Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 12/152/01. The contractual start date was in September 2013. The draft report began editorial review in December 2014 and was accepted for publication in March 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Luke Vale is a member of the funding panel for the National Institute for Health Research (NIHR) Programme Grants for Applied Research and NIHR Health Technology Assessment. He is also a Director of the NIHR Research Design Service in the North East. Stephen C Robson is a panel member of NIHR Efficacy and Mechanism Evaluation. Catherine Nelson-Piercy is a co-developer of the Royal College of Obstetricians and Gynaecologists green-top guideline on management of nausea vomiting and hyperemesis gravidarum.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by O’Donnell et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
Background
Nausea and vomiting in pregnancy (NVP) is one of the most common symptoms of pregnancy affecting 50–85% of all women during the first half of pregnancy. 1 Symptoms usually start between 6 and 8 weeks of gestation, rise to a peak before the end of the first trimester and, in the majority of women, resolve by 20 weeks. 2 Most women (65–70%) self-manage their symptoms with avoidance of dietary triggers and oral hydration. 2 However, in the remainder, symptoms are more severe and/or protracted, leading to physical and psychosocial sequelae. These can include reduced quality of life (QoL), lost work time and negative effects on relationships with family and friends. 3
The most severe form of NVP is referred to as hyperemesis gravidarum (HG), and is reported to affect 0.3–1.0% of pregnant women. 1 It is characterised by intractable vomiting, dehydration, ketosis, electrolyte imbalance, nutritional deficiencies and weight loss (usually defined as > 5% of pre-pregnancy weight). However, there is no widely accepted point at which NVP becomes HG. Likewise, the distinction between studies of women with NVP and HG is generally not possible as the degree of dehydration and weight loss prior to the intervention are rarely reported. Furthermore, although some studies report baseline symptom severity using a validated scale, this is insufficient to make a diagnosis of HG. For these reasons, study populations are seldom described as having HG, and are more frequently defined in terms of the severity of NVP. Therefore, for the purposes of this review, studies on interventions for both NVP and HG have been included.
Aetiology
The underlying pathophysiology of NVP/HG is poorly understood but is thought to involve a combination of biological, physiological, psychological and sociocultural factors. 4
Genetic factors increase the risk of occurrence: results from a Norwegian study which included over 500,000 women found that the risk of HG was 15.2% in the second pregnancy of women who had a previous history of HG compared with 0.7% in women who did not [odds ratio (OR) 26.4, 95% confidence interval (CI) 24.2 to 28.7]. 5 The risk of developing HG is also increased threefold in the daughters of women who suffered from HG (unadjusted OR 2.9, 95% CI 2.4 to 3.6). 6
Endocrine factors, especially higher levels of human chorionic gonadotropin, as is the case in multiple or molar pregnancies, have been associated with more severe forms of NVP/HG. A recent observational study found that free human chorionic gonadotropin and pappalysin-1 (also known as pregnancy-associated plasma protein A) were higher in women suffering from HG than in non-sufferers. 7
Gestational transient thyrotoxicosis, has been reported in 60% of women suffering from HG8 and thyroid-stimulating hormone levels are raised in women with HG. 9 Certain human chorionic gonadotropin subtypes can stimulate thyroid-stimulating hormone receptors and so contribute to the hyperthyroidism. The degree of hyperthyroidism has been found to correlate with the severity of NVP/HG. 10 Higher levels of oestrogen, progesterone and leptin, and lower levels of adrenocorticotrophic hormone and prolactin have also been associated with HG. 11
Delayed gastric emptying related to relaxation of smooth muscle during pregnancy may influence NVP symptoms. Furthermore, higher rates of Helicobacter pylori infection have been noted in women suffering from HG:11 in a meta-analysis of 25 studies investigating the association of H. pylori and HG, 14 studies demonstrated an increased risk of HG in infected women (with OR between 2.42 and 109.3), and 11 studies found no association. 12
Lack of a definitive physiological trigger for HG has, in the past, led to numerous psychosomatic and psychological theories such as resentment or ambivalence towards the pregnancy, immaturity, conversion disorder, symptom of hysteria, neurosis or depression. 13 It is now more commonly accepted that psychological afflictions are a consequence of the condition rather than a cause. 4,9
Impact on patients
Severe NVP causes emotional and psychological distress and can have a profound effect on a women’s QoL, behavioural and cognitive function, affecting work capacity, household activities and interaction with children. 14–16 Women with HG report feeling isolated, depressed and lonely, unable to cope with routine daily interactions or simple tasks. Two recent observational studies found higher incidences of depression, anxiety and stress in women diagnosed with HG compared with controls. 17,18 Following cessation of symptoms the depression, anxiety and stress scores took several weeks to resolve,18 not returning to control values until the third trimester. 17 However, in some women these psychological symptoms do not fully resolve and can result in post-traumatic stress disorder. 19
As a result women make greater use of health-care resources. Based on Hospital Episode Statistics data for England, there were nearly 26,000 admissions for NVP/HG in 2010–11 with an average length of stay of 2 days. 20 These NHS costs are likely to underestimate the full costs as women may purchase a variety of products over the counter, pay for alternative therapies, receive treatment in primary care settings or as a hospital outpatient, and may incur extra child care, living costs and lost earnings. In addition, the associated increased risk of cognitive, behavioural and emotional dysfunction in pregnancy18 may prompt the use of further services and resources.
In the absence of a definitive cause, management of NVP/HG tends to focus on the alleviation of symptoms and prevention of serious morbidity. Typically, women are admitted to hospital, prescribed intravenous (i.v.) fluid therapy and antiemetic medication, but there is little time spent dealing with their psychological, social and emotional needs or providing information and guidance about the condition. The result is that women can feel unsupported, dissatisfied with care and experience negative interpersonal interactions with health-care providers. 21
Finally, severe NVP/HG has implications for offspring. A recent systematic review and meta-analysis reported that women with HG were more likely to deliver preterm (OR 1.32, 95% CI 1.04 to 1.68) and to have a baby that was small for gestational age (OR 1.28, 95% CI 1.02 to 1.60), although there was no evidence of an association with congenital anomalies (pooled results from three studies: OR 1.17, 95% CI 0.68 to 2.03) or perinatal death (OR 0.92, 95% CI 0.61 to 1.41). 22 A large Swedish birth cohort reported that women with HG who had their first admission in the second trimester were at increased risk of preterm pre-eclampsia (OR 2.09, 95% CI 1.38 to 3.16), placental abruption (OR 3.07, 95% CI 1.88 to 5.00) and to have a baby that was small for gestational age (OR 1.39, 95% CI 1.06 to 1.83), suggesting an association between HG and placental-mediated disease. 23
Assessment and diagnosis
The diagnosis of NVP/HG is made after excluding differential diagnoses, including gastrointestinal disorders, urinary tract infection, metabolic and endocrine disorders, drugs, psychological disorders (such as eating disorders) and other pregnancy-associated conditions (in particular molar pregnancy). However, there is currently no widely accepted approach to measuring the severity of symptoms in women. The most commonly used tools for the assessment of NVP/HG severity are presented in Table 1, with actual examples of the tools provided in Appendix 1.
| Tool | Description |
|---|---|
| PUQE score | Three questions regarding nausea, vomiting and retching during previous 12 hours (PUQE-24 = previous 24 hours) For each component: 0 = no symptoms, 5 = worst possible symptoms Maximum score = 15 Scores of ≥ 13 indicate severe symptoms24–26 |
| RINVR | Contains total of eight questions about duration/amount, frequency and distress caused by symptoms of nausea, vomiting and retching For each component: 0 = no symptoms, 5 = worst possible symptoms Maximum score = 40 Scores of ≥ 33 indicated severe symptoms27–29 |
| McGill Nausea Questionnaire (measures nausea only) | Contains a nausea rating index (nine sets of words which describe sensory, affective, evaluative and miscellaneous afferent feelings related to nausea that patients rank) An overall nausea index (0–5, where 0 = no symptoms, 5 = excruciating symptoms) Plus a VAS: 0 cm = no nausea, 10 cm = extreme nausea30,31 |
| NVPI | Three questions relating to nausea, retching and vomiting over the past 7 days For each component: 0 = no symptoms, 5 = worst possible symptoms Maximum score = 15 A score of ≥ 8 indicates severe symptoms32,33 |
| VAS | Patients rate their symptoms on a scale of 0–10, where 0 = no symptoms, 10 = extreme symptoms |
However, although the measurement of NVP/HG symptom severity is the main aim for women and practitioners, other wider outcomes are also relevant when assessing the broader effectiveness of interventions. Thus, key secondary outcomes in studies to date have included both measures related to maternal physical and psychosocial health, and fetal or neonatal outcomes (Table 2).
| Maternal: physical | Maternal: psychosocial | Fetal/neonatal |
|---|---|---|
| Admission/readmission rate | QoL (SF-12 or SF-36 score) | Congenital abnormality |
| Length of hospital stay | General Health Questionnaire | Low birthweight (< 2.5 kg) |
| Antiemetic/other medication use | Pregnancy-specific QoL measure | Small for gestational age (< 10th centile) |
| Amount/duration i.v. fluid administration | NVP specific questionnaire | Preterm birth (before 37 weeks’ gestation) |
| Enteral/TPN | Satisfaction with care | 5-minute APGAR score |
| Side effects | Direct costs to woman/family | Stillbirth/intrauterine death |
| Economic costs (hospital/medical care) | Time lost from work | Neonatal death |
| Adverse pregnancy outcomes | Edinburgh Postnatal Depression Scale | Spontaneous miscarriage |
| Weight loss | Admission to special care baby unit | |
| Therapeutic termination of pregnancy | Infant development outcomes |
Current interventions for nausea and vomiting in pregnancy/hyperemesis gravidarum
For the purposes of this report, interventions are considered in three broad groups:
-
First-line interventions, usually initiated by women before seeking medical care and hence tend to be used in less severe NVP.
-
Second-line interventions, typically prescribed when a women presents to medical care. Initially this is likely to be a general practitioner (GP) in primary care but may involve referral of women with more severe symptoms for inpatient, outpatient or day case care in hospital.
-
Third-line interventions, reserved for women in hospital with persistent or recurrent symptoms despite second-line therapies.
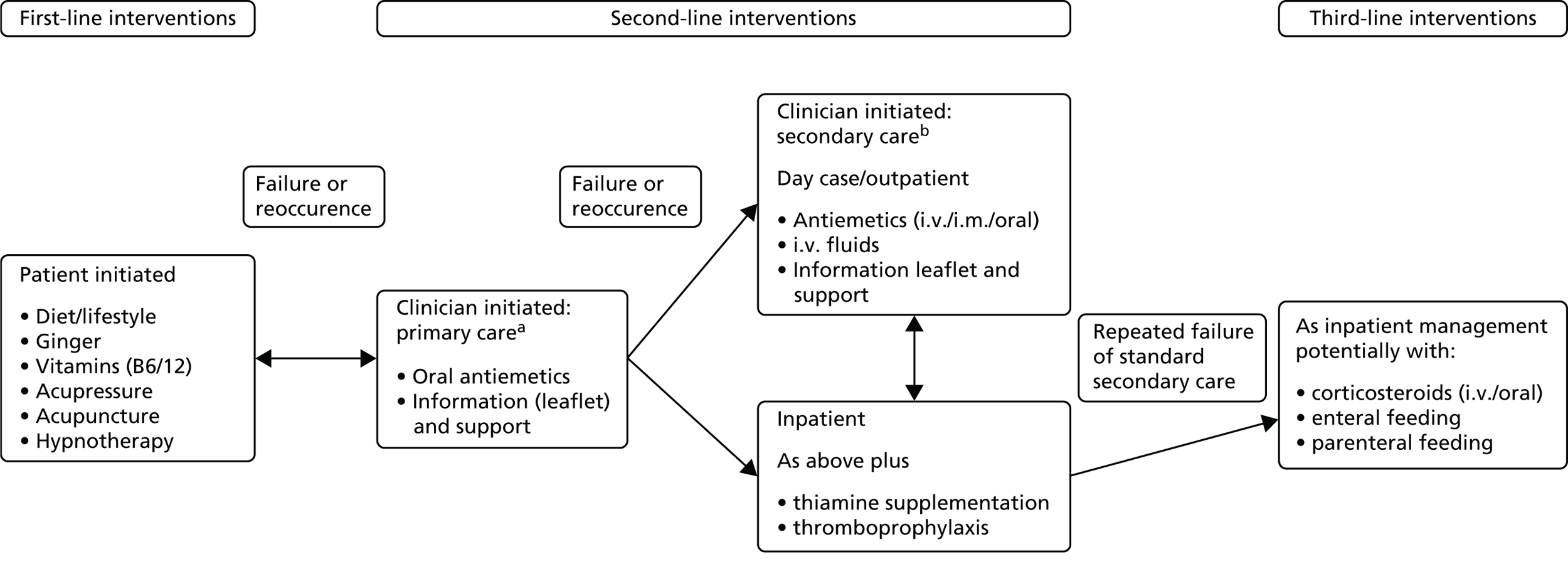
The relationship between these three intervention groups is described in Figure 1, with key individual interventions described in detail in the following sections.
FIGURE 1.
Treatments for NVP. a, Care may also involve urine ± blood tests, weight and maternal observations; and b, care will involve urine and blood tests, weight, maternal observations and pelvic ultrasound. i.m., intramuscular.
Patient-initiated first-line interventions
When first experiencing the symptoms of NVP, women often access information, advice and services from a variety of sources. Information is readily available regarding simple lifestyle changes, dietary modifications and alternative therapies via the internet and in pregnancy magazines. ‘Self-help’ interventions also include a range of supplements that are available ‘over the counter’. Many women try one or more of these before seeking medical advice.
Dietary/lifestyle interventions
Women report using a range of dietary/lifestyle interventions (e.g. increasing oral fluid intake, eating small frequent meals, eating bland foods/protein-predominant meals and avoiding spicy, odorous and fatty foods, and stopping iron-containing multivitamins). 2,34
Vitamins
Vitamins are vital nutrients. They are available over the counter as single vitamin or multivitamin preparations.
Vitamin B6 (pyridoxine) A water-soluble vitamin essential for many metabolic processes within the body. Usually taken in doses of 10–50 mg up to four times daily to treat NVP.
Vitamin B12 (cyanocobalamin) A water-soluble vitamin essential for normal function of the nervous system, red blood cell formation and many other metabolic processes.
Ginger
Ginger (Zingiber officinale) is considered a food supplement (not a drug) and is available in several preparations; powdered fresh root, tablets, capsules and syrup. Its antinausea properties were first described in traditional Chinese medicine. 35
Acupressure/acupuncture
Acupressure involves the application of physical pressure to specific acupuncture points; with respect to NVP this involves the pericardium 6 (P6) point near the wrist.
Acupuncture involves the manipulation of thin needles inserted into acupuncture points in the skin.
Hypnotherapy
Hypnotherapy employs direct suggestion of symptom removal with the subject under hypnosis.
Aromatherapy
Aromatherapy was first used by ancient civilisations for cosmetics, perfumes and drugs. It involves the use of plant materials, aromatic plant and essential oils to alter mood, cognitive, psychological or physical well-being. Oils can either be applied topically via massage, via inhalation or via emersion mixed with water. Common uses include stress and anxiety relief, to uplift mood or counter depression. Evidence surrounding efficacy and safety remains unclear for some treatments.
Clinician-prescribed second-line interventions
Second-line interventions tend to be used for more severe symptoms either instead of or, less frequently, in addition to, first-line interventions. These may be initiated either in primary care by the GP or in a secondary care hospital setting.
Antiemetic drugs
Antiemetic drugs include antagonists to histamine, acetylcholine, dopamine and 5-hydroxytryptamine (5-HT3) receptors in the chemoreceptor trigger zone, vestibular apparatus and visceral afferents. Dyspepsia symptoms which often accompany NVP are also often treated with H2 receptor blockers (e.g. ranitidine) or proton pump inhibitors (e.g. omeprazole). 2
Antihistamines (H1 receptor blockers) are probably the most widely used antiemetics and include doxylamine, meclizine, diphenhydramine, hydroxyzine, dimenhydrinate and cyclizine. Doxylamine is sometimes used in combination with vitamin B6 (pyridoxine). This combined therapy could be used as a treatment option in countries where Diclectin® (Duchesnay Inc.; delayed release doxylamine, 10 mg, plus pyridoxine, 10 mg, available in Canada and the USA but not the UK) is not available. 36
Dopamine antagonists are known to stimulate gastrointestinal motility, so encouraging the transit of substances through the stomach. They also work centrally by antagonising the action on D2 receptors in the chemoreceptor trigger zone. Several phenothiazines including promethazine and prochlorperazine have been used to treat NVP/HG. Other drugs in this class used to treat NVP/HG include metoclopramide, domperidone, droperidol and trimethobenzamide.
5-HT3 receptor antagonists (selective serotonin receptor antagonists) are commonly used to treat chemotherapy and post-operative induced nausea and vomiting which is caused by release of 5-HT3 from the upper small intestine. The action of 5-HT3 receptor antagonists are mediated through the central chemoreceptor trigger zone and peripheral (intestinal and spinal) 5-HT3 receptors.
Intravenous fluids
Administration of i.v. fluids treats the consequences of NVP/HG rather than the symptoms. Women who are severely dehydrated and ketotic need hospital admission and i.v. fluid and electrolyte replacement. This is routinely carried out in either a day care ‘outpatient’ setting or on an inpatient ward.
Clinician-prescribed third-line interventions
Third-line interventions are reserved for women who have severe and persisting symptoms and associated weight loss and dehydration (although latter may have been corrected). Although commenced while the women are in hospital, some of these interventions may be continued on an outpatient basis.
Corticosteroids
Steroids are being increasingly used in refractory cases of NVP/HG which have been unresponsive to other treatments (i.v. hydrocortisone 100 mg twice daily, followed by oral prednisolone 40–50 mg, reducing to a maintenance dose).
Enteral feeding and total parenteral nutrition
Enteral feeding refers to the delivery of nutrients directly into the stomach, duodenum or jejunum. For women who cannot tolerate enteral nutrition, the use of total parenteral nutrition (TPN) has been reported in case series but use is associated with significant maternal morbidity. 37
Interventions presented in the report but not routinely used to treat nausea and vomiting in pregnancy
Diazepam
Diazepam in a benzodiazepine drug used to treat, for example, anxiety, panic attacks, insomnia and seizures. It enhances the effects of the neurotransmitter gamma-aminobutyric acid which leads to central nervous system depression. Its use results in sedation, long-term use results in physical dependence.
Clonidine
Clonidine is a centrally acting α2 adrenergic agonist and imidazoline receptor agonist. It is usually used to treat hypertension, attention deficit hyperactivity disorder and, less commonly, anxiety disorders, withdrawal, migraine and certain chronic pain conditions. Observational data suggests that it may be effective in the treatment of refractory nausea and vomiting. 38
Gabapentin
Gabapentin was originally synthesised to mimic the action of the neurotransmitter gamma-aminobutyric acid, but acts on various brain receptors. It is generally used to treat seizures and neuropathic pain, with less common uses including the treatment of generalised anxiety disorders, restless leg syndrome and itching caused by various aetiologies. It has previously been associated with improvements in refractory nausea in a small study of breast cancer patients. 39
Current guidance and use of therapies within the NHS
Currently there are no national guidelines within the NHS pertaining to NVP/HG; however, the Royal College of Obstetricians and Gynaecologists are in the process of producing said guidelines which should be published in early 2016. Initially, GPs may try different antiemetics before referring women to hospital. Traditionally, secondary care would involve admission to either an antenatal or gynaecology ward for treatment with i.v. fluids, antiemetics and vitamin supplements. Oral intake would gradually be resumed followed by discharge back into the community. Resumption of symptoms would result in readmission and a repeat of previous care, possibly trying different antiemetics or a combination thereof.
Increasingly, more obstetric and gynaecology units are using ‘day case’ management as the first option for initial referrals. Care usually involves some form of rapid rehydration and treatment with an i.v. antiemetic, followed by discharge with oral antiemetics, ideally with advice, support and guidance regarding self-help measures. However, assessing symptom severity, as well as the packages of care, vary substantially and lack a strong evidence base.
When available, day case, outpatient management does result in fewer admissions to hospital. Consequently, women who are admitted tend to be suffering from more severe symptoms. These women are likely to have had repeated hospital attendances and to have tried a number of different combinations of interventions. This latter group of women are likely to experience persistent severe symptoms, weight loss, electrolyte imbalance and failure to cope. In some of these women corticosteroid therapy may be considered an appropriate option when more conventional options have failed. In rare circumstances where this proves unsuccessful, enteral or parenteral nutrition may be instigated and, as a last resort, some women will opt for termination of pregnancy.
Aims and objectives
This study aimed to:
-
review systematically the evidence of the clinical effectiveness and cost-effectiveness of each treatment for NVP/HG
-
determine which therapies are most likely to be cost-effective for implementation into the UK NHS
-
identify and prioritise future research needs.
Structure of the report
The following chapter (see Chapter 2) describes the methods employed for the systematic review and synthesis of evidence for interventions for HG and/or NVP. Chapter 3 provides an overview of the identified evidence, including the quality of the included studies, and a brief discussion of the issues that arose in attempting to synthesise the emergent data. Chapters 4–17 detail the findings for each individual intervention, focussing on the evidence for their effectiveness in terms of nausea, vomiting and retching. Chapter 18 presents the methods and results of the economic evaluation. Key issues considered likely to be important from the perspective of both patients and health-care practitioners are described in Chapters 19 and 20. The implications of the results of this review are discussed in depth in Chapter 21, with the final conclusions outlined in Chapter 22.
Chapter 2 Methods for the systematic review of effectiveness
General methodology
The systematic review followed the approach suggested by the Evidence for Policy and Practice Information and Co-ordinating Centre at the Institute of Education, London. The review protocol was registered with PROSPERO, the International Prospective Register of Systematic Reviews,40 and it aimed to systematically appraise and summarise the evidence on available interventions for NVP/HG within the three broad groups described in Chapter 1:
-
first-line interventions
-
second-line interventions
-
third-line inpatient interventions.
The review examined the evidence for these groups of interventions in relation to their clinical effectiveness and associated adverse events, and their cost-effectiveness.
Inclusion criteria
Types of studies
Randomised controlled trials (RCTs), non-randomised comparative studies and population-based case series were deemed eligible for inclusion. The latter design was included primarily to facilitate calculation of estimates of rare adverse events and fetal outcomes, and for treatments reserved for the most severe cases such as TPN.
Types of participants
Participants were women experiencing nausea, vomiting and/or retching in pregnancy where recruitment to a trial took place before 20 weeks’ gestation. As HG is difficult to differentiate from severe or intractable NVP, two approaches were used initially to identify relevant populations of women. First, studies were selected where their study samples were reported as suffering severe symptoms using published scales and cut-points for severity [e.g. Pregnancy-Unique Quantification of Emesis and Nausea (PUQE)25 ≥ 13, the Rhodes Index of Nausea, Vomiting and Retching (RINVR)27 ≥ 33]. These cut-off points are well correlated. 25 For studies of mixed levels of severity, the study was included if > 80% of participants exceeded these cut-offs. Second, studies were selected if, using the authors’ definition, women in the study sample were defined as having severe symptoms. Similarly, studies were included if > 80% of the sample met this definition. However, due to the inconsistent application of severity scales both within and across studies, and to ensure completeness, a broader selection of studies was deemed eligible for inclusion than originally anticipated. Details of the method used by authors to define severity were recorded for all eligible studies.
Types of interventions and comparators
All pharmacological and non-pharmacological interventions relevant to the NHS for delivery in the community, and in hospital, either as an inpatient or an outpatient, were deemed relevant for this evidence synthesis. These interventions included dietary/lifestyle interventions; vitamins such as vitamin B6 and vitamin B12; ginger; acupressure/acupuncture; hypnosis; antiemetic drugs [such as antihistamines; dopamine antagonists, hydroxytryptamine (5-HT3) receptor antagonists]; corticosteroids; i.v. fluids; enteral feeding; and TPN. Studies were included that had a comparative group for assessment of relative effectiveness. This was either a no treatment group, a treatment as usual group or an alternative intervention group. For the treatment as usual group we endeavoured to clearly define what this entailed. For rare fetal or adverse outcomes and for studies investigating treatments for women with the most severe symptoms (e.g. TPN), no comparator group was defined as the target studies were population-based series.
Types of outcome measures
Primary outcomes
Severity of symptoms [such as PUQE,25 RINVR,27 McGill Nausea Questionnaire,30 Nausea and Vomiting of Pregnancy Instrument (NVPI) and34 visual analogue scales (VASs)41–43] (see Table 1).
Secondary outcomes
Duration of symptoms (reported period of symptoms, date of symptom relief); study-specific measures of NVP; health-related QoL; health-care utilisation (including admission and length of stay of the woman, readmission to hospital of the women, admission and length of stay on special care baby units); patient satisfaction; maternal weight; fetal outcomes [fetal or neonatal death, congenital abnormalities, low birthweight (< 2.5 kg), preterm birth (before 37 weeks’ gestation) or small for gestational age (birthweight < 10th centile)]; adverse events, for example pregnancy complications (as reported in the study), but including haemorrhage, hypertension, pre-eclampsia and proteinuria; costs (as defined by the study authors); and cost-effectiveness (as defined by the study authors) (see Table 2).
Search strategy
The search strategy was designed and executed by an experienced information specialist in collaboration with the rest of the research team. The original protocol stated that the search strategy would combine the two main conditions of pregnancy and NVP/HG with associated interventions and QoL outcomes. However, given both the extensive array of interventions used to address NVP/HG, and the relatively small available literature in this field, it was subsequently decided not to restrict the scope of the review by including key interventions or outcomes as search terms. Although such a strategy increases the number of papers to be reviewed; it minimises the risk of missing any relevant studies. The search was therefore structured around two core concepts: (1) nausea, vomiting and HG; and (2) pregnancy. Key words for both concepts were coupled with relevant medical subject heading (MeSH) and thesaurus terms. The search strategy was designed in MEDLINE and translated as appropriate to the other databases. All terms were truncated as appropriate and variant spellings were used. In order to reduce the number of studies returned, search filters for the relevant study types (RCTs or case series studies) were applied where possible. No time or language limit was set.
The full list of search terms for MEDLINE is presented in Table 3.
| A. HG | B. Pregnancy | C. Nausea/vomiting | D. Exclusions |
|---|---|---|---|
| exp Morning Sickness/ | Pregnancy/ Pregnancy Complications/ |
Nausea/ Vomiting/ Sialorrhea/ |
Animals/ not humans Letter/ Editorial/ News/ exp Historical Article/ Anecdotes as Topic/ Comment/ |
| (morning sickness or hyperemesis gravidarum).ti,ab. | (pregnan$ adj5 (sick or sickness or nause$ or vomit$ or retch$ or dry heave or heaving or emesis or hyperemesis or ptyalism or hypersalivat$ or sialorrh$ or spitting)).ti,ab. | ||
We searched the following electronic bibliographic databases on the dates described below, with update searches executed between the 11 and 16 September 2014 unless otherwise stated. As our initial scoping search highlighted the number of complementary medicine interventions for NVP/HG, the search was extended to include additional key databases of non-English-language studies44 (Latin American and Caribbean Health Sciences Literature and China National Knowledge Infrastructure).
-
MEDLINE (Ovid) 1946–November 2013, searched 10 December 2013.
-
EMBASE (Ovid) 1980–2013 week 50, searched 12 December 2013.
-
Cochrane Central Register of Controlled Trials (Wiley) issue 11 2013, searched 16 December 2013.
-
Cochrane Database of Systematic Reviews (Wiley) issue 11 2013, searched 16 December 2013.
-
Database of Abstracts of Reviews of Effects (Wiley) issue 11 2013, searched 16 December 2013.
-
Cumulative Index to Nursing and Allied Health Literature (EBSCOhost) 1981–November 2013, searched 17 December 2013.
-
British Nursing Index (NHS Healthcare Databases) 1992–January 2014, searched 22 January 2014.
-
PsycINFO (Ovid) 1806–December week 2 2013, searched 17 December 2013.
-
Commonwealth Agricultural Bureaux (CAB) Abstracts (Ovid) 1910–2013 week 49, searched 18 December 2013.
-
Latin American and Caribbean Health Sciences Literature (http://regional.bvsalud.org), searched 18 December 2013.
-
Allied and Complementary Medicine Database (NHS Healthcare Databases) 1985–January 2014, searched 22 January 2014.
-
Science Citation Index (Web of Knowledge) 1970–November 2013, searched 18 December 2013.
-
Social Science Citation Index (Web of Knowledge) 1970–November 2013, searched 18 December 2013.
-
Scopus, searched 8 January 2014.
-
Conference Proceedings Index – Science (Web of Knowledge) 1990–November 2013, searched 18 December 2013.
-
ClinicalTrials.gov searched 8 January 2014.
-
NHS Economic Evaluation Database (Wiley) issue 11 2013, searched 16 December 2013.
-
Health Economic Evaluations Database (Wiley), searched 30 January 2014.
-
China National Knowledge Infrastructure (http://eng.cnki.net/grid2008/index.htm), searched 14 March 2014.
In addition, the reference lists of included papers and key relevant literature reviews identified during the search process were also examined for additional relevant studies, and Obstetric Medicine vol. 1(1) (September 2008) and vol. 7(2) (June 2014) were hand-searched. Furthermore, the following websites of relevant organisations were also searched in order to source as much unpublished literature as possible:
-
Motherisk (URL: www.motherisk.org/women/drugs.jsp; accessed September 2014).
-
American Congress of Obstetricians and Gynecologists (URL: www.acog.org/; accessed September 2014).
-
Pregnancy Sickness Support (PSS) (URL: www.pregnancysicknesssupport.org.uk; accessed September 2014).
-
National Institute for Health and Care Excellence Clinical Knowledge Summaries (URL: http://cks.nice.org.uk/nauseavomiting-in-pregnancy; accessed September 2014).
-
Hyperemesis Education and Research (URL: www.helpher.org/health-professionals/treatments/index.php; accessed September 2014).
-
UK Teratology Information Service (UKTIS) (URL: www.uktis.org/) including checking the references of the following relevant documents:
-
treatment of NVP (December 2013)
-
use of promethazine in pregnancy (October 2010)
-
use of vitamin B12 in pregnancy (September 2013)
-
use of pyridoxine (vitamin B6) in pregnancy (January 2011)
-
use of ginger in pregnancy (March 2013).
-
-
European Medicines Agency (URL: www.ema.europa.eu/ema/; accessed September 2014).
-
ProQuest Dissertations and Theses – UK & Ireland (URL: www.theses.com/; accessed September 2014).
-
e-thesis online service (URL: http://ethos.bl.uk/; accessed September 2014).
-
Trip (URL: www.tripdatabase.com/; accessed September 2014).
-
System for Information on Grey Literature in Europe (URL: www.opengrey.eu/; accessed September 2014).
-
Google Scholar (URL: https://scholar.google.co.uk; accessed September 2014).
First exclusion process
All records were imported into a bibliographic referencing software programme (EndNote v.X7; Thomson Reuters, CA, USA). Duplicate records were identified and deleted. The remaining references were assessed for relevancy by two independent investigators on the basis of the title and abstract (or title only if abstract not available). Papers were considered relevant to the systematic review if they met the inclusion criteria detailed in Inclusion criteria.
All of the titles and abstracts of all references were read by both investigators and classified as potentially eligible, not eligible or unclear within EndNote. Reconciliation of the resultant EndNote databases was conducted via Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA, USA) and any discrepancies were discussed. In case of doubt, papers went through to the next stage of the exclusion process. Full-text copies of those papers identified as of potential relevance were obtained.
Second exclusion process
All full-text English-language papers obtained were assessed by two investigators independently and classified as relevant, not relevant or unclear on the basis of the same inclusion criteria. Any disagreements at this stage were resolved by discussion between the two researchers. Full-text papers published in languages other than English (German, French, Portuguese, Arabic, Chinese, Korean, Danish and Spanish) were assessed by native speakers of the relevant languages, working alongside one of the two investigators to ensure consistency and adequate compliance against the specified inclusion criteria. Tables of studies excluded at this stage were prepared, detailing reasons for exclusion.
Data extraction
Information from all papers identified as meeting the specified inclusion criteria was extracted using a structured data abstraction form. Key data extracted from eligible papers included:
-
study characteristics (bibliographic details, setting, intervention type, study population including definition of severity)
-
methodology and reporting
-
quantitative findings and conclusions.
For English-language papers, data extraction was carried out by one researcher and checked by another. For papers published in languages other than English, data extraction was carried out by a native speaker working alongside an investigator to identify and translate the relevant information. The data abstraction form for clinical effectiveness is presented as Appendix 2.
Risk of bias in included studies and quality assessment
The quality of the included studies was evaluated in accordance with the comprehensive approach advised by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group. 45 The risk of bias of included RCTs was assessed with the Cochrane Collaboration’s tool46 (see Appendix 3 for full details). This included assessment of sequence generation; allocation concealment; blinding; selective reporting of outcomes; incomplete outcome data; and other possible sources of bias. For the incomplete outcome data item, we coded the satisfactory level of loss to follow-up for each outcome as ‘low risk of bias’, if fewer than 20% of patients were lost to follow-up and reasons for loss to follow-up were similar in all study arms. Disputes were resolved by discussion with another member of the review team. The risk of bias for case series studies was assessed using the component-based tool developed by the Effective Public Health Practice Project (EPHPP), Canada47 (see Appendix 4), which possesses a relatively high degree of inter-rater reliability in comparison to alternative tools. 48,49 For English-language papers, quality assessment was conducted independently by two investigators, with any disputes resolved by discussion. For papers published in languages other than English, quality assessment was carried out by a native speaker working alongside an investigator.
We had initially used an objective approach to make decisions about overall risk of bias; if at least one item was adjudged as being at high risk of bias then the trial was given a high risk of bias overall rating. Similarly, a trial that had no items scored as being at high risk of bias, but at least one was at an unclear risk of bias, then the trial was deemed to be at an unclear risk of bias. This meant that only trials that were scored at low risk of bias for all six risk of bias items could get an overall low risk judgement. Instead, we used a robust approach to assess overall risk of bias in a study, and which did not simply rely on a vote counting approach. This approach gave careful consideration to all six risk of bias item judgements, and the impact of unclear and high risk of bias in individual items, given the scope and context of the trial. For example, if a study had adequately addressed five of the six individual risk of bias items, but a placebo-controlled trial was unblinded in some capacity (either patients, personnel or both), then we scored this trial as being at high overall risk of bias, as this flaw in the conduct of such a trial could seriously impact on the results. However, in some trials blinding was not possible due to the type of interventions being compared so although the individual ‘blinding’ risk of bias item was scored as being at high risk of bias, this did not necessary mean the overall risk of bias in the study would follow. If other items were generally at low risk of bias, and we deemed blinding to be of little relevance, then we scored the study as being at low overall risk of bias. Justification for overall decisions has been provided where necessary.
In addition, two researchers independently assessed all included studies for the potential for imprecision, inconsistency and indirectness of results, using GRADE guidelines. 50–54 Summary of findings (SoF) tables were not presented due to the narrative nature of the review and the heterogeneity of the outcomes.
Data synthesis
First, the range of interventions, populations and outcomes that have been studied were described. The direction and size of the reported effects from effectiveness studies were presented overall, as well as grouped according to population, intervention type, outcomes and study design. Results are summarised in tables. Groups of studies using similar definitions of severity were identified, based on the data extracted and expert opinion. A coding frame was developed for the different definitions used, which was checked by the second systematic reviewer. Two clinical specialists within the research team then grouped the studies into the coding frame. The grouping produced was compared and any discrepancies, including definitions that did not fit into the coding frame, were resolved by discussion.
Meta-analysis was considered to be inappropriate due to heterogeneity, as will be illustrated in the overview of included studies chapter (see Chapter 3). This judgement was made after consideration of interventions, trial populations, and especially the reporting and definitions of outcome measures and methods. We also explored whether data from different studies could be transformed on to a common scale (e.g. symptom severity might be recoded into number no longer experiencing severe symptoms) using imputation and subject to sensitivity analysis and methods, but this was not possible. Therefore it was not necessary for the team to investigate the validity of performing mixed-treatment (indirect) comparisons, using appropriate methods to compare interventions that have not been compared directly with each other. 55,56 Heterogeneity could not be assessed by visualisation of results or, where relevant in statistical terms, by the chi-squared test for homogeneity and the I2 statistic as specified a priori. Instead, a narrative synthesis was conducted, with the effects split into numerous categories and classes of intervention comparison described in the following chapter (see Chapter 3, Interventions and comparators and Table 6). Trials with more than two randomised groups may appear in more than one category depending on the comparisons made.
Data on effectiveness, fetal outcomes and adverse events were tabulated and described narratively, including variation in the form, setting, study population and delivery of the interventions. Given the inconsistencies in the application of both published and author-defined severity scales, studies were recategorised by clinical experts on the review team according to whether the participants were predominantly suffering from mild, moderate or severe NVP/HG. The effects are generally presented in terms of whether or not there were statistically significant differences between randomised groups at the last time point at which outcomes were assessed. However, where possible, magnitude of effects was reported such as a mean difference or risk ratio with corresponding 95% CIs. All studies are included in the narrative synthesis, irrespective of their risk of bias but the weight of evidence is discussed accordingly. Where necessary, comments are made in the text to advise caution for serious methodological shortcomings as well as applying the GRADE approach50–54 in the overall assessment of the quality of the evidence, although SoF tables were not constructed (see Risk of bias in included studies and quality assessment).
Owing to limited available data, it was not possible to examine publication bias using funnel plots as specified in the original review protocol. We were also unable to conduct subgroup analyses to explore the variation with pre-determined factors (e.g. the setting in which the intervention was applied and the severity and duration of symptoms at baseline) or sensitivity analyses to explore the impact of study design, including variation in definitions of outcomes, on measures of effectiveness due to lack of suitable data.
Chapter 3 Clinical effectiveness: overview of included studies
Studies identified
A flow chart of the studies is shown in Figure 2. In total, 11,830 papers were identified from the combination of standard electronic databases (n = 11,659), specialist Chinese databases (n = 102) and various sources of grey literature (n = 69). Of these, 5152 duplicate papers were identified and deleted (5150 from the standard electronic databases, and two from the grey literature).
FIGURE 2.
Flow chart of clinical effectiveness literature.
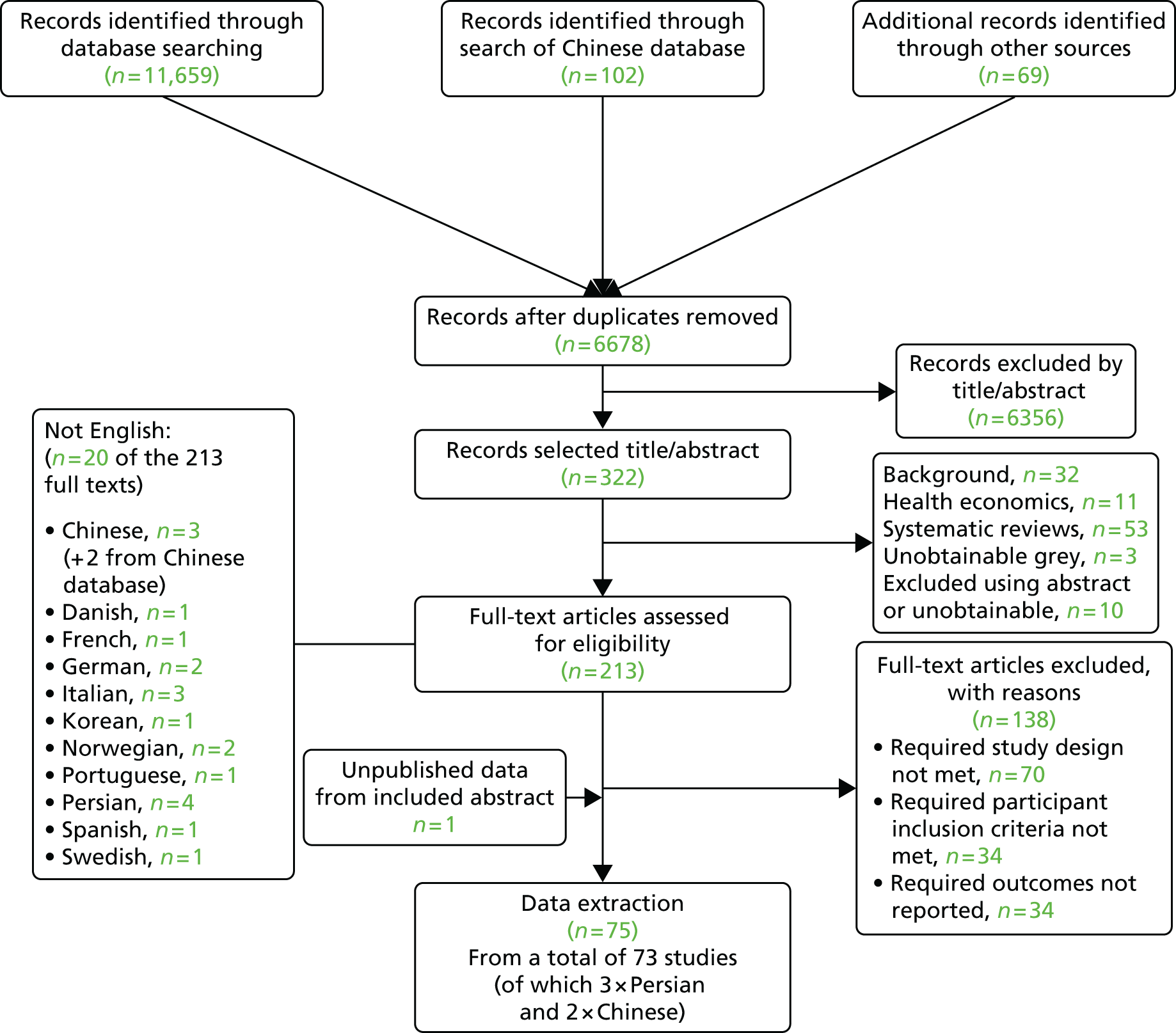
The deletion of duplicate papers left 6678 individual papers for assessment. After screening titles and abstracts, 322 papers were identified as of potential relevance and full-text copies of 309 papers were obtained (with the remainder unobtainable). Of these, 96 were judged ineligible for the effectiveness review and immediately excluded (narrative overviews, systematic literature reviews or economic evaluations). After the second exclusion process, comprising more detailed reading of each full-text paper, a further 138 papers were judged not to meet the inclusion criteria of the review and were also excluded.
Key reasons for exclusion were duplicate paper already included; participant inclusion criteria for the identified study judged not relevant to our review; did not include any of the pre-specified outcomes; or ineligible study design (no comparator group).
As a result, 75 papers were identified for data extraction, from a total of 73 separate studies. A full list of included studies is provided as Appendix 5. A table of excluded studies detailing reasons for exclusion is provided as Appendix 6.
Quality of included studies
Randomised controlled trials
Overall risk of bias
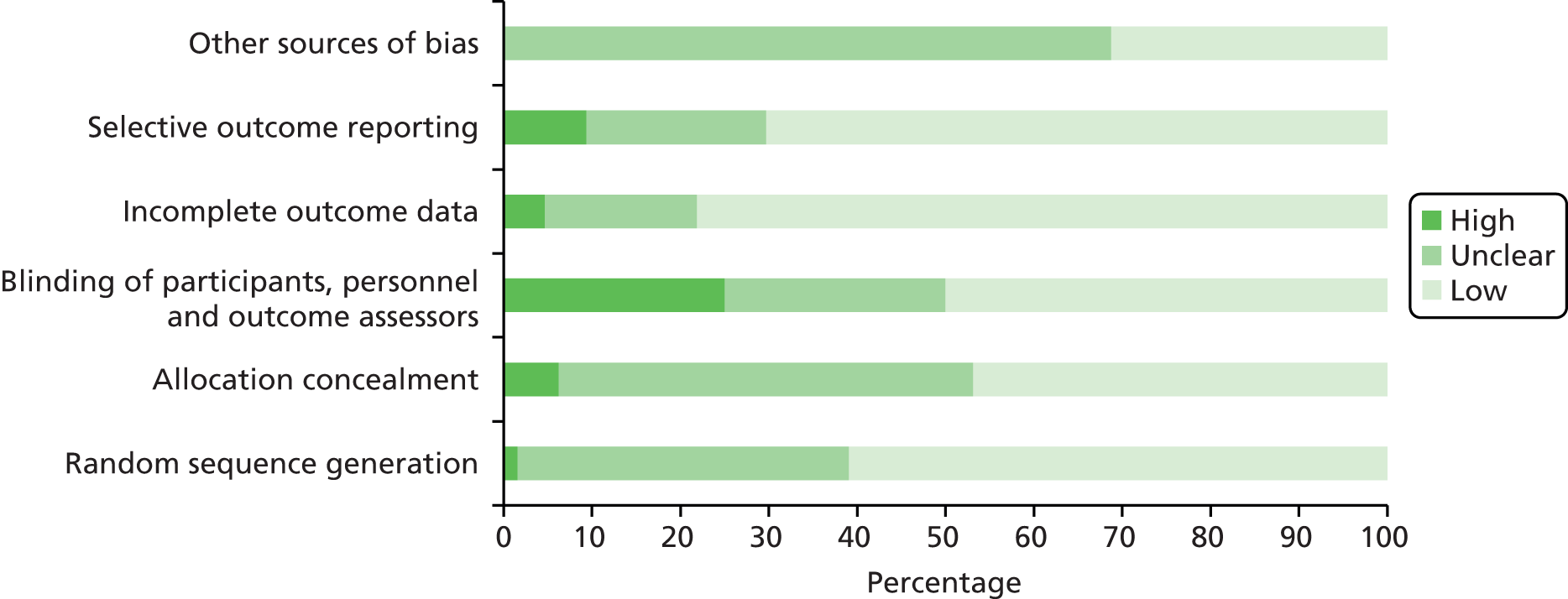
The results of the quality assessment procedure for the 64 included RCTs (reported in 66 papers) are displayed in Figure 3 and Table 4. There was variation both in terms of the quality of the studies and the quality of the reporting. In a large number of papers, there was insufficient detail provided to permit clear judgement of risk of bias in a range of key areas. Overall, 33 RCTs were classed as having low within-study risk of bias, 11 RCTs were classed as having high within-study risk of bias, and the remainder (n = 20) were classed as unclear in this respect. The high proportion of studies at unclear risk of bias was due to poor reporting and a lack of detail, particularly in the methods section. There were also a number of publications in abstract form only. As an unclear judgement was often due to poor reporting rather than specific methodological concerns, it was not judged appropriate to categorise studies with those deemed at high risk of bias as a result of more serious methodological flaws. Our robust approach to the assessment of the overall risk of bias within individual studies is described in more detail in Chapter 2, Risk of bias in included studies and quality assessment. More detail is provided below to illustrate the range in quality in terms of each individual component of the Cochrane’s risk of bias tool. 46
FIGURE 3.
Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included RCT studies.
| Study | Random sequence generation | Allocation concealment | Blinding of participants, personnel and outcome assessors | Incomplete outcome data | Selective outcome reporting | Other sources of bias | Within study risk of bias | Comments |
|---|---|---|---|---|---|---|---|---|
| Abas 201457 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Adamczak 200758 | ? | ? | ✗ | ? | ? | ? | Unclear | Abstract form only, blinding of participants and personnel not possible |
| Babaei 201459 | ? | ? | ✓ | ✓ | ✓ | ? | Unclear | Double-blind RCT, but methods of sequence generation and allocation concealment not reported |
| Basirat 200960 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Bayreuther 199461 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Belluomini 199462 | ✓ | ? | ✓ | ✗ | ✓ | ✓ | Low | Most women lost to follow-up and attrition between groups was similar |
| Biswas 201163 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Bondok 200664 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Can Gurkan 200843 | ? | ? | ? | ? | ✓ | ? | Unclear | Study at unclear risk of bias |
| Capp 201465 | ? | ? | ? | ✓ | ✓ | ? | Unclear | Study at unclear risk of bias |
| Carlsson 200066 | ✓ | ✓ | ✗ | ? | ✓ | ? | Low | Not possible to blind personnel to acupuncture and acupuncture placebo |
| Chittumma 200767 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Diggory 196268 | ? | ? | ✗ | ✗ | ? | ? | High | Study at high risk of bias |
| Ditto 199969 | ✓ | ? | ? | ? | ? | ? | Unclear | Study at unclear risk of bias |
| Ensiyeh 200970 | ✓ | ? | ? | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Erez 197171 | ? | ? | ✓ | ✓ | ✓ | ✓ | Low | Labelled as double-blind crossover RCT and predates 1996 CONSORT statement |
| Eftekhari 201372 | ? | ✗ | ✓ | ✓ | ✓ | ? | Unclear | Study at unclear risk of bias |
| Evans 199373 | ? | ✓ | ? | ? | ? | ? | Unclear | Study at unclear risk of bias |
| Fischer-Rasmussen 199174 | ? | ? | ✓ | ✓ | ✓ | ✓ | Low | Labelled as double-blind crossover RCT and predates 1996 CONSORT statement |
| Ghahiri 201175 | ? | ? | ✗ | ✓ | ✓ | ? | Unclear | Study at unclear risk of bias |
| Ghani 201376 | ✓ | ✓ | ? | ✓ | ✓ | ? | Low | Study at low risk of bias overall, but did not report control results |
| Haji Seid Javadi 201377 | ? | ? | ✗ | ? | ? | ? | High | Vitamin B6 tablets and ginger capsules given so trial unblinded |
| Heazell 200678 | ? | ✓ | ✗ | ✓ | ✓ | ? | Unclear | Study at unclear risk of bias |
| Hsu 200379 | ? | ? | ✓ | ? | ? | ? | Unclear | Study at unclear risk of bias |
| Jamigorn 200780 | ✓ | ✓ | ✗ | ✓ | ✓ | ? | Low | Not possible to blind personnel to acupressure and acupressure placebo |
| Kashifard 201381 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Keating 200282 | ✓ | ✓ | ✓ | ✓ | ? | ? | Low | Study at low risk of bias |
| Knight 200183 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Koren 201084 | ? | ✓ | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Maina 201485 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Maltepe 201386 | ✓ | ? | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Mao 200987 | ✓ | ✗ | ✗ | ✓ | ✗ | ? | High | Study at high risk of bias |
| McParlin 200888 | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | Low | Not possible to blind patients or personnel to interventions in this trial |
| Mohammadbeigi 201189 | ✓ | ✓ | ✗ | ✓ | ✓ | ? | High | Personnel member gave medicines to patients and conducted randomisation |
| Monias 195790 | ? | ? | ✓ | ? | ✗ | ? | High | Unclear whether or not this was truly a RCT and outcomes selectively reported |
| Naeimi Rad 201291 | ✓ | ? | ✗ | ✓ | ✓ | ? | Low | Not possible to blind personnel, but patients were blinded to sham devices |
| Narenji 201292 | ? | ✗ | ✗ | ✓ | ✓ | ? | High | Study at high risk of bias |
| Nelson-Piercy 200193 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Neri 200594 | ✓ | ? | ? | ✓ | ✗ | ? | High | Selective reporting of outcomes and just 2/6 core risk of bias items satisfied |
| Oliveira 201395 | ? | ? | ? | ? | ? | ? | Unclear | Study at unclear risk of bias |
| Ozgoli 200996 | ? | ? | ✗ | ✓ | ✓ | ✓ | Unclear | Unclear details on whether or not trial was truly randomised, personnel unblinded |
| Pasha 201297 | ? | ? | ? | ✓ | ✓ | ? | Unclear | Study at unclear risk of bias |
| Pongrojpaw 200742 | ? | ? | ? | ✓ | ? | ✓ | Unclear | Study at unclear risk of bias |
| Rosen 200398 | ✓ | ✓ | ? | ✓ | ✓ | ? | Low | Not possible to blind personnel, but patients were blinded to sham devices |
| Saberi 201313 | ✓ | ? | ✗ | ✓ | ✓ | ✓ | Low | Trial of acupressure, ginger and no treatment so blinding not possible |
| Safari 199899 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Sahakian 1991100 | ✓ | ? | ✓ | ? | ? | ? | Unclear | Study at unclear risk of bias |
| Smith 2002101 | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | Low | Not possible to blind personnel to sham control, but possible to blind patients |
| Smith 2004102 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Sripramote 2003103 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Steele 2001104 | ? | ? | ? | ✓ | ✓ | ? | Unclear | Study at unclear risk of bias |
| Sullivan 1996105 | ? | ✓ | ✓ | ✓ | ? | ? | Unclear | If no change in nausea or emesis was observed after 48 hours of medication and hydration, patient was considered a treatment failure, but unclear if included in final analyses |
| Tan 2010106 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Tan 2009107 | ✓ | ✓ | ? | ✓ | ✓ | ? | Unclear | Placebo used Tic Tac® (Ferrero UK Ltd, Greenford, UK) which could potentially lead to unblinding |
| Tan 2013108 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | Low | Study at low risk of bias |
| Veciana 2001109 | ? | ? | ? | ? | ? | ? | Unclear | Study at unclear risk of bias |
| Vutyavanich 199541 | ✓ | ? | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Vutyavanich 2001110 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Werntoft 2001111 | ✗ | ? | ? | ✗ | ? | ? | High | Study at high risk of bias |
| Wibowo 2012112 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Low | Study at low risk of bias |
| Willetts 2003113 | ✓ | ? | ✓ | ✓ | ✗ | ? | High | Selective reporting of outcomes and just 3/6 core risk of bias items satisfied |
| Yost 2003114 | ✓ | ? | ? | ✓ | ✗ | ? | High | Selective reporting of outcomes and just 2/6 core risk of bias items satisfied |
| Zhang 2005115 | ✓ | ✗ | ✗ | ✓ | ✗ | ? | High | Study at high risk of bias |
| Ziaei 2004116 | ? | ? | ✓ | ✓ | ✓ | ? | Unclear | Study at unclear risk of bias |
Random sequence generation
The risk of bias arising from the method of generation of the allocation sequence was low in 39 of the included RCTs. 13,41,57,60,62–64,66,67,69,70,76,80–83,85–89,91,93,94,98–104,106–108,110,112–115 Methods employed included random number tables, computer-generated sequence generation61,63,64,81–83,88,93,94,98,99,106,108,112,114 and randomised block design. 62,67,80,87,89,91,101,102,107,113,115,117 One trial was classed as high risk because women were asked to draw an envelope from a box with the same appearance but with different contents. 111 It was categorised as unclear in the remaining 24 RCTs due to insufficient information provided by the authors to permit judgement either way. 42,43,58,59,65,68,71–75,77–79,84,90,92,95–97,104,105,109,116
Allocation concealment
Thirty studies employed allocation concealment methods judged to carry low risk of bias, such as the use of sequentially numbered sealed opaque envelopes containing allocation assignment. 57,60,61,63,64,66,67,73,76,78,80–85,88,89,93,98,99,102,103,105–108,112,118 Thirty studies did not provide sufficient information to allow a judgement of low or high risk and were therefore classed as unclear. 13,41–43,58,59,62,65,68–71,74,75,77,79,90,91,94–97,100,104,109,111,113,114,116,117 The remaining four RCTs were judged as having high risk of allocation concealment bias. 72,87,92,115 For example, one study stated that patients were randomly divided into two groups by those involved in the study,72 or the nature of the intervention being tested meant it was not possible to conceal allocation. 87,92,115
Blinding of participants, personnel and outcome assessors
Of the included RCT studies, 32 were judged to have low risk of bias in relation to the blinding of participants and other personnel involved in the trial,41,57,59–64,67,71,72,74,79,81–85,90,93,99,100,102,103,105,106,108,110,112,113,116,117 generally through the provision of medication in identical formats for both active and placebo. Sixteen studies were judged to have high risk of bias in this respect, for example due to clear differences in either the appearance, dosage rates or mode of delivery between intervention and placebo comparator, or as a result of evidence that the research staff involved were aware of allocation status. 13,58,66,68,75,77,78,80,87–89,91,92,96,101,115 In some instances, however, despite lack of blinding, the nature of the intervention meant that this was not relevant; for example, in McParlin and colleagues88 where blinding of participants and staff was not possible as the packages of care delivered to the intervention and control groups varied in content. However, it is important to highlight that although it might not have been possible to blind patients or clinicians, outcome assessors and analysts handling the resultant data may nevertheless have been blinded. The remaining 16 studies did not provide sufficient information to permit a judgement of low or high bias, often due to imprecise, poor reporting, and were thus classed as unclear. 42,43,65,69,70,73,76,94,95,97,98,104,107,109,111,114
Incomplete outcome data
Most studies (n = 50) were judged as carrying low risk of bias in relation to this component. 13,41,42,57,59–61,63–65,67,70–72,74–76,78,80–85,87–89,91–94,96–99,102–108,110,112–118 Although published protocols were rarely available, all data for the primary outcomes pre-specified in the paper were reported for all randomised participants, or rates of drop-out were either sufficiently low (< 20%), or proportionately comparable between groups, so that it was not considered likely to result in a clinically relevant bias. Three studies displayed a high risk of bias in this regard, all as a result of high numbers of participant drop-outs. 62,68,111 The remainder (11 studies in total) were judged as unclear due to lack of sufficient information. 43,58,66,69,73,77,79,90,95,100,109
Selective outcome reporting
Six studies were judged as having high risk of bias in terms of selective outcome reporting, due to either not reporting data for pre-specified outcomes, or for reporting data in the results that were not pre-specified in either the original study protocol or methods section. 87,90,94,113–115 Forty-five studies were classed as having low risk of bias, with all outcomes specified and subsequently reported. 13,41,43,57,59–67,70–72,74–76,78,80,81,83–85,88,89,91–93,96–99,101–104,106–108,110,112,116,117 Risk of bias was judged as unclear for the final 13 studies. 42,58,68,69,73,77,79,82,95,100,105,109,111
Other sources of bias
Twenty of the included RCT studies were judged as having low risk of bias in this area. 13,41,42,61,62,64,67,70,71,74,81,83,88,96,101–103,106,110,112 However, a substantial number (n = 44) were classed as unclear, due to lack of sufficient information in the paper to permit detailed assessment of whether or not an important risk of bias existed, or due to insufficient rationale or evidence that an identified problem had introduced serious levels of bias to the study. 43,57–60,65,66,68,69,72,73,75–80,82,84,85,87,89–95,97–100,104,105,107–109,111,113–117,119 For example, in one paper,76 lack of reporting of full results for the control group resulted in an unclear judgement in this area.
Case series studies
The nine case series or non-randomised studies were quality assessed using the component-based EPHPP tool,47 which appraises studies on the basis of six core components, rated 1–4 (where 1 is deemed to be the highest quality of study). These areas are selection bias; strength of overall study design; extent to which confounders were identified and controlled for in the study; blinding of participants and/or research personnel; approach to data collection; and rate of withdrawals/drop-outs from study. As shown in the Table 5, all studies were judged as weak in terms of quality (which corresponds to a high risk of bias judgement using the standard Cochrane approach for RCTs).
| Study | Selection bias | Study design | Confounders | Blinding | Data collection method | Withdrawals and drop-outs | Overall rating |
|---|---|---|---|---|---|---|---|
| Alalade 2007120 | 2 | 3 | 3 | 3 | 1 | 4 | Weak |
| Ashkenazi-Hoffnung 201336 | 2 | 3 | 3 | 2 | 3 | 1 | Weak |
| Einarson 2004121 | 1 | 3 | 3 | 3 | 1 | 1 | Weak |
| Ferreira 2003122 | 2 | 3 | 3 | 3 | 1 | 1 | Weak |
| Guttuso 201039 | 1 | 3 | 3 | N/A | 1 | 1 | Weak |
| Hsu 1996123 | 2 | 3 | 3 | 3 | 1 | 1 | Weak |
| Markose 2004124 | 2 | 3 | 3 | 3 | 1 | 3 | Weak |
| Moran 2002125 | 3 | 3 | 3 | 3 | 3 | 1 | Weak |
| Saha 2009126 | 3 | 3 | 3 | 2 | 2 | 4 | Weak |
Interventions and comparators
The included studies were grouped into the three broad groups of interventions outlined in Chapter 1: patient-initiated first-line interventions; clinician-prescribed second-line interventions; and clinician-prescribed third-line interventions. It should be noted that, for patient-initiated first-line interventions, the only studies identified that could be classified as lifestyle interventions were those which trialled ginger preparations and/or vitamin B6. No studies of dietary- or hypnotherapy-based interventions were identified. However, studies of a number of novel therapies not covered by our original review protocol were identified, namely the use of aromatherapy, transdermal clonidine and gabapentin. The studies comprising the evidence base for each group of interventions are detailed in Table 6. Note that all studies are two-arm RCTs unless otherwise stated.
| Intervention/comparator | Number of studies | Studies |
|---|---|---|
| Patient-initiated first-line intervention | ||
| Ginger vs. placebo | 7a | Basirat 200960 (biscuit) Fischer-Rasmussen 199174 Keating 200282 (syrup) aMohammadbeigi 201189 (also ginger vs. metoclopramide) Ozgoli 200996 Vutyanvanich 2001110 Willetts 2003113 |
| Ginger vs. acupressure | 1 | Saberi 201313 |
| Ginger vs. vitamin B6 | 6 | Chittumma 200767 Ensiyeh 200970 Narenji 201292 Haji Seid Javadi 201377 Smith 2004102 Sripramote 2003103 |
| Ginger vs. doxylamine/pyridoxine | 1 | Biswas 201163 |
| Ginger vs. antihistamine | 1 | Pongrojpaw 200742 |
| Ginger vs. metoclopramide | 1a | aMohammadbeigi 201189 (also ginger vs. placebo) |
| Vitamin B6 vs. placebo | 3 | Tan 2009107 [metoclopramide ± vitamin B6 (dopamine receptor antagonist)] Sahakian 1991100 Vutyavanich 199541 |
| High- vs. low-dose vitamin B6 | 1 | Wibowo 2012112 (high- vs. low-dose vitamin B6) |
| Antihistamine ± vitamin B6 | 2 | Babaei 201459 Diggory 196268 (four-arm RCT) |
| Aromatherapy | 2 | Ghani 201376 Pasha 201297 |
| Acupressure vs. nocebo | 8 | Bayreuther 199461 Belluomini 199462 Can Gurkan 200843 Heazell 200678 Hsu 200379 Naeimi Rad 201291 Steele 2001104 Werntoff 2001111 (three-arm RCT) |
| Acupressure | 1 | Markose 2004124 (case series) |
| Acupressure vs. vitamin B6 | 1 | Jamigorn 200780 |
| Nerve stimulation vs. placebo | 3 | Evans 199373 Rosen 200398 Veciana 2001109 |
| Acupuncture vs. placebo | 3 | Carlsson 200066 Knight 200183 Smith 2002101 (four-arm RCT) |
| Acupuncture vs. metoclopramide | 1 | Neri 200594 |
| Acupuncture ± moxibustion vs. Chinese herbal medicine vs. Western medicine | 2 | Mao 200987 Zhang 2005115 |
| Clinician-prescribed second-line intervention | ||
| Doxylamine/pyridoxine (Diclectin) vs. placebo | 1 | Koren 201084 |
| Pre-emptive Diclectin vs. Diclectin once symptoms begin | 1 | Maltepe 2013117 (pre-emptive therapy) Koren 2013127 |
| Doxylamine/pyridoxine vs. metoclopramide | 1 | Ashkenazi-Hoffnung 201336 (cohort study) |
| Doxylamine/pyridoxine vs. ondansetron | 2 | Oliveira 201395 Capp 201465 |
| i.v. fluids (D-Saline vs. N-Saline) | 1 | Tan 2013108 |
| i.v. fluids ± diazepam | 1 | Ditto 199969 |
| Antihistamine vs. placebo | 1 | Erez 197171 |
| Antihistamine + vitamin B6 vs. placebo | 1 | Monias 195790 |
| Droperidol/antihistamine combination vs. other medication (dopamine receptor antagonist) | 1 | Ferreira 2003122 (cohort study) |
| Metoclopramide vs. antihistamine (phenothiazine) (dopamine receptor antagonist) | 1 | Tan 2010106 |
| Serotonin antagonist (ondansetron) vs. antihistamines | 2 | Eftekhari 201372 Sullivan 1996105 |
| Serotonin antagonist (ondansetron) vs. metoclopramide | 3 | Abas 201457 Ghahiri 201175 Kashifard 201381 |
| Serotonin antagonist (ondansetron) vs. other | 1 | Einarson 2004121 (cohort study) |
| Transdermal clonidine vs. placebo patch | 1 | Maina 201485 |
| Out patient management vs. routine inpatient care | 1 | McParlin 200888 and McParlin unpublished |
| Out patient management | 1 | Alalade 2007120 (case series) |
| Clinician-prescribed third-line intervention | ||
| Steroids vs. ‘treatment as usual’ | 7 | Adamczak 200758 Bondok 200664 Moran 2002125 (case series) Nelson-Piercy 200193 Safari 1998128 Yost 2003114 Ziaei 2004116 |
| Nasogastric feeding | 1 | Hsu 1996123 (case series) |
| Jejunostomy | 1 | Saha 2009126 (case series) |
| Gabapentin | 1 | Guttuso 201039 (case series) |
In addition, the network plot (Figure 4) shows the range of interventions from all comparative studies included in the review. Individual interventions have been grouped where appropriate.
FIGURE 4.
Network plot of range of interventions and comparisons for NVP/HG. Size of node is proportional to frequency of intervention and width of line to frequency of comparisons between two interventions. Plot does not include one pre-emptive trial,117 outpatient care trial127 and two four-arm trials. 68,101

The size of the nodes in the network plot is proportional to the frequency of the intervention in the review, and the width of the lines indicates the frequency of the comparisons made between two interventions. These nodes and lines, however, do not represent the weight of evidence in the review as this would also be influenced by sample size and the precision of estimates, as well as other factors. The plot did not include a trial on pre-emptive treatment of doxylamine/pyridoxine combination, outpatient versus inpatient care117,127 or two four-arm trials,68,101 which would have over-reported the number of comparisons in the network plot. These interventions included dietary instructions only, or together with either placebo, antihistamines or antihistamine/vitamin B6 combination in one trial68 and traditional acupuncture, P6 acupuncture, placebo or no acupuncture in another trial. 101 Ginger, vitamin B6, antihistamines, acupressure, metoclopramide, corticosteroids, doxylamine/pyridoxine combination and the serotonin antagonist ondansetron are more widely reported than other interventions, but there is also information on interventions such as acupuncture, nerve stimulation therapy and aromatherapy oils which have been considered as treatments for NVP/HG. Evidence on the effects of interventions such as Chinese herbal medicine, dextrose saline, transdermal clonidine and diazepam is very limited and in most cases is reported in single trials. As expected, placebo interventions are most widely reported as comparators, and so this has the biggest node on the network plot (emphasised by the square node). The most commonly reported treatment comparisons are ginger capsules versus placebo; acupressure versus placebo; ginger capsules versus vitamin B6 capsules; corticosteroids versus ‘treatment as usual’; metoclopramide versus ondansetron; and acupuncture versus nocebo (nocebo is an inert intervention that creates comparable side effects/harmful effects in a patient, as opposed a placebo, which is an inert substance that creates either a beneficial response or no response in a patient).
Participants and symptom severity
In addition to substantial variation in terms of the range of interventions and comparators evident within the literature, it is also important to highlight the heterogeneity of symptom severity found among patient populations.
It was initially intended that as part of this review only studies that recruited women with severe NVP or HG would be included. However, assessment of symptom severity varied within and across studies, and it was not possible to easily place every participant population into categories. We therefore attempted to categorise the symptom severity of participants for each study, using the description of severity in the inclusion criteria and, if available, any severity score given at baseline. These two items of information were assessed by two independent assessors (CMP and SCR) to assign severity as mild, moderate, severe or unclear. Agreement was reached for all but one study, which was classified as unclear.
This classification was then used in each results chapter to describe symptoms and outcomes in terms of severity.
Outcome measures
Finally, and linked to the issues discussed above, the identified literature in this field was also characterised by the range of symptom severity scales employed from study to study to assess intervention outcomes. Out of the 73 included studies (reported in 75 papers), only 23 used validated NVP/HG assessment scales such as PUQE (10 studies), RINVR (11 studies) or the McGill Nausea Questionnaire (one study). Thirty-one studies assessed nausea and/or vomiting severity using a 10-point VAS. Twenty-one studies employed either a study-specific, non-validated author-defined assessment scale (including, for example, numbers of episodes of vomiting combined with the use of a Likert scale to assess subjective feelings of symptom severity among participants), or used the various proxy measures of symptom severity outlined in our protocol [e.g. percentage weight loss, length of hospital stay, or hospital (re-)admission episodes]. Table 7 illustrates the primary symptom severity outcome measures employed by each included study.
| Study | PUQE | RINVR | McGill Nausea Questionnaire | NVPI | VAS | Other scale/proxy measure |
|---|---|---|---|---|---|---|
| Abas 201457 | ✓ | ✓ | ||||
| Adamczak 200758 | ✓ | |||||
| Alalade 2007120 | ✓ | |||||
| Ashkenazi-Hoffnung 201336 | ✓ | |||||
| Babaei 201459 | ✓ | |||||
| Basirat 200960 | ✓ | |||||
| Bayreuther 199461 | ✓ | |||||
| Belluomini 199462 | ✓ | |||||
| Biswas 201163 | ✓ | |||||
| Bondok 200664 | ✓ | |||||
| Can Gurkan 200843 | ✓ | |||||
| Capp 201465 | ✓ | ✓ | ||||
| Carlsson 200066 | ✓ | |||||
| Tan 2010106 | ✓ | |||||
| Tan 2013108 | ✓ | |||||
| Tan 2009107 | ✓ | |||||
| Chittumma 200767 | ✓ | |||||
| Diggory 196268 | ✓ | |||||
| Ditto 199969 | ✓ | |||||
| Einarson 2004121 | ✓ | |||||
| Ensiyeh 200970 | ✓ | |||||
| Erez 197171 | ✓ | |||||
| Evans 199373 | ✓ | |||||
| Ferreira 2003122 | ✓ | |||||
| Fischer-Rasmussen 199174 | ✓ | |||||
| Ghahiri 201175 | ✓ | |||||
| Ghani 201376 | ✓ | |||||
| Guttuso 201039 | ✓ | |||||
| Heazell 200678 | ✓ | |||||
| Hsu 1996123 | ✓ | |||||
| Hsu 200379 | ✓ | |||||
| Jamigorn 200780 | ✓ | |||||
| Kashifard 201381 | ✓ | |||||
| Keating 200282 | ✓ | |||||
| Knight 200183 | ✓ | |||||
| Koren 201084 | ✓ | |||||
| Maina 201485 | ✓ | ✓ | ||||
| Maltepe 201386 | ✓ | |||||
| Mao 200787 | ✓ | |||||
| Markose 2004124 | ✓ | |||||
| McParlin 200888 | ✓ | |||||
| Mohammadbeigi 201189 | ✓ | |||||
| Monias 195790 | ✓ | |||||
| Moran 2002125 | ✓ | |||||
| Naeimi Rad 201291 | ✓ | |||||
| Narenji 201292 | ✓ | |||||
| Nelson-Piercy 200193 | ✓ | |||||
| Neri 200594 | ✓ | |||||
| Oliveira 201395 | ✓ | |||||
| Ozgoli 200996 | ✓ | |||||
| Pasha 201297 | ✓ | |||||
| Pongrojpaw 200742 | ✓ | |||||
| Rosen 200398 | ✓ | |||||
| Saberi 201313 | ✓ | |||||
| Safari 199899 | ✓ | |||||
| Saha 2009126 | ✓ | |||||
| Sahakian 1991100 | ✓ | |||||
| Haji Seid Javadi 201377 | ✓ | |||||
| Smith 2004102 | ✓ | |||||
| Smith 2002101 | ✓ | |||||
| Sripramote 2003103 | ✓ | |||||
| Steele 2001104 | ✓ | |||||
| Sullivan 1996105 | ✓ | |||||
| Eftekhari 201472 | ✓ | |||||
| Veciana 2001109 | ✓ | |||||
| Vutyavanich 2001110 | ✓ | |||||
| Vutyavanich 199541 | ✓ | |||||
| Werntoft 2001111 | ✓ | |||||
| Wibowo 2012112 | ✓ | |||||
| Willetts 2003113 | ✓ | |||||
| Yost 2003114 | ✓ | |||||
| Zhang 2005115 | ✓ | |||||
| Ziaei 2004116 | ✓ |
Additional sources of outcome data on medications
The UKTIS is currently commissioned by Public Health England to provide advice to UK health professionals on the fetal effects of therapeutic, poisoning and chemical exposures in pregnancy, and to conduct surveillance of known and emerging teratogens. The UKTIS database currently contains a record of just under 60,000 enquiries dating back to 1978, of which 320 relate to use of specific drugs in the treatment of HG (period of enquiry 18 June 1978 to 18 March 2014). Surveillance data collected by the UKTIS are reviewed periodically and published in UKTIS monographs through the National Poisons Information Service database (www.TOXBASE.org). Data collected by the UKTIS in relation to medications for NVP/HG, including specific monograph data on ginger, vitamin B6, vitamin B12, promethazine and olanzapine, are provided in Table 43, Appendix 7 for information.
Meta-analysis of included randomised controlled trials
As highlighted in the previous sections, there was wide variation across studies. Specifically, there was considerable heterogeneity between interventions within each of the categories of comparisons, and in terms of how interventions were administered/delivered. The measurement of outcomes also differed substantially between trials reporting the same comparisons, so in most cases the trials were not directly comparable. In a meta-analysis it is important not to combine outcomes that are too diverse; even if it had been possible to extract data for a meta-analysis, such an analysis is likely to produced misleading results due to the considerable heterogeneity between studies. 46 Furthermore, many of these trials were extremely poorly reported and their conduct was often uncertain. In summary, clinical and methodological variations between studies were considerable, and the intervention effect was likely to be affected by the factors that varied across studies. Consequently, we have not conducted a meta-analysis of findings from the RCTs.
Structure of individual results chapters
The following chapters present more detailed findings from the evidence review for each individual intervention. As already indicated, given it was not possible to meta-analyse the data from individual studies for any group of interventions and comparators, the results are summarised in narrative form. The narrative content of each chapter focuses on the findings from the included studies in terms of their reported effectiveness for addressing our primary outcomes of interest, that is, the key symptoms associated with HG/NVP. Thus, where available, effectiveness is reported in terms of the validated overall HG/NVP assessment scales (PUQE, RINVR or McGill Nausea Questionnaire). Otherwise, the effectiveness of interventions is reported in relation to their impact on the three key symptoms: nausea, vomiting and retching. Data illustrating significant results in relation to these key symptoms are detailed in the narrative text; otherwise, results are described as not significance or not clear. Data for case series studies are not included in the narrative but available in the accompanying results tables for information. Additional secondary outcome data reported by included studies (see Table 2 for a full list) are presented in Appendix 8.
Chapter 4 Clinical effectiveness: ginger
Introduction
Ginger was used as an intervention to treat HG, NVP or various forms of pregnancy sickness in a total of 16 RCTs. 13,42,60,63,67,70,74,77,82,89,92,96,102,103,110,113 Heterogeneity was observed in relation to the clinical setting and patient populations in which the studies were conducted, as well as the interventions, comparators and outcomes reported in each trial. As previously described (see Chapter 3, Meta-analysis of included randomised controlled trials) given the differences between trials in patient populations, settings, interventions and, in particular, the heterogeneous nature of the reported outcomes across trials, we did not attempt to perform meta-analyses and have thus reported a narrative summary only for each intervention and comparator set, with additional outcome data presented in Table 8.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Ginger vs. placebo | |||||||||
| Basirat 200960 | Antenatal clinic, Babol University of Medical Sciences, Iran | Effect of ginger in a biscuit form on NVP, double-blind RCT | 65 (I = 35, C = 35), 7–17 weeks | Author defined, women with nausea and vomiting of pregnancy | Nausea VAS score: I = 5.88 ± 1.83, C = 4.67 ± 1.97 Episodes of vomiting I = 1.63 ± 1.18, C = 1.3 ± 1.3 (MILD) |
Ginger biscuits (0.5 mg of ginger, five biscuits daily for 4 days) | Non-ginger containing biscuits (five biscuits daily for 4 days) | VAS for nausea Episodes of vomiting |
Nausea: average change in scores over 4 days in the ginger group = 2.57 ± 1.77, placebo group = 1.39 ± 1.62; p = 0.01 Vomiting: average change in episodes over 4 days in ginger group = 0.96 ± 0.2, placebo group = 0.62 ± 0.19; p = 0.243 |
| Fischer-Rasmussen 199174 | Obstetrics and Gynaecology Department, University Hospital of Copenhagen, Denmark | Effectiveness of ginger capsules on the symptoms of HG, double-blind randomised crossover trial | 30 (I = 15, C = 15), I = 11 weeks (7–17), C = 10.8 weeks (7–16) | Women admitted to the hospital with HG before 20th week of gestation and with symptoms persisting after 2 days | 70% of participants reported constant nausea at baseline 66.6% of women reported vomiting two to six times per day 33.3% of women reported vomiting seven or more times per day (MILD–MODERATE) |
Ginger capsules (250 mg of powdered root ginger) four times daily for 4 days, followed by a 2-day wash out before alternate treatment | Placebo capsules (250 mg of lactose) four times daily for 4 days, followed by a 2-day wash out before alternate treatment | Author-defined severity score for nausea (1–3) Author-defined relief score for nausea and vomiting (–3 to 3) Episodes of vomiting |
Mean severity scores decreased equally in the two groups Mean relief scores highlighted greater relief of symptoms after ginger treatment compared to placebo (p = 0.035) |
| Keating 200282 | Department of Obstetrics and Gynaecology, University of South Florida, FL, USA, private practice office | Effectiveness of ginger syrup mixed in water in treating NVP in the first trimester of pregnancy, double-blind RCT | 26 (I = 14, C = 12),7–11 weeks | Women complaining of nausea with and without vomiting either at a planned or ad hoc obstetric visit and were not taking a prescribed or over-the-counter antiemetic | NR (MILD) |
250 mg ginger + honey and water. One table spoon mixed with 4–8 ounces water taken four times a day for 2 weeks. Both groups received verbal and written dietary advice | Placebo syrup = water, honey and lemon oil. One table spoon mixed with 4–8 ounces water taken four times a day for 2 weeks | VAS for nausea Episodes of vomiting |
Ten women in ginger group had ≥ 4-point improvement on VAS by day 9. Placebo group: two women had same improvement by day 9 Eight women in the ginger group stopped vomiting by day 6. Only two women in the placebo group stopped by day 6 No statistical analysis |
| Ozgoli 200996 | Isfahan City Hospitals, Iran | Effects of ginger in nausea and vomiting of pregnancy, single-blind RCT | 70 (I = 35, C = 35) | Women with mild and moderate nausea, with or without vomiting | Nausea intensity moderate I = 56% C = 54%; mild I = 18.7% C = 25.7%; severe I = 8% C = 7% (MILD–MODERATE) |
Capsules containing 250 mg of ginger extract taken four times daily for 4 days. Dietary advice given. Twice daily VAS score completed | Identical placebo capsules containing lactose taken following same regime. Dietary advice given. Twice daily VAS score completed | VAS for vomiting symptoms VAS for nausea intensity |
Nausea intensity: ginger group had a higher rate of improvement (85% vs. 56%; p < 0.01) Vomiting: 50% decrease in the ginger group vs. 9% in the placebo group; p < 0.05 |
| Vutyavanich 2001110 | Antenatal clinic, Maharaj Nakorn Chiang Mai University Hospital, Chiang Mai, Thailand | Effectiveness of ginger for the treatment of NVP, double-masked RCT | 70 (I = 32, C = 38), I = 10.3 ± 2.6 | First attended the clinic before 17 weeks’ gestation and had nausea of pregnancy, with or without vomiting | Baseline nausea scores (cm): I = 4.7 ± 2.1, C = 5.4 ± 2.1(MILD) | Capsules containing 250 mg of ginger taken three times/day following meals and another before bed for 4 days. Dietary advice given | Identical placebo capsules following the same regime. Dietary advice given | VAS for nausea Episodes of vomiting |
Decrease in nausea score: ginger group (2.1 ± 1.9) vs. placebo group (0.9 ± 2.2; p = 0.014) Decrease in vomiting episodes: ginger group (1.4 ± 1.3) vs. placebo group (0.3 ± 1.1; p < 0.001) |
| Willetts 2003113 | Antenatal clinic, Royal Hospital for Women, Sydney, NSW, Australia | Effect of a ginger extract (EV.EXT35) on the symptoms of morning sickness, double-blind RCT | 120 (I = 60, C = 60) | Women who have experienced morning sickness daily for at least a week which had failed to respond to dietary measures | Nausea experience score presented as a figure, no numerical values available (MILD) | Capsules containing 125 mg of ginger extract taken four times daily for 4 days. RINVR score completed 1 hour later | Identical placebo capsules containing soya oil taken following same regime | RINVR score | Nausea experience score: significantly less for the ginger extract group relative to the placebo group after the first day and each subsequent treatment day Retching: reduced by the ginger extract although to a lesser extent Vomiting: no significant effect observed |
| Ginger vs. vitamin B6 | |||||||||
| Chittumma 200767 | Antenatal clinic, Vajira Hospital, Bangkok, Thailand | Effectiveness of ginger in comparison with vitamin B6 for treatment of NVP, double-blind RCT | 126 (I = 63, C = 63), I = 12 (SD 2) C = 11 (SD 2) | Women who had nausea with or without vomiting and required treatment | RINVR score: I = 8.7 (SD 2.2), C = 8.3 (SD 2.5) (MILD) |
Ginger capsules, 2 × 325 mg four times daily for 4 days. Dietary advice given | Vitamin B6 capsules, 2 × 12.5 mg four times daily for 4 days. Dietary advice given | RINVR score | Symptoms reduced in both groups. Ginger from 8.7 ± 2.2 to 5.4 ± 2.0 and vitamin B6 from 8.3 ± 2.5 to 5.7 ± 2.3 (p < 0.05). The mean score change with ginger was greater than with vitamin B6 (3.3 ± 1.5 vs. 2.6 ± 1.3) (p < 0.05) |
| Ensiyeh 200970 | Antenatal clinic, Fatemieh Hospital, Hamedan, Iran | Effectiveness of ginger in comparison with vitamin B6 for the treatment of NVP, double-blind RCT | 70 (I = 35, C = 35), NR | Women’s first attendance at clinic and experienced nausea, with or without vomiting | VAS for nausea: I = 5.4 cm ± 2.6, C = 4.6 cm ± 2.3 (MILD) |
Ginger capsules, 500 mg, twice daily for 4 days. VAS completed three times daily | Vitamin B6 capsules, 20 mg twice daily for 4 days. VAS completed three times daily | VAS to assess nausea Episodes of vomiting |
Mean change in nausea score over 4 days: ginger 2.2 ± 1.9 compared with vitamin B6 group 0.9 ± 1.7 (p = 0.024) Vomiting episodes decreased in both groups, but no difference between groups. Ginger mean change 0.6 ± 0.7, vitamin B6 mean change 0.5 ± 1.1 (p = 1.101) |
| Haji Seid Javadi 201377 | Health centres, University of Medical Sciences of Qazvin, Iran | Effectiveness of ginger in comparison with vitamin B6 for the treatment of NVP, RCT | 95 (I = 47, C = 48), ginger 9 (SD 1.1) weeks, vitamin B6 9 (SD 1.6) weeks | Women suffering from pregnancy induced nausea | NR (NOT CLEAR) |
Ginger tablets, 250 mg, 6-hourly for 4 days | Vitamin B6 tablets, 40 mg, 12-hourly for 4 days | PUQE score | Mean change of PUQE score over 4 days: ginger group 8.32 (SD 2.19), vitamin B6 group 7.77 (SD 1.80); p = 0.172 Retching in vitamin B6 group had a greater, non-significant reduction; p = 0.333 |
| Narenji 201292 | Antenatal clinic, Arak University of Medical Sciences, Iran | Effectiveness of ginger syrup in comparison with vitamin B6 for the treatment of NVP, RCT | 100 (I = 50, C = 50) states < 17 weeks | Women attending clinic suffering from at least 24 hours of nausea | VAS mean (SE): nausea I = 5.6 (1.94), C = 6.04 (2.55); vomiting I = 5.6 (1.94), C = 6.66 (2.41) (MILD–MODERATE) |
Given i.v. fluids to rehydrate. Ginger syrup (mix of ginger and honey), one teaspoon twice daily for 4 days | Given i.v. fluids to rehydrate, vitamin B6 capsules, 40 mg twice daily for 4 days | VAS to assess nausea Episodes of vomiting |
Nausea score: vitamin B6 mean change 0.7 (SD 1.99), ginger mean change 1.0 (SD 1.32); p = 0.8 Vomiting decreased in both groups but no significant difference between groups |
| Smith 2004102 | University, Women’s and Childrens Hospital, Adelaide, SA, Australia, referrals from GPs and health-care providers | Comparison of ginger with pyridoxine hydrochloride (vitamin B6) in the treatment of NVP, randomised, controlled equivalence trial | 301 (I = 146, C = 145), I median = 8.5, range 8–15; C median = 8.6, range 8–15 | Women with nausea or vomiting | Use of antiemetics: I = 33 (44%), C = 42 (56%) (MILD–MODERATE) |
Ginger capsules, (350 mg) three times a day for 3 weeks. (Participants could also take any other antiemetics they wanted) | Vitamin B6 capsules (25 mg) three times a day for 3 weeks. (Participants could also take any other anti-emetics they wanted) | RINVR score | Nausea: equivalent reduction in score for both treatments. Mean difference 0.2 (90% CI –0.3 to 0.8) Retching: mean difference 0.3 (90% CI 0.0 to 0.6) Vomiting: mean difference 0.5 (90% CI 0.0 to 0.9), averaged over time, with no evidence of different effects at the three time points (7, 14 and 21 days) |
| Sripramote 2003103 | Antenatal clinic, Vajira Hospital, Thailand, and Obstetrics and Gynaecology Department, Bangkok Metropolitan Administration Medical College, Bangkok | Efficacy of ginger in comparison with vitamin B6 in the treatment of NVP, double-blind RCT | 138 (I = 68, C = 70), I = 10.1 (SD 2.74), C = 10.3 (SD 2.95) | Women with nausea of pregnancy, with or without vomiting and requesting antiemetics | Nausea scores: I = 5.0 cm (SD 1.99), C = 5.3 cm (SD 2.08). Episodes of vomiting in last 24 hours: I = 1 (range 0–10), C = 1 (range 0–10) (MILD–MODERATE) |
Ginger capsules, 500 mg, three times daily for 3 days. Dietary advice given. VAS for nausea completed three times daily, plus record of vomiting episodes | Vitamin B6 capsules, 10 mg, following the same regime | VAS for nausea Episodes of vomiting |
Nausea: decreased in both groups Ginger: 5.0 (SD 1.99) to 3.6 (SD 2.48) Vitamin B6: 5.3 (SD 2.08) to 3.3 (SD 2.07); p < 0.001 Vomiting: reduced in both groups Ginger: 1.9 (SD 2.06) to 1.2 (SD 1.75) Vitamin B6: 1.7 (SD 1.81) to 1.2 (SD 1.50); p < 0.01 |
| Ginger vs. acupressure | |||||||||
| Saberi 201313 | Antenatal clinic, Naghvi Hospital, Kashan, Iran | Effectiveness of acupressure in comparison with ginger in the treatment of NVP, three-arm RCT | 159 (I = 53, C = 53, control = 53), ginger = 8.78 (SD 2.32), acupressure = 9.32 (SD 2.38), control = 9.11 (SD 0.18) | Women having mild to moderate nausea and/or vomiting | RINVR score: ginger = 17.91 (SD 6.11); acupressure = 17.91 (SD 5.90), C = 17.90 (SD 5.30) (MILD–MODERATE) |
Ginger capsules, 250 mg, three times daily for 4 days. n = 53 acupressure: sea-bands given, to be worn continuously for 4 days | C group received no I | RINVR score | Mean difference in improvement pre and post I: ginger 8.61 (SD 5.24), acupressure 4.17 (SD 5.53), C –0.84 (SD 3.72) p < 0.001 for differences in total score and for each component (nausea, vomiting and retching) |
| Ginger vs. vitamin B6 combination | |||||||||
| Biswas 201163 | Seth Sukhlal Karnani Memoria Hospital, Kolkata, India and R.G. Kar Medical College Hospitals, Kolkata, India | Efficacy and tolerability of ginger extract in comparison with a combination of doxylamine 10 mg + pyridoxine 10 mg, single-blind RCT | 78 (I = 42, C = 36), I = 10.25 (SD 2.8), C = 9.3 (SD 3.1) | Women who sought treatment for the symptoms of morning sickness between 6 and 16 weeks of pregnancy without having received any previous treatment | Median (IQR) VAS score nausea: I = 34.5 mm (IQR 25.0), C = 30.4 mm (IQR 34.0). Vomiting: I = 14.5 mm (IQR 33.0), C = 22.0 mm (IQR 35.0) (MILD) |
Ginger tablets, 150 mg, three daily | Doxinate (Sigma Laboratories, PVT LTD, Mumbai) (doxylamine 10 mg plus pyridoxine 10 mg) three times daily | VAS for nausea Episodes of vomiting |
Both groups had a significant decline in severity of nausea and vomiting from baseline to week 2 Nausea persisted, but with reduced severity median values tending towards zero at study end No significant difference between groups |
| Ginger vs. antihistamine | |||||||||
| Pongrojpaw 200742 | Hospital antenatal clinic, Thammasat University Hospital, Thailand | To study the efficacy of ginger and dimenhydrinate in the treatment of NVP, double-blind RCT | 170 (I = 85, C = 85), I = 10.25 (SD 2.8), C = 9.3 (SD 3.1) | Pregnant women with nausea and vomiting less than 16 weeks of gestation | NR (NOT CLEAR) |
Ginger capsules, 500 mg, twice daily for 1 week | Dimenhydrate capsules, 50 mg twice daily for 1 week | VAS to assess nausea Episodes of vomiting |
Nausea: mean score on days 1–7 decreased in both groups. Daily score between groups not statistically different (p > 0.05) Vomiting episodes: on days 1–7 decreased in both groups. Dimenhydrinate significantly more effective on days 1–2 (p < 0.05). Days 3–7 scores similar |
| Ginger vs. metoclopramide | |||||||||
| Mohammadbeigi 201189 | B’esat Hospital, Kurdistan, Iran | To study the effects of ginger NVP with metoclopramide, three-arm RCT | 102 (I = 34, C = 34, placebo = 34), ginger 9.5 ± 2.02, metoclopramide 10.03 ± 1.99, placebo 10.32 ± 2.25 | Women with inefficacy of food regimens in controlling vomiting and nausea | NR (MILD) |
Ginger capsules, 200 mg, three times daily for 5 days | Metoclopramide capsules, 10 mg, three times daily, and placebo (200 mg flour) for 5 days | RINVR score | Trend in symptom improvement to the 5th day in all three groups Nausea: ginger (p = 0.003) and metoclopramide (p = 0.001) had significantly better improvement than placebo, but no difference between ginger and metoclopramide (p = 0.683) Vomiting: ginger (p = 0.046) and metoclopramide (p = 0.018) had significantly better improvement than placebo. No difference between ginger and metoclopramide group (p = 0.718) |
Of the included trials, half (n = 8) described the women participants as experiencing symptoms categorised at the mild end of the NVP severity scale. 60,63,67,70,82,89,110,113 Six were classed as including participants with mild–moderate symptom severity. 13,74,92,96,102,103 The information provided by the remainder was insufficient to categorise objectively severity, although the authors describe the women as experiencing pregnancy-related nausea and vomiting. 42,77 Of the 16 studies, 4 were judged to carry a high risk of bias,77,89,92,113 10 low risk,13,60,63,67,70,74,82,102,103,110 and the remainder, unclear due to lack of information. 42,96
Ginger capsules versus placebo capsules
Five trials74,89,96,110,113 compared ginger and placebo capsules for the treatment of NVP. The trial by Mohammadbeigi and colleagues89 was a three-arm RCT which compared ginger, metoclopramide and placebo. 89 Only one trial74 explicitly reported the effects of ginger in the treatment of HG (which they define as vomiting occurring during pregnancy, presenting prior to the 20th week and of sufficient severity to require hospital admission). However, it is important to note that this deviates from the standard definition of HG (see Chapter 1, Background). Three of these trials were judged to carry a low risk of bias, two high risk due to issues regarding blinding of personnel administering the treatment89 or selective outcome reporting113 and the risk of bias in the remaining trial was unclear. 96
Rhodes Index of Nausea, Vomiting and Retching
In the Mohammadbeigi and colleagues89 trial, the observed differences in the RINVR score on the second day (ginger: 26.41 ± 4.12; metoclopramide: 25.56 ± 5.51; placebo: 27.35 ± 3.36) and the fifth day (ginger: 18.71 ± 2.81; metoclopramide: 18.53 ± 5.18; placebo: 23.15 ± 4.03) compared with the first day of treatment (ginger: 31.68 ± 5.32; metoclopramide: 30.00 ± 8.29; placebo: 30.53 ± 4.64) were statistically significant in all groups (p < 0.001). 89 Although there was a reduction in scores in all three groups, the authors stated that the intensity of changes was different in ginger (p < 0.01) and metoclopramide (p = 0.03) groups compared with placebo, but did not differ between the ginger and metoclopramide groups (p = 0.51). However, it was not clear from the paper how differences in the intensity of changes were established.
Author-defined symptom severity/relief scales
Fischer-Rasmussen and colleagues74 devised a study-specific severity/relief score based on the degree of nausea, duration and number of episodes of vomiting and change in body weight, and a subjective assessment of the extent to which these symptoms had improved, worsened or stayed the same. In this randomised crossover trial, the authors compared relief scores at day 5 and day 11, following 4 days of treatment with either ginger or placebo capsules. Fischer-Rasmussen and colleagues74 reported that the mean severity scores decreased equally in the two groups. However, given the differences in gestational age at baseline, the scores at points 1 and 11 were not considered directly comparable, and therefore no statistical analysis was carried out. Mean relief scores showed greater relief of symptoms after ginger treatment than after placebo (p = 0.035), with analyses of single-item components demonstrating a particular reduction in vomiting episodes and nausea in the ginger group.
Vutyavanich and colleagues110 used 5-item Likert scales to assess patients’ subjective response to treatment in terms of whether general nausea and vomiting symptoms had worsened, improved or stayed the same. Of the 67 women surveyed, 28 out of 32 (88%) treated with ginger reported that their symptoms improved, compared with only 10 out of 35 (29%) in the placebo group (p < 0.001).
Nausea outcomes
Willetts and colleagues113 examined the effect of a ginger extract on pregnancy-induced nausea. 113 The RINVR was used to assess nausea experience in terms of frequency, duration and distress (in addition to vomiting and retching) 1 hour after treatment was administered. For both the ginger extract and placebo groups, there was a reduction in the overall nausea experience score from baseline to day 1 of treatment, which then remained at this reduced level until day 4 of treatment. The effect of ginger extract relative to placebo on nausea experience was calculated as a difference parameter for 4 consecutive days of treatment post baseline. On days 1, 2 and 4, the authors state that the difference parameter was significantly less than zero, and that results showed a significant effect for ginger on nausea experience by/on day 4. However, the authors did not report p-values and added a note of caution as results were considered likely to be confounded by a regression-to-the-mean effect.
Mohammadbeigi and colleagues89 also measured nausea severity with the RINVR. The observed difference in nausea severity between the second to the fifth days of the intervention and the first day was significant in all three groups (p < 0.001). However, there were differences observed in the intensity of changes in the ginger (p < 0.01) and metoclopramide (p = 0.01) groups compared with the placebo group. The difference in intensity was not different between the ginger and metoclopramide groups (p = 0.68).
Ozgoli and colleagues96 investigated the effect of ginger capsules on NVP. 96 They measured nausea intensity twice a day for 4 days using a 10-point VAS, which was converted into author-defined categories of severe, moderate, mild and no nausea (where 10 = most severe and 0 = absence of nausea). Based on these categories, nausea improved in the ginger group compared with the placebo group: after treatment, 28% of women who had taken ginger capsules had no nausea compared with 10% in the placebo group (p < 0.05). There were also more women who reported severe nausea in the placebo group (15%) than in the ginger group (9%) (p < 0.05).
Vutyavanich and colleagues110 also used a VAS to assess severity of nausea. The mean change in nausea scores (baseline minus average post-therapy nausea scores for all women) was greater in the ginger group than in the placebo group (p = 0.014). To account for three missing patients in the placebo group, the authors assumed that their nausea scores changed as much as subjects with the best improvement for the purposes of intent-to-treat analysis. These results were sensitive to plausible extreme value sensitivity analysis and differences in nausea scores were no longer significant (p = 0.08). When the mean change in nausea scores were compared at baseline and at the end of the trial at day 4, there was a greater reduction in nausea scores in the ginger group than in the placebo group (p = 0.035 and p = 0.005 in analyses that did and did not impute for three missing placebo values respectively).
Vomiting outcomes
In the Willetts and colleagues113 trial there was no difference between ginger extract and placebo groups for vomiting symptoms assessed using the RINVR.
Mohammadbeigi and colleagues89 also measured vomiting severity with the RINVR. 89 Vomiting severity decreased in the ginger, metoclopramide and placebo arms between the second to fifth days of intervention compared with the first day (p < 0.01). There was an observed difference between the ginger (p < 0.05) and metoclopramide (p = 0.02) groups compared with the placebo group. However, there was no difference between the ginger and metoclopramide groups (p = 0.72).
In the trial of Ozgoli and colleagues,96 there was a 50% decrease in the number of vomiting episodes in the ginger group post-treatment period (p < 0.05). In the control group, a 9% reduction was reported, which was not statistically significant. The between-group rate of reduction in number of vomiting episodes was also significant (p < 0.05).
After 4 days of treatment, the proportion of women in the Vutyavanich and colleagues trial110 who had vomiting was lower in the ginger compared with the placebo group (37.5% vs. 68.0%; p = 0.021). Similarly, a greater reduction in vomiting episodes was found in the ginger group compared with placebo (based on baseline number of episodes minus average number of vomiting episodes over the 4 days of treatment) (p < 0.001).
Retching outcomes
In the Willetts and colleagues113 trial, using the RINVR to assess symptoms, ginger extract was shown to lower retching symptom scores compared with the placebo group for the first 2 of 4 consecutive days of treatment.
Safety outcomes
Fetal outcomes and maternal adverse events were reported in four out of five included trials. 74,89,96,110 Fischer-Rasmussen and colleagues74 reported one miscarriage and one termination in trial participants. These data are summarised in the text following but it should be noted that given the anticipated rarity of these events, small trials are likely to provide unreliable estimates. No congenital anomalies were reported and the mean birthweight/gestation at delivery were within normal ranges. No adverse effects were reported in the trial of Ozgoli and colleagues96 Vutyavanich and colleagues110 reported one miscarriage in the intervention ginger and three in placebo group, delivery at term in the majority of pregnancies in both groups (placebo = 91.4%, ginger = 96.9%; no p-value reported) and no congenital anomalies. See Appendix 8, Secondary outcome data for full details, with additional UKTIS ginger data provided in Appendix 7.
Ginger syrup versus placebo syrup
The trial of Keating and Chez82 reported on the effect of ginger syrup versus non-ginger-containing placebo syrup on nausea and vomiting in early pregnancy. This trial was judged as carrying a low risk of bias.
Combined severity score
No combined score reported.
Nausea outcomes
Nausea severity was measured using the 10-point VAS: 10 out of 13 (77%) women who received ginger had at least a 4-point improvement on the 10-point nausea scale by day 9; whereas only 2 out of 10 (20%) of the women in the placebo group had the same improvement. Conversely, no woman in the ginger group, but seven (70%) in the placebo group, had a ≤ 2-point improvement on the nausea scale at both 9 and 14 days. It was not reported whether or not these differences were statistically significant.
Vomiting outcomes
Eight out of 12 women in the ginger group who were vomiting daily at the beginning of treatment stopped vomiting by day 6 compared with 2 out of 10 (20%) women in the placebo. Again, it was not reported whether or not this difference was statistically significant.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No safety-related outcome data were reported by Keating and Chez. 82 See Appendix 7 for additional UKTIS ginger data.
Ginger biscuit versus placebo biscuit
We identified one trial,60 judged at low risk of bias, which reported on the effect of ginger biscuits on nausea and vomiting in early pregnancy.
Author-defined symptom severity/relief scales
Basirat and colleagues60 used a 5-item Likert scale to assess patients’ subjective response to treatment in terms of whether symptoms had worsened, improved or remained the same. They found that a higher proportion of women consuming ginger compared with placebo biscuits reported improved symptoms: 28 out of 32 (88%) compared with 21 out of 30 (70%) (p = 0.043).
Nausea outcomes
Nausea severity was assessed via a 10-point VAS. The average improvement in nausea scores (baseline minus average post-therapy nausea scores of day 1–4 for all subjects) in the ginger group was significantly greater than that in the placebo group. The nausea score [standard deviation (SD)] on day 4 in the placebo and ginger groups decreased to 3.03 (SD 2.47) from 4.67 (SD 1.97) and 3.03 (SD 2.19) from baseline score of 5.88 (SD 1.83), respectively (p = 0.01).
Vomiting outcomes
The average reduction in the number of vomiting episodes (baseline minus average post-therapy nausea scores of day 1–4 for all subjects) was greater in the ginger biscuit group (0.96 ± 0.21) than in the placebo biscuit group (0.62 ± 0.19). However, this difference was not significant (p = 0.243). After 4 days of treatment, the proportion of women who had no vomiting in the ginger group (11/32, 34%) was greater than that in the placebo group (6/30, 20%). It was not reported whether or not this difference was statistically significant.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No safety-related outcome data were reported by Basirat and colleagues. 60 See Appendix 7 for additional UKTIS ginger data.
Ginger versus vitamin B6
Six trials compared ginger with vitamin B6 capsules for the treatment of NVP in pregnancy. 67,70,77,92,102,103 Most of these trials were judged as being at a low risk of bias. 67,70,102,103 However, risk of bias in the trial of Haji Seid Javari and colleagues77 was judged as unclear, and Nanreji and colleagues92 was judged as being at a high risk of bias due to concerns with regard to the blinding process and allocation concealment.
Rhodes Index of Nausea, Vomiting and Retching
Chittumma and colleagues67 used a modified version of the RINVR to assess change in nausea and vomiting severity (comprised episodes of nausea, duration of nausea and numbers of vomits). The trial found a reduction in symptoms in both groups [ginger from 8.7 (SD 2.2) to 5.4 (SD 2.0); vitamin B6 from 8.3 (SD 2.5) to 5.7 (SD 2.3); p < 0.05]. However, the mean score reduction (i.e. improvement in symptoms) with ginger was greater than with vitamin B6 (3.3 ± 1.5 vs. 2.6 ± 1.3) (p < 0.05).
Pregnancy-Unique Quantification of Emesis and Nausea scale
Haji Seid Javadi and colleagues77 measured changes in symptoms using the PUQE scoring system (capturing numbers of nausea, vomiting and retching episodes, along with severity). The study found an improvement in PUQE scores between baseline and the subsequent 4 days of treatment [ginger 8.32 (SD 2.19), vitamin B6 7.77 (SD 1.80); p < 0.001]. However, this difference between groups was not significant (p = 0.172).
Author-defined symptom severity/relief scales
At the 1-week follow-up point, Ensiyeh and Sakineh70 used a 5-point Likert scale (much worse, worse, same, better, much better) to assess overall treatment response. On day 7, 29 out of 35 (82.9%) women in the ginger group reported an improvement in general symptoms, compared with 23 out of 34 (67.6%) in the vitamin B6 group. However, this difference was not significant (p = 0.52).
Nausea outcomes
Sripramote and Lekhyananda103 used a 10-point VAS to measure nausea severity at baseline (pre treatment) and days 1–3 (post treatment). 103 Comparing baseline and post treatment, there was a reduction in mean score change in both ginger (1.4, SD 2.22) and vitamin B6 groups (2.0, SD 2.19) (p < 0.001 for both groups). However, the difference between groups was not statistically significant (p = 0.136).
Ensiyeh and Sakineh70 also used a 10-point VAS to assess nausea severity between baseline and the first 4 days of treatment. They found a greater mean change in nausea score over the 4 days in the ginger group (2.2 ± 1.9) compared with the vitamin B6 group (2.2 ± 1.9) (p = 0.024).
Smith and colleagues102 used the RINVR to assess differences in nausea severity between baseline and at days 7, 14 and 21. Equivalent reductions in mean differences over time were reported for both treatment groups (mean difference 0.2, 90% CI –0.3 to 0.8).
Narenji and colleagues92 used a 10-point VAS to assess nausea severity. However, although both groups reduced their mean nausea scores [vitamin B6 mean change 0.7 (SD 1.99), ginger mean change 1.0 (SD 1.32)], there was no difference between groups (p = 0.8).
Vomiting outcomes
Sripramote and Lekhyananda103 assessed vomiting severity by the change in number of vomiting episodes. Both groups showed a reduction in the mean number of vomiting episodes [ginger group 0.7 (SD 2.18), p = 0.003; vitamin B6 group 0.5 (SD 1.44), p = 0.008]. However, the mean change difference between groups was not significant.
Ensiyeh and Sakineh70 also assessed the change in number of vomiting episodes between baseline and the first 4 days of treatment. Although number of vomiting episodes decreased in both groups (ginger 0.6 ± 0.7, vitamin B6 0.5 ± 1.1), this difference was not statistically significant (p-value reported as p = 1.101 in the paper, which we assume is a reporting error).
Narenji and colleagues92 also found a reduction in the number of episodes of vomiting in both groups. However, they reported no difference between groups (although did not provide a p-value).
Smith and colleagues102 used the RINVR to assess differences in vomiting severity between baseline and at days 7, 14 and 21. Equivalent reductions in mean differences over time were reported for both treatment groups (mean difference 0.5, 90% CI 0.0 to 0.9).
Retching outcomes
Smith and colleagues102 used the RINVR to assess differences in retching severity between baseline and at days 7, 14 and 21. Equivalent reductions in mean differences over time were reported for both treatment groups (mean difference 0.3, 90% CI –0.0 to 0.6).
In the trial of Haji Seid Javadi and colleagues,77 changes in retching severity were assessed by PUQE scores. There was no difference in the reduction of retching between the vitamin B6 group and ginger groups (p = 0.333).
Safety outcomes
Fetal outcomes and maternal adverse events were reported in four out of the six included trials. 67,70,102,103 These data are summarised in the text following but as noted previously, given the anticipated rarity of these events, small trials are likely to provide unreliable estimates.
No pregnancy outcomes were reported by either Sripramote and Leekhyananda103 or Chittumma and colleagues,67 and both trials found only minor side effects in both groups. Sripramote and Leekhyananda103 found no difference in rates of sedation (ginger 26.6% vs. vitamin B6 32.8%; p = 0.439), or heartburn (ginger 9.4% vs. vitamin B6 6.3%; p = 0.510). In the trial of Chittumma and colleagues,67 minor side effects such as sedation, heartburn and arrhythmia were reported, but the difference between groups was not significant (% experiencing side effects: ginger 25.4%, vitamin B6 23.8%; p = 0.80).
Ensiyeh and Sakineh70 reported slight drowsiness in 7% of the hydroxyzine-treated patients. In terms of miscarriages, the ginger group reported two events and the vitamin B6 group reported one event. However, no congenital abnormalities or neonatal problems were reported in either group. Smith and colleagues102 reported no differences between groups in terms of live births, congenital abnormalities or birthweight (p > 0.05). See Appendix 8, Secondary outcome data for full details, with additional UKTIS ginger data provided in Appendix 7.
Ginger capsules versus acupressure
The trial of Saberi and colleagues13 reported a randomised comparison of the effectiveness of ginger capsules versus acupressure to relieve NVP. A control arm was also included where no intervention was performed during the 7 days of the trial. Analysis was performed on all participants. This study was judged as carrying low risk of bias.
Rhodes Index of Nausea, Vomiting and Retching
The authors calculated the mean difference in the overall RINVR scores between the three groups by subtracting the pre-intervention (3 days before intervention) from the post-intervention (4 days after treatment) scores. It was significantly greater (p < 0.001) in the ginger group (8.61 ± 5.32) than in the acupressure (4.17 ± 5.53) and control groups (–0.84 ± 3.72). The authors reported that the total RINVR scores was reduced by 49% in the ginger group and by 29% in the acupressure group. There was little change in the control group (raised to 0.06%). It was not reported if the difference between these three groups was significant.
Nausea outcomes
The difference in nausea severity (as assessed by the RINVR in the same way as above) was found to be lower in the ginger group (3.94 ± 2.58) compared with the acupressure (2.00 ± 2.37) or control groups (0.18 ± 1.24) (p = 0.001 for differences between groups). A similar trend was observed in the reduction percentage of scores (ginger 48%, acupressure 29%, control 0.03%), although it was not reported if this difference was significant.
Vomiting outcomes
The difference in vomiting severity (as assessed by the RINVR in the same way as above) was found to be lower in the ginger group (2.66 ± 2.64) compared with the acupressure (0.64 ± 2.14) or control groups (–0.17 ± 2.12) (p = 0.001). A similar trend was observed in the reduction percentage of scores (ginger, –52%; acupressure, 19%; control, –0.24%), although it was not reported if this difference was significant.
Retching outcomes
The difference in retching severity (assessed as above) was also found to be lower in the ginger group (2.01 ± 1.56) compared with the acupressure (1.52 ± 1.86) or control groups (0.31 ± 1.36) (p = 0.001 for differences between groups). A similar trend was observed in the percentage reduction of scores (ginger 46%, acupressure 37%, control –0.09%), although it was not reported if this difference was significant.
Safety outcomes
Saberi and colleagues13 did not report pregnancy-related outcomes and found no side effects in trial participants. See Appendix 7 for additional UKTIS ginger data.
Ginger versus doxylamine–pyridoxine
Biswas and colleagues63 reported a randomised, comparison of ginger extract tablets versus doxinate (doxylamine 10 mg plus pyridoxine 10 mg) in the treatment of nausea and vomiting during pregnancy. Patients were blinded to the treatment, whereas investigators were not. However, overall, this study was judged to have a low risk of bias.
Combined severity score
No combined score reported.
Nausea outcomes
Nausea was assessed in terms of severity (using the 10-point VAS) and number of spells. Both groups showed a significant decline in nausea severity median score {ginger from 34.5 [interquartile range (IQR) 0.0–91.0] to 0.00 [IQR 0.0–52.0]; doxylamine–pyridoxine from 30.4 [IQR 0.0–100.0] to 0.0 [IQR 0.0–65.0]} and number of nausea spells {ginger from 3.0 [IQR 1.0–10.0] to 0.43 [IQR 0.00–12.00]; doxylamine-pyridoxine from 4.0 [IQR 0.0–12.00(sic)] to 0.6 [IQR 0.0–7.7]} (p = 0.001). However, between group differences were not significant at any time point.
Vomiting outcomes
Vomiting was assessed in terms of severity (using the 10-point VAS) and number of episodes. Again, both groups showed a decline in severity [ginger from median 14.00 (range 0.00–73.00) to median 0.00 (range 0.00–30.00); doxylamine–pyridoxine from median 22.00 (range 0.00–87.00) to median 0.00 (range 0.00–47.00)] and vomiting episodes [ginger from median 0.14 (range 0.00–5.50) to median 0.15 (range 0.00–5.50); doxylamine–pyridoxine from median 2.00 (range 0.00–6.00) to median 0.00 (range 0.00–2.80)]. However, as above, between group differences were not significant at any time point.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No stillbirths, congenital anomalies, neonatal or fetal complications were reported in the trial of Biswas and colleagues63 See Appendix 7 for additional UKTIS ginger data.
Ginger versus antihistamine (dimenhydrinate) capsules
Pongrojpaw and colleagues42 examined the effect of ginger versus antihistamine (dimenhydrinate) capsules in the treatment of NVP. Risk of bias was unclear due to lack of information provided in this abstract.
Combined severity score
No combined score reported.
Nausea outcomes
The mean nausea score during days 1–7 of the treatment decreased in both groups. There was no significant difference in the daily mean nausea scores between both groups (p > 0.05).
Vomiting outcomes
The frequency of vomiting episodes during days 1–7 of the treatment decreased in both groups. There was no significant difference in the daily mean number of vomiting episodes between days 3–7 post treatment (p > 0.05), although the daily mean number of vomiting episodes in the dimenhydrinate group during days 1 and 2 of the treatment was less than in the ginger group (p < 0.05).
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes were reported; however, Pongrojpaw and colleagues42 found a significant difference in drowsiness after treatment (dimenhydrinate 77.6% compared with ginger 5.9%; p < 0.01). These data are summarised in the text following, but it should be noted that given the anticipated rarity of these events small trials are likely to provide unreliable estimates. See Appendix 8, Secondary outcome data for full details, noting the aforementioned caveat in relation to generalisability of this safety data, with additional UKTIS ginger data provided in Appendix 7.
Ginger versus metoclopramide
The 2011 trial of Mohammadbeigi and colleagues89 randomised women to ginger, metoclopramide or placebo capsules for the treatment of pregnancy sickness. Details are reported in Ginger capsules versus placebo capsules concerning ginger versus placebo. In summary, both were found to be were efficacious but there was no evidence that one treatment was superior to the other. Furthermore, as detailed above, the trial was judged as carrying a high risk of bias due to concerns over lack of blinding of trial personnel.
Summary
-
The evidence available for ginger was predominantly at low risk of bias or the risk of bias was unclear, with four exceptions. 77,89,92,113
-
Ginger is one of the most widely reported interventions but the evidence is limited and generalisability relates to women with less severe nausea and vomiting symptoms receiving ginger treatment.
-
The quality of the evidence for ginger versus placebo is low and was downgraded due to clinical heterogeneity and imprecision. Further research is very likely to have an important impact on our confidence in the estimate of effect and may change the estimate. There was a sparseness of data in the other comparisons, so they were further downgraded to very low quality of evidence and we are very uncertain about the estimates.
-
The identified studies comparing ginger preparations with placebo generally reported evidence of an improvement over a range of symptoms with the use of ginger.
-
When consideration is restricted to those studies at low risk of bias, the results are less clear cut. Ginger looks promising in reducing symptoms, but the findings are not conclusive.
-
For the comparison of ginger preparations with acupressure, ginger again looks promising, but the evidence is very limited in both quantity and quality.
-
For the comparison of ginger versus vitamin B6 there are some higher-quality studies, but in general there was little evidence of a difference in the severity of symptoms between groups. There were few data for the comparisons of ginger against doxylamine–pyridoxine or antihistamine or metoclopramide, and minimal evidence suggesting any difference between groups.
-
Overall, there is a suggestion that ginger might be better than placebo in reducing the severity of symptoms, but more larger, better-quality studies are required for this and all other comparators.
Chapter 5 Clinical effectiveness: acupressure, acupuncture and nerve stimulation
Introduction
Acupuncture or acupressure was used as an intervention for NVP in a total of 18 RCTs and one case series study. The majority (n = 13) of studies compared acupressure, acupuncture or nerve stimulation against placebo or sham treatment. However, heterogeneity was observed in relation to the clinical setting and patient populations in which the studies were conducted, as well as the interventions, comparators and outcomes reported in each trial. As previously described (see Chapter 3, Meta-analysis of included randomised controlled trials), given the differences between trials in patient populations, settings, interventions and, in particular, the heterogeneous nature of the reported outcomes across trials, we did not attempt to perform meta-analyses. We have thus reported a narrative summary only for each intervention and comparator set, with additional outcome data presented in Table 9.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Acupressure vs. placebo | |||||||||
| Bayreuther 199461 | General practices, Southampton, UK | Effectiveness of acupressure at P6, RCT | n = 23 (I n = 11; comparator n = 12) | Patients presenting with early morning sickness | NR (MILD) |
Sea-bands at P6 point for 7 consecutive days followed by 2 days no treatment | Sea-bands at placebo position for 7 consecutive days followed by 2 days no treatment | VAS for nausea Episodes of emesis |
Mean levels of nausea between conditions/treatment difference: (1) paired t-test 1.69; (2) two-sample t-tests 1.67; (3) Wilcoxon signed-rank test 1.65; (4) Mann–Whitney U-test 1.61 |
| Belluomini 199462 | Physician and midwife practices, San Francisco, CA | Effectiveness of acupressure in reducing nausea and vomiting of pregnancy, RCT | n = 60 (I n = 30; comparator n = 30). At study entry: (1) I 8.5 ± 1.4; (2) comparator 8.6 ± 1.4 | Women complaining of nausea with or without emesis | Baseline nausea scores: I = 8.38 ± 2.2, C = 7.99 ± 2.5; baseline emesis scores: I = 2.09 ± 2.5, C = 1.83 ± 2.7 Total scores baseline: (1) I 12.64 ± 5.7; (2) comparator 11.47 ± 4.9 (MILD) |
3-day control period (no treatment) then self-administered acupressure for 10 minutes four times a day for 7 consecutive days at point PC-6 | 3-day control period (no treatment) followed by self-administered acupressure for 10 minutes four times a day for 7 consecutive days at a placebo point | RINVR | Nausea scores post treatment: (1) I 5.80 ± 2.9 (p ≤ 0.001); (2) comparator 7.04 ± 2.6 (p ≤ 0.001) Emesis scores post treatment: (1) I 1.28 ± 1.9 (p = 0.03); (2) comparator 1.63 ± 2.3 (p-value not reported) Total scores post treatment: (1) I 8.69 ± 5.0 (p ≤ 0.001); (2) comparator 10.03 ± 4.6 (p = 0.019) |
| Can Gurkan 200843 | Antenatal polyclinic of a maternity and child hospital in Istanbul, Turkey | Effect of acupressure on nausea and vomiting during pregnancy, RCT | n = 75 (I n = 26; C n = 25; placebo n = 24) | Women with a nausea severity of at least 50 using VAS, with or without vomiting in the last 24 hours | NR (MILD–MODERATE) |
Three-step process: (1) days 1–3 no treatment; (2) days 4–6 acupressure wristbands applied to the P6 point to be only taken off at night when going to sleep and replaced before leaving their beds in the morning; and (3) days 7–9 no treatment (bands were not worn) | Three-step process: (1) days 1–3 no treatment; (2) days 4–6 acupressure wristbands applied to a placebo point (upper side of the wrist, being the opposite direction of the P6 point) to be only taken off at night when going to sleep and replaced before leaving their beds in the morning; and (3) days 7–9 no treatment (bands were not worn) | VAS for nausea Episodes of vomiting |
Frequency of nausea: First 3 days compared with second 3 days: (1) I z = –3.35 (p < 0.001); (2) placebo z = –0.28 (p < 0.05); (3) C z = –0.92 (p > 0.05) Second 3 days compared with third 3 days: (1) I z = –1.28 (p > 0.05); (2) placebo z = 10.18 (p > 0.05); (3) C z = –1.40 (p > 0.05) Severity of nausea: First 3 days compared with second 3 days: (1) I z = –3.04 (p < 0.05); (2) placebo z = –2.96 (p < 0.05); (3) C z = –1.02 (p > 0.05) Second 3 days compared with third 3 days: (1) I z = –1.48 (p > 0.05); (2) placebo z = –1.26 (p > 0.05); (3) C z = 0 (p > 0.05) Intensity of discomfort felt from nausea: First 3 days compared with second 3 days: (1) I z = –3.7 (p < 0.001); (2) placebo z = –2.4 (p < 0.05); (3) C z = –1.2 (p > 0.05) Second 3 days compared with third 3 days: (1) I z = –0.22 (p > 0.05); (2) placebo z = –1.4 (p > 0.05); (3) C z = –0.44 (p > 0.05) Number of vomiting episodes: First 3 days compared with second 3 days: (1) I z = –1.38 (p > 0.05); (2) placebo z = –1.85 (p > 0.05); (3) C z = –0.37 (p > 0.05) Second 3 days compared with third 3 days: (1) I z = –1.3 (p > 0.05); (2) placebo z = –0.7 (p > 0.05); (3) C z = –0.57 (p > 0.05) Cross-comparison of symptoms in treatment group and placebo group on days 4–6: Number of nausea: (1) I MR = 24.52; (2) placebo group MR = 26.56, p > 0.05 Severity of nausea: (1) I MR = 24.9, U = 296.5, p > 0.05; (2) placebo MR = 26.15, U = 296.5, p > 0.05 Intensity of discomfort: (1) I MR = 23.98, U = 272.5, p > 0.05; (2) placebo MR = 27.15, U = 272.5, p > 0.05 Number of vomiting: (1) I MR = 22.67, U = 238.5, p > 0.05; (2) placebo MR = 28.56, U = 238.5, p > 0.05 |
| Heazell 200678 | Inner city secondary care centre, Manchester, UK | Efficacy of acupressure at the P6 point for the inpatient treatment of severe nausea and vomiting in early pregnancy, RCT | n = 80 (I n = 40; comparator n = 40). At study entry: (1) I – 8.5 (standard error of the mean 0.32, range 6–14); (2) comparator – 9.0 (standard error of the mean 0.36, range 5–14) | Women with NVP on their first inpatient admission (at least 2+ of ketonuria on urinalysis, an inability to tolerate oral fluids, and a requirement for antiemetic medication) | NR (MODERATE) |
Acupressure bead placed at the P6 meridian point for 8 hours a day, from 9 a.m. to 5 p.m. In addition, patients were treated according to a standard protocol: 3 l of i.v. fluid in 24 hours and parenteral antiemetic medication while the patient was unable to tolerate oral fluids and thiamine (100 mg) that was taken orally once daily. When the patient could tolerate oral fluids, the antiemetic medication was administered orally. There was a defined antiemetic protocol that used cyclizine as a first-line agent, prochlorperazine as a second-line agent and metoclopramide, ondansetron or phenothiazine as a third-line agent | Patients assigned to the placebo group had the beads placed at a site on the dorsal aspect of the forearm which is not thought to be effective for 8 hours a day, from 9 a.m. to 5 p.m. In addition, patients were treated according to a standard protocol: 3 l of i.v. fluid in 24 hours and parenteral antiemetic medication while the patient was unable to tolerate oral fluids and thiamine (100 mg) that was taken orally once daily. When the patient could tolerate oral fluids, the antiemetic medication was administered orally. There was a defined antiemetic protocol that used cyclizine as a first-line agent, prochlorperazine as a second-line agent and metoclopramide, ondansetron or phenothiazine as a third-line agent | Not reported | Not reported |
| Hsu 200379 | Emergency department (triage), hospital setting, USA | Effect of acupressure wristband on pregnancy-related nausea/vomiting during the initial period of emergency department evaluation, RCT | n = 77 (I n = 38; comparator n = 39). At study entry: (1) I = 9 (range 3–18); (2) comparator = 9 (range 3–18) | Women with nausea/vomiting related to pregnancy | NR (NOT CLEAR) |
Acupressure device placed over the P6 point for 60 minutes | Acupressure device placed over the sham site for 60 minutes | McGill Nausea Questionnaire | No difference between I and comparator was detected at baseline, 30 or 60 minutes for any of the indexes (p < 0.2 for all) |
| Naeimi Rad 201291 | Prenatalogy clinic, Rouhani Hospital, Babol University of Medical Science, Iran | Efficacy of KID21 point (Youmen) acupressure on nausea and Vomiting of pregnancy, RCT | n = 80 (I = 40; comparator = 40). At study entry: (1) I 9.55 ± 1.81; (2) comparator 9.45 ± 2.02 | Women with moderate to severe nausea and vomiting, but normal electrolytes | Nausea intensity before acupressure: median I = 8 (IQR 10–7); median C = 8 (IQR 9–7). Vomiting intensity before acupressure: median I = 2 (IQR 4–1); median C = 2 (IQR 3–1) (MILD–MODERATE) |
Provision of routine advice to reduce nausea and vomiting via educational pamphlets. All women took vitamin B6 (40 mg twice daily). Acupressure to the two symmetrical KID21 points for 20 minutes for 4 consecutive days. Women were also advised to self-administer acupressure whenever they felt nausea and vomiting to the KID21 point | Provision of routine advice to reduce nausea and vomiting via educational pamphlets. All women took vitamin B6 (40 mg twice daily). Acupressure to a false point, gradually increasing in pressure, for 20 minutes for 4 consecutive days | VAS for nausea | Intensity of nausea, median VAS scores (IQR): (1) I first day = 7 (IQR 8–6), second day = 6 (IQR 7.75–4), third day = 5 (IQR 5–3), fourth day = 4 (IQR 5–2); (2) comparator first day = 7 (IQR 8–6), second day = 7 (IQR 8–6), third day = 7 (IQR 8–5), fourth day = 7 (IQR 8–5) Frequency of nausea, median VAS scores (IQR): (1) I first day = 1 (IQR 2–0), second day = 0 (IQR 1–0), third day = 0 (IQR 1–0), fourth day = 0 (IQR 0.75–0); (2) comparator first day = 1 (IQR 2–1), second day = 1 (IQR 2–0.25), third day = 1 (IQR 2–0), fourth day = 1 (IQR 2–0) |
| Steele 2001104 | Obstetric and gynaecology offices and clinics, Michigan, MI, USA | Effect of acupressure by sea-bands on nausea and vomiting of pregnancy, RCT | n = 110 (I = 68; comparator = 42) | Women who self-report of one or more episodes of pregnancy-related nausea and/or vomiting | NR (MILD) |
Sea-bands with acupressure buttons on each wrist for 7 consecutive days (removed only when bathing) followed by a 72-hour no-treatment control period | Placebo sea-bands without acupressure buttons on each wrist for 7 consecutive days (removed only when bathing) followed by a 72-hour no-treatment control period | Author defined (four closed-ended questions on frequency and severity of nausea with responses recorded on a 5-point Likert scale) | Nausea frequency (days 1–4): (1) I MR = 40.30; (2) comparator MR = 72.82 Nausea severity (days 1–4): (1) I MR = 40.13; (2) comparator MR= 73.09 Vomiting frequency (days 1–4): (1) I MR = 41.51; (2) comparator MR = 70.94 Vomiting severity (days 1–4): (1) I MR = 39.28: (2) comparator MR = 73.65 Nausea frequency (days 5–7): (1) I MR = 47.18; (2) comparator MR = 58.47 Nausea severity (days 5–7): (1) I MR = 49.46; (2) comparator MR = 54.79 Vomiting frequency (days 5–7): (1) I MR = 50.44; (2) comparator MR = 53.22 Vomiting severity (days 5–7): (1) I MR = 46.63; (2) comparator MR = 58.24 |
| Werntoft 2001111 | Antenatal clinics, Sweden | Effect of acupressure on nausea and vomiting during pregnancy, three-arm RCT | n = 60 (I = 20; placebo = 20; no treatment = 20). At onset: (1) I = 5.8 (SD 2.3); (2) placebo = 5.6 (SD 1.2); (3) no treatment = 5.6 (SD 2.0). At study entry: (1) I = 9.8 (SD 1.9); (2) placebo = 9.6 (SD 1.6); (3) no treatment = 10.8 (SD 2.2) | Women described as experiencing NVP | VAS: P6 = 8.4 (SD 1.2); placebo = 8.4 (SD 1.4); no treatment = 8.0 (SD 1.5) (MODERATE–SEVERE) |
Acupressure wristbands with button at P6 point worn for 2 weeks, removing it only when showering | Acupressure wristbands with button at placebo point on the upper side of the wrist, worn for 2 weeks, removing it only when showering. A third group received no treatment | VAS for nausea | Before pregnancy: (1) I 1.4 (SD 1.4); (2) placebo 1.1 (SD 0.9); (3) no treatment 1.5 (SD 2.4) Before treatment: (1) I 8.4 (SD 1.2); (2) placebo 8.4 (SD 1.4); (3) no treatment 8.0 (SD 1.5) After 1 day: (1) I 5.2 (SD 2.7); (2) placebo 5.6 (SD 2.5); (3) no treatment 7.6 (SD 1.6) After 3 days: (1) I 5.6 (SD 2.3); (2) placebo 5.5 (SD 2.8); (3) no treatment 7.2 (SD 1.3) After 6 days: (1) I 4.9 (SD 2.4); (2) placebo 6.3 (SD 2.4); (3) no treatment 6.9 (SD 2.0) After 14 days: (1) I 4.2 (SD 2.6); (2) placebo 5.9 (SD 2.4); (3) no treatment 6.5 (SD 2.2) |
| Nerve stimulation vs. placebo | |||||||||
| Evans 199373 | Obstetrics clinic, University of California, CA, USA | Effect of stimulation of a region on the wrist by either surface pressure or micro-voltage electrical current on NVP, randomised crossover trial | n = 25 | Women diagnosed with NVP by their physician | NR (NOT CLEAR) |
An active battery-powered SAS wrist unit was provided to participants which they were told would produce a perceptible tingling sensation in the wrist and hand when active, while the inactive unit would produce only a pressure sensation on the wrist when stimulating the median nerve Each subject was instructed to wear the device continually for 48 hours successively | Not applicable | Author-defined subjective change in nausea and vomiting (improved, worsened, no change) | Average nausea score: (1) active unit 2.4; (2) placebo 2.7 (p < 0.05) Improvement in nausea: (1) active unit 15; (2) placebo 10 (p < 0.05) |
| Rosen 200398 | Hospital clinics and physicians’ private offices, Morristown, New Jersey, NJ, USA, Eastern Virginia Medical School, Norfolk, VA, USA, University of Arizona Health Sciences Centre, Arizona, AZ, USA, and New York University School of Medicine, New York, NY, USA | To evaluate the effectiveness of low-level nerve stimulation therapy over the volar aspect of the wrist at the P6 point to treat nausea and vomiting in early pregnancy, multicentre RCT | n = 230 | Women with symptoms of mild to severe nausea and vomiting | RINVR score: I = 13.5 (SD 6.0); C = 12.0 (SD 5.3) (MILD–MODERATE) |
Nerve stimulation for 3 weeks via a ReliefBand Model WB-R (Woodside Biomedical Inc., Carlsbad, CA, USA) [a non-invasive, portable (34 g), battery-powered, watch-like acustimulation device]. A rotary dial on the device allows users to select between five intensities (n = 117) | Participants given an identical non-stimulating device (n = 113) | RINVR | Mean change from baseline: I = 6.48 (95% CI 5.31 to 7.66), C = 4.65 (95% CI 3.67 to 5.63); p = 0.02 |
| Veciana 2001109 | Obstetrics and gynecology, Eastern Virgina Medical School, Norfolk, VA, USA | RCT | n = 460 (I = 230; comparator = 230). At study entry: all 6–12 weeks | Women with symptoms of mild to severe nausea and vomiting | NR (NOT CLEAR) |
Nerve stimulation device worn at P6 point | Non-stimulating device worn at P6 point | RINVR | No significant difference in RINVR score between groups |
| Jamigorn 200780 | Antenatal clinic, department of obstetrics and gynaecology, faculty of medicine, Chulalongkorn University, Bangkok, Thailand | Effectiveness of acupressure compared with vitamin B6 in reducing NVP, RCT | n = 66 (I = 33; comparator = 33) At onset: (1) I 8.1 ± 1.7; (2) comparator 8.9 ± 3.5 At study entry: (1) I 6.2 ± 1.0; (2) comparator 6.8 ± 1.5 |
Women who suffered from mild to moderate nausea and/or vomiting | RINVR score: I = 14.3 ± 3.3; C = 15.4 ± 3.0 (MILD–MODERATE) |
Acupressure wristbands (sea-bands) with a button on P6 point worn continuously as possible on days 1–5 plus a placebo tablet to mimic vitamin B6. Also instructed to use oral dimenhydrinate (50 mg) every 6 hours when they had nausea and vomiting, to divide their meals into frequent small ones rich in carbohydrates and low fat and advised not to take any other medications | Sea-bands with a button on a dummy point and 50 mg-tablets of vitamin B6 were prescribed every 12 hours for 5 days. Also advised to divide their meals into frequent small ones rich in carbohydrates and low fat and not to take any other medications | RINVR | Significant improvement of nausea, retching and vomiting symptoms in both acupressure (p < 0.001) and vitamin B6 groups (p < 0.001) No statistically significant differences in scores between baseline and end of treatment (evening of the fifth day) between both groups (p > 0.05) |
| Acupuncture vs. metoclopramide/vitamin B12 | |||||||||
| Neri 200594 | Department of obstetrics and gynaecology, University of Modena and Reggio Emilia, University of Turin, Italy | Efficacy of acupuncture sessions plus acupressure compared with metoclopramide/vitamin B12 treatment, RCT | n = 81 (I = 43; C = 38). (Both groups less than 12 weeks’ gestation) | Diagnosis of HG following the commonly accepted criteria of nausea and vomiting leading to clinical symptoms of dehydration and > 5% weight loss | NR. States no difference between groups at baseline (MODERATE–SEVERE) |
Twice-weekly (for 2 weeks) acupuncture with 0.3 mm diameter sterile disposable steel needles (length 52 mm) to a depth of 10–30 mm to points PC6, CV12 and ST36, manipulated until the patient reported the characteristic irradiating sensation, then left in situ for 20 minutes without any further manual stimulation. Patients also advised to wear an acupressure device (sea-band) at the PC6 point for 6–8 hours a day at home | Metoclopramide infusion (20 mg/500 ml saline for 60 minutes) at the hospital twice a week for 2 weeks plus oral supplementation with vitamin B12 complex [pyridoxine, hydroxycobalamine, 30 mg/day (Benadon®, Roche)] was prescribed at home | Author defined (intensity of nausea, number of vomiting episodes and rate of food intake) | Nausea intensity, number of cases improved (%): (1) I first session 1 (2.3%); second session 11 (25.5%); third session 19 (44.1%); (2) comparator first session 1 (2.3%); second session 9 (23.6%); third session 12 (31.5%) Vomiting episodes, number of cases improved: (1) I first session 7 (16.2%); second session 15 (34.8%); third session 24 (55.8%); (2) comparator first session 4 (10.5%); second session 12 (31.5%); third session 14 (36.8%) |
| Acupuncture vs. placebo | |||||||||
| Carlsson 200066 | University hospital, department of obstetrics and gynaecology in Uppsala, Sweden | Effect of acupuncture plus standard treatment on HG, randomised crossover study | n = 33 (group A n = 17; group B n = 16) | Women suffering from HG and not responding to conventional outpatient treatment | No numerical values for severity at baseline provided. However, 25 women had previously tried antihistamines (MODERATE–SEVERE) |
Group A: on days 1 and 2, active acupuncture was performed at point PC6 for 30 minutes three times per day. No acupuncture was performed on days 3 and 4 (wash-out period). On days 5 and 6, sham acupuncture (needles were inserted only 1–2 mm in the skin) was performed for 30 minutes three times per day. During the study, the women also received parenteral nutrition with 5% glucose and patients were discharged on day 7 | Group B: on days 1 and 2, sham acupuncture (needles were inserted only 1–2 mm in the skin) was performed for 30 minutes three times per day. No acupuncture was performed on days 3 and 4 (wash-out period). On days 5 and 6, active acupuncture was performed at point PC6 for 30 minutes three times per day. During the study, the women also received parenteral nutrition with 5% glucose and patients were discharged on day 7 | VAS for nausea Episodes of vomiting |
Nausea in active acupuncture: (1) group A pre-acupuncture, post-VAS reduction = 4; (2) group B pre-acupuncture, post-VAS reduction = 3 Nausea in placebo acupuncture: (1) group B pre-placebo, post-VAS-reduction = 1.7; (2) group A pre-acupuncture, post-VAS reduction = 0.1 Vomiting occurrence: (1) I 7 out of 17 women were still vomiting after 2 acupuncture days; (2) comparator 12 out of 16 women were still vomiting after 2 placebo treatment days |
| Knight 200183 | Maternity unit, Royal Devon and Exeter Hospital, Devon, UK | Effectiveness of acupuncture compared with placebo acupuncture for treatment of nausea of pregnancy, RCT | n = 55 (I n = 28; comparator n = 27) (1) I 7.8 ± 1.0; (2) comparator 8.0 ± 1.0 |
Women complaining of nausea, with or without vomiting, who approached a community midwife | Nausea scores, median (IQR): I = 85.5 (IQR 71.25–89.75); sham = 87.0 (IQR 73.0–90.0) (MILD–MODERATE) |
At the first visit a traditional Chinese medical diagnosis was made and each woman was allocated one of three categories and treated with acupuncture to a combination of the following points: stomach 36; conception vessel 12; spleen 4; P6; stomach 44; and stomach 34 and P6. 40 × 0.25-mm needles (Seirin, Japan) inserted to a depth of 0.5–1.0 cm with the assistance of a guide tube, then manipulated. Needles were left in place for 15 minutes, given twice in the first week and once weekly for 2 weeks | Sham treatment consisted of tapping a blunt cocktail stick, supported by a plastic guide tube, over a bony prominence in the region of each acupuncture point. Sham needles were left in place for 15 minutes, given twice in the first week and once weekly for 2 weeks | VAS for nausea Episodes of vomiting |
Median nausea score (IQR): (1) I day 1 85.5 (IQR 71.25–89.75), 3 days after session one 63.0 (IQR 50.75–86.5), 3 days after session two 65.0 (IQR 36.25–79.5), 3 days after session three 44.0 (IQR 29.0–77.25), 3 days after session four 47.5 (IQR 29.25–69.5); (2) comparator day 1 87.0 (IQR 73.0–90.0), 3 days after session one 69.0 (IQR 45.0–87.0), 3 days after session two 61.0 (IQR 30.0–80.0), 3 days after session three 53.0 (IQR 25.0–80.0), 3 days after session four 48.0 (IQR 14.0–80.0) |
| Smith 2002101 | Women’s and children’s hospital in Adelaide, SA, Australia | Effectiveness of acupuncture (traditional and P6) compared with sham (placebo) acupuncture or no acupuncture on NVP, RCT | I n = 148; comparator n = 148; sham n = 148; C n = 149 | Women with symptoms of nausea or vomiting | RINVR score, I = nausea 8.3 (SD 2.5), dry retching 2.5, (SD 1.9) vomiting 2.3 (SD 2.7); C = nausea 8.2 (SD 2.6), dry retching 2.5 (SD 2.2), vomiting 2. (SD 2.8) (MILD–MODERATE) |
(1) Serin (Japan) 0.2 × 30 mm needles were inserted to a depth 0.5–1.0 cun using a guide tube (maximum of six needles per session) then manipulated and left for a 20-minute period. Treatment was based on a traditional Chinese medicine diagnosis. Treatment points included stomach points 19, 20, 21; kidney points 21, 20; and conception vessel points 14, 13, 12, 11, or 10 plus points to treat the traditional Chinese medicine diagnosis | (2) comparator – women allocated to the P6 study group received acupuncture to this single point only for a 20-minute period (twice during the first week and then weekly for 3 further weeks); (3) sham – women allocated to the sham acupuncture group received acupuncture needles inserted into an area close to, but not on, acupuncture points over similar time points; (4) C – a standardised information sheet was made available about advice on diet, lifestyle and the use of vitamin B6 during the 4-week study period. Women in this group received a weekly 10-minute telephone call from the study investigator to assess their general sense of well-being and to encourage compliance with participating in the trial | RINVR | Nausea: (1) I – day 7: 5.0 (SD 3.0), day 14: 4.6 (SD 3.1), day 21: 3.8 (SD 3.1), day 26: 3.4 (SD 3.0); (2) comparator – day 7: 5.4 (SD 3.3), day 14: 4.8 (SD 3.6), day 21: 4.3 (SD 3.3), day 26: 4.0 (SD 3.3); (3) sham – day 7: 5.7 (SD 2.8), day 14: 5.0 (SD 3.0), day 21: 4.4 (SD 2.7), day 26: 3.7 (SD 2.8); (4) C – day 7: 6.1 (SD 2.9), day 14: 6.0 (SD 3.1), day 21: 5.8 (SD 3.1), day 26: 5.0 (SD 3.0). (p-values – day 7 p = 0.05, day 14 p = 0.01, day 21 p = 0.001, day 26 p = 0.001) Dry retching: (1) I – day 7: 1.3 (SD 1.4), day 14: 0.9 (SD 1.3), day 21: 0.9 (SD 1.4), day 26: 0.8 (SD 1.4); (2) comparator – day 7: 1.6 (SD 1.7), day 14: 1.3 (SD 1.5), day 21: 0.9 (SD 1.3), day 26: 0.9 (SD 1.3); (3) sham – day 7: 1.5 (SD 1.8), day 14: 1.3 (SD 1.7), day 21: 0.9 (SD 1.3), day 26: 0.9 (SD 1.4); (4) C – day 7: 1.7 (SD 1.7), day 14: 1.3 (SD 1.7), day 21: 1.6 (SD 1.7), day 26: 1.6 (SD 1.7). (p-values – day 7 p = ns, day 14 p = 0.01, day 21 p = 0.001, day 26 p = 0.001) Vomiting: (1) I – day 7: 1.4 (SD 2.0), day 14: 1.1 (SD 1.8), day 21: 0.9 (SD 1.6), day 26 0.9 (SD 1.5); (2) comparator – day 7: 1.2 (SD 2.0), day 14: 1.3 (SD 2.2), day 21: 1.2 (SD 2.1), day 26 = 0.9 (SD 1.8); (3) sham – day 7: 1.5 (SD 2.2), day 14: 1.4 (SD 2.1), day 21: 1.0 (SD 1.7), day 26 = 1.0 (SD 1.6); (4) C – day 7: 1.5 (SD 2.1), day 14: 1.6 (SD 2.2), day 21: 1.1 (SD 2.1), day 26 = 1.4 (SD 2.0). (p-values – all non-significant) |
| Acupuncture vs. Chinese herbal medicine vs. Western medicine | |||||||||
| Mao 200987 | Jiuquan Hospital of Traditional Chinese Medicine, Jiuquan, China | Effectiveness of acupuncture vs. Chinese herbal medicine vs. Western medicine, three-arm RCT | n = 90 (I n = 30; comparator 1 n = 30; comparator 2 n = 30) (1) I 8.30 (SD 1.60); (2) comparator 1 8.33 (SD 1.38); (3) comparator 2 8.57 (SD 1.66) |
Women attending hospital clinic with vomiting and unable to tolerate oral intake | I mean number of vomiting episodes per 24 hours = 18.20 (8.54); comparator 1 mean number of vomiting episodes per 24 hours = 17.57 (7.06); comparator 2 mean number of vomiting episodes per 24 hours = 17.27 (8.50) (MODERATE–SEVERE) |
All women given i.v. fluids to rehydrate and correct electrolyte imbalance. Traditional Chinese acupuncture twice daily for 7 days | Comparator 1, i.v. fluids given to rehydrate, phenobarbitol given (30 mg) three times a day for 7 days Comparator 2, i.v. fluids given to rehydrate, traditional herbal remedy made daily and given in small doses through the day. Aim for three doses but if difficult to swallow then split into smaller more frequent doses |
Author-defined scale (change in symptoms) | Symptom severity on day 4: (1) I complete recovery 12 (40%), obvious improvement 8 (26.7%), slight improvement 9 (30.0%), no effect 1 (3.3%); (2) comparator 1 complete recovery 2 (6.7%), obvious improvement 10 (10.0%), slight improvement 7 (23.3%), no effect 18 (60.0%); (3) comparator 2 complete recovery 3 (10.0%), obvious improvement 1 (3.3%), slight improvement 8 (26.7%), no effect 18 (60.0%) Day 4, proportion of women with symptom relief: (1) I 96.7%; (2) comparator 1 40.0%; (3) comparator 2 40.0% Symptom severity on day 8: (1) I complete recovery 27 (90.0%), obvious improvement 2 (6.7%), slight improvement 0 (0%), no effect 1 (3.3%); (2) comparator 1 complete recovery 1 (3.3%), obvious improvement 6 (20.0%), slight improvement 4 (13.3%), no effect 16 (53.4%); (3) comparator 2 complete recovery 3 (10.0%), obvious improvement 10 (33.0%), slight improvement 5 (16.7%), no effect 12 (40%) Proportion of women gaining some benefit at day 8: (1) I 96.7%; (2) comparator 1 46.6%; (3) comparator 2 60.0.% Acupuncture significantly better than other two groups, no significant differences between other two groups |
| Zhang 2005115 | Dongguan City, Zhangmutou Hospital, Guangdone, China | Effectiveness of Chinese acupuncture plus moxibustion vs. Chinese herbal medicine vs. Western medicine, three-arm RCT | n = 150 (I n = 50; comparator 1 n = 50; comparator 2 n = 50) At study entry: (1) I 6–8 weeks n = 30, 8–12 weeks n = 17, > 12 weeks n = 3; (2) comparator 1 6–8 weeks n = 28, 8–12 weeks n = 20, > 12 weeks n = 2; (3) comparator 3 6–8 weeks n = 25, 8–12 weeks n = 22, > 12 weeks n = 3 |
Women attending hospital with abnormal vomiting and unable to tolerate oral intake | Number of women per severity of vomiting: I < 5 times/day n = 15, 6–10 times/day n = 30, > 10 times/day n = 5; comparator 1 < 5 times/day n = 11, 6–10 times/day n = 27, > 10 times/day n = 12; comparator 2 < 5 times/day n = 13, 6–10 times/day n = 32, > 10 times/day n = 5 (MODERATE) |
Traditional Chinese acupuncture at specific points plus gentle warming moxibustion for 10–15 minutes twice daily for 7 days. If the first round of treatment is ineffective a 3-day rest period was given before repeating the 7 days | Comparator 1, specific traditional formula of herbs boiled and made into drink. Full daily dose given in two parts over 7 days (repeated if not effective for further 7 days) Comparator 2, 2500–3000 mls i.v. fluids given daily to correct dehydration and electrolyte imbalance. Phenobarbitol (30 mg) given orally three times daily for 7 days. If not effective treatment repeated for another 7 days after a 3-day rest period |
Author-defined scale (change in symptoms) | (1) I acupuncture plus moxibustion complete recovery 21 (42%), obvious improvement 13 (26%), slight improvement 9 (18%), no effect 7 (14%); (2) comparator 1 complete recovery 9 (18%), obvious improvement 7 (14%), slight improvement 5 (10%), no effect 29 (58%); (3) comparator 2 complete recovery 5 (10%), obvious improvement 8 (16%), slight improvement 6 (12%), no effect 31 (62%) |
| Acupressure vs. no comparator | |||||||||
| Markose 2004124 | Christian Medical College Hospital, Vellore, India | To evaluate the effect of P6 acupressure in women who were given reassurance about the natural regression of nausea and who were not under any medication, case series | n = 35 recruited, n = 17 completed | Women experiencing nausea with or without vomiting | Percentage of women experiencing symptoms and distress: frequency of nausea 52.9%; frequency of vomiting 88.2%; frequency of dry retches 58.8%; distress due to nausea 58.8%; distress due to vomiting 82.3%; distress due to dry retches 70.5% (MILD–MODERATE) |
Acupressure on point P6 from the fourth day (the first 3 days being the control phase), four times a day for 10 minutes on each hand | None, days 1–3 classed as a control period | RINVR | Frequency of nausea: day 1 52.9%, day 3 58.8%, day 7 11.7%; p = 0.008 Frequency of vomiting: day 1 88.2%, day 3 100%, day 7 17.6%; p < 0.001 Frequency of dry retches: day 1 58.8%, day 3 58.8%, day 7 5.8%; p = 0.004 Distress due to dry retches: day 1 70.5%, day 3 64.7%, day 7 23.5%; p = 0.016 Distress due to vomiting: day 1 82.3%, day 3 76.4%, day 7 29.4%; p = 0.008 Distress due to nausea: day 1 58.8%, day 3 70.5%, day 7 11.7%; p = 0.002 |
Of the identified trials, eight were judged as being low risk of bias,61,62,66,80,83,91,98,101 with a further six unclear due to lack of sufficient information on the research process. 43,73,78,79,104,109 Four were judged as carrying high risk of bias on the basis of incomplete outcome data and weak randomisation process,115 lack of blinding,87 or selective outcome reporting. 94,111,115 We also identified a case series which evaluated the effect of P6 acupressure by Markose and colleagues,124 which was categorised as weak based on the EPHPP tool.
The severity of symptoms for patient participants in the studies comprising this group of interventions varied substantially. Three studies were classed as focussing on women with mild NVP,61,62,104 seven with mild to moderate,43,80,83,91,98,101,124 two with moderate severity,78,115 four with moderate to severe,66,87,94,111 and a final three for which severity was not possible to classify. 73,79,109
Acupressure versus placebo
Eight trials compared acupressure with placebo or sham treatment. 43,61,62,78,79,91,104,111 Seven trials43,61,62,78,79,104,111 involved the comparison of acupressure administered to the P6 acupoint, which lies between the tendons of the palmaris longus and flexor carpi radialis muscles, four centimetres proximal to the wrist crease. 129 Six of these trials examined the application of acupressure to point P6 by the use of pressure bands worn by study participants;43,61,78,79,104,111 one comprised self-administered acupressure at the P6 acupoint. 62 A final acupressure versus placebo trial compared acupressure self-administered with the two KID21 acupoints, which are located above the navel. 91 The placebo comparison intervention came in a two formats. The vast majority of studies (7/8) compared the active acupressure intervention with the application of acupressure to a sham acupoint (i.e. at which there is no known acupressure point or meridian pathway). 43,61,62,78,79,91,111 One final study compared the use of pressure bands with the wearing of placebo pressure bands which did not have a pressure button. 104 Three of these trials were judged as having low risk of bias61,62,91 and four were judged to be unclear. 43,78,79,104 Werntoff and Dykes111 was judged as having high risk of bias on the basis of incomplete outcome data and weak randomisation process.
Rhodes Index of Nausea, Vomiting and Retching
Belluomini and colleagues62 used the RINVR as a combined measure of change in nausea, vomiting and retching between the pre-treatment period (mean of days 1–3) and the post-treatment period (mean of days 5–7). The study found a significant reduction in combined scores for both groups (intervention from 12.64 ± 5.7 to 8.69 ± 5.0; p ≤ 0.001; placebo from 11.47 ± 4.9 to 10.03 ± 4.6; p = 0.019).
McGill Nausea Questionnaire
Only one trial used the McGill Nausea Questionnaire (a combined measure of various nausea severity indices) to assess symptom relief. Hsu and colleagues79 reported no difference between intervention and sham comparator at baseline, 30 or 60 minutes for any of the indices (p = 0.2 for all).
Nausea outcomes
The trial of Bayreuther and colleagues61 used the 10-point VAS to assess the difference in mean levels of nausea severity between groups. They reported that the mean level of nausea was significantly lower for the intervention group (3.23 points on the VAS) than for the placebo group (4.92 points on the VAS) (p = 0.019).
Can Gurkan and Arslan43 assessed the frequency, severity and discomfort from nausea using the VAS. They compared the difference in mean VAS scores between (1) the first 3 days and the second 3 days of the study; and (2) the second 3 days and the third 3 days for the each study group (intervention, placebo and a third no-treatment control arm). For frequency of nausea, a significant difference was reported between the first and second 3 days in both intervention (z = –3.35; p < 0.001) and placebo groups (z = –0.28; p < 0.05), but not in the control group (z = –0.92; p > 0.05). For frequency of nausea between the second and third 3 days of the study, no significant difference was found in any group (intervention z = –1.28, placebo z = 10.18, control z = –1.40; p > 0.05). For severity of nausea, the difference between the first and second 3 days was significant in the intervention and placebo group (z = –0.04 and z = –2.96, respectively; p < 0.05), but not in the control group (z = –1.02; p > 0.05). No significant difference was found in any group between the second and third 3 days (intervention z = –1.48; placebo z = –1.26, control z = 0; p > 0.05). The difference in the intensity of discomfort felt from nausea was significant for both the intervention group (z = –3.7; p < 0.001) and placebo group (z = –2.4; p < 0.05) but not control (z = –1.2; p > 0.05) between the first and second 3 days. However, the difference for any group for the second to third 3 was not significant (intervention z = –0.22; p > 0.05; placebo z = –1.4, p > 0.05; control z = –0.44; p > 0.05).
Naeimi Rad and colleagues91 also used the 10-point VAS to assess nausea severity between intervention (acupressure at point KID21) and placebo (‘false’ point) groups. Median VAS scores showed no significant difference between groups at day 1 [intervention 7 (IQR 8–6), comparator 7 (IQR 8–6); p = 0.473]. However, the difference was significant at day 2 [intervention 6 (IQR 7.75–4), comparator 7 (IQR 8–6); p = 0.012] and highly significant at days 3 [intervention 5 (IQR 5–3), comparator 7 (IQR 8–5); p < 0.001] and 4 [intervention 4 (IQR 5–2), comparator 7 (IQR 8–5); p < 0.001].
Werntoft and Dykes111 assessed the difference in nausea severity using the 10-point VAS between an intervention group receiving acupressure at the P6 acupoint compared with either a placebo treatment group or a third control group receiving no treatment at all. Although significant differences were observed between both intervention and placebo group compared with control at days 1 and 3 (p = 0.005 and p = 0.038, respectively), no differences in favour of the intervention group compared with the placebo and control groups were found at days 6 and 14 of treatment (p = 0.17 and p = 0.11 respectively).
Belluomini and colleagues62 measured nausea via the RINVR between the pre-treatment period (mean of days 1–3) and the post-treatment period (mean of days 5–7). Both intervention and comparator groups reported a significant reduction in nausea scores [intervention from 8.38 ± 2.2 to 5.80 ± 2.9 (p ≤ 0.001); comparator from 7.99 ± 2.5 to 7.04 ± 2.6 (p ≤ 0.001)].
An author-defined assessment scale composed of number of episodes and self-reported severity of nausea was used in Steele and colleagues104 to determine impact of acupressure at point P6 against placebo. During the 4 days of treatment, significant differences in favour of the intervention group were detected on both measures (mean rank for nausea frequency: intervention 40.30, comparator 72.82, p < 0.001; nausea severity: intervention 40.13, comparator 73.09, p < 0.001). However, when comparing the mean differences between the treatment period (days 1–4) and the post-treatment period (days 5–7), only the frequency of nausea showed a significant reduction (p < 0.05).
Vomiting outcomes
Emesis was measured with the RINVR in the trial of Belluomini and colleagues62 [change between the pre-treatment period (mean of days 1–3) and the post-treatment period (mean of days 5–7)]. A significant reduction was reported for the intervention group (from 2.09 ± 2.5 to 1.28 ± 1.9; p = 0.03). However, although the comparator group showed a reduction (from 1.83 ± 2.7 to 1.63 ± 2.3), it was not reported if this change was significant.
Naeimi Rad and colleagues91 used the 10-point VAS to compare vomiting frequency91 between intervention (acupressure at point KID21) and placebo (‘false’ point) groups. Increasingly significant differences between intervention and placebo groups were recorded on all days of treatment [day 1, intervention 1 (IQR 2–0), comparator 1 (IQR 2–1), p = 0.012; day 2, intervention 0 (IQR 1–0), comparator 1 (IQR 2–0.25), p = 0.003; day 3, intervention 0 (IQR 1–0), comparator 1 (IQR 2–0), p = 0.001; day 4, intervention 0 (IQR 0.75–0), comparator 1 (IQR 2–0), p < 0.001].
Can Gurkan and Arslan43 assessed the difference in number of vomiting episodes between (1) the first and second 3 days of the study; and (2) the second and third 3 days for the each study group (intervention, placebo and a third no-treatment control arm). 43 No significant difference was observed at either time point in any of the three study groups [first 3 days compared with second 3 days: intervention z = –1.38, placebo z = –1.85 and control z = –0.37 (p > 0.05); second 3 days compared with third 3 days: intervention z = –1.3, placebo z = –0.7 and control z = –0.57 (p > 0.05)]. Bayreuther and colleagues61 recorded episodes of vomiting in both intervention and comparator groups but did not report those findings in their paper.
As above, Steele and colleagues104 employed an author-defined assessment scale composed of number of episodes and self-reported severity of vomiting to measure the effectiveness of acupressure at point P6 against placebo. Significant differences favouring intervention were reported for both the frequency (intervention mean rank 41.51, comparator mean rank 70.94; p < 0.001) and severity (intervention mean rank 39.28, comparator mean rank 73.65; p < 0.001) of vomiting during the 4 intervention days. However, only the difference between groups for the severity of vomiting was significant when comparing days 1–4, with days 5–7 (p < 0.05).
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes or adverse events were reported for any of the included trials. There were no relevant data on this intervention from the UKTIS.
Acupressure versus vitamin B6
One trial (Jamigorn and Phupong80), judged as having a low risk of bias, compared the use of acupressure administered via a pressure band at acupoint P6 against vitamin B6 taken in tablet form.
Rhodes Index of Nausea, Vomiting and Retching
Jamigorn and Phupong80 used the RINVR to measure changes in combined nausea, vomiting and retching scores. They reported significant improvements in overall scores in both the acupressure (p < 0.001) and vitamin B6 groups (p < 0.001) (see Figure 2). However, there were no statistically significant differences in the reduction of RINVR scores between baseline and end of treatment score between groups (p > 0.05).
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes or adverse events were reported in any of the included trials. There were no relevant data on this intervention from the UKTIS.
Acupressure (case series)
Markose and colleagues124 was a case series study that evaluated the effect of P6 acupressure on women with mild to moderate nausea following an initial control phase of 3 days without treatment (categorised as weak in terms of quality).
Rhodes Index of Nausea, Vomiting and Retching
The RINVR was used to assess symptoms, but the actual RINVR score was not presented. Results for individual components of score (nausea, vomiting and retching) are presented below.
Nausea outcomes
The RINVR was used to measure nausea outcomes. A significant reduction in the frequency of nausea (defined as percentage of women experiencing three or more adverse events) (day 1 52.9%, day 3 58.8%, day 7 11.7%; p = 0.008) and distress due to nausea (day 1 58.8%, day 3 70.5%, day 7 11.7%; p = 0.002) was reported.
Vomiting outcomes
Emesis outcomes were measured using the RINVR in terms of both the frequency of vomiting and the vomiting-related distress reported by the women themselves. 124 As with vomiting, the authors report a significant trend of reduced vomiting frequency by day 7 (defined as percentage of women reporting three or more events) (day 1 88.2%, day 3 100%, day 7 17.6%; p < 0.001). A similar positive trend was reported for distress experienced as a result of vomiting (defined as percentage of women self-reporting moderate to severe distress) (day 1 82.3%, day 3 76.4%, day 7 29.4%; p = 0.008).
Retching outcomes
Finally, Markose and colleagues124 also measured the frequency of, and distress caused by, dry retches using the RINVR. A significant reduction in both retching outcomes (defined as percentage of women reporting three or more events, and distress from moderate to severe) was reported (retching frequency: day 1 58.8%, day 3 58.8%, day 7 5.8%, p = 0.004; distress due to dry retches: day 1 70.5%, day 3 64.7%, day 7 23.5%, p = 0.016).
Safety outcomes
No pregnancy outcomes or adverse events were reported in any of the included trials. There were no relevant data available on these interventions from the UKTIS.
Nerve stimulation versus placebo
Three studies compared the effect of a nerve stimulation device administered at pressure point P6 (as described in Acupressure versus placebo) against an identical inactive unit. 73,98,109 Of these trials, two provided insufficient data to permit a clear judgement of bias,73,109 and the other trial was judged as having a low risk of bias. 98 Given the differences between trials in patient populations, settings, interventions and in particular the heterogeneous nature of the reported outcomes across trials, we did not attempt to perform meta-analyses and have outlined individual trial results in a narrative.
Rhodes Index of Nausea, Vomiting and Retching
Rosen and colleagues98 used the RINVR to assess overall change in symptom severity. They determined that the time-averaged change in the RINVR score for total experience was significantly better in the study group than in the control group [6.48 (95% CI 5.31 to 7.66) vs. 4.65 (95% CI 3.67 to 5.63); p = 0.02]. Veciana and colleagues109 also used the RINVR to detect the difference symptom severity scores between the intervention and control groups. However, they found no significant difference in RINVR score between groups (p-value not reported).
Author-defined scale
Evans and colleagues73 measured subjective change in nausea and vomiting between those wearing active versus inactive nerve stimulation units via an author-defined scale (improved, worsened, no change). A significant change favouring the intervention group was detected in terms of both average nausea score (active unit 2.4, placebo 2.7; p < 0.05) and improvement in nausea score (active unit 15, placebo 10; p < 0.05).
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
The trial of Rosen and colleagues98 did not report pregnancy outcomes, but three dehydration events were reported in the study group compared with 12 events in the control group (p = 0.013). 98 Neither of the other two trials reported pregnancy outcomes or side effects,73,109 and there were no UKTIS data available on this intervention.
Acupuncture versus placebo
The trials of Carlsson and colleagues66 and Knight and colleagues83 both compared acupuncture at various treatment points with placebo (sham) treatment. Smith and colleagues101 was a four-arm RCT comparing a combination of various treatment points (group 1); with comparators including single point acupuncture to P6 (group 2); sham acupuncture to ineffective points (group 3); and a control comprising a standard information sheet and telephone support (group 4). Smith and colleagues101 and Knight and colleagues83 were both judged as carrying a low risk of bias; however, Carlsson and colleagues66 was judged as high due to lack of blinding.
Combined severity score
No combined score reported.
Nausea outcomes
Carlsson and colleagues66 assessed nausea severity between day 0 and day 1, and day 4 and day 5, in their crossover trial with the 10-point VAS. Focussing on ‘speed’ of change, the VAS reductions were calculated as the difference between the VAS estimates the day before acupuncture and those the day following the 2 acupuncture days for each patient. This intergroup crossover analysis showed a significantly faster reduction of nausea when giving the patients active acupuncture than when giving them placebo acupuncture (p = 0.032). However, they found no time effect (p = 0.138). The VAS was also used by Knight and colleagues83 to measure changes in nausea outcomes. They found evidence of a time effect (p < 0.001) in all groups [intervention scores reduced from 85.50 (IQR 71.25–89.75) on day 1 to 47.5 (IQR 29.25–69.5) at 3 days after session four; comparator scores reduced from 87.0 (IQR 73.0–90.0) on day 1 to 48.0 (IQR 14.0–80.0) at 3 days after session four. However, the authors reported that they found no evidence of a group effect (p = 0.9) or a group–time interaction (p = 0.8).
Smith and colleagues101 measured nausea severity with the RINVR. They found that women in the traditional acupuncture group were more likely to be free from nausea compared with women in the no acupuncture control group (relative risk 0.93, 95% CI 0.88 to 0.99) at the end of their first week of treatment. During the second week of the trial, women who received traditional acupuncture (p < 0.001), and P6 acupuncture (p < 0.05) reported lower nausea scores compared with women in the no acupuncture control group. This improvement in nausea continued for women receiving traditional acupuncture (p < 0.001) and P6 acupuncture (p < 0.01) into the third week compared with women in the no acupuncture control group. From the third week, women in the sham acupuncture group also reported lower nausea scores compared with women in the no acupuncture control group (p < 0.01). In the final week of the study, improvements in nausea continued for women in the traditional acupuncture (reported in the paper as p < 001, but actual value is not clear), P6 acupuncture (p < 0.05) and sham acupuncture (p < 0.01) groups compared with women in the no acupuncture group.
Vomiting outcomes
In the crossover trial of Carlsson and colleagues,66 occurrence of vomiting (i.e. emesis vs. no emesis) was compared between study groups. For active acupuncture treatment, they reported that 7 out of 17 women were still vomiting after 2 acupuncture days. For the placebo group, 12 out of 16 women were still vomiting at the same time point. They did not report if this difference was significant. Knight and colleagues83 measured number of vomiting episodes, but did not report these data.
Smith and colleagues101 measured vomiting severity with the RINVR. Lowered vomiting scores were recorded in all groups [intervention: day 7, mean 1.4 (SD 2.0) to day 26, mean 0.9 (SD 1.5); single point acupuncture: day 7, mean 1.2 (SD 2.0) to day 26, mean 0.9 (SD 1.8); placebo: day 7, mean 1.5 (SD 2.2) to day 26, mean 1.0 (SD 1.6)], including a small reduction in the control arm [day 7, mean 1.5 (SD 2.1) to day 26, mean 1.4 (SD 2.0)]. However, the differences between groups were not significant.
Retching outcomes
Smith and colleagues101 measured retching severity with the RINVR. They found that women in the traditional acupuncture (p < 0.001), P6 acupuncture (p < 0.01) and sham acupuncture (p < 0.001) groups all experienced fewer periods of dry retching compared with women in the no acupuncture control group at the end of the study. Sixty-eight (56%) women in the traditional acupuncture group were free from dry retching compared with 46 (39%) women in the no acupuncture control group by the end of the third week (relative risk 0.72, 95% CI 0.56 to 0.93; p < 0.01; number needed to treat 6, 95% CI 3 to 22). In the sham acupuncture group, 72 (59%) women were free from dry retching compared with 46 (39%) women in the no acupuncture control group (relative risk 0.68, 95% CI 0.52 to 0.87; p < 0.001; number needed to treat 6, 95% CI 3 to 13). These improvements continued to the end of the trial. In the P6 acupuncture group, no difference occurred in women free from dry retching compared with women in the no acupuncture control group.
Safety outcomes
No pregnancy outcomes or adverse events were reported in any of the included trials. There was no relevant data on this intervention from the UKTIS.
Acupuncture versus metoclopramide
The trial of Neri and colleagues94 compared acupuncture to acupoints PC6, Central Venter 12 and Stomach 36 plus the wearing of an acupressure device at the PC6 point against the administration of a metoclopramide infusion at hospital plus oral supplementation with a vitamin B12 complex. The trial was judged as carrying a high risk of bias due to selective outcome reporting.
Combined severity score
No combined score reported.
Nausea outcomes
Neri and colleagues94 measured the number of cases self-reporting improvements in the intensity of nausea (scored as 0 = no nausea; 1 = low intensity, no discomfort; 2 = high intensity, discomfort). Improvements were reported for both interventions [n (%) per session] [acupuncture: first session 1 (2.3%); second session 11 (25.5%); third session 19 (44.1%); metoclopramide: first session 1 (2.3%); second session 9 (23.6%); third session 12 (31.5%)], and the difference between groups was not reported as being non-significant (first session p = 0.3; second session p = 0.6; third session p = 0.2).
Vomiting outcomes
Neri and colleagues94 measured improvements in the number of cases reporting improvements in vomiting episodes (grouped as 0 = no episodes, 1 = 1–3/day, 2 = > 3/day). Both groups showed improvements [n (%) per session] [acupuncture: 7 (16.2%) for the first session; 15 (34.8%) for the second session; and 24 (55.8%) for the third session; metoclopramide: 4 (10.5%) for the first session; 12 (31.5%) for the second session; 14 (36.8%) for the third session]. However, the difference between groups was not found to be significant (p = 0.4 for first session and p = 0.5 for the second), although it approached significance after the third treatment session, in favour of acupuncture (p = 0.07).
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes or adverse events were reported in by Neri and colleagues. 94 There were no relevant data on this intervention from the UKTIS.
Acupuncture versus Chinese herbal medicine versus barbiturates
Two studies compared acupuncture against both Chinese herbal medicine and Western medicine. In the Mao and Liang trial,87 all women were given i.v. fluids for rehydration purposes and to correct electrolyte imbalance. The following interventions were then compared: (1) traditional Chinese acupuncture at acupoints BL11, ST37, PC6 and SP4; (2) a traditional herbal remedy; and (3) phenobarbital. In the Zhang 2005 trial,115 traditional Chinese acupuncture was compared with a traditional herbal drink and i.v. fluids plus phenobarbitol. Both trials were found to have a high risk of bias due to inadequate blinding and/or selective outcome reporting.
Author-defined scale
Mao and Liang87 assessed symptom severity using an author-defined scale (complete recovery, obvious improvement, slight improvement, no effect) on days 4 and 8, alongside the proportion of women with symptom relief in each group. They reported that the acupuncture performed significantly better than comparator intervention groups (with no significant difference between those other two groups). However, they did not report p-values. In the trial of Zhang,115 a similar author-defined scale was also used to assess symptom relief. It reported the highest proportion of complete recovery (21 patients, 42%) among the acupuncture group [compared with herbal medicine 9 (18%) or Western medicine 5 (10%)], but did not report if this difference was significant. The lowest numbers of patients reporting no effect were also found in the acupuncture group compared with either the herbal remedy or Western medicine groups [7 (14%) vs. 29 (58%) vs. 31 (62%) respectively]. However, again, it was not reported if this difference was significant.
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes or adverse events were reported in the included trials. There were no relevant data on this intervention from the UKTIS.
Summary
-
The quality of evidence available for this group of interventions varied considerably, from low (eight studies61,62,66,80,83,91,98,101) to high (five studies87,94,111,115,124) risk of bias.
-
Comparisons with placebo were equivocal: two studies (both where participants had mild symptoms and at low risk of bias)61,62 found no evidence of a difference or did not report the outcome for nausea and vomiting symptoms respectively.
-
Acupressure at the KID21 acupoint reduced both nausea and vomiting compared with placebo.
-
No evidence of a difference between acupressure and vitamin B6. 80
-
Two studies73,98 of nerve stimulation at the P6 acupressure point reported better outcomes versus a non-stimulating device [one study = participants with mild–moderate severity with low risk of bias,98 one study = unclear severity and risk of bias73]. A third study found no evidence of a difference (unclear severity and risk of bias). 109
-
Three studies66,83,101 compared acupuncture with placebo. There was no evidence of an effect on vomiting but one study (mild–moderate symptoms, low risk of bias)101 reported reduced nausea and retching in both traditional and P6 acupuncture groups.
-
No evidence of a difference between acupuncture compared with metoclopramide, but symptoms improved from baseline in both groups (one study: high risk of bias, severity assessed as moderate–severe94).
-
Comparisons of traditional Chinese acupuncture and herbal medicine with Western medicine were at high risk of bias and impossible to emulate within the UK NHS setting.
-
Overall conclusions are limited by the quality of included studies. Many participants appear to have improved symptoms from baseline in all treatment arms.
-
There is some suggestion that acupressure may have some beneficial effect in women with mild symptoms of NVP.
-
Acupressure at the KID21 point appears to improve symptoms of nausea and vomiting compared with acupressure to a false point, but data are limited.
-
The evidence for nerve stimulation is mixed.
-
Acupuncture may reduce symptoms of nausea and retching in women with mild–moderate symptoms, but data are limited and inconclusive.
-
More larger, better-quality studies are required for these interventions.
Chapter 6 Clinical effectiveness: aromatherapy
Introduction
Aromatherapy was used as an intervention to treat nausea and/or vomiting in two pilot RCTs. 76,97 Heterogeneity was observed in relation to the clinical setting and patient populations in which the studies were conducted, as well as the interventions, comparators and outcomes reported in each trial. As previously described (see Chapter 3, Meta-analysis of included randomised controlled trials) given these, we did not attempt to perform meta-analyses, and have thus reported a narrative summary only for each intervention and comparator set.
One trial compared aromatherapy with placebo in pre-natal wards97 whereas the other trial compared aromatherapy with routine antenatal care. 76 Both trials were at unclear risk of bias: mainly due to poor reporting in the trial of Pasha and colleagues;97 and for uncertainty surrounding whether the trial was truly randomised or was a quasi-RCT in Ghani and Ibrahim. 76 The women were described as experiencing symptoms at the mild to moderate end of the severity spectrum at baseline in both trials (Table 10).
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Pasha 201297 | Pre-natal wards of seven health clinics, Iran | To evaluate the effect of mint oil on nausea and vomiting during pregnancy, pilot RCT | n = 67; I = 9.07 (SD 1.31), C = 9.73 (SD 2.2) | Women complaining of nausea and vomiting | Mean of nausea and vomiting intensity was: I = 4.78 ± 1.62, C = 3.00 ± 2.19 and I = 4.85 ± 1.82, C = 2.52 ± 2.4, 7 days before treatment (MILD) |
Assigned to use a bowl of water with four drops of pure mint oil placed on the floor near their beds for 4 consecutive nights before sleeping. Dietary advice also given (n = 33) | As I except given saline instead of mint oil (n = 34) | VAS for nausea Episodes of vomiting |
Trend towards improvement by day 4 in mint group Mint group, mean scores over the 4 days: nausea 3.50 (SD 1.95), vomiting 2.23 (SD 1.88) Placebo, mean scores over the 4 days: nausea 4.38 (SD 2.18), vomiting 2.55 (SD 2.55) Not significant |
| Ghani 201376 | Outpatient department, maternity teaching hospital plus three maternal and child health centres in Abha Kingdom, Saudi Arabia | To estimate the effect of mixed essential oils inhalation on nausea and vomiting in early pregnancy, pilot RCT | n = 101; I = 10 (SD 2.61), C = 10.2 (SD 2.29) | Women who had nausea and/or vomiting and required antiemetics but were not hospitalised | RINVR score: I = 23.06 (SD 6.37), C = 21.74 (SD 7.30) (MILD–MODERATE) |
Four drops of lavender oils plus one drop peppermint oil in one spoon of water (ratio 4 : 1 : 1) heated using an oil burner. Perform twice a day for 3 days before sleep. Women were instructed to breathe deeply for 20 minutes. No other medication taken, diet/lifestyle advice given (n = 50) | Routine care, no treatment/oils given, no medication taken, diet/lifestyle advice given (n = 51) | RINVR score | Treatment group: change in score from 23.06 (SD 6.37) to 17.60 (SD 6.08); p < 0.001 Results from the C group not reported |
Aromatherapy versus no aromatherapy
One trial97 compared mint oil aromatherapy against placebo for the treatment of mild NVP. 97 Another trial compared mixed essential oils (lavender and peppermint) and routine antenatal care, where no treatment oils were given, in women with mild to moderate nausea and/or vomiting (i.e. requiring antiemetics but not hospitalisation).
Rhodes Index of Nausea, Vomiting and Retching
In the trial of Ghani and Ibrahim,76 the observed difference in the overall change from baseline RINVR score in the aromatherapy group was reduced to 17.60 (SD 6.08) from 23.06 (SD 6.37) at the end of the 3-day trial (p < 0.001). The change score in the no aromatherapy control group was not reported so it is unclear if the aromatherapy was effective in reducing nausea and vomiting or if it was due to the time lag.
Nausea outcomes
Pasha and colleagues97 examined the effectiveness of mint aromatherapy on pregnancy-induced nausea intensity using a VAS. There was no significant difference between the two groups. However, the authors reported a trend towards improvement by day 4 in the mint group, where the score had reduced to 3.50 (SD 1.95) from 4.78 (SD 1.62) at baseline, and an increase in nausea score at the end of day 4 from baseline score in the placebo group [mean 4.38 (SD 2.18) at day 4 compared with mean 3.00 (SD 2.19) at baseline].
Vomiting outcomes
The trial of Pasha and colleagues97 also examined the effect of mint aromatherapy on the number of vomiting episodes. 97 There was no significant difference between the two groups. However, there was a reported trend towards improvement by day 4 in the mint group where the mean number of episodes had reduced to 2.23 (SD 1.88) from 4.85 (SD 1.82) at baseline. In the placebo group there was no significant difference between the number of vomiting episodes at the end of day 4 and baseline [mean 2.55 (SD 2.55) at day 4 compared with mean 2.52 (SD 2.4) at baseline].
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes or adverse events were reported in either of the included trials. There were no relevant data on this intervention from the UKTIS.
Summary
-
The evidence from the two trials76,97 available for aromatherapy was predominantly at an unclear risk of bias.
-
The identified studies reported evidence of an improvement in symptoms over time, but there was no evidence of a difference compared with placebo or routine antenatal care.
-
Overall, few data are available with no evidence of an effect.
-
More larger, better-quality studies are required for to make any conclusions about this intervention.
Chapter 7 Clinical effectiveness: vitamin B6 (pyridoxine)
Introduction
Five trials compared the effectiveness of pyridoxine (vitamin B6) for the treatment of NVP. 41,59,100,107,112 Two trials compared doses of vitamin B6 against placebo tablets,41,100 and they were at low41 and unclear100 risk of bias, respectively. Tan and colleagues107 examined the effect of vitamin B6 and metoclopramide combination versus metoclopramide alone and was at an unclear risk of bias, mainly due to the use of a dubious placebo (Tic Tac®, Ferrero UK Ltd, Greenford, UK). The trial of Wibowo and colleagues112 compared high and low doses of vitamin B6, and was at low risk of bias. Babaei and Foghaha59 compared the effectiveness of vitamin B6 against dimenhydrinate in the treatment of NVP and was at an unclear risk of bias.
In all five studies,41,59,100,107,112 women were described as experiencing mild to moderate symptoms at baseline (Table 11). However, as previously described (see Chapter 3, Meta-analysis of included randomised controlled trials), given the differences between trials in patient populations, settings, interventions and, in particular, the heterogeneous nature of the reported outcomes across trials, we did not attempt to perform meta-analyses. Thus we reported a narrative summary only for each intervention and comparator set.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Vitamin B6 vs. placebo | |||||||||
| Vutyavanich 199541 | Antenatal clinic, Maharaj Nakorn Chiang Mai Hospital, Chiang Mai University, Thailand | To determine the effectiveness of pyridoxine for NVP, double-blind RCT | n = 342; I 10.9 (± 2.7), C 10.9 (± 2.8) | Women with nausea, with or without vomiting | Nausea and vomiting pregnancy instrument: I 5.2 (± 5.3), C 4.9 (± 2.4) Episodes of vomiting in past 24 hours: I 1.8 ± 2.3, C 1.6 ± 2.0 (MILD–MODERATE) |
Vitamin B6: 10-mg tablets of pyridoxine hydrochloride 8-hourly for 5 days. Dietary advice given, advised not to take any other medication (n = 173) | Placebo: identical tablets 8-hourly for 5 days. Dietary advice given, advised not to take any other medication (n = 169) | VAS for nausea Episodes of vomiting |
Nausea mean change in score: pyridoxine 2.9 (SD 2.2) vs. placebo 2.0 (SD 2.7) (p < 0.001) Vomiting episodes change: pyridoxine 1.22 (SD 2.0) vs. placebo 0.65 (SD 2.4) (p = 0.055) |
| Sahakian 1991100 | General obstetric clinic, Iowa, IA, USA | To determine the efficacy of pyridoxine for the treatment of NVP, double-blind RCT | n = 74; I 9.3 (range 6–15.5), C 9.7 (range 6–19) | Women suffering from nausea and vomiting but not requiring hospitalisation | VAS for nausea: I 6.4 (SD 1.8), C 6.6 (SD 1.9) (MILD–MODERATE) |
Vitamin B6 25-mg tablets of pyridoxine 8-hourly for 3 days. Dietary advice given (n = 31) | Placebo: identical tablets 8-hourly for 3 days. Dietary advice given (n = 28) | VAS for nausea Episodes of vomiting |
Nausea mean change: pyridoxine 2.9 (SD 2.4), placebo 1.9 (SD 2.0), p-value non-significant Severe nausea mean change: pyridoxine 4.3 (SD 2.1), placebo 1.8 (SD 2.2); p < 0.01 Vomiting: improvement in total pyridoxine group (p < 0.05) and severe symptoms (p < 0.05). Crude OR for vomiting vs. no vomiting in pyridoxine vs. placebo = 0.3014 (95% CI 0.102 to 0.893); p < 0.05 |
| Wibowo 2012112 | Cipto Mangunkusumo National Hospital, University of Indonesia, Indonesia | To determine if supplementation with vitamin B6 improves NVP (and to compare circulating plasma vitamin B6 between sufferers and non-sufferers), RCT | 60 sufferers (+60 non-sufferers who did not receive any treatment but acted as comparison for plasma B6 concentrations) C: < 8 weeks’ gestation (n = 12); 8–12 weeks’ gestation (n = 18) I: < 8 weeks’ gestation (n = 8); 8–12 weeks’ gestation (n = 22) |
Women suffering nausea and vomiting | PUQE: I 7 (range 4–15), C 6 (range 4–11) (MILD) |
Pyridoxine (5 mg) mixed with 40 g of powdered milk twice a day for 2 weeks. Dose of pyridoxine was equivalent to 10 mg per day. Women were asked not to take other medications | As I but equivalent dose of pyridoxine (0.64 mg) twice daily for 2 weeks ( = 1.28 mg per day). Women were asked not to take any other medications (n = 30) | PUQE score | Change in score: high-dose vitamin B6 3.86 ± 2.12 vs. low-dose vitamin B6 2.80 ± 1.78; p < 0.05 |
| Tan 2009107 | University of Malaya Medical Centre, Malaysia | To evaluate the oral use of pyridoxine in conjunction with standard therapy in women hospitalised for HG, RCT | n = 94; I 10.5 ± 3.1, C 9.6 ± 2.8 | Women with severe nausea and vomiting during pregnancy with clinical features | Nausea score via VAS: I median 7 (IQR 5), C median 7 (IQR 4) (MODERATE) |
i.v. rehydration with saline (± potassium chloride), pyridoxine two 10 mg-tablets given plus i.v. metoclopramide (10 mg) given three times daily plus oral thiamine (10 mg) daily. Discharged with pyridoxine, two tablets three times daily plus oral metoclopramide and thiamine (n = 48) | As I group, except instead of pyridoxine two mint Tic Tac® (Ferrero UK Ltd, Greenford, UK) given (n = 46) | VAS for nausea Episodes of vomiting |
Nausea score after 2 weeks: I median 2 (IQR 3), usual care median 2.5 (IQR 4); p = 0.69 Vomiting after 2 weeks: I mean 1.4 (SD 1.3), usual care mean 1.4 (SD 1.6); p = 0.98 |
| Vitamin B6 vs. serotonin antagonists | |||||||||
| Babaei 201459 | Two antenatal clinics of referral hospitals affiliated to Shiraz University of Medical Sciences, Shiraz, Southern Iran | To compare effectiveness of vitamin B6 and dimenhydrinate in the treatment of NVP, double-blind RCT | 140 participants, gestation < 16 weeks | Not reported (exclusion criteria included hospitalisation for severe vomiting) | RINVR nausea vomiting scores mean (SD) at baseline were 8.6 (SD 2.9) for vitamin B6 (group A) and 8.3 (SD 7.4) for dimenhydrinate (group B) (MILD) |
Vitamin B6 tablet (50 mg) orally every morning for 1 week (n = 70). Both vitamin B6 and dimenhydrinate tablets were identical in size, colour and odour | Dimenhydrinate tablet (50 mg) orally every morning for 1 week (n = 70) | RINVR | Both groups decreased nausea and vomiting scores from baseline values Average score change in the vitamin B6 group was less than that in the dimenhydrinate group [mean 4.4 (SD 1.6) vs. mean 5.7 (SD 5.5); p < 0.05] Each day, there were significant differences in score change of vitamin B6 group vs. dimenhydrinate group |
Vitamin B6 versus placebo
Pregnancy-Unique Quantification of Emesis and Nausea scale
Wibowo and colleagues112 measured the change in overall symptom severity using the PUQE scale for lower versus higher doses of vitamin B6. They found a higher mean change for the high dosage compared with lower, and there was a statistically significant improvement in PUQE score with the higher dose.
Nausea outcomes
The trial of Vutyavanich and colleagues41 used the 10-point VAS to assess mean change in nausea symptoms. 41 The study determined a higher mean change in the pyridoxine group [2.9 (SD 2.2) vs. placebo 2.0 (SD 2.7)], and this difference was significant (p < 0.001). The Sahakian and colleagues100 trial also employed the VAS to assess mean change in nausea. Overall, the study did not detect a significant difference between groups. However, for patients experiencing severe nausea, a significant mean change was observed in favour of the pyridoxine group (p < 0.001).
Vomiting outcomes
The change in the number of vomiting episodes was measured by Vutyavanich and colleagues. 41 However, although a greater reduction was observed in the pyridoxine group, this was not significant (p = 0.055). Sahakian and colleagues100 also assessed vomiting outcomes via number of vomiting episodes. 100 They observed a significant improvement both in the pyridoxine group as a whole (p < 0.05), and for the subgroup of women experiencing severe symptoms (p < 0.055).
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
None of the included trials reported on pregnancy outcomes or adverse events. UKTIS data on vitamin B6 enquiries are provided in Appendix 7.
Vitamin B6 and metoclopramide combination versus metoclopramide alone
The trial of Tan and colleagues107 used the 10-point VAS to assess median nausea scores in women with severe nausea and vomiting during pregnancy with clinical features. The trial also reported the mean number of daily vomiting episodes. 107
Combined severity score
No combined score reported.
Nausea outcomes
Tan and colleagues107 reported no significant difference in nausea score after 2 weeks between the pyridoxine (vitamin B6) and metoclopramide as a combination treatment and metoclopramide alone [combination median 2 (IQR 3), metoclopramide alone median 2.5 (IQR 4); p = 0.69].
Vomiting outcomes
Tan and colleagues107 reported no significant difference in the mean number of daily vomiting episodes after 2 weeks between the vitamin B6 and metoclopramide as a combination treatment and metoclopramide alone [combination mean 1.4 (SD 1.3), metoclopramide alone mean 1.4 (SD 1.6); p = 0.98].
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
Tan and colleagues107 did not report on pregnancy outcomes or adverse events. UKTIS data on vitamin B6 enquiries are provided in Appendix 7.
Vitamin B6 versus serotonin antagonist
The trial of Babaei and Foghaha59 compared effectiveness of vitamin B6 against dimenhydrinate in the treatment of NVP in a double-blind RCT which was adjudged as being at unclear risk of bias.
Rhodes Index of Nausea, Vomiting and Retching
Babaei and Foghaha59 compared nausea and vomiting scores at baseline and post treatment using the RINVR. Results showed that both vitamin B6 and dimenhydrinate groups decreased nausea and vomiting scores from baseline. However, the average score change in the vitamin B6 group was less than that in the dimenhydrinate group [mean 4.4 (SD 1.6) vs. mean 5.7 (SD 5.5); p < 0.05].
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
Babaei and Foghaha59 did not report on pregnancy outcomes. Occurrence of drowsiness was significantly lower in the vitamin B6 group compared with the dimenhydrinate group [5 (4.5%) as opposed to 36 (53%); p < 0.01]. No other adverse effect was observed in either group during the 1-week follow-up. UKTIS data on vitamin B6 enquiries are provided in Appendix 7.
Summary
-
The evidence available for vitamin B6 was predominantly at low risk of bias or the risk of bias was unclear.
-
Participants in the five studies41,59,100,107,112 had symptoms categorised as mild to moderate at baseline.
-
Comparisons of vitamin B6 preparations with placebo generally reported evidence of a reduction in symptoms of nausea, especially in women with more severe symptoms, and vomiting.
-
Higher doses of vitamin B6 preparations resulted in a greater improvement in NVP symptoms.
-
There was no evidence to suggest that vitamin B6 and metoclopramide as a combination treatment had an advantage over metoclopramide alone.
-
Overall, there is a suggestion that vitamin B6 might be better than placebo in reducing the severity of symptoms especially at higher doses, but more studies are required using a range of comparators.
Chapter 8 Clinical effectiveness: pyridoxine/doxylamine combination
Introduction
Four trials65,84,95,117 assessed the effectiveness of vitamin B6 in combination with doxylamine for the treatment of NVP in comparison with a placebo (Koren and colleagues84), ondansetron (Capp and colleagues65 and Oliveira and colleagues95) or when administered pre-emptively versus following symptom onset (Maltepe and Koren117). In the Koren and colleagues84 and Maltepe and Koren117 studies this took the form of Diclectin (delayed-release doxylamine/pyridoxine combination), while Oliveira and colleagues95 and Capp and colleagues65 gave pyridoxine and doxylamine as separate preparations.
One of the trials95 was only available in abstract form and risk of bias was unclear, whereas the trial of Koren and colleagues84 was at a low risk of bias. Another trial117 examined pre-emptive treatment with Diclectin and this trial appeared to be at low risk of bias but some items were unclear. Capp and colleagues65 was at unclear risk of bias due to lack of provided details across a number of measures. 65 The reporting of severity of symptoms was not possible for the Maltepe and Koren117 pre-emptive study, poor for the Oliveira and colleagues95 study and unclear for the Capp and colleagues65 study, but in the Koren and colleagues84 study, severity appeared to range from mild to moderate. As previously described (see Chapter 3, Meta-analysis of included randomised controlled trials), given the differences between trials in patient populations, settings, interventions and, in particular, the heterogeneous nature of the reported outcomes across trials, we did not attempt to perform meta-analyses, and have thus reported a narrative summary only for each intervention and comparator set.
We also identified a non-randomised prospective observational study (Ashkenazi-Hoffnung and colleagues36) which compared a combination regimen of doxylamine and pyridoxine versus metoclopramide only (control group). This study is prone to extreme selection bias and there was a noticeable difference at baseline: moderate to severe symptoms were present in 97% of the intervention group women versus 69% of control group women (p < 0.01). A summary of study conduct and results is depicted in Table 12 for completeness.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Pyridoxine/doxylamine vs. placebo | |||||||||
| Koren 201084 | Three university medical centres: the University of Texas, Texas, TX, USA; University of Pittsburgh, Pittsburgh, PA, USA; and Georgetown University, Washington, DC, USA | The effectiveness of Diclectin [doxylamine succinate (10 mg), pyridoxine hydrochloride (10 mg), delayed-release preparation] vs. placebo for NVP, double-blind RCT | n = 280; I 9.3 ± 2.0, C 9.3 ± 1.8 | Women suffering from NVP with a PUQE score of ≥ 6 and had not responded to conservative management (dietary/lifestyle advice) | Mean PUQE: I 9.0 ± 2.1, C 8.8 ± 2.1 Median PUQE: I 9.0, C 8.0 (MODERATE) |
Diclectin, two tablets at night, increasing up to four tablets daily as needed. Follow-up clinic visits and telephone calls (n = 140) | Identical placebo tablet: two tablets at night, increasing up to four tablets daily as needed. Follow-up clinic visits and telephone calls (n = 140) | PUQE score | Greater improvement in mean score change in Diclectin group vs. placebo (PUQE score: –4.8 ± 2.7 vs. 3.9 ± 2.6; p = 0.006) The mean area under the curve of the change in PUQE score from baseline was significantly larger with Diclectin as compared with placebo (61.5 ± 36.9 vs. 53.5 ± 37.5; p < 0.001) |
| Maltepe 2013117 | Women recruited who were calling the Motherisk NVP Helpline for counselling, Canada | Does pre-emptive treatment before the symptoms begin vs. when the symptoms begin improve symptoms in patients at a high risk for recurrence of severe NVP, RCT | n = 60, NR | N/A (recruited onto study before symptoms stated) | Not applicable – see Severity inclusion criteria | Diclectin, two tablets at bedtime following pregnancy confirmation, gradual increase if symptoms escalate. Frequent additional counselling provided, Motherisk algorithm of treatment followed (n = 31) | Diclectin, two tablets at bedtime on first day of NVP symptoms with gradual increase if symptoms escalated. Frequent additional counselling provided, Motherisk algorithm of treatment followed (n = 29) | PUQE score | Pre-emptive group, 43.3% reduction in HG between the previous pregnancy (19/30) and the present one (6/30), vs. 17.2% reduction (from 11/29 to 6/29) in the C group (p = 0.047) Pre-emptive group: 70% fewer cases of moderate–severe NVP (PUQE ≥ 11) [4/26 (15.4%) vs. 9/23 (39.13%)] in the C group during the first 3 weeks of NVP (p < 0.04) |
| Pyridoxine/doxylamine vs. metoclopramide | |||||||||
| Ashkenazi-Hoffnung 201336 | Recruitment via BELTIS, a free call-in centre for queries regarding drug use during pregnancy and lactation, CA, USA | To evaluate the efficacy and safety of pyridoxine (50 mg twice daily) and doxylamine (25–50 mg) as an alternative treatment for NVP, described as a prospective case–controlled observational study | 58, NR | Women who contacted the BELTIS regarding treatment of NVP were eligible for inclusion | Categorised as having moderate–severe NVP: I = 28/29 (97%), C = 18/26 (69%) (NOT CLEAR) |
Pyridoxine (50 mg) twice daily. If vomiting persisted plus doxylamine (25 mg) at night, with two additional doses of 12.5 mg if required (n = 29) | Metoclopramide (10 mg) 8-hourly as needed (n = 29) | Maternal report on the severity of NVP (mild, moderate, severe) and efficacy of treatment (no or mild, moderate, high) | Moderate/severe symptoms in 28/29 of treatment group (97%) vs. 18/26 in the C group (69%) (p < 0.01) at baseline Comparison of the treatment vs. C following treatment = similar efficacy in 20/29 (69%) vs. 18/25 (72%) of women (p = 0.65) |
| Pyridoxine/doxylamine vs. ondansetron | |||||||||
| Capp 201465 | Naval Medical Centre, San Diego, CA, USA | To determine whether ondansetron or the combination of doxylamine plus pyridoxine was superior for treatment of NVP, double-blind RCT | Trial was only available in abstract form so reporting lacks detail. Severity was NR so likely to have included all ranges from mild to severe | NR | Thirty-six women were enrolled in the trial with 30 fully completing the study. Presumably 18 were randomised in each group initially, gestation in weeks NR – authors stated first trimester of pregnancy only (UNCLEAR) |
4-mg ondansetron plus a placebo tablet every 8 hours for 5 days | 25-mg pyridoxine plus 12.5-mg doxylamine every 8 hours for 5 days | VAS for nausea and vomiting | Patients randomised to ondansetron demonstrated a greater reduction in nausea as compared with those taking pyridoxine and doxylamine (p < 0.05) Furthermore, women taking ondansetron reported less vomiting (p < 0.05) |
| Oliveira 2013 (abstract)95 | Naval Medical Centre, San Diego, CA, USA | Is ondansetron or the combination of doxylamine plus pyridoxine superior for treating NVP, double-blind RCT | 17, first trimester | Women with nausea and vomiting during first trimester and present at the emergency department | NR (MILD–MODERATE) |
One tablet of pyridoxine (25 mg) plus one tablet of doxylamine (12.5 mg) (P + D group) every 8 hours for 5 days (n = 9) | One tablet of ondansetron (4 mg) plus a second (placebo) tablet (O group) (n = 8) | VAS for nausea, and vomiting | Greater mean reduction in nausea with ondansetron (56–15 mm) vs. pyridoxine plus doxylamine (27–29 mm); p = 0.02 No difference in vomiting between groups (28–25 mm for ondansetron vs. 10–31 mm for pyridoxine plus doxylamine; p = 0.38) |
Doxylamine/pyridoxine versus placebo
One double-blind, multicentre placebo-controlled trial84 compared treatment with Diclectin, a combination preparation of doxylamine succinate (10 mg) and pyridoxine hydrochloride (10 mg), to placebo in women with symptoms of NVP and a PUQE score ≥ 7. Women in the trial had not previously responded to conservative management.
Pregnancy-Unique Quantification of Emesis and Nausea scale
Diclectin led to significantly greater improvement in NVP symptoms as compared with placebo (PUQE score: –4.8 ± 2.7 vs. 3.9 ± 2.6; p = 0.006). The mean area under the curve of the change in PUQE from baseline as measured day-by-day was significantly larger with Diclectin compared with placebo (61.5 ± 36.9 in the Diclectin group vs. 53.5 ± 37.5 in the placebo group; p < 0.001).
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
Koren and colleagues84 did not report on pregnancy outcomes or adverse events. UKTIS data on doxylamine/pyridoxine combination treatment are provided in Appendix 7.
Doxylamine/pyridoxine versus ondansetron
The double-blind RCT of Oliveira and colleagues95 was in abstract form only and randomised women in the first trimester of pregnancy requesting treatment for NVP to either one tablet of ondansetron (4 mg) plus a second (placebo) tablet or one tablet of pyridoxine (25 mg) plus one tablet of doxylamine (12.5 mg) administered every 8 hours for 5 days. 95 All study medications were identical in appearance. Capp and colleagues65 also compared 4-mg ondansetron plus a placebo tablet administered every 8 hours for 5 days against 25-mg pyridoxine plus 12.5-mg doxylamine. 65
Combined severity score
No combined score reported.
Nausea outcomes
Oliveira and colleagues95 found a significantly greater mean reduction in nausea (p = 0.02) using the VAS in patients using ondansetron (56 ± 15 mm) compared with those taking pyridoxine plus doxylamine (27 ± 29 mm). A significant difference in favour of ondansetron was also reported by Capp and colleagues. 65 However, no detailed scores were provided as the paper was in abstract form only (p < 0.05).
Vomiting outcomes
There was no significant difference in vomiting between the two groups reported by Oliveira and colleagues95 (28 ± 25 mm for ondansetron vs. 10 ± 31 mm for pyridoxine plus doxylamine; p = 0.38). However, Capp and colleagues65 found a significant improvement in the ondansetron groups in terms of reduction in vomiting using the VAS (p < 0.05), although, as with nausea scores, no exact values were reported in the abstract.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
Oliveira and colleagues95 did not report on pregnancy outcomes or adverse events. The trial of Capp and colleagues65 did not report on pregnancy outcomes either but found no statistically significant difference between groups with respect to sedation or constipation (p > 0.05) (see Appendix 8). UKTIS data on doxylamine/pyridoxine combination treatment are provided in Appendix 7.
Pre-emptive doxylamine/pyridoxine
One RCT117 compared pre-emptive treatment with Diclectin before the onset of symptoms of NVP, versus when the symptoms first began in patients at high risk for recurrence of severe NVP.
Pregnancy-Unique Quantification of Emesis and Nausea scale
In the pre-emptive group there were 70% fewer cases of moderate–severe NVP (PUQE score of ≥ 11) compared with the control group [4/26 (15.4%) vs. 9/23 (39.13%)] during the first 3 weeks of NVP (p = 0.05). In addition, in the pre-emptive group there was a 43% reduction in HG between the previous pregnancy (19/30) and the present one (6/30) compared with a 17% reduction (from 11/29 to 6/29) in the control group (p = 0.047).
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
The trial of Maltepe and Koren117 did not report either pregnancy outcomes or adverse events. UKTIS data on doxylamine/pyridoxine combination treatment are provided in Appendix 7.
Summary
-
The evidence available for pyridoxine/doxylamine combinations is varied, but two trials appeared to be at low risk of bias84,117 with the other two having an unclear risk of bias profile. 65,95
-
The quality of the evidence is low and was downgraded due to clinical heterogeneity and sparseness of data in most comparisons. Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimates.
-
Diclectin appears to be more effective at relieving symptoms of NVP than placebo.
-
Ondansetron appears more effective at reducing nausea than pyridoxine plus doxylamine but there was no difference for vomiting.
-
Limited data from a single small study36 showed no difference in efficacy between pyridoxine plus vitamin B6 versus metoclopramide but was subject to selection bias.
-
Pre-emptive treatment with Diclectin appears to result in a reduced risk of moderate/severe NVP compared with treatment initiation once symptoms begin.
-
Further larger, well-conducted trials are required to test the effectiveness of Diclectin or pyridoxine/doxylamine in combination compared with other treatment options.
Chapter 9 Clinical effectiveness: antihistamines
Introduction
Antihistamines were used as an intervention to treat nausea and/or vomiting in three RCTs. 68,71,90 Heterogeneity was observed in relation to the clinical setting, and the patient populations in which the studies were conducted, but most notably there were differences in interventions, comparators and outcomes reported in each trial. As previously described (see Chapter 3, Meta-analysis of included randomised controlled trials), given these differences, we did not attempt to perform meta-analyses and have thus reported a narrative summary only for each intervention and comparator set.
The three trials had varying risk of bias profiles, with just one of the trials appearing to be at low risk of bias,71 and the remaining two at high risk of bias due to concerns with regard to blinding and incomplete outcome reporting,68 and selective outcome reporting. 90 The women were described as experiencing mild symptoms at baseline in all three trials (Table 13).
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Antihistamines vs. placebo | |||||||||
| Erez 197171 | Prenatal clinics, Kasimpasa Naval Hospital and Golcuk Naval Hospital, Ismit, Turkey | To investigate the effectiveness of hydroxyzine hydrochloride as an antiemetic in pregnancy and its effect on fetal outcomes, RCT | n = 150 (I n = 100, C n = 50); states treatment in first 2 months of pregnancy only | Women reporting recurrent nausea and had vomited at least three times per week over the previous 2 weeks | NR (MILD) |
Hydroxyzine hydrochloride capsules (25 mg) two times a day (a.m. and 2 p.m. for 3 weeks) (n = 100) | Identical placebo capsules two times a day (a.m. and 2 p.m. for 3 weeks) (n = 50) | Patient assessment: (1) complete relief; (2) partial relief; and (3) no relief | Hydroxyzine, partial or complete relief in 82% of the patients; placebo, some effect in 22% of the patients (p < 0.01) |
| Antihistamines ± vitamin B6 | |||||||||
| Diggory 196268 | Antenatal clinic, Queen Charlotte’s and Chelsea Hospital, London, UK | To compare meclozine hydrochloride ± pyridoxine with placebo and simple dietary advice, four-arm RCT | n = 139 (group 1 n = 29, group 2 n = 34, group 3 n = 41, group 4 n = 35); ≤ 14 weeks | Women attending antenatal clinics who were experiencing nausea or vomiting | NR (MILD) |
Group 3 = dietary info sheet plus antihistamines (25 mg a.m., 50 mg p.m.). Group 4 = dietary info sheet plus antihistamines (25 mg a.m., 50 mg a.m. plus pyridoxine 50 mg a.m., 100 mg p.m.) | Group 1 = dietary info sheet only. Group 2 = dietary info sheet plus placebo | Author-defined severity scale based on disruption to life (good, fair, poor) | Group 1 good (n = 6), fair (n = 4); poor (n = 19); group 2 good (n = 5), fair (n = 11), poor (n = 18); group 3 good (n = 28), fair (n = 12), poor (n = 1); group 4 good (n = 22), fair (n = 11), poor (n = 2) No differences between groups 1 and 2 or 3 and 4, but both groups 3 and 4 significantly improved compared with groups 1 and 2; p < 0.001 in all cases |
| Monias 195790 | Military hospital, Massachusetts, MA, USA | To evaluate the effectiveness of cyclizine plus pyridoxine in treating NVP, RCT | n = 200 (n = 100 each arm); 6–20 weeks | Women complaining of nausea and/or vomiting | NR (MILD) |
Instructed to take two cyclizine plus pyridoxine tablets half an hour before breakfast and an additional tablet before lunch if required for 10 days. Dose not reported (n = 100) | Instructed to take two placebo tablets half an hour before breakfast and an additional tablet before lunch if felt it was required, for 10 days (n = 100) | Author defined (complete, partial or no relief) | I group: complete relief n = 78, partial relief n = 5, no relief n = 17 Comparator: complete relief n = 13, partial relief n = 5, no relief n = 82 |
Antihistamines versus placebo
Two trials71,90 compared antihistamines and placebo: one trial71 in women with mild recurrent nausea and who had vomited at least three times per week over the previous 2 weeks; and the other trial90 in women complaining of nausea and/or vomiting. Hydroxyzine hydrochloride (25 mg) capsules were given twice daily for 3 weeks in the trial of Erez and colleagues,71 and cyclizine pyridoxine (dose not reported) tablets twice daily for 2 weeks in the Monias90 trial.
Author-defined symptom severity/relief scale
Hydroxyzine significantly relieved symptoms of nausea and vomiting compared with placebo in the trial of Erez and colleagues,71 resulting in partial or initial or complete relief in 82% of women, whereas the placebo produced some effect in only 22% of women (p < 0.01). This trial was at low risk of bias.
In the trial of Monias,90 78, 5 and 17 out of 100 women experienced complete, partial and no relief in the intervention group, respectively. In the placebo group (also n = 100), only 13 women experienced complete relief, five partial relief, and in 82 women no relief of symptoms was observed. The intervention relieved symptoms in a higher percentage of women than the placebo group; however, no formal statistical analysis was undertaken.
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting scores reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
The trial of Erez and colleagues71 found no statistically significant differences in terms of miscarriage, perinatal outcomes and fetal outcomes between groups (p > 0.05), and only minor side effects (slight drowsiness) were reported by 7% of the intervention group. No pregnancy outcomes or adverse events were reported by Monias. 90 See Appendix 8 for details, with UKTIS data on hydroxyzine reported in Appendix 7.
Antihistamines alone or in combination with Vitamin B6 versus control
One four-arm trial68 compared antihistamines (meclizine hydrochloride) with and without vitamin B6 (pyridoxine) with a placebo group and a no treatment group in women experiencing mild nausea or vomiting. In the intervention arms, meclizine hydrochloride was given at doses of 25 mg and 50 mg in the morning and evening, respectively. In the combination group, pyridoxine was given at 50 mg in the morning and 100 mg in the evening.
Author-defined scale
The trial used an author-defined severity scale based on disruption to life whereby women were asked to judge symptoms on the basis of whether the impact of the treatment on restoring disrupted routine could be categorised as good, fair or poor. No differences between the control groups or the two intervention groups were observed (p > 0.05). However, based on subjective assessments of restoration of disrupted routine, both the antihistamine alone and antihistamine with vitamin B6 groups significantly improved (p < 0.001) in comparison to the two control groups (no treatment group: good n = 6, fair n = 4, poor n = 19; placebo group: good n = 5, fair n = 11, poor n = 18; antihistamine alone: good n = 28, fair n = 12, poor n = 1; antihistamine with vitamin B6: good n = 22, fair n = 11, poor n = 2).
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting scores reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes or adverse events were reported by Diggory and Tomkinson68 and there were no UKTIS data relating to meclizine hydrochloride.
Summary
-
Of the three studies available for antihistamines, two were at high risk of bias68,90 while one was at low risk. 71 The quality of the evidence was very low and was downgraded due to the reporting of author-defined scales to measure symptom severity, and other concerns about the overall risk of bias in included RCTs. We are very uncertain about the effectiveness estimates in terms of validation and estimates may change in future trials.
-
Participants in all three studies68,71,90 had mild symptoms so generalisability is restricted.
-
Use of antihistamines resulted in an improvement over a range of symptoms.
-
The addition of vitamin B6 does not appear to improve effectiveness.
-
Evidence is limited in both quantity and quality.
-
Antihistamines appear to be better than placebo in reducing the severity of symptoms, but better-quality, large studies are required for this and all other comparators.
Chapter 10 Clinical effectiveness: dopamine antagonists
Introduction
Dopamine antagonists were used as an intervention to treat HG in the trial of Tan and colleagues. 106 The trial was a head-to-head comparison of two interventions (promethazine vs. metoclopramide) and was at low risk of bias. We will focus on the results from this trial here. We also identified a non-randomised prospective study122 which examined two study groups (67 patients treated with i.v. droperidol 1 mg/hour plus diphenhydramine 25–50 mg every 6 hours; and 34 patients treated with i.v. droperidol 0.5 mg/hour plus diphenhydramine 50 mg every 6 hours; and a historical control of 54 patients receiving conventional antiemetic treatment). The study groups were then gradually weaned onto oral hydroxyzine and metoclopramide. This study is prone to extreme selection bias and other biases, and classified as ‘weak’ according to the EPHPP quality assessment tool. A summary of study conduct and results is depicted in Table 14, with safety data reported in Appendix 8.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Dopamine antagonists vs. conventional treatment | |||||||||
| Ferreira 2003122 | Sainte-Justine Hospital, Montréal, Québec, Canada | To compare the efficacy of the droperidol/diphenhydramine combination with other conventional treatments used. Described as a case–control study but actually a cohort study | Group A n = 54, group B n = 67, group C n = 34 Group A = 11.1 ± 4.6, group B = 10.3 ± 3.9, group C = 10.4 ± 2.8 |
Women hospitalised for HG with at least one of the three following criteria: weight loss ≥ 5% of pre-pregnancy weight, ketonuria (objectified on urinary test strips), or hypokalemia (< 3.5 mEq/l) | Mean score National Cancer Institute’s Common Toxicity Criteria scale: nausea (scale 0–3) group A = 2.24 ± 0.8, group B = 1.33 ± 1.05, group C = 1.03 ± 1.00; vomiting (scale 0–4) group A = 1.06 ± 1.00, group B = 0.34 ± 0.66, group C = 0.41 ± 0.74 (MODERATE) |
Two groups (groups B, C). Both groups received i.v. rehydration plus multivitamins. Group B: i.v. droperidol infusion at 1 mg/hour plus i.v. diphenhydramine (25–50 mg) 6-hourly Group C: i.v. droperidol at 0.5 mg/hour plus i.v. diphenhydramine (50 mg) 6-hourly. Gradually oral antiemetic treatment consisting of hydroxyzine and metoclopramide was started |
A retrospective control group (A), treated with a variety of antiemetic treatments (i.m. chlorpromazine, i.v. dimenhydrinate, i.v. metoclopramide, or a combination of doxylamine–pyridoxine (Diclectin) taken orally) according to the physicians’ choice | National Cancer Institute’s Common Toxicity Criteria scale: nausea analogue scale varies from 0 to 3, and the vomiting scale varies from 0 to 4 | Mean score on day 1 (SD) to during hospitalisation: Nausea (n = 155): group A = 2.24 (SD 0.87) to 1.48 (SD 0.49); group B = 1.33 (SD 1.05) to 0.78 (SD 0.70); group C = 1.03 (SD 1.00) to 0.58 (SD 0.60); p < 0.001 Vomiting: group A = 1.06 (SD 1.00) to 0.62 (SD 0.54); group B = 0.34 (SD 0.66) to 0.25 (SD 0.36); group C = 0.41 (SD 0.74) to 0.24 (SD 0.39). p < 0.001 in favour of group B This trend continued through the hospital stay, although it was not clear whether or not analysis accounted for group differences at baseline |
| Dopamine antagonists vs. metoclopramide | |||||||||
| Tan 2010106 | Gynaecology ward, university hospital in Kuala Lumpur, Malaysia | To compare the effects of promethazine with those of metoclopramide for HG, double-blind RCT | n = 159; metoclopramide 9.2 ± 2.3, promethazine 9.3 ± 2.6 | Women hospitalised with presumed hyperemesis who were determined clinically to require i.v. antiemetic therapy | Nausea score via VAS: I = median 5 (IQR 2.75–7), C = median 5 (IQR 1.5–7) (MODERATE) |
Metoclopramide (10 mg) given i.v. after randomisation, at 8, 16 and 24 hours (n = 79) | Promethazine (25 mg) given i.v. after randomisation and at 8, 16 and 24 hours (n = 80) | VAS for nausea Episodes of vomiting |
Vomiting: metoclopramide = 1 (IQR 0–5), promethazine = 2 (IQR 0–3); p = 0.81 Nausea at 24 hours: metoclopramide = 2 (IQR 1–5), promethazine = 2 (IQR 1–4); p = 0.99 (Nausea scores at 8 and 16 hours also showed no significant difference) Repeated measures analysis of variance for nausea score: p = 0.95 |
Promethazine versus metoclopramide
The trial of Tan and colleagues106 randomised women in early pregnancy (gestation of ≤ 16 weeks) with clinical HG to either 25-mg promethazine (n = 76) or 10-mg metoclopramide (n = 73), administered intravenously every 8 hours for 24 hours.
Combined severity score
No combined score reported.
Nausea outcomes
There were no significant differences in median nausea scores during all monitored time points (at baseline and at 8, 16 and 24 hours) between the promethazine and metoclopramide groups (p = 0.95). The median nausea score at 24 hours was 2 (IQR 1–4) in the promethazine group and 2 (IQR 1–5) in the metoclopramide group (p = 0.99).
Vomiting outcomes
There was no significant difference in the median number of vomiting episodes between the promethazine and metoclopramide groups [median episodes were 2 (range 0–3) and 1 (range 0–5) in the promethazine and metoclopramide groups respectively; p = 0.8].
Retching score
No independent retching score reported.
Safety outcomes
No pregnancy outcomes were reported by Tan and colleagues106 and only minor side effects, with significantly more women in the promethazine group reporting drowsiness (p = 0.001) and dizziness (p < 0.001). Additional UKTIS data on promethazine are reported in Appendix 7.
Summary
-
Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP.
-
The quality of evidence was very low and was downgraded due to sparseness of data and imprecision, although the one trial106 that reported a comparison on promethazine and metoclopramide was at low risk of bias.
-
We are very uncertain about the estimates of effectiveness. Further, well-conducted studies are required to compare the effectiveness of metoclopramide against other comparators.
Chapter 11 Clinical effectiveness: serotonin antagonists (ondansetron)
Introduction
A total of five trials57,72,75,81,105 and one cohort study121 compared the serotonin antagonist (ondansetron) against a range of alternatives for the treatment of women experiencing various severities of nausea in pregnancy. Of these, one study focussed on the safety of ondansetron versus the usual treatment regimen,121 with symptom severity not specified. Three trials tested ondansetron against metoclopramide, with participants’ symptoms classified as mild to moderate in two trials,75,81 and severe in one trial. 57 The remaining two trials compared ondansetron with antihistamines,72,105 with women classed as experiencing symptoms at the moderate to severe end of the spectrum.
Two of the identified trials were found to have a low risk of bias. 57,81 The trial of Sullivan and colleagues105 was classed as unclear due to insufficient information, with the remaining two found to carry a high risk of bias. 72,75 The included cohort study of Einarson and colleagues121 was classed as ‘weak’ according to the EPHPP quality assessment tool. As previously described (see Chapter 3, Meta-analysis of included randomised controlled trials), given the differences between trials in patient populations, settings, interventions and, in particular, the heterogeneous nature of the reported outcomes across trials, we did not attempt to perform meta-analyses and have thus reported a narrative summary only for each intervention and comparator set. A summary of study conduct and results is depicted in Table 15, with safety data reported in Appendix 8.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Ondansetron vs. usual treatment | |||||||||
| Abas 201457 | Full-service, state-funded university hospital, Kuala Lumpur, Malaysia | To compare effectiveness of ondansetron with metoclopramide in the treatment of HG | n = 160; ≤ 16 weeks with clinical dehydration and ketonuria (of 2+ or greater) | Presence of nausea and intractable vomiting sufficient to cause dehydration and metabolic disturbance of a severity to require hospitalisation | Nausea score: ondansetron median 8 (IQR 7–9); metoclopramide median 8 (IQR 7–10) (SEVERE) |
4-mg ondansetron was diluted in 100-ml normal saline and standard 100-ml normal saline packs were labelled as A or B (n = 80) | 10-mg metoclopramide was diluted in 100-ml normal saline and the standard 100-ml normal saline packs were labelled as A or B (n = 80) | VAS for nausea Episodes of vomiting |
Nausea visual numeric rating scale scores [median (IQR)] at 8 hours [4 (IQR 3–6) vs. 5 (IQR 4–6)], 16 hours [3 (IQR 1–4) vs. 3 (IQR 2–4.75)], and 24 hours [1 (IQR 1–3) vs. 2 (IQR 1–3)] after randomisation were not significantly different when assessed separately at each time point Vomiting episodes in the first 24 hours were median 1 (IQR 0–2) vs. median 2 (IQR 0–2.75) (p = 0.38) for ondansetron and metoclopramide respectively Repeated measures analysis of variance also showed no difference across the trial arms (p = 0.22) for nausea visual numeric rating scale scores, although generally across both arms, nausea score lessened significantly over at 24 hours (12.5% compared with 30%; p = 0.01; number needed to treat to benefit, 6) for the ondansetron arm |
| Einarson 2004121 | Women calling the Helpline or TIS at the Motherisk Program in Toronto, Canada, or the MotherSafe Program in Sydney, Australia | To determine whether or not the use of ondansetron during pregnancy is associated with an increased risk for major malformations. Prospective, three-arm, comparative study | Group 1 n = 188 (ondansetron), group 2 n = 176 (antiemetics), group 3 n = 176 (non-teratogen) | Women who called either the Motherisk and MotherSafe counselling services, who were taking ondansetron for NVP | NR (NOT CLEAR) |
Group 1: women who called either service and were taking ondansetron at the time of call within a 2-year period were enrolled | Group 2: women who called one of the helplines but were not exposed to ondansetron (used other antiemetics including Diclectin, metoclopramide, phenothiazines and ginger) Group 3: women exposed to other drugs considered safe to use in pregnancy or those who had not used any medication |
PUQE | NR |
| Ondansetron vs. metoclopramide | |||||||||
| Kashifard 201381 | Ruhani Hospital of Babol University of Medical Sciences, North Iran | To compare the effectiveness of ondansetron vs. metoclopramide in the treatment of HG, double-blind RCT | n = 83, gestational age in weeks 8.7 (SD 2.6) both groups | Women vomiting three times a day with weight loss > 3 kg and presence of ketonuria | NR (MILD–MODERATE) |
Ondansetron hydrochloride tablets (4 mg), three times a day for 1 week. Dose gradually reduced and discontinues: two times a day for 3 days; once a day for 4 days. Medication stopped after second week | Metoclopramide (10 mg), three times daily following same regime | VAS for nausea Episodes of vomiting |
Nausea was significantly less in the ondansetron group on third and fourth days of treatment vs. metoclopramide group (p = 0.024 and p = 0.023, respectively) Vomiting episodes in the ondansetron group were fewer than the metoclopramide group from the second to the eighth days Trend of change for vomiting in the ondansetron group was lower (p = 0.045) No difference in nausea trend |
| Ghahiri 201175 | Shahid Beheshti Hospital, Iran | To compare the effectiveness of ondansetron vs. metoclopramide in the treatment of NVP, RCT | n = 70; metoclopramide 12 weeks (SD 3.8), ondansetron 10.8 weeks (SD 3.3) | Women suffering from chronic NVP, requiring hospitalisation and treatment | Mean (SE): nausea VAS I 3.14 (SE 0.55), C 3.09 (SE 0.66); vomiting VAS I 2.29 (SE 0.71), C 2.09 (SE 0.78) (MILD–MODERATE) |
All participants rehydrated with i.v. fluids plus 10-mg metoclopramide twice daily orally for 3 weeks (n = 35) | All participants rehydrated with i.v. fluids plus ondansetron (4 mg) orally twice daily for 3 weeks (n = 35) | VAS for nausea Episodes of vomiting |
No difference in severity of NVP at 3 days or 1 week At 2 weeks nausea was less in ondansetron group, (p = 0.05) and vomiting was less in the metoclopramide group (p = 0.04) At 3 weeks vomiting was less in the ondansetron group (p = 0.02) |
| Ondansetron vs. antihistamines | |||||||||
| Sullivan 1996105 | Women admitted to the University of Mississippi Medical Centre, MS, USA | To investigate whether or not ondansetron may be an effective antiemetic in pregnancy, RCT | n = 30, (n = 15 in each arm); I 11.0 (SD 2.7), C 10.2 (SD 3.8) | Women admitted to hospital with severe HG, > 5 lb weight loss, ketonuria > 80 mg/dl, hypokalemia < 3.0 mEq/dl, hyponatremia < 134 mEq/dl requiring i.v. replacement, positive serum acetone, two or more visits to obstetric emergency department for HG which required i.v. hydration or promethazine suppositories, as an outpatient | NR (MODERATE–SEVERE) |
i.v. hydration. Ondansetron (10 mg) given intravenously in 50 ml of compatible i.v. fluid over 30 minutes. First dose mandatory, then as needed 8-hourly. I.v. hydration continued until patient ingesting a bland diet. Discharged with promethazine suppositories plus dietary instructions. Seen in clinic on a weekly basis. If no change after 48 hours patient considered treatment failure and was excluded | As I except promethazine (50 mg) given intravenously in 50 ml of compatible i.v. fluid over 30 minutes for initial and subsequent inpatient doses | VAS for nausea | Daily VAS score presented graphically, no numerical values presented No significant difference between treatments over 5 days of treatment via p-values |
| Eftekhari 201372 | University hospital, Kerman, Iran | To compare the effectiveness of treating HG with either ondansetron or promethazine, RCT | n = 60 (n = 30 in each group); I 71.56 days (SD 15–125), C 80.06 days (SD 35–128) | Women with chronic vomiting, not able to take oral fluids, dehydration, weight loss, in need of hospitalisation | NR (MODERATE–SEVERE) |
All participants rehydrated with i.v. fluids. The ondansetron group received 8 mg i.m. 8-hourly for 48 hours | All participants rehydrated with i.v. fluids. Promethazine group received 25 mg i.m. 6-hourly for 48 hours | Author-defined symptom and relief scales | Mean change severity: ondansetron = 6.4 (SD 202), promethazine = 5.34 (SD 3.1); p = 0.46 Relief: ondansetron = 12.16 (SD 3.7), promethazine = 11.65 (SD 3.4); p = 0.178 |
Ondansetron versus usual treatment
Einarson and colleagues121 examined ondansetron versus the usual treatment regimen. 121 As this involved a telephone survey of women already taking ondansetron, however, no direct measures of symptom relief were assessed. The outcomes of interest related to the incidence of fetal abnormalities in the surveyed patient population. These data are provided in Appendix 8, with additional UKTIS data on the intervention detailed in Appendix 7.
Ondansetron versus metoclopramide
Combined severity score
No combined score reported.
Nausea outcomes
All three trials comparing ondansetron against metoclopramide assessed nausea severity using the 10-point VAS. 57,75,81
The trial of Kashifard and colleagues81 (classed as low risk of bias), measured nausea in a group of women taking ondansetron versus a comparison group taking metoclopramide for pregnancy-related nausea and vomiting. They found that nausea scores for the ondansetron group were significantly less on the third and fourth days of treatment in comparison with those taking metoclopramide (p = 0.024 and p = 0.023 respectively). However, there was no significant difference between groups in the overall nausea trend over time.
Ghahiri and colleagues75 (classified as unclear risk of bias), compared women taking metoclopramide versus a comparison group taking ondansetron for pregnancy-related nausea and vomiting. They found no difference in symptom severity at either 3 days or 1 week. However, nausea was significantly lower in the ondansetron group at 2 weeks (p = 0.05).
Finally, the trial of Abas and colleagues57 compared the effectiveness of ondansetron with metoclopramide in the treatment of HG. No significant difference in the median (IQR) of well-being VAS scores were found between treatment arms [intervention = 9 (IQR 8–10) vs. comparator = 9 (IQR 7–10) (p = 0.33)].
Vomiting outcomes
Kashifard and colleagues81 measured vomiting outcomes using the number of episodes of vomiting recorded per group. They reported that both fewer episodes of vomiting were found in the ondansetron group compared with the metoclopramide group, and that the trend over time for vomiting in the ondansetron group was significantly lower compared with the comparator (p = 0.045). Ghahiri and colleagues75 found no differences in episodes of vomiting between groups until 2 weeks, when episodes were lower in the metoclopramide group (p = 0.04). However, by 3 weeks episodes of vomiting were significantly lower in the ondansetron group (p = 0.02). Finally, no significant difference was reported by Abas and colleagues57 in terms of median (IQR) number of vomiting episodes in the first 24 hours between treatment arms [intervention median 1 (IQR 0–2) compared with comparator median 2 (IQR 0–2.75); p = 0.38].
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No adverse events were reported in the trial of Kashifard and colleagues,81 in terms of either pregnancy outcomes or side effects. Ghahiri and colleagues75 found no significant difference between groups in relation to minor side effects [headaches, dizziness, sedation or anxiety (p > 0.05)]. However, although Abas and colleagues57 also reported some minor side effects (difficulty sleeping, dizziness, diarrhoea, headache, palpitations and skin rash) in similar proportions across the trial arms (p > 0.5), significant differences were found in self-reported drowsiness (p = 0.011) and dry mouth (p = 0.003) in favour of ondansetron. Full details are presented in Appendix 8 (although as previously emphasised, given the anticipated rarity of these events small trials are likely to provide unreliable estimates). Additional UKTIS data on ondansetron and metoclopramide enquiries can be found in Appendix 7.
Ondansetron versus antihistamines
Author-defined relief scale
The study by Eftekhari and Mehralhasani72 used an author-defined scale to assess change in symptom severity and relief. No significant difference between treatment groups was found for either category (severity p = 0.46, relief p = 0.178). Furthermore, this trial was found to have a high risk of bias due to inadequate allocation concealment procedures.
Nausea outcomes
Sullivan and colleagues105 (classified as unclear risk of bias due to lack of information), assessed daily scores using the VAS. No significant difference between ondansetron and antihistamine was reported during the 5-day treatment period (data presented graphically, therefore no specific p-value is available).
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes or adverse event data were reported in the trial of Eftekhari and Mehralhasani. 72 In the trial of Sullivan and colleagues,105 eight women reported sedation versus none in the ondansetron group (p = 0.002). UKTIS data on ondansetron related inquiries are presented in Appendix 7.
Summary
-
The evidence available for serotonin receptor antagonists, specifically ondansetron, was predominantly at high or unclear risk of bias with only one at low risk. 81
-
Evidence for the comparison of ondansetron with metoclopramide was mixed, with both drugs improving symptoms.
-
Low risk of bias studies found ondansetron more effective at reducing symptoms of vomiting compared with metoclopramide after 4 days.
-
Both ondansetron and antihistamine improved symptoms with no evidence of a difference between them.
-
Overall, ondansetron does reduce the severity of symptoms, but more larger, better-quality studies are required to assess benefit over other comparators.
Chapter 12 Clinical effectiveness: intravenous fluids
Introduction
Two studies compared the effectiveness of i.v. fluids for the treatment of women with HG. 69,108 One trial by Tan and colleagues108 tested different compositions of i.v. solution (dextrose plus saline vs. saline only)108 and was judged as low risk of bias. The other study compared the use of diazepam against i.v. fluids containing vitamins69 but was judged as carrying an unclear risk of bias due to lack of sufficient information in a number of areas. Both papers described the trial participants as suffering from HG; however, we classified severity as either moderate,69 or moderate to severe108 based on the participant data provided. As previously described (see Chapter 3, Meta-analysis of included randomised controlled trials), given the differences between trials in patient populations, settings, interventions and, in particular, the heterogeneous nature of the reported outcomes across trials, we did not attempt to perform meta-analyses and have thus reported a narrative summary only for each intervention and comparator set. A summary of study conduct and results is depicted in Table 16, with safety data reported in Appendix 8.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| I.v. fluids D-Saline vs. N-Saline | |||||||||
| Tan 2013108 | University hospital, Kuala Lumpur, Malaysia | To compare 5% dextrose, 0.9% saline against 0.9% saline solution in the i.v. rehydration of HG, double-blind RCT | n = 222 (n = 111 each group); I 9.8 ± 2.8, C 9.8 ± 2.5 | Women at their first hospitalisation for HG (intractable nausea and vomiting of pregnancy with dehydration and starvation clinically judged to require hospitalisation for i.v. rehydration and antiemetic drug administration) | VAS median nausea score 9 (IQR 7–10) for both groups (MODERATE–SEVERE) |
5% dextrose, 0.9% saline by i.v. infusion, 125 ml/hour over 24 hours plus potassium chloride (9.5 mmol) as required, plus multivitamin containing 250-mg thiamine given intraveniously. I.v. antiemetic prescribed according to health-care providers’ preference. If capillary glucose > 8 mmol/l, infusion fluid changed to open-label standard 0.9% saline | 0.9% saline by i.v. infusion, 125 ml/hour over 24 hours plus potassium chloride (9.5 mmol) as required, plus multivitamin containing 250-mg thiamine given intraveniously. I.v. antiemetic prescribed according to health-care providers’ preference. If capillary glucose > 8 mmol/l, infusion fluid changed to open-label standard 0.9% saline | Numerical scale 0–10 for nausea Episodes of vomiting |
Median vomiting episodes both groups 0 (IQR 0–2); p = 0.66 Nausea in D-Saline group at 24 hours = 2 (IQR 1–4), N-Saline group = 2 (IQR 2–4); p = 0.39 Repeated-measures analysis of variance of nausea score: p = 0.046 in favour of D-Saline |
| i.v. fluids ± diazepam | |||||||||
| Ditto 199969 | Department of obstetrics and gynaecology, Siena University Hospital, Italy | The efficacy of parenteral fluids with vitamins with or without diazepam sedation in cases of HG | n = 50; i.v. fluids plus diazepam group 11.2 weeks ± 3.17, i.v. fluids only 11.5 weeks ± 2.96 | Women with HG | Numerical values for nausea and baseline not provided. Proportion of women who had lost > 5% of pre-pregnancy weight: I 52%, C 56% (MODERATE) |
i.v. fluids plus multivitamins given plus diazepam (10 mg) i.v. twice daily. Discharged with oral diazepam tablets (5 mg), twice daily (n = 25) | i.v. fluids plus multivitamins only. Discharged with placebo tablets (n = 25) | VAS for nausea Episodes of vomiting |
There was a significant decrease in nausea in both groups but for women on diazepam the reduction was significantly greater on day 2 (p < 0.002) and day 3 than for the comparator group |
Dextrose saline versus saline only
Combined severity score
No combined score reported.
Nausea outcomes
The 10-point VAS was used by Tan and colleagues108 to assess nausea in their trial comparing dextrose plus saline versus saline only i.v. fluids. Although the difference after 24 hours between groups was not found to be significant [dextrose plus saline, VAS score = 2 (SD 1–4), saline only, VAS score = 2 (SD 2–4); p = 0.39], repeated-measures of the analysis of variance for nausea scores detected a significantly greater reduction in favour of the dextrose plus saline preparation (p = 0.046).
Vomiting outcomes
Tan and colleagues108 measured number of episodes of emesis to assess vomiting outcomes and did not detect a difference in the median change in episodes between groups [both groups = 0 (IQR 0–2); p = 0.66].
Retching outcomes
No independent retching scores reported.
Safety outcomes
Tan and colleagues108 did not report any pregnancy outcomes or side effects. No specific UKTIS data were available on this intervention.
Intravenous fluids versus intravenous fluids plus diazepam
Combined severity score
No combined score presented.
Nausea outcomes
For patients with a nausea score of 4+ (classed by the authors as severe nausea), significant reductions for both groups were found on the second and third days of therapy using the VAS (p < 0.05) in the trial of Ditto and colleagues69 They reported that on day 2, this reduction was significantly greater in the diazepam group (p < 0.002); however, post treatment, the difference between groups was not significant (no p-value reported).
Vomiting outcomes
Ditto and colleagues69 assessed vomiting outcomes via number of vomiting episodes. No significant difference between groups was observed (exact p-value not provided).
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No side effects were reported in the trial of Ditto and colleagues,69 and no statistically significant differences were reported in terms of gestation at delivery; preterm delivery; caesarean section rate; mean birthweight or neonatal abnormalities (p-value not reported). As above, no specific UKTIS data were available on this intervention.
Summary
-
The evidence available for i.v. fluids was at low108 or unclear69 risk of bias.
-
i.v. fluid improves reported symptoms. Dextrose saline may be more effective at improving nausea over time for those with moderate nausea.
-
Diazepam appears to be more effective than i.v. fluids alone at reducing nausea on day 2 but there was no evidence post treatment for those with moderate/severe nausea.
-
Overall, i.v. fluids help correct dehydration and improve symptoms, dextrose saline may be more effective at reducing nausea than normal saline. (The lower concentration of sodium in dextrose saline may exacerbate any pre-existing hyponatraemia. High doses/concentrations of dextrose solutions may increase the risk of Wernicke’s encephalopathy, but concentrations in dextrose saline are unlikely to provoke this response.)
-
Future studies are required which focus on interventions given alongside rehydration therapy.
Chapter 13 Clinical effectiveness: transdermal clonidine
Introduction
One trial by Maina and colleagues85 studied the efficacy of a 5-mg transdermal clonidine patch in the treatment of HG, in a double-blind, placebo-controlled, crossover RCT. Patients were classified at the severe end of the HG spectrum, with the trial judged as having a low risk of bias. A summary of study conduct and results is depicted in Table 17, with safety data reported in Appendix 8.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Maina 201485 | The trial was carried out in a single hospital setting (Ospedale Sant’Anna, Italy) after admission of patients | To study the efficacy of transdermal clonidine in the treatment of severe refractory HG, randomised, double-blind, placebo-controlled, crossover design (RCT) | Major grade of HG clinical severity who were unresponsive to standard antiemetic treatment (e.g. pyridoxine, metoclopramide or ondansetron plus an antireflux medication such as ranitidine or omeprazole) | Clinical severity was defined by a PUQE score index ≥ 13 | Twelve women of gestational age 6–12 weeks (SEVERE) |
With and without transdermal clonidine (5-mg clonidine patch or sham patch) for two consecutive periods of 5 days, other antiemetic drugs and antireflux drugs (ranitidine, omeprazole) being administered on a scheduled or as-needed basis. All women received i.v. hydration and supplementation with thiamine during both periods. The use of steroids was allowed as a rescue medication in the case of further worsening of symptoms | Sham patch crossover trial, see column 7 | PUQE VAS |
Clonidine vs. placebo, mean (95% CI): PUQE score 6.3 (95% CI 5.5 to 7.1), 8.5 (95% CI 7.7 to 9.3); p = 0.001 Mann–Whitney U-test, VAS score 22 (95% CI 19 to 26), 29 (95% CI 25 to 32); p = 0.009 |
Transdermal clonidine versus placebo patch
Pregnancy-Unique Quantification of Emesis and Nausea scale
Maina and colleagues85 assessed overall improvements in symptom severity using the PUQE scale. They reported that the transdermal clonidine patch led to a greater improvement in PUQE score [mean 6.3 (95% 5.5 to 7.1) vs. mean 8.5 (95% CI 7.7 to 9.3); p = 0.001].
Nausea outcomes
The 10-point VAS was also used to assess nausea severity. As above, the study found an improvement in VAS scores favouring the intervention group [mean 22 (95% CI 19 to 26) vs. mean 29 (95% CI 25 to 32); p = 0.009].
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
A number of pregnancy outcomes were reported in the trial of Maina and colleagues. 85 These included two major pregnancy complications: a central venous catheter-related sepsis and a postpartum haemorrhage. In addition, one baby was small for gestational age. However, no adverse fetal outcomes were reported (defined as miscarriage, stillbirth, preterm delivery or low birthweight) and no major or minor birth defects were detected. In addition, there was no significant association to an increase of adverse effects such as lassitude, drowsiness, dry mouth, headache, dizziness, fainting or skin intolerance in comparison with the placebo group (p = 0.2). These data are reported in Appendix 8 (with the proviso that this was a small trial in terms of the generalisabilty of the results). No UKTIS data were available on transdermal clonidine patches.
Summary
-
Evidence from one study85 suggests that the use of transdermal clonidine patches may be effective for the treatment of severe HG, but more and larger studies are required to compare effectiveness against comparators.
Chapter 14 Clinical effectiveness: outpatient/day case management
Introduction
One study compared the effectiveness of either midwife-led outpatient management versus standard inpatient care,88 while another examined the feasibility of day case management,120 for the treatment of moderate to severe HG/NVP. The trial of McParlin and colleagues88 was judged as having a low risk of bias, while a 2007 case series study by Alalade and colleagues120 was classed as of weak quality. A summary of study conduct and results is depicted in Table 18, with safety data reported in Appendix 8.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| McParlin 200888 | Maternity assessment unit, Newcastle upon Tyne Hospitals, UK | To compare the effectiveness of midwife-led outpatient management versus standard inpatient care, RCT | n = 53, (I n = 27, C n = 26); I = 9.3 (SD 2.8), C = 10.3 (SD 2.9) | Women attending the maternity assessment unit with severe NVP/PUQE score of ≥ 9 | Mean PUQE score: I 12.6 (2.2), C 11.5 (2.2) (MODERATE–SEVERE) |
Cyclizine (50 mg, i.v.), given followed by 3 l of Hartmann’s solution over 6 hours (i.e. 1 hour, 2 hours and 3 hours). 50 mg of oral thiamine given, discharged home with prescription for oral cyclizine (50 mg), three times daily. Women telephoned on day 3 and day 7 to offer ongoing support and advice | Admission to antenatal ward for routine care, i.v. fluids, i.v. cyclizine, oral thiamine | PUQE score | Mean change in PUQE score: I 6.9 (SD 4.1), C 6.2 (SD 2.3); p > 0.05 |
| Alalade 2007120 | Whipps Cross University Hospital, London, UK | Feasibility and clinical efficacy of day case management of HG and patients’ satisfaction | 27; 8.8 weeks | Women suffering from NVP with severe dehydration; inability to retain fluids orally; urine dipstick 4+ ketones and electrolyte imbalance | Not applicable (MODERATE–SEVERE) |
Direct admission to the gynaecological day ward. 2 l of normal saline were infused over 4 hours with 20 mmol of potassium chloride in each bag. Regular i.m./i.v. antiemetics were given. Discharged with oral antiemetics, folic acid and thiamine | N/A | Not assessed | Not reported |
Outpatient management versus standard inpatient care
Pregnancy-Unique Quantification of Emesis and Nausea scale
In the trial of McParlin and colleagues,88 the effectiveness of the same treatments (i.v. cyclizine and i.v. fluids), administered via an outpatient management setting versus standard inpatient care was assessed via mean change in PUQE scores. 88 No significant difference was found between groups [intervention = 6.9 (SD 4.1), comparator = 6.2 (SD 2.3); p > 0.05] when followed up for 7 days from initiation of treatment.
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No adverse events were reported in the trial of McParlin and colleagues88 and no significant differences between groups were found in the rates of miscarriage, termination of pregnancy, gestation at delivery, birthweight, incidence of small for gestational age, or admissions to a special care baby unit (see Appendix 8 for full data). There were no UKTIS data available for this intervention and, given the anticipated rarity of these events, small trials are unlikely to provide unreliable estimates.
Day case management
The feasibility and efficacy of day case management of HG was assessed by Alalade and colleagues120 using rates of patient discharges within a 24-hour period. These case series data are reported in Appendix 8.
Summary
-
The evidence available for day case management was at low risk88 and high risk120 of bias.
-
The identified studies indicate that day case management of women with moderate to severe symptoms is feasible and acceptable to women.
-
The results indicate that day case management is as effective at improving severity scores as inpatient management for some women.
-
More, larger studies are required to provide definitive results and women’s views.
Chapter 15 Clinical effectiveness: corticosteroids
Introduction
Corticosteroids were tested against a variety of alternative treatments in seven individual studies. 58,64,93,99,114,116,125 Two trials compared the effectiveness of corticosteroids against placebo tablets in patient populations categorised as experiencing moderate to severe symptoms. 93,114 Three trials compared corticosteroids with either promethazine99,116 or phenergan suppositories58 in patients classed as experiencing moderate, unclear or moderate to severe level symptoms respectively. One trial tested the effectiveness of steroids against metoclopramide for women with moderate to severe HG. 116 As previously described (see Chapter 3, Meta-analysis of included randomised controlled trials), given the differences between trials in patient populations, settings, interventions and, in particular, the heterogeneous nature of the reported outcomes across trials, we did not attempt to perform meta-analyses and have thus reported a narrative summary only for each intervention and comparator set.
Of these trials, three were classed as carrying a low risk of bias64,93,99 and two were unclear due to lack of information. 58,116 One study was judged to have a high risk of bias due to lack of blinding and unclear outcome reporting. 114 A final case series study examined the effect of corticosteroids in comparison with the usual treatment regimen in women with severe HG. 125 A summary of study conduct and results is depicted in Table 19, with safety data reported in Appendix 8.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Corticosteroids vs. placebo | |||||||||
| Nelson-Piercy 200193 | Inpatient gynaecology wards in eight collaborating centres in the UK | To test the hypothesis that corticosteroids would lead to rapid and complete remission of the symptoms of NVP in cases of severe HG, RCT | n = 25, I n = 13, C n = 12 | Onset NVP < 12 weeks, dependent on i.v. fluids for at least 1 week (first admission for HG) or 24 hours (second or subsequent admission), receiving regular treatment with at least 1 antiemetic, ketonuria on admission, vomiting at least two times per day or nausea so severe that unable to eat or drink, receiving regular treatment with oral thiamine or a single dose of parenteral thiamine | I: number vomiting five or more times per day = 6; number requiring one or more antiemetics = 4 C: number vomiting five or more times per day = 6; number requiring one or more antiemetics = 2 (MODERATE–SEVERE) |
A 1-week course of prednisolone, 20 mg (four 5-mg tablets) orally 12-hourly, If, following 72 hours, a woman was still vomiting or vomiting tablets, and still dependent on i.v. fluids and electrolyte replacement, the therapy was changed to an i.v. equivalent [i.e. hydrocortisone (100 mg) 12-hourly] | A 1-week course of placebo (four 5-mg tablets) orally 12-hourly. If, following 72 hours, a woman was still vomiting or vomiting tablets, and still dependent on i.v. fluids and electrolyte replacement, the therapy was changed to an i.v. equivalent (i.e. N-Saline) | VAS for nausea Episodes of vomiting |
Number still vomiting at 1 week: I 5, C 7; relative risk 1.4 (95% CI 0.6 to 3.2) Number vomiting five or more times per day: I 2, C 5; relative risk 2.5 (95% CI 0.6 to 10.5) Reduction in vomiting score: I median 2.0 (range –1.0 to 4.0), C median 1.5 (range –3.0 to 4.0) Nausea score improvement I = 6.5 (range 2.0–10.0), C = 4.0 (range –5.0 to 9.0), relative risk 0.10 for proportion with nausea |
| Yost 2003114 | Parkland Memorial Hospital, Dallas, TX, USA | To estimate the effect of corticosteroids in reducing the number of women requiring rehospitalisation for HG, RCT | n = 126, I n = 64, C n = 62 | Women who previously had not responded to outpatient therapy and had three or four dipstick urinary ketones as evidence of severe dehydration | NR (MODERATE–SEVERE) |
All women: i.v. rehydration with crystalloid until ketonuria cleared [first litre included thiamine (100 mg)]. Conventional treatment: promethazine (25 mg) and metoclopramide (10 mg) intravenously every 6 hours for 24 hours, followed by the same regimen orally until discharge from the hospital. The women were also randomised, I = methylprednisolone (125 mg, i.v.). This was followed by a tapering regimen of oral prednisone (40 mg for 1 day, 20 mg for 3 days, 10 mg for 3 days, and 5 mg for 7 days) | All women: i.v. rehydration with crystalloid until ketonuria cleared [first litre included thiamine (100 mg)]. Conventional treatment: promethazine (25 mg) and metoclopramide (10 mg) intravenously every 6 hours for 24 hours, followed by the same regimen orally until discharge from the hospital. The women were also randomised, C = i.v. placebo. This was followed by an identical tapering regimen) | N/A | Not reported |
| Corticosteroids vs. phenothiazines/promethazine/Phenergan® (Sanofi-Aventis) | |||||||||
| Adamczak 200758 | Unclear, obstetrics and gynaecology department, hospital, New Jersey, NJ, USA | To compare SDP with Phenergan suppositories in the treatment of symptomatic NVP, RCT | n = 110, I n = 55, C n = 55; states 8–14 weeks | Patients presenting with NVP | Diagnosed with NVP (NOT CLEAR) |
SDP included 8-mg t.i.d. tapered over 6 days | Phenergan suppositories were dosed at 25-mg q.i.d. | Episodes of vomiting | I (SDP), number of vomiting episodes: day 1: 7.1 (SD 1.8), day 3: 3.0 (SD 1.9), day 7: 1.8 (SD 1.6), day 14: 0.6 (SD 0.8) C, number of vomiting episodes: day 1: 6.6 (SD 1.9), day 3: 4.7 (SD 1.8), day 7: 3.9 (SD 1.7), day 14: 2.5 (SD 1.4) p-values for differences: day 1 p = 0.2, days 3, 7 and 14 p < 0.05 |
| Safari 199899 | Women’s and children’s hospital, Los Angeles, CA, USA | To compare the efficacy of methylprednisolone with that of promethazine for the treatment of HG, RCT | n = 40, I n = 20, C n = 20; I gestational age in weeks = 9.8 (SD 2.1), C gestational age in weeks = 9.5 (SD 2.7) | Diagnosed with HG, given i.v. hydration but with no resolution of symptoms, or second admission for HG | NR. The duration of HG before admission was longer in the promethazine group than in the methylprednisolone group (p = 0.03) (MODERATE–SEVERE) |
Methylprednisolone (16 mg) orally three times a day for 3 days, followed by a tapering regimen, halving of dose every 3 days, to none during the course of 2 weeks (10 a.m., 2 p.m., 8 p.m.). After 2 days women were discharged with their study medication. If no improvement study allocation unblinded and patients withdrawn from further data collection | Promethazine (25 mg) orally three times a day for 2 weeks (10 a.m., 2 p.m., 8 p.m.). After 2 days women were discharged with study medication. If no improvement study allocation unblinded and patients withdrawn from further data collection | NR | Not reported |
| Ziaei 2004116 | Najmieh Hospital, Iran | To determine whether or not low dosages of prednisolone are effective in the treatment of outpatients with HG, RCT | n = 80, I n = 40, C n = 40 | Vomiting more than three times per day during the last 72 hours or ketonoria that did not respond to dietary manipulation and caused weight loss | Episodes of vomiting/day: I 3 (range 2–5), C 3 (range 2–6) (MODERATE) |
Prednisolone, (5 mg) given once in the morning for 10 days | Promethazine was administered (25 mg), three times daily for 10 days | VAS for nausea Episodes of vomiting |
Severity of nausea: Mild/moderate: first 48 hours, I = 20 (50%), C = 30 (75%); third to tenth day, I = 6 (65%), C = 25 (62.5%); seventeenth day, I = 17 (43.6%), C = 12 (30.8%) Severe: first 48 hours, I = 20 (50%), C = 10 (25%); third to tenth day, I = 14 (35%), C = 15 (37.5%); seventeenth day, I = 22 (56.4%), C = 27 (69.2%) For prednisolone group OR (95% CI) of nausea: during first 48 hours OR 0.33 (95% CI 0.13 to 0.86); between third and tenth days OR 1.11 (95% CI 0.14 to 2.6); seventeenth day OR 1.7 (95% CI 0.68 to 4.4) Episodes of vomiting: first 48 hours, I median 3 (range 1–7), C median 1 (range 0–4), p = 0.04; third to tenth day, I median 1.5 (range 1–5), C median 1 (range 0–5), p = 0.80; tenth to seventeenth day, I median 3 (range 0–6), C median 3 (range 0–5), p = 1.0 |
| Corticosteroids vs. metoclopramide | |||||||||
| Bondok 200664 | Intensive care unit of Ain Shams University Maternity Hospital, Cairo, Egypt | To compare the efficacy of pulsed hydrocortisone therapy with that of metoclopramide for the management of intractable HG, prospective double-blind study | n = 40, I n = 20, C n = 20; I = 10 ± 2.68, C = 11 ± 2.44 | Women admitted to the intensive care unit with intractable hyperemesis (defined as severe persistent vomiting, ketonuria and weight loss > 5% of pre-pregnancy weight) | NR (MODERATE–SEVERE) |
300 mg of i.v. hydrocortisone for 3 days, followed by a tapering regimen of 200 mg for 2 days, then 100 mg for another 2 days. Patients received three syringes, each every 8 hours, 10 ml each, one containing the drug diluted in normal saline and the other two containing normal saline. Nursing services recorded the daily number of emetic episodes | 10 mg of metoclopramide, in a 10-ml syringe diluted in normal saline, intravenously every 8 hours for the same 7-day period | Episodes of vomiting | Mean vomiting episodes: hydrocortisone group reduced by 40.9% on second day, 71.6% on third day, and 95.8% on seventh day. Metoclopramide group reduced by 16.5% on second day, 51.2% on third day, and 76.6% on seventh day (p < 0.001) |
| Corticosteroids vs. usual treatment | |||||||||
| Moran 2002125 | Inpatient antenatal ward, hospital, Newcastle upon Tyne, UK | To document the effect of prednisolone therapy in women with defined severity of HG, case series | Thirty pregnancies in 25 women in treatment group, matched with 25 women treated with conventional therapy (i.v. fluids and antiemetics), treatment group median age in weeks = 9.6 (range 8.6–11.1) | HG requiring hospital admission plus weight loss > 5 kg and/or evidence of muscle wasting; onset of nausea and vomiting before 6 weeks; ketonuria on admission; i.v. fluids for > 1 week or > 24 hours if a repeat admission; failure of traditional antiemetic treatment; vomiting at least twice per day or severe nausea precluding any oral intake; gestation over 8 weeks | Assessed by physician and deemed severe enough to meet inclusion criteria (SEVERE) |
Oral prednisolone (10 mg) 8-hourly prescribed, replacing traditional antiemetics. If unable to tolerate tablets stabilisation achieved with i.v. hydrocortisone (50 mg) 8-hourly. Prednisolone dosage was reduced in a stepwise fashion. Typically dosage decreased to 15 mg daily within 5 weeks, remaining between 12.5 mg and 15 mg for a further 3–8 weeks | Retrospective case series of 25 consecutive women hospitalised for hyperemesis but judged not to require steroid therapy | VAS for nausea | Six women completed VAS for nausea over 1 week Data for intensity show a clear pattern of resolution in the active group Three comparator group women received steroids Median number of in patient days pre-steroid treatment = 8 (range 4–14) and after commencement = 3 (range 1–6.5) |
Corticosteroids versus placebo
Combined severity score
No combined score reported.
Nausea outcomes
Nelson-Piercy and colleagues93 assessed the effect of corticosteroids compared with placebo tablets on nausea symptoms using the VAS. However, although the observed change was greater in the intervention group [median 6.5 (range 2.0–10.0) compared with median 4.0 (range –5.0 to 9.0)], this difference was not significant (relative risk for proportion with nausea 0.10; CI not reported).
Vomiting outcomes
In the trial of Nelson-Piercy and colleagues,93 changes in vomiting status were assessed using numbers of patients still vomiting at 1 week of treatment; numbers of patients vomiting more than five times a day at day 5 of treatment; and via an author-defined scale which coded severity from 0 to 4. 93 Overall, although reported scores favoured the steroid treatment group across all three measures, the difference in effect sizes was not found to be significant [number still vomiting at 1 week, relative risk 1.4 (range 0.6–3.2); number vomiting more than five times per day, relative risk 2.5 (range 0.6–10.5); median reduction in vomiting score intervention 2.0 (range –1.0 to 4.0) vs. comparator 1.5 (range –3.0 to 4.0)].
The trial of Yost and colleagues114 assessed the difference in the impact on readmission rates between groups. These data are presented in Appendix 8.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
Nelson-Piercy and colleagues93 did not report side effects, but found no difference in birthweight or gestational age at delivery (excluding the triplet pregnancy) between groups (p > 0.05), or in terms of the numbers of babies born with birthweights less than the 5th centile (p > 0.05). Yost and colleagues114 reported no significant differences between groups in terms of spontaneous abortion (p = 0.6); gestational diabetes (p = 0.96); hypertension (p = 0.2); preterm delivery (p = 0.4); or primary or repeat caesarean delivery (p = 0.06 and p = 0.5 respectively). Full data are reported in Appendix 8. No UKTIS data were available on this intervention and it should be noted that given the anticipated rarity of these events, small trials are unlikely to provide unreliable estimates.
Corticosteroids versus promethazine (Phenergan)
Combined severity score
No combined score reported.
Nausea outcomes
Ziaei and colleagues116 used the VAS to assess severity of nausea and found that women who received promethazine responded better in the first 48 hours of treatment (p = 0.02). However, with continuation of the treatment, the difference decreased, and 1 week after completion of the treatment, the subjects who had received corticosteroids had fewer symptoms, although this difference was not significant (p = 0.23).
Vomiting outcomes
Number of episodes of vomiting was assessed in the trials of Zaiei and colleagues116 and Adamczak and colleagues. 58 In the Zaiei and colleagues116 study, median episodes of vomiting in the first 4 hours were lower in the promethazine group. 116 However, as with nausea severity, by the end of the study period, there was no significant difference between groups (p = 1.0). In contrast, Adamczak and colleagues58 reported that episodes of emesis were significantly lower in the steroid intervention group compared with those receiving Phenergan suppositories at days 3, 7 and 14 (p < 0.05 at all time points). 58
The primary outcome in the Safari and colleagues99 study related to numbers of patients for whom therapy had failed at different points in the treatment period. These are reported in detail in Appendix 8.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcomes or side effects were reported by Adamczak and colleagues. 58 Safari and colleagues99 reported no significant difference between the two groups in relation to birthweight or American Pediatric Gross Assessment Record scores at 1 and 5 minutes (p > 0.05). One patient in the methylprednisolone group was delivered at 35 weeks’ gestation of a male infant with Smith–Lemli–Opitz syndrome. No pregnancy outcomes were reported by Zaiei and colleagues,116 but significant differences were found in terms of drowsiness during the first 48 hours, and between the third and tenth days (p = 0.026 in both instances in favour of the intervention). These data are detailed in Appendix 8, but it should be noted that given the anticipated rarity of these events, small trials are unlikely to provide unreliable estimates. No UKTIS data were available on this intervention.
Corticosteroids versus metoclopramide
Combined severity score
No combined score reported.
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
One trial by Bondok and colleagues64 compared the effectiveness of corticosteroids against metoclopramide in terms of recorded episodes of emesis. A significant improvement was observed in favour of the corticosteroid group (p < 0.001).
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No pregnancy outcome or side effect data were reported in the trial of Bondok and colleagues,64 and no UKTIS data were available.
Corticosteroids against usual treatment
Combined severity score
No combined score reported.
Nausea outcomes
Moran and Taylor125 assessed the change in nausea symptoms in 6 out of the 25 case series patients who were treated with oral or i.v. corticosteroids for severe HG using the VAS. Data presented graphically suggested that the intensity of nausea experienced showed a pattern of improvement in the intervention group. However, no precise numerical scores were provided.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
Moran and Taylor125 did not report any side effects and there was no difference in mean gestation at delivery or birthweight for term infants. Full data are reported in Appendix 8.
Summary
-
Evidence available for corticosteroids was predominantly at low risk of bias (three studies64,93,99), or the risk of bias was unclear/high (three studies58,114,116).
-
Steroids versus placebo had a trend towards improved symptoms, but results were not statistically significant.
-
For steroids versus promethazine, there was no evidence of a difference in improvement by 1 week.
-
Steroids were more effective at reducing vomiting episodes than Phenergan suppositories or metoclopramide.
-
Overall, treatment with corticosteroids reduces the severity of symptoms, but more and larger studies are required to compare effectiveness against comparators.
Chapter 16 Clinical effectiveness: nasogastric enteral/jejunostomy feeding
Introduction
Two case series of nasogastric123 and jejunostomy126 feeding for women experiencing HG at the severe end of the spectrum were found. Both studies were judged as weak in quality. A summary of study conduct and results is depicted in Table 20, with safety data reported in Appendix 8.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Nasogastric feeding | |||||||||
| Hsu 1996123 | The Genesee Hospital, Rochester, NY, USA | To report experiences of treating HG with nasogastric enteral feeding, case series | Seven participants (reported as individual not as mean) | Hospitalised due to intractable nausea, vomiting and weight loss, symptoms present at 1–4 weeks and had failed to respond to dietary manipulation and antiemetics | NR (SEVERE) |
Enteral feeding via an 8-Fr Dobbhoff nasogastric tube, of Jevity or Osmolite incrementally to meet daily caloric requirements. Initial rate of 25 ml/hour, increasing as tolerated by 25 ml/hour/day. Patients were discharged once stabilised. Six women continued enteral feedings at home. Patients were instructed to eat when they felt able. Nasogastric feedings were discontinued when nutritional needs were being met orally | NA | NR | NR |
| Jejunostomy | |||||||||
| Saha 2009126 | Women and Infants Hospital, Providence, RI, USA | To assess the feasibility and efficacy of surgically placed feeding jejunostomy (J-tube) in women with HG refractory to standard therapy, case series | Five patients (covering 6 pregnancies), 16.3 weeks | Persistent severe nausea and vomiting and one of the following: weight loss of > 5% of pre-pregnancy weight, ketonuria, multiple ER visits for dehydration, and/or inability to tolerate oral intake, despite i.v. hydration/ondansetron/ranitidine or pantoprazole, and metoclopramide | NR (SEVERE) |
The J-tubes were placed between 12 and 26 weeks’ gestation (median 14 weeks). The J-tubes were in place for a mean duration of 19 weeks (range 8–28 weeks). Four J-tubes remained in place until delivery. One tube was removed at 34 weeks at the patient’s request because of emotional distress (patient 1) and one tube fell out at 30 weeks’ gestation and was not replaced (patient 2) | NA | NR | All patients had continued nausea and vomiting |
Nasogastric enteral feeding
Hsu and colleagues123 reported their experience of treating HG with nasogastric enteral feeding in a case study with seven women conducted at the Genesee Hospital, Rochester, New York. Enteral feeding was administered via an 8-Fr Dobbhoff nasogastric tube (Ross Products Division, Abbott Laboratories, Columbus, OH), delivering Jevity or Osmolite incrementally to meet daily caloric requirements (initial rate of 25 ml/hour, increasing as tolerated by 25 ml an hour per day). Patients were discharged once stabilised. Six women continued enteral feedings at home with nasogastric feedings discontinuing when nutritional needs were being met orally. Key outcomes of interest were the period of time (in days) after which patients were discharged and the mean duration of feedings (see Appendix 8).
Combined severity score
No combined scores reported.
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No UKTIS data were available on this intervention.
Jejunostomy feeding
A further case series study by Saha and colleagues126 looked at the feasibility and efficacy of feeding via jejunostomy in five women with HG compared with standard therapy at the Women and Infants Hospital, Providence, Rhode Island. Participants all displayed persistent severe nausea and vomiting plus one of the following: weight loss of > 5% of pre-pregnancy weight; ketonuria; multiple emergency room visits for dehydration; and/or inability to tolerate oral intake, despite i.v. hydration, i.v. ondansetron, i.v. ranitidine or pantoprazole, and i.v. metoclopramide. The J-tubes were placed between 12 and 26 weeks’ gestation (median 14 weeks) for a mean duration of 19 weeks (range 8–28 weeks). Four J-tubes remained in place until delivery. One tube was removed at 34 weeks at the patient’s request because of emotional distress and one tube fell out at 30 weeks’ gestation and was not replaced. They reported that all patients had continued nausea and vomiting over the study period which required continued standard therapy in addition to J-tube feedings. Outcomes measured by the study included use of additional medication and adverse events (see Appendix 8).
Combined severity score
No combined scores reported.
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes reported.
Safety outcomes
No UKTIS data were available on this intervention.
Summary
-
Enteral feeding is an effective but extreme method of supporting women suffering from very severe symptoms as a last resort.
Chapter 17 Clinical effectiveness: gabapentin
Introduction
No controlled trials of gabapentin use in the treatment of HG were identified. The only available data were derived from one uncontrolled pilot study by Guttuso and colleagues39 which enrolled seven consecutive women of 20 weeks’ gestation with HG to examine gabapentin therapy. This study was classed as ‘weak’ by the EPHPP quality assessment tool.
Author-defined scale
The authors concluded that gabapentin appeared to be well-tolerated and may be effective in the treatment of HG but that they did not recommend the use of gabapentin in the treatment of HG until larger controlled trials have properly assessed gabapentin’s efficacy in HG. This is only a very small pilot study, but a summary of study conduct and results is depicted in Table 21.
| Study | Setting, location | Research question, study design | Number of participants, gestation | Severity inclusion criteria | Severity scores (reviewers’ assessment) | Intervention | Comparator | Outcome assessment scale | Symptom relief outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Guttuso 201039 | Combination of inpatients and outpatients included, Buffalo, NY, USA | To perform an open-label pilot study examining the safety, tolerability and effectiveness of gabapentin in the treatment of HG, case series | Seven participants, 8 weeks | Eligible subjects needed to have severe nausea and vomiting, refractory to at least one antiemetic, causing at least 3+ ketonuria or 5% weight loss compared with the pre-pregnancy weight | All seven subjects had at least 3+ ketonuria and 5% weight loss from their pre-pregnancy weight at baseline (MODERATE–SEVERE) |
Gabapentin initiated at 300 mg orally, three times daily. Every day the total dose could be increased by 300 mg (maximum of 3600 mg/day) if the subject was still experiencing nausea or emesis and was not experiencing bothersome side effects. After 14 days of therapy, gabapentin was discontinued for 2 days and could then be resumed on day 17 and for the remainder of the pregnancy, if necessary | N/A | PUQE scale | Mean reductions in nausea and emesis from baseline to days 12–14 of 80% and 94%, respectively, and 84% and 98%, respectively, from baseline to days 19–21. There was a 3 times increase in mean nausea and a seven times increase in mean emesis scores associated with discontinuing gabapentin during days 15–16 |
Nausea outcomes
No independent nausea outcomes reported.
Vomiting outcomes
No independent vomiting outcomes reported.
Retching outcomes
No independent retching outcomes.
Safety outcomes
Guttuso and colleagues39 reported two serious congenital defects among seven of the subjects’ infants (tethered spinal cord and hydronephrosis). Four subjects experienced mild–moderate side effects of sleepiness or dizziness when first starting gabapentin. It is important to highlight that this was a very small trial so unlikely to provide reliable estimates; however, the authors did conclude that gabapentin’s safety during pregnancy needed to be further assessed. No UKTIS data were available on this intervention but full details are reported in Appendix 8, Secondary outcome data.
Summary
-
We identified only one very small pilot trial which examined gabapentin therapy in women with HG.
-
More research is needed, including monitoring of safety, in light of the reported cases of congenital anomalies among the seven exposed infants.
Chapter 18 Economic analysis
Introduction
This chapter has two aims: (i) to review systematically the published evidence relating to the cost-effectiveness of interventions used in the treatment of NVP/HG; and (ii) to assess the relative cost-effectiveness of such interventions from a NHS and Personal Social Services perspective. To assess cost-effectiveness, an economic model was developed in the first instance. However, due to the lack of evidence required to populate the economic model, an alternative method of economic evaluation was used. The methods and findings of the systematic review are presented first, followed by those of the economic evaluation.
Systematic review of economic evaluations
Methods
The broad methods of this systematic review were similar to those presented in Chapter 2 and thus, only key details relevant to the economic review are given here.
Search strategy
Searches for economic studies were run on MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature, PsycInfo, Allied and Complementary Medicine Database, British Nursing Index, Cochrane Central Register of Controlled Trials, Scopus, Web of Science, NHS Economic Evaluation Database and Health Economic Evaluations Database. The same terms as used for the main review were used, with the addition of health economic-related terms (included in Appendix 9).
Study selection
As part of the main review, titles and abstracts were screened for relevance and any potentially relevant articles were to be obtained for scrutiny against the full selection criteria by the health economics lead. The criteria were:
Study design Cost–consequence analysis, cost-effectiveness analysis, cost–benefit analysis, cost–utility analysis, cost studies.
Population Women experiencing severe nausea, vomiting and/or retching in pregnancy where recruitment to a trial took place up to 20 weeks’ gestation. Owing to the difficulty in differentiating between HG and severe or intractable NVP, specific approaches were used to identify relevant populations of women (described in Chapter 3). Studies with mixed populations were to be included as long as data for relevant patients were extractable.
Intervention All pharmacological and non-pharmacological interventions relevant to the NHS in the community and in hospital as either an inpatient or an outpatient. The list of eligible interventions has been outlined previously in Chapter 2.
Comparator A no treatment group, a treatment as usual group or an alternative intervention group.
Outcome Cost-effectiveness, cost estimates, utilisation estimates, QoL estimates.
Data extraction and quality assessment strategy
Data on the following, where available, were to be extracted from included studies by one health economic reviewer and checked by another:
-
study characteristics, such as study question, form of economic analysis, populations, interventions, comparators, perspective, time horizon and form of modelling used
-
clinical effectiveness and cost parameters, such as effectiveness data, health state valuations (utilities), resource use data, unit cost data, price year, discounting and key assumptions; and
-
results and sensitivity analyses.
Studies were to be quality assessed using the following tools as part of the data extraction process: the Consensus on Health Economic Criteria list130 for economic evaluations and the checklist by Philips and colleagues131 for model-based analyses.
Results
From the main systematic review, 11 papers (no duplicates) were identified. None of the records were deemed relevant to this economic review and, as such, no hard copies were obtained for scrutiny against the inclusion criteria for the review. A flow diagram presenting the process of selecting studies can be found in Figure 5.
FIGURE 5.
Flow diagram showing study selection for economic evaluations review.
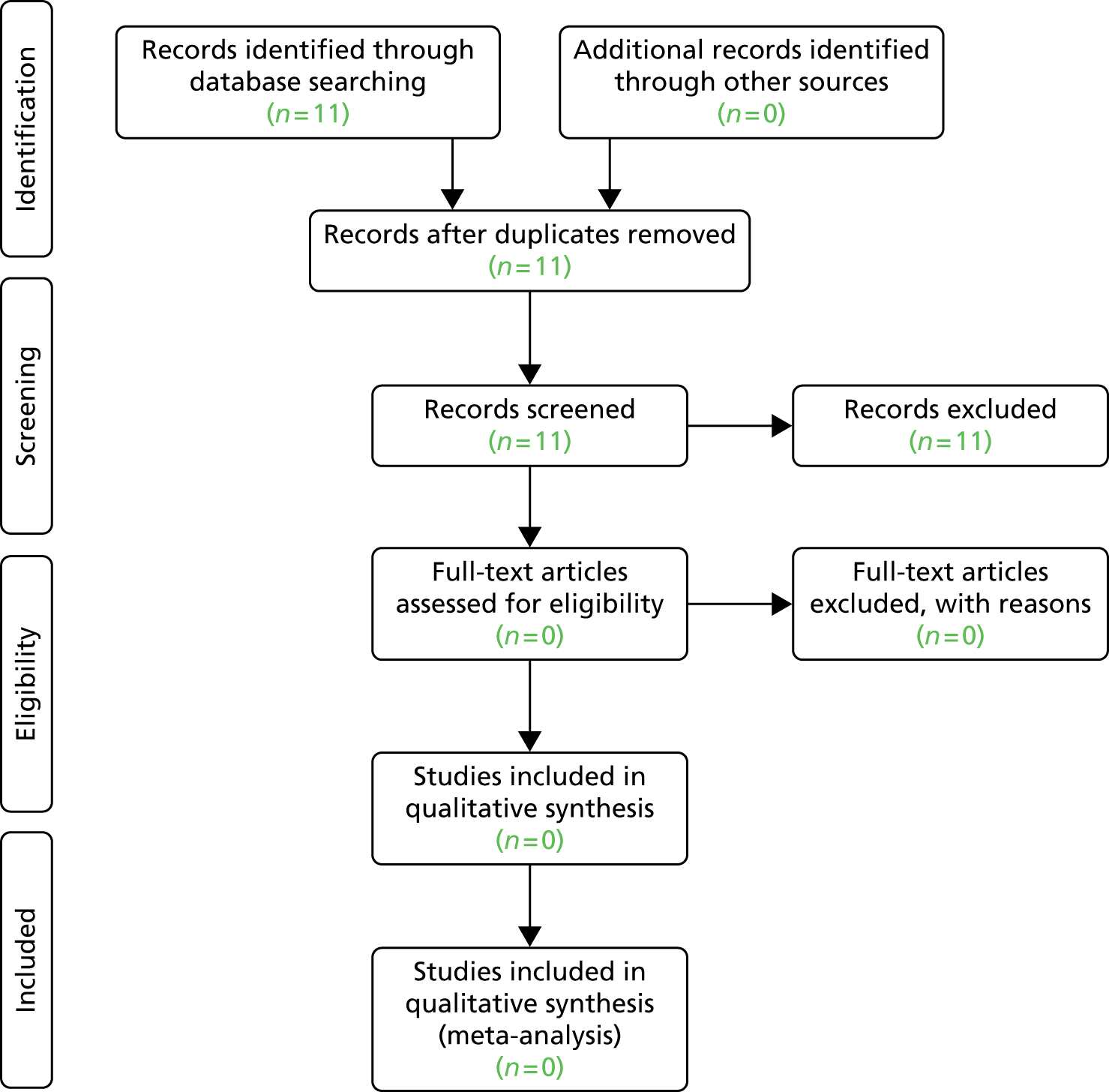
Discussion
No economic evaluations were found during the search for literature on the cost and cost-effectiveness of interventions used in the treatment of NVP/HG.
Economic modelling
Introduction
This section provides a detailed description of the economic model developed to estimate the relative cost-effectiveness of interventions used to treat pregnant women suffering from NVP/HG. The model describes the potential care pathways experienced by patients at different levels of severity (mild, moderate and severe). A separate, identical model was created for each group, with the plan to adjust probabilities and outcomes in each model to reflect reality. Unfortunately, due to the lack of available clinical evidence it was not possible to populate the economic model. However, a model now exists for analysis should additional information become available. An overview of the key characteristics of the proposed cost-effectiveness analysis is presented in Box 1.
Intervention: All clinically relevant interventions used to treat pregnant women suffering from NVP and HG.
Comparator: Alternative interventions used in the treatment of NVP/HG.
Population: Cohort of patients suffering from mild, moderate or severe NVP/HG and who are receiving a clinically relevant intervention in response.
Time frame: Lifetime time horizon, 3-month time cycle.
Perspective: NHS/Personal Social Services.
Effects: Any adverse events and necessary hospital treatments related to NVP/HG.
Costs: Pharmacological costs associated with medical treatment and changing medical treatment and the non-pharmacological costs associated with treating patients who have experienced a progression of symptoms or an adverse event.
Outcomes: Mortality, QoL, QALYs.
Assessment of cost-effectiveness: Cost per additional QALY gained.
QALY, quality-adjusted life-year.
Methods
Outline of model
We initially proposed to develop an economic model to estimate costs, long-term effects and relative cost-effectiveness of the alternative interventions for NVP and HG from the perspective of the UK NHS and Personal Social Services. The model was to describe the pathways of individuals who have different severities of symptoms and have treatment initiated in different sectors of the health service (primary care, hospital outpatients and hospital inpatients). It was to cover the period of initial intervention and the costs and consequences of any subsequent outcomes including further interventions. Some of the effects of NVP and HG are short term; however, there may be some persisting impact on the mother and longer-term effects on the child. It was the intention to model the cumulative costs and quality-adjusted life-years for the mother and longer-term effects on the child (reported either in natural units or, if data allowed, quality-adjusted life-years). An outline structure of the core pathways for this proposed model is presented in Figure 6. The full model is available from the authors.
FIGURE 6.
Structure of the decision model.
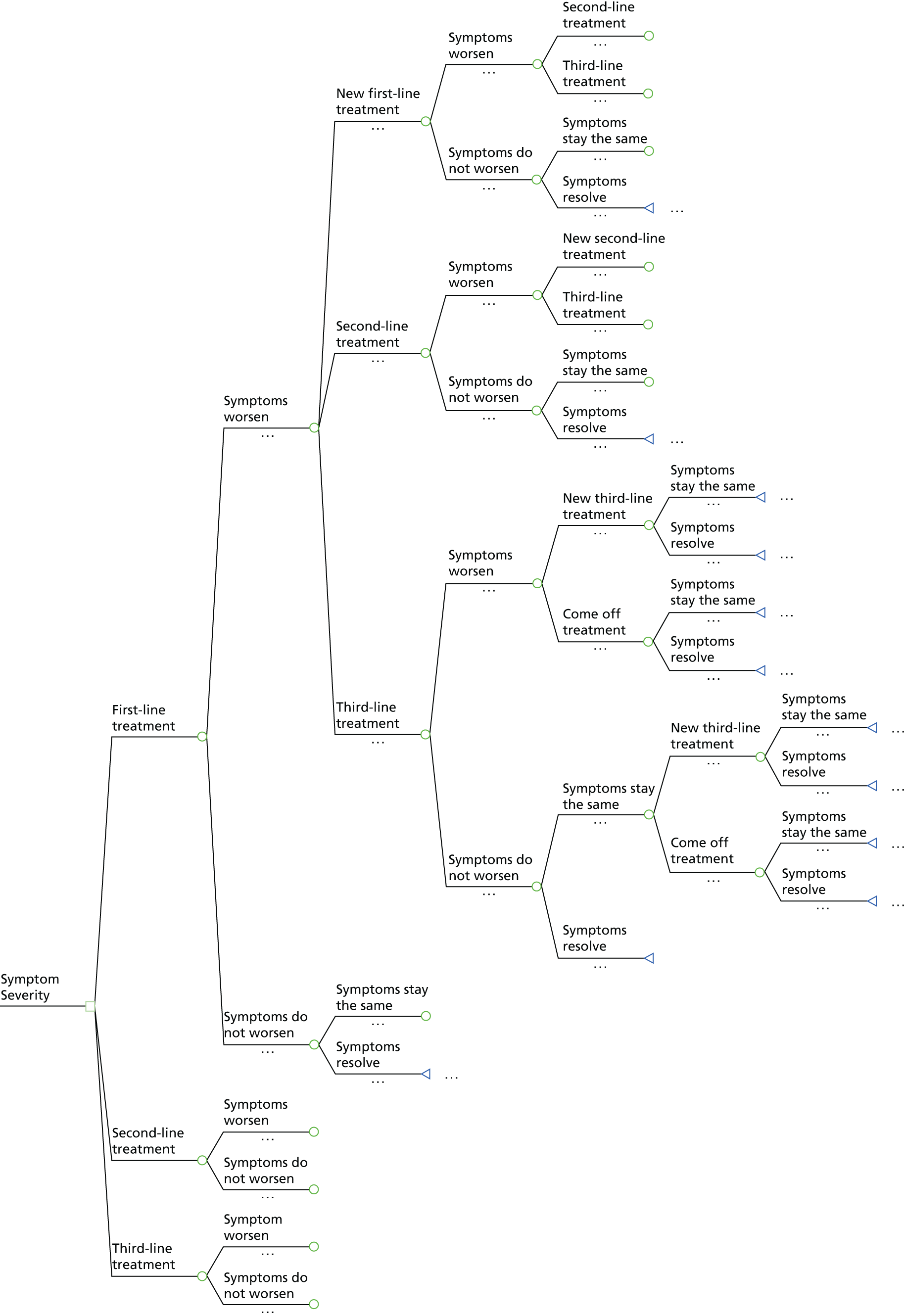
The economic model was built in TreeAge Pro® 2014 (TreeAge Software, Inc., Williamstown, MA, USA) to estimate the relative cost-effectiveness of the pharmacological and non-pharmacological interventions used to treat NVP/HG. The populations considered were women experiencing mild, moderate and severe nausea, vomiting and/or retching in pregnancy.
The decision tree structure can be described as follows. Depending on the severity of symptoms, patients began treatment on first-, second- or third-line treatment. The categorisation of interventions is described in detail in Chapter 2 but can be distinguished loosely as patient-initiated treatments (first line), clinician-prescribed antiemetics (second line) and clinician-prescribed corticosteroids (third line). The categorisation of these treatments as first line, second line and third line is not medically recognised and there may be discrepancies in how clinicians describe particular interventions. However, such a hierarchy allows us to compare the relative cost-effectiveness of categories of treatments rather than the multiple individual treatments that exist, while allowing us to think through the sequence of treatments that are likely to be relevant to patients at the different levels of severity of symptoms.
Beginning at ‘first-line treatment’, symptoms may worsen or not worsen. If symptoms worsened, patients moved to a ‘new first-line treatment’, ‘second-line treatment’ or ‘third-line treatment’. From each of these points, symptoms may again worsen or not worsen. If symptoms worsened, patients moved to the next hierarchical treatment strategy. This sequence was followed until patients reached ‘third-line treatment’, at which point symptoms may worsen or not worsen. If symptoms worsened, patients moved to a ‘new third-line treatment’ or ‘came off treatment’, at which point symptoms could either ‘stay the same’ or ‘resolve’ (terminal nodes). Beginning at the same starting point (‘first-line treatment’), if symptoms did not worsen, symptoms could ‘stay the same’ or ‘resolve’ (terminal node). If ‘symptoms stayed the same’, the pathways described at the same point as symptoms worsening were replicated.
For those patients beginning at ‘second-line’ and third-line’ treatment, the subsequent care pathways were broadly similar to those previously described. However, the model assumes that those patients starting at second- and third-line treatments are unable to progress to less severe treatment strategies. Therefore, the care pathways are progressively shorter as we move through the hierarchy of treatments. The decision model allows one to assess costs and effects across the three alternative treatment strategies and to assess the relative cost-effectiveness of interventions used to treat NVP/HG.
Economic evaluation
Introduction
Unfortunately, as described in previous chapters, the evidence base supporting alternative treatments was not sufficiently robust to support an informative model. Therefore, the focus of the economic component was to estimate the cost of delivering each of the interventions and then use these data in a disaggregated form of economic evaluation. The differences between interventions, in terms of resource use (costs) and natural and clinical measures of effectiveness are presented. Such an approach serves to highlight the choices and trade-offs between the various treatments. Nonetheless, any decision based on this approach is made using an implicit (rather than explicit) synthesis of the available data. These differences between interventions are presented for each of the comparisons presented in Chapters 4–17.
The cost data are used to estimate the implied value for the benefits of treatment should a decision be made to adopt one treatment over another. The approach relies on the conditions required for an efficient allocation of resources. When resources are efficiently allocated the ratio of marginal costs to marginal benefits for all interventions a to n must be equal, that is:
Rearranging the above and simplifying shows that when there is an efficient allocation of resources the ratio of costs is equal to the ratio of benefits, such that:
Although benefits may not be clearly known, it is possible to use information about the costs of interventions a and b to imply how much more effective a needs to be compared with b to be considered efficient. For example, if the ratio of the costs of a to b is 1.2 : 1 then this means that a is 20% more costly than b and for a to be considered a worthwhile use of resources compared with b it should provide at least 20% more benefits. This implied value is then compared with the evidence on effectiveness reported in Chapters 4–17 to inform judgements made on the relative cost-effectiveness of treatments. This section provides a detailed description of the costs of interventions used in the treatment of NVP/HG.
Estimation of costs of interventions
In order to inform the economic evaluation, a detailed cost analysis of interventions used in the treatment of NVP/HG was performed. The interventions considered were categorised as follows: (1) patient-initiated first-line interventions; (2) clinician-prescribed second-line interventions; and (3) clinician-prescribed third-line interventions. The cost of interventions includes both the pharmacological (medication) and non-pharmacological (GP visits, outpatient care, inpatient care, medical tests and management) costs of treatment. The weekly pharmacological costs of clinically relevant interventions (as advised by clinical experts) are listed in Table 22, whereas non-pharmacological costs are listed in Table 23. A full table of interventions included in the analysis can be seen in Appendix 10. These additional treatments were included for completeness but are rarely prescribed in the NHS.
| Preparation | Patient-initiated first-line intervention | Low-estimate weekly cost | High-estimate weekly cost |
|---|---|---|---|
| Tablets | Vitamin B6: pyridoxine hydrochloride (non-proprietary) | £0.12 | £2.59 |
| Tablets | Vitamin B12: cyanocobalamin (non-proprietary) | £0.87 | £2.62 |
| Solution | Ginger (FortiCare) | NE | £2.21 (assumes 125 ml per week)a |
| Physical therapy | Acupressure/acupuncture | NE | First appointment: £50–70 Subsequent appointments: £35–50a |
| Hypnosis | Hypnotherapy | NE | £50–90 for a private hypnotherapy sessiona |
| Preparation | Clinician-prescribed second-line interventions | Low-estimate weekly cost | High-estimate weekly cost |
| Antihistamines | |||
| Tablets | Cyclizine (non-proprietary) | £0.74 | £2.22 |
| i.v./i.m. injection | Cyclizine: Valoid® (Amdipharm Mercury Company Ltd) | NE | £13.65 |
| Tablets | Chlorpromazine (non-proprietary) | NE | £1.55 |
| i.v./i.m. injection | Chlorpromazine (non-proprietary) | £12.60 | £33.60 |
| Dopamine antagonists | |||
| Tablets | Promethazine: Phenergan | £0.74 | £2.22 |
| i.v./i.m. injection | Promethazine (non-proprietary) | £0.68 (daily)a | £1.20 (daily)a |
| Tablets | Prochlorperazine (non-proprietary) | £0.47 | £1.42 |
| i.v./i.m. injection | Prochlorperazine (non-proprietary) | NE | £0.52 (daily)a |
| Tablets | Domperidone (non-proprietary) | £0.39 | £1.17 |
| Tablets | Metoclopramide (non-proprietary) | £0.22 | £0.66 |
| i.v./i.m. injection | Metoclopramide (non-proprietary) | £2.24 | £6.72 |
| Serotonin antagonists | |||
| Tablets | Ondansetron (non-proprietary) | NE | £8.69 (daily)a |
| i.v./i.m. injection | Ondansetron (non-proprietary) | NE | £1.00 (daily)a |
| Preparation | Clinician-prescribed third-line interventions | Low-estimate weekly cost | High-estimate weekly cost |
| Corticosteroids | |||
| i.v./i.m. injection | Methylprednisolone: Solu-Medrone® (Pharmacia) | NE | £17.30 (daily)a |
| Tablets | Prednisone: Lodotra® (Napp Pharmaceuticals Limited) | £12.46 | £24.92 |
| Tablets | Prednisolone (non-proprietary) | £0.67 | £1.33 |
| i.v./i.m. injection | Hydrocortisone: Efcortesol® (Amdipharm Mercury Company Ltd) | £3.24 (daily)a | £19.56 (daily)a |
| Primary care | Costs |
|---|---|
| GP consultation | |
| Per surgical consultation lasting 11.7 minutes | £45 |
| Ketone Reagent Strips: Ketosis (Bayer Diabetes Care) (50 pack) | £2.50 |
| Secondary care | |
| Outpatient | |
| Obstetrics | £122 |
| Ultrasound scan in obstetrics (less than 20 minutes) | £38 |
| Urinary test (urine culture) | £8.51 |
| Ketone Reagent Strips: Ketosis (Bayer Diabetes Care) (50 pack) | £2.50 |
| Liver function test | £6.80 |
| Thyroid function test | £13.55 |
| Glucose | £2.96 |
| Urea and electrolytes | £5.84 |
| Full blood count | £4.94 |
| Sodium chloride i.v. infusion | £1.29 per litre |
| Potassium chloride concentrate, sterile (non-proprietary) (10-ml ampoule) | £0.48 |
| Cost of administering the fluid | £50.42 per day |
| Thiamine supplements | £0.05 per day/£0.35 per week (low estimate) £0.08 per day/£0.56 per week (high estimate) |
| Inpatient | |
| Non-elective inpatient (long stay) excess bed-days | £265 |
| Urinary test (urine culture) | £8.51 |
| Ketone Reagent Strips: Ketosis (Bayer Diabetes Care) (50 pack) | £2.50 |
| Liver function test | £6.80 |
| Thyroid function test | £13.55 |
| Glucose | £2.96 |
| Urea and electrolytes | £5.84 |
| Full blood count | £4.94 |
| Sodium chloride i.v. infusion | £1.29 per litre |
| Potassium chloride concentrate, sterile (non-proprietary) (10-ml ampoule) | £0.48 |
| Cost of administering the fluid | £50.42 per day |
| Pabrinex® (Archimedes Pharma) (10 ml) | £2.25 per week |
| Treatment for thromboembolism: | |
| Clexane® (Sanofi-Aventis) (40 mg) | £3.03 per day |
| Tinzaparin (Innohep®, Leo Laboratories) (4500 units) | £3.56 per day |
| Fragmin® (Pfizer) (5000 units) | £2.56 per day £9.15 per day |
The costs of medication were sourced from the British National Formulary 2014. 132 For all medications, the non-proprietary costs were sought in the first instance. However, if these were unavailable the patented drug costs were used. Where available, the costs of medications which have been incorporated into a tablet or capsule were obtained. Clinical experts in the study team were able to advise on which medications are also commonly administered by i.v. or intramuscular (i.m.) injection and through suppositories, and the relevant costs were included. The overall cost of medication and the average daily dose were used to calculate a low- and high-estimate weekly cost of medication, unless otherwise stated. Where average daily dose was presented as a minimum and maximum, the minimum was used to calculate the low-estimate cost and the maximum was used to calculate the high-estimate cost. Where average daily dose was not presented over a range, costs have been included under high-estimate weekly cost. These drug costs and the recommended daily doses are included in Appendix 10.
Non-pharmacological costs included the unit costs of health and social care services, as well as any tests and medication administered, in a primary and secondary care setting. Clinical experts advised on the tests and treatments which are commonly given to women suffering from NV/HG in each setting. Standard sources such as the NHS Reference Healthcare Research Group tariffs 2012–13,133 the British National Formulary 2014132 for medications and the Personal Social Services Research Unit Unit Costs of Health and Social Care 2013134 were used to obtain these costs.
Estimation of total cost of care
In order to estimate the total cost of interventions, the pharmacological and non-pharmacological costs were combined together in informative packages of care. All likely scenarios experienced by patients suffering from NVP/HG, based on the advice of clinical experts, were included. These scenarios ranged from treatments initiated before consultation with a medical professional to treatments prescribed in primary and secondary care. The flow chart presented in Figure 1 shows the treatments that patients are likely to receive at each level of care and the scenarios presented in this section are based on these care pathways. The costs of managing patients in each setting, as well as the costs of treatment, were used to estimate the overall cost of care. For patient-initiated interventions and medication prescribed in a primary care setting, costs were estimated on a weekly basis. For all other interventions administered in a secondary care setting, costs were estimated according to length of stay. The packages of care are described in scenarios 1–7 below, and total costs for all clinically relevant interventions, as advised by clinical experts, are displayed in Tables 24–30. The estimation of total costs for all interventions is included in Appendix 10.
Packages of care
Scenario 1
Initially, we assumed that the patient does not visit her GP. Rather, she initiates treatment herself. The patient may seek advice from a community midwife or GP at this stage. However, costs are for the medication or treatment costs alone. These costs are outlined in Table 24.
| Pharmacological preparation | Patient-initiated first-line intervention | Total low-estimate weekly cost | Total high-estimate weekly cost |
|---|---|---|---|
| Tablets | Vitamin B6: pyridoxine hydrochloride (non-proprietary) | £0.12 | £2.59 |
| Tablets | Vitamin B12: cyanocobalamin (non-proprietary) | £0.87 | £2.62 |
| Solution | Ginger (FortiCare) | NE | £2.21 (assuming 125 ml per week) |
| Physical therapy | Acupressure/acupuncture | £35 | £50 |
| Hypnosis | Hypnotherapy | £50 | £90 |
Scenario 2
We assumed that the patient visits her GP and receives a urinary test. The GP decides to reassure the patient and advises her to remain on one of the patient-initiated first-line interventions. It was judged unlikely that the GP would advise on acupressure/acupuncture or hypnosis at this stage as these therapies are not routinely available on the NHS. Costs are displayed in Table 25.
| Pharmacological preparation | Patient-initiated first-line intervention | Total low-estimate weekly cost | Total high-estimate weekly cost | GP clinic consultation | Urine ketones strip | Total |
|---|---|---|---|---|---|---|
| Tablets | Vitamin B6: pyridoxine hydrochloride (non-proprietary) | £0.12 | £2.59 | £45 | £0.05 | £45.17–47.64 |
| Tablets | Vitamin B12: cyanocobalamin (non-proprietary) | £0.87 | £2.62 | £45 | £0.05 | £45.92–47.67 |
| Solution | Ginger (FortiCare) | NE | £2.21 (assuming 125 ml per week) | £45 | £0.05 | £47.26 |
Scenario 3
We assumed that the patient visits her GP and receives a urinary test. Symptoms are severe enough that the GP prescribes one of the clinician-prescribed second-line interventions (oral antiemetic only). Costs are displayed in Table 26.
| Pharmacological preparation | Clinician-prescribed second-line intervention | Total low-estimate weekly cost | Total high-estimate weekly cost | GP clinic consultation | Urine ketones strip | Total |
|---|---|---|---|---|---|---|
| Antihistamines | ||||||
| Tablets | Cyclizine (non-proprietary) | £0.74 | £2.22 | £45 | £0.05 | £45.79–47.27 |
| Tablets | Chlorpromazine (non-proprietary) | NE | £1.55 | £45 | £0.05 | £46.60 |
| Dopamine antagonists | ||||||
| Tablets | Domperidone (non-proprietary) | £0.39 | £1.17 | £45 | £0.05 | £45.44–46.22 |
| Tablets | Metoclopramide (non-proprietary) | £0.22 | £0.66 | £45 | £0.05 | £45.27–45.71 |
| Tablets | Prochlorperazine (non-proprietary) | £0.47 | £1.42 | £45 | £0.05 | £45.52–46.47 |
| Tablets | Promethazine: Phenergan | £0.74 | £2.22 | £45 | £0.05 | £45.79–47.27 |
| Serotonin antagonists | ||||||
| Tablets | Ondansetron (non-proprietary) | NE | £60.83 | £45 | £0.05 | £105.88 |
Scenario 4
If the patient is in a serious enough condition that they cannot be managed in primary care, the GP may refer the woman to secondary care (or alternatively, women may refer themselves to hospital maternity services). The following costs reflect those costs that might be incurred in a secondary care setting. In Table 27 we include the costs of the woman attending hospital as a ‘day case’, receiving the relevant outpatient tests, receiving an antiemetic and then being discharged. Included also are the daily cost of receiving a thiamine supplement (high estimate) and the cost of receiving 3 l (in severe cases) of sodium chloride i.v. infusion along with the appropriate amount of potassium chloride. All costs are calculated on a daily basis.
| Pharmacological preparation | Clinician-prescribed second-line intervention | Total low-estimate daily cost (£) | Total high-estimate daily cost (£) | Obstetrics unit (£) | Ultrasound scan (< 20 minutes) (£) | Urinary test (urine culture) (£) | Urine ketones strip (£) | Liver function test (£) | Thyroid function test (£) | Glucose (£) | Urea and electrolytes (£) | Full blood count (£) | Thiamine supplement (£) | Normal saline + a proportional amount of potassium chloride + cost of administering the fluid (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antihistamines | |||||||||||||||
| Tablets | Cyclizine (non-proprietary) | 0.11 | 0.32 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.93–286.14 |
| i.v./i.m. injection | Cyclizine: Valoid | NE | 1.95 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 287.77 |
| Tablets | Chlorpromazine (non-proprietary) | NE | 0.22 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.04 |
| i.v./i.m. injection | Chlorpromazine (non-proprietary) | 1.80 | 4.80 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 287.62–290.62 |
| Dopamine antagonists | |||||||||||||||
| Tablets | Promethazine: Phenergan | 0.11 | 0.32 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.93–286.14 |
| i.v./i.m. injection | Promethazine (non-proprietary) | 0.68 | 1.20 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.50–287.02 |
| Tablets | Prochlorperazine (non-proprietary) | 0.07 | 0.20 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.89–286.02 |
| i.v./i.m. injection | Prochlorperazine (non-proprietary) | NE | 0.52 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.34 |
| Tablets | Domperidone (non-proprietary) | 0.06 | 0.17 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.88–285.99 |
| Tablets | Metoclopramide (non-proprietary) | 0.03 | 0.09 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.85–285.91 |
| i.v./i.m. injection | Metoclopramide (non-proprietary) | 0.32 | 0.96 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.14–286.78 |
| Serotonin antagonists | |||||||||||||||
| Tablets | Ondansetron (non-proprietary) | NE | 8.69 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 294.51 |
| i.v./i.m. injection | Ondansetron (non-proprietary) | NE | 1.00 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.82 |
Scenario 5
In very severe cases, or where the patient refuses outpatient treatment, or if outpatient treatment fails (i.e. the patient feels as unwell at the end of outpatient treatment), the woman may be admitted as an inpatient. In Table 28 the assumption is that the woman is admitted as an inpatient for 2 days (based on expert opinion). In this scenario, it is assumed that the woman would have received a one-off ultrasound scan prior to being admitted as an inpatient and thus, this cost is not included. Based on expert clinical advice, we have assumed that the patient receives all relevant tests on day of admission and day of discharge, medication used in the prevention of venous thromboembolism, i.v. infusion of 3 l of sodium chloride solution every day along with the appropriate amount of potassium chloride, i.v. thiamine (Pabrinex, 10 ml) once a week, and appropriate antiemetics (as advised by clinical experts) (no steroids) over the course of the 2-day admission before being discharged.
| Pharmacological preparation | Clinician-prescribed second-line interventions | Total low-estimate daily cost × 2 (£) | Total high-estimate daily cost × 2 (£) | Inpatient excess bed-days × 2 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Treatment for thromboembolism (1-night stay) (£) | Thiamine supplement (Pabrinex) × 1 (£) | Normal saline + a proportional amount of potassium chloride × 2 + cost of administering the fluid over 2 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antihistamines | |||||||||||||||
| i.v./i.m. injection | Cyclizine: Valoid | NE | 3.90 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 796.78 |
| Tablets | Chlorpromazine (non-proprietary) | NE | 0.44 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.32 |
| i.v./i.m. injection | Chlorpromazine (non-proprietary) | 3.60 | 9.60 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 796.48–802.48 |
| Dopamine antagonists | |||||||||||||||
| i.v./i.m. injection | Metoclopramide (non-proprietary) | 0.64 | 1.92 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.52–794.80 |
| Tablets | Prochlorperazine (non-proprietary) | 0.13 | 0.41 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.01–793.29 |
| i.v./i.m. injection | Prochlorperazine (non-proprietary) | NE | 1.04 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.92 |
| Tablets | Domperidone (non-proprietary) | 0.11 | 0.33 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 792.99–793.21 |
| Serotonin antagonists | |||||||||||||||
| i.v./i.m. injection | Ondansetron (non-proprietary) | NE | 2.00 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 794.88 |
Scenario 6
In this scenario, it is assumed that the patient has not responded to the single antiemetic prescribed while admitted as an inpatient and so has been admitted as an inpatient for 2 days (based on expert opinion) with two antiemetics prescribed. Based on expert clinical advice, we have assumed that the patient receives all relevant tests on day of admission and day of discharge, i.v. infusion of 3 l of sodium chloride solution every day along with the appropriate amount of potassium chloride, medication used in the prevention of venous thromboembolism, i.v. thiamine (Pabrinex, 10 ml) once a week, and a combination of two antiemetics (no steroids) over the course of the 2-day admission before being discharged. Owing to the minimal difference in cost between antiemetics, the low- and high-estimate costs represent combinations of the two cheapest and two most expensive medications (based on high-estimate daily cost). These costs are displayed in Table 29.
| Clinician-prescribed second-line intervention | Total daily cost (two antiemetics) × 2 (£) | Inpatient excess bed-days × 2 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Treatment for thromboembolism (1-night stay) (£) | Thiamine supplement (Pabrinex) × 1 (£) | Normal saline + a proportional amount of potassium chloride × 2 + cost of administering the fluid over 2 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Least costly | 0.50 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.38 |
| Most costly combination | 50.70 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 843.58 |
Scenario 7
In this scenario, it is assumed that the patient has so far not responded to any antiemetics prescribed while admitted as an inpatient. In the following table of costs (see Table 30), the assumption is that the woman has been admitted as an inpatient for 5 days (based on expert opinion) to follow a regime of multiple antiemetics and steroids. Up until this point the woman has experienced (a) weight loss, (b) failed second-line interventions, or (c) difficulty coping. As the condition of the patient is so severe, it is assumed that she receives all relevant tests on each day of admission (following the guidance of clinical experts). It is assumed that i.v. infusion of 3 l of sodium chloride solution is given every day along with the appropriate amount of potassium chloride, medication used in the prevention of venous thromboembolism is given for each night of stay, i.v. thiamine (Pabrinex, 10 ml) is given once over the course of the admission, and a combination of three antiemetics is given to the patient for the first 3 days before a steroid is provided in days 4 and 5, before discharge. Owing to the minimal difference in cost between antiemetics, the low- and high-estimate costs represent combinations of the three cheapest and three most expensive medications (based on high-estimate daily cost). Similarly, there is little difference in cost between steroids and so, the low- and high-estimate costs are representative of packages including the cheapest and most expensive steroid (based on high-estimate daily cost). These costs are displayed in Table 30.
| Clinician-prescribed third-line intervention | Total daily cost (three antiemetics) × 3 (£) | Total daily cost (corticosteroid) × 2 (£) | Inpatient excess bed-days × 5 (£) | Urinary test (urine culture) × 5 (£) | Urine ketones strip × 5 (£) | Liver function test × 5 (£) | Thyroid function test × 5 (£) | Glucose × 5 (£) | Urea and electrolytes × 5 (£) | Full blood count × 5 (£) | Treatment for thromboembolism (4-night stay) (£) | Thiamine supplement (Pabrinex) × 1 (£) | Normal saline + a proportional amount of potassium chloride × 5 + cost of administering the fluid over 5 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Least costly combination | 1.26 | 0.38 (prednisolone tablets) | 1325 | 42.55 | 0.25 | 34.00 | 67.75 | 14.80 | 29.20 | 24.70 | 36.60 | 2.25 | 415.45 | 1994.19 |
| Most costly combination | 82.86 | 39.12 (hydrocortisone injection) | 1325 | 42.55 | 0.25 | 34.00 | 67.75 | 14.80 | 29.20 | 24.70 | 36.60 | 2.25 | 415.45 | 2114.53 |
The packages of care presented above are representative scenarios that combine the pharmacological and non-pharmacological costs of interventions used in the treatment of patients suffering from NVP and HG. If symptoms have not resolved following scenario 7, extreme measures such as enteral or parenteral nutrition may sometimes be used. However, this is quite rare and the costs can be significant. Kilonzo estimated the mean cost of treatment for standard parenteral nutrition to be £337 among a group of patients in intensive care units and high-dependency units for ≥ 48 hours, with gastrointestinal failure and requiring parenteral nutrition (Kilonzo M, University of Aberdeen, 2014, personal communication). Enteral and parenteral feeding is a last-resort therapy among women suffering from NVP/HG and would usually only ever be used as a last resort.
The packages of care indicate that the costs of treatment increase rapidly as women move through the hierarchy of treatments. In scenario 1, we see that in less severe cases, where women initiate treatment themselves, costs may be as low as £0.12 per week. Alternative patient-initiated treatment strategies such as acupressure/acupuncture or hypnosis are significantly more expensive, but may only be required on a one-off basis. If symptoms are persistent, it is likely that the woman would seek the advice of a clinician and begin to take oral prescribed medication. In scenarios 2 and 3, we see the cost of attending a GP and taking oral medication for 1 week. Following this first week, costs would revert back to the cost of medication alone, which is small in comparison with the cost of attending the GP, provided no further consultations are required. In scenario 4, we see the costs that would be incurred if the woman was to be referred to hospital as a ‘day case’. This is the woman’s first point of contact with secondary care services, and a number of tests, including an ultrasound scan and relevant bloods, are likely to be done at this stage. When we factor in the costs of hospital care and medication that is likely to be administered at this stage, costs range from £286 in the least costly scenario to £295 in the most costly (based on high-estimate costs). Again, the cost of managing the woman in this setting is the main cost driver, with medication costs becoming less significant in comparison. Finally, scenarios 5–7 are representative of scenarios where the woman has been admitted to hospital as an inpatient due to the extremity of her symptoms. This is the point at which costs escalate rapidly, largely driven by length of stay. This is reflected in the fact that there is very little difference in the total cost of care between scenarios 5 and 6, despite antiemetics being doubled in the latter scenario. Similarly, in the most severe cases, where women are admitted for a 5-day period, < 6% of the total cost of care is accounted for by the medication costs.
As we have seen, the cost of medication used in the treatment of NVP/HG is less important when compared with the cost of managing women with the condition in a primary and secondary care setting. One issue which may be of importance to decision-makers is whether it is more economical to manage women with NVP/HG as day cases or as inpatients. In Table 31, the cost of first-, second- and third-line interventions is omitted and the focus is placed solely on the hospital management costs. The cost of managing women as day cases on 2 separate days is presented alongside the cost of managing women as inpatients over a 2-day period. All treatment costs relevant to each scenario are presented.
| Day case | Obstetrics unit × 2 (£) | Ultrasound scan (< 20 minutes) × 1 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Thiamine supplement × 2 (£) | Normal saline and a proportional amount of potassium chloride and cost of administering the fluid on 2 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 244 | 38 | 17.02 | 0.10 | 13.60 | 27,10 | 5.92 | 11.68 | 9.88 | 0.16 | 166.18 | 533.64 | |
| Inpatient | Inpatient excess bed-days × 2 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Treatment for thromboembolism (1-night stay) (£) | Thiamine supplement (Pabrinex) (£) | Normal saline and a proportional amount of potassium chloride and cost of administering the fluid over 2 days (£) | Total (£) |
| 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 792.88 |
The difference in cost between inpatient management and day case management is largely driven by the fact that inpatient bed-days are substantially more expensive than the obstetrics unit day case costs. The only other major cost differentials are that an ultrasound scan is likely to initially be carried out on day case patients, whereas it is assumed that patients would have received a scan prior to being admitted as an inpatient. Additionally, clinical experts have advised that inpatients would require prophylactic treatment to prevent deep-vein thrombosis and pulmonary embolism, whereas this cost is not incurred when treating day case patients. The total cost difference is £259, with inpatient treatment significantly more expensive than day case treatment in the 2-day scenario presented in Table 31.
Methods
The total cost data were used to estimate the implied value for the benefits of treatment should a decision be made to adopt one treatment over another. Within each package of care, the ratio of the cost of one treatment to another was calculated, with the results informing us as to the increase in benefits that the more expensive option would need to provide in order to be considered a worthwhile use of resources. Benefits of treatment are not clearly known, but these results were used to imply how much more effective one treatment needs to be compared with another to be considered efficient. The implied value was then used to compare with the evidence on effectiveness reported in Chapters 4–17, in a disaggregated form of economic evaluation. Each comparison presented in Chapters 4–17 is included. The implied value for the benefits of treatments is presented in the subsequent section.
Results
Implied value for the benefits of treatment
Within each package of care, the ratio of the cost of one treatment to another was calculated. The size of the ratio was indicative of the increase in benefits that the more costly option would need to provide in order to be considered efficient compared with the less costly option. Effect sizes were categorised according to Grimshaw and colleagues’135 review of guideline dissemination and implementation strategies and, in particular, the description of the size of effect for process dichotomous measures. The effects sizes were categorised as follows:
-
‘small’ to describe effect sizes ≤ 5%
-
‘modest’ to describe effect sizes > 5% and ≤ 10%
-
‘moderate’ to describe effect sizes > 10% and ≤ 20%
-
‘large’ to describe effect sizes > 20%.
Cost comparisons for all clinically relevant interventions in the UK, as advised by clinical experts, were based on the high-estimate costs and are presented in Tables 32–39. Unfortunately, in a large number of cases, while a comparison of costs could be made between interventions within each package of care, evidence on effect was unavailable. Cost comparisons for all interventions included in the analysis can be seen in Appendix 10.
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Vitamin B6 : ginger | 1.2 : 1 | Moderate | No evidence of a difference between groups |
| Vitamin B12 : vitamin B6 | 1.01 : 1 | Small | Unknown |
| Vitamin B12 : ginger | 1.2 : 1 | Moderate | Unknown |
| Acupressure/acupuncture: vitamin B12 | 19.1 : 1 | Large | Unknown |
| Acupressure/acupuncture : vitamin B6 | 19.3 : 1 | Large | No evidence of a difference between groups |
| Acupressure/acupuncture : ginger | 22.6 : 1 | Large | Ginger looks promising in reducing symptoms when compared with acupressure but findings are not conclusive |
| Hypnotherapy : acupressure/acupuncture | 1.8 : 1 | Large | Unknown |
| Hypnotherapy : vitamin B12 | 34.4 : 1 | Large | Unknown |
| Hypnotherapy : vitamin B6 | 34.7 : 1 | Large | Unknown |
| Hypnotherapy : ginger | 40.7 : 1 | Large | Unknown |
| Ginger : placebo | Not assessable | Not assessable | Ginger looks more effective when compared with placebo. Additional cost of ginger is small |
| Acupressure/acupuncture : placebo | Not assessable | Not assessable | Acupressure looks promising in reducing symptoms when compared with placebo in a small number of studies, while the rest show no difference between the groups |
| Vitamin B6 : placebo | Not assessable | Not assessable | Vitamin B6 looks more effective when compared with placebo. Additional cost of vitamin B6 is small |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Vitamin B6 : ginger | 1.008 : 1 | Small | No evidence of a difference in effect |
| Vitamin B12 : vitamin B6 | 1.0006 : 1 | Small | Unknown |
| Vitamin B12 : ginger | 1.009 : 1 | Small | Unknown |
| Ginger : placebo | Not assessable | Not assessable | Ginger looks promising in reducing symptoms when compared with placebo, but findings are not conclusive |
| Vitamin B6 : placebo | Not assessable | Not assessable | Vitamin B6 looks promising in reducing symptoms when compared with placebo, but findings are not conclusive |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Domperidone : metoclopramide | 1.01 : 1 | Small | Unknown |
| Prochlorperazine : domperidone | 1.005 : 1 | Small | Unknown |
| Prochlorperazine : metoclopramide | 1.02 : 1 | Small | Unknown |
| Chlorpromazine : prochlorperazine | 1.003 : 1 | Small | Unknown |
| Chlorpromazine : domperidone | 1.008 : 1 | Small | Unknown |
| Chlorpromazine : metoclopramide | 1.02 : 1 | Small | Unknown |
| Cyclizine : chlorpromazine | 1.01 : 1 | Small | Unknown |
| Cyclizine : prochlorperazine | 1.02 : 1 | Small | Unknown |
| Cyclizine : domperidone | 1.02 : 1 | Small | Unknown |
| Cyclizine : metoclopramide | 1.03 : 1 | Small | Unknown |
| Promethazine : cyclizine | 1 : 1 | Small | Unknown |
| Promethazine : chlorpromazine | 1.01 : 1 | Small | Unknown |
| Promethazine : prochlorperazine | 1.02 : 1 | Small | Unknown |
| Promethazine : domperidone | 1.02 : 1 | Small | Unknown |
| Promethazine : metoclopramide | 1.03 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Ondansetron : promethazine | 2.2 : 1 | Large | Unknown |
| Ondansetron : cyclizine | 2.2 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no evidence of significant difference in effects |
| Ondansetron : chlorpromazine | 2.3 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no evidence of significant difference in effects |
| Ondansetron : prochlorperazine | 2.3 : 1 | Large | Unknown |
| Ondansetron : domperidone | 2.3 : 1 | Large | Unknown |
| Ondansetron : metoclopramide | 2.3 : 1 | Large | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Antihistamines : placebo | Not assessable | Not assessable | Antihistamines appear to be better than placebo in reducing the severity of symptoms, but more larger, better-quality studies are required |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Domperidone (tablets) : metoclopramide (tablets) | 1.0003 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : domperidone (tablets) | 1.0001 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : metoclopramide (tablets) | 1.0004 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : prochlorperazine (tablets) | 1.00007 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : domperidone (tablets) | 1.0002 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : metoclopramide (tablets) | 1.0005 : 1 | Small | Unknown |
| Cyclizine (tablets) : chlorpromazine (tablets) | 1.0003 : 1 | Small | Unknown |
| Cyclizine (tablets) : prochlorperazine (tablets) | 1.0004 : 1 | Small | Unknown |
| Cyclizine (tablets) : domperidone (tablets) | 1.0005 : 1 | Small | Unknown |
| Cyclizine (tablets) : metoclopramide (tablets) | 1.0008 : 1 | Small | Unknown |
| Promethazine (tablets) : cyclizine (tablets) | 1 : 1 | Small | Unknown |
| Promethazine (tablets) : chlorpromazine (tablets) | 1.0003 : 1 | Small | Unknown |
| Promethazine (tablets) : prochlorperazine (tablets) | 1.0004 : 1 | Small | Unknown |
| Promethazine (tablets) : domperidone (tablets) | 1.0005 : 1 | Small | Unknown |
| Promethazine (tablets) : metoclopramide (tablets) | 1.0008 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Prochlorperazine (injection) : promethazine (tablets) | 1.0007 : 1 | Small | Unknown |
| Prochlorperazine (injection) : cyclizine (tablets) | 1.0007 : 1 | Small | Unknown |
| Prochlorperazine (injection) : chlorpromazine (tablets) | 1.001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : prochlorperazine (tablets) | 1.001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : domperidone (tablets) | 1.001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : metoclopramide (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : prochlorperazine (injection) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : promethazine (tablets) | 1.002 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Metoclopramide (injection) : cyclizine (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : chlorpromazine (tablets) | 1.003 : 1 | Small | Unknown |
| Metoclopramide (injection) : prochlorperazine (tablets) | 1.003 : 1 | Small | Unknown |
| Metoclopramide (injection) : domperidone (tablets) | 1.003 : 1 | Small | Unknown |
| Metoclopramide (injection) : metoclopramide (tablets) | 1.003 : 1 | Small | Unknown |
| Ondansetron (injection) : metoclopramide (injection) | 1.0001 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron (injection) : prochlorperazine (injection) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : promethazine (tablets) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : cyclizine (tablets) | 1.002 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : chlorpromazine (tablets) | 1.003 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : prochlorperazine (tablets) | 1.003 : 1 | Small | Unknown |
| Ondansetron (injection) : domperidone (tablets) | 1.003 : 1 | Small | Unknown |
| Ondansetron (injection) : metoclopramide (tablets) | 1.003 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Promethazine (injection) : ondansetron (injection) | 1.0007 : 1 | Small | Unknown |
| Promethazine (injection) : metoclopramide (injection) | 1.0008 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Promethazine (injection) : prochlorperazine (injection) | 1.002 : 1 | Small | Unknown |
| Promethazine (injection) : promethazine (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : cyclizine (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : chlorpromazine (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : prochlorperazine (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : domperidone (tablets) | 1.004 : 1 | Small | Unknown |
| Promethazine (injection) : metoclopramide (tablets) | 1.004 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Cyclizine (injection) : promethazine (injection) | 1.003 : 1 | Small | Unknown |
| Cyclizine (injection) : ondansetron (injection) | 1.003 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Cyclizine (injection) : metoclopramide (injection) | 1.003 : 1 | Small | Unknown |
| Cyclizine (injection) : prochlorperazine (injection) | 1.005 : 1 | Small | Unknown |
| Cyclizine (injection) : promethazine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : cyclizine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : chlorpromazine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : prochlorperazine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : domperidone (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : metoclopramide (tablets) | 1.007 : 1 | Small | Unknown |
| Chlorpromazine (injection) : cyclizine (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : promethazine (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : ondansetron (injection) | 1.01 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Chlorpromazine (injection) : metoclopramide (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : prochlorperazine (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : promethazine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : cyclizine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : chlorpromazine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : prochlorperazine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : domperidone (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : metoclopramide (tablets) | 1.02 : 1 | Small | Unknown |
| Ondansetron (tablets) : chlorpromazine (injection) | 1.01 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : cyclizine (injection) | 1.02 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : promethazine (injection) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : ondansetron (injection) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : metoclopramide (injection) | 1.03 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron (tablets) : prochlorperazine (injection) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : promethazine (tablets) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : cyclizine (tablets) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : chlorpromazine (tablets) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : prochlorperazine (tablets) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : domperidone (tablets) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : metoclopramide (tablets) | 1.03 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Antihistamines : placebo | Not assessable | Not assessable | Antihistamines appear to be better than placebo in reducing the severity of symptoms, but more larger, better-quality studies are required |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Prochlorperazine (tablets) : domperidone (tablets) | 1.0001 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : prochlorperazine (tablets) | 1.00004 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : domperidone (tablets) | 1.0001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : chlorpromazine (tablets) | 1.0008 : 1 | Small | Unknown |
| Prochlorperazine (injection) : prochlorperazine (tablets) | 1.0008 : 1 | Small | Unknown |
| Prochlorperazine (injection) : domperidone (tablets) | 1.0009 : 1 | Small | Unknown |
| Metoclopramide (injection) : prochlorperazine (injection) | 1.001 : 1 | Small | Unknown |
| Metoclopramide (injection) : chlorpromazine (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : prochlorperazine (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : domperidone (tablets) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : metoclopramide (injection) | 1.0001 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron (injection) : prochlorperazine (injection) | 1.001 : 1 | Small | Unknown |
| Ondansetron (injection) : chlorpromazine (tablets) | 1.002 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : prochlorperazine (tablets) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : domperidone (tablets) | 1.002 : 1 | Small | Unknown |
| Cyclizine (injection) : ondansetron (injection) | 1.002 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Cyclizine (injection) : metoclopramide (injection) | 1.002 : 1 | Small | Unknown |
| Cyclizine (injection) : prochlorperazine (injection) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : chlorpromazine (tablets) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : prochlorperazine (tablets) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : domperidone (tablets) | 1.005 : 1 | Small | Unknown |
| Chlorpromazine (injection) : cyclizine (injection) | 1.007 : 1 | Small | Unknown |
| Chlorpromazine (injection) : ondansetron (injection) | 1.01 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Chlorpromazine (injection) : metoclopramide (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : prochlorperazine (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : chlorpromazine (tablets) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : prochlorperazine (tablets) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : domperidone (tablets) | 1.01 : 1 | Small | Unknown |
| Antihistamines : placebo | Not assessable | Not assessable | Antihistamines appear to be better than placebo in reducing the severity of symptoms, but more larger, better-quality studies are required |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Most expensive : least expensive | 1.06 : 1 | Modest | Unknown |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Most expensive : least expensive | 1.06 : 1 | Modest | Unknown |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Inpatient : day case | 1.5 : 1 | Large | Results indicate that day case management is as effective at improving severity scores as inpatient management for some women. However, more, larger studies are required to provide definitive results |
For patient-initiated first-line interventions, the ratio of the cost of vitamin B6 to ginger was 1.2 : 1. Therefore, in order to be considered a worthwhile use of resources, vitamin B6 would need to provide at least 20% more in benefits than ginger. It is feasible that such a difference in effect could exist. However, there was no evidence to support a difference of this magnitude. The ratio of the cost of acupressure/acupuncture to both vitamin B6 and ginger is extremely large and it is inconceivable that an equally large difference in effectiveness could exist to justify this. The evidence on effect showed no significant difference between the interventions, although the evidence was limited. Finally, ginger, acupressure/acupuncture and vitamin B6 were all compared with placebo. Although an implied valuation was not assessable, evidence on effect showed that all three treatments looked promising in reducing symptoms compared with placebo, but the findings were not conclusive. With respect to ginger and vitamin B6 the cost of these therapies might be considered modest and were quite similar. From an economics perspective, this suggests that we are indifferent about which is used as a first treatment.
For patient-initiated first-line interventions following a GP visit, the ratio of the cost of vitamin B6 to ginger was 1.008 : 1. Therefore, vitamin B6 would only need to provide 0.8% more in benefits than ginger in order to be considered a worthwhile use of resources within this package of care. Unfortunately, there was little evidence on effect available and a conclusion could not be drawn. Both ginger and vitamin B6 look promising in reducing symptoms compared with placebo, but the findings from the effectiveness review were not conclusive. The main difference in cost between the use of vitamin B6 and ginger was the difference in medications. The cost of these therapies might be considered modest and were quite similar. From an economics perspective this suggests that we are indifferent about which is used.
Although this may not be considered acceptable to women or clinically, the results from Tables 32 and 33 allow comparisons to be drawn whether or not women are encouraged to self-medicate before seeking medical treatment from primary care. For example, as an initial response to NVP, seeking advice from a GP who goes on to recommend vitamin B6 as opposed to self-medicating with vitamin B6 implies that the benefits of advice and treatment from the GP are at least 17 times more than the benefits of self-medication. The question for decision-makers is whether or not the benefits from the advice and reassurance gained from contacting a GP are of sufficient value to be worth the additional cost.
Cost comparisons were carried out for all clinician-prescribed second-line interventions (oral antiemetics only) following a GP visit. In the comparison between promethazine and metoclopramide the implied valuation was 1.03 : 1, meaning that in order to be considered efficient, promethazine would need to provide at least 3% more benefits than metoclopramide. No difference in effectiveness was reported from the review; however, it is feasible that such a difference in effect could exist. Ondansetron was compared with both antihistamines (cyclizine and chlorpromazine) within this package of care. Although ondansetron is more expensive (2.2 : 1 and 2.3 : 1, respectively), no difference in effects was shown in the review. In the cost comparison between ondansetron and metoclopramide, the ratio of the cost of ondansetron to the cost of metoclopramide was 2.3 : 1. While the evidence on effect showed that ondansetron was more effective at reducing the symptoms of vomiting than metoclopramide after 4 days, it would need to provide at least 1.3 times more in benefits than metoclopramide in order to be considered a worthwhile use of resources. Finally, antihistamines were compared with placebo and, while an implied valuation was not assessable, the limited information available from the effectiveness review showed that antihistamines appear to be better than placebo in reducing the severity of symptoms.
Within this package of care, it is the patient management costs which are the main cost drivers. Therefore, the difference in cost between all interventions in this package of care was extremely small. The cost comparison ratios ranged from 1 : 1 to 1.03 : 1. From the evidence on effect, ondansetron was more effective at reducing the symptoms of vomiting than metoclopramide after 4 days. Antihistamines also appear to be better than placebo in reducing the severity of symptoms. Other than this, there was no significant difference in effect between any of the comparators included in the effectiveness review within this package of care. Owing to the small difference in cost between all comparators, it is conceivable that any of the more costly options could provide sufficient benefit in order to be worthwhile. However, the limited data available on clinical effectiveness mean that a definitive conclusion cannot be drawn.
As before, it is the patient management costs which are the main cost drivers within this package of care. Cost comparison ratios ranged from 1.00004 : 1 in the smallest instance to 1.01 : 1 in the largest. From the evidence on effect, ondansetron was more effective at reducing the symptoms of vomiting than metoclopramide after 4 days. Antihistamines also appear to be better than placebo in reducing the severity of symptoms. Other than this, there was no significant difference in effect between any of the comparators included in the effectiveness review within this package of care. Again, because of the small difference in cost between all comparators, it is conceivable that any of the more costly options could provide sufficient benefit in order to be considered worthwhile. However, the limited data available on clinical effectiveness mean that a definitive conclusion cannot be drawn.
In order to be considered a worthwhile use of resources, the more expensive option of second-line inpatient care would need to provide at least 6% more in benefits than the less expensive option. Evidence on effect is unknown but it is not implausible that such a difference could exist.
In order to be considered a worthwhile use of resources, the more expensive option would need to provide at least 6% more in benefits than the less expensive option. Evidence on effect is unknown.
The cost of inpatient management compared with day case management in the 2-day scenario presented is almost 50% greater. This means that the benefits of inpatient management would need to be at least 50% greater than those of day case management in order for it to be considered a worthwhile use of resources. Although the results are not definitive due to limited data, the evidence on effectiveness indicates that day case management is as effective at improving severity scores as inpatient management for some women. Therefore, the additional cost of inpatient management in the scenario presented may represent an inefficient use of resources.
For a large number of comparators included in this section, evidence on effect is unknown. All clinically relevant interventions in the UK were included in each package of care; however, clinical evidence is unavailable for many interventions. The ratio of the cost of one intervention to another was calculated within packages of care to determine the increase in effectiveness that the more costly option would need to provide in order to be considered a worthwhile use of resources. However, as illustrated above, this technique could also be applied to treatments in separate packages of care. This would allow one to, for instance, compare a patient-initiated first-line intervention with a clinician-prescribed second-line intervention to calculate the implied valuation. This information may be of interest to decision-makers.
Summary
-
Currently, there are no economic evaluations on the cost-effectiveness of interventions used in the treatment of NVP/HG.
-
An economic model has been developed to estimate the relative cost-effectiveness of interventions used in the treatment of NVP/HG and may be used in a model-based economic evaluation once additional information becomes available.
-
Pharmacological and non-pharmacological costs of treatment have been combined together to develop informative packages of care. The cost of treatment increases rapidly as patients move from patient-initiated first-line interventions to clinician-prescribed second-line interventions to clinician-prescribed third-line interventions. The cost of medication is small in comparison with the cost of care.
-
An implied valuation form of economic evaluation has been used to assess cost-effectiveness. Within each package of care, cost comparisons have been carried out in order to determine the increase in benefits that the more costly option would need to provide in order to be considered efficient.
-
For patient-initiated first-line interventions, the cost comparison ratios ranged from 1.01 : 1 in the comparison between vitamin B12 and vitamin B6 to 41 : 1 for the comparison between hypnotherapy and ginger.
-
The final cost comparison between inpatient management and day case management indicated that inpatient management would need to provide at least 50% more benefits than day case management to be considered worthwhile. The results on clinical effectiveness indicate that day case management is equally as effective.
-
The economic evaluation requires additional information on clinical effectiveness for a large number of interventions in order to make definitive conclusions on cost-effectiveness.
Chapter 19 Issues of importance to patients
Introduction
Nausea and vomiting of pregnancy is a frequently occurring, often debilitating condition which can result in physical, emotional and psychological distress, and a reduced QoL for sufferers. Management of the condition by health-care providers is inconsistent, with many women reporting a poor experience of the health-care system. It is therefore essential to consider the views and opinions of previous sufferers alongside research evidence for clinical effectiveness if the care and the treatment of this condition is to be improved.
Key to carrying out this review was the role played by practitioners and service user members of the research team. Women who had suffered from NVP and/or HG were members of our Project Steering Group along with representatives of key patient advocacy groups in the field. These members represented their own views, not necessarily the views of the advocacy groups. These representatives were consulted at the start of the study, when we informed them about the evidence review and invited their comments on how the project could be improved. Engagement continued throughout the project, so that they were able contribute to meetings in the latter stages of the review when we sought their input to help the research team generate ideas for dissemination.
Background
Previous research and an online survey carried out by the PSS Group (unpublished data, 2014, www.pregnancysicknesssupport.co.uk/), has highlighted the problems women face when seeking advice, support and care from health-care professionals (HCPs). Tables 40 and 41 represent themes and examples drawn from comments made to women that were reported as part of this survey.
| Theme | Explanation | Quotes |
|---|---|---|
| Knowledge and beliefs |
|
Biggest difficulty trying to find GP who understood or would prescribe helpMedical care awful if I’d been diagnosed earlier and given medication earlier I wouldn’t have terminated three babiesI felt that they dismissed my symptoms, even tried to convince me I had gastroenteritisI was responsible for researching all options regarding drugs and asking for thingsThe total lack of understanding and support from the medical profession both during and after my pregnancyDespair at lack of understanding or clear direction from GP and hospital staffHad to see 4 doctors before I was prescribed Buccastem. Previous doctors refused to prescribe me any medication |
| Attitudes |
|
Told (by GP) that only ‘stupid people’ need admitted to hospitalI was very much treated as weak and hysterical by hospital staff and when I asked for injectionsI was made to feel like I was wasting their [community midwife and consultant] time and that it was a normal part of pregnancyDespair at lack of understanding or clear direction from GP and hospital staffI was treated by medical professionals as though HG was a matter of my mind and not realHis [GP] exact words were ‘you can’t expect pregnancy to be a walk in the park’ |
| Lack of sympathy/understanding |
|
Made to feel as if should just get on with itI regret the termination and feel if the medical profession had shown any empathy I might have been able to get through the HG that first timeNo empathy from GPs. Felt as though I had to beg for medicationI was ignored by my GP, turned away from the hospital due to no ketones in my urine. Little to no support from healthcare professionals until I found a consultant who specialised in HG |
| Theme | Explanation | Quotes |
|---|---|---|
| Communication and attitude |
|
When my GP did see me, she was fantastic but had to rush me into hospital due to dehydrationMidwife was awful and ended up complaining and changing at 30 weeks, wish I’d done it sooner as the next midwife was amazing! |
| Knowledge and understanding |
|
I was lucky to have an excellent GP who was quick to diagnose, quick to treat, and got me through |
Relating what patients want to review findings
The remit of this systematic review was to evaluate the available research evidence surrounding interventions to treat NVP/HG. It is hoped that results from this review can be used to make suggestions as to how to address some of the problems women face.
Women want HCPs to acknowledge that NVP/HG is a chronic condition and that symptoms can vary dramatically between individuals, from mild to very severe, with no time limit on when symptoms will cease. The review has highlighted inconsistencies with assessing severity of symptoms in many of the included studies. This is likely to be the case within the wider health-care system. HCPs need to acknowledge and be able to assess the wide spectrum of symptoms severity that can be experienced. The introduction of a validated, standard method of assessment may help, so enabling HCPs to discuss the most appropriate treatment options with women. This decision-making process should take into consideration the individual woman’s situation, experience, knowledge and past history. Pre-emptive therapy may be appropriate in some cases where women have a history of HG in a previous pregnancy.
The review results will inform clinical guidelines which in turn will support HCPs to advise and prescribe the most effective treatment depending on location, gestation and severity. Different pathways of care make it clear that not all treatments work for all women and that there are different options which should be tried.
The results from this review can also provide women with evidence-based information about different treatment options. Women experiencing NVP for the first time may want to try ‘patient initiated’ options before seeking medical support. For example, trying preparations of fresh root ginger or acupressure regularly for 3–4 days may help to reduce mild symptoms. Similarly, vitamin B6 taken regularly for at least 3 days may help to reduce mild to moderate symptoms in some women.
If women do seek medical support, prior knowledge relating to treatment effectiveness may then help to empower them, enabling a more satisfactory interaction and outcome.
Summary
Although it is beyond the scope of this review to address all the problems and issues sufferers of NVP/HG have had with their care, it will add to the body of evidence-based knowledge surrounding treatment. This in turn should inform clinical guidelines, so leading to improved care, attitudes and advice for women suffering from NVP/HG. Similarly, if women also have this information they will hopefully be less likely to be treated dismissively and inappropriately.
Dissemination of findings to appropriate audiences will be essential. As well as the published report, the findings will be presented at conferences (medical, midwifery, service users so that women have access to the information) and submitted to peer-reviewed journals.
Chapter 20 Issues of importance to practitioners
Introduction
When providing care and support to women suffering from moderate or severe NVP, HCPs need to consider the evidence on effectiveness and safety as well as the direct and indirect costs to the NHS and to the women. The effectiveness of any intervention is likely to be dependent on the severity of symptoms. Ideally, the severity of NVP should be assessed in a reliable and valid way (e.g. using the PUQE, RINVR or Nausea Questionnaire score). A mild, moderate or severe score, alongside an assessment of how the individual woman is coping, will help HCPs make appropriate recommendations.
The following findings include evidence of effectiveness from the results of the review and associated treatment costs from the economic evaluation presented in Chapter 18, Economic evaluation. No reliable data on fetal outcomes [fetal or neonatal death, congenital abnormalities, low birthweight (< 2.5 kg), preterm birth (before 37 weeks’ gestation) or small for gestational age (birthweight < 10th centile)] were identified as part of the systematic review. All safety data presented below are derived from large population-based observational studies. This evidence is indirect in that it relates to pregnancy but not specifically to NVP.
The interventions that can be recommended to women fall into three categories:
-
Self-help, ‘over-the-counter’ interventions which can be recommended by GPs, midwives, practice nurses and pharmacists, in information leaflets and on NHS approved websites.
-
Primary care interventions which can be prescribed by GPs. These may be in addition to or instead of self-help interventions.
-
Secondary care interventions which are delivered in a hospital setting. Some women are referred to hospital by primary care/community HCPs after failure of self-help and/or primary care interventions. However, increasingly, women refer themselves to hospital maternity services (via day/maternity assessment units) often without any prior intervention. Depending on symptom severity and duration, sufferers may need to progress from one category to another and possibly try a number of different, or combinations of interventions.
Findings
First-line ‘over-the-counter’ interventions and alternative therapies
Ginger
Fresh root ginger may be effective in improving mild symptoms, especially nausea, but findings are not conclusive. When compared with acupressure, ginger may be more effective, but the quality and quantity of evidence is limited. There are too few data to suggest ginger is any better or worse than vitamin B6 or pharmacological interventions.
Ginger appears to be safe for women during pregnancy. Data from two birth cohorts and several small RCTs suggest there is no evidence of an increased risk of congenital anomalies or adverse perinatal outcomes. 136,137 In a birth cohort of 68,522 women, 1020 reported using ginger, with no associated increased risks of congenital malformations, stillbirth, perinatal death, preterm birth or low birthweight babies. 137
The estimated weekly cost of using a ginger preparation was £2.20.
Acupressure at pericardium point P6
Acupressure using correctly placed ‘sea-bands’ may be effective in improving symptoms of NVP in women with mild to moderate symptoms. Acupressure at KID21 may also be effective but data are limited. The quality of the evidence is low and it is difficult to ascertain whether acupressure is more or less effective than other interventions.
Acupressure is a non-invasive intervention and no safety data are available. The price of sea-bands is approximately £10.
Acupuncture
The evidence of effectiveness of acupuncture is inconclusive. The cost of acupuncture consultations and treatments range between £35 and £70. These data suggest that acupuncture should not be recommended.
Vitamin B6 (pyridoxine)
Vitamin B6 appears to have some effectiveness at improving NVP in women with mild to moderate symptoms, especially at higher doses (≥ 10 mg three times daily for at least 3–4 days).
There is little information regarding the safety of vitamin B6 in isolation. However, the safety of vitamin B6 in combination with antihistamines (doxylamine) has been studied extensively. The results of two meta-analyses, which involved over 200,000 women, found no evidence of increased risk of congenital malformations (relative risk 0.95, 95% CI 0.88 to 1.04138 and OR 1.02, 95% CI 0.66 to 1.55). 139 These findings have since been confirmed by several epidemiological studies.
The weekly cost of vitamin B6 preparations has been estimated at between £0.12 and £2.60.
Second-line interventions prescribed by general practitioners in primary care settings
All quoted medication costs will require the addition of £45 for the GP consultation.
Doxylamine plus pyridoxine
A combination of high-dose pyridoxine and doxylamine may be as effective as metoclopramide at relieving moderate symptoms of NVP. However, a combination of these medications has not been shown to be as effective as ondansetron. Given other data, it can be inferred that this therapy is more effective than no treatment (proxied by placebo in trials).
Evidence suggests that the combined therapy of doxylamine and pyridoxine is safe to use during pregnancy (see Appendix 7).
The cost of this combined therapy would be £0.12–2.60 plus cost of doxylamine [price currently not available as not routinely used in the UK NHS, price of alternative antihistamine (e.g. cyclizine) is £0.74–2.22].
Diclectin (delayed release doxylamine 10 mg plus pyridoxine 10 mg) appears to be more effective than placebo when given to treat moderate symptoms and when given pre-emptively to women with a history of moderate NVP in a previous pregnancy. However, Diclectin is currently not available in the UK.
Antihistamines (hydroxyzine, meclizine, cyclizine)
Evidence from the review suggests that these drugs appear to be more effective in treating mild symptoms of NVP compared with no treatment.
A large meta-analysis which involved over 200,000 women who took antihistamines during pregnancy found no evidence of an increased risk of teratogenicity (OR for major malformations was 0.76, 95% CI 0.60 to 0.94), with no other serious maternal or fetal outcomes. 140
Estimated weekly cost of treatment with oral cyclizine was £0.74–2.22.
Dopamine receptor antagonists
There was no evidence of a difference between metoclopramide and promethazine in improving symptoms in moderate cases of NVP. There was also very low-quality evidence from a non-randomised study that droperidol may be effective, especially at higher doses but higher-quality evidence is needed to confirm or refute this.
Dopamine antagonists such as the phenothiazines promethazine and prochlorperazine are regarded as safe: a meta-analysis of eight studies (n = 2948) identified no difference in the risk of major malformations (pooled relative risk 1.03, 95% CI 0.89 to 1.22). 141 Other drugs in this class used to treat NVP/HG include domperidone, droperidol, trimethobenzamide and metoclopramide. Limited evidence suggests that trimethobenzamide is safe while a recent large study of metoclopramide used during the first trimester of pregnancy (n = 3458) found no evidence of an increased risk of major malformations (OR 1.04, 95% CI 0.89 to 1.14) or adverse obstetric outcome. 142 These findings agreed with those of a large, Danish birth cohort (exposed cases n = 28,486), which reported no increased risk of congenital malformations (OR 0.95, 95% CI 0.88 to 1.03), miscarriages or stillbirths. 143 The estimated weekly costs of these drugs are metoclopramide £0.22–0.66, promethazine £0.74–2.22, prochlorperazine £0.47–1.42, domperidone £0.39–1.17.
Serotonin receptor antagonists (ondansetron)
Ondansetron appears to be effective at all levels of symptom severity. However, there is little evidence to say that it is more effective than metoclopramide or antihistamines.
Serotonin antagonists may be safe in pregnancy but experience is limited. One recent case–control study reported an increased risk of cleft palate (adjusted OR 2.37, 95% CI 1.18 to 4.76). 144 However, another Danish study, involving over 600,000 pregnancies, found no association with any adverse fetal outcomes. 145 Concerns have been raised regarding the risk of cardiac arrhythmias [time between start of the Q wave and of the T wave in the heart’s electrical cycle (QT) prolongation] with large doses of i.v. ondansetron. A recent systematic review identified that out of all cases of QT prolongation, 67% of patients had a significant medical history or were using a concomitant QT prolonging medication. The study concluded that prior screening of electrocardiogram (ECG) and electrolytes should be limited to high risk patients receiving ondansetron intravenously. 146
The estimated weekly cost of prescribing oral ondansetron was £60.83.
Second- and third-line interventions delivered in secondary care settings
Outpatient/day case management
Limited evidence suggests that this could be an effective alternative to inpatient admission for women with moderate to severe symptoms where i.v. rehydration is required.
There is no population-based safety data regarding pregnancy outcomes following outpatient/day case management.
The estimated cost of an outpatient attendance, which would involve i.v. rehydration, i.v. antiemetics, appropriate blood and urine tests and an ultrasound scan, would be approximately £290.
Inpatient management costs
The estimated cost of a 2-night inpatient admission, which would involve i.v. rehydration, i.v./oral antiemetics, appropriate blood and urine test, an ultrasound scan, thromboprophylaxis and thiamine supplementation, was approximately £800. If a combination of, or alternative antiemetics were required this cost could rise to £850.
Corticosteroids
Evidence is limited but corticosteroids appear to reduce symptom severity, and appear to be more effective at reducing episodes of vomiting than metoclopramide and Phenergan.
Concerns remain about the safety of corticosteroids. In one meta-analysis, the pooled risk ratio for cohort and case–control studies combined revealed no increased risk of major malformations associated with first trimester exposure (cumulative OR 1.45, 95% CI 0.81 to 2.60). However, a subanalysis of case–control studies revealed an increase in the risk of the fetus developing an oral cleft palate (OR 3.35, 95% CI 1.97 to 5.69) and the results were homogeneous between studies. 147 However, other studies do not show this association with cleft palate formation. 148,149
Treatment with corticosteroids would generally be initiated following failure of other antiemetic therapies, when the woman is suffering from severe symptoms and during an inpatient admission. The estimated cost of a 5-day inpatient admission in which corticosteroid therapy was given was estimated at £2000–2100.
Enteral nutrition
Enteral feeding appears to be a potentially effective but extreme method of supporting women suffering from very severe symptoms, but no comparative studies were identified.
Costs were not available for enteral feeding but in a recent economic evaluation of total parental feeding the cost per patient of the intervention itself and excluding other hospital based costs was approximately £340 per patient (Kilonzo M, personal communication).
Summary
Overall, there are some data to guide the choice of therapy, but there is little information to guide the choice between therapies. The evidence reviewed suggests that treatments tend to improve symptoms quickly – over a small number of days. Therefore, if a woman gets insufficient relief from a first treatment then this suggests an alternative treatment could be tried. For some treatments there are no data currently available to support their use. Thus, while there may be few safety concerns with some of these treatments, lack of robust effectiveness data can nevertheless guide practitioners in the advice that is given to women.
One obvious concern is around safety. In part this is prompted by the legacy of thalidomide. No reliable evidence directly applicable to the target group of pregnant women was found although evidence from large population sources exists. These data have generally suggested that there is no evidence of any safety concerns with the medications, but this is not the same as ruling out any important differences in safety outcomes. In many cases the CIs are sufficiently wide to include clinically important differences both in favour and against the treatments. Although women need reassurance that treatments are safe, this should not offer false reassurance, therefore advice on safety should be tempered by these findings.
Chapter 21 Discussion
Clinical effectiveness and harms
This study aimed to systematically identify and assess the evidence on the clinical effectiveness and cost-effectiveness of treatments for severe NVP and HG. This review was complicated because there is no agreed point where severe NVP becomes HG, and because studies in this area were both poorly indexed and generally poorly described in terms of severity of symptoms. Scoping searches indicated that the total size of the evidence base in this area was, for a systematic review, relatively small. For this reason the search strategy adopted was unusually comprehensive and included terms related to NVP and HG, but made no restrictions around study design, intervention or language. As such it considers all studies related to NVP and HG.
The study aimed to conduct both a fixed- or random-effect model meta-analysis as well as a Bayesian mixed-treatment comparison. Full details of the proposed methods are reported in the review protocol (PROSPERO CRD42013006642). However, these planned analyses were not performed due to heterogeneity in interventions, trial populations, reporting and definitions of outcome measures and methods. As a consequence the data on effectiveness, fetal outcomes and adverse events were tabulated and reported in narrative fashion. The implication of this is that summary quantitative statistics of the relative performance of different treatments against each other are not available. Rather the focus has been on the consistency of the direction of effect and on the quality of the evidence available. Where possible we have attempted to draw out the implications for both women and practitioners.
In total, 11,830 papers were identified from the combination of standard electronic databases, specialist Chinese databases and various sources of grey literature. From these, 75 papers were identified for data extraction, based on a total of 73 separate studies. The key reasons for exclusion were duplicate papers already included; participant inclusion criteria for the identified study judged not relevant to our review; not including any of the pre-specified outcomes; or as ineligible study design (no comparator group) for effectiveness data or not a population-based case series for rarer maternal and fetal outcomes. The 73 included studies were made up of 64 RCTs and nine case series or non-randomised studies.
With respect to overall quality of the evidence, there was variation both in terms of the quality of the studies and the quality of the reporting. For almost half of all RCTs identified there was insufficient detail provided to permit clear judgement of risk of bias in a range of key areas. Overall, 33 RCTs were classed as having a low within-study risk of bias, 11 RCTs were classed as having a high within-study risk of bias, and the remainder (n = 20) were classed as unclear in this respect. The high proportion of studies at unclear risk of bias was due to poor reporting and a lack of detail, particularly in the methods section. All the case series or non-randomised studies were judged as weak methodologically.
The included studies were grouped into the three broad groups of interventions outlined in Chapter 1:
-
First-line ‘over-the-counter’ interventions, which can be recommended by HCPs, in information leaflets and on NHS approved websites, for women to try before seeking medical care. Alternative therapies were included in this group and there were 17 comparisons drawn from 43 studies.
-
Second-line interventions, usually delivered in primary health-care settings and prescribed by a GP, but may also involve referral of women with more severe symptoms for inpatient, outpatient or day case care in hospital. There were 16 comparisons from 20 studies.
-
Third-line interventions reserved for women in hospital with persistent or recurrent symptoms, despite second-line therapies, which are prescribed in hospital settings. There were four comparisons, drawn from 10 studies.
First-line ‘over-the-counter’ interventions
The most common comparisons drawn were acupressure versus nocebo (n = 8); steroid versus usual treatment (n = 7); ginger versus placebo (n = 7); and ginger versus B6 (n = 6). Other comparators were considered in only one or two studies. A common finding was that symptoms in all arms (including placebo) improved from baseline.
The evidence on the use of ginger came from 16 RCTs13,42,60,63,67,70,74,77,82,89,92,96,102,103,110,113 which were predominantly at low or unclear risk of bias, with four exceptions. 77,89,92,113 Seven studies compared ginger preparations with placebo60,74,82,89,96,110,113 and these generally reported a statistically significant improvement over a range of nausea and vomiting symptoms. However, these data are potentially unreliable because of the number of studies that were judged to have a high or unclear risk of bias. When the comparison was restricted just to those studies at low risk of bias the results were not conclusive. For the comparison of ginger with vitamin B667,70,77,92,102,103 there are some higher-quality studies, but little evidence of a difference in effectiveness. There was a similar finding for the comparison of ginger with the other active treatments (doxylamine–pyridoxine63 or antihistamine42 or metoclopramide89). For the comparison of ginger versus acupressure,13 ginger again looked promising but the evidence was very limited. Overall, ginger might be better than placebo in reducing the severity of symptoms, but these data are limited to less severe symptoms.
A similar picture emerged for vitamin B6. Comparisons of B6 preparations with placebo41,100 generally reported evidence of reduced symptoms of nausea, especially for women with more severe symptoms and vomiting. Higher doses of vitamin B6 resulted in a greater improvement in symptoms. However, for other head-to-head comparisons of treatments there were few data identified that suggested a difference in performance. 59,107,112 Furthermore, for the comparatively well researched acupuncture or acupressure (data were available from 18 trials43,61,62,66,73,78–80,83,87,91,94,98,101,104,109,111,115), there is a suggestion that acupressure may reduce symptoms of nausea and retching in women with mild–moderate symptoms; however, the data are limited and inconclusive. A similar situation was observed for nerve stimulation73,98,109 and aromatherapy. 76,97 Comparisons of traditional Chinese acupuncture and herbal medicine with Western medicine were at high risk of bias and impossible to emulate within the NHS. 87,115
No reliable direct evidence was identified in the review on the impact on maternal weight; fetal outcomes [fetal or neonatal death, congenital abnormalities; low birthweight (< 2.5 kg), preterm birth (before 37 weeks’ gestation) or small for gestational age (birthweight < 10th centile)]; or adverse events (e.g. pregnancy complications). The identified studies were all too small to provide any reliable data. Indirect evidence came from a variety of large population studies and these data suggested that there was no evidence of any increased risk of adverse fetal or maternal outcomes.
Overall, it is disappointing that the evidence base to guide women in the choice of therapy and practitioners in the advice is so severely lacking. What evidence did exist mainly related to those with milder symptoms and not severe NVP/HG.
Second-line interventions prescribed by general practitioners in primary care settings
For antihistamines, their use resulted in an improvement compared with placebo or no treatment over a range of symptoms. 68,71,90 Diclectin (a vitamin B6 and antihistamine combination), which is not currently available within the UK, also appears to be more effective than placebo. 65,84,117 Further, pre-emptive treatment with Diclectin before symptoms of NVP begin in women at high risk of severe NVP recurrence appears to result in a reduced risk of moderate/severe NVP compared with women who take Diclectin once symptoms begin. 117
Dopamine antagonists were used in one trial which was judged to be at low risk of bias106 and one poor-quality non-randomised study. 122 These studies provided limited evidence suggesting that promethazine is as effective as metoclopramide in reducing the symptoms of NVP. Five trials57,72,75,81,105 and one case series study121 compared serotonin antagonists (ondansetron) against a range of alternatives. Three trials tested ondansetron against metoclopramide: symptoms were classified as mild to moderate in two trials75,81 and severe in one trial. 57 The identified studies comparing ondansetron with metoclopramide had mixed results, with both drugs improving symptoms. However, the evidence from one study81 with low risk of bias found ondansetron more effective at reducing vomiting compared with metoclopramide after 4 days. There was some suggestion that ondansetron appears more effective at reducing nausea than vitamin B6 plus doxylamine, but with equivocal evidence for vomiting. However, evidence from two trials72,105 comparing ondansetron with antihistamines among women whose symptoms were classified as being moderate to severe found there was no evidence of a significant difference between treatments. The data from one small study85 also suggests that the use of transdermal clonidine patches may be effective for the treatment of severe NVP/HG.
With respect to safety, the only data available was indirect sources from large population-based observational studies relating to pregnancy rather than NVP or HG. These sources found no evidence of increased risk of congenital malformations, miscarriages or stillbirths (see Chapter 20 for details). For ondansetron, concerns have been raised regarding the risk of cardiac arrhythmias (QT prolongation), relating to the administration of large doses of i.v. ondansetron. However, a recent systematic review146 concluded that prior screening of an ECG and electrolytes should be limited to high risk patients receiving ondansetron intravenously.
Second- and third-line interventions delivered in secondary care settings
For interventions provided in secondary care, one issue is whether they should be provided as inpatient therapy, or can be provided in a day case or outpatient setting. For women with moderate to severe symptoms day case care is feasible and acceptable, and the data suggest that day case management is as effective at improving severity scores as inpatient management for some women.
In terms of specific therapies, there were two studies69,108 identified that compared i.v. fluids. One108 compared different compositions of i.v. solution (dextrose + saline vs. saline only, which was at low risk of bias), and one69 compared i.v. fluids containing vitamins with diazepam. The findings suggest that i.v. fluid improves reported symptoms and that dextrose saline may be more effective at improving nausea over time for those with moderate nausea. The lower concentration of sodium in dextrose saline may exacerbate any pre-existing hyponatraemia. High doses/concentrations of dextrose solutions may increase the risk of Wernicke’s encephalopathy. However, concentrations in dextrose saline are unlikely to provoke this response. Diazepam appears to be more effective than i.v. fluids at reducing nausea on day 2, but there was no evidence post treatment for those with moderate/severe nausea or HG.
The use of corticosteroids was better researched with seven studies58,64,93,99,114,116,125 identified (three at low risk of bias,64,93,99 three where the risk of bias was unclear/high58,114,116 and one weak case series study125). The evidence suggested a trend towards improved symptoms with steroids compared with placebo, but the results were not statistically significant. There was a small amount of evidence suggesting steroids were more effective at reducing vomiting episodes than Phenergan suppositories or metoclopramide. Nevertheless, the overall evidence base on effectiveness is limited and there are concerns over safety. As reported in Chapter 20, a subanalysis of case–control studies identified an increase in the risk of the fetus developing an oral cleft palate (OR 3.35, 95% CI 1.97 to 5.69) and the results were homogeneous between studies,147 although other studies did not show this association. 148,149 Few data were found on the use of assisted feeding in this patient group, but the limited data showed that enteral feeding is an effective, but extreme, method of supporting women suffering from very severe symptoms as a last resort.
In summary, the evidence on effectiveness of all treatments was severely limited by the poor quality of the evidence available. Although there appears to be some evidence that some treatments (ginger preparations, vitamin antihistamines, metoclopramide, B6) were better than placebo for mild disease, there is little on the effectiveness of treatments for more severe disease. Evidence on differences in effectiveness was available for few other comparisons.
Cost-effectiveness
As part of the systematic review, a review of the economic evaluations was planned but no studies that met the inclusion criteria were identified. Likewise, an economic evaluation based on a modelling exercise was planned. Given the paucity of the effectiveness data this proved not to be possible. As a consequence, a simpler analysis was conducted that estimated the cost of the intervention and then used these data to consider the difference in effectiveness that would be implied if a more costly intervention was used instead of a less costly intervention. This form of analysis is based on the theoretical conditions required for an efficient allocation of resources. The implied relative effectiveness estimated along with information on cost were then set alongside the limited evidence on effectiveness.
The results of the economic analysis indicate that the cost of treating patients with NVP/HG increases rapidly with severity. The ranges of costs are as follows: patient-initiated first-line interventions, cost between £0.12 and £90 per week; patient-initiated first-line interventions following a GP visit, cost between £45 and £47 per week; and clinician-prescribed second-line interventions (e.g. antihistamines), cost between £45 and £106 per week, including the cost of the GP visit itself.
Some women are referred to hospital by primary care/community HCPs after failure of self-help and/or primary care interventions. Women may also self-refer themselves to hospital maternity services (via day/maternity assessment units), often without any prior intervention. This opens up a range of other potential interventions and potentially greatly increases costs. For example, for a clinician-prescribed second-line intervention when a woman attends hospital as a day case the cost would be between almost £300 per day. Whereas if the woman were admitted to hospital as an inpatient, the cost for a 2-day admission would be approximately £800. For those women with the most severe or intractable symptoms, combinations of medications may be administered and should the woman be admitted for 5 days, the cost was estimated to be between £2000 and £2100. However, the actual medication costs as a component of total cost is relatively small, with the majority of cost incurred for the inpatient stay itself.
These data on costs are not of much practical value without information on effectiveness (although they may help in assessing budget impacts). As noted, data on effectiveness are very limited. Nevertheless, what data there is can be interpreted, along with the cost data. For patient-initiated first-line interventions, the cost comparison ratios ranged from 1.01 : 1 for the comparison between vitamin B12 and vitamin B6 (i.e. vitamin B12 would only need to be 1% more effective than vitamin B6 to be considered cost-effective) to 41 : 1 for the comparison between hypnotherapy and ginger. In cost terms there is little difference between possible medications and some evidence that ginger and vitamin B6 may provide some relief. Therefore, in economic terms the results suggest that we are indifferent between these treatments. There is also evidence that acupressure may be effective, but the cost of acupressure consultations and treatments range from £35 to £70. Comparing this with the cost of a medication like ginger or vitamin B6, therefore, choosing acupressure over either ginger or vitamin B6, would imply that acupressure is at least 13 times better (taking the costs most in favour of acupressure, £35 for acupressure and £2.60 for the weekly cost of ginger or vitamin B6). A judgement is required whether or not this is plausible. If it is not judged plausible then this suggests that acupressure should not be adopted as an initial treatment, but it does not rule it out as a second treatment if the first does not provide sufficient symptom relief.
The relatively small medication costs in comparison to the cost of accessing primary or secondary care had a direct impact on the results of the implied value method of economic evaluation. For the majority of cost comparisons in the remaining packages of care, the difference in cost was so small that only a marginal increase in clinical effectiveness would be required in order for the more costly interventions to be considered a worthwhile use of resources. Nevertheless, the same sort of judgement described above still applies.
A final cost comparison considered was between inpatient management and day case management. The results of this analysis indicated that inpatient management would need to be 1.5 times more effective than day case management. The question for decision-makers is whether or not this difference is plausible given that the evidence from the systematic review provided no evidence of a difference in effectiveness between inpatient and day case care.
Overall, however, even though costs for the different treatments can be estimated, it must be emphasised that the evidence on cost-effectiveness is constrained by the very limited data available on effectiveness.
Strengths and limitations
The main strength of this review was the comprehensive and systematic approach taken to review the literature. The searches sought to be exhaustive, and have included the major electronic databases, grey literature sources and non-English-language databases. The search strategy itself was broadly defined and included terms related to NVP and HG, but made no restrictions on language, study design or type of intervention. Taken together, the searches should have identified all relevant studies. It is possible, however, that there exist some relevant data that remains hidden because of non-publication, but it is questionable about what this might add given the generally very small size of identified studies and their often very limited methodology. Thus, it seems implausible that a large high-quality study was missed.
The process of assembling data on interventions was also rigorous. As noted above, no studies were excluded on the basis of language, and where necessary translations were sought. Risk of bias assessments were conducted for included RCTs and for non-randomised studies using high-quality tools. Data were extracted for pre-specified outcomes onto a standard form to prevent biases caused by selective data extraction. The choice of outcomes for the systematic review was itself based on the advice of our expert clinical panel and from advice from women themselves and patient representative groups.
The study included a pre-planned economic component and although the proposed economic modelling was not possible, information were rigorously assembled and presented in such a way as to help facilitate judgements about alternative therapies. As such, although less sophisticated than the proposed model, it is entirely consistent with the role of economic evaluation as an aid to decision-making.
The review itself identified 73 studies but very few were available for most comparisons and not every study contributed data to each outcome, including our pre-specified primary outcome of severity of symptoms (such as PUQE, RINVR, McGill Nausea Questionnaire, NVPI, VASs). This was compounded by the differences in reporting of studies that precluded the opportunity for meta-analysis. As a consequence, we were restricted to a narrative review that was not able to produce summary measures that quantified the effect on outcomes. Rather we were restricted to reporting on the likely direction of effect. This problem will remain and there is a need for future studies to use standardised measures of severity and include patient-centric outcomes such as QoL. The development of a standardised set of outcomes that would be measured and reported for all studies is required.
One set of outcome measures that are likely to be very important to women and practitioners are around safety. In this study we sought to assemble data on fetal outcomes and adverse events to both the mother and child. No reliable data meeting our inclusion criteria were identified. To partially overcome this limitation we looked at large population-based observational studies. This evidence is indirect in that it relates to pregnancy but not specifically to NVP. Nevertheless, it does provide some reassurance that many of the treatments are not clearly associated with an increase in adverse events. However, by the same token, these data do not rule out differences that would be considered important by the women themselves or by practitioners.
With respect to the economic element of the research, this element shares many of the strengths and limitations already described. The main manifestation of this limitation is that the planned economic modelling was not possible. An alternative approach was used and although this may provide some useful data for decision-making its value is limited.
Chapter 22 Conclusions
Introduction
In developing these conclusions, we worked with a range of individuals and organisations to ensure their relevancy to patients and practitioners. Women who had suffered from NVP and/or HG and representatives of key patient advocacy groups in the field were members of our Project Steering Group, and were consulted in shaping both the review implications and our recommendations for future research. Our Steering Group and Project Management Group also included a number of clinicians working with women sufferers of NVP and/or HG in a range of health-care settings, representing midwifery, general practice, obstetrics, teratology, paediatrics and clinical pharmacology.
Implications for women and for practitioners
-
Nausea and vomiting in pregnancy occurs frequently. Even without treatment, the symptoms for some women will resolve. For women who do experience more persistent problems there are some simple approaches that they could adopt themselves that might improve symptoms and/or QoL. These could include increasing oral fluid intake, eating small frequent meals, eating bland foods/protein-predominant meals, avoiding spicy, odorous and fatty foods and stopping iron-containing multivitamins. However, for others there are a range of treatments available to women where there is some evidence that they might help.
-
Where symptoms are mild, there are a number of first-line over-the-counter or self-purchased therapies where there is some evidence that they work. These therapies may also be considered as initial treatments if a woman sees a doctor, nurse, midwife or other HCP. These treatments are ginger supplements and vitamin B6. These are generally low cost and there is no evidence that they are a risk to the health of the mother or baby. There is no proof that a more expensive version of either ginger or vitamin B6 is any better than a lower cost option. Higher doses of vitamin B6 were found to be more effective than lower doses in reducing symptoms (0.64 mg twice daily vs. 1.28 mg per day). There is also some evidence that acupressure may be effective, but the evidence is very limited. The available evidence suggests that any benefit derived from these over-the-counter therapies will be evident within 3–4 days. Thus, women need to know that, in such cases, it is worth trying something else or consulting with a GP as there are other treatments available via prescription. There is no evidence that these treatments are unsafe to use. Further details on dosage and effects are in Chapters 4–7 and Tables 8–11.
-
Where symptoms are mild to moderate and/or if the above over-the-counter therapies have not proved helpful to women, a number of second-line interventions are available via prescription. Of the drugs that a GP might prescribe there is evidence that an antihistamine can help reduce symptoms (either alone or combined with vitamin B6) compared with no treatment. Limited data suggests that metoclopramide and promethazine may also help when symptoms are moderate. Droperidol may also be effective, especially at higher doses. Available evidence indicates these treatments are likely to be safe, but more research is needed to clarify this (further details on dosage and effects are in Chapter 9 and Table 13).
-
A GP may also prescribe ondansetron when other treatments have failed. This treatment may be effective for some women in reducing symptoms. The drug appears to be safe in pregnancy but experience is limited and more research is needed. Where women are given large doses of ondansetron and have a risk of some cardiac conditions, they may need an ECG and to have their blood chemistry checked (further details on dosage and effects are in Chapter 8 and Table 12).
-
Where symptoms are more severe or persistent, based on assessment using a validated measurement scale, care may be provided in hospital, and for these women a further range of treatments are available. Evidence suggests that where available these treatments can be provided as an outpatient or day case patient rather than requiring an admission, and usually involve rehydration with i.v. fluids. Dextrose saline appears to be more effective at reducing nausea when compared with normal saline, but must be administered with care as excessive dextrose can exacerbate the potential problem of Wernicke’s encephalopathy (see Chapter 12 and Table 16 for more details).
-
Treatment with corticosteroids does work but would generally only be used following failure of other treatments, when the woman is suffering from severe symptoms and during an inpatient admission. This is because doctors and other HCPs are cautious about the safety of these treatments and the side effect they may have for both the mother and the fetus. Therefore, doctors would like to use other options first if possible. Ideally, more evidence is needed comparing corticosteroids to other antisickness medications (further details on dosage and effects are in Chapter 15 and Table 19).
-
Where symptoms are extremely severe, and when the prolonged effects of severe nausea and vomiting have made women extremely ill, assisted feeding either by tube directly into the stomach or, in very rare cases, by i.v. catheter may be effective. As there are risks associated with this type of treatment, it is restricted to women suffering from very severe symptoms (see Chapter 16 and Table 20 for more details).
Recommendations for research
Trajectory of research
Any recommendations for further research need to take into account the trajectory of new research. Research on treatments and management of NVP/HG is ongoing: since the date of the last systematic update of published research for this study (September 2014) new evidence has been published. Although not assembled systematically, scoping searches conducted in early December 2014 identified two potentially relevant studies. The first was a review of the use of gabapentin in pregnancy150 and the second was a RCT comparing day care with inpatient management. 151 Neither study was formally assessed, but the authors’ conclusions were that further clinical trials were needed on the use of gabapentin for HG, and that day case care was acceptable and reduced length of stay. These conclusions are consistent with the findings reported in this review.
There are also a number of studies recorded as ongoing on searches of ClinicalTrials.gov (www.clinicaltrials.gov) and the International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/default.aspx) (searches of both were conducted in December 2014). Ongoing studies are investigating:
-
gabapentin versus ondansetron for HG in a double-blind RCT of 80 women with HG (NCT02163434, due to finish in May 2018)
-
Diclectin as a pre-emptive treatment for NVP versus treatment with Diclectin when symptoms occur in a RCT (NCT00293644, due to end in April 2015)
-
rapid hydration with hospital admission for HG (ISRCTN24659467)
-
enteral feeding with oral rehydration for the treatment of HG.
Research recommendations
Given the trajectory of research and the evidence gaps identified by this study, in order of priority, the following recommendations for research are made:
-
A well-designed multicentre RCT to determine which second-line, hospital-prescribed therapy should be adopted as mainstream provision for the treatment of NVP in the UK NHS. This could compare day case or inpatient delivery of (a) a combination of antiemetic therapy (antihistamines or dopamine receptor antagonists or serotonin receptor antagonists) with i.v. rehydration (rapid i.v. hydration or standard inpatient care) as required; against (b) alternative antiemetic therapy (antihistamines or dopamine receptor antagonists or serotonin receptor antagonists) with i.v. rehydration (rapid i.v. hydration or standard inpatient care).
-
A well-designed multicentre RCT to test the use of subsequent treatments, such as steroids, as a third-line therapy. This could examine, for example, the effectiveness of corticosteroids versus serotonin receptor antagonists (ondansetron). In this trial, the indication for steroid use could also be investigated. For example, failure of successful treatment following three admissions for i.v. rehydration and medication. The dose, duration of treatment and effectiveness could also be examined.
-
A well-designed multicentre RCT to determine which second-line, GP-prescribed therapy should be adopted as mainstream provision for the treatment of NVP in UK primary care. This could compare the effectiveness and cost-effectiveness of vitamin B6–antihistamine combination against, for example, a dopamine receptor antagonist.
-
Six key factors should be incorporated within any future research trial of second-line, third-line or GP-initiated NVP/HG therapies:
-
Stakeholder co-design: all stakeholders and, in particular, the women themselves, should be involved in the design of future studies to ensure that future research produces information of relevance to them as well as to health services.
-
Embedded process evaluation in order to examine the views of women participants on the intervention/therapy being trialled, study how the intervention is implemented in practice, investigate contextual factors that affect the delivery of an intervention, and study the way effects vary in subgroups.
-
Mental health and well-being outcomes: we know from other sources that severe NVP has an impact on mental health both ante- and post-natally. Therefore consideration needs to be given as to how to capture the impact on women regarding these factors. A variety of approaches are possible, but it may for example include qualitative work and/or the use of existing validated tools such as (a) QoL indices such as Short Form questionnaire-36 items (total and subscales); (b) measures of mental health and well-being such as Edinburgh Postnatal Depression Scale; and (c) satisfaction with care as measured by Client Satisfaction Questionnaire-8.
-
Validated symptom severity scale: given the problems identified in this review with the lack of consistent outcome measures in the existing evidence base, entry to future trials should be based on PUQE criteria as an objective means of establishing severity, with subsequent outcome measurements also based on the same score.
-
Standard reporting criteria for adverse events, maternal and fetal outcomes: all studies of drugs administered during the first trimester of pregnancy should have obligatory reporting of rates of adverse events and maternal/fetal outcomes to the UKTIS central database to support the availability of reliable prospective controlled data. In addition, all trials of NVP/HG interventions in the UK NHS should include sufficiently long-term participant follow-up periods to enable the capture of relevant maternal and fetal outcomes given the safety profile of the therapies compared. These outcome data should be analysed to determine whether or not there are any associations between particular therapies and/or characteristics of women, in order to guide further research into stratified care.
-
Economic evaluation of NVP/HG therapies: as there may be trade-offs between cost and effects, future studies should also include an economic evaluation.
-
-
A large simple RCT of self-medication. The choice of interventions should be informed by the preferences of women about which treatments are of most relevance to them. Points 1–5 listed above also apply, but the inclusion of an economic component would also need to be justified given the anticipated low cost of the intervention and that a more effective treatment would save subsequent management costs.
Acknowledgements
We thank Professor Gideon Koren (Director, the Motherisk Program; Professor of Pediatrics, Pharmacology, Pharmacy, Medicine and Medical Genetics at The University of Toronto; Senior Scientist at The Research Institute Hospital for Sick Children; and The Ivey Chair in Molecular Toxicology, at the University of Western Ontario Canada) for advice on clinical aspects of the research. We thank our patient and public representatives, Dr Nicolette Rousseau and Juliet Hall, for providing ongoing advice and support as part of the Review Steering Group. We thank Dr Margaret O’Hara and the other women volunteers from PSS for sharing their views and experiences on the review topic, and for the contribution of survey data to the chapter on patient issues. We thank the UKTIS for the provision of enquiry data relating to medications for HG/NVP. We thank Astrid McIntyre for secretarial support and assistance with obtaining full-text papers. The views expressed are those of the authors and not necessarily those of the funding bodies. Any errors are the responsibility of the authors.
Contributions of authors
Amy O’Donnell (Research Associate) and Catherine McParlin (Senior Research Midwife) took the role as co-first authors. They screened the search results, assessed full-text studies for inclusion, undertook data extraction and quality assessment, drafted the introduction and background chapter, methods, overview of included studies, individual intervention results chapters and co-ordinated the review.
Stephen C Robson (Professor of Fetal Medicine), Catherine Nelson-Piercy (Professor of Obstetric Medicine), Justine Norman (GP) and Laura Yates (Consultant in Clinical Genetics and Head of Teratology) provided expert advice on clinical aspects of the review.
Fiona Beyer (Information Scientist) developed and ran the search strategies, reconciled search results, obtained papers and managed the reference database.
Eoin Moloney drafted the chapter on the economic evaluation, supervised by Luke Vale (Professor of Health Economics).
Andrew Bryant undertook quality assessment and data extraction, contributed to the drafting of the overview chapter, individual results chapters, with particular responsibility for the sections on risk of bias including the production of the SoF tables, supervised by Colin Muirhead (Lecturer in Medical Statistics).
Jennifer Bradley (Research Assistant) and Emma Simpson (Research Assistant) undertook data extraction and quality assessment of included papers, supervised by Amy O’Donnell.
Dorothy Newbury-Birch (Lecturer in Public Health) provided expert advice on the systematic review process.
Brian Swallow (Expert Advisor) provided expert advice in relation to the patient perspective.
Stephen C Robson and Luke Vale were coprinciple investigators and take overall responsibility for the study.
All authors assisted in preparing the manuscript, reading and commenting on drafts, and reading the final draft.
Publication
McParlin C, O’Donnell A, Robson SC, Beyer F, Moloney E, Bryant A, et al. Treatments for hyperemesis gravidarum and nausea and vomiting in pregnancy: a systematic review. JAMA 2016;316:1392–401.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Niebyl JR. Clinical practice. Nausea and vomiting in pregnancy. N Engl J Med 2010;363:1544-50. http://dx.doi.org/10.1056/NEJMcp1003896.
- Jarvis S, Nelson-Piercy C. Management of nausea and vomiting in pregnancy. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d3606.
- Attard CL, Kohli MA, Coleman S, Bradley C, Hux M, Atanackovic G, et al. The burden of illness of severe nausea and vomiting of pregnancy in the United States. Am J Obstet Gynecol 2002;186:S220-7. http://dx.doi.org/10.1067/mob.2002.122605.
- Jueckstock JK, Kaestner R, Mylonas I. Managing hyperemesis gravidarum: a multimodal challenge. BMC Med 2010;8. http://dx.doi.org/10.1186/1741-7015-8-46.
- Trogstad LIS, Stoltenberg C, Magnus P, Skjaerven R, Irgens LM. Recurrence risk in hyperemesis gravidarum. Br J Obstet Gynaecol 2005;112:1641-5. http://dx.doi.org/10.1111/j.1471-0528.2005.00765.x.
- Vikanes AV, Skjaerven R, Grijibovski AM, Gunnes N, Vangen S, Magnus P. Recurrence of hyperemesis gravidarum across generations: population based cohort study. BMJ 2010;340. http://dx.doi.org/10.1097/ogx.0b013e3182021d24.
- Derbent AU, Yanik FF, Simavli S, Atasoy L, Urun E, Kuscu UE, et al. First trimester maternal serum PAPP-A and free beta-HCG levels in hyperemesis gravidarum. Prenat Diagn 2011;31:450-3. http://dx.doi.org/10.1002/pd.2715.
- Goodwin TM, Poursharif B, Korst LM, MacGibbon KW, Romero R, Fejzo MS. Secular trends in the treatment of hyperemesis gravidarum. Am J Perinatol 2008;25:141-7. http://dx.doi.org/10.1055/s-2008-1040344.
- Ismail SK, Kenny L. Review on hyperemesis gravidarum. Baillieres Best Pract Res Clin Gastroenterol 2007;21:755-69. http://dx.doi.org/10.1016/j.bpg.2007.05.008.
- Yamazaki K, Sato K, Shizume K, Kanaji Y, Ito Y, Obara T, et al. Potent thyrotropic activity of human chorionic gonadotrophin variants in terms of 125I incorporation and de novo synthesized thyroid hormone release in human thyroid follicles. J Clin Endocrinol Metab 1995;80:473-9.
- Verberg MF, Gillott DJ, Al-Fardan N, Grudzinskas JG. Hyperemesis gravidarum, a literature review. Hum Reprod Update 2005;11:527-39. http://dx.doi.org/10.1093/humupd/dmi021.
- Sandven I, Abdelnoor M, Nesheim B-I, Melby KK. Helicobacter pylori infection and hyperemesis gravidarum: a systematic review and meta-analysis of case–control studies. Acta Obstet Gynecol Scand 2009;88:1190-200. http://dx.doi.org/10.3109/00016340903284927.
- Saberi F, Sadat Z, Abedzadeh-Kalahroudi M, Taebi M. Acupressure and ginger to relieve nausea and vomiting in pregnancy: a randomized study. Iran Red Crescent Med J 2013;15:854-61. http://dx.doi.org/10.5812/ircmj.12984.
- Mazzotta P, Maltepe C, Navioz Y, Magee LA, Koren G. Attitudes, management and consequences of nausea and vomiting of pregnancy in the United States and Canada. Int J Gynaecol Obstet 2000;70:359-65. http://dx.doi.org/10.1016/S0020-7292(00)00255-1.
- Smith C, Crowther C, Beilby J, Dandeaux J. The impact of nausea and vomiting on women: a burden of early pregnancy. Aust N Z J Obstet Gynaecol 2000;40:397-401. http://dx.doi.org/10.1111/j.1479-828X.2000.tb01167.x.
- Poursharif B, Korst LM, MacGibbon KW, Fejzo MS, Romero R, Goodwin TM. Elective pregnancy termination in a large cohort of women with hyperemesis gravidarum. Contraception 2007;76:451-6. http://dx.doi.org/10.1016/j.contraception.2007.08.009.
- Tan PC, Zaidi SN, Azmi N, Omar SZ, Khong SY. Depression, anxiety, stress and hyperemesis gravidarum: temporal and case controlled correlates. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0092036.
- McCarthy FP, Khashan AS, North RA, Moss-Morris R, Baker PN, Dekker G, et al. A prospective cohort study investigating associations between hyperemesis gravidarum and cognitive behavioural and emotional well-being in pregnancy. PLOS ONE 2011;6. http://dx.doi.org/10.1371/journal.pone.0027678.
- Ayyavoo A, Derraik JGB, Hofman PL, Cutfield WS. Hyperemesis gravidarum and long-term health of the offspring. Am J Obstet Gynecol 2014;210:521-5. http://dx.doi.org/10.1016/j.ajog.2013.11.035.
- Hospital Episode Statistics for England. In-Patient Statistics – Diagnosis. Leeds: NHS Information Centre; 2012.
- Locock L, Alexander J, Rozmovitz L. Women’s responses to nausea and vomiting in pregnancy. Midwifery 2008;24:143-52. http://dx.doi.org/10.1016/j.midw.2006.12.001.
- Veenendaal MV, van Abeelen AF, Painter RC, van der Post JA, Roseboom TJ. Consequences of hyperemesis gravidarum for offspring: a systematic review and meta-analysis. BJOG 2011;118:1302-13. http://dx.doi.org/10.1111/j.1471-0528.2011.03023.x.
- Bolin M, Akerud H, Cnattingius S, Stephansson O, Wikstrom AK. Hyperemesis gravidarum and risks of placental dysfunction disorders: a population-based cohort study. Br J Obstet Gynaecol 2013;120:541-7. http://dx.doi.org/10.1111/1471-0528.12132.
- Koren G, Boskovic R, Hard M, Maltepe C, Navioz Y, Einarson A. Motherisk-PUQE (pregnancy-unique quantification of emesis and nausea) scoring system for nausea and vomiting of pregnancy. Am J Obstet Gynecol 2002;186:S228-31. http://dx.doi.org/10.1067/mob.2002.123054.
- Koren G, Piwko C, Ahn E, Boskovic R, Maltepe C, Einarson A. Validation studies of the Pregnancy Unique-Quantification of Emesis (PUQE) scores. J Obstet Gynaecol 2005;25:241-4. http://dx.doi.org/10.1080/01443610500060651.
- Lacasse A, Rey E, Ferreira E, Morin C, Berard A. Validity of a modified Pregnancy-Unique Quantification of Emesis and Nausea (PUQE) scoring index to asses severity of nausea and vomiting of pregnancy. Am J Obstet Gynecol 2008;198:71.e1-7. http://dx.doi.org/10.1016/j.ajog.2007.05.051.
- Rhodes V, Watson P, Johnson M. Development of reliable and valid measures of nausea and vomiting. Cancer Nurs 1984;7:33-41. http://dx.doi.org/10.1097/00002820-198402000-00003.
- Zhou Q, O’Brien B, Soeken K. Rhodes Index of nausea and vomiting-Form 2 in pregnant women. A confirmatory factor analysis. Nurs Res 2001;50:251-7. http://dx.doi.org/10.1097/00006199-200107000-00009.
- O’Brien B, Relyea MJ, Taerum T. Efficacy of P6 acupressure in the treatment of nausea and vomiting during pregnancy. Am J Obstet Gynecol 1996;174:708-15. http://dx.doi.org/10.1016/S0002-9378(96)70454-4.
- Melzack R, Rosberger Z, Hollingsworth M. New approaches to measuring nausea. CMAJ 1985;133:755-8.
- Lacroix R, Eason E, Melzack R. Nausea and vomiting during pregnancy: a prospective study of its frequency, intensity, and patterns of change. Am J Obstet Gynecol 2000;182:931-7. http://dx.doi.org/10.1016/S0002-9378(00)70349-8.
- Swallow BL, Lindow SW, Masson EA, Hay DM. Women with nausea and vomiting in pregnancy demonstrate worse health and are adversely affected by odours. J Obstet Gynaecol 2005;25:544-9. http://dx.doi.org/10.1080/01443610500230783.
- Swallow BL, Lindow SW, Masson EA, Hay DM. Development of an instrument to measure nausea and vomiting in pregnancy. J Obstet Gynaecol 2002;22:481-5. http://dx.doi.org/10.1080/0144361021000003582.
- Chandra K, Magee L, Einarson A, Koren G. Nausea and vomiting in pregnancy: results of a survey that identified interventions used by women to alleviate their symptoms. J Psychosom Obstet Gynaecol 2003;24:71-5. http://dx.doi.org/10.3109/01674820309042804.
- Thomson M, Corbin R, Leung L. Effects of ginger for nausea and vomiting in early pregnancy: a meta-analysis. J Am Board Fam Med 2014;27:115-22. http://dx.doi.org/10.3122/jabfm.2014.01.130167.
- Ashkenazi-Hoffnung L, Merlob P, Stahl B, Klinger G. Evaluation of the efficacy and safety of bi-daily therapy with pyridoxine and doxylamine for nausea and vomiting of pregnancy. IMAJ 2013;15:23-6.
- American Congress of Obstetricians and Gynecologists . American Congress of Obstetricians and Gynecologists (ACOG) practice bulletin #52: nausea and vomiting of pregnancy. Obstet Gynecol 2004;103:803-16.
- Maina A, Todros T. A novel approach to hyperemesis gravidarum: evaluation by a visual analogue scale score and treatment with transdermal clonidine. Obstetric Medicine 2011;4:156-9. http://dx.doi.org/10.1258/om.2011.110050.
- Guttuso T, Robinson LK, Amankwah KS. Gabapentin use in hyperemesis gravidarum: a pilot study. Early Hum Dev 2010;86:65-6. http://dx.doi.org/10.1016/j.earlhumdev.2009.11.003.
- O’Donnell A, Vale L, Moloney E, Muirhead C, Bryant A, Beyer F, et al. A Systematic Review and Economic Modelling of the Relative Clinical- and Cost-Effectiveness of Interventions for Hyperemesis Gravidarum n.d. www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42013006642 (accessed on 4 September 2014).
- Vutyavanich T, Wongtra-ngan S, Ruangsri R. Pyridoxine for nausea and vomiting of pregnancy: a randomized, double-blind, placebo-controlled trial. Am J Obstet Gynecol 1995;173:881-4. http://dx.doi.org/10.1016/0002-9378(95)90359-3.
- Pongrojpaw D, Somprasit C, Chanthasenanont A. A randomized comparison of ginger and dimenhydrinate in the treatment of nausea and vomiting in pregnancy. J Med Assoc Thai 2007;90:1703-9.
- Can Gurkan O, Arslan H. Effect of acupressure on nausea and vomiting during pregnancy. Complement Ther Clin Pract 2008;14:46-52. http://dx.doi.org/10.1016/j.ctcp.2007.07.002.
- Pham B, Klassen TP, Lawson ML, Moher D. Language of publication restrictions in systematic reviews gave different results depending on whether the intervention was conventional or complementary. J Clin Epidemiol 2005;58:769-76. http://dx.doi.org/10.1016/j.jclinepi.2004.08.021.
- GRADE Working Group . Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490-4. http://dx.doi.org/10.1136/bmj.328.7454.1490.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011.
- Quality Assessment Tool for Quantitative Studies Method. Hamilton, ON: McMaster University; 2008.
- Armijo-Olivio S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J Eval Clin Pract 2010;18:12-8. http://dx.doi.org/10.1111/j.1365-2753.2010.01516.x.
- Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs 2004;1:176-84. http://dx.doi.org/10.1111/j.1524-475X.2004.04006.x.
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence – imprecision. J Clin Epidemiol 2011;64:1283-93. http://dx.doi.org/10.1016/j.jclinepi.2011.01.012.
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines 8. Rating the quality of evidence – indirectness. J Clin Epidemiol 2011;64:1303-10. http://dx.doi.org/10.1016/j.jclinepi.2011.04.014.
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines 7. Rating the quality of evidence – inconsistency. J Clin Epidemiol 2011;64:1294-302. http://dx.doi.org/10.1016/j.jclinepi.2011.03.017.
- Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines 5. Rating the quality of evidence – publication bias. J Clin Epidemiol 2011;64:1277-82. http://dx.doi.org/10.1016/j.jclinepi.2011.01.011.
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines 4. Rating the quality of evidence – study limitations (risk of bias). J Clin Epidemiol 2011;64:407-15. http://dx.doi.org/10.1016/j.jclinepi.2010.07.017.
- Jones B, Roger J, Lane PW, Lawton A, Fletcher C, Cappelleri JC, et al. Statistical approaches for conducting network meta-analysis in drug development. Pharmaceut Stat 2011;10:523-31. http://dx.doi.org/10.1002/pst.533.
- Salanti G, Higgins JP, Ades AE, Ioannidis JP. Evaluation of networks of randomized trials. Stat Methods Med Res 2008;17:279-301. http://dx.doi.org/10.1177/0962280207080643.
- Abas MN, Tan PC, Azmi N, Omar SZ. Ondansetron compared with metoclopramide for hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol 2014;123:1272-9. http://dx.doi.org/10.1097/AOG.0000000000000242.
- Adamczak J, Kasdaglis J, Rinehart B, Antebi Y, Wolf E, Terrone D. A prospective randomized trial of solumedrol dose pack vs. Phenergan for the treatment of symptomatic nausea and vomiting in pregnancy. Am J Obstet Gynecol 2007;197. http://dx.doi.org/10.1016/j.ajog.2007.10.292.
- Babaei AH, Foghaha MH. A randomized comparison of vitamin B6 and dimenhydrinate in the treatment of nausea and vomiting in early pregnancy. Iran J Nurs Midwifery Res 2014;19:199-202.
- Basirat Z, Moghadamnia AA, Kashifard M, Sarifi-Razavi A. The effect of ginger biscuit on nausea and vomiting in early pregnancy. Acta Med Iran 2009;47:51-6.
- Bayreuther J, Lewith GT, Pickering R. A double–blind cross-over study to evaluate the effectiveness of acupressure at pericardium 6 (P6) in the treatment of early morning sickness (EMS). Complement Ther Med 1994;2:70-6. http://dx.doi.org/10.1016/0965-2299(94)90002-7.
- Belluomini J, Litt RC, Lee KA, Katz M. Acupressure for nausea and vomiting of pregnancy: a randomized, blinded study. Obstet Gynecol 1994;84:245-8.
- Biswas SC, Dey R, Kamliya GS, Bal R, Hazra A, Tripathi SK. A single-masked, randomized, controlled trial of ginger extract in the treatment of nausea and vomiting of pregnancy. JIMSA 2011;24:167-9.
- Bondok RS, El Sharnouby NM, Eid HE, Abd Elmaksoud AM. Pulsed steroid therapy is an effective treatment for intractable hyperemesis gravidarum. Crit Care Med 2006;34:2781-3. http://dx.doi.org/10.1097/01.CCM.0000242156.15757.70.
- Capp S, Oliveira L, Carstairs S, You W. Ondansetron versus doxylamine/pyridoxine for treatment of nausea and vomiting in pregnancy: a prospective randomized double-blind trial. Am J Obstet Gynecol 2014;210. http://dx.doi.org/10.1016/j.ajog.2013.10.092.
- Carlsson CP, Axemo P, Bodin A, Carstensen H, Ehrenroth B, Madegard-Lind I, et al. Manual acupuncture reduces hyperemesis gravidarum: a placebo-controlled, randomized, single-blind, crossover study. J Pain Symptom Manage 2000;20:273-9. http://dx.doi.org/10.1016/S0885-3924(00)00185-8.
- Chittumma P, Kaewkiattikun K, Wiriyasiriwach B. Comparison of the effectiveness of ginger and vitamin B6 for treatment of nausea and vomiting in early pregnancy: a randomized double-blind controlled trial. J Med Assoc Thai 2007;90:15-20.
- Diggory PL, Tomkinson JS. Nausea and vomiting in pregnancy. A trial of meclozine dihydrochloride with and without pyridoxine. Lancet 1962;2:370-2. http://dx.doi.org/10.1016/S0140-6736(62)90228-3.
- Ditto A, Morgante G, la Marca A, De Leo V. Evaluation of treatment of hyperemesis gravidarum using parenteral fluid with or without diazepam. A randomized study. Gynecol Obstet Invest 1999;48:232-6. http://dx.doi.org/10.1159/000010189.
- Ensiyeh J, Sakineh MA. Comparing ginger and vitamin B6 for the treatment of nausea and vomiting in pregnancy: a randomised controlled trial. Midwifery 2009;25:649-53. http://dx.doi.org/10.1016/j.midw.2007.10.013.
- Erez S, Schifrin BS, Dirim O. Double-blind evaluation of hydroxyzine as an antiemetic in pregnancy. J Reprod Med 1971;7:35-7.
- Eftekhari N, Mehralhasani Y. A comparison of ondansetron and promethasin in treating hyperemesis gravidarum. JKUMS 2013;20:354-65.
- Evans AT, Samuels SN, Marshall C, Bertolucci LE. Suppression of pregnancy-induced nausea and vomiting with sensory afferent stimulation. J Reprod Med 1993;38:603-6.
- Fischer-Rasmussen W, Kjaer SK, Dahl C, Asping U. Ginger treatment of hyperemesis gravidarum. Eur J Obstet Gynecol Reprod Biol 1991;38:19-24. http://dx.doi.org/10.1016/0028-2243(91)90202-V.
- Ghahiri AA, Abdi F, Mastoo R, Ghasemi M. The effect of ondansetron and metoclopramide in nausea and vomiting of pregnancy. JIMS 2011;29:259-65.
- Ghani RMA, Ibrahim ATA. The effect of aromatherapy inhalation on nausea and vomiting in early pregnancy: a pilot randomized controlled trial. J Nat Sci Res 2013;3:10-22.
- Haji Seid Javadi E, Salehi F, Mashrabi O. Comparing the effectiveness of vitamin B6 and ginger in treatment of pregnancy-induced nausea and vomiting. Obstet Gynecol Int 2013. http://dx.doi.org/10.1155/2013/927834.
- Heazell A, Thorneycroft J, Walton V, Etherington I. Acupressure for the in-patient treatment of nausea and vomiting in early pregnancy: a randomized control trial. Am J Obstet Gynecol 2006;194:815-20. http://dx.doi.org/10.1016/j.ajog.2005.08.042.
- Hsu E, Pei V, Shofer FS, Abbuhl SB. A prospective randomized controlled trial of acupressure vs. sham for pregnancy-related nausea and vomiting in the emergency department. Acad Emerg Med 2003;10. http://dx.doi.org/10.1197/aemj.10.5.437.
- Jamigorn M, Phupong V. Acupressure and vitamin B6 to relieve nausea and vomiting in pregnancy: a randomized study. Arch Gynecol Obstet 2007;276:245-9. http://dx.doi.org/10.1007/s00404-007-0336-2.
- Kashifard M, Basirat Z, Kashifard M, Golsorkhtabar-Amiri M, Moghaddamnia A. Ondansetrone or metoclopromide? Which is more effective in severe nausea and vomiting of pregnancy? A randomized trial double-blind study. Clin Exp Obstet Gynecol 2013;40:127-30.
- Keating A, Chez RA. Ginger syrup as an antiemetic in early pregnancy. Altern Ther Health Med 2002;8:89-91.
- Knight B, Mudge C, Openshaw S, White A, Hart A. Effect of acupuncture on nausea of pregnancy: a randomized, controlled trial. Obstet Gynecol 2001;97:184-8. http://dx.doi.org/10.1016/S0029-7844(00)01152-2.
- Koren G, Clark S, Hankins GD, Caritis SN, Miodovnik M, Umans JG, et al. Effectiveness of delayed-release doxylamine and pyridoxine for nausea and vomiting of pregnancy: a randomized placebo controlled trial. Am J Obstet Gynecol 2010;203:571.e1-7. http://dx.doi.org/10.1016/j.ajog.2010.07.030.
- Maina A, Arrotta M, Cicogna L, Donvito V, Mischinelli M, Todros T, et al. Transdermal clonidine in the treatment of severe hyperemesis. A pilot randomised control trial: CLONEMESI. BJOG 2014;121:1556-62. http://dx.doi.org/10.1111/1471-0528.12757.
- Maltepe C, Koren G. The management of nausea and vomiting of pregnancy and hyperemesis gravidarum – a 2013 update. J Popul Ther Clin Pharmacol 2013;20:e184-92.
- Mao ZN, Liang CE. Observation on therapeutic effect of acupuncture on hyperemesis gravidarum. Zhongguo Zhen Jiu 2009;29:973-6.
- McParlin C, Carrick-Sen D, Steen IN, Taylor P, Robson SC. Hyperemesis in pregnancy study: a randomised controlled trial of midwife-led ‘outpatient’ care. Arch Dis Child Fetal Neonatal Ed 2008;93.
- Mohammadbeigi R, Shahgeibi S, Soufizadeh N, Rezaiie M, Farhadifar F. Comparing the effects of ginger and metoclopramide on the treatment of pregnancy nausea. Pak J Biol Sci 2011;14:817-20. http://dx.doi.org/10.3923/pjbs.2011.817.820.
- Monias M. Evaluation of cyclizine with pyridoxine in vomiting of pregnancy. Mil Med 1957;121:403-4.
- Naeimi Rad M, Lamyian M, Heshmat R, Jaafarabadi MA, Yazdani S. A randomized clinical trial of the efficacy of KID21 point (youmen) acupressure on nausea and vomiting of pregnancy. Iran Red Crescent Med J 2012;14:697-701. http://dx.doi.org/10.5812/ircmj.2153.
- Narenji F, Delavar M, Rafiei M. Comparison the effects of the ginger fresh root and vitamin B6 on the nausea and vomiting in pregnancy. IJOGI 2012;15:39-43.
- Nelson-Piercy C, Fayers P, Swiet M. Randomised, double-blind, placebo-controlled trial of corticosteroids for the treatment of hyperemesis gravidarum. BJOG 2001;108:9-15. http://dx.doi.org/10.1016/s0306-5456(00)00017-6.
- Neri I, Allais G, Schiapparelli P, Blasi I, Benedetto C, Facchinetti F. Acupuncture versus pharmacological approach to reduce Hyperemesis gravidarum discomfort. Minerva Ginecol 2005;57:471-5.
- Oliveira LG, Capp S, You WB, Carstairs SD. Ondansetron versus doxylamine/pyridoxine for treatment of nausea and vomiting in first trimester pregnancy: a prospective randomized double-blind controlled study. Acad Emerg Med 2013;1. http://dx.doi.org/10.1097/AOG.0000000000000479.
- Ozgoli G, Goli M, Simbar M. Effects of ginger capsules on pregnancy, nausea, and vomiting. J Altern Complement Med 2009;15:243-6. http://dx.doi.org/10.1089/acm.2008.0406.
- Pasha H, Behmanesh F, Mohsenzadeh F, Hajahmadi M, Moghadamnia AA. Study of the effect of mint oil on nausea and vomiting during pregnancy. Iran Red Crescent Med J 2012;14:727-30. http://dx.doi.org/10.5812/ircmj.3477.
- Rosen T, de Veciana M, Miller HS, Stewart L, Rebarber A, Slotnick RN. A randomized controlled trial of nerve stimulation for relief of nausea and vomiting in pregnancy. Obstet Gynecol 2003;102:129-35. http://dx.doi.org/10.1016/S0029-7844(03)00375-2.
- Safari HR, Fassett MJ, Souter IC, Alsulyman OM, Goodwin TM. The efficacy of methylprednisolone in the treatment of hyperemesis gravidarum: a randomized, double-blind, controlled study. Am J Obstet Gynecol 1998;179:921-4. http://dx.doi.org/10.1016/S0002-9378(98)70189-9.
- Sahakian V, Rouse D, Sipes S, Rose N, Niebyl J. Vitamin B6 is effective therapy for nausea and vomiting of pregnancy: a randomized, double-blind placebo-controlled study. Obstet Gynecol 1991;78:33-6.
- Smith C, Crowther C, Beilby J. Acupuncture to treat nausea and vomiting in early pregnancy: a randomized controlled trial. Birth 2002;29:1-9. http://dx.doi.org/10.1046/j.1523-536X.2002.00149.x.
- Smith C, Crowther C, Willson K, Hotham N, McMillian V. A randomized controlled trial of ginger to treat nausea and vomiting in pregnancy. Obstet Gynecol 2004;103:639-45. http://dx.doi.org/10.1097/01.AOG.0000118307.19798.ec.
- Sripramote M, Lekhyananda N. A randomized comparison of ginger and vitamin B6 in the treatment of nausea and vomiting in pregnancy. J Med Assoc Thai 2003;86:846-53.
- Steele NM, French J, Gatherer-Boyles J, Newman S, Leclaire S. Effect of acupressure by sea-bands on nausea and vomiting of pregnancy. J Obstet Gynecol Neonatal Nurs 2001;30:61-70. http://dx.doi.org/10.1111/j.1552-6909.2001.tb01522.x.
- Sullivan CA, Johnson CA, Roach H, Martin RW, Stewart DK, Morrison JC. A pilot study of intravenous ondansetron for hyperemesis gravidarum. Am J Obstet Gynecol 1996;174:1565-8. http://dx.doi.org/10.1016/S0002-9378(96)70607-5.
- Tan PC, Khine PP, Vallikkannu N, Omar SZ. Promethazine compared with metoclopramide for hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol 2010;115:975-81. http://dx.doi.org/10.1097/AOG.0b013e3181d99290.
- Tan PC, Yow CM, Omar SZ. A placebo-controlled trial of oral pyridoxine in hyperemesis gravidarum. Gynecol Obstet Invest 2009;67:151-7. http://dx.doi.org/10.1159/000181182.
- Tan PC, Norazilah MJ, Omar SZ. Dextrose saline compared with normal saline rehydration of hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol 2013;121:291-8. http://dx.doi.org/10.1097/AOG.0b013e31827c5e99.
- Veciana M, Stewart L, Miller H, Slotnick R, Rebarber A, Rosen T. Multicenter randomized controlled trial of nerve stimulation therapy for the relief of nausea and vomiting in pregnancy. Am J Obstet Gynecol 2001;185. http://dx.doi.org/10.1016/S0002-9378(01)80402-6.
- Vutyavanich T, Kraisarin T, Ruangsri R. Ginger for nausea and vomiting in pregnancy: randomized, double-masked, placebo-controlled trial. Obstet Gynecol 2001;97:577-82. http://dx.doi.org/10.1016/S0029-7844(00)01228-X.
- Werntoft E, Dykes AK. Effect of acupressure on nausea and vomiting during pregnancy. A randomized, placebo-controlled, pilot study. J Reprod Med 2001;46:835-9.
- Wibowo N, Purwosunu Y, Sekizawa A, Farina A, Tambunan V, Bardosono S. Vitamin B6 supplementation in pregnant women with nausea and vomiting. Int J Gynaecol Obstet 2012;116:206-10. http://dx.doi.org/10.1016/j.ijgo.2011.09.030.
- Willetts KE, Ekangaki A, Eden JA. Effect of a ginger extract on pregnancy-induced nausea: a randomised controlled trial. Aust N Z J Obstet Gynaecol 2003;43:139-44. http://dx.doi.org/10.1046/j.0004-8666.2003.00039.x.
- Yost NP, McIntire DD, Wians FH, Ramin SM, Balko JA, Leveno KJ. A randomized, placebo-controlled trial of corticosteroids for hyperemesis due to pregnancy. Obstet Gynecol 2003;102:1250-4. http://dx.doi.org/10.1016/j.obstetgynecol.2003.08.013.
- Zhang HH. Observation on therapeutic effect of acupuncture and moxibustion on hyperemesis gravidarum. Zhongguo Zhen Jiu 2005;25:469-70.
- Ziaei S, Hosseiney FS, Faghihzadeh S. The efficacy low dose of prednisolone in the treatment of hyperemesis gravidarum. Acta Obstet Gynecol Scand 2004;83:272-5. http://dx.doi.org/10.1111/j.0001-6349.2004.0141.x.
- Maltepe C, Koren G. Preemptive treatment of nausea and vomiting of pregnancy: results of a randomized controlled trial. Obstet Gynecol Int 2013. http://dx.doi.org/10.1155/2013/809787.
- Smith C, Crowther C, Beilby J. Pregnancy outcome following women’s participation in a randomised controlled trial of acupuncture to treat nausea and vomiting in early pregnancy. Complement Ther Med 2002;10:78-83. http://dx.doi.org/10.1054/ctim.2002.0523.
- Biswas SC, Bal R, Kamilya GS, Mukherjee J, Hazra A, Narender S, et al. A Single-Masked, Randomized, Controlled Trial of Ginger Extract in the Treatment of Nausea and Vomiting of Pregnancy 2006. http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/832/CN-00582832/frame.html (accessed 28 November 2014).
- Alalade AO, Khan R, Dawlatly B. Day-case management of hyperemesis gravidarum: feasibility and clinical efficacy. J Obstet Gynaecol 2007;27:363-4. http://dx.doi.org/10.1080/01443610701327396.
- Einarson A, Maltepe C, Navioz Y, Kennedy D, Tan MP, Koren G. The safety of ondansetron for nausea and vomiting of pregnancy: a prospective comparative study. BJOG 2004;111:940-3. http://dx.doi.org/10.1111/j.1471-0528.2004.00236.x.
- Ferreira E, Bussieres JF, Turcotte V, Duperron L, Ouellet G. Case-control study comparing droperidol plus diphenhydramine with conventional treatment in hyperemesis gravidarum. JPT 2003;19:349-54. http://dx.doi.org/10.1177/875512250301900602.
- Hsu JJ, Clark-Glena R, Nelson DK, Kim CH. Nasogastric enteral feeding in the management of hyperemesis gravidarum. Obstet Gynecol 1996;88:343-6. http://dx.doi.org/10.1016/0029-7844(96)00174-3.
- Markose MT, Ramanathan K, Vijayakumar J. Reduction of nausea, vomiting, and dry retches with P6 acupressure during pregnancy. Int J Gynaecol Obstet 2004;85:168-9. http://dx.doi.org/10.1016/j.ijgo.2003.09.008.
- Moran P, Taylor R. Management of hyperemesis gravidarum: the importance of weight loss as a criterion for steroid therapy. QJM 2002;95:153-8. http://dx.doi.org/10.1093/qjmed/95.3.153.
- Saha S, Loranger D, Pricolo V, Degli-Esposti S. Feeding jejunostomy for the treatment of severe hyperemesis gravidarum: a case series. J Parenter Enteral Nutr 2009;33:529-34. http://dx.doi.org/10.1177/0148607109333000.
- Koren G, Maltepe C. Preemptive Diclectin therapy for the management of nausea and vomiting of pregnancy and hyperemesis gravidarum. Am J Obstet Gynecol 2013;208. http://dx.doi.org/10.1016/j.ajog.2012.10.205.
- Safari HR, Fassett MJ, Souter IC, Goodwin TM. Randomized double-blind trial of methylprednisolone versus promethazine in the treatment of hyperemesis gravidarum. Am J Obstet Gynecol 1998;178.
- Yang LC, Jawan B, Chen CN, Ho RT, Chang KA, Lee JH. Comparison of P6 acupoint injection with 50% glucose in water and intravenous droperidol for prevention of vomiting after gynecological laparoscopy. Acta Anaesthesiol Scand 1993;37:192-4. http://dx.doi.org/10.1111/j.1399-6576.1993.tb03699.x.
- Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care 2005;21:240-5.
- Philips Z, Bojke L, Sculpher M, Claxton K, Golder S. Good practice guidelines for decision-analytic modelling in health technology assessment: a review and consolidation of quality assessment. Pharmacoeconomics 2006;24:355-71. http://dx.doi.org/10.2165/00019053-200624040-00006.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2014.
- Department of Health . Payment by Results in the NHS: Tariff for 2012 to 2013 n.d. www.gov.uk/government/publications/confirmation-of-payment-by-results-Pbr-arrangements-for-2012–13 (accessed 28 November 2014).
- Curtis L. Unit Costs of Health and Social Care 2013. University of Kent: Personal Social Services Research Unit; 2013.
- Grimshaw J, Thomas R, MacLennan G, Fraser C, Ramsay C, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 2004;8. http://dx.doi.org/10.3310/hta8060.
- Portnoi G, Chng L, Karimi-Tabesh L, Koren G, Tan MP, Einarson A. Prospective comparative study of the safety and effectiveness of ginger for the treatment of nausea and vomiting in pregnancy. Am J Obstet Gynecol 2003;190:1140-374. http://dx.doi.org/10.1067/s0002-9378(03)00649-5.
- Heitmann K, Nordeng H, Holst L. Safety of ginger use in pregnancy: results from a large population-based cohort study. Eur J Clin Pharmacol 2013;69:269-77. http://dx.doi.org/10.1007/s00228-012-1331-5.
- Einarson T, Leeder J, Koren G. A method for metaanalysis of epidemiological studies. Drug Intell Clin Pharm 1988;22:813-24.
- McKeigue PM, Lamm SH, Linn S, Kutcher JS. Bendectin and birth defects: I. A meta-analysis of the epidemiologic studies. Teratology 1994;50:27-3. http://dx.doi.org/10.1002/tera.1420500105.
- Seto A, Einarson T, Koren G. Pregnancy outcome following first trimester exposure to antihistamines: meta-analysis. Am J Perinatol 1997;14:119-24. http://dx.doi.org/10.1055/s-2007-994110.
- Mazzotta P, Magee LA. A risk-benefit assessment of pharmacological and nonpharmacological treatments for nausea and vomiting of pregnancy. Drugs 2000;59:781-800. http://dx.doi.org/10.2165/00003495-200059040-00005.
- Matok I, Gorodischer R, Koren G, Sheiner E, Wiznitzer A, Levy A. The safety of metoclopramide use in the first trimester of pregnancy. N Engl J Med 2009;360:2528-35. http://dx.doi.org/10.1056/NEJMoa0807154.
- Pasternak B, Svanstrom H, Molgaard-Nielsen D, Melbye M, Hviid A. Metoclopramide in pregnancy and risk of major congenital malformations and fetal death. JAMA 2013;310:1601-11. http://dx.doi.org/10.1001/jama.2013.278343.
- Anderka M, Mitchell AA, Louik C, Werler MM, Hernandez-Diaz S, Rasmussen SA, et al. Medications used to treat nausea and vomiting of pregnancy and the risk of selected birth defects. Birth Defects Res A Clin Mol Teratol 2012;94:22-30. http://dx.doi.org/10.1002/bdra.22865.
- Pasternak B, Svanstrom H, Hviid A. Ondansetron in pregnancy and risk of adverse fetal outcomes. N Engl J Med 2013;368:814-23. http://dx.doi.org/10.1056/NEJMoa1211035.
- Freedman SB, Uleryk E, Rumantir M, Finkelstein Y. Ondansetron and the risk of cardiac arrhythmias: a systematic review and postmarketing analysis. Ann Emerg Med 2014;64:19-25. http://dx.doi.org/10.1016/j.annemergmed.2013.10.026.
- Park-Wyllie L, Mazzotta P, Pastuszak A, Moretti M, Beique L, Hunnisett L, et al. Birth defects after maternal exposure to corticosteroids: prospective cohort study and meta-analysis of epidemiological studies. Teratology 2000;62:385-92. http://dx.doi.org/10.1002/1096-9926(200012)62:6<385::AID-TERA5>3.0.CO;2-Z.
- Czeizel AE, Rockenbauer M. Population-based case-control study of teratogenic potential of corticosteroids. Teratology 1997;56:335-40. http://dx.doi.org/10.1002/(SICI)1096-9926(199711)56:5<335::AID-TERA7>3.0.CO;2-W.
- Tata LJ, Lewis SA, McKeever TM, Smith CJP, Doyle P, Smeeth L, et al. Effect of maternal asthma, exacerbations and asthma medication use on congenital malformations in offspring: a UK population-based study. Thorax 2008;63:981-7. http://dx.doi.org/10.1136/thx.2008.098244.
- Guttuso T, Shaman M, Thornburg LL. Potential maternal symptomatic benefit of gabapentin and review of its safety in pregnancy. Eur J Obstet Gynecol Reprod Biol 2014;181:280-3. http://dx.doi.org/10.1016/j.ejogrb.2014.08.013.
- McCarthy FP, Murphy A, Khashan AS, McElroy B, Spillane N, Marchocki Z, et al. Day care compared with inpatient management of nausea and vomiting of pregnancy: a randomized controlled trial. Obstet Gynecol 2014;124:743-8. http://dx.doi.org/10.1097/AOG.0000000000000449.
- Use of Ginger in Pregnancy. London: UKTIS; 2013.
- Use of Vitamin B12 in Pregnancy. London: UKTIS; 2013.
- Use of Vitamin B6 in Pregnancy. London: UKTIS; 2011.
- Use of Promethazine in Pregnancy. London: UKTIS; 2010.
- Use of Ondansetron in Pregnancy. London: UKTIS; 2014.
Appendix 1 Examples of hyperemesis gravidarum/nausea and vomiting in pregnancy assessment tools
This assessment has been reproduced with permission from Professor Gideon Koren, Director, The Motherisk Program; Professor of Pediatrics, Pharmacology, Pharmacy, Medicine and Medical Genetics at The University of Toronto; Senior Scientist at The Research Institute Hospital for Sick Children; and The Ivey Chair in Molecular Toxicology at the University of Western Ontario Canada, 2014, personal communication.
Appendix 2 Data abstraction form: clinical effectiveness
Appendix 3 Risk of bias for randomised controlled trials
| Domain | Description | Review authors’ judgement |
|---|---|---|
| Sequence generation | Describe the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether or not it should produce comparable groups | Was the allocation sequence adequately generated? |
| Allocation concealment | Describe the method used to conceal the allocation sequence in sufficient detail to determine whether or not intervention allocations could have been foreseen in advance of, or during, enrolment | Was allocation adequately concealed? |
| Blinding of participants, personnel and outcome assessors Assessments should be made for each main outcome (or class of outcomes) |
Describe all measures used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. Provide any information relating to whether the intended blinding was effective | Was knowledge of the allocated intervention adequately prevented during the study? |
| Incomplete outcome data Assessments should be made for each main outcome (or class of outcomes) |
Describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. State whether attrition and exclusions were reported, the numbers in each intervention group (compared with total randomised participants), reasons for attrition/exclusions where reported, and any reinclusions in analyses performed by the review authors | Were incomplete outcome data adequately addressed? |
| Selective outcome reporting | State how the possibility of selective outcome reporting was examined by the review authors, and what was found | Are reports of the study free of suggestion of selective outcome reporting? |
| Other sources of bias | State any important concerns about bias not addressed in the other domains in the tool If particular questions/entries were pre-specified in the review’s protocol, responses should be provided for each question/entry |
Was the study apparently free of other problems that could put it at a high risk of bias? |
Possible approach for summary assessments outcome (across domains) within and across studies
| Risk of bias | Interpretation | Within a study | Across studies |
|---|---|---|---|
| Low risk of bias | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information is from studies at low risk of bias |
| Unclear risk of bias | Plausible bias that raises some doubt about the results | Unclear risk of bias for one or more key domains | Most information is from studies at low or unclear risk of bias |
| High risk of bias | Plausible bias that seriously weakens confidence in the results | High risk of bias for one or more key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of the results |
Criteria for judging risk of bias in the ‘risk of bias’ assessment tool
| Sequence generation | |
|---|---|
| Was the allocation sequence adequately generated? [Short form: Adequate sequence generation?] | |
| Criteria for a judgement of ‘YES’ (i.e. low risk of bias) | The investigators describe a random component in the sequence generation process such as:
|
| Criteria for the judgement of ‘NO’ (i.e. high risk of bias) | The investigators describe a non-random component in the sequence generation process. Usually, the description would involve some systematic, non-random approach, for example:
|
| Criteria for the judgement of ‘UNCLEAR’ (uncertain risk of bias) | Insufficient information about the sequence generation process to permit judgement of ‘YES’ or ‘NO’ |
| Allocation concealment | |
| Was allocation adequately concealed? [Short form: Allocation concealment?] | |
| Criteria for a judgement of ‘YES’ (i.e. low risk of bias) | Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation:
|
| Criteria for the judgement of ‘NO’ (i.e. high risk of bias) | Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on:
|
| Criteria for the judgement of ‘UNCLEAR’ (uncertain risk of bias) | Insufficient information to permit judgement of ‘YES’ or ‘NO’. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement; for example, if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed |
| Blinding of participants, personnel and outcome assessors | |
| Was knowledge of the allocated interventions adequately prevented during the study? [Short form: Blinding?] | |
| Criteria for a judgement of ‘YES’ (i.e. low risk of bias) | Any one of the following:
|
| Criteria for the judgement of ‘NO’ (i.e. high risk of bias) | Any one of the following:
|
| Criteria for the judgement of ‘UNCLEAR’ (uncertain risk of bias) | Any one of the following:
|
| Incomplete outcome data | |
| Were incomplete outcome data adequately addressed? [Short form: Incomplete outcome data addressed?] | |
| Criteria for a judgement of ‘YES’ (i.e. low risk of bias) | Any one of the following:
|
| Criteria for the judgement of ‘NO’ (i.e. high risk of bias) | Any one of the following:
|
| Criteria for the judgement of ‘UNCLEAR’ (uncertain risk of bias) | Any one of the following:
|
| Selective outcome reporting | |
| Are reports of the study free of suggestion of selective outcome reporting? [Short form: Free of selective reporting?] | |
| Criteria for a judgement of ‘YES’ (i.e. low risk of bias) | Any of the following:
|
| Criteria for the judgement of ‘NO’ (i.e. high risk of bias) | Any one of the following:
|
| Criteria for the judgement of ‘UNCLEAR’ (uncertain risk of bias) | Insufficient information to permit judgement of ‘YES’ or ‘NO’. It is likely that the majority of studies will fall into this category |
| Other potential threats to validity | |
| Was the study apparently free of other problems that could put it at a risk of bias? [Short form: Free of other bias?] | |
| Criteria for a judgement of ‘YES’ (i.e. low risk of bias) | The study appears to be free of other sources of bias |
| Criteria for the judgement of ‘NO’ (i.e. high risk of bias) | There is at least one important risk of bias. For example, the study:
|
| Criteria for the judgement of ‘UNCLEAR’ (uncertain risk of bias) | There may be a risk of bias, but there is either:
|
Appendix 4 Quality of case series studies
Appendix 5 Included papers
Abas 2014
Abas MN, Tan PC, Azmi N, Omar SZ. Ondansetron compared with metoclopramide for hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol 2014;123:1272–9.
Adamczak 2007
Adamczak J, Kasdaglis J, Rinehart B, Antebi Y, Wolf E, Terrone D. A prospective randomized trial of solumedrol dose pack vs. Phenergan for the treatment of symptomatic nausea and vomiting in pregnancy. Am J Obstet Gynecol 2007;197:S88.
Alalade 2007
Alalade AO, Khan R, Dawlatly B. Day-case management of hyperemesis gravidarum: feasibility and clinical efficacy. J Obstet Gynaecol 2007;27:363–4.
Ashkenazi-Hoffnung 2013
Ashkenazi-Hoffnung L, Merlob P, Stahl B, Klinger G. Evaluation of the efficacy and safety of bi-daily combination therapy with pyridoxine and doxylamine for nausea and vomiting of pregnancy. Isr Med Assoc J 2013;15:23–6.
Babaei 2014
Babaei AH, Foghaha MH. A randomized comparison of vitamin B6 and dimenhydrinate in the treatment of nausea and vomiting in early pregnancy. Iran J Nurs Midwifery Res 2014;19:199–202.
Basirat 2009
Basirat Z, Moghadamnia AA, Kashifard M, Sarifi-Razavi A. The effect of ginger biscuit on nausea and vomiting in early pregnancy. Acta Medica Iranica 2009;47:51–6.
Bayreuther 1994
Bayreuther J, Lewith GT, Pickering R. A double-blind cross-over study to evaluate the effectiveness of acupressure at pericardium 6 (P6) in the treatment of early morning sickness (EMS). Complement Ther Med 1994;2:70–6.
Belluomini 1994
Belluomini J, Litt RC, Lee KA, Katz M. Acupressure for nausea and vomiting of pregnancy: a randomized, blinded study. Obstet Gynecol 1994;84:245–8.
Biswas 2011
Biswas SC, Dey R, Kamliya GS, Bal R, Hazra A, Tripathi SK. A single-masked, randomized, controlled trial of ginger extract in the treatment of nausea and vomiting of pregnancy. JIMSA 2011;24:167–9.
Bondok 2006
Bondok RS, El Sharnouby NM, Eid HE, Abd Elmaksoud AM. Pulsed steroid therapy is an effective treatment for intractable hyperemesis gravidarum. Crit Care Med 2006;34:2781–3.
Capp 2014
Capp S, Oliveira L, Carstairs S, You W. Ondansetron versus doxylamine/pyridoxine for treatment of nausea and vomiting in pregnancy: a prospective randomized double-blind trial. Am J Obstet Gynecol 2014;210:S39.
Can Gurkan 2008
Can Gurkan O, Arslan H. Effect of acupressure on nausea and vomiting during pregnancy. Complement Ther Clin Pract 2008;14:46–52.
Carlsson 2000
Carlsson CP, Axemo P, Bodin A, Carstensen H, Ehrenroth B, Madegard-Lind I, et al. Manual acupuncture reduces hyperemesis gravidarum: a placebo-controlled, randomized, single-blind, crossover study. J Pain Symptom Manage 2000;20:273–9.
Chittumma 2007
Chittumma P, Kaewkiattikun K, Wiriyasiriwach B. Comparison of the effectiveness of ginger and vitamin B6 for treatment of nausea and vomiting in early pregnancy: a randomized double-blind controlled trial. J Med Assoc Thai 2007;90:15–20.
Diggory 1962
Diggory PL, Tomkinson JS. Nausea and vomiting in pregnancy. A trial of meclozine dihydrochloride with and without pyridoxine. Lancet 1962;2:370–2.
Ditto 1999
Ditto A, Morgante G, la Marca A, De Leo V. Evaluation of treatment of hyperemesis gravidarum using parenteral fluid with or without diazepam. A randomized study. Gynecol Obstet Invest 1999;48:232–6.
Eftekhari 2013
Eftekhari N, Mehralhasani Y. A comparison of ondansetron and promethasin in treating hyperemesis gravidarum. JKUMS 2013;20:354–65.
Einarson 2004
Einarson A, Maltepe C, Navioz Y, Kennedy D, Tan MP, Koren G. The safety of ondansetron for nausea and vomiting of pregnancy: a prospective comparative study. BJOG 2004;111:940–3.
Ensiyeh 2009
Ensiyeh J, Sakineh MA. Comparing ginger and vitamin B6 for the treatment of nausea and vomiting in pregnancy: a randomised controlled trial. Midwifery 2009;25:649–53.
Erez 1971
Erez S, Schifrin BS, Dirim O. Double-blind evaluation of hydroxyzine as an antiemetic in pregnancy. J Reprod Med 1971;7:35–7.
Evans 1993
Evans AT, Samuels SN, Marshall C, Bertolucci LE. Suppression of pregnancy-induced nausea and vomiting with sensory afferent stimulation. J Reprod Med 1993;38:603–6.
Ferreira 2003
Ferreira E, Bussieres JF, Turcotte V, Duperron L, Ouellet G. Case-control study comparing droperidol plus diphenhydramine with conventional treatment in hyperemesis gravidarum. JPT 2003;19:349–54.
Fischer-Rasmussen 1991
Fischer-Rasmussen W, Kjaer SK, Dahl C, Asping U. Ginger treatment of hyperemesis gravidarum. Eur J Obstet Gynecol Reprod Biol 1991;38:19–24.
Ghahiri 2011
Ghahiri AA, Abdi F, Mastoo R, Ghasemi M. The effect of ondansetron and metoclopramide in nausea and vomiting of pregnancy. JIMS 2011;29:259–65.
Ghani 2013
Ghani RMA, Ibrahim ATA. The effect of aromatherapy inhalation on nausea and vomiting in early pregnancy: a pilot randomized controlled trial. J Nat Sci Res 2013;3:10–22.
Guttuso 2010
Guttuso T Jr, Robinson LK, Amankwah KS. Gabapentin use in hyperemesis gravidarum: a pilot study. Early Hum Dev 2010;86:65–6.
Haji Seid Javadi 2013
Haji Seid Javadi E, Salehi F, Mashrabi O. Comparing the effectiveness of vitamin B6 and ginger in treatment of pregnancy-induced nausea and vomiting. Obstet Gynecol Int 2013;927834.
Heazell 2006
Heazell A, Thorneycroft J, Walton V, Etherington I. Acupressure for the inpatient treatment of nausea and vomiting in early pregnancy: a randomized control trial. Am J Obstet Gynecol 2006;194:815–20.
Hsu 1996
Hsu JJ, Clark-Glena R, Nelson DK, Kim CH. Nasogastric enteral feeding in the management of hyperemesis gravidarum. Obstet Gynecol 1996;88:343–6.
Hsu 2003
Hsu E, Pei V, Shofer FS, Abbuhl SB. A prospective randomized controlled trial of acupressure vs sham for pregnancy-related nausea and vomiting in the emergency department. Acad Emerg Med 2003;10:437.
Jamigorn 2007
Jamigorn M, Phupong V. Acupressure and vitamin B6 to relieve nausea and vomiting in pregnancy: a randomized study. Arch Gynecol Obstet 2007;276:245–9.
Kashifard 2013
Kashifard M, Basirat Z, Kashifard M, Golsorkhtabar-Amiri M, Moghaddamnia A. Ondansetrone or metoclopromide? Which is more effective in severe nausea and vomiting of pregnancy? A randomized trial double-blind study. Clin Exp Obstet Gynecol 2013;40:127–30.
Keating 2002
Keating A, Chez RA. Ginger syrup as an antiemetic in early pregnancy. Altern Ther Health Med 2002;8:89–91.
Knight 2001
Knight B, Mudge C, Openshaw S, White A, Hart A. Effect of acupuncture on nausea of pregnancy: a randomized, controlled trial. Obstet Gynecol 2001;97:184–8.
Koren 2010
Koren G, Clark S, Hankins GD, Caritis SN, Miodovnik M, Umans JG, et al. Effectiveness of delayed-release doxylamine and pyridoxine for nausea and vomiting of pregnancy: a randomized placebo controlled trial. Am J Obstet Gynecol 2010;203:571.e1–7.
Koren 2013
Koren G, Maltepe C. Preemptive Diclectin therapy for the management of nausea and vomiting of pregnancy and hyperemesis gravidarum. Am J Obstet Gynecol 2013;208:S20.
Maina 2014
Maina A, Arrotta M, Cicogna L, Donvito V, Mischinelli M, Todros T, et al. Transdermal clonidine in the treatment of severe hyperemesis. A pilot randomised control trial: CLONEMESI. BJOG 2014;121:1556–62.
Maltepe 2013
Maltepe C, Koren G. Preemptive treatment of nausea and vomiting of pregnancy: results of a randomized controlled trial. Obstet Gynecol Int 2013;809787.
Mao 2009
Mao ZN, Liang CE. [Observation on therapeutic effect of acupuncture on hyperemesis gravidarum.] Zhongguo Zhenjiu 2009;29:973–6.
Markose 2004
Markose MT, Ramanathan K, Vijayakumar J. Reduction of nausea, vomiting, and dry retches with P6 acupressure during pregnancy. Int J Gynaecol Obstet 2004;85:168–9.
McParlin 2008
Primary reference
McParlin C, Carrick-Sen D, Steen IN, Taylor P, Robson SC. Hyperemesis in pregnancy study: a randomised controlled trial of midwife-led ‘outpatient’ care. Arch Dis Child Fetal Neonatal Ed 2008;93:Fa9.
Secondary reference
McParlin C, Carrick-Sen D, Steen IN, Taylor P, Robson SC. Hyperemesis in pregnancy study: a randomised controlled trial of midwife-led ‘outpatient’ care. Unpublished.
Mohammadbeigi 2011
Mohammadbeigi R, Shahgeibi S, Soufizadeh N, Rezaiie M, Farhadifar F. Comparing the effects of ginger and metoclopramide on the treatment of pregnancy nausea. Pak J Biol Sci 2011;14:817–20.
Monias 1957
Monias M. Evaluation of cyclizine with pyridoxine in vomiting of pregnancy. Mil Med 1957;121:403–4.
Moran 2002
Moran P, Taylor R. Management of hyperemesis gravidarum: the importance of weight loss as a criterion for steroid therapy. QJM 2002;95:153–8.
Naeimi Rad 2012
Naeimi Rad M, Lamyian M, Heshmat R, Jaafarabadi MA, Yazdani S. A randomized clinical trial of the efficacy of KID21 point (youmen) acupressure on nausea and vomiting of pregnancy. Iran 2012;14:697–701.
Narenji 2012
Narenji F, Delavar M, Rafiei M. Comparison the effects of the ginger fresh root and vitamin B6 on the nausea and vomiting in pregnancy. IJOGI 2012;15:39–43.
Nelson-Piercy 2001
Nelson-Piercy C, Fayers P, Swiet M. Randomised, double-blind, placebo-controlled trial of corticosteroids for the treatment of hyperemesis gravidarum. BJOG 2001;108:9–15.
Neri 2005
Neri I, Allais G, Schiapparelli P, Blasi I, Benedetto C, Facchinetti F. Acupuncture versus pharmacological approach to reduce hyperemesis gravidarum discomfort. Minerva Ginecol 2005;57:471–5.
Oliveira 2013
Oliveira LG, Capp S, You WB, Carstairs SD. Ondansetron versus doxylamine/pyridoxine for treatment of nausea and vomiting in first trimester pregnancy: a prospective randomized double-blind controlled study. Acad Emerg Med 2013;1:S101.
Ozgoli 2009
Ozgoli G, Goli M, Simbar M. Effects of ginger capsules on pregnancy, nausea, and vomiting. J Altern Complement Med 2009;15:243–6.
Pasha 2012
Pasha H, Behmanesh F, Mohsenzadeh F, Hajahmadi M, Moghadamnia AA. Study of the effect of mint oil on nausea and vomiting during pregnancy. Iran Red Crescent Med J 2012;14:727–30.
Pongrojpaw 2007
Pongrojpaw D, Somprasit C, Chanthasenanont A. A randomized comparison of ginger and dimenhydrinate in the treatment of nausea and vomiting in pregnancy. J Med Assoc Thai 2007;90:1703–9.
Rosen 2003
Rosen T, de Veciana M, Miller HS, Stewart L, Rebarber A, Slotnick RN. A randomized controlled trial of nerve stimulation for relief of nausea and vomiting in pregnancy. Obstet Gynecol 2003;102:129–35.
Saberi 2013
Saberi F, Sadat Z, Abedzadeh-Kalahroudi M, Taebi M. Acupressure and ginger to relieve nausea and vomiting in pregnancy: a randomized study. Iran Red Crescent Med J 2013;15:854–61.
Safari 1998
Safari HR, Fassett MJ, Souter IC, Alsulyman OM, Goodwin TM. The efficacy of methylprednisolone in the treatment of hyperemesis gravidarum: a randomized, double-blind, controlled study. Am J Obstet Gynecol 1998;179:921–4.
Saha 2009
Saha S, Loranger D, Pricolo V, Degli-Esposti S. Feeding jejunostomy for the treatment of severe hyperemesis gravidarum: a case series. J Parenter Enteral Nutr 2009;33:529–34.
Sahakian 1991
Sahakian V, Rouse D, Sipes S, Rose N, Niebyl J. Vitamin B6 is effective therapy for nausea and vomiting of pregnancy: a randomized, double-blind placebo-controlled study. Obstet Gynecol 1991;78:33–6.
Smith 2002
Smith C, Crowther C, Beilby J. Acupuncture to treat nausea and vomiting in early pregnancy: a randomized controlled trial. Birth 2002;29:1–9.
Smith 2004
Smith C, Crowther C, Willson K, Hotham N, McMillian V. A randomized controlled trial of ginger to treat nausea and vomiting in pregnancy. Obstet Gynecol 2004;103:639–45.
Sripramote 2003
Sripramote M, Lekhyananda N. A randomized comparison of ginger and vitamin B6 in the treatment of nausea and vomiting in pregnancy. J Med Assoc Thai 2003;86:846–53.
Steele 2001
Steele NM, French J, Gatherer-Boyles J, Newman S, Leclaire S. Effect of acupressure by sea-bands on nausea and vomiting of pregnancy. J Obstet Gynecol Neonatal Nurs 2001;30:61–70.
Sullivan 1996
Sullivan CA, Johnson CA, Roach H, Martin RW, Stewart DK, Morrison JC. A pilot study of intravenous ondansetron for hyperemesis gravidarum. Am J Obstet Gynecol 1996;174:1565–8.
Tan 2009
Tan PC, Yow CM, Omar SZ. A placebo-controlled trial of oral pyridoxine in hyperemesis gravidarum. Gynecol Obstet Invest 2009;67:151–7.
Tan 2010
Tan PC, Khine PP, Vallikkannu N, Omar SZ. Promethazine compared with metoclopramide for hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol 2010;115:975–81.
Tan 2013
Tan PC, Norazilah MJ, Omar SZ. Dextrose saline compared with normal saline rehydration of hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol 2013;121:291–8.
Veciana 2001
Veciana M, Stewart L, Miller H, Slotnick R, Rebarber A, Rosen T. Multicenter randomized controlled trial of nerve stimulation therapy for the relief of nausea and vomiting in pregnancy. Am J Obstet Gynecol 2001;185:S182.
Vutyavanich 1995
Vutyavanich T, Wongtra-ngan S, Ruangsri R. Pyridoxine for nausea and vomiting of pregnancy: a randomized, double-blind, placebo-controlled trial. Am J Obstet Gynecol 1995;173:881–4.
Vutyavanich 2001
Vutyavanich T, Kraisarin T, Ruangsri R. Ginger for nausea and vomiting in pregnancy: randomized, double-masked, placebo-controlled trial. Obstet Gynecol 2001;97:577–82.
Wentoft 2001
Werntoft E, Dykes AK. Effect of acupressure on nausea and vomiting during pregnancy. A randomized, placebo-controlled, pilot study. J Reprod Med 2001;46:835–9.
Wibowo 2012
Wibowo N, Purwosunu Y, Sekizawa A, Farina A, Tambunan V, Bardosono S. Vitamin B6 supplementation in pregnant women with nausea and vomiting. Int J Gynaecol Obstet 2012;116:206–10.
Willetts 2003
Willetts KE, Ekangaki A, Eden JA. Effect of a ginger extract on pregnancy-induced nausea: a randomised controlled trial. Aust N Z J Obstet Gynaecol 2003;43:139–44.
Yost 2003
Yost NP, McIntire DD, Wians FH Jr, Ramin SM, Balko JA, Leveno KJ. A randomized, placebo-controlled trial of corticosteroids for hyperemesis due to pregnancy. Obstet Gynecol 2003;102:1250–4.
Zhang 2005
Zhang HH. [Observation on therapeutic effect of acupuncture and moxibustion on hyperemesis gravidarum.] Zhongguo Zhenjiu 2005;25:469–70.
Ziaei 2004
Ziaei S, Hosseiney FS, Faghihzadeh S. The efficacy low dose of prednisolone in the treatment of hyperemesis gravidarum. Acta Obstet Gynecol Scand 2004;83:272–5.
Appendix 6 Excluded papers and reasons for exclusion
Required study design not met (n = 70)
Abas MN, Tan PC, Azmi N, Omar SZ. Ondansetron compared with metoclopramide for hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol 2013;123:1272–9.
Agren A, Berg M. Tactile massage and severe nausea and vomiting during pregnancy – women’s experiences. Scand J Caring Sci 2006;20:169–76.
Ajufo I. Four-year retrospective review of day admission service provision for hyperemesis gravidarum (HG) at St Thomas’ Hospital London [UK]. BJOG 2013;120:534–5.
Bailit JL. Hyperemesis gravidarium: epidemiologic findings from a large cohort. Am J Obstet Gynecol 2005;193:811–14.
Balestri F. [Treatment of hyperemesis gravidarum with combined inositol and pyridoxine.] Gazz Med Ital 1955;114:225–7.
Bond S. Large study finds metoclopramide can be safely used for nausea and vomiting in early pregnancy. J Midwifery Womens Health 2009;54:510–11.
Boone SA, Shields KM. Treating pregnancy-related nausea and vomiting with ginger. Ann Pharmacother 2005;39:1710–13.
Boskovic R, Einarson A, Maltepe C, Wolpin J, Koren G. Diclectin therapy for nausea and vomiting of pregnancy: effects of optimal dosing. J Obstet Gynaecol Can 2003;25:830–3.
Bozzo P, Koren G, Nava-Ocampo AA, Einarson A. The incidence of nausea and vomiting of pregnancy (NVP): a comparison between depressed women treated with antidepressants and non-depressed women. Clin Invest Med 2006;29:347–50.
Brill JR. Acupressure for nausea and vomiting of pregnancy: a randomized, blinded study (4). Obstet Gynecol 1995;85:159–60.
Brodbaek HB, Damkier P. [The treatment of hyperemesis gravidarum with chlorobutanol-caffeine rectal suppositories in Denmark: practice and evidence.] Ugeskr Laeger 2007;169:2122–3.
Bufano G, Cervellin G, Calderini MC, Coscelli C. [Enteral nutrition in hyperemesis gravidarum.] Rivista Italiana di Nutrizione Parenterale ed Enterale 1992;10:260–5.
Buttino L Jr, Coleman SK, Bergauer NK, Gambon C, Stanziano GJ. Home subcutaneous metoclopramide therapy for hyperemesis gravidarum. J Perinatol 2000;20:359–62.
Charlin V, Borghesi L, Hasbun J, Von Mulenbrock R, Moreno MI. Parenteral nutrition in hyperemesis gravidarum. Nutrition 1993;9:29–32; discussion 68.
Crawford-Faucher A. Which drug is more effective for treating hyperemesis gravidarum? Am Fam Physician 2011;83:842.
Fejzo MS, Magtira A, Schoenberg FP, MacGibbon K, Mullin P, Romero R, et al. Antihistamines and other prognostic factors for adverse outcome in hyperemesis gravidarum. Eur J Obstet Gynecol Reprod Biol 2013;170:71–6.
Fuchs K, Paldi E, Abramovici H, Peretz BA. Treatment of hyperemesis gravidarum by hypnosis. Int J Clin Exp Hyp 1980;28:313–23.
Gordon GH. Dextrose saline compared with normal saline rehydration of hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol 2013;121:1360.
Heitmann K, Holst L, Maltepe C, Lupattelli A, Nordeng H. Treatment of nausea during pregnancy – results from a multinational, cross-sectional, internet-based study. Res Soc Adm Pharm 2014;10:e57–8.
Gill SK, Maltepe C, Mastali K, Koren G. The effect of acid-reducing pharmacotherapy on the severity of nausea and vomiting of pregnancy. Obstet Gynecol Int 2009;585269.
Golaszewski T, Frigo P, Mark HE, Rattay F, Schaller A. [Treatment of hyperemesis gravidarum by electrostimulation of the vestibular apparatus.] Z Geburtshilfe Neonatol 1995;199:107–10.
Goodwin TM, Poursharif B, Korst LM, MacGibbon KW, Romero R, Fejzo MS. Secular trends in the treatment of hyperemesis gravidarum. Am J Perinatol 2008;25:141–7.
Gulley RM, Pleog NV, Gulley JM. Treatment of hyperemesis gravidarum with nasogastric feeding. Nutr Clin Pract 1993;8:33–5.
Hordern CE, Medina Lucena H, Stanley KP, Sule MM. HARP – Hyperemesis Ambulatory Rehydration Project: development, implementation and improvement to minimise hospital stay. BJOG 2013;120:432–3.
Hyde E. Acupressure therapy for morning sickness. A controlled clinical trial. J Nurse Midwifery 1989;34:171–8.
Jednak MA, Shadigian EM, Kim MS, Woods ML, Hooper FG, Owyang C, et al. Protein meals reduce nausea and gastric slow wave dysrhythmic activity in first trimester pregnancy. Am J Physiol 1999;277:G855–61.
Jewell D, Young G, Hall PF. Review: antiemetic drugs reduce nausea in early pregnancy. Evid-Based Med 2002;7:155.
Jungmayr P. [Pregnancy hyperemesis: a cohort study confirms safety of metoclopramide.] Deutsche Apotheker Zeitung 2009;149:42–3.
Kawakami SI, Furuki Y, Kubota T, Souda Y, Souda T, Kyono K, et al. Effect of Chinese Herbal Medicine Suppositories for Hyperemesis Gravidarum by Using an Index for Nausea and Vomiting of Pregnancy. In Koren G, Bishai R, editors. Nausea and Vomiting of Pregnancy: State of the Art 2000. Toronto: Hospital Sick Children, Motherisk Program; 2000. pp. 122–7.
Khan TN, Karpate S, Shehmar M. Hyperemesis day centre audit. BJOG 2013;120:527–8.
King TL, Murphy PA. Evidence-based approaches to managing nausea and vomiting in early pregnancy. J Midwifery Womens Health 2009;54:430–44.
Koren G. Appraisal of drug therapy for nausea and vomiting of pregnancy: I. The placebo effect – methodological and practical considerations. Can J Clin Pharmacol 2000;7:135–7.
Lacasse A, Rey E, Ferreira E, Morin C, Bérard A. Validity of a modified Pregnancy-Unique Quantification of Emesis and Nausea (PUQE) scoring index to assess severity of nausea and vomiting of pregnancy. Am J Obstet Gynecol 2008;198:71.e1–7.
Lacasse A, Berard A. Validation of the nausea and vomiting of pregnancy specific health related quality of life questionnaire. Health Qual Life Outcomes 2008;6:32.
Long MA, Simone SS, Tucher JJ. Outpatient treatment of hyperemesis gravidarum with stimulus control and imagery procedures. J Behav Ther Exp Psychiatry 1986;17:105–9.
Low KG. Nausea and vomiting in pregnancy: a review of the research. J Gender Culture Health 1996;1:151–72.
Magee LA, Chandra K, Mazzotta P, Stewart D, Koren G, Guyatt GH. Development of a health-related quality of life instrument for nausea and vomiting of pregnancy. Am J Obstet Gynecol 2002;186:S232–8.
Maina A, Todros T. A novel approach to hyperemesis gravidarum: evaluation by a visual analogue scale score and treatment with transdermal clonidine. Obstet Med 2011;4:156–9.
Matok I, Umans J, Feghali MN, Clark S, Caritis S, Miodovnik M, et al. Characteristics of women with nausea and vomiting of pregnancy who chose to continue compassionate use of placebo after a randomised trial. J Obstet Gynaecol 2013;33:557–60.
Maxwell CI, Hilden K, Delegge MH, Kinikini MM, Olafsson S, Fang JC. Feasibility of percutaneous direct jejunal feeding tubes in pregnant patients. Gastrointest Endosc 2010;71:AB268–9.
McCauley L, Coleman S, Jacques D, Palmer B, Stanziano G. Safety and efficacy of ondansetron therapy for nausea and vomiting of pregnancy. Obstet Gynecol 2002;99:24S.
Milkovich L, van den Berg BJ. An evaluation of the teratogenicity of certain antinauseant drugs. Am J Obstet Gynecol 1976;125:244–8.
Munch S. A qualitative analysis of physician humanism: women’s experiences with hyperemesis gravidarum. J Perinatol 2000;20:540–7.
Munch S, Schmitz MF. The Hyperemesis Beliefs Scale (HBS): a new instrument for assessing beliefs about severe nausea and vomiting in pregnancy. J Psychosom Obstet Gynaecol 2007;28:219–29.
Nelson-Piercy C, De Swiet M. Corticosteroids for the treatment of hyperemesis gravidarum. Br J Obstet Gynaecol 1994;101:1013.
Norheim AJ, Pedersen EJ, Fonnebo V, Berge L. Acupressure treatment of morning sickness in pregnancy. A randomised, double-blind, placebo-controlled study. Scand J Prim Health Care 2001;19:43–7.
Nulman I, Rovet J, Barrera M, Knittel-Keren D, Feldman BM, Koren G. Long-term neurodevelopment of children exposed to maternal nausea and vomiting of pregnancy and diclectin. J Pediatr 2009;155:45–50,e1–2.
Onghena G, De ROM. [Clinical study of prochlorperazine in hyperemesis gravidarum.] Brux Med 1960;40:1551–4.
Palatty PL, Haniadka R, Valder B, Arora R, Baliga MS. Ginger in the prevention of nausea and vomiting: a review. Clin Rev Food Sci Nutr 2013;53:659–69.
Pasquinucci C. [Association of vitamins B 1 and B 6 in high doses in therapy of hyperemesis gravidarum.] Ann Ostet Ginecol Med Perinat 1965;87:65–70.
Pasternak B, Svanstrom H, Molgaard-Nielsen D, Melbye M, Hviid A. Metoclopramide in pregnancy and risk of major congenital malformations and fetal death. JAMA 2013;310:1601–11.
Pasternak B, Svanstrom H, Hviid A. Ondansetron in pregnancy and risk of adverse fetal outcomes. N Engl J Med 2013;368:814–23.
Portnoi G, Chng LA, Karimi-Tabesh L, Koren G, Tan MP, Einarson A. Prospective comparative study of the safety and effectiveness of ginger for the treatment of nausea and vomiting in pregnancy. Am J Obstet Gynecol 2003;189:1374–7.
Puangsricharern A, Mahasukhon S. Effectiveness of auricular acupressure in the treatment of nausea and vomiting in early pregnancy. J Med Assoc Thai 2008;91:1633–8.
Seidner HM. Nausea and vomiting of pregnancy; preliminary trial of bonamine in sixteen patients. Ill Med J 1956;109:20–1.
Shrim A, Boskovic R, Maltepe C, Navios Y, Garcia-Bournissen F, Koren G. Pregnancy outcome following use of large doses of vitamin B6 in the first trimester. J Obstet Gynaecol 2006;26:749–51.
Slotnick RN. Safe, successful nausea suppression in early pregnancy with P-6 acustimulation. J Reprod Med 2001;46:811–14.
Smith C, Crowther C. The placebo response and effect of time in a trial of acupuncture to treat nausea and vomiting in early pregnancy. Complement Ther Med 2002;10:210–16.
Smith C, Crowther C, Beilby J. Pregnancy outcome following women’s participation in a randomised controlled trial of acupuncture to treat nausea and vomiting in early pregnancy. Complement Ther Med 2002;10:78–83.
Sorensen HT, Nielsen GL, Christensen K, Tage-Jensen U, Ekbom A, Baron J. Birth outcome following maternal use of metoclopramide. The Euromap study group. Br J Clin Pharmacol 2000;49:264–8.
Stainton MC, Neff EJ. The efficacy of SeaBands for the control of nausea and vomiting in pregnancy. Health Care Women Int 1994;15:563–75.
Subramaniam R, Soh EB, Dhillon HK, Abidin HZ. Total parenteral nutrition (TPN) and steroid usage in the management of hyperemesis gravidarum. Aust N Z J Obstet Gynaecol 1998;38:339–41.
Taylor R. Successful management of hyperemesis gravidarum using steroid therapy. QJM 1996;89:103–7.
Tompsett H, Ajala T, Dixon G, Kelly T. The implementation of an ambulatory care bundle for the treatment of hyperemesis gravidarum. BJOG 2013;120:477.
Trovik J, Haram K, Berstad A, Flaatten H. [Nasoenteral tube feeding in hyperemesis gravidarum. An alternative to parenteral nutrition.] Tidsskr Nor Laegeforen 1996;116:2442–4.
Vaisman N, Kaidar R, Levin I, Lessing JB. Nasojejunal feeding in hyperemesis gravidarum – a preliminary study. Clin Nutr 2004;23:53–7.
Wang Y, Lin Y, Wu X. The effect of total parenteral nutrition on hyperemesis gravidarum and pregnancy ending. Clin Med China 2001;8:63–4.
Weinstein BB, Wohl Z, Mitchell GJ, Sustendal GF. Oral administration of pyridoxme hydrochloride in the treatment of nausea and vomiting of pregnancy. Amur J Obstet Gynecol 1944;47:389–94.
Westfall RE, Janssen PA, Lucas P, Capler R. Survey of medicinal cannabis use among childbearing women: patterns of its use in pregnancy and retroactive self-assessment of its efficacy against ‘morning sickness’. Complement Ther Clin Pract 2006;12:27–33.
Whittaker R. Randomised, Double-Blind, Placebo-Controlled Trial of Corticosteroids for the Treatment of Hyperemesis Gravidarum. 2003. URL: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/519/CN-00473519/frame.html
Required participant inclusion criteria not met (n = 34)
Atanackovic G, Navioz Y, Moretti ME, Koren G. The safety of higher than standard dose of doxylamine-pyridoxine (Diclectin) for nausea and vomiting of pregnancy. J Clin Pharmacol 2001;41:842–5.
Bethea RC. Evaluation of a combination of meclizine and pyridoxine in the control of nausea and vomiting in pregnancy. Int Rec Med 1960;173:283–7.
Bisley BL, Kay CR. Anti-emetic effects of a phenothiazine compared with an antihistamine. Practitioner 1964;193:358–60.
Boneva RS, Moore CA, Botto L, Wong LY, Erickson JD. Nausea of Pregnancy, Antinausea Preparations and Congenital Heart Defects: A Population-Based Case–Control Study. In Koren G, Bishai R, editors. Nausea and Vomiting of Pregnancy: State of the Art 2000. Toronto: Hospital Sick Children, Motherisk Program; 2000. pp. 60–72.
Christer C. Manual acupuncture at pc6 reduces hyperemesis gravidarum-a placebo-controlled randomised crossover study. Akupunktur 1998;26:261–2.
Coleman L, O’Sullivan M, Dilloway L, Sinha A, Epee M. An innovative ambulatory care service for women suffering with hyperemesis gravidarum. BJOG 2014;121:19.
Cottin J, Beghin D, Jonville-Bera AP, Boyer M, Zenut M, Damase-Michel C, et al. First trimester exposure to domperidone: a comparative prospective study. Fundam Clin Pharm 2013;27:44.
Czeizel AE, Dudas I, Fritz G, Tecsoi A, Hanck A, Kunovits G. The effect of periconceptional multivitamin-mineral supplementation on vertigo, nausea and vomiting in the first trimester of pregnancy. Arch Gynecol Obstet 1992;251:181–5.
Dorsey CW. The use of pyridoxine and suprarenal cortex combined in the treatment of nausea and vomiting of pregnancy. Am J Obstet Gynecol 1949;58:1073–8.
Duggar CR, Carlan SJ. The efficacy of methylprednisolone in the treatment of hyperemesis gravidarum: a randomized double-blind controlled study. Obstet Gynecol 2001;97:45.
Dundee JW, Sourial FB, Ghaly RG, Bell PF. P6 acupressure reduces morning sickness. J R Soc Med 1988;81:456–7.
Durham MP. Clinical trial of buclizine hydrochloride for vomiting of pregnancy. Br Med J 1956;2:1276–7.
Eriksson G, Jullig D, Tysk U. [Postadoxin-a new remedy for nausea and emesis gravidarum. A clinical test with the double-blind method.] Sven Lakartidn 1961;58:1722–5.
Fletcher SJ, Waterman H, Nelson L, Carter LA, Chuang LH, Roberts C, et al. The effectiveness and cost-effectiveness of a holistic assessment and individualised package of care of women with hyperemesis gravidarum: randomised controlled trial. BJOG 2013;120:552–3.
Ge Q. The therapeutic effect of intravenous nutritional solution combined with psychological interventions on 100 cases of hyperemesis gravidarum. China J Health Psychol 2012;9:1322–4.
Gill SK, Maltepe C, Koren G. The effectiveness of discontinuing iron-containing prenatal multivitamins on reducing the severity of nausea and vomiting of pregnancy. J Obstet Gynaecol 2009;29:13–16.
Hart BF, McConnell WT, Pickett AN. Vitamin and endocrine therapy in nausea and vomiting of pregnancy. Am J Obstet Gynecol 1944;48:251–3.
He XL, Zhong G, He Y. [Clinical observation on treatment of hyperemesis gravidarum by integrative Chinese and Western medicine and its influence on serum motilin.] Zhongguo Zhong Xi Yi Jie He Za Zhi 2009;29:872–4.
Henker FO III. Psychotherapy as adjunct in treatment of vomiting during pregnancy. South Med J 1976;69:1585–7.
Klauser CK, Fox NS, Istwan N, Rhea D, Rebarber A, Desch C, et al. Treatment of severe nausea and vomiting of pregnancy with subcutaneous medications. Am J Perinatol 2011;28:715–21.
Koren G, Maltepe C. Pre-emptive therapy for severe nausea and vomiting of pregnancy and hyperemesis gravidarum. J Obstet Gynaecol 2004;24:530–3.
Lacasse A, Lagoutte A, Ferreira E, Berard A. Metoclopramide and diphenhydramine in the treatment of hyperemesis gravidarum: effectiveness and predictors of rehospitalisation. Eur J Obstet Gynecol Reprod Biol 2009;143:43–9.
Lacasse A, Lagoutte A, Ferreira E, Berard A. Metoclopramide and diphenhydramine in the treatment of hyperemesis gravidarum: effectiveness, safety, and predictors of rehospitalisation. Pharmacoepidem Dr S 2007;16:S146–S7.
Liu S-J. Clinical study on TCM and acupuncture combined treating hyperemesis gravidarum. LNUTCM 2007;6:145–6.
Modares M, Besharat S, Kian FR, Besharat S, Mahmoudi M, Sourmaghi HS. Effect of ginger and chamomile capsules on nausea and vomiting in pregnancy. J Gorgan Uni Med Sci 2012;14:e46–e50.
Mulla NP. Evaluation of trimethobenzamide with pyridoxine in nausea and vomiting of pregnancy. Clin Med 1963;70:2052–4.
Newlinds JS. Nausea and vomiting in pregnancy: a trial of thiethylperazine. Med J Aust 1964;1:234–6.
O’Brien B, Relyea MJ, Taerum T. Efficacy of P6 acupressure in the treatment of nausea and vomiting during pregnancy. Am J Obstet Gynecol 1996;174:708–15.
Price JJ, Barry MC. A double blind study of fluphenazine with pyridoxine. Pa Med J 1964;67:37–40.
Shin HS, Song YA, Seo S. Effect of Nei-Guan point (P6) acupressure on ketonuria levels, nausea and vomiting in women with hyperemesis gravidarum. J Adv Nurs 2007;59:510–19.
Shin HS, Song YA. [The effect of P6 acupressure for symptom control in pregnant women having hyperemesis gravidarum.] Taehan Kanho Hakhoe Chi 2005;35:593–601.
Sullivan CL. Treatment of nausea and vomiting of pregnancy with chlorpromazine; a report of 100 cases. Postgrad Med 1957;22:429–32.
Yavari Kia P, Safajou F, Shahnazi M, Nazemiyeh H. The effect of lemon inhalation aromatherapy on nausea and vomiting of pregnancy: a double-blinded, randomized, controlled clinical trial. Iran 2014;16:e14360.
Zhu Z-N, Fa Y-H, Wang C-R. Injection plus acupuncture clinical observation hyperemesis gravidarum 44 cases. J Pract Tradit Chinese Intern Med 2011;6:129–30.
Required outcomes not reported (n = 34)
Albertazzi E, Bellodi P, Guerzoni G. Phosphorate carbohydrate solutions in the treatment of vomiting in pregnancy. Curr Ther Res Clin E 1989;46:1059–67.
Anderka M, Mitchell AA, Louik C, Werler MM, Hernandez-Diaz S, Rasmussen SA, et al. Medications used to treat nausea and vomiting of pregnancy and the risk of selected birth defects. Birth Defects Res Part A Clin Mol Teratol 2012;94:22–30.
Andersen JT, Jimenez-Solem E, Andersen NL, Poulsen HE. Ondansetron use in early pregnancy and the risk of congenital malformations-a register based nationwide cohort study. Pharmacoepidem Dr S 2013;22:13–14.
Aselton P, Jick H, Chentow SJ, Perera DR, Hunter JR, Rothman KJ. Pyloric stenosis and maternal Bendectin exposure. Am J Epidemiol 1984;120:251–6.
Asker C, Norstedt Wikner B, Kallen B. Use of antiemetic drugs during pregnancy in Sweden. Eur J Clin Pharmacol 2005;61:899–906.
Babaee PAG. Determining the effect of pyridoxine on nausea and vomiting in pregnancy. J Matern Fetal Neonatal Med 2010;23:129.
Balsamo SB, Sampaio LF, Nobre Nde S, Rozas A, Barros HC, Neme B. [Clinical trial of thiethylperazine (Torecan).] Hospital (Rio J) 1966;70:451–7.
Berkovitch M, Mazzota P, Greenberg R, Elbirt D, Addis A, Schuler-Faccini L, et al. Metoclopramide for nausea and vomiting of pregnancy: a prospective multicenter international study. Am J Perinatol 2002;19:311–16.
Bsat FA, Hoffman DE, Seubert DE. Comparison of three outpatient regimens in the management of nausea and vomiting in pregnancy. J Perinatol 2003;23:531–5.
Costantine MM, Matok I, Chiossi G, Clark S, Miodovnik M, Umans JG, et al. Determinants of adherence to delayed-release doxylamine and pyridoxine in patients with nausea and vomiting of pregnancy. Ther Drug Monit 2012;34:569–73.
de Aloysio D, Penacchioni P. Morning sickness control in early pregnancy by Neiguan point acupressure. Obstet Gynecol 1992;80:852–4.
Farazmand T, Khadem N. Comparison of the effect of methylprednisolone and promethazine in the treatment of hyperemesis gravidarum (2001–2002). Int J Gynecol Obstet 2009;107:S523.
Folk JJ, Leslie-Brown HF, Nosovitch JT, Silverman RK, Aubry RH. Hyperemesis gravidarum: outcomes and complications with and without total parenteral nutrition. J Reprod Med 2004;49:497–502.
Fuchs K, Paldi E, Abramovici H, Peretz BA. Treatment of hyperemesis gravidarum by hypnosis. Int J Clin Exp Hyp 1980;28:313–23.
Gant H, Reinken L, Dapunt O, Scholz K. Vitamin B-6 depletion in hyperemesis gravidarum. Wiener Klinische Wochenschrift 1975;87:510–13.
Gawande S, Vaidya M, Tadke R, Kirpekar V, Bhave S. Progressive muscle relaxation in hyperemesis gravidarum. SAFOG 2011;3:28–32.
Habek D, Barbir A, Habek JC, Janculiak D, Bobic-Vukovic M. Success of acupuncture and acupressure of the Pc 6 acupoint in the treatment of hyperemesis gravidarum. Forsch Komplementarmed Klass Naturheilkd 2004;11:20–3.
Hasbun J, Charlin V, Von Mulhenbrock R, Munoz H, Yuri C. [Total parenteral nutrition in severe hyperemesis gravidarum.] Rev Chil Obstet Ginecol 1994;59:378–82.
Heazell AEP, Langford N, Judge JK, Heazell MA, Downey GP. The use of levomepromazine in hyperemesis gravidarum resistant to drug therapy – a case series. Reprod Toxicol 2005;20:569–72.
Holmgren C, Aagaard-Tillery KM, Silver RM, Porter TF, Varner M. Hyperemesis in pregnancy: an evaluation of treatment strategies with maternal and neonatal outcomes. Am J Obstet Gynecol 2008;198:56.e1–4.
Kutcher JS, Engle A, Firth J, Lamm SH. Bendectin and birth defects. II: Ecological analyses. Birth Defects Res Part A Clin Mol Teratol 2003;67:88–97.
Lacasse A, Rey E, Ferreira E, Morin C, Berard A. Nausea and vomiting of pregnancy: what about quality of life? BJOG 2008;115:1484–93.
Levine MG, Esser D. Total parenteral nutrition for the treatment of severe hyperemesis gravidarum: maternal nutritional effects and fetal outcome. Obstet Gynecol 1988;72:102–7.
Lombardi DG, Istwan NB, Rhea DJ, O’Brien JM, Barton JR. Measuring outpatient outcomes of emesis and nausea management in pregnant women. Manag Care 2004;13:48–52.
Matok I, Gorodischer R, Koren G, Sheiner E, Wiznitzer A, Levy A. The safety of metoclopramide use in the first trimester of pregnancy. N Engl J Med 2009;360:2528–35.
Moessner GF. Clinical evaluation of a meprobamate–promazine combination for control of nausea and vomiting in pregnancy; a preliminary report. West J Surg Obstet Gynecol 1959;67:180–2.
Paridokht A, Gholamreza B. Determine effect VB6 on nausea and vomiting of pregnancy. J Matern Fetal Neonatal Med 2010;23:127–8.
Reyhani M, Eskandari M. Evaluation of the achillea millefolum effect in nausea and vomiting of early pregnancy. Iran J Pharmaceut Res 2013;12:232.
Rotman J. [Clinical trial of plitican in vomiting of pregnancy.] Semaine des Hopitaux 1986;62:138–40.
Tabatabaii A, Sekhavat L, Mojibian M. A randomized, placebo-controlled trial of corticosteroids for hyperemesis gravidarum. J Matern Fetal Neonatal Med 2008;21:225.
Tasci Y, Demir B, Dilbaz S, Haberal A. Use of diazepam for hyperemesis gravidarum. J Matern Fetal Neonatal Med 2009;22:353–6.
Wheatley D. Treatment of pregnancy sickness. Br J Obstet Gynaecol 1977;84:444–7.
Xu C-Z. The clinical study of 654-II in treating hyperemesis gravidarum. Hebei Medicine 2005;10:923–4.
Ylikorkala O, Kauppila A, Ollanketo ML. Intramuscular ACTH or placebo in the treatment of hyperemesis gravidarum. Acta Obstet Gynecol Scand 1979;58:453–5.
Appendix 7 UK Teratology Information Service enquiries and follow-ups relating to hyperemesis gravidarum/nausea and vomiting in pregnancy medication
UK Teratology Information Service follow-up data
Ginger
The UKTIS has followed up a single prospective case of ginger exposure during pregnancy. Ginger exposure occurred at an unknown stage of pregnancy and the outcome was a live-born infant with no reported congenital malformations or neonatal problems. 152
Vitamin B12
The UKTIS has followed up 21 cases of vitamin B12 (hydroxocobalamin and cyanocobalamin) exposure during pregnancy. There were 20 prospective therapeutic exposures and one retrospective case. 153
Prospective therapeutic exposure data
The frequency of congenital malformations in live-born infants (0/21; 0%, 95% CI 0% to 19.2%) was not significantly higher than the background rate. However, due to the small numbers of cases and wide CIs due to the consequent uncertainty, the conclusions that can be drawn from these data are limited.
Retrospective therapeutic exposure data
The UKTIS occasionally receives retrospective information on the outcome of pregnancies. Although retrospective reports are biased in that adverse outcomes are more likely to be reported, these data may be useful in identifying patterns of malformations that may be suggestive of a teratogenic syndrome and are therefore analysed periodically.
The UKTIS have retrospective follow-up data for one pregnancy following therapeutic exposure to vitamin B12 at 5 weeks. The infant had microcephaly and dysmorphic facial features.
Vitamin B6 (pyridoxine)
The UKTIS has followed up 23 cases of pyridoxine exposure during pregnancy including 18 prospective therapeutic exposures, three overdoses and two retrospective cases. 154
Prospective therapeutic exposure data
The frequency of congenital malformations in live-born infants (3/15; 20%, 95% CI 5.3% to 48.6%) was significantly higher than the background rate; however, the numbers involved are very small and no pattern of malformation was observed. One of the malformations reported is an inherited disorder (Apert syndrome) and not expected to be linked to the maternal exposure.
Prospective overdose data
The UKTIS have collected prospective follow up data on three pregnancies in which pyridoxine was taken in overdose (amounts ingested ranged from 1250 mg to 3500 mg). The outcomes were two healthy babies and one elective termination.
Retrospective therapeutic exposure data
The UKTIS have retrospective follow-up data for two pregnancies following therapeutic exposure to pyridoxine. In the first case, exposure to an unreported amount of pyridoxine occurred between 11 and 15 weeks’ gestation. The outcome was an infant with multiple congenital anomalies including a bent ulna with a malformed hand, polydactyly on the other hand, and one leg with talipes and abnormal digits. In the second case maternal use of 50-mg pyridoxine per day throughout pregnancy resulted in an infant delivered with polydactyly. In addition to the pyridoxine, 20-mg paroxetine was taken each day throughout pregnancy, and 600-mg rifampicin and 300-mg isoniazid was administered per day from 0 to 12 weeks’ gestation.
Promethazine
The UKTIS has followed up 67 cases of promethazine exposure during pregnancy. There were 45 prospective therapeutic exposures, 15 overdoses and seven retrospective cases. 155
Prospective therapeutic exposure data
The frequency of congenital malformations in live-born infants (2/41; 4.9%, 95% CI 0.85% to 17.8%) was not significantly higher than the background rate.
Retrospective exposure data
The UKTIS have retrospective follow-up data for seven pregnancies following exposure to promethazine, six therapeutic and one overdose. Malformations were reported in all cases but showed no consistent pattern suggestive of teratogenesis.
Ondansetron
The UKTIS has followed up 48 cases of ondansetron exposure during pregnancy. There were 42 prospective therapeutic exposures and six retrospective cases. 156
Prospective therapeutic exposure data
The frequency of live-born infants with one or more major congenital malformation (1/34; 2.9%, 95% CI 0.15% to 17.1%) was not significantly higher than the background rate (2–3%).
Retrospective therapeutic exposure data
The UKTIS occasionally receives retrospective information on the outcome of pregnancies. These data are analysed periodically to look for patterns of malformations (Table 42). No specific pattern has been observed for ondansetron. The UKTIS have retrospective follow-up data for six pregnancies following therapeutic exposure to ondansetron.
| Drugs | Total number of enquiries | Annual enquiries by 5-year period | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total number of enquiries for exposure | Enquiries for which indication was HG | HG enquiries for which pregnancy outcome knowna | Pre 1990 | 1990–4 | 1995–9 | 2000–4 | 2005–9 | 2010–14b | |
| Calcium carbonate | 188 | 1 | 0 | – | – | – | – | 1 | – |
| Cetirizine | 356 | 6 | 3 | – | – | 1 | – | 3 | 2 |
| Cyclizine (Valoid) | 433 | 221 | 58 | – | – | 7 | 36 | 79 | 99 |
| Dimenhydrinate (Dramamine®, Prestige Brands Holdings, Inc.) | 4 | 1 | 1 | – | – | – | – | – | 1 |
| Diphenhydramine | 68 | 2 | 1 | – | 1 | 1 | – | – | – |
| Doxylamine | 12 | 3 | 1 | – | – | – | – | 1 | 2 |
| Doxylamine succinate-pyridoxine hydrochloride | 2 | 1 | 0 | – | – | – | – | 1 | – |
| Hydroxyzine | 62 | 2 | 0 | – | – | – | 1 | 1 | – |
| Hydrocortisone | 265 | 19 | 4 | – | – | – | 6 | 12 | 1 |
| Methylprednisolone | 58 | 2 | 0 | – | – | – | 1 | – | 1 |
| Metoclopramide | 278 | 108 | 33 | – | 2 | 7 | 17 | 43 | 39 |
| Ondansetron | 235 | 140 | 33 | – | – | 8 | 17 | 53 | 62 |
| Peppermint | 76 | 1 | 0 | – | – | – | – | 1 | – |
| Prednisolone | 559 | 21 | 8 | – | – | 1 | 5 | 10 | 5 |
| Prochlorperazine (Stemetil, Sanofi) | 426 | 207 | 43 | – | 9 | 11 | 35 | 92 | 60 |
| Promethazine (Avomine, Manx Healthcare Ltd, Phenergan) | 405 | 93 | 28 | 1 | 7 | 4 | 16 | 31 | 34 |
| Pyridoxine (vitamin B6) | 100 | 12 | 6 | 1 | – | – | – | 8 | 3 |
| Ranitidine | 377 | 35 | 17 | – | 2 | 7 | 8 | 10 | 8 |
| Thiamine | 97 | 18 | 7 | – | – | 2 | 3 | 12 | 1 |
| Vitamin B12 (cyanocobalamin) | 144 | 2 | 2 | – | – | – | – | – | 2 |
| Total enquiries | – | – | 219a | 2 | 21 | 49 | 145 | 358 | 320a |
Appendix 8 Secondary outcome data
| Study | Pregnancy outcomes | Other outcomes |
|---|---|---|
| Abas 201457 |
|
|
| Adamczak 200758 |
|
|
| Alalade 2007120 |
|
|
| Ashkenazi-Hoffnung 201336 |
|
|
| Babaei 201459 |
|
|
| Basirat 200960 |
|
|
| Bayreuther 199461 |
|
|
| Belluomini 199462 |
|
|
| Biswas 201163 |
|
|
| Bondok 200664 |
|
|
| Capp 201465 |
|
|
| Can Gurkan 200843 |
|
|
| Carlsson 200066 |
|
|
| Chittumma 200767 |
|
|
| Diggory 196268 |
|
|
| Ditto 199969 |
|
|
| Eftekhari 201372 |
|
|
| Einarson 2004121 |
|
|
| Ensiyeh 200970 |
|
|
| Erez 197171 |
|
|
| Evans 199373 |
|
|
| Ferreira 2003122 |
|
|
| Fischer-Rasmussen 199174 |
|
|
| Ghahiri 201175 |
|
|
| Ghani 201376 |
|
|
| Guttuso 201039 |
|
|
| Haji Seid Javadi 201377 |
|
|
| Heazell 200678 |
|
|
| Hsu 1996123 |
|
|
| Hsu 200379 |
|
|
| Jamigorn 200780 |
|
|
| Kashifard 201381 |
|
|
| Keating 200282 |
|
|
| Knight 200183 |
|
|
| Koren 201084 |
|
|
| Koren 2013127 |
|
|
| Maina 201485 |
|
|
| Maltepe 201386 |
|
|
| Mao 200987 |
|
|
| Markose 2004124 |
|
|
| McParlin 200888 |
|
|
| Mohammadbeigi 201189 |
|
|
| Monias 195790 |
|
|
| Moran 2002125 |
|
|
| Naeimi Rad 201291 |
|
|
| Narenji 201292 |
|
|
| Nelson-Piercy 200193 |
|
|
| Neri 200594 |
|
|
| Oliveira 201395 |
|
|
| Ozgoli 200996 |
|
|
| Pasha 201297 |
|
|
| Pongrojpaw 200742 |
|
|
| Rosen 200398 |
|
|
| Saberi 201313 |
|
|
| Safari 199899 |
|
|
| Saha 2009126 |
|
|
| Sahakian 1991100 |
|
|
| Smith 2002101 |
|
|
| Smith 2004102 |
|
|
| Sripramote 2003103 |
|
|
| Steele 2001104 |
|
|
| Sullivan 1996105 |
|
|
| Tan 2009107 |
|
|
| Tan 2010106 |
|
|
| Tan 2013108 |
|
|
| Veciana 2001109 |
|
|
| Vutyavanich 199541 |
|
|
| Vutyavanich 2001110 |
|
|
| Werntoft 2001111 |
|
|
| Wibowo 2012112 |
|
|
| Willetts 2003113 |
|
|
| Yost 2003114 |
|
|
| Zhang 2005115 |
|
|
| Ziaei 2004116 |
|
|
Appendix 9 Systematic review of published economic evaluations: inclusion criteria
A systematic review to identify any existing economic studies will be undertaken. The method will be similar to the review of clinical effectiveness studies except that (i) the inclusion criteria for study design will target cost analysis, cost-effectiveness, cost–utility, cost–consequence and cost–benefit studies; decision model-based analyses and outcomes will be QoL, costs and incremental cost-effectiveness ratios; (ii) quality assessment will be appropriate to the study design, for example the Consensus on Health Economic Criteria list130 for economic evaluations and the Philips checklist131 for model-based analyses; (iii) data considered relevant will be extracted. If available, economic models will be reviewed and utilised where appropriate to inform a model-based economic evaluation based on the above proposed systematic review.
Appendix 10 Cost of drug interventions and recommended daily doses
| Preparation | Patient-initiated first-line intervention | Low-estimate weekly cost | High-estimate weekly cost |
|---|---|---|---|
| Tablets | Vitamin B6: pyridoxine hydrochloride (non-proprietary) | £0.12 | £2.59 |
| Tablets | Vitamin B12: cyanocobalamin (non-proprietary) | £0.87 | £2.62 |
| Solution | Ginger (FortiCare) | NE | £2.21 (assumes 125 ml per week) |
| Physical therapy | Acupressure/acupuncture | NE | First appointment: £50–70a Subsequent appointments: £35–50a |
| Hypnosis | Hypnotherapy | NE | £50–90 for a private hypnotherapy sessiona |
| Preparation | Clinician-prescribed second-line interventions | Low-estimate weekly cost | High-estimate weekly cost |
| Antihistamines | |||
| Tablets | Hydroxyzine: Atarax® (Alliance) | £0.91 | £1.22 |
| Tablets | Cyclizine (non-proprietary) | £0.74 | £2.22 |
| i.v./i.m. injection | Cyclizine: Valoid | NE | £13.65 |
| Tablets | Dimenhydrinate: Arlevert® (Hennig Arzneimittel) | NE | £5.04 |
| Tablets | Chlorpromazine (non-proprietary) | NE | £1.55 |
| i.v./i.m. injection | Chlorpromazine (non-proprietary) | £12.60 | £33.60 |
| Tablets | Codeine phosphate (non-proprietary) | £1.09 | £2.24 |
| i.v./i.m. injection | Codeine phosphate (non-proprietary) | £24.89 | £49.77 |
| Capsules | Benadryl: acrivastine (non-proprietary) | NE | £4.16 |
| Tablets | Cetirizine (non-proprietary) | NE | £0.24 |
| Dopamine antagonists | |||
| Tablets | Promethazine: Phenergan | £0.74 | £2.22 |
| i.v./i.m. injection | Promethazine (non-proprietary) | £0.68 (daily)a | £1.20 (daily)a |
| Tablets | Prochlorperazine (non-proprietary) | £0.47 | £1.42 |
| i.v./i.m. injection | Prochlorperazine (non-proprietary) | NE | £0.52 (daily)a |
| Tablets | Domperidone (non-proprietary) | £0.39 | £1.17 |
| Tablets | Metoclopramide (non-proprietary) | £0.22 | £0.66 |
| i.v./i.m. injection | Metoclopramide (non-proprietary) | £2.24 | £6.72 |
| Serotonin antagonists | |||
| Tablets | Ondansetron (non-proprietary) | NE | £8.69 (daily)a |
| i.v./i.m. injection | Ondansetron (non-proprietary) | NE | £1.00 (daily)a |
| Other drugs | |||
| Tablets | Antiepileptic: gabapentin (non-proprietary) | £0.34 | £1.03 |
| Tablets | Diazepam | £0.64 | £0.70 |
| i.v./i.m. injection | Diazepam (non-proprietary) | £0.90 (daily)a | £1.80 (daily)a |
| Rectal tubes | Diazepam (non-proprietary): assume weight of 60 kg | NE | £41.10 (every 12 hours as required)a |
| Tablets | Dicycloverine (non-proprietary) | £12.64 | £15.88 |
| Preparation | Clinician-prescribed third-line interventions | Low-estimate weekly cost | High-estimate weekly cost |
| Corticosteroids | |||
| Tablets | Methylprednisolone: medrone | £0.91 | £10.02 |
| i.v./i.m. injection | Methylprednisolone: Solu-Medrone | NE | £17.30 (daily)a |
| Tablets | Prednisone: Lodotra | £12.46 | £24.92 |
| Tablets | Prednisolone (non-proprietary) | £0.67 | £1.33 |
| i.v./i.m. injection | Prednisolone acetate: Deltastab® (Amdipharm Mercury Company Ltd) | £6.87 | £54.96 |
| Rectal foam | Prednisolone (non-proprietary) | £34 | £68 |
| Tablets | Hydrocortisone (non-proprietary) | £17.03 | £29.05 |
| i.v./i.m. injection | Hydrocortisone: Efcortesol | £3.24 (daily)a | £19.56 (daily)a |
| Preparation | Patient-initiated first-line interventions | Recommended daily dose (low estimate) | Recommended daily dose (high estimate) | Unit cost |
|---|---|---|---|---|
| Tablets | Vitamin B6 | 20 mg × 3 | 50 mg × 3 | 10 mg, net price 500 = £8.48; 20 mg, net price 500 = £8.53; 50 mg, net price 28 = £3.46 |
| Tablets | Vitamin B12 | 50 µg | 150 µg | 50 µg, net price 50 = £6.24 |
| Solution | Ginger (FortiCare) | 125 ml weeklya | NE | Bottle, 4 × 125 ml = £8.84 |
| Antihistamines | ||||
| Tablets | Hydroxyzine: Atarax | 25 mg × 3 | 25 mg × 4 | 10 mg, net price 84 = £2.18; 25 mg, net price 28 = £1.22 |
| Tablets | Cyclizine (non-proprietary) | 50 mg | 50 mg × 3 | 50 mg, net price 100 = £10.58 |
| i.v./i.m. injection | Cyclizine: Valoid | NE | 50 mg × 3 | 50 mg/ml, 1-ml ampoule = £0.65 |
| Tablets | Dimenhydrinate: Arlevert | NE | 30 mg × 3 | Cinnarizine 20 mg, dimenhydrinate 40 mg, net price 100 = £24.00 |
| Tablets | Chlorpromazine (non-proprietary) | NE | 25 mg × 3 | 25 mg, net price 28 = £2.07; 50 mg, net price 28 = £2.21; 100 mg, net price 28 = £2.21 |
| i.v./i.m. injection | Chlorpromazine (non-proprietary) | 25 mg × 3 | 50 mg × 4 | 25 mg/ml, 1-ml ampoule = £0.60 |
| Tablets | Codeine phosphate (non-proprietary) | 30 mg × 3 | 60 mg × 3 | 15 mg, net price 28 = £1.23; 30 mg, net price 28 = £1.46; 60 mg, net price 28 = £2.99 |
| i.v./i.m. injection | Codeine phosphate (non-proprietary) | 30 mg × 3 | 60 mg × 3 | 60 mg/ml, 1-ml ampoule = £2.37 |
| Capsules | Benadryl: Acrivastine (non-proprietary) | NE | 8 mg × 3 | 8 mg, 12 capsule pack = £2.75; 8 mg, 24 capsule pack = £4.76 |
| Tablets | Cetirizine (non-proprietary) | NE | 10 mg | 10 mg, net price 30 = £1.01 |
| Dopamine antagonists | ||||
| Tablets | Promethazine: Phenergan | 10 mg × 2 | 20 mg × 3 | 10 mg, net price 56 = £2.96; 25 mg, net price 56 = £4.65 |
| i.v./i.m. injection | Promethazine (non-proprietary) | 25 mg | 50 mg | 25 mg/ml, 1-ml ampoule = £0.68; 25 mg/ml, 2-ml ampoule = £1.20 |
| Tablets | Prochlorperazine (non-proprietary) | 5 mg × 2 | 10 mg × 3 | 5 mg, net price 28 = £0.95; 5 mg, net price 84 = £1.37 |
| i.v./i.m. injection | Prochlorperazine (non-proprietary) | 12.5 mg (when required)a | NE | 12.5 mg/ml, 1-ml ampoule = £0.52 |
| Tablets | Domperidone (non-proprietary) | 10 mg | 10 mg × 3 | 10 mg, net price 30 = £1.67; 10 mg, net price 100 = £5.57 |
| Tablets | Metoclopramide (non-proprietary) | 10 mg | 10 mg × 3 | 10 mg, net price 28 = £0.88 |
| i.v./i.m. injection | Metoclopramide (non-proprietary) | 10 mg | 10 mg × 3 | 5 mg/ml, 2-ml ampoule = £0.32 |
| Serotonin antagonists | ||||
| Tablets | Ondansetron (non-proprietary) | NE | 16 mg | 4 mg, net price 30 = £5.37; 8 mg, net price 10 = £43.43 |
| i.v./i.m. injection | Ondansetron (non-proprietary) | NE | 4 mg | 2 mg/ml, 2-ml ampoule = £1.00 |
| Other drugs | ||||
| Tablets | Antiepileptic: gabapentin (non-proprietary) | 300 mg | 300 mg × 3 | 600 mg, net price 100 = £9.81; 800 mg, net price 100 = £32.22 |
| Tablets | Diazepam | 2 mg × 3 | 30 mg | 2 mg, net price 28 = £0.86; 5 mg, net price 28 = £0.88; 10 mg, net price 28 = £0.94 |
| i.v./i.m. injection | Diazepam (non-proprietary) | 5 mg × 4 | 10 mg × 4 | 5 mg/ml, 2-ml ampoule = £0.45 |
| Rectal tubes | Diazepam (non-proprietary): assume weight of 60 kg | 500 µg/kg (repeated after 12 hours as required)a | NE | 2 mg/ml, net price 1.25 ml (2.5 mg) tube = £1.13; 2.5 ml (5 mg) tube = £1.09; 4 mg/ml, 2.5 ml (10 mg) tube = £1.37 |
| Tablets | Dicycloverine (non-proprietary) | 10 mg × 3 | 20 mg × 3 | 10 mg, net price 100 = £60.19; 20 mg, net price 84 = £63.52 |
| Preparation | Clinician-prescribed third-line interventions | Recommended daily dose (low estimate) | Recommended daily dose (high estimate) | Unit cost |
| Corticosteroids | ||||
| Tablets | Methylprednisolone: Medrone | 2 mg | 40 mg | 2 mg, net price 30 = £3.88; 4 mg, net price 30 = £6.19; 16 mg, net price 30 = £17.17; 100 mg, net price 20 = £48.32 |
| i.v./i.m. injection | Methylprednisolone: Solu-Medrone | NE | 1 g | 40-mg vial = £1.58; 125-mg vial = £4.75; 500-mg vial = £9.60; 1-g vial = £17.30; 2 g vial = £32.86 |
| Tablets | Prednisone: Lodotra | 10 mg | 20 mg | 1 mg, net price 30 = £26.70; 2 mg, net price 30 = £26.70; 2 mg, net price 100 = £89.00; 5 mg, net price 30 = £26.70; 5 mg, net price 100 = £89.00 |
| Tablets | Prednisolone (non-proprietary) | 10 mg | 20 mg | 1 mg, net price 28 = £1.25; 5 mg, net price 28 = £1.33; 25 mg, net price 56 = £50.00 |
| i.v./i.m. injection | Prednisolone acetate: Deltastab | Varies according to sizea | NE | 25 mg/ml, 1-ml ampoule = £6.87 |
| Rectal foam | Prednisolone (non-proprietary) | 1-metred application (20 mg) | 1-metred application (20 mg) × 2 | 20 mg, 14 application canister = £68.00 |
| Tablets | Hydrocortisone (non-proprietary) | 20 mg | 30 mg | 10 mg, net price 30 = £51.46; 20 mg, net price 30 = £73.00 |
| i.v./i.m. injection | Hydrocortisone: Efcortesol | 100 mg × 3 | 500 mg × 4 | 100 mg/ml, 1-ml ampoule = £1.08; 5-ml ampoule = £4.89 |
| Pharmacological preparation | Patient-initiated first-line intervention | Total low-estimate weekly cost (£) | Total high-estimate weekly cost (£) |
|---|---|---|---|
| Tablets | Vitamin B6: pyridoxine hydrochloride (non-proprietary) | 0.12 | 2.59 |
| Tablets | Vitamin B12: cyanocobalamin (non-proprietary) | 0.87 | 2.62 |
| Solution | Ginger (FortiCare) | NE | 2.21 (assuming 125 ml per week) |
| Physical therapy | Acupressure/acupuncture | 35 | 50 |
| Hypnosis | Hypnotherapy | 50 | 90 |
| Pharmacological preparation | Patient-initiated first-line intervention | Total low-estimate weekly cost (£) | Total high-estimate weekly cost (£) | GP clinic consultation (£) | Urine ketones strip (£) | Total (£) |
|---|---|---|---|---|---|---|
| Tablets | Vitamin B6: pyridoxine hydrochloride (non-proprietary) | 0.12 | 2.59 | 45 | 0.05 | 45.17–47.64 |
| Tablets | Vitamin B12: cyanocobalamin (non-proprietary) | 0.87 | 2.62 | 45 | 0.05 | 45.92–47.67 |
| Solution | Ginger (FortiCare) | NE | 2.21 (assuming 125 ml per week) | 45 | 0.05 | 47.26 |
| Pharmacological preparation | Clinician-prescribed second-line intervention | Total low-estimate weekly cost (£) | Total high-estimate weekly cost (£) | GP clinic consultation (£) | Urine ketones strip (£) | Total (£) |
|---|---|---|---|---|---|---|
| Antihistamines | ||||||
| Tablets | Cyclizine (non-proprietary) | 0.74 | 2.22 | 45 | 0.05 | 45.79–47.27 |
| Tablets | Hydroxyzine: Atarax | 0.91 | 1.22 | 45 | 0.05 | 45.96–46.27 |
| Tablets | Dimenhydrinate: Arlevert | NE | 5.04 | 45 | 0.05 | 50.09 |
| Tablets | Chlorpromazine (non-proprietary) | NE | 1.55 | 45 | 0.05 | 46.60 |
| Tablets | Codeine phosphate (non-proprietary) | 1.09 | 2.24 | 45 | 0.05 | 46.14–47.29 |
| Capsules | Benadryl: acrivastine (non-proprietary) | NE | 4.16 | 45 | 0.05 | 49.21 |
| Tablets | Cetirizine (non-proprietary) | NE | 0.24 | 45 | 0.05 | 45.29 |
| Dopamine antagonists | ||||||
| Tablets | Domperidone (non-proprietary) | 0.39 | 1.17 | 45 | 0.05 | 45.44–46.22 |
| Tablets | Metoclopramide (non-proprietary) | 0.22 | 0.66 | 45 | 0.05 | 45.27–45.71 |
| Tablets | Prochlorperazine (non-proprietary) | 0.47 | 1.42 | 45 | 0.05 | 45.52–46.47 |
| Tablets | Promethazine: Phenergan | 0.74 | 2.22 | 45 | 0.05 | 45.79–47.27 |
| Serotonin antagonists | ||||||
| Tablets | Ondansetron (non-proprietary) | NE | 60.83 | 45 | 0.05 | 105.88 |
| Pharmacological preparation | Clinician-prescribed second-line interventions | Total low-estimate daily cost × 2 (£) | Total high-estimate daily cost × 2 (£) | Inpatient excess bed-days × 2 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Treatment for thromboembolism (1-night stay) (£) | Thiamine supplement (Pabrinex) × 1 (£) | Normal saline + a proportional amount of potassium chloride × 2 + cost of administering the fluid over 2 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antihistamines | |||||||||||||||
| Tablets | Hydroxyzine: Atarax | 0.13 | 0.17 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.95–285.99 |
| Tablets | Cyclizine (non-proprietary) | 0.11 | 0.32 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.93–286.14 |
| i.v./i.m. injection | Cyclizine: Valoid | NE | 1.95 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 287.77 |
| Tablets | Chlorpromazine (non-proprietary) | NE | 0.22 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.04 |
| i.v./i.m. injection | Chlorpromazine (non-proprietary) | 1.80 | 4.80 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 287.62–290.62 |
| Tablets | Dimenhydrinate: Arlevert | NE | 0.72 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.54 |
| Tablets | Codeine phosphate (non-proprietary) | 0.16 | 0.32 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.98–286.14 |
| i.v./i.m. injection | Doxylamine: codeine phosphate (non-proprietary) | 3.56 | 7.11 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 289.38–292.93 |
| Capsules | Benadryl: Acrivastine (non-proprietary) | NE | 0.59 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.41 |
| Tablets | Cetirizine (non-proprietary) | NE | 0.03 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.85 |
| Dopamine antagonists | |||||||||||||||
| Tablets | Promethazine: Phenergan | 0.11 | 0.32 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.93–286.14 |
| i.v./i.m. injection | Promethazine (non-proprietary) | 0.68 | 1.20 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.50–287.02 |
| Tablets | Prochlorperazine (non-proprietary) | 0.07 | 0.20 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.89–286.02 |
| i.v./i.m. injection | Prochlorperazine (non-proprietary) | NE | 0.52 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.34 |
| Tablets | Domperidone (non-proprietary) | 0.06 | 0.17 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.88–285.99 |
| Tablets | Metoclopramide (non-proprietary) | 0.03 | 0.09 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 285.85–285.91 |
| i.v./i.m. injection | Metoclopramide (non-proprietary) | 0.32 | 0.96 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.14–286.78 |
| Serotonin antagonists | |||||||||||||||
| Tablets | Ondansetron (non-proprietary) | NE | 8.69 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 294.51 |
| i.v./i.m. injection | Ondansetron (non-proprietary) | NE | 1.00 | 122 | 38 | 8.51 | 0.05 | 6.80 | 13.55 | 2.96 | 5.84 | 4.94 | 0.08 | 83.09 | 286.82 |
| Pharmacological preparation | Clinician-prescribed second-line interventions | Total low-estimate daily cost × 2 (£) | Total high-estimate daily cost × 2 (£) | Inpatient excess bed-days × 2 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Treatment for thromboembolism (1-night stay) (£) | Thiamine supplement (Pabrinex) × 1 (£) | Normal saline + a proportional amount of potassium chloride × 2 + cost of administering the fluid over 2 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antihistamines | |||||||||||||||
| i.v./i.m. injection | Cyclizine: Valoid | NE | 3.90 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 796.78 |
| Tablets | Chlorpromazine (non-proprietary) | NE | 0.44 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.32 |
| i.v./i.m. injection | Chlorpromazine (non-proprietary) | 3.60 | 9.60 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 796.48–802.48 |
| Dopamine antagonists | |||||||||||||||
| i.v./i.m. injection | Metoclopramide (non-proprietary) | 0.64 | 1.92 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.52–794.80 |
| Tablets | Prochlorperazine (non-proprietary) | 0.13 | 0.41 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.01–793.29 |
| i.v./i.m. injection | Prochlorperazine (non-proprietary) | NE | 1.04 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.92 |
| Tablets | Domperidone (non-proprietary) | 0.11 | 0.33 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 792.99–793.21 |
| Serotonin antagonists | |||||||||||||||
| i.v./i.m. injection | Ondansetron (non-proprietary) | NE | 2.00 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 794.88 |
| Other drugs | |||||||||||||||
| Tablets | Antiepileptic: gabapentin (non-proprietary) | 0.10 | 0.29 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 792.98–793.17 |
| Tablets | Benzodiazepines: diazepam (non-proprietary) | 0.18 | 0.20 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.06–793.08 |
| i.v./i.m. injection | Diazepam (non-proprietary) | 1.80 | 3.60 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 794.68–796.48 |
| Rectal tubes | Diazepam (non-proprietary) | NE | 41.10 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 833.98 |
| Tablets | Dicycloverine (non-proprietary) | 3.61 | 4.54 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 796.49–797.42 |
| Clinician-prescribed second-line intervention | Total daily cost (two antiemetics) × 2 (£) | Inpatient excess bed-days × 2 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Treatment for thromboembolism (1-night stay) (£) | Thiamine supplement (Pabrinex) × 1 (£) | Normal saline + a proportional amount of potassium chloride × 2 + cost of administering the fluid over 2 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cheapest combination | 0.50 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 793.38 |
| Most expensive combination | 50.70 | 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 843.58 |
| Clinician-prescribed third-line intervention | Total daily cost (three antiemetic) × 3 (£) | Total daily cost (corticosteroid) × 2 (£) | Inpatient excess bed-days × 5 (£) | Urinary test (urine culture) × 5 (£) | Urine ketones strip × 5 (£) | Liver function test × 5 (£) | Thyroid function test × 5 (£) | Glucose × 5 (£) | Urea and electrolytes × 5 (£) | Full blood count × 5 (£) | Treatment for thromboembolism (4-night stay) (£) | Thiamine supplement (Pabrinex) × 1 (£) | Normal saline + a proportional amount of potassium chloride × 5 + cost of administering the fluid over 5 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cheapest combination | 1.26 | 0.38 (prednisolone tablets) | 1325 | 42.55 | 0.25 | 34.00 | 67.75 | 14.80 | 29.20 | 24.70 | 36.60 | 2.25 | 415.45 | 1994.19 |
| Most expensive combination | 82.86 | 39.12 (hydrocortisone injection) | 1325 | 42.55 | 0.25 | 34.00 | 67.75 | 14.80 | 29.20 | 24.70 | 36.60 | 2.25 | 415.45 | 2114.53 |
| Day case | Obstetrics unit × 2 (£) | Ultrasound Scan (< 20 minutes) × 1 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Thiamine supplement × 2 (£) | Normal saline and a proportional amount of potassium chloride and cost of administering the fluid on 2 days (£) | Total (£) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 244 | 38 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 0.16 | 166.18 | 533.64 | |
| Inpatient | Inpatient excess bed-days × 2 (£) | Urinary test (urine culture) × 2 (£) | Urine ketones strip × 2 (£) | Liver function test × 2 (£) | Thyroid function test × 2 (£) | Glucose × 2 (£) | Urea and electrolytes × 2 (£) | Full blood count × 2 (£) | Treatment for thromboembolism (1-night stay) (£) | Thiamine supplement (Pabrinex) (£) | Normal saline and a proportional amount of potassium chloride and cost of administering the fluid over 2 days (£) | Total (£) |
| 530 | 17.02 | 0.10 | 13.60 | 27.10 | 5.92 | 11.68 | 9.88 | 9.15 | 2.25 | 166.18 | 792.88 |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Vitamin B6 : ginger | 1.2 : 1 | Moderate | Little evidence on effect |
| Vitamin B12 : vitamin B6 | 1.01 : 1 | Small | Unknown |
| Vitamin B12 : ginger | 1.2 : 1 | Moderate | Unknown |
| Acupressure/acupuncture : vitamin B12 | 19.1 : 1 | Large | Unknown |
| Acupressure/acupuncture : vitamin B6 | 19.3 : 1 | Large | In the comparison between acupressure and vitamin B6, there was an improvement in both groups but no difference between groups |
| Acupressure/acupuncture : ginger | 22.6 : 1 | Large | Ginger looks promising in reducing symptoms when compared with acupressure, but findings are not conclusive |
| Hypnotherapy : acupressure/acupuncture | 1.8 : 1 | Large | Unknown |
| Hypnotherapy : vitamin B12 | 34.4 : 1 | Large | Unknown |
| Hypnotherapy : vitamin B6 | 34.7 : 1 | Large | Unknown |
| Hypnotherapy : ginger | 40.7 : 1 | Large | Unknown |
| Ginger : placebo | Not assessable | Not assessable | Ginger looks promising in reducing symptoms when compared with placebo, but findings are not conclusive |
| Acupressure/acupuncture : placebo | Not assessable | Not assessable | Acupressure looks promising in reducing symptoms when compared with placebo in a small number of studies while the rest show no difference between the groups |
| Vitamin B6 : placebo | Not assessable | Not assessable | Vitamin B6 looks promising in reducing symptoms when compared with placebo but findings are not conclusive |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Vitamin B6 : ginger | 1.008 : 1 | Small | Little evidence on effect |
| Vitamin B12 : vitamin B6 | 1.0006 : 1 | Small | Unknown |
| Vitamin B12 : ginger | 1.009 : 1 | Small | Unknown |
| Ginger : placebo | Not assessable | Not assessable | Ginger looks promising in reducing symptoms when compared with placebo, but findings are not conclusive |
| Vitamin B6 : placebo | Not assessable | Not assessable | Vitamin B6 looks promising in reducing symptoms when compared with placebo, but findings are not conclusive |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Metoclopramide : cetirizine | 1.009 : 1 | Small | Unknown |
| Domperidone : metoclopramide | 1.01 : 1 | Small | Unknown |
| Domperidone : cetirizine | 1.02 : 1 | Small | Unknown |
| Hydroxyzine : domperidone | 1.001 : 1 | Small | Unknown |
| Hydroxyzine : metoclopramide | 1.01 : 1 | Small | Unknown |
| Hydroxyzine : cetirizine | 1.02 : 1 | Small | Unknown |
| Prochlorperazine : hydroxyzine | 1.004 : 1 | Small | Unknown |
| Prochlorperazine : domperidone | 1.005 : 1 | Small | Unknown |
| Prochlorperazine : metoclopramide | 1.02 : 1 | Small | Unknown |
| Prochlorperazine : cetirizine | 1.03 : 1 | Small | Unknown |
| Chlorpromazine : prochlorperazine | 1.003 : 1 | Small | Unknown |
| Chlorpromazine : hydroxyzine | 1.007 : 1 | Small | Unknown |
| Chlorpromazine : domperidone | 1.008 : 1 | Small | Unknown |
| Chlorpromazine : metoclopramide | 1.02 : 1 | Small | Unknown |
| Chlorpromazine : cetirizine | 1.03 : 1 | Small | Unknown |
| Cyclizine : chlorpromazine | 1.01 : 1 | Small | Unknown |
| Cyclizine : prochlorperazine | 1.02 : 1 | Small | Unknown |
| Cyclizine : hydroxyzine | 1.02 : 1 | Small | Unknown |
| Cyclizine : domperidone | 1.02 : 1 | Small | Unknown |
| Cyclizine : metoclopramide | 1.03 : 1 | Small | Unknown |
| Cyclizine : cetirizine | 1.04 : 1 | Small | Unknown |
| Promethazine : cyclizine | 1 : 1 | Small | Unknown |
| Promethazine : chlorpromazine | 1.01 : 1 | Small | Unknown |
| Promethazine : prochlorperazine | 1.02 : 1 | Small | Unknown |
| Promethazine : hydroxyzine | 1.02 : 1 | Small | Unknown |
| Promethazine : domperidone | 1.02 : 1 | Small | Unknown |
| Promethazine : metoclopramide | 1.03 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Promethazine : cetirizine | 1.04 : 1 | Small | Unknown |
| Codeine phosphate : promethazine | 1.0004 : 1 | Small | Unknown |
| Codeine phosphate : cyclizine | 1.0004 : 1 | Small | Unknown |
| Codeine phosphate : chlorpromazine | 1.01 : 1 | Small | Unknown |
| Codeine phosphate : prochlorperazine | 1.02 : 1 | Small | Unknown |
| Codeine phosphate : hydroxyzine | 1.02 : 1 | Small | Unknown |
| Codeine phosphate : domperidone | 1.02 : 1 | Small | Unknown |
| Codeine phosphate : metoclopramide | 1.03 : 1 | Small | Unknown |
| Codeine phosphate : cetirizine | 1.04 : 1 | Small | Unknown |
| Benadryl : codeine phosphate | 1.04 : 1 | Small | Unknown |
| Benadryl : promethazine | 1.04 : 1 | Small | Unknown |
| Benadryl : cyclizine | 1.04 : 1 | Small | Unknown |
| Benadryl : chlorpromazine | 1.06 : 1 | Modest | Unknown |
| Benadryl : prochlorperazine | 1.06 : 1 | Modest | Unknown |
| Benadryl : hydroxyzine | 1.06 : 1 | Modest | Unknown |
| Benadryl : domperidone | 1.06 : 1 | Modest | Unknown |
| Benadryl : metoclopramide | 1.08 : 1 | Modest | Unknown |
| Benadryl : cetirizine | 1.09 : 1 | Modest | Unknown |
| Dimenhydrinate : benadryl | 1.02 : 1 | Small | Unknown |
| Dimenhydrinate : codeine phosphate | 1.06 : 1 | Modest | Unknown |
| Dimenhydrinate : promethazine | 1.06 : 1 | Modest | Unknown |
| Dimenhydrinate : cyclizine | 1.06 : 1 | Modest | Unknown |
| Dimenhydrinate : chlorpromazine | 1.07 : 1 | Modest | Unknown |
| Dimenhydrinate : prochlorperazine | 1.08 : 1 | Modest | Unknown |
| Dimenhydrinate : hydroxyzine | 1.08 : 1 | Modest | Unknown |
| Dimenhydrinate : domperidone | 1.08 : 1 | Modest | Unknown |
| Dimenhydrinate : metoclopramide | 1.1 : 1 | Modest | Unknown |
| Dimenhydrinate : cetirizine | 1.1 : 1 | Modest | Unknown |
| Ondansetron : dimenhydrinate | 2.1 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron : benadryl | 2.2 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron : codeine phosphate | 2.2 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron : promethazine | 2.2 : 1 | Large | Unknown |
| Ondansetron : cyclizine | 2.2 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron : chlorpromazine | 2.3 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron : prochlorperazine | 2.3 : 1 | Large | Unknown |
| Ondansetron : hydroxyzine | 2.3 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron : domperidone | 2.3 : 1 | Large | Unknown |
| Ondansetron : metoclopramide | 2.3 : 1 | Large | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron : cetirizine | 2.3 : 1 | Large | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Antihistamines : placebo | Not assessable | Not assessable | Antihistamines appear to be better than placebo in reducing the severity of symptoms, but more larger, better-quality studies are required |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Metoclopramide (tablets) : cetirizine (tablets) | 1.0002 : 1 | Small | Unknown |
| Domperidone (tablets) : metoclopramide (tablets) | 1.0003 : 1 | Small | Unknown |
| Domperidone (tablets) : cetirizine (tablets) | 1.0005 : 1 | Small | Unknown |
| Hydroxyzine (tablets) : domperidone (tablets) | 1 : 1 | Small | Unknown |
| Hydroxyzine (tablets) : metoclopramide (tablets) | 1.0003 : 1 | Small | Unknown |
| Hydroxyzine (tablets) : cetirizine (tablets) | 1.0005 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : hydroxyzine (tablets) | 1.0001 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : domperidone (tablets) | 1.0001 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : metoclopramide (tablets) | 1.0004 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : cetirizine (tablets) | 1.0006 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : prochlorperazine (tablets) | 1.00007 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : hydroxyzine (tablets) | 1.0002 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : domperidone (tablets) | 1.0002 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : metoclopramide (tablets) | 1.0005 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : cetirizine (tablets) | 1.0007 : 1 | Small | Unknown |
| Cyclizine (tablets) : chlorpromazine (tablets) | 1.0003 : 1 | Small | Unknown |
| Cyclizine (tablets) : prochlorperazine (tablets) | 1.0004 : 1 | Small | Unknown |
| Cyclizine (tablets) : hydroxyzine (tablets) | 1.0005 : 1 | Small | Unknown |
| Cyclizine (tablets) : domperidone (tablets) | 1.0005 : 1 | Small | Unknown |
| Cyclizine (tablets) : metoclopramide (tablets) | 1.0008 : 1 | Small | Unknown |
| Cyclizine (tablets) : cetirizine (tablets) | 1.001 : 1 | Small | Unknown |
| Codeine phosphate (tablets) : cyclizine (tablets) | 1 : 1 | Small | Unknown |
| Codeine phosphate (tablets) : chlorpromazine (tablets) | 1.0003 : 1 | Small | Unknown |
| Codeine phosphate (tablets) : prochlorperazine (tablets) | 1.0004 : 1 | Small | Unknown |
| Codeine phosphate (tablets) : hydroxyzine (tablets) | 1.0005 : 1 | Small | Unknown |
| Codeine phosphate (tablets) : domperidone (tablets) | 1.0005 : 1 | Small | Unknown |
| Codeine phosphate (tablets) : metoclopramide (tablets) | 1.0008 : 1 | Small | Unknown |
| Codeine phosphate (tablets) : cetirizine (tablets) | 1.001 : 1 | Small | Unknown |
| Promethazine (tablets) : codeine Phosphate (tablets) | 1 : 1 | Small | Unknown |
| Promethazine (tablets) : cyclizine (tablets) | 1 : 1 | Small | Unknown |
| Promethazine (tablets) : chlorpromazine (tablets) | 1.0003 : 1 | Small | Unknown |
| Promethazine (tablets) : prochlorperazine (tablets) | 1.0004 : 1 | Small | Unknown |
| Promethazine (tablets) : hydroxyzine (tablets) | 1.0005 : 1 | Small | Unknown |
| Promethazine (tablets) : domperidone (tablets) | 1.0005 : 1 | Small | Unknown |
| Promethazine (tablets) : metoclopramide (tablets) | 1.0008 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Promethazine (tablets) : cetirizine (tablets) | 1.001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : promethazine (tablets) | 1.0007 : 1 | Small | Unknown |
| Prochlorperazine (injection) : codeine phosphate (tablets) | 1.0007 : 1 | Small | Unknown |
| Prochlorperazine (injection) : cyclizine (tablets) | 1.0007 : 1 | Small | Unknown |
| Prochlorperazine (injection) : chlorpromazine (tablets) | 1.001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : prochlorperazine (tablets) | 1.001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : hydroxyzine (tablets) | 1.001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : domperidone (tablets) | 1.001 : 1 | Small | Unknown |
| Prochlorperazine (injection) : metoclopramide (tablets) | 1.002 : 1 | Small | Unknown |
| Prochlorperazine (injection) : cetirizine (tablets) | 1.002 : 1 | Small | Unknown |
| Benadryl (capsules) : prochlorperazine (injection) | 1.0002 : 1 | Small | Unknown |
| Benadryl (capsules) : promethazine (tablets) | 1.0009 : 1 | Small | Unknown |
| Benadryl (capsules) : codeine phosphate (tablets) | 1.0009 : 1 | Small | Unknown |
| Benadryl (capsules) : cyclizine (tablets) | 1.0009 : 1 | Small | Unknown |
| Benadryl (capsules) : chlorpromazine (tablets) | 1.001 : 1 | Small | Unknown |
| Benadryl (capsules) : prochlorperazine (tablets) | 1.001 : 1 | Small | Unknown |
| Benadryl (capsules) : hydroxyzine (tablets) | 1.001 : 1 | Small | Unknown |
| Benadryl (capsules) : domperidone (tablets) | 1.001 : 1 | Small | Unknown |
| Benadryl (capsules) : metoclopramide (tablets) | 1.002 : 1 | Small | Unknown |
| Benadryl (capsules) : cetirizine (tablets) | 1.002 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : benadryl (capsules) | 1.0005 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : prochlorperazine (injection) | 1.0007 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : promethazine (tablets) | 1.001 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : codeine phosphate (tablets) | 1.001 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : cyclizine (tablets) | 1.001 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : chlorpromazine (tablets) | 1.002 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : prochlorperazine (tablets) | 1.002 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : hydroxyzine (tablets) | 1.002 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : domperidone (tablets) | 1.002 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : metoclopramide (tablets) | 1.002 : 1 | Small | Unknown |
| Dimenhydrinate (tablets) : cetirizine (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : dimenhydrinate (tablets) | 1.0008 : 1 | Small | Unknown |
| Metoclopramide (injection) : benadryl (capsules) | 1.001 : 1 | Small | Unknown |
| Metoclopramide (injection) : prochlorperazine (injection) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : promethazine (tablets) | 1.002 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Metoclopramide (injection) : codeine phosphate (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : cyclizine (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : chlorpromazine (tablets) | 1.003 : 1 | Small | Unknown |
| Metoclopramide (injection) : prochlorperazine (tablets) | 1.003 : 1 | Small | Unknown |
| Metoclopramide (injection) : hydroxyzine (tablets) | 1.003 : 1 | Small | Unknown |
| Metoclopramide (injection) : domperidone (tablets) | 1.003 : 1 | Small | Unknown |
| Metoclopramide (injection) : metoclopramide (tablets) | 1.003 : 1 | Small | Unknown |
| Metoclopramide (injection) : cetirizine (tablets) | 1.003 : 1 | Small | Unknown |
| Ondansetron (injection) : metoclopramide (injection) | 1.0001 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron (injection) : dimenhydrinate (tablets) | 1.001 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : benadryl (capsules) | 1.001 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : prochlorperazine (injection) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : promethazine (tablets) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : codeine phosphate (tablets) | 1.002 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : cyclizine (tablets) | 1.002 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : chlorpromazine (tablets) | 1.003 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : prochlorperazine (tablets) | 1.003 : 1 | Small | Unknown |
| Ondansetron (injection) : hydroxyzine (tablets) | 1.003 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : domperidone (tablets) | 1.003 : 1 | Small | Unknown |
| Ondansetron (injection) : metoclopramide (tablets) | 1.003 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron (injection) : cetirizine (tablets) | 1.003 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Promethazine (injection) : ondansetron (injection) | 1.0007 : 1 | Small | Unknown |
| Promethazine (injection) : metoclopramide (injection) | 1.0008 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Promethazine (injection) : dimenhydrinate (tablets) | 1.002 : 1 | Small | Unknown |
| Promethazine (injection) : benadryl (capsules) | 1.002 : 1 | Small | Unknown |
| Promethazine (injection) : prochlorperazine (injection) | 1.002 : 1 | Small | Unknown |
| Promethazine (injection) : promethazine (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : codeine phosphate (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : cyclizine (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : chlorpromazine (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : prochlorperazine (tablets) | 1.003 : 1 | Small | Unknown |
| Promethazine (injection) : hydroxyzine (tablets) | 1.004 : 1 | Small | Unknown |
| Promethazine (injection) : domperidone (tablets) | 1.004 : 1 | Small | Unknown |
| Promethazine (injection) : metoclopramide (tablets) | 1.004 : 1 | Small | Limited data suggest that promethazine is as effective as metoclopramide in reducing the symptoms of NVP |
| Promethazine (injection) : cetirizine (tablets) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : promethazine (injection) | 1.003 : 1 | Small | Unknown |
| Cyclizine (injection) : ondansetron (injection) | 1.003 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Cyclizine (injection) : metoclopramide (injection) | 1.003 : 1 | Small | Unknown |
| Cyclizine (injection) : dimenhydrinate (tablets) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : benadryl (capsules) | 1.005 : 1 | Small | Unknown |
| Cyclizine (injection) : prochlorperazine (injection) | 1.005 : 1 | Small | Unknown |
| Cyclizine (injection) : promethazine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : codeine phosphate (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : cyclizine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : chlorpromazine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : prochlorperazine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : hydroxyzine (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : domperidone (tablets) | 1.006 : 1 | Small | Unknown |
| Cyclizine (injection) : metoclopramide (tablets) | 1.007 : 1 | Small | Unknown |
| Cyclizine (injection) : cetirizine (tablets) | 1.007 : 1 | Small | Unknown |
| Chlorpromazine (injection) : cyclizine (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : promethazine (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : ondansetron (injection) | 1.01 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Chlorpromazine (injection) : metoclopramide (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : dimenhydrinate (tablets) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : benadryl (capsules) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : prochlorperazine (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : promethazine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : codeine phosphate (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : cyclizine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : chlorpromazine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : prochlorperazine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : hydroxyzine (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : domperidone (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : metoclopramide (tablets) | 1.02 : 1 | Small | Unknown |
| Chlorpromazine (injection) : cetirizine (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : chlorpromazine (injection) | 1.008 : 1 | Small | Unknown |
| Doxylamine (injection) : cyclizine (injection) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : promethazine (injection) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : ondansetron (injection) | 1.02 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Doxylamine (injection) : metoclopramide (injection) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : dimenhydrinate (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : benadryl (capsules) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : prochlorperazine (injection) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : promethazine (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : codeine phosphate (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : cyclizine (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : chlorpromazine (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : prochlorperazine (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : hydroxyzine (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : domperidone (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : metoclopramide (tablets) | 1.02 : 1 | Small | Unknown |
| Doxylamine (injection) : cetirizine (tablets) | 1.02 : 1 | Small | Unknown |
| Ondansetron (tablets) : doxylamine (injection) | 1.005 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : chlorpromazine (injection) | 1.01 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : cyclizine (injection) | 1.02 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : promethazine (injection) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : ondansetron (injection) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : metoclopramide (injection) | 1.03 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron (tablets) : dimenhydrinate (tablets) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : benadryl (capsules) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : prochlorperazine (injection) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : promethazine (tablets) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : codeine phosphate (tablets) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : cyclizine (tablets) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : chlorpromazine (tablets) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : prochlorperazine (tablets) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : hydroxyzine (tablets) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (tablets) : domperidone (tablets) | 1.03 : 1 | Small | Unknown |
| Ondansetron (tablets) : metoclopramide (tablets) | 1.03 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron (tablets) : cetirizine (tablets) | 1.03 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Antihistamines : placebo | Not assessable | Not assessable | Antihistamines appear to be better than placebo in reducing the severity of symptoms, but more larger, better-quality studies are required |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Gabapentin (tablets) : diazepam (tablets) | 1.0001 : 1 | Small | Unknown |
| Domperidone (tablets) : gabapentin (tablets) | 1.00005 : 1 | Small | Unknown |
| Domperidone (tablets) : diazepam (tablets) | 1.0002 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : domperidone (tablets) | 1.0001 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : gabapentin (tablets) | 1.0002 : 1 | Small | Unknown |
| Prochlorperazine (tablets) : diazepam (tablets) | 1.0003 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : prochlorperazine (tablets) | 1.00004 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : domperidone (tablets) | 1.0001 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : gabapentin (tablets) | 1.0002 : 1 | Small | Unknown |
| Chlorpromazine (tablets) : diazepam (tablets) | 1.0003 : 1 | Small | Unknown |
| Prochlorperazine (injection) : chlorpromazine (tablets) | 1.0008 : 1 | Small | Unknown |
| Prochlorperazine (injection) : prochlorperazine (tablets) | 1.0008 : 1 | Small | Unknown |
| Prochlorperazine (injection) : domperidone (tablets) | 1.0009 : 1 | Small | Unknown |
| Prochlorperazine (injection) : gabapentin (tablets) | 1.0009 : 1 | Small | Unknown |
| Prochlorperazine (injection) : diazepam (tablets) | 1.001 : 1 | Small | Unknown |
| Metoclopramide (injection) : prochlorperazine (injection) | 1.001 : 1 | Small | Unknown |
| Metoclopramide (injection) : chlorpromazine (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : prochlorperazine (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : domperidone (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : gabapentin (tablets) | 1.002 : 1 | Small | Unknown |
| Metoclopramide (injection) : diazepam (tablets) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : metoclopramide (injection) | 1.0001 : 1 | Small | Evidence comparing ondansetron with metoclopramide showed mixed results, with both improving symptoms. Ondansetron was found to be more effective at reducing symptoms of vomiting than metoclopramide after 4 days |
| Ondansetron (injection) : prochlorperazine (injection) | 1.001 : 1 | Small | Unknown |
| Ondansetron (injection) : chlorpromazine (tablets) | 1.002 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Ondansetron (injection) : prochlorperazine (tablets) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : domperidone (tablets) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : gabapentin (tablets) | 1.002 : 1 | Small | Unknown |
| Ondansetron (injection) : diazepam (tablets) | 1.002 : 1 | Small | Unknown |
| Diazepam (injection) : ondansetron (injection) | 1.002 : 1 | Small | Unknown |
| Diazepam (injection) : metoclopramide (injection) | 1.002 : 1 | Small | Unknown |
| Diazepam (injection) : prochlorperazine (injection) | 1.003 : 1 | Small | Unknown |
| Diazepam (injection) : chlorpromazine (tablets) | 1.004 : 1 | Small | Unknown |
| Diazepam (injection) : prochlorperazine (tablets) | 1.004 : 1 | Small | Unknown |
| Diazepam (injection) : domperidone (tablets) | 1.004 : 1 | Small | Unknown |
| Diazepam (injection) : gabapentin (tablets) | 1.004 : 1 | Small | Unknown |
| Diazepam (injection) : diazepam (tablets) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : diazepam (injection) | 1.0004 : 1 | Small | Unknown |
| Cyclizine (injection) : ondansetron (injection) | 1.002 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Cyclizine (injection) : metoclopramide (injection) | 1.002 : 1 | Small | Unknown |
| Cyclizine (injection) : prochlorperazine (injection) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : chlorpromazine (tablets) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : prochlorperazine (tablets) | 1.004 : 1 | Small | Unknown |
| Cyclizine (injection) : domperidone (tablets) | 1.005 : 1 | Small | Unknown |
| Cyclizine (injection) : gabapentin (tablets) | 1.005 : 1 | Small | Unknown |
| Cyclizine (injection) : diazepam (tablets) | 1.005 : 1 | Small | Unknown |
| Dicycloverine (tablets) : cyclizine (injection) | 1.0008 : 1 | Small | Unknown |
| Dicycloverine (tablets) : diazepam (injection) | 1.001 : 1 | Small | Unknown |
| Dicycloverine (tablets) : ondansetron (injection) | 1.003 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Dicycloverine (tablets) : metoclopramide (injection) | 1.003 : 1 | Small | Unknown |
| Dicycloverine (tablets) : prochlorperazine (injection) | 1.004 : 1 | Small | Unknown |
| Dicycloverine (tablets) : chlorpromazine (tablets) | 1.005 : 1 | Small | Unknown |
| Dicycloverine (tablets) : prochlorperazine (tablets) | 1.005 : 1 | Small | Unknown |
| Dicycloverine (tablets) : domperidone (tablets) | 1.005 : 1 | Small | Unknown |
| Dicycloverine (tablets) : gabapentin (tablets) | 1.005 : 1 | Small | Unknown |
| Dicycloverine (tablets) : diazepam (tablets) | 1.005 : 1 | Small | Unknown |
| Chlorpromazine (injection) : dicycloverine (tablets) | 1.006 : 1 | Small | Unknown |
| Chlorpromazine (injection) : cyclizine (injection) | 1.007 : 1 | Small | Unknown |
| Chlorpromazine (injection) : diazepam (injection) | 1.008 : 1 | Small | Unknown |
| Chlorpromazine (injection) : ondansetron (injection) | 1.01 : 1 | Small | Both ondansetron and antihistamines improve symptoms, with no significant difference in effects |
| Chlorpromazine (injection) : metoclopramide (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : prochlorperazine (injection) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : chlorpromazine (tablets) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : prochlorperazine (tablets) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : domperidone (tablets) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : gabapentin (tablets) | 1.01 : 1 | Small | Unknown |
| Chlorpromazine (injection) : diazepam (tablets) | 1.01 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : chlorpromazine (injection) | 1.04 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : dicycloverine (tablets) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : cyclizine (injection) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : diazepam (injection) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : ondansetron (injection) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : metoclopramide (injection) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : prochlorperazine (injection) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : chlorpromazine (tablets) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : prochlorperazine (tablets) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : domperidone (tablets) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : gabapentin (tablets) | 1.05 : 1 | Small | Unknown |
| Diazepam (rectal tubes) : diazepam (tablets) | 1.05 : 1 | Small | Unknown |
| Antihistamines : placebo | Not assessable | Not assessable | Antihistamines appear to be better than placebo in reducing the severity of symptoms, but more larger, better-quality studies are required |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Most expensive : least expensive | 1.06 : 1 | Modest | Unknown |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Most expensive : least expensive | 1.06 : 1 | Modest | Unknown |
| Comparison | Implied valuation | Effect size | Evidence on effect |
|---|---|---|---|
| Inpatient : day case | 1.5 : 1 | Large | Results indicate that day case management is as effective at improving severity scores as inpatient management for some women. However, more, larger studies are required to provide definitive results |
List of abbreviations
- 5-HT3
- 5-hydroxytryptamine
- CI
- confidence interval
- ECG
- electrocardiogram
- EPHPP
- Effective Public Health Practice Project
- GP
- general practitioner
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- HCP
- health-care professional
- HG
- hyperemesis gravidarum
- i.m.
- intramuscular
- IQR
- interquartile range
- i.v.
- intravenous
- MeSH
- medical subject heading
- NVP
- nausea and vomiting in pregnancy
- NVPI
- Nausea and Vomiting of Pregnancy Instrument
- OR
- odds ratio
- P6
- pericardium 6
- PSS
- Pregnancy Sickness Support
- PUQE
- Pregnancy-Unique Quantification of Emesis and Nausea
- QoL
- quality of life
- QT
- time between start of the Q wave and of the T wave in the heart’s electrical cycle
- RCT
- randomised controlled trial
- RINVR
- Rhodes Index of Nausea, Vomiting and Retching
- SD
- standard deviation
- SoF
- summary of findings
- TPN
- total parenteral nutrition
- UKTIS
- UK Teratology Information Service
- VAS
- visual analogue scale