Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 14/151/01. The contractual start date was in May 2015. The draft report began editorial review in November 2015 and was accepted for publication in March 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
The BMJ Technology Assessment Group (BMJ-TAG) and the editorial team of the BMJ work independently of one another.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Edwards et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Description of the health problem
Fibrin sealants are commercial products used during surgical procedures in many sites of the body (including the liver, breast, pancreas, thorax and nervous system) and are widely regarded as useful adjuncts to make blood clot, seal tissues and help the body repair mechanisms that can aid haemostasis and reduce seroma formation. However, the benefits and harms of fibrin sealants remain controversial and seem to be dependent on the surgical procedure.
Seroma and repair
Seroma is formed by acute inflammatory exudates in response to surgical trauma and in the acute phase of wound healing. 1 After surgery, the body’s natural response to the removal of organs or tissues is to fill the space with fluid and blood cells. During this process, a collection of fluid and cells can result in the formation of a seroma (collection of a clear, yellow fluid). Some parts of the body are especially prone to seroma, for example the breasts and parts of the digestive tract.
Avoidance of post-operative drains
Post-operative drains are intended to prevent the build-up of fluid or seroma after some types of surgery by filling ‘dead space’. The main concerns with seroma are that they can become infected or leak fluid and, if they remain, over time become swollen, hard and uncomfortable. Both additional surgery to remove the seroma and fine-needle aspiration are associated with increased resource use, such as nursing time, hospital stay and analgesic or antibiotic use. There is contradictory evidence from two small randomised controlled trials (RCTs)2,3 (n = 100 and n = 75) about the use of fibrin sealants as an alternative to post-operative drains during thyroid surgery. In one trial, patient outcomes were best in the fibrin sealant group; pain was significantly reduced, as was the length of time spent in hospital. 2 However, no statistically different effects on any outcome was observed in a second trial. 3 The findings from individual RCTs also suggest that post-operative pain can be reduced when fibrin sealants are used in skin graft surgery.
Fibrin sealants are not recommended for surgical use in some sites; they were reported to be ineffective in reducing post-operative leakage from oesophago-gastric anastomoses. 4
Tissue adhesion or sealing
A systematic review summarised the evidence for fibrin glue in the repair of pilonidal disease (the invasion of hair into the skin of the natal cleft). 5 The review included five RCTs in which fibrin glue was used to fill dead space and sinus tracks during surgery. The reviewers reported equivalent or better healing times at an average of 2–6 weeks and low recurrence rates between 0% and 17% at follow-up periods between 4 and 28 months for all patients treated with fibrin glue than for those treated with conventional therapies. However, no statistically significant differences between those who received fibrin glue and those who did not were observed. Furthermore, fibrin sealants are commonly used to prevent fistula during pancreatic surgery. 6–8
Hernia repair
A systematic review of randomised and non-randomised studies evaluating fibrin sealants used in the surgical management of hernia repair concluded that fibrin sealants are an effective alternative to mechanical approaches. 9
Dural repair in neurosurgery
Fibrin sealants can be used as an adjunct to dura (the outer-most layer of the brain and spinal cord) repair to achieve intraoperative watertight closure of the dura and to reduce post-operative cerebrospinal fluid leak. A RCT (n = 139) showed the fibrin sealant EVICEL® (Ethicon, Livingston, UK) to be effective as an adjunct to dural sutures. Intra-operative watertight closure was achieved in 82 out of 89 participants (92.1%) in the EVICEL group, compared with 19 out of 50 participants (38.0%) in the control group (p < 0.001). 10
Haemorrhage (bleeding)
Perioperative or post-operative haemorrhage is a common complication of surgery. Unexpected, excessive perioperative bleeding can be due to a pre-existing undetected bleeding disorder, or to coagulation abnormalities arising from massive blood loss and/or various coexisting pathologies. 11 It can be related to the nature of the operation itself. Red blood cell transfusion is often required as a result of perioperative bleeding, but this resource can be scarce and there has been worldwide concern regarding its safety.
Assisting the arrest of haemorrhage (haemostasis) perioperatively is an important function of fibrin sealant preparations. In a previous systematic review12 researchers demonstrated that fibrin use during the removal of uterine fibroids in premenopausal women reduced blood loss and, consequently, the rate of blood transfusions. However, the quality of evidence was assessed as low. This effect was also reported in a systematic review of surgical interventions for liver, orthopaedic, vascular, prostate, thoracic, renal, pancreatic and cardiac conditions. 13 A RCT evaluating the use of fibrin sealants in total knee arthroplasty procedures also demonstrated statistically significant reductions in blood loss. 14
Aetiology, pathology and prognosis
Incidence and/or prevalence and impact of the health problem
Seroma and repair
The development of seroma formation depends on the site of surgery. Approximately 50% of inpatients with a closed suction drain develop post-operative seroma,15 and the incidence after breast cancer surgery and axillary node dissections ranges from 15% to 60%. 16 The most common complication of abdominoplasty is seroma formation, and the incidence in abdominal procedures, including abdominoplasty, panniculectomy and transverse rectus abdominis myocutaneous flap abdominal donor sites, ranges from 1% to 38%. 17 In a study of incisional hernia repair involving a combined fascial and prosthetic mesh repair in 35 patients (16 males and 19 females), the incidence of post-operative seroma formation was 17%. 18 One of the most common and serious complications of pancreatic surgery is post-operative pancreatic fistula, defined as a drain output of any measurable volume or fluid on or after post-operative day 3, with an amylase content greater than three times the serum amylase activity. 19–21 The estimated incidence of post-operative pancreatic fistula ranges between 2% and 24% based on different studies. 19,22
Haemorrhage (bleeding)
The incidence of perioperative or post-operative bleeding also depends on the site or type of surgery. Severe bleeding occurs in about 7% of patients undergoing cardiac surgery. 23 Excess perioperative bleeding following surgery results in the increased use of red blood cell transfusions: between 60% and 70% of all red blood cell transfusions are used in surgical settings. 24,25 Moreover, bleeding perioperatively or post-operatively increases the risk of morbidity and mortality. 11 The mortality rate among patients undergoing elective vascular surgery who experience severe bleeding has been reported to be approximately 20%. 26 Uncontrolled bleeding has been reported to be the cause of 30–40% of all trauma-related deaths. 27
Significance for patients in terms of ill health (burden of disease)
A seroma may cause problems because it can become infected or leak fluid and, over time, may also become swollen, hard and uncomfortable. After thoracic surgery the placement of a post-surgical drain can increase the length of hospital stay and cause discomfort. Problems arise when the drains do not work properly and, as a result, become blocked and infected.
Current service provision
Management of condition
Seroma and repair
To try to stop seroma formation, surgeons sometimes leave a drain (tube) in the wound to make sure fluid can escape and does not build up after the operation. Occasionally, the only way to cure the problem is further surgery to remove the seroma or drainage with a fine needle, which might increase the time spent in hospital.
To prevent post-operative pancreatic fistulas, a number of methods have been proposed, including application of duct stents, modification of anastomotic techniques and administration of somatostatin (a hormone that inhibits the secretion of pancreatic juice). 20,21,28,29
Haemorrhage (haemostasis)
To look for ways to minimise the need for perioperative blood transfusion, a number of systematic reviews assessed the efficacy and safety of different interventions for the International Study of Perioperative Transfusion. 30–34 These reviews showed that techniques for reinfusing patients’ own blood provided only relatively small reductions in the need for blood transfusion. However, interventions to reduce surgical blood loss resulted in significant improvements in reducing the need for blood transfusion. 35
Variation in services and/or uncertainty about best practice
Relevant national guidelines
In 2012, a European review of the safety of sprayable fibrin sealants was started after reports of life-threatening events and deaths following administration of fibrin sealants using a pressure regulator. 36 The European Medicines Agency (EMA)’s Committee for Medicinal Products for Human Use (CHMP) stated that the benefits of fibrin sealants outweigh their risks, but that appropriate procedures have to be undertaken to optimise the safe use of fibrin sealant sprays during surgery. 36
In 2013, four sprayable fibrin sealants were authorised in the UK: EVICEL, Tisseel Lyo® (Baxter Healthcare, Norfolk, UK), Tisseel Ready® to Use (Baxter Healthcare, Norfolk, UK) and Artiss® [Solutions for Sealant], deep frozen (Baxter Healthcare, Norfolk, UK). In all cases, the surface area of the wound should be dried with standard procedures before applying the fibrin sealants spray with a pressure regulator device. 37
Description of technology under assessment
Summary of intervention
Fibrin sealants are commercial products that usually comprise two substances that occur naturally in mammals: (1) fibrinogen, a protein; and (2) thrombin, an enzyme that acts on fibrinogen to produce a fibrin clot, exactly as in normal blood clotting. The components used in these products are derived from either human or animal blood. There are different preparations of fibrin sealants: patches, sponges and bandage formulations, which can all be impregnated with fibrinogen and thrombin. Alternatively, fibrin glue is a mixture of the two substances in liquid form, which is dispensed via a ‘gun’ and there is also a liquid ‘droplet’ formulation that is delivered in an aerosol spray. 38
Fibrin sealants are used during surgical procedures in many sites of the body (including the liver, breast, pancreas, thorax and nervous system) and are widely regarded as useful adjuncts to aid haemostasis and reduce seroma formation. They are used to seal tissues and prevent the accumulation of post-operative fluid and blood loss. Aerosol sprays, sponges, bandages and pad preparations are available, and all contain elements that make blood clot and help the body repair.
Concerns about safety
Fibrin sealants have been found to stop fluid collecting in the body after operations, but it is unclear if this ‘good effect’ works for all types of operations. There is concern that some types of fibrin sealants can have harmful effects, such as leaving pockets of air in the body, which can be dangerous.
The Food and Drug Administration (FDA) in the USA has issued warnings about life-threatening air or gas emboli developing after the use of fibrin sealant aerosol sprays during surgery. Users of the products have been advised about the dangers of using sprays too close to exposed tissue surfaces and at higher pressures than those recommended by the manufacturers. 39 However, despite concerns about safety, data from RCTs about harms are scarce. 40 A multicentre RCT41 conducted in three Italian hospitals compared the rate of adverse events in a group of patients receiving fibrin sealants as an adjuvant for air leak control in patients undergoing lung resection. Air leakage and broncopleural fistulas in the lungs are both common complications after these procedures. With a follow-up period of 30–40 days the investigators found that the rate of adverse events was not statistically significantly different between patients who received fibrin sealant and those who did not. 41
A review conducted in 201042 on the risks and complications of spinal fibrin sealants, included the two fibrin glues EVICEL and Tisseel. It concluded that Tisseel had been used in clinical studies without adverse events. However, the review found a lack of large clinical studies on the safety of EVICEL for neurosurgery. A more recent RCT evaluating the safety of EVICEL found that the incidence of adverse events and cerebrospinal leakage up to 30 days post surgery was similar in the EVICEL and control groups. No deaths or suspected unexpected serious adverse drug reactions occurred during the trial. 10
The authors of a systematic review of RCTs have suggested that the beneficial patient outcomes that have been observed when using fibrin sealants are dependent on surgeon training in their use. 40
Identification of important subgroups
Surgical specialties
The efficacy of fibrin sealants in different surgical specialties has been reported to differ. Therefore, where possible, after carrying out a meta-analysis combining all surgical specialties, additional subgroup analysis was carried out according to identified surgical specialties.
Type of intervention
For assessing the efficacy of fibrin sealant in reducing operative time, subgroup analysis according to interventions and comparators was carried out, as application times of different interventions was expected to vary.
Current usage in the NHS
Fibrin sealants are believed to be widely used by surgeons from many different disciplines working in the UK. There are no data collected at a national level about the cost of fibrin products to the NHS; costs data are likely to be available only at the level of NHS trust (NHS England, 2015, personal communication). It is anticipated that variations in the use of fibrin sealants are likely.
Chapter 2 Definition of the decision problem
Decision problem
The eligibility criteria pertaining to population, intervention, comparators and outcomes are summarised in Table 1.
| PICOS | Criteria |
|---|---|
| Population | People aged ≥ 18 years undergoing non-emergency surgery at any site in secondary care (hospital) |
| Intervention | Any fibrin sealant product including
|
| Comparators | Standard care |
| Outcomes | Primary outcomes
|
Secondary outcomes
|
|
Resource use
|
|
| Health-related quality of life | |
| Adverse events related to the use of fibrin sealant (attributed by the primary study authors and/or reviewers) | |
| In addition, an important output of the review will include an overview of gaps in knowledge to inform recommendations for future primary research, including specific outcomes for different conditions | |
| Study design | RCTs and observational studies |
Overall aims and objectives of assessment
Objectives
-
To map the evidence of benefits (clinical effectiveness) of use of fibrin sealants from RCTs.
-
To map the evidence of harms (adverse events) related to the use of fibrin sealants from RCTs, observational studies and regulatory body reports.
Chapter 3 Assessment of clinical effectiveness
Methods for reviewing clinical effectiveness
Evidence on the clinical effectiveness of fibrin sealants was identified by conducting a systematic review of the published research literature. The review was undertaken following the general principles published by the Centre for Reviews and Dissemination (CRD) and the Cochrane Collaboration. 43,44 The protocol for the systematic review is registered on PROSPERO (registration number CRD42015020710). 45 The protocol and review were developed with clinical experts who had experience with using fibrin sealants (Professor John MacFie, University of Hull, Hull, and Mr Alexander Green, John Radcliffe Hospital, Oxford). Guidance for systematic review reporting on benefits46 and harms47 was followed where possible.
Eligibility criteria
Eligibility criteria for the review of clinical effectiveness were as specified in the decision problem (see Table 1 for a summary). The review included RCTs to assess both the benefits and harms, and observational studies and regulatory body reports to assess adverse events related to fibrin sealants in the view of primary study investigators and/or reviewers. Systematic reviews and other types of studies were excluded. The interventions of interest were any type of fibrin sealant. RCTs and observational studies were included if the treatments were evaluated in an adult population undergoing non-emergency surgery in a secondary care setting and compared with standard care. Regulatory body reports were included if they reported on deaths or serious adverse events related to fibrin sealants. RCTs were excluded if none of the outcomes of interest was reported. Observational studies were excluded if they did not report on adverse events that were thought to be related to the use of fibrin sealants.
Identification of studies
Search strategy
Two search strategies, one for RCTs and one for observational studies, were developed (see Appendix 1). Information on benefits and harms were extracted from RCTs. The searches for RCTs combined terms for the technology being assessed and the study design using the Cochrane Collaboration RCT filter. 44 Evidence of harms was obtained from observational studies with a search strategy focused on adverse events. For observational studies, the searches combine both controlled vocabulary terms (medical subject heading and EMTREE) and free-text terms for general adverse events from the CRD43 and Cochrane guidance,43,44 including the following: safe, safety, side effect, undesirable effect, treatment emergent, adverse effects, contraindications and complications. 48–51 Both search strategies for RCTs and observational studies included terms for the technology, which used both controlled vocabulary terms (medical subject heading and EMTREE) and free-text terms including the following: fibrin sealant, fibrin adhesive, fibrin glue, fibrin sponges, fibrin bandages or aerosol and commercial names. The search strategies were refined by scanning key papers identified during the review, through discussion with the review team, clinical experts and information specialists (see Appendix 1). No limits relating to inception date or language were applied to the searches.
The following searches were conducted in May 2015. The following electronic sources were searched: MEDLINE, EMBASE and The Cochrane Library (including the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effects, the Health Technology Assessment database and the Cochrane Central Register of Controlled Trials). Ongoing and unpublished RCTs were searched for in the following websites: clinicaltrials.gov, controlled-trials.com and clinicaltrialsregister.eu. For observational studies websites from the following organisations were searched: Medicines and Healthcare products Regulatory Agency (MHRA) (www.gov.uk/search?q=fibrin+sealants), the EMA (www.ema.europa.eu/ema/index.jsp?curl=search.jsp&q=FIBRIN+SEALANT&spell=1&site=pfoi_collection&client=pfoi_frontend&ie=UTF-8&output=xml_no_dtd&proxystylesheet=pfoi_frontend&access=p) and the FDA (www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/detail.cfm?mdrfoi__id=4277068). Relevant reviews and guidelines were identified through searching additional resources, including Clinical Evidence, National Institute for Health and Care Excellence, National Institute for Health Research Health Technology Assessment programme and the University of York Database of Abstracts for Reviews of Effectiveness. Additionally, reference lists of included papers were assessed and the abstracts from key conference proceedings were screened. Furthermore, clinical experts in the relevant therapy area were contacted to request details of RCTs and observational studies (published and unpublished) of which they may be aware.
Abstract appraisal
Titles and abstracts of studies identified by the search process were assessed for inclusion independently by two reviewers (GOA and MvV). In cases where the reviewers were unable to reach a consensus regarding whether or not the full text should be obtained for further appraisal, the full text was obtained. When potentially relevant data were identified, corresponding authors were contacted to obtain the full publications. A deadline for response to the initial contact of 1 calendar month was imposed. Studies were not screened on the basis of the presence or absence of harms-related terms in title or abstract as harms were expected to be reported in other sections of the primary study publications. 47
Study inclusion assessment
Two teams of two reviewers (GOA and MvV, FSa and MB) independently assessed the full text of the RCTs and observational studies identified during the abstract assessment stage for inclusion, and differences in opinion were arbitrated by a third reviewer (FC). Studies rejected at this or subsequent stages were recorded in a ‘characteristics of excluded studies table’ and reasons for exclusion recorded. 46 Only RCTs reporting on one of the outcomes specified in Table 1 and only observational studies or regulatory body reports of adverse events related to the use of fibrin sealants were included.
Data extraction and management
Data were extracted by one reviewer using a standardised data extraction form (items for which data were reported are presented in Appendix 2) and independently checked by another reviewer. Information extracted included details of the study’s design and methodology; the intervention and comparators; baseline characteristics of participants and outcome measures, including clinical efficacy outcomes (variables for which data were sought are reported in Table 20 in Assessment of benefits) and any type of adverse event related to the use of fibrin sealants as attributed by the primary study authors of studies or regulatory organisations. No data were sought for patient-underlying risk factors or for practitioner training or qualifications. When there was incomplete information, attempts were made to contact authors to request for further details. Discrepancies in the data extraction were resolved by discussion with involvement of a third reviewer.
Data from intention-to-treat (ITT) analyses were extracted. When a trial did not report ITT data for dichotomous outcomes, missing data were treated as treatment failures to allow analysis to conform to an ITT analysis. 50 For the purpose of this review, ITT analysis was defined as the analysis of patients according to the treatment group to which they were allocated at randomisation, irrespective of whether they received the allocated intervention, withdrew or were lost to follow-up.
Quality assessment strategy
The quality of included studies was assessed by one reviewer and independently checked by another. Any disagreements were resolved by consensus and the opinion of a third reviewer was sought. 43,46
Randomised controlled trials were assessed according to the guidance published by the CRD43 and the Cochrane Handbook for Systematic Reviews of Interventions,44 and recorded using the Cochrane risk-of-bias tool. Seven domains were assessed for each included study:
-
random sequence generation
-
allocation concealment
-
blinding of participants and personnel
-
blinding of outcomes assessment
-
incomplete outcome data (study level)
-
selective reporting
-
‘other bias’.
Three bias assessment categories were used: low, high and unclear risk. Unclear risk was assigned because of poor reporting of how the trial was conducted rather than a poorly conducted trial. RCTs that were deemed to be at low or unclear risk of bias were included in the main analysis.
Within a study, a summary assessment of low risk of bias was given when there was a low risk of bias for all key domains, unclear risk of bias when there was an unclear risk of bias for one or more key domains and high risk of bias when there was a high risk of bias for one or more key domains. Across studies, a summary assessment of the risk of bias for the primary outcome (across domains) was undertaken.
For observational studies, guidance from the CRD43 was used to inform the quality assessment of adverse event reporting in observational studies. Although criteria for quality assessment of adverse event data from observational studies are currently being developed, most tools have not been validated and there is currently no agreement on how these quality assessments should be used in systematic reviews. 49,51 Tools that have been validated for different types of observational studies seemed inadequate for the purpose of this systematic review. 51,52 Therefore, the relevant questions for quality assessment from the CRD43 guidance were used:
-
Is there an adequate explanation of how adverse effects were identified?
-
Were the adverse effects assessed independently by someone other than the surgeon performing the procedure?
-
Are the measurement instruments described?
-
Is the timing and duration of follow-up reported?
-
Was a standardised or validated measurement instrument used?
-
How was the adverse effect(s) attributed to the intervention?
-
Was the process was blinded to assigned treatment?
-
Are the terms clearly explained?
The following question that was deemed relevant was also added: Are all adverse events from the population reported?
Publication bias
For each of the primary pairwise meta-analyses, a funnel plot was assessed for publication bias when at least 10 studies were included. A regression of normalised effect versus precision was calculated as a test for small study effects (using p < 0.10 as an indicator of a significant result), and Egger bias values are presented in Quantity and quality of research available. 53
Methods of analysis/synthesis
For all study designs (RCTs and observational studies) data were tabulated and discussed in a narrative analysis. In this narrative the evidence is grouped according to shared characteristics relevant to the review question. A meta-analysis was performed to estimate a summary measure of effect on relevant outcomes based on ITT analyses. For dichotomous outcomes, odds ratios (ORs) were used as the summary statistic. For continuous outcomes, mean difference (MD) was the summary statistic. Meta-analyses were conducted when clinically homogeneous studies of similar comparisons reporting the same outcome measures were identified. Standard pairwise meta-analysis was conducted when more than one RCT was identified. Meta-analysis of continuous outcomes was carried out with the inverse variance method. 44 For dichotomous outcomes meta-analysis was carried out using a fixed-effects model with the Mantel–Haenszel method. 54 Sensitivity analysis was conducted using a random-effects model with the DerSimonian and Laird method. 55 Subgroup analyses were performed for specific surgical indications, when possible. Studies with zero events in both the intervention and control group were reported in a narrative.
In RCTs with more than one control group, the control that was reported as standard care was included. However, in RCTs where standard care was unclear or variable, all control groups were included. In cases for which standard care was unclear or variable, the different control groups were compared with a respective proportion of patients of the intervention group; for example if there were three control groups, the fibrin population was divided by three and compared in a pairwise meta-analysis with each control. The same approach was undertaken in RCTs with more than one fibrin group (i.e. different concentrations) and one control group; all the fibrin sealant groups were included and the number of patients in the control group was divided appropriately. This procedure was followed to avoid double counting of events.
Heterogeneity
For pairwise meta-analysis, heterogeneity was explored through consideration of the study populations, methods and interventions, by visual inspection of results and, in statistical terms, by the chi-squared test for homogeneity and the I2 statistic. Statistically significant heterogeneity was defined as p < 0.10. Levels of inconsistency were assessed using I2 and were defined as follows: I2 of 0–25% = low level of inconsistency; 26–50% = moderate level of inconsistency; and > 50% = high level of inconsistency. 56 In instances when statistically significant heterogeneity was detected in the analyses, a hypothesis-generating subgroup analysis was conducted. 57
Sensitivity analysis
The sensitivity analysis was conducted using a random-effects model with the DerSimonian and Laird method. 55
Changes between protocol and systematic review
Systematic reviews were not included and, therefore, the quality of systematic reviews was not assessed as was mentioned in the protocol. Haematoma is an additional post hoc primary outcome that was not reported in protocol. As the mechanism of haematoma and seroma formation is similar and is reported in some studies interchangeably, it was deemed important to include haematoma as a primary outcome. In addition, a post hoc analysis of combined seroma and haematoma development was undertaken. Haemorrhage, pain levels and infections were described in the protocol as adverse events, but have been moved to secondary outcomes as these were found to be adverse events of surgery, but not adverse events related to fibrin sealant (and fibrin sealants are used to reduce these adverse events related to surgery). Duration of the operation was used to reflect the outcome ‘nurse or doctor time’ instead of the previously mentioned ‘dressing or fine-needle aspirations’. Sensitivity analyses were planned for aspects of the review that might have an impact on the results; for example, including studies where there is a high risk of bias. 53 However, most studies were assessed as having an unclear risk of bias and, therefore, these analyses were not deemed to be appropriate. Sensitivity analysis using a random-effects model was conducted, but because of the large number of RCTs identified in the review, it was not possible to perform additional analyses in the time available.
Results
Quantity and quality of research available
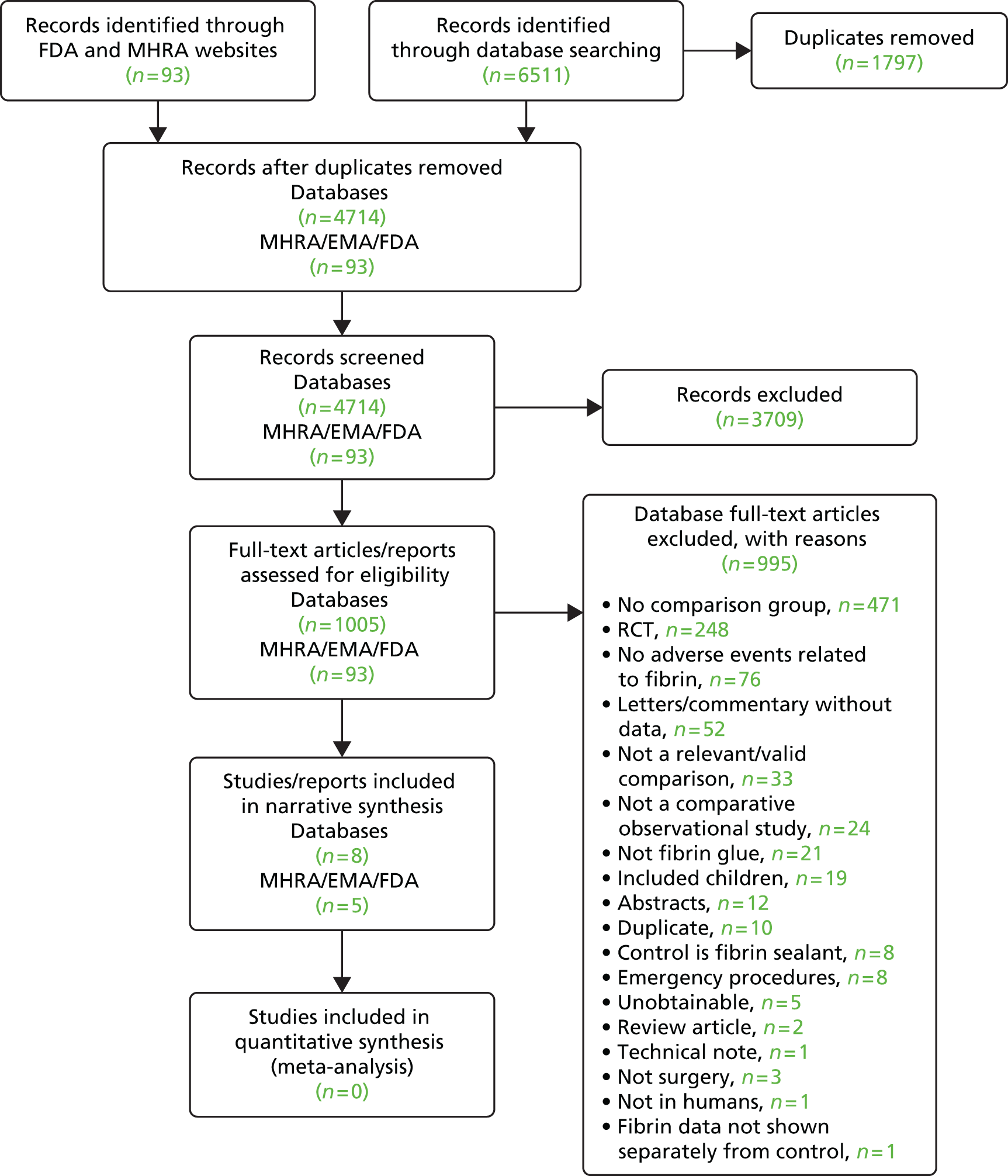
Quantity of randomised controlled trials
A total of 2509 records were identified by searching MEDLINE, EMBASE and The Cochrane Library (Figure 1). After deduplication and screening records, 443 full-text papers were assessed for inclusion. After reviewing the full text, 257 studies were excluded for various reasons, as outlined in Figure 1 (for details of excluded studies see Appendix 3). We included 186 RCTs, which are summarised in Table 2. These RCTs were undertaken in 14 different surgical specialties (classification based on the Royal College of Surgeons of England58) or included a mix of different surgical specialties (four papers combined different surgical specialties), and are presented in Table 2.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for RCTs.

| Surgical area | Number of RCTs |
|---|---|
| Upper GI tract (digestive system) | 33 |
| Stomach | 11 |
| Liver | 13 |
| Gallbladder | 3 |
| Pancreas | 6 |
| Breast and lymph nodes | 30 |
| Breast and/or axillary lymph nodes | 19 |
| Inguinal and/or axillary lymph nodes | 9 |
| Pelvic and/or para-aortic lymph nodes | 1 |
| Thorax/oesophagus lymph nodes | 1 |
| Cardiothoracic | 20 |
| Lung | 16 |
| Heart | 4 |
| Orthopaedic (joints) | 17 |
| Shoulder | 1 |
| Hip | 5 |
| Knee | 11 |
| Eye | 15 |
| Hernia | 14 |
| Otolaryngology (ENT) | 7 |
| Nose | 6 |
| Tonsils | 1 |
| Vascular | 13 |
| Plastic or reconstructive | 10 |
| Skin (graft and ulcer) | 5 |
| Buttock (pilonidal disease) | 2 |
| Abdomen (lipoabdominoplasty) | 2 |
| Ischial region | 1 |
| Colorectal (anus) | 5 |
| Urology (urinary tract) | 5 |
| Kidney | 3 |
| Prostate | 1 |
| Urethra | 1 |
| Oral (mouth) and maxillofacial | 7 |
| Mixed | 4 |
| Gynaecological | 4 |
| Neurological | 2 |
| Total | 186 |
Sample sizes ranged from seven participants in Nativ et al. 59 to 1436 participants in Tavilla et al. ,60 with a median sample size of 62 participants and most values at the lower end. RCTs were published over the past 30 years, since 1985. The main fibrin sealants used were Tisseel (n = 37)/Tissucol® (ImmunoAG, Vienna, Austria) (n = 16), Quixil® (Johnson & Johnson Wound Management, Somerville, NJ, USA) (n = 23), TachoSil® (Takeda Austria GmbH, Linz, Austria) (n = 18), Beriplast® (Behringwerke, Marburg, Germany; FSBP, Aventis Behring, Strasbourg, France) (n = 12), Vivostat® (Vivolution A/S, Birkerød, Denmark) (n = 8) and EVICEL (n = 6).
In addition, 87 RCTs from clinicaltrials.gov were identified, of which 11 relevant trials started since January 2013 (see Appendix 4). Seven trials from controlled-trials.com were found, of which none was recent (since January 2013). A total of 26 trials from clinicaltrialsregister.eu were found, of which 4 were relevant, recent RCTs (see Appendix 4).
In the following subsections the quantity of RCTs and their characteristics for each of the 14 surgical specialties are described.
Upper gastrointestinal (digestive system) surgery
A total of 33 upper gastrointestinal (GI) tract surgery RCTs were identified:61–93 13 liver surgeries,65–75,77,250 three cholecystectomies,78–80 seven pancreatic surgeries,81–86,93 five gastric surgeries63,64,89,90,92 and five surgeries in other areas of the digestive tract61,62,87,88,91 (Table 3). Fibrin sealants had a range of indications in the RCTs reporting GI tract surgeries: improving haemostasis, reducing leakage and wound drainage, and preventing post-operative complications. A variety of different fibrin sealants were used. The sample size ranged from 1361 to 32062 participants, with a mean size of 116 participants. The follow-up duration varied from approximately 7 days in Fernandez et al. 63 to 53 months in Huang et al. ,64 but was infrequently reported.
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Bektas et al., 201465 | 31 | Liver resection | Tisseel spray | Compression |
| de Boer et al., 201266 | 45 | Liver resection | Quixil/Crosseal (Johnson & Johnson Wound Management, Somerville, NJ, USA) | Standard care |
| Chapman et al., 200067 | 60 | Hemihepatectomy or segmental liver resection | CoStasis Surgical Hemostat (Cohesion Technologies Inc., Palp Alto, CA, USA) | Standard care |
| Uetsuji et al., 199468 | 96 | Hepatectomy | IMMUNOAG spray (IMMUNO AG, Vienna, Austria) | Liver mobilisation |
| Liu and Lui, 199369 | 118 | Liver resection | Fibrin sponge/bandage | Standard care |
| Noun et al., 199670 | 137 | Liver resection | Biocol glue (Bio-transfusion, Lille, France) | Standard care |
| Figueras et al., 200771 | 143 | Liver and contralateral resection | Tissucol | Standard care |
| Fischer et al., 201172 | 146 | Liver resection | TachoSil patch | Argon beam coagulation |
| Frilling et al., 200573 | 148 | Liver resection | TachoSil | Argon beam coagulation |
| Kakaei et al., 201374 | 166 | Liver resection | TachoSil patch | Surgicel (Ethicon, Somerville, NJ, USA) |
| Kohno et al., 199275 | 174 | Liver resection | Beriplast | Bovine microcrystalline collagen powder |
| Moench et al., 201476 | 187 | Liver resection | TachoSil patch | Collagen hemostat sangustop fleeces (B. Braun Surgical S.A., Barcelona, Spain) |
| Schwartz et al., 200477 | 207 | Liver resection | Crosseal/Quixil spray | Haemostatic agents |
| Fu et al., 200978 | 60 | Laparoscopic cholecystectomy | Fibrin sealant | Fibrin sealant and ropivacaine hydrochloride |
| Danielsen et al., 201079 | 51 | Laparoscopic cholecystectomy | Vivostat | Human albumin |
| Dimo et al., 198980 | 80 | Cholecystectomy | Beriplast spray | Standard care |
| Carter et al., 201381 | 101 | Pancreatectomies | Vitagel injection (Stryker, Kalamazoo, MI, USA) | Staples or sutures |
| Suzuki et al., 199582 | 56 | Distal pancreatectomy | Tisseel glue | Standard care |
| Lillemoe et al., 200483 | 124 | Pancreaticoduodenectomy | Hemaseel glue (Baxter Healthcare Corp, Deerfield, MA, USA) | Standard care |
| Montorsi et al., 201284 | 275 | Pancreatectomy | TachoSil patch | Standard suturing or stapling |
| Suc et al., 200385 | 182 | Pancreaticoduodenectomy | Tissucol spray | Standard care |
| Martin and Au, 201386 | 57 | Pancreaticoduodenectomy | Tisseel adhesive | Standard care |
| Hwang and Chen, 199661 | 13 | Closure of low-output enterocutaneous fistula | Fibrin tissue glue, infused | Conservative treatment |
| Huang et al., 201564 | 42 | Locally advanced gastric cancer without peritoneal metastases | Fibrin sealant spray | Cisplatin hyperthermic intraoperative chemotherapy |
| Fernandez Fernandez et al., 199663 | 86 | Total gastrectomy for gastric adenocarcinoma | Tissucol fibrin glue | Standard care |
| Oliver et al., 201287 | 104 | Anastomosis of the digestive tract | Tissucol Duo (1 ml) | Standard care |
| Musella et al., 201488 | 100 | Laparoscopic sleeve gastrectomy | Tiseel spray | Standard care |
| Silecchia et al., 200862 | 320 | Laparoscopic Roux-en-Y antecolic antegastric gastric bypass | Tissucol/Tisseel | Sutures |
| Pilone et al., 201289 | 30 | Laparoscopic sleeve gastrectomy for bariatric surgery | TachoSil spray | Standard care |
| Sroka et al., 201590 | 165 | Laparoscopic sleeve gastrectomy | EVICEL spray | Sutures |
| Fékété et al., 199291 | 100 | Surgery requiring oesophageal anastomosis | Quick-setting fibrin glue | Standard care |
| Bulbuller et al., 201392 | 65 | Gastrectomy | Tisseel | Without suture |
| Huang and Qian, 201493 | 95 | Radical gastrectomy | Fibrin spray | Standard care |
Breast and lymph node surgery
A total of 30 breast and lymph nodes surgery RCTs94–123 were identified: 19 in breast and/or axillary lymph nodes,95–112,123 nine in inguinal and/or axillary lymph nodes,94,113–120 one in pelvic and/or para-aortic lymph nodes121 and one in thorax/oesophagus lymph nodes122 (Table 4). Fibrin sealants were used as a wound sealant in all RCTs apart from Zhibo and Miaobo,95 when a local anaesthetic was incorporated into the fibrin sealant. A variety of different fibrin sealants were used in different forms, such as patches [TachoComb (Takeda Pharma, Apotekerstien, Denmark) and TachoSil] and sprays (Vivostat, Tisseel and Beriplast). Control-group interventions included standard closure, lidocaine only, no fibrin and no drain. The sample size ranged from 26114 to 159110 participants, with a mean size of 66 participants. Individual randomisation took place in all the RCTs. The follow-up duration varied from approximately 3 days in Moore et al. 106 to 46 months in Swan et al. ,113 but was infrequently reported.
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Zhibo and Miaobo, 200995 | 30 | Breast: surgical augmentation | Fibrin glue and lidocaine | Lidocaine only |
| Ulusoy et al., 200396 | 54 | Breast: mastectomy | Fibrin sealant, spray | Standard closure |
| Dinsmore et al., 200097 | 27 | Breast: mastectomy | Autologous fibrin glue, spray | Standard closure |
| Nielsen et al., 1985123 | 38 | Breast: mastectomy | Tisseel, spray | Standard care |
| Udén et al., 199398 | 68 | Breast and axillary lymph nodes | Tisseel, adhesive | Standard closure |
| Jain et al., 200499 | 116 | Breast and axillary lymph nodes | Tisseel spray; no drains | No fibrin, no drain |
| Johnson et al., 2005100 | 82 | Breast and axillary lymph nodes | Hemaseel APR, spray | Standard closure |
| Llewellyn-Bennett et al., 2012101 | 101 | Breast and axillary lymph nodes | Tisseel, spray | Standard closure |
| Ko et al., 2009102 | 95 | Breast and axillary lymph nodes | Greenplast kit (Green Cross Corp., Seoul, Korea), spray | Standard closure |
| Miri Bonjar et al., 2012103 | 60 | Breast and axillary lymph nodes | Hemaseel, spray | Standard closure |
| Mustonen et al., 2004104 | 40 | Breast and axillary lymph nodes | Tisseel, spray | Standard closure |
| Segura-Castillo et al., 2005105 | 45 | Breast and axillary lymph nodes | Quixil, spray | Standard closure |
| Moore et al., 1997106 | 63 | Breast and axillary lymph nodes | Autologous fibrin sealant, spray | Standard closure |
| Berger et al., 2001107 | 60 | Axillary lymph nodes | TachoComb H, patch | Standard closure |
| GiIlly et al., 1998108 | 108 | Axillary lymph nodes | Tissucol, unclear application | Standard closure |
| Benevento et al., 2014109 | 60 | Axillary lymph nodes | Fibrin sealant | Standard closure |
| Cipolla et al., 2010110 | 159 | Axillary lymph nodes | Fibrin sealant, spray | Standard closure |
| Moore et al., 2001111 | 80 | Axillary lymph nodes | Fibrin sealant VI Guard spray (V.I. Technologies, Inc. Vitex, Watertown, MA, USA) 4/8/16 ml | Standard closure |
| Vaxman et al., 1995112 | 40 | Axillary lymph nodes | Tisseel, spray | Standard closure |
| Swan et al., 2011113 | 74 | Axillary or inguinal lymph nodes | Tisseel, spray | Standard closure |
| Siim et al., 1994114 | 26 | Axillary or inguinal lymph nodes | Tisseel, unclear application | Standard closure |
| Gilly et al., 1994115 | 40 | Axillary or inguinal lymph nodes | Tissucol, spray | Standard closure |
| Furrer et al., 1993116 | 30 | Axillary or inguinal lymph nodes | Tissucol, spray | Standard closure |
| Di Monta et al., 2012117 | 70 | Axillary or ilioinguinal lymph nodes | TachoSil, patch | Standard closure |
| Neuss et al., 2009118 | 58 | Inguinal lymph nodes | Tissucol, spray | Standard closure |
| Simonato et al., 2009119 | 60 | Inguinal lymph nodes | TachoSil, patch | Standard closure |
| Carlson et al., 200894 | 137 | Inguinal lymph nodes | Tisseel, spray | Standard closure |
| Mortenson et al., 2008120 | 30 | Inguinofemoral lymph nodes | Tisseel, unclear application | Standard closure |
| Scholz et al., 2002121 | 93 | Pelvic or pelvic and para-aortic lymph nodes | Tissucol, spray | Standard closure |
| Tachibana et al., 2003122 | 43 | Thorax/oesophagus lymph nodes | Bohleal (Kaketsuken Pharmaceutical, Kumamoto, Japan), spray | Standard closure |
Cardiothoracic surgery
A total of 18 cardiothoracic surgery RCTs60,124–140 were identified, of which 14 were in lung surgery124–137 and four were in heart surgery60,138–140 (Table 5). In lung surgery, fibrin sealants were used to prevent or reduce air leakage, whereas in heart surgery the indication for fibrin sealants was to stop bleeding. A variety of different fibrin sealants were used, such as patches (TachoComb and TachoSil) and sprays (Vivostat, Tisseel or Beriplast). Control-group interventions included sutures, stapling, clips, standard patches, fleece material, electrocautery or no additional procedures. The sample size ranged from 23138 to 346129 participants, with a mean size of 115 participants.
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Lung | ||||
| Fabian et al., 2003128 | 100 | Pulmonary resection | Fibrin glue spray | Stapling |
| Droghetti et al., 2008124 | 40 | Pulmonary resection | Fibrin patch | Stapling |
| Lopez et al., 2013129 | 346 | Pulmonary resection | TachoSil patch | Suturing |
| Rena et al., 2009127 | 60 | Pulmonary resection | TachoSil patch | Standard treatment |
| Gonfiotti et al., 2011130 | 186 | Pulmonary resection | Fibrin sealant | No additional interventions |
| Moser et al., 2008126 | 25 | Pulmonary resection | Vivostat system | No additional interventions |
| Belcher et al., 2010131 | 102 | Pulmonary resection | Vivostat system, spray | BioGlue (CryoLife, Kennesaw, GA, USA) |
| Mouritzen et al., 1993132 | 114 | Pulmonary resection (pneumonectomies, lobectomies, bilobectomies, segmental resections, subsegmental resections or decortications) | Beriplast P spray | Not specified |
| Belboul et al., 2004133 | 40 | Pulmonary resection (lobectomy) | Vivostat system | No additional interventions |
| Lang et al., 2004134 | 186 | Pulmonary resection (lobectomy) | TachoComb, fleece-bound sealant | Sutures |
| Anegg et al., 2007125 | 152 | Pulmonary resection (lobectomy, segmentectomy) | TachoSil, fleece-bound sealant patch | Sutures with absorbable patches or staples |
| Marta et al., 2010135 | 299 | Pulmonary resection (lobectomy) | TachoSil, surgical patch | Resuturing, stapling or no treatment |
| Filosso et al., 2013136 | 24 | Pulmonary resection (thoracotomy, lobectomy) | TachoSil, patch | Stapling/suturing |
| Czerny et al., 2004137 | 80 | Lobectomy and mediastinal lymph node dissection | TachoComb, bandage/patch | Conventional surgical haemostasis |
| Heart | ||||
| Kjaergard and Trumbull, 1998138 | 23 | Primary coronary artery bypass surgery/grafting | Vivostat system | Sutures, clips and electrocautery |
| Kjaergard and Trumbull, 2000139 | 60 | Median sternotomy | Vivostat system | No additional interventions |
| Maisano et al., 2009140 | 119 | Elective surgery on the heart, ascending aorta or arch requiring a cardiopulmonary bypass procedure | TachoSil, patch | Standard haemostatic fleece material |
Orthopaedic (joint) surgery
A total of 17 RCTs14,141–156 in orthopaedic surgery were identified (Table 6). Eleven reported fibrin usage for knee arthroplasty,14,142–151 whereas five reported on hip arthroplasty141,152–154,156 and one on shoulder surgery. 155 In knee and hip arthroplasty, fibrin was used as a haemostatic agent. The most commonly reported sealant used was Quixil spray, which was used in eight RCTs. 14,144–148,154,156 The remaining RCTs reported using EVICEL,149–151 Vivostat141 and Omrixil® spray (Omrix Biopharmaceuticals, Tel Hashomer, Israel),153 whereas two RCTs did not specify the product that was used. 152,155 Control groups mostly constituted patients receiving standard care. The sample size ranged from 24145 to 198142 participants, with a mean size of 81 participants. Within-patient randomisation took place in Kjaergard and Trumbull139 and individual randomisation was undertaken in the remaining RCTs. Duration of follow-up ranged from 7 days in Randelli et al. 149 to 3 years in Mawatari et al. 152
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Knee | ||||
| Aguilera et al., 2013143 | 166 | Total knee arthroplasty | Fibrin glue, Tissucol | None |
| Levy et al., 199914 | 58 | Total knee arthroplasty | Quixil, spray | Standard care |
| Wang et al., 2001144 | 46 | Knee arthroplasty | Quixil, spray | Standard care |
| Kluba et al., 2012145 | 24 | Total knee arthroplasty | Quixil, spray | Anaesthesia and fluid regimen |
| McConnell et al., 2012146 | 65 | Knee arthroplasty | Quixil, spray | Tranexamic acid |
| Molloy et al., 2007147 | 150 | Total knee arthroplasty | Quixil, spray | Tranexamic acid |
| Sabatini et al., 2012148 | 70 | Total knee, cement-less arthroplasty | Quixil | Dideco blood recovery device (Liva Nova, London, UK) |
| Randelli et al., 2014149 | 62 | Total knee arthroplasty | EVICEL, spray | Electrocautery |
| Skovgaard et al., 2013150 | 48 | Total knee arthroplasty | EVICEL, spray | Saline |
| Choufani et al., 2015151 | 60 | Total knee arthroplasty | EVICEL, spray | Standard care |
| Heyse et al., 2014142 | 198 | Total knee arthroplasty | Fibrin, spray | Standard care |
| Hip | ||||
| Mawatari et al., 2006152 | 100 | Total hip arthroplasty | Autologous fibrin tissue adhesive, spray | Standard care |
| Wang et al., 2003153 | 81 | Total hip arthroplasty | Omrixil, spray | Standard care |
| Lassen et al., 2006141 | 58 | Hip arthroplasty | Vivostat, spray | Standard care |
| Falez et al., 2013154 | 95 | Hip arthroplasty | Quixil, spray | Bipolar sealer (Medtronic, Minneapolis, MN, USA) |
| McConnell et al., 2011156 | 66 | Hip arthroplasty | Quixil, spray | Tranexamic acid |
| Shoulder | ||||
| Antuña et al., 2013155 | 28 | Arthroscopic massive rotator cuff tears repair | Platelet-rich fibrin | Standard care |
Eye surgery
A total of 15 eye surgery RCTs157–171 were identified, of which 13 were on pterygium surgeries,157–163,165–169,171 one was a cataract surgery170 and one a corneal perforation surgery164 (Table 7). In pterygium surgery, fibrin adhesives were used to attach conjunctival autografts. For cataracts and perforation, fibrin sealants were used for wound closure and perforation closure, respectively. The most commonly reported sealant used within the RCTs was Tisseel (used in seven RCTs157,160–163,167,171). Quixil159,166,169 and Beriplast158,168 were also used, whereas the product was not specified in three RCTs. 164,165,170 Control group interventions were sutures in all the RCTs except for one in which cyanoacrylate tissue adhesive was used (Sharma et al. 164). The sample size ranged from 22168 to 116165 participants, with a mean size of 63 participants.
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Ocular surface | ||||
| Kucukerdonmez et al., 2010157 | 70 | Pterygium surgery with autograft | Tisseel VH, glue | Sutures |
| Eye | ||||
| Yüksel et al., 2010158 | 58 | Pterygium surgery with autograft | Beriplast P/Combi-set (Aventis Hehring GmbH, Marburg, Germany) | Sutures |
| Bahar et al., 2006159 | 65 | Pterygium surgery | Quixil | Sutures |
| Rubin et al., 2011166 | 42 | Pterygium surgery with autograft | Quixil, glue | Sutures |
| Conjunctiva | ||||
| Hall et al., 2009160 | 50 | Pterygium surgery with autograft | Tisseel, glue | Sutures |
| Karalezli et al., 2008161 | 50 | Pterygium surgery with autograft | Tisseel, glue | Sutures |
| Koranyi et al., 2005162 | 43 | Pterygium surgery with autograft | Tisseel, glue | Sutures |
| Sati et al., 2014163 | 90 | Pterygium surgery with autograft | Tisseel, spray | Sutures |
| Ratnalingam et al., 2010165 | 137 | Pterygium surgery with autograft | Fibrin, glue | Sutures |
| Srinivasan et al., 2009167 | 40 | Pterygium surgery with autograft | Tisseel | Sutures |
| Uy et al., 2005168 | 22 | Pterygium surgery with autograft | Beriplast P, glue | Sutures |
| Mellin and Kondler, 1989170 | 100 | Cataract surgery | Fibrin, glue | Sutures |
| Malik and Kumar, 2010171 | 50 | Pterygium surgery with autograft | Tisseel Duo Quick | Sutures |
| Cornea | ||||
| Sharma et al., 2003164 | 40 | Corneal perforation | Fibrin, glue | Cyanoacrylate tissue adhesive |
| Bahar et al., 2007169 | 81 | Pterygium surgery with autograft | Quixil | Sutures |
Hernia surgery
A total of 14 hernia surgery RCTs172–185 were identified (Table 8). Fibrin sealants were used mostly for prosthetic mesh fixation (12 RCTs172–176,178,181–186). The most commonly reported sealant used was Tisseel/Tissucol (10 RCTs172,176–178,180–185). Quixil (two RCTs174,179) and Vivostat (one RCT173) were also used, whereas one RCT did not report which fibrin product was used. 175 Three papers reported using fibrin sealant in spray form176,177,179 and three reported using laparoscopic applicators. 172,178,180 One paper reported using a needle applicator,174 another reported using a manual application catheter183 and the remaining six papers did not specify how it was applied. 173,175,181,182,184,185 Fibrin was compared with a range of interventions across the RCTs including sutures, staples, tacks and self-gripping mesh. The sample size ranged from 22173 to 600185 participants, with a mean size of 172 participants. Within-patient randomisation took place in Boldo173 and individual randomisation was undertaken in the remaining RCTs. The follow-up duration varied from approximately 3 months in Cambal et al. 175 to 26 months in Olmi et al. 185
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Inguinal canal | ||||
| Lau, 2005172 | 93 | Endoscopic totally extraperitoneal inguinal hernioplasty | Tisseel VH | Staples |
| Boldo, 2008173 | 22 | Laparoscopic hernioplasty | Vivostat | Staples |
| Bracale et al., 2014174 | 102 | Hernioplasty | Quixil | Sutures |
| Cambal et al., 2012175 | 100 | Laparoscopic hernioplasty | Fibrin glue | Self-gripping (or self-anchoring) mesh |
| Campanelli et al., 2012176 | 316 | Hernioplasty | Tissucol/Tisseel | Sutures |
| Canonico et al., 1999177 | 50 | Hernioplasty | Tissucol | Standard care |
| Chan et al., 2014178 | 129 | Total extraperitoneal hernioplasty | Tisseel spray | Staples |
| Lionetti et al., 2012179 | 148 | Hernioplasty | Quixil spray | Sutures |
| Wong et al., 2011182 | 56 | Hernioplasty | Tisseel glue | Sutures |
| Damiano et al., 2014184 | 468 | Herniorrhaphy | Tissucol | Sutures |
| Olmi et al., 2007185 | 600 | Laparoscopic transabdominal pre-peritoneal hernia repair | Tissucol/Tisseel | Staples |
| Inguinal and femoral canals | ||||
| Lovisetto et al., 2007180 | 197 | Hernioplasty | Tissucol/Tisseel | Staples |
| Tolver et al., 2013181 | 100 | Laparoscopic groin hernia | Tisseel spray | Tacks |
| Umbilicus | ||||
| Eriksen et al., 2013183 | 34 | Laparoscopic ventral hernia repair | Tisseel Duo Quick | Tacks |
Ear, nose and throat surgery
Seven RCTs186–192 were identified in ear, nose and throat (ENT) surgery: six nasal surgeries186–191 and one tonsillectomy192 (Table 9). Fibrin adhesives were mostly used to aid haemostasis (five RCTs188–192) and to improve healing. The most commonly reported sealant used was Quixil (spray/glue) and was used in four RCTs,188,189,191,192 whereas Beriplast187 and EVICEL186 were also used. Control-group interventions included packing, compression, sutures and standard care. The sample size ranged from 10186 to 513191 participants, with a mean size of 133 participants. Within-patient randomisation took place in two RCTs,186,190 whereas individual randomisation was undertaken in the remaining RCTs. The follow-up duration varied from approximately 21 days in Pryor et al. 186 to 1 year in Prado et al. 187
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Nose | ||||
| Prado et al., 2006187 | 22 | Rhinoplasty | Beriplast | Standard care |
| Pryor et al., 2008186 | 10 | Rhinoplasty | EVICEL | Compression |
| Vaiman et al., 2005189 | 64 | Endoscopic sinus surgery | Quixil/Crosseal (Johnson & Johnson Wound Management, Somerville, NJ, USA) spray | Nasal packing |
| Yu et al., 2014190 | 41 | Rhinosinusitis refractory | Fibrin spray | Sponge packing |
| Vaiman et al., 2005191 | 513 | Endonasal surgery | Quixil glue | Nasal packing |
| Nose and septum | ||||
| Vaiman et al., 2002188 | 204 | Septoplasty and conchotomy | Quixil aerosol glue | Quixil aerosol glue and trans-septal suturing |
| Tonsils | ||||
| Vaiman et al., 2006192 | 80 | Tonsillectomy | Quixil spray | Electrocautery |
Vascular surgery
A total of 13 vascular surgery RCTs193–205 were identified (Table 10). Fibrin sealant was used in all cases to control suture hole bleeding from placing the graft for vascular access or vascular reconstruction surgery. In Bajardi et al. 194 Poly(ethyl benzene-1,4-dicarboxylate) [Dacron® (Ethicon Inc., Somerville, NJ, USA)] grafts were used, whereas in all other RCTs193,195–204 polytetrafluoroethylene grafts were used. These materials are frequently used for vascular replacement or bypass when no autologous venae are available. All RCTs used different fibrin sealants apart from the Joseph et al. 200 and Czerny et al. 205 RCTs that used TachoComb patches. Control group interventions were manual compression194,196–198,200,204,205 or use of thrombin,196 thrombin-soaked materials,196,199 Surgicel195,196 or Kalkostat. 202 The sample size ranged from 24200 to 199199 participants, with a mean size of 66 participants. Individual randomisation was undertaken in all RCTs. Follow-up duration varied from approximately 30 days in Sintler et al. 202 to 6 months in Schenk et al. ,195 but was infrequently reported.
| Study (author, year) | Sample size | Surgical area | Surgery | Intervention | Control |
|---|---|---|---|---|---|
| Schenk et al., 2003195 | 48 | Upper extremity; artery and vein in the upper arm or forearm | Vascular access surgery using PTFE graft placement (dialysis required for end-stage renal failure) | Bioplasma (ZLB, Bioplasma AG, Bern, Switzerland) glue | Surgicel (Johnson & Johnson, Somerville, NJ, USA) |
| Schenk et al., 2002196 | 28 | Upper extremity; artery and vein in the upper arm or forearm | Vascular access surgery using PTFE graft placement | Hemaseel spray (Haemacure Corp., Sarasota, FL, USA) | Thrombin (n = 8); pressure (n = 6); thrombin-soaked Gelfoam (Pfizer Inc., New York City, NY, USA) (n = 2); Surgicel (n = 2) |
| Saha et al., 2012197 | 140 | Upper and lower extremity: axillofemoral, iliofemoral, femorofemoral, iliopopliteal, proximal femoropopliteal, distal femoropopliteal and femorotibial vessel bypass | Arterio-arterial bypasses and arteriovenous shunting for dialysis access with expanded PTFE graft placement | Fibrin sealant | Compression |
| Chalmers et al., 2010198 | 147 | Femoral or upper extremity arteries | PTFE grafts | EVICEL | Compression |
| Taylor et al., 2003199 | 199 | Femoral artery | PTFE grafts | Beriplast P gel | Thrombin-soaked gelatin sponge |
| Joseph et al., 2004200 | 24 | Femoral or carotid artery | Femoral anastomosis and femoral or carotid patch angioplasty with PTFE grafts | TachoComb patch | Compression |
| Jackson et al., 1999193 | 47 | Carotid artery | Elective carotid endarterectomy with expanded PTFE patch angioplasty (atherosclerotic occlusive diseases) | Investigational new drug number 4353, human fibrin sealant | Gelfoam |
| Milne et al., 1995201 | 17 | Carotid artery | Endarterectomy with a PTFE patch | Fibrin spray | No treatment |
| Sintler et al., 2005202 | 20 | Carotid artery | Endarterectomy with an expanded PTFE patch | Quixil | Kaltostat (ConvaTec, Flintshire, UK) |
| Milne et al., 1996203 | 39 | Artery or aorta | Arterial bypass surgery with a PTFE bypass graft and aortic aneurysm repair with a woven Dacron graft | Fibrin injection | No treatment |
| Saha et al., 2011204 | 73 | Anastomoses (junction) of arterio-arterial bypasses and arteriovenous shunts | Bypass vessel PTFE grafts | Tisseel | Compression |
| Czerny et al., 2000205 | 60 | Aortofemoral, femoropopliteal and crossover bypasses, femoral artery, arteria carotis interna | Vascular reconstruction; anastomoses or patch angioplasties with PTFE prostheses | TachoComb H patch | Compression |
| Bajardi et al., 2009194 | 20 | Infrarenal abdominal aorta | Elective infrarenal abdominal aortic aneurysm replacement with a Dacron graft | TachoSil patch | Compression |
Plastic or reconstructive surgery
Ten RCTs206–215 in plastic/reconstructive surgery in various body sites were found (Table 11). Fibrin sealant had different indications within plastic/reconstructive surgery: haemostasis (four RCTs207,208,211,212), reduction of seroma formation (two RCTs213,214), reduction of drainage (two RCTs210,215) and wound healing (two RCTs206,209). Various types of fibrin sealants were used across the RCTs: sprays (Tisseel,210,211 Cryoseal,206,212 Quixil213 and autologous sealant using a spraypen207) and a Bioseed fibrin net. 208 Control-group interventions included standard care,206,210,212,214,215 pressure,208,209 thrombogen kit,207 fabric dressing211 and suction drains. 213 The sample size ranged from 10210 to 225208 participants, with a mean size of 58 participants. Individual randomisation was undertaken in all RCTs except Drake and Wong,207 which reported within-patient randomisation. The follow-up duration varied from 1 week207 to 12 months210 and was not reported in Oliver et al. 215
| Study (author, year) | Sample size | Surgical area | Surgery | Intervention | Control |
|---|---|---|---|---|---|
| Drake and Wong, 2003207 | 34 | Skin | Skin graft | Vivolution spraypen (Vivolution A/S, Birkerød, Denmark) | Thrombogen Kit (Johnson & Johnson Wound Management, Somerville, NJ, USA) |
| Vanscheidt et al., 2007208 | 225 | Lower legs | Treatment of recalcitrant venous leg ulcers | BioSeed fibrin net (BioTissue Technologies GmbH, Freiburg, Germany) | Pressure dressing pad |
| Danielsen et al., 2008209 | 39/40 | Legs | Treatment of leg ulcers | Vivolution | Gauze and pressure |
| Erba et al., 2010210 | 10 | Ischial region | Seal fasciocutaneous flaps to cover ischial pressure sore | Tisseel spray | Standard care |
| Healy et al., 2013211 | 40 | Thigh | Treat split skin graft donor sites | Tisseel spray | Mefix self-adhesive fabric dressing (MoInlycke Healthcare, Lancashire, UK) |
| Altinli et al., 2007206 | 32 | Buttock | Limberg flap procedure in pilonidal disease | CryoSeal spray (Thermogenesis, Rancho Cordova, CA, USA) | Standard care |
| Sözen et al., 2011212 | 50 | Buttock | Karydakis flap operation for pilonidal sinus | CryoSeal spray | Standard care |
| Bercial et al., 2012213 | 43 | Abdomen | Abdominoplasty | Quixil spray | Suction drains |
| Mabrouk et al., 2013214 | 60 | Abdomen | Lipoabdominoplasty | Fibrin glue | Standard care |
| Oliver et al., 2002215 | 44 | Axilla, groin, back and abdomen | Axillary dissection, groin dissection, latissimus dorsi flaps and abdominoplasty | Beriplast spray | Standard care |
Colorectal surgery
Five RCTs were found in colorectal surgery216–220 (Table 12). Fibrin sealant was used mainly to minimise recurrence and prevent incontinence after anal fistula surgery. Three RCTs216,217,219 reported the use of Tisseel/Tissucol in the fibrin group, whereas Beriplast was used in one RCT218 and the remaining RCT220 did not specify the product used. The sample size ranged from 28219 to 62217 participants and the mean number of patients was 44. Individual randomisation was undertaken in all RCTs. The follow-up duration varied from approximately 1 year217 to 60 months. 220
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Ellis and Clark, 2006216 | 57 | Mucosal or anodermal advancement flap for surgical management of anal fistulas | Tisseel injection | Flap repair |
| Altomare et al., 2011217 | 62 | Treatment of trans-sphincteric anal fistulas | Tissucol | Seton treatment |
| Lindsey et al., 2002218 | 42 | Treatment of anal fistulas | Beriplast glue | Fistulotomy or loose seton insertion |
| Hammond et al., 2011219 | 28 | Treatment of idiopathic anal fistula | Tisseel glue | Permacol (Covidien, Dublin, Ireland) |
| van der Hagen et al., 2011220 | 30 | Treatment of complex perianal fistulas | Fibrin sealant glue | Seton drainage |
Urology (urinary tract)
Five RCTs59,221–224 were found in urological surgery (Table 13). Fibrin sealant was used for haemostasis in all the RCTs except for Schultz and Christiansen224 in which it was used to reduce the post-operative drainage period. Various fibrin sealants were used across the RCTs: Siemer et al. 221 and Cormio et al. 222 used a TachoSil patch, Nativ et al. 59 used an Ethicon pad, Luke et al. 223 used Beriplast and Schultz and Christiansen224 used Tisseel. Control groups received standard care in all the RCTs. The sample size ranged from 759 to 185221 participants, and the mean number of patients was 67. Individual randomisation was undertaken in all RCTs. The follow-up duration varied from 159,221 to 3 months223 but was not reported for Cormio et al. 222 and Schultz and Christiansen. 224 Randomisation was carried out at an individual level in all RCTs.
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Kidney | ||||
| Nativ et al., 201259 | 7 | Open partial nephrectomy | Ethicon pad (Johnson & Johnson Wound Management, Somerville, NJ, USA) | Standard care |
| Siemer et al., 2007221 | 185 | Resection of small, superficial kidney tumours not extending into the collecting duct system; nephron-sparing surgery | TachoSil patch | Standard suturing |
| Cormio et al., 2012222 | 96 | Percutaneous nephrolithotomy | TachoSil patch | Nephrostomy tube |
| Prostate | ||||
| Luke et al., 1986223 | 30 | Transurethral resection of the prostate | Beriplast glue | Standard care |
| Urethra | ||||
| Schultz and Christiansen, 1985224 | 16 | Closure of the ureterotomy after ureteral stone surgery | Tisseel adhesive | Dexon sutures (Syneture, Mansfield, MA, USA) |
Oral and maxillofacial surgery
Seven RCTs225–231 were found in oral and maxillofacial surgery (Table 14). Fibrin sealant was used mostly to reduce post-operative wound drainage in different types of procedures. A variety of fibrin sealants were used across RCTs: Tisseel,225,226,230 Crosseal,227 Beriplast spray,228 autologous fibrin glue229 and Artiss. 231 Control-group interventions included ‘no sealant’,225,228,231 tranexamic acid229 and sutures. 230 The sample size ranged from 9227 to 75231 participants, with a mean size of 41 participants. Within-patient randomisation was carried out in four RCTs,226–228,231 whereas the remaining three reported individual-level randomisation. 225,229,230 The follow-up duration varied from 24 hours in Oliver et al. 228 to 3 weeks in Maharaj et al. 230
| Study (author, year) | Sample size | Surgery | Intervention | Control |
|---|---|---|---|---|
| Face | ||||
| Marchac and Greensmith, 2005226 | 29 | Rhytidectomy | Tisseel spray | Rhytidectomy using the vertical U incision technique without glue |
| Oliver et al., 2001228 | 20 | Rhytidectomy | Beriplast spray | No sealant |
| Face and neck | ||||
| Lee et al., 2009227 | 9 | Rhytidectomy | Crosseal | No Crosseal treatment |
| Hester et al., 2013231 | 75 | Rhytidectomy | Artiss | No application of fibrin sealant |
| Thyroid gland | ||||
| Uwiera et al., 2005225 | 56 | Hemithyroidectomy and total thyroidectomy | Tisseel | No sealant |
| Tooth socket | ||||
| Carter et al., 2003229 | 49 | Dental extraction | Autologous fibrin glue | Active 4.8% tranexamic acid solution |
| Parotid glands | ||||
| Maharaj et al., 2006230 | 50 | Superficial and total parotidectomy | Tisseel fibrin glue | Vicryl and Monocryl sutures (Johnson & Johnson Wound Management, Somerville, NJ, USA) |
Gynaecological surgery
Four RCTs232–235 were found in gynaecological surgery (Table 15). Fibrin sealant was indicated for the following: the prevention of post-operative adhesions,232,234 haemostasis around myomectomy suture sites233 and prevention of a vesicovaginal fistula. 235 A variety of fibrin sealants were used across RCTs and control group patients received ‘no sealant’ procedures. The sample size ranged from 16232 to 91 participants,234 with a mean size of 54 participants. Follow-up duration was 3 months235 to 1 year,233 but not reported in Diamond et al. 232 and Takeuchi et al. 234
| Study (author, year) | Sample size | Surgical area | Surgery | Intervention | Control |
|---|---|---|---|---|---|
| Diamond et al., 2011232 | 16 | Ovaries | Bilateral ovarian surgery | Adhexil spray/drip (Johnson & Johnson Wound Management, Somerville, NJ, USA) | Standard care |
| Maggiore et al., 2011233 | 70 | Uterus/endometrium | Laparoscopic removal of myomas (neoplasm) | TachoSil sponge | Standard care |
| Takeuchi et al., 2005234 | 91 | Uterus/abdomen | Laparoscopic myomectomy | Beriplast spray | TachoComb sheet |
| Safan et al., 2009235 | 38 | Vesicovaginal region | Treatment of vesicovaginal fistula | Fibrin adhesive | Standard care |
Neurosurgery
Two RCTs236,237 reporting on fibrin sealant for prevention of cerebrospinal fluid leakage were found in neurosurgery (Table 16). Beriplast adhesive was compared with autologous fibrin sealant in Nakamura et al. ,236 whereas collagen sponge was compared with standard care in Hutter et al. 237 Nakamura et al. 236 reported a sample size of 30 participants, whereas the sample size in Hutter et al. 237 was 229 participants, giving a mean sample size of 134 participants. Individual randomisation was undertaken in both RCTs. The follow-up duration was 32 days in Hutter et al. 237 and 8 weeks in Nakamura et al. 236
| Study (author, year) | Sample size | Surgical area | Surgery | Intervention | Control |
|---|---|---|---|---|---|
| Nakamura et al., 2005236 | 39 | Dura layer of spinal cord | Spinal cord tumours and related illnesses | Beriplast adhesive | Autologous fibrin sealant |
| Hutter et al., 2014237 | 229 | Dura mater of the brain | Elective cranial surgery involving a dural incision | Collagen sponge | Standard care |
Mixed surgery
Four RCTs238–241 across more than one surgical area were found (Table 17): Bochicchio et al. 239 and Verhoef et al. 240 were in spinal and vascular surgery, hepatic resection and soft tissue dissection; Hanks et al. 238 was cardiothoracic, general, obstetric and gynaecological and vascular surgery; and Fischer et al. 241 was in abdominal, retroperitoneal, pelvic and non-cardiac thoracic surgeries. Fibrin sealant was used for haemostasis in all the RCTs and different products were used across them. Raplixa fibrocaps powder was used in Bochiccio et al. 239 and Verhoef et al. 240 In Hanks et al. 238 autologous fibrin sealant derived from patients’ blood was used, whereas in Fischer et al. 241 fibrin pads were used. The sample size ranged from 69238 to 719239 participants, with a mean size of 263 participants. Individual randomisation was undertaken in all RCTs. The follow-up duration was around 1 month in Bochicchio et al. 239 and Fischer et al. ,241 but was not reported in the other two RCTs.
| Study (author, year) | Sample size | Surgical specialties | Surgery | Interventions | Control |
|---|---|---|---|---|---|
| Bochicchio et al., 2015239 | 719 | Spine, liver, arteries, soft tissues | Spinal procedures; vascular procedures with suture hole bleeding; hepatic resection; soft tissue dissection | Raplixa fibrocaps powder (ProFibrix BV – The Medicines Company, Leiden, The Netherlands) | Gelatin sponge |
| Verhoef et al., 2015240 | 122 | Spine, liver, arteries, soft tissues | Hepatic resections (46%), spinal procedures (30%), vascular procedures (24%) and soft tissue dissection (1%) | Raplixa fibrocaps powder | Pressure dressing pad |
| Hanks et al., 2003238 | 69 | Cardiothoracic, general, obstetric and gynaecological, and vascular | Not reported | Vivostat system | Dry surgical sponge |
| Fischer et al., 2013241 | 90/141 | Abdomen, retroperitoneum, pelvis and non-cardiothoracic surgery | Surgical operations in the abdomen, retroperitoneum, pelvis and non-cardiothoracics | Fibrin pad | Surgicel |
Quality of randomised controlled trials
A risk-of-bias table for RCTs can be found in Appendix 5. Overall, 154 studies were assessed as having an ‘unclear risk of bias’, eight RCTs as having a ‘high risk of bias’ and 24 RCTs as having a ‘low risk of bias’ (see Table 37). The risk-of-bias table (see Table 37) shows a high level of uncertainty about the validity of data collected across all parameters, especially regarding the blind collection of patient outcomes. Owing to the nature of the intervention, surgeons could not be blinded to the intervention, as they had to apply the fibrin sealant; however, patients and outcome assessors who could be blinded to the intervention were frequently not blinded either.
Most of the funnel plots did not show publication bias (see Appendix 6); however, the funnel plot for development of haematoma meta-analysis [Egger bias –0.63, 95% confidence interval (CI) –1.20 to –0.06; p = 0.03] (see Figure 43) and duration of drainage for breast surgery meta-analysis (Egger bias –3.34, 95% CI –6.75 to –0.05; p = 0.05) (see Figure 47) showed a skewed figure of publications, which indicated the presence of small study effects.
Quantity of observational studies and regulatory body reports
The search of electronic databases identified 4714 potentially relevant articles about harms related to the use of fibrin sealants, of which 3709 references were excluded and 1005 full-text papers assessed (Figure 2 and Appendix 7). There were an additional 93 reports, reviews or notifications about harms from the use of these products from the MHRA, EMA and FDA websites.
FIGURE 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of observational studies and regulatory body reports.
After screening and applying the eligibility criteria, eight observational studies were included242–249 (Table 18). Three observational studies were in eye surgery,242–244 three in upper GI tract surgery,245–247 one in plastic/reconstructive surgery248 and one in vascular surgery. 249 There were three cohort studies,243,245,249 three comparative studies242,244,247 and two reviews of patient records. 246,248 The following fibrin sealants were used: unspecified fibrin glue in eye surgery,242–244 Tiseel,245 Beriplast,247 aerosolised fibrin glue248 and platelet-enriched fibrin glue sealant. 249 Comparator interventions were standard care245–249 or sutures in eye surgery. 242–244 Sample sizes ranged from 40243 to 529246 participants.
| Study (author, year) | Sample size | Type of comparative study | Surgery | Intervention | Control |
|---|---|---|---|---|---|
| Eye surgery | |||||
| Cagatay et al., 2014242 | 103 | Comparative study (consecutive sample) | Conjunctival autografting for pterygium surgery | Fibrin glue | Sutures |
| Jiang et al., 2008243 | 40 | Cohort study | Conjunctival autografting for pterygium surgery | Fibrin glue | Sutures |
| Choi et al., 2010244 | 126 | Comparative study | Pars plana vitrectomy (eye) | Fibrin glue | Sutures |
| Upper GI tract surgery | |||||
| Efthimiou et al., 2010245 | 474 | Cohort (consecutive sample supplemented with clinical observations and chart reviews) | Laparoscopic Roux-en-Y gastric bypass | Tisseel | Standard care |
| Ibele et al., 2014246 | 529 | Review of patient records (consecutive sample) | Laparoscopic Roux-en-Y gastric bypass | Autologous fibrin sealant | Standard care |
| Nanashima et al., 2012247 | 341 | Comparative study (consecutive sample) | Hepatobiliary pancreas surgery; hepatectomy and pancreatectomy | Beriplast fibrin glue spray | Standard care |
| Plastic/reconstructive surgery | |||||
| Marchac and Sándor, 1994248 | 200 | Review of patient records (consecutive sample) | Rhytidectomy | Aerosolised fibrin glue | Standard care |
| Vascular surgery | |||||
| Sakic et al., 2013249 | 418 | Cohort study (consecutive sample) | Bilateral internal thoracic artery grafting | Platelet-enriched fibrin glue sealant | Standard care |
Five reports from the regulatory body websites that reported on harms related to the use of fibrin sealants were included (see Table 43).
Quality of observational studies
The validity of the eight observational studies was compromised owing to a general failure to report whether or not adverse events were assessed independently and whether or not blinding to the assigned was performed (Table 19). Cagatay et al. 242 reported that harms were assessed independently. Five studies described measurement instruments,243,245,246,248,249 but only three studies reported timing and duration of follow-up. 243,246,249 Only Sakic et al. 249 appeared to have used objective measures. All eight studies, except that by Jiang et al. ,243 attributed the harms to the use of fibrin sealants and seven studies explained terms used to identify harms. 242–246,248,249 No studies reported to have blinded the collection of outcomes to the treatment assignment.
| Study (author, year) | AEs assessed independently? | Measurement instruments described? | Timing and duration of follow-up reported? | Standard or validated measurement instrument used? | Objective measures? | AEs attributed to the intervention? | Collection of outcomes blinded to assigned treatment? | Terms used to identify AEs clearly explained? | All AEs from the population reported? |
|---|---|---|---|---|---|---|---|---|---|
| Cagatay et al., 2014242 | Y | N | N | N | N | Y | N | Y | Y |
| Jiang et al., 2008243 | N | Y | Y | Y | UC | N | NA | Y | Y |
| Choi et al., 2010244 | N | N | N | N | N | Y | N | Y | Y |
| Efthimiou et al., 2010245 | N | Y | N | UC | UC | Y | UC | Y | Y |
| Ibele et al., 2014246 | N | Y | Y | Y | UC | Y | N | Y | Y |
| Nanashima et al., 2012247 | N | N | N | N | UC | Y | N | N | N |
| Marchac and Sándor, 1994248 | N | Y | N | N | N | Y | N | Y | Y |
| Sakic et al., 2013249 | Y | Y | Y | Y | Y | Y | N | Y | Y |
Assessment of benefits
The following sections present the analyses of benefits for the primary and secondary outcomes (Table 20). Fixed-effects model results are presented in the text and random-effects model results in Appendix 8. Data on primary and secondary outcomes used in the meta-analysis for all RCTs are presented in Appendix 9.
| Outcomes | Variables |
|---|---|
| Primary outcomes (dichotomous) | |
| Seroma development | Number of patients who developed seroma |
| Haematoma development | Number of patients who developed haematoma and a post hoc analysis in which the development of seroma and haematoma are combined |
| Secondary outcomes (dichotomous) | |
| Haemorrhage (blood loss) | Number of patients with bleeding |
| Reoperation | Number of patients with reoperation |
| Infections | Number of patients with wound infection |
| Use of analgesics | Number of patients (no meta-analysis as the data from RCTs were too heterogeneous) |
| Complications arising from the use of drains | Number of patients with complications (no data in RCTs reported) |
| Secondary outcomes (continuous) | |
| Duration of operation | Mean duration in minutes |
| Length of hospital stay | Mean duration in days |
| Use of drains | Mean duration of drainage in days |
| Pain levels | Mean level of pain (no meta-analysis as the data from RCTs were too heterogeneous) |
| Health-related quality of life | Mean health-related quality-of-life value (no data in RCTs reported) |
Primary outcomes
Seroma development
Development of seroma was reported in 37 RCTs, of which 33 (n = 3472) were included in the meta-analysis (Figure 3). The remaining four RCTs were excluded for the following reasons: Cipolla et al. 110 as all participants in the fibrin and control groups developed seroma; Erba et al. 210 and Uwiera et al. 225 because no patients developed seroma; and Siim et al. 114 because seroma development was not reported separately but combined with other complications reported as ‘post-operative complications’. The included RCTs were across different surgical specialties: breast and axillary/inguinal (19 RCTs94,96–105,107–109,111,113,115,118,120), hernia (8 RCTs172–174,178,181,182,184,185), plastic, hepatic and otolayrngology. 202,204,227
FIGURE 3.
Seroma development in all surgical specialties: fibrin sealant vs. standard care.
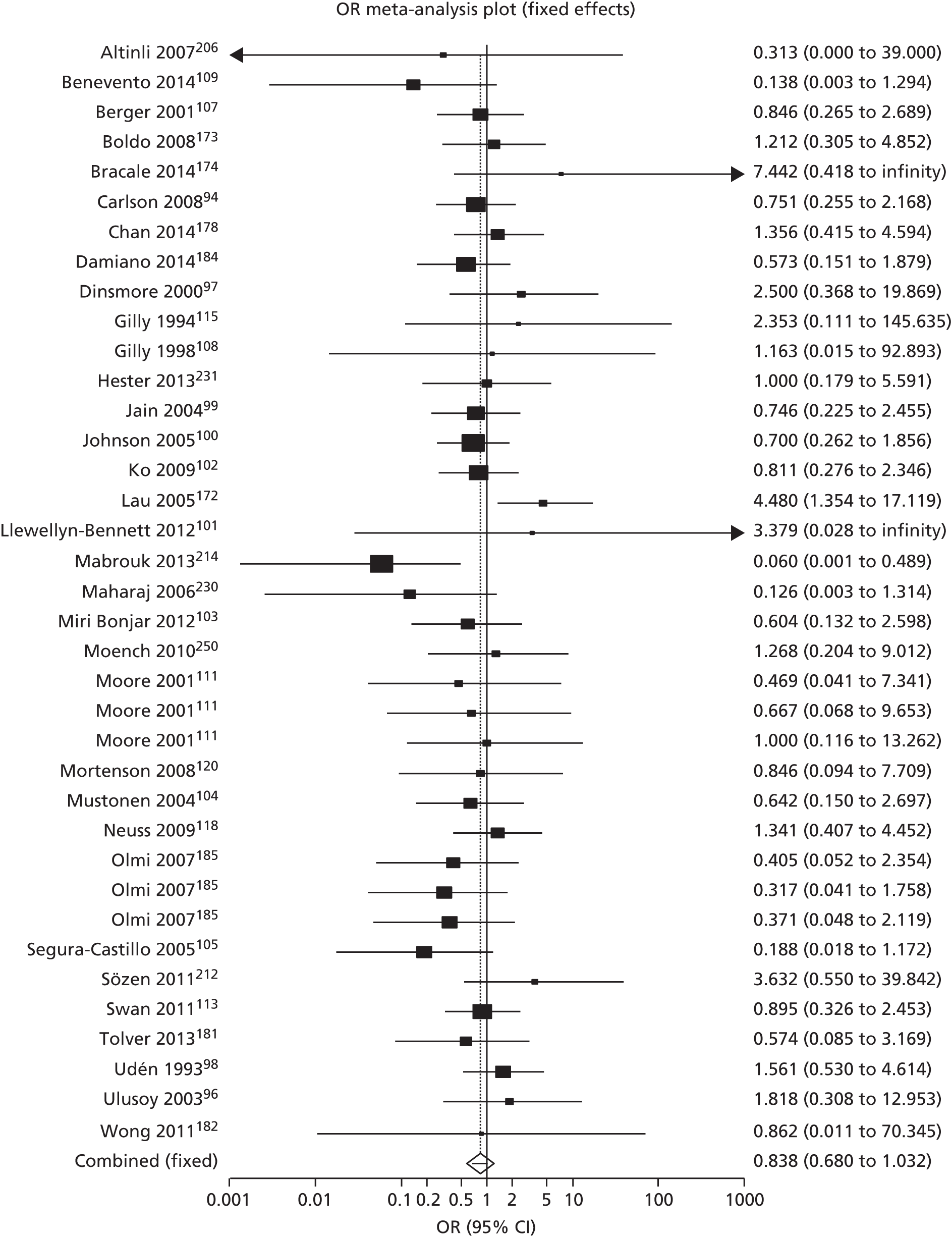
Patients receiving fibrin sealants rather than the control had a statistically non-significant reduced risk of developing seroma (OR 0.84, 95% CI 0.68 to 1.04; p = 0.13; I2 = 12.7%, fixed-effects model). The random-effects model showed a similar result (see Appendix 8). Two of the 32 RCTs with an unclear risk of bias showed a statistically significant difference in seroma development: Mabrouk et al. 214 reported a significant benefit of fibrin sealant, whereas Lau172 reported more seroma development in patients receiving fibrin sealants.
There were some differences in how seroma was defined and at which time point it was reported; the data used in the meta-analysis were the first point at which seroma was reported for the hernia RCTs. 144,172–174,178,181,184,185 Jain et al. 99 had two control groups: (1) no drain and no fibrin, and (2) drain and no fibrin. The first was deemed to be most appropriate for analysis as the only difference from the intervention group was the addition of fibrin. In Moore et al. 111 three intervention groups were reported in which different amounts of fibrin were used; therefore, the control group was divided into three and compared accordingly. Olmi et al. 185 reported one intervention group and three control groups which were different types of fixation, and so the fibrin group was divided into three and compared with each control group. In cases where seroma development was reported at different time points, only the development at the first time point was included in the analysis.
Subgroup analysis was conducted for two surgical specialties that were deemed comparable: breast surgery RCTs (Figure 4) and hernia RCTs (Figure 5). In breast RCTs, patients (n = 1277) receiving fibrin sealants had a statistically non-significantly reduced risk of developing seroma than control group patients (OR 0.84, 95% CI 0.64 to 1.11; p = 0.26; I2 = 0.0%, fixed-effects model). In hernia RCTs, patients (n = 1592) receiving fibrin sealants had no difference in risk of developing seroma than control group patients (OR 0.98, 95% CI 0.66 to 1.46; p = 1.00; I2 = 0.0%, fixed-effects model). The random-effects models showed similar results for these subgroups (see Appendix 8). These results are broadly consistent with the primary analysis that showed an apparent trend of a decrease in the risk of seroma development in patients receiving fibrin sealants.
FIGURE 4.
Seroma development in breast surgery: fibrin sealant vs. standard care.
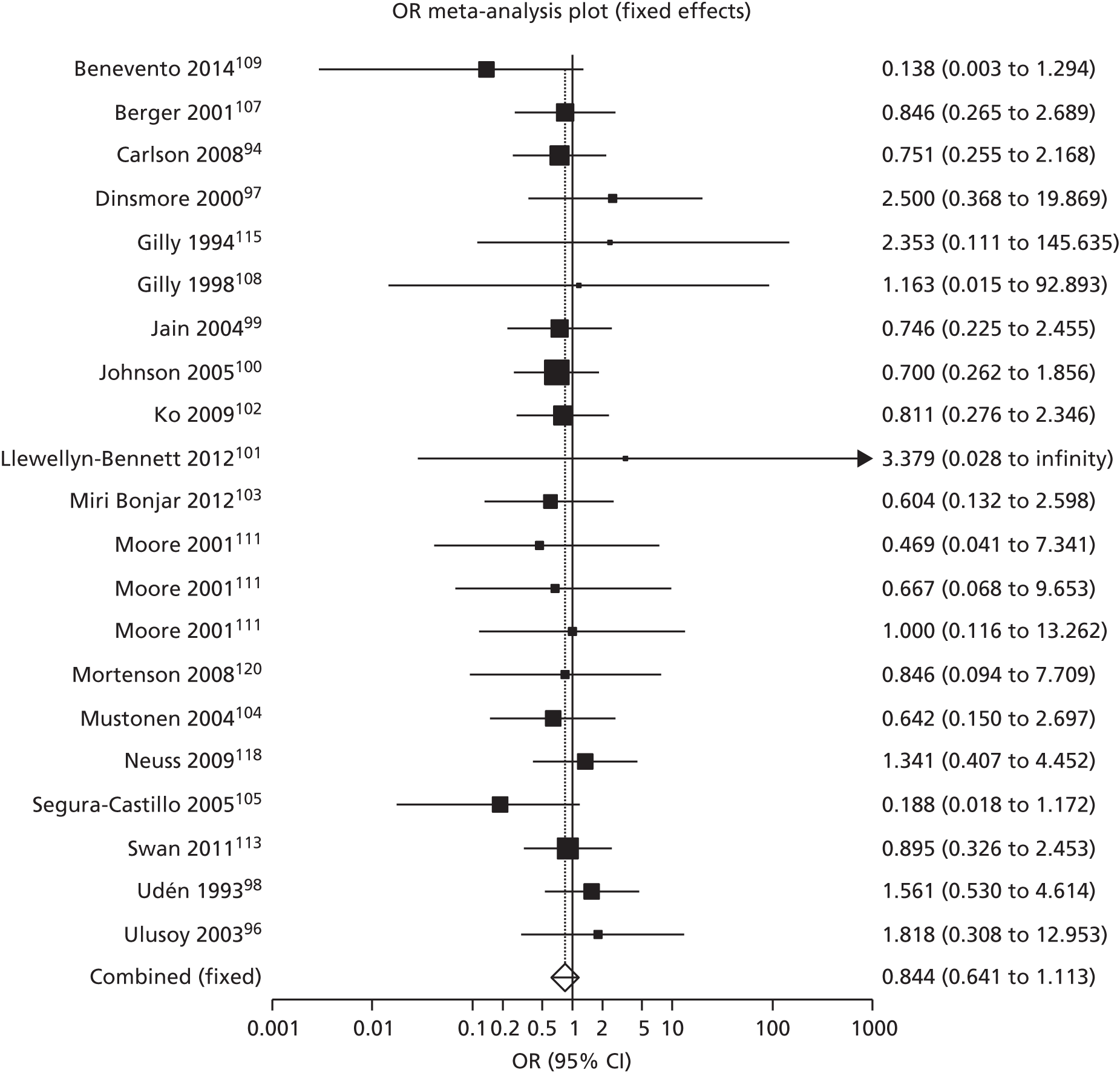
FIGURE 5.
Seroma development in hernia surgery: fibrin sealant vs. standard care.

Haematoma development
Development of haematoma was reported in 26 RCTs, of which 24 were included in the meta-analysis (Figure 6). Two RCTs were excluded from the primary analysis for following reasons: Prado et al. 187 reported only median, quartiles and ranges across a 12-month period and Lovisetto et al. 180 reported haematoma and seroma combined and not separately. The 24 included RCTs65,70,90,100,101,103,110,111,113,118,141,143,144,148,173,177,181,185,188,221,222,227,228,231 (n = 2665) were within the following surgical specialties: breast and axillary/inguinal lymph nodes, hernia, plastic, orthopaedic, upper GI tract, oral and otolaryngology. Patients receiving fibrin sealant had a statistically significant lower risk of developing haematomas than control patients (n = 2403, OR 0.62, 95% CI 0.44 to 0.86; p = 0.01; I2 = 0%, fixed-effects model). The random-effects model showed a similar result (see Appendix 8).
FIGURE 6.
Haematoma development in all surgical specialties: fibrin sealant vs. standard care.

Overall haematoma development was calculated by combining groin and axillary haematomas in Swan et al. ,113 and by combining hepatic and post procedural haematomas in Bektas et al. 65 Reviewers checked that different haematomas did not occur in the same person and, therefore, that data were not double-counted. Data from multiple intervention and control groups in Olmi et al. 185 and Moore et al. 111 were dealt with in the same manner as in the seroma analysis. As two different fibrin groups and two controls were reported in Aguilera et al. 143 it was decided for analysis purposes to compare fibrin glue to control and Tissucol to tranexamic acid.
Subgroup analyses were conducted for the following areas: breast (Figure 7), hernia (Figure 8), orthopaedics (Figure 9) and upper GI tract (Figure 10). A statistically significant reduction in the risk of haematoma formation due to fibrin use occurred only in a meta-analysis of four hernia surgery RCTs173,177,181,185 (n = 794, OR 0.22, 95% CI 0.06 to 0.74; p = 0.01; I2 = 0%, fixed-effects model). There was a trend of a decreased risk of haematoma when using fibrin sealants within the remaining surgical specialties, but these reductions were not statistically significant: p = 0.87 (seven breast RCTs,100,101,103,110,111,113,118 n = 588), p = 0.20 (four orthopaedic RCTs,141,143,144,148 n = 347) and p = 0.88 (three upper GI tract RCTs,65,70,90 n = 243). The random-effects models showed similar results (see Appendix 8).
FIGURE 7.
Haematoma development in hernia surgery: fibrin sealant vs. standard care.
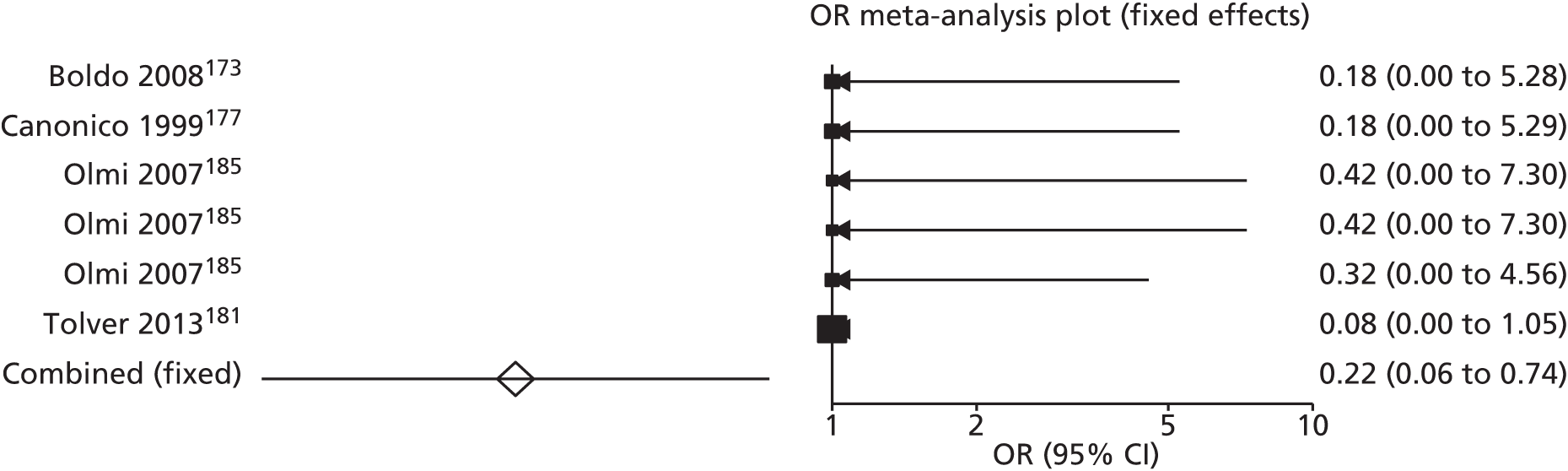
FIGURE 8.
Haematoma development in breast surgery: fibrin sealant vs. standard care.
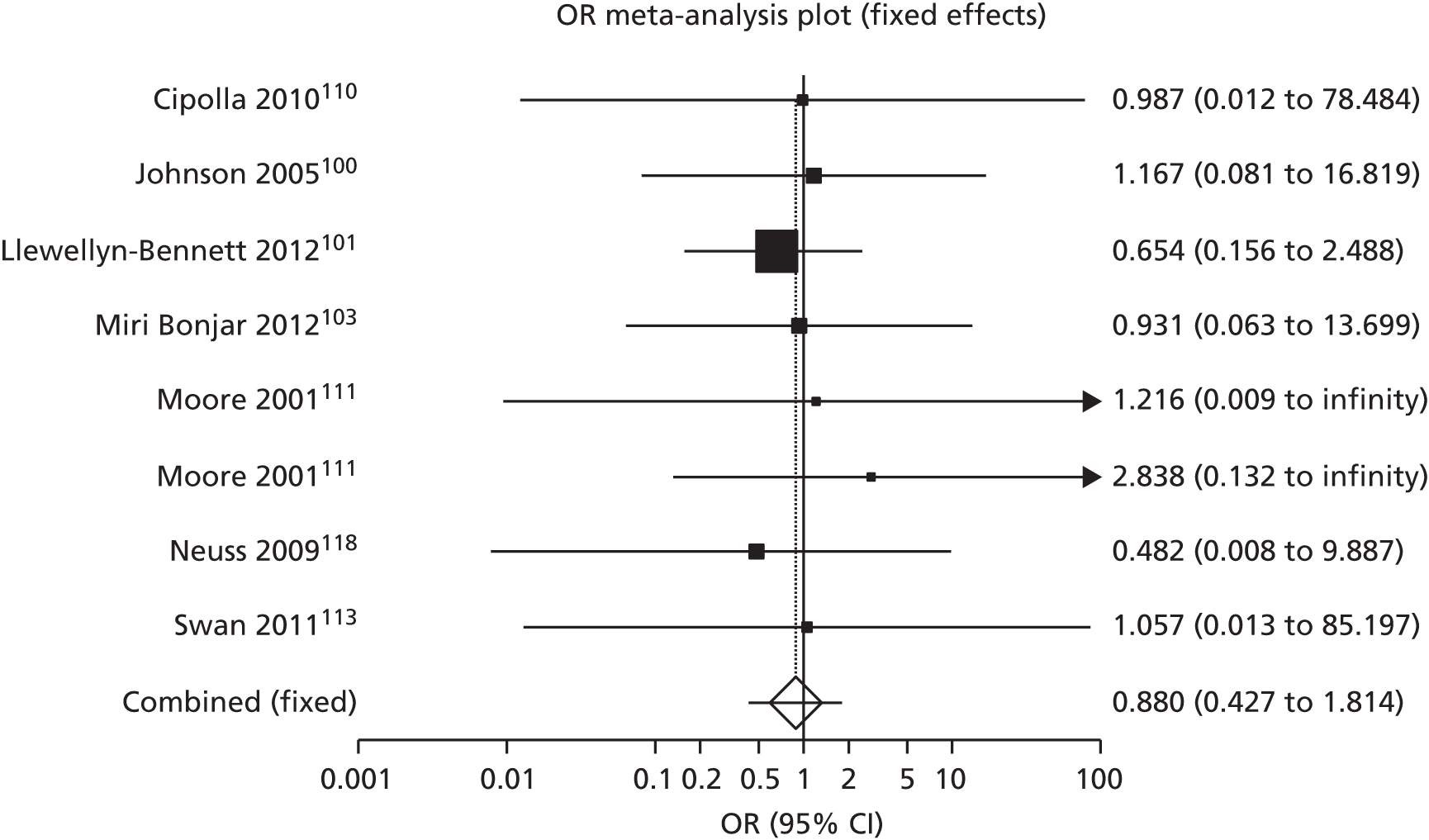
FIGURE 9.
Haematoma development in orthopaedic surgery: fibrin sealant vs. standard care.

FIGURE 10.
Haematoma development in upper GI tract surgery: fibrin sealant vs. standard care.

A post hoc analysis including 48 RCTs65,70,90,94,96–105,107–111,113,115,118,120,141,143,144,148,172–174,177,178,180–182,184,185,188,206,212,214,221,222,227,228,230,231,250 (n = 4876) was carried out to explore impact of combining seroma and haematoma as an outcome (Figure 11). The study by Lovisetto et al. ,180 who reported only combined haematoma and seroma rates (and, therefore, was excluded from the haematoma analysis), was included in the combined analysis. This meta-analysis demonstrated a statistically significant reduction in the risk of developing seroma or haematoma with fibrin sealant compared with control (OR 0.77, 95% CI 0.64 to 0.92; p = 0.01; I2 = 6.7%, fixed-effects model). The random-effects model showed a similar result (see Appendix 8).
FIGURE 11.
Seroma and haematoma development combined in all surgical specialties: fibrin sealant vs. standard care.

Secondary dichotomous outcomes
The following sections present the five dichotomous outcomes: haemorrhage (bleeding), reoperation, infections, use of analgesics and complications arising from the use of drains.
Haemorrhage (bleeding)
Haemorrhage was reported in 19 RCTs, of which 1759,62,74,75,84,85,99,102,134,135,158,168,177,197,199,205,250 (n = 2125) were included in the meta-analysis (Figure 12). Two RCTs (Neuss et al. 118 and Jackson et al. 193) were excluded because they reported that none of the participants experienced post-operative bleeding. The included RCTs were within several surgical specialties: cardiothoracic,134,135,205 breast and axillary/inguinal lymph nodes,99,102 hernia,177 vascular,197,199 eye,158,168 upper GI tract62,74,75,84,85,250 and urology. 59 There was statistically non-significant reduction in risk of post-operative bleeding between patients receiving fibrin sealants versus standard care (OR 0.64, 95% CI 0.40 to 1.02; p = 0.08; I2 = 0%, fixed-effects model). The random-effects model showed a similar result (see Appendix 8).
FIGURE 12.
Haemorrhage (bleeding) in all surgical specialties: fibrin sealant vs. standard.

Randomised controlled trials that did not report the number of patients and only reported bleeding as total number of blood units were also excluded. In Jain et al. 99 two control groups (no drain and no fibrin; drain and no fibrin) were reported and the first group was deemed to be most appropriate for analysis as the only difference between the intervention and control group was the addition of fibrin.
Subgroup analyses were conducted for the following surgical specialties: upper GI tract (Figure 13), cardiothoracic lung (Figure 14), breast (Figure 15), vascular (Figure 16) and eye (Figure 17). There was a statistically significant reduction in risk of haemorrhage when using fibrin sealants compared with standard care within upper GI tract surgery (six RCTs,62,74,75,84,85,250 n = 995, OR 0.39, 95% CI 0.19 to 0.80; p = 0.01; I2 = 0%, fixed-effects model) and no significant difference in the remaining surgical specialties: p = 0.84 (three cardiothoracic lung RCTs,134,135,205 n = 501), p = 0.69 (two breast RCTs,99,102 n = 153), p = 0.76 (two vascular RCTs,197,199 n = 339) and p = 0.61 (two eye RCTs,158,168 n = 80). The random-effects models showed similar results (see Appendix 8).
FIGURE 13.
Haemorrhage (bleeding) in upper GI tract surgery: fibrin sealant vs. standard.

FIGURE 14.
Haemorrhage (bleeding) in cardiothoracic lung surgery: fibrin sealant vs. standard care.
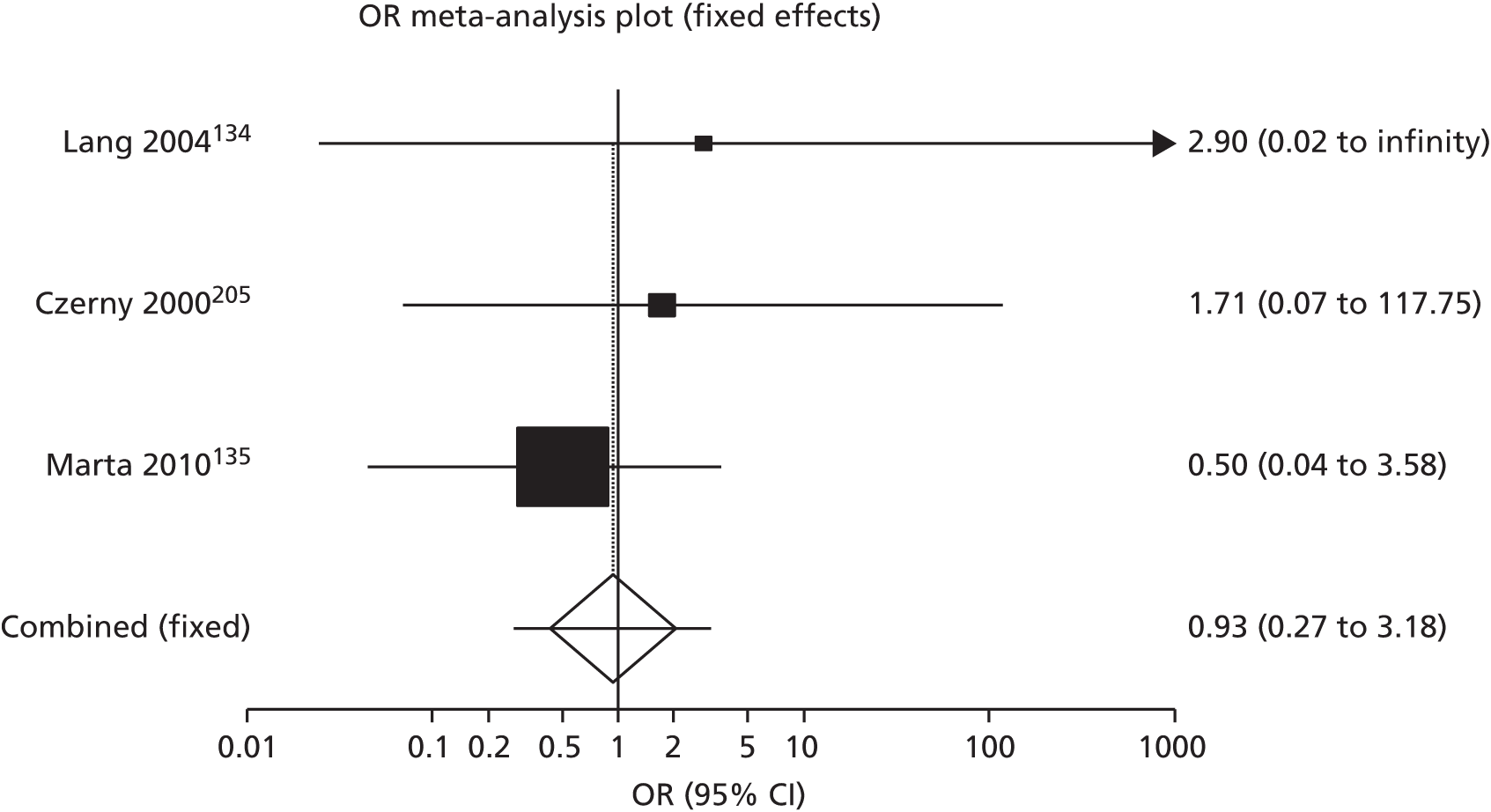
FIGURE 15.
Haemorrhage (bleeding) in breast surgery: fibrin sealant vs. standard care.

FIGURE 16.
Haemorrhage (bleeding) in vascular surgery: fibrin sealant vs. standard care.
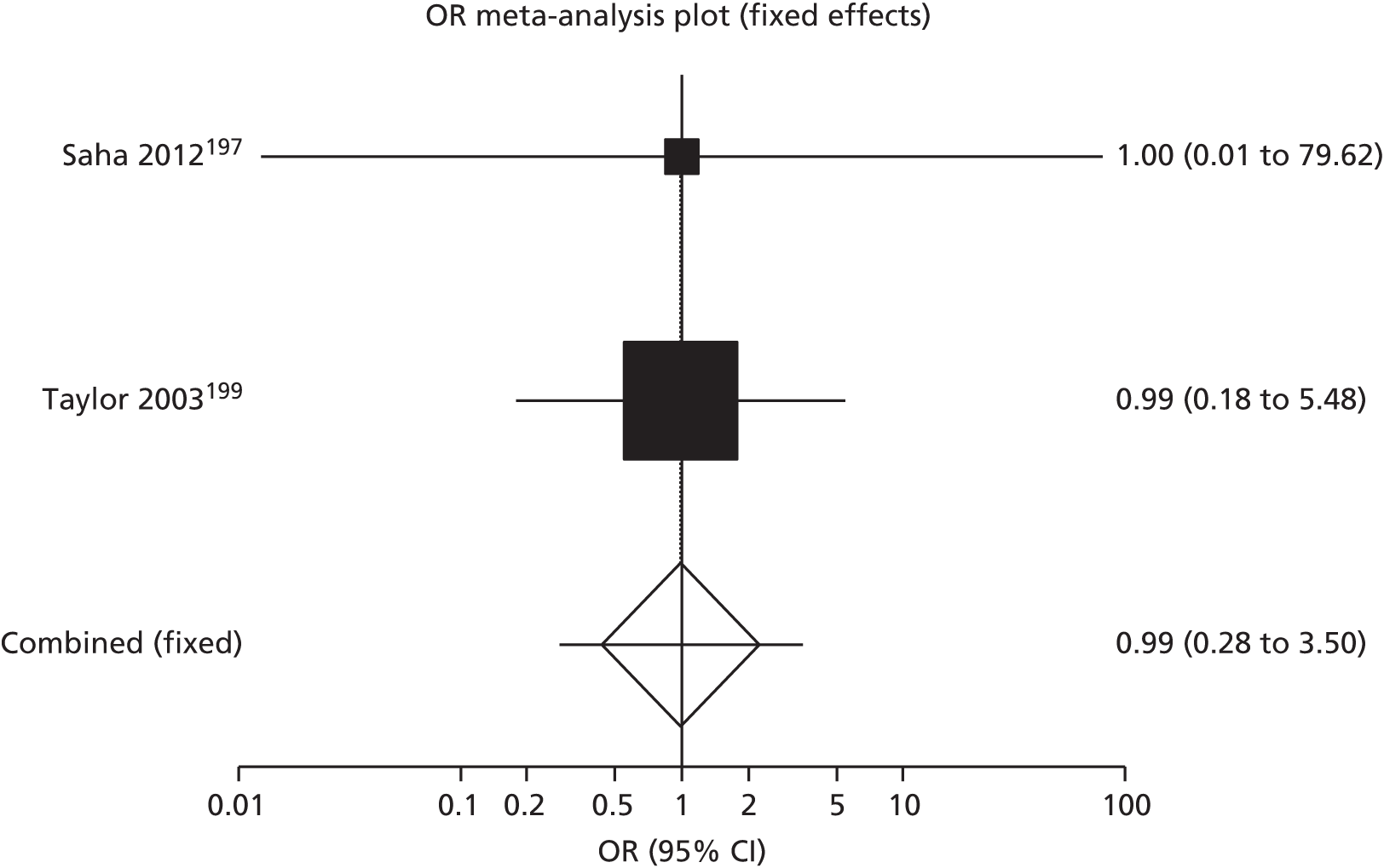
FIGURE 17.
Haemorrhage (bleeding) in eye surgery: fibrin sealant vs. standard care.
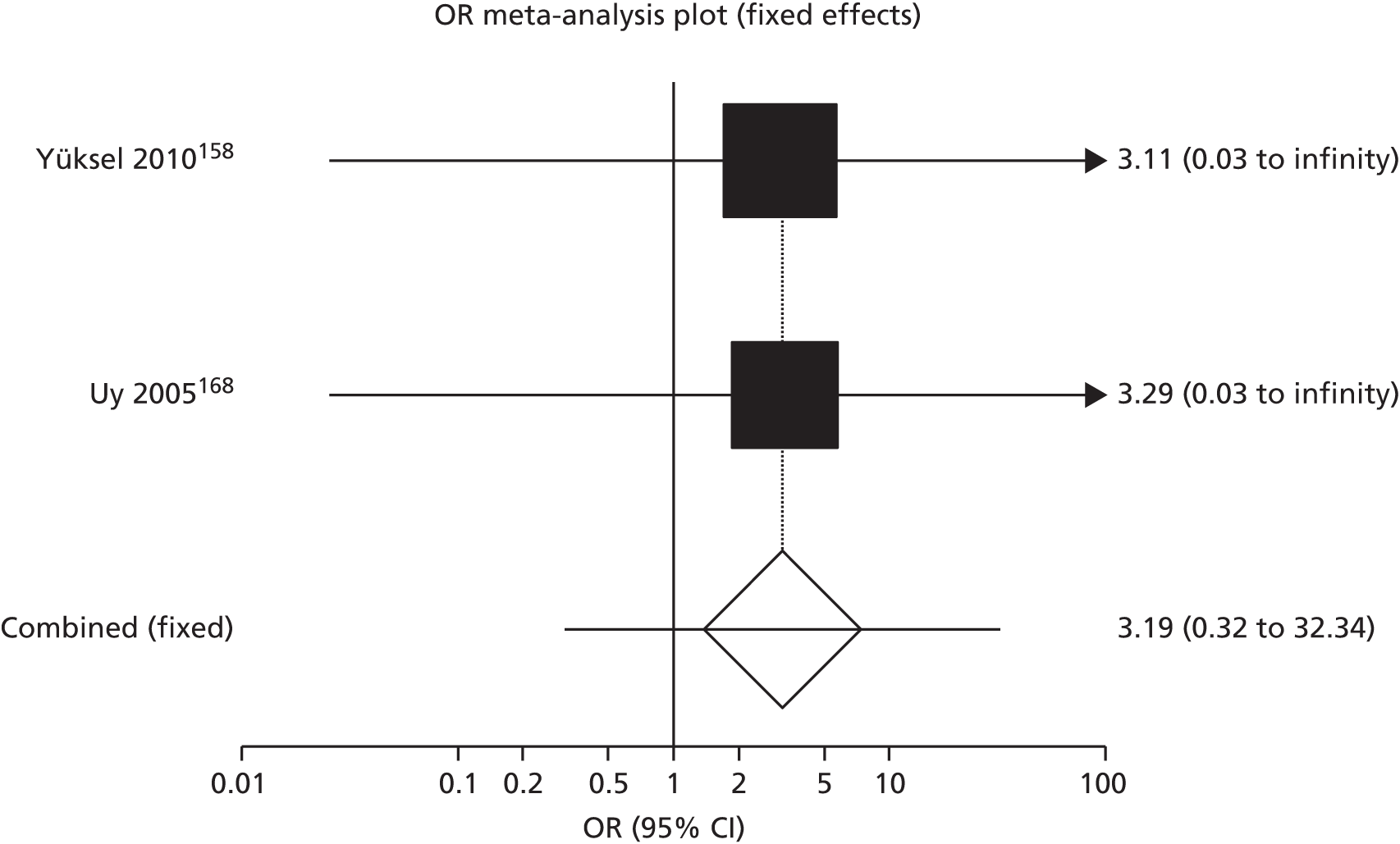
Reoperation
A total of 20 RCTs reported reoperation as an outcome, of which 1560,77,85,86,93,101,107,116,125,135,138,140,143,237,239 were included in the meta-analysis (Figure 18). Five RCTs were excluded for the following reasons: Droghetti et al. ,124 Milne et al. 201 and Dimo et al. 80 reported that none of the trial patients had a reoperation; Bulbuller et al. 92 reported that the only patients who had a reoperation were in an additional intervention arm and not in the fibrin or standard care arms; and Moser et al. 126 did not report any data for the fibrin group.
FIGURE 18.
Reoperation in all surgical specialties: fibrin sealant vs. standard care.

The RCTs included in the meta-analysis reported fibrin use within four surgical specialties: cardiothoracic lung and heart, breast and axillary/inguinal lymph nodes, orthopaedics and neurosurgery. Patients receiving fibrin sealants had a statistically significant lower risk of reoperation than those in the control group (15 RCTs,60,77,85,86,93,101,107,116,125,135,138,140,143,237,239 n = 3789, OR 0.65, 95% CI 0.48 to 0.87; p ≤ 0.01; I2 = 0%, fixed-effects model). The random-effects model showed a similar result (see Appendix 8).
A subgroup analysis was conducted for the following surgical specialties: upper GI tract (Figure 19), cardiothoracic lung (Figure 20), cardiothoracic heart (Figure 21) and breast (Figure 22). The decrease in reoperations associated with using fibrin sealants was only statistically significant in upper GI tract (four RCTs,77,85,86,93 n = 455, OR 0.43, 95% CI 0.27 to 0.70; p = 0.0009; I2 = 51.4%, fixed-effects model). There was a statistically non-significant decrease in the risk of reoperation in cardiothoracic heart surgery (three RCTs,60,138,140 n = 1578; OR 0.71, 95% CI 0.43 to 1.19; p = 0.24; I2 = 0%, fixed-effects model), whereas in cardiothoracic lung surgery (two RCTs,125,135 n = 451; OR 1.38, 95% CI 0.47 to 4.04; p = 0.76; no I2, fixed-effects model) and breast surgery (three RCTs,101,107,116 n = 191; OR 1.21, 95% CI 0.51 to 2.90; p = 0.83; I2 = 0%, fixed-effects model) there was a non-significant increase in risk of reoperation for fibrin sealant compared with standard care.
FIGURE 19.
Reoperation in upper GI tract surgery: fibrin sealant vs. standard care.
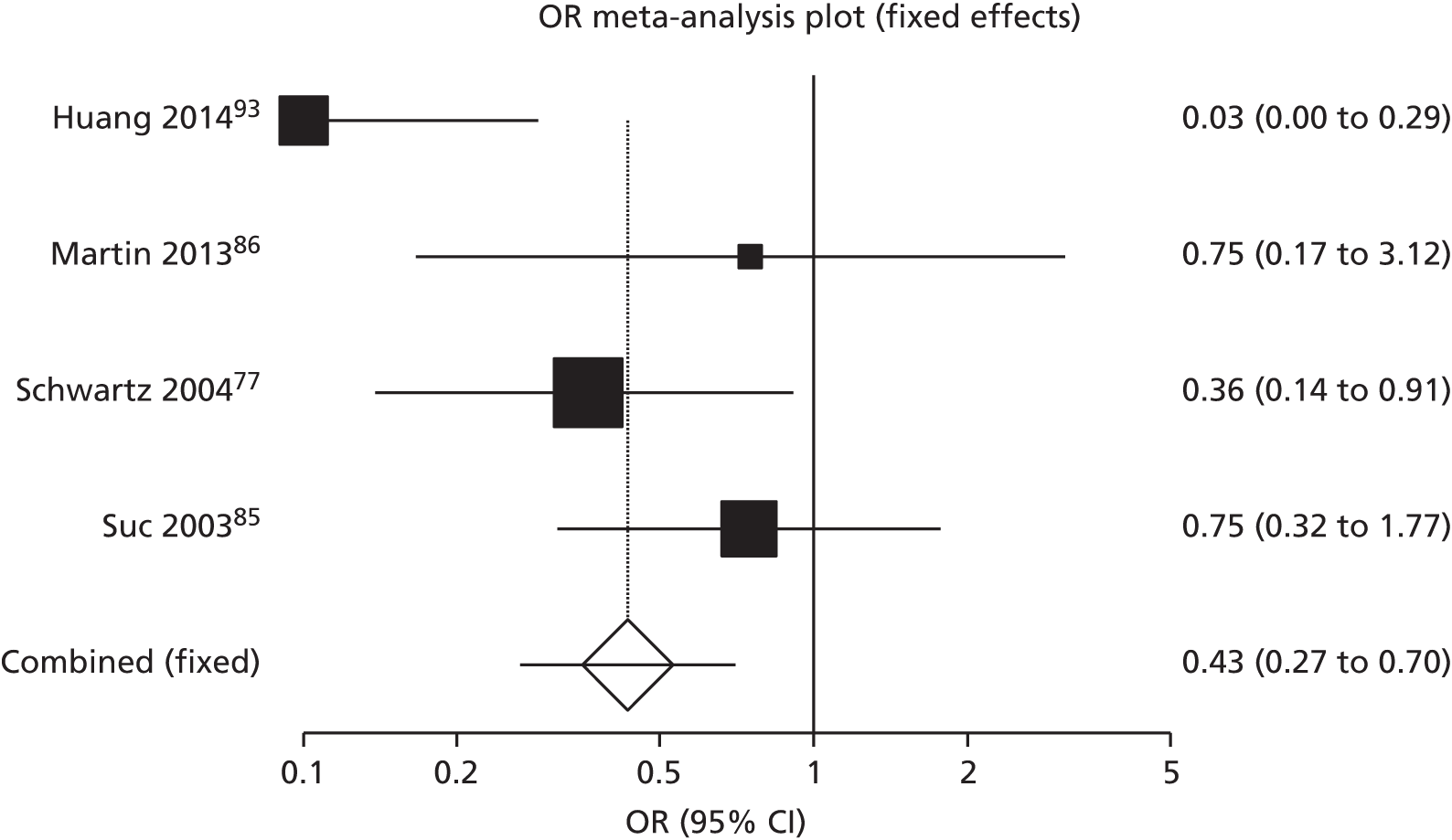
FIGURE 20.
Reoperation in cardiothoracic lung surgery: fibrin sealant vs. standard care.
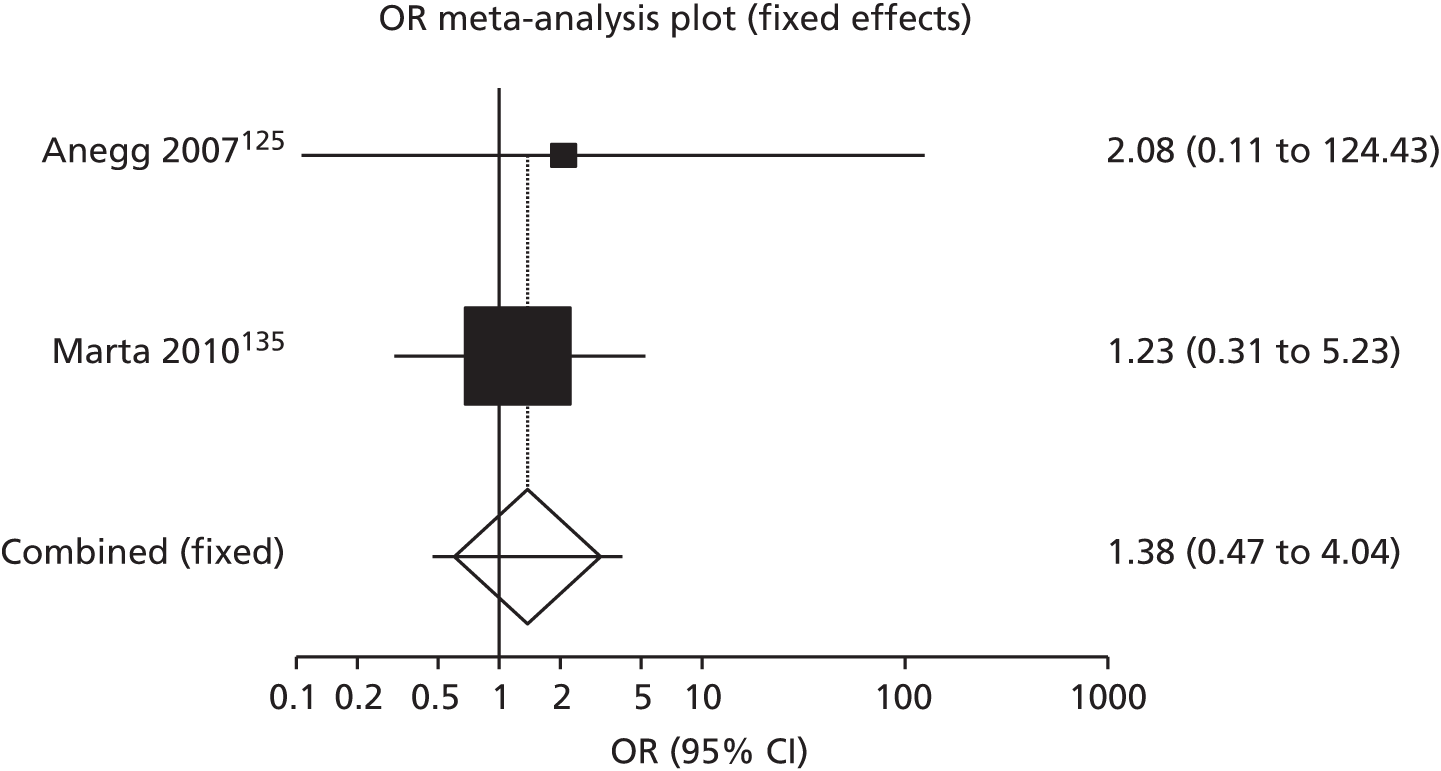
FIGURE 21.
Reoperation in cardiothoracic heart surgery: fibrin sealant vs. standard care.
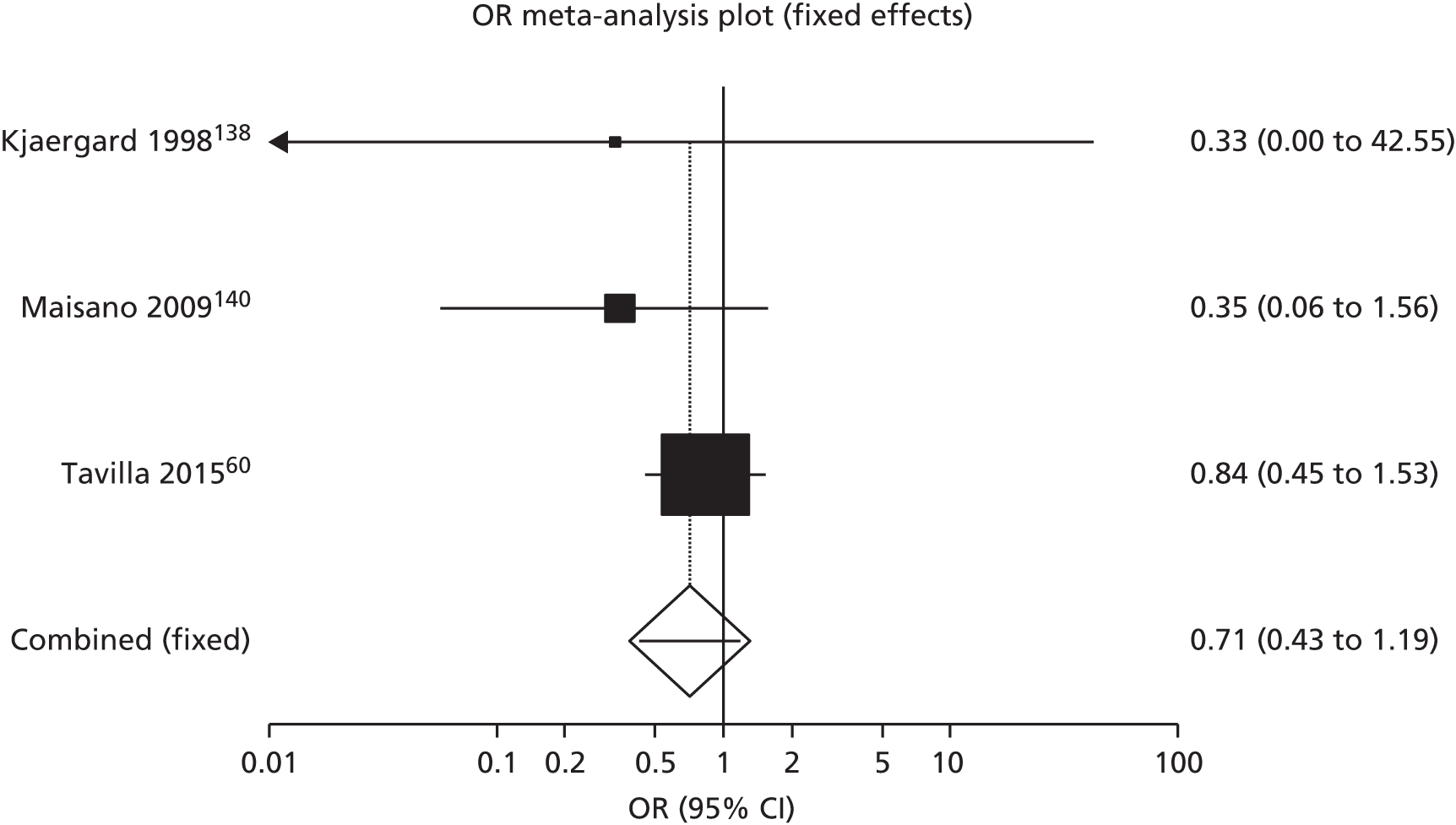
FIGURE 22.
Reoperation in breast surgery: fibrin sealant vs. standard care.
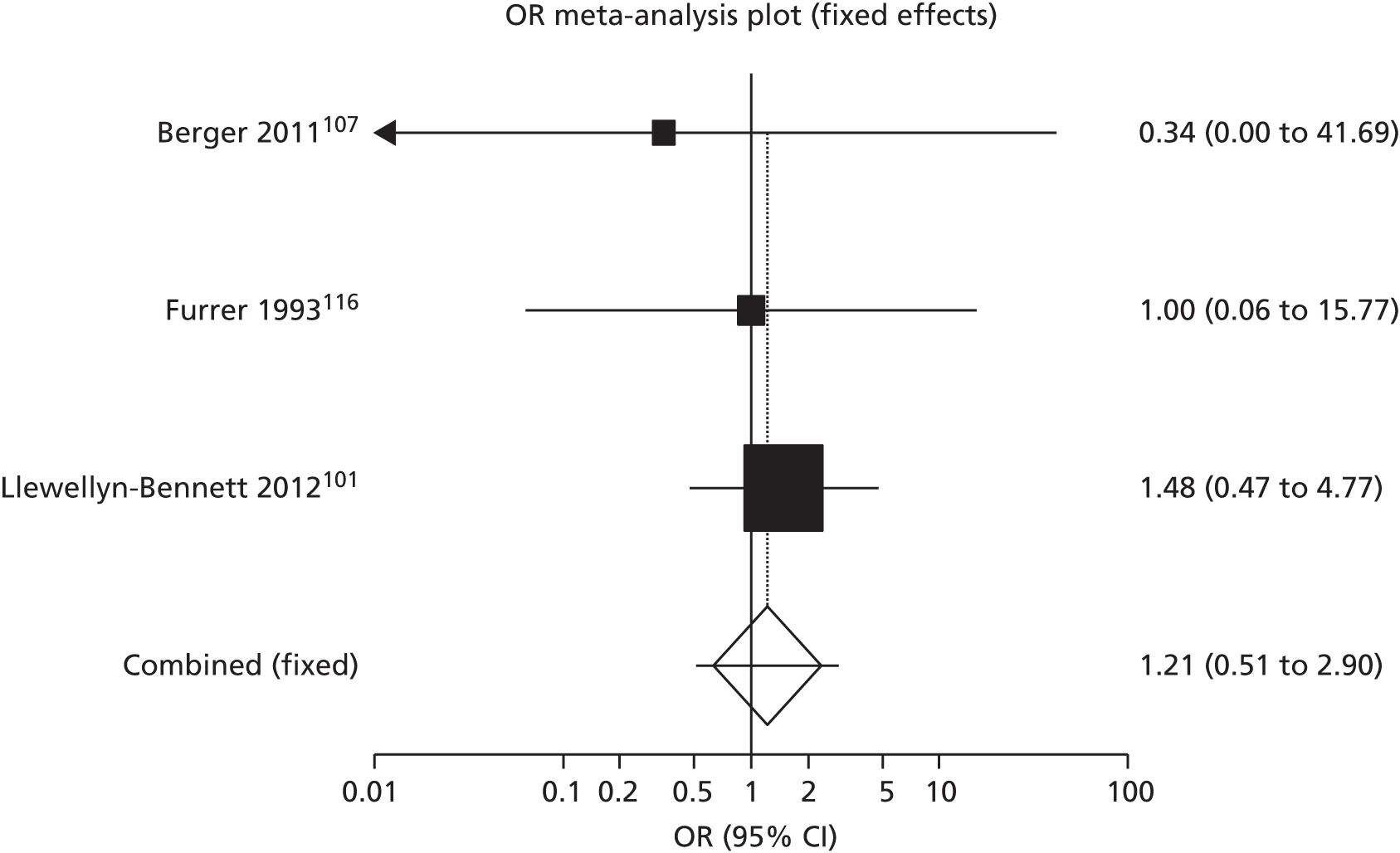
Infection
Wound infections were reported by 30 RCTs, of which 2514,59,60,64,72,73,75,83,84,86,96,99,102,111,118,120,122,130,135,143,170,178,198,230,250 were included in meta-analysis (Figure 23). The RCTs included in the meta-analysis reported fibrin use within four surgical specialties: upper GI tract (eight RCTs),64,72,73,75,83,84,86,250 breast (seven RCTs),96,99,102,111,118,120,122 cardiothoracic lung (two RCTs)130,135 and heart (one RCT),60 orthopaedic knee (two RCTs),14,143 vascular (one RCT),198 eye (one RCT),170 urology (one RCT),59 oral (one RCT)230 and hernia (one RCT). 178 The following five RCTs were excluded because they reported no wound infections in the fibrin sealant and standard care group: Udén et al. ,98 Sabatini et al. ,148 Danielsen et al. ,79 Lovisetto et al. 180 and Lau. 172 Patients receiving fibrin sealants did not have a statistically significant lower risk of wound infection than control patients (25 RCTs, n = 3902, OR 0.76, 95% CI 0.54 to 1.06; p = 0.12; I2 = 0%, fixed-effects model). The random-effects model showed a similar result (see Appendix 8).
FIGURE 23.
Infections in all surgeries: fibrin sealant vs. standard care.
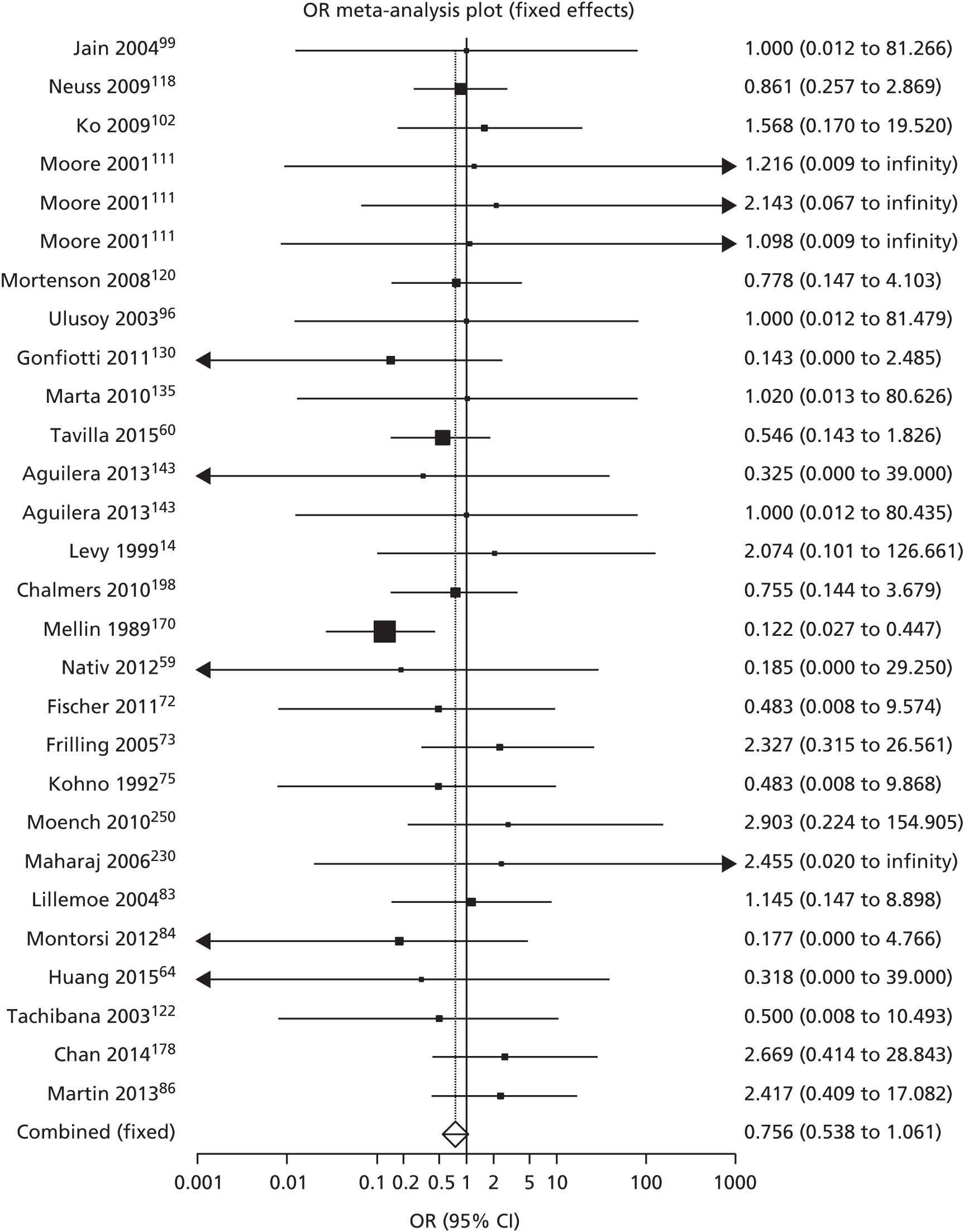
A subgroup analysis was conducted for the following surgical specialties: upper GI tract (Figure 24), breast (Figure 25), cardiothoracic lung (Figure 26) and orthopaedic knee (Figure 27). The risk of wound infection appeared not to be statistically significantly different in upper GI tract surgery (n = 917, OR 1.15, 95% CI 0.59 to 2.27; p = 0.81; I2 = 0%, fixed-effects model), cardiothoracic lung surgery (n = 484, OR 0.34, 95% CI 0.05 to 2.16; p = 0.43; I2 = 0%, fixed-effects model), breast surgery (n = 418, OR 0.95, 95% CI 0.50 to 1.81; p = 0.99; I2 = 0%, fixed-effects model) or orthopaedic surgery (n = 224, OR 1.00, 95% CI 0.22 to 4.51; p = 0.70; I2 = 0%, fixed-effects model).
FIGURE 24.
Infections in upper GI tract surgery: fibrin sealant vs. standard care.

FIGURE 25.
Infections in breast surgery: fibrin sealant vs. standard care.

FIGURE 26.
Infections in cardiothoracic lung surgery: fibrin sealant vs. standard care.
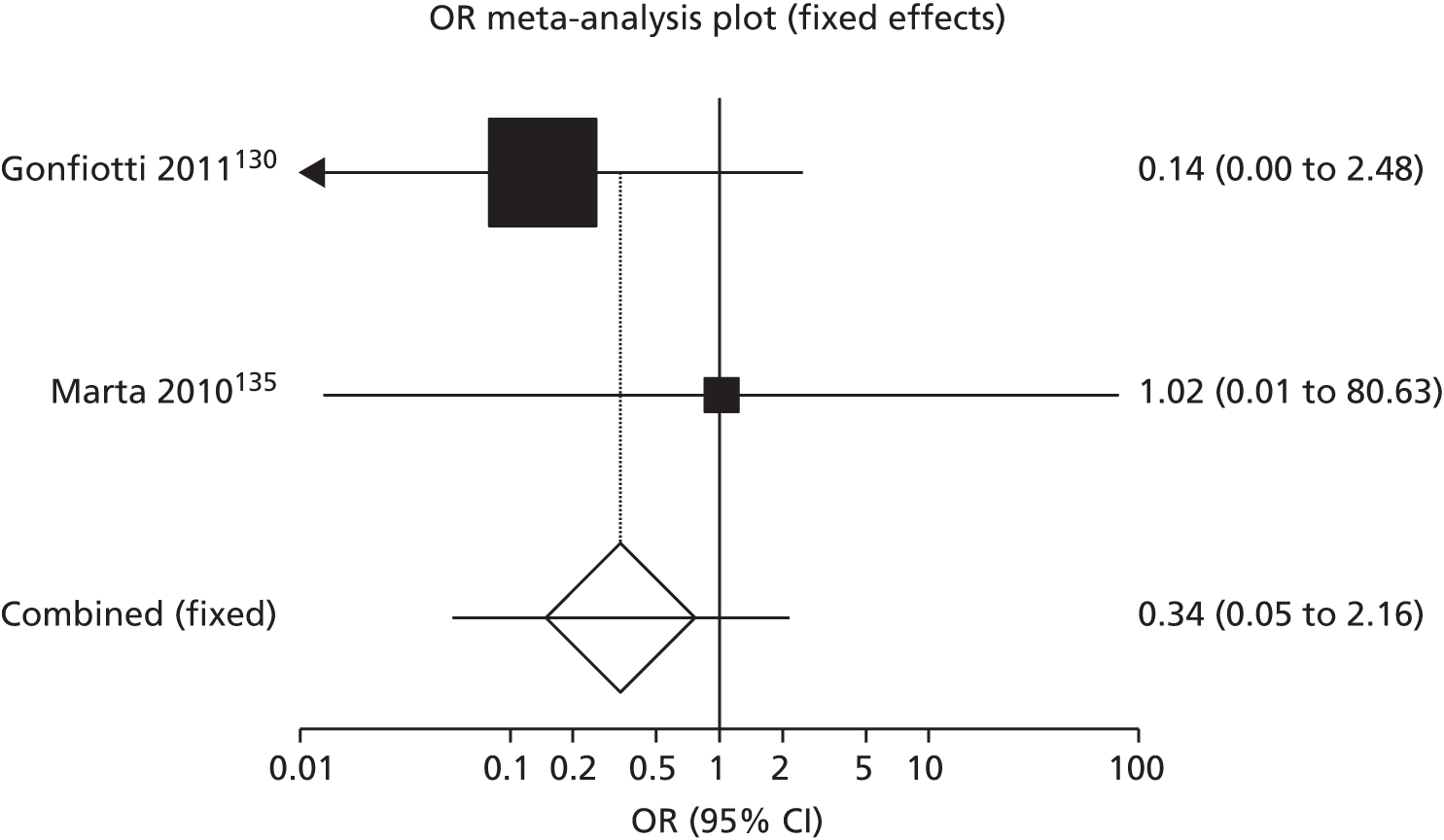
FIGURE 27.
Infections in orthopaedic knee surgery: fibrin sealant vs. standard care.

Use of analgesics
Three RCTs133,217,222 reported on use of analgesics, but the data were too heterogeneously reported for meta-analysis. Belboul et al. 133 (cardiothoracic lung) reported on the number of days of post-operative thoracic epidural analgesia, which was 2 days in the fibrin group and 3 days in the standard care group. Altomare et al. 217 (colorectal) reported that no patients were on analgesics in the fibrin group and almost all patients in the standard care group received analgesics. Cormio et al. 222 (kidney) reported on the number of doses of analgesic required during the first 24 hours post operation, which was 1.2 [standard deviation (SD) 1.69] in the fibrin group and 1.17 (SD 1.56) in the control group.
Complications arising from the use of drains
No RCTs reported on complications arising from the use of drains.
Continuous secondary outcomes
Continuous outcomes were analysed separately for each surgical area for RCTs with similar interventions and comparators as the type of intervention (e.g. staples vs. stitches). The following continuous outcomes are reported below: duration of operation, length of hospital stay, duration of drainage, pain levels and health-related quality of life.
Duration of operation (minutes)
Duration of operation was reported in the following surgical specialties: upper GI tract (gastric and liver), eye and hernia.
Mean duration of operation was reported in five gastric surgery RCTs,62,88–90,92 of which two were included in the meta-analysis88,90 (Figure 28). As operation time was expected to be dictated by the type of surgery and interventions, only Sroka et al. 90 and Musella et al. ,88 who reported on use of fibrin in laparoscopic sleeve gastrectomies, were comparable. Sroka et al. 90 compared sealant application with both sutures and not applying sealant and Musella et al. 88 compared fibrin sealant with no sealant. A non-significantly shorter mean time of –2.03 minutes (95% CI –4.12 to 0.14 minutes; p = 0.07) was found for fibrin sealant versus no sealant (n = 198).
FIGURE 28.
Mean duration of gastric surgery in minutes: fibrin sealant vs. no sealant.
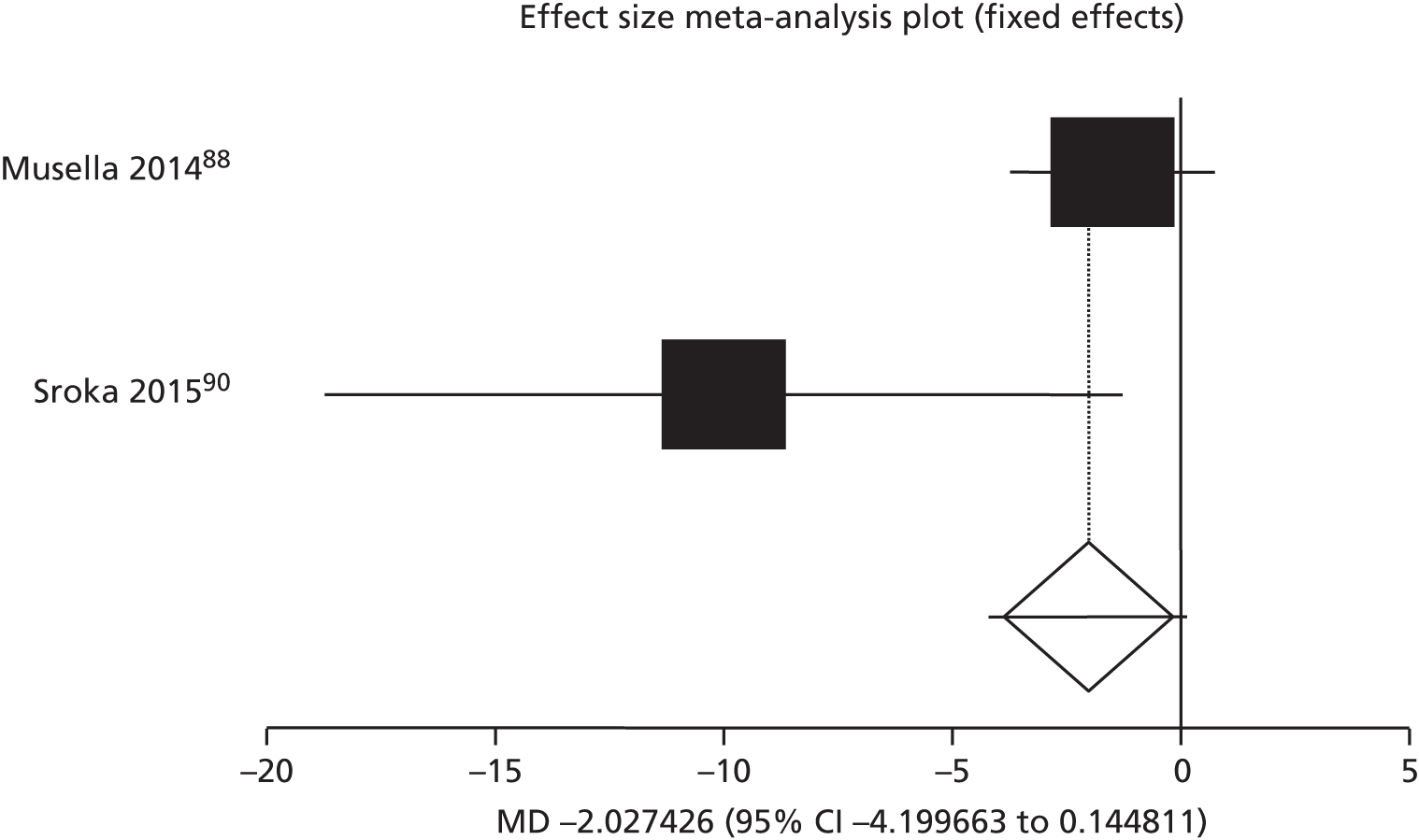
Three RCTs were excluded from the meta-analysis: Pilone et al. 89 compared fibrin sealant with no sealant, Silecchia et al. 62 compared sealant application with sutures and Bulbuller et al. 92 compared sealant application with both sutures and not applying sealant. SDs were reported only by Silecchia et al.,62 who investigated the use of fibrin in laparoscopic gastric bypass and reported no statistically significant difference in operative time. Challenges faced in interpreting these data are that duration of operation was not explicitly defined in the papers and the type of sealant applied may have an effect on the time taken.
Mean duration of surgery was reported by four RCTs68–71 using fibrin in hepatic resection surgery: Liu and Liu69 and Noun et al. 70 seemed comparable as hepatic resection was carried out without liver mobilisation (Figure 29). Without liver mobilisation, the MD of the duration of surgery for fibrin sealant compared with standard care is a decrease of 14 minutes (two RCTs,69,70 n = 117, 95% CI –54.2 to 24.3 minutes; p = 0.46), but this is not statistically significant.
FIGURE 29.
Mean duration of hepatic resection without liver mobilisation in minutes: fibrin sealant vs. standard care.

In Figueras et al. ,71 liver mobilisation was carried out in both intervention and comparator groups. Uetsuji et al. 68 had three groups: (1) liver mobilisation and no sealant, (2) liver mobilisation with sealant and (3) no liver mobilisation or sealant. Figueras et al. 71 and the ‘liver mobilisation’ groups were combined in a separate meta-analysis. In liver with mobilisation, the MD increased by 19.07 minutes (two RCTs,68,71 n = 364, 95% CI 2.75 to 35.38 minutes; p = 0.02) for fibrin sealant compared with standard care (Figure 30). This result indicates a statistically significant increase in surgery time associated with the use of fibrin sealants compared with standard care in hepatic resection with liver mobilisation.
FIGURE 30.
Mean duration of hepatic resection with liver mobilisation in minutes: fibrin sealant vs. standard care.

Duration of surgery was reported in 12 RCTs157–163,165,166,168,169,171 that all compared fibrin sealant with sutures and eight RCTs were included in the meta-analysis (Figure 31). Three RCTs159,160,169 did not report variability around the means and, thus, were excluded from the analysis.
FIGURE 31.
Duration of eye surgery in minutes: fibrin sealant vs. sutures.
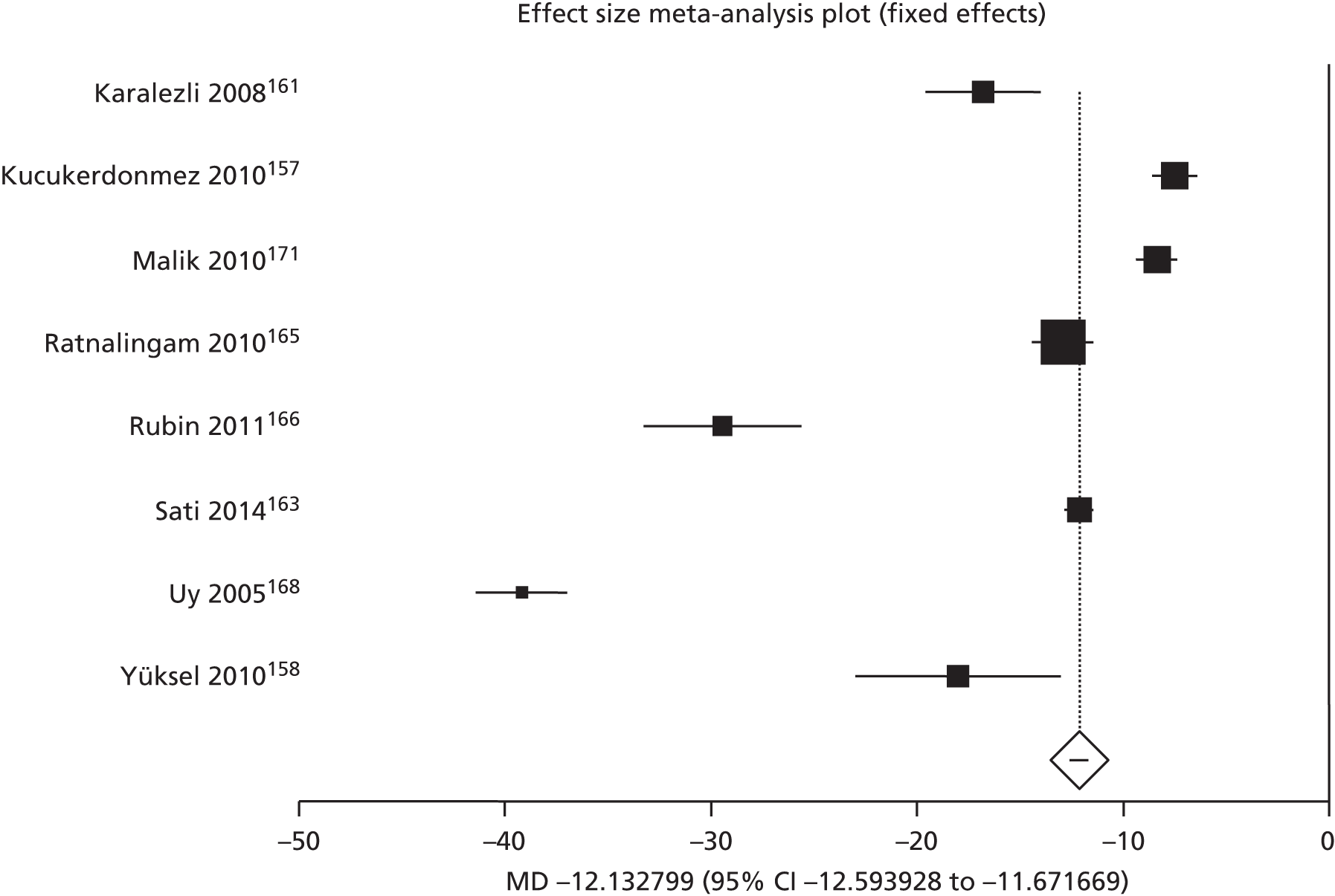
The mean duration was statistically significant shorter in the fibrin group than the sutures group, with a MD of –12.13 minutes (95% CI –12.59 to –11.67 minutes; p < 0.01; I2 = 99.1%, fixed-effects model, eight RCTs,157,158,161,163,165,166,168,171 n = 519). The high level of heterogeneity was explored by sequentially excluding individual RCTs to identify if the potential cause of the heterogeneity was caused by any individual RCT. This was found not to be the case as I2 always remained > 90%. The random-effects model showed a MD of –17.19 minutes (95% CI –23.35 to –12.50 minutes; p < 0.0001; I2 = 99.1%, see Appendix 8). Furthermore, the RCTs excluded from the meta-analysis also reported a shorter mean duration of surgery in the fibrin group than the sutures group: Hall et al. 160 (12.04 vs. 26.04 minutes, respectively), Bahar et al. 159 (16 vs. 20 minutes, respectively) and Bahar et al. 169 (16 vs. 28 minutes, respectively).
Five RCTs175,176,178,180,184 reported mean duration of surgery, of which four176,178,180,184 reported means and SDs and were included in two separate meta-analyses. Campanelli et al. 176 and Damiano et al. 184 compared fibrin sealant with sutures (Figure 32). Surgery time was statistically significantly shorter for fibrin sealant than sutures in the meta-analysis (n = 784), with a MD of –2.56 minutes (95% CI –3.57 to –1.56 minutes; p < 0.01). Lovisetto et al. 180 and Chan et al. 178 compared fibrin with staples (Figure 33). Surgery time was statistically significantly longer with fibrin than with staples (n = 326), with a MD in surgery time of 13.22 minutes (95% CI 11.59 to 15.26 minutes; p < 0.01). The excluded RCT175 reported on a using self-gripping mesh instead of fibrin and, therefore, could not be compared with either intervention.
FIGURE 32.
Duration of hernia surgery in minutes: fibrin sealant vs. sutures.
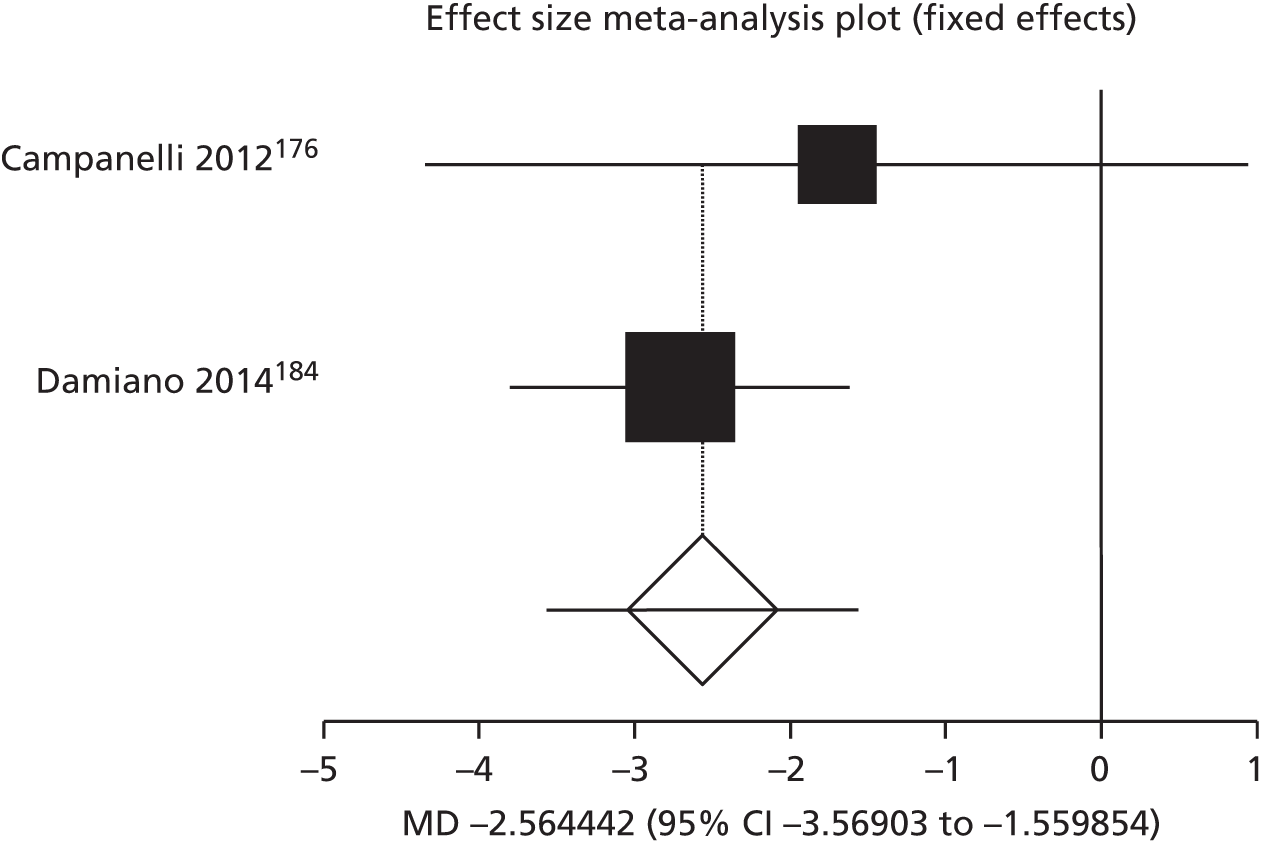
FIGURE 33.
Duration of hernia surgery in minutes: fibrin sealant vs. staples.

Length of hospital stay (days)
Length of hospital stay was reported in the following surgical specialties: upper GI tract (pancreas, gastric and bowel), cardiothoracic (lung and heart), breast and joint (knee).
Three RCTs81,83,86 reported mean length of hospital stay for pancreatic surgery when using fibrin sealant and two83,86 were included in the meta-analysis (Figure 34). The study by Carter et al. 81 was excluded because the authors did not report variability around the mean. Fibrin sealants statistically significantly decreased hospital stay for fibrin sealant compared with standard care in a meta-analysis (n = 181), with a MD of –1.40 days (95% CI –1.72 to –1.09 days; p < 0.01). Carter et al. 81 reported that mean hospital stay was shorter in the fibrin sealant group (6.4 days) than in the control group (7.3 days), which is consistent with the results of the meta-analysis.
FIGURE 34.
Length of hospital stay in days in pancreatic surgery: fibrin sealant vs. standard care.
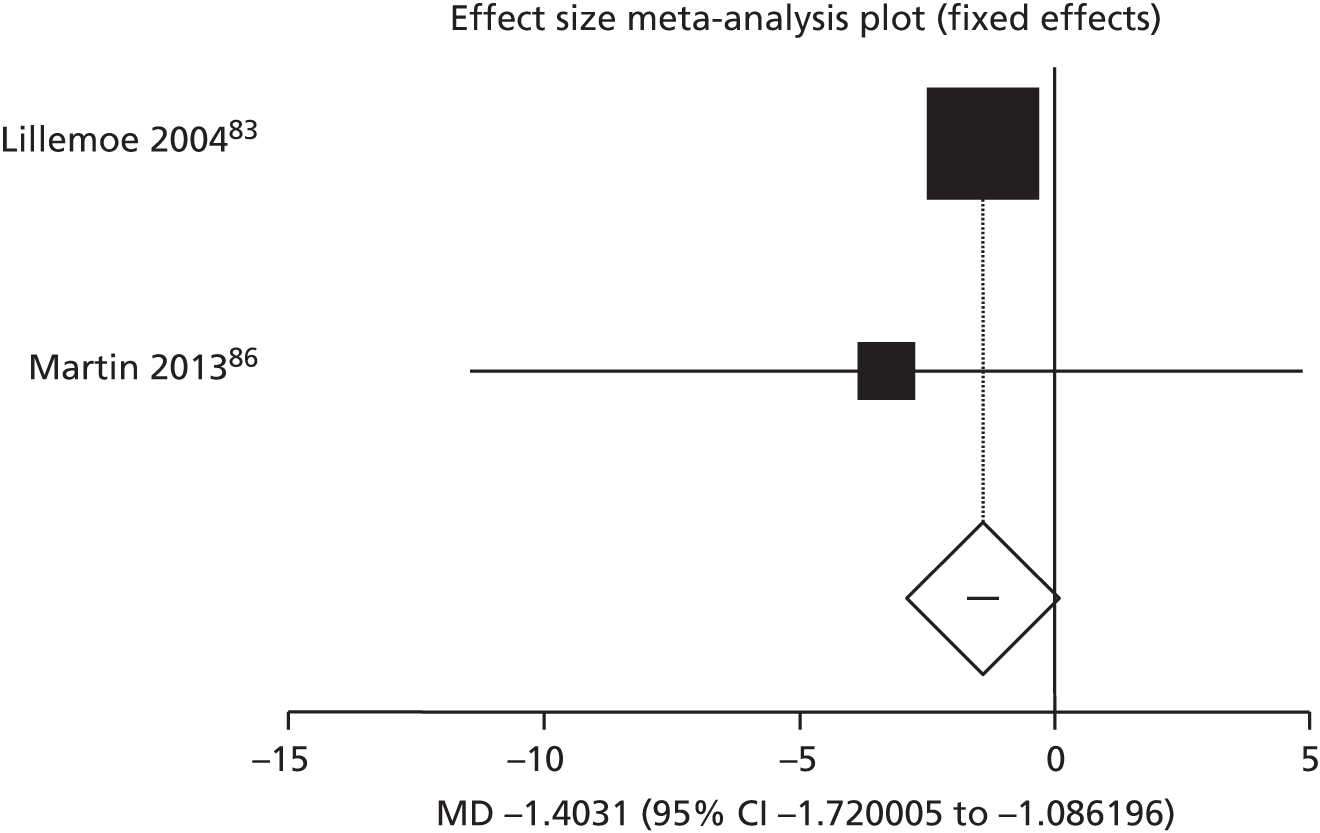
Three RCTs62,88,89 reported mean length of hospital stay: two for surgery around the gastric region88,89 and one for stay after bowel surgery,62 utilising fibrin sealant. The three RCTs were considered sufficiently similar to be analysed together; however, Pilone et al. 89 did not report variability around the mean and was therefore excluded. Silecchia et al. 62 and Musella et al. 88 were combined in meta-analysis (Figure 35). There was not a statistically significant increase in hospital stay for fibrin sealant compared with standard care in the meta-analysis (n = 420), which had a MD of 0.04 days (95% CI –0.34 to 0.42 days; p = 0.82). Pilone et al. 89 reported a mean hospital stay of 6.5 days and 7 days for the fibrin sealant and control groups, respectively.
FIGURE 35.
Length of hospital stay in days in pancreatic surgery: fibrin sealant vs. standard care.

Six RCTs124,125,127,128,130,136 reported mean hospital stay for lung surgery and were considered similar enough to be included in a meta-analysis. However, only three RCTs127,130,136 reported variability around the mean and were analysed (Figure 36). Mean length of hospital stay was statistically significantly reduced for fibrin sealant compared with standard care in the meta-analysis (n = 269), with a MD of –1.37 days (95% CI –1.93 to –0.81 days; p < 0.01; I2 = 91.9%). However, there is a high level of heterogeneity between the RCTs, and the significant result becomes non-significant in a random-effects meta-analysis (MD –1.20 days, 95% CI –3.22 to 0.81 days; p = 0.24). The studies excluded from the meta-analysis reported a lower mean hospital stay for the fibrin group than the control group: Fabian et al. 128 reported 4.6 versus 4.9 days, respectively; Droghetti et al. 124 reported 11 versus 14.3 days, respectively; and Anegg et al. 125 reported 6.2 versus 7.7 days, respectively.
FIGURE 36.
Length of hospital stay in days in cardiothoracic lung surgery: fibrin sealant vs. standard care.

Tavilla et al. 60 (n = 1436) reported a mean length of hospital stay of 5.99 days (SD 3.95 days) and 6.07 days (SD 4.21 days) between fibrin and control groups, respectively, and p-value of 0.71 indicating no statistically significant difference.
Ten RCTs reported mean hospital stay following breast surgery using fibrin sealants, of which eight104,106–109,112,115,116 were included in the meta-analysis (Figure 37). Two RCTs were excluded for the following reasons: Udén et al. 98 did not report variability around the mean and Jain et al. 99 did not report mean duration separately for two of the groups. Mean length of hospital stay was statistically significantly reduced in the meta-analysis (n = 440), with a MD of –0.73 days (95% CI –0.95 to –0.50 days; p < 0.01; I2 = 88.7%). The high level of heterogeneity was explored by sequentially excluding individual RCTs to identify if the potential cause of the heterogeneity was caused by any individual RCT. This was found not to be the case as I2 always remained > 80%. However, the statistically significant result became non-significant in a random-effects meta-analysis (MD –0.87 days, 95% CI –1.75 to 0.01 days; p = 0.05).
FIGURE 37.
Length of hospital stay in days in breast surgery: fibrin sealant vs. standard care.
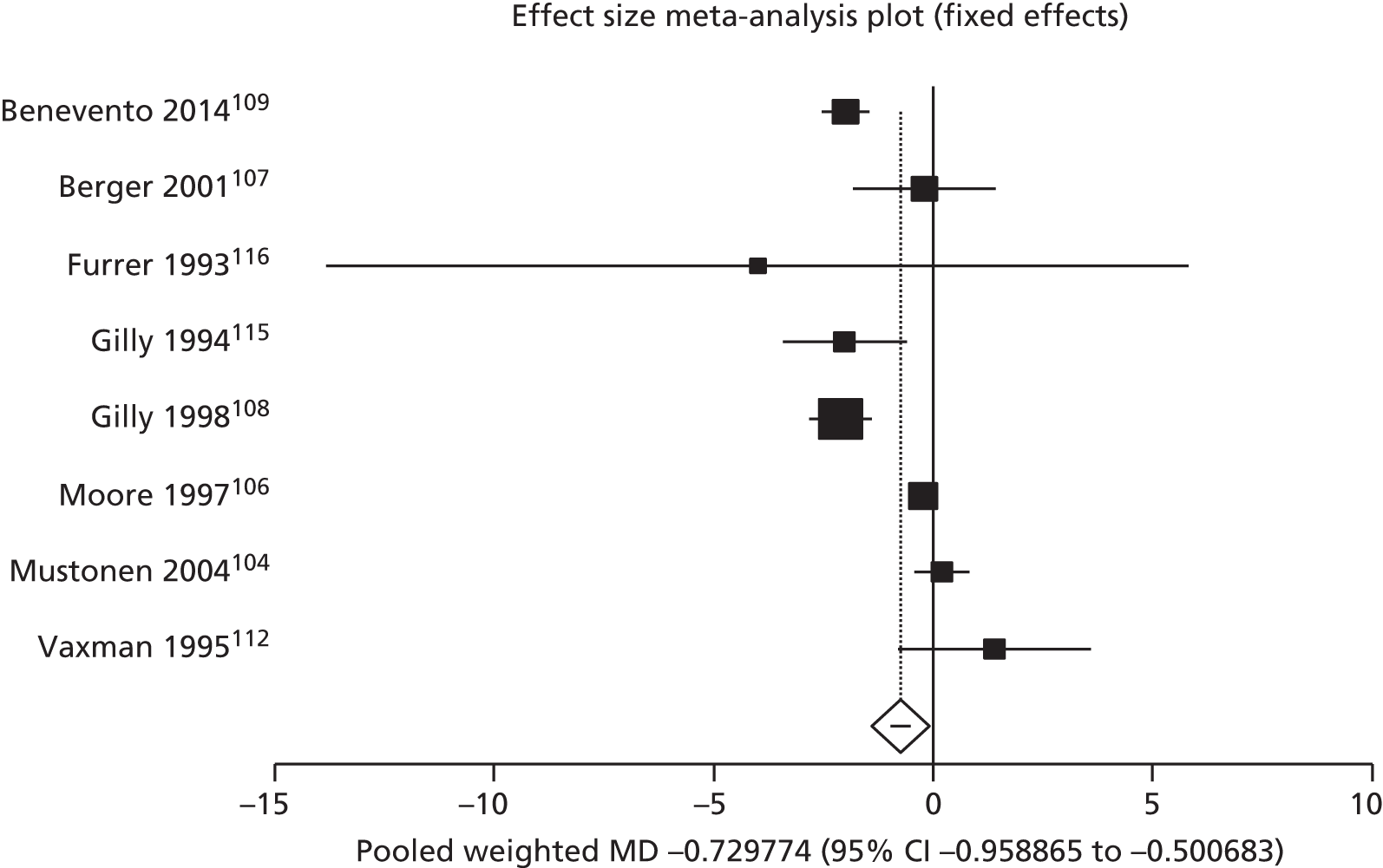
Four RCTs reported mean hospital stay following knee surgery using fibrin sealants, of which three143,145,149 were included in the meta-analysis (Figure 38). Molloy et al. 147 was excluded from the meta-analysis because they did not report variability around the mean. There was no significant effect on the mean duration of hospitalisation for knee surgery for fibrin sealant compared with standard care in the meta-analysis (n = 251), giving a MD of 0.07 days (95% CI –0.74 to 0.88 days; p = 0.87; I2 = 0%, fixed-effects model).
FIGURE 38.
Length of hospital stay in days for knee surgery: fibrin sealant vs. standard care.

Duration of drainage was reported in the following surgical specialties: breast and axillary lymph nodes, liver and lung surgery.
A total of 15 RCTs reported mean duration of drainage, of which 1396,102,104–107,109,110,112,115–117,251 were included in the meta-analysis (Figure 39). Two RCTs did not report variability around the means97,123 and were excluded from the meta-analysis. In the meta-analysis (n = 953), there was a statistically significantly lower mean number of days of drainage of –0.50 days (95% CI –0.68 to –0.33 days; p < 0.01; I2 = 90.6%, fixed-effects model) when fibrin sealant was used than standard care. The high level of heterogeneity was explored by sequentially excluding individual RCTs to identify if the potential cause of the heterogeneity was caused by any individual RCT. This was found not to be the case as I2 always remained > 90%. However, the random-effects model showed an increased MD of –1.06 days (95% CI –1.69 to –0.42 days; p = 0.01; see Appendix 8).
FIGURE 39.
Duration of drainage in days in breast and axillary lymph nodes surgery: fibrin sealant vs. standard care.

Mean duration of drainage after liver surgery was reported by four RCTs65,69,74,75 and combined in a meta-analysis (Figure 40). In the meta-analysis (n = 202) there was a not a statistically significant difference in the number of drainage days for fibrin sealant compared with standard care, with a MD of –0.27 days (95% CI –0.82 to 0.27 days; p = 0.33; I2 = 0%, fixed-effects model).
FIGURE 40.
Duration of drainage in days for liver surgery: fibrin sealant vs. standard care.
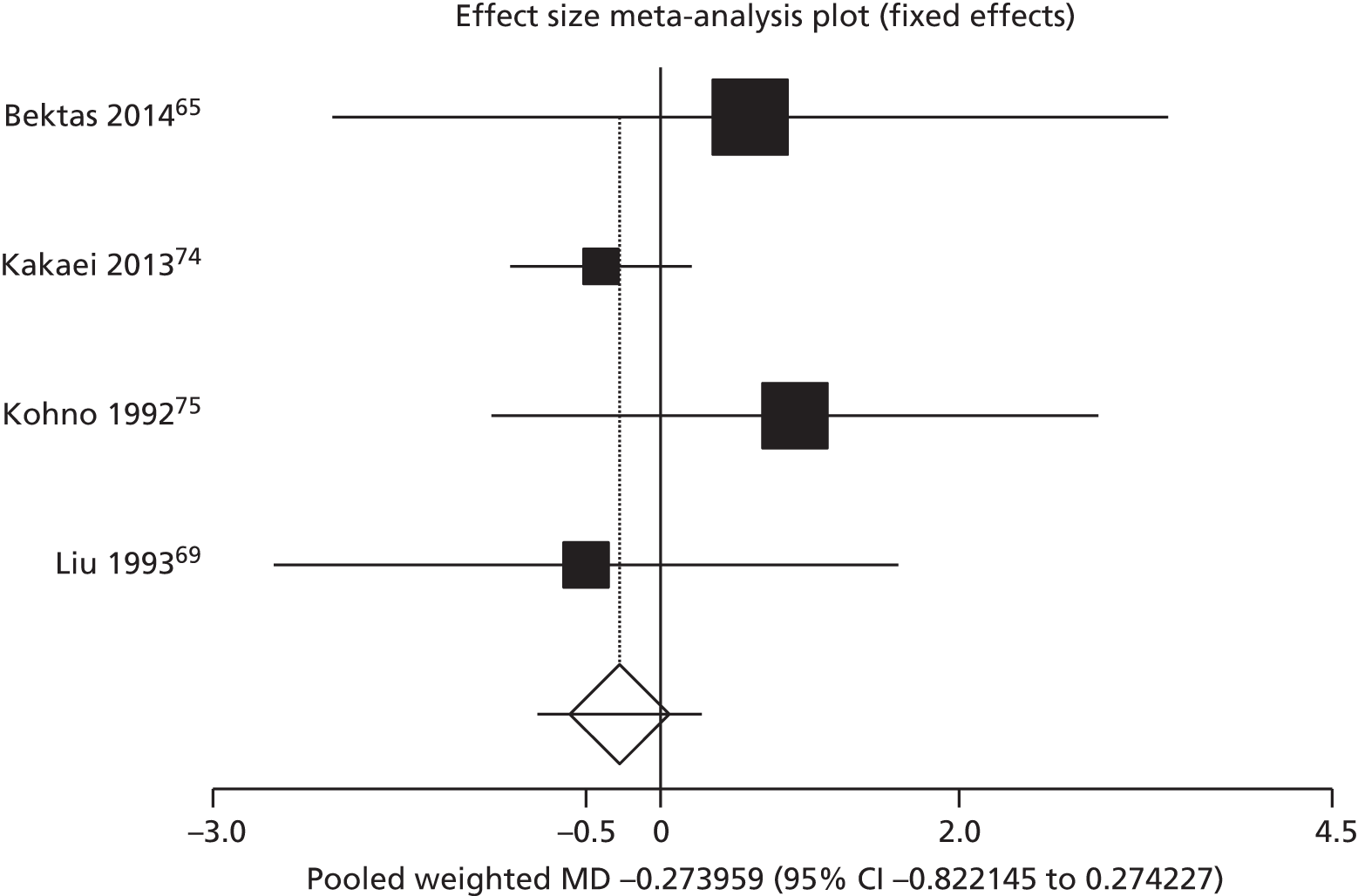
Mean duration of drainage after lung surgery was reported by five RCTs126,127,130,136,137 that were combined in a meta-analysis (Figure 41). In the meta-analysis (n = 399) there was a statistically significant lower number of drainage days for fibrin sealant than standard care, with a MD of –0.46 days (95% CI –0.53 to –0.39 days; p < 0.01; I2 = 91%, fixed-effects model). The high level of heterogeneity was explored by sequentially excluding individual RCTs to identify if the potential cause of the heterogeneity was caused by any individual RCT. This was found not to be the case as I2 always remained > 80%. The random-effects model also showed a statistically significant MD of –2.10 days (95% CI –3.65 to –0.56 days; p = 0.01; see Appendix 8).
FIGURE 41.
Duration of drainage in days for lung surgery: fibrin sealant vs. standard care.
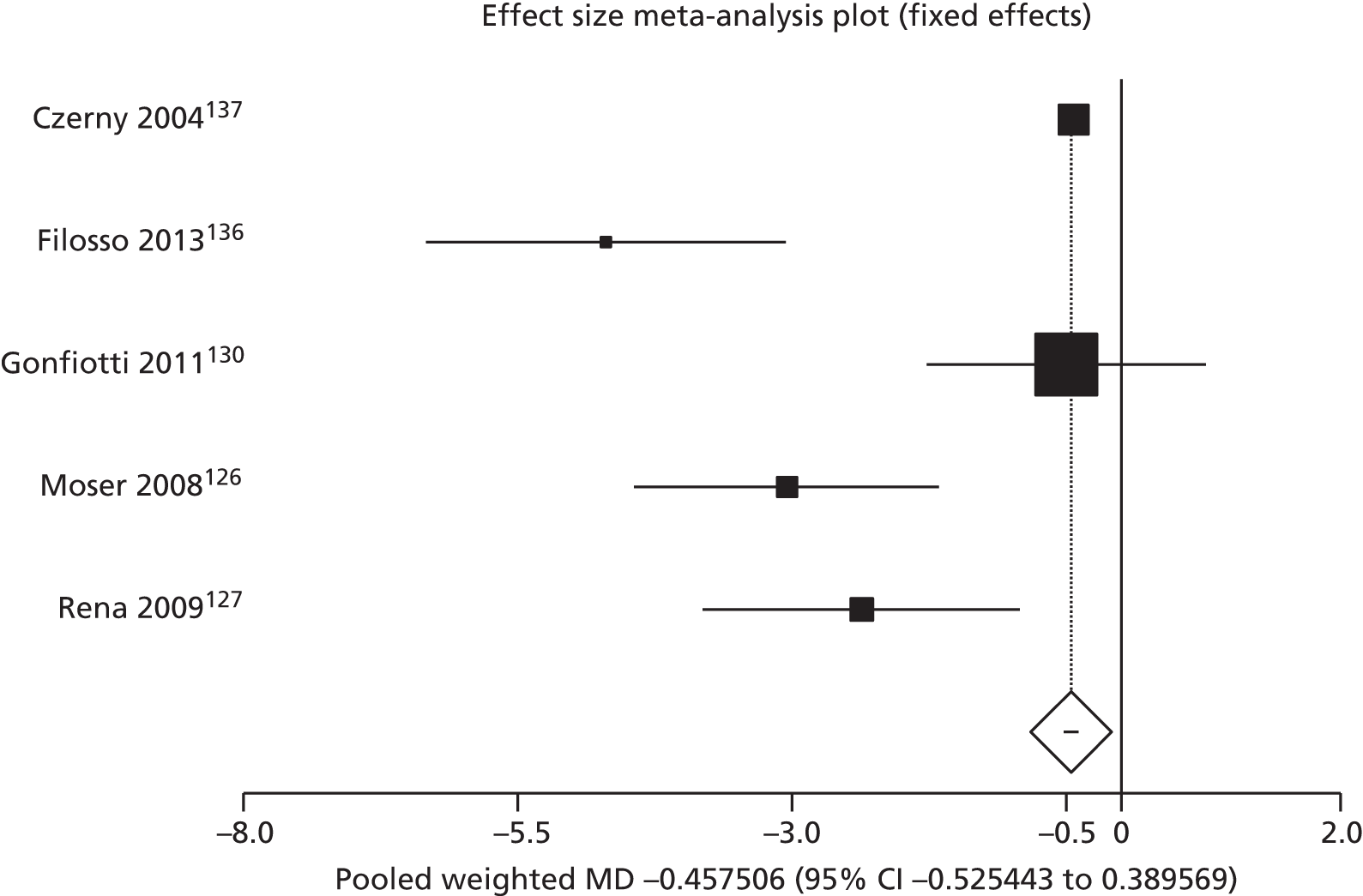
Pain levels
Pain was reported by 20 RCTs in six surgical specialties: breast,95,99,101 joint,142,147,150 ENT,187,190,192 plastic and reconstructive,209,211 eye157,159,161,165,166,168,169,171 and urology. 222 The large differences in the different scales used, time points at which assessments took place and lack of variability data did not permit a meta-analysis. When RCTs measured pain at different time intervals, pain is reported for the first mentioned measurement point after surgery (Table 21).
| Study (author, year) | Fibrin sealant and standard care group description | Number of patients | Pain score and variability description | Pain score | Variability around score |
|---|---|---|---|---|---|
| Breast | |||||
| Jain et al., 200499 | Fibrin sealant (Tisseel), no drain | 29 | Mean post-operative pain at 24 hours (not reported separately for Tisseel, no drain and no glue, no drain groups) | 3.2 | SD 0.9 |
| No glue, no drain | 29 | 3.2 | SD 0.9 | ||
| No glue, drain | 58 | 4.5 | SD 1.5 | ||
| Llewellyn-Bennett et al., 2012101 | Fibrin sealant (Tisseel) | 48 | Donor-site pain visual analogue scale score over 15 days | 27 | Range: 0–89 |
| Standard closure | 53 | 34 | Range: 7–79 | ||
| Zhibo and Miaobo, 200995 | Fibrin sealant and lidocaine | 10 | Post-operative pain during first week post operation (day 1); self-reported pain recorded on a scale of 0–3, where 0 = no pain, 1 = light pain, 3 = worst pain | 1 | NR |
| Standard care (lidocaine only) | 10 | 9 | NR | ||
| Fibrin sealant only | 10 | 10 | NR | ||
| Joint (knee) | |||||
| Skovgaard et al., 2013150 | Fibrin sealant (EVICEL), spray | 24 | Visual analogue scale score for rest and flexion at day 1 post surgery | Rest: 22; flexion: 45 | Rest: range 8.5–58; flexion: range 22–71 |
| Standard care (saline) | 24 | Rest: 26; flexion: 44 | Rest: range 12–51; flexion: range 29–67 | ||
| Molloy et al., 2007147 | Fibrin sealant (Quixil) | 50 | Pain scores at 6 hours using a 100-mm visual analogue scale, in which 0 represented no pain and 100 the most severe pain | 17.6 | 15.9 |
| Tranexamic acid | 50 | 19.4 | 17.9 | ||
| Standard care | 50 | 20.03 | 20.4 | ||
| Heyse et al., 2014142 | Fibrin sealant spray | 98 | Pain (on visual analogue scale) at 6 weeks | 4.3 | NR |
| Standard care | 100 | 3.9 | NR | ||
| ENT (nose) | |||||
| Vaiman et al., 2006192 | Fibrin sealant (Quixil) | 40 | Visual analogue scale pain scores at peak for saliva swallow, normal swallow, drinking and dysphagia severity score | Approximately 6.5–7.0 | NR |
| Standard care (electrocautery) | 40 | Approximately 6.8–7.6 | NR | ||
| Prado et al., 2006187 | Fibrin sealant (Beriplast) | 11 | Pain (10-cm visual analogue scale) | 4 | 25% quartile: 3; 75% quartile: 4 |
| Standard care | 11 | 4 | 25% quartile: 3; 75% quartile: 5 | ||
| Yu et al., 2014190 | Fibrin sealant spray | 41 | Pain during packing; pain on removal of packing | 4.2; 4.5 | 1.4; 1.0 |
| Standard care (sponge packing) | Within patienta | 3.1; 8.3 | 0.9; 1.1 | ||
| Plastic and reconstructive | |||||
| Danielsen et al., 2008209 | Fibrin sealant (Vivolution) | 20/19 | Pain score on day 5 post surgery | 3 | Range: 2.0–5.0 |
| Standard care (gauze and pressure) | 20 | 4 | Range: 3.0–5.0 | ||
| Healy et al., 2013211 | Fibrin sealant (Tisseel) | 20 | Mean daily pain score at 14 days post surgery | 0.42 | 95% CI 0.19 to 0.65 |
| Mefix self-adhesive fabric dressing | 20 | 1.6 | 95% CI 1.11 to 2.08 | ||
| Eye | |||||
| Rubin et al., 2011166 | Fibrin sealant | 21 | Overall mean post-operative pain as recorded on visual analogue scale | 5.1 | SD 1.26 |
| Standard care (sutures) | 26 | 4.77 | SD 1.21 | ||
| Uy et al., 2005168 | Fibrin sealant (Beriplast) | 11 | Pain on day 1; using a five-point scale adapted from Lim-Bon-Siong et al.:252 0 = none, no pain; 1 = very mild, presence of pain but easily tolerated; 2 = mild, pain causing some discomfort; 3 = moderate, pain that partially interferes with usual activity or sleep; 4 = severe, pain that completely interferes with usual activity or sleepb | ≈2.2 | NR |
| Standard care (sutures) | 11 | ≈3.1 | NR | ||
| Bahar et al., 2007169 | Fibrin sealant (Quixil) | 42 | Mean pain score on day 1 post surgery; grading symptoms and signs on a scale of 0–4a | ≈37 | NR |
| Standard care (sutures) | 39 | ≈66 | NR | ||
| Malik and Kumar, 2010171 | Fibrin sealant (Tisseel duo-quick) | 25 | Pain score, based on Wong Baker FACES® Pain Rating Scale253 | 0.44 | SD 0.583 |
| Standard care (sutures) | 25 | 3.32 | SD 0.802 | ||
| Kucukerdonmez et al., 2010157 | Fibrin sealant | 32 | Five-point scale assessment of degree of paina | ≈2.4 | ≈1 |
| Standard care (Vicryl sutures) | 38 | ≈3.6 | ≈1 | ||
| Bahar et al., 2006159 | Fibrin sealant (Quixil) | 39 | Mean pain score on day 2 post surgery; grading symptoms and signs on a scale of 0–4a | ≈48 | NR |
| Standard care (sutures) | 26 | ≈22 | NR | ||
| Karalezli et al., 2008161 | Fibrin sealant (Tisseel) | 25 | Pain on day 1 post surgery using a five-point scale, adapted from Lim-Bon-Siong et al.252: 0 = none, no pain; 1 = very mild, presence of pain but easily tolerated; 2 = mild, pain causing some discomfort; 3 = moderate, pain that partially interferes with usual activity or sleep; 4 = severe, pain that completely interferes with usual activity or sleepb | ≈2.5 | NR |
| Standard care (sutures) | 25 | ≈3.1 | NR | ||
| Ratnalingam et al., 2010165 | Fibrin sealant | 68 | Median pain score day 1 post surgery | 1 | NR |
| Standard care (sutures) | 69 | 2 | NR | ||
| Urology | |||||
| Cormio et al., 2012222 | Fibrin sealant (TachoSil patch) | 49 | Visual analogue scale pain score at day 1 post operation | 4.24 | SD 2.32 |
| Standard care (nephrostomy tube) | 47 | 4.77 | SD 2.28 | ||
No data on pain assessments could be reported for five RCTs for the following reasons: Antuña et al. 155 reported values only for the entire group; Mabrouk et al. 214 reported only that ‘all of the patients suffered from pain, ecchymosis, and oedema postoperatively, but to varying degrees’; Diamond et al. 232 reported only that ‘the most common adverse event reported was abdominal pain’; Hall et al. 160 did not report values; and Pryor et al. 186 reported only ‘no significance difference for overall rate of pain or recovery (p = 0.06)’. Furthermore, eight RCTs78,107,108,151,153,221,239,250 only reported the number of patients with pain.
Health-related quality of life
No RCTs reported on health-related quality of life.
Assessment of harms
Randomised controlled trials
Ten RCTs in various surgical specialties (liver, two RCTs;73,77 kidney, two RCTs;59,221 mixed, one RCT;241 oral and maxillofacial, one RCT;231 hernia, one RCT;176 plastic and reconstructive, one RCT;208 vascular, one RCT;204 and orthopaedic, one RCT143) reported adverse events that were thought to be related to the use of fibrin sealants (Table 22). Sample sizes varied from 759 to 316176 participants. Only Fischer et al. 241 reported a death as possibly related to fibrin sealant application in upper GI tract surgery caused by a large bleed, but bleeding did not occur at the target bleeding site and no further information was provided. Other RCTs reported on various non-severe adverse events: mild cellulitis and mild seroma,231 anaemia,73 extravasation of urine,221 incision site complications204 and mild generalised skin rash. 143 Severity was unclear for the following: excessive pain, scar pain and testicular pain hydrocele in Campanelli et al. ,176 post-procedural haemorrhage in Nativ et al. 59 and antibodies to hepatitis B in Schwartz et al. 77 It was not reported how adverse events were related to the application of fibrin sealant or how severity was determined. The time when adverse events occurred after surgery was immediately in Aguilera et al. ,143 2 hours later in Nativ et al. ,59 1 and 14 days later in Hester et al. 231 and 32 days later in Saha et al. ,204 but was not reported in Fischer et al. ,241 Campanelli et al. ,176 Schwartz et al. ,77 Frilling et al. 73 and Siemer et al. 221 Furthermore, another 21 RCTs explicitly reported that there were no complications or adverse events related to fibrin. 14,62,65,67,88,94,124–127,141,142,193–195,206,207,225,227,232,238
| Study (author, year) | Sample size | Surgery | Adverse event |
|---|---|---|---|
| Fischer et al., 2013241 | 90/141 | Mixed | Of the patients who received fibrin pads, 2.7% (3/11) experienced a related or possibly related AE, compared with 6.7% (2/30) of patients who received absorbable haemostat. These events include operative haemorrhage, ascites and suspected pulmonary embolism. There was no confirmation to rule out relatedness, therefore these AEs were attributed as related to the assigned treatment Seven serious AEs resulted in death: six (5.4%) in the fibrin group and one (3.3%) in the absorbable haemostat group. One of the deaths in the fibrin pad group was considered possibly related to treatment (massive intraluminal GI bleed, although bleeding did not occur at the target bleeding site) |
| Hester et al., 2013231 | 75 | Oral and maxillofacial | Two of the non-SAE were considered related to treatment: 1 patient had mild cellulitis on the side of the face treated with FS VH S/D 4 s-apr (14 days postoperatively), and 1 patient had mild seroma on postoperative day 1 |
| Campanelli et al., 2012176 | 316 | Hernia | Adverse events were attributed to study product in three patients in the fibrin sealant group (1.9%: one excessive pain; one scar pain; one testicular pain hydrocele) |
| Schwartz et al., 200477 | 207 | Liver | One patient developed antibodies to hepatitis B after being treated with Crosseal. The patient had also received 16 units of allogeneic blood and, in view of the recognised effectiveness against hepatitis B virus of the viral inactivation techniques used in the manufacture of Crosseal, this event was considered unlikely to be related to the fibrin sealant. No further information was available regarding blood donors |
| Frilling et al., 200573 | 148 | Liver | Four adverse events were considered to be possibly related to the test treatment. Three of them were considered to be serious: postoperative haemorrhage (TachoSil), abscess and pleural effusion (argon beamer), while one was considered not to be serious: anaemia (TachoSil) |
| Siemer et al., 2007221 | 185 | Kidney | Two severe adverse events were related to treatments in the trial. In a subject who received TachoSil extravasation of urine, a non-serious event was reported. One patient who received standard treatment reported subileus, a serious event. The patient was treated successfully with analgesics, laxatives, and diet. Both patients recovered fully |
| Nativ et al., 201259 | 7 | Kidney | One case was haemodynamically instable and post-procedural haemorrhage was observed in the drain 2 hours after surgery. This required the patient to be reoperated, and the source of bleeding was the resection area beneath the fibrin pad. The fibrin pad was removed and haemostasis was achieved using a standard surgical technique. A total of 10 units of blood were administered in the post-operative period and the patient was discharged from the hospital without sequelae |
| Vanscheidt et al., 2007208 | 225 | Plastic or reconstructive | One patient was found to have a ‘certain’ adverse event (application site disorders) related to the study treatment; this was in the Bio Seed-Ss group. Two AEs (general disorders, n = 1; skin and appendages, n = 1) reported in the BioSeeds treatment group were ‘probably’ related to treatment. Six AEs (general disorders, n = 2; skin and appendages, n = 2; secondary terms, n = 2) were ‘possibly’ related |
| Saha et al., 2011204 | 73 | Vascular | One non-serious AE that was considered possibly related to FS was incision site complications. The complication occurred 32 days after application of FS and raised concerns of possible graft occlusion. An angiogram indicated venous stenosis in the area of the anastomosis. The investigator stated that a causal relationship to FS was unlikely but could not be completely ruled out |
| Aguilera et al., 2013143 | 166 | Orthopaedic (joint) | A 67-year-old man who received Tissucol developed a mild generalized skin rash in the immediate postoperative period. This rash resolved after the administration of an oral antihistamine and topical corticosteroid treatment |
Observational studies
Eight included observational studies reported adverse events that appear to be fibrin related (Table 23). There were no reports of death or serious adverse events from the observational studies included in the systematic review. Cagatay et al. 242 and Choi et al. 244 thought that the application of too much fibrin sealant caused discomfort for patients undergoing eye surgery, but this was expected to be solved by surgeons gaining more expertise with fibrin sealant application. Jiang et al. 243 reported a slighter higher proportion of patients with graft oedema in eyes treated with fibrin sealant. In upper GI tract surgery statistically significantly more events were seen in patients treated with fibrin sealants (i.e. inflammation,245 strictures requiring dilatation246 and uncontrolled ascites247). In Marchac et al. 248 trapped pockets of air were only found in the fibrin group and Sakic et al. 249 reported more superficial sternal infections in patients treated with fibrin sealant.
| Study (author, year) | Sample size | Surgery | Adverse event |
|---|---|---|---|
| Cagatay et al., 2014242 | 103 | Conjunctival autografting for pterygium surgery (eye) | One patient experienced serious discomfort post operatively as a result of excess glue. The excess was removed from the ocular surface using scissors to trim it under slit lamp biomicroscopy The development of Tenon’s cyst was not higher in patients in the fibrin group (5/53) than in the control group (3/53) in a statistically significant manner (p = 0.71) |
| Jiang et al., 2008243 | 40 | Conjunctival autografting for pterygium surgery (eye) | A yellowish graft edema was observed in some eyes in the first few days post operatively, which resolved gradually and spontaneously. There were more cases of edema in the fibrin sealant group than in the sutures group (8/20 vs. 3/20, respectively). However, the difference between the two groups in graft edema development was not statistically significant (p = 0.077) |
| Choi et al., 2010244 | 126 | Pars plana vitrectomy (eye) | Three patients reported discomfort, possibly caused by the application of too much glue, and two cases showed wound dehiscence, probably caused by too little solution. However, such problems can be overcome with further experience |
| Efthimiou et al., 2010245 | 474 | Laparoscopic Roux-en-Y gastric bypass (upper GI tract) | Patients had an increased inflammatory response with the application of fibrin sealant, indicated by statistically significant higher temperature, white blood count and heart rate in the fibrin group compared to the two control groups (p = 0.001). There was an increased rate of fever (six patients in fibrin group vs. none in the control group) and abdominal collection (two patients in fibrin group vs. none in the control groups) |
| Ibele et al., 2014246 | 529 | Laparoscopic Roux-en-Y gastric bypass (upper GI tract) | The rate of stricture requiring dilation was a significantly increased in the sealant group (11.3%, compared with 4.8% stricture rate in patients who did not receive sealant; p = 0.04) Patients in the fibrin sealant group showed a notable stricture delay with strictures occurring an average of 4.1 weeks following surgery without sealant and 9.2 weeks after surgery (p = 0.3), suggesting that the mechanism of stricture formation may have differed between the two groups |
| Nanashima et al., 2012247 | 341 | Hepatobiliary pancreas surgery; hepatectomy and pancreatectomy (upper GI tract) | In the hepatectomy group, uncontrolled ascites were more frequent in the fibrin glue group (145/228) than in the non-fibrin glue group (6/94) (p < 0.05) |
| Marchac et al., 1994248 | 200 | Rhytidectomy (plastic) | One complication unique to the fibrin glue treated group was the postoperative finding of trapped pockets of air. These had the appearance of small haematomas and yielded 3–5 cc of air on aspiration |
| Sakic et al., 2013249 | 418 | Bilateral internal thoracic artery grafting (vascular) | The use of platelet-enriched-fibrin glue (PRF) sealant, however, was associated with more superficial sternal infections (OR: 3.7, 95% CI: 1.3 to 10.5, p = 0.02) |
Regulatory body reports
Five reports from the MHRA (one report), EMA (one report) and FDA (three reports) websites reported on deaths associated with the use of fibrin sealants, as either case series or single case reports (Table 24).
| Regulatory body | Fibrin sealant name | Date | Subject | Findings | Source |
|---|---|---|---|---|---|
| MHRA254 | EVICEL, Tisseel and Artiss | February 2013 | Drug safety update | The MHRA notes the findings from the EMA | www.gov.uk/drug-safety-update/sprayable-fibrin-sealants-evicel-tisseel-and-artiss-updated-guidance (accessed 11 November 2015) |
| EMA255 | Artiss, Beriplast P, EVICEL, Tisseel, Tissucol spray applications | 15 March 2013 | Questions and answers | Risk of air or gas embolism; recommendations for surgeons | www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Fibrinogen-containing_solutions_for_sealant_authorised_for_administration_by_spray_application/human_referral_000332.jsp&mid=WC0b01ac05805c516f (accessed 11 November 2015) |
| FDA256 | Artiss and Tisseel | 5 October 2009 | Important drug warning: fatality reported | Risk of life-threatening air or gas embolism with the use of spray devices employing pressure regulator to administer fibrin sealants | www.fda.gov/biologicsbloodvaccines/safetyavailability/ucm209778.htm (accessed 11 November 2015) |
| FDA257 | Tisseel | 2014 | Fatalities reported | Three deaths thought to have occurred as a result of the use of Tisseel fibrin sealant | www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/pediatricadvisorycommittee/ucm386895.doc (accessed 11 November 2015) |
| FDA258 | Tisseel | February 2015 | Medical device report analysis | An analysis of nine reports of adverse events involving one death | www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/pediatricadvisorycommittee/ucm388149.pdf (accessed 11 November 2015) |
Medicines and Healthcare products Regulatory Agency
The MHRA notes the findings from the EMA, namely the number of life-threatening or fatal air embolisms. A total of six reports of such events have been reported worldwide according to the EMA – EVICEL (five reports), Tisseel (four reports), Quixil (four reports)254 – although Quixil is no longer available in the UK. In 2013, the MHRA provided updated guidance for the use of sprayable fibrin sealants. Four sprayable fibrin sealants are authorised for use in the UK:254
-
EVICEL
-
Tisseel Lyo
-
Tisseel Ready to use
-
Artiss solution for sealant, deep frozen.
European Medicines Agency
In 2012, the EMA completed a review of the safety and effectiveness of four fibrin sealants (Tisseel, Tissucol, Artiss and Beriplast P) used in spray formation. 254 The agency’s CHMP considered the evidence for the development of gas embolisms and concluded that the benefits outweigh the risks. The CHMP recommended that the wording on product information be strengthened; the manufacturers of the products should ensure that they are used with pressure regulators that do not exceed the maximum pressure necessary for the delivery of the fibrin sealant; and labelling with the recommended pressure and distance. Furthermore, the EMA report suggests that the product information should include a warning that the risk of gas embolism appears to be higher when sprayed with air than with carbon dioxide (CO2). The report also recommends patients to be closely monitored for signs of possible gas embolism (heart rate, blood pressure, oxygen and CO2 levels in blood) during procedures using sprayable fibrin sealants.
Food and Drug Administration
The FDA website contained reports of five fatalities arising from the use of fibrin sealants.
The FDA reported:
Air or gas embolism has occurred with the use of spray devices employing pressure regulator to administer fibrin sealants. This event appears to be related to the use of the spray device at higher than recommended pressures and in close proximity to the tissue surface. When applying fibrin sealants using a spray device, be sure to use the pressure within the pressure range recommended by the spray device manufacturer. In the absence of a specific recommendation avoid using pressure above 20–25 psi. Do not spray closer than the distance recommended by the spray device manufacturer. In the absence of a specific recommendation avoid spraying closer than 10–15 cm from the surface of the tissue. When spraying the fibrin sealant, changes in blood pressure, pulse, oxygen saturation and end tidal CO2 should be monitored because of the possibility of occurrence of air or gas embolism.
Recommendations for surgeons are similar those previously mentioned for the EMA:
Specifically, the safety update includes the following instructions for sealant application using a spray device to help prevent air or gas embolism:
utilize spray pressure that is within the recommended guidelines by the device manufacturer
ensure that distance between the spray head and the application bed is within the recommended guidelines of the device manufacturer;
monitor patients for air or gas embolism.
The FDA reported a fatal air embolism after the use of an EVICEL spray device. EVICEL was being used to arrest a haemorrhage using a spray device (wall unit) at a higher than recommended pressure. Additionally, the spray head was held at a distance from the bleeding area that was closer than the recommended guidelines suggest. The website also advises the use of fibrin sealant spray at pressures of < 20–25 pounds/inch2.
A safety review for Tiseel/Tissucol by the Centre for Biologics Evaluation and Research of the FDA identified three adult deaths considered likely to be associated with the use of the fibrin sealant. In one case (reference 9283933) from Columbia, a fatal thrombosis and colon necrosis was observed in a male aged 60 years. Tissucol was sprayed after a right hepatectomy. After the operation the patient underwent a repeat laparotomy and a mesenteric thrombosis was found; after a hepatectomy the patient died. Underlying liver disease is a risk factor for development of mesenteric thrombosis. In a second case (reference 9540751), from Germany (in 1990), a male experienced a fatal air embolism after gastropic sealing for the closure of a fistula. It is reported that:
. . . seconds after the Tissucol immune gas flow, the patient lost consciousness and had a cardiac arrest. Autopsy showed the right ventricle filled with air and death was assumed to be due to air embolism.
The third death associated with Tissucol (case 8815161) was of a male aged 37 years from the UK who suffered a fatal cardiac arrest during revision laminectomy. The device was held closer than the recommended distance to the tissue, with the tip of the applicator being located within the wound.
Furthermore, the FDA Manufacturer and User Safety Device Experience database reports one death of a patient who lost consciousness and experienced a cardiac arrest:
Autopsy showed the right ventricle was filled with air, and death was assumed to be due to an air embolism.
However, the source is reported to be published literature from 1990 and, as the wording is similar to that of case reference 9540751 from the safety review, the researchers of this report consider it highly likely to be a duplicate report.
Chapter 4 Discussion
Statement of principal findings
This review included 186 RCTs to assess the benefits of fibrin sealants during non-emergency surgery in adults. The RCTs, eight observational studies and five reports from regulatory bodies were used to inform a review of harms caused by the use of fibrin sealants. Studies were found in the following 15 surgical specialties: upper GI tract (digestive system), breast and lymph nodes, orthopaedic (joints), eye, hernia, otolaryngology (ENT), vascular, plastic or reconstructive, colorectal (anus), oral (mouth) and maxillofacial, mixed, gynaecological, urology, neurology and cardiothoracic.
Evidence of effectiveness
A series of meta-analyses carried out over different populations and different formulations of fibrin sealant to assess the effectiveness of fibrin sealants on improving various post-operative outcomes shows that the effectiveness of fibrin sealants does not appear to vary according to surgical procedures, as there was virtually no heterogeneity in the meta-analyses of primary and secondary dichotomous outcomes. The results from the fixed-effects analyses are presented below. However, the results of secondary continuous outcomes should be interpreted with caution because of the uncertain quality of included studies and the large amount of statistical heterogeneity identified in the meta-analyses. Where high levels of heterogeneity were identified, the results from the random-effects analyses are reported (i.e. duration of eye surgery, length of hospital stay for breast surgery and duration of post-operative drainage for breast and lungs surgery).
The primary outcomes of this review were seroma and haematoma development. The most frequently reported indication for fibrin sealant use was the prevention of post-operative seroma (37 RCTs) in surgical procedures for breast and axillary/inguinal, hernia, plastic, liver and otolaryngology. A meta-analysis of data from 3472 patients (32 RCTs) did not identify a significant benefit for fibrin sealant over standard procedures (OR 0.84, 95% CI 0.68 to 1.04; p = 0.13; I2 = 12.7%). Development of haematoma was reported by 26 RCTs in breast and axillary/inguinal lymph nodes, hernia, plastic, orthopaedic, upper GI tract, oral and otolaryngology. A meta-analysis of 24 RCTs (n = 2403) demonstrated a statistically significant effect for fibrin sealant compared with standard care (OR 0.62, 95% CI 0.44 to 0.86; p = 0.01; I2 = 0%) that was driven by the results for hernia surgery in four RCTs (OR 0.22 95% CI 0.06 to 0.74; p = 0.01; I2 = 0%). Furthermore, there was a trend of haematoma risk reduction in the remaining surgical specialties that was not statistically significant (p = 0.87 for breast, p = 0.20 for orthopaedic and p = 0.88 for upper GI tract). A post hoc analysis was conducted that combined both seroma and haematoma as it was plausible that these events were broadly similar, and in some studies they were combined in a single outcome. This meta-analysis of 48 RCTs to explore the impact of combining seroma and haematoma showed a statistically significant benefit for fibrin sealant use compared with control (OR 0.77, 95% CI 0.64 to 0.92; p = 0.01; I2 = 6.7%).
Secondary dichotomous outcomes included in this review were haemorrhage (bleeding), reoperation, infections, use of analgesics and complications arising from the use of drains. There was no statistically significant difference in the risk of post-operative bleeding between patients receiving fibrin sealants and standard care (18 RCTs, OR 0.64, 95% CI 0.40 to 1.02; p = 0.08; I2 = 0%) and the risk of developing infections (25 RCTs, OR 0.76, 95% CI 0.54 to 1.06; p = 0.12; I2 = 0%). However, there was a statistically significant reduction in risk of haemorrhage when using fibrin sealants within upper GI tract surgery (six RCTs, OR 0.39, 95% CI 0.19 to 0.80; p = 0.01). The risk of reoperation was significantly lower among patients receiving fibrin sealants than among control patients (17 RCTs, OR 0.65, 95% CI 0.48 to 0.87; p = 0.00; I2 = 0%). However, a non-statistically significant higher risk of reoperation was found in breast surgery (three RCTs, OR 1.21, 95% CI 0.51 to 2.90; p = 0.83; I2 = 0%) and lung surgery (two RCTs, OR 1.38, 95% CI 0.47 to 4.04; p = 0.76). Use of analgesics was reported by only four RCTs. No RCTs reported on complications arising from the use of drains.
Secondary continuous outcomes included duration of operation, length of hospital stay, use of drains, pain levels and health-related quality of life. There was evidence of statistically significant benefit of fibrin sealants compared with standard care in the mean duration of operation for eye surgery in eight RCTs (fixed-effects model: MD –12.13 minutes, 95% CI –12.59 to –11.67 minutes; p < 0.01; I2 = 99.1%; random-effects model: MD –17.19 minutes, 95% CI –23.35 to –12.50 minutes; p < 0.0001; I2 = 99.1%) and hernia surgery in two RCTs (MD –2.56 minutes, 95% CI –3.57 to –1.56 minutes; p < 0.01; no I2). However, in surgery with liver mobilisation, a meta-analysis of two RCTs showed a statistically significant longer duration of operation when fibrin sealants were used (MD 19.07 minutes, 95% CI 2.75 to 35.38 minutes; p = 0.02; no I2). Fibrin sealants were shown to reduce the length of hospital stay for people undergoing upper GI tract surgery involving the pancreas in two RCTs (MD –1.40 days, 95% CI –1.72 to –1.09 days; p < 0.01; no I2), cardiothoracic lung surgery in two RCTs (MD –1.37 days, 95% CI –1.93 to –0.81 days; p < 0.01; no I2) and breast surgery in eight RCTs (fixed-effects model: MD –0.73 days, 95% CI –0.95 to –0.50 days; p < 0.01; I2 = 88.7%; random-effects model: MD –0.87 days, 95% CI –1.75 to 0.01 days; p = 0.05). The duration of post-operative drainage for breast and axillary lymph nodes was slightly reduced (12 RCTs, fixed-effects model: MD –0.50 days, 95% CI –0.68 to –0.33 days; p < 0.01; I2 = 90.6%; random-effects model: MD –1.06 days, 95% CI –1.69 to –0.42 days; p = 0.01), as well as the duration of drainage for lung surgery (five RCTs, fixed-effects model: MD –0.46 days, 95% CI –0.53 to –0.39 days; p < 0.01; I2 = 91.0%; random-effects model: MD –2.10 days, 95% CI –3.65 to –0.56 days; p = 0.01), for fibrin sealants than standard care. These results were not consistent across surgical specialties, with fibrin sealants showing no beneficial effect when compared to standard care in the following surgical specialties: duration of operation in surgery without liver mobilisation (four RCTs; p = 0.46), gastric surgery (two RCTs; p = 0.07); length of hospital stay in gastric and bowel surgery (two RCTs; p = 0.82), joint surgery (four RCTs; p = 0.871) and duration of drainage in liver surgery (four RCTs; p = 0.33). However, the high level of heterogeneity warrants caution with interpreting the results of these analyses. This might be expected when the likely duration of different operations conducted is being considered (e.g. a longer duration of upper GI tract surgery than eye surgery). Pain levels were reported in 20 RCTs, but the large differences in the various scales used and time points at which assessments took place, as well as lack of variability data, did not permit a meta-analysis. No RCT reported on health-related quality of life.
Overall, 154 studies were assessed as having an ‘unclear risk of bias’, eight RCTs as having a ‘high risk of bias’ and 24 RCTs as having a ‘low risk of bias’. The risk-of-bias table (see Table 37) shows a high level of uncertainty about the validity of data collected across all parameters, especially regarding the blind collection of patient outcomes.
Evidence of harms
This review considered the evidence that fibrin sealants cause serious adverse events from data contained in reports from the RCTs, observational studies and the regulatory bodies (MHRA, EMA and FDA).
Ten RCTs in various surgical specialties (liver, kidney, mixed, oral and maxillofacial, hernia, plastic and reconstructive, vascular, orthopaedic) reported adverse events that were thought to be related to the use of fibrin sealants by primary study investigators or reviewers. Only one RCT reported a death as possibly related to fibrin sealant application in upper GI tract surgery caused by a large bleed, but bleeding did not occur at the target bleeding site and no further information was provided. Other RCTs reported on various non-severe adverse events including mild cellulitis and mild seroma, anaemia, extravasation of urine, incision site complications and mild generalised skin rash. Severity was unclear for excessive pain, scar pain, testicular pain hydrocele and post-procedural haemorrhage antibodies to hepatitis B. It was not reported how adverse events were related to the application of fibrin sealant or how severity was determined. The time at which adverse events occurred after surgery was immediate,143 2 hours,59 1 and 14 days231 or 32 days,204 but not reported in five RCTs. 73,91,95,110,187 Another 22 RCTs explicitly reported that there were no complications or adverse events related to fibrin.
Eight observational studies reported adverse events that appear to be fibrin related by primary study investigators or reviewers, but there were no reports of death or serious adverse events. In eye surgery, the application of too much fibrin sealant was thought to cause discomfort for patients, but this was expected to be solved by surgeons gaining more expertise with fibrin sealant application. It was reported that the proportion of eyes that developed graft oedema was higher in the fibrin sealant group (8/20) that in the. in the standard care group (3/20). In upper GI tract surgery more of the following events were seen in patients treated with fibrin sealants: inflammation, strictures requiring dilatation and uncontrolled ascites. In plastic or reconstructive surgery trapped pockets of air were only found in the fibrin group. Furthermore, in vascular surgery more superficial sternal infections were found in patients treated with fibrin sealant. The evidence from observational studies did not produce evidence of causality about fibrin sealants resulting in potentially serious adverse events. The validity of the eight observational studies was compromised by a general failure to report whether or not adverse events were assessed independently, whether or not blinding to the assigned allocation was performed and at which time point the adverse event occurred.
Five MHRA, EMA and FDA reports warned about deaths from air emboli as a result of fibrin sealants, in aerosol form, being held too close to tissues and used at higher than recommended pressures.
Strengths and limitations of the assessment
This research reviewed the evidence on the benefits and harms from the use of fibrin sealants compared with standard care for adults undergoing non-emergency surgery. The large number of RCTs allowed analysis of results for the most common and consistently measured outcomes, and the strength of this systematic review is that the findings are based on increased statistical power from these meta-analyses. It was not possible to provide a detailed evaluation of individual RCTs in their respective contexts because of the limited resources that were available for this research. In addition, the number of RCTs that were identified made it impractical to conduct independent data extraction by two reviewers in the time available. Another consequence of the resource constraints imposed by the identification of such a large number of RCTs was our limited ability to perform a thorough evaluation of the source of heterogeneity in meta-analyses where this was identified at high levels of inconsistency. However, the high level of heterogeneity in continuous secondary outcomes was explored by sequentially excluding individual RCTs to identify if the potential cause of the heterogeneity was caused by any individual RCT. This was often found not to be the case as I2 remained >80% or >90%. Had additional time been available, analyses to assess the impact of different fibrin glues and delivery mechanisms would have been evaluated. However, all RCTs that met the eligibility criteria were included in order to create a repository for future researchers.
A second strength of the review is the inclusion of evidence regarding harms arising from the use of fibrin sealants, a methodologically challenging approach for those engaged in evidence-based research. However, poor reporting of adverse events in RCTs and observational studies limited our ability to provide a comprehensive overview of harms. The review cites only reported outcomes that are likely to be considered important in clinical practice but were not part of the scope of the review; one example is that the data for the use of fibrin sealant to prevent cerebrospinal fluid leakage in neurology RCTs could not be included in meta-analyses. Although individual RCTs are referenced, their findings are not discussed because of the three RCTs evaluating the effect of fibrin sealants for the prevention of cerebrospinal fluid leakage after neurosurgery,10,236,237 one measured cerebrospinal fluid in ml,236 one categorised data into minor, moderate or major cerebrospinal fluid leakage and presented absolute numbers237 and another RCT presented outcome data as the absolute number of patients with watertight closure of the dura. 10 The findings of these RCTs did not converge and the inconsistencies make any interpretation difficult. Furthermore, cost-effectiveness was not assessed and would be a relevant outcome for policy-makers and budget-holders.
As mentioned in Chapter 3, Methods of analysis/synthesis, there were changes between the protocol and this review. Systematic reviews were not included and, therefore, the quality of systematic reviews was not assessed, as was mentioned in the protocol. 45 Haematoma is an additional post hoc primary outcome that was not included in the protocol. As the mechanism of haematoma and seroma formation is similar, and is reported in some studies interchangeably, it was deemed important to include haematoma as a primary outcome. In addition, a post hoc analysis of combined seroma and haematoma development was undertaken. Haemorrhage, pain levels and infections were described in the protocol as adverse events – but have been moved to secondary outcomes as these were found to be adverse events of surgery and not related to fibrin sealant (and fibrin sealants are used to reduce these adverse events related to surgery). The duration of operation was used to reflect the outcome ‘nurse or doctor time’ instead of the previously mentioned ‘dressing or fine-needle aspirations’. Sensitivity analyses were planned to be carried out for aspects of the review that might have an impact on the results, for example, including studies in which there is a high risk of bias. 53 However, most studies were assessed as having an unclear risk of bias and, therefore, these analyses were not deemed to be appropriate. Sensitivity analysis using a random-effects model was conducted, but as a result of the large number of RCTs identified in the review it was not possible to perform additional analyses in the time available. Furthermore, overall risk of bias in included RCTs was deemed to be ‘unclear’, which may reflect poor reporting of primary studies in published papers rather than potentially flawed methods employed.
The overall results for haematoma development show a significant benefit for using fibrin sealants over standard care, and are supported by the trends in all of the subgroup analyses. However, despite the large number of RCTs included in this systematic review, there remains uncertainty with regard to reducing the risk of post-operative seroma for most of the secondary outcomes considered. In some cases the direction of the non-statistically significant trend suggested that fibrin sealants might be harmful; for example, data from the meta-analyses of RCTs showed a non-statistically significant effect in breast and lung surgery suggestive of an increase in the risk of reoperation.
Clinical opinion noted that most patients are now managed within enhanced recovery programmes and may not stay in hospital with drains, as they did previously. Therefore, data on length-of-stay reduction may not reflect current practice (Mr Kurinchi Gurusamy, UCL and Royal Free NHS Trust, 2016, personal communication).
The researchers were unable to obtain information about the use and costs of fibrin sealants to the NHS in England. NHS England replied to our request indicating that it does not hold this information but that individual hospital trusts may be able to provide these data. It was beyond the scope of the current research to perform a survey of NHS trusts to provide results that would be representative for the NHS in England.
Chapter 5 Conclusions
Implications for service provision
Fibrin sealants statistically significantly reduce the risk of development of haematoma when used in non-emergency surgical procedures compared with standard care, but the reduction in risk of post-operative seroma remains unproven.
We found reports254 stating that the spraying of fibrin sealants caused the formation of air emboli which resulted in perioperative deaths during elective surgical procedures. Surgeons should follow the detailed safely recommendations when using fibrin sealants and they are advised by regulatory bodies that prior to applying fibrin sealants by spray application, a pressure regulator device should be used and the surface area of the wound should be dried. The patient’s blood pressure, heart rate, oxygen saturation and end-tidal CO2 should be closely monitored when spraying fibrin sealants because of the potential to create an air embolism. The use of air in the spray device is considered more dangerous than CO2, and warnings to this effect are issued by the regulatory bodies.
Recommendations about how and for which procedures certain products should be used are available. EVICEL spray should be used with CO2 gas (not pressurised air) and in laparoscopic procedures should be used only when the spray distance is at least 4 cm; it is not recommended for use in any other endoscopic procedures. 37 The recommended spray distance for Tisseel is even shorter, at 2 cm from the tissue. 37 Artiss is recommended for use only in open-wound surgery and not during laparoscopic or any other endoscopic procedures,37 and there is no risk of gas embolism with Beriplast P when used in accordance with the prescribing advice and with the recommended device, although this product is not used in the UK. Surgeons are advised to utilise spray pressure that is within the recommended guidelines by the device manufacturer; to ensure that the distance between the spray head and the application bed is within the recommended guidelines of the device manufacturer; and to monitor patients for air or gas embolism.
Suggested research priorities
The search carried out for this review (May 2015) identified only a small number of RCTs (< 10) that showed statistically significant differences between fibrin and comparators. No evidence of a statistically significant effect of fibrin sealants compared with standard care was found for the outcomes listed for the following surgical indications:
-
all surgical specialties (seroma development)
-
neurological, gynaecological, oral and maxillofacial, urology, colorectal and orthopaedics knees or hips (for any outcome)
-
breast surgery (haematoma development)
-
upper GI tract (haematoma development)
-
cardiothoracic heart or lung surgery (reoperation rates).
The most appropriate study type to assess outcomes would be a RCT in which outcome assessors and, potentially, patients, but not surgeons, are blind to intervention. In general, RCTs of fibrin sealants in non-emergency surgery are small and involve fewer than 100 people; an a priori sample size that is adequate to ensure that a statistically significant effect can be detected should be used.
The findings of this review are based on data that show inconsistent effects as a result of the large number of small RCTs that evaluated different outcomes, sometimes for the same surgical area. It is necessary that those who undertake future RCTs capture all important outcomes in the same population of patients. Researchers should plan RCTs that collect data for biological outcomes, such as seroma, haematoma, duration of drainage and more service-related outcomes, such as length of hospital stay and rates of reoperations, in order to reach a balanced view of the benefits and harms arising from fibrin sealants. A variety of units of analysis were used within the same surgical specialties and this limited the number of studies included in each meta-analysis. The work of other researchers should be evaluated using, for example, this review to inform the design of new RCTs and employ units of analysis that are consistent with those used in previous RCTs to enable the conduct of meta-analyses.
Furthermore, adverse events of the use of fibrin sealants were poorly and infrequently reported in both RCTs and observational studies. Only Fischer et al. 241 reported a death as possibly related to fibrin sealant application in upper GI tract surgery caused by a large bleed, but bleeding did not occur at the target bleeding site and no further information was provided. Researchers need to test a biologically plausible hypothesis when testing whether or not adverse events are related to the use of fibrin sealants. Both RCTs and observational studies on the use of fibrin sealants in all surgical specialties need to assess harms relevant to the specific surgical area.
Acknowledgements
Clinical experts
-
Professor John MacFie, professor of surgery and consultant surgeon at the University of Hull and Scarborough Hospital.
-
Mr Alexander Green, consultant neurosurgeon at the Department of Neurosurgery, John Radcliffe Hospital, Oxford.
-
Mr Kurinchi Gurusamy, Reader in Surgery, UCL and Royal Free NHS Trust, London.
Translations
-
Kaori Dezaki, BMJ, London.
-
Yen Chau, BMJ, London.
-
Alan Thomas, BMJ, London.
-
Elin Goodwin, BMJ, London.
Contributions of authors
Steven J Edwards (Head of Clinical and Economic Evidence) was the project lead, supervised the production of the final report, advised on the protocol and the analyses carried out, and was guarantor of the report.
Fay Crawford (Senior Health Technology Assessment Analyst) wrote the protocol and carried out searches, screening, assessment of studies for eligibility and data extraction.
Michelle Helena van Velthoven (Health Technology Assessment Analyst) carried out searches, screening, assessment of studies for eligibility, data extraction, preparation of data for analysis and data analysis.
Andrea Berardi (Health Economist Lead) carried out data extraction and preparation of data for analysis.
George Osei-Assibey (Health Technology Assessment Analyst) carried out screening, assessment of studies for eligibility and data extraction.
Mariana Bacelar (Senior Health Economist) carried out screening, assessment of studies for eligibility and data extraction.
Fatima Salih (Health Economist) carried out screening, assessment of studies for eligibility, data extraction and data analysis.
Victoria Wakefield (Senior Health Technology Assessment Analyst) advised on the protocol and created the search strategies.
All authors read and commented on draft versions of the report.
Publications
Crawford F, Edwards S, van Velthoven M, Osei-Assibey G. The Use of Fibrin Sealants During Non-Emergency Surgery: A Systematic Review of the Evidence of Benefits and Harms. CRD, University of York; 2015. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015020710 (accessed 19 May 2015).
Data sharing statement
This is a systematic review and, therefore, the data used for each analysis are present within the report. Further information and requests for access to the data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Pogson CJ, Adwani A, Ebbs SR. Seroma following breast cancer surgery. Eur J Surg Oncol 2003;29:711-17. http://dx.doi.org/10.1016/S0748-7983(03)00096-9.
- Sözen S, Topuz O, Tükenmez M, Keçeli M. The use of fibrin sealant after total thyroidectomy for benign disease obviates the need for routine drainage. Results of a randomized controlled trial. Hippokratia 2011;15:247-51.
- Kim TW, Choi SY, Jang MS, Lee GG, Nam ME, Son YI, et al. Efficacy of fibrin sealant for drainage reduction in total thyroidectomy with bilateral central neck dissection. Otolaryngol Head Neck Surg 2012;147:654-60. http://dx.doi.org/10.1177/0194599812449315.
- Hsu HK, Hsu WH, Huang MH. Prospective study of using fibrin glue to prevent leak from esophagogastric anastomosis. J Surg Assoc 1992;25:1248-52.
- Handmer M. Sticking to the facts: a systematic review of fibrin glue for pilonidal disease. ANZ J Surg 2012;82:221-4. http://dx.doi.org/10.1111/j.1445-2197.2011.05752.x.
- Cheng Y, Xiong X, Peng S, Wu Hong M, Cheng N. Fibrin sealants for the prevention of postoperative pancreatic fistula following pancreatic surgery. Cochrane Database Syst Rev 2012;2. http://dx.doi.org/10.1002/14651858.cd009621.
- Fingerhut A, Veyrie N, Ata T, Alexakis N, Leandros E. Use of sealants in pancreatic surgery: critical appraisal of the literature. Dig Surg 2009;26:7-14. http://dx.doi.org/10.1159/000191284.
- Ohwada S, Ogawa T, Tanahashi Y, Nakamura S, Takeyoshi I, Ohya T, et al. Fibrin glue sandwich prevents pancreatic fistula following distal pancreatectomy. World J Surg 1998;22:494-8. http://dx.doi.org/10.1007/s002689900423.
- Morales-Conde S, Barranco A, Socas M, Alarcón I, Grau M, Casado MA. Systematic review of the use of fibrin sealant in abdominal-wall repair surgery. Hernia 2011;15:361-9. http://dx.doi.org/10.1007/s10029-011-0809-x.
- Green AL, Arnaud A, Batiller J, Eljamel S, Gauld J, Jones P, et al. A multicentre, prospective, randomized, controlled study to evaluate the use of a fibrin sealant as an adjunct to sutured dural repair. Br J Neurosurg 2015;29:11-7. http://dx.doi.org/10.3109/02688697.2014.948808.
- Koh MB, Hunt BJ. The management of perioperative bleeding. Blood Rev 2003;17:179-85. http://dx.doi.org/10.1016/S0268-960X(02)00062-0.
- Kongnyuy EJ, Wiysonge CS. Interventions to reduce haemorrhage during myomectomy for fibroids. Cochrane Database Syst Rev 2011;11. http://dx.doi.org/10.1002/14651858.cd005355.pub4.
- Liu J, Cao JG, Wang L, Ma XL. Effect of fibrin sealant on blood loss following total knee arthroplasty: a systematic review and meta-analysis. Int J Surg 2014;12:95-102. http://dx.doi.org/10.1016/j.ijsu.2013.11.011.
- Levy O, Martinowitz U, Oran A, Tauber C, Horoszowski H. The use of fibrin tissue adhesive to reduce blood loss and the need for blood transfusion after total knee arthroplasty. A prospective, randomized, multicenter study. J Bone Joint Surg Am 1999;81:1580-8. http://dx.doi.org/10.2106/00004623-199911000-00010.
- Petrek JA, Peters MM, Nori S, Knauer C, Kinne DW, Rogatko A. Axillary lymphadenectomy. A prospective, randomized trial of 13 factors influencing drainage, including early or delayed arm mobilization. Arch Surg 1990;125:378-82. http://dx.doi.org/10.1001/archsurg.1990.01410150100018.
- Terrell GS, Singer JA. Axillary versus combined axillary and pectoral drainage after modified radical mastectomy. Surg Gynecol Obstet 1992;175:437-40.
- Smith MM, Lin MP, Hovsepian RV, Wood D, Nguyen T, Evans GR, et al. Postoperative seroma formation after abdominoplasty with placement of continuous infusion local anesthetic pain pump. Can J Plast Surg 2009;17:127-9. http://dx.doi.org/10.4172/plastic-surgery.1000624.
- Khaira HS, Lall P, Hunter B, Brown JH. Repair of incisional hernias. J R Coll Surg Edinb 2001;46:39-43.
- Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13. http://dx.doi.org/10.1016/j.surg.2005.05.001.
- Dong Z, Xu J, Wang Z, Petrov MS. Stents for the prevention of pancreatic fistula following pancreaticoduodenectomy. Cochrane Database Syst Rev 2013;6. http://dx.doi.org/10.1002/14651858.cd008914.pub2.
- Gurusamy KS, Koti R, Fusai G, Davidson BR. Somatostatin analogues for pancreatic surgery. Cochrane Database Syst Rev 2010;2. http://dx.doi.org/10.1002/14651858.cd008370.
- Connor S, Alexakis N, Garden OJ, Leandros E, Bramis J, Wigmore SJ. Meta-analysis of the value of somatostatin and its analogues in reducing complications associated with pancreatic surgery. Br J Surg 2005;92:1059-67. http://dx.doi.org/10.1002/bjs.5107.
- Shander A. Financial and clinical outcomes associated with surgical bleeding complications. Surgery 2007;142:20-5. http://dx.doi.org/10.1016/j.surg.2007.06.025.
- Hasley PB, Lave JR, Hanusa BH, Arena VC, Ramsey G, Kapoor WN, et al. Variation in the use of red blood cell transfusions. A study of four common medical and surgical conditions. Med Care 1995;33:1145-60. http://dx.doi.org/10.1097/00005650-199511000-00007.
- Hebert PC, Schweitzer I, Calder L, Blajchman M, Giulivi A. Review of the clinical practice literature on allogeneic red blood cell transfusion. CMAJ 1997;156:9-26.
- Marietta M, Facchini L, Pedrazzi P, Busani S, Torelli G. Pathophysiology of bleeding in surgery. Transplant Proc 2006;38:812-14. http://dx.doi.org/10.1016/j.transproceed.2006.01.047.
- Spahn DR, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernandez-Mondejar E, et al. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Crit Care 2013;17. http://dx.doi.org/10.1186/cc12685.
- Schulick RD, Yoshimura K. Stents, glue, etc.: is anything proven to help prevent pancreatic leaks/fistulae?. J Gastrointest Surg 2009;13:1184-6. http://dx.doi.org/10.1007/s11605-009-0866-y.
- Wente MN, Shrikhande SV, Müller MW, Diener MK, Seiler CM, Friess H, et al. Pancreaticojejunostomy versus pancreaticogastrostomy: systematic review and meta-analysis. Am J Surg 2007;193:171-83. http://dx.doi.org/10.1016/j.amjsurg.2006.10.010.
- Bryson GL, Laupacis A, Wells GA. Does acute normovolemic hemodilution reduce perioperative allogeneic transfusion? A meta-analysis. The International Study of Perioperative Transfusion. Anesth Analg 1998;86:9-15.
- Forgie MA, Wells PS, Laupacis A, Fergusson D. Preoperative autologous donation decreases allogeneic transfusion but increases exposure to all red blood cell transfusion: results of a meta-analysis. International Study of Perioperative Transfusion (ISPOT) Investigators. Arch Intern Med 1998;158:610-16. http://dx.doi.org/10.1001/archinte.158.6.610.
- Huët C, Salmi LR, Fergusson D, Koopman-van Gemert AW, Rubens F, Laupacis A. A meta-analysis of the effectiveness of cell salvage to minimize perioperative allogeneic blood transfusion in cardiac and orthopedic surgery. International Study of Perioperative Transfusion (ISPOT) Investigators. Anesth Analg 1999;89:861-9. http://dx.doi.org/10.1213/00000539-199910000-00009.
- Laupacis A, Fergusson D. Drugs to minimize perioperative blood loss in cardiac surgery: meta-analyses using perioperative blood transfusion as the outcome. The International Study of Peri-operative Transfusion (ISPOT) Investigators. Anesth Analg 1997;85:1258-67. http://dx.doi.org/10.1213/00000539-199712000-00014.
- Laupacis A, Fergusson D. Erythropoietin to minimize perioperative blood transfusion: a systematic review of randomized trials. The International Study of Peri-operative Transfusion (ISPOT) Investigators. Transfus Med 1998;8:309-17. http://dx.doi.org/10.1046/j.1365-3148.1998.00171.x.
- Henry DA, Carless PA, Moxey AJ, O’Connell D, Stokes BJ, Fergusson DA, et al. Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2011;1. http://dx.doi.org/10.1002/14651858.cd001886.pub3.
- EMA . Fibrinogen-Containing Solutions for Sealant Authorised for Administration by Spray Application 2012. www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Fibrinogen-containing_solutions_for_sealant_authorised_for_administration_by_spray_application/human_referral_000332.jsp&mid=WC0b01ac05805c516f (accessed 19 May 2015).
- Sprayable Fibrin Sealants (Evicel, Tisseel and Artiss): Updated Guidance. London: MHRA; 2013.
- Carless PA, Henry DA, Anthony DM. Fibrin sealant use for minimising peri-operative allogeneic blood transfusion. Cochrane Database Syst Rev 2003;2. http://dx.doi.org/10.1002/14651858.cd004171.
- Food and Drugs Administration . Risk of Life Threatening Air or Gas Embolism With the Use of Spray Devices Employing Pressure Regulator to Administer Fibrin Sealants (Baxter Health Care Corporation) 2009. www.fda.gov/biologicsbloodvaccines/safetyavailability/ucm209778.htm (accessed 19 May 2015).
- Kjaergard HK, Fairbrother JE. Controlled clinical studies of fibrin sealant in cardiothoracic surgery – a review. Eur J Cardiothorac Surg 1996;10:727-33. http://dx.doi.org/10.1016/S1010-7940(96)80332-0.
- Cardillo G, Carleo F, Carbone L, De Massimi AR, Lococo A, Santini PF, et al. Adverse effects of fibrin sealants in thoracic surgery: the safety of a new fibrin sealant: multicentre, randomized, controlled, clinical trial. Eur J Cardiothorac Surg 2012;41:657-62. http://dx.doi.org/10.1093/ejcts/ezr083.
- Epstein NE. Dural repair with four spinal sealants: focused review of the manufacturers’ inserts and the current literature. Spine J 2010;10:1065-8. http://dx.doi.org/10.1016/j.spinee.2010.09.017.
- Systematic Reviews: Centre for Reviews and Dissemination (CRD) Guidance for Undertaking Systematic Reviews in Health Care. York: CRD; 2010.
- Higgins JPT, Green S. Cochrane Handbook Version 5.1.0. 2011.
- Crawford F, Edwards S, van Velthoven M, Osei-Assibey G. The Use of Fibrin Sealants During Non-Emergency Surgery: A Systematic Review of the Evidence of Benefits and Harms. CRD, University of York; 2015.
- Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b2535.
- Zorzela L, Golder S, Liu Y, Pilkington K, Hartling L, Joffe A, et al. Quality of reporting in systematic reviews of adverse events: systematic review. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.f7668.
- Loke YK, Price D, Herxheimer A. Cochrane Adverse Effects Methods Group . Systematic reviews of adverse effects: framework for a structured approach. BMC Med Res Methodol 2007;7. http://dx.doi.org/10.1186/1471-2288-7-32.
- McIntosh HM, Woolacott NF, Bagnall AM. Assessing harmful effects in systematic reviews. BMC Med Res Methodol 2004;4. http://dx.doi.org/10.1186/1471-2288-4-19.
- Higgins JPT, Green S. Intention-to-Treat Issues for Dichotomous Data 2011. http://handbook.cochrane.org/chapter_16/16_2_2_intention_to_treat_issues_for_dichotomous_data.htm (accessed 19 May 2015).
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses 2014. www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 19 May 2015).
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377-84. http://dx.doi.org/10.1136/jech.52.6.377.
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. http://dx.doi.org/10.1136/bmj.315.7109.629.
- Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 1959;22:719-48.
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. http://dx.doi.org/10.1016/0197-2456(86)90046-2.
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. http://dx.doi.org/10.1136/bmj.327.7414.557.
- Thompson SG, Higgins JP. How should meta-regression analyses be undertaken and interpreted?. Stat Med 2002;21:1559-73. http://dx.doi.org/10.1002/sim.1187.
- Royal College of Surgeons . Surgical Specialties n.d. www.rcseng.ac.uk/patients/the-surgical-team/surgical-specialties (accessed October 2015).
- Nativ O, Patel B, Shen J, Batiller J, Horn S, Hart JC. Safety and hemostatic efficacy of fibrin pad in partial nephrectomy: results of an open-label phase I and a randomized, standard-of-care-controlled phase I/II study. BMC Nephrol 2012;13. http://dx.doi.org/10.1186/1471-2369-13-147.
- Tavilla G, Bruggemans EF, Gielen CL, Brand A, van den Hout WB, Klautz RJ, et al. Multicentre randomized clinical trial to investigate the cost-effectiveness of an allogeneic single-donor fibrin sealant after coronary artery bypass grafting (FIBER Study). Br J Surg 2015;102:1338-47. http://dx.doi.org/10.1002/bjs.9877.
- Hwang TL, Chen MF. Randomized trial of fibrin tissue glue for low output enterocutaneous fistula. Br J Surg 1996;83. http://dx.doi.org/10.1002/bjs.1800830135.
- Silecchia G, Boru CE, Mouiel J, Rossi M, Anselmino M, Morino M, et al. The use of fibrin sealant to prevent major complications following laparoscopic gastric bypass: results of a multicenter, randomized trial. Surg Endosc 2008;22:2492-7. http://dx.doi.org/10.1007/s00464-008-9885-0.
- Fernandez Fernandez L, Tejero E, Tieso A. Randomized trial of fibrin glue to seal mechanical oesophagojejunal anastomosis. Br J Surg 1996;83:40-1. http://dx.doi.org/10.1002/bjs.1800830111.
- Huang O, Lu X, Xu X, Shi Y. Fibrin-sealant-delivered cisplatin chemotherapy versus cisplatin hyperthermic intraperitoneal perfusion chemotherapy for locally advanced gastric cancer without peritoneal metastases: a randomized phase-II clinical trial with a 40-month follow-up. Cell Biochem Biophys 2015;71:1171-80. http://dx.doi.org/10.1007/s12013-014-0326-5.
- Bektas H, Nadalin S, Szabo I, Ploder B, Sharkhawy M, Schmidt J. Hemostatic efficacy of latest-generation fibrin sealant after hepatic resection: a randomized controlled clinical study. Langenbecks Arch Surg 2014;399:837-47. http://dx.doi.org/10.1007/s00423-014-1227-1.
- de Boer MT, Klaase JM, Verhoef C, van Dam RM, van Gulik TM, Molenaar IQ, et al. Fibrin sealant for prevention of resection surface-related complications after liver resection: a randomized controlled trial. Ann Surg 2012;256:229-34. http://dx.doi.org/10.1097/SLA.0b013e3182602819.
- Chapman WC, Clavien PA, Fung J, Khanna A, Bonham A. Effective control of hepatic bleeding with a novel collagen-based composite combined with autologous plasma: results of a randomized controlled trial. Arch Surg 2000;135:1200-4. http://dx.doi.org/10.1001/archsurg.135.10.1200.
- Uetsuji S, Komada Y, Kwon AH, Imamura A, Takai S, Kamiyama Y. Prevention of pleural effusion after hepatectomy using fibrin sealant. Int Surg 1994;79:135-7.
- Liu M, Lui WY. The use of fibrin adhesive for hemostasis after liver resection. Zhonghua Yi Xue Za Zhi 1993;1:19-22.
- Noun R, Elias D, Balladur P, Bismuth H, Parc R, Lasser P, et al. Fibrin glue effectiveness and tolerance after elective liver resection: a randomized trial. Hepatogastroenterology 1996;43:221-4.
- Figueras J, Llado L, Miro M, Ramos E, Torras J, Fabregat J, et al. Application of fibrin glue sealant after hepatectomy does not seem justified: results of a randomized study in 300 patients. Ann Surg 2007;245:536-42. http://dx.doi.org/10.1097/01.sla.0000245846.37046.57.
- Fischer L, Seiler CM, Broelsch CE, de Hemptinne B, Klempnauer J, Mischinger HJ, et al. Hemostatic efficacy of TachoSil in liver resection compared with argon beam coagulator treatment: an open, randomized, prospective, multicenter, parallel-group trial. Surgery 2011;149:48-55. http://dx.doi.org/10.1016/j.surg.2010.02.008.
- Frilling A, Stavrou GA, Mischinger HJ, De Hemptinne B, Rokkjaer M, Klempnauer J, et al. Effectiveness of a new carrier-bound fibrin sealant versus argon beamer as haemostatic agent during liver resection: a randomised prospective trial. Langenbecks Arch Surg 2005;390:114-20. http://dx.doi.org/10.1007/s00423-005-0543-x.
- Kakaei F, Seyyed Sadeghi MS, Sanei B, Hashemzadeh S, Habibzadeh A. A randomized clinical trial comparing the effect of different haemostatic agents for haemostasis of the liver after hepatic resection. HPB Surg 2013;2013. http://dx.doi.org/10.1155/2013/587608.
- Kohno H, Nagasue N, Chang YC, Taniura H, Yamanoi A, Nakamura T. Comparison of topical hemostatic agents in elective hepatic resection: a clinical prospective randomized trial. World J Surg 1992;16:966-9. http://dx.doi.org/10.1007/BF02067005.
- Moench C, Mihaljevic AL, Hermanutz V, Thasler WE, Suna K, Diener MK, et al. Randomized controlled multicenter trial on the effectiveness of the collagen hemostat Sangustop® compared with a carrier-bound fibrin sealant during liver resection (ESSCALIVER study, NCT00918619). Langenbecks Arch Surg 2014;399:725-33. http://dx.doi.org/10.1007/s00423-014-1203-9.
- Schwartz M, Madariaga J, Hirose R, Shaver TR, Sher L, Chari R, et al. Comparison of a new fibrin sealant with standard topical hemostatic agents. Arch Surg 2004;139:1148-54. http://dx.doi.org/10.1001/archsurg.139.11.1148.
- Fu JZ, Li J, Yu ZL. Effect of implanting fibrin sealant with ropivacaine on pain after laparoscopic cholecystectomy. World J Gastroenterol 2009;15:5851-4. http://dx.doi.org/10.3748/wjg.15.5851.
- Danielsen PL, Agren MS, Jorgensen LN. Platelet-rich fibrin versus albumin in surgical wound repair: a randomized trial with paired design. Ann Surg 2010;251:825-31. http://dx.doi.org/10.1097/SLA.0b013e3181d3548c.
- Dimo B, Jørgensen T, Kjaergaard J, Luke M, Kvist E, Hjortrup A. Randomized trial of fibrin adhesive for reduction of drained secretion after elective cholecystectomy. Acta Chir Scand 1989;155:177-8.
- Carter TI, Fong ZV, Hyslop T, Lavu H, Tan WP, Hardacre J, et al. A dual-institution randomized controlled trial of remnant closure after distal pancreatectomy: does the addition of a falciform patch and fibrin glue improve outcomes?. J Gastrointest Surg 2013;17:102-9. http://dx.doi.org/10.1007/s11605-012-1963-x.
- Suzuki Y, Kuroda Y, Morita A, Fujino Y, Tanioka Y, Kawamura T, et al. Fibrin glue sealing for the prevention of pancreatic fistulas following distal pancreatectomy. Arch Surg 1995;130:952-5. http://dx.doi.org/10.1001/archsurg.1995.01430090038015.
- Lillemoe KD, Cameron JL, Kim MP, Campbell KA, Sauter PK, Coleman JA, et al. Does fibrin glue sealant decrease the rate of pancreatic fistula after pancreaticoduodenectomy? Results of a prospective randomized trial. J Gastrointest Surg 2004;8:766-72. http://dx.doi.org/10.1016/j.gassur.2004.06.011.
- Montorsi M, Zerbi A, Bassi C, Capussotti L, Coppola R, Sacchi M, et al. Efficacy of an absorbable fibrin sealant patch (TachoSil) after distal pancreatectomy: a multicenter, randomized, controlled trial. Ann Surg 2012;256:853-9. http://dx.doi.org/10.1097/SLA.0b013e318272dec0.
- Suc B, Msika S, Fingerhut A, Fourtanier G, Hay JM, Holmières F, et al. Temporary fibrin glue occlusion of the main pancreatic duct in the prevention of intra-abdominal complications after pancreatic resection: prospective randomized trial. Ann Surg 2003;237:57-65. http://dx.doi.org/10.1097/00000658-200301000-00009.
- Martin I, Au K. Does fibrin glue sealant decrease the rate of anastomotic leak after a pancreaticoduodenectomy? Results of a prospective randomized trial. HPB 2013;15:561-6. http://dx.doi.org/10.1111/hpb.12018.
- Oliver JL, Medina IA, Garcıa-Almenta EM, Martin GJ, Sanchez MS, Diaz P. Use of fibrin based biological adhesives in the prevention of anastomotic leaks in the high risk digestive tract: preliminary results of the multicentre, prospective, randomised, controlled, and simple blind phase IV clinical trial: Protissucol001. CIR ESP 2012;10:647-55. http://dx.doi.org/10.1016/j.ciresp.2012.05.007.
- Musella M, Milone M, Maietta P, Bianco P, Pisapia A, Gaudioso D. Laparoscopic sleeve gastrectomy: efficacy of fibrin sealant in reducing postoperative bleeding. A randomized controlled trial. Updates Surg 2014;66:197-201. http://dx.doi.org/10.1007/s13304-014-0257-0.
- Pilone V, Di Micco R, Monda A, Villamaina E, Forestieri P. Use of Tachosil® in bariatric surgery: preliminary experience in control of bleeding after sleeve gastrectomy. Minerva Chir 2012;67:241-8.
- Sroka G, Milevski D, Shteinberg D, Mady H, Matter I. Minimizing hemorrhagic complications in laparoscopic sleeve gastrectomy – a randomized controlled trial. Obes Surg 2015;25:1577-83. http://dx.doi.org/10.1007/s11695-015-1580-3.
- Fékété F, Gayet B, Panis Y. Contribution of fibrin glue to the reinforcement of esophageal anastomoses. Presse Med 1992;21:157-9.
- Bulbuller N, Aslaner A, Oner OZ, Oruc MT, Koc U, Ongen NA, et al. Comparison of four different methods in staple line reinforcement during laparascopic sleeve gastrectomy. Int J Clin Exp Med 2013;6:985-90.
- Huang J, Qian L. The study on the efficacy of fibrin glue in preventing post-traumatic focal pancreatitis (PTFP) after radical gastrectomy. J Gastrointest Surg 2014;18:476-80. http://dx.doi.org/10.1007/s11605-013-2442-8.
- Carlson JW, Kauderer J, Walker JL, Gold MA, O’Malley D, Tuller E, et al. A randomized phase III trial of VH fibrin sealant to reduce lymphedema after inguinal lymph node dissection: a Gynecologic Oncology Group study. Gynecol Oncol 2008;110:76-82. http://dx.doi.org/10.1016/j.ygyno.2008.03.005.
- Zhibo X, Miaobo Z. Effect of sustained-release lidocaine on reduction of pain after subpectoral breast augmentation. Aesthet Surg J 2009;29:32-4. http://dx.doi.org/10.1016/j.asj.2008.10.008.
- Ulusoy AN, Polat C, Alvur M, Kandemir B, Bulut F. Effect of fibrin glue on lymphatic drainage and on drain removal time after modified radical mastectomy: a prospective randomized study. Breast J 2003;9:393-6. http://dx.doi.org/10.1046/j.1524-4741.2003.09506.x.
- Dinsmore RC, Harris JA, Gustafson RJ. Effect of fibrin glue on lymphatic drainage after modified radical mastectomy: a prospective randomized trial. Am Surg 2000;66:982-5.
- Udén P, Aspegren K, Balldin G, Garne JP, Larsson SA. Fibrin adhesive in radical mastectomy. Eur J Surg 1993;159:263-5.
- Jain PK, Sowdi R, Anderson AD, MacFie J. Randomized clinical trial investigating the use of drains and fibrin sealant following surgery for breast cancer. Br J Surg 2004;91:54-60. http://dx.doi.org/10.1002/bjs.4435.
- Johnson L, Cusick TE, Helmer SD, Osland JS. Influence of fibrin glue on seroma formation after breast surgery. Am J Surg 2005;189:319-23. http://dx.doi.org/10.1016/j.amjsurg.2005.01.004.
- Llewellyn-Bennett R, Greenwood R, Benson JR, English R, Turner J, Rayter Z, et al. Randomized clinical trial on the effect of fibrin sealant on latissimus dorsi donor-site seroma formation after breast reconstruction. Br J Surg 2012;99:1381-8. http://dx.doi.org/10.1002/bjs.8874.
- Ko E, Han W, Cho J, Lee JW, Kang SY, Jung SY, et al. Fibrin glue reduces the duration of lymphatic drainage after lumpectomy and level II or III axillary lymph node dissection for breast cancer: a prospective randomized trial. J Korean Med Sci 2009;24:92-6. http://dx.doi.org/10.3346/jkms.2009.24.1.92.
- Miri Bonjar MR, Maghsoudi H, Samnia R, Saleh P, Parsafar F. Efficacy of fibrin glue on seroma formation after breast surgery. Int J Breast Cancer 2012;2012. http://dx.doi.org/10.1155/2012/643132.
- Mustonen PK, Härmä MA, Eskelinen MJ. The effect of fibrin sealant combined with fibrinolysis inhibitor on reducing the amount of lymphatic leakage after axillary evacuation in breast cancer. A prospective randomized clinical trial. Scand J Surg 2004;93:209-12.
- Segura-Castillo JL, Estrada-Rivera O, Castro-Cervantes JM, Cortés-Flores AO, Velázquez-Ramírez GA, González-Ojeda A. Reduction of lymphatic drainage posterior to modified radical mastectomy with the application of fibrin glue. Cir Cir 2005;73:345-50.
- Moore MM, Nguyen DH, Spotnitz WD. Fibrin sealant reduces serous drainage and allows for earlier drain removal after axillary dissection: a randomized prospective trial. Am Surg 1997;63:97-102.
- Berger A, Tempfer C, Hartmann B, Kornprat P, Rossmann A, Neuwirth G, et al. Sealing of postoperative axillary leakage after axillary lymphadenectomy using a fibrin glue coated collagen patch: a prospective randomised study. Breast Cancer Res Treat 2001;67:9-14. http://dx.doi.org/10.1023/A:1010671209279.
- Gilly FN, Francois Y, Sayag-Beaujard AC, Glehen O, Brachet A, Vignal J. Prevention of lymphorrhea by means of fibrin glue after axillary lymphadenectomy in breast cancer: prospective randomized trial. Eur Surg Res 1998;30:439-43. http://dx.doi.org/10.1159/000008611.
- Benevento R, Santoriello A, Pellino G, Sciaudone G, Candilio G, De Fatico GS, et al. The effects of low-thrombin fibrin sealant on wound serous drainage, seroma formation and length of postoperative stay in patients undergoing axillary node dissection for breast cancer: a randomized controlled trial. Int J Surg 2014;12:1210-15. http://dx.doi.org/10.1016/j.ijsu.2014.10.005.
- Cipolla C, Fricano S, Vieni S, Graceffa G, Licari G, Torcivia A, et al. Does the use of fibrin glue prevent seroma formation after axillary lymphadenectomy for breast cancer? A prospective randomized trial in 159 patients. J Surg Oncol 2010;101:600-3. http://dx.doi.org/10.1002/jso.21531.
- Moore M, Burak WE, Nelson E, Kearney T, Simmons R, Mayers L, et al. Fibrin sealant reduces the duration and amount of fluid drainage after axillary dissection: a randomized prospective clinical trial. J Am Coll Surg 2001;192:591-9. http://dx.doi.org/10.1016/S1072-7515(01)00827-4.
- Vaxman F, Kolbe A, Stricher F, Zund D, Volkmar P, Gros D, et al. Does fibrin glue improve drainage after axillary lymph node dissection? Prospective and randomized study in humans. Eur Surg Res 1995;27:346-52. http://dx.doi.org/10.1159/000129419.
- Swan MC, Oliver DW, Cassell OC, Coleman DJ, Williams N, Morritt DG, et al. Randomized controlled trial of fibrin sealant to reduce postoperative drainage following elective lymph node dissection. Br J Surg 2011;98:918-24. http://dx.doi.org/10.1002/bjs.7462.
- Siim E, Dahlstrom K, Drzewiecki KT, Andersson AP. The effect of fibrin adhesive on postoperative wound secretion after lymph node dissection. Reg Cancer Treat 1994;1:51-3.
- Gilly FN, Carry PY, Brachet A, Curtil A, Burgard G, Buisson L, et al. Efficacity of fibrin glue on lymphostasis during lymph node dissection. Prospective randomised study in 40 patients. Annales De Chirurgie 1994;48:194-6.
- Furrer M, Inderbitzi R, Nachbur B. Does administration of fibrin glue prevent development of lymphoceles after radical lymphadenectomy?. Chirurg 1993;64:1044-9.
- Di Monta G, Caracò C, Crispo A, Marone U, Mozzillo N. Collagen sealant patch to reduce lymphatic drainage after lymph node dissection. World J Surg Oncol 2012;10. http://dx.doi.org/10.1186/1477-7819-10-275.
- Neuss H, Raue W, Koplin G, Schwenk W, Reetz C, Mall JW. A prospective randomized trial: the influence of intraoperative application of fibrin glue after radical inguinal/iliacal lymph node dissection on postoperative morbidity. Eur J Surg Oncol 2009;35:884-9. http://dx.doi.org/10.1016/j.ejso.2008.09.016.
- Simonato A, Varca V, Esposito M, Venzano F, Carmignani G. The use of a surgical patch in the prevention of lymphoceles after extraperitoneal pelvic lymphadenectomy for prostate cancer: a randomized prospective pilot study. J Urol 2009;182:2285-90. http://dx.doi.org/10.1016/j.juro.2009.07.033.
- Mortenson MM, Xing Y, Weaver S, Lee JE, Gershenwald JE, Lucci A, et al. Fibrin sealant does not decrease seroma output or time to drain removal following inguino-femoral lymph node dissection in melanoma patients: a randomized controlled trial (NCT00506311). World J Surg Oncol 2008;6. http://dx.doi.org/10.1186/1477-7819-6-63.
- Scholz HS, Petru E, Benedicic C, Haas J, Tamussino K, Winter R. Fibrin application for preventing lymphocysts after retroperitoneal lymphadenectomy in patients with gynecologic malignancies. Gynecol Oncol 2002;84:43-6. http://dx.doi.org/10.1006/gyno.2001.6462.
- Tachibana M, Kinugasa S, Yoshimura H, Dhar DK, Ueda S, Fujii T, et al. Does fibrin glue reduce lymph leakage (pleural effusion) after extended esophagectomy? Prospective randomized clinical trial. World J Surg 2003;27:776-81. http://dx.doi.org/10.1007/s00268-003-6989-5.
- Nielsen BP, Willumsen H, Rashmussen OV. The secretion inhibition effect of fibrin glue in mastectomy scars. A prospective, randomized, clinically controlled study. Ugeskr Laeger 1985;147:1995-6.
- Droghetti A, Schiavini A, Muriana P, Folloni A, Picarone M, Bonadiman C, et al. A prospective randomized trial comparing completion technique of fissures for lobectomy: stapler versus precision dissection and sealant. J Thorac Cardiovasc Surg 2008;136:383-91. http://dx.doi.org/10.1016/j.jtcvs.2008.04.014.
- Anegg U, Lindenmann J, Matzi V, Smolle J, Maier A, Smolle-Jüttner F. Efficiency of fleece-bound sealing (TachoSil) of air leaks in lung surgery: a prospective randomised trial. Eur J Cardiothorac Surg 2007;31:198-202. http://dx.doi.org/10.1016/j.ejcts.2006.11.033.
- Moser C, Opitz I, Zhai W, Rousson V, Russi EW, Weder W, et al. Autologous fibrin sealant reduces the incidence of prolonged air leak and duration of chest tube drainage after lung volume reduction surgery: a prospective randomized blinded study. J Thorac Cardiovasc Surg 2008;136:843-9. http://dx.doi.org/10.1016/j.jtcvs.2008.02.079.
- Rena O, Papalia E, Mineo TC, Massera F, Pirondini E, Turello D, et al. Air-leak management after upper lobectomy in patients with fused fissure and chronic obstructive pulmonary disease: a pilot trial comparing sealant and standard treatment. Interact Cardiovasc Thorac Surg 2009;9:973-7. http://dx.doi.org/10.1510/icvts.2009.202770.
- Fabian T, Federico JA, Ponn RB. Fibrin glue in pulmonary resection: a prospective, randomized, blinded study. Ann Thorac Surg 2003;75:1587-92. http://dx.doi.org/10.1016/S0003-4975(02)04994-9.
- Lopez C, Facciolo F, Lequaglie C, Rendina EA, Saita S, Dell’Amore D, et al. Efficacy and safety of fibrin sealant patch in the treatment of air leakage in thoracic surgery. Minerva Chir 2013;68:559-67.
- Gonfiotti A, Santini PF, Jaus M, Janni A, Lococo A, De Massimi AR, et al. Safety and effectiveness of a new fibrin pleural air leak sealant: a multicenter, controlled, prospective, parallel-group, randomized clinical trial. Ann Thorac Surg 2011;92:1217-25. http://dx.doi.org/10.1016/j.athoracsur.2011.05.104.
- Belcher E, Dusmet M, Jordan S, Ladas G, Lim E, Goldstraw P. A prospective, randomized trial comparing BioGlue and Vivostat for the control of alveolar air leak. J Thorac Cardiovasc Surg 2010;140:32-8. http://dx.doi.org/10.1016/j.jtcvs.2009.11.064.
- Mouritzen C, Drömer M, Keinecke HO. The effect of fibrin glueing to seal bronchial and alveolar leakages after pulmonary resections and decortications. Eur J Cardiothorac Surg 1993;7:75-80. http://dx.doi.org/10.1016/1010-7940(93)90184-D.
- Belboul A, Dernevik L, Aljassim O, Skrbic B, Radberg G, Roberts D. The effect of autologous fibrin sealant (Vivostat) on morbidity after pulmonary lobectomy: a prospective randomised, blinded study. Eur J Cardiothorac Surg 2004;26:1187-91. http://dx.doi.org/10.1016/j.ejcts.2004.08.009.
- Lang G, Csekeo A, Stamatis G, Lampl L, Hagman L, Marta GM, et al. Efficacy and safety of topical application of human fibrinogen/thrombin-coated collagen patch (TachoComb) for treatment of air leakage after standard lobectomy. Eur J Cardiothorac Surg 2004;25:160-6. http://dx.doi.org/10.1016/j.ejcts.2003.11.018.
- Marta GM, Facciolo F, Ladegaard L, Dienemann H, Csekeo A, Rea F, et al. Efficacy and safety of TachoSil® versus standard treatment of air leakage after pulmonary lobectomy. Eur J Cardiothorac Surg 2010;38:683-9. http://dx.doi.org/10.1016/j.ejcts.2010.03.061.
- Filosso PL, Ruffini E, Sandri A, Lausi PO, Giobbe R, Oliaro A. Efficacy and safety of human fibrinogen-thrombin patch (TachoSil®) in the treatment of postoperative air leakage in patients submitted to redo surgery for lung malignancies: a randomized trial. Interact Cardiovasc Thorac Surg 2013;16:661-6. http://dx.doi.org/10.1093/icvts/ivs571.
- Czerny M, Fleck T, Salat A, Zimpfer D, Klepetko W, Wolner E, et al. Sealing of the mediastinum with a local hemostyptic agent reduces chest tube duration after complete mediastinal lymph node dissection for stage I and II non-small cell lung carcinoma. Ann Thorac Surg 2004;77:1028-32. http://dx.doi.org/10.1016/j.athoracsur.2003.08.041.
- Kjaergard HK, Trumbull HR. Vivostat system autologous fibrin sealant: preliminary study in elective coronary bypass grafting. Ann Thorac Surg 1998;66:482-6. http://dx.doi.org/10.1016/S0003-4975(98)00470-6.
- Kjaergard HK, Trumbull HR. Bleeding from the sternal marrow can be stopped using Vivostat patient-derived fibrin sealant. Ann Thorac Surg 2000;69:1173-5. http://dx.doi.org/10.1016/S0003-4975(99)01560-X.
- Maisano F, Kjaergård HK, Bauernschmitt R, Pavie A, Rábago G, Laskar M, et al. TachoSil surgical patch versus conventional haemostatic fleece material for control of bleeding in cardiovascular surgery: a randomised controlled trial. Eur J Cardiothorac Surg 2009;36:708-14. http://dx.doi.org/10.1016/j.ejcts.2009.04.057.
- Lassen MR, Solgaard S, Kjersgaard AG, Olsen C, Lind B, Mittet K, et al. A pilot study of the effects of Vivostat patient-derived fibrin sealant in reducing blood loss in primary hip arthroplasty. Clin Appl Thromb Hemost 2006;12:352-7. http://dx.doi.org/10.1177/1076029606291406.
- Heyse TJ, Haas SB, Drinkwater D, Lyman S, Kim HJ, Kahn BA, et al. Intraarticular fibrinogen does not reduce blood loss in TKA: a randomized clinical trial. Clin Orthop Relat Res 2014;472:272-6. http://dx.doi.org/10.1007/s11999-013-3036-1.
- Aguilera X, Martinez-Zapata MJ, Bosch A, Urrutia G, Gonzalez JC, Jordan M, et al. Efficacy and safety of fibrin glue and tranexamic acid to prevent postoperative blood loss in total knee arthroplasty: a randomized controlled clinical trial. J Bone Joint Surg Am 2013;95:2001-7. http://dx.doi.org/10.2106/JBJS.L.01182.
- Wang GJ, Hungerford DS, Savory CG, Rosenberg AG, Mont MA, Burks SG, et al. Use of fibrin sealant to reduce bloody drainage and hemoglobin loss after total knee arthroplasty: a brief note on a randomized prospective trial. J Bone Joint Surg Am 2001;83–A:1503-5. http://dx.doi.org/10.2106/00004623-200110000-00007.
- Kluba T, Fiedler K, Kunze B, Ipach I, Suckel A. Fibrin sealants in orthopaedic surgery: practical experiences derived from use of QUIXIL® in total knee arthroplasty. Arch Orthop Trauma Surg 2012;132:1147-52. http://dx.doi.org/10.1007/s00402-012-1519-2.
- McConnell JS, Shewale S, Munro NA, Shah K, Deakin AH, Kinninmonth AW. Reducing blood loss in primary knee arthroplasty: a prospective randomised controlled trial of tranexamic acid and fibrin spray. Knee 2012;19:295-8. http://dx.doi.org/10.1016/j.knee.2011.06.004.
- Molloy DO, Archbold HA, Ogonda L, McConway J, Wilson RK, Beverland DE. Comparison of topical fibrin spray and tranexamic acid on blood loss after total knee replacement: a prospective, randomised controlled trial. J Bone Joint Surg Br 2007;89:306-9. http://dx.doi.org/10.1302/0301-620X.89B3.17565.
- Sabatini L, Trecci A, Imarisio D, Uslenghi MD, Bianco G, Scagnelli R. Fibrin tissue adhesive reduces postoperative blood loss in total knee arthroplasty. J Orthop Traumatol 2012;13:145-51. http://dx.doi.org/10.1007/s10195-012-0198-7.
- Randelli F, D’Anchise R, Ragone V, Serrao L, Cabitza P, Randelli P. Is the newest fibrin sealant an effective strategy to reduce blood loss after total knee arthroplasty? A randomized controlled study. J Arthroplasty 2014;29:1516-20. http://dx.doi.org/10.1016/j.arth.2014.02.024.
- Skovgaard C, Holm B, Troelsen A, Lunn TH, Gaarn-Larsen L, Kehlet H, et al. No effect of fibrin sealant on drain output or functional recovery following simultaneous bilateral total knee arthroplasty: a randomized, double-blind, placebo-controlled study. Acta Orthop 2013;84:153-8. http://dx.doi.org/10.3109/17453674.2013.769082.
- Choufani C, Barbier O, Bajard X, Ollat D, Versier G. Medical and economic impact of a haemostatic sealant on the rate of transfusion after total knee arthroplasty. Transfus Clin Biol 2015;22:22-9. http://dx.doi.org/10.1016/j.tracli.2015.01.001.
- Mawatari M, Higo T, Tsutsumi Y, Shigematsu M, Hotokebuchi T. Effectiveness of autologous fibrin tissue adhesive in reducing postoperative blood loss during total hip arthroplasty: a prospective randomised study of 100 cases. J Orthop Surg (Hong Kong) 2006;14:117-21. http://dx.doi.org/10.1177/230949900601400202.
- Wang GJ, Goldthwaite CA, Burks S, Crawford R, Spotnitz WD. Orthopaedic Investigators Group . Fibrin sealant reduces perioperative blood loss in total hip replacement. J Long Term Eff Med Implants 2003;13:399-411. http://dx.doi.org/10.1615/JLongTermEffMedImplants.v13.i5.50.
- Falez F, Meo A, Panegrossi G, Favetti F, La Cava F, Casella F. Blood loss reduction in cementless total hip replacement with fibrin spray or bipolar sealer: a randomised controlled trial on ninety five patients. Int Orthop 2013;37:1213-17. http://dx.doi.org/10.1007/s00264-013-1903-8.
- Antuña S, Barco R, Martínez Diez JM, Sánchez Márquez JM. Platelet-rich fibrin in arthroscopic repair of massive rotator cuff tears: a prospective randomized pilot clinical trial. Acta Orthop Belg 2013;79:25-30.
- McConnell JS, Shewale S, Munro NA, Shah K, Deakin AH, Kinninmonth AW. Reduction of blood loss in primary hip arthroplasty with tranexamic acid or fibrin spray. Acta Orthop 2011;82:660-3. http://dx.doi.org/10.3109/17453674.2011.623568.
- Kucukerdonmez C, Karalezli A, Akova YA, Borazan M. Amniotic membrane transplantation using fibrin glue in pterygium surgery: a comparative randomised clinical trial. Eye 2010;24:558-66. http://dx.doi.org/10.1038/eye.2009.136.
- Yüksel B, Unsal SK, Onat S. Comparison of fibrin glue and suture technique in pterygium surgery performed with limbal autograft. Int J Ophthalmol 2010;3:316-20.
- Bahar I, Weinberger D, Dan G, Avisar R. Pterygium surgery: fibrin glue versus Vicryl sutures for conjunctival closure. Cornea 2006;25:1168-72. http://dx.doi.org/10.1097/01.ico.0000240087.32922.ee.
- Hall RC, Logan AJ, Wells AP. Comparison of fibrin glue with sutures for pterygium excision surgery with conjunctival autografts. Clin Exp Ophthalmol 2009;37:584-9. http://dx.doi.org/10.1111/j.1442-9071.2009.02105.x.
- Karalezli A, Kucukerdonmez C, Akova YA, Altan-Yaycioglu R, Borazan M. Fibrin glue versus sutures for conjunctival autografting in pterygium surgery: a prospective comparative study. Br J Ophthalmol 2008;92:1206-10. http://dx.doi.org/10.1136/bjo.2008.139600.
- Koranyi G, Seregard S, Kopp ED. The cut-and-paste method for primary pterygium surgery: long-term follow-up. Acta Ophthalmol Scand 2005;83:298-301. http://dx.doi.org/10.1111/j.1600-0420.2005.00465.x.
- Sati A, Shankar S, Jha A, Kalra D, Mishra S, Gurunadh VS. Comparison of efficacy of three surgical methods of conjunctival autograft fixation in the treatment of pterygium. Int Ophthalmol 2014;34:1233-9. http://dx.doi.org/10.1007/s10792-014-0013-y.
- Sharma A, Kaur R, Kumar S, Gupta P, Pandav S, Patnaik B, et al. Fibrin glue versus N-butyl-2-cyanoacrylate in corneal perforations. Ophthalmology 2003;110:291-8. http://dx.doi.org/10.1016/S0161-6420(02)01558-0.
- Ratnalingam V, Eu AL, Ng GL, Taharin R, John E. Fibrin adhesive is better than sutures in pterygium surgery. Cornea 2010;29:485-9. http://dx.doi.org/10.1097/ICO.0b013e3181c29696.
- Rubin MR, Dantas PE, Nishiwaki-Dantas MC, Felberg S. Efficacy of fibrin tissue adhesive in the attachment of autogenous conjuntival graft on primary pterygium surgery. Arq Bras Oftalmol 2011;74:123-6. http://dx.doi.org/10.1590/S0004-27492011000200011.
- Srinivasan S, Dollin M, McAllum P, Berger Y, Rootman DS, Slomovic AR. Fibrin glue versus sutures for attaching the conjunctival autograft in pterygium surgery: a prospective observer masked clinical trial. Br J Ophthalmol 2009;93:215-18. http://dx.doi.org/10.1136/bjo.2008.145516.
- Uy HS, Reyes JM, Flores JD, Lim-Bon-Siong R. Comparison of fibrin glue and sutures for attaching conjunctival autografts after pterygium excision. Ophthalmology 2005;112:667-71. http://dx.doi.org/10.1016/j.ophtha.2004.08.028.
- Bahar I, Weinberger D, Gaton DD, Avisar R. Fibrin glue versus vicryl sutures for primary conjunctival closure in pterygium surgery: long-term results. Curr Eye Res 2007;32:399-405. http://dx.doi.org/10.1080/02713680701294723.
- Mellin KB, Kondler R. Management of conjunctival wounds with suture or fibrin glue following intraocular lens implantation – a comparative study. Fortschr Ophthalmol 1989;86:129-31.
- Malik VK, Kumar S. Use of fibrin glue in the management of recurrent pterygium by conjunctival autograft. Saudi Med J 2010;31:1326-30.
- Lau H. Fibrin sealant versus mechanical stapling for mesh fixation during endoscopic extraperitoneal inguinal hernioplasty: a randomized prospective trial. Ann Surg 2005;242:670-5. http://dx.doi.org/10.1097/01.sla.0000186440.02977.de.
- Boldo E. Pain after laparascopic bilateral hernioplasty: early results of a prospective randomized double-blind study comparing fibrin versus staples. Surg Endosc 2008;22:1206-9. http://dx.doi.org/10.1007/s00464-007-9587-z.
- Bracale U, Rovani M, Picardo A, Merola G, Pignata G, Sodo M, et al. Beneficial effects of fibrin glue (Quixil) versus Lichtenstein conventional technique in inguinal hernia repair: a randomized clinical trial. Hernia 2014;18:185-92. http://dx.doi.org/10.1007/s10029-012-1020-4.
- Cambal M, Zonca P, Hrbaty B. Comparison of self-gripping mesh with mesh fixation with fibrin-glue in laparoscopic hernia repair (TAPP). Bratisl Lek Listy 2012;113:103-7. http://dx.doi.org/10.4149/bll_2012_024.
- Campanelli G, Pascual MH, Hoeferlin A, Rosenberg J, Champault G, Kingsnorth A, et al. Randomized, controlled, blinded trial of Tisseel/Tissucol for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: results of the TIMELI trial. Ann Surg 2012;255:650-7. http://dx.doi.org/10.1097/SLA.0b013e31824b32bf.
- Canonico S, Sciaudone G, Pacifico F, Santoriello A. Inguinal hernia repair in patients with coagulation problems: prevention of postoperative bleeding with human fibrin glue. Surgery 1999;125:315-17. http://dx.doi.org/10.1016/S0039-6060(99)70242-4.
- Chan MS, Teoh AY, Chan KW, Tang YC, Ng EK, Leong HT. Randomized double-blinded prospective trial of fibrin sealant spray versus mechanical stapling in laparoscopic total extraperitoneal hernioplasty. Ann Surg 2014;259:432-7. http://dx.doi.org/10.1097/SLA.0b013e3182a6c513.
- Lionetti R, Neola B, Dilillo S, Bruzzese D, Ferulano GP. Sutureless hernioplasty with light-weight mesh and fibrin glue versus Lichtenstein procedure: a comparison of outcomes focusing on chronic postoperative pain. Hernia 2012;16:127-31. http://dx.doi.org/10.1007/s10029-011-0869-y.
- Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, et al. Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg 2007;245:222-31. http://dx.doi.org/10.1097/01.sla.0000245832.59478.c6.
- Tolver MA, Rosenberg J, Juul P, Bisgaard T. Randomized clinical trial of fibrin glue versus tacked fixation in laparoscopic groin hernia repair. Surg Endosc 2013;27:2727-33. http://dx.doi.org/10.1007/s00464-012-2766-6.
- Wong JU, Leung TH, Huang CC, Huang CS. Comparing chronic pain between fibrin sealant and suture fixation for bilayer polypropylene mesh inguinal hernioplasty: a randomized clinical trial. Am J Surg 2011;202:34-8. http://dx.doi.org/10.1016/j.amjsurg.2010.05.004.
- Eriksen JR, Bisgaard T, Assaadzadeh S, Jorgensen LN, Rosenberg J. Fibrin sealant for mesh fixation in laparoscopic umbilical hernia repair: 1-year results of a randomized controlled double-blinded study. Hernia 2013;174:511-14. http://dx.doi.org/10.1007/s10029-013-1101-z.
- Damiano G, Gioviale MC, Palumbo VD, Spinelli G, Buscemi S, Ficarella S, et al. Human fibrin glue sealing versus suture polypropylene fixation in Lichtenstein inguinal herniorrhaphy: a prospective observational study. Chirurgia 2014;109:660-3.
- Olmi S, Scaini A, Erba L, Guaglio M, Croce E. Quantification of pain in laparoscopic transabdominal preperitoneal (TAPP) inguinal hernioplasty identifies marked differences between prosthesis fixation systems. Surgery 2007;142:40-6. http://dx.doi.org/10.1016/j.surg.2007.02.013.
- Pryor SG, Sykes J, Tollefson TT. Efficacy of fibrin sealant (human) (Evicel) in rhinoplasty: a prospective, randomized, single-blind trial of the use of fibrin sealant in lateral osteotomy. Arch Facial Plast Surg 2008;10:339-44. http://dx.doi.org/10.1001/archfaci.10.5.339.
- Prado A, Andrades P, Danilla S, Benitez S, Wisnia P. Use of aerosolized bovine-prepared fibrin glue for skin fixation after primary open rhinoplasty: a prospective randomized and controlled trial. Aesthetic Plast Surg 2006;30:568-73. http://dx.doi.org/10.1007/s00266-006-0020-0.
- Vaiman M, Eviatar E, Segal S. The use of fibrin glue as hemostatic in endonasal operations: a prospective, randomized study. Rhinology 2002;40:185-8.
- Vaiman M, Sarfaty S, Shlamkovich N, Segal S, Eviatar E. Fibrin sealant: alternative to nasal packing in endonasal operations. A prospective randomized study. Isr Med Assoc J 2005;7:571-4.
- Yu MS, Kang SH, Kim BH, Lim DJ. Effect of aerosolized fibrin sealant on hemostasis and wound healing after endoscopic sinus surgery: a prospective randomized study. Am J Rhinol Allergy 2014;28:335-40. http://dx.doi.org/10.2500/ajra.2014.28.4047.
- Vaiman M, Eviatar E, Shlamkovich N, Segal S. Use of fibrin glue as a hemostatic in endoscopic sinus surgery. Ann Otol Rhinol Laryngol 2005;114:237-41. http://dx.doi.org/10.1177/000348940511400313.
- Vaiman M, Krakovski D, Gavriel H. Fibrin sealant reduces pain after tonsillectomy: prospective randomized study. Ann Otol Rhinol Laryngol 2006;115:483-9. http://dx.doi.org/10.1177/000348940611500701.
- Jackson MR, Gillespie DL, Longenecker EG, Goff JM, Fiala LA, O’Donnell SD, et al. Hemostatic efficacy of fibrin sealant (human) on expanded poly-tetrafluoroethylene carotid patch angioplasty: a randomized clinical trial. J Vasc Surg 1999;30:461-6. http://dx.doi.org/10.1016/S0741-5214(99)70073-X.
- Bajardi G, Pecoraro F, Mirabella D. Efficacy of TachoSil patches in controlling Dacron suture-hole bleeding after abdominal aortic aneurysm open repair. J Cardiothorac Surg 2009;4. http://dx.doi.org/10.1186/1749-8090-4-60.
- Schenk WG, Burks SG, Gagne PJ, Kagan SA, Lawson JH, Spotnitz WD. Fibrin sealant improves hemostasis in peripheral vascular surgery: a randomized prospective trial. Ann Surg 2003;237:871-6. http://dx.doi.org/10.1097/01.SLA.0000071565.02994.DA.
- Schenk WG, Goldthwaite CA, Burks S, Spotnitz WD. Fibrin sealant facilitates hemostasis in arteriovenous polytetrafluoroethylene grafts for renal dialysis access. Am Surg 2002;68:728-32.
- Saha SP, Muluk S, Schenk IW, Dennis JW, Ploder B, Grigorian A, et al. A prospective randomized study comparing fibrin sealant to manual compression for the treatment of anastomotic suture-hole bleeding in expanded polytetrafluoroethylene grafts. J Vasc Surg 2012;56:134-41. http://dx.doi.org/10.1016/j.jvs.2012.01.009.
- Chalmers RT, Darling Iii RC, Wingard JT, Chetter I, Cutler B, Kern JA, et al. Randomized clinical trial of tranexamic acid-free fibrin sealant during vascular surgical procedures. Br J Surg 2010;97:1784-9. http://dx.doi.org/10.1002/bjs.7235.
- Taylor LM, Mueller-Velten G, Koslow A, Hunter G, Naslund T, Kline R. Prospective randomized multicenter trial of fibrin sealant versus thrombin-soaked gelatin sponge for suture- or needle-hole bleeding from polytetrafluoroethylene femoral artery grafts. J Vasc Surg 2003;38:766-71. http://dx.doi.org/10.1016/S0741-5214(03)00474-9.
- Joseph T, Adeosun A, Paes T, Bahal V. Randomised controlled trial to evaluate the efficacy of TachoComb H patches in controlling PTFE suture-hole bleeding. Eur J Vasc Endovasc Surg 2004;27:549-52. http://dx.doi.org/10.1016/j.ejvs.2004.01.018.
- Milne AA, Murphy WG, Reading SJ, Ruckley CV. Fibrin sealant reduces suture line bleeding during carotid endarterectomy: a randomised trial. Eur J Vasc Endovasc Surg 1995;10:91-4. http://dx.doi.org/10.1016/S1078-5884(05)80203-5.
- Sintler MP, Mahmood A, Smith SRG, Simms MH, Vohra RK. Randomized trial comparing quixil surgical sealant with kaltostat hemostatic dressing to control suture line bleeding after carotid endarterectomy with ePTFE patch reconstruction. World J Surg 2005;29:1259-62. http://dx.doi.org/10.1007/s00268-005-7863-4.
- Milne AA, Murphy WG, Reading SJ, Ruckley CV. A randomised trial of fibrin sealant in peripheral vascular surgery. Vox Sang 1996;70:210-12. http://dx.doi.org/10.1111/j.1423-0410.1996.tb01328.x.
- Saha SP, Muluk S, Schenk W, Burks SG, Grigorian A, Ploder B, et al. Use of fibrin sealant as a hemostatic agent in expanded polytetrafluoroethylene graft placement surgery. Ann Vasc Surg 2011;25:813-22. http://dx.doi.org/10.1016/j.avsg.2010.12.016.
- Czerny M, Verrel F, Weber H, Müller N, Kircheis L, Lang W, et al. Collagen patch coated with fibrin glue components. Treatment of suture hole bleedings in vascular reconstruction. J Cardiovasc Surg 2000;41:553-7.
- Altinli E, Koksal N, Onur E, Celik A, Sumer A. Impact of fibrin sealant on Limberg flap technique: results of a randomized controlled trial. Tech Coloproctol 2007;11:22-5. http://dx.doi.org/10.1007/s10151-007-0320-7.
- Drake DB, Wong LG. Hemostatic effect of Vivostat patient-derived fibrin sealant on split-thickness skin graft donor sites. Ann Plast Surg 2003;50:367-72. http://dx.doi.org/10.1097/01.SAP.0000041484.22953.6D.
- Vanscheidt W, Ukat A, Horak V, Bruning H, Hunyadi J, Pavlicek R, et al. Treatment of recalcitrant venous leg ulcers with autologous keratinocytes in fibrin sealant: a multinational randomized controlled clinical trial. Wound Repair Regen 2007;15:308-15. http://dx.doi.org/10.1111/j.1524-475X.2007.00231.x.
- Danielsen P, Jørgensen B, Karlsmark T, Jorgensen LN, Agren MS. Effect of topical autologous platelet-rich fibrin versus no intervention on epithelialization of donor sites and meshed split-thickness skin autografts: a randomized clinical trial. Plast Reconstr Surg 2008;122:1431-40. http://dx.doi.org/10.1097/PRS.0b013e318188202c.
- Erba P, di Summa PG, Wettstein R, Raffoul W, Kalbermatten DF. Fibrin sealant for fasciocutaneous flaps. J Reconstr Microsurg 2010;26:213-17. http://dx.doi.org/10.1055/s-0030-1247716.
- Healy C, Greig AV, Murphy AD, Powell C, Pinder RJ, Saour S, et al. Prospective randomized controlled trial: fibrin sealant reduces split skin graft donor-site pain. Plast Reconstr Surg 2013;132:139e-46e. http://dx.doi.org/10.1097/PRS.0b013e318299c6f4.
- Sözen S, Emir S, Güzel K, Ozdemir CS. Are postoperative drains necessary with the Karydakis flap for treatment of pilonidal sinus? (Can fibrin glue be replaced to drains?) A prospective randomized trial. Ir J Med Sci 2011;180:479-82. http://dx.doi.org/10.1007/s11845-010-0549-4.
- Bercial ME, Sabino Neto M, Calil JA, Rossetto LA, Ferreira LM. Suction drains, quilting sutures, and fibrin sealant in the prevention of seroma formation in abdominoplasty: which is the best strategy?. Aesthetic Plast Surg 2012;36:370-3. http://dx.doi.org/10.1007/s00266-011-9807-8.
- Mabrouk AA, Helal HA, Al Mekkawy SF, Mahmoud NA, Abdel-Salam AM. Fibrin sealant and lipoabdominoplasty in obese grade 1 and 2 patients. Arch Plast Surg 2013;40:621-6. http://dx.doi.org/10.5999/aps.2013.40.5.621.
- Oliver DW, Hamilton SA, Figle AA, Wood SH, Lamberty GB. Can fibrin sealant be used to prevent postoperative drainage? A prospective randomized double blind trial. Eur J Plast Surg 2002;24:387-90. http://dx.doi.org/10.1007/s00238-001-0317-9.
- Ellis CN, Clark S. Fibrin glue as an adjunct to flap repair of anal fistulas: a randomized, controlled study. Dis Colon Rectum 2006;49:1736-40. http://dx.doi.org/10.1007/s10350-006-0718-8.
- Altomare DF, Greco VJ, Tricomi N, Arcana F, Mancini S, Rinaldi M, et al. Seton or glue for trans-sphincteric anal fistulae: a prospective randomized crossover clinical trial. Colorectal Dis 2011;13:82-6. http://dx.doi.org/10.1111/j.1463-1318.2009.02056.x.
- Lindsey I, Smilgin-Humphreys MM, Cunningham C, Mortensen NJ, George BD. A randomized, controlled trial of fibrin glue vs. conventional treatment for anal fistula. Dis Colon Rectum 2002;45:1608-15. http://dx.doi.org/10.1007/s10350-004-7247-0.
- Hammond TM, Porrett TR, Scott SM, Williams NS, Lunniss PJ. Management of idiopathic anal fistula using cross-linked collagen: a prospective phase 1 study. Colorectal Dis 2011;13:94-104. http://dx.doi.org/10.1111/j.1463-1318.2009.02087.x.
- van der Hagen SJ, Baeten CG, Soeters PB, van Gemert WG. Staged mucosal advancement flap versus staged fibrin sealant in the treatment of complex perianal fistulas. Gastroenterol Res Pract 2011;2011. http://dx.doi.org/10.1155/2011/186350.
- Siemer S, Lahme S, Altziebler S, Machtens S, Strohmaier W, Wechsel HW, et al. Efficacy and safety of TachoSil as haemostatic treatment versus standard suturing in kidney tumour resection: a randomised prospective study. Eur Urol 2007;52:1156-63. http://dx.doi.org/10.1016/j.eururo.2007.04.027.
- Cormio L, Perrone A, Di Fino G, Ruocco N, De Siati M, de la Rosette J, et al. TachoSil® sealed tubeless percutaneous nephrolithotomy to reduce urine leakage and bleeding: outcome of a randomized controlled study. J Urol 2012;188:145-50. http://dx.doi.org/10.1016/j.juro.2012.03.011.
- Luke M, Kvist E, Andersen F, Hjortrup A. Reduction of post-operative bleeding after transurethral resection of the prostate by local instillation of fibrin adhesive (Beriplast). Br J Urol 1986;58:672-5. http://dx.doi.org/10.1111/j.1464-410X.1986.tb05910.x.
- Schultz A, Christiansen LA. Fibrin adhesive sealing of ureter after ureteral stone surgery. A controlled clinical trial. Eur Urol 1985;11:267-8.
- Uwiera TC, Uwiera RR, Seikaly H, Harris JR. Tisseel and its effects on wound drainage post-thyroidectomy: prospective, randomized, blinded, controlled study. J Otolaryngol 2005;34:374-8. http://dx.doi.org/10.2310/7070.2005.34603.
- Marchac D, Greensmith AL. Early postoperative efficacy of fibrin glue in face lifts: a prospective randomized trial. Plast Reconstr Surg 2005;115:911-16. http://dx.doi.org/10.1097/01.PRS.0000153219.32665.D5.
- Lee S, Pham AM, Pryor SG, Tollefson T, Sykes JM. Efficacy of Crosseal fibrin sealant (human) in rhytidectomy. Arch Facial Plast Surg 2009;11:29-33. http://dx.doi.org/10.1001/archfacial.2008.511.
- Oliver DW, Hamilton SA, Figle AA, Wood SH, Lamberty BG. A prospective, randomized, double-blind trial of the use of fibrin sealant for face lifts. Plast Reconstr Surg 2001;108:2101-5. http://dx.doi.org/10.1097/00006534-200112000-00044.
- Carter G, Goss A, Lloyd J, Tocchetti R. Tranexamic acid mouthwash versus autologous fibrin glue in patients taking warfarin undergoing dental extractions: a randomized prospective clinical study. J Oral Maxillofac Surg 2003;61:1432-5. http://dx.doi.org/10.1016/j.joms.2003.01.001.
- Maharaj M, Diamond C, Williams D, Seikaly H, Harris J. Tisseel to reduce postparotidectomy wound drainage: randomized, prospective, controlled trial. J Otolaryngol 2006;35:36-9. http://dx.doi.org/10.2310/7070.2005.4032.
- Hester TR, Shire JR, Nguyen DB, Gerut ZE, Chen AH, Diamond J, et al. Randomized, controlled, phase 3 study to evaluate the safety and efficacy of fibrin sealant VH S/D 4 s-apr (Artiss) to improve tissue adherence in subjects undergoing rhytidectomy. Aesthet Surg J 2013;33:487-96. http://dx.doi.org/10.1177/1090820X13479969.
- Diamond MP, Korell M, Martinez S, Kurman E, Kamar M, Freeman M, et al. A prospective, controlled, randomized, multicenter, exploratory pilot study evaluating the safety and potential trends in efficacy of Adhexil. Fertil Steril 2011;95:1086-90. http://dx.doi.org/10.1016/j.fertnstert.2010.11.024.
- Maggiore ULR, Alessandri F, Ferrero S. Tachosil application after laparoscopic myomectomy: a prospective randomized trial. Ital J Gynaecol Obstet 2011;23:147-54.
- Takeuchi H, Kitade M, Kikuchi I, Shimanuki H, Kumakiri J, Kinoshita K. Adhesion-prevention effects of fibrin sealants after laparoscopic myomectomy as determined by second-look laparoscopy: a prospective, randomized, controlled study. J Reprod Med 2005;50:571-7.
- Safan A, Shaker H, Abdelaal A, Mourad MS, Albaz M. Fibrin glue versus martius flap interpositioning in the repair of complicated obstetric vesicovaginal fistula. A prospective multi-institution randomized trial. Neurourol Urodyn 2009;28:438-41. http://dx.doi.org/10.1002/nau.20754.
- Nakamura H, Matsuyama Y, Yoshihara H, Sakai Y, Katayama Y, Nakashima S, et al. The effect of autologous fibrin tissue adhesive on postoperative cerebrospinal fluid leak in spinal cord surgery: a randomized controlled trial. Spine 2005;30:347-51. http://dx.doi.org/10.1097/01.brs.0000167820.54413.8e.
- Hutter G, von Felten S, Sailer MH, Schulz M, Mariani L. Risk factors for postoperative CSF leakage after elective craniotomy and the efficacy of fleece-bound tissue sealing against dural suturing alone: a randomized controlled trial. J Neurosurg 2014;121:735-44. http://dx.doi.org/10.3171/2014.6.JNS131917.
- Hanks JB, Kjaergard HK, Hollingsbee DA. A comparison of the haemostatic effect of Vivostat patient-derived fibrin sealant with oxidised cellulose (Surgicel) in multiple surgical procedures. Eur Surg Res 2003;35:439-44. http://dx.doi.org/10.1159/000072229.
- Bochicchio GV, Gupta N, Porte RJ, Renkens KL, Pattyn P, Topal B, et al. The FINISH-3 trial: a phase 3, international, randomized, single-blind, controlled trial of topical fibrocaps in intraoperative surgical hemostasis. J Am Coll Surg 2015;220:70-81. http://dx.doi.org/10.1016/j.jamcollsurg.2014.09.019.
- Verhoef C, Singla N, Moneta G, Muir W, Rijken A, Lockstadt H, et al. Fibrocaps for surgical hemostasis: two randomized, controlled phase II trials. J Surg Res 2015;194:679-87. http://dx.doi.org/10.1016/j.jss.2014.12.011.
- Fischer CP, Bochicchio G, Shen J, Patel B, Batiller J, Hart JC. A prospective, randomized, controlled trial of the efficacy and safety of fibrin pad as an adjunct to control soft tissue bleeding during abdominal, retroperitoneal, pelvic, and thoracic surgery. J Am Coll Surg 2013;217:385-93. http://dx.doi.org/10.1016/j.jamcollsurg.2013.02.036.
- Cagatay HH, Gokce G, Ekinci M, Koban Y, Daraman O, Ceylan E. Long-term comparison of fibrin tissue glue and vicryl suture in conjunctival autografting for pterygium surgery. Postgrad Med 2014;126:97-103. http://dx.doi.org/10.3810/pgm.2014.01.2729.
- Jiang J, Yang Y, Zhang M, Fu X, Bao X, Yao K. Comparison of fibrin sealant and sutures for conjunctival autograft fixation in pterygium surgery: one-year follow-up. Ophthalmologica 2008;222:105-11. http://dx.doi.org/10.1159/000112627.
- Choi SH, Lee EK, Nam KY, Kim JY. Fibrin glue-assisted conjunctival closure in pars plana vitrectomy where conjunctival closure with a suture would be difficult. Retina 2010;30:688-91. http://dx.doi.org/10.1097/IAE.0b013e3181cdf398.
- Efthimiou E, Al-Sabah S, Sampalis JS, Christou NV. Fibrin sealant associated with increased body temperature and leukocytosis after laparoscopic gastric bypass. Surg Obes Relat Dis 2010;6:46-9. http://dx.doi.org/10.1016/j.soard.2009.03.002.
- Ibele AR, Bendewald FP, Mattar SG, McKenna DT. Incidence of gastrojejunostomy stricture in laparoscopic Roux-en-Y gastric bypass using an autologous fibrin sealant. Obes Surg 2014;24:1052-6. http://dx.doi.org/10.1007/s11695-014-1204-3.
- Nanashima A, Tobinaga S, Kunizaki M, Nonaka T, Takeshita H, Hidaka S, et al. Does fibrin glue prevent biliary and pancreatic fistula after surgical resection?. Hepatogastroenterology 2012;59:1544-7.
- Marchac D, Sándor G. Face lifts and sprayed fibrin glue: an outcome analysis of 200 patients. Br J Plast Surg 1994;47:306-9. http://dx.doi.org/10.1016/0007-1226(94)90087-6.
- Sakic A, Chevtchik O, Kilo J, Schistek R, Mueller LC, Ulmer H, et al. Simple adaptations of surgical technique to critically reduce the risk of postoperative sternal complications in patients receiving bilateral internal thoracic arteries. Interact Cardiovasc Thorac Surg 2013;17:378-82. http://dx.doi.org/10.1093/icvts/ivt089.
- Moench C, Bechstein WO, Hermanutz V, Hoexter G, Knaebel H. Comparison of the collagen haemostat Sangustop versus a carrier-bound fibrin sealant during liver resection; ESSCALIVER-Study. Trials 2010;11. http://dx.doi.org/10.1186/1745-6215-11-109.
- Vaxman F, Kolbe R, Stricher F, Boullenois JN, Volkmar P, Gros D, et al. Fibrin glue does not reduce lymphorrhoea after axillary lymph node dissection. Annales De Chirurgie 1995;49:411-16.
- Lim-Bon-Siong R, Valluri S, Gordon M, Pepose J. Efficacy and safety of the ProTek (Vifilcon A) therapeutic soft contact lens after photorefractive keratectomy. Am J Ophthalmol 1998;125:169-76. http://dx.doi.org/10.1016/S0002-9394(99)80087-7.
- Wong DL, Hockenberry-Eaton M, Wilson D, Winkelstein ML, Schwartz P. Wong’s Essentials of Pediatric Nursing. St Louis, MO: Mosby; 2001.
- MHRA . Sprayable Fibrin Sealants (Evicel, Tisseel and Artiss): Updated Guidance 2013. www.gov.uk/drug-safety-update/sprayable-fibrin-sealants-evicel-tisseel-and-artiss-updated-guidance (accessed 11 November 2015).
- EMA . Fibrinogen-Containing Solutions for Sealant Authorised For Administration by Spray Application 2013. www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Fibrinogen-containing_solutions_for_sealant_authorised_for_administration_by_spray_application/human_referral_000332.jsp&mid=WC0b01ac05805c516f (accessed 11 November 2015).
- FDA . Risk of Life-Threatening Air or Gas Embolism With the Use of Spray Devices Employing Pressure Regulator to Administer Fibrin Sealants (Baxter Healthcare Corporation) 2009. www.fda.gov/biologicsbloodvaccines/safetyavailability/ucm209778.htm (accessed 11 November 2015).
- FDA . Pediatric Safety and Utilization Review for the Pediatric Advisory Committee (PAC) Meeting 2014. www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/pediatricadvisorycommittee/ucm386895.doc (accessed 11 November 2015).
- FDA . MDR Analysis of Tisseel Fibrin Sealant Delivery Systems 2014. www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/pediatricadvisorycommittee/ucm388149.pdf (accessed 11 November 2015).
- Olmi S, Scaini A, Erba L, Bertolini A, Croce E. Laparoscopic repair of inguinal hernias using an intraperitoneal onlay mesh technique and a Parietex composite mesh fixed with fibrin glue (Tissucol). Personal technique and preliminary results. Surg Endosc 2007;21:1961-4. http://dx.doi.org/10.1007/s00464-007-9355-0.
- Eriksen JR, Bisgaard T, Assaadzadeh S, Nannestad Jorgensen L, Rosenberg J. Randomized clinical trial of fibrin sealant versus titanium tacks for mesh fixation in laparoscopic umbilical hernia repair. Br J Surg 2011;98:1537-45. http://dx.doi.org/10.1002/bjs.7646.
- Shiono N, Koyama N, Watanabe Y, Tokuhiro K, Suzuki N, Fujii T. Application of cryoprecipitate as a hematostatic glue. J Cardiovasc Surg 1998;39:609-12.
Appendix 1 Literature search strategies
Randomised controlled trial search MEDLINE In-Process & Other Non-Indexed Citations and Ovid MEDLINE search strategy
Date searched: 19 May 2015.
Date range searched: inception to 2015.
Search strategy
-
exp Fibrin tissue adhesive/ (3992)
-
Fibrin Foam/ (155)
-
(fibrin adj2 glu$).tw. (3415)
-
(fibrin adj2 seal$).tw. (1546)
-
(fibrin adj2 adhesi$).tw. (676)
-
fibrin spong$.tw. (38)
-
fibrin bandag$.tw. (7)
-
fibrin aerosol$.tw. (1)
-
(biological adj2 glu$).tw. (541)
-
(biological adj2 seal$).tw. (76)
-
Beriplast.tw. (87)
-
Bolheal.tw. (10)
-
Collaseal.tw. (1)
-
Tissucol.tw. (302)
-
Tisseel.tw. (281)
-
Quixil.tw. (36)
-
Biocol.tw. (6)
-
Omrixil.tw. (1)
-
Vivostat.tw. (36)
-
Hemaseel.tw. (10)
-
Crosseal.tw. (8)
-
Tachocomb.tw. (112)
-
Tachosil.tw. (137)
-
Tissel.tw. (5)
-
Transglutine.tw. (4)
-
or/1-25 (6775)
-
Randomized Controlled Trials as Topic/ (96,124)
-
randomized controlled trial/ (387,346)
-
Random Allocation/ (82,288)
-
Double Blind Method/ (128,148)
-
Single Blind Method/ (19,993)
-
clinical trial/ (490,948)
-
clinical trial, phase i.pt. (14,761)
-
clinical trial, phase ii.pt. (23,777)
-
clinical trial, phase iii.pt. (9622)
-
clinical trial, phase iv.pt. (994)
-
controlled clinical trial.pt. (88,856)
-
randomized controlled trial.pt. (387,346)
-
multicenter study.pt. (181,269)
-
clinical trial.pt. (490,948)
-
exp Clinical Trials as topic/ (285,725)
-
or/27-41 (1,059,020)
-
(clinical adj trial$).tw. (229,125)
-
((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw. (133,359)
-
PLACEBOS/ (32,653)
-
placebo$.tw. (164,245)
-
randomly allocated.tw. (18,131)
-
(allocated adj2 random$).tw. (20,780)
-
or/43-48 (440,148)
-
42 or 49 (1,217,384)
-
case report.tw. (215,419)
-
letter/ (867,687)
-
historical article/ (311,107)
-
or/51-53 (1,382,196)
-
50 not 54 (1,186,930)
-
26 and 55 (788)
Observational study search MEDLINE In-Process & Other Non-Indexed Citations and Ovid MEDLINE search strategy
Date searched: 19 May 2015.
Date range searched: inception to 2015.
Search strategy
-
exp Fibrin tissue adhesive/ (3992)
-
Fibrin Foam/ (155)
-
(fibrin adj2 glu$).tw. (3415)
-
(fibrin adj2 seal$).tw. (1546)
-
(fibrin adj2 adhesi$).tw. (676)
-
fibrin spong$.tw. (38)
-
fibrin bandag$.tw. (7)
-
fibrin aerosol$.tw. (1)
-
(biological adj2 glu$).tw. (541)
-
(biological adj2 seal$).tw. (76)
-
Beriplast.tw. (87)
-
Bolheal.tw. (10)
-
Collaseal.tw. (1)
-
Tissucol.tw. (302)
-
Tisseel.tw. (281)
-
Quixil.tw. (36)
-
Biocol.tw. (6)
-
Omrixil.tw. (1)
-
Vivostat.tw. (36)
-
Hemaseel.tw. (10)
-
Crosseal.tw. (8)
-
Tachocomb.tw. (112)
-
Tachosil.tw. (137)
-
Tisseel.tw. (5)
-
Transglutine.tw. (4)
-
or/1-25 (6775)
-
adverse effects.mp. (88,922)
-
contraindications.mp. (15,525)
-
Intraoperative Complications/ or Postoperative Complications/ (312,034)
-
ae.fs. (1,395,438)
-
co.fs. (1,642,251)
-
safe.ti,ab. (235,639)
-
safety.ti,ab. (304,730)
-
side effect$.ti,ab. (184,400)
-
treatment emergent.ti,ab. (2294)
-
undesirable effect$.ti,ab. (2173)
-
adrs.ti,ab. (2252)
-
(adverse adj2 (effect or effects or reaction or reactions or event or events or outcome or outcomes)).ti,ab. (267,285)
-
or/27-38 (359,9151)
-
26 and 39 (2592)
Footnote
‘ae’ denotes the subheading ‘adverse effects’.
‘co’ denotes the subheading ‘complications’.
Appendix 2 Tables of study characteristics and data tables
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Liver | |||||
| Bektas et al., 201465 | 70 | Aged ≥ 18 years scheduled for elective resection of at least one anatomical liver segment | Tisseel Spray (applied from a distance of 10–15 cm) | Manual compression | Proportion of subjects with intraoperative haemostasis; failure to achieve haemostasis within 4 minutes; intraoperative rebleeding after 4 minutes |
| de Boer et al., 201266 | 310 | Aged ≥ 18 years who underwent resection of at least one liver segment or a non-anatomical resection | Quixil (Crosseal in the USA) | Conventional technique such as suture, clip or coagulation | Occurrence of a resection surface-related complication; bleeding or evidence of a haematoma in proximity to the resection surface |
| Chapman et al., 200067 | 67 | Male or non-pregnant female patients scheduled for hemihepatectomy or segmental resection of the liver by tangential excision | CoStasis Surgical Hemostat (Cohesion Technologies Inc., Palo Alto, CA, USA) | Collagen sponge applied with pressure | Primary end point: haemostatic success; secondary end point: time to bleeding |
| Uetsuji et al., 199468 | 87 | Not reported | ‘Spray’ manufactured by IMMUNOAG (Vienna, Austria) | Liver mobilisation without fibrin sealant | Presence or absence of liver cirrhosis; operative procedure; time required for operation; duration of anaesthesia; amount of bleeding; amount of blood transfused |
| Liu and Liu, 199369 | 40 | Patients with diagnoses of benign or malignant disease of the liver scheduled for liver resection | Fibrin adhesive | No fibrin adhesive | Operation time; blood loss; post-operative bloody discharge; removal of drain tube; blood transfusion |
| Noun et al., 199670 | 82 | Patients undergoing elective hepatic resection. Patients with associated biliary reconstruction/GI procedure were excluded | Glue (Biocol; Bio-transfusion, Lille, France) | No fibrin sealant | Fluid drainage; haemoglobin concentration; bilirubin concentration; complications |
| Figueras et al., 200771 | 300 | Patients undergoing hepatic resection and patients who required contralateral hepatic resection, concomitant bowel resection or bilioenteric anastomosis | 5 ml of Tissucol | No fibrin sealant or collagen | Patients with intraoperative transfusion (%); blood transfusion units; post-operative transfusion; hospital mortality; duration of operation (minutes) |
| Frilling et al., 200573 | 121 | Patients undergoing elective hepatic resection. All patients gave their written informed consent before any trial-specific procedures | TachoSil | Argon beamer (argon beam coagulator) | Time to haemostasis was the primary outcome measure |
| Fischer et al., 201172 | 119 | Aged ≥ 18 years, elective liver resection, at least segmental resection of the liver and only minor (oozing) or moderate haemorrhage persisting after primary procedures | TachoSil | Argon beam coagulation | Primary end point: haemostasis; secondary end points: total drainage volume, post-operative duration of drainage, content of haemoglobin and bilirubin in the drainage |
| Kakaei et al., 201374 | 45 | All patients with resectable liver lesions of any size during this period were included in this study | TachoSil is an absorbable surgical patch | Glubran 2 (GEM SrI, Viareggio, Italy) is a synthetic surgical glue | The primary objective was to compare time to haemostasis between groups. Secondary outcomes were blood loss calculated; amount of blood substitute administered; sponges used; and total amount of blood in the suction |
| Kohno et al., 199275 | 62 | Not reported | Beriplast solution | Microcrystalline collagen powder from bovine | Primary end point: (efficacy of the fibrin tissue adhesive). The primary efficacy end point was haemostatic efficacy during surgery, post-operative rebleeding, bile leakage and other complications |
| Moench et al., 201476 | 128 | Patients aged > 18 years scheduled for an elective, open liver resection (segmental or non-segmental) | Patch (Tachosil) | Collagen hemostat Sangustop fleeces (Aesculap AG, Tuttlingen, Germany) | Haemostasis within 3 minutes after application of haemostat; haemostasis after 5 and 10 minutes of application of haemostat; time to haemostasis; blood transfusions |
| Schwartz et al., 200477 | 121 | Adult patients (aged > 18 years) were candidates for entry if they required liver resection for any reason except trauma and underwent no major surgical intervention beyond the liver | Spray (Crosseal/Quixil) | Actifoam (Davol Inc., Cranston, RI, USA), Avitene (CR Bard, Murray Hill, NJ, USA), Gelfoam (Pfizer Inc., New York City, NY, USA), Oxycel (Parke-Davis, Detroit, MI, USA), Surgicel and Surgicel Nu-Knit (Johnson & Johnson, Somerville, NJ, USA), and Thrombinar (King Pharmaceuticals, Bristol, TN, USA) | Time to haemostasis; percentage achieving haemostasis within 10 seconds; volume of blood loss; duration of post-operative bilious drainage; occurrence of abdominal fluid collection |
| Pancreas | |||||
| Carter et al., 201381 | 109 | Not reported | Fibrin glue was injected | The remnant could be stapled or mattress sutured | Post-operative complications; development of a pancreatic fistula; percutaneous drain placement; drain amylase values |
| Suzuki et al., 199582 | 56 | Patients undergoing distal pancreatectomy | Tisseel, glue (applied over suture) | No application of fibrin glue | Occurrence of post-operative pancreatic fistula |
| Lillemoe et al., 200483 | 124 | Patients with pancreatic-enteric anastomosis considered to be at high risk for the development of pancreatic leak | Hemaseel (glue) | No such fibrin application | Pancreatic fistula; complications; length of stay; reoperation; death; cost savings |
| Montorsi et al., 201284 | 275 | Adults aged ≥ 18 years undergoing elective distal pancreatectomy, with or without spleen preservation, for pancreatic disease other than chronic pancreatitis | Absorbable fibrin sealant patch (TachoSil) | Standard suturing or stapling | Primary end point: occurrence of post-operative pancreatic fistula; number of days until drain removal, volume of fluid drained; and length of hospital stay. Adverse events and post-operative complications were also reported |
| Suc et al., 200385 | 182 | Patients undergoing pancreatic resection | Tissucol | Resection without ductal occlusion | Post-operative abdominal complications; post-operative mortality; reoperation |
| Martin and Au, 201386 | 57 | Patients undergoing pancreaticoduodenectomy | Tisseel | No application of Tisseel | Drain lipase levels; anastomotic leak; all complications; length of hospital stay; death |
| Gall bladder | |||||
| Fu et al., 200978 | 60 | All patients whose American Society of Anaesthetists physical status was I or II | Fibrin sealant | Laparoscopic cholecystectomy | Post-operative pain. Secondary efficacy parameters: amount of pethidine hydrochloride used per capita |
| Danielsen et al., 201079 | 51 | Patients aged ≥ 18 years subjected to elective laparoscopic cholecystectomy | Autologous platelet-rich fibrin (Vivostat) | Human albumin | Wound infection |
| Dimo et al., 198980 | 80 | Patients admitted to the surgical department for elective simple cholecystectomy | Beriplast, spray | No application of Beriplast | Secretion volume and total at day 1 post surgery; number of days until drain removal |
| Mixed GI | |||||
| Hwang and Chen, 199661 | 13 | Patients with low output (< 20 ml/day) enterocutaneous fistulas that had been present for 2–4 weeks | Fibrin tissue glue, infused | Conservative treatment with total parenteral nutrition | Fistula closure time; time to discharge; recurrence; adverse reactions |
| Huang et al., 201564 | 42 | Aged 16–70 years with locally advanced gastric cancer confirmed by pathological testing and confined to the abdominal cavity | Cisplatin loaded into a syringe and sprayed | Standard care | Disease-specific overall survival; local and/or systemic infections; abdominal leakage; death as a result of the procedure; biochemical differences over time |
| Oliver et al., 201287 | 61 | Patients undergoing high-risk anastomosis of the digestive tract with or without GI surgery, intestinal anastomosis | Tissucol Duo | No fibrin adhesive in the suture line | Incidence of anastomotic leakage; incidence of further surgical intervention and mortality |
| Bulbuller et al., 201392 | 65 | Adult patients aged 18–60 years undergoing classical laparoscopic sleeve gastrectomy | 4 ml of Tisseel fibrin sealant | Without suture or with suture | Post-operative complications: bleeding; anastomosis leakage; wound site infection; abscess formation; duration of hospital stay; reoperation |
| Fernandez Fernandez et al., 199663 | 86 | Patients undergoing total gastrectomy for gastric adenocarcinoma | Tissucol | Curative resection without fibrin glue | Number of fistulas; post-operative complications; length of hospital stay; death |
| Musella et al., 201488 | 100 | Men and women aged 18–65 years with a BMI ranging from 40 to 55 kg/m2 | Spray (Tisseel) | No fibrin sealant | Occurrence of complications; operative time; length of hospital stay; time to oral diet initiation |
| Silecchia et al., 200862 | 320 | Aged 21–65 years, morbidly obese (BMI 40–59 kg/m2), undergoing laparoscopic gastric bypass | Tissucol/Tisseel fibrin sealant | Closure of the mesentery defects and the Petersen space was carried out using stitches | Proportion of complication-free patients; length of hospital stay; occurrence of anastomotic stenosis; weight loss; occurrence of early complications; adverse effects directly related to fibrin sealant |
| Pilone et al., 201289 | 30 | Candidates for sleeve gastrectomy | Tachosil | Spray (Tachosil) | Operation time; length of hospital stay (time of discharge); complications; change in haemoglobin and red blood cells |
| Sroka et al., 201590 | 165 | Aged > 18 years and had clear indication for bariatric surgery | EVICEL | Suture | Operating time; change in haemoglobin level; drain amount; patients receiving packed cells; late, infected haematoma |
| Fékété et al., 199291 | 100 | Patients undergoing surgery and requiring oesophageal anastomosis | Quick-setting fibrin glue | No application of fibrin glue | Operative mortality rate; fistulas incidence rate and severity; anastomotic stenosis |
| Huang and Qian, 201493 | 95 | Patients diagnosed with gastric carcinoma by preoperative gastric endoscopy and pathological examination | Fibrin glue | Standard surgery procedure | Operative time; intraoperative blood loss; post-operative drainage volume; complications; wound healing conditions |
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Antuña et al., 2013155 | 28 | Patients with a diagnosis of a massive rotator cuff tear of the posterosuperior rotator cuff (two tendons, > 5 cm) made by clinical examination and magnetic resonance imaging | Platelet-rich fibrin | No additional treatment was applied | Primary end point: shoulder function; secondary end points: self-report scale to evaluate the upper-extremity of disability, pain and degree of satisfaction |
| Aguilera et al., 2013143 | 172 | Adult patients (aged ≥ 18 years) scheduled for elective primary total knee arthroplasty | Tissucol | Tranexamic acid or routine haemostasis | Post-operative drain blood; total blood loss; rate of perioperative blood transfusion; haemoglobin; rate of surgical infections; length of hospital stay; rate of venous thrombosis; mortality |
| Wang et al., 2003153 | 71 | Aged > 18 years with diagnosis of osteoarthritis of the hip, scheduled for primary unilateral total hip replacement | Omrixil, spray | Standard haemostatic techniques | Intraoperative blood loss; blood loss for the post-operative period; volume of blood in the drains |
| Lassen et al., 2006141 | 69 | Patients (aged > 18 years) undergoing elective primary hip arthroplasty surgery in one Danish hospital | Vivostat (spray) | No topical haemostatic treatment | Intraoperative blood loss; drain volume; auto-transfusion; hospitalisation times; oozing; haematoma |
| Levy et al., 199914 | 46 | Patients who had osteoarthritis of the knee scheduled to have unilateral total knee arthroplasty with cement (cruciate-sparing implants) | Octacol F15 (Quixil); spray | No fibrin adhesive | Reduction in blood loss; reduction in haemoglobin levels; reduction in blood transfusion; development of haematoma; functional recovery; range of motion |
| Skovgaard et al., 2013150 | 24 | Adults aged > 18 years with symptomatic and radiographic bilateral knee osteoarthritis | EVICEL, spray | Saline as placebo | Blood loss; pain; range of movement; swelling; readmission within 90 days from the operation |
| Falez et al., 2013154 | 57 | Aged between 45 and 75 years; pre-operative haemoglobin levels equal to 11 g/dl and fibrinogen levels within normal range | Fibrin spray | Standard care: electrocautery to seal the vessels | Blood loss (ml) at 6, 24, 48 and 72 hours; measured using autologous blood transfusion device (BellovacTM, Astra Tech Ltd, Gloucestershire, UK) |
| Kluba et al., 2012145 | 24 | Patients diagnosed with primary osteoarthritis of the knee and scheduled for primary bicondylar knee arthroplasty with cement | Quixil (topical spraying) | Standardised general anaesthesia and fluid regiment control | Post-operative fluid loss; maximum flexion; length of stay; complications |
| McConnell et al., 2011156 | 66 | Patients were eligible if they were scheduled to undergo elective primary unilateral cemented hip arthroplasty | Fibrin spray | Tranexamic acid | Median intraoperative blood loss |
| Molloy et al., 2007147 | 100 | Pre-operative haemoglobin level ≤ 13.0 g/dl prior to total knee replacement | Quixil spray | Tranexamic acid intravenously | Post-operative pain scores; total blood loss; post-operative haemoglobin level; length of hospital stay; complications |
| Sabatini et al., 2012148 | 70 | Patients treated for osteoarthritis of the knee with total knee cement-less arthroplasty | Quixil | Blood recovery device | Blood loss; haemoglobin decrease; surgical time; transfusions; complications |
| Randelli et al., 2014149 | 114 | Patients with a diagnosis of osteoarthritis of the knee scheduled for primary total knee arthroplasty | EVICEL | Electrocautery after the release of the tourniquet | Total blood loss; time to drain removal; changes in haemoglobin levels; mean haemoglobin level and haemoglobin loss; drained blood loss; length of hospital stay |
| Wang et al., 2001144 | 53 | Patients with osteoarthritis and a baseline haemoglobin level of ≤ 110 g/l and evidence of a bleeding or metabolic-based haemolytic disorder were excluded from the study | Spray | No placebo was used in the control group | Amount of post-operative drainage in 12 hours; haemoglobin level on the first post-operative day; transfusion requirements; adverse events; hematoma; seroconversion |
| Choufani et al., 2015151 | 60 | Patients undergoing elective total knee replacement | EVICEL, spray | No fibrin sealant | Post-operative blood transfusion, difference in haemoglobin levels between pre and post operation; total blood loss at third post-operative day; adverse events |
| Heyse et al., 2014142 | 198 | Patients aged > 18 years who were able and willing to give informed consent | Spray applicator | Standard care – no fibrin sealant | Drain output 24 hours after surgery; transfusions; haemoglobin levels; haematocrit levels; range of motion; pain scores |
| Mawatari et al., 2006152 | 100 | Total hip arthroplasty patients | Autologous fibrin tissue adhesive, spray | No application of fibrin sealant | Intra- and post-operative blood loss; complications such as infection, deep-vein thrombosis, pulmonary embolism |
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Bajardi et al., 2009194 | 20 | Patients with intact infrarenal abdominal aortic aneurysm | TachoSil haemostatic surgical patch | Compression | Primary outcome: time to achieve haemostasis; secondary outcomes: blood loss, duration of the operation, drain volume, requirement for blood transfusion |
| Schenk et al., 2003195 | 38 | Patients who were undergoing PTFE graft placement for dialysis access | Glue (Bioplasma) | Cellulose (surgical) | Time to haemostasis; occurrence of haemostasis; time of application plus time to haemostasis; duration of graft implant procedure |
| Jackson et al., 1999193 | 47 | Patients undergoing elective carotid endarterectomy with expanded PTFE patch closure | Human fibrin sealant, applied as a liquid | Thrombin-soaked gelatine sponge | Haemostasis within 15 minutes; amount of blood loss; time to haemostasis |
| Milne et al., 1995201 | 16 | Patients undergoing a carotid endocardectomy | Spray | Nothing was applied to the suture line | Operative blood loss; time to achieve haemostasis; total operative time; drop in haemoglobin level; post-operative cerebrovascular accident |
| Milne et al., 1996203 | 39 | Patients undergoing either arterial bypass surgery with a PTFE bypass graft or aortic aneurysm repair with a woven Dacron graft | Injection (applied using a syringe) | Nothing was applied to the suture line | Time to achieve haemostasis; operation time; intraoperative blood loss; proportion achieving haemostasis; post-operative virology/infection |
| Saha et al., 2012197 | 140 | Patients scheduled for arterio-arterial bypasses with expanded PTFE grafts. Patients with moderate or severe anastomotic suture-hole bleeding that could not be controlled with additional suturing | A soluble mixture that transforms to form a matrix | Continuous manual compression with surgical gauze pads | Proportion of patients who achieved haemostasis at the study suture line of the graft; incidence of intraoperative rebleeding; incidence of post-operative rebleeding |
| Joseph et al., 2004200 | 24 | Patients undergoing femoral anastomosis and femoral or carotid patch angioplasty with PTFE grafts | TachoComb, moistened patches | Compression with 10 × 10 cm2 surgical swabs | Time to haemostasis; blood loss during the operation; duration of operation; drain volume; requirement for blood transfusion; surgeons rating of efficacy; coagulation parameters |
| Sintler et al., 2005202 | 20 | Primary procedure, normal clotting profile and on aspirin (75 mg) for at least 2 weeks prior to surgery | Quixil | Kaltostat | Time to achieve haemostasis; blood loss; adverse events |
| Taylor et al., 2003199 | 128 | Male or non-pregnant, non-lactating females, aged > 18 years, scheduled for elective extruded PTFE grafting | Beriplast P gel | Thrombin-soaked gelatin sponge | Haemostasis at 4 minutes post randomisation; volume of blood loss at the anastomosis; incidence of repeat bleeding; duration of intensive care unit stay; length of hospital stay; mortality |
| Chalmers et al., 2010198 | 70 | Aged ≥ 18 years, scheduled for vascular procedure using uncoated or heparin-coated PTFE prosthetic graft material with at least one end-to-side anastomosis to a femoral or upper-extremity artery | EVICEL | Manual compression | Primary end point: absence of bleeding at the anastomosis at 4 minutes after randomisation; secondary end point: absence of bleeding at the anastomosis |
| Czerny et al., 2000205 | 60 | Vascular reconstruction surgery with PTFE prosthesis, aged ≥ 18 years | TachoComb H patch | Surgical compresses only to control suture hole bleedings | Time to haemostasis; intraoperative blood loss; intraoperative blood substitutes; duration of the operation |
| Saha et al., 2011204 | 73 | Patients undergoing PTFE graft placement surgery, including arterio-arterial bypasses and arteriovenous dialysis access shunts | Fibrin sealant (Tisseel) | Manual compression | Proportion of patients achieving haemostasis; incidence of intraoperative rebleeding after achievement of haemostasis; incidence of post-operative rebleeding that required surgical exploration; transfusion requirements |
| Schenk et al., 2002196 | 28 | Aged ≥ 18 years who required placement of a PTFE graft with arterial and venous anastomoses using non-filament non-absorbable suture to obtain an arteriovenous fistula for renal dialysis access | Hemaseel | Commercial topical bovine thrombin (thrombogen), oxidised cellulose (Surgicel) | Time to haemostasis |
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Berger et al., 2001107 | 61 | Primary breast cancer, no previous breast surgery or neo-adjuvant chemotherapy or prior locoregional radiotherapy | TachoComb | Standard closure (not described) | Duration of axillary drainage; length of post-operative hospital stay; drainage volume; presence of local infection; use of antibiotics; use of local wound treatments; seroma formation at discharge |
| Udén et al., 199398 | 68 | Women undergoing modified radical mastectomy with axillary clearance for breast cancer | Tisseel | Control group had no glue applied | Seroma formation; wound infection; necrosis of skin flaps |
| Benevento et al., 2014109 | 60 | Female sex, aged ≥ 25 years, absences of anticoagulopathy, and/or liver disease, BMI ≤ 35 kg/m2, indication to axillary lymph node dissection | Artiss | All patients received a percutaneous vacuum drain | Volume of serous fluid; time to remove drain (days); length of post-operative hospital stay (hours); seroma; number of patients with lymphoedema |
| Jain et al., 200499 | 116 | Patients presenting with newly diagnosed carcinoma of the breast who required primary excision and axillary lymphadenectomy | Tisseel spray | Suction drain, and no drain and no fibrin | Frequency and volume of seroma; post-operative length of hospital stay; post-operative pain and wound infection; bleeding complication |
| Johnson et al., 2005100 | 82 | Females aged ≥ 18 years scheduled for elective breast procedure | Hemaseel | Placement of one or two Jackson–Pratt drains in their wound and/or axilla | Incidence of seroma formation and volume; blood loss; length of hospital stay; complications; interval to seroma resolution; number of post-operative visits |
| Llewellyn-Bennett et al., 2012101 | 101 | Women with newly diagnosed invasive or non-invasive breast cancer who required mastectomy and axillary staging | Tisseel | Standard closure of the back skin wound | Total seroma volume; total back seroma volumes aspirated after drain removal over 3 months; volume of donor-site seromas; number of seroma aspirations after drain removal; post-operative complications |
| Nielsen et al., 1985123 | 38 | NR | 2 ml of Tisseel vs. 4 ml of Tisseel | Standard/control group not defined | Wound secretion |
| Ko et al., 2009102 | 95 | Newly diagnosed breast cancer, female sex, scheduled for elective breast lumpectomy and axillary dissection | Greenplast kit (Green Cross Corp., Seoul, Korea) (spray) | Control group (non-fibrin glue) | Duration of drainage; overall drain output; incidence of seroma formation; wound-related complications |
| Di Monta et al., 2012117 | 70 | Candidates for surgical treatment of metastatic melanoma stage III by axillary or ilioinguinal radical lymph node dissection | Tachosil | Standard treatment alone | Post-operative duration of drainage; incidence of drainage removal; daily drainage volume |
| Miri Bonjar et al., 2012103 | 60 | Female aged > 18 years scheduled for elective breast procedure, had platelet counts ≥ 100,000/ml, no diabetes or advanced liver disease, not severely obese, not had axillary lymph surgery | Hemaseel | Conventional drain placement (Jackson–Pratt drain) | Estimated blood loss; length of hospital stay; post-operative day drain removal; complications; incidence of seroma; interval to seroma resolution; seroma aspirate volume; number of post-operative visits |
| Moore et al., 2001111 | 80 | Patients who were about to undergo axillary node dissection with either a lumpectomy or a modified radical mastectomy procedure | 4, 8 or 16 ml of fibrin | Use of no therapeutic agent | Time of wound drainage; volume of drainage after treatment; adverse events; serological presence of hepatitis A, B or C virus |
| Mortenson et al., 2008120 | 30 | Patients scheduled to undergo a superficial inguinofemoral lymph node dissection | Tisseel | One or two closed suction drains are inserted | Time to drain removal (days); estimated blood loss; operative time (minutes); complications |
| Mustonen et al., 2004104 | 40 | Patients undergoing modified radical mastectomy (including axillary evacuation) for breast cancer | Tisseel | Non-fibrin sealant group | Axillary drain volume and time; breast drain volume and time; length of hospital stay; seroma incidence; number of aspirations |
| Segura-Castillo et al., 2005105 | 45 | Women diagnosed with breast cancer who underwent modified radical mastectomy | Quixil | Standard mastectomy using electrocauterisation and sutures | Time to drain removal; volume of lymphatic fluid days 1–6 post surgery; seroma formation |
| Vaxman et al., 1995112 | 20 | Patients with breast cancer requiring axillary lymph node dissection with lumpectomy or a modified radical mastectomy | Tisseel | Standard mastectomy technique (cutaneous suture) | Total drainage fluid volume and duration of axillary drainage fluid; mastectomy drainage fluid and duration; hospital stays; complications |
| Zhibo and Miaobo, 200995 | 30 | Women undergoing surgical breast augmentation procedures | Fibrin glue only | Fibrin glue and lidocaine, or lidocaine only | Self-reported pain |
| Swan et al., 2011113 | 74 | Patients aged ≥ 18 years or who required elective lymph node dissection | Tisseel | No fibrin sealant | Total volume of wound drainage before drain removal; duration of drainage; seroma formation; total number of aspirations and volume; wound cellulitis; locoregional recurrence; survival |
| Ulusoy et al., 200396 | 54 | Patients who underwent modified radical mastectomy because of breast cancer | Fibrin glue | Siliconised suction drain | Drainage volumes; drain removal times; seroma formation frequency; seroma formation volume |
| Cipolla et al., 2010110 | 160 | Diagnosis of N1 breast carcinoma, and aged ≥ 18 years | Fibrin sealant | Placement of a Jackson–Pratt suction drain only | Post-operative day of drainage removal; total volume of drained serum; total volume of evacuated seroma; number of seroma aspirations needed |
| Dinsmore et al., 200097 | 27 | Women diagnosed with breast cancer who had selected radical mastectomy for treatment | Fibrin glue | Standard closure of wound | Drain output |
| Gilly et al., 1994115 | 40 | Patients undergoing inguinal or axillary lymphadenectomy | Tissucol | Same surgical procedure without the application of fibrin glue | Drainage volume; number of drainage days; number of hospitalisation days; occurrence of parietal suppuration; occurrence of post-operative seroma; post-operative comfort of the patient; skin state 1 month after the operation |
| Gilly et al., 1998108 | 108 | Patients scheduled for axillary lymphadenectomy for breast cancer, with no previous irradiation or chemotherapy | Tissucol | Same intervention without application of fibrin glue | Daily and cumulative drainage volume over the first 6 post-operative days; time to hospital discharge |
| Moore et al., 1997106 | 21 | Women who elected modified radical mastectomy for carcinoma, with level I and II axillary node dissections for an infiltrating ductal or lobular breast carcinoma | Autologous fibrin sealant | No fibrin sealant | Cumulative drainage; number of days to the first drainage reading of ≤ 40 ml (length of time the patient needed to retain a wound drain) |
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Lau, 2005172 | 93 | People aged ≥ 18 years with bilateral inguinal hernia | Tisseel | Endoscopic stapler | Post-operative pain; analgesic requirement; incidence of seroma; operative time; length of hospital stay; number of days required to resume normal activities; recurrence rate; pain |
| Boldo, 2008173 | 27 | Patients with bilateral hernia | Autologous fibrin sealant, Vivostat | Staples | Post-operative seroma; post-operative haematoma; hernia recurrence |
| Bracale et al., 2014174 | 102 | Adult aged ≥ 18 years primary uncomplicated inguinal hernia | Quixil | Conventional Lichtenstein technique | Operative time; inguinal pain recurrence; numbness |
| Cambal et al., 2012175 | 100 | Patients with unilateral inguinal hernia | Fibrin glue | Self-gripping mesh | Operative time; local complications; recurrence; ease of product use |
| Campanelli et al., 2012176 | 315 | Men aged 18–60 years | Tissucol/Tisseel drops and spray | Lichtenstein technique | Prevalence of moderate to severe pain or numbness and groin discomfort |
| Canonico et al., 1999177 | 50 | Patients with coagulation disorders | Tissucol | Lichtenstein technique | Haemorrhagic complications |
| Eriksen et al., 2011260 | 40 | Patients with umbilical hernia defects aged 18–85 years | Tisseel | Tack fixation | Acute post-operative pain |
| Lionetti et al., 2012179 | 148 | Aged > 18 years, male and with groin hernia | Quixil | Lichtenstein technique | Post-operative pain score; recurrences; proportion of patients with chronic pain |
| Lovisetto et al., 2007180 | 197 | Aged > 18 years with a diagnosis of inguinal or femoral hernia | Tissucol/Tisseel | Endopath multifeed stapler | Post-operative neuralgia |
| Chan et al., 2014178 | 130 | Male patients aged 18–70 years | Tisseel spray | Staples | Incidence of chronic pain |
| Tolver et al., 2013181 | 112 | Mean aged 18–80 years with unilateral inguinal or femoral hernia | Tisseel spray | Protacks fixation devices | Pain, discomfort, fatigue, nausea or vomiting; seroma formation; haematoma formation; hernia recurrence |
| Wong et al., 2011182 | 56 | Primary inguinal hernia, aged > 20 years | Glue (Tissucol, Tisseel) | Sutures | Post-operative pain; seroma or haematoma formation; infection; mortality |
| Damiano et al., 2014184 | 468 | Patients with primary unilateral inguinal hernia | Tisscol fibrin glue | Sutures | Operating time; intra- and post-operative complications |
| Olmi et al., 2007259 | 600 | Patients undergoing laparoscopic hernia repair | Tissucol/Tisseel | Endopath multifeed stapler | Operating time; time to return to work; rates of conversion; morbidity; mortality; recurrence |
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Carlson et al., 200894 | 137 | Female patients with a vulvar malignancy undergoing a radical vulvectomy or hemivulvectomy | Tisseel, spray | No fibrin sealant | Incidence of grade 2 and 3; incidence of wound complications; infections; number of days of drainage; discontinuation; incidence of wound separation |
| Furrer et al., 1993116 | 30 | Patients undergoing inguinal or axillary radical lymph node dissection. Lymphadenectomy-relapsed interventions, however, were excluded | Tissucol spray | Radical lymph node dissection | Drainage volume and time; lymphocele volume; hospitalisation; wound healing (clinical follow-up) |
| Siim et al., 1994114 | 30 | Patients with malignant melanoma lymph node metastases | Fibrin adhesive glue | Standard lymphadenectomy | Daily amount of wound secretion; total amount of wound secretion; number of days with drains; duration of hospital stay; post-operative, complications (i.e. hematomas, seromas, infections and flap necrosis) |
| Neuss et al., 2009118 | 58 | Patients with malignant melanoma with stage III or IV disease with lymph node metastases of the groin | Tissomat spray | Low-molecular-weight heparin | Amount and quality of the drained fluids were recorded every 24 hours; duration of drain placement |
| Simonato et al., 2009119 | 60 | The only exclusion criterion was any evidence of coagulation disorders and such cases were, in fact, excluded from study | TachoSil patch | Standard technique only | Development of symptomatic or asymptomatic lymphoceles; drainage volume and duration; all complications; need for further surgical intervention |
| Tachibana et al., 2003122 | 43 | Patients with primary carcinoma of the thoracic oesophagus undergoing one-stage transthoracic oesophagectomy | Bohleal (Kaketsuken Pharmaceuticals, Kumamoto, Japan), spray | Same surgical procedure without the application of the fibrin sealant | Reduction in the interval until the thoracic drain can be removed; incidence of post-operative complications and viral infectious diseases |
| Scholz et al., 2002121 | 93 | Patients with gynaecological malignancies undergoing surgery including pelvic or pelvic and para-aortic lymphadenectomy | Tissucol spray | Sutures | Incidence of lymphocysts; incidence of lymphoedema; incidence of deep-vein thrombosis; time to diagnosis of lymphocysts; time to regression of lymphocysts; time to diagnosis of lymphoedema; time to thrombosis |
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Nose | |||||
| Prado et al., 2006187 | 22 | Patients undergoing primary open rhinoplasty | Fibrin sealant glue (Beriplast) | No fibrin sealant glue | Post-operative pain; oedema; ecchymosis; skin adherence; average operating time; patient satisfaction |
| Pryor et al., 2008186 | 10 | Patients undergoing rhinoplasty involving lateral osteotomy | EVICEL | Gentle manual compression | Swelling, bruising and pain |
| Vaiman et al., 2002188 | 204 | Patients undergoing septoplasty | Fibrin aerosol glue (Quixil) | Merocel foam packing (Medtronic Inc., Minneapolis, MN, USA) | Number of post-operative bleeds |
| Vaiman et al., 2005189 | 64 | Patients with excessive intraoperative or immediate bleeding | Aerosol spray (Quixil/Crosseal) | Nasal packing | Bleeding |
| Yu et al., 2014190 | 82 | Patients aged > 18 years undergoing bilateral functional endoscopic sinus surgery | Fibrin sealant aerosol spray | Polyvinyl acetyl sponge packing | Severity of symptoms |
| Tonsils | |||||
| Vaiman et al., 2005191 | 513 | Patients undergoing endonasal surgeries | Fibrin glue (Quixil) | Merocel nasal packing | Unclear |
| Vaiman et al., 2006192 | 102 | Patients undergoing tonsillectomy | Spray (Quixil) | Electrocautery | Pain; dysphagia |
| Skin | |||||
| Drake and Wong, 2003207 | 46 | Patients requiring harvest of a split thickness skin graft | Spray pen | Thrombin solution and manual pressure | Time to haemostasis; differences of rates; safety of Vivostat sealant |
| Vanscheidt et al., 2007208 | 215 | Patients aged 18–90 years with a history of leg ulceration of at least 3 months | Bioseed | Compression bandage | Time to complete healing; number of patients achieving healing |
| Danielson et al., 2008209 | 40 | Patients aged > 18 years and scheduled for surgical debridement of ulcer | Autologous platelet-rich fibrin | Epithelial resurfacing; pain scores | Venous insufficiency |
| Erba et al., 2010210 | 10 | Patients with paraplegia and decubitus ulcers stage IV (Daniel’s classification) | Fibrin glue | No fibrin glue | Drainage volume; time of drain removal |
| Healy et al., 2013211 | 50 | Patients aged > 18 years undergoing split skin grafting from a lateral thigh donor site | Fibrin sealant (spray) | Self adhesive fabric dressing (Mefix) | Pain; incapacity |
| Colorectal | |||||
| Ellis and Clark, 2006216 | 58 | Patients with trans-sphincteric anal fistulas | Tisseel | Sutures | Fistula recurrence |
| Altomare et al., 2011217 | 101 | Patients with trans-sphincteric anal fistulas | Tissucol | No fibrin sealant | Healing rate; hospital stay; healing time; faecal incontinence |
| Lindsey et al., 2002218 | 42 | Patients aged ≥ 18 years with cryptoglandular or Crohn’s anal fistulas | Beriplast | Current standard fistula practice | Pain score; time to return to work; satisfaction |
| Hammond et al., 2011219 | 29 | Patients with anal fistulas | Tisseel glue | Permacol, collagen sheet | Wound healing time; return to work; patient satisfaction; continence disturbance; recurrence; proportion of symptoms |
| van der Hagen et al., 2011220 | 30 | Patients with perianal fistulas | Fibrin glue | No fibrin | Treatment failure; recurrent fistulas; soiling after treatment; quality of life; incontinence score |
| Prostate | |||||
| Luke et al., 1986223 | 30 | Patients undergoing transurethral prostatectomy | Beriplast fibrin glue | No fibrin glue | Blood loss; urine volume; concentration of haemoglobin |
| Schultz and Christiansen, 1985224 | 16 | Patients with obstruction caused by a ureteral stone | Tisseel adhesive | Interrupted sutures | Median drainage of urine postoperatively |
| Facelift | |||||
| Marchac and Greensmith, 2005226 | 29 | Patients undergoing rhytidectomy | Tisseel aerosol spray | No fibrin glue | Post-operative drainage; haematoma; degree of ecchymosis; degree of oedema |
| Lee et al., 2009227 | 9 | Patients undergoing rhytidectomy | Crosseal | No Crosseal treatment | Seroma formation; ecchymosis score |
| Oliver et al., 2001228 | 40 | Rhytidectomy procedures | Beriplast fibrin spray | No fibrin glue | Median drainage; post-operative haematoma |
| Thyroid | |||||
| Uweria et al., 2005225 | 56 | Patients with anterior neck dissection in conjunction with thyroid surgery | Tisseel | No Tisseel treatment | Drainage from surgical site; wound drainage; drain removal |
| Carter et al., 2003229 | 49 | Patients undergoing dental extractions who were therapeutically anticoagulated for comorbidities | Autologous fibrin glue | Tranexamic acid solution | Pain; discomfort haematoma; oedema |
| Maharaj et al., 2006230 | 60 | Patients aged > 18 years planned to receive superficial or total parotidectomy | Tisseel fibrin glue | Sutures | Wound drainage; duration of percutaneous drainage; length of hospital stay; frequency of complications |
| Hester et al., 2013231 | 75 | Healthy patients aged 18–75 years undergoing full rhytidectomy | Artiss sealant | No fibrin glue | Total drainage volume; incidence of adverse events |
| Mixed | |||||
| Bochicchio et al., 2015239 | 721 | Patients undergoing spinal vascular, hepatic and soft tissue procedures | Fibrocaps (Raplixa, The Medicines Company, Leiden, the Netherlands) | No fibrin glue | Gelatin sponge |
| Fischer et al., 2013241 | 90 | Patients aged > 18 years requiring non-emergency surgical procedures | Fibrin pad | Surgical original absorbable hemostat | Haemostasis |
| Verhoef et al., 2015240 | 126 | Patients with mild or moderate bleeding during a surgical procedure | Fibrocaps | Gelatin sponge | Haemostasis |
| Hanks et al., 2003238 | 73 | Patients aged 18–75 years undergoing elective surgery | Spray pen | Dry surgical sponge | Time to haemostasis; success of treatment |
| Oliver et al., 2002215 | 50 | Patients undergoing mixed surgical procedures | Beriplast | No fibrin sealant | Average drainage |
| Gynaecology (uterus) | |||||
| Diamond et al., 2011232 | 34 | Patients with bilaterally documented ovarian disease scheduled for laparoscopy | Adhexil (Johnson & Johnson, Somerville, NJ, USA) sprayed or dipped | No fibrin sealant | Incidence of adhesions; serious adverse events |
| Maggiore et al., 2011233 | 70 | Patients with intraurine uterine fibroma | Tachosil fibrin-coated sponge | No haemostatic agent used | Surgery duration; intraoperative blood loss; post-operative drainage; length of hospital stay |
| Takeuchi et al., 2005234 | 83 | Women with symptomatic uterine myomas | Beriplast spray | No application of fibrin sealant | Occurrence of post-operative adhesions |
| Safan et al., 2009235 | 40 | Patients with vesicovaginal fistulas | Autologous fibrin preparation | No fibrin preparation | Fistula size and location; fibrosis; dryness |
| Neurosurgery | |||||
| Nakamura et al., 2005236 | 39 | Patients with spinal cord tumours | Beripast-P autologous fibrin sealant | No fibrin sealant | Volume of drainage; coagulation; mean post-operative cerebrospinal fluid leakage |
| Hutter et al., 2014237 | 229 | Patients scheduled for elective cranial surgery, aged > 18 years | Collagen sponge coated with a dry layer of fibrinogen and thrombin | Standard care | Incidence of cerebrospinal fluid leakage; incidence of meningitis |
| Green et al., 201510 | 139 | Patients undergoing elective craniotomy in the supraentorial region or the processes in the posterior fossa, aged > 18 years | EVICEL | Closure with sutures | Watertight closure of the dura |
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Heart | |||||
| Kjaergard and Trumbull, 1998138 | 24 | Aged 18–80 years with coronary artery disease demonstrated by arteriogram and suitable candidate for coronary artery bypass grafting | Vivostat | Traditional methods of haemostasis alone (sutures, clips and electrocautery) | Survival (death); atrial fibrillation; anaemia; pleural effusion; pneumothoraxes; post-operative transfusions; chest tube drainage; reoperations |
| Kjaergard and Trumbull, 2000139 | 30 | Aged > 18 years admitted for elective cardiac operation requiring median sternotomy | Vivostat | No application of fibrin sealant | Time to haemostasis |
| Maisano et al., 2009140 | 119 | Aged ≥ 18 years with planned elective heart surgery, ascending aorta or arch requiring a cardiopulmonary bypass procedure | TachoSil | Standard haemostatic fleece material | Haemostasis; duration of surgery; need for intraoperative transfusions; duration of drainage; post-operative drainage volume; incidence of reoperation; post-operative transfusion and other post-operative complications |
| Shiono et al., 1998261 | 32 | Adult patients undergoing elective cardiac surgery | Fibrin glue | Cryoprecipitate from patients’ own fresh-frozen plasma | Post-operative haemoglobin concentration; platelet levels; cardiac index; rate of homologous transfusion; homologous transfusion volume |
| Tavilla et al., 201560 | 1445 | Patients undergoing elective isolated coronary artery bypass graft (either on pump or off pump) | CryoSeal | No CryoSeal treatment | Number of transfused blood products; duration of stay in intensive care unit; amount of blood loss within 48 hours post surgery; reoperations; 30-day mortality; duration of hospital stay |
| Lung | |||||
| Fabian et al., 2003128 | 100 | Patients undergoing planned open anatomic pulmonary resection or wedge resection | HemaMyst system (Haemacure Corp., Sarasota, FL, USA) | Stapling techniques | Mean duration of AAL; mean time to chest tube removal; incidence of prolonged AAL; mean first 24-hour drainage; percentage of patients discharged with valve; mean post-operative length of stay |
| Droghetti et al., 2008124 | 40 | Early stage non-small-cell lung cancer patients scheduled for elective pulmonary lobectomy | TachoSil | Routine surgical procedure with staplers | Intraoperative alveolar air leaks; percentage of patients free of air leaks throughout hospitalisation; last post-operative day when an air leak was observed; costs of procedure and hospitalisation |
| Lang et al., 2004134 | 186 | Lung cancer patients undergoing elective standard lobectomy with or without mediastinal lymphadenectomy | TachoComb | Single or continuous running sutures | Incidence of air leakage 48 hours after lobectomy; post-operative mortality and morbidity pattern was recorded in all patients |
| Anegg et al., 2007125 | 152 | Patients undergoing lobectomy or segmentectomy for non-small-cell lung cancer | TachoSil | Standard treatment | Post-operative mean air leakage (volume in ml/min); efficacy outcome; incidence of post-operative air leakage; rate of complications |
| Belboul et al., 2004133 | 40 | Adult patients with lung tumour limited to one lobe, undergoing elective lobectomy | Vivostat system | Patients assigned to the control group underwent no additional interventions (after randomisation) | Time to chest tube removal; volume at removal of chest tube; duration of thoracic epidural analgesia treatment; post-operative length of hospital stay; post-operative haemorrhage; post-operative leucocyte counts; adverse events |
| Belcher et al., 2010131 | 113 | Patients undergoing elective open thoracic procedures likely to result in a post-operative air leak | Vivostat | Reducing AAL after pulmonary resection | Duration of air leak; time to drain removal; length of hospital stay; post-operative complications |
| Lopez et al., 2013129 | 346 | Aged ≥ 18 years; patients undergoing pulmonary resection (anatomical segmental resection for lung cancer) | TachoSil | Manual suturing | Intraoperative air leakage; duration of post-operative air leakage: time to removal of last chest drain; duration of surgery; volume of drained pleural effusion; hospital length; adverse events; post-operative complications |
| Filosso et al., 2013136 | 24 | Aged ≥ 18 years who had previously undergone pulmonary resection for a thoracic malignancy | TachoSil | Stapling/suturing | Duration of air leaks; time to first and second chest tube removal; possible post-operative complications; duration of hospital stay |
| Gonfiotti et al., 2011130 | 185 | Aged 18–75 years; lung resection; primitive/secondary neoplastic pulmonary pathology | Fibrin sealant used is obtained from human plasma | The standard treatment | Mean duration of AAL from the wound closure; mean duration of drainage; percentage of patients without AALs for the entire hospitalisation time; duration of post-operative hospitalisation |
| Moser et al., 2008126 | 25 | Patients with severe airflow obstruction | Vivostat | No additional treatment | Incidence and intensity of air leaks |
| Mouritzen et al., 1993132 | 114 | Patients undergoing pulmonary resections | Spray (Beriplast P) | Suture alone | Airway tolerance pressure; rate of post-operative air leakages; duration of post-operative air leakages; length of hospital stay |
| Rena et al., 2009127 | 60 | Patients requiring a lobotomy | Fibrin patch | Suture | Intraoperative air leak |
| Czerny et al., 2004137 | 40 | Patients with clinical stage I | TachoComb | Conventional surgical haemostasis | Cumulative chest drain volume; duration of test tubes |
| Marta et al., 2010135 | 299 | Patients aged ≥ 18 years with lung cancer | TachoSil | Resuturing, stapling or no treatment | Number of patches used; success of lung inflation; need for rescue treatment; air leakage; atrial fibrillation; deaths |
| Study (author, year) | Sample size (n) | Population (inclusion criteria) | Intervention | Comparator | Outcomes |
|---|---|---|---|---|---|
| Kucukerdonmez et al., 2010157 | 70 | Patients with primary nasal pterygium who underwent pterygium excision | Tisseel (two-component fibrin glue) | 8–0 Vicryl sutures (8–10 sutures) | Procedure outcome (photographic images, graded); post-operative symptoms; operative time; recurrence |
| Yüksel et al., 2010158 | 61 | Patients with primary nasal pterygium | Beriplast P/Combi-set Aventis 1 ml | Silk (Surgisilk, Sutures Ltd, Wrexham, UK) | Complications; haemorrhage under graft; conjunctival cyst; granuloma; recurrence; surgery time; mean surgery cost; objective signs; hyperaemia |
| Bahar et al., 2006159 | 65 | Patients undergoing primary pterygium removal | Quixil | Interrupted 8–0 Vicryl sutures | Best corrected visual acuity; intraocular pressure; pain; photophobia; foreign body sensation; irritation; epiphora; local hyperaemia; conjunctival chemosis; dry-eye sensation; operative time; recurrence |
| Hall et al., 2009160 | 50 | Patients with primary nasal pterygia booked for surgery with conjunctival autograft | Tisseel (glue) | Standard sutured interrupted (Vicryl) | Surgical time; patient discomfort; recurrence; complications; post-operative pain |
| Karalezli et al., 2008161 | 50 | Patients with primary nasal pterygium | Tisseel (glue) | Vicryl 8–10 sutures | Operation time; recurrence; intensity of post-operative complaints (pain, irritation, foreign body, epiphora) |
| Koranyi et al., 2005162 | 43 | Patients with nasal primary pterygium and if informed consent was obtained | Tisseel (glue/spray) | Absorbable sutures | Post-operative pain; surgical times; recurrences |
| Sati et al., 2014163 | 60 | Eyes with ocular pterygia of grade 1, 2 and 3, and at least 2-mm extension from the limbus | Spray (Tisseel) | Vicryl suture group: I, 8/0 Vicryl | Rate of recurrence; surgical time; post-operative discomfort |
| Sharma et al., 2003164 | 40 | Patients (eyes) treated for corneal perforation | Glue | Cyanoacrylate tissue adhesive | Anterior chamber depth; inflammatory reaction; glue adherence |
| Ratnalingam et al., 2010165 | 113 | Patients with pterygium | Adhesive | Vicryl 8/0 | Duration of surgery; recurrence rate; pain scores; complications (displaced graft, conjunctival cysts) |
| Rubin et al., 2011166 | 47 | Aged 18–70 years, patients diagnosed with primary medial located pterygium | Quixil | Mononylon 10–0 (Ethicon) suture | Efficacy of the fibrin tissue adhesive; mean surgery time; ocular discomfort measured with the visual analogue scale; ocular hyperaemia was also measured |
| Srinivasan et al., 2009167 | 40 | Patients with primary pterygium | Tisseel, dripped on the graft | Polygactin sutures | Grading of Adobe Photoshop-edited eye pictures (version 7.0, Adobe Systems Inc., San Jose, CA, USA) on the degree of graft inflammation, subconjunctival haemorrhage and stability |
| Uy et al., 2005168 | 22 | Patients with primary pterygia undergoing primary pterygium excision at the Philippine General Hospital, Manila | Fibrin glue | Nylon sutures | Graft success; recurrence; subjective sensations of pain; foreign body sensation; tearing; discomfort |
| Bahar et al., 2007169 | 81 | Patients undergoing primary pterygium removal | Quixil | For excessive bleeding, one drop of adrenaline 10% solution or small amounts of sodium hyaluronate 10 mg/ml | Mean operative time (minutes); intraocular pressure; post-operative signs and symptoms (mean score); overall patient satisfaction (mean score); complications (incidence); recurrence (number of eyes) |
| Mellin and Kondler, 1989170 | 100 | Aged > 70 years, without other eye diseases such as cataract, or maculopathy | Fibrin glue | 2 8/0 silk sutures from the limbus, nasally | Foreign body sensation; wound closure |
| Malik and Kumar, 2010171 | 50 | Patients with recurrent pterygium | Tisseel Duo Quick | Three interrupted 8–0 Vicryl sutures | Pterygium recurrence; surgical time; post-operative discomfort |
Appendix 3 Tables of excluded randomised controlled trials
| Study excluded | Reason for exclusion |
|---|---|
| Agresta F, Tordin C. Laparoscopic transabdominal inguinal hernia repair: a randomized study of fibrin sealant versus absorbable tack to fix the mesh. Surg Endosc 2015;29:S35 | Abstract/full text unavailable |
| Ak G, Alpkılıç Başkırt E, Kürklü E, Koray M, Tanyeri H, Zülfikar B. The evaluation of fibrin sealants and tissue adhesives in oral surgery among patients with bleeding disorders. Turk J Haematol 2012;29:40–7 | Did not meet population/intervention criteria |
| Albala DM, Wood C, Fischer C, Hart J, Batiller J, Shen J. A randomized trial of aprotinin free fibrin sealant versus absorbable hemostat. J Endourol 2011;25:A95 | Abstract/full text unavailable |
| Albillos A, Calleja JL. Randomised trial of fibrin glue versus polidocanol for bleeding peptic ulcer. Lancet 1997;350:1397–8 | Not a RCT |
| Al-Fayez M. Fibrin Glue vs. Suture Fixation of Limbal Conjunctival Autograft for Pterygium. American Academy of Ophthalmology; 2008. URL: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/968/CN-00745968/frame.html (accessed 19 May 2015) | Abstract/full text unavailable |
| Alió JL, Mulet E, Sakla HF, Gobbi F. Efficacy of synthetic and biological bioadhesives in scleral tunnel phacoemulsification in eyes with high myopia. J Cataract Refract Surg 1998;24:983–8 | Outcomes not of interest |
| Anghelacopoulos SE, Tagarakis GI, Pilpilidis I, Kartsounis C, Chryssafis G. Albumin-glutaraldehyde bioadhesive (‘Bioglue’) for prevention of postoperative complications after stapled hemorrhoidopexy: a randomized controlled trial. Wien Klin Wochenschr 2006;118:469–72 | Did not meet population/intervention criteria |
| Anon. TISSEEL Fibrin Sealant. 2013. URL: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/847/CN-00862847/frame.html (accessed July 2013) | Not a RCT |
| Arslani N, Patrlj L, Kopljar M, Rajkovic Z, Altarac S, Papes D, et al. Advantages of new materials in fascia transversalis reinforcement for inguinal hernia repair. Hernia 2010;14:617–21 | Not a RCT |
| Ayala M. Results of pterygium surgery using a biologic adhesive. Cornea 2008;27:663–7 | Not a RCT |
| Babicki A, Dobosz M. Second-look endoscopy with repeated injection of thrombin with adrenaline vs fibrin glue in bleeding peptic ulcer. Br J Surg 1988;85(Suppl. 2):113 | Abstract/full text unavailable |
| Babicki A, Dobosz M, Marczewski R, Wajda Z. [Evaluation of using fibrin tissue adhesive (Beriplast) and preparations of thrombin and adrenalin in injection hemostasis methods for gastric and duodenal ulcer hemorrhage. Randomized, prospective clinical trial.] Wiad Lek 1997;50(Suppl. 1):383–7 | Did not meet population/intervention criteria |
| Bailey SH, Oni G, Guevara R, Wong C, Saint-Cyr M. Latissimus dorsi donor-site morbidity: the combination of quilting and fibrin sealant reduce length of drain placement and seroma rate. Ann Plast Surg 2012;68:555–8 | Not a RCT |
| Ben-Rafael Z, Ashkenazi J, Shelef M, Farhi J, Voliovitch I, Feldberg D, et al. The use of fibrin sealant in in vitro fertilization and embryo transfer. Int J Fertil Menopausal Stud 1995;40:303–6 | Did not meet population/intervention criteria |
| Benyamini OG, Barkana Y, Hartstein M, Attas L, Avni I, Zadok D. Biological glue in pterygium surgery with a rotational flap or sliding flaps. Cornea 2008;27:911–15 | Did not meet population/intervention criteria |
| Beppu T, Iwatsuki M, Okabe H, Okabe K, Masuda T, Hayashi H, et al. A new approach to percutaneous transhepatic portal embolization using ethanolamine oleate iopamidol. J Gastroenterol 2010;45:211–17 | Not a RCT |
| Berg P, Born P, Barina W, Simon W, Zellmer R, Paul F. [Fibrin glue versus Polidocanol by upper gastrointestinal bleeding.] Gastroenterol 1990;28:467 | Abstract/full text unavailable |
| Berg PL, Barina W, Born P. Endoscopic injection of fibrin glue versus polidocanol in peptic ulcer hemorrhage: a pilot study. Endoscopy 1994;26:528–30 | Did not meet population/intervention criteria |
| Bernardo L, Bernardo WM, Shu EB, Roz LM, Almeida CC, Monaco BA, et al. Does the use of DuraSeal in head and spinal surgeries reduce the risk of cerebrospinal fluid leaks and complications when compared to conventional methods of dura mater closure? Rev Assoc Med Bras 2012;58:402–3 | Review |
| Bernasek TL, Burris RB, Fujii H, Levering MF, Polikandriotis JA, Patterson JJ. Effect on blood loss and cost-effectiveness of pain cocktails, platelet-rich plasma, or fibrin sealant after total knee arthroplasty. J Arthroplasty 2012;27:1448–51 | Not a RCT |
| Biedner B, Rosenthal G. Conjunctival closure in strabismus surgery: Vicryl versus fibrin glue. Ophthalmic Surg Lasers 1996;27:967 | Not a RCT |
| Blinder D, Manor Y, Martinowitz U, Taicher S, Hashomer T. Dental extractions in patients maintained on continued oral anticoagulant: comparison of local hemostatic modalities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:137–40 | Not a RCT |
| Bochicchio G, Singla N, Gupta NY, Porter R, Renkens KL, Pattyn P, et al. An international, multicenter, randomized, single-blind, controlled trial of a dry-powder, fibrin sealant for mild to moderate perioperative surgical bleeding. J Am Coll Surg 2014;219(Suppl. 1):e13–14 | Abstract/full text unavailable |
| Boereboom C, Watson NFS, Liptrot SA, Lund JN, Tierney GM. A randomised trial of fibrin glue versus surgery for pilonidal disease: results and long term follow up. Colorectal Dis 2010;12:20 | Abstract/full text unavailable |
| Buciarelli P, Ginelli G, Misani M, Moia M. Fibrin glue plus tranexamic acid mouthwashing in patients on oral anticoagulants undergoing dental extractions: a randomised study. Thrombosis Haemostasis 1997;(Suppl.):37 | Abstract/full text unavailable |
| Calabrò B, Ponsetto M, Greco R, Peradotto F, Personnettaz E, Obialero M. [Treatment of leg ulcers with fibrin glue.] Minerva Chir 1995;50:569–74 | Not a RCT |
| Caldas Neto S, Oliveira RL, Caldas N. Use of in fibrin glue in the prevention of postoperative bleeding and hematomas after septoplasty. Revista Brasileira de Otorrinolaringologia 2002;68:635–8 | Did not meet population/intervention criteria |
| Calvet X, Vergara M, Brullet E, Gisbert JP, Campo R. Addition of a second endoscopic treatment following epinephrine injection improves outcome in high-risk bleeding ulcers. Gastroenterology 2004;126:441–50 | Review |
| Campanelli G, Champault G, Pascual MH, Hoeferlin A, Kingsnorth A, Rosenberg J, et al. Randomized, controlled, blinded trial of Tissucol/Tisseel for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: rationale and study design of the TIMELI trial. Hernia 2008;12:159–65 | Not a RCT |
| Canonico S. The use of human fibrin glue in the surgical operations. Acta Bio-Medica 2003;74(Suppl. 2):21–5 | Not a RCT |
| Cardillo G, Lococo A, De Massimi AR, D’Agostino A, Carleo F, Larocca V, et al. Adverse effects of fibrin sealants in thoracic surgery. The safety of a new fibrin sealant: multicentre, controlled, prospective, parallel group randomised clinical trial. Interact Cardiovasc Thorac Surg 2011;13:S56 | Did not meet population/intervention criteria |
| Carter TI, Fong ZV, Hyslop T, Lavu H, Tan WP, Hardacre J, et al. A dual-institution randomized controlled trial of remnant closure after distal pancreatectomy: Does the addition of falciform patch and fibrin glue improve outcomes? Gastroenterology 2012;142(Suppl. 1):1042–3 | Abstract/full text unavailable |
| Cedin AC, Atallah ÁN, Andriolo RB, Cruz OL, Pignatari SN. Surgery for congenital choanal atresia. Cochrane Database Syst Rev 2012;2:CD008993 | Review |
| Cesana G, Olmi S, Croce E. Trans-abdominal pre-peritoneal laparoscopic inguinal hernia repair versus classical inguinotomic repair: a randomized study. Surg Endosc 2011;25:S7 | Abstract/full text unavailable |
| Chan MS, Melissa CS, Teoh AY, Bun TA, Chan KW, Wing CK, et al. Randomized double-blinded prospective trial of fibrin sealant spray versus mechanical stapling in laparoscopic total extraperitoneal hernioplasty. Ann Surg 2014;259:432–7 | Letter/commentary/erratum |
| Chang YR, Jang JY, Kwon W, Kang MJ, Choi DW, Choi SH, et al. Interim analysis of prospective randomized controlled study comparing clinical early outcome including pancreatic fistula between external and internal pancreatic drainage in pancreaticoduodenectomy. HPB 2014;16:112 | Abstract/full text unavailable |
| Charles JF, Barra JA, Leroy JP. [Mesenteric fold by biological glue. Experimental study and clinical application (author’s translation).] Ann Chir 1976;30:651–5 | Not a RCT |
| Chiu CC. Randomized clinical trial of techniques for closure of the pancreatic remnant following distal pancreatectomy (Br J Surg 2009;96:602–7). Br J Surg 2009;96:1222 | Review |
| Chou D, Cheng J, Chesnut R, Choudhri H, Gopinath S, Scott Graham R, et al. A prospective, multi-center, randomized controlled study to compare a low swell formulation of a PEG hydrogel spinal sealant as an adjunct to sutured dural repair with common dural sealing methods. Spine J 2010;10(Suppl. 1):80 | Did not meet population/intervention criteria |
| Chu FCK, Yao P, Morris DL. A randomized controlled study of the efficacy of fibrin glue in reducing fluid collections following liver surgery. ANZ J Surg 2008;78:A71 | Abstract/full text unavailable |
| Codispoti M, Mankad PS. Significant merits of a fibrin sealant in the presence of coagulopathy following paediatric cardiac surgery: randomised controlled trial. Eur J Cardiothorac Surg 2002;22:200–5 | Did not meet population/intervention criteria |
| Conboy P, Brown DH. Use of tissue sealant for day surgery parotidectomy. J Otolaryngol Head Neck Surg 2008;37:208–11 | Not a RCT |
| Copuroğlu C, Ercan S, Ozcan M, Ciftdemir M, Turan FN, Yalniz E. Comparison of autogenous bone graft donor site haemostatic agents used in spinal surgery. Acta Orthop Traumatol Turc 2011;45:359–64 | Did not meet population/intervention criteria |
| Cormio L, Perrone A, Pentimone S, Selvaggio O, Lorusso F, Di Fino G, et al. Tachosil-sealed tubeless percutaneous nephrolithotomy in supine antero-lateral position: a prospective study. Eur Urol Suppl 2010;9:35 | Abstract/full text unavailable |
| Corral M, Ferko N, Hollmann S, Jamous N, Batiller J, Shen JX, et al. Clinician reported ease of use for a novel fibrin sealant patch for hemostasis: results from three randomized controlled trials. J Thromb Haemost 2014;12:31–2 | Abstract/full text unavailable |
| Cruz-Korchin N, Korchin L. The use of fibrin sealant (Tisseel) in abdominoplasty. Plastic Reconstruct Surg 2005;116(Suppl. 3):23–5 | Abstract/full text unavailable |
| Czerny et al. 2004137 | Did not meet population/intervention criteria |
| D’Andrea AA, Costantino V, Sperti C, Pedrazzoli S. Human fibrin sealant in pancreatic surgery: it is useful in preventing fistulas? A prospective randomized study. Ital J Gastroenterol 1994;26:283–6 | Did not meet population/intervention criteria |
| De Boer MT, Porte RJ. Reply: Re: Fibrin sealant for prevention of resection surface-related complications after liver resection: a randomized controlled trial. Ann Surg 2015;261:e78 | Letter/commentary/erratum |
| Di Saverio S, Masetti M, Zanello M, De Blasiis MG, Jovine E. Re: Fibrin sealant for prevention of resection surface-related complications after liver resection: a randomized controlled trial. Ann Surg 2015;261:e77–8 | Letter/commentary/erratum |
| Dobrilla G, Rutgeerts P, Rauws EAJ, Wara P, Hoos A, Dobrilla G, et al. Fibrin sealant (Beriplast) vs polidocanol 1% in the endoscopic treatment of bleeding gastroduodenal ulcers: final results of a phase III clinical trial on adjuvant intraportal infusion with heparin and 5 fluorouracil (5 FU) in resectable colon cancer (EORTC GITCCG 1983 1987). European Organization for Research and Treatment of Cancer Gastrointestinal Tract Cancer Cooperative Group. Eur J Cancer 1997;33:1209–15 | Letter/commentary/erratum |
| Dovellini EV, Taddeucci E, Trapani M, Valenti R, Moschi G, Cerisano G, et al. Pocket haematoma prevention in patients who required implantation/replacement of a pacemaker or implantable cardiac defibrillator. The PHP Study. Eur Heart J 2011;32:305 | Abstract/full text unavailable |
| Draus JM, Huss SA, Harty NJ, Cheadle WG, Larson GM. Enterocutaneous fistula: are treatments improving? Surgery 2006;140:570–6 | Not a RCT |
| Ebbehoj J, Gavrilyuk BK, Menzul VA, Paklin EL, Rochev YuA. Controlled trial of Biocol versus Jelonet on donor sites. Burns 1996;22:557–9 | Did not meet population/intervention criteria |
| Eimiller A, Berg P, Born P, Barina W, Paul F, Homann J. [Fibrin glue as a sclerotherapeutic agent.] Gastroenterol 1988;26:458 | Abstract/full text unavailable |
| El Nakeeb A. Influence of fibrin glue on seroma formation after modified radical mastectomy: a prospective randomized study. Breast J 2009;15:671–2 | Letter/commentary/erratum |
| Eriksen JR. Pain and convalescence following laparoscopic ventral hernia repair. Danish Med Bulletin 2011;58:B4369 | Pre-results for Eriksen et al.183 |
| Everts PA, Devilee RJ, Brown Mahoney C, Eeftinck-Schattenkerk M, Box HA, Knape JT, et al. Platelet gel and fibrin sealant reduce allogeneic blood transfusions in total knee arthroplasty. Acta Anaesthesiol Scand 2006;50:593–9 | Not a RCT |
| Foster K, Greenhalgh D, Gamelli RL, Mozingo D, Gibran N, Neumeister M, et al. Efficacy and safety of a fibrin sealant for adherence of autologous skin grafts to burn wounds: results of a phase 3 clinical study. J Burn Care Res 2008;29:293–303 | Did not meet population/intervention criteria |
| Fullarton G, Galloway D. Randomised trial of fibrin glue versus polidocanol for bleeding peptic ulcer. Lancet 1997;350:1397–8 | Letter/commentary/erratum |
| Fuller CW, Gillespie MB, Nguyen SA, Jones T, Hornig JD. A double-blind, randomized, placebo-controlled clinical trial evaluating fibrin sealant in thyroidectomy closure. Otolaryngol Head Neck Surg 2014;151(Suppl. 1):P160–1 | Abstract/full text unavailable |
| Garcia-Olmo D, Herreros M, Guadalajara H, DeLaQuintana P, Trebol J, Georgiev-Hristov T, et al. Expanded adipose derived autologous stem cells for the treatment of complex cryptoglandular fistulas. A phase III clinical trial (fatt1: Fistulaadvanced therapy trial 1) and longterm evaluation (LTE). Dis Colon Rectum 2011;54:e68–e9 | Abstract/full text unavailable |
| Genyk Y, Kato T, Pomposelli JJ, Lophaven KW, Chapman WC. Tachosil versus surgicel original for the secondary treatment of local bleeding in adult patients undergoing hepatic resection. HPB 2014;16:27 | Abstract/full text unavailable |
| Gibran N, Luterman A, Herndon D, Lozano D, Greenhalgh DG, Grubbs L, et al. Comparison of fibrin sealant and staples for attaching split-thickness autologous sheet grafts in patients with deep partial- or full-thickness burn wounds: a phase 1/2 clinical study. J Burn Care Res 2007;28:401–8 | Did not meet population/intervention criteria |
| Gilly FN, Sayag-Beaujard AC, Francois Y. Efficacy of fibrin glue (Tisseel) in axillary lymph node removal for breast cancer: prospective randomized trial. Eur J Surg Oncol 1996;22:397–8 | Abstract/full text unavailable |
| Gioffrè Florio MA, Mezzasalma F, Manganaro T, Pakravanan H, Cogliandolo A. [The use of fibrin glue in the surgery of breast carcinoma.] G Chir 1993;14:239–41 | Unobtainable |
| Giovannacci L, Eugster T, Stierli P, Hess P, Gürke L. Does fibrin glue reduce complications after femoral artery surgery? A randomised trial. Eur J Vasc Endovasc Surg 2002;24:196–201 | Did not meet population/intervention criteria |
| Gipponi M, Reboa G, Testa T, Giannini G, Strada P. Tension-free primary closure with autologous platelet gel versus VivostatTM for the definitive treatment of chronic sacrococcygeal pilonidal disease. In Vivo 2010;24:583–9 | Did not meet population/intervention criteria |
| Giusti G, Maugeri O, Piccinelli A, Graziotti P. Is sealing of percutaneous tract with hemostatic sealant really necessary after tubeless procedure? Eur Urol Suppl 2009;8:263 | Abstract/full text unavailable |
| Glickman M, Gheissari A, Money S, Martin J, Ballard JL. A polymeric sealant inhibits anastomotic suture hole bleeding more rapidly than gelfoam/thrombin: results of a randomized controlled trial. Arch Surg 2002;137:326–31 | Did not meet population/intervention criteria |
| González HD, Figueras Felip J. [Topical hemostatic devices in surgery: between science and marketing.] Cir Esp 2009;85(Suppl. 1):23–8 | Review |
| Gopal SC, Gangopadhyay AN, Mohan TV, Upadhyaya VD, Pandey A, Upadhyaya A, et al. Use of fibrin glue in preventing urethrocutaneous fistula after hypospadias repair. J Pediatr Surg 2008;43:1869–72 | Did not meet population/intervention criteria |
| Greenhalgh DG, Gamelli RL, Lee M, Delavari M, Lynch JB, Hansbrough JF, et al. Multicenter trial to evaluate the safety and potential efficacy of pooled human fibrin sealant for the treatment of burn wounds. J Trauma 1999;46:433–40 | Did not meet population/intervention criteria |
| Grimaud JC, Munoz-Bongrand N, Siproudhis L, Abramowitz L, Sénéjoux A, Vitton V, et al. Fibrin glue is effective healing perianal fistulas in patients with Crohn’s disease. Gastroenterology 2010;138:2275–81 | Did not meet population/intervention criteria |
| Grimm C, Polterauer S, Helmy S, Cibula D, Zikan M, Reinthaller A, et al. A collagen-fibrin patch (Tachosil) for the prevention of symptomatic lymphoceles after pelvic lymphadenectomy in women with gynecologic malignancies: a randomized clinical trial. BMC Cancer 2014;14:1–7 | Not a RCT |
| Grossman JA, Capraro PA, Atagi T. A prospective, randomized, double-blind trial of the use of fibrin sealant for face lifts. Plast Reconstr Surg 2002;110:1371–2 | Letter/commentary/erratum |
| Grund KE, Salm R, Fischer H, Becker HD. Endoscopic therapy of heavy ulcerous bleeding: obvious advantages of fibrin glue against polidocanol in a controlled randomised study. Endoskopie Heute 1993;6:46 | Abstract/full text unavailable |
| Gugenheim J, Bredt LC, Iannelli A. A randomized controlled trial comparing fibrin glue and PlasmaJet on the raw surface of the liver after hepatic resection. Hepatogastroenterology 2011;58:922–5 | Did not meet population/intervention criteria |
| Günay H. [Transplantation of allogeneic freeze-preserved bone spongiosa into periodontal bone defects: clinical results.] Schweiz Monatsschr Zahnmed 1988;98:611–18 | Did not meet population/intervention criteria |
| Gust R, Kleine P, Fabel H. [Fibrin glue and tetracycline pleurodesis in recurrent malignant pleural effusions. A randomized comparative study.] Med Klin 1990;85:18–23 | Unobtainable |
| Hammond TM, Grahn MF, Lunniss PJ. Fibrin glue in the management of anal fistulae. Colorectal Dis 2004;6:308–19 | Review |
| Hayes Inc. InteguSeal Microbial Sealant (Kimberly-Clark Worldwide Inc.) for Prevention of Surgical Site Infection (Structured Abstract). 2009. URL: www.hayesinc.com/hayes/crd/?crd=10164 (accessed 19 May 2015) | Abstract/full text unavailable |
| Hayes Inc. Tisseel VH (Baxter Healthcare Corp.) for Cardiac Surgery (Structured Abstract). 2008. URL: www.hayesinc.com/hayes/crd/?crd=7985 (accessed 19 May 2015) | Abstract/full text unavailable |
| Hayes Inc. Tisseel VH (Baxter Healthcare Corp.) for Noncardiac Surgeries with Problematic Hemostasis (Structured Abstract). 2008. URL: www.hayesinc.com/hayes/crd/?crd=7986 (accessed 19/05/15) | Abstract/full text unavailable |
| Heldwein W, Avenhaus W, Schönekäs H, Kaess H, Müller-Lissner S, Hasford B, et al. Injection of fibrin tissue adhesive versus laser photocoagulation in the treatment of high-risk bleeding peptic ulcers: a controlled randomized study. Endoscopy 1996;28:756–60 | Did not meet population/intervention criteria |
| Herreros MD, Garcia-Arranz M, Guadalajara H, De-La-Quintana P, Garcia-Olmo D, FATT Collaborative Group. Autologous expanded adipose-derived stem cells for the treatment of complex cryptoglandular perianal fistulas: a phase III randomized clinical trial (FATT 1: fistula Advanced Therapy Trial 1) and long-term evaluation. Dis Colon Rectum 2012;55:762–72 | Did not meet population/intervention criteria |
| Hickey NC. Randomized clinical trial of tranexamic acid-free fibrin sealant during vascular surgical procedures. Br J Surg 2010;97:1790 | Letter/commentary/erratum |
| Hidalgo M, Castillo MJ, Eymar JL, Hidalgo A. Lichtenstein inguinal hernioplasty: sutures versus glue. Hernia 2005;9:242–4 | Not a RCT |
| Hilten JA, Verra WC, Honohan A, Wildt-Eggen J, Nelissen R. The effectiveness of a single-donor allogeneic fibrin sealant on functional knee recovery: a multicenter randomized controlled trial. Transfusion 2014;54:201a | Abstract/full text unavailable |
| Holle J. Early postoperative efficacy of fibrin glue in face lifts: a prospective randomized trial. Plast Reconstr Surg 2005;115:917–18 | Discussion paper |
| Huang QS, Hong GX, Wang FB, Kang H, Weng YX, Chen ZB. Dynamic changes in countertraction intensity of the peripheral nerve repaired with the adhesion of fibrin glue. Chin J Clin Rehabil 2005;9:192–4 | Not a RCT |
| Imhof M, Ohmann C, Röher HD, Glutig H, DUESUC study group. Endoscopic versus operative treatment in high-risk ulcer bleeding patients – results of a randomised study. Langenbecks Arch Surg 2003;387:327–36 | Did not meet population/intervention criteria |
| Inghilleri G, Aloni A, Santoleri L, Mancini L, Fonti E, Rondinara G, et al. Home-made versus commercial fibrin glue in liver surgery. Transfus Altern Transfus Med 2005;7(Suppl. 1):103 | Not a RCT |
| Jackson MR. Tissue sealants: current status, future potential. Nat Med 1996;2:637–8 | Review |
| Jain AK, Sukhija J. Comparison of Cut-and-Paste with Cut-and-Suture Technique of Pterygium Surgery. Poster session presented at American Academy of Ophthalmology, 2006, Las Vegas, TX, USA | Abstract/full text unavailable |
| Jiang J, Yang Y, Zhang M, Fu X, Bao X, Yao K. Comparison of fibrin sealant and sutures for conjunctival autograft fixation in pterygium surgery: one-year follow-up. Ophthalmologica 2008;222:105–11 | Not a RCT |
| Jones BM, Grover R. Early postoperative efficacy of fibrin glue in face lifts: a prospective randomized trial. Plast Reconstr Surg 2007;119:433–4 | Discussion paper |
| Kamal HM, Goda HAEB. Epidural fibrin glue for treatment of post-dural puncture headache (PDPH): comparative study with epidural blood patch. Eg J Anaesth 2009;25:41–7 | Did not meet population/intervention criteria |
| Kanemaru S, Umeda H, Kitani Y, Nakamura T, Hirano S, Ito J. Regenerative treatment for tympanic membrane perforation. Otol Neurotol 2011;32:1218–23 | Did not meet population/intervention criteria |
| Kim A, Lopez MA, Rojas V, Broman AT, Chuck RS, Batlle JF. Comparison of preserved amniotic membrane and dehydrated amniotic membrane allografting using fibrin glue or sutures for attachment after excision of primary pterygium. IOVS 2007;48:5316 | Abstract/full text unavailable |
| Kitajiri S, Tabuchi K, Hiraumi H, Kaetsu H. Relief of post-tonsillectomy pain by release of lidocaine from fibrin glue. Laryngoscope 2001;111:642–4 | Did not meet population/intervention criteria |
| Klecker C, Knoll S, Moller T. [Adrenalin versus adrenalin and Beriplast as primary therapy of acute bleeding in the upper gastrointestinal tract]. Gastroenterol 2004;42:1219 | Did not meet population/intervention criteria |
| Klinfelder JW, Lange DE. Application of hydroxyapatite combined with fibrin glue in periodontal surgery. J Dent Res 1989;68:643 | Abstract/full text unavailable |
| Kokesch-Häuser S, Beer M, Staehler G. [Effect of intraoperative fibrin gluing on lymph flow and lymphocele formation after kidney transplantation.] Urologe A 1993;32:334–8 | Did not meet population/intervention criteria |
| Kraus TW, Mehrabi A, Schemmer P, Kashfi A, Berberat P, Büchler MW. Scientific evidence for application of topical hemostats, tissue glues, and sealants in hepatobiliary surgery. J Am Coll Surg 2005;200:418–27 | Review |
| Kurian A, Reghunadhan I, Nair KG. Autologous blood versus fibrin glue for conjunctival autograft adherence in sutureless pterygium surgery: a randomised controlled trial. Br J Ophthalmol 2015;99:464–70 | Did not meet population/intervention criteria |
| Lantis JC 2nd, Marston WA, Farber A, Kirsner RS, Zhang Y, Lee TD, et al. The influence of patient and wound variables on healing of venous leg ulcers in a randomized controlled trial of growth-arrested allogeneic keratinocytes and fibroblasts. J Vasc Surg 2013;58:433–9 | Outcomes not of interest |
| Larsen T, Devantier A, Iversen E, Fischer A, Hansen R, Dragsted J. [Treatment of testicular hydrocele with fibrin adhesive.] Ugeskr Laeg 1986;148:896–7 | Not a RCT |
| Lee S, Kim HR, Cho S, Huh DM, Lee EB, Ryu KM, et al. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 2014;98:2005–11 | Did not meet population/intervention criteria |
| Lei QF, Cai W. Clinical observation on fibrin glue application during pterygium surgery. Int Eye Sci 2015;15:364–6 | Not a RCT |
| Lesur G. Upper gastrointestinal hemorrhages not related to portal hypertension. Hepatogastro 2002;9:445–54 | Review |
| Levitsky S. Further information on the fibrin sealant conference. Transfusion 1996;36:845–6 | Letter/commentary/erratum |
| Levy O, Martinowitz U, Oran A, Tauber H, Liberman N, Salai M, et al. The use of fibrin tissue adhesive reduces blood loss and blood transfusion after total knee arthroplasty: a prospective, randomized, multi-centre study. J Bone Joint Surg Am 2000;82(Suppl. 3):221–2 | Abstract/full text unavailable |
| Lin HJ, Hsieh YH, Tseng GY, Perng CL, Chang FY, Lee SD. Endoscopic injection with fibrin sealant versus epinephrine for arrest of peptic ulcer bleeding: a randomized, comparative trial. J Clin Gastroenterol 2002;35:218–21 | Did not meet population/intervention criteria |
| Lindsey I, Smilgin-Humphreys MM, Cunningham C, Mortensen NJ, George BD. Randomised trial of fibrin glue vs. conventional treatment for anal fistula. Colorectal Dis 2001;3(Suppl. 1):Oral 78 | Abstract/full text unavailable |
| Liptrot S, Leveson S, Lund J. A prospective randomized controlled trial of fibrin glue versus surgery in the treatment of pilonidal sinus. Br J Surg 2007;94:5 | Abstract/full text unavailable |
| Liptrot S, Leveson S, Lund J. Fibrin glue may be better than surgery for pilonidal sinus: results of a prospective, randomized, controlled trial and 2-year follow up. Dis Colon Rectum 2008;51:P80 | Abstract/full text unavailable |
| Liu H, Wei RH, Huang Y, Yang RB, Zhang C, Zhao SZ. Clinical observation on fibrin glue technique in pterygium surgery under surface anaesthesia. Int Eye Sci 2014;14:1527–8 | Did not meet population/intervention criteria |
| Liu H, Wei RH, Huang Y, Yang RB, Zhang C, Zhao SZ. Clinical observation on fibrin glue technique in pterygium surgery performed with limbal autograft transplantation. Int Eye Sci 2013;13:1498–9 | Chinese |
| Liu W, Zhang YP, Xie MF, Liu Y. Application of fibrin glue with bandage contact lens in pterygium surgery. Int Eye Sci 2014;14:879–81 | Chinese |
| Llewellyn-Bennett R, English R, Turner J, Tsim N, Rayter Z, Winters Z. A randomised controlled trial to evaluate the role of Tisseel, a fibrin sealant on seroma formation in Latissimus dorsi breast reconstruction. Eur J Surg Oncol 2011;37:S16 | Abstract/full text unavailable |
| Lockhart K, Teo E, Teo S, Dhillon M, van Driel Mieke L. Mesh versus non-mesh for inguinal and femoral hernia repair. Cochrane Database Syst Rev 2015;2:CD011517 | Protocol |
| Lowe J, Luber J, Levitsky S, Hantak E, Montgomery J, Schiestl N, et al. Evaluation of the topical hemostatic efficacy and safety of TISSEEL VH S/D fibrin sealant compared with currently licensed TISSEEL VH in patients undergoing cardiac surgery: a phase 3, randomized, double-blind clinical study. J Cardiovasc Surg 2007;48:323–31 | Did not meet population/intervention criteria |
| Luke et al. 1986223 | Not a RCT |
| Maca TH, Mlekusch W, Ahmadi A, Al AM, Haumer M, Sabeti S, et al. Treatment of iatrogenic pseudoaneurysms with injection of thrombin and fibrin glue. Ann Hematol 2003;82:S59 | Abstract/full text unavailable |
| Malhotra C, Jain AK, Sawhney A, Nawani N, Ram J. Outcomes of fibrin glue-assisted conjunctival versus conjunctivolimbal autograft in primary pterygia with a new technique of conjunctival resection and tenon extended removal. Cornea 2015;34:193–8 | Did not meet population/intervention criteria |
| Martinazzoli A, Cangemi V, Cammarata A, Ceccobelli M, Costanzo F, Corradi R, et al. [Use of fibrin glue in breast prosthesis implantation immediately after bilateral adenectomy.] G Chir 1995;16:457–8 | Did not meet population/intervention criteria |
| Martinowitz U, Levy O, Tauber H, Horoszowski H. Prospective randomized multicenter study on efficacy and safety of fibrin tissue adhesive in knee arthroplasty. Thromb Haemost 1997;78:661–6 | Abstract/full text unavailable |
| Martinowitz U, Levy O, Oran A, Tauber H, Heroszowski H. Fibrin tissue adhesive reduces blood loss and blood transfusion requirements after total knee arthroplasty: a prospective, randomized, multicenter study. Haemophilia 1998;4:186 | Abstract/full text unavailable |
| Mercuriali F, Inghilleri G, Aloni A, Santoleri L, Angeloro D, Capitani D, et al. Autologous fibrin glue (AFG) reduces blood loss in patients submitted to total hip replacement (THR). Vox Sang 2004;87(Suppl. 3):35 | Abstract/full text unavailable |
| Milic DJ, Perisic ZD, Zivic SS, Stanojkovic ZA, Stojkovic AM, Karanovic ND, et al. Prevention of pocket related complications with fibrin sealant in patients undergoing pacemaker implantation who are receiving anticoagulant treatment. Europace 2005;7:374–9 | Did not meet population/intervention criteria |
| Milne AA. Clinical impact of fibrin sealants. Vox Sang 2004;87(Suppl. 2):29–30 | Letter/commentary/erratum |
| Miyamoto H, Sakao Y, Sakuraba M, Oh S, Takahashi N, Miyasaka Y, et al. The effects of sheet-type absorbable topical collagen hemostat used to prevent pulmonary fistula after lung surgery. Ann Thorac Cardiovasc Surg 2010;16:16–20 | Did not meet population/intervention criteria |
| Mohindra S, Mohindra S, Gupta K. Endoscopic repair of CSF rhinorrhea: necessity of fibrin glue. Neurol India 2013;61:396–9 | Did not meet population/intervention criteria |
| Moon YM, Kang JK, Park IS, Chon CY, Chung JB, Han KH. Comparison of hemostatic effect of endoscopic injection with fibrin glue (FG) and hypertonic saline – epinephrine (HSE) for peptic ulcer bleeding: a prospective randomized trial. Korean J Gastrointest Endosc 1995;15:12–25 | Did not meet population/intervention criteria |
| Moralee SJ, Carney AS, Cash MP, Murray JA. The effect of fibrin sealant haemostasis on post-operative pain in tonsillectomy. Clin Otolaryngol Allied Sci 1994;19:526–8 | Did not meet population/intervention criteria |
| Mulet Homs ME, Alio YSJL, Gobby F. Efficacy of fibrinogen as bioadhesive in cataract surgery through scleral tunnel. Arch Soc Esp Oftalmol 1997;72:427–30 | Outcomes not of interest |
| Murphy WG, Milne AA, Ruckley CV, Kubba AK, Palmer KR. Fibrin sealant: update on clinical studies. Transfus Sci 1996;17:341–2 | Not a RCT |
| Muzi MG, Nigro C, Cadeddu F, Andreoli F, Farinon AM. Randomized clinical trial of Lichtenstein’s operation versus mesh plug for inguinal hernia repair. Br J Surg 2007;94:647 | Did not meet population/intervention criteria |
| Naga MI, Goubran HA, Said M, Burnouf-Radosevich M, Burnouf T, Huart JJ. A comparison between endoscopic injection of bleeding esophageal varices using ethanolamine oleate and fibrin glue sealant in patients with bilharzial liver fibrosis. Endoscopy 1999;31:405 | Letter/commentary/erratum |
| NCT0212065. Effect of the Fibrin Monomer in the Integrity of the Graft during Tympanoplasty Compared with the Effect of the Hemostatic Sponge. Clinicaltrials.gov, 2012. URL: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/034/CN-01001034/frame.html (accessed 19 May 2015) | Insufficient data |
| Negro P, Basile F, Brescia A, Buonanno GM, Campanelli G, Canonico S, et al. Open tension-free Lichtenstein repair of inguinal hernia: use of fibrin glue versus sutures for mesh fixation. Hernia 2011;15:7–14 | Not a RCT |
| Nervi C, Gamelli RL, Greenhalgh DG, Luterman A, Hansbrough JF, Achauer BM, et al. A multicenter clinical trial to evaluate the topical hemostatic efficacy of fibrin sealant in burn patients. J Burn Care Rehabil 2001;22:99–103 | Did not meet population/intervention criteria |
| Niekisch R. [Application possibilities of fibrin glue in dentistry and maxillofacial surgery.] Zahn Mund Kieferheilkd Zentralbl 1980;68:555–61 | Not a RCT |
| Novik B. Randomized trial of fixation vs nonfixation of mesh in total extraperitoneal inguinal hernioplasty. Arch Surg 2005;140:811–12 | Letter/commentary/erratum |
| Novik B. Fibrin glue mesh fixation in hernia repair. Ann Surg 2007;246:906–8 | Letter/commentary/erratum |
| Öllinger R, Mihaljevic AL, Schuhmacher C, Bektas H, Vondran F, Kleine M, et al. A multicentre, randomized clinical trial comparing the Veriset haemostatic patch with fibrin sealant for the management of bleeding during hepatic surgery. HPB (Oxford) 2013;15:548–58 | Did not meet population/intervention criteria |
| Osbun JW, Ellenbogen RG, Chesnut RM, Chin LS, Connolly PJ, Cosgrove GR, et al. A multicenter, single-blind, prospective randomized trial to evaluate the safety of a polyethylene glycol hydrogel (Duraseal Dural Sealant System) as a dural sealant in cranial surgery. World Neurosurg 2012;78:498–504 | Did not meet population/intervention criteria |
| Ota Y, Ikemiyagi Y, Takizawa K, Yamada C, Rikitake R, Suzuki M. Efficacy of covering mucosal defects with polyglycolic acid sheets after ear or nose surgery. Laryngoscope 2015;125:567–70 | Not a RCT |
| Oz MC, Rondinone JF, Shargill NS. FloSeal Matrix: new generation topical hemostatic sealant. J Card Surg 2003;18:486–93 | Not a RCT |
| Pal Singh B, Dhakad U. Re: TachoSil Sealed tubeless percutaneous nephrolithotomy to reduce urine leakage and bleeding: outcome of a randomized controlled study: L. Cormio, A. Perrone, G. di Fino, N. Ruocco, M. de Siati, J. de la Rosette and G. Carrieri. J Urol 2012;188:145–50. J Urol 2013;189:777–8 | Letter/commentary/erratum |
| Pan I, Dendukuri N, McGregor M. Efficacy and Cost-Effectiveness of Collatamp-G for Infection Prophylaxis in Cardiac Surgery. 2009. URL: www.mcgill.ca/files/tau/COLLATAMP_ CARDIAC_ REPORT.pdf (accessed 19 May 2015) | Review |
| Park DH, Iwashita T, Samarasena JB, Nakai Y, Chang KJ, Chao HH. Prospective randomized comparative study using hemoclip, endoloop, and fibrin sealant for endoscopic closure of iatrogenic duodenal perforation in a porcine model: HELLP study. Gastrointest Endosc 2011;73(Suppl. 1):AB156 | Did not meet population/intervention criteria |
| Park DH, Han JH, Jang JY, Lee SY. Effect of fibrin glue on post-tonsillectomy pain. Korean J Otorhinolaryngol-Head Neck Surg 2009;52:591–3 | Korean |
| Patel MR, Caruso PA, Yousuf N, Rachlin J. CT-guided percutaneous fibrin glue therapy of cerebrospinal fluid leaks in the spine after surgery. Am J Roentgenol 2000;175:443–6 | Not a RCT |
| Pescatore P, Jornod P, Borovicka J, Pantoflickova D, Suter W, Meyenberger C, et al. Epinephrine versus epinephrine plus fibrin glue injection in peptic ulcer bleeding: a prospective randomized trial. Gastrointest Endosc 2002;55:348–53 | Did not meet population/intervention criteria |
| Petersen B, Barkun A, Carpenter S, Chotiprasidhi P, Chuttani R, Silverman W, et al. Tissue adhesives and fibrin glues. Gastrointest Endosc 2004;60:327–33 | Review |
| Petrov DB, Manolov EP, Minchev TR, Alexov SB, Botev CN. Additional intraoperative aerostasis with a 100% autologous fibrin glue in thoracic surgery. Eur Respir J 2001;18(Suppl. 33):524 | Outcomes not of interest |
| Petter Puchner AH, Khakpour Z, May C, Mika K, Glaser KS, Redl H. The impact of atraumatic fibrin sealant vs. staple mesh fixation in tapp hernia repair on chronic pain and quality of life – results of a randomized controlled study. Surg Endosc 2010;24(Suppl. 1):S618 | Abstract/full text unavailable |
| Pichon R, Augustovski GM, Garcia MS, Glujovsky D, Alcaraz A, Lopez A, et al. Biological Tissue Adhesive Versus Standard Suture in Conjuctival Autograft for the Surgical Treatment of Pterygium. 2012. URL: www.iecs.org.ar/iecs-visor-publicacion.php?cod_ publicacion=1324& amp;origen_%20publicacion=publicaciones (accessed 19 May 2015) | Abstract/full text unavailable |
| Pini Prato GP, Cortellini P, Agudio G, Clauser C. Human fibrin glue versus sutures in periodontal surgery. J Periodontol 1987;58:426–31 | Not a RCT |
| Porte RJ, Verhoef C, De Wilt JHW, Rijken AM, Klaase JM, Ayez N, et al. FibrocapsTM, a novel fibrin sealant, for bleeding during hepatic resection: results of a phase 2, randomized, controlled study. HPB 2012;14:133 | Abstract/full text unavailable |
| Pulikkotil SJ, Nath S. Fibrin sealant as an alternative for sutures in periodontal surgery. J Coll Physicians Surg Pak 2013;23:164–5 | Outcomes not of interest |
| Pulikkotil SJ, Nath S. Effect on interleukin-1beta and interleukin-8 levels following use of fibrin sealant for periodontal surgery. Aust Dent J 2014;59:156–64 | Not a RCT |
| Raborn GW, Hohn FI, Grace MG, Arora BK. Tisseel, a two component fibrin tissue sealant system: report of a trial involving anticoagulated dental patients. J Can Dent Assoc 1990;56:779–81 | Review |
| Rauws EAJ, Rutgeerts P, Wara P, Hoos A, Solleder E, Halttunen J, et al. Fibrin sealant (Beriplast®) v.s. polidocanol 1% in the endoscopic treatment of bleeding gastroduodenal ulcers. Endoscopy 1996;28:S19 | Abstract/full text unavailable |
| Rehder J, Bosnardo CA, Kraft MB, Frade MA, Guillaumon AT, Batista FR. A comparative study of cell therapy and fibrin glue applied to chronic venous ulcers. Procedia Engineering 2013;59:85–91 | Outcomes not of interest |
| Richter G, Prassler R, Rutgeerts P, Rauws E, Warn P, Hoos A, et al. Fibrin glue versus Polidocanol 1% in ulcerous bleeding therapy – results of a multi-centre study. Endoskopie Heute 1997;10:93 | Abstract/full text unavailable |
| Robertson L, Kesteven P, McCaslin JE. Oral direct thrombin inhibitors or oral factor Xa inhibitors for the treatment of pulmonary embolism. Cochrane Database Syst Rev 2015;12:CD010957 | Protocol |
| Rodig J, Dinkelaker F, Rahmanzadeh R. Reduction of ossification after cement-free hip replacement using fibrin glue. Hefte zur Unfallheilkunde 1990;212:465–6 | Abstract/full text unavailable |
| Rodin IuV. [Local hemostasis during the carotid endarterectomy under condition of antithrombocytic therapy.] Klin Khir 2007;10:32–4 | Not a RCT |
| Rousou J, Levitsky S, Gonzalez-Lavin L, Cosgrove D, Magilligan D, Weldon C, et al. Randomized clinical trial of fibrin sealant in patients undergoing resternotomy or reoperation after cardiac operations. A multicenter study. J Thorac Cardiovasc Surg 1989;97:194–203 | Cross-over |
| Rutgeerts P, Rauws E, Wara P, Swain P, Hoos A, Solleder E, et al. Randomised trial of single and repeated fibrin glue compared with injection of polidocanol in treatment of bleeding peptic ulcer. Lancet 1997;350:692–6 | Did not meet population/intervention criteria |
| Sakoda T, Shibano A, Saitoh Y, Dake Y, Sogo H, Fujimura S, et al. [An office technique for myringoplasty without the use of fibrin glue.] Nippon Jibiinkoka Gakkai Kaiho 2000;103:836–9 | Did not meet population/intervention criteria |
| Sánchez M, Anitua E, Orive G, Mujika I, Andia I. Platelet-rich therapies in the treatment of orthopaedic sport injuries. Sports Med 2009;39:345–54 | Abstract/full text unavailable |
| Sandrock D, Steinröder M, Emrich D. [Fibrin agglutination of thyroid gland cysts after fine needle puncture.] Dtsch Med Wochenschr 1993;118:1–5 | Did not meet population/intervention criteria |
| Santini F, Luciani GB, Pessotto R, Petrilli G, Fabbri A, Mazzucco A. Current techniques to reduce blood loss after the Ross procedure. J Heart Valve Dis 1997;6:343–6 | Not a RCT |
| Scheer M, Steveling H, Schweigert HG, Neugebauer J, Kubler AC, Zoller JE. Efficacy of fibrinogen and thrombin coated collagen sponge (TachoComb) in anticoagulated patients undergoing dental surgery. Chirug Dtsch Zahnarztl Z 2004;59:220–6 | Abstract/full text unavailable |
| Segal N, Puterman M, Rotem E, Niv A, Kaplan D, Kraus M, et al. A prospective randomized double-blind trial of fibrin glue for reducing pain and bleeding after tonsillectomy. Int J Pediatr Otorhinolaryngol 2008;72:469–73 | Did not meet population/intervention criteria |
| Segura-Castillo JL, Aguirre-Camacho H, González-Ojeda A, Michel-Perez J. Reduction of bone resorption by the application of fibrin glue in the reconstruction of the alveolar cleft. J Craniofac Surg 2005;16:105–12 | Did not meet population/intervention criteria |
| Sener BC, Saysel MY. The comparison between alloplastic bone chips with and without fibrin glue used in maxillary sinus lifting operations. J Craniomaxillofac Surg 1998;26(Suppl. 1):3–21 | Abstract/full text unavailable |
| Shah HN, Hegde S, Shah JN, Mohile PD, Yuvaraja TB, Bansal MB. A prospective, randomized trial evaluating the safety and efficacy of fibrin sealant in tubeless percutaneous nephrolithotomy. J Urol 2006;176:2488–92 | Did not meet population/intervention criteria |
| Shcherba SN, Polovinkin VV. [Use of Tachocomb for prevention of postoperative lymphatic leaks in the abdomen.] Vopr Onkol 2011;57:269–70 | Unobtainable |
| Shen L, Luo H, Tan S. Effect of fibrin glue on patients after high frequency electrocoagulatomy for gastrointestinal protuberant lesions. Med J Wuhan Uni 2003;24:377 | Chinese |
| Simons MP. Randomized clinical trial of fibrin sealant versus titanium tacks for mesh fixation in laparoscopic umbilical hernia repair. Br J Surg 2011;98:1537–45 | Letter/commentary/erratum |
| Singer M, Cintron J, Nelson R, Orsay C, Bastawrous A, Pearl R, et al. Treatment of fistulas-in-ano with fibrin sealant in combination with intra-adhesive antibiotics and/or surgical closure of the internal fistula opening. Dis Colon Rectum 2005;48:799–808 | Did not meet population/intervention criteria |
| Singh PK, Singh S, Vyas C, Singh M. Conjunctival autografting without fibrin glue or sutures for pterygium surgery. Cornea 2013;32:104–7 | Did not meet population/intervention criteria |
| Soumian S, Al-Ani S, Sterne G. Randomized clinical trial on the effect of fibrin sealant on latissimus dorsi donor-site seroma formation after breast reconstruction (Br J Surg 2012;99:1381–1388). Br J Surg 2013;100:1671 | Letter/commentary/erratum |
| Spinzi G, Minoli G. Injection of fibrin tissue adhesive versus laser photocoagulation in the treatment of high-risk bleeding peptic ulcers: a controlled randomized study. Gastrointest Endosc 1997;46:198–9 | Did not meet population/intervention criteria |
| Stabilini C, Fornaro R, Lazzara F, Mandolfino F, Imperatore M, Gianetta E. Suturless-lightweight hernioplasty vs traditional Lichtenstein repair. One year results on chronic postoperative pain. Eur Surg Res 2010;45:197 | Abstract/full text unavailable |
| Stephens J, Robless P, Jenkins M, Cheshire N. Re: Does fibrin glue reduce complications after femoral artery surgery? A randomised trial. Eur J Vasc Endovasc Surg 2003;25:596 | Letter/commentary/erratum |
| Stevens MH, Stevens DC. Pain reduction by fibrin sealant in older children and adult tonsillectomy. Laryngoscope 2005;115:1093–6 | Letter/commentary/erratum |
| Stiller-Timor L, Goldbart AD, Segal N, Amash A, Huleihel M, Leiberman A, et al. Circulating cytokines in patients undergoing tonsillectomy with fibrin glue. Int J Pediatr Otorhinolaryngol 2012;76:419–22 | Did not meet population/intervention criteria |
| Stoeckli SJ, Moe KS, Huber A, Schmid S. A prospective randomized double-blind trial of fibrin glue for pain and bleeding after tonsillectomy. Laryngoscope 1999;109:652–5 | Did not meet population/intervention criteria |
| Strohm WD, Römmele UE, Barton E, Paul-Martin C. [Injection therapy of bleeding peptic ulcer with fibrin or polidocanol.] Dtsch Med Wochenschr 1994;119:249–56 | Did not meet population/intervention criteria |
| Stutz H, Hempelmann HCG. The use of autologous fibrin glue to reduce perioperative blood loss in total knee arthroplasty – results of a controlled study. Orthopadische Praxis 2004;40:1–3 | Not a RCT |
| Suc B, Msika S, Piccinini M, Fourtanier G, Hay JM, Flamant Y, et al. Octreotide in the prevention of intra-abdominal complications following elective pancreatic resection: a prospective, multicenter randomized controlled trial. Arch Surg 2004;139:288–94 | Did not meet population/intervention criteria |
| Szczesny T, Kubiszewska I, Rybak A, Michalkiewicz J, Szymankiewicz M, Kowalewski J. The role of Tachosil in lymphostasis after mediastinal lymphadenectomy in lung cancer patients. J Thorac Oncol 2011;6(Suppl. 2):876–7 | Abstract/full text unavailable |
| Tabatabaei S, Talab SS, Kloc LS, Siddiqui MM, Akhavein A, Vazquez R, et al. Use of evicel fibrin sealant for improving hemostasis following transurethral prostate debulking surgery in patients with BPH. J Endourol 2014;28:A131 | Abstract/full text unavailable |
| Takeuchi J, Suzuki H, Murata M, Kakei Y, Ri S, Umeda M. Clinical evaluation of application of polyglycolic acid sheet and fibrin glue spray for partial glossectomy. J Oral Maxillofac Surg 2013;71:e126–31 | Not a RCT |
| Tamaki H, Fukushima H, Nakamura H, Kanemaru S, Fukuyama Y, Tamura Y. Control of postoperative pain with Beriplast P in tonsillectomy. Practica Otologica 1996;89:1027–30 | Did not meet population/intervention criteria |
| Taylor et al. 2003199 | Not a RCT |
| Testini M, Lissidini G, Poli E, Gurrado A, Lardo D, Piccinni G. A single-surgeon randomized trial comparing sutures, N-butyl-2-cyanoacrylate and human fibrin glue for mesh fixation during primary inguinal hernia repair. Can J Surg 2010;53:155–60 | Did not meet population/intervention criteria |
| Tian BY, Zhang H. Limbal stem cell transplantation with fibrin sealant for the treatment of recurrent pterygium. Int J Ophthalmol 2011;11:1066–7 | Chinese |
| Tocchhetti EV, Carter G, Goss A, Lloyd JV. Local management of haemostasis with fibrin adhesive in patients with coagulopathies undergoing surgery. Vox Sang 2000;79(Suppl. 1):220 | Abstract/full text unavailable |
| Tofuku K, Koga H, Yanase M, Komiya S. The use of antibiotic-impregnated fibrin sealant for the prevention of surgical site infection associated with spinal instrumentation. Eur Spine J 2012;21:2027–33 | Not a RCT |
| Topiwala P, Bansal RK. Comparative evaluation of cyanoacrylate and fibrin glue for muscle recession in strabismus surgery. J Pediatr Ophthalmol Strabismus 2014;51:349–54 | Did not meet population/intervention criteria |
| Troisi RI, Bektas H, Pratschke J, Topal B, Buchler M, Schuhmacher CP, et al. A prospective, multi-center, randomized, single-blind study to compare the VerisetTM hemostatic patch to fibrin sealant (Tachosil) in subjects undergoing hepatic surgery. HPB 2012;14:104–5 | Abstract/full text unavailable |
| Trombelli L, Scabbia A, Wikesjö UM, Calura G. Fibrin glue application in conjunction with tetracycline root conditioning and coronally positioned flap procedure in the treatment of human gingival recession defects. J Clin Periodontol 1996;23:861–7 | Outcomes not of interest |
| Trombelli L, Scabbia A, Calura G. Effect of topical application of a fibrin-fibronectin sealing system on healing response following periodontal surgical procedures. Clin Drug Invest 1997;14:268–75 | Outcomes not of interest |
| Trombelli L, Scabbia A, Scapoli C, Calura G. Clinical effect of tetracycline demineralization and fibrin-fibronectin sealing system application on healing response following flap debridement surgery. J Periodontol 1996;67:688–93. [Erratum published in J Periodontol 1996;67:1368.] | Outcomes not of interest |
| Tsai CH, Hsu HC, Chen YJ, Lin MJ, Chen HT. Using the growth factors-enriched platelet glue in spinal fusion and its efficiency. J Spinal Disord Tech 2009;22:246–50 | Not a RCT |
| Upadhyaya VD, Gopal SC, Gangopadhyaya AN, Gupta DK, Sharma S, Upadyaya A, et al. Role of fibrin glue as a sealant to esophageal anastomosis in cases of congenital esophageal atresia with tracheoesophageal fistula. World J Surg 2007;31:2412–15 | Did not meet population/intervention criteria |
| Uy HS, Reyes JMG, Flores JP, Limbonsiong R. Human plasma derived fibrin glue (Beriplast P) in conjunctival autografts for pterygia. IOVS 2002;43:129 | Not a RCT |
| Vaiman et al. 2002188 | Not a RCT |
| Vaiman M, Eviatar E, Shlamkovich N, Segal S. Effect of modern fibrin glue on bleeding after tonsillectomy and adenoidectomy. Ann Otol Rhinol Laryngol 2003;112:410–14 | Did not meet population/intervention criteria |
| Valentini MF, Lissidini G, Gurrado A, Poli E, Ruggiero L, Piccinni G, et al. Comparison among three different methods of mesh fixation in patients undergoing plug and mesh technique for primary inguinal hernia repair: a prospective randomised controlled study. Eur Surg Res 2010;45:198–9 | Abstract/full text unavailable |
| Visna P, Pasa L, Cizmár I, Hart R, Hoch J. Treatment of deep cartilage defects of the knee using autologous chondrograft transplantation and by abrasive techniques – a randomized controlled study. Acta Chir Belg 2004;104:709–14 | Did not meet population/intervention criteria |
| Wagner W, Wiltfang J, Pistner H, Yildirim M, Ploder B, Chapman M, et al. Bone formation with a biphasic calcium phosphate combined with fibrin sealant in maxillary sinus floor elevation for delayed dental implant. Clin Oral Implants Res 2012;23:1112–17 | Did not meet population/intervention criteria |
| Ware P, Rutgeerts P, Rauws EAJ, Hoos A, Solleder E. Endoscopic injection therapy of bleeding gastro-duodenal ulcers: fibrin glue (beriplast) vs. polidocanol 1%. Gut 1996;39(Suppl. 1):A5 | Abstract/full text unavailable |
| Winters ZE, Llewellyn-Bennett R, English R, Turner J, Rayter Z, Greenwood R. A randomised controlled trial to evaluate the role of Tisseel, a fibrin sealant on seroma formation in latissimus dorsi breast reconstruction. Cancer Res 2011;71(Suppl. 3):P2-16-07 | Abstract/full text unavailable |
| Wong K, Goldstraw P. Effect of fibrin glue in the reduction of postthoracotomy alveolar air leak. Ann Thorac Surg 1997;64:979–81 | Did not meet population/intervention criteria |
| Wurtz A, Chambon JP, Sobecki L, Batrouni R, Huart JJ, Burnouf T. [Use of a biological glue in partial pulmonary excision surgery. Results of a controlled trial in 50 patients.] Ann Chir 1991;45:719–23 | Did not meet population/intervention criteria |
| Yasumizu Y, Miyajima A, Maeda T, Hasegawa M, Takeda T, Shinoda K, et al. What prevents lymphocele development after laparoscopic radical prostatectomy? J Endourol 2011;25:A227 | Abstract/full text unavailable |
| Yeung SN, Lichtinger A, Kim P, Elbaz U, Ku JY, Amiran MD, et al. Superior versus inferior conjunctival autografts combined with fibrin glue in the management of primary pterygia. Cornea 2013;32:1582–6 | Did not meet population/intervention criteria |
| Yoshimura M, Tsubota N, Matsuoka H, Sakamoto T. Efficacy of a pedicled pericardial fat pad fixed with fibrin glue on postoperative alveolar air leakage. Surg Today 2002;32:26–8 | Did not meet population/intervention criteria |
| Yuasa K, Shimizu T, Matsubara J, Toyoda T. [Sealing effect of fibrin adhesive by various method on protection of air leakage in lung surgery.] Kyobu Geka 1998;51:1001–5 | Did not meet population/intervention criteria |
| Zhang SP, Cao B, Xiu XG, Wu BB. Local application of fibrin glue carrying gatifloxacin. J Clin Rehabil Tissue Engin Res 2011;15:431–5 | Abstract/full text unavailable |
| Zhou LB, Guo SY, Zhang W, Du KH, Gong DQ. The efficacy of fibrin glue in radical mastectomy. Acta Medicinae Sinica 2003;16:14–15 | Unobtainable |
| Ziaee SA, Sarhangnejad R, Abolghasemi H, Eshghi P, Radfar MH, Ahanian A, et al. Autologous fibrin sealant in tubeless percutaneous nephrolithotomy; a prospective study. Urol J 2013;10:999–1003 | Not a RCT |
| Zimmer T, Rucktäschel F, Stölzel U, Liehr RM, Schuppan D, Stallmach A, et al. Endoscopic sclerotherapy with fibrin glue as compared with polidocanol to prevent early esophageal variceal rebleeding. J Hepatol 1998;28:292–7 | Did not meet population/intervention criteria |
| Zimmer TJ, Faiss S, Liehr RM, Breitkreutz C, Klein M, Stolzel U, et al. [Fibrin glue versus endoscopic ligature to stop acute bleeding and in the prophylaxis of early relapse of oesophagus varices. Results of a German multi-centre study.] Gastroenterol 2005;43:828 | Abstract/full text unavailable |
Other
Chiu PWY, Lau TS, Kwong KH, Suen DTK, Kwok PY. Impact of programmed second endoscopy with appropriate re-treatment on peptic ulcer re-bleeding: a systematic review. Ann Coll Surg Hong Kong 2003;7:106–15.
Appendix 4 Tables of recent and ongoing studies
| NCT Number | Title | Recruitment | Start date | URL |
|---|---|---|---|---|
| NCT01828892 | Glue application in the treatment of low-output fistulas | Recruiting | March 2014 | http://ClinicalTrials.gov/show/NCT01828892 |
| NCT02094885 | The Bioseal vascular study | Completed | February 2014 | http://ClinicalTrials.gov/show/NCT02094885 |
| NCT01613664 | Efficiency of TISSEEL for sleeve gastrectomy complications | Recruiting | February 2014 | http://ClinicalTrials.gov/show/NCT01613664 |
| NCT02040428 | The Fibrin pad CV phase III study | Recruiting | January 2014 | http://ClinicalTrials.gov/show/NCT02040428 |
| NCT02034799 | Phase IV Bioseal study in brain tumour surgery | Completed | November 2013 | http://ClinicalTrials.gov/show/NCT02034799 |
| NCT01993888 | The EVARREST fibrin sealant patch liver study | Completed | October 2013 | http://ClinicalTrials.gov/show/NCT01993888 |
| NCT02011698 | Absorbable sutures, non absorbable sutures or biologic fibrin glue for protesic mesh fixing in Lichtenstein technique for primitive groin hernia repair: a randomised prospective multicentric trial | Recruiting | October 2013 | http://ClinicalTrials.gov/show/NCT02011698 |
| NCT01902459 | EVARREST fibrin sealant patch post-market study | Recruiting | July 2013 | http://ClinicalTrials.gov/show/NCT01902459 |
| NCT02153593 | Postoperative bleeding prevention in massive bone tumour resection: a multicentric, randomised, parallel, controlled trial | Recruiting | March 2013 | http://ClinicalTrials.gov/show/NCT02153593 |
| NCT02150720 | Prevention of postoperative bleeding in subcapital femoral fractures: a multicenter, randomised, controlled, parallel clinical trial | Recruiting | February 2013 | http://ClinicalTrials.gov/show/NCT02150720 |
| NCT01641718 | Use of human fibrin glue versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty | Active, not recruiting | January 2013 | http://ClinicalTrials.gov/show/NCT01641718 |
| EudraCT number | Title | Recruitment | Start date | URL |
|---|---|---|---|---|
| 2014–003954–15 | A single blinded, randomised, controlled study to evaluate the safety and effectiveness of EVICEL® fibrin sealant (Human) compared to a hydrogel sealant as an adjunct to sutured dural repair | Ongoing | May 2015 | www.clinicaltrialsregister.eu/ctr-search/trial/2014-003954-15/GB/ |
| 2013–004353–24 | Wound management in post-bariatric surgery investigation for the reduction of the mean drainage volume in patients after abdominoplasty/lower body lift using Artiss fibrin sealant in comparison to the standard procedure | Ongoing | May 2014 | www.clinicaltrialsregister.eu/ctr-search/trial/2013-004353-24/DE/ |
| 2013–002579–16 | PHASE III clinical trial, single-centre, randomised, double blind in two groups parallel to compare the efficacy and safety of rich plasma growth factors (PRGF) in front of fibrin glue (Tissucol®) for sealing anal and criptoglandular fistula after 48 weeks | Ongoing | December 2014 | www.clinicaltrialsregister.eu/ctr-search/trial/2013-002579-16/ES/ |
| 2013–002535–24 | A phase iii randomised, controlled, superiority study evaluating EVARREST™ fibrin sealant patch versus standard of care treatment in controlling parenchymal bleeding during hepatic surgery | Ongoing | September 2013 | www.clinicaltrialsregister.eu/ctr-search/trial/2013-002535-24/GB/ |
Appendix 5 Quality assessment
| Study (author, year) | Random sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective reporting | ‘Other bias’ | Overall bias | |
|---|---|---|---|---|---|---|---|---|
| Patient | Outcome assessor | |||||||
| Aguilera et al., 2013143 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Altinli et al., 2007206 | ✗ | ✗ | ? | ? | ? | ? | ? | ✗ |
| Altomare et al., 2011217 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Anegg et al., 2007125 | ? | ? | ? | ? | ? | ? | ? | ? |
| Antuña et al., 2013155 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Bahar et al., 2006159 | ✗ | ? | ? | ? | ? | ? | ? | ? |
| Bahar et al., 2007169 | ✗ | ? | ? | ? | ? | ? | ? | ✗ |
| Bajardi et al., 2009194 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Bektas et al., 201465 | ✓ | ✓ | ? | ? | ✓ | ? | ? | ✓ |
| Belboul et al., 2004133 | ✓ | ✓ | ? | ✓ | ? | ? | ? | ✓ |
| Belcher et al., 2010131 | ✓ | ? | ✓ | ✗ | ? | ? | ? | ? |
| Benevento et al., 2014109 | ✓ | ? | ✓ | ✓ | ? | ? | ? | ? |
| Bercial et al., 2012213 | ? | ? | ? | ? | ? | ? | ? | ? |
| Berger et al., 2001107 | ✓ | ? | ✗ | ✗ | ? | ? | ? | ? |
| Bochicchio et al., 2015239 | ? | ? | ✓ | ✗ | ? | ? | ? | ? |
| de Boer et al., 201266 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ? | ✓ |
| Boldo, 2008173 | ✓ | ? | ✓ | ✓ | ? | ? | ? | ? |
| Bracale et al., 2014174 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Bulbuller et al., 201392 | ? | ? | ? | ? | ? | ? | ? | ? |
| Cambal et al., 2012175 | ? | ? | ? | ? | ? | ? | ? | ? |
| Campanelli et al., 2012176 | ✓ | ✓ | ✓ | ✓ | ✗ | ? | ? | ✓ |
| Canonico et al., 1999177 | ? | ? | ? | ? | ? | ? | ? | ? |
| Carlson et al., 200894 | ? | ? | ? | ? | ? | ? | ? | ? |
| Carter et al., 2003229 | ? | ? | ? | ? | ? | ? | ? | ? |
| Carter et al., 201381 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Chalmers et al., 2010198 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Chan et al., 2014178 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Chapman et al., 200067 | ✓ | ✓ | ? | ✓ | ? | ? | ? | ✓ |
| Choufani et al., 2015151 | ✗ | ✗ | ✓ | ✗ | ? | ? | ? | ✗ |
| Cipolla et al., 2010110 | ? | ? | ? | ? | ? | ? | ? | ? |
| Cormio et al., 2012222 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Czerny et al., 2000205 | ? | ? | ? | ? | ? | ? | ? | ? |
| Czerny et al., 2004137 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Damiano et al., 2014184 | ? | ? | ? | ? | ? | ? | ? | ? |
| Danielsen et al., 2008209 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Danielsen et al., 201079 | ✓ | ✓ | ? | ✓ | ? | ? | ? | ✓ |
| Diamond et al., 2011232 | ? | ? | ? | ✓ | ? | ? | ? | ? |
| Dimo et al., 198980 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Dinsmore et al., 200097 | ? | ? | ? | ? | ? | ? | ? | ? |
| Drake and Wong, 2003207 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Droghetti et al., 2008124 | ? | ? | ? | ? | ? | ? | ? | ? |
| Ellis and Clark, 2006216 | ? | x | ? | ? | ? | ? | ? | ? |
| Erba et al., 2010210 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Eriksen et al., 2013183 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Fabian et al., 2003128 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Falez et al., 2013154 | ? | ? | ✓ | ✗ | ? | ? | ? | ? |
| Fékété et al., 199291 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Fernandez Fernandez et al., 199663 | ? | ? | ? | ? | ? | ? | ? | ? |
| Figueras et al., 200771 | ? | ✗ | ? | ? | ? | ? | ? | ? |
| Filosso et al., 2013136 | ? | ? | ? | ? | ? | ? | ? | ? |
| Fischer et al., 201172 | ✓ | ✓ | ✗ | ✗ | ✓ | ? | ? | ? |
| Fischer et al., 2013241 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Frilling et al., 200573 | ? | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Fu et al., 200978 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Furrer et al., 1993116 | ? | ? | ? | ? | ? | ? | ? | ? |
| Gilly et al., 1994115 | ✓ | ? | ✗ | ✗ | ? | ? | ? | ? |
| Gilly et al., 1998108 | ? | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Gonfiotti et al., 2011130 | ? | ? | ✗ | ✗ | ? | ? | ? | ? |
| Hall et al., 2009160 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Hammond et al., 2011219 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Hanks et al., 2003238 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Healy et al., 2013211 | ✓ | ✓ | ✓ | ✗ | ? | ? | ? | ✓ |
| Hester et al., 2013231 | ? | ? | ✓ | ✗ | ? | ? | ? | ? |
| Heyse et al., 2014142 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Huang and Qian, 201493 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Huang et al., 201564 | ? | ? | ? | ? | ? | ? | ? | ? |
| Hutter et al., 2014237 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Hwang and Chen, 199661 | ? | ? | ✗ | ✗ | ? | ? | ? | ? |
| Jackson et al., 1999193 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Jain et al., 200499 | ✓ | ✓ | ✓ | ✗ | ? | ? | ? | ? |
| Johnson et al., 2005100 | ? | ? | ? | ? | ? | ? | ? | ? |
| Joseph et al., 2004200 | ? | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Kakaei et al., 201374 | ✓ | ✓ | ? | ✓ | ? | ? | ? | ✓ |
| Karalezli et al., 2008161 | ? | ? | ✓ | ? | ? | ? | ? | ? |
| Kjaergard and Trumbull, 1998138 | ? | ? | ? | ? | ? | ? | ? | ? |
| Kjaergard and Trumbull, 2000139 | ✗ | ✗ | ✗ | ✗ | ? | ? | ? | ✗ |
| Kluba et al., 2012145 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Ko et al., 2009102 | ✓ | ✓ | ? | ✓ | ? | ? | ? | ? |
| Kohno et al., 199275 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Koranyi et al., 2005162 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Kucukerdonmez et al., 2010157 | ✓ | ✓ | ✓ | ? | ? | ? | ? | ✓ |
| Lang et al., 2004134 | ? | ? | ✗ | ✗ | ? | ? | ? | ? |
| Lassen et al., 2006141 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Lau, 2005172 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Lee et al., 2009227 | ? | ? | ✗ | ✓ | ? | ? | ? | ? |
| Levy et al., 199914 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Lillemoe et al., 200483 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Lindsey et al., 2002218 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Lionetti et al., 2012179 | ? | ? | ? | ? | ? | ? | ? | ? |
| Liu and Lui, 199369 | ? | ? | ? | ? | ? | ? | ? | ? |
| Llewellyn-Bennett et al., 2012101 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Lopez et al., 2013129 | ✓ | ? | ✗ | ✗ | ? | ? | ? | ? |
| Lovisetto et al., 2007180 | ✓ | ? | ✓ | ✓ | ? | ? | ? | ? |
| Luke et al., 1986223 | ? | ? | ? | ? | ? | ? | ? | ? |
| Mabrouk et al., 2013214 | ? | ? | ? | ? | ? | ? | ? | ? |
| Maggiore et al., 2011233 | ✓ | ✓ | x | ✓ | ? | ? | ? | ? |
| Maharaj et al., 2006230 | ? | ✓ | ✓ | ✓ | ? | ? | ? | ? |
| Maisano et al., 2009140 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Malik and Kumar, 2010171 | ? | ? | ? | ? | ? | ? | ? | ? |
| Marchac and Greensmith, 2005226 | ✗ | ✗ | ✗ | ✗ | ? | ? | ? | ✗ |
| Marta et al., 2010135 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Martin and Au, 201386 | ✗ | ✓ | ✗ | ✗ | ? | ? | ? | ✗ |
| Mawatari et al., 2006152 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| McConnell et al., 2011156 | ? | ✓ | ✓ | ✗ | ? | ? | ? | ? |
| McConnell et al., 2012146 | ? | ✓ | ✗ | ✓ | ? | ? | ? | ? |
| Mellin and Kondler, 1989170 | ? | ? | ? | ? | ? | ? | ? | ? |
| Milne et al., 1995201 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Milne et al., 1996203 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Miri Bonjar et al., 2012103 | ? | ? | ? | ? | ? | ? | ? | ? |
| Moench et al., 2010250 | ✓ | ✓ | ✓ | ? | ? | ? | ? | ✓ |
| Molloy et al., 2007147 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Di Monta et al., 2012117 | ? | ? | ✗ | ✓ | ? | ? | ? | ? |
| Montorsi et al., 201284 | ✗ | ? | ✗ | ✗ | ? | ? | ? | ✗ |
| Moore et al., 1997106 | ✓ | ? | ✓ | ✗ | ? | ? | ? | ? |
| Moore et al., 2001111 | ? | ? | ? | ? | ? | ? | ? | ? |
| Mortenson et al., 2008120 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Moser et al., 2008126 | ? | ✓ | ✗ | ✓ | ? | ? | ? | ? |
| Mouritzen et al., 1993132 | ? | ? | ? | ? | ? | ? | ? | ? |
| Musella et al., 201488 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Mustonen et al., 2004104 | ? | ? | ? | ? | ? | ? | ? | ? |
| Nakamura et al., 2005236 | ? | ? | ? | ? | ? | ? | ? | ? |
| Nativ et al., 201259 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Neuss et al., 2009118 | ✓ | ? | ✓ | ? | ? | ? | ? | ? |
| Nielsen et al., 1985123 | ? | ? | ? | ? | ? | ? | ? | ? |
| Noun et al., 199670 | ? | ? | ? | ? | ? | ? | ? | ? |
| Oliver et al., 2001228 | ✓ | ✓ | ? | ✓ | ? | ? | ? | ✓ |
| Oliver et al., 2002215 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Oliver et al., 201287 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Olmi et al., 2007259 | ? | ? | ✓ | ✓ | ? | ? | ? | ? |
| Pilone et al., 201289 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Prado et al., 2006187 | ✓ | ? | ? | ✓ | ? | ? | ? | ? |
| Pryor et al., 2008186 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Randelli et al., 2014149 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Ratnalingam et al., 2010165 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Rena et al., 2009127 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Rubin et al., 2011166 | ? | ? | ? | ? | ? | ? | ? | ? |
| Sabatini et al., 2012148 | ? | ? | ? | ? | ? | ? | ? | ? |
| Safan et al., 2009235 | ? | ? | ? | ? | ? | ? | ? | ? |
| Saha et al., 2011204 | ? | ? | ✓ | ? | ? | ? | ? | ? |
| Saha et al., 2012197 | ? | ? | ✓ | ? | ? | ? | ? | ? |
| Sati et al., 2014163 | ✓ | ? | ✓ | ? | ? | ? | ? | ? |
| Schenk et al., 2002196 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Schenk et al., 2003195 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Scholz et al., 2002121 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Schultz and Christiansen, 1985224 | ? | ? | ? | ? | ? | ? | ? | ? |
| Schwartz et al., 200477 | ✓ | ✓ | ? | ✓ | ? | ? | ? | ✓ |
| Segura-Castillo et al., 2005105 | ? | ? | ? | ? | ? | ? | ? | ? |
| Sharma et al., 2003164 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Shiono et al., 1998261 | ✓ | ? | ? | ? | ? | ? | ? | ? |
| Siemer et al., 2007221 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Siim et al., 1994114 | ? | ? | ? | ? | ✗ | ? | ? | ? |
| Silecchia et al., 200862 | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? |
| Simonato et al., 2009119 | ? | ? | ? | ? | ? | ? | ? | ? |
| Sintler et al., 2005202 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Skovgaard et al., 2013150 | ✓ | ✓ | ? | ✓ | ? | ? | ? | ✓ |
| Sözen et al., 2011212 | ? | ? | ? | ? | ? | ? | ? | ? |
| Srinivasan et al., 2009167 | ? | ✗ | ? | ✓ | ? | ? | ? | ? |
| Sroka et al., 201590 | ✓ | ✓ | ✓ | ? | ? | ? | ? | ✓ |
| Suc et al., 200385 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Suzuki et al., 199582 | ? | ✓ | ? | ? | ✗ | ? | ? | ? |
| Swan et al., 2011113 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Tachibana et al., 2003122 | ? | ? | ? | ✓ | ? | ? | ? | ? |
| Takeuchi et al., 2005234 | ✗ | ? | ? | ? | ? | ? | ? | ? |
| Tavilla et al., 201560 | ? | ? | ? | ? | ? | ? | ? | ? |
| Taylor et al., 2003199 | ? | ✓ | ✓ | ? | ? | ? | ? | ? |
| Tolver et al., 2013181 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Udén et al., 199398 | ? | ? | ? | ? | ? | ? | ? | ? |
| Uetsuji et al., 199468 | ? | ? | ? | ? | ✗ | ? | ? | ? |
| Ulusoy et al., 200396 | ? | ? | ? | ? | ? | ? | ? | ? |
| Uwiera et al., 2005225 | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ |
| Uy et al., 2005168 | ✗ | ✓ | ? | ? | ? | ? | ? | ? |
| Vaiman et al., 2002188 | ? | ? | ? | ? | ? | ? | ? | ? |
| Vaiman et al., 2005189 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Vaiman et al., 2005191 | ? | ✓ | ? | ? | ? | ? | ? | ? |
| Vaiman et al., 2006192 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| van der Hagen et al., 2011220 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Vanscheidt et al., 2007208 | ? | ? | ✗ | ✗ | ? | ? | ? | ? |
| Vaxman et al., 1995251 | ? | ? | ? | ? | ? | ? | ? | ? |
| Verhoef et al. 2015240 | ? | ? | ? | ? | ? | ? | ? | ? |
| Wang et al., 2001144 | ? | ? | ? | ? | ? | ? | ? | ? |
| Wang et al., 2003153 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Wong et al., 2011182 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Yu et al., 2014190 | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Yüksel et al., 2010158 | ✗ | ✗ | ? | ? | ? | ? | ? | ✗ |
| Zhibo and Miaobo, 200995 | ? | ? | ? | ? | ? | ? | ? | ? |
| Study (author, year) | Were the adverse events assessed independently? | Are the measurement instruments described? | Is the timing and duration of follow-up reported? | Was a standard or validated measurement instrument used? | Were the measurements objective? | Was the adverse effect(s) attributed to the intervention? | Was the process blinded to the assigned treatment? | Are the terms used to identify adverse events clearly explained? | Are all adverse events from the population reported? |
|---|---|---|---|---|---|---|---|---|---|
| Cagatay et al., 2014242 | ✓ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ |
| Jiang et al., 2008243 | ✗ | ✓ | ✓ | ✓ | ? | ✗ | ? | ✓ | ✓ |
| Choi et al., 2010244 | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ |
| Efthimiou et al., 2010245 | ✗ | ✓ | ✗ | ? | ? | ✓ | ? | ✓ | ✓ |
| Ibele et al., 2014246 | ✗ | ✓ | ✓ | ✓ | ? | ✓ | ✗ | ✓ | ✓ |
| Nanashima et al., 2012247 | ✗ | ✗ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ |
| Marchac and Sándor, 1994248 | ✗ | ✓ | ✗ | ✗ | ✗ | ✓ | ✗ | ✓ | ✓ |
| Sakic et al., 2013249 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ |
Appendix 6 Funnel plots for meta-analyses
Primary outcomes
FIGURE 42.
Funnel plot for the seroma. Egger bias = –0.47 (95% CI –1.50 to 0.56; p = 0.36).

FIGURE 43.
Funnel plot for haematoma. Egger bias = –0.63 (95% CI –1.20 to –0.06; p = 0.03).

FIGURE 44.
Funnel plot for combined seroma and haematoma. Egger bias = –0.67 (95% CI –1.38 to 0.03; p = 0.06).
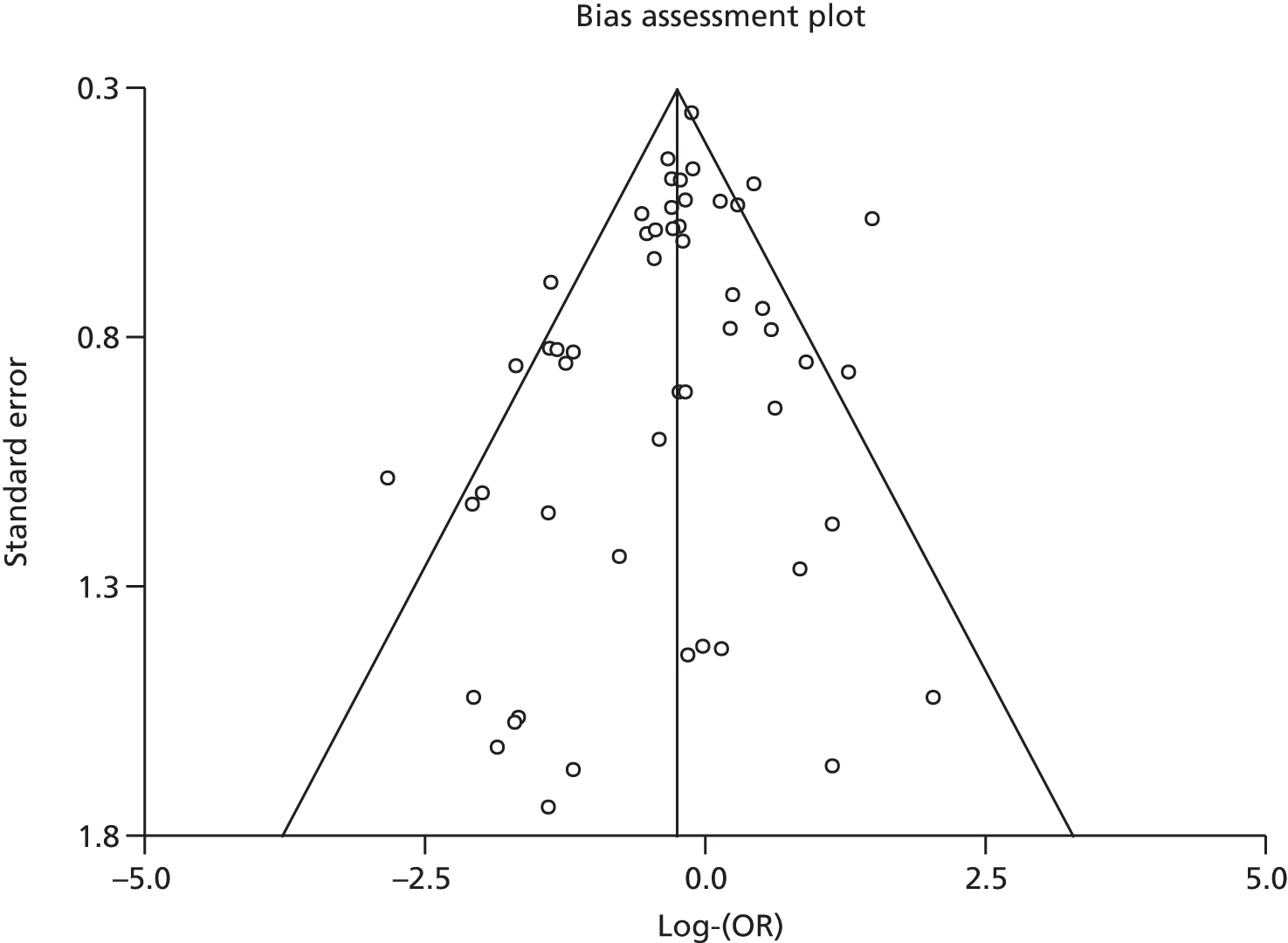
Secondary outcomes
FIGURE 45.
Funnel plot for haemorrhage (bleeding). Egger bias = 0.65 (95% CI –0.53 to 1.82; p = 0.26).
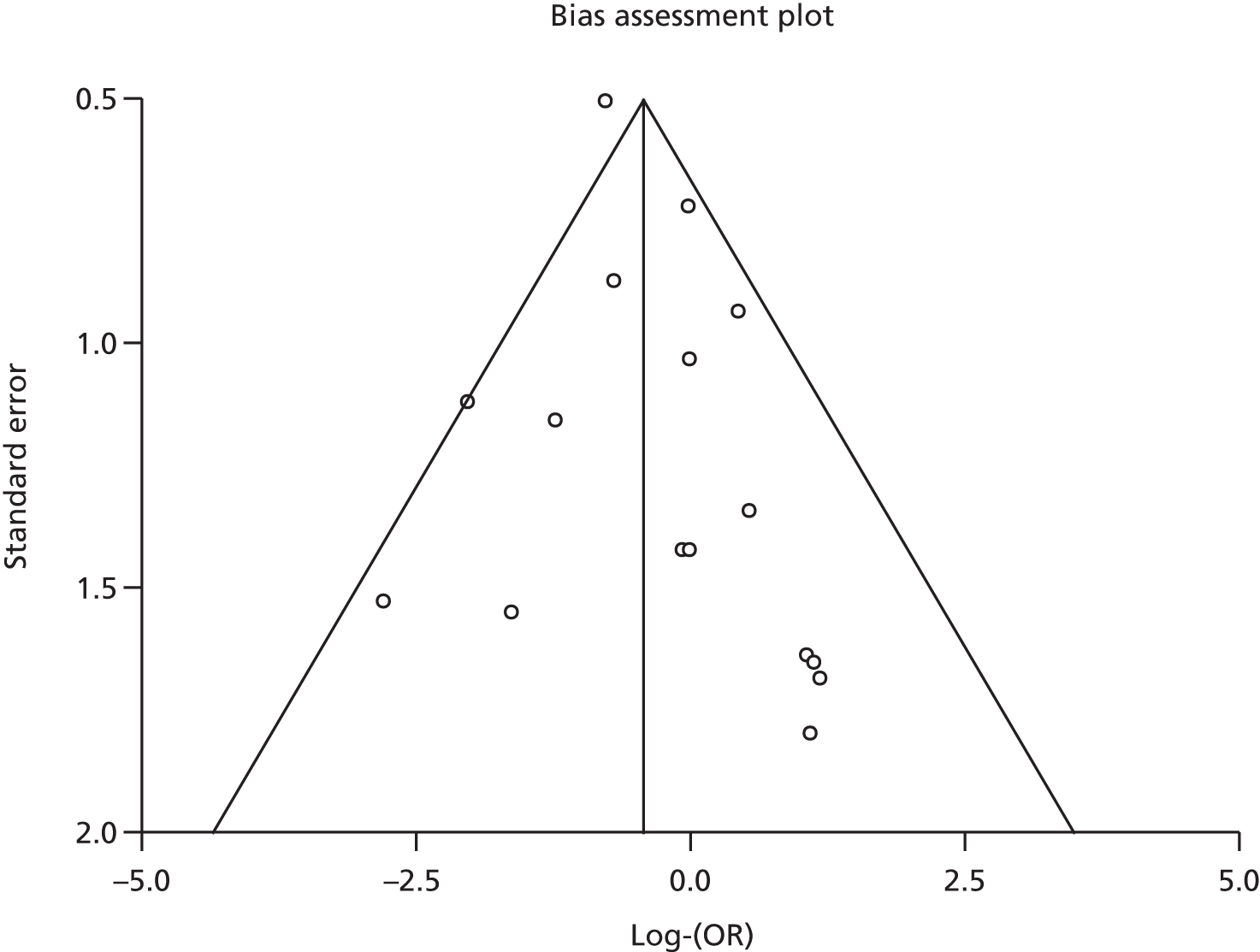
FIGURE 46.
Funnel plot for reoperation. Egger bias = –0.47 (95% CI –1.47 to 0.53; p = 0.33).

FIGURE 47.
Funnel plot for infections. Egger bias = 0.22 (95% CI –0.74 to 1.18; p = 0.64).
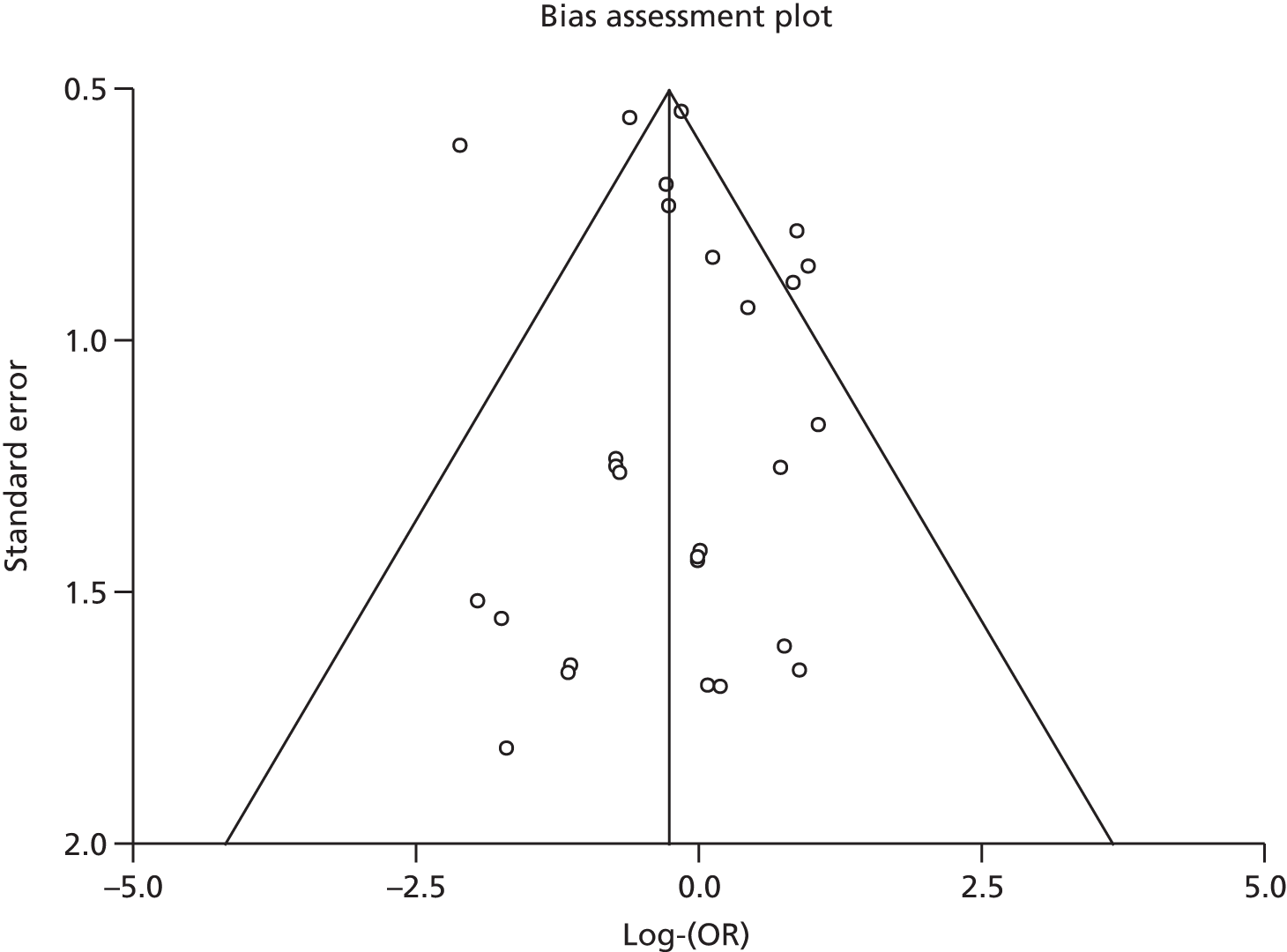
FIGURE 48.
Funnel plot for duration of drainage in breast surgery. Egger bias = –3.40 (95% CI –6.75 to –0.05; p = 0.05).
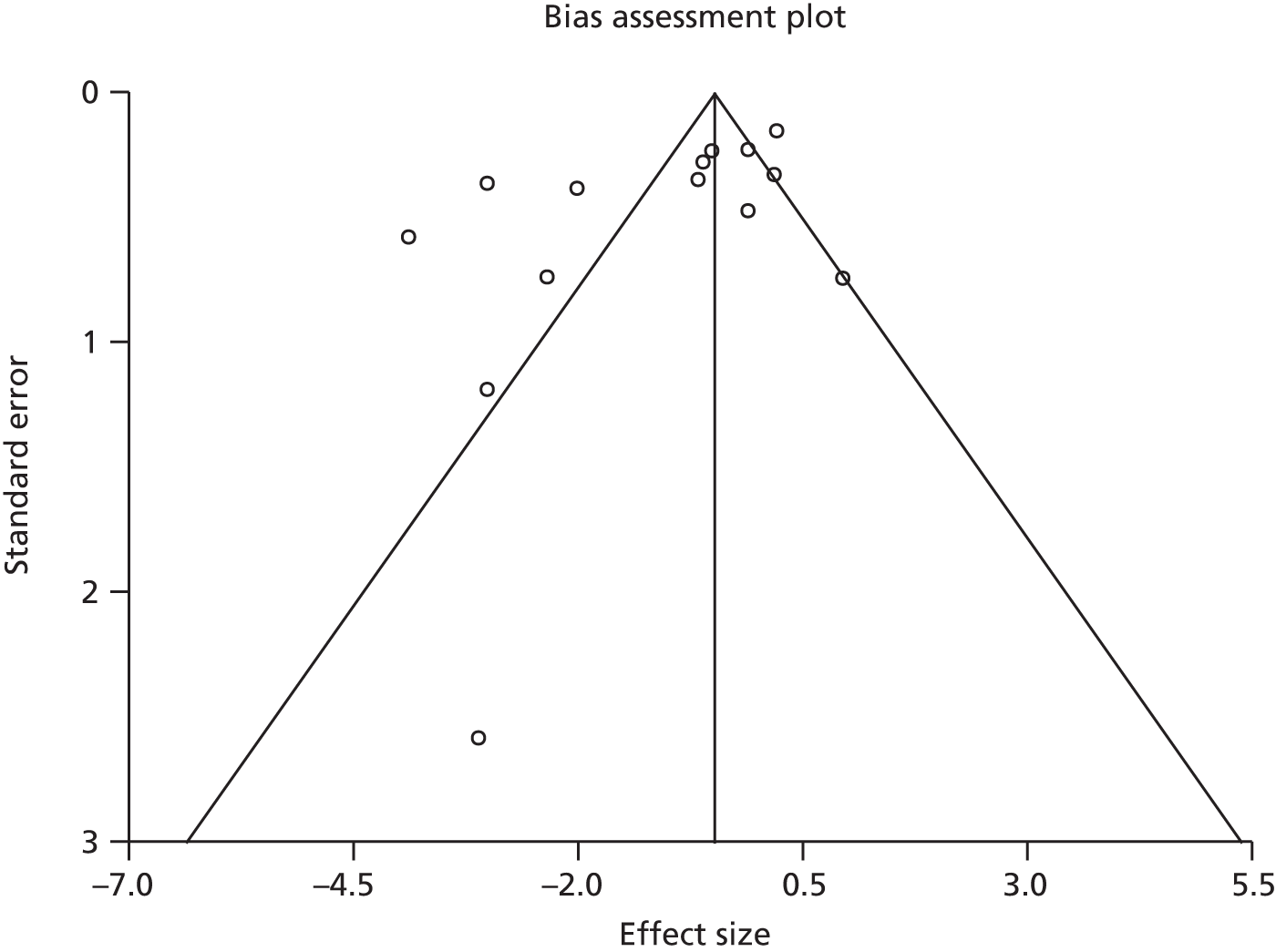
No funnel plot for the duration of operation and length of hospital stay meta-analysis is reported as there was an insufficient number of studies (< 10).
Appendix 7 Tables of excluded observational studies
| Study excluded | Reason for exclusion |
|---|---|
| Abdeen K, Kato Y, Kiya N, Yoshida K, Kanno T. Neuroendoscopy in microvascular decompression for trigeminal neuralgia and hemifacial spasm: technical note. Neurol Res 2000;22:522–6 | No comparison group |
| Abdulla A, Neff M. Laparoscopic repair of perforated duodenal ulcer in child’s class C cirrhotic patient. Surg Endosc 2011;25:S364 | No comparison group |
| Abe T, Goda M, Kamida T, Fujiki M, Kobayashi H, Nakano T, et al. Overlapping free bone graft with galea-pericranium in reconstruction of the anterior skull base to prevent CSF leak and sequestrum formation. Acta Neurochir 2007;149:771–5 | Not a comparative observational study |
| Abel ME, Chiu YS, Russell TR, Volpe PA. Autologous fibrin glue in the treatment of rectovaginal and complex fistulas. Dis Colon Rectum 1993;36:447–9 | No comparison group |
| Abu Hilal M, Hallam MJ, Zeidan BA, Pearce NW. Management of a ruptured pseudoaneurysm of common hepatic artery following pancreaticoduodenectomy. Sci World J 2007;7:1658–62 | No comparison group |
| Abuzayed B, Kafadar AM, Oğuzoğlu SA, Canbaz B, Kaynar MY. Duraplasty using autologous fascia lata reinforced by on-site pedicled muscle flap: technical note. J Craniofac Surg 2009;20:435–8 | No comparison group |
| Achauer BM, Miller SR, Lee TE. The hemostatic effect of fibrin glue on graft donor sites. J Burn Care Rehabil 1994;15:24–8 | RCT |
| Acholonu E, Eckstein J, Patel S, Abu-Jaish W, Szomstein S. Indications, complications and long term outcomes of remnant gastrectomy for gastrogastric fistula after divided Roux-en-Y gastric bypass for morbid obesity. Surg Endosc 2010;24(Suppl. 1):300 | No comparison group |
| Acholonu E, Eckstein J, Patel S, Szomstein S, Rosenthal RJ. Indications, complications and long term outcomes of remnant gastrectomy for gastro-gastric fistula after divided Roux-en-Y gastric bypass for morbid obesity. Obes Surg 2010;20:1005 | Duplicate |
| Adamian LV, Mynbaev OA, Dzhakhan I. [The use of fibrin glue in obstetrics and gynecology.] Akush Ginekol 1991;11:3–4 | Not a comparative observational study |
| Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg 2008;34:1433–8 | Not a comparative observational study |
| Aghamir SM, Khazaeli MH, Meisami A. Use of Surgicel for sealing nephrostomy tract after totally tubeless percutaneous nephrolithotomy. J Endourol 2006;20:293–5 | RCT |
| Agha-Mir-Salim P, Beck R, Bloching M, Berghaus A. [Endoscopic treatment of iatrogenic esophageal perforation.] Laryngorhinootologie 2000;79:39–42 | No comparison group |
| Agresta F. Re: Spray application of fibrin glue as risk factor for subcutaneous emphysema in laparoscopic transabdominal inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 2007;17:222 | Letter/commentary/reply |
| Agresta F, Baldazzi GA, Ciardo LF, Trentin G, Giuseppe S, Ferrante F, et al. Lightweight partially absorbable monofilament mesh (polypropylene/poliglecaprone 25) for TAPP inguinal hernia repair: Initial experience. Surg Laparosc Endosc Percutan Tech 2007;17:91–4 | No comparison group |
| Agresta F, Bedin N. Transabdominal laparoscopic inguinal hernia repair: is there a place for biological mesh? Hernia 2008;12:609–12 | No comparison group |
| Aguilar PH, De Oliveira EP. The use of fibrin glue to stop venous bleeding in the epidural space, vertebral venous plexus, and anterior cavernous sinus: Technical note – commentary. Neurosurgery 2007;61(Suppl.):E51 | Letter/commentary/reply |
| Aguilera et al. 2013143 | RCT |
| Agus GB, Bono AV, Mira E, Olivero S, Peilowich A, Homdrum E, et al. Hemostatic efficacy and safety of TachoComb in surgery. Ready to use and rapid hemostatic agent. Int Surg 1996;81:316–19 | No comparison group |
| Aida H, Kagaya S. [Successful repair of left ventricular free wall rupture with repeated mydriasis and loss of light reflex.] Kyobu Geka 2011;64:1168–71 | No comparison group |
| Aigner C, Wolner E, Mohl W. Management of central coronary sinus ruptures using the pericardial patch repair technique. Ann Thorac Surg 2006;81:1275–8 | No comparison group |
| Aitola P, Hiltunen KM, Matikainen M. Fibrin glue in perianal fistulas – a pilot study. Ann Chir Gynaecol 1999;88:136–8 | No comparison group |
| Ak G, Alpkılıç Başkırt E, Kürklü E, Koray M, Tanyeri H, Zülfikar B. The evaluation of fibrin sealants and tissue adhesives in oral surgery among patients with bleeding disorders. Turk J Haematol 2012;29:40–7 | RCT |
| Akaogi E, Mitsui K, Sohara Y, Endo S, Ishikawa S, Hori M. Treatment of postoperative chylothorax with intrapleural fibrin glue. Ann Thorac Surg 1989;48:116–18 | No comparison group |
| Akhras J, Tobi M, Zagnoon A. Endoscopic fibrin sealant injection with application of hemostatic clips: a novel method of closing a refractory gastrocutaneous fistula. Dig Dis Sci 2005;50:1872–4 | No comparison group |
| Al Harakeh AB. Complications of laparoscopic Roux-en-Y gastric bypass. Surg Clin North Am 2011;91:1225–37 | Not fibrin sealant |
| Alashwal AH, Yaakub A, Noor RAM, Tajudin LSA. Fibrin glue for sealing early bleb leak: a case report. Int J Ophthalmol 2009;9:831–2 | No comparison group |
| Albala DM, Wood C, Fischer C, Hart J, Batiller J, Shen J. A randomized trial of aprotinin free fibrin sealant versus absorbable hemostat. J Endourol 2011;25:A95 | RCT |
| Albéniz Arbizu E, López San Román A, Garcia González M, Foruny Olcina JR, Garcia-Hoz Rosales F, Bárcena Marugán R, et al. Fibrin-glue sealed liver biopsy in patients with a liver transplantation or in liver transplantation waiting list: preliminary results. Transplant Proc 2003;35:1911–12 | No comparison group |
| Albera R, Canale A, Lacilla M, Cavalot AL, Ferrero V. Delayed vertigo after stapes surgery. Laryngoscope 2004;114:860–2 | No comparison group |
| Albert JG. Closure of an ischemic duodenal fistula with an over-the-scope clip. Video J Encyclopedia GI Endosc 2013;1:219–20 | No comparison group |
| Ali A, Zayed H, Kizilates K, El Sakka K, Brown J, Halawa M, et al. The feasibility and safety of drainless carotid endarterectomy. Interact Cardiovasc Thorac Surg 2009;8:S72 | No comparison group |
| Ali SN, Gill P, Oikonomou D, Sterne GD. The combination of fibrin glue and quilting reduces drainage in the extended latissimus dorsi flap donor site. Plast Reconstr Surg 2010;125:1615–19 | RCT |
| Alibai EA, Rahmanian AK, Razmkon A, Nabavizadeh SA. Tension pneumocephalus following pterional craniotomy for treatment of intracavernous internal carotid artery aneurysm. Emerg Radiol 2008;15:441–4 | No comparison group |
| Alio JL, Mulet E, Sakla HF, Gobbi F. Efficacy of synthetic and biological bioadhesives in scleral tunnel phacoemulsification in eyes with high myopia. J Cataract Refract Surg 1998;24:983–8 | RCT |
| Alio JL, Rodriguez AE, Martinez LM, Rio AL. Autologous fibrin membrane combined with solid platelet-rich plasma in the management of perforated corneal ulcers: a pilot study. JAMA Ophthalmol 2013;131:745–51 | No comparison group |
| Alizadeh Ghavidel A, Mirmesdagh Y, Samiei N, Gholampour Dehaki M. Haemostatic role of TachoSil surgical patch in cardiac surgery. J Cardiovasc Thorac Res 2014;6:91–5 | No adverse effects related to fibrin reported |
| Al-khudari S, Vitale L, Ghanem T, McLean S. Recurrent high output chyle fistula post neck dissection resolution with conservative management. Laryngoscope 2010;120(Suppl. 4):141 | No comparison group |
| Allende CA, Allende BT, Allende BL, Bitar I, Gonzalez G. Intercondylar distal humerus fractures – surgical treatment and results. Chir Main 2004;23:85–95 | No adverse effects related to fibrin reported |
| Alleyne Jr CH, Pearce JE. Nonsuture dural repair using polyglycolic acid mesh and fibrin glue: clinical application to spinal surgery – commentary. Surg Neurol 2006;65:142–3 | Letter/commentary/reply |
| Almer ZE, Miller NR. Delayed third cranial nerve palsy after aneurysm wrapping. J Neuroophthalmol 2008;28:359 | Letter/commentary/reply |
| Al-Mutairi M, AlEnezi F, Al-Einati T. Left main coronary artery ostial stenosis with biologic glue post-Bentall procedure. Kuwait Med J 2008;40:321–3 | No comparison group |
| Al-Qahtani K. Initial experience with hemostatic fibrin glue as adjuvant during drainless parotidectomy. Saudi Dent J 2011;23:67–71 | No comparison group |
| Altomare et al. 2011217 | RCT |
| Alvarez JA, Bermejo F, Algaba A, Hernandez MP, Grau M. Surgical repair and biological therapy for fecal incontinence in Crohn’s disease involving both sphincter defects and complex fistulas. J Crohns Colitis 2011;5:598–607 | No comparison group |
| Rubio Alvarez J, Sierra Quiroga J, Martinez de Alegria A, Delgado Dominguez C. Pulmonary embolism due to biological glue after repair of type A aortic dissection. Interact Cardiovasc Thorac Surg 2011;12:650–1 | No comparison group |
| Al-Yamany M, Del Maestro RF. Prevention of subdural fluid collections following transcortical intraventricular and/or paraventricular procedures by using fibrin adhesive. J Neurosurg 2000;92:406–12 | Included children |
| Amano J, Suzuki A. Surgical treatment of cardiac involvement in Takayasu arteritis. Heart Vessels 1992;7(Suppl. 7):168–78 | No comparison group |
| Ambriz-Gonzalez G, Velazquez-Ramirez GA, Garcia-Gonzalez JL, De Leon-Gomez JMG, Mucino-Hernandez MI, Gonzalez-Ojeda A, et al. Use of fibrin sealant in hypospadias surgical repair reduces the frequency of postoperative complications. Urol Int 2007;78:37–41 | Included children |
| Ambruoso G, Aimè G, Borsa R, Cordara G, Governa G, Polledro P, et al. [Urethro-vesical anastomosis after radical prostatectomy and bladder replacement with the Camey II approach.] Minerva Urol Nefrol 1994;46:159–61 | No comparison group |
| Anagiotos A, Feyka M, Gostian AO, Lichtenstein T, Henning TD, Guntinas-Lichius O, et al. Endoscopic laser-assisted diverticulotomy without versus with wound closure in the treatment of Zenker’s diverticulum. Eur Arch Otorhinolaryngol 2014;271:765–70 | No comparison group |
| Anderson NJ, Hardten DR. Fibrin glue for the prevention of epithelial ingrowth after laser in situ keratomileusis. J Cataract Refract Surg 2003;29:1425–9 | No comparison group |
| Andree C, Munder BIJ, Behrendt P, Hellmann S, Audretsch W, Voigt M, et al. Improved safety of autologous breast reconstruction surgery by stabilisation of microsurgical vessel anastomoses using fibrin sealant in 349 free DIEP or fascia-muscle-sparing (fms)-TRAM flaps: a two-centre study. Breast 2008;17:492–8 | No comparison group |
| Andress HJ, Mewes A, Lange V. Endoscopic hemostasis of a bleeding diverticulum of the sigma with fibrin sealant. Endoscopy 1993;25:193 | Letter/commentary/reply |
| Andrychowski J, Czernicki Z, Taraszewska A, Frontczak-Baniewicz M, Przytula E, Zebala M. Granulomatous inflammation of dura mater – a rare side effect after application of hemostatic and insulation materials in case of two-stage operation of huge meningioma. Folia Neuropathol 2012;50:417–24 | No comparison group |
| Angioli R, Plotti F, Ricciardi R, Terranova C, Zullo MA, Damiani P, et al. The use of novel hemostatic sealant (Tisseel) in laparoscopic myomectomy: a case-control study. Surg Endosc 2012;26:2046–53 | RCT |
| Anonymous. [Additional aerostasis with a 100% autologous fibrin glue in lung surgery – a prospective randomised trial.] Khirurgiia 2009;1:10–18 | RCT |
| Anonymous. Additional aerostasis with a 100% autologous fibrin glue in lung surgery – a prospective randomised trial. Khirurgiia 2009;1:10–18 | No comparison group |
| Anwar HM, El-Danasoury A, Hashem AN. The use of fibrin glue to seal Descemet membrane microperforations occurring during deep anterior lamellar keratoplasty. Cornea 2012;31:1193–6 | No comparison group |
| Apestegui C, Breitenstein S, Dutkowski P, Clavien PA. Control of severe portal bleeding by carrier-bound fibrin sealant. Surg Today 2009;39:363–5 | No comparison group |
| Arbes H, Bosch P, Lintner F, Salzer M. First clinical experience with heterologous cancellous bone grafting combined with the fibrin adhesive system (F.A.S.). Arch Orthop Trauma Surg 1981;98:183–8 | No comparison group |
| Argiriou M, Patris V, Lama N, Argiriou O, Charitos C. Off pump repair of left ventricular rupture following mitral valve replacement: the crucial assistance of the intraaortic balloon pump. Int J Surg Case Rep 2013;4:5–6 | No comparison group |
| Arlt F, Trantakis C, Krupp W, Renner C, Winkler D, Strauss G, et al. Cerebrospinal fluid leak after microsurgical surgery in vestibular schwannomas via retrosigmoidal craniotomy. Neurol Res 2011;33:947–52 | No comparison group |
| Arndt S, Maier W, Aschendorff A, Klenzner T, Schipper J. [Ethisorb/Ethisorb durapatch for the transnasal duraplasty procedure?] Laryngorhinootologie 2006;85:260–4 | No comparison group |
| Asato R, Honda K, Tsuji J, Kanda T, Ushiro K, Wtanabe Y. A new method of covering mucosal defect after oral cancerresection – a combination of polyglycolic acid (PGA) sheet and sprayed fibrin glue. Oral Oncol 2011;47:S150–1 | Not fibrin sealant |
| Asensio Samper JM, Fabregat Cid G, Valia-Vera JC, De Andres JA. [Epidural fibrin glue injection as a conservative treatment for persistent cerebrospinal fluid leakage after spinal catheterization.] Rev Esp Anestesiol Reanim 2011;58:391–3 | Letter/commentary/reply |
| Asrani SG, Wilensky JT. Management of bleb leaks after glaucoma filtering surgery. Use of autologous fibrin tissue glue as an alternative. Ophthalmology 1996;103:294–8 | No comparison group |
| Assalia A. A novel method for the management of gastric fistula complicating laparoscopic sleeve gastrectomy: biological glue application in a combined percutaneous and endoscopic approach. Obes Surg 2014;24:1145 | No comparison group |
| Atallah J, Gage E, Koning J, Duggan J, Ramsey-Williams V, Scott S, et al. Treatment of post-dural puncture headache using epidural injection of fibrin sealant as an alternative to autologous epidural blood patch (case report). Scand J Pain 2014;5:170–2 | No comparison group |
| Athanasiadis S, Kuhlgatz C, Girona I. [Experiences with fibrin adhesives in surgery of the rectum and colon.] Zentralbl Chir 1984;109:1107–11 | No comparison group |
| Athanassiadi K, Kalavrouziotis G, Bellenis I. Bronchopleural fistula after pneumonectomy: a major challenge. Acta Chir Hung 1999;38:5–7 | Not fibrin sealant |
| Aurangzeb A, Ahmed E, Khan SA, Ali A, Ihsan A, Mehmood S. Outcome of transcranial repair of traumatic CSF rhinorrhea. J Ayub Med Coll Abbottabad 2012;24:47–9 | No comparison group |
| Avalos-Gonzalez J, Portilla-deBuen E, Leal-Cortes CA, Orozco-Mosqueda A, Estrada-Aguilar MC, Velazquez-Ramirez GA, et al. Reduction of the closure time of postoperative enterocutaneous fistulas with fibrin sealant. World J Gastroenterol 2010;16:2793–800 | No adverse effects related to fibrin reported |
| Avanoglu A, Celik A, Ulman I, Ozcan C, Kavakli K, Nişli G, et al. Safer circumcision in patients with haemophilia: the use of fibrin glue for local haemostasis. BJU Int 1999;83:91–4 | Included children |
| Avisar R, Vaiman M, Sarfaty S, Shlamkovich N, Segal S, Eviatar E, et al. Using fibrin glue in endonasal surgery (multiple letters). Isr Med Assoc J 2005;7:823–4 | Letter/commentary/reply |
| Aydin A, Ozden BC, Mersa B. Complications of microsurgical reconstruction of obstetrical brachial plexus palsy. Plast Reconstr Surg 2005;115:353–4 | Letter/commentary/reply |
| Aydin K, Cokluk C, Kocabicak E, Celik B, Taslak Sengul A. Cervical screw extrusion into the trachea leading to perforation: a case report. Chirurgia 2012;25:355–7 | Not fibrin sealant |
| Ayloo S, Bueno R. Band erosion: laparoscopic removal of lap-band. Surg Endosc 2009;23:657–8 | No comparison group |
| Bacciu A, Falcioni M, Pasanisi E, Di Lella F, Lauda L, Flanagan S, et al. Intracranial facial nerve grafting after removal of vestibular schwannoma. Am J Otolaryngol 2009;30:83–8 | No comparison group |
| Bachet J, Gigou F, Laurian C, Bical O, Goudot B, Guilmet D. Four-year clinical experience with the gelatin-resorcine-formol biological glue in acute aortic dissection. J Thorac Cardiovasc Surg 1982;83:212–17 | Not fibrin sealant |
| Bachleda P, Utikal P, Kalinova L, Herman J. TachoSil® in the treatment of postoperative groin lymphatic fistula. Ann Acad Med Singap 2012;41:534–5 | Letter/commentary/reply |
| Bagot d’Arc M, Daculsi G, Emam N. Biphasic ceramics and fibrin sealant for bone reconstruction in ear surgery. Ann Otol Rhinol Laryngol 2004;113:711–20 | No comparison group |
| Bahar et al. 2006159 | RCT |
| Bahar et al. 2007169 | RCT |
| Bailey SH, Oni G, Guevara R, Wong C, Saint-Cyr M. Latissimus dorsi donor-site morbidity: the combination of quilting and fibrin sealant reduce length of drain placement and seroma rate. Ann Plast Surg 2012;68:555–8 | No adverse effects related to fibrin reported |
| Baiocchi G, Portolani N, Gheza F, Giulini SM. Collagen-based biological glue after Appleby operation for advanced gastric cancer. World J Gastroenterol 2011;17:4044–7 | No comparison group |
| Bajardi et al. 2009194 | RCT |
| Bakeer M, Abd El-Gawad T, El-Metwaly Ali R, El-Morsi A, El-Badrawy M, El-Sharawy S. Low cost biological lung volume reduction therapy for advanced emphysema. Eur Respir J 2014;44(Suppl. 58):P3705 | Abstract |
| Balint B, Gazivoda D, Todorovic-Balint M, Lazic Z, Pavlovic M, Kanjuh V. ‘Triple-way’ approach for the treatment of dry socket: surgery and drugs plus fibrin sealant – as a biomatrix for ‘ultra-concentrated’ platelets. Transfus Apher Sci 2014;51:221–2 | Letter/commentary/reply |
| Bänninger H, Hardegger T, Tobler A, Barth A, Schüpbach P, Reinhart W, et al. Fibrin glue in surgery: frequent development of inhibitors of bovine thrombin and human factor V. Br J Haematol 1993;85:528–32 | No comparison group |
| Barbagli G, De Stefani S, Sighinolfi MC, Annino F, Micali S, Bianchi G. Bulbar urethroplasty with dorsal onlay buccal mucosal graft and fibrin glue. Eur Urol 2006;50:467–74 | No comparison group |
| Barbosa MD, Gregh SL, Passanezi E. Fibrin adhesive derived from snake venom in periodontal surgery. J Periodontol 2007;78:2026–31 | No adverse effects related to fibrin reported |
| Bardaxoglou E, Campion JP, Landen S, Manganas D, Siriser F, Chareton B, et al. Oesophageal perforation: primary suture repair reinforced with absorbable mesh and fibrin glue. Br J Surg 1994;81:399 | No comparison group |
| Barthelemy C, Fayard MO, Etaix JP, Audigier JC, Fraisse H. [Esophagobronchial fistula following sclerosis of esophageal varices. Treatment by injection of biological glue.] Gastroenterol Clin Biol 1984;8:772–3 | Unobtainable |
| Basmak H, Erdogan H, Sahin A, Gürsoy H. Scleral dellen after fibrin glue use in strabismus surgery. J Pediatr Ophthalmol Strabismus 2010;47:e1–3 | No comparison group |
| Basmak H, Gursoy H, Cakmak Aİ, Niyaz L, Yildirim N, Sahin A. Tissue adhesives as an alternative for conjunctival closure in strabismus surgeries. Strabismus 2011;19:59–62 | Included children |
| Basso N. Staple-line leaks management after laparoscopic sleeve gastrectomy. Obes Surg 2009;19:1050 | Not fibrin sealant |
| Batman C, Ozdamar Y, Aslan O, Sonmez K, Mutevelli S, Zilelioglu G. Tissue glue in sutureless vitreoretinal surgery for the treatment of wound leakage. Ophthalmic Surg Lasers Imaging 2008;39:100–6 | No comparison group |
| Batman C, Ozdamar Y, Mutevelli S, Sonmez K, Zilelioglu G, Karakaya J. A comparative study of tissue glue and vicryl suture for conjunctival and scleral closure in conventional 20-gauge vitrectomy. Eye 2009;23:1382–7 | Not a comparative observational study |
| Baumann P, Schumacher H, Husing J, Luntz S, Knaebel HP. A randomized, controlled, prospective trial to evaluate the haemostatic effect of Lyostypt versus Surgicel in arterial bypass anastomosis: ‘COBBANA’ trial. 2009;10:91 | RCT |
| Baumann WR, Ulmer JL, Ambrose PG, Garvey MJ, Jones DT. Closure of a bronchopleural fistula using decalcified human spongiosa and a fibrin sealant. Ann Thorac Surg 1997;64:230–3 | No comparison group |
| Bazan A, Samper A, Lasso JM. The use of fibrin glue in vaginal reconstruction with a pudendal thigh flap. Ann Plast Surg 1999;43:576 | Letter/commentary/reply |
| Beer GM, Goldscheider E, Weber A, Lehmann K. Prevention of acute hematoma after face-lifts. Aesthetic Plast Surg 2010;34:502–7 | Not a valid comparison |
| Beese RC, Tomlinson MA, Buckenham TM. Endoluminal embolization of bilateral atherosclerotic common iliac aneurysms with fibrin tissue glue (Beriplast). Cardiovasc Intervent Radiol 2000;23:239–41 | No comparison group |
| Beierlein W, Scheule AM, Antoniadis G, Braun C, Schosser R. An immediate, allergic skin reaction to aprotinin after reexposure to fibrin sealant. Transfusion 2000;40:302–5 | No comparison group |
| Beitzke M, Leber KA, Deutschmann H, Gattringer T, Poltrum B, Fazekas F. Cerebrovascular complications and granuloma formation after wrapping or coating of intracranial aneurysms with cotton gauze and human fibrin adhesives: results from a single-center patient series over a 5-year period. J Neurosurg 2013;119:1009–14 | Not a valid comparison |
| Bekkers JA, Raap GB, Takkenberg JJ, Bogers AJ. Acute type A aortic dissection: long-term results and reoperations. Eur J Cardiothorac Surg 2013;43:389–96 | Not a valid comparison |
| Bektas H, Nadalin S, Schmidt J, Szabo I, Ploder B, Sharkhawy M. Hemostatic efficacy of latest generation fibrin sealant after hepatic resection; a randomized controlled clinical study. HPB 2013;15:6–7 | RCT |
| Bektas et al. 201465 | RCT |
| Belboul et al. 2004133 | RCT |
| Belcher et al. 2010136 | RCT |
| Bellini LP, Brum GS. Cataract incision closure using fibrin adhesive. J Cataract Refract Surg 2008;34:343–4 | Letter/commentary/reply |
| Benevento et al. 2014109 | No comparison group |
| Benfatto G, Benfatto SM, Strazzanti A, Giovinetto RM, Jiryis A, Salina GM, et al. [Fibrin sealant in tension free hernioplasty: our experience.] G Chir 2006;27:392–4 | No adverse effects related to fibrin reported |
| Benizri EI, Rahili A, Avallone S, Balestro JC, Caï J, Benchimol D. Open inguinal hernia repair by plug and patch: the value of fibrin sealant fixation. Hernia 2006;10:389–94 | No adverse effects related to fibrin reported |
| Benkó I, Molnár TF, Horváth OP. A case of fibrin sealant application for closing benign trachea-esophageal fistula (TEF). Acta Chir Hung 1997;36:25–6 | No comparison group |
| Bense L. Intrabronchial selective coagulative treatment of hemoptysis. Report of three cases. Chest 1990;97:990–6 | RCT |
| Benyamini OG, Barkana Y, Hartstein M, Attas L, Avni I, Zadok D. Biological glue in pterygium surgery with a rotational flap or sliding flaps. Cornea 2008;27:911–15 | No comparison group |
| Beppu T, Iwatsuki M, Okabe H, Okabe K, Masuda T, Hayashi H, et al. A new approach to percutaneous transhepatic portal embolization using ethanolamine oleate iopamidol. J Gastroenterol 2010;45:211–17 | Not a valid comparison |
| Bercial et al. 2012213 | RCT |
| Berg PL, Barina W, Born P. Endoscopic injection of fibrin glue versus polidocanol in peptic ulcer hemorrhage: a pilot study. Endoscopy 1994;26:528–30 | RCT |
| Berger et al. 2001107 | RCT |
| Bergeron E, Roux A, Demers J, Vanier LE, Moore L. A 40-year-old woman with cauda equina syndrome caused by rectothecal fistula arising from an anterior sacral meningocele. Neurosurgery 2010;67:E1464–7 | No comparison group |
| Berkoff DJ, Kanaan M, Kamath G. Fibrin glue as a non-invasive outpatient treatment for post-arthroscopic knee seromas. Knee Surg Sports Traumatol Arthrosc 2013;21:1922–4 | No comparison group |
| Bernal JM, Naranjo S, Trugeda M, Sarralde A, Diago C, Revuelta JM. [Cardiac surgery in Jehovah’s Witnesses. Experience in Santander, Spain.] Rev Esp Cardiol 2006;59:507–9 | No comparison group |
| Bernard RW, Greenwald JA, Beran SJ, Morello DC. Enhancing upper lid aesthetics with the lateral subcutaneous brow lift. Aesthet Surg J 2006;26:19–23 | No comparison group |
| Bernardo L, Bernardo WM, Shu EB, Roz LM, Almeida CC, Monaco BA, et al. Does the use of DuraSeal in head and spinal surgeries reduce the risk of cerebrospinal fluid leaks and complications when compared to conventional methods of dura mater closure? Rev Assoc Med Bras 2012;58:402–3 | Not fibrin sealant |
| Bernasek TL, Burris RB, Fujii H, Levering MF, Polikandriotis JA, Patterson JJ. Effect on blood loss and cost-effectiveness of pain cocktails, platelet-rich plasma, or fibrin sealant after total knee arthroplasty. J Arthroplasty 2012;27:1448–51 | No adverse effects related to fibrin reported |
| Berney CR. The Endoloop technique for the primary closure of direct inguinal hernia defect during the endoscopic totally extraperitoneal approach. Hernia 2012;16:301–5 | No comparison group |
| Berney CR, Yeo AE. Mesh fixation with fibrin sealant during endoscopic totally extraperitoneal inguinal hernia approach: a review of 640 repairs. Hernia 2013;17:709–17 | No comparison group |
| Berruyer M, Amiral J, Ffrench P, Belleville J, Bastien O, Clerc J, et al. Immunization by bovine thrombin used with fibrin glue during cardiovascular operations. Development of thrombin and factor V inhibitors. J Thorac Cardiovasc Surg 1993;105:892–7 | No comparison group |
| Berzofsky CE, Holiday RA, Pitman MJ. Variability of postoperative esophagrams after endoscopic cricopharyngeal myotomy: technique dependence. Ann Otol Rhinol Laryngol 2012;121:145–50 | Not fibrin sealant |
| Bhavana K, Kumar R, Keshri A, Aggarwal S. Minimally invasive technique for repairing CSF leaks due to defects of posterior table of frontal sinus. J Neurol Surg B Skull Base 2014;75:183–6 | No comparison group |
| Binenbaum SJ, Dressner RM, Borao FJ. Laparoscopic repair of a free perforation of a marginal ulcer after Roux-en-Y gastric bypass: a safe alternative to open exploration. JSLS 2007;11:383–8 | No comparison group |
| Birmingham B. TEE diagnosis of mechanical AVR dysfunction associated with biological glue. Anesth Analg 2001;93:1627–8 | Letter/commentary/reply |
| Birth M, Figueras J, Bernardini S, Troen T, Gunther K, Mirza D, et al. Collagen fleece-bound fibrin sealant is not associated with an increased risk of thromboembolic events or major bleeding after its use for haemostasis in surgery: a prospective multicentre surveillance study. Patient Saf Surg 2009;3:13 | No comparison group |
| Bischoff G, Muehling B, Orend K, Bischoff M, Sunder-Plassmann L. A new treatment concept for bronchial stump insufficiency. Thorac Cardiovasc Surg 2010;58:169–74 | Not a valid comparison |
| Bittner R, Gmähle E, Gmähle B, Schwarz J, Aasvang E, Kehlet H. Lightweight mesh and noninvasive fixation: an effective concept for prevention of chronic pain with laparoscopic hernia repair (TAPP). Surg Endosc 2010;24:2958–64 | No adverse effects related to fibrin reported |
| Bittner R, Leibl BJ, Kraft B, Schwarz J. One-year results of a prospective, randomised clinical trial comparing four meshes in laparoscopic inguinal hernia repair (TAPP). Hernia 2011;15:503–10 | RCT |
| Black P. Cerebrospinal fluid leaks following spinal or posterior fossa surgery: use of fat grafts for prevention and repair. Neurosurg Focus 2000;9:e4 | No comparison group |
| Black P. Cerebrospinal fluid leaks following spinal surgery: use of fat grafts for prevention and repair. Technical note. J Neurosurg 2002;96(Suppl. 2):250–2 | No comparison group |
| Blinder D, Manor Y, Martinowitz U, Taicher S, Hashomer T. Dental extractions in patients maintained on continued oral anticoagulant: comparison of local hemostatic modalities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:137–40 | No adverse effects related to fibrin reported |
| Blumenkranz MS, Ohana E, Shaikh S, Chang S, Coll G, Morse LS, et al. Adjuvant methods in macular hole surgery: intraoperative plasma-thrombin mixture and postoperative fluid-gas exchange. Ophthalmic Surg Lasers 2001;32:198–207 | No comparison group |
| Blute ML. Fibrin sealant for retrograde ureteroscopic closure of urine leak after partial nephrectomy. French DB, Marcovich R, Department of Urology, University of Texas Health Science Center, San Antonio, TX. Urol Oncol Seminars Orig Invest 2006;24:554–5 | No comparison group |
| Boadas A, Fernandez-Palazzi F, De Bosch NB, Cedeno M, Ruiz-Saez A. Elective surgery in patients with congenital coagulopathies and inhibitors: experience of the National Haemophilia Centre of Venezuela. Haemophilia 2011;17:422–7 | No comparison group |
| Boaventura PN, Sobreira ML, Yoshida WB, Rollo HA. Treatment of postoperative inguinal lymphocele with fibrin glue injection: case report. J Vasc Brasileiro 2007;6:190–2 | No comparison group |
| Bochicchio G, Singla N, Gupta NY, Porter R, Renkens KL, Pattyn P, et al. An international, multicenter, randomized, single-blind, controlled trial of a dry-powder, fibrin sealant for mild to moderate perioperative surgical bleeding. J Am Coll Surg 2014;219(Suppl. 1):e13–14 | RCT |
| Bochicchio et al. 2015239 | RCT |
| Bock HC, Cohnen J, Keric N, Kantelhardt SR, Giese A. Occlusion of surgical opening of the ventricular system with fibrinogen-coated collagen fleece: a case collection study. Acta Neurochir 2011;153:533–9 | RCT |
| Bodner L, Weinstein JM, Baumgarten AK. Efficacy of fibrin sealant in patients on various levels of oral anticoagulant undergoing oral surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;86:421–4 | No comparison group |
| Boenisch M, Nolst Trenité GJ. [Fibrin glue for operative correction of septal deviations.] HNO 2004;52:963–7 | No comparison group |
| Boldo 2008173 | RCT |
| Boldo E, Armelles A, Perez de Lucia G, Martin F, Aracil JP, Miralles JM, et al. Pain after laparascopic bilateral hernioplasty : Early results of a prospective randomized double-blind study comparing fibrin versus staples. Surg Endosc 2008;22:1206–9. [Erratum appears in Surg Endosc 2008;22:1210] | Duplicate |
| Boonstra EA, Molenaar IQ, Porte RJ, de Boer MT. Topical haemostatic agents in liver surgery: do we need them? HPB 2009;11:306–10 | Not a comparative observational study |
| Borgeskov S, Balslev E. [Use of fibrin adhesive (Tisseel) in pacemaker pockets. An experimental study.] Ugeskr Laeg 1987;149:1059–61 | Not a comparative observational study |
| Born P, Ott R, Rösch T. Endoscopic hemostasis using fibrin sealant for postsphincterotomy bleeding: report of two cases. Gastrointest Endosc 2000;51:731–3 | No comparison group |
| Borowiec AM, McCall M, Lees GM. The trans-sphincteric posterior sagittal repair of recto-urinary and recto-vaginal fistulae using Surgisis™ mesh and fibrin sealant. Tech Coloproctol 2014;18:201–3 | No comparison group |
| Botti G, Pascali M, Botti C, Bodog F, Gentile P, Cervelli V. Comparison of commercial fibrin sealants in facelift surgery: a prospective study. Clin Cosmet Investig Dermatol 2013;6:273–80 | Letter/commentary/reply |
| Bou Monsef J, Buckup J, Waldstein W, Cornell C, Boettner F. Fibrin sealants or cell saver eliminate the need for autologous blood donation in anemic patients undergoing primary total knee arthroplasty. Arch Orthop Trauma Surg 2014;134:53–8 | No adverse effects related to fibrin reported |
| Bouchot O, Bouchot-Hermouet FB, Karam G, Glemain P, Pannier M, Auvigne J. [Prevention of complications in inguinal lymphadenectomy.] J Urol 1990;96:279–83 | No comparison group |
| Boulos PR, Harissi-Dagher M, Kavalec C, Hardy I, Codere F. Intralesional injection of Tisseel fibrin glue for resection of lymphangiomas and other thin-walled orbital cysts. Ophthal Plast Reconstr Surg 2005;21:171–6 | No comparison group |
| Bouwmeester SJ, Beckers JM, Kuijer R, van der Linden AJ, Bulstra SK. Long-term results of rib perichondrial grafts for repair of cartilage defects in the human knee. Int Orthop 1997;21:313–17 | No comparison group |
| Boylu U, Basatac C, Tahra A, Onol FF, Gumus E. Laparoscopic ureterolithotomy with fibrin sealant in the treatment of large impacted proximal ureteral stone. J Endourol 2013;27:A432–3 | No comparison group |
| Bozorg Grayeli A, Mosnier I, Julien N, El Garem H, Bouccara D, Sterkers O. Long-term functional outcome in facial nerve graft by fibrin glue in the temporal bone and cerebellopontine angle. Eur Arch Otorhinolaryngol 2005;262:404–7 | No comparison group |
| Bracale et al. 2014174 | RCT |
| Bradford TJ, Wolf JS. Percutaneous injection of fibrin glue for persistent nephrocutaneous fistula after partial nephrectomy. Urology 2005;65:799 | No comparison group |
| Bradley JP, Gabbay JS, Taub PJ, Heller JB, O’Hara CM, Benhaim P, et al. Monobloc advancement by distraction osteogenesis decreases morbidity and relapse. Plast Reconstr Surg 2006;118:1585–97 | Not fibrin sealant |
| Brady AP, Malone DE, Deignan RW, O’Donovan N, McGrath FP. Fibrin sealant in interventional radiology: a preliminary evaluation. Radiology 1995;196:573–8 | Not a comparative observational study |
| Brady AP, Malone DE, Tam P, McGrath FP. Closure of a duodenal fistula with fibrin sealant. J Vasc Interv Radiol 1993;4:525–7 | No comparison group |
| Braga Ade F, Rousselet MS, Zambelli H, Sbragia L, Barini R. [Anesthesia for intrauterine myelomeningocele correction: case report.] Rev Bras Anestesiol 2005;55:329–35 | No comparison group |
| Brandão RA, Costa BS, Dellaretti MA, de Carvalho GT, Faria MP, de Sousa AA. Efficacy and safety of a porcine collagen sponge for cranial neurosurgery: a prospective case-control study. World Neurosurg 2013;79:544–50 | Not fibrin sealant |
| Breda A, Stepanian SV, Lam JS, Liao JC, Gill IS, Colombo JR, et al. Use of haemostatic agents and glues during laparoscopic partial nephrectomy: a multi-institutional survey from the United States and Europe of 1347 cases. Eur Urol 2007;52:798–803 | Not a comparative observational study |
| Brega Massone PP, Magnani B, Conti B, Lequaglie C, Cataldo I. Cauterization versus fibrin glue for aerostasis in precision resections for secondary lung tumors. Ann Surg Oncol 2003;10:441–6 | No adverse effects related to fibrin reported |
| Breugem SJM, Rijcken THP, Albers GHR. Recurrent hemarthrosis after total knee arthroplasty caused by pseudoaneurysm. Curr Orthop Pract 2011;22:382–4 | No comparison group |
| Briceño J, Naranjo A, Ciria R, Díaz-Nieto R, Sánchez-Hidalgo JM, Luque A, et al. A prospective study of the efficacy of clinical application of a new carrier-bound fibrin sealant after liver resection. Arch Surg 2010;145:482–8 | No adverse effects related to fibrin reported |
| Briones-Estebanez JL, Zaragoza-Garcia JM, Martinez-Parreno C, Al-Raies Bolanos B, Plaza-Martinez A, Blanes-Mompo JI, et al. The treatment of iatrogenic pseudoaneurysms: a comparison of the ultrasound compression technique with the ultrasound-guided injection of human thrombin. Angiologia 2006;58:445–50 | Not surgery |
| Brolin RE, Lin JM. Treatment of gastric leaks after Roux-en-Y gastric bypass: a paradigm shift. Surg Obes Relat Dis 2013;9:229–33 | Not surgery |
| Brountzos EN, Malagari K, Papathanasiou MA, Gougoulakis A, Kelekis DA. Internal iliac artery aneurysm embolization with fibrin sealant: a simple and effective solution. Cardiovasc Intervent Radiol 2003;26:76–80 | No comparison group |
| Brown JA, Hubosky SG, Gomella LG, Strup SE. Hand assisted laparoscopic partial nephrectomy for peripheral and central lesions: a review of 30 consecutive cases. J Urol 2004;171:1443–6 | No comparison group |
| Brown NE, Grundfast KM, Jabre A, Megerian CA, O’Malley BW, Rosenberg SI. Diagnosis and management of spontaneous cerebrospinal fluid-middle ear effusion and otorrhea. Laryngoscope 2004;114:800–5 | Not a valid comparison |
| Bruck HG. Fibrin tissue adhesion and its use in rhytidectomy: a pilot study. Aesthetic Plast Surg 1982;6:197–202 | No comparison group |
| Brückner M, Grimm H, Nam VC, Soehendra N. Endoscopic treatment of a pancreatic abscess originating from biliary pancreatitis. Surg Endosc 1990;4:227–9 | No comparison group |
| Bruner JP, Richards WO, Tulipan NB, Arney TL. Endoscopic coverage of fetal myelomeningocele in utero. Am J Obstet Gynecol 1999;180:153–8 | No comparison group |
| Bruns J, Klima H. [Osteochondritis dissecans of the knee joint. Results of follow-up.] Z Orthop Ihre Grenzgeb 1993;131:413–19 | Included children |
| Buchanan GN, Bartram CI, Phillips RK, Gould SW, Halligan S, Rockall TA, et al. Efficacy of fibrin sealant in the management of complex anal fistula: a prospective trial. Dis Colon Rectum 2003;46:1167–74 | No comparison group |
| Buckley RC, Breazeale EE, Edmond JA, Brzezienski MA. A simple preparation of autologous fibrin glue for skin-graft fixation. Plast Reconstr Surg 1999;103:202–6 | No comparison group |
| Buda A, Fruscio R, Pirovano C, Signorelli M, Betti M, Milani R. The use of TachoSil for the prevention of postoperative complications after groin dissection in cases of gynecologic malignancy. Int J Gynaecol Obstet 2012;117:217–19 | No adverse effects related to fibrin reported |
| Buda A, Pirovano C, Fruscio R, Betti M, Cuzzocrea M, Dell’Orto F, et al. Tachosil patch for the prevention of postoperative complications after inguinofemoral lymphadenectomy in gynecological malignancy: a single institution case-control study. Ital J Gynaecol Obstet 2011;23:133–8 | No adverse effects related to fibrin reported |
| Buda A, Pirovano C, Giuliani D, Signorelli M, Lissoni AA, Chiappa V, et al. Tachosil patch plus surgical clips for prevention of postoperative complications after inguinofemoral lymphadenectomy for vulvar cancer: a single institution experience. Int J Gynecol Cancer 2011;21(Suppl. 3):S894 | No adverse effects related to fibrin reported |
| Bulajic P, Savic N, Djordjevic Z, Kecmanovic D, Bulajic M, Milicevic M, et al. Role of autologous fibrin tissue adhesive in abdominal surgery. Acta Chir Iugosl 1999;46:43–5 | Not a comparative observational study |
| Bulbuller et al. 201392 | RCT |
| Bullocks JM, Echo A, Guerra G, Stal S, Yuksel E. A novel autologous scaffold for diced-cartilage grafts in dorsal augmentation rhinoplasty. Aesthetic Plast Surg 2011;35:569–79 | No comparison group |
| Burnouf T, Chen TM, Tsai JC. A novel technique combining single-donor platelet gel and fibrin glue with skin graft to heal recalcitrant lower extremity ulcers. Vox Sanguinis 2010;99:264 | No comparison group |
| Busuttil RW. A comparison of antifibrinolytic agents used in hemostatic fibrin sealants. J Am Coll Surg 2003;197:1021–8 | Not a comparative observational study |
| Butler CE. Treatment of refractory donor-site seromas with percutaneous instillation of fibrin sealant. Plast Reconstr Surg 2006;117:976–85 | No comparison group |
| Bylund JR, Clark CJ, Crispen PL, Lagrange CA, Strup SE. Hand-assisted laparoscopic partial nephrectomy without formal collecting system closure: perioperative outcomes in 104 consecutive patients. J Endourol 2011;25:1853–7 | No comparison group |
| Byrne DJ, Hardy J, Wood RA, McIntosh R, Hopwood D, Cuschieri A. Adverse influence of fibrin sealant on the healing of high-risk sutured colonic anastomoses. J R Coll Surg Edinb 1992;37:394–8 | Not fibrin sealant |
| Byun CS, Hwang JJ, Choi JH. Single-incision vats bullectomy with suture-lift method in primary spontaneous pneumothorax. Innovations 2013;8:145–6 | No comparison group |
| Caccavale A, Romanazzi F, Imparato M, Negri A, Porta A, Ferentini F. Ropivacaine for topical anesthesia in pterygium surgery with fibrin glue for conjunctival autograft. Cornea 2010;29:375–6 | No comparison group |
| Cachaldora-del Rio JA, Hernandez-Lahoz Ortiz I, Sanchez-Abuin J, Rielo-Arias FJ, Gallegos-Vidal M, Fernandez-Fernandez JC, et al. Treatment of iatrogenic arterial pseudoaneurysms with human thrombin injections. Angiologia 2002;54:390–6 | No comparison group |
| Caers J, Reekmans A, Jochmans K, Naegels S, Mana F, Urbain D, et al. Factor V inhibitor after injection of human thrombin (tissucol) into a bleeding peptic ulcer. Endoscopy 2003;35:542–4 | No comparison group |
| Calabrò B, Ponsetto M, Greco R, Peradotto F, Personnettaz E, Obialero M. [Treatment of leg ulcers with fibrin glue.] Minerva Chir 1995;50:569–74 | Not surgery |
| Calado E, Ayres-de-Campos D. Premature rupture of membranes at 20 weeks: report of a successful outcome after transcervical application of fibrin glue. Fetal Diagn Ther 2007;22:14–17 | No comparison group |
| Caldas Neto S, Oliveira RL, Caldas N. Use of in fibrin glue in the prevention of postoperative bleeding and hematomas after septoplasty. Rev Bras Otorrinolaringol 2002;68:635–8 | RCT |
| Callari C, Perretta S, Diana M, Dagostino J, Dallemagne B, Marescaux J. Multimedia manuscript. Thoracoscopic management of chylothorax after esophagectomy. Surg Endosc 2012;26:1160 | Not fibrin sealant |
| Cambal et al. 2012175 | RCT |
| Campanelli G, Champault G, Pascual MH, Hoeferlin A, Kingsnorth A, Rosenberg J, et al. Randomized, controlled, blinded trial of Tissucol/Tisseel for mesh fixation in patients undergoing Lichtenstein technique for primary inguinal hernia repair: rationale and study design of the TIMELI trial. Hernia 2008;12:159–65 | RCT |
| Campanelli et al. 2012176 | RCT |
| Campanelli G, Sfeclan C, Cavalli M, Biondi A. Reducing postoperative pain: the use of Tisseel for mesh fixation in inguinal hernia repair. Surg Technol Int 2012;22:134–9 | RCT |
| Campbell ML, Abboud EC, Dolberg ME, Sanchez JE, Marcet JE, Rasheid SH. Treatment of refractory perianal fistulas with ligation of the intersphincteric fistula tract: preliminary results. Am Surg 2013;79:723–7 | No comparison group |
| Campos F, Fujio S, Sugata S, Tokimura H, Hanaya R, Bohara M, et al. Effect of thrombin concentration on the adhesion strength and clinical application of fibrin glue-soaked sponge. Neurol Med Chir (Tokyo) 2013;53:17–20 | No comparison group |
| Campos JM, Pereira EF, Evangelista LF, Siqueira L, Neto MG, Dib V, et al. Gastrobronchial fistula after sleeve gastrectomy and gastric bypass: endoscopic management and prevention. Obes Surg 2011;21:1520–9 | No comparison group |
| Campos JM, Siqueira LT, Meira MR, Ferraz AA, Ferraz EM, Guimaraes MJ. Gastrobronchial fistula as a rare complication of gastroplasty for obesity: a report of two cases. J Bras Pneumol 2007;33:475–9 | No comparison group |
| Canby-Hagino ED, Morey AF, Jatoi I, Perahia B, Bishoff JT. Fibrin sealant treatment of splenic injury during open and laparoscopic left radical nephrectomy. J Urol 2000;164:2004–5 | No comparison group |
| Canonico S, Benevento R, Della Corte A, Fattopace A, Canonico R. Sutureless tension-free hernia repair with human fibrin glue (Tissucol) in soccer players with chronic inguinal pain: initial experience. Int J Sports Med 2007;28:873–6 | No comparison group |
| Canonico S, Benevento R, Perna G, Guerniero R, Sciaudone G, Pellino G, et al. Sutureless fixation with fibrin glue of lightweight mesh in open inguinal hernia repair: effect on postoperative pain: a double-blind, randomized trial versus standard heavyweight mesh. Surgery 2013;153:126–30 | RCT |
| Canonico S, Pacifico F, Santoriello A. The prophylaxis of haemocoagulative complications after prosthetic surgery of inguinal hernias. Chirurgia 1995;8:88–92 | No adverse effects related to fibrin reported |
| Canonico S, Santoriello A, Campitiello F, Fattopace A, Corte AD, Sordelli I, et al. Mesh fixation with human fibrin glue (Tissucol) in open tension-free inguinal hernia repair: a preliminary report. Hernia 2005;9:330–3 | No comparison group |
| Canonico et al. 1999177 | RCT |
| Canziani M, Agrusti S, Bertocchi V, Cavalli M, Campanelli G, Cavaliere D, et al. The tailored surgery in incisional hernia repair. Eur Surg Res 2010;45(3–4):168 | Abstract |
| Canziani M, Frattini F, Cavalli M, Agrusti S, Somalvico F, Campanelli G. Sutureless mesh fibrin glue incisional hernia repair. Hernia 2009;13:625–9 | No comparison group |
| Cappabianca P. The awake endoscope-guided sealant technique with fibrin glue in the treatment of postoperative cerebrospinal fluid leak after extended transsphenoidal surgery: technical note. World Neurosurg 2014;82:e479–85 | No comparison group |
| Cappabianca P, Cavallo LM, Valente V, Romano I, D’Enza AI, Esposito F, et al. Sellar repair with fibrin sealant and collagen fleece after endoscopic endonasal transsphenoidal surgery. Surg Neurol 2004;62:227–33 | Fibrin was used in both groups |
| Cappabianca P, Esposito F, Cavallo LM, Messina A, Solari D, di Somma LG, et al. Use of equine collagen foil as dura mater substitute in endoscopic endonasal transsphenoidal surgery. Surg Neurol 2006;65:144–8 | No comparison group |
| Capussotti L, Ferrero A, Viganò L, Sgotto E, Muratore A, Polastri R. Bile leakage and liver resection: where is the risk? Arch Surg 2006;141:690–4 | Included children |
| Carbon RT, Baar S, Waldschmidt J, Huemmer HP, Simon SI. Innovative minimally invasive pediatric surgery is of therapeutic value for splenic injury. J Pediatr Surg 2002;37:1146–50 | Included children |
| Cardillo G, Carbone L, Carleo F, Batzella S, Jacono RD, Lucantoni G, et al. Tracheal lacerations after endotracheal intubation: a proposed morphological classification to guide non-surgical treatment. Eur J Cardiothorac Surg 2010;37:581–7 | No comparison group |
| Cardillo et al. 201241 | RCT |
| Cardillo G, Galetta D, van Schil P, Zuin A, Filosso P, Cerfolio RJ, et al. Completion pneumonectomy: a multicentre international study on 165 patients. Eur J Cardiothorac Surg 2012;42:405–9 | RCT |
| Carey JN, Sheckter CC, Watt AJ, Lee GK. Intra-abdominal pedicled rectus abdominis muscle flap for treatment of high-output enterocutaneous fistulae: case reports and review of literature. J Plast Reconstr Aesthet Surg 2013;66:1145–8 | No comparison group |
| Carini M, Serni S, Lapini A, Selli C, Menchi I. Endoscopic treatment of refluxing ureteric stump following nephrectomy with Tissucol and teflon injection. Eur Urol 1989;16:312–14 | No comparison group |
| Carlson et al. 200894 | RCT |
| Carter et al. 2003229 | RCT |
| Carter G, Goss AN, Lloyd J, Tocchetti R. Local haemostasis with autologous fibrin glue following surgical enucleation of a large cystic lesion in a therapeutically anticoagulated patient. Br J Oral Maxillofac Surg 2003;41:275–6 | No comparison group |
| Carter et al. 201381 | No comparison group |
| Caruso A, Manta R, Melotti G, Conigliaro R. Endoscopic treatment of a large post-surgical fistula using combined fibrin glue spray and vicryl mesh. Dig Liver Dis 2012;44:85–6 | No comparison group |
| Casarotto A, Militello V, Piatto G, Gruppo M, Militello C. Hernioplasty in elderly high-risk adults: efficacy of fibrin glue. J Am Geriatr Soc 2012;60:1193–4 | Letter/commentary/reply |
| Casas VE, Kheirkhah A, Blanco G, Tseng SC. Surgical approach for scleral ischemia and melt. Cornea 2008;27:196–201 | Not a valid comparison |
| Casella G, Soricelli E, Rizzello M, Trentino P, Fiocca F, Fantini A, et al. Nonsurgical treatment of staple line leaks after laparoscopic sleeve gastrectomy. Obes Surg 2009;19:821–6 | Duplicate |
| Cavallini M, Tallerini A, Stipa F. [Occlusion of the duct with a fibrin glue and preservation of the pylorus after resection of the duodenum and head of the pancreas for periampullary carcinoma.] Minerva Chir 1991;46:733–9 | No comparison group |
| Cavallo LM, Messina A, Esposito F, de Divitiis O, Dal Fabbro M, de Divitiis E, et al. Skull base reconstruction in the extended endoscopic transsphenoidal approach for suprasellar lesions. J Neurosurg 2007;107:713–20 | No comparison group |
| Cavallo LM, Solari D, Somma T, Di Somma A, Chiaramonte C, Cappabianca P. Use of equine pericardium sheet (LYOMESH) as dura mater substitute in endoscopic endonasal transsphenoidal surgery. Transl Med USA 2013;7:23–8 | No comparison group |
| Cavallo LM, Solari D, Somma T, Savic D, Cappabianca P. The awake endoscope-guided sealant technique with fibrin glue in the treatment of postoperative cerebrospinal fluid leak after extended transsphenoidal surgery: technical note. World Neurosurg 2014;82:e479–85 | No comparison group |
| Ceccarelli G, Casciola L, Pisanelli MC, Bartoli A, Di Zitti L, Spaziani A, et al. Comparing fibrin sealant with staples for mesh fixation in laparoscopic transabdominal hernia repair: a case control-study. Surg Endosc 2008;22:668–73 | No adverse effects related to fibrin reported |
| Cecchi M, Sepich CA, Pagni G, Ippolito C, Minervini R, Fiorentini L. Painless treatment of hydrocele: EMLA cream anaesthesia and fibrin adhesive sclerotherapy. Int Urol Nephrol 1997;29:457–9 | No comparison group |
| Cederholm-Williams SA. Benefits of adjuvant fibrin glue in skin grafting. Med J Aust 1994;161:575 | Letter/commentary/reply |
| Cederholm-Williams SA, Dean MG, Nicholls MD. Benefits of adjuvant fibrin glue in skin grafting. Med J Aust 1994;161:575 | Duplicate |
| Cedin AC, Fujita R, Cruz OL. Endoscopic transeptal surgery for choanal atresia with a stentless folded-over-flap technique. Otolaryngol Head Neck Surg 2006;135:693–8 | No comparison group |
| Celia A, Zeccolini G, Guazzoni G, Pansadoro V, Disanto V, Porpiglia F, et al. Laparoscopic nephron sparing surgery: a multi-institutional European survey of 592 cases. Arch Ital Urol Androl 2008;80:85–91 | No comparison group |
| Celiento M, Scioti G, Pratali S, Bortolotti U. Repair of coronary artery perforation following angioplasty using TachoSil patches. Interact Cardiovasc Thorac Surg 2010;10:328–30 | No comparison group |
| Cellier C, Landi B, Faye A, Wind P, Frileux P, Cugnenc PH, et al. Upper gastrointestinal tract fistulae: endoscopic obliteration with fibrin sealant. Gastrointest Endosc 1996;44:731–3 | No comparison group |
| Cellini C, Manta R, Caruso A, Mirante VG, Bertani H, Manno M, et al. Endoscopic treatment of post-surgical gastrointestinal fistulas: experience of a tertiary referral centre. Dig Liver Dis 2014;46:S139 | Not a valid comparison |
| Cennamo V, Fuccio L, Giampalma E, Terzi E, Eusebi LH, Mosconi C, et al. Choledochoscope-assisted percutaneous fibrin glue sealing of bile leak complicating transarterial chemoembolization of hepatocellular carcinoma after liver transplantation. Endoscopy 2011;43(Suppl. 2):E238–9 | No comparison group |
| Cerfolio RJ, Allen MS, Deschamps C, Trastek VF, Pairolero PC. Postoperative chylothorax. J Thorac Cardiovasc Surg 1996;112:1361–5 | No comparison group |
| Cernea CR, Hojaij FC, De Carlucci D Jr, Tavares MR, Araujo-Filho VJ, Silva-Filho GB, et al. Abdominal compression: a new intraoperative manoeuver to detect chyle fistulas during left neck dissections that include level IV. Head Neck 2012;34:1570–3 | No comparison group |
| Cerný M, Havlícek K, Sákra L, Flasar J. [Massive hemothorax following canylation of the subcalvian vein – a case review.] Rozhl Chir 2008;87:376–9 | No comparison group |
| Cerwenka H, Bacher H, Werkgartner G, El-Shabrawi A, Mischinger HJ. Massive liver haemorrhage and rupture caused by HELLP-syndrome treated by collagen fleeces coated with fibrin glue. Eur J Surg 1998;164:709–11 | No comparison group |
| Cesana G, Olmi S, Croce E. Trans-abdominal pre-peritoneal laparoscopic inguinal hernia repair versus classical inguinotomic repair: a randomized study. Surg Endosc 2011;25:S7 | RCT |
| Cestaro G, De Rosa M, Gentile M. Treatment of fistula in ano with fibrin glue: preliminary results from a prospective study. Minerva Chir 2014;69:225–8 | RCT |
| Cha HG, Kang SG, Shin HS, Kang MS, Nam SM. Does fibrin sealant reduce seroma after immediate breast reconstruction utilizing a latissimus dorsi myocutaneous flap? Arch Plast Surg 2012;39:504–8 | No adverse effects related to fibrin reported |
| Cha HS, Kim A, Nowzari H, Chang HS, Ahn KM. Simultaneous sinus lift and implant installation: prospective study of consecutive two hundred seventeen sinus lift and four hundred sixty-two implants. Clin Implant Dent Relat Res 2014;16:337–47 | Not fibrin sealant |
| Chabok SY, Safaie M, Ashraf A, Emamhadi M, Behzadnia H, Alijani B, et al. Effect of fat graft on dural tear repair in lumbar spine laminectomy surgery. Neurosurg Q 2014;24:1–4 | Not a valid comparison |
| Chalmers et al. 2010198 | RCT |
| Chan K, Dickinson J. Surgical results following full-thickness skin grafting with tisseel in the periocular region-cosmetic outcomes and incidence of complications. Clin Experiment Ophthalmol 2013;41:88 | No comparison group |
| Chan et al. 2014178 | RCT |
| Chapman WC, Clavien P, Fung JJ, Block JE. Managing hepatic bleeding with autologous plasma/collagen-based fibrin sealant. Arch Surg 2001;136:967 | Letter/commentary/reply |
| Chapman et al. 200067 | RCT |
| Chartrand C, Dumont L, Stanley P. Value of fibrin sealant in heart transplantation. Transplant Proc 1989;21:3347–8 | Not in humans |
| Chawla B, Tandon R. Sutureless amniotic membrane fixation with fibrin glue in symptomatic bullous keratopathy with poor visual potential. Eur J Ophthalmol 2008;18:998–1001 | No comparison group |
| Chen ML, Tomaszewski JJ, Matoka DJ, Ost MC. Management of urine leak after laparoscopic cyst decortication with retrograde endoscopic fibrin glue application and ureteral stent placement. J Endourol 2011;25:71–4 | No comparison group |
| Chen RJ, Fang JF, Lin BC, Hsu YB, Kao JL, Kao YC, et al. Selective application of laparoscopy and fibrin glue in the failure of nonoperative management of blunt hepatic trauma. J Trauma 1998;44:691–5 | No comparison group |
| Chen TM, Tsai JC, Burnouf T. A novel technique combining platelet gel, skin graft, and fibrin glue for healing recalcitrant lower extremity ulcers. Dermatol Surg 2010;36:453–60 | No comparison group |
| Chen WL, Huang ZQ, Chai Q, Zhang DM, Wang YY, Wang HJ, et al. Percutaneous sclerotherapy of massive macrocystic lymphatic malformations of the face and neck using fibrin glue with OK-432 and bleomycin. Int J Oral Maxillofac Surg 2011;40:572–6 | Included children |
| Chen WL, Huang ZQ, Li JS, Chai Q, Zhang DM. Percutaneous sclerotherapy of juvenile nasopharyngeal angiofibroma using fibrin glue combined with OK-432 and bleomycin. Int J Pediatr Otorhinolaryngol 2010;74:422–5 | No comparison group |
| Chen WL, Huang ZQ, Zhang DM, Chai Q. Percutaneous sclerotherapy of massive venous malformations of the face and neck using fibrin glue combined with OK-432 and pingyangmycin. Head Neck 2010;32:467–72 | No comparison group |
| Chen WL, Zhang LP, Huang ZQ, Zhou B. Percutaneous sclerotherapy of sialoceles after parotidectomy with fibrin glue, OK-432, and bleomycin. Br J Oral Maxillofac Surg 2013;51:786–8 | No comparison group |
| Cheng HT, Hsu YC, Wu CI. Quilting sutures, fibrin tissue adhesive or both in reducing the incidence of seroma in the latissimus dorsi flap donor site? An evidence-based analysis. J Plast Reconstr Aesthet Surg 2014;67:881–2 | Letter/commentary/reply |
| Chernousov AF, Khororykh TV, Urzhumtseva GA, Urakova IaCh. [Endoscopic hemostasis of erosive-ulcerous gastroduodenal bleeding with fibrin glue at critically ill patients.] Khirurgiia 2006;8:17–20 | No comparison group |
| Chi JH, Sughrue M, Kunwar S, Lawton MT. The ‘yo-yo’ technique to prevent cerebrospinal fluid rhinorrhea after anterior clinoidectomy for proximal internal carotid artery aneurysms. Neurosurgery 2006;59:ONS–101 | No comparison group |
| Chin Ai, Ragavendra N, Hilborne L, Gritsch HA. Fibrin sealant sclerotherapy for treatment of lymphoceles following renal transplantation. J Urol 2003;170:380–3 | No comparison group |
| Chin CJ, Kus L, Rotenberg BW. Use of duraseal in repair of cerebrospinal fluid leaks. J Otolaryngol Head Neck Surg 2010;39:594–9 | Letter/commentary/reply |
| Chirletti P, Caronna R, Fanello G, Schiratti M, Stagnitti F, Peparini N, et al. Pancreaticojejunostomy with application of fibrinogen/thrombin-coated collagen patch (TachoSil) in Roux-en-Y reconstruction after pancreaticoduodenectomy. J Gastrointest Surg 2009;13:1396–8 | Letter/commentary/reply |
| Chisholm RA, Jones SN, Lees WR. Fibrin sealant as a plug for the post liver biopsy needle track. Clin Radiol 1989;40:627–8 | No comparison group |
| Cho JM, Ahn JY, Chang JH, Kim SH. Prevention of cerebrospinal fluid rhinorrhea after transsphenoidal surgery by collagen fleece coated with fibrin sealant without autologous tissue graft or postoperative lumbar drainage. Neurosurgery 2011;68(Suppl.):130–6 | No comparison group |
| Cho S, Huh DM, Kim BH, Lee S, Kwon OC, Ahn WS, et al. Staple line covering procedure after thoracoscopic bullectomy for the management of primary spontaneous pneumothorax. Thorac Cardiovasc Surg 2008;56:217–20 | No comparison group |
| Cho S, Ryu KM, Jheon S, Sung SW, Kim BH, Huh DM. Additional mechanical pleurodesis after thoracoscopic wedge resection and covering procedure for primary spontaneous pneumothorax. Surg Endosc 2009;23:986–90 | Not a valid comparison |
| Choi et al. 2010244 | No comparison group |
| Chou D, Cheng J, Chesnut R, Choudhri H, Gopinath S, Scott Graham R, et al. A prospective, multi-center, randomized controlled study to compare a low swell formulation of a PEG hydrogel spinal sealant as an adjunct to sutured dural repair with common dural sealing methods. Spine J 2010;10:80S | RCT |
| Chou D, Wang VY, Khan AS. Primary dural repair during minimally invasive microdiscectomy using standard operating room instruments. Neurosurgery 2009;64(Suppl. 2):356–8 | No comparison group |
| Choudhari NS, Neog A, Sharma A, Iyer GK, Srinivasan B. Our experience of fibrin sealant-assisted implantation of Ahmed glaucoma valve. Indian J Ophthalmol 2013;61:23–7 | No comparison group |
| Choufani et al. 2015151 | RCT |
| Chouillard EK, Fingerhut AL. Sutureless repair of bronchial tears using fibrin sealant-reinforced Vicryl bridge. ANZ J Surg 2006;76:419 | Letter/commentary/reply |
| Christenson JT, Kalangos A. Autologous fibrin glue reinforced by platelets in surgery of ascending aorta. Thorac Cardiovasc Surg 2004;52:225–9 | RCT |
| Christine B, Carson CC. The use of adjunct hemostatic agents during peyronie’s plaque incision and grafting: Less frequent complications secondary to hematoma formation at the site of the graft may be possible. J Sex Med 2012;9:28 | Not a valid comparison |
| Chryssagis K, Klugl S, Liangos A, Gutleben KJ, Brachmann J, Diegeler A. Surgical feasibility of the injection of fibrin sealant in cardiac fat pads to reduce the incidence of postoperative atrial fibrillation after coronary artery bypass grafting or valve surgery a pilot study. Innovations 2008;3:151–4 | No comparison group |
| Chu W, Chien GW, Finley DS. Novel ureteroscopic technique for treatment of prolonged caliceal leak after partial nephrectomy. J Endourol 2015;29:397–400 | No comparison group |
| Chung HW, Mehta JS. Fibrin glue for Gundersen flap surgery. Clin Ophthalmol 2013;7:479–84 | No comparison group |
| Chung SG, Lee SY, Kim W. Treatment of lateral epicondylitis using allogeneic adipose-derived mesenchymal stem cells. PMR 2014;6(Suppl. 1):177 | RCT |
| Chung W, Ko D, Sun C, Raval MJ, Brown CJ, Phang PT. Outcomes of anal fistula surgery in patients with inflammatory bowel disease. Am J Surg 2010;199:609–13 | No adverse effects related to fibrin reported |
| Ciavarella N, Schiavoni M, Valenzano E, Mangini F, Inchingolo F. Use of recombinant factor VIIa (NovoSeven) in the treatment of two patients with type III von Willebrand’s disease and an inhibitor against von Willebrand factor. Haemostasis 1996;26(Suppl. 1):150–4 | No comparison group |
| Cintron JR, Park JJ, Orsay CP, Pearl RK, Nelson RL, Abcarian H. Repair of fistulas-in-ano using autologous fibrin tissue adhesive. Dis Colon Rectum 1999;42:607–13 | No comparison group |
| Cipolla et al. 2010110 | RCT |
| Citardi MJ, Cox AJ 3rd, Bucholz RD. Acellular dermal allograft for sellar reconstruction after transsphenoidal hypophysectomy. Am J Rhinol 2000;14:69–73 | No comparison group |
| Ciurtin DH, Maghiar AM, Sfirlea M, Sookha PR, Suta A, Purza A, et al. Intraoperative complications in laparoscopic cholecystectomy. Surg Endosc 2011;25:S119 | No comparison group |
| Clajus C, Stockhammer F, Rohde V. The intra- and postoperative management of accidental durotomy in lumbar spine surgery: results of a German survey. Acta Neurochir 2015;157:525–30 | Not a comparative observational study |
| Cleaveland P, Tang V, Pollard A, Adeyoju A. Management of a patient with a chronic nephrocutaneous fistula after partial nephrectomy using a novel technique. Int J Urol 2015;22:232–3 | No comparison group |
| Cocero N, Pucci F, Messina M, Pollio B, Mozzati M, Bergamasco L. Autologous plasma rich in growth factors in the prevention of severe bleeding after teeth extractions in patients with bleeding disorders: a controlled comparison with fibrin glue. Blood Transfus 2015;13:287–94 | RCT |
| Codispoti M, Mankad PS. Significant merits of a fibrin sealant in the presence of coagulopathy following paediatric cardiac surgery: randomised controlled trial. Eur J Cardiothorac Surg 2002;22:200–5 | RCT |
| Coenen VA, Gilsbach JM. Effect of arachnoid plasty using fibrin glue membrane after clipping of ruptured aneurysm on the occurrence of complications and outcome in the elderly patients: commentary. Acta Neurochir 2006;148:631 | Letter/commentary/reply |
| Cohen I, Heim M, Martinowitz U, Chechick A. Orthopaedic outcome of total knee replacement in haemophilia A. Haemophilia 2000;6:104–9 | No comparison group |
| Cohen J, Jayram G, Mullins JK, Ball MW, Allaf ME. Do fibrin sealants impact negative outcomes after robot-assisted partial nephrectomy? J Endourol 2013;27:1236–9 | No adverse effects related to fibrin reported |
| Cohen-Gadol AA, Bellew MP, Akard W, Payner TD. The application of n-butyl 2-cyanoacrylate to repair CSF fistulas for 221 patients who underwent transsphenoidal surgery. Minim Invasive Neurosurg 2010;53:207–9 | Not fibrin sealant |
| Cohen-Gadol AA, Mokri B, Piepgras DG, Meyer FB, Atkinson JL. Surgical anatomy of dural defects in spontaneous spinal cerebrospinal fluid leaks. Neurosurgery 2006;58(Suppl. 4):ON238–45 | Not fibrin sealant |
| Colm SJ. The use of a fibrin sealant to control intraoperative bleeding during a Le Fort I osteotomy: report of a case. J Oral Maxillofac Surg 1996;54:1014–16 | No comparison group |
| Conboy P, Brown DH. Use of tissue sealant for day surgery parotidectomy. J Otolaryngol Head Neck Surg 2008;37:208–11 | No comparison group |
| Conde SM, Aguilar LT, Moreno AB, Macias MS, Garcia DM, Borrero IS, et al. A new technique for laparoscopic ventral hernia repair: double crown with one /third of tackers and fibrin glue. Surg Endosc 2011;25:S6 | No comparison group |
| Copuroğlu C, Ercan S, Ozcan M, Ciftdemir M, Turan FN, Yalniz E. Comparison of autogenous bone graft donor site haemostatic agents used in spinal surgery. Acta Orthop Traumatol Turc 2011;45:359–64 | RCT |
| Coral-Ghanem R, Oliveira RF, Furlanetto E, Ghanem MA, Ghanem VC. [Conjunctival autologous transplantation using fibrin glue in primary pterygium.] Arq Bras Oftalmol 2010;73:350–3 | No adverse effects related to fibrin reported |
| Cormio L, Perrone A, Pentimone S, Selvaggio O, Lorusso F, Di Fino G, et al. Tachosil-sealed tubeless percutaneous nephrolithotomy in supine antero-lateral position: a prospective study. Eur Urol Suppl 2010;9:35 | RCT |
| Correa ME, Annicchino-Bizzacchi JM, Jorge J, Paes de Almeida O, Ozelo MC, Aranha FJ, et al. Clinical impact of oral health indexes in dental extraction of hemophilic patients. J Oral Maxillofac Surg 2006;64:785–8 | No comparison group |
| Cothren CC, McIntyre RC, Johnson S, Stiegmann GV. Management of low-output pancreatic fistulas with fibrin glue. Am J Surg 2004;188:89–91 | No comparison group |
| Crawford RW, Giangrande P, Murray D. Fibrin sealant reduces blood loss in total hip arthroplasty. Hip Int 1999;9:127–32 | No adverse effects related to fibrin reported |
| Crul BJ, Gerritse BM, van Dongen RT, Schoonderwaldt HC. Epidural fibrin glue injection stops persistent postdural puncture headache. Anesthesiology 1999;91:576–7 | No comparison group |
| Curcio G, Badas R, Miraglia R, Barresi L, Tarantino I, Traina M. Duodenal stump fistula following Roux-en-Y gastrectomy, treated with single-balloon enteroscopy using the tulip bundle technique and fibrin glue injection. Endoscopy 2012;44(Suppl 2 UCTN):E364–5 | No comparison group |
| Czepko R, Kwinta B. [The use of TachoComb for the rhinorrhea repair in pituitary transsphenoidal surgery.] Polim Med 2006;36:3–9 | No adverse effects related to fibrin reported |
| Czerny et al. 2000205 | RCT |
| Dadeya S, Ms K. Strabismus surgery: fibrin glue versus vicryl for conjunctival closure. Acta Ophthalmol Scand 2001;79:515–17 | Included children |
| Dagnini G, Caldironi MW, Marin G, Patella M. Fibrin sponge plugging of hemorrhage from laparoscopic biopsy. Gastrointest Endosc 1985;31:35–6 | Technical note |
| Dal Pizzol MM, Roggia MF, Kwitko S, Marinho DR, Rymer S. [Use of fibrin glue in ocular surgery.] Arq Bras Oftalmol 2009;72:308–12 | No comparison group |
| Damiano et al. 2014184 | RCT |
| D’Andrea AA, Costantino V, Sperti C, Pedrazzoli S. Human fibrin sealant in pancreatic surgery: it is useful in preventing fistulas? A prospective randomized study. Ital J Gastroenterol 1994;26:283–6 | RCT |
| Daneshrad P, Chin GY, Rice DH. Fibrin glue prevents complications of septal surgery: findings in a series of 100 patients. Ear Nose Throat J 2003;82:196–7 | No comparison group |
| D’Arcy FT, Jaffry SQ. A review of 100 consecutive Sutureless child and adult circumcisions. Ir J Med Sci 2011;180:51–3 | No comparison group |
| Darnis E, Mutungwa I, Guillaume M, Pagneux JM. Conization with fibrin sealant: retrospective study of 150 cases. Ref Gynecol Obstet 2002;9:60–5 | No comparison group |
| Datta D, Vlavianos P, Alisa A, Westaby D. Use of fibrin glue (beriplast) in the management of bleeding gastric varices. Endoscopy 2003;35:675–8 | No comparison group |
| Dattola A, Alberti A, Parisi A, Maccarone P, Dattola P, Celi S, et al. [Minimally invasive percutaneous ultrasonography-guided treatment of postoperative splenic abscess. Personal experience with 5 clinical cases.] Chir Ital 1999;51:451–7 | Not a valid comparison |
| Davis BR, Sándor GK. Use of fibrin glue in maxillofacial surgery. J Otolaryngol 1998;27:107–12 | No comparison group |
| de Boer MT, Boonstra EA, Lisman T, Porte RJ. Role of fibrin sealants in liver surgery. Dig Surg 2012;29:54–61 | Not a comparative observational study |
| de Boer et al. 201266 | Not a comparative observational study |
| de Boer MT, Porte RJ. Reply to letter: ‘Fibrin sealants do not prevent resection surface-related complications after liver resection’. Ann Surg 2015;261:e82–3 | Not a comparative observational study |
| de Boer MT, Porte RJ. Reply: Re: Fibrin sealant for prevention of resection surface-related complications after liver resection: A randomized controlled trial. Ann Surg 2015;261:e78 | RCT |
| de Boer MT, Porte RJ. Reply: Fibrin sealant for prevention of resection surface-related complications after liver resection in living liver donors. Ann Surg 2015;261:e82–3 | Letter/commentary/reply |
| de Gracia J, de la Rosa D, Catalán E, Alvarez A, Bravo C, Morell F. Use of endoscopic fibrinogen-thrombin in the treatment of severe hemoptysis. Respir Med 2003;97:790–5 | No comparison group |
| de Hingh IH, Nienhuijs SW, Overdevest EP, Scheele K, Everts PA. Mesh fixation with autologous platelet-rich fibrin sealant in inguinal hernia repair. Eur Surg Res 2009;43:306–9 | No comparison group |
| de la Garza JL, Rumsey E. Fibrin glue and hemostasis in liver trauma: a case report. J Trauma 1990;30:512–13 | No comparison group |
| de Oca J, Del Rio C, Millan M, Fraccalvieri D, Kreisler E, Golda T, et al. Long-term results of fibrin glue for treatment of transsphincteric perianal fistula: a prospective cohort study. Colorectal Dis 2011;13:37 | No comparison group |
| de Oca J, Millán M, Jiménez A, Golda T, Biondo S. Long-term results of surgery plus fibrin sealant for anal fistula. Colorectal Dis 2012;14:e12–15 | No comparison group |
| De Stefano A, Bettarini F, Di Mare G, Neri A. [Enteric anastomosis and Tachosil®.] Minerva Chir 2011;66:183–8 | No adverse effects related to fibrin reported |
| de Vries J, Menovsky T, Grotenhuis JA, van Overbeeke JJ. Protective coating of cranial nerves with fibrin glue (Tissucol) during cranial base surgery: technical note. Neurosurgery 1998;43:1242–6 | No comparison group |
| de Wit D, Athanasiadis I, Sharma A, Moore J. Sutureless and glue-free conjunctival autograft in pterygium surgery: a case series. Eye 2010;24:1474–7 | No comparison group |
| Defrere J, Franckart A. Teflon/polyurethane arthroplasty of the knee: the first 2 years preliminary clinical experience in a new concept of artificial resurfacing of full thickness cartilage lesions of the knee. Acta Chir Belg 1992;92:217–27 | No comparison group |
| Delanois RE, Mont MA. Does tranexamic acid reduce blood loss in total knee arthroplasty? Commentary on an article by X. Aguilera, MD, et al.: ‘Efficacy and safety of fibrin glue and tranexamic acid to prevent postoperative blood loss in total knee arthroplasty. A randomized controlled clinical trial’. J Bone Joint Surg Am 2013;95:e179 | RCT |
| Della Corte A, Baldascino F, La Marca F, Scardone M, Nappi G, Cefarelli M, et al. Hemostatic modifications of the Bentall procedure: imbricated proximal suture and fibrin sealant reduce postoperative morbidity and mortality rates. Tex Heart Inst J 2012;39:206–10 | No comparison group |
| Dello Russo N. Questions concerning the safety of the tissue adhesive (Tissucol). J Periodontol 1986;57:652 | Letter/commentary/reply |
| Depondt J, Koka VN, Nasser T, Portier F, Guedon C, Barry B, et al. Use of fibrin glue in parotidectomy closure. Laryngoscope 1996;106:784–7 | Included children |
| Descottes B, Bagot d’Arc M. Fibrin sealant in inguinal hernioplasty: an observational multicentre study in 1,201 patients. Hernia 2009;13:505–10 | No comparison group |
| Deutsch M, Meinhart J, Zilla P, Howanietz N, Gorlitzer M, Froeschl A, et al. Long-term experience in autologous in vitro endothelialization of infrainguinal ePTFE grafts. J Vasc Surg 2009;49:352–62 | Not a valid comparison |
| Di Carlo I, Pulvirenti E, Toro A, Ardiri A, Bertino G. Localized fluid collection after carrier-bound fibrin sealant application on liver: complication or proof of efficacy? A long-term clinical observational study. Hepatogastroenterology 2011;58:937–42 | No comparison group |
| DiMonta et al. 2012117 | RCT |
| Di Saverio S, Masetti M, Zanello M, De Blasiis MG, Jovine E. Re: Fibrin sealant for prevention of resection surface-related complications after liver resection: a randomized controlled trial. Ann Surg 2015;261:e77–8 | RCT |
| Diamond et al. 2011232 | RCT |
| Dick B, Kohnen T, Hessemer V. Fibrin glue in temporal clear corneal tunnel incision. Eur J Implant Refract Surg 1995;7:224–8 | No comparison group |
| Dimaio CJ, Dorfman MP, Gardner GJ, Nash GM, Schattner MA, Markowitz AJ, et al. The use of covered esophageal self-expanding metal Stents (CSEMS) for the management of post-operative colo-rectal anastomotic leaks. Gastrointest Endosc 2012;75(Suppl. 1):AB425–6 | No comparison group |
| Dimitrakakis G, Podila SR, O’Keefe PA, Kulatilake NE. Biological glue: a word of careful assessment! Interact Cardiovasc Thorac Surg 2011;13:244–5 | Letter/commentary/reply |
| Dimitrakakis G, von Oppell UO. The use of biological glues in cardiothoracic surgery. Interact Cardiovasc Thorac Surg 2011;13:118 | Letter/commentary/reply |
| Dimo et al. 198980 | RCT |
| Diner EK, Patel SV, Kwart AM. Does fibrin sealant decrease immediate urinary leakage following radical retropubic prostatectomy? J Urol 2005;173:1147–9 | RCT |
| Dinsmore et al. 200097 | RCT |
| Docimo G, Limongelli P, Conzo G, Gili S, Bosco A, Rizzuto A, et al. Axillary lymphadenectomy for breast cancer in elderly patients and fibrin glue. BMC Surg 2013;13(Suppl. 2):8 | No adverse effects related to fibrin reported |
| Dolay K, Aras B, Tuğcu V, Ozbay B, Aygün E, Taşçi AI. Combined treatment of iatrogenic rectourethral fistula with endoscopic fibrin glue application and clipping. J Endourol 2007;21:433–6 | No comparison group |
| Dong N, Li C, Chen WS, Qin WJ, Xue YH, Wu HP. Fibrin glue-assisted for the treatment of corneal perforations using glycerin-cryopreserved corneal tissue. Int J Ophthalmol 2014;7:62–5 | No comparison group |
| Donnez J, Nisolle M. Laparoscopic management of large ovarian endometrial cyst: use of fibrin sealant. J Gynecol Surg 1991;7:163–6 | No adverse effects related to fibrin reported |
| Dovellini EV, Taddeucci E, Trapani M, Valenti R, Cerisano G, Moschi G, et al. Pocket haematoma prevention in patients who required implantation/replacement of a pacemaker or implantable cardiac defibrillator. The PHP study. G Ital Cardiol 2011;12(Suppl. 1):140S | RCT |
| Dovellini EV, Taddeucci E, Trapani M, Valenti R, Moschi G, Cerisano G, et al. Pocket haematoma prevention in patients who required implantation/replacement of a pacemaker or implantable cardiac defibrillator. The PHP Study. Eur Heart J 2011;32:305 | Duplicate |
| Doyama H, Tominaga K, Yoshida N, Takemura K, Yamada S. Endoscopic tissue shielding with polyglycolic acid sheets, fibrin glue and clips to prevent delayed perforation after duodenal endoscopic resection. Dig Endosc 2014;26(Suppl. 2):41–5 | No comparison group |
| Draus JM, Huss SA, Harty NJ, Cheadle WG, Larson GM. Enterocutaneous fistula: are treatments improving? Surgery 2006;140:570–6 | No adverse effects related to fibrin reported |
| Droghetti et al. 2008124 | RCT |
| Drumheller GW. Fibrin glue. Ear Nose Throat J 2003;82:483 | Letter/commentary/reply |
| Du J, Qiu B, Tao J, Ou S, Wang Y. Sellar reconstruction using biomaterials after transsphenoidal surgery in 449 cases of pituitary adenomas. Neurosurg Q 2014;24:22–6 | No comparison group |
| Du X, Guo W, Liu XP, Jia X, Zhang MH, Yin T, et al. [Treatment of type II endoleak after abdominal aortic aneurysm endovascular repair.] Zhonghua Yi Xue Za Zhi 2011;91:2955–8 | No comparison group |
| Duchesne B, Tahi H, Galand A. Use of human fibrin glue and amniotic membrane transplant in corneal perforation. Cornea 2001;20:230–2 | No comparison group |
| Dumonceau JM, Cremer M, Lalmand B, Devière J. Esophageal fistula sealing: choice of stent, practical management, and cost. Gastrointest Endosc 1999;49:70–8 | No comparison group |
| Ebner FM, Paul A, Peters J, Hartmann M. Venous air embolism and intracardiac thrombus after pressurized fibrin glue during liver surgery. Br J Anaesth 2011;106:180–2 | No comparison group |
| Edelman DS. Fibrin glue fixation of bioactive extracellular matrix mesh compared with soft prolene mesh for laparoscopic hernia repair. Surg Laparosc Endosc Percutan Tech 2008;18:569–72 | No comparison group |
| Edelman DS. Robotic, laparoscopic inguinal hernia repair. Surg Endosc 2015;29:S467 | No comparison group |
| Edelman DS, Selesnick H. ‘Sports’ hernia: treatment with biologic mesh (Surgisis): a preliminary study. Surg Endosc 2006;20:971–3 | No comparison group |
| Eden CG, Sultana SR, Murray KH, Carruthers RK. Extraperitoneal laparoscopic dismembered fibrin-glued pyeloplasty: medium-term results. Br J Urol 1997;80:382–9 | No comparison group |
| Eder F, Meyer F, Nestler G, Halloul Z, Lippert H. Sealing of the hepatic resection area using fibrin glue reduces significant amount of postoperative drain fluid. World J Gastroenterol 2005;11:5984–7 | No adverse effects related to fibrin reported |
| Ederle A, Scattolini C, Vantgini I, Bulighin G, Scuro LA. Human fibrin sealant in upper G.I. tract bleeding. Endoscopy 1989;21:112 | Letter/commentary/reply |
| Eichler C, Dahdouh F, Sauerwald A, Warm M. Seroma suppression using TissuGlu® in a high-risk patient post-mastectomy: a case report. J Med Case Rep 2013;7:138 | No comparison group |
| Eide E, Jurgeit H. [Use of fibrin glue in pronounced Dupuytren contracture.] Handchir Mikrochir Plast Chir 1985;17:145–6 | No comparison group |
| El Feghaly M, Chahine E, Abi Ghanem M, Abou Zahr O, Alayli M, Abu Khalil B. Acute limb ischaemia due to embolisation of biological glue 45 days after surgery. Eur J Vasc Endovasc Surg 2011;41:518–20 | No comparison group |
| El Nakeeb A. Influence of fibrin glue on seroma formation after modified radical mastectomy: a prospective randomized study. Breast J 2009;15:671–2 | RCT |
| El-Banhawy OA, Halaka AN, El-Hafiz Shehab El-Dien A, Ayad H. Subcranial transnasal repair of cerebrospinal fluid rhinorrhea with free autologous grafts by the combined overlay and underlay techniques. Minim Invasive Neurosurg 2004;47:197–202 | Included children |
| Elderkin SJ, Epstein RJ, Seldomridge DL. Successful treatment of recurrent epithelial ingrowth associated with interface fluid syndrome, flap necrosis, and epithelial defects following LASIK. J Refract Surg 2011;27:70–3 | No comparison group |
| Eleftheriadis E, Kotzampassi K. Therapeutic fistuloscopy: an alternative approach in the management of postoperative fistulas. Dig Surg 2002;19:230–5 | Not a valid comparison |
| Eleftheriadis E, Tzartinoglou E, Kotzampassi K, Aletras H. Early endoscopic fibrin sealing of high-output postoperative enterocutaneous fistulas. Acta Chir Scand 1990;156:625–8 | No comparison group |
| El-Gazzaz G, Hull T, Mignanelli E, Hammel J, Gurland B, Zutshi M. Analysis of function and predictors of failure in women undergoing repair of Crohn’s related rectovaginal fistula. J Gastrointest Surg 2010;14:824–9 | Not a valid comparison |
| Ellis DA, Pelausa EO. Fibrin glue in facial plastic and reconstructive surgery. J Otolaryngol 1988;17:74–7 | Not a comparative observational study |
| Ellis DA, Shaikh A. The ideal tissue adhesive in facial plastic and reconstructive surgery. J Otolaryngol 1990;19:68–72 | No adverse effects related to fibrin reported |
| Ellis DA, Pelausa EO. Fibrin glue in facial plastic and reconstructive surgery. J Otolaryngol 1988;17:74–7 | Duplicate |
| Ellis DA, Shaikh A. The ideal tissue adhesive in facial plastic and reconstructive surgery. J Otolaryngol 1990;19:68–72 | Duplicate |
| Eloy JA, Choudhry OJ, Friedel ME, Kuperan AB, Liu JK. Endoscopic nasoseptal flap repair of skull base defects: is addition of a dural sealant necessary? Otolaryngol Head Neck Surg 2012;147:161–6 | Not fibrin sealant |
| Eltorai IM, Montroy RE, Kaplan SL, Ho WH. Pneumocephalus secondary to cerebrospinal fluid leak associated with a lumbar pressure ulcer in a man with paraplegia. J Spinal Cord Med 2003;26:262–9 | No comparison group |
| Emmert MY, Salzberg SP, Theusinger OM, Felix C, Plass A, Hoerstrup SP, et al. How good patient blood management leads to excellent outcomes in Jehovah’s witness patients undergoing cardiac surgery. Interact Cardiovasc Thorac Surg 2011;12:183–8 | No comparison group |
| Engler S, Dorlars D, Riemann JF. [Endoscopic fibrin gluing of a pancreatic duct fistula following acute pancreatitis.] Dtsch Med Wochenschr 1996;121:1396–400 | No comparison group |
| Enoki C, Higashi S, Oohata M, Tanaka T. [A case of acute erythroblastic anemia due to infection with human parvovirus B19 after coronary artery bypass grafting.] Kyobu Geka 2002;55:116–19 | No comparison group |
| Epstein NE. Wound-peritoneal shunts: part of the complex management of anterior dural lacerations in patients with ossification of the posterior longitudinal ligament. Surg Neurol 2009;72:630–4 | No comparison group |
| Epstein NE. Tisseel utilized as hemostatic in spine surgery impacts time to drain removal and length of stay. Surg Neurol Int 2014;5(Suppl. 7):354–61 | Not a relevant comparison |
| Epstein NE. Hemostasis and other benefits of fibrin sealants/glues in spine surgery beyond cerebrospinal fluid leak repairs. Surg Neurol Int 2014;5(Suppl. 7):304–14 | Not a comparative observational study |
| Erba et al. 2010210 | RCT |
| Erbagci I, Bekir N. Sutureless closure of the conjunctiva with a commercial fibrin sealant in extraocular muscle surgery for strabismus. Strabismus 2007;15:89–94 | No comparison group |
| Erdogan A, Gurses G, Keskin H, Demircan A. The sealing effect of a fibrin tissue patch on the esophageal perforation area in primary repair. World J Surg 2007;31:2199–203 | Emergency surgery |
| Erdogru T, Sanli A, Celik O, Baykara M. Laparoscopic transvesical repair of recurrent vesicovaginal fistula using with fleece-bound sealing system. Arch Gynecol Obstet 2008;277:461–4 | No comparison group |
| Eriksen JR. Pain and convalescence following laparoscopic ventral hernia repair. Dan Med Bull 2011;58:B4369 | Not a relevant comparison |
| Eriksen et al. 2013183 | Not a comparative observational study |
| Esposito F, Cappabianca P, Fusco M, Cavallo LM, Bani GG, Biroli F, et al. Collagen-only biomatrix as a novel dural substitute. Examination of the efficacy, safety and outcome: clinical experience on a series of 208 patients. Clin Neurol Neurosurg 2008;110:343–51 | No comparison group |
| Esposito F, Grimod G, Cavallo LM, Lanterna L, Biroli F, Cappabianca P. Collagen-only biomatrix as dural substitute: what happened after a 5-year observational follow-up study. Clin Neurol Neurosurg 2013;115:1735–7 | No comparison group |
| Esquenazi S, Rand W, Velazquez G, Grunstein L. Novel therapeutic approach in the management of band keratopathy using amniotic membrane transplantation with fibrin glue. Ophthalmic Surg Lasers Imaging 2008;39:418–21 | No comparison group |
| Esteban F, Delgado-Rodríguez M, Mochón A, Solano J, Soldado L, Solanellas J. [Study of in-patient hospital stay following total laryngectomy: multivariable retrospective analysis of a 442 total laryngectomies.] Acta Otorrinolaringol Esp 2006;57:176–82 | Not a relevant comparison |
| Etienney I, Rabahi N, Cuenod CA, Hoffmann P, Charachon A, Bauer P. Fibrin glue sealing in the treatment of a recto-urethral fistula in Crohn’s disease: a case report. Gastroenterol Clin Biol 2009;33:1094–7 | No comparison group |
| Evans LA, Ferguson KH, Foley JP, Rozanski TA, Morey AF. Fibrin sealant for the management of genitourinary injuries, fistulas and surgical complications. J Urol 2003;169:1360–2 | No comparison group |
| Evaristo-Méndez G, Sánchez-Hernández AT, Melo-Velázquez A, Ventura-Sauceda FA, Sepúlveda-Castro RR. [Sigmoido-buttock fistula by diverticulitis: report of a rare complication.] Cir Cir 2013;81:158–62 | No comparison group |
| Everts PA, Devilee RJ, Brown Mahoney C, Eeftinck-Schattenkerk M, Box HA, Knape JT, et al. Platelet gel and fibrin sealant reduce allogeneic blood transfusions in total knee arthroplasty. Acta Anaesthesiol Scand 2006;50:593–9 | Not a relevant comparison |
| Fabian et al. 2003128 | RCT |
| Falavarjani KG, Modarres M, Foroutan A, Bakhtiari P. Fibrin glue-assisted sutureless scleral fixation. J Cataract Refract Surg 2009;35:795 | Letter/commentary/reply |
| Falez et al. 2013154 | RCT |
| Falsaperla M, Autorino R, Puglisi M, Damiano R, Salerno GL, Motta M, et al. Haemostatic agents during laparoscopic nephron-sparing surgery: what about TachoSil? BJU Int 2009;104:270–1 | Letter/commentary/reply |
| Falworth MS, Butler PM, Powell BW. The use of fibrin glue to prevent seroma formation following sentinel node biopsy. Plast Reconstr Surg 1999;104:2331–2 | Letter/commentary/reply |
| Fanari M, Serra S, Corona A, De Lisa A. [Use of TachoSil in laparoscopic enucleoresection of renal masses smaller than 4 cm: our preliminary experience of 41 cases.] Urologia 2012;79(Suppl. 19):131–3 | No comparison group |
| Farhat F, Durand M, Delahaye F, Jegaden O. Prosthetic valve sewing-ring sealing with antibiotic and fibrin glue in infective endocarditis. A prospective clinical study. Interact Cardiovasc Thorac Surg 2007;6:16–20 | No comparison group |
| Farr IJ, Cole BJ, Tabet S. Prospective study of particulated juvenile allograft cartilage to treat knee femoral cartilage lesions. Arthroscopy 2013;29(Suppl. 1):e27 | No comparison group |
| Farrag TY, Boahene KD, Agrawal N, Turner L, Byrne PJ, Earnest L, et al. Use of fibrin sealant in closing mucocutaneous fistulas following head and neck cancer surgery. Otolaryngol Head Neck Surg 2007;137:159–61 | No adverse effects related to fibrin reported |
| Faust A, Aguillard R, Finch C. Use of fibrin glue administered during bronchoscopy to seal a persistent bronchopleural fistula: a case report. Crit Care Med 2010;38:A266 | No comparison group |
| Fava MA, Choi CJ, El Mollayess G, Melki SA. Sandwich fibrin glue technique for attachment of conjunctival autograft during pterygium surgery. Can J Ophthalmol 2013;48:516–20 | Not a relevant comparison |
| Federici AB, Sacco R, Stabile F, Carpenedo M, Zingaro E, Mannucci PM. Optimising local therapy during oral surgery in patients with von Willebrand disease: effective results from a retrospective analysis of 63 cases. Haemophilia 2000;6:71–7 | Included children |
| Fékété et al. 199291 | RCT |
| Felipetto R, Vigano L, Cecchi M, Florentini L, Minervini R. Use of fibrin sealant in the treatment of prostatic cutaneous fistula in a case of Pseudomonas prostatitis. Int Urol Nephrol 1995;27:563–5 | No comparison group |
| Feng JX, Lu QS, Jing ZP, Yang Y, Nie B, Bao JM, et al. [Fibrin glue embolization treating intra-operative type I endoleak of endovascular repair of abdominal aortic aneurysm: long-term result.] Zhonghua Wai Ke Za Zhi 2011;49:883–7 | No comparison group |
| Ferlitsch A, Puspok A, Wewalka F, Schoefl R, Brownstone E, Madl C, et al. A multi-centre proof of concept study to assess efficacy and safety of a new liquid endoscopic hemostatic agent (Seraseal/Fastact) in patients with active gastrointestinal bleeding. Gastrointest Endosc 2014;79(Suppl. 1):AB151–2 | Not fibrin sealant |
| Fernández Lobato R, García Septiem J, Ortega Deballon P, Martín Lucas FJ, Ruíz de Adana JC, Limones Esteban M. Tissucol application in dermolipectomy and incisional hernia repair. Int Surg 2001;86:240–5 | RCT |
| Fernandez-Esparrach G, Lautz DB, Thompson CC. Peroral endoscopic anastomotic reduction improves intractable dumping syndrome in Roux-en-Y gastric bypass patients. Surg Obes Relat Dis 2010;6:36–40 | No comparison group |
| Fernandez-Lobato R, Angulo-Morales F, Garcia-Septiem J, Hernandez-Matias A, Marin-Lucas J, Limones-Esteban M. Ten years of experience about laparoscopic ventral hernia repair. Surg Endosc 2011;25:S56 | No comparison group |
| Fernandez-Lobato R, Bagot D’Arc M, Krishnan S. An economic evaluation of fibrin sealants used during incisional hernia with dermolipectomy procedures in Spain. Value Health 2010;13:A103 | Not a comparative observational study |
| Ferrarese A, Marola S, Surace A, Borello A, Bindi M, Cumbo J, et al. Fibrin glue versus stapler fixation in laparoscopic transabdominal inguinal hernia repair: a single center 5-year experience and analysis of the results in the elderly. Int J Surg 2014;12(Suppl. 2):94–8 | No adverse effects related to fibrin reported |
| Ferrer-Puchol MD, Gil-Romero J, Laso-Pablos S, Guijarro-Rosaleny J. Treatment of oesophago-cutaneous fistula with covered stent and percutaneous fibrin tissue sealant. J Intervent Radiol 1999;14:222–5 | No comparison group |
| Figueras et al. 200771 | RCT |
| Filosso et al. 2013136 | RCT |
| Finch CK, Pittman AL. Use of fibrin glue to treat a persistent pneumothorax with bronchopleural fistula. Am J Health Syst Pharm 2008;65:322–4 | No comparison group |
| Finck C, Lefebvre P. Implantation of esterified hyaluronic acid in microdissected Reinke’s space after vocal fold microsurgery: first clinical experiences. Laryngoscope 2005;115:1841–7 | No comparison group |
| Fine AP. Laparoscopic repair of inguinal hernia using Surgisis mesh and fibrin sealant. JSLS 2006;10:461–5 | No comparison group |
| Fink D, Klein JJ, Kang H, Ergin MA. Application of biological glue in repair of intracardiac structural defects. Ann Thorac Surg 2004;77:506–11 | No comparison group |
| Fiore A, Grandmougin D, Maureira JP, Elfarra M, Laurent N, Andronache M, et al. Efficacy of TachoSil® as a sutureless hemostatic patch to repair a perforation of the interventricular groove during endocardial radiofrequency ablation. J Cardiovasc Surg 2014;55:295–8 | No comparison group |
| Fischer A, Benz S, Baier P, Hopt UT. Endoscopic management of pancreatic fistulas secondary to intraabdominal operation. Surg Endosc 2004;18:706–8 | No comparison group |
| Fischer et al. 2013241 | RCT |
| Fischer CP, Wood CG, Shen J, Batiller J, Hart JC, Patel B, et al. A randomized trial of aprotinin-free fibrin sealant versus absorbable hemostat. Clin Appl Thromb Hemost 2011;17:572–7 | RCT |
| Fischer et al. 201172 | RCT |
| Fleisher AG, Evans KG, Nelems B, Finley RJ. Effect of routine fibrin glue use on the duration of air leaks after lobectomy. Ann Thorac Surg 1990;49:133–4 | RCT |
| Flemming I. Fibrin glue in face lifts. Facial Plast Surg 1992;8:79–88 | RCT |
| Fortelny RH, Petter-Puchner AH, Glaser KS. Fibrin sealant (Tissucol) for the fixation of hiatal mesh in the repair of giant paraesophageal hernia: a case report. Surg Laparosc Endosc Percutan Tech 2009;19:e91–4 | No comparison group |
| Fortelny RH, Petter-Puchner AH, Khakpour Z, May C, Mika K, Glaser KS, et al. Spray application of fibrin sealant with an angled spray tip device in laparoscopic inguinal hernia repair. Eur Surg 2010;42:171–6 | No comparison group |
| Fortelny RH, Petter-Puchner AH, May C, Jaksch W, Benesch T, Khakpour Z, et al. The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc 2012;26:249–54 | RCT |
| Fortunato G, Bonucci E. Two cases of reconstruction of large defects of the facial skeleton with hydroxyapatite-fibrin glue. Rivista Italiana di Chirurgia Plastica 1996;28:17–29 | No comparison group |
| Foster JA, Holck DE, Perry JD, Wulc AE, Burns JA, Cahill KV, et al. Fibrin sealant for Müller muscle-conjunctiva resection ptosis repair. Ophthal Plast Reconstr Surg 2006;22:184–7 | No comparison group |
| Foster K, Greenhalgh D, Gamelli RL, Mozingo D, Gibran N, Neumeister M, et al. Efficacy and safety of a fibrin sealant for adherence of autologous skin grafts to burn wounds: results of a phase 3 clinical study. J Burn Care Res 2008;29:293–303 | RCT |
| Fountas KN, Kapsalaki EZ, Johnston KW. Cerebrospinal fluid fistula secondary to dural tear in anterior cervical discectomy and fusion: case report. Spine 2005;30:E277–80 | No comparison group |
| Fraioli RE, Hirsch BE, Kassam AB. Fibrin sealant for control of cerebrospinal fluid otorrhea. Am J Otolaryngol 2008;29:135–7 | No comparison group |
| Franco-Vidal V, Daculsi G, Bagot d’Arc M, Sterkers O, Smail M, Robier A, et al. Tolerance and osteointegration of TricOs(TM)/MBCP in association with fibrin sealant in mastoid obliteration after canal wall-down technique for cholesteatoma. Acta Oto-Laryngologica 2014;134:358–65 | No comparison group |
| Frena A, Martin F. How to improve bilio-stasis in liver surgery. Chir Ital 2006;58:793–5 | No comparison group |
| French DB, Marcovich R. Fibrin sealant for retrograde ureteroscopic closure of urine leak after partial nephrectomy. Urology 2006;67:1085.e1–3 | No comparison group |
| Frilling et al. 200573 | RCT |
| Fu et al. 200978 | RCT |
| Fuks D, Bréhant O, Dumont F, Viart L, Manaouil D, Bartoli E, et al. [Tissue adhesive treatment of persistent recto-cutaneous fistula following Hartmann procedure.] J Chir 2007;144:35–8 | No comparison group |
| Fuks D, Bréhant O, Dumont F, Viart L, Manaouil D, Bartoli E, et al. [Tissue adhesive treatment of persistent recto-cutaneous fistula following Hartmann procedure.] J Chir 2007;144:35–8 | Duplicate |
| Fuks D, Verhaeghe P, Brehant O, Sabbagh C, Dumont F, Riboulot M, et al. Results of laparoscopic sleeve gastrectomy: a prospective study in 135 patients with morbid obesity. Surgery 2009;145:106–13 | No comparison group |
| Fullarton G, Galloway D, Albillos A, Calleja JL, Rutgeerts P, Wara P, et al. Randomised trial of fibrin glue versus polidocanol for bleeding peptic ulcer (multiple letters). Lancet 1997;350:1397–8 | Letter/commentary/reply |
| Fuller CW, Gillespie MB, Nguyen SA, Jones T, Hornig JD. A double-blind, randomized, placebo-controlled clinical trial evaluating fibrin sealant in thyroidectomy closure. Otolaryngol Head Neck Surg 2014;151(Suppl. 1):P160–1 | RCT |
| Fullum TM, Aluka KJ, Turner PL. Decreasing anastomotic and staple line leaks after laparoscopic Roux-en-Y gastric bypass. Surg Endosc 2009;23:1403–8 | RCT |
| Furey CG, Sadowski K, Ahn NU. Recurrent CSF leak following repair of incidental durotomy. Spine J 2014;14(Suppl. 1):113 | Abstract |
| Furrer et al. 1993116 | RCT |
| Furuse M, Ishikawa M, Nishida N, Aoki T, Takahashi JA. Transposition of the vertebral artery with fibrin glue adhesive in microvascular decompression: a case report. Neurosurg Q 2010;20:170–2 | No comparison group |
| Gaertner WB, Madoff RD, Spencer MP, Mellgren A, Goldberg SM, Lowry AC. Results of combined medical and surgical treatment of recto-vaginal fistula in Crohn’s disease. Colorectal Dis 2011;13:678–83 | No comparison group |
| Gagarine A, Urschel JD, Miller JD, Bennett WF, Young JE. Effect of fibrin glue on air leak and length of hospital stay after pulmonary lobectomy. J Cardiovasc Surg 2003;44:771–3 | No adverse effects related to fibrin reported |
| Gage EA, Jones GE, Powelson JA, Johnson MS, Goggins WC, Fridell JA. Treatment of enterocutaneous fistula in pancreas transplant recipients using percutaneous drainage and fibrin sealant: three case reports. Transplantation 2006;82:1238–40 | No comparison group |
| Galajda Z, Fulop T, Peterffy A, Alamanni F, Parolari A, Biglioli P. Subacute left ventricular rupture complicated by free wall rupture: repair with a TachoComb sheet and Tissucol glue (multiple letters). J Thorac Cardiovasc Surg 2002;123:1014–6 | Letter/commentary/reply |
| Gallego JM, Barcia JA, Barcia-Mariño C. Fatal outcome related to carmustine implants in glioblastoma multiforme. Acta Neurochir 2007;149:261–5 | No comparison group |
| Galor A, Yoo SH, Piccoli FV, Schmitt AJ, Chang V, Perez VL. Phase I study of subconjunctival ranibizumab in patients with primary pterygium undergoing pterygium surgery. Am J Ophthalmol 2010;149:926–31.e2 | RCT |
| Galosi AB, Lacetera V, Tiroli M, Conti A, Muzzonigro G. Haemostatic sponge application on Denonvillier fascia after open nerve-sparing prostatectomy. Anticancer Res 2010;30:1430 | No comparison group |
| Gammon RR, Prum BE Jr, Avery N, Mintz PD. Rapid preparation of small-volume autologous fibrinogen concentrate and its same day use in bleb leaks after glaucoma filtration surgery. Ophthalmic Surg Lasers 1998;29:1010–12 | No comparison group |
| Ganekal S, Venkataratnam S, Dorairaj S, Jhanji V. Comparative evaluation of suture-assisted and fibrin glue-assisted scleral fixated intraocular lens implantation. J Refract Surg 2012;28:249–52 | No adverse effects related to fibrin reported |
| Garcia-Caballero M, Carbajo M, Martinez-Moreno JM, Sarria M, Osorio D, Carmona JA. Drain erosion and gastro-jejunal fistula after one-anastomosis gastric bypass: endoscopic occlusion by fibrin sealant. Obes Surg 2005;15:719–22 | No comparison group |
| Garcia-Olmo D, Herreros M, Guadalajara H, DeLaQuintana P, Trebol J, Georgiev-Hristov T, et al. Expanded adipose derived autologous stem cells for the treatment of complex cryptoglandular fistulas. A phase III clinical trial (fatt1: Fistulaadvanced therapy trial 1) and longterm evaluation (LTE). Dis Colon Rectum 2011;54:e68–9 | RCT |
| Garcia-Villarreal OA, Casillas-Covarrubias LE. Fibrin sealant for left ventricular rupture after mitral valve replacement. Asian Cardiovasc Thorac Ann 2008;16:152–3 | No comparison group |
| Garçon C, Cavaillon JP, Girard P. [The use of Tissucol in oral surgery in problems of hemostasis.] Chir Dent Fr 1986;56:49–55 | Included children |
| Gatti MAN, Vieira LM, Barraviera B, Barraviera S. Treatment of venous ulcers with fibrin sealant derived from snake venom. J Venom Anim Toxins 2011;17:226–9 | RCT |
| Gauthier L, Lagoutte F. [Use of a fibrin glue (Tissucol) for treating perforated or pre-perforated corneal ulcer.] J Fr Opthalmol 1989;12:469–76 | No comparison group |
| Gazzeri R, Fiore C, Galarza M. (EVICEL) for augmentation of dural closure: results of a preliminary clinical study. Surg Technol Int 2014;25:265–70 | No adverse effects related to fibrin reported |
| Gazzeri R, Galarza M, Alfieri A, Neroni M, Roperto R. Simple intraoperative technique for minor dural gap repair using fibrin glue and oxidized cellulose. World Neurosurg 2011;76:173–5 | No comparison group |
| Gazzeri R, Galarza M, Fiore C, Callovini G, Alfieri A. Use of tissue-glue-coated collagen sponge (TachoSil) to repair minor cerebral dural venous sinus lacerations: technical note. Neurosurgery 2015;11(Suppl. 2):32–6 | No comparison group |
| Gazzeri R, Neroni M, Alfieri A, Galarza M, Faiola A, Esposito S, et al. Transparent equine collagen biomatrix as dural repair. A prospective clinical study. Acta Neurochir 2009;151:537–43 | No comparison group |
| Gentili ME. Epidural fibrin glue injection stops postdural puncture headache in patient with long-term intrathecal catheterization. Reg Anesth Pain Med 2003;28:70 | No comparison group |
| Genyk Y, Kato T, Pomposelli JJ, Lophaven KW, Chapman WC. Tachosil versus surgicel original for the secondary treatment of local bleeding in adult patients undergoing hepatic resection. HPB 2014;16:27 | RCT |
| Germanidis G, Papavramidis TS, Mantzoukis K, Sapalidis K, Divanis D, Kalevrosoglou I, et al. Fibrin glue as a protective biomembrane for a duodenal ulcer vessel. Endoscopy 2010;42(Suppl. 2):E348–9 | No comparison group |
| Gerritse BM, van Dongen RT, Crul BJ. Epidural fibrin glue injection stops persistent cerebrospinal fluid leak during long-term intrathecal catheterization. Anesth Analg 1997;84:1140–1 | No comparison group |
| Ghavanini AA, Scott CA, Chan DK, Tang-Wai DF. Management of patients with spontaneous intracranial hypotension causing altered level of consciousness: report of two cases and review of literature. Cephalalgia 2013;33:43–51 | No comparison group |
| Ghelardi A, di Stefano C, Galante L, Guelfi F, Migliorini P. Inguinofemoral lymphadenectomy in patients undergoing radical vulvectomy for vulvar cancer. A new patch is able to reduce lymphatic complications. Ital J Gynaecol Obstet 2011;23:139–46 | No adverse effects related to fibrin reported |
| Ghotb A, Shah JN, Binmoeller KF, Weilert F, Bhat YM. Efficacy of endoscopic treatment of symptomatic upper gastrointestinal leaks and fistulas post-bariatric surgery: report of 25 cases. Gastrointest Endosc 2011;73(Suppl. 1):AB395 | No comparison group |
| Giampapa VC, Bitar GJ. Use of fibrin sealant in neck contouring. Aesthet Surg J 2002;22:519–25 | No comparison group |
| Gibran N, Luterman A, Herndon D, Lozano D, Greenhalgh DG, Grubbs L, et al. Comparison of fibrin sealant and staples for attaching split-thickness autologous sheet grafts in patients with deep partial- or full-thickness burn wounds: a phase 1/2 clinical study. J Burn Care Res 2007;28:401–8 | RCT |
| Gidaro S, Cindolo L, Lipsky K, Zigeuner R, Schips L. Efficacy and safety of the haemostasis achieved by Vivostat system during laparoscopic partial nephrectomy. Arch Ital Urol Androl 2009;81:223–7 | No comparison group |
| Gilat H, Rappaport Z, Yaniv E. Endoscopic transnasal cerebrospinal fluid leak repair: a 10 year experience. Isr Med Assoc J 2011;13:597–600 | Included children |
| Gille J, Schuseil E, Wimmer J, Gellissen J, Schulz AP, Behrens P. Mid-term results of autologous matrix-induced chondrogenesis for treatment of focal cartilage defects in the knee. Knee Surg Sports Traumatol Arthrosc 2010;18:1456–64 | No comparison group |
| Gilly et al. 1998108 | RCT |
| Gioffrè Florio MA, Mezzasalma F, Manganaro T, Pakravanan H, Cogliandolo A. [The use of fibrin glue in the surgery of breast carcinoma.] G Chir 1993;14:239–41 | RCT |
| Giovannacci L, Eugster T, Stierli P, Hess P, Gürke L. Does fibrin glue reduce complications after femoral artery surgery? A randomised trial. Eur J Vasc Endovasc Surg 2002;24:196–201 | RCT |
| Giovannacci L, Renggli JC, Eugster T, Stierli P, Hess P, Gürke L. Reduction of groin lymphatic complications by application of fibrin glue: preliminary results of a randomized study. Ann Vasc Surg 2001;15:182–5 | RCT |
| Girard S, Sideman M, Spain DA. A novel approach to the problem of intestinal fistulization arising in patients managed with open peritoneal cavities. Am J Surg 2002;184:166–7 | No comparison group |
| Gisbertz SS, Sosef MN, Festen S, Gerhards MF. Treatment of fistulas in ano with fibrin glue. Dig Surg 2005;22:91–4 | No comparison group |
| Giugno A, Maugeri R, D’Arpa S, Visocchi M, Iacopino DG. Complex reconstructive surgery following removal of extra-intracranial meningiomas, including the use of autologous fibrin glue and a pedicled muscle flap. Interdisc Neurosurg 2014;1:84–7 | No comparison group |
| Giuliani G, Coletta D, Farina A, Guerra F, Velluti F, Iaquinandi F, et al. Perineal surgical approach to treat rectourethral fistula with Tachosil© patch apposition: a case report. Tech Coloproctol 2013;17:138 | No comparison group |
| Glimåker H, Björck CG, Hallstensson S, Ohlsén L, Westman B. Avoiding blow-out of the aortic stump by reinforcement with fibrin glue. A report of two cases. Eur J Vasc Surg 1993;7:346–8 | No comparison group |
| Glitsch A, von Bernstorff W, Seltrecht U, Partecke I, Paul H, Heidecke CD. Endoscopic transanal vacuum-assisted rectal drainage (ETVARD): an optimized therapy for major leaks from extraperitoneal rectal anastomoses. Endoscopy 2008;40:192–9 | No comparison group |
| Glover W, Chavis TV, Daniel TM. Fibrin glue application through the flexible fiberoptic bronchoscope: closure of bronchopleural fistulas. J Thorac Cardiovasc Surg 1987;93:470–2 | No comparison group |
| Godeberge P, Blain A, Christidis C, Denet C, Levard H, Mal F, et al. Biological glue in the treatment of postoperative fistula in colorectal surgery. Acta Endoscopica 2009;39:424–8 | No comparison group |
| Goerler H, Oppelt P, Abel U, Haverich A. Safety of the use of Tissucol Duo S in cardiovascular surgery: retrospective analysis of 2149 patients after coronary artery bypass grafting. Eur J Cardiothorac Surg 2007;32:560–6 | Includes emergency surgery; overall 9.3% of patients |
| Gonfiotti et al. 2011130 | RCT |
| González-Ojeda A, Avalos-González J, Muciño-Hernández MI, López-Ortega A, Fuentes-Orozco C, Sánchez-Hochoa M, et al. Fibrin glue as adjuvant treatment for gastrocutaneous fistula after gastrostomy tube removal. Endoscopy 2004;36:337–41 | No adverse effects related to fibrin reported |
| Gopal SC, Gangopadhyay AN, Mohan TV, Upadhyaya VD, Pandey A, Upadhyaya A, et al. Use of fibrin glue in preventing urethrocutaneous fistula after hypospadias repair. J Pediatr Surg 2008;43:1869–72 | RCT |
| Grau AE, Durán JA. Treatment of a large corneal perforation with a multilayer of amniotic membrane and TachoSil. Cornea 2012;31:98–100 | No comparison group |
| Graziano F, Certo F, Basile L, Maugeri R, Grasso G, Meccio F, et al. Autologous fibrin sealant (Vivostat) in the neurosurgical practice: part I: intracranial surgical procedure. Surg Neurol Int 2015;6:77 | No comparison group |
| Greco DP, Fei L, Guerriero L, Pradella P, Mazzola M, Magistro C, et al. Feasibility and effectiveness of primary umbilical hernia repair with biologic graft: preliminary study. Acta Chir Belg 2014;114:125–30 | No comparison group |
| Greco S, Tringali A, Familiari P, Boskoski I, Perri V, Costamagna G. A rescue therapy for refractory post-sphincterotomy and post-papillectomy bleeding: fibrin glue injection. Dig Liver Dis 2015;47:e153 | Not a relevant comparison |
| Greenberg R, Kashtan H, Skornik Y, Werbin N. Treatment of pilonidal sinus disease using fibrin glue as a sealant. Tech Coloproctol 2004;8:95–8 | No comparison group |
| Greenberg R, Werbin N, Skornik Y, Kaplan O. [Repair of anorectal fistulas using fibrin glue tissue adhesive – preliminary experience in 15 patients.] Harefuah 2002;141:1021–4, 1091 | No comparison group |
| Greenhalgh DG, Gamelli RL, Lee M, Delavari M, Lynch JB, Hansbrough JF, et al. Multicenter trial to evaluate the safety and potential efficacy of pooled human fibrin sealant for the treatment of burn wounds. J Trauma 1999;46:433–40 | RCT |
| Grewing R, Mester U. Fibrin sealant in the management of complicated hypotony after trabeculectomy. Ophthalmic Surg Lasers 1997;28:124–7 | No comparison group |
| Grimaud JC, Munoz-Bongrand N, Siproudhis L, Abramowitz L, Sénéjoux A, Vitton V, et al. Fibrin glue is effective healing perianal fistulas in patients with Crohn’s disease. Gastroenterology 2010;138:2275–81 | RCT |
| Groitl H, Scheele J. Initial experience with the endoscopic application of fibrin tissue adhesive in the upper gastrointestinal tract. Surg Endosc 1987;1:93–7 | No comparison group |
| Grossman JA, Capraro PA, Atagi T. A prospective, randomized, double-blind trial of the use of fibrin sealant for face lifts. Plast Reconstr Surg 2002;110:1371–2 | RCT |
| Gubitosi A, Docimo G, Parmeggiani D, Pirozzi R, Vitiello C, Schettino P, et al. Acellular bovine pericardium dermal matrix in immediate breast reconstruction after skin sparing mastectomy. Int J Surg 2014;12(Suppl. 1):205–8 | No comparison group |
| Gubitosi A, Ruggiero R, Docimo G, Avenia N, Villaccio G, Esposito A, et al. Hepatic cirrhosis and groin hernia: binomial or dichotomy? Our experience with a safe surgical treatment protocol. Ann Ital Chir 2011;82:197–204 | No comparison group |
| Gugenheim J, Bredt LC, Iannelli A. A randomized controlled trial comparing fibrin glue and PlasmaJet on the raw surface of the liver after hepatic resection. Hepatogastroenterology 2011;58:922–5 | RCT |
| Guilmet D, Bachet J, Goudot B, Laurian C, Gigou F, Bical O, et al. Use of biological glue in acute aortic dissection. Preliminary clinical results with a new surgical technique. J Thorac Cardiovasc Surg 1979;77:516–21 | Emergency surgery |
| Gündoğdu AG, Yazicioğlu A, Kara M, Kanbak M, Doğan R. [The use of tissue glue and its effect on hospital cost in patients undergoing pulmonary surgery.] Tuberk Toraks 2006;54:157–60 | No adverse effects related to fibrin reported |
| Guo S, Wagner RS, Forbes BJ, DeRespinis PA, Caputo AR. Cut and paste: sutureless conjunctival closure in strabismus surgery. J Pediatr Ophthalmol Strabismus 2010;47:228–30 | No comparison group |
| Gürer B, Kertmen H, Akturk UD, Kalan M, Sekerci Z. Use of the bovine pericardial patch and fibrin sealant in meningomyelocele closure. Acta Neurochir 2014;156:1345–50 | No comparison group |
| Gursoy S, Yapucu MU, Ucvet A, Yazgan S, Basok O, Ermete S. Fibrin glue administration to support bronchial stump line. Asian Cardiovasc Thorac Ann 2008;16:450–3 | No comparison group |
| Gutierrez C, Barrios JE, Lluna J, Vila JJ, Garcia-Sala C, Roca A, et al. Recurrent tracheoesophageal fistula treated with fibrin glue. J Pediatr Surg 1994;29:1567–9 | Not fibrin sealant |
| Gutiérrez Calzada JL, Burgos Rodríguez R. [Partial transplantectomy combined with substitution of the urinary tract, in the treatment of segmental renal infarction after transplantation.] Arch Esp Urol 1996;49:1093–9 | No comparison group |
| Gutiérrez San Román C, Barrios JE, Lluna J, Ibañez V, Hernández E, Ayuso L, et al. Long-term assessment of the treatment of recurrent tracheoesophageal fistula with fibrin glue associated with diathermy. J Pediatr Surg 2006;41:1870–3 | No comparison group |
| Gutiérrez-Calzada JL, Ramos-Titos J, González-Bonilla JA, Garcia-Vaquero AS, Martin-Morales A, Burgos-Rodríguez R. Caliceal fistula formation following renal transplantation: management with partial nephrectomy and ureteral replacement. J Urol 1995;153:612–14 | No comparison group |
| Haas S. The use of a surgical patch coated with human coagulation factors in surgical routine: a multicenter postauthorization surveillance. Clin Appl Thromb Hemost 2006;12:445–50 | No comparison group |
| Habesoglu TE, Kulekci S, Habesoglu M, Deveci I, Deveci S, Toros S, et al. Comparative outcomes of using fibrin glue in septoplasty and its effect on mucociliary activity. Otolaryngol Head Neck Surg 2010;142:394–9 | No adverse effects related to fibrin reported |
| Hadzhiev B. [Treatment of chronic anorectal fistulas by fibrin sealant.] Khirurgiia 2008;3:41–5 | No comparison group |
| Haga T, Kurihara M, Kataoka H. Spontaneous pneumothorax with persistent air leakage and invasive procedures. Intern Med 2013;52:2189–92 | No comparison group |
| Haim N, Neufeld D, Ziv Y, Tulchinsky H, Koller M, Khaikin M, et al. Long term success of fibrin glue in the treatment of perianal fistulae – a multicenter study. Colorectal Dis 2010;12:52 | No comparison group |
| Haim N, Neufeld D, Ziv Y, Tulchinsky H, Koller M, Khaikin M, et al. Long-term success of fibrin glue in the treatment of perianal fistulas – a multicenter study. Dis Colon Rectum 2010;53:576 | No comparison group |
| Haim N, Neufeld D, Ziv Y, Tulchinsky H, Koller M, Khaikin M, et al. Long-term results of fibrin glue treatment for cryptogenic perianal fistulas: a multicenter study. Dis Colon Rectum 2011;54:1279–83 | No comparison group |
| Haim N, Neufeld D, Ziv Y, Tulchinsky H, Koller M, Khaikin M, et al. Long-term results of fibrin glue in the treatment of perianal fistulas: a multicenter study. Tech Coloproctol 2011;15:240 | No comparison group |
| Haim N, Neufeld D, Ziv Y, Tulchinsky H, Koller M, Khaikin M, et al. Long-term success of fibrin glue in the treatment of perianal fistulas-a multicenter study. Tech Coloproctol 2011;15:121 | Duplicate |
| Halfpenny W, Fraser JS, Adlam DM. Comparison of 2 hemostatic agents for the prevention of postextraction hemorrhage in patients on anticoagulants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:257–9 | RCT |
| Hall et al. 2009160 | RCT |
| Halverson AL, Hull TL, Fazio VW, Church J, Hammel J, Floruta C. Repair of recurrent rectovaginal fistulas. Surgery 2001;130:753–7 | No comparison group |
| Hammond et al. 2011219 | RCT |
| Hanai M, Kobayashi Y, Miyata K, Yoneyama F, Hattori T, Yuas N. Gastric tube-pulmonary fistula after esophageal reconstruction treated by endoscopic fibrin glue injection: a case report. Nihon Shokaki Geka Gakkai Zasshi 2001;34:329–33 | No comparison group |
| Harries K, Masoud A, Brown TH, Richards DG. Endoscopic placement of fibrin sealant as a treatment for a long-standing Boerhaave’s fistula. Dis Esophagus 2004;17:348–50 | No comparison group |
| Hashimoto K, Shirakashi M, Watanabe J, Fukuchi T, Sawaguchi S, Kushiro M, et al. A case of the use of fibrin glue in leaking filtering bleb. Nihon Ganka Kiyo 1997;48:357–61 | No comparison group |
| Hata N, Hisada K, Torisu R, Suzuki SO, Kameda K, Sasaki T. Foreign body granuloma associated with dura-cranioplasty after resection of convexity meningioma with extracranial extension: case report. Neurol Med Chir 2011;51:236–8 | No comparison group |
| Hatzichristodoulou G, Fiechtner S, Gschwend JE, Lahme S. Long-term results after partial plaque excision and grafting with collagen fleece in Peyronie’s disease. Eur Urol Suppl 2015;14:e133 | No comparison group |
| Hatzichristodoulou G, Gschwend JE, Lahme S. Surgical correction of Peyronie’s curvature by partial plaque excision or incision and grafting with collagen fleece – first results of a prospective, multicenter study. Eur Urol Suppl 2011;10:317 | No comparison group |
| Hausmann M, Keller R. [Thoracoscopic pleurodesis in spontaneous pneumothorax.] Schweiz Med Wochenschr 1994;124:97–104 | No comparison group |
| Hayashi K, Nagano J, Hattori S. Adhesive arachnoiditis after percutaneous fibrin glue treatment of a sacral meningeal cyst. J Neurosurg Spine 2014;20:763–6 | No comparison group |
| Hayward PJ, Mackay IS. Fibrin glue in nasal septal surgery. J Laryngol Otol 1987;101:133–8 | No comparison group |
| Heldwein W, Avenhaus W, Schönekäs H, Kaess H, Müller-Lissner S, Hasford B, et al. Injection of fibrin tissue adhesive versus laser photocoagulation in the treatment of high-risk bleeding peptic ulcers: a controlled randomized study. Endoscopy 1996;28:756–60 | RCT |
| Helvind NM, Andresen K, Rosenberg J. Lower reoperation rates with the use of fibrin sealant versus tacks for mesh fixation. Surg Endosc 2013;27:4184–91 | Emergency surgery |
| Hennis HL, Stewart WC, Jeter EK. Infectious disease risks of fibrin glue. Ophthalmic Surg 1992;23:640 | Letter/commentary/reply |
| Herbrig K, Pistrosch F, Gross P, Palm C. Resumption of peritoneal dialysis after transcutaneous treatment of a peritoneal leakage using fibrin glue. Nephrol Dial Transplant 2006;21:2037–8 | Letter/commentary/reply |
| Hernandez C, Romero RJ, Lamoureux J, Seetharamaiah R, Garcia PE, Gallas M, et al. Gastric bypass postoperative clinical parameters using fibrin sealant. Bariatr Surg Pract Patient Care 2014;9:102–5 | No comparison group |
| Herold G, Danz B. Endoscopic (-ERC) fibrin sealing and histoacryl sealing of an abscess induced bilio-hepatico-cutaneous and a bilio-hepatico-phrenico-bronchial fistulous system. Z Gastroenterol 1995;33:605–9 | No comparison group |
| Herold G, Preclik G, Stange F. Gastroduodenal ulcer hemorrhage: endoscopic injection therapy using a fibrin sealant. Hepatogastroenterology 1994;41:116–19 | No comparison group |
| Hester TR Jr, Gerut ZE, Shire JR, Nguyen DB, Chen AH, Diamond J, et al. Exploratory, randomized, controlled, phase 2 study to evaluate the safety and efficacy of adjuvant fibrin sealant VH S/D 4 S-Apr (ARTISS) in patients undergoing rhytidectomy. Aesthet Surg J 2013;33:323–33 | RCT |
| Hester et al. 2013231 | RCT |
| Heusse JL, Hivelin M, Lepage C, Santini C, Lantieri L. [Fibrin sealant significantly decrease postoperative drainage in breast reconstruction by deep inferior epigastric perforator (DIEP) flap.] Ann Chir Plast Esthet 2012;57:50–8 | No adverse effects related to fibrin reported |
| Hevia M, Abascal-Junquera JM, Sacristan R, Suarez J, Lobo B, Mendez S, et al. [Haemostasis control during laparoscopic partial nephrectomy without parenchymal renorrhaphy: the VIVOSTAT experience.] Actas Urol Esp 2013;37:47–53 | No comparison group |
| Hick EJ, Morey AF. Initial experience with fibrin sealant in pendulous urethral reconstruction. Is early catheter removal possible? J Urol 2004;171:1547–9 | No adverse effects related to fibrin reported |
| Hick S, Demers PE, Brunette I, La C, Mabon M, Duchesne B. Amniotic membrane transplantation and fibrin glue in the management of corneal ulcers and perforations: a review of 33 cases. Cornea 2005;24:369–77 | Not a relevant comparison |
| Hickey NC. Randomized clinical trial of tranexamic acid-free fibrin sealant during vascular surgical procedures. Br J Surg 2010;97:1790 | RCT |
| Hida K, Yamaguchi S, Seki T, Yano S, Akino M, Terasaka S, et al. Nonsuture dural repair using polyglycolic acid mesh and fibrin glue: clinical application to spinal surgery. Surg Neurol 2006;65:136–42 | No comparison group |
| Hidalgo M, Castillo MJ, Eymar JL, Hidalgo A. Lichtenstein inguinal hernioplasty: sutures versus glue. Hernia 2005;9:242–4 | RCT |
| Hidalgo MP, Ferrero EH, Ortiz MA, Castillo JM, Hidalgo AG. Incisional hernia in patients at risk: can it be prevented? Hernia 2011;15:371–5 | No comparison group |
| Higashiyama M, Takami K, Higaki N, Kodama K. Pulmonary middle lobe fixation using TachoComb in patients undergoing right upper lobectomy with complete oblique fissure. Interact Cardiovasc Thorac Surg 2004;3:107–9 | No comparison group |
| Hillerdal G, Gustafsson G, Wegenius G, Englesson S, Hedenström H, Hedenstierna G. Large emphysematous bullae. Successful treatment with thoracoscopic technique using fibrin glue in poor-risk patients. Chest 1995;107:1450–3 | No comparison group |
| Hino M, Ishiko O, Honda KI, Yamane T, Ohta K, Takubo T, et al. Transmission of symptomatic parvovirus B19 infection by fibrin sealant used during surgery. Br J Haematol 2000;108:194–5 | No comparison group |
| Hino M, Yamamura R, Nishiki S, Ohta K, Yamane T, Takubo T, et al. [Human parvovirus B19-induced aplastic crisis in a patient treated with fibrin sealant.] Rinsho Ketsueki 1999;40:145–9 | No comparison group |
| Hivelin M, Heusse JL, Matar N, Lepage C, Lantieri L. Fibrin sealant decreases postoperative drainage in immediate breast reconstruction by deep inferior epigastric perforator flap after mastectomy with axillary dissection. Microsurgery 2011;31:18–25 | No comparison group |
| Hjortrup A, Moesgaard F, Kjaergård J. Fibrin adhesive in the treatment of perineal fistulas. Dis Colon Rectum 1991;34:752–4 | No comparison group |
| Höckel M, Klose KJ. Treatment of non-neoplastic nipple discharge with fibrin adhesive. Lancet 1987;2:331–2 | Letter/commentary/reply |
| Hodges SD, Humphreys SC, Eck JC, Covington LA. Management of incidental durotomy without mandatory bed rest. A retrospective review of 20 cases. Spine 1999;24:2062–4 | No comparison group |
| Hofmann HS, Rettig G, Radke J, Neef H, Silber RE. Iatrogenic ruptures of the tracheobronchial tree. Eur J Cardiothorac Surg 2002;21:649–52 | No comparison group |
| Hofstetter C, Segovia E, Vara-Thorbeck R. Treatment of uncomplicated hydatid cyst of the liver by closed marsupialization and fibrin glue obliteration. World J Surg 2004;28:173–8 | No comparison group |
| Hohendorff B, Siepen W, Spiering L, Staub L, Schmuck T, Boss A. Long-term results after operatively treated Achilles tendon rupture: fibrin glue versus suture. J Foot Ankle Surg 2008;47:392–9 | Included children |
| Hölscher AH, Schröder W, Bollschweiler E, Beckurts KT, Schneider PM. [How safe is high intrathoracic esophagogastrostomy?] Chirurg 2003;74:726–33 | No comparison group |
| Holub Z, Kliment Jr L. The effectiveness of collagen fleece combined with a fibrin glue in hemostasis during laparoscopic surgery. J Gynecol Surg 1999;15:185–91 | No adverse effects related to fibrin reported |
| Honda K, Asato R, Tsuji J, Kanda T, Ushiro K, Watanabe Y. Extended application of polyglycolic acid sheet combined with sprayed fibrin glue to advanced oral cancers. Oral Oncol 2011;47:S151 | No comparison group |
| Honda K, Ishiko O, Tsujimura A, Hino M, Hirai K, Itoh F, et al. Neutropenia accompanying parvovirus B19 infection after gynecologic surgery. Acta Haematol 2000;103:186–90 | No comparison group |
| Hong CK, Kim YB, Hong JB, Lee KS. Sealing of cerebrospinal fluid leakage during conventional transsphenoidal surgery using a fibrin-coated collagen fleece. J Clin Neurosci 2015;22:696–9 | No adverse effects related to fibrin reported |
| Huang and Qian 201493 | RCT |
| Huang et al. 201564 | RCT |
| Huguier M, Barrier A, Gouillat C, Suc B, Jaeck D, Launois B. [Pancreaticoduodenectomy for cancer of the head of the pancreas.] J Chir 2008;145:9–15 | Not a comparative observational study |
| Huh JW, Kim HR, Kim YJ. Anastomotic leakage after laparoscopic resection of rectal cancer: the impact of fibrin glue. Am J Surg 2010;199:435–41 | No adverse effects related to fibrin reported |
| Hurtgen M, Linder A, Friedel G, Toomes H. Video-assisted thoracoscopic pleurodesis. A survey conducted by the German Society for Thoracic Surgery. Thorac Cardiovasc Surg 1996;44:199–203 | Emergency surgery |
| Hutter et al. 2014237 | RCT |
| Hvass U, Chatel D, Assayag P, Juliard JM, Caliani J, Oroudji M, et al. [Repair of post-infarction left ventricular wall ruptures by biological glue and a flap from the pericardium. Results from 2 to 10 years.] Arch Mal Coeur Vaiss 1996;89:1255–8 | No comparison group |
| Hvass U, Chatel D, Assayag P, Juliard JM, Caliani J, Oroudji M, et al. [Repair of post-infarction left ventricular wall ruptures by biological glue and a flap from the pericardium. Results from 2 to 10 years.] Arch Mal Coeur Vaiss 1996;89:1255–8 | Duplicate |
| Iankin AV. [Tachocomb plates efficacy in prevention of lymphorrhea in radical operations for gastric cancer.] Khirurgiia 2006;11:44–6 | Unobtainable |
| Ikeda T, Sasaki M, Yamada N, Takamori A, Tanabe S, Okada A, et al. Controlling air leaks using free pericardial fat pads as surgical sealant in pulmonary resection. Ann Thorac Surg 2015;99:1170–5 | Not a relevant comparison |
| Imai K, Taniguchi M, Watanabe K, Einama T, Karasaki H, Kono T, et al. Efficacy of fibrin glue spray and polyglycolic acid sheet for the protection of transection surface after liver resection. HPB (Oxford) 2012;14:517–18 | Abstract |
| Imhof M, Ohmann C, Roher HD, Glutig H, Duesuc study g. Endoscopic versus operative treatment in high-risk ulcer bleeding patients – results of a randomised study. Langenbecks Arch Surg 2003;387:327–36 | RCT |
| Inderbitzi RG, Krebs T, Stirneman T, Ulrich A. Treatment of postoperative chylothorax by fibrin glue application under thoracoscopic view with use of local anesthesia. J Thorac Cardiovasc Surg 1992;104:209–10 | Letter/commentary/reply |
| Inghilleri G, Santoleri L, Cristallo A, Aloni A, Mancini L, Rondinara G, et al. Homemade vs commercial fibrin glue in liver surgery. Blood Transfus 2006;4:81–91 | Fibrin was used in both groups |
| Ishikura Y, Odagiri S, Shimazu A, Yoshimatsu H. Left ventricular rupture following mitral valve replacement – a report of two cases. Jpn J Surg 1990;20:699–703 | No comparison group |
| Ishio K. Delayed postoperative labyrinthine fistula. Otolaryngol Head Neck Surg (Tokyo) 1995;67:1024–9 | No comparison group |
| Ito H, Kimura T, Sameshima T, Aiyama H, Nishimura K, Ochiai C, et al. Reinforcement of pericranium as a dural substitute by fibrin sealant. Acta Neurochir 2011;153:2251–4 | No comparison group |
| Ito H, Nakayama H, Arai H, Karita S, Shotsu A, Fujita A. [Prevention of parenchymal air leakage after lung resection; comparison of effectiveness in drug formation of fibrin adhesive.] Kyobu Geka 2003;56:1014–16 | Fibrin was used in both groups |
| Izzo F, Palaia R, Albino V, Amore A, di Giacomo R, Piccirillo M, et al. Hepatocellular carcinoma and liver metastases: clinical data on a new dual-lumen catheter kit for surgical sealant infusion to prevent perihepatic bleeding and dissemination of cancer cells following biopsy and loco-regional treatments. Infectious Agents Cancer 2015;10:11 | No comparison group |
| Jabłoński S, Brocki M, Klejszmit P, Kutwin L, Wawrzycki M, Śmigielski J. Repair of postpneumonectomy bronchopleural fistula using pedicled pericardial flap supported by fibrin glue. Int Wound J 2015;12:154–9 | Not a relevant comparison |
| Jackson et al. 1999193 | RCT |
| Jain et al. 200499 | RCT |
| Johnsen S, Ermuth T, Tanczos E, Bannasch H, Horch RE, Zschocke I, et al. Treatment of therapy-refractive ulcera cruris of various origins with autologous keratinocytes in fibrin sealant. VASA 2005;34:25–9 | No comparison group |
| Johnson et al. 2005100 | RCT |
| Johnston WK, Montgomery JS, Seifman BD, Hollenbeck BK, Wolf JS. Fibrin glue v sutured bolster: lessons learned during 100 laparoscopic partial nephrectomies. J Urol 2005;174:47–52 | No adverse effects related to fibrin reported |
| Jones BM, Grover R. Avoiding hematoma in cervicofacial rhytidectomy: a personal 8-year quest. Reviewing 910 patients. Plast Reconstr Surg 2004;113:381–7 | Not a relevant comparison |
| Jones BM, Grover R. Early postoperative efficacy of fibrin glue in face lifts: a prospective randomized trial. Plast Reconstr Surg 2007;119:433–4 | RCT |
| Jonk A, van Dongen JA, Kroon BB. Prevention of seroma following axillary lymph node dissection or radical mastectomy; ineffectiveness of fibrin glue sealing technique. Neth J Surg 1987;39:135 | Unobtainable |
| Joseph et al. 2004200 | RCT |
| Jurczak F, Laridon JY, Raffaitin P, Redon Y, Pousset JP. [Long-term follow-up of the treatment of high anal fistulas using fibrin glue.] J Chir 2009;146:382–6 | No comparison group |
| Kahook MY, Noecker RJ. Fibrin glue-assisted glaucoma drainage device surgery. Br J Ophthalmol 2006;90:1486–9 | No adverse effects related to fibrin reported |
| Kamal HM, Goda HAEB. Epidural fibrin glue for treatment of post-dural puncture headache (PDPH): comparative study with epidural blood patch. Egypt J Anaesth 2009;25:41–7 | RCT |
| Kamer FM, Nguyen DB. Experience with fibrin glue in rhytidectomy. Plast Reconstr Surg 2007;120:1045–51 | RCT |
| Kanazawa R, Sato S, Iwamoto N, Teramoto A. Allergic reaction following arachnoid plasty with a fibrin sealant. Neurol Med Chir 2010;50:608–10 | No comparison group |
| Kanemaru S, Umeda H, Kitani Y, Nakamura T, Hirano S, Ito J. Regenerative treatment for tympanic membrane perforation. Otol Neurotol 2011;32:1218–23 | RCT |
| Kang GC, Sng KW, Tay AG. Modified technique for frontal sinus obliteration using calvarial bone and Tisseel glue. J Craniofac Surg 2009;20:528–31 | No comparison group |
| Kaplonyi G, Zimmerman I, Frenyo AD, Farkas T, Nemes G. The use of fibrin adhesive in the repair of chondral and osteochondral injuries. Injury 1988;19:267–72 | No comparison group |
| Karim MA, Ali A. Simple technique to manage redundant skin after laparoscopic ventral hernia repair. Asian J Endosc Surg 2013;6:137–9 | No comparison group |
| Karlikaya C, Ucan E, Oto O, Akkoclu A, Cimrin A, Akpinar O. Successful fibrin glue repair of iatrogenic bronchial rupture. Respir Med 1993;87:397–8 | Letter/commentary/reply |
| Karvonen JA, Gronroos JM, Nikulainen V, Gullichsen R, Salminen P. Endoscopic treatment of internal gastrointestinal fistulas with fibrin glue. Surg Laparosc Endosc Percutan Tech 2013;23:37–40 | No comparison group |
| Kaseda S, Aoki T, Hangai N, Omoto T, Yamamoto S, Sugiura H. Treating bullous lung disease with Holmium YAG laser in conjunction with fibrin glue and DEXON mesh. Lasers Surg Med 1998;22:219–22 | No comparison group |
| Kaseda S, Aoki T, Hangai N, Shimizu K, Kiguchi H. One hundred consecutive treatments with holmium: YAG laser for pulmonary bullae: especially in conjunction with gelatin-resorcinol formaldehyde-glutaraldehyde glue adhesion. Lasers Surg Med 2001;28:255–8 | Not fibrin sealant |
| Kassam A, Horowitz M, Carrau R, Snyderman C, Welch W, Hirsch B, et al. Use of tisseel fibrin sealant in neurosurgical procedures: incidence of cerebrospinal fluid leaks and cost-benefit analysis in a retrospective study. Neurosurgery 2003;52:1102–5 | Included children |
| Katkhouda N. Application of fibrin glue after hepatectomy might still be justified. Ann Surg 2008;247:399-400 | RCT |
| Katoch CD, Chandran VM, Bhattacharyya D, Barthwal MS. Closure of bronchopleural fistula by interventional bronchoscopy using sealants and endobronchial devices. Med J Armed Forces India 2013;69:326–9 | No comparison group |
| Kauer WKH, Stein HJ, Dittler HJ, Siewert JR. Stent implantation as a treatment option in patients with thoracic anastomotic leaks after esophagectomy. Surg Endosc 2008;22:50–3 | No comparison group |
| Kavanagh MC, Ohr MP, Czyz CN, Cahill KV, Perry JD, Holck DE, et al. Comparison of fibrin sealant versus suture for wound closure in Muller muscle-conjunctiva resection ptosis repair. Ophthal Plast Reconstr Surg 2009;25:99–102 | No adverse effects related to fibrin reported |
| Kawamura M, Kase K, Sawafuji M, Watanabe M, Horinouchi H, Kobayashi K. Staple-line reinforcement with a new type of polyglycolic acid felt. Surg Laparosc Endosc Percutan Tech 2001;11:43–6 | No comparison group |
| Kawamura M, Sawafuji M, Watanabe M, Horinouchi H, Kobayashi K. Frequency of transmission of human parvovirus B19 infection by fibrin sealant used during thoracic surgery. Ann Thorac Surg 2002;73:1098–100 | No comparison group |
| Keller R. [Thoracoscopic pleurodesis in persistent and recurrent pneumothorax.] Zentralbl Chir 1992;117:267–9 | No comparison group |
| Khafagy W, Zedan S, Setiet A, El-Awady S, El-Shobaky MT. Autologous fibrin glue in treatment of fistula in ano. Coloproctology 2001;23:17–21 | No adverse effects related to fibrin reported |
| Khaleal F, Berney C. The role of fibrin glue in decreasing chronic pain in laparoscopic totally extraperitoneal (TEP) inguinal hernia repair: a single surgeon’s experience. ANZ J Surg 2011;81:154–8 | No comparison group |
| Kheirkhah A, Casas V, Blanco G, Li W, Hayashida Y, Chen YT, et al. Amniotic membrane transplantation with fibrin glue for conjunctivochalasis. Am J Ophthalmol 2007;144:311–13 | No comparison group |
| Kheirkhah A, Casas V, Sheha H, Raju VK, Tseng SC. Role of conjunctival inflammation in surgical outcome after amniotic membrane transplantation with or without fibrin glue for pterygium. Cornea 2008;27:56–63 | No adverse effects related to fibrin reported |
| Kheirkhah A, Ghaffari R, Kaghazkanani R, Hashemi H, Behrouz MJ, Raju VK. A combined approach of amniotic membrane and oral mucosa transplantation for fornix reconstruction in severe symblepharon. Cornea 2013;32:155–60 | No comparison group |
| Kiejna N, Lubocki M, Wegrzyn K, Rzepecki P. Laparoscopic nephron sparing surgery (LNSS) using a clamp on the renal parenchyma and haemostatic material on the loge of the tumor. Eur Urol Suppl 2011;10:653 | No comparison group |
| Kilic B, Turna A, Demirkaya A, Kaynak K. A prospective randomized trial comparing heterologous and autologous fibrin sealants for the control of alveolar air leak. Interact Cardiovasc Thorac Surg 2013;17(Suppl. 1):1–62 | RCT |
| Kim HH, Mun HJ, Park YJ, Lee KW, Shin JP. Conjunctivolimbal autograft using a fibrin adhesive in pterygium surgery. Korean J Ophthalmol 2008;22:147–54 | No comparison group |
| Kim HJ, Huh JW, Kim HR, Kim YJ. Oncologic impact of anastomotic leakage in rectal cancer surgery according to the use of fibrin glue: case-control study using propensity score matching method. Am J Surg 2014;207:840–6 | No comparison group |
| Kim HK, Park HS. Fibrin glue-assisted augmented amniotic membrane transplantation for the treatment of large noninfectious corneal perforations. Cornea 2009;28:170–6 | No comparison group |
| Kim TS, Oh JH, Rhew HY. ‘Off-clamp, non-renorrhaphy’ laparoscopic partial nephrectomy with perirenal fat and gerota’s fascia reapproximation: initial experience and perioperative outcomes. J Laparoendosc Adv Surg Tech A 2014;24:339–44 | No comparison group |
| Kim YA, Steinbacher DM. Demineralized bone-fibrin sandwich for genioplasty. Aesthetic Plast Surg 2014;38:755–8 | RCT |
| Kim YA, Steinbacher DM. Demineralized bone-fibrin sandwich for genioplasty. Aesthet Plast Surg 2014;38:755–8 | No comparison group |
| Kimura N, Kawahito K, Murata S, Yamaguchi A, Adachi H, Ino T. Pitfalls of sutureless repair of a blow-out type left ventricular free wall rupture. Jpn J Thorac Cardiovasc Surg 2005;53:382–5 | No comparison group |
| Kinahan TJ, Johnson HW. Tisseel in hypospadias repair. Can J Surg 1992;35:75–7 | No adverse effects related to fibrin reported |
| Kingsnorth AN, Shahid MK, Valliattu AJ, Hadden RA, Porter CS. Open onlay mesh repair for major abdominal wall hernias with selective use of components separation and fibrin sealant. World J Surg 2008;32:26–30 | Fibrin data not shown separately from control |
| Kinoshita T. Usefulness of intrapleural administration of a large amount of diluted fibrin glue for intractable pneumothoraces. J Wakayama Med Soc 1998;49:289–96 | No comparison group |
| Kinoshita T, Miyoshi S, Suzuma T, Sakurai T, Enomoto K, Yoshimasu T, et al. Intrapleural administration of a large amount of diluted fibrin glue for intractable pneumothorax. A clinical study based on 57 cases: including 2 unsuccessful cases. Jpn J Thorac Cardiovasc Surg 2003;51:41–7 | No comparison group |
| Kirkegaard P, Madsen PV. [Closure of fistula with fibrin-glue.] Ugeskr Laeg 1982;144:3832–4 | Unobtainable |
| Kirkegaard P, Madsen PV. Perineal sinus after removal of the rectum. Occlusion with fibrin adhesive. Am J Surg 1983;145:791–4 | No comparison group |
| Kitago M, Matsui J, Tanabe M, Kawachi S, Itano O, Shinoda M, et al. Pylorus-preserving pancreatoduodenectomy with gastrointestinal reconstruction by the imanaga method enable the endoscopic examination of pancreatojejunostomy or choledochojejunostomy anastomosis. HPB (Oxford) 2012;14:672 | No comparison group |
| Kjaergard and Trumbull 1998138 | RCT |
| Kjølhede P, Rydén G, Hewardt P. Abdominal urethrocystopexy using fibrin sealant. A prospective study of long-term efficacy. Int Urogynecol J Pelvic Floor Dysfunct 2000;11:93–6 | No comparison group |
| Kluba et al. 2012145 | RCT |
| Knox Cartwright NE, Tole DM. Potential complication of fibrin sealant. J Cataract Refract Surg 2008;34:881–2 | Letter/commentary/reply |
| Kobayashi M, Suzuki K, Ichinose Y, Hashimoto K, Matsumoto K, Yamanaka H. Intractable fecal fistula cured by a combination of conservative therapy using fibrin adhesive agent and complicating. Jpn J Clin Urol 1989;43:815–17 | No comparison group |
| Kobayashi S, Nagano H, Marubashi S, Wada H, Eguchi H, Takeda Y, et al. Fibrin sealant with PGA felt for prevention of bile leakage after liver resection. Hepatogastroenterology 2012;59:2564–8 | Fibrin was used in both groups |
| Kohno et al. 199275 | RCT |
| Kon NF, Masumo H, Nakajima S, Tozawa R, Kimura M, Maeda S. [Anaphylactic reaction to aprotinin following topical use of biological tissue sealant.] Masui 1994;43:1606–10 | No comparison group |
| Konety BR. Fibrin glue v sutured bolster: lessons learned during 100 laparoscopic partial nephrectomies. Urol Oncol 2006;24:88 | Letter/commentary/reply |
| Koranyi et al. 2005162 | No adverse effects related to fibrin reported |
| Korotin DP, Pavlunin AV, Artifexova AA. Surgical prevention technique of the primary bronchus stump insufficiency using a fibrin-collagenic plate. Sovrem Tekhnologii Med 2011;2011:61–6 | No adverse effects related to fibrin reported |
| Kosmidis C, Efthimiadis C, Anthimidis G, Levva S, Prousalidis J, Papapolychroniadis K, et al. Combined left hepatectomy with fenestration and using a harmonic scalpel, fibrin glue and closed suction drainage to prevent bile leakage and ascites in the management of symptomatic polycystic liver disease: a case report. J Med Case Rep 2009;3:7442 | No comparison group |
| Kowalski C, Kastuar S, Mehta V, Brolin RE. Endoscopic injection of fibrin sealant in repair of gastrojejunostomy leak after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 2007;3:438–42 | No adverse effects related to fibrin reported |
| Kram HB, Nathan RC, Stafford FJ, Fleming AW, Shoemaker WC. Fibrin glue achieves hemostasis in patients with coagulation disorders. Arch Surg 1989;124:385–7 | No comparison group |
| Kram HB, Ocampo HP, Yamaguchi MP, Nathan RC, Shoemaker WC. Fibrin glue in renal and ureteral trauma. Urology 1989;33:215–18 | No comparison group |
| Krämer SC, Görich J, Rilinger N, Siech M, Aschoff AJ, Vogel J, et al. Embolization for gastrointestinal hemorrhages. Eur Radiol 2000;10:802–5 | No comparison group |
| Kruger T, Lisy M, Kalhil M, Nagy C, Stock UA, Wildhirt SM. Matrix-based repair of acute type-a aortic dissections as an alternative to conventional glue repair. Innovations 2012;7:105 | No comparison group |
| Kudo H, Sakagami Y, Kawamura A, Tamaki N. Delayed cerebrospinal fluid rhinorrhea seven months after transsphenoidal surgery for pituitary adenoma – case report. Neurol Med Chir 2000;40:160–3 | No comparison group |
| Kumar A, Maartens NF, Kaye AH. Evaluation of the use of BioGlue in neurosurgical procedures. J Clin Neurosci 2003;10:661–4 | No comparison group |
| Kurian A, Reghunadhan I, Nair KG. Autologous blood versus fibrin glue for conjunctival autograft adherence in sutureless pterygium surgery: a randomised controlled trial. Br J Ophthalmol 2015;99:464–70 | RCT |
| Lalos O, Berglund AL, Bjerle P. The long-term outcome of retropubic urethrocystopexy (sutures and fibrin sealant) and pubococcygeal repair. Acta Obstet Gynecol Scand 2000;79:135–9 | No comparison group |
| Lam FC, Kasper E. Augmented autologous pericranium duraplasty in 100 posterior fossa surgeries – a retrospective case series. Neurosurgery 2012;71(Suppl. 2):ons302–7 | No comparison group |
| Lam FC, Penumaka A, Chen CC, Fischer EG, Kasper EM. Fibrin sealant augmentation with autologous pericranium for duraplasty after suboccipital decompression in Chiari 1 patients: a case series. Surg Neurol Int 2013;4:6 | No comparison group |
| Lamm P, Adelhard K, Juchem G, Weitkunat R, Milz S, Kilger E, et al. Fibrin glue in coronary artery bypass grafting operations: casting out the Devil with Beelzebub? Eur J Cardiothorac Surg 2007;32:567–72 | No valid comparison |
| Lamont JP, Hooker G, Espenschied JR, Lichliter WE, Franko E. Closure of proximal colorectal fistulas using fibrin sealant. Am Surg 2002;68:615–18 | No comparison group |
| Lang et al. 2004134 | RCT |
| Lange V, Meyer G, Wenk H, Schildberg FW. Fistuloscopy – an adjuvant technique for sealing gastrointestinal fistulae. Surg Endosc 1990;4:212–16 | RCT |
| Lassen et al. 2006141 | RCT |
| Lau 2005172 | RCT |
| Laws ER. Sellar repair with fibrin sealant and collagen fleece after endoscopic endonasal transsphenoidal surgery. Commentary. Surg Neurol 2004;62:233 | Letter/commentary/reply |
| Lebowitz RA, Hoffman RA, Roland JT, Cohen NL. Autologous fibrin glue in the prevention of cerebrospinal fluid leak following acoustic neuroma surgery. Am J Otol 1995;16:172–4 | Fibrin was used in both groups |
| Lee FY, Leung KL, Lai PB, Lau JW. Selection of patients for laparoscopic repair of perforated peptic ulcer. Br J Surg 2001;88:133–6 | Emergency surgery |
| Lee S, Kim HR, Cho S, Huh DM, Lee EB, Ryu KM, et al. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 2014;98:2005–11 | RCT |
| Lee JH, Kang NY. Comparison of fibrin glue and sutures for conjunctival wound closure in strabismus surgery. Korean J Ophthalmol 2011;25:178–84 | RCT |
| Lee et al. 2009227 | RCT |
| Lehnhardt M, Hauser J, Daigeler A, Fredersdorf S, Dragieva G, Ploder B, et al. A variant PDGF incorporated into fibrin sealant for treatment of burn patients undergoing autologous mesh skin grafting. Burns 2009;35:S43 | RCT |
| Lei QF, Cai W. Clinical observation on fibrin glue application during pterygium surgery. Int Eye Sci 2015;15:364–6 | RCT |
| Leonardo C, De Mayo E, Franco G, Zampelli A, Tiesi A, Tartaglia N, et al. Modified ‘pluck’ technique with tissucol for the management of distal ureter during nephroureterectomy. Eur Urol Suppl 2009;8:347 | No comparison group |
| Levy O, Martinowitz U, Oran A, Tauber C, Horoszowski H. The use of fibrin tissue adhesive to reduce blood loss and the need for blood transfusion after total knee arthroplasty. A prospective, randomized, multicenter study. J Bone Joint Surg 1999;81:1580–8 | RCT |
| Lewandowski B. [Topical treatment of bleeding post removed teeth in patients with prosthetic heart valves whose receiving long-term of oral anticoagulant therapy.] Pol Merkur Lekarski 2002;12:20–4 | No comparison group |
| Liang HS, Hu M, Zhu XS, Zhao HB. Fibrin glue plus danshen injection in the prevention of postoperative lower back pain due to epidural adhesion: a synchronous controlled study. Chin J Clin Rehabil 2005;9:16–17 | RCT |
| Lillemoe et al. 200483 | RCT |
| Lin JM, Brolin RE. Treatment of gastric leaks after roux-en-y gastric bypass: a paradigm shift. Surg Obes Relat Dis 2011;7:373–4 | No comparison group |
| Lin R, Zhang FJ, Yu BW. Fibrin sealant and anaphylactic shock. Chin J New Drugs 2010;19:203–6 | Review |
| Lippert E, Klebl FH, Schweller F, Ott C, Gelbmann CM, Scholmerich J, et al. Fibrin glue in the endoscopic treatment of fistulae and anastomotic leakages of the gastrointestinal tract. Int J Colorectal Dis 2011;26:303–11 | No comparison group |
| Liu H, Wei RH, Huang Y, Yang RB, Zhang C, Zhao SZ. Clinical observation on fibrin glue technique in pterygium surgery performed with limbal autograft transplantation. Int Eye Sci 2013;13:1498–9 | RCT |
| Liu et al. 201413 | Not a comparative observational study |
| Liu W, Zhang YP, Xie MF, Liu Y. Application of fibrin glue with bandage contact lens in pterygium surgery. Int Eye Sci 2014;14:879–81 | RCT |
| Llewellyn-Bennett et al. 2012101 | RCT |
| Lobel B, Ordonez O, Olivo JF, Cipolla B, Milon D, Leveque JM, et al. [Radical prostatectomy and biologic glue.] Prog Urol 1991;1:440–4 | No adverse effects related to fibrin reported |
| Locatelli D, Vitali M, Custodi VM, Scagnelli P, Castelnuovo P, Canevari FR. Endonasal approaches to the sellar and parasellar regions: closure techniques using biomaterials. Acta Neurochir 2009;151:1431–7 | No adverse effects related to fibrin reported |
| Lopez et al. 2013129 | RCT |
| Lovisetto et al. 2007180 | RCT |
| Low JC, von Niederhäusern B, Rutherford SA, King AT. Pilot study of perioperative accidental durotomy: does the period of postoperative bed rest reduce the incidence of complication? Br J Neurosurg 2013;27:800–2 | No comparison group |
| Lowe J, Luber J, Levitsky S, Hantak E, Montgomery J, Schiestl N, et al. Evaluation of the topical hemostatic efficacy and safety of TiSSEEL VH S/D fibrin sealant compared with currently licensed TISSEEL VH in patients undergoing cardiac surgery: a phase 3, randomized, double-blind clinical study. J Cardiovasc Surg 2007;48:323–31 | RCT |
| Lu Q, Feng J, Yang Y, Nie B, Bao J, Zhao Z, et al. Treatment of type I endoleak after endovascular repair of infrarenal abdominal aortic aneurysm: success of fibrin glue sac embolization. J Endovasc Ther 2010;17:687–93 | No comparison group |
| Lund JN, Leveson SH. Fibrin glue in the treatment of pilonidal sinus: results of a pilot study. Dis Colon Rectum 2005;48:1094–6 | No comparison group |
| Mabrouk et al. 2013214 | RCT |
| Macias CA, Sandler B, Barajas-Gamboa JS, Valero M, Cheverie J, Talamini MA, et al. Standardized protocol utilization decreases rate of complications: A study of laparoscopic sleeve gastrectomy in 189 consecutive patients. Surg Endosc 2013;27:S489 | No comparison group |
| Maharaj et al. 2006230 | RCT |
| Mahdy RA, Wagieh MM. Safety and efficacy of fibrin glue versus vicryl sutures in recurrent pterygium with amniotic membrane grafting. Ophthalmic Res 2012;47:23–6 | RCT |
| Maisano et al. 2009140 | RCT |
| Makiyama K, Sakata R, Sano F, Yamanaka H, Nakaigawa N, Yao M, et al. Clinical comparison between microporrus polysaccharide hemispheres (MPH) and fibrin glue during laparoscopic partial nephrectomy. J Endourol 2012;26:A258–9 | Abstract |
| Malik and Kumar 2010171 | RCT |
| Mammis A, Agarwal N, Mogilner AY. Alternative treatment of intracranial hypotension presenting as postdural puncture headaches using epidural fibrin glue patches: two case reports. Int J Neurosci 2014;124:863–6 | No comparison group |
| Maralcan G, Başkonuş I, Aybasti N, Gökalp A. The use of fibrin glue in the treatment of fistula-in-ano: a prospective study. Surg Today 2006;36:166–70 | No comparison group |
| Maralcan G, Başkonuş I, Gökalp A, Borazan E, Balk A. Long-term results in the treatment of fistula-in-ano with fibrin glue: a prospective study. J Korean Surg Soc 2011;81:169–75 | No comparison group |
| Marangos IP, Rosok BI, Kazaryan AM, Rosseland AR, Edwin B. Effect of TachoSil patch in prevention of postoperative pancreatic fistula. J Gastrointest Surg 2011;15:1625–9 | No comparison group |
| Marchac and Greensmith 2005226 | RCT |
| Marta et al. 2010135 | RCT |
| Martin and Au 201386 | RCT |
| Martin II, Yuen L, Au K. Does fibrin glue sealant decrease the rate of anastomotic leak following pancreaticoduodenectomy? Results of a prospective randomized trial. HPB 2012;14:84 | RCT |
| Martin-Mateos RM, Lopez-San Roman A, García-Sánchez C, Garcia-Hoz F, Gil-Grande LA, Gómez EG, et al. Fibrin-glue-sealed liver biopsy: indications, complications and results. J Gastrointestin Liver Dis 2014;23:100–1 | Letter/commentary/reply |
| Matsuse S, Maruyama A, Hara Y. Nitrogenous subcutaneous emphysema caused by spray application of fibrin glue during retroperitoneal laparoscopic surgery. J Anesth 2011;25:426–30 | No comparison group |
| Matthews TW, Briant TD. The use of fibrin tissue glue in thyroid surgery: resource utilization implications. J Otolaryngol 1991;20:276–8 | No adverse effects related to fibrin reported |
| McConnell et al. 2012146 | RCT |
| McGoldrick JP, White RW. Fibrin sealant in coronary artery surgery – the devil is always in the detail! Eur J Cardiothorac Surg 2008;33:949–50 | Letter/commentary/reply |
| Meister T, Kuhlgatz J, Floer M. Over-the-Scope Clip (OTSC) application as rescue therapy for postoperative enterocutaneous fistula closure. Acta Chir Belg 2014;114:87–9 | No comparison group |
| Melissa CS, Bun TAY, Wing CK, Chung TY, Wai NEK, Tat LH. Randomized double-blinded prospective trial of fibrin sealant spray versus mechanical stapling in laparoscopic total extraperitoneal hernioplasty. Ann Surg 2014;259:432–7 | RCT |
| Menegolo M, Frigatti P, Antonello M, Lepidi S, Morelli I, Scrivere P, et al. Prevention of type ii endoleaks by coils and fibrin glue embolization of the aneurysmatic sac. Interact Cardiovasc Thorac Surg 2011;12:S52–3 | Abstract |
| Menovsky T. Editorial note on: the clinical study of repairing cauda equina fibres with fibrin glue after lumbar fracture and dislocation. Spinal Cord 2010;48:638 | Letter/commentary/reply |
| Mentens R, Stalmans P. Comparison of fibrin glue and sutures for conjunctival closure in pars plana vitrectomy. Am J Ophthalmol 2007;144:128–31 | No adverse effects related to fibrin reported |
| Mentens R, Stalmans P. Comparison of postoperative comfort in 20 gauge versus 23 gauge pars plana vitrectomy. Bull Soc Belge Ophtalmol 2009;311:5–10 | Not a relevant comparison |
| Messmann H, Schaller P, Andus T, Lock G, Vogt W, Gross V, et al. Effect of programmed endoscopic follow-up examinations on the rebleeding rate of gastric or duodenal peptic ulcers treated by injection therapy: a prospective, randomized controlled trial. Endoscopy 1998;30:583–9 | RCT |
| Mikhail AA, Kaptein JS, Bellman GC. Use of fibrin glue in percutaneous nephrolithotomy. Urology 2003;61:910–14 | Included children |
| Mikulas J, Laurinc P, Kazik P, Mraz R. Haemostatic use of Tachosil in partial nephrectomy – initial experience. Eur Urol Suppl 2010;9:636 | No comparison group |
| Milde LN. An anaphylactic reaction to fibrin glue. Anesth Analg 1989;69:684–6 | No comparison group |
| Milic DJ, Perisic ZD, Zivic SS, Stanojkovic ZA, Stojkovic AM, Karanovic ND, et al. Prevention of pocket related complications with fibrin sealant in patients undergoing pacemaker implantation who are receiving anticoagulant treatment. Europace 2005;7:374–9 | RCT |
| Milne et al. 1995201 | RCT |
| Milne et al. 1996203 | RCT |
| Minami K, Saito Y, Shomura Y, Imamura H. [A device to prevent an air-leakage after a thoracoscopic surgery for spontaneous pneumothorax.] Kyobu Geka 2003;56:904–7 | Emergency surgery |
| MiriBonjar et al. 2012103 | RCT |
| Miscusi M, Polli FM, Forcato S, Coman MA, Ricciardi L, Ramieri A, et al. The use of surgical sealants in the repair of dural tears during non-instrumented spinal surgery. Eur Spine J 2014;23:1761–6 | No adverse effects related to fibrin reported |
| Mishra A, Shah S, Nar AS, Bawa A. The role of fibrin glue in the treatment of high and low fistulas in ano. J Clin Diagn Res 2013;7:876–9 | Not a relevant comparison |
| Mita K, Ito H, Fukumoto M, Murabayashi R, Koizumi K, Hayashi T, et al. Pancreaticojejunostomy using a fibrin adhesive sealant (TachoComb) for the prevention of pancreatic fistula after pancreaticoduodenectomy. Hepatogastroenterology 2011;58:187–91 | No comparison group |
| Mita K, Ito H, Fukumoto M, Murabayashi R, Koizumi K, Hayashi T, et al. A fibrin adhesive sealing method for the prevention of pancreatic fistula following distal pancreatectomy. Hepatogastroenterology 2011;58:604–8 | No comparison group |
| Mithal C, Agarwal P, Mithal N. Pterygium surgery with conjunctival limbal autograft with fibrin glue under topical anaesthesia with lignocaine 2% jelly. Nepal J Ophthalmol 2011;3:151–4 | No comparison group |
| Mitsuhata H, Horiguchi Y, Saitoh J, Saitoh K, Fukuda H, Hirabayasi Y, et al. An anaphylactic reaction to topical fibrin glue. Anesthesiology 1994;81:1074–7 | No comparison group |
| Miyamoto H, Futagawa T, Wang Z, Yamazaki A, Morio A, Sonobe S, et al. Fibrin glue and bioabsorbable felt patch for intraoperative intractable air leaks. Jpn J Thorac Cardiovasc Surg 2003;51:232–6 | No comparison group |
| Mizuno H, Hitomi S, Nakamura T, Shimizu Y. [Clinical experience of the combined use of polyglycolide non-woven felt with fibrin glue to prevent postoperative pulmonary fistula.] Nihon Kyobu Geka Gakkai Zasshi 1995;43:1559–64 | Not a relevant comparison |
| Moench et al. 2010250 | RCT |
| Molloy et al. 2007147 | RCT |
| Montorsi et al. 201284 | RCT |
| Moore et al. 2001111 | RCT |
| Moralee SJ, Carney AS, Cash MP, Murray JA. The effect of fibrin sealant haemostasis on post-operative pain in tonsillectomy. Clin Otolaryngol Allied Sci 1994;19:526–8 | RCT |
| Morita Y, Nishii O, Kido M, Tsutsumi O. Parvovirus infection after laparoscopic hysterectomy using fibrin glue hemostasis. Obstet Gynecol 2000;95:1026 | No comparison group |
| Morris MS, Morey AF, Stackhouse DA, Santucci RA. Fibrin sealant as tissue glue: preliminary experience in complex genital reconstructive surgery. Urology 2006;67:688–91 | No comparison group |
| Mortenson et al. 2008120 | RCT |
| Moser et al. 2008126 | RCT |
| Mueller TJ, DaJusta DG, Cha DY, Kim IY, Ankem MK. Ureteral fibrin sealant injection of the distal ureter during laparoscopic nephroureterectomy – a novel and simple modification of the pluck technique. Urology 2010;75:187–92 | No comparison group |
| Muntean W, Zenz W, Edlinger G, Beitzke A. Severe bleeding due to factor V inhibitor after repeated operations using fibrin sealant containing bovine thrombin. Thromb Haemost 1997;77:1223 | Letter/commentary/reply |
| Muramatsu T, Ohmori K, Shimamura M, Furuichi M, Takeshita S, Negishi N. Staple line reinforcement with fleece-coated fibrin glue (TachoComb) after thoracoscopic bullectomy for the treatment of spontaneous pneumothorax. Surg Today 2007;37:745–9 | Emergency surgery |
| Murphy WG, Milne AA, Ruckley CV, Kubba AK, Palmer KR. Fibrin sealant: update on clinical studies. Transfus Sci 1996;17:341–2 | Review |
| Mustonen et al. 2004104 | RCT |
| Nakahira J, Ishii H, Sawai T, Minami T. Fibrin glue on an aortic cusp detected by transesophageal echocardiography after valve-sparing aortic valve replacement: a case report. J Med Case Rep 2015;9:53 | No comparison group |
| Nakamura et al. 2005236 | RCT |
| Narotam PK, José S, Nathoo N, Taylon C, Vora Y. Collagen matrix (DuraGen) in dural repair: analysis of a new modified technique. Spine 2004;29:2861–7 | No comparison group |
| Nativ et al. 201259 | RCT |
| Navarro-Rodriguez E, Gomez-Luque I, Diaz-Jimenez N, Rioja-Torres P, Bascunana-Estudillo G, Ruiz-Rabelo JF, et al. Effectiveness of an absorbable fibrin sealant patch to reduce lymphoceles formation after axillary lymphadenectomy for breast cancer: a matched-pair analysis. Am J Surg 2014;208:824–30 | No adverse effects related to fibrin reported |
| Nelson RL, Cintron J, Abcarian H. Dermal island-flap anoplasty for transsphincteric fistula-in-ano: assessment of treatment failures. Dis Colon Rectum 2000;43:681–4 | No comparison group |
| Nervi C, Gamelli RL, Greenhalgh DG, Luterman A, Hansbrough JF, Achauer BM, et al. A multicenter clinical trial to evaluate the topical hemostatic efficacy of fibrin sealant in burn patients. J Burn Care Rehabil 2001;22:99–103 | RCT |
| Neuss H, Raue W, Koplin G, Schwenk W, Reetz C, Mall JW. Intraoperative application of fibrin sealant does not reduce the duration of closed suction drainage following radical axillary lymph node dissection in melanoma patients: a prospective randomized trial in 58 patients. World J Surg 2008;32:1450–5 | RCT |
| Neuss et al. 2009118 | RCT |
| Nieuwendaal CP, van der Meulen IJ, Mourits M, Lapid-Gortzak R. Long-term follow-up of pterygium surgery using a conjunctival autograft and Tissucol. Cornea 2011;30:34–6 | No comparison group |
| Nishizawa S, Yokota N, Yokoyama T, Mukodaka H, Watanabe T, Hoshino T, et al. Prevention of postoperative complications in skull base surgery for nasal or paranasal sinus carcinoma invading the skull base. J Clin Neurosci 2001;8(Suppl. 1):67–70 | No comparison group |
| Nistor RF. Fibrin sealant in coronary artery bypass grafting surgery; reflection on risk and benefit. Eur J Cardiothorac Surg 2008;33:317 | Letter/commentary/reply |
| Notarnicola A, Moretti L, Martucci A, Spinarelli A, Tafuri S, Pesce V, et al. Comparative efficacy of different doses of fibrin sealant to reduce bleeding after total knee arthroplasty. Blood Coagul Fibrinolysis 2012;23:278–84 | RCT |
| Novik B, Hagedorn S, Mörk UB, Dahlin K, Skullman S, Dalenbäck J. Fibrin glue for securing the mesh in laparoscopic totally extraperitoneal inguinal hernia repair: a study with a 40-month prospective follow-up period. Surg Endosc 2006;20:462–7 | No comparison group |
| Ochiai T, Sonoyama T, Soga K, Inoue K, Ikoma H, Shiozaki A, et al. Application of polyethylene glycolic acid felt with fibrin sealant to prevent postoperative pancreatic fistula in pancreatic surgery. J Gastrointest Surg 2010;14:884–90 | No comparison group |
| Ochsner MG, Maniscalco-Theberge ME, Champion HR. Fibrin glue as a hemostatic agent in hepatic and splenic trauma. J Trauma 1990;30:884–7 | No comparison group |
| Ofikwu GI, Sarhan M, Ahmed L. EVICEL glue-induced small bowel obstruction after laparoscopic gastric bypass. Surg Laparosc Endosc Percutan Tech 2013;23:e38–40 | No comparison group |
| Ohta M, Komatsu F, Abe H, Sakamoto S, Tsugu H, Oshiro S, et al. Complication caused by use of fibrin glue in vessel transposition for trigeminal neuralgia. Neurol Med Chir 2008;48:30–2 | No comparison group |
| Ohwada et al. 19988 | Not a relevant comparison |
| Oliver et al. 2001228 | RCT |
| Oliver et al. 2002215 | RCT |
| Öllinger R, Mihaljevic AL, Schuhmacher C, Bektas H, Vondran F, Kleine M, et al. A multicentre, randomized clinical trial comparing the Veriset™ haemostatic patch with fibrin sealant for the management of bleeding during hepatic surgery. HPB 2013;15:548–58 | RCT |
| Olmi S, Erba L, Bertolini A, Scaini A, Croce E. Fibrin glue for mesh fixation in laparoscopic transabdominal preperitoneal (TAPP) hernia repair: indications, technique, and outcomes. Surg Endosc 2006;20:1846–50 | No comparison group |
| Olmi S, Erba L, Bertolini A, Scaini A, Mastropasqua E, Conti M, et al. [Use of fibrin glue (Tissucol) for mesh fixation in laparoscopic transabdominal hernia repair.] Chir Ital 2005;57:753–9 | No comparison group |
| Olmi et al. 2007259 | No comparison group |
| Olmi S, Scaini A, Erba L, Croce E. Use of fibrin glue (Tissucol) in laparoscopic repair of abdominal wall defects: preliminary experience. Surg Endosc 2007;21:409–13 | No comparison group |
| Olsen TW, Sternberg P Jr, Capone A Jr, Martin DF, Lim JI, Grossniklaus HE, et al. Macular hole surgery using thrombin-activated fibrinogen and selective removal of the internal limiting membrane. Retina 1998;18:322–9 | No comparison group |
| Olsha O, Hadar T, Dalo RA, Verocherinsky N, Ashkenazi I. Fibrin sealant to reduce drainage after axillary dissection. Ann Surg Oncol 2014;21:92–3 | Not a relevant comparison |
| Olsha O, Hadar T, Noy V, Verocherinsky N, Abu Dalo R, Ashkenazi I. Fibrin sealant to reduce lymphatic drainage after axillary dissection. Eur J Cancer 2014;50:S130–1 | No comparison group |
| Omote Y, Kubo Y. [Effectiveness of fibrin glue in preventing postoperative pulmonary air leakage.] Kyobu Geka 1994;47:355–9 | No adverse effects related to fibrin reported |
| Orsel I, Guillaume A, Feiss P. [Anaphylactic shock caused by fibrin glue.] Ann Fr Anesth Reanim 1997;16:292–3 | No comparison group |
| Oswald AM, Joly LM, Gury C, Disdet M, Leduc V, Kanny G. Fatal intraoperative anaphylaxis related to aprotinin after local application of fibrin glue. Anesthesiology 2003;99:762–3 | Letter/commentary/reply |
| Ozdamar Y, Mutevelli S, Han U, Ileri D, Onal B, Ilhan O, et al. A comparative study of tissue glue and vicryl suture for closing limbal-conjunctival autografts and histologic evaluation after pterygium excision. Cornea 2008;27:552–8 | RCT |
| Ozeki M, Watanabe N, Miyamoto N, Takahashi M, Murakami S, Sekiya Y, et al. Prevention of postoperative meningitis in cochlear implantation: the advantage of the use of temporal muscles and fibrin glue for the shield of cochleostomy. Cochlear Implants Int 2004;5(Suppl. 1):73–5 | Abstract |
| Palacios Jaraquemada JM, Pesaresi M, Nassif JC, Hermosid S. Anterior placenta percreta: surgical approach, hemostasis and uterine repair. Acta Obstet Gynecol Scand 2004;83:738–44 | Not a relevant comparison |
| Parker MC, Pohlen U, Borel Rinkes IH, Delvin T. The application of TachoSil® for sealing colorectal anastomosis: a feasibility study. Colorectal Dis 2013;15:252–7 | No comparison group |
| Pavlik Marangos I, Røsok BI, Kazaryan AM, Rosseland AR, Edwin B. Effect of TachoSil patch in prevention of postoperative pancreatic fistula. J Gastrointest Surg 2011;15:1625–9 | No adverse effects related to fibrin reported |
| Pescatore P, Jornod P, Borovicka J, Pantoflickova D, Suter W, Meyenberger C, et al. Epinephrine versus epinephrine plus fibrin glue injection in peptic ulcer bleeding: a prospective randomized trial. Gastrointest Endosc 2002;55:348–53 | RCT |
| Petersen B, Barkun A, Carpenter S, Chotiprasidhi P, Chuttani R, Silverman W, et al. Tissue adhesives and fibrin glues. Gastrointest Endosc 2004;60:327–33 | Not a comparative observational study |
| Petsas T, Siamblis D, Giannakenas C, Tepetes K, Dougenis D, Spiropoulos K, et al. Fibrin glue for sealing the needle track in fine-needle percutaneous lung biopsy using a coaxial system: Part II – Clinical study. Cardiovasc Intervent Radiol 1995;18:378–82 | RCT |
| Petter Puchner AH, Khakpour Z, May C, Mika K, Glaser KS, Redl H. The impact of atraumatic fibrin sealant vs. staple mesh fixation in tapp hernia repair on chronic pain and quality of life – results of a randomized controlled study. Surg Endosc 2010;24(Suppl. 1):618 | RCT |
| Pfuhl JP, Rucker KJ, Schafer D, Baumann R. Extrauterine pregnancy after tubal anastomosis with fibrin glue-light microscopy. Arch Gynecol Obstet 1989;245:436–7 | Abstract |
| Phillips AW, Viswanath YK, Burns JK, Hall CE, Horgan AF. Use of fibrin glue for fixation of mesh and approximation of Peritoneum in Transabdominal Preperitoneal (TAPP) inguinal hernia repair: technical feasibility and early surgical outcomes. Surg Laparosc Endosc Percutan Tech 2014;24:e43–5 | No comparison group |
| Pilon F, Tosato F, Danieli D, Campanile F, Zaramella M, Milite D. Intrasac fibrin glue injection after platinum coils placement: the efficacy of a simple intraoperative procedure in preventing type II endoleak after endovascular aneurysm repair. Interact Cardiovasc Thorac Surg 2010;11:78–82 | No adverse effects related to fibrin reported |
| Pilone et al. 201289 | RCT |
| Por YM, Tan YL, Mehta JS, Tan DT. Intracameral fibrin tissue sealant as an adjunct in tectonic lamellar keratoplasty for large corneal perforations. Cornea 2009;28:451–5 | No comparison group |
| Porpiglia F, Fiori C, Bertolo R, Mele F, Valentino F, Di Stasio A, et al. Complications after laparoscopic partial nephrectomy in a recent series. J Urol 2011;185:e314–15 | No comparison group |
| Porpiglia F, Renard J, Billia M, Morra I, Terrone C, Scarpa RM. Biological glues and collagen fleece for hemostasis during laparoscopic partial nephrectomy: technique and results of prospective study. J Endourol 2007;21:423–8 | No adverse effects related to fibrin reported |
| Porte RJ, Verhoef C, De Wilt JHW, Rijken AM, Klaase JM, Ayez N, et al. FibrocapsTM, a novel fibrin sealant, for bleeding during hepatic resection: results of a phase 2, randomized, controlled study. HPB (OXFORD) 2012;14:133 | RCT |
| Powell BS, Wandrey D, Voeller GR. A technique for placement of a bioabsorbable prosthesis with fibrin glue fixation for reinforcement of the crural closure during hiatal hernia repair. Hernia 2013;17:81–4 | No comparison group |
| Prado et al. 2006187 | RCT |
| Probst EN, Grzyska U, Westphal M, Zeumer H. Preoperative embolization of intracranial meningiomas with a fibrin glue preparation. Am J Neuroradiol 1999;20:1695–702 | No comparison group |
| Pruthi RS, Chun J, Richman M. The use of a fibrin tissue sealant during laparoscopic partial nephrectomy. BJU Int 2004;93:813–17 | No comparison group |
| Pugao R, Perenack J. Delayed reaction to fibrin sealant after facelift surgery: a case report and literature review. J Oral Maxillofac Surg 2012;70:e44–5 | No comparison group |
| Rábago LR, Ventosa N, Castro JL, Marco J, Herrera N, Gea F. Endoscopic treatment of postoperative fistulas resistant to conservative management using biological fibrin glue. Endoscopy 2002;34:632–8 | No comparison group |
| Ramon Rabago L, Moral I, Delgado M, Guerra I, Quintanilla E, Castro JL, et al. [Endoscopic treatment of gastrointestinal fistulas with biological fibrin glue.] Gastroenterologia y Hepatologia 2006;29:390–6 | No comparison group |
| Randelli F, Banci L, Ragone V, Pavesi M, Randelli G. Effectiveness of fibrin sealant after cementless total hip replacement: a double-blind randomized controlled trial. Int J Immunopathol Pharmacol 2013;26:189–97 | RCT |
| Randelli et al. 2014149 | RCT |
| Raquel SS, Gonzalez S, Nicolas R, Crego R, Tome C, Estevez S, et al. Staple line reinforcement with tissue glue sealant (Tissucol) during the learning curve of laparoscopic bariatric surgery. Obes Surg 2009;19:1045 | No comparison group |
| Reddy M, Schöggl A, Reddy B, Saringer W, Weigel G, Matula C. A clinical study of a fibrinogen-based collagen fleece for dural repair in neurosurgery. Acta Neurochir 2002;144:265–9 | No comparison group |
| Reppenhagen S, Reichert JC, Rackwitz L, Rudert M, Raab P, Daculsi G, et al. Biphasic bone substitute and fibrin sealant for treatment of benign bone tumours and tumour-like lesions. Int Orthop 2012;36:139–48 | No comparison group |
| Richmon JD, Tian Y, Husseman J, Davidson TM. Use of a sprayed fibrin hemostatic sealant after laser therapy for hereditary hemorrhagic telangiectasia epistaxis. Am J Rhinol 2007;21:187–91 | Included children |
| Romeo F, Pagano N, Carlino A, Rando G, Strangio G, Vitetta E, et al. Multimodal endoscopic approach to postsurgical gastro-esophageal anastomotic leaks. Gastrointest Endosc 2010;71:AB132 | No comparison group |
| Rousou J, Levitsky S, Gonzalez-Lavin L, Cosgrove D, Magilligan D, Weldon C, et al. Randomized clinical trial of fibrin sealant in patients undergoing resternotomy or reoperation after cardiac operations. A multicenter study. J Thorac Cardiovasc Surg 1989;97:194–203 | RCT |
| Rudelstorfer B, Loidl K, Heider R. [Wound closure of the fallopian tube with fibrin glue: endoscopic organ preserving therapy of extrauterine pregnancy.] Gynakol Geburtshilfliche Rundsch 1997;37:62–7 | No comparison group |
| Ruggiero R, Procaccini E, Gili S, Cremone C, Parmeggiani D, Conzo G, et al. New trends on fibrin glue in seroma after axillary lymphadenectomy for breast cancer. G Chir 2009;30:306–10 | RCT |
| Ruggiero R, Procaccini E, Piazza P, Docimo G, Iovino F, Antoniol G, et al. Effectiveness of fibrin glue in conjunction with collagen patches to reduce seroma formation after axillary lymphadenectomy for breast cancer. Am J Surg 2008;196:170–4 | No adverse effects related to fibrin reported |
| Sabatini et al. 2012148 | RCT |
| Sadik KW, Bonatti H, Schmitt T. Injection of fibrin glue for temporary treatment of an ascites leak from a ruptured umbilical hernia in a patient with liver cirrhosis. Surgery 2008;143:574 | Letter/commentary/reply |
| Sadik KW, Laibstain S, Northup PG, Kashmer D, Schmitt TM, Bonatti HJR. Closure of ascites leaks with fibrin glue injection in patients with end-stage liver disease. J Laparoendosc Adv Surg Tech A 2011;21:609–14 | No comparison group |
| Sáenz Medina J, Redondo González E, Hernández-Atance JM, Crespo Martínez L, Llanes González L, Rendón Sánchez D, et al. Renocolic fistula as a complication of radiofrequency in the treatment of renal cell carcinoma. Arch Esp Urol 2010;63:74–7 | No comparison group |
| Safan et al. 2009235 | RCT |
| Saha et al. 2011204 | RCT |
| Saha et al. 2012197 | RCT |
| Salgado W, Rosa GV, Nonino-Borges CB, Ceneviva R. Prospective and randomized comparison of two techniques of staple line reinforcement during open Roux-en-Y gastric bypass: oversewing and bioabsorbable Seamguard®. J Laparoendosc Adv Surg Tech A 2011;21:579–82 | RCT |
| Samimi DB, Hamilton DR. Recalcitrant epithelial ingrowth in patients with compromised eyelid function. J Refract Surg 2008;24:544–6 | No comparison group |
| Sanal M. Does fibrin glue cause foreign body reactions? Eur J Pediatr Surg 1993;3:190 | Letter/commentary/reply |
| Sanchez-Mendez JI, Lopez-Rodriguez MJ, Sanchez-Martinez C, Martinez-Garcia MT, Iniesta Donate MD, Ordas Santotomas J. Fibrin sealant for the prevention of axillary seroma formation after axillary lymph node dissection. A prospective randomized study. Cancer Res 2009;69:4139 | RCT |
| Santoro E, Agresta F, Buscaglia F, Mulieri G, Mazzarolo G, Bedin N, et al. Preliminary experience using fibrin glue for mesh fixation in 250 patients undergoing minilaparoscopic transabdominal preperitoneal hernia repair. J Laparoendosc Adv Surg Tech A 2007;17:12–15 | No adverse effects related to fibrin reported |
| Santulli P, Marcellin L, Touboul C, Ballester M, Darai E, Rouzier R. Experience with TachoSil in obstetric and gynecologic surgery. Int J Gynaecol Obstet 2011;113:112–15 | No comparison group |
| Sapala JA, Wood MH, Schuhknecht MP. Anastomotic leak prophylaxis using a vapor-heated fibrin sealant: report on 738 gastric bypass patients. Obes Surg 2004;14:35–42 | No comparison group |
| Sarnicola V, Vannozzi L, Motolese PA. Recurrence rate using fibrin glue-assisted ipsilateral conjunctival autograft in pterygium surgery: 2-year follow-up. Cornea 2010;29:1211–14 | No comparison group |
| Satoi S, Toyokawa H, Yanagimoto H, Yamamoto T, Hirooka S, Yui R, et al. Reinforcement of pancreticojejunostomy using polyglycolic acid mesh and fibrin glue sealant. Pancreas 2011;40:16–20 | No adverse effects related to fibrin reported |
| Sautter NB, Batra PS, Citardi MJ. Endoscopic management of sphenoid sinus cerebrospinal fluid leaks. Ann Otol Rhinol Laryngol 2008;117:32–9 | No comparison group |
| Savva A, Taylor MJ, Beatty CW. Management of cerebrospinal fluid leaks involving the temporal bone: report on 92 patients. Laryngoscope 2003;113:50–6 | No adverse effects related to fibrin reported |
| Schaller B, Baumann A. Headache after removal of vestibular schwannoma via the retrosigmoid approach: a long-term follow-up-study. Otolaryngol Head Neck Surg 2003;128:387–95 | No comparison group |
| Scheele J, Schricker KT, Goy RD, Lampe I, Panis R. [Risk of hepatitis in fibrin gluing in general surgery.] Med Welt 1981;32:783–8 | Unobtainable |
| Schenk et al. 2003195 | RCT |
| Schenk et al. 2002196 | RCT |
| Schettino AM, Franco D, Franco T, Filho JM, Vendramin FS. Use of autologous fibrin glue (platelet-poor plasma) in abdominal dermolipectomies. Aesthetic Plast Surg 2012;36:1296–301 | Not fibrin sealant |
| Scheule AM, Beierlein W, Lorenz H, Ziemer G. Repeated anaphylactic reactions to aprotinin in fibrin sealant. Gastrointest Endosc 1998;48:83–5 | No comparison group |
| Schlenker M, Ringelstein EB. Epidural fibrin clot for the prevention of post-lumbar puncture headache: a new method with risks. J Neurol Neurosurg Psychiatr 1987;50:1715 | Letter/commentary/reply |
| Schmidt SC, Langrehr JM. Re: Spray application of fibrin glue as risk factor for subcutaneous emphysema in laparoscopic transabdominal inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 2007;17:221–2 | Letter/commentary/reply |
| Scholz et al. 2002121 | RCT |
| Schopf SK, von Ahnen M, von Ahnen T, Schardey HM. [Observations on the use of TachoSil® in cholecystectomy – a multicentre, prospective, single-arm cohort study.] Zentralbl Chir 2012;137:55–60 | No comparison group |
| Schwartz et al. 200477 | RCT |
| Segal N, Puterman M, Rotem E, Niv A, Kaplan D, Kraus M, et al. A prospective randomized double-blind trial of fibrin glue for reducing pain and bleeding after tonsillectomy. Int J Pediatr Otorhinolaryngol 2008;72:469–73 | RCT |
| Séguin JR, Frapier JM, Colson P, Chaptal PA. Fibrin sealant improves surgical results of type A acute aortic dissections. Ann Thorac Surg 1991;52:745–8 | Emergency surgery |
| Séguin JR, Picard E, Frapier JM, Chaptal PA. Repair of the aortic arch with fibrin glue in type A aortic dissection. J Card Surg 1994;9:734–8 | No comparison group |
| Seiler RW, Mariani L. Sellar reconstruction with resorbable vicryl patches, gelatin foam, and fibrin glue in transsphenoidal surgery: a 10-year experience with 376 patients. J Neurosurg 2000;93:762–5 | No comparison group |
| Sentovich SM. Fibrin glue for anal fistulas: long-term results. Dis Colon Rectum 2003;46:498–502 | No comparison group |
| Seo JK, Kim HJ, Koh JK, Hong SK, Jung SY, Hwang SH, et al. The use of fibrin glue in osmidrosis surgery with a cartilage shaver: 18 patients. J Am Acad Dermatol 2013;68(Suppl. 1):AB223 | No comparison group |
| Seok Y, Cho S, Lee E. Bronchial stump coverage with fibrin glue-coated collagen fleece in lung cancer patients who underwent pneumonectomy. Ann Thorac Cardiovasc Surg 2014;20:117–22 | No adverse effects related to fibrin reported |
| Shah HN, Hegde S, Shah JN, Mohile PD, Yuvaraja TB, Bansal MB. A prospective, randomized trial evaluating the safety and efficacy of fibrin sealant in tubeless percutaneous nephrolithotomy. J Urol 2006;176:2488–92 | RCT |
| Shah HN, Kausik V, Hedge S, Shah JN, Bansal MB. Initial experience with hemostatic fibrin glue as adjuvant during tubeless percutaneous nephrolithotomy. J Endourol 2006;20:194–8 | No adverse effects related to fibrin reported |
| Sharma et al. 2003164 | RCT |
| Sharma SK, Perry KT, Turk TM. Endoscopic injection of fibrin glue for the treatment of urinary-tract pathology. J Endourol 2005;19:419–23 | No comparison group |
| Shehadeh-Mashor R, Srinivasan S, Boimer C, Lee K, Tomkins O, Slomovic AR. Management of recurrent pterygium with intraoperative mitomycin C and conjunctival autograft with fibrin glue. Am J Ophthalmol 2011;152:730–2 | No comparison group |
| Shen L, Luo H, Tan S. Effect of fibrin glue on patients after high frequency electrocoagulatomy for gastrointestinal protuberant lesions. Med J Wuhan Uni 2003;24:377 | RCT |
| Shimada Y, Hongo M, Miyakoshi N, Sugawara T, Kasukawa Y, Ando S, et al. Dural substitute with polyglycolic acid mesh and fibrin glue for dural repair: technical note and preliminary results. J Orthop Sci 2006;11:454–8 | Fibrin was used in both groups |
| Shin IS, Lee DW, Lew DH. Efficacy of quilting sutures and fibrin sealant together for prevention of seroma in extended latissimus dorsi flap donor sites. Arch Plast Surg 2012;39:509–13 | Fibrin was used in both groups |
| Shinohara H, Koizumi T, Aoki T, Yoshiya K, Koike T, Tsuchida M. Intrapleural administration of a combination of cisplatin and fibrin glue for pleural lavage cytology-positive patients with non-small cell lung cancer. J Thorac Oncol 2013;8:S508 | Not a relevant comparison |
| Siemer et al. 2007221 | RCT |
| Silas AM, Forauer AR, Perrich KD, Gemery JM. Sclerosis of postoperative lymphoceles: avoidance of prolonged catheter drainage with use of a fibrin sealant. J Vasc Interv Radiol 2006;17:1791–5 | No comparison group |
| Silecchia et al. 200862 | RCT |
| Silecchia G, Boru CE, Mouiel J, Rossi M, Anselmino M, Tacchino RM, et al. Clinical evaluation of fibrin glue in the prevention of anastomotic leak and internal hernia after laparoscopic gastric bypass: preliminary results of a prospective, randomized multicenter trial. Obes Surg 2006;16:125–31 | RCT |
| Silecchia G, Iossa A, Cavallaro G, Rizzello M, Longo F. Reinforcement of hiatal defect repair with absorbable mesh fixed with non-permanent devices. Minim Invasive Ther Allied Technol 2014;23:302–8 | Not a comparative observational study |
| Singer M, Cintron J, Nelson R, Orsay C, Bastawrous A, Pearl R, et al. Treatment of fistulas-in-ano with fibrin sealant in combination with intra-adhesive antibiotics and/or surgical closure of the internal fistula opening. Dis Colon Rectum 2005;48:799–808 | RCT |
| Sintler et al. 2005202 | RCT |
| Skovgaard et al. 2013150 | RCT |
| Slupski P, Jarzemski P, Listopadzki S, Wisniewski P. Suture-free laparoscopic partial nephrectomy - improvement of hemostasis with human fibrinogen and thrombin-coated collagen patch (TachoSil). Eur Urol Suppl 2010;9:636 | Abstract |
| Sokullu O, Sanioglu S, Orhan G, Kut MS, Hastaoglu O, Karaca P, et al. New use of teflon to reduce bleeding in modified bentall operation. Tex Heart Inst J 2008;35:147–51 | No comparison group |
| Soumian S, Al-Ani S, Sterne G. Randomized clinical trial on the effect of fibrin sealant on latissimus dorsi donor-site seroma formation after breast reconstruction (Br J Surg 2012;99:1381–8). Br J Surg 2013;100:1671 | RCT |
| Sozen et al. 2011212 | RCT |
| Sozen S, Topuz O, Keceli M, Tukenmez M, Onceken O, Tuna O. The use of fibrin glue in surgical treatment of pilonidal sinus disease: a prospective study in the limberg flap procedure. Pak J Med Sci 2011;27:537–40 | RCT |
| Spotnitz WD, Dalton MS, Baker JW, Nolan SP. Successful use of fibrin glue during 2 years of surgery at a university medical center. Am Surg 1989;55:166–8 | No comparison group |
| Srinivasan et al. 2009167 | RCT |
| Stanojkovic Z, Milic D, Zivic S, Perisic Z. Application effect of fibrin sealant in patients undergoing pacemaker implantation. Vox Sang 2009;96:238 | Abstract |
| Sterkers O, Becherel P, Sterkers JM. [Repair of the facial nerve exclusively by fibrin glue. 56 cases.] Ann Otolaryngol Chir Cervicofac 1989;106:176–81 | No comparison group |
| Stoeckli SJ, Moe KS, Huber A, Schmid S. A prospective randomized double-blind trial of fibrin glue for pain and bleeding after tonsillectomy. Laryngoscope 1999;109:652–5 | RCT |
| Sugg U. [Risk of transmission of hepatitis through human fibrin adhesives.] Dtsch Med Wochenschr 1985;110:1161–2 | No adverse effects related to fibrin reported |
| Suzuki A, Amano J, Tanaka H, Sakamoto T, Sunamori M. Surgical consideration of aortitis involving the aortic root. Circulation 1989;80:I222–32 | Not a relevant comparison |
| Swain BT, Ellis CN. Fibrin glue treatment of low rectal and pouch-anal anastomotic sinuses. Dis Colon Rectum 2004;47:253–5 | No comparison group |
| Swan et al. 2011113 | RCT |
| Szczesny T, Kubiszewska I, Rybak A, Michalkiewicz J, Szymankiewicz M, Kowalewski J. The role of Tachosil in lymphostasis after mediastinal lymphadenectomy in lung cancer patients. J Thorac Oncol 2011;6(Suppl. 2):876–7 | RCT |
| Tachibana et al. 2003122 | RCT |
| Taguchi Y, Suzuki R, Okada M, Sekino H. Spinal arachnoid cyst developing after surgical treatment of a ruptured vertebral artery aneurysm: a possible complication of topical use of fibrin glue. Case report. J Neurosurg 1996;84:526–9 | No comparison group |
| Takeuchi et al. 2005234 | RCT |
| Tan LA, Takagi I, Straus D, O’Toole JE. Management of intended durotomy in minimally invasive intradural spine surgery: clinical article. J Neurosurg Spine 2014;21:279–85 | No comparison group |
| Tan QT, Lee CM, Tan VKM, Ong KW. The use of Tisseel fibrin sealant in seroma reduction after mastectomy – a pilot study. Breast 2015;24:S133 | Abstract |
| Târcoveanu E, Lupaşcu C, Moldovanu R, Vlad N, Bradea C, Vasilescu A. [Fibrin-collagen patch (TachoComb) in general surgery. Indications and results.] Rev Med Chir Soc Med Nat Iasi 2007;111:396–401 | No comparison group |
| Terasaka S, Iwasaki Y, Kuroda S, Uchida T. [A novel method of dural repair using polyglycolic acid non-woven fabric and fibrin glue: clinical results of 140 cases.] No Shinkei Geka 2006;34:1109–17 | No comparison group |
| Terashima M, Fujiwara S, Yaginuma GY, Takizawa K, Kaneko U, Meguro T. Outcome of percutaneous intrapericardial fibrin-glue injection therapy for left ventricular free wall rupture secondary to acute myocardial infarction. Am J Cardiol 2008;101:419–21 | No comparison group |
| Than KD, Baird CJ, Olivi A. Polyethylene glycol hydrogel dural sealant may reduce incisional cerebrospinal fluid leak after posterior fossa surgery. Neurosurgery 2008;63(Suppl. 1):ON182–6 | Not fibrin sealant |
| Tirindelli MC, Flammia G, Cudillo L, Dentamaro T, Picardi A, Annibali O, et al. Fibrin glue directly applied on damaged bladder mucosa during cystoscopy is highly effective to treat severe, refractory, haemorrhagic cystitis after allogeneic transplant. Bone Marrow Transplant 2010;45:S12 | No comparison group |
| Tirindelli MC, Flammia G, Sergi F, Cerretti R, Cudillo L, Picardi A, et al. Fibrin glue for refractory hemorrhagic cystitis after unrelated marrow, cord blood, and haploidentical hematopoietic stem cell transplantation. Transfusion 2009;49:170–5 | No comparison group |
| Tirindelli MC, Flammia GP, Bove P, Cerretti R, Cudillo L, de Angelis G, et al. Fibrin glue therapy for severe hemorrhagic cystitis after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2014;20:1612–17 | No comparison group |
| Tiscione D, Cicuto S, Luciani L, Vattovani V, Coccarelli F, Malossini G. Use of fibrin gel (Tissucol) as hemostatic agent during laparoscopic partial nephrectomy: our experience. Anticancer Res 2010;30:1520–1 | No comparison group |
| Toman N, Buschmann A, Muehlberger T. [Fibrin glue and seroma formation following abdominoplasty.] Chirurg 2007;78:531–5 | Fibrin was used in both groups |
| Tomizawa Y, Endo M, Kitamura M, Shiikawa A, Yagi Y, Koyanagi H. [Coronary artery bypass graft stenosis suspected to be due to hemostatic agents: a case report.] Kyobu Geka 1991;44:764–6 | No comparison group |
| Topart P, Vandenbroucke F, Lozac’h P. Tisseel versus tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias: a retrospective analysis. Surg Endosc 2005;19:724–7 | No adverse effects related to fibrin reported |
| Topgül K, Anadol AZ, Güngör B, Malazgirt Z. Laparoscopic bilateral hernia repair using fibrin sealant: technical report of two cases. J Laparoendosc Adv Surg Tech A 2005;15:638–41 | No comparison group |
| Topiwala P, Bansal RK. Comparative evaluation of cyanoacrylate and fibrin glue for muscle recession in strabismus surgery. J Pediatr Ophthalmol Strabismus 2014;51:349–54 | RCT |
| Tournoux F, Karila-Cohen D, Hvass U, Peytavin G, Phelippeau G, Vahanian A. [Neutropenia and fever after aorto-coronary bypasses.] Ann Chir 2004;129:174–6 | No comparison group |
| Tredwell SJ, Sawatzky B. The use of fibrin sealant to reduce blood loss during Cotrel-Dubousset instrumentation for idiopathic scoliosis. Spine 1990;15:913–15 | RCT |
| Tripoloni DE, Schierano MC. Comments about the article ‘Open tension-free Lichtenstein repair of inguinal hernia: use of fibrin glue versus sutures for mesh fixation’ by Negro et al. Hernia 2012;16:235–6 | Letter/commentary/reply |
| Troisi RI, Bektas H, Pratschke J, Topal B, Buchler M, Schuhmacher CP, et al. A prospective, multi-center, randomized, single-blind study to compare the VerisetTM hemostatic patch to fibrin sealant (Tachosil) in subjects undergoing hepatic surgery. HPB 2012;14:104–5 | RCT |
| Truong S, Bohm G, Klinge U, Stumpf M, Schumpelick V. Results after endoscopic treatment of postoperative upper gastrointestinal fistulas and leaks using combined Vicryl plug and fibrin glue. Surg Endosc 2004;18:1105–8 | No comparison group |
| Tsuji Y, Fujishiro M, Kodashima S, Ono S, Niimi K, Mochizuki S, et al. Polyglycolic acid sheets and fibrin glue decrease the risk of bleeding after endoscopic submucosal dissection of gastric neoplasms (with video). Gastrointest Endosc 2015;81:906–12 | Not a comparative observational study |
| Tsuji Y, Ohata K, Gunji T, Shozushima M, Hamanaka J, Ohno A, et al. Endoscopic tissue shielding method with polyglycolic acid sheets and fibrin glue to cover wounds after colorectal endoscopic submucosal dissection (with video). Gastrointest Endosc 2014;79:151–5 | No comparison group |
| Udén et al. 199398 | RCT |
| Ulusoy et al. 200396 | RCT |
| Ussat S, Lodes U, Wex C, Rapp L, Schulz HU, Meyer F. [Successful closure of a postoperative esophagobronchial fistula following esophageal resection using fibrin glue.] Dtsch Med Wochenschr 2013;138:1406–9 | RCT |
| Uy HS, Reyes JMG, Flores JDG, Lim-Bon-Siong R. Comparison of fibrin glue and sutures for attaching conjunctival autografts after pterygium excision. Ophthalmology 2005;112:667–71 | No comparison group |
| Vaiman M, Eviatar E. Lymphatic fistulae after neck dissection: the fibrin sealant treatment. J Surg Oncol 2008;98:467–71 | RCT |
| Vaiman et al. 2002188 | No comparison group |
| Vaiman M, Eviatar E, Shlamkovich N, Segal S. Effect of modern fibrin glue on bleeding after tonsillectomy and adenoidectomy. Ann Otol Rhinol Laryngol 2003;112:410–14 | RCT |
| Vaiman et al. 2005191 | RCT |
| Vaiman et al. 2005189 | RCT |
| Vaiman M, Segal S, Eviatar E. Fibrin glue treatment for epistaxis. Rhinology 2002;40:88–91 | RCT |
| Valenti A, Rivkin E, Carandina S, Steiger A, Polliand C, Rizk N, et al. Laparoscopy sleeve gastrectomy: 220 cases in a comparative study with three buttressing methods applied on stapler line. Obes Surg 2013;23:1053 | Not a comparative observational study |
| Van Velthoven V, Clarici G, Auer LM. Fibrin tissue adhesive sealant for the prevention of CSF leakage following transsphenoidal microsurgery. Acta Neurochir 1991;109:26–9 | No comparison group |
| Vaxman et al. 1995112 | RCT |
| Vaxman et al. 1995251 | RCT |
| Verhoef et al. 2015240 | RCT |
| Vichare N, Choudhary T, Arora P. A comparison between fibrin sealant and sutures for attaching conjunctival autograft after pterygium excision. Med J Armed Forces India 2013;69:151–5 | No adverse effects related to fibrin reported |
| Vitton V, Gasmi M, Barthet M, Desjeux A, Orsoni P, Grimaud JC. Long-term healing of Crohn’s anal fistulas with fibrin glue injection. Aliment Pharmacol Ther 2005;21:1453–7 | No comparison group |
| Waclawiczek HW, Boeckl O. [Clinical experience with fibrin gluing in general and thoracic surgery.] Zentralbl Chir 1986;111:16–24 | No comparison group |
| Wang et al. 2003153 | RCT |
| Wang et al. 2001144 | RCT |
| Wang X, Ren J, Zhu W, Li N, Li J. Fibrin sealant prevents gastrointestinal anastomosis dehiscence in intra-abdominal sepsis. Int Surg 2007;92:27–31 | No comparison group |
| Watanabe G, Haverich A, Speier R, Dresler C, Borst HG. Surgical treatment of active infective endocarditis with paravalvular involvement. J Thorac Cardiovasc Surg 1994;107:171–7 | No comparison group |
| White N, Carver ED, Rodrigues D, Dover S, Magdum S, Nishikawa H, et al. Calvarial remodelling for sagittal synostosis: does fibrin glue (Tisseel) reduce post-operative blood transfusion requirements? Childs Nerv Syst 2009;25:867–9 | Included children |
| Willecocq C, Pizzoferrato AC, Fauconnier A, Bader G. [Use of glue in laparoscopic sacrocolpopexy. A comparative study about 32 cases.] Gynecol Obstet Fertil 2014;42:822–6 | No adverse effects related to fibrin reported |
| Wong K, Goldstraw P. Effect of fibrin glue in the reduction of postthoracotomy alveolar air leak. Ann Thorac Surg 1997;64:979–81 | RCT |
| Yeom JS, Buchowski JM, Shen HX, Liu G, Bunmaprasert T, Riew KD. Effect of fibrin sealant on drain output and duration of hospitalization after multilevel anterior cervical fusion: a retrospective matched pair analysis. Spine 2008;33:E543–7 | No adverse effects related to fibrin reported |
| Yildirim AE, Dursun E, Ozdol C, Divanlioglu D, Nacar OA, Koyun OK, et al. Using an autologous fibrin sealant in the preventing of cerebrospinal fluid leak with large skull base defect following endoscopic endonasal transsphenoidal surgery. Turk Neurosurg 2013;23:736–41 | No comparison group |
| Yin W, Pauza K, Olan W, Doerzbacher J. Long-term outcomes from a prospective, multicenter investigational device exemption (IDE) pilot study of intradiscal fibrin sealant for the treatment of discogenic pain. Pain Med 2011;12:1446–7 | No comparison group |
| Yu L, Gu T, Song L, Shi E, Fang Q, Wang C, et al. Fibrin sealant provides superior hemostasis for sternotomy compared with bone wax. Ann Thorac Surg 2012;93:641–4 | No comparison group |
| Yuan Q, Bai XM, Cheng L, Gu XS, Jin Y. Efficacy of fibrin glue in percutaneous transhepatic obliteration for the management of upper gastrointestinal bleeding in patients with portal hypertension. Shijie Huaren Xiaohua Zazhi 2012;20:3397–402 | RCT |
| Yüksel et al. 2010158 | No comparison group |
| Zacharias T, Ferreira N. Carrier-bound fibrin sealant compared to oxidized cellulose application after liver resection. HPB 2012;14:839–47 | No adverse effects related to fibrin reported |
| Zhang YH, Gu TX, Zhang GW, Wang C, Liu Y, Yu Y. Injection of fibrin glue directly into the sternum for sternal bleeding in old patients with osteoporosis during coronary artery bypass. J Clin Rehabil Tiss Engin Res 2011;15:4735–8 | RCT |
| Zhou D, Shen L, Jin Y, Bennet S, Wang W, McLennan G. Efficacy and safety of selective arterial embolization with fibrin glue in the treatment of primary postpartum hemorrhage: a prospective study of 61 cases. J Vasc Interv Radiol 2012;23(Suppl. 1):105–6 | Abstract |
| Zmora O, Neufeld D, Ziv Y, Tulchinsky H, Scott D, Khaikin M, et al. Prospective, multicenter evaluation of highly concentrated fibrin glue in the treatment of complex cryptogenic perianal fistulas. Dis Colon Rectum 2005;48:2167–72 | No comparison group |
| Zoumalan R, Rizk SS. Hematoma rates in drainless deep-plane face-lift surgery with and without the use of fibrin glue. Arch Facial Plast Surg 2008;10:103–7 | No adverse effects related to fibrin reported |
Appendix 8 Sensitivity analysis random-effects model (DerSimonian and Laird55)
Primary outcomes
Seroma development
FIGURE 49.
Seroma development in all surgical specialties: fibrin sealant vs. standard care. Pooled OR 0.86 (95% CI 0.68 to 1.10; p = 0.23).
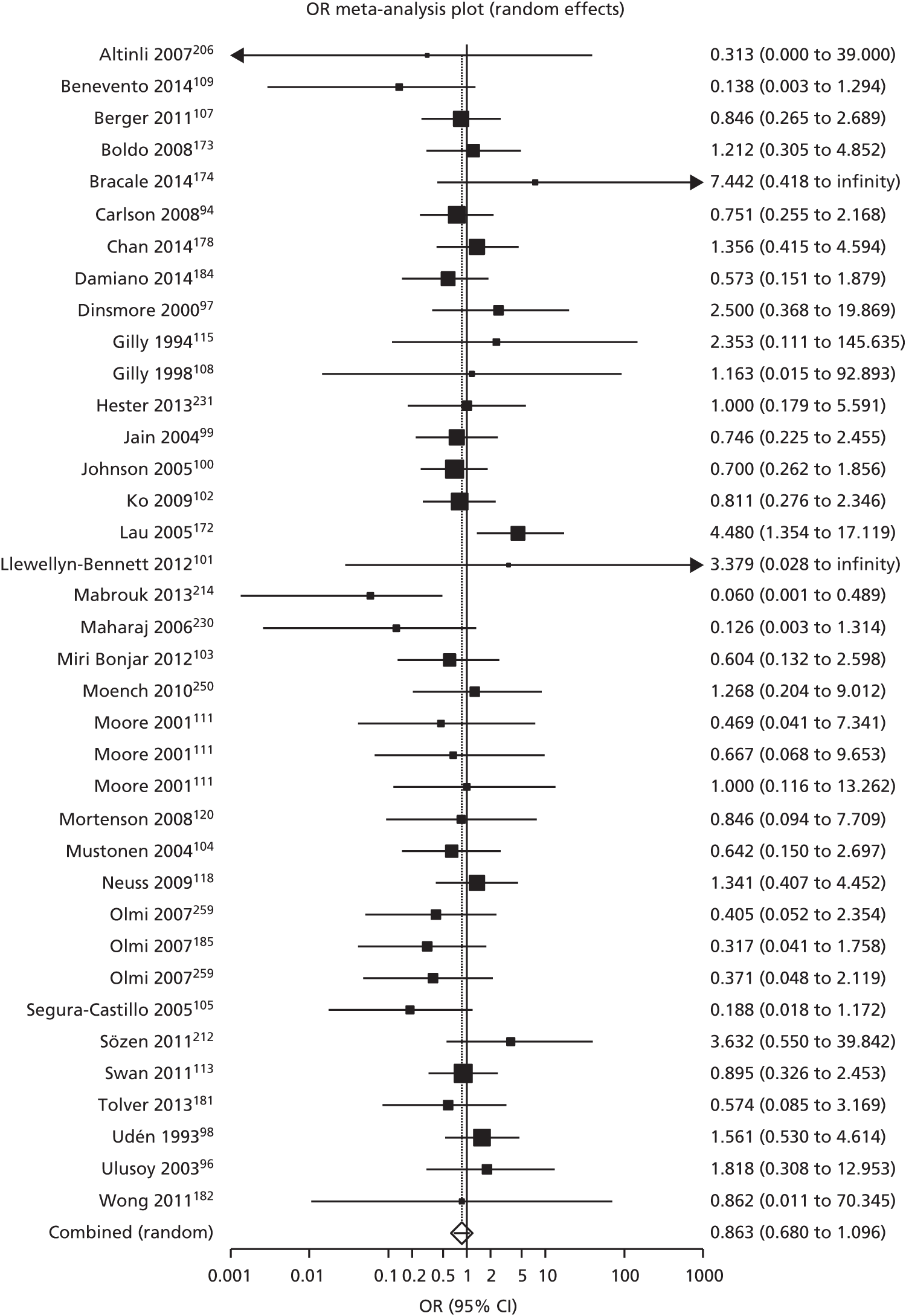
FIGURE 50.
Seroma development in breast surgery: fibrin sealant vs. standard care. Pooled OR 0.86 (95% CI 0.65 to 1.14; p = 0.30).
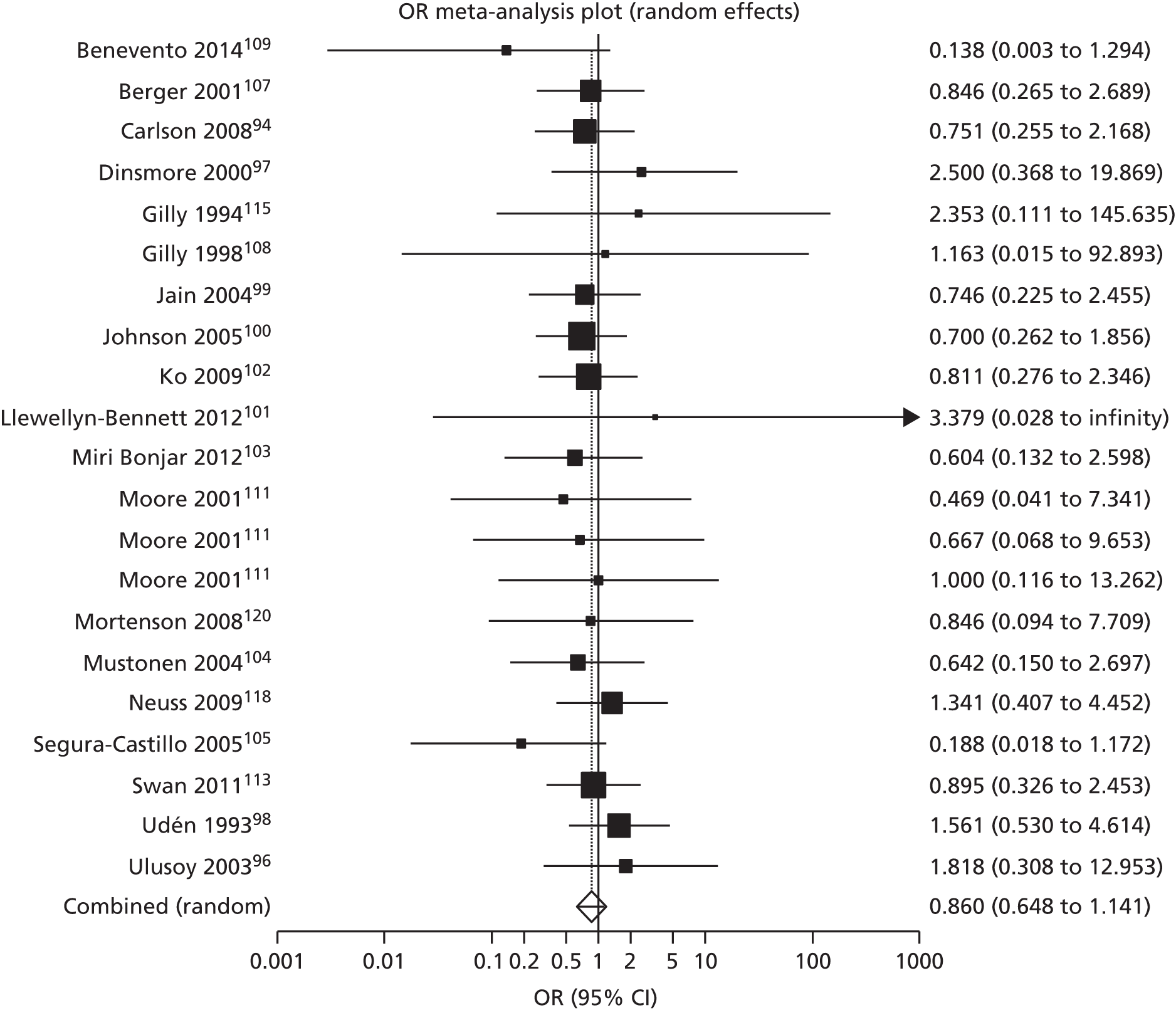
FIGURE 51.
Seroma development in hernia surgery: fibrin sealant vs. standard care. Pooled OR 0.93 (95% CI 0.51 to 1.72; p = 0.825).

Haematoma development
FIGURE 52.
Haematoma development in all surgical specialties: fibrin sealant vs. standard care. Pooled OR 0.66 (95% CI 0.46 to 0.94; p = 0.023).
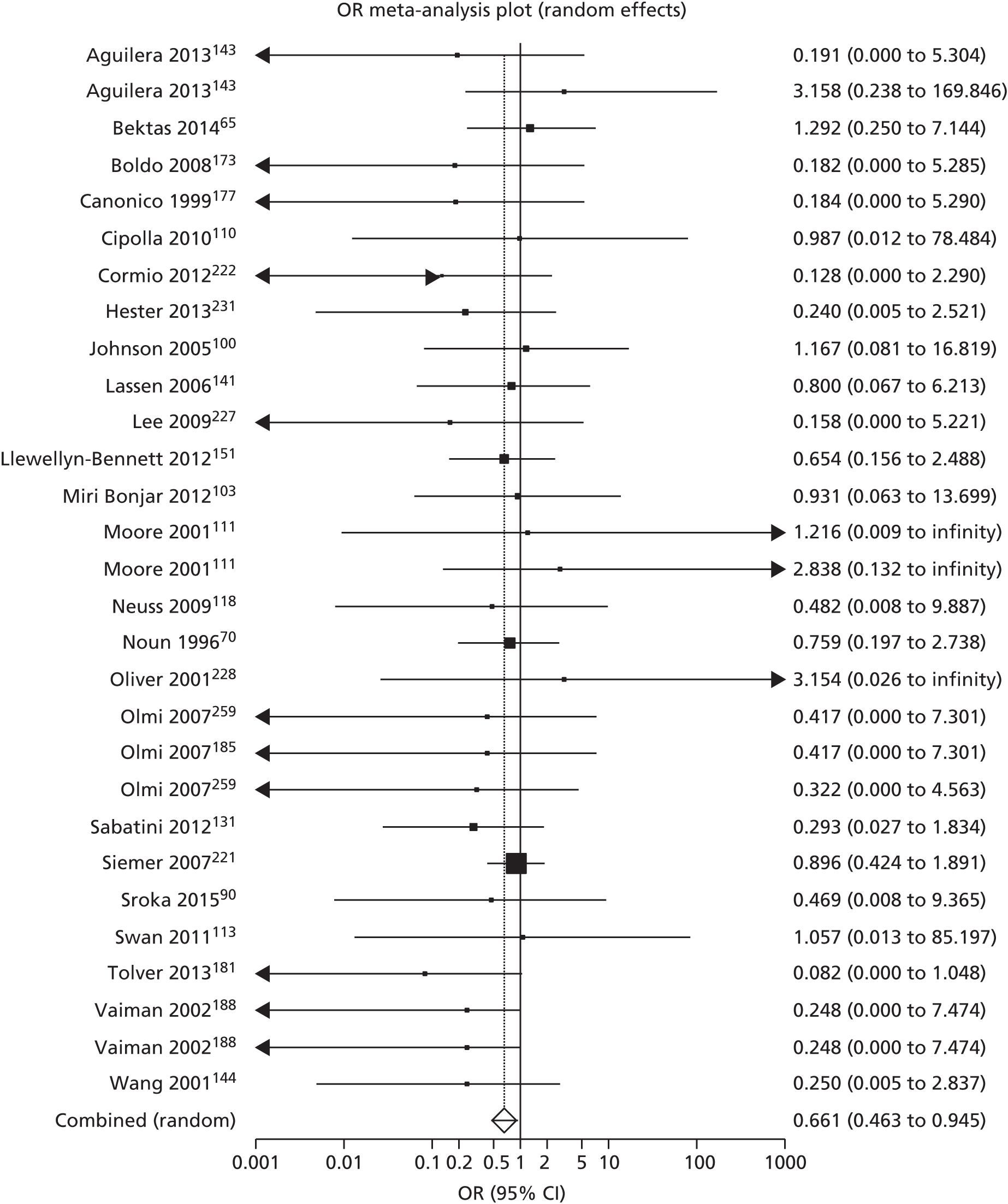
FIGURE 53.
Haematoma development in breast surgery: fibrin sealant vs. standard care. Pooled OR 0.86 (95% CI 0.41 to 1.82; p = 0.70).
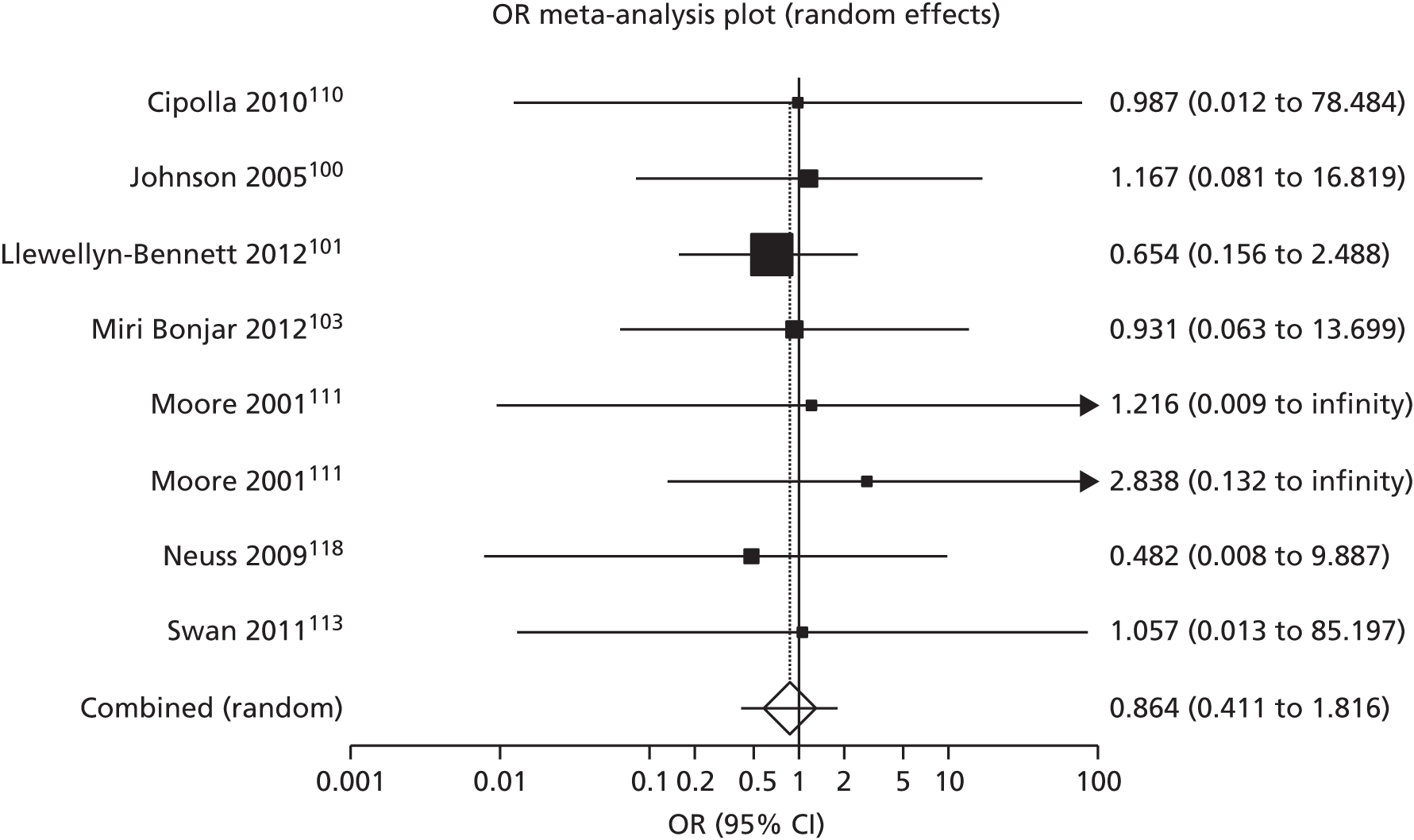
FIGURE 54.
Haematoma development in hernia surgery: fibrin sealant vs. standard care. Pooled OR 0.23 (95% CI 0.07 to 0.79; p = 0.02).
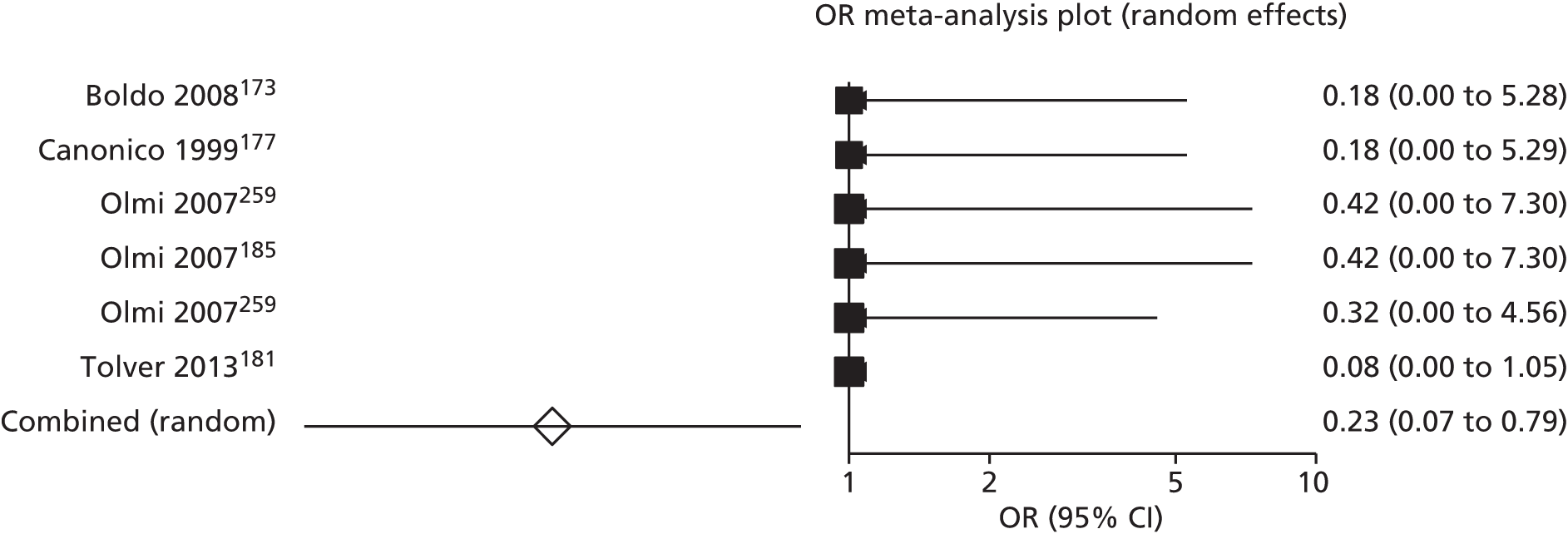
FIGURE 55.
Haematoma development in orthopaedic surgery: fibrin sealant vs. standard care. Pooled OR 0.53 (95% CI 0.21 to 1.34; p = 0.18).
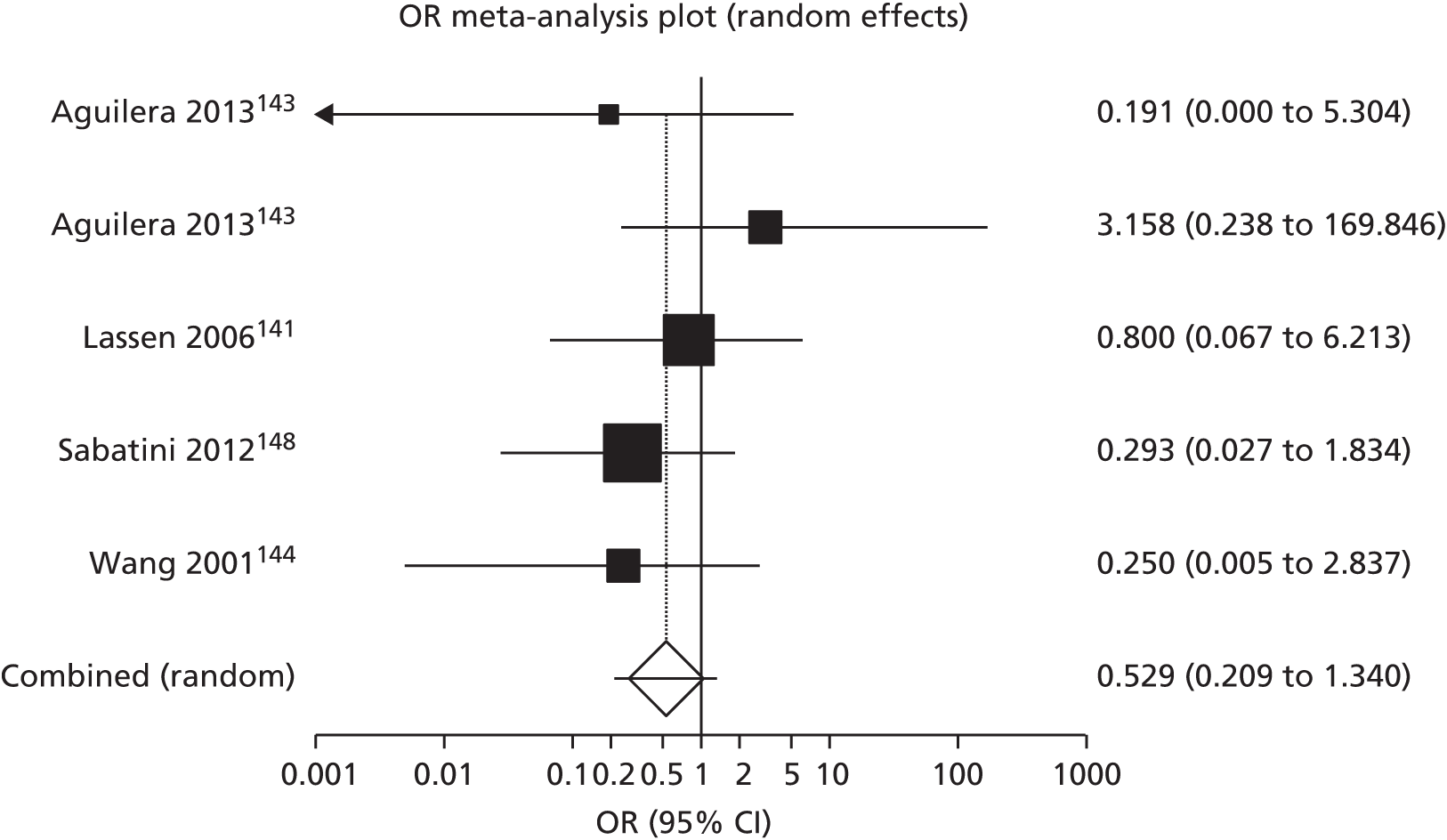
FIGURE 56.
Haematoma development in upper GI tract surgery: fibrin sealant vs. standard care. Pooled OR 0.86 (95% CI 0.38 to 1.99; p = 0.73).
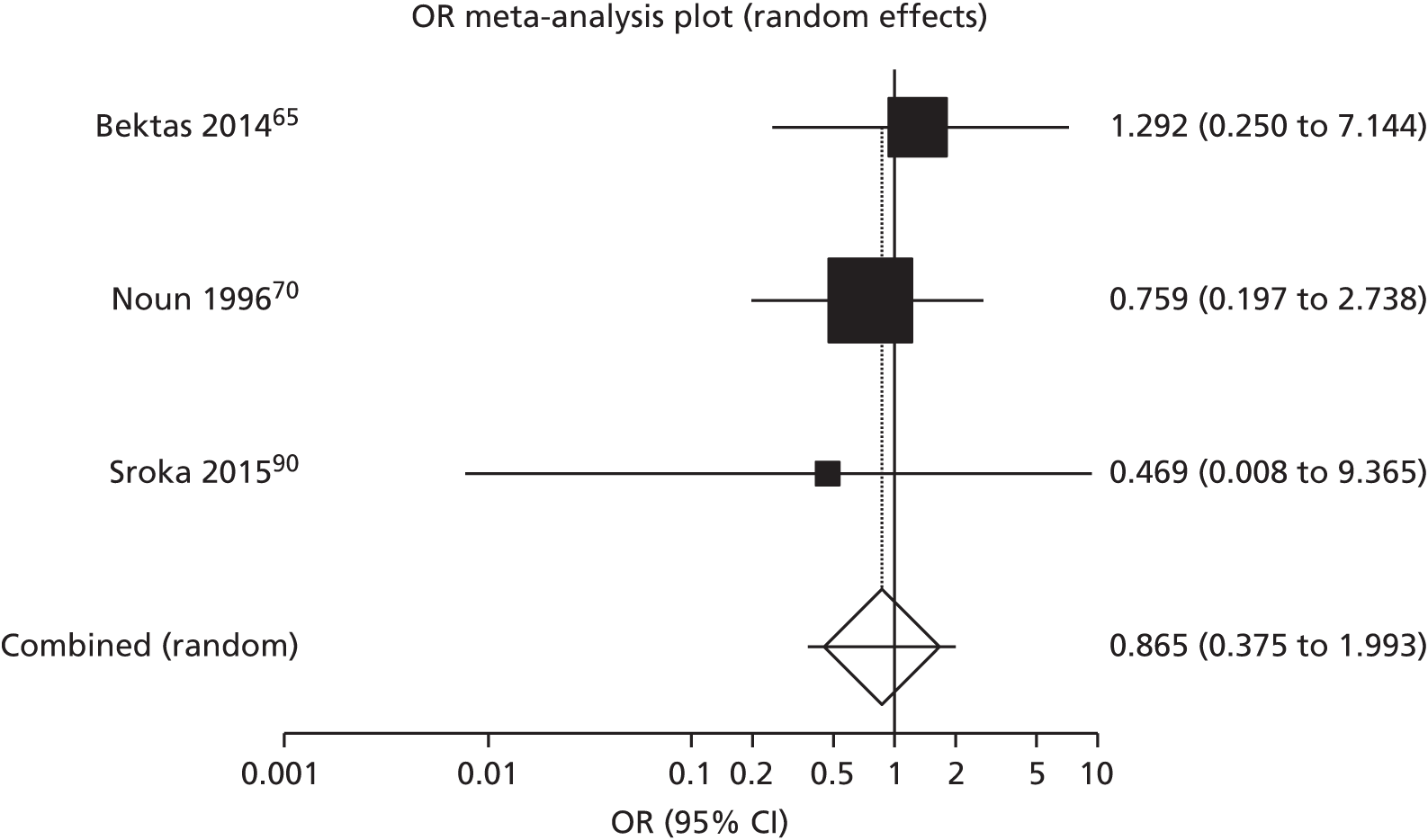
Seroma and haematoma combined
FIGURE 57.
Seroma and haematoma development combined in all surgical specialties: fibrin sealant vs. standard care. Pooled OR 0.80 (95% CI 0.65 to 0.98; p = 0.03).

Secondary dichotomous outcomes
Haemorrhage (bleeding)
FIGURE 58.
Haemorrhage (bleeding) in all surgical specialties: fibrin sealant vs. standard care. Pooled OR 0.69 (95% CI 0.41 to 1.15; p = 0.15).
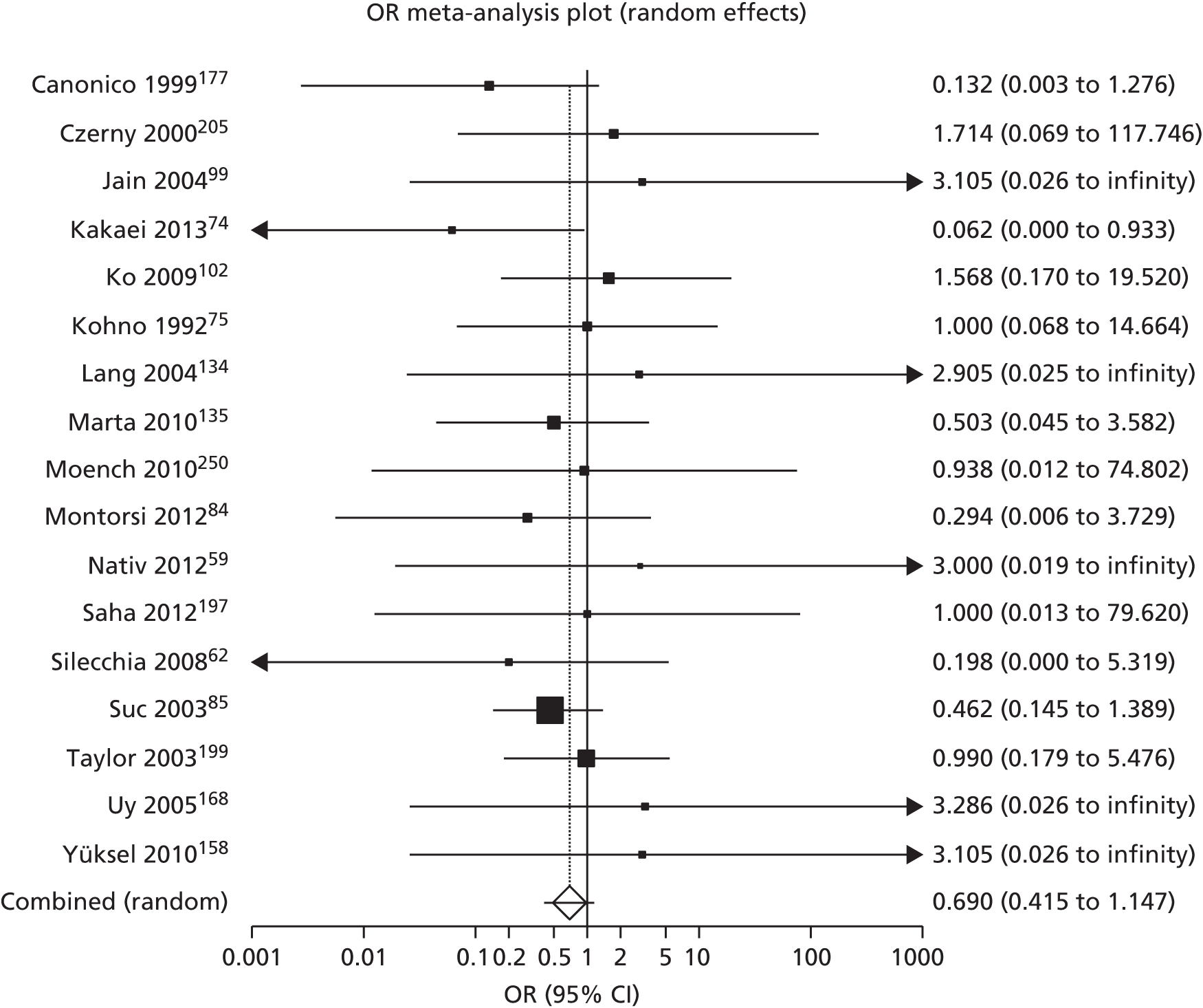
FIGURE 59.
Haemorrhage (bleeding) in upper GI tract surgery: fibrin sealant vs. standard care. Pooled OR 0.43 (95% CI 0.20 to 0.91; p = 0.03).
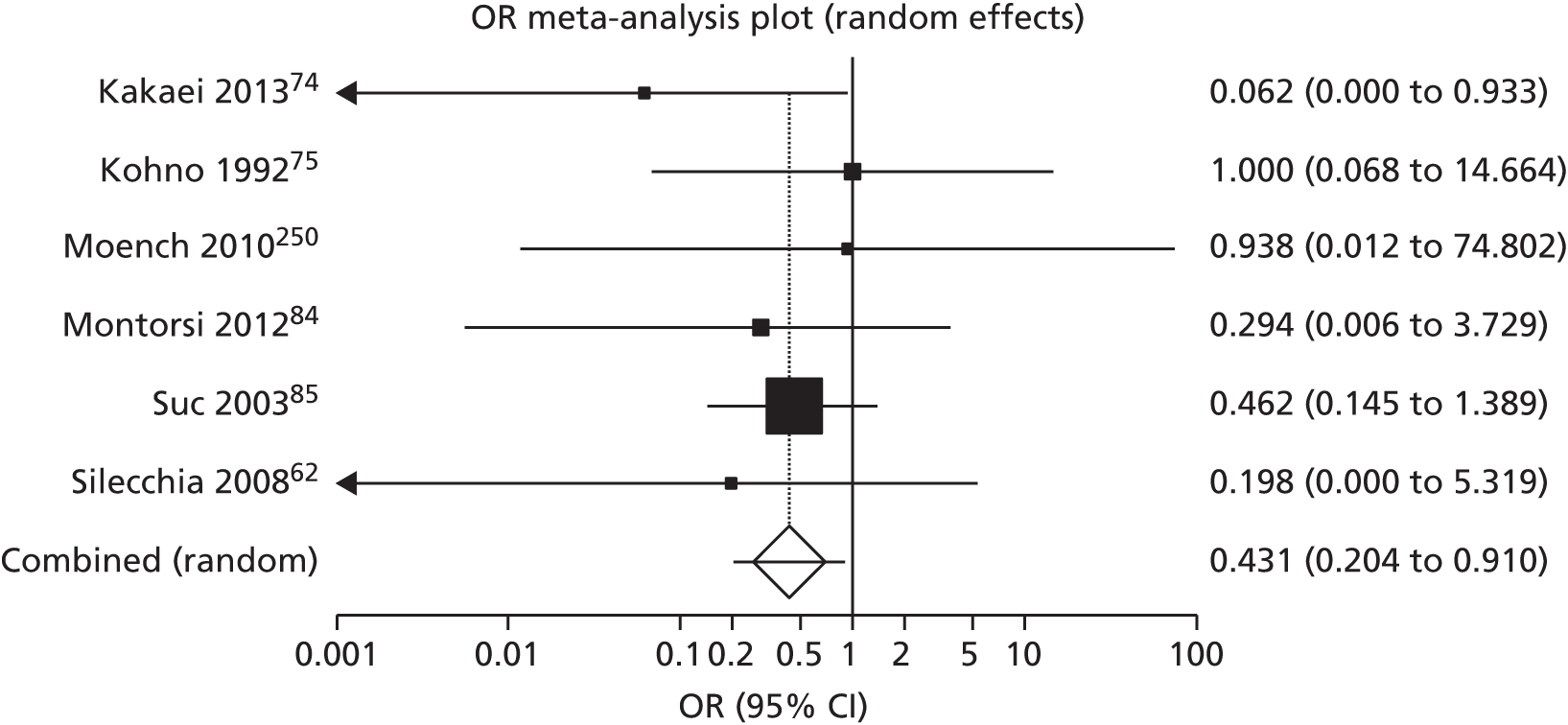
FIGURE 60.
Haemorrhage (bleeding) in cardiothoracic surgery: fibrin sealant vs. standard care. Pooled OR 0.91 (95% CI 0.25 to 3.39; p = 0.89).

FIGURE 61.
Haemorrhage (bleeding) in vascular surgery: fibrin sealant vs. standard care. Pooled OR 1.85 (95% CI 0.37 to 9.15; p = 0.45).

FIGURE 62.
Haemorrhage (bleeding) in vascular surgery: fibrin sealant vs. standard care. Pooled OR 0.99 (95% CI 0.28 to 3.50; p = 0.99).
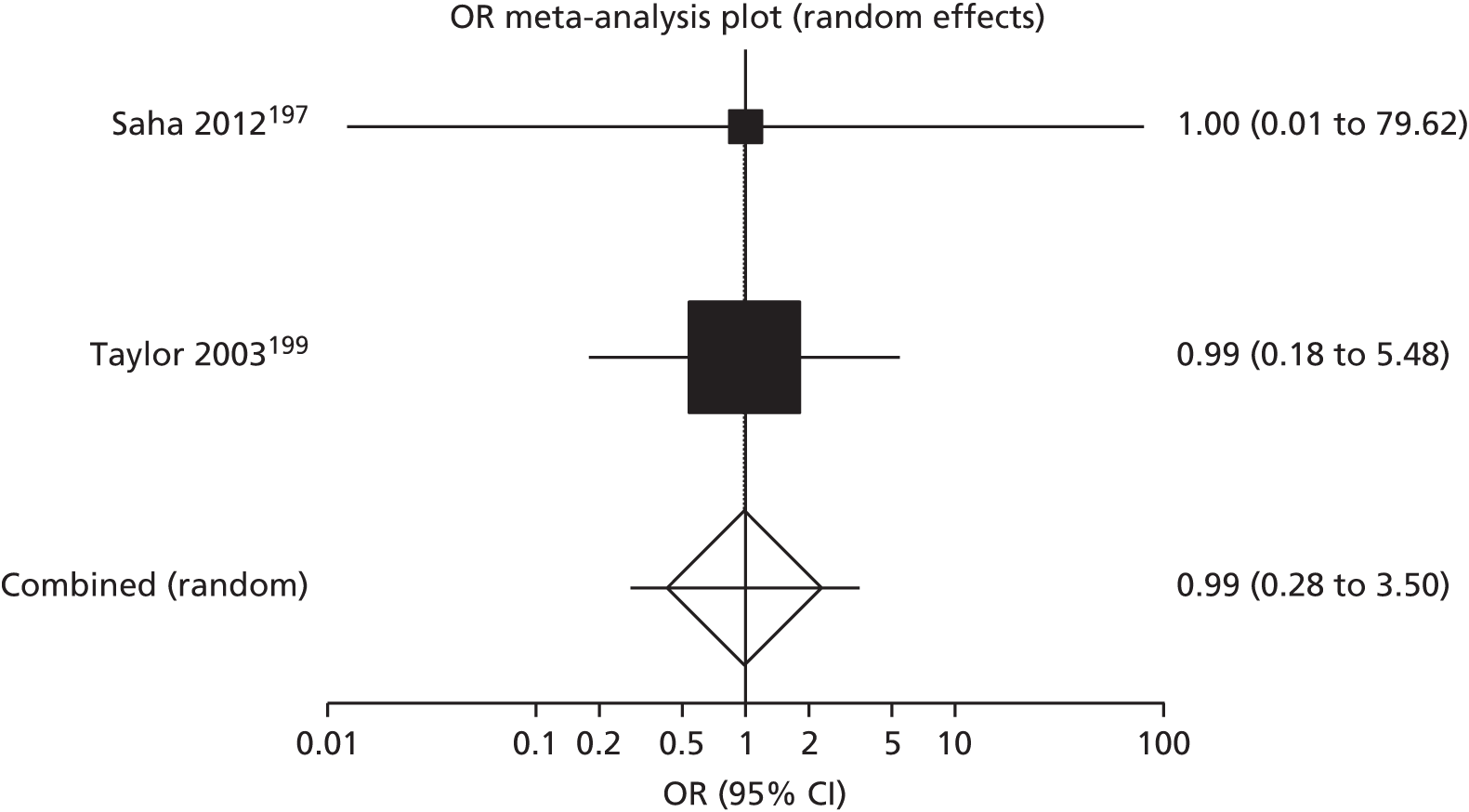
FIGURE 63.
Haemorrhage (bleeding) in eye surgery: fibrin sealant vs. standard care. Pooled OR 3.19 (95% CI 0.32 to 32.33; p = 0.33).

Reoperation
FIGURE 64.
Reoperation in all surgical specialties: fibrin sealant vs. standard care. Pooled OR 0.71 (95% CI 0.52 to 0.95; p = 0.02).

FIGURE 65.
Reoperation in cardiothoracic lung surgery: fibrin sealant vs. standard care. Pooled OR 1.37 (95% CI 0.46 to 4.04; p = 0.57).

FIGURE 66.
Reoperation in cardiothoracic heart surgery: fibrin sealant vs. standard care. Pooled OR 0.72 (95% CI 0.43 to 1.21; p = 0.22).

FIGURE 67.
Reoperation in upper GI tract surgery: fibrin sealant vs. standard care. Pooled OR 0.46 (95% CI 0.20 to 1.06; p = 0.07).

FIGURE 68.
Reoperation in breast surgery: fibrin sealant vs. standard care. Pooled OR 1.24 (95% CI 0.51 to 3.00; p = 0.64).
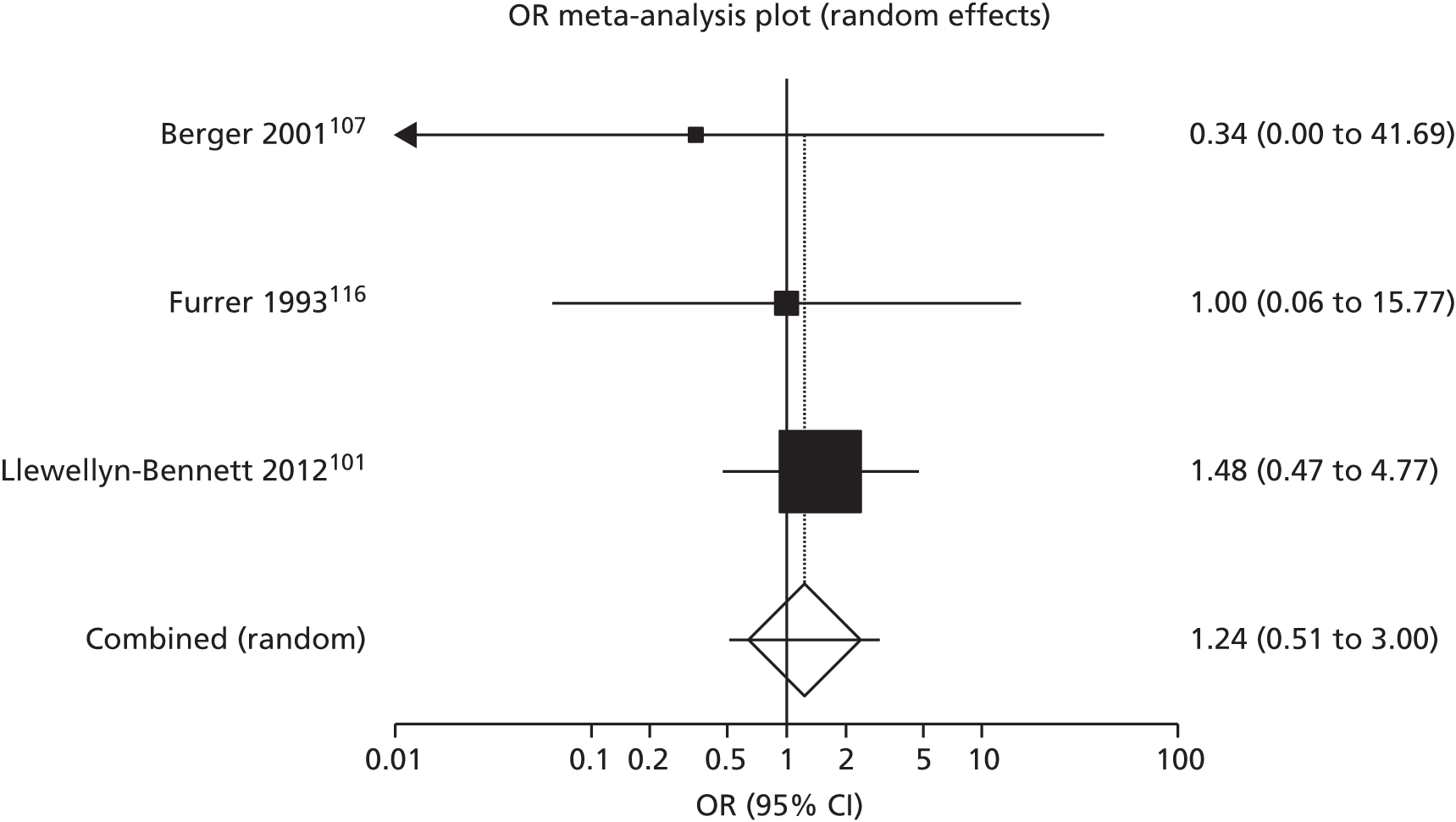
Infections
FIGURE 69.
Infections in all surgeries: fibrin sealant vs. standard care. Pooled OR 0.79 (95% CI 0.55 to 1.14; p = 0.20).

FIGURE 70.
Infections in upper GI tract surgery: fibrin sealant vs. standard care. Pooled OR 1.22 (95% CI 0.58 to 2.54; p = 0.60).

FIGURE 71.
Infections in breast surgery: fibrin sealant vs. standard care. Pooled OR 0.95 (95% CI 0.49 to 1.82; p = 0.87).

FIGURE 72.
Infections in orthopaedic surgery: fibrin sealant vs. standard care. Pooled OR 1.034 (95% CI 0.21 to 5.15; p = 0.97).

FIGURE 73.
Infections in cardiothoracic lung surgery: fibrin sealant vs. standard care. Pooled OR 0.41 (95% CI 0.05 to 3.12; p = 0.39).

Secondary continuous outcomes
Duration of operation
FIGURE 74.
Mean duration of gastric surgery in minutes: fibrin sealant vs. no sealant. Pooled MD –4.66 (95% CI –12.71 to 3.39; p = 0.26). DL, DerSimonian and Laird. 55
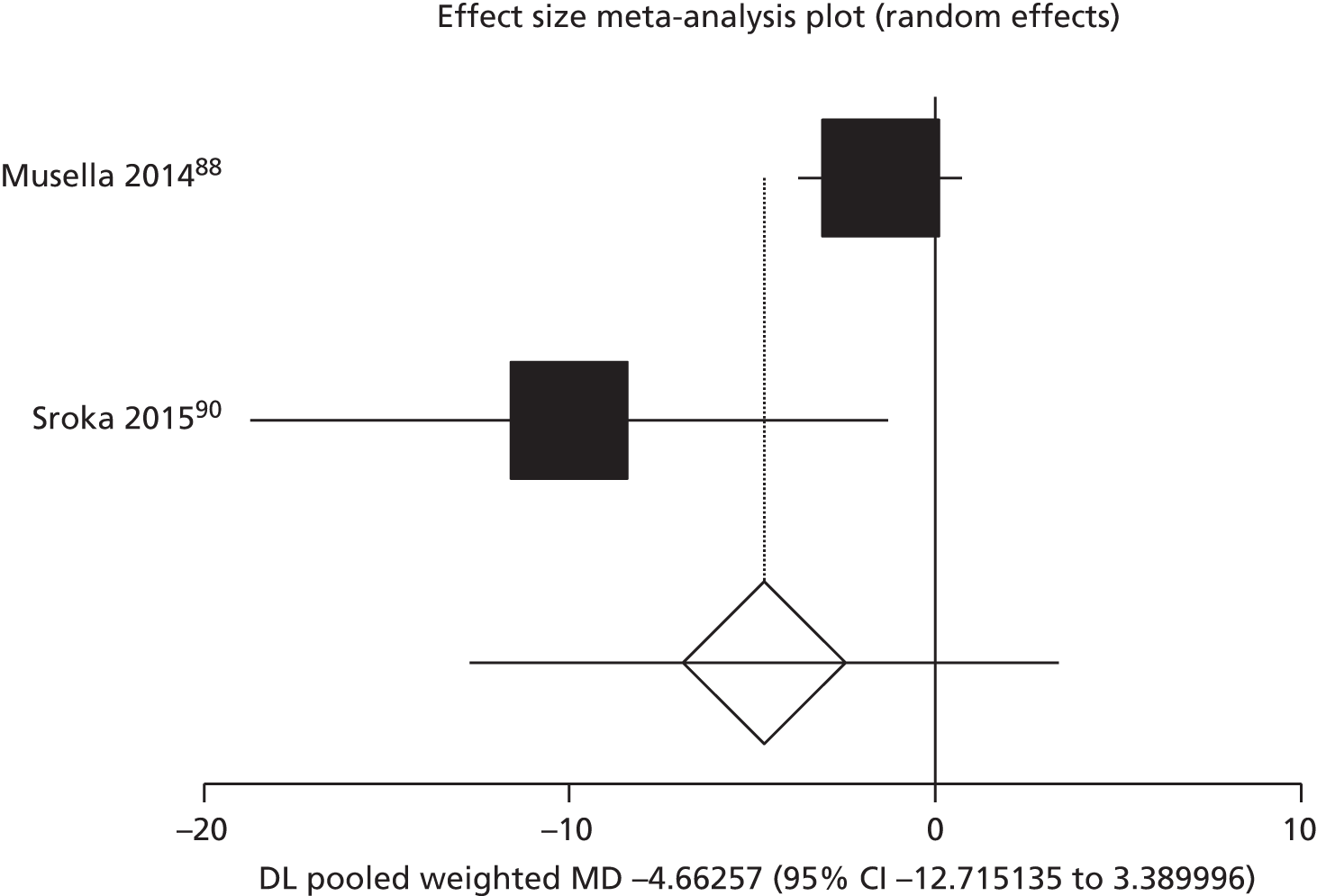
FIGURE 75.
Mean duration of hepatic resection without liver mobilisation in minutes: fibrin sealant vs. standard care. Pooled MD –14.96 (95% CI –54.2 to 24.3; p = 0.46). DL, DerSimonian and Laird. 55
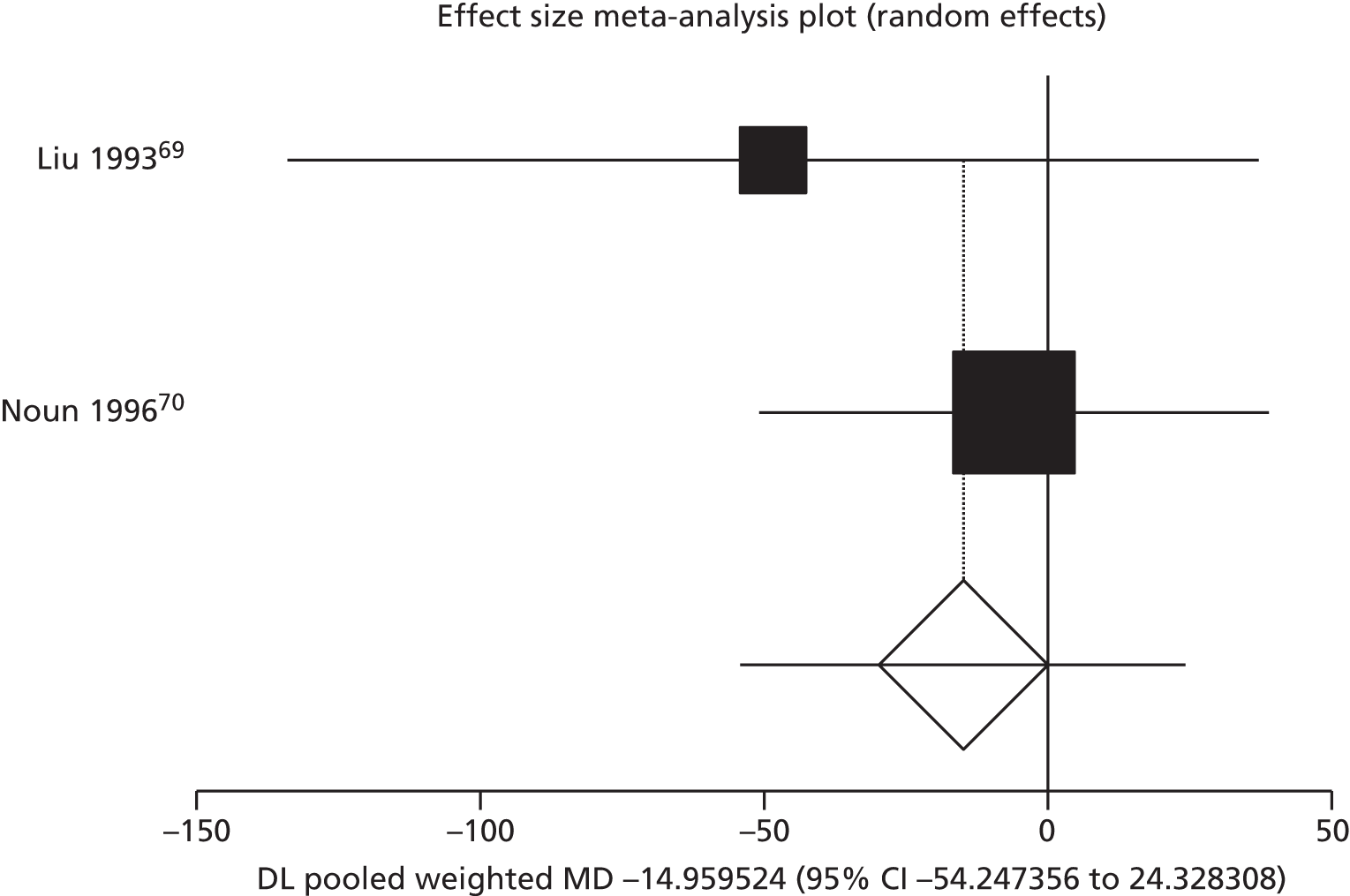
FIGURE 76.
Mean duration of hepatic resection with liver mobilisation in minutes: fibrin sealant vs. standard care. Pooled MD 19.07 (95% CI 2.75 to 35.38; p = 0.02). DL, DerSimonian and Laird. 55
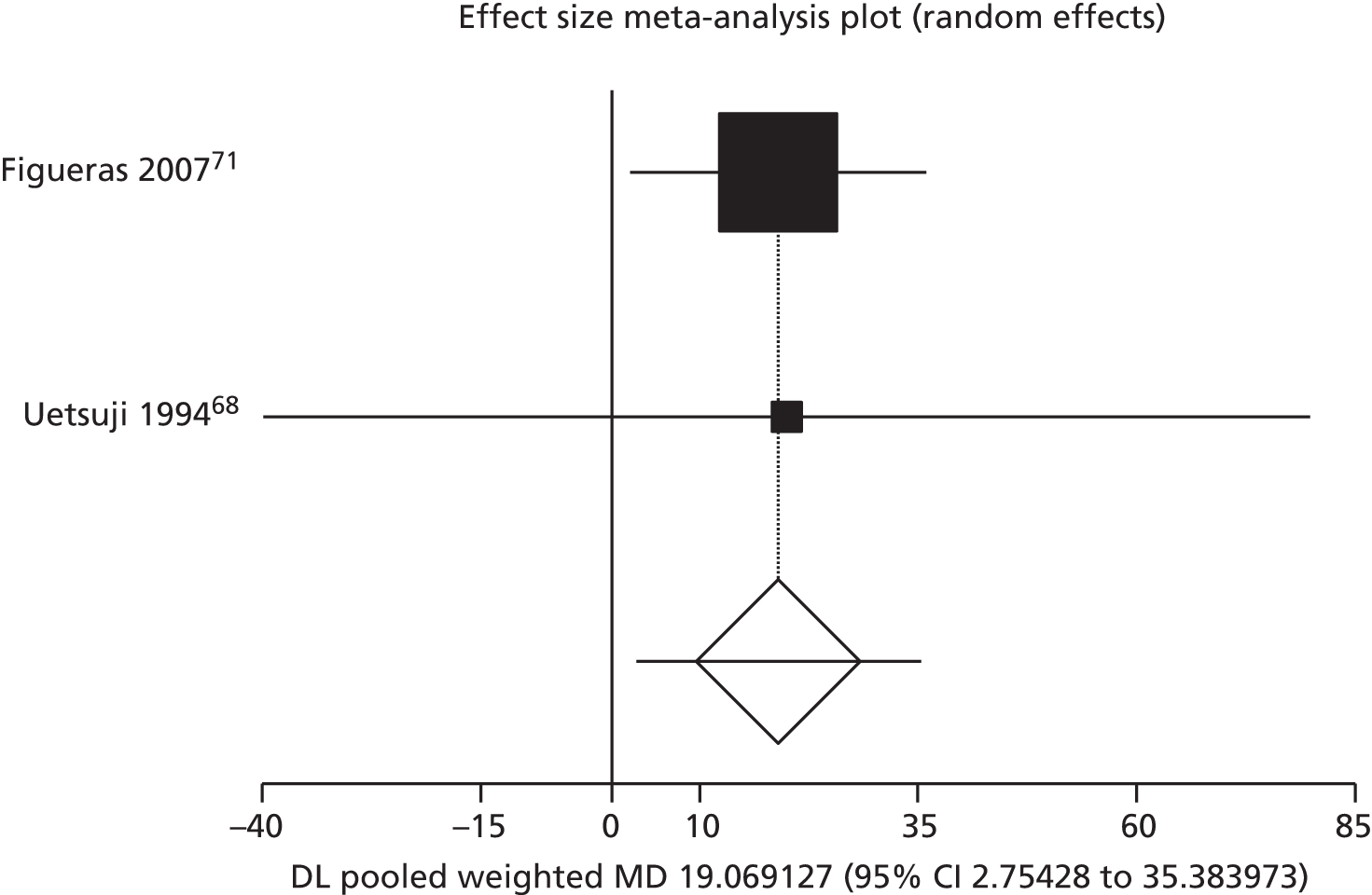
FIGURE 77.
Mean duration of eye surgery in minutes: fibrin sealant vs. sutures. Pooled MD –17.93 (95% CI –23.35 to –12.50; p < 0.01). DL, DerSimonian and Laird. 55
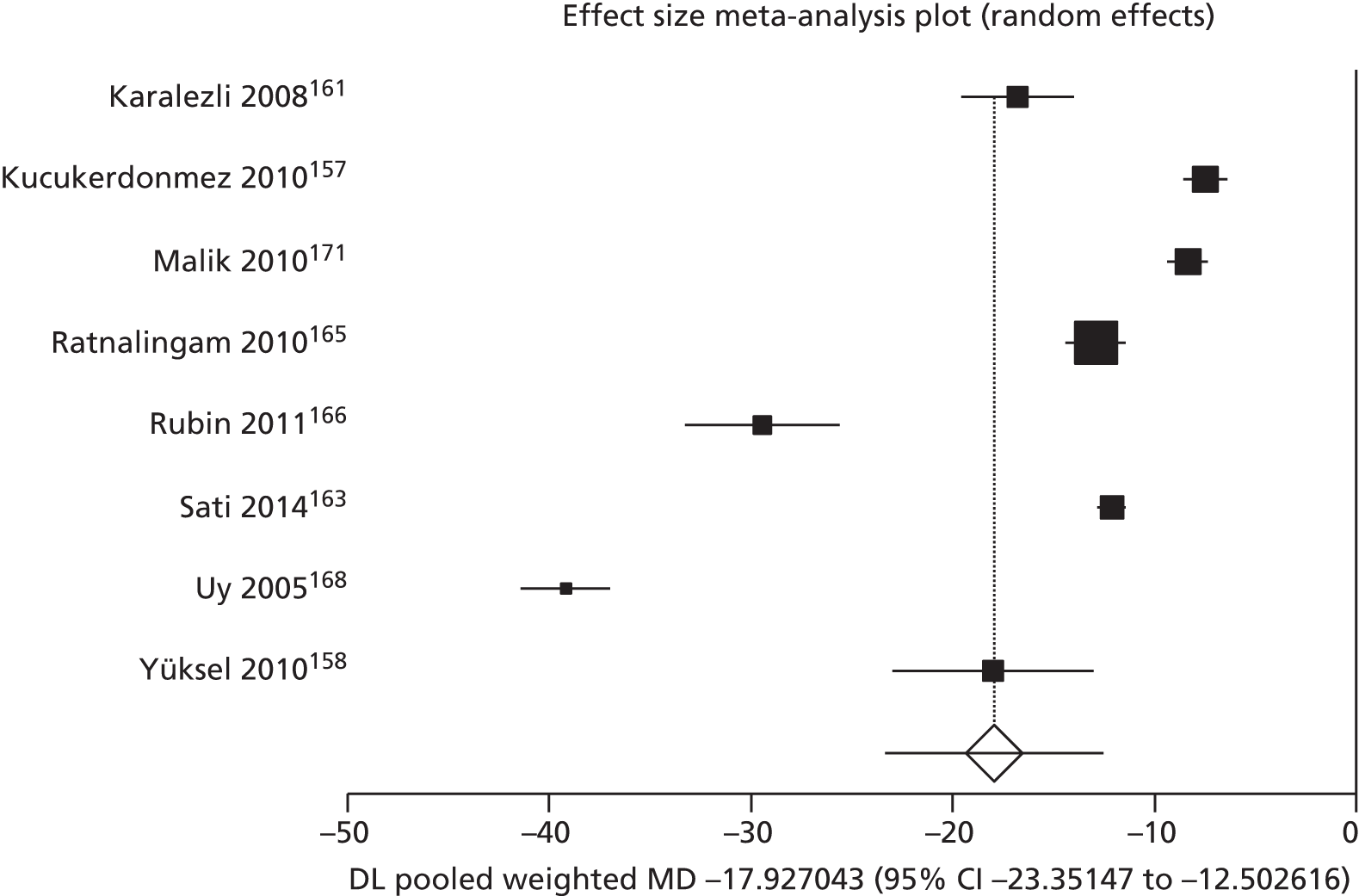
FIGURE 78.
Mean duration of hernia surgery in minutes: fibrin sealant vs. sutures. Pooled MD –2.56 (95% CI –3.57 to –1.56; p < 0.01). DL, DerSimonian and Laird. 55
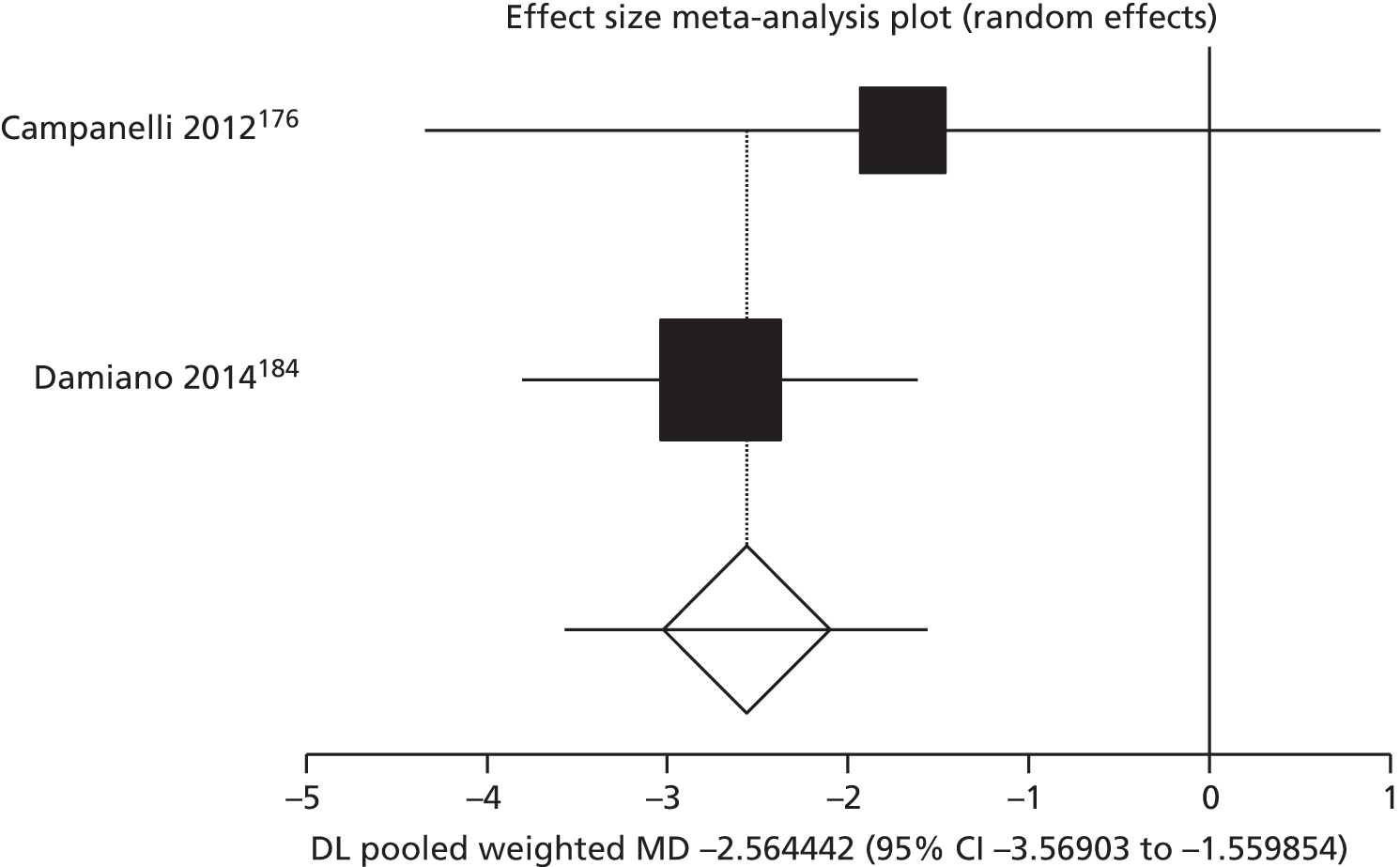
FIGURE 79.
Mean duration of hernia surgery in minutes: fibrin sealant vs. staples. Pooled MD 8.98 (95% CI –2.20 to 20.15; p = 0.12). DL, DerSimonian and Laird. 55
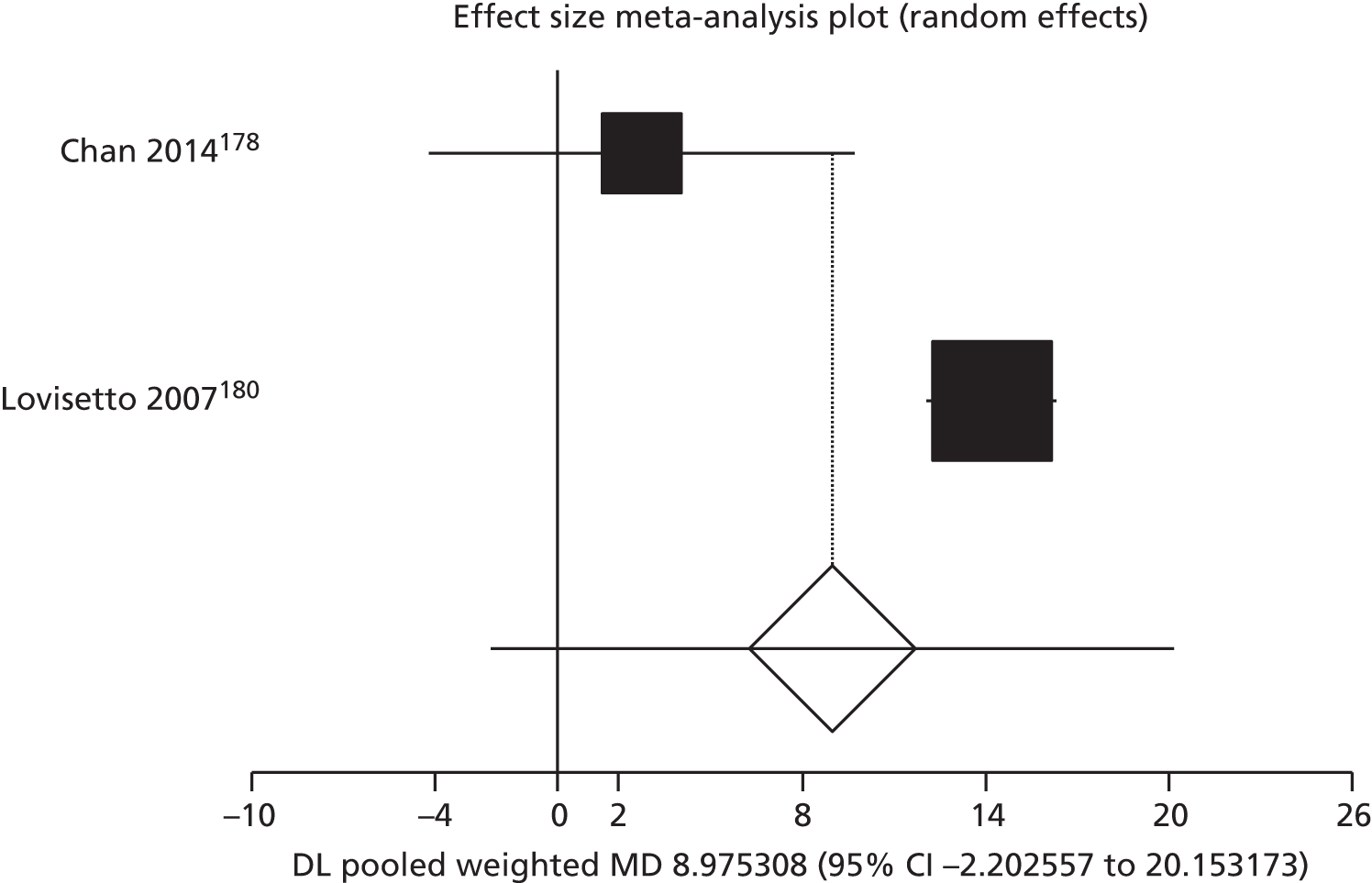
Length of hospital stay
FIGURE 80.
Length of hospital stay in days in pancreatic surgery: fibrin sealant vs. standard care. Pooled MD –1.40 (95% CI –1.72 to –1.09; p < 0.01). DL, DerSimonian and Laird. 55

FIGURE 81.
Length of hospital stay in days in gastric surgery: fibrin sealant vs. standard care. Pooled MD 0.07 (95% CI –0.39 to 0.54; p = 0.76). DL, DerSimonian and Laird. 55

FIGURE 82.
Length of hospital stay in days in cardiothoracic lung surgery: fibrin sealant vs. standard care. Pooled MD –1.20 (95% CI –3.22 to 0.81; p = 0.24). DL, DerSimonian and Laird. 55
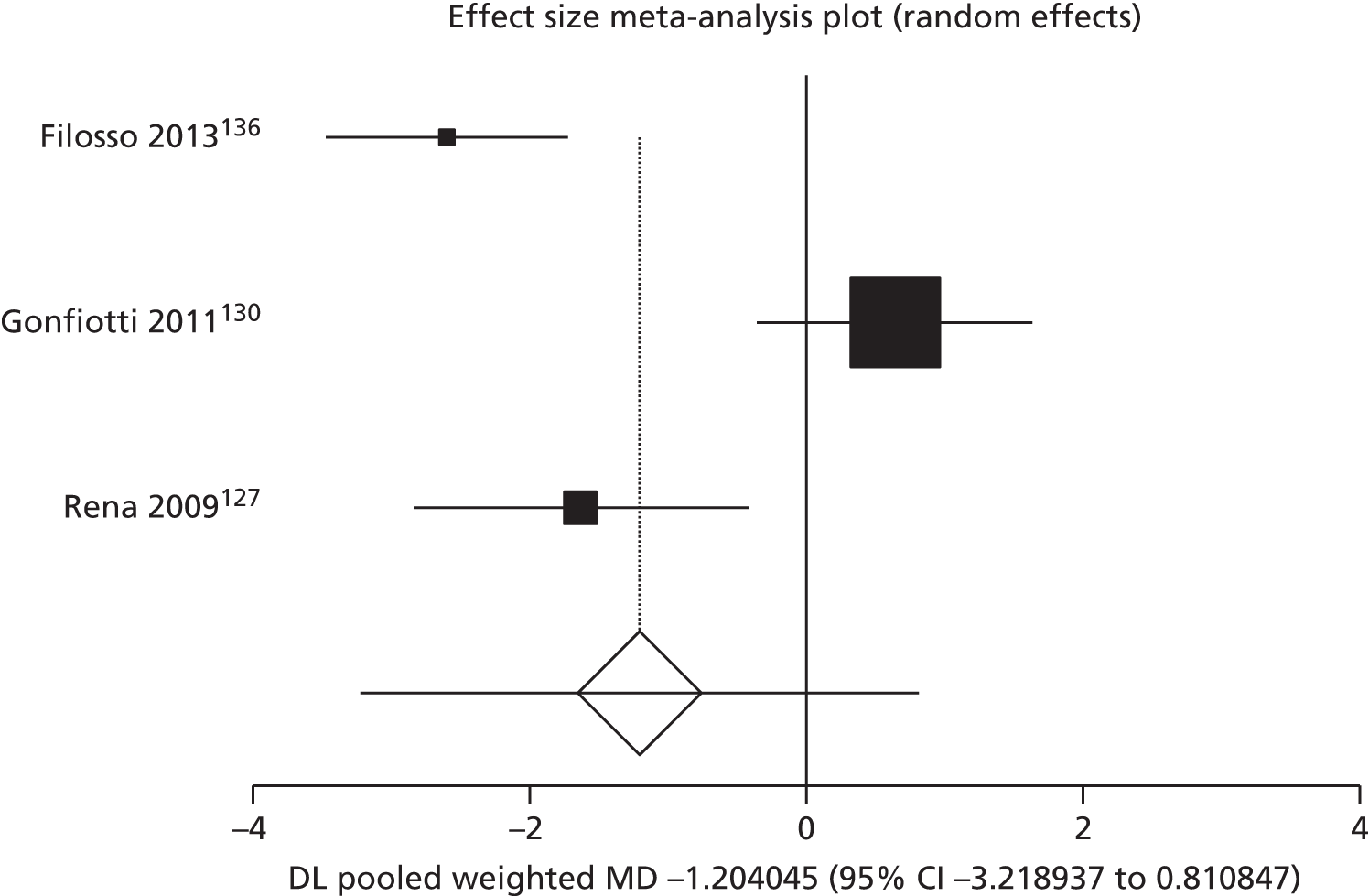
FIGURE 83.
Length of hospital stay in days in breast surgery: fibrin sealant vs. standard care. Pooled MD –0.87 (95% CI –1.75 to 0.01; p = 0.05). DL, DerSimonian and Laird. 55
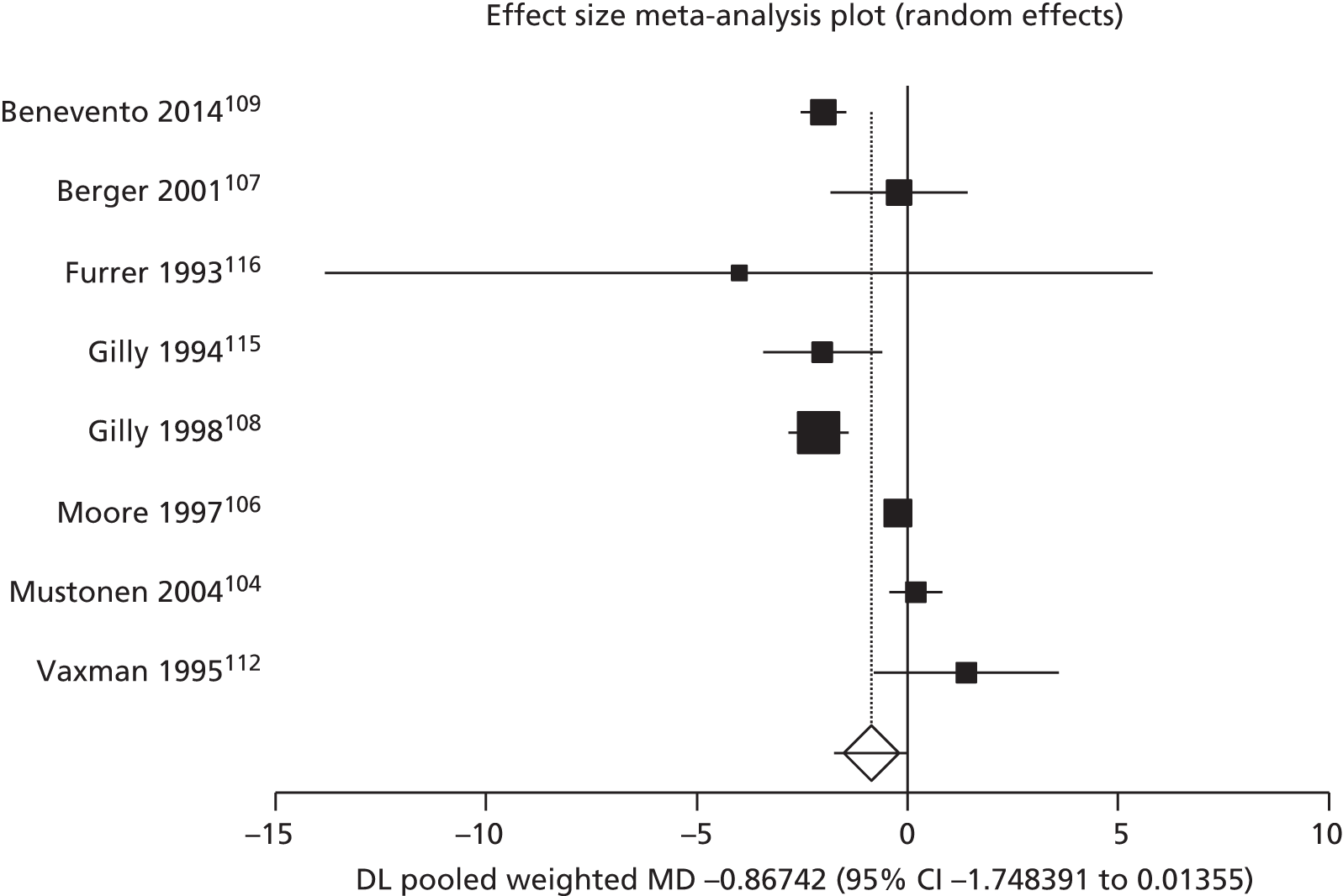
FIGURE 84.
Length of hospital stay in days for knee surgery: fibrin sealant vs. standard care. Pooled MD 0.07 (95% CI –0.74 to 0.88; p = 0.87). DL, DerSimonian and Laird. 55

Duration of drainage
FIGURE 85.
Duration of drainage in days in breast and axillary lymph nodes surgery: fibrin sealant vs. standard care. Pooled MD –1.06 (95% CI –1.69 to –0.42; p = 0.00). DL, DerSimonian and Laird. 55

FIGURE 86.
Duration of drainage in days for liver surgery: fibrin sealant vs. standard care. Pooled MD –0.27 (95% CI –0.82 to 0.27; p = 0.33). DL, DerSimonian and Laird. 55
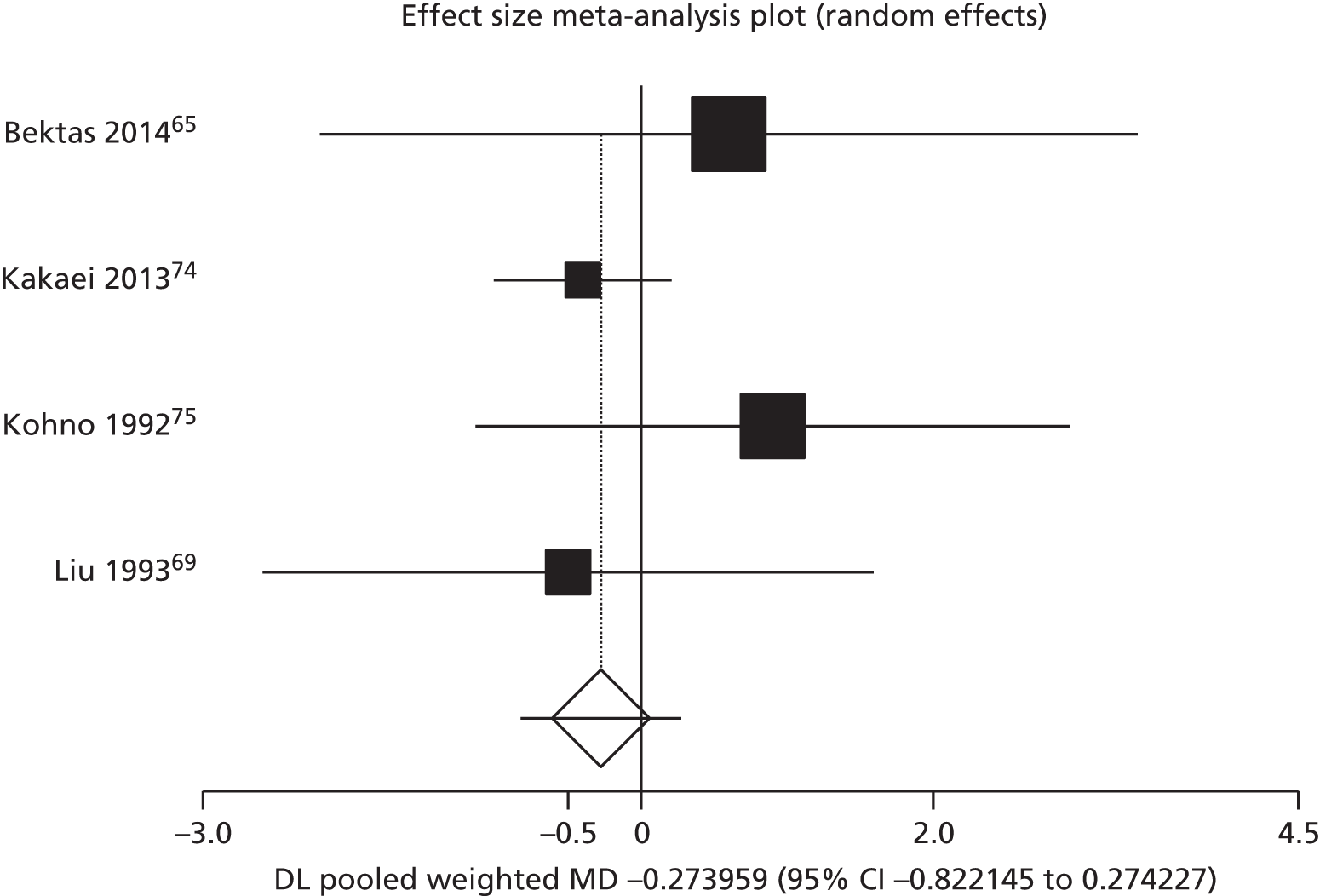
FIGURE 87.
Duration of drainage in days for lung surgery: fibrin sealant vs. standard care. Pooled MD –2.10 (95% CI –3.65 to –0.56; p = 0.01). DL, DerSimonian and Laird. 55

Appendix 9 Data tables for randomised controlled trials
| Study (author, year) | Group (n/N) | Total population size across all studies | |
|---|---|---|---|
| Fibrin sealant | Standard care | ||
| Altinli et al., 2007206 | 0/16 | 1/16 | – |
| Benevento et al., 2014109 | 1/30 | 6/30 | – |
| Berger et al., 2001107 | 11/29 | 13/31 | – |
| Boldo, 2008173 | 9/22 | 8/22 | – |
| Bracale et al., 2014174 | 3/50 | 0/50 | – |
| Carlson et al., 200894 | 9/70 | 11/67 | – |
| Chan et al., 2014178 | 9/64 | 7/65 | – |
| Damiano et al., 2014184 | 5/216 | 10/252 | – |
| Dinsmore et al., 200097 | 6/14 | 3/13 | – |
| Gilly et al., 1994115 | 2/19 | 1/21 | – |
| Gilly et al., 1998108 | 1/50 | 1/58 | – |
| Hester et al., 2013231 | 4/75 | 4/75 | – |
| Jain et al., 200499 | 10/29 | 12/29 | – |
| Johnson et al., 2005100 | 14/38 | 20/44 | – |
| Ko et al., 2009102 | 10/47 | 12/48 | – |
| Lau, 2005172 | 16/46 | 5/47 | – |
| Llewellyn-Bennett et al., 2012101 | 1/48 | 0/53 | – |
| Mabrouk et al., 2013214 | 1/30 | 11/30 | – |
| Maharaj et al., 2006230 | 1/28 | 5/22 | – |
| Miri Bonjar et al., 2012103 | 5/31 | 7/29 | – |
| Moench et al., 201476 | 4/65 | 3/61 | – |
| Moore et al., 2001111 | 3/19 | 2/7 | – |
| Moore et al., 2001111 | 4/19 | 2/7 | – |
| Moore et al., 2001111 | 6/21 | 2/7 | – |
| Mortenson et al., 2008120 | 3/16 | 3/14 | – |
| Mustonen et al., 2004104 | 7/19 | 10/21 | – |
| Neuss et al., 2009118 | 12/29 | 10/29 | – |
| Olmi et al., 2007259 | 1.7/50 | 12/150 | – |
| Olmi et al., 2007259 | 1.7/50 | 15/150 | – |
| Olmi et al., 2007259 | 1.7/50 | 13/150 | – |
| Segura-Castillo et al., 2005105 | 2/22 | 8/23 | – |
| Sözen et al., 2011212 | 6/25 | 2/25 | – |
| Swan et al., 2011113 | 17/36 | 19/38 | – |
| Tolver et al., 2013181 | 3/50 | 5/50 | – |
| Udén et al., 199398 | 23/36 | 17/32 | – |
| Ulusoy et al., 200396 | 5/27 | 3/27 | – |
| Wong et al., 2011182 | 1/30 | 1/26 | – |
| Total | 228/1586 | 275/1886 | 3472 |
| Study (author, year) | Group (n/N) | Total population size across all studies | |
|---|---|---|---|
| Fibrin sealant | Standard care | ||
| Aguilera et al., 2013143 | 0/42 | 2/42 | – |
| Aguilera et al., 2013143 | 3/41 | 1/41 | – |
| Bektas et al., 201465 | 5/35 | 4/35 | – |
| Boldo, 2008173 | 0/22 | 2/22 | – |
| Canonico et al., 1999177 | 0/25 | 2/25 | – |
| Cipolla et al., 2010110 | 1/80 | 1/79 | – |
| Cormio et al., 2012222 | 0/49 | 3/47 | – |
| Hester et al., 2013231 | 1/75 | 4/75 | – |
| Johnson et al., 2005100 | 2/38 | 2/44 | – |
| Lassen et al., 2006141 | 2/22 | 4/36 | – |
| Lee et al., 2009227 | 0/9 | 2/9 | – |
| Llewellyn-Bennett et al., 2012101 | 5/48 | 8/53 | – |
| Miri Bonjar et al., 2012103 | 2/31 | 2/29 | – |
| Moore et al., 2001111 | 1/19 | 0/7 | – |
| Moore et al., 2001111 | 3/21 | 0/7 | – |
| Neuss et al., 2009118 | 1/29 | 2/29 | – |
| Noun et al., 199670 | 6/35 | 9/42 | – |
| Oliver et al., 2001228 | 1/20 | 0/20 | – |
| Olmi et al., 2007259 | 0/50 | 3/150 | – |
| Olmi et al., 2007259 | 0/50 | 3/150 | – |
| Olmi et al., 2007259 | 0/50 | 4/150 | – |
| Sabatini et al., 2012148 | 2/35 | 6/35 | – |
| Siemer et al., 2007221 | 40/92 | 22/93 | – |
| Sroka et al., 201590 | 1/49 | 2/47 | – |
| Swan et al., 2011113 | 1/36 | 1/38 | – |
| Tolver et al., 2013181 | 0/50 | 5/50 | – |
| Vaiman et al., 2002188 | 0/68 | 0.5/34 | – |
| Vaiman et al., 2002188 | 0/68 | 0.5/34 | – |
| Wang et al., 2001144 | 1/25 | 4/28 | – |
| Total | 58/1214 | 99/1451 | 2665 |
| Study (author, year) | Group (n/N) | Total population size across all studies | |
|---|---|---|---|
| Fibrin sealant | Standard care | ||
| Aguilera et al., 2013143 | 0/42 | 2/42 | – |
| Aguilera et al., 2013143 | 3/41 | 1/41 | – |
| Altinli et al., 2007206 | 0/16 | 1/16 | – |
| Bektas et al., 201465 | 5/35 | 4/35 | – |
| Benevento et al., 2014109 | 1/30 | 6/30 | – |
| Berger et al., 2001107 | 11/29 | 13/31 | – |
| Boldo, 2008173 | 9/22 | 10/22 | – |
| Bracale et al., 2014174 | 3/50 | 0/52 | – |
| Canonico et al., 1999177 | 0/25 | 2/25 | – |
| Carlson et al., 200894 | 9/70 | 11/67 | – |
| Chan et al., 2014178 | 9/64 | 7/65 | – |
| Cipolla et al., 2010110 | 1/80 | 1/79 | – |
| Cormio et al., 2012222 | 0/49 | 3/47 | – |
| Damiano et al., 2014184 | 5/216 | 10/252 | – |
| Dinsmore et al., 200097 | 6/14 | 3/13 | – |
| Gilly et al., 1994115 | 2/19 | 1/21 | – |
| Gilly et al., 1998108 | 1/50 | 1/58 | – |
| Hester et al., 2013231 | 5/75 | 8/75 | – |
| Jain et al., 200499 | 10/29 | 12/29 | – |
| Johnson et al., 2005100 | 16/38 | 22/44 | – |
| Ko et al., 2009102 | 10/47 | 12/48 | – |
| Lassen et al., 2006141 | 2/22 | 4/36 | – |
| Lau, 2005172 | 16/46 | 5/47 | – |
| Lee et al., 2009227 | 0/9 | 2/9 | – |
| Llewellyn-Bennett et al., 2012101 | 6/48 | 8/53 | – |
| Lovisetto et al., 2007180 | 5/99 | 3/98 | – |
| Mabrouk et al., 2013214 | 1/30 | 11/30 | – |
| Maharaj et al., 2006230 | 1/28 | 5/22 | – |
| Miri Bonjar et al., 2012103 | 7/31 | 9/29 | – |
| Moench et al., 2010250 | 4/65 | 3/61 | – |
| Moore et al., 2001111 | 4/19 | 2/7 | – |
| Moore et al., 2001111 | 4/19 | 2/7 | – |
| Moore et al., 2001111 | 9/21 | 2/7 | – |
| Mortenson et al., 2008120 | 3/16 | 3/14 | – |
| Mustonen et al., 2004104 | 7/19 | 10/21 | – |
| Neuss et al., 2009118 | 13/29 | 12/29 | – |
| Noun et al., 199670 | 6/35 | 9/42 | – |
| Oliver et al., 2001228 | 1/20 | 0/20 | – |
| Olmi et al., 2007259 | 1.67/50 | 15/150 | – |
| Olmi et al., 2007259 | 1.67/50 | 18/150 | – |
| Olmi et al., 2007259 | 1.67/50 | 17/150 | – |
| Sabatini et al., 2012148 | 2/35 | 6/35 | – |
| Segura-Castillo et al., 2005105 | 2/22 | 8/23 | – |
| Siemer et al., 2007221 | 20/92 | 22/93 | – |
| Sözen et al., 2011212 | 6/25 | 2/25 | – |
| Sroka et al., 201590 | 1/49 | 2/47 | – |
| Swan et al., 2011113 | 18/36 | 20/38 | – |
| Tolver et al., 2013181 | 3/50 | 10/50 | – |
| Udén et al., 199398 | 23/36 | 17/32 | – |
| Ulusoy et al., 200396 | 5/27 | 3/27 | – |
| Vaiman et al., 2002188 | 0/68 | 0.5/34 | – |
| Vaiman et al., 2002188 | 0/68 | 0.5/34 | – |
| Wang et al., 2001144 | 1/25 | 4/28 | – |
| Wong et al., 2011182 | 1/30 | 1/26 | – |
| Total | 282/2310 | 366/2566 | 4876 |
| Study (author, year) | Group (n/N) | Total population size across all studies | |
|---|---|---|---|
| Fibrin sealant | Standard care | ||
| Canonico et al., 1999177 | 1/25 | 6/25 | – |
| Czerny et al., 2000205 | 2/9 | 1/7 | – |
| Jain et al., 200499 | 1/29 | 0/29 | – |
| Kakaei et al., 201374 | 0/15 | 5/15 | – |
| Ko et al., 2009102 | 3/47 | 2/48 | – |
| Kohno et al., 199275 | 2/31 | 2/31 | – |
| Lang et al., 2004134 | 1/95 | 0/91 | – |
| Marta et al., 2010135 | 2/148 | 4/151 | – |
| Moench et al., 2010250 | 1/65 | 1/61 | – |
| Montorsi et al., 201284 | 1/145 | 3/130 | – |
| Nativ et al., 201259 | 1/4 | 0/3 | – |
| Saha et al., 2012197 | 1/70 | 1/70 | – |
| Silecchia et al., 200862 | 0/160 | 2/160 | – |
| Suc et al., 200385 | 7/102 | 11/80 | – |
| Taylor et al., 2003199 | 4/100 | 4/99 | – |
| Uy et al., 2005168 | 1/11 | 0/11 | – |
| Yüksel et al., 2010158 | 1/29 | 0/29 | – |
| Total | 29/1085 | 42/1040 | 2125 |
| Study (author, year) | Group (n/N) | Total population size across all studies | |
|---|---|---|---|
| Fibrin sealant | Standard care | ||
| Aguilera, 2013143 | 1/42 | 1/42 | – |
| Aguilera, 2013143 | 1/41 | 1/41 | – |
| Anegg et al., 2007125 | 2/75 | 1/77 | – |
| Berger et al., 2001107 | 0/29 | 1/31 | – |
| Bochicchio et al., 2015239 | 0/480 | 1/239 | – |
| Furrer et al., 1993116 | 2/15 | 2/15 | – |
| Hutter et al., 2014237 | 6/113 | 10/116 | – |
| Huang and Qian, 201493 | 0/48 | 12/47 | – |
| Kjaergard and Trumbull, 1998138 | 0/11 | 1/12 | – |
| Llewellyn-Bennett et al., 2012101 | 10/48 | 8/53 | – |
| Maisano et al., 2009140 | 3/59 | 8/60 | – |
| Marta et al., 2010135 | 6/148 | 5/151 | – |
| Martin and Au, 201386 | 5/25 | 8/32 | – |
| Schwartz et al., 200477 | 10/58 | 23/63 | – |
| Suc et al., 200385 | 15/102 | 15/80 | – |
| Tavilla et al., 201560 | 23/722 | 27/714 | – |
| Total | 84/2016 | 124/1773 | 3789 |
| Study (author, year) | Group (n/N) | Total population size across all studies | |
|---|---|---|---|
| Fibrin sealant | Standard care | ||
| Aguilera et al., 2013143 | 0/42 | 1/42 | – |
| Aguilera et al., 2013143 | 1/41 | 1/41 | – |
| Chalmers et al., 2010198 | 4/75 | 5/72 | – |
| Chan et al., 2014178 | 5/64 | 2/65 | – |
| Fischer et al., 201172 | 1/60 | 2/59 | – |
| Frilling et al., 200573 | 4/53 | 2/59 | – |
| Gonfiotti et al., 2011130 | 0/91 | 3/94 | – |
| Huang et al., 201564 | 0/21 | 1/21 | – |
| Jain et al., 200499 | 1/29 | 1/29 | – |
| Ko et al., 2009102 | 3/47 | 2/48 | – |
| Kohno et al., 199275 | 1/31 | 2/31 | – |
| Levy et al., 199914 | 2/29 | 1/29 | – |
| Lillemoe et al., 200483 | 3/58 | 3/66 | – |
| Maharaj et al., 2006230 | 1/28 | 0/22 | – |
| Marta et al., 2010135 | 1/148 | 1/151 | – |
| Martin and Au 201386 | 5/25 | 3/32 | – |
| Mellin and Kondler 1989170 | 4/51 | 16/39 | – |
| Moench et al., 2010250 | 3/65 | 1/61 | – |
| Montorsi et al., 201284 | 0/145 | 2/130 | – |
| Moore et al., 2001111 | 1/19 | 0/7 | – |
| Moore et al., 2001111 | 2/19 | 0/7 | – |
| Moore et al., 2001111 | 1/21 | 0/7 | – |
| Mortenson et al., 2008120 | 7/16 | 7/14 | – |
| Nativ et al., 201259 | 0/4 | 1/3 | – |
| Neuss et al., 2009118 | 10/29 | 11/29 | – |
| Tachibana et al., 2003122 | 1/21 | 2/22 | – |
| Tavilla et al., 201560 | 5/722 | 9/714 | – |
| Ulusoy et al., 200396 | 1/27 | 1/27 | – |
| Total | 67/1981 | 80/1921 | 3902 |
| Study (author, year) | Group | Note | Surgery area | |||||
|---|---|---|---|---|---|---|---|---|
| Fibrin sealant | Standard care | |||||||
| n | Mean | SD | n | Mean | SD | |||
| Bulbuller et al., 201392 | 6 | 138.2 | 21.57 | 15 | 138.1 | 19.77 | C | Upper GI tract: bowel |
| Bulbuller et al., 201392 | 6 | 138.2 | 21.57 | 16 | 196 | 19.77 | C | Upper GI tract: bowel |
| Bulbuller et al., 201392 | 6 | 138.2 | 21.57 | 16 | 166.4 | 19.77 | C | Upper GI tract: bowel |
| Musella et al., 201488 | 50 | 82.8 | 5.2 | 50 | 84.3 | 6.2 | Upper GI tract: bowel | |
| Pilone et al., 201289 | 15 | 108 | 21.57 | 15 | 102 | 19.77 | C | Upper GI tract: bowel |
| Silecchia et al., 200862 | 160 | 149.4 | 36.5 | 160 | 142.7 | 34.1 | Upper GI tract: bowel | |
| Sroka et al., 201590 | 49 | 64 | 23 | 47 | 54 | 19 | Upper GI tract: bowel | |
| Sroka et al., 201590 | 49 | 64 | 23 | 49 | 74 | 21 | Upper GI tract: bowel | |
| Uetsuji, 199468 | 25 | 362 | 131 | 39 | 280 | 85 | Upper GI tract: liver | |
| Liu and Lui, 199369 | 20 | 294.5 | 65.3 | 20 | 343 | 184 | Upper GI tract: liver without mobilisation | |
| Noun et al., 199670 | 35 | 252 | 90 | 42 | 258 | 108 | Upper GI tract: liver without mobilisation | |
| Uetsuji et al., 199468 | 25 | 362 | 131 | 39 | 342 | 111 | Upper GI tract: liver with mobilisation | |
| Figueras et al., 200771 | 150 | 282 | 76.3 | 150 | 263 | 73.1 | Upper GI tract: liver with mobilisation | |
| Mortenson et al., 2008120 | 16 | 227 | 16.2 | 14 | 261 | 16.8 | Breast/lymph | |
| Moore et al., 1997106 | 32 | 135 | 16.2 | 31 | 132 | 16.8 | Breast/lymph | |
| Cambal et al., 2012175 | 50 | 48.5 | 11.11 | 50 | 44 | 11.77 | Hernia | |
| Campanelli et al., 2012176 | 158 | 39.8 | 12.1 | 158 | 41.5 | 11.9 | Hernia | |
| Damiano et al., 2014184 | 216 | 48.89 | 5.71 | 252 | 51.6 | 6.27 | Hernia | |
| Lovisetto et al., 2007180 | 99 | 53.8 | 7.61 | 98 | 39.6 | 7.61 | Hernia | |
| Chan et al., 2014178 | 64 | 75.84 | 19.01 | 65 | 73.09 | 21.31 | Hernia | |
| Bahar et al., 2007169 | 42 | 16 | 3.94 | 39 | 28 | 4 | C | Eye |
| Bahar et al., 2006159 | 39 | 16 | 3.94 | 26 | 20 | 4 | C | Eye |
| Hall et al., 2009160 | 25 | 12.04 | 3.94 | 25 | 26.04 | 4 | C | Eye |
| Karalezli et al., 2008161 | 25 | 15.7 | 2.4 | 25 | 32.5 | 6.7 | Eye | |
| Kucukerdonmez et al., 2010157 | 32 | 11.22 | 2.4 | 38 | 18.7 | 2.2 | Eye | |
| Malik and Kumar, 2010171 | 50 | 18.24 | 2.2 | 25 | 26.6 | 1.93 | Eye | |
| Ratnalingam et al., 2010165 | 68 | 16.93 | 2.85 | 69 | 29.84 | 5.65 | Eye | |
| Rubin et al., 2011166 | 21 | 19.05 | 6.12 | 26 | 48.5 | 7.13 | Eye | |
| Sati et al., 2014163 | 30 | 15.5 | 1.2 | 30 | 27.63 | 1.63 | Eye | |
| Uy et al., 2005168 | 11 | 27.8 | 1 | 11 | 67 | 3.6 | Eye | |
| Yüksel et al., 2010158 | 29 | 23.42 | 13.34 | 29 | 41.45 | 3.2 | Eye | |
| Filosso et al., 2013136 | 13 | 216 | 24 | 11 | 240 | 30 | Cardiothoracic: lung | |
| Lopez et al., 2013129 | 179 | 165.6 | 82.6 | 167 | 155.5 | 81.6 | Cardiothoracic: lung | |
| Maisano et al., 2009140 | 59 | 249 | 77 | 60 | 235 | 59 | Cardiothoracic: heart | |
| Fischer et al., 2013241 | 60 | 247.8 | 140.4 | 30 | 253.4 | 141.8 | Mixed | |
| Maggiore et al., 2011233 | 35 | 98.4 | 7.8 | 35 | 98 | 9.5 | Gynaecological | |
| Takeuchi et al., 2005234 | 29 | 112 | 45.8 | 16 | 103 | 30.6 | Gynaecological | |
| Takeuchi et al., 2005234 | 30 | 108 | 41.7 | 16 | 103 | 30.6 | Gynaecological | |
| Study (author, year) | Group | Note | Surgery area | |||||
|---|---|---|---|---|---|---|---|---|
| Fibrin sealant | Standard care | |||||||
| n | Mean | SD | n | Mean | SD | |||
| Noun et al., 199670 | 35 | 10.8 | 4 | 42 | 11.3 | 5 | Upper GI tract: liver | |
| Carter et al., 201381 | 50 | 6.4 | 51 | 7.3 | 6.75 | Check values | Upper GI tract: pancreas | |
| Lillemoe et al., 200483 | 58 | 12.2 | 0.8 | 66 | 13.6 | 1 | Upper GI tract: pancreas | |
| Martin and Au, 201386 | 25 | 14.1 | 12.7 | 32 | 17.4 | 17.5 | Upper GI tract: pancreas | |
| Musella et al., 201488 | 50 | 5.1 | 1.1 | 50 | 5.2 | 1.2 | Upper GI tract: bowel | |
| Pilone et al., 201289 | 15 | 6.5 | 2.65 | 15 | 7 | 1.5 | C | Upper GI tract: bowel |
| Schwartz et al., 200477 | 58 | 9 | 4 | 63 | 10.5 | 5 | Values taken from Noun et al.70 (reporting on SD for liver surgery) | Upper GI tract: bowel |
| Silecchia et al., 200862 | 160 | 7.1 | 4.2 | 160 | 6.7 | 1.8 | Upper GI tract: bowel | |
| Aguilera et al., 2013143 | 42 | 7.6 | 5.3 | 42 | 7.5 | 2.6 | Joints: knee | |
| Aguilera et al., 2013143 | 41 | 7.2 | 4.5 | 41 | 6.8 | 2.4 | Joints: knee | |
| Kluba et al., 2012145 | 12 | 12.67 | 5.1 | 12 | 13.67 | 2.7 | Joints: knee | |
| Molloy et al., 2006147 | 50 | 4.82 | 4.3 | 50 | 5.86 | 2.55 | C | Joints: knee |
| Randelli et al., 2014149 | 31 | 9 | 2.3 | 31 | 9 | 2.5 | Joints: knee | |
| Lassen et al., 2006141 | 22 | 7 | 36 | 7 | Joints: hip | |||
| Wang et al., 2003153 | 38 | 4.9 | 43 | 5.3 | Joints: hip | |||
| Benevento et al., 2014109 | 30 | 2.08 | 1.06 | 30 | 4.08 | 1.05 | Breast/lymph | |
| Berger et al., 2001107 | 29 | 9.1 | 2.7 | 31 | 9.3 | 3.6 | Breast/lymph | |
| Furrer et al., 1993116 | 15 | 18 | 11 | 15 | 22 | 16 | Breast/lymph | |
| Mustonen et al., 2004104 | 19 | 3.9 | 1 | 21 | 3.7 | 1 | Breast/lymph | |
| Vaxman et al., 1995251 | 20 | 10.8 | 3.5 | 19 | 9.4 | 3.5 | Breast/lymph | |
| Gilly et al., 1994115 | 19 | 6.46 | 1.85 | 21 | 8.47 | 2.62 | Breast/lymph: inguinal or axillary lymph nodes | |
| Udén et al., 199398 | 36 | 5.7 | 32 | 4.3 | Breast/lymph: inguinal or axillary lymph nodes | |||
| Gilly et al., 1998108 | 50 | 8 | 1.6 | 58 | 10.1 | 2.1 | Breast/lymph: axillary lymph nodes | |
| Moore et al., 1997106 | 32 | 1.18 | 0.6 | 31 | 1.41 | 0.69 | Breast/lymph: breast and axillary lymph nodes | |
| Lovisetto et al., 2007180 | 99 | 1 | 98 | 1 | Hernia | |||
| Olmi et al., 2007259 | 50 | 1 | 150 | 1.1 | Hernia | |||
| Olmi et al., 2007259 | 50 | 1 | 150 | 1.1 | Hernia | |||
| Olmi et al., 2007259 | 50 | 1 | 150 | 1.2 | Hernia | |||
| Cormio et al., 2012222 | 49 | 2.75 | 1.68 | 47 | 5.15 | 1.74 | Urology | |
| Czerny et al., 2000205 | 9 | 10 | 7 | 10.5 | Vascular | |||
| Anegg et al., 2007125 | 75 | 6.2 | 2 | 77 | 7.7 | 2.2 | C | Cardiothoracic: lung |
| Droghetti et al., 2008124 | 20 | 11 | 2 | 20 | 14.3 | 2.2 | C | Cardiothoracic: lung |
| Fabian et al., 2003128 | 50 | 4.6 | 2 | 50 | 4.9 | 2.2 | C | Cardiothoracic: lung |
| Filosso et al., 2013136 | 13 | 6.9 | 1.4 | 11 | 9.5 | 0.5 | Cardiothoracic: lung | |
| Gonfiotti et al., 2011130 | 91 | 7.64 | 3.56 | 94 | 7 | 3.33 | Cardiothoracic: lung | |
| Rena et al., 2009127 | 30 | 5.87 | 1.07 | 30 | 7.5 | 3.2 | Cardiothoracic: lung | |
| Tavilla et al., 201560 | 722 | 5.99 | 3.95 | 714 | 6.07 | 4.21 | Cardiothoracic: heart | |
| Study (author, year) | Group | Note | Surgery area | |||||
|---|---|---|---|---|---|---|---|---|
| Fibrin sealant | Standard care | |||||||
| n | Mean | SD | n | Mean | SD | |||
| Maisano et al., 2009140 | 59 | 3.9 | 7.4 | 60 | 2.8 | 4.4 | Cardiothoracic: heart | |
| Berger et al., 2001107 | 29 | 3.8 | 1.9 | 31 | 3.9 | 1.8 | Breast/lymph | |
| Benevento et al., 2014109 | 30 | 2 | 1.4 | 30 | 4 | 1.6 | Breast/lymph | |
| Cipolla et al., 2010110 | 80 | 4.5 | 1.7 | 79 | 5.1 | 1.9 | Breast/lymph | |
| Di Monta et al., 2012117 | 37 | 20 | 5 | 33 | 23 | 5 | Breast/lymph | |
| Dinsmore et al., 200097 | 14 | 16.5 | 1.9 | 13 | 12.3 | 2.3 | C | Breast/lymph |
| Furrer et al., 1993116 | 15 | 8.6 | 4.2 | 15 | 11.7 | 9.1 | Breast/lymph | |
| Gilly et al., 1994115 | 19 | 4.85 | 2.06 | 21 | 7.19 | 2.59 | Breast/lymph | |
| Ko et al., 2009102 | 47 | 3.3 | 0.9 | 48 | 3.8 | 1.4 | Breast/lymph | |
| Moore et al., 1997106 | 32 | 3.9 | 1.7 | 31 | 6.9 | 1.19 | Breast/lymph | |
| Mustonen et al., 2004104 | 19 | 3.3 | 1.2 | 21 | 3.1 | 0.9 | Breast/lymph | |
| Mustonen et al., 2004104 | 19 | 2.2 | 0.8 | 21 | 2.3 | 0.7 | Breast/lymph | |
| Nielsen et al., 1985123 | 10 | 4.4 | 1.9 | 20 | 4.4 | 2.3 | C | Breast/lymph |
| Nielsen et al., 1985123 | 8 | 6.5 | 1.9 | 20 | 4.4 | 2.3 | C | Breast/lymph |
| Segura-Castillo et al., 2005105 | 22 | 5.09 | 1.48 | 23 | 8.96 | 2.33 | Breast/lymph | |
| Ulusoy et al., 200396 | 27 | 9.88 | 0.59 | 27 | 9.66 | 0.58 | Breast/lymph | |
| Vaxman et al., 1995112 | 20 | 5.85 | 2.7 | 19 | 4.89 | 1.9 | Breast/lymph | |
| Vaxman et al., 1995112 | 20 | 2.3 | 1 | 19 | 2.95 | 1.2 | Breast/lymph | |
| Erba et al., 2010210 | 5 | 4 | 1 | 5 | 6 | 1 | Plastic | |
| Oliver et al., 2002215 | 5 | 8.2 | 5 | 6.3 | Plastic | |||
| Oliver et al., 2002215 | 4 | 9.5 | 4 | 9.3 | Plastic | |||
| Oliver et al., 2002215 | 5 | 4.6 | 5 | 9.6 | Plastic | |||
| Oliver et al., 2002215 | 8 | 4.1 | 8 | 4.9 | Plastic | |||
| Czerny et al., 2000205 | 9 | 2 | 7 | 2 | Vascular | |||
| Randelli et al., 2014149 | 31 | 0.81 | 0.16 | 31 | 0.8 | 0.11 | Joints | |
| Bektas et al., 201465 | 35 | 8.7 | 7.4 | 35 | 8.1 | 4.1 | Upper GI tract: liver | |
| Fischer et al., 201172 | 60 | 6.6 | 4.33 | 59 | 7.6 | 2.58 | C | Upper GI tract: liver |
| Frilling et al., 200573 | 53 | 8.2 | 4.33 | 59 | 5.7 | 2.58 | C | Upper GI tract: liver |
| Kakaei et al., 201374 | 15 | 3.66 | 0.97 | 15 | 4.06 | 0.7 | Upper GI tract: liver | |
| Kohno et al., 199275 | 31 | 7.2 | 5.1 | 31 | 6.3 | 2.7 | Upper GI tract: liver | |
| Liu and Lui, 199369 | 20 | 7.85 | 3.85 | 20 | 8.35 | 2.81 | Upper GI tract: liver | |
| Czerny et al., 2004137 | 40 | 2.53 | 0.17 | 40 | 2.97 | 0.14 | Cardiothoracic: lung | |
| Filosso et al., 2013136 | 13 | 6.1 | 1.7 | 11 | 10.8 | 2.4 | Cardiothoracic: lung | |
| Gonfiotti et al., 2011130 | 91 | 6 | 3.1 | 94 | 6.5 | 5.4 | Cardiothoracic: lung | |
| Moser et al., 2008126 | 25 | 2.83 | 1.96 | 25 | 5.88 | 2.96 | Cardiothoracic: lung | |
| Rena et al., 2009127 | 30 | 3.53 | 1.59 | 30 | 5.9 | 3.72 | Cardiothoracic: lung | |
List of abbreviations
- CHMP
- Committee for Medicinal Products for Human Use
- CI
- confidence interval
- CO2
- carbon dioxide
- CRD
- Centre for Reviews and Dissemination
- EMA
- European Medicines Agency
- ENT
- ear, nose and throat
- FDA
- Food and Drug Administration
- GI
- gastrointestinal
- ITT
- intention to treat
- MD
- mean difference
- MHRA
- Medicines and Healthcare products Regulatory Agency
- OR
- odds ratio
- RCT
- randomised controlled trial
- SD
- standard deviation