 in the USA.
Sample sizes
All studies had small samples sizes. The COSs170,171 had sample sizes at baseline, ranging from a total of 12 participants171 to 70 participants. 170 Monck et al. 169 included 47 participants.
Participants
Age
Verleur et al. 173 focused on teenagers with an age range of 13–17 years. The other studies focused on younger age groups, with ages ranging from 4 to 13 years. 169–172
Maltreatment
All five169–173 studies recruited children and young people who had been sexually abused. De Luca et al. 170 and McGain and McKinzey172 recruited only girls; Grayston and De Luca171 recruited only boys and Monck et al. 169 recruited both boys and girls, although the sample included mainly girls (85%).
Interventions and comparisons
In the De Luca et al. 170 study, participants in the intervention (sexually abused girls) were compared with girls with no known history of sexual abuse. Control group participants in the remaining studies received either TAU, or were placed on a wait-list control.
In four170–173 studies, the intervention was described as ‘group therapy’. Verleur et al. 173 assessed the impact of group-based sexual education combined with group psychotherapy (no further information) led by same-sex (female) therapists. McGain and McKinzey172 set out the goals of the group-based programme, but do not detail the nature of the therapy/group process, other than to observe that it was ‘similar to hundreds of treatment programs provided to children who have been sexually abused’172 (p. 1168) and to differentiate it from other treatment programmes, such as those that are more behaviourally orientated, brief therapy programmes and crisis intervention programmes. The group intervention for boys in the study by Grayston and De Luca171 was run by therapists of both genders, supervised by a registered clinical psychologist. Sessions were said to follow ‘a consistent four-part format’ (described by De Luca and her associates717). Behaviour management techniques were used throughout to reduce disruptive behaviour and increase acceptable conduct. At the midpoint, the therapists also implemented a fixed-interval reinforcement schedule to further manage behaviour (described by Hack et al. 535).
Monck et al. 169 assessed the effectiveness of a family network treatment programme with or without group treatment.
Number and duration of sessions
Sessions in Grayston et al. 171 and De Luca et al. 170 were 90 minutes in duration, and were provided for 12 weeks171 and between 9 and 12 weeks. 170
The group work programme evaluated by McGain and McKinzey172 continued weekly for 6 months, with the possibility for children to continue on to another cycle. Some children are reported to have spent between 9 months to 1 year in treatment.
The number of sessions ranged considerably, from 9–12 weekly sessions170,171 to 6–9 months of weekly sessions. 172,173
No information was available on the structure of group work in Monck et al. 169
Outcomes: group work with children
These studies169–173 had few outcomes in common, and, those that did, used different measures.
Anxiety
Anxiety was assessed in De Luca et al. ,170 using the RCMAS/What I Think and Feel Questionnaire. 293
Behaviour
Problem behaviours were assessed by three170–172 studies. De Luca et al. 170 and Grayston and De Luca171 both used the CBCL,257 McGain and McKinzey172 used the Revised Behavior Problem Checklist438 and the ECBI. 439
Risk of bias: randomised controlled trials of group work for children
A graphic summary of the risk of bias of the one group work trial is provided in Figures 35 and 36, Appendix 10.
Sequence generation and allocation concealment
Monck et al. 169 stated that ‘allocation was made without the direct involvement of the researchers or the clinical team, and was achieved by blind choice of marked cards drawn from an envelope’169 (p. 12). Judgements of low risk of bias were made for both sequence generation and allocation concealment.
Blinding of participants, personnel and outcome assessors
This study169 did not make any reference to procedures to blind the participants or outcomes assessors. However, because of the nature of the intervention, it is unlikely to have been feasible to blind participants. The use of self-report and parent-reported measures also indicates that it was not possible to blind outcome assessors, suggesting this study169 had a high risk of bias.
Incomplete outcome data
This study169 analysed only the available data of 47 participants. However, there was insufficient information provided in the study169 regarding how many participants were originally assigned to each group. Therefore, this study169 was judged to be of unclear risk of bias.
Selective outcome reporting
There appears to be no evidence that other outcomes were planned and then omitted from the results, but, in the absence of prospective registration, we judged this aspect to be of ‘unclear’ risk of bias.
Other sorces of bias
No other identical sources of bias were identified in these studies.
Summary details of the risk-of-bias assessments of these trials can be found in Appendix 10.
Quality assessment of quasi-experimental and controlled observational studies of group work for children
The quality of the COSs was low. All five169–173 studies provided a clear description of the objectives and outcomes in their studies, with the exception of De Luca et al. ,170 who did not clearly describe their outcomes. Only two171,172 studies provided clear descriptions of the characteristics of the patients included in the study,171,172 and only Grayston and De Luca171 provided a clear description of the intervention. Neither Grayston and De Luca171 nor De Luca et al. 170 clearly described their main findings. No study adequately addressed potential adverse effects, nor did they report probability values for the main outcomes. Only one study172 provided information on recruitment of participants, the characteristics of patients lost to follow-up, and the representativeness of the staff (satisfactory). Determinations of the representativeness of others studies were not possible as a result of inadequate information. Blinding of participants and outcome assessors was not attempted in any of the studies.
Results: group work for children
No meta-analyses were possible for these interventions. There was only one randomised trial169 and a very heterogeneous group of COSs.
Depression
Monck et al. 169 found no significant difference in depression between children participating in the family network treatment programme with group treatment and those participating in the family network treatment programme alone.
Anxiety
In the only study to assess anxiety, De Luca et al. 170 found that, although anxiety scores for both intervention group (sexually abused) and the comparison group (no sexual abuse) decreased following the intervention, there was no significant difference between the two groups. The authors note that anxiety scores for both groups were low at baseline.
Self-esteem
The results of analyses in De Luca et al. 170 indicated a statistically significant impact of group treatment for self-esteem for those girls who completed therapy. Monck et al. 169 found no difference in measures of self-esteem following the intervention tested in the RCT.
Behavioural problems
Two170,172 of the three169,170,172 studies that examined the impact of group therapy on problem behaviour reported post-treatment improvement. Only in De Luca et al. 170 were participants followed up for 1 year. In this study,170 parents reported sustained improvements in internalising and externalising behaviour problems at 9–12 months’ follow-up, although this reached statistical significance only for internalising behaviours. However, data were not collected on the behaviour of those in the comparison group.
Grayson and De Luca171 also found larger changes in pre–post treatment scores for problem behaviours among children in the intervention group, but the between-group differences were not statistically significant.
Sexual behaviour
Only Grayston and De Luca171 examined the impact of group therapy on sexual behaviour, finding that, although sexualised behaviour tended to decline following treatment, the changes – as measured by the Child Sexual Abuse Inventory – were not statistically different between treatment and control children. Verleur et al. 173 reported that children in the experimental group improve significantly compared with the control group with regards to the measure of sexual awareness used in the study.
Self-esteem
One173 study assessed participants’ self-esteem following the intervention and found that, although the self-esteem for both intervention and control groups increased, there was a larger increase in the treatment group than the control group.
Effectiveness of group work interventions for maltreated children
Summary
We identified just five169–173 studies of group work (all with sexually abused children), of which only one169 study was a randomised trial. The trial169 found no evidence of the effectiveness of adding a group work component to a family network treatment in terms of reducing depression or improving children’s self-esteem. For the other studies, the limited information provided about the interventions, combined with heterogeneity in outcomes assessed and measures used, make it impossible to draw conclusions about the effectiveness of therapeutic group work for sexually abused children.
Completeness and applicability
The trial169 was conducted in the UK. The remaining four170–173 studies were conducted in North America. All focused on children who have been sexually abused. As indicated above, the studies provide little information that would allow these interventions to be replicated or to explore possible reasons for differences in reported effects.
Quality of the evidence
The trial conducted by Monck et al. 169 ‘scored’ well in terms of risk of bias, and was one of the few studies that reported an adequate sequence generation and concealment of allocation. The COSs were judged to be overall of poor quality.
Economic evidence
No economic evaluations of group work with children who have been maltreated were located.
Psychotherapy/counselling
In this section, we review those studies that either stated that they were studies of psychotherapy or counselling per se, or that described an eclectic RBI. We deal with these together simply because it was not possible clearly to differentiate between the included studies in relation to the content of the therapies assessed.
Four155,174,178,179 studies assessed the effectiveness of psychotherapy without clearly describing their theoretical underpinnings. One178 study explored the value added of group psychotherapy when added to individual psychotherapy. One155 study is also described in the section on psychoeducation. The other two studies of interventions described as psychotherapy are those of Sullivan179 and Thun et al. 174
We identified four175–177,180 studies that assessed the effectiveness of counselling interventions. Two assessed, respectively, the effectiveness of specific techniques for children in foster care, life story work175 and a mindfulness-based intervention. 176 The other two studies are those of Cadol et al. 177 and Downing et al. 180
Description of studies
Study design
Four studies were randomised trials. 155,174–176 Cadol et al. 177 was a QEx study.
The Downing et al. ,180 Sullivan179 and Nolan et al. 178 studies were COSs.
Location
Nolan et al. 178 was conducted in Ireland, and Trowell et al. 155 in the UK. The other six studies174–177,179,180 were conducted in North America.
Sample sizes
Of the four trials, two were very small. Haight et al. 175 was a feasibility study, with a small sample of just 23 randomised participants (15 completers). Thun et al. 174 recruited 13 participants, but only 11 participants completed the intervention and follow-up assessments. Reddy et al. 176 and Trowell et al. 155 randomised 71 and 75 participants, respectively.
Cadol et al. 177 recruited 140 participants and Sullivan179 recruited 72 participants. The remaining COSs were very small. Downing et al. 180 had a sample size of 22 participants and Nolan et al. 178 had a sample of 38 participants.
Participants
Age
Nolan et al. 178 recruited children aged between 6 and 17 years old, and Trowell et al. 155 recruited children aged 6–14 years. Thun et al. 174 focused on teenage girls aged 16–18 years. Participants were aged 7–14 years in the study by Haight et al. ,175 and 13–17 years in the Reddy et al. 176 study. Downing et al. 180 focused on children aged 6–12 years, and Cadol et al. 177 focused on a slightly older population, with a mean age of 17.2 years. In the study by Sullivan179 participants were deaf children, aged 12–16 years, living in a residential school, who had been sexually abused by either dormitory staff or older pupils. This was the only CS179 that focused on disabled children.
Gender
The majority of children in the Nolan et al. 178 study were female (92%). There were more males than females in Cadol et al. 177 (69 males, 37 females). In the studies by Downing et al. ,180 Haight et al. 175 and Reddy et al. 176 the samples were more evenly split, with girls being in the majority in Downing et al. 180 and Reddy et al. 176 and boys being in the majority in the Haight et al. 175 study (nine, and six completers). All participants in the Trowell et al. 155 study were girls.
Referral
Participants in the study by Nolan et al. 178 were referred from eight urban and rural services for sexually abused children and adolescents. Those in the study by Trowell et al. 155 were recruited from the authors’ own clinics and from professionals’ agencies in the community.
Haight et al. 175 recruited children from Department of Children and Family Services caseworkers. Case managers approached eligible young people in foster care to invite them to participate in the study conducted by Reddy et al. 176 Participants in Cadol et al. 177 and Downing et al. 180 studies were recruited from hospitals and private practitioners. Teenagers in the Thun et al. 174 study were referred by the staff of the military-based programme to which they had signed up to assist them in getting their Graduate Equivalency Degree (having previously dropped out of school).
Maltreatment
Children in the Haight et al. 175 study were in foster care and came from families in which they had experienced multiple forms of abuse, and whose parents misused methamphetamine. In Cadol et al. ,177 the children had experienced both physical abuse and neglect. Downing et al. 180 recruited children who had experienced sexual abuse. Reddy et al. 176 provides no detailed information on maltreatment histories.
Participants in the studies by Trowell et al. ,155 Thun et al. ,174 Sullivan179 and Nolan et al. 178 had all been subjected to sexual abuse.
Interventions and comparisons
Nolan et al. 178 compared the effectiveness of IT with combined individual and group therapy (IGT). The purpose of these two interventions was to treat the ‘psychological sequelae of child sexual abuse’. Both interventions drew on the principles of a broad range of individual and group therapies (psychodynamic, client centred, CBT, etc.) and implementation varied between therapies and across clients. All therapists sought to provide their clients with a supportive therapeutic relationship that would enable them to process the psychological consequences of sexual abuse, and help them to develop the insights and skills needed to prevent further abuse. Those receiving group therapy also had the opportunity to realise that they were not alone in experiencing CSA, to enjoy peer support, and to benefit from peer-to-peer feedback on their experiences and their behaviour. On average, the duration of intervention ranged from 18 to 20 hours. This was the only intervention received by participants in the comparison group (those in the intervention group also received group psychotherapy).
Sullivan179 compared group psychotherapy developed at the Boys Town National Research Hospital with individual psychotherapy for survivors of abuse. After listing treatment goals, the reader is referred to an earlier paper for further information. 718 Children in the Sullivan179 study met weekly with their therapist for 2 hours (because of the communication problems and need for signing) for 36 weeks. Control group participants received no treatment.
Thun et al. 174 state that the group curriculum ‘followed a modified multidimensional model proposed by Lindon and Nourse (1994544) that incorporated a skills component, a psychotherapeutic component and an educative component’174 (p. 8) and, arguably, this study174 might, with additional information, have been included in the psychoeducational or group treatment grouping. In describing the intervention, Thun et al. 174 emphasise the benefits of groups as a means of alleviating feelings of isolation and alienation, and fostering trust. Those in the comparison group had the option to avail of individual counselling, but none did.
The intervention used by Haight et al. 175 was ‘Life Story Intervention’ (LSI), described by the study authors as a narrative and relationship-based mental health intervention. LSI was delivered in and around the children’s homes, on a one-to-one basis, by a range of professionals, including teachers, child welfare professionals and counsellors. The intervention was delivered over the course of a series of weekly 1-hour sessions for approximately 7 months. Control group participants were placed on a wait-list and received the intervention at the conclusion of the study.
Reddy et al. 176 assessed the impact of Cognitively-Based Compassion Training (CBCT), described by the authors as a type of contemplative practice that is built on mindfulness practice and teaches active contemplation of loving kindness, empathy and compassion towards loved ones, strangers and enemies. 719 It uses a variety of cognitive restructuring and asset-generating practices, with the long-term goal of developing the equanimity of mind that fosters acceptance and understanding of others. Participants were assigned to classes that met twice a week, for 1 hour, for 6 weeks. The control group was a wait-list control.
The interventions used in studies by Cadol et al. 177 and Downing et al. 180 were described as one-to-one counselling. No information was provided on the duration or number of counselling sessions, other than Downing et al. 180 stating that sessions took place ‘near-weekly for approximately 1 year’. In Cadol et al. 177 children in all arms received developmental testing, regular medical care and co-ordination of services, but only those in the experimental arm received the counselling. Participants in the control group in the Downing et al. 180 study received reinforcement treatment (helping parents to focus on positive behaviour).
Trowell et al. 155 compared brief, focused, individual psychoanalytic psychotherapy with group psychotherapy (comprising both psychotherapeutic and psychoeducational components).
Outcomes: psychotherapy/counselling
Post-traumatic stress disorder
Trowell et al. 155 used the 1982 version of Orvaschel’s PTSD scale – an extension of the KSADS instruments. 406 Reddy et al. 176 used the Childhood Trauma Questionnaire (CTQ448).
Trauma symptoms in Nolan et al. 178 were assessed using the TSCC. 260 Specific subscales used included anxiety, depression, anger, post-traumatic stress, dissociation, overt dissociation, fantasy dissociation, sexual concerns, sexual preoccupation and sexual distress.
Depression, anxiety, emotional disorder and conduct disorder
Trowell et al. 155 used a shortened version of the KSADS. 268 Reddy et al. 176 used the Quick Inventory of Depressive Symptomatology–Self-Report442 to assess depression. Reddy et al. 176 also assessed non-suicidal self- injurious behaviour using the Functional Assessment of Self-Mutilation (FASM443).
Nolan et al. 178 assessed depression using the CDI. 258 Specific subscales used included negative mood, interpersonal difficulties, ineffectiveness, anhedonia and negative self-esteem.
Child behaviour
Nolan et al. 178 and Sullivan179 both assessed problem behaviours using the CBCL. 294,418;720 Specific subscales used in Nolan et al. 178 included total problems, externalising, internalising, withdrawn, somatic complaints, anxious/depressed, social problems, thought problems, attention problems, delinquent behaviour and aggressive behaviour.
Cadol et al. 177 assessed cognitive, physical, social, and emotional functioning of their participants using a range of measures, including the Bayley’s Scales of Infant Development,449 Bayley Infant Behavior Record451 and Child Behavioral Characteristics Questionnaire.
Downing et al. 180 used parents’ and teachers’ behavioural observations to record sleep disturbance, sexual play with other children, enuresis, general misbehaviour and sexual self-stimulation.
Emotional self-regulation
Reddy et al. 176 used the Difficulties with Emotion Regulation Scale (DERS446) to assess participants’ awareness and understanding of emotional experience, acceptance of emotions, ability to modulate emotional arousal and effective action in the presence of intense emotions.
Self-efficacy
Reddy et al. 176 used the Children’s Hope Scale445 to assess agency and pathways (belief in one’s ability to develop successful call planning).
Self-esteem
Thun et al. 174 assessed participants’ self-image using four subscales (see Results: psychotherapy/counselling) of the Offer Self-Image Questionnaire-Revised (OSIQ-R440), a personality test designed to measure self-image of adolescents aged 13–18 years.
Risk of bias: randomised controlled trials of psychotherapy/counselling
Figures 37 and 38, Appendix 10, present an overview of the risk of bias of RCTs of psychotherapy and counselling.
Sequence generation and allocation concealment
Thun et al. 174 stated that participants were ‘randomly assigned’ but gave no other information and Trowell et al. 155 simply said participants were randomised. Both studies were therefore assessed as ‘unclear’ for each domain.
Both Reddy et al. 176 and Haight et al. 175 were assessed as ‘unclear’ risk of bias for each of these domains. Although Reddy et al. 176 state that the study used block randomisation to equalise numbers in each group, no information was provided that shed light on the sequence generation or allocation concealment.
Blinding of participants and personnel
Owing to the nature of the intervention, neither staff nor participants were likely to have been ‘blinded’ in the study by Thun et al. ,174 and the study was therefore assessed as high risk of bias. In Trowell et al. ,155 the authors state it was not possible to blind participants. Haight et al. 175 stated that caregivers were not blind whether or not the child was receiving the intervention, and it would not have been possible to blind the children. Both studies were155,174 were therefore assessed as high risk of bias. The same judgement was made for Reddy et al. 176
Blinding of outcome assessors
Assessors in Thun et al. 174 were a faculty member and selected graduate students from a Marriage and Family Therapy programme at the University of Southern Mississippi but it is not clear whether or not they were blind to experimental conditions. This item was therefore assessed as unclear.
Reddy et al. 176 provide no information on the blinding of outcome assessors. Haight et al. 175 state that assessments were conducted by master’s level professionals who were not serving as the child’s community clinician, but it is not clear that they were unaware of the allocation status of the children. Both were therefore assessed as ‘unclear’.
Trowell et al. 155 state that blinding of assessors was probably compromised because the children and their mother often mentioned the specific therapy during assesment, so was judged high risk of bias.
Incomplete outcome data
Thun et al. 174 analysed only the available data, as two of the six participants randomised to the treatment arm dropped out. Haight et al. 175 suffered significant attrition and analysed only the available data. Both studies174,175 were therefore judged as high risk of bias for incomplete outcome reporting.
No information is provided by Reddy et al. 176 other than that caregivers in the wait-list control did not complete, post-treatment, the Inventory of Callous and Unemotional Traits-Parent Report (ICU-P447) – one out of six measures of children’s psychosocial functioning. This was therefore assessed as unclear risk of bias.
Trowell et al. 155 was judged low risk of bias on these grounds.
Selective outcome reporting
There appears to be no evidence that other outcomes were planned and then omitted from the results from any of these four174–176 trials. However, in the absence of a published protocol or trial registration, we have judged all four to be of ‘unclear’ risk of bias.
Other sources of bias
No other potential sources of bias were identified in these studies.
Summary details of the risk-of-bias assessments of these trials can be found in Appendix 10.
Risk of bias: controlled observational studies of psychotherapy/counselling
Nolan et al. 178 provided a clear description of the objectives, participants, intervention and outcomes in the study, and addressed potential confounders in their research. The study178 provided a good description of the characteristics of patients who were lost to follow-up. Statistical tests used were appropriate; however, actual probability values for the main outcomes were not reported.
Cadol et al. 177 and Downing et al. 180 provided a clear description of the objectives and participants in their studies, but only Downing et al. 180 provided a clear description of the outcomes. Only Cadol et al. 177 at least partially addressed potential confounders in their research. Although both of these studies177,180 provided a clear description of their findings, only Cadol et al. 177 addressed the potential adverse effect of repeat abuse. Neither study described the characteristics of patients lost to follow-up; only Cadol et al. 177 reported probability values for the main outcomes. It was not possible to determine whether or not the participants were asked to participate, or whether those that did, and the staff members involved in the study, were representative of the entire population from which they were recruited. Blinding of participants and of outcome assessors did not appear to be attempted by either study.
Sullivan179 failed to provide a clear description of the objectives, outcomes and participants in the study. The study179 did describe the characteristics of patients lost to follow-up, and reported actual probability values for the main outcome, and at least partially addressed potential confounders, but did not address potential adverse effects. It was not possible to determine whether or not participants had been asked to participate, or, whether they, or the staff involved in the study, were representative of the population from which they were recruited.
Results: psychotherapy/counselling
It was not possible to conduct a meta-analysis for any of the outcomes. We provide a short summary of the findings of each study, given their heterogeneity, their small samples, risk of bias and limited coverage of outcomes of interest.
Post-traumatic stress disorder
In Trowell et al. ,155 univariate analyses failed to identify a difference between those receiving group and those receiving IT on the PTSD dimension of ‘persistent symptoms of increased arousal’ used in the study405 (data not provided, but the authors, following Cohen et al. ,716 used an effect size of 0.5 as a threshold of moderate effect). No further analyses relating to this indicator of PTSD were undertaken.
Controlling for the impairment score on the KGAS405 in a multivariate analysis, the authors report a significant effect of IT for ‘the re-experiencing of trauma’ dimension of PTSD (baseline to 1- and 2-year follow up, and baseline to exit), and – for the ‘persistence/avoidance of stimuli’ dimension – at baseline to first-year follow-up. When KGAS is replaced by the baseline score on the same dimensions, the significance of the effects is attenuated.
For trauma symptoms, assessed by Nolan et al. 178 using the TSCC,325 the only scores to improve were depression (p < 0.05) and anger (p < 0.01), and these improved for participants in both treatments, with no significant difference between the groups. No changes were detected for anxiety, post-traumatic symptoms, dissociation, overt dissociation, dissociation–fantasy, sexual concerns, sexual preoccupation and sexual distress.
Depression
In Nolan et al. ,178 total depression score (p < 0.01), interpersonal problems (p < 0.05) and anhedonia (p < 0.01) all improved for both interventions, but there was no significant difference between groups. ‘Ineffectiveness’ was improved only in the combined IGT group (p < 0.01). Between-group difference in Trowell et al. 155 failed to reach the threshold size of 0.5 adopted by the authors (KGAS).
Behavioural problems
Results in the study by Haight et al. 175 indicate a significant group (experimental or control) by time (pre- or post-test) interaction on child externalising behaviour (p < 0.05), but no main effects. Results indicated that although experimental group externalising scores decreased, control group externalising increased over time. There were no other significant group or time effects for internalising behaviour scores or total problem scores.
Sullivan179 concluded that participants in the intervention group of this COS had significantly fewer behaviour problems than children not receiving individual psychotherapy. For boys, the treatment main effect was statistically significant for 10 of the 12 dependent variables assessed (total CBL; external and internal composite scales; nine CBL subscale scores). For girls, the main effect was significant for 5 of the 11 relevant variables (total CBL; external and internal composite scales; eight subscale scores). The numbers were very small, particularly for girls, and the authors point to a non-significant main effect for girls for the remaining variables.
Nolan et al. 178 reported that total CBCL scores were reduced for both of the interventions (p < 0.01). In addition, internalising (p < 0.01) and externalising scores (p < 0.05) were also significantly improved by both interventions. CBCL subscales: withdrawn, somatic complaints, anxious/depressed, social problems, attention problems and aggressive behaviour all improved with both interventions (p < 0.01). There was no significant difference between groups. Delinquent behaviour and thought problems remained unchanged. Results from the YSR indicated that there was no significant time or group effect on any YSR scales, indicating that there was no impact of therapy on any of the YSR scales.
Downing et al. 180 reported that for the children in the counselling intervention group, parents reported a decrease in sleep disturbance, sexual play with other children, enuresis and general misbehaviour. However, there was no evident decrease in sexual self-stimulation.
Six weeks after the end of treatment, Reddy et al. 176 found no differences on any measure of psychosocial functioning following CBCT, although the authors suggest that practice frequency was associated with increased hopefulness and trend for decrease in generalised anxiety.
Self-image
Thun et al. 174 found no significant differences between the two groups on the four subscales of the OSIQ-R (Offer et al. 440) used to measure self-image: impulse control, self-confidence, self-reliance and body image. Negative self-esteem remained unchanged in Nolan et al. 178 (as assessed by the CDI).
For Cadol et al. 177 results of comparisons of the three experimental groups and control indicate significant differences between the groups in the cognitive, physical, social and emotional areas. However, results also indicated that treatment techniques tested do not significantly affect the developmental performance of the participants.
Effectiveness of psychotherapy/counselling for maltreated children
Summary
A relatively small body of evidence was found pertaining to the effectiveness of psychotherapy/counselling interventions. Four155,174–176 studies were randomised trials, one177 study was a QEx study and three178–180 studies were COSs.
Five155,174,178,180,186 of the eight included studies recruited children who had been sexually abused. The remaining three studies recruited children who had experienced a variety of forms of maltreatment. The interventions were disparate, ranging from life story work with children in foster care, to cognitive-based compassion training – intervention built on mindfulness practice and cognitive restructuring.
Most studies compared psychotherapy with supportive counselling or no treatment, including wait-list controls. Nolan et al. 178 compared the effectiveness of IT with combined IGT, and Trowell et al. 155 compared individual psychotherapy with a group therapy that combined psychotherapuetic and psychoeducational components.
One study176 examined six outcome domains to assess the impact of compassion training, only one of which (depression) was examined in another study,178 which used a different measure. Four177–180 studies examined child behaviour as an outcome, but again all used different measures and had very different samples. It is therefore not possible, meaningfully, to draw any overall conclusions about the effectiveness of psychotherapy for maltreated children.
Completeness and applicability
All but Nolan et al. 178 and Trowell et al. 155 were conducted in the USA. Nolan et al. 178 was conducted in Ireland and Trowell et al. 155 in the UK. Most of the interventions described have residents with therapies available in the UK, for example one-to-one counselling,177,180 the therapies provided in Nolan et al. 178 for sexually abused girls and the LSI described by Haight et al. 175 Given the dominance of counselling and current recommendations to increase access to counselling for troubled children, the dearth of evidence to support the effectiveness of psychotherapy or counselling for maltreated children is of concern.
Quality of the evidence
Four174,175,178,180 of the studies, including two174,175 of the three trials, were extremely small. The trials were poorly reported, with low risk of judgements made only in relation to selective outcome reporting (and this is probably generous). The overall quality of the non-randomised studies was judged to be poor.
Economic evidence
No economic evaluations of psychotherapy/counselling for children who have been maltreated were located.
Peer mentoring
We identified two181,182 studies that assessed the effectiveness of peer-mentoring interventions.
Description of studies
Sample sizes
Both181,182 studies had baseline sample sizes of just 36 and 46 participants, respectively.
Participants
Maltreatment
Children in both studies had experienced both physical abuse and neglect.
Interventions and comparisons
The intervention used in both studies181,182 was resilient peer treatment (RPT), designed to promote the development of social competencies of preschool children in the context of classroom play mediated by a resourceful peer.
In Fantuzzo 1988181 the control group pairs met in the same setting as the treatment group pairs for the same number of play sessions under identical conditions, except that their peer was instructed to respond positively to social initiations but to refrain from initiating social interactions. In Fantuzzo 1996,182 control group participants were paired with a classmate of average interactive play ability.
Number and duration of sessions
In both181,182 studies, sessions lasted 15 minutes each, and were spread out over a 2-month period, with no more than three sessions occurring per week.
Outcomes
Interactive peer play was assessed by Fantuzzo 1996182 using an observational coding system.
Social skills were assessed in the Fantuzzo 1996182 study, using the Social Skills Rating System (SSRS). 379
Problem behaviours were also assessed in Fantuzzo 1996182 using the SSRS. 379
Positive social behaviours were assessed by Fantuzzo 1988181 through the use of the same observational coding system, the SSRS. 379
Psychological adjustment was assessed by Fantuzzo 1988181 using the Preschool Behavior Questionnaire. 455
Pre-academic progress was assessed in Fantuzzo et al. 181 using the Brigance Diagnostic Inventory of Early Development. 456
Risk of bias: randomised controlled trials of peer-mentoring interventions
The risk of bias across the two181,182 included trials of peer mentoring is summarised in Figures 39 and 40 in Appendix 10.
Sequence generation and allocation concealment
Both trials181,182 stated their participants were ‘randomly assigned’, but gave no other information on the method of random allocation and allocation concealment. Both were judged ‘unclear’ risk of bias for each of these domains.
Blinding of participants and personnel
One181 study made no reference to procedures to blind participants or personnel, but the other study182 stated that ‘teachers, play supporters and data collectors were not informed of the maltreatment status of the participants throughout the study’182 (p. 1284). Fantuzzo et al. 182 was therefore judged to be of low risk of bias. The other181 study was assessed as being of unclear risk of bias.
Blinding of outcome assessors
Both181,182 studies stated that children were observed by trained raters who were blind to both the assignment of children to conditions and the specific hypotheses of the study, resulting in judgements of low risk of bias.
Incomplete outcome data
Both181,182 studies were assessed being of low risk of bias, as both were able to minimise potential attrition bias by analysing participants based on ‘assigned treatment’ rather than ‘treatment completed’.
Selective outcome reporting
Both181,182 studies differed in their choice of outcomes, and there appears to be no evidence that other outcomes were planned and then omitted from the results. However, in the absence of a published protocol or trial registration, we categorised these studies181,182 as ‘unclear’ risk of bias.
Other sources of bias
No other potential sources of bias were identified in these studies.
Summary details of the risk-of-bias assessments of these trials can be found in Appendix 10.
Results: peer-mentoring interventions
It was not possible to conduct a meta-analysis for any of the outcomes.
Interactive peer play
Children assigned to the RPT intervention showed significantly higher levels of interactive play and significantly less solitary play post test than the children in the control condition. No significant group differences were found for the social attention and non-play categories by Fantuzzo 1996. 182
Social skills
Children in the RPT group scored significantly higher than those in the control group on the Self-Control subscale and the Interpersonal Skills subscale. However, no significant group differences were found on the Verbal Assertion subscale (Fantuzzo 1996182).
In Fantuzzo 1988,181 results indicated that children in the peer-mentoring group demonstrated significantly increased levels of positive social interaction, whereas levels of social interaction remained the same for the control group.
Problem behaviours
Children who received the RPT intervention displayed significantly lower levels of both internalising and externalising behaviour problems (Fantuzzo 1996182).
In Fantuzzo 1988,181 results indicated that, post test, the children in the peer group demonstrated either a similar, or a decreased, level of problematic behaviours, whereas control groups seemed to demonstrate an increase in problematic behaviour.
Preacademic progress
Results indicated that there was no significant group effect for pre-academic progress (Fantuzzo 1988181).
Effectiveness of peer mentoring for maltreated children
Summary
The two studies of peer mentoring identified in our search were both randomised trials, were both conducted in the USA by the same researcher. The results provide evidence of a range of benefits of peer mentoring for maltreated children, although both studies were small and the follow-up periods were short.
Completeness and applicability
Evidently this evidence base is limited, but it represents the only rigorous evaluation of therapeutic day care programmes aimed at addressing the needs of neglected of physically abused children. This could be of relevance to the UK, where there is an increasing move to intervene with children in the school setting.
Quality of the evidence
Compared with most of the included trials, the quality of these peer-mentoring studies is moderately good.
Economic evidence
No economic evaluations of peer-mentoring for children who have been maltreated were located.
Intensive service models
Covered in this section are a number of interventions designed to help children in substitute care or children in specialist day-care settings. They fall into three broad categories:
-
co-ordinated care. 198
In this context, treatment foster care is used to describe a number of intensive interventions targeted at children in foster care, rather than – as is sometimes done – as the name of an intervention. Because of the heterogeneity of these studies,145,183–198 we discuss each group of studies separately, beginning with treatment foster care.
Description of studies
Study design
Four of the controlled studies were randomised trials. 145,183–191 Fisher et al. 192 and Graham et al. 193 were COSs. Graham et al. 193 used a subsample recruited from the trial conducted by Fisher et al. 183–188 Biehal et al. 145 embedded a small randomised trial within a QEx case–control study.
Location
Five studies183–193 were conducted in the USA, whereas the study by Biehal et al. 145,146 was conducted in the UK.
Sample sizes
Three trials183–191 had moderate baseline sample sizes of 100, 117 and 156 participants, respectively. Sample sizes in the COSs were small, with just 30 participants in the Fisher et al. 192 study and 37 participants in the Graham et al. 193 study. Biehal et al. 145,146 randomised just 34 young people; a further 185 were included in the QEx sample. 145
Participants
Age
For the treatment foster care studies, the mean ages of participants in the RCTs were 5.94 years;183–188 11.54 years;189 and 10.46 years. 190,191 In the study by Biehal et al. ,145,146 the young people were aged 10–17 years (although the intended recruitment age range was 11–16 years).
The mean age of participants across the COSs was 2.35 years in the Fisher et al. 192 study and 6.11 years in the Graham et al. 193 study. In Taiissig et al. 190,191 the age range was 9–11 years.
Maltreatment
All studies145,183–193 focused on children who had experienced a combination of physical abuse, emotional abuse, sexual abuse and neglect.
Interventions and comparisons
Control group participants included those who had received RFC in four183–189,192,193 studies. In the studies by Biehal et al. 145,146 and Taussig et al. 190,191 they received services as usual.
Four145,146,183–188,193 studies were of MTFC. MTFC has been described as a community-based, multimodal ‘wraparound’ intervention for children and young people with challenging behaviour. It makes use of a ‘team approach’, by which foster parents (and, where applicable, biological parents/future carers) are trained to provide a therapeutic home environment for children. Foster parents received intensive preservice training and post placement they received support and supervision by means of daily telephone contacts, weekly home visits by foster parent consultant, a weekly support group and 24-hour on-call crisis intervention. Children received services from a behaviour specialist. When appropriate, the family therapist worked with the biological family to teach the same parenting skills used by programme foster parents in order to promote generalisation of treatment gains and facilitate reunification.
Three183–188,192,193 of the four MTFC studies used the Multidimensional Treatment Foster Care Program for Preschoolers (MTFC-P).
Smith et al. 189 evaluated the effectiveness of a manualised intervention targeting the prevention of behaviour problems for girls in foster care at the point of transition to middle school. In the summer prior to middle school entry, both foster parents and the girls they were caring for participated in separate six-session, group-based interventions, followed by ongoing training and support to foster carers and girls throughout the first year of middle school. The girls groups focused on ‘setting personal goals; establishing and maintaining positive relationships with peers and adults; effective decision-making and problem-solving strategies; developing support systems for reaching goals; and modelling, practising, and reinforcing adaptive behaviours’ (p. 271). Foster parents groups were focused on establishing and maintaining stability in the home, preparing the girls for school and preventing early adjustment problems during the transition. They were taught how to use a behavioural reinforcement system modelled after systems used in MTFC.
The intervention evaluated in the Taussig et al. 190 trial was called Fostering Healthy Futures (FHF), which the authors describe as a preventative mental health intervention, consisting of two components, specifically a manualised skills group and one-on-one mentoring.
Number and duration of sessions
In the Biehal et al. 145,146 study, the duration of an MTFC placement was intended to be around 9 months, prior to a young person’s return to his or her birth family or to an alternative placement. With one exception, young people in the study145,146 spent between 5 and 11 months in MTFC placements.
In the Taussig et al. 190,191 study the skills groups met for approximately 30 weeks for 1.5-hour weekly sessions. The mentoring component of Taussig et al. ’s190,191 FHF programme provided 30 weeks of one-on-one mentoring for each child. Mentors spent 2–4 hours of individual time each week with their mentees.
In the Fisher et al. 183–188 study, children are said usually to receive services for between 6 and 9 months. Information on number and duration of sessions is unavailable from Fisher et al. 192 (other than that reported above). No information on ‘dose’ was provided by Graham et al. 193
In the Smith et al. 189 study, the summer groups comprised six sessions across 3 weeks, followed by weekly 2-hour meetings (foster parent meeting; one-on-one session for girls) throughout the first year of middle school.
Outcomes: treatment foster care
Post-traumatic stress disorder
No study assessed the impact of the intervention on PTSD, but the primary outcome in Taussig et al. 190,191 was mental health functioning, measured using two scales from the TSCC,325 specifically the post-traumatic stress scale, and the dissociation scales (see Child behaviour, below).
A multi-informant index of mental health problems was also derived in this study, based on TSCC325 scores, the internalising scales of the CBCL269 and the Teacher Report Form (TRF269).
Salivary cortisol
Children’s salivary cortisol levels were used to assess hypothalamic–pituitary–adrenal axis activity in three183–188,192,193 of the four included studies.
Child behaviour
Smith et al. 189 assessed children’s internalising problems, externalising problems and prosocial behaviour using the Parent Daily Report Checklist. 458 Taussig et al. 190,191 used the Internalising scales of the CBCL269 – Youth Report and TRFs. Data were combined with TSCC325 scores to create a mental health index (see Results: treatment foster care).
As one of two primary outcomes in the RCT, Biehal et al. 145,146 used the standardised Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA382) as a measure of emotional and behavioural difficulties. It was selected because it enabled the synthesis of large quantities of data gathered from multiple informants and sources including a range of standardised measure (and which could accommodate variable completeness of information).
Biehal et al. 145,146 also used a range of standardised measures, including the CBCL,257 SDQ721 and DAWBA-AD.
One of the COSs192 assessed child behaviours problems using the Early Childhood Inventory (ECI462).
Attachment-related behaviour
Children’s attachment-related behaviour towards foster parents was assessed by Fisher et al. 183–188 using the PAD. 221
Biehal et al. 145,146 used the Development and Well-Being Assessment-Attachment Disorder (Minnis et al. , unpublished manuscript), consisting of 26 items about behaviours associated with the International Classification of Diseases-Tenth Edition diagnoses of attachment disorder.
Children’s social functioning
Participants’ coping skills were measured in Taussig et al. 190,191 using the Positive and Negative Coping scales of the CSI. 459 In this study,190,191 participants’ perceived self-competence was also measured using the social acceptance and global self-worth scales of the SPPC. 413,431
Biehal et al. 145,146 used the CGAS292 to assess children’s general adaptive functioning.
Permanency
Placement outcomes were assessed by three145,146,183–188,190,191 studies. Taussig et al. 190,191 recorded the number of placement changes over the 18-month study period of the study, whether or not a child had experienced a new placement in a residential treatment centre (RTC) during that time or had attained permanency by 1-year post intervention, plus the types of permanence attained (i.e. adoption or reunification with family). Fisher et al. 183–188 recorded the type of permanent placement, and success or failure of a subsequent permanent placement. Biehal et al. 145,146 recorded care placement type.
Quality of life
Taussig et al. 190,191 assessed children’s quality of life using the Life Satisfaction Survey. 402 Related to quality of life, the authors also recorded children’s recent and current use of mental health services and psychotropic medications (based on caregiver and self-report), and their levels of social support, using scores from The People in My Life-Short Form. 460
Other
Biehal et al. 145,146 also gathered data relating to children’s engagement in education and training, including type of provision received.
Cognitive control
Cognitive control and response monitoring was assessed by Fisher et al. 183–188 using a computerised flanker task, which includes red and green circles as stimuli and trial-by-trial performance feedback. 722 We include a brief description, taken from one of the papers, as this outcome measure is not commonplace. A small fixation point was displayed in the centre of a computer screen.
For each trial, a warning cue is presented for 200 ms before a horizontal row of five 1-in. circles, with the central circle directly above the fixation point, is shown for 700 ms. The task comprises congruent trials, which consist of five red circles or five green circles, and incongruent trials, which consist of a central red circle flanked by green circles or a central green circle flanked by red circles. A 30:70 ratio (congruent trials–incongruent trials) is used. Participants are required to respond within 1100 ms. Performance feedback, which consists of a 1-in. face, is then presented for 1050 ms; a smiling face indicates a correct response and a frowning face indicates an incorrect response. The intertrial interval varies in length from 0 to 500 ms. The 20-min task consists of three blocks of 60 trials each. In the current study, the STIM stimulus presentation system (James Long Company, Caroga Lake, NY) was used to control the task presentation and to record the behavioral and electrophysiological measures for each trial. The children sat approximately 24 in. from a 14 in. computer monitor and held a button box with a red pushbutton and a green pushbutton. Prior to beginning the task, color vision, color familiarity, and comprehension of task terminology were assessed. The children were instructed to press the button that corresponded with the color of the central circle regardless of the color of the flanking circles. They were told to respond quickly and correctly. The children completed eight practice trials to ensure task comprehension.
Reproduced with permission from Bruce et al. ,183 p. 5
Risk of bias: randomised trials of Treatment Foster Care models
Sequence generation
Smith et al. 189 stated that a coin flip was used, and for the randomised part of the Biehal et al. 145,146 study, the authors state that the randomisation sequence was generated by a computer-generated random numbers. Both were therefore assessed as ‘low risk of bias’. Fisher et al. 183–188 provide no information on sequence generation, and Taussig et al. 190,191 stated that all children were manually randomised, by cohort (five), but provided no further information. Both183–189 studies were therefore judged unclear risk of bias.
Allocation concealment
No study provided information on allocation concealment, and all were judged unclear risk of bias.
Blinding of participants and personnel
No study made any reference to procedures to blind the participants or personnel, and judgements of high risk of bias were allocated to each.
Blinding of outcome assessors
Smith et al. 189 and Fisher et al. 183–188 state that research staff and interviewers were blind to participants’ group assignment. Biehal et al. 145,146 describe the study as single blind, with outcome assessors blind to which arm data belonged (although the assessors were not those who provided/gathered the information). Taussig et al. 190,191 attempted to mask independent interviewers to condition but records that some children did spontaneously disclose treatment condition which could not be controlled for. All studies were judged low risk of bias.
Incomplete outcome data
Fisher et al. 183–188 was able to minimise potential attrition bias by making use of a full information maximum likelihood estimator in Mplus (Muthén & Muthén, Los Angeles, CA, USA) which allows for the inclusion of participants with partial data on dependent variables, and was judged to be of low risk of bias. Smith et al. 189 provided insufficient information regarding dropouts and missing data and was judged unclear risk of bias. Taussig et al. 190,191 undertook data analyses using ITT principles and the study was judged to be of low risk of bias. Biehal et al. 145,146 state that data from the RCT sample was analysed on ITT principles (subject to the availability of outcome data), with imputation for missing data. Although this study145,146 suffered from differential attrition (12 of the 34 young people randomised to MTFC did not receive it) the data sources meant that only one person was lost to follow-up. Overall, we judged this study to be of low risk of bias for incomplete outcome data.
Selective outcome reporting
Two trials were registered: Taussig et al. 190,191 (NCT00809315) and Fisher et al. 183–188 (NCT00701194). Both were judged to be of low risk of bias, as the authors report on all outcomes listed in the trial registration (although specific measures were not identified). In the absence of a published protocol, the studies by Biehal et al. ,145,146 and Smith et al. 189 were judged to be ‘unclear’.
Other sources of bias
A potential additional bias was noted in Fisher et al. ,183–188 in which randomisation occurred prior to recruitment into the study, and performance was not assessed prior to the intervention. Therefore, differences between the two groups may have existed prior to the intervention. No other potential sources of bias were identified in this studies.
Summary details of the risk-of-bias assessments of these trials can be found in Appendix 10.
Quality assessment of controlled observational studies of intensive service models
The quality of the two192,193 COSs was very similar. Both provided a clear description of the objectives of the study, the outcomes, the participants and the interventions. Both addressed potential confounders in their research, and both provided a clear description of their findings. Both studies reported actual probability values for the main outcomes.
However, neither study addressed potential adverse effects, nor described the characteristics of patients lost to follow-up.
It was not possible to determine whether or not participants were asked to participate, or whether or not those who did participate, and the staff members involved in the study were representative of the entire population from which they were recruited for any of the studies. Statistical tests used to assess the main outcomes appeared appropriate. Blinding of participants or outcome assessors was not attempted and it seems unlikely it would have been feasible owing to the psychosocial nature of the intervention.
Results: treatment foster care
There were no common outcomes recorded across any of the included RCTs. Therefore, it was not possible to conduct a meta-analysis for any of the outcomes.
Post-traumatic stress disorder
Post-traumatic stress disorder symptomatology was assessed only in the Taussig et al. 190,191 study, which reported no significant effect post intervention or 6 months’ follow-up. The study190,191 results indicate that intervention participants had significantly fewer dissociation symptoms than control group participants, as measured by the TSCC at the 6-month follow-up (p = 0.02).
Mental health
Taussig et al. 190,191 reported that intervention participants had significantly fewer mental health problems than control group participants at the 6-month follow-up (p = 0.003), as measured by the multi-informant index of mental health problems. There was no significant difference between intervention and control participants for recent or current use of psychotropic medications (post test or 6-month follow-up) but there was a significantly lower rate of recent mental health therapy usage at the 6-month follow-up for intervention participants (p = 0.04). Intervention participants also had significantly better quality of life at the end of the intervention (p = 0.006) but this difference failed to reach significance at 6 months (p = 0.38).
Children’s behaviour problems
Smith et al. 189 (RCT) indicated that the participants who were part of the MTFC intervention demonstrated significantly lower internalising problems (p < 0.01) and lower externalising problems (p < 0.01) at 6 months post baseline than the control participants. However, this study189 found that intervention participants did not have higher prosocial behaviour than the control participants (p > 0.05).
Fisher et al. 192 (RCT) found that participants who were part of the MTFC intervention demonstrated significantly improved behavioural adjustment scores (p < 0.05), as measured by the ECI.
Taussig et al. 190,191 reported no significant difference between intervention and control groups for Positive and Negative Coping skills, perceived self-competence, or social support at post test or 6-month follow-up.
In the study by Biehal et al. ,145,146 MTFC participants had slightly better outcomes at follow-up than UC, as measured by HoNOSCA (adjusted MD –1.04, 95% CI –6.21 to 4.13) but this was not statistically significant (p = 0.68).
Children’s attachment-related behaviour
Children’s attachment-related behaviour towards foster parents was assessed by Fisher et al. ,183–188 and indicated that children in the intervention condition made significant increases in secure attachment behaviour (p < 0.05) and significant decreases in avoidant behaviour (p < 0.05) compared with children in the RFC condition. However, treatment was not associated with changes in resistant behaviour. No between-group differences were found in the Biehal et al. 145,146 study.
Salivary cortisol
Children’s salivary cortisol levels were taken by three of the included studies. 183–188,192,193 Although the results of these studies indicated some improvement over time, including daytime patterns, which showed the salivary cortisol levels of the intervention group becoming closer to the community comparison group of non-maltreated children,192 and a distinct pattern of change in cortisol slope across the days,189 none of these results reached statistical significance. Moreover, Fisher et al. 183–188 indicated that control group participants showed significantly greater morning-to-evening cortisol level decreases following placement changes than the experimental group (p < 0.05), a negative outcome.
Permanent placement outcomes
Permanent placement outcomes were assessed by the studies of Fisher et al. 183–188 and Taussig et al. 190,191 In Fisher et al. ,183–188 participants in both groups entered permanent placements at approximately equal rates, but the number of placement failures between the two groups was significantly different, with 10% (n = 3) failing in the intervention group compared with 36% (n = 9) in RFC [χ2(1) = 5.11; p = 0.02]. One child in the RFC group experienced two placement failures (no child had two placement failures in the early intervention fostering group).
In the study by Taussig et al. ,190,191 the results indicated a significantly lower rate of placement changes for the intervention group than the control group (p = 0.04), and a significantly lower rate of new placements in a RTC (p = 0.03). There was also a higher rate of permanency attained for intervention group participants than for the control group participants (p = 0.004).
For children whose parents retained parental rights, significantly more intervention youth had reunified at 1 year post intervention than the control youth (p < 0.05). Taussig et al. 190,191 also report that 26% of intervention children had been adopted 1 year post intervention, compared with 8% of control children, but numbers were too small for conventional statistical tests.
Children’s social functioning
In the study by Biehal et al. ,145,146 MTFC participants had slightly better outcomes at follow-up than UC participants (adjusted MD 1.3, 95% CI –7.1 to 9.7) but this was not statistically significant (p = 0.75). Biehal et al. 145,146 also found no differences for school engagement or school exclusion.
No between-group differences were found in Taussig et al. 190,191 in relation to the Coping Inventory or the Self-Perception Profile.
Cognitive control and response monitoring
Cognitive control and response monitoring was assessed by Fisher et al. 183–188 using a computerised flanker task. There were no group differences on the behavioural measures of cognitive control (p > 0.05) or response monitoring (p > 0.05). A significant group effect was indicated observed on the electrophysiological measures of response monitoring. Children who received the intervention were significantly more responsive to performance feedback than foster children who received services as usual (p < 0.05).
Economic evidence
Two economic evaluations of intensive service models of care for children who have been maltreated were located in the systematic review (Wood et al. 616 and Lynch et al. 615), both carried out in the USA.
Wood et al. 616 was a cohort study comparing the costs and outcomes for families receiving a child abuse prevention service (n = 26) and families receiving UC (n = 24). The intervention was home-based counselling/psychology and the therapists were available 24 hours a day, 7 days a week, for a period of 4–6 weeks, providing practical help, FT and liaison with schools other community services in order to reduce the risk of out-of-home placement.
The evaluation, most accurately described as a cost–consequences analysis, had a 1-year follow-up and took a limited economic perspective, focusing on the service provider and including the cost of the interventions and any out-of-home placements. Outcomes were measured in terms of family functioning and whether or not the children stayed at home. Methods of costing were not outlined.
Children in the families that received the intensive intervention were significantly more likely to remain at home than families receiving UC and costs were significantly lower, as a result of the lower use of placements. However, this study616 was carried out some years ago and the methods are severely limited, with no random allocation, small sample sizes, failure to report the results for all measures of outcome, lack of incremental analysis and no assessment of uncertainty.
Lynch et al. 615 evaluated the net benefit of MTFC-P entering new foster placements. The study615 used data from the Fisher et al. 186 RCT (see subsection Intensive service models, Description of studies) and compared MTFC-P (n = 57) with RFC (n = 60) for children aged between 3 and 5 years.
The evaluation was conducted from a public agency perspective, including health, social care and education. Resources used were valued using nationally applicable published unit costs and were reported in 2008 US dollars (US$). Outcomes were assessed in terms of the primary measure for the clinical trial – the rate of placement permanency for each group, where permanent placement included reuniting with the biological parent, adoption by a relative or non-relative adoption. Costs and outcomes were assessed over a 24-month period and did not appear to be discounted.
Permanent placement rates were higher for the MTFC-P group than the RFC group, although the difference was not significant. Average total costs were significantly lower for MTFC-P and the incremental average net benefit was positive for all levels of willingness to pay for improvements in outcome, indicating that the value of the benefits of MTFC-P was greater than the costs. The authors conclude that MTFC-P is highly likely to have a positive net benefit for increasing permanent placements in comparison with RFC. Although no agreed level of willingness to pay for increases in placement permanence exists, the authors note that lack of permanent placement is associated with a variety of negative outcomes for young people, and suggest that willingness to pay for reductions in neglect and abuse is high. The study615 suffers from relatively small sample sizes and the lack of a generic measure of outcome associated with an agreed level of willingness to pay.
Therapeutic residential and day care services
No controlled studies that assessed the effectiveness of therapeutic residential care interventions were identified. We found three controlled studies194–197 that assessed the effectiveness of Therapeutic Day Programme interventions, of which only one was a randomised trial. 194 The others195–197 were COSs.
Description of studies
Sample sizes
The randomised trial had a sample size of 61 participants at baseline and 35 participants assessed at follow-up. The COSs195–197 had sample sizes of 34 and 70 participants, respectively.
Location
All three therapeutic day programme studies were conducted in the USA.
Participants
Age
At recruitment, the mean age of participants in the RCT was 11 months (SD 7 months) for the intervention group and 13 months (SD 8 months) for the control group. Participants were followed up to a mean age of 12 years (SD 7 months) for the intervention group and 13 years (SD 7 months) for the control group. 194 The mean age of participants across the COSs195–197 ranged from 3 years195,196 to 4.8 years. 197
Maltreatment
All three194–197 studies recruited children who had experienced a combination of physical abuse and neglect.
Interventions and comparisons
Two195–197 of the interventions were identified by the study authors as ‘therapeutic day treatment program’. The third194 was identified as the Childhaven therapeutic child care program. All three194–197 studies aimed to improve outcomes for children who had experienced maltreatment.
Control group participants in the included studies received either CPS as usual,194 no intervention,195,196 or were part of a wait-list control group. 197
Number and duration of sessions/treatment
Limited information was provided by the RCT study194 regarding the duration and number of treatment sessions.
The therapeutic day-treatment programme195–197 was described as a classroom-based therapy lasting 6 hours per day, 5 days per week, for approximately 8–9 months.
Outcomes
Behaviour problems
Moore et al. 194 used all three report forms (caregivers, teachers and youth report) of the CBCL269,294,418 to assess the impact of intervention on children’s behaviour.
Moore et al. 194 also measured drug and alcohol use with the Winters Personal Experience Screening Questionnaire723: participants’ involvement in the legal system, using juvenile court files, and – using school files – their involvement in special classes, their grades, special help, disciplinary actions, suspensions, or expulsions.
Risk of bias: randomised trial
Sequence generation and allocation concealment
In the absence of information about sequence generation or allocation concealment, a judgement of unclear risk of bias was made in relation to Moore et al. 194
Blinding of participants and personnel
No information was provided on the blinding of participants or personnel, and the study194 was judged as being of high risk, as neither is likely to have been feasible.
Blinding of outcome assessors
Interviewers were initially blind to group assignment, but caregivers did have the opportunity to mention their treatment experiences, which is likely to have indicated group assignment. A judgement of high risk of bias was therefore made.
Incomplete outcome data
There is a high risk of bias related to incomplete outcomes data, as this study194 analysed only available case data.
Selective outcome reporting
There is no evidence that other outcomes were planned and then omitted from the results, but, in the absence of trial registration or a published protocol, we judged Moore et al. 194 as being ‘unclear’. See Appendix 10.
Quality assessment of controlled observational studies
The quality of the two COSs was variable. Both provided a clear description of the objectives of the study, the outcomes, the participants, the interventions and the findings. Only Culp 1991197 addressed potential confounders in the research. Neither study addressed potential adverse effects, nor did they describe the characteristics of patients lost to follow-up. Only Culp 1991197 reported actual probability values for the main outcomes. It was not possible to determine whether the subjects asked to participate, the subjects who did participate, and the staff members involved in the study were representative of the entire population from which they were recruited for any of the studies. Statistical tests used to assess the main outcomes appeared appropriate. Blinding of participants or outcome assessors was not attempted and it seems unlikely it would have been feasible owing to the psychosocial nature of the intervention.
Results: therapeutic day care
It was not possible to conduct a meta-analysis for any of the outcomes, as only one relevant randomised trial was found.
Children’s problem behaviour
Moore et al. 194 found that for the CBCL (YSR), more children in the control group than in the intervention group scored in the clinical range, but this difference reached significance only for the aggressive behaviour subscale (p < 0.05). However, teachers perceived a higher rate of problems for children in the intervention group, although these differences failed to reach significance.
This study194 found that a significantly higher percentage of control youths showed drug and alcohol use (p < 0.05). Furthermore, control group youths were first arrested at a significantly younger age than intervention youths (p < 0.01). There was no significant difference between groups for delinquency records or delinquency episodes and no significant difference for property crime. However, control youths were arrested significantly more often for serious/violent crimes than intervention group youths (p < 0.05).
This study194 found no significant difference between groups for special classes, grades and special help. Although there was a higher rate of disciplinary actions, suspensions or expulsions for control group participants, this difference reached significance only for disciplinary actions for fighting (p < 0.05).
Children’s developmental progress
Culp 1987195,196 measured children’s developments progress on all five subscales of the EIDP, and found that children who were enrolled in the day-treatment programme scored significantly higher than control children on perception/fine motor skills (p < 0.001), cognition (p < 0.001), gross motor skills (p < 0.01), social/emotional (p < 0.001) and language development (p < 0.05). Culp 1991197 found similar results for perception/fine motor (p = 0.05), cognition (p = 0.01) and social/emotional (p = 0.01). However, this study197 found no significant difference for gross motor skills (p = 0.07).
Children’s self-concept
Children’s self-concept was measured by Moore et al. 194 (RCT) and Culp 1991197 (COS). Culp 1991197 found children receiving the intervention scored significantly better in cognitive competence (p = 0.05), physical competence (p = 0.01) and maternal acceptance (p = 0.02). However, there was no significant group effect for peer acceptance (p = 0.59). Likewise, in the Moore et al. 194 study, results indicate that intervention youths rated themselves higher than control youths on the Social Acceptance Scale [F(1,32) = 3.8; p < 0.07].
Economic evidence
No economic evaluations of therapeutic residential or day-care services for children who have been maltreated were located.
Co-ordinated care
We identified just one example of co-ordinated care evaluated with a CS. 198
Description of studies
Study design and location
The study was a randomised trial198 that took place in the USA.
Sample size
This study198 recruited 45 families with 72 children.
Participants
Children ranged from birth to 17 years old, with a relatively even split of males and females (47% male, 53% female). Participants were recruited from the Department of Social Services.
Maltreatment
Children had experienced multiple forms of abuse, including physical abuse, sexual abuse, emotional abuse and neglect.
Intervention and comparisons
This interagency intervention established a partnership between one private provider and three state agencies that served maltreated children who were compulsorily removed to out-of-home care, named the ‘Charleston Collaborative Project’, which aimed to:
-
reduce risk factors to promote child safety and child functioning and caregiving functioning, thereby allowing return of children to their families in a timely fashion
-
provide cost savings by delivering effective and focused interventions at the time children enter care to reduce both the number of children requiring more intensive and costly services and the length of time children remain in state custody
-
improve service system efficiency by co-ordinating care.
These goals were to be achieved by creating a single point of entry and a ‘seamless system for providing services’. 198 The providers of Charleston Collaborative Project included an assessment worker, a therapist and a service co-ordinator. Control group participants in this study received TAU.
Risk of bias: randomised controlled trial of co-ordinated care
Sequence generation
Low: participants were randomly assigned using a table of random numbers.
Allocation concealment
Unclear: inadequate information provided.
Blinding of participants and personnel
High: the study198 did not discuss this issue, but blinding these parties is not possible in such an intervention.
Blinding of outcome assessors
High: some data were collected from the child’s caseworker, and the study198 does not indicate that the researcher who interviewed family members or caseworkers was blind to allocation status of families.
Incomplete outcome data
Low: only available data were analysed but attrition was low (42/45 families were retained at last data collection point, and no family dropped out of treatment).
Selective outcome reporting
Unclear: there appears to be no evidence that other outcomes were planned and then omitted from the results. However, the study198 did not provide post intervention means for any of the outcomes, only latent growth curve data.
Other sources of bias
Unclear: where multiple children in one family were abused, one child was randomly selected for inclusion in the analyses of child functioning. No further details were provided.
Summary details of the risk-of-bias assessments of these trials can be found in Appendix 10.
Results: co-ordinated care
Although this study198 found total behaviour problems (as measured by the CBCL) to decrease significantly for both intervention and control groups, there was no significant difference between the two groups for any of the measures post test.
The effectiveness of intensive service models
Summary
There is growing evidence for the effectiveness of MTFC for children who have experienced one or more of physical, emotional, sexual abuse and neglect. The evidence suggests that MTFC can exert a positive influence on children’s internalising and externalising problems, and may be able to improve children’s emotional self-regulation (as measured by saliva cortisol), but more evidence is required. The study by Fisher et al. 183–188 suggests that MTSC may increase a child’s chances of a successful permanent placement for children in out-of-home care. MTSC children in this study198 also made significant increases in secure attachment behaviour towards foster carers and significant decreases in avoidant behaviour when compared with children in RFC.
Although included within the group of TFC studies, the intervention evaluated by Taussig et al. 190,191 is more accurately described as enhanced foster care, in contrast with the MTFC examined in the other three studies. Overall, the findings by Taussig et al. 190,191 provide limited support for the effectiveness of the mentoring and skills group intervention evaluated in improving children’s mental health. Taussig et al. 190,191 reports a lower rate of placement changes and lower rates of new placements in RTCs for children who participated in the mentoring and skills group.
The results of Moore’s evaluation194 of the Childhaven Therapeutic Early Intervention suggest some improvement in children’s self-concept, in reduced drug and alcohol use and age at first arrest, and in self-reported levels of aggression. However, the evidence is limited, and no differences were found for other measures (e.g. school performance) to support its effectiveness. In contrast, the two studies by Culp et al. 195–197 suggest that therapeutic day care of the kind provided can improve children’s development across a variety of domains and also (perhaps as a consequence) improve their self-concept.
There is no evidence for the effectiveness of the model of co-ordinated care assessed by Swenson et al. 198
Completeness and applicability
All183–196 but one145 of the studies were conducted in the USA. The UK study145 was a replication of MTFC. This study,145 conducted in difficult circumstances, failed to reproduce the results reported from the USA studies, but this may be due to design and implementation features (not necessarily the responsibility of the research team) and the quality of the comparison group: MTFC was compared with routine services in the UK, compared with limited provision of custodial care in the USA. The evidence from Fisher et al. ,183–188 although limited, suggests that intensive fostering support such as that provided in MTFC might well be able to improve the success rates for permanent placements following foster care, although this also needs to be tested in locations in which the profile of provision is closer to that of the UK than the USA.
Quality of the evidence
Overall, the quality of the evidence from trials is moderate.
Economic evidence
One economic evaluation,198 carried out in the USA, explored the costs and outcomes of a co-ordinated model of care, the Charleston Collaborative Project, for maltreated children. The paper is also reported in the effectiveness section above, as it is a combined effectiveness and economic paper. The study used a RCT design to compare the collaborative model of care (n = 48) to UC (n = 24) for maltreated children aged between 1 and 16 years.
The paper presents costs and outcomes separately, so would best be described as a cost–consequences analysis. Participants were followed up post treatment and 3 months post treatment. Effects included caregiver and child psychosocial functioning. Costs focused on the interventions under consideration, out-of-home placements and health services. Costs are reported in US dollars but the financial year applied was not reported.
Despite the collaborative project being more expensive than UC, total costs were lower as a result of lower placement and other service-use costs. Statistical analyses were not reported for all cost categories or total costs, so it is unclear if this difference is significant. The authors note that much of the difference in out-of-home placement costs was due to two young people in the UC group, which, given very small sample sizes (total n = 39 for cost data), may be the result of chance. The authors caution against drawing any firm conclusions from the cost data. Outcomes were similar across the two groups and as no formal economic evaluation, combining costs and outcomes, was undertaken no clear conclusion can be drawn.
Activity-based therapies
We identified six studies199–204 that assessed the effectiveness of interventions that engaged the child in activity-based interventions, grouped as follows:
Proponents of these therapies would possibly emphasise the differences between them, as opposed to the similarities. For this reason, we provide a ‘grouped but differentiated’ account of the descriptive elements of the studies (designs, sample sizes, etc.) and separate accounts of the findings of the included studies.
Description of studies
Study design
Play therapy
One of the three studies of play therapy was a randomised trial202 and one a quasi-experimental study. 203 The third was a COS. 201
Animal therapy
The only study of animal therapy204 was a COS.
Location
Arts therapy
Pretorius and Pfeifer200 took place in South Africa and Brillantes-Evangelista199 was conducted in the Philippines.
Play therapy
The Udwin203 study (QEx) was conducted in the UK. The other two201,202 studies took place in the USA.
Animal therapy
The Dietz et al. 204 study took place in the USA.
Sample sizes
Arts therapy
Pretorius and Pfeifer200 and Brillantes-Evangelista199 recruited samples of just 25 and 33 participants, respectively.
Play therapy
Both the RCT203 and QEx study202 were very small, with samples of just 34203 and 38. 202 The COS201 had a somewhat larger sample of 88 participants.
Animal therapy
Dietz et al. 204 recruited 153 participants.
Participants
Arts therapy
Pretorius and Pfeifer200 recruited girls aged 8–11 years. Brillantes-Evangelista199 focused on a slightly older population of both girls and boys (64% female), aged 13–18 years. Participants in both199,200 studies were recruited from either children’s homes200 or shelters for abused children. 199
Play therapy
The QEx study203 focused on younger children, aged 3–6 years. The remaining studies201,202 focused, respectively, on populations with age ranges of 8–17 years202 and 12–21 years. 201 Although the COS201 focused solely on girls, the remaining two202,203 studies focused on a fairly equal numbers of males and females.
Participants in the studies by McDonald and Howe202 and D’Andrea et al. 201 were recruited from residential facilities. No information was provided by Udwin203 on how participants were recruited.
Animal therapy
Dietz et al. 204 focused on children and adolescents aged 7–17 years, the majority of whom (94%) were female. Participants were recruited from CPS, law enforcement, the county district attorney’s office, and the local children’s hospital.
Maltreatment
Arts therapy
One study200 focused on girls who had been sexually abused, whereas the other study199 focused on children who had experienced both physical and sexual abuse.
Play therapy
There was limited information regarding the specific types of maltreatment across all three play therapy studies. 201–203 The children were identified as having been ‘abused’,202 as having experienced ‘parental neglect and/or abuse’,203 or a mixture of ‘physical abuse, sexual abuse, or neglect’. 201
Animal therapy
The intervention in Dietz et al. 204 was directed at children who had experienced sexual abuse.
Intervention and comparison
Arts therapy
This intervention used in Pretorius and Pfeifer200 was a structured group art therapy programme, aimed at reducing depression, anxiety, sexual trauma and low self-esteem. Brillantes-Evangelista199 had two experimental groups: (1) a visual arts group and (2) a poetry group. Both studies included a ‘no treatment’ control group.
Play therapy
The intervention used in the RCT202 was a challenge/initiative programme that aimed to enhance self-concept using co-operative and adventure games. The QEx study203 assessed the effects of imaginative play training. The COS201 assessed the impact of a sports-based intervention called ‘Do the Good’ (DtG), which was designed using trauma-informed treatment principles. Control group participants across all three play therapy studies201–203 received some form of active comparison, including playing other games with the same researcher but with no debriefing,202 engaging in a variety of activities unrelated to make-believe203 and structured activities part of participant’s TAU routine. 201
Animal therapy
Dietz et al. 204 used canine animal-assisted therapy (AAT). Two forms of treatment were compared with a ‘no treatment control’. The treatments were an ‘AAT with therapeutic stories’ group and an ‘AAT without therapeutic stories’ group.
Frequency and duration of sessions
Arts therapy
Both199,200 art therapy studies aimed at alleviating depression and PTSD and provided treatment over the course of eight weekly sessions.
Play therapy
All three play therapy interventions used a group-based approach, the duration of which ranged from 30 minutes203 to 60 minutes. 201,202
Animal therapy
Both treatments were provided in 12 weekly sessions.
Outcomes: activity-based interventions
Post-traumatic stress disorder
Depression
Depression was assessed in Pretorius and Pfeifer200 using both the TSCC473 and human figure drawing (HFD474). It was also assessed in Brillantes-Evangelista199 using the Self-Rating Depression Scale (as cited in Coroner and Fischer472).
Behaviour
Self-concept
Children’s imaginary play
Play therapy
Udwin203 assessed dimensions of children’s imaginative play by recording observations of (1) imagination, (2) positive affect, (3) concentration, (4) aggression, (5) peer interaction, (6) adult interaction, (7) peer co-operation, and (8) adult co-operation. Udwin et al. 203 also assessed participant’s fantasy predisposition, using Guilford’s Unusual Uses Test477 and a storytelling task using Children’s Apperception Test. 478
Risk of bias: randomised controlled trial of play therapy
Sequence generation and allocation concealment
Unclear risk: McDonald and Howe202 simply stated that participants were ‘randomly assigned’ but gave no other information on the method of random allocation or allocation concealment.
Blinding of participants, personnel and outcome assessors
High risk: McDonald and Howe202 made no reference to procedures to blind the participants or personnel (unlikely to have been feasible) or to outcomes assessors. The study202 was judged high risk of bias on each domain (participants and personnel, and outcome assessors).
Incomplete outcome data
Low risk: there is nothing to suggest that outcome data were incomplete for this study.
Selective outcome reporting
Unclear risk: there is no evidence that outcomes were planned and then omitted from the results, but we have only the paper to rely on, and it is an older paper.
Other sources of bias
The same researcher was the ‘recreation leader’ for both groups, leading to a judgement of high risk of bias.
Summary details of the risk-of-bias assessments of these trials can be found in Appendix 10.
Quality assessment of quasi-experimental and controlled observational studies of activity-based interventions
Arts therapy
The quality of the two199,200 QEx studies was very similar. Both studies provided a clear description of the objectives, intervention and outcomes in the study, although neither study adequately described their participants. Neither study addressed potential confounders in their research. Although both studies provided a clear description of their findings, neither addressed potential adverse effects. Both studies failed to describe the characteristics of patients lost to follow-up. Statistical tests used were appropriate and both studies reported actual probability values for the main outcomes. It was not possible to determine whether or not the subjects asked to participate, or whether or not those who did participate, or the staff members involved in the study, were representative of the population from which they were recruited. Blinding of participants and of outcome assessors did not appear to have been attempted by either study.
Play therapy
The quality of the QEx study203 and COS201 was variable. Both studies provided a clear description of the objectives, participants and outcomes in the study. Both studies only partially addressed potential confounders in their research. Although both studies provided a clear description of their findings, neither study addressed potential adverse effects. Both studies failed to describe the characteristics of patients lost to follow-up, and only one study203 reported actual probability values for the main outcomes. It was not possible to determine whether the subjects asked to participate, the subjects who did participate, and the staff members involved in the study, were representative of the entire population from which they were recruited for any of the studies. Blinding of participants and of outcome assessors did not appear to have been attempted by either study.
Animal therapy
The quality of Dietz et al. 204 was variable. The study provided a clear description of the objectives, participants, intervention and outcomes, and addressed potential confounders. But, despite providing a clear description of findings, the study failed to address potential adverse effects. The study also failed to describe the characteristics of patients lost to follow-up. Statistical tests used were appropriate and actual probability values for the main outcomes were reported. It was not possible to determine whether the subjects asked to participate, the subjects who did participate, and the staff members involved in the study were representative of the entire population from which they were recruited for any of the studies. Blinding of participants and of outcome assessors did not appear to have been attempted.
Results: activity-based interventions
It was not possible to conduct a meta-analysis for any of the outcomes, as only one RCT was identified.
Post-traumatic stress disorder
Arts therapy
In the study by Pretorius and Pfeifer,200 no statistically significant difference was found between the intervention and control group for trauma as measured by the TSCC or the HFD. In the Brillantes-Evangelista199 study, trauma scores decreased for both intervention groups and increased for the control group, but this change reached statistical significance only for the visual arts group (p = 0.011).
Animal therapy
The scores for the children in the animal therapy (dogs) with stories group decreased significantly more than the animal therapy (dogs) without stories group for all of the subscales of the TSCC, except sexual concerns (p < 0.001). This included subscales of anxiety, depression, anger, PTSD and dissociation. In addition, the animal therapy without stories group decreased significantly more than the no animal therapy (dogs) group (p < 0.001).
In the sexual concerns group, children in the animal therapy (dogs) with stories group had scores that decreased significantly more than those in either the no animal therapy or animal therapy (dogs) without stories groups (p < 0.001).
Depression
Arts therapy
Although the intervention group participants demonstrated a greater improvement in depression across both199,200 studies, this difference reached statistical significance only in the Pretorius and Pfeifer200 study (p = 0.001) when measured by the HFD. The scores on the TSCC failed to reach statistical significance in Pretorius and Pfeifer. 200
In the study by Brillantes-Evangelista199 the improvement in scores reached statistical significance only for the poetry intervention group (p = 0.0445). Improvement in scores for the visual arts intervention group and the control group failed to reach statistical significance.
Anxiety
Arts therapy
Pretorius and Pfeifer200 found no statistically significant difference between groups for anxiety as measured by the TSCC, although the experimental group evidenced statistically significantly lower post-test scores than the control group on anxiety (p = 0.000) as measured by the HFD.
Effectiveness of activity-based interventions
Summary
We were able to identify only two199,200 studies of art therapy, two201,203 studies of play therapy and one204 study of an animal therapy. One202 of these was a randomised trial, three199,200,203 were QEx and two203,204 were COSs. The outcomes targeted in these studies were heterogeneous, as were the interventions, making it extremely difficult to draw conclusions about their effectiveness. The small samples in these studies and the generally poor quality exacerbate this problem.
Completeness and applicability
Given the popularity of activity-based therapies in the UK and elsewhere, it is striking that we were able to identify so few studies. Even more striking is the absence of rigorous studies of music therapy, which appears to be extremely popular in the treatment of traumatised children, particularly young children.
Economic evidence
No economic evaluations of activity-based therapies for children who have been maltreated were located.
Chapter 5 Acceptability
Introduction
In this chapter we present evidence on the acceptability of therapeutic interventions to maltreated children, their families and other carers. The chapter draws on three sources of evidence:
-
data from studies that are designed to investigate factors associated with treatment engagement and dropout, and data from outcome studies that provide information on these issues, irrespective of study design
-
data from qualitative studies designed to investigate the experiences of children and young people, their carers and service providers
-
the views of members of our Young People’s Advisory Groups, and our PAG.
The issue of acceptability was addressed in a variety of ways in these included studies, and the heterogeneity in the methods of data collection used was further complicated by overall study quality. We used a systematic approach to reviewing the evidence about acceptability, first summarising the available data on treatment engagement and completion then summarising qualitative evidence on the views and experiences of children and young people, their carers and those providing the interventions. The available studies varied considerably in number, design and quality for each group of interventions (CBT, relationship-based, etc.), with the result that sometimes there is only a very thin evidence base, sometimes the evidence is largely sourced from carers or service providers and sometimes there are data from a range of sources.
We consider some of the key issues in defining acceptability, particularly in relation to quantitative data on engagement and dropout. We then consider the information on acceptability in relation to studies of particular interventions and groups of interventions. We present the views of children and young people about what they want from professionals, and examine the synergies, discrepancies and gaps in the findings from the published literature. On the basis of the evidence as a whole, we identify some of the key messages which, we believe, raise some important issues about the acceptability of service provision to this group of young people, and which are relevant to the development of effective and cost-effective service provision.
Overview of included studies
Please refer to Chapter 2 for details of the search strategy and approach taken to this area of the review. Seventy-three studies (see Table 12) were identified that addressed the issue of intervention acceptability. Thematic analysis of the qualitative data was conducted and discussed by members of the research team. Analysis of the data and identification of key themes was simultaneously deductive (based on key research questions for this review) and inductive (emerging from the reported data). Table 12 lists the studies, and provides an overview of the information available within each that relate to particular aspects of acceptability.
| Intervention type | Study | Children – satisfaction | Caregiver – satisfaction | Clinician – satisfaction | Profile of completers/attriters | Therapy difficult but worthwhile | Caregivers’ shared experience | Early termination | Parent–therapist tension | Secondary impact of abuse | Client–therapist relationship | Parent–child tension | Gender | Race | Practical considerations | Resources | Quality assessment | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT | aBarker 2005481 | |||||||||||||||||
| Buschbacher 2002629 | ||||||||||||||||||
| aChasson 2008482 | ✓ | |||||||||||||||||
| Chasson 2013630 | ✓ | |||||||||||||||||
| Eslinger 2014631 | ✓ | |||||||||||||||||
| Fraynt 2014632 | ✓ | |||||||||||||||||
| aHubel 2014492 | ||||||||||||||||||
| aKolko 1996107 | ||||||||||||||||||
| aLange 2010497 | ✓ | |||||||||||||||||
| McPherson 2012633 | ✓ | |||||||||||||||||
| aSalloum 2014504 | ||||||||||||||||||
| San Diego 2011680 | ||||||||||||||||||
| aSilovsky 2007505 | ||||||||||||||||||
| aSmith 2008506 | ||||||||||||||||||
| Relationship-based | Cross 2013634 | ✓ | ||||||||||||||||
| Ducharme 2000510 | ✓ | |||||||||||||||||
| aGolding 2004511 | ||||||||||||||||||
| aOsofsky 2007515 | ✓ | |||||||||||||||||
| Powell 2010662 | ||||||||||||||||||
| Sudbery 2010663 | ||||||||||||||||||
| Taban 2001635 | ||||||||||||||||||
| Timmer 2004656 | ✓ | |||||||||||||||||
| Systemic | Conran 1993621 | |||||||||||||||||
| Costa 2009678 | ||||||||||||||||||
| aDanielson 2010526 | ||||||||||||||||||
| Tjersland 2006673 | ||||||||||||||||||
| aWoodworth 1991533 | ||||||||||||||||||
| Psychoeducation | aBarth 1994161 | |||||||||||||||||
| Boisvert 2008658 | ✓ | |||||||||||||||||
| aHyde 1995538 | ||||||||||||||||||
| Rushton 2000664 | ||||||||||||||||||
| Group therapy | Ashby 1987636 | |||||||||||||||||
| Baker 2001637 | ||||||||||||||||||
| aDe Luca 1995170 | ||||||||||||||||||
| Grayston 1996659 | ||||||||||||||||||
| Gustafsson 1995676 | ||||||||||||||||||
| aMonck 1996169 | ||||||||||||||||||
| Nelson-Gardell 2001638 | ||||||||||||||||||
| Peled 1992639 | ||||||||||||||||||
| Counselling | Baginsky 2001640 | |||||||||||||||||
| Fowler 1992641 | ||||||||||||||||||
| Fowler 1993642 | ||||||||||||||||||
| Haight 2010175 | ||||||||||||||||||
| Haskett 1991657 | ✓ | |||||||||||||||||
| Kilcrease-Fleming 1992643 | ||||||||||||||||||
| Kolko 1999644 | ✓ | |||||||||||||||||
| Overlien 2011674 | ||||||||||||||||||
| Porter 1996645 | ||||||||||||||||||
| aReddy 2013176 | ||||||||||||||||||
| Scott 1996677 | ||||||||||||||||||
| Deb 2011679 | ✓ | |||||||||||||||||
| Thompson 2011646 | ||||||||||||||||||
| Psychotherapy | Davies 2009665 | |||||||||||||||||
| Horowitz 1997647 | ✓ | |||||||||||||||||
| Jensen 2010675 | ||||||||||||||||||
| Lippert 2008648 | ✓ | |||||||||||||||||
| Peer mentoring | Alaggia 1999660 | |||||||||||||||||
| Intensive service models | Biehal 2012145 | |||||||||||||||||
| Cunningham 2009649 | ||||||||||||||||||
| Gallagher 2012666 | ||||||||||||||||||
| Laan 2001671 | ✓ | |||||||||||||||||
| Leenarts 2013672 | ✓ | |||||||||||||||||
| Shennum 1995650 | ||||||||||||||||||
| Staines 2011667 | ||||||||||||||||||
| West 2014651 | ||||||||||||||||||
| Activity-based therapies | Bannister 1996668 | |||||||||||||||||
| Burgon 2011669 | ||||||||||||||||||
| Gilbert 1988652 | ||||||||||||||||||
| Hill 2009670 | ||||||||||||||||||
| Mishna 2012661 | ||||||||||||||||||
| General relevance | Koverola 2007653 | ✓ | ||||||||||||||||
| Murphy 2014654 | ✓ | |||||||||||||||||
| Risser 2013655 | ✓ |
There is considerable difficulty making any meaningful comparisons across the different therapeutic approaches, given the diverse range of research methodologies and treatment modalities investigated. However, a brief summary of the nature and quality of the data (by intervention group) is presented in Appendix 13, and a more detailed description of each study is available in Appendix 14.
Defining acceptability
What makes a treatment acceptable? For cancer patients, treatment may be experienced as highly unpleasant, requiring major disruptions to daily life, and with evident adverse effects for the individual and their family. Nonetheless, the treatment may be considered acceptable if there are few alternatives. The ‘costs’ to the individual, and those close to them, may be outweighed by the anticipated benefits.
For maltreated children and their carers, the costs and benefits may seem very different. Children may initially present with no problems, either emotionally or behaviourally, rendering the apparent cost of pursuing or accepting services as unnecessary or unnecessarily high, especially if one of the ‘costs’ of therapy is reliving or retelling experiences that are deeply personal, distressing and often traumatic. Even when the need for therapy is evident, it may not be easy to persuade either the child or caregivers to accept help, or to continue accepting help until problems are sufficiently ameliorated, if not resolved.
Possibly one of the most significant issues is that acceptability is rarely considered from the standpoint of the child or young person. Most of the quantitative studies examining engagement with treatment do so in relation to child or caregiver characteristics (e.g. maltreatment type, behaviour, age or mental health) but rarely from the perspective of the child. Among the qualitative studies, most examine issues from the perspectives of children’s caregivers.
What young people said
At the outset of this study, our consultations with young people focused on three issues: the outcomes they considered important from therapy; what they felt made it easier to ask for help, or easier to get it; and what they felt made it harder. We described the methodology in Chapter 2. The two groups with whom we consulted approached the Q-sort task (used to facilitate discussion) in rather different ways, but all took it very seriously (see Appendix 15).
Outcomes that matter
In relation to the outcomes they felt were important for maltreated children, one of the two groups felt that 18 of the 25 outcomes listed on the Q-sort cards were too specific to particular problems (such as anger or eating disorder) and would entail inappropriate generalisations, so they removed them. In this group, this left only seven outcomes to discuss, to which the young people themselves added an eighth. Despite differences in approach, there were clear similarities in the views of both groups. The items ranked most highly across the two groups were as follows:
Helping the person to:
-
learn skills to handle life’s ups and downs (group 1)
-
understand what being ‘treated badly’ is, and learning to recognise when things are not OK (group 2)
-
learn ways to keep themselves safe (e.g. knowing when to report something and to whom to report it) (group 2)
-
feel safe (groups 1 and 2)
-
‘bounce back’ if things in their life go wrong (groups 1 and 2).
Asking for, and receiving, help
The young people also viewed individuality as central to understanding what things might be important in making it easier for someone to ask for help, or might make some forms of help more acceptable than others. For example, two of the cards in the Q-sort were ‘person was still living with their family’ and ‘the person was no longer living with their family’. The young people pointed out, quite appropriately, that it was not easy to rank these cards one against the other because their importance would depend on whether the young person had experienced maltreatment within the family or outside it. One of the things that they emphasised in their discussions was the importance of choice, both in relation to starting and ending a service or therapy. Young people in one of the groups were unanimous in the view that the most important factor for a young person was the opportunity to meet a professional beforehand and to decide whether or not they would be happy to begin getting help from them. Furthermore, the group wanted the format of this preliminary meeting to be determined by the young person themselves, because some might want an opportunity to meet a potential therapist informally (e.g. meeting for a cup of coffee) without any mention of the therapy, whereas others might prefer a formal discussion of what to expect from the intervention. Clearly these alternatives are not mutually exclusive, but reflect different concerns. The opportunity to meet someone informally speaks to a concern about the likely quality of the therapeutic relationship. It may also be a proxy for choice and commitment, both of which may increase the likelihood of someone engaging with therapy, or staying with a course of treatment. A formal discussion of expectations can provide an opportunity to allay anxieties, to negotiate boundaries and to make an informed decision about the acceptability of what the therapist is offering.
Other things that mattered to young people included confidentiality (accessing help in ways that maintained their confidentiality) and trust in the help-giver. Making their own decisions about whether or not to get help, or at least being involved in that decision (rather than these decisions being taken by their parents or carers) was also ranked highly, along with not feeling judged or criticised – and, perhaps surprisingly, not having to worry about paying for the service. Clearly, many of these issues are of most relevance to older children and young people, such as those in the advisory groups, but, in terms of engagement with therapeutic services, they are probably salient to children of most age groups.
Things that get in the way
One group found it particularly difficult to identify a single factor that they regarded as the most significant barrier to young people accessing therapy. This group identified two things that they thought might deter young people from seeking help. The first was a worry that their situation was too complicated for anyone to be able to help with, and the second was that some children might think that those offering help would not believe them. Other factors identified were as follows.
The person does not:
-
want to be seen as having mental health problems (group 1)
-
know who to ask about getting help (group 2)
-
think they need any help (group 1)
-
trust the people/services offering help (group 2)
-
think that the help available will work for them (group 1).
This is a percipient list from these groups of young people. Children whose families have been engaged with social services for reasons of maltreatment, some of whom may have been removed from home as a consequence, may well have ambivalent feelings about public services. It is not unusual for children to feel responsible for a family break-up, and some are blamed by their parents for the involvement of Child Protection Services. Together, these point to the importance of services anticipating, and addressing, feelings of stigma and concerns about the likely effectiveness of services, and ensuring that those who need help know where and how to access it. The barriers that can be created by parents who prevent children from accessing services was also identified as an issue.
Most of these concerns or issues surface in the studies included in our acceptability review, although few have been systematically investigated. We return to these issues after following a review of the included studies.
Cognitive–behavioural interventions
Fourteen107,108,481,482,492,497,504–506,629–633,680 studies addressed issues relating to the acceptability of a range of cognitive/behavioural interventions. Details can be found in Table 13.
| Study/location | PICO | Sample size; response rate | Data collection – acceptability | Analysis | Findings |
|---|---|---|---|---|---|
| Barker 2005481 UK |
The Sunrise Project P Children aged 4–18 (mean 9.2) years, with histories of physical, emotional, sexual abuse and neglect; 45% female I Individual CBT approach, 1–25 sessions of 1 hour; emphasis on psychoeducation (older children) and therapeutic play plus age-appropriate psychoeducation for younger children C N/A O Pre–post changes in therapist’s rating of HoNOSCA scores382 |
14/67 children seen by project and/or their parents; five social services staff | Interviews | Summary overview |
Parent views
|
| Buschbacher 2002629 USA |
Individualised Support Project P Physically abused and neglected male in foster care, aged 2.5 years I Family-centred, communication-based approach to challenging behaviour. 1- to 2-hour sessions, increasing to 3 hours C N/A O Improved child behaviour |
n = 1 | Interviews with foster parent and two staff members of three-person team |
Foster/adoptive parent’s views
|
|
| Chasson 2008482 USA |
Individual Exposure-based CBT P Child victims or covictims of trauma: sexual or physical abuse, witness to murder/sexual assault; aged 5–19 (mean 10.88, SD 5.3) years 68% female; 31% Hispanic, 30% African American, 29% Caucasian, 9% Other I 20 × 1-hour sessions of TF-CBT C N/A O Avoidance, intrusive thoughts, (IES279), depression (CDI258) |
n = 99 | Withdrawal metrics | Multiple regression analysis | Dropout was defined as failing to complete the PTAP
|
| Chasson 2013630 USA |
Individual Exposure-based CBT P Child victims or covictims of trauma: sexual or physical abuse, witness to murder/sexual assault. Aged 5–19 (mean 11.03, SD 3.6) years 63% female; 34% Hispanic, 28% African American, 29% Caucasian, 9% Other I 20 × 1-hour sessions of TF-CBT C N/A O Avoidance, intrusive thoughts, depression |
n = 134 (99 from Chasson 2008482) |
Withdrawal metrics | Regression analysis of trauma characteristics as predictors of attrition | In this study, premature treatment termination defined in terms of number of accumulated sessions Participants more likely to terminate treatment prematurely were those who had:
|
| Eslinger 2014631 USA |
Individual TF-CBT P Children who were sexually, physically and emotionally abused, or neglected (75%), or who experienced death of a caretaker (9%), catastrophic event or terrorism (16%); aged 5–19 (M = 9.7, SD 4.5) years 57% female; 84% Caucasian I 20 × 1-hour sessions of TF-CBT C PCIT O child behaviour (CBCL297,349); PTSD (TSCC-A,325); parenting stress (PSI725) |
n = 115 | Baseline, post treatment and 3 months | Multinomial logistic regression of predictors of dropout | Three levels of treatment attendance: early dropout, moderate dose of treatment and full completion (see p. 125)
For every year of increase in caregiver’s age, the odds of receiving a moderate dose of treatment increases by 10% For every point rise in PTS score the odds that a child and caregiver will receive a moderate does increases by 4% |
| Fraynt 2014632 USA |
Individual, group and/or family P Physically and sexually abused children aged 2–18 (M = 12; SD 3.5) years; 49.3% female; 100% African American or Latino I Trauma-focused treatment in a mental health agency; average number of sessions = 34 (SD 32.8) C N/A O Treatment engagement |
n = 562 | Factors predicting treatment engagement | Binominal regression; multinomial logistic regression | African American children had significantly shorter trauma-informed treatment duration and higher rates of premature termination than Spanish-speaking Latino children, even when accounting for other variables associated with treatment duration and completion (e.g. child’s age, level of functional impairment, and receipt of group and field services) |
| Hubel 2014492 USA |
Project SAFE P Sexually abused children aged 6–12 (M = 10; SD 1.63) years; 77% female; 80% Caucasian and their non-offending parents I 12 × 90 minutes of parallel group CBT to explore and cope with feelings about abuse and empower against future victimisation C N/A O CHILD: depression (CDI430), anxiety (RCMAS256), loneliness (CLQ,726), impact of trauma (CITES-R,414), fear of victimisation (CFRV255 + Wolfe and Wolfe 1986, unpublished) |
n = 99; n = 67 analysed | Child and parent client evaluation form (six-point Likert scale, 6 = extremely unfavourable) | Child scores Satisfaction with group therapists:
Satisfaction with group environment:
|
|
| Kolko 1996107,108 USA |
Individual CBT P Physically abused children; mean age = 8.6 (SD 2.2) years; 28% female I 12 × 1 hours of CBT C FT and TAU O Child to parent violence, child externalising behaviour, parental distress and child abuse risk; family conflict and cohesion (see Chapter 4) |
n = 25 CBT, n = 18 FT, n = 12 control | Treatment expectancy (five-point Likert scale) Brief phone call to each parent between sessions 3 and 5 to determine initial treatment satisfaction Post-treatment 10-item CEI |
Treatment status and satisfaction
|
|
| Lange 2010497 The Netherlands |
Therapist-assisted web-based treatment P Sexually abused children aged 14–25 (M = 20, SD 3.5) years I Web-based treatment based on CBT for PTSD in adults comprising 11 virtual contacts over 8 weeks C N/A – baseline controlled O Impact of events (IES, Dutch adaptation727); depression (subscale of SCL-90-R728,729); client satisfaction plus routine outcome monitoring |
Sampling via advertisement and online application n = 24 | Client satisfaction: general, with treatment and with therapists; interviews plus 10-point rating scale (1 = high) Attrition |
Quantitative findings
Qualitative findings
|
|
| McPherson 2012633 USA |
FSP P Sexually abused children aged 3–16 years. 74% female I Trauma-focused counselling including individual treatment, group therapy and/or FT; TF-CBT most common treatment model used C N/A O Linkage to mental health services plus patient-achieved goals (retrospective chart review) |
n = 254 | Treatment completion | Univariate analysis and multivariate logistic regression models |
|
| Salloum 2014504 USA |
Stepped Care TF-CBT P Physically and sexually abused children aged 3–7 (M = 4.7, SD 0.87) years; 22.2% female; 77.8% Caucasian I Step 1: 3 × 1-hour parent-led sessions; if insufficient, therapy moves to 9 × 1.5-hour sessions led by therapist C N/A O Children: PTSD (DIPA730 + TSCYC–PTS731); severity of psychopathology (CGI-Severity732); treatment improvement rating (CGI-I)733 |
n = 6 | Parents completed:
|
Parent acceptability
|
|
| San Diego 2011680 The Philippines |
TF-CBT P Sexually abused female children aged 16–18 years I 15 × 1–2 hours sessions of TF-CBT C N/A O N/A |
5/6 referred adolescents participated Referrals came from College Dean and students in General Psychiatry & Personality Department |
Participants’ journals; therapy notes and interviews | IPA |
|
| Silovsky 2007505 USA |
Treatment for Preschool Children with Sexual Behaviour Problems P Sexually abused children aged 3–7 (M = 4.9, SD 1.1) years; 58% F and the non-offending parent I 12 × 90-minute parallel group sessions followed by a conjoint session for parents and child. Treatment protocol uses behavioural, cognitive–behavioural and psychoeducational approaches C N/A O Children: sexual behaviour (CSBI-3734); behaviour problems and social competence (CBCL,294; Parents; stress (PSI471) |
n = 85 | CSBP Preschool Group Satisfaction and Social Validity Questionnaire (CSBP-PGSQ). Fata et al. 1989, unpublished measure |
|
|
| Smith 2008506 Australia |
SAS-CBT P Sexually abused children aged 11–16 (M = 14) years and non-offending guardians; 66% female I 12 × 1.5-hour weekly of SAS-CBT conducted for adolescents and guardians in parallel. C N/A O Trauma (TSCC258); depression (CDI258) 12 weekly sessions |
n = 6 | Client Satisfaction Questionnaire | Adolescents All adolescents attended every therapy session apart from one dropout Adolescent Satisfaction Questionnaire scores indicated that 4/5 strongly agreed that the programme was of high quality, it helped them make progress, it met their needs, they would recommend it and it would help them to deal more effectively with trauma Adolescents felt understood by therapists and free to express thoughts and feelings related to abuse Guardians
|
Description of studies
Study design
One107,108 of the included studies was a randomised trial. The rest were uncontrolled studies.
Sample sizes
Sample sizes varied. They included a single case629 and four497,504,506,680 studies with very small samples of six504,506,680 and 25. 497 Five107,108,481,482,492,505 studies had samples numbering between 50 and 100, and four studies630–633 had samples of > 100. McPherson et al. 633 recruited 254. Fraynt et al. 632 had the largest sample of 562 children, but was a study based on data from a core data set in the USA.
Location
These were mostly US based (nine107,108,482,492,504,505,629–633 studies), with two Australasian studies (Australia,506 Philippines680), two European studies (UK,481 The Netherlands497) and one South African study. 200
Participants
The age ranges of children varied from 2.5 years to 25 years. Six492,497,504,505,633,680 studies reported on interventions that were solely treating children for sexual abuse history. Kolko 1996107,108 focused solely on children who had been physically abused. The other studies recruited children with had experienced one or more types of maltreatment.
Interventions
Interventions covered individual, group- or family-based therapy. Lange and Ruwaard497 explored the impact and acceptability of a web-based version of cognitive/behavioural approaches with no face-to-face contact at all between therapist and client.
The number of sessions ranged from 8 to 34, with most interventions lasting 12 sessions (eight studies);107,108,481,492,497,504–506,632,680 three629,631,633 studies did not specify the length of treatment. Interventions in the two Chasson et al. 482,630 studies comprised 20 sessions.
Fraynt et al. 632 reported variable attendance rates which differed in relation to ethnicity, the focus of treatment (family treatment vs. no family treatment), group treatment compared with no group treatment, and location of treatment (office vs. community).
Characteristics of those who complete treatment
Pre-treatment withdrawal was the main focus of the study497 reported by Lange and Ruwaard.
Four482,630,631,633 studies focused on treatment compliance. Factors predicting treatment engagement were analysed in the Fraynt et al. 632 study.
Pre-treatment withdrawal
Lange and Ruwaard497 set out to explore the effects of an online treatment for young victims of sexual abuse. In light of significant pre-treatment withdrawal in an earlier uncontrolled study, the authors introduced a number of measures that they hoped would reduce this in the context of a controlled (within-subject baseline-controlled) study. In common with other online treatment studies, the previous study had experienced a pre-treatment withdrawal rate of 90%.
In Lange and Ruwaard497 there remained a high level (77%) of pre-treatment withdrawal (82 out of 106 applicants not excluded by the research team), despite the steps taken to minimise it, namely no randomisation, parental consent required only for children of < 16 years rather than < 18 years (Dutch law for RCTs of new interventions), raising the upper age level for participants from 18 to 25 years, and providing the alternative of a structured interview by ‘chat’ if they were reticent to answer screening questions on the telephone.
Data available to the researchers indicated that pre-treatment withdrawal was strongly correlated with biographic questions, suggesting that anonymity may be an important factor, although whether for treatment or as an artefact of the study is not clear. The lowest pre-treatment withdrawal was among the oldest group, among which 46% (19/41) of those aged ≥ 18 years started treatment. All but one of the eight adolescents aged 14–15 years (and who required parental consent) withdrew, and 12 of the 16 young people aged 16–17 years withdrew (75%). Once engaged in treatment, there were few subsequent dropouts. The authors conclude that ‘fear of losing anonymity is important for both young and old participants, whereas the fear of needing parental consent is more or less decisive for younger age groups’497 (≤ 16 years). Once engaged in treatment, there were few subsequent dropouts.
These findings need to be interpreted against the context of a very small study. One of the recommendations of the authors is to change the intervention from a therapist-led online treatment to a wholly ‘self-help’ model, which may resolve the anxieties about loss of anonymity, while not dealing with some of the legal dilemmas associated with professional accountability and so on.
Treatment engagement
Fraynt et al. 632 used regression analysis to investigate factors associated with treatment engagement in trauma-informed therapies. The paper632 includes no detailed description of the therapies offered these children, but the interventions they identify as trauma-informed interventions include TF-CBT, cognitive–behavioural intervention for trauma in schools, CPP, and EMDR therapy.
Although the study632 is set in the USA, its findings raise potentially important issues for the successful engagement of children and young people in therapy within the UK. Fraynt et al. 632 found that age, functional impairment and the receipt of group and community-based (as opposed to office-based) services were correlated with increased engagement. Younger children who received more group sessions, and children who received services in places other than the office, were more likely to engage in treatment, as were children with more functional impairments, although children with more impairments were also more likely to be deemed by their therapist to have dropped out of treatment involuntarily.
When these things were controlled for, ethnicity remained a significant predictor of engagement, with Spanish-speaking Latino clients being most engaged in treatment (an average of 34 sessions) and African American clients being least engaged (an average of 25 sessions). The authors hypothesise that because of their language preference, Spanish-speaking Latinos may be more likely to get a therapist of the same cultural background to themselves, which may enhance treatment engagement compared with African American families. Furthermore, they hypothesise that the latter may be less engaged in treatment because they may mistrust or have had negative experiences of mental health treatment services (p. 72). These findings underline the importance of addressing language and culture in the context of mental health services. They also highlight the importance of ensuring that services communicate relevance and sensitivity to families from minority ethnic groups, and to all families who may have found engagement with Child Protection Services itself a traumatic experience, leaving them reluctant to seek help or engage with available treatment.
Treatment completion
Regression analyses were used in four482,630,631,633 studies to examine treatment completion. Caregivers’ perceptions of the severity of abuse appear to be a common theme relating to treatment completion. Chasson et al. 482 reported that higher levels of depressive symptoms and feelings of intrusion during treatment were associated with dropout from TF-CBT. In a later study,630 in which they analysed data from the same group of children augmented with additional cases, the authors found that children who had been abused by another child (not by a parental/adult figure), or had experienced a single event and had not suffered a life-threatening or serious injury, were more likely to drop out than those children exposed to multiple, physical injurious abuse by an adult.
Eslinger et al. 631 found that the odds of dropout were greater for children with younger parents. The authors also found a relationship between age and dropout, with the odds of dropout being greater for older children. Children in foster care were more likely to complete treatment than those living with biological or adoptive parents, although the authors augur some caution as the parents in this study were more likely to be younger than foster carers. When children’s and parents’ scores were high for PTSD (which the authors interpret as ‘acknowledgement’) then the odds of children completing at least a moderate ‘dose’ of treatment were improved. Children who were the only victim in the family were also more likely to complete at least a moderate dose if their caregivers were involved in the treatment process. McPherson et al. 633 also found that caregiver involvement was positively associated with treatment completion and achievement of mental health treatment goals among a sample of sexually abused children who were referred to a hospital-based children’s centre that provided assessment and therapy. This issue of how seriously the abuse is viewed will be discussed in more detail.
Acceptability
Children’s views
Four107,108,492,497,506 studies used data from rating scales to quantify children’s satisfaction levels. Scores indicated moderate to high levels of satisfaction, both with therapists and with CBT interventions. When studies also reported caregiver ratings, children’s reported levels of satisfaction were lower than those of their parents.
Lange and Ruwaard497 asked participants about their satisfaction with treatment in general and also specific aspects of treatment. Their participants rated the therapeutic alliance, and were asked questions about the nature of the online contact, whether or not they missed face-to-face contact with their therapists, and how they perceived the effectiveness of treatment. Participants generally expressed satisfaction with their online treatment, and, although 22% did miss face-to-face contact, all were highly satisfied with their therapists, and all but 2 of the 23 said that they would recommend the treatment to others. Significantly, although all modules were well received, the module that focused on the exposure was most highly rated.
This study497 (which used baselines as a source of historical control) found a steep drop in scores on the IES279 during the control phase, which Lange and Ruwaard,497 attributed to an effect of screening (which asked questions that required participants to focus on their trauma and current situations). They hypothesise that, in combination with the psychoeducation and expectation of treatment, this might have resulted in increases of awareness and hope.
The studies by Smith and Kelly506 and Kolko107,108 used questionnaires to assess perceptions of treatment acceptability and treatment expectations. Four of the five participants in the Smith and Kelly study506 agreed that the programme was of high quality, it met their needs and they would recommend it to others. Children and parents in the study by Kolko107,108 were asked to rate the overall acceptability of the key components of the interventions allocated to them. At the end of treatment children completed the 10-item Child Evaluation Inventory (CEI301). Mean ratings suggested moderate to high acceptability of treatment at the outset of treatment, with all but one item scoring a mean rating of > 3 (out of 5). Ratings tended to be higher than those for FT in relation to participants interested in the material learned that session (4.6 vs. 3.8) and confidence that therapists could help minimise abuse potential (4.2 vs. 2.8).
The mean ratings for children’s responses on the CEI suggest moderate to high acceptability (25.1 for CBT, 22.6 for FT) and utility (15.1 for CBT, 14.0 for FT).
Barker and Place481 and San Diego680 report qualitative data on children’s and young people’s views of their treatment. Most of the children were generally positive about the experience, but Barker and Place481 described the children as having some difficulty in articulating what they found most and least useful about the therapy. The analyses of the progress of five young women through the course of therapy by San Diego680 illustrated the women’s reluctance at the start of treatment, initial loathing of re-experiencing trauma and being unsure that therapy would help, but becoming more positive as therapy progressed.
Caregivers’ views
Six107,108,481,492,504,505,629 studies reported caregivers’ views of treatment and provided both qualitative and quantitative data, using a range of data collection methods, from qualitative interviews to focus groups and evaluation forms. Details are provided in Table 13.
All used rating scales to collect data on satisfaction, and some on caregiver treatment expectancy. In five107,108,481,504,505,629 of these studies, parents were recruited by a convenience sample, as parents of children involved in treatment; it is unclear how the caregiver sample was selected in the Project Safe programme. 492
Parents rated treatment satisfaction as ‘high’ in all studies that used treatment rating scales. 107,108,492,504,505 The sample sizes in these studies varied from 6504 to 85. 41 Some parents in the Barker and Place481 study felt that the CBT intervention had ended sooner than expected.
Two481,629 studies presented qualitative findings from interviews with parents and carers. Both studies481,629 reported positive experiences of the interventions, including a clear understanding of treatment aims and their expectations for the therapy, appreciating having someone neutral to whom their child could talk;481 Buschbacher’s single-case study629 found that the mother felt part of the therapeutic team that treated her son, although this study is particularly vulnerable to bias, as it was effectively (as its title indicates) a testimonial sought from a selected parent by a clinical team, one of whom conducted the interviews. The quantitative evidence presented supports the positive reports from the qualitative data.
In the Kolko107,108 study, parents were telephoned between the third and the first treatment sessions and asked to answer 10 questions using a five-point Likert scale (e.g. how much did the counsellor listen to you?, how much do you like your counsellor?). At the end of treatment they completed a 16-item consumer satisfaction questionnaire. Responses indicated high levels of acceptability with both treatments (53.8 for CBT, 50.9 for FT) and overall satisfaction (27.7 for CBT, 27.4 for FT).
Staff views
Qualitative evidence of staff views was also presented by Barker and Place481 and Buschbacher and Place,629 both of whom report positive findings. However, in both studies,481,629 staff expressed concerns about resource constraints, or strain, that was felt to threaten the viability of the service. The Sunrise Project481 relied on one worker, and staff referring children to the project worried about the security of this post, the overall lack of resources and the lack of potential to increase capacity. Concerns about capacity were also raised by Buschbacher. 629
The importance of parents and caregivers in securing successful outcomes in therapy was generally recognised in all studies, and is a recurring theme that will be discussed in more detail.
Summary: acceptability of cognitive–behavioural therapy interventions
Cognitive–behavioural interventions appear to be broadly acceptable to both children and caregivers, but the studies reviewed raise some issues for consideration.
Trauma exposure (by a number of means) is a central component of most CBT interventions. Although its proponents would argue that this is a significant factor in its effectiveness, there is some evidence that this aspect of CBT might be correlated with treatment dropout, and it is clearly something that parents and caregivers are anxious about. It suggests that therapist should perhaps be more mindful of the potential impact of traumatic reactions to exposure and take steps to ensure that therapy does not impose more of a demand on children and young people than they can tolerate. A guiding principle of early desensitisation interventions was to ensure that no patient left a session without experiencing ‘coping’.
Although generally ‘one-study stories’, the evidence suggests that the location of therapy should perhaps receive more consideration than is usual. Most services are offered in clinics or hospitals, but it is possible that if services were to be offered in the home then this might be more acceptable to some children and families. The same study632 that found an advantage for community-based treatments among ethnically diverse, urban children in the USA also found that children who participated in group treatments were more likely to complete treatment. Groups may address some of the anxieties that children feel about engaging in therapy (although of course they may engender some of their own fears).
Most CBT interventions include an element of psychoeducation, and it is notable that Lange and Ruwaard497 reported a steep decrease in scores on the IES,279 which the authors attribute to an unplanned consequence of screening, which comprised a combination of exposure and learning about abuse and its consequences. As well as reinforcing the potential of online interventions, this finding suggests that engagement in treatment might be enhanced by investing time in explaining the treatment rationale to potential patients.
Although a modest study that highlights significant challenges with engagement, Lange and Ruwaard497 indicate the potential for developing web-based CBT interventions, at least for specific sequelae of sexual abuse. Given the role of these media in young people’s lives, this might be an important delivery mode for further consideration. However, it raises complex issues around confidentiality and anonymity, and the ethical obligations placed on therapists.
Relationship-based interventions
Eight510,511,515,634,635,656,662,663 studies were included that reported RBIs. One656 study described PCIT, and three510,511,635 studies were concerned with parent training interventions. Two515,663 studies were of attachment-based interventions. Although not strictly attachment-based interventions, we consider two634,662 other studies under this heading. Powell and Cheshire662 explored the benefits of massage by ‘non-offending’ parents for children who had been sexually abused; we include it in this group because it aims to improve bonding and communication. Cross et al. 634 analysed data on study and intervention retention in a multisite evaluation of projects providing services to children exposed to violence, two-thirds of whom received interventions focused on dyadic therapy or FT. 735
Attachment-based interventions
Details of these studies can been found in Table 14.
| Study and location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Findings |
|---|---|---|---|---|---|
| Cross 2013634 USA |
Safe Start Promising Approaches (SSPA) P Maltreated children aged 1–17 (50% 3–7) years; mean age of retained group = 5.56 (SD 3.03) years, mean age of not-retained group = 4.99 (2.81) years Retained 53.3% female Not retained 50.7% female I CPP, one-to-one and group C N/A O N/A |
n = 1085; 60% retained | Predictors of study retention defined as follows:
|
Single predictors of study retention – logistic regression Multivariate predictors of study retention – multivariate regression remodelling |
Children more likely to be retained in the study were those:
Caregivers of intervention and comparison children were more likely to be retained if they :
|
| Osofsky 2007515 USA |
CPP P High risk parents at risk of maltreating or had maltreated their children aged 2–52 months at intake (M = 27, SD 10.91 months); 35% female I Number of treatment sessions ranged from 8 to 92 (M = 27) C N/A O N/A |
n = 346 children, n = 57 dyads | Caregivers’ and therapists’ qualitative impressions of treatment | Caregivers:
|
|
| Sudbery 2010663 UK |
Attachment and ‘holding’ therapy P Children aged 6–21 years who experienced multiple abuse I Therapy using ‘holding’ techniques C N/A O N/A |
n = 45 children | Individual and group interviews with current and former residents in residential care Interviews with employees and company directors; content analysis of files and organisational documents; survey of parents, social workers and children |
|
|
| Powell 2010662 UK |
MOSAC Massage P Sexually abused children and their mothers and one grandmother; age range 5–18 years, 80% female I Nine sessions using massage to help address problems associated with children’s sexual abuse C N/A O N/A |
n = 5 children, n = 4 mothers and 1 grandmother attended one-to-one sessions with children (one mother attended with two children) | Semistructured qualitative interviews | At follow-up, all mothers were happy with the practical considerations of the programme, most found it easy to learn and aimed to continue at home. They also felt less isolated meeting similar mothers Difficulties:
|
Description of studies
Location
The studies by Cross et al. 634 and Osofsky et al. 515 were set in the USA, whereas the studies by Sudbery et al. 663 and Powell and Cheshire662 were undertaken in the UK.
Study designs
The four515,634,662,663 studies vary widely in design.
Cross et al. 634 used data from a multiyear, multisite, national evaluation of 15 sites providing services to children exposed to violence. They examined retention at 6 months post baseline, using logistic regression to analyse the characteristics of those retained in treatment.
Osofsky et al. 515 report on a multisite study of a pilot infant mental health programme. Interviews were used to obtain caregivers’ and therapists’ qualitative impressions of treatment.
The Sudbery et al. 663 study is the only study of the three that presents children’s views of the intervention. As well as a focus group, semistructured interviews and survey methodology, case file analysis and organisational documentation were used, and two members of the research team were embedded within the organisation as participant observers.
The Powell and Cheshire662 study was a pilot evaluation that used qualitative methods.
Sample sizes
Pooling data from 15 sites, the sample in the Cross et al. 634 study was 1085. Osofsky et al. 515 recruited 75 mother–child dyads: 25 from each of three sites. The sample size in the Sudbury et al. 663 study is difficult to ascertain, but the authors appear to have scrutinised the files of 113 children, conducted a focus group of eight young people and interviewed a further four. Powell and Cheshire662 conducted semistructured interviews with four mothers and one grandmother.
Participants
Cross et al. 634 reported an age range of 1–17 years, with the majority of participants aged between 3 and 7 years. Children in the Osofsky et al. 515 study were maltreated young children aged < 5 years, or young children at risk of maltreatment. Their mean age was 20.19 months (SD 10.91 months).
Sudbery et al. 663 report on an older population with an age range of between 6 and 19 years, using purposive sampling to achieve a demographic mix of participants. Powell and Cheshire662 conducted interviews with four non-abusing mothers and a grandmother of children aged 5–18 years who had been sexually abused.
Interventions
Services in the Cross et al. 634 study differed across sites but all provided therapy to children, caregivers or both. Eight of the 15 sites provided a form of CPP,129 often in addition to other services. Detailed information of the interventions is not reported but the reader is referred to other sources of information.
Osofsky et al. 515 describe a model of intervention designed to identify families with children at risk and provide clinical evaluation and treatment, with a view to enhancing children’s development. The treatment provided was CPP.
Sudbery et al. 663 were focused on the holding therapy techniques used in a therapeutic residential setting for children, all of whom had been assessed as experiencing disordered attachment, some with an attachment disorder diagnosis.
The MOSAC Massage Programme (MMP) aims to equip mothers with simple massage routines that will ‘enable them to relax and calm their child, reintroduce positive touch in a safe environment, enable bonding/rebuilding of the mother-child relationship and work towards replacing memories of touch as fearful, painful, and distressing with memories of touch as loving, nurturing, and trusting’. 662
Characteristics of treatment completers
Cross et al. 634 examined five different predictors of study retention: demographics; violence exposure; child mental health; caregiver demographics; and engagement in intervention. Using logistic regression, they found, as in other studies, that those with older caregivers and those reporting higher levels of maltreatment were more likely to be retained. Physical health also had a relationship with retention, with those who rated their health as ‘poor’ or ‘fair’ also being more likely to maintain treatment. However, this study634 did not set out to examine treatment retention and thus the methodology falls somewhat short of exploring the factors related to treatment completion comprehensively, including motivation to change.
Osofsky et al. 515 reported that, of 129 child–caregiver pairs referred over 3 years, 75 were non-compliant from the outset or dropped out of treatment. Some families were court ordered and others were referred by child welfare or primary care providers. The authors observe that attrition is not surprising in samples in which substance abuse, parental mental illness or low functioning and homelessness are common. Of the 57 dyads that completed treatment, mother’s age at intake and maternal education (completed high school) were significantly correlated with treatment completion.
Acceptability
Children’s views
In the Sudbery et al. 663 study, children reported feeling safer in this setting than they had done in previous placements (many had experienced multiple placements over a short period of time). The use of restraint was sometimes seen as important, to keep everyone safe. Some children found it difficult to develop secure attachments with staff. The data are, however, very limited. The sample is unlikely to be representative, and the study663 was poorly designed and executed, and fewer children participated than indicated interest in doing so.
Caregivers’ views
In the Osofsky et al. 515 study, 45% of participants who completed treatment also completed a satisfaction survey, including one participant who did not comply with treatment and one who was still in treatment. On investigation, the only factor correlated with survey completion was programme site (site 1, 72%; site 2, 58%; and site 3, 28%). Parents were asked eight questions about the effectiveness of the programme and their satisfaction with the intervention. Those who responded were extremely positive. It is not made clear whether these questions were asked face to face or anonymously, which may have an impact on responses; it is also unclear whether or not those who did not complete the survey (56%) did not do so because of dissatisfaction with the programme. The differential completion across the three sites may also suggest variation in delivery.
Sudbery et al. 663 briefly mention parents’ views of holding therapy as mixed, but no data are reported. Powell and Cheshire662 report that mothers were generally happy with the practical aspects of MMP. They appreciated the ground rules that were established for the group sessions that preceded massage and the safeguards taken to protect the vulnerability of participants, for example no clothes removed. One of the five carers felt that because her children were teenagers it was difficult to get them to 10 sessions (they did not want to spend time with their mother).
Staff views
Therapists involved in the infant mental health programme515 noted positive outcomes in both caregiver–child interactions and other treatment outcomes, for example assistance with the early identification of possible developmental delays and subsequent follow-up with primary care, and helping mothers to understand and establish support systems around them. An additional positive outcome that may be associated with the intervention was that no further reports of abuse or neglect were reported during treatment and up to post assessment, and there was a major reduction in reports during the first 3 years of the pilot. Although Sudbery et al. 663 interviewed staff, this evidence is not presented in any detail in the paper.
Parent–child interaction therapy
Only one656 study addressed the acceptability of PCIT (Table 15).
| Study and location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Timmer 2004656 USA |
PCIT P Foster carers of children aged 2–8 (M = 4.4) years, who experienced multiple maltreatment; 36% children female; 95% foster carers female; 33% Caucasian I PCIT C N/A O Child behaviour (CBCL;297,736 ECBI311,737); caregiver stress (PSI297,725,736); caregiver depression (SCL-90-R705); child abuse potential (CAPI366) |
102 kin foster carers, 157 non-kin foster carers | Treatment completion | Treatment completers – 13.6 sessions (SD 7.4) Early termination – 7.1 sessions (SD 6.7) 54.9% of kin foster carers completed treatment, 36.9% of non-kin foster carers completed χ2 (1, n = 259) = 8.09; p < 0.01 Non-kin foster carers were more likely to report externalising behaviour in of their foster child |
Location
The study656 was conducted in the USA.
Study design and sample size
Timmer et al. 656 used social exchange theory as a framework within which to examine foster parents’ perceptions of their foster children, their relationships with them and their own functioning, comparing the views of 102 kin and 157 non-kin foster carers. The rationale for the study656 was that such perceptions might impact on the investment that foster carers make in their foster children, all of whom had been referred to PCIT on account of their behaviour problems.
Participants
The children were aged 2–8 years (M = 4.37 years) and were victims of multiple maltreatment. The majority were male (64%), cared for by women (95%) and one-third were Caucasian.
Intervention
The study656 report contains no detailed description of the intervention, but provides a brief outline of standard PCIT, that is, a two-phase therapy that begins with a focus on enhancing the parent–child relationships (CDirI) followed by a focus on enhancing child compliance (PDI). Both phases (which each last around 7–10 sessions) begin with a didactic component followed by therapist coaching, conducted by a ‘bug in the ear’ from a separate observation room.
Characteristics of treatment completers
Treatment completion and withdrawal metrics were reported. Dyads were considered to have completed treatment if they had mastered the relationship enhancement element of the programme, and could demonstrate sustained child’s compliance to commands and successful discipline approaches. If dyads did not attend treatment after the initial session, or if a parent chose to terminate therapy before the treatment goals had been met, then these were considered as early terminators. The average number of treatment sessions to treatment completion was 13.6 (SD 7.4). The average number of coaching sessions for dyads terminating early was 7.1 (SD 6.7). There were few demographic differences between the kin and non-kin carer groups.
Kin foster carers were significantly more likely to complete treatment than non-kin carers: 54.9% of kin carers completed treatment, compared with 36.9% non-kin carers completed [χ2(1, n = 259) = 8.09; p < 0.01].
Of the 145 foster carers who terminated treatment early, approximately two-thirds of kin and non-kin carers left treatment during phase 1 (CDirI). Of the rest, around half terminated treatment during the second phase (parent directed) and half never started. Of the early terminations, 40% were as a result of Child Welfare Services moving the child to a pre-adoptive home (more likely to happen in non-kin care settings). Some 43% were initiated by caregivers. In almost 28% of cases termination was triggered by the therapist and an 11% early treatment termination was categorised as ended by ‘other’ (not specified).
The results of binary logistic regressions suggest that kin caregivers with clinical levels of parental distress were more likely to stay in treatment than non-kin foster carers or kin caregivers scoring in the normal range on this indicator, although this effect was only marginally significant (p < 0.06). From their analyses the authors conclude that ‘parental distress’ explains some of the differences in overall attrition between kin and non-kin caregivers, and hypothesise that kin caregivers’ distress reflects their frustration and helplessness in the face of their foster children’s behavioural challenges and may motivate them to seek and continue with treatment.
Given that this was a study of foster parents, the authors note their concern about the relationship between elevated scores on the CAPI and early termination. If so, then this is yet another study that suggests that those who need help most are those who are least likely to access help or complete treatment. Similarly, those foster parents who avoided completing the Parenting Stress Index (PSI) were also more likely to leave treatment early, perhaps because they interpreted this as a measure of their mental health rather than that of their child, and therefore as a threat.
Parent training interventions
Three510,511,635 studies presented data for parent training interventions. Details are shown in Table 16.
| Study and location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Ducharme 2000510 USA |
Group Parent Training P Children aged 3–10 years who experienced physical abuse and witnessed domestic violence and their mothers I Two group and then individual (parent–child) sessions of errorless compliance therapy C Multiple baseline controls O Compliance (event recording plus Compliance Probability Checklist) |
n = 28 parents n = 15 children from n = 9 families |
n = 8 mothers completed a satisfaction questionnaire (scale 0–5, 5 most positive) | Mean satisfaction with:
n = 13 families dropped out citing severe stressors: child apprehension; commitment to psychiatric unit; suicidal ideation; father refused treatment |
|
| Golding 2004511 UK |
Parent Training P Foster parents of children aged 5–15 years, who experienced abuse or neglect and who had challenging behaviour; 43% female I 18 × 2-hour, monthly sessions of Fostering Attachments C IY plus psychoeducational component O SDQ;721 Knowledge Quiz, Symptom checklist (attachment group only) |
n = 44 children, n = 41 foster carers | Participant satisfaction questionnaire, qualitative evaluation, group facilitator feedback |
Parent Training Group
|
|
| Taban 2001635 USA |
Project SafeCare P Parents of children from birth to 5 (M = 4.9) years, who experienced multiple abuse; 64% Latino, 28% Caucasian, 7% African American I Eco-behavioural programme (partial replication of Project 12-Ways); 15 sessions, three areas of intervention: home safety; infant and child health care; bonding and stimulation C N/A O Not covered in this paper, but covered in other reports |
n = 45 families health training, n = 37 home accident prevention; n = 31 PCIT | Three social validity questionnaires developed specifically for the study |
Positive
|
Study design
The study by Ducharme et al. 510 was a multiple baseline study of the effects of an intervention to help parents manage oppositional behaviour. The Golding and Picken511 study was a qualitative evaluation of two forms of group work. The Taban and Lutzker635 study was a study of parental satisfaction and acceptability of a parent training programme, exploring parental preference for different models of training.
Sample sizes
Sample sizes were small, with just 15 children from nine families in the Ducharme et al. 510 study and 44 children and 41 carers in the Golding and Picken511 study. In the study by Taban and Lutzker635 data were collected from the 31 parents provided with parent training in Project SafeCare.
Participants
Children in the Taban and Lutzker635 study ranged in age from birth to 5 years old (M = 4.9 years). The studies by Ducharme et al. 510 and Golding and Picken511 examined an older population aged between 3 and 12 years, and the foster carers in the Golding and Picken511 study were caring for school-aged children.
Participants in the Taban and Lutzker635 study were drawn mainly from the Latino population (68%). Golding and Picken511 suggest that the children fostered by their participants were white British (like the carers). No information is provided by Ducharme et al. 510
Children had been victims of physical abuse and witnessed domestic violence in the Ducharme et al. 510 study, and victims of physical abuse and neglect in the Golding and Picken511 study. Eighty per cent of those who received the parent interaction training in Taban and Lutzker635 were from a sample of maltreated children referred by the Department of Child and Family Services.
Intervention
Golding and Picken’s511 study compared two parent training interventions for foster carers. The first was based around the IY programme, with an additional psychoeducational component. This was compared with an intervention designed to develop emotional understanding and give skills in providing empathetic discipline, entitled Fostering Attachments. The IY intervention was delivered in 2-hour sessions over 9 weeks. Fostering Attachments was delivered in monthly, 2-hour sessions over an 18-month period.
In the Ducharme et al. 510 study, parents were taught ‘errorless compliance training’ in a five-session group format. Errorless compliance training is designed to improve children’s compliance while minimising non-compliance and associated risks of confrontation. The study510 reported generalised improvements in compliance that were maintained at 6 months’ follow-up.
Project SafeCare was a 15-session programme that targeted home safety, infant and child health care, bonding and stimulation, and which included a parent–child interaction training component that was offered to those parents who needed it. 635
Characteristics of treatment completers
Only Ducharme et al. 510 addressed the issue of treatment completion. However, in this small study510 the focus was on attrition, which in this study was significant: 13 children out of 28 children failed to complete treatment. Reasons for attrition were attributed to severe stressors for the child, including child apprehension, commitment to psychiatric unit and suicide ideation. In one case, the father refused treatment.
Acceptability
All three510,511,635 studies used a parent satisfaction questionnaire, which we have used as an indicator of acceptability. The views of children were not reported in any of the studies. Golding and Picken511 concede that limited evaluation was built in to the research design because it was not a formal research study.
Caregivers’ views
Using a five-point rating scale, mothers in the Ducharme et al. 510 study indicated a high degree of satisfaction with the intervention and therapist, and rated their children as being significantly more co-operative after treatment. However, as indicated above, almost half of the original sample did not complete treatment. Foster parents receiving the IY parent training intervention were more satisfied than those having the Fostering Attachments intervention in the study by Golding and Picken,511 with 84% saying that they found the programme to be very helpful, compared with 60% in the fostering attachment group. Only half of each intervention group stated that they had some increase in their understanding and confidence.
Participants in the study by Taban and Lutzker635 also reported positive feedback; parents reported high levels of satisfaction and training procedures and also rated staff highly. There are some limitations using these non-standardised measures.
Staff views
Group facilitator feedback was described by Golding and Picken511 Facilitators stated that attendance had been good, with a high degree of participation. They emphasised the importance of trainers having a sound understanding of the needs of looked-after children. Many of the foster carers in the Fostering Attachments group spoke about their own histories of abuse and neglect, probably because of the focus of the intervention and the duration (over 18 months), and this also required skilful handling.
Summary: acceptability of relationship-based interventions
There is a surprising lack of evidence about the acceptability of RBIs. The one515 study that specifically explored treatment dropout and failure to engage with an attachment-orientated treatment found that mothers who had completed high school were most likely to complete treatment. The authors also estimate that every hour of treatment required around 10 hours of ‘engagement’ effort, including ‘frequent telephone calls, home visits, child care visits, and other efforts to build a trusting relationships with the parent’. 515 They note that ‘cooperation, collaboration, and communication with foster care workers was essential, both to retain parents and children in the program and help with engagement activities’515 (p.18). Notwithstanding these efforts, 72 of the 129 child–caregiver dyads referred to the programme being evaluated, refused to engage or dropped out of treatment. These dyads were either referred from child welfare/primary care providers or were court ordered to attend. This is of some concern: the typical profile of children for whom a child protection plan is in place in the UK.
One issue of concern identified by Timmer et al. 656 (not for the first time) is that kin foster carers lack much-needed support in managing the challenging behaviour of the children whom they are fostering.
The parent training interventions in the included studies were generally welcomed by parents/caregivers, with the exception of the Ducharme et al. 510 study. Here, although attrition was significant, it was attributable to events outside the intervention, such as the child’s admission to a psychiatric unit. One father refused treatment and, although it would be a mistake to generalise from this study,510 it is the case that few studies of interventions even mention the involvement of fathers.
Systemic interventions
Five526,533,621,673,678 very different studies addressed issues of the acceptability of systemic interventions. Details of these studies can be found in Table 17.
| Study/location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Conran 1993621 USA |
FT P Single case of a sexually abused girl I FT unspecified C N/A O N/A |
n = 2, mother and daughter | Child’s experience of intervention, interview transcribed | Child did not feel forced into talking Uncomfortable using two-way mirror at first Ambivalent about use of group approach Child suggested therapist being more ‘child-like’ in approach – using jokes, tricks and games |
|
| Costa 2009678 Brazil |
Multifamilial Group Sessions P Action research of participation of extremely socially excluded families (living in settlements); sexual abuse I Not specified C N/A O N/A |
n = 28; n = 8 families interviewed | Benefits and limits of psychosocial interventions – parents/adolescents questionnaire, children’s drawings, evaluation of the effects of conversations and actions in families | Qualitative epistemology | Families as a whole feel unprotected and vulnerable to other violence Group therapy and shared experiences made it easier to talk More sessions were required Involving other social institutions to support the family’s welfare and help to prepare them for humiliating process of police and court process |
| Danielson 2010526 USA |
RRFT P Sexual abuse and comorbid substance abuse: mean age = 15.0 (SD 1.7, range 13–17) years; 100% female; 40% Caucasian, 40% African American, 10% Hispanic I Individual therapy and FT; 14–34 × 90-minute sessions; mean number of sessions = 24 (SD 8.0) C N/A O Substance use; UCLA-A PTSD374 CDI (Kovacs M, 1983, unpublished manuscript); FES-Con-A; FES-Con-C; FES-Coh-A; FES-Coh-C, post, 3-month and 6-month follow-up375 |
n = 10 Treatment completers five out of seven sessions (n = 9 completed all seven sessions, n = 1 completed five sessions) |
3–6 months post treatment Participants rated their satisfaction with each component of RRFT on a scale of 1–5, with 5 being the most positive rating |
90% of participants completed ratings on the utility of RRFT components (rating scale of 1–5, 5 most positive): psychoeducation (M = 3.89, SD 0.93) Coping/family communication (M = 4.78, SD 0.44) Substance abuse (M = 4.56, SD 0.73) PTSD (M = 4.33, SD 1.11) Healthy dating/sexual decision-making (M = 4.78, SD 0.44) Sexual victimisation risk reduction (M = 4.44, SD 0.42) |
|
| Tjersland 2006673 Norway |
Eclectic – FT based on crisis and narrative theory P Sexual abuse allegations; age range 3–16 years; 75% female I FT based on crisis and narrative theory, which may involve confronting alleged perpetrators of CSA; ≥ 6 sessions (M = 20) C N/A O N/A |
n = 23 families, n = 32 children | Data collected from therapeutic session observation and follow-up interviews with mothers, children and alleged perpetrators | Descriptive coding developed by two therapists, independently rated to verify categorisation | Children Majority were reluctant to discuss abuse – at follow-up reasons were given why: threatened by abuser; fear of upsetting mother; fear of not being believed The children in 21 families had symptoms at start of treatment – this was reduced to three families at end In 18 cases, mental health improved. Children from four families still had severe symptoms Children reported positive comments and, from observations of child/therapists exchanges, these were rated as positive, playful and talkative Caregivers Mother participated in most sessions. Reluctant to discuss abuse in case it had not happened. Felt vulnerable to how therapists perceived them. Majority of mothers described help positively – felt they understood their children better and valued contributions from team Alleged perpetrator For those who engaged in the process, it was described as a relief to talk to someone in a non-judgemental setting. Those who were discontented with the process felt that the mother had formed a coalition with the therapist |
| Woodworth 1991533 USA |
The Family Project P Sexual abuse; mean age 14.5 years; typically female; 100% Caucasian I Multiple Family Incest Treatment Program – group therapy for multiple families with multiple therapists; peer groups also for men, women, couples and children; all family members also offered IT, couple therapy and individual FT C N/A O Interviews and questionnaire covering personal/family adjustment, friendship, employment and education client satisfaction |
n = 22; n = 16 interviewed, n = 5 refused, n = 1 could not be found |
n = 40 interviews with n = 13 incest victims, n = 12 offenders, n = 2 siblings | 75% of victims and 83% of mothers considered intervention personally helpful Clients appreciated the support received from each other and their counsellors Two clients complained that counsellors left too soon Mothers favoured more direct confrontation of perpetrators Respondents recommended more use of smaller groups 88% of siblings refused to participate: mothers often refused for non-victim children; siblings were clinically hard to reach and less convinced that therapy had benefits |
Description of studies
Study design
The five526,533,621,673,678 studies examined family or multisystemic therapies. The Conran and Love621 study was a case study, the Costa et al. 678 study was an action research project, and the studies by Danielson et al. 526 Tjersland et al. 673 and Woodworth533 were uncontrolled studies (see Table 17).
Sample sizes
The FT/MST interventions all had small sample sizes, ranging from a single case621 or samples of just eight678 and 10 families. 526 The sample of Woodworth533 comprised 22 families completing treatment; Tjersland et al. 673 had the largest sample of 31 families.
Location
The studies by Conran and Love,621 Danielson et al. 526 and Woodworth533 were US based, whereas the Costa et al. 678 study was set in Brazil and the Tjersland et al. 673 study was conducted in Norway.
Participants
Interventions in all five526,533,621,673,678 studies were directed at victims of sexual abuse. Danielson et al. ’s526 sample had comorbid substance misuse. Woodworth et al. ’s programme533 was for victims of incest. Participants in the Tjersland et al. 673 study were referred by agencies concerned that a child aged < 18 years was being sexually abused by a family member. Participants in the Costa et al. 678 study were extremely socially excluded, drawn from a population of settlement/dump dwellers with a high level of mobility.
Only Danielson et al. 526 reported the age of participants (mean 15.0 years, SD 1.7 years).
Intervention
Conran and Love621 did not provide any information about the FT intervention provided in the single case. Costa et al. 678 briefly describes a Multifamilial Group Therapy intervention and Danielson et al. 526 reported on RRFT, which was a combination of individual therapy and FT. RRFT was delivered by a university-based clinic and consisted of weekly 60–90 sessions over 14–34 weeks (M = 24 weeks, SD 8.0 weeks); participants were recruited through the university-based urban clinic, which specialises in adult/child trauma. The FT for suspected familial sexual abuse673 was delivered by one therapist, with a second therapist observing and reflecting on every session. It was anticipated that each family would be at crisis point at the start of treatment and this informed the development of the programme: narrative therapy techniques and relationship-building were used and could include confronting alleged perpetrators. The Multiple Family Incest Treatment Program533 provided support and therapy for all family members and included sibling support as one of its priorities, a group that they found particularly hard to reach.
Acceptability
Children’s views
Conran 1993621 reports qualitative findings from a transcribed interview with the single female participant. Although not feeling forced to talk to the therapist, she said she found the two-way mirror uncomfortable at the start of treatment, but got used to it once treatment was established. She preferred IT and was ambivalent about group therapy. She also suggested that the therapist should take a more ‘child-like’ approach, by introducing games, jokes or tricks to engage the young person.
Costa et al. 678 describe young people’s feelings of shame, anxiety, fear and pain and sadness; group therapy with other children with shared experience made it easier for the young people to talk about their problems.
The study by Danielson et al. 526 was the only one to report results from a treatment satisfaction measure. Out of a total of 10 participants, nine completed ratings on the perceptions of the usefulness of treatment components: psychoeducation; coping/family communication; substance abuse; PTSD; healthy dating/sexual decision-making; and sexual revictimisation risk reduction. Each domain was rated positively. A total of 90% of participants completed all seven sessions; one participant ended treatment after five sessions.
Tjersland et al. 673 collected data through observations from therapist sessions and follow-up interviews with children, mothers and alleged perpetrators of sexual abuse. In most cases, the abuse had not been substantiated at that time, and the majority of children were reluctant to discuss the abuse at follow-up interview. The reasons given for this reluctance included the following: they had been threatened by the abuser; they were afraid of upsetting their mother; and they feared not being believed. The majority of children displaying symptoms at the start of treatment had made progress by the end. Children expressed generally positive comments, and therapy observations reported positive exchanges between child and therapist.
Data were collected using interviews with 13 incest victims, 12 offenders and two siblings in the Woodworth533 study. Overall, three-quarters of victims found the group therapy to be helpful. The most commonly appreciated aspect of the groups was mutual support and the support provided by the counsellors. Two clients complained that counsellors left too soon. This may have been as a result of the use of interns to provide therapy (with shorter tenure), resulting in a negative impact on children who had formed bonds with them. Out of the 26 siblings, only three agreed to participate in the therapy. Reasons given for this 88% refusal rate were that mothers often refuse on behalf of non-victim children or that siblings were less convinced that therapy had benefits for them.
Caregivers’ views
Parents in the study by Costa et al. 678 described how they felt their families were unprotected and vulnerable to further violence. Some expressed fears for their child’s future sexuality, including concern that the sexual abuse would negatively impact on the child’s sexuality (homosexuality) and how they might interact physically (i.e. sexually) with other children. The mothers in this action research study valued the group therapy with other families because it created an opportunity for them to talk to other women with similar experiences, but there was some criticism that treatment ended prematurely. Financial constraints impacted adversely on parents’ access to support – for most of the families the male perpetrator (and primary earner) had been removed from the home.
Tjersland et al. 673 reported the conflicting interests expressed by participant mothers about treatment: they wanted help for their child but were concerned about revisiting the abuse by getting their child to talk about it. Concern for the alleged perpetrator was also observed: fear of criminal prosecution or negative reactions to the allegations; this was particularly relevant if an immediate family member (husband or son) had been implicated in the abuse. Some mothers felt vulnerable to being perceived negatively by the therapist because of their implicit role in the abuse, or acting in an over-protective way. In client satisfaction ratings, mothers were generally very contented with the treatment. In the Woodworth533 study, 83% of mothers found the group therapy to be helpful but they also favoured more direct confrontation with perpetrators and smaller group work.
Mothers were generally satisfied with the therapy received in the study by Woodworth 1991,533 with 83% feeling that it had helped them personally. Three-quarters of respondents in this study533 considered that the multiple-family group (several families meeting together for therapy) had been helpful. Comments indicated that some respondents thought that the group needed more guidance from the facilitators, and that offenders should have been confronted more, and some thought that the group was too large.
Staff views
Staff involved in the Costa et al. 678 study recognised the limitations of the intervention in providing protection to vulnerable young people living in a potentially dangerous environment. They stressed the need for a wider network of support for these socially excluded families, ranging from the extended family of parents, grandparents to the social institutions responsible for their care and supervision during the investigation of child abuse. The process of dealing with criminal justice system can be humiliating and may have implications for the wider family network, by witnessing ongoing contact with the police, hospital staff, forensic teams and court officials.
Alleged perpetrators
Alleged perpetrators in the Tjersland et al. 673 study were confronted about the abuse during treatment, one-third of whom were unaware of the suspicions prior to therapy starting. Reactions to the allegations presented elicited three different kinds of response: confirmation of the abuse; abuse was denied and the alleged perpetrator withdrew from the mother and child; and abuse was denied but the alleged perpetrator tried to maintain contact with the family. Six of the alleged perpetrators rated the treatment positively, and valued the objective role of the therapist. Those who were critical of the therapy (n = 2, an additional n = 2 were both contented and discontented) were unhappy that they had not been involved from the start and felt that the therapists had formed a coalition with the mother. At the end of treatment, conflicts associated with the question of abuse had been clearly reduced in 20 cases; three families were still facing significant conflict, with two cases brought to court.
In the Woodworth533 study, the offenders were by far the most positive in their satisfaction with the programme, with 88% saying that they were ‘strongly satisfied’ and 83% describing the therapy as ‘very helpful’ to them personally.
Summary: acceptability of systemic interventions
The heterogeneity of these five526,533,621,673,678 studies makes it very difficult draw out clear messages. Generally, participants appear to find these interventions acceptable, with the exception of a high refusal rate amongst siblings in the intervention studied by Woodworth. 533 This was a multiple family incest treatment programme and it is perhaps unsurprising that siblings who had not experienced maltreatment would be unenthusiastic at participating in an intervention that exposed their family difficulties to strangers. Participants in the Tjersland et al. 673 study reinforced the concerns of young people in the advisory group of this study673 about the potential adverse consequences of disclosing or sharing their experiences. Mothers in this study673 were also apprehensive about the negative consequences of therapy: they wanted help for their child but did not want them retraumatised, and they were worried about the consequences for family members when these were implicated in abuse. The potential value of group work for children is evident in several of these studies.
Psychoeducation
Four161,538,658,664 studies considered issues relevant to the acceptability of psychoeducation interventions. See Table 18.
| Study/location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Barth 1994161 USA |
P Foster parents of sexually abused children (mean age 8.2 years); 87% female; 69% black; 18% Caucasian; 13% Latino I 11 structured group sessions with homework C N/A O Child behaviour (CBCL257 and CSI423) |
n = 15 | Brief client satisfaction survey | High levels of endorsement, overall group ratings:
Providing child care encouraged them to come and made them feel appreciated Travel expenses helped – foster carers are often financially burdened |
|
| Boisvert 2008658 Canada |
P Foster parents of sexually abused children aged 12–17 (M = 14.63) years I 8–22 × 2-hour sessions of group-based psychoeducation C N/A O N/A |
n = 116 | Dropout (defined as someone who agrees to therapy and participates in at least one session and stops before the half-way point without therapist approval or an agreement that treatment is finished) | Univariate and multivariate analyses exploring relationships between dropout and sexual abuse, individual and family characteristics | 19.8% did not complete treatment Higher dropout was associated with higher levels of:There were no family characteristic differences between completers and non-completers |
| Hyde 1995538 UK |
P Sexually abused children aged 4–16 years; 85% female I Family network PLUS age-group for children, stratified by age; single-sex groups for abused teenage girls; separate groups for teenage boy perpetrators, adult perpetrators, caretakers and couples in which a partner was an abuser C Family network treatment O Children: All – Health and behaviour (20-item maternal report/interview738) ; Teacher’s Behaviour Checklist289) Children 8–16 years: Self-esteem (SPCC/A401,432); Depression (CDI430); Health and behaviour (12-item self-report/interview738) Children 6–7 years: Pictorial Scale of Perceived Competence and Social Acceptance for children (PSPCSA467); Family Relationships (FRT739) Mothers: Self-esteem (ICHSEQ435); psychiatric state (GHQ740) |
Interview and rating | Positive 71% of children and all of the mothers felt that meeting others with similar experiences was positive 78% of children rated the programme highly for preventing further abuse 65% found it useful for guilt resolution 41% better understood origins of abuse Negative < 50% of children felt positive talking about abuse 62% of mothers felt positive Mothers rated helpfulness of treatment lower than children |
||
| Rushton 2000664 UK |
P Sexually abused children; 75% of mothers and 70% of foster mothers were white British I Psychoeducational Group Therapy (girls) plus carer support C Focused individual therapy (girls) plus carer support O Girls: KSADS,405 CGAS;261 carers: interview schedules designed for the study |
n = 58; n = 46 mothers, n = 19 foster/adoptive mothers; 14 carers attended a total of three groups | Carer interviews: 1- and 2-year follow-up; follow-up interviews with carers’ workers 1 year after start of treatment | Carers rated the intervention largely positively: 30% found it very beneficial, 48% beneficial Mothers who were in a relationship with the abuser were more likely to have negative/mixed views of treatment. Those who reported positively on help for themselves attended on average 8.8 months; those who had mixed/negative views attended for less than half this time (4.3 months) Foster carers/adoptive mothers attended for longer (9.2 months) but birth mothers reported higher levels of satisfaction Most caregivers reported continued improvement of children at both 1- and 2-year follow-up Would have liked longer period of treatment and ongoing support available to help deal with isolation and stigma |
Description of studies
Study design
The study by Hyde et al. 538 was related to a randomised trial. 169 Although the carers in the Rushton and Miles664 study were not randomised, the study was part of a trial in which the sexually abused adolescent girls for whom they cared were randomised, and the carers offered either a carers’ group or individual support. 116 The study by Barth et al. 161 was a COS with a control group. The Boisvert et al. 658 study was an uncontrolled study, designed to investigate attrition rates amongst sexually abused children who were referred to mental health services.
Sample sizes
The total sample in the Barth et al. 161 study was 27, with 15 foster carers assigned to the intervention group. Hyde et al. 538 had a sample of 47 adolescents and their families and Rushton et al. 658 had a sample of 65 carers. Boisvert et al. 658 analysed data relating to 116 adolescents.
Location
The study by Boisvert et al. 658 was based in Canada, whereas the Barth et al. 161 study was based in the USA. The studies by Hyde et al. 538 and Rushton et al. 664 were conducted in the UK.
Participants and maltreatment
All participants had a history of sexual abuse. Participants in the Hyde et al. 538 study were the youngest, ranging from 4 to 16 years. Both Barth et al. 161 and Boisvert et al. 658 report data relating to adolescents aged 12–17 years. Although Rushton et al. ’s664 study was focused on carers, the children in the original trial were aged 6–14 years at recruitment.
Ethnicity was reported for the participants in the Barth et al. 161 study (69% black people). Carers and mothers in the Rushton et al. 664 study were largely white and UK born (75%), with another 10% being African Caribbean and 7% Mediterranean.
The studies by Barth et al. 161 and Hyde et al. 538 had a predominantly female sample. The Boisvert et al. 647 study did not provide any data on gender.
Interventions
All of the interventions were group based, although Barth et al. 161 also included some individual work, and Rushton et al. 664 compared group-based support with individual support. Hyde et al. 538 also incorporated some family network meetings.
Groups typically ran for at least 8 weeks and, for some young people, groups ran for around 20 weeks. 538,647 In the Rushton et al. 664 study, treatment was planned for 30 weekly sessions for the girls, and the work with carers lasted for the same duration, but the authors note that it was not uniform because of limited resources. Birth and adoptive parents were usually seen weekly; foster carers were usually seen fortnightly.
Characteristics of treatment completers
In the study by Boisvert et al. ,647 those who had attended 15 sessions were considered to have completed treatment; non-completers attended no more than four sessions. There was a 19.8% dropout rate. Higher dropout was associated with higher levels of sexual abuse impact, behavioural difficulties, social difficulties and delinquency. There were no family characteristic differences between treatment completers and non-completers.
Acceptability
Two161,538 studies collected data on the acceptability of the intervention using client questionnaires. Hyde et al. 538 supplemented questionnaire data with data from interviews. Rushton et al. 664 gathered data from foster carers, using two established schedules at baseline and follow-up (1 and 2 years). Boisvert et al. 647 presented a profile of treatment completers.
Children’s views
The rating scale used to measure participant satisfaction is not described in Hyde 1995538 but, as indicated above, ratings were supplemented with qualitative interviews. Feedback was generally positive, but fewer than half the children were positive about talking about the abuse or felt that, as a result of the group work, they understood the origins of the abuse any better. Seventy-eight per cent said that they did find it useful for preventing further abuse and dealing with feelings of guilt. The helpfulness of treatment was generally rated higher by children than by their mothers.
Children in this study538 generally welcomed the opportunity provided by the groups to meet with others with similar experiences, but not all, and less than half of those interviewed felt positively about talking about the abuse.
Neither the Boisvert et al. 658 study nor the Rushton et al. 664 study report the views of children.
Caregivers’ views
A brief client satisfaction questionnaire was given to foster parents in the study by Barth et al. 161 and the programme received high levels of endorsement for the group, but the length and intensity of the intervention were insufficient to observe any measurable changes of effectiveness.
Rushton et al. 664 report that most carers were positive about the support provided to them (30% ‘very beneficial’, 48% ‘beneficial’). Mothers who were still in a relationship with the abuser were more likely to have negative or mixed views of the help provided to them and their daughter. Analyses indicate that those who reported positively on the help provided to them attended for an average of 8.8 months compared with those who had a mixed negative response, who attended just half of this time (4.3 months). This might mean that mothers who were not helped dropped out sooner, or that those who attended fewer sessions (perhaps for different reasons) did not receive enough help to find it beneficial. The authors note that both foster carers and adopters attended for significantly longer periods (M 9.2 months) than the birth parents (M 6.1 months), although, when levels of satisfaction were explored, birth mothers appeared to benefit more than foster carers, but the difference was not significant; few respondents said they received little benefit and foster carers were few in number.
The authors hypothesise that ‘mothers who clearly valued the support provided would probably have benefited from an independent professional listening to their difficulties and dealing with feelings such as guilt and anxiety’664 (p. 425), which, in turn, may have prevented deterioration in their relationships with their children. This study664 was primarily designed to examine the relationship between kinds of support to carers and outcomes for children hence the rather speculative reflections on what the help meant to carers themselves.
Summary: acceptability of psychoeducational Interventions
The available evidence presents a rather tenuous and fragmented picture of the acceptability of psychoeducational interventions. The one658 study to explore attrition identified severity of sexual abuse impact and behavioural problems as associated with dropout, but this was just one study, with a modest sample size, providing psychoeducation in a group format.
Where solicited, feedback from children and caregiver was generally positive with the exception of participants who were still in a relationship with the alleged perpetrator. The authors of this study664 speculate that mothers who valued the support provided might have benefited form further, personalised support. Again, there is support for the value of group work for children who have experienced sexual abuse.
Group work with children
Seven169–171,636,637,639,676 studies explored the acceptability of children/young persons’ group interventions. For details, see Table 19.
| Study/location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Ashby 1987636 USA |
Group Treatment Program P Sexually abused girls aged referred by tribal social services; 100% American Indian I 10 × 2-hour sessions led by an female Indian therapist C N/A O N/A |
n = 9 | Acceptability and usefulness evaluation rating on numerical scale – midway and final group; school counsellor reports | Programme rated on average 9.8, on a scale of 1 (poor) to 11 (outstanding) Indian talking circle was rated as most useful Data from school reports saw positive behaviour change in 70% of participants |
|
| Baker 2001637 USA |
Family Learning Program P Sexually abused children aged 3–18 years I Individual, group (sibling) and family programme, including child abuse prevention skills and reunification therapy if required C N/A O N/A |
n = 5–14 | Satisfaction ratings; evaluations conducted in 1997, 1998 and 2000; four group evaluations and follow-up telephone survey of n = 7 terminated clients | Satisfaction ratings generally high Reasons for including siblings in treatment:
Additional resources required |
|
| De Luca 1995170 Canada |
Children’s Group P Sexually abused girls, age range 7–12 years; I Circle time and activities designed to address issues around sexual abuse, groups of six to eight children 90 minutes × 9–12 weeks C Group of girls with no abuse history O SEI436; RCMAS293; CBLC257 |
n = 35 intervention, n = 35 control | Child-report measures | Positive Children liked group members, leaders and activities Group helped children deal with issues, ‘taught me how to say yes, no and who to tell and taught me that abuse was not my fault’ Parent feedback was generally positive Negative Disliked some group members/disagreements Frightened by puppets and idea that abuse might recur Some parents would have liked to observe the group and receive more feedback |
|
| Grayston 1996171 Canada |
P Sexually abused boys aged 8–10 years I 12 × 90-minute weekly group sessions C Wait-list O CBCL;707 CSBI;259 frequency counts of up to three problem behaviours identified by caregivers |
n = 6 | Child feedback and parent feedback questionnaires | Most parents and children found intervention helpful All children enjoyed attending the programme Children liked feeling safe and were satisfied with the group and level of parental involvement Half of parents suggested more feedback would be helpful |
|
| Gustafsson 1995676 Sweden |
Psycho-pedagogical Group Therapy P Physical abuse and domestic violence witnesses, children of alcoholics; age range 5–20 years, 53% F I Based on Alcoholics Anonymous family systems theory, weekly group meeting C N/A O N/A |
n = 19 | Semistructured interviews with group therapists | Working with the whole family diminished dropout rate Children of alcoholics need specific help – group work was sometimes difficult because children had relational problems and were fearful of discussing parent’s abuse |
|
| Monck 1996169 UK |
Family Network Treatment Programme P Sexual abuse; 85% female I Family treatment meeting every 4–6 weeks; group treatment by age ranging from 6 to 8 weeks (mixed gender groups for ages 6–10 years, parents, perpetrators) to 20 weeks for adolescent girls C Family treatment only O Children: CDI;430 SPPC/A;431 FSC-R433; CBCL294 Parents: GHQ434; ASEP435 |
n = 47 | Participant rating | Children rated the programme Positive Therapist’s interview style, gender, feeling understood Meeting others with similar experiences Talking to the abuser Most helpful: preventing further abuse; raising self-esteem; offering understanding and resolving guilt Negative Talking to a parent or family about the abuse Mixed/no effects Relations with current family; enabling further disclosures; planning for the future; understanding the origins of abuse Mothers found it helpful preventing further abuse, offering support and dealing with their role in the abuse It was rated unhelpful/no effect for accepting the abuse has happened; discovery of future abuse; resolving own guilt; relating to family; future planning; relating to perpetrator; understanding origins of abuse; relating to managing abused child |
|
| Peled 1992639 USA |
Support and education P Children aged 4–12 years who had witnessed domestic violence, four children also physically abused; one sexually abused. 60% female; 73% white, 27% mixed race I 1 hour × 10 weeks, children’s group and concurrent therapy group for adults 1 hour × one final family group session C N/A O N/A |
n = 30 | Interviews with n = 16 mothers, n = 5 fathers, n = 4 group leaders, n = 30 children; observations of one group | Findings highlighted four major group goals: ‘breaking the secret’ of abuse in the children’s families; learning to protect oneself; having a positive experience; and strengthening self-esteem. Under a positive experience, children described needing to feel safe in the group and their negative expectations of the group, which improved over time |
Description of studies
Study design
All but two171,636,637,639,676 studies were uncontrolled studies. The De Luca et al. 170 study was a COS, and the Monck et al. 169 study was a quasi-randomised trial.
Sample sizes
Sample sizes were all small, ranging respectively from just six and nine, respectively, in the studies by Grayston and De Luca171 and Ashby et al. ,636 to a sample of 95 in the study by Monck et al. 169
Location
Three636,637,639 studies were based in North America and two170,171 in Canada. The study by Gustafsson 1995676 was conducted in Sweden, and the Monck et al. 169 study was UK based.
Participants
Interventions were delivered to children as young as 3 years, and up to 20 years. In five169–171,636,637 studies, all of the children had been sexually abused. Children in the Peled and Edleson639 were in treatment as a result of witnessing domestic violence. The participants in the study by Gustafsson 1995676 had suffered physical abuse, parental alcohol misuse and had witnessed domestic violence.
In two170,636 studies the participants were sexually abused girls and in the study by Grayston and De Luca171 the participants were sexually abused boys. The remaining four169,639,676 studies had mixed gender groups. Ashby et al. 636 describe a population that was 100% American Indian, referred by tribal social services.
Intervention
Interventions comprised group activities (including art activities/circle time), abuse prevention skills, family reunification therapy and psychotherapeutic approaches. Interventions were delivered in group settings for children with similar abuse histories or, as in one study,637 a sibling/victim group setting.
In four170,171,636,639 studies treatment lasted between 10 and 12 weeks. Treatment in Monck et al. 169 could last up to 12 months. No information was available in the remaining two studies. 63,637
Acceptability
Four169,171,636,637 studies used questionnaires or rating scales to measure satisfaction.
Baker et al. 637 reported findings from telephone surveys, used to interview treatment completers, drawing on four different group evaluations conducted in 1997, 1998 and 2000. Ashby et al. 636 augmented data from children with data from school counsellor reports. Gustafsson et al. 676 interviewed group therapists using semistructured schedules and De Luca et al. 170 collected data using child report measures and a social validation scale. Peled and Edelson639 used interviews and group observations.
Children’s views
Using a child feedback questionnaire, Grayston and De Luca171 found that most children found the group helpful, enjoyed attending, liked feeling safe and were satisfied with the level of parental involvement. They had no suggestions for changes. No objective measures were used to assess satisfaction levels, and this is a limitation of this study. 171
Participants in the studies by Ashby et al. ,636 Monck et al. 169 and De Luca et al. 170 rated the programmes positively. On a scale of 1–11 (11 = outstanding), the group treatment programme in the Ashby et al. 636 study scored 9.8 on average. Data from school counsellor reports saw positive behaviour change in school for 70% of participants. Children rated therapists highly in the Monck et al. 169 study and valued meeting others with similar experiences; they also valued being able to talk to their abuser. Some reported negative feelings about talking about the abuse, their family and the hospital location of the therapy. The majority felt that it was helpful in preventing further abuse, raising their self-esteem, understanding and feelings of guilt surrounding the abuse. There was mixed effects for relations with their family, planning for the future and understanding the origins of the abuse. The children in the De Luca et al. 170 study also reported similar positive and negative responses, plus some elements that frightened them, for example using puppets and the idea that abuse could recur.
Child-reported benefits of treatment identified in the study by Peled and Edleson639 included self-protection and strengthening self-esteem.
Caregivers’ views
Parents surveyed in the study by Baker et al. 637 viewed the sibling group intervention positively, and, in the 2000 survey, parents’ mean score rating was 1.9 (on a scale of 1 to 4, with ‘4’ = unsatisfactory). Parents felt that their children had learnt how to deal with inappropriate advances (score 1.5) but helping the child to cope with stress was rated less positively (score 2.8).
Monck et al. 169 also report mothers rating the prevention of further abuse as helpful, but the intervention fared less well when trying to deal with issues including understanding why and accepting abuse has happened, resolving guilt relating to the family and managing the abused child. In the De Luca et al. 170 study, parents believed that the children liked feeling understood and having somewhere to talk about the abuse and someone to talk to, but would have liked to have received more feedback or observe the treatment.
Staff views
The importance of involving siblings in treatment is discussed by Baker et al. 637 – siblings have a high risk of being abused too and often there are unresolved feelings of anger, jealousy and guilt, particularly if a family member is the perpetrator. On a purely practical level, involving all family members enables therapy to happen as no child-care issues arise. Sibling therapy also adds to the costs of the treatment, which may not be covered by the provider; it also has implications for rooms, materials and staffing.
Summary: acceptability of group work interventions
Generally, evidence for the acceptability of group-based interventions for maltreated children is very positive. Although, superficially, group work may appear to be a very efficient way of providing therapy, it requires a great deal of planning, special training and resources. Generally, these issues are not considered in one-off studies of this intervention, although the lack of attention to such issues is not unique to group work.
Counselling/psychotherapy interventions
Fourteen175,176,638,640–646,657,674,677,679 studies addressed issues of the acceptability of counselling interventions.
Four647,648,665,675 studies did so for psychotherapy interventions. In reality, there appears to be little difference between these two groups of interventions, other than how the authors describe them.
Counselling interventions
Details of the 14 studies of counselling interventions can be found in Table 20.
| Study/location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Baginsky 2001640 Italy, the Netherlands and UK |
Looks at pattern of provision in three countries and the reaction of young people who had or had not received services | n = 130 | Italy: n = 36 telephone interviews The Netherlands: n = 25 face to face, letters, telephone and questionnaires UK: n = 41 face-to-face group and parent interviews |
Summary overview | Provision Not enough support available Range of provision required for variety of needs Provision at local and national level needs to be mapped and made available to young people, parents and professionals Multiprofessional interventions and co-ordination required Open-door policy if clients need to return to counselling Sexual abuse Not enough awareness of damage of sexual abuse Schools have a role to play in prevention and harm reduction |
| Fowler 1992641 USA |
P Sexual abuse; mean age 11.83 (SD 3.17) years; 100% female I Counselling C N/A O Comfort ratings of male vs. female examiner |
n = 35 | Seven-point Likert scale | n = 19 were examined by a male counsellor, n = 16 by a female counsellor Pre-consultation: n = 25 preferred a female, n = 7 had no preference, n = 3 preferred a male Post-examination: No significant differences in ratings of comfort with examiner [χ2(2,35) = 0.50; p > 0.77] |
|
| Fowler 1993642 USA |
P Sexually abused; age range 1–17 (M = 8.24) years; 83% female; 77% Caucasian, 22.5% African American I Psychoeducationally based individual counselling; 50 minutes × six sessions C N/A O N/A |
n = 20 | Pre- and post-treatment preference for male or female counsellor | Pre treatment, all participants stated a preference for female counsellor Post treatment, 3/10 (30%) of the girls treated by male counsellors reported a preference for male counsellors 10/10 (100%) of the girls treated by female counsellors continued to indicated a preference for female counsellors |
|
| Haight 2010175 USA |
P Physical, emotional, sexual abuse and neglect – children of methamphetamine-misusing parents placed in foster care; age range 7–14 (M = 9.6) years; 60% male; 100% Caucasian I 7-month, LSI 1 hour per week C Wait-list O CBLC297; PPVT-III441 |
n = 15 children from n = 12 families | Views from children, caregivers and community clinicians; field notes | Emic coding | Children’s views:
|
| Haskett 1991657 USA |
P Sexual abuse; mean age 8.24 (range 1–17) years; 83% female; 77% white, 22.5% African American I Long-term counselling C N/A O N/A |
n = 129 children referred for counselling in a 6-month period | Factors associated with treatment entry | Factors associated with successful treatment entry Attenders: n = 84, mean age 8.5 years Non-attenders: n = 45, mean age 7.7 years Higher percentage of males than females attended Higher percentage of Caucasians attended Attenders and non-attenders did not differ in parental educational level, marital status or SES Children in homes with telephones more likely to attend first session and if mothers felt entire family required counselling Referrals to private centres more likely to attend first session |
|
| Kilcrease-Fleming 1992643 USA |
P Sexually abused; age range 7–17 years, 100% female I Six sessions of individual counselling C N/A O N/A |
n = 20; n = 18 videos analysed | Three counselling process rating scales of videotaped interviews | MANOVA results found no significant differences in counsellor gender; however, a significantly higher verbalisation by female counsellors than their clients was observed Conclude that female victims do not necessarily need to be treated by female counsellors |
|
| Kolko 1999644 USA |
P Neglect, maltreatment, physical and sexual abuse; mean age 11.6 (SD 5.29) years; 62% female; 54% African American, 38% Caucasian, 8% biracial I Various individual and group counselling treatments C N/A O N/A |
n = 86 | Children and parents completed an evaluation of the level of perceived service needs, motivation and interests, goals or expectations and obstacles; interviewed at study intake and 4–8 months after initial service Services used Prediction of total service involvement: Child: CBCL269 Parent: CANIS432 BSI741 CAPI366 Family: SOCSS742 FES710 CTS743 CLEI744 |
Predictors of service use computed using Pearson correlations or chi-squared tests | Variables associated with overall service involvement:
Children perceived to have a high level of motivation to participate in services. Children identified parent factors as the largest obstacle to treatment completion. Sexually abused children were more likely to have received services at post-service assessment |
| Nelson-Gardell 2001638 USA |
P Sexual abuse; age range 10–18 (M = 13.7) years; 100% female; 70% white, 21% black, 9% other race or ethnicity I Not specified C N/A O N/A |
n = 34; five focus groups | Focus group methodology to address the issues of interest | Thematic analysis | Four themes emerged:
|
| Overlien 2011674 Norway |
P Physically abused children, aged 4–18 years, in women’s refuges; 73% female; mostly non-Norwegian ethnicity I Life in refuge, including unspecified counselling C N/A O N/A |
n = 50 women’s refuges directors, n = 22 children | Face-to-face interviews, age-appropriate schedules | Grounded theory approach | Counselling valued and considered helpful by most children Play/leisure time was an important element of intervention, as well as the physical safety of the environment as real life and school routine activities can be disrupted by move Some language difficulties, as majority of population are immigrants |
| Porter 1996645 USA |
P Sexually abused; mean age 12.65 (SD 2.79) years; 100% female; 63% Caucasian, 37% African American I Six sessions of psychoeducation-based individual counselling; 10 male, 8 female Caucasian counsellors; C N/A O N/A |
n = 27 | Client Behavior System745 – verbalisation measure | Girls were rated as verbalising more resistance in response to sexual abuse questions regardless of the sex of the counsellor. Verbalisation may be more influenced by the type of question than the gender of the counsellor | |
| Reddy 2013176 USA |
P Children aged 13–17 years, subject to physical, emotional and sexual abuse or neglect; 65% female; 89% African American I Cognitive Based Compassion Training C Wait-list O CBCL;297 QUIDS-SR;442 STAI-T;333 FASM;443 SQFI;444 DERS;446 ICU-P;447 CTQ;448 cortisol and C-reactive protein levels |
n = 70 | Qualitative post-treatment feedback | 62% found the programme to be very helpful; 30% a little helpful Frequency of thinking about CBCT principles or lessons outside class? 41% a lot, 46% once in a while 87% would recommend to friends Like programme to be offered in schools? 40% yes, 46% not sure, 14% no Programme length? 60% just right, 27% too many, 11% not enough Participants felt moderately connected to their classmates (M = 6.86, SD 2.49) Participants felt more strongly connected to their instructors (M = 7.14, SD 2.07) |
|
| Scott 1996677 Australia |
P 80% sexually abused; age range 15 months to 10 years I Individual and group counselling C N/A O N/A |
n = 10 families (n = 17 children) | In-depth interviews with parents | Mixed views about value of child expressing painful feelings Parent/professional tension – alienated and ambivalent about professional’s role, plus personal guilt and distress Contamination of normal sexuality in family and fear of future sexual/relationship problems Disintegration of social network support and impact on parental relations. Propose holistic approach to supporting child, which includes immediate and wider family |
|
| Deb 2011679 India |
P Sexually abused children rescued from red-light areas; aged 13–18 years, 100% female I Basic support services plus individual and group counselling in rehabilitation homes; 2–3 months’ duration with weekly-plus counselling C Non-abused comparison group O The Adjustment Inventory (Paul 1995)746 |
n = 120 Purposive sampling from four randomly selected shelters (one government run, three private) Non-abused control group from local schools |
Quantitative and qualitative data | Desruptive statistics and t-tests | 58.3% found counselling beneficial, 41.7% found it ‘non-facilitative’ |
| Thompson 2011646 USA |
P 55% had a history of child abuse or neglect; mean age of youth 15.20 (SD 1.38) years, mean age of mothers 41.1 (SD 6.16) years; 65% female youth I Various mental health services C N/A O N/A |
n = 40 | Semistructured interviews developed to elicit information about mothers and youth experiences and satisfaction with mental health services | Mothers’ views 48% generally satisfied 21% dissatisfied – feeling service providers were not invested or interested in them 40% both satisfied and dissatisfied – felt that some counsellors did not act professionally Youth views 52.4% were satisfied, liked being able to talk to someone, learn to deal with anger 23.8% were dissatisfied – medicating was seen as a short cut, relationship with counsellor also important |
Study design
The study reported by Haight et al. 175 was a randomised trial.
Baginsky640 conducted a review of the pattern of provision in the UK, the Netherlands and Italy and the reaction of young people who had or had not received services. The literature review was followed by interviews (both face to face and telephone), group discussions, questionnaires and letters to collect additional data.
Deb and Mukherjee679 used purposive sampling from four randomly selected shelters across Kolkata, India, and sourced a non-abused control group from local schools, which were also randomly selected. Both qualitative and quantitative data collection were used.
The other studies176,638,641–643,645,646,674,677 were uncontrolled designs, each using a purposive sample of those engaged in treatment. The studies by Fowler et al. 641,642 examined the acceptability of counsellor gender for treatment for sexual abuse. Kilcrease-Fleming et al. 643 also investigated counsellor gender using a standardised rating scale of video-taped interviews analysing differences in verbalisation between male and female counsellors. Porter et al. 645 used the Client Behavior System verbalisation measure to assess gender differences in counsellors. Thompson et al. 646 used two semistructured interview guides to interview both mothers and youths. Scott 677 also conducted in-depth interviews with parents. Nelson-Gardell638 conducted focus groups. Overlien’s674 investigation of counselling provision in women’s refuges used a grounded theory approach to conduct face-to-face interviews while using age-appropriate schedules. Reddy et al. 176 relied on qualitative post-treatment feedback to assess intervention acceptability.
Kolko et al. 644 conducted quantitative analyses to predict service use and Haskett et al. 657 used regression analysis to investigate treatment entry.
Sample sizes
Sample size varied. Haight et al. 175 recruited 17 children from 10 families, and Scott677 recruited 15 children from 12 families. Nelson-Gardell638 recruited 34 participants, and four641,643,645,674 studies had samples of around 50. The largest study640 had 130 participants. The studies by Fowler and Wagner,642 Haskett et al. ,657 Reddy et al. ,176 Kolko et al. 644 and Deb and Mukherjee679 all had between 70 and 100 participants.
Location
Most of the studies were USA based. One677 was set in Australia, one679 in India and another in Norway. 674 Baginsky640 examined counselling provision for young people across three nations: the UK, the Netherlands and Italy.
Participants
All studies focused on participants with a sexual abuse history, apart from Overlien,674 who examined physically abused children who had witnessed domestic violence. The sample in Kolko et al. 644 had also been subjected to neglect, and those in the studies by Haight et al. 175 and Reddy et al. 176 had been exposed to a range of abuse and neglect. Baginsky640 did not specify type of abuse, but sexual abuse recovery was included in the findings; therefore, an assumption has been made that at least part of the sample had been sexually abused.
Interventions
Four644,674,677,679 studies reported on IGT – concurrent with individual counselling. The group therapy included counselling with other sexually abused girls,679 family members644,677 and play therapy within a women’s refuge setting. 674
Five640–643,645,657 studies examined individual counselling, four of which specifically analysed counsellor gender preferences pre and post treatment. 641–643,645 Haskett et al. 657 examined factors associated with successful treatment entry for long-term counselling and, last, Baginsky640 reviewed varied counselling provision in Europe.
Counselling for sexually abused girls in Kolkata679 was based around basic support services, as many of these girls had been living on the streets and had been sexually exploited; provision included nutrition, safety and security, education and training, and medical care, as well as counselling. The intervention lasted between 2 and 3 months, and individual and group counselling were delivered on a weekly basis, with more if required.
Participants in the study by Nelson-Gardell638 had received therapy from a range of counsellors, the details of whom are not provided. In this study638 the researchers wanted to know what and whom the participants had found helpful in recovery.
Fowler and Wagner,642 Kilcrease-Fleming et al. 643 and Porter et al. 645 all report a psychoeducation/psychological treatment programme, which lasted for six sessions. Adolescents in the study by Reddy et al. 176 were provided with CBCT. Haight et al. 175 describe the LSI for children who were living with parental methamphetamine misuse.
Haskett et al. 657 describe the intervention as ‘long-term counselling’. Additional content of counselling intervention is not described in detail.
Young people in the study by Thompson et al. 646 received a range of individual and group-based counselling services in a range of service settings. The families of these participants also received a range of other counselling services, as well as – for some – FT, drug counselling and inpatient services (mothers).
Characteristics of treatment completers
Only two studies644,657 examined the characteristics of those who remained in therapy or dropped out.
Haskett et al. 657 presented factors associated with successful treatment entry for long-term counselling in a convenience sample. A higher percentage of males attended, as did a higher percentage of white Americans, but attenders and non-attenders did not differ in parental education level, marital status or socioeconomic status (SES). Children in homes with telephones were more likely to attend the first session, as were those referred to a private centre. When mothers felt that the entire family needed counselling, attendance was also more likely.
In the study by Kolko et al. ,644 children and parents were interviewed at study intake and at 4–8 months after receiving an initial service. Potential predictors of service use were computed using Pearson‘s correlations or chi-squared tests to determine the relationships between several key clinical characteristics. Four variables were found to be significant, and these were used to perform multiple regression analyses. Four variables predicted the number of services received at intake: white American children with lower levels of anxiety and parents with heightened distress and with more abusive experiences when they themselves were children received more services at intake. Three of these variables also predicted number of services at post-service assessment: white American child, parental distress and low child anxiety.
Acceptability
Children’s views
Highlighting issues raised by the young people they surveyed, Baginsky640 concluded that not enough support was available, and greater awareness was needed of the damage inflicted by sexual abuse. Young people also stressed the need for open-door policies for clients to return for help if necessary.
Another conclusion of those surveyed was that schools have a greater role to play in prevention through protective education and better sexual education.
Four641–643,645 studies considered counsellor gender preference using rating scales (including verbalisation measures and counselling process rating scales) and statement of counsellor gender preference pre and post intervention. The all-female samples in the studies by Fowler et al. 641,642 and Porter 1996645 expressed a preference for a female counsellor pre treatment: 71%, 100% and 100%, respectively. However, only Fowler and Wagner642 re-tested gender preference post treatment and found that 30% of girls treated by a male stated a preference for a male counsellor, while 100% of girls treated by a female stated a preference for a female counsellor.
The studies by Kilcrease-Fleming et al. 643 and Porter et al. 645 examined client behaviour during a counselling session. Kilcrease-Fleming et al. 643 collected data at the initial counselling session using three different counselling process rating scales, which were scored by observers. Data were gathered on verbalisation frequency, overall participation, willingness to return and disclosures made during the session. MANOVA results found no significant differences in counsellor gender; however, a significantly higher verbalisation rate was observed in female counsellors than in their clients. Kilcrease-Fleming et al. 643 conclude that female victims do not necessarily need to be treated by female counsellors. Porter et al. 645 found that the type of questions asked may influence verbalisation, regardless of counsellor gender; girls in this study were found to be more resistant to questions about sexual abuse than other types.
Fifty-eight per cent of the sample in the study by Deb and Mukherjee679 said they found counselling beneficial, although some caveats were made about the limitations of the study design and the potential for sensitive data to be suppressed. The qualitative summary findings in Overlien674 conclude that, with very few exceptions, counselling was valued and considered helpful by the children interviewed. Using a grounded theory approach, children identified the play element of the therapy as important, creating a safe and fun place to play with other children.
Kolko et al. 644 reported some barriers to successful treatment participation. In this study, the young people interviewed identified parental factors as among the largest obstacles to accessing therapy, including ‘parent was too busy to attend’ and ‘parent does not think counselling will help’. Children acknowledged greater obstacles to parental treatment than parents.
Most children in the study by Reddy et al. 176 found the programme to be helpful and 87% said they would recommend the intervention to others. They were less enamoured of undertaking homework tasks and opinion was split about the desirability of offering the programme within schools. They reported that their alliances with instructors were stronger than those with their peers. Similarly, the children participating in the LSI described by Haight et al. 175 mostly characterised the experience as enjoyable, particularly the relationships that they had developed with the community clinicians. Most found having someone to talk to helpful, but they also expressed anxiety at the early stages of the treatment, particularly talking about their experiences.
Nelson-Gardell638 identified four important themes, of which ‘being believed’ was considered to be so important by the focus group participants that they conflated it with ‘being helped’. The other three themes were that talking about what happened is not easy but it helps; talking about feelings helps and – although no one had wanted to go to a therapy group – the groups help. Concern was expressed that if the abuse was not talked about, it would impact on them negatively in the future. In brief, group therapy was found to be difficult but useful.
Caregivers’ views
In the study by Kolko et al. ,644 caregivers rated the severity of family problems higher than children did, and stressed the importance of targeting behaviour and competence as treatment goals.
Scott677 used in-depth interviews with parents to explore family counselling. Parents expressed mixed views about the value of talking about painful feelings and many worried about their children having to relive the experiences through therapy, although other parents felt that this was helpful. Managing parents’ expectations was also raised as an issue: therapy was referred to by some parents as a cathartic process, but children may not see it in the same way or wish to talk. There were also some tensions highlighted in the parent–therapist relationship.
-
Some parents had high levels of anxiety but felt unable to discuss these with the therapist because they were unaware of what was being discussed with their child.
-
As discussed previously, issues of parental guilt that the abuse was able to happen – once this issue was addressed, it became easier to talk about.
-
Some parents felt ambivalent about the therapist’s ‘authority’; counselling for some families was compulsory; once social services were involved, things were taken out of their control.
Scott677 also reports concerns about the impact of secondary abuse. Parents worried about the contamination of normal sexuality in the home, particularly at bath times and getting dressed/undressed. The potential threat to masculinity in fathers was also raised, and some parents expressed anxiety about their child’s future sexual adjustment. Scott677 suggests that female social workers are often unaware of fathers’ concerns, which can lead to further tension between the professional and the family. In their study of family group therapy, Costa et al. 678 highlighted similar concerns amongst parents regarding their child’s future sexuality, with some parents afraid that the sexual abuse would result in homosexuality or lead to inappropriate sexual behaviour with other children.
Secondary abuse also impacted on families’ extended social networks; views of the wider family and local community became coloured by a significant mistrust of adults; this, in turn, put additional pressure on their marital relationships. Investigations by social services and police also attached considerable stigma, which, in turn, negatively impacted on the immediate social support networks of family and friends. Scott677 recommends that the wider family unit is included in the disclosure and subsequent intervention.
Caregiver perspectives were sought in the study by Haight et al. 175 using open-ended questionnaires. Like the children, their views were largely positive, with the relationship between their child and the community clinician considered to one of the most beneficial elements of the programme. Caregivers also recommended that the treatment length should have been extended.
Staff views
Baginsky640 suggests that provision needs to be mapped at both local and national level and made available to young people, parents and other professionals, and that a multiprofessional response is also required.
Kolko et al. 644 found that sexually abused children were more likely to receive child-directed treatment and physically abusive families were more likely to receive in-home crisis services, such as family preservation. At post-service assessment, sexually abused children were more likely to have received services – Kolko et al. 644 attribute this to caseworker perceptions that the sexually abused were at greater risk.
In their interviews, directors of 50 of the 51 women’s shelters in Norway stressed the value of normal and fun activities within the shelter environment. 674 They saw this as especially important when normal family life has been shattered. Scott677 highlighted that professional staff were sometimes unaware of some of the therapist–parent tensions emerging from compulsory counselling.
The clinician field notes analysed in the study by Haight et al. 175 describe the positive benefits of the non-clinical setting, but also suggest some difficulties in maintaining professional boundaries within a community setting while working with vulnerable children. Confidentiality was inevitably breached at times, when clinicians were made aware of risk factors facing these children.
Psychotherapy interventions
Details of these studies647,648,665,675 and the interventions can be found in Table 21.
| Study/location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Davies 2009665 UK |
P Neglect/abuse; age range 8–10 years; 100% female I Individual psychotherapy lasting between 4 months and 3.5 years C N/A O N/A |
n = 4 | Children: Single interview of their experiences of participation in therapy, using age-appropraite methodologies Carers: Interview |
IPA | Children valued feeling able to make their own contributions to therapy; rated importance of non-verbal communication; saw therapists as attachment figures Practical considerations The waiting room was important as it gave time with familiar others; increase level of contact; recommend that physical facilities could be improved |
| Horowitz 1997647 USA |
P Sexually abused children; aged 6–16 years; 100% female; 40% minority ethnic I Psychotherapy including individual and group or FT C N/A O N/A |
n = 81 | Therapy experiences gathered from parents | Regression analyses | Abuse variables were powerful predictors of total sessions of therapy: earlier onset predicted more sessions; child psychopathology – more disturbance was associated with more treatment; family functioning did not predict treatment Non-minority subjects received more therapy than minority subjects, who were typically older, of lower SES and age at onset of abuse was later |
| Jensen 2010675 Norway |
P Sexual abuse; mean age = 8.3 years; 64% female I 3 to 17 (M = 7.5) weekly sessions of individual psychotherapy C N/A O CBCL294 |
n = 15 | Video-taped therapy sessions Separate interviews with children and their carers at the end of therapy and 7 years later |
Content analysis, guided by Bordin’s conceptualisation of the working alliance | Negotiation of goals depended on children’s caregiver. No child could articulate therapy goals at onset but could articulate gradually gained understanding of the purpose of therapy Therapists need to build a positive bond with caregivers, as this relationship may be a reference point for children in interpreting their own relationship with the therapist |
| Lippert 2008648 USA |
P Sexually abused children aged 3–17 years I Psychotherapy based at an urban Child Advocacy Centre C N/A O N/A |
n = 101 | Case record review Caregiver interviews (n = 45) including ‘perceptions related to therapy’, including the ECBI311 and SFI747 |
54% had at least one therapy session, 47% did not begin therapy Initiators of therapy Less likely to be black (33%) than decliners (50%) More likely to report maternal neglect (24%) than decliners (4%) Closer in time to forensic interview Caregivers who declined scored lower on measures of conflict, competence and expressiveness Reasons for declining Work conflict (50%) DCAC was inaccessible (40%) Child was symptom free (15%) Caregiver was busy (15%) Caregiver wanted to forget abuse or let child forget (15%) |
Study design
All studies647,648,665,675 were uncontrolled. In the study by Horowitz et al. 647 the data analysed were collected as part of a longitudinal study of the psychobiological effects of CSA (Putnam and Trickett, 1987–1988748). The studies by Davies et al. 665 and Jensen et al. 675 used qualitative methodologies, and Lippert et al. 648 reviewed case records with additional qualitative data collection.
Sample sizes
There were just four participants in the Davies et al. 665 study and 15 in the Jensen et al. 675 study. The other studies647,648 had samples sizes of 81 participants647 and 101 participants,648 respectively.
Location
The studies by Horowitz et al. 647 and Lippert et al. 648 were US-based studies, the Davies et al. 665 study was a UK study and the Jensen et al. 675 study was set in Norway.
Participants
Sexual abuse history was the maltreatment experienced by children in three647,648,675 studies, and in the Davies et al. 665 study the four participants had been neglected/abused. The sample was 100% female in the studies by Jensen et al. 675 and Davies et al. ,665 whereas in the study by Horowitz et al. 647 60% of participants were female. Lippert et al. 648 did not present a gender breakdown. Forty per cent of the participants in the study by Horowitz et al. 647 were described as non-white and the entire sample in the Jensen et al. 675 study was of Norwegian ethnic origin.
Intervention
Davies et al. 665 and Jensen et al. 675 describe individual psychotherapy, but details of intervention delivery are not reported in the studies by Horowitz et al. 647 or Lippert et al. 648 Children in the Davies et al. 665 study had been in receipt of psychotherapy for between 4 months and 3.5 years, and in the Jensen et al. 675 study weekly sessions were provided for a mean of 7.5 weeks.
Characteristics of treatment completers
Horowitz et al. 647 reported that non-minority children received more therapy. Abuse variables were found to be powerful predictors of the total number of therapy sessions, and earlier onset predicted more sessions. Children who experienced higher levels of psychopathological disturbance also received more treatment. Family functioning did not predict level of treatment in the model.
Lippert et al. 648 profiled those who failed to participate in treatment: 46% of the sample of 101 did not begin therapy and 54% had at least one therapy session (therapy initiators). Initiators of therapy were less likely to be ethnically black (33%) than decliners (50%), and were more likely to have been subject to maternal neglect (24%) than decliners (4%). Decliners were those whose first appointments were twice as long from the initial forensic interview following abuse report. Caregivers who declined treatment reported lower scores on the Self-Report Family Inventory (SFI) conflict, competence and expressiveness scales. Reasons for declining included ‘work conflict’ (50%); ‘inaccessible venue’ (40%); ‘child was symptom free’ (15%); ‘caregiver was busy’ (15%); and ‘caregiver wanted to forget about abuse or let their child forget’ (15%).
Acceptability
Interviews exploring children’s experiences of therapy were conducted in the study by Davies et al. 665 Jensen et al. 675 interviewed children and their caregivers, separately, at two different points in time: just after the last therapy session and 1 year later. Lippert et al. 648 relied on parents’ accounts, and presented a profile of non-participation and data from case record reviews. Horowitz et al. 647 collected data from therapists’ reports and ran multiple regression analyses to examine the correlates of therapy usage.
Children’s views
Davies et al. 665 used a range of age-appropriate methodologies to garner children’s experiences of psychotherapy. This was an extremely small sample size (just four), but the children interviewed valued feeling able to make their own contributions to therapy, and they appeared to view their therapists as attachment figures. The importance of non-verbal communication was stressed. Physical space was also raised as an issue: children stated that the waiting room environment was important as it became a familiar place, but they also felt that it could have been improved. There were no measures of therapy outcome in this study. 665 Jensen et al. 675 was designed to explore therapy goals and whether or not these were achieved. Of the 15 children interviewed, none had therapy goals at the outset, and expectations of therapy were low, but, through the course of treatment, a better understanding of the therapy was gained. The play therapy element was also recognised as being enjoyable.
Caregivers’ views
Jensen et al. 675 reports mothers’ fears of feeling condemned by the therapist, and anxiety that they were losing control over the situation. Three aspects were identified as being important in developing a positive bond with the therapist: the therapists’ personal qualities (in contrast to parents identifying qualifications as the most important); the collaborative process between therapist and caregiver (identified as the gatekeeper); and developing a systemic three-way relationship between therapist, child and parent.
Staff views
In the study by Jensen et al. ,675 the parent is described as the ‘gatekeeper’ who enables the child to participate in therapy, and the importance of this three-way relationship is stressed.
Summary: acceptability of psychotherapy/counselling interventions
From the available evidence, we know very little about the factors that predict the engagement of children with counselling or psychotherapy, or what differentiates those who complete therapy from those who do not.
Generally, children and caregivers are positive about counselling and psychotherapy and the therapists delivering them. However, it is largely from these studies that parents’ and caregivers’ concerns about ‘knowing what is happening in therapy’ emerge.
There is no strong evidence to suggest that children have marked gender preferences for counsellors, but it would be a mistake to draw conclusions from this particular set of studies, none of which is very rigorous, and most of which are very small. Those studies emphasise the importance of addressing caregivers’ concerns about the wider impact of sexual abuse on family functioning.
As with all interventions considered in this review, most of the studies were undertaken outside the UK, and there is a need to determine the views of children and young people within the UK.
Peer mentoring
One660 study provided acceptability evidence for peer mentoring (Table 22).
| Study/location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Alaggia 1999660 Canada |
PSP P Sexually abused young people aged 14–21 years I Parent- and youth-led peer support groups, 12-week cycle with open-ended membership C N/A O N/A |
24 families, 26 children | Interviewed a sample of parents, youths and professionals | Summary overview | Parent feedback Respectful, sensitive staff Outreach service was unique; group gave them coping strategies and they felt that they were not alone Youth feedback Enthusiastic endorsement Outreach and staff availability highly rated One-to-one support most important, group work less so Professional feedback PSP fills gaps in services No other agency provides similar support |
Overview of this study
This was a qualitative study,660 undertaken in Canada, with a sample of 24 families with 26 children.
Participants
Participants had experienced sexual abuse and were aged between 14 and 21 years.
Intervention
The ‘Peer Support Program for Parents and Youths’ was led by parents and young people, and was delivered on a 12-week cycle but with open-ended membership. It brought to implement and change existing normal treatment service and was targeted at families that did not benefit from mainstream support or services. Specialising in child sex abuse issues, the group offered flexible delivery and outreach support, and also offered practical advice with legal procedures and child welfare.
Acceptability
A sample of parents, youths and professionals were interviewed to collect data.
Children’s views
Young people ‘enthusiastically endorsed’ (p. 70) provision and found the outreach service to be very helpful. Staff were available by phone during evenings, which was valued. One-to-one support was considered to be the most important element and the youth-led support group was less favourably viewed.
Caregivers’ views
Parents found staff to be respectful and sensitive and identified the outreach service as unique. Parents felt that the parent-led group gave them information and coping strategies and appreciated hearing that they were not alone.
Staff views
Staff felt that the group filled services gaps and that no other agency provided similar support.
Summary: acceptability of peer-mentoring interventions
The evidence base for the effectiveness of peer mentoring is relatively slim (see Chapter 4) but these interventions receive a strong endorsement from children and carers.
Intensive service models
Eight studies provided information relevant to the acceptability of a variety of intensive service provision for maltreated children, details of which can be found in Table 23 (see also Table 24).
| Study/location | PICO | Sample size; response rate | Data collection – acceptability | Analysis method | Findings |
|---|---|---|---|---|---|
| Cunningham 2009649 USA |
Therapeutic residential care P Young people in need of supervision (PINS), with a mean age of 15.5 (SD 1.1) years; 45% female, 38% white, 35% African American I Therapeutic residential care, average length of stay 88 months C N/A O N/A |
n = 130 | Action research 44 semistructured interviews with RTC staff Interviews with primary caregiver (T1a and T4a) School, clinical and residential treatment team questionnaires (T2a and T3a) Data from client case files |
Inductive thematic coding; confirmatory factor analysis | Engaging youth required continual efforts – type of engagement varies and can be unstable The authors conclude that engagement needs to be measured at multiple time points across treatment Staff qualities of client-centred communication and the use of positive reinforcement were strongly correlated with the composite measure of engagement |
| Leenarts 2013672 The Netherlands |
Compulsory residential treatment P Severely traumatised female children aged 12–19 years I Stapstenen stabilisation training psychoeducation and non-exposure CBT C N/A O N/A |
n = 154 | Multiple linear regression for treatment motivation logistic regression to identify possible predictors for dropout | Age and ethnicity associated with motivation for treatment; non-Dutch ethnicity and younger age had significantly higher levels of distress Emotional abuse predicted motivation for treatment more strongly than other types of maltreatment. The study found no significant prediction for (time to) dropout |
|
| Gallagher 2012666 UK |
Therapeutic children’s homes P 8 facilities, each with three to five children aged 16–22 years, subject to multiple maltreatment; 63% female; 94% white I Therapeutic parenting, formal therapy sessions, life story work C N/A O N/A |
Target n = 34 Achieved n = 16 |
Semistructured interviews covering three domains:
|
Summary overview |
Positive
|
| Shennum 1995650 USA |
Therapeutic residential care P Neglected or abused children with comorbid depression, anxiety, attention deficit, CD; mean age 11.8 (SD 2) years; 32.5% female I 1.5–2 years C N/A O N/A |
n = 80 | Interviews with children, 58 of whom were interviewed after discharge Onsite observations; including video and audio tapes Interviews with staff |
Summary overview |
Positive
|
| West 2014651 USA |
Modified curriculum and ‘Monarch Room’ P Abused and neglected court-involved girls attending a residential school; age range 14–18 years; 100% female; 23% white, 69% black, 8% other I Trauma-informed alternative to traditional school discipline policies and ‘Monarch Room’ intervention designed to develop problem-solving, emotional regulation and sensorimotor activities to de-escalate problem behaviour C N/A O N/A |
n = 39 | Focus group | Thematic analysis | Six focus groups were conducted to help understand the lived experiences of trauma-exposed students and how this impedes classroom learning There were 16 total behaviours identified by the students as behaviours displayed in the classroom or school group Students also identified 23 probable causes for those behaviours and provided 20 recommendations for improving policies and practices in schools Student data were used to build the trauma-informed training intervention for school stuff |
Residential treatment Five649–651,666,671 studies described residential facilities that provided care for maltreated young people with behavioural and conduct problems. West et al. 651 examined the views of young people about a trauma-informed alternative to traditional school policies in a residential care setting, so we include that study651 in this section.
Enhanced fostering Three145,146,667,671 studies reported on enhanced foster care interventions carers.
No study explored the acceptability of, or satisfaction with, therapeutic day care services.
Therapeutic residential care
Details of the five649–651,666,672 studies exploring different types of therapeutic residential care interventions can be found in Table 23.
Location
One672 study was based in the Netherlands and three in the USA. 649–651 The Gallagher and Green666 study was undertaken in the UK.
Study design
Cunningham et al. 649 described the development of a measure of youth engagement that was suitable for use with young people in RTCs. In collaboration with staff from two RTCs, the research team established a programme logic model, which they used to develop a multidimensional measure of engagement, adapting items from existing measures of readiness to change and the therapeutic alliance. The tools were then piloted drawing on data from interviews with young people at four time points, interviews with primary caregivers at the first and last time points, questionnaires to the school, clinical and residential members of the young people’s treatment teams, and data from the client’s case files and school records. Confirmatory factor analysis using maximum likelihood estimation was the primary analytic method used for analysis, and informed subsequent modifications of the measure.
Leenarts et al. 672 examined motivation for change among girls in compulsory residential care, using a range of standardised measures of child maltreatment, trauma and treatment motivation, which they analysed in relation to motivation for treatment, using multiple linear regression analyses, and treatment dropout, using logistic regression.
Both Shennum and Carlo650 and Gallagher and Green666 used semistructured interviews. Both interviewed children who had previously lived in therapeutic residential care; the sample in the Shennum and Carlo study650 included some children still resident at the time of interview.
West et al. 651 used focus groups to explore the views of young people in a school that they attended under court order.
Sample sizes
A total of 154 adolescent girls participated in the Leenarts et al. 672 study and 130 young people were interviewed on four occasions by the researchers in the study by Cunningham et al. 649 Shennum and Carlo650 recruited a sample of 80 young people and Gallagher and Green666 achieved a sample of just 16. Thirty-nine girls participated in focus groups in the study by West et al. 651
Participants
Characteristically, the children served by these interventions were described as ‘unfosterable’ or difficult to place, because of behavioural issues or physical and psychological conditions and/or disability.
The young people in the study by Gallagher and Green666 had experienced severe sexual, physical and emotional abuse and neglect, by one or more members of their family, and sometimes others, which had left them with significant problems of attachment. Previous placements had broken down, often because of challenging (including sexualised) behaviour. Some had experienced subsequent maltreatment in foster care.
Shennum and Carlo650 described residential facilities that were providing care for maltreated young people who were also presenting with behavioural and conduct problems.
Young people in the study by Cunningham et al. 649 had a somewhat different profile in that the majority were in residential care (‘congregate foster care’) as the result of being in need of supervision (53%), and it is not entirely clear whether or not they had a history of maltreatment. A further 38% were adjudicated delinquents and 9% had been referred for reasons including abuse, neglect and special educational needs. It is possible that – with additional information – this study649 would fail to meet our inclusion criteria in respect of participants.
Those in the Leenarts et al. 672 study were in compulsory residential treatment facilities. All had experienced prior traumas, and their histories were characterised by several out-of-home placements (60%), homelessness (30%), police contact of family members (45%) and histories of physical or psychological problems of family members (62%).
The girls in the West et al. 651 study were maltreated girls who were involved in the criminal justice system.
Interventions
The therapeutic residential settings ranged from a compulsory treatment facility for severely traumatised girls651,672 through residential treatment649,650 to a small domestic-style setting described as a Therapeutic Children’s Home,666 where children lived in ‘families’ of three or four children with two adult staff acting in loco parentis. In this setting, the therapeutic model comprised three components: therapeutic parenting (to address attachment issues and a secure base), formal therapy sessions (based on play and expressive arts) and life story work.
The larger residential facilities provided a range of individual and group therapies as well as education. Typically, the environment was structured in ways designed to promote prosocial and to adaptive behaviour. 649,650,672
The treatment setting in West 2014651 was a residential school, which offered a modified training curriculum (The Heart of Teaching and Learning: Compassion, Resiliency and Academic Success) and a ‘Monarch Room’ facility, which promoted emotion regulation and skills to de-escalate problem situations through problem-solving techniques, talk therapy and sensorimotor activities, and avoid student suspensions and expulsions, which are recognised as counterproductive.
Characteristics of treatment completers
One649 study specifically examined factors associated with engagement, but does not provide relevant data, as the study concerned the development of a measure appropriate to residential treatment settings. We discuss the issues raised by Cunningham et al. 649 in our concluding discussion. One672 study explored the factors associated with treatment engagement and dropout, and, given the risks associated with running away from residential care, this study – although conducted in the Netherlands – addresses an important UK-wide issue.
Leenarts et al. 672 report that several demographic variables predicted motivation for treatment, as assessed by the Nijmegen Motivation List 2 (NML-2749). The 34 items in this self-report questionnaire ask respondents to answer using a five-point Likert-type scale, ranging from one (‘not at all applicable’) to five (‘highly applicable’). The NML-2 generates three subscales: (1) preparedness to engage in treatment, (2) level of distress and (3) doubt about treatment. Data on dropout consisted of a total of five possible outcomes: ‘client left: runaway’; ‘judge did not extend stay’, ‘transfer to another facility’, ‘regular termination: end treatment’ and ‘stay not terminated: adolescent is still a resident’. Girls who terminated their stay by running away were identified as dropouts, that is, those who ran away and stayed away for > 14 days and, as a result, were discharged from the facility. In this study,672 23 girls (15%) ended their first uninterrupted stay by dropping out. One girl was transferred to another facility but dropped out after return, resulting in a total number of girls dropping out of 24. Girls with a non-Dutch ethnic background and a younger age reported significantly higher levels of distress and were more likely to engage in treatment.
Level of distress was predicted by a history of out-of-home placements when considering demographics only, and predicted doubt about treatment when considering demographics and childhood maltreatment. The authors point out that out-of-home placements and separating children from their parents may adversely affect their functioning. Out-of-home placements no longer predicted level of distress and doubt once emotional abuse, anxiety, depression and dissociation were taken into account. The authors conclude that the relationship between out-of-home placements and motivation is mediated by emotional abuse and trauma-related symptoms.
Emotional abuse was the type of maltreatment most strongly correlated with motivation to engage with treatment. Girls who reported internalising symptoms (anxiety, depression) were more likely to experience high levels of distress than those with fewer such problems. Girls with dissociative symptoms were more likely to have doubts about treatment. Adolescents are generally more willing to change their internalising problems than their externalising problems, and the authors point out that dropping out of treatment by running away may be attributable to externalising symptoms and antisocial behaviour. They go on to suggest that this is perhaps why the study672 did not find a significant association between dropout and a history of child maltreatment. The authors suggest that as dropout often occurs when adolescents are on leave from residential care; future research should investigate whether or not going on leave adversely affects girls’ motivation for treatment and also the relationship between motivation to change and motivation for treatment.
Acceptability
Three650,651,666 of these five649–651,666,672 studies specifically explored the view of children and young people.
Children’s views
From the qualitative evidence, young people in the study by Gallagher and Green666 valued the therapeutic home-like setting provided, but pointed to limits on the extent to which it felt like a real family home; for example, friends had difficulty calling in if they had not been officially vetted. Participants stressed the need for developing a special relationship with an adult, so that they felt ‘loved’, and that within the constraints of the working environment this was sometimes difficult. They liked the life story work. There was also some evidence of poorly managed transitions, with little or no preparation for leaving care. This intervention is costly and there is currently an absence of robust effectiveness data to support its use.
Therapists were considered helpful and, in the most part, viewed positively by young people in another residential setting,650 but, here too, there were negative views reported: 20% felt that their therapist was too busy to deal with them; 30% disliked the milieu of therapy, as they considered it to be a means of controlling young people; and 60% disliked the behaviour management approach. Only 20% of the sample felt that they had a good relationship with the staff.
The six focus groups convened in the study by West et al. 651 were used to understand the lived experiences of students who had difficulties with their own externalising behaviour and that of others. The girls, over half of whom had a history of maltreatment (just under half were placed for reasons of delinquency), attended a school that aimed to ‘treat, heal, and educate its students by following a school discipline system that incorporates the students’ treatment goals and strategies . . . [and which emphasises] . . . reducing student disciplinary issues by providing an effective social-emotional learning environment’651 (p. 60). Students were asked to identify behaviours that they saw in themselves or others (displayed in the classroom or in the school grounds) and describe the kinds of experiences that led to these behaviours and to say what advice they would give to teachers working with students like themselves. The girls identified 16 behaviours and 23 likely causes. They made 20 recommendations for improving policies and practices in schools. The authors observe that these respondents were very aware of their behaviour and that of their fellow students. They were able to identify triggers from past experience that they felt resulted in highly charged emotional and behavioural reactions that are common among those who have experienced complex trauma. The kinds of linkages that students made included unwanted or unexpected touch, raised voices and references to relatives, as well as triggers unique to particular individuals. They conclude that schools need more trauma-informed teaching practices in order to manage these behaviours.
Enhanced foster care
Details of the three145,146,667,671 studies of enhanced foster care can be found in Table 24.
| Study and location | PICO | Sample size; response rate | Data collection – acceptability | Analysis | Findings |
|---|---|---|---|---|---|
| Biehal 2012145,146 UK |
MTFC-A P Care sample: multiple maltreatment; ages 7–17 (mean 13.06) years; 46% female I Wrap-around multimodal intervention for children in care aimed at reinforcing positive behaviour C TAU O Placement stability; CGAS,479 CBLC,257 DAWBA-RAD |
N = 219; two arms: RCT, n = 34 (experimental MTFC, n = 20; control TAU, n = 14) Observational arm: MTFC, n = 92; comparison, n = 93 Qualitative purposively sampled case studies n = 20 |
Quantitative and qualitative evidence; postal questionnaires, face-to-face interviews, telephone interviews, reports and parent records | Bivariate and multivariate analyses of qualitative data. Thematic analyses of qualitative data In-depth case study analyses |
Children’s views
|
| Laan 2001671 The Netherlands |
Project Intensieve Pleegzorg P Foster parents caring for abused and neglected children; mean length in placement = 5.2 years; comorbid: learning disabled – 32% mild, 22% moderate, 4% severe, 3% profound; physically disabled or disease 37%; ‘deviant conduct behaviour’ 80% I Intensive foster care C N/A O N/A |
n = 78 | Case notes and questionnaire data | Analysis of questionnaire data; thematic analysis of case notes | 74% of children remained with their foster family 2 years after the counselling Foster care is more likely to end prematurely for girls, children with psychiatric problems and for children who had experienced neglect or sexual abuse in their biological family Foster parent views
|
| Staines 2011667 UK |
Therapeutic Team Parenting P Physically, sexually and emotionally abused and neglected children aged 5–14 (M = 12) years, in foster care; 44% female; 87% white; 77% difficult behaviour, 26% school excludes, 20% in trouble with police I Intensive foster care C N/A O N/A |
n = 450 Demographic information for: 299 children; 177 foster carers fostering 221 children |
Questionnaires – foster parents and social workers; at placement start and 1 year on | Summary overview |
Foster carer views
|
No study explored the acceptability of, or satisfaction with, therapeutic day care services.
Location
The studies by Staines et al. 667 and Biehal et al. 145,146 were conducted in the UK. The Laan et al. 671 study was undertaken in the Netherlands.
Study design
Staines et al. 667 used a prospective, repeated-measures design to investigate the supports and services provided to children and carers in an Independent Fostering Agency (IFA), and the relationship between these and children’s progress and placement outcomes over a 12-month period. They used questionnaires to obtain data from carers, children and social workers, at two time points (at the start of a placement and 1 year later). The included paper reports the views of foster parents.
Biehal et al. 145,146 undertook a small randomised trial of the effectiveness of MTFC, embedded in a larger, observational QEx case–control study (see Chapter 4 for details of the RCT).
Laan et al. 671 used data from case notes, together with data from a questionnaire completed by foster carers, to explore the characteristics of children included in an enhanced fostering programme, the content of counselling provided within the service, placement outcomes, and relationships between children’s characteristics and placement outcomes.
Sample size
The achieved sample in the study by Biehal et al. 145,146 was 219 participants (with 34 participants in the RCT). Laan et al. 671 examined case files for 78 children, and secured questionnaire data from 64 of the 78 foster parents. Staines et al. 667 received completed questionnaires from 49% (221) of the IFA foster carers and 66% of the IFA social workers (299) at time 1 – when child was first placed. At time 2 – either 1 year following the start of the placement or when the placement ended, the team secured completed questionnaires from 50% (227) of foster carers and 69% (312) of the IFA social workers. For only 138 placements at time 1 and 80 placements at time 2, were completed questionnaires received from both IFA social workers and foster carers
Participants
Respondents in the study by Laan et al. 671 were foster parents looking after learning disabled children with challenging behaviour. It was the only study671 of disabled children identified. Participants in the study by Biehal et al. 145,146 were children and young people in foster care, aged 10–17 years, who were showing complex or severe emotional difficulties or challenging behaviours, and whose placements were unstable, at risk of breakdown, or not meeting their assessed needs. Children in the study by Staines et al. 667 were aged 5–14 years, who had been in a placement and provided by the IFA participating in the study for > 1 year. All of the children had been maltreated, with most having experienced more than one form of abuse.
Interventions
Biehal et al. 145,146 evaluated Multidimensional Treatment Foster Care for Adolescents (MTFC-A), described as a ‘wrap-around multimodal foster care intervention for children with challenging behaviour’.
The IFA in the study by Staines et al. 667 incorporated a therapeutic approach to its service provision, which recognised the importance of individual therapeutic work with children, but focused the efforts of therapists on supporting foster parents and other staff within the agency. As the authors note, local authorities typically use IFAs for their more difficult-to-place children and this, together with the therapeutic focus, is why this study667 was categorised as one that was concerned with enhanced fostering provision.
Intensive Foster Care [Project Intensieve Pleegzorg (PIP): project for intensive foster care] was the focus of Laan et al. 671 PIP provided foster carers with intensive and specialised counselling by a counsellor who also had access to an educational psychologist, and a psychiatrist or psychotherapist from a multidisciplinary PIP support team.
Characteristics of treatment completers
In Laan et al. ’s671 analysis, intensive foster care placements were more likely to end prematurely for girls, for children with psychiatric problems and for children who had experienced neglect or sexual abuse in their biological family. 671 Staines et al. 667 and Biehal et al. 145,146 do not present systematic data on this issue.
Acceptability
Of the three studies, Biehal et al. 145,146 was the only one to canvass children’s views of the intervention. All three studies considered the views of staff and caregivers.
Children’s views
Using 20 purposively sampled and anonymised case studies, Biehal et al. 145,146 provide qualitative evidence of the acceptability of the intervention to young people. Two young people described the benefits of the points and levels system integrated in MTFC-A, as both had been experiencing considerable problems in care and at school, displaying anti-social behaviour. One boy explained how beneficial the programme was:
I thought it was quite good. It was sort of a target to reach, sort of expectation, and it was sort of good, cos I wanted to sort of beat the expectation, sort of double it. So it was sort of a thing to push myself.
Young male; Biehal 2012, p. 180145
Both boys interviewed felt secure and cared for in their new foster care setting and by the end of year both were retained in the placement. The other boy stated:
They treat me nice and all that and they look after me, make sure I’ve got the right things . . . Like they’re all kind to me.
Young male; Biehal 2012, p. 178145
Biehal et al. 145 reported that there was a sense of genuine affection demonstrated by many carers, which can be absent in other residential care settings. One young person who had been referred for treatment for risk-taking behaviour had initially found it hard to adapt because of the contrast of the MTFC-A placement with previous care settings:
It was hard . . . stricter, like trying to keep in your head certain things that you have to do every day . . . and for someone who’s just come from a house where you had to look after their parents then to a children’s home where you just run riot basically then come into this structured programme, it was very puzzling, difficult to get your head round, but then you get used to it (p. 182) . . . . Mary concludes that ‘Treatment foster care was the best thing ever, I can put my hand on my heart, if it wasn’t for TFC I would probably be in a secure unit by now.
Young woman participant; Biehal 2012, p. 183145
Some children reacted negatively to the points system during the early stages of the programme:
It’s really strict, it’s really rubbish, I had all my stuff taken off me and I have to do stupid things I would have done anyway for points.
Young female participant; Biehal 2012, p. 195145
One child felt that the system was artificial and refused to participate, as the system would not be introduced in a ‘normal family’. Some less successful placements were included in the case studies, including young people with outcome scores that had showed little change or had deteriorated at follow-up. In three of the cases that demonstrated mixed outcomes for the children, all had experienced behavioural difficulties alongside serious emotional problems. Biehal et al. 145 conclude that, in some cases, MTFC may be less effective for young people with serious emotional problems. Although the programme does offer therapeutic support, the main focus is on behavioural change, which may not be the most appropriate intervention for these children. Placements that were disrupted early on, were also less likely to lead to positive changes in the children’s outcome scores.
Caregivers’ views
The Staines et al. 667 study reports high levels of success, with 77% of foster carers reporting that the placement was going well after 12 months. Laan et al. 671 reported similar satisfaction levels (79%) with foster carers identifying the emotional support element of the counselling as the most useful.
In the study by Biehal et al. 145,146 many carers found the points and levels system to be a key contributor to the programme’s success. Typical questionnaire feedback at the 3-month follow up included:
Points and levels rewards are brilliant for her. See this on daily basis. It’s a good thing, gives a second chance . . . Points system motivates the young person. Spending points, buying privileges brings the desired reward for good behaviour.
Foster carer; Biehal 2012, p. 192145
A few carers felt that the programme did not suit some young people: children who did not accept that their behaviour was a problem.
Foster carers in this study145 felt very supported, with the points and levels system creating a distance between the carer and the sanction for poor behaviour. Responsibility for discipline was shared with the team, and the carers were less likely to feel ultimately responsible for invoking punishment. This helped maintain positive relationships. There was also some evidence of carers feeling less stressed because of the ‘depersonalisation of discipline’ (Carer’s view, p. 197).
Resource pressure was cited as a programme difficulty, in particular, staff shortages, which hampered delivery.
Finding appropriate education placements was also considered extremely important by caregivers. Children who had been excluded from school were found an environment to suit their needs, although there was no evidence of improvement in truancy or exclusion rates by follow-up.
Factors that helped placement progress included removing the young person to a new environment in a single placement away from antisocial influences; developing a warm and caring relationship with his/her foster carer; and the child accepting, and being motivated to participate in, the programme. Conversely, the programme could be hindered by the negative influence of birth families and the placement setting at follow-up.
Staff views
The research by Staines et al. 667 on a therapeutic team parenting approach in an IFA found that social workers considered resource limitations, poor planning and lengthy decision-making to have a direct negative impact on the child.
Summary: acceptability of intensive service interventions
We have very little research intelligence about the acceptability of intensive service provision, such as therapeutic residential care or treatment foster care, from the perspective of children and young people, and not much more from the perspective of carers. The data from West et al. 651 indicate that young people are more aware of their behaviour and its likely triggers (and distal causes) than one might imagine, and that training teachers to better appreciate the ways in which trauma impacts on behaviour might help to improve social and educational outcomes for maltreated children, particularly when combined with approaches to the curriculum and behaviour problems that minimise the adverse consequences of externalising behaviour (school expulsion) while maximising the opportunities to develop self-regulation and problem-solving, etc. (the Monarch Room).
The studies indicate that foster carers are able to better care for challenging children when provided with similar support and training. Although the results of the UK study of MTFC-A145 were – at best – mixed, the majority of young people and carers were positive about them.
The study by Cunningham et al. 649 is of interest because of what it has to say about treatment engagement, and we discuss this later.
Activity-based therapies
Five652,661,668–670 studies presented qualitative data in relation to the acceptability of the three types of activity-based intervention: art and creative therapies, play therapies and equine-assisted therapy.
Description of studies
Study designs
All five studies were qualitative studies. The study of art therapy651 was primarily a descriptive account of a group for children in women’s refuges, but included analyses of children’s drawings and reports of the children’s written evaluations of their group experiences. The study of equine-assisted therapy669 incorporated participant observation, field notes and interviews (semistructured, ethnographic conversational plus unstructured interviews). Bannister and Gallagher668 investigated the case histories of children referred to the NSPCC. Hill670 examined case records, supplemented with 48 interviews with parents, therapists and children. Mishna et al. 661 interviewed children’s parents and professionals using semistructured interviews at 6, 12 and 18 months following the start of treatment. Both Burgon669 and Gilbert652 wrote from the perspective of practitioner researchers.
Samples
Samples were extremely small: just seven children in the study by Burgon669 and six in the Bannister and Gallagher668 study. Mishna et al. 661 interviewed the parents, teachers and therapists of 11 children who were undergoing play therapy. Hill670 examined the cases of 13 children who were seen by four therapists. No sample size was available in the study by Gilbert. 652
Setting
Bannister and Gallagher,668 Burgon669 and Hill670 conducted their studies in the UK. The studies undertaken by Gilbert652 and Mishna et al. 661 were based in North America.
Participants
The seven children in the study by Burgon669 were in foster care; they had all experienced multiple abuse and presented with additional problems, such as school exclusion or involvement with youth justice. Those described by Bannister and Gallagher668 were children who had, themselves, been sexually abused and who were sexually abusing other children.
The children in the study by Gilbert652 had been exposed to domestic violence exposure, and those in the study by Mishna et al. 661 included children who had been exposed to domestic violence, plus children who experienced serious verbal, physical and/or sexual abuse, neglect by parents or neglect prior to international adoption by their present parents. The children in the study by Hill670 had also been subjected to physical and/or sexual abuse and neglect.
Intervention
The length of treatment varied with each intervention and population but in three of the studies, the therapy could last up to 2 years. 661,669,670 The weekly group art therapy reported in the Gilbert652 study ran for 8 weeks.
In the study by Bannister and Gallagher668 the treatment could last up to 8 months, although one child withdrew from treatment after 6 weeks, and, at the time of the study, some children were still receiving treatment.
Two interventions were based around creative activity. 652,668 The play therapy interventions described in the studies by Hill670 and Mishna et al. 661 also involved parents. Burgon669 helped to deliver an equine-assisted therapeutic intervention.
The intervention in the Bannister and Gallagher668 study drew on art, play and drama therapy techniques, and included an educative–behavioural intervention to treat offending behaviour; carers were involved as much as possible in the treatment. Two of the six children were seen for 3 months, purely for assessment, but the authors regarded assessment as intrinsically therapeutic.
Acceptability
None of these five652,661,668–670 studies has anything relevant to say about treatment engagement or completion. Hill670 notes that ‘gate-keeping’ was an issue when trying to access children’s views in his research and feels that children’s voices were not adequately represented.
Children’s views
The ethnographic study of equine-assisted therapy by Burgon669 presented some data on children’s experiences of this therapeutic approach. Working as practitioner–observer, Burgon669 identified some positive feedback from the seven children with whom she worked, interpreting these experiences as empowering for them. One young person expressed this as follows: ‘[the horse] kind of made me feel like, you know, I’m the queen of the world kind of thing because I was higher up’669 (p .171). Another child described how she learnt to deal with feelings of anger because she knew that she had to be calm around the horses in case she frightened them. Two other participants demonstrated how trying something new had helped them explore new opportunities with the confidence that they had gained from riding horses. These young people had gone on to begin training in an equine-related career.
Using written feedback from the final meeting of an art therapy group housed in a women’s refuge, Gilbert652 gives positive examples of some children’s experiences, but the data are sparse and it is difficult to draw any conclusions about either acceptability or effectiveness for this group of children who had witnesses domestic violence. She notes that the children raised multiple issues of concern through the weekly art tasks, suggesting that the children were comfortable about doing this and that such group work might provide a fruitful platform for therapeutic work. Unfortunately, this was not the purpose of the group, and no information is provided that addresses the group’s effectiveness, which Gilbert652 acknowledges as a significant gap.
Bannister and Gallagher668 report mostly positive views of the intervention but one child had found it difficult to discuss the abuse and felt that the intervention had not helped their own abuse to stop.
Caregivers’ views
The art therapy for child witnesses of domestic violence was timed to coincide with their mothers attending a therapy session (which meant that babysitters were not required). From a practical point of view, carers thought that this was helpful. 651
Hill’s670 study of parent–therapist interactions highlighted the importance of therapists thinking carefully about the parents’ needs, when and how it is appropriate to involve them in therapy, and when not, and the skills required to do so effectively. One parent described how betrayed she felt following the sexual abuse of her child, and how this had impacted negatively on her trust of all professionals. The ability to follow the parent’s lead at the start of the therapy was identified as important by one therapist, and Hill670 refers to this as ‘interactional expertise’ – valuing the expertise of others and combining it with professional expertise. It is also clear from Hill’s paper670 that parents also needed to be ‘taught’ how to engage with therapy and to recognise that they were part of the therapeutic process too.
Tensions were clear in the study by Mishna et al. ,661 who reported that it took parents some time to develop a relationship with the play therapists working with their children, typically around 1 year. The parents in this study661 had a history of school failure, and were reluctant to engage with parent/teacher consultations; building a relationship with therapists who were school based was considered important in re-engaging the parents in a relationship with the school community.
In the study by Bannister and Gallagher,668 caregivers observed improved behaviour, but this was not sustained in all cases. No acceptability data per se were obtained from carers or children.
Staff views
Burgon669 described positive interactions with young people using horses as a means of initially communicating with them, with a shared goal of riding the horse safely and with enjoyment. She documented the growing confidence of the young people, who were very withdrawn at the start of the therapy, arguing that the children developed empathy and a strong bond with the animals with which they were involved.
The therapist delivering the art therapy intervention in the study by Gilbert652 expressed frustration about the fluctuating membership of her group, with only two children regularly attending the group over an 8-week period. This is perhaps because it was an add-on intervention that was timed to coincide with the maternal therapy group.
The therapists in Hill’s670 study viewed parents as generally supportive, but in need of advice and support in how to deal with the complex difficulties that are associated with sexual abuse. Feelings of guilt and blame are common in parents of sexually abused children, and the therapists in this study670 described how they worked to develop parent confidence in their own parenting skills. Only three fathers were involved in this study,670 but the therapists interviewed described how they took a proactive approach in involving them in their child’s therapy.
Therapists in the study by Mishna et al. 661 identified some practical considerations. Staff agreed that delivering the play therapy intervention within a school setting facilitated the development of rapport with teachers and school administration staff, which was felt to be important to facilitate treatment. Further work was required to develop relationships with parents. During the first year, therapists reported difficulties with parents, which might be attributable to feelings of mistrust and guilt (e.g. as described by Hill670) or reluctance to deal with the school environment. Therapists describe how learning to engage and build trust with the parent ‘typically took up to a full year before regular contact and a degree of trust was established’ (p. 79). 661 There was also evidence of relationship strain between therapists and the teaching staff, which took time to resolve. Teachers valued therapist input into classroom behaviour management and also appreciated knowing more about the child’s family life. More experienced therapists were able to develop a more effective relationship with teaching staff, which, in turn, helped teachers to develop some empathy for the child’s family situation.
Summary: acceptability of activity-based interventions
There are surprisingly few studies of the acceptability of this group of interventions, which, almost by definition, are designed to be attractive to children and young people. Possibly their acceptability is taken for granted. No study of the effectiveness of these interventions incorporated any data that were relevant to any dimension of acceptability, and the evidence base is also rather weak (see Chapter 4). The limited data available within these five studies (Table 25) suggest that children are amenable to engaging in these types of therapy (although we know nothing about those who decline). The most helpful data relate to the important issue of how therapists relate to parents about their involvement in their child’s therapy, emphasising the importance of establishing rapport and being inclusive rather than exclusive about the content of therapy. The study by Mishna et al. 661 raises the possibility about the potential use of schools as settings for therapy, but no more than this. It does remind one of how difficult it can be for parents, who may themselves have had difficult experiences with education, to find liaison with teachers. Given the impact of maltreatment on children’s educational progress, this is an important issue that is too rarely addressed.
| Study and location | PICO | Sample size; response rate | Data collection – acceptability | Analysis | Findings |
|---|---|---|---|---|---|
| Bannister 1996668 UK |
P Maltreated children sexually offending against other children; aged 11–12 years; 17% female; 83% Caucasian I Creative therapy intervention (art, play, drama therapy techniques) with educative/behavioural intervention to treat offending behaviour; treatment lasted up to 8 months C N/A O N/A |
N = 6; n = 1 child refused treatment after 6 weeks | Pre- and post-treatment interviews with social worker, carer and child | Children’s views Five children viewed the intervention positively Most felt treatment length was ‘OK’ They enjoyed the creative elements and videotaping their progress One child found it difficult to talk about abuse, the treatment failed to stop their continued abuse and more help was needed Carers’ views Two carers felt the treatment was too short All observed that the children were calmer/less aggressive but this was not sustained in all cases. Also reported a decrease or cessation in sexualised behaviour There was no follow-up included in the design but some progress was observed in two children, over time, who had received both creative and behavioural aspects of treatment. One child was investigated for sexually abusive behaviour during treatment and for violent behaviour post treatment |
|
| Burgon 2011669 UK |
P Maltreated children in foster and residential care; 71% female I 1–3 hours of equine-assisted learning and therapy/therapeutic horsemanship; weekly, fortnightly or intermittently over 2 years C N/A O N/A |
Agency referred, n = 7 | Qualitative interviews, field note observations | Qualitative, participative and reflexive ethnography; thematic analysis | Motivation to work with horses led to:
|
| Gilbert 1988652 USA |
P Children aged 2–14 years, who had witnessed or been victims of family violence I 8 × I hour weekly behavioural group therapy, delivered in a women’s refuge C N/A O N/A |
Group attendance ranged from two to six children (average attendance n = 4) | Art qualitative feedback | The children were found to process a number of their concerns through the modality of art Behavioural approaches and developmental and curative factors provided the therapist with mechanisms for structure and role Positive group evaluations were received from the children, the therapist, the shelter director and the parents |
|
| Hill 2009670 UK |
P Physically and sexually abused children aged 2–17 years; 46% female I Individual play therapy with children; individual sessions with parents, joint sessions with parents and children: parent peer support group, individual parent support; variety of models ranging from 6 weeks to 2 years C N/A O N/A |
13 families: Mothers, n = 12 Fathers/stepfathers, n = 4 Children, n = 28 |
Qualitative case study of 13 cases comprising in-depth interviews with therapists (n = 27), parents (n = 18) and children (n = 3); plus examination of case files | Thematic analysis | ‘Interactional expertise’ involves valuing the expertise of others (e.g. family member) and combining it with one’s professional expertise It is important, particularly in building trust, to negotiate parental guilt and sensitivity to potential blame, enabling reluctant parents to become involved, and involving fathers |
| Mishna 2012661 Canada |
P Physically or sexually abused/neglected children plus those who witnessed domestic violence; age 4–10 years; 27% female I School-based ecological treatment – independent play therapy 2–3 times weekly, 1 hour of therapist time with parents and teachers over 18–24 months C N/A O N/A |
n = 11 | 63 interviews were conducted at 6, 12 and 18 months with parents, teachers and therapists | Grounded theory approach | School location viewed positively by all: easy to attend; could view child in context Some tensions reported between therapists, teachers and parents, which required resolution, which took up to 1 year Proposed guidelines for best practice |
Studies of general relevance
Three653–655 studies focused on issues relating to children and families receiving a range of services (Table 26).
| Study/location | Intervention; population | Sample size; response rate | Data collection – acceptability | Analysis method | Qualitative findings |
|---|---|---|---|---|---|
| Murphy 2014654 USA |
P Physical and sexual abuse; mean age 12.1 years; 57% female; 58% white, 19% black; 24% other minority or multiracial background; 41% were of Hispanic or Latin American heritage I Community treatment centres across USA, specialising in childhood trauma, providing EBTs C N/A O N/A |
n = 928 | Examined the direct and indirect associations among physical and sexual trauma, child PTSD symptomatology (PTSD-RI750) and treatment completion controlling for demographic variables and treatment site | Mediation analyses; linear and logistic regression modelling | Maltreatment not directly related to the treatment completion Indirect associations
|
| Risser 2013655 USA |
P Children aged 1–11 (M = 3.82) years, exposed to domestic violence and/or child abuse; 54% male; 51% white, 15.9% black, 15.4% Hispanic, 16.1% biracial, 0.8% Native American; 0.8% Asian American, 0.3% other I Individual/family and multimodal therapy and psychoeducation; service length ranged from 0 to 55 (M 6.3, SD 5.4) months C N/A O N/A |
n = 529 treatment completers | Background Information (BI) Completion of Services form (CSF) CBCL349 PSI367 |
ANOVA, MANOVA and regression analysis | Child emotional and behavioural problems, general parent stress and income not correlated with treatment engagement Type of violence exposure, parent–child stress and race differed by category of treatment engagement Children exposed to both domestic violence and child abuse demonstrated higher rates of treatment completion and attended more sessions than children exposed to either domestic violence or child abuse Caregivers with higher levels of parent–child stress were more likely to engage in treatment White children in the full sample completed treatment at higher rates than minority children |
| Koverola 2007653 USA |
Eclectic – individual and group both child and caregiver and FT (including siblings, spouses and grandparents) P Physical, sexual abuse and neglect (41.5% also witnessed domestic violence); mean age 9.6 (SD 3.76) years; 44.2% female; 73% African American, 24% Caucasian; 1% Hispanic I Paediatric outpatient mental health clinic C N/A O Treatment engagement |
n = 118 | Withdrawal metrics Children:Caregivers: |
Three treatment groups identified:
Very few differences in caregivers were observed, but caregivers reporting high child-related parental distress and high psychological distress were least likely to engage in treatment Families receiving multimodal treatment compared with individual/family-only treatment were more likely to comply Comprehensive study design and data collection methodology Measures used had evidence of reliability and validity Interventions clearly described although the eclectic nature of the IT makes results hinders generalisations Data analysis was appropriate and clearly presented |
Description of studies
Study design
All three653–655 studies analysed factors associated with treatment engagement and completion.
Sample sizes
Kolverola et al. 653 analysed the records of 118 children and their caregivers.
Risser and Schewe655 collected data on 1365 children (and their caregivers) for whom services were sought from one of 12 sites between 2001 and 2010.
Murphy et al. 654 used data on 928 youth from the National Child Traumatic Stress Network (NCTNS) Core Data Set (CDS).
Participants included children from birth to age 21 years who received assessment and treatment services from one of 56 community sites between 2004 and 2010.
Location
All of the interventions were USA based.
Participants
The participants in the study by Murphy et al. 654 had suffered physical as well as sexual abuse. In the Koverola et al. 653 study the children had been referred to outpatients with a history of intrafamilial violence, and those in the Risser and Schewe655 study had been exposed to violence, including domestic violence. Ethnicity was reported in all studies, with the majority being white American.
Acceptability
Quantitative analysis was undertaken to examine the direct and indirect associations among physical and sexual trauma, child PTSD symptomology and treatment completion in Murphy et al. 654 The data reported in the study by Koverola et al. 653 were collected through an archival chart review process. Data contained in the charts were drawn from comprehensive assessment protocols completed by the child and his/her primary caregiver, referral forms, progress notes and discharge summaries. Risser and Schewe655 examined factors associated with treatment engagement and child outcome. No data are available on children’s views.
Characteristics of treatment completers
Murphy et al. 654 concluded that neither physical nor sexual trauma was directly related to the probability of treatment completion. Indirect associations were found: physical trauma was associated with hyperarousal, but hyperarousal did not predict treatment completion. Sexual trauma was significantly associated with higher avoidance symptoms, which, in turn, were associated with lower likelihood of treatment completion. Sexual trauma was also associated significantly with overall PTSD symptoms, which, in turn, were associated with treatment completion at a marginally significant level.
In the study by Risser and Schewe,655 children were categorised into groups based on whether or not they attended any therapy session after the intake, terminated prematurely from therapy or completed treatment. Results demonstrated that child emotional and behavioural problems at intake, general parent stress and income did not differ by treatment engagement. Type of violence exposure, parent–child stress and race differed by category of treatment engagement. Children exposed to both domestic violence and child abuse demonstrated higher rates of treatment completion and attended more sessions than children exposed to either domestic violence or child abuse. Caregivers with higher levels of parent–child stress were more likely to engage in treatment. White children in the full sample completed treatment at higher rates than minority children.
Koverola et al. 653 found no differences in children’s race, gender or caregivers’ gender by treatment attrition type; 60.5% of the sample were legally mandated to participate in treatment, but whether treatment was court mandated or voluntary was not associated with a likelihood of engaging in, or completing, treatment [χ2(2) = 0.1; p = 0.95].
There were some baseline differences in compliers, dropouts and non-engagers in Koverola et al. 653 The mean age in the three groups was significantly different [F(2,116) = 4.0; p = 0.02]. Non-engagers were older than both attriters and compliers (M = 11.1, 9.5 and 8.0 years). Attriters were more likely to be in the family of origin than non-engagers or compliers. Families referred for child abuse in this study were also more likely to comply with treatment than those who were referred for domestic violence (67% vs. 33%, respectively) [χ2(2) = 5.6; p = 0.06]. There were very few differences found among caregivers of attriters, completers and non-engagers. Caregivers’ self-reports revealed that caregivers of completers do not experience significantly higher levels of social support and daily stress than caregivers of attriters or non-engagers (F = 0.5; p = 0.63; F = 0.7; p = 0.52). In addition, they do not report higher levels of internalising or externalising behaviour problems or post-traumatic symptoms in their children (F = 0.5; p = 0.59; F = 2.9; p = 0.05; F = 1.8; p = 0.17). Differences were found in relation to psychological distress and parental distress. Caregivers reporting high child-related parental distress [F(2,32) = 3.9; p = 0.03] and high psychological distress [F(2,70) = 3.3; p = 0.04) were least likely to engage in treatment. No differences were found with regard to children’s self-report of post-traumatic symptoms or cognitive functioning (F = 0.3; p = 0.71; F = 0.7; p = 0.49). When treatment modality was examined, findings revealed that families were more likely to complete treatment successfully if they received multimodal treatment relative to individual or family-only treatment [χ2(2) = 7.6; p = 0.01].
Caregivers’ views
The majority of the mothers interviewed by Koverola et al. 653 were reluctant to discuss the abuse because of fear that it had not happened. Some also felt vulnerable because of how therapists perceived their reactions – they either felt overprotective or too careless that abuse had happened. Most expressed positive opinions about treatment and felt that they understood their children better, had new ideas about possible solutions and valued the contributions made by the team.
Staff views
Conflicts associated with alleged abuse had been reduced in n = 20 cases in the study by Koverola et al. 653 Alleged perpetrators who had engaged in therapy expressed relief being able to talk about it in a non-judgemental setting. Those who did not view the intervention positively felt that mothers had formed a coalition with the therapist.
Summary
We consider the relevance of these data in the concluding section of this chapter.
Summary: key messages about acceptability
Insofar as the evidence permits, we have summarised data on the acceptability of particular kinds of treatment above. In this final section, we consider overall messages from the evidence presented above.
What the studies said
The included studies approached acceptability in a number of ways. Some framed it in terms of client satisfaction, often using questionnaires that required respondents (usually caregivers) to answer by scoring statements on a Likert scale, representing views from ‘not at all (satisfied)’ to ‘completely (satisfied)’. Typically, they covered issues such as the respondent’s relationship with the therapist, the perceived relevance of the therapy and the perceived helpfulness of the therapy and therapist. But, of course, this measures acceptability only for those who accept services. Findings from these studies tell us nothing about how acceptable a service or therapy is to those who have not taken up the offer. Did they not accept help because the help on offer was not something they saw as relevant, or otherwise acceptable to them? Or was it for other reasons, such as an inability to travel to the service, to secure time off work or because someone else stopped them attending? Few studies have investigated the reasons why maltreated children and their carers decline services.
Engaging with therapy is often deemed to be an implicit marker of acceptability, and dropping out of therapy an implicit marker of dissatisfaction or unacceptability. Again, without asking them, one cannot be sure why people drop out of therapy or other kinds of help, and relatively few studies present such information, if indeed they obtained it. Furthermore, engagement [and disengagement (or ‘dropout’)] are defined in different ways. Often, in the studies we reviewed, researchers excluded from the final analyses all of those who did not receive a certain ‘dose’ of therapy. Although this might make sense from the point of view of assessing impact, it leaves unanswered questions about why some people complete therapy and others leave early. Is it because the therapy is not helping, or is it because the client feels better and in no further need of help? Or is it for reasons unconnected with the therapy? And do those who drop out of this therapy continue without further support or do they seek it, and accept it, elsewhere?
In controlled studies of the effectiveness of psychosocial interventions, concerns about group equivalence is often the driving force behind those that document reasons for dropout. Researchers are concerned to identify any evidence of differential dropout between the intervention and comparison groups, and any evidence to suggest that the reasons for dropout are attributable to factors associated with a particular intervention or study arm, both of which might confound the results of the study. Rarely, however, do the lists of reasons include attitudes towards the therapy. Rather, they concentrate on factors such as moving placement, lost contact, refusal, all of which – from the point of view of acceptability – raise more questions than they answer.
Examining dropout in controlled effectiveness studies is further complicated because it is often difficult to disinter the effect of the interventions offered from those of participating in the study, that is, are the demands of therapy unacceptable or the demands of the study design? This may be particularly true of randomised trials, for which potential participants may hope to be randomised to receive (or not receive) the intervention, and opt with their feet when allocated to the unwanted arm of the study. This is one reason why uncontrolled studies are helpful in exploring acceptability.
Definitions matter
The studies in this review examined the phenomena of treatment engagement, dropout and completion using differing definitions, ranging from percentage of client-attended sessions to ‘last appointment missed’. This needs to be borne in mind when considering their results, as variations in definition impact on the apparent evidence base relating to the prevalence and predictors of attrition. 756
In addition to the inherent heterogeneity across studies (in relation to location, samples, settings, staff profiles, factors explored, etc.), differential approaches to defining core concepts make it particularly challenging to synthesise the findings of the included studies.
Treatment completion and dropout
How one conceptualises treatment completion dictates how one defines premature treatment termination or dropout. This, in turn, can change the answers that research studies provide to questions about treatment acceptability. Even defining completion is not straightforward. Some researchers define it in terms of attending all sessions. Although one cannot assume that full attendance is equivalent to engaging with treatment (turning up at a lecture is not synonymous with listening or learning), it may be a reasonable indicator that someone is finding therapy helpful or expecting it to be helpful. It may indicate that someone is probably an active participant, although this may not be a reasonable assumption for children who might have no choice. In contrast, defining lack of success as lack of engagement is, at best, tautologous. Timmer et al. 656 provide an example of the problem. In this study656 of PCIT, parents were considered to have completed treatment once they:
-
had met the mastery criteria for the relationship enhancement element of the programme
-
could demonstrate compliance commands from their children
-
could successfully implement a discipline procedure, and
-
could show maintenance of skills that they had acquired in the first phase of the programme.
In this study,756 failure to comply with all of these tasks was categorised as early termination, but this was essentially synonymous with programme effectiveness, thereby stacking the odds in favour of a positive result for the efficacy of the treatment being assessed.
Some studies define completion in terms of ‘dosage’, by calculating the average number of sessions attended and setting a minimum threshold. Theoretically, this is often argued on the basis of evidence from earlier studies suggesting that a minimum level of exposure is necessary for a certain intervention to have an effect. 757 So, for example, Laan et al. 671 defined premature termination of intensive foster care placement as those placements that ended within 2 years of inclusion within the intensive fostering service. In this case, the authors acknowledge that this is ‘something of an arbitrary criterion’, based on the belief that fostering can postpone a residential placement and postponement of at least 2 years is deemed a success. The children in this study757 were predominantly learning disabled children, the remainder having serious physical impairments or health problems. All were in out-of-home placements as a result of maltreatment or inadequate parenting. Yet others use definitions such as ‘termination with therapist approval or mutual agreement’. Some might see these definitions of completion as a source of bias. Taken as a whole, these factors probably account for some of the contradictory messages that appear across studies, but perhaps make some of the consistent messages more important.
Although no intervention can demonstrate 100% effectiveness, the odds of success should arguably not be estimated without consideration of the factors that cause those it is designed to help to decline or drop out early. The reasons for both might reflect factors that are only indirectly linked to the intervention (relationship with therapist, service setting, time of day) but are important to know and understand.
Treatment engagement
Almost no study addressed the issue of treatment engagement, which is also subject to various definitions, some of which can run the risk of being used almost interchangeably with treatment success, that is, failure is explained in terms of failure to engage, when – in some circumstances at least – engagement might be a function of service or therapist attitude and behaviour.
Engagement can be used to refer to a variety of closely related things. Most usually it refers to someone’s commitment to the therapeutic process and active participation in it. As Cunningham et al. 649 point out, it is ‘related to other concepts such as readiness to change, rapport, motivation, working alliance, and collaboration and compliance’ (p. 64). As such, measures of engagement (the focus of this study) have looked variously at clients’ motivation for, and expectations about, treatment; the client–therapist relationship; and client behaviour within therapy.
Expectations of treatment may act as facilitators or barriers to participation in treatment, for example believing that treatment will – or will not – be helpful, recognising the need for treatment compared with failing to see a problem to be resolved.
On the basis of the wider therapeutic literature, establishing rapport with the therapist or with care staff is probably a necessary prerequisite of achieving therapeutic change, but it may present particular challenges with reluctant, ambivalent or involuntary clients. Cunningham et al. 649 noted that engagement by young people in the RTCs they studied required continual effort because the process of engagement was unstable and required constant ‘refreshing’. Few studies in this review of psychosocial interventions gave much attention to this aspect of effective interventions, with only a handful referring (in passing) to strategies such as motivational interviewing, and none to the wider challenges of engaging young people in therapeutic interventions.
What the study by Cunningham et al. 649 emphasises is the importance of professionals thinking theoretically and strategically about what they need to do to facilitate engagement, and how this might vary with context (service setting, timing, voluntary/compulsory and therapy type) and indeed, influence service outcomes. For the population of seriously maltreated children, engagement may require particular thought and care, given the fracturing of trust and the damaged ability to form relationships that is so much a feature of these young people’s lives.
Key themes
We first consider some of the findings from the studies that were designed to explore issues of engagement and treatment exposure. We then summarise some of the key themes to emerge from our thematic analysis of all included acceptability studies, recognising that these need to be considered in light of the issues discussed above. The studies discussed in this section are illustrative – further detail can be found in the relevant sections dealing with intervention groups. As indicated above, studies that used data from key stakeholders typically gathered information from parents or other caregivers and therapists, rather than children themselves. However, parent and therapist reports of experiences raised a number of issues that could clearly impact on a child’s engagement or retention in therapy.
Keeping the first appointment
Many children who require help do not receive it because they are not referred for appropriate services (see Chapter 6). It is also the case, however, that significant numbers of those referred for therapy do not avail themselves of it.
The study by Haskett et al. 657 was one of a few studies that were concerned specifically with understanding the reasons why children referred for treatment following abuse failed to keep their first scheduled therapy session. This early American study of referrals for children who had been sexually abused found that ethnicity (African American) was significantly associated with failure to attend, together with whether or not the referral was to a public or private centre, whether or not clients had access to a telephone and whether or not the mother agreed that the family needed counselling. However, these factors accounted for only some 11% of the total variance between families who failed to keep that first appointment (45 out of 129) and those who turned up. This points to the importance of factors not measured in this study, such as practical obstacles, for example parental illness or forgetting appointments. Mothers who felt that the whole family could benefit from counselling were more likely to attend the first treatment session, and the authors highlight the potential significance of mediating variables that might inhibit attendance, such as failing fully to understand the abuse or feelings of guilt and self-blame.
More recently, Lippert et al. 648 undertook a study of the factors differentiating those families who decline therapy from those who initiate therapy. In this study,648 46% of families of sexually abused children who were referred over a 6-month period did not commence therapy within 2 months. In addition to measures of child behaviour, family functioning, data from child protection service records and information provided by caregivers, this study648 also used semistructured interviews to explore caregivers’ support networks; their perceptions of, and relationship with, the child; and perceptions of therapy. Analyses of the administrative data indicated only two significant variables, namely the child’s ethnicity and neglectful supervision by the mother. The odds of entry to therapy were just over two times greater for non-black children than for black children (p < 0.099) and just under 14 times greater for children whose mothers were accused of neglectful supervision (p < 0.01). Caregivers from both groups reported low levels of child problem behaviours as measured by the ECBI,311 but those who declined therapy had lower scores on the SFI,747 indicating higher functioning. Interview data suggest that mothers who declined therapy were possibly less child centred than those who attended, that is, ‘decliners’ more often talked about ‘going places’ as what they enjoy doing with their children, in contrast to ‘attenders’, who more often talked about playing with the child, talking, singing or engaging in other activities, such as reading or doing homework. Although most caregivers (80%) initially saw the relevance of therapy, the authors hypothesise that ‘those who decline child therapy may overlook its emotional benefits’, as these caregivers less frequently described therapy in terms of emotional help or change (p. 866). Perceived barriers to therapy identified by caregivers were practical ones, such as location (see below). Although neither of these studies648,657 was conducted in the UK, both indicate the importance of addressing sociocultural factors, such as class and ethnicity.
In the study by Koverola et al. ,653 caregivers who, at intake, reported high levels of stress related to the caregiver role (as opposed to general stress) and high levels of psychological distress were least likely to keep the first therapy appointment after assessment. In this study,653 concerned with children with a history of intrafamilial violence, the majority of participants (61%) were legally compelled to attend, but this was neither associated with a likelihood of engaging in, or completing, treatment. Few studies found any impact of mandatory, compared with voluntary, referral on subsequent engagement or attendance.
Starting but not finishing
Of those who start treatment, significant numbers cease attending before therapy is scheduled to end. We identified a number of studies that specifically explored factors associated with dropout from therapy, and a number that undertook post hoc explorations of those children who dropped out of therapy in the course of the effectiveness study (see above). These studies simultaneously explored the factors associated with retention. Studies that explored treatment dropout or retention did so in very different ways, making it difficult to draw generalisable conclusions. This general problem is exacerbated by the fact that most of these studies have been conducted outside the UK, most usually in the USA.
Among the factors reported by individual studies or groups of studies are those in four key domains: (1) sociodemographic variables (age, ethnicity, family status); (2) maltreatment variables (age at onset, duration and severity); (3) child symptomatology/psychopathology (depression, PTSD, behaviour problems); and (4) family functioning/caregiver attributes or involvement. Typically, these were explored in relation to children who have experienced one kind therapy (e.g. CBT) or one kind of maltreatment (e.g. sexual abuse).
Correlates of treatment engagement and attrition
An early study647 used regression analyses to investigate factors associated with the amount of therapy (unspecified) received by 81 girls who had been sexually abused (primarily by male family members). Horowitz et al. 647 found that earlier onset of abuse predicted more sessions of therapy, and more disturbance was associated with more treatment. Non-minority ethnic status also appeared to be associated with increased treatment, but this failed to approach significance once age at onset was added to the equation. Around 33% of the variance in total numbers of sessions attended could be explained by variables from three of the above domains, namely age at onset, number of types of sexual abuse (severity) and child depression.
The authors noted that their study647 was biased towards families who had engaged with therapy, most of whom were recruited through Child Protection Services and who may have felt that they had little choice about attending. Bearing that in mind their findings raise some interesting issues, both for researchers and for clinicians. They speculate that the significance of children’s abuse history may be attributable to therapists’ expectations that children who are more seriously abused require more sessions, or indirectly from the ways in which their abuse influences their behaviour and affect. Although children’s views were not sought, their parents reported a general pattern of initial reluctance or hostility towards therapy, which became more positive as therapy got under way, something reported in other studies. This may reflect children’s initial fearfulness or anxiety when faced with something unknown to them, and which attenuates as they establish a relationship with the therapist. In this study, the same pattern was noted by the children’s therapists. In contrast, parents may initially see treatment as something to be welcomed but subsequently feel threatened by the child’s developing relationship with the therapist and the issues that therapy might raise within the family. From a research perspective, the authors noted that, in contrast to other studies of treatment dropouts, ‘family functioning’ did not appear to be correlated with length of time and treatment. They suggest that researchers may be assessing different family characteristics using the same general term, and that multiple measures of family functioning would be useful in helping to identify which families are at risk of dropping out, and how this might be prevented.
Other studies identify maltreatment severity as predictive of treatment completion. In Boisvert 2008,658 higher dropout (those completing fewer than 15 sessions) was associated with higher levels of sexual abuse impact, behavioural difficulties, social difficulties and delinquency. There were no family characteristic differences identified between treatment completers and non-completers. In Chasson 2013,630 children who had been abused by an adult figure, had been physically injured, and had been subjected to more than one event, were more likely to complete treatment. Even if true of all studies or interventions, knowing these associations is not sufficient to enable one to know what steps to take to enhance treatment completion.
Two631,634 studies report correlations between the child and/or caregiver’s age and treatment completion, although it is worth noting that the study by Cross et al. 634 is primarily a report of study retention rather than treatment retention, and it is particularly difficult to disinter the relative effect of study requirements. Eslinger et al. 631 found that as caregivers’ age increased by 1 year, the likelihood that both child and caregiver would fully complete treatment increased by 11%, whereas the chance of completing treatment decreased by 80% as the child’s age increased by 1 year. Similar findings were reported by Cross et al. ,634 who found that older caregivers were more likely to continue with treatment, but that the older the child was, the less likely they were to engage in treatment (see also the study by Koverola et al. 653).
In a study633 comprising a retrospective chart review of a sample of children referred for TF-CBT following sexual abuse, only 254 of 490 referred for therapy (52%) started treatment and only 98 (38% of the 254) completed therapy. The authors found no evidence that ethnicity, severity and duration of abuse, SES or placement in foster care influenced use of therapy, which the authors attribute to agency factors, for example a sliding scale of payment, accepting all insurance plans and an integrated model of assessment and treatment. What was significant was whether or not the caregiver themselves participated in counselling services, either individual therapy or FT. When this happened, the young person was more likely successfully to complete the recommended therapy. The authors attributed this to the fact that non-offending caregivers often have mental health problems that negatively impact on family functioning in ways that can interfere with treatment completion. In this agency, the psychosocial assessment was designed to identify such risk factors and, when identified, referral was made for the caregiver. When these carers ‘bought in’ to therapy, they believed that this was associated with enhanced motivation to continue with counselling (for the child) and provide them with important support. Of course, it may also be simply that parents who received help for the negative impact of sexual abuse on themselves were more able to provide adequate care and attention to the child. The bottom line is that in this study,633 48% families referred to this agency did not start treatment and, of those who did, 62% did not complete therapy. Another 532 families were referred to other services, but the study collected no data on service engagement for these families. The evidence about parental involvement resonates with a trend in the review of effectiveness studies – that parental involvement is associated with better outcomes.
Ambivalence about the value of therapy
Parents whose children are referred for therapy following maltreatment may be apprehensive for a number of reasons. Non-offending parents may feel guilty at having failed to protect their child, and may be fearful of how they will be viewed by others. Those implicated in maltreatment may be even more trepidatious, anticipating censure. All parents may be concerned about what their child will share with the therapist, and how this might influence their relationship with their son or daughter. A number of studies have confirmed the importance of these, and other issues that matter to parents, which, if unaddressed, may prevent engagement with therapy, lead to premature termination or undermine its effectiveness. Few studies explored these issues, and none did so with respect to the interventions that appear most promising from the point of view of effectiveness. Here are some examples.
In a study of the involvement of parents in their children’s play therapy (seen primarily through the eyes of therapists), Hill670 notes that some parents expressed an initial lack of trust in the professionals and concludes that rapport and trust is something that the therapist needs explicitly to address. One mother described her experience as a parent of a sexually and physically abused child receiving play therapy as follows.
You are going through such emotional upheaval that you don’t trust anyone. And there are definitely some real difficulties with some professionals. You need honesty . . . you need to be sure that they will be open with you.
Hill 2009, p. 1670
Therapists decided whether or not mothers should be involved in the child’s therapy, sometimes deciding against it because of problems in the mother–child relationship. Clearly, communicating those decisions to mothers in ways that do not result in them withdrawing the child from therapy is a complex business. The guilt that mothers may experience may lead them to imagine that professionals are developing very negative assessments of their parenting, even when therapists are saying otherwise:
I felt so bad about myself that I thought they must be thinking the same thing even if they were smiling nicely. I think I was very frightened.
Mother; Hill 2009, p. 390670
Hill670 also found that, for some mothers, relief at securing help may result in a metaphorical ‘handing over of responsibility’ to the therapist, when their involvement is essential to securing a good outcome. In Hill’s study,670 involving fathers presented particular challenges. There were only three fathers in his small sample, none of whom had much to do with therapy. The singleton father who became involved did so because the therapist conveyed a clear expectation that he should be there, rather than leaving it as an open invitation.
Scott677 used in-depth interviews to explore the views of a small group of parents (n = 10) whose children were receiving counselling. Twelve of the 17 children in these families had been sexually abused. Parents expressed mixed views about the value of talking about painful feelings. Some worried about their children having to relive traumatic experiences in therapy, whereas others felt that this process was helpful. Scott677 highlights the importance of managing parents’ expectations, as some parents clearly had quite unrealistic expectations. For example, some parents expected particular changes in children’s behaviour as a result of therapy and were frustrated and disappointed when these did not occur. Typical concerns described by parents included the following.
-
Some parents had high levels of anxiety, but felt unable to discuss these with the therapist because they were unaware of what was being discussed with their child.
-
As discussed previously, issues of parental guilt that the abuse had been able to happen – once this issue was addressed, it became easier to talk about.
-
Some parents felt ambivalent about the therapist’s ‘authority’; counselling for some families was compulsory once social services were involved, and they felt that things were taken out of their control.
-
Parents also reported being distanced from the criminal justice process; once legal action was taken, it was important for parents to be briefed about any progress on this front.
Similar concerns about ‘wanting to know what was happening’ in the therapy were reported by De Luca et al. 170 and Grayston and De Luca171 Parents interviewed by De Luca et al. 170 wanted more feedback from therapists about their child’s group therapy, and would have welcomed the opportunity to observe treatment and receive regular updates by phone. Half of those surveyed in the study by Grayston and De Luca171 said that more feedback would have been helpful.
Tjersland et al. 673 reported how vulnerable some parents felt, worried that the therapist would think they were too overprotective or too careless that abuse had been allowed to happen.
Where parents had clear expectations of treatment, satisfaction levels were higher. Parents who felt part of the therapeutic team or part of the treatment process experienced less tension with the team. 629 Evidence from studies of the effectiveness of cognitive–behavioural studies confirm the value of parental involvement.
Addressing the needs of caregivers
There is some evidence that caregiver distress is correlated with treatment attrition and that, if this is addressed, children are more likely to complete therapy. For example, Koverola et al. 653 conducted an exploratory study examining the association between attrition and retention and (1) demographic and referral characteristics; (2) child functioning; and (3) caregiver functioning. The sample included 118 children, aged 4–17 years, referred for treatment of child abuse and/or exposure to domestic violence. They classified children into three distinct groups: those who failed to engage with treatment at all (n = 24; 20%); those who started but failed to complete treatment (n = 19; 16%); and those who completed treatment (defined as those who were ‘compliant with treatment and who completed their recommended course of treatment’653 p. 26). The 75 children who completed treatment completed between 1 and 55 sessions (median eight sessions). Data were collected through an archival chart review. The only factors that predicted treatment completion were high levels of child externalising behaviour and receipt of multimodal treatment, rather than individual or family-only treatment. In this agency, all children and their caregivers received one of three treatment modalities: IT for both child and caregiver, FT or multimodal therapy. Multimodal therapy included individual therapy and FT, and family advocacy services, aimed at helping families deal with practical issues such as court orders, housing, financial assistance, job training and school resources. Essentially, the family advocate worked with families and community agencies to ensure that nothing prevented the family from engaging in treatment. This included providing in-home services during crises. The authors hypothesise that high levels of externalising behaviour may essentially ensure that the child’s voice is heard and may generate more concern from parents, teachers and indeed juvenile justice agencies. Conversely, the authors suggest that caregivers (and others) may underestimate the adverse consequences of internalising or PTSD symptoms, and that it might be important to provide psychoeducation regarding the importance of intervention for such children, even when their symptoms do not interfere with day-to-day life. Similarly, using multinomial logistic regression, Eslinger et al. 631 were able to predict whether a family would complete treatment, receive a ‘moderate dose’ or drop out early, using the variables age of child, age of caregiver, child’s baseline score for externalising behaviour (CBCL297,349) and child’s baseline maximum post-traumatic stress score (TSCCA325). Older caregivers with younger children were more likely to complete treatment, and older caregivers who identified higher ratings of post-traumatic stress and externalising behaviour were more likely to receive a moderate dose.
Many of the qualitative studies canvassing the views of caregivers stressed the importance of speaking to other parents with similar crises in their own families, and the strength they could draw on sharing these similar experiences, knowing that they were not alone (see, for example, the studies by Powell and Cheshire662 and Costa et al. 678):
I always find it very helpful to meet other mums who’ve been through this. You automatically kind of feel like you belong. It is a terribly isolating experience, and though you may have friends you can talk to, they don’t really understand the true horror or the system or what you’ve been through.
Powell 2010 (reproduced with permission), p. 149662
On a rather different note, Mishna et al. 661 described difficulty in forming alliances between the teacher and therapist, and between the therapist and parent, in a play therapy intervention based in a school. These difficulties took up to a year to resolve, but once the needs of the parents were considered as part of the therapeutic process, relationships improved – one therapist described their thoughts, thus:
I started realising that something had to shift in my relationship with this parent and I think it shifted because I was able to hold her in my mind as well as him.
Mishna 2012, p. 79661
Talking to therapists
It is clear that a good relationship between a young person and therapist will benefit treatment. However, respondents in the included studies reported mixed experiences of the client–therapist relationship. Some participants reported difficulties with this relationship, which required significant investment, and some considered that therapists were too analytical and not adequately child focused. Children valued the personality characteristics of therapists highly, whereas parents were more interested in evidence of appropriate qualifications.
A number of children and young people were initially resistant towards therapy and found it difficult to articulate their feelings and talk about what had happened to them (see, for example, Haight 2010175). One child in the study by Sudbery et al. 663 put it like this:
Having to talk to people about your problems. Having to share your feelings with them as well, which brings out a lot. I don’t like doing talking about stuff when they want you to talk about it, it feels sad. It really upsets me, scares me.
Sudbery 2010, p. 1543663
The respondents in this study663 had spent time in residential care and were being interviewed some years later. Young people in the study conducted by Nelson-Gardell638 also said how difficult they had found it to talk about their abuse but that doing so was helpful.
In the study by San Diego et al. ,680 there was some suggestion that children may have had low treatment expectations, and felt that therapy would not help them. If this is a problem (and the young people in our advisory groups identified it as an issue) then it is something that could be improved by placing a greater emphasis on preparation for treatment. However, no study appears to have explored the treatment expectations of maltreated children.
For children and young people living in a therapeutic care setting, the issue of acceptability is perhaps more complex. Although by no means always the case, young people in therapeutic residential care are often not there by choice, and the (often very troubled) experiences that lead to their placement make it extremely difficult for them to engage with care staff or those offering a specific therapeutic service. One UK study666 interviewed 16 young people who had previously lived in a therapeutic children’s home. These former residents were almost certainly not a representative sample but they were generally positive about their experiences. They valued the relationships with staff, and many of the leisure and therapeutic activities provided during their time in the home. Here too, some respondents commented on the length of time it took to build up trust with staff but, having done so, their ongoing contact with them remained important. Only one interviewee expressed a different view, pointing to something that goes to the heart of the adverse consequences of severe maltreatment and the challenges facing those providing substitute care and therapy.
. . . in care, you are craving this kind of love but you never really get it . . . The one thing you need most is to feel genuinely loved. You never quite got that.
Gallagher 2012, p. 440666
Four641–643,645 studies examined young people’s gender preference for their counsellor. Most female participants expressed a preference for a female counsellor pre treatment; however, in those studies641–643,645 that measured preferences post treatment, gender appeared to matter less. One643 study presented evidence that female counsellors verbalised more than their male counterparts but concluded that gender did not play a significant factor in treating girls. Another study645 suggested that the type of questions asked (specifically sexual abuse-focused ones) was more important than counsellor gender. Young people in one of our advisory group consultations said that they thought gender might not matter per se, but that a young person might wish to talk to someone of a different gender than the person who had maltreated them – again, choice being important.
Children in foster and adoptive placements
Eslinger et al. 631 found that children in foster care were more likely to complete treatment than those living with biological or adoptive parents, perhaps because of the degree of external scrutiny by social workers of these children and their progress. As Koverola et al. 653 observe, in order to ensure that children attend therapy, there needs to be at least one caregiver who is sufficiently motivated to take them (or ensure that they are taken) and possibly to participate in treatment. In violent families, there may be no-one able or willing to do this, and this may be true of families in which children are presenting with other forms of maltreatment. However, not all studies found such a clear relationship between treatment completion and living with foster carers.
In a UK study conducted by Staines et al. ,667 the research team investigated the supports and services provided to children and their foster carers by one IFA. Children placed in IFAs are typically particularly challenging, and IFAs make much of the additional support they provide to parents compared with those foster carers registered with the local authority. This IFA described its approach to fostering as inherently therapeutic and, although recognising the importance of individual therapeutic work, IFA therapists focus their attention on ‘helping to create ‘therapeutic placements’ through the application of their particular skills in assessment and consultation to carers and staff’667 (p. 319). In this broad definition of therapy (seen as the impact of the whole organisation on the young person), foster carers have a formally recognised role as members of the therapeutic parenting team. The approach seemed to address concerns often expressed by foster carers that they are not adequately informed about the child or what is happening, not consulted, and excluded from therapeutic work.
The parenting team was seen to be an essential part of the information-sharing/decision-making process and many carers commented on the inclusive and respectful nature of the team: ‘We are always discussing things together and we all make decisions on how to meet the child’s needs. We always feel equal.’
Staines 2010 (reproduced with permission), p. 8667
Providing foster care for children with a challenging placement profile, the majority of whom displayed difficult behaviour, this approach contributed to providing stable and successful placements, with 77% of foster parents feeling the placement was going ‘very well’ after 12 months. Almost all (97%) foster carers felt that they were a valued member of the team and that their opinions mattered, although the authors suggest that this is perhaps more reflective of the experience of independent foster agencies rather than local authority-led foster care.
Other barriers to treatment engagement and completion
A variety of practical obstacles can conspire to prevent children accessing therapy or benefiting from it. The physical environment – in terms of location and quality of meeting space – was raised in a small number of studies. Other practical considerations, such as transport costs, child-care facilities or expenses, were also reported.
Lippert et al. 648 examined the reasons given for non-participation (46%) in a sample of 101 children who were referred for psychotherapy following CSA. Reasons for declining included some factors we have already discussed, but also covered some important practical obstacles: work conflict (50%); inaccessible venue (40%); child was symptom free (15%); caregiver was busy (15%); and caregiver wanted to forget about abuse or let their child forget (15%).
The mothers of sexually abused children in the study of FT reported by Costa et al. 678 identified financial constraints as a barrier to support – particularly viewed in the context of primary earner perpetrators (fathers) being removed from the home.
The young people surveyed in the study by Kolko et al. 644 were perceived to be highly motivated to participate in services, and the children themselves reported moderate ratings about the need to address child and family goals during treatment. They identified parent factors as the largest obstacles to participating in therapy, selecting reasons such as ‘parent was too busy to attend’ and ‘parent does not think counselling will help’. Clearly, this is relevant to the issue of accessibility of therapy for some young people. Although caregiver ratings were generally similar to those of the children, they assigned higher ratings to the severity of family problems and the importance of targeting child behaviour and competencies as treatment goals. Commenting on the limited number of children who were offered IT in this study, Kolko et al. 644 hypothesise that this may reflect caseworkers’ perceptions that family or parent services are more important for the improvement of children’s adjustment, partly as a result of the risk assessment tool used by caseworkers. They suggest that, in this agency, some children who probably required services to address specific abuse sequelae or risk factors associated with their own behaviour did not receive it.
Children in the Tjersland et al. 673 study talked about other issues that made them reluctant to discuss their abuse, including having been threatened by the abuser; being afraid of telling their mother; and being concerned that that they would not be believed. Nelson-Gardell638 reported that ‘being believed’ by someone was considered by the sexually abused girls she interviewed as the thing that mattered most to them, experiencing it as intrinsically therapeutic.
Woodworth533 highlights the problem of staff turnover. In this study,533 as part of a move to be more cost-effective, college interns were used to provide therapy. Although keeping costs down, one unintended consequence is the increased risk, for some children, that the departure of someone with whom they had begun to develop a therapeutic bond may have a detrimental effect.
Summary
The studies
Understanding what makes a therapy acceptable is complex. The immense heterogeneity in those (relatively few) studies that have sought to ascertain what factors encourage people to seek therapy, to accept an offer of therapy, to actively engage with therapy and to ‘stick with’ therapy’ means that few unequivocally clear answers are to be found. The different ways of defining engagement, completion and attrition make synthesising the data very challenging, but this variation may be indicative of the need to take a more nuanced approach to thinking about attrition.
Chasson et al. 482 point out that treatment is not static and neither is symptom severity (and possibly other factors that influence engagement). In their study,482 which explored the predictive value for dropout (from exposure-based CBT) of trauma-related symptom severity, they found that baseline symptom severity failed to predict dropout. In contrast, symptom severity measured just before termination was significantly associated with the number of attended sessions, and higher severity of depression, measured just before termination, was correlated with fewer treatment sessions, that is, immediate distress may be a trigger for dropping out of treatment. The implication for therapists working with children with mental disorders is that monitoring those factors that might impact on future attendance on a session-by-session basis could possibly help to prevent premature termination. This might be particularly relevant for exposure-based psychological interventions.
Synergies with the views of young people
Some of the studies focused on issues that mattered to the young people in our advisory group, and some of the findings resonate with their concerns. For example, their concern that some children might be deterred from seeking help because they felt their situation too complicated or too serious for anybody to be able to help with is in keeping with findings that severity of abuse is an important factor in differentiating those who start (and complete) therapy from those who do not. The studies note the connection, but generally do little more than speculate about the mechanism of effect. It is possible that caregivers, as well as children, may have doubts about the ability of therapy to ‘fix’ what they may regard as ‘unfixable’.
The pivotal role that parents and other caregivers play in ensuring the availability of therapy to young people, particularly younger children, was also recognised as an issue in our consultations, and was mirrored in the findings from the included studies. Some young people identified parents as a potential barrier to accessing therapy. Younger children are particularly dependent on having someone reliable and willing to get them to the therapist, but even older children may be unable to avail of therapy if their parent objects, for whatever reason.
Only one of the studies included in this review mentioned the importance of being believed, but the concern about not being believed was a very significant issue for some of the young people with whom we talked.
Issues of confidentiality and trust appear not to have been systematically examined in studies of therapy for maltreated children. It is possible that both researchers and therapists take this for granted, and it is difficult to say how widespread a concern this might be for young people, but it perhaps merits more attention, from therapists if not researchers.
Given the limited resources available in children’s mental health services, it is perhaps unsurprising that no study examined the issue of choice, but the potential benefits of involving children in discussions of therapy is something that young people identified as one way of enhancing engagement in therapy and might therefore be worth exploring further. Several studies talk about the process of therapy, and the considerable anxiety that some children experience at the outset. The suggestions made by the young people may help to alleviate these concerns for some children.
Chapter 6 Discussion
Aim of the review
This review sought to bring the highest standards of evidence synthesis to bear on a significant area of public health. Maltreatment adversely affects the development of children and young people in many ways, over long periods of time, and the cumulative consequences of maltreatment in early childhood can be particularly devastating. Despite recent emphases on the importance of early intervention, significant numbers of children continue to have to deal with the realities of physical and emotional abuse, physical and emotional neglect, and sexual abuse, whether directly or indirectly as the result of witnessing the abuse of others.
The review aimed to achieve a number of objectives. The first was to identify those interventions that are most effective for maltreated children, and the study was designed so that we might be able to address the issue of whether or not certain interventions were more effective than others for children with particular profiles of maltreatment, for example children who have been sexually abused, than for those who have been physically abused, and those who have experienced more than one form of maltreatment. Second, when the evidence suggested that two or more interventions might both be appropriate, we aimed to explore which might be the most likely to be effective. Again, we were mindful that some interventions might be more suitable than others for particular groups of children or for children and families in particular circumstances. Third, we sought to identify those interventions for which there was no evidence of benefit, or when the evidence suggested that they might result in harm. Fourth, we wanted to know whether different interventions were more accessible and acceptable than others, from the perspectives of both children and young people, and their caregivers. Finally, we aimed to present evidence about the economic benefits of available interventions, and to identify the potential value of undertaking future research.
In this final chapter, we present an overview of the evidence identified, which we discuss in the light of consultations with our advisory groups of young people, and with a PAG whose members came from a range of disciplines and service contexts, including foster parents. We conclude with a summary of what the evidence permits us to conclude in relation to the original objectives of the review, and identify implications for research and practice.
Evidence base
The details of all of the included studies are presented in Chapters 3 and 4. Altogether, we identified 198 studies assessing the effectiveness of psychosocial interventions for maltreated children. Sixty-one of the studies were randomised or quasi-randomised trials; eight studies used a QEx design and a further 26 controlled observational designs. A total of 101 studies were uncontrolled. We drew on data from controlled studies when synthesising the evidence for the effectiveness of interventions. Only three116,145,146,155 of the controlled studies were conducted in the UK.
The consequences of maltreatment have considerable implications for public services, including not only health, but also social services, education, criminal justice, employment and welfare. Despite this, we were able to identify only six studies assessing the cost-effectiveness of relevant psychosocial interventions, four198,613–615 of which used data from a randomised trial and one612 a decision-analytic model. Only two613,614 of these studies were conducted in the UK (Box 1).
Two of the 61 controlled trials identified were conducted in the UK.
Two out of the 10 economic evaluations were conducted in the UK.
Fourteen of all 73 studies providing information on acceptability were conducted in the UK.
For studies of accessibility and acceptability, we cast a wider net, and drew on evidence from studies irrespective of design. In total, we identified 73 studies, 19 of which also addressed the effectiveness of intervention. Some of these studies were specifically designed to systematically investigate the factors associated with treatment engagement and completion, and treatment satisfaction, but many of the studies were small, qualitative studies that explored the experiences of small numbers of respondents. Surprisingly, relatively few of the studies talked to children or young people. Fourteen145,146,169,481,538,662–670 of the 73 studies were undertaken in the UK, or included UK participants. 640 Many of these studies were conducted by researchers with social care backgrounds, reflecting a long tradition of client opinion research in this field. 758
Coverage of maltreatment and relevance to the UK
Maltreatment severity
For the most part, these studies focus on children who have been seriously maltreated, irrespective of whether the study recruited children who had been sexually abused, physically abused or neglected or had experienced multiple forms of maltreatment. Generally, the profile of participants closely resembles that of children who come to the attention of UK Child Protection Services, and in respect of whom child protection plans are made and care proceedings sometimes undertaken. Most of the study participants were children living with their birth parents; relatively few studies focused on children living in substitute care, whether foster care, adoptive families or residential care. Many looked-after children have particularly complex needs, particularly those in residential care. Their maltreatment histories are often amongst the most severe, and their out-of-home placements have often compounded trauma and loss. Those who have experienced multiple placements will have had particularly limited opportunities to develop secure relationships, with either adults or peers. Overall, the picture is one of very complex need, and rigorous evaluations of therapeutic services aimed at this group are few and far between.
Maltreatment focus
There is unevenness in the available evidence base for the effectiveness of interventions for different kinds of maltreatment (Box 2). Of the 101 controlled effectiveness studies, almost one-third (3289–105,120,143,150,155,159–163,166–174,178–180,204) focused solely on children who had experienced sexual abuse, usually girls. These included all five169–173 studies of group work interventions, 1289–104 of the 24 CBT studies (excluding EMDR), seven155,159,161–163,166–168 of the 17 studies of psychoeducational interventions, and four of the eight studies of psychotherapy and counselling. 174,178–180 The majority of other studies recruited children who had experienced any form of maltreatment. These sometimes included children who had experienced sexual abuse, but on the whole the profile was of children who had experienced a combination of physical and emotional abuse and neglect. Five151–154,156 of the RCTs specifically recruited children who had been exposed to domestic violence.
We found no controlled studies of interventions for children in which maltreatment took the form of fabricated or induced illness, and only one uncontrolled study. 523
The 2010 NSPCC prevalence survey found that, across the UK, 8.9% of children aged < 11 years, 21.9% of 11- to 17-year-olds and 24.5% of 18- to 24-year-olds had one or more experiences of physical violence, sexual or emotional abuse and neglect by a parent or guardian during their childhood. 21 Similar rates of multiple and repeated maltreatment have been found in surveys of family violence conducted elsewhere. 317,759 One therefore needs to be cautious about interpreting the results of studies that are designed to examine the consequences of particular types of maltreatment, or the effectiveness of interventions for particular types of maltreatment. As Saunders et al. 760 observed, different research teams, studying different types of violence (physical abuse, sexual abuse, domestic violence), may well be studying many of the same children, but simply catching them at different times of their lives and subsequently categorising them according to their particular protocol.
-
Controlled studies cover a range of interventions for maltreated children, with a bias towards interventions for sexually abused children.
-
There is a paucity of controlled studies focusing on improving outcomes for looked-after children.
-
There are no controlled studies of interventions for children whose maltreatment takes the form of fabricated or induced illness.
-
More studies are needed that address the reality for many children of multiple experiences of different forms of maltreatment.
Interventions evaluated
Clearly, the profile of investment in intervention types presented in this review would look somewhat different had we grouped the included interventions differently. For example, we might have combined relationship interventions with systemic interventions or combined multisystemic FT with MTFC. We hope that clarity within the review will mean that readers can make their own judgements, but there does seem to be a marked unevenness in the available evidence (positive or negative) among the interventions that might currently be offered to maltreated children and their caregivers.
As anticipated, the intervention that was most frequently studied was CBT, followed by interventions that sought to improve the relationship between parent and child, interventions that we grouped together as ‘relationship-based interventions’. They included four attachment-orientated interventions (ABC,122,125,126,130,132 CPP,123,124,127–129,133 PFR131 and dyadic developmental therapy134,135), PCIT131–138 and two139,140 studies of parenting-focused interventions.
Focus of interventions
Irrespective of whether or not studies were focusing on a group of children recruited for one particular form of maltreatment, the interventions studied concentrated primarily on defined disorders associated with maltreatment, rather than on the broader consequences of maltreatment per se (Box 3). This is possibly one of the reasons why, with few exceptions, interventions were brief, with the majority comprising weekly therapeutic sessions over a period of between 10 and 20 weeks. Few studies examined interventions designed to tackle the more complex and longer-term consequences of maltreatment, which may, arguably, require a longer-term and broader-based approach to intervention, as well as to the evaluation of its effectiveness (see below, particularly Conclusions).
-
Some interventions have been more frequently subjected to rigorous evaluation than others.
-
These differences cannot be explained in terms of some being easier to evaluate than others.
-
Few interventions have an explicit theory of change; those that do are more likely to have been rigorously evaluated.
-
Most studies are focused on interventions that are designed to address specific diagnosable disorders, such as depression or PTSD.
-
Few studies examine the effectiveness of interventions that are designed to address the wider consequences of maltreatment for children’s social functioning or quality of life.
One area that is somewhat underdeveloped is that dealing with the provision of residential care. This is not surprising, given the challenges that are inherent in evaluating ‘whole-service’ interventions, but it would be possible. In recent years, a number of initiatives have been taken across the UK to introduce more therapeutic regimens into residential care settings. Interventions have ranged from social pedagogy to interventions anchored squarely in theories of attachment and social learning [e.g. ARC (Attachment, Regulation and Competency); Sanctuary; CARE (Children and Residential Experiences)]. All are designed to address the complex needs of this very vulnerable population in residential care settings, and the particular challenges faced by the staff that run them. Unfortunately, the opportunity to conduct controlled studies of these important initiatives was not seized, and a review of the evidence concluded that there was no robust evidence of their effectiveness as ‘programmes’. Macdonald and Millen761 conclude that if one was to ‘drill down’ into particular aspects of these service models (many of which are shared), one would find a strong evidence base in favour of component parts, but this does not obviate the need for rigorous evaluation.
Theories of change
Some studies provided (or referenced) a clear theory of change (‘logic model’) to outline how the intervention was thought to bring about change, but these were in a minority. Those that did were over-represented among studies that subjected interventions to a randomised trial, and included therapies that were not tightly manualised, such as CPP. Conceptualisations of maltreatment as trauma informed a number of the cognitive–behavioural interventions; attachment theory and developing understanding of the impact of maltreatment on children’s neurological development informed some of the RBIs; and systems and ecological transactional theory provided the rationale for interventions such as MTFC. Such conceptual grounding was noticeable, however, in its absence from many of the studies, underpinned by taken-for-granted assumptions that the intervention in question was an appropriate therapy for addressing specific sequelae of maltreatment which would not bring about any harm.
However, the very specificity of some interventions is problematic, given the impact of maltreatment on children’s lives. Children who have experienced severe maltreatment present with complex psychopathology, which is ‘characterised by attachment difficulties, relationship insecurity, problematic sexual behaviour, trauma-related anxiety, inattention/hyperactivity, and conduct problems and defiance’ (p. 614). 61 For this reason, Tarren-Sweeney61 has argued that we need to reconceptualise the mental health needs of children in care and adopted, if we are adequately to address their needs, and this may also apply to significant numbers of children who become subject to child protection plans, but who remain at home. These children simply do not have single mental health problems, such as PTSD or depression, and many of the problems with which they present do not fall under the auspices of any diagnostic classification system; the following are just a selection – smearing faeces, hoarding, eating problems, hiding and storing food, speech and language delays, sexualised behaviour, low self-esteem and poor social functioning. 61,431,762 The design and implementation of effective therapeutic services for maltreated children requires both researchers and clinicians to develop and understand the potentially varied and pervasive consequences of maltreatment, particularly during sensitive periods; how even similar histories of maltreatment can lead to a variety of different outcomes (the principle of multifinality) and the same outcome can arise from very different maltreatment histories (the principle of equifinality), and that ensuring a ‘logical fit’ between a child’s needs and the choice of an intervention or interventions depends critically on a detailed assessment. We return to this issue later, as it is a crucial factor in interpreting the evidence presented in this review.
No study included the investigation of adverse effects as part of the study design. This suggests an unfounded confidence in the benefit of therapy, which, as evidence from related fields suggests, may be misplaced. 763,764
Comparisons
Few studies used a no-treatment or wait-list control. When the desirability of using a no-treatment control group to determine the effectiveness of an intervention was reported (and rejected), this was usually because it was deemed inappropriate to withhold intervention. However, it perhaps also reflects the assumption that therapy is necessarily helpful. Most studies compared a particular intervention with TAU, which was sometimes minimal, but often quite considerable. Among the CBT studies, where there is a growing confidence in the effectiveness of TF-CBT in particular, some studies were designed to manipulate treatment dose (e.g. number of sessions) or intervention components (e.g. TNs, child only vs. parent plus child) to explore their particular contribution to the intervention’s effectiveness.
Although TF-CBT interventions perform well in controlled evaluations, most of the best evaluations have been undertaken by the teams who developed the programmes. Independent evaluations are necessary to consolidate (or test) their effectiveness, and also to determine their effectiveness in locations outside the USA. This is particularly important in the UK context, for which the profile of ‘comparison’ public services is very different from, and possibly better than, that of the USA. 145,146 The same is true for a number of other interventions that have been rigorously evaluated either only in the USA and/or in evaluations conducted by the programme developers, or where programme developers have been heavily involved in the evaluation.
Outcomes and measures
As in many other areas, the choice of outcomes and outcome measures appears to be the ‘Wild West’ in relation to studies of the effectiveness of psychosocial interventions. Table 5 provides an overview of the lack of consensus around what outcomes matter and, perhaps more importantly in this area, how they are best measured at particular developmental stages. In contrast with, for example, a Cochrane systematic review, we were not able to establish a small set of primary and secondary outcomes for this review. This reflects the multiplicity of ways in which maltreatment can impact on children’s lives and who is determining which outcomes matter, and this was also evident in our consultations with young people and with the PAG established for this study. It is likely that the concept of a core outcomes set for maltreated children is a nonsense. However, a core outcomes set for assessing the effectiveness of interventions designed to address for instance, PTSD or depression among maltreated children, together with agreement on how these are best measured, would be highly desirable.
The absence of such a consensus is a major reason why, despite identifying a large number of outcome studies in this area, we were unable to synthesise the available evidence in ways that would strengthen the cumulative evidence base. This was true even when studies were sufficiently homogeneous to reasonably combine their data in a meta-analysis, for example among the CBT trials. Furthermore, measures were predominantly self-report or caregiver/teacher report, although some made use of multiple sources of information or observational data, for example the Strange Situation Test. 336
Even when standardised measures have been used, it is not always evident that they are psychometrically sound or developmentally appropriate. Most focus on problems rather than strengths or competencies, and so the impact of interventions on promoting optimal child functioning, development and well-being is unknown. 182 Fantuzzo et al. 182 also draw attention to the fact that the external validity of many measures has not been tested in relation to low income and or minority children. Few studies assess the progress of children and their families in ecologically valid settings; those that do include some of the relationship-based therapies and intensive fostering support for preschool children.
Relevance of outcomes and measures
The most insidious consequences of early or chronic maltreatment are those that undermine a child’s capacity to reach their potential and to develop into a well-adjusted adult, but – as indicated above – a focus on these consequences of maltreatment is almost absent in the intervention studies in this field. Unsurprisingly, given the focus of the interventions studies, scrutiny of the outcome domains and measures used highlights a dominant focus on mental health measures, such as measures of PTSD, depression and anxiety, rather than measures of overall child development and functioning. Given the consequences of maltreatment on a wide spectrum of children’s behaviour, some have highlighted the inadequacy of some of the most commonly used standardised measures of behaviour, such as the CBCL260 and the ECBI. 310 Tarren-Sweeney765 has developed a behavioural rating scale for children in out-of-home placements which more accurately reflects the range of problems that such seriously maltreated children can present, and which would also be relevant to some groups of maltreated children who remain with their parents. It includes 10 clinical and two self-esteem scales, covering sexual behaviour, pseudo-mature interpersonal behaviour, non-reciprocal interpersonal behaviour, indiscriminate interpersonal behaviour, insecure interpersonal behaviour, anxious–distrustful, abnormal pain response, food maintenance, self injuries, suicide discourse, negative self-image, and low confidence. Initial research suggests that the instrument has good content construct and criterion-related validity, and certainly it seems more adequately to capture the range of problem behaviours commonly presented by maltreated children.
Few studies assess the impact of intervention on children’s physical or cognitive development, speech and language development, social functioning, self-esteem or educational achievement. In the UK, governments have for some time been concerned about the underperformance of looked-after children in relation to educational achievement and employment, and their over-representation among the homeless, sexually exploited and those involved in substance misuse and offending. The difficulties responsible for these over-representations start long before children become looked after, and suggest that effective interventions need to be targeted ‘upstream’, even if resources permit extension of service provision only to those families whose children are subject to child protection plans and where there is a possibility of care proceedings.
There is some evidence that the choice of outcome measure might unduly favour experimental interventions, as when a PTSD measure is used to evaluate the effectiveness of an intervention specifically geared to address PTSD in comparison with an intervention that is not. Selecting measures that are meaningful measures of the intended effect of the intervention, but which do not unduly favour it, is not something that is given due consideration in this area. Particularly in the absence of study protocols, it is worrying that researchers sometimes opt post hoc to report data from total measure scores, and sometimes from subscales. In the absence of an a priori analysis plan, it is difficult not to be concerned about the possibility of selective outcome reporting.
Few studies included follow-up periods that extended for even a year following the intervention, and most had follow-up periods lasting only months or none at all. This will, in part, be a function of available funding, and the challenges of retaining these families in a study, but it also reflects the treatment focus of the majority of studies and the changes sought. Even so, the absence of longer-term follow-up is a weakness in the current body of evidence, given the importance of examining the maintenance of change, and also the reality that problems (re-)emerge for maltreated children at different times.
Synergies with the views of young people and professionals
As indicated in Chapter 5, young people in our Young People’s Advisory Groups gave their views regarding the outcomes that they thought would matter most to children and young people like themselves. Very often, the interventions evaluated in this review focused on, or resonated with, their concerns, but rarely did they feature in the measures of effectiveness chosen by the researchers. For example, equipping young people to secure their future safety and to feel safe was a component part of most, if not all, of the CBT interventions, the psychoeducation interventions and the group work interventions. However, none of these studies used ‘safety’ or ‘perceived safety’ as an outcome, nor did they examine repeat maltreatment. Many of the interventions (predominantly those focused on children who had been sexually abused) included content designed to help children recognise ‘what being treated badly is’ but none evaluated this.
The views of professionals were, unsurprisingly, varied. Like young people, they recognised the importance of keeping children safe, but they were more inclined to focus on common, maltreatment-associated mental health problems, such as attachment, depression and consequences for healthy development, such as emotional development and peer relationships. Although at first glance these views differed from those of the young people we consulted, the differences seemed primarily to reflect a difference in developmental perspectives, that is, professionals have the benefit of a knowledge base, their (generally broad) clinical experience and a sense of how different things matter more at different stages of development. The outcomes identified by professionals as being important generally reflected their broader knowledge base of the adverse consequences of maltreatment. Specific outcomes, such as attachment and depression, are represented in one or more of the included studies that specifically address these sequelae of maltreatment, but, as indicated earlier, fewer studies monitor broader outcomes, such as emotional development and peer relationships, not least because very few interventions focus on these outcome domains, even when the interventions might improve them.
Relevance to clinicians
Research evidence is one of a number of factors that influence clinical decisions regarding the use of particular psychosocial interventions. The weight afforded to research may depend on many factors, including the perceived match between the characteristics of research samples and those of patients or clients seen in ‘real life’; the appropriateness of manualised treatments that might be thought not to address the very individual needs of each patient; and the view that treatments that do well in the research literature are biased towards those interventions that are most easily manualised. 431 In addition, there may be challenges to implementation that are not evident from the included studies, particularly when these are conducted in policy contexts other than the UK. Clinicians may not have the requisite skills or training opportunities; resources may be such that, of two effective interventions, the one that is the less effective of the two might, nonetheless, be more likely to be of use in a particular clinical setting. These were issues that we raised with our Professionals’ Advisory Group when we reported the draft findings of the review. We asked colleagues whether or not there were any surprises about the coverage of maltreatment topics or the profile or evidence, whether or not the findings matched their professional experience and, if not, what might account for this. We asked how clinicians might respond to the key messages of the report, particularly the weight of evidence relating to CBT, and what barriers might impede the implementation of the study findings.
Quality of the overall evidence base
Throughout this report we have considered and presented the quality of the evidence base in the context of the specific psychosocial intervention being evaluated. Although we have been able to draw some specific conclusions about the effectiveness of individual therapeutic approaches, and to make some important observations about the features and applicability of the evidence, it is important to comment on the quality of the body of literature as a whole, and to consider its ability to inform policy and practice recommendations, as well as decisions about future research investment. Here we provide some broad observations about the evidence, based on our assessment of the limitations of the evidence base, the overall strength of the evidence provided, how applicable it is to the children and young people and services in the UK, and how reliable it is.
We considered the best available evidence for each part of our evidence synthesis and, while respecting the hierarchy of evidence, the breadth and scope of our review objectives determined the need to include studies other than RCTs. To help mitigate concerns about over-interpretation of findings from poor-quality studies, we assessed the potential impact of design and conduct problems using quality assessment tools that were appropriate to the type of study. We have also acknowledged the complex nature of studies of psychosocial interventions in these populations and the difficulties that commonly arise. The following comments on the overall evidence base are more general and are intended to indicate the level of confidence that we can have about our findings, based on the sorts of considerations that form a GRADE assessment (Grading of Recommendations Assessment, Development and Evaluation766) and that therefore might be useful to guideline developers and policy-makers. Any decisions taken or recommendations made on the basis of the evidence presented here will need to take account of these general concerns.
Throughout this report, we have identified weaknesses in the studies that we found. The nature of these interventions means that blinding of personnel and participants in these studies is problematic and usually not possible, rendering them open to the effects of performance bias. We have tended not to focus attention on this potential limitation, as most, if not all, studies of psychosocial interventions will suffer from this difficulty, but it is a limitation. Although blinding of outcome assessment is not always possible (e.g. in the case of self-reported rating scales), the lack of independent evaluation, even in well-conducted studies, is an important flaw, leaving them open to the effects of detection bias. We also found extensive evidence of incomplete data in the reports we looked at. Resource constraints mean that we were not able routinely to contact study authors about the omission of post-treatment and follow-up data, and the reasons for this. We attempted to provide an indication of the level of attrition based on the available data points (see Appendix 11), however, and, as we were basing these assessments on the data available from published reports, these are also illustrative of the level of incomplete outcome data in these studies.
We have outlined our concerns about the selective reporting and associated reporting bias in the studies that we found, much of which stems from an inability to access study protocols. As well as reporting bias, the evidence presented here is very likely to be prone to the effects of publication bias. Owing to the limited outcome data available for meta-analysis, we were unable to formally assess the impact of publication bias on our findings using funnel plots. However, it should be noted that many of the studies that we identified (and studies undertaken on this field more generally) are small and underpowered, and prone to the biases associated with small studies. Thus, it is likely that these biases are operating in our analyses.
The frequent lack of detailed descriptions about the children who participated in these studies, and also what was offered to participants by way of experimental or comparison treatment, is problematic, not least because the choice of comparator impacts directly on the apparent effectiveness of the experimental treatment.
As noted in the preceding chapters, the evidence base in this field stems from a highly variable array of primary studies differing, sometimes quite markedly, on multiple aspects of content. For example, study populations (where they were described in sufficient detail) varied in age, experience of maltreatment, and other key factors, making it difficult to arrive at the most appropriate way of grouping them. It was only rarely possible to organise our evidence summaries for each intervention according to the abuse type experienced by the child, but, even when possible, there was considerable heterogeneity across studies in the range of participants with differing experiences and histories. Similarly, interventions were highly variable in their purpose, approach, content and delivery. Even within our broad categories of interventions there will be multiple differences between the therapies offered. The outcomes reported were also highly variable and, in many cases, not comparable with one another. In the relatively few instances where we were able to pool studies in a meta-analyses, the majority of the pooled estimates indicated moderate to substantial unexplained heterogeneity and, in these analyses, we identified few outcomes in which we had confidence to draw clear conclusions (Table 27).
| Therapeutic approach and outcome | Effect size | 95% CI |
|---|---|---|
| CBT for sexual abuse (n = 11) | ||
| Post-treatment PTSD | SMD –0.44 | –4.43 to –1.53 |
| Post-treatment depression CDI | MD –02.83 | –4.53 to –1.13 |
| Post-treatment anxiety | SMD –0.23 | –0.03 to –0.42 |
| Post-treatment sexualised behaviour | MD –0.65 | –3.53 to 2.24 |
| Post-treatment externalising behaviour | SMD –0.12 | –0.40 to 0.17 |
| One-year behaviour management skills of parent | MD –0.89 | –4.89 to 3.11 |
| Post-treatment parental support to child | SMD 0.30 | 0.03 to 0.57 |
| Attachment-focused interventions (n = 14) | ||
| Secure attachment | OR 0.14 | 0.03 to 0.70 |
| Disorganised behaviour | SMD 0.23 | 0.13 to 0.42 |
| Avoidant attachment | OR 0.90 | 0.13 to 6.37 |
| Externalising behaviour | SMD 0.10 | –0.011 to 0.32 |
Attrition from RCTs was assessed to provide a proxy measure of acceptability of treatment. The available data did not allow for a formal analysis of dropout from treatment. To estimate treatment attrition, the risk ratios were calculated based on the number of people randomised in each group and the number contributing data post intervention. All available data are presented for transparency. We acknowledge the possibility that not everybody contributing data post intervention actually completed treatment, and that some people who did complete treatment may not have contributed data during the post-treatment phase; however, these analyses are still likely to provide a broad indication of attrition from different interventions. The forest plots for these analyses are provided in Appendix 11.
Based on the amount of management, oversight and monitoring often provided in these studies, they resemble attempts at generating information about ‘efficacy’ (where interventions are tested to see if they work under controlled circumstances) rather than ‘effectiveness’ in real-world settings. Important features of the majority of studies also differ markedly from the UK context in terms of comparisons, and organisation and delivery of care, and, as indicated in Box 4, some of the studies reviewed here are likely to be of limited relevance to the UK context. Only 3116,145,146,155 of the 61 trials and two613,614 cost-effectiveness studies were conducted in the UK and, therefore, only a limited body of evidence is available that provides any direct consideration of the health and social care environment and context.
Most of the available studies have been conducted in the USA.
Many of the evaluations of particular interventions (such as TF-CBT, CPP and MTFC) have been undertaken by programme developers.
There is a preponderance of interventions targeted at specific mental disorders rather than the more pervasive impacts on children’s general functioning and development.
Independent evaluations of interventions, delivered in the UK, are important for deciding their relevance and effectiveness in this particular policy context.
It is also difficult to make any reliable judgement about the applicability of the studies that were undertaken elsewhere due to the lack of detailed descriptions of what was offered to participants. During this project and through the work of the advisory groups, we acknowledged that we know little about what is routinely offered to children and young people experiencing maltreatment in the UK, although we do know that this is highly variable. Thus, even the generalisability of ‘TAU’ or ‘standard care comparisons’ (including those used in studies undertaken in the UK) is hard to judge. Similarly, the mismatch between the interventions evaluated and those provided in the UK limit our confidence in their applicability. Finally, our work with Young Persons and PAGs confirm that key outcomes (and ways of measuring these) are frequently not measured and/or not reported.
In summary, despite the large numbers of studies available to inform decisions about the psychosocial treatment and support of children and young people who have experienced sexual abuse, or physical and emotional abuse or neglect, the broad concerns outlined above indicate the need for caution in the interpretation of the available data.
Summary of findings
In light of the above, what does this body of evidence tell us about the questions we set out to answer?
What interventions are effective for which children, with what maltreatment profiles, in what circumstances?
The available evidence provides only partial answers to these questions. The use of other-treatment control group participants, plus susceptibility to bias, may account for the evidence being less than clear-cut in relation to some interventions (which is not to say that better-designed and better-implemented studies would necessarily confirm effectiveness). In other circumstances, the results of studies are unequivocally positive, but they are few in number and some also suffer from weaknesses in design and implementation. In almost all cases they have been conducted in policy and practice contexts that differ markedly from the circumstances in which interventions might be offered in the UK. Furthermore, the intervention has been monitored and quality assured to an extent that they are closer to efficacy trials than effectiveness trials. This means that even where we have identified evidence of positive outcomes following specific therapeutic approaches, there can be no expectation that these results would necessarily be observed in practice.
Some of these interventions focus on particular sequelae of maltreatment, and would be appropriate for children when an assessment has identified particular mental health disorders, such as PTSD, depression or anxiety. Others have more promise as broader-based interventions, the impact of which could potentially improve children’s overall development and function. These are typically interventions designed for use with families with young children. An overview of those interventions that enjoy some degree of empirical support is provided below (see Table 28), indicating the age range and focus of intervention. The numbers of asterisks represent purely a judgement call on the perceived strength of evidence, based on the same considerations that one would use in constructing a GRADE Summary of Findings (SOF) table, namely (1) study limitations; (2) inconsistency; (3) indirectness; (4) imprecision; and (5) publication bias. One asterisk was allocated to each GRADE domain. Interventions that appear to have only very weak, or no, evidence of effectiveness on these criteria are not mentioned.
Cognitive–behavioural therapy
As Chapter 4 makes clear, the results sometimes favour the experimental group (e.g. for depression and anxiety) but are generally very mixed. Although we were able to combine some of the data from these trials to an extent that we were unable to do elsewhere, the meta-analyses were less comprehensive than would have been desirable. Looking at the body of evidence as a whole, for children who had been sexually abused, CBT outperformed non-directive or supportive therapies in ameliorating symptoms of PTSD and anxiety. It did less well when compared with (1) conventional sexual abuse therapy, which was, in every respect, the same except for two elements [SIT and GE], for which the focus was fear and anxiety but the children recruited presented with only moderate levels of both, and where elements of SIT and GE were said to be present in both interventions;89 and (2) supportive therapy for parents plus a form of psychoeducation for children. 99 In both of these trials, significant improvements were reported for both groups.
For children who had been physically abused, the evidence indicated that CBT may be effective for addressing PTSD symptoms109 and child behaviour problems,106,109 but, in a third study107,108 that examined its effect on behavior problems, CBT did not outperform FT.
In studies recruiting children with a variety of maltreatment histories, those that assessed the impact of CBT on PTSD reported significant differences in favour of CBT compared with TAU,111,120 no treatment111 or active listening. 121 Two of these were studying EMDR. There is mixed evidence of the effectiveness of CBT for children’s behaviour problems in those studies that examined this outcome.
Relationship-based interventions
We identified four122,125,126,130,132 studies of ABC data, two of which we were able to combine in a meta-analysis with one study of CPP. 123 We also identified four123,124,127–129,133 studies of CPP. Both interventions are designed to promote sensitive and responsive caregiving to children who are adversely affected by maltreatment, with the focus on the carer–child relationship. Meta-analyses indicate significant increases in attachment security and decreases in disorganised attachment, and this pattern of findings was reported in those studies whose data we could not combine. These interventions both focus on relationship changes that could potentially have significant preventative capacity in stemming potentially cumulative impact of the maltreatment experienced by children at the point of referral.
Systemic interventions
There was very little evidence from which to draw conclusions about the effectiveness of systemic interventions. As indicated earlier, FT and CBT were both reported as effective in addressing child behaviour problems, compared with routine services, in the one107,108 study that compared these two interventions, but neither significantly outperformed the other. Only one of the three studies of MST assessed its impact on PTSD, reporting a significant, positive impact. 144 The same study144 also reported a significant improvement in parent-reported internalising behaviour for MST youth, but no between-group differences for externalising behaviour. As in the study by Kolko,107,108 the sample in this study144 had experienced physical abuse or neglect.
Psychoeducation
Group-based psychoeducation appears to be a promising intervention for alleviating PTSD in children, and possibly ameliorating behaviour problems. Whilst it is difficult to disinter the potentially beneficial influences of a group (e.g. sharing experiences, reducing stigma) and the findings are not uniformly positive, there is sufficient evidence to indicate consideration of group-based psychoeducation for sexually abused children and children exposed to IPV.
Peer mentoring
Only two181,182 studies of peer mentoring have been conducted, but the results of each indicate the potential of this day-care intervention for maltreated preschool children who have been physically abused and neglected.
Enhanced foster care
For young children in foster care there is indicative evidence of benefit to maltreated children from three studies that compared enhanced foster care with RFC. 183–189,191 A pilot study183–188 of treatment foster care for preschool maltreated children suggests that this form of care may facilitate children’s attachment to their foster parents, improve the behaviour management strategies used by foster carers, and – perhaps relatedly – improve the behaviour of these challenging children.
Providing mentoring and skills training to children aged 9–11 years, in foster care (including kinship care), was reported to impact positively on children’s mental health and better manage the transition to senior school. 190 This intervention,191 which was provided over 9 months (30 weeks), also resulted in fewer placement changes, fewer placements in residential care and higher rates of permanency, including adoption.
There is tentative evidence that MTFC may be able to help foster parents to help children to improve their ability to self-regulate,193 but further evidence is required.
Improving attachment to caregivers, reducing behaviour problems and promoting placement stability are all significant achievements for maltreated children in out-of-home care, and are likely to represent significant improvements with cumulative benefits. Further studies of this intervention in the UK are, however, required. The less significant results from the UK study of MTFC may be attributable to the older age range of children in the study and the nature of routine services. The authors concluded – from the RCT and data from the wider QEx trial in which the RCT was nested – that the intervention might be more beneficial for young people with antisocial behaviour, but less beneficial than usual treatment for those without.
Therapeutic day care
Although only a small number of studies have evaluated the effectiveness of therapeutic day care, all three studies (one trial) indicate the potential of this intervention to address some of the behavioural difficulties of maltreated children and enhance their overall development.
Summary overview of what works, for whom, in what circumstances?
For treating the symptoms of PTSD, TF-CBT currently enjoys the strongest evidence of effectiveness, although there have been few independent evaluations of this intervention. The most effective CBT interventions for children who have been sexually abused appear to be those that involve the non-offending parents. Therapeutic day care and peer mentoring may also provide opportunities to address developmental and social specific sequelae of maltreatment in preschool children.
For infants and preschool children, the evidence suggests that interventions that target parental sensitivity and responsiveness (ABC, CPP, MTFC-P) are effective in promoting secure attachments with birth parents and foster carers. Given the importance of secure attachment in promoting children’s overall development and well-being, these are important findings. Table 28 provides a summary overview.
| Intervention | Evidence of effectiveness | PSEa | Focus of intervention | Age |
|---|---|---|---|---|
| TF-CBT | PTSD | * | Designed specifically to address a trauma associated with maltreatment, particularly sexual abuse, TF-CBT combines psychoeducation (see Psychoeducation) with skills training in affect modulation, stress management, and personal safety Participants are helped to understand the relationships between thoughts, feelings and behaviour GE (by means of creating a TN) is used to enable the child to describe (confront) and process increasingly distressing details of their maltreatment Parents are seen separately and receive similar interventions together with training in parenting skills that can help parent and child The intervention includes some joint sessions |
Children and young people aged ≥ 4 years |
| Anxiety | * | |||
| Depression | * | |||
| ABC | Promoting secure attachments | ** | Enhances attachment by promoting sensitive and responsive caregiving Coaches use ‘in the moment’ opportunities to provide information, shape parental understanding of, and responsiveness to, the child, and help the parent to avoid maladaptive, automatic responses learned from prior experiences The focus of intervention is the child–parent dyad |
Children aged 6 months to 4 years |
| Reducing avoidant attachment | ** | |||
| Promoting self-regulation | *** | |||
| CPP (IPP, PPP) | Promoting secure attachments | ** | Enhances attachment by promoting sensitive and responsive caregiving Focus is on translating the parent’s and child’s feelings and experiences to one another as a means of enhancing emotional reciprocity The focus of intervention is the child–parent dyad, and includes interventions designed to help the traumatised individuals (child and carer) to (re)learn ways of coping with stress without undue, dysfunctional, levels of arousal |
Children aged 0–4 years |
| Reducing avoidant attachment | ** | |||
| Promoting self-regulation | *** | |||
| Psychoeducation | PTSD | *** | Reduces trauma of abuse and promotes healthy development by providing information about maltreatment (how common it is, the impact it often has, and how people typically react, including unhelpful ways of coping); reduces stigma and provides an opportunity for parents and children to know that they are not ‘alone’ and that their reactions are normal (validation) Psychoeducation interventions are varied, and many include a focus on developing effective ways of dealing with their experiences, and ensuring their future safety |
Children and young people aged ≥ 4 years |
| Peer mentoring | Behaviour problems | *** | Peer mentoring aims to help those children whose social functioning has been adversely affected by maltreatment to acquire key developmental skills, namely the ability to form and maintain effective peer relationships Maltreated peers with high levels of prosocial behaviour are paired with withdrawn maltreated children and trained to involve them in their play |
Preschool children |
| Social behaviour | *** | |||
| MTFC-P | Behavioural problems | *** | Facilitates attachment with caregivers, by helping to establish an optimal environment for child development, by helping foster carers provide a responsive, consistent and predictable daily routine, with preparation for transitions between activities Foster carers receive extensive training, including the management of challenging behaviour, and children receive behavioural support in preschool or day care, as well as in home-based settings, and attend weekly sessions at a therapeutic playgroup where their behavioural, social and developmental progress is monitored and addressed |
Preschool children (MTFC-P) |
| Placement permanence | *** | |||
| Self-regulation | *** | |||
| Therapeutic day care | Behaviour | *** | Teachers provide children with the environment designed to facilitate the development of strong teacher–child relationships and caring peer relationships; children are helped to recognise and deal with their own feelings organised around ordinary preschool activities, and receive a variety of individual treatments such as play therapy, speech therapy and physical therapy, designed to address developmental impairments associated with maltreatment Parents also receive services, including counselling and education |
Preschool children |
| Child development | *** | |||
| Peer relationships | *** | |||
| Parent–child relationships |
Where two or more interventions might be appropriate, which is the most likely to be effective?
Although a number of studies compared an intervention with TAU, few studies compared treatments ‘head to head’. In order to shed light on the relative effectiveness of alternate interventions for maltreated children, we consider the results of ‘other-treatment’ controlled studies in relation to children who have been sexually abused, those who have been physically abused and/or neglected, and those who have experienced multiple forms of maltreatment. In this section, with two exceptions, we draw only on studies in which at least one intervention enjoys evidence of effectiveness, that is, those interventions considered above. The exceptions are (1) a study of AAT,204 in which the evidence indicates the value added of so-called ‘therapy animals’ as an adjunct to group work with children; and (2) a small (and generally poor-quality) study180 comparing psychoanalytic therapy with reinforcement therapy. We include this last study180 as it provides a rare illustration of an intervention that targeted both school and parents while comparing the two treatments.
Children who have been sexually abused
Cognitive–behavioural therapy
Two studies95,96,102 compared a cognitive–behavioural intervention for sexually abused children with child-centred psychotherapy95,96 and EMDR. 102 The results of the study102 comparing EMDR and CBT suggest that both were equally effective in reducing PTSD symptoms in a small sample of 14 Iranian girls aged 12–13 years. However, as well as having only a very small sample, data were available only at 2 weeks post treatment; as the authors observe, it is difficult to disinter therapist effects and no steps were taken to ensure therapist adherence to either manualised treatment.
The results of the study95,96 comparing TF-CBT and CCT indicate that CBT is superior to CCT in alleviating PTSD. Most studies of CBT used non-directive, supportive therapy as a comparison. In this study,95,96 CCT was a manualised (non-directive) treatment in which therapists provided active listening, reflection, accurate empathy, and encouraged parents and children to talk about their feelings. The authors state that the treatment was ‘based on the empirically supported premise that these children and their parents develop difficulties because they have experienced a violation of trust and disempowerment (Barker-Collo & Read, 2003;767 Finkelhor, 1987205)’ (p. 398). 95 Although manualised in this study,95,96 the non-directive/supportive therapy provided to participants in the control group was comparable with other studies in which the treatment was not manualised.
One89 study assessed the value added of including SIT and GE to a conventional sexual abuse treatment. The results did not confirm the hypothesis that participants receiving SIT and GE would demonstrate a greater reduction in fear and anxiety symptoms than those in the control group. No differences were found between the two groups. Reflecting on these results, the authors consider a number of explanations, including the problem of floor effects (children in this study89 were recruited on the basis of their abuse rather than reaching a particular clinical threshold for anxiety) and the fact that elements of SIT and GE were present in both treatment programmes.
Finally, Deblinger et al. 99 compared CBT with and without the construction of a TN, alongside an examination of the impact of eight-session therapy compared with 16-session therapy. The authors99 conclude that TF-CBT was effective irrespective of the number of sessions or the inclusion of a TN component. Furthermore, they conclude that the eight-session condition with TN seemed most effective (and efficient) at ameliorating parents’ abuse-specific distress and children’s abuse-related fear and general anxiety, although parents assigned to the 16-session, no TN, condition reported greater increases in effective parenting and fewer externalising child behaviour problems post treatment. At the 1-year follow-up, improvements were sustained among those for whom data were available, and between-group differences were no longer evident.
Relationship-based interventions and multisystemic therapy
Sexually abused children were rarely included in any RBI, and no study directly compared a systemic intervention with other interventions for this group of children. Danielson et al. 526 compared MST and TAU in a specialist clinic in which evidence-based interventions were said to be commonly used. In this small study (n = 30), Danielson et al. 526 reported that the young people who received MST fared better than young people in the control group in terms of significant reductions in substance use and specific substance use risk factors (substance use was the primary focus of this MST intervention), parent-reported PTSD, depression and general internalising symptoms. No effects were found for youth-reported PTSD or externalising behaviour, and the authors526 note that randomisation failed to produce equivalent groups and that baseline differences existed between the two groups on most variables. We judged that no firm conclusions should be drawn from this study526 on the probable superiority of MST, particularly in the absence of detailed information on the interventions received by young people and their families in the control group.
The one155 UK study that compared psychoeducation with an alternative treatment compared psychoeducational group therapy with brief, focused, individual psychoanalytic psychotherapy. In this study,155 substantial reductions in psychological pathology are reported for girls in both treatment groups, assessed by the Schedule for Affective Disorders and Schizophrenia for School-Age Children (KD-SADS405) and the Orvaschel scale for assessing PTSD. 406 No between-group differences were reported except for ‘manifestations of post-traumatic stress disorder’, where the authors report greater improvement for girls receiving individual psychotherapy. In the absence of baseline data, the results of this study155 are difficult to interpret, and there are indications of post hoc selection of subscales in the analyses reported.
Counselling/psychotherapy
One180 small study (n = 22) compared psychoanalytic psychotherapy with reinforcement therapy (essentially contingent reinforcement advice to parents and teachers) for sexually abused children aged 6–12 years. This study180 used no standardised measures, relying on parent and teacher verbal report, and the authors provide no details of the procedures used to assign children to each condition. Based on parent report, children in the reinforcement group made more and faster improvements in behaviour. No child in this group presented with sleep problems or engaged in sexual play with others at the end of treatment, whereas such improvements were noted in only a few children in the psychodynamic group. Three out of seven children in the reinforcement group continued to suffer from enuresis, compared with seven out of eight children in the psychodynamic group. Neither intervention made a difference to sexual self-stimulation. Teachers reported the elimination of acting out behaviour among children in the reinforcement group, whereas 67% of those in the psychoanalytic group continued to disrupt their own and others’ learning after treatment. Most of the parents in the psychodynamic group reported tension between themselves and school personnel; in contrast, with one exception, parents in the reinforcement group reported positive relationships with school staff. Similar differences emerged in school staff perceptions of parents in each group. Perhaps most significantly, all parents participating in the psychodynamic group, but only 20% in the reinforcement group, believed that their child would be adversely affected for life as a result of sexual abuse. Reinforcement therapy has now largely been superseded by TF-CBT.
Animal-assisted therapy
Dietz et al. 204 compared three group therapies for sexually abused children aged between 7 and 17 years: no animal therapy; animal therapy (dogs) without stories; and animal therapy (dogs) with stories. In the animal therapy (dogs) without stories condition, therapy dogs and handlers were available in the lobby for 30 minutes before the group started, to interact with the children. Dogs and handlers then joined the group for 10–15 minutes as part of the introductory activity of the group and then left. In the animal therapy (dogs) with stories condition, therapeutic stories about the dogs were developed specifically for the session topics. This was designed to add structure and depth to therapy dog visits. A set of questions, developed to enable the therapist to make a smooth transition from the dog’s visit to the specific topic from the group, helped to clarify the purpose of the dog’s visit. The results indicate that children in the groups that involved therapy dogs showed significant decreases in trauma symptoms, with those in the animal therapy (dogs) with stories condition showing most improvement. This COS204 was of a reasonable size and quality but the findings, although positive, identify a need for replication using a randomised design.
Other treatments
There were no other treatment comparisons among the five studies168–173 of group work for sexually abused girls.
Table 29 summarises the evidence available on the comparative effectiveness of interventions for children who have been sexually abused.
| Study | Interventions compared | Outcome | Findings favour | |||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| Jaberghaderi 2004102 | CBT | EMDR | N/A | N/A | PTSD | Both groups improved |
| Cohen 200495 | CBT | CCP | N/A | N/A | PTSD | CBT |
| Berliner 199689 | Conventional sexual abuse treatment plus SIT and GE | Conventional sexual abuse | N/A | N/A | Fear Anxiety |
Both groups improved |
| Deblinger 2011100 | CBT × 8 | CBT × 8 + TN | CBT × 16 | CBT × 16 + TN | Parents’ abuse-related stress | CBT × 8 + TN |
| Children’s abuse-related fear and general anxiety | CBT × 8 + TN | |||||
| Effective parenting | CBT × 16 | |||||
| Externalising child behaviours | CBT 16 | |||||
| Danielson 2010526 | MST | Unspecified evidence-based practices | N/A | N/A | Substance misuse | MST |
| Substance misuse risk factors | MST | |||||
| Parent-reported PTSD | MST | |||||
| Parent-reported depression | MST | |||||
| Internalising | MST | |||||
| Youth-reported PTSD | Neither | |||||
| Externalising | Neither | |||||
| Trowell 2002155 | Psychoeducational GP | Brief IP | N/A | N/A | Psychopathological symptoms | Both groups improved |
| PTSD manifestations | Individual PT | |||||
| Dietz 2012204 | GT | GTD | GTDS | Trauma symptoms | GTDS followed by GTD All groups improved |
|
| Downing 1986180 | PP | RT | N/A | N/A | Sleep | RT |
| Sexual play with others | RT | |||||
| Sexual self-stimulation | Neither group improved | |||||
| Disruption in school | RT | |||||
| Enuresis | RT | |||||
Children who have been physically abused
Cognitive–behavioural therapy
Runyon et al. 109 compared two CBT interventions, one involving just parents and the other involving parents and children (see Chapter 4 for further details). Significant improvements were reported for both groups on parent- and child-reported corporal punishment, total number of PTSD symptoms and parents’ reports on children’s internalising behaviour problems; only in the CPC-CBT group (CBT for both parents and children) were significant MDs found in the pre- and post-test measure of positive parenting, and significant improvements in the pre- and post-test mean scores for externalising behaviour were found only for those in the parent-only CBT group. Improvements were maintained 3 months after treatment. In a comparison between CBT and FT, Kolko107,108 found no significant differences between the two groups, although overall levels of parental anger and use of physical discipline/force were lower in CBT than in FT families.
Multisystemic therapy
In the study by Swenson et al. ,144 MST was compared with enhanced outpatient treatment, which included the standard services offered at the centre (including a range of therapies and outward referrals) plus special measures to maximise the engagement and retention of families in treatment (including telephone reminders, the scheduling of appointments). The STEP-TEEN768 was provided for all parents. The results indicated that MST-CAN was more effective than enhanced outpatient treatment in reducing youth mental health symptoms, parental psychiatric stress, those parenting behaviours associated with maltreatment, youth out-of-home placements and changes in new placements.
Table 30 summarises the evidence available on the comparative effectiveness of interventions for children who have been physically abused.
| Study | Interventions compared | Outcome | Findings favour | |
|---|---|---|---|---|
| 1 | 2 | |||
| Runyon 2010109 | CBT-PO | CPC-CBT | PTSD Internalising behaviour |
CPC-CBT |
| Externalising behaviour | CBT-PO | |||
| Kolko 1996108 | CBT | FT | Both groups improved | |
| Swenson 2010144 | MST | Enhanced outpatient treatment | Youth mental health | MST |
| Parental psychiatric stress | MST | |||
| Parenting behaviour | MST | |||
| Permanency in placement | MST | |||
Children who have experienced different kinds of maltreatment
Cognitive–behavioural therapy
Rushton and Miles664 compared a cognitive–behavioural parent training intervention based upon (but not replicating) Webster-Stratton’s IY programme, with an educational programme that was designed to improve adopters’ understanding of the meaning of children’s current behaviour and to help them see how this might reflect their past experiences. No differences were found in child behaviour problems between the two groups at 6 months’ follow-up, although there was greater satisfaction with the behavioural intervention than with the educational comparison.
Scheck et al. 121 compared EMDR with an active-listening intervention, and reported a significant effect for EMDR on depression and self-concept.
Attachment and Biobehavioral Catch-up
Attachment and Biobehavioral Catch-up (ABC) was compared in two122,125,126 studies with a home-based educational intervention designed to enhance cognitive and linguistic development, which was stripped of components that promoted parental sensitivity to child cues. Different outcome measures were used in each study. Results favoured ABC in promoting secure attachment in the Bernard et al. 122 study and in the Dozier et al. 125,126 study, in which parents reported fewer behaviour problems among older children, and improvements in foster children’s regulatory capabilities (assessed by saliva cortisol).
Child–parent psychotherapy
Child–parent psychotherapy (CPP) was compared with PPI in three123,124,133 studies and with psychotherapy plus case management in a fourth study. 127–129 Results from the study by Toth et al. 133 indicated children in the CPP group evidenced fewer maladaptive maternal representations and fewer negative self-representations over time than those in the psychoeducational home-visiting condition or in a community standard. Similarly, mother–child relationship expectations of children in the CPP group became more positive than for children in the other groups. The majority of these children had experienced multiple forms of maltreatment, typically physical abuse, neglect and emotional maltreatment.
In a sample of families in which children had witnessed domestic violence, Lieberman et al. 127–129 reported a significant impact of CPP compared with case management plus community referral for individual treatment. Results indicate significant improvements in children’s behaviour problems and maternal psychiatric symptoms of distress for those who completed CPP, compared with case management plus community referral for IT. Cicchetti et al. 123 reported improvement in secure attachment in both those children allocated to CPP and those allocated to a PPI. Significant results were also reported for both these interventions in a study examining their impact on normalising biological regulatory processes. 124
Other
No studies of treatment foster care, therapeutic day care or psychoeducation included other treatment controls (Table 31).
| Study | Interventions compared | Outcome | Findings favour | |
|---|---|---|---|---|
| 1 | 2 | |||
| Rushton 2000664 | CB/PT | EPT | Child behaviour | CB/PT |
| Parental satisfaction | EPT | |||
| Scheck 1998121 | EMDR | Active listening | Depression | EMDR |
| Self-concept | EMDR | |||
| Bernard 2012122 | ABC | Home-based educational intervention | Secure attachment | ABC |
| Dozier 2006125,126 | Regulatory ability | ABC | ||
| Toth 2002133 | CPPa | PPI | Improvements in children’s maternal representations | CPP |
| Improvements in children’s negative self-representations | CPP | |||
| Improvements in mother–child relationship expectations | CPP | |||
| Cicchetti 2006123 | CPPa | PPI | Secure attachments | Both groups improved |
| Maternal psychiatric symptoms | CPP | |||
| Cicchetti 2011124 | CPP | PPI | Biological regulatory processes | CPP |
| Lieberman 2006129 | CPP | Psychotherapy and case management | Secure attachment | CPP |
What interventions are of no benefit or may result in harm?
On the basis of the studies identified in this review, it is not currently possible to answer this question. In some areas there is little or no evidence about the effectiveness of interventions, some of which are routinely used in the UK. Examples of this would be non-directive counselling, supportive therapy, music therapy, art therapy and some other activity-based interventions. Unfortunately, ‘intelligence’ from our PAG suggests that these are the therapies that are most likely to be offered to maltreated children.
Very few studies address the issue of harm. One89 1996 study of CBT noted that the symptoms of 5–15% of children in both treatment groups actually got worse over time. The authors note that, in the absence of a no treatment control, it is not possible to know whether improvement or deterioration may have occurred without treatment. Equally, treatment may have limited the level of deterioration but, again, it is not possible to tell from an ‘other treatment’ control design. This attention to the important issue of deterioration was the exception rather than the rule. No study appeared to have been designed with the explicit aim of tracking unintended consequences of treatment.
What interventions are most accessible and acceptable to carers, children and young people?
One of the key messages to emerge from this body of research is that researchers routinely miss the opportunity to consider issues of accessibility and acceptability. Although additional dimensions increase the cost of research, there are some low-cost strategies that could be deployed to explore the barriers and facilitators both of engagement and of retention in therapy. Given the difficulty of disinterring retention in a study from retention in an intervention, there is also a research gap in relation to these important issues within the UK.
One of the things to emerge from the studies, and which drew comment from the PAG, was that in the included studies many users were recruited by research teams into specialist centres, and, even where the setting was a mainstream service setting, little was said about normal referral pathways. Together with the fact that very few studies were conducted in the UK, this means that, at a very basic level, we currently know little about who receives services in the UK, who is and who is not referred, and what factors determine referral and the acceptance of those referrals by services.
Caregiver support
One factor to emerge from the literature and from the Young People’s Advisory Groups is the important role that parents and other caregivers play in determining whether or not children and young people engage with therapeutic services when these are offered. Young children need their parents to take them, and most children look to their parents for messages, both verbal and non-verbal, about the acceptability of treatment, in terms of both its probable helpfulness and its acceptability within the family. Although not discussed in these terms, this may be one reason why therapies generally appear to be more effective when they involve parents, although the primary reason is likely that such interventions are more ecologically valid and maximise the opportunities for influence.
Relatively few studies addressed the issue of the relationship between therapist and parent, or indeed the impact of the therapist’s relationship with the child. We know from the broader psychotherapy literature that the latter is an important factor, and in this area, both are important influences on the likelihood of engagement with services and on outcome. Among the PAG there were different opinions as to how parents’ own prior history of therapy might influence their decisions about seeking treatment for a child, or accepting it if offered. It is very probable that parents who had been deemed to have maltreated their children may need some persuasion and skilled workers. Some of the techniques described in studies of ABC and CPP provide useful illustrations of the skills required to work with these families.
In the absence of studies addressing this, one can only speculate, but the studies included in this review illustrate (if at times only by omission) the importance of addressing these interpersonal issues. As we discussed in Chapter 5, young adolescents would clearly like the opportunity to influence decisions about seeking help, and negotiating the form that this help might take.
The basics
Although largely conducted in America, studies examining service engagement and retention consistently point to the probable importance of some very basic considerations, such as location of services, the extent to which people feel welcome, the importance placed on confidentiality, and knowing what to expect. The length of the waiting list was a factor implicated as a probable cause of ‘no shows’ in those studies which examined treatment engagement.
Groups and psychoeducation
Although the results for studies of therapeutic group work were generally disappointing, there was evidence across the studies that bringing children and parents together in (separate) groups was a useful adjunct to other therapeutic approaches, such as cognitive–behavioural interventions, psychoeducation and in some of the intensive service models, such as treatment foster care. Therapeutic day-care settings offer some of the same characteristics. Groups provide an opportunity for children – and parents – to realise that they are not alone in coping with difficult circumstances; they provide an opportunity to share experiences with others whose own circumstances are closer to their own than those of the typical professional or therapist, and this also provides opportunities for problem-solving and skill development that are not so readily available in IT. Groups can be organised around activities which can attenuate the awkwardness that some people feel in one-to-one counselling, or in therapeutic interventions that depend wholly on talking. As the study by Diez et al. 204 suggests, animals may provide one such opportunity. The studies that have consulted with children and young people participating in groups, make clear that the prospect of joining a group is not necessarily less intimidating than that of talking alone to a therapist, and for some children it may be more so. Groups may be cost-effective, but require considerable planning. Ensuring their effectiveness also requires attending to the issues discussed above.
Psychoeducational group therapy and CBT (which includes a strong component of psychoeducation) may appeal to parents and children because they represent a sharing of expert knowledge and offer very concrete strategies for dealing with present and future difficulties. It is possible (although no study has investigated this, as far as we can tell) that the processing content of psychoeducational interventions provides participants with a language and a means to address the consequences of maltreatment. This has certainly been the experience in other fields (e.g. psychoeducational interventions for people with schizophrenia and their families), which is why it is often referred to as an empowering intervention.
What do we know about the economic benefits?
Little is known about the cost-effectiveness of alternative interventions for maltreated children. Only six economic evaluations that could be considered ‘full’ economic evaluations (comparative analysis of alternative interventions in terms of both costs and effects) were located, and the results are conflicting. Evidence from an Australian decision-analytic model suggests economic benefits for TF-CBT compared with no treatment and non-directive counselling, particularly when combined with a SSRI antidepressant. 612 In contrast, a UK-based study613 found no evidence of cost-effectiveness of parenting programmes that included a cognitive–behavioural approach. Another UK-based study614 found economic advantages for a group-based psychoeducation intervention compared with individual psychotherapy for girls who had been sexually abused. Two615,616 US-based studies support the cost-effectiveness of intensive service models of care and the final study,198 also US based, was inconclusive when evaluating a co-ordinated model of care.
In addition to conflicting results, all studies suffered from a number of limitations, primarily small sample sizes and narrow cost perspectives, but also the lack of generic measures of outcome, incremental analysis and exploration of uncertainty. None of the studies was scientifically robust enough to have strong confidence in the results reported and no economic evidence was found for CBT for physical abuse, RBIs, systemic therapies, activity-based therapies, psychotherapy/counselling, peer mentoring or therapeutic residential or day-care services.
Exploration of the cost-effectiveness of the most promising intervention, CBT for children who had been sexually abused, using outcome data from meta-analysis, was still unable to provide a clear conclusion. The results for all analyses, apart from one, showed no clear economic advantage for CBT. The only exception was for post-treatment depression outcomes. However, any potential advantage for CBT disappeared by the 12-month follow-up.
Overall, it is clear that there is a serious lack of robust evidence of cost-effectiveness of interventions for children who have been maltreated and further good-quality research is needed.
Conclusions
The multiple and different effects of maltreatment vary with maltreatment type; maltreatment characteristics (duration, intensity, frequency); the nature of support available to the child (during and after maltreatment); and the child’s innate/genetic vulnerability. It follows that what is needed before offering therapy (resource-led approach) is an assessment of the child’s current and probable future therapeutic needs. The needs of looked-after children, in particular, require regular review, albeit in ways that are acceptable to the children and non-stigmatising. Some children will need treatment for specific psychiatric sequelae, such as PTSD, anxiety and depression. Most will need services that can minimise the adverse consequences that maltreatment often has on children’s emotional, social, behavioural and physical development.
For children in out-of-home placements, in particular, assessments need to include assessments of the child’s ‘caregiving system’ and how this is influenced by wider systems, such as education and social welfare. 769 It should include an assessment of motivations for caregiving and the factors that impact on carers’ roles, including how secure they feel in the permanence of their relationships with the child. As this review makes clear, foster and adoptive parents are a fundamental therapeutic resource for the children for whom they are caring. Although residential workers are clearly in a different relationship with children, these factors underline the importance of thinking therapeutically and strategically about this form of care which, although serving only around 11% of children in care, is usually caring for some of the most troubled young people.
A rather different, but fundamental, consideration is the need for a comprehensive assessment of the needs of any seriously maltreated child and his/her family. A point repeatedly made in the sexual abuse literature is that sexual abuse is an event and not a disorder. Not all children who are sexually abused, or are the victims of excessive physical punishment, go on to develop PTSD or depression, or behaviour problems. The consequences of maltreatment differ because every child is different. 770 Furthermore, the consequences of significant maltreatment manifest themselves at different stages of a child’s development and often in different ways. If PTSD becomes a problem for a child then it is important to address this. For some children PTSD or depression may not be a problem until triggered by something later in their lives, or may be a problem that recurs at significant transition points.
Those children whose maltreatment history is such that they are made subject to a child protection plan, or are placed in out-of-home care, need to have their circumstances comprehensively reviewed (by the responsible social worker and the core team) and require an overall assessment of the impact of their experiences – not just in terms of mental disorder, but in relation to their general development and functioning. They may also need to be kept under periodic review, although managing this without stigmatising children (particularly those in care) needs very careful handling if it is to be acceptable to them.
For example, speech and language delay are not unusual amongst maltreated children, and maltreatment frequently impacts adversely on social and emotional functioning and on educational progress. If not addressed, the cumulative damage of these developmental deficits may well be as costly to the child and to society as particular psychiatric disorders. Yet relatively few studies examined interventions designed to address these longer-term problems. Exceptions are the peer-mentoring interventions studied by Fantuzzo et al. ;182 the therapeutic day care evaluated by Culp et al. ;197 and the MTFC developed by Fisher et al. 183–188 for preschool children. Both Culp et al. 196 and Fantuzzo et al. 182 paid considerable attention to the involvement of parents (directly or indirectly). RBIs, such as those mentioned above, are well placed to improve developmental outcomes for infants.
The families of children who come to the attention of Child Protection Services in the UK typically have a wide range of needs, as do their children. An unintended consequence of the Children Act 1989,771 exacerbated by resource shortages, is that many of the children in care, and many of those who are subject to a child protection plan, have been exposed to maltreatment for many years before services respond adequately. Their needs are very complex and most are long-term and may be exacerbated by moves within the care system. One of weaknesses in the current evidence base is that there are few studies of complex and longer interventions (such as service configurations) designed to address the realities facing Child Protection Services and partner agencies. It is difficult, on the base of the existing evidence, to identify interventions with a strong evidence base, but even if this were not the case we would argue that in this area the choice of therapeutic intervention (such as group work or CBT) needs to be driven as much by the conclusions of a good-quality assessment as by the occurrence of maltreatment, however serious. In short, child maltreatment, particularly when chronic or severe, disrupts normal development, and children who have been adversely affected by maltreatment carry a particular ‘handicap’ (to coin sporting jargon) in the negotiation of developmental transitions. Beyond therapeutic interventions, they require good caregiving.
Access to therapy
This review generally confirms the relevance to maltreated children in the UK of the interventions examined in the included studies, but highlights significant gaps that are consequent on the narrow focus of these studies on particular clinical sequelae of maltreatment, such as PTSD. But, whatever help children need, it is not easy for them to know where or how to access it.
CAMHS in the UK are currently a scarce resource, with high thresholds and significant waiting lists. Little is known about the profile of services provided or to whom they are provided. A survey of provision in the UK would be extremely helpful in ascertaining the extent to which maltreated children, including children in care, are offered, and are accessing, this provision.
A survey ascertaining the kinds of interventions used in this service would also facilitate a systematic investigation of a problem reported by our PAG, namely that there would appear to be a mismatch between the services children are most likely to receive in the UK (as indicated by the PAG) and those interventions that have been rigorously evaluated in relation to maltreated children, or indeed evaluated at all. The interventions most rigorously evaluated, and whose results are most promising (CBT, CPP, ABC), either appear to be very patchy in the UK or, if practised (CBT), not necessarily practised to a high standard (i.e. with fidelity). In contrast, therapies that have not been subjected to rigorous evaluation, and for which the evidence base is extremely weak, appear to be routinely available, for example creative therapies and play therapies. Some of these therapies may be effective; they may be particularly relevant for children unable to express themselves verbally, either for reasons of trauma or because of their developmental age, but at the moment they cannot be said to be evidence based. In some cases, interventions in use have simply not been evaluated and entirely lack empirical support for use with maltreated children (e.g. non-directive play therapy, art therapy). In the absence of evidence for their use, policy initiatives, such as the Department for Education’s decision to provide adoptive parents with vouchers to purchase therapeutic services (the Adoptive Support Fund), may serve only to exacerbate this situation, as such therapies are also the easiest to access. Adopters need support to help their children access not specialist services, but effective services.
Children need access to relevant sources of help when they need it. This suggests that sources of help need to extend beyond those provided by CAMHS. Some of the studies in this review emphasised the specialist knowledge that is required when working with maltreated children, which is not necessarily included in qualifying or even post-qualifying training. We return to this issue in the next section.
There was only one497 study of a web-based therapeutic support identified in this review and, despite the many concerns facing professionals who wish to provide therapeutic help through this medium, the general principle of using social media as means of communicating and encouraging sources of help, and providing sources of help, should not be dismissed.
Evidence-based interventions
Compared with the evident need for effective interventions to address the consequences of maltreatment, the number of interventions for which there is strong empirical support is relatively small. For symptoms such as PTSD and anxiety, cognitive–behavioural interventions appear to enjoy most support. The evidence for their effectiveness for depression is less clear. There is promising support for the effectiveness of relatively brief, focused, manualised interventions to help address insecure attachments among maltreated infants and toddlers. An even smaller, but also promising, evidence base suggests that therapeutic day care can help with some of the social interactional problems experienced by some maltreated children. Psychoeducation, both as part of an intervention such as CBT or as a central component in organising groups of children, may be effective in reducing trauma and helping children to cope and move forward. One183–188 study of MTFC for preschool children suggests that this may be an effective strategy for promoting placement stability.
Increasing capacity to deliver evidence-based intervention
In a survey of relevant mental health clinicians in the USA (including social work, counselling, clinical psychology and ‘other’) Allen et al. 772 provided respondents with a list of 15 interventions, and asked them to identify those interventions that they commonly used in practice; for which they had received specialist training; for which they would like to receive training or more advanced training; and that they saw, regardless of the targeted presenting problem, as empirically supported for use with maltreated children (maximum of five interventions). The research team did not define empirical support in an attempt to increase ecological validity. The list was constructed by 10 experts in the field of research with maltreated children, some of whom might well be deemed to have been a conflict of interest, but the list is broadly consistent with the conclusions of this review. Irrespective of experience, primary practice setting or self-reported theoretical orientation, few respondents were able to identify interventions that the expert advisory group identified as empirically supported, with the exception of TF-CBT, in which 73% of the 262 clinicians said they were trained. Aside from this, no more than one-third were able to identify any other empirically supported treatments and were not trained in their use. Most reported being trained in, on average, two non-empirically supported treatments, and many indicated that they used interventions that they knew were not empirically supported. The more experienced the clinician, the greater the number of non-empirically supported training interventions undertaken (and the greater the number of non-empirically supported interventions identified as empirically supported).
These findings reflect common challenges that are inherent in developing and maintaining evidence-based practice among busy clinicians, namely how best to make the findings of research accessible to them and how to facilitate their use, with concomitant implications for qualifying training, continuing professional development and organisational support. For UK clinicians, a further challenge might be scepticism about the perceived relevance of evidence produced outside the UK.
Concerns were expressed by the PAG that a similar situation exists in the UK, but, to our knowledge, no such research has been conducted in the UK. Robustly gathered, such information would, alongside information on the profile of children accessing services from CAMHS, facilitate an evidence-informed approach to workforce planning, training strategies and the identification of research gaps.
Enhancing placement stability for looked-after children
For maltreated children whose histories require out-of-home placements for long periods of time, the importance of placement stability in a home where they can develop close relationships with their caregivers cannot be overstated. It is evident from the studies included in this review that placement stability can be enhanced by providing foster and adoptive parents with the skills and support needed to understand and address the problems that result from maltreatment and insecure attachments.
Tarren-Sweeney61 has argued for a clinical workforce that specialises in children in care or adopted. There are two strong arguments for this. The first is that such a workforce – which would extend beyond CAMHS (e.g. including specialist social workers, therapists working with adoption and fostering agencies) – would go some way to ensuring that children who have experienced maltreatment and, importantly, their caregivers would have ready access to appropriate services. For some children, such a person might provide an anchor point in the world where social workers come and go, and placements often change. This is perhaps optimistic, but it is more difficult to take issue with the second argument, which is that those working with looked-after children, irrespective of disciplinary background, require specialist training. He suggests that such training should reflect a broader conceptualisation of practice that incorporates enhanced expertise in the assessment and formulation of attachment- and trauma-related psychopathology among vulnerable children, and a greater focus on ‘the nature of family life that sustains and promotes the development of children who have experienced chronic social adversity; children’s felt experiences and worldview; child welfare systemic influences; and more detailed consideration of children’s developmental histories, with particular reference to attachment and trauma theories’61 (p. 619). All of these also need to be understood by the children’s caregivers, who are the crucial agents of positive change for the children, alongside therapeutic interventions. In the UK, Golding60 makes a similar point, albeit in the context of multiagency working. Training in evidence-based, psychosocial interventions is necessary, but not sufficient, training for practitioners working with the majority of children in the UK who have experienced abuse and neglect.
Strengths and limitations of this evidence synthesis
Strengths
This review is largest and most comprehensive review of what is known about the effectiveness of psychosocial interventions for maltreated children. The searches were thorough and comprehensive, unrestricted either by language or by time. This should have ensured that we have missed little, but the body of evidence was larger and more complex than we anticipated. Our method of judging study eligibility should have ensured that we did not exclude studies inappropriately.
The study benefited from a multidisciplinary Steering Group of very actively engaged individuals from a variety of professional backgrounds, from statutory, voluntary and research user organisations. The involvement of key stakeholders is, we believe, a major strength in this report. Although we were able to consult with only relatively small numbers of young people, their views provided an important lens through which to consider the available evidence, and the same is true of the – somewhat more representative – group of professionals in our PAG.
Limitations
This evidence synthesis was developed to be of value to decision-makers. We have therefore tried, throughout this report, to consider the five factors influencing quality that are judged as part of a GRADE assessment. In view of the relatively sparse data available for pooled analyses, the added value of presenting separate SOF tables for all comparisons was deemed limited, although for illustrative purposes we have developed a SOF table for CBT alternatives compared with non-CBT-based alternatives for children who have been sexually abused (see Appendix 11).
Another limitation of the available evidence (rather than the review itself) is the generalisability of findings from studies that were largely conducted outside the UK. This applies particularly to the effectiveness studies and studies of economic evaluations, but it also applies to studies of acceptability of interventions and services. Here, there are marginally more UK studies, and, although their quality is acceptable in respect of their aims, one would not wish to generalise from the findings of most of these studies, wherever they are conducted. Their major contribution is shining a spotlight on important issues that researchers have rarely taken seriously, and which could merit both from dedicated research on these issues and from being embedded in studies of effectiveness.
A key limitation is the restricted focus of most studies on outcomes deployed in studies of effectiveness. For this population, it may well be appropriate for a study of CBT or psychoeducation to focus on specific clinical outcomes, such as anxiety or PTSD, but such a narrow focus on clinical outcomes assumes that, if these are addressed, so too will be the wider and – we have argued – more serious effects of maltreatment on the lives of many children and young people.
Given the large number of heterogeneous studies, the time and resource constraints under which we were working limited our ability to investigate a number of issues that emerged as hypotheses, for example the extent to which certain intervention components are important irrespective of intervention type. The role of parents, the role of groups and the contribution of psychoeducation are three such candidates.
Implications for practice
This review cast a wide net in seeking evidence of ‘what works’ in addressing the adverse consequence of child maltreatment. The field is certainly challenging, for both technical and ethical reasons, and for this reason we did not seek to restrict our inclusion criteria to randomised trials. It is therefore particularly disappointing that the available evidence does not lend itself to unequivocal guidance on what therapeutic approaches are best suited to this population. The key reasons for this stem from the poor quality and reporting of the available research, and we address this in the final section, Future research. It would appear also to indicate something of a ‘disconnect’ between the focus of researchers and the reality of clinical practice, particularly in relation to the populations served by the latter and the inclusion criteria of the former.
However, reviewing and critically appraising these studies has highlighted a number of implications for practice. First, although no evidence of effectiveness is not evidence of ineffectiveness, those interventions that appear to have some benefit share some common features, such as an educational component (helping children and parents to understand what has happened and to appropriately allocate responsibility for maltreatment), the importance of being believed and supported, helping children and parents to establish strategies to ensure their future safety, and – where necessary – addressing the direct psychological sequelae of trauma, such as post-traumatic stress or depression (where cognitive–behavioural approaches outperform others). Studies have focused predominantly on the psychological sequelae of maltreatment, neglecting other areas of functioning and development that may be less dramatic (failing to fall into a diagnostic category) but, which, nonetheless, can have significant, cumulative effects on a young person’s development and quality of life.
When studies have inclusion criteria that (rightly) do not simply rely on the ‘fact’ of maltreatment, they usually apply criteria that draw on mental health diagnoses, for example PTSD. This is clearly a difficult issue. In order to maximise the chances of detecting an effect, studies often (and rightly) recruit only children with evidence of an adverse impact of maltreatment. However, the recruitment strategies of these (mainly North American) studies suggest that the samples are not typical of those children routinely presenting at UK clinics or indeed clinics worldwide. Many are victims of sexual abuse, often when the non-offending parent has believed the child and engaged in therapy. Some studies examine the impact of interventions on children in foster care, and these samples are probably more typical of the wider population of children who have experienced significant maltreatment, that is, of such a serious nature that they have been placed in out-of-home care. For these children, adding CBT to the management of challenging behaviour and (for infants) attachment-based approaches seem to have most promise.
More broadly, evidence from the included studies points to the following.
-
Many children have experienced more than one form of maltreatment and the harmful effects are heterogeneous. It is therefore necessary for any therapeutic intervention to be preceded by a full assessment of the child’s functioning, which goes beyond a search for diagnosable mental health disorders and includes physical and cognitive development, speech and language development, interpersonal/social functioning, behaviour, self-esteem and educational attainment.
-
Therapy provided for identified mental health disorders, such as anxiety, PTSD and depression, may be necessary but will often not be sufficient to meet the child’s overall needs.
-
Therapeutic intervention may be required at different times in the child’s life, as opposed to a single time-limited intervention.
-
Whatever the nature of the intervention, parents or other primary caregivers need to be included, at the very least to support the child’s participation, but interventions may also include carers’ participation in the child’s therapy, parallel work with the caregivers, work directed at the caregivers’ interaction with the child, or parenting work to enhance the child’s behaviour difficulties.
-
Attention needs to be paid to the expressed needs and wishes of children and their caregivers regarding the setting of the therapeutic work to be provided.
-
There are benefits, both for children and for caregivers, to providing therapeutic work in groups, which allow for sharing of experiences and reducing of stigma and guilt.
-
For symptoms such as PTSD and anxiety, trauma-focused cognitive–behavioural interventions appear to be most effective. The evidence for their effectiveness for depression is less clear.
-
Therapeutic day care and peer mentoring may also provide opportunities to address developmental and social specific sequelae of maltreatment in preschool children.
-
There is promising support for the effectiveness of relatively brief, focused, manualised interventions to help address insecure attachments among maltreated infants and toddlers.
-
MTFC for preschool children suggests that this may be an effective strategy for promoting placement stability. Its impact on improving outcomes for older children is less clear.
-
Many interventions currently used in the UK have no empirical evidence to support their use.
Future research
Given the paucity of evidence directly relevant to the needs of maltreated children and young people in the UK, the primary recommendation from this review must be for research investment in this area. This should include robust evaluations of those therapies most commonly used with this group of children. In identifying these, we have no UK data, and draw only on the knowledge of the research team and the PAG. The interventions most likely to be offered to maltreated children for identified mental health problems are cognitive–behavioural therapies (for those suffering from PTSD or depression), attachment-based interventions (for infants), music therapy (and other activity-based therapies, such as art or play therapy) and group-based interventions.
There is a need for independent evaluation of these interventions, as well as primary research into the profile of needs and provision of therapeutic services – including, but not confined to, clinical interventions – for maltreated children. A particular focus should be on those children looked after by the state, where there is some evidence that interventions designed to support foster parents, and adopters can enhance placement stability.
Studies should focus on issues beyond those readily assessed by clinical measures, and address the more pervasive consequences of maltreatment. Urgently needed is the development and evaluation of interventions that can address the broader psychosocial needs of maltreated children across the range of systems that have the potential to mitigate the adverse effects of their experiences. Significantly, these include schools and day-care settings.
The underdeveloped profile of UK research in this field suggests that commissioners should require researchers to pay careful attention to the growing literature on how best to conduct studies of complex interventions, beginning with the development of logic models or theories of change (clearly specifying why and how proposed interventions are expected to improve outcomes for children who have experienced maltreatment), using appropriate comparisons, and outcome measures that have ecological validity, that is, that address the wider impacts of maltreatment and include measures beyond those of psychological adjustment (e.g. school readiness, well-being, daily life skills, family functioning, academic achievement). Importantly, studies need to be better designed, with adequate sample sizes (probably requiring multisite trials), recruiting participants who reflect those presenting routinely to CAMHS, and that address the wider range of opportunities for dealing with the consequences of maltreatment, for example school-based interventions, and support to foster and adoptive parents.
The reporting of studies should adhere to CONSORT guidelines, which now include a guideline extension for the reporting of complex social interventions. 773
Acknowledgements
We are extremely grateful to all of the young people and professionals who assisted us in this review. It made an important contribution to our understanding of what is important to young people and those delivering services, including foster care. It also assisted in our interpretation of the data.
Further information about the data underpinning this report can be obtained from Geraldine Macdonald.
Contributions of authors
All authors were involved in the conception and design of the study, the acquisition of data or analysis, data interpretation, drafting and/or revising the report and final approval of the version to be published. All members of the Steering Committee helped to search the grey literature. Individual contributions were as follows.
Geraldine Macdonald drafted the original proposal and comanaged the project. Responsible for the work of the research team. Contributed to screening of studies, quality assured data extraction and risk-of-bias judgements. Drafted Chapters 1, 2 and 4–6 on the basis of preparatory work from NL, JH, CMcC and TB, with subsequent contributions from others, particularly DG. With RC, drafted the scientific summary, abstract and plain English summary.
Nuala Livingstone helped to draft the original proposal. Responsible for the day-to-day management of the study and the study team (JH, CMcC and TB). Took a lead role in planning the consultations with young people and the PAGs. Undertook screening of citations, data extraction, risk-of-bias assessments, meta-analyses of data and SOF tables. Contributed to Chapters 2–6.
Jennifer Hanratty planned and conducted consultations with young people; helped plan the consultations with the PAGs; drafted reports following the consultations (with RC, NL and CMcC); and undertook screening of studies, data extraction and quality assessment of included studies. Prepared and maintained Excel spreadsheet from which tables were produced. Prepared draft of Chapter 3 and contributed to draft of Chapter 4.
Claire McCartan undertook screening of studies, data extraction and quality assessment of non-randomised studies. Conducted thematic analyses for synthesis of acceptability data. Drafted Chapter 5 of the report, and contributed to Chapter 6. Managed all referencing in the final report.
Richard Cotmore was a member of the Steering Group. Took a lead role in planning and implementing consultations with the Young People’s Advisory Group. Contributed to planning and implementation of professional liaison group. Drafted sections of the final report relating to the Young People’s Advisory Group. Commented on, and contributed to, Chapters 1, 3, 5 and 6. Provided advice and assistance in relation to young people’s views.
Maria Cary assisted with searching the grey literature. Contributed to screening of all studies. Responsible for data extraction and quality assessment of studies that were relevant to the economic evaluation, and contributed to the screening of the effectiveness studies. Undertook the economic analysis. Helped draft the economic sections of the report.
Danya Glaser was a member of the project Steering Committee. Contributed to planning all advisory groups. Provided expert clinical advice throughout the project. Ensured that the team was up to date with relevant developments. Helped to draft Chapters 1, 4 and 6.
Sarah Byford helped to draft the original proposal. Responsible for the economic component of the work, including supervision of the health economist (MC). Drafted the economic sections of Chapters 2–4. Commented on, and contributed to, Chapters 2–5.
Nicky J Welton was responsible for providing advice on evidence synthesis for use in economic evaluation. Performed sensitivity analysis for quantitative meta-analyses in Chapter 4, and read and commented on the economic evaluation and Chapters 2 and 4.
Tania Bosqui undertook screening of studies, data extraction and quality assessment of included studies. Helped to prepare descriptions of included interventions, and prepared section on results of attachment-based interventions.
Lucy Bowes contributed to the original proposal and to Chapter 1.
Suzanne Audrey assisted in organising the Young People’s Advisory Group, contributed to the study design as a member of the Steering Group, and contributed to Chapter 5.
Gill Mezey assisted in planning and organisation the first PAG. Contributed to Chapters 4 and 6.
Helen L Fisher helped to critically revise the original proposal. Assisted with facilitation of first PAG and commented on the subsequent report. Assisted with searching the grey literature and commented on the final report.
Wendy Riches was a member of the project Steering Group. Took a key role in planning and implementing consultations with the young people’s advisory group, and those with the professional liaison group. Commented on Chapters 1 and 4. Provided advice throughout on ensuring relevance to key stakeholders, such as the National Institute for Health and Care Excellence, and policy-makers.
Rachel Churchill Contributed to the original proposal, managed the contract at the University of Bristol and co-chaired Steering Group/team meetings. Helped to plan consultation with young people and the PAG. Conducted attrition analyses with assistance from NL; contributed to the structure of the final report, and drafted Chapter 3, following preparatory work from NL and JH. Contributed to Chapters 2 and 6. With GM, drafted the abstract and scientific summary.
Data sharing statement
The data in the systematic review reported here can be obtained from the corresponding author on request.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- European Report on Preventing Child Maltreatment. Copenhagen: WHO Regional Office for Europe; 2013.
- Munro E. The Munro Review of Child Protection: Final Report – A Child-centred System. London: The Stationery Office; 2011.
- Brandon M, Sidebotham P, Bailey S, Belderson P, Hawley C, Ellis C, et al. New Learning from Serious Case Reviews: A Two-Year Report for 2009–11. London: Department for Education; 2012.
- Parton N. Child protection and safeguarding in England: changing and competing conceptions of risk and their implications for social work. Br J Soc Work 2011;41:854-75. http://dx.doi.org/10.1093/bjsw/bcq119.
- Howarth E, Moore T, Welton N, Lewis N, Stanley N, MacMillan H, et al. IMPRoving Outcomes for Children exposed to domestic ViolencE (IMPROVE): an evidence synthesis. Public Health Res 2016.
- Working Together to Safeguard Children. London: The Stationery Office; 2006.
- National Institute for Health and Care Excellence . When to Suspect Child Maltreatment 2009. www.nice.org.uk/CG89 (accessed 23 November 2011).
- Safeguarding Children in Whom Illness is Fabricated or Induced: Supplementary Guidance to Working Together to Safeguard Children. London: Department of Health; 2002.
- Safeguarding Children in Whom Illness is Fabricated or Induced: Supplementary Guidance to Working Together to Safeguard Children. Nottingham: DCSF Publications; 2008.
- Incredibly Caring (DVD plus booklet). A Training Resource for Professionals in Fabricated or Induced Illness (FII) in children. Milton Keynes: Radcliffe Publishing; 2008.
- Lazenbatt A, Taylor J. Fabricated or Induced Illness in Children: A Rare Form of Child Abuse? NSPCC Research Briefing 2011. www.nspccc.org.uk/inform (accessed 5 January 2012).
- Bass C, Jones D. Fabricated or induced illness. Psychiatry 2006;5:60-5. http://dx.doi.org/10.1383/psyt.2006.5.2.60.
- Jones D, Byrne G, Newbold C, Eminson MPR. Munchausen Syndrome by Proxy Abuse: A Practical Approach. Oxford: Butterworth Heinemann; 2002.
- Postlethwaite R. Fabricated or induced illness. Paediatr Child Health 2010;20:561-5. http://dx.doi.org/10.1016/j.paed.2010.08.003.
- Glaser D. How to deal with emotional abuse and neglect: further development of a conceptual framework (FRAMEA). Child Abuse Negl 2011;35:866-75. http://dx.doi.org/10.1016/j.chiabu.2011.08.002.
- Pears KC, Hyoun K, Fisher P. Psychosocial and cognitive functioning of children with specific profiles of maltreatment. Child Abuse Negl 2008;32:958-71. http://dx.doi.org/10.1016/j.chiabu.2007.12.009.
- McCrae J, Chapman M, Christ S. Profile of children investigated for sexual abuse: association with psychopathology symptoms and services. Am J Orthopsychiatry 2006;76:468-81. http://dx.doi.org/10.1037/0002-9432.76.4.468.
- Lau AS, Leeb RT, English D, Graham JC, Briggs EC, Brody KE, et al. What’s in a name? A comparison of methods for classifying predominant type of maltreatment. Child Abuse Negl 2005;29:533-51. http://dx.doi.org/10.1016/j.chiabu.2003.05.005.
- Gilbert R, Fluke J, O’Donnell M, Gonzalez-Izquierdo A, Brownett M, Gulliver P, et al. Child Maltreatment: variation in trends and policies in six developed countries. Lancet 2012;379:758-72. http://dx.doi.org/10.1016/S0140-6736(11)61087-8.
- Sidebotham P, Aktins B, Hutton J. Changes in rates of violent child deaths in England and Wales between 1974 and 2008: an analysis of national mortality data. Arch Dis Child 2012;97:193-9. http://dx.doi.org/10.1136/adc.2010.207647.
- Child Abuse and Neglect in the UK Today. London: NSPCC; 2011.
- McCrory E, De Brito S, Viding E. Research review: the neurobiology and genetics of maltreatment and adversity. J Child Psychol Psychiatry 2010;51:1079-95. http://dx.doi.org/10.1111/j.1469-7610.2010.02271.x.
- Van Harmelen A, van Tol M, van der Wee N, Veltman D, Aleman A, Spinhoven P, et al. Reduced medical prefrontal cortex volume in adults reporting childhood emotional maltreatment. Biol Psychiatry 2010;68:832-8. http://dx.doi.org/10.1016/j.biopsych.2010.06.011.
- Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D. Reduced medial prefrontal cortex volume in adults reporting childhood emotional maltreatment. Biol Psychiatry 2012;71:286-93. http://dx.doi.org/10.1016/j.biopsych.2011.10.021.
- Huang-Storms L, Bodenhamer-Davis E, Davis R, Dunn J. QEEG-guided neurofeedback for children with histories of abuse and neglect: neurodevelopmental rationale and pilot study. J Neurother 2006;10:3-16. http://dx.doi.org/10.1300/J184v10n04_02.
- Mehta D, Klengel T, Conneely K, Smith A, Altmann A, Pace T. Childhood maltreatment is associated with distinct genomic and epigenetic profiles in posttraumatic stress disorder. Proc Natl Acad Sci USA 2013;110:8302-7. http://dx.doi.org/10.1073/pnas.1217750110.
- Yang B, Zhang H, Ge W, Weder N, Douglas-Palumberi H, Perepletchikova F. Child abuse and epigenetic mechanisms of disease risk. Am J Prev Med 2013;44:101-7. http://dx.doi.org/10.1016/j.amepre.2012.10.012.
- Gilbert R, Widom CA, Browne K, Fergusson D, Webb E, Janson S. Child Maltreatment. 1. Burden and consequences of child maltreatment in high-income countries. Lancet 2009;373:68-81. http://dx.doi.org/10.1016/S0140-6736(08)61706-7.
- Mills R, Alati R, O’Callaghan M, Najman J, Williams G, Bor W, et al. Child abuse and neglect and cognitive function at 14 years of age: findings from a birth cohort. Pediatrics 2011;127:4-10. http://dx.doi.org/10.1542/peds.2009-3479.
- Zielinski D. Child maltreatment and adult socioeconomic well-being. Child Abuse Negl 2009;33:666-78. http://dx.doi.org/10.1016/j.chiabu.2009.09.001.
- Cicchetti D, Toth S. Child maltreatment. Ann Rev Clin Psychol 2005;1:409-38. http://dx.doi.org/10.1146/annurev.clinpsy.1.102803.144029.
- Colman R, Widom C. Childhood abuse and neglect and adult intimate relationships: a prospective study. Child Abuse Negl 2004;28:1133-51. http://dx.doi.org/10.1016/j.chiabu.2004.02.005.
- Veltman M, Browne K. Three decades of child maltreatment research: implications for the school years. Trauma Violence Abuse 2001;2:215-39. http://dx.doi.org/10.1177/1524838001002003002.
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry 2003;160:1453-60. http://dx.doi.org/10.1176/appi.ajp.160.8.1453.
- Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: a neglected component in child victimization. Child Abuse Negl 2007;31:7-26. http://dx.doi.org/10.1016/j.chiabu.2006.06.008.
- Herrenkohl T, Herrenkohl R. Examining the overlap and prediction of multiple forms of Child Maltreatment, stressors, and socioeconomic status: a longitudinal analysis of youth outcomes. J Fam Violence 2007;22:553-70. http://dx.doi.org/10.1007/s10896-007-9107-x.
- Widom C, DuMont K, Czahja S. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry 2007;64:49-56. http://dx.doi.org/10.1001/archpsyc.64.1.49.
- Kotch JB, Lewis T, Jussey JM, English D, Thompson R, Litrownik AJ, et al. Importance of early neglect for childhood aggression. Pediatrics 2008;121:725-31. http://dx.doi.org/10.1542/peds.2006-3622.
- Manly J, Kim J, Rogosch F, Cicchetti D. Dimensions of Child Maltreatment and children’s adjustment: contributions of developmental timing and subtype. Dev Psychopathol 2001;13:759-82.
- Briere J, Jordan C. Childhood maltreatment, intervening variables, and adult psychological difficulties in women: an overview. Trauma Violence Abuse 2009;10:375-88. http://dx.doi.org/10.1177/1524838009339757.
- Cicchetti D, Rogosch F. Adaptive coping under conditions of extreme stress: multilevel influences on the determinants of resilience in maltreated children. New Dir Child Adolesc Dev 2009;124:47-59. http://dx.doi.org/10.1002/cd.242.
- Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: evidence from a community sample. Child Abuse Negl 2007;31:211-29. http://dx.doi.org/10.1016/j.chiabu.2007.02.004.
- Jaffee S, Gallop R. Social, emotional, and academic competence among children who have had contact with child protective services: prevalence and stability estimates. J Am Acad Child Adolesc Psychiatry 2007;46:757-65. http://dx.doi.org/10.1097/chi.0b013e318040b247.
- Koenen KC, Harley RM, Lyons MJ, Wolfe J, Simpson JC, Goldberg J, et al. A twin registry study of familial and individual risk factors for trauma exposure and posttraumatic stress disorder. J Nerv Ment Dis 2002;190:209-18. http://dx.doi.org/10.1097/00005053-200204000-00001.
- Koenen KC, Moffitt TE, Poulton R, Martin J, Caspi A. Early childhood factors associated with the development of post-traumatic stress disorder: results from a longitudinal birth cohort. Psychol Med 2007;37:181-92. http://dx.doi.org/10.1017/S0033291706009019.
- Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP. The effect of child sexual abuse on social, interpersonal, and sexual function in adult life. Br J Psychiatry 1994;165:35-47. http://dx.doi.org/10.1192/bjp.165.1.35.
- Widom CS, Dohrenwend BP. Adversity, Stress, and Psychopathology. New York, NY: Oxford University Press; 1998.
- Hyman B. The economic consequences of child sexual abuse for adult lesbian women. J Marriage Fam 2000;62:199-211. http://dx.doi.org/10.1111/j.1741-3737.2000.00199.x.
- Currie J, Widom C. Long-term consequences of child abuse and neglect on adult economic well-being. Child Maltreat 2010;15:111-20. http://dx.doi.org/10.1177/1077559509355316.
- Corso PS, Edwards VJ, Fang X, Mercy JA. Health-related quality of life among adults who experienced maltreatment during childhood. Am J Public Health 2008;98:1094-140. http://dx.doi.org/10.2105/AJPH.2007.119826.
- Corso P, Lutzker J. The need for economic analysis in research on child maltreatment. Child Abuse Negl 2006;30:727-38. http://dx.doi.org/10.1016/j.chiabu.2005.12.006.
- Currie J, Tekin E. ‘Does Child Abuse Cause Crime?’. Nation Bureau of Economic Research (NBER); 2006.
- Lansford JE, Berlin L, Bates J, Pettit GS. Early physical abuse and later violent delinquency: a prospective longitudinal study. Child Maltreat 2007;12:233-45. http://dx.doi.org/10.1177/1077559507301841.
- Fundudis T, Kaplan C, Dickinson H. A comparison study of characteristics of parents of abused and non-abused children. Educ Child Psychol 2003;20:90-108.
- Berger L, Waldfogel J. Economic Determinants and Consequences of Child Maltreatment. Paris: OECD Publishing; 2011.
- Allnock D, Bunting L, Price A, Morgan-Klein N, Illis J, Radford L, et al. Mapping the Provision of Therapeutic Services to Children and Young People who have been Sexually Abused in the UK. London: NSPCC; 2009.
- Stafford A, Morgan-Klein N, Kelly S. Mapping Therapeutic Services to Children and Young People who have been Sexually Abused: Services in Scotland. Summary Report. Edinburgh: University of Edinburgh/NSPCC; 2009.
- Radford L, Aitken R, Miller P, Ellis J, Roberts J, Firkic A. Meeting the Needs of Children Living with Domestic Violence in London: Research Report. London: Refuge/NSPCC; 2011.
- Shaw M, De Jong M. Child abuse and neglect: a major public health issue and the role of child and adolescent mental health services. Psychiatrist 2012;36:321-5. http://dx.doi.org/10.1192/pb.bp.111.037135.
- Golding K. Multi-agency and specialist working to meet the mental health needs of children in care and adopted. Clin Child Psychol Psychiatry 2010;15:573-87. http://dx.doi.org/10.1177/1359104510375933.
- Tarren-Sweeney M. It’s time to re-think mental health services for children in care, and those adopted from care. Clin Child Psychol Psychiatry 2010;15:613-26. http://dx.doi.org/10.1177/1359104510377702.
- Macdonald G, Livingstone N, Davidson G, Sloan S, Fargas M, McSherry D. Improving the Mental Health of Northern Ireland’s Children and Young People: Priorities for Research. Northern Ireland: ICCR/HSC; 2011.
- Oates R, Bross D. What have we learned from treating physical abuse. Child Abuse Negl 1995;19:463-73. http://dx.doi.org/10.1016/0145-2134(95)00005-S.
- Macdonald G. Effective Interventions for Child Abuse and Neglect: An Evidence Based Approach to Assessment, Planning and Intervention. Chichester: John Wiley; 2001.
- Morrell C, Siby H, Stewart P, Walters S, Morgan A. Costs and effectiveness of community postnatal support workers: randomised controlled trial. BMJ 2002;321:593-8. http://dx.doi.org/10.1136/bmj.321.7261.593.
- Olds D, Kitzman H, Cole R, Hanks C, Arcoleo K, Anson E, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med 2010;164:419-24. http://dx.doi.org/10.1001/archpediatrics.2010.49.
- McIntosh E, Barlow J, Davis H, Stewart-Brown S. Economic evaluation of an intensive home visiting programme for vulnerable families: a cost-effectiveness analysis of a public health intervention. J Public Health 2009;31:423-33. http://dx.doi.org/10.1093/pubmed/fdp047.
- Goldhaber-Fiebert JD, Snowden LR, Wulcyn F, Landsverk J, Horwitz SM. Economic evaluation research in the context of Child Welfare policy: a structured literature review and recommendations. Child Abuse Negl 2011;35:722-40. http://dx.doi.org/10.1016/j.chiabu.2011.05.012.
- Undertaking Systematic Reviews of Research on Effectiveness: CRD’s Guidance for Those Carrying Out or Commissioning Reviews. York: CRD; 2008.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011.
- Churchill R, Macdonald G, Bowes L, Campbell R, Mezey G, Fisher H, et al. The Effectiveness, Acceptability and Cost-Effectiveness of Psychosocial Interventions for Maltreated Children and Adolescents: An Evidence Synthesis 2013. www.nets.nihr.ac.uk/__data/assets/pdf_file/0019/81190/PRO-11-110-01.pdf (accessed 4 May 2016).
- Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4: Software for Research Synthesis. EPPI-Centre Software. London: Social Science Research Unit, Institute of Education; 2010.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011.
- Downs S, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non-randomized studies of health care interventions. J Epidemiol Community Health 1998;52:377-84. http://dx.doi.org/10.1136/jech.52.6.377.
- Critical Appraisal Skills Programme (CASP) . Ten Questions to Help You Make Sense of Qualitative Research n.d. http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf (accessed 7 August 2013).
- Drummond M, Sculpher M, Torrance GW, O’Brien BJ, Stoddart G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Riley R, Higgins J, Deeks J. Interpretation of random effects meta-analyses. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d549.
- Moreno S, Sutton A, Ades A, Cooper N, Abrams K. Adjusting for publication biases across similar interventions performed well when compared with gold standard data. J Clin Epidemiol 2011;64:1230-41. http://dx.doi.org/10.1016/j.jclinepi.2011.01.009.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. A Product from the ESRC Methods Programme. Lancaster: University of Lancaster; 2006.
- Kovacs M. The Children’s Depression Inventory (CDI). Psychopharmacol Bull 1985;21:995-8.
- Curtis L. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2014.
- Van Hout B, Al M, Gordon G, Rutten F. Costs, effects and C/E-ratios alongside a clinical trial. Health Econ 1994;3:309-19. http://dx.doi.org/10.1002/hec.4730030505.
- Briggs A, Claxton K, Sculpher M. Decision Analytic Modelling for the Evaluation of Health Technologies. Oxford: Oxford University Press; 2006.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. http://dx.doi.org/10.1002/hec.635.
- Welton N, Caldwell D, Adamopoulos E, Vedhara K. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am J Epidemiol 2009;169:1158-65. http://dx.doi.org/10.1093/aje/kwp014.
- Chen Y-F, Madan J, Welton N, Yahaya I, Aveyard P, Bauld L, et al. Effectiveness and cost-effectiveness of computer and other electronic aids for smoking cessation: a systematic review and network meta-analysis. Health Technol Assess 2012;16. http://dx.doi.org/10.3310/hta16380.
- May M, Housley W. The effects of group counselling on the self-esteem of sexually abused female adolescents. Guid Couns 1996;11:38-42.
- Shanan Y. Teaching maladjusted children. M’gamot 1951;3:111-36.
- Berliner L, Saunders BE. Treating fear and anxiety in sexually abused children: results of a controlled 2-year follow-up study. Child Maltreat 1996;1:294-309. http://dx.doi.org/10.1177/1077559596001004002.
- Celano M, Hazzard A, Webb C, McCall C. Treatment of traumagenic beliefs among sexually abused girls and their mothers: an evaluation study. J Abnorm Child Psych 1996;24:1-17. http://dx.doi.org/10.1007/BF01448370.
- Cohen JA, Mannarino AP. A treatment outcome study for sexually abused preschool children: Initial findings. J Am Acad Child Adolesc Psychiatry 1996;35:42-50. http://dx.doi.org/10.1097/00004583-199601000-00011.
- Cohen JA, Mannarino AP. A treatment study for sexually abused preschool children: Outcome during a one-year follow-up. J Am Acad Child Adolesc Psychiatry 1997;36:1228-35. http://dx.doi.org/10.1097/00004583-199709000-00015.
- Cohen JA, Mannarino AP. Interventions for sexually abused children: initial treatment outcome findings. Child Maltreat 1998;3:17-26. http://dx.doi.org/10.1177/1077559598003001002.
- Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse Negl 2005;29:135-45. http://dx.doi.org/10.1016/j.chiabu.2004.12.005.
- Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry 2004;43:393-402. http://dx.doi.org/10.1097/00004583-200404000-00005.
- Deblinger E, Mannarino AP, Cohen JA, Steer RA. A follow-up study of a multisite, randomized, controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry 2006;45:1474-84. http://dx.doi.org/10.1097/01.chi.0000240839.56114.bb.
- Deblinger E, Lippmann J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: initial treatment outcome findings. Child Maltreat 1996;1:310-21. http://dx.doi.org/10.1177/1077559596001004003.
- Deblinger E, Steer RA, Lippmann J. Two-year follow-up study of cognitive behavioral therapy for sexually abused children suffering post-traumatic stress symptoms. Child Abuse Negl 1999;23:1371-8. http://dx.doi.org/10.1016/S0145-2134(99)00091-5.
- Deblinger E, Stauffer LB, Steer RA. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreat 2001;6:332-43. http://dx.doi.org/10.1177/1077559501006004006.
- Deblinger E, Mannarino AP, Cohen JA, Runyon MK, Steer RA. Trauma-focused cognitive behavioral therapy for children: impact of the trauma narrative and treatment length. Depress Anxiety 2011;28:67-75. http://dx.doi.org/10.1002/da.20744.
- Foa EB, McLean CP, Capaldi S, Rosenfield D. Prolonged exposure vs supportive counseling for sexual abuse-related PTSD in adolescent girls: a randomized clinical trial. JAMA 2013;310:2650-7. http://dx.doi.org/10.1001/jama.2013.282829.
- Jaberghaderi N, Greenwald R, Rubin A, Zand SO, Dolatabadi S. A comparison of CBT and EMDR for sexually-abused Iranian girls. Clin Psychol Psychot 2004;11:358-68. http://dx.doi.org/10.1002/cpp.395.
- King NJ, Tonge BJ, Mullen P, Myerson N, Heyne D, Rollings S, et al. Treating sexually abused children with posttraumatic stress symptoms: a randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2000;39:1347-55. http://dx.doi.org/10.1097/00004583-200011000-00008.
- Paquette G, Tourigny M, Joly J. Effects of a group therapy program led by social workers for adolescent girls who have experienced sexual abuse. Can Soc Work Rev 2011;13:93-110.
- Paquette G, Tourigny M, Joly J, Tardif M. L’agression Sexuelle: Transformations et Paradoxes. Montréal, QC: CIFAS-Institute Philippe-Pinel de Montréal; 2009.
- LeSure-Lester GE. An application of cognitive-behavior principles in the reduction of aggression among abused African American adolescents. J Interpers Violence 2002;17:394-402. http://dx.doi.org/10.1177/0886260502017004003.
- Kolko DJ. Clinical monitoring of treatment course in child physical abuse: psychometric characteristics and treatment comparisons. Child Abuse Negl 1996;20:23-4. http://dx.doi.org/10.1016/0145-2134(95)00113-1.
- Kolko DJ. Individual cognitive behavioral treatment and family therapy for physically abused children and their offending parents: a comparison of clinical outcomes. Child Maltreat 1996;1:322-42. http://dx.doi.org/10.1177/1077559596001004004.
- Runyon MK, Deblinger E, Steer RA. Group cognitive behavioral treatment for parents and children at-risk for physical abuse: an initial study. Child Fam Behav Ther 2010;32:196-218. http://dx.doi.org/10.1080/07317107.2010.500515.
- Champion JD, Collins JL. Comparison of a theory-based (AIDS Risk Reduction Model) cognitive behavioral intervention versus enhanced counseling for abused ethnic minority adolescent women on infection with sexually transmitted infection: results of a randomized controlled trial. Int J Nurs Stud 2012;49:138-50. http://dx.doi.org/10.1016/j.ijnurstu.2011.08.010.
- Church D, Pina O, Reategui C, Brooks A. Single-session reduction of the intensity of traumatic memories in abused adolescents after EFT: a randomized controlled pilot study. Traumatology 2012;18:73-9. http://dx.doi.org/10.1177/1534765611426788.
- Holt T, Jensen TK, Wentzel-Larsen T. The change and the mediating role of parental emotional reactions and depression in the treatment of traumatized youth: results from a randomized controlled study. Child Adolesc Psychiatry Ment Health 2014;8. http://dx.doi.org/10.1186/1753-2000-8-11.
- Jensen TK, Holt T, Ormhaug SM, Egeland K, Granly L, Hoaas LC, et al. Randomized effectiveness study comparing trauma-focused cognitive behavioral therapy with therapy as usual for youth. J Clin Child and Adolescent Psychol 2014;43:356-69. http://dx.doi.org/10.1080/15374416.2013.822307.
- Linares OL, Montalto D, Li M, Oza VS. A promising parenting intervention in foster care. J Consult Clin Psychol 2006;74:32-41. http://dx.doi.org/10.1037/0022-006X.74.1.32.
- Linares OL, Li M, Shrout PE. Child training for physical aggression? Lessons from foster care. Child Youth Serv Rev 2012;34:2416-22. http://dx.doi.org/10.1016/j.childyouth.2012.08.010.
- Rushton A, Monck E, Leese M, McCrone P, Sharac J. Enhancing adoptive parenting: a randomized controlled trial. Clin Child Psychol Psychiatry 2010;15:529-42. http://dx.doi.org/10.1177/1359104510365041.
- Shirk SR, DePrince AP, Crisostomo PS, Labus J. Cognitive behavioral therapy for depressed adolescents exposed to interpersonal trauma: an initial effectiveness trial. Psychotherapy 2014;51:167-79. http://dx.doi.org/10.1037/a0034845.
- Kolko DJ, Iselin A-MR, Gully KJ. Evaluation of the sustainability and clinical outcome of Alternatives for Families: a Cognitive-Behavioral Therapy (AF-CBT) in a child protection center. Child Abuse Negl 2011;35:105-16. http://dx.doi.org/10.1016/j.chiabu.2010.09.004.
- Rondeau C. The Efficacy of Reward vs. Punishment: A Comparison of Two Cottage Units. Beaumont, CA: Childhelp USA/International; 1983.
- Farkas L, Cyr M, Lebeau T, Lemay J, McDuff P. Treatment effectiveness of MASTR-EMDR therapy for sexually abused adolescents. Revue Québécoise De Psychologie 2008;29:101-15.
- Scheck MM, Schaeffer JA, Gillette C. Brief psychological intervention with traumatized young women: the efficacy of eye movement desensitization and reprocessing. J Trauma Stress 1998;11:25-44. http://dx.doi.org/10.1023/A:1024400931106.
- Bernard K, Dozier M, Bick J, Lewis-Morrarty E, Lindhiem O, Carlson E. Enhancing attachment organization among maltreated children: results of a randomized clinical trial. Child Dev 2012;83:623-36. http://dx.doi.org/10.1111/j.1467-8624.2011.01712.x.
- Cicchetti D, Rogosch F, Toth S. Fostering secure attachment in infants in maltreating families through preventive interventions. Dev Psychopathol 2006;18:623-49. http://dx.doi.org/10.1017/s0954579406060329.
- Cicchetti D, Rogosch F, Toth S, Sturge-Apple M. Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Dev Psychopathol 2011;23:789-800. http://dx.doi.org/10.1017/S0954579411000307.
- Dozier M, Peloso E, Lindhiem O, Gordon MK, Manni M, Sepulveda S, et al. Developing evidence-based interventions for foster children: an example of a randomized clinical trial with infants and toddlers. J Soc Issues 2006;62:767-85. http://dx.doi.org/10.1111/j.1540-4560.2006.00486.x.
- Dozier M, Lindhiem O, Lewis E, Bick J, Bernard K, Peloso E. Effects of a foster parent training program on young children’s attachment behaviors: preliminary evidence from a randomized clinical trial. Child Adolesc Soc Work J 2009;26:321-32. http://dx.doi.org/10.1007/s10560-009-0165-1.
- Lieberman AF, Van Horn P, Ghosh Ippen C. Toward evidence-based treatment: child-parent psychotherapy with preschoolers exposed to marital violence. J Am Acad Child Adolesc Psychiatry 2005;44:1241-8. http://dx.doi.org/10.1097/01.chi.0000181047.59702.58.
- Ghosh Ippen C, Harris W, Van Horn P, Lieberman A. Traumatic and stressful events in early childhood: can treatment help those at highest risk?. Child Abuse Negl 2011;35:504-13. http://dx.doi.org/10.1016/j.chiabu.2011.03.009.
- Lieberman AF, Ghosh Ippen C, Van Horn P. Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2006;45:913-18. http://dx.doi.org/10.1097/01.chi.0000222784.03735.92.
- Moss E, Dubois-Comtois K, Cyr C, Tarabulsy GM, St-Laurent D, Bernier A. Efficacy of a home-visiting intervention aimed at improving maternal sensitivity, child attachment, and behavioral outcomes for maltreated children: a randomized control trial. Dev Psychopathol 2011;23:195-210. http://dx.doi.org/10.1017/S0954579410000738.
- Spieker SJ, Oxford ML, Kelly JF, Nelson EM, Fleming CB. Promoting first relationships: randomized trial of a relationship-based intervention for toddlers in child welfare. Child Maltreat 2012;17:271-86. http://dx.doi.org/10.1177/1077559512458176.
- Sprang G. The efficacy of a relational treatment for maltreated children and their families. Child Adolesc Ment Health 2009;14:81-8. http://dx.doi.org/10.1111/j.1475-3588.2008.00499.x.
- Toth SL, Maughan A, Manly J, Todd, Spagnola M, Cicchetti D. The relative efficacy of two interventions in altering maltreated preschool children’s representational models: Implications for attachment theory. Dev Psychopathol 2002;14:877-908. http://dx.doi.org/10.1017/S095457940200411X.
- Becker-Weidman A. Treatment of children with trauma-attachment disorders: dyadic developmental psychotherapy. Child Adolesc Soc Work J 2006;23:147-71. http://dx.doi.org/10.1007/s10560-005-0039-0.
- Becker-Weidman A, Stuart SM. New Developments in Child Abuse Research. New York, NY: Nova; 2006.
- Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, et al. Parent–child interaction therapy with physically abusive parents: efficacy for reducing future abuse reports. J Consult Clin Psychol 2004;72:500-10. http://dx.doi.org/10.1037/0022-006X.72.3.500.
- Thomas R, Zimmer-Gembeck MJ. Accumulating evidence for parent-child interaction therapy in the prevention of child maltreatment. Child Dev 2011;82:177-92. http://dx.doi.org/10.1111/j.1467-8624.2010.01548.x.
- Thomas R, Zimmer-Gembeck MJ. Parent–child interaction therapy: an evidence-based treatment for child maltreatment. Child Maltreat 2012;17:253-66. http://dx.doi.org/10.1177/1077559512459555.
- Hughes JR, Gottlieb LN. The effects of the Webster-Stratton parenting program on maltreating families: fostering strengths. Child Abuse Negl 2004;28:1081-97. http://dx.doi.org/10.1016/j.chiabu.2004.02.004.
- Valentino K, Comas M, Nuttall AK, Thomas T. Training maltreating parents in elaborative and emotion-rich reminiscing with their preschool-aged children. Child Abuse Negl 2013;37:585-95. http://dx.doi.org/10.1016/j.chiabu.2013.02.010.
- Linares OL, Jimenez J, Nesci C, Pearson E, Beller S, Edwards N, et al. Reducing sibling conflict in maltreated children placed in foster homes. Prev Sci 2015;16:211-21. http://dx.doi.org/10.1007/s11121-014-0476-0.
- Brunk MA, Henggeler SW, Whelan JP. Comparison of multisystemic therapy and parent training in the brief treatment of child abuse and neglect. J Consult Clin Psychol 1987;55:171-8. http://dx.doi.org/10.1037/0022-006X.55.2.171.
- Danielson C, McCart M, Walsh K, De Arellano M, White D, Resnick H. Reducing substance use risk and mental health problems among sexually assaulted adolescents: a pilot randomized controlled trial. J Fam Psychol 2012;26:628-35. http://dx.doi.org/10.1037/a0028862.
- Swenson CC, Schaeffer CM, Henggeler SW, Faldowski R, Mayhew AM. Multisystemic therapy for child abuse and neglect: a randomized effectiveness trial. J Fam Psychol 2010;24:497-50. http://dx.doi.org/10.1037/a0020324.
- Biehal N, Dixon J, Parry E, Sinclair I, Greenlaw J, Roberts C, et al. The Care Placements Evaluation (CaPE) of Multidimensional Treatment Foster Care for Adolescents (MTFC-A). London: Department for Education; 2012.
- Green J, Biehal N, Roberts C, Dixon J, Kay C, Parry E, et al. Multidimensional treatment foster care for adolescents in English care: randomised trial and observational cohort evaluation. Br J Psychiatry 2014;204:214-21. http://dx.doi.org/10.1192/bjp.bp.113.131466.
- Schaeffer CM, Swenson CC, Tuerk EH, Henggeler SW. Comprehensive treatment for co-occurring child maltreatment and parental substance abuse: outcomes from a 24-month pilot study of the MST-Building Stronger Families program. Child Abuse Negl 2013;37:596-607. http://dx.doi.org/10.1016/j.chiabu.2013.04.004.
- Meezan W, O’Keefe M. Multifamily group therapy: impact on family functioning and child behavior. Fam Soc 1998;79:32-44. http://dx.doi.org/10.1606/1044-3894.1796.
- Meezan W, O’Keefe M. Evaluating the effectiveness of multifamily group therapy in child abuse and neglect. Res Soc Work Pract 1998;8:330-53. http://dx.doi.org/10.1177/104973159800800306.
- Bagley C, LaChance M. Evaluation of a family-based programme for the treatment of child sexual abuse. Child Fam Soc Work 2000;5:205-13. http://dx.doi.org/10.1046/j.1365-2206.2000.00162.x.
- Graham-Bermann SA, Lynch S, Banyard V, De Voe ER, Halabu H. Community-based intervention for children exposed to intimate partner violence: an efficacy trial. J Consult Clin Psychol 2007;75:199-20. http://dx.doi.org/10.1037/0022-006X.75.2.199.
- Howell KH, Miller LE, Lilly MM, Graham-Bermann SA. Fostering social competence in preschool children exposed to intimate partner violence: evaluating the Preschool Kids’ Club intervention. J Aggress Maltreat Trauma 2013;22:425-45. http://dx.doi.org/10.1080/10926771.2013.775986.
- Overbeek MM, de Schipper JC, Lamers-Winkelman F, Schuengel C. Effectiveness of specific factors in community-based intervention for child-witnesses of interparental violence: a randomized trial. Child Abuse Negl 2013;37:1202-14. http://dx.doi.org/10.1016/j.chiabu.2013.07.007.
- Sullivan CM, Bybee DI, Allen NE. Findings from a community-based program for battered women and their children. J Interpers Violence 2002;17:915-36. http://dx.doi.org/10.1177/0886260502017009001.
- Trowell J, Kolvin I, Weeramanthri T, Sadowski H, Berelowitz M, Glaser D, et al. Psychotherapy for sexually abused girls: psychopathological outcome findings and patterns of change. Br J Psychiatry 2002;180:234-47. http://dx.doi.org/10.1192/bjp.180.3.234.
- Wagar JM, Rodway MR. An evaluation of a group treatment approach for children who have witnessed wife abuse. J Fam Violence 1995;10:295-306. http://dx.doi.org/10.1007/BF02110994.
- Wolfe DA, Wekerle C, Scott K, Straatman A-L, Grasley C, Reitzel-Jaffe D. Dating violence prevention with at-risk youth: a controlled outcome evaluation. J Consult Clin Psychol 2003;71:279-91. http://dx.doi.org/10.1037/0022-006X.71.2.279.
- Noether CD, Brown V, Finkelstein N, Russell LA, Van De Mark NR, Morris LS, et al. Promoting resiliency in children of mothers with co-occurring disorders and histories of trauma: Impact of a skills-based intervention program on child outcomes. J Community Appl Soc 2007;35:823-43. http://dx.doi.org/10.1002/jcop.20184.
- Simoneau AC, Hebert M, Tourigny M. Evaluation of a group therapy for 6–13 year old sexually abused children. Revue Québécoise De Psychologie 2008;29:27-43.
- Tourigny M, Hebért M. Comparison of open versus closed group interventions for sexually abused adolescent girls. Violence Vict 2007;22:334-49. http://dx.doi.org/10.1891/088667007780842775.
- Barth R, Yeaton J, Winterfelt N. Psychoeducational groups with foster care of sexually abused children. Child Adolesc Soc Work J 1994;11:405-24. http://dx.doi.org/10.1007/BF01876590.
- Duffany A, Panos PT. Outcome evaluation of a group treatment of sexually abused and reactive children. Res Soc Work Pract 2009;19:291-303. http://dx.doi.org/10.1177/1049731508329450.
- Hébert M, Tourigny M. Effects of a psychoeducational group intervention for children victims of sexual abuse. J Child Adolesc Trauma 2010;3:143-60. http://dx.doi.org/10.1080/19361521003726930.
- Holland P, Gorey KM, Lindsay A. Prevention of mental health and behaviour problems among sexually abused aboriginal children in care. Child Adolesc Soc Work J 2004;21:109-15. http://dx.doi.org/10.1023/B:CASW.0000022726.59560.6c.
- Santibáñez R. Effects of an educational intervention programme on self-control and moral development in foster-home children. Infanc Aprendiz 2000;92:85-107.
- Tourigny M, Hébert M, Daigneault I, Simoneau AC. Efficacy of a group therapy for sexually abused adolescent girls. J Child Sex Abuse 2005;14:71-93. http://dx.doi.org/10.1300/J070v14n04_04.
- Tourigny M. A six month follow-up study of psychoeducative group therapy for sexually abused female adolescents. Revue Québécoise De Psychologie 2008;29:117-31.
- Tourigny M, Boisvert I, Jacq B. Effectiveness of a short group intervention for sexually abused adolescents. Intervention 2008;129:27-38.
- Monck E, Bentovim A, Goodall G, Hyde C, Lwin R, Sharland E, et al. Child Sexual Abuse: A Descriptive and Treatment Study. Studies in Child Protection. London: HMSO; 1996.
- De Luca R, Boyes D, Grayston A, Romano E. Sexual abuse: effects of group therapy on pre-adolescent girls. Child Abuse Rev 1995;4:263-77. http://dx.doi.org/10.1002/car.2380040406.
- Grayston AD, De Luca RV. Group therapy for boys who have experienced sexual abuse: is it the treatment of choice?. J Child Adolesc Group Ther 1995;5:57-82. http://dx.doi.org/10.1007/BF02548959.
- McGain B, McKinzey R. The efficacy of group treatment in sexually abused girls. Child Abuse Negl 1995;19:1157-69. http://dx.doi.org/10.1016/0145-2134(95)00076-K.
- Verleur D, Hughes RE, de Rios MD. Enhancement of self-esteem among female adolescent incest victims: a controlled comparison. Adolescence 1986;21:843-54.
- Thun D, Sims PL, Adams MA, Webb T. Effects of group therapy on female adolescent survivors of sexual abuse: a pilot study. J Child Sex Abuse 2002;11:1-16. http://dx.doi.org/10.1300/J070v11n04_01.
- Haight W, Black J, Sheridan K. A mental health intervention for rural, foster children from methamphetamine-involved families: experimental assessment with qualitative elaboration. Child Youth Serv Rev 2010;32:1446-57. http://dx.doi.org/10.1016/j.childyouth.2010.06.024.
- Reddy SD, Negi LT, Dodson-Lavelle B, Ozawa-de S, Pace TWW, Cole SP, et al. Cognitive-based compassion training: a promising prevention strategy for at-risk adolescents. J Child Fam Stud 2013;22:219-30. http://dx.doi.org/10.1007/s10826-012-9571-7.
- Fitch MJ, Cadol EJ, Goldson EK, Jackson DF, Swartz Wendell TP. Prospective Study in Child Abuse: The Child Study Program 1975.
- Nolan M, Carr A, Fitzpartrick C, O’Flaherty A, Keary K, Turner R, et al. A comparison of two programmes for victims of child sexual abuse: a treatment outcome study. Child Abuse Rev 2002;11:103-23. http://dx.doi.org/10.1002/car.727.
- Sullivan PM. The effects of psychotherapy on behavior problems of sexually abused deaf children. Child Abuse Negl 1992;16:297-30. http://dx.doi.org/10.1016/0145-2134(92)90036-Q.
- Downing J, Jenkins SJ, Fisher GL. A comparison of psychodynamic and reinforcement treatment with sexually abused children. Elementary School Guidance &Amp; Counseling 1988;22:291-8.
- Fantuzzo JW, Jurecic L, Stovall A, Hightower AD, Goins C, Schachtel D. Effects of adult and peer social initiations on the social behavior of withdrawn, maltreated preschool children. J Consult Clin Psychol 1988;56:34-9. http://dx.doi.org/10.1037/0022-006X.56.1.34.
- Fantuzzo JW, Sutton-Smith B, Meyers R, Atkins M, Stevenson H, Coolahan K, et al. Community-based resilient peer treatment of withdrawn maltreated preschool children. J Consult Clin Psychol 1996;64:1377-86. http://dx.doi.org/10.1037/0022-006X.64.6.1377.
- Bruce J, McDermott JM, Fisher PA, Fox NA. Using behavioral and electrophysiological measures to assess the effects of a preventive intervention: a preliminary study with preschool-aged foster children. Prev Sci 2009;10:129-40. http://dx.doi.org/10.1007/s11121-008-0115-8.
- Fisher PA, Burraston B, Pears KC. The early intervention foster care program: permanent placement outcomes from a randomized trial. Child Maltreat 2005;10:61-7. http://dx.doi.org/10.1177/1077559504271561.
- Fisher PA, Kim HK. Intervention effects on foster preschoolers’ attachment-related behaviors from a randomized trial. Prev Sci 2007;8:161-70. http://dx.doi.org/10.1007/s11121-007-0066-5.
- Fisher PA, Kim HK, Pears KC. Effects of multidimensional treatment foster care for preschoolers (MTFC-P) on reducing permanent placement failures among children with placement instability. Child Youth Serv Rev 2009;31:541-6. http://dx.doi.org/10.1016/j.childyouth.2008.10.012.
- Fisher PA, Stoolmiller M, Gunnar MR, Burraston BO. Effects of a therapeutic intervention for foster preschoolers on diurnal cortisol activity. Psychoneuroendocrinology 2007;32:892-905. http://dx.doi.org/10.1016/j.psyneuen.2007.06.008.
- Fisher PA, Van Ryzin MJ, Gunnar MR. Mitigating HPA axis dysregulation associated with placement changes in foster care. Psychoneuroendocrinology 2011;36:531-9. http://dx.doi.org/10.1016/j.psyneuen.2010.08.007.
- Smith DK, Leve LD, Chamberlain P. Preventing internalizing and externalizing problems in girls in foster care as they enter middle school: impact of an intervention. Prev Sci 2011;12:269-77. http://dx.doi.org/10.1007/s11121-011-0211-z.
- Taussig HN, Culhane SE. Impact of a mentoring and skills group program on mental health outcomes for maltreated children in foster care. Arch Pediatr Adolesc Med 2010;164:739-46. http://dx.doi.org/10.1001/archpediatrics.2010.124.
- Taussig HN, Culhane SE, Garrido E, Knudtson MD. RCT of a mentoring and skills group program: placement and permanency outcomes for foster youth. Pediatrics 2012;130:E33-9. http://dx.doi.org/10.1542/peds.2011-3447.
- Fisher PA, Gunnar MR, Chamberlain P, Reid JB. Preventive intervention for maltreated preschool children: impact on children’s behavior, neuroendocrine activity, and foster parent functioning. J Am Acad Child Adolesc Psychiatry 2000;39:1356-64. http://dx.doi.org/10.1097/00004583-200011000-00009.
- Graham AM, Yockelson M, Kim Hyoun K, Bruce J, Pears Katherine C, Fisher PA. Effects of maltreatment and early intervention on diurnal cortisol slope across the start of school: a pilot study. Child Abuse Negl 2012;36:666-70. http://dx.doi.org/10.1016/j.chiabu.2012.07.006.
- Moore E, Armsden G, Gogerty PL. A twelve-year follow-up study of maltreated and at-risk children who received early therapeutic child care. Child Maltreat 1998;3:3-16. http://dx.doi.org/10.1177/1077559598003001001.
- Culp R. Differential developmental progress of maltreated children in day treatment. Social Work 1987;32:497-9.
- Culp RE. Maltreated children’s developmental scores: treatment versus nontreatment. Child Abuse Negl 1987;11:29-34. http://dx.doi.org/10.1016/0145-2134(87)90030-5.
- Culp RE, Little V, Letts D, Lawrence H. Maltreated children’s self-concept: effects of a comprehensive treatment program. Am J Orthopsychiatry 1991;61:114-21. http://dx.doi.org/10.1037/h0079233.
- Swenson CC, Randall J, Henggeler SW, Ward D. The outcomes and costs of an interagency partnership to serve maltreated children in state custody. Child Serv Soc Pol Res Pract 2000;3:191-209. http://dx.doi.org/10.1207/S15326918CS0304_1.
- Brillantes-Evangelista G. An evaluation of visual arts and poetry as therapeutic interventions with abused adolescents. Art Psychother 2013;40:71-84. http://dx.doi.org/10.1016/j.aip.2012.11.005.
- Pretorius G, Pfeifer N. Group art therapy with sexually abused girls. S Afr J Psychol 2010;40:63-7. http://dx.doi.org/10.1177/008124631004000107.
- D’Andrea W, Bergholz L, Fortunato A, Spinazzola J. Play to the whistle: a pilot investigation of a sports-based intervention for traumatized girls in residential treatment. J Fam Violence 2013;28:739-49. http://dx.doi.org/10.1007/s10896-013-9533-x.
- McDonald RG, Howe CZ. Challenge/initiative recreation programs as a treatment for low self-concept children. J Leisure Res 1989;21:242-53.
- Udwin O. Imaginative play training as an intervention method with institutionalised preschool children. Br J Clin Psychol 1983;53:32-9. http://dx.doi.org/10.1111/j.2044-8279.1983.tb02533.x.
- Dietz TJ, Davis D, Pennings J. Evaluating animal-assisted therapy in group treatment for child sexual abuse. J Child Sex Abuse 2012;21:665-83. http://dx.doi.org/10.1080/10538712.2012.726700.
- Hamama L, Hamama-Raz Y, Dagan K, Greenfeld H, Rubinstein C, Ben-Ezra M. A preliminary study of group intervention along with basic canine training among traumatized teenagers: a 3-month longitudinal study. Child Youth Serv Rev 2011;33:1975-80. http://dx.doi.org/10.1016/j.childyouth.2011.05.021.
- Finkelhor D, Browne A. The traumatic impact of child sexual abuse: a conceptualization. Am J Orthopsychiatry 1985;55:530-41.
- Finkelhor D. The trauma of child sexual abuse: two models. J Interpers Violence 1987;2:348-66. http://dx.doi.org/10.1177/088626058700200402.
- Deblinger E, Heflin AH. Treating sexually abused children and their nonoffending parents: a cognitive behavioral approach. Thousand Oaks, CA: Sage Publications, Inc.; 1996.
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: an AIDS risk reduction model (ARRM). Health Educ Q 1990;17:53-72.
- Webster-Stratton C. Incredible Years: The Parents, Teachers, and Children Training Series. Seattle, WA: Carolyn Webster-Stratton; 2001.
- Webster-Stratton C. The Children’s Videotape Series: Dina Dinosaur’s Curriculum for Young Children 2004.
- Webster-Stratton C. The Incredible Years: A Trouble Shooting Guide for Parents of Children Aged 3–8. Toronto, ON: The Umbrella Press; 2003.
- Webster-Stratton C, Hancock L, Briesmeister JM, Schaefer CE. Handbook of Parent Training: Parents as Co-Therapists for Children’s Behavior Problems. Hoboken, NJ: John Wiley & Sons Inc.; 1998.
- Shapiro F. Eye movement desensitization and reprocessing procedure: from EMD to EMDR: a new treatment model for anxiety and related traumata. Behavior Therapist 1991;14:133-5.
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of Attachment: Assessed in the Strange Situation and at Home. Hillsdale, NJ: Erlbaum; 1978.
- Olds DL, Eckenrode J, Henderson CR, Kitzman H, Powers J, Cole R, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect: fifteen-year follow-up of a randomized trial. JAMA 1997;278:637-43. http://dx.doi.org/10.1001/jama.1997.03550080047038.
- Olds D, Henderson C, Kitzman H, Eckenrode J, Cole R, Tatelbaum R. The promise of home visitation: Results of two randomized trials. J Commun Psychol 1998;26:5-21.
- Olds DL, Kitzman H. Can home visitation improve the health of women and children at environmental risk?. Pediatrics 1990;86:108-16.
- Bakermans-Kranenburg MJ, Juffer F, Van Ijzendoorn MH. Interventions with video feedback and attachment discussions: does type of maternal insecurity make a difference?. Infant Ment Health J 1998;19:202-19. http://dx.doi.org/10.1002/(SICI)1097-0355(199822)19:2<202::AID-IMHJ8>3.0.CO;2-P.
- Moran G, Pederson DR, Krupka A. Maternal unresolved attachment status impedes the effectiveness of interventions with adolescent mothers. Infant Ment Health J 2005;26:231-49. http://dx.doi.org/10.1002/imhj.20045.
- Stovall-McClough KC, Dozier M. Forming attachments in foster care: infant attachment behaviors during the first 2 months of placement. Dev Psychopathol 2004;16:253-71.
- Eyberg S. Parent-child interaction therapy: integration of traditional and behavioral concerns. Child Family Behavior Therapy 1988;10:33-46.
- Hembree-Kigin TL, McNeil CB. Parent–Child Interaction Therapy. New York, NY: Plenum Press; 1995.
- Bandura A. Social Learning Theory. Engelwood Cliffs, NJ: Prentice Hall; 1977.
- Alexander J, Parsons B. Functional Family Therapy. Monterey, CA: Brooks/Cole Publishing; 1982.
- Robin A, Foster S. Negotiating Adolescence: A Behavioral Family Systems Approach to Parent-adolescent Conflict. New York, NY: Guilford Publications; 1989.
- Belsky J. Etiology of child maltreatment: a developmental ecological analysis. Psychol Bull 1993;114. http://dx.doi.org/10.1037/0033-2909.114.3.413.
- Mowrer O. Learning Theory and Behavior. Hoboken, NJ: Wiley; 1960.
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psycholog Rev 2004;111:33-51.
- Henggeler SW, Schoenwald SK, Borduin CM, Rowland MD, Cunningham PB. Multisystemic Therapy for Antisocial Behavior in Children and Adolescents. New York, NY: Guilford Press; 2009.
- Perry DB. Neurodevelopment and the neurophysiology of trauma II: clinical work along the alarm-fear-terror continuum. The APSAC Advisor 1993;6:1-20.
- Jaffe P, Wilson S, Wolfe DA. Promoting changes in attitudes and understanding of conflict resolution among child witnesses of family violence. Can J Behav Sci 1986;18.
- Dobash RE, Dobash RP. Women, Violence and Social Change. New York, NY: Routledge; 2003.
- Kanfer FH, Kanfer FH, Goldstein AP. Helping People Change. New York, NY: Academic Press; 1975.
- Karoly P, Hersen M, Eisler RM, Miller RM. Progress in Behavior Modification. New York, NY: Academic Press; 1977.
- BANDURA A. Principles of Behavior Modification. New York, NY: Holt Rinehart Winston; 1969.
- Giarretto H, Mrazek PB, Kempe HC. Sexually Abused Children and Their Families. Oxford: Pergamon Press; 1981.
- Furniss T. Mutual influence and interlocking professional-family process in the treatment of child sexual abuse and incest. Child Abuse Negl 1983;7:207-23.
- Rogoff B. The Cultural Nature of Human Development. New York, NY: Oxford University Press; 2003.
- Shweder RA, Goodnow JJ, Hitano G, LeVine RA, Markus HR, Miller PJ, et al. Handbook of Child Psychology, Vol 1: Theoretical Models of Human Development 6. Hoboken, NJ: Wiley; 2006.
- Salzberg S, Kabat-Zinn J. Lovingkindness: The Revolutionary Art of Happiness. Shambhala Publications; 2004.
- Gogerty PL, Durkin RP. Help the child tirst: the Seattle Day nursery/childhaven approach. Caring 1981;7:10-1.
- Miller JL, Whittaker JK. Social services and social support: blended programs for families at risk of child maltreatment. Child Welfare 1988:161-74.
- DePanfilis D. Social isolation of neglectful families: a review of social support assessment and intervention models. Child Maltreat 1996;1:37-52.
- Durkin R. The use of therapeutic day care to resolve the legal dilemma of protecting the rights of both children and parents in equivocal cases of abuse and neglect. Child and Youth Care Forum 1986;15:138-40.
- Ralston ME, Swenson CC. The Charleston Collaborative Project Intervention Manual. Unpublished Manual. Charleston SC: Lowcountry Children’s Center; 1998.
- Narango C. Gestalt Therapy: The Attitude and Practice of an Atheoretical Experientialism. Carmarthen: UK Crown Publishing; 2000.
- Perls FS, Hatcher C, Himelstein P. The Handbook of Gestalt Therapy. New York, NY: Jason Aronson; 1990.
- Rogers CR. On Becoming a Person, A Therapist’s View of Psychotherapy. USA: Constable; 1967.
- Du Toit AS, Grobler HD, Schenck CJ. Person-Centered Communication: Theory and Practice. Johannesburg: International Thomson Publishing; 1998.
- Briere J. Child Abuse Trauma: Theory and Treatment of the Lasting Effects. Thousand Oaks, CA: SAGE Publications; 1992.
- Feitelson D, Ross GS. The neglected factor – play. Hum Dev 1973;16:202-23. http://dx.doi.org/10.1159/000271276.
- Freyberg T, Singer TL. The Child’s World of Make Believe. New York, NY: Academic Press; 1973.
- Delta Society . Improving Human Health Through Service and Therapy Animals 2012. www.deltasociety.org/Page.aspx?pid=320.
- Ollendick TH. Reliability and validity of the revised fear survey schedule for children (FSSC-R). Behav Res Ther 1983;21:685-92. http://dx.doi.org/10.1016/0005-7967(83)90087-6.
- Reynolds CR, Richmond BO. Revised Children’s Manifest Anxiety Scale (RCMSAS) Manual. Los Angeles, CA: Western Psychological Services; 1985.
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1983.
- Kovacs M. Children’s Depression Inventory Manual. North Tonawanda, NY: Multi-Health Systems; 1992.
- Friedrich WN, Grambsch P, Damon L, Hewitt SK, Koverola C, Lang RA, et al. Child Sexual Behavior Inventory: normative and clinical comparisons. Psychol Assess 1992;4. http://dx.doi.org/10.1037/1040-3590.4.3.303.
- Achenbach TM, Edelbrock C. Child Behavior Checklist. Burlington, VT: University of Vermont; 1991.
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A children’s global assessment scale (CGAS). Arch Gen Psychiatry 1983;40:1228-31. http://dx.doi.org/10.1001/archpsyc.1983.01790100074010.
- Everson MD, Hunter WM, Runyon DK, Edelsohn GA, Coulter ML. Maternal support following disclosure of incest. Am J Orthopsychiatry 1989;59:197-20. http://dx.doi.org/10.1111/j.1939-0025.1989.tb01651.x.
- Martini DR, Strayhorn JM, Puig-Antich J. A symptom self-report measure for preschool children. J Am Acad Child Adolesc Psychiatry 1990;29:594-600. http://dx.doi.org/10.1097/00004583-199007000-00013.
- Cohen JA, Mannarino AP. A treatment model for sexually abused preschoolers. J Interpers Violence 1983;8:115-31.
- Spielberger CD, Edwards CD. STAIC Preliminary Manual for the State-Trait Anxiety Inventory for Children (‘How I feel questionnaire’). Palo Alto, CA: Consulting Psychologists Press; 1973.
- Achenbach TME. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1983.
- Cohen JA, Mannarino AP, Deblinger E. Treating Trauma and Traumatic Grief in Children and Adolescents. New York, NY: Guildford Press; 2006.
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997;36:980-8. http://dx.doi.org/10.1097/00004583-199707000-00021.
- Achenbach TM. Integrative Guide for the 1991 CBCL/4-18. YSR and TRF Profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 1991.
- Mannarino AP, Cohen JA, Berman SR. The Children’s Attributions and Perceptions Scale: a new measure of sexual abuse-related factors. J Clin Child Psychol 1994;23:204-11. http://dx.doi.org/10.1207/s15374424jccp2302_9.
- Feiring C, Taska L, Lewis M. Adjustment following sexual abuse discovery: the role of shame and attributional style. Dev Psychol 2002;38:79-92. http://dx.doi.org/10.1037/0012-1649.38.1.79.
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory. San Antonio, TX: The Psychological Corporation; 1996.
- Mannarino AP, Cohen JA. Family-related variables and psychological symptom formation in sexually abused girls. J Child Sex Abuse 1996;5:105-20. http://dx.doi.org/10.1300/J070v05n01_06.
- Strayhorn JM, Weidman CS. A parent practices scale and its relation to parent and child mental health. J Am Acad Child Adolesc Psychiatry 1988;27:613-18. http://dx.doi.org/10.1097/00004583-198809000-00016.
- Orvaschel H, Puig-Antich J, Chambers W, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J Am Acad Child Adolesc Psychiatry 1982;21:392-7. http://dx.doi.org/10.1016/S0002-7138(09)60944-4.
- Sarno JA, Wurtele SK. Effects of a personal safety program on preschoolers’ knowledge, skills, and perceptions of child sexual abuse. Child Maltreat 1997;2:35-4. http://dx.doi.org/10.1177/1077559597002001004.
- Miller SM, Rosenbaum M. Learned Resourcefulness on Coping Skills, Self Regulation and Adaptive Behaviour. New York, NY: Spring Press; 1990.
- Derogatis LR. Symptom Checklist-90-R: Administration, Scoring, and Procedures Manual. Minneapolis, MN: National Computer Systems; 1994.
- Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom Med 1979;41:209-18. http://dx.doi.org/10.1097/00006842-197905000-00004.
- Cohen J, Mannarino A. Factors that mediate treatment outcome of sexually abused preschool children: six- and 12-month follow-up. J Am Acad Child Adolesc Psychiatry 1998;37:44-51. http://dx.doi.org/10.1097/00004583-199801000-00016.
- Zich J, Temoshok L. Perceptions of social support in men with AIDS and ARC: relationships with distress and hardiness 1. J Appl Soc Psychol 1987;17:193-215. http://dx.doi.org/10.1111/j.1559-1816.1987.tb00310.x.
- Hersen ME, Bellack AS. Dictionary of Behavioral Assessment Techniques. Oxford: Pergamon Press; 1988.
- March JS, Parker JDA, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry 1997;36:554-65. http://dx.doi.org/10.1097/00004583-199704000-00019.
- Feiring C, Taska L, Lewis M. Age and gender differences in children’s and adolescents’ adaptation to sexual abuse. Child Abuse Negl 1999;23:115-28. http://dx.doi.org/10.1016/S0145-2134(98)00116-1.
- McCarthy D. Manual for the McCarthy Scales of Children’s Abilities. New York, NY: Psychological Corporation; 1972.
- Foa EB, Johnson KM, Feeny NC, Treadwell KR. The child PTSD symptom scale: a preliminary examination of its psychometric properties. J Clin Child Psychol 2001;30:376-84. http://dx.doi.org/10.1207/S15374424JCCP3003_9.
- Gillihan S, Aderka I, Conklin P, Capaldi S, Foa E. The Child PTSD Symptom Scale: psychometric properties in female adolescent sexual assault survivors. Psychol Assessment 2013;25:23-31. http://dx.doi.org/10.1037/a0029553.
- Greenwald R, Rubin A. Brief assessment of posttraumatic symptoms in children: development and preliminary validation of parent and child scales. Res Soc Work Pract 1999;9:61-75. http://dx.doi.org/10.1177/104973159900900105.
- Rutter M. A children’s behaviour questionnaire for completion by teachers: preliminary findings. J Child Psychol Psychiatry 1967;8:1-11. http://dx.doi.org/10.1111/j.1469-7610.1967.tb02175.x.
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. San Antonio, TX: The Psychological Corporation; 1996.
- Kleinknecht RA, Bernstein DA. Fear Thermometer. Dictionary of Behavioral Assessment Techniques n.d.
- Schafer DS, Moesch MS. Developmental Programming for Infants and Young Children. Ann Arbor, MI: University of Michigan Press; 1981.
- Reynolds CR, Richmond BO. What I think and feel: a revised measure of children’s manifest anxiety. J Abnorm Child Psych 1978;6:271-80. http://dx.doi.org/10.1007/BF00919131.
- Achenbach TM. Manual of the Child Behavior Checklist: 4-18 and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991.
- Wolfe VV, Gentile C, Wolfe DA. The impact of sexual abuse on children: a PTSD formulation. Behavior Therapy 1989;20:215-28. http://dx.doi.org/10.1016/S0005-7894(89)80070-X.
- Diagnostic and Statistical Manual of Mental Disorders, 3rd edition-revised (DSM-III-R). Washington, DC: American Psychiatric Association; 1987.
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001.
- Knussen C, Sloper P, Cunningham CC, Turner S. The use of the Ways of Coping (Revised) questionnaire with parents of children with Down’s syndrome. Psychol Med 1992;22:775-86. http://dx.doi.org/10.1017/S0033291700038216.
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatr 1981;46:305-15.
- Bierman KL, McCauley E. Children’s descriptions of their peer interactions: useful information for clinical child assessment. J Clin Child Psychol 1987;16:9-18. http://dx.doi.org/10.1207/s15374424jccp1601_2.
- Kazdin AE, Rodgers A, Colbus D, Siegel T. Children’s hostility inventory: measurement of aggression and hostility in psychiatric inpatient children. J Clin Child Psychol 1987;16:320-8. http://dx.doi.org/10.1207/s15374424jccp1604_5.
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the parent-child conflict tactics scales: development and psychometric data for a national sample of American parents. Child Abuse Negl 1998;22:249-70. http://dx.doi.org/10.1016/S0145-2134(97)00174-9.
- Báguena MJV, Villaroya E, Beleña A, Díaz A, Roldán C, Reig R. Psychometric Properties of the Spanish Version of the Impact of Events Scale Revised (IES-R) 1998. www.uv.es/baguena/art-IES-R.pdf (accessed 4 May 2016).
- Nader KO, Kriegler J, Blake D, Pynoos R, Newman E, Weathers F. Clinician-administered PTSD Scale for Children and Adolescents. White River Junction, VT: National Center for PTSD; 1996.
- Nadar K, Newman E, Weathers F, Kaloupek DG, Kriegler J, Blake D. Clinician Administered PTSD Scale for Children and Adolescents (CAPS-CA). Los Angeles, CA: Western Psychological Press; 2004.
- Angold A, Costello EJ, Messer SC, Pickles A. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res 1995;5:237-49.
- Birmaher B, Brent DA, Chiapetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry 1999;38:1230-6. http://dx.doi.org/10.1097/00004583-199910000-00011.
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45. http://dx.doi.org/10.1097/00004583-200111000-00015.
- Achenbach TM. Manual for the Child Behavior Checklist/2–3 and 1992 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1992.
- Eyberg S, Boggs SR, Reynolds LA. Eyberg Child Behavior Inventory. Eugene, OR: University of Oregon Health Sciences Center; 1980.
- Eyberg SM, Pincus D. ECBI–: Eyberg Child Behavior Inventory. SESBI– Sutter–Eyberg Student Behavior Inventory-Revised. Odessa, FL: Psychological Assessment Resources; 1999.
- Webster-Stratton C. Preventing conduct problems in Head Start children: strengthening parenting competencies. J Consult Clin Psychol 1998;66:715-30. http://dx.doi.org/10.1037/0022-006X.66.5.715.
- Caldwell B, Bradley R. Home Observation for the Measurement of the Environment (revised edition). Little Rock, AR: University of Arkansas at Little Rock; 1984.
- Wills TA, Isasi CR, Mendoza D, Ainette MG. Self-control constructs related to measures of dietary intake and physical activity in adolescents. J Adolesc Health n.d.;41:551-8. http://dx.doi.org/10.1037/0893-164X.20.3.265.
- Quinton D, Rushton A, Dance C, Mayes D. Joining New Families: A Study of Adoption and Fostering in Middle Childhood. Hoboken, NJ: John Wiley & Sons; 1998.
- Davis H, Spurr P. Parent counselling: an evaluation of a community child mental health service. J Child Psychol Psychiatry 1998;39:365-76. http://dx.doi.org/10.1017/S002196309700214X.
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. J Clin Child Psychol 1989;18:167-75. http://dx.doi.org/10.1207/s15374424jccp1802_8.
- Ohan JL, Leung DW, Johnston C. The parenting sense of competence scale: evidence of a stable factor structure and validity. Can J Behav Sci 2000;32. http://dx.doi.org/10.1037/h0087122.
- Crnic KA, Booth CL. Mothers’ and fathers’ perceptions of daily hassles of parenting across early childhood. J Marriage Fam 1991;53:1042-50. http://dx.doi.org/10.2307/353007.
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories – IA and – II in psychiatric outpatients. J Pers Asses 1996;67:588-97. http://dx.doi.org/10.1207/s15327752jpa6703_13.
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann 1979;2:197-20. http://dx.doi.org/10.1016/0149-7189(79)90094-6.
- Kazdin AE, French NH, Sherick RB. Acceptability of alternative treatments for children: evaluations by inpatient children, parents, and staff. J Consult Clin Psychol 1981;49. http://dx.doi.org/10.1037/0022-006X.49.6.900.
- Kazdin AE. Acceptability of alternative treatments for deviant child behavior. J Appl Behav Anal 1980;13:259-73. http://dx.doi.org/10.1901/jaba.1980.13-259.
- Friedrich WN, Fisher, JL, Dittner CA, Acton R, Berliner L, Butler J, et al. Child Sexual Behavior Inventory: normative, psychiatric, and sexual abuse comparisons. J Am Prof Soc Abuse Child 2001;6:37-49. http://dx.doi.org/10.1177/1077559501006001004.
- Briere J. Trauma Symptom Checklist for Children. Odessa, FL: Psychological Assessment Resources; 1996.
- Gully KJ. Expectations test: trauma scales for sexual abuse, physical abuse, exposure to family violence and posttraumatic stress. Child Maltreatment 2003;8:218-29.
- Gully KJ. The Social Behavior Inventory for children in a child abuse treatment program: development of a tool to measure interpersonal behavior. Child Maltreat 2001;6:260-70. http://dx.doi.org/10.1177/1077559501006003007.
- Briere J. Trauma Symptom Checklist for Children (TSC-C). Los Angeles, CA: University of Southern California Press; 1989.
- Greenwald R. Child Trauma Measures for Research and Practice n.d.
- Greenwald R, Rubin A, Russell A, O’Connor MB. Brief Assessment of Children’s and Adolescents’ Trauma Loss Exposure n.d.
- Watson CG, Juba MP, Manifold V, Kucala T, Anderson PE. The PTSD interview: rationale, description, reliability, and concurrent validity of a DSM-III-based technique. J Clin Psychol 1991;47:179-88. http://dx.doi.org/10.1002/1097-4679(199103)47:2<179::AID-JCLP2270470202>3.0.CO;2-P.
- Beck AT, Steer RA. Beck Depression Inventory Manual. San Antonio, TX: The Psychological Association; 1993.
- Spielberger CD, Gorsuch RL, Lushene PR, Vagg PR, Jacobs G. Manual for the State-Trait Anxiety Inventory: STAI (Form Y. Palo Alto, CA: Consulting Psychologists Press Inc.; 1983.
- Hammarberg M. Penn Inventory for Posttraumatic Stress Disorder: psychometric properties. Psychol Assessment 1992;4:67-76. http://dx.doi.org/10.1037/1040-3590.4.1.67.
- Roid G, Fitts W. Tennessee Self-Concept Scale Manual (revised). Los Angeles, CA: Western Psychological Services; 1991.
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of Attachment: A Psychological Study of the Strange Situation. Hillsdale, NJ: Erlbaum; 1978.
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry 1994;151:1132-6. http://dx.doi.org/10.1176/ajp.151.8.1132.
- Lichtenstein J, Cassidy J. The Inventory of Adult Attachment: Validation of a New Measure n.d.
- Pederson DR, Moran G. Maternal behavior Q-set. Monogr Soc Res Child Dev 1995;60:247-54. http://dx.doi.org/10.2307/1166182.
- Bavolek SJ, Keene RG. The Adult–Adolescent Parenting Inventory: AAPI-2: Assessing High-risk Parenting Attitudes and Behaviors. Park City, UT: Family Development Resources; 1999.
- Vaux A, Riedel S, Stewart D. Modes of social support: the Social Support Behaviors (SS-B) Scale. Am J Community Psychol 1987;15:209-37. http://dx.doi.org/10.1007/BF00919279.
- Abidin RR. Parenting Stress Index: Short Form. Charlottesville, VA: Pediatric Psychology Press; 1990.
- Diagnostic Classification: 0–3. Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood. Washington, DC: Zero to Three: National Center for Clinical Infant Programs; 1994.
- Achenbach TM. Manual for the Teacher’s Report Form and the 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991.
- Wolfe JW, Kimerling R, Brown PJ, Chrestman KR, Levin K, Stamm BH. Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran Press; 1996.
- Blake DD, Weathers F, Nagy L, Kaloupek DG, Klauminzer G, Charney D, et al. Clinician administered PTSD scale. Behav Ther 1990;18:12-4.
- Spitzer RL, Williams JB, Gibbon M. Structured Clinical Interview for DSM-III-R. New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1987.
- Weathers FW, Litz BT. Psychometric properties of the clinician administered PTSD scale. PTSD Res Q 1994;5:2-6.
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Department of Psychiatry; 2000.
- Kirkland J, Bimler D, Drawneek A, McKim M, Schölmerich A. An alternative approach for the analyses and interpretation of attachment sort items. Early Child Dev Care 2004;174:701-19. http://dx.doi.org/10.1080/0300443042000187185.
- Baggett K, Carta JJ, Horn EM. Indicator of Parent-Child Interaction (IPCI) User’s Manual. Lawrence, KA: Special Education, University of Kansas; 2009.
- Briggs-Gowan MJ, Carter AS. Brief Infant-Toddler Social and Emotional Assessment (BITSEA) Manual. New Haven, CT: Yale University; 2002.
- Achenbach T, Rescorla L. Child Behavior Checklist for Ages 1 1/2–5. Burlington, VT: ASEBA, University of Vermont; 2000.
- Bayley N. Bayley Scales of Infant and Toddler Development: Bayley-III. New York, NY: Harcourt Assessment, The Psychological Corporation; 2006.
- Bayley N. Bayley Scales of Infant and Toddler Development (Bayley-III) Screening Test. San Antonio, TX: Harcourt Assessment; 2005.
- Bayley N. Bayley Scales of Infant Development 2. San Antonio, TX: The Psychological Corporation; 1993.
- Barnard K. The Nursing Child Assessment Satellite Training (NCAST) Teaching Scale. Seattle, WA: NCAST Programs; 1994.
- Barnard KE, Sumner GS, Pietz A. NCAST: Caregiver/Parent-Child Interaction teaching manual. Seattle, WA: University of Washington, NCAST Publications; 1994.
- Dozier M, Lindhiem O. This is my child: differences among foster parents in commitment to their young children. Child Maltreat 2006;11:338-45. http://dx.doi.org/10.1177/1077559506291263.
- Abidin RA. Parenting Stress Index: Short Form (PSI-SF). Lutz, FL: Psychological Assessment Resources Inc.; 1995.
- Milner JS. An interpretive model for the Child Abuse Potential Inventory. Dekalb, IL: Pstec Inc.; 1990.
- Bretherton I, Ridgeway D, Cassidy J, Greenberg M, Cicchetti E, Cummings E. Attachment in the Preschool Years: Theory, Research and Intervention. Chicago, IL: University of Chicago Press; 1990.
- Weschler D. Weschler Preschool and Primary Scale of Intelligence. New York, NY: Psychological Corporation; 1989.
- Randolph E. Manual for the Randolph Attachment Disorder Questionnaire. Evergreen, CO: The Attachment Centre Press; 2000.
- Reynolds CR, Kamphaus RW. BASC: Behavior Assessment System for Children: Manual. Circle Pines, MN: American Guidance Service; 1992.
- Milner JS. The Child Abuse Potential Inventory: Manual. Webster, NC: Psytec; 1986.
- Abidin RA. Parenting Stress Index. Virginia, CA: Pediatric Psychology Press; 1990.
- Biringen Z, Robinson JL, Emde RN. Appendix B: the emotional availability scales (3rd edn; an abridged infancy/early childhood version). Attach Hum Dev 2000;2:257-70. http://dx.doi.org/10.1080/14616730050085626.
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385-401. http://dx.doi.org/10.1177/014662167700100306.
- Smith J, Ross H. Training parents to mediate sibling disputes affects children’s negotiation and conflict understanding. Child Dev 2007;78:790-805. http://dx.doi.org/10.1111/j.1467-8624.2007.01033.x.
- Derogatis L, Lipman R, Covi DM. SCL-90: an outpatient psychiatric rating scale – preliminary report. Psychopharmacol Bull 1973;9:13-20.
- Moos RH, Moos BS. Family Environment Scale Manual. Palo Alto, CA: Consulting Psychologists Press; 1981.
- McCubbin HI, Patterson JM, Wilson LR, Olsen DH, McCubbin HI, Barnes H, et al. Family Inventories: Inventories Used in a National Survey of Families Across the Family Life Cycle. St Paul, MN: Family Social Science, University of Minnesota; 1985.
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles post-traumatic stress disorder reaction index. Curr Psychiatry Rep 2004;6:96-100. http://dx.doi.org/10.1007/s11920-004-0048-2.
- Moos R, Moos B. Family Environment Scale Manual. Palo Alto, CA: Consulting Psychologists Press; 1986.
- Sobell LC, Sobell MB. Timeline Follow Back: A Calendar Method for Assessing Alcohol and Drug Use (Users Guide). Toronto, ON: Addiction Research Foundation; 1996.
- Ruggiero KJ, McLeer SV. PTSD scale of the child behavior checklist: concurrent and discriminant validity with non-clinic-referred sexually abused children. J Trauma Stress 2000;13:287-99. http://dx.doi.org/10.1023/A:1007710828777.
- Briere J. Trauma Symptom Checklist for Children. Odessa, FL: Psychological Assessment; 1989.
- Gresham FM, Elliott SN. Social Skills Rating System: Manual. Circle Pines, MN: American Guidance Service; 1990.
- Derogatis L. Brief Symptom Inventory. Baltimore, MD: Clinical Psychometric Research; 1975.
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the Functional Components of Social Support. Social Support: Theory, Research and Applications. The Hague: Holland, Martin Nexjhoff; 1985.
- Gowers SG, Harrington RC, Whitton A, Lelliott P, Beevor A, Wing J, et al. Brief scale for measuring the outcomes of emotional and behavioural disorders in children. Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA). Br J Psychiatry 1999;174:413-6. http://dx.doi.org/10.1192/bjp.174.5.413.
- Briere J. Trauma Symptom Checklist for Children (TSCC): Professional Manual. Odessa, FL: Psychological Resources Inc.; 1996.
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat 1992;9:199-213. http://dx.doi.org/10.1016/0740-5472(92)90062-S.
- Deluty RH. Children’s action tendency scale: a self-report measure of aggressiveness, assertiveness, and submissiveness in children. J Consult Clin Psychol 1979;47. http://dx.doi.org/10.1037/0022-006X.47.6.1061.
- Hudson W, Nurios PS, Daley JC, Newcombe RD. A short-form scale to measure peer relations dysfunction. J Soc Serv Res 1990;13:57-69. http://dx.doi.org/10.1300/J079v13n04_04.
- Telleen S. Parenting Social Support Index: Reliability and Validity (Tech. Rep. No 1). Chicago, IL: University of Illinois, School of Public Health; 1985.
- Heppner PP, Petersen CH. The development and implications of a personal problem-solving inventory. J Couns Psychol 1982;29. http://dx.doi.org/10.1037/0022-0167.29.1.66.
- Olson DH, Portner J, Lavee Y. Family Adaptability and Cohesion Evaluation Scales (FACES III). St Paul, MN: University of Minnesota, Family Social Science; 1985.
- McCroskey J, Sladen S, Meezan W. Family Assessment Form: A Practice Based Approach to Assessing Family Functioning. Washington, DC: Child Welfare League of America Press; 1997.
- Bagley C, Burrows B, Yaworski C, Hornick N, Volpe R. Canadian Child Welfare Law: Children, Families and the State. Toronto, ON: Thompson Educational Publishing Inc.; 1999.
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) scales. J Marriage Fam 1979;41:75-88. http://dx.doi.org/10.2307/351733.
- Marshall LL. Development of the severity of violence against women scales. J Fam Violence 1992;7:103-21. http://dx.doi.org/10.1007/BF00978700.
- Graham-Bermann S. Attitudes About Family Violence (AAFV) Scale. Ann Arbor, MI: University of Michigan, Department of Psychology; 1994.
- Group CPPR. Psychometric Properties of the Social Competence Scale: Teacher and Parent Ratings. Fast Track Project Technical Report. University Park, PA: Pennsylvania State University; 1995.
- Frick PJ, Christian RE, Wootton JM. Age trends in the association between parenting and conduct problems. Behavior Modification 1999;23:106-28. http://dx.doi.org/10.1177/0145445599231005.
- Foa E. Posttraumatic Stress Diagnostic Scale Manual. Minneapolis, MN: National Computer Systems, Pearson; 1995.
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. J Fam Issue 1996;17:283-316. http://dx.doi.org/10.1177/019251396017003001.
- Briere J. Trauma Symptoms Checklist for Young Children. Lutz, FL: Psychological Assessment Resources; 1997.
- Verhulst EC, Ende vdJ, Koot HM. Manual for the CBCL/4-18. Rotterdam, the Netherlands: Sophia Kinderziekenhuis/Academisch Ziekenhuis Rotterdam/Erasmus Universiteit Rotterdam; 1996.
- Harter S. Manual for the Self-Perception Profile for Children. Denver, CO: University of Denver; 1985.
- 4326.0 - National Survey of Mental Health and Wellbeing: Summary of Results. Canberra, ACT: ABS; 2007.
- Bogat GA, Chin R, Sabbath W, Schwartz C. The Adult’s Social Support Questionnaire. East Lansing, MI: Michigan State University; 1983.
- Rosenberg M. Rosenberg Self-Esteem Scale (RSE). Acceptance and Commitment Therapy Measures Package 61 1965. https://socy.umd.edu/about-us/rosenberg-self-esteem-scale.
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, et al. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode Version. Arch Gen Psychiatry 1985;42:696-702. http://dx.doi.org/10.1001/archpsyc.1985.01790300064008.
- Kiddies SADS-E Section. Designed to Assess PTSD. Philadelphia, PA: Medical College of Pennsylvania; 1989.
- Wolfe DA, Scott K, Reitzel-Jaffe D, Wekerle C, Grasley C, Straatman A-L. Development and validation of the conflict in adolescent dating relationships inventory. Psychol Assessment 2001;13:277-99. http://dx.doi.org/10.1037/1040-3590.13.2.277.
- Elliott DM, Briere J. Sexual abuse trauma among professional women: validating the Trauma Symptom Checklist-40 (TSC-40). Child Abuse Negl 1992;16:391-8. http://dx.doi.org/10.1016/0145-2134(92)90048-V.
- Buhrmester D. Intimacy of friendship, interpersonal competence, and adjustment during preadolescence and adolescence. Child Dev 1990;61:1101-11. http://dx.doi.org/10.2307/1130878.
- Epstein MH, Sharma JM. Behavioral and Emotional Rating Scale: A Strength-Based Approach to Assessment: Examiner’s Manual. Austin, TX: ProEd; 1998.
- Tutty LM. The revised Children’s Knowledge of Abuse Questionnaire: development of a measure of children’s understanding of sexual abuse prevention concepts. Soc Work Res 1995;19:112-20.
- Wurtele SK, Kast LC, Miller-Perrin CL, Kondrick PA. Comparison of programs for teaching personal safety skills to preschoolers. J Consult Clin Psychol 1989;57:505-11. http://dx.doi.org/10.1037/0022-006X.57.4.505.
- Harter S. The perceived competence scale for children. Child Dev 1982;53:87-9. http://dx.doi.org/10.2307/1129640.
- Wolfe VV, Gentile C, Michienzi T, Sas L, Wolfe DA. The Children’s Impact of Traumatic Events Scale: a measure of post-sexual abuse PTSD symptoms. Behaviol Assess 1991;13:359-83.
- Wright J, Sabourin S. Traduction française du ‘Trauma symptom checklist for children.’ Document inédit. Montréal, QC: Département de Psychologie, Université de Montréal; 1996.
- Hébert MD. Traduction francaise du ‘Child Post-Traumatic Stress Reaction Index’ de CJ Frederick, RS Pynoos et KO Nader (CPTS-RI; 1992). Montreal, QC: Département de sexologie, Université du Québec a Montréal; 2002.
- Putnam FW. Child Dissociative Checklist. Bethesda, MD: National Institute of Mental Health; 1988.
- Achenbach TM. Manual for the Youth Self Report and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991.
- Bouchard G, Sabourin S, Lussier Y, Richer C, Wright J. Nature des stratégies d’adaptation au sein des relations conjugales: présentation d’une version abrégée du Ways of Coping Questionnaire. Can J Behav Sci 1995;27. http://dx.doi.org/10.1037/0008-400X.27.3.371.
- Folkman SL, Lazarus RS. Ways of Coping Questionnaire: Research Edition. Palo Alto, CA: Consulting Psychologists Press; 1988.
- Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer-constructed scale to measure empowerment among users of mental health services. Psych Serv 1997;48:1042-7. http://dx.doi.org/10.1176/ps.48.8.1042.
- Giuli CA, Hudson WW. Assessing parent–child relationship disorders in clinical practice: the child’s point of view. J Soc Serv Res 1977;1:77-92. http://dx.doi.org/10.1300/J079v01n01_06.
- Friedrich WN, Urquiza AJ, Beilke RL. Behavior problems in sexually abused young children. J Pediatr Psychol 1986;11:47-5. http://dx.doi.org/10.1093/jpepsy/11.1.47.
- Brown G, Burlingame G, Lambert M, Jones E, Vaccaro J. Pushing the quality envelope: a new outcomes management system. Psych Serv 2001;52:925-34. http://dx.doi.org/10.1176/appi.ps.52.7.925.
- Causey DL, Dubow EF. Development of a self-report coping measure for elementary school children. J Clin Child Psychol 1992;21:47-59. http://dx.doi.org/10.1207/s15374424jccp2101_8.
- Putnam FW, Helmers K, Trickett PK. Development, reliability, and validity of a child dissociation scale. Child Abuse Negl 1993;17:731-41. http://dx.doi.org/10.1016/S0145-2134(08)80004-X.
- Diaz-Aguado MJ. Niños Con Dificultades Socioemocionales: Instrumentos de Evaluación. Madrid: Ministerio de Asuntos Sociales; 1995.
- Shapiro DH. Shapiro Control Inventory (SCI). Palo Alto, CA: Behaviordyne; 1992.
- Kohlberg L. Estadios morales y moralización. El enfoque andomiza-evolutivo [Moral stages and moralization. A cognitive developmental approach]. Infancia Y Aprendizaje 1982;18:33-51.
- Kovacs M, Beck AT, Schulterbrandt JG, Raskin A. Depression in Children: Diagnosis, Treatment and Conceptual Models. New York, NY: Raven; 1977.
- Harter S. Self-perception Profile for Children (Revision of the Perceived Competence Scale for Children). Denver, CO: University of Denver; 1985.
- Harter S. The Self-Perception Profile for Adolescents. Denver, CO: University of Denver; 1987.
- Ollendick TH. Reliability and validity of the Fears Schedule for Children-Revised (FSSC-R). Behav Res Ther 1993;21:685-92.
- Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med 1979;9:139-45. http://dx.doi.org/10.1017/S0033291700021644.
- Messer BA, Harter S. The Adult Self-Perception Profile. Denver, CO: University of Denver; 1986.
- Coopersmith S. Self-esteem Inventory. Palo Alto, CA: Consulting Psychologists Press; 1981.
- Minden HA. Two Hugs for Survival: Strategies for Effective Parenting. Toronto: McClelland and Stewart; 1982.
- Quay H, Peterson D. Manual for the Revised Behaviour Checklist. Coral Gables, FL: University of Miami, Department of Psychology; 1987.
- Eyberg S. Eyberg Child Behavior Inventory. Portland, OR: University of Oregon; 1980.
- Offer D, Ostrov E, Howard KI, Dolan S. Offer Self-Image Questionnaire, Revised. Los Angeles, CA: Western Psychological Services; 1992.
- Dunn DM, Dunn LM. Peabody Picture Vocabulary Test. Circle Pines, MN: American Guidance Service; 1977.
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry 2003;54:573-83. http://dx.doi.org/10.1016/S0006-3223(02)01866-8.
- Lloyd EE, Kelley ML, Hope T. Self-Mutilation in a Community Sample of Adolescents: Descriptive Characteristics and Provisional Prevalence Rates 1997.
- Kraus S, Sears S. Measuring the immeasurables: development and initial validation of the Self-Other Four Immeasurables (SOFI) scale based on Buddhist teachings on loving kindness, compassion, joy, and equanimity. SOCI 2009;92:169-81. http://dx.doi.org/10.1007/s11205-008-9300-1.
- Snyder CR, Hoza B, Pelham WE, Rapoff M, Ware L, Danovsky M, et al. The will and the ways: Development and validation of an individual differences measure of hope. J Pediatr Psychol 1997;22:399-421. http://dx.doi.org/10.1093/jpepsy/22.3.399.
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess 2004;26:41-54. http://dx.doi.org/10.1023/B:JOBA.0000007455.08539.94.
- Essau CA, Sasagawa S, Frick PJ. Callous-unemotional traits in a community sample of adolescents. Assessment 2006;13:454-69. http://dx.doi.org/10.1177/1073191106287354.
- Fink LA, Bernstein D, Handelsman L, Foote J. Initial reliability and validity of the Childhood Trauma Interview: a new multidimensional measure of childhood interpersonal trauma. Am J Psychiatry 1995;152:1329-35. http://dx.doi.org/10.1176/ajp.152.9.1329.
- Bayley N. Bayley Scales of Infant Development: Manual. New York, NY: Harcourt Assessment, The Psychological Corporation; 1993.
- Fitts WH, Roid GH. Tennessee Self Concept Scale. Nashville, TN: Counselor Recordings and Tests; 1964.
- Matheny AP. Bayley’s Infant Behavior Record: behavioral components and twin analyses. Child Dev 1980;51:1157-67. http://dx.doi.org/10.2307/1129557.
- Briere J. Professional Manual for the Trauma Symptom Checklist for Children. (TSCC). Odessa, FL: Psychological Assessment Resources; 1996.
- Strain PS, Timm MA. An experimental analysis of social interaction between a behaviorally disordered preschool child and her classroom peers. J Appl Behav Anal 1974;7:583-90. http://dx.doi.org/10.1901/jaba.1974.7-583.
- Strain PS, Shores RE, Kerr MM. An experimental analysis of “spillover” effects on the social interaction of behaviorally handicapped preschool children. J Appl Behav Anal 1976;9:31-40. http://dx.doi.org/10.1901/jaba.1976.9-31.
- Behar L, Stringfield S. Manual for the Preschool Behavior Questionnaire. Chapel Hill, NC: University of North Carolina; 1974.
- Brigance AH. Brigance™ Diagnostic Inventory of Early Development. North Billerica, MA: Curriculum; 1978.
- Fantuzzo JW, Sutton-Smith B, Coolahan KC, Manz PH, Canning S, Debnam D. Resilient peer training: assessment of preschool play interaction behaviours in young low-income children: Penn Interactive peer Play Scale. Early Childhood Res Quarterly 1995;10:105-20.
- Chamberlain P, Reid JB. Parent observation and report of child symptoms. Behavioral Assessment 1987;9:97-109.
- Dise-Lewis JE. The life events and coping inventory: an assessment of stress in children. Psychosom Med 1988;50:484-99. http://dx.doi.org/10.1097/00006842-198809000-00005.
- Gifford-Smith M. People in My Life 2000. www.fasttrackproject.org (accessed June 2002).
- Chamberlain P, Fisher PA. The Child Caregiver Interviewer Impressions Form n.d.
- Gadow KD, Sprafkin J. Early Childhood Inventories Manual. Stony Brook, NY: Checkmate Plus; 1994.
- Winters KC, Henly GA. The Personal Experience Inventory Test and Manual. Los Angeles, CA: Western Psychological Services; 1999.
- Bradley RH, Caldwell BM. Using the HOME inventory to assess the family environment. Pediatr Nurs 1988;14:97-102.
- Bricker DD, Bricker DD. Intervention with At-risk and Handicapped Infants. Baltimore, MD: University Park Press; 1982.
- Schafer DS, Moesch M. Developmental Programming for Infants and Young Children. Ann Arbor, MI: University of Michigan Press; 1981.
- Harter S, Pike R. The pictorial scale of perceived competence and social acceptance for young children. Child Dev 1984;55:1969-82. http://dx.doi.org/10.2307/1129772.
- Frankenburg WK, Dodds J, Archer P, Shapiro H, Bresnick B. The Denver II: a major revision and restandardization of the Denver Developmental Screening Test. Pediatrics 1992;89:91-7.
- McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, et al. New data from the Addiction Severity Index. Reliability and validity in three centers. J Nerv Ment Dis 1985;173:412-23. http://dx.doi.org/10.1097/00005053-198507000-00005.
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients. The Addiction Severity Index. J Nerv Ment Dis 1980;168:26-33. http://dx.doi.org/10.1097/00005053-198001000-00006.
- Abidin RA. Parenting Stress Index: Short Form (PSI-SF). Odessa, FL: Psychological Assessment Resources Inc.; 1990.
- Corcoran K, Fischer J. Measures of Clinical Practice: A Source Book. New York, NY: Simon & Schuster Inc.; 2000.
- Briere J, Stamm BH. Measurement of Stress, Trauma, and Adaptation. Lutherville, MD: Sidran Press; 1996.
- Koppitz EM. Psychological Evaluation of Children’s Human Figure Drawings. University of Michigan, Ann Arbor, MI: Grune and Stratton; 1968.
- Piers EV, Harris DB. The Piers-Harris Children’s Self Concept Scale. Nashville, TN: Counselor Recordings and Tests; 1969.
- Singer JL. The Child’s World of Make-Believe. New York, NY: Academic Press; 1973.
- Guilford JP. Creativity. Am Psychol 1950;5:444-54. http://dx.doi.org/10.1037/h0063487.
- Bellak L. The Thematic Apperception Test and the Children’s Apperception Test in Clinical Use. Oxford: Grune & Stratton; 1954.
- Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist-Civilian Version. J Trauma Stress 2003;16:495-502. http://dx.doi.org/10.1023/A:1025714729117.
- Arnold E, Kirk R, Roberts A, Griffith D, Meadows K, Julian J. Treatment of incarcerated, sexually-abused adolescent females: an outcome study. J Child Sex Abuse 2003;12:123-39. http://dx.doi.org/10.1300/J070v12n01_06.
- Barker R, Place M. Working in collaboration: a therapeutic intervention for abused children. Child Abuse Rev 2005;14:26-39. http://dx.doi.org/10.1002/car.867.
- Chasson G, Vincent J, Harris G. The use of symptom severity measured just before termination to predict child treatment dropout. J Clin Psychol 2008;64:891-904. http://dx.doi.org/10.1002/jclp.20494.
- Clarke S, Llewelyn S. Personal constructs of survivors of childhood sexual abuse receiving cognitive analytic therapy. Br J Med Psychol 1994;67:273-89. http://dx.doi.org/10.1111/j.2044-8341.1994.tb01796.x.
- Cohen JA, Mannarino AP, Perel JM, Staron V. A pilot randomized controlled trial of combined trauma-focused CBT and sertraline for childhood PTSD symptoms. J Am Acad Child Adolesc Psychiatry 2007;46:811-19. http://dx.doi.org/10.1097/chi.0b013e3180547105.
- Deblinger E, McLeer SV, Henry D. Cognitive behavioral treatment for sexually abused children suffering post-traumatic stress: preliminary findings. J Am Acad Child Adolesc Psychiatry 1990;29:747-52. http://dx.doi.org/10.1097/00004583-199009000-00012.
- Feather J, Ronan K. Trauma-focused cognitive-behavioural therapy for abused children with posttraumatic stress disorder: a pilot study. NZ J Psychol 2006;35:132-45.
- Feather JS, Ronan KR. Trauma-focused CBT with maltreated children: a clinic-based evaluation of a new treatment manual. Aust Psychol 2009;44:174-94. http://dx.doi.org/10.1080/00050060903147083.
- Habib M, Labruna V, Newman J. Complex histories and complex presentations: implementation of a manually-guided group treatment for traumatized adolescents. J Fam Violence 2013;28:717-28. http://dx.doi.org/10.1007/s10896-013-9532-y.
- Habigzang Luisa F, Hatzenberger R, Corte Fabiana D, Stroeher F, Koller S. Assessment of a psychology intervention model effect on sexual abused girls. Psicologia: Teoria E Pesquisa 2008;24:67-76.
- Habigzang Luisa F, Stroeher Fernanda H, Hatzenberger R, Cunha Rafaela C, Ramos Michele da S, Koller Silvia H. Cognitive behavioral group therapy for sexually abused girls. Rev Saude Publ 2009;43:70-8.
- Habigzang LF, Damasio BF, Koller SH. Impact evaluation of a cognitive behavioral group therapy model in Brazilian sexually abused girls. J Child Sex Abuse 2013;22:173-90. http://dx.doi.org/10.1080/10538712.2013.737445.
- Hubel G, Campbell C, West T, Friedenberg S, Schreier A, Flood M, et al. Child advocacy center based group treatment for child sexual abuse. J Child Sex Abuse 2014;23:304-25. http://dx.doi.org/10.1080/10538712.2014.888121.
- Jarero I, Roque-Lopez S, Gomez J. The provision of an EMDR-based multicomponent trauma treatment with child victims of severe interpersonal trauma. J EMDR Pract Res 2013;7:17-28. http://dx.doi.org/10.1891/1933-3196.7.1.17.
- Kirsch V, Fegert Jorg M, Seitz Diana C, Goldbeck L. Trauma-focused cognitive behavioral therapy (Tf-CBT) for children and adolescents after abuse and maltreatment: results of a pilot study. Kindh Entwickl 2011;20:95-102. http://dx.doi.org/10.1026/0942-5403/a000045.
- Kjellgren C, Svedin C, Nilsson D. Child physical abuse-experiences of combined treatment for children and their parents: a pilot study. Child Care Pract 2013;19:275-90. http://dx.doi.org/10.1080/13575279.2013.785934.
- Kruczek T, Vitanza S. Treatment effects with an adolescent abuse survivor’s group. Child Abuse Negl 1999;23:477-85. http://dx.doi.org/10.1016/S0145-2134(99)00023-X.
- Lange A, Ruwaard J. Ethical dilemmas in online research and treatment of sexually abused adolescents. J Med Internet Res 2010;12. http://dx.doi.org/10.2196/jmir.1455.
- Lanktree CB, Briere J. Outcome of therapy for sexually abused children: a repeated measures study. Child Abuse Negl 1995;19:1145-55. http://dx.doi.org/10.1016/0145-2134(95)00075-J.
- Matulis S, Resick P, Rosner R, Steil R. Developmentally adapted cognitive processing therapy for adolescents suffering from posttraumatic stress disorder after childhood sexual or physical abuse: a pilot study. Clin Child Fam Psychol Rev 2014;17:173-90. http://dx.doi.org/10.1007/s10567-013-0156-9.
- Misurell J, Springer C, Tryon W. Game-based cognitive-behavioral therapy (GB-CBT) group program for children who have experienced sexual abuse: a preliminary investigation. J Child Sex Abuse 2011;20:14-36. http://dx.doi.org/10.1080/10538712.2011.540000.
- Misurell J, Springer C, Acosta L, Liotta L, Kranzler A. Game-based cognitive-behavioral therapy individual model (GB-CBT-IM) for child sexual abuse: a preliminary outcome study. Psychol Trauma 2014;6:250-8. http://dx.doi.org/10.1037/a0033411.
- Rosenberg HJ, Jankowski MK, Fortuna LR, Rosenberg SD, Mueser KT. A pilot study of a cognitive restructuring program for treating posttraumatic disorders in adolescents. Psychol Trauma 2011;3:94-9. http://dx.doi.org/10.1037/a0019889.
- Runyon M, Deblinger E, Schroeder C. Pilot evaluation of outcomes of combined parent-child cognitive-behavioral group therapy for families at risk for child physical abuse. Cogn Behav Pract 2009;16:101-18. http://dx.doi.org/10.1016/j.cbpra.2008.09.006.
- Salloum A, Robst J, Scheeringa MS, Cohen JA, Wang W, Murphy TK, et al. Step one within stepped care trauma-focused cognitive behavioral therapy for young children: a pilot study. Child Psychiatry Hum Dev 2014;45:65-77. http://dx.doi.org/10.1007/s10578-013-0378-6.
- Silovsky J, Niec L, Bard D, Hecht D. Treatment for preschool children with interpersonal sexual behavior problems: a pilot study. J Clin Child Adolesc Psychol 2007;36:378-91. http://dx.doi.org/10.1080/15374410701444330.
- Smith A, Kelly A. An exploratory study of group therapy for sexually abused adolescents and nonoffending guardians. J Child Sex Abuse 2008;17:101-16. http://dx.doi.org/10.1080/10538710801913496.
- Stauffer L, Deblinger E. Cognitive behavioral groups for nonoffending mothers and their young sexually abused children: a preliminary treatment outcome study. Child Maltreat 1996;1:65-76. http://dx.doi.org/10.1177/1077559596001001007.
- Sullivan M, Egan M, Gooch M. Conjoint interventions for adult victims and children of domestic violence: a program evaluation. Res Soc Work Pract 2004;14:163-70. http://dx.doi.org/10.1177/1049731503257881.
- Timmons-Mitchell J. Containing aggressive acting out in abused children. Child Welfare 1986;65:459-68.
- Ducharme JM, Atkinson L, Poulton L. Success-based, noncoercive treatment of oppositional behavior in children from violent homes. J Am Acad Child Adolesc Psychiatry 2000;39:995-1004. http://dx.doi.org/10.1097/00004583-200008000-00014.
- Golding K, Picken W. Group work for foster carers caring for children with complex problems. Adopt Foster 2004;28:25-37. http://dx.doi.org/10.1177/030857590402800105.
- Jackson A, Frederico M, Tanti C, Black C. Exploring outcomes in a therapeutic service response to the emotional and mental health needs of children who have experienced abuse and neglect in Victoria, Australia. Child Fam Soc Work 2009;14:198-212. http://dx.doi.org/10.1111/j.1365-2206.2009.00624.x.
- Lanier P, Kohl PL, Benz J, Swinger D, Drake B. Preventing maltreatment with a community-based implementation of parent-child interaction therapy. J Child Fam Stud 2014;23:449-60. http://dx.doi.org/10.1007/s10826-012-9708-8.
- Lanier P, Kohl PL, Benz J, Swinger D, Moussette P, Drake B. Parent–child interaction therapy in a community setting: examining outcomes, attrition, and treatment setting. Res Soc Work Prac 2011;1:689-98. http://dx.doi.org/10.1177/1049731511406551.
- Osofsky JD, Kronenberg M, Hammer JH, Lederman C, Katz L, Adams S, et al. The development and evaluation of the intervention model for the Florida Infant Mental Health Pilot Program. Infant Ment Health J 2007;28:259-80. http://dx.doi.org/10.1002/imhj.20135.
- Puckering C, Connolly B, Werner C, Toms-Whittle L, Thompson L, Lennox J, et al. Rebuilding relationships: a pilot study of the effectiveness of the Mellow Parenting Programme for children with Reactive Attachment Disorder. Clin Child Psychol Psychiatry 2011;16:73-87. http://dx.doi.org/10.1177/1359104510365195.
- Timmer S, Urquiza A, Zebell N, McGrath J. Parent–child interaction therapy: application to maltreating parent–child dyads. Child Abuse Negl 2005;29:825-42. http://dx.doi.org/10.1016/j.chiabu.2005.01.003.
- Timmer S, Urquiza A, Zebell N. Challenging foster caregiver-maltreated child relationships: the effectiveness of parent-child interaction therapy. Child Youth Serv Rev 2006;28:1-19. http://dx.doi.org/10.1016/j.childyouth.2005.01.006.
- Timmer S, Ware L, Urquiza A, Zebell N. The effectiveness of parent–child interaction therapy for victims of interparental violence. Violence Vict 2010;25:486-503. http://dx.doi.org/10.1891/0886-6708.25.4.486.
- Winton M. An evaluation of a support group for parents who have a sexually abused child. Child Abuse Negl 1990;14:397-405. http://dx.doi.org/10.1016/0145-2134(90)90011-H.
- Arabgol F, Derakhshanpour F, Panaghi L, Sarjami S, Hajebi A. Effect of therapeutic interventions on behavioral problems of abused children. IJPCP 2014;19:202-10.
- Bentovim A, Boston P, Van E. Child sexual abuse: children and families referred to a treatment project and the effects of intervention. Br Med J 1987;29:1453-7. http://dx.doi.org/10.1136/bmj.295.6611.1453.
- Berg B, Jones DPH. Outcome of psychiatric intervention in factitious illness by proxy (Munchausen’s syndrome by proxy). Arch Dis Child 1999;81:465-72. http://dx.doi.org/10.1136/adc.81.6.465.
- Coren E, Thomae M, Hutchfield J, Iredale W. Report on the implementation and results of an outcomes-focused evaluation of child sexual abuse interventions in the UK. Child Abuse Rev 2013;22:44-59. http://dx.doi.org/10.1002/car.2200.
- Crusto C, Lowell D, Paulicin B, Reynolds J, Feinn R, Friedman S, et al. Evaluation of a wraparound process for children exposed to family violence. Best Pract Ment Health 2008;4:1-18.
- Danielson C, McCart M, de Arellano M, Macdonald A, Doherty L, Resnick H. Risk reduction for substance use and trauma-related psychopathology in adolescent sexual assault victims: findings from an open trial. Child Maltreat 2010;15:261-8. http://dx.doi.org/10.1177/1077559510367939.
- De Paul J, Arruabarrena I. Evaluation of a treatment program for abusive and high-risk families in Spain. Child Welfare 2003;82:413-42.
- Donohue B, Van Hasselt V. Development and description of an empirically based ecobehavioral treatment program for child maltreatment. Behav Intervent 1999;14:55-82. http://dx.doi.org/10.1002/(SICI)1099-078X(199904/06)14:2<55::AID-BIN31>3.0.CO;2-%23.
- Forbes F, Duffy John C, Mok J, Lemvig J. Early intervention service for non-abusing parents of victims of child sexual abuse: Pilot study. Br J Psychiatry 2003;183:66-72. http://dx.doi.org/10.1192/bjp.183.1.66.
- McClure EB, Connell AM, Zucker M, Griffith JR, Kaslow NJ, Hibbs ED, et al. Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. Washington, DC: American Psychological Association; 2005.
- Staff I, Fein E. Stability and change: Initial findings in a study of treatment foster care placements. Child Youth Serv Rev 1995;17:379-89. http://dx.doi.org/10.1016/0190-7409(95)00023-6.
- Tourigny M, Peladeau N, Doyon M, Bouchard C. Efficacy of a treatment program for sexually abused children. Child Abuse Negl 1998;22:25-43. http://dx.doi.org/10.1016/S0145-2134(97)00117-8.
- Woodworth DL, Patton M. Family Sexual Abuse: Frontline Research and Evaluation. Thousand Oaks, CA: Sage Publications; 1991.
- Grosz CA, Kempe RS, Kelly M. Extrafamilial sexual abuse: treatment for child victims and their families. Child Abuse Negl 2000;24:9-23. http://dx.doi.org/10.1016/S0145-2134(99)00113-1.
- Hack T, Osachuk T, De Luca R. Group treatment for sexually abused preadolescent boys. Fam Soc 1994;75:217-28.
- Harbeck C, Peterson L, Starr L. Previously abused child victims’ response to a sexual abuse prevention program: a matter of measures. Behav Ther 1992;23:375-87. http://dx.doi.org/10.1016/S0005-7894(05)80164-9.
- Hiebert-Murphy D, de Luca R, Runtz M. Group treatment for sexually abused girls: evaluating outcome. Fam Soc 1992;73:205-13.
- Hyde C, Bentovim A, Monck E. Some clinical and methodological implications of a treatment outcome study of sexually abused children. Child Abuse Negl 1995;19:1387-99. http://dx.doi.org/10.1016/0145-2134(95)00096-Q.
- Lee J, Kolomer S, Thomsen D. Evaluating the effectiveness of an intervention for children exposed to domestic violence: a preliminary program evaluation. Child Adolesc Social Work J 2012;29:357-72. http://dx.doi.org/10.1007/s10560-012-0265-1.
- MacMillan K, Harpur L. An examination of children exposed to marital violence accessing a treatment intervention. J Emot Abuse 2003;3:227-52. http://dx.doi.org/10.1300/J135v03n03_04.
- Merrick MV, Allen BM, Crase SJ. Variables associated with positive treatment outcomes for children surviving sexual abuse. J Child Sex Abuse 1994;3:67-8. http://dx.doi.org/10.1300/J070v03n02_05.
- Mukaddes N, Bilge S, Alyanak B, Kora M. Clinical characteristics and treatment responses in cases diagnosed as reactive attachment disorder. Child Psychiatry Hum Dev 2000;30:273-87. http://dx.doi.org/10.1023/B:CHUD.0000037154.77861.21.
- Nelki J, Watters J. A group for sexually abused young children: unravelling the web. Child Abuse Negl 1989;13:369-77. http://dx.doi.org/10.1016/0145-2134(89)90077-X.
- Lindon J, Nourse C. A multi-dimensional model of groupwork for adolescent girls who have been sexually abused. Child Abuse Negl 1994;18:341-8. http://dx.doi.org/10.1016/0145-2134(94)90036-1.
- Reeker J, Ensing D. An evaluation of a group treatment for sexually abused young children. J Child Sex Abuse 1998;7:65-8. http://dx.doi.org/10.1300/J070v07n02_04.
- Sinclair J. Outcome of group treatment for sexually abuse adolescent females living in a group home setting. J Interpers Violence 1995;10:533-42. http://dx.doi.org/10.1177/088626095010004011.
- Friedrich WN, Luecke WJ, Beilke RL, Place V. Psychotherapy outcome of sexually abused boys: an agency study. J Interpers Violence 1992;7:396-409. http://dx.doi.org/10.1177/088626092007003008.
- Rust J, Troupe P. Relationships of treatment of child sexual abuse with school achievement and self-concept. J Early Adolesc 1991;11:420-9. http://dx.doi.org/10.1177/0272431691114002.
- Jarvis KL, Novaco RW. Postshelter adjustment of children from violent families. J Interpers Violence 2006;21:1046-62. http://dx.doi.org/10.1177/0886260506290205.
- Wagner W, Kilcrease-Fleming D, Fowler W, Kazelskis R. Brief-term counseling with sexually abused girls: the impact of sex of counselor on clients’ therapeutic involvement, self-concept, and depression. J Couns Psychol 1993;40:490-50. http://dx.doi.org/10.1037/0022-0167.40.4.490.
- Brown A, McCauley K, Navalta C, Saxe G. Trauma systems therapy in residential settings: improving emotion regulation and the social environment of traumatized children and youth in congregate care. J Fam Violence 2013;28:693-70. http://dx.doi.org/10.1007/s10896-013-9542-9.
- Cross T, Leavey J, Mosley P, White A, Andreas J. Outcomes of specialized foster care in a managed child welfare services network. Child Welfare 2004;83:533-64.
- Gallagher B, Green A. Outcomes among young adults placed in therapeutic residential care as children. J Child Serv 2013;8:31-5. http://dx.doi.org/10.1108/17466661311309772.
- Gray J, Nielsen DR, Wood LE, Andresen M, Dolce K. Academic progress of children who attended a preschool for abused children: a follow-up of the Keepsafe Project. Child Abuse Negl 2000;24:25-32. http://dx.doi.org/10.1016/S0145-2134(99)00111-8.
- Heede T, Runge H, Storebo OJ, Rowley E, Hansen KG. Psychodynamic milieu-therapy and changes in personality: what is the connection?. J Child Psychother 2009;35:276-89. http://dx.doi.org/10.1080/00754170903237286.
- Hussey D, Guo S. Characteristics and trajectories of treatment foster care youth. Child Welfare 2005;84:485-506.
- Jones C, Chancey R, Lowe L, Risler E. Residential treatment for sexually abusive youth: an assessment of treatment outcomes. Res Soc Work Pract 2010;20:172-82. http://dx.doi.org/10.1177/1049731509333349.
- Oates K. A therapeutic preschool for abused children: the Keepsafe Project. Child Abuse Negl 1995;19:1379-86. http://dx.doi.org/10.1016/0145-2134(95)00102-E.
- Parish R. Developmental milestones in abused children and their improvement with a family-oriented approach to the treatment of child abuse. Child Abuse Negl 1985;9:245-50. http://dx.doi.org/10.1016/0145-2134(85)90017-1.
- Pugh R, Tepper F, Halpern-Felsher B, Howe T, Tomlinson-Keasey C, Parke R. Changes in abused children’s social and cognitive skills from intake to discharge in a residential treatment center. Resid Treat Child Youth 1997;14:65-83. http://dx.doi.org/10.1300/J007v14n03_06.
- Ray J, Smith V, Peterson T, Gray J, Schaffner J, Houff M. A treatment program for children with sexual behavior problems. Child Adolesc Social Work J 1995;12:331-43. http://dx.doi.org/10.1007/BF01876734.
- Schram D, Giovengo M. Evaluation of threshold: an independent living program for homeless adolescents. J Adolesc Health 1991;12:567-72. http://dx.doi.org/10.1016/0197-0070(91)90089-5.
- Stubenbort K, Cohen M, Trybalski V. The effectiveness of an attachment-focused treatment model in a therapeutic preschool for abused children. Clin Soc Work J 2010;38:51-60. http://dx.doi.org/10.1007/s10615-007-0107-3.
- Vernberg EM, Jacobs AK, Nyre JE, Puddy RW, Roberts MC. Innovative treatment for children with serious emotional disturbance: preliminary outcomes for a school-based intensive mental health program. J Clin Child Adolesc Psychol 2004;33:359-65. http://dx.doi.org/10.1207/s15374424jccp3302_17.
- Coulter S. Effect of song writing versus recreational music on posttraumatic stress disorder (PTSD) symptoms and abuse attribution in abused children. J Poet Ther 2000;13:189-208. http://dx.doi.org/10.1023/A:1021402618865.
- Ernst A, Weiss S, Enright-Smith S, Hansen J. Positive outcomes from an immediate and ongoing intervention for child partner violence. Am J Emerg Med 2008;26:389-94. http://dx.doi.org/10.1016/j.ajem.2007.06.018.
- Hall-Marley Susan E, Damon L. Impact of structured group therapy on young victims of sexual abuse. J Child Adolesc Group Ther 1993;3:41-8. http://dx.doi.org/10.1007/BF00973642.
- Kemp K, Signal T, Botros H, Taylor N, Prentice K. Equine facilitated therapy with children and adolescents who have been sexually abused: a program evaluation study. J Child Fam Stud 2013;23:558-66. http://dx.doi.org/10.1007/s10826-013-9718-1.
- MacKay B, Gold M, Gold E. A pilot study in drama therapy with adolescent girls who have been sexually abused. Art Psychother 1987;14:77-84. http://dx.doi.org/10.1016/0197-4556(87)90037-2.
- Clausen JM, Ruff S, von Wiederhold W, Heineman T. For as long as it takes: relationship-based play therapy for children in foster care. Psychoanal Soc Work 2012;19:43-5. http://dx.doi.org/10.1080/15228878.2012.666481.
- Nilsson D, Wadsby M. Symboldrama, a psychotherapeutic method for adolescents with dissociative and PTSD symptoms: a pilot study. J Trauma Dissociation 2010;11:308-21. http://dx.doi.org/10.1080/15299731003781075.
- Pifalo T. Pulling out the thorns: art therapy with sexually abused children and adolescents. Art Ther 2002;19:12-2. http://dx.doi.org/10.1080/07421656.2002.10129724.
- Pifalo T. Art therapy with sexually abused children and adolescents: extended research study. Art Ther 2006;23:181-5. http://dx.doi.org/10.1080/07421656.2006.10129337.
- Purvis K, Cross D. Improvements in salivary cortisol, depression, and representations of family relationships in at-risk adopted children utilizing a short-term therapeutic intervention. Adopt Q 2007;10:25-43. http://dx.doi.org/10.1300/J145v10n01_02.
- Purvis K, Cross D, Federici R, Johnson D, McKenzie B. The hope connection: a therapeutic summer day camp for adopted and at-risk children with special socio-emotional needs. Adopt Foster 2007;31:38-4. http://dx.doi.org/10.1177/030857590703100406.
- Reyes C, Asbrand J. A longitudinal study assessing trauma symptoms in sexually abused children engaged in play therapy. Int J Play Ther 2005;14:25-47. http://dx.doi.org/10.1037/h0088901.
- Schultz P, Remick-Barlow G, Robbins L. Equine-assisted psychotherapy: a mental health promotion/intervention modality for children who have experienced intra-family violence. Health Soc Care Comm 2007;15:265-71. http://dx.doi.org/10.1111/j.1365-2524.2006.00684.x.
- Scott T, Burlingame G, Starling M, Porter C, Lilly J. Effects of individual client-centered play therapy on sexually abused children’s mood, self-concept, and social competence. Int J Play Ther 2003;12:7-30. http://dx.doi.org/10.1037/h0088869.
- Amaya-Jackson L, Reynolds V, Murray M, Nelson A, Cherney M, Lee R, et al. Cognitive-behavioral treatment for pediatric posttraumatic stress disorder: protocol and application in school and community settings. Cogn Behav Pract 2003;10:204-13. http://dx.doi.org/10.1016/S1077-7229(03)80032-9.
- Barton K. In-home treatment of child abuse: healing at home can be effective and cost-effective. Calif Agricult 1994;48:36-8.
- Barton K, Baglio C, Braverman M. Stress reduction in child-abusing families: global and specific measures. Psychol Rep 1994;75:287-304. http://dx.doi.org/10.2466/pr0.1994.75.1.287.
- Brook J, McDonald T. Evaluating the effects of comprehensive substance abuse intervention on successful reunification. Res Soc Work Pract 2007;17:664-73. http://dx.doi.org/10.1177/1049731507300148.
- Cohen J, Mannarino A. Predictors of treatment outcome in sexually abused children. Child Abuse Negl 2000;24:983-94. http://dx.doi.org/10.1016/S0145-2134(00)00153-8.
- Coleman H, Jenson JM. A longitudinal investigation of delinquency among abused and behavior problem youth following participation in a family preservation program. J Offender Rehabil 2000;31:143-62. http://dx.doi.org/10.1300/J076v31n01_10.
- Collado C, Levine P. Reducing transfers of children in family foster care through onsite mental health interventions. Child Welfare 2007;86:133-50.
- Currier LL, Wurtele SK. A pilot study of previously abused and non-sexually abused children’s responses to a personal safety program. J Child Sex Abuse 1996;5:71-87. http://dx.doi.org/10.1300/J070v05n01_04.
- DeSena A, Murphy R, Douglas-Palumberi H, Blau G, Kelly B, Horwitz S, et al. SAFE Homes: is it worth the cost? An evaluation of a group home permanency planning program for children who first enter out-of-home care. Child Abuse Negl 2005;29:627-43. http://dx.doi.org/10.1016/j.chiabu.2004.05.007.
- Edinburgh LD, Saewyc EM. A novel, intensive home-visiting intervention for runaway, sexually exploited girls. J Spec Pediatr Nurs 2009;14:41-8. http://dx.doi.org/10.1111/j.1744-6155.2008.00174.x.
- Friman P, Jones M, Smith G, Daly D, Larzelere R. Decreasing disruptive behavior by adolescent boys in residential care by increasing their positive to negative interactional ratios. Behav Modif 1997;21:470-86. http://dx.doi.org/10.1177/01454455970214005.
- Graham-Bermann S, Miller L. Intervention to reduce traumatic stress following intimate partner violence: an efficacy trial of the Moms’ Empowerment Program (MEP). Psychodyn Psychiatry 2013;41:329-49. http://dx.doi.org/10.1521/pdps.2013.41.2.329.
- Hakman M, Chaffin M, Funderburk B, Silovsky J. Change trajectories for parent-child interaction sequences during parent-child interaction therapy for child physical abuse. Child Abuse Negl 2009;33:461-70. http://dx.doi.org/10.1016/j.chiabu.2008.08.003.
- Harder J. Prevention of child abuse and neglect: an evaluation of a home visitation parent aide program using recidivism data. Res Soc Work Pract 2005;15:246-56. http://dx.doi.org/10.1177/1049731505275062.
- Harold GT, Kerr DCR, Van R, DeGarmo DS, Rhoades KA, Leve LD. Depressive symptom trajectories among girls in the juvenile justice system: 24-month outcomes of an RCT of multidimensional treatment foster care. Prev Sci 2013;14:437-46. http://dx.doi.org/10.1007/s11121-012-0317-y.
- Howes C, Ritchie S. Changes in child-teacher relationships in a therapeutic preschool program. Early Educ Dev 1998;9:411-22. http://dx.doi.org/10.1207/s15566935eed0904_6.
- Iwaniec D, Sneddon H, Allen S. The outcomes of a longitudinal study of non-organic failure-to-thrive. Child Abuse Rev 2003;12:216-26. http://dx.doi.org/10.1002/car.805.
- Kirk R, Griffith D. Intensive family preservation services: demonstrating placement prevention using event history analysis. Soc Work Res 2004;28:5-16. http://dx.doi.org/10.1093/swr/28.1.5.
- Lewis C, Simons A, Nguyen L, Murakami J, Reid M. Impact of childhood trauma on treatment outcome in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry 2010;49:132-40.
- Lorber R, Felton D, Reid J. A social learning approach to the reduction of coercive processes in child abusive families: a molecular analysis. Adv Behav Res Ther 1984;6:29-45. http://dx.doi.org/10.1016/0146-6402(84)90011-0.
- MacMillan H. Effectiveness of home visitation by public-health nurses in prevention of the recurrence of child physical abuse and neglect: a randomised controlled trial. Lancet 2005;365:1786-93. http://dx.doi.org/10.1016/S0140-6736(05)66388-X.
- Mersky J, Topitzes J, Reynolds A. Maltreatment prevention through early childhood intervention: a confirmatory evaluation of the Chicago Child-Parent Center preschool program. Child Youth Serv Rev 2011;33:1454-63. http://dx.doi.org/10.1016/j.childyouth.2011.04.022.
- Overbeek M, de Schipper J, Lamers-Winkelman F, Schuengel C. Risk factors as moderators of recovery during and after interventions for children exposed to interparental violence. Am J Orthopsychiatry 2014;84:295-306. http://dx.doi.org/10.1037/ort0000007.
- Pereira P, D’Affonseca S, Williams L. A feasibility pilot intervention program to teach parenting skills to mothers of poly-victimized children. J Fam Violence 2013;28:5-15. http://dx.doi.org/10.1007/s10896-012-9490-9.
- Rivara FP. Physical abuse in children under two: a study of therapeutic outcomes. Child Abuse Negl 1985;9:81-7. http://dx.doi.org/10.1016/0145-2134(85)90095-X.
- Sagatun I, Prince L. Incest family dynamics: family members’ perceptions before and after therapy. J Soc Work Hum Sex 1988;7:69-87. http://dx.doi.org/10.1300/J291v07n02_04.
- Sullivan P, Scanlan J. Psychotherapy with handicapped sexually abused children. Dev Disabil Bull 1990;18:21-34.
- Swart J, Apsche J. Family Mode Deactivation Therapy (FMDT): a randomized controlled trial for adolescents with complex issues. Int J Behav Consult Ther 2014;9:14-22. http://dx.doi.org/10.1037/h0101010.
- Swart J, Apsche J. A comparative treatment efficacy study of conventional therapy and Mode Deactivation Therapy (MDT) for adolescents with conduct disorders, mixed personality disorders, and experiences of childhood trauma. Int J Behav Consult Ther 2014;9:23-9. http://dx.doi.org/10.1037/h0101011.
- Szykula S, Fleischman M. Reducing out-of-home placements of abused children: two controlled field studies. Child Abuse Negl 1985;9:277-83. http://dx.doi.org/10.1016/0145-2134(85)90020-1.
- Vitulano LA, Nagler S, Adnopoz J, Grigsby RK. Preventing out-of-home placement for high-risk children. Yale J Biol Med 1990;63:285-91.
- Waxman H, Houston W, Profilet S, Sanchez B. The long-term effects of the Houston Child Advocates, Inc., program on children and family outcomes. Child Welfare 2009;88:23-46.
- Iwaniec D. Evaluating parent training for emotionally abusive and neglectful parents: comparing individual versus individual and group intervention. Res Social Work Pract 1997;7:329-49.
- Gospodarevskaya E, Segal L. Cost-utility analysis of different treatments for post-traumatic stress disorder in sexually abused children. Child Adolesc Psychiatry Ment Health 2012;6:1-15. http://dx.doi.org/10.1186/1753-2000-6-15.
- Sharac J, McCrone P, Rushton A, Monck E. Enhancing adoptive parenting: a cost-effectiveness analysis. Child Adolesc Ment Health 2011;16:110-15. http://dx.doi.org/10.1111/j.1475-3588.2010.00587.x.
- McCrone P, Weeramanthri T, Knapp M, Rushton A, Trowell J, Miles G, et al. Cost-effectiveness of individual versus group psychotherapy for sexually abused girls. Child Adolesc Ment Health 2005;10:26-31. http://dx.doi.org/10.1111/j.1475-3588.2005.00113.x.
- Lynch F, Dickerson JF, Saldana L, Fisher PA. Incremental net benefit of early intervention for preschool-aged children with emotional and behavioral problems in foster care. Child Youth Serv Rev 2014;36:213-19. http://dx.doi.org/10.1016/j.childyouth.2013.11.025.
- Wood S, Barton K, Schroeder C. In-home treatment of abusive families: cost and placement at one year. Psychotherapy 1988;29:409-14. http://dx.doi.org/10.1037/h0085362.
- Lynch F, Fisher P, Dickerson JF, Saldana L. Incremental cost-effectiveness of multidimensional treatment foster care for pre-schoolers. J Ment Health Policy Econ 2011;14:S19-20.
- Blazey A. Reducing the Risk, Cutting the Cost: An Assessment of the Potential Savings on Barnardo’s Interventions for Young People who have been Sexually Exploited. Barkingside: Barnardo’s; 2011.
- Clark C, Yampolskaya S, Robst J. Mental health services expenditures among children placed in out-of-home care. Admin Policy Ment Health Ment Health Serv Res 2011;38:430-8. http://dx.doi.org/10.1007/s10488-010-0330-z.
- Cohen M, Miller TR. The cost of mental health care for victims of crime. J Interpers Violence 1998;13:92-110. http://dx.doi.org/10.1177/088626098013001006.
- Conran T, Love J. The talkative chair: a child’s experience of sexual abuse intervention. J Systemic Ther 1993;12:68-85.
- DePanfilis DDH, Kunz J. Assessing the cost-effectiveness of family connections. Child Abuse Negl 2008;32:335-51. http://dx.doi.org/10.1016/j.chiabu.2007.06.005.
- Florence C, Brown DS, Fang X, Thompson HF. Health care costs associated with child maltreatment: impact on Medicaid. Pediatrics 2013;132:312-18. http://dx.doi.org/10.1542/peds.2012-2212.
- Foster EM, Prinz RJ, Sanders MR, Shapiro CJ. The costs of a public health infrastructure for delivering parenting and family support. Child Youth Serv Rev 2008;30:493-501. http://dx.doi.org/10.1016/j.childyouth.2007.11.002.
- Maher EJ, Corwin TW, Hodnett R, Faulk K. A cost-savings analysis of a statewide parenting education program in child welfare. Res Soc Work Pract 2012;22:615-25. http://dx.doi.org/10.1177/1049731512449873.
- New M, Berliner L. Mental health service utilization by victims of crime. J Trauma Stress 2000;13:693-707. http://dx.doi.org/10.1023/A:1007818402277.
- Reynolds AJ, Temple JA, Robertson DL, Mann EA. Age 21 of the cost-benefit analysis of the Title I Chicago Child-parent centers. Educ Eval Policy Anal 2002;24:267-303. http://dx.doi.org/10.3102/01623737024004267.
- Rovi S, Chen P, Johnson MS. The economic burden of hospitalizations associated with child abuse and neglect. Am J Public Health 2004;94:586-90. http://dx.doi.org/10.2105/AJPH.94.4.586.
- Buschbacher PW. Positive behavior support for a young child who has experienced neglect and abuse: testimonials of a family member and professionals. J Posit Behav Interv 2002;4:242-8. http://dx.doi.org/10.1177/10983007020040040701.
- Chasson G, Mychailyszyn M, Vincent J, Harris G. Evaluation of trauma characteristics as predictors of attrition from cognitive-behavioral therapy for child victims of violence. Psychol Rep 2013;113:734-53. http://dx.doi.org/10.2466/16.02.PR0.113x30z2.
- Eslinger JG, Sprang G, Otis MD. Child and caregiver dropout in child psychotherapy for trauma. J Loss Trauma 2014;19:121-36. http://dx.doi.org/10.1080/15325024.2012.742720.
- Fraynt R, Ross L, Baker BL, Rystad I, Lee J, Briggs EC. Predictors of treatment engagement in ethnically diverse, urban children receiving treatment for trauma exposure. J Trauma Stress 2014;27:66-73. http://dx.doi.org/10.1002/jts.21889.
- McPherson P, Scribano P, Stevens J. Barriers to successful treatment completion in child sexual abuse survivors. J Interpers Violence 2012;27:23-39. http://dx.doi.org/10.1177/0886260511416466.
- Cross A, Jaycox L, Hickman L, Schultz D, Barnes-Proby D, Kofner A, et al. Predictors of study retention from a multisite study of interventions for children and families exposed to violence. J Community Appl Soc 2013;41:743-57. http://dx.doi.org/10.1002/jcop.21568.
- Taban N, Lutzker J. Consumer evaluation of an ecobehavioral program for prevention and intervention of child maltreatment. J Fam Violence 2001;16:323-30. http://dx.doi.org/10.1023/A:1011194417691.
- Ashby MR, Gilchrist LD, Miramontez A. Group treatment for sexually abused American Indian adolescents. Soc Work Groups 1987;10:21-32. http://dx.doi.org/10.1300/J009v10n04_03.
- Baker JN, Tanis HJ, Rice JB. Including siblings in the treatment of child sexual abuse. J Child Sex Abuse 2001;10:1-16. http://dx.doi.org/10.1300/J070v10n03_01.
- Nelson-Gardell D. The voices of victims: surviving child sexual abuse. Child Adolesc Social Work J 2001;18:401-16. http://dx.doi.org/10.1023/A:1012936031764.
- Peled E, Edleson JL. Multiple perspectives on groupwork with children of battered women. Violence Vict 1992;7:327-46.
- Baginsky M. Counselling and Support Services for Young People Aged 12–16 who have Experienced Sexual Abuse: A Study of the Provision in Italy, the Netherlands and the United Kingdom. London: NSPCC; 2001.
- Fowler W, Wagner W, Iachini A, Johnson J. The impact of sex of psychological examiner on sexually abused girls’ preference for and anticipated comfort with male versus female counselors. Child Study J 1992;22:1-10.
- Fowler W, Wagner W. Preference for and comfort with male versus female counselors among sexually abused girls in individual treatment. J Couns Psychol 1993;40:65-72. http://dx.doi.org/10.1037/0022-0167.40.1.65.
- Kilcrease-Fleming D, Wagner W, Fowler W. Sexually abused girls’ behavior during an initial counseling session. J Fam Violence 1992;7:179-87. http://dx.doi.org/10.1007/BF00979026.
- Kolko D, Selelyo J, Brown E. The treatment histories and service involvement of physically and sexually abusive families: description, correspondence, and clinical correlates. Child Abuse Negl 1999;23:459-76. http://dx.doi.org/10.1016/S0145-2134(99)00022-8.
- Porter R, Wagner W, Johnson J, Cox L. Sexually abused girls’ verbalizations in counseling: an application of the client behavior system. J Couns Psychol 1996;43:383-8. http://dx.doi.org/10.1037/0022-0167.43.4.383.
- Thompson R, Dancy BL, Wiley TRA, Perry SP, Najdowski CJ. The experience of mental health service use for African American mothers and youth. Issues Ment Health Nurs 2011;32:678-86. http://dx.doi.org/10.3109/01612840.2011.595534.
- Horowitz L, Putnam F, Noll J, Trickett P. Factors affecting utilization of treatment services by sexually abused girls. Child Abuse Negl 1997;21:35-48. http://dx.doi.org/10.1016/S0145-2134(96)00129-9.
- Lippert T, Favre T, Alexander C, Cross TP. Families who begin versus decline therapy for children who are sexually abused. Child Abuse Negl 2008;32:859-68. http://dx.doi.org/10.1016/j.chiabu.2008.02.005.
- Cunningham WS, Duffee DE, Huang YF, Steinke CM, Naccarato T. On the meaning and measurement of engagement in youth residential treatment centers. Res Soc Work Pract 2009;19:63-76. http://dx.doi.org/10.1177/1049731508314505.
- Shennum W, Carlo P. A look at residential treatment from the child’s point of view. Resid Treat Child Youth 1995;12:31-44. http://dx.doi.org/10.1300/J007v12n03_03.
- West SD, Day AG, Somers CL, Baroni BA. Student perspectives on how trauma experiences manifest in the classroom: engaging court-involved youth in the development of a trauma-informed teaching curriculum. Child Youth Serv Rev 2014;38:58-65. http://dx.doi.org/10.1016/j.childyouth.2014.01.013.
- Gilbert CM. Children in women’s shelters: a group intervention using art. J Child Adolesc Psychiatr Ment Health Nurs 1988;1:7-13. http://dx.doi.org/10.1111/j.1744-6171.1988.tb00220.x.
- Koverola C, Murtaugh CA, Connors KM, Reeves G, Papas MA. Children exposed to intra-familial violence: predictors of attrition and retention in treatment. J Aggress Maltreat Trauma 2007;14:19-42. http://dx.doi.org/10.1300/J146v14n04_02.
- Murphy RA, Sink HE, Ake GS, Carmody KA, Amaya-Jackson LM, Briggs EC. Predictors of treatment completion in a sample of youth who have experienced physical or sexual trauma. J Interpers Violence 2014;29:3-19. http://dx.doi.org/10.1177/0886260513504495.
- Risser HJ, Schewe PA. Predictors of treatment engagement for young children exposed to violence. J Aggress Maltreat Trauma 2013;22:87-108. http://dx.doi.org/10.1080/10926771.2013.743946.
- Timmer S, Sedlar G, Urquiza A. Challenging children in kin versus nonkin foster care: perceived costs and benefits to caregivers. Child Maltreat 2004;9:251-62. http://dx.doi.org/10.1177/1077559504266998.
- Haskett M, Nowlan N, Hutcheson J, Whitworth J. Factors associated with successful entry into therapy in child sexual abuse cases. Child Abuse Negl 1991;15:467-76. http://dx.doi.org/10.1016/0145-2134(91)90030-H.
- Boisvert I, Tourigny M, Paquette G. Characteristics associated with group therapy dropout for sexually abused female adolescents. Revue Québécoise De Psychologie 2008;29:133-45.
- Grayston A, De Luca R. Social validity of group treatment for sexually abused boys. Child Fam Behav Ther 1996;18:1-16. http://dx.doi.org/10.1300/J019v18n02_01.
- Alaggia R, Michalski J, Vine C. The use of peer support for parents and youth living with the trauma of child sexual abuse: an innovative approach. J Child Sex Abuse 1999;8:57-75. http://dx.doi.org/10.1300/J070v08n02_04.
- Mishna F, Morrison J, Basarke S, Cook C. Expanding the playroom: school-based treatment for maltreated children. Psychoanal Soc Work 2012;19:70-9. http://dx.doi.org/10.1080/15228878.2012.666483.
- Powell L, Cheshire A. A preliminary evaluation of a massage program for children who have been sexually abused and their nonabusing mothers. J Child Sex Abuse 2010;19:141-55. http://dx.doi.org/10.1080/10538711003627256.
- Sudbery J, Shardlow SM, Huntington AE. To have and to hold: questions about a therapeutic service for children. Br J Soc Work 2010;40:1534-52. http://dx.doi.org/10.1093/bjsw/bcp078.
- Rushton A, Miles G. A study of a support service for the current carers of sexually abused girls. Clin Child Psychol Psychiatry 2000;5:411-26. http://dx.doi.org/10.1177/1359104500005003010.
- Davies J, Wright J, Drake S, Bunting J. ‘By listening hard’: developing a service-user feedback system for adopted and fostered children in receipt of mental health services. Adopt Foster 2009;33:19-33. http://dx.doi.org/10.1177/030857590903300404.
- Gallagher B, Green A. In, out and after care: young adults’ views on their lives, as children, in a therapeutic residential establishment. Child Youth Serv Rev 2012;34:437-50. http://dx.doi.org/10.1016/j.childyouth.2011.11.014.
- Staines J, Farmer E, Selwyn J. Implementing a therapeutic team parenting approach to fostering: the experiences of one independent foster-care agency. Br J Soc Work 2011;41:314-32. http://dx.doi.org/10.1093/bjsw/bcq043.
- Bannister A, Gallagher E. Children who sexually abuse other children. J Sex Aggress 1996;2:87-98. http://dx.doi.org/10.1080/13552609608413259.
- Burgon HL. ‘Queen of the world’: experiences of ‘at-risk’ young people participating in equine-assisted learning/therapy. J Soc Work Pract 2011;25:165-83. http://dx.doi.org/10.1080/02650533.2011.561304.
- Hill A. Combining professional expertize and service user expertize: negotiating therapy for sexually abused children. Br J Soc Work 2009;39:261-79. http://dx.doi.org/10.1093/bjsw/bcm120.
- Laan N, Loots G, Janssen C, Stolk J. Foster care for children with mental retardation and challenging behaviour: a follow-up study. Br J Dev Disabil 2001;47:3-13. http://dx.doi.org/10.1179/096979501799155675.
- Leenarts L, Hoeve M, Van de Ven P, Lodewijks H, Doreleijers T. Childhood maltreatment and motivation for treatment in girls in compulsory residential care. Child Youth Serv Rev 2013;35:1041-7. http://dx.doi.org/10.1016/j.childyouth.2013.04.001.
- Tjersland O, Mossige S, Gulbrandsen W, Jensen T, Reichelt S. Helping families when child sexual abuse is suspected but not proven. Child Fam Soc Work 2006;11:297-306. http://dx.doi.org/10.1111/j.1365-2206.2006.00409.x.
- Overlien C. Women’s refuges as intervention arenas for children who experience domestic violence. Child Care in Practice 2011;17:375-91. http://dx.doi.org/10.1080/13575279.2011.596816.
- Jensen T, Haavind H, Gulbrandsen W, Mossige S, Reichelt S, Tjersland O. What constitutes a good working alliance in therapy with children that may have been sexually abused?. Qual Soc Work 2010;9:461-78. http://dx.doi.org/10.1177/1473325010374146.
- Gustafsson PA, Anlen AS, Lannestrom G, Nilsson M, Rolling G. Group-therapy for children of alcoholics. Nord J Psychiatry 1995;49:209-15. http://dx.doi.org/10.3109/08039489509011908.
- Scott D. Parental experiences in cases of child sexual abuse: a qualitative study. Child Fam Soc Work 1996;1:107-14. http://dx.doi.org/10.1111/j.1365-2206.1996.tb00015.x.
- Costa L, de Almeida M, Ribeiro M, Penso M. Multifamiliar group: space for listening to the families in situation of sexual abuse. Psicol Estud 2009;14:21-30.
- Deb S, Mukherjee A. Background and adjustment capacity of sexually abused girls and their perceptions of intervention. Child Abuse Rev 2011;20:213-30. http://dx.doi.org/10.1002/car.1153.
- San Diego R. Healing the invisible wounds of trauma: a qualitative analysis. Asia Pac J Counsell Psychother 2011;2:151-70. http://dx.doi.org/10.1080/21507686.2011.588243.
- Fureman B, Parikh G, Bragg A, McLellan AT. Addiction Severity Index. A Guide to Training and Supervising ASI Interviews. Philadelphia, PA: University of PA/Philadelphia VAMC, Center for Studies of Addiction; 1990.
- Spielberger CD, Gorsuch RL. State-Trait Anxiety Inventory for Adults: Sampler Set: Manual, Text Booklet and Scoring Key. Palo Alto, CA: Consulting Psychologists Press; 1983.
- Twenge JM, Nolen-Hoeksema S. Age, gender, race, socioeconomic status, and birth cohort difference on the children’s depression inventory: a meta-analysis. J Abnorm Psychol 2002;111. http://dx.doi.org/10.1037/0021-843X.111.4.578.
- Smucker M, Craighead W, Craighead L, Green B. Normative and reliability data for the Children’s Depression Inventory. J Abnorm Child Psych 1986;14:25-39. http://dx.doi.org/10.1007/BF00917219.
- Macdonald G, Higgins JPT, Ramchandani P, Valentine JC, Bronger LP, Klein P, et al. Cognitive-behavioural interventions for children who have been sexually abused. Cochrane Database Syst Rev 2012;5. http://dx.doi.org/10.1002/14651858.cd001930.pub3.
- Harvey ST, Taylor JE. A meta-analysis of the effects of psychotherapy with sexually abused children. Clin Psychol Rev 2010;30:517-35. http://dx.doi.org/10.1016/j.cpr.2010.03.006.
- de Medeiros Passarela C, Mendes DD, de Jesus Mari J. A systematic review to study the efficacy of cognitive behavioral therapy for sexually abused children and adolescents with posttraumatic stress disorder. Rev Psiq Clín 2010;37:60-5.
- Frankel F, Weiner H. The Child Conflict Index: factor analysis, reliability, and validity for clinic referred and nonreferred children. J Clin Child Psychol 1990;19:239-48. http://dx.doi.org/10.1207/s15374424jccp1903_6.
- Linehan M. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, NY: Guilford Press; 1993.
- Shapiro F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols and Procedures. New York, NY: Guilford Publications; 2001.
- Greenwald R. Treating Problem Behaviors. New York, NY: Routledge; 2009.
- Diagnostic and Statistical Manual of Mental Disorders (DSM) fourth edition. Washington, DC: American Psychiatric Association; 1994.
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry 2000;39:28-3. http://dx.doi.org/10.1097/00004583-200001000-00014.
- Angold A, Costello EJ. Mood and Feelings Questionnaire (MFQ). Durham, NC: Developmental Epidemiology Program, Duke University; 1987.
- Ramey CT, McGinness GD, Cross L, Collier AM, Barrie-Blackley S, Borman K. The Social Life of Children in a Changing Society. Hillsdale, NJ: Lawrence Erlbaum Associates; 1982.
- Ramey CT, Yeates KO, Short EJ. The plasticity of intellectual development: insights from preventive intervention. Child Dev 1984;55:1913-25. http://dx.doi.org/10.2307/1129938.
- Stovall KC, Dozier M. The development of attachment in new relationships: single subject analyses for 10 foster infants. Dev Psychopathol 2000;12:133-56. http://dx.doi.org/10.1017/S0954579400002029.
- Waters E. Attachment Behavior Q-Set (Revision 3.0). Stony Brook, NY: State University of New York at Stony Brook, Department of Psychology; 1987.
- Deci EL, Ryan RM, Dienstbier R. Nebraska Symposium on Motivation Perspectives on Motivation. Lincoln, NE: University of Nebraska Press; 1991.
- Deci EL, Ryan RM. Intrinsic Motivation and Self-Determination in Human Behaviour. New York, NY: Plenum Press; 1985.
- Eyberg SM, Duke M, McDiarmid M, Boggs S, Robinson E, Washington E. Dyadic Parent–Child Interaction Coding System. Gainesville, FL: Clinical and Health Psychology Publishing; 2004.
- Eyberg S, Bessmer J, Newcomb K, Edwards D, Robinson E. Dyadic Parent–Child Coding System-II (DPICS–II). Corte Madera, CA: Select Press; 1994.
- Dunn DM, Dunn LM. Peabody Picture Vocabulary Test. Minneapolis, MN: NCS Pearson; 2007.
- Bagley C, King K. Child Sexual Abuse: The Search for Healing. London: Tavistock-Routledge; 1990.
- Derogatis LR. SCL-90-R, Symptom Checklist-90-R. Minneapolis, MN: Psychological Assessment Resources; 1994.
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1986.
- Achenbach TM, Edlebrock C. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991.
- Milner JS. Applications and limitations of the CAP inventory. Early Child Develop Care 1989;42:85-7. http://dx.doi.org/10.1080/0300443890420106.
- Bavolek SJ. Handbook for the Adult–Adolescent Parenting Inventory (AAPI). Park City, UT: Family Developmental Resources, Inc.; 1984.
- Moos RH, Insel PM, Humphrey B. Family Work and Group Environment Scales. Palo Alto, CA: Consulting Psychologists Press; 1974.
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. J Marital Fam Ther 1983;9:17-80.
- Bank L, Burraston B, Snyder J. Sibling conflict and ineffective parenting as predictors of adolescent boys’ antisocial behavior and peer difficulties: additive and interactional effects. J Res Adolesc 2004;14:99-125. http://dx.doi.org/10.1111/j.1532-7795.2004.01401005.x.
- Graham-Bermann S. The Kids’ Club: A Preventive Intervention Program for Children of Battered Women. Ann Arbor, MI: Department of Psychology, University of Michigan; 1992.
- Frappier JY, Roy É. HIV Seroprevalence and Risk Behaviors Study among Adolescents with Maladaptive and Social Problems in Montréal, in rapport de randomiza–projet #5505-3744-AIDS, PNRDS. Montréal, QC: Unité de maladies infectieuses; 1995.
- Seisdedos N. AC: Antisocial and Criminal Behavior Questionnaire. Madrid: TEA Ediciones; 1988.
- Cohen J. A power primer. Psychol Bull 1992;112:155-9. http://dx.doi.org/10.1037/0033-2909.112.1.155.
- De Luca RV, Boyes DA, Furer P, Grayston AD, Hiebert-Murphy D. Group treatment for child sexual abuse. Can Psychol 1992;33:168-79. http://dx.doi.org/10.1037/h0078711.
- Sullivan PM, Scanlon JM, Garbarino J, Brookhouser PE, Authier KJ. Special Children–Special Risks: The Maltreatment of Children with Disabilities. New York, NY: de Gruyter; 1987.
- Ozawa-de Silva B, Dodson-Lavelle B, Raison C, Negi L. Compassion and ethics: scientific and practical approaches to the cultivation of compassion as a foundation for ethical subjectivity and well-being. JHSH 2012;2:145-61.
- Achenbach TM, Edelbrock CS. Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991.
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Eriksen BA, Eriksen CW. Effects of noise letters upon the identification of a target letter in a nonsearch task. Percept Psychophys 1974;16:143-9. http://dx.doi.org/10.3758/BF03203267.
- Winters KC. Development of an adolescent alcohol and other drug abuse screening scale: Personal Experience Screening Questionnaire. Addict Behav 1992;17:479-90. http://dx.doi.org/10.1016/0306-4603(92)90008-J.
- Achenbach TM, Edelbrock CS. The child behavior profile: II. Boys aged 12-16 and girls aged 6-11 and 12-16. J Consult Clin Psychol 1979;47:223-33. http://dx.doi.org/10.1037/0022-006X.47.2.223.
- Abidin RR. Parenting Stress Index: Professional Manual (3rd edition). Odessa, FL: Psychological Assessment Resources; 1995.
- Asher SR, Wheeler VA. Children’s loneliness: a comparison of rejected and neglected peer status. J Consult Clin Psychol 1985;53:500-5. http://dx.doi.org/10.1037/0022-006X.53.4.500.
- Brom D, Kleber RJ. De SchokVerwerkingslijst [Impact of Events Scale – Dutch version]. Nederlands Tijdschrift Psychologie 1985;40:164-8.
- Arrindell WA, Ettema JHM. S [SCL-90: revised manual of a multi-faceted measures of psychopathology.]. Lisse, The Netherlands: Swets and Zeitlinger; 2003.
- Schmitz N, Kruse J, Heckrath C, Alberti L, Tress W. Diagnosing mental disorders in primary care: the General Health Questionnaire (GHQ) and the Symptom Check List (SCL-90-R) as screening instruments. Soc Psychiatry Psychiatr Epidemiol 1999;34:360-6. http://dx.doi.org/10.1007/s001270050156.
- Scheeringa MS, Haslett N. The reliability and criterion validity of the Diagnostic Infant and Preschool Assessment: a new diagnostic instrument for young children. Child Psychiatry Hum Dev 2010;41:299-312. http://dx.doi.org/10.1007/s10578-009-0169-2.
- Briere J. Trauma Symptom Checklist for Young Children: Professional Manual. Lutz, FL: Psychological Assessment Resources Inc; 2005.
- National Institute of Mental Health Clinical global impressions . Psychopharmacol Bull 1985;21:839-43.
- Guy W. ECDELL Assesment Manual for Psychopharmacology. Washington, DC: US Department of Health, Education and Welfare; 1976.
- Friedrich WN. Child Sexual Behavior Inventory: Professional Manual. Odessa. FL: Psychological Assessment Resources; 1997.
- Jaycox LH, Hickman LJ, Schultz D, Barnes-Proby D, Setodji CM, Kofner A, et al. National Evaluation of Safe Start Promising Approaches. Santa Monica, CA: RAND Corporation; 2011.
- Achenbach TM. Manual for the Child Behavior Checklist 4-18 and 1994 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1994.
- Eyberg S, Ross AW. Assessment of child behavior problems: the validation of a new inventory. J Clin Child Psychol 1978;7:113-16. http://dx.doi.org/10.1080/15374417809532835.
- Jenkins J, Smith M. Factors protecting children living in disharmonious homes: maternal reports. J Am Acad Child Adolesc Psychiatry 1990;29:60-9. http://dx.doi.org/10.1097/00004583-199001000-00011.
- Bene E, Anthony J. Manual for the Children’s Version of the Family Relations Test (rev.). Windsor: NFER Publishing Co. Ltd; 1978.
- Goldberg D. The Manual of the General Health Questionnaire. Windsor: NFER Publishing Co. Ltd; 1978.
- Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychol Med 1983;13:595-60. http://dx.doi.org/10.1017/S0033291700048017.
- Dubow EF, Ullman DG. Assessing social support in elementary school children: the survey of children’s social support. J Clin Child Psychol 1989;18:52-64. http://dx.doi.org/10.1207/s15374424jccp1801_7.
- Straus MA, Strau MA, Gelles RJ. Physical Violence in American families: Risk factors and Adaptations to Violence in 8,145 families. New Brunswick, NH: Transaction; 1990.
- Chandler LA, Million ME, Shermis MD. The incidence of stressful life events of elementary school-aged children. Am J Community Psychol 1985;13:743-6. http://dx.doi.org/10.1007/BF00929799.
- Hill CE, Corbet MM, Kanitz B, Rios P, Lightsey R, Gomez M. Client behavior in counseling and therapy sessions: development of a pantheoretical measure. J Counsel Psychol 1992;39:539-9. http://dx.doi.org/10.1037/0022-0167.39.4.539.
- Paul R. Adjustment Inventory. Agra: Agra Psychological Research Cell; 1995.
- Beavers W, Hampson R. Successful Families: Assessment and Intervention. New York, NY: WW Norton; 1990.
- Putnam FW, Trickett PK. The Psychobiological Effects of Sexual Abuse. National Institute of Mental Health, Division of Intramural Research Program. Bethesda, MD: US Department of Health and Human Services, Public Health Service, Alcohol, Drug Abuse and Mental Health Administration; n.d.
- Keijsers GP, Schaap CP, Hoogduin C, Hoogsteyns B, de Kemp E. Preliminary results of a new instrument to assess patient motivation for treatment in cognitive-behaviour therapy. Behav Cogn Psychother 1999;27:165-79.
- Pynoos RS, Rodriguez N, Steinberg A. PTSD Index for DSM-IV. Los Angeles, LA: University of California Los Angeles; 2000.
- Brown L, Sherbenou RJ, Johnsen SK. Test of Non Verbal Intelligence. Austin, TX: PRO-ED; 1997.
- Greenwald R. Child Report of Posttraumatic Symptoms. Towson, MD: Sidran; 1999.
- Greenwald R. Parent Report of Posttraumatic Symptoms. Towson, MD: Sidran; 1999.
- Derogatis LR, Goldberger L, Breznitz S. Handbook of Stress. New York, NY: Free Press; 1982.
- Broadhead WE, Gehlbach SH, DeGruy FV, Kaplan BH. The Duke-UNC functional social support questionnaire: measurement of social support in family medicine patients. Med Care 1988;26:161-71. http://dx.doi.org/10.1097/00005650-198807000-00006.
- Warnick E, Gonzalez A, Robin Weersing V, Scahill L, Woolston J. Defining dropout from youth psychotherapy: how definitions shape the prevalence and predictors of attrition. Child Adolesc Ment Health 2012;17:76-85. http://dx.doi.org/10.1111/j.1475-3588.2011.00606.x.
- Howard KI, Kopta SM, Krause MS, Orlinsky DE. The dose–effect relationship in psychotherapy. Am Psychol 1986;41. http://dx.doi.org/10.1037/0003-066X.41.2.159.
- Macdonald G, Sheldon B, Gillespie J. Contemporary studies of the effectiveness of social work. Br J Soc Work 1992;22:615-43.
- Hansen DJ, Sedlar G, DeRoma V. Manual for the PAI: The Parental Anger Inventory. Lincoln, NE: University of Nebraska, Clinical Psychology Training Program; 1998.
- Saunders BE. Understanding children exposed to violence: toward an integration of overlapping fields. J Interpers Violence 2003;18:356-76.
- Macdonald G, Millen S. Therapeutic Approaches to Social Work in Residential Child Care Settings: Literature Review. London: Social Care Institute of Excellence; 2012.
- DeJong M. Some reflections on the use of psychiatric diagnosis in the looked after or ‘in care’ child population. Clin Child Psychol Psychiatry 2010;15:589-99. http://dx.doi.org/10.1177/1359104510377705.
- Fonaghy P, Bateman A. Progress in the treatment of borderline personality disorder. Br J Psychiatry 2006;188:1-3. http://dx.doi.org/10.1192/bjp.bp.105.012088.
- Jonsson U, Alaie I, Parling T, Arnberg F. Reporting of harms in randomized controlled trials of psychological interventions for mental and behavioral disorders: a review of current practice. Contemp Clin Trials 2014;38:1-8. http://dx.doi.org/10.1016/j.cct.2014.02.005.
- Tarren-Sweeney M. The Assessment Checklist for Children—ACC: a behavioral rating scale for children in foster, kinship and residential care. Child Youth Serv Rev 2007;29:672-91. http://dx.doi.org/10.1016/j.childyouth.2007.01.008.
- Schünemann H, Brozek J, Guyatt G, Oxman A. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations 2013.
- Barker-Collo S, Read J. Models of response to childhood sexual abuse their implications for treatment. Trauma Violence Abuse 2003;4:95-111. http://dx.doi.org/10.1177/1524838002250760.
- Dinkmeyer S, McKay GD, McKay JL, Dinkmeyer D. Systematic Training for Effective Parenting of Teens. Circle Pines, MN: American Guidance Services; 1998.
- Simmonds J. The making and breaking of relationships – organisational and clinical questions in providing services for looked after children?. Clin Child Psychol Psychiatry 2010;15:601-12. http://dx.doi.org/10.1177/1359104510375930.
- Cicchetti D, Lynch M. Toward an ecological/transactional model of community violence and child maltreatment: consequences for children’s development. Psychiatry 1993;56:95-118.
- The Children Act. London: HMSO; 1989.
- Allen B, Gharagozioo L, Johnson J. Clinician knowledge and utilization of empirically-supported treatments for maltreated children. Child Maltreat 2012;17:11-2. http://dx.doi.org/10.1177/1077559511426333.
- Montgomery P, Grant S, Hopewell S, Macdonald G, Moher D, Michie S, et al. Protocol for CONSORT-SPI: an extension for social and psychological interventions. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-99.
- De Luca R, Hazen A, Cutler J. Evaluation of a group counseling program for preadolescent female victims of incest. Element Sch Guid Couns 1993;28:104-14.
- Springer C, Misurell J, Hiller A. Game-based cognitive-behavioral therapy (GB-CBT) group program for children who have experienced sexual abuse: a three-month follow-up investigation. J Child Sex Abuse 2012;21:646-64. http://dx.doi.org/10.1080/10538712.2012.722592.
- Iwaniec D, Sneddon H. The quality of parenting of individuals who failed to thrive as children. Brit J Soc Work 2002;32:283-98. http://dx.doi.org/10.1093/bjsw/32.3.283.
- Conrad C. Measuring costs of child abuse and neglect: a mathematic model of specific cost estimations. J Health Hum Serv Adm 2006;29:103-23.
- Widom CS, Wilson HW. Intergenerational Transmission of Violence. Netherlands: Springer Netherlands; 2015.
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guildford Press; 1979.
- Bowlby J. Attachment: Attachment and Loss. New York, NY: Basic Books; 1969.
- Stronach EP, Toth SL, Rogosch F, Cicchetti D. Preventive interventions and sustained attachment security in maltreated children. Dev Psychopathol 2013;256:919-30. http://dx.doi.org/10.1017/S0954579413000278.
- Oxford ML, Fleming CB, Nelson EM, Kelly JF, Spieker SJ. Randomized trial of Promoting First Relationships: effects on maltreated toddlers’ separation distress and sleep regulation after reunification. Child Youth Serv Rev 2013;35:1988-992. http://dx.doi.org/10.1016/j.childyouth.2013.09.021.
- van Ijzendoorn MH, Schuengel C, Bakermans-Kranenburg MJ. Disorganized attachment in early childhood: meta-analysis of precursors, concomitants, and sequelae. Dev Psychopathol 1999;11:225-49. http://dx.doi.org/10.1017/S0954579499002035.
- Nelson EM, Spieker SJ. Intervention effects on morning and stimulated cortisol responses among toddlers in foster care. Infant Ment Health J 2013;34:211-21. http://dx.doi.org/10.1002/imhj.21382.
- Lieberman AF. Infant–parent psychotherapy with toddlers. Develop Psychopathol 1992;4:559-74. http://dx.doi.org/10.1017/S0954579400004879.
- Madigan S, Moran G, Schuengel C, Pederson DR, Otten R. Unresolved maternal attachment representations, disrupted maternal behavior and disorganized attachment in infancy: Links to toddler behavior problems. J Child Psychol Psychiatry 2007;48:1042-50. http://dx.doi.org/10.1111/j.1469-7610.2007.01805.x.
- Dozier M, Dozier D, Manni M. Attachment and biobehavioral catch-up: ABCs of helping foster infants cope with early adversity. Zero Three 2002;22:7-13.
- Cicchetti D, Valentino K, Cicchetti D, Cohen D. Developmental Psychopathology Volume 3 Risk, Disorder, and Adaptation. New Jersey, NJ: John Wiley & Sons; 2006.
- Hughes D. An attachment-based treatment of maltreated children and young people. Attach Hum Dev 2004;6:263-78. http://dx.doi.org/10.1080/14616730412331281539.
- Hughes D, Becker-Weidman A, Shell D. Creating Capacity for Attachment. Oklahoma City, OK: Wood N Barnes; 2005.
- Becker-Weidman A, Hughes D. Dyadic developmental psychotherapy: an evidence-based treatment for children with complex trauma and disorders of attachment. Child Fam Soc Work 2006;13:329-37. http://dx.doi.org/10.1111/j.1365-2206.2008.00557.x.
- Carr A. Evidence-based practice in family therapy and systemic consultation. I. Child-focused problems. J Fam Ther 2000;22:29-60. http://dx.doi.org/10.1111/1467-6427.00137.
- Minuchin S. Families and Family Therapy. Cambridge, MA: Harvard University Press; 1974.
- Henggeler SW, Cunningham PB, Pickrel SG, Schoenwald SK, Brondino MJ. Multisystemic therapy: an effective violence prevention approach for serious juvenile offenders. J Adolesc 1996;19:47-61. http://dx.doi.org/10.1006/jado.1996.0005.
- Luthar SS, Suchman NE, Altomare M. Relational psychotherapy mothers’ group: a randomized clinical trial for substance abusing mothers. Develop Psychopathol 2007;19:243-61.
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry 1997;36:340-8. http://dx.doi.org/10.1097/00004583-199703000-00012.
- Kaufman J, Birmaher B, Brent D, Rao U, Ryan N. The Schedule for Affective Disorders and Schizophrenia for School-Age Children Present and Lifetime Version (version 1.0). Pittsburgh, PA: University of Pittsburgh School of Medicine, Department of Psychiatry; 1996.
- Zung WWK. A self-rating depression scale. Arch Gen Psychiatry 1965;12:63-70. http://dx.doi.org/10.1001/archpsyc.1965.01720310065008.
- Spielberger CD. Manual for the State-Trait Anxiety Inventory for Children. Palo Alto, CA: Consulting Psychologists Press; 1973.
- Briere J. Trauma Symptom Checklist for Children (TSC-C) Professional Manual. Odessa Los Angeles, CA: University of Southern California Press; 1989.
- Eyberg S, Bessmer J, Newcomb K, Edwards D, Robinson E, . Dyadic Parent–Child Interaction Coding System-II: A Manual. Social and Behavioural Sciences Documents. San Rafael, CA: Select Press; 1994.
- Selzer ML, Vinokur A, Rooijen LV. A self-administered short Michigan alcoholism screening test (SMAST). J Stud Alcohol Drugs 1975;36. http://dx.doi.org/10.15288/jsa.1975.36.117.
- Georgiou SN. Parental attributions as predictors of involvement and influences on child achievement. Br J Clin Psychol 1999;69:409-29. http://dx.doi.org/10.1348/000709999157806.
- Garfield SL. Handbook of Psychotherapy and Behaviour Change. Oxford: Wiley; 1994.
Appendix 1 Research team and Steering Group members
Geraldine Macdonald (SG)
Nuala Livingstone (SG)
Jennifer Hanratty (ExO)
Claire McCartan (ExO)
Richard Cotmore (SG)
Maria Cary
Danya Glaser (SG)
Sarah Byford (SG)
Nicola J. Welton
Tania Bosqui
Lucy Bowes
Suzanne Audrey
Gill Mezey
Helen Fisher
Wendy Riches (SG)
Rachel Churchill (SG)
Note: SG, Steering Group member; ExO, Ex Officio Steering Group member
Appendix 2 Professional Advisory Group members
Professional Advisory Group meeting attendees: Wednesday 1 May 2013
|
Voluntary sector/social work
Facilitator: Richard Cotmore, NSPCC |
Educational Psychology
Facilitator: Wendy Riches |
||
| Dorit Braun | The College of Social Work | Catherine Kelly | University of Manchester |
| Laurence Guinness | Kids Company | Louise Lightfoot | University of Salford |
| Kate Mulley | Action for Children | Patrick McArdle | University of Salford |
| Jonathon Rallings | Barnardo’s | Eamon McCrory | University College London |
| Suzanne Watts | Oxford Brookes University | Joanne Snee | University of Salford |
|
Health Economics
Facilitator: Sarah Byford, Institute of Psychiatry, King’s College London |
Social Science
Facilitator: Rachel Churchill, University of Bristol |
||
| Jennifer Beecham | University of Kent | Cheryl Burgess | University of Stirling |
| Farhat R Rasul | Hounslow Social Services | Elaine Farmer | University of Bristol |
| Maria Violato | University of Oxford | Corinne May-Chahal | Lancaster University |
|
Clinical Psychology/Psychiatry
Facilitator: Helen Fischer, Institute of Psychiatry, King’s College London |
Julie Mytton | University of the West of England | |
| Foster carers | |||
| Rachel Calum | The University of Manchester | Facilitator: Nuala Livingstone, Queen’s University, Belfast | |
| Andrea Danese | King’s College London | Marrion Collins | Foster carer |
| Margaret DeJong | Great Ormond Street Hospital | Sharon Galway | Foster carer |
| Emilio Lemoniatis | The Tavistock and Portman NHS Foundation Trust | Tracey Gibbons | Foster carer |
| Kavita Misra | Salford CAMHS | Helen Harpum | Foster carer |
| Helen Stain | Durham University | Chris Ingram | Foster carer |
| Health Professionals | Foster carers | ||
| Facilitator: Gill Mezey, St George’s, University of London | Facilitator: Geraldine Macdonald, Queen’s University, Belfast | ||
| Celina Grant | Lambeth CAMHS | Julie Kee | Foster carer |
| Christine Habgood | General practitioner | Cherry Largie | Foster carer |
| Narad Mathura | St David’s Children’s Centre, St David’s Hospital | Annie Nugent | Foster carer |
| Aideen McLaughlin | Belfast Trust, Health & Social Care Services in Northern Ireland | Zena Richards | Foster carer |
| Colin Michie | Ealing Hospital NHS Trust | Doreen Sylvester | Foster carer |
| Catherine Powell | NHS Portsmouth | ||
Professional Advisory Group meeting attendees: Thursday 27 November 2014
| Number | Forename | Surname | Organisation |
|---|---|---|---|
| 1 | Jennifer | Beecham | University of Kent |
| 2 | Sarah | Byford | King’s College London |
| 3 | Rona | Campbell | University of Bristol |
| 4 | Maria | Cary | King’s College London |
| 5 | Rachel | Churchill | University of Bristol |
| 6 | Marrion | Collins | Foster carer |
| 7 | Paula | Cooper-Neville | Foster team |
| 8 | Richard | Cotmore | NSPCC |
| 9 | Tracey | Gibbons | Foster carer |
| 10 | Danya | Glaser | University College London |
| 11 | Laurence | Guinness | Kids Company |
| 12 | Jennifer | Hanratty | Queen’s University, Belfast |
| 13 | Sarah | Howcutt | Oxford Brookes University |
| 14 | Nuala | Livingstone | Queen’s University, Belfast |
| 15 | Geraldine | Macdonald | Queen’s University, Belfast |
| 16 | Gill | Mezey | St George’s, University of London |
| 17 | Annie | Nugent | Foster carer |
| 18 | Jonathon | Rallings | Barnardo’s |
| 19 | Wendy | Riches | University College London |
| 20 | Maria | Violato | University of Oxford |
Appendix 3 Examples of search strategies for different database types
Core search strategy (Ovid MEDLINE)
-
exp Child Abuse/
-
(child$ adj3 (abuse$ or cruelty or maltreat$ or mal-treat$ or neglect$ or victimi#$)].tw.
-
child protection.tw.
-
or/1-3
-
[(emotion$ or psychological$) adj3 (abuse$ or harm or neglect$ or trauma$ or victimi#$)].tw.
-
(physical$ adj3 (abuse$ or assault$ or harm$ or neglect$ or trauma$ or victimi#$)].tw.
-
(sex$ adj3 (abuse$ or assault$ or trauma$ or victimi#$)].tw.
-
Incest/
-
incest$.tw.
-
(maltreat$ or mal-treat$).tw.
-
(intentional$ adj3 injur$).tw.
-
(non-accidental adj3 injur$).tw.
-
or/5-12
-
exp infant/
-
exp child/
-
adolescent/
-
young adult/
-
(child$ or infant$ or teenage$ or adolescen$ or youth$ or young person$ or young adult$ or young people or preschool$ or pre-school$ or baby or babies).tw.
-
or/14-18
-
13 and 19
-
4 or 20
-
exp Psychotherapy/
-
exp Mind-Body Therapies/
-
(psycho$ therap$ or psychotherap$).tw.
-
(psychoanalytic$ or psycho-analytic$ or psychodynamic$ or psycho-dynamic$).tw.
-
Cognitive Therapy/
-
[(cognitive-behav$ or cognitive or cognition) adj3 (program$ or intervention$ or therap$ or treatment$)].tw.
-
CBT.tw.
-
counsel?ing.tw.
-
(psychodrama or acting out or role play).tw.
-
(meditation or mindfulness or mind training).tw.
-
(Relax$ adj3 (training$ or treatment$ or therap$)].tw.
-
(multisystemic or multi-systemic).tw.
-
[(psychosocial or psycho-social or psychoeducation$ or psychoeducation$) adj3 (intervention$ or program$ or support$ or therap$ or treatment$)].tw.
-
[(family or group or systemic$ or multimodal$ or multi-modal$) adj3 (program$ or intervention$ or therap$ or treatment$)].tw.
-
Mental health/
-
exp Behavior Therapy/
-
(behavio?r$ adj3 (program$ or intervention$ or therap$ or treatment$)].tw.
-
[(exposure or abreaction or desensitization) adj3 therap$).tw.
-
(‘Eye Movement Desensitization and Reprocessing’ or EMDR).tw.
-
Foster Home Care/
-
[(foster$ or residential or out-of-home) adj3 (care$ or therapeutic$ or treatment$)].tw.
-
peer mentor$.tw.
-
[(gestalt or milieu or residential) adj therap$).tw.
-
(therapeutic adj (alliance or relationship)].tw.
-
dramatherapy.tw.
-
Feedback, Psychological/
-
[(biofeedback or feedback or imagery) adj3 (intervention$ or therap$ or treatment$ or train$)].tw.
-
(hypnosis or hypno-therapy or hypnotherapy or breathing exercise$).tw.
-
object attachment/
-
[(attachment or bond$) adj3 (infant$ or child$ or mother$ or maternal$ or father$ or paternal$ or parental$)].tw.
-
[(insecure adj2 attachment$) or attachment disorder).tw.
-
[(solution focus$ or trauma$ or talking) adj3 therap$).tw.
-
sensory art therapies/
-
[(art or creative or drama or music or narrative or play$ or sensory) adj3 (program$ or intervention$ or therap$)].tw.
-
or/22-55
-
21 and 56
-
(autobiography or biography or comment or editorial or letter or news).pt.
-
57 not 58
Search strategy for Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews and Database of Abstracts of Reviews of Effects (via The Cochrane Library)
| ID | Search |
|---|---|
| #1 | medical subject heading (MeSH) descriptor: [Child Abuse] 2 tree(s) exploded |
| #2 | (child* near/3 (abuse* or cruelty or maltreat* or mal next treat* or neglect* or victimi*)]:ti,ab |
| #3 | (child next protection):ti,ab |
| #4 | #1 or #2 or #3 |
| #5 | [(emotion* or psychological*) near/3 (abuse* or harm or neglect* or trauma* or victimi*)]:ti,ab |
| #6 | (physical* near/3 (abuse* or assault* or harm* or neglect* or trauma* or victimi*)]:ti,ab |
| #7 | (sex* near/3 (abuse* or assault* or trauma* or victimi*)]:ti,ab |
| #8 | MeSH descriptor: [Incest] this term only |
| #9 | incest*:ti,ab |
| #10 | (maltreat* or mal-treat*):ti,ab |
| #11 | (intentional* near/3 injur*):ti,ab |
| #12 | (non-accidental near/3 injur*):ti,ab |
| #13 | {or #5-#12} |
| #14 | MeSH descriptor: [Infant] 1 tree(s) exploded |
| #15 | MeSH descriptor: [Child] explode all trees |
| #16 | MeSH descriptor: [Adolescent] this term only |
| #17 | MeSH descriptor: [Young Adult] this term only |
| #18 | (infant* or child* or baby or babies* or adolescen* or teen* or youth* or young next person* or young next people or young next adult* or pre next school* or preschool* or baby or babies):ti,ab |
| #19 | {or #14-#18} |
| #20 | #13 and #19 |
| #21 | #4 or #20 |
| #22 | MeSH descriptor: [Psychotherapy] 1 tree(s) exploded |
| #23 | MeSH descriptor: [Mind-Body Therapies] 1 tree(s) exploded |
| #24 | (psycho next therap* or psychotherap*):ti,ab |
| #25 | (psychoanalytic* or psycho next analytic* or psychodynamic* or psycho next dynamic*):ti,ab |
| #26 | MeSH descriptor: [Cognitive Therapy] this term only |
| #27 | [(cognitive next behav* or cognitive or cognition) near/3 (program* or intervention* or therap* or treatment*)]:ti,ab |
| #28 | ‘CBT’:ti,ab |
| #29 | (counselling or counseling):ti,ab |
| #30 | (psychodrama or ‘acting out’ or ‘role play’):ti,ab |
| #31 | (meditation or mindfulness or ‘mind training’):ti,ab |
| #32 | (Relax* near/3 (training* or treatment* or therap*)]:ti,ab |
| #33 | (multisystemic or multi next systemic):ti,ab |
| #34 | [(psychosocial or psycho next social or psycho NEXT education* or psychoeducation*) near/3 (intervention* or program* or support* or therap* or treatment*)]:ti,ab |
| #35 | [(family or group or systemic* or multimodal* or multi-modal*) near/3 (program* or intervention* or therap* or treatment*)]:ti,ab |
| #36 | MeSH descriptor: [Mental Health] this term only |
| #37 | MeSH descriptor: [Cognitive Therapy] 1 tree(s) exploded |
| #38 | (behav* near/3 (program* or intervention* or therap* or treatment*)]:ti,ab |
| #39 | [(exposure or abreaction or desensitization) near/3 therap*):ti,ab |
| #40 | (‘Eye Movement Desensitization and Reprocessing’ or EMDR):ti,ab |
| #41 | MeSH descriptor: [Foster Home Care] this term only |
| #42 | [(foster* or residential or out-of-home) near/3 (care* or therapeutic* or treatment*)]:ti,ab |
| #43 | (peer next mentor*):ti,ab |
| #44 | [(gestalt or milieu or residential) next therap*):ti,ab |
| #45 | (therapeutic next (alliance or relationship*)]:ti,ab |
| #46 | MeSH descriptor: [Feedback, Psychological] 2 tree(s) exploded |
| #47 | [(biofeedback or feedback or imagery) near/3 (intervention* or therap* or treatment* or train*)]:ti,ab |
| #48 | (hypnosis or hypno next therapy or hypnotherapy or breathing next exercise*):ti,ab |
| #49 | MeSH descriptor: [Object Attachment] this term only |
| #50 | [(attachment or bond*) near/3 (infant* or child* or mother* or maternal* or father* or paternal* or parental*)]:ti,ab |
| #51 | [(solution focus* or trauma* or talking) near/3 therap*):ti,ab |
| #52 | MeSH descriptor: [Sensory Art Therapies] 1 tree(s) exploded |
| #53 | [(art or creative or drama or music or narrative or play* or sensory) near/3 (program* or intervention* or therap*)]:ti,ab |
| #54 | dramatherapy:ti,ab |
| #55 | {or #22-#54} |
| #56 | #55 and #21 |
Search strategy for Social Sciences Abstracts (ProQuest)
[(SU.EXACT.EXPLODE(‘Behavior Modification’) OR SU.EXACT.EXPLODE(‘Role Playing’) OR SU.EXACT.EXPLODE(‘Group Therapy’) OR SU.EXACT.EXPLODE(‘Psychotherapy’) OR SU.EXACT.EXPLODE(‘Family Therapy’) OR SU.EXACT.EXPLODE(‘Hypnosis’) OR SU.EXACT.EXPLODE(‘Sociotherapy’) OR SU.EXACT(‘Group Therapy’) OR SU.EXACT(‘Family Therapy’) OR SU.EXACT(‘Counseling’) OR TI,AB(counselling OR counseling) OR SU.EXACT(‘Foster Care’) OR SU.EXACT(‘Residential Institutions’) OR (TI,AB(psycho-therap[*5] OR psychotherap[*5] OR psychoanalytic[*2] OR psycho-analytic[*2] OR psychodynamic[*3] OR psycho-dynamic[*3]) OR TI,AB[(psychosocial OR ‘psycho-social’ OR psychoeducation[*3] OR ‘ psychoeducation[*3]’) NEAR/3 (program[*3] OR intervention[*1] OR therap[*5] OR treatment[*1])] OR TI,AB[(behavior[*2] OR behavour[*2]) NEAR/3 (program[*3] OR intervention[*1] OR therap[*5] OR treatment[*1])] OR TI,AB[(‘cognitive-behav[*3]’ OR cognitive OR cognition) NEAR/3 (program[*3] OR intervention[*1] OR therap[*5] OR treatment[*1])] OR TI,AB(relaxation OR multisystemic OR ‘multi-systemic’ OR psychodrama OR ‘acting out’ OR ‘role play’) OR TI,AB[(family OR group OR systemic[*3] OR multimodal[*3] OR ‘multi-modal’) NEAR/3 (program[*3] OR intervention[*1] OR therap[*5] OR treatment[*1])] OR TI,AB[(exposure OR abreaction OR desensitization) NEAR/3 (therap[*5])] OR TI,AB(‘Eye Movement Desensitization and Reprocessing’ OR EMDR) OR TI,AB [(foster[*3] OR residential OR out-of-home) NEAR/3 (care[*3] OR therapeutic[*3] OR treatment)] OR ‘peer mentor[*3]’ OR TI,AB[(gestalt OR milieu OR residential) NEAR/3 (therap[*5])] OR TI,AB[(therapeutic) NEAR/2 (alliance OR relationship[*3])] OR TI,AB(biofeedback OR imagery OR hypnosis OR ‘breathing exercises’) OR TI,AB[(‘solution focus[*2]’ OR trauma[*3] OR talking) NEAR/3 (therap[*5])] OR TI,AB[(attachment OR bond[*3]) NEAR/3 (infant[*1] OR child[*3] OR mother[*3] OR maternal[*3] OR father[*3] OR paternal[*3] OR parental[*3])] OR TI,AB [(insecure NEAR/2 attachment[*3]) OR attachment disorder) OR TI,AB[(art OR creative OR drama OR music OR narrative OR play[*3] OR sensory) NEAR/3 (program[*3] OR intervention[*1] OR therap[*5])] OR TI,AB(dramatherap[*3])]) AND [(SU.EXACT.EXPLODE(‘Child Sexual Abuse’) OR SU.EXACT.EXPLODE(‘Child Abuse’) OR TI,AB[(child[*3]) NEAR/3 (abuse[*3] OR ‘at risk’ OR maltreat[*4] OR mal-treat[*4] OR neglect[*3])] OR TI,AB(‘child protection’) OR TI,AB[(emotion[*3] OR psychological[*3]) NEAR/3 (abuse[*3] OR harm OR neglect[*3] OR trauma[*3] OR victim[*5])] OR TI,AB(physical[*3] NEAR/3 (abuse[*3] OR assault[*3] OR harm[*3] OR neglect[*3] OR trauma[*3] OR victim[*5])] OR TI,AB(sex[*5] NEAR/3 (abuse[*3] OR assault[*3] OR trauma[*3] OR victim[*5])] OR TI,AB(maltreat[*4] OR mal-treat[*4]) OR TI,AB(‘intentional injur[*3]’ OR ‘non-accidental injur[*3]’) OR TI,AB(incest)] AND (SU.EXACT(‘Children’) OR SU.EXACT(‘Adolescents’) OR SU.EXACT(‘Infants’) OR TI,AB(child[*3] OR infant[*1] OR teen[*5] OR adolescen[*3] OR youth[*1] OR ‘young person’ OR ‘young adult[*1]’ OR ‘young people’ OR preschool[*3] OR pre-school[*3] OR baby OR babies)])]
Search strategy for EconLit (via EBSCOhost)
S13 S4 OR S12
S12 S10 AND S11
S11 TI(child* or infant* or teenage* or adolescen* or youth* or young person* or young adult* or young people or preschool* or pre school* or baby or babies) OR AB(child* or infant* or teenage* or adolescen* or youth* or young person* or young adult* or young people or preschool* or pre school* or baby or babies)
S10 S5 OR S6 OR S7 OR S8 OR S9
S9 TI(maltreat* or mal-treat*) OR AB(maltreat* or mal-treat*)
S8 TI(incest*) or AB(incest*)
S7 TI (sex* N3 (abuse* or assault* or trauma* or victim*)] OR AB(sex* N3 (abuse* or assault* or trauma* or victim*)]
S6 TI(physical* N3 (abuse* or assault* or harm* or neglect* or trauma* or victim*)] OR AB(physical* N3 (abuse* or assault* or harm* or neglect* or trauma* or victim*)]
S5 TI [(emotion* or psychological*) N3 (abuse* or harm or neglect* or trauma* or victim*)] OR AB [(emotion* or psychological*) N3 (abuse* or harm or neglect* or trauma* or victim*)]
S4 S1 OR S2 OR S3
S3 ‘at risk register’
S2 ‘child protection’
S1 (child* or adolescen* or teen or infant*) N3 (abuse* or cruelty or maltreat* or mal-treat* or neglect* or trauma or victimis* or victimiz*)
Database of Promoting Health Effectiveness Reviews (DoPHER) (eppi.ioe.ac.uk/webdatabases/)
Keyword/categorical search
#2 Characteristics of the study population: children OR young people
#4 Focus of the report: child neglect OR emotional abuse OR physical abuse OR sexual abuse
#5 2 AND 4
Appendix 4 Citations of included and excluded studies
Included controlled studies (citations): effectiveness studies
1. Bagley C, LaChance M. Evaluation of a family-based programme for the treatment of child sexual abuse. Child Fam Soc Work 2000;5:205–13. 150
2. Barth R, Yeaton J, Winterfelt N. Psychoeducational groups with foster care of sexually abused children. Child Adolesc Soc Work J 1994;11:405–24. 161
3. Becker-Weidman A. Dyadic developmental psychotherapy: a multi-year follow-up. In Stuart S, editor. New Developments in Child Abuse Research. New York, NY: Nova; 2006. 135
4. Becker-Weidman A. Treatment of children with trauma-attachment disorders: dyadic developmental Psychotherapy. Child Adolesc Soc Work J 2006;23:147–71. 134
Berliner L, Saunders BE. Treating fear and anxiety in sexually abused children: results of a controlled 2-year follow-up study. Child Maltreat 1996;1:294–309. 89
5. Bernard K, Dozier M, Bick J, Lewis-Morrarty E, Lindhiem O, Carlson E. Enhancing attachment organization among maltreated children: results of a randomized clinical trial. Child Dev 2012;83:623–36. 122
6. Biehal N, Dixon J, Parry E, Sinclair I, Green J, Roberts C, et al. The Care Placements Evaluation (CaPE) Evaluation of Multidimensional Treatment Foster Care for Adolescents (MTFC-A): Research Brief, DFE-RB194. London: Department for Education; 2012. 145
Green J, Biehal N, Roberts C, Dixon J, Kay C, Parry E, et al. Multidimensional treatment foster care for adolescents in English care: randomised trial and observational cohort evaluation. Br J Psychiatry 2013;204:214–21. 146
7. Brillantes-Evangelista G. An evaluation of visual arts and poetry as therapeutic interventions with abused adolescents. Arts Psychother 2013;40:71–84. 199
8. Brunk MA, Henggeler SW, Whelan JP. Comparison of multisystemic therapy and parent training in the brief treatment of child abuse and neglect. J Consult Clin Psychol 1987;55:171–8. 142
9. Fitch MJ, Cadol EJ, Goldson EK, Jackson DF Swartz, Wendell TP. Prospective Study in Child Abuse: the Child Study Program. Final Report. OCD-CR-371. 1975. 177
10. Celano M, Hazzard A, Webb C, McCall C. Treatment of traumagenic beliefs among sexually abused girls and their mothers: an evaluation study. J Abnorm Child Psych 1996;24:1–17. 90
11. Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, et al. Parent–child interaction therapy with physically abusive parents: efficacy for reducing future abuse reports. J Consult Clin Psychol 2004;72:500–10. 136
12. Champion JD, Collins JL. Comparison of a theory-based (AIDS Risk Reduction Model) cognitive behavioral intervention versus enhanced counseling for abused ethnic minority adolescent women on infection with sexually transmitted infection: results of a randomized controlled trial. Int J Nurs Stud 2012;49:138–50. 110
13. Church D, Pina O, Reategui C, Brooks A. Single-session reduction of the intensity of traumatic memories in abused adolescents after EFT: a randomized controlled pilot study. Traumatology 2012;18:73–9. 111
14. Cicchetti D, Rogosch F, Toth S. Fostering secure attachment in infants in maltreating families through preventive interventions. Dev Psychopathol 2006;18:623–49. 123
15. Cicchetti D, Rogosch F, Toth S, Sturge-Apple M. Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Dev Psychopathol 2011;23:789–800. 124
16. Cohen JA, Mannarino AP. A treatment outcome study for sexually abused preschool children: initial findings. J Am Acad Child Adolesc Psychiatry 1996;35:42–50. 91
Cohen JA, Mannarino AP. A treatment study for sexually abused preschool children: outcome during a one-year follow-up. J Am Acad Child Adolesc Psychiatry 1997;36:1228–35. 92
17. Cohen JA, Mannarino AP. Interventions for sexually abused children: initial treatment outcome findings. Child Maltreat 1998;3:17–26. 93
Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse Negl 2005;29:135–45. 94
18. Cohen JA, Deblinger E, Mannarino AP, Steer RA. A multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry 2004;43:393–402. 95
Deblinger E, Mannarino AP, Cohen JA, Steer RA. A follow-up study of a multisite, randomized controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry 2006;45:1474–84. 96
19. Culp RE. Maltreated children’s developmental scores: treatment versus nontreatment. Child Abuse Negl 1987;11:29–34. 196
20. Culp RE, Little V, Letts D, Lawrence H. Maltreated children’s self-concept: effects of a comprehensive treatment program. Am J Orthopsychiatry 1991;61:114–21. 197
21. D’Andrea W, Bergholz L, Fortunato A, Spinazzola J. Play to the whistle: a pilot investigation of a sports-based intervention for traumatized girls in residential treatment. J Fam Violence 2013;28:739–49. 201
22. Danielson CK, McCart MR, Walsh K, De Arellano MA, White D, Resnick HS. Reducing substance use risk and mental health problems among sexually assaulted adolescents: a pilot randomized controlled trial. J Fam Psychol 2012;26:628–35. 143
23. De Luca RV, Boyes DA, Grayston AD, Romano E. Sexual abuse: effects of group therapy on pre-adolescent girls. Child Abuse Rev 1995;4:263–77. 170
24. Deblinger E, Lippmann J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: initial treatment outcome findings. Child Maltreat 1997;1:310–21. 97
Deblinger E, Steer RA, Lippmann J. Two-year follow-up study of cognitive behavioral therapy for sexually abused children suffering post-traumatic stress symptoms. Child Abuse Negl 1999;23:1371–8. 98
25. Deblinger E, Stauffer LB, Steer RA. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreat 2001;6:332–43. 99
26. Deblinger E, Mannarino AP, Cohen JA, Runyon MK, Steer RA. Trauma-focused cognitive behavioral therapy for children: impact of the trauma narrative and treatment length. Depress Anxiety 2011:28;67–75. 100
27. Dietz TJ, Davis D, Pennings J. Evaluating animal-assisted therapy in group treatment for child sexual abuse. J Child Sex Abuse 2012;21:665–83. 204
28. Downing J, Jenkins SJ, Fisher GL. A comparison of psychodynamic and reinforcement treatment with sexually abused children. Element School Guid Couns 1988;22:291–8. 180
29. Dozier M, Peloso E, Lindhiem O, Gordon MK, Manni M, Sepulveda S, et al. Developing evidence-based interventions for foster children: an example of a randomized clinical trial with infants and toddlers. J Soc Issues 2006;62:767–85. 125
30. Duffany A, Panos PT. Outcome evaluation of a group treatment of sexually abused and reactive children. Res Social Work Prac 2009;19:291–303. 162
31. Fantuzzo JW, Jurecic L, Stovall A, Hightower AD, Goins C, Schachtel D. Effects of adult and peer social initiations on the social behavior of withdrawn, maltreated preschool children. J Consult Clin Psychol 1988;56:34–9. 181
32. Fantuzzo JW, Sutton-Smith B, Meyers R, Atkins M, Stevenson H, Coolahan K, Weiss A, Manz P. Community-based resilient peer treatment of withdrawn maltreated preschool children. J Consult Clin Psychol 1996;64:1377–86. 182
33. Farkas L, Cyr M, Lebeau T, Lemay J, McDuff P. Treatment effectiveness of MASTR-EMDR therapy for sexually abused adolescents. Revue Québécoise de Psychologie 2008;29:101–15. 120
34. Fisher PA, Gunnar MR, Chamberlain P, Reid JB. Preventive intervention for maltreated preschool children: impact on children’s behavior, neuroendocrine activity, and foster parent functioning. J Am Acad Child Adolesc Psychiatry 2000;39:1356–64. 192
Fisher PA, Burraston B, Pears KC. The Early Intervention Foster Care Program: permanent placement outcomes from a randomized trial. Child Maltreat 2005;10:61–71. 184
Bruce J, McDermott JM, Fisher PA, Fox NA. Using behavioral and electrophysiological measures to assess the effects of a preventive intervention: a preliminary study with preschool-aged foster children. Prev Sci 2009;10:129–40. 183
Fisher PA, Kim HK. Intervention effects on foster preschoolers’ attachment-related behaviors from a randomized trial. Prev Sci 2007;8:161–70. 185
Fisher PA, Kim HK, Pears KC. Effects of multidimensional treatment foster care for preschoolers (MTFC-P) on reducing permanent placement failures among children with placement instability. Child Youth Serv Rev 2009:31;541–6. 186
Fisher PA, Stoolmiller M, Gunnar MR, Burraston BO. Effects of a therapeutic intervention for foster preschoolers on diurnal cortisol activity. Psychoneuroendocrinology 2007;32:892–905. 187
Fisher PA, Van Ryzin MJ, Gunnar MR. Mitigating HPA axis dysregulation associated with placement changes in foster care. Psychoneuroendocrinology 2011;36:531–9. 188
35. Foa EB, McLean CP, Capaldi S, Rosenfield D. Prolonged exposure vs. supportive counseling for sexual abuse-related PTSD in adolescent girls: a randomized clinical trial. JAMA 2013:310;2650–7. 101
36. Graham AM, Yockelson M, Kim Hyoun K, Bruce J, Pears KC, Fisher PA. Effects of maltreatment and early intervention on diurnal cortisol slope across the start of school: a pilot study. Child Abuse Negl 2012;36:666–70. 193
37. Graham-Bermann SA, Lynch S, Banyard V, De Voe ER, Halabu H. Community-based intervention for children exposed to intimate partner violence: an efficacy trial. J Consult Clin Psychol 2007;75:199–209. 151
38. Grayston AD, De Luca RV. Group therapy for boys who have experienced sexual abuse: is it the treatment of choice? J Child Adolesc Group Ther 1995;5:57–82. 171
39. Haight W, Black J, Sheridan K. A mental health intervention for rural, foster children from methamphetamine-involved families: experimental assessment with qualitative elaboration. Child Youth Serv Rev 2010:32;1446–57. 175
40. Hamama L, Hamama-Raz Y, Dagan K, Greenfeld H, Rubinstein C, Ben-Ezra M. A preliminary study of group intervention along with basic canine training among traumatized teenagers: a 3-month longitudinal study. Child Youth Serv Rev 2011:33;1975–80. 205
41. Hébert M, Tourigny M. Effects of a psychoeducational group intervention for children victims of sexual abuse. J Child Adolesc Trauma 2010;3:143–60. 163
42. Holland P, Gorey KM, Lindsay A. Prevention of mental health and behaviour problems among sexually abused aboriginal children in care. Child Adolesc Social Work J 2004:21;109–15. 164
43. Holt T, Jensen TK, Wentzel-Larsen T. The change and the mediating role of parental emotional reactions and depression in the treatment of traumatized youth: results from a randomized controlled study. Child Adolesc Psychiatry Ment Health 2014;8:11. 112
44. Howell KH, Miller LE, Lilly MM, Graham-Bermann SA. Fostering social competence in preschool children exposed to intimate partner violence: evaluating the Preschool Kids’ Club intervention. J Aggress Maltreat Trauma 2013;22:425–45. 152
45. Hughes JR, Gottlieb LN. The effects of the Webster-Stratton parenting program on maltreating families: fostering strengths. Child Abuse Negl 2004;28:1081–97. 139
46. Jaberghaderi N, Greenwald R, Rubin A, Zand SO, Dolatabadi S. A comparison of CBT and EMDR for sexually-abused Iranian girls. Clin Psychol Psychother 2004;11:358–68. 102
47. King NJ, Tonge BJ, Mullen P, Myerson N, Heyne D, Rollings S, et al. Treating sexually abused children with posttraumatic stress symptoms: a randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2000;39:1347–55. 103
48. Kolko DJ. Clinical monitoring of treatment course in child physical abuse: psychometric characteristics and treatment comparisons. Child Abuse Negl 1996;20;23–43. 107
Kolko DJ. Individual cognitive behavioral treatment and family therapy for physically abused children and their offending parents: a comparison of clinical outcomes. Child Maltreat 1996;1:322–42. 108
49. Kolko DJ, Iselin A-MR, Gully KJ. Evaluation of the sustainability and clinical outcome of Alternatives for Families: a Cognitive-Behavioral Therapy (AF-CBT) in a child protection center. Child Abuse Negl 2011;35:105–16. 118
50. LeSure-Lester GE. An application of cognitive-behavior principles in the reduction of aggression among abused African American adolescents. J Interpers Violence 2002;17:394–402. 106
51. Lieberman AF, Van Horn P, Ghosh Ippen C. Toward evidence-based treatment: child-parent psychotherapy with preschoolers exposed to marital violence. J Am Acad Child Adolesc Psychiatry 2005;44:1241–8. 127
52. Ghosh Ippen C, Harris WW, Van H, Lieberman AF. Traumatic and stressful events in early childhood: can treatment help those at highest risk? Child Abuse Negl 2011;35:504–13. 128
53. Lieberman AF, Ghosh Ippen C, Van Horn P. Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. Am Acad Child Adolesc Psychiatry 2006;45:913–18. 129
54. Linares OL, Jimenez J, Nesci C, Pearson E, Beller S, Edwards N, et al. Reducing sibling conflict in maltreated children placed in foster homes. Prev Sci 2015;16:211–21. 141
55. Linares OL, Li M, Shrout PE. Child training for physical aggression?: Lessons from foster care. Child Youth Serv Rev 2012;34:2416–22. 115
56. Linares OL, Montalto D, Li M, Oza VS. A promising parenting intervention in foster care. J Consult Clin Psychol 2006:74;32–41. 114
57. McDonald RG, Howe CZ. Challenge/initiative recreation programs as a treatment for low self-concept children. J Leisure Res 1989;21:242–53. 202
58. McGain B, McKinzey R. The efficacy of group treatment in sexually abused girls. Child Abuse Negl 1995;19:1157–69. 172
59. Meezan W, O’Keefe M. Evaluating the effectiveness of multifamily group therapy in child abuse and neglect. Res Social Work Prac 1998;8:330–53. 149
Meezan W, O’Keefe M. Multifamily group therapy: impact on family functioning and child behavior. Fam Soc 1998;79:32–44. 148
60. Monck E, Bentovim A, Goodall G, Hyde C, Lwin R, Sharland E, et al. Child Sexual Abuse: A Descriptive & Treatment Study. Studies in Child Protection. London: Her Majesty’s Stationary Office; 1996. 169
61. Moore E, Armsden G, Gogerty PL. A twelve-year follow-up study of maltreated and at-risk children who received early therapeutic child care. Child Maltreat 1998;3:3–16. 194
62. Moss E, Dubois-Comtois K, Cyr C, Tarabulsy GM, St-Laurent D, Bernier A. Efficacy of a home-visiting intervention aimed at improving maternal sensitivity, child attachment, and behavioral outcomes for maltreated children: a randomized control trial. Dev Psychopathol 2011;23:195–210. 130
63. Noether CD, Brown V, Finkelstein N, Russell LA, Van De Mark NR, Morris LS, et al. Promoting resiliency in children of mothers with co-occurring disorders and histories of trauma: Impact of a skills-based intervention program on child outcomes. J Commun Psychol 2007;35:823–43. 158
64. Nolan M, Carr A, Fitzpartrick C, O’Flaherty A, Keary K, Turner R, et al. A comparison of two programmes for victims of child sexual abuse: a treatment outcome study. Child Abuse Rev 2002;11:103–23. 178
65. Overbeek MM, de Schipper JC, Lamers-Winkelman F, Schuengel C. Effectiveness of specific factors in community-based intervention for child-witnesses of interparental violence: a randomized trial. Child Abuse Negl 2013;37:1202–14. 153
66. Paquette G, Tourigny M, Joly J. Effects of a group therapy program led by social workers for adolescent girls who have experienced sexual abuse. Can Soc Work 2011;13:93–110. 104
Paquette G, Tourigny M, Joly J. Programme d’intervention de groupe pour des adolescentes agressées sexuellement: étude des effets spécifiques et exploration du lien avec l’implantation. 2011. In Tardif M, editor. L’agression Sexuelle: Transformations et Paradoxes. CIFAS. 2009. pp. 56–78. 105
67. Pretorius G, Pfeifer N. Group art therapy with sexually abused girls. S Afr J Psychol 2010;40:63–73. 200
68. Reddy SD, Negi LT, Dodson-Lavelle B, Ozawa-de S, Pace TWW, Cole SP, et al. Cognitive-based compassion training: a promising prevention strategy for at-risk adolescents. J Child Fam Stud 2013;22:219–30. 176
69. Rondeau C. The Efficacy of Reward vs. Punishment: a Comparison of Two Cottage Units. Monograph Series No. 2:3/83. Beaumont, CA: Childhelp USA; 1983. 119
70. Runyon MK, Deblinger E, Steer RA. Group cognitive behavioral treatment for parents and children at-risk for physical abuse: an initial study. Child Fam Behav Ther 2010;32:196–218. 109
71. Rushton A, Monck E, Leese M, McCrone P, Sharac J. Enhancing adoptive parenting: a randomized controlled trial. Clin Child Psychol Psychiatry 2010;15:529–42. 116
72. Santibáñez R. Effects of an educational intervention programme on self-control and moral development in foster-home children. Infanc Aprendiz 2000;92:85–107. 165
73. Schaeffer CM, Swenson CC, Tuerk EH, Henggeler SW. Comprehensive treatment for co-occurring child maltreatment and parental substance abuse: outcomes from a 24-month pilot study of the MST-Building Stronger Families program. Child Abuse Negl 2013;37:596–607. 147
74. Scheck MM, Schaeffer JA, Gillette C. Brief psychological intervention with traumatized young women: the efficacy of eye movement desensitization and reprocessing. J Trauma Stress 1998;11:25–44. 121
75. Shirk SR, DePrince AP, Crisostomo PS, Labus J. Cognitive behavioral therapy for depressed adolescents exposed to interpersonal trauma: an initial effectiveness trial. Psychotherapy 2014;51:167–79. 117
76. Simoneau AC, Hébert M, Tourigny M. Evaluation of a group therapy for 6–13 year old sexually abused children. Revue Québécoise de Psychologie 2008;29:27–43. 159
77. Smith DK, Leve LD, Chamberlain P. Preventing internalizing and externalizing problems in girls in foster care as they enter middle school: impact of an intervention. Prev Sci 2011;12:269–77. 189
78. Spieker SJ, Oxford ML, Kelly JF, Nelson EM, Fleming CB. Promoting First Relationships: randomized trial of a relationship-based intervention for toddlers in child welfare. Child Maltreat 2012;17:271–86. 131
79. Sprang G. The efficacy of a relational treatment for maltreated children and their families. Child Adolesc Ment Health 2009;14:81–8. 132
80. Sullivan CM, Bybee DI, Allen NE. Findings from a community-based program for battered women and their children. J Interpers Violence 2002;17:915–36. 154
81. Sullivan PM. The effects of psychotherapy on behavior problems of sexually abused deaf children. Child Abuse Negl 1992;16:297–307. 179
82. Swenson CC, Randall J, Henggeler SW, Ward D. The outcomes and costs of an interagency partnership to serve maltreated children in state custody. Child Serv Soc Pol Res Pract 2000;3:191–209. 198
83. Swenson CC, Schaeffer CM, Henggeler SW, Faldowski R, Mayhew AM. Multisystemic therapy for child abuse and neglect: a randomized effectiveness trial. J Fam Psychol 2010;24:497–507. 144
84. Taussig HN, Culhane SE. Impact of a mentoring and skills group program on mental health outcomes for maltreated children in foster care. Arch Pediatr Adolesc Med 2010;164:739–46. 190
85. Taussig HN, Culhane SE, Garrido E, Knudtson MD. RCT of a mentoring and skills group program: placement and permanency outcomes for foster youth. Pediatrics 2012;130:E33–9. 191
86. Thomas R, Zimmer-Gembeck MJ. Accumulating evidence for parent-child interaction therapy in the prevention of child maltreatment. Child Dev 2011;82:177–92. 137
87. Thomas R, Zimmer-Gembeck MJ. Parent–child interaction therapy: an evidence-based treatment for child maltreatment. Child Maltreat 2012;17:253–66. 138
88. Thun D, Sims PL, Adams MA, Webb T. Effects of group therapy on female adolescent survivors of sexual abuse: a pilot study. J Child Sex Abuse 2002;11:1–16. 174
89. Toth SL, Maughan A, Manly JT, Spagnola M, Cicchetti D. The relative efficacy of two interventions in altering maltreated preschool children’s representational models: Implications for attachment theory. Dev Psychopathol 2002;14:877–908. 133
90. Tourigny M, Hébert M, Daigneault I, Simoneau AC. Efficacy of a group therapy for sexually abused adolescent girls. J Child Sex Abuse 2005;14:71–93. 166
Tourigny M. A six month follow-up study of psychoeducative group therapy for sexually abused female adolescents. Revue Québécoise de Psychologie 2008;29:117–31. 167
91. Tourigny M, Hébert M. Comparison of open versus closed group interventions for sexually abused adolescent girls. Violence Victims 2007;22:334–49. 160
92. Tourigny M, Boisvert I, Jacq B. Effectiveness of a short group intervention for sexually abused adolescents. Intervention 2008;129:27–38. 168
93. Trowell J, Kolvin I, Weeramanthri T, Sadowski H, Berelowitz M, Glaser D, et al. Psychotherapy for sexually abused girls: psychopathological outcome findings and patterns of change. Br J Psychiatry 2002;180:234–47. [Erratum appears in Br J Psychiatry 2002;180:553.]155
94. Udwin O. Imaginative play training as an intervention method with institutionalised preschool children. Br J Clin Psychol 1983;53:32–9. 203
95. Valentino K, Comas M, Nuttall AK, Thomas T. Training maltreating parents in elaborative and emotion-rich reminiscing with their preschool-aged children. Child Abuse Negl 2013;37:585–95. 140
96. Verleur D, Hughes RE, de Rios MD. Enhancement of self-esteem among female adolescent incest victims: a controlled comparison. Adolescence 1986;21:843–54. 173
97. Wagar JM, Rodway MR. An evaluation of a group treatment approach for children who have witnessed wife abuse. J Fam Violence 1995;10:295–306. 156
98. Wolfe DA, Wekerle C, Scott K, Straatman A-L, Grasley C, Reitzel-Jaffe D. Dating violence prevention with at-risk youth: a controlled outcome evaluation. J Consult Clin Psychol 2003;71:279–91. 157
Included uncontrolled studies (citations): effectiveness studies
1. Arabgol F, Derakhshanpour F, Panaghi L, Sarjami S, Hajebi A. Effect of therapeutic interventions on behavioral problems of abused children. Iran J Psychiatry Clin Psychol 2004;19:202–10. 521
2. Arnold EM, Kirk RS, Roberts AC, Griffith DP, Meadows K, Julian J. Treatment of incarcerated, sexually-abused adolescent females: an outcome study. J Child Sex Abuse 2003;12:123–39. 480
3. Barker R, Place M. Working in collaboration: a therapeutic intervention for abused children. Child Abuse Review 2005;14:26–39. 481
4. Bentovim A, Boston P, Van E. Child sexual abuse: children and families referred to a treatment project and the effects of intervention. Br Med J 1987;295:1453–7. 522
5. Berg B, Jones DPH. Outcome of psychiatric intervention in factitious illness by proxy (Munchausen’s syndrome by proxy). Arch Dis Child 1999;81:465–72. 523
6. Brown A, McCauley K, Navalta C, Saxe G. Trauma systems therapy in residential settings: improving emotion regulation and the social environment of traumatized children and youth in congregate care. J Fam Violence 2013;28:693–703. 551
7. Chasson GS, Vincent JP, Harris GE. The use of symptom severity measured just before termination to predict child treatment dropout. J Clin Psychol 2008;64:891–904. 482
8. Clarke S, Llewelyn S. Personal constructs of survivors of childhood sexual abuse receiving cognitive analytic therapy. Br J Med Psychol 1994;67:273–89. 483
9. Clausen JM, Ruff SC, Wiederhold WV, Heineman TV. For as long as it takes: relationship-based play therapy for children in foster care. Psychoanal Soc Work 2012;19:43–53. 570
10. Cohen JA, Mannarino AP, Perel JM, Staron V. A pilot randomized controlled trial of combined trauma-focused CBT and sertraline for childhood PTSD symptoms. J Am Acad Child Adolesc Psychiatry 2007;46:811–19. 484
11. Coren E, Thomae M, Hutchfield J, Iredale W. Report on the implementation and results of an outcomes-focused evaluation of child sexual abuse interventions in the UK. Child Abuse Rev 2013;22:44–59. 524
12. Coulter SJ. Effect of Song Writing versus Recreational Music on Posttraumatic Stress Disorder (PTSD) Symptoms and Abuse Attribution in Abused Children. J Poet Ther 2000;13:189–208. 565
13. Cross TP, Leavey J, Mosley PR, White AW, Andreas JB. Outcomes of specialized foster care in a managed child welfare services network. Child Welfare 2004;83:533–64. 552
14. Crusto CA, Lowell DI, Paulicin B, Reynolds J, Feinn R, Friedman SR, Kaufman JS. Evaluation of a Wraparound Process for Children Exposed to Family Violence. Best Pract Ment Health 2008;4:1–18. 525
15. Culp RE. Differential Developmental Progress of Maltreated Children in Day Treatment. Social Work 1987;32:497–9. 195
16. Danielson CK, McCart MR, de A, Michael A, Macdonald A, Doherty LS, Resnick HS. Risk reduction for substance use and trauma-related psychopathology in adolescent sexual assault victims: findings from an open trial. Child Maltreatment 2010;15:261–8. 526
17. De Luca RV, Hazen A, Cutler J. Evaluation of a group counseling program for preadolescent female victims of incest. Element School Guid Couns 1993;28:104–14. 774
18. De Paúl PJ, Arruabarrena I. Evaluation of a treatment program for abusive and high-risk families in Spain. Child Welfare 2003;82:413–42. 527
19. Deblinger E, McLeer SV, Henry D. Cognitive behavioral treatment for sexually abused children suffering post-traumatic stress: preliminary findings. J Am Acad Child Adolesc Psychiatry 1990;29:747–52. 485
20. Donohue B, Van HVB. Development and description of an empirically based ecobehavioral treatment program for child maltreatment. Behav Intervent 1999;14:55–82. 528
21. Ducharme JM, Atkinson L, Poulton L. Success-based, noncoercive treatment of oppositional behavior in children from violent homes. J Am Acad Child Adolesc Psychiatry 2000;39:995–1004. 510
22. Ernst AA, Weiss SJ, Enright-Smith S, Hansen JP. Positive outcomes from an immediate and ongoing intervention for child partner violence. Am J Emerg Med 2008;26:389–94. 566
23. Feather JS, Ronan KR. Trauma-focused cognitive-behavioural therapy for abused children with posttraumatic stress disorder: a pilot study. NZ J Psychol 2006;35:132–45. 486
24. Feather JS, Ronan KR. Trauma-focused CBT with maltreated children: a clinic-based evaluation of a new treatment manual. Aust Psychol 2009;44:174–94. 487
25. Forbes F, Duffy JC, Mok J, Lemvig J. Early intervention service for non-abusing parents of victims of child sexual abuse: pilot study. Br J Psychiatry 2003;183:66–72. [Erratum appears in Br J Psychiatry 2003;183.]529
26. Friedrich WN, Luecke WJ, Beilke RL, Place V. Psychotherapy outcome of sexually abused boys: an agency study. J Interpers Violence 1992;7:396–409. 547
27. Gallagher B, Green A. Outcomes among young adults placed in therapeutic residential care as children. J Child Serv 2013;8:31–51. 553
28. Golding K, Picken W. Group work for foster carers caring for children with complex problems. Adopt Foster 2004;28:25–37. 511
29. Gray J, Nielsen DR, Wood LE, Andresen M, Dolce K. Academic progress of children who attended a preschool for abused children: a follow-up of the Keepsafe project. Child Abuse Negl 2000;24:25–32. 554
30. Grosz CA, Kempe RS, Kelly M. Extrafamilial sexual abuse: Treatment for child victims and their families. Child Abuse Negl 2000;24:9–23. 534
31. Habib M, Labruna V, Newman J. Complex histories and complex presentations: implementation of a manually-guided group treatment for traumatized adolescents. J Fam Violence 2013;28:717–28. 488
32. Habigzang LF, Damasio BF, Koller SH. Impact evaluation of a cognitive behavioral group therapy model in Brazilian sexually abused girls. J Child Sex Abuse 2013;22:173–90. 491
33. Habigzang LF, Hatzenberger R, Corte FD, Stroeher F, Koller S. Assessment of a psychology intervention model effect on sexual abused girls. Psicologia: Teoria e Pesquisa 2008;24:67–76. 489
34. Habigzang LF, Stroeher FH, Hatzenberger R, Cunha RC, da Ramos MS, Koller SH. Cognitive behavioral group therapy for sexually abused girls. Rev Saude Publica 2009;43:70–8. 490
35. Hack TF, Osachuk TAG, De L, Rayleen V. Group treatment for sexually abused preadolescent boys. Fam Soc 1994;75:217–28. 535
36. Hall-Marley SE, Damon L. Impact of structured group therapy on young victims of sexual abuse. J Child Adolesc Group Ther 1993;3:41–8. 567
37. Hamama L, Hamama-Raz Y, Dagan K, Greenfeld H, Rubinstein C, Ben-Ezra M. A preliminary study of group intervention along with basic canine training among traumatized teenagers: a 3-month longitudinal study. Child Youth Serv Rev 2011;33:1975–80. 205
38. Harbeck C, Peterson L, Starr L. Previously abused child victims’ response to a sexual abuse prevention program: a matter of measures. Behav Ther 1992;23:375–87. 536
38. Heede T, Runge H, Storebo OJ, Rowley E, Hansen KG. Psychodynamic milieu-therapy and changes in personality: what is the connection? J Child Psychother 2009;35:276–89. 555
40. Hiebert-Murphy D, de L, Rayleen V, Runtz M. Group treatment for sexually abused girls: evaluating outcome. Families in Society 1992;73:205–13. 537
41. Huang-Storms L, Bodenhamer-Davis E, Davis R, Dunn J. QEEG-guided neurofeedback for children with histories of abuse and neglect: neurodevelopmental rationale and pilot study. J Neurother 2006;10:3–16. 25
42. Hubel G, Campbell C, West T, Friendenberg S, Schreier A, Flood M, et al. Child advocacy center based group treatment for child sexual abuse. J Child Sex Abuse 2014;23:304–25. 492
43. Hussey DL, Guo S. Characteristics and trajectories of treatment foster care youth. Child Welfare 2005;84:485–506. 556
44. Hyde C, Bentovim A, Monck E. Some clinical and methodological implications of a treatment outcome study of sexually abused children. Child Abuse Negl 1995;19:1387–99. 538
45. Jackson A, Frederico M, Tanti C, Black C. Exploring outcomes in a therapeutic service response to the emotional and mental health needs of children who have experienced abuse and neglect in Victoria, Australia. Child Fam Soc Work 2009;14:198–212. 512
46. Jarero I, Roque-Lopez S, Gomez J. The provision of an EMDR-based multicomponent trauma treatment with child victims of severe interpersonal trauma. J EMDR Pract Res 2013;7:17–28. 493
47. Jarvis KL, Novaco RW. Postshelter adjustment of children from violent families. J Interpers Violence 2006;21:1046–62. 549
48. Jones CD, Chancey R, Lowe LA, Risler EA. Residential treatment for sexually abusive youth: an assessment of treatment outcomes. Res Soc Work Pract 2010;20:172–82. 557
49. Kemp K, Signal T, Botros H, Taylor N, Prentice K. Equine facilitated therapy with children and adolescents who have been sexually abused: a program evaluation study. J Child Fam Stud 2013;23:558–66. 568
50. Kirsch V, Fegert JM, Seitz DC, Goldbeck L. Trauma-focused cognitive behavioral therapy (Tf-CBT) for children and adolescents after abuse and maltreatment: results of a pilot study. Kindh Entwickl 2011;20:95–102. 494
51. Kjellgren C, Svedin CG, Nilsson D. Child Physical Abuse-Experiences of combined treatment for children and their parents: a pilot study. Child Care in Practice 2013;19:275–90. 495
52. Kruczek T, Vitanza S. Treatment effects with an adolescent abuse survivor’s group. Child Abuse Negl 1999;23:477–85. 496
53. Lange A, Ruwaard J. Ethical dilemmas in online research and treatment of sexually abused adolescents. J Med Internet Res 2010;12. 497
54. Lanier P, Kohl PL, Benz J, Swinger D, Drake B. Preventing maltreatment with a community-based implementation of parent-child interaction therapy. J Child Fam Stud 2014;23:449–60. 513
Lanier P, Kohl PL, Benz J, Swinger D, Moussette P, Drake B. Parent-child interaction therapy in a community setting: examining outcomes, attrition, and treatment setting. Res Soc Work Prac 2011;1:689–98. 514
55. Lanktree CB, Briere J. Outcome of therapy for sexually abused children: a repeated measures study. Child Abuse Negl 1995;19:1145–55. 498
56. Lee J, Kolomer S, Thomsen D. Evaluating the effectiveness of an intervention for children exposed to domestic violence: a preliminary program evaluation. Child Adolesc Soc Work J 2012;29:357–72. 539
57. Lindon J, Nourse CA. A multi-dimensional model of groupwork for adolescent girls who have been sexually abused. Child Abuse Negl 1994;18:341–8. 544
58. MacKay B, Gold M, Gold E. A pilot study in drama therapy with adolescent girls who have been sexually abused. Art Psychother 1987;14:77–84. 569
59. MacMillan KM, Harpur LL. An examination of children exposed to marital violence accessing a treatment intervention. J Emot Abuse 2003;3:227–52. 540
60. Matulis S, Resick PA, Rosner R, Steil R. Developmentally adapted cognitive processing therapy for adolescents suffering from posttraumatic stress disorder after childhood sexual or physical abuse: a pilot study. Clin Child Fam Psychol Rev 2014;17:173–90. 499
61. McClure EB, Connell AM, Zucker M, Griffith JR, Kaslow NJ. The Adolescent Depression Empowerment Project (ADEPT): a Culturally Sensitive Family Treatment for Depressed African American Girls. In Hibbs ED, Jensen PS, editors. Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. 2nd edn. Washington, DC: American Psychological Association; 2005. pp.149–64. 530
62. Merrick MV, Allen BM, Crase SJ. Variables associated with positive treatment outcomes for children surviving sexual abuse. J Child Sex Abuse 1994;3:67–87. 541
63. Misurell J, Springer C, Acosta L, Liotta L, Kranzler A. Game-based cognitive-behavioral therapy individual model (GB-CBT-IM) for child sexual abuse: a preliminary outcome study. Psychol Trauma 2014;6:250–8. 501
Misurell JR, Springer C, Tryon WW. Game-based cognitive-behavioral therapy (GB-CBT) group program for children who have experienced sexual abuse: a preliminary investigation. J Child Sex Abuse 2011;20:14–36. 500
64. Mukaddes NM, Bilge S, Alyanak B, Kora ME. Clinical characteristics and treatment responses in cases diagnosed as reactive attachment disorder. Child Psychiatry and Human Development 2000;30:273–87. 542
65. Nelki JS, Watters J. A group for sexually abused young children: unravelling the web. Child Abuse Negl 1989;13:369–77. 543
66. Nilsson D, Wadsby M. Symboldrama, a psychotherapeutic method for adolescents with dissociative and PTSD symptoms: a pilot study. J Trauma Dissoc 2010;11:308–21. 571
67. Oates KR. A therapeutic preschool for abused children: The Keepsafe Project. Child Abuse Negl 1995;19:1379–86. 558
68. Osofsky JD, Kronenberg M, Hammer JH, Lederman C, Katz L, Adams S, Graham M, Hogan A. The development and evaluation of the intervention model for the Florida Infant Mental Health Pilot Program. Infant Ment Health 2007;28:259–80. 515
69. Parish RA. Developmental milestones in abused children and their improvement with a family-oriented approach to the treatment of child abuse. Child Abuse Negl 1985;9:245–250. 559
70. Pifalo T. Pulling out the thorns: art therapy with sexually abused children and adolescents. Art Therapy 2002;19:12–22. 572
Pifalo T. Art therapy with sexually abused children and adolescents: extended research study. Art Therapy 2006;23:181–5. 573
71. Puckering C, Connolly B, Werner C, Toms-Whittle L, Thompson L, Lennox J, Minnis H. Rebuilding relationships: a pilot study of the effectiveness of the Mellow Parenting Programme for children with Reactive Attachment Disorder. Clin Child Psychol Psychiatry 2011;16:73–87. 516
72. Pugh Robin H, Tepper FL, Halpern-Felsher BL, Howe TR, Tomlinson-Keasey C, Parke RD. Changes in abused children’s social and cognitive skills from intake to discharge in a residential treatment center. Resid Treat Child Youth 1997;14:65–83. 560
73. Purvis KB, Cross DR. Improvements in salivary cortisol, depression, and representations of family relationships in at-risk adopted children utilizing a short-term therapeutic intervention. Adopt Q 2007;10:25–43. 574
Purvis KB, Cross DR, Federici RA, Johnson D, McKenzie BL. The Hope Connection: a therapeutic summer day camp for adopted and at-risk children with special socio-emotional needs. Adopt Foster 2007;31:38–48. 575
74. Ray J, Smith V, Peterson T, Gray J, Schaffner J, Houff M. A treatment program for children with sexual behavior problems. Child Adolesc Social Work J 1995;12:331–43. 561
75. Reeker J, Ensing D. An evaluation of a group treatment for sexually abused young children. J Child Sex Abuse 1998;7:65–85. 545
76. Reyes CJ, Asbrand JP. A longitudinal study assessing trauma symptoms in sexually abused children engaged in play therapy. Int J Play Ther 2005;14:25–47. 576
77. Rosenberg HJ, Jankowski MK, Fortuna LR, Rosenberg SD, Mueser KT. A pilot study of a cognitive restructuring program for treating posttraumatic disorders in adolescents. Psychol Trauma 2011;3:94–9. 502
78. Runyon MK, Deblinger E, Schroeder CM. Pilot evaluation of outcomes of combined parent-child cognitive-behavioral group therapy for families at risk for child physical abuse. Cogn Behavior Pract 2009;16:101–18. 503
79. Rust JO, Troupe PA. Relationships of treatment of child sexual abuse with school achievement and self-concept. J Early Adolesc 1991;11:420–9. 548
80. Salloum A, Robst J, Scheeringa MS, Cohen JA, Wang W, Murphy TK, et al. Step one within stepped care trauma-focused cognitive behavioral therapy for young children: a pilot study. Child Psychiatry Hum Dev 2014;45:65–77. 504
81. Schram DD, Giovengo MA. Evaluation of threshold: an independent living program for homeless adolescents. J Adolesc Health 1991;12:567–72. 562
82. Schultz PN, Remick-Barlow GA, Robbins L. Equine-assisted psychotherapy: a mental health promotion/intervention modality for children who have experienced intra-family violence. Health Soc Care Comm 2007;15:265–71. 577
83. Scott TA, Burlingame G, Starling M, Porter C, Lilly JP. Effects of individual client-centered play therapy on sexually abused children’s mood, self-concept, and social competence. Int J Play Ther 2003;12:7–30. 578
84. Silovsky JF, Niec L, Bard D, Hecht DB. Treatment for preschool children with interpersonal sexual behavior problems: a pilot study. J Clin Child Adolesc Psychol 2007;36:378–91. 505
85. Sinclair JJ. Outcome of group treatment for sexually abuse adolescent females living in a group home setting. J Interpers Violence 1995;10:533–42. 546
86. Smith AP, Kelly AB. An exploratory study of group therapy for sexually abused adolescents and nonoffending guardians. J Child Sex Abuse 2008;17:101–16. 506
87. Springer C, Misurell JR, Hiller A. Game-based cognitive-behavioral therapy (GB-CBT) group program for children who have experienced sexual abuse: a three-month follow-up investigation. J Child Sex Abuse 2012;21:646–64. 775
88. Staff I, Fein E. Stability and change: Initial findings in a study of treatment foster care placements. Child Youth Serv Rev 1995;17:379–89. 531
89. Stauffer LB, Deblinger E. Cognitive behavioral groups for nonoffending mothers and their young sexually abused children: a preliminary treatment outcome study. Child Maltreatment 1996;1:65–76. 507
90. Stubenbort K, Cohen MM, Trybalski V. The effectiveness of an attachment-focused treatment model in a therapeutic preschool for abused children. Clin Soc Work J 2010;38:51–60. 563
91. Sullivan M, Egan M, Gooch M. Conjoint interventions for adult victims and children of domestic violence: a program evaluation. Res Social Work Pract 2004;14:163–70. 508
92. Timmer SG, Urquiza AJ, Zebell N. Challenging foster caregiver-maltreated child relationships: the effectiveness of parent-child interaction therapy. Child Youth Serv Rev 2006;28:1–19. 518
93. Timmer SG, Urquiza AJ, Zebell NM, McGrath JM. Parent–child interaction therapy: application to maltreating parent-child dyads. Child Abuse Negl 2005;29:825–42. 517
94. Timmer SG, Ware LM, Urquiza AJ, Zebell NM. The effectiveness of parent-child interaction therapy for victims of interparental violence. Violence Vict 2010;25:486–503. 519
95. Timmons-Mitchell J. Containing aggressive acting out in abused children. Child Welfare 1986;65:459–68. 509
96. Tourigny M, Peladeau N, Doyon M, Bouchard C. [Efficacy of a treatment program for sexually abused children.] Child Abuse Negl 1998;22:25–43. 532
97. Vernberg EM, Jacobs AK, Nyre JE, Puddy RW, Roberts MC. Innovative treatment for children with serious emotional disturbance: preliminary outcomes for a school-based intensive mental health program. J Clin Child Adolesc Psychol 2004;33:359–65. 564
98. Wagner WG, Kilcrease-Fleming D, Fowler WE, Kazelskis R. Brief-term counseling with sexually abused girls: the impact of sex of counselor on clients’ therapeutic involvement, self-concept, and depression. J Couns Psychol 1993;40:490–500. 550
99. Winton MA. An evaluation of a support group for parents who have a sexually abused child. Child Abuse Negl 1990;14:397–405. 520
100. Woodworth DL. Evaluation of a Multiple-Family Incest Treatment Program. In Patton M, editor. Family Sexual Abuse: Frontline Research and Evaluation. Thousand Oaks, CA: SAGE Publications;1991:121–34. 533
Excluded studies (citations): effectiveness studies
1. Amaya-Jackson LRV, Murray MC, Nelson A, Cherney MS, Lee R, Foa E, et al. Cognitive-behavioral treatment for pediatric posttraumatic stress disorder: protocol and application in school and community settings. Cogn Behav Pract 2003;10:204–13. 579
2. Barton K. In-home treatment of child abuse: healing at home can be effective and cost-effective. Calif Agricult 1994;48:36–8. 580
3. Barton K, Baglio C. Braverman M. Stress reduction in child-abusing families: global and specific measures. Psychol Rep 1994;75:287–304. 581
4. Brook J, McDonald TP. Evaluating the effects of comprehensive substance abuse intervention on successful reunification. Res Soc Work Pract 2007;17:664–73. 582
5. Cohen J, Mannarino AP. Factors that mediate treatment outcome of sexually abused preschool children: six- and 12-month follow-up. J Am Acad Child Adolesc Psychiatry 1998;37:44–51. 280
6. Cohen JA, Mannarino AP. Predictors of treatment outcome in sexually abused children. Child Abuse Negl 2000;24:983–94. 583
7. Coleman H, Jenson JM. A longitudinal investigation of delinquency among abused and behavior problem youth following participation in a family preservation program. J Offender Rehabil 2000;31:143–62. 584
8. Collado C, Levine P. Reducing transfers of children in family foster care through onsite mental health interventions. Child Welfare 2007;86:133–50. 585
9. Currier LL, Wurtele SK. A pilot study of previously abused and non-sexually abused children’s responses to a personal safety program. J Child Sex Abuse 1996;5:71–87. 586
10. DeSena AD, Murphy RA, Douglas-Palumberi H, Blau G, Kelly B, Horwitz SM, et al. SAFE homes: is it worth the cost? An evaluation of a group home permanency planning program for children who first enter out-of-home care. Child Abuse Negl 2005;29:627–43. 587
11. Edinburgh LD, Saewyc EM. A novel, intensive home-visiting intervention for runaway, sexually exploited girls. J Spec Pediatr Nurs 2009;14:41–8. 588
12. Friman PC, Jones M, Smith G, Daly DL, Larzelere R. Decreasing disruptive behavior by adolescent boys in residential care by increasing their positive to negative interactional ratios. Behav Modif 1997;21:470–86. 589
13. Graham-Bermann SA, Miller LE. Intervention to reduce traumatic stress following intimate partner violence: an efficacy trial of the Moms’ Empowerment Program (MEP). Psychodyn Psychiatry 2013;41:329–49. 590
14. Hakman M, Chaffin M, Funderburk B, Silovsky JF. Change trajectories for parent-child interaction sequences during parent-child interaction therapy for child physical abuse. Child Abuse Negl 2009;33:461–70. 591
15. Harder J. Prevention of child abuse and neglect: an evaluation of a home visitation parent aide program using recidivism data. Res Soc Work Pract 2005;15:246–56. 592
16. Harold GT, Kerr DCR, Van R, DeGarmo DS, Rhoades KA, Leve LD. Depressive symptom trajectories among girls in the juvenile justice system: 24-month outcomes of an RCT of multidimensional treatment foster care. Prev Sci 2013;14:437–46. 593
17. Howes C, Ritchie S. Changes in child–teacher relationships in a therapeutic preschool program. Early Educ Dev 1998;9:411–22. 594
18. Iwaniec D, Sneddon H. The quality of parenting of individuals who failed to thrive as children. Br J Soc Work 2002;32:283–98. 776
19. Iwaniec D, Sneddon H, Allen S. The outcomes of a longitudinal study of non-organic failure-to-thrive. Child Abuse Rev 2003;12:216–26. 595
20. Kirk Raymond S, Griffith DP. Intensive family preservation services: demonstrating placement prevention using event history analysis. Soc Work Res 2004;28:5–16. 596
21. Lewis CC, Simons AD, Nguyen LJ, Murakami JL, Reid MW. Impact of childhood trauma on treatment outcome in the treatment for adolescents with depression study (TADS). J Am Acad Child Adolesc Psychiatry 2010;49:132–40. 597
22. Lorber R, Felton DK, Reid JB. A social learning approach to the reduction of coercive processes in child abusive families: a molecular analysis. Adv Behav Res Ther 1984;6:29–45. 598
23. MacMillan HL. Effectiveness of home visitation by public-health nurses in prevention of the recurrence of child physical abuse and neglect: a randomised controlled trial. Lancet 2005;365:1786–93. 599
24. Mersky JP, Topitzes JD, Reynolds AJ. Maltreatment prevention through early childhood intervention: a confirmatory evaluation of the Chicago Child-Parent Center preschool program. Child Youth Serv Rev 2011;33:1454–63. 600
25. Overbeek MM, de S, Lamers-Winkelman F, Schuengel C. Risk factors as moderators of recovery during and after interventions for children exposed to interparental violence. Am J Orthopsychiatry 2014;84:295–306. 601
26. Pereira P, D’Affonseca S, Williams L. A feasibility pilot intervention program to teach parenting skills to mothers of poly-victimized children. J Fam Violence 2013;28:5–15. 602
27. Rivara FP. Physical abuse in children under two: a study of therapeutic outcomes. Child Abuse Negl 1985;9:81–7. 603
28. Sagatun IJ, Prince L. Incest family dynamics: family members’ perceptions before and after therapy. J Soc Work Hum Sex 1988;7:69–87. 604
29. Sullivan PM, Scanlan JM. Psychotherapy with handicapped sexually abused children. Dev Disabil Bull 1990;18:21–34. 605
30. Swart J, Apsche J. A comparative treatment efficacy study of conventional therapy and mode deactivation therapy (MDT) for adolescents with conduct disorders, mixed personality disorders, and experiences of childhood trauma. Int J Behav Consult Ther 2014;9:23–9. 607
31. Swart J, Apsche J. Family mode deactivation therapy (FMDT): a randomized controlled trial for adolescents with complex issues. Int J Behav Consult Ther 2014;9:14–22. 606
32. Szykula SA, Fleischman MJ. Reducing out-of-home placements of abused children: two controlled field studies. Child Abuse Negl 1985;9:277–83. 608
33. Vitulano LA, Nagler S, Adnopoz J, Grigsby RK. Preventing out-of-home placement for high-risk children. Yale J Biol Med 1990;63:285–91. 609
34. Waxman H, Houston W, Profilet S, Sanchez B. The long-term effects of the Houston Child Advocates, Inc., program on children and family outcomes. Child Welfare 2009;8:23–46. 610
Included economic studies (citations)
1. Gospodarevskaya E, Segal L. Cost-utility analysis of different treatments for post-traumatic stress disorder in sexually abused children. Child Adolesc Psychiatry Ment Health 2012;6:1–15. 612
2. Lynch F, Dickerson JF, Saldana L, Fisher PA. Incremental net benefit of early intervention for preschool-aged children with emotional and behavioral problems in foster care. Child Youth Serv Rev 2014;36:213–19. 615
3. McCrone P, Weeramanthri T, Knapp M, Rushton A. Trowell J, Miles G, Kolvin, I. Cost-effectiveness of individual versus group psychotherapy for sexually abused girls. Child Adolesc Ment Health 2005;10:26–31. 614
4. Sharac J, McCrone P, Rushton A, Monck E. Enhancing adoptive parenting: a cost-effectiveness analysis. Child Adolesc Ment Health 2011;16:110–15. 613
5. Swenson CC, Randall J, Henggeler SW, Ward D. The outcomes and costs of an interagency partnership to serve maltreated children in state custody. Child Serv Soc Pol Res Pract 2000;3:191–209. 198
6. Wood S, Barton K, Schroeder C. In-home treatment of abusive families: cost and placement at one year. Psychotherapy 1988;25:409–14. 616
Excluded economic studies (citations)
1. Blazey A. Reducing the Risk, Cutting the Cost: an Assessment of the Potential Savings on Barnardo’s Interventions for Young People Who Have Been Sexually Exploited. London: Barnardo’s; 2011. URL: www.barnardos.org.uk/ (accessed 16 June 2015). 618
2. Clark C, Yampolskaya S, Robst J. Mental health services expenditures among children placed in out-of-home care. Admin Policy Ment Health 2011;38:430–9. 619
3. Cohen MA, Miller TR. The cost of mental health care for victims of crime. J Interpers Violence 1998;13:93–110. 620
4. Conrad C. Measuring costs of child abuse and neglect: a mathematic model of specific cost estimations. J Health Hum Serv Adm 2006;29:103–23. 777
5. DePanfilis D, Dubowitz H, Kunz J. Assessing the cost-effectiveness of family connections. Child Abuse Negl 2008;32:335–51. 622
6. DeSena AD, Murphy RA, Douglas-Palumberi H, Blau G, Kelly B, Horwitz SM, et al. SAFE Homes: Is it worth the cost? An evaluation of a group home permanency planning program for children who first enter out-of-home care. Child Abuse Negl 2005;29:627–43. 587
7. Edinburgh LD, Saewyc EM. A novel, intensive home-visiting intervention for runaway, sexually exploited girls. J Spec Pediatr Nurs 2009;14:41–8. 588
8. Florence C, Brown DS, Fang X, Thompson HF. Health care costs associated with child maltreatment: impact on Medicaid. Pediatrics 2013;132:312–18. 623
9. Foster EM, Prinz RJ, Sanders MR, Shapiro CJ. The costs of a public health infrastructure for delivering parenting and family support. Child Youth Serv Rev 2008;30:493–501. 624
10. Lynch F, Fisher P, Dickerson JF, Saldana L. Incremental cost-effectiveness of multidimensional treatment foster care for pre-schoolers. J Ment Health Policy Econ 2011;14:S19–20. 617
11. Maher EJ, Corwin TW, Hodnett R, Faulk K. A cost-savings analysis of a statewide parenting education program in child welfare. Res Soc Work Pract 2012;22:615–25. 625
12. New M, Berliner L. Mental health service utilization by victims of crime. J Trauma Stress 2000;13:693–707. 626
13. Reynolds AJ, Temple JA, Robertson DL, Mann EA. Age 21 cost-benefit analysis of the title I Chicago child-parent centers. Educ Eval Policy Anal 2002;24:267–303. 627
14. Rovi S, Chen P, Johnson MS. The economic burden of hospitalizations associated with child abuse and neglect. Am J Public Health 2004;94:586–90. 628
15. Rushton A, Monck E, Leese M, McCrone P, Sharac J. Enhancing adoptive parenting: a randomized controlled trial. Clin Child Psychol Psychiatry 2010;15:529–42. 116
16. Salloum A, Robst J, Scheeringa MS, Cohen JA, Wang W, Murphy TK, et al. Step one within stepped care trauma-focused cognitive behavioral therapy for young children: a pilot study. Child Psychiatry Hum Dev 2014;45:65–77. 504
Included acceptability studies (citations)
1. Alaggia R, Michalski J, Vine C. The use of peer support for parents and youth living with the trauma of child sexual abuse: an innovative approach. J Child Sex Abuse 1999;8:57–75. 660
2. Ashby MR, Gilchrist LD, Miramontez A. Group treatment for sexually abused American Indian adolescents. Soc Work Groups 1987;10:21–32. 636
3. Baginsky, M. Counselling and support services for young people aged 12 – 16 who have experienced sexual abuse: a study of the provision in Italy, the Netherlands and the United Kingdom. National Society for the Prevention of Cruelty to Children 2001;11:333–4. 640
4. Baker JN, Tanis HJ, Rice JB. Including siblings in the treatment of child sexual abuse. J Child Sex Abuse 2001;10:1–16. 637
5. Bannister A, Gallagher E. Children who sexually abuse other children. J Sex Aggress 1996;2:87–98. 668
6. Barker R, Place M. Working in collaboration: a therapeutic intervention for abused children. Child Abuse Rev 2005;14:26–39. 481
7. Barth R, Yeaton J, Winterfelt N. Psychoeducational groups with foster care of sexually abused children. Child Adolesc Soc Work J 1994;11:405–24. 161
8. Biehal N, Dixon J, Parry E, Sinclair I, Greenlaw J, Roberts C, et al. The Care Placements Evaluation. (CaPE) of Multidimensional Treatment Foster Care for Adolescents (MTFC-A). London: Department for Education: 2012. 145
9. Boisvert I, Tourigny M, Paquette G. Characteristics associated with group therapy dropout for sexually abused female adolescents. Revue Québécoise de Psychologie 2008;29:133–45. 658
10. Burgon HL. ’Queen of the world’: experiences of ‘at-risk’ young people participating in equine-assisted learning/therapy. J Soc Work Pract 2011;25:165–83. 669
11. Buschbacher PW. Positive behavior support for a young child who has experienced neglect and abuse: testimonials of a family member and professionals. J Posit Behav Interv 2002;4:242–8. 629
12. Chasson G, Mychailyszyn M, Vincent J, Harris G. Evaluation of trauma characteristics as predictors of attrition from cognitive-behavioral therapy for child victims of violence. Psychol Rep 2013;113:734–53. 630
13. Chasson GSP, Vincent J, Harris G. The use of symptom severity measured just before termination to predict child treatment dropout. J Clin Psychol 2008;64:891–904. 482
14. Conran T, Love J. The talkative chair: a child’s experience of sexual abuse intervention. J Systemic Ther 1993;12:68–85. 621
15. Costa L, de Almeida M, Ribeiro M, Penso M. Multifamiliar group: space for listening to the families in situation of sexual abuse. Psicologia em Estudo 2009;14:21–30. 678
16. Cross A, Jaycox L, Hickman L, Schultz D, Barnes-Proby D, Kofner A, et al. Predictors of study retention from a multisite study of interventions for children and families exposed to violence. J Community Appl Soc 2013;41:743–57. 634
17. Cunningham WS, Duffee DE, Huang YF, Steinke CM, Naccarato T. On the meaning and measurement of engagement in youth residential treatment centers. Res Soc Work Pract 2009;19:63–76. 649
18. Danielson CKR, McCart M, de Arellano M, Macdonald A, Doherty L, Resnick H. Risk reduction for substance use and trauma-related psychopathology in adolescent sexual assault victims: Findings from an open trial. Child Maltreatment 2010;15:261–8. 526
19. Davies J, Wright J, Drake S, Bunting J. ‘By listening hard’: developing a service-user feedback system for adopted and fostered children in receipt of mental health services. Adopt Foster 2009;33:19–33. 665
20. De Luca R, Boyes D, Grayston A, Romano E. Sexual abuse: effects of group therapy on pre-adolescent girls. Child Abuse Rev 1995;4:263–77. 170
21. Deb S, Mukherjee A. Background and adjustment capacity of sexually abused girls and their perceptions of intervention. Child Abuse Rev 2011;20:213–30. 679
22. Ducharme JM, Atkinson L, Poulton L. Success-based, noncoercive treatment of oppositional behavior in children from violent homes. J Am Acad Child Adolesc Psychiatry 2000;39:995–1004. 510
23. Eslinger JG, Sprang G, Otis MD. Child and caregiver dropout in child psychotherapy for trauma. J Loss Trauma 2014;19:121–36. 631
24. Fowler WE, Wagner WG. Preference for and comfort with male versus female counselors among sexually abused girls in individual treatment. J Counsel Psychol 1993;40:65–72. 642
25. Fowler W, Wagner W, Iachini A, Johnson J. The impact of sex of psychological examiner on sexually abused girls’ preference for and anticipated comfort with male versus female counselors. Child Study J 1992;22:1–10. 641
26. Fraynt R, Ross L, Baker BL, Rystad I, Lee J, Briggs EC. Predictors of treatment engagement in ethnically diverse, urban children receiving treatment for trauma exposure. J Trauma Stress 2014;27:66–73. 632
27. Gallagher B, Green A. In, out and after care: young adults’ views on their lives, as children, in a therapeutic residential establishment. Child Youth Serv Rev 2012;34:437–50. 666
28. Gilbert CM. Children in women’s shelters: a group intervention using art. J Child Adolesc Psychiatry Ment Health Nurs 1988;1:7–13. 652
29. Golding K, Picken W. Group work for foster carers caring for children with complex problems. Adopt Foster 2004;28:25–37. 511
30. Grayston A, De Luca R. Social validity of group treatment for sexually abused boys. Child Fam Behav Ther 1996;18:1–16. 659
31. Gustafsson PA, Anlen AS, Lannestrom G, Nilsson M, Rolling G. Group-therapy for children of alcoholics. Nord J Psychiatry 1995;49:209–15. 676
32. Haight W, Black J, Sheridan K. A mental health intervention for rural, foster children from methamphetamine-involved families: Experimental assessment with qualitative elaboration. Child Youth Serv Rev 2010;32:1446–57. 175
33. Haskett M, Nowlan N, Hutcheson J, Whitworth J. Factors associated with successful entry into therapy in child sexual abuse cases. Child Abuse Negl 1991;15:467–76. 657
34. Hill A. Combining professional expertize and service user expertize: negotiating therapy for sexually abused children. Br J Soc Work 2009;39:261–79. 670
35. Horowitz L, Putnam F, Noll J, Trickett P. Factors affecting utilization of treatment services by sexually abused girls. Child Abuse Negl 1997;21:35–48. 647
36. Hubel G, Campbell C, West T, Friedenberg S, Schreier A, Flood M, et al. Child advocacy center based group treatment for child sexual abuse. J Child Sex Abuse 2014;23:304–25. 492
37. Hyde C, Bentovim A, Monck E. Some clinical and methodological implications of a treatment outcome study of sexually abused children. Child Abuse Negl 1995;19:1387–99. 538
38. Jensen T, Haavind H, Gulbrandsen W, Mossige S, Reichelt S, Tjersland O. What constitutes a good working alliance in therapy with children that may have been sexually abused? Qual Soc Work 2010;9:461–78. 675
39. Kilcrease-Fleming D, Wagner W, Fowler W. Sexually abused girls’ behavior during an initial counseling session. J Fam Violence 1992;7:179–87. 643
40. Kolko DJ. Individual cognitive behavioral treatment and family therapy for physically abused children and their offending parents: a comparison of clinical outcomes. Child Maltreat 1996;1:322–42. 108
41. Kolko D, Selelyo J, Brown E. The treatment histories and service involvement of physically and sexually abusive families: description, correspondence, and clinical correlates. Child Abuse Negl 1999;23:459–76. 644
42. Koverola C, Murtaugh CA, Connors KM, Reeves G, Papas MA. Children exposed to intra-familial violence: predictors of attrition and retention in treatment. J Aggress Maltreat Trauma 2007;14:19–42. 653
43. Laan N, Loots G, Janssen C, Stolk J. Foster care for children with mental retardation and challenging behaviour: a follow-up study. Brit J Dev Disabil 2001;47:3–13. 671
44. Lange A, Ruwaard J. Ethical dilemmas in online research and treatment of sexually abused adolescents. J Med Internet Res 2010;12:e58. 497
45. Leenarts L, Hoeve M, Van de Ven P, Lodewijks H, Doreleijers T. Childhood maltreatment and motivation for treatment in girls in compulsory residential care. Child Youth Serv Rev 2013;35:1041–7. 672
46. Lippert T, Favre T, Alexander C, Cross Theodore P. Families who begin versus decline therapy for children who are sexually abused. Child Abuse Negl 2008;32:859–68. 648
47. McPherson P, Scribano P, Stevens J. Barriers to successful treatment completion in child sexual abuse survivors. J Interpers Violence 2012;27:23–39. 633
48. Mishna F, Morrison J, Basarke S, Cook C. Expanding the playroom: school-based treatment for maltreated children. Psychoanal Soc Work 2012;19:70–90. 661
49. Monck E, Bentovim A, Goodall G, Hyde C, Lwin R, Sharland E, et al. Child Sexual Abuse: A Descriptive & Treatment Study. Studies in Child Protection. London: Her Majesty’s Stationary Office; 1996. 169
50. Murphy RA, Sink HE, Ake GS, Carmody KA, Amaya-Jackson LM, Briggs EC. Predictors of treatment completion in a sample of youth who have experienced physical or sexual trauma. J Interpers Violence 2014;29:3–19. 654
51. Nelson-Gardell D. The voices of victims: surviving child sexual abuse. Child Adolesc Social Work J 2001;18:401–16. 638
52. Osofsky JD, Kronenberg M, Hammer JH, Lederman C, Katz L, Adams S, et al. The development and evaluation of the intervention model for the Florida Infant Mental Health Pilot Program. Infant Ment Health J 2007;28:259–80. 515
53. Overlien C. Women’s refuges as intervention arenas for children who experience domestic violence. Child Care Pract 2011;17:375–91. 674
54. Peled EM, Edleson JL. Multiple perspectives on groupwork with children of battered women. Violence Vict 1992;7:327–46. 639
55. Porter R, Wagner W, Johnson J, Cox L. Sexually abused girls’ verbalizations in counseling: an application of the client behavior system. J Couns Psychol 1996;43:383–8. 645
56. Powell L, Cheshire A. A preliminary evaluation of a massage program for children who have been sexually abused and their nonabusing mothers. J Child Sex Abuse 2010;19:141–55. 662
57. Reddy SD, Negi LT, Dodson-Lavelle B, Ozawa-de S, Pace TWW, Cole SP, et al. Cognitive-based compassion training: a promising prevention strategy for at-risk adolescents. J Child Fam Stud 2013;22:219–30. 176
58. Risser HJ, Schewe PA. Predictors of treatment engagement for young children exposed to violence. J Aggress Maltreat Trauma 2013;22:87–108. 655
59. Rushton A, Miles G. A study of a support service for the current carers of sexually abused girls. Clin Child Psychol Psychiatry 2000;5:411–26. 664
60. Salloum A, Robst J, Scheeringa MS, Cohen JA, Wang W, Murphy TK, et al. Step one within stepped care trauma-focused cognitive behavioral therapy for young children: a pilot study. Child Psychiatry Hum Dev 2014;45:65–77. 504
61. San Diego RJS, Ryan JS. Healing the invisible wounds of trauma: a qualitative analysis. Asia Pac J Counsel Psychother 2011;2:151–70. 680
62. Scott DA. Parental experiences in cases of child sexual abuse: a qualitative study. Child Fam Soc Work 1996;1:107–14. 677
63. Shennum WA, Carlo P. A look at residential treatment from the child’s point of view. Resid Treat Child Youth 1995;12:31–44. 650
64. Silovsky J, Niec L, Bard D, Hecht D. Treatment for preschool children with interpersonal sexual behavior problems: a pilot study. J Clin Child Adolesc Psychol 2007;36:378–91. 505
65. Smith AP, Kelly AB. An exploratory study of group therapy for sexually abused adolescents and nonoffending guardians. J Child Sex Abuse 2008;17:101–16. 506
66. Staines J, Farmer E, Selwyn J. Implementing a therapeutic team parenting approach to fostering: the experiences of one independent foster-care agency. Brit J Soc Work 2011;41:314–32. 667
67. Sudbery J, Shardlow SM, Huntington AE. To have and to hold: questions about a therapeutic service for children. Br J Soc Work 2010;40:1534–52. 663
68. Taban N, Lutzker JR. Consumer evaluation of an ecobehavioral program for prevention and intervention of child maltreatment. J Fam Violence 2001;16:323–30. 635
69. Thompson R, Dancy BL, Wiley TRA, Perry SP, Najdowski CJ. The experience of mental health service use for African American mothers and youth. Issues Ment Health Nurs 2011;32:678–86. 646
70. Timmer S, Sedlar G, Urquiza A. Challenging children in kin versus nonkin foster care: perceived costs and benefits to caregivers. Child Maltreat 2004;9:251–62. 656
71. Tjersland O, Mossige S, Gulbrandsen W, Jensen T, Reichelt S. Helping families when child sexual abuse is suspected but not proven. Child Fam Soc Work 2006;11:297–306. 673
72. West SD, Day AG, Somers CL, Baroni BA. Student perspectives on how trauma experiences manifest in the classroom: engaging court-involved youth in the development of a trauma-informed teaching curriculum. Child Youth Serv Rev 2014;38:58–65. 651
73. Woodworth DL. Evaluation of a Multiple-Family Incest Treatment Program. In Patton M, editor. Family Sexual Abuse: Frontline Research and Evaluation. Thousand Oaks, CA: SAGE Publications;1991. pp. 121–34. 533
Appendix 5 Types of interventions
We identified therapies according to 10 different therapeutic approaches, as summarised below. Detailed descriptions of each approach are also provided.
Cognitive–behavioural therapies:
-
cognitive–behavioural therapy (CBT)
-
behavioural therapies
-
modelling and skills training
-
trauma-focused CBT (TF-CBT)
-
eye movement desensitization and reprocessing (EMDR).
Relationship-based interventions (RBIs):
-
attachment-orientated interventions
-
Attachment and Biobehavioral Catch-up (ABC)
-
parent–child interaction therapy (PCIT)
-
parenting interventions
-
dyadic developmental psychotherapy (DDP).
Systemic interventions:
-
systemic family therapy (FT)
-
transtheoretical intervention
-
multisystemic FT
-
multigroup FT
-
family-based programme.
Psychoeducation
Group work with children
Psychotherapy (unspecified)
Counselling
Peer mentoring
Intensive service models:
-
treatment foster care
-
therapeutic residential/day care
-
co-ordinated care.
Activity-based therapies
-
arts therapy
-
play/activity interventions
-
animal therapy.
Cognitive–behavioural therapies
Cognitive–behavioural therapies are a group of interventions that draw on a number of theories of learning, both to account for, and address a range of, emotional, psychological and behavioural problems. They have a wide application, ranging from addressing health and mental health problems to more interpersonal and social problems, such as social skills deficits and delinquency. As such, they have considerable relevance to the problems associated with child maltreatment. Before describing the core features of a cognitive–behavioural approach, we briefly describe the therapeutic approaches associated with earlier behavioural and social learning theories, as these continue to form important components of complex cognitive–behavioural interventions.
Behavioural therapies
The earliest interventions were essentially behavioural, drawing on operant (instrumental) and classical (respondent) conditioning paradigms of learning, associated, respectively, with BF Skinner and I Pavlov. Operant conditioning focuses on how behaviour changes with changes in the environment, as when a child’s antisocial behaviour increases as a result of adult attention (reinforcement). Classical conditioning focuses on associative learning, whereby a person learns to respond in a particular way (e.g. becoming anxious) to a neutral stimulus (e.g. a place) by dint of the pairing of the neutral stimulus with a traumatic event (e.g. sexual assault, humiliation).
Although now rarely viewed as adequate conceptualisations of human behaviour, operant and classical conditioning continue to inform the interventions required to address complex social and psychological problems, such as those associated with child maltreatment. Strategies drawing on both operant and classical conditioning are used in psychosocial treatments. The most commonly used classical or respondent-based technique is relaxation training. Children are trained to relax in the face of a hitherto stressful stimulus (e.g. a memory of sexual abuse) either as a way of neutralising the impact of the stimulus (where it forms part of an exposure therapy) or as the means of providing an opportunity to practise other ways of coping, such as ‘reframing’ (locating the responsibility for the maltreatment with the perpetrator rather than blaming themselves; practising positive self-talk). Some of the included studies evaluate a purely respondent approach to anxiety management. Operant techniques, such as differential reinforcement (essentially ensuring unwanted behaviour is not reinforced and positively reinforcing prosocial or wanted behaviour) form an important part of interventions that are designed to address the behavioural problems that are often associated with maltreatment, particularly for younger infants and children.
Modelling and skills training
Social learning theory224,241 recognises that we are not simply the product of our environments: we do not simply respond to stimuli – we interpret them. What we think influences what we do and how we respond to other people and events, and our experiences lead us to expect certain outcomes from certain courses of action under certain circumstances. Furthermore, a large proportion of our behavioural repertoire (e.g. our social skills, our ability to problem solve) comes not from simple respondent or operant processes, but by learning from others. We learn how to do things and how to behave by watching other people or via processes of vicarious learning (e.g. by books or verbal instruction). Reinforcement will play a part in determining whether or not we adopt or use certain responses, and some may find it difficult to manage particular situations if they have not had the opportunity to develop the appropriate skills, including social skills. Social learning theory informs our understanding of how certain forms of maltreatment may be associated with the certain outcomes, for example in understanding how witnessing intimate partner violence can exert a ‘modelling effect’ on children, particularly boys, which – in the absence of opportunities to learn alternate ways of managing conflict or frustration (for example) – can lead to intergenerational cycles of violence. 778 The understanding of the importance of modelling and behaviour rehearsal (with feedback and positive reinforcement) is used to inform a number of psychosocial therapies that aim to help individuals find more adaptive ways of responding to situations.
Cognitive–behavioural therapies
In contrast with traditional learning theory, cognitive theories afford the mind a central role in understanding behaviour, and in developing interventions designed to address psychosocial problems. Unlike the behaviour therapies, which emerged from laboratory-based experiments, cognitive therapies developed from clinical practice, largely in the field of depression, and thus predated the empirical data that have subsequently accrued. For example, Beck 1979779 argued that depression resulted from the reciprocal interaction of three things: a negative way of viewing oneself, one’s situation and one’s prospects (cognitive triad), rigid ways of thinking about the world (schema) that often develop early in life or based on the interpretation of prior experience, and which result in negative, automatic thoughts, and biased and erroneous thinking (faulty information processing). It is thought that children who have experienced maltreatment may well develop unhelpful ways of thinking about themselves, their situation and their prospects, which may cause them difficulties or prevent them overcoming associated problems. For example, children who have been maltreated may well blame themselves for what has happened to them; they may have internalised a negative self-image; they may have ‘learned’ that nothing they do can bring about a sought-after outcome (to be loved, thought well of), resulting in poor self-efficacy or indeed depression. Many of the psychosocial interventions designed to address the problems experienced by maltreated children are concerned to influence these cognitive sequelae. Cognitive–behavioural therapies seek to do so quite directly by helping individuals to identify maladaptive beliefs and ways of thinking, to challenge them (reality testing) and to replace them with more realistic and positive ways of thinking.
Trauma-focused cognitive–behavioural therapy
Trauma-focused CBT (TF-CBT) is a manualised intervention developed by Cohen, Mannarino and Deblinger. 267 TF-CBT directly addresses traumatic symptoms, alongside other components that are typical of CBT interventions, such as coping skill training and symptom management, cognitive restructuring and gradual exposure. However, key differences are a greater focus on graded exposure, creating an appropriate account of the trauma [a trauma narrative (TN)] and cognitive processing of experiences. This focus builds on findings from research that support a model of trauma in which traumatic memories and related symptoms are maintained by cognitive biases and avoidance strategies. The TN component aims to address this in order to reduce symptomology and process traumatic memories. 100 TF-CBT combines joint child–parent sessions and individual sessions for both child and non-offending parents. Parent involvement provides opportunities to address misperceptions and to validate parental reactions to their child’s traumatic experiences, to train parents to support their child’s therapeutic work and to provide a supportive environment at home (e.g. the studies by Cohen et al. 95,96 and Cohen and Mannarino93).
Eye movement desensitisation and reprocessing
We identified two controlled studies (both randomised trials) of EMDR. EMDR is a manualised intervention developed by Shapiro et al. 690 Because its core features combine strategies from the learning theories outlines above, we have included it in the group of cognitive–behavioural interventions. EMDR involves the identification and processing of traumatic memories using bilateral stimulation, desensitisation through imaginal exposure, and challenging and replacing maladaptive beliefs about the trauma. The information processing model suggests that this helps to process traumatic memories into long-term memory, thereby reducing trauma-related symptoms, such as hypervigilance, as well as replacing unhelpful beliefs, related to the trauma, with more adaptive ones. 120
Relationship-based interventions
Attachment-orientated Interventions
Attachment describes an infant’s strong disposition ‘to seek proximity to and contact with a specific figure and to do so in certain situations, notably when . . . frightened, tired, or ill’. 780 It is a behavioural system that is a product of human evolution, designed to trigger protection in the face of perceived danger and to alleviate its associated response, fear. Most infants develop an attachment to their primary carers, and, for most infants, the relationship with the mother is the first intimate relationship in which they engage. From these attachment relationships children start to form a sense of who they are, what they can expect from others, and what behaviour it is useful or dangerous to engage in. Infants whose primary carer provides sensitive and responsive care develop what is called a secure attachment. Carer sensitivity and responsiveness to their infant’s needs helps to ‘shape their physiological regulation and biobehavioral patterns of response’ (p. 624),123 and, as infants develop a secure attachment (sometime towards the end of their first year), they use that attachment and associated feelings as a secure base from which to explore their worlds.
Emotional and physical neglect or abuse, and exposure to violence, can result in insecure attachments or sometimes disorganised attachments, which, if unresolved, will contribute to a wide range of problems in later development, including poor socioemotional development, self-regulation difficulties, maladaptive behaviour, sleep disturbance, language delays, poor peer relationships, school underachievement, and psychopathology and delinquency in later life. 130,781,782 It has also been associated with a disturbed hypothalamic–pituitary–adrenal axis, which is important for self-regulation and stress management. 124 Disorganised attachment styles develop when children are emotionally and physically depending on someone who is also a source of fear and anxiety. Unsurprisingly, disorganised attachments styles are prevalent among children living in families in which there is child maltreatment, parental depression, parental history of loss or trauma, parental dissociation, parental frightening behaviour or marital discord. 783 The cascade of negative outcomes associated with a disturbed attachment has been referred to as ‘toxic stress’. 784
There is a sizeable literature focused on interventions that are designed to promote maternal sensitivity and responsiveness (see van Ijzendoorn et al. 783). In this review, we included only those interventions that specifically focused on families when maltreatment was deemed to be an issue. Although these interventions might arguably also be viewed as secondary prevention (and therefore not appropriate for this review), the nature of attachment is such that interventions designed to promote secure attachments inevitably focus on the primary caregiver. Given the significant impact on subsequent development, these interventions were judged to meet the inclusion criteria of a psychosocial intervention dealing with the adverse consequences of maltreatment for children.
Attachment interventions generally involve caregiver–infant sessions, and aim to enhance parental sensitivity to emotional and behavioural cues in order to improve a child’s attachment security (e.g. Moss et al. 130). This may involve child development training, parenting skills, coping strategies, developing social support networks, enhancing the caregiver’s capacity to provide safety, child–caregiver joint narrative of trauma experiences, addressing negative maternal representational models in the parent–child interaction, providing a corrective emotional experience for caregivers or addressing a caregiver’s own attachment difficulties stemming from childhood. 123,124,127–130 In attachment-based interventions, the focus of the intervention is not the caregiver or the child but rather the caregiver–child relationship. 785 This relationship is used as a vehicle to address a child’s emotional, cognitive and social functioning difficulties. 127–129
Attachment and biobehavioral catch-up
Attachment and Biobehavioral Catch-up (ABC) is informed by both attachment theory780 and neurobiology. 125,126 ABC focuses specifically on disorganised attachment styles, which are associated with frightening or frightened parental behaviour rather than purely a lack of attunement or insensitivity by the parent. 122 This form of attachment has been found to mediate disrupted maternal behaviour and children’s behavioural difficulties and dysregulation. 786 Children’s behavioural level and biobehavioural level dysregulation is characterised by externalising behaviour problems, conduct difficulties and disrupted cortisol patterns (which are associated with stress reactivity). 125,126
Attachment and Biobehavioral Catch-up (ABC) is a manualised didactic intervention which was designed to decrease parental frightening behaviour and increase parental sensitivity. 787 In contrast with more general attachment-based interventions, the focus of ABC is on parental behaviour change rather than changing parental internal representations. 122 The aim of the intervention is to help children learn self-regulatory skills by changing the way parents interpret their children’s behaviour, over-riding their own issues that interfere with their caregiving and providing an enabling environment for developing self-regulation skills. 125,126
Parent–child interaction therapy
Parent–child interaction therapy (PCIT) was developed by Sheila Eyberg. 222 PCIT draws on the work of Diana Baumrind (on parenting styles), as well as attachment theory and learning theory. In its original form it was designed to help parents to establish a secure and nurturing relationships with their child, and enhance prosocial behaviour while decreasing undesirable behaviour. Unlike parent training, PCIT involves in vivo child–parent dyadic sessions in which parents are taught behaviour management techniques, often being coached through a one-way mirror. 138 To an extent, PCIT resembles a behavioural version of play therapy [Children’s Depression Inventory (CDI)] and behavioural parent training (parent-directed interaction).
Most studies of PCIT seek to minimise the risk of maltreatment or future maltreatment and secure children’s well-being by promoting nurturing parenting and reducing those parental practices that have been linked to maltreatment and attachment disorders, such as inappropriate discipline, coercive cycles of behaviour and negative communication. 137,788
Dyadic developmental psychotherapy
Dyadic developmental psychotherapy (DDP) is designed to address the impairments associated with attachment disorders and complex childhood trauma. 789,790 The intervention uses the child–therapist relationship to establish a relational context in which the child can learn how to engage with, and benefit from, relationships with others. The therapist seeks to establish a relationship that mirrors the general principles characteristic of parent–child relationships that facilitate secure attachments, for example attunement, reflecting back to the child his/her subjective experiences (including the trauma s/he has experienced) and helping him/her to make sense of these ‘with acceptance, curiosity and empathy’. In the same way that attachments develop as a result of experience (preverbally), DDP emphasises the importance of healing experiences. In order to benefit from DDP, children need to be in a safe and secure environment (at home or in substitute care) and parents (or carers) are active participants in the therapy, either being with the child in the sessions or watching the therapy through a one-way mirror. 791
Child–parent psychotherapy
Child–parent psychotherapy (CPP) is a home-based, manualised intervention provided on a weekly basis for 1 year by trained master’s level therapists. 124 It is described as a ‘supportive, non-directive, and nondidactic’ intervention that ‘includes developmental guidance based on the mother’s concerns’ (p. 794). 124 When children are aged ≤ 1 year, this therapy is referred to as Infant–Parent Psychotherapy; when they are older, the intervention is called, alternately, Pre-School Parent Psychotherapy or Toddler–Parent Psychotherapy.
Parenting interventions
In general, parent training interventions aim to change unhelpful or maladaptive parenting practices in order to improve child development and well-being. As such, most parenting programmes that address maltreatment are concerned with secondary prevention, but we found three studies114,139,140 with a specific focus on improving outcomes for children who have been exposed to maltreatment, and these studies were included. One study114 evaluated the effectiveness of a parenting programmes designed to help foster parents and parents to co-parent children in foster care, with a view to ameliorating the child behaviour problems associated with, and return the children to, the care of their biological parents. A second assessed the impact of training maltreating mothers in elaborative and supportive reminiscing about positive and negative everyday past events with young children, as a means of addressing multiple sequelae of maltreatment. 140 The third specifically examined the impact of the Webster-Stratton IY programme on children’s autonomy, as well as positive parenting, recognising that autonomy is an important subjective state and a critical behaviour acquired in the early years, and which is related to the quality of parenting. 139
Systemic interventions
Systems theory posits that individuals are embedded in, and influenced by, a number of interacting systems, including – most importantly – the family. Within systems theory, the problems affecting an individual are conceptualised as a function of the relationships and patterns of interaction that surround him or her, with the resulting implication that effective interventions necessitate locating individual problems within that context and – in many circumstances – directing intervention at the family, rather than simply the individual. Systemic analyses can also be applied to other social systems, such as wider family networks, groups or organisations. Given the inclusion criteria, systemic interventions were included only when they directly focused on ameliorating the consequences of maltreatment for the children in the family (as opposed to halting it and creating a supportive family system that was capable of promoting optimal child development).
Systemic family therapy
There are many forms of FT,792 most of which are informed primarily by structural family systems theory793 and drawing on a wide range of techniques from other interventions, such as CBT. This can make assessing its effectiveness quite challenging, as some forms of therapy are essentially systems-focused cognitive–behavioural interventions.
Multisystemic therapy
Multisystemic therapy (MST) is a short-term, multifaceted intervention for children and young people with serous psychosocial and behavioural problems. It differs from FT in that it includes a combination of multiple systems in the treatment focus, such as family, peers, school, neighbourhood or community. Consistent with social ecological theories of human development, this broader focus is based on the view of the programme developers – that children’s difficulties are caused and maintained by multiple factors within these systems and their interaction. The intervention therefore focuses on identifying and targeting these factors in order to reduce symptoms and distress142,794 and promote health.
Psychoeducational interventions
At the heart of psychoeducational interventions is the view that helping people to understand how their problems have arisen and how they are maintained is an important first step in empowering them to address those problems. Information or education is therefore at the heart of psychoeducational interventions. It may include information about available resources that people might access and direct instruction on coping strategies or change strategies. The educational component is often combined with other activities designed to support change, and psychoeducational interventions are often run in group formats in order to enable the modelling of acceptable behaviour, modifying of inappropriate behaviour and the development of social competencies. 152
Group work with children
Group psychotherapies (or therapeutic groups) are interventions in which the group format is central. The group itself is deemed to be ‘therapeutic’, providing a number of essential components, such as a feeling of universality, reducing isolation, extending social networks, social skills practice, healthy relationship building170 and normalising. 171
The interventions’ group content includes psychoeducation, as well as skills training and experiential learning. This may include assertiveness training, narrative therapeutic activities, such as storytelling169 or body image and self-esteem enhancement. 170 Many of these interventions are based on social learning theory. 169
Psychotherapy/counselling
Common to all psychotherapeutic interventions that address individual, familial and community-level issues, is a non-judgemental, insight-orientated approach with a strong focus on the therapeutic alliance795 and dynamic relational processes with therapists or group members. Using these processes to work through past and current relationships, losses and disruptions, is thought to address underlying psychological processes in relation to traumatisation and to enable long-term change. 155 Many the studies we identified provided only very general descriptions of these talking-based therapies (such as ‘psychotherapy’ or ‘counselling’), often with little or no information on the underpinning theory of the approach used.
Peer mentoring
Peer mentoring aims to help those children whose social functioning has been adversely affected by maltreatment to acquire key developmental skills, namely the ability to form and maintain effective peer relationships. Maltreated peers with high levels of prosocial behaviour are paired with withdrawn maltreated children and trained to involve them in their play.
Intensive service provision
Treatment foster care
Enhanced Foster Care is designed specifically to meet the developmental, social and emotional needs of children in foster care with particularly challenging behaviour. A multidisciplinary team works with specially trained foster parents to reduce behavioural difficulties, increase regulatory abilities and increase a young person’s secure attachment-related behaviour through a consistent and predictable environment. It involves high rates of positive reinforcement for desirable behaviours, clear limit setting, 24-hour crisis intervention for foster parents, support groups for foster parents, group therapeutic support for children and FT for relationships with biological family. 183
Therapeutic residential/day care
Like milieu therapy, therapeutic residential care entails creating a nurturing, stable and consistent environment and a predictable routine for children and young people who need specialist help, and whose problems make it difficult to provide that help in any other way. Indeed, for some maltreated children their experiences of maltreatment, combined with adverse care experiences, may mean they cannot be managed in substitute home-based care settings, such as adoption and fostering. A variety of specific interventions are used in the therapeutic residential care studies included in this review, among which are therapeutic parenting, life story work,553 trauma-focused psychological therapy,551 addressing cognitive distortions, improving impulse control, social skills training, risk management, sex education and behaviour modification,557 as well as preparation for independence for older adolescents. 562
Therapeutic day programmes aim to meet the developmental needs of children in terms of fine motor, language, and social and emotional skills. 559 Therapeutic day programmes are held in classroom environments and usually run intensively over numerous full days per week. The programmes can include milieu therapy (see below), developmentally appropriate play and activities, structured interaction, individual and parent counselling, and education services, within a psychologically safe environment that is consistent and predictable. 195,196,558,563
Milieu therapy is a therapeutically planned approach to a residential or day-care environment that is designed to provide a safe environment in which adults can assist children to address the consequences of maltreatment. Safety, containment, structure, support, involvement and validation are key therapeutic activities. Like therapeutic communities (the terms are sometimes used interchangeably), the aim is to provide a safe, nurturing environment that can engage the ‘whole child’ in processes of psychological change. Through multiple and repeated experiences that are carefully controlled (safe), children can learn about their behaviour and how to discuss distressing feelings and find alternative ways of expressing these. They can develop their self-esteem, learn to trust others, and learn to negotiate relationships and to acquire problem-solving skills. Milieu therapy draws on a range of theoretical frameworks, including attachment theory and object relations theory. Staff use their understanding of transference and countertransference to identify how a child’s feelings and behaviour towards others reflect those with parents, siblings and significant others in their lives, and use this to facilitate change.
Co-ordinated care
Co-ordinated care refers to interventions designed to provide a single point of entry to services, combined with a seamless system of service delivery. It has much in common with initiatives designed to improve interagency working. It is designed to address some of the weaknesses that are inherent in a reliance solely on case management.
Activity-based therapies
Arts therapy
Children who have been maltreated can find it difficult to verbalise their experience, and may feel intimidated by the therapeutic environment and overwhelmed by the verbalisation of abuse experiences. Using a variety of media – such as paint, clay, photos, poems, storytelling or music – arts-based therapies are thought to help facilitate the non-verbal and verbal expression of thoughts, feelings and life narratives. In this way, arts can provide a non-verbal medium for therapeutic communication and cognitive processing for children for whom verbal forms of therapy are not possible. It can help to bridge the gap between the internal world and the limitations of verbal language, particularly in latency age children,199 and provide a mode of communication for children who are unwilling or unable to talk about what has happened to them. 200
Play/activity interventions
Play or activity interventions, depending on the age of the target population, are based on the premise that play and activity are vital for healthy development. Play therapy views play as a ‘natural medium in which children express themselves’ (p. 28). 576 It therefore provides a way to communicate complex ideas that would be otherwise difficult, through verbal means and helps children make sense of their internal and external worlds. 576 Furthermore, deficits in imaginative play have been observed in children who have experienced maltreatment that have been negatively associated with positive affect, peer interaction and problem-solving. 203 Activity-based interventions, such as sports or game based interventions, view activity as an appropriate medium for adolescents because it is more enjoyable than one-to-one office-based therapy, requires the development of social skills and peer relations, has physiological benefits through physical exercise and requires cognitive skills, such as impulse inhibition and planning. 201
Interventions included under this category are those identified by the author as imaginative play training, challenge/initiative games and the sports-based intervention ‘Do the Good’.
Animal therapy
Animal therapy (or animal-assisted therapy) uses animals as part of the therapeutic process. Animals (from dogs through to horses) are used to assist with the therapeutic process and strengthen treatment strategies. They are thought to aid the therapeutic environment through the provision of warmth, acceptance, empathy and unconditional love. 204 Animal therapy is based on research that has found that the presence of animals has improved the communication skills of children participating in therapy, lowered anxiety while undergoing therapy and improved motivation for therapy, as well providing opportunities to teach boundaries and appropriate touch in maltreated populations. 205
Appendix 6 List of databases searched, with dates
| Cochrane Central Register of Controlled Trials (CENTRAL) | Issue 4 of 12 April 2014 |
| Ovid MEDLINE | 1946 to May Week 3 2014 |
| EMBASE (Ovid) | 1980 TO 2014 Week 21 |
| Cumulative Index to Nursing and Allied Health Literature (CINAHL Plus) (EBSCOhost) | 1937 to current |
| PsycINFO (Ovid) | 1967 to May Week 4 2014 |
| Science Citation Index Expanded (SCIE) and Social Sciences Citation Index (SSCI) (Web of Science) | 1970 to 28 May 2014 |
| Social Care Online | All available years |
| Social Services Abstracts (ProQuest) | 1979 to current |
| Education Resources Information Centre (ERIC) (ProQuest) | 1966 to current |
| British Education Index (ProQuest) | 1975 to current |
| Australian Education Index (ProQuest) | 1977 to current |
| Health Technology Assessment (HTA) database | Issue 2 of 4, 2014 |
| Health Management Information (HMIC) Consortium (Ovid) | 1979 to March 2014 |
| Trials Register of Promoting Health Interventions (TRoPHI) | All available years |
| EconLit (EBSCOhost) | 1886 to current |
| NHS Economic Evaluation Database (NHS EED) | Issue 2 of 4, 2014 |
| Health Economic Evaluations Database (HEED) | All years |
| Paediatric Economic Database Evaluation (PEDE) | 1980 to 2012 |
| IDEAS | All available years |
| The Campbell Library | All available years |
| Database of Promoting Health Effectiveness Reviews (DoPHER) | All available years |
| Database of Abstracts of Reviews of Effects (DARE) | Issue 2 of 4 April 2014 |
| Cochrane Database of Systematic Reviews (CDSR) | Issue 5 of 12 May 2014 |
Appendix 7 Other searches
| Resource | Website | Searcher |
|---|---|---|
|
www.mentalhealth.org.uk/ | DG |
|
www.barnardos.org.uk/ | NW |
|
www.carersuk.org/ | GM |
|
www.childline.org.uk | NL |
|
www.childrenssociety.org.uk/ | RC |
|
www.depressionalliance.org/ | RCh |
|
www.mind.org.uk/ | HF |
|
www.anxietyuk.org.uk/ | NL |
|
www.nspcc.org.uk/ | RC |
|
www.carers.org/ | NL |
|
www.sane.org.uk/ | NL |
|
www.thesite.org/ | NL |
|
www.turning-point.co.uk/ | MC |
|
www.youngminds.org.uk/ | SB |
|
www.nctsn.org/ | NL |
|
www.opengrey.eu/ | SA |
|
www.google.com | All |
Appendix 8 Checklist: quality of data within economic evaluations
Drummond’s checklist for the critical appraisal of economic evaluations
1 Was a well-defined question posed in answerable form?
1.1 Did the study examine both costs and effects of the service(s) or programme(s)?
1.2 Did the study involve a comparison of alternatives?
1.3 Was a viewpoint for the analysis stated and was the study placed in any particular decision-making context?
2 Was a comprehensive description of the competing alternatives given ( i.e. can you tell who, did what, to whom, where and how often )?
2.1 Were any important alternatives omitted?
2.2 Was (Should) a do-nothing alternative (be) considered?
3 Was the effectiveness of the programmes or services established?
3.1 Was this done through a randomised controlled clinical trial? If so, did the study protocol reflect what would happen in regular practice?
3.2 Was effectiveness established through an overview of clinical studies (systematic review/meta-analysis)?
3.3 Were observational data or assumptions used to establish effectiveness? If so, what are the potential biases in results?
4 Were all the important and relevant costs and consequences for each alternative identified?
4.1 Was the range wide enough for the research question at hand?
4.2 Did it cover all relevant viewpoints? (possible viewpoints include the community or social viewpoint, and those of patients and third-party payers)
4.3 Were capital costs, as well as operating costs, included?
5 Were costs and consequences measured accurately in appropriate physical units ( e.g. hours of nursing time, number of physician visits, lost work days, gained life-years )?
5.1 Were any of the identified items omitted from measurement? If so, does this mean that they carried no weight in the subsequent analysis?
5.2 Were there any special circumstances (e.g. joint use of resources) that made measurement difficult? Were these circumstances handled appropriately?
6 Were costs and consequences valued credibly?
6.1 Were the sources of all values clearly identified? (possible sources include market values, patient preferences and views, policy-makers’ views and health professionals’ judgements)
6.2 Were market values employed for changes involving resources gained or depleted?
6.3 Where market values were absent (e.g. volunteer labour), or market values did not reflect actual values (such as clinic space donated at a reduced rate), were adjustments made to approximate market values?
6.4 Was the valuation of consequences appropriate for the question posed (i.e. has the appropriate type or types of analysis – cost-effectiveness, cost–benefit, cost–utility – been selected)?
7 Were costs and consequences adjusted for differential timing?
7.1 Were costs and consequences that occur in the future ‘discounted’ to their present values?
7.2 Was any justification given for the discount rate used?
8 Was an incremental analysis of costs and consequences of alternatives performed?
8.1 Were the additional (incremental) costs generated by one alternative over another compared with the additional effects, benefits, or utilities generated?
9 Was allowance made for uncertainty in the estimates of costs and consequences?
9.1 If data on costs or consequences were stochastic, were appropriate statistical analyses performed?
9.2 If a sensitivity analysis was employed, was justification provided for the ranges of values (for key study parameters)?
9.3 Were study results sensitive to changes in the values (within the assumed range for sensitivity analysis, or within the CI around the ratio of costs to outcomes)?
10 Did the presentation and discussion of study results include all issues of concern to users?
10.1 Were the conclusions of the analysis based on some overall index or ratio of costs to consequences (e.g. cost-effectiveness ratio)? If so, was the index interpreted intelligently or in a mechanistic fashion?
10.2 Were the results compared with those of others who have investigated the same question? If so, were allowances made for potential differences in study methodology?
10.3 Did the study discuss the generalisability (external validity) of the results to other settings and patient/client groups?
10.4 Did the study allude to, or take account of, other important factors in the choice or decision under consideration (e.g. distribution of costs and consequences, or ethical issues)?
10.5 Did the study discuss issues of implementation, such as the feasibility of adopting the ‘preferred’ programme given existing financial or other constraints, and whether any freed resources could be redeployed to other worthwhile programmes?
Appendix 9 Outcome domains and measures used
Primary outcome domains
Psychological distress/mental health
-
Adult Self-Esteem Profile (adapted from the ASEP). 435
-
Anxiety Disorders interview Schedule DSM-IV. 290
-
Avoidance Symptoms (Impact of Events Scale; IES). 279
-
Behavioral and Emotional Rating Scale (BERS). 410
-
Brief Infant Toddler Social and Emotional Assessment (BITSEA). 352
-
Child Attachment: Ainsworth Strange Situation Procedure. 336
-
Child Post Traumatic Stress Reaction Index French version). 416
-
Child post-traumatic stress disorder (PTSD) Symptom Scale – Interview. 287
-
Child PTSD Symptom Scale. 286
-
Child Report of Post-traumatic Symptoms (CROPS). 288
-
Child Witness to Violence Questionnaire (CWVQ). 156
-
Childhood Trauma Questionnaire. 796
-
Children’s Apperception Test. 478
-
Children’s Attributions and Perceptions Scale (CAPS). 270
-
Children’s Impact of Traumatic Events Scale (Wolfe and Gentile, 1991, unpublished). Children’s Impact of Traumatic Events Scale-Revised (CITES-R; Wolfe and Gentile, 1991). 414
-
Children’s Knowledge of Abuse Questionnaire (CKAQ). 411
-
Clinician Administered PTSD Scale for Children and Adolescents (CAPS-CA). 305
-
Coopersmith Self-Esteem Inventory. 436
-
Cortisol.
-
Difficulties with Emotion Regulation Scale (DERS). 446
-
Emotional Regulation Bayley-III. 354
-
Expectations Test. 327
-
Family Inventory of Life Events and Changes. 373
-
Fear Survey Schedule for Children-Revised. 255
-
Fear Thermometer for Sexually Abused Children. 291
-
Global functioning (Children’s Global Assessment Scale, CGAS). 261
-
Global Severity Index of the Brief Symptom Inventory. 380
-
Health of the Nation Outcome Scales for Children and Adolescents. 382
-
Impact of Events Scale (intrusive thoughts and avoidant thoughts; IES). 279
-
Kiddie Schedule for Schizophrenia and Affective Disorders (KSADS). 268,797
-
McCarthy Scales of Children’s Abilities. 285
-
Mood and Feelings Questionnaire. 694
-
Multidimensional Anxiety Scale for Children. 283
-
Number of placement changes.
-
Offer Self-Image Questionnaire-Revised. 440
-
Parental Support Questionnaire (PSQ). 273
-
Penn Inventory for Posttraumatic Stress Disorder. 334
-
Perceived Competence and Social Acceptance Scale. 467
-
Piers–Harris Children’s Self-Concept Scale. 475
-
Post-traumatic Stress Disorder Interview. 331
-
Posttraumatic Stress Diagnostic Scale. 397
-
Preschool Symptom Self-report. 263
-
PTSD Subscale. 295
-
Randolph Attachment Disorder Questionnaire. 364
-
Reabuse/Abuse.
-
Revised Children’s Manifest Anxiety Scale (RCMAS). 256
-
Rosenberg Self-Esteem Scale. 404
-
Self-Perception Profile for Children (SPPC; 8- to 12-year-old version). 413
-
SPPC. 413
-
Self-Perception Profiles for Children and Adolescents (adapted). 448
-
Self-Rating Depression Scale (SDS). 798
-
SDS. 798
-
Self-representation scores (MacArthur Narrative Coding Manual-Rochester Revision, Robinson, Mantz-Simmons and Macfie, 1996, unpublished).
-
Self–Other Four Immeasurables Scale (SOFI). 444
-
Semistructured Interview for Diagnostic Classification. 343
-
Sexual Abuse Fear Evaluation (SAFE) scale (Wolfe VV, Wolfe DA. University of Western Ontorio, London, ON, 1989, unpublished questionnaire).
-
Shame Questionnaire (Feiring). 284
-
Short Center for Epidemiologic Studies Depression Scale. 369
-
State-Trait Anxiety Inventory for Children. 799
-
Strengths and Difficulties Questionnaire (SDQ). 308
-
Subjective wellbeing.
-
Tennessee Self-Concept Scale (Roid). 335
-
The Preschool Separation–Reunion Procedure unpublished.
-
The Screen for Child Anxiety Related Disorders. 106
-
Trauma Symptom Checklist for Children (TSCC). 325,383,415,452,473,800
-
Treatment Outcome Questionnaire. 142
-
University of California Los Angeles PTSD Index for Diagnostic and Statistical Manual of Mental Disorders. 374
Behaviour (particularly internalising and externalizing behaviours)
-
Attitudes About Family Violence (AAFV). 394
-
Bayley Infant Behavior Record. 451
-
Behavior Assessment System for Children. 365
-
Behavior Problem Checklist. 438
-
Behavior Problem Checklist-Revised. 438
-
BERS. 410
-
Brigance Diagnostic Inventory of Early Development. 456
-
Child Behavior Checklist (CBCL). 257,260,269,294,297,309,344,349,353,418,706,707,720,724,736
-
Child Behaviour Characteristics Questionnaire (Mother’s perceptions of child’s behaviour).
-
Children’s Action Tendency Scale. 385
-
CAPS. 270
-
Cognitive Mediators of Aggression Questionnaire. 427
-
Early Childhood Inventory (behaviour problems). 462
-
ECI. 462
-
Functional Assessment of Self-Mutilation. 443
-
Global functioning (KGAS). 405
-
Hostility (Children’s Hostility Inventory). 301
-
Inventory of Callous and Unemotional Traits-Parent Report. 447
-
McCarthy Scales of Children’s Abilities. 285
-
Miller Behaviour Style Scale. 277
-
Parent and Therapist Perceptions of Adjustment (devised by author). 119
-
Parent Daily Report. 458
-
Parent, social worker and self-report of problem/delinquent behaviours.
-
Preschool Behavior Questionnaire. 455
-
Risky Sexual Behaviour (n sexual partners in previous 3 months plus any diagnosis of sexually transmitted infection).
-
Rutter Teacher Scale. 289
-
Self-Injurious Behavior Questionnaire (Sadovsky, unpublished).
-
Semi-Structured Interview for Diagnostic Classification DC: 0-3 for Clinicians, Traumatic Stress Disorder. 343
-
Shapiro Control Inventory (SCI). 428
-
Social Behavior Inventory (SBI). 327
-
SDQ. 308
-
Sutter–Eyberg Student Behaviour Inventory-Revised. 311
-
Symptom Checklist-90-Revised (Post traumatic symptom scale). 278
-
Visual analogue scales (used to gauge improvement). 116
-
Weekly Behaviour Record. 91
-
Youth Outcomes Questionnaire. 424
Social functioning, including attachment and relationships with family and others
-
Adolescent Interpersonal Competence Questionnaire (AICQ). 409
-
BITSEA. 352
-
Child’s Attitude to Mother (CAM) and Child’s Attitude to Father (CAF) questionnaires. 422
-
CAPS. 270
-
Children’s Global Assessment Scale. 261
-
CHI. 301
-
Conflict in Adolescent Dating Relationships Inventory (CADRI). 407
-
Dyadic Parent–Child Interaction Coding System II (DPICS-II). 701,702,801
-
Family Adaptability and Cohesion Scale II. 389
-
Family Assessment Device. 711
-
Family Assessment Form (FAF). 390
-
Family Relations Test. 739
-
Friendship Questionnaire. 300
-
Global Assessment Functioning Scale, APA 1987. 296
-
Global functioning (KGAS). 261
-
Index of Peer Relations. 386
-
Indicator of Parent-Child Interaction. 351
-
Interactive peer play observational coding system. 181
-
Level of Moral Reasoning. 429
-
McCarthy Scales of Children’s Abilities. 285
-
Parent Attachment Diary. 697
-
Parent-Child Conflict Tactics Scale (CTSPC). 302
-
Parenting Social Support Index. 387
-
Peer Play Interactive Checklist (PPIC). 457
-
Personal Safety Questionnaire. 412
-
Preschool Social Skills Rating System (SSRS). 144
-
Randolf Attachment Disorder Questionnaire. 364
-
SCI. 428
-
Sibling Interaction Quality (unpublished).
-
SBI. 327
-
Social Competence Scale (Conduct Problems Prevention Research Group). 395
-
SSRS (Parent functioning). 379
-
Social Support Factor Score [derived from principal components factor analysis of scales scores from ‘The People in My Life-Short Form’]. 460
-
Social Support Questionnaire. 281
-
SDQ. 308
-
Toddler-Attachment Sort-45. 350
-
‘What If’ Situations Test. 276
Cognitive/academic attainment
-
Anatomy/Physiology Sexual Awareness Scale. 173
-
Cognitive Mediators of Aggression Questionnaire. 427
-
Guilford’s Unusual Uses Test. 477
-
McCarthy Scales of Children’s Abilities. 285
-
Peabody Picture Vocabulary Test-Third Edition. 441
-
Problem-Solving Inventory. 388
-
Wechsler Preschool and Primary Scale of Intelligence-Revised. 363
Quality of life
-
Life Satisfaction Survey. 402
Secondary outcome domains
Substance misuse
Delinquency
-
Juvenile and court reports.
-
Parent, social worker and self-report of problem/delinquent behaviours.
Resilience
-
Children’s Hope Scale. 445
-
Coping Questionnaire for Sexually Abused Children. 103
-
Coping Scales Inventory (Positive and Negative Coping scales). 459
-
Coping with stressful life events (ask participants to rate their perception of coping with daily life on a five-point Likert scale).
-
Empowerment Scale (23-item). 421
-
Self-Report Coping Scale. 425
-
Ways of Coping Questionnaire. 420
Acceptability
-
Brief Client Satisfaction Inventory. 161
-
Child Feedback Questionnaire (developed by University of Manitoba to assess acceptability of treatment). 659
-
Client Satisfaction Questionnaire Treatment. 321
-
Expectancy of Therapeutic Outcome for Adolescents (Enhanced Outpatient Treatment Assessment, EOT-A).
-
Parent Feedback Questionnaire (developed by University of Manitoba to assess acceptability of treatment).
-
PSQ. 273
-
Treatment Evaluation Inventory. 323
Other outcome domains
Parent/carer outcomes
-
Adults SSQ (Mothers). 403
-
Alabama Parenting Questionnaire (Frick PJ, University of Alabama, Tuscaloosa, AL, 1991, unpublished).
-
Brief Symptom Inventory (BSI). 380
-
Child Abuse Potential Inventory (CAPI). 366
-
Child Caregiver Interviewer Impressions Form (Parenting strategies). 461
-
CAPS-CA. 346
-
Life Stressor Checklist-Revised. 345
-
Maternal Sensitivity: Maternal Behaviour Q-Set. 339
-
Mother’s perceived quality of life (nine-item scale adapted from Andrews and Withey). 402
-
Parent Daily Report (parental stress measure). 458
-
Parent Emotional Reaction Questionnaire. 273
-
Parenting Practices Questionnaire (PPQ). 274
-
Parent Report of Post-traumatic Symptoms. 288
-
CTSPC. 302
-
Parental Attribution Scale. 803
-
Parental Problem Solving. 388
-
Parental Reaction to Incest Disclosure Scale. 262
-
Parenting Daily Hassles Scale. 319
-
Parenting Sense of Competence Scale. 318
-
Perceptions of Adult Attachment Scale. 338
-
Raising a Baby (Kelly JF, Korfmacher J. University of Washington, Seattle, WA, unpublished).
-
Revised Conflict Tactics Scale (CTS-R). 398
-
The Conflict Checklist. 370
-
The Parent Feedback Questionnaire (developed by University of Manitoba to assess acceptability of treatment).
-
The Rosenberg Self-Esteem Inventory (Mothers’ self-esteem). 404
-
This Is My Baby. 359
-
Treatment Evaluation Inventory. 323
-
A subscale of the Emotional Availability Scales. 368
Placement stability
Appendix 10 Risk-of-bias graphs for included randomised trials
FIGURE 23.
Risk-of-bias graph: cognitive–behavioural studies (sexual abuse).

FIGURE 24.
Risk-of-bias summary: cognitive–behavioural studies (sexual abuse).

FIGURE 25.
Risk-of-bias graph: cognitive–behavioural studies (physical abuse).

FIGURE 26.
Risk-of-bias summary: cognitive–behavioural studies (physical abuse).

FIGURE 27.
Risk-of-bias graph: cognitive–behavioural studies (multiple abuse).

FIGURE 28.
Risk-of-bias summary: cognitive–behavioural studies (multiple abuse).
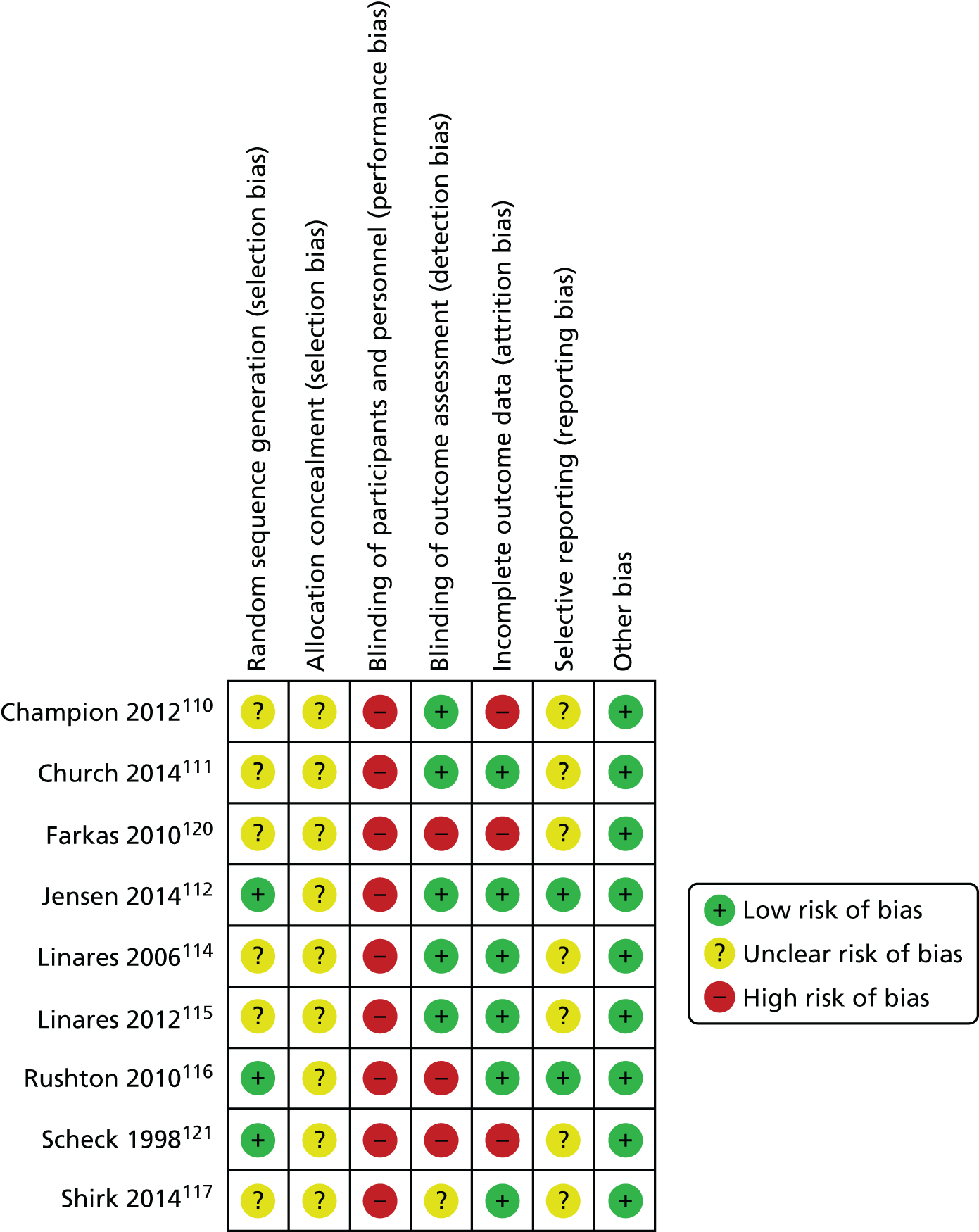
FIGURE 29.
Risk-of-bias graph: RBIs.
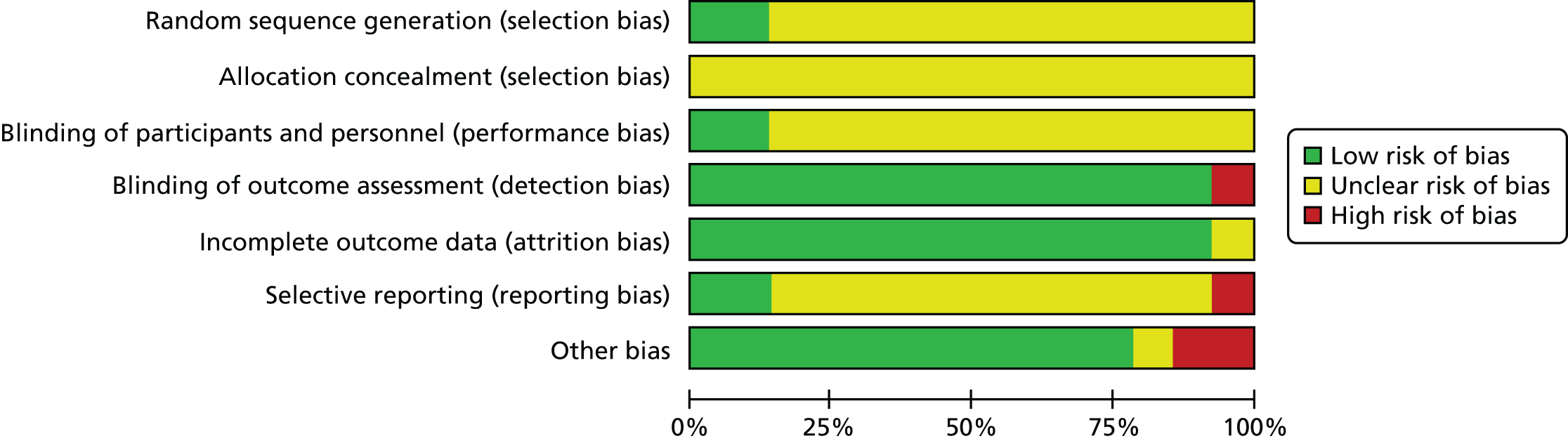
FIGURE 30.
Risk-of-bias summary: RBIs.
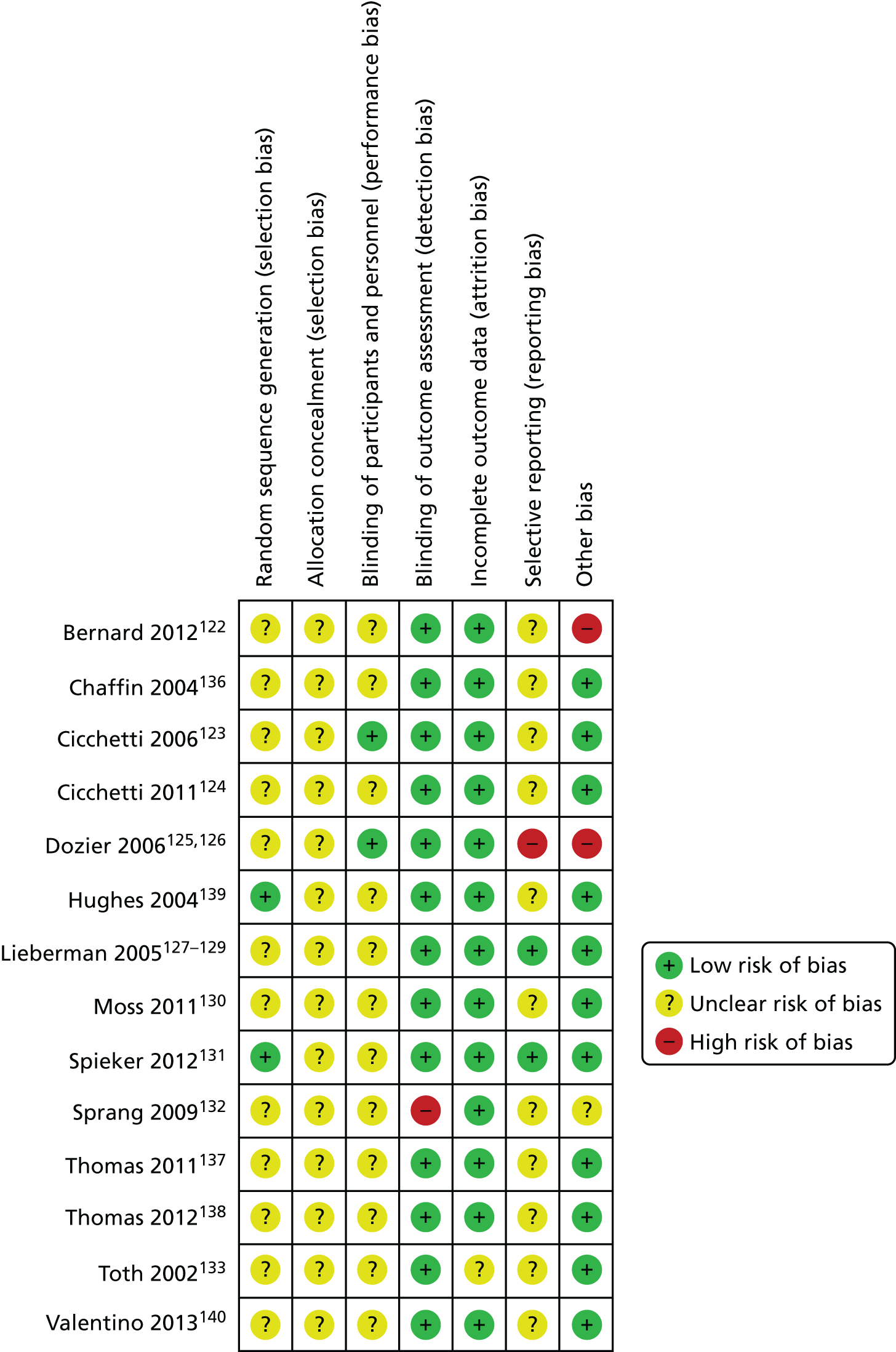
FIGURE 31.
Risk-of-bias graph: systemic interventions.

FIGURE 32.
Risk-of-bias summary: systemic interventions.

FIGURE 33.
Risk-of-bias graph: psychoeducation.

FIGURE 34.
Risk-of-bias summary: psychoeducation.

FIGURE 35.
Risk-of-bias graph: group work with children.
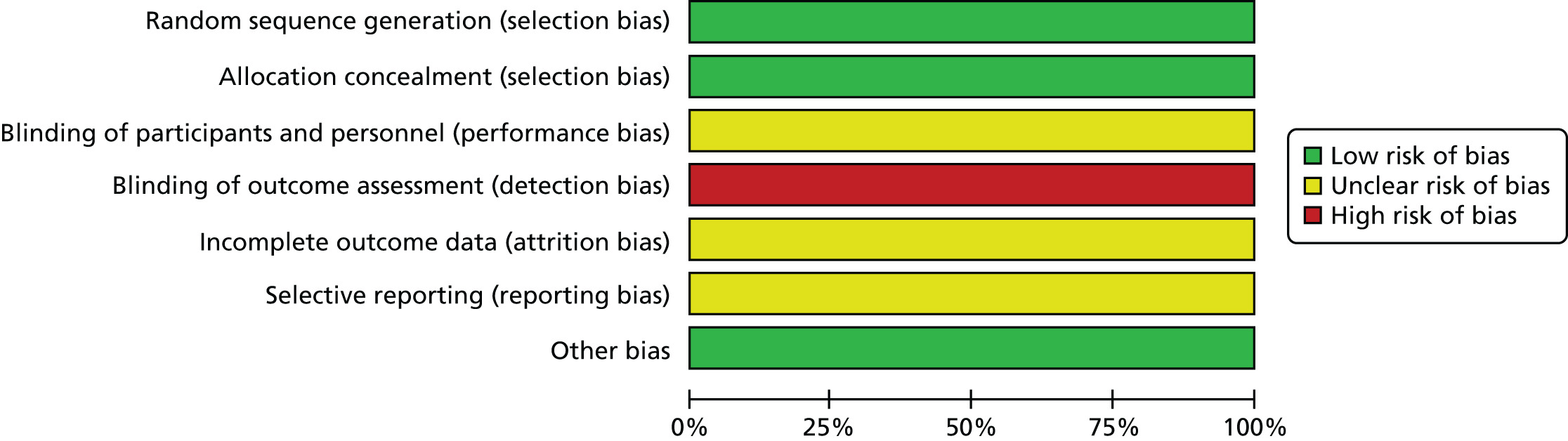
FIGURE 36.
Risk-of-bias summary: group work with children.
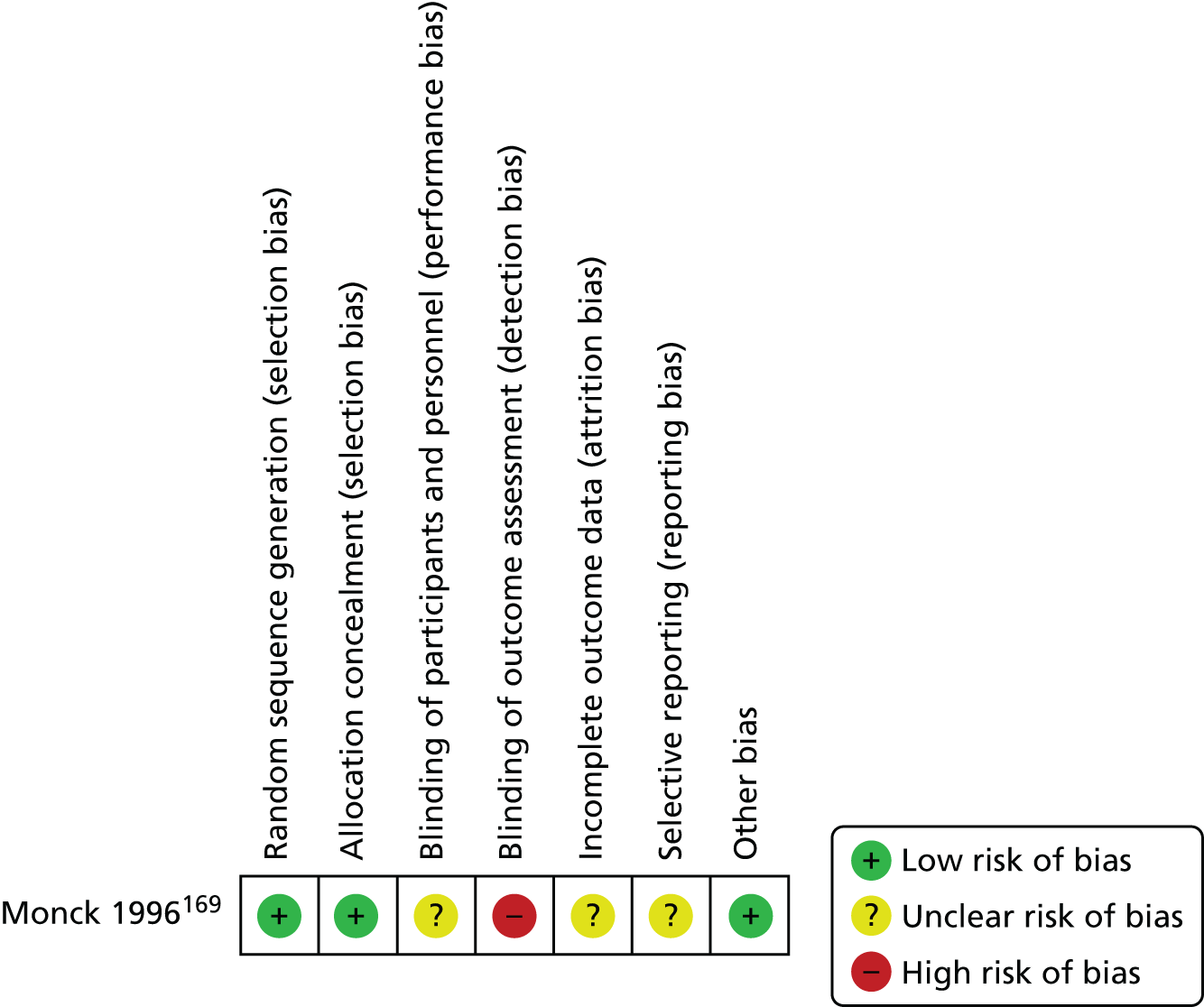
FIGURE 37.
Risk-of-bias graph: psychotherapy/counselling.
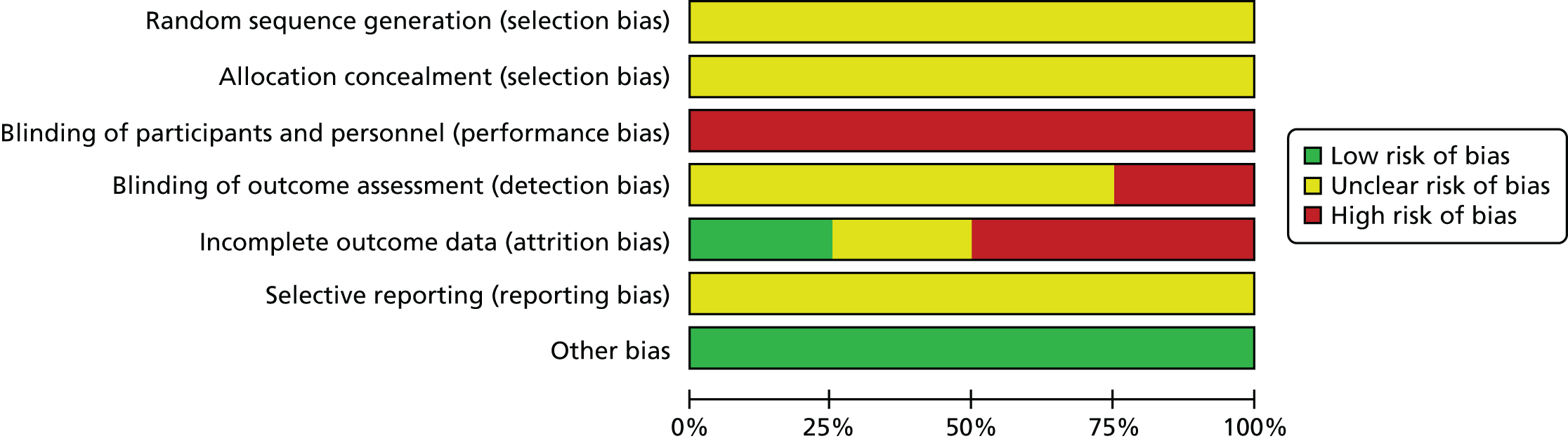
FIGURE 38.
Risk-of-bias summary: psychotherapy/counselling.
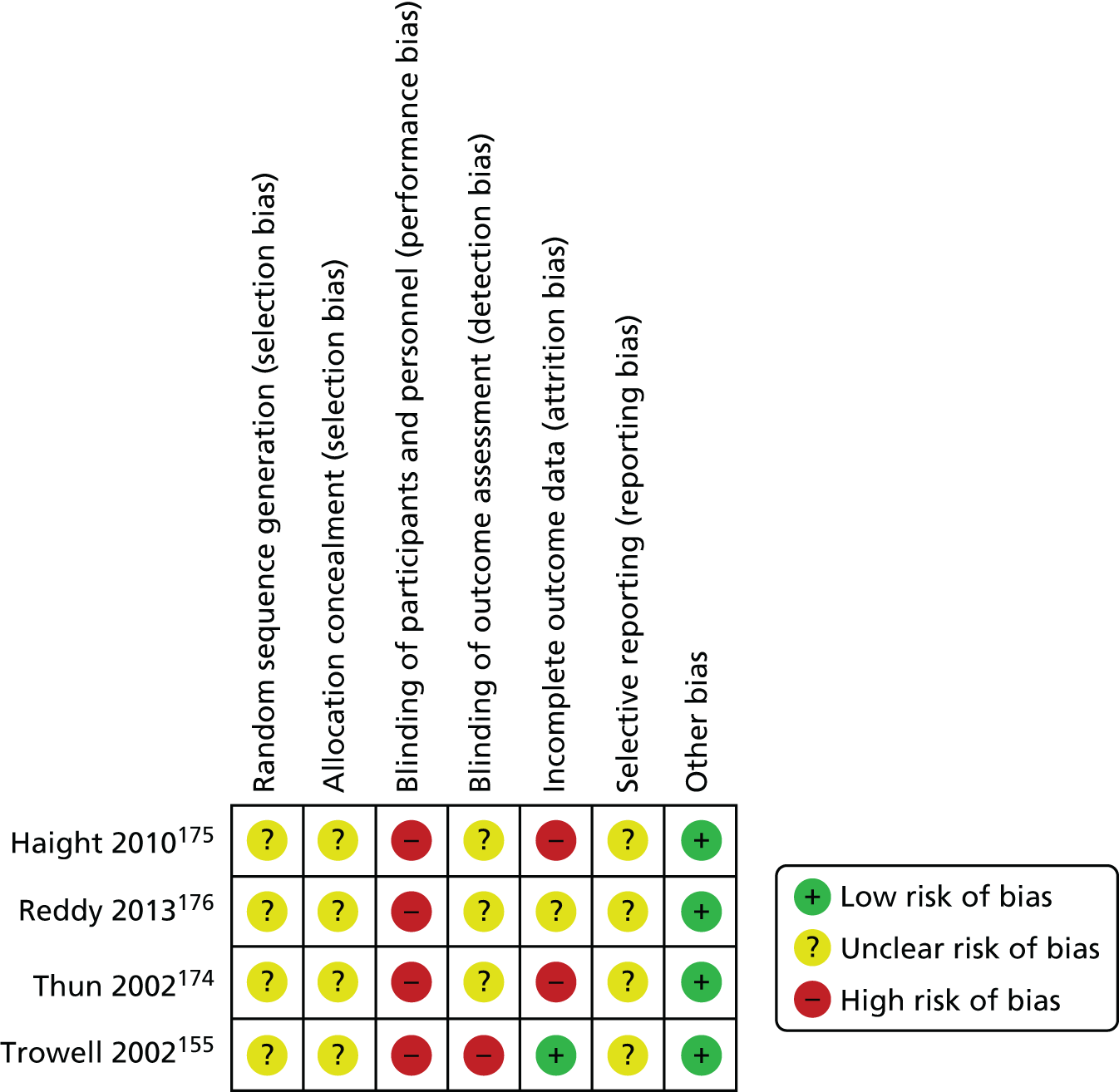
FIGURE 39.
Risk-of-bias graph: peer mentoring.
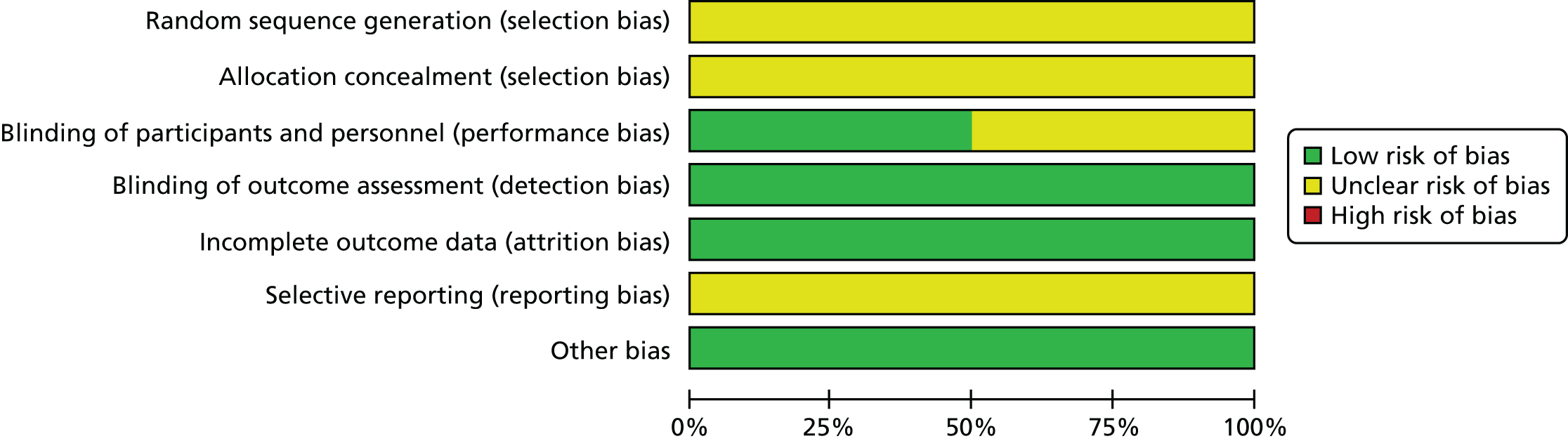
FIGURE 40.
Risk-of-bias summary: peer mentoring.

FIGURE 41.
Risk-of-bias graph: intensive service models.
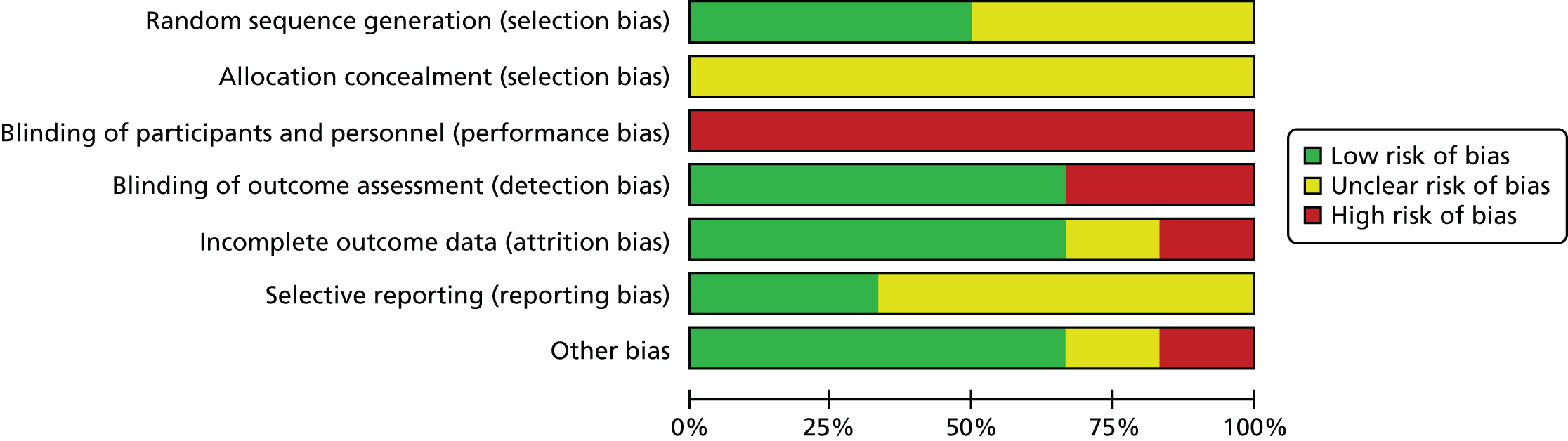
FIGURE 42.
Risk-of-bias summary: intensive service models.
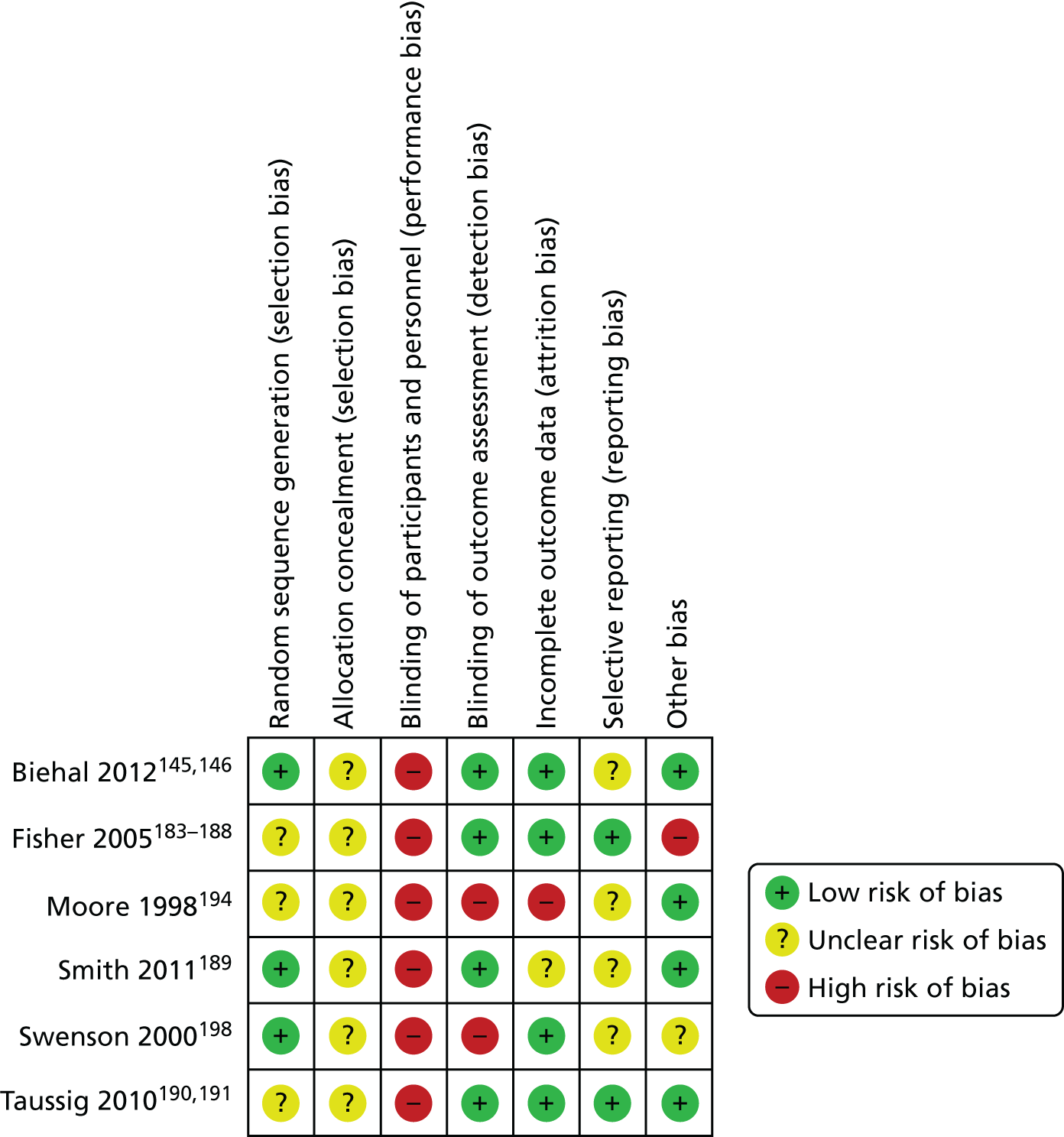
FIGURE 43.
Risk-of-bias graph: activity-based interventions.

FIGURE 44.
Risk-of-bias summary: activity-based interventions.
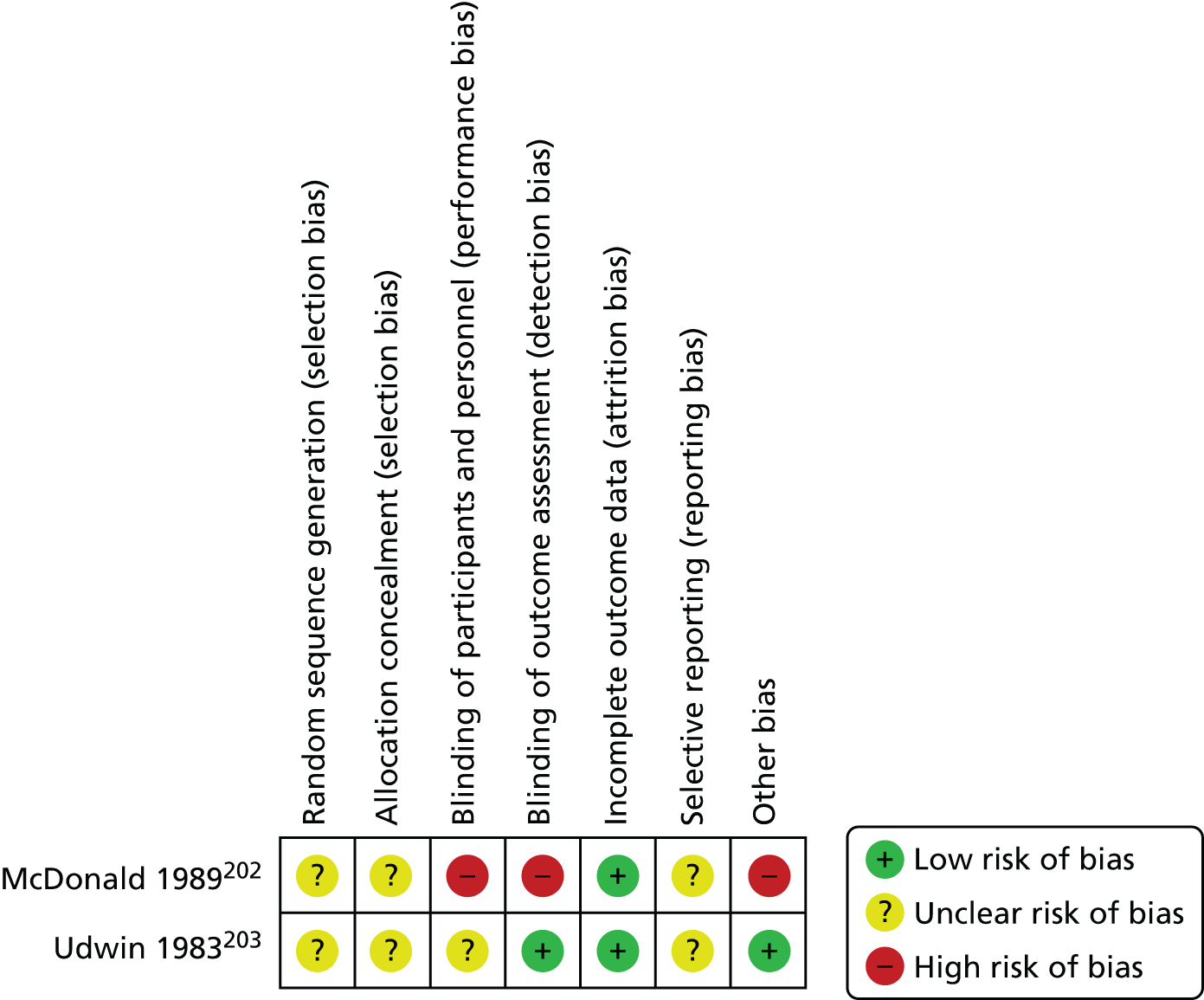
Appendix 11 Summary of findings: cognitive–behavioural therapy for sexually abused children
Cognitive–behavioural therapy compared with non-cognitive–behavioural therapy-based alternatives for children who have been sexually abused
Patient or population Patients with children who have been sexually abused.
Settings Health service/hospital, and community.
Intervention CBT [CBT interventions include group treatment approaches, Recovering from Abuse Program, sexual abuse-specific CBT, and TF-CBT].
Comparison Non-CBT-based alternatives (non-CBT-based alternatives include non-directive supportive therapy, CCT, standard community care and wait-list control).
| Outcomes | Illustrative comparative risksa (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | ||||
| Non-CBT-based alternatives | CBT | ||||
| Child depression (CDI) | |||||
| Short term (immediately after treatment) CDI Scale from 0 to 100 |
The mean child depression (CDI), short-term (immediately after treatment) ranged across control groups from 7 to 15.5 | The mean child depression (CDI), short term (immediately after treatment), in the intervention groups was 2.83 lower (4.53 to 1.13 lower)b | 421 (five studiesc) | ++–– lowd,e,f | MD –2.83 (95% CI –4.53 to –1.13) |
| Intermediate term (3–6 months after treatment) CDI Scale from 0 to 100 Follow-up: 3–6 months |
The mean child depression (CDI), intermediate term (3–6 months after treatment) in the control groups was 5.77–13.83 | The mean child depression (CDI), intermediate term (3–6 months after treatment), in the intervention groups was 1.76 lower (3.33 to 0.2 lower)b | 288 (four studiesc) | ++–– lowd,f,g | MD –1.76 (95% CI –3.33 to –0.20) |
| Long term (at least 1 year) Child Depression Inventory CDI Scale from 0 to 100 Follow-up: 1 year |
The mean child depression (CDI), long term (at least 1 year) ranged across control groups from 5.25 to 10.17 | The mean child depression (CDI), long term (at least 1 year), in the intervention groups, was 1.32 lower (2.84 lower to 0.19 higher)b | 301 (four studiesc) | ++–– lowd,f,g | MD –1.42 (95% CI –2.91 to 0.06) |
| Child PTSD (various scales) | |||||
| Short term (immediately after treatment) Various scalesh |
The mean child PTSD (various scales), short term (immediately after treatment) ranged across control groups from 2.32 to 41.8 | The mean child PTSD (various scales), short term (immediately after treatment), in the intervention groups was 0.44 SDs lower (0.73 to 0.16 lower)b | 442 (six studiesi) | ++–– lowd,f,j | SMD –0.44 (95% CI –0.73 to –0.16) |
| Intermediate term (3–6 months after treatment) Various scalesh Follow-up: 3–6 months |
The mean child PTSD (various scales), intermediate term (3–6 months after treatment) ranged across control groups from 1.91 to 10.92 | The mean child PTSD (various scales), intermediate term (3–6 months after treatment), in the intervention groups was 0.39 SDs lower (0.74 to 0.04 lower)b | 327 (five studiesi) | +––– very lowd,f,g,k | SMD –0.39 (95% CI –0.74 to –0.04) |
| Long term (at least 1 year) various scalesh Follow-up: 1 year |
The mean child PTSD (various scales), long term (at least 1 year) ranged across control groups from 1.33 to 9.58 | The mean child PTSD (various scales), long term (at least 1 year), in the intervention groups was 0.38 SDs lower (0.65 to 0.11 lower)b | 246 (three studiesi) | ++–– lowd,f,g | SMD –0.38 (95% CI –0.65 to –0.11) |
| Child anxiety | |||||
| Short term (immediately after treatment) Various scalesl |
The mean child anxiety, short term (immediately after treatment) ranged across control groups from 12.8 to 55.08 | The mean child anxiety, short term (immediately after treatment), in the intervention groups was 0.23 SDs lower (0.42 to 0.03 lower)b | 434 (five studies) | +++– moderated,f | SMD –0.23 (95% CI –0.42 to –0.03) |
| Intermediate term (3–6 months after treatment) Various scalesl Follow-up: 3–6 months |
The mean child anxiety, intermediate term (3–6 months after treatment), ranged across control groups from 26.14 to 55.08 | The mean child anxiety, intermediate term (3–6 months after treatment), in the intervention groups was 0.38 SDs lower (0.61 to 0.14 lower)b | 296 (four studies) | ++–– lowd,f,g | SMD –0.38 (95% CI –0.61 to –0.14) |
| Long term (at least 1 year) Various scalesl Follow-up: 1 years |
The mean child anxiety, long term (at least 1 year) ranged across control groups from 12.4 to 32.38 | The mean child anxiety, long term (at least 1 year), in the intervention groups was 0.28 SDs lower (0.52 to 0.04 lower)b | 278 (four studies) | ++–– lowd,f,g | SMD –0.28 (95% CI –0.52 to –0.04) |
| Child sexualised behaviour (CSBI) | |||||
| Short term (immediately after treatment) CSBI |
The mean child sexualised behaviour (CSBI), short term (immediately after treatment) ranged across control groups from 3.74 to 17.85 | The mean child sexualised behaviour (CSBI), short term (immediately after treatment), in the intervention groups was 0.65 lower (3.53 lower to 2.24 higher)b | 451 (five studies) | ++–– lowd,f,m | MD –0.65 (95% CI –3.53 to 2.24) |
| Intermediate term (3–6 months after treatment) CSBI Follow-up: 3–6 months |
The mean child sexualised behaviour (CSBI), intermediate term (3–6 months after treatment) ranged across control groups from 3.91 to 16.78 | The mean child sexualised behaviour (CSBI), intermediate term (3–6 months after treatment), in the intervention groups was 0.46 lower (5.68 lower to 4.76 higher)b | 133 (three studies) | +––– very lowd,f,g,n | MD –0.46 (95% CI –5.68 to 4.76) |
| Long term (at least 1 year) CSBI Follow-up: 1 years |
The mean child sexualised behaviour (CSBI), long term (at least 1 year) ranged across control groups from 7.5 to 16.79 | The mean child sexualised behaviour (CSBI), long term (at least 1 year), in the intervention groups was 1.61 lower (5.72 lower to 2.49 higher)b | 161 (three studies) | +––– very lowd,f,g,o | MD –1.61 (95% CI –5.72 to 2.49) |
| Child externalising behaviour (CBCL Externalising) | |||||
| Short term (immediately after treatment) CBCL |
The mean child externalising behaviour (CBCL Externalising), short term (immediately after treatment) ranged across control groups from 10.7 to 59.04 | The mean child externalising behaviour (CBCL Externalising), short term (immediately after treatment), in the intervention groups was 0.12 SDs lower (0.4 lower to 0.17 higher)b | 537 (seven studies) | ++–– lowd,f,p | SMD –0.12 (95% CI –0.4 to 0.17) |
| Intermediate term (3–6 months after treatment) CBCL Follow-up: 3–6 months |
The mean child externalising behaviour (CBCL Externalising), intermediate term (3–6 months after treatment) ranged across control groups from 13.04 to 65.44 | The mean child externalising behaviour (CBCL Externalising), intermediate term (3–6 months after treatment), in the intervention groups was 0.11 SDs lower (0.42 lower to 0.21 higher)b | 175 (four studies) | ++–– lowd,f,g | SMD –0.11 (95% CI –0.42 to 0.21) |
| Long term (at least 1 year) CBCL Follow-up: 1 year |
The mean child externalising behaviour (CBCL Externalising), long term (at least 1 year) ranged across control groups from 10.34 to 59.84 | The mean child externalising behaviour (CBCL Externalising), long term (at least 1 year) in the intervention groups, was 0.05 SDs higher (0.16 lower to 0.27 higher)b | 355 (five studies) | ++–– lowd,f,g | SMD 0.05 (95% CI –0.16 to 0.27) |
| Parent’s belief of child | |||||
| Short term (immediately after treatment) Various scalesq |
The mean parent’s belief of child, short term (immediately after treatment) ranged across control groups from 22.8 to 87.95 | The mean parent’s belief of child, short term (immediately after treatment), in the intervention groups was 0.3 SDs higher (0.03 to 0.57 higher)r | 211 (two studies) | ++ – lowd,f,g | SMD 0.3 (95% CI 0.03 to 0.57) |
| Intermediate term (3–6 months after treatment) Various scalesq Follow-up: 3–6 months |
The mean parent’s belief of child, intermediate term (3–6 months after treatment) in the control groups was 33.75 | The mean parent’s belief of child, intermediate term (3–6 months after treatment), in the intervention groups was 0.32 SDs lower (0.65 lower to 0.01 higher)r | 143 (one study) | + – very lowd,f,g | SMD –0.32 (95% CI –0.65 to 0.01) |
| Long term (at least 1 year) various scalesq Follow-up: 1 year |
The mean parent’s belief of child, long term (at least 1 year) in the control groups was 87.01 | The mean parent’s belief of child, long term (at least 1 year), in the intervention groups was 0.1 SDs lower (0.43 lower to 0.23 higher)r | 146 (one study) | ++ – lowd,f,g | SMD –0.1 (95% CI –0.43 to 0.23) |
| Parenting skills (PPQ) | |||||
| Short term (immediately after treatment) PPQ |
The mean parenting skills (PPQ), short term (immediately after treatment) ranged across control groups from 136.81 to 139.19 | The mean parenting skills (PPQ), short term (immediately after treatment), in the intervention groups was 3.86 higher (0.47 to 7.26 higher)r | 278 (three studies) | ++ – lowd,f,g | MD 3.86 (95% CI 0.47 to 7.26) |
| Intermediate term (3–6 months after treatment) PPQ Follow-up: 3–6 months |
The mean parenting skills (PPQ), intermediate term (3–6 months after treatment) ranged across control groups from 132.86 to 148.39 | The mean parenting skills (PPQ), intermediate term (3–6 months after treatment), in the intervention groups was 2.36 higher (1.55 lower to 6.28 higher)r | 231 (three studies) | ++ – lowd,f,g | MD 2.36 (95% CI –1.55 to 6.28) |
| Long term (at least 1 year) PPQ Follow-up: 1 year |
The mean parenting skills (PPQ), long term (at least 1 year) ranged across control groups from 133.93 to 143.08 | The mean parenting skills (PPQ), long term (at least 1 year), in the intervention groups was 0.89 lower (4.89 lower to 3.11 higher)r | 193 (two studies) | ++ – lowd,f,g | MD –0.89 (95% CI –4.89 to 3.11) |
Appendix 12 Attrition analyses
Attrition from cognitive–behavioural therapy studies. df, degrees of freedom; M–H, Mantel–Haenszel.

Relationship-based interventions. df, degrees of freedom; M–H, Mantel–Haenszel.

Systemic therapies. df, degrees of freedom; M–H, Mantel–Haenszel.

Psychoeducation compared with control. df, degrees of freedom; M–H, Mantel–Haenszel.

Group work. M–H, Mantel–Haenszel.
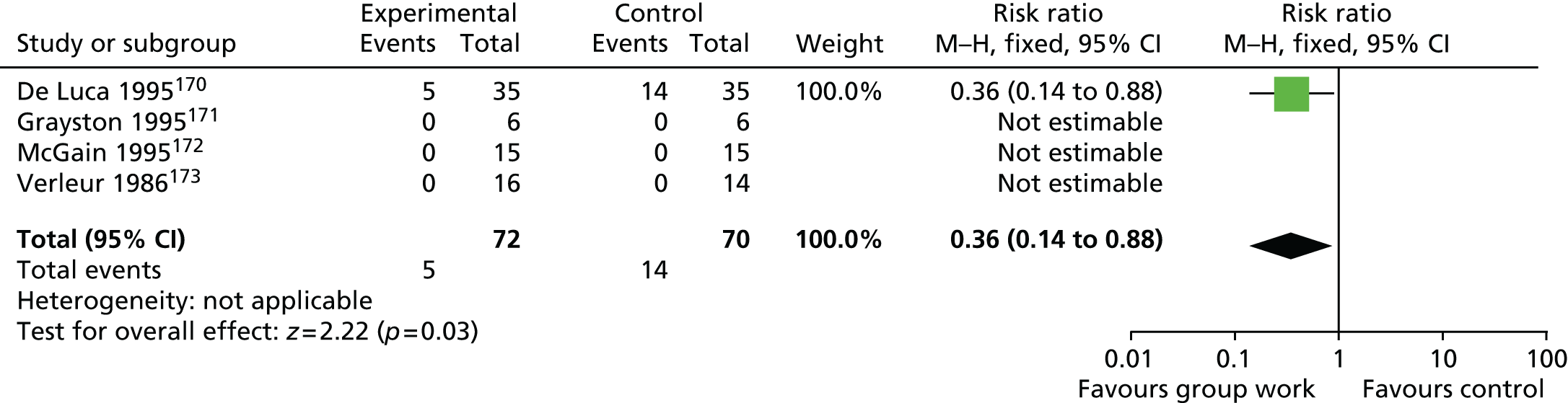
Psychotherapy/counselling. df, degrees of freedom; M–H, Mantel–Haenszel.
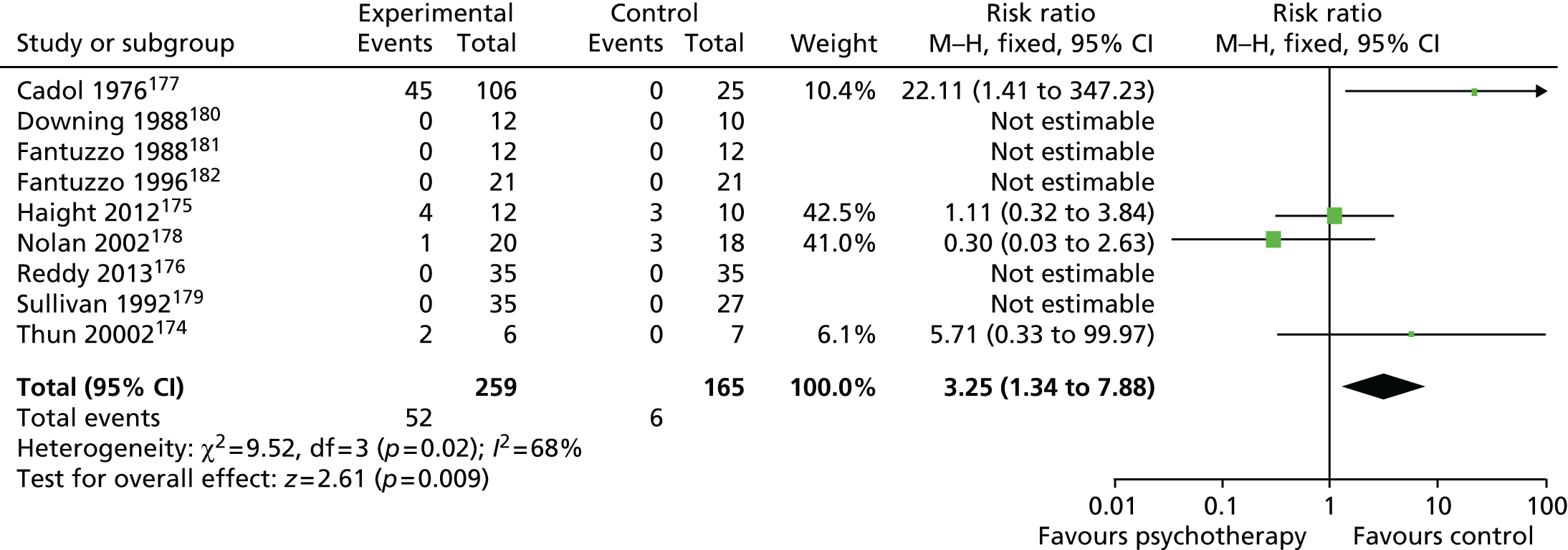
Peer mentoring. M–H, Mantel–Haenszel.
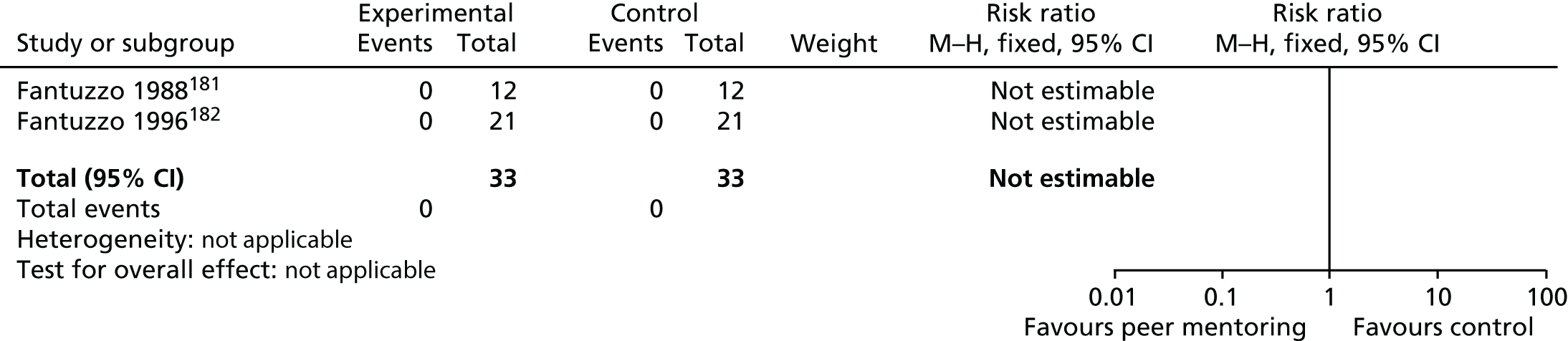
Intensive service models. df, degrees of freedom; M–H, Mantel–Haenszel.
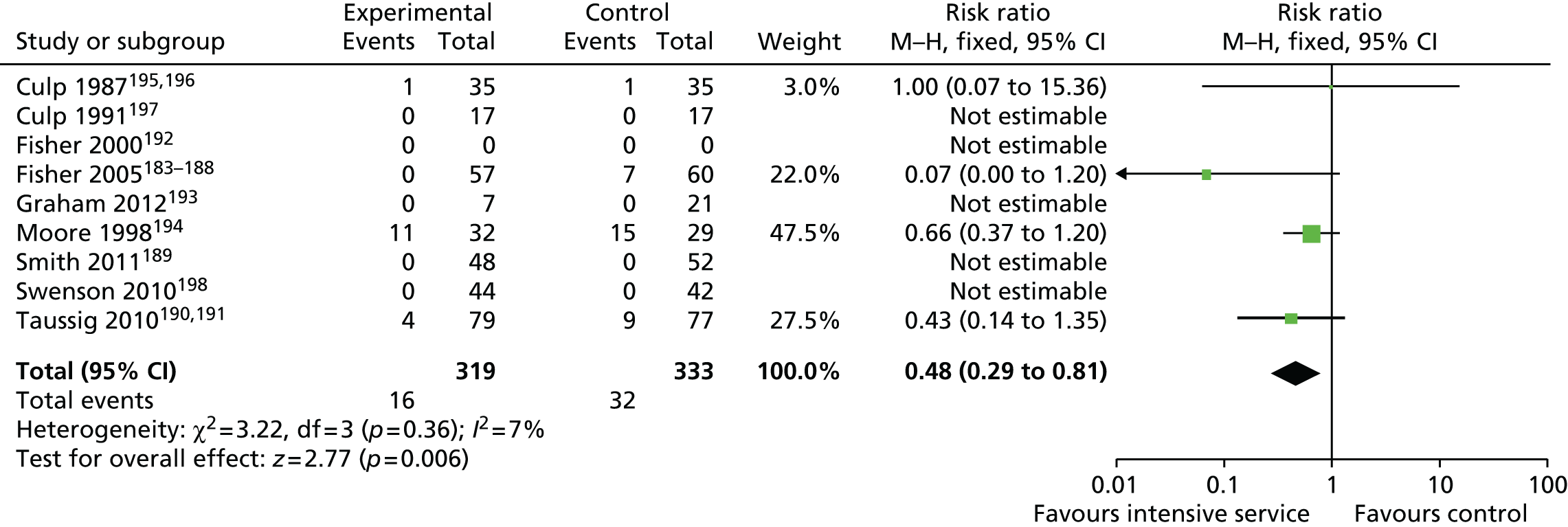
Activity-based interventions. df, degrees of freedom; M–H, Mantel–Haenszel.

Appendix 13 Overview of acceptability evidence by intervention group
| Intervention type (number of studiesb) | Quantitative evidence | Quantitative overview | Qualitative evidence | Qualitative overview | Quality |
|---|---|---|---|---|---|
| Cognitive–behavioural approaches (15) | Nine studies (two smalla; seven mediuma sample size) | Attrition and treatment completion profile – perceived severity of abuse associated with completion | Six studies (four small; two medium) | Children mostly viewed interventions positively; four studies reported mixed views Parents tended to rate interventions more positively than child Staff reported mixed views |
Generally good quality |
| Activity based (5) | – | – | Five studies (all small) | Received positive evaluations Therapist views expressed including some tension between parents/therapists |
Adequate quality |
| Attachment based (3) | One study (large) | Treatment completers – older caregivers with poorer health, perceived severity of abuse | Two studies (one small; one large) | Parents and children viewed positively | Mixed quality |
| Therapeutic residential care (4) | One study (medium) | Treatment completion – age/ethnicity factors | Three studies (one small; two medium) | Importance of re-engaging youth during treatment process Children had very positive and some negative experiences |
Generally good quality |
| Enhanced foster care (2) | One study (medium) | Evidence of placement stability following intervention | Two studies (one medium; one large) | Foster carers very positive about both interventions | Generally good quality |
| Family/systemic (4) | One study (small) | Positive ratings | Three studies (all small) | Children and parents expressed mixed views One study reported high rate of sibling refusal in family intervention |
Mixed quality |
| PCIT (1) | One study (medium) | Kin foster carers more likely to complete than non-kin foster carers | – | – | Good quality |
| Counselling (10) | Seven studies (three small; four medium) | Therapist gender not significant White children more likely to enter therapy |
Four studies (two small; two medium) | Children mostly positive One study reported mixed parental views including pain of talking about abuse and negative impact on family and social networks |
Generally good quality |
| Children/young people’s groups (6) | Three studies (all small) | Mostly positive ratings from children, parents and school counsellors, but some mixed views also expressed | Five studies (all small) | Mixed views from children, parents and therapists | Mixed quality |
| Psychoeducational (4) | Two studies (one small; one medium) | Children who had suffered more abuse and had behavioural/social difficulties more likely to drop out | Three studies (all small) | Foster parents expressed positive views Children and parents also mostly positive Parents wanted more feedback from therapists |
Mixed quality |
| Psychotherapy (4) | Two studies (all medium) | Initiators of therapy and predictors of total sessions | Three studies (two small; one medium) | Children rated positively Three-way process of therapy between child, parent and therapist |
Generally good quality |
| Peer mentoring (1) | – | – | One study (small) | Children rated intervention highly Parent and staff positive reports |
Good quality |
| Eclectic (3) | One study (medium) | Attrition/treatment completers | Two studies (all small) | Children reported positive and some negative views Caregivers more positive One study presented alleged perpetrators experiences of therapy, mixed views |
Mixed quality |
| Other (9) | Four studies (one medium; three large) | Ethnicity associated with early termination Profile of treatment completers |
Five studies (all small) | Varied range of interventions described, both positive and negative views expressed by children, parents and clinicians | Good quality |
Appendix 14 Overview of acceptability evidence by study interventions
Cognitive–behavioural interventions
| Study | Sample size | Data collection | Analysis | Quality overview |
|---|---|---|---|---|
| Barker 2005481 | 14/67 children; 5 staff | Interviews | Summary overview | Aims of the research were clearly stated Methodology and research design were appropriate for qualitative data Data collection was not adequately described The findings not clearly described |
| Buschbacher 2002629 | n = 1 | Interviews with foster parent and staff members | Aims clearly described but this was a testimonial rather than a research study One of the treatment team conducted interviews with foster mother and colleagues Retrospective interview in one successful case High risk of bias |
|
| Chasson 2008482 | n = 99 | Withdrawal metrics | Multiple regression analysis | Aims were clearly stated and the methodology and research design were appropriate Data collection was adequately described Potential confounders not added to statistical model Findings were clearly described |
| Chasson 2013630 | n = 134 (99 from Chasson 2008) | Withdrawal metrics | Regression analysis of trauma characteristics as predictors of attrition | Aims were clearly stated and the methodology and research design were appropriate Data collection was adequately described Potential confounders were not added to statistical model Findings clearly described |
| Eslinger 2014631 | n = 115 | Baseline, post treatment and 3 months | Multinomial logistic regression of predictors of dropout | Study design was appropriate Sampling methods were not sufficiently clear; age range was quite wide and sample heterogeneous Data analysis was appropriate |
| Fraynt 2014632 | n = 562 | Factors predicting treatment engagement | Binominal regression; multinomial logistic regression | Study design and sampling was appropriate; however, the study did not measure the type of intervention received other than individual or group treatment, which limited the validity of the study Data collection methods and measures were appropriate for the population and the analysis was adequate for the aim of the study |
| Hubel 2014492 | n = 99; n = 67 analysed | Child and parent client evaluation form | Study design was appropriate but the acceptability questionnaire lacks validity, as it relied on satisfaction ratings Findings were clearly reported |
|
| Kolko 1996108 | n = 25 CBT, n = 18 FT, n = 12 control | Treatment expectancy (Likert scale) Brief telephone calls to parents Post-treatment CEI |
Study design appropriate and procedure were clearly described Standardised measures were used with evidence of reliability and validity Findings were reported clearly |
|
| Lange 2010497 | n = 24 | Client satisfaction: general, with treatment and with therapists Interviews plus 10-point rating scale (1 = high) Attrition |
Study design appropriate and procedure were clearly described Sampling through the media open to bias Standardised measures were used with evidence of reliability and validity; however, acceptability was measured using subjective satisfaction ratings Findings were clearly presented |
|
| McPherson 2012633 | n = 254 | Treatment completion | Univariate analysis and multivariate logistic regression models | Appropriate study design and sampling Data collection based on electronic medical files which relies on accuracy of record-keeping Data analysis was appropriate and clearly described |
| Salloum 2014504 | n = 6 | Parents completed expectancy rating form; client satisfaction questionnaire plus treatment costs calculated with the time tracking system | Study design was appropriate Acceptability measure relied on satisfaction ratings, although used a questionnaire that used in other research; however, no ‘depth’ of data was captured by this measure, such as why caregivers were or were not satisfied with treatment Findings were clearly reported |
|
| San Diego 2011680 | 5/6 of those referred | Participants’ journals, therapy notes, and interviews | IPA | Study was well designed, and appropriate data collection methods and analysis were used Findings were clearly reported Ethical considerations were not clearly outlined |
| Silovsky 2007505 | n = 85 | CSBP preschool group satisfaction and social validity questionnaire – caregiver satisfaction | Study design was appropriate but measure of acceptability relies on satisfaction ratings Findings were clearly reported |
|
| Smith 2008506 | n = 6 | Client satisfaction questionnaire | Study design was appropriate but measure of acceptability relies on satisfaction ratings Findings only partially reported descriptively |
Acceptability of attachment-based interventions
| Study | Sample size | Data collection | Analysis method | Quality overview |
|---|---|---|---|---|
| Cross 2013634 | n = 1085; 60% retained | Case file data | Single predictors of study retention – logistic regression Multivariate predictors of study retention – multivariate regression remodelling |
One site was excluded because it did not comply with study protocol Programme content and delivery varied across the 15 sites |
| Osofsky 2007515 | n = 346 children; n = 57 dyads | Caregivers’ and therapists’ qualitative impressions of treatment | Study design suffered from differing procedures across sites Some measures used were standardised and had evidence of reliability and validity, although impressions of treatment was measured using satisfaction ratings of ‘yes’ or ‘no’ Findings were clearly presented but lacked depth |
|
| Sudbery 2010663 | Experiences reports of n = 45 children | Interviews; content analysis of files and organisational documents; children; surveys of social workers and others | Study was adequately designed and described and the findings were clearly reported | |
| Powell 2010662 | n = 5 children, n = 4 mothers and 1 grandmother | Semistructured qualitative interviews | Methodology and research design were appropriate for the research aims Data were reported clearly and thoroughly It is unclear whether or not ethical issues were considered |
Acceptability of parent–child interaction therapy
| Study | Sample size | Data collection | Analysis method | Quality overview |
|---|---|---|---|---|
| Timmer 2004656 | 102 kin; 157 non-kin foster carers | Treatment completion | The study design was limited by having no control group Patterns of termination of treatment were measured by clinician discharge sheets Results were reported in full and the analysis is appropriate |
Acceptability of parent training interventions
| Study | Sample size | Data collection | Analysis method | Quality overview |
|---|---|---|---|---|
| Ducharme 2000510 | n = 28 parents n = 15 children from n = 9 families |
Eight mothers completed the satisfaction questionnaire | The study design was limited by not having a control group Treatment satisfaction was measured using mother’s self-report rating scales It is unclear how perceptions of treatment was measured and analysed Results were limited by not reporting variance |
|
| Golding 2004511 | n = 44 children, n = 41 foster carers | Participant satisfaction questionnaire, qualitative evaluation, group facilitator feedback | Study design and methodology were appropriate Findings were clearly reported |
|
| Taban 2001635 | n = 45 families health training, n = 37 home accident prevention; n = 31 PCIT | Three social validity questionnaires developed specifically for the study | Study design was appropriate Social validity questionnaire was well developed, but relied on satisfaction ratings as a measure of acceptability Findings were partially reported |
Acceptability of family/systemic interventions
| Study | Sample size | Data collection | Analysis method | Quality overview |
|---|---|---|---|---|
| Conran 1993621 | n = 2, mother and daughter | Interviews | This single case study was not adequately designed or reported | |
| Costa 2009678 | n = 28; n = 8 families interviewed | Questionnaires, children drawings, evaluation of the effects of conversations and actions in families | Qualitative epistemology | The study aims and objectives were clearly stated and the research methodology was appropriate Reporting of findings was appropriate |
| Danielson 2010526 | n = 10 | 3–6 months post treatment Ecological functioning measure treatment satisfaction and adherence |
Study was well designed, and the data collection, analysis and findings were clearly reported | |
| Tjersland 2006673 | n = 23 families, n = 32 children | Observational data from therapeutic sessions; interviews with mothers, children and alleged perpetrators | Descriptive coding developed by two therapists, independently rated to verify categorisation | Some relevant points about the tension that mothers feel between not wanting to talk about the abuse/suspected abuse to protect their child, but also wanting to help them Nothing useful on children’s perspectives |
| Woodworth 1991533 | n = 16/22 | N = 40 interviews with n = 13 incest victims, n = 12 offenders, n = 2 siblings | Poorly described Opportunistic sampling, insufficient methodological information to be able to properly assess the quality of the work |
Acceptability of psychoeducation interventions
| Study and location | Sample size; response rate | Data collection: acceptability | Analysis method | Quality overview |
|---|---|---|---|---|
| Barth 1994161 | n = 15 | Brief client satisfaction survey | Study design was appropriate but acceptability measures relied on satisfaction ratings with no other detail Findings were clearly reported |
|
| Boisvert 2008658 | n = 116 | ‘Dropout’ defined as someone who agrees to therapy and participates in at least one session and then stops before the half-way point without the therapists approval or an agreement that treatment is finished (Garfield 1994804) | Univariate and multivariate analyses exploring relationships between dropout and sexual abuse, individual and family characteristics | Study design did not include a control group and compared characteristics of only treatment completers and those who dropped out Standardised measures were used but the study did not describe the treatment in any detail or measure effectiveness, which limited the conclusions of the study |
| Hyde 1995538 | Interview and rating | Study procedure is unclear Measures used had evidence of reliability and validity and were age appropriate Analysis of data is unclear |
||
| Rushton 2000664 | n = 58; n = 46 mothers, n = 19 foster/adoptive mothers; 14 carers | Carer interviews – 1- and 2-year follow-up Follow-up interviews with carers’ workers 1 year after start of treatment |
Methodology and research design were appropriate for the research aims The research findings were reported clearly |
Acceptability of group work for children
| Study and location | Sample size | Data collection: acceptability | Analysis method | Quality overview |
|---|---|---|---|---|
| Ashby 1987636 | n = 9 | Acceptability and usefulness evaluation rating on numerical scale – midway and final group; school counsellor reports | The research aims were clearly described but the methodology, analysis and findings were not clearly reported | |
| Baker 2001637 | n = 5–14 | Satisfaction ratings; evaluations conducted in 1997, 1998 and 2000 Four group evaluations and follow-up telephone survey of n = 7 terminated clients |
The research aims were clearly described but the methodology, analysis and findings were not clearly reported | |
| De Luca 1995170 | n = 35 intervention n = 35 control |
Child-report measures | Study design was limited by no control group Treatment satisfaction was measured using self-report social validation ratings by children and parents Presentation of results was limited to percentages Unclear how themes responded to were identified |
|
| Grayston 1996659 | n = 6 | Child feedback and parent feedback questionnaires | Research aims were clearly defined and methodology is appropriate Data collection and ethical considerations were not described in detail Findings were reported clearly |
|
| Gustafsson 1995676 | n = 19 | Semistructured interviews with group therapists | Research was well designed but findings were not clearly reported | |
| Monck 1996169 | n = 47 | Participant rating | Study design was appropriate but the wide scope means that interventions lack specificity in terms of aims and theoretical underpinning Although randomised, small sample size Data collection lacked detail in description and appeared to lack sophistication in terms of non-standardised measures and the use of subjective rating scales Data analysis lacked complexity and included a simplistic presentation of ratings |
|
| Peled 1992639 | n = 30 | Interviews plus observations | Aims and methodology were well explained, and data collection and analysis appropriate Findings were clearly reported |
Acceptability of counselling interventions
| Study and location | Sample size; response rate | Data collection: acceptability | Analysis method | Quality overview |
|---|---|---|---|---|
| Baginsky 2001640 | n = 130 | Telephone interviews (Italy) Interviews, letters, telephone and questionnaires (the Netherlands) Individual and group interviews (UK) |
Summary overview | Research was well designed but data collection methods were not similar across the three countries and may not have been representative Findings were clearly reported |
| Fowler 1992641 | n = 35 | Seven-point Likert scale | The study design is appropriate for the research aims although is limited by a sample that includes only girls Gender preference was measured using only self-reported rating scores Results were reported in full and the analysis was appropriate |
|
| Fowler 1993642 | n = 20 | Pre- and post-treatment preference stated | Although the study design was appropriate, sampling methods may not be representative of the typical population The method of data collection is questionable, as data were collected post intervention but longer-term follow-up may have been more informative Age range was wide and may have been too heterogeneous The type of data analysis conducted was appropriate |
|
| Haight 2010175 | n = 15 | Views from children, caregivers and community clinicians; field notes | Emic coding | |
| Haskett 1991657 | n = 129 | Factors associated with treatment entry | Study design was appropriate and the sampling included all referred cases within a set time frame Data relied on parents self-reports with no use of standardised questionnaires The same therapists were also used as researchers; however, the analysis was appropriate and thorough |
|
| Kilcrease-Fleming 1992643 | n = 20 | Three counselling process rating scales of videotaped interviews | An innovative design using observer ratings but with an unclear methodology in terms of participant recruitment, intervention type Although measures were designed for the study and lack prior use or testing, clear efforts were made to improve the reliability of the measures The analysis was appropriate but the small sample size hampered generalisations |
|
| Kolko 1999644 | n = 86 | Children and parents completed an evaluation of the level of perceived service needs, motivation and interests, goals or expectations and obstacles; interviewed at study intake and 4–8 months after initial service | Predictors of service use computed using Pearson’s correlations or chi-squared tests | A clear study design, participant recruitment strategy and assessment schedule Measures included standardised and non-standardised measures Analysis was appropriate and findings were clearly presented |
| Nelson-Gardell 2001638 | n = 34 plus five focus groups | Focus group methodology to address the issues of interest | Thematic analysis | The aims of the research were clearly defined and the methodology was appropriate to meet these aims Data analysis was not fully described Findings were reported clearly |
| Overlien 2011674 | n = 50 women’s refuges directors, n = 22 children | Face-to-face interviews, age-appropriate schedules | Grounded theory approach | Study design was appropriate, analysis was adequate and findings were clearly reported Unclear if all ethical considerations were made |
| Porter 1996645 | n = 27 | Client Behavior System745 – verbalisation measure | Study design was appropriate overall but relies on the measurement of verbalisation within one specific session; however, attempts were made to blind therapists to the study aims and observer raters were recruited externally and trained to standardise ratings using a predetermined protocol (the Client Behavior System) Findings were clearly reported, although descriptions lack direction, such as reporting that non-abuse-related questions elicited significantly more non-abuse-related answers |
|
| Reddy 2013176 | n = 70 | Qualitative post-treatment feedback | Study design was appropriate as was sampling. However, data collection for treatment acceptability relied on non-standardised rating scales. Findings were reported clearly | |
| Scott 1996677 | n = 10 families (n = 17 children) | In-depth interviews with parents | Research aims were not clearly stated but research design and data collection clearly described Findings were clearly reported |
|
| Deb 2011679 | n = 120 | Quantitative and qualitative data | The study design was appropriate for the aims of the research It is unclear how perceptions of treatment were measured and analysed Results were limited to descriptive narratives and percentages |
|
| Thompson 2011646 | n = 40 | Semistructured interviews developed to elicit information about mothers and youth experiences and satisfaction with mental health services – Mother Interview Guide and Youth Interview Guide | The methodology and research design were appropriate for the research aims The research findings were reported clearly |
Acceptability of psychotherapy interventions
| Study and location | Sample size; response rate | Data collection: acceptability | Analysis method | Quality overview |
|---|---|---|---|---|
| Davies 2009665 | n = 4 | Single time point interview of children’s experiences of participation | IPA | Aims of the research were clearly defined and the methodology was appropriate to meet these aims Findings were reported clearly |
| Horowitz 1997647 | n = 81 | Therapy experiences gathered from parents | Regression analyses | Study was part of a larger longitudinal study but the design suffers from a reliance on therapists’ own feedback, lacking child feedback and a lack of clarity on the type of intervention other than the format (individual, family or group); however, the analysis of data was appropriate and findings were clearly reported |
| Jensen 2010675 | n = 15 | Follow-up interview in child’s home | Content analysis guided by Bordin’s conceptualisation of the working alliance | Aims of the research were clearly defined and the methodology was appropriate to meet these aims Findings were reported clearly |
| Lippert 2008648 | n = 101 | Case record review Caregiver interview including ‘perceptions related to therapy’ |
Systematic and appropriate study design, including both quantitative and qualitative components Measures used were standardised and interviews used a predetermined protocol Data analysis was appropriate, although reported results lacked qualitative depth |
Acceptability of peer-mentoring interventions
| Study and location | Sample size; response rate | Data collection: acceptability | Analysis method | Quality overview |
|---|---|---|---|---|
| Alaggia 1999660 | 24 families, 26 children | Interviewed a sample of parents, youths and professionals | Summary overview | Aims of the research were clearly defined and the methodology was appropriate to meet these aims Data analysis was not fully described Findings were reported clearly |
Acceptability of therapeutic residential care interventions
| Study and location | Sample size; response rate | Data collection: acceptability | Analysis method | Quality overview |
|---|---|---|---|---|
| Cunningham 2009649 | n = 130 | Semistructured interviews with RTC staff; school, clinical and residential treatment team questionnaires (T2 and T3); data from client case files | Inductive thematic coding; confirmatory factor analysis | Study design was adequate, and method was clearly described and appropriate Data were collected over a number of time points (weeks after admission, the approximate midpoint of the client’s stay, immediately prior to discharge and 4 months after discharge) and from multiple sources Clear thought was given to the age-appropriateness and ethics of data collection from young people Thematic analysis and factor analysis were both appropriate and reported in detail |
| Gallagher 2012666 | 16/34 | Semistructured interviews | Summary overview | Study was well designed and described, and the findings were clearly reported |
| Leenarts 2013672 | n = 154 | Multiple linear regression for treatment motivation. Logistic regression to identify possible predictors for dropout | Appropriate study design and sampling Measures had evidence of reliability and validity Appropriate data analysis and findings were clearly reported |
|
| Shennum 1995650 | n = 80 | Qualitative interviews with participants | Summary overview | Appropriate study design but sampling was unclear Measures had evidence of reliability and validity Data analysis could have been more rigorous but findings were clearly reported |
| West 2014651 | n = 39 | Focus group | Thematic analysis | Aims, methodology, data collection and analysis were all good quality; however, the content may not be very relevant to our review – it is more focused on the components that a good intervention for externalising behaviour in a school setting should contain |
Acceptability of enhanced foster care interventions
| Study and location | Sample size; response rate | Data collection: acceptability | Analysis | Quality overview |
|---|---|---|---|---|
| Biehal 2012145,146 | n = 219; RCT n = 34; observational n = 185 Case studies n = 20 |
Postal questionnaires; interviews; reports; parent records | Bivariate and multivariate analyses plus thematic analyses of interview data and more in-depth analyses of case study data | Aims and progress of the study clearly stated Criteria for case study selection clear and appropriate Data analyses appropriate and findings clearly described |
| Laan 2001671 | n = 78 | Case notes and questionnaire data | Analysis of questionnaire data; thematic analysis of case notes | Study design was appropriate Data collection relied on satisfaction ratings, although bias was addressed by matching with qualitative answers when given Satisfaction ratings were clearly presented but there is limited reporting of qualitative findings |
| Staines 2011667 | n = 450 | Questionnaires – foster parents and social workers; at placement start and 1 year on | Summary overview | A well-designed study with appropriate data collection measures Questionnaires were anonymised to prevent bias Findings were clearly reported |
Acceptability of activity-based Interventions
| Study and location | Sample size; response rate | Data collection: acceptability | Analysis | Quality overview |
|---|---|---|---|---|
| Bannister 1996668 | n = 6 | Pre- and post-treatment interviews with social worker, carer and child | Aims, methodology, analysis and findings were not clearly described | |
| Burgon 2011669 | n = 7 | Qualitative interviews, field note observations | Qualitative, participative and reflexive ethnography; thematic analysis | Aims, methods and design of the study were appropriate Recruitment of sample was unclear and author was participant researcher, which may be subject to bias Reporting of findings were clear |
| Gilbert 1988652 | Group attendance ranged from two to six children (average attendance n = 4) | Art qualitative feedback | Aims and methodology were clearly described but data collection and analysis were lacking in depth | |
| Hill 2009670 UK |
13 families: mothers n = 12, fathers/stepfathers n = 4 Children n = 28 |
Qualitative case study of 13 cases files plus in-depth interviews with therapists (n = 27), parents (n = 18) and children (n = 3) | Thematic analysis | Aims, methods and design of the study were appropriate Data analysis was adequate Reporting of findings are clear |
| Mishna 2012661 | n = 11 | 63 interviews were conducted at 6, 12 and 18 months with parents, teachers and therapists | Grounded theory approach | Aims of the research were clearly stated, and the methodology and research design were appropriate Data collection was adequate described and the findings were clearly described |
Appendix 15 Report of consultations with young people and professionals
Introduction
The involvement of young people and professionals was seen as important for helping to:
-
shape the review
-
interpret the evidence
-
draw conclusions from it.
It was hoped that engagement with a range of stakeholders would help to ensure the relevance of the review report to the UK practice and policy contexts. In addition, it would help to identify the potential barriers and facilitators to the implementation and use of the review findings from the following perspectives:
-
children and young people who have been maltreated and who could benefit from psychosocial interventions
-
those involved in the identification of such young people
-
those responsible for referring them
-
those who deliver the interventions.
Approach and methods
The plan that was outlined in the proposal consisted of an advisory group process with young people and professionals that would reflect the different above purposes. Consultations took place at two points:
-
early in the review process to help ‘shape’ the review planning
-
late in the review process to help with interpretation and conclusion forming.
An overview of the advisory group sessions that were held is provided in Table 32. The key questions and methods for the ‘early’ advisory groups for young people and professionals were the same. There were three sets of questions around:
-
outcomes for maltreated young people from psychosocial interventions
-
factors that would facilitate them getting the help they needed
-
factors that would act as barriers to them getting that help.
| Early | Young people | Group 1 Voice of Young People in Care, Belfast: seven young people aged between 16 and 24 years, 27 March 2013 Group 2 Voices from Care, Cardiff: seven young people aged 18+ years, 9 April 2013 |
| Professionals | Group of 39 professionals, 1 May 2013, from a range of professional groupings: voluntary sector/social work; health economics; clinical psychology/psychiatry; health professionals; educational psychology; social science; and foster carers | |
| Late | Young people | Group of six young people at NSPCC participation event, 27 October 2014, aged 15–19 years |
| Professionals | Group of 20 professionals, 27 November 2014, from a range of professional groupings |
More specifically, the questions that the young people addressed were:
-
What difference would ‘helpful help’ make for a child or young person who had been treated badly?
-
What would make it easier to ask for help or get help?
-
What would make it harder to ask for help or get help?
A sorting and ranking exercise was conducted with the early Young People’s Advisory Groups and Professional Advisory Groups (PAGs), called the Q-Set. Group members were presented with a set of cards, each of which had a different possible outcome/facilitator/barrier, generated by the Steering Group from knowledge of the research and from professional experience. Group members were first asked to review the cards individually and consider their own opinions on where each card should be placed on the large Q-sort pyramidal grid. They were then asked to discuss their opinions in the group and to work together to create one single, group-agreed, Q-sort pyramid. Cards placed to the right of the grid would be those that were the most important outcomes/facilitators/barriers, and the least important were placed to the left. Group members were informed that they could amend the cards if necessary. They were also welcome to add new cards if they felt that any potential factors were missing, and to remove any cards that they felt were irrelevant.
The two Young People’s Groups were cofacilitated by a member of the project team and an existing group facilitator who was well known to the young people. The Q-Set process proved to be quite effective at engaging the young people and serving as a basis for discussion, although there were some limitations to this in both groups. It became clear that the task for the young people was a demanding one, and we had been a bit optimistic as to what could be achieved in one session. In one group the energy levels noticeably dipped as the session wore on. In the other, only three or four of the group were well engaged with the task at any one time, although those who were engaged changed during the course of the discussion. As a result of the experience of the first group, the second group was run a little differently, including revision of the sequence of issues (which had started with a discussion of facilitator factors originally) and part of the session was spent in smaller subgroup discussions. It is notable that groups responded so differently to the same task. This is encouraging, as it suggests that, despite the limitations noted above, the young people felt an ownership of the task and hence that the engagement process was meaningful for them.
The early PAG session also used the Q-Set process in a similar way. Given the large size of the group, it had to be organised into smaller groups to enable meaningful discussion and the steering group decided to organise the groups by professional discipline. This was principally to enable all groups to have a say, but it was hoped that it would also highlight any differences between the groups and reasons for this, as well as areas of agreement. Groups were facilitated by members of the project team/steering group. Given the intensity of debate across all groups, this exercise seems to have been effective at promoting engagement and participation.
The ‘later’ consultations with young people and professionals focused on responses to evidence from the review, although the focus and methods were different. The Young Persons’ Group was cofacilitated by members of the research team and steering group, without an adult present that the young people knew well. This session was part of a broader participation event, for which known and trusted adults were available to support the young people should they become distressed. We explained to them that during the session they would hear quotations from young people that were quite powerful and which they might find unsettling. In such an event we told them that they could let us know if they wanted a break or simply take themselves off to the agreed point to find their identified adult supporter. One young person, who had been the only one to struggle to engage with the process, seemed to become bored and did ask to leave the session.
In the first part of the session, members of the research team provided an overview of the key intervention types that were identified through the review: CBT; counselling/psychotherapy; family intervention; attachment therapy; activity-based interventions; and therapeutic residential care. In addition to talking about these, pictures were provided, on large laminated sheets, to help illustrate key features of these approaches. The main part of the session was focused around three sets of questions:
-
Prioritising between interventions:
-
Which of these intervention types would young people want more?
-
Some therapies have a lot of evidence showing that they work, but others do not. If you were the government, which ones would you give the money to?
-
-
Responses to ‘acceptability’ statements:
-
Therapy does not help people to forget about abuse – they just make them talk about it over and over again
-
In some situations when the child starts therapy, he/she can get upset, and the parent then does not want them to go. What advice would you give a parent if their child was upset for the first time?
-
It’s not just the child that needs help – parents do too.
-
Do other people need to know what the therapist and child talk about?
-
Does a young person have to like their therapist for treatment to help?
-
-
Disseminating research evidence and findings to young people:
-
Suggestions for how to do this most effectively.
-
The group was given a range of tools to help the discussion. For example, they were given a pile of fake bank notes to help them allocate the funds to different intervention types. The visual component to this was important, and the young people ensured that they distributed the money carefully to reflect their priorities. They were also given voting cards with which to respond to the acceptability statements, with different colours representing different options.
A much longer, detailed and technical presentation of the findings was provided for the ‘later’ PAG. Given the smaller size of this compared with the earlier group, the whole session was held as one group, without splitting into subgroups, as this seemed unnecessary. A series of questions was developed to focus the discussion:
-
Do you think there is anything missing?
-
Are there any:
-
surprises about the coverage of maltreatment types?
-
surprises about the profile of evidence across different types of intervention?
-
disappointments or puzzles?
-
-
To what extent do the findings match your experience of what is offered by clinicians?
-
If different, what might account for this?
-
training
-
therapeutic context
-
therapeutic preferences
-
resource constraints
-
other.
-
-
How do you think clinicians will respond to the messages about the weight of evidence in favour of CBT interventions (broadly defined)?
-
What are the barriers to implementing the findings, and how might these be addressed in the final report?
-
What do you see as the priorities for research?
Findings from early advisory group process
Outcomes
There were striking differences between the two Young People’s Groups in how they ranked outcomes. This, in part, reflected differences in how they approached the task. One group did the rankings as outlined, whereas the other group felt that it would be inappropriate to rank the majority of outcomes. Their reasoning for this was because they felt that those outcomes were too specific to an individual’s particular problems and circumstances, such as anger or an eating disorder. They were unhappy about the task as originally outlined, as they felt it made them ‘generalise’ inappropriately about the population of maltreated young people. Therefore, they removed those cards, leaving only seven plus one that they added, as they felt that those remaining were more general and could apply to the majority of young people. As a result, one group ranked many more outcomes than the other. The full lists of outcomes rankings are provided in the appendix.
There were some similarities between groups in the highest ranking outcomes, as shown in Table 33. There is an emphasis on safety (both keeping and feeling safe) and resilience. There is also a similarity in the absence of positive rankings for interpersonal relationship outcomes. In other words, they were defining the outcomes more narrowly, as for the young person only. For the group that ranked a large majority of the outcomes, their rationale for ranking, as least important, the outcomes around stealing and drug use, for example, was that these represented individuals’ situations and choices, and hence were less generally applicable. This resonates closely with the rationale of the other group for removing many of those cards. In other words, although the groups approached the task very differently, there was an important similarity in their narratives, which formed a link with the later consultation exercise, as young people argued for the importance of each individual to be assessed according to their needs and circumstances, rather than just as part of a wider grouping.
| Rank | Group 1 | Group 2 |
|---|---|---|
| +4 | Helping the person to learn skills to handle life’s ‘ups’ and ‘downs’ | Helping the person to understand what being ‘treated badly’ is, learning to recognise when things are not OK Helping the person to learn ways to keep themselves safe (e.g. knowing when to report something and to whom to report it) |
| +3 | Helping the person to feel safe Helping the person to ‘bounce back’ if things in their life go wrong |
Helping the person to feel safe Helping the person to ‘bounce back’ if things in their life go wrong Helping the person to stop worrying |
The highest-ranked outcomes by the professional groups were well-being; attachment; emotional development; keeping safe; placement stability; peer relationships; and depression. The least important outcomes were socioeconomic; suicide prevention; violence/aggression; self-harm; criminality/legal; mental health literacy; substance abuse; and eating disorders (see appendix to this report for a full listing).
There were significant differences between the eight professional groupings, as shown both by their different rankings and their reasoning for these. Placement stability is an example of an outcome that attracted a wide range of rankings. This was generally ranked high, except for one group, which did not rank it at all – reasoning that this was not because it was unimportant, but because it did not represent an outcome, but rather a facilitator. This is significant in raising a definitional question about outcomes and also in focusing on the relationship between different types of outcome; for example, that placement stability could be seen as an intermediate outcome that would enable other outcomes to be achieved.
The relationship between outcomes was reflected in the high ranking for ‘well-being’, as two groups both referred to this as an ‘overarching’ outcome that other outcomes would feed into. Even here, though, with the highest-ranked outcome across all professional groups, there was disagreement, as neither of the foster carer groups rated it as an important outcome. Reasons given for the low ranking of some outcomes included:
-
A question of timescale, such that these more ‘tangible’ outcomes would feed into broader outcomes ‘downstream’.
-
The framing of the outcomes, either in that they could prove to be negative for the young person as well as positive (e.g. they may adopt coping skills that have negative effects) or that they were too much of an ‘adult concept’, such as intimate relationships.
-
Neurodevelopmental outcomes can be very difficult to change.
-
Not understanding what was meant by ‘mental health literacy’.
Facilitating factors
As with the outcomes discussion above, the two groups of young people approached the task differently, with one group removing a large number of cards. An example concerned the two cards: ‘the person was still living with their family’ and ‘the person was no longer living with their family’. They argued that these could not be ranked against each other, as the importance of each would differ, depending on whether the young person had experienced abuse from within or from outside their family. As with the outcomes, this group argued that such factors would be dependent on an individual’s circumstances and that it would be wrong to generalise. The facilitating factors ranked highest by the two groups are presented in Table 34. The key similarity across the groups is the importance of choice for the young person, both in starting and ending the service. Group 1 created the factor that was their most highly ranked, focusing on what would help the young person decide to start to receive the service. The group added to this that the format of the preliminary meeting should be determined by the young person, for example that he/she should have the option of either having an informal chat over coffee without any mention of the intervention, or a formal discussion of what to expect from the intervention.
| Rank | Group 1 | Group 2 |
|---|---|---|
| +4 | The person could meet the person giving help beforehand, to decide if they would be happy to begin getting help from them | The person knows that the person giving the help would not judge them or criticise them The person knows that the help will not stop before they are ready for it to stop |
| +3 | The person knows that no one would see them getting this help (e.g. no one would see them in that room, or see them through the window from the street) The person knows that it is their own decision whether to get the help or not, and not the decision of their parents or carers |
The person knows that they could trust the person/people that they would be getting the help from The person did not have to worry abut having money to pay for the services |
Other highly ranked factors reflect the importance of the ‘boundaries’ of the service in relation to confidentiality, trust in the help-giver, a quality to the experience such that they do not feel judged or criticised, and not having to worry about paying for the service (see Table 34). The lowest ranked factors included:
-
what other people think, such as parents or social workers
-
characteristics of the help-provider, such as gender.
The factors that were ranked the highest as facilitators by the PAGs were interventions tailored to individual needs and providing ‘young person-friendly’ information about services. Other factors to rank highly were high-quality research evidence; services are free to use; knowing where to find help; support for family/carers; and help/interventions available online. There was generally a high level of agreement among the PAGs on these, although there was some disagreement over ‘services are free to use’, with the range from high ranking to not being ranked at all. In the latter case, a group member explained that this was because it was ‘taken for granted’.
There was some disagreement too over ‘reducing stigma’. This was rated as the most important (4) by both foster carer groups, as they saw that getting the child/young person to engage with services and actually attend was most important. Other groups saw reducing stigma as less important, particularly the voluntary sector/social work group. Discussions indicated that this group felt that if services were well designed and delivered then the service would overcome any barriers created by stigma.
The factors that the professionals rated as being the least important in facilitating change were: child/young person can meet the service provider before therapy begins; choice of location of service delivery; child/young person can choose when the service ends; mental health literacy; and school-based interventions. Three of these five factors relate to the young person’s choice and represent a striking contrast with the importance given by young people to choice. A factor that young people and professionals agreed on, however, was in the importance of tailoring the intervention to the individual.
Barriers
As with outcomes and facilitators, the two groups of young people approached the task a little differently. One group found it difficult to agree on which factor was the most likely barrier, and felt that several of the cards held an equal status and were equally important. It was agreed that they could have more than one highest-ranked barrier, and these were moved into a specially created ‘+5’ column. This is significant in showing how the young people took ownership of the task and responded creatively when faced with their own barrier. The factors rated as the most likely barriers by the two groups of young people are presented in Table 35.
| Rank | Group 1 | Group 2 |
|---|---|---|
| +5 | The person thinks that their situation is too complicated for anyone to help The person thinks that the people offering help will not believe them |
|
| +4 | The person does not want to be seen as having mental health problems The person does not think they need any help The person does not think that the help available will work for them The person does not trust the people/services offering help |
The person does not know who to ask about getting help |
| +3 | The person does not trust the people/services offering help The person’s parents or carers will not allow it |
A range of factors is highlighted, including suspicion and concern over the service being offered; implications of receiving the service, such as feeling judged or being labelled; feelings about one’s own needs and situation, and barriers created by others, such as parents. The point about not knowing where to look for information reflects the points made under facilitators about the importance of child-friendly information. There was agreement between the two groups about the relative lack of importance of practical issues. A facilitator noted, for example, that one group had a remarkable trust that the services would accommodate them as necessary, for example coming to where they were if they could not travel, services were free so money was not a concern, and translators or someone who speaks your language would be made available if that was a problem for you.
The factors that were ranked the highest as the most likely barriers by the professionals were embarrassment; inadequate resources; stigma; lack of trust in service providers; fear; negative attitude; and lack of training for staff. Themes of stigma and lack of resources come strongly through the professionals’ responses. There is a significant difference between the professionals’ focus on lack of resources and the trust that young people put in the system to make the necessary service available.
There was generally a high degree of agreement between groups of professionals as to the relative significance of the various barriers. Groups generally ranked items related to the theme of stigma/fear highly, with the exception of the social work/voluntary sector group. They ranked all items relating to the child or young person as less important than items relevant to service providers and wider structural barriers, such as lack of training for staff, inadequate resources and ineffective health system structures. They indicated that if services are effective then they will be designed so that barriers relating to the child/young person would be eliminated. Other groups disagreed with this approach, as they saw stigma and fear as a wider social issue. Barriers relating to the child/young person were seen as equally important, and in some cases more important, than the barriers that were relevant for service providers.
The relative importance of ‘negative attitude’ also caused some disagreement. The majority saw this as the negative attitude of the child/young person towards the service, although the educational psychology group were clear that they saw the negative attitudes of other professionals as an important barrier. The educational psychology group also differed in their ranking of continuity of service. They ranked high staff turnover and continuity of service as the most important barriers. Other groups ranked these barriers as of medium importance (range –2 to 2). Money was ranked as a barrier by half of the groups. Those who did not rank it saw it as too broad/generic a barrier and so excluded it. Those groups who did rank it indicated that it was an important barrier, with the exception of one of the foster carer groups, which felt that ‘they would always find the money’ if necessary.
Findings from later advisory group process
Of the intervention types that were presented, the Young People’s Group felt that the most widely known among young people were CBT; counselling; and FT. The initial response from the group when starting the resource allocation exercise was that they found it hard to answer, as they suggested that it was important to know the individual before judging what interventions would be effective. Looking across the interventions, the group felt that all the interventions could potentially be useful, but again the judgement about this for an individual would have to be made in the light of that individual’s circumstances, their experience and environment. For example, if they had suffered ‘bad’ abuse, they may not want counselling – they may prefer CBT and attachment-based work. Hence on this basis, the group considered that all the different therapies should be made available.
The group considered different ways of completing the task, for example allocating the available resource equally across all intervention types and to the intervention types with fewer well-developed evidence bases. The group was very thoughtful about what sorts of information they would need to help make the judgement, including:
-
asking people what service they would prefer
-
having a choice, as some young people may prefer not to talk but would find ‘doing’ things helpful
-
the nature of evidence that is available
-
the need to ascertain as much information about an individual at the beginning as possible, with a suggestion that a ‘survey’ could be done with them.
They were concerned that focusing all of the resource to CBT, for which there is already evidence, does not help the other interventions to establish their own evidence bases. Nevertheless, they did not want to lose the benefits from CBT, given the evidence of its effectiveness. The group finally decided that they would want to continue to deliver CBT, but would also want to invest resources in the lesser-known therapies – attachment, activity based and therapeutic residential care – to see if it was possible to generate an evidence base for those.
Table 36 shows a high degree of consensus among the young people as to their views on a range of statements. The statements had been framed based on views expressed within the review of studies for the acceptability of interventions. The group disagreed with statement 1, from a parent who was critical of the therapeutic process for their family member, for two reasons:
-
It is not possible to forget about the abuse. The best thing is to talk about it to get it in the open. It should be the child’s decision as to what works best for them.
-
Therapy does not mean going over it again and again. It means going over it once, thinking about the experience, learning how they feel about it, but then doing different things.
| Statement | Red | Amber | Green |
|---|---|---|---|
| 1. Therapy doesn’t help people to forget about abuse, they just make them talk about it over and over again | 5 | 0 | 0 |
| 2. It’s not just the child that needs help, parents do too | 0 | 1 | 4 |
| 3. Do other people need to know what the therapist and child talk about? | 0 | 5 | 0 |
| 4. Does a young person have to like their therapist for treatment to help? | 0 | 0 | 5 |
The group could understand why it may be difficult for a parent, as they may take it personally and feel that it is their fault. They suggested that parents can need reassurance and it may help them to talk through the process. This could mean that the parents could meet the therapist first, or even get some therapy first, as they may need it. This led neatly into their consideration of the second statement, with a large majority of the group agreeing that parents may also need therapy. The group member who had selected ‘amber’ said that this was because the parent may not need therapy as such, but may instead need some guidance. The rest of the group agreed that support, rather than therapy, may be more appropriate in some situations. Meeting other parents was seen as potentially helpful, possibly with mothers’ and fathers’ groups run separately before being brought together.
The reason for the middle ‘amber’ position to statement 3 was that the group felt that it would depend on the child’s views as to who their information should be shared with, including parents. However, they did agree that other services would need to be informed if the child was in danger. There was agreement too in response to statement 4. Group members felt that young people would have to feel comfortable with their therapist for the therapy to be effective and this would mean feeling listened to and not feeling judged. A downside to this, however, is that if the therapist leaves, as this could result in the young person going back to their ‘old ways’. This led to a discussion about the nature of the therapeutic relationship: that it should not be too personal, as it is a job for the therapist; they are not a ‘friend’, so the young person should not become too attached to them.
The Professionals’ Advisory Group reflected on the significance of some of the factors that had been identified as facilitators, including parental involvement in the therapeutic process, as results have indicated that parent-plus-child therapy may be more effective than child-focused therapy alone. The foster carers stressed that the parent/carer must be involved in the process and be aware of what’s happening. For example, if a child wakes up at night having nightmares following a revelation made during therapy, the parent/carer must know how to deal with this. It was acknowledged that carers can be involved in different ways. One foster carer shared his/her experience of regular update meetings with the child’s therapist, in which they do not hear about the details of the sessions but can consider any implications arising from them. He/she felt that this arrangement had represented a balance between being sufficiently ‘in the loop’ and maintaining client confidentiality. A voluntary sector representative reminded the group that many children do not have a ‘functioning adult’ in their lives, and that this would have to be considered in any push towards greater carer involvement in the therapeutic process.
There was a nuanced discussion about the possibility of increasing the young person’s choice-making in relation to their own therapy. There was some resistance to the idea that young people should be more involved in deciding which type of therapy they should have, on the basis that they do not know or understand enough about the choices with which they are presented. A suggestion from this followed – that it may be more important to involve young people in discussions about the options for their therapy rather than simply seeing it as their choice. The group confirmed the importance, underlined by the first PAG, about the need to tailor interventions to individual children’s needs: ‘We cannot look at a child as a set of symptoms, we must look at each individual as a whole.’ This discussion was grounded by the view that choice and tailoring may not actually matter, given that young people are probably offered only whatever intervention is available locally. Despite these constraints and the caveats above about choice-making, the group considered that not enough was known about what outcomes children wanted and that this should be a future research priority.
The Professionals’ Advisory Group considered implications arising from the lack of evidence of effectiveness of interventions. A concern was raised about how any decisions on resource allocation or priorities could be made based on such a limited evidence base. It was agreed that, other than for CBT, it was important to emphasise for the other interventions that they should not be seen as ineffective, but that there is currently no evidence of their effectiveness. Some group members were not surprised at the lack of evidence of effectiveness for CBT at follow-up, for a couple of reasons:
-
CBT is very limited in duration (often delivered over 12 weeks), which may not be sufficient given the complexity of needs experienced by maltreated children.
-
CBT may be inappropriate for children, given that it was originally designed for adults.
The group considered the importance that young people had attached to the outcome of safety. They were concerned, however, to be careful when talking about ‘safety’ as an outcome, as it may be more related to prevention, and this could be misunderstood, given some confusion between prevention and early intervention. The group agreed that early intervention should be defined as an intervention that occurs at ‘the first recognition of trouble’, regardless of the child’s age. It was suggested that the review findings should be situated carefully within these discourses to avoid confusion and because of their current salience in government policy.
The group also highlighted practice contexts that the review findings will be seen within. The issue that came across most strongly concerned the pressures under which professionals are operating, including budget cuts for local authorities, a large-scale turnover of social workers and a large number of vacancies in social work departments. It was suggested that there is a risk that this review could add to the pressure on professionals by promoting criticism of them from the lack of evidence of their effectiveness, and the group was keen that this should be avoided.
Pressures on the professional system can help to explain, in part, why there can be little choice for the service user as to the type of intervention offered, such that there is a risk that the service is offered because it is available rather than because it is needed. There is also potentially a gap between the services that are researched and reported on in this review and those that are offered more widely in practice. There was agreement in the group that an urgent next step should be to conduct a survey of what services are currently being offered to maltreated young people. This was one of a range of future research priorities identified by the group, which included:
-
access to psychosocial interventions and impact of different referral routes on the effectiveness of interventions
-
children’s views concerning desired outcomes
-
mechanisms of change in therapy
-
importance of therapist persona
-
effects of the age of child on outcomes achieved by different interventions
-
experience of maltreated children who are asymptomatic.
Summary
The advisory group process was arguably quite limited. Nevertheless, it achieved the purpose for which it was designed. The early consultations provided a very helpful reminder of the range and diversity of views about desired outcomes for psychosocial interventions. There were different narratives for the relationships between different types of outcome and a definitional question about outcomes and facilitators. This was a further reminder of the contested nature of this field. There was a range of views too over the factors that were seen as facilitators of, and barriers to, change. This fed through into the later consultation phase, which considered different possible interpretations of the findings. The later consultation phase helped the project team to situate the findings within current policy and practice contexts, which is essential for promoting engagement with, and use of, the findings.
Appendix
Young People’s Advisory Group 1: 27 March 2013, Belfast
| ‘What difference would ‘helpful help’ make: | Rank | Notes |
|---|---|---|
| Helping the person to learn skills to handle life’s ‘ups’ and ‘downs’ | +4 | |
| Helping the person to feel safe | +3 | |
| Helping the person to ‘bounce back’ if things in their life go wrong | +3 | |
| Helping the person to stop going over and over in their mind the bad things that have happened to them | +2 | |
| Helping the person to feel better about themselves | +2 | |
| NEW CARD – Helping the person to not feel alone and to recognise that they are not ‘different’ to other people | +2 | |
| (The group did not place any cards in the ‘+1’ column) | +1 | |
| (The group did not place any cards in the ‘0’ column) | 0 | |
| (The group did not place any cards in the ‘–1′ column) | –1 | |
| (The group did not place any cards in the ‘–2′ column) | –2 | |
| Helping the person to stop taking their problems out on other people | –3 | |
| Helping the person to look after their physical health | –4 | |
|
CARDS REMOVED
The group removed all of the following cards because they felt that they were all too specific to an individual situation, e.g. it is not possible to rank whether eating properly is more important than not using drugs. A person with an eating disorder would rank addressing that as a more important outcome than a person who was using drugs, and so forth |
||
| Helping the person to stop feeling sad or unhappy | ||
| Helping the person to stop worrying | ||
| Helping the person to stop wanting to hurt himself or herself | ||
| Helping the person to eat well and not overeat or eat too little | ||
| Helping the person to stop bullying other people | ||
| Helping the person to stop using too much alcohol | ||
| Helping the person to get on better with their friends | ||
| Helping someone who was stealing to stop | ||
| Helping the person to do their best at school | ||
| Helping the person to get on better with their family | ||
| Helping the person to stop using drugs | ||
| Helping the person to be happier | ||
| Helping the person to stop getting in fights | ||
| Helping to stop the person being bullied | ||
| Helping the person to feel less angry | ||
| Helping the person to control their temper | ||
| Helping the person to understand what being ‘treated badly’ is, learning to recognise when things are not OK | ||
| Helping to person to learn ways to keep themself safe (e.g. knowing when to report something and to whom to report it) | ||
Young People’s Advisory Group 2: 9 April 2013, Cardiff
| What would ‘helpful help’ help with? | Rank | Notes |
|---|---|---|
| Helping the person to understand what being ‘treated badly’ is, learning to recognise when things are not OK | 4 | Both +4 rankings were made by one more-senior member of the group There was little discussion of these two rankings by the rest of the group |
| Helping the person to learn ways to keep themself safe (e.g. knowing when to report something and to whom to report it) | 4 | Both +4 rankings were made by one, more senior member of the group There was little discussion of these two rankings by the rest of the group |
| Helping the person to ‘bounce back’ if things in their life go wrong | 3 | |
| Helping the person to feel safe | 3 | |
| Helping the person to stop worrying | 3 | This was seen as a big problem for many in the group They expressed how they often or always felt anxious and worried about everything |
| Helping the person to control their temper | 2 | More than half of the group made reference to that being relevant for them, or joked about needing ‘anger management’ |
| Helping the person to stop feeling sad or unhappy | 2 | A number of people in the group said they suffered badly with depression |
| Helping the person to feel better about themselves | 1 | Ranked highest of the ‘+1’ rankings |
| Helping the person to stop going over and over in their mind the bad things that have happened to them | 1 | |
| Helping the person to stop taking their problems out on other people | 1 | |
| Helping the person to be happier | 0 | Being happy was seen as a choice: ‘some people are happy being miserable’ |
| Helping the person to do their best at school | 0 | This was not seen as overly important by the majority, but two participants expressed the view that doing well at school is important to help you ‘get out’ or get away from the bad situation you are in and make a better life for yourself in the future |
| Helping the person to eat well and not overeat or eat too little | 0 | A number of people in the group mentioned not eating right but this was not seen as a particularly important problem to overcome It was seen as being related to other bigger issues, such as the overall stresses of their lives |
| Helping the person to look after their physical health | 0 | The items on drugs, alcohol and food were all seen as relating to physical health and also a form of self-harm They felt that looking after your physical health would include eating well, not abusing drugs and alcohol |
| Helping to stop the person being bullied | 0 | |
| Helping the person to learn skills to handle life’s ‘ups’ and ‘downs’ | –1 | This one came out surprisingly low compared with the rating from Young People’s Advisory Group 1 |
| Helping the person to stop using drugs | –1 | The items on drugs, alcohol and food were all seen as relating to physical health and also a form of self-harm They felt that looking after your physical health would include eating well, not abusing drugs and alcohol |
| Helping the person to stop using too much alcohol | –1 | ‘That’s a personal choice, some people can enjoy drinking. It’s not always a problem for most people’ |
| Helping the person to stop wanting to hurt himself or herself | –1 | |
| Helping the person to feel less angry | –2 | Controlling your temper was seen as more important because sometimes getting angry is a good thing. It can help you protect yourself and stop people taking advantage of you |
| Helping the person to stop bullying other people | –2 | |
| Helping the person to stop getting in fights | –2 | ‘That’s a personal choice’ |
| Helping the person to get on better with their family | –3 | |
| Helping the person to get on better with their friends | –3 | ‘If your friends don’t understand then you’ve got the wrong friends’ |
| Helping someone who was stealing to stop | –4 | This was not seen as a problem related to maltreatment . . . ‘That’s an individual choice’, ‘If you can get something for free then get it’ One person rated this as more important than the rest of the group as ‘getting into trouble or getting caught could mess up your whole future’ |
Professional Advisory Group: 1 May 2013
| Outcome domain | Average ranking | SD | Number of groups | Theme |
|---|---|---|---|---|
| Well-being | 2.83 | 1.47 | 6 | Well-being |
| Attachment | 2.63 | 1.19 | 8 | Attachment/emotion |
| Emotional development | 1.88 | 1.73 | 8 | Attachment/emotion |
| Keeping safe | 1.86 | 1.95 | 7 | Being/keeping safe |
| Placement stability | 1.57 | 2.57 | 7 | Placement stability |
| Peer relationships | 1.50 | 1.20 | 8 | Relationships |
| Depression | 1.25 | 1.91 | 8 | Mental health |
| Cognitive | 1.17 | 0.98 | 6 | Neurological/cognitive |
| Anxiety | 1.13 | 2.10 | 8 | Mental health |
| Coping skills | 1.13 | 1.64 | 8 | Well-being |
| Academic | 1.00 | 1.15 | 7 | Attainment |
| Conduct/behaviour | 0.88 | 1.55 | 8 | Externalising behaviour |
| Intimate relationships | 0.75 | 1.75 | 8 | Relationships |
| Post-traumatic stress | 0.75 | 2.05 | 8 | Mental health |
| Physical health | 0.57 | 2.30 | 7 | Physical health |
| Family relationships | 0.50 | 1.85 | 8 | Relationships |
| Self-efficacy | 0.50 | 1.85 | 8 | Well-being |
| Self-regulation | 0.29 | 1.11 | 7 | Attachment/emotion |
| Neurodevelopmental | 0.25 | 3.10 | 4 | Neurological/cognitive |
| Socioeconomic | 0.00 | 0.82 | 7 | Attainment |
| Suicide prevention | 0.00 | 2.00 | 8 | Internalising behaviour |
| Violence/aggression | –0.14 | 1.57 | 7 | Externalising behaviour |
| Self-harm | –0.38 | 1.92 | 8 | Internalising behaviour |
| Criminality/legal | –0.50 | 1.51 | 8 | Externalising behaviour |
| Mental health literacy | –0.60 | 1.14 | 5 | Well-being |
| Substance abuse | –0.86 | 1.35 | 7 | Internalising behaviour |
| Eating disorders | –1.80 | 1.48 | 5 | Internalising behaviour |
List of abbreviations
- AAT
- animal-assisted therapy
- ABC
- Attachment and Biobehavioral Catch-up
- ANCOVA
- analysis of covariance
- ARRM
- AIDS Risk Reduction Model
- BDI
- Beck Depression Inventory
- BDI-II
- Beck Depression Inventory-Second Edition
- BPC
- Behavior Problem Checklist
- BSI
- Brief Symptom Inventory
- CAMHS
- Child and Adolescent Mental Health Services
- CAPI
- Child Abuse Potential Inventory
- CBCL
- Child Behavior Checklist
- CBCT
- Cognitively-Based Compassion Training
- CBT
- cognitive–behavioural therapy
- CCI
- Child Conflict Index
- CCT
- child-centred therapy
- CD
- conduct disorder
- CDI
- Children’s Depression Inventory
- CDirI
- child-directed interaction
- CEAC
- cost-effectiveness acceptability curve
- CEI
- Child Evaluation Inventory
- CES-D
- Center for Epidemiologic Studies Depression Scale
- CGAS
- Children’s Global Assessment Scale
- CI
- confidence interval
- CITES-R
- Children’s Impact of Traumatic Events Scale-Revised
- CONSORT
- Consolidated Standards of Reporting Trials
- COS
- controlled observational study
- CPC-CBT
- combined parent–child cognitive–behavioural therapy
- CPP
- child–parent psychotherapy
- CPS
- Child Protective Services
- CPSS
- Child PTSD Symptom Scale
- CROPS
- Child Report of Post-traumatic Symptoms
- CS
- controlled study
- CSA
- child sexual abuse
- CSATP
- Child Sexual Abuse Treatment Program
- CSBI
- Child Sexual Behavior Inventory
- CSI
- Coping Scales Inventory
- CTQ
- Childhood Trauma Questionnaire
- CTS
- Conflict Tactics Scale
- DDP
- dyadic developmental psychotherapy
- DERS
- Difficulties with Emotion Regulation Scale
- DISC
- Diagnostic Interview Schedule for Children
- DPICS
- Dyadic Parent–Child Interaction Coding System
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition
- ECBI
- Eyberg Child Behavior Inventory
- ECI
- Early Childhood Inventory
- EFT
- emotional freedom techniques
- EMDR
- eye movement desensitisation and reprocessing
- FAD
- Family Assessment Device
- FAF
- Family Assessment Form
- FASM
- Functional Assessment of Self-Mutilation
- FES
- Family Environment Scale
- FHF
- Fostering Healthy Futures
- FT
- family therapy
- GE
- gradual exposure
- GP
- general practitioner
- HFD
- human figure drawing
- HoNOSCA
- Health of the Nation Outcome Scales for Children and Adolescents
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- ICU-P
- Inventory of Callous and Unemotional Traits-Parent Report
- IES
- Impact of Events Scale
- IFA
- Independent Fostering Agency
- IGT
- individual and group therapy
- IPP
- infant–parent psychotherapy
- IPV
- intimate partner violence
- IT
- individual therapy
- ITT
- intention to treat
- IY
- Incredible Years Program
- KGAS
- Kiddie Global Assessment Scale
- KSADS
- Kiddie Schedule for Schizophrenia and Affective Disorders
- KSADS-PL
- Kiddie Schedule for Schizophrenia and Affective Disorders, Present and Lifetime Version
- LMM
- linear mixed model
- LSI
- Life Story Intervention
- LSS
- Life Satisfaction Survey
- M
- mean
- m-CBT
- modified CBT intervention
- MANOVA
- multivariate analysis of variance
- MASTR
- motivation–adaptive skills–trauma resolution
- MD
- mean difference
- MFGT
- multifamily group therapy
- MMP
- MOSAC Massage Programme
- MST
- multisystemic therapy
- MST-CAN
- Multisystemic Therapy for Child Abuse and Neglect
- MTFC
- Multidimensional Treatment Foster Care
- MTFC-A
- Multidimensional Treatment Foster Care for Adolescents
- MTFC-P
- Multidimensional Treatment Foster Care Program for Preschoolers
- NML-2
- Nijmegen Motivation List 2
- NSPCC
- National Society for the Prevention of Cruelty to Children
- OR
- odds ratio
- OSIQ-R
- Offer Self-Image Questionnaire-Revised
- PAD
- Parent Attachment Diary
- PAG
- Professional Advisory Group
- PCIT
- parent–child interaction therapy
- PDI
- parent-directed interaction
- PENN
- Penn Inventory for Posttraumatic Stress Disorder
- PERQ
- Parent Emotional Reaction Questionnaire
- PFR
- Promoting First Relationships
- PHV
- psychoeducational home visitation
- PI
- Project Image
- PPI
- psychoeducational parenting intervention
- PPP
- Pre-School–Parent Psychotherapy
- PPQ
- Parenting Practices Questionnaire
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROPS
- Parent Report of Post-traumatic Symptoms
- PSI
- Parenting Stress Index
- PTSD
- post-traumatic stress disorder
- QALY
- quality-adjusted life-year
- QEx
- quasi-experimental
- RBI
- relationship-based intervention
- RCMAS
- Revised Children’s Manifest Anxiety Scale
- RCT
- randomised controlled trial
- RET
- reminiscing and emotion training
- RFC
- regular foster care
- RPT
- resilient peer treatment
- RRFT
- Risk Reduction through Family Therapy
- RSES
- Rosenberg Self-Esteem Scale
- RTC
- residential treatment centre
- SAFE
- Sexual Abuse Fear Evaluation scale
- SAS-CBT
- Sexual Abuse-Specific Cognitive–Behavioural therapy
- SCARED
- Screen for Child Anxiety Related Disorders
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SEI
- Self-Esteem Inventory
- SES
- socioeconomic status
- SESBI-R
- Sutter–Eyberg Student Behaviour Inventory-Revised
- SFI
- Self-Report Family Inventory
- SIT
- stress inoculation therapy
- SMD
- standarised mean difference
- SOF
- Summary of Findings
- S/PCIT
- standard parent–child interaction therapy
- SPPC
- Self-Perception Profile for Children
- SSRI
- selective serotonin reuptake inhibitor
- SSRS
- Social Skills Rating System
- STAI
- State-Trait Anxiety Inventory
- STAI-C
- State-Trait Anxiety Inventory for Children
- STEP-TEEN
- Systematic Training for Effective Parenting of Teens
- STI
- sexually transmitted infection
- T3
- time 3
- TAU
- treatment as usual
- TF-CBT
- trauma-focused cognitive behavioural therapy
- TN
- trauma narrative
- TRF
- Teacher Report Form
- TSC-40
- Trauma Symptom Checklist-40
- TSCC
- Trauma Symptom Checklist for Children
- TSCYC
- Trauma Symptom Checklist for Young Children
- TV/PCIT
- time-variable parent–child interaction therapy
- UC
- usual care
- UCLA-A
- University of California Los Angeles PTSD Index for DSM-IV (Adolescent version)
- VOYPIC
- Voice of Young People in Care
- YSR
- Youth Self-Report