Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 12/17/05. The contractual start date was in September 2013. The draft report began editorial review in January 2016 and was accepted for publication in April 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Julie Mytton is a member of the Health Technology Assessment Maternal, Neonatal and Child Health Panel.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Jackson et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
The focus of this study was Gypsy, Traveller and Roma communities in England and Scotland. Throughout this report we use the term ‘Traveller’ to include distinct and diverse Gypsy, Traveller and Roma communities, who may be settled or nomadic or live on authorised or unauthorised sites or in houses.
Traveller identity and history
Travellers in the UK are a heterogeneous group consisting of North Welsh Kale, South Welsh and English Romanichals, Irish Travellers (Pavees, or Mincéirs), Scottish Travellers and, increasingly, European Roma. 1 There is an ongoing debate in the UK concerning the definition of Travellers, whether they are defined by their ethnicity or their nomadic lifestyle. As Clark2 suggests, the continuing question of who are Travellers may, in part, be because of the lack of neutrality of the terms ‘Gypsy’ and ‘Traveller’ either within or outside the communities. In the Caravan Sites Act,3 Travellers are defined as ‘people of nomadic habit and lifestyle whatever their race or origin’. This definition, however, does not include those who live on permanent private sites or in houses. In contrast, Oakley4 suggests a definition of Travellers based on descent. She argues that a Traveller’s status is ascribed at birth and reinforced by their upbringing and commitment to Travellers’ values and lifestyle.
Gypsies have a very long history and are believed to have moved from India to Persia at the end of the ninth century, moving across the Middle East and becoming established all over Europe by the fifteenth century. 5 They are said to be one of the oldest ethnic minorities in the UK and were thought to have established themselves in Britain by the sixteenth century. The first official reference of Gypsies in the UK was in Scotland in 1505. 4,5 However, by 1554, Gypsies were considered ‘felons’ and executed. 2 Irish Travellers are thought to have originated from itinerant craftsmen and peasants who were forced on the road by war, famine and poverty. 6
In the twentieth century, Travellers again were a persecuted group. During the period between 1938 and late 1943, they were subjected to an extreme form of exclusion in Germany, which has been described as ‘The Great Devouring’ or ‘Gypsy Holocaust’,2 with an estimated 250,000 to 500,000 killed during this episode in history. 7 As recently as 2004, the forced sterilisation of Traveller women in Eastern Europe during communist rule has been reported. 8,9
Travellers hold a strong sense of their cultural identity, viewing themselves as separate from non-Traveller communities. 10 Nickson and Sudbery11 describe persecution as being at the ‘heart’ of Traveller identity, considering that the continued persecution of Travellers throughout history to the present day contributes to the maintenance of this. This identity based on persecution has implications for understanding the relationship between Travellers and the wider community, and the importance of ‘understanding the ethnic and cultural context’ in delivering services. 10
Traveller communities in England and Scotland
There are an estimated 54,895 ‘white: Gypsy or Irish Traveller’12 and 193,297 ‘migrant Roma’ living in England. 13 The Scottish Traveller population has been estimated at 421212 to 15,000. 14 The diversity of Travellers in the UK is increasing with greater ease of movement of populations within Europe. There are now an estimated 4400 Eastern European Roma across the UK. 15 All of these are likely to be underestimations because of the poor recording of Traveller ethnicity on public service systems, a reluctance to self-identify attributed to the history of persecution and rapidly changing inward migration. The figure of 360,000 Travellers in the UK is commonly cited. 16
The health of Travellers
Travellers typically experience significantly poorer health and shorter life expectancy than the general population. 17–24 For example, Parry et al. 20 reported that Travellers in England were 11% more likely than their age- and sex-matched comparators in the general population to have a self-reported long-term illness which limited daily activities. The life expectancy of Irish Travellers is 15 years shorter than the national average for men, and 12 years shorter for women. 25 Despite this greater health need, there is low uptake of health services by Travellers, including preventative health care. 17–22,24 As an example, individuals living in Roma communities in England were found to be less likely than non-Roma to visit a dentist, chiropodist or practice nurse, to contact NHS Direct or to be registered with a general practitioner (GP). 26 Barriers to uptake stem partly from a lack of consideration of Traveller culture by health providers when developing services, for example, reluctance by GP practices to register transient Travellers. 27 Further barriers include a history of discrimination leading to mistrust of people and institutions, poverty, low health literacy, language barriers, lack of knowledge of health systems in new countries to which they travel,21 and, in some communities, strong beliefs of ‘stoicism’, ‘self-reliance’ and ‘fatalism’ about health. 27
The UK immunisation programme
The public health benefits and cost-effectiveness of immunisation are well established,28 preventing globally between 2 and 3 million deaths each year in children and adults from diphtheria, tetanus, whooping cough, measles, mumps and rubella. 29 In the UK, effective and safe vaccines against 13 potentially damaging infections [diphtheria, tetanus, poliomyelitis, pertussis (hereafter referred to as whooping cough), Haemophilus influenzae type b, meningococcal ACWY, meningococcal B, pneumococcal, measles, mumps, rubella, influenza and rotavirus] are routinely offered to children and young people up to 18 years as part of the UK childhood immunisation programme. 30 Since 2008, girls aged 12–13 years are also offered the human papillomavirus (HPV) vaccine to protect against infections that can lead to cervical cancer. Children in specific at-risk groups are offered additional vaccines; for example, the bacillus Calmette–Guérin (BCG) vaccine is offered to infants in areas where the incidence of tuberculosis is above a specific rate or whose parents or grandparents were born in a country with high rates of tuberculosis. 31
The uptake of immunisations across the population needs to be sufficiently high so that the few individuals who are unable to be immunised, because of genuine contraindications, are protected from disease by living in a community in which there is very little circulating infection. This concept is known as herd immunity. The UK uptake rates for most of the routine vaccines in children up to 6 years are generally high and stable, approaching or meeting the 95% target required for herd immunity. 32,33 A notable exception is the seasonal flu vaccine for which 2014/15 uptake rates in England for children aged 2, 3 and 4 years were 38.5%, 39.5% and 32.9%, respectively. 34 Yet, even with good national coverage, social clustering of unprotected individuals (unimmunised/partially immunised) can lead to outbreaks of vaccine-preventable diseases. 35 Coverage of the routine three-dose HPV vaccination programme was consistently over 86% in England from 2012 to 201436 and over 80% in Scotland. 37
In addition to routine flu vaccination for children aged 2 to 17 years, which was introduced in 2013 and is gradually being rolled out and offered to the youngest children first,30 the flu vaccine is recommended for all adults over 65 years and for adults/children with chronic health conditions which put them at higher risk of serious complications of the illness, for example pregnant women, children/adults with underlying disease particularly chronic respiratory or cardiac conditions. 38 In the winter of 2014/15 uptake in England in those aged over 65 years was 73%34 and 76% in Scotland,39 close to the 75% target. However, among those at-risk under 65 years, uptake was just 50% and 54% in England 34 and Scotland,39 respectively, with the uptake by pregnant women even lower (44% and 47%, respectively). 34,39 Following a rise in cases of whooping cough in all ages and, in particular, among babies < 3 months old with deaths in infants too young to have been protected by their own immunisation course, it has been recommended since 2012 that pregnant women be offered the whooping cough vaccine between 28 and 38 weeks of pregnancy. Current uptake is 58% and 65% in England and Scotland, respectively. 40,41
One of the challenges for ensuring that groups at risk of poor immunisation uptake are targeted effectively is their identification. Until the 2011 census, ethnic group classifications did not provide for Travellers to ‘self-identify’. 42 Indeed, ethnic group is not routinely collected during registration with a GP and, even now, may be incomplete or poorly coded. 43 There is, therefore, a lack of accurate information about immunisation uptake in Traveller communities. A small number of local studies using parent self-report1,44–46 and NHS records1,47 suggest low or variable uptake of childhood immunisation. These patterns mirror data for other disadvantaged groups who are more likely to be unimmunised or not up to date, significantly increasing their risk (and consequent spread) of vaccine-preventable disease. 35,48,49 Indeed, there have been several, well-documented, outbreaks of measles and whooping cough in Traveller communities. 50,51 Adolescent girls from Traveller communities may no longer be attending school,52,53 reducing the likelihood of receiving sufficient doses of the HPV vaccine (which is now given in two doses). 30 Traveller girls were identified in a recent report54 as one of the target groups to ensure equitable uptake of the HPV vaccine. Unfortunately, most of the studies of vaccine uptake in Traveller communities are dated and it is unclear if these reflect current uptake rates in Traveller communities. In terms of adult vaccines, we found no adult whooping cough or flu vaccine uptake data for Travellers; however, they tend to have larger families,20,22,55 which is a risk factor for reduced vaccine uptake and higher prevalence of asthma20,22 and bronchitis20 (both indications for flu vaccine). This coupled with low uptake of health care, including maternity services,18 suggests uptake of both vaccines may be low.
Factors influencing the uptake of immunisation
A large body of literature56–63 identifies two broad categories of parental factors influencing uptake of childhood immunisation in the general population and high-risk groups. The first relates to socioeconomic disadvantage for which, despite not objecting to vaccines, parents lack access to resources and support to overcome logistical barriers such as having no private transport. The second relates to parents’ concerns about the safety or beliefs about the necessity of vaccines. There are differences in parents who accept immunisation but do not complete the course (partial immunisers), those who have concerns about the safety of some vaccines but not others (selective immunisers) and those who reject immunisation altogether (non-immunisers). 64 These different groups are likely to require different support and information to enable them to take up immunisation opportunities. Regardless of parental position on immunisation, trust in health professionals and services is paramount. 63,65 Studies have also explored factors influencing uptake of immunisation in adults 66,67 including those with high-risk conditions,68 pregnant women69,70 and minority ethnic groups. 71 The barriers appear to broadly fall into the same two categories, access and beliefs, including the perception that healthy people do not need immunisations. 72
Although many of the issues influencing vaccine uptake described in the literature are likely to be similar for Travellers, further research is needed to understand the specific issues affecting diverse Traveller communities to inform the development of interventions tailored to their needs and cultural context. To date, only a few studies1,44–47 have explored the barriers specific to immunisation uptake in Traveller communities. These identify multiple issues reflecting the difficulties in accessing wider health services experienced by marginalised, socially excluded communities. 17–21,24,73–75 Issues particular to immunisation include barriers to accessing primary care services (e.g. the absence of a permanent postal address for recall letters),45 parental concerns about the safety of vaccines46,76 and objection to immunisation arising from strongly held cultural beliefs and traditions. 18 A reluctance to ‘self-identify’ as Travellers for fear of discrimination77 and the challenge of maintaining reliable health records for transient communities19 hinder record keeping of immunisation uptake in Traveller communities.
These studies are typically small, dated or focused on one Traveller community. Although Traveller communities may share similar features of lifestyle that distinguish them from the general population, beliefs and cultural traditions can vary. 77 It is, therefore important to understand whether or not, and how, factors that promote or inhibit immunisation differ between specific communities. Moreover, immunisation has often been only one small part of studies exploring several health issues with Travellers. This limits the extent to which the complex nature of barriers to and facilitators of immunisation is explored. For example, barriers may be specific to particular vaccines [e.g. measles, mumps and rubella (MMR) vaccine], differ for adult and childhood vaccines or be specific for different Traveller communities. Many vaccines have been introduced in the last three decades (MMR in 1988; Haemophilus influenzae type b in 1992; meningococcal C in 1999; pneumococcal conjugate in 2006; HPV in 2008; rotavirus in 2013; and childhood flu in 2013) or indications for established vaccines have expanded (e.g. pregnancy flu and whooping cough vaccines in 2010 and 2012, respectively). Since several studies among Travellers were conducted in 1980/90s, issues associated with these newer vaccines have not always been considered, neither have evolving views about previously controversial vaccines (e.g. whooping cough, MMR) or the views of more recent migrant communities in the UK (e.g. Romanian and Slovakian Roma). Finally, we were unable to locate any studies on immunisation uptake in adults living in Traveller communities.
Interventions to increase the uptake of immunisation
The effectiveness of interventions to increase immunisation uptake among children48,78–82 and adults68,78,83,84 have also been reviewed and there are many examples of innovative health- and social-care provisions aimed at improving the health of Travellers. 17,18,85,86 Some target immunisation specifically (e.g. outreach immunisation programmes, tailored health promotion resources), whereas others are generic yet relevant to immunisation (hand-held patient records, specialist health visitors17 and cultural competence training of health professionals). 87 These interventions are rarely rigorously evaluated so it is unclear which are feasible, acceptable and (cost-)effective, in which communities they work and how they may or may not work. Finally, existing interventions are rarely informed by theoretical frameworks which can increase effectiveness by aiding understanding of the likely mechanisms of change. 88 This study set out to advance the understanding by addressing these limitations of previous research.
Research aims and objectives
Aims
-
To investigate the barriers to and facilitators of acceptability and uptake of immunisations among six Traveller communities across four UK cities.
-
To identify possible interventions to increase uptake of immunisations in these Traveller communities that could be tested in a subsequent feasibility study.
Objectives
-
To investigate the views of Travellers on the barriers to and facilitators of acceptability and uptake of immunisations and explore their ideas for improving immunisation uptake.
-
To investigate the views of service providers on the barriers to and facilitators of uptake of immunisations within the Traveller communities with whom they work, and explore their ideas for improving immunisation uptake.
-
To examine whether or not and how these responses by Travellers and service providers vary within and across communities and for different vaccines (childhood and adult).
-
To use the data collected from (1–3) to identify possible interventions to increase uptake of immunisations in the six Traveller communities.
-
To conduct workshops in each community to discuss findings and to produce a prioritised list of potentially feasible and acceptable interventions to be considered for testing in a subsequent feasibility study.
Chapter 2 Methods
Approvals and registration
The National Research Ethics Service Committee Yorkshire and The Humber – Leeds East approved the study on 23 August 2013. Research and development approval was secured from the relevant NHS organisations: Bristol Clinical Commissioning Group (CCG), York Teaching Hospital NHS Foundation Trust, Vale of York CCG, NHS Greater Glasgow and Clyde, Great Ormond Street Hospital for Children NHS Trust, Homerton University Hospital NHS Foundation Trust, Lewisham and Greenwich NHS Trust and Guys’ and St Thomas’ NHS Foundation Trust. The study was assigned the International Standard Randomised Controlled Trials Number of ISRCTN20019630 and UK Clinical Research Network Portfolio number 15182.
Study design
This was a three-phase qualitative study. The three phases and the aims they each address are presented in Figure 1. The study design comprised the first stage of the Medical Research Council’s framework for developing and evaluating complex interventions. 88 The aim of this stage is to ensure that a complex intervention ‘can reasonably be expected to have a worthwhile effect’. To this end, this stage is used to identify the components of the intervention and the mode of delivery. Questions of whether or not and how the content and delivery of the intervention might need to differ within and across populations and settings, and what are the potential barriers to and facilitators of implementation are also addressed. This stage of the framework also includes identification of an appropriate theoretical framework to inform the intervention and to aid understanding of the likely mechanisms of change. This increases the likelihood of an intervention being effective. 88
FIGURE 1.
Mapping of study aims against the phases of the UNderstanding uptake of Immunisations in TravellIng aNd Gypsy communities (UNITING) study.

Theoretical framework
The theoretical framework underpinning the research was the social ecological model (SEM),89 which recognises that individuals’ behaviour is affected by, and affects, multiple levels of influence (intrapersonal, interpersonal, institutional, community, policy; Table 1). Levels are interactive and reinforcing. 90 This multilevel focus is consistent with the World Health Organization (WHO)’s conceptualisation of health. 90 The model also identifies intervention strategies for each level of influence and it is proposed that, to achieve long-term health improvements, all five levels should be targeted simultaneously. If this is not possible, then at least two levels should be targeted. 90 We used the SEM to ensure that all levels of potential influence on immunisation behaviours were considered and we proposed to identify interventions at all five levels. Although we did not anticipate designing interventions to change national immunisation policy in a subsequent feasibility study, we considered it possible that there may be local policies and/or approaches to communicating national initiatives that fail to meet the needs of these communities and we would identify strategies to tackle this. Acknowledging these complex multifaceted determinants on behaviour is considered to be of particular relevance to understanding health behaviours (to inform future interventions) in socially excluded communities with specific health needs such as Travellers. The SEM has previously been used in the context of flu immunisation,91 child health92 and with culturally diverse93 and disadvantaged populations. 94
| Level | Level-specific influences on health behaviour | Examples of level-specific influences on immunisation behaviour | Level-specific intervention strategies |
|---|---|---|---|
| Intrapersonal | Characteristics of the individual, for example knowledge, attitudes, behaviour, self-concept and skills | Perceptions of risk from disease and effectiveness of vaccine, attitudes towards immunisation, past immunisation behaviour, perceived membership of a vaccine priority group and trust in ‘experts’ | Education, training and skill enhancement of target population |
| Interpersonal | Formal and informal social networks and social support systems, for example family and friendship groups | Beliefs that friends and families (do not) want them to vaccinate, number of people vaccinating in the social network (social norm) and social capital | Education, training and skill enhancement of people who interact with target population (e.g. family members, friends, teachers) |
| Institutional | Social institutions with organisational characteristics and (in)formal rules and regulations for operation | Access to a health-care provider, reminders and amount of information from health-care provider, and recommendation to vaccinate by health-care provider | Education, training and skill enhancement of general community beyond target population and immediate contacts including institutional leaders |
| Modifications to institutional environments, policies or services | |||
| Community | Relationships among organisations, institutions and informal networks within defined boundaries | Presence of disease in community, perceived risk for self and of infecting others | Education, training and skill enhancement of general community beyond target population and immediate contacts including community leaders |
| Modifications to institutional environments or services | |||
| Policy | Local, state and national polices | Presence in vaccine priority group and access to immunisation (free of charge, location of services) | Education, training and skill enhancement of general community beyond target population and immediate contacts specific to policy change |
| Creation or modification of public policies |
Setting
The research was undertaken in four UK cities and focused on six Traveller communities (see Table 2), who predominantly, but not exclusively, lived in houses or on authorised sites (privately owned, council managed). This was a complex, multisite study working with socially excluded, marginalised communities who are traditionally considered to be hard to engage in research. 95 For reasons of practicality, and to enable our approach to be refined in the light of experience, we conducted the study in two waves (wave 1, York and Bristol; and wave 2, Glasgow and London). This enabled us to learn important lessons in wave 1 to inform wave 2, for example about gaining the trust of communities to facilitate recruitment and about the organisation of the phase 3 workshops.
A description of the six Traveller communities is presented in Table 2. The English Gypsy, European Roma and Irish Traveller communities are recognised in the Race Relations Act 197696 as ethnic minorities, replaced now by the Equality Act 2010. 97 Although they have different beliefs, customs and languages, they share common features of lifestyle and culture,27 and are genealogically and linguistically related. 98 In contrast, the Scottish Showpeople are not recognised in the Race Relations Act 197696 or by the aforementioned communities to be part of the ‘traditional Travellers’ ethnic group. Indeed, it is reported that they do not want to have recognised ethnic minority status, self-defining as business/cultural communities. It is only their traditionally nomadic lifestyle that means that, legally, they are labelled as Travellers. 99
| City | Community | Overview |
|---|---|---|
| Bristol | Romanian Roma | Descended from the same people as British Romany Gypsies and have recently moved to the UK from Central and Eastern Europe. Recognised as the same ethnic category as British Gypsies, yet distinct from the UK community. A total of 40 families in shared rented accommodation in relative proximity to each other. Families are mainly Romanian |
| English Gypsy | Recognised in British law as an ethnic group. More than 100 families living on two council-managed sites (one a transit site) in Bristol. Families live on a privately owned site in North Somerset (117 caravans) and a council run site (250 caravans) in South Gloucestershire. These are all mixed sites, home to both English Gypsies and Irish Travellers | |
| Irish Traveller | ||
| York | English Gypsy | Recognised in British Law as an ethnic group. More than 350 families living across three official sites and some in housing |
| Glasgow | Romanian and Slovakian Roma | Descended from the same people at British Romany Gypsies and have recently moved to the UK from Central and Eastern Europe. Recognised as the same ethnic category as British Gypsies, yet distinct from the UK community. An estimated 3500 Roma live in Glasgow,15 mainly in a small geographical area (6–8 streets) in the Govanhill area of the city. The settled population in Govanhill are mainly Slovakian. However, there has been an increase in the Romanian population since migration restrictions were lifted in January 2014 |
| Scottish Showpeople | Scottish Showmen/Showpeople or travelling show, circus and fairground families. Not recognised in British law as an ethnic group. Approximately 300 live in fixed sites in the north-east of Glasgow (these numbers are likely to be an underestimate; accurate numbers are not available). Some sites are council owned, others privately owned. Travelling with shows is becoming less common, and many families own and run snack vans and children’s fun rides in shopping malls, etc. | |
| London | Irish Traveller | Traditionally nomadic people of Celtic descent arriving in Britain in 1850s. Recognised in British law as an ethnic group. A total of 17,000 live in London. Most are in rented accommodation and on local authority sites. Three areas were included: Hackney, Lewisham and Southwark. In Hackney, 17 families live across five official sites and 54 families live in houses (temporary/emergency, private and social housing). Lewisham currently has no official Traveller sites and the population live in either social or private housing. Researchers were advised that the vast majority live in privately rented accommodation and are now being significantly impacted on by the introduction of the ‘benefit cap’ with rental costs being high. In Southwark, there are four official Traveller sites, but many more families live in social and private housing |
We included two English Gypsy (Bristol and York) and two Eastern European Roma communities (Bristol and Glasgow). This enabled us to consider whether or not Travellers’ views and experiences of immunisation were specific to those particular communities (e.g. English Gypsy people living in York) or reflected more widely the experiences of communities of the same descent (e.g. English Gypsy communities across the UK). Romanian Roma participated in Bristol, whereas both Romanian and Slovakian families were included in Glasgow. The intention at the outset was to work with the English Gypsy community in the Bristol area and sites were selected for recruitment where predominantly English Gypsy populations reside. However, as members of the Irish Traveller community also live on the same sites, it was not considered equitable by the gatekeeper to recruit solely English Gypsies which meant we included Irish Travellers in Bristol in the study. Therefore, we also included two Irish Traveller communities (Bristol and London), which facilitated further cross-community comparison.
Participants
Phase 1
Within each Traveller community we recruited both men and women living in extended families across generations. We included young women planning families, parents and grandparents to capture a lifespan/cross-generational perspective, as well as adolescents eligible for their three-in-one booster (diphtheria, tetanus, poliomyelitis, given at age 13–18 years), girls eligible for HPV vaccine (given at age 12 or 13 years in school); and adults eligible for the flu vaccine (pregnant women, over 65 years and with specified long-term conditions) and whooping cough vaccine (pregnant women). Childhood immunisation decisions are typically made by mothers;56,57 however, we were keen to recruit both men and women to explore any potential gender differences in views. We aimed for one-quarter of participants to be male. We also purposively sought to recruit a mix of full immunisers/partial immuniser and non-immunisers (based on self-report). We planned to interview approximately 22–32 participants in each of the six Traveller communities (total 132–192 participants). The upper limit was subsequently increased to 45 (see Chapter 3, Participants). An overview of the target sample for each Traveller community is presented in Table 3. We were confident that this sample size would enable us to look for potential differences and similarities in views within a community as well as draw out meaningful comparisons across Traveller communities, both across gender and for different vaccines (childhood and adult) to allow robust conclusions to be made.
| Gender | Total | ||||
|---|---|---|---|---|---|
| Male | Female | ||||
| Fathers | Grandfathers | Adolescents/young women | Mothers | Grandmothers | |
| 2–4 | 2–4 | 6–8 | 6–8 | 6–8 | 22–32 |
Phase 2
Service providers able to influence local policy making, drive health improvement, and/or providing or commissioning services for Traveller communities in the four cities were recruited to the study. We purposively sampled service providers in each of the four cities to ensure we interviewed a mix of ‘frontline workers’ (e.g. health visitors, practice nurses, community midwives, school nurses, GPs, range of community workers including third sector) and those working in more strategic/commissioning roles (e.g. local decision-makers in health protection/public health/health and wellbeing boards/CCGs). We set out to interview 6–8 service providers in each city (total 24–32 participants). In Bristol and Glasgow, where we were working with two Traveller communities, some of the service provider participants worked specifically with one Traveller community, whereas others had a more city-wide role.
Phase 3
A subsample of participants from phases 1 and 2 who had agreed to be reapproached were recruited to take part in the workshops. We aimed to include 10–12 Traveller participants per community, comprising a mix of Traveller men and women, across generations. We set out to recruit three or four service providers to each workshop, both frontline workers and those with a more strategic role. When we were unable to recruit sufficient numbers of phase 1 and phase 2 participants, other Travellers and service providers who had not been interviewed were invited to attend. The target participant numbers for the workshops were 13–16 per workshop, with a total of 78–96 participants.
Access and recruitment
Phase 1
We were aware that the ‘outsider’ position of researchers, with few similarities of experience and no ‘network connections’ with Traveller communities, might lead to mistrust meaning that gaining access could be difficult and time-consuming. 95 Therefore, our research team included gatekeepers in all four cities who had long-standing trustful relationships with the communities and who could ‘vouch’ for our trustworthiness, enable access and help recruit participants to the study. Our proposed approach in each Traveller community was based on the experience of these gatekeepers, as well as drawing on established good practice. 100
Recruitment and data collection in wave 1 (Bristol and York) occurred from December 2013 to March 2014. In wave 2, recruitment was March to April 2014 (Glasgow Roma), July 2014 to April 2015 (Glasgow Scottish Showpeople) and June to November 2014 (London Irish Travellers). A description of the approach to access and recruitment for each Traveller community is presented in Table 4. In all communities the gatekeepers (e.g. a member of the Bristol City Council Gypsy and Traveller Team who is an English Gypsy, a health visitor who works with Roma families in Glasgow) first spoke with community members about the study, and handed out the participant information sheet (PIS) for people to take away with them and discuss with others. These documents had been developed with the community partners (see Community partners) and used simple language and pictures (see Appendix 1). Documents were translated for the Roma communities in Bristol and Glasgow. Roma language, Romani, is predominantly oral with a wide number of dialects. Roma people from one area may not speak or understand a dialect spoken in another area; however, they often understand languages such as those spoken in the country from which they migrated. For this reason study documents were translated into Romanian and Slovakian for the Roma communities to improve accessibility to the study, although it was recognised that the primary route to engagement for these communities was oral. The gatekeepers then identified potential participants for the study and either booked interviews on behalf of the local researcher or passed on the contact details of participants for the researcher to book the interviews. Throughout the recruitment phase these gatekeepers continued to promote the study with community members, discussing it with them and reminding them to attend interviews they had booked. Snowballing95 occurred in the Bristol English Gypsy/Irish Traveller, York English Gypsy, Glasgow Roma, Glasgow Scottish Showpeople and London Irish Travellers communities, with community members telling others about the study. We constantly reviewed our sampling to ensure that we met our target for different family roles (see Table 3). Participants were given a £15 gift voucher to thank them for their time. The shop for which the voucher could be redeemed was recommended by the community partners (see Community partners), so as to be the most useful for the community.
| City | Community | Overview |
|---|---|---|
| Bristol | Romanian Roma | Phase 1: a member of Bristol City Council Gypsy and Traveller Team who is an English Gypsy and part of the research team attended the existing Roma drop-in centre, handed out the PISs and explained the project. She returned a week later to compile a list of people willing to be interviewed. The drop-in centre manager and interpreter/advisor also told people about the project using the PISs. The interpreter/advisor further discussed the study with Roma families who she met as a bilingual family mentor. The drop-in centre manager and interpreter/advisor booked appointments for the next few weeks on behalf of the local researchers and the advisor/interpreter reminded participants to attend on the morning prior to the interview (by telephone or text) |
| Phase 3: the interpreter from the Roma drop-in centre telephoned phase 1 participants and then visited them at home to deliver the PISs about the workshop. She then reminded participants to attend on the morning prior to the workshop (by telephone or text) | ||
| English Gypsy and Irish Traveller | Phase 1: a member of Bristol City Council Gypsy and Traveller Team who is an English Gypsy and part of the research team spoke to Travellers on two sites, both close to the Bristol local authority boundary, but located in neighbouring authorities. On the north Somerset site, she handed out the PISs and explained the project. She then visited the site with the local researcher, introduced her to some participants who then suggested others to be interviewed | |
| In South Gloucestershire the health visitor for Travellers used the same approach on the local sites and passed on the details of potential participants to the local researcher. The researcher then visited the site, initially with the health visitor. The researcher was known to the community as she had previously worked on this site as a health professional and knew key members of the community. Snowball sampling was again used as some participants suggested others to be interviewed. In this way some housed Travellers were accessed | ||
| Phase 3: the same gatekeeper from phase 1 (who no longer worked for Bristol City Council by this stage of the study) spoke to phase 1 participants and handed out the PISs about the workshop. She then brought the participants to the event on the day | ||
| York | English Gypsy | Phase 1: the chief officer of YTT and a member of the community (both part of the research team) spoke to people attending YTT about the project and handed out the PIS. The community member passed on the study information to others who did not attend YTT. Interview sessions were organised on ‘busy’ days when lots of people attended for literacy and other classes. The local researchers attended YTT on those mornings to interview participants who turned up. Snowballing also occurred at this time with families telling other families to attend the interview sessions. Later in the study when we were interviewing the final few people (to meet our sampling criteria) interviews were booked with specific participants. Throughout recruitment YTT staff encouraged participants to attend for interviews when they saw them |
| Phase 3: the chief officer of YTT spoke to phase 1 participants and handed out the PISs about the workshop, compiled a list of participants and reminded people to attend | ||
| Glasgow | Romanian and Slovakian Roma | Phase 1: members of the local EU Team (i.e. a health visitor with a specialist role and a bilingual support worker) spoke to people about the project and handed out the PISs. The local researcher then attended a ‘drop-in’ clinic run by the EU team to answer questions. Interview slots were booked at particular dates/times. Those wishing to participate/hear more about the study were asked to attend at these dates/times. Adolescent girls were recruited with the assistance of the Deputy Head and bilingual support workers in the local secondary school. Those who wished to participate attended an interview on an agreed date. Snowballing occurred within the Roma community |
| Phase 3: the EU team discussed the workshop with families and handed out the PISs. They then invited the families to attend on an agreed date/time | ||
| Scottish Showpeople | Phase 1: two community partners shared the PISs with potential participants and asked for permission to pass on contact details to the local researcher of those who may be interested in taking part in the study. The researcher then contacted these potential participants (by text, telephone call, e-mail) discussed the study, answered any questions and booked an interview. The researcher also asked participants if they had contacts who might be interested in taking part | |
| Phase 3: the researcher recontacted phase 1 participants who had agreed to be recontacted. The PISs were provided and participants were invited to attend on an agreed date/time | ||
| London | Irish Traveller | Phase 1: in Lewisham, the gatekeeper and/or a local researcher who was known to the community approached individuals about the study, gave them copies of the PIS and booked interviews. In Southwark, a member of the Irish Traveller community who worked as a volunteer with Southwark Travellers’ Action Group was particularly influential in promoting the study and organising and encouraging participation. The Southwark Travellers’ Action Group Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) page was also used. In Hackney and Southwark, the local researchers were invited to attend established groups for Traveller women and girls to promote the study |
| Phase 3: the researchers and gatekeepers recontacted participants. The PIS was provided and participants were invited to attend on an agreed date/time. As it was decided that the workshop would be held in Hackney, transport was provided for the Travellers who were coming from the other side of the city |
We did not formally record how many Travellers were approached and then agreed/declined to be interviewed in each city. The gatekeepers in Bristol reported that one adolescent Roma girl refused to take part having asked for permission from her mother-in law, and one man (who turned up in place of the two women booked for interviews) refused to be interviewed as he did not wish to sign a consent form or be audio-recorded. No English Gypsy or Irish Travellers in Bristol, York or London were reported to have declined to participate. In Glasgow, gatekeepers observed that the majority of the Roma people approached agreed to take part. Approximately 25 Scottish Showpeople were approached and 14 were recruited.
Phase 2
Recruitment and data collection in wave 1 occurred from April to June 2014 (Bristol) and from June 2014 to February 2015 (York). In wave 2, recruitment was from October 2014 to April 2015 (Glasgow) and from February to August 2015 (London). In each of the four cities we drew up a list of relevant service providers (their organisations and roles). These lists were derived from conversations with gatekeepers and local service providers (e.g. lead for children and families in north-east Glasgow, health improvement practitioner specialist at York City Council), interviews with Travellers and service providers as well as our own knowledge and professional practice. Potential participants were approached by telephone, e-mail or face to face, and given the PIS (see Appendix 2) to review before an interview was booked. In Bristol, York and London service providers were not offered financial reimbursement for their time. In Glasgow, financial reimbursement was offered, in order to facilitate recruitment of GPs and practice nurses.
As in phase 1, we did not formally record how many service providers were approached and subsequently agreed/declined to be interviewed. In Bristol and London everyone who was approached agreed to participate. In York, with the exception of health professionals at two GP practices, everyone approached agreed to be interviewed or suggested a colleague to participate in their place. In Glasgow, 20 were approached and 14 were recruited.
Phase 3
Recruitment and the workshops in wave 1 took place in November 2014 (combined workshop for Roma and English Gypsy/Irish Traveller communities in Bristol) and March 2015 (York English Gypsy). The wave 2 workshops took place in June 2015 (Glasgow Roma), August 2015 (Glasgow Scottish Showpeople) and September 2015 (London Irish Travellers). Traveller participants from phase 1 who had agreed to be recontacted about phase 3 were approached by the gatekeepers to take part in the workshop and given a PIS about the workshop (see Table 4). As in phase 1, these documents had been developed with the community partners (see Community partners) and used simple language and pictures (see Appendix 3). They were translated into Romanian and Slovakian for the Roma communities. The gatekeepers then confirmed the participants for the workshop and reminded them to attend. Service providers from phase 2 were recontacted by telephone or e-mail and invited to attend the workshop (see Appendix 3 for PIS). Traveller participants were given a certificate of attendance and a £25 gift voucher (the shop was decided by the community partners; see Community partners) to thank them for their time. Service providers also received a certificate of attendance. They did not receive financial reimbursement for their time.
We did not formally record how many Travellers were reapproached and subsequently attended the workshop. Two service providers in Bristol declined to attend the workshop, as they were too busy or their work no longer focused on the Traveller communities. They were replaced by people in similar roles. In York, all of the participants in phase 2 attended or sent a colleague in their place. In Glasgow, three service providers working with the Roma community who were interviewed attended or sent a colleague in their place. One service provider working with the Scottish Showpeople attended a workshop. In London, one participant identified a replacement. One of the three London localities was not represented by any service providers.
Data collection
A data collection protocol was developed to ensure that a consistent approach was employed across the research team.
Phase 1
A mix of one-to-one and small-group interviews with members of the same family/peer groups were conducted. The number of people in the interview depended on participant preference and who attended for the interview. As recommended in the literature95,100 and by the local gatekeepers, the interviews were held in locations known to participants: at the Roma drop-in (Bristol Roma), at home (Bristol English Gypsy and Irish Travellers), at the York Travellers Trust (YTT) premises and at home (York English Gypsy), in a building adjacent to the local health centre or in the local secondary school (Glasgow Roma) and at home or a local café (Glasgow Scottish Showpeople). In London, interviews were carried out in people’s homes, the café of a local library, a community organisation office and a community centre. Interviews with the Roma participants were conducted with the assistance of an interpreter. In York, two Travellers (one of whom is a member of the research team) were trained by a researcher to conduct the interviews on one of the Traveller sites considered by the gatekeeper to be inaccessible to the researchers.
With the consent of participants, interviews were recorded digitally. For the group interviews the researcher took brief notes to identify who was speaking to facilitate accurate transcription. Prior to commencing the interview written consent was collected from participants. If Traveller participants reported that they struggled with reading, the researcher read out the PIS and each item on the consent form (see Appendix 4) and asked participants to mark or initial the item if they consented.
Phase 2
Interviews with service providers were predominantly one to one, with the exception of a small number of small-group interviews. They were conducted in the participants’ workplace or at the university leading the study in that city. With consent, interviews were recorded digitally. Prior to commencing the interview written consent was obtained from participants (see Appendix 5).
Focus of the interviews
In this study we focused primarily on issues arising from the UK childhood immunisation schedule30 and also, to better understand issues relating to adult immunisation, we explored views on flu and whooping cough vaccinations in adults either identified at risk of developing serious complications of flu themselves, or, in the case of whooping cough vaccine, to prevent potentially life-threatening infection in their newborn infants.
Topic guides for the interviews (individual and small group) were developed to ensure consistency both within and across the six communities (see Appendices 6 and 7), although the format was flexible to allow participants to generate naturalistic data on what they viewed as important. An overview of the interview topics is presented in Table 5. Throughout, the SEM89 informed the questions that we asked, ensuring that we explored all five levels of influence on immunisation behaviour. Researchers’ local knowledge of immunisation and of the Traveller community also fed into the development of the topic guides to prompt dialogue of particular local issues (e.g. outbreaks of measles and whooping cough in the community, introduction/removal of specialist services). The topic guides for phase 1 were reviewed and piloted with the community partners in York (see Community partners) and questions were reworded to improve comprehension.
| Phase of study | Interview topics |
|---|---|
| Phase 1 interviews with Travellers |
|
| Phase 2 interviews with service providers |
|
The original intention was to integrate paper-based vignettes into the phase 2 interviews with service providers and to present verbatim quotations87 from the Traveller interviews on key issues that emerged in each of the five levels of the SEM, in terms of both the influences (barriers and facilitators) on immunisation behaviour and ideas for interventions to increase uptake. This was to stimulate discussion of local issues identified as important by the Traveller communities, as well as the service providers who have responsibility for designing and delivering immunisation programmes locally. Following discussion at a research team meeting, a decision was taken not to do this as it might influence the expressed views of the service providers. Instead, key emerging issues from phase 1 were integrated into the topic guide for phase 2 (see Table 5).
Phase 3
The workshops were held in local venues known and accessible to the Travellers: a church hall in Bristol, YTT premises, a local neighbourhood centre in Govanhill, Glasgow, a function suite in a local Glasgow hotel and a children’s centre in London. The workshops with the Roma participants were conducted with the assistance of interpreters (Romanian and Slovak). To capture the discussions at the workshops, local researchers (who were not facilitating the sessions) took detailed notes. Prior to commencing each workshop, written consent was collected from participants (see Appendix 8). As before, with those Traveller participants who offered that they struggle with reading, the researcher read out the PIS and each item on the consent form and asked participants to mark or initial the item if they consented.
The aim of the workshops was to disseminate the findings of phases 1 and 2 and to discuss and ‘co-produce’95 ideas for the content and delivery of potentially feasible and acceptable interventions at all five levels of the SEM, with a view to then identifying one priority intervention at each level (intrapersonal, interpersonal, institutional, community and policy). The duration of the five workshops varied slightly depending on the availability of participants, ranging from 2 hours (Glasgow) to 3 hours (York and London).
Following the spoken presentation of the key findings of the phase 1 and phase 2 interviews, a structured two-step process101 was used to prioritise the interventions. On the advice of our independent project advisory group (IPAG; see Independent project advisory group), this approach replaced the nominal group technique102 that we had originally planned to use. It was considered that the revised method involved more detailed discussion of the importance and feasibility of potential interventions to increase uptake of immunisation.
First, the Travellers and service providers worked in two separate groups. The researcher presented the ideas for interventions to improve uptake of immunisations that had emerged from the interviews. To do this, each idea for an intervention to improve uptake of immunisations was written on an A4 sheet of coloured paper and read out to the group. The idea was then discussed and scored in terms of potential impact (If this idea happened how much of a difference would it make to your/the local Traveller community in having injections? 1 = no difference to 5 = a lot of difference). At the end of this session, each group had a ranked list of interventions based on their impact scores. The Travellers and service providers then came together and presented their ranked list of interventions to each other. The final workshop session was a facilitated discussion to jointly agree a prioritised list of potentially feasible and acceptable interventions which could positively impact on immunisation uptake in their community.
Data analysis
Within-community analysis
Phase 1 and 2 interviews were transcribed verbatim and data subjected to thematic analysis using the framework approach103 which is designed to address applied policy-related questions. All of the transcripts were checked for accuracy against the audio-recording by the researcher who conducted the interview. The certainty that the data represent the views of participants is very important, particularly so in cross-cultural research in which interpreters are required. 104 A randomly selected sample of audio-recordings (four Bristol Romanian Roma, two Glasgow Romanian Roma and one Glasgow Slovakian Roma) were checked against the transcripts by an independent interpreter, and the level of accuracy deemed satisfactory overall. A small number of errors revealed by this process were corrected in the transcript or the data were removed from the analysis; for example, in one of the Glasgow interviews, the HPV vaccine was incorrectly translated in the interview as flu and so could not be included.
The stages of framework analysis, detailed below, were undertaken independently for each of the six Traveller communities and for both phase 1 and phase 2 data. Participant-based group analysis105 was used to analyse the group interviews, with the contribution of each individual within the interview being analysed separately. The analysis was undertaken by seven researchers. Other members of the research team were involved at different stages to enhance rigour and to ensure that the local context in which the data were collected was retained. A data analysis protocol was developed to ensure consistency across the research team. NVivo version 10 (QSR International, Warrington, UK) and Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA) software packages facilitated data management.
Familiarisation
Two researchers read the interview transcripts to record emerging ideas and recurrent themes that were relevant to the aims of the study.
Constructing a thematic framework
A thematic framework for the Traveller data was developed using 16 phase 1 interview transcripts (four from Bristol, 12 from York). The framework was applied to a further four transcripts (from Bristol) by a second researcher and refined as necessary (see Appendix 9). A second framework was developed in the same way for the phase 2 service provider interviews using all eight interview transcripts from Bristol and then applied to three transcripts from York (see Appendix 10). At this point, the SEM89 was put to one side so that the data were organised by the views expressed by participants rather than forced into a prespecified framework.
Indexing and charting
The thematic frameworks (one for Travellers, one for service providers) were systematically applied to the interview data by a team of seven researchers. On the rare occasion when the data did not easily fit into the framework, the ‘other’ category within each theme was used to ensure that these data were captured. Charts were produced in NVivo for each theme and summaries of responses from participants and verbatim quotations were entered. A subsample of the completed charts for each Traveller community and group of service providers (by city) was reviewed by a second researcher to check the detail and sufficiency of the summaries and quotations.
Mapping and interpretation
The completed charts were exported from NVivo into Microsoft Excel. These were then reviewed and interrogated to compare and contrast views and to seek patterns, connections and explanations within the data (by a team of four researchers). Descriptive findings documents were written up for each Traveller community and the service providers in each city focusing on the barriers to and facilitators of uptake of immunisation and ideas for interventions for improving uptake. The local research teams then reviewed their documents (1) to check that the interpretation of the local data by the analysis team reflected the intended meaning spoken during the interviews and (2) when necessary to provide local context; for example, the Glasgow team provided information on the role of the European Union (EU) team in working with the Roma community.
Cross-community synthesis
The next step of the analysis of the phase 1 and 2 data was a thematic cross-community synthesis that took account of the inferences derived from all the interview data for the sample as a whole. 106 Using the descriptive findings documents and the charts created in the charting stage of analysis for each Traveller community (both Traveller participants and service providers), the data across all six communities were synthesised to explore similarities and difference in views on barriers to and facilitators of immunisation. We particularly looked for similarities and difference by gender and vaccine (within the UK childhood immunisation schedule, adult flu/whooping cough). The SEM89 was reintroduced into the process at this stage in that the themes and subthemes were mapped to the five levels of influence.
Identifying the interventions to take to the workshops
A modified intervention mapping approach107 was used to identify the interventions to take to the phase 3 workshops. This method ‘maps the path from recognition of a need or problem to the identification of a solution’. First, a matrix was developed using the descriptive findings documents for the Bristol Roma and English Gypsy/Irish Traveller communities. This matrix combined the barriers to and facilitators of immunisation uptake that had emerged from the phase 1 and phase 2 interviews with ideas for interventions to increase uptake of immunisation. In order to generate as many ideas as possible for interventions, these were drawn from interviews with Travellers and service providers for that particular community, knowledge and experience of the research team and the IPAG, as well as existing literature. Two researchers then independently matched interventions to potentially relevant barriers and facilitators and then met to agree a final list of interventions to take to the first workshop (see Chapter 4, Identifying the interventions to take to the workshops) which was held in Bristol. At this point, detail from the phase 1 and phase 2 interviews pertinent to each intervention were included; for example, for the intervention ‘Identify Travellers in health records’ specific suggestions about how to do this in GP practices and across immunisation databases were added. This process enabled us to produce a detailed list of interventions to take to the workshop that we were confident addressed the identified issues for both the Bristol Romanian Roma and English Gypsy/Irish Traveller communities.
To identify the interventions to take to the workshops for the other Traveller communities, the descriptive findings documents were discussed by the local research teams with the lead researcher to agree the barriers to and facilitators of immunisation uptake. When these were the same as for Bristol, the interventions identified for the Bristol workshop were chosen. When additional issues emerged for a community, additional interventions were taken to the workshop. This meant that many of the interventions were considered at several workshops, whereas others were only discussed at one workshop (see Chapter 4, Table 34).
Community partners
In each Traveller community we worked in partnership with ‘community partners’ for the duration of the study in that city. Our approach in each community (Table 6) was based on the experience of the local gatekeepers. Community partners were offered a £40 gift voucher of their choice per meeting that they attended. The number of meetings held ranged from two (Glasgow Roma, London Irish Travellers) to four (Bristol – across both communities). Over the duration of the study the community partners changed in Bristol and London, and were the same people in York and Glasgow.
| City | Community | Overview |
|---|---|---|
| Bristol | Romanian Roma, English Gypsy and Irish Traveller | Meeting 1 (October 2013, Bristol City Council premises): local researchers and an interpreter met with three English Gypsies/Irish Travellers, one Roma person and one Showperson. Discussed how best to work with the local Traveller communities in terms of recruitment and conduct of interviews. Commented on the phase 1 PIS. Decided on gift voucher |
| Meeting 2 (March 2014, local health centre): a researcher and interpreter met with four Roma people. Plan was to discuss themes emerging from the phase 1 interviews and to identify key issues to be taken forward into the phase 2 interviews with service providers. In reality, it became more a focus group about immunisation as the purpose of the meeting was difficult for attendees to grasp | ||
| Meeting 3 (October 2014, local secondary school): local researchers and an interpreter met with seven community partners, a mix of English Gypsies/Irish Travellers (including the member of the research team) and Roma. Discussed location and organisation of the phase 3 workshop | ||
| Meeting 4 (May 2015, local Traveller site – local church for Roma): a researcher and specialist health visitor met with five English Gypsies. A researcher and an interpreter met with five Roma mothers. Discussed how to disseminate study findings to community | ||
| York | English Gypsy | Meeting 1 (October 2013, YTT premises): a researcher met with the YTT Advisory Steering Group (nine Travellers, including the research team member) who were willing to act as community partners. Discussed how best to work with the local community in terms of recruitment and conduct of interviews. Commented on the phase 1 PIS and study flyer. Decided on gift voucher |
| Meeting 2 (January 2015, YTT premises): a researcher met with the YTT Trust Advisory Steering Group (eight Travellers including the research team member) to feedback a summary of the phase 1 and 2 interview findings and discuss how best to run the phase 3 workshop | ||
| Meeting 3 (June 2015, YTT premises): a researcher met with one community partner to discuss how to disseminate the findings of the study across the community | ||
| Glasgow | Romanian and Slovakian Roma | Meeting 1 (September 2013, South Sector Health Board premises): two researchers met with a group of service providers including two members of the community who worked as bilingual support workers. Discussed how best to work with the Roma community in terms of recruitment, conducting interviews and collaborating with community partners |
| Meeting 2 (November 2013, South Sector Health Board premises): two researchers met with the same group (only one member of the community attended) to further discuss the logistics of recruitment and to comment on the phase 1 PIS | ||
| Scottish Showpeople | Meeting 1 (October 2013, Glasgow Caledonian University): a researcher met with one member of the community to discuss how the community partner group would work, discussed approach to recruitment and commented on the phase 1 PIS. Decided on gift voucher | |
| Meeting 2 (November 2013, Glasgow Caledonian University): two researchers met with two community partners to finalise approach to recruitment to phase 1 interviews | ||
| Meeting 3 (May 2015, Glasgow Caledonian University): two researchers met with one community partner to feedback a summary of the phase 1 and 2 interview findings and discuss location and organisation of the phase 3 workshop | ||
| London | Irish Traveller | Meeting 1 (May 2014, London Gypsy and Traveller Forum, City Hall): a researcher attended and identified/met with potential gatekeepers for the study |
| Meeting 2 (September 2015, London Gypsy and Traveller Forum, Kings Place): a researcher discussed the plans for the phase 3 workshop with some Travellers at the meeting |
Across the six communities, community partners advised on participant information about the study, recruitment, choice of gift voucher, the location/organisation of the workshops and dissemination of study findings across the community. Feedback on the PIS (see Appendix 1) was to use pictures that illustrate the type of people who need immunisations; and in York we learnt that while the photo of a man wearing glasses was acceptable, Travellers would know he was not a Traveller as they do not have their photo taken wearing glasses. In terms of recruitment, the community partners in York suggested conducting the phase 1 interviews on a day when lots of Travellers attend YTT for literacy classes and in Glasgow the community partners offered to publicise the study with others in the community and distribute the PIS. The community partners in all four cities informed our choice of venue for the phase 3 workshops by suggesting venues that were well known, and accessible, to their community. The community partners in Glasgow attended the workshops. Finally, for dissemination of the study findings to the community (see Appendix 11) in York a poster was developed by the community partners and displayed at YTT. Further dissemination ideas were to use gatekeeper organisation websites and Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) pages. In Bristol ideas about dissemination included a leaflet, a YouTube (YouTube, LLC, San Bruno, CA, USA; www.youtube.com) video that included members of the community so that the link could be shared via Facebook, and via link workers.
Independent project advisory group
The IPAG was set up at the start of the study to provide independent advice on all stages of the study. The group comprised:
-
Dr Martin Schweiger (chairperson), Public Health Consultant, Public Health England
-
Dr Jill Edwards, research fellow, University of Leeds, experienced in research with ‘marginalised’ communities
-
Dr Patrice Van Cleemput, freelance research consultant, previously a health visitor with experience of conducting research with Travellers.
A fourth member of the group did not attend any meetings, so is not named here.
The group met four times over the duration of the study (July 2014, October 2014, June 2015 and October 2015). The group’s input focused on signposting the research team to up-to-date literature, relevant Traveller or immunisation projects/policy documents and key individuals with useful expertise; offering views on the emerging interview findings; suggesting ideas for interventions to be taken to the phase 3 workshops; and inputting on the discussion chapter of this final report.
Chapter 3 Barriers to and facilitators of uptake of immunisation: interviews with Travellers and service providers
Participants
Travellers
We interviewed 174 Traveller participants from six Traveller communities in four UK cities. These communities were identified as Romanian Roma and English Gypsy/Irish Traveller in Bristol; English Gypsy in York; Romanian Roma/Slovakian Roma and Scottish Showpeople in Glasgow; and Irish Travellers in London. Thirty-eight participants participated in individual interviews, while the remainder took part in group interviews. Three-quarters (n = 47) of the interviews with the Roma participants were conducted using an interpreter. A summary of the demographic characteristics of Traveller participants is presented in Figure 2 and Table 7.
FIGURE 2.
Travellers by community. (a) Traveller community by city; (b) gender by community; (c) housing by community; and (d) family role by community. EG, English Gypsy; IT, Irish Traveller.




| Characteristic | All (N) | Traveller community by city (n) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Bristol | York | Glasgow | London | ||||||
| Romanian Roma | English Gypsya | Irish Travellerb | English Gypsy | Romanian Roma | Slovakian Romac | Scottish Showpeopled | Irish Traveller | ||
| Total | 174 | 24 | 15 | 9 | 48 | 17 | 20 | 14 | 27 |
| Used interpreter | 47 | 19 | 0 | 0 | 0 | 12 | 16 | 0 | 0 |
| Gender | |||||||||
| Female | 139 | 14 | 10 | 7 | 37 | 17 | 17 | 10 | 27 |
| Male | 35 | 10 | 5 | 2 | 11 | 0 | 3 | 4 | 0 |
| Family role | |||||||||
| Mother | 64 | 9 | 5 | 4 | 19 | 8 | 7 | 5 | 7 |
| Grandmother | 33 | 3 | 4 | 1 | 6 | 3 | 5 | 3 | 8 |
| Pregnant woman | 5 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 3 |
| Woman, no children | 8 | 0 | 1 | 1 | 3 | 0 | 0 | 1 | 2 |
| Adolescent girl with children | 5 | 2 | 0 | 0 | 0 | 1 | 1 | 1 | 0 |
| Adolescent girl, no children | 24 | 0 | 0 | 1 | 7 | 4 | 5 | 0 | 7 |
| Father | 19 | 6 | 2 | 2 | 5 | 0 | 2 | 2 | 0 |
| Grandfather | 5 | 1 | 0 | 0 | 2 | 0 | 0 | 2 | 0 |
| Male, no children | 11 | 3 | 3 | 0 | 4 | 0 | 1 | 0 | 0 |
| Marital status | |||||||||
| Single | 62 | 6 | 5 | 3 | 22 | 6 | 5 | 2 | 13 |
| Married | 74 | 16 | 8 | 6 | 17 | 8 | 6 | 6 | 7 |
| Common law partner | 19 | 1 | 0 | 0 | 6 | 2 | 8 | 2 | 0 |
| Engaged | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 |
| Widowed | 9 | 1 | 2 | 0 | 1 | 1 | 1 | 1 | 2 |
| Separated | 5 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 4 |
| Divorced | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Missing | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Housing | |||||||||
| House/flat | 112 | 23 | 0 | 6 | 24 | 17 | 20 | 3 | 19 |
| Authorised site – caravan/trailer | 45 | 0 | 11 | 3 | 23 | 0 | 0 | 8 | |
| Authorised site – chalet | 15 | 0 | 4 | 0 | 0 | 0 | 0 | 11 | 0 |
| Bed and breakfast | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Missing | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Self-reported immunisation status of participants | |||||||||
| Full | 59 | 7 | 4 | 2 | 24 | 5 | 4 | 11 | 2 |
| Partial | 40 | 5 | 7 | 2 | 7 | 4 | 4 | 3 | 8 |
| None | 11 | 1 | 0 | 3 | 4 | 1 | 0 | 0 | 2 |
| Missing | 64 | 11 | 4 | 2 | 13 | 7 | 12 | 0 | 15 |
| Self-reported immunisation status of participants’ children | |||||||||
| Full | 69 | 10 | 8 | 6 | 20 | 7 | 10 | 0 | 8 |
| Partial | 17 | 4 | 0 | 1 | 2 | 0 | 2 | 0 | 8 |
| None | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| N/A | 44 | 3 | 4 | 2 | 16 | 5 | 4 | 1 | 9 |
| Missing | 42 | 7 | 1 | 0 | 10 | 5 | 4 | 13 | 2 |
| Employment | |||||||||
| Employed | 19 | 4 | 1 | 0 | 6 | 3 | 1 | 4 | 0 |
| Self-employed | 9 | 1 | 4 | 0 | 0 | 0 | 0 | 4 | 0 |
| Unemployed | 43 | 12 | 5 | 5 | 1 | 0 | 4 | 0 | 16 |
| Stay at home parent | 43 | 1 | 2 | 2 | 11 | 9 | 11 | 2 | 5 |
| Student | 24 | 3 | 0 | 2 | 6 | 5 | 4 | 2 | 2 |
| Disabled | 3 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 0 |
| Retired | 4 | 0 | 1 | 0 | 0 | 0 | 0 | 2 | 1 |
| Missing | 29 | 3 | 0 | 0 | 23 | 0 | 0 | 0 | 3 |
| Age (years), mean (SD); range | 32.34 (4.93); 13–82 | 33.42 (12.56); 16–65 | 33.80 (18.90); 18–82 | 28.34 (12.25); 17–50 | 34.62 (15.08); 14–65 | 25.35 (10.89); 13–44 | 25.90 (12.56); 14–60 | 42.64 (17.73); 18–72 | 32.33 (14.47); 14–63 |
| Number of children,e mean (SD); range | 3.18 (2.14); 1–12 | 3.14 (2.11); 1–8 | 2.38 (1.60); 1–6 | 3.00 (1.79); 1–6 | 3.56 (1.97); 1–10 | 4.08 (2.94); 0–12 | 1.80 (1.21); 1–5 | 1.85 (0.90); 1–4 | 4.34 (2.35); 1–9 |
| Number of grandchildren,e mean (SD); range | 7.26 (8.29); 1–41 | 7.67 (5.77); 1–11 | 7.33 (2.31); 1–10 | 5.00 (N/A); N/Af | 5.50 (4.31); 1–16 | 7.33 (3.21); 1–11 | 8.00 (10.30); 1–26 | 2.80 (2.68); 1–7 | 12.00 (15.08); 1–41 |
| Years of residency, mean (SD); range | 10.67 (9.70); 0.17–41.00 | 3.97 (1.94); 0.25–7.00 | 20.00 (1.48); 18.00–24.00 | 16.56 (9.74); 2.00–30.00 | 17.48 (9.76); 1.00–41.00 | 1.97 (1.74); 0.17–5.00 | 1.71 (1.71); 0.40–8.00 | 13.32 (12.16); 2.00–31.00 | 11.15 (7.23); 2.00–28.00 |
Our original recruitment target was 22–32 Traveller participants from each of the six communities. The upper limit was later increased to 45 to ensure that the sampling criteria were met following the large number of York English Gypsy Travellers attending for an interview on 1 day. The target sample was achieved for all of the communities, except for the Glasgow Scottish Showpeople. The Bristol English Gypsy and Irish Traveller community were viewed as one community, as were the Glasgow Romanian and Slovakian Roma (see Chapter 2, Setting).
A total of 139 Traveller participants were female and 35 were male. This ratio of female to male participants (3 : 1) achieved our proposed sampling aim for one-quarter of all participants to be male. We did not manage to recruit any men from the Irish Traveller community in London. As intended, we spoke to women across generations, including grandmothers (n = 33), mothers (n = 64), pregnant women (n = 5), women without children (n = 8), adolescent girls with children (n = 5) and adolescent girls with no children (n = 24). We achieved our target of 6–8 mothers in all but the Glasgow Scottish Showpeople community (n = 5). We achieved the targets of 6–8 grandmothers and 6–8 adolescent/young women in three communities (York English Gypsy, Glasgow Roma and London Irish Traveller). The men were a mix of grandfathers (n = 5), fathers (n = 19) and young men with no children (n = 11). We achieved our target of 2–4 grandfathers in two communities (York English Gypsy and Glasgow Scottish Showpeople). We did not set out to recruit young men without children; however, 11 took part across four communities (not Glasgow Scottish Showpeople or London Irish Travellers). Interviewing grandparents, parents and young people enabled us to explore intergenerational differences in attitudes and beliefs; speaking to pregnant women and older adults helped us to gain awareness of views relating to the adult whooping cough and flu vaccines. Adolescents gave us an insight into attitudes towards the HPV vaccine (girls only) and three-in-one booster.
We met our aim to interview a mix of full, partial and non-immunisers. Approximately one-third of participants (n = 59) self-reported that they were fully immunised, 40 were partially immunised and 11 had had no vaccinations. There were missing data from over one-third of participants (n = 64). We did not recruit any Glasgow Roma participants who reported having had no immunisations themselves. Parents (n = 130) self-reported the immunisation status of their children as follows: half (n = 69) said that their children were fully immunised, 17 reported partial immunisation and two said that their children had had no vaccinations. Once again there were missing data for one-third of participants (n = 42). We spoke with participants with non-immunised children only in the Bristol English Gypsy community (none self-identified as this in the other five communities). These immunisation status data should be viewed with caution. They were based on self-report, may be subject to recall and response bias and for some participants did not tie in with their accounts in the interviews. Validation of self-reported immunisation status against external sources was beyond the scope of this study.
Of the 145 adult participants, 74 were married, 62 were single and 19 had a common law partner. There were nine widowed participants, five were separated and one was divorced. Traveller participants predominantly described themselves as unemployed (n = 43), a stay-at-home parent (n = 43), student (n = 24) or employed (n = 19). Employment data were missing for half of the York participants (n = 23). Finally, the vast majority of those interviewed lived in either a house or flat (n = 112) or on an authorised caravan, trailer or chalet site (n = 60). One participant was in bed and breakfast accommodation. The Roma (Bristol and Glasgow) and Irish Travellers (Bristol and London) interviewed in this study tended to live in houses and flats, whereas the Bristol English Gypsy and York English Gypsy participants were more often living on official Traveller sites. We did not recruit any Travellers living on the roadside or on unauthorised encampments. Traveller participants’ ages ranged from 13 to 82 years (mean 32 years), and those with children had on average three children (range 1–12 children); those with grandchildren had on average seven grandchildren (range 1–41 grandchildren). The average number of years of residency was 11 years (range 2 months–41 years), noticeably shorter for the Roma participants. These characteristics (marital status, employment, housing, age, number of children/grandchildren and residency) were not part of the sampling strategy.
Service providers
We interviewed 39 service providers from four cities: Bristol (n = 8), York (n = 9), Glasgow (n = 14) and London (n = 8). Three of the interviews were group interviews (two in York and one in London), the rest were individual interviews. A summary of the demographic characteristics of service provider participants is presented in Figure 3 and Table 8.
FIGURE 3.
Service providers by city. (a) Service providers by city; and (b) service provider role by city.
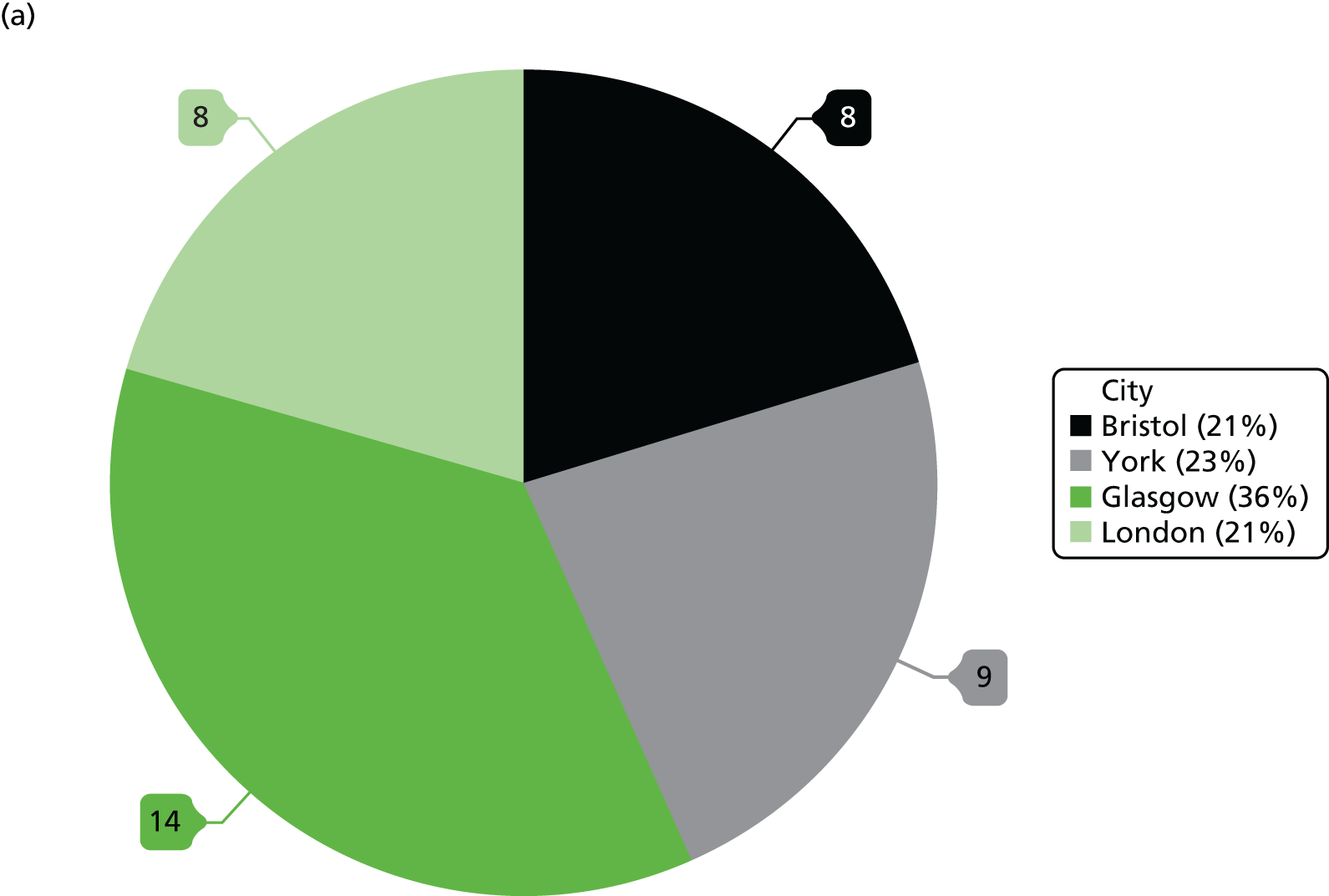

| Title, role, community reach | All (N) | City (n) | |||
|---|---|---|---|---|---|
| Bristol | York | Glasgow | London | ||
| Total | 39 | 8 | 9 | 14 | 8 |
| Frontline workers | |||||
| Primary care | |||||
| GP | 2 | 1 | 0 | 1 | 0 |
| Health visitor | 6 | 2 | 1 | 3 | 0 |
| Practice nurse | 3 | 0 | 1 | 1 | 1 |
| Practice manager | 1 | 0 | 0 | 1 | 0 |
| Other NHS | |||||
| Outreach nurse | 1 | 0 | 0 | 0 | 1 |
| Local authority | |||||
| Traveller team | 2 | 1 | 0 | 0 | 1 |
| Children’s services | 2 | 0 | 1 | 1 | 0 |
| Education | |||||
| Head teacher | 1 | 0 | 0 | 1 | 0 |
| Outreach worker | 1 | 0 | 1 | 0 | 0 |
| School nurse | 1 | 0 | 0 | 1 | 0 |
| Voluntary sector | |||||
| Traveller support services | 2 | 0 | 0 | 0 | 2 |
| Strategic roles | |||||
| NHS | |||||
| Children’s services | 2 | 0 | 0 | 2 | 0 |
| Health improvement | 1 | 0 | 0 | 1 | 0 |
| Primary care and community services | 1 | 0 | 0 | 1 | 0 |
| Screening and immunisation | 9 | 2 | 3 | 1 | 3 |
| Local authority | |||||
| Public health | 4 | 2 | 2 | 0 | 0 |
| Community work witha | |||||
| Whole population | 16 | 6 | 6 | 1 | 3 |
| Minority ethnic groups | 1 | 0 | 0 | 0 | 1 |
| All local Travellers | 1 | 0 | 0 | 0 | 1 |
| Romanian/Slovakian Roma | 12 | 1 | 0 | 10 | 1 |
| English Gypsies/Roma | 4 | 1 | 3 | 0 | 0 |
| Irish Travellers | 5 | 1 | 0 | 0 | 4 |
| Scottish Showpeople | 3 | 0 | 0 | 3 | 0 |
Twenty-two participants were frontline workers employed across a wide range of roles in the NHS (n = 13), local authorities (n = 5), education (n = 2) and the voluntary sector (n = 2). Seventeen participants were in more strategic roles in the NHS (n = 13) and local authorities (n = 4). We exceeded our recruitment target of 24 to 32 participants overall and our target of interviewing 6–8 service providers in each city. We also achieved our aim to recruit a mix of frontline workers and those working in more strategic/commissioning roles for every city.
The service providers were often in immunisation, public health or health professional roles and nearly half had a remit to work with the general population which included working with local Traveller communities. Approximately one-quarter worked with Roma communities, predominantly based in Glasgow. In each of the four cities we interviewed at least one person who had a remit to specifically work with the Traveller community of interest to this research.
Barriers to and facilitators of uptake of immunisation
The findings from the interviews with Travellers and service providers are presented below. These themes and subthemes emerged from the thematic frameworks (one for Travellers and one for service providers; see Appendices 9 and 10) which were organised by the views expressed by participants rather than by the SEM89 which underpinned the study. The link between the themes, subthemes and the five levels of the model is summarised at the end of the chapter. For some themes and subthemes, both Travellers and service providers offered their views and so both perspectives are presented. For others, only Travellers or service providers spoke of them and so only those accounts are included. The majority of views expressed by Travellers were in the presence of family members or friends. Where there are differences in views for particular Traveller communities (and the ‘sub’ communities, i.e. Romanian vs. Slovakian Roma), specific vaccinations or by gender these are highlighted. Summary boxes are provided for each theme. We use a variety of terms for immunisation to reflect the range of words that participants used (see Table 5).
Knowledge about immunisation
Levels of knowledge
Overall, there was widespread understanding among Traveller participants across all six communities that immunisation provides protection against diseases. (We use the terms ‘knowledge’ and ‘understanding’ interchangeably.) Most were able to talk generally about vaccinations, in terms of them fighting against illnesses and preventing the spreading of infection:
It’s a very good thing because it protects them from diseases, from illnesses. When they come into contact with the viruses, the body can fight it if they have the right vaccines.
BT203a, Romanian Roma, grandfather, Bristol
A minority appeared to have a good understanding about how a vaccine works, developing immunity and the schedule for childhood vaccinations. They described how they believed vaccines prevented diseases.
It’s a bit of that virus to stop that virus spreading through your body.
BT108a, married to an Irish Traveller, father, Bristol
[Vaccines work by injecting] a little bit of that stuff . . . to make them immune to it.
YT005d, English Gypsy, adolescent girl with no children, York
There was very little reference to herd immunity. A small number of mothers and grandmothers in the Bristol English Gypsy/Irish Traveller and London Irish Traveller communities talked about how they or their children had experienced no ill effects from non-vaccination (sometimes speaking of a particular vaccine rather than more generally), attributing this as evidence that immunisation is not necessary and that their decision not to vaccinate is the right one.
I ain’t got the BCG and nothing’s happened to me, so [laughs] can’t be that bad.
LT009b, Irish Traveller, mother, London
Yeah . . . I would say no [to needles for children] . . . I would be scared about it, you know . . . ‘cos I think how I brought my children up, I think they should bring them up the same way, ‘cos I never had no trouble in things like that with my children.
BT111b, Irish Traveller, mother, Bristol
Only one Glasgow Scottish Showperson mother referred explicitly to the need to immunise children for the health of the community. A Roma father in Bristol understood the need to have the adult flu vaccination to prevent the spread of infection in vulnerable older adults, as his wife worked as a care assistant.
If my child got something and it went round the school and lots ended up sick because she didn’t immunise.
GT204a, married to a Scottish Showperson, mother, Glasgow
Yes, for older people . . . most of them, they got their flu jabs and even us, as workers, we . . . we do the flu jabs [so we] . . . don’t spread the virus.
BT204b, Romanian Roma, father, Bristol
In contrast to knowledge of vaccinations in general, knowledge of specific childhood vaccinations, appeared to be variable and sometimes misinformed. Tetanus, BCG, whooping cough, MMR and polio vaccinations and the diseases they aim to prevent were frequently mentioned by Traveller participants in all six communities, although within each community, the level of awareness and knowledge of these vaccinations was uneven. Service provider participants in all four cities suggested that when Travellers have limited understanding about immunisation, this is often related to language and literacy barriers (see Language and literacy).
Most of the Romanian Roma participants in Bristol and Glasgow appeared to have limited understanding of specific vaccines, the diseases they protect against and the time at which they are routinely provided.
I don’t know if there are vaccinations. The doctor don’t . . . make appointments for, so I don’t know if you can go yourself and do them.
BT212a, Romanian Roma, mother, Bristol
Some Slovakian Roma participants in Glasgow seemed more knowledgeable than the Romanian Roma, mentioning the names of the different vaccines and diseases. This difference was confirmed by service providers, who commented that the Slovakian Roma families are slightly better informed than the Romanian Roma community because they arrive in the UK with more experience of vaccinations, and have now been settled in the UK over a longer period of time, and so have more experience of accessing health services.
A minority of participants within the Bristol English Gypsy/Irish Traveller and York English Gypsy communities acknowledged their own limited or lack of understanding of one or more of the childhood vaccinations and/or the diseases they aim to prevent. In the London Irish Traveller community over half described themselves as having no or poor knowledge. In contrast, only two Scottish Showpeople, both women, discussed having a lack of knowledge.
No, I don’t know. I just remember a couple of years ago, it was the same injection, I don’t know what it was, but they changed it a bit. It was like, for side effects, I don’t, it was like two out of three chance, I don’t know, at first it was a lower chance and then it was a bigger chance with something bad, I don’t know. I don’t know if they changed it back.
LT003a, Irish Traveller, adolescent girl with no children, London
Knowledge of specific vaccines
Awareness and knowledge of the whooping cough and the MMR vaccinations were particularly evident in the English-speaking Traveller communities, which appeared to be a consequence of the controversies surrounding their safety in past decades. There was also generally good awareness of the existence of the HPV vaccination among young women and their mothers, although there were examples of limited understanding of the purpose of this vaccine.
Didn’t really know what the HPV vaccine [was] for at the time, just had it.
YT004b, English Gypsy, young woman with no children, York
In contrast to young women in the other communities, adolescent girls from the London Irish Traveller community appeared to be less aware of the existence of the HPV vaccine as well as its purpose.
Have you heard of the injections that young girls get, girls in particular at school?
No, no.
No. I don’t know what they’re called. What’s it [HPV] for then?
A minority of participants in the Bristol Roma, York English Gypsy and Glasgow Roma communities were unclear about the type of cancer the HPV vaccine protected against, or believed it prevents all cancers. For example, a Bristol Roma mother thought HPV prevented ovarian cancer and a mother in the Glasgow Scottish Showpeople community referred to HPV preventing breast as well as womb cancer; while two adolescent girls from the Glasgow Roma community referred to HPV preventing cancer of the ‘belly’ (GT112a, Romanian Roma, adolescent girl with no children, Glasgow) and ‘all types’ of cancer (GT112b, Romanian Roma, adolescent girl with no children, Glasgow). One adolescent from the Glasgow Slovakian Roma community believed that the HPV vaccination might affect her ability to have children in the future (information given to her by her mother) and, as consequence, did not have the vaccination. The idea that cancer is in the system and, therefore, cannot be prevented by a vaccination was voiced by a Bristol Irish Traveller mother who had not accepted the HPV vaccination offered to her daughter in school.
I don’t think that anything can prevent cancer ‘cos it’s in your system so I don’t think that it [HPV vaccination] would stop it [you] having it.
BT111b, Irish Traveller, mother, Bristol
There was infrequent reference in any of the communities to the newer vaccinations that have been recently added to the NHS childhood immunisation programme. For example, the rotavirus vaccine was rarely mentioned, although the vaccine was not always explicitly asked about in every interview. Similarly, few Traveller participants mentioned the recently introduced flu vaccination for babies and young children, in contrast to the adult flu vaccination targeting older or vulnerable people, awareness of which was generally greater.
Across all six communities, (with the exception of flu) awareness and knowledge of adult vaccinations tended to be less than for childhood vaccinations. The flu vaccination offered in pregnancy was referred to more often than the whooping cough vaccination in pregnancy. However, both vaccines were mentioned by a minority of women who had either taken up the offer of one or both vaccinations and those who had not, either through choice or because the vaccine was not offered at the time of their pregnancy (the NHS has recommended antenatal flu vaccine since 2010 and antenatal whooping cough vaccine since 2012).
Awareness of the availability of an annual flu jab to protect older people and those with particular disabilities or long-term conditions, such as diabetes, asthma and heart disease, was widespread among the English-speaking communities. Compared with the other communities, the Bristol and Glasgow Roma participants appeared less familiar with the availability and purpose of adult vaccinations.
He says he has not heard of immunisation for adults which is why he was surprised when his brother said ‘he has done one’ . . . he knew about vaccinations for children but not for adults.
BT202, Romanian Roma, father, Bristol (via his wife who was translating on his behalf)
Changes in knowledge
A common perception among the English-speaking communities was that, although the older generation have poor understanding of immunisation, the current generation of parents of young children have better levels of literacy enabling them to have access to more information and hence are more knowledgeable. This was not mentioned by Roma participants in Bristol and Glasgow.
A lot of the Travelling community like you saw today are starting to read and write so they’ll be able to look and read the leaflets properly . . . I think it’s the old people they don’t really understand what injections are for because they probably didn’t get their kids done but the younger ones these days what’s having kids, they are having them done.
LT001a, Irish Traveller, mother, London
Impact of knowledge on uptake of immunisation
Across all six communities, a basic level of understanding (together with trust in health professionals; see Relationships with health professionals) appeared to be sufficient to encourage most Traveller participants to take their children for vaccinations.
I don’t really know much about injections, if I was sent for the kids to have their injections I would just take ‘em.
YT001a, English Gypsy, grandmother, York
Similarly, in terms of adult vaccines, a lack of understanding did not appear to be a deterrent to uptake of the whooping cough vaccination or flu vaccination among pregnant women, although attitudes about vaccinations in pregnancy and the belief that flu vaccination causes flu were a deterrent for some Traveller participants (see Beliefs about specific vaccines).
A summary of this theme is provided in Table 9.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Sources of information and advice about immunisation
Health professionals
Traveller participants obtained their information and advice about immunisations from similar sources for all vaccinations (childhood and adult). Across all six communities participants overwhelmingly identified health professionals as their key sources of written and verbal information about both childhood (GP, health visitor, midwife, support worker) and adult [GP, practice nurse (flu), midwife (flu) and whooping cough] immunisation. This was observed to be different from previous generations (in which family was the significant source) and typically because health professionals are trusted to be knowledgeable because of their medical training and it is assumed that the NHS ‘will surely know what they’re doing’ (GT209a, Scottish Showperson, grandmother, Glasgow).
Well the medical professionals . . . know what they’re talking about rather than somebody that’s talking about it on the news, ‘cos they could be telling you anything.
GT205a, Scottish Showperson, father, Glasgow
The information you need for whichever injection you are getting the doctors will provide you with . . . anyway so you wouldn’t need to go and have a look anywhere else would you?
YT007a, English Gypsy, mother, York
Another important reason for relying on health professionals for information about immunisation appeared to be related to experiences of good-quality, relational continuity with health professionals, particularly with GPs and health visitors that led to trusting long-term relationships with individuals in families (see Relationships with health professionals). Having faith and trust in health professionals was reflected in responses that indicated a belief that they will do the right thing for them as patients.
They [health professionals] must think they [vaccinations] are good as they give them.
LT001a, Irish Traveller, mother, London
Most Traveller participants across all six communities appeared to be content with the written information leaflets about immunisations or the verbal information provided in conversations with health professionals. Indeed, three Roma participants from Bristol commented that health professionals in England take more time to explain immunisations to them than do health professionals in Romania. That said, some described difficulties in understanding the information that is provided (see Language and literacy).
Schools
A small number of mothers and adolescent girls across all six communities described receiving invitation letters and information about immunisations delivered in schools (flu, HPV and three-in-one booster) from their schools (see Immunisation recall and reminders, and local initiatives). The information they received was written as well as verbal, for example presentations by the school nurse in assembly. Again, most participants seemed content with the information provided; an exception was a Scottish Showperson adolescent girl who said that the school had told her about the HPV vaccination in assembly but she would have liked a leaflet or a presentation providing more detail. A school nurse described how she runs sessions for Roma parents using a digital versatile disc (DVD) and an interpreter about the new flu vaccination programme for primary school-aged children as well as assemblies about HPV vaccination. A Glasgow head teacher described how over the years trust has built up with the Roma community and suggested that the school provides information about the flu vaccination programme in a way that is understandable for parents, to enable good uptake.
We’ve built up good relationships of trust with parents and they trust the school, and the school is now a kinda place where they come for everything you know.
GH310, head teacher, Glasgow
Media, social media and the internet
The media [television (TV), newspapers], social media [e.g. Facebook, Mumsnet (Mumsnet Ltd, London, UK; www.mumsnet.com)] and the internet more generally [e.g. Google (Google Inc., Mountain View, CA, USA), YouTube] were identified as both positive and negative sources of information by several Traveller participants in all six communities. For some, TV campaigns (e.g. promoting the flu vaccine) were seen as useful for those who cannot read, a good way to reach lots of people, especially if shown between episodes of Coronation Street, and a powerful method of encouraging people to have vaccinations.
I call it scaremongering, to be honest, because if you see pictures of a child who hasn’t had it [vaccination] and the effects of what can happen, that really wakes people up.
BT108a, married to an Irish Traveller, father, Bristol
Concerns expressed about TV campaigns were that not everybody watches TV, that there was the possibility of scaring people off from having vaccinations, that some people would be sceptical about whether or not the campaign was telling the truth and that TV as a medium for communication was inappropriate for HPV as it is a private matter for girls.
If it was on the television . . . boys shouldn’t be watching it or seeing it.
YT014b, English Gypsy, mother, York
Facebook was by far the most commonly discussed form of social media and again there were mixed views on its value as a source of information for immunisation. In the London Irish Traveller and Bristol English Gypsy/Irish Traveller communities several participants commented that Facebook is used by people of all ages, so is a good method of disseminating information.
You’re on Facebook . . . I think it’s, it’s good, because they never leaves the phone out of their hands, they’re always on Facebook so they always, so I think that’s good.
LT005a, Irish Traveller, grandmother, London
It emerged that in Bristol Facebook had been used recently, with success, for a campaign to educate Travellers on the dangers of leaving their children in car seats for too long. The limitations of Facebook (and other forms of social media) offered by a few Traveller participants across communities were that immunisation is a private matter and not appropriate for social media, that people would just scroll past posts about immunisation, and that many Traveller people do not have internet access (observed particularly by Roma participants in Glasgow).
[You would not want] everybody and their grannies commenting.
GT209b, married to a Scottish Showperson, mother, Glasgow
The internet more widely, particularly Google, was identified by small numbers of Traveller participants as a useful source of immunisation information. People talked about using it to make sense of advice provided by health professionals, checking out side effects of vaccinations, symptoms of diseases and to translate immunisation information into their first language. As an example a young York English Gypsy woman talked about Googling the symptoms of swine flu in an attempt to persuade her GP practice to give her the vaccination. Several participants observed that it is the ‘young people’ who mainly use the internet and will often help their parents who do not have the information technology or literacy skills to access information in this way. All of the Glasgow Slovakian Roma and London Irish Traveller adolescent girls who were interviewed said that they use the internet to obtain information about immunisation.
Do you Google things as well?
No, my love, I can’t even use a computer . . . me daughter does it all.
My generation yes because if I hear something new and I don’t understand what I’m being told then I do Google it, I can’t help it. If someone says a word to me and I think, right I don’t want to sound dumb in front of you, but I will Google this when I get home to find out what it means. So the younger generation yes we do like know a lot about the internet and we can all read and write because we have all done our schooling . . . What if a new jab came out? I’d Google it and see what it was all about first.
YT004b, English Gypsy, adolescent girl with no children, York
Traveller participants who talked about these media and internet sources often acknowledged that they cannot necessarily be trusted to provide unbiased information. The exception was NHS websites, which were seen by a few Traveller participants as trustworthy.
The internet’s just full of nonsense, people making stories up . . . that could be anybody that’s put that on there. No, I definitely don’t trust, I would never ever rely on information on the internet unless it was a proper NHS website or summat like that.
GT205a, Scottish Showperson, father, Glasgow
Noticeably, over half of the women from the Scottish Showpeople discussed negative information in the media/on the internet about the MMR vaccine. This had caused them concern and prompted them to do more research: specifically, media coverage of Tony Blair’s refusal to discuss whether or not his son had had the MMR vaccine, Andrew Wakefield’s Facebook page and other Facebook pages about the MMR vaccine–autism link.
I’m on autism Facebook pages and there’s all the mothers and there’s been plenty . . . of discussion on that; I don’t normally comment on it, I just, I’m just nosey, and I read what they write, and if they’re having issues I’ll look into it . . . There’s a few mothers that will say definitely [there is a link between MMR vaccine and autism], but I just feel that there’s more . . . that says ‘no’. . . There’s a Facebook page for kids with autism in the community ‘Show kids with autism.’
GT204a, married to a Scottish Showperson, mother, Glasgow
Community
A strong theme to emerge across all six Traveller communities was the assimilation and sharing of informal or experiential knowledge through the community through ‘word of mouth’ (GT203a, Scottish Showperson, mother, Glasgow) and passed down knowledge. This occurred through intergenerational relations (grandmothers, mothers and children) and female community members (in the Bristol English Gypsy/Irish Traveller and Glasgow Scottish Showpeople communities) who served as immunisation advocates, providing information and advice on immunisation.
All the younger ones, they go and take the children and they’ll have the needles and we’ll advise them as well and we’ll say it’s a good thing, because there’s a lot more chat about things now than what there used to be years ago.
BT105a, English Gypsy, grandmother, Bristol
Several Traveller participants acknowledged the powerful influence of hearsay and rumour within the community in rapidly spreading negative messages about immunisation when someone is reported to have had a poor experience and/or experienced illness symptoms which they attributed to vaccination (correctly or incorrectly). As a counter to this, the influence of seeing people with disease symptoms was a motivator to vaccinate (see Acceptance of immunisation).
From whispering, hearing rumours . . . you can hear a friend, a neighbour, someone and look what happens, and gossiping ‘somebody had a vaccination against the flu and look what happened, she was really ill.’
BT211a, Romanian Roma, grandmother, Bristol
I never got the MMR [vaccination] . . . because I got so afraid of it and in our community . . . us being Travellers when you hear one thing everyone believes it . . . they just believe it automatically, that it’s not safe.
LT008b, Irish Traveller, mother, London
In all four cities these rumours were commonly and historically about the MMR vaccination being implicated in causing autism.
There’s a group of Travellers at this moment will not vaccinate their children [with MMR vaccine] . . . because they’re saying . . . some of the children is getting autistic, there’s something happening to the children afterwards.
LT013b, Irish Traveller, grandmother, London
An immunisation co-ordinator in London acknowledged how quickly the MMR vaccine–autism rumours spread in the Irish Traveller community in the late 1990s/2000s. In Bristol, a health visitor and immunisation co-ordinator also talked about hearsay in the community of a link between MMR vaccine and autism.
A lot of them would say they know someone who’s had a bad reaction; you know, ‘oh little Johnny was real bad after that, and my mother said never to let, she’d never let them have it again’, sort of thing. They don’t know all the facts . . . they think they do . . . they very much react to what they hear on the television . . . or what someone else on site has told them.
BH301, health visitor, Bristol
In the Bristol English Gypsy/Irish Traveller, York English Gypsy and London Irish Traveller communities, young people (males and females) relied principally on their mothers for information, as well as receiving information about HPV from school. Several daughters and granddaughters described obtaining their information principally from their mothers, who were also the prime influences on their subsequent vaccination behaviour. This transfer of knowledge from grandmother to mother to daughter was a particular feature of conversations with Irish Traveller participants in Bristol and London, and was reinforced in the corresponding service provider interviews in these communities (see Interpersonal influences on beliefs about immunisation and Decision-making about immunisation).
A summary of this theme is provided in Table 10.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
Acceptance of immunisation
The majority of Traveller participants across all six communities appeared to believe that, on balance, the protective benefits of immunisation outweigh the risks such as minor side effects or short-lived discomfort and upset, meaning that they take up the offer of vaccinations for themselves and their children.
The way I look at it, the benefits outweigh it [the risks]. So I’ve had all my kids done. I’ve always made sure they’ve had everything done.
LT010b, Irish Traveller, grandmother, London
It’s not nice putting them through it, but I guess they need it don’t they, so that they don’t catch anything. I know if I didn’t take her and then anything did happen what could have protected her . . . I think she’d be worse off.
YT006b, English Gypsy, mother, York
Many service provider participants in all four cities similarly spoke of their perception that most of the Travellers who they work with, in the main, accept vaccinations, although some were cautious in offering an opinion on this because of the absence of uptake data for Travellers within routine immunisation data collection systems (see Record keeping and monitoring).
There’s very, very few people in my opinion, who actually really don’t want it. I think I have only probably come across one that actually says to me ‘we don’t want it, and we’ve thought about it’.
BH308, health visitor, Bristol
Within this generally positive disposition towards immunisation there were differences in Traveller participants’ levels of confidence in and acceptance of immunisation generally as well as for particular vaccines. There was also recognition by service providers that there are some vaccinations, such as MMR and HPV, for which uptake is more selective.
Many Traveller participants reported that they follow the advice of their GP and other health professionals because they trust them when they say that the vaccinations are beneficial and safe (see Relationships with health professionals). These participants often acknowledged that there are minor side effects, for example bruising or a red lump at the injection site, which they considered to be normal, and they shared experiences of their children having a minor reaction to a vaccination and being reassured by health professionals not to worry.
But she does get really swollen legs with injections like really badly. One time her full top leg had gone massive, but we rang doctors up and they just said that was just the reaction for the injection.
YT006b, English Gypsy, mother, York
They also described vaccination as a normal part of bringing up children these days and something that everybody was doing.
I think for us it’s natural to get injections for the babies, it’s natural, it’s what you do . . . it’s all part of rearing ‘em up and keeping ‘em safe innit? We’ve never heard of no-one [in Ireland] not getting their children injections or needles . . . until we came here.
BT112b, Irish Traveller, mother, Bristol
This general acceptance of immunisation based on trust and social norms was expressed by approximately half of the participants from the York English Gypsy and London Irish Traveller communities; three-quarters of the Bristol English Gypsy/Irish Traveller community and Glasgow Scottish Showpeople; and almost all of the Bristol and Glasgow Roma participants.
The other Traveller participants appeared to have mixed feelings about immunisation. They talked about worrying about the discomfort to their child of having the injection, their potential side effects, not always believing that a vaccination works and uncertainty of what the vaccines contain.
My granddaughter is five and . . . my daughter didn’t have all her inoculations because she took very high temperatures as a small child; she was actually in the Sick Children’s [hospital] twice . . . and in a bath of cold water and a fan, fairly, fairly scary stuff, and they didn’t know whether she should get inoculations or not, because they didn’t know what had caused it. They gave her every test that they had and they never ever found out. But if my daughter was going to be not well, sometimes she had a fairly bad reaction to whatever it was that she had.
GT208a, Scottish Showperson, grandmother, Glasgow
Rather than uncritically accepting vaccinations, many of these participants described weighing up the advantages and disadvantages before usually deciding to go ahead, believing that the diseases they protect against are more dangerous than the vaccines themselves.
Yeah I mean if it, if you’re told this is gonna protect your child against something that is potentially fatal then obviously you’re gonna do it. But then . . . you’ve got . . ., ‘oh but something could be wrong with your baby if you give her that’, do you know what I mean, it’s a lot to weigh up that. Obviously I gave mine them and, touch wood, mine are all fine.
LT007a, Irish Traveller, mother, London
These needles are really to help the children against getting polio or meningitis or stuff like that because that’s more dangerous than actually getting the needles.
BT106a, Irish Traveller, grandmother, Bristol
A few spoke of being mindful of not wanting to regret a decision not to vaccinate should their child catch a preventable disease at a later date.
Well you don’t want nowt to happen to your bairns do you? I’d never forgive myself if I took them to the hospital and they said ‘have they had their injections’ ‘No’. ‘Well they should have had that and it could have stopped whatever from happening’.
YT011b, English Gypsy, mother, York
Concerns about ‘overload’ to the immune system from multiple or combined childhood vaccines in general and more specifically about the triple-dose MMR vaccination were mentioned by a small number of participants in each of the English-speaking Traveller communities, and by one Bristol Roma mother.
Like I said, they [some other families in the community] are scared . . . if they have two immunisations one time they think something happen bad.
BT201a, Romanian Roma, mother, Bristol
In some instances, families in the Scottish Showpeople, Bristol Irish Traveller/English Gypsy and York English Gypsy communities had previously paid privately for single vaccines, instead of accepting the combined MMR vaccine for their children.
You’ve worried for months about getting jags and then it takes two seconds for that virus in your child and it’s in it canna come out. It’s horrible, it’s not nice to think about. It’s the three live viruses in the one needle . . . too much.
GT202a, Scottish Showperson, mother, Glasgow
One mother from the Scottish Showpeople community had a daughter with autism and, while she did not attribute this to the MMR vaccine directly, she pronounced herself as less pro-immunisation than before her daughter’s diagnosis and was mindful that not everything in vaccines ‘is ideal’ (GT204a, married to a Scottish Showperson, mother, Glasgow).
Explanations behind acceptance of immunisation
Irrespective of their levels of confidence in immunisation, many Traveller participants across all six communities spoke about wanting to do the best for their children, with one English Gypsy mother from Bristol describing Travellers as superstitious and overly protective about their children.
We wanna do everything for our children, so if they need their needles, its gonna help them, of course we’re gonna be first there to get ‘em done.
LT009b, Irish Traveller, mother, London
[Travellers are] very superstitious and very funny about their children . . . overly protective. In a Gypsy’s eyes there’s no other child like your own.
BT109a, English Gypsy, mother, Bristol
Small numbers of Roma participants in Glasgow said that they had been asked if they were up to date with their vaccinations when applying for work and believed that their children would not be allowed to attend school unless they had all their childhood vaccinations. Two Bristol participants commented that they see having vaccinations as a way to integrate in the UK society in which having your vaccinations is the accepted norm. A manager of a local authority community centre in Bristol spoke of younger Roma parents wanting to have the same opportunities, such as immunisation, for their children as British families.
When you speak to them they want to live here, they want their children to go through schools here, they want their children to have opportunities. It’s not like them going like, ‘oh yeah, we’re Roma, we want to be one place here, one place today, another place tomorrow’.
BH307, manager in the voluntary sector, Bristol
Another motivator to vaccinate among older participants was personal experience or seeing others’ experience of preventable diseases, particularly measles, whooping cough and meningitis. For a minority, the memory of seeing a friend or member of their family suffer from diseases such as polio and the concern of family members at the time had been a stimulus to have their own children vaccinated.
I remember my nieces and nephews used to get . . . whooping cough, and you’d never hear about any vaccination for it, it’s frightening ‘cos they keeps coughing and they go blue coughing the whole time . . . And my child had . . . measles at that time. I had to keep him in, in the caravan but I had to put him into darkness . . . it was my mother used to be telling me, keep him in darkness, don’t leave him out in the light, and get Calpol® [Johnson & Johnson Ltd, Maidenhead, UK] or whatever you can get for him . . . he was about 2 weeks like that.
LT005a, Irish Traveller, grandmother, London
There were one or two stories of when a child had died from measles. Several Irish Travellers in London talked about the measles outbreak in their community in 2007, with one mother saying that she went against the majority community belief at that time and took her children for the MMR vaccination.
At that time all the Travellers were saying to me ‘what did you do, what did you do, you got the children the MMR [vaccination]’. . . they said to me ‘do you know that can make children sick?’, and I said, ‘it’s either sick or dead’.
LT008b, Irish Traveller, mother, London
For some, these experiences of witnessing outbreaks or experiencing a vaccine-preventable disease themselves had changed their minds about having vaccinations. For example, measles outbreaks subsequently triggered a change in attitude, leading to a local demand for the MMR vaccination. A grandmother from the York English Gypsy community who had previously not had the flu vaccination, because she believed it made you ill, then experienced flu and stated that she would have the vaccination in the future.
I am all for injections I agree with them 100%, just had a bad experience with the flu one. But now I have the pros and cons a lot of good things out of it, so I think I will start having it.
YT001a, English Gypsy, mother, York
A history of cancer in general or cervical cancer in the family was mentioned by several women in the Glasgow Scottish Showpeople and London Irish Traveller communities as the reason for ensuring that their daughters have the HPV vaccine.
The girls need this, cervical cancer’s rife in my family, so all my aunties had had pre-cancerous cells, apart from one, she’s had full blown cervical cancer. She was only 32 [with] three kids . . . so I would definitely be sending, as much as I don’t like them to be getting injections, but . . . that would be an important one for us.
GT204a, Married to a Scottish Showperson, mother, Glasgow
Experience of having vaccinations and not being harmed by them also encouraged some Traveller participants to take them up. Four London Irish Travellers spoke of this for the MMR vaccination and explained that community thinking had changed from believing that children will get sick from MMR vaccination to seeing it as an important injection to have. They attributed this shift in thinking to either having the vaccination themselves or seeing no ill effects in other children after having it.
‘Cos where my mum brought me to get mine done, so I thought nothing happened to me so it’s not gonna happen to my kids like.
LT009b, Irish Traveller, mother, London
A summary of this theme is provided in Table 11.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Concerns about Immunisation
Fear of injections
A very small number of Traveller participants (sometimes just one person) across all six communities referred to a fear of injections (needles) in terms of anxiety for themselves and their partners or perceived pain for their children. For most of these individuals it did not appear to deter them from having their vaccinations or taking their children to be vaccinated. The exception was a York English Gypsy man who said that he did not have his adult vaccinations because needles make him pass out and give him ‘sweats’ (YT010d, English Gypsy, young man, no children, York). Three women (one Bristol English Gypsy adolescent, one Glasgow Scottish Showpeople mother and one York English Gypsy grandmother) described overcoming their fear of needles to benefit their children; one described having the flu jab when pregnant because of the baby.
I had my flu jab when I was pregnant though. I had to ‘cos of the baby.
Now, you see, you do things for the baby but not for yourself?
Not for yourself. Babies are more important though aren’t they?
A second talked about needing to have blood taken when she was pregnant, while the other said she takes her children to be immunised but looks away from the injection.
I’m scared to death of a needle but I know that it is important to have them so I do have them. I probably look the other way while I have them but I still have them because I know it is important to have them.
YT006a, English Gypsy, grandmother, York
Another woman from the Glasgow Scottish Showpeople community explained how her husband’s fear of needles means that she has to take the children on her own to the GP practice for their vaccinations and so she finds it more convenient that they are given at school.
Reference to fear of injections was also connected with beliefs about contamination from needles and what you can ‘catch off’ (BT101a, English Gypsy, mother, Bristol) them. This was referred to by a very small minority of participants in the Bristol English Gypsy/Irish Traveller and York English Gypsy communities.
There’s a lot of people who are afraid of injections and there’s so many things you can pick up off injections.
BT101a, English Gypsy, mother, Bristol
Scepticism about immunisation
A very small minority of Traveller participants (sometimes just one person) in the four English-speaking communities said that they seriously question the value of immunisation but, on balance, do still have them. This scepticism was usually because of a belief that someone they were aware of in their community or their own family had been seriously harmed by a vaccination. For example, an Irish Traveller mother in Bristol said that she had seen a small boy end up in a wheelchair after vaccination. Another Irish Traveller mother, this time in London, spoke about how someone she knew believed that her children’s development was delayed by vaccination.
They were kids at the time and they lost their voice, they lost everything, and now they’re very behind over it. They do assure you that it doesn’t happen, but if you’ve seen it happen, people’s witnessed it, then it’s very scary to go and bring your kids for immunisation. That’s what stopped me half the time.
LT014b, Irish Traveller, mother, London
An Irish Traveller grandmother in London talked about it not being the ‘Travellers’ way’ (LT006a, Irish Traveller, grandmother, London) to have injections, although she did accept vaccinations herself.
And especially Travellers would be frightened of them. We’re not into putting needles or testing you for this and that. It’s not the Travellers’ way of doing things.
LT006a, Irish Traveller, grandmother, London
Only three Traveller participants in the sample as a whole talked about completely rejecting immunisation. A Bristol Irish Traveller mother explained that she had not had her children vaccinated because she follows how her mother had brought up her children. She thinks that childhood vaccines contain too many chemicals, preferring to look after her children with aspirin and calamine lotion for chickenpox (not recommended practice) as her mother did.
Today it’s a lot of chemicals. When my children had it [chickenpox] I done the same with them, how my mother treated us I treated my children, and there was nowt wrong with my children.
BT112b, Irish Traveller, mother, Bristol
She added that she hoped that her grown-up children would do the same for their children. In the York English Gypsy community, a mother said that she did not believe in the value of injections, describing them as ‘parasites’ that cause brain damage.
I’ve got three bairns and none of them has had, and I haven’t had no injections . . . I don’t believe in them. Because I think that a lot of ‘em do give ‘em [children] brain damage, and er I don’t know the word for it, some make ‘em slow and things. And er I just didn’t believe in it. None of me family has had any injections.
Where do you get your knowledge about injections from?
Me granny . . . She says you don’t need, she called them parasites, you don’t need foreign parasites in your body.
She explained that none of her family had ever had any vaccinations and that she trusts her parents’ views above others. Her unvaccinated daughter commented that she also trusts her own mother’s judgement about immunisation.
A summary of this theme is provided in Table 12.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
Beliefs about specific vaccines
Vaccinations in pregnancy were largely accepted for the same reasons offered above (see Explanations behind acceptance of immunisation). Interestingly, while some women were fairly ambivalent about adult vaccinations for themselves, knowledge that the whooping cough and flu vaccinations given in pregnancy would protect the health of their child appeared to be the stimulus to have these vaccinations in pregnancy.
Yeah it’s very important for, for my family, it’s very important and me, when I was pregnant I have all the immunisation.
BT201b, Romanian Roma, mother, Bristol
There was noticeable variability of beliefs among the English Gypsy/Irish Traveller community in Bristol. Although some had accepted vaccinations during their pregnancy, a number of women in the community stated that they had declined them or indicated they would not accept them if offered during a future pregnancy. This seemed to stem from a common belief, expressed by both men and women, that the ‘immune system is low’ (BT102a, Irish Traveller, mother, Bristol) in pregnancy and ‘needles’ (BT108b, Irish Traveller, young woman with no children, Bristol) should be given after the baby is born as well as, for some, the adoption of a fatalistic attitude.
These [whooping cough] are needles that the women don’t take when they are pregnant because to them it’s God’s fate, you just don’t inject when a woman’s having a baby . . . you just leave it alone and leave it in God’s hands. What will be will be.
BT108d, Irish Traveller, father, Bristol
Concerns that were raised about specific vaccines largely related to whooping cough, MMR, HPV and flu (adult) vaccinations. Issues about these specific vaccinations were mentioned across all six communities; however, some were a particular point of discussion for particular communities.
The anxieties surrounding the whooping cough and MMR vaccines derived largely from the negative publicity of the 1970s and late 1990s/2000s alleging links to brain damage and autism for the two vaccinations, respectively.
The second big driver was MMR [vaccine], because, you know, the autism story hit . . . but prior to that there’d been resistance to MMR [vaccination] in, in the Traveller community . . . I think it came from the difficulty in distinguishing what was genuinely vaccine-related reactions from intercurrent illness, and the fact that it was a live vaccine, and the fear associated with, with giving a live vaccine. Then of course the autism story broke and that just reinforced all those prejudices. So we had a lot of trouble getting MMR [vaccination] accepted.
BH304, former immunisation co-ordinator, Bristol
Whooping cough
Concerns about the whooping cough vaccine being given in pregnancy were voiced by a minority of women in the York English Gypsy and London Irish Traveller communities but not in the Roma communities in Bristol and Glasgow nor by Glasgow Scottish Showpeople. This vaccination was a particular issue for the Bristol English Gypsy/Irish Travellers, with more than half of the women interviewed stating that they did not or would not have it when pregnant. One family in the community attributed the whooping cough vaccine as having caused their (now grown-up) son’s disability. A strong, long-held community belief that the whooping cough jab leads to brain damage and disability seemed to be pervasive among some older sections of the community, although there was recognition that this belief may be fading, particularly among younger people. Similarly, reference to fears of the whooping cough vaccination causing brain damage was also made by some in the London Irish Traveller community.
Travellers strongly believe in these, especially tetanus and polio and all those injections [for children] . . . but not a lot of Travellers believe in those whooping cough injections. Some used to say it could like [lead to] brain damage or something. We wouldn’t have whooping cough injections. That’s the one we was strongly against.
BT109a, English Gypsy, mother, Bristol
Measles, mumps and rubella
Measles, mumps and rubella vaccination was a particular point for discussion for women in the Scottish Showpeople community in Glasgow, where unease was greater (almost half voiced concerns) than in the other communities. This may have been a consequence of the fact that two mothers in the Scottish Showpeople community had a child with autism, one of whom attributed the MMR vaccination to be the cause. She was active in the Scottish Autism network and on social media (Facebook) and acted as a lay advisor for other women in the close-knit community, who sought her advice about the MMR vaccination.
I’ve had people coming to me now saying that their child’s going for the MMR [vaccination] ‘what should I do’ and I said ‘I can’t tell you what to do . . . I can advise you and I can tell you what I think but it’s your child and I can’t tell you what to do’ . . . and I’ve said ‘look go with your heart’.
GT202a, Scottish Showperson, mother, Glasgow
With regard to the other communities, although a few Travellers still retained mixed views about the MMR vaccine, most now considered the benefits of the vaccination outweighed the effects of measles.
You have to weigh up the pros and cons and, to be honest, I think the good outweigh the bad and because none of the rest of my kids had a negative effect from it [MMR vaccination].
LT010b Irish Traveller, grandmother, London
Some Traveller participants (mostly women) and service providers (mainly health visitors and immunisation co-ordinators) described how MMR vaccination delays and refusals in some families in the Bristol English Gypsy/Irish Traveller, Bristol Roma, York English Gypsy and London Irish Traveller communities had resulted in measles outbreaks 3 or 4 years earlier.
Everyone in the whole community ended up, ended up getting the measles ‘cos we were on a Traveller site and it was very small and everyone got measles on the Traveller site, so it went like wild fire through the community and at the same time no one no one no one had their children immunised with MMR [vaccine].
LT008a, Irish Traveller, mother, London
The service providers in these communities referred to considerable challenges with getting MMR vaccination accepted in the Traveller communities in the recent past but believed that, generally, the level of community concern about MMR vaccination was now not dissimilar to that of the general population.
The MMR [vaccination] is quite a big one that I noticed that quite a few [Traveller children] don’t have it but we had recent outbreak of measles and I think a lot of the families that didn’t, children that didn’t have the injection, they went and had it.
YH001, teaching assistant, York
As discussed above (see Explanations behind acceptance of immunisation), measles outbreaks in Bristol, York and London had served as a trigger for the majority of families to have their children vaccinated.
I didn’t give one of my children MMR [vaccination] because there was a scare on TV, but then I looked at kids who did get ill . . . I realised it was the wrong thing to do.
BT106a, Irish Traveller, mother, Bristol
Human papillomavirus vaccine
Safety concerns about HPV vaccine were mentioned by a few women who had read stories of serious side effects in the media (for example, one Roma mother in Glasgow and one mother from the London Irish Traveller community) but the more common issue raised, across the English-speaking Traveller communities (not the Glasgow Scottish Showpeople), related to the belief that having the vaccination would imply that Traveller girls are promiscuous.
There’s a new one we are all a bit wary about, the HPV for the young ones. And our young ones, they’re clean when they get married so we don’t, we’re not into than kinda giving that one to the young ones . . . our girls aren’t promiscuous, look after the girl’s reputations do you know what I mean?
LT008b: Irish Traveller, mother, London
This cautiousness about the HPV vaccination was voiced among a minority of mothers and fathers/grandfathers, mainly in the English Gypsy/Irish Traveller community in Bristol, York English Gypsy women and Irish Traveller women in London. Within these accounts, HPV elicited strong views with respect to the moral overtones of accepting the HPV vaccination and how this would be viewed by their community in which no sex before marriage and a partner for life were powerfully held beliefs. In this sense, fathers had a duty by virtue of their position in the household to protect their daughters from being viewed as promiscuous by others in the community. Although mothers tended to be viewed as the primary decision-makers about childhood vaccination, in general (see Decision-making about immunisation), with respect to the HPV decision, it appeared that men’s views may have been more influential in the decision-making process in these communities.
I don’t think men, the Traveller men would approve of the teenage girls having this particular needle, and we don’t talk about what’s it about . . . we won’t go into detail . . . the men have a very stronger view about that than the women of the Travelling community, because they feel it would be an insult to offer that needle to their daughters.
BT108c Irish Traveller, adolescent girl, Bristol
They’ve no business of it anyway . . . you don’t cross that line till you get married.
BT108a, married to an Irish Traveller, father, Bristol
Service providers working with the English-speaking Traveller communities also spoke about attitudes towards the HPV vaccination leading to resistance in some families. In these circumstances, they would frame the vaccination message as a cancer prevention measure rather than preventing a sexually transmitted infection.
One of the grandmas who’s also got young children and she’s very worried about the HPV for kids and she’s said there was a lot of gossip going on and a lot of sort of information going round the community and that her, the girls in their community didn’t need it because they were going to be virgins when they married.
LH303, practice nurse, London
These views were also counterbalanced by other Traveller participants, particularly mothers, their adolescent daughters and grandmothers, who were positively predisposed to the HPV vaccination as a preventative measure for cancer.
I would definitely be sending, as much as I don’t like them getting injections, but for that [HPV] that would be an important one for us.
GT204a, Scottish Show People, mother, Glasgow
I know obviously it’s [HPV vaccination] aimed at people that’s more sexually active, you know Traveller girls are less likely to be that, but I think it’s good because obviously it’s not just yourself you have to worry about, I think it’s your partner . . . you don’t know where they have been (laughs) . . .
LT010b, Irish Traveller, grandmother, London
In addition, decisions about HPV were often viewed as more sensitive, a private matter for the family and not a topic for discussion outside the family, in contrast, for example, to other vaccines, around which there were concerns for some Travellers, such as MMR or whooping cough, which were openly discussed within the community. This may have been a reason why a minority of mothers who were positively predisposed to their daughters having the vaccination expressed a preference for them to have it at their GP practice rather than in school (see Relationships with health professionals).
Flu
Concerns about becoming ill by having the adult flu vaccination were raised by a minority across all the English-speaking Traveller communities. This vaccination appeared to be declined on the basis that it was either not important, in relation to other vaccine-preventable diseases, or because of concerns about it giving the person flu (based on personal experience or observations of others who had received the vaccination).
When I went and had it [flu vaccination] I was bad for days after the needle, but I haven’t had it since . . . it put me off having it to be honest.
BT108a, married to an Irish Traveller, father, Bristol
A summary of this theme is provided in Table 13.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Intergenerational change in beliefs about immunisation
There appeared to be an intergenerational shift in beliefs about immunisation, with the current generation of parents tending to being more positive than their grandparents, and sometimes their parents, had previously been. There was reference to ‘old people’s stories’ (BT105a, English Gypsy, grandmother, Bristol) and the traditional view of using natural remedies to cure illness as well as Travellers being frightened of immunisation in the past. This change in attitudes from seeing immunisation as dangerous to viewing it as a protective measure was mentioned by several Travellers and service providers for five of the Traveller communities. A shift in beliefs was not mentioned by any Glasgow Scottish Showpeople participants or their service providers.
A number of reasons were offered for this shift in beliefs. It was suggested that Traveller communities are now more integrated into society because many Travellers are settled and are influenced by their associations with non-Travellers through working locally and sending their children to local schools. This may have increased their confidence to access health services.
The ones who are settled and in bricks and who are in more established communities appear to engage more consistently and comfortably with the whole concept of health care and immunisation; so more commonly will be registered with a local practice and will turn up as and when appropriate.
BH302, GP, Bristol
Many Traveller participants spoke about a move over time towards trusting health professionals as a key source of information about immunisation (see Sources of information and advice about immunisation and Relationships with health professionals).
I think our generation, up to about 30, 35 years old, we accept the idea of immunisation. The older ones . . . they are a bit [uncertain] . . . because they didn’t go to the doctor so often.
BT218a, Romanian Roma, father, Bristol
Improved literacy (see Language and literacy) in the younger generations was also seen as a reason for the change in attitudes, with parents now proactively accessing information about immunisation from a variety of sources. This has led to younger generations having far greater knowledge and understanding about immunisations than their parents and grandparents (see Knowledge about immunisation).
The families are very, very clued up about it and so I believe they access it more you know . . . from my experience they more take their children now, it’s getting a lot better I believe.
LH306, team leader in the voluntary sector, London
A summary of this theme is provided in Table 14.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Interpersonal influences on beliefs about immunisation
Family
Traveller participants across all six communities acknowledged that the influence of family on beliefs about immunisation was less than for previous generations. However, several mothers (and indeed fathers) talked about being influenced by their own mothers, mothers-in-law and their grandmothers in their beliefs about childhood immunisation (see Sources of information and advice about immunisation and Decision-making about immunisation). For most of these parents, they spoke of having their immunisations when they were children and growing up believing that it was the right thing to do.
Mother said we had to have it [polio immunisation] and that was that.
GT208a, Scottish Showperson, grandmother, Glasgow
Just obviously my mum got all ours [vaccinations] done, so it’s that type of thing where you pass it down, so obviously I got theirs, then probably they have kids they’ll get theirs done . . . like when you are getting baptised, obviously it’s just something that when it happens to you also, you just pass it down to yours then.
LT011a, Irish Traveller, mother, London
A small number of Travellers spoke of how their family did not accept immunisation when they were children and continued not to do so now. The three Traveller participants who completely rejected all immunisation (see Concerns about immunisation) clearly stated that they trusted and followed their mother’s or grandmother’s judgement.
We keep the rules. What my mother done, we done. How my mother treated us I treated my children and there is nowt wrong with my children.
BT112b, Irish Traveller, mother, Bristol
In contrast, there were also examples of mothers, daughters and female siblings choosing to do differently from their mothers, grandmothers or sisters, in terms of their acceptance regarding vaccinations generally, or specific vaccinations (e.g. MMR, HPV, whooping cough).
When we were all little me mum wouldn’t let us have needles, because it was, if you give the children them they’ll give them the meningitis and it would kill ‘em and all this. But I . . . they’ve [her children] gotta have ‘em there’s that many diseases in the world now, they’ve got to have ‘em.
BT101a, English Gypsy, mother, Bristol
A small number of Traveller participants referred to not involving their own parents in the vaccination decisions that they make for their children; for some this was associated with current parents having more evidence-based information about immunisation than their parents had had (see Knowledge about immunisation).
I didn’t get any information from my mother . . . I don’t think she had any information herself . . . Travellers know a lot more now . . . not when I was growing up.
LT010b, Irish Traveller, grandmother, London
Friends
A minority of Traveller participants (sometimes just one or two people) across the six communities commented on their friends’ views about immunisation, and this was usually prompted by a direct question from the interviewer. A father from the York English Gypsy community and one father and a mother from two different families in the Glasgow Scottish Showpeople community suggested that immunisation is a private family issue and not discussed with others.
What I chat about like injections . . . for my kids, it just keeps between me, me missus and the three kids, no-one else, that’s it.
YT012a, English Gypsy, father, York
Of the few Traveller participants who mentioned their friends, some said that they are not particularly aware of what their friends think about immunisation; others spoke of friends with positive views as well as those with negative views. A couple of female Scottish Showpeople described how they had ignored their friends’ concerns about the flu vaccine being a waste of time and causing a heavy cold, and had gone ahead with having the vaccination. Two mothers, a Bristol Roma and a Glasgow Scottish Showperson, explained how they try to advise their friends about vaccination; one tried to encourage them and the other (who attributed her son’s autism to the MMR vaccine) told people to ‘follow their heart’ (GT202a, Scottish Showperson, mother, Glasgow) and provided information on the single injections for measles, mumps and rubella.
Some of them, they are not very happy doing it because they don’t understand the benefit of it . . ., but the people I spoke with I advise them to do it because my children are . . . bigger and they had it and everything was alright. Then everybody decides for their [own] children.
BT214a, Romanian Roma, mother, Bristol
A summary of this theme is provided in Table 15.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
Decision-making about immunisation
Several mothers from five communities talked about being the main decision-maker about childhood immunisation (Bristol Roma participants did not actively volunteer information on this). This was considered the norm within the community principally because mothers were considered more knowledgeable than fathers about vaccination and had the main responsibility for bringing up their children.
Do you ever consult your husband on health things and health decisions? I mean if, if you were unsure about a vaccine, like the MMR [vaccination] we’ve talked about, would you say, you know, to your husband?
No, I mean, no, I mean . . . No, he mainly leaves everything to me.
In the York English Gypsy and Glasgow Scottish Showpeople communities, most of the men either described not discussing immunisations with their family or concurred with the view that their female partner knows more about childhood immunisation than they do. These men described immunisation as ‘more a woman’s thing’ (YT013a, English Gypsy, father, York).
Well the men went out and done the jobs and done all the rest and women watched the kids and made meals, did the home, home cleaning and kept the kids clean, that was it.
Has that changed over your lifetime?
No
Similar small numbers of Traveller mothers, in all six communities, described making the decision with or seeking agreement from their partners. Two Bristol Irish Traveller mothers spoke of persuading their husbands to allow their children to have their vaccinations.
He thought it was wrong to get . . . [MMR vaccination] as there was a history of Travelling people . . . their child got disabilities. He said no but after a long while of persuading I finally get him [the son] the jab.
BT107a, Irish Traveller, mother, Bristol
A summary of this theme is provided in Table 16.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
Language and literacy
Language barriers for the Roma communities in Bristol and Glasgow were acknowledged by Roma participants themselves and by service providers. Challenges were identified in terms of being able to communicate with health professionals within consultations as well as understanding written information and invitation letters for immunisation.
Several Roma participants in Bristol and Glasgow who do not speak English recalled their struggles to make themselves understood to health professionals during health encounters in the absence of interpreters.
I take my son twice . . . I didn’t know what they were actual saying, I didn’t know what it was for; I didn’t understood. If I go somewhere I do manage to make myself understood; that time I didn’t . . . I did not know exactly where to go to get the flu injection.
GT102a, Slovakian Roma, mother, Glasgow
All of the service providers in Glasgow who work with Roma talked about the importance of having an interpreter in consultations, although for some there were challenges in these consultations even when an interpreter is present. For example, the appointment takes much longer and, at times, they lack confidence that interpreters are translating all that is spoken. An example of this was reference to a home visit when a family member spoke for 40 seconds and the interpreter said one word. Furthermore, the interpreters and community link workers speak Slovakian and Romanian, whereas many of the adults who did not go to school speak only Roma and there is only one Roma interpreter in the city. Some Roma participants commented that interpreters are often not available when they attend for appointments. This was also confirmed by the service providers in Glasgow. The health visitors and a school nurse all spoke of a shortage of interpreters who speak Romanian, meaning that they often struggle to do basic health visiting and health promotion with parents. A school nurse further described how the flu immunisation programme was cancelled in one school which was to be a pilot site, as she could not access the right interpreter because there was no dedicated budget for this.
And the frustrations are at times that people just don’t listen. You know last year we pulled [name of school] from immunisations because of, at that point there were more Slovakian families with Slovakian children and yet this year . . . they gave us Roma . . . they gave us Romanian, gave us Polish . . . didn’t give us Slovakian. Slovakian was the one that I needed. So it’s just really hard.
GH303, school nurse, Glasgow
A minority of service providers in Glasgow spoke of an alternative translation service, which is available to use over the telephone. However, they explained that this service is not practical to use in consultations because, as well as being time-consuming, there might be a wait of up to 12 minutes to access it. One local authority team leader expressed frustration that some receptionists in GP practices fail to use this service.
I mean we routinely hear about receptionists being rude to people, and doing the kind of shouting at people as if raising their voice could help with the communication . . . when in fact all they need to do is type a number into their phone, pick it up and it’s a speak phone system.
GH302, social services team leader, Glasgow
Service providers working with the Bristol Roma community spoke less about the use of interpreters, although a former immunisations manager suggested that more is needed than ‘just’ (BH303, former immunisation manager, Bristol) interpreters as they often come from a different, usually middle-class background. They believed that using an interpreter does not always work very well because a dialogue about immunisation is not just about language translation.
But I think the perception is, often, with public health commissioners . . . especially sort of with Roma gypsies, that you can just translate materials into that language and I think it’s not always acknowledged that perhaps it is more [an] oral culture and especially when you’ve got communities, if there’s not you know, low levels of literacy.
BH303, former immunisation manager, Bristol
Many of the Roma participants in both cities expressed a preference for spoken information rather than written in terms of being informed of appointments and learning about immunisation.
It’s better to, if someone told them, like personally speaking, rather than a leaflet.
BT205a, Romanian Roma, mother, Bristol
A GP in Glasgow agreed with this approach, describing how take-up of childhood immunisations is good because of the face-to-face work that the specialist EU health visiting team does with Roma families; in contrast, adults are sent a letter, in English, about immunisations, which they do not understand and so they do not attend. A school nurse expressed her concerns that parents sign consent forms written in English for their child’s flu vaccination without understanding what they are consenting to. In Bristol and Glasgow, bilingual link workers, based within GP practices, agencies who work with under-fives and in schools, were seen as highly valuable as they are trusted by the community and can interpret as well as follow up families for immunisation by telephoning them or visiting them at home (see Immunisation recall and reminders).
The idea was really that the health link worker would phone them up; we trained the health link workers so they were able to talk about child immunisations . . . and then the idea was that they would contact the family, try a few times, and then yeah, if they wanted support, to be with them when they attended for the appointment, and then . . . if people didn’t turn up, to do follow-up and also to ring up before the appointment.
BH303, former immunisation manager, Bristol
When information needs to be written, translating it was seen as one solution for some.
It would be better is they could send a letter . . . in Romanian because some people can’t, don’t understand what it’s all about . . . some people who don’t know how to write and read it’s difficult and then they don’t understand what the letter is about so then they don’t turn up for vaccination or they think it’s something worse, being scared.
BT203a, Romanian Roma, grandfather, Bristol
Although for some Roma participants and most service providers from different sectors (health, education and social) language translation was not seen as sufficient as literacy difficulties in a Traveller’s own language present a key barrier to understanding written information, limiting the value of the information. However, they considered this to be a relatively easy barrier to overcome, for example, by using pictures of the vaccine-preventable diseases, of someone being vaccinated, as well as a way of getting an appointment without a letter.
Pictures would be helpful for the older ones.
BT209a, Romanian Roma, father, Bristol
They can’t read the letters to start with, all they want is an appointment to know when they can go.
BH301, health visitor, Bristol
Low levels of literacy were also seen as an issue for the English-speaking Traveller communities in Bristol and York. Nearly all of the women and half of the men from the Bristol English Gypsy/Irish Traveller community talked about low levels of literacy among their community. In York, a minority of participants discussed literacy. For both communities, it was suggested that, although low levels of literacy are more common among older Travellers, it is not a problem that is exclusive to older community members.
Half of these women can’t read or write and they’re embarrassed, and not to talk big talk with the big words, to make it basic so as a Traveller woman can understand what they’re on about.
BT108c, Irish Traveller, adolescent girl with no children, Bristol
I don’t like reading anything at all. I think it looks posh anything writ down for me . . . everything looks like I can’t understand it.
BT112b, Irish Traveller, mother, Bristol
Some service providers working with these Traveller communities offered a similar view that low levels of literacy remain a problem with the current generation of parents. A teaching assistant in York with a remit for developing literacy in young children explained that many young parents with whom she works can read but struggle with writing.
Of those Traveller and service provider participants who discussed literacy, many described how low levels of literacy result in people being unable to read immunisation leaflets or letters/texts about appointments. They may struggle to make sense of conversations with health professionals, particularly GPs, if they use technical terms or medical jargon, and may feel embarrassed. A Bristol Irish Traveller mother explained that she does not understand the language her GP uses, for example ‘hepatitis B’, but that she pretends that she can so as not to look stupid. She prefers to see the health visitor, who explains things more clearly.
She’s good, I like her [the health visitor]. You’re worried about things and you say to her like ‘I don’t know what, what I should do’. She, she’ll tell you, but she’ll tell you in our words that we understand . . . whereas if you go to a doctor . . . you’ll sit there and you’re thinking ‘I don’t know what you’re saying but I’ll pretend I know otherwise I’ll look stupid’, you know what I mean?
BT112a, Irish Traveller, mother, Bristol
Like you go up to the hospital you see all these leaflets . . . about needles . . . if you could read, you could sit and read them. But you go up to a GP they’ve got nothing up like that in . . . the waiting room . . . They’ve got leaflets but it’s got no pictures of what they mean.
YT003a, English Gypsy, mother, York
Those Travellers who spoke of their own difficulty with reading and writing described how they rely on family and other community members for information about immunisation, to read out letters about appointments and to accompany them to consultations with health professionals.
If we don’t understand it because we are trying to learn to read because we could never read or write we couldn’t even put our own name until we started to study. Her daughter would read so many words out to us and tell us like what to do.
YT003b, English Gypsy, woman with no children, York
Scottish Showpeople in Glasgow and Irish Travellers in London did not mention their own literacy levels or those of their family and wider community. However, some service providers in both cities said they had observed low literacy levels among these Traveller communities. A health visitor knew of some Scottish Showpeople mothers in their twenties and thirties who struggle to read. In London, a service provider working in the voluntary sector suggested that low levels of literacy hold Travellers back from advocating for their way of life on sites. A practice nurse stated that literacy is the biggest barrier working with Traveller communities and health professionals have an expectation that service users have appropriate literacy skills.
And the other thing . . . that’s really important is the level of literacy and literacy expectations. That isn’t considered quite often at commissioning level, because people don’t understand functional literacy and they don’t understand the sort of ideas about literacy and the truth of text embedded in a non-graphical, still a non-graphical society; it’s still not focused on text in the same way as the majority culture in the UK which means that giving information [on] posters or that sort of public health campaign, isn’t as appropriate . . . and that’s a sociological anthropological thing that often isn’t taken into account when you’re trying to engage people with information.
LH303, practice nurse, London
As with the Roma communities, there was widespread support from Traveller and service providers for simple written information with pictures and a preference for verbal information from health professionals either alongside, or instead, of written information.
We’re Travellers, we can’t read or write . . . I don’t understand the big words, you’ve gotta break it down a bit for me and I don’t think that is much to ask.
BT105a, English Gypsy, grandmother, Bristol
You’ve got to put it over simple but you have to give them all the information . . . not treating them like idiots but not treating them as though they’re academics.
GT208a, Scottish Showperson, grandmother, Glasgow
I think your nurses at your doctors . . . they should have leaflets to explain everything about every injection . . . Not in big words what people can understand. If they’d just give some more information on what’s going on, put a leaflet explaining what it is instead of just ‘you need an injection, make an appointment’.
YT001a, English Gypsy, mother, York
A small minority in Bristol and York commented that Travellers will not pick up or keep leaflets because of a cultural preference for oral traditions. A similar minority emphasised the importance of health professionals verbally explaining about the side effects of immunisation.
A summary of this theme is provided in Table 17.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Discrimination
A few female participants from the English-speaking Traveller communities (sometimes just one person) described discrimination and marginalisation from health services. This included discrimination from health professionals as well as support staff in NHS premises. A Bristol English Gypsy grandmother spoke of how a nurse had dealt badly with her granddaughter’s sore throat, failing to examine her, instead chastising the grandmother for letting the young girl drink cola. She perceived this to be because she is a Traveller who ‘all get tarred with the same brush’ (BT105a, English Gypsy, Grandmother, Bristol). In York, two participants suggested that there is less discrimination by health professionals nowadays, although some remains, as it does for any minority group.
They’d get more than the sack they would be sued for absolutely thousands and thousands of pounds . . . if they was being racist and they weren’t going to treat you just because of the culture you come from.
YT007a, English Gypsy, mother, York
A York grandmother described how when her children were young their GP practice registered their family as temporary; this meant that they had to complete a form each time they attended, even though they had lived on a site for 20 years. She suggested that this was because the GP practice wanted them to go elsewhere but added that it is not like this now. One of the Glasgow Scottish Showpeople mothers reported that she did not want to discuss her problems with the nurse working at her GP practice because she ‘looked down her nose at her’ (GT208a, Scottish Showperson, grandmother, Glasgow). She added that she was not sure if this was because she is a Traveller as they are seen as ‘thieves, vagabonds, unhygienic and would steal children’ (GT208a, Scottish Showperson, grandmother, Glasgow). A mother from the London Irish Traveller community reported a lack of consideration when she missed an appointment for her child.
The health visitor was rude but I said ‘I’m here now, it’s not like I’m holding back the needles, my child is up to date with everything, she’s just 2 or 3 weeks late this time because I couldn’t get appointment from the doctors’.
LT009b, Irish Traveller, mother, London
No Roma participants in Bristol or Glasgow described experiencing discrimination from health services. Indeed two Slovakian Roma, a grandmother and a father, commented that they are treated more kindly in Scotland, ‘normally like the others’ (GT103d, Slovakian Roma, grandmother, Glasgow), than in Slovakia, where racism towards Roma is a problem.
Service providers in all four cities similarly expressed a number of concerns about discrimination against Travellers. Several Bristol service provider participants were aware of how a lack of cultural competence had an adverse effect on Travellers’ experience of health services.
I have been in meetings where particular sort of practice managers seem to think that, you know, that people are irresponsible and don’t care about their children and don’t make the effort and are lazy and that sort of thing. So I have come across those kind of attitudes.
BH303, former immunisation manager, Bristol
Some service providers suggested that doctors and nurses lack understanding of cultural differences and can feel resentful about responding to Travellers’ needs, questioning how much effort they should give to ‘chasing people round the country’ (BH304, former immunisation co-ordinator, Bristol). Indeed, one participant offered this view:
I’m not sure how appropriate it is for us to commission somebody to go trundling round sites for people who can’t be bothered to come in, because actually these folk do have transport, that’s how they travel, by definition they’ve got transport, they don’t think it’s a priority or important.
BH302, GP, Bristol
Another spoke of a colleague who did not want to take on Travellers in her caseload and attributed that to her being nervous about taking on new challenges and fearful of the ‘unknown’ (BH308, health visitor, Bristol). A manager of a local authority community centre in Bristol commented that he sees a lot of stereotyping of the Roma community but that this is done in an appropriate way, as it is seen as a way to ensure that this community, perceived to be at risk, is supported.
I think it is for good reasons because they see, as they should, legally, the Roma community as this protected characteristics element and they obviously want to be very vigilant to any risk of discrimination, that’s why they say . . . we have to provide quite a lot for this community.
BH307, manager of local authority community centre, Bristol
There was a view from the service providers in York that those who work routinely with Travellers are more understanding and less judgemental than other workers. A practice nurse described how the English Gypsy patients are regarded as part of the practice community and highly accepted within her GP practice, although she had witnessed rude comments by some patients, leading to her view that stigma and lack of respect towards the Traveller community persists.
I think people [other patients] just look at them as Gypsies and don’t look at them very highly . . . making comments about the ‘gypos’.
YH004, practice nurse, York
A teaching assistant described how a health professional (who does not usually work with Travellers) was surprised to see that Travellers’ houses and children are clean, and that they wear school uniform. She referred to other health professionals assuming that English Gypsy children will be dirty and neglected to some extent.
It’s almost making the assumption that Travellers are dirty and the children are dirty.
YH001, teaching assistant, York
A children’s centre support worker explained how she was asked for advice by Traveller parents on how to approach a teacher who they consider to be discriminating against Traveller children.
In Glasgow, service providers expressed their own views about the challenges of working with the Roma community. A GP expressed negative views, which he suggested was a response to the frustration felt when individuals fail to attend hospital appointments. A health visitor suggested that GP practices may feel that the Roma take up too much of their time because they attend at busy times and they do not speak English. As in York, the view was that those who work with Traveller families have more positive attitudes. There was also a view that discrimination is now more likely to be challenged and there is an increase in both Roma understanding of the NHS and an improvement in the attitudes of health professionals and others towards Roma people.
I think there are still pockets where they’re very much treated as ‘these people’ but I think, I think staff are more careful about what they would say about it ‘cos . . . we do have individuals that challenge within the team and say, ‘well that’s not appropriate to say that’.
GH304, NHS service team leader, Glasgow
Finally, in London, a practice nurse perceived impatience from health professionals when Travellers attended the accident and emergency (A&E) department for non-emergency conditions. A project manager from the voluntary sector described a Facebook page set up by the police about Travellers that was discriminatory but reported that Irish Travellers who participated in a recent focus group did not feel that health professionals discriminated against them.
And so in terms of . . . our focus group recently, which was about health . . . they said they had never felt discriminated against . . . and I think perhaps . . . those caring professionals would tend to treat people reasonably well.
LH307, project manager in the voluntary sector, London
A summary of this theme is provided in Table 18.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
| – |
|
| Service providers | |
|
|
Housing
The vast majority of Traveller participants lived in caravans or chalets on official Traveller sites or in rented houses, flats or bungalows. No participants lived on the roadside (see Table 7). Two Traveller participants, one Bristol Roma father and a York English Gypsy mother, specifically spoke of how their housing (a house and caravan on an official site, respectively) facilitates take-up of immunisations because their families are more integrated into society and are located close to the local GP practice.
Housing was also identified by a minority of Traveller and service provider participants as a barrier to immunisation for a number of reasons: ensuring that recall and reminder letters reach people is challenging; health professionals visiting sites are sometimes unable to find the families they are looking for; and worry about housing means that immunisation is not a priority.
Two Glasgow Scottish Showpeople mothers explained how immunisation letters sometimes go missing because of the community postbox on site. A health visitor working with this community also described how, when visiting a family for the first time, she can struggle to identify the correct chalet as they are not numbered.
In terms of worrying about the housing itself, an Irish Traveller grandmother referred to a young single mother who lives in a flat away from her family, describing her as isolated and sleep deprived, with the result that immunisations ‘go off her radar’ (LT010b, Irish Traveller, grandmother, London). Service provider participants in Bristol, York and London similarly spoke of their perception that Traveller families living in houses can be more isolated from their community and less engaged with health services, including immunisation, than those who live on sites. In Bristol a service provider from the city council also spoke of families being moved on within privately rented accommodation. In London, the problem with housing was considered to be a lack of local authority sites and houses for Travellers as well as housing benefit being insufficient to cover private rents, leading to a fear of eviction.
The local authorities just haven’t got the properties or the accommodation so a lot of the families are being shipped out . . . they’re losing their family network, they’re losing all their support networks . . . One [barrier] is the lack of sites. Families who are placed in houses . . . they feel quite isolated and they’re, you know, away from their community and their culture . . . it’s really sad.
LH306, team leader in the voluntary sector, London
Finally, there were accounts from several Glasgow service providers of Romanian Roma families living in particularly poor, crowded housing. They described how they live in ‘wee ghettos’ (GH302, social services team leader, Glasgow) in a particular area of Glasgow, with large families sharing small spaces.
Families who are suffering from really, really unsanitary conditions, cockroaches, appalling living conditions.
GH309, NHS community health manager, Glasgow
But the Roma community in particular, because I suppose the way they live, like lots of people living together, the heat’s full on, you know, it’s always really warm when you go in, The conditions . . . make it more [likely] . . . that they’d be at risk of infestation, so you’ve got all these things going on.
GH301, health visitor, Glasgow
A summary of this theme is provided in Table 19.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
| – |
|
| Service providers | |
| – |
|
Travelling
The travelling culture was discussed by several Traveller participants across the four English-speaking communities. The English Gypsies in York and Glasgow Scottish Showpeople reported living more or less permanently in their locality and travelling to fairs only in the summer months.
Are there many Travellers in York who are moving around a lot?
No we are all stable.
Obviously some of the Travellers . . .
They only travel around in the six week [school] holidays the rest [of the time] have got their own place. That’s when they mostly go away for the big horse fairs and stuff like that.
Yes but it’s not really like it used to be. They don’t really travel as much as what they used to. Like when I was at home me and my sister . . . used to travel up and down road sides a lot. Now they don’t.
These York Traveller participants identified the advantages of being settled as being close to a GP practice, routinely accessing their services, including immunisation, and developing a trustful relationship with doctors and nurses at the GP practice (see Relationships with health professionals). A York English Gypsy mother explained that, in contrast, she knew of roadside Travellers without a permanent address and who, she believes, have to reregister every 6 months with a GP practice, even if it is with the same practice.
The Scottish Showpeople participants were clear in their view that their travelling is not a barrier to immunisation because families do not travel for long periods of time, and they either change the date of the appointment or go to another GP practice for the immunisation in the same way that their children previously changed schools when travelling for long periods of time.
If you was offered a jag and you wasn’t here and you was out travelling, you would probably make another appointment wouldn’t you? You wouldn’t miss it. If you wanted it [immunisation] you wouldn’t miss it.
GT201b, Scottish Showperson, mother, Glasgow
Service providers in York and Glasgow also spoke of the English Gypsy and Scottish Showpeople communities being more settled now. A children’s centre support worker commented that families travel for only up to 6 weeks as they do not want to lose their space on the site; she added that they come back to the same GP practice. A challenge for roadside Travellers offered by a teaching assistant in York is that they are moved on by the council every 6 weeks, so are unlikely to have their immunisations. A health visitor working with the Scottish Showpeople described how families come back from travelling so that their babies can have their vaccinations and that some arrange to have their mail opened when they are away so that they know when they are due to attend.
When it’s a baby and they know their baby’s getting three lots of immunisations a month apart, they will, even if it is within the summer, they’ll make sure they come back.
GH306, health visitor, Glasgow
Among the Bristol English Gypsy/Irish Traveller and London Irish Traveller participants, views on levels of travelling and the impact on having immunisations were more mixed. In Bristol, an English Gypsy mother and an Irish Traveller grandmother spoke about how travelling makes it difficult to get to appointments for children’s vaccinations because they may not receive the invitation letter, forget about appointments, or the appointment may be for when they are away and, therefore, it is a ‘hassle’ to attend.
When Travellers have to book things, they never keep to it if they’re travelling about . . . We think injections are good but they just can’t be arsed with the hassle . . . ‘cos they’re never in one place more than, well, a couple of weeks . . . ‘cos the doctor won’t see you half the time, will he?
BT111b, English Gypsy, mother, Bristol
Two other Bristol English Gypsy mothers mentioned that, although they missed their own immunisations when pregnant because of travelling, they ensured that they came back for their children’s appointments. Similarly, in London, five mothers said their daughters had missed their HPV vaccination (see Attendance at school) as they were travelling, whereas others talked about travelling in the past, rather than nowadays, being a barrier to take-up of immunisation.
Service providers in Bristol described the English Gypsy/Irish Traveller community as ‘static’ (BH305, strategic lead for public health, Bristol), with high levels of GP registration and immunisation. The few who continue to travel were suggested by a GP to be less accepting of vaccinations, as well as needing to move on every few weeks, making it difficult to access health services.
The ones who are settled and in bricks and who are in more established communities appear to engage more consistently and comfortably with the whole concept of healthcare and immunisation, so more commonly will be registered with a local practice and will turn up as and when appropriate . . . There is a subset, and [in] my experience [this] relates actually more . . . to the Irish Travellers than to either the English or the Roma, they seem to be more itinerant, travel around a lot more [and] appear to be more suspicious of healthcare providers and the whole concept of immunisations.
BH302, GP, Bristol
No service providers in London offered a view about the level of travelling in the Irish Traveller community.
No Bristol Roma participants talked about travelling, except in the context of arriving in the UK. Service providers in Bristol observed that the Roma community are now fairly stable, having moved a few years ago to Birmingham for housing benefit and employment reasons and then coming back. Travelling was mentioned by just one Glasgow Romanian Roma adolescent, who said that she had missed her HPV as a result of being away. A health visitor thought that the Slovakian Roma families tend to travel to England from Glasgow regularly, whereas Romanian families travel around Europe and so are more likely to have incomplete immunisations. These families often arrive in the UK having had no vaccinations because of a need to pay for them in Romania (see Local and national strategies). A school nurse described her frustration about the travelling lifestyle of the Glasgow Roma, explaining that she gets so far with families in terms of engagement and relationship building and then they move on.
I think there’s a frustration at times that we get so far into a piece of work with a family and then they take off.
GH303, school nurse, Glasgow
A summary of this theme is provided in Table 20.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
| – |
|
| Service providers | |
|
|
Attendance at school
A small number of female Traveller participants discussed how some adolescent girls are not at secondary school, which can present a barrier to school-based immunisations such as HPV. This was evident across Traveller communities, with the exception of the Glasgow Scottish Showpeople, among whom school attendance appeared to be good. A number of reasons were offered for this non-attendance. There was a view from some York English Gypsy participants that some girls are withdrawn from school as they enter puberty because their fathers do not like them mixing with non-Traveller boys. A young woman from York said that nowadays girls want to complete their education so that they can go on and get a job, but that this is met with resistance from some of the older generation, particularly the men.
When they [girls] get to a certain age they do not go to school because of all the bother with the boys.
YT017a, English Gypsy, grandmother, York
Slovakian Roma in Glasgow reported experiencing racism and discrimination at school. One Slovakian adolescent girl gave an example of being sworn at, saying how it made her feel.
You don’t want to talk to anyone now . . . you’re not interested about them . . . it feels like you’re different from them, like you have different, like everything different, not like them.
GT111a, Slovakian Roma, adolescent girl with no children, Glasgow
However, some London Irish Traveller mothers said their daughters had missed HPV as they were travelling or were simply just not in school that day. One spoke of how she is struggling to access the HPV injection for her home-schooled daughter.
Poor school attendance was also alluded to in the accounts from service providers in Bristol, Glasgow and London. In Glasgow, service providers said that nowadays most Roma children go to primary school and have their flu vaccination.
Certainly the ones who are in school tend to be the ones who are motivated for everything, so they tend to have their immunisations, they tend to attend school, they tend to have slightly better English, they tend to integrate a wee bit better.
GH303, school nurse, Glasgow
Their concern is low attendance by girls at secondary school, particularly for the Romanian Roma. A senior NHS manager in Glasgow admitted that some Roma social norms, including keeping children off school, are quite challenging to health workers. A service provider working for a third-sector organisation in London reported that their organisation tries to work with schools to remove barriers for Travellers and finds that schools are hard to engage with in this work.
A summary of this theme is provided in Table 21.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Poverty
Poverty was described by service providers and less so by Traveller participants for four of the Traveller communities (Bristol Roma, York English Gypsy, Glasgow Roma and London Irish Traveller). This was seen as linked to language, employment, benefit systems and housing.
In Bristol, two Roma mothers described how a lack of language skills in the community and a reluctance of employers to take on Roma workers results in limited job opportunities, leading to self-employment and unsociable hours. One described life as hard. A commissioner from Bristol City Council suggested that poverty and lack of any or skilled employment is the key issue for the Roma community, while the manager of a local authority community centre in Bristol suggested that employment is how Roma people manage to escape ‘exclusion and discrimination’.
This is a pattern that we see in economic migrants quite a lot, that they start at the very bottom and work their way up. I started in a kind of [laughs] very lowly job when I came to the UK . . . My first job was dishwashing, and I, relied on this kind of work for [a] good 6 months, even though I had a degree; so, you know, so, so it is a quite common theme. But those that we consider fairly successful are say self-employed delivery drivers, that’s pretty good, ‘cos we, do see quite a lot of that stereotypical . . . scrap metal collector, Big Issue selling, Roma as well . . . very much kind of day-to-day struggle for existence. There, there, there are people who do building work, decorating, delivery drivers, that’s, and, and it’s all within the self-employed kind of, rather than, rather than being employed.
BH307, manager of a local authority community centre, Bristol
In York, an English Gypsy mother described how the new requirement for a licence to collect and sell scrap metal now limits the work that men in the community can do and their earning potential. Service providers also spoke about limited income and increasing rent charges on official sites as issues for the community, and a children’s centre support worker spoke of the vulnerable families she sees:
We’ve got some very, very vulnerable Travellers and we’ve also got some very able Travellers, and those able ones, their voices are heard because they shout the loudest and they go to the meetings ‘cos they’re able to get there, and the more vulnerable ones, they just kinda sit quiet in the background . . . we’ve got obviously the unemployment, the poor education, the poor health, you’ve got your prison families, and you’ve got families that marry family relatives.
YH005, children’s centre support worker, York
Several service providers in Glasgow gave accounts of poverty, particularly among the Romanian Roma. Some observed that the Romanians coming to Glasgow are different from the Slovakians: they are ‘destitute with many problems’ (GH301, health visitor, Glasgow). According to another:
They’ve [the Slovakians] got a bit more money than the Romanian families that are coming. They’re much poorer, they’ve got nothing, they come here initially, they’re not entitled to anything, so sometimes you go into houses and they literally have nothing you know.
GH304, NHS team leader, Glasgow
A school nurse described how Roma families often live in ‘horrible conditions and have to wait for their benefits’ (GH303, school nurse, Glasgow). She also mentioned that Roma children are not entitled to free school meals. Another NHS service provider explained the impact of high levels of poverty on Roma families’ diet. The lack of free school meals results in children leaving school at lunchtime and ‘going to Lidl to buy doughnuts’ (GH305, NHS heath improvement worker, Glasgow), and some Romanian Roma families rely on food from the food bank. A local authority frontline worker gave a detailed account of the structural problems that contribute to Romanian Roma poverty. Romanians were granted accession rights only in January 2014 and, since then, there has been a clamp-down to limit benefits. Slovakians were granted accession rights in May 2011 and, therefore, can work and are more established. In addition, there was a belief that the numbers of Slovakian migrants has levelled off, whereas the number of Romanians arriving is increasing. This service provider also believed that the Roma come from a poorer area at home, which may mean they have a lower educational level and fewer resources to deal with the impact of migration.
In contrast, there was no mention of low incomes among the Glasgow Scottish Showpeople community either by the Travellers themselves or by service providers. Indeed, some self-identified themselves as business people and talked about their work in the interviews. In London, two service providers talked about the challenge to London Traveller communities of changes to benefit systems: a cap on housing benefit and increasing private rents, leading to families being evicted (see Housing). No Irish Travellers themselves discussed this issue.
A summary of this theme is provided in Table 22.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
| – |
|
| Service providers | |
|
|
Access to health services
A minority of Traveller participants across all six communities described problems accessing health services. They talked about the difficulty of registering with a GP practice for those without a fixed address or living on an unofficial site (mentioned only in York and London), a frustration in getting through to the GP practice on a mobile phone to book an appointment, and being unable to get an appointment quickly, with some reporting that they had to wait for up to 2 weeks for an appointment, a particular problem for those who are travelling.
It’s very hard to get an appointment innit?
LT014b, Irish Traveller, mother, London
Yeah, it is hard. They might give you an appointment for 2 weeks’ time, by 2 weeks’ time I’m forgetting about it anyway.
LT014a, Irish Traveller, mother, London
A further complaint was about having to wait for long periods of time in the waiting room, often with tired and grumpy children. As an example, one Irish Traveller mother in London described feeling stressed as she waited for an appointment in a drop-in baby clinic.
I find it very stressful when I go in there because it’s full . . . it’s like they [other mothers] fight over who’s to get there first and they’re arguing.
LT012a, Irish Traveller, mother, London
The key consequence of this was that some Traveller participants would use out-of-hours doctors or A&E, which some described as providing a better service – ‘you are seen quicker, the doctor looks at you more carefully’ (YH005b, children’s centre support worker, York) – and this involves less paperwork, important for those who struggle to fill in forms. A London Irish Traveller mother also explained that a delay in securing an appointment meant that she sometimes forgot to attend, particularly as she has three children and many appointments to remember.
Other frustrations with health services offered by small numbers of Traveller participants were the difficulty of using the touch screen on arrival at the GP practice and the lack of time with some GPs, and to a lesser extent health visitors, because they are busy.
The doctor I like, he just told you straight . . . and you could talk to him . . . but these other two it’s like you’re trying to get a conversation with them . . . it’s just quick answers, bang, gone.
GT206a, Scottish Showperson, grandfather, Glasgow
Service providers in Bristol, York and London similarly observed that some of the Travellers they work with prefer to go to A&E and use out-of-hours services for reasons similar to those outlined above. A health visitor further suggested that ‘they tend to be reactive rather than proactive’ (YH006, health visitor, York) in using health services, using them when they are ill rather than for prevention, except in the case of childhood immunisations. Other reasons offered by service providers in London were that GP practices have long waiting lists so people cannot register, a problem worsened by the housing crisis (see Housing), and that Travellers still feel excluded by health services.
I think there’s still a great deal of feeling excluded and that’s not just ‘cos of our service. It’s because . . . any small group . . . are gonna feel that other people are making assumptions . . . and that will put up barriers, so you always need to take . . . into account that there will be negative views about Traveller communities and that needs to be recognised when any plans are being made.
LH303, practice nurse, London
Frontline service providers working with Roma communities in Bristol and Glasgow described how, when Roma arrive in the UK, they are unfamiliar with the NHS system and the need to register with a GP practice and book appointments; this, they said, results in many people turning up at the GP practice and assuming that they can wait for an appointment. The perception in Glasgow was that this has improved as Roma families have begun to understand the systems better.
But I think as time goes on, you know, it’s better, ‘cos they’ve got a better understanding, but I think that initial, you know when they’re registering and they’re initially trying to get appointments and things like that.
GH301, health visitor, Glasgow
They also identified some service delivery barriers: Roma women who are pregnant can arrive in the UK without having received any antenatal care (including immunisations) and they cannot access this care in the UK until they are registered with a GP practice and have a Community Health Index number (a registration number for patients in NHS Scotland); and one GP practice operates a policy of striking patients off its list if they do not attend three appointments. Accessing health services was not perceived to be a problem for the Glasgow Scottish Showpeople, with two NHS frontline workers suggesting that members of the community access health care when they need it and are not overly involved with health services.
Finally, several service providers explained how they tried to support Travellers in accessing health services (see Local initiatives).
A summary of this theme is provided in Table 23.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
– |
| Service providers | |
|
|
Relationships with health professionals
Relationships with health professionals, with GPs and health visitors particularly, appeared to be very important. Many Travellers, predominantly women, across all six communities described positive relationships based on trust and respect that had usually developed by attending the same GP practice and seeing the same health professionals over a long period of time.
It’s the same practice so we know the doctors and I really wouldn’t want to move myself or my kids from them because they know us as if you’re equal, if you know what I mean. [I’m] not just a patient, they know our history and get on with them.
YT002a, English Gypsy, mother, York
Other positive features that were mentioned were regular chasing by GP practices to remind families to attend appointments, which was seen as evidence that they care, and the confidence to telephone the GP practice to ask about anything they had concerns about. Two Roma mothers in Glasgow described how health professionals are ‘nice to us’ (GT102a, Slovakian Roma, mother, Glasgow), while an Irish Traveller mother in Bristol spoke fondly of a health visitor who visits their site and helps with that anything her family needs.
[She is] more like a friend than a health visitor.
BT112b, Irish Traveller, mother, Bristol
Specific to immunisation, positive examples of relationships with health professionals included a GP who had encouraged a distressed child to sit still to have an injection; and practice nurses and health visitors taking the time to discuss with parents the importance of having a particular immunisation. A Bristol English Gypsy mother explained how her health visitor had reassured her husband that MMR vaccination was safe for their child, as he was concerned about possible side effects.
A few Traveller participants explicitly spoke of preferring to see the same health professional each time for continuity of care and to build a trusting relationship so that they feel comfortable discussing their health. As an example, an English Gypsy father described that his GP had changed and he felt uncomfortable with his new GP and reluctant to talk about his concern that the flu jab makes him ill.
When I go to the doctors I ask for a specific doctor . . . so it’s like we kinda know each other . . . she lets me explain and I feel like she looks after the kids . . . better. But if you just see any doctor, ‘cos they’re not used to you, they just like diagnose you straight away, give you this and go, but I feel more comfortable with the one [doctor].
LT009a, Irish Traveller, grandmother, London
A small number of English Gypsy Travellers in York, Irish Travellers in London and Glasgow Scottish Showpeople commented that they prefer to have their vaccinations administered by a GP in the practice rather than by an outreach health visitor, a school nurse or a pharmacist. This appeared to be based on either having a more established relationship with the GP or seeing the GP as having greater expertise and being in a position of authority.
‘Cos when I got it [flu injection] proper GP give it. Proper one, yeah.
LT003b, Irish Traveller, adolescent girl with no children, London
One York English Gypsy adolescent girl commented that she does not mind whether a GP or practice nurse gives a vaccination; more important to her is the sex of the person giving the injection if it is to be administered in a place that she believes only her husband should see.
If it was just your arms or summat then that’d be alright if it was a man, but like other places like, well it’s just like you should be seeing like your husband then a woman should be doing it.
YT014a, English Gypsy, adolescent girl with no children, York
A few Traveller participants from the English-speaking communities had negative perceptions of health professionals. They spoke about wanting health professionals to spend more time with them to discuss the immunisations, specifically the pros and cons, rather than assuming that their attendance implies they are content to proceed with vaccination.
If the doctor said ‘Could you make an appointment to discuss having the [adult] flu jab’ I think more people would have it.
YT005a, English Gypsy, grandmother, York
A small number of Travellers in the Bristol English Gypsy/Irish Traveller and London Irish Traveller communities described a general lack of trust in doctors, while a ‘frustrating’ (YT005a, English Gypsy, grandmother, York) lack of continuity of care at the GP practice was mentioned in York.
There were also accounts of negative encounters and experiences with health professionals which had damaged relationships and broken down trust. Some of these were directly related to immunisation and others were not. For example, an English Gypsy grandmother spoke of how in the past a GP had called her an uncaring parent when she would not have her children immunised because she was concerned about vaccination safety.
It was only out of care that we were doing it, it wasn’t that you wanted to neglect them.
BT105a, English Gypsy, grandmother, Bristol
Two York English Gypsy mothers talked about health visitors interfering and treating them with a lack of respect, while a mother from the London Irish Traveller community described how a health visitor had directly asked some adolescent girls if they were sexually active, which she considered to be disrespectful of their culture. A Scottish Showperson mother talked about how her GP and health visitor had made her feel stupid about worrying about the MMR vaccination so she had changed health visitor. Several London Irish Travellers offered examples of health visitors not taking time to discuss immunisations fully.
The health visitors, doctors and [said], ‘don’t be so stupid, course it [MMR vaccination] didn’t cause his autism’, and you’re made to feel basically that you’re just an over-paranoid mother and you’re just looking for something to blame, and I’ll say to ‘em ‘My, my son’s got autism’. And I tell everybody that, but I’m telling you here and now that’s what caused it, and they just look at you like you’re stupid, don’t be ridiculous, don’t be ridiculous . . . I got a different health visitor and she was lovely ‘You do what you, we can’t force you what to do’. So she was, she was great.
GT202a, Scottish Showperson, mother, Glasgow
Some examples of perceived poor practice were also identified in York. Individual participants described having been given the wrong prescription, notes being lost by a GP practice and a grandfather going blind because of a mistake with an operation.
So it’s that silly little mistake . . . and that puts a lot of distrust in doctors when they start doing things like that.
YT008a, English Gypsy, mother, York
It’s frustrating though isn’t it, I don’t know, it’s like you feel neglected don’t you, you’re putting your trust in them and you want answers from them because they are the doctors.
YT005a, English Gypsy, grandmother, York
Interestingly, the Roma participants in Bristol and Glasgow did not identify any negative experiences with health professionals; and only two participants from the Scottish Showpeople referred to poor experiences.
Service providers in all four cities also talked about the importance of developing trustful relationships with Travellers. Some offered reasons why they perceive Travellers may not trust health services. Three service providers in York suggested that, on occasions, Traveller parents can feel judged by health visitors about their approach to parenting, and particularly about the norm not to breastfeed in the English Gypsy community. A NHS manager and a health visitor in Glasgow both wondered if Roma people may not trust primary care services in the UK because they associate something that is free with poor quality, either because they have no experience of free primary care provision in Romania or because in Slovakia they get specialist services from a paediatrician rather than a generalist GP.
Several of the service providers described their own good relationships with Travellers, evidenced by people coming to them for help with ‘arranging things’ (BH301, health visitor, Bristol), for reassurance about different vaccinations, asking lots of questions about health (Bristol), their drop-in clinics being very busy, people stopping them in the street to ask questions and inviting them into their homes (in Glasgow) and all of their clients being self-referrals (in London). The considerable time taken to develop these relationships was commonly acknowledged and some ways of achieving this were offered. Continuity of care was seen as paramount, as well as having the right person in specialist roles (see Local initiatives).
I think having a relationship in a GP practice that’s an ongoing thing so the same GP practice has been there for people and that’s the shift being settled, that will make a difference. Because you’ve got that point of reference, you’ve got that person to come back to.
LH303, practice nurse, London
I think if you get the right people in those jobs that build up a rapport and relationship with the community.
BH303, former immunisation manager, Bristol
In York, a practice nurse explained that she is the only person who does vaccinations with Travellers and that this continuity of care ‘works really well’ (YH004, practice nurse, York), and a children’s centre support worker described how the Traveller parents she works with bypass her colleagues to ask for her, adding that it took a year for these parents to acknowledge her by name.
Once they trust you, you’re fine.
YH005, children’s centre support worker, York
A local authority outreach worker in London runs a ‘Travellers Forum’, which Travellers and a range of service providers from health and other sectors, including the police, are invited to attend. She explained that a key aim of the forum is for Travellers to have access to these service providers so that they begin to build trust.
Conversely one-off outreach visits by health professionals who do not have a relationship with a Traveller community, for example immunisation teams going into Bristol Traveller sites to promote the flu vaccine, was considered not to have increased take up of the vaccination. A health visitor in Glasgow suggested that their Roma drop-in clinic had helped because people know where to seek them out.
I think probably the drop-in clinic itself has probably been a blessing, because that has been our way into the community. Although . . . maybe that would have happened through time, just visiting them. But I think the fact they’ve got somewhere to seek us out . . . that’s probably led like into kinda different things.
GT301, health visitor, Glasgow
Another explained how being in the role for over 5 years means that parents recognise her. She also suggested that working with interpreters who become known to families is useful as this provides some consistency. In London, several frontline workers talked about the importance of getting the face-to-face encounter with Travellers right by using eye contact, being straight talking while as the same time not dictatorial, as ‘that starts engagement in trust and relationships’ (LH303, practice nurse, London).
Conversely, two health visitors in Bristol and a NHS manager in Glasgow spoke of health visitors, on occasion, feeling threatened by large groups of young Roma men as they go to visit homes. A similar account was offered about a health visitor in York on her first visit to a Traveller site when residents surrounded her car until she explained who she was.
Sometimes the health visitors, when they’re going in to visit families, they’re going where close knit groups of young Roma men gather together, and we’ve had incidents where staff have said ‘I feel too threatened to go in there’. And we’ve had to ask the Police occasionally to sort of be a little bit more present, because sometimes . . . the health visitors were saying ‘They spoke about me in Roma, I know they were talking about me because they were looking at me and laughing at me’ you know. So there’s the element of the young male population which our health visitors find a bit threatening sometimes.
GH309, NHS community health manager, Glasgow
A summary of this theme is provided in Table 24.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Immunisation recall and reminders
Traveller participants, particularly women, across all six communities, reported a range of methods by which they are prompted to attend for immunisations for their children or themselves. Most commonly, they referred to letters from their GP practice or from school to inform them that a vaccination is due. Some spoke about receiving texts and telephone calls as a reminder to attend or to rebook a missed appointment. These recall and reminder systems appeared to be seen as effective for the majority of people, including those who travel (when texts are useful), and those facing literacy and language barriers (see Language and literacy), who described how they manage with these systems. For example, a Romanian Roma father talked about how he uses Google Translate to understand the letter, another accessed a translator at the GP practice and a York English Gypsy mother had asked a receptionist and a health visitor at the GP practice to read out the letter.
Because like the dates on the letter and which we couldn’t read because I wasn’t attending these [literacy] classes then so I took the letter to the receptionist and she read it out, have a seat until the nurse calls you through, she called us through we went through and she read the letter out and she says, ‘oh it’s just because you are asthmatic and this is to like stop you getting infections and that from the weather’.
YT003a, English Gypsy, mother, York
Ideas for improving the recall and reminder systems offered by individual Traveller participants included having texts and telephone call reminders in Romanian rather than English, and GP practices being more proactive in reminding people to attend for vaccinations they have missed.
Contact with the patients more often ‘cos they know our files and what is wrong with us, what we’ve had, what we haven’t had. It clicks up on their system that you rang for a visit and it came up on their system that you haven’t had certain jabs they should be saying to you ‘you’re missing this jab, is there any sort of time that you can arrange to come in and have it?’ Instead of just ignoring it when it comes onto their system or thinking ‘well they must know that they haven’t had that’.
YT004b, English Gypsy, adolescent girl with no children, York
Service providers in York and London described how the system of recall and reminders for immunisation is the same for everyone, Travellers and non-Travellers alike, with some acknowledgement that this does not always work for those Travellers who are not registered with a GP practice, whose children are not in school and those who move on (and so access multiple health professionals).
Child health, the, the thing to, the other thing to think about is that we hold certain records so any child who’s been given an immunisation without obviously it’s been recorded at the time on our clinical software, but if a child’s had a vaccination with another health professional, health visiting team, it goes onto a different database and we don’t automatically get informed when they have had it, we do get informed if they haven’t.
LH303, practice nurse, London
In Bristol and Glasgow, some NHS frontline service providers described the strategies they have used to tailor the recall and reminder systems to the needs of the local Traveller communities which they considered had improved uptake of immunisations. Specifically, in Bristol, a GP talked about how in her practice they identify ‘particularly challenging [to immunise]’ (BH302, GP, Bristol) families and the receptionists then contact them by text or telephone to attend for immunisation appointments. Those working with Roma families in Glasgow had set up a specific recall system so that these families are automatically recalled by letter or text to attend specialist clinics. A head teacher explained how he sends texts in different languages to Roma parents to tell them that a consent form for their child’s vaccination is being sent home and asking them to sign it. A health visitor identifies letters by caravan (e.g. first on the right) to avoid them being lost in communal postboxes.
Several Traveller women in every community also referred to being reminded about immunisations through home visits from midwives, health visitors and bilingual support workers, through their Red Books (personal child health records) and by attending the GP practice for other reasons (e.g. getting a child weighed). A small number of men and women described how when they attended for appointments for blood tests and check-up appointments for long-term conditions health professionals took the opportunity to check whether or not their immunisations were due. These face-to-face reminders appeared to be particularly well received, offering the opportunity for an explanation of the vaccinations to be provided as well as overcoming language and literacy barriers.
When she [health visitor] comes over, she tells us. It’s very good when she comes and tells us.
GT105a, Romanian Roma, adolescent girl with children, Glasgow
Yeah, with the little, little children when they were babies your, your health visitor would remind yer, and she’d keep on. Now that they’re older it’s harder, it’s harder to get, you don’t know what ones they need or what ones they don’t need, because you’ve just mentioned there about vaccine for the older ones, I didn’t know that, so it’s kinda hard to keep up when they’re older.
LT006a, Irish Traveller, grandmother, London
Service providers in all four cities also described how they use every opportunity to remind people about immunisation within their everyday face-to-face contact, which might be through outreach visits, appointments at the GP practice as well as in non-health settings, for example mother and baby groups in a children’s centre. A Bristol health visitor described how she always looks at the Red Book when she visits families, and helps families to book appointments for immunisations, going as far as reminding those who have moved away by finding a telephone number and telephoning them. In Glasgow, a GP described how valuable the EU team (who work specifically with Roma families) is in reminding parents about their children’s vaccinations, whereas this support is not available for adult immunisations, resulting in lower uptake. Some explained how they work with other health professionals, usually health visitors, to identify those who have missed their immunisations and remind them to attend. For example, a manager of a local authority community centre, a teaching assistant in York and a practice nurse in London all said that they contacted a health visitor when they identified families who were missing some immunisations.
If people come up on the defaulters list, we get a list every quarter I think and if it’s somebody who does look as though they might need more sort of close attention, having a chat, whatever, then we can talk to the health visitors and ask them to do a home visit or get in touch in another way and that would be across, that wouldn’t be special for Travellers. That’d be anybody who maybe didn’t understand or had missed that, seemed always too busy or their family was too big or whatever.
LH303, practice nurse, London
A summary of this theme is provided in Table 25.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Attending appointments for immunisations
Most Traveller participants across all six communities, the Glasgow Scottish Showpeople participants particularly, did not appear to have problems with attending appointments for immunisations.
Just take your child to the doctors, wait for your name to be shout, take ‘em in, and within seconds she’d be jabbed, out, that’s it, all over with.
BT101a, English Gypsy, mother, Bristol
We are pleased with what is happening because we have appointments and we’ve got the GP and . . . they call us to go.
GT106a, Romanian Roma, mother, Glasgow
Only two Traveller participants (both Bristol Irish Travellers) suggested that it is not usual for Travellers to follow appointments within their travelling culture.
Travellers don’t like working on appointments because they’re either moving away or the timing is wrong or they haven’t got a way of going.
BT106a, Irish Traveller, grandmother, Bristol
An alternative view was offered by some service providers. In Bristol, several NHS service providers spoke of some Travellers struggling to use an appointment system, particularly when an appointment is in 2 weeks’ time, suggesting that this is not how they live.
I think it’s because Travellers live very much in the here and now, so if they’re given an appointment say for 2 weeks’ time which is not unusual, 2 weeks is a long time in the life of, of some Travellers.
BH308, health visitor, Bristol
In York, a local authority teaching assistant suggested that it is not uncommon to have four children, meaning that it is easy to forget about immunisation appointments, especially if they are too far in the future, while another expressed concern for the ‘vulnerable’ families who are ‘busy with other things’ (YH005, teaching assistant, York).
A few Traveller participants talked about how they found it easy to change immunisation appointments when they found themselves unable to attend or if a child is unwell, although a similar small number of people described problems with rebooking appointments and having to wait several weeks for the new appointment.
It’s just like [name of son]’s not well at the moment and I rang ‘em yesterday I said ‘He’s not well, he’s got the flu’ ‘cos the doctor told me it was flu . . . so they won’t give ‘em their injections when they’re sick so I said ‘can I reschedule it?’. And it’s 2 weeks’ time I’ve gotta wait for it.
LT006a, Irish Traveller, grandmother, London
One London Irish Traveller mother said that she had had to wait 3 weeks to rebook an immunisation appointment for her child and was told off by the health visitor for delaying protecting her child.
As with general appointments, similar small numbers of participants commented on their frustration of having to wait in the waiting room with small children for immunisations, either for prebooked appointments or within a drop-in clinic. A London Irish Traveller did not like waiting for up to 3 hours with many other families in a drop-in immunisation clinic and said that her daughters were only partially immunised because of this, while a Roma adolescent girl commented that waiting times are an issue in the UK compared with Slovakia.
Because obviously if you’re going to get sick here you must wait and something can happen to you, but in Slovakia if you’re sick, you go, you are not waiting.
GT111b, Slovakian Roma, adolescent girl with no children, Glasgow
Drop-in or walk-in clinics for immunisations were seen as a sensible approach to free up appointments in GP practices, prevent people having to wait 2 weeks for an appointment and for groups of mothers to share transport as well as meet other mothers to share their concerns and experiences with. They were seen as particularly convenient for those who struggle to get to the GP practice for prebooked appointments, for example mothers with many children, people working long, antisocial hours (mentioned by a Romanian Roma mother in Bristol) and those who regularly travel.
Or a walk-in, if we have a walk-in we could just do it there and then and say right, we’re walking in today, we’re getting it done today.
LT014b, Irish Traveller, mother, London
Outreach was also discussed by some Traveller participants. In York, the general perception appeared to be that while visits from health visitors and midwives provided a good opportunity to discuss immunisations, they should only be administering vaccinations for those who struggle to attend the GP practice, for example older people. A Bristol Irish Traveller adolescent girl and Scottish Showperson mother both offered the same view.
Because like new mums they should be able to get to a doctor shouldn’t they? Most people do this in this day and age doctors are accessible but like the elderly, it’s even if they only live maybe half a mile from the doctors for an old person that half a mile can seem like 10 miles to them. So for the elderly I think there should be a nurse for a couple of hours that could go out and give them their immunisation.
YT005a, English Gypsy, grandmother, York
In London, while some preferred attending the GP practice for immunisations, a few Irish Travellers valued the health visitors who came to their sites to do vaccinations (including during the time of a measles outbreak). They suggested that this is less stressful for the children and easier for those who travel as well as those who do not have a car to get to the GP practice, and that the health visitor takes more time over discussing and giving the vaccination than happens in the GP practice.
Service providers in all four cities talked about the importance of being flexible in providing immunisation appointments for Travellers. They described several strategies that they use, adopting an opportunistic approach, delivering outreach services, tailoring appointments to be more accessible and providing specific clinics.
You know, the problem is if you, if you don’t adapt to the communities you’re working with then you end up missing people and people will not get preventative care.
GH302, social services team leader, Glasgow
Two frontline providers in Bristol and in Glasgow spoke of how they opportunistically vaccinate older children, adolescents and adults when they attend other appointments at the GP practice, as they are not sure when they will see them again.
So we used to, if we saw a young person we’d give them tetanus and polio and hope for the best. But it was not part of any co-ordinated campaign to improve coverage it was entirely opportunistic.
BH304, former immunisation co-ordinator, Bristol
These participants suggested that opportunistic vaccinations in A&E and in the non-immunisation drop-in clinic for Roma (run by the EU team in Glasgow) would be a good idea for those who are not accessing them in the GP practice.
I know this would never happen in a million years but I probably think personally the best thing to do is when you get families with, just to immunise them, whether it’s in the house or in the community clinic . . . we would just go and visit them once a month and just immunise them for that 3 months.
GH301, health visitor, Glasgow
Service providers in Bristol, York and London, in discussing outreach, all described how health visitors had previously routinely done immunisations on sites but that the approach these days is to provide that service only for those who are the ‘hardest to reach’ (YH002a, immunisation manager, York), meaning those who cannot or will not ever attend GP practices to have their immunisations, for example those who regularly travel. The general view, consistent with the view of most Travellers, seemed to be that this is a more appropriate approach as it encourages people to attend mainstream services and ‘take responsibility’ (YH006, health visitor, York) for their family’s health.
[Outreach is] spoon feeding and not encouraging them to take responsibility for their health or child’s health.
YH006, health visitor, York
There were also many examples of having a flexible approach to appointments in GP practices. A Bristol health visitor described an initiative whereby GP practices were encouraged to offer a more flexible approach in which Travellers could come in at a non-designated time for immunisations and book appointments as soon as they can, which had worked well and improved uptake in those practices that had adopted it. However, there had been some resistance in some GP practices, as it requires two nurses to be working.
I think, yeah, having, keep keep appointments so that your more opportunistic appointment system, a drop-in, a drop-in would be good but if you can’t, if they can’t quite manage the drop-in, keep it today or tomorrow. I think that sort of time, you know today or tomorrow.
BH308, health visitor, Bristol
A practice nurse in York explained how the GP practice she works with has long opening hours and puts on lots of clinics for childhood immunisations, which she considers to be more flexible than other local GP practices working with Travellers. A health visitor in Glasgow who works with Scottish Showpeople described how she often gives immunisations before families head off travelling; and, in London, a practice nurse explained that she keeps a stock of the HPV vaccine so that she can provide HPV injections for Traveller girls who do not have it in school.
Some short-term initiatives for Travellers to increase uptake of immunisations were also offered (see Local initiatives). In Glasgow, a more permanent solution had been put in place when it was found that Roma families were not attending regular immunisation clinics: two GP practices now run monthly specialist clinics and are flexible in how they work, for example they provide appointments times like 9 a.m. rather than 9.05 a.m. as this is seen to work better as people attend and health professionals have more control over the immunisations they give, to make up for those which have been missed.
There’s always this about being PC you know, about like everybody should have the same service and whatever, but I think sometimes you’ve just got to look at you know what’s best for the community as a whole. I think, as a community as a whole is to have everyone immunised isn’t it?
GH301, health visitor, Glasgow
A summary of this theme is provided in Table 26.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
|
|
Record keeping and monitoring
Several service providers in all four cities observed that NHS services do not routinely have a way of recording that someone is a Traveller. As a result they do not have accurate records of uptake levels of different vaccinations to inform the funding and targeting of services. The reasons offered for this were that GP practice records typically use the 2001 census ethnicity categories,42 which do not include a Traveller option, and the Child Health Information (CHI) system does not record ethnicity. Two frontline service providers in York were concerned that recording Traveller status could be seen as discrimination.
Have to be very careful about being discriminatory, surely if you identified a certain group of the population.
YH002b, immunisation co-ordinator, York
In all four cities, service providers described employing a range of strategies to try to identify and follow up Travellers in their GP practices and health visitor caseloads. A health visitor and immunisation manager in Bristol both spoke of using the postcodes of Traveller sites and common Roma surnames to try to identify people in GP records. They spoke highly of the CHI system in terms of checking the immunisation status of Traveller families and had contacted the CHI system in other regions to enquire about families who had moved into their area; as well as using ‘verbal handovers’ (BH301, health visitor, Bristol) between health professionals to keep track of families (which was also used in York and London). A commissioner in Bristol described how previously, as part of a Roma project, they had put flags on Roma patients’ GP records to identify them, and a practice manager in Glasgow also used this system. The EU team in Glasgow reported that information about its drop-in clinic was spread by word of mouth, with the result that Roma families came to them and so were known to them and, therefore, recording ethnicity was not a problem. For them the challenge was families arriving without a record of the immunisations that they or their children have had in other countries.
Another challenge of achieving accurate immunisation uptake data was identified as the time lag from administering an immunisation in a GP practice or school and it being recorded on the CHI system, as well as a time lag in informing GP practices of immunisations given in hospital. As a York health visitor commented, Travellers may have moved on before these data were recorded. Lack of co-ordination across data systems also appeared to cause problems. A practice nurse in London described how vaccinations are recorded on different systems by different health professionals, which can mean the information cannot be accessed. Similarly, a health visitor in Bristol spoke of her frustration of not being able to access the records on Traveller families who register temporarily with a GP practice, and sharing immunisation records between midwifery and GP practices was seen as an issue. There was a general perception in Bristol, York and Glasgow that local authority and school records capture Traveller ethnicity and that sharing of these records is helpful.
I’ve been working with the immunisation team that are now responsible for imms and vaccines and screening as part of NHS England, they’ve recently been, well we’ve recently been looking at MMR [vaccination] uptake in the inner city, but not specifically Roma, Roma Gypsy communities; and some of the learning from that has been absolutely brilliant, where we’ve been able to look at those children that, that are unimmunised, and also to profile those children by using pupil-level data provided at the local authority that we don’t have within the NHS.
BH306, local authority commissioning manager, Bristol
A summary of this theme is provided in Table 27.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Service providers | |
|
|
Local initiatives
Service providers in all four cities talked about current or previous local Traveller health or immunisation initiatives. These included programmes that were developed to raise awareness of, and increase access to, health services and uptake of immunisations as well as specialist posts to work with Travellers. Some were perceived as effective, others less so.
The health board in Glasgow had produced a ‘Pathways to Health’ resource in Romanian and Slovakian, which explained how to access health services, and information about infant feeding using pictures was being developed through ROMA-net (see Local and national strategies). A health visitor in Bristol explained that she was in the process of preparing drop-in health education sessions for home-educated children that would include immunisations, while another in London described how she gives talks about immunisation to parents at community centres where Travellers attend, adding that she takes any opportunity she can to speak to parents about immunisation.
We can never stop talking about immunisations and what I say to professionals that as long as we know that we’ve given them an informed choice and ensure that parents do understand, but we can never stop talking about immunisations ‘cos we know that it’s protected so many lives and we know that it’s saved so many lives, so we can never stop.
LH305, immunisation co-ordinator, London
There were also examples of raising awareness about particular vaccination programmes. In Bristol, an immunisations manager recalled how, in 2012, the local immunisation team had gone onto the Traveller sites with health visitors to promote MMR vaccination, and more recently a community development worker had visited Traveller families about the flu vaccine. Neither was well received, and he did not perceive this approach to be effective in increasing uptake. A similar approach in York was seen as facilitating few additional MMR vaccinations and in London promoting MMR vaccination had resulted in having doors slammed in a health visitor’s face.
I’ve just remembered when we were doing the flu actually we had someone who was our community development worker and he actually went onto the site to talk about flu and he got a lot of resistance and closed doors and that, that it wasn’t an issue, or it wasn’t important.
BH303, former immunisation manager, Bristol
On a more positive note, a school nurse in Glasgow explained that she runs school assembly sessions about HPV vaccination and meetings with Romanian and Slovakian parents about the flu immunisation using a DVD and interpreters. She believed that these sessions worked well as she was asked to attend a Roma community meeting a week later to run the session again (see Sources of information and advice about immunisation).
In terms of initiatives to facilitate access to health services, a project manager in the voluntary sector in London remembered the drive by their organisation to work with GP practices and increase registration of Travellers.
So I think that a lot of people are registered and that there was a big [name of organisation] something like 5, 10 years ago and they did a big drive and a lot of people at the point registered with GPs . . . if you speak to people they’re, they’re using the health services.
LH307, project manager in the voluntary sector, London
In Glasgow, there were several examples of current and past programmes designed to improve the health of the Roma communities, including a welfare rights campaign in primary schools to increase the number of children having free school meals, ‘Keep Well’ preventative health checks in GP practices and stop smoking services for Slovakians. The EU team ran general drop-in clinics for Roma families.
At the moment it it’s just anything that comes through the door and we are gonna try and change that around as well, you know so it is a baby clinic.
GH301, health visitor, Glasgow
There were also several examples of initiatives or changes in services specifically designed to increase the take-up of immunisations by local Travellers. In Bristol, a Travellers immunisation project organised by the community health services ran from 1990 to 2004 (until funding cuts), which had included funding a specialist health visitor and a converted van that was used to do immunisations on site. There was also a drive to encourage GP practices to be more flexible in the appointments they offer Travellers for immunisations (see Attending appointments for immunisation) and Irish Travellers were targeted for the BCG vaccination, as levels of tuberculosis are higher in this community. More recently, the health visitors had run MMR vaccination pop-up clinics for Roma families and had discussed organising this for other vaccinations, for example school-delivered injections. A screening and immunisations manager questioned whether these clinics are cost-effective. In London, an immunisation co-ordinator offered that there is now a lot of local support to enable Travellers to have immunisations, including a Red Book day when parents are invited to bring their children into the site office to have their vaccinations.
In Glasgow, a NHS manager explained that there are no specialist services for Scottish Showpeople because services are based on need and not on Traveller status.
On an individual basis. So what we haven’t done is taken a blanket approach to say that is you’re a Traveller or a Showperson then you get that, that’s different. What we’ve said is it’s based on individualised needs, and there will be individualised needs for families. So that’s really how we look at it.
GH311, NHS manager, Glasgow
Specialist health visitor roles were unanimously recognised as beneficial for Travellers. Many service providers in all four cities explained how individuals in this role were able to develop long-term trustful relationships with Travellers, supporting them to access health and welfare information and services, including the Healthy Child Programme, and assessing vulnerable families to see if they need an enhanced service. They also used to give vaccinations in people’s home.
Their primary function was to be notified if there was any new families or children coming into the area and then try and make contact with them, to liaise from a child health perspective . . . they worked very closely with other parts of the Council which might become aware of a family moving into an area and then that would get a referral triggered to the health visitor who would alert the practice or contact the family directly.
BH305, strategic lead for public health, Bristol
In Bristol and Glasgow, specialist health visitors are still funded and are clearly highly regarded. In contrast, there are currently no such posts in York and London. In these cities some service providers spoke highly of previous specialist health visitors who had done valuable work, but observed that once these individuals had left there was no longer funding made available for that post, which was seen as detrimental to the service provided now.
[Name] worked with really vulnerable families . . . whereas I think now they’re kind of skirting round the edges. Health visitors aren’t getting stuck right in.
YH001, teaching assistant, York
Community health link worker was another specialist role funded to work with Roma families in Bristol and Glasgow. These individuals were also highly valued and described as working with GP practices and schools to liaise with families and remind them/support them to attend for immunisations (see Language and literacy).
A summary of this theme is provided in Table 28.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Service providers | |
|
|
Joined-up working
The importance of working in partnership with colleagues within one’s own organisation and sector as well as with those working in other sectors was unanimously acknowledged by service providers in all four cities.
A lot of the work is local and it’s all about local relationships.
YH002a, immunisation manager, York
This collaborative working tended to be around sharing information on Travellers with other service providers and sometimes jointly visiting families so that the appropriate professional can act, as well as taking the opportunity when coming into contact with Travellers to encourage those families to access other services. Some challenges of this joint working were offered as described below.
There were many examples of health service providers working together in order to better support Traveller families in having their immunisations (see Immunisation recall and reminders, and Record keeping and monitoring and Local initiatives). There were also several non-immunisation examples. A health visitor in Bristol explained how at one point she had accompanied a colleague who had experienced a breakdown in relationship with some families to ensure that these families received a health visiting service. She described how initially there had been friction between herself and other health visitors based on different views of her role (which others saw as larger than she did), but that this is now resolved. In Glasgow, a health visitor said that the EU team is telephoned if a Roma person turns up in the A&E department or if it is necessary to organise follow-up care for a Roma child who presents as unwell. Another health visitor who works with Roma families explained how, previously, the health visitors in the EU team picked up Roma families for 16 weeks and then passed them on to regular health visitors, which did not work too well as often families were not seen again. Now EU health visitors work with children until they go to school. This is perceived to work much better, providing continuity of care and developing trust with families.
Links between health and schools and Traveller Education Services were also described. In Bristol, a health visitor talked about how she works with the co-ordinator of the immunisation programmes in local schools, as they can identify who has not had their immunisations and she can then follow up those individuals who are Travellers. A senior manager in education spoke of how they encourage Roma families to register with GP practices. Another health visitor in Bristol spoke of liaising closely with the Traveller Education Service, which informs her if an adolescent girl who is eligible for the HPV vaccination is not in school so that she can speak to the family about alternative ways to have the injection. She also visits unauthorised encampments with someone from the Traveller Education Service to address any health needs of the children living there. The Traveller Education Service also lets her know if a family self-reports not being registered with a GP practice so she can act on that. She acknowledged that there were initially tensions in this working relationship, as she believed that the Traveller Education Service was doing things outside its remit, for example giving out leaflets about MMR vaccination despite being unable to answer questions about it. In York, a health visitor spoke of someone from the Traveller Education Service being part of her wider team. A local authority frontline worker in London described previously working with the Traveller Education Service, but noted that this service was no longer funded.
There were examples of health service providers sharing information with social care and housing teams. In Bristol, a senior manager in the local authority described how members of the social services team who are in touch with transient families communicate with health visitors so that they can go and visit new families. This was also described as happening in Glasgow as part of ROMA-Net, with health and social workers sharing information on new Roma families arriving in the city. In London, a voluntary sector frontline worker spoke of working with landlords.
There were also some links between the NHS and the local authorities. Some of these were evident in joint strategies (see Local and national strategies) and others as a result of the NHS restructure in that public health directorates now have a quality assurance role for immunisations. As an example, in York, an immunisation manager spoke of how the city council now has representation on the strategic immunisation group and three district immunisation groups. A city council teaching assistant explained that she works alongside a health visitor in attending a mother and baby group as well as doing joint home visits. This health visitor had telephoned her during a measles outbreak and asked her to remind families to have the MMR vaccination when she visited them. A children’s centre support worker (YH005, York) described herself as a ‘go-between’ for Traveller families and health visitors, she lets the health visitors know if she has concerns about children’s weight or speech and language development. In Bristol, part of the role of the Roma drop-in was seen as supporting people to book appointments with a GP, dentist and hospital consultant. A health visitor pops in to speak with families to help with this, as well as to remind families to have their immunisations (see Immunisation recall and reminders).
Finally, the children’s centre support worker in York said that the police give her advance warning of when they are going onto one of the Traveller sites so that she can be sure that she is not there at the time, for her own safety. A health visitor in Glasgow described how the police contact her if a Roma person goes missing; and a voluntary sector project manager in London reported links with the Traveller officer in the police.
A summary of this theme is provided in Table 29.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Service providers | |
|
– |
Local and national strategies
A small minority of Traveller participants, all women, talked about policy-level influences on the uptake of immunisations, and this was usually prompted by a direct question from the interviewer. Most of these participants were positive about the UK government’s policy of free immunisation explaining that, if they had to pay for them, they could not afford them.
It’s a very good thing [that immunisation is free], because there is a lot more than the Travelling community out there that would need these needles and they couldn’t afford it.
BT108c, Irish Traveller, adolescent girl with no children, Bristol
Some Bristol Roma mothers and fathers observed that UK health policies are better than in Romania, where immunisations have to be paid for.
It was difficult sometimes, because some immunisation, they need to be paid, and have some immunisation free, but it’s very important here because it’s free.
BT201a, Romanian Roma, mother, Bristol
There were suggestions from a few Traveller participants that childhood immunisations should be mandatory for school attendance, or people should be fined for not having them. An alternative view, also offered by just a few, was that the government does not care about people, is doing a bad job and so is not a credible source of motivation for immunisation.
The new government doesn’t care if you die or not.
LT001a, Irish Traveller, mother, London
They’re not doing a very good job now are they the government, making the poor richer . . . you must be bloody joking they’re making the poor poorer you know.
YT011a, English Gypsy, mother, London
Some service providers spoke of national and local strategies that drove their work with Travellers. This was particularly evident among those working with the Roma community in Glasgow, who spoke of EU funding for marginalised communities; ROMA-Net, which has local action plans for education, health, housing and employability; the Romani Local Action Plan, with 50 recommendations, some of which are health and social care; and a local area partnership. A NHS manager spoke of their frustration that, while Scotland has a national Traveller strategy, it does not have a national strategy for housed Roma, which limits access to funding. In Bristol, a senior manager in the local authority spoke of the current strategy for Gypsy, Roma and Travellers and a NHS frontline worker remembered the joint needs assessment that had been done by Bristol City Council that led to funding for improvement work on the Traveller sites. In York, a senior public health manager, the teaching assistant and community centre support worker all knew of a city council strategy for Travellers and of two community needs assessments (one very recent) which had been done with the English Gypsy community. Most of the NHS service providers had not heard of these documents. There was no mention of any national or local strategies for Scottish Showpeople or London Irish Travellers (it may be that this was simply not discussed in the interviews).
A summary of this theme is provided in Table 30.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Travellers | |
|
|
| Service providers | |
| – |
|
Funding
Several service providers in all four cities spoke of a lack of funding which inhibited their work. Those working with Roma communities in both Bristol and Glasgow suggested that the reason was a lack of understanding of the complex nature of this work by senior managers and commissioners.
A local authority public health manager in York and the immunisation co-ordinators in York and London talked about cuts in funding for national immunisation campaigns and for preparing schools to deliver the flu immunisation programme. The public health manager also expressed concern that no one now funds immunisation training and had concerns about the lack of trained professionals should an outbreak occur.
There’s accidents waiting to happen really.
YH003a, acting strategic lead for public health, York
Others described having insufficient funding to do their targeted work with Travellers. Service providers in England commented on how, since the NHS restructure, budgets that had historically been protected for targeted work with Travellers, including funding for specialist health visitors, had been cut or reduced (see NHS reforms).
In Scotland, where there was no NHS restructure in 2013, funding was still an issue. A school nurse in Glasgow expressed her frustration about the lack of funding to pay for staff to carry out health education work with Roma families. She also explained that there is no budget for schools to print information and consent forms for immunisations in other languages. A head teacher concurred, offering that his school had not taken part in the pilot flu immunisation programme the year before as there had been no money to produce the consent forms in other languages and hence it was considered to be too risky to go ahead. A senior manager in the NHS in Glasgow stated that there had never been a budget for a specialist health visitor post to work with Roma families and that the resource allocation formula does not reflect how challenging and time-consuming this work is.
So we’ve always had it sitting here as an unfunded line in the budget, just to say to people look we’ve never had any money for this but its needed . . . I think what we’re left with is this EU team in the [name of Department] no funding and not an awful lot else.
GH309, NHS community health manager, Glasgow
Financial targets for GP practices were mentioned by two service providers. A Bristol City Council commissioner suggested that a historical ‘transactional’ relationship, in which the primary care trust (PCT) paid GP practices, was not helpful in achieving sustainable changes, as the work ends when resources run out. A practice manager in Glasgow commented that the GP practice suffers financially because it struggles to meet targets as a result of having Roma patients.
A summary of this theme is provided in Table 31.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Service providers | |
|
|
NHS reforms
The 2013 NHS reforms in England, and the associated changes in commissioning and delivery of public health services, were identified by service providers in Bristol, York and London as a barrier to delivering immunisation and health visiting services generally, as well threatening the provision of specialist health services for Travellers.
Those who discussed the impact of the reforms on immunisation services generally described how the whole system has changed, with the result that it is difficult for individuals responsible for service delivery to know who to contact in the CCGs and local authorities.
I mean it was all very coherent and now it’s not. Local authorities are mandated to provide a public health advisory service to the local CCGs but exactly what that means isn’t defined, and because there’s been such a lack of capacity here, there’s hardly been any input at all, and there’s certainly been none around immunisation, that’s just not happened.
YH003a, acting strategic lead for public health, York
This also makes it difficult to understand who does what, which can mean that important services, for example provision of immunisation training (see Funding), fall through the gaps. A local authority manager in York spoke of her frustration that, although the local authority, and specifically the strategic lead for public health, has responsibility for commissioning and quality assuring the school flu immunisation programme, it actually has no direct involvement in that work.
The Director of Public Health has responsibility for the local public health system delivery but not power at all.
YH003a, acting strategic lead for public health, York
A few service providers in Bristol, York and London also mentioned the plan to move the commissioning of health visitor services for 0 to 19 years from NHS England to local authorities in October 2015. They all admitted to feeling nervous about funding cuts in local authority budgets leading to cuts in services, for example no funding for a specialist health visitor role.
Are there particular barriers to engaging the communities, improving immunisation uptake that we haven’t spoken about?
Well money is always the big one, you know, just to keep the, the funding for the health visitors is, well it’s, it’s not actually our responsibility, it will be in the future, as you know, it’ll be coming back to local authority, but just keeping the, the funding for those posts.
Finally, the NHS reforms had appeared to have had a negative impact on targeted services for Travellers and health inequalities work more widely. In Bristol, the recommendations from a Traveller Review ‘got lost’ (BH303, former immunisation manager, Bristol) when the public health team moved from the PCT to the local authority and resources were diverted from delivering the Gypsy, Roma and Traveller service, resulting in this team becoming smaller.
There’s been a massive restructuring at the city council while the Public Health was moving into the city council, and, and this alone created quite a lot of problems, so; and obviously those problems divert resources from delivering the service, so, so there was an issue with, and there is an issue with things changing so fast that you actually have to spend quite a lot of time to keep up with those changes.
BH307, project manager in the voluntary sector, Bristol
In York, an immunisation manager suggested that the current government places less emphasis on health inequalities than was the case 5–10 years ago, with the result that their service is very reactive. For example, a catch-up MMR vaccination programme would be implemented if there is a measles outbreak, rather than working proactively with the community to target services on the basis of need.
We might expect some challenge from NHS England about what are you doing about immunisation uptake in Travellers, we haven’t had that, but there’s something about, general tenure of the world, certainly this government seems to have been less emphasis on inequalities, to be frank, you know, its variations, its, it, you imagine, think back 5, 10 years there was a lot more focus on inequalities in general, you know . . . quite driven stuff, which is fine, that all just seems to have gone very quiet.
And have the funding cuts had any impact?
Well they will have done, I think. It doesn’t, it doesn’t help; if you like the extra bits, all the, the additional bits above and beyond a core service tend to go when, when you have funding.
Yeah, it’s very much pared down to core services really.
A summary of this theme is provided in Table 32.
| Views that are similar across Traveller communities | Views that differ by community, gender or vaccination |
|---|---|
| Service providers | |
|
|
Linking the barriers to and facilitators of uptake of immunisation to the social ecological model
Many of the themes were considered to be relevant to more than one level of the SEM. 89 Six themes were classified as intrapersonal (knowledge, sources of information and advice, acceptance of immunisation, concerns about immunisation, beliefs about specific vaccines and intergenerational change in beliefs about immunisation). Five were classified as interpersonal (intergenerational change in beliefs about immunisation, interpersonal influences on beliefs about immunisation, decision-making about immunisation, discrimination and poverty). The institutional level was linked to 14 themes (sources of information and advice, language and literacy, discrimination, travelling, attendance at school, access to health services, relationships with health professionals, immunisation recall and reminders, attending appointments for immunisation, record keeping and monitoring, local initiatives, joined-up working, local and national strategies, and funding). Community was linked to four themes (sources of information and advice, discrimination, poverty and interpersonal influences on beliefs about immunisation). Three themes (national and local strategies, funding and NHS reforms) were classified as policy.
Chapter 4 Interventions to increase the uptake of immunisation: workshops with Travellers and service providers
This chapter will first outline the ideas for interventions to improve uptake of immunisation that were taken to the workshops. We then describe the workshop participants and present the interventions which were agreed as ‘top priority’ at the workshops for future testing and/or implementation.
Identifying the interventions to take to the workshops
Table 33 presents the ideas for interventions to improve uptake of immunisation mapped against the key barriers to and facilitators of uptake. As described earlier (see Chapter 2, Identifying the interventions to take to the workshops) this matrix was developed using the interview data from the two Traveller communities and their service providers in Bristol. The source (English Gypsy/Irish Travellers, Roma and service providers) of the ideas, barriers and facilitators are indicated. Twelve intervention ideas were identified to be taken forward to the first workshop (in Bristol). These fell into three categories: promoting awareness and understanding of immunisation in the Traveller community, developing trust and respect towards Travellers, and improving health services.
| Intervention idea | Barriers to and facilitators of uptake of immunisation |
|---|---|
| Promoting awareness and understanding of immunisation in the Traveller community | |
| Combined written and verbal information: package of appropriate leaflets (simple language with pictures) and verbal communication with a trusted health professional |
|
| Social media: accurate and culturally appropriate information in a popular medium, for example Facebook, other popular websites within Traveller communities | |
| Community champions: community champions to promote widespread support for immunisation and address knowledge gaps and fears | |
| Outreach: trusted health professionals to raise awareness of the importance and safety of immunisation and connect Travellers with health services | |
| Developing trust and respect towards Travellers | |
| Staff training: cultural competence training for health professionals and frontline staff |
|
| Designated person in GP practice: named person who is trusted by community who they can ask to see |
|
| Improving health services | |
| Multisectorial working (e.g. health, schools, children services, housing) to raise community awareness of immunisation and identify Travellers |
|
| Flexible and diverse recall and reminder systems: combination of text, telephone or face-to-face recall and reminders |
|
| Flexible and diverse appointment systems: variety of appointment options, for example drop-in clinics, outreach, after-hours |
|
| Improve system of temporary registration at GP practices |
|
| Identify Travellers in health records: to record immunisation uptake and tailor support |
|
| Commissioning of immunisation services: improve organisation of service commissioning, delivery and monitoring of immunisations (within new NHS delivery structure) |
|
Following the subsequent completion of the phase 1 and 2 interviews in York, Glasgow and London, each local research team adapted and added to the original 12 interventions, depending on the interview data generated locally (see Chapter 2, Identifying the interventions to take to the workshops). This typically resulted in the addition of one or two interventions for consideration. An exception was the Scottish Showpeople in Glasgow, for whom only six intervention ideas were taken to the workshop. This reflected the view from the Scottish Showpeople and service provider interview participants that the needs of Scottish Showpeople are similar to those of the general population in Glasgow and that they require minimal specialist intervention. Conversely, the additional interventions included for consideration by Roma participants in Glasgow reflected their specific needs for increased access to language support services (see Chapter 3, Barriers to and facilitators of uptake of immunisation). The ideas for interventions taken forward for consideration at each of the phase 3 workshops are presented in Table 34. Five workshops were held: one workshop in Bristol which both the Roma and English Gypsy/Irish Traveller communities attended, one workshop in York, one in London, and two workshops in Glasgow (one for the Roma community and one for Scottish Showpeople).
| Intervention idea | City | ||||
|---|---|---|---|---|---|
| Bristol | York | Glasgow | London | ||
| Roma | Scottish Showpeople | ||||
| Promoting awareness and understanding of immunisation in the Traveller community | |||||
| Appropriate and accessible information about new vaccinations | ✗ | ||||
| Awareness-raising campaigns using social media, magazines, smartphone applications | ✗ | ✗ | ✗ | ✗ | ✗ |
| Insert into Red Book that is clear and simple, designed by Travellers | ✗ | ✗ | |||
| Appropriately designed leaflets and verbal personalised information from trusted health professional in GP practice and/or outreach setting | ✗ | ✗ | ✗ | ✗ | ✗ |
| Training for health professionals to identify those most concerned about immunisations to discuss their fears and concerns | ✗ | ✗ | |||
| Community champions | ✗ | ✗ | ✗ | ||
| General information about using NHS in Scotland | ✗ | ||||
| Developing trust and respect towards Travellers | |||||
| Cultural competence training for health professionals, frontline staff and other service providers who work with Travellers | ✗ | ✗ | ✗ | ✗ | ✗ |
| Named person in GP practice who is trusted by the community for frontline service at reception desk and link to health professionals | ✗ | ✗ | ✗ | ✗ | |
| Multisectorial working led by health professionals to raise understanding of cultural issues among professionals in all sectors | ✗ | ✗ | ✗ | ✗ | |
| Improving health services | |||||
| Ensure agenda of patient choice is delivered for Travellers | ✗ | ||||
| Flexible and diverse approach to booking appointments, recall and reminder systems | ✗ | ✗ | ✗ | ✗ | |
| Flexible delivery of immunisation services to meet specific needs of most socially excluded Travellers, for example drop-in clinics, outreach | ✗ | ✗ | |||
| Protect funding of specialist roles, for example health visitor post dedicated to Traveller community | ✗ | ✗ | ✗ | ✗ | |
| Improve joined-up working and planning between diverse organisations involved in commissioning and delivery of immunisation services | ✗ | ✗ | ✗ | ||
| Improved joined-up working to target specific groups, for example young people in schools and health services | ✗ | ||||
| Representation from Traveller community at meetings of CCG/immunisation committees | ✗ | ✗ | ✗ | ||
| Identify Travellers in health records to record immunisation uptake and tailor support | ✗ | ✗ | ✗ | ✗ | |
| Improve system of temporary registration for roadside Travellers | ✗ | ✗ | |||
| Increased recognition that providing good services (e.g. with interpreters) for Roma community has resource implications | ✗ | ||||
| Increased provision of interpreters and/or bilingual support workers, especially Romanian speakers | ✗ | ||||
| Maintain and improve links with health services in Slovakia and Romania for sharing of health record information | ✗ | ||||
Workshop participants
Travellers
A total of 51 Travellers attended a workshop (Figure 4 and Table 35). Our recruitment target was 10–12 Traveller participants from each community. This was achieved for three of the six communities (Bristol Roma, York English Gypsy and London Irish Traveller). We set out to include Traveller men and women across generations. A total of 41 participants were female; 10 were male. Overall, we included women across several generations: grandmothers (n = 13), mothers (n = 18), women without children (n = 4) and adolescent girls (n = 6). No grandmothers or adolescent girls attended from the Glasgow Roma community and no adolescent girls from the Scottish Showpeople community. No men from the Glasgow Scottish Showpeople community or the Irish Traveller community in London and no fathers from the Bristol English Gypsy/Irish Traveller or York English Gypsy communities attended a workshop. Two grandfathers were present (one Bristol Roma and one York English Gypsy). Finally, just over half (n = 29) of the participants had taken part in a phase 1 interview.
FIGURE 4.
Traveller workshop participants. (a) Participants by community; (b) gender by community; and (c) family role by community.

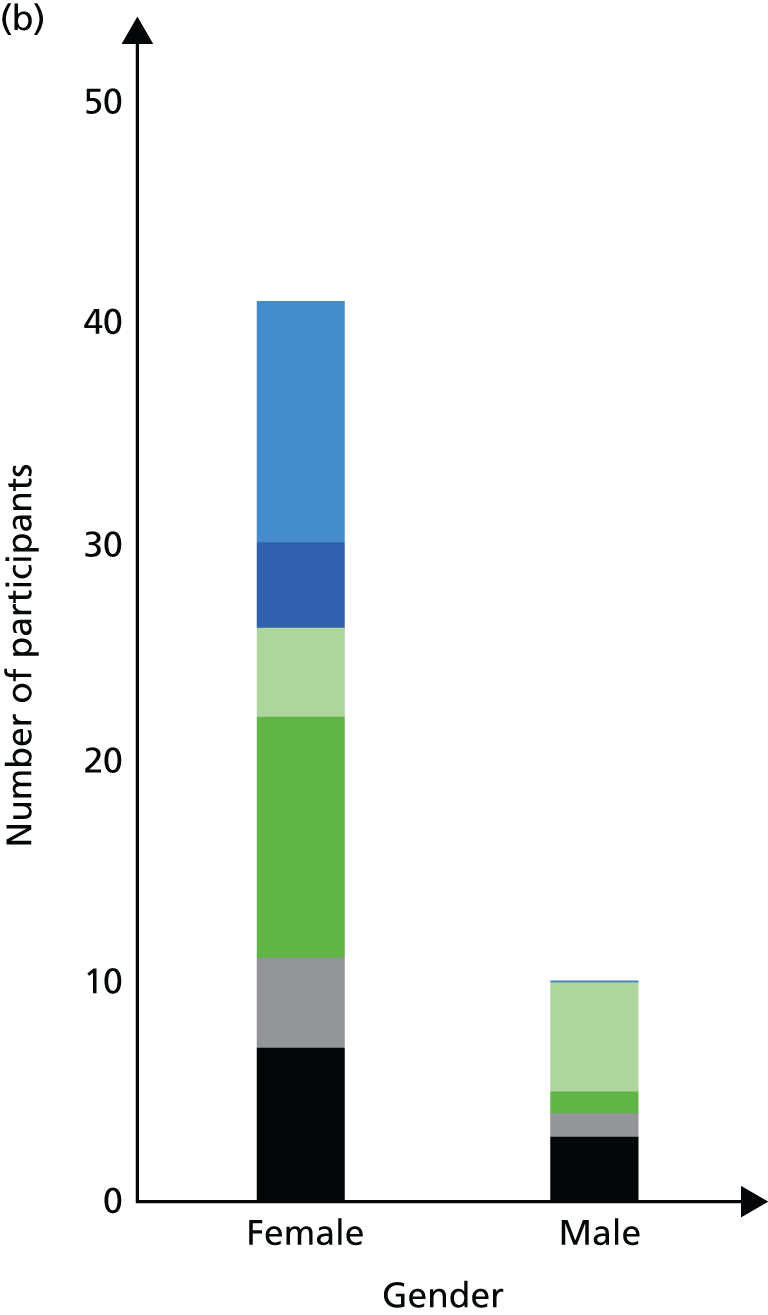

| Characteristic | All | City | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Bristol | York | Glasgow | London | ||||||
| Roma | English Gypsy | Irish Traveller | English Gypsy | Romanian Roma | Slovakian Roma | Scottish Showpeople | Irish Traveller | ||
| Total | 51 | 10 | 5 | 0 | 12 | 7 | 2 | 4 | 11 |
| Female | 41 | 7 | 4 | 0 | 11 | 3 | 1 | 4 | 11 |
| Male | 10 | 3 | 1 | 0 | 1 | 4 | 1 | 0 | 0 |
| Mother | 18 | 5 | 2 | 0 | 4 | 3 | 1 | 2 | 1 |
| Grandmother | 13 | 2 | 1 | 0 | 4 | 0 | 0 | 1 | 5 |
| Woman, no children | 4 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 2 |
| Adolescent girl | 6 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 3 |
| Father | 7 | 2 | 0 | 0 | 0 | 4 | 1 | 0 | 0 |
| Grandfather | 2 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Male, no children | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Took part in phase 1 interview | |||||||||
| Yes | 29 | 9 | 3 | 0 | 9 | 0 | 0 | 3 | 5 |
Service providers
We met our recruitment target of three to four service providers with the exception of the workshop with the Glasgow Scottish Showpeople, which only one health visitor attended (Figure 5 and Table 36). Fifteen participants were frontline workers employed across a wide range of roles in the NHS (n = 10), local authorities (n = 1), education (n = 3) and the voluntary sector (n = 1). Nine participants were in more strategic roles in the NHS (n = 6) and local authorities (n = 3), and one was a student working with Travellers. We achieved our aim to recruit a mix of frontline workers and those working in more strategic/commissioning roles for every city. Approximately two-thirds (n = 16) of the service provider participants had taken part in a phase 2 interview.
FIGURE 5.
Service provider workshop participants. (a) Service providers by city; and (b) service provider role by city.


| Characteristic | All | City | ||||
|---|---|---|---|---|---|---|
| Bristol | York | Glasgow | London | |||
| Roma | Scottish Showpeople | |||||
| Total | 25 | 6 | 10 | 4 | 1 | 4 |
| Frontline workers | ||||||
| Primary care | ||||||
| Health visitor | 6 | 2 | 2 | 1 | 1 | 0 |
| Practice nurse | 2 | 0 | 1 | 0 | 0 | 1 |
| Other NHS | ||||||
| Bilingual support worker | 1 | 0 | 0 | 1 | 0 | 0 |
| Outreach nurse | 1 | 0 | 0 | 0 | 0 | 1 |
| Local authority | ||||||
| Children’s services | 1 | 0 | 1 | 0 | 0 | 0 |
| Education | ||||||
| School nurse | 1 | 0 | 0 | 1 | 0 | 0 |
| Outreach worker | 2 | 1 | 1 | 0 | 0 | 0 |
| Voluntary sector | ||||||
| Traveller support services | 1 | 0 | 0 | 0 | 0 | 1 |
| Strategic roles | ||||||
| NHS | ||||||
| Children’s services | 1 | 0 | 0 | 1 | 0 | 0 |
| Screening and immunisation | 5 | 1 | 3 | 0 | 0 | 1 |
| Local authority | ||||||
| Public health | 3 | 1 | 2 | 0 | 0 | 0 |
| Other | ||||||
| Student | 1 | 1 | 0 | 0 | 0 | 0 |
| Took part in phase 2 interview? | ||||||
| Yes | 16 | 3 | 6 | 3 | 1 | 3 |
Prioritised interventions to improve uptake of immunisation
The interventions presented below were identified by Traveller and/or service provider participants within their top six ‘potentially feasible and acceptable interventions’ which could positively impact on immunisation uptake in their community. The majority of these interventions were ranked as top three interventions.
Interventions for Travellers who are housed or settled on an authorised site
Figures 6 and 7 illustrate the most important interventions to improve uptake of immunisations among Travellers who are housed or settled on an authorised site. These characteristics were typical of the Traveller participants within the UNderstanding uptake of Immunisations in TravellIng aNd Gypsy communities (UNITING) study (see Chapter 3, Participants). As such, these interventions are considered to be relevant to the vast majority of Traveller participants in the four study cities (see Chapter 5, Generalisability). The key difference between the interventions presented in Figure 6 and those in Figure 7 is the level of agreement across Travellers and service providers for each intervention. In Figure 6, the five interventions have been prioritised by all or most of the Traveller communities and/or service provider groups as within their top six interventions. In Figure 7, each of the 10 interventions has been prioritised as within the top six interventions by Travellers and/or service providers in particular communities/cities.
FIGURE 6.
Top priority interventions to improve uptake of immunisation by Travellers who are housed or settled on an authorised site, identified across communities. ‘Top priority’ intervention is defined as within the top six most important interventions to potentially improve uptake of immunisation.

FIGURE 7.
Top priority interventions to improve uptake of immunisation by Travellers who are housed or settled on an authorised site, identified by particular communities. ‘Top priority’ intervention is defined as within the top six most important interventions to potentially improve uptake of immunisation.
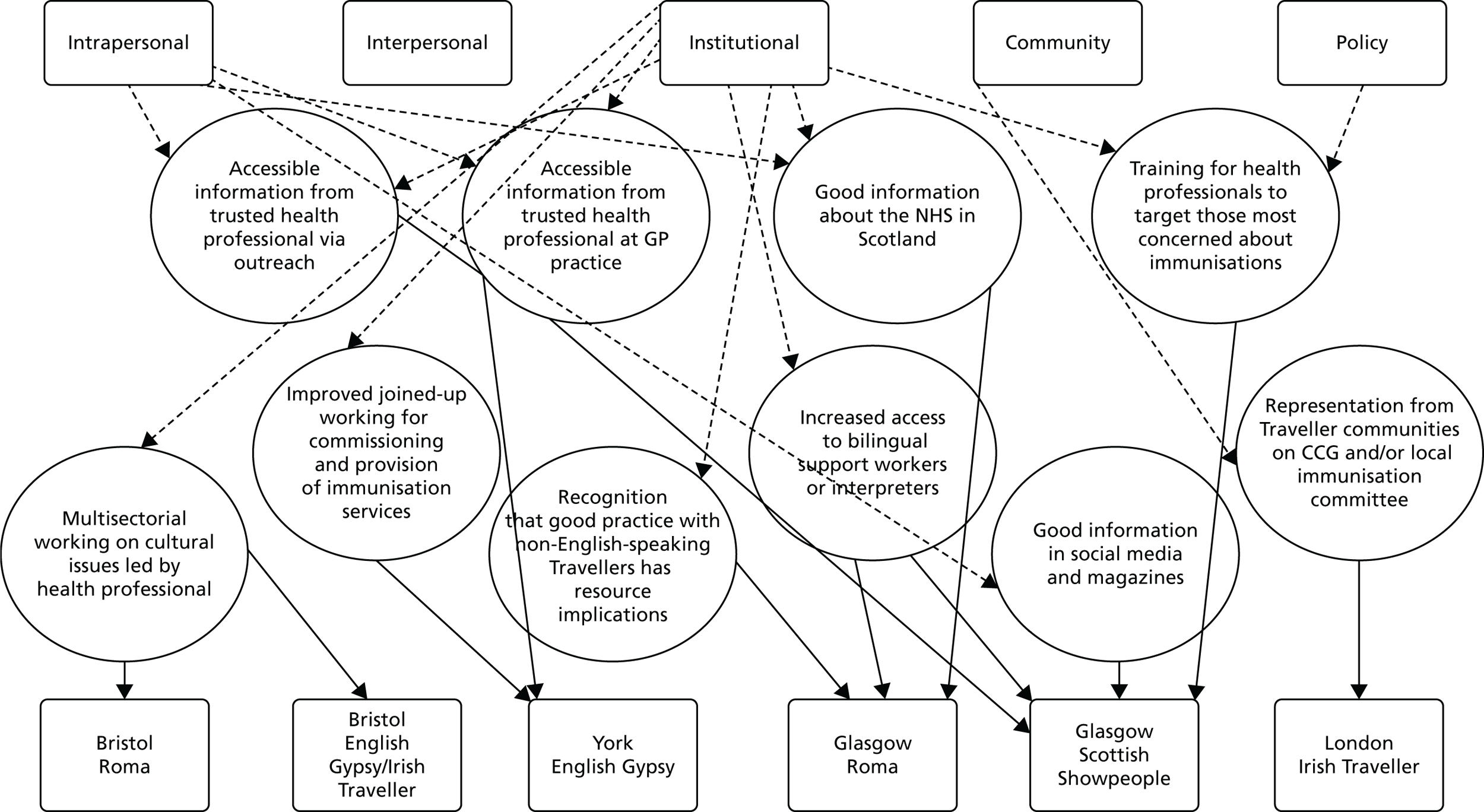
Five interventions were prioritised by all or most of the Traveller communities and/or service provider groups. Based on the SEM,89 these five interventions all fell within the institutional and policy levels of influence. In Figure 6, the smallest, most central circle represents the single intervention most supported by both Traveller communities and service providers; the surrounding larger circles indicate prioritised interventions with increasingly less consensus. The most supported intervention was ‘cultural competence training for health professionals and frontline staff’. The next most supported interventions were ‘identify Travellers in health records to record immunisation uptake and tailor support’ and ‘named person in GP practice who is trusted by the community for frontline service at reception desk and link to health professionals’.
-
National policy intervention to include cultural competence training as a key performance indicator to improve standards and best practice across all GP practices.
-
Cultural competence training of health professionals and frontline staff on:
-
cultural norms of different Traveller communities towards immunisation in general; these should include positive and negative norms, for example, prioritising children and their good health within the family
-
cultural concerns regarding specific immunisations to enable staff to openly and confidently discuss these issues with Travellers
-
awareness and understanding of the prejudice that Travellers can face in general
-
removal of negative stereotypes towards Travellers and ensure trust and respect is shown towards Travellers
-
culturally appropriate methods of collecting ethnicity data from different Traveller communities
-
cultural understanding of Traveller lifestyle and values for interpreters who are often middle class and may not have previously worked with Travellers.
-
-
As a minimum standard, training to target GPs, practice nurses, health visitors, midwives, specialist health workers and receptionists.
-
Widespread support warrants national policy and guidance to achieve universal implementation and standards of service.
-
Culturally informed concerns about pregnancy vaccines and HPV were particularly evident in the Bristol English Gypsy/Irish Traveller community.
-
Existing resources may be available via some local training schemes but long-term core funding needed to enable consistency of standards and practice.
-
This intervention to be closely linked with and supported by implementation of interventions 2 and 3.
-
Policy mandate (as for 2001 census) for electronic identification of Travellers based on 2011 census which included a Traveller ethnicity category, with additional categories for Roma and Occupational Travellers.
-
NHS England to provide guidance on codes for Traveller identification as part of broader guidance on codes for ethnicity.
-
Central government targets for routine data collection so recording Traveller ethnicity becomes part of the ‘data dictionary’.
-
National standards and protocols to provide clarity regarding confidentiality and sharing of information.
-
Improved joined-up working and cross-referencing records held by NHS, schools, social services and education, for example the annual school census held by local authorities includes a Traveller code, local health worker knowledge, postcode data, distinctive surnames.
-
New registration forms for GP practices to include 2011 census classification of ethnicity.
-
Local health workers to check immunisation status opportunistically to update Travellers’ health records.
-
Local health workers to encourage effective use of patient-held records (Red Book) as an up-to-date immunisation record.
-
As a minimum, public bodies including GP practices and immunisation data sets [e.g. Cover of Vaccination Evaluated Rapidly (COVER) programme, KC50] to adopt 2011 categories, with additional categories for Roma and Occupational Travellers as indicated above.
-
All childhood and adult vaccines should be recorded on the electronic record for each identified Traveller.
-
Widespread support and complexity of intervention warrants national policy and guidance to achieve universal implementation and minimum standards for data protection and confidentiality.
-
Although there is widespread support for this intervention to improve service provision and record keeping, a sensitive approach is needed to take this intervention forward, with particular attention to:
-
fears of prejudice if identified as Travellers
-
a general reluctance to self-identification by Romanian and Slovakian Roma.
-
-
The Romanian and Slovakian Roma community in Glasgow were particularly interested in improving links with health services in Romania and Slovakia so that information on ‘immunisation’ status can be shared across countries.
-
This intervention was not taken to the workshop for consideration by the Scottish Showpeople community and their service providers in Glasgow as it was not supported as a potentially useful intervention based on their interview data. This is consistent with the overarching view of this Traveller community as an integral part of the local community with good access to mainstream services.
-
A lack of national policy and guidance is likely to result in variation in practice between cities.
-
Existing recording systems for data on Romanian and Slovakian Roma are considered to be poor in Bristol.
-
This intervention to be closely linked with, and supported by, implementation of interventions 1 and 3.
-
Existing high levels of trust in individual GPs, practice nurses and health visitors across all Traveller communities provide a strong foundation on which to build this intervention.
-
The named person(s) should be able to provide a consistently positive and culturally appropriate experience for the Traveller on his or her arrival at the GP practice. In many cases, this simply refers to being spoken to with respect and politeness; in other cases, Travellers may require support with literacy or language issues to complete a form or identify the appropriate care pathway.
-
Receptionists or practice administrators have been identified as potentially suitable to provide this basic standard of service.
-
The frontline service should include a timely referral to a health professional who has the appropriate training, competency and local knowledge to provide a culturally appropriate immunisation service.
-
Culturally appropriate frontline and health-care services within the GP practice will provide continuity of care for any outreach services targeting the most socially excluded Travellers.
-
Widespread support warrants national policy and guidance to achieve universal implementation and standards of care.
-
Good practice should be identified and shared with other GP practices.
-
This intervention was not taken to the workshop for consideration by the Scottish Showpeople community and their service providers in Glasgow as, based on interview data, it was not considered a potentially useful intervention. This is consistent with the overarching view of this Traveller community as an integral part of the local community with good access to mainstream services.
-
Creation of a culturally appropriate and accessible primary care service will be of potential benefit to all childhood and adult health services for Traveller populations.
-
This intervention to be closely linked with, and supported by implementation of, interventions 1 and 2.
-
The core component of this intervention is inclusion of a SMS text-based approach for immunisation recall systems, booking the appointment and regular reminders, in addition to existing letter systems.
-
A combined system of both letter and SMS text communication is required because of differing literacy needs and fluctuating credit levels on mobile telephones.
-
The core SMS text intervention should be demanded as standard through national policy and potentially as a quality indicator of ‘access and flexibility’ as per disability indicators.
-
Appointments within 1 or 2 days of booking are more likely to be attended than appointments booked for a fortnight’s time because of some Travellers’ broad concepts of time and difficulty with the commitment of a fixed appointment.
-
Existing annual reminder systems, for example for the flu vaccine, are considered to work well and should remain an integral part of any adapted system.
-
This intervention was not discussed by service providers working with the Roma community in Glasgow. Discussion regarding a more flexible system for delivering the immunisations, for example out-of-hours appointments, was not supported.
-
Although this intervention was not ranked within the top six priority interventions by Traveller communities and service providers in York and London, these groups did identify this intervention as very important and within their top eight priority interventions. Service providers in York ranked this as their top priority of all interventions.
-
Widespread support warrants consideration for national policy and guidance to achieve universal implementation and standards of care.
-
Travellers working in low-paid employment, for example Romanian and Slovakian Roma in Bristol, often work long and antisocial hours, making it difficult to attend for immunisations within usual clinic times.
-
Health visitors or other health professionals working with Traveller communities could usefully provide additional, face-to-face reminders when possible.
-
Good practice should be identified and shared with other GP practices.
-
Outreach service provided by a specialist health visitor would support any letter and text system (see intervention 5).
-
This intervention to be closely linked with, and supported by, implementation of interventions 2 and 5.
-
The specialist service provides an important outreach component to target those families who do not access mainstream services.
-
The outreach service increases access to culturally appropriate and personalised information and service support, referral to immunisation services within the GP practice and improved linkages between Traveller families and the GP practice.
-
Practice-based services delivered by a specialist health visitor identified as important to improve uptake of immunisation include drop-in clinics for specific population groups within Traveller communities, for example adolescent girls, and/or specific vaccines (e.g. HPV) and out-of-hours appointments.
-
A specialist health visitor has detailed local knowledge of existing and new families within the Traveller community. This has typically resulted in a targeted and timely service and would inform identification of Travellers in their health records for improved monitoring of uptake (see intervention 2).
-
Widespread support across all Traveller communities warrants national policy and guidance to achieve universal implementation and minimum standards of care.
-
Continuity of high-quality care from a trusted service provider, typically a health visitor, has been identified as one of the services considered most important and most valued by all Traveller communities.
-
Loss of protected funding for this post in the past.
-
Additional resources are required with appropriate policy guidance to prioritise this service within the face of local budget constraints.
-
This intervention to be closely linked with, and supported by, implementation of interventions 1 and 2.
Ten interventions were prioritised by particular Traveller communities and/or their service providers (see Figure 7). Based on the SEM89 these interventions fell into four levels of influence. Most were at the intrapersonal and institutional levels, reflecting a focus on providing good information on immunisation to Travellers and the key role of the NHS in improving immunisation uptake.
Interventions for Travellers living on the roadside or on an unauthorised encampment
Two interventions were identified as top priority to improve uptake of immunisations among Travellers who live on the roadside or on an unauthorised encampment.
-
flexible delivery of immunisation services
-
an improved system of temporary registration at GP practices.
This small but important population within each community has been characterised as frequently travelling and, therefore, is less likely to access health care and other services. It is important to note this characterisation has been generated from interviews with typically settled Travellers and service providers in just two cities (Bristol and York) rather than by these Travellers themselves. Both prioritised interventions were at the institutional and policy levels of the SEM. 89
Detailed description of the five prioritised interventions for Travellers who are housed or settled on an authorised site
A detailed description of the five interventions that were prioritised across the Traveller communities is presented in Box 1. The nature of each intervention is analysed in accordance with the Medical Research Council’s guidance on developing and evaluating complex interventions:88 components; mode and intensity of delivery; differences in content, and delivery, within and across populations and settings; and potential barriers and facilitators. This description is based on data we collected in the interviews and workshops with Traveller and service provider participants and subsequent academic input from the IPAG (see Chapter 2, Independent project advisory group) and the research team. In presenting the detail for each intervention, we have commented on its applicability for delivery at the national and/or local level.
Chapter 5 Discussion
The UNITING study set out to (1) investigate the barriers to and facilitators of acceptability and uptake of childhood and selected adult (flu, whooping cough) immunisations among six Traveller communities across four UK cities; and (2) identify possible interventions to increase uptake of immunisations in these Traveller communities that could be tested in a subsequent feasibility study. This chapter will first consider the strengths and limitations of the study, including an assessment of our confidence in the generalisability of the findings. We then discuss the key findings on the barriers to and facilitators of immunisation uptake and potential interventions to increase immunisation uptake in the context of existing literature, policy and practice. Finally, we present recommendations for future research, including the feasibility testing of the identified interventions, as well as implications for health professionals and policy-makers.
Strengths and limitations
To our knowledge this is the first in-depth, qualitative study in which the views on childhood and selected adult immunisation of Travellers across multiple communities and cities in the UK have been investigated. Furthermore, this was a large study, with 174 Travellers and 39 service providers interviewed and 51 Travellers and 25 service providers attending a workshop. This enabled us to identify differences and similarities in views within each community as well as draw out meaningful comparisons across the six Traveller communities, both for gender and for different vaccines (childhood and adult). A small number of studies have reported the uptake of immunisation by different groups of Travellers in the UK1,44,45,47 and Roma communities in Europe;108–110 and an extensive literature exists on Travellers’ experiences of health services more generally. 17–22,24 However, there is very little research on Travellers’ views on, and experiences of, immunisation specifically. 46,74,76,111 Moreover, these studies tend to include a small number of Travellers, often from one community, or immunisation is only part of a larger study exploring health and health care.
In reflecting on the strengths and limitations of this work and to assess our confidence in the validity and generalisability of our results (see Generalisability), we applied a comprehensive set of evaluative criteria for qualitative research112 to our methods and findings. These criteria were most relevant to the interviews conducted in phases 1 and 2, but were also applied to the phase 3 workshops when appropriate. Our detailed evaluation is presented in Appendix 12 and summarised in Table 37 (criteria 1 to 5).
| Number | Criterion | Evidence | Criterion met? |
|---|---|---|---|
| 1 | Evidence of responsiveness to the social context and flexibility of design |
|
Yes |
| 2 | Evidence of theoretical or purposeful sampling |
|
Mostly |
| 3 | Evidence of adequate description |
|
Yes |
| 4 | Evidence of data quality |
|
Yes |
| 5 | Evidence of theoretical and conceptual adequacy |
|
Yes |
| 6 | Potential for assessing typicality | Representational generalisation is evidenced by:105
|
Mostly |
For the phase 1 and 2 interviews, we achieved consistency and rigour in our data collection methods across the four cities and local research teams through the use of a data collection protocol. This was balanced with an element of flexibility to ensure that the methods, for example our initial approach and the interview topic guides, were best suited to the social circumstances of each community and acknowledged important community differences. There is likely to have been some ‘social desirability’ in participants’ accounts, and responses may have been influenced by family members present during the interviews. Indeed, a limitation of focus groups and group interviews (used in this study) is the risk that participants may not disclose any views or hide their true views, particularly if the topic is sensitive or personal. In this study our gatekeepers advised that the most sensitive topic was HPV so we ensured that the adolescent girls were not asked to discuss this in the company of men (and when possible not with their mother present). We suggest that the concern about ‘social desirability’ is counterbalanced by the frank exchanges in many interviews and the emergence of several strong themes which were similar across communities and had a range of views within them. We also worked to a data analysis protocol, followed the precise steps of the framework approach105 and drew on recognised procedures (triangulation, constant comparison, deviant case105,114) to ensure that the analysis of the interview data was carried out systematically and comprehensively. In presenting the findings we took care to ensure that we remained ‘true’ to the interview data105 by describing in detail the range of participants’ views with the extensive use of direct quotations. In terms of the phase 3 workshops, we ensured consistency through the use of a standard programme for the event and we employed established methods of intervention mapping107 and prioritisation. 101 We suggest that these research processes demonstrate a high level of scientific rigour and we are confident in the validity (authenticity105) of our study findings.
Generalisability
Generalisability in qualitative research, namely considering whether or not the findings are relevant beyond the study sample and context, is ‘important and much contested’. 105 Other terms commonly used are ‘transferability’, ‘external validity’ or ‘typicality’. 105 This is not to be confused with the quantitative notion of generalisability based on achieving samples that are statistically representative of the population from which they are derived. Several tools and structured approaches for assessing the quality of qualitative research now exist,115–118 including the one we have used for this study112 (see Table 37 and Appendix 12). These tools provide specific criteria on how to reflect on the quality of a study to then assess the generalisability of the findings. In assessing our confidence in the generalisability of the UNITING study findings, we discuss two types of generalisation proposed by Ritchie et al:105
-
representational generalisation – how far the findings from a study can be inferred to the specific population from which the sample is drawn
-
inferential generalisation – how far the findings from a study can be inferred to other settings and populations beyond the sampled one.
We did not set out to achieve theoretical generalisation (a third type of generalisation105) as this was an applied research study with a very large number of qualitative data and, as such, the findings are predominantly descriptive rather than explanatory (theory generating).
Representational generalisation
-
Are the views of the Traveller participants generalisable to other Travellers in the six study communities?
-
Are the views of the service provider participants generalisable to other service providers working with these six Traveller communities?
It is proposed105 that this type of generalisation can be evidenced by the quality of the fieldwork, analysis and interpretation (which we discuss above; see criteria 1, 3–5 in Table 37) and the degree to which we have achieved the diversity in characteristics that we consider to be important (see criteria 2 and 6 in Table 37).
There were some gaps in our community samples that should be acknowledged. We are not overly concerned about the lack of grandfathers in all six communities and of fathers in both Glasgow communities and the London Irish Travellers as our findings, and those of others,119,120 suggest that men are unlikely to be the primary immunisation decision-makers. Low numbers of adolescent girls/young women in the Bristol Roma and English Gypsy/Irish Travellers communities and the inclusion of few self-reported non-immunisers may mean that the perspectives of these population groups are not adequately represented. That said, interviews were conducted with Travellers with a mix of family roles across generations and immunisation status in all six communities and we observed many consistent views within communities (few gender differences, some intergenerational differences). Overall, we are confident that our interview findings are generalisable within the six communities to Travellers who are housed or settled on an authorised site. We are less confident that the study findings should be generalised to Traveller families who relocate frequently. Local gatekeepers have confirmed that these more mobile Travellers are a minority in the six study communities; however, they are an important group, as we might expect them to be less likely to access immunisation, and health service providers may find it harder to reach these Traveller families (see Access to health and immunisation services and Interventions to increase uptake of immunisation). There may also be some Travellers within the York and London communities who, although settled in a location, may be more socially excluded or resistant to accessing services. We relied on snowballing methods95 and trained two Travellers to conduct some interviews in York in order to include these families; however, they are likely to be under-represented in this study.
In terms of service providers, a diverse mix of frontline workers and those in strategic roles in each city were interviewed producing consistent views on common topics of relevance to this study. We are, therefore, confident in the generalisability of these findings within Bristol, York, Glasgow and London.
Regarding the workshops, we presented the interview findings at the start of each workshop, so are not concerned that our intention that all workshop participants had been interviewed was not achieved because they will have had the opportunity to hear and discuss the phase 1/phase 2 findings before undertaking the prioritisation activity. There were low numbers of Traveller participants at the workshops for the Bristol English Gypsy/Irish Travellers and two Glasgow communities; no men from the Glasgow Scottish Showpeople and London Irish Travellers; and a lack of service providers for the workshop with Glasgow Scottish Showpeople. However, despite this, there was consistent agreement across the communities on the five ‘top priority’ interventions to increase uptake of immunisation (see Interventions to increase immunisation uptake).
Inferential generalisation
-
Are the views of the Traveller participants generalisable to other Traveller communities?
-
Are the views of the service provider participants generalisable to other service providers working with other Traveller communities?
-
This is evidenced by the ‘degree of congruence’105 or typicality of the features between the study sample/context and the sample/context to which the findings are to be applied.
We observed considerable similarities within the ‘pairs’ of communities in the study (e.g. two Roma communities, two English Gypsy communities) in terms of their views on immunisation (see Acceptance of vaccines) as well as their broader social circumstances: travelling, housing, language and literacy and attendance at school (see Access to health and immunisation services). Furthermore, we have no reason to believe that the six communities in the study are markedly different from other Traveller communities of the same descent (e.g. from other English Gypsy communities) either in their acceptance of immunisation46,74,76,111 or their social contexts which impact on access to immunisation services. 12,13,15,18 Therefore, we are confident that our interview findings are generalisable to members of other Traveller communities of English, Irish, Romanian/Slovakian Roma and Scottish Showpeople descent who are housed or settled on an authorised site.
Barriers to and facilitators of immunisation uptake
The barriers and facilitators that emerged from the interviews with Travellers and service providers are discussed in terms of the two broad categories of factors that are considered to influence the uptake of childhood and adult immunisation in the general population and high-risk groups:56–60,62 acceptance of vaccines and access to health services. Together, these two categories capture the five levels of the SEM,89 the theoretical framework underpinning this study.
In discussing the barriers and facilitators, we identify where they are similar to the general population and other minority ethnic groups and issues that appear particularly relevant to Travellers, as well as to specific Traveller communities. For example, there were many common issues for the English-speaking communities, whereas the two Roma communities noticeably experienced additional barriers in terms of language and being in a new country. The Scottish Showpeople appeared most similar to the general population in their views and experiences. We also conducted an analysis of our data by gender in five out of the six communities in our study (no male London Irish Travellers were interviewed). On the whole, men and women described similar barriers to and facilitators of immunisation uptake. The few gender differences suggested by our analysis are discussed, where appropriate. In short, similar to the general population,89,119 childhood immunisation was often regarded as an area in which women took more interest, and for which they took more responsibility, than men. In addition, women were more likely than men to discuss community facilitators of immunisation (such as intergenerational change) and barriers to immunisation (such as discrimination and low levels of literacy).
Acceptance of vaccines
The majority of Traveller participants were generally positive towards immunisation. This was particularly evident among Roma communities in Bristol and Glasgow, followed closely by the Bristol English Gypsies/Irish Travellers and Glasgow Scottish Showpeople. Within these communities there were differences in the levels of acceptance. Many described following the advice of health professionals and viewed childhood immunisation as a normal part of bringing children up, whereas others thought carefully about the advantages and disadvantages of each vaccination before usually going ahead; there were particular concerns voiced about multiple/combined vaccines, as well as specific vaccines (discussed below).
Internationally, parental uncertainty about the safety and efficacy of some or all of the recommended vaccines in childhood schedules is a key driver of vaccine delay, selective vaccination or refusal. 121,122 Moreover, there is extensive evidence to show that the determinants of vaccine acceptance are multiple, complex and often interlinked57,123,124 necessitating a broad range of approaches on the individual, provider, health system and national levels to ensure optimum vaccination uptake. 48 The WHO Strategic Advisory Group of Experts on Immunisation123 working group found that vaccine determinants cluster predominantly around three domains: vaccine and vaccine-specific issues; individual and social group processes; and contextual influences. The findings from our study in different Traveller communities reflect many of the same issues that have been found consistently to influence vaccination uptake in the general population in the UK and elsewhere. 56–60,62,122
‘Vaccine hesitancy’, a term increasingly used in the literature, refers to a parent who is unsure whether or not to have their child vaccinated or is intentionally delaying or refusing one or more immunisations for non-medical reasons. 61,123 It usefully challenges the assumption that individuals or groups are either anti-vaccine or pro-vaccine but may be somewhere in the middle of a continuum from total acceptance to complete refusal. 122 A very small minority in the four English-speaking communities in our study were sceptical about immunisation in general, and only three participants (a Bristol Irish Traveller mother and a York English Gypsy mother and daughter) expressed views suggesting outright rejection of vaccinations. Leask et al. ,61 based on a review of the literature, identify five parental positions towards immunisation with approximate estimates of the proportion of each group: the ‘unquestioning acceptor’ (30–40%); the ‘cautious acceptor’ (25–35%); the ‘hesitant’ (20–30%); the ‘late or selective vaccinator’ (2–27%); and the ‘refuser’ of all vaccines (< 2%). These positions, based on the general population, were all clearly evident among the Travellers we interviewed for childhood as well as adult vaccines. The small number of published studies exploring Travellers’ (predominantly English Gypsy and Welsh Traveller communities) views on childhood immunisation also report mixed acceptance. 46,74,111 In those studies resistance to immunisations was associated with concerns about the potential side effects and a lack of belief in the value of vaccination. We found no studies investigating Travellers’ views on adult immunisation with which to compare our findings.
It has been suggested that Travellers traditionally favour natural remedies over modern medicine,25,125 and have cultural pride in self-reliance and stoicism,20,77,111 as well as a ‘fatalistic’ approach to health, suggesting that they may not believe in the value of preventative health care. 25,125 Consequently, we may have expected to find widespread overt resistance to immunisation, but this was not typically the case for our participants. Among the English Gypsy and Irish Traveller communities (in Bristol, York and London) an intergenerational shift towards ‘normalising’ immunisation was consistently acknowledged, with a move away from traditional, natural remedies preferred by older generations towards increasing acceptance of modern medicine among younger generations. Both Travellers and service providers discussed how, compared with the older community members, the current generation of parents have better knowledge about immunisation and more trustful relationships with health professionals (see Access to health and immunisation services), with the result that they rely less on family/community influence. That said, for a small minority of young parents, mothers and grandmothers remained influential in shaping their beliefs about immunisation, evident most strongly among the Irish Traveller communities in Bristol and London. The intergenerational change towards greater acceptance of immunisation was attributed to improved literacy, access to education and Traveller communities becoming more integrated into wider society (see Access to health and immunisation services). Other authors have similarly reported younger Travellers engaging more readily with maternity services125 and health services more generally. 24 Intergenerational change was discussed less among the Roma communities and not at all by the Scottish Showpeople. It could be that the Scottish Showpeople had already adopted similar values to the general population and made the shift towards normalising immunisation in previous generations. Some participants in the Roma communities, particularly those that have recently arrived from the EU, may not have been exposed to the UK health system for very long. There was evidence among these Roma communities that a motivating factor to immunise was driven by a desire to integrate into their local community and to be able to work.
Concerns about the safety of specific vaccines were primarily around the MMR and the whooping cough vaccines. This is not surprising given the historical context of these vaccinations, with controversies over their safety in the late 1990s/2000s (MMR vaccine) and 1970s (whole-cell whooping cough vaccine – which is no longer used). A feature of Traveller communities is the close proximity in which people live, with close contact with extended family, close-knit community networks as well as a strong oral tradition. 126 As is the case in the general population, the spread of information and misinformation can result in the ‘social amplification of risk’ that quickly influences perceptions and behaviours. 127 Indeed, this had occurred in the past for MMR vaccination in Bristol, York and London. However, the data suggested that views had changed over time, with the majority now accepting this combination vaccine, which, again, has parallels with the general population. 32,128 Just a minority of Travellers in all communities voiced their concerns about MMR vaccination, particularly in the York English Gypsy, Glasgow Scottish Showpeople and London Irish Traveller communities, in which some parents had opted to have the single vaccines. We found only one other Traveller study111 exploring views on MMR vaccination, which reported that nearly half of the 100+ participants (predominantly English Gypsy Romany) had partially immunised children, which most said was a result of avoiding the MMR vaccination. That study was published in 2009 and so will not reflect the recent national upwards trend in MMR vaccination acceptance and uptake to almost pre-1998 levels. Anxiety about the whooping cough vaccine was strongest among Bristol English Gypsies/Irish Travellers and some York English Gypsies and London Irish Travellers. These concerns, were more often about the effects of the vaccine in pregnant women rather than in infants and were related to a fear that the vaccine may cause brain damage as well as a belief that injections should not be given during pregnancy as the immune system is ‘low’ and pregnancy is in ‘God’s hands’. Among the other communities, vaccinations in pregnancy appeared to be widely accepted and seen as important in protecting the health of the child, which is consistent with the view of general population. 129 That said, in the general population uptake of the antenatal vaccines remains suboptimal (whooping cough – England 58%, Scotland 65%; flu vaccine – England 44%, Scotland 47%), with evidence of significant differences in uptake of the whooping cough vaccine by ethnic group of up to 25% between the highest uptake group (white British) and the lowest (black Caribbean). 40,130
Safety concerns about the HPV vaccine were mentioned by a few women and adolescent girls in all six communities, but on balance its importance in preventing cancer led to general acceptance of this vaccination. Missing school was a barrier to some adolescent girls having the HPV vaccination (see Access to health and immunisation services). Access to GP services for a ‘catch-up’ HPV vaccination, or because of parental choice because of the greater privacy a GP practice affords in providing this vaccination, was not always forthcoming. We had been advised by our research team member (AC) who is an English Gypsy that cancer and sexual behaviour are topics that Travellers would not want to talk about and that we should not ask girls under 16 years of age about the HPV vaccine. This was not particularly evident in terms of people’s willingness to discuss HPV vaccination in the interviews (although in one group interview a mother did not wish to discuss the topic in front of her adolescent daughter). However, it was acknowledged that the HPV vaccination was different from other vaccinations, as it was regarded as a ‘private issue’ and not to be discussed outside the family. In other minority ethnic groups, cultures ‘advocating monogamy and prohibiting sexual contact outside of marriage’131 have prevented HPV vaccination uptake by young women. 132 In our study there were some concerns that having the HPV vaccination would imply that adolescent girls are promiscuous; however, this was a minority view, most strongly discussed in the Bristol English Gypsy/Irish Traveller community, and not mentioned at all by the Glasgow Scottish Showpeople.
Finally, consistent with the general population133 there was variable acceptance of the adult flu vaccination among the English-speaking communities. Some Traveller participants across all four English-speaking communities believed that it caused flu and is less important than other immunisations. The perception that vaccination can cause flu and concerns about side effects have both been identified as deterrents to uptake in high-risk older people and the general population. 134 Views on the childhood flu vaccination appeared to be more positive across all six communities, although the programme was only introduced in 201338 with gradual roll-out so that only the youngest children were being targeted at the time of the study; hence this vaccine was under-investigated.
Access to health and immunisation services
Accounts from Traveller and service providers suggested that the majority of English-speaking Traveller participants in this study experienced no problems registering with a GP practice, being notified and reminded of immunisations (via letters, texts, telephone calls, face-to-face contact with health professionals) and attending appointments for immunisations in primary care and schools. This is likely to be related to the ‘settled’ and ‘integrated’ nature of our sample, who were housed or settled on authorised Traveller sites, often over many years, with established, long-term relationships with GP practices and health professionals; as well as the specialist work done by service providers to support their local Travellers to take up immunisations (discussed below). Indeed, the apparent satisfaction may reflect that the services are ‘enhanced’ for some communities, rather than routine services being ‘fit for purpose’ for Travellers. The All Ireland Traveller Health Study Team25 suggests that understanding access to health services is complex and, although many of the Travellers in its study (and in other studies20,111,135) report using health services, it is the ‘experience’ of that engagement that is important and too often is suboptimal. In our study there were some Traveller participant accounts of frustrations with getting through on the telephone to make a GP appointment, the length of time, often several weeks, to get an appointment (including for immunisation), as well as having to wait lengthy periods in busy clinics to be seen by a health professional. This led to a minority preferring to use A&E or out-of-hours doctors, which has also been observed elsewhere. 25,27 These criticisms of primary care similarly feature in national surveys for England and Scotland136 and are known to impact on people’s use of services. As up to 40% of A&E attendances have been reported to be ‘inappropriate or avoidable’,137 the reasons for using A&E are complex138,139 and clearly are not solely the domain of Travellers.
With the exception of language barriers (discussed below), the Romanian and Slovakian Roma participants did not talk about the difficulties they faced accessing health services, which may be because of restrictions on freedom of free expression within Romania and, to a lesser extent, Slovakia. 140,141 In contrast, service providers working with those communities spoke at length of how Roma people arrive in the UK and, because they have not been advised how the NHS works, will turn up without an appointment at the GP practice to wait to be seen, which puts pressure on the frontline staff. Service providers described ‘system’ barriers that pose challenges for Roma people, for example the requirement in Scotland to register with a GP practice in order to access maternity services (including immunisations) and GP practices striking patients off the register after three missed appointments. These barriers to accessing health services have been reported in other studies with Roma21,23 as well as existing for other migrant142 and minority ethnic communities. 143 The implication is that those with the greatest health need are least likely to access health services144 including immunisation.
There were other examples of difficulties in using immunisation services which were associated with broader, inter-related, socioeconomic barriers that exist for Travellers and are known to impact on their access to health services more widely. 17,19,20,24,25,55,85 These were typically discussed by service providers and only a minority of Travellers, often speaking of other Travellers’ experiences rather than their own. Across the six Traveller communities, the Romanian Roma (and to a lesser extent Slovakian Roma) families appeared to live with the highest levels of socioeconomic deprivation, which is well documented. 21,23,73 In contrast, the Glasgow Scottish Showpeople and their service providers spoke much less about these challenges, again resonating with existing reports. 18 Showpeople generally run businesses, live in permanent homes in privately owned or leased yards and travel out to set up and run fairground attractions. Consistent with other studies,19,74,111 living on the roadside was perceived to make it difficult to register with a GP practice, receive health visitor services and to be informed of forthcoming immunisation appointments. Travelling less frequently, for example to summer fairs, was not seen as a barrier to immunisation by York English Gypsy or Glasgow Scottish Showpeople participants, who said that they would return to a known health professional for a scheduled immunisation appointment. Views on this were more mixed among the Bristol English Gypsy/Irish Traveller and London Irish Traveller communities.
As reported elsewhere,54 poor attendance or non-attendance at school was identified as a barrier to having the HPV vaccination for some adolescent girls. In September 2014 the schedule for the HPV vaccine changed from three to two doses, which may facilitate take-up of the vaccine in those girls who are not regular school attenders. This is important given that socioeconomically disadvantaged women are more likely to develop cervical cancers145 and less likely to attend screening. 146 Low levels of literacy were also identified as a barrier, even among the current generation of parents, to understanding written information and invitation letters for immunisation, as well as communicating with health professionals, especially GPs, in consultations. There was widespread preference for simple written information with pictures and jargon-free spoken communication by health professionals. The Roma communities and their service providers also spoke at length about the additional language barriers they face in accessing health services, relying heavily on interpreters and bilingual health workers, who are often in short supply, particularly Roma speakers (rather than Romanian or Slovakian). These literacy and language barriers have been found to affect Travellers’ confidence in attending appointments and engaging in conversations with health professionals24,25,85 for fear of feeling humiliated and shamed. 27 Finally, poor housing conditions, worrying about eviction from local authority accommodation, working long unsociable hours and living in poverty mean that for some Travellers immunisation is simply not the most important issue. Prioritising food and shelter, the first level of basic human needs,147 is rational human behaviour.
Trust in health professionals, particularly GPs, health visitors and bilingual workers, and relational continuity143 were important factors influencing immunisation acceptance and experience. This is also the case for the general population61,63 although it is perhaps more pertinent to Travellers because of their history of not accessing health services and of long-standing discrimination. 27 Many English-speaking Travellers spoke of attending the same GP practice and preferring to see the same health professional over many years. A very small minority of Traveller participants from the English-speaking communities described a general lack of trust of health professionals or negative experiences, for example medical notes being lost or health visitors being perceived to be judgemental about Travellers’ cultural beliefs. These experiences appeared to have damaged their relationship with health professionals and eroded trust. For some women these experiences were seen as examples of discrimination because of their Traveller status. These findings resonate strongly with other studies of Travellers’ experiences of health services,20,25,27,86,111,135 which have reported that health professionals who are culturally well informed and respectful are highly valued,20,77 that outreach workers foster trust by mediating between health services and Travellers25 and that Travellers attribute past medical errors to discriminatory lack of care based on being a Traveller. 77 Service providers in this study also acknowledged the importance of developing trustful relationships with Travellers and the considerable time and commitment required for this. Some had observed discrimination among colleagues towards Travellers and attributed this to a lack of understanding of cultural differences and resentment about the additional work created by responding to Travellers’ needs. Van Cleemput27 concurs that discrimination by health professionals is often associated with a lack of personal contact with Travellers, leading to assumptions based on stereotypes. Van Cleemput and other authors15,18,20,24,87,111,148 identify a clear need for cultural awareness training for service providers.
What was clearly evident was the considerable work that service providers were doing to support Travellers to access health services and immunisation, working in partnership within and outside the NHS, and often going beyond the ‘call of duty’. Activities ranged from supporting Travellers to register with GP practices, searching GP records to identify Travellers who are missing some immunisations, using every opportunity to remind Travellers to have their immunisations and developing specific recall systems and clinics that are flexible to the needs of the local Traveller communities. Specialist health-care provision for Travellers has long been advocated. 86,149 This work is challenging for service providers because Traveller ethnicity status is not routinely recorded in GP or CHI systems, and recent cuts in funding and dispersal of public health expertise since the 2013 NHS reforms (in England)47 are hindering the co-ordinated and multiagency approach advocated by those with the knowledge of the health needs of these communities. In our study the most intensive specialist work was with the Romanian and Slovakian Roma families in Bristol and Glasgow. There was little or no targeted work specific to immunisation in York or with the Glasgow Scottish Showpeople, which was the case for different reasons. In York, there had previously been a specialist heath visitor for the English Gypsy community who had not been replaced once she retired, whereas the Scottish Showpeople were perceived to not require specialist services.
Interventions to increase immunisation uptake
Priority interventions for Travellers who are housed or settled on an authorised site, identified across communities
Five ‘top priority’ interventions were agreed across communities to improve the uptake of immunisation among Travellers who reflect the profile of our study participants, namely are housed or settled on an authorised site (see Generalisability).
-
cultural competence training for health professionals and frontline staff
-
identification of Travellers in health records to tailor support and monitor uptake
-
provision of a named frontline person in GP practices to provide respectful and supportive service
-
flexible and diverse systems for booking appointments, recall and reminders
-
protected funding for health visitors specialising in Traveller health, including immunisation.
The detail of these interventions in terms of their suggested components, mode and intensity of delivery, differences in content and delivery of the intervention within and across populations and settings88 are presented in Chapter 4 (see Table 37). All five interventions are at the institutional and policy levels of the SEM (see Chapter 2, Theoretical framework) and as such are ‘upstream’ interventions, which are suggested to have greater potential for reducing health inequalities than ‘downstream’ programmes, which are commonly delivered by frontline public health practitioners and focus on individuals and communities. 150 It is recommended that, to achieve long-term health improvements, all five levels of the SEM should be targeted simultaneously and, if this is not possible, then at least two levels. 90 What emerged in the workshops was the complementary nature of these interventions, with the suggestion that their impact would be enhanced if delivered as a combined package. This is consistent with National Institute for Health and Care Excellence (NICE) guidance, which recommends the delivery of ‘multifaceted, co-ordinated’ programmes to increase timely uptake of immunisation;48 and with the findings of a recent review of 181 studies that found multicomponent interventions to be most effective in increasing vaccine uptake. 82 It also parallels the package of interventions recommended to promote the uptake of breastfeeding initiation and duration of breastfeeding within the NICE evidence into practice briefing. 151 This briefing identified eight evidence-based actions that were considered as a whole and decisions made for each locality regarding the most relevant and important interventions to meet the diverse needs of local population groups. Importantly, the recommendations included a key national policy, namely routine implementation of the United Nation’s International Children’s Emergency Fund (UNICEF) UK Baby Friendly Initiative across all NHS hospitals151 and PCTs152 in England to provide the essential foundation on which to build the complementary, locally delivered, interventions as appropriate. 153
What is clear is that these five interventions are not novel. The Equality Act 201097 recommends that organisations provide training to their employees on the protected characteristics (one of which is race, which includes ethnicity), acceptable/non-acceptable behaviour and the impact of discrimination. Many reports and strategies focusing on Travellers recommend cultural competence training for service providers including frontline reception staff in GP practices15,18,20,24,25,87,111,148,154 and an economic review by Carr et al. 86 concluded that this can be delivered by Traveller community members for ‘modest costs’.
In the NICE guidance for reducing differences in the uptake of immunisations among children and young people48 (former) PCTs and GP practices are recommended to ‘have a structured, systematic method for recording, maintaining and transferring accurate information status of all children and young people’. NHS England proposes that the 2011 census categories for ethnicity, which included the category ‘Gypsy or Irish Traveller’, are routinely used in NHS health systems, for example in GP practice and CHI systems. 155 Other authors call for this to be mandated, with an additional category for Roma 23,156 and Occupational Travellers. This would mean that patterns of health services utilisation, including immunisation, could be monitored to identify health inequalities155 and tailor service provision to reduce inequalities. 19,22,25,155 The Information Services Division in Scotland has already adopted the 2011 classification for health service data collection. 22 Other service providers, for example local authorities, education services, could usefully use the same monitoring system to share information and facilitate joined-up working. 148 Of course Travellers may choose not to self-identify for fear of discrimination25 which reinforces the importance of delivering these interventions alongside each other.
Offering flexibility in terms of inviting people for immunisation, booking and then attending the appointments is a further recommendation of NICE. 48 Carr et al. 86 suggest that this should be a ‘minimum acceptable action to facilitate access to healthcare’ for Travellers. There is an increasing body of evidence on the effectiveness of different recall, reminder and appointment systems for childhood and adult vaccinations78,83,84,134,157 to draw on. Clearly, exactly how this is done should be informed by the particular needs of each Traveller community and could be informed by local joint strategic needs assessments. 158 Many reports recommend making health care more accessible to Travellers,17,19,20,23,154,159 and this is a stated national priority. 49,160,161 This may not be about providing specific immunisation services including outreach for Travellers, but areas may focus on ensuring that mainstream provision is signposted and accessible. 15,86,154 The key issue is that provision should be embedded into mainstream planning and commissioning,17,86,160 for example through health and well-being strategies of English local authorities and their partner CCGs158 and by health and social care partnerships in Scotland. 162 The WHO’s Guide to Tailoring Immunization Programmes163 offers a useful framework to increasing infant and childhood immunisation among diverse communities. It aims to provide proven methods and tools to assist national and local immunisation programmes to design targeted strategies that increase uptake of infant and childhood vaccinations, through identifying susceptible populations, determining barriers to vaccination and implementing evidence-based interventions. 163
Finally, specialist health visitors are consistently highly valued by Travellers and considered to play an important role in facilitating access to health services including immunisation,17,18,20,86 although this is rarely formally evaluated. 86 In an era of restricted NHS164 and public health funding,165 these roles have largely been lost.
In the light of the existing body of evidence, current practice and guidance for these five priority interventions for Travellers and the general population, we suggest that they could usefully inform the development of a national policy plan to promote uptake of immunisation among culturally diverse Traveller communities in the UK, which could be evaluated alongside its implementation. An accompanying national practice guidance plan could be developed to aid the effective implementation of the national policy and organisational interventions at the local level. This would describe what each intervention should comprise and how it might vary between communities.
Priority interventions for Travellers who are housed or settled on an authorised site, identified by particular communities
Ten interventions were identified by particular Traveller communities and/or their service providers to improve the uptake of immunisation within their own communities (see Figure 7, Chapter 4). To be clear, these interventions were not as broadly supported across communities as the five interventions discussed above. That said, we would suggest that they could be relevant to other communities of the same ‘descent’ (see Inferential generalisation); for example, ‘Increased access to bilingual support workers or interpreters’, which was prioritised by the Glasgow Roma and their service providers, would be potentially relevant to all Roma communities. The 10 interventions fell across all five levels of the SEM,89 so are a mix of ‘upstream’ and ‘downstream’ interventions. 150
Five of these 10 interventions focused on the provision of accessible, evidence-based information about immunisation (and the NHS in Scotland for the Glasgow Roma community) from trusted, well-trained health professionals (prioritised by York English Gypsy, Glasgow Scottish Showpeople), as well as from reliable social media and media sources (prioritised by Glasgow Scottish Showpeople). Provision of ‘tailored information, advice and support’ with ‘an opportunity to discuss concerns’ is a recommendation of NICE48 and also a quality criterion for effective immunisation programmes. 166 Importantly, immunisation information tailored to specific populations and their particular concerns can increase immunisation knowledge, awareness, attitudes,82 intentions to immunise,81 and help address vaccine hesitancy,81,82 especially when part of a dialogue with a health professional. 82,163 Involving the target audience, in this case Travellers, to co-produce information is key to success. 17,157 Our interview findings, consistent with other research,17,20 demonstrated that Travellers with low levels of literacy struggle to understand immunisation information, and the routine translation of NHS resources into minority ethnic languages is therefore unhelpful, particularly for Roma people, for whom these languages, for example Romanian, are their second language. There are many examples of good practice of developing accessible health information for Travellers17 as well as guidance on communicating about immunisation167 on which to draw to deliver this prioritised intervention. More research is needed on delivering immunisation information through different media. 81 Social media are suggested to be a potential way of addressing vaccine hesitancy for individuals who have already started their vaccination schedule or are familiar with social media. 82 UNICEF suggests that training for service providers should include skills to react to anti-vaccination sentiments in social media to enable them to discuss this with their patients. 168 This is worth considering given the large amount of ill-informed or anti-vaccination material now available on the internet.
Two interventions were about improving service delivery, in terms of improving access to bilingual support workers or interpreters, and recognising the resource issues for good practice with non-English-speaking Travellers (both prioritised by Glasgow Roma). As identified elsewhere in this report, the needs of the Roma community are quite specific in many ways. Other authors acknowledge the pressures on bilingual support services for Roma15,23 and the importance of sharing good practice more extensively to avoid scarce resources being used to redesign existing practices which work. 15 The final three interventions, better joined-up working for immunisation services (prioritised by York English Gypsies), multisectorial working on cultural issues led by health professionals (prioritised by Bristol Roma) and representation from the Traveller community on the CCG and or immunisation committee (prioritised by London Irish Travellers), are linked. The Health and Social Care Act 2012169 should have been a driver for more joined-up working; however, for immunisation, services are now separate from public health (based in local authorities) which, service providers’ accounts in this study suggest, have worked against collaborative working. Involving people, and in this case Travellers, in decisions about their own health and health care is now considered a hallmark of good-quality care,159 and there are many good practice examples of Travellers being members of multiagency groups. 20,24 That said, people from socially excluded groups, such as Travellers, face barriers to taking part in committees and forums that rely on traditional structures and procedures. 159 An alternative approach might be to set up a Traveller forum,148,160 which discusses issues broader than immunisation and which can include more members of the community, from which a champion for the community could then sit on the more formal CCG or immunisation committee. 86 Importantly, this forum would need to be culturally appropriate, in familiar surroundings160 and use creative strategies159 to take time to build group dynamics and develop Travellers’ confidence in voicing their views. 24 Such forums promoting joined-up working, and including Traveller community members, already exist. 170
As with the five priority interventions identified across communities, these 10 interventions for particular Traveller communities are not novel. We suggest that they would be included in the aforementioned national practice guidance plan to aid the effective implementation of the national policy plan at the local level, and ensure that immunisation programmes address the needs of the local Traveller communities.
Interventions for Travellers living on the roadside or on an unauthorised encampment
Two interventions were identified as important to improve the uptake of immunisation among these groups of Travellers:
-
flexible delivery of immunisation services (prioritised by the York English Gypsy community)
-
an improved system of temporary registration at GP practices (prioritised by Bristol English Gypsy/Irish Traveller community).
Neither of these ideas, nor their prioritisation, came from roadside Travellers themselves, although they parallel issues identified in a small number of reports which mention roadside Travellers. 86,111,160 A flexible approach might use outreach immunisation services160 and GP practices could receive financial reimbursement for registering frequently mobile Travellers. We suggest that more research is needed to understand the particular needs and preferences for immunisation interventions of these less researched, ‘most vulnerable’, families,160 as they are likely to be different from those of more settled Travellers. 160
Recommendations for research
-
Mixed-methods research to explore the challenges and opportunities of ethnic identification of Travellers in primary care and maternity health services, including:
-
exploratory qualitative research with health professionals and Travellers (men and women across generations) to explore their views on their barriers to and facilitators of recording Traveller ethnicity
-
quantitative analysis of immunisation uptake by ethnicity (if recording of Traveller ethnicity improves to a level to enable this) to explore inequality in uptake by ethnic group (and aid further targeting of services).
-
-
Evaluation of the implementation of a national policy plan (and accompanying practice guidance plan) to promote uptake of immunisation among culturally diverse Traveller communities in the UK.
-
Methodological research to identify appropriate methods to capture the views and experiences of immunisation of roadside Travellers and those living on unauthorised encampments (men and women across generations).
-
Informed by (3), exploratory qualitative research with roadside Travellers and those living on unauthorised encampments to identify acceptable and feasible interventions to improve uptake of immunisation, including views on:
-
– flexible delivery of immunisation services
-
– improving the system of temporary registration with GP practices.
-
-
Exploratory qualitative research with Travellers to explore their views on the barriers to and facilitators of the uptake of vaccines newly introduced to the routine schedule, such as rotavirus and meningitis B.
Implications for policy and practice
Evidence from this study points to ways to promote uptake of immunisation among English Gypsy, Irish Traveller, Eastern European Roma and Showpeople Traveller communities in the UK.
-
The development and implementation of a national policy plan (and accompanying practice guidance plan) which comprises:
-
cultural competence training for health professionals and frontline staff
-
identification of Travellers in health records to tailor support and monitor uptake
-
provision of a named person in GP practices to provide a consistently respectful and supportive frontline service
-
flexible and diverse systems for booking appointments and follow-up reminders and recalls
-
protected funding for a designated health visitor specialising in Traveller health including immunisation.
-
-
The development of national targets to support the effective implementation of a national policy plan (and accompanying practice guidance plan), including:
-
national target for GP practices for the collection of immunisation status data for local Traveller communities within routine Quality and Outcomes framework data collection requirements
-
national target for GP practices to achieve an agreed per cent coverage of full immunisation uptake among local Traveller communities.
-
-
The integration of a national policy plan (and accompanying practice guidance plan) into key guidance and policy documents, including:
-
NICE guidance for reducing differences in the uptake of immunisations among children and young people48
-
the Department of Health’s Healthy Child Programme171
-
the Scottish Government’s Healthy Child Programme172
-
NHS England’s National Health Visitor Core Service Specification173
-
the Scottish Government’s Universal Health Visiting Pathway in Scotland174
-
NHS England’s Public Health Section 7a Commissioning Intentions. 175
-
Acknowledgements
The UNITING research team would like to thank all the Travellers and service providers who took part in the interviews and the workshops. We are also very grateful to our community partners and the IPAG who guided us throughout the study; and to our collaborators who facilitated our contact with the Traveller communities. These individuals are listed below. Without this support, our study would not have been possible. Thanks also to Paula Cowan (University of York) for providing administrative support, and to Colin Clark and Lynn Poole (University of the West of Scotland) for their advice at the start of the study.
Community partners
-
Shirell Johnson, member of Glasgow Scottish Showpeople community.
-
Danielle Thomas, member of Glasgow Scottish Showpeople community.
-
London Gypsy and Traveller Forum.
-
York Travellers Trust Advisory Steering Group.
Independent project advisory group
-
Martin Schweiger (chairperson), Public Health Consultant, Public Health England.
-
Jill Edwards, Research Fellow, University of Leeds.
-
Patrice Van Cleemput, Freelance Research Consultant.
Collaborators
-
Hilary Beach, University of the West of England.
-
Sarah Bridgman, North Somerset Community Partnership Community Interest Company.
-
Gill Francis, North East London Foundation Trust.
-
Bridget Gallagher, NHS Greater Glasgow and Clyde.
-
Jacob Jablonowski, formerly Wellspring Healthy Living Centre, Bristol.
-
Sheila Lally, North Bristol NHS Trust.
-
Anne Marie McCulloch, NHS Greater Glasgow and Clyde.
-
Luiza McRae, Freelance Interpreter.
-
Gillian Thomson, NHS Greater Glasgow and Clyde.
-
Linda Vousden, North Bristol NHS Trust.
-
Lewisham Irish Community Centre.
-
Local Planning Group, Glasgow.
-
London Gypsy and Traveller Unit.
-
Southwark Traveller Action Group.
-
York Travellers Trust.
Contributions of authors
Dr Cath Jackson (Senior Research Fellow, Public Health) was the principal investigator. She conceived, designed and led the study, contributed to data collection in York and to data analysis and prepared the final report.
Ms Lisa Dyson (Research Fellow, Maternal and Child Health) contributed to study design, data collection in York and data analysis and drafted sections of the final report.
Dr Helen Bedford (Senior Lecturer, Children’s Health) contributed to study conception and design, led the data collection in London and contributed to the preparation of the final report.
Professor Francine M Cheater (Professor, Public Health and Implementation Science) contributed to study conception and design and to data analysis and drafted sections of the final report.
Dr Louise Condon (Associate Professor, Nursing) contributed to study conception and design, co-led the data collection in Bristol and drafted sections of the final report.
Ms Annie Crocker (Member of English Gypsy community in Bristol) contributed to study conception and design, facilitated recruitment in Bristol and contributed to the preparation of the final report.
Dr Carol Emslie (Reader, Public Health) contributed to study conception and design, data collection and data analysis and drafted sections of the final report.
Dr Lana Ireland (Researcher, Psychology) contributed to data collection in Glasgow and to the preparation of the final report.
Ms Philippa Kemsley (Research Health Visitor) facilitated recruitment and contributed to data collection in London and to the preparation of the final report.
Dr Susan Kerr (Reader, Public Health) contributed to study conception and design, led the data collection in Glasgow and contributed to the preparation of the final report.
Dr Helen J Lewis (Research Fellow, Mental Health) contributed to study conception and design, to data collection in York and to the preparation of the final report.
Dr Julie Mytton (Associate Professor, Child Health) contributed to study conception and design, co-led the data collection in Bristol and drafted sections of the final report.
Ms Karen Overend (Research Fellow, Mental Health) contributed to data analysis and drafted sections of the final report.
Professor Sarah Redsell (Professor, Public Health) contributed to study conception and design and to data analysis and drafted sections of the final report.
Miss Zoe Richardson (Trial Support Officer) contributed to data analysis and drafted sections of the final report.
Miss Christine Shepherd (Chief Officer, Gypsy Travellers) contributed to study conception and design, facilitated recruitment in York and contributed to the preparation of the final report.
Mrs Lesley Smith (Member of English Gypsy Traveller community in York) contributed to study conception and design, facilitated recruitment in York and contributed to the preparation of the final report.
Publication
Jackson C, Bedford H, Condon L, Crocker A, Emslie C, Dyson L, et al. UNderstanding uptake of Immunisations in TravellIng aNd Gypsy communities (UNITING): protocol for an exploratory, qualitative study. BMJ Open 2015;5:e008564.
Data sharing statement
Data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Feder GS, Vaclavik T, Streetly A. Traveller Gypsies and childhood immunization: a study in east London. Br J Gen Pract 1993;43:281-4.
- Clark C, Greenfields M. Here to Stay: The Gypsies and Travellers of Britain. Hatfield: University of Hertfordshire Press; 2006.
- Caravan Sites Act 1968. London: The Stationery Office; 1968.
- Oakley J. The Traveller-Gypsies. Cambridge: Cambridge University Press; 1983.
- Jarman A, Jarman E. The Welsh Gypsies, Children of Abram Wood. Cardiff: Cardiff University Press; 1991.
- Gmelch G. The Irish Tinkers. Prospect Heights, IL: Waveland Press Inc.; 1985.
- Kenrick D. In the Shadow of the Swastika: The Gypsies during the Second World War. Hatfield: University of Hertfordshire Press; 1999.
- Krosnar K. Roma women were unlawfully sterilised. BMJ 2006;332. http://dx.doi.org/10.1136/bmj.332.7534.138-d.
- Kovac C, Hajnal A. Roma woman goes to UN claiming sterlisation without consent. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.328.7441.662-c.
- Lewis H. A Multi-Method Evaluation of a Community Initiative Intended to Improve the Quality of Healthcare in the Gypsy and Traveller Communities. Cardiff: Cardiff University; 2007.
- Nickson K, Sudbery J. Education social work with a Traveller woman. J Soc Pract 1997;11:91-102. http://dx.doi.org/10.1080/02650539708415117.
- What Does the 2011 Census Tell us about the Characteristics of Gypsy or Irish Travellers in England and Wales?. London: ONS; 2014.
- Brown P, Scullion L, Martin P. Migrant Roma in the United Kingdom. Population size and Experiences of Local Authorities and Partners. Final Report. Manchester: University of Salford; 2013.
- Equal Opportunities Committee 1st Report, 2012 (Session 4) Where Gypsy/Travellers Live. Edinburgh: The Scottish Parliament; 2012.
- Mapping the Roma Community in Scotland. Final Report. Glasgow: The Social Marketing Gateway; 2013.
- Inclusion Health: Improving the Way We Meet the Primary Healthcare Needs of the Socially Excluded. London: Cabinet Office; 2010.
- Aspinall P. Report for Health ASERT programme Wales. Cardiff: Welsh Assembly Government; 2005.
- Cemlyn S, Greenfields M, Burnett S, Matthews Z, Whitwell C. Inequalities Experienced by Gypsy and Traveller Communities: A Review. Manchester: Equality and Human Rights Commission; 2009.
- Matthews Z. The Health of Gypsies and Travellers in the UK. London: Race Equality Foundation; 2008.
- Parry G, Van Cleemput P, Peters J, Walters S, Thomas K, Cooper C. Health status of Gypsies and Travellers in England. J Epidemiol Community Health 2007;61:198-204. http://dx.doi.org/10.1136/jech.2006.045997.
- Cook B, Wayne GF, Valentine A, Lessios A, Yeh E. Revisiting the evidence on health and health care disparities among the Roma: a systematic review 2003–2012. Int J Public Health 2013;58:885-911. http://dx.doi.org/10.1007/s00038-013-0518-6.
- Aspinall P. Hidden Needs Identifying Key Vulnerable Groups in Data Collections: Vulnerable Migrants, Gypsies and Travellers, Homeless People, and Sex Workers. Canterbury: University of Kent; 2014.
- Lane P, Spencer S, Jones A. Gypsy, Traveller and Roma: Experts by Experience. Cambridge: Anglia Ruskin University; 2014.
- Jenkins L. Preparation Study of Gypsy/Traveller Needs. Canterbury: University of Kent; 2010.
- All Ireland Traveller Health Study Our Geels. Dublin: University College Dublin; 2010.
- Peters J, Parry GD, Van Cleemput P, Moore J, Cooper CL, Walters SJ. Health and use of health services: a comparison between Gypsies and Travellers and other ethnic groups. Ethn Health 2009;14:359-77. http://dx.doi.org/10.1080/13557850802699130.
- Van Cleemput P. Social exclusion of Gypsies and Travellers: health impact. J Res Nurs 2010;15:315-27. http://dx.doi.org/10.1177/1744987110363235.
- Global Immunization Vision and Strategy, 2006–2015. Geneva: WHO and UNICEF; 2005.
- Global Immunization Vision and Strategy. Geneva: WHO; 2011.
- NHS . The Routine Immunisation Schedule 2015. www.gov.uk/government/uploads/system/uploads/attachment_data/file/473570/9406_PHE_2015_Complete_Immunisation_Schedule_A4_21.pdf (accessed 11 November 2015).
- Immunisation Against Infectious Disease. Tuberculosis (Chapter 32). London: Department of Health; 2013.
- Quarterly Vaccination Coverage Statistics for Children Aged up to Five Years in the UK (COVER programme): January to March 2015. London: Public Health England; 2015.
- Health Protection Scotland . Measles, Mumps, Rubella and Whooping Cough Illness and Routine Childhood Vaccine Uptake (Quarter Ending Week 12 2015) 2015. www.hps.scot.nhs.uk/immvax/wrdetail.aspx?id=63406&wrtype=6 (accessed 11 November 2015).
- Seasonal Influenza Vaccine Uptake Amongst GP Patients in England Provisional Monthly Data for 1 September 2014 to 31 January 2015. London: Public Health England; 2015.
- Vaccination Services Reducing Inequalities in Uptake. London: DH; 2005.
- Human Papillomavirus (HPV) Vaccine Coverage in England, 2008/09 to 2013/14: A Review of the Full Six Years of the Three-Dose Schedule. London: Public Health England; 2015.
- Sinka K, Kavanagh K, Gordon R, Love J, Potts A, Donaghy M, et al. Achieving high and equitable coverage of adolescent HPV vaccine in Scotland. J Epidemiol Community Health 2014;68:57-63. http://dx.doi.org/10.1136/jech-2013-202620.
- The National Flu Immunisation Programme 2015/16. London: DH, Public Health England and NHS England; 2015.
- HPS Weekly National Influenza Report Summary of Surveillance of Influenza and other Seasonal Respiratory Illnesses. Glasgow: Health Protection Scotland; 2015.
- Pertussis Vaccination Programme for Pregnant Women: Vaccine Coverage Estimates in England, June to September 2015. London: Public Health England; 2015.
- Public Health Protection Unit Newsletter November 2015. Glasgow: NHS Greater Glasgow and Clyde; 2015.
- Office for National Statistics . Census: Ethnicity and National Identity in England and Wales 2011 2011. www.ons.gov.uk/ons/rel/census/2011-census/key-statistics-for-local-authorities-in-england-and-wales/rpt-ethnicity.html (accessed 20 December 2015).
- Kumarapeli P, Stepaniuk R, de Lusignan S, Williams R, Rowlands G. Ethnicity recording in general practice computer systems. J Public Health 2006;28:283-7. http://dx.doi.org/10.1093/pubmed/fdl044.
- Gordon M, Gorman DR, Hashem S, Stewart DG. The health of Travellers’ children in Northern Ireland. Public Health 1991;105:387-91. http://dx.doi.org/10.1016/S0033-3506(05)80598-0.
- Pahl J, Vaile M. Health and health care among travellers. J Soc Policy 1988;17:195-213. http://dx.doi.org/10.1017/S0047279400016639.
- Moreton J. HIB. Educating parents and professionals. Health Visit 1992;65:266-7.
- Dar O, Gobin M, Hogarth S, Lane C, Ramsay M. Mapping the Gypsy Traveller community in England: what we know about their health service provision and childhood immunization uptake. J Public Health 2013;35:404-12. http://dx.doi.org/10.1093/pubmed/fdt052.
- Reducing Differences in the Uptake of Immunisations (Including Targeted Vaccines) Among Children and Young People Aged Under 19 years. London: NICE; 2009.
- Equal Opportunities Committee 3rd Report, 2013 (Session 4) Gypsy/Travellers and Care. Edinburgh: The Scottish Parliament; 2012.
- Maduma-Butshe A, McCarthy N. The burden and impact of measles among the Gypsy-Traveller communities, Thames Valley, 2006-09. J Public Health 2013;35:27-31. http://dx.doi.org/10.1093/pubmed/fds052.
- Measles Outbreaks in Gypsy and Travellers Communities. Gateway Reference Number: 14614. London: DH; 2010.
- Wilkin A, Derrington C, White R, Foster B. Improving the Outcomes for Gypsy, Roma and Traveller Pupils Literature Review. London: National Foundation for Educational Research; 2009.
- Wilkin A, Derrington C, White R, Martin K, Foster B, Kinder K, et al. Improving the Outcomes for Gypsy, Roma and Traveller Pupils: Final Report Research Report DFE-RR043. London: Department for Education; 2010.
- Bentley C. Systematically Addressing Inequalities in Human Papillomavirus (HPV) Vacination Coverage. London: Sanofi Pasteur MSD; 2015.
- Smart H, Titterton M, Clark C. A literature review of the health of Gypsy/Traveller families in Scotland: the challenges for health promotion. Health Educ 2003;103:156-65. http://dx.doi.org/10.1108/09654280310472379.
- Falagas ME, Zarkadoulia E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review. Curr Med Res Opin 2008;24:1719-41. http://dx.doi.org/10.1185/03007990802085692.
- Brown K, Kroll J, Hudson M, Ramsay M, Green J, Long S, et al. Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine 2010;28:4235-48. http://dx.doi.org/10.1016/j.vaccine.2010.04.052.
- Tickner S, Leman PJ, Woodcock A. Factors underlying suboptimal childhood immunisation. Vaccine 2006;24:7030-6. http://dx.doi.org/10.1016/j.vaccine.2006.06.060.
- Mills E, Jadad A, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol 2005;8:1081-8. http://dx.doi.org/10.1016/j.jclinepi.2005.09.002.
- Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med 2014;112:1-11. http://dx.doi.org/10.1016/j.socscimed.2014.04.018.
- Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatr 2012;12. http://dx.doi.org/10.1186/1471-2431-12-154.
- Pearce A, Marshall H, Bedford H, Lynch J. Barriers to childhood immunisation: findings from the Longitudinal Study of Australian Children. Vaccine 2015;33:3377-83. http://dx.doi.org/10.1016/j.vaccine.2015.04.089.
- Rapid literature Review on Motivating Hesitant Population Groups in Europe to Vaccinate. Stockholm: ECDC; 2015.
- Samad L, Butler N, Peckham C, Bedford H. Incomplete immunisation uptake in infancy: maternal reasons. Vaccine 2006;24:6823-9. http://dx.doi.org/10.1016/j.vaccine.2006.06.039.
- Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics 2006;117:1532-41. http://dx.doi.org/10.1542/peds.2005-1728.
- Eilers R, Krabbe PF, de Melker HE. Factors affecting the uptake of vaccination by the elderly in Western society. Prev Med 2014;69:224-34. http://dx.doi.org/10.1016/j.ypmed.2014.10.017.
- Wheelock A, Thomson A, Sevdalis N. Social and psychological factors underlying adult vaccination behavior: lessons from seasonal influenza vaccination in the US and the UK. Expert Rev Vaccines 2013;12:893-901. http://dx.doi.org/10.1586/14760584.2013.814841.
- Ahmed F, Friedman C, Franks A, Latts LM, Nugent EW, France EK, et al. Effect of the frequency of delivery of reminders and an influenza tool kit on increasing influenza vaccination rates among adults with high-risk conditions. Am J Manag Care 2004;10:698-702.
- Bödeker B, Walter D, Reiter S, Wichmann O. Cross-sectional study on factors associated with influenza vaccine uptake and pertussis vaccination status among pregnant women in Germany. Vaccine 2014;32:4131-9. http://dx.doi.org/10.1016/j.vaccine.2014.06.007.
- Wiley KE, Massey PD, Cooper SC, Wood NJ, Ho J, Quinn HE, et al. Uptake of influenza vaccine by pregnant women: a cross-sectional survey. Med J Aust 2013;198:373-5. http://dx.doi.org/10.5694/mja12.11849.
- Chen JY, Fox SA, Cantrell CH, Stockdale SE, Kagawa-Singer M. Health disparities and prevention: racial/ethnic barriers to flu vaccinations. J Community Health 2007;32:5-20. http://dx.doi.org/10.1007/s10900-006-9031-7.
- Johnson DR, Nichol KL, Lipczynski K. Barriers to adult immunization. Am J Med 2008;121:28-35. http://dx.doi.org/10.1016/j.amjmed.2008.05.005.
- Sivic S, Huremovic A, Djerzic H. Social exclusion as a determining health factor of the Roma population. Med Arch 2013;67:60-2. http://dx.doi.org/10.5455/medarh.2013.67.60-62.
- Papadopoulos I, Lay M. The health promotion needs and preferences of Gypsy Travellers in Wales. Divers Health Soc Care 2007;4:167-76.
- Hawes D. Travellers and the Health Service. Bristol: The Policy Press; 1997.
- Rechel B, Blackburn CM, Spencer NJ, Rechel B. Access to health care for Roma children in Central and Eastern Europe: findings from a qualitative study in Bulgaria. Int J Equity Health 2009;8. http://dx.doi.org/10.1186/1475-9276-8-24.
- Van Cleemput P, Parry G, Thomas K, Peters J, Cooper C. Health-related beliefs and experiences of Gypsies and Travellers: a qualitative study. J Epidemiol Community Health 2007;61:205-10. http://dx.doi.org/10.1136/jech.2006.046078.
- Jacobson Vann JC, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates. Cochrane Database Syst Rev 2005;3. http://dx.doi.org/10.1002/14651858.cd003941.pub2.
- Kaufman J, Synnot A, Ryan R, Hill S, Horey D, Willis N, et al. Face to face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev 2013;5. http://dx.doi.org/10.1002/14651858.cd010038.pub2.
- Cairns G, MacDonald L, Angus K, Walker L, Cairns-Taylor T, Bowdler T. Systematic Literature Review of the Evidence for Effective National Immunisation Schedule Promotional Communications. Stockholm: European Centre for Disease Prevention and Control; 2012.
- Sadaf A, Richards JL, Glanz J, Salmon DA, Omer SB. A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine 2013;31:4293-304. http://dx.doi.org/10.1016/j.vaccine.2013.07.013.
- Jarrett C, Wilson R, O’Leary M, Larson H. the Sage Working Group on Vaccine Hesitancy . Strategies for addressing vaccine hesitancy – a systematic review. Vaccine 2015;33:4180-90. http://dx.doi.org/10.1016/j.vaccine.2015.04.040.
- Thomas R, Lorenzetti D. Interventions to increase inflenza vaccination rates of those 60 years and older. Cochrane Database Syst Rev 2014;7.
- Lau D, Hu J, Majumdar S, Storie D, Rees S, Johnson J. Interventions to improve influenza and pneumococcal vaccination rates among community-dwelling adults: a systematic review and meta-analysis. Ann Fam Med 2012;10:538-46. http://dx.doi.org/10.1370/afm.1405.
- Van Cleemput P, Bissell P, Harris J. Pacesetters Programme – Gypsy, Roma and Traveller Core Strand. Sheffield: University of Sheffield; 2010.
- Carr S, Lhussier M, Forster N, Goodall D, Geddes L, Pennington M, et al. Outreach programmes for health improvement of Traveller Communities: a synthesis of evidence. Public Health Res 2014;2.
- Francis G. Developing the Cultural Completence of Health Professionals Working with Gypsy Travellers Report for Mary Seacole Development Award. London: Department of Health; 2010.
- Developing and Evaluating Complex Interventions: New Guidance. London: MRC; 2008.
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q 1988;15:351-77. http://dx.doi.org/10.1177/109019818801500401.
- Golden SD, Earp JA. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav 2012;39:364-72. http://dx.doi.org/10.1177/1090198111418634.
- Kumar S, Quinn SC, Kim KH, Musa D, Hilyard KM, Freimuth VS. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Educ Behav 2012;39:229-43. http://dx.doi.org/10.1177/1090198111415105.
- Quinn LA, Thompson SJ, Ott MK. Application of the social ecological model in folic acid public health initiatives. J Obstet Gynecol Neonatal Nurs 2005;34:672-81. http://dx.doi.org/10.1177/0884217505281877.
- Documét PI, Green HH, Adams J, Weil LA, Stockdale J, Hyseni Y. Perspectives of African American, Amish, Appalachian And Latina women on breast and cervical cancer screening: implications for cultural competence. J Health Care Poor Underserved 2008;19:56-74. http://dx.doi.org/10.1353/hpu.2008.0018.
- Larson C, Schlundt D, Patel K, Goldzweig I, Hargreaves M. Community participation in health initiatives for marginalized populations. J Ambul Care Manage 2009;32:264-70. http://dx.doi.org/10.1097/JAC.0b013e3181ba6f74.
- Emmel N, Hughes K, Greenhalgh J, Sales A. Accessing socially excluded people – trust and the gatekeeper in the researcher–participant relationship. Sociol Res Online 2007;12. http://dx.doi.org/10.5153/sro.1512.
- Race Relations Act 1976. London: The Stationery Office; 1976.
- Equality Act 2010. London: The Stationery Office; 2010.
- Travellers Aid Trust . Grant Makers Fact Sheet on Gypsies and Travellers n.d. www.travellersaidtrust.org/pdfs/grant%20makers%20fact%20sheet%2009.pdf (accessed 11 November 2015).
- Scottish Traveller Education Programme . Travelling Communities in Scotland 2013. www.step.education.ed.ac.uk/travelling-communities-in-scotland/ (accessed 11 November 2015).
- Moffett L. Extending our Reach: Promoting Good Practice in Engaging Marginalised and Hard to Reach Groups. Coleraine: North East Peace III Partnership; 2010.
- Renfrew M, Dyson L, Herbert G, McFadden A, McCormick F, Thomas J, et al. Developing evidence-based recommendations in public health – incorporating the views of practitioners, service users and user representatives. Health Expectations 2008;11:3-15. http://dx.doi.org/10.1111/j.1369-7625.2007.00471.x.
- Gaining Consensus Among Stakeholders Through the Nominal Group Technique. Atlanta, GA: Centers for Disease Control and Prevention; 2012.
- Bryman A, Bryman A. Analysing Qualitative Data. London: Routledge; 1984.
- Ovretveit J. Comparative and Cross-cultural Health Research: A Practical Guide. Oxford: Radcliffe Medical Press; 1998.
- Ritchie J, Lewis J, McNaughton Nicholls C, Ormston R. Qualitative Research Practice. London: Sage; 2014.
- Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol 2009;9. http://dx.doi.org/10.1186/1471-2288-9-59.
- Bartholomew LK, Parcel GS, Kok G. Intervention mapping: a process for developing theory- and evidence-based health education programs. Health Educ Behav 1998;25:545-63. http://dx.doi.org/10.1177/109019819802500502.
- Stefanoff P, Orlikova H, Rogalska J, Kazanowska-Zielinska E, Slodinski J. Mass immunisation campaign in a Roma settled community created an opportunity to estimate its size and measles vaccination uptake, Poland 2009. Eurosurveillance 2010;33:16-21.
- Stojanovski K, McWeeney G, Emiroglu N, Ostlin P, Koller T, Licari L, et al. Risk factors for low vaccination coverage among Roma children in disadvantaged settlements in Belgrade, Serbia. Vaccine 2012;30:5459-63. http://dx.doi.org/10.1016/j.vaccine.2012.06.072.
- Kraigher A, Vidovic M, Kustec T, Skaza A. Vaccination coverage in hard to reach Roma children in Slovenia. Coll Antropol 2006;30:789-94.
- Twiselton I, Huntington F. Health Needs Assessment: Cumbria Gypsy Travellers. Penrith: NHS Cumbria; 2009.
- Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative literature in health services research. Qual Health Res 1998;8:341-51. http://dx.doi.org/10.1177/104973239800800305.
- Richards H, Emslie C. The ‘doctor’ or the ‘girl from the University’? Considering the influence of professional roles on qualitative interviewing. Fam Pract 2000;17:71-5. http://dx.doi.org/10.1093/fampra/17.1.71.
- Silverman D. Interpreting Qualitative Data: Methods for Analysing Talk, Text and Interaction. London: Sage; 2006.
- Horsburgh D. Evaluation of qualitative research. J Clin Nurs 2003;12:307-12. http://dx.doi.org/10.1046/j.1365-2702.2003.00683.x.
- Dixon-Woods M, Shaw RL, Agarwal S, Smith JA. The problem of appraising qualitative research. Qual Saf Health Care 2004;13:223-5. http://dx.doi.org/10.1136/qshc.2003.008714.
- Spencer L, Ritchie J, Lewis J, Dillon L. Quality in Qualitative Evaluation: A Framework for Assessing Research Evidence. London: Government Chief Social Researcher’s Office; 2003.
- Critical Appraisal Skills Programme . Qualitative Research: Appraisal Tool 2006. www.casp-uk.net/#!checklists/cb36 (accessed 15 December 2015).
- Ranji U, Salganicoff A. Balancing on Shaking Ground: Women, Work and Family Health. California: The Henry J Kaiser Family Foundation; 2014.
- McMurray R, Cheater FM, Weighall A, Nelson C, Schweiger M, Mukherjee S. Managing controversy through consultation: a qualitative study of communication and trust around MMR vaccination decisions. Br J Gen Pract 2004;54:520-5.
- Stefanoff P, Mamelund S, Robinson M, Netterlid E, Tuells J, Bergsaker MA, et al. Tracking parental attitudes on vaccination across European countries: The Vaccine Safety, Attitudes, Training and Communication Project (VACSATC). Vaccine 2010;28:5731-7. http://dx.doi.org/10.1016/j.vaccine.2010.06.009.
- Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine 2014;32:2150-9. http://dx.doi.org/10.1016/j.vaccine.2014.01.081.
- Report of the SAGE Working Group on Vaccine Hesitancy. Geneva: WHO; 2014.
- Salmon D, Dudley M, Glanz J, Omer S. Vaccine hesitancy: causes, consequences, and a call to action. Vaccine 2015;33:D66-D71. http://dx.doi.org/10.1016/j.vaccine.2015.09.035.
- Dartnall L, Ganguly N, Batterham J. Access to Maternity Services Research Report. London: Department of Health; 2005.
- Liégeois J-P. Roma in Europe. Strasbourg: Council of Europe; 2007.
- Larson H, Smith D, Paterson P, Cumming M, Eckersberger E, Freifeld C, et al. Measuring vaccine confidence: analysis of data obtained by a media surveillance system used to analyse public concerns about vaccines. Lancet Infect Dis 2013;13:606-13. http://dx.doi.org/10.1016/S1473-3099(13)70108-7.
- Brown KF, Long SJ, Ramsay M, Hudson MJ, Green J, Vincent CA, et al. U.K. parents’ decision-making about measles-mumps-rubella (MMR) vaccine 10 years after the MMR–autism controversy: a qualitative analysis. Vaccine 2012;30:1855-64. http://dx.doi.org/10.1016/j.vaccine.2011.12.127.
- ECDC Scientific Advice on Seasonal Influenza Vaccination of Children and Pregnant Women. Stockholm: European Centre for Disease Prevention and Control; 2012.
- Donaldson B, Jain P, Holder B, Lindsay B, Regan L, Kampmann B. What determines uptake of pertussis vaccine in pregnancy? A cross sectional survey in an ethnically diverse population of pregnant women in London. Vaccine 2015;33:5822-8. http://dx.doi.org/10.1016/j.vaccine.2015.08.093.
- Batista Ferrer H, Trotter CL, Hickman M, Audrey S. Barriers and facilitators to uptake of the school-based HPV vaccination programme in an ethnically diverse group of young women [published online ahead of print June 7 2015]. J Public Health 2015. http://dx.doi.org/10.1093/pubmed/fdv073.
- Wong L. Young multiethnic women’s attitudes toward the HPV vaccine and HPV vaccination. Int J Gynecol Obstetr 2008;103:131-5. http://dx.doi.org/10.1016/j.ijgo.2008.07.005.
- Nagata J, Hernández-Ramos I, Kurup A, Albrecht D, Vivas-Torrealba C, Franco-Paredes C. Social determinants of health and seasonal influenza vaccination in adults ≥ 65 years: a systematic review of qualitative and quantitative data. BMC Public Health 2013;13. http://dx.doi.org/10.1186/1471-2458-13-388.
- Brondi L, Higgins M, Gorman D, McCormick D, McCallum A, Fisken S. Review of the Scientific Literature on Drivers and Barriers of Seasonal Influenza Coverage in the EU/EEA. Stockholm: European Centre for Disease Prevention and Control; 2013.
- Travellers’ Perceptions and Experiences of Maternity & Child Health Services. Limerick: Mid Western Health Board; 2009.
- NHS England . GP Patient Survey 2014–15 2015. www.england.nhs.uk/statistics/2015/07/02/gp-patient-survey-2014-15/ (accessed 15 December 2015).
- Ismail SA, Gibbons DC, Gnani S. Reducing inappropriate accident and emergency department attendances: a systematic review of primary care service interventions. Br J Gen Pract 2013;63:e813-20. http://dx.doi.org/10.3399/bjgp13X675395.
- Penson R, Coleman P, Mason S, Nicholl J. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department?. Emerg Med J 2012;29:487-91. http://dx.doi.org/10.1136/emj.2010.107276.
- Time to Act. London: The Royal College of Emergency Medicine; 2015.
- Stan M. Romania’s Threatened Freedom of Speech 2015. www.publicseminar.org/2015/10/romanias-threatened-freedom-of-speech/#.VmAmHnbhDIU (accessed 15 December 2015).
- Hvizdos J. Slovakia 2015. https://freespeechfreepress.wordpress.com/slovakia/ (accessed 15 December 2015).
- Stagg HR, Jones J, Bickler G, Abubakar I. Poor uptake of primary healthcare registration among recent entrants to the UK: a retrospective cohort study. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-001453.
- Burt J, Lloyd C, Campbell J, Roland M, Abel G. Variations in GP-patient communication by ethnicity, age, and gender: evidence from a national primary care patient survey. Br J Gen Pract 2016;66:e47-52. http://dx.doi.org/10.3399/bjgp15X687637.
- Hart JT. The inverse care law. Lancet 1971;1:405-12. http://dx.doi.org/10.1016/S0140-6736(71)92410-X.
- Shack L, Jordan C, Thomson CS, Mak V, Møller H. UK Association of Cancer Registries . Variation in incidence of breast, lung and cervical cancer and malignant melanoma of skin by socioeconomic group in England. BMC Cancer 2008;8. http://dx.doi.org/10.1186/1471-2407-8-271.
- Sutton S, Rutherford C. Sociodemographic and attitudinal correlates of cervical screening uptake in a national sample of women in Britain. Soc Sci Med 2005;61:2460-5. http://dx.doi.org/10.1016/j.socscimed.2005.07.017.
- Maslow A. A theory of human motivation. Psychol Rev 1943;50:370-96. http://dx.doi.org/10.1037/h0054346.
- Cullen S, Hayes P, Hughes L. Good Practice Guide: Working with Housed Gypsies and Travellers. London: Shelter; 2008.
- Van Cleemput P. Health care needs of travellers. Arch Dis Child 2000;82:32-7. http://dx.doi.org/10.1136/adc.82.1.32.
- Freudenberg N, Franzosa E, Chisholm J, Libman K. New approaches for moving upstream: how state and local health departments can transform practice to reduce health inequalities. Health Educ Behav 2015;42:46S-56S. http://dx.doi.org/10.1177/1090198114568304.
- Dyson L, Renfrew M, McFadden A, McCormick F, Herbert G, Thomas J. Promotion of Breastfeeding Initiation and Duration. Evidence into Practice Briefing. London: National Institute for Health and Care Excellence; 2006.
- Routine Postnatal Care of Women and their Babies. London: NICE; 2006.
- Dyson L, Renfrew MJ, McFadden A, McCormick F, Herbert G, Thomas J. Policy and public health recommendations to promote the initiation and duration of breast-feeding in developed country settings. Public Health Nutr 2010;13:137-44. http://dx.doi.org/10.1017/S136898000999067X.
- Gill P, Macleod U, Lester H, Hegenbarth A. Improving Access to Healthcare for Gypsies and Travellers, Homeless People and Sex Workers. London: Royal College of General Practitioners; 2013.
- Monitoring Equalities and Health Inequalities: A Position Paper. London: NHS England; 2015.
- Ryder A, Cemlyn S. Civil Society Monitoring on the Implementation of the National Roma Integration Strategy in the United Kingdom. Budapest: Decade of Roma Inclusion Secretariat Foundation; 2014.
- Dempsey AF, Zimet GD. Interventions to improve adolescent vaccination: what may work and what still needs to be tested. Am J Prev Med 2015;49:445-54. http://dx.doi.org/10.1016/j.amepre.2015.04.013.
- Commissioning Inclusive Services. London: Department of Health; 2013.
- Wemyss R, Matthews Z, Jones H. The National Gypsy and Traveller Health Inclusion Project 2012–2015. Brighton: Leeds GATE and Friends Families and Travellers; 2015.
- Travelling to a Better Future. Gypsy and Traveller Framework for Action and Delivery. Cardiff: Welsh Government; 2013.
- Progress Report by the Ministerial Working Group on Tackling Inequalities Experienced by Gypsies and Travellers. London: Department for Communities and Local Government; 2012.
- Public Bodies (Joint Working) (Scotland) Act 2014. London: The Stationery Office; 2014.
- Butler R, MacDonald NE. Diagnosing the determinants of vaccine hesitancy in specific subgroups: The Guide to Tailoring Immunization Programmes (TIP). Vaccine 2015;33:4176-9. http://dx.doi.org/10.1016/j.vaccine.2015.04.038.
- Budget 2015. London: HM Treasury; 2015.
- Local Authority Public heaLth Allocations 2015/16: In-Year Savings a Consultation. London: DH; 2015.
- Quality Criteria for an Effective Immunisation Programme. London: Health Protection Agency; 2012.
- Conducting Health Communication Activities on MMR Vaccination. Stockholm: European Centre for Disease Prevention and Control; 2010.
- Tracking Anti Vaccination Sentiment in Eastern European Social Media Networks. Geneva: UNICEF; 2012.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- Annual Report 2010/11. Bristol: West of England Strategic Partnership for Travellers Health and Wellbeing; 2011.
- Healthy Child Programme: Pregnancy and the First Five Years. London: DH; 2009.
- Guidance Setting out the Way Forward for the Successful Delivery of Health for All Children (Hall 4) in the Early Years. Edinburgh: The Scottish Government; 2011.
- 2014–15 National Health Visiting Service Specification. London: NHS England; 2014.
- Universal Health Visiting Pathway in Scotland. Edinburgh: The Scottish Government; 2015.
- Public Health Section 7A Commissioning Intentions 2015/16. London: NHS England; 2014.
Appendix 1 Phase 1 participant information sheet
Leaflet for adults
We would like to invite you to take part in our research project.
This leaflet gives information about the project so you can decide if you want to take part.
If you have any questions please ask the person who gave you this leaflet or contact …………………… who is leading the study in York.
This research project is being organised by:


Why are you doing this research project?
We want to find out what Gypsies, Roma and Travellers have to say about vaccinations for their children and for themselves. Some people call vaccinations jabs, jags, needles or immunisations.
Why have I been asked to take part?
We are talking to Gypsies, Roma and Travellers in York, Bristol, Glasgow and London. We would like to talk to young people, parents and grandparents.

What will I have to do?
If you want to take part we will arrange a convenient time and place for us to talk. We can talk to you alone or with others in a group, whichever you prefer. We would like to hear your stories about vaccinations for you, your children and your grandchildren. We would also like to hear your ideas about how we can make it easier for Gypsies, Roma and Travellers to have vaccinations if they want to. We will ask you if it is OK for us to record what you say to us. If you do not want to be recorded, we can take notes instead. We will type up the recording or notes and keep them in a locked filing cupboard. They will not have your name on.

Do I have to take part?
No. It is up to you. If you decide to take part you can still change your mind without saying why. This will not affect the care you receive from the NHS.
What are the good things about taking part?
This research project will help health care workers to understand what is important for Gypsies, Roma and Travellers, and show that it is important to listen to what you have to say. We cannot promise the project will change things for you and your community.
We will give you a £15 gift voucher to thank you for your time.
Are there bad things about taking part?
It takes up some of your time. If we speak to you on your own this will take between 30 minutes and 1 hour. If we speak to you in a group it will take a bit longer, between 1 hour and 1 ½ hours.
Will my doctor be told I am taking part?
No.
Will other people know what I say?
Only our UNITING research team will know what you have said to us. We will write about what Gypsies, Roma and Travellers have to say about vaccination but we will not give your name to anyone.
What do I do now?
If you want to take part in the research project you can tell the person who gave you this leaflet. If you want to you can phone or email our researcher: …………………………………………………………………

If you are unhappy with the project you can contact (name of PI) who is leading it. Tel. xx Email. xx.
Appendix 2 Phase 2 participant information sheet
Participant Information Sheet for Commissioners and Providers of Health Services
We would like to invite you to take part in our study. Before you decide we will explain what the study is about and what it involves. Please read this information. If you have any questions please ask us. Our contact details are at the end of the information sheet.
Why are you doing this study?
The aim of this study is to explore the barriers and facilitators to immunisation uptake in Gypsy and Traveller communities; with a view to identifying ways to improve uptake that are feasible and acceptable to different Gypsy and Traveller communities.
Why have I been asked to take part?
We are working with the English Gypsy community in York. You have been invited to take part because you either provide or commission health services for this community. The UNITING study is also running in Bristol, Glasgow and London.
What does it involve?
If you agree to take part, our researcher will arrange a time and a place of your choice to interview you.
We will ask you about your experiences of providing or commissioning health services for the English Gypsy community, your views on the barriers and facilitators to uptake of childhood and adult immunisations; and your ideas for improving uptake which are appropriate for this community. We will also share with you what we have learnt from interviewing members of the community.
We will ask you if we can record the interview.
Do I have to take part?
No. It is up to you. Even if you decide to take part you can still change your mind without giving a reason why. If we have already started recording the interview we will ask your permission to use that information.
What are the benefits of taking part?
You will be helping the NHS to understand what different Gypsy and Traveller communities think about immunisations and why they choose or choose not to have them. There is very little good research on this.
The aim is to improve immunisation services for Gyspy and Traveller communities in the UK but we don’t promise that the UNITING study will change these for the local English Gypsy community.
What are the disadvantages of taking part?
It takes up some of your time. The interview will take up to 1 hour.
We do not think that the questions we want to ask you are embarrassing or upsetting. If you don’t want to answer a question that is fine. You can choose to stop the interview at any time.
Is the interview confidential?
What you tell us will be strictly confidential. Only our UNITING study team will listen to the interview recording and read the transcript. Your name will not appear in any written reports of the study.
We may ask if we can quote you in our reports and other study outputs (e.g. conference presentations). If you agree to this your name will not be used. We will not share anything you have told us outside the UNITING study team without your permission.
Who has reviewed the study?
All research studies are looked at by an independent group of people called a Research Ethics Committee. This is to protect your safety, rights, wellbeing and dignity. The UNITING study has been approved by the (name of Committee) on behalf of all the study locations.
What happens after the interview?
When we have finished interviewing people who provide or commission health services for the English Gypsy community we will analyse these interview data.
After that we will organise a half day meeting to present about what we have learnt from both the local community and from you. We will invite you to come to that meeting.
At the end of the study we will write a report for our funder and present our findings at conferences and in journal publications. We will send you a summary of the findings.
What do I do now?
A researcher will contact you within the next two weeks to discuss the study. Alternatively if you are interested in taking part or have some questions about the study you can contact (name of researcher, Email. xx. Tel. xx). We will then arrange a time and place for the interview.
Who is organising and funding this study?
This study is being organised by researchers at the University of York and York Travellers Trust. It is being led by (name of PI) at the University of York. You can contact her if you have any concerns about the study.
Email xx. Tel. xx.
The research has been funded by the Department of Health, National Institute for Health Research Health Technology Assessment programme.
Thank you for reading this information.
This study is organised by:


Appendix 3 Phase 3 participant information sheet

Leaflet about a meeting
We would like to invite you to come to a meeting to talk about how we can make getting vaccinations as easy as possible for Gypsies, Roma and Travellers.
This leaflet gives information about the meeting so you can decide if you want to come.
If you have any questions please ask the person who gave you this leaflet or contact Lisa who is running the meeting in York.
This research project is being organised by:


Why are you holding this meeting?
Last year we spoke to over 50 Gypsies, Roma and Travellers in York and asked you to tell us your stories about vaccinations. If you spoke to us last year, thank you! We also spoke to some doctors, health visitors and others who provide vaccinations in York. At this meeting we will tell you what we have learnt and talk about ideas to make getting vaccinations as easy as possible for Gypsies, Roma and Travellers in York.
Why have I been asked to take part?
We want to talk to Gypsies, Roma and Travellers as well as doctors, health visitors and others who provide vaccinations in York.

What will I have to do?
We would like you to come to a meeting on xx to xx at xx. At the meeting there will be about 20 people: some from the local Gypsy, Roma and Traveller community; as well as doctors, health visitors and others who provide vaccinations in York.
There will be coffee and teas when you arrive. Then we will go into small groups to talk about ideas to make getting vaccinations as easy as possible. People from the Gypsy, Roma and Traveller community will be in one group. The doctors and health visitors will be in a different group. After that both groups will come together to share their ideas and we will have lunch.

Do I have to come to the meeting?
No. It is up to you. If you decide to come you can still change your mind without saying why. This will not affect the care you receive from the NHS.
What are the good things about taking part?
You will be able to help the NHS understand how to make getting vaccinations they need as easy as possible for Gypsies, Roma and Travellers in York. We cannot promise the project will change things for you and your community.
We will give you a £25 gift voucher to thank you for your time.
Are there bad things about taking part?
It takes up some of your time. If you come to the meeting it will take up 3 hours of your time.
Will my doctor be told I am taking part?
No.
Will other people know what I say?
Only our UNITING research team will know what you have said to us. We will write about what Gypsies, Roma and Travellers have to say about vaccinations but we will not give your name to anyone.
What do I do now?
If you want to come to the meeting you can tell the person who gave you this leaflet or you can contact (name of researcher, Email x. Tel. x). If you are unhappy with the project you can contact (name of PI) who is leading it Email xx. Tel. xx.
Appendix 4 Phase 1 consent form

Consent Form for Adults
The researcher will read out all of the information on this form to you. Please put your initials or a mark in each box if you agree with the information.
All the information on this form will be kept confidential which means it will not be given to anyone outside the UNITING team.
| I have read/have had read to me and understand the UNITING Leaflet for Adults (Short Version - Version 1.0 Dated 27-08-2013). | |
| My questions have been answered OK. | |
| I understand that taking part is voluntary and that I am free to stop at any time without giving a reason. | |
| I agree to take part. | |
| I agree to let our conversation be recorded. | |
| I understand that things I say may be used in reports and that my name will not be used. | |
| I agree to the University of York keeping a copy of this form that I have signed. | |
| I understand that what I say will be looked at by the UNITING team. I agree to this. | |
| I agree to being invited to take part in a meeting for the UNITING research project. |
Please sign your name or place a mark in the box *.
| Name | Date | * |
| Name of researcher | Date | * |
[One copy to be kept by participant, one copy to be kept by the researcher]
Appendix 5 Phase 2 consent form
Consent Form for Commissioners and Providers of Health and Community Services
Please initial each of the boxes below, then sign and date this form. The information in this form will be kept confidential and will not be given to anyone outside the UNITING study team.
| I confirm I have read and understand the Participant Information Sheet for Commissioners and Providers of Health and Community Services Version 2.0 dated 02-01-2014 for the UNITING study. | |
| I understand that my taking part is voluntary and that I am free to withdraw at any time without giving any reason. | |
| I have had the opportunity to consider the information, ask questions have had these answered to my satisfaction. | |
| I agree to the University of York holding copies of my consent form(s). | |
| I understand that the information I provide in the interview may be used in reports and other study outputs. I understand I will not be identifiable. | |
| I agree to take part in the UNITING study. | |
| I agree that if I end the interview, what I have said up to that time will be used for the study. | |
| I understand that the information I provide will be looked at by the UNITING study team. I agree to this. | |
| I agree to be re-contacted to take part in a workshop for the UNITING study. | |
| I agree to the interview being recorded using a digital recorder. |
Please sign your name in the box *.
| Name | Date | * |
| Name of researcher | Date | * |
[One copy to be kept by participant, one copy to be kept by the researcher]
Appendix 6 Phase 1 topic guide
We want to hear about what you think about jabs, your experiences and how things might be improved. Can I just check do you call them jabs or something else?
Story about jabs
Perhaps you could tell us a story about one of your experiences to do with jabs, anything at all that sticks in your mind.
Interviewer to note what term the participant uses to describe immunisation.
Interviewer to note key issues emerging from story and follow those up using questions and prompts below to ensure all topics are covered (rather than going through the questions below).
What you think about jabs
Have you heard about jabs before today?
Prompts
-
Where have you heard about jabs from?
-
What have you heard?
What do you think jabs are for?
Prompts
-
What do they do?
-
Are they a good or bad idea? Why is that?
-
Do you think the same about all jabs? (for children/adults) Why is that?
-
Where/who do you go to get your ideas from? / Where have you learnt this?
-
Have you always thought the same about jabs?
What do your family think about jabs?
Prompts
-
Are they a good or bad idea? Why is that?
-
Do they think the same about all jabs? (for children/adults) Why is that?
-
Where/who do they get their ideas from? / Where have they learnt this?
-
Do you think the same as them? Why/why not?
What do your friends think about jabs?
Prompts
-
Are they a good or bad idea? Why is that?
-
Do they think the same about all jabs? (for children/adults) Why is that?
-
Where/who do they get their ideas from? / Where have they learnt this?
-
Do you think the same as them? Why/why not?
Can you tell me who you think of as your community?
What does your community think about jabs?
Prompts
-
Are they a good or bad idea? Why is that?
-
Do they think the same about all jabs? (for children/adults) Why is that?
-
Where/who do they get their ideas from? / Where have they learnt this?
-
Do you think the same as them? Why/why not?
What do you think doctors and nurses think about jabs?
Prompts
-
Are they a good or bad idea? Why is that?
-
Do they think the same about all jabs? (for children/adults) Why is that?
-
Where/who do they get their ideas from? / Where have they learnt this?
-
Do you think the same as them? Why/why not?
-
What’s your relationship like with your doctor or any of the other staff at your surgery?
-
Do you trust the health professionals there?
-
How long have you been with that surgery?
-
Do you sometimes go to A&E instead? Why is that? (the health issue or about the people)
-
Who do you prefer to give you your jabs (Dr, Nurse, HV, school nurse, drop in clinic staff, A&E . . .)
-
What’s your relationship like with other authorities in the community (e.g. teachers at school, the police, housing people at local council . . .)
What do you think about or local or national policy about jabs? (by this I mean the local NHS Trust/Foundation Trust/ Health Board (Scotland) and/or the Government)
Prompts
-
Does policy say they are good or bad? What leads you to think that?
-
Where do the people who make local or national policies get their ideas from?
Whose views about jabs are most important to you?
Prompts
Why is that?
Jabs for children
-
Can I just check, does your daughter go to secondary school?
-
If not, when did she stop going to school?
-
Can you tell me a bit about why that is – who makes that decision?
-
What does your daughter do at home? (home schooled, work, etc.)
I would like to now ask you about the jabs your (grand) child/children may have been offered.
Have your (grand) children have been offered any jabs by their doctor or nurse?
Prompts
-
Can you tell me which ones?
-
Did he/she have the jab (s)? Why was that?
-
Who decides in your family about whether your (grand) children have their jabs?
-
Is that the same for any decision about your (grand) children’s health? How/why?
-
Have your (grand) children had all the jabs (s) they have been offered? Why is that?
If ‘yes’ they have had jabs , thinking about the last jab they were offered, can you please tell me what happened.
-
How did you know they were being invited for a jab?
-
Did you get any information about it? If so, what information did you get? How did you get this?
-
What did you do next?
-
What happened in the end? (child had jab / did not have jab)?
-
If they had the jab – where? (clinic/home)
-
Who made that decision? - If not you, why did you decide to agree to it?
-
Overall was it a good or bad experience? Why is that?
Is that what normally happens?
-
If not, can you tell me what normally happens
If ‘no’ they haven’t had jabs:
-
What do you know about the jabs that children are offered?
-
Is it a good or bad idea? Why is that?
-
Do you know anyone whose children have had their jabs? What was their experience?
Jabs for adults
I would like to move on now to ask you about 2 jabs you may have been offered as an adult. Let’s start with flu.
Have you have been offered the flu jab?
If ‘yes’:
Prompts
-
Can you tell me why you think you were offered it?
Thinking about the last time you were offered the flu jab, can you please tell me what happened?
Prompts
-
How were you invited for the flu jab?
-
Did you get any information about it? If so, what information did you get? How did you get this?
-
What did you do next?
-
What happened in the end? (child had jab / did not have jab)?
-
If they had the jab – where? (clinic/home)
-
Who made that decision? - If not you, why did you decide to agree to it?
-
Overall was it a good or bad experience? Why is that?
Is that what normally happens?
-
If not, can you tell me what normally happens
If ‘no’ they haven’t been offered the flu jab:
Prompts
-
What do you know about the flu jab?
-
Who do you think should be offered it?
-
Is it a good idea? Why/Why not?
-
Do you know anyone who has had this jab? What was their experience?
Now let’s talk about the whooping cough vaccine that is given to pregnant women.
Ask the same questions for whooping cough vaccine (if relevant – probably more focus of interviews with young women).
Ideas for increasing take up of immunisations
The last thing I’d like to do is ask you about is your ideas to increase take up of jabs (if you would like to have them), both for your (grand) children and for you.
What makes it hard for you and your (grand) children to have jabs?
Prompts
-
Pick up on points raised earlier in interview (make sure ask about travelling/being settled community views/norms)
-
Has this changed over time?
-
Can I ask has the work you do changed over time? (idea from Christine that harder now to make money from scrapping)
-
Has that made a difference to your (grand) children’s health (immunisations)? How?
What would help you and your (grand) children to have jabs?
Make sure ask about each of these.
Is there anything about the GP practices and the doctor/nurses could do differently?
-
Access – invitations, location (at surgery or at home), timing (scheduled appointments versus drop in)
-
Information about the jabs
-
Reminders about jabs
-
Relationships with doctor/nurse
-
Registering with GP practices
-
Changing GP practices – moving medical records, seeing different doctors/nurses
At a higher level (those in charge) is there anything that the NHS could do differently?
-
The way they plan the jabs they offer and tell people about them
-
Benefits
-
Use social media (e.g. Facebook) to tell people about jabs
-
Advertising campaigns (e.g. TV adverts) to tell people about jabs
Is there anything your community could do differently?
Is there anything your family could do differently?
Is there anything you could do differently?
Is there anything you could do differently?
Of all the ideas you’ve suggested, which ones would you say are the most important to help you and your children get your jabs?
Is there anything else about jabs for children or adults that you want to tell me before we finish?
Collect participant background information.
End interview
Refer to ‘Protocol for Data Collection’ - Interviews.
Appendix 7 Phase 2 topic guide
Introductory question
Can you please tell me about your role?
Prompts
-
How are you involved with the local (name of community)?
-
How is your role linked to health (more specifically immunisations)?
-
How long have you been in this role?
-
Has it changed? – How?
-
Who do you work with and how? (within name of community itself/other commissioners and providers)
-
How does your work link to the City of York Strategy for Travellers/ Recent Health Needs Assessment? (insert similar local documents)
-
How does it link to national policies/strategies? (e.g. Quality Improvement Joint Strategic Needs Assessment in which Travellers are identified as one of 4 vulnerable groups to prioritise)
-
How have you seen local and national (non-health) policies (e.g. housing, rents, scrap metal permits) affect the local (name of community) (ask for examples)
-
What do you think are the key issues for the local (name of community) and how have these been addressed (well or not so well) by your organisation/other local organisations?
If work NOT associated with immunisations, spend time exploring their role in working with Travellers more broadly and ask who should speak with)
Attitudes
How would you describe the attitudes of Travellers from (name of community) towards immunisation?
Can you think of a recent example to share with me?
Prompts
-
Do attitudes vary across different childhood immunisations (e.g. MMR, HPV) – How?
-
Are they different for adult immunisations – How?
-
Have attitudes changed over the generations - How?
-
Have you seen attitudes change within individuals based on their family experience – How?
More generally, how would you describe the attitudes of Travellers from (name of community) towards the professionals in your organisation / take up of healthcare services?
Can you think of a recent example to share with me?
Prompts
-
Strong trust / lack of trust
-
Differences between health professionals
-
Respectful
-
Continuity of relationship important?
Again generally, how would you describe the attitudes of service providers within your organisation towards Travellers from (name of community)
Can you think of a recent example to share with me?
Prompts
-
Respectful
-
Aware of and willing to address literacy and social barriers
-
Have the attitudes of service providers changed towards Travellers over time? – How?
Service provision
Thinking first about childhood immunisations
What childhood immunisation services are provided to/commissioned for the local (name of community) by your organisation?
Prompts
-
Are there specialist services/policies for Travellers?
-
How do these differ for those who are ‘settled’ versus ‘on the road’?
-
How have services changed over time?
-
How good is uptake? – How does this vary across different childhood immunisations? What about HPV?
-
How do you identify and follow-up Travellers who are not up-to-date with their child’s immunisations?
-
Who is targeted as main decision maker for childhood vaccines and how? (i.e. is it Mum?)
-
Have there been any vaccine ‘scares’ locally / any outbreaks of diseases (e.g. measles, whooping cough)? What happened?
What strategies are used to promote and deliver HPV and other teenage immunisations (Tetanus/diphtheria/polio and Men C)?
Prompts
-
Traveller girls who’ve been withdrawn from secondary education
-
Traveller girls whose family don’t want them having the HPV vaccine at school/at all
-
Who is targeted as main decision maker for these teenage vaccines and how?
-
What about Traveller teenage boys? How do you reach them to attend for their teenage injections?
Thinking now about adult immunisations
We are interested particularly in- adult flu and whooping cough for pregnant women.
What adult immunisation services are provided to/commissioned for the local (name of community) by your organisation?
Prompts
-
Are there specialist services/policies for Travellers?
-
How do these differ for those who are ‘settled’ versus ‘on the road’?
-
How have services changed over time?
-
How good is uptake? (across groups of eligible adults – over 65, pregnant, certain health conditions) Why do you think that is?
-
How do you identify and follow-up Travellers who are not up-to-date?
What do you think works well in terms of providing/commissioning immunisation services for the (name of community)? – both childhood and adult
What works less well?
Can you think of recent examples to share with me?
Prompts
Systems to improve access/increase attendance:
-
Outreach / drop-in
-
Registration with GP practice
-
Little red book
-
Overcome literacy barriers,
-
Contact to invite attendance for immunisations
-
Reminders to attend prior to appointment (e.g. when coming for growth monitoring, SMS)
-
Follow ups if don’t attend, rebooking, respectful
-
‘Telling’ people to do it rather than offering immunisation as a choice (emerged as Bristol Roma issue and is important in terms of shared decision-making policy agenda more widely)
Providing information:
-
Taking time to explain reason for immunisation, provide reassurance etc.
-
Gender sensitive (e.g. HPV in girl magazines)
-
Literacy (simple language with illustrations)
-
Interpreters
-
Role of media in GP practices
-
Leaflets at GP practices
-
Links to further information if needed (e.g. clearly explained evidence base)
Is there anything else about immunisations for Traveller children or adults that you want to tell me before we finish?
Or anything about the local (name of community) that we haven’t discussed?
End interview
Collect participant background information.
Appendix 8 Phase 3 consent forms

Consent Form for a Meeting for Travellers
The researcher will read out all of the information on this form to you. Please put your initials or a mark in each box if you agree with the information.
All the information on this form will be kept confidential which means it will not be given to anyone outside of the UNITING team.
| I have read/have had read to me and understand the UNITING Leaflet about a Meeting (Version 2.0 Dated 07-10-2014). | |
| My questions have been answered OK. | |
| I understand that taking part is voluntary and that I am free to stop at any time without giving a reason. | |
| I agree to take part. | |
| I understand that things I say may be used in reports and that my name will not be used. | |
| I agree to the University of York keeping a copy of this form that I have signed. | |
| I understand that what I say will be looked at by the UNITING team. I agree to this. |
Please sign your name or place a mark in the box *.
| Name | Date | * |
| Name of researcher | Date | * |
[One copy to be kept by participant, one copy to be kept by the researcher]
Consent Form for a Workshop for Commissioners and Providers of Health and Community Services
Please initial each of the boxes below, then sign and date this form. The information in this form will be kept confidential and will not be given to anyone outside of the UNITING study team.
| I confirm I have read and understand the Participant Information Sheet for Commissioners and Providers of Health and Community Services -Workshop Version 2.0 dated 29-10-2014 for the UNITING study. | |
| I understand that my taking part is voluntary and that I am free to withdraw at any time without giving any reason. | |
| I have had the opportunity to consider the information, ask questions have had these answered to my satisfaction. | |
| I agree to the University of York holding copies of my consent form(s). | |
| I understand that the information I provide in the workshop may be used in reports and other study outputs. I understand I will not be identifiable. | |
| I agree to take part in the UNITING study workshop. | |
| I agree that if I leave the workshop, what I have said up to that time will be used for the study. | |
| I understand that the information I provide will be looked at by the UNITING study team. I agree to this. |
Please sign your name in the box *.
| Name | Date | * |
| Name of researcher | Date | * |
[One copy to be kept by participant, one copy to be kept by the researcher]
Appendix 9 Phase 1 thematic framework
Theme 1: immunisation and health status
| ID | Age | Immunisation status | Immunisation status of children | Immunisation status of grandchildren | Terminology (jabs, needles, immunisations) | General health status (participant and family) | Literacy |
Theme 2: indirect positive influences on immunisation attitudes/behaviour
| ID | First hand | Second hand (relative) | Second hand (friend) | Second hand (health professional) | Second hand (community) | Other |
Theme 3: indirect negative influences on immunisation attitudes/behaviour
| ID | First hand | Second hand (relative) | Second hand (friend) | Second hand (health professional) | Second hand (community) | Other |
Theme 4: knowledge of immunisation
| ID | Existing/prior knowledge | Source | Knowledge at time of decision | Source | Knowledge at time of having immunisation | Source |
Theme 5: reason(s) for general immunisation behaviour
| ID | Protection against disease | Friends all have them | Advised by health professional | What my parents did | Other |
Theme 6: reason(s) for behaviour for a specific immunisation (if different from general)
| ID | Name of immunisation | Protection against disease | Friends all have them | Advised by health professional | What my parents did | Other |
Theme 7: reason(s) for immunisation beliefs or behaviour for a family member
| ID | Name of immunisation | Protection against disease | Friends all have them | Advised by health professional | What my parents did | Other |
Theme 8: prompt for attending for immunisation
| ID | Name of immunisation | Letter from GP practice | Previously booked appointment | Knew it was due from record | Follow-up for missed appointment | Attended with someone else visiting GP practice | Provided at school | Visit by outreach health professional | Other |
Theme 9: family’s, friends’ and others’ immunisation attitudes and behaviour
| ID | Family member | Partner | Friend | Health professional | School | Community | Media | Intergenerational change |
Theme 10: Barriers to immunisation(s)
| ID | Lack of awareness of need for immunisation | Information difficult to understand | Lack of time from health professional | Hostility/lack of respect towards Travellers | Negative image of Travellers in media | Difficulty accessing services as travelling | Difficulty of registration at GP practice when travelling | Daughter not at school | Mistrust of school-based immunisation | Other |
Theme 11: ideas for interventions – information and culture
| ID | Increased acceptance/integration of Travellers in community | Positive portrayal of Travellers within media | Verbal Information to promote awareness | Simple leaflets including pictures and appropriate text explaining benefits and side effects | Adverts on TV to promote specific immunisation campaigns | Role of older generations to promote immunisations and support attendance for younger generations | Other |
Theme 12: ideas for interventions – access to and quality of health care services
| ID | Increased access to drop-in centres | Outreach services | Availability of GP as trusted health professional | Out-of-hours services | Red Book | Invitation letter/text to attend appointment | Reminder letter/text to attend appointment | Follow-up by health professionals if miss appointment | Being treated with respect by health professional | Easier temporary registration | Other |
Appendix 10 Phase 2 thematic framework
Theme 1: role
| ID | City, job title, organisation, Travellers full/part of role | Communities work with | Time in role/how role changed | Commission services | Provide/manage services | Face-to-face contact | Other |
Theme 2: how work links with other organisations/individuals and national/local strategies
| ID | Nurses, health visitors, school nurses/midwives | GP practices | Housing | Education | Social/welfare services | Public health | Local strategies | National strategies | Other |
Theme 3: previous/current immunisation/Traveller initiatives/programmes and their impact
| ID | Specialist HV for Travellers | Drop-in/pop-up clinics | Flexible appointments | Awareness campaigns | Identify and target Travellers | Community health link worker/peer support | Mobile clinic | Opportunistic immunisation | Other |
Theme 4: perception of level of uptake of immunisations in community (general and specific)
| ID | Name of community | High | Mixed | Low | Changed over time | Settled vs. travelling | Other |
Theme 5: attitudes/behaviours towards Travellers they see health professionals/services have/do
| ID | Stereotype | Frustration | Don’t prioritise/tailor | Unfriendly | Supportive | Other |
Theme 6: community barriers to immunisation (general)
| ID | Large, busy families | Community norms/knowledge | Distrust of services | Don’t self-identify | Poverty | Literacy/language | Housing | Unemployment | Discrimination | Use of health systems | Other |
Theme 7: community barriers to specific immunisations (if different)
| ID | MMR vaccine–autism link | HPV vaccine–sex/cancer link | BCG vaccine | Flu vaccine | Other |
Theme 8: community facilitators of immunisation (general)
| ID | Travel less | Good relationship with health professionals | Experience of the disease/outbreak of disease | Desire for children to be healthy | Integrated into society | Community influencer | Other |
Theme 9: community facilitators of specific immunisations (if different)
| ID | Name of immunisation | See it as important | Other |
Theme 10: service delivery barriers to immunisation
| ID | Poor access to Sites | Breakdown in relationships with community | Staff/funding cuts/cost-effective | Service restructure/changing priorities | Lack of confidence/skills | Lack of linked up working | Inflexible services | Lack of follow-up | Other |
Theme 11: service delivery facilitators of immunisation
| ID | Known to community | Flexible approach | Part of role to work with community | Can-do attitude | Prompt Travellers | Other |
Theme 12: record keeping and monitoring
| ID | CHI system | Red book | Identifying Traveller status in record | Identifying current location of family | Local authority/school data | Patient-held records | Other |
Theme 13: ideas for interventions – information and culture
| ID | Tailored information (content/format/delivery) | Verbal information | Community champions | Pictorial record cards | Word of mouth | Other |
Theme 14: ideas for interventions – service delivery
| ID | Outreach services | Reminders for Travellers | Computer prompts for GP practices | Opportunistic immunisations | Improved follow-up of ‘did not attends’ | Flexibility of services | Linked up working across organisations/professionals | Drop-in clinics/different settings | Sustained funding | Other |
Theme 15: ideas for interventions – commissioning and higher-level policy/development
| ID | Specialist roles | Outreach services | Targeting funding/strategies | Uptake targets for Travellers | Improve access to mainstream services | Other |
Appendix 11 Examples of Feedback to Participants
A YouTube videoclip to present the findings from Bristol is available here: www.youtube.com/watch?v=6AE0EzWZR_I
Summary Report for Service Providers in York
Why was the study undertaken?
There is some evidence of lower levels of immunisation uptake in Traveller communities than in the wider population. Our aim was to explore the barriers and facilitators to immunisation uptake in these communities and to identify possible ideas for interventions to increase uptake.
Who took part in the study?
We interviewed 174 Traveller participants from six Traveller communities in four UK cities: Bristol Romanian Roma, Bristol English Gypsy/Irish Travellers, York English Roma, Glasgow Roma, Glasgow Scottish Show People and London Irish Travellers.
Who took part in York?
In York, we spoke to 48 people from the English Roma community including mothers (19), grandmothers (6), pregnant women (2) and women with no children (3), teenage girls (7), fathers (5), grandfathers (2) and men with no children (4).
Half of those interviewed lived in either a house or flat and half of the participants lived on an official caravan site.
We also interviewed 37 Service Providers in all four cities.
In York we spoke to 9 Service Providers working in a range of services from Public Health, Children’s Services, Screening and Immunisation and Primary Care.
What did we find in York?
Facilitators to immunisation uptake
-
General community view that immunisations are beneficial and protect children
-
Most trust their GP’s advice
-
The majority are happy with written or spoken information received at time of vaccination
-
Current generation of mothers have greater knowledge than previous generations
-
Most receive relevant information from GPs, Health Visitors or family (not friends)
Barriers to immunisation uptake
-
Difficulties for travelling English Roma (discrimination/difficulty in registering with GP practices)
-
Girls not going to secondary school
-
Breakdown in relationship with Health Professionals
-
Problems booking appointments
-
Seeing different Health Professionals hinders trust
-
Community gossip about negative immunisation experiences
-
Discrimination
-
Some concerns about particular vaccinations: adult flu vaccine, HPV, MMR and whooping cough
What was the outcome of the study?
We ran workshops in all 4 cities with Travellers and Service Providers. In York we agreed 5 interventions to increase immunisation uptake:
-
Specialist Health Visitor for Travellers
-
Identify Travellers in health records to tailor support and record take-up of vaccinations
-
Cultural competence training (for GPs, nurses and others who work with Travellers)
-
Accessible immunisation information from GPs and nurses
-
Improved joined-up working among organisations that plan and deliver immunisations
What happens next?
A report of the findings from the 6 Traveller communities is currently being prepared for the funder. Results will be disseminated locally and nationally and published in peer-reviewed journals.
Thank you
We would like to thank all study participants, including York Service Providers for sharing their views and experiences.
This study was organised by:


It was funded by:

Appendix 12 Evidence of meeting the evaluative criteria for qualitative research112
-
The research team across the four cities worked to a data collection protocol, which was developed to ensure consistency of approach. However, from the outset it was recognised that local adaptations would occur and, indeed, these were encouraged. For example, the initial approach to Travellers about the study (see Chapter 2, Access and recruitment) and how the work with community partners was undertaken (see Chapter 2, Community partners) varied across the six Traveller communities to ensure that the most appropriate and acceptable methods were employed for each community. Changes to protocol occurred following deliberation within the research team/with the IPAG, which led to decisions being taken to strengthen the rigour of the study. Specifically, a decision was taken to integrate key issues from phase 1 interviews into the phase 2 topic guides rather than using verbatim quotations, so as not to influence the expressed views of the service providers (see Chapter 2, Data collection). The original method for prioritising the interventions in the phase 3 workshops (nominal group technique)102 was replaced by a method considered to involve more detailed discussion by workshop participants (see Chapter 2, Data collection).
-
Flexibility is also evidenced by two other changes to protocol which occurred directly from a ‘social circumstance’ of the study. Specifically, the upper limit for the sample size for phase 1 interviews was increased to ensure that the sampling criteria were met following the large number of York English Gypsy participants attending for interviews on 1 day; and payment (£75) was needed to recruit primary care professionals in Glasgow (this is the accepted approach in Scotland).
A clear description of the target sample for the three phases of the study, a rationale and how we set out to achieve this is provided (see Chapter 2, Participants).
b. Does the sample produce the type of knowledge necessary to understand the structures and processes within which the individuals or situations are located?To address this question, we reflect on whether or not our recruitment approaches for the three phases of the study allowed for all perspectives to be captured, the characteristics of the sample and any known features of non-participation (see Chapter 3, Interview participants, and Chapter 4, Workshop participants). 105
Phase 1: Travellers-
Recruitment approaches were developed based on the advice of local gatekeepers and community partners (see Chapter 2, Data collection). In four communities (Bristol Roma, York English Gypsy, Glasgow Roma and London Irish Traveller), the Travellers who were approached to take part in the study were those accessing Traveller services, for example an Irish Community Centre in London. To recruit Bristol English Gypsy/Irish Traveller participants, two gatekeepers visited official Travellers sites and for Glasgow Scottish Showpeople a community partner distributed study information among the community. These methods may have led to some selection bias in that those taking part were those who attend services or are known to gatekeepers. However, we saw evidence of snowballing for five communities (all but the Bristol Roma). In York, two Travellers were trained to do interviews on a site in which residents do not tend to access YTT.
-
We achieved our target sample size overall and for five of the six Traveller communities. We did not meet our recruitment target for Glasgow Scottish Showpeople.
-
Bristol Roma: while fewer grandmothers/grandfathers/adolescent girls than intended, there were some from these participant groups.
-
Bristol English Gypsy/Irish Traveller: no grandfathers, only three adolescent girls/young women, grandfathers perhaps less important as unlikely to be decision-makers for immunisations, although data suggested may have views on HPV vaccine, and might have offered a view on adult flu.
-
York English Gypsy: only two grandfathers, again, perhaps not an important gap as unlikely to be decision-makers for immunisations.
-
Glasgow Roma: only three men, so lack of fathers’ and grandfathers’ perspectives.
-
Glasgow Scottish Showpeople: only 14 participants, of whom four were men. No sample targets achieved, but did have participants in each of the targeted family roles.
-
London Irish Traveller: no men, but targets for female roles all met.
-
-
In all six communities, we achieved a good mix of self-reported immunisation status for participants themselves and their children; again, there were some gaps and missing data. Low numbers with no immunisations but might expect them to be a minority? One-third of these data were missing so these data should be viewed with caution. Furthermore, they were based on self-report and sometimes did not tie in with accounts in the interviews.
-
Bristol Roma: no participants reported having children with no immunisations, which is likely to reflect that once Roma families are accessing the NHS they tend to have their children immunised.
-
Bristol English Gypsy/Irish Traveller: no gaps.
-
York English Gypsy: no participants reported having children with no immunisations, but within the interview accounts there clearly was one person.
-
Glasgow Romanian/Slovakian Roma: no participants reported having children with no immunisations which local gatekeepers believe is likely to reflect that once Roma families are accessing the NHS they tend to have their children immunised
-
Glasgow Scottish Showpeople: no participants reported having children with no immunisations, which local gatekeepers suggest is likely to reflect that immunisation is well accessed in this community.
-
London Irish Traveller: no participants reported having children with no immunisation, which local gatekeepers suggest is likely to reflect that immunisation is well accessed in this community.
-
-
For other demographic characteristics which we did not sample on (marital status, employment and housing, age, number of children/grandchildren and residency), we achieved a mix overall and within each community. With the exception that we did not recruit any Travellers who live in unauthorised roadside encampments or unauthorised private sites (no planning permission in place) in any of the six communities so we cannot be sure that our findings are transferable to them. Is this important for each community? In all four cities the majority of Travellers live in the type of accommodation that the study participants lived in, so a very small minority view is missing.
-
We have no reason to believe that the Traveller participants differed to their wider local Traveller community.
-
We did not formally record how many people who were approached declined to take part and the reasons why, so we cannot say if those who declined were different from those who took part.
-
In five of the communities, the same gatekeepers who had approached Travellers about phase 1 interviews, reapproached people (who had agreed to be recontacted) to attend the workshops. For the Glasgow Scottish Showpeople, the researcher who had done the phase 1 interviews made this approach. The intention was to recruit a sample of phase 1 participants, so in that regard, the same issues of selection bias apply here in that we are likely to not have attracted those who do not attend services or those who would not feel confident to participant in a workshop.
-
Our recruitment target was achieved for three of the six communities (Bristol Roma, York English Gypsy and London Irish Traveller). We set out to include Traveller men and women across generations, this was achieved overall. No grandmothers or adolescent girls attended from the Roma community and no Scottish Showpeople adolescent girls. No men from the Glasgow Scottish Showpeople or the Irish Traveller community in London and no fathers from the Bristol English Gypsy/Irish Traveller or York English Gypsy communities attended a workshop. Two grandfathers were present (one Bristol Roma and one York English Gypsy).
-
Just over half (n = 29) of the participants had taken part in a phase 1 interview. At least half in each community except Glasgow Romanian/Slovakian Roma in which none had previously been interviewed. To address this we presented and briefly discussed the findings of the local phase 1 interviews before commencing the prioritisation activity.
-
We did not formally record how many people who were approached declined to take part and the reasons why so we cannot say if those who declined were different from those who took part.
-
To identify potential service provider participants, we drew up a list based on conversations with gatekeepers and local service providers, the interviews with Travellers and service providers and our own knowledge/professional practice. The types of roles and organisations varied across the four cities and we were confident that this was comprehensive.
-
Individuals were then approached using a mix of e-mail and telephone calls.
-
We achieved our target sample size overall and within each city. We aimed to recruit a mix of frontline workers and those in more strategic roles; this was achieved overall as well as an approximate 50–50 spilt in each city.
-
For the other characteristics (which we did not sample on) in each city we included a mix of people with a remit to work with the general population which included working with local Traveller communities as well as those with a specific remit for working with Traveller families.
-
All of those approached in Bristol and London agreed to take part, all except two GP practices in York agreed or found someone else in a similar role to be interviewed, and 14 of 20 approached agreed in Glasgow. Those who declined often suggested that others were better placed to input (for Roma) or that they did not see the needs of the Showpeople to be any different from those of the general population.
-
Individuals were reapproached using the same approach as for phase 2, a mix of e-mail and telephone calls.
-
We met our recruitment target of three or four service providers, with the exception of the workshop with the Glasgow Scottish Showpeople. We achieved our aim to recruit a mix of frontline workers and those working in more strategic/commissioning roles for every city. Sixteen of the service provider participants had taken part in a phase 2 interview. To address this we presented and briefly discussed the findings of the local phase 2 interviews before commencing the prioritisation activity.
-
Two service providers from phase 2 in Bristol declined to attend the workshop as their role had changed; all of those invited in York took part or found a replacement; eight declined in London as they were too busy, not working on that day or it was too far to travel.
To address these questions, we reflect on the ‘richness of the findings and interpretation of data that the research produces’112 by considering whether or not we have adequately displayed the ‘qualitative evidence’ (p. 385)105 specifically the range and diversity of the phenomena (e.g. attitudes, beliefs and behaviours) being studied, associations between phenomena, and our use of visual representations (see Chapter 3, Barriers to and facilitators of uptake of immunisation).
-
For each theme and subtheme we present in detail the range of views that emerged from the Traveller and service provider data. When a view is consistent across Traveller communities this is stated; similarly differences in views across and within communities (by gender, vaccination), as well as between Travellers and service providers, are highlighted. Examples of the data on which these descriptions are based are provided through the use of illustrative quotations.
-
We highlight throughout the chapter when there are linkages between phenomena and present evidence of how these are linked, for example how an intergenerational change towards being more accepting of immunisation is associated with improvements in literacy and development of trustful relationships with health professionals over time. We also identify when particular phenomena are attached to particular Traveller communities or groups of people within those communities. An example here is language barrier faced by the Romanian and Slovakian Roma participants.
-
The themes and subthemes, how they interlink with each other and with the five levels of the SEM are described at the end of Chapter 3. Summary boxes for each theme are included to display the range and diversity in views as well as linkages.
Three types of triangulation105 were used in the study to produce an account that is ‘rich, robust, comprehensive and well-developed’.
-
Methods triangulation: we investigated Travellers and service providers’ views on interventions to increase immunisation uptake in the phase 1 and 2 interviews and the phase 3 workshops and so were able to assess the consistency in views across these different methods.
-
Triangulation of sources: we explored views on the barriers to and facilitators of immunisation uptake expressed by Travellers and service providers across four cities within the phase 1 and 2 interviews, and then compared and contrasted these perspectives from different sources.
-
Analyst triangulation: a team of 13 researchers conducted interviews for the study, seven researchers were directly involved in the data analysis, the descriptive findings documents were reviewed by all of the local researchers, and the final write up of the interview and workshop findings were reviewed by the entire research team. As such, we incorporated the perceptions of multiple team members on these key research processes. These steps will have provided ‘a check on selective perception and illuminate blind spots in an interpretive analysis’.
The views, stories and experiences of Traveller and service provider participants are presented throughout Chapter 3 (see Barriers to and facilitators of uptake of immunisation) along with direct quotations. When participants are talking about their own views, stories and experiences this is clearly distinguished from when people are talking about their perceptions of others’ views, stories and experiences. For example, presentation of Travellers’ own views on their knowledge about, and attitudes towards, immunisation is distinct (and far more extensive) from service providers’ ‘second-hand’ views on this.
4c. To what extent has the researcher rendered transparent the processes by which data were collected, analysed and presented?To address this question, we reflect on whether or not our fieldwork (interviews and workshops) was carried out consistently, if our questioning allowed sufficient opportunity to cover relevant ground, how data were recorded and the completeness and accuracy of this, as well as reflexivity. 105
Phases 1 and 2-
We developed a data collection protocol to ensure consistency across the four cities, while recognising that some differences would be necessary (see Q2 above).
-
The topic guides (for Travellers and service providers) were the same across all four cities while flexible enough to enable local details to emerge. They were informed by the SEM to ensure that we were sure we were asking about immunisation across all five levels of influence (see Chapter 2, Data collection). The Traveller topic guide was reviewed and piloted with community partners (see Chapter 2, Community partners) in York and questions reworded where necessary to be clearer. We used a story-telling approach with the Travellers so that they started with their own story about immunisation rather than being led by the researcher. In the group interviews each participant was asked to tell their own story. We used open-ended questions and prompts, and local terms for the word immunisation to encourage conversation. Some of the interviews using an interpreter were shorter and less detailed than those with English-speaking participants, providing less-rich data.
-
To ensure that we covered the relevant issues with the service providers, we integrated key emerging issues from phase 1 interviews to ensure that issues that were important to the Travellers, with whom these service providers worked with, were discussed (see Chapter 2, Data collection).
-
Response bias may have occurred with participants offering views that they perceived were ‘correct’ rather than what they genuinely thought. Also, most of the interviews were group interviews, usually with family members, meaning that participant responses may have been constrained by others in the interviews.
-
All transcripts were checked for accuracy by the interviewer and corrected when necessary (see Chapter 2, Data analysis). A sample of transcripts of interviews where an interpreter was used was checked for accuracy against the audio-recordings by an independent interpreter. Where the data were incorrect, these were not included in the analysis. Therefore, we are confident that all of the transcripts accurately capture the conversations within the interviews.
-
We developed a programme (see Chapter 2, Data collection) which outlined the steps of the workshop to ensure consistency across the four cities, while recognising that some differences would be necessary, owing to time constraints and the numbers of participants and the use of interpreters. With the exception of the workshop with the Glasgow Scottish Showpeople (for which only one service provider attended), the first session of the workshop where Travellers and service providers worked in two separate groups was the same in each city (ideas for interventions were presented to the group on A4 sheets of paper and prioritised for impact). The second ‘joint’ approach to final prioritisation did not occur in Bristol, and this was done post hoc.
-
The two stages of prioritisation of the interventions were recorded by observers of the workshop sessions and they also took notes to provide background context to those decisions. We are confident that the ranking of the interventions were recorded accurately.
In terms of a reflexive study design, the research team was large (17 people), scattered across the UK, very mixed in terms of experience of working with Travellers and in the field of immunisation as well as personal experience (two team members were Travellers). This encouraged healthy dialogue, throughout the duration of the study, about different team members’ understanding of the study as well as their own beliefs about immunisation and Travellers. Individual’s own perspectives will undoubtedly have impacted on all stages of the study and influenced, for example, how interview questions were asked, and how illustrative quotations were selected.
5. Evidence of theoretical and conceptual adequacy: interpretive validity How does the researcher move from a description of the data to quotation of examples, to analysis and interpretation of the meaning of data: what kind of method is used?A methodical, comprehensive and transparent approach was used for the data analysis for both the interview and the workshop data (see Chapter 2, Data analysis).
Phases 1 and 2-
The data analysis process followed the precise steps of the framework approach105 which enabled the analytic routes to be transparent. A data analysis protocol was produced so that all of the researchers involved in the analysis worked in the same, systematic way.
The constant comparative method114 and deviant case analysis105 are recommended methods for ensuring that data analysis is systematically carried out.
-
The constant comparison method114 was used at three points in the analysis. First, the thematic frameworks (one for Travellers, one for service providers) were developed using the data from Bristol and York and we ensured that the themes and categories within both frameworks applied to both cities. Moreover, constant checks were made to ensure that data for the two cities were adequately captured by the framework. Second, the production of the descriptive findings documents for each Traveller community and for service providers in each city occurred over 2 years. This meant that we could constantly compare the themes within these documents as they were developed with those produced earlier, observe where there were differences and modify them as necessary. Third, in the interpretation/cross-synthesis and write-up stages, for every theme and subtheme the data were interrogated for each Traveller community (and their associated service providers) and compared both within communities (by gender and vaccination) and against other communities meaning that we could be confident in our conclusions of when views are common within and across Traveller communities and when there are important differences.
-
Deviant case analysis105 was also used at two points in the analysis. First, within the descriptive findings documents, any participants with views that appeared different from the majority view for that Traveller community or group of service providers were identified. Second, in the interpretation/cross-synthesis and write-up stages, for every theme and subtheme the majority view and alternative views were identified and presented.
-
To identify the interventions for increasing uptake of immunisations to take to the workshop for discussion we drew on an established method for planning health promotion interventions from a needs assessment (in this study, the phase 1 and 2 interview data). Two independent researchers ‘mapped’ potential strategies to address the barriers to and facilitators of immunisation uptake to produce the list of interventions to take to the first workshop. For the subsequent workshops the interventions (a combination of those taken from the initial list of interventions and additional interventions) were discussed and agreed by the lead researcher and the local research teams.
-
The constant comparison method114 was also used in this process. The initial list of interventions was drawn from the data for the Bristol Romanian and English Gypsy/Irish Traveller communities. For the subsequent communities, the key barriers, facilitators and potential strategies to address these were reviewed against the Bristol list and modified based on local findings.
-
At the workshops we used an established method of prioritising the interventions. 101
To address these questions we consider two types of generalisation that are suggested to have relevance for qualitative research. 105
Representational generalisation-
How far the findings from a study can be generalised to the specific population from which the sample is drawn. Specifically, are we confident that the views of the Traveller and service provider participants in this study can be generalised to the other members of those six communities and other service providers in the four cities?
-
This can be evidenced by the quality of the fieldwork, analysis and interpretation (see criteria 1 and 3–5) and the degree to which the sample is representative of the parent population, not in terms of a statistical match but rather have we achieved the diversity in characteristics that we consider to be important? (See criterion 2. 105)
-
For Travellers (phases 1 and 3) and service providers (phases 2 and 3) we did not record why people declined to take part so we cannot know if they were different from those who participated.
-
In all six communities, we achieved a good mix of family roles across generations (our sampling criteria) and the addition of males with no children in four communities. There were some gaps, some of which may be more important than others.
-
No grandfathers in Bristol English Gypsy/Irish Traveller and London Irish Traveller communities were interviewed, and less than intended participated in the other four communities. We cannot be confident we have sufficiently captured the grandfather view in any community. Suggest that unlikely to be decision-makers for childhood and pregnancy immunisation so not too important. Views on adult flu might be different.
-
No fathers in London Travellers and less than intended (n = 2) for Glasgow Roma and Glasgow Scottish Showpeople. We cannot know what the father perspective is for these communities. Suggest that unlikely to be sole decision-makers for childhood and pregnancy immunisation so not too important.
-
Fewer adolescent girls/young women than intended in Bristol Roma (n = 2) and Bristol English Gypsy/Irish Traveller (n = 3). We cannot generalise on views about HPV vaccination.
-
Fewer grandmothers than intended for Bristol Roma.
-
Consistent views across family roles within communities (very few gender differences, some intergenerational differences) so perhaps should not be too concerned with some gaps.
-
-
We do not have confidence in the immunisation status data, as many data were missing and self-reports were not always consistent with accounts in interviews. In five communities, we had no participants who said that their children had had no immunisations, and only one in the Bristol English Gypsy/Irish Traveller community. We would expect 2% in the general population and perhaps more in Travellers, so should not generalise findings to this non-immunising group in any community.
-
We did not recruit any Travellers who live in unauthorised roadside encampments or unauthorised private sites in any of the six communities, so we cannot be sure that our findings are transferable to them. Our knowledge of these communities suggests this is a small minority view that is missing.
-
Overall, we have no reason to believe that the Traveller participants were particularly different from the rest of their local community.
-
Low numbers of workshop participants for Bristol English Gypsy/Irish Traveller community and two Glasgow communities.
-
No grandfathers attended from four communities and fewer than intended participated in other four communities. Only one Bristol Roma and one York English Gypsy Grandfather were present. We cannot be confident we have sufficiently captured the grandfather view in any community. Suggest that unlikely to be decision-makers for childhood and pregnancy immunisation so not too important. No fathers from any English-speaking communities.
-
No grandmothers or adolescent girls attended from the Glasgow Roma community and no Scottish Showpeople adolescent girls attended.
-
Just over half (n = 29) of the participants had taken part in a phase 1 interview. At least half in each community participated, except for the Glasgow Roma, none of whom had previously been interviewed. Presenting the findings of the local phase 1 and 2 interviews at the start of each workshop meant that ‘new’ participants were informed.
-
We achieved our target sample size overall and within each city. We aimed to recruit a mix of frontline workers and those in more strategic roles; this was achieved overall as well as an approximate 50–50 spilt in each city. These roles varied by city, but participants were identified as ‘key players’. Also in each city we included a mix of people with a remit to work with the general population which included working with local Traveller communities, as well as those with a specific remit for working with Traveller families. Consistent views were evident across professional roles within cities where they had common ground.
-
We met our recruitment target of three or four service providers with the exception of the workshop with the Glasgow Scottish Showpeople. We achieved our aim to recruit a mix of frontline workers and those working in more strategic/commissioning roles for every city. Two-thirds of the service provider participants had taken part in a phase 2 interview. Presenting the findings of the local phase 1 and 2 interviews at the start of each workshop meant that ‘new’ participants were informed.
-
Whether or not the findings from a particular study can be generalised, or inferred, to other settings or contexts beyond the sampled one. Are we confident that the views of the Traveller and service provider participants in this study can be generalised to other Traveller communities across the UK, for example are the views of the Romanian Roma in Bristol generalisable to other Romanian Roma Travellers? Can they be generalised to other minority ethnic groups/disadvantaged groups in society?
-
This can be evidenced by congruence between the ‘sending context’ within which the research is conducted and the ‘receiving context’ to which it is to be applied. To demonstrate this congruence, it is necessary to provide a detailed description of the characteristics of the participants and the setting so can assess the similarity.
-
Pairs of communities, that is Romanian Roma participants in Bristol and Glasgow, Irish Travellers in Bristol and London, and English Gypsies in Bristol and York, appear to have similar social circumstances.
-
All six communities appear to have similar social circumstances (housing/travelling, discrimination, poverty, education, literacy, language) to other communities of the same descent, for example Irish Travellers, Roma,12,13 across the UK.
List of abbreviations
- A&E
- accident and emergency
- BCG
- bacillus Calmette–Guérin
- CCG
- Clinical Commissioning Group
- CHI
- Child Health Information
- DVD
- digital versatile disc
- EU
- European Union
- GP
- general practitioner
- HPV
- human papillomavirus
- IPAG
- independent project advisory group
- MMR
- measles, mumps and rubella
- NICE
- National Institute for Health and Care Excellence
- PCT
- primary care trust
- PIS
- participant information sheet
- SEM
- social ecological model
- TV
- television
- UNICEF
- United Nations International Children’s Emergency Fund
- UNITING
- UNderstanding uptake of Immunisations in TravellIng aNd Gypsy communities study
- WHO
- World Health Organization
- YTT
- York Travellers Trust