Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/67/01. The contractual start date was in August 2015. The draft report began editorial review in March 2016 and was accepted for publication in August 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Rumona Dickson is on the Health Technology Assessment Evidence Synthesis Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Aslam et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Decision problem
The aim of this review was to determine whether or not automated computerised tests accurately identify patients with progressive cognitive impairment and, if so, to investigate their role in monitoring disease progression and/or response to treatment.
Specifically, the research objectives were to:
-
determine the performance of automated computerised tests in detecting mild cognitive impairment (MCI) and early dementia
-
determine the performance of automated computerised tests in the monitoring of the disease post diagnosis, specifically in detecting disease progression
-
identify future research needs.
Chapter 2 Background and rationale for review
Cognitive impairment in dementia is progressive, and is a growing public health concern. 1 It is one of the most distinctive characteristics of all dementias. Consequently, the assessment of cognitive impairment is an essential element in the diagnosis of dementia. 2
The timely recognition of dementia syndromes can be beneficial because some causes of dementia are treatable and are fully or partially reversible, for example dementias caused by vitamin B12 deficiency,3 side effects of medications,4 metabolic abnormality and certain brain tumours. 5 There is also some evidence from the USA that early recognition and treatment may delay the subsequent need for nursing home care and may reduce the risk of misdiagnosis and inappropriate management. 6 In the UK, the results of a recent trial showed that patients with moderate to severe Alzheimer’s disease (AD) who continued donepezil treatment were at reduced risk of nursing home placement. 7 Early diagnosis can also assist in addressing anxiety about changes in memory, thinking, mood or behaviour for people with suspected dementia and their carers. 8
A number of pen-and-paper-based tools for cognitive assessment are currently used in the UK, for example the Mini-Mental State Examination (MMSE) and the General Practitioner Assessment of Cognition. 9 A few automated cognitive assessment tools for assessing MCI and early dementia are now also available; however, their use in the diagnosis and/or in monitoring the progression of cognitive impairment or response to treatment has not been evaluated. 10
The rationale for this review is to determine whether or not these automated computerised tests for cognitive impairment have the potential to contribute to early diagnosis and simplify the current monitoring and assessment process compared with standard NHS clinical practice.
Population
This review addresses patients in two specific diagnostic categories: those with MCI and those suffering from early dementia.
Mild cognitive impairment
Evidence from neuropathological and neuroimaging studies suggests that biological changes associated with dementia occur long before the onset of symptoms. 11 Extensive research has been devoted to identifying the characteristics of incipient dementia, which presents before the onset of the full dementia syndrome. 12,13
This research has given rise to the concept of MCI, which is the state between the cognitive changes of normal ageing and very early dementia. 14,15 The transitional period has been described using a variety of terms such as MCI, dementia prodrome, incipient dementia, isolated memory impairment16 and, more recently, mild neurocognitive disorder. 12 For the purposes of this report, the term ‘mild cognitive impairment’ or MCI has been used.
Mild cognitive impairment refers to the clinical condition used to describe people whose cognitive function is below that of the normal population for their educational level and age but who do not have any loss of functional abilities or skills. 17–20 The diagnosis of MCI is complicated by the fact that complaints of memory loss in people over the age of 65 years are common. 21 Some of the indicators of dementia, such as a reduction in activities of daily living, decreased attention or ability to plan, are absent in people with MCI. 20
Mild cognitive impairment is a heterogeneous state, with possible trajectories including AD, other dementias, and even reversion to normal cognitive functioning. 12 It is also worth noting that the authors of a meta-analysis22 of 41 inception cohort studies reported that the annual conversion rate from defined MCI to dementia was approximately 5–10%. The overall conversion rate from MCI to AD has been estimated to be between 6% and 25% of cases per year. 23 However, these rates vary by subtype of disease. The variation in the conversion rates could be explained by the differing disease processes13,24 and the heterogeneity which comes from different populations being studied. 25 In epidemiological samples, MCI has often been classified by applying a psychometric cut-off point to a proportion of cases without in-depth clinical examination, and a large proportion of these cases subsequently revert to normality. 25 In contrast, cases of MCI diagnosed in secondary care services, following detailed and comprehensive examination and investigations by a specialist, reveal fewer cases reverting to normality and much higher rates of progression. Therefore, the concept of MCI depends on how thoroughly the pre-diagnostic assessment is performed.
Mild cognitive impairment is subtyped in terms of the type and number of cognitive domains affected. 16 The classification of MCI is described in Table 1.
| Variable | Amnestic | Non-amnestic |
|---|---|---|
| Aetiology | Neurodegenerative disease | Vascular damage |
| Apolipoprotein E | Cerebrovascular disease | |
| Presentation | Memory impairment present | Impairment in non-memory domains |
| Long-term outcomes | Alzheimer’s dementia (AD) | Non-Alzheimer dementias: vascular dementia, Lewy body dementia, frontotemporal dementia |
Different types of MCI have now been proposed, including ‘amnestic form of MCI’, when memory is affected, and non-amnestic form of MCI, when impairment is in a non-memory domain. 16 MCI is also classified as single-domain or multiple-domain according to the number of cognitive domains with objectively verified impairment. 26
Early dementia
Early dementia is differentiated from MCI by the level of cognitive decline and changes in mood and behaviour. The common changes experienced by people with dementia can be understood in three stages: early, middle and late dementia (Table 2). Individuals diagnosed with early dementia present with multiple cognitive deficits and their memory loss is sufficient to impact on everyday social and occupational functioning. In the later stages, there is a noticeable deterioration in perception, comprehension and language. This is also often accompanied by an impaired ability to recognise objects (agnosia) and an inability to think abstractly and plan, initiate, sequence, monitor and stop complex behaviour. 28,29
| Stages of dementia | Common changes experienced by people with dementia |
|---|---|
| Early stage |
|
| Middle stage |
|
| Late stage |
|
There are a number of conditions that result in dementia. The three most common reasons are AD vascular conditions (e.g. multiple cortical/subcortical infarcts), frontotemporal atrophy and Lewy body disease. Some rare causes of dementia include inherited metabolic disorders (e.g. porphyria), infectious causes, autoimmune causes and neoplasms (e.g. meningioma). 30,31 Irrespective of the primary cause, the outlook for people with most types of dementia is usually poor. Irreversible or untreated dementia usually continues to worsen over time until the person’s death. 32,33
There are subtle neuropsychological differences in patterns of cognitive deficit in different types of dementia but, as far as we are aware, there are no dedicated automated tests to specifically diagnose different types of dementia, such as vascular dementia, alcohol-related dementia or Lewy body dementia. Furthermore, this is complicated by the fact that authors of studies often use terms inconsistently and erroneously when describing dementia.
Epidemiology
Obtaining accurate incidence and prevalence figures for MCI is difficult, as people with memory decline may go undiagnosed. Prevalence and incidence estimates can also vary significantly depending on the definitions that are used. The variance in these estimates then poses a challenge to the understanding of the social burden of this disease. For example, the authors of a study utilising data from the Medical Research Council Cognitive Function and Ageing Study of people aged ≥ 65 years29 estimated the prevalence of MCI to range from 2.5% to 41.0% in the UK. In addition, the rates of progression from MCI to dementia varied from 3.7% to 30.0%. 29
The most common form of dementia in the UK is AD. 34 There are an estimated 163,000 new cases of dementia identified each year in England and Wales. The risk of being diagnosed with dementia rises with increasing age; however, a significant portion of people who are diagnosed with dementia are younger than 65 years. 35 The incidence of dementia ranges from 6.7 per 1000 person-years at age 65–69 years to 68.5 per 1000 person-years at age ≥ 85 years. Prevalence increases with age; it is estimated to be 3% by 70 years and then to double every 5.1 years thereafter. 36 A report published by the Alzheimer’s Society predicts that there will be 1 million people living with dementia in the UK by 2025. 35
Current diagnostic practice
The 2006 guidelines from the National Institute for Health and Care Excellence (NICE)8 place emphasis on the early diagnosis of people with dementia to allow for effective management and planning with patients and carers. The projected increase35 in the prevalence of dementia by the Alzheimer’s Society highlights the importance of equitable and easy access to diagnosis in the UK patient population.
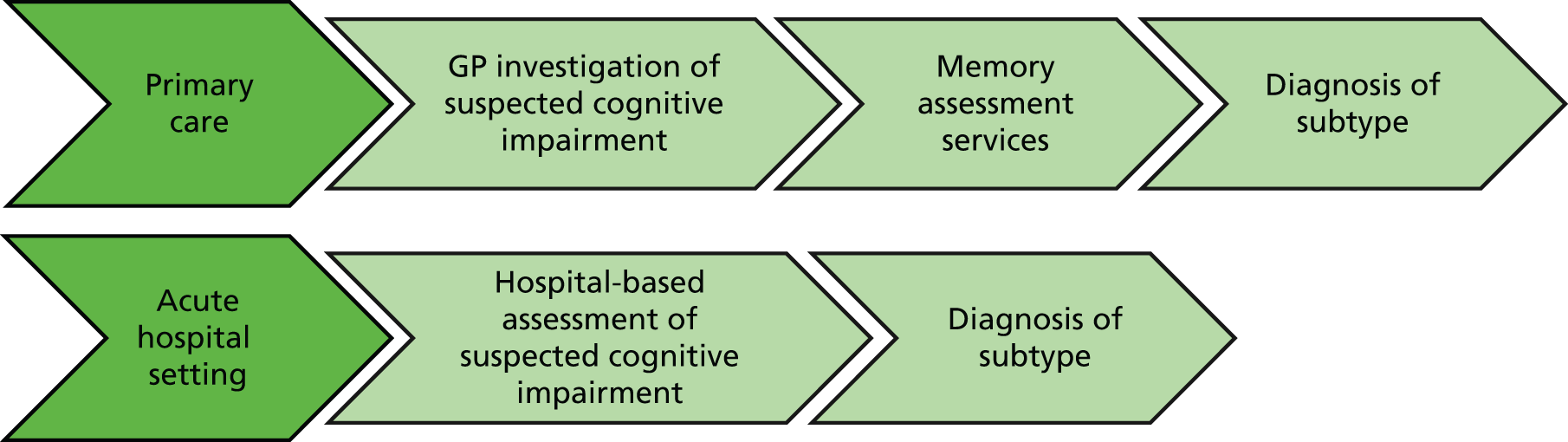
A schema of the pathway for assessing cognitive impairment in the UK is presented in Figure 1. The first point of contact with health-care services for a person with suspected cognitive impairment is with a health-care professional in primary care or in an acute hospital setting. In primary care, the general practitioner (GP) usually takes a brief history, conducts a physical examination and conducts a short test of cognitive function to establish a differential diagnosis for cognitive impairment. The NICE guidelines8 recommend the use of the MMSE when aiming to diagnose people with dementia. It is possible to offer a diagnosis of dementia at this point if it is in an established state. 37 However, MMSE is insensitive to early-stage dementia38 and does not effectively map the transition from MCI to early dementia. 39 The NICE guidelines8 also recommend a number of pen-and-paper-based tools as suitable tests for screening people for cognitive impairment. Some of these tests, along others with others used in clinical practice, are further outlined in Table 3.
FIGURE 1.
Adapted pathway for assessing cognitive impairment.
| Test | Administration time (minutes) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| GPCOG8 | 5 | 82–8540 | 82–8540 |
| 6CIT8 | 3–4 | 78.5–8341 | 77–10041 |
| Mini-Cog assessment instrument42 | 2–4 | 76–9940 | 89–9640 |
| AMT8 | 2–4 | Not validated in a primary care setting | Not validated in a primary care setting |
| Memory Impairment Screen43 | 4 | 74–8640 | 96–9740 |
After this initial screening, the GP refers patients with suspected MCI or early dementia to a memory assessment service, which is usually based in secondary care and can involve the examination of older adults by community mental health teams. Memory assessment service teams play an important role in clarifying the diagnosis (MCI or dementia, subtype and severity of dementia), identifying which patients with MCI are at greatest risk of developing dementia and determining who are most in need of follow-up. Diagnoses are clarified by taking a detailed clinical history from the patient and a family member or carer, interpreting scan results (if needed) and interpreting the findings from cognitive function pen-and-paper diagnostic tests. 44
In an acute hospital setting, patients can be ‘incidentally’ discovered to be living with cognitive impairment through routine testing for another medical condition, and/or patients may present with acute confusion secondary to a medical problem. 44 There are many different pen-and-paper tests used to aid diagnosis for MCI and early dementia available for use in a secondary setting; three of the tests most commonly used in the NHS are described in Table 4.
Reference standard
A reference standard can be described as being the best available method for identifying patients who have the target condition. 50 The reference standard for this research is the clinical diagnosis of MCI and early dementia. It is recognised that clinical diagnosis itself has a degree of variability, but this is not unique to dementia studies and does not invalidate the basic diagnostic test accuracy approach. Any recognised diagnostic criteria (e.g. International Classification of Diseases, Tenth Edition;2 Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition51 or -Fifth Edition52) can be used. 53 Dementia diagnosis may specify a pathological subtype. Clinicians may use imaging, biomarkers or other data to aid diagnosis, for example the Clinical Dementia Rating54 which is a gold-standard research criterion against which most rating scales have been compared. 55 However, in this report, diagnoses based only on these tests, without corresponding clinical assessment, were not included. It is recognised that different iterations of diagnostic criteria may not be directly comparable and that diagnosis may vary with the degree or manner in which the criteria have been operationalised (e.g. individual clinician vs. algorithm vs. consensus determination).
Index test
For the purpose of this report, the index test is any automated computerised assessment of cognitive impairment, which can either be self-administered or interviewer administered. In self-administered tests, patients may require help with accessing the necessary computer programs, login identification and simple start-up explanation. It is important to ensure that the patient can see and/or hear the instructions and test stimuli.
There are several automated tests available to help identify patients with MCI and early dementia. An accurate automated cognitive assessment tool would be clinically valuable if it were shown to work as well as clinician-delivered tests. However, there is limited clinical evidence to demonstrate their equivalence or superiority over standard practice.
The authors of a UK-based review56 investigated the use of several available computerised automated tests and assessed their sensitivity and specificity for detection of MCI compared with two well-validated pen-and-paper tests: the Hopkins Verbal Learning Test and the MMSE. 56 The authors of the review concluded that the Hopkins Verbal Learning Test had better sensitivity for the detection of MCI in older adults than the computerised tests. They also identified that one automated test, CogState, enabled the identification of cognitive deficits beyond mild impairments in memory; for example, CogState detected more functional deficits than the Hopkins Verbal Learning Test or MMSE. 56 The authors, however, did not address if these tests had the potential to facilitate timely diagnosis or if they were effective in monitoring disease progression. Appendix 1 explains measures for assessing an index test against a reference standard.
Table 5 provides a list of automated computerised tests that were identified during the initial scoping search that was conducted to inform the development of the protocol for this review.
| Tool | Condition | Administration | Duration (minutes) | Domains |
|---|---|---|---|---|
| ANAM56,57 | Cognitively impaired elderly; AD | Mouse/keyboard Self-administered |
NR | Memory, attention, psychomotor speed, language, reaction time |
| CAMCI56 | MCI | Touchscreen computer Self-administered |
20 | Attention, memory, executive function, working memory |
| CANS-MCI56,57 | MCI | Touchscreen Self-administered |
30 | Memory, executive function, symbol fluency |
| CANTAB56,57 | Early-stage AD; Parkinson’s disease | Touchscreen Self-administered |
30 | Executive function, memory, attention, visuospatial function |
| CNSVS56,57 | MCI; mild dementia | Keyboard Self-administered |
30 | Memory, psychomotor speed, reaction time, complex attention, cognitive flexibility |
| CNTB56 | AD | Keyboard Technician administered |
NR | Language, information processing, motor speed, attention, spatial, memory |
| COGDRAS-D56,57 | Dementia; AD; Huntington’s disease | Yes/no button Technician administered | 20–25 | Attention, memory, reaction time |
| CogState™56,57 | MCI | Keyboard Self-administered |
15–20 | Working memory, attention, visuospatial memory |
| CSI56,57 | Dementia | Keyboard Self-administered |
25–35 | Memory, attention, response speed, processing speed |
| CST57 | NR | Technician assisted | 15 | Learning, memory, executive function |
| MCIS56,57 | MCI | Technician records responses via telephone | 10 | Memory, executive function, language |
| MicroCog™56,57 | MCI | Keyboard/pad Self-administered |
> 60a | Reaction time, memory, attention, mental control, reasoning, spatial processing |
| Mindstreams™56,57 | MCI; dementia | Mouse/pad Technician administered |
45–60 | Memory, executive function, visual and special ability |
Chapter 3 Methods
The methods used in the review followed the systematic review principles outlined in the Centre for Reviews and Dissemination’s58 guidance for undertaking reviews in health care, the NICE Diagnostic Assessment Programme Manual59 and publications from the Cochrane Collaboration Diagnostic Test Accuracy60 Working Group.
Search strategy
The following electronic databases were searched for the period from 2005 to the latest available version (August 2015).
-
MEDLINE (via OvidSP)
-
MEDLINE In Process & Other Non-Indexed Citations (via OvidSP)
-
-
EMBASE (via OvidSP)
-
The Cochrane Library
-
Central Register of Controlled Trials
-
Cochrane Database of Systematic Reviews
-
Database of Abstracts of Reviews of Effects
-
Health Technology Assessment database
-
NHS Economic Evaluation Database
-
-
ISI Web of Science
-
Proceedings (via Index to Scientific and Technical Proceedings)
-
ISI Web of Science – Science Citation Index Expanded
-
-
PsycINFO.
The search terms for electronic databases comprised a combination of medical subject heading terms and free-text words. The search had no language restrictions and there were no limits on specific study design. Animal studies were excluded, as were case reports, comments, editorials and letters. The details of the search strategies and the number of references retrieved are provided in Appendix 2.
Grey literature
Theses or PhD abstracts were accessed from ProQuest.
Reference lists
Backwards and forwards citation tracking for all relevant studies and reviews for further possible titles was undertaken.
Hand-searching
Trial and research registers were hand-searched for ongoing studies and reviews, including:
-
ClinicalTrials.gov
-
Register of Controlled Trials and International Standard Randomized Controlled Trial Number Register
-
World Health Organization International Clinical Trials Registry Platform
-
PROSPERO systematic review register
-
Epistemonikos.
The resulting database of potentially relevant studies was managed in EndNote X7 (Thomson Reuters, CA, USA). After individual tests were identified, a second search was run to identify individual test costs.
Study selection
The citations identified were assessed for inclusion through two stages using Covidence systematic review software (Veritas Health Innovation Ltd, Melbourne, VIC, Australia). 61 Two reviewers independently scanned all of the titles and abstracts and identified the potentially relevant articles to be retrieved. Full-text copies of the selected studies were subsequently obtained and assessed independently by two reviewers. Disagreements were resolved by consensus or in discussions with a third reviewer.
The eligibility criteria are listed in Table 6 for the diagnostic accuracy studies and in Table 7 for the studies monitoring disease progression.
| Criteria | Included | Excluded |
|---|---|---|
| Study design | Index test and reference tests are evaluated in the same study population which are fully paired (all study participants receive the index test and the reference standard) | Any case studies, qualitative studies or studies with sample size of < 10 participants |
| Patient population | Adults (aged > 18 years) with suspected MCI or early dementia | Patients diagnosed with neurological damage caused by stroke or head injury, learning disabilities or brain tumours |
| Studies that report on both late and early stages of dementia were included only if both the populations were reported separately | ||
| Setting | Primary care, secondary care, memory clinics, acute care settings, care homes, tertiary or community-based setting | |
| Index test | Any commercial or non-commercial computer-based cognitive diagnostic tool with automated interpretation, addressing one or more domains of cognitive impairment | Automated cognitive diagnostic tool in a language other than English |
| Outcomes | Diagnostic accuracy (e.g. specificity, sensitivity, likelihood ratios, diagnostic odds ratio, intrapatient variability) | Studies not reporting on at least one diagnostic accuracy outcome |
| Acceptability (any studies recording a measure of acceptability) |
| Criteria | Included | Excluded |
|---|---|---|
| Study design | Index test and reference tests are evaluated in the same study population which are fully paired (all study participants receive the index test and the reference standard) | Any case studies, qualitative studies or studies with sample size of < 10 participants |
| Patient population | Adults (aged > 18 years) with diagnosed MCI and early dementia | Patients diagnosed with neurological damage caused by stroke or head injury, learning disabilities or brain tumours |
| Studies that report on both late and early stages of dementia were included only if both the populations were reported separately | ||
| Setting | Primary care, secondary care, memory clinics, acute care settings, care homes, tertiary or community-based setting | |
| Index test | Any commercial or non-commercial computer-based cognitive monitoring tool with automated interpretation, addressing one or more domains of cognitive impairment used for monitoring disease progression and treatment | Automated cognitive diagnostic tool in a language other than English |
| Outcomes | Monitoring accuracy (e.g. specificity, sensitivity, likelihood ratios, diagnostic odds ratio, intrapatient variability) | Studies not reporting on at least one monitoring outcome |
| Acceptability (any studies recording a measure of acceptability) |
Data extraction
Two reviewers developed, piloted and standardised two sets of data extraction forms. One form was designed to collect data on diagnostic accuracy and the other was designed to collect data related to monitoring disease progression. One reviewer extracted details of study design, participants, index and reference standard tests, outcome data and other relevant data, and a second reviewer checked the data extraction. Any discrepancies were resolved by consensus or in discussions with a third reviewer.
Assessment of methodological quality
The quality assessment of studies meeting the inclusion criteria was carried out by one reviewer and independently checked for accuracy by a second reviewer. The methodological quality of the included studies was assessed using the QUADAS-2 (Quality Assessment Tool for Diagnostic Accuracy Studies) tool. 62 This tool is designed to evaluate the risk of bias and applicability of primary diagnostic accuracy studies. The results of the quality assessment are presented in summary tables and as a narrative synthesis.
Outcomes
We recorded the following diagnostic accuracy outcome measures of automated computerised tests for MCI and early dementia:
-
sensitivity and specificity
-
area under the receiver operating characteristic curve (AUC).
Method of analysis/synthesis
Statistical analysis and data synthesis
Individual study results
The results of the individual diagnostic studies were tabulated and sensitivity, specificity, predictive values, likelihood ratios (LRs) and diagnostic odds ratios were calculated for the index test for each study where true-positive (TP), true-negative (TN), false-positive (FP) and false-negative (FN) data were available (see Appendix 1). These data were required to establish the actual sensitivity and specificity of a test for a given cut-off value. From this point onwards, TP, TN, FP and FN data will be referred to as 2 × 2 data. These terms are explained in detail in Appendix 1.
The authors of all of the studies included in this review were individually approached with a request for specific 2 × 2 data whether or not they were available in the published report. Out of 15 authors, only two responded and were able to provide these data.
Meta-analysis
It was not possible to perform a meta-analysis owing to non-comparable data; for example, study designs varied, the primary outcome measure cut-off points were heterogeneous, the likelihood of bias differed across the studies and the summary statistics were often inconsistently reported. The results of the included studies have been synthesised narratively and in tables. The possible effects of study quality (based on the assessment of risk of bias) on the 2 × 2 data and review findings have been considered.
Patient and public involvement
The review team was guided during the review by an Advisory Group comprising clinicians and service users. Building trusted contacts with service users led us to believe that the most effective way to obtain engagement with service users was through frontline agencies, for example the Alzheimer’s Society and Dementia UK. We sent out a call for participation through these frontline groups to identify people interested in giving feedback on the results of the review and on the final report. We took guidance from these agencies when we planned and facilitated our meetings and consulted the guidance available from INVOLVE on the principles of involving the public in research from the National Institute for Health Research. 63
Chapter 4 Results
Initial searches and application of inclusion criteria
The results of the searches and study selection are presented in Figure 2. The initial electronic search was conducted in August 2015 and 13,352 records were retrieved. An additional 5444 records were identified through ProQuest, hand-searching and citation tracking. After deduplication, 13,542 titles and abstracts were screened and 399 articles were shortlisted for full-text assessment. Four trials were identified during hand-searching:64–67 two are still recruiting participants,64,67 one has been completed but the results have not been published66 and the status of one trial65 is unknown. The authors of these studies were approached by e-mail and telephone for results, but no responses were received. These studies are tabulated in Table 21 in Appendix 2.
FIGURE 2.
The PRISMA flow diagram.
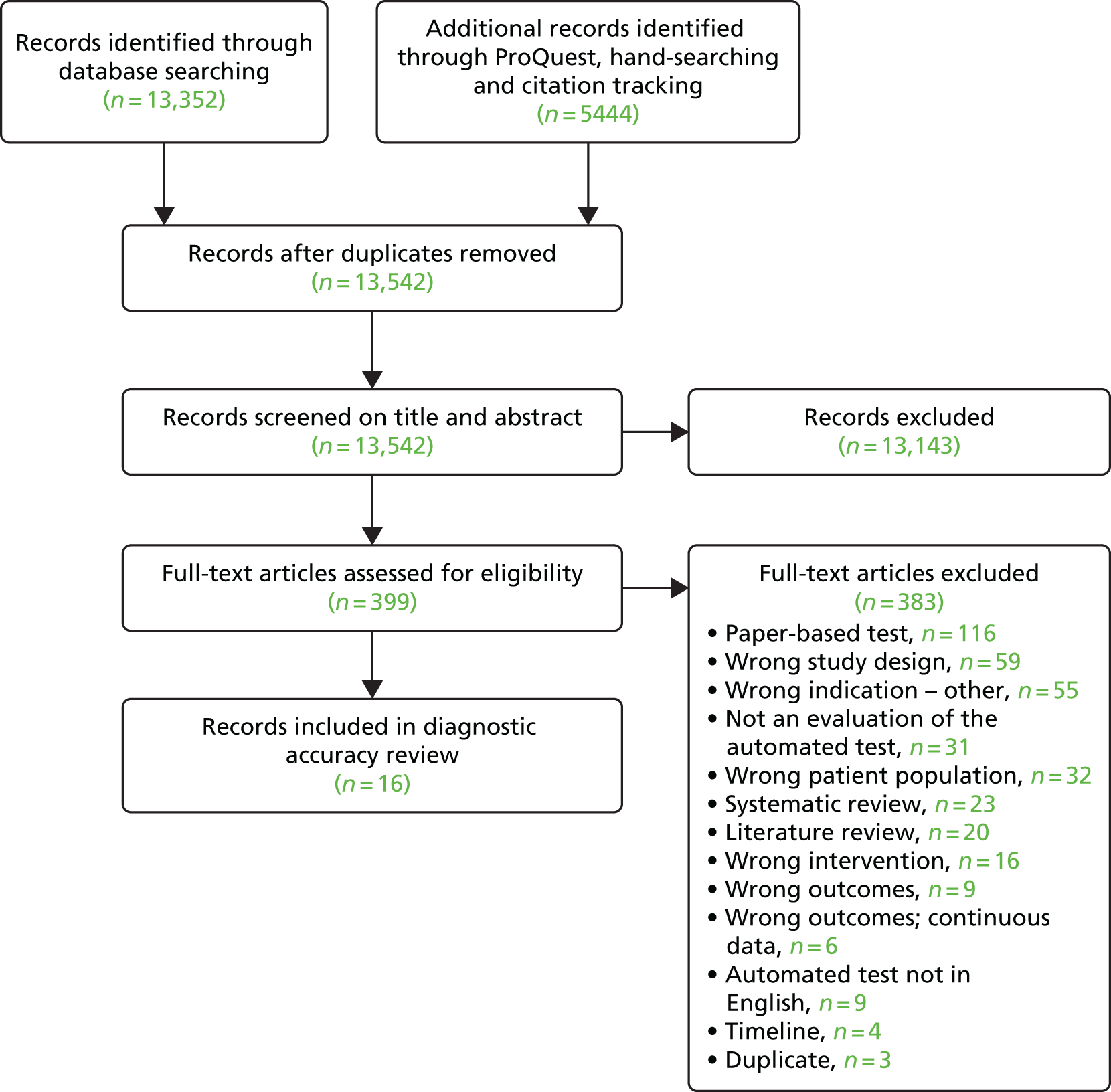
The reasons for excluding studies are tabulated in Appendix 3.
All of the tests (computerised and pen-and-paper) identified during screening are listed in Appendix 4.
Included studies
In total, 16 studies68–72,74–81,83,85,86 were included in the diagnostic accuracy review.
No studies met the review inclusion criteria for monitoring progression in MCI or early dementia and, therefore, there is no further mention of monitoring disease progression in the results section.
The details of the 16 included studies68–72,74–81,83,85,86 are summarised in Tables 8–10. Five studies reported results for more than two groups of participants: three included healthy controls, MCI and early dementia,71,76,86 and two included healthy controls, early dementia and early dementia/MCI combined. 70,74
| Study and year | Condition | Irrelevant study groups | Index test | Reference test | Company funding/financial interest |
|---|---|---|---|---|---|
| Ahmed et al.68 2012 | MCI | NA | CANS-MCI | Clinical diagnosis using Petersen’s criteria | No |
| de Jager et al.69 2009 | MCI | NA | CogState | Clinical diagnosis using battery of neurocognitive tests | No |
| Doniger et al.70 2005 | MCI MCI/mild dementia |
NA | Mindstreams | Clinical diagnosis using Petersen’s criteria20 for MCI and DSM-IV51 for dementia | Yes Not-for-profit |
| Dwolatzky et al.71 2003 | MCI Mild AD |
No relevant results reported for mild AD group | Mindstreams | Clinical diagnosis using Petersen’s criteria20 for MCI and DSM-IV51 for mild AD | Yes |
| Juncos-Rabadán et al.72 2014 | aMCI | NA | CANTAB | Clinical diagnosis using neurocognitive tests and Albert criteria73 and Peterson criteria20 for aMCI | No |
| Junkkila et al.74 2012 | aMCI/mild/probable dementia Mild/probable dementia |
NA | CANTAB-PAL | Clinical diagnosis using Petersen’s criteria20 and neurocognitive tests | No |
| Kingsbury et al.75 2010 | MCI | Depressed | CogniScreen | Clinical diagnosis using Petersen’s criteria20 | NR |
| Kluger et al.76 2009 | MCI Early dementia |
Other dementias | No name | Diagnosed by a consensus of at least two clinicians | No |
| Lichtenberg et al.77 2006 | MCI/early dementia | CST | Clinical diagnosis using Petersen’s criteria;20 clinical diagnosis of dementia using DSM-V52 | NR | |
| Maruff et al.79 2013 | MCI | Mild to moderate AD | CBB | Clinical diagnosis using Peterson criteria20 | Yes |
| Mundt et al.80 2001 | Dementia | Moderate stage of dementia | Computer-automated telephone screening | Clinical diagnosis using CDR score | No |
| O’Connell et al.81 2004 | Probable AD | NA | CANTAB-PAL | Clinical diagnosis using NINCDS-ADRDA82 criteria | NR |
| Rosenthal et al.83 2013 | HAND | HIV-negative people; HIV-positive people with asymptomatic neurocognitive impairment and minor neurocognitive disorder | CAMCI modified for use in HIV-positive population | HAND category using the Frascati criteria84 | Yes |
| Saxton et al.85 2009 | MCI | NA | CAMCI | Clinical diagnosis by consensus using battery of neurocognitive tests and functional and medical information | Yes |
| Tierney et al.78 2014 | MCI | NA | CAMCI | Clinical diagnosis using battery of neurocognitive tests | No |
| Vacante et al.86 2013 | MCI Early dementia |
NA | TPT | Clinical diagnosis using Petersen’s criteria20 | No |
| Study and year | Test name | Cognitive domains tested | Details of test platform used | Time (minutes) | Method of administration |
|---|---|---|---|---|---|
| Ahmed et al.68 2012 | CANS-MCI | Memory Language Visuospatial Executive function |
Desktop computer, a touchscreen system with both oral (loud speakers) and on-screen instructions | 30 | Self-administered Researcher in room |
| de Jager et al.69 2009 | CogState | Memory Executive function Attention Processing speed |
Internet | ≈20 | Self-administered Practice session with a psychologist |
| Doniger et al.70 2005 | Mindstreams (abridged) | Memory Executive function Visuospatial Motor skills |
Computer and mouse | 30 | Self-administered Practice session |
| Dwolatzky et al.71 2003 | Mindstreams | Memory Executive function Visuospatial Verbal Attention Information processing Motor skills |
Designed for use with the elderly. Mouse with the number pad on the keyboard (similar to the telephone keypad) | 45 | Self-administered Practice session with feedback prior to testing Research assistant |
| Juncos-Rabadán et al.72 2014 | CANTAB-R (DMS, PAL and PRM) | Memory | Touchscreen computer | NR | Self-administered Researcher present |
| Junkkila et al.74 2012 | CANTAB-PAL | Memory | Touchscreen computer | NR | Self-administered |
| Kingsbury et al.75 2010 | CogniScreen | Memory | Laptop, headset with microphone | 20–40 | Self-administered Experimenter in room |
| Kluger et al.76 2009 | Computerised test (no name) | Memory Praxis Naming Executive function |
Laptop | 12–15 | Self-administered Screening test for computer competency |
| Lichtenberg et al.77 2006 | CST | Learning Memory Executive function |
Internet based, interface with both written and oral instructions | 15 | Self-administered Keyboard proficiency test Administered by graduate psychology student |
| Maruff et al.79 2013 | CBB | Memory | Desktop computer, yes/no button attached through USB port | 10 | Self-administered Verbal instructions by supervisor Practice session |
| Mundt et al.80 2001 | Computer-automated telephone screening | Memory Spatial (auditory) Executive function Orientation Language |
Standard touch-tone telephones | 11–15 | Self-administered Researcher provided assistance in dialling the number |
| O’Connell et al.81 2004 | CANTAB-PAL | Memory | Touchscreen computer | 10 | NR |
| Rosenthal et al.83 2013 | CAMCI Modified | Memory Attention Executive function Processing speed |
Tablet with stylus | 25 | Self-administered |
| Saxton et al.85 2009 | CAMCI | Memory Attention Executive function Processing speed |
Desktop computer | ≈20 | Self-administered |
| Tierney et al.78 2014 | CAMCI | Memory Attention Executive function Processing speed |
Tablet computer | 30 | Self-administered some required researcher assistance |
| Vacante et al.86 2013 | TPT | Memory | Computer | 20 | Self-administered Including practice pages |
| Study and year | Country, setting | n | Exclusion criteria | Mean age, years (SD, range) | Gender (male, %) | Mean education, years (SD, range) | Race/ethnicity (%) |
|---|---|---|---|---|---|---|---|
| Ahmed et al.68 2012 | UK, primary care (Oxford OPTIMA Study)a | 35 (control: 20; MCI: 15) | A history of any disease which in the investigator’s opinion might confound the results of the study or pose an additional risk to the patient (e.g. diagnosis of psychiatric or endocrine disease, central neurological disorder, problems with eyesight, dementia treatment medication) | Control: 77.4 (4); MCI: 80.9 (7.2) | Control: 55.0; MCI: 33.3 | Control: 14.7 (2.9); MCI: 13.1 (3) | NR |
| de Jager et al.69 2009 | UK, community | 119 (control: 98; MCI: 21) | NR | Control: 77.18 (5.9); MCI: 81.95 (5.4) | NR | Unclear | NR |
| Doniger et al.70 2005 | USA, Israel and Canada, tertiary care, memory clinic | 161 (control: 71; MCI: 58; mild AD: 32) | Diagnosis of neurological or psychiatric disease or colour-blindness Missing information on age and education levels |
Entire group: 76.0 (8.2) | Entire group: 37.5 | Entire group: 13.3 (3.6) | Entire group White American: 1.2 African American: 4.3 Afro-Caribbean American: 7.5 White Canadian: 36 White Hispanic: 0.6 Israeli: 50.3 |
| Dwolatzky et al.71 2003 | Canada/Israel, two tertiary care memory clinics | 98 (control: 39; MCI: 30; mild AD: 29) | Prior history of major psychiatric disorder, major depression or any neurological disorder | Control: 73.41 (8.00); MCI: 77.15 (6.43); mild AD: 80.55 (4.91) | Control: 33.3; MCI: 56.7; mild AD: 44.8 | Control: 14.95 (3.5); MCI: 13.07 (2.86); mild AD: 11.31 (2.85) | NR |
| Juncos-Rabadán et al.72 2014 | Spain, primary care | 162 (control: 85; mda-MCI: 29; sda-MCI: 48) | History of clinical stroke, traumatic brain injury, motor–sensory defects, alcohol or drug abuse/dependence, diagnosed with any significant medical or psychiatric illnesses | Control: 62.25 (8.26, 50–82); mda-MCI: 71.68 (7.74, 54–87); sda-MCI: 68.02 (9.04, 50–84) | All participants: 36.4 | Control: 10.83 (5, 2–21); mda-MCI: 10.06 (3.99, 3–20); sda-MCI: 9.83 (3.96, 2–20) | NR |
| Junkkila et al.74 2012 | Finland, hospital | 58 (control: 22; aMCI: 17; AD: 19) | Depression, known or suspected cerebral ischaemic event, alcohol abuse, head injury and other significant neurological or psychiatric illness | Control: 70 (4.48, 65–80); aMCI: 73 (6.3, 61–83); AD: 73 (6.76, 61–83) | Control: 36.36; aMCI: 64.7; AD: 26.35 | Control: 10 (3.25); aMCI: 8 (3); AD: 8 (2.88) | NR |
| Kingsbury et al.75 2010 | Australia, community, memory clinic | 140 (control: 95; MCI: 30)b | Comorbidity of MCI and/or late-life depression, poor literacy, inability to give informed written consent | Controls: 68.85 (7.96, 53–89); MCI: 77.62 (7.45, 51–87) | Control: 37; MCI: 43 | Controls: 4.93 (1.71); MCI: 3.07 (1.71) Unclear what is measured |
NR |
| Kluger et al.76 2009 | USA, memory clinic | 101 (control: 39; MCI: 19; probable AD: 17; no diagnosis: 25) | Control participants were excluded if they had any history of significant neurological or psychiatric disease or if they scored < 27/30 on the MMSE | Control: 64 (11); MCI: 72 (10); probable AD: 78 (9) | NR | NR | NR |
| Lichtenberg et al.77 2006 | USA, specialised geriatric clinic | 102 (control: 55; MCI: 11; mild dementia: 36) | Significant motor, visual or cognitive impairments that prevented participants from using a computer or understanding directions, and individuals who were not fluent in English | All participants: 79.3 (6.6) | All participants: 46.1 | All participants: 13.5 (2.9) | African American: 5.9; European American: 94.1 European American: 94.1 |
| Maruff et al.79 2013 | Australia, primary care Some participants were part of Australian Imaging, Biomarkers and Lifestyle Study of Ageing |
766 (control: 659; aMCI: 107) | Schizophrenia, depression (15-item Geriatric Depression Score of ≥ 6), Parkinson’s disease, cancer (except basal cell skin carcinoma) within the last 2 years, symptomatic stroke, uncontrolled diabetes, or current regular alcohol use exceeding two standard drinks per day for women or four per day for men | Control: 69.5 (6.6); MCI: 75.7 (7.5) | Control: 42.2; MCI: 49.5 | Control: 12c (9–15); MCI: 12c (9–15) | NR |
| Mundt et al.80 2001 | USA, specialised geriatric clinic | 116 (control: 74; mild dementia: 42 | NR | All participants: 76.7 (7.0, 56–93) | All participants: 36.7 | All participants: 13.3 (3, 6–22) | NR |
| O’Connell et al.81 2004 | Ireland, memory clinic | 50 (control: 16; probable AD: 34) | NR | Control: 72.6 (7.7); probable AD: 73 (5.9) | Control: 12.5; probable AD: 32.4 | NR | NR |
| Rosenthal et al.83 2013 | USA, General Clinical Research Clinic | 55 (HIV positive: 16; HAD: 39) | History or current opportunistic central nervous system infection, history or current schizophrenia, current severe affective disorder believed to explain a subject’s cognitive impairment, history of a chronic neurological disorder including multiple sclerosis and epilepsy, and current intoxication on illegal drugs or alcohol | HIV-positive controls: 45.4 (6); HAD: 48.3 (6.3) | HIV-positive controls: 75.0; HAD: 71.8 | HIV-positive controls: 12.3 (1.8); HAD: 12.6 (2.1) | Black people/ African American/Caribbean: HIV-positive control; 81.3, HAD: 94.9 |
| Saxton et al.85 2009 | USA, primary care and community | 524 (control: 296; MCI: 228) | Diagnosis of alcohol abuse, stroke, mental health disorder, presence of neurological disease and significant sensory deficit or physical limitation precluding performance on cognitive tests | Control: 71.84 (5.95); MCI: 75.18 (6.76) | MCI: 37.7; control: 32.8 | Control 13.74 (2.69); MCI: 13.10 (2.61) | Control: white people (95.9); MCI: white people (92.1) |
| Tierney et al.78 2014 | Canada, tertiary care | 263 NR |
Under 65 years old, documented diagnosis of dementia or who had been referred to, and worked up by, a specialist for a cognitive concern. Current diagnoses of major depressive disorder, schizophrenia, or bipolar disorder, those not fluent in English, unable to read normal print with or without glasses, unable to hear normal conversation with or without hearing aids, acutely ill, delirious or had a life expectancy of < 1 year | Completed without assistance: 78.7 (6.9); completed with assistance: 81.8 (6.5) | All participants: 41.4 | Completed without assistance: 15.2 (3.2); completed with assistance: 13.9 (4.0) | White people 87 |
| Vacante et al.86 2013 | UK, primary care (Oxford OPTIMA Study)a | 78 (controls: 40; MCI: 20; early AD: 18) | NR | Traditional version Control: 74.7 (7.78); MCI: 78.3 (8.4); early AD: 73.67 (6.28) Novel version Control: 73.67 (7.14); MCI: 79.7 (6.07); early AD: 77.22 (4.94) |
Traditional version Control: 50; MCI: 60; early AD: 66.7 Novel version Control: 45; MCI: 60; early AD: 77.8 |
Traditional version Control: 15.85 (3.36); MCI: 15.9 (3.32); early AD: 15 (3.04) Novel version Control:16.35 (3.18); MCI: 15 (2.66); early AD: 16.11 (2.97) |
NR |
In total, 10 studies68,69,71,72,75,76,78,79,85,86 evaluated the use of automated computerised tests to detect MCI alone, seven studies70,71,74,76,80,81,86 reported results for early dementia, three studies70,74,77 reported results for combined MCI/early dementia and one study83 reported results for human immunodeficiency virus (HIV)-associated neurocognitive disorder (HAND).
The information in Table 8 shows that the index tests assessed in the included studies varied. However, the references tests used in the studies were generally consistent across studies for patients with MCI and for patients with early dementia.
Study quality assessment
A summary of the quality assessment conducted is presented in Figures 3 and 4.
FIGURE 3.
Risk of bias and applicability concerns: summary.
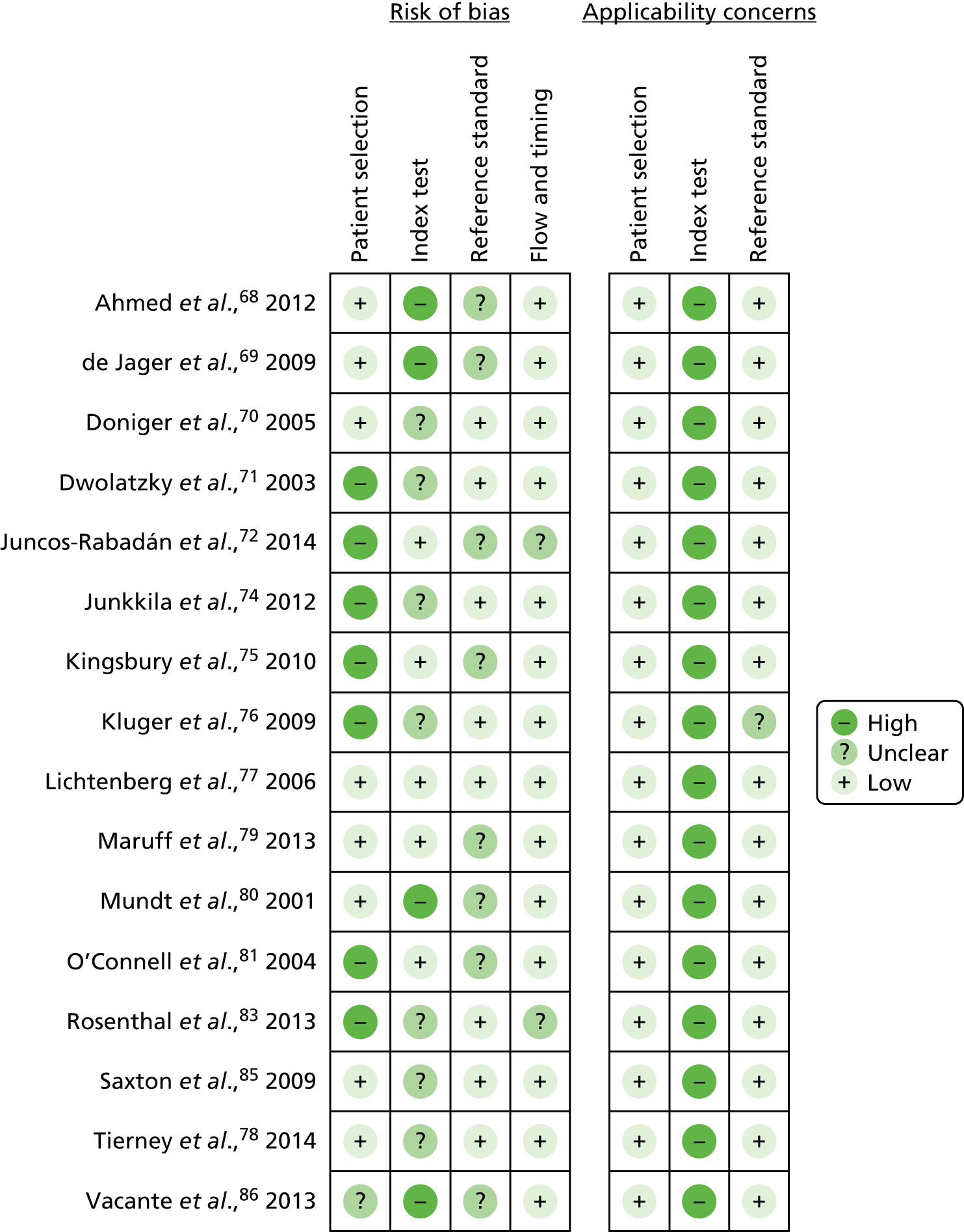
FIGURE 4.
Risk of bias and applicability concerns graph: presented as percentages.
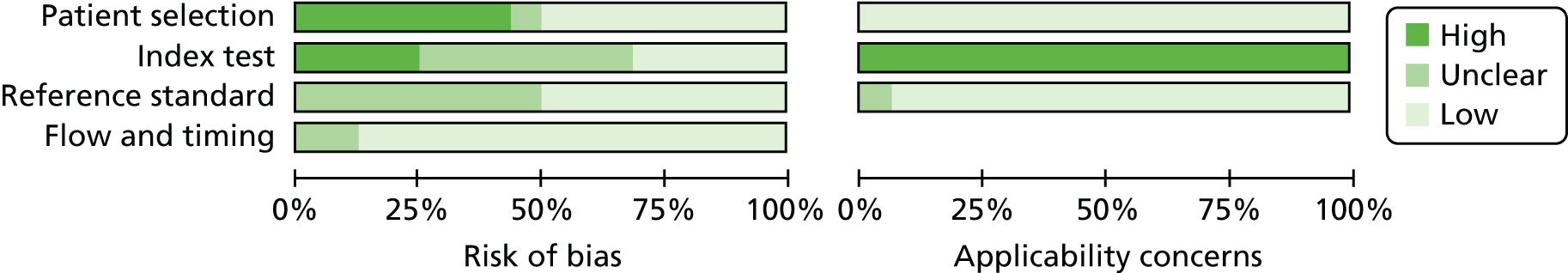
We used the modified form of QUADAS-2,62 which is recommended by the Cochrane Diagnostic Test Accuracy Reviews Guidelines,87 to assess the quality of the included studies. Concerns regarding the risk of bias and applicability have been presented as a summary and as percentages in Figures 3 and 4, respectively.
The risk-of-bias criterion for patient selection was high for seven studies,71,72,74–76,81,83 unclear for one study86 and low for eight studies. 68–70,77–80,85 The studies were judged to be at high risk for this criterion because a case–control study design was used.
Regarding the index test criteria for risk of bias, seven studies70,71,74,76,78,83,85 were judged to be at unclear risk. In these studies, the threshold values for the index tests were not pre-specified. However, for all of these studies, except Dwolatzky et al.,71 it was clear that the index test results had been interpreted without knowledge of the results of the reference standard.
We gave a judgement of high concern regarding applicability of the index test for all of the studies68–72,74–81,83,85,86 because the interpretation of the index test was different from the review question, as it is not possible to diagnose MCI and early dementia using automated computerised tests in isolation; specialist expertise is necessary to establish a diagnosis.
The reference standard domain for the risk of bias was unclear in eight studies,68,69,72,75,79–81,86 as it was not possible to ascertain whether or not reference standard results were interpreted without knowledge of the results of the index tests. However, the reference standard used in each of the studies was likely to correctly classify the target condition. All studies but one76 were judged to have low concern for applicability regarding the reference standard. The one study76 used a consensus of two clinicians’ opinions as the reference standard.
In the flow and timing domain for the risk of bias, a judgement of unclear risk of bias was given to two studies72,83 as a result of there being no details of timing or attrition described in the published papers. Not all of the studies (n = 11)68–71,74,76,77,79,80,85,86 reported whether or not there had been an appropriate interval between the index test and the reference standard. However, 14 studies68–71,74–81,85,86 were assessed as being at low risk owing to all patients having received the same reference standard and all patients being included in the analysis.
Although only one study77 was judged to be at low risk of bias across the four domains, the studies were considered to be of good quality. Patient selection issues were the most likely to introduce bias.
The only concern for applicability was the one previously mentioned, that is the interpretation of the index test was different from the review question as it is not possible to diagnose MCI and early dementia using automated computerised tests in isolation.
Index test details
The time required to self-administer the different index tests ranged from 10 minutes79,81 to 45 minutes. 71 A range of cognitive domains was tested across the different tests, memory and executive function being the most common. Even though all of the tests were self-administered, a practice session was offered to participants in five studies69–71,79,86 to make sure that patients were familiar with the software and platform for the index test. Nine studies68,69,71,72,75,77–80 reported that support staff were present in the room to address any questions from participants about the software or platform.
Study and participant characteristics
The characteristics of the included studies are presented in Table 10. A total of 2832 people were included in the studies, with the number of people in each study ranging from 5085 to 766. 81
Two studies were multicentred71,85 and one study71 was carried out internationally, in Canada and Israel. The earliest study was published in 200180 and two were recently conducted in 2014. 72,78 The study participants were generally similar across the studies (owing to relatively similar study inclusion and exclusion criteria), although four studies69,80,81,86 did not report their exclusion criteria.
The participants were mainly recruited through primary care68,72,79,85,86 or from a memory clinic. 71,75,76,81 Six studies were based in the USA,70,76,77,80,83,85 three were based in the UK,68,69,86 two were based in Australia,75,79 one was based in Ireland,81 one was based in Canada and Israel,71 one was based in Canada,78 one was based in Spain72 and one was based in Finland. 74 Participants in 13 studies68,70–72,74,75,77–80,83,85,86 had 874 to 2280 years of education; for the other three studies, data describing the education of the participants were not reported. 69,76,81 Only five studies70,72,77,83,85 reported data on ethnicity. There is a lack of demographic data in two studies69,76 for participants who were tested for MCI. Fifteen studies reported on cognitive impairment without comorbidities. 68–72,74–81,85,86 One of the included studies reported on cognitive impairment with a comorbidity (i.e. HIV). 83
Results from studies on cognitive impairment without comorbidities
The diagnostic accuracy of 11 automated computerised tests for the detection of MCI and/or early dementia without comorbidities was evaluated in 15 studies. 68–72,74–81,85,86 One study76 evaluated a test which did not have a name. Three studies72,74,81 reported on multiple or singular domains of the Cambridge Neuropsychological Test Automated Battery (CANTAB). The pooling of data from these 15 included studies was considered inappropriate as there were few studies evaluating the same index test in the same population, and it was possible to extract 2 × 2 data from only five72,74,80,81,85 of the 15 studies.
Studies reporting on diagnostic accuracy outcomes with 2 × 2 table
There were five studies72,74,80,81,85 that reported diagnostic accuracy outcomes in a 2 × 2 table. Two studies72,85 reported the diagnostic accuracy outcomes for MCI, three studies74,80,81 reported outcomes for early dementia and one study74 reported combined outcomes for both MCI/early dementia. When possible, the positive predictive value (PPV), negative predictive value (NPV), positive LR (LR+) and negative LR (LR–) were calculated using 2 × 2 data.
Mild cognitive impairment
The diagnostic accuracy outcomes for the two studies72,85 reporting 2 × 2 data for MCI are presented in Table 11. The study by Juncos-Rabadán et al. 72 evaluated three different visual episodic memory tests included in the CANTAB; these memory tests were Pattern Recognition Memory, Delayed Matching to Sample and Paired Associated Learning. The overall sensitivity and specificity for the three visual episodic memory tests was moderate, at 79.7% and 76.3%, respectively. The AUC ranged from 0.623 to 0.747, which shows poor ability to discriminate between the MCI group and the non-MCI group. This test had a high overall PPV of 71.4%; this means that 71.4% of the people who tested positive for MCI with the reference standard actually had MCI. Similarly, the overall NPV for this test was 83.3%, meaning that 83.3% of people who tested negative for MCI on the reference standard did not have MCI. This test had a low overall LR+ of 3.4, which shows a low likelihood of the test to establish the presence of disease. It also had a low overall LR– of 0.3, which shows a low likelihood of the test to establish the absence of disease.
| Study and year | Index test | Cut-off point | Sensitivity (%) | Specificity (%) | AUC | TP | FN | TN | FP | PPV (%) | NPV (%) | LR+ | LR– |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Juncos-Rabadán et al.72 2014 | CANTAB | ||||||||||||
| Overalla | 79.7 | 76.3 | NR | 55 | 14 | 71 | 22 | 71.4 | 83.3 | 3.4 | 0.3 | ||
| PRM | 1.5 SD below controls | 45.5b | 92.9b | 0.704b | 35 | 42 | 79 | 6 | 85.4b | 65.3b | 6.44b | 0.59b | |
| DMS | 1.5 SD below controls | 23.4b | 97.6b | 0.623b | 18 | 59 | 83 | 2 | 90.0b | 58.5b | 9.94b | 0.78b | |
| PAL | 1.5 SD below controls | 58.4b | 89.4b | 0.747b | 45 | 32 | 76 | 9 | 83.3b | 70.4b | 5.52b | 0.46b | |
| Saxton et al.85 2009 | CAMCI | Final tree model | 86 | 94 | 91.22b | 201 | 27 | 277 | 19 | 91.4b | 91.1b | 13.7b | 0.127b |
The study by Saxton et al. 85 evaluated the Computer Assessment of Mild Cognitive Impairment (CAMCI) and reported good sensitivity (86%) and exceptional specificity (94%), with an exceptional AUC of 0.91.
Early dementia
The diagnostic accuracy outcomes for the three studies74,80,81 reporting 2 × 2 data for patients with early dementia are presented in Table 12. The Cambridge Neuropsychological Test Automated Battery Paired Associated Learning (CANTAB-PAL) was evaluated in two of the studies. 74,81 The authors of one study74 reported high sensitivity (81.8%) and specificity (97.2%) and an AUC of exceptional discrimination (0.914) for early dementia. It also had a PPV of 94.7% and a NPV of 89.7%.
| Study and year | Index test | Cut-off point | Sensitivity (%) | Specificity (%) | AUC | TP | FN | TN | FP | PPV (%) | NPV (%) | LR+ | LR– |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Junkkila et al.74 2012 | CANTAB-PAL | NR | 81.8a | 97.2a | 0.914a | 18 | 4 | 35 | 1 | 94.7a | 89.7a | 5.35a | 0.0.3a |
| Mundt et al.80 2001 | Computer Automated Telephone System | A derived scoring algorithm | 79.17a | 83.8a | 0.819a | 38 | 10 | 62 | 12 | 76.0a | 86.1a | 4.88a | 0.249a |
| O’Connell et al.81 2004 | CANTAB-PAL | 32 errors | 67.6 | 100 | 0.780 | 23 | 11 | 16 | 0 | 100 | 59.3 | 0.324 |
The study by O’Connell et al. 81 reported poor sensitivity (67.6%) and high specificity (100%) and an AUC of moderate discrimination between the early dementia group and non-early dementia group (0.78). The authors also reported a PPV of 100.0% and a NPV of 59.3%. This test also had a low LR– of 0.324 for early dementia.
Mundt et al. 80 assessed the Computer Automated Telephone System and reported moderate sensitivity (79.17%) and high specificity (83.8%) for this test. The authors reported an AUC of 0.819, which shows good discrimination. The test also had a PPV of 76.0%, a NPV of 86.1%, a low LR+ of 4.88 and a low LR– of 0.249 for dementia.
Mild cognitive impairment/early dementia
The diagnostic accuracy outcomes for the one study74 reporting 2 × 2 data for MCI/early dementia are presented in Table 13. This study evaluated CANTAB-PAL. The authors reported high sensitivity (96.9%) and high specificity (80.8%), with an AUC of good discrimination (0.897) between the MCI/early dementia group and non-MCI/early dementia group. The test had a PPV of 86.1% and a NPV of 95.5%; it also had a low LR+ of 5.04 and low LR– of 0.04 for MCI/early dementia.
Studies reporting on diagnostic accuracy outcomes without 2 × 2 table
The authors of 10 studies68–71,75–79,86 reported diagnostic accuracy outcomes for nine different index tests without using 2 × 2 data. Instead, the authors of the studies calculated optimal sensitivity and specificity values using receiver operating characteristic curve analysis. The authors of seven studies reported the optimal sensitivity and specificity. 68,69,75,77–79,86 There were seven studies that reported AUC values. 68–71,75,76,79 Two studies reported PPV and NPV,68,77 and no study reported LR+ and LR– results. The outcome measures presented in these studies are tabulated in Tables 14–16.
| Study and year | Index test | Cut-off point | Sensitivity (%) | Specificity (%) | AUC (95% CI) | PPV (%) | NPV (%) | LR+ | LR– |
|---|---|---|---|---|---|---|---|---|---|
| Ahmed et al.68 2012 | CANS-MCI | 0.5 | 89.0 | 73.0 | 0.867 (0.743 to 0.990) | 60 | 84 | NR | NR |
| de Jager et al.69 2009 | CogState | ||||||||
| Accuracy | 82.6 | 78.0 | 90.0 | 0.86 (NR) | NR | NR | NR | NR | |
| Accuracy–speed ratio | 3.54 | 76.0 | 79.0 | 0.84 (NR) | NR | NR | NR | NR | |
| Dwolatzky et al.71 2003 | Memory | ||||||||
| Verbal memory (accuracy, first rep. trial) | NA for AUC | NR | NR | 0.779 (0.668 to 0.890) | NR | NR | NR | NR | |
| Verbal memory (accuracy, second rep. trial) | NR | NR | 0.838 (0.741 to 0.936) | NR | NR | NR | NR | ||
| Verbal memory (accuracy, third rep. trial) | NR | NR | 0.752 (0.629 to 0.876) | NR | NR | NR | NR | ||
| Verbal memory (accuracy, final rep. trial) | NR | NR | 0.783 (0.662 to 0.904) | NR | NR | NR | NR | ||
| Verbal memory (accuracy, all rep. trials) | NR | NR | 0.859 (0.765 to 0.953) | NR | NR | NR | NR | ||
| Verbal memory (accuracy, delayed recognition) | NR | NR | 0.771 (0.651 to 0.890) | NR | NR | NR | NR | ||
| Non-verbal memory (accuracy, first rep. trial) | NR | NR | 0.654 (0.522 to 0.786) | NR | NR | NR | NR | ||
| Non-verbal memory (accuracy, second rep. trial) | NR | NR | 0.698 (0.563 to 0.833) | NR | NR | NR | NR | ||
| Non-verbal memory (accuracy, third rep. trial) | NR | NR | 0.712 (0.585 to 0.839) | NR | NR | NR | NR | ||
| Non-verbal memory (accuracy, final rep. trial) | NR | NR | 0.773 (0.654 to 0.892) | NR | NR | NR | NR | ||
| Non-verbal memory (accuracy, all rep. trials) | NR | NR | 0.756 (0.633 to 0.879) | NR | NR | NR | NR | ||
| Non-verbal memory (accuracy, delayed recognition) | NR | NR | 0.728 (0.601 to 0.854) | NR | NR | NR | NR | ||
| Executive function | |||||||||
| Go/no go (accuracy) | NA for AUC | NR | NR | 0.736 (0.608 to 0.863) | NR | NR | NR | NR | |
| Go/no go (performance index) | NR | NR | 0.810 (0.701 to 0.920) | NR | NR | NR | NR | ||
| Problem-solving (accuracy) | NR | NR | 0.768 (0.653 to 0.884) | NR | NR | NR | NR | ||
| Stroop interference (performance index) | NR | NR | 0.703 (0.551 to 0.854) | NR | NR | NR | NR | ||
| Catch game (accuracy) | NR | NR | 0.696 (0.548 to 0.843) | NR | NR | NR | NR | ||
| Visual spatial | |||||||||
| Visual spatial imagery (accuracy) | NA for AUC | NR | NR | 0.765 (0.648 to 0.881) | NR | NR | NR | NR | |
| Verbal | |||||||||
| Verbal function (accuracy, naming) | NA for AUC | NR | NR | 0.716 (0.584 to 0.848) | NR | NR | NR | NR | |
| Verbal function (accuracy, rhyming) | NR | NR | 0.824 (0.724 to 0.923) | NR | NR | NR | NR | ||
| Attention | |||||||||
| Go/no go (RT) | NA for AUC | NR | NR | 0.771 (0.648 to 0.893) | NR | NR | NR | NR | |
| Go/no go (SD of RT) | NR | NR | 0.706 (0.576 to 0.835) | NR | NR | NR | NR | ||
| Choice RT (performance index) | NR | NR | 0.490 (0.326 to 0.653) | NR | NR | NR | NR | ||
| Information processing | |||||||||
| Staged information processing, low load (performance index) | NA for AUC | NR | NR | 0.579 (0.416 to 0.743) | NR | NR | NR | NR | |
| Staged information processing, medium load (performance index) | NR | NR | 0.783 (0.646 to 0.920) | NR | NR | NR | NR | ||
| Staged information processing, high load (performance index) | NR | NR | 0.688 (0.515 to 0.860) | NR | NR | NR | NR | ||
| Motor skills | |||||||||
| Finger tapping (inter-tap interval) | NA for AUC | NR | NR | 0.595 (0.446 to 0.744) | NR | NR | NR | NR | |
| Finger tapping (SD of inter-tap interval) | NR | NR | 0.625 (0.469 to 0.782) | NR | NR | NR | NR | ||
| Catch game (time to first move) | NR | NR | 0.521 (0.360 to 0.682) | NR | NR | NR | NR | ||
| Kingsbury et al.75 2010 | CogniScreen | ||||||||
| Pair recognition | 0.47 | 76.0 | 60.0 | 0.72 (0.62 to 0.83) | NR | NR | NR | NR | |
| Cued recall | 0.305 | 82.1 | 76.7 | 0.87 (0.80 to 0.95) | NR | NR | NR | NR | |
| Immediate and delayed serial recall | 0.385 | 92.6 | 80.0 | 0.89 (0.81 to 0.97) | NR | NR | NR | NR | |
| Kluger et al.76 2009 | Computerised test (no name) | NR | NR | NR | 0.89 | NR | NR | NR | NR |
| Tierney et al.78 2014 | CAMCI | 2 | 80.0 | 74.0 | NR | NR | NR | NR | NR |
| Maruff et al.79 2013 | CBB | ||||||||
| Psychomotor/attention | 90 | 41.1 | 85.7 | 0.67 (0.6 to 0.73) | NR | NR | NR | NR | |
| Learning/working memory | 90 | 80.4 | 84.7 | 0.91 (0.87 to 0.94) | NR | NR | NR | NR | |
| Vacante et al.86 2013 | Computerised total (novel and traditional) | 19.5 | 70.0 | 76.2 | NR | NR | NR | NR | NR |
| Computerised objects and faces (novel and traditional) | 12.5 | 50 | 64.3 | NR | NR | NR | NR | NR | |
| Computerised objects and faces (novel and traditional) | 75 | 52.4 | NR | NR | NR | NR | NR | ||
| Study and year | Index test | Cut-off point | Sensitivity (%) | Specificity (%) | AUC (95% CI) | PPV (%) | NPV (%) | LR+ | LR– |
|---|---|---|---|---|---|---|---|---|---|
| Doniger et al.70 2005 | Mindstreams (abridged) | ||||||||
| Overall | NA for AUC | NR | NR | 0.886 | NR | NR | NR | NR | |
| Memory | |||||||||
| Verbal memory | NA for AUC | NR | NR | 0.830 (0.762 to 0.898) | NR | NR | NR | NR | |
| Non-verbal memory | NA for AUC | NR | NR | 0.825 (0.756 to 0.893) | NR | NR | NR | NR | |
| Executive function | |||||||||
| Go/no go | NA for AUC | NR | NR | 0.733 (0.640 to 0.826) | NR | NR | NR | NR | |
| Stroop interference | NA for AUC | NR | NR | 0.790 (0.690 to 0.890) | NR | NR | NR | NR | |
| Catch game | NA for AUC | NR | NR | 0.748 (0.670 to 0.827) | NR | NR | NR | NR | |
| Visual spatial | |||||||||
| Visual spatial imagery | NA for AUC | NR | NR | 0.678 (0.567 to 0.789) | NR | NR | NR | NR | |
| Dwolatzky et al.71 2003 | Mindstreams Computerised Cognitive Testing | NR | NR | NR | NR | NR | NR | NR | NR |
| Kluger et al.76 2009 | Computerised test (no name) | NR | NR | NR | 0.97 | NR | NR | NR | NR |
| Vacante et al.86 2013 | TPT | ||||||||
| Computerised total (novel and traditional) | 15.5 | 88.9 | 92.9 | NR | NR | NR | NR | NR | |
| Computerised objects and faces (novel and traditional) | 94.4 | 78.6 | NR | NR | NR | NR | NR | ||
| Computerised objects and faces (novel and traditional) | 13.5 | 94.4 | 52.4 | NR | NR | NR | NR | NR | |
| Study and year | Index test | Cut-off point | Sensitivity (%) | Specificity (%) | AUC (95% CI) | PPV (%) | NPV (%) | LR+ | LR– |
|---|---|---|---|---|---|---|---|---|---|
| Doniger et al.70 2005 | Mindstreams (abridged) | ||||||||
| Overall | NA for AUC | NR | NR | 0.823 (0.757 to 0.888) | NR | NR | NR | NR | |
| Memory | |||||||||
| Verbal memory | NA for AUC | NR | NR | 0.773 (0.697 to 0.849) | NR | NR | NR | NR | |
| Non-verbal memory | NA for AUC | NR | NR | 0.767 (0.690 to 0.844) | NR | NR | NR | NR | |
| Executive function | |||||||||
| Go/no go | NA for AUC | NR | NR | 0.719 (0.639 to 0.800) | NR | NR | NR | NR | |
| Stroop interference | NA for AUC | NR | NR | 0.671 (0.575 to 0.766) | NR | NR | NR | NR | |
| Catch game | NA for AUC | NR | NR | 0.685 (0.595 to 0.776) | NR | NR | NR | NR | |
| Visual spatial | |||||||||
| Visual spatial imagery | NA for AUC | NR | NR | 0.721 (0.638 to 0.803) | NR | NR | NR | NR | |
| Lichtenberg et al.77 2006 | CST | 1.5 | 80.0 | 87.0 | NR | 88.0 | 79.0 | NR | NR |
Mild cognitive impairment
The diagnostic accuracy outcomes reported in eight studies68,69,71,75,76,78,79,86 for MCI are presented in Table 14. Ahmed et al. 68 evaluated Computer-Administered Neuropsychological Screen for Mild Cognitive Impairment and reported high sensitivity (89.0%) and moderate specificity (73.0%) with an AUC of 0.867, which shows a good ability to discriminate between the MCI group and the non-MCI group.
Tierney et al. 78 evaluated the CAMCI test and reported a high sensitivity (80.0%) and a moderate specificity (74.0%); the authors did not report AUC PPV, NPV, LR+ or LR– values.
Maruff et al. 79 evaluated the CogState Brief Battery. The CogState Brief Battery has two composite scores for four tasks: psychomotor function, attention function, learning memory and working memory. The psychomotor/attention function had poor discrimination, as its AUC was 0.67. It also had poor sensitivity (41.1%) but high specificity (85.7%). The AUC for the learning/working memory was 0.91, which shows exceptional ability to discriminate between the MCI group and the non-MCI group. It also had high sensitivity (80.4%) and high specificity (84.7%). The overall sensitivity, specificity and AUC were not reported.
Early dementia
The diagnostic accuracy outcomes for early dementia were assessed in four studies70,71,76,86 and are presented in Table 15.
Dwolatzky et al. 71 did not report any results for early dementia patients, despite relevant data for this group having been collected during the study. Doniger et al. 70 evaluated an abridged version of Mindstreams and reported an overall AUC of 0.886, which showed a good ability to discriminate between the early dementia group and the non-early dementia group.
Kluger et al. 76 evaluated an automated computerised test, which did not have a specific name. This automated test examined the domains of memory, praxis, temporal, orientation, naming and crossed response inhibition. The authors reported an AUC of 0.97, which shows exceptional ability to discriminate between patients with early dementia and healthy control subjects.
Mild cognitive impairment/and early dementia
The diagnostic accuracy outcomes in two studies70,77 for MCI/early dementia are presented in Table 16.
Doniger et al. 70 reported an overall AUC of 0.823, which showed a good ability to discriminate between the cognitively healthy group and the cognitive unhealthy group. AUC values for individual test results ranged from 0.671 to 0.773.
Lichtenberg et al. 77 reported values for sensitivity and specificity (80.0% and 87.0%, respectively), PPV (88.0%) and NPV (79.0%).
Results from studies on cognitive impairment with comorbidities
The diagnostic accuracy of one automated computerised test was evaluated in one study83 that included people with cognitive impairment with comorbidities. This study examined HAND and used the automated test CAMCI. CAMCI assessed multiple domains with different tasks, which included simple reaction time, recurring picture, go/no go rule 1, go/no go rule 2, word recall, digit span forward, digit span reverse, shopping trip directions task, shopping list task, errand – bank, errand – post office, completion of the shopping list task and incidental recall task. The study set out to examine a range of diagnostic accuracy outcomes, but did not report the values for all of them.
The study authors state that the AUC analyses indicate that the digit span, forward digit span size and functional driving task differentiated between HIV-positive individuals with and without HAND. 83 However, the results presented show a low to moderate sensitivity but poor specificity. The authors of the study presented values for several, but not all, tests. It was reported that, in the forward digit span, a raw score cut-off point of ≥ 6 gives a sensitivity of 63.0% and a specificity of 19.0% and a forward span size raw score cut-off point of ≥ 5 gave a sensitivity of 80.0% and a specificity of 9.0%. The study also reported that the raw score on the shopping trip directions task of ≥ 13 gave a sensitivity of 75.0% and a specificity of 18.0%. 83
Patient and public involvement
Data from the included studies describing the index test details, characteristics of study participants and diagnostic accuracy outcomes were presented and discussed with a service user. The structure of this meeting is described in Appendix 5. As some of the index tests showed high sensitivity and specificity when used to examine one or two cognitive domains, the service user thought that all of the index text domains ought to have been explored by the authors of the studies to enable a comprehensive overview of any cognitive impairment identified. In addition, the service user considered that more information on key domains would help clinicians and patients to address the challenges faced by patients with MCI or early dementia as they carry out their everyday activities. The service user thought that the studies covered different populations very well, but raised concerns about the age of the study participants, as none of the tests evaluated cognitive impairment in people older than 90 years of age. A further concern was that the level of education of the person being tested might affect his or her performance on the test.
The discussion with the service user was mostly centred around the importance of the index tests being user-friendly and acceptable to patients. In a conversation about the different kinds of platforms used for the tests, the service user noted that if a patient had tremors then a desktop computer would be preferred to a touchscreen test, especially if the touchscreen test was very sensitive to touch.
When discussing the different types of tests available, the service user also highlighted the importance of ensuring that the test had a clear contrast between colours because it is likely that older people will have cataracts, colour blindness or other problems with their eyesight.
The service user also stated that some people might become frustrated with tests that lasted longer than 40 minutes, especially people who are not familiar with modern technology and people who are considered to be very elderly. The service user suggested that a patient’s GP might be the best person to make a decision about whether or not the patient would be able to complete an automated test and generate meaningful results, as some people are more comfortable than others when using technology.
Individual test costs
After identifying the individual index tests via searching, a second search was run to identify the total costs of using these computerised tests and, where possible, to determine the acquisition costs of the tests. A number of grey literature sources generated some cost data, but it was not clear if these costs were yearly subscription costs for an organisation that had planned to use the test or if they were one-off costs for the use of one test by one person. 88–91 The authors of the publications did not state whether or not the costs also included the costs associated with training or administering the test, and the need for a health-care specialist to score/interpret the test was not discussed.
Chapter 5 Discussion
Summary of main results
We identified 16 studies68–72,74–81,83,85,86 for inclusion in the diagnostic accuracy review of automated computerised tests to detect MCI or early dementia; only one study83 included patients with comorbidities. No studies met the review inclusion criteria for monitoring disease progression.
Ten studies68,69,71,72,75,76,78,79,85,86 evaluated the use of automated computerised tests to detect MCI alone, seven studies70,71,74,76,80,81,86 reported results for early/mild dementia, three studies70,74,77 reported results for combined MCI/early dementia and one study83 reported results for HAND.
Eleven different index tests were evaluated. The only study which evaluated the diagnostic accuracy of automated computerised tests for people with cognitive impairment with comorbidities was conducted by Rosenthal et al. 83
Most of the included studies had small sample sizes; 10 studies68,69,71,72,74–77,81,86 had fewer than 150 participants and only two studies79,85 had more than 500 participants. Differences in study design, primary outcome measure cut-off points, the likelihood of bias, the reporting of summary statistics (e.g. 2 × 2 data) and disparity in the index tests precluded a meta-analysis of the data reported in the included studies. Meaningful synthesis of the diagnostic outcomes from the included studies was not possible.
Of the 16 studies,68–72,74–81,83,85,86 only one77 was judged to be at low of risk of bias across the four domains examined; despite this, the overall quality of the included studies was considered to be good. Patient selection issues were the most likely to introduce bias. The only concern for applicability was the one previously mentioned, that is, the interpretation of the index test was different from the review question as it is not possible to diagnose MCI and early dementia using automated computerised tests in isolation.
Applicability of findings to the review question
Ideally, for diagnostic purposes, an index test with high specificity is preferable, and high sensitivity is preferred for screening. 92 When diagnosing patients with MCI and/or early dementia, an index test with both high sensitivity and specificity is needed to be able to appreciate a distinctive pattern of cognitive impairment in MCI and early dementia.. This distinctive pattern of cognitive impairment is different from the cognitive impairment caused by other disease processes (e.g. cognitive impairment as presented in depression or HIV). The distinctive pattern of cognitive impairment caused by other conditions such as depression requires the use of elaborate scales such as the Cambridge Cognitive Examination,93–95 the Alzheimer’s Disease Assessment Scale96,97 or the Repeatable Battery for the Assessment of Neuropsychological Status. 98,99 Current pen-and-paper tests screening instruments for MCI cannot do this.
In the case of HIV, however, it is difficult to draw a clearer distinction in the pattern of cognitive impairment, as no attempt has been made to adapt the diagnostic criteria for HAND to the pattern of cognitive domains that are affected in HIV. 84,100,101 Although it is difficult to find robust data, the dominant theory is that HAND causes deficits primarily in executive function, psychomotor speed and attention. Language is not thought to be affected, and neither are learning nor recall, although deficits in the other domains can present themselves to the patient as communication and memory difficulties in the ‘real-life’ scenario (as opposed to the testing environment). 102 This makes it difficult to separate it from or equate it to MCI or early dementia.
Most studies were not conducted in samples representative of the usual clinical population in which these tests might be used (e.g. patients coming to memory clinics with a mix of MCI and dementia of various aetiologies, some were the ‘worried well’ and others were depressed) but were conducted in convenience samples of patients with limited diagnoses (mostly MCI and AD). Furthermore, only three studies68,69,86 out of 16 were conducted in the UK.
It is difficult to draw a clear picture of the diagnostic accuracy of the index tests that were assessed in this review, as there is not enough evidence to support the use of one test over another.
It is not clear from reviewing the included studies if these computerised tests ought to be used in primary and/or secondary care. In the UK, some GP practices take part in ‘case finding’ for dementia, for example specifically targeting ‘high-risk’ groups (e.g. older adults, or patients with high vascular risk, learning disability or Parkinson’s disease), and hospital staff undertake brief cognitive assessments during all acute admissions for older adults.
The pen-and-paper tests currently used in clinical practice not only help clinicians differentiate between normal cognition, MCI and dementia,45,46,48 but also assist in staging severity of illness. In contrast, CANTAB was the only automated test in this review that could stage severity. 72,74,81 The time taken to complete these computerised tests varied between 10 and 45 minutes but was not reported in two studies. 72,74 In contrast, pen-and-paper-based tests typically range from 7 to 10 minutes to complete. 45,46,48 Concern for the time it takes to complete the tests was raised by the service user, who pointed out the possibility of people becoming frustrated with tests that lasted for more than 40 minutes, especially if they were not familiar with using technology.
The data in the included papers did not describe the time required for training, administration, scoring and interpreting the test results.
Comparisons with previous research
None of the previously conducted relevant reviews56,57,103 in this area carried out a diagnostic accuracy review. They were narrative reviews56,57,103 that provided a summary of the battery of tests used and then rated this evidence on validity and reliability, comprehensiveness, and usability. Our review focused on automated computerised tests that were self-administered and had a minimum level of involvement from health-care professionals. In line with our review findings, the authors of the other reviews56,57,103 concluded that there are significant differences in automated computerised tests and hence they must be judged on a case-by-case basis. 57
Strengths and weaknesses of the review
The search strategy for this review was extensive and included multiple databases and grey literature sources. The majority of studies were identified by terms related to the index test, the terminology for which is reasonably standardised. To capture the difficult-to-locate studies where the index test is not referred to in the parts of the electronic record available for search retrieval, we searched the Cochrane Dementia and Cognitive Improvement Group’s register of diagnostic test accuracy studies. The methodological rigour of the review process was enhanced by the use of two assessors to perform citation screening, quality assessment and data extraction/checking. We also contacted all of the primary study authors and asked them to fill in the actual values of a 2 × 2 table. Out of 15 authors, only two were able to send in the requested details. We also conducted a patient and public involvement exercise, but were able to receive feedback on our review findings from only one service user representative.
We excluded studies in which the automated tests or the studies evaluating the automated test were not described in English. The utility of this review is limited in part by the heterogeneity of the automated computerised tests assessed in the included studies. Owing to substantial diversity in the index tests and the characteristics of the participants, it was not appropriate to pool the data. The poor reporting of the diagnostic accuracy outcomes by the authors also hampered data extraction, quality assessment and meaningful synthesis.
We were also unable to identify any studies that reported on any measure of test acceptability. We did not identify any studies that reported outcomes related to monitoring disease progression.
Chapter 6 Conclusions
Implications for practice
The overall quality and quantity of information is insufficient to be able to make recommendations on the clinical use of the computerised tests for diagnosing and monitoring MCI and early dementia progression. The suitability of these tests also depends on the costs of the test, training, administration and scoring. Increased effectiveness of a test could offset the costs of the test, equipment and staff training.
The diagnosis of patients with MCI and early dementia is currently based on clinical judgement and medical history as well as on the results of cognitive tests. However, a ‘definitive’ diagnosis of dementia can be made only after a post-mortem analysis of the brain. We also note that autopsy studies in dementia have shown that there is little correlation of these results with the clinical diagnosis made when patients were alive. Therefore, the reference standard remains a clinical diagnosis based on history and physical and cognitive examination. For this reason, we would recommend against approaches that use computerised tests in isolation. Even with pre-specified cut-off values for a particular population, any cognitive testing measure alone is insufficient to render a diagnostic classification: other relevant clinical information must be taken into account.
Older people are more likely to have motor limitations (e.g. as a result of strokes, pain or tremor) or vision and hearing impairments that may render computerised testing impractical. This raises the issue of whether or not these tests can be truly self-administered and valid. For these patients, automated computerised tests may not offer benefits over current practice.
Implications for research
Further research is required in order to establish stable cut-off points for each automated computerised test used to diagnose patients with MCI or early dementia. These cut-off points need to be tested in specific patient populations, for example in patients of different age groups or education levels and from different geographical regions.
The prevalence of dementia and alternative diagnoses in the study populations should be clearly reported and make reference to standardised checklists for diagnostic reviews such as Standards for Reporting Diagnostic Accuracy104 or Standards for Reporting Diagnostic Accuracy – dementia. 105 Investigators might consider evaluating automated computerised test performance at different cut-off points, across populations with varying prevalence of MCI and early dementia. Once sufficient studies in the defined populations are conducted, further reviews and meta-analyses can be carried out.
Future research in this area should also focus on providing more information on the costs of computerised tests and include time for training, administration and scoring of the different tests, as these are important factors for their use in routine clinical practice. This type of information is currently lacking in the published studies describing computerised tests used to diagnose or monitor people with MCI or early dementia.
Acknowledgements
The authors are pleased to acknowledge the contributions of Mr Robert Little, who was the representative for public and patient involvement for this report. We are also appreciative of Professor John O’Brien (University of Cambridge), who reviewed the final draft of the report. We would also like to thank Dr Lewis Haddow (University College London) for his advice on the role of HIV in cognitive impairment.
Contributions of authors
Dr Rabeea’h W Aslam drafted the review protocol, managed the process of study selection, data extraction and data checking, facilitated the service user feedback and drafted the final report.
Dr Vickie Bates commented on the protocol, contributed to study selection and data extraction and provided input into the final report.
Dr Yenal Dundar contributed to the initial search strategy, commented on the protocol, contributed to data checking and provided input into the final report.
Ms Juliet Hounsome commented on the protocol, contributed to data extraction and provided input into the final report.
Miss Marty Richardson commented on the protocol, contributed to the discussion on possible statistical analysis and provided input into the final report.
Mrs Ashma Krishan commented on the protocol, contributed to the discussion on possible statistical analysis and provided input into the final report.
Professor Rumona Dickson commented on the protocol and provided input into final report.
Dr Angela Boland provided input into the draft and final reports.
Ms Eleanor Kotas conducted the literature searches for studies and costs.
Miss Joanne Fisher contributed to data extraction.
Dr Sudip Sikda was clinical consultant, reviewed the protocol and provided input into the final report.
Professor Louise Robinson was clinical consultant, reviewed the protocol and provided input into the final report.
Data sharing statement
All available data can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement 2013;9:63-75.e2. http://dx.doi.org/10.1016/j.jalz.2012.11.007.
- World Health Organization (WHO) . International Classification of Diseases – Classification of Diseases, Functioning, and Disability 2010. www.who.int/classifications/icd/en/ (accessed 16 July 2015).
- O’Neill D, Barber RD. Reversible dementia caused by vitamin B12 deficiency. J Am Geriatr Soc 1993;41:192-3. http://dx.doi.org/10.1111/j.1532-5415.1993.tb02058.x.
- Meador KJ. Cognitive side effects of medications. Neurol Clin 1998;16:141-55. http://dx.doi.org/10.1016/S0733-8619(05)70371-6.
- Muangpaisan W, Petcharat C, Srinonprasert V. Prevalence of potentially reversible conditions in dementia and mild cognitive impairment in a geriatric clinic. Geriatr Gerontol Int 2012;12:59-64. http://dx.doi.org/10.1111/j.1447-0594.2011.00728.x.
- Chang CY, Silverman DH. Accuracy of early diagnosis and its impact on the management and course of Alzheimer’s disease. Expert Rev Mol Diagn 2004;4:63-9. http://dx.doi.org/10.1586/14737159.4.1.63.
- Howard R, McShane R, Lindesay J, Ritchie C, Baldwin A, Barber R, et al. Nursing home placement in the Donepezil and Memantine in Moderate to Severe Alzheimer's Disease (DOMINO-AD) trial: secondary and post-hoc analyses. Lancet Neurol 2015;14:1171-81. http://dx.doi.org/10.1016/S1474-4422(15)00258-6.
- National Institute for Health and Care Excellence . Dementia. Supporting People With Dementia and Their Carers in Health and Social Care 2006. www.nice.org.uk/guidance/cg42 (accessed 21 July 2015).
- National Institute for Health and Care Excellence . Dementia Diagnosis and Assessment 2015. http://pathways.nice.org.uk/pathways/dementia (accessed 21 July 2015).
- Brooks LG, Loewenstein DA. Assessing the progression of mild cognitive impairment to Alzheimer’s disease: current trends and future directions. Alzheimers Res Ther 2010;2.
- Braak H, Braak E, Jellinger K, Fazekas F, Windisch M. Ageing and Dementia. Vienna: Springer; 1998.
- Petersen RC, Caracciolo B, Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution. J Intern Med 2014;275:214-28. http://dx.doi.org/10.1111/joim.12190.
- Watkin A, Sikdar S, Majumdar B, Richman AV. New diagnostic concepts in Alzheimer’s disease. Adv Psychiatr Treat 2013;19:242-9. http://dx.doi.org/10.1192/apt.bp.112.010462.
- Bruscoli M, Lovestone S. Is MCI really just early dementia? A systematic review of conversion studies. Int Psychogeriatr 2004;16:129-40. http://dx.doi.org/10.1017/S1041610204000092.
- Busse A, Angermeyer MC, Riedel-Heller SG. Progression of mild cognitive impairment to dementia: a challenge to current thinking. Br J Psychiatry 2006;189:399-404. http://dx.doi.org/10.1192/bjp.bp.105.014779.
- Roberts R, Knopman DS. Classification and epidemiology of MCI. Clin Geriatr Med 2013;29:753-72. http://dx.doi.org/10.1016/j.cger.2013.07.003.
- Gauthier S, Reisberg B, Zaudig M, Petersen RC, Ritchie K, Broich K, et al. Mild cognitive impairment. Lancet 2006;367:1262-70. http://dx.doi.org/10.1016/S0140-6736(06)68542-5.
- Feldman HH, Jacova C. Mild cognitive impairment. Am J Geriatr Psychiatry 2005;13:645-55. http://dx.doi.org/10.1097/00019442-200508000-00003.
- Forlenza OV, Diniz BS, Stella F, Teixeira AL, Gattaz WF. Mild cognitive impairment. Part 1: clinical characteristics and predictors of dementia. Rev Bras Psiquiatr 2013;35:178-85. http://dx.doi.org/10.1590/1516-4446-2012-3503.
- Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 1999;56:303-8. http://dx.doi.org/10.1001/archneur.56.3.303.
- Jonker C, Geerlings MI, Schmand B. Are memory complaints predictive for dementia? A review of clinical and population-based studies. Int J Geriatr Psychiatry 2000;15:983-91. http://dx.doi.org/10.1002/1099-1166(200011)15:11<983::AID-GPS238>3.0.CO;2-5.
- Mitchell AJ, Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia – meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand 2009;119:252-65. http://dx.doi.org/10.1111/j.1600-0447.2008.01326.x.
- Petersen RC. Clinical practice. Mild cognitive impairment. N Engl J Med 2011;364:2227-34. http://dx.doi.org/10.1056/NEJMcp0910237.
- Bischkopf J, Busse A, Angermeyer MC. Mild cognitive impairment – a review of prevalence, incidence and outcome according to current approaches. Acta Psychiatr Scand 2002;106:403-14. http://dx.doi.org/10.1034/j.1600-0447.2002.01417.x.
- Launer LJ. Counting dementia: there is no one ‘best’ way. Alzheimers Dement 2011;7:10-4. http://dx.doi.org/10.1016/j.jalz.2010.11.003.
- Sachdev PS, Lipnicki DM, Crawford J, Reppermund S, Kochan NA, Trollor JN, et al. Risk profiles of subtypes of mild cognitive impairment: the Sydney memory and ageing study. J Am Geriatr Soc 2012;60:24-33. http://dx.doi.org/10.1111/j.1532-5415.2011.03774.x.
- World Health Organization (WHO) . Dementia: A Public Health Priority 2012. www.who.int/iris/handle/10665/75263#sthash.yy7M37Ka.dpuf (accessed 21 July 2015).
- Finkel SI. Behavioral and psychologic symptoms of dementia. Clin Geriatr Med 2003;19:799-824. http://dx.doi.org/10.1016/S0749-0690(03)00046-6.
- Kales HC, Gitlin LN, Lyketsos CG. Assessment and management of behavioral and psychological symptoms of dementia. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h369.
- Harvey RJ, Skelton-Robinson M, Rossor MN. The prevalence and causes of dementia in people under the age of 65 years. J Neurol Neurosurg Psychiatr 2003;74:1206-9. http://dx.doi.org/10.1136/jnnp.74.9.1206.
- Marosi C, Hassler M, Roessler K, Reni M, Sant M, Mazza E, et al. Meningioma. Crit Rev Oncol Hematol 2008;67:153-71. http://dx.doi.org/10.1016/j.critrevonc.2008.01.010.
- Patient . Dementia 2015. http://patient.info/doctor/dementia-pro (accessed 27 July 2015).
- National Institute for Health and Care Excellence . Dementia – Clinical Knowledge Summary 2015. http://cks.nice.org.uk/dementia (accessed 21 July 2015).
- National Audit Office . Improving Services and Support for People With Dementia 2007. www.nao.org.uk/report/improving-services-and-support-for-people-with-dementia/ (accessed 24 November 2015).
- Alzheimer’s Society . Dementia UK: The Full Report 2007. www.alzheimers.org.uk/site/scripts/download_info.php?fileID=2 (accessed 21 July 2015).
- Prince M, Knapp M, Guerchet M, McCrone P, Prina M, Comas-Herrera A, et al. Alzheimer’s Society . Dementia UK: Update 2014. www.cfas.ac.uk/files/2015/07/P326_AS_Dementia_Report_WEB2.pdf (accessed 22 November 2015).
- Alzheimer’s Society . Dementia – Assessment and Diagnosis 2014. www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=260.
- Herlitz A, Small BJ, Fratiglioni L, Almkvist O, Viitanen M, Bäckman L. Detection of mild dementia in community surveys. Is it possible to increase the accuracy of our diagnostic instruments?. Arch Neurol 1997;54:319-24. http://dx.doi.org/10.1001/archneur.1997.00550150075019.
- Morris JC, Storandt M, Miller JP, McKeel DW, Price JL, Rubin EH, et al. Mild cognitive impairment represents early-stage Alzheimer disease. Arch Neurol 2001;58:397-405. http://dx.doi.org/10.1001/archneur.58.3.397.
- Yokomizo JE, Simon SS, Bottino CM. Cognitive screening for dementia in primary care: a systematic review. Int Psychogeriatr 2014;26:1783-804. http://dx.doi.org/10.1017/S1041610214001082.
- Brooke P, Bullock R. Validation of a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatry 1999;14:936-40. http://dx.doi.org/10.1002/(SICI)1099-1166(199911)14:11%3C936::AID-GPS39%3E3.0.CO;2-1.
- Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry 2000;15:1021-7. http://dx.doi.org/10.1002/1099-1166(200011)15:11%3C1021::AID-GPS234%3E3.0.CO;2-6.
- Buschke H, Kuslansky G, Katz M, Stewart WF, Sliwinski MJ, Eckholdt HM, et al. Screening for dementia with the memory impairment screen. Neurology 1999;52:231-8. http://dx.doi.org/10.1212/WNL.52.2.231.
- Longmore M, Wilkinson I, Baldwin A, Wallin E, Longmore M, Wilkinson I, et al. Oxford Handbook of Clinical Medicine. Oxford: Oxford University Press; 2014.
- Kalbe E, Kessler J, Calabrese P, Smith R, Passmore AP, Brand M, et al. DemTect: a new, sensitive cognitive screening test to support the diagnosis of mild cognitive impairment and early dementia. Int J Geriatr Psychiatry 2004;19:136-43. http://dx.doi.org/10.1002/gps.1042.
- Velayudhan L, Ryu SH, Raczek M, Philpot M, Lindesay J, Critchfield M, et al. Review of brief cognitive tests for patients with suspected dementia. Int Psychogeriatr 2014;26:1247-62. http://dx.doi.org/10.1017/S1041610214000416.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695-9. http://dx.doi.org/10.1111/j.1532-5415.2005.53221.x.
- Tariq SH, Tumosa N, Chibnall JT, Perry MH, Morley JE. Comparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive disorder – a pilot study. Am J Geriatr Psychiatry 2006;14:900-10. http://dx.doi.org/10.1097/01.JGP.0000221510.33817.86.
- Kansagara D, Freeman M. A Systematic Evidence Review of the Signs and Symptoms of Dementia and Brief Cognitive Tests Available in VA Department of Veterans Affairs (US) 2010. www.ncbi.nlm.nih.gov/books/NBK49021/ (accessed 22 November 2015).
- Leeflang MM, Deeks JJ, Gatsonis C, Bossuyt PM. Cochrane Diagnostic Test Accuracy Working Group . Systematic reviews of diagnostic test accuracy. Ann Intern Med 2008;149:889-97. http://dx.doi.org/10.7326/0003-4819-149-12-200812160-00008.
- Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2000.
- Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2013.
- Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry 2003;160:4-12. http://dx.doi.org/10.1176/appi.ajp.160.1.4.
- Chang YL, Bondi MW, McEvoy LK, Fennema-Notestine C, Salmon DP, Galasko D, et al. Global clinical dementia rating of 0.5 in MCI masks variability related to level of function. Neurology 2011;76:652-9. http://dx.doi.org/10.1212/WNL.0b013e31820ce6a5.
- Sheehan B. Assessment scales in dementia. Ther Adv Neurol Disord 2012;5:349-58. http://dx.doi.org/10.1177/1756285612455733.
- Tierney MC, Lermer MA. Computerized cognitive assessment in primary care to identify patients with suspected cognitive impairment. J Alzheimers Dis 2010;20:823-32.
- Wild K, Howieson D, Webbe F, Seelye A, Kaye J. Status of computerized cognitive testing in aging: a systematic review. Alzheimers Dement 2008;4:428-37. http://dx.doi.org/10.1016/j.jalz.2008.07.003.
- Centre for Reviews and Dissemination (CRD) . Systematic Reviews: CRD’s Guidance on Undertaking Reviews in Health Care 2009. www.york.ac.uk/media/crd/Systematic_Reviews.pdf (accessed 22 November 2015).
- National Institute for Health and Care Excellence . Diagnostics Assessment Programme Manual 2011. www.nice.org.uk/Media/Default/About/what-we-do/NICE-guidance/NICE-diagnostics-guidance/Diagnostics-assessment-programme-manual.pdf (accessed 27 July 2015).
- Macaskill P, Gatsonis C, Deeks JJ, Harbord RM, Takwoingi Y, Deeks JJ, et al. Analysing and Presenting Results . Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy 2010. http://methods.cochrane.org/sdt/sites/methods.cochrane.org.sdt/files/uploads/Chapter%2010%20-%20Version%201.0.pdf (accessed 22 November 2015).
- Babineau J. Product review: Covidence (systematic review software). J Can Health Libr Assoc 2014;35.
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529-36. http://dx.doi.org/10.7326/0003-4819-155-8-201110180-00009.
- Caress AL, Ford A, Roberts L, Turner K, Ward D, Williamson T. INVOLVE: Briefing Notes for Researchers 2012. www.invo.org.uk/resource-centre/resource-for-researchers/ (accessed 22 November 2015).
- Janssen Research & Development, LLC . A Study of a Self-Administered Memory Screening Test With Automated Reporting (SAMSTAR) in Subjects With Mild Cognitive Impairment 2015. www.clinicaltrials.gov/ct2/show/NCT02419183.
- Singer A. Pilot Testing a New Computer-Based Screening Tool to Detect Cognitive Impairment 2011. https://clinicaltrials.gov/ct2/show/NCT01220674.
- Martin CK. Feasibility and Validity of A Novel Computer Based Battery of Assessments in the Elderly (HHT) 2014. https://clinicaltrials.gov/ct2/show/NCT02109419 (accessed 24 November 2015).
- Soininen H. Computational Tools for Early Diagnosis of Memory Disorders (ProsKuopio) 2014. https://clinicaltrials.gov/ct2/show/NCT02050464 (accessed 24 November 2015).
- Ahmed S, de Jager C, Wilcock G. A comparison of screening tools for the assessment of mild cognitive impairment: preliminary findings. Neurocase 2012;18:336-51. http://dx.doi.org/10.1080/13554794.2011.608365.
- de Jager CA, Schrijnemaekers AC, Honey TE, Budge MM. Detection of MCI in the clinic: evaluation of the sensitivity and specificity of a computerised test battery, the Hopkins Verbal Learning Test and the MMSE. Age Ageing 2009;38:455-60. http://dx.doi.org/10.1093/ageing/afp068.
- Doniger GM, Zucker DM, Schweiger A, Dwolatzky T, Chertkow H, Crystal H, et al. Towards practical cognitive assessment for detection of early dementia: a 30-minute computerized battery discriminates as well as longer testing. Curr Alzheimer Res 2005;2:117-24. http://dx.doi.org/10.2174/1567205053585792.
- Dwolatzky T, Whitehead V, Doniger GM, Simon ES, Schweiger A, Jaffe D, et al. Validity of a novel computerized cognitive battery for mild cognitive impairment. BMC Geriatr 2003;3. http://dx.doi.org/10.1186/1471-2318-3-4.
- Juncos-Rabadán O, Pereiro AX, Facal D, Reboredo A, Lojo-Seoane C. Do the Cambridge Neuropsychological Test Automated Battery episodic memory measures discriminate amnestic mild cognitive impairment?. Int J Geriatr Psychiatry 2014;29:602-9. http://dx.doi.org/10.1002/gps.4042.
- Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:270-9. http://dx.doi.org/10.1016/j.jalz.2011.03.008.
- Junkkila J, Oja S, Laine M, Karrasch M. Applicability of the CANTAB-PAL computerized memory test in identifying amnestic mild cognitive impairment and Alzheimer’s disease. Dement Geriatr Cogn Disord 2012;34:83-9. http://dx.doi.org/10.1159/000342116.
- Kingsbury R, Pachana NA, Humphreys M, Tehan G, Byrne GJA. Utility of a computerised cognitive screen in MCI and depression in an older population. Aust J Rehabil Counsell 2010;16:14-26.
- Kluger BM, Saunders LV, Hou W, Garvan CW, Kirli S, Efros DB, et al. A brief computerized self-screen for dementia. J Clin Exp Neuropsychol 2009;31:234-44. http://dx.doi.org/10.1080/13803390802317559.
- Lichtenberg PA, Johnson AS, Erlanger DM, Kaushik T, Maddens ME, Imam K, et al. Enhancing cognitive screening in geriatric care: Use of an internet-based system. Int J Healthcare Inf Sysinformatics 2006;1:47-5. http://dx.doi.org/10.4018/jhisi.2006070103.
- Tierney MC, Naglie G, Upshur R, Moineddin R, Charles J, Jaakkimainen RL. Feasibility and validity of the self-administered computerized assessment of mild cognitive impairment with older primary care patients. Alzheimer Dis Assoc Disord 2014;28:311-19. http://dx.doi.org/10.1097/WAD.0000000000000036.
- Maruff P, Lim YY, Darby D, Ellis KA, Pietrzak RH, Snyder PJ, et al. Clinical utility of the Cogstate Brief Battery in identifying cognitive impairment in mild cognitive impairment and Alzheimer’s disease. BMC Psychol 2013;1. http://dx.doi.org/10.1186/2050-7283-1-30.
- Mundt JC, Ferber KL, Rizzo M, Greist JH. Computer-automated dementia screening using a touch-tone telephone. Arch Intern Med 2001;161:2481-7. http://dx.doi.org/10.1001/archinte.161.20.2481.
- O’Connell H, Coen R, Kidd N, Warsi M, Chin AV, Lawlor BA. Early detection of Alzheimer’s disease (AD) using the CANTAB paired Associates Learning Test. Int J Geriatr Psychiatry 2004;19:1207-8. http://dx.doi.org/10.1002/gps.1180.
- McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:263-9. http://dx.doi.org/10.1016/j.jalz.2011.03.005.
- Rosenthal LS, Skolasky RL, Moxley RT, Roosa HV, Selnes OA, Eschman A, et al. A novel computerized functional assessment for human immunodeficiency virus-associated neurocognitive disorder. J Neurovirol 2013;19:432-41. http://dx.doi.org/10.1007/s13365-013-0195-5.
- Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology 2007;69:1789-99. http://dx.doi.org/10.1212/01.WNL.0000287431.88658.8b.
- Saxton J, Morrow L, Eschman A, Archer G, Luther J, Zuccolotto A. Computer assessment of mild cognitive impairment. Postgrad Med 2009;121:177-85. http://dx.doi.org/10.3810/pgm.2009.03.1990.
- Vacante M, Wilcock GK, de Jager CA. Computerized adaptation of The Placing Test for early detection of both mild cognitive impairment and Alzheimer’s disease. J Clin Exp Neuropsychol 2013;35:846-56. http://dx.doi.org/10.1080/13803395.2013.825235.
- Reitsma JB, Rutjes AWS, Whiting P, Vlassov VV, Leeflang MMG, Deeks JJ, et al. Assessing Methodological Quality . Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy 2009. http://srdta.cochrane.org/ (accessed 24 July 2015).
- Gualtieri C. Computerized Neurocognitive Test Batteries for Dementia Screening 2004. www.ncneuropsych.com/research/ALZscreen_AAIC_pres.pdf (accessed 22 November 2015).
- Neurocare . Cambridge Neuropsychological Test Automated Battery 2012. www.neurocare.org.uk/2012/09/cambridge-neuropsychological-test-automated-battery/ (accessed 13 December 2015).
- Psychology Software Tools I . CAMCI® Overview 2015. www.pstnet.com/software.cfm?ID=98 (accessed 22 November 2015).
- NeuroTrax Corporation . Advanced Computerized Test Detects Early Signs of Dementia 2004. www.prnewswire.com/news-releases/advanced-computerized-test-detects-early-signs-of-dementia-74997062.html (accessed 22 November 2015).
- Gilbert R, Logan S, Moyer VA, Elliott EJ. Assessing diagnostic and screening tests: part 1. Concepts. West J Med 2001;174:405-9. http://dx.doi.org/10.1136/ewjm.174.6.405.
- Burns A, Jacoby R, Levy R. Progression of cognitive impairment in Alzheimer’s disease. J Am Geriatr Soc 1991;39:39-45. http://dx.doi.org/10.1111/j.1532-5415.1991.tb05904.x.
- Roth M, Huppert FA, Mountjoy CQ, Tym E. CAMDEX: The Cambridge Examination for Mental Disorders of the Elderly. Cambridge: Cambridge University Press; 1988.
- Lozano-Gallego M, Vilalta-Franch J, Llinàs-Reglà J, López-Pousa S. The Cambridge Cognitive Examination as a tool for detection of dementia. Rev Neurol 1999;28:348-52.
- Rozzini L, Chilovi BV, Peli M, Conti M, Rozzini R, Trabucchi M, et al. Anxiety symptoms in mild cognitive impairment. Int J Geriatr Psychiatry 2009;24:300-5. http://dx.doi.org/10.1002/gps.2106.
- Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer's disease. Am J Psychiatr 1984;141:1356-64.
- Johnson LA, Mauer C, Jahn D, Song M, Wyshywaniuk L, Hall JR, et al. Cognitive differences among depressed and non-depressed MCI participants: a project FRONTIER study. Int J Geriatr Psychiatry 2013;28:377-82. http://dx.doi.org/10.1002/gps.3835.
- Randolph C, Tierney MC, Erich Mohr E, Chase TN. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. J Clin Exper Neuropsychol 1998;20:310-19. http://dx.doi.org/10.1076/jcen.20.3.310.823.
- Blackstone K, Moore DJ, Franklin DR, Clifford DB, Collier AC, Marra CM, et al. Defining neurocognitive impairment in HIV: deficit scores versus clinical ratings. Clin Neuropsychol 2012;26:894-908. http://dx.doi.org/10.1080/13854046.2012.694479.
- Gisslén M, Price RW, Nilsson S. The definition of HIV-associated neurocognitive disorders: are we overestimating the real prevalence?. BMC Infect Dis 2011;11. http://dx.doi.org/10.1186/1471-2334-11-356.
- Cysique LA, Maruff P, Brew BJ. Prevalence and pattern of neuropsychological impairment in human immunodeficiency virus-infected/acquired immunodeficiency syndrome (HIV/AIDS) patients across pre- and post-highly active antiretroviral therapy eras: a combined study of two cohorts. J Neurovirol 2004;10:350-7. http://dx.doi.org/10.1080/13550280490521078.
- Zygouris S, Tsolaki M. Computerized cognitive testing for older adults: a review. Am J Alzheimers Dis Other Demen 2015;30:13-28. http://dx.doi.org/10.1177/1533317514522852.
- Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015;351. http://dx.doi.org/10.1136/bmj.h5527.
- Noel-Storr AH, McCleery JM, Richard E, Ritchie CW, Flicker L, Cullum SJ, et al. Reporting standards for studies of diagnostic test accuracy in dementia. The STARDdem Initiative. Neurology 2014;83:364-73. http://dx.doi.org/10.1212/WNL.0000000000000621.
- Nicholson A, Mahon J, Boland A, Beale S, Dwan K, Fleeman N, et al. The Clinical and Cost-Effectiveness of the PROGENSA PCA3 Assay and the Prostate Health Index (phi) in the Diagnosis of Prostate Cancer: A Systematic Review and Economic Evaluation 2014. www.nice.org.uk/guidance/DG17/documents/diagnosing-prostate-cancer-progensa-pca3-assay-and-prostate-health-index-diagnostics-assessment-report2 (accessed 22 November 2015).
- Macaskill P, Gatsonis C, Deeks JJ, Harbord RM, Takwoingi Y, Deeks JJ, et al. Analysing and Presenting Results . Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy 2010. http://srdta.cochrane.org/ (accessed 22 November 2015).
Appendix 1 Measures for assessing an index test against a reference standard
The following section outlines the different methods of assessing diagnostic outcomes. It is adapted from a previous piece of work conducted by the Liverpool Review and Implementation Group (LRiG) and is reproduced here with permission. 106
The classic presentation of the results of a clinical validity study is the so-called 2 × 2 table, as shown in Table 17.
| Test result | Clinical diagnosis (reference standard) | |
|---|---|---|
| MCI | No MCI | |
| New test positive | a | b |
| New test negative | c | d |
The number entered into cell ‘a’ is the number of patients for whom the new test correctly diagnoses MCI (as determined by the reference standard, in this case a clinical diagnosis of MCI). For these people, the new test is positive as is the reference standard; these are TPs.
The number entered into cell ‘b’ is the number of patients for whom the new test is positive (i.e. indicates the presence of MCI) but who do not, according to the reference standard (clinical diagnosis), have MCI. The new test has incorrectly diagnosed MCI; these are FPs.
The number entered into cell ‘c’ is the number of patients who are identified through the reference standard (clinical diagnosis) as having MCI but for whom the new test gave negative results. The new test has incorrectly labelled the patient as having MCI; these are FNs.
The number in cell ‘d’ is the number of patients who do not, according to the reference standard (clinical diagnosis), have MCI and who are also shown by the new test to be free from disease; these are TNs.
The numbers displayed in a 2 × 2 table are used to generate other summary measures. These are set out in Table 18.
| Term | Formula | Notes |
|---|---|---|
| Sensitivity | a/(a + c) | Proportion of those who actually have disease and are correctly identified with positive test results. TP rate |
| High sensitivity = few FNs | ||
| Specificity | d/(b + d) | Proportion of those who do not actually have the disease who are correctly identified with negative test results. 1–FP rate |
| High specificity = few FPs | ||
| PPV | a/(a + b) | The proportion of those with positive test results who actually have the disease |
| NPV | d/(c + d) | The proportion of those with negative test results who do not have the disease |
In an ideal world, a test would be 100% sensitive and 100% specific. However, in reality there is often a trade-off between the two, with tests that have high sensitivity having low specificity and vice versa.
The use of a 2 × 2 tables requires that the test results are dichotomous, that is, they can be divided into two groups: test positive and test negative.
Receiver operating characteristic curve
When an intervention test has a range of possible thresholds that could be used to divide results into test positive and test negative, the relationship between the threshold used and the performance of the test can be examined in a receiver operating characteristic curve. This is a graphical plot of the sensitivity (TP rate) against 1 – specificity or the FP rate for each threshold; examples of a receiver operating characteristic curve are shown in Figure 5, with the associated distribution of the index tests in diseased and non-diseased populations. An ideal test would have a point in the top-left corner with 100% specificity and 100% sensitivity.
FIGURE 5.
Examples of a receiver operating characteristic curve. (Image reproduced from Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy with permission. 107)
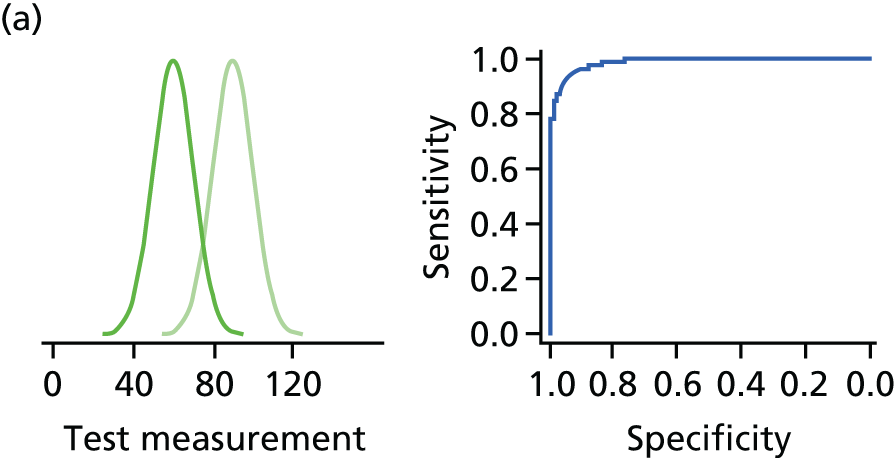
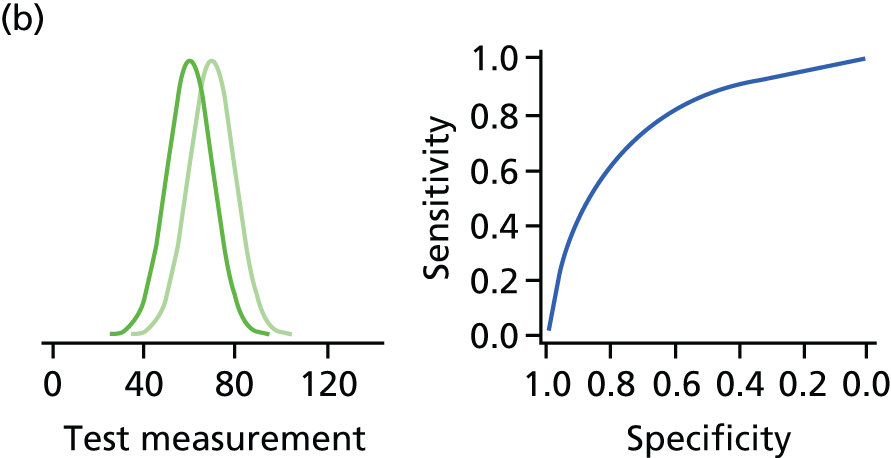
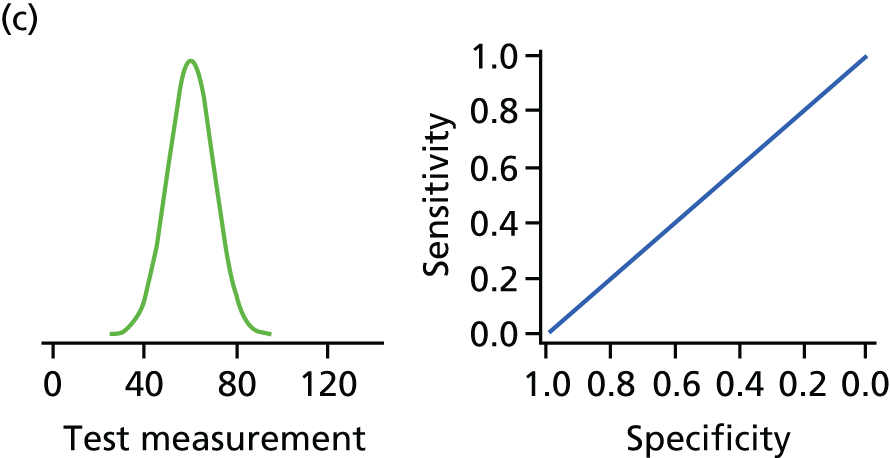

Area under a receiver operating characteristic curve
The receiver operating characteristic curve can be used to assess the degree to which sensitivity changes at different levels of specificity or vice versa. Some studies report AUC as a proportion of the total area of the graph. This is a measure of the predictive accuracy or discrimination of the diagnostic test, that is, the ability of the test to discriminate between those who have (or will develop) MCI from those who do not have (or will not develop) MCI.
The AUC can also be expressed as the probability that someone with the disease will have a higher test result than someone without the disease. It is also referred to as the c-statistic. An AUC of 1.0 indicates a perfect test, and an AUC of 0.5 (the diagonal line) indicates that the test is no better than chance (i.e. 50% probability) in predicting whether or not the disease is present. An AUC of 0.5 to 0.7 is considered as poor discrimination, 0.7 to 0.8 acceptable discrimination, 0.8 to 0.9 excellent discrimination and > 0.9 exceptional discrimination.
Positive predictive value and negative predictive value
The PPV is the probability that subjects with a positive screening test truly have the disease.
The NPV is the probability that subjects with a negative screening test truly do not have the disease.
The PPV and NPV are clinically significant, as they give probabilities that an individual is truly MCI/early dementia positive given that they tested positive or truly MCI/early dementia negative given that they tested negative.
Likelihood ratio
The LR gives another measure of performance for the disease, and is described in chapter 10 of the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy,107 as follows:
The LR+ describes how many times more likely positive index test results were in the diseased group than in the non-diseased group. The LR+, which should be > 1 if the test informative, is defined as:
(where T+ is index test positive, T– is index text negative, D+ is diseased, D– is non-diseased, P means probability and | means ‘given that’ or ‘on condition that’) and is estimated as:
The LR– describes how many times less likely negative index test results were in the diseased group than in the non-diseased group. The LR–, which should be < 1 if the test is informative, is defined as:
and is estimated as:
Appendix 2 Search strategies
A draft search strategy for MEDLINE was prepared and run on 15 July 2015 as part of the scoping searches. The search was updated on 6 August 2015 alongside a search of additional databases. The search strategies for each database are reported in Tables 19–22 and Boxes 1–4.
| Search terms | Results | |
|---|---|---|
| 1 | exp mild cognitive impairment/ | 3249 |
| 2 | ((early* or onset* or initial* or young* or incipient*) adj2 (dementia* or Alzheimer* or AD)).tw. | 9646 |
| 3 | ((Mild* or early* or onset* or initial* or progress* or minor or young* or moderat* or suspect*) adj2 Cognit* adj1 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)).tw. | 11,933 |
| 4 | MCI.tw. | 11,603 |
| 5 | NCD.tw. | 1233 |
| 6 | ((memory* or neurocognitiv*) adj2 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)).tw. | 29,085 |
| 7 | (“preclinical alzheimer*” or “pre-clinical alzheimer*”).tw. | 293 |
| 8 | (prodrom* adj2 dement*).tw. | 84 |
| 9 | *dementia/ or *alzheimer disease/ or *dementia, vascular/ or *dementia, multi-infarct/ or *frontotemporal dementia/ | 88,482 |
| 10 | or/1-9 | 129,676 |
| 11 | ((computer* or automate*) adj2 (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)).tw. | 19,607 |
| 12 | (automat* adj2 (interpretat* or test*)).tw. | 2445 |
| 13 | *Neuropsychological Tests/ | 13,160 |
| 14 | ((neuropsychological or neuro-psychological or psychometric*) adj5 (computer* or automate*) adj5 (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)).tw. | 831 |
| 15 | psychometrics/ | 58,160 |
| 16 | or/11-15 | 87,870 |
| 17 | 10 and 16 | 5551 |
| 18 | Diagnosis, Computer-Assisted/ | 19,850 |
| 19 | ((computer* or automate*) adj4 (diagnos* or detect*)).tw. | 13,645 |
| 20 | or/18-19 | 30,836 |
| 21 | 10 and 20 | 366 |
| 22 | disease progression/ | 114,210 |
| 23 | ((test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*) adj3 diseas* adj3 (progress* or exacerbat*)).tw. | 4249 |
| 24 | or/22-23 | 117,390 |
| 25 | 17 and 24 | 342 |
| 26 | “cambridge Neuropsychology Test*”.tw. | 0 |
| 27 | Computerised Neuropsychological Test Battery.tw. | 38 |
| 28 | Six Item Cognitive Impairment Test.tw. | 11 |
| 29 | “Computer Assessment of Mild Cognitive Impairment”.tw. | 3 |
| 30 | MindStream*.tw. | 27 |
| 31 | “Mild Cognitive Impairment Screen*”.tw. | 11 |
| 32 | Computer Administered Neuropsychological Screen for Mild Cognitive Impairment.tw. | 2 |
| 33 | Automated Neuropsychological Assessment Metrics.tw. | 90 |
| 34 | CANS-MCI.tw. | 2 |
| 35 | “CNS Vital Signs”.tw. | 33 |
| 36 | Cognitive Drug Research Computerised Assessment System for Dementia.tw. | 1 |
| 37 | CogState.tw. | 93 |
| 38 | “Cognitive Stability Index*”.tw. | 6 |
| 39 | “Cognitive Screening Test*”.tw. | 183 |
| 40 | Microcog.tw. | 28 |
| 41 | (COGDRAS-D or COGDRASD or COGDRAS).tw. | 0 |
| 42 | MCIS.tw. | 167 |
| 43 | (CAMCI or CNTB).tw. | 20 |
| 44 | 6CIT.tw. | 11 |
| 45 | (CANTAB-A or CANTABA or CANTAB).tw. | 343 |
| 46 | ANAM.tw. | 128 |
| 47 | CADi2.tw. | 1 |
| 48 | or/26-46 | 1103 |
| 49 | 17 or 21 or 25 or 48 | 6733 |
| 50 | animals/ not humans/ | 3,996,470 |
| 51 | 49 not 50 | 6691 |
| 52 | comment/ or editorial/ or letter/ | 1,496,207 |
| 53 | case reports/ | 1,764,849 |
| 54 | (comment or editorial or letter or journal correspondence or opinion).pt. | 1,496,207 |
| 55 | or/52-54 | 3,069,853 |
| 56 | 51 not 55 | 6360 |
| 57 | limit 56 to yr=“2005 -Current” | 3779 |
| Searches | Results | |
|---|---|---|
| 1 | exp mild cognitive impairment/ | 12,572 |
| 2 | ((early* or onset* or initial* or young* or incipient*) adj2 (dementia* or Alzheimer* or AD)).tw. | 12,911 |
| 3 | ((Mild* or early* or onset* or initial* or progress* or minor or young* or moderat* or suspect*) adj2 Cognit* adj1 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)).tw. | 18,245 |
| 4 | MCI.tw. | 18,975 |
| 5 | NCD.tw. | 1481 |
| 6 | ((memory* or neurocognitiv*) adj2 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)).tw. | 38,383 |
| 7 | (“preclinical alzheimer*” or “pre-clinical alzheimer*”).tw. | 374 |
| 8 | (prodrom* adj2 dement*).tw. | 124 |
| 9 | *dementia/ or *alzheimer disease/ or *dementia, vascular/ or multiinfarct dementia/ or *frontotemporal dementia/ | 125,217 |
| 10 | or/1-9 | 181,482 |
| 11 | ((computer* or automate*) adj2 (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)).tw. | 24,195 |
| 12 | (automat* adj2 (interpretat* or test*)).tw. | 3310 |
| 13 | *Neuropsychological Test/ | 6554 |
| 14 | ((neuropsychological or neuro-psychological or psychometric*) adj5 (computer* or automate*) adj5 (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)).tw. | 1174 |
| 15 | psychometry/ | 46,698 |
| 16 | or/11-15 | 76,781 |
| 17 | 10 and 16 | 3845 |
| 18 | computer assisted diagnosis/ | 36,170 |
| 19 | ((computer* or automate*) adj4 (diagnos* or detect*)).tw. | 16,191 |
| 20 | or/18-19 | 48,801 |
| 21 | 10 and 20 | 503 |
| 22 | disease course/ | 323,960 |
| 23 | ((test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*) adj3 diseas* adj3 (progress* or exacerbat*)).tw. | 6175 |
| 24 | or/22-23 | 326,786 |
| 25 | 17 and 24 | 215 |
| 26 | “cambridge Neuropsychology Test*”.tw. | 0 |
| 27 | Computerised Neuropsychological Test Battery.tw. | 50 |
| 28 | Six Item Cognitive Impairment Test.tw. | 14 |
| 29 | “Computer Assessment of Mild Cognitive Impairment”.tw. | 4 |
| 30 | MindStream*.tw. | 76 |
| 31 | “Mild Cognitive Impairment Screen*”.tw. | 17 |
| 32 | Computer Administered Neuropsychological Screen for Mild Cognitive Impairment.tw. | 3 |
| 33 | Automated Neuropsychological Assessment Metrics.tw. | 120 |
| 34 | CANS-MCI.tw. | 4 |
| 35 | “CNS Vital Signs”.tw. | 63 |
| 36 | Cognitive Drug Research Computerised Assessment System for Dementia.tw. | 1 |
| 37 | CogState.tw. | 232 |
| 38 | “Cognitive Stability Index*”.tw. | 10 |
| 39 | “Cognitive Screening Test*”.tw. | 288 |
| 40 | Microcog.tw. | 33 |
| 41 | (COGDRAS-D or COGDRASD or COGDRAS).tw. | 1 |
| 42 | MCIS.tw. | 257 |
| 43 | (CAMCI or CNTB).tw. | 33 |
| 44 | 6CIT.tw. | 22 |
| 45 | (CANTAB-A or CANTABA or CANTAB).tw. | 626 |
| 46 | ANAM.tw. | 199 |
| 47 | CADi2.tw. | 1 |
| 48 | or/26-46 | 1917 |
| 49 | 17 or 21 or 25 or 48 | 5930 |
| 50 | nonhuman/ not human/ | 3,604,816 |
| 51 | 49 not 50 | 5870 |
| 52 | comment/ or editorial/ or letter/ | 1,363,574 |
| 53 | case reports/ | 2 |
| 54 | (comment or editorial or letter or journal correspondence or opinion).pt. | 1,375,197 |
| 55 | or/52-54 | 1,407,178 |
| 56 | 51 not 55 | 5756 |
| 57 | limit 56 to yr=“2005 -Current” | 4134 |
| 58 | limit 57 to embase | 3228 |
| 59 | remove duplicates from 58 | 3191 |
| Databases | Date searched | Version/files | Number retrieved |
|---|---|---|---|
| Cochrane Database of Systematic Reviews (via Cochrane) | 6 August 2015 | Issue 7 of 12, July 2015 | 684 |
| Database of Abstracts of Reviews of Effects (via Cochrane) | 6 August 2015 | Issue 7 of 12, July 2015 | 32 |
| HTA database (via Cochrane) | 6 August 2015 | Issue 7 of 12, July 2015 | 4 |
| Cochrane Central Database of Controlled Trials (via Cochrane) | 6 August 2015 | Issue 7 of 12, July 2015 | 1136 |
| NHS Economic Evaluation Database | 6 August 2015 | Issue 7 of 12, July 2015 | 7 |
| MEDLINE (via Ovid) and MEDLINE In-Process & Other Non-Indexed Citations (via Ovid) | 6 August 2015 | Ovid MEDLINE(R) 1946 to week 5 July 2015, Database Field Guide Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations 5 August 2015 | 3779 |
| EMBASE (via Ovid) | 6 August 2015 | 1980 to 2015 Week 31 | 3191 |
| Web of Science | 6 August 2015 | N/A | 3586 |
| PsycINFO | 6 August 2015 | N/A | 541 |
| PubMed | 3 September 2015 | N/A | 392 |
| ProQuest theses and dissertations | 3 September 2015 | N/A | 197 (main search); 1919 (search for test names) |
| Hand-searching | 26 August 2015 | N/A | 4 |
| Citation tracking | 19 September 2015 | N/A | 3324 |
| Databases | Date searched | Links to results |
|---|---|---|
| ClinicalTrials.gov | 26 August 2015 | A Study of a Self-Administered Memory Screening Test With Automated Reporting (SAMSTAR) in Participants With Mild Cognitive Impairment64 |
| Pilot Testing a New Computer-based Screening Tool to Detect Cognitive Impairment65 | ||
| Feasibility and Validity of A Novel Computer Based Battery of Assessments in the Elderly (HHT)66 | ||
| Computational Tools for Early Diagnosis of Memory Disorders (ProsKuopio)67 | ||
| metaRegister of Controlled Trials and ISRCTN Register | 26 August 2015 | None found |
| World Health Organization International Clinical Trials Registry Platform | 26 August 2015 | None found |
| PROSPERO systematic review register | 26 August 2015 | None found |
| Epistemonikos | 26 August 2015 | No new references found |
TI “Cognitive Stability Index*” OR TI “Cognitive Screening Test*” OR TI Microcog OR TI ( (COGDRAS-D or COGDRASD or COGDRAS) ) OR TI MCIS OR TI ( (CAMCI or CNTB) ) OR TI 6CIT OR TI ( (CANTAB-A or CANTABA or CANTAB) ) OR TI ANAM OR TI CADi2
TI “cambridge Neuropsychology Test*” OR TI Computerised Neuropsychological Test Battery OR TI Six Item Cognitive Impairment Test OR TI “Computer Assessment of Mild Cognitive Impairment” OR TI MindStream* OR TI “Mild Cognitive Impairment Screen*” OR TI Computer Administered Neuropsychological Screen for Mild Cognitive Impairment OR TI Automated Neuropsychological Assessment Metrics OR TI CANS-MCI OR TI “CNS Vital Signs” OR TI Cognitive Drug Research Computerised Assessment System for Dementia OR TI CogState
TI ( ((early* or onset* or initial* or young* or incipient*) near2 (dementia* or Alzheimer* or AD)) ) OR TI ( ((Mild* or early* or onset* or initial* or progress* or minor or young* or moderat* or suspect*) near2 Cognit* near1 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)) ) OR TI ( MCI or NCD ) OR TI ( ((memory* or neurocognitiv*) near2 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)) ) OR TI ( (“preclinical alzheimer*” or “pre-clinical alzheimer*”) ) OR TI (prodrom* near2 dement*) AND TI ( ((computer* or automate*) near4 (diagnos* or detect*)) )
TI ( ((early* or onset* or initial* or young* or incipient*) near2 (dementia* or Alzheimer* or AD)) ) OR TI ( ((Mild* or early* or onset* or initial* or progress* or minor or young* or moderat* or suspect*) near2 Cognit* near1 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)) ) OR TI ( MCI or NCD ) OR TI ( ((memory* or neurocognitiv*) near2 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)) ) OR TI ( (“preclinical alzheimer*” or “pre-clinical alzheimer*”) ) OR TI (prodrom* near2 dement*) AND TI ( ((computer* or automate*) near2 (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)) ) OR TI ( (automat* near2 (interpretat* or test*)) ) OR TI ( ((neuropsychological or neuro-psychological or psychometric*) near5 (computer* or automate*) near5 (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)) )
TITLE: (((early* or onset* or initial* or young* or incipient*) near2 (dementia* or Alzheimer* or AD))) OR TITLE:(((Mild* or early* or onset* or initial* or progress* or minor or young* or moderat* or suspect*) near2 Cognit* near1 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*))) OR TITLE: (MCI or NCD)OR TITLE: (((memory* or neurocognitiv*) near2 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)))OR TITLE: ((“preclinical alzheimer*” or “pre-clinical alzheimer*”)) ORTITLE: ((prodrom* near2 dement*))OR TITLE: (*dementia/ or *alzheimer disease/ or *dementia, vascular/ or *dementia, multi-infarct/ or *frontotemporal dementia/) ANDTITLE: (Diagnosis, Computer-Assisted/) OR TITLE: (((computer* or automate*) near4 (diagnos* or detect*)))
Refined by: PUBLICATION YEARS: ( 2013 OR 2011 OR 2014 OR 2010 OR 2009 OR 2012 OR 2005 OR 2008 OR 2007 OR 2006 OR 2015 )
TITLE: (((early* or onset* or initial* or young* or incipient*) near2 (dementia* or Alzheimer* or AD))) OR TITLE:(((Mild* or early* or onset* or initial* or progress* or minor or young* or moderat* or suspect*) near2 Cognit* near1 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*))) OR TITLE: (MCI or NCD)OR TITLE: (((memory* or neurocognitiv*) near2 (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)))OR TITLE: ((“preclinical alzheimer*” or “pre-clinical alzheimer*”)) ORTITLE: ((prodrom* near2 dement*))OR TITLE: (*dementia/ or *alzheimer disease/ or *dementia, vascular/ or *dementia, multi-infarct/ or *frontotemporal dementia/) ANDTITLE: (((computer* or automate*) near2 (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*))) OR TITLE: ((automat* near2 (interpretat* or test*))) ORTITLE: (((neuropsychological or neuro-psychological or psychometric*) near5 (computer* or automate*) near5 (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)))
Refined by: PUBLICATION YEARS: ( 2013 OR 2011 OR 2014 OR 2010 OR 2009 OR 2012 OR 2005 OR 2008 OR 2007 OR 2006 OR 2015 )
TITLE:(“cambridge Neuropsychology Test*”) OR TITLE: (Computerised Neuropsychological Test Battery) ORTITLE: (Six Item Cognitive Impairment Test) OR TITLE:(“Computer Assessment of Mild Cognitive Impairment”) OR TITLE:(MindStream*) OR TITLE: (“Mild Cognitive Impairment Screen*”) ORTITLE: (Computer Administered Neuropsychological Screen for Mild Cognitive Impairment) OR TITLE:(Automated Neuropsychological Assessment Metrics) OR TITLE:(CANS-MCI) OR TITLE: (“CNS Vital Signs”) OR TOPIC: (Cognitive Drug Research Computerised Assessment System for Dementia) OR TITLE:(CogState) OR TITLE: (“Cognitive Stability Index*”) OR TITLE:(“Cognitive Screening Test*”) ORTITLE: (Microcog) OR TITLE:((COGDRAS-D or COGDRASD or COGDRAS)) OR TITLE: (MCIS) ORTITLE: ((CAMCI or CNTB)) ORTITLE: (6CIT) OR TITLE: ((CANTAB-A or CANTABA or CANTAB)) ORTITLE: (ANAM) OR TITLE: (CADi2)
Refined by: PUBLICATION YEARS: ( 2014 OR 2012 OR 2005 OR 2013 OR 2007 OR 2006 OR 2010 OR 2009 OR 2011 OR 2015 OR 2008 )
SearchAdd to builderQueryItems foundTime#10AddSearch (#8 and #9)39206:19:55#9AddSearch (“2015/03/03”[Date - Entrez] : “3000”[Date - Entrez])55757506:09:00#8AddSearch (#3 or #5 or #6)780906:08:27#7AddSearch (#3 and #5 and #6)38906:07:46#6AddSearch (((((((((((((((((((((“cambridge Neuropsychology Test*”) OR Computerised Neuropsychological Test Battery) OR Six Item Cognitive Impairment Test) OR “Computer Assessment of Mild Cognitive Impairment”) OR MindStream*) OR “Mild Cognitive Impairment Screen*”) OR Computer Administered Neuropsychological Screen for Mild Cognitive Impairment) OR Automated Neuropsychological Assessment Metrics) OR CANS-MCI) OR “CNS Vital Signs".) OR Cognitive Drug Research Computerised Assessment System for Dementia) OR CogState) OR “Cognitive Stability Index*”) OR “Cognitive Screening Test*”) OR Microcog) OR (COGDRAS-D or COGDRASD or COGDRAS)) OR MCIS) OR ((CAMCI or CNTB))) OR 6CIT) OR ((CANTAB-A or CANTABA or CANTAB))) OR ANAM) OR CADi2395306:06:42#5AddSearch (#1 and #4)266706:03:29#4AddSearch ((computer* or automate*)) AND (diagnos* or detect*)20789406:03:01#3AddSearch (#1 and #2)352806:02:34#2AddSearch (((((((computer* or automate*)) AND (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)) OR automat*) AND (interpretat* or test*)) OR (neuropsychological or neuro-psychological or psychometric*)) AND (computer* or automate*)) AND (test* or assess* or evaluat* or screen* or battery or monitor* or identif* or assess* or evaluat* or interpret*)15364006:01:47#1AddSearch ((((((((early* or onset* or initial* or young* or incipient*)) AND (dementia* or Alzheimer* or AD)) OR (Mild* or early* or onset* or initial* or progress* or minor or young* or moderat* or suspect*)) AND Cognit*) AND (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)) AND (MCI OR NCD)) OR (memory* or neurocognitiv*)) AND (impair* or disord* or diseas* or declin* or deteriorat* or fail* or complain* or dysfunct* or degenerat* or deficit*)11603206:00:22
“cambridge Neuropsychology Test*” OR (“Computerised Neuropsychological Test Battery” OR “Six Item Cognitive Impairment Test”) OR (“Computer Assessment of Mild Cognitive Impairment” OR (CANTAB-A or CANTABA or CANTAB)) OR (“Mild Cognitive Impairment Screen*” OR “Computer Administered Neuropsychological Screen for Mild Cognitive Impairment”) OR (“Automated Neuropsychological Assessment Metrics” OR CANS-MCI) OR (“CNS Vital Signs” OR “Cognitive Drug Research Computerised Assessment System for Dementia”) OR (CogState or microcog OR “Cognitive Stability Index*”) OR (“Cognitive Screening Test*” OR (CAMCI or CNTB)) OR ((COGDRAS-D or COGDRASD or COGDRA) OR MCIS or 6CIT or ANAM or CADi2 or MindStream*) AND (dementia or alzheimers or MCI OR “Mild cognitive impairment”)
((early* OR onset* OR initial* OR young* OR incipient*) NEAR/2 (dementia* OR Alzheimer* OR AD)) AND (((computer* or automate*) near/2 (test* or assess* or evaluate* or screen* or battery or monitor* or identif* or ssess* or evaluate* or interpret*)) OR (automat* near/2 (interpret* or test*)) )
Appendix 3 Studies excluded, with reasons
The full list of excluded studies is available from the authors.
| Reason for exclusion | Number of studies |
|---|---|
| Exclusion reason: paper-based test | 116 |
| Exclusion reason: wrong study design | 59 |
| Exclusion reason: not an evaluation of the automated test | 31 |
| Exclusion reason: wrong patient population | 32 |
| Exclusion reason: systematic review | 23 |
| Exclusion reason: literature review | 20 |
| Exclusion reason: wrong intervention | 16 |
| Exclusion reason: wrong indication – other | 55 |
| Exclusion reason: wrong outcome | 9 |
| Exclusion reason: wrong outcomes; continuous data | 6 |
| Exclusion reason: automated test not in English | 9 |
| Exclusion reason: timeline | 4 |
| Exclusion reason: duplicate | 3 |
Appendix 4 Names of all of the tests identified
| Test | Paper or computer or other |
|---|---|
| ANAM | Computer |
| Automated Cognitive Test | Computer |
| Automated Neuropsychological Assessment Metrics | Computer |
| CADi2 | Computer |
| CAMCI | Computer |
| CANTAB | Computer |
| Central Nervous System Vital Signs Brief Clinical Evaluation Battery | Computer |
| CNS vital signs | Computer |
| CNTB | Computer |
| COAD | Computer |
| COGDRAS-D | Computer |
| Cognitive Drug Research Computerised Assessment System for Dementia | Computer |
| CogState MCI/AD battery | Computer |
| Community Screening Instrument for Dementia | Computer |
| Computer Assessment of MCI | Computer |
| Computer Self Test | Computer |
| Computer-Administered Neuropsychological Screen for MCI | Computer |
| CSI | Computer |
| CST | Computer |
| Dr Oz | Computer |
| Florida Brief Memory Scale | Computer |
| GrayMatters Assessment System | Computer |
| Groton Maze Learning Test | Computer |
| IntegNeuro and WebNeuro | Computer |
| MCIS | Computer |
| MCI Screen | Computer |
| MicroCog | Computer |
| Mindstreams | Computer |
| NeuroTrax | Computer |
| Nonverbal Medical Symptom Validity Test | Computer |
| Poon-Baro-Wens | Computer |
| TDAS | Computer |
| TPSP | Computer |
| Scenery Picture Memory Test | Other |
| Sweet 16 | Other |
| 3MS | Paper |
| 3TD | Paper |
| 6CIT | Paper |
| AD8 | Paper |
| ADAS-COG | Paper |
| Albert Einstein Health Self-Assessment Form | Paper |
| Animal Naming Test | Paper |
| BDRS | Paper |
| BEHAVE-AD | Paper |
| Benton Fluency Test | Paper |
| CAMCOG | Paper |
| CAMDEX | Paper |
| CERAD | Paper |
| CERAD-BRSD | Paper |
| Clock Drawing Test | Paper |
| Cued-Recall Retrieval Speed Task | Paper |
| GPCOG | Paper |
| Hopkins Verbal Learning Test-Revised | Paper |
| KICA-Cog | Paper |
| MIS | Paper |
| MMSE | Paper |
| MoCA | Paper |
| National Institutes of Health Toolbox | Paper |
| Neuropsychological Test Battery | Paper |
| Nishimura Mental State | Paper |
| NPI-NH | Paper |
| PAS | Paper |
| PBAC | Paper |
| RBANS | Paper |
| RUDAS | Paper |
| SIS | Paper |
| SLUMS | Paper |
| Social Cognition and Emotional Assessment | Paper |
| The Mini-Kingston Standardized Cognitive Assessment | Paper |
| Trail Making Test | Paper |
| Verbal Category Cued Memory Test | Paper |
| Verbal Fluency Test | Paper |
| Wechsler Adult Intelligence Scale | Paper |
| Cognistat | Paper/computer |
| MOST | Paper/computer |
| Rey-Osterrieth Figure Copy | Paper/computer |
| CUSPAD | Paper/other |
Appendix 5 Patient and public involvement: structure of meeting
Brief chat, any difficulties with train trip, any questions he may have. Check for comfort with recording device, assure recording will be deleted. If not, use tablet for quick typing. He mentioned his caring responsibilities. Talk slowly, pay attention to ability to retain and analyse information. Simple language.
What is LRiG. Overview of the project. Brief discussion background MCI and dementia. Explain the review process very briefly.
Intro questions from protocol.
-
Was the purpose of the review clear?
-
Was the purpose of the review appropriate/valid/important?
Questions relating to technology.
Explain what computerised tests are briefly. Compare to tests used in his and/or carer’s diagnosis.
-
About the tests (show table on test, discuss table, clarify, make sure it is understood)
-
– Different types of tests (show table), some tests look at 1–2 aspects of memory and thinking, others look at all aspects of memory and thinking (cognitive domains).
-
– 2 tests look at the visual aspect (PAL), and make an assessment with a clinician present about existence of challenges with memory and thinking.
-
– Our findings say it works well. Does he have any thoughts about this?
-
-
Platform used
-
– Internet-based test, iPad versus computer touchscreen versus desktop. Rating 1–4.
-
– Comfort in using platform (create flow from previous questions so would talk about use of technology in the elderly).
-
-
Professionals involved
-
– Different papers used professionals differently.
-
– For test administration it was (1) self-administered with minimum assistance with nurse or technician; (2) self-administered with minimum assistance with nurse or technician, which also included them typing or using the mouse to manipulate the mouse or arrows for the patient or facilitate the typing and entering of patient responses; (3) verbal directions from administration; (4) interactive system provided oral instruction through speakers and written instructions on screen; (5) self-administration, but carer can assist needed them typing or using the mouse to manipulate the mouse or arrows for the patient or facilitate the typing and entering of patient responses.
-
– Rate tests from 1–5 with 1 being most preferable. Enter sixth option manually if a combination.
-
– Feedback on professionals conducting the test (who).
-
– What did he think of the level of involvement of the assessor in these scenarios in conducting the tests?
-
– What about monitoring?
-
-
Patient characteristics
-
– Disease progression, do they go to the doctor
-
– Follow-up
-
– Study sample
-
– Where people were recruited from
-
– Only included patients (summary and variance of inclusion criteria)
-
– Summary of age, gender, education, ethnicity (race).
-
-
Follow-up questions in the end
-
– Do we report on all of the important aspects of the research (show tables) (e.g. age of participants, practicality of computer tests for this age group)?
-
– Was the purpose of the review clear?
-
– Was the purpose of the review appropriate/valid/important?
-
– What do they see as the implications for clinical practice?
-
– What value do you see in the use of diagnostic tests for MCI?
-
– Do you feel that the inclusion of computerised tests is a good one?
-
– Should they be used instead of pen-and-paper tests?
-
– When do you think they should be used?
-
– What areas need further research?
-
Appendix 6 Organisations approached for service user involvement
-
Liverpool Service User Reference Forum for Dementia.
-
North West People in Research Forum.
-
Salford Citizen Scientist – Francine Jury at People In Research Involve.
-
Join Dementia Research – National Institute for Health Research.
-
Dementias and Neurodegeneration National Institute for Health Research Clinical Research Network.
-
National Institute for Health Research Clinical Research Network for Ageing.
-
The Alzheimer’s Society.
Using Twitter (Twitter Inc., San Francisco, CA, USA; www.twitter.com), we also sent out mass tweets to 72 other relevant organisations.
Appendix 7 Sample letter sent to organisations to invite service users
Advisory group members: computer based tests for mild cognitive impairment and dementia
By Aslam, 19 August 2015.
Do you want to get involved in research to find out whether computer-based tests for assessing a person’s memory and thinking work?
The Liverpool Reviews and Implementation Group specialises in using a research method called a systematic review of the literature. This method provides an overview of the relevant research in the subject area.
The Liverpool Reviews and Implementation Group is currently working on a research project funded by the National Institute for Health Research. They are currently looking for people living with mild cognitive impairment (MCI) or early dementia as well as their carers who have an interest in assessment tools for thinking and memory.
As part of the research process, they would like to form an advisory group. The advisory group will have 2–3 service users or carers who have an interest in assessment tools for thinking and memory. The advisory group would be expected to attend two meetings between August 2015 and December 2015, and will need to be available for consultation via e-mail or face to face between meetings. They will pay a fee for consultation and travel expenses for all meetings. To apply, please complete the application form and return to the Liverpool Reviews and Implementation Group.
For more information contact:
Dr Rabeea’h Waseem Aslam, Liverpool Reviews and Implementation Group, University of Liverpool.
Telephone: XXX
E-mail: XXX
Deadline: 20 September 2015.
Glossary
- Accuracy
- A measure of the closeness of the experimental value to the actual amount of the substance in the matrix.
- Area under the curve
- A measure of the diagnostic accuracy of a technology, which is based on the geometric inspection of a receiver operating characteristic curve. A receiver operating characteristic curve is a plot of the true-positive rate against the false-positive rate at different threshold settings. A technology with perfect diagnostic accuracy will have an area under the curve of 1; a technology that is no better than chance will have an area under the curve of 0.5; and a technology that miscategorises on every occasion will have an area under the curve of 0.
- Cut-off point
- See Threshold.
- Diagnostic accuracy
- The effectiveness of a diagnostic test to correctly categorise patients as either ‘positive’ or ‘negative’. There are several ways that this can be expressed, for example as the area under the curve or as sensitivity and specificity.
- False negative
- When a patient has been diagnosed with, for example, mild cognitive impairment using a standard test but the index test fails to detect this.
- False positive
- When a patient has been diagnosed with, for example, mild cognitive impairment using the index test but they do not have this condition.
- Index test
- The diagnostic test that is being evaluated.
- Likelihood ratio
- A description of how many times more likely it is that a person with the disease will have a particular test result than a person without the disease.
- National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association criteria
- The prevalent criteria for the diagnosis of Alzheimer’s disease, proposed by the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association. These criteria require the presence of cognitive impairment and a suspected dementia syndrome to be confirmed by neuropsychological testing for a clinical diagnosis of possible or probable Alzheimer’s disease, while histopathologic confirmation is needed for the definitive diagnosis. These criteria specify eight cognitive domains that may be impaired in Alzheimer’s disease: memory, language, perceptual skills, attention, constructive abilities, orientation, problem solving and functional abilities.
- Negative predictive value
- The proportion of people with negative test results who do not have the disease, for example the probability that a patient who is test negative on an index test does not have mild cognitive impairment or dementia on clinical diagnosis.
- Petersen’s criteria
- The criteria for mild cognitive impairment, as defined by Petersen, which include the following: memory problems, objective memory disorder, absence of other cognitive disorders or repercussions on daily life, normal general cognitive function and absence of dementia.
- Positive predictive value
- The proportion of people with positive test results who actually have the disease, for example the probability that a patient who tests positive on an index test has mild cognitive impairment or dementia on clinical diagnosis.
- Precision
- Measures how close individual measurements of a sample are to each other.
- Receiver operating characteristic curve
- A plot of the true-positive rate against the false-positive rate of a test at different threshold settings.
- Reference standard
- A diagnostic test used to estimate the sensitivity and specificity of another diagnostic test, known as an index test. The reference standard is assumed to have perfect sensitivity and specificity, and so in cases when both tests categorise something differently, the reference standard test categorisation is assumed to be correct (either true negative or true positive).
- Sensitivity
- Also called the true-positive rate, measures the proportion of those who actually have the disease correctly identified with positive test results, for example the proportion of patients with mild cognitive impairment or dementia at clinical diagnosis identified by the index test.
- Specificity
- The proportion of people who do not have the disease, correctly identified as having a negative test result, for example the proportion of patients without mild cognitive impairment or dementia on clinical diagnosis who are test negative on the index test.
- Threshold (clinical)
- A value, within a range of values, used to categorise observations into one of two mutually exclusive groups. For example, guidelines suggest that the decision of whether or not to investigate for possible mild cognitive impairment or dementia is influenced by cognitive test scores (e.g. in the Mini-Mental State Examination, the threshold for mild Alzheimer’s disease is a score of 21–26, whereas the threshold for moderate Alzheimer’s disease is a score of 10–20).
- True negative
- In the case of mild cognitive impairment, a patient who has been correctly identified by the index test as not having mild cognitive impairment.
- True positive
- In the case of mild cognitive impairment, a patient who has been correctly identified by the index test as having mild cognitive impairment.
List of abbreviations
- AD
- Alzheimer’s disease
- AUC
- area under the receiver operating characteristic curve
- CAMCI
- Computer Assessment of Mild Cognitive Impairment
- CANTAB
- Cambridge Neuropsychological Test Automated Battery
- CANTAB-PAL
- Cambridge Neuropsychological Test Automated Battery Paired Association Learning
- FN
- false negative
- FP
- false positive
- GP
- general practitioner
- HAND
- HIV-associated neurocognitive disorder
- HIV
- human immunodeficiency virus
- LR
- likelihood ratio
- LRiG
- Liverpool Review and Implementation Group
- MCI
- mild cognitive impairment
- MMSE
- Mini-Mental State Examination
- NICE
- National Institute for Health and Care Excellence
- NPV
- negative predictive value
- PPV
- positive predictive value
- QUADAS-2
- Quality Assessment Tool for Diagnostic Accuracy Studies
- TN
- true negative
- TP
- true positive