Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA programme on behalf of NICE as project number 13/177/01. The protocol was agreed in March 2015. The assessment report began editorial review in February 2016 and was accepted for publication in July 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
David McGrane has spoken at educational meetings sponsored by AstraZeneca, Eli Lilly, Sanofi, MSD, Takeda Pharmaceutical Company, Novo Nordisk, Janssen, and has served on Advisory Boards for Eli Lilly, Sanofi, Novo Nordisk. J Paul O’Hare has received lecture fees, advisory board meeting fees, and grants for research from Novo Nordisk and Sanofi. All fees are paid through University of Warwick to fund access to insulin projects in sub-Saharan Africa.
Corrections
-
This article was corrected in February 2018. See Johnston R, Uthman O, Cummins E, Clar C, Royle P, Colquitt J, et al. Corrigendum: Canagliflozin, dapagliflozin and empagliflozin monotherapy for treating type 2 diabetes: systematic review and economic evaluation. Health Technol Assess 2018;21(2):219–220. http://dx/doi.org/10.3310/hta21020-c201802
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Johnston et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
The York and Humber Public Health Observatory (YHPHO) estimates that, in 2015, around 3.5 million people in England had type 2 diabetes, with a prevalence of about 8%. 1 The prevalence has been increasing, partly due to demographic change, partly due to better detection, but mainly due to increased prevalence of overweight and obesity. Diabetes is costly to the UK NHS, with a recent study estimating that 10% of all NHS expenditure is on diabetes. 2
The report, Prescribing for Diabetes, from the Health and Social Care Information Centre estimated that in 2013–14, 9.5% of prescribing costs were for diabetes, including drugs and blood glucose testing strips. 3
There are two characteristics of type 2 diabetes: insulin resistance and a loss of insulin-producing capacity in the pancreas. Insulin resistance is the initial state, which the pancreas initially copes with by increased production of insulin from its beta cells. Over time, pancreatic insulin production falls. It is generally accepted that by the time type 2 diabetes is diagnosed, the pancreas has lost half of its insulin-producing capacity.
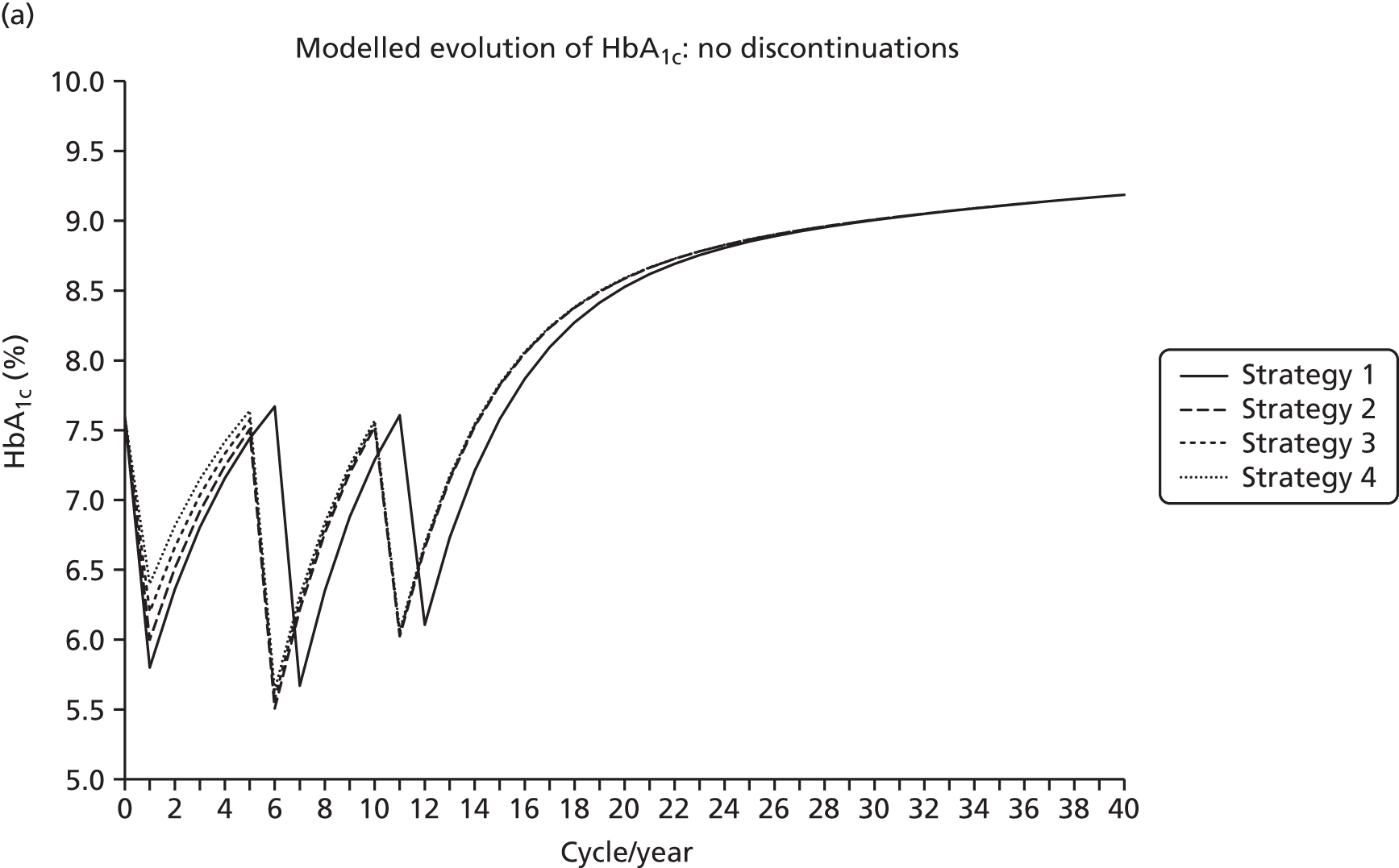
Type 2 diabetes is regarded as a progressive disease. The United Kingdom Prospective Diabetes Study (UKPDS) trial showed a deterioration in glycated haemoglobin (HbA1c) of about 0.2% a year. 4 The UKPDS495 paper reported that, by 3 years, only 50% could maintain HbA1c under 7% on monotherapy and that this proportion fell to 25% after 9 years.
However, some people with early type 2 diabetes, who manage to lose weight and increase physical activity, may then have enough beta cell capacity to remain well controlled on diet alone or on diet plus monotherapy. They are probably a small minority, though a study in Trent region in 2003 found that 31% of people with type 2 diabetes were being managed on diet alone with over 80% achieving HbA1c of 7.5% or under. 6 Most patients do not lose sufficient weight and so their diabetes is expected to progress over time. They will require additional drug therapies, with about one-third progressing to requiring insulin injections to try to control blood glucose levels. Progression may be slow. In a population-based study in Denmark, 79% of people with type 2 diabetes who started metformin were still on metformin monotherapy 3 years later. 7
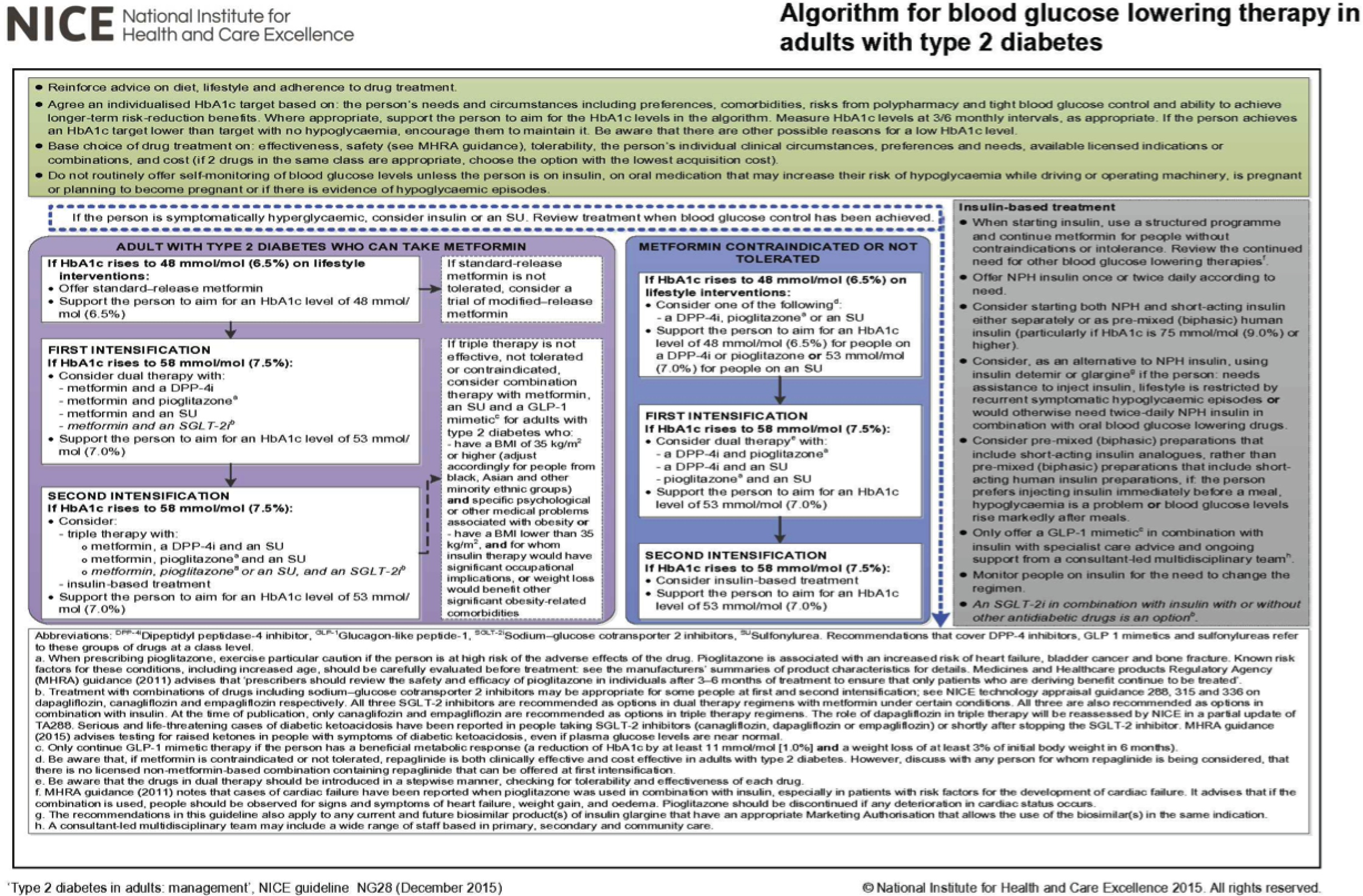
National Institute for Health and Care Excellence clinical guideline 2015
The updated National Institute for Health and Care Excellence (NICE) clinical guideline (CG) for type 2 diabetes (CG28)8 was issued in December 2015. The recommendations include:
-
Start drug treatment with metformin in patients who are overweight or obese, and whose control is inadequate with lifestyle measures (diet and physical activity) alone.
-
If metformin is contraindicated or not tolerated, consider monotherapy with one of a dipeptidyl peptidase-4 (DPP-4) inhibitor, pioglitazone or a sulfonylurea (SU).
-
Do not use pioglitazone in patients who have heart failure, hepatic impairment, a history of bladder cancer or haematuria.
-
When glycaemic control becomes unsatisfactory on metformin, consider dual therapy by adding a SU, pioglitazone or a DPP-4 inhibitor.
-
In patients who cannot take metformin, and if monotherapy does not control HbA1c, consider dual therapy with two of a DPP-4 inhibitor, pioglitazone or a SU.
-
Consider a DPP-4 inhibitor or pioglitazone in triple therapy with metformin and a SU when dual therapy was insufficient to achieve adequate control.
-
Addition of another drug, referred to as intensification of treatment, was recommended when HbA1c was 7.5% or over (though with a recommendation that targets be adjusted for individual circumstances).
The guideline dealt only briefly with the sodium–glucose co-transporter 2 (SGLT2) inhibitors, mentioning that they may be appropriate for some people and referring readers to the guidances on canagliflozin (Invokana, Janssen, High Wycombe, UK), dapagliflozin (Farxiga, Bristol-Myers Squibb, Luton, UK) and empagliflozin (Jardiance, Boehringer Ingelheim, Ingelheim, Germany/Eli Lilly and Company, Indianapolis, IN, USA) in combination therapy.
We prefer to use the terms ‘dual therapy’ and ‘triple therapy’ to ‘second-line’ and ‘third-line’ because these last terms could cover substitution as well as addition.
Drugs for type 2 diabetes
We now have nine classes of glucose-lowering drugs for type 2 diabetes, though some contain only a single drug. Those that are used in monotherapy are:
-
Metformin.
-
SUs: usually second- or third-generation drugs – gliclazide, glimepiride and glipizide.
-
Pioglitazone.
-
Acarbose.
-
Meglitinides: nateglinide and repaglinide, though only the latter is licensed for monotherapy. These drugs act in the same way as the SUs, promoting release of insulin.
-
The DPP-4 inhibitors, also known as the ‘gliptins’, not currently recommended by NICE8 for monotherapy (because of cost). There are now five available: sitagliptin, vildagliptin (Galvus, Novartis Frimley, UK), saxagliptin (Onglyza, Bristol-Myers Squibb, Luton, UK), alogliptin (Vipidia, Takeda Pharmaceutical Company, High Wycombe, UK) and linagliptin (Trajenta, Boehringer Ingelheim, Bracknell, UK).
-
The SGLT2 receptor inhibitors. In the UK, dapagliflozin, empagliflozin and canagliflozin have been approved by NICE9–11 in combination therapy.
There are two classes that are injectable treatments. Neither is commonly used in monotherapy. Because of both cost and the need to be injected, they appear later in the treatment pathway:
-
The glucagon-like peptide-1 (GLP-1) analogues exenatide (Bydureon, AstraZeneca, Luton, UK), albiglutide (Eperzan, GlaxoSmithKline, Brentford UK) and dulaglutide (Trulicity, Eli Lilly, Basingstoke, UK) given once weekly, and liraglutide (Victoza, Novo Nordisk, Crawley, UK) and lixisenatide (Lixilan, Sanofi, Guildford, UK) given once daily. There is also a form of exenatide given twice daily. Exenatide, liraglutide and lixisenatide were covered in the update of the NICE guideline on type 2 diabetes,8 but dulaglutide and albiglutide were not. Both dulaglutide and albiglutide are licensed in Europe for use in monotherapy, when metformin cannot be used, as well as for combination therapy. 12,13
-
Insulins In type 2 diabetes, insulin treatment starts with once-daily basal insulin [NICE recommends neutral protamine Hagedorn (NPH) insulin as first choice8], but if intensification is needed, short-acting insulins may be added at mealtimes, or twice-daily biphasic insulin may be used.
There are now combinations of GLP-1 analogues with basal insulins, such as insulin degludec combined with liraglutide, and insulin glargine and lixisenatide.
There are quite marked differences in costs of GLP-1 analogues, ranging from daily lixisenatide at around £690 to weekly dulaglutide at almost £1200. Patients may prefer to inject once a week. There may be differences in adverse effects (AEs). Longer-acting drugs increase heart rate more than shorter-acting ones, though the importance of this is, as yet, uncertain. 14
Despite the number of classes, there is still a need for drugs that that will lower glucose without causing hypoglycaemia or weight gain, and that can improve cardiovascular outcomes. The SUs, repaglinide and insulin cause varying degrees of weight gain, which may worsen insulin resistance. They can cause hypoglycaemia. The gliptins do not cause weight gain or hypoglycaemia, but have not been shown to improve cardiovascular outcomes.
The 2015 NICE guideline first draft recommended that patients who cannot take or tolerate metformin should take repaglinide, a meglitinide analogue (NICE Internal Clinical Guidelines Team. Type 2 Diabetes in Adults. URL: www.nice.org.uk/guidance/NG28/documents/type-2-diabetes-guideline2). The meglitinide analogues are insulin secretagogues, shorter acting than the SUs. 15 They have not been widely used in the UK.
Pioglitazone is recognised as causing weight gain and oedema, with a risk of heart failure and fractures, but does not cause hypoglycaemia. Metformin does not cause either weight gain or hypoglycaemia.
Box 1 shows the flow chart from the NICE guideline. 16
The rational for including repaglinide was twofold:
-
a network meta-analysis (NMA) showed that repaglinide reduced HbA1c more than SUs, by 0.19%, and was non-significantly safer than SUs in terms of hypoglycaemia. However, the NICE modelling included a mixture of SUs, including tolbutamide, glibenclamide, glipizide, glimepiride and gliclazide. The largest number of trials comparing repaglinide with SUs featured glibenclamide. Gliclazide has been reported to cause less hypoglycaemia than other SUs, so a direct comparison of repaglinide with gliclazide might not have given the same results. Gliclazide is the SU that is preferred by clinicians in the UK.
-
costing that assumed self-monitoring of blood glucose (SMBG) was required because of risk of hypoglycaemia on SUs and pioglitazone, but not for repaglinide, which is odd, given that repaglinide causes hypoglycaemia and pioglitazone does not. If this assumption is reversed, pioglitazone becomes the choice if metformin cannot be taken, though only just.
One drawback to using repaglinide in monotherapy in people who cannot take metformin is that it is licensed only in dual therapy with metformin. So if repaglinide monotherapy was insufficient, dual therapy would mean starting two new drugs.
Sulfonylureas
The SUs are insulin secretagogues, which means that they work largely by stimulating insulin release by the beta cells in the pancreas. Once the beta cell capacity falls, the SUs become less effective. There is some evidence that the duration of effectiveness is longer with gliclazide than glibenclamide. 17
The main AEs of the SUs are weight gain and hypoglycaemia. A population-based study from Tayside found an incidence of severe hypoglycaemia amongst people on SUs of 0.9 per 100 patient-years. 18 This rate is similar to the 0.8% seen in the meta-analysis by Schopman et al. 19 Monami et al. ,20 in a good-quality meta-analysis of 69 trials involving SUs, reported a cumulative incidence of at least one episode of severe hypoglycaemia of 1.2%, but this was based on 24 trials because the others did not report any severe hypoglycaemia. There was some evidence that hypoglycaemia was less common with gliclazide than with other SUs. 20 Schopman et al. 19 reported that 0.1% of patients on gliclazide had severe hypoglycaemia and that 1.4% had plasma glucose (PG) under 3.1 mmol/l at some point in trials that ranged in duration from 24 to 104 weeks. Schernthaner et al. 21 from the 27-week GUIDE (GlUcose control in type 2 diabetes: Diamicron MR vs. glimEpiride trial), using modified-release (MR) gliclazide, reported that 3.7% of patients had at least one PG of < 3 mmol/l, but that none needed assistance. Compared with the glimepiride arm, there were about 50% fewer hypoglycaemic episodes, despite a reduction in HbA1c of 1.2% on gliclazide and 1.0% on glimepiride.
The Schopman meta-analysis19 reported that, overall, 0.8% of patients on SUs had a severe hypoglycaemic episode, but the proportions ranged from 0.1% for gliclazide to 2.1% for glipizide. In the ORIGIN trial, 75% of patients on standard treatment (25% of whom were on SUs) never had any hypoglycaemia. 22
In the very large (11,140 patients) ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation) trial, gliclazide MR was used in two arms, intensive and standard. In the intensive arm, the aim was to achieve HbA1c of 6.5% or less. 23 This was achieved in 65% in the intensive arm and 29% in the standard arm. Severe hypoglycaemia event rates were 0.07 per 1000 patient-years in the intensive arm and 0.04 per 1000 patient-years in the standard arm. Minor hypoglycaemic events occurred at rates of 12 and 9 per 1000 patient-years in intensive and standard arms, respectively.
These rates of hypoglycaemia on SUs are much lower than the 7% reported for severe hypoglycaemia by the UK Hypoglycaemia Study Group,24 but the patients in that study were recruited only from secondary care clinics.
In the Netherlands, the guideline for the management of type 2 diabetes advises that gliclazide is the SU of choice, partly because of its safety in renal failure. 25,26 A meta-analysis of SU trials concluded that severe hypoglycaemia was rare with gliclazide, especially if the dose does not exceed 240 mg daily. Non-severe hypoglycaemia was seen mainly in those on 320 mg daily. 25
Simpson et al. 27 argued that as different SUs had different tissue selectivity and risk of hypoglycaemia, the cardiovascular risk might also vary. They carried out a systematic review and NMA, and used glibenclamide as the reference risk. Compared with people taking glibenclamide, those on gliclazide had a relative risk for total mortality of 0.65 [95% credible interval (CrI) 0.53 to 0.79]. For cardiovascular mortality, the risk ratio (RR) for gliclazide was 0.60 (95% CrI 0.45 to 0.84), whereas other SUs showed no significant difference from glibenclamide.
Schramm et al. 28 used Danish record linkage data to compare the mortality and cardiovascular risks amongst patients on monotherapy with SUs and repaglinide, with those on metformin. The risks were higher on most SUs, but not for gliclazide or repaglinide.
The risk of severe hypoglycaemia with SUs may have been overestimated, but it remains a problem that can lead to hospital admission, as well causing anxiety and interrupting usual activities.
The Scottish Intercollegiate Guidelines Network (SIGN) recommends that SUs should be considered as first line in patients who cannot take metformin. 29 The 2015 American Diabetes Association (ADA) position statement expresses no preference amongst SUs, pioglitazone, flozins and gliptins in people who cannot take metformin. 30
If SUs were the same price as the newer drugs such as the gliptins or the flozins, they would probably be superceded. But they are very cheap, and have been used for so long that all their AEs are known.
In this report, based on the evidence reported above, we use gliclazide as the SU of choice. There are two forms of gliclazide, standard and MR. The Diamicron Study Group reported these to be clinically equivalent in a 10-month study in 800 patients. 31 The MR form was given once a day, and 30–120 mg was equivalent to 80–320 mg of the standard form taken twice daily. No severe hypoglycaemia occurred. Mild or moderate hypoglycaemia was seen in 5% of those on the MR form. Once-daily administration may help adherence, but the MR form costs more – £62 a year at 60 mg a day, £89 at 90 mg. The standard form costs about £28 a year.
Pioglitazone
Pioglitazone, the only glitazone used in the UK, can cause oedema, which can precipitate congestive heart failure (CHF) and fractures. CHF is a common cause of admission to hospital, and the second commonest first presentation of cardiovascular disease (CVD) (after peripheral arterial disease). 32 A fivefold risk of macular oedema (MO) has also been reported. 33
There is an increased risk of fractures amongst people taking pioglitazone. The fractures were originally reported as being atypical fractures of long bones,34 but Scottish data also show an increase in hip fractures. 35
More recently there has been concern over bladder cancer. Pioglitazone use has now been discontinued in France.
However, the evidence is inconsistent. A Canadian study using UK data36 reported an increased risk of 1.83 (95% confidence interval (CI) 1.10 to 3.05). A French study37 reported a doubling of a very small risk of bladder cancer. The large Kaiser Permanente study from the USA reported an increase in risk with pioglitazone with RR of 1.18 but this was not statistically significant. 38 The PrOactive (PROspective pioglitAzone Clinical Trial In macroVascular Events) trial reported a RR of 2.83 (p = 0.04) but once cases of bladder cancer diagnosed in the first year were excluded there was no difference. 39 It was argued that cancers diagnosed within a year of starting the drug must have been there before. However, Gale has argued that pioglitazone could be acting as a growth promoter in latent tumours. 40
A very large study by Levin et al. ,41 mainly in the UK, Finland and British Columbia (one million people with type 2 diabetes, almost 6 million person-years of observation), found no increased risk of bladder cancer, providing further reassurance.
It should be noted that diabetes itself has been reported in a very large meta-analysis to increase the risk of bladder cancer with RR 1.35 (95% CI 1.17 to 1.56), though this applied only to those within 5 years of diagnosis. 42 Amongst those with duration of over 5 years, the RR was 1.08.
The European Medicines Agency (EMA) issued a statement in 2011 saying that there was a small increased risk of bladder cancer, but that, on balance, pioglitazone could still be used as a second- and third-line treatment. 43 The Medicines & Healthcare products Regulatory Agency (MHRA) concurred. 44
Patients should be screened for haematuria before starting pioglitazone and then at least annually afterwards.
There are some cardiovascular benefits from pioglitazone (the reverse of what was seen with rosiglitazone) with a reported reduced risk of myocardial infarction (MI), but there is clearly an increased risk of heart failure,34,39 and regular monitoring with B-type natriuretic peptide (BNP) seems advisable for the safest use of this drug. 45 Patients are advised of possible side effects and advised to stop if oedema or shortness of breath develops. If there are concerns regarding heart failure, echocardiography is often carried out, to check that left ventricular function is satisfactory, before starting pioglitazone.
Despite its side effects, including progressive weight gain by as much as 5 kg, pioglitazone can be a valuable diabetes therapy, as it is an insulin sensitiser and allows reduction in insulin resistance, still known to be a major factor in the pathogenesis of type 2 diabetes and glucose intolerance. Early studies using genetic profiling showed that the Pro12Ala of the peroxisome proliferator-activated receptor gamma (PPARG) gene showed a population attributable risk of approximately 50% and, taken together with clinical risk factors, might define those most at risk of renal sodium retention and oedema. Unfortunately, probably because of the fact that the PPARG agonists also show greater metabolic efficacy in those with the Pro12Ala variant, this approach has not been developed in clinical practice, as those who would benefit most would have to be excluded. 46
Many people with type 2 diabetes are considerably overweight and may develop non-alcoholic fatty liver disease (NAFLD). Pioglitazone has been reported to improve NAFLD,47 so if attempts at weight loss are unsuccessful and the NAFLD is progressing, pioglitazone may need to be considered for this group of patients. NAFLD is a spectrum of disease ranging from an increased fat content in the liver (steatosis) to inflammation (non-alcoholic steatohepatitis) and possibly on to cirrhosis. NAFLD is strongly associated with insulin resistance.
Despite its AEs, pioglitazone is still widely used, though its use may be declining, with new initiations falling in recent years. The Health and Social Care Information Centre Report gives figures for items prescribed in 2013–143 (Table 1).
| Drug | No. of prescriptions |
|---|---|
| Metformin | 18,100,000 |
| SUs | 8,400,000 |
| Sitagliptin | 2,020,100 |
| Pioglitazone | 1,408,600 |
| Linagliptin | 329,400 |
| Vildagliptin | 173,200 |
| Repaglinide | 83,800 |
The strongest argument for using pioglitazone is the very low cost, but the costs of AEs need to be considered.
Dipeptidyl peptidase-4 inhibitors
The first two of these to reach the market, sitagliptin and vildagliptin, were appraised for NICE CG87, and recommended for use in combination therapy. 8 There are now five DPP-4 inhibitors with slightly different licensed indications. Others are coming, including two that are taken only once a week, trelagliptin and omarigliptin, both now licensed in Japan.
The CG87 guidance8 is reproduced in Box 2.
1.6.1.1 Consider adding a DPP-4 inhibitor (sitagliptin, vildagliptin) instead of a sulfonylurea as second-line therapy to first-line metformin when control of blood glucose remains or becomes inadequate (HbA1c ≥ 6.5%, or other higher level agreed with the individual) if:
-
the person is at significant risk of hypoglycaemia or its consequences (for example, older people and people in certain jobs [for example, those working at heights or with heavy machinery] or people in certain social circumstances [for example, those living alone]), or
-
the person does not tolerate a sulfonylurea or a sulfonylurea is contraindicated.
1.6.1.2 Consider adding a DPP-4 inhibitor (sitagliptin, vildagliptin) as second-line therapy to first-line sulfonylurea monotherapy when control of blood glucose remains or becomes inadequate (HbA1c ≥ 6.5%, or other higher level agreed with the individual) if:
-
the person does not tolerate metformin, or metformin is contraindicated.
1.6.1.3 Consider adding sitagliptin5 as third-line therapy to first-line metformin and a second-line sulfonylurea when control of blood glucose remains or becomes inadequate (HbA1c ≥ 7.5% or other higher level agreed with the individual) and insulin is unacceptable or inappropriate. 6
1.6.1.4 Only continue DPP-4 inhibitor therapy (sitagliptin, vildagliptin) if the person has had a beneficial metabolic response (a reduction of at least 0.5 percentage points in HbA1c in 6 months).
A DPP-4 inhibitor (sitagliptin, vildagliptin) may be preferable to pioglitazone if:
-
further weight gain would cause or exacerbate significant problems associated with a high body weight, or
-
pioglitazone is contraindicated, or
-
the person has previously had a poor response to, or did not tolerate, a TZD.
TZD, thiazolidinedione.
Repaglinide
Repaglinide acts on the same receptor in the pancreas as the SUs (and another receptor) but is shorter-acting and was therefore thought to be particularly useful in controlling hyperglycaemia after meals. Like the SUs, its AEs include significant weight gain and hypoglycaemia.
The relevant recommendation in CG878 was ‘to consider offering a rapid-acting insulin secretagogue to a person with an erratic lifestyle’. This presumably related to unpredictability of mealtimes, when there would be a case for using a shorter-acting meglitinide analogue instead of a SU.
The cost of repaglinide treatment will depend on dosages used. It was designed to be taken to reduce postprandial hyperglycaemia, which means it should be taken at mealtimes. The NICE guideline costing16 assumes a total daily dose of 4 mg. If that comprised 2 × 2-mg tablets twice a day, the annual cost would be about £48. However, that assumes that people take it at only two meals. If a third 2-mg dose was added, the annual cost would be £72. But if the third dose was only 1 mg (say to cover a small breakfast or lunch), the annual cost would be £92, because the 1-mg tablets are almost double the price of the 2-mg ones. The variability in doses used in the repaglinide studies makes comparison with the SUs difficult.
Sodium–glucose co-transporter 2 inhibitors
The SGLT2 inhibitors, hereafter referred to as the flozins, have a unique mechanism of action. In the non-diabetic state glucose is allowed through the filter in the renal glomeruli but is fully reabsorbed in the renal tubules through sodium–glucose co-transporter mechanisms. Glycosuria (glucose in the urine) occurs when the renal threshold for glucose (blood glucose of approximately 10 mmol/l) is exceeded. The main transport mechanism responsible for glucose reabsorption, SGLT2, is found in the proximal kidney tubule. This is encoded by the gene for the solute carrier family 5 (sodium–glucose co-transporter), member 2 (SLC5A2). Some people have a mutation in the SLC5A2 gene that causes a defective SGLT2 protein, resulting in glycosuria. Individuals who have this mutation do not have significant problems related to the glycosuria, such as urinary tract infections (UTIs), and they have a normal life expectancy with no increase in cardiovascular mortality or urogenital cancers. 48 This implies that blocking the transport mechanism should not cause problems.
The flozins block the SGLT2 system and so mimic the effect of the SLC5A2 mutation and reduce the reabsorption of renal filtered glucose back into the bloodstream, thereby lowering blood glucose levels. Owing to their insulin-independent mode of action, they do this without weight gain or hypoglycaemia. 49
For uncertain reasons, the SGLT2 inhibitors do not block all glucose reabsorption. Around 160–180 mg of glucose is filtered into the urine each day, and the SGLT2 system reabsorbs 80–90% of that. The amount blocked appears to vary amongst the different drugs, with dapagliflozin 10 mg blocking only about a third of reabsorption. 50,51 Even very large doses of dapagliflozin (such as 100 mg) do not block all glucose reabsorption in people with type 2 diabetes. 52 But none of the SGLT2 inhibitors block reabsorption of over half of the filtered glucose load.
There is also a sodium–glucose co-transporter 1 (SGLT1) transport mechanism, which is present both in the kidney and the gut. In the kidney, it is much less important than SGLT2. Inhibition of gut SGLT1 reduces absorption of glucose there, and it has been suggested that canagliflozin may have a dual action. This was reported first in healthy volunteers53 but has since been reported in a study of people with type 2 diabetes. 54
Because these drugs act through an insulin-independent mechanism, they can be effective when other drugs that depend entirely (sulfonylureas and meglitinides) or in part (gliptins and GLP-1 analogues) on stimulating insulin release have lost effectiveness. In type 2 diabetes, the capacity of the pancreatic beta cells to produce insulin often falls over time.
In addition to improving glycaemic control, the SGLT2 inhibitors also reduce blood pressure (BP). In a meta-analysis of 27 randomised controlled trials (RCTs) with 12,960 patients, Baker et al. 55 reported a mean reduction in systolic blood pressure (SBP) of 4 mmHg.
Marketing authorisations
The indications for the three flozins are similar – for adults with type 2 diabetes, when diet and physical activity do not provide good control (or adherence is poor) and metformin cannot be tolerated or is contraindicated.
The NICE recommendations differ slightly for the three flozins as shown in Box 3.
-
In a dual therapy regimen in combination with metformin, only if it is used as described for DPP-4 inhibitors in Type 2 diabetes: The Management of Type 2 Diabetes (NICE CG87).
-
Dapagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option for treating type 2 diabetes.
Dapagliflozin in a triple therapy regimen in combination with metformin and a sulfonylurea is not recommended for treating type 2 diabetes, except as part of a clinical trial. This was because at the time of the dapagliflozin appraisal, there was insufficient evidence on its use in triple therapy.
Canagliflozin has been approved by NICE, as follows10-
In a dual therapy regimen in combination with metformin is recommended as an option for treating type 2 diabetes, only if a sulfonylurea is contraindicated or not tolerated or the person is at significant risk of hypoglycaemia or its consequences.
-
Canagliflozin in a triple therapy regimen is recommended as an option for treating type 2 diabetes in combination with metformin and either a sulfonylurea or pioglitazone.
-
Canagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option for treating type 2 diabetes.
1.1 Empagliflozin in a dual therapy regimen in combination with metformin is recommended as an option for treating type 2 diabetes, only if:
-
A sulphonylurea is contraindicated or not tolerated.
-
The person is at significant risk of hypoglycaemia or its consequences.
1.2 Empagliflozin in a triple therapy regimen is recommended as an option for treating type 2 diabetes in combination with:
-
metformin and a sulphonylurea.
-
metformin and pioglitazone.
1.3 Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option for treating type 2 diabetes.
Renal impairment
The dapagliflozin, canagliflozin and empagliflozin guidances differ also in use in moderate renal impairment. The guidance on dapagliflozin says that it should not be used in patients with glomerular filtration rates (GFRs) of below 60 ml/minute, whereas the guidances on canagliflozin and empagliflozin say that if started before renal function declined to an estimated glomerular filtration rate (eGFR) of 60 ml/minute, it may be continued until eGFR falls below 45 ml/minute.
Age
Dapagliflozin is not recommended in people aged over 75 years but there is no such restriction for canagliflozin or empagliflozin. However, empagliflozin is not recommended for people over 85 years due to lack of data in this group.
Pioglitazone
Dapagliflozin is not licensed for use in combination with pioglitazone. Both canagliflozin and empagliflozin are.
Dosages
There are two doses of canagliflozin and empagliflozin. Canagliflozin comes as 100 mg and 300 mg. The licence states that the 300-mg dose may be used in those who tolerate the 100-mg dose – so ruling out canagliflozin 300 mg as a starting dose. Similarly, with empagliflozin, the 25-mg dose is licensed for those who can tolerate the 10 mg starting dose. A 5 mg starting dose of dapagliflozin is recommended for patients with severe hepatic impairment.
Newer SGLT2 inhibitors include luseogliflozin (Taisho Pharmaceutical, Tokyo, Japan, and Novartis), ipragliflozin (Suglat®, Astella Pharma, Chertsey, UK), tofogliflozin (Sanofi, Guildford, UK; Takeda Pharmaceutical Company, High Wycombe, UK) and remogliflozin (GlaxoSmithKline, Research Triangle Park, NC, USA) but these are not included in the NICE scope. Some are still in pre-licensing trials.
Therapeutic pathway
Where should SGLT2 inhibitors fit into the therapeutic pathway? Factors to be considered include:
-
Effect on glycaemic control as reflected in HbA1c reductions.
-
Effect on weight, compared with other drugs, some of which cause marked weight gain.
-
Effect on cardiovascular risk, including on BP and lipid levels, and ideally as reflected in longer-term cardiovascular outcomes.
-
AEs, particularly increased genital and urinary infections.
-
Duration of diabetes. In long-standing type 2 diabetes, the efficacy of the flozins will not be affected by a fall in endogenous insulin production.
-
Interactions with other drugs, especially in patients on treatment for comorbidities.
-
Ease of use, by oral administration rather than injection.
-
Cost.
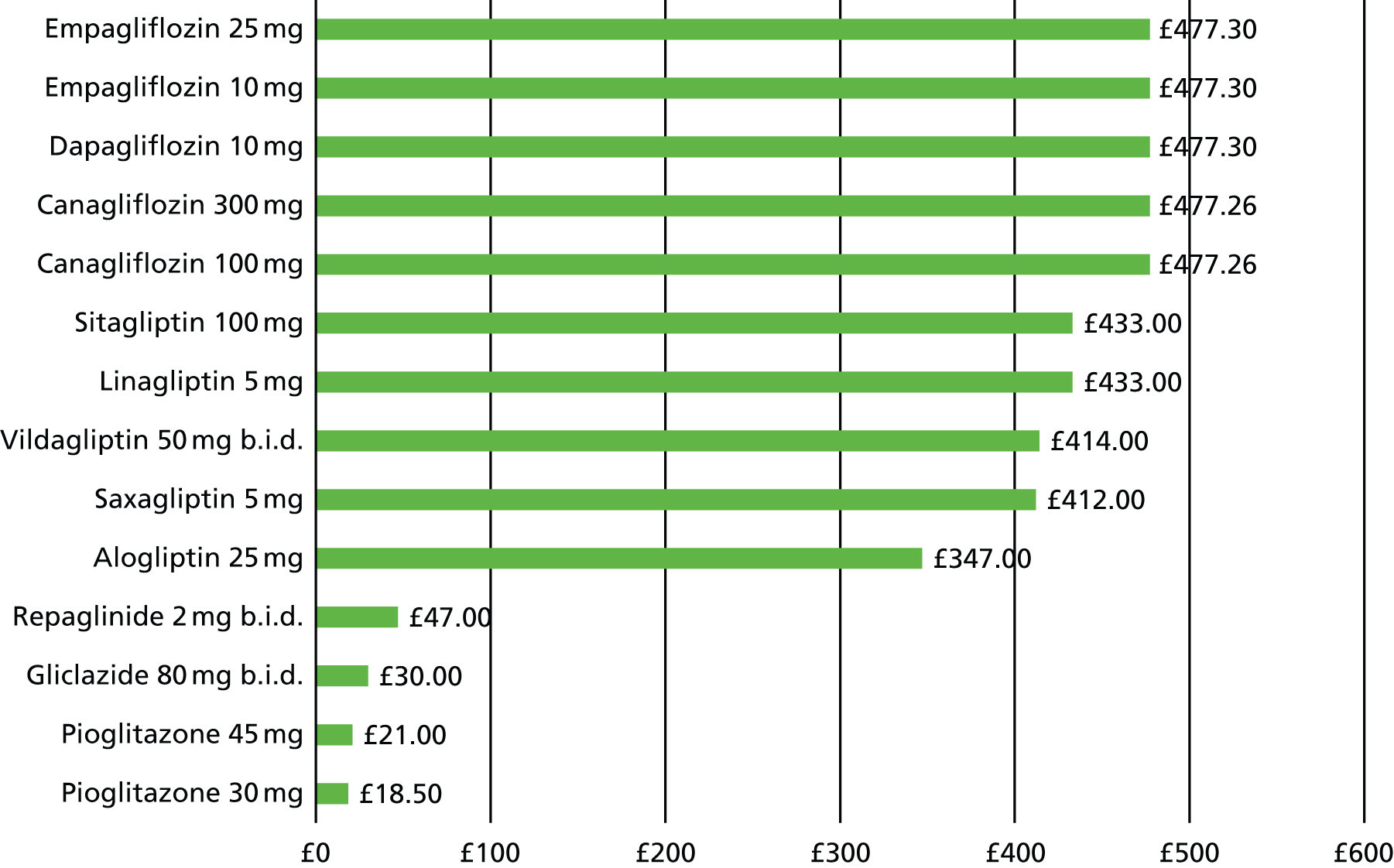
Figure 1 shows the annual costs of the drugs for type 2 diabetes (drug costs only).
FIGURE 1.
Costs of different pharmacological interventions for diabetes. Source: Drug Tariff;56 MS/ERG report on canagliflozin. b.i.d., twice daily; MS, manufacturer submission. ERG, Evidence Review Group.
Decision problem
The objective of the appraisal as stated by NICE57 is:
To appraise the clinical and cost-effectiveness of canagliflozin, dapagliflozin and empagliflozin monotherapy within their licensed indications for treating type 2 diabetes.
In PICO (Population, Intervention, Comparator, Outcomes) terms:
-
The population is people with type 2 diabetes, not currently on glucose-lowering drugs, but requiring a glucose-lowering agent, but who cannot take metformin.
-
The interventions are the SGLT2 inhibitors dapagliflozin, canagliflozin and empagliflozin.
-
The comparators listed in the NICE scope are repaglinide, sulfonylureas, pioglitazone and the DPP-4 inhibitors, hereafter referred to as the gliptins.
-
The outcomes would ideally be the rates of complications of diabetes, but most trials of new diabetes drugs are short term, and rely on modelling changes in HbA1c, BP, weight and lipids to predict longer-term outcomes.
As noted above, the NICE guideline CG878 recommends starting with diet and lifestyle, adding metformin if lifestyle change is insufficient. However, 5–15% of people with type 2 diabetes cannot take metformin, either because they cannot tolerate it, or because of contraindications to use. The intolerance is usually because of gastrointestinal (GI) side effects such as diarrhoea, especially with higher doses. Faecal incontinence can occur. Bailey and Turner58 reported that 5% of people could not tolerate any dose of metformin, and Garber et al. 59 also reported that 5% had to stop. Of those who could take it, over half could manage the maximum dose (2250 mg/day). De Fronzo and Goodman60 reported that with gradual dose escalation, 85% could take 2250 mg per day. The AEs are reduced by using slow-release metformin: diarrhoea from 18% to 8%; any GI AEs from 26% to 12%. 61 So the slow-release form should be tried before abandoning metformin. Scarpello et al. 62,63 reported that use of bile acid sequestrants could improve tolerance to metformin, but many patients find these drugs unpalatable.
The main contraindication to metformin use is chronic renal impairment, and NICE recommends that metformin should not be used once eGFR falls below 30 ml/minute, and used with caution if eGFR is in the range of < 45 to > 30 ml/minute.
The guidance on contraindications may be overcautious, and are largely with lactic acidosis in mind. Emslie-Smith et al. ,64 using population-based data in Tayside, found 621 episodes of contraindications, but in only 10% of patients was metformin stopped. Overall, 25% of people on metformin had contraindications but AEs were rare. The fear of lactic acidosis with metformin use may be a carry-over from problems with phenformin, the other biguanide, which increases lactate levels – metformin does not. 60 Phenformin was withdrawn from use in the UK many years ago because of the lactic acidosis risk. The Cochrane review of metformin and lactic acidosis concluded that there was no increase in lactic acidosis with metformin. 65
For those who cannot tolerate metformin or in whom it is contraindicated, the usual next drug has been a SU such as gliclazide. CG878 recommended that a sulfonylurea may be considered as first-line monotherapy if the person is not overweight, or if
-
metformin is not tolerated or is contraindicated, or
-
a rapid therapeutic response is required because of hyperglycaemic symptoms.
It also listed acarbose as being considered if a person is unable to use other oral glucose-lowering agents.
Issues
The patients involved will be those who cannot take metformin. One issue is that trials of flozins and other drugs as monotherapy have not been restricted to patients who have not been able to tolerate metformin. A literature search found few studies comparing people who got diarrhoea on metformin with those who did not. A study from Japan66 identified several factors that increased the incidence of diarrhoea (often transient, in the first few days): female gender, initial dose of 750 mg, age under 65 years, and BMI of over 25 kg/m2.
Given the lack of data, it is necessary to assume that the effectiveness of other drugs, and the effect on long-term complications, is no different in those who get GI AEs with metformin than from those who can tolerate it. However, some renal function restrictions also apply to other drugs such as the flozins.
Some previous appraisals of diabetes drugs have often found very little differences in lifetime quality-adjusted life-year (QALY) gains and sometimes in lifetime costs. For example, table 38 of the Evidence Review Group (ERG) report on empagliflozin in combination therapy noted a difference in lifetime cost of £40 and in QALYs of 0.030 – which means 11 days. Another QALY difference noted was 0.003 – 1.1 days. There are two problems with such differences. Firstly, they result in very unstable incremental cost-effectiveness ratios (ICERs). Secondly, and more importantly, such differences are effectively meaningless over a lifetime. It would be useful if NICE could decide what the smallest meaningful difference in QALYs is. A QALY difference of 0.1 would equate to 36 days. If we are modelling over an average 20 years of expected life (most modelling is done over a 40-year time span), those 36 days represent 0.5% of the lifespan. Any difference of 0.1 or fewer QALYs could be regarded as no difference. Perhaps 0.1 QALY is too small and 0.2 or 0.3 would be better, over a mean expected lifespan of 20 years. The meaningful difference should be expressed as a proportion of expected life expectancy.
Similarly, small cost differences should be discarded, especially as many costs will change over the modelling timescale, including drug prices. Current methods assume that drug prices remain constant for the duration.
Targets
The NICE type 2 diabetes guideline update suggests that a HbA1c of 7.5% should be the switching point for intensification (as in CG878) aiming at a target of 7.0% (see section 1.3.4). In section 1.5, Recommendation 38, the target of 6.5% is suggested for most adults managed on the combination of diet and a single drug not associated with hypoglycaemia. However, the draft notes the need for individualised setting of targets.
These individual targets may take the following factors into account:67
-
The duration of diabetes. Patients who have not developed complications such as retinopathy after 20 years’ duration are unlikely to do so, and have less to gain from tight control.
-
Age and life expectancy, and hence time to develop complications. Intensification may be unnecessary and possibly harmful in people over 75 years of age with no symptoms of diabetes.
-
The risk of severe hypoglycaemia.
-
Comorbidities.
-
Patient preferences.
Glycaemic targets are based mainly on reducing the risk of microvascular disease. With a greater number of younger people being diagnosed with type 2 diabetes, glycaemic control becomes increasingly important to reduce the potential microvascular disease burden. There is less evidence that tight control using existing treatments reduces macrovascular disease or overall mortality,68 though this may be because trials are not long enough. In the UKPDS, there was no difference in macrovascular outcomes at study end69 but with the longer-term follow-up, a significant difference emerged70 despite a considerable narrowing of the difference in glycaemic control. However, neither the ACCORD (Action to Control Cardiovascular Risk in Diabetes ) trial71 nor the ADVANCE trial72 showed that intensive control (HbA1c 6.4% and 6.3%, respectively) reduced cardiovascular outcomes compared with standard therapy (HbA1c 7.5% and 7.0%). A meta-analysis by Boussageon et al. 73 showed no reduction in all-cause mortality or cardiovascular death in trials of intensive versus standard regimens.
Targets also need to take account of potential benefits and harms. Vijan et al. 74 used data from the UKPDS to model probable benefits of improving glycaemic control at different ages and by different means (metformin, insulin), taking into account the burden of treatment. For older people the benefits of intensifying treatment could be outweighed by even minor AEs and other inconvenience. A reduction of 1% in HbA1c in a 45-year-old might gain 0.8 QALYs (10 months) but the same reduction in someone aged 75 years might gain 0.06 QALYs (22 days). If that was achieved using insulin, the AEs on quality of life (QoL) from insulin treatment could mean that the net effect was a QALY loss.
Chapter 2 Clinical effectiveness
Methods
Inclusion criteria
Types of studies
We included RCTs with a minimum duration of 24 weeks. Observational studies were included to assess safety data. Some of these were open-label extensions of the trials, but we obtained other studies in two ways. First, we checked the Food and Drug Administration (FDA) and EMA websites for alerts of possible AEs. Second (and more productively), we had auto-alerts running throughout the review, which picked up concerns about diabetic ketoacidosis (DKA) and fractures.
Types of participants
We included trials in people with type 2 diabetes on diet and exercise therapy only or in people on monotherapy with a glucose-lowering agent after a washout period. The target group was patients with type 2 diabetes, unable to take metformin, but this distinction was not made in the trials.
A search was carried out for studies comparing people who can and cannot tolerate metformin, looking for any differences in factors that might affect the modelling, such as weight, BP and cholesterol. Nothing significant was found.
Types of interventions
Only trials of monotherapy were included.
To be included, trials had to investigate canagliflozin (100 mg or 300 mg), dapagliflozin (10 mg) or empagliflozin (10 mg or 25 mg). Eligible comparators were repaglinide, gliclazide as representative of the sulfonylureas, pioglitazone, DPP-4 inhibitors (the gliptins) or placebo.
The three flozins were also compared with each other. As there were no head-to-head trials of the flozins, data from a NMA were required.
Types of outcomes
Studies were eligible if they investigated at least one of the following outcomes:
-
mortality
-
complications of diabetes, including cardiovascular, renal and eye
-
HbA1c/glycaemic control
-
body mass index (BMI)
-
frequency and severity of hypoglycaemia
-
changes in cardiovascular risk factors
-
AEs of treatment, including UTIs, genital infections and malignancies
-
health-related QoL.
Search strategy
Searches were run in Ovid MEDLINE, EMBASE and Web of Science from the inception of the databases until February 2015. Thereafter, weekly auto-alerts were run in PubMed in process and EMBASE until September 2015 to check for newly emerging studies. The searches were not restricted by language or publication type. The full search strategy is shown in Appendix 1.
Selection of studies
Two reviewers independently checked titles and abstracts of the search results against the inclusion criteria. Studies were retrieved in full if they appeared to fulfil the inclusion criteria or when eligibility could not be determined from the search results alone.
Assessment of study quality
The quality of the RCTs was assessed using the Cochrane risk of bias tool, which included the following items (rated as adequate, unclear, not reported or inadequate):
-
method of randomisation
-
allocation concealment
-
blinding of participants and personnel
-
blinding of outcome assessment
-
incomplete outcome data (> 20% dropout regarded as inadequate)
-
intention-to-treat (ITT) analysis
-
selective reporting
-
similarity at baseline
-
other (e.g. power analysis).
Overall quality was expressed in terms of proportion of items rated as ‘adequate’.
Quality was assessed by one reviewer and checked by a second reviewer.
Data extraction
Data were extracted using a predesigned data extraction table, with one reviewer extracting and another reviewer checking the data.
Results were expressed as means and standard deviations (SDs). Standard errors (SEs) and CIs were converted to SDs using the equations provided in the Cochrane handbook. 75 Results for lipids were expressed as millimoles per litre (mmol/l). Cholesterol values expressed in milligrams per decilitre (mg/dl) were converted to mmol/l by dividing by 38.67 and lipid values expressed in milligrams per decilitre were converted to millimoles per litre by dividing by 88.57.
Data summary
Data were summarised using text and tables.
The following subgroup analyses were considered:
-
BMI < 25, 25–29, 30 kg/m2 and over
-
baseline HbA1c.
Results
Search results
Seven studies76–84 were included in the final analysis. We will usually refer to them by first author and year. They were:
Canagliflozin:
Dapagliflozin:
Empagliflozin:
A list of excluded studies, and reasons for exclusion, is in Appendix 2.
Characteristics of included studies
A summary of study characteristics is shown in Table 2.
| Study | Intervention | n | Age (years) | Diabetes duration (years) | HbA1c (%) | BMI (kg/m2) |
|---|---|---|---|---|---|---|
| Canagliflozin | ||||||
| CANTATA-M (Stenlöf 2013) 84 | Canagliflozin 100 mg/day | 195 | 55.1, SD 10.8 | 4.5, SD 4.4 | 8.1, SD 1.0 | 31.3, SD 6.6 |
| Quality 5/9 criteria adequate | Canagliflozin 300 mg/day | 197 | 55.3, SD 10.2 | 4.3, SD 4.7 | 8.0, SD 1.0 | 31.7, SD 6.0 |
| Placebo | 192 | 55.7, SD 10.9 | 4.2, SD 4.1 | 8.0, SD 1.0 | 31.8, SD 6.2 | |
| 100 mg/day HbA1c > 10% | 47 | 49.7, SD 11.1 | 4.6, SD 4.6 | 10.6, SD 0.9 | 30.4, SD 7.1 | |
| 300 mg/day HbA1c > 10% | 44 | 48.8, SD 10.8 | 5.2, SD 4.8 | 10.6, SD 0.6 | 30.5, SD 5.5 | |
| Inagaki 2014 76 | Canagliflozin 100 mg/day | 90 | 58.4, SD 10.4 | 4.7, SD 4.6 | 8.0, SD 0.7 | 25.6, SD 4.2 |
| Quality 8/9 criteria adequate | Placebo | 93 | 58.2, SD 11.0 | 5.6, SD 5.8 | 8.0, SD 0.7 | 25.9, SD 4.4 |
| Dapagliflozin | ||||||
| Ferrannini 2010/Bailey 2015 77 , 78 | Dapagliflozin 10 mg/day a.m. | 70 | 50.6, SD 10.0 | 0.45 (0.1–3.4) (median, IQR) | 8.0, SD 0.9 | 33.6, SD 5.4 |
| Quality 8/9 adequate | Dapagliflozin 10 mg/day p.m. | 76 | 50.7, SD 9.7 | 0.40 (0.1–2.45) | 8.0, SD 1.1 | 33.3, SD 5.6 |
| Placebo | 75 | 52.7, SD 10.3 | 0.5 (0.1–3.4) | 7.8, SD 0.9 | 32.3, SD 5.5 | |
| Dapagliflozin 10 mg/day HbA1c > 10% | 39 | 47.9, SD 12.1 | 1.4 (0.2–3.5) | 10.7, SD 0.9 | 31.1, SD 5.9 | |
| Ji 2014 79 | Dapagliflozin 10 mg/day | 133 | 51.2, SD 9.9 | 1.7, SD 2.8 | 8.3, SD 1.0 | 25.8, SD 3.4 |
| Quality 9/9 adequate | Placebo | 132 | 49.9, SD 10.9 | 1.3, SD 2.0 | 8.4, SD 1.0 | 25.9, SD 3.6 |
| Kaku 2014 80 | Dapagliflozin 10 mg/day | 88 | 57.5, SD 9.3 | 4.9, SD 4.5 | 7.5, SD 0.6 | 26.1, SD 4.5 |
| Quality 6/9 adequate | Placebo | 87 | 60.4, SD 9.7 | 5.3, SD 6.2 | 7.5, SD 0.6 | 25.2, SD 4.4 |
| Empagliflozin | ||||||
| Lewin 2015 81 | Empagliflozin 10 mg/day | 132 | 53.9, SD 10.5 | 32.6% ≤ 1 year | 8.1, SD 1.0 | 31.5, SD 5.7 |
| 45.5% > 1–5 years | ||||||
| 11.4% > 5–10 years | ||||||
| 10.6% > 10 years | ||||||
| Quality 6/9 adequate | Empagliflozin 25 mg/day | 133 | 56.0, SD 9.3 | 36.1% ≤ 1 year | 8.0, SD 1.0 | 31.2, SD 5.7 |
| 36.1% > 1–5 years | ||||||
| 18.8% > 5–10 years | ||||||
| 9.0% > 10 years | ||||||
| Linagliptin 5 mg/day | 133 | 53.8, SD 11.5 | 37.6% ≤ 1 year | 8.1, SD 0.9 | 31.9, SD 5.9 | |
| 42.9% > 1–5 years | ||||||
| 16.5% > 5–10 years | ||||||
| 3.0% > 10 years | ||||||
| Roden 2013/14 82 , 83 | Empagliflozin 10 mg/day | 224 | 56.2, SD 11.6 | 39% ≤ 1 year | 7.9, SD 0.9 | 28.3, SD 5.5 |
| 41% 1–5 years | ||||||
| 13% 5–10 years | ||||||
| 7% > 10 years | ||||||
| Quality 9/9 adequate | Empagliflozin 25 mg/day | 224 | 53.8, SD 11.6 | 41% ≤ 1 year | 7.9, SD 0.9 | 28.2, SD 5.5 |
| 37% 1–5 years | ||||||
| 17% 5–10 years | ||||||
| 6% > 10 years | ||||||
| Sitagliptin 100 mg/day | 223 | 55.1, SD 9.9 | 42% ≤ 1 year | 7.9, SD 0.8 | 28.2, SD 5.2 | |
| 39% 1–5 years | ||||||
| 14% 5–10 years | ||||||
| 5% > 10 years | ||||||
| Placebo | 228 | 54.9, SD 10.9 | 32% ≤ 1 year | 7.9, SD 0.8 | 28.7, SD 6.2 | |
| 46% 1–5 years | ||||||
| 15% 5–10 years | ||||||
| 8% > 10 years | ||||||
| Empagliflozin 25 mg/day HbA1c > 10% | 87 | 50.2, SD 11.3 | 52% ≤ 1 year | 11.5, SD 1.4 | 28.2, SD 5.5 | |
| 25% 1–5 years | ||||||
| 14% 5–10 years | ||||||
| 8% > 10 years | ||||||
Details can be found in Appendix 3.
Study design
The studies were all double-blind multicentre trials and only the two empagliflozin trials had active comparators (Roden 2013/1482,83 and Lewin 201581). Four studies were carried out in centres around the world (CANTATA-M 2013,84 Ferrannini 2010,77 Lewin 2015,81 Roden 2013/1482,83), while three (Inagaki 2014,76 Ji 2014,79 Kaku 201480) were in Asian populations. Primary end points were generally reported at 24 or 26 weeks, but four trials had extensions, following participants up to 52 weeks (CANTATA-M 2013,84 Lewin 201581) or 76–78 weeks (Ferrannini 2010,77 Roden 2013/1482,83). However, the CANTATA-M study (2013)84 did not report results for the placebo group for the extension period, so results were not considered here. All studies were sponsored by industry.
Participants
The studies included between 183 and 986 participants, with 70–228 participants in the main comparison groups. Three studies77,82,84 included small exploratory groups of patients (n = 39–87) with HbA1c > 10%; however, these were not randomised groups (it being unethical not to treat such high levels) and no relevant comparison group existed. Between 34.1% and 58.7% of participants in the main comparison groups were women and mean age was between 50 and 60 years. In most studies, the entry HbA1c of patients was restricted to between 7% and 10% or 10.5%. Most participants had duration of diabetes of less than 5 years. Mean baseline HbA1c was between 7.5% and 8.4% in the main comparison groups and between 10.6% and 11.5% in the high HbA1c groups. BMI was between 25 and 34 kg/m2. Four studies had ethnically mixed populations (CANTATA-M 2013,84 Ferrannini 2010,77 Lewin 2015,81 Roden 2013/14),82,83 while three studies included only Asian participants (Japanese in the Inagaki and Kaku studies,76,80 mainly Chinese in Ji 201479).
Interventions
Two studies76,84 examined canagliflozin. The CANTATA-M (2013) study84 compared 100 or 300 mg/day with placebo. After the main intervention period of 26 weeks, placebo was replaced with 100 mg/day of sitagliptin (double blind) for another 26 weeks. Inagaki 201476 compared 100 mg/day of canagliflozin with placebo. They also included a 200-mg/day group, but this is not considered here because it is not a marketed dose.
Three studies77,79,80 examined dapagliflozin. Ferrannini 201077 compared 10 mg/day of dapagliflozin given in the morning with the same amount given in the evening and with placebo. The trial also included groups receiving 2.5 or 5 mg/day of dapagliflozin, but these were not included in the current analysis as they are not recommended doses. After the main intervention period of 24 weeks, participants in the placebo group were switched to low-dose metformin (500 mg/day, double blind). Both Ji 201479 and Kaku80 compared 10 mg/day of dapagliflozin given in the morning with placebo. Both also included a 5-mg/day group which is not considered here.
Two trials studied empagliflozin. Lewin 201581 compared 10 or 25 mg/day of empagliflozin with 5 mg/day of linagliptin. The trial also included groups receiving a fixed combination of empagliflozin and linagliptin (10 or 25 mg/day of empagliflozin and 5 mg/day of linagliptin), but these were not considered here. Roden 2013/1482,83 compared 10 or 25 mg/day of empagliflozin with 100 mg/day of sitagliptin and with placebo.
Some studies included run-in periods for washout of previous medication (if required) and to establish a diet/exercise regime.
Rescue therapy was provided as outlined in the detailed data tables (see Appendix 3).
Outcomes
The primary outcome in all trials was change in HbA1c from baseline to the end of the main intervention period. Most studies also reported on body weight, blood lipids and BP, as well as on safety parameters including hypoglycaemia. Outcomes with respect to complications of diabetes were not reported, and neither was health-related QoL.
Three trials defined hypoglycaemia as PG levels of ≤ 3.9 mmol/l with or without symptoms (CANTATA-M 2013,84 Lewin 2015,81 Roden 2013/147983). Inagaki 201476 distinguished between symptomatic (typical hypoglycaemic symptoms irrespective of blood glucose levels) and asymptomatic (blood glucose ≤ 3.9 mmol/l without symptoms) hypoglycaemia. In Ji 201479 and Ferrannini 2010,77 hypoglycaemia was defined as PG levels of ≤ 3.5 mmol/l. Only three trials defined major hypoglycaemia (CANTATA-M 2013,84 Ferrannini 2014,77 Ji 201479). All three trials defined major hypoglycaemia as requiring external assistance and two specified associated blood glucose levels of < 3.0 mmol/l (Ferrannini 2014;77 Ji 201479). Kaku et al. 201480 did not define hypoglycaemia.
Note that the 3.9-mmol/l cut-off is above the lower end of the normal range for PG (3.5 mmol/l). It is the threshold for action to avoid hypoglycaemia in people on drugs that may cause it.
Quality of included studies
Details of study quality can be found in Appendix 4.
Two studies fulfilled all the quality criteria (Ji 2014,79 Roden 2013/1482,83), two fulfilled eight of the nine quality criteria (Inagaki 201476 and Ferrannini 201077), one only fulfilled six of nine criteria (Kaku 201480) and two only fulfilled five (CANTATA-M 2013,84 Lewin 201581).
Two studies80,84 did not report on the method of randomisation and three studies80,81,84 did not report on allocation concealment. All studies were double blind, but in three studies80,81,84 it was not clearly reported whether or not outcome assessors were also blinded to study treatment. Rates of discontinuation were reported by all studies and were between 7% and 20%. In most studies, rates of discontinuation were lower than 20% and balanced between groups. In Inagaki 2014,76 only 7% discontinued in the canagliflozin group, whereas 20% discontinued in the placebo group. Only one study77 did not clearly carry out an ITT analysis, and studies gave no evidence of selective reporting, except that in two studies81,84 some results were shown only in graphs and numeric values were not provided. Baseline characteristics were similar for the main comparison groups in all studies, and all studies reported on a power analysis.
Outcomes
A summary of results is shown in Table 3.
| Trials | Time (weeks) | ΔHbA1c (%) | Δ weight (kg) | ΔSBP (mmHg) | ΔTC (mmol/l) | ΔLDL (mmol/l) | ΔHDL (mmol/l) |
|---|---|---|---|---|---|---|---|
| Canagliflozin | |||||||
| CANTATA-M (Stenlöf 2013)84 | |||||||
| Canagliflozin 100 mg/day | 26 | –0.77, SD 0.7 | –2.5, SD 2.4 | –3.3, SD 11.1 | NR | 0, SD 0.67 | 0.11, SD 0.27 |
| Canagliflozin 300 mg/day | 26 | –1.03, SD 0.7 | –3.4, SD 2.4 | –5.0, SD 11.2 | NR | 0.12, SD 0.67 | 0.11, SD 0.27 |
| Placebo | 26 | 0.14, SD 0.7 | –0.5, SD 2.4 | 0.4, SD 11.0 | NR | –0.07, SD 0.65 | 0.04, SD 0.26 |
| Inagaki 201476 | |||||||
| Canagliflozin 100 mg/day | 24 | –0.74, SD 0.66 | –2.6, SD 2.3 | –7.9, SD 10.3 | NR | 0.15, SD 0.51 | 0.07, SD 0.18 |
| Placebo | 24 | 0.29, SD 0.68 | –0.5, SD 2.3 | –2.7, SD 10.1 | NR | –0.01, SD 0.50 | –0.03, SD 0.18 |
| Dapagliflozin | |||||||
| Ferrannini 2010/Bailey 201577,78 | |||||||
| Dapagliflozin 10 mg/day a.m. | 24 | –0.89, SD 0.92 | –3.20, SD 4.18 | –3.6, SD 15.9 | NR | NR | NR |
| Dapagliflozin 10 mg/day p.m. | 24 | –0.79, SD 0.87 | –3.10, SD 3.49 | –2.3, SD 12.2 | NR | NR | NR |
| Placebo | 24 | –0.23, SD 0.87 | –2.20, SD 3.46 | –0.9, SD 15.6 | NR | NR | NR |
| Dapagliflozin 10 mg/day a.m. | 102 | –0.61, SD 0.70 | –3.94, SD 3.52 | 3.9, SD 14.7 | NR | NR | NR |
| Placebo/metformin | 102 | –0.17, SD 0.67 | –1.34, SD 3.34 | 2.1, SD 18.6 | NR | NR | NR |
| Ji 201479 | |||||||
| Dapagliflozin 10 mg/day | 24 | –1.11, SD 0.76 | –2.25, SD 2.60 | –2.3, SD 11.7 | 0.06, SD 0.41 | 0.19, SD 0.72 | 0.30, SD 0.44 |
| Placebo | 24 | –0.29, SD 0.79 | –0.27, SD 2.64 | 0.8, SD 12.8 | –0.04, SD 0.40 | –0.03, SD 0.67 | 0.11, SD 0.41 |
| Kaku 201480 | |||||||
| Dapagliflozin 10 mg/day | 24 | –0.45, SD 0.57 | –2.22, SD 2.44 | –3.2, SD 11.2 | 0.01, SD 0.34 | –0.03, SD 0.57 | 0.16, SD 0.38 |
| Placebo | 24 | –0.06, SD 0.57 | –0.84, SD 2.47 | –0.5, SD 11.4 | 0.02, SD 0.33 | 0.12, SD 0.59 | 0.07, SD 0.40 |
| Empagliflozin | |||||||
| Lewin 201581 | |||||||
| Empagliflozin 10 mg/day | 24 | –0.83, SD 0.56 | –2.3, SD 4.0 | NR | 0.2, SD 1.2 | 0.1, SD 1.2 | 0.1 SE0.0 |
| Empagliflozin 25 mg/day | 24 | –0.95, SD 0.57 | –2.2, SD 4.0 | NR | 0.2, SD 1.2 | 0, SD 1.2 | 0.1 SE0.0 |
| Linagliptin 5 mg/day | 24 | –0.67, SD 0.57 | –0.8, SD 4.0 | NR | –0.1, SD 1.2 | –0.1, SD 1.2 | 0 SE0.0 |
| Empagliflozin 10 mg/day | 52 | –0.85, SD 0.65 | –2.3, SD 4.3 | –2.2, SD 10.5 | NR | NR | NR |
| Empagliflozin 25 mg/day | 52 | –1.01, SD 0.66 | –2.4, SD 4.3 | –2.1, SD 10.5 | NR | NR | NR |
| Linagliptin 5 mg/day | 52 | –0.51, SD 0.66 | –0.3, SD 4.3 | –0.4, SD 10.5 | NR | NR | NR |
| Roden 2013/1482,83 | |||||||
| Empagliflozin 10 mg/day | 24 | –0.66, SD 0.76 | –2.3, SD 2.6 | –2.9, SD 12.2 | 0.07, SD 0.75 | 0.06, SD 0.6 | 0.11, SD 0.15 |
| Empagliflozin 25 mg/day | 24 | –0.78, SD 0.80 | –2.5, SD 2.6 | –3.7, SD 12.2 | 0.15, SD 0.75 | 0.11, SD 0.6 | 0.13, SD 0.15 |
| Sitagliptin 100 mg/day | 24 | –0.66, SD 0.76 | 0.18, SD 2.6 | 0.5, SD 12.2 | 0.08, SD 0.75 | 0.03, SD 0.6 | 0.02, SD 0.15 |
| Placebo | 24 | 0.08, SD 0.81 | –0.33, SD 2.58 | –0.3, SD 12.3 | 0.05, SD 0.75 | 0.04, SD 0.6 | 0.04, SD 0.15 |
Glycated haemoglobin
Canagliflozin
Canagliflozin at 100 mg/day reduced HbA1c by between 0.74% (Inagaki76) and 0.77% (CANTATA-M84) from baseline, which amounted to between 0.91 and 1.03% more than with placebo (p < 0.001 for both). Between 31.5% and 44.6% reached HbA1c < 7%. With 300 mg/day, HbA1c was reduced by 1.03%, which was 1.17% more than with placebo (p < 0.001). In this group, 62.4% reached HbA1c < 7%. In both studies,76,84 reductions in HbA1c were significantly greater in participants with higher HbA1c values.
Dapagliflozin
Dapagliflozin at 10 mg/day reduced HbA1c by between 0.45% (Kaku80) and 1.11% (Ji:79 p < 0.0001) from baseline, which amounted to between 0.39 and 0.82% more than with placebo. Between 48.8% and 51.4% of participants reached HbA1c < 7% compared with between 20.5% and 32.0% in the placebo group. There was no significant difference in HbA1c results depending on whether dapagliflozin was given in the morning or in the evening (Ferrannini 201077). Reductions in HbA1c were greater in the exploratory group with HbA1c > 10% (Ferrannini 201077), as well as in higher HbA1c subgroups of the main study cohorts (Ferrannini 2010,77 Ji 2014,79 Kaku 201480). In Ji 2014, results were similar for the exclusively Chinese cohort. In Ferrannini 2010,77 at 102 weeks, HbA1c reductions were still significantly greater with 10 mg/day dapagliflozin than with low-dose metformin (–0.61% compared with baseline and –0.44% compared with placebo).
Empagliflozin
Empagliflozin at 10 mg/day reduced HbA1c by between 0.66 (Roden,82,83 the monotherapy trial) and 0.83% (Lewin,81 the fixed dose trial) from baseline, which amounted to 0.16% more than with linagliptin, no difference to sitagliptin, and 0.58% more than with placebo. Empagliflozin at 25 mg/day reduced HbA1c by between 0.78 (Roden82,83) and 0.95% (Lewin81) from baseline, which amounted to between 0.28% more than with linagliptin, 0.12% more than with sitagliptin and 0.86% more than with placebo (p < 0.0001 for comparisons with placebo). Between 35.3% and 38.8% of participants reached HbA1c < 7% with 10 mg/day of empagliflozin, 41.5% to 43.6% with 25 mg/day of empagliflozin, 37.5% with sitaglipitin, 32.3% with linagliptin and 12.0% with placebo. Reductions in HbA1c were greater in the exploratory group with HbA1c > 10% (Roden 2013/1482,83), as well as in higher HbA1c subgroups of the main study cohorts (Roden 2013/14,82,83 Lewin 201581). In Lewin 2015,81 at 52 weeks, HbA1c was reduced by 1.01% from baseline, which amounted to 0.5% more than with placebo.
Weight
Canagliflozin
Canagliflozin at 100 mg/day reduced weight by between 2.5 and 2.6 kg from baseline, which amounted to between 1.9 and 2.1 kg more than with placebo (p < 0.001 for both). With 300 mg/day, weight was reduced by 3.4 kg, which was 2.9 kg more than with placebo.
Dapagliflozin
Dapagliflozin at 10 mg/day reduced weight by between 2.2 and 3.2 kg from baseline, which amounted to between 0.9 and 2.0 kg more than with placebo. In the study by Ji et al. 2014,79 results were similar for the exclusively Chinese cohort. In Ferrannini 2010,77 at 102 weeks, weight reductions were still significantly greater with 10 mg/day dapagliflozin than with low-dose metformin (–3.9 kg compared with baseline and –2.6 kg compared with placebo).
Empagliflozin
Empagliflozin at 10 or 25 mg/day reduced weight by between 2.2 and 2.5 kg from baseline, which amounted to 1.4–1.5 kg more than with linagliptin, 2.5–2.7 kg more than with sitagliptin, and 2.0 and 2.2 kg more than with placebo. In Lewin 2015,81 weight was reduced by 2.3 and 2.4 kg with 10 and 25 mg/day of empagliflozin after 52 weeks, which was 2.0 and 2.1 kg more than with linagliptin.
The weight loss on the SGLT2 inhibitors is less than might be expected from the glucose loss in the urine. Rajeev et al. 85 have reviewed possible explanations, such as a compensatory increase in food intake, but the mechanism is uncertain. Ferrannini et al. 86 reported that patients in an empagliflozin trial lost only 38% of the weight loss predicted from the calories lost via glycosuria, and suggested that this was due to an increase in food intake.
Lipids
Canagliflozin
Canagliflozin at 100 mg/day increased low-density lipoprotein cholesterol (LDL-C) levels by between 0 and 0.15 mmol/l from baseline, which amounted to between 0.07 and 0.16 mmol/l more than with placebo. The corresponding high-density lipoprotein cholesterol (HDL-C) levels showed increases of between 0.07 and 0.11 mmol/l from baseline and 0.07–0.1 mmol/l of difference from placebo (p < 0.01). With 300 mg/day, LDL-C was increased by 0.12 mmol/l, which was 0.19 mmol/l more than with placebo, and HDL-C was increased by 0.11 mmol/l, which was 0.07 mmol/l different from placebo. The two studies76,84 did not report total cholesterol (TC) levels.
Dapagliflozin
Ferrannini 201077 did not report on lipid levels. In the other studies, TC changed by 0.01–0.06 mmol/l from baseline in the 10-mg/day dapagliflozin groups, the difference from placebo was between –0.01 and 0.1 mmol/l. LDL-C changed by between 0.19 and –0.03 mmol/l from baseline (difference to placebo between 2.2 and –0.15 mmol/l). HDL-C changed by between 0.16 and 0.3 mmol/l from baseline (difference to placebo between 0.19 and 0.09 mmol/l).
Empagliflozin
Total cholesterol changed by 0.07–0.2 mmol/l from baseline in the 10- or 25-mg/day empagliflozin groups, the difference from control was between 0.02 and 0.3 mmol/l. LDL-C changed by between 0.06 and 0.11 mmol/l from baseline (difference to control 0.02 mmol/l). HDL-C changed by between 0.10 and 0.13 mmol/l from baseline (difference to control between 0.07 and 0.1 mmol/l).
Systolic blood pressure
Canagliflozin
Canagliflozin at 100 mg/day reduced SBP by between 3.3 and 7.9 mmHg from baseline, which amounted to between 3.7 and 5.2 mmHg more than with placebo (p < 0.001). With 300 mg/day, SBP was reduced by 5.0 mmHg, which was 5.4 mmHg more than with placebo.
Dapagliflozin
Dapagliflozin at 10 mg/day reduced SBP by between 2.3 and 3.6 mmHg from baseline, which amounted to between 1.4 and 3.1 mmHg more than with placebo. In Ji 2014,79 results were similar for the exclusively Chinese cohort. In Ferrannini 2010,77 at 102 weeks, SBP was increased by 3.9 mmHg from baseline, which was 1.8 mmHg more than with placebo/low-dose metformin.
Empagliflozin
In Roden 2013,83 empagliflozin at 10 or 25 mg/day reduced SBP by between 2.9 and 3.7 mmHg from baseline, which amounted to between 2.6 and 3.3 mmHg more than in the placebo group. In patients with previously uncontrolled hypertension, the reductions were greater at 3.9 and 5.0 mmHg.
Hypoglycaemia
The definition of hypoglycaemia varied amongst trials, with most using 4.0 mmol/l as the threshold, which seems a little high, when the lower limit of normal is 3.5 mmol/l. 87 The threshold of 4.0 mmol/l is used as an indicator of the need for corrective action, and is also relevant for driving. The three dapagliflozin trials used 3.5 mmol/l to define minor hypoglycaemic events.
Canagliflozin
Rates of hypoglycaemia were not substantially different between canagliflozin and placebo groups. The CANTATA-M study (2013)84 defined hypoglycaemia as PG of under 4.0 mmol/l. They reported rates of hypoglycaemia of 3.6% in the 100-mg/day canagliflozin group, 3.0% in the 300-mg/day group and 2.6% in the placebo group. There were no cases of major hypoglycaemia.
In Inagaki 2014,76 there were two cases of symptomatic (2.2%) and four cases of asymptomatic (4.4%) hypoglycaemia (PG under 4.0 mmol/l) in the 100-mg/day canagliflozin group, and one case of asymptomatic (1.1%) and two cases of symptomatic (2.2%) hypoglycaemia in the placebo group.
Dapagliflozin
Rates of hypoglycaemia were not substantially different between the dapagliflozin and placebo groups. Over 24 weeks, not more than two cases of hypoglycaemia occurred in any of the comparison groups. There were no cases of major hypoglycaemia.
Empagliflozin
In Roden 2013/14,82,83 there was one case of hypoglycaemia (defined as below 4.0 mmol/l or requiring assistance) in each of the comparison groups over 24 weeks (none of them was symptomatic) and two cases in each group at 76 weeks or more (only one of these in the 10-mg/day empagliflozin group was symptomatic). In Lewin 2015,81 there was one case of hypoglycaemia (also defined as under 4.0 mmol/l) in the linagliptin group and the 25-mg/day empagliflozin group, and four cases in the 10-mg/day empagliflozin group. None of these required assistance.
Given the infrequency of reported hypoglycaemia, the similarities of the frequencies of hypoglycaemia in active and placebo arms, and the cut-off level used, the Assessment Group (AG) considers that it would be reasonable to assume that the flozins do not cause hypoglycaemia.
Tables 4 and 5 summarise the occurrence of UTIs and genital tract infections (GTIs), respectively, in the studies considered for this review.
| Inagaki 201476 | Canagliflozin 100 mg | Canagliflozin 200 mg | Placebo | |
|---|---|---|---|---|
| 24 weeks | 1/90 (1.1%) | 1/89 (1.1%) | 1/93 (1.1%) | |
| Stenlöf 2013, 201484,92 | Canagliflozin 100 mg | Canagliflozin 300 mg | Placebo | Canagliflozin 100 mg (high HbA1c) |
| 26 weeks | 14/195 (7.2%) | 10/197 (5.1%) | 8/192 (4.2%) | 3/47 (6.4%) |
| 52 weeks | 16/195 (8.2%) | 14/197 (7.1%) | 12/192 (6.3%) | |
| Kaku 201480 | Dapagliflozin 10 mg | Placebo | ||
| 24 weeks | 2/88 (2.3%) | 2/87 (2.3%) | ||
| Ji 201479 | Dapagliflozin 10 mg | Placebo | ||
| 24 weeks | 7/133 (5.3%) | 4/132 (3.0%) | ||
| 24 weeks (Chinese) | 6/110 (5.5%) | 4/110 (3.6%) | ||
| Ferrannini/Bailey 2010, 201577,78 | Dapagliflozin 10 mg (a.m.) | Placebo | Dapagliflozin 10 mg (p.m.) | |
| 24 weeks | 4/70 (5.7%) | 3/75 (4.0%) | 5/76 (6.6%) | |
| 102 weeks | 6/70 (8.6%) | 3/75 (4.0%) | ||
| 102 weeks (men) | 2/34 (5.9%) | 0/31 (0.0%) | ||
| 102 weeks (women) | 4/36 (11.1%) | 3/44 (6.8%) | ||
| Roden 2013, 201482,83 | Empagliflozin 10 mg | Empagliflozin 25 mg | Placebo | Sitagliptin 100 mg |
| 24 weeks | 15/224 (6.7%) | 12/223 (5.4%) | 12/229 (5.2%) | 11/223 (4.9%) |
| 24 weeks (men) | 3/142 (2.1%) | 2/144 (1.4%) | 3/124 (2.4%) | 4/141 (2.8%) |
| 24 weeks (women) | 12/82 (14.6%) | 10/79 (12.7%) | 9/105 (8.6%) | 7/82 (8.5%) |
| ≥ 76 weeks | 21/224 (9.4%) | 20/224 (8.9%) | 25/228 (11.0%) | 20/223 (9.0%) |
| Lewin 201381 | Empagliflozin 10 mg | Empagliflozin 25 mg | Linagliptin 5 mg | |
| 52 weeks | 22/135 (16.3%) | 14/135 (10.4%) | 14/135 (10.4%) | |
| 52 weeks (men) | 6/77 (9.2%) | 3/64 (3.8%) | 2/75 (2.7%) | |
| 52 weeks (women) | 16/58 (22.9%) | 11/71 (19.3%) | 12/60 (20.0%) |
| Inagaki 201476 | Canagliflozin 100 mg | Canagliflozin 200 mg | Placebo | ||
|---|---|---|---|---|---|
| 24 weeks | 2/90 (2.2%) | 1/89 (1.1%) | 1/93 (1.1%) | ||
| 24 weeks (men) | 0/59 (0.0%) | 0/73 (0.0%) | 1/60 (1.7%) | ||
| 24 weeks (women) | 2/31 (6.5%) | 1/16 (6.3%) | 0/33 (0.0%) | ||
| Stenlöf 2013;84 201492 | Canagliflozin 100 mg | Canagliflozin 300 mg | Placebo | Canagliflozin 100 mg (high HbA1c) | Canagliflozin 300 mg (high HbA1c) |
| 26 weeks | 12/195 (6.2%) | 13/197 (6.6%) | 4/192 (2.1%) | 6/47 (12.8%) | 2/44 (4.5%) |
| 26 weeks (men) | 2/195 (2.5%) | 5/197 (5.6%) | 0/192 (0.0%) | ||
| 26 weeks (women) | 10/195 (8.8%) | 8/197 (7.4%) | 4/192 (3.8%) | ||
| 52 weeks | 18/195 (9.2%) | 18/197 (9.1%) | 5/192 (2.6%) | ||
| 52 weeks (men) | 5/195 (6.2%) | 8/197 (9.0%) | 0/192 (0.0%) | ||
| 52 weeks (women) | 13/195 (11.4%) | 10/197 (9.3%) | 5/192 (4.8%) | ||
| Kaku 201480 | Dapagliflozin 10 mg | Placebo | |||
| 24 weeks | 2/88 (2.3%) | 1/87 (1.1%) | |||
| Ji 201479 | Dapagliflozin 10 mg | Placebo | |||
| 24 weeks | 6/133 (4.5%) | 1/132 (0.8%) | |||
| 24 weeks (Chinese) | 4/110 (3.6%) | 0/110 (0.0%) | |||
| Ferrannini 201077/Bailey 201578 | Dapagliflozin 10 mg (a.m.) | Placebo | Dapagliflozin 10 mg (p.m.) | Dapagliflozin 10 mg (high HbA1c) | |
| 24 weeks | 9/70 (12.9%) | 1/75 (1.3%) | 2/76 (2.6%) | 7/39 (17.9%) | |
| 102 weeks | 11/70 (15.7%) | 1/75 (1.3%) | |||
| 102 weeks (men) | 2/34 (5.9%) | 0/31 (0.0%) | |||
| 102 weeks (women) | 9/36 (25.0%) | 1/44 (2.3%) | |||
| Roden 2013/1482,83 | Empagliflozin 10 mg | Empagliflozin 25 mg | Placebo | Sitagliptin 100 mg | Empagliflozin 25 mg (open-label) |
| 24 weeks | 7/224 (3.1%) | 9/223 (4.0%) | 0/229 (0.0%) | 2/223 (0.9%) | 1/87 (1.1%) |
| 24 weeks (men) | 4/142 (2.8%) | 2/144 (1.4%) | 0/124 (0.0%) | 1/141 (0.7%) | 1/64 (1.6%) |
| 24 weeks (women) | 3/82 (3.7%) | 7/79 (8.9%) | 0/105 (0.0%) | 1/82 (1.2%) | 0/23 (0.0%) |
| ≥ 76 weeks | 13/224 (5.8%) | 14/24 (6.3%) | 4/228 (1.8%) | 2/223 (0.9%) | |
| Lewin 201581 | Empagliflozin 10 mg | Empagliflozin 25 mg | Linagliptin 5 mg | ||
| 52 weeks | 7/135 (5.2%) | 6/135 (4.4%) | 4/135 (3.0%) | ||
| 52 weeks (men) | 2/77 (3.1%) | 1/64 (1.3%) | 1/75 (1.3%) | ||
| 52 weeks (women) | 5/58 (7.1%) | 5/71 (8.8%) | 3/60 (5.0%) |
Adverse events
In this section, we include data from trials and other studies in combination therapy as well as monotherapy.
Urogenital tract infections
Although most UTIs are mild and easily resolved with appropriate antibiotic treatment, more severe infections can be devastating, resulting in bacteraemia, sepsis and death. Because of the frequency with which they occur, UTIs also impose a substantial economic burden on health-care systems. 88
Symptoms of UTI include dysuria (a burning feeling when urinating); frequency of urination; urgency (a feeling of an intense urge to urinate); pain or pressure in the back or lower abdomen; nausea and/or vomiting; cloudy, dark, bloody or strange-smelling urine; feeling tired or shaky; and fever or chills.
The presence of glucose in the urine (glycosuria) creates a suitable environment for the growth and proliferation of bacteria. Glycosuria also promotes increased adherence of bacteria to uroepithelial cells, in particular Escherichia coli. 89 By blocking renal glucose reabsorption, SGLT2 inhibitors cause glycosuria, and increase the risk of UTI in patients. 89
Glycosuria in patients with type 2 diabetes predisposes these patients to develop GTIs, in particular genital mycotic infections, that is vulvovaginal candidiasis in women and candida balanitis in men, as it provides a favourable growth environment for otherwise commensal genital microorganisms. Candida albicans is the most common cause, but Candida glabrata is also an important cause in women with type 2 diabetes. 90
Symptoms of genital candidiasis can include itching; burning; genital discharge; pain during sexual intercourse; soreness; redness in the genital area; and rash.
Both UTIs and GTIs are more common in females. 91
Canagliflozin
In the Inagaki study of Japanese patients with type 2 diabetes,76 urogenital tract infections were infrequent, mild, managed with standard treatments and did not recur in any of the patients. The low incidence may be at least partly because patients with a history of such infections were excluded from the trial. The incidence of UTIs was similar across all groups. 76 GTIs were more frequent in the canagliflozin groups compared with placebo, and mostly occurred in women.
In the Stenlöf study (CANTATA-M study) of predominantly white people,84,92 there were small increases in UTIs with canagliflozin 100 mg (7.2% at 24 weeks, 8.2% at 52 weeks) and 300 mg (5.1% and 7.1%) compared with placebo (4.2% and 6.3%). All UTIs were mild to moderate in severity and no patients discontinued treatment because of a UTI.
Lavalle-González et al. 93 examined the efficacy and safety of canagliflozin 100 mg and canagliflozin 300 mg versus placebo and sitagliptin, for 26 weeks, in patients with type 2 diabetes who were being treated with background metformin; interestingly, the incidence of UTIs was higher only in the canagliflozin-100 mg group. The incidence of genital mycotic infections was higher in females and males with canagliflozin than with placebo, but all were mild to moderate in severity, and responded to standard antifungal treatment. Once again, the incidence was higher in females than males, as expected;93 furthermore, the incidence of genital mycotic infections was higher in patients with high HbA1c. 93 No patients discontinued treatment because of a GTI.
In a separate 52-week, open-label study by Inagaki94 of canagliflozin alone or as add-on to other oral antihyperglycaemic drugs in Japanese patients with diabetes, UTI was present in 2 out of 127 (1.6%) with canagliflozin 100 mg and 5 out of 253 (2.0%) with canagliflozin 200 mg, and none was severe (9). GTIs mostly occurred in females; most of the events were mild in severity and the patients recovered after antifungal therapy.
Leiter et al. 95 also compared canagliflozin 100 mg and canagliflozin 300 mg with glimepiride over 104 weeks in patients with type 2 diabetes that was inadequately controlled with metformin, and found the incidence of UTIs to be higher in the canagliflozin groups.
Interestingly, Neal et al. 96 looked at canagliflozin 100 mg and canagliflozin 300 mg when used together with insulin treatment over a 52-week time period and found no increase in the incidence of UTIs.
Further, in a double-blind, Phase III clinical study,97 patients aged > 55 years to < 80 years inadequately controlled with their current treatment regimen (n = 714) were randomised to receive canagliflozin 100 mg, canagliflozin 300 mg or placebo. Over 2 years, the incidence of GTIs was higher with canagliflozin 100 mg (23.9%) or canagliflozin 300 mg (18.7%) than placebo (4.3%) in women and men (5.6% and 10.9% vs. 1.4%, respectively). The largest number of events occurred within 6 months of treatment initiation and declined with time. Most GTIs were mild to moderate in intensity and responded to standard treatment.
In a pooled analysis by Nicolle et al. ,98 the association between UTIs and canagliflozin treatment based on data from patients with type 2 diabetes enrolled in Phase III clinical studies, and on data from individual Phase III clinical studies in special patient populations, showed that the incidence of UTIs tended to be higher with canagliflozin 100 mg and canagliflozin 300 mg than with placebo, but with no dose dependence.
Finally, a recent report99 based on pooled data from patients with type 2 diabetes enrolled in Phase III clinical studies supports the notion of higher incidences of genital mycotic infections with canagliflozin compared with control patients with type 2 diabetes, GTIs being generally mild to moderate in intensity and responding to standard treatments.
In summary, canagliflozin treatment (≥ 24 weeks) is associated with a higher incidence of urogenital tract infections, but there is no evidence of a dose-dependent response. UTIs were mild to moderate in severity and were amenable to standard treatment with no recurrence. This was also true in patients on pre-existing diabetic medication, that is metformin. GTIs were also more frequent in females, and in older patients (> 55 years but < 80 years) – the risk of GTIs with canagliflozin use is increased mostly early after treatment initiation, that is within the first 6 months. GTIs were also mild to moderate in severity and were amenable to standard treatment.
Dapagliflozin
Dapagliflozin has been shown to have a dose-dependent effect on glycosuria in patients with type 2 diabetes,50 and treatment with dapagliflozin 10 mg as add-on to metformin showed that increased glycosuria with dapagliflozin was maintained for up to 102 weeks. 100 However, there is no demonstrable dose relationship between glycosuria and UTIs. 101
In the Kaku monotherapy study in Japanese patients,80 after 24 weeks, two patients each in the dapagliflozin 10 mg and placebo groups experienced at least one event suggestive of UTIs, but they were mild to moderate in severity. 80 Two patients in the dapagliflozin-10 mg group and one patient in the placebo group experienced one or more GTI events, and GTIs were mild to moderate in severity. 80
In a separate 52-week, open-label Phase III study by Kaku,102 consisting of a single treatment arm with no comparator, dapagliflozin (initiated at 5 mg/day and titrated to 10 mg/day as required) was administered as monotherapy (n = 249) or combination therapy (n = 479) with other antihyperglycaemic agents (AHAs: sulfonylurea, glinides, metformin, alpha-glucosidase inhibitors, thiazolidinediones (TZDs), DPP-4 inhibitors, or GLP-1 receptor agonists) in Japanese patients with type 2 diabetes with inadequate glycaemic control. 102 Urogenital infections were rare, mild to moderate in intensity, and rates were similar in the monotherapy and combination therapy groups. 102
In the study by Ji et al. 79 in predominantly Chinese patients, urogenital tract infections were few, with higher incidence in the dapagliflozin group (5.3%) compared with placebo (3.0%). All reported events were predominantly of mild or moderate intensity. One patient had urethritis of moderate intensity, which resolved with antibiotic treatment; the patient continued with the study.
In the 24-week study by Ferrannini et al. ,77 there was an increased incidence of urogenital tract infections with dapagliflozin treatment compared with placebo. The incidence of urogenital tract infections in the exploratory evening-dose cohort was similar to the morning-dose cohort. Urogenital tract infections resolved with standard treatment and rarely led to discontinuation. 77
In the 102-week Bailey study,100 which is an extension of the 24-week Ferrannini study,77 low-dose metformin 500 mg/day was added to the placebo group. 100 Once again, the incidence of urogenital tract infections with dapagliflozin treatment was higher than with the placebo-plus-low-dose-metformin group. 100 Urogenital tract infections occurred during the first 6 months of dapagliflozin therapy, were more common in women, and most were single episodes of mild or moderate severity. All urogenital tract infections responded to standard management. 103 One patient on dapagliflozin discontinued the study because of UTI.
In triple therapy, dapagliflozin as add-on to metformin plus sulfonylurea, in a 24-week trial, was associated with a higher incidence of urogenital tract infections than in the placebo group. 104
Rosenstock et al.,105 in a 24-week trial against saxagliptin, reported that urogenital infections were more frequent in the dapagliflozin/metformin arm than either saxagliptin/metformin or saxagliptin/dapagliflozin/metformin groups.
In a recent report by Ptaszynska et al. ,106 the association between urogenital tract infections and dapagliflozin treatment based on pooled analyses from 12 placebo-controlled studies of Phase IIb or Phase III clinical studies in patients with type 2 diabetes receiving comparator or dapagliflozin as monotherapy, add-on to antidiabetic therapy or as initial combination with metformin, showed that urogenital tract infections occurred more often with dapagliflozin treatment than with placebo, but were mild or moderate in severity. Pyelonephritis was rare and balanced among treatments.
In summary, dapagliflozin monotherapies and combination therapies (≥ 24 weeks) are associated with a higher incidence of urogenital tract infections. Urogenital infections were generally mild to moderate in severity, tended to occur during the first 6 months of dapagliflozin therapy, were more common in women and were amenable to standard treatment. Urogenital infection rates were similar between monotherapy and combination therapy groups in all studies, with the exception of combination therapies involving saxagliptin. 105
Empagliflozin
Roden et al. 83,107 found that after 24 weeks UTIs were mild to moderate in intensity (only one patient in the empagliflozin-25 mg group discontinued the study) and more common in women but similar in all arms. After 76 weeks, the frequency of UTIs was again similar in all groups. However, the frequency of GTIs was higher in the empagliflozin groups (3.1% and 4.0%) than the placebo (0%) and sitagliptin (0.9%) groups. GTIs were once again more common in women. GTI events were of moderate intensity in three patients in the empagliflozin-25 mg group (one patient discontinued the study); all other events were mild.
Barnett et al. ,108 in the EMPA-REG RENAL (Efficacy and Safety of Empagliflozin in Patients With Type 2 diabetes and Renal Impairment) study of empagliflozin versus placebo in patients with renal impairment, found that both UTIs and GTIs were more frequent in patients with type 2 diabetes with stage 3 chronic kidney disease (CKD) and stage 4 CKD, but not stage 2 CKD.
In the Lewin trial,81 after 52 weeks, urogenital infections were more common in women, and empagliflozin treatment was usually associated with a higher incidence of urogenital infections compared with the placebo group. The exceptions were empagliflozin 25 mg versus placebo for UTI, and empagliflozin 10 mg/linagliptin 5 mg versus placebo for GTI. One patient (receiving empagliflozin 25 mg) had a UTI of severe intensity, but which did not lead to discontinuation of the study drug, and one patient (receiving empagliflozin 10 mg) had chronic pyelonephritis that was mild in intensity and was not considered to be related to the study drug. 81 There were no severe GTI events, but two patients (one patient on empagliflozin 25 mg/linagliptin 5 mg and one patient on empagliflozin 10 mg) discontinued the study because of GTIs.
DeFronzo et al. 109 evaluated combinations of empagliflozin/linagliptin (empagliflozin 10 mg/linagliptin 5 mg and empagliflozin 25 mg/linagliptin 5 mg) as second-line therapy in subjects with type 2 diabetes that was inadequately controlled on metformin. They found that after 52 weeks, the incidence of UTIs was similar across the empagliflozin-25 mg, empagliflozin-10 mg and linagliptin-5 mg groups. In contrast with UTIs, the frequency of GTIs was higher in the empagliflozin-25 mg and empagliflozin-10 mg groups than with the linagliptin-5 mg group; interestingly, the two combinations of empagliflozin/linagliptin therapies had a lower frequency of urogenital infections compared with these three groups.
Similar findings were reported from the Rosenstock placebo-controlled trial in obese (BMI ≥ 30 kg/m2 and ≤ 45 kg/m2), inadequately controlled (HbA1c ≥ 7.5% to ≤ 10%) patients with type 2 diabetes, when empagliflozin was added on to multiple daily injections (MDI) of insulin for 52 weeks, that is similar rates of UTIs and higher rates of GTIs in the empagliflozin groups compared with the placebo group. 110 However, in the EMPA-REG BASAL (Impact of empagliflozin added on to basal insulin in type 2 diabetes inadequately controlled on basal insulin) study, which enrolled patients with type 2 diabetes with BMI ≤ 45 kg/m2, inadequately controlled (HbA1c > 7% to ≤ 10%), despite treatment with basal glargine or detemir insulin (≥ 20 IU/day) or NPH insulin (≥ 14 IU/day), with or without metformin and/or sulfonylurea use, Rosenstock et al. 111 observed that both UTIs as well as GTIs were more frequent in the empagliflozin groups than with the placebo group.
Häring et al. 112 studied the effect of adding either empagliflozin 10 mg or empagliflozin 25 mg or placebo for 24 weeks in patients with type 2 diabetes, inadequately controlled (HbA1c ≥ 7% to ≤ 10%), on metformin and sulfonylurea [EMPA-REG METSU (Empagliflozin as add-on to metformin plus sulfonylurea in patients with type 2 diabetes)] or on metformin alone [EMPA-REG MET]. 113 In both studies, the incidence of UTIs was slightly higher and the incidence of GTIs higher in the empagliflozin groups than in the placebo groups, respectively. 71.2% of patients of the EMPA-REG METSU study continued in a double-blind extension for ≥ 52 weeks, named the EMPA-REG EXTEND METSU study,114 and 72.7% of patients of the EMPA-REG MET study continued in a double-blind extension study for ≥ 52 weeks, named the EMPA-REG EXTEND MET study. 115 Both of these studies demonstrated that UTIs were not more frequent in the empagliflozin groups than the placebo groups, but GTIs were reported in more patients on empagliflozin therapies than placebo. 114,115 Similar findings were found in the 104-week randomised, active-controlled, double-blind, parallel-group Phase III trial comparing empagliflozin and glimepiride as add-on therapy to metformin treatment in patients with type 2 diabetes, the EMPA-REG H2H-SU study. 116
The EMPA-REG PIOGLITAZONE study compared empagliflozin as add-on therapy to pioglitazone (≥ 30 mg/day) with or without metformin (≥ 1500 mg/day), at unchanged doses for ≥ 12 weeks, in patients with type 2 diabetes. 117 Afterwards, 61.2% of patients who completed 24 weeks of treatment continued in a double-blind extension trial for ≥ 52 weeks (total duration ≥ 76 weeks), the EMPA-REG EXTEND™ PIO study. 118 Both of these studies found that UTIs were not more frequent in the empagliflozin groups compared with the placebo arms. However, GTIs were reported in more patients on empagliflozin therapies than placebo. 117,118
In summary, empagliflozin monotherapies and combination therapies (≥ 24 weeks) are associated with a higher incidence of GTIs but not UTIs, as almost all studies reported similar rates of UTI across all treatment and placebo groups. Urogenital infections were more common in women, generally mild to moderate in severity and amenable to standard treatment.
Some trials show little difference in UTI results between the SGTL2 inhibitor and placebo arms. A possible explanation is that the placebo group had glycosuria, due to poor diabetes control, leading to an increased risk of UTI. We note that in a trial of dapagliflozin against an active comparator, glipizide, the difference in UTI rates was greater than in most of the trials against placebo. 119
Frequencies of urinary tract infections
The trials of different drugs reported different rates of UTIs, but a recent meta-analysis of 19 trials found no significant differences in risk amongst the three drugs. 120
When do urinary tract infections occur?
Several trials report cumulative incidence of UTIs. Kaku80 reports 2.3% at 24 weeks and 3.6% by 52 weeks. So 1.3% of UTIs occur in months 7–12. Ferrannini77 reports 5.7% at 24 weeks and 8.6% at 102 weeks. So 2.9% occur from week 24 to week 102. Roden82,83 reports 6.7% at week 24 and 9.4% by week 76. So 2.7% occurred from week 24 to week 76.
Patients on SGLT2 inhibitors who have more than one UTI will be switched to another drug. For modelling purposes, we will assume that:
-
Sixty per cent of flozin-induced UTIs will occur in the first 6 months.
-
All flozin-induced UTIs will occur in the first 2 years.
-
Two UTIs will trigger a change of therapy.
Diabetic ketoacidosis
Diabetic ketoacidosis (DKA) is a serious complication of diabetes, seen predominantly, but not exclusively, in type 1 diabetes. It is life-threatening. It requires admission to hospital for intensive treatment with intravenous infusion and insulin. It is therefore costly to health care.
Cases of DKA have been reported associated with treatment with SGLT2 inhibitors. The EMA has announced a review of the risk of DKA amongst people who are treated with these drugs. 121 It notes that 101 cases of DKA had been reported worldwide in patients who are treated with SGLT2 inhibitors, which, based on an estimated 500,000 patient-years of use, would be a risk of 1 in 5000 patient-years. The EMA also notes that in some cases the level of blood glucose was much lower than is usually seen in DKA (‘euglycaemic DKA’) and expressed concern that this might lead to delays in diagnosis.
In the USA, the FDA has also announced a review and has issued a safety announcement. 122 The FDA had received notifications of DKA in patients treated with SGLT2 inhibitors.
The manufacturers of canagliflozin, Janssen, have reported that in their series of trials, the incidence of DKA was very low – 0.5 per 1000 patient-years on canagliflozin 100 mg daily, 0.8 on canagliflozin 300 mg daily and 0.2 per 1000 patient-years on placebo. 123 The other manufacturers have yet to publish data, but enquiries by Rosenstock and Ferrannini124 for a commentary in Diabetes Care elicited rates from the manufacturer for dapagliflozin and empagliflozin of under 0.1%, though no details are given of time period. Rosenstock and Ferrannini124 suggest that some of the cases reported in the USA may have been in patients with type 1 diabetes.
With greater use of the SGLT2 inhibitors, rare adverse events can be expected. Acute pancreatitis has been reported shortly after canagliflozin was started,125 but cause and effect is not proven. A case of severe hypercalcaemia has been reported,126 possibly linked to the osmotic diuresis and ingestion of calcium-containing indigestion tablets.
Late reporting of adverse events is not unusual. The FDA have also recently issued a safety alert on the gliptins, the DPP-4 inhibitors, after reports of severe joint pain. 127
What is becoming clearer as evidence accumulates, is that the SGLT2 inhibitors have actions beyond the kidney, for example on the pancreas, with an increase in plasma glucagon levels, and effects on blood lipids. 128
Cardiovascular safety
All three of the SGLT2 inhibitors reviewed in this report are in large, long-term cardiovascular studies, mandated by the FDA to satisfy the post-marketing requirements in the USA. The results of these (CANVAS129 for canagliflozin and DECLARE130 for dapagliflozin) are awaited but there have been early reports of reductions in cardiovascular events. 131 The results of the empagliflozin study are reported below.
Bone health
The FDA has issued a warning on decreases in bone density and an increased risk of fractures in people taking canagliflozin, possibly through effects on phosphate metabolism involving parathyroid hormone, fibroblast growth factor 23 and vitamin D. 132 Fractures have also been reported amongst people taking dapagliflozin. Kohan et al. 133 randomised 252 people with moderate renal impairment (94% in the range 30–59 ml/minute) to placebo or dapagliflozin. HbA1c fell by 0.44% on dapagliflozin 10 mg daily and by 0.32% on placebo, but there was good weight loss on dapagliflozin (reduction by 1.89 kg) and a useful reduction in SBP (6.8 mmHg). However, 8 of 85 (9.4%) people on dapagliflozin 10 mg suffered fractures, compared with none on placebo.
Kwon134 reviewed bone safety and canagliflozin for the FDA, using data from the canagliflozin Phase 3 programme, for 6177 patients on the drug and 3262 on other treatments. The proportions suffering fractures were 2.1% and 1.6% for canagliflozin and others, respectively, with most of the difference being in low trauma fractures (1.6% and 1.2%), with the main difference being in the upper limb (0.7% vs. 0.3%). The incidence per 1000 patient-years was 18.1 for canagliflozin regimens and 14.2 for other regimens. So the risk of fracture is small but increased by around 30% in people taking canagliflozin.
The mechanism by which canagliflozin increases fracture risk is uncertain. 135 An important issue is that the fracture rate is not increased in the first year of treatment, but appears later. So any increase in fracture risk may not be detected in short trials (Taylor 2015135). (The FDA warning, however, states that fractures can occur as early as 12 weeks after starting canagliflozin.)
EMPA-REG OUTCOME study
The results of this trial were published on 17 September 2015. 136 The trial recruited 7020 patients at high risk of CVD. High risk included having a history of MI or stroke, coronary artery stenosis of 50% or more, previous coronary revascularisation and peripheral vascular disease (PVD). The trial scores quite well with the Cochrane risk of bias score (see Appendix 5) with the deficiencies probably due to failure to provide details rather than design or execution flaws.
Patients were randomised to placebo, and empagliflozin 10 mg or 25 mg. Patients were recruited from 590 sites in 42 countries, an average of 12 per site: 72% were white, 21% Asian and 5% black, including African-Americans. Of the 21% Asian, 19% were from 10 countries with a mix of South and East Asian centres, ranging from India to Japan and Korea. There were no centres in China except Hong Kong, but there were centres in Taiwan and Singapore. Numbers are not given by country. There were 12 UK centres, and 41% of all recruits were from Europe, including Russia. The mean HbA1c at baseline was just under 8.1%. In 57% of patients, duration of diabetes was over 10 years. At baseline, 74% were on metformin, 48% on insulin, 43% on sulfonylureas and 11% on DPP-4 inhibitors. About 29% were on monotherapy, 2% on no drugs and 45% on dual therapy, implying that 24% were on more complex regimens with three drugs or more. Discontinuation from trial medication occurred in 29% of the placebo group and 23% of the empagliflozin group, with 13% and 11.5% being due to adverse events (which did not include need for rescue therapy).
After 12 weeks, other glucose-lowering drugs could be adjusted or added. Targets were not specified centrally but left to local guidelines. Changes were made in 31.5% of the placebo group and 19.5% of the empagliflozin group. The changes in the empagliflozin group included the introduction of insulin (5.8%), a DPP-4 inhibitor (5.4%), a sulfonylurea (3.8%), metformin (3.7%), a TZD (1.2%) or a GLP-1 analogue (1.4%). This means that we cannot use the drift upwards of HbA1c of 0.1% per year in the empagliflozin group as a guide to progression of diabetes. Despite the addition of other glucose-lowering drugs, the mean HbA1c at week 206 was 7.81% in the empagliflozin group and 8.16% in the placebo group, a difference of 0.35%.
Being a high-risk group, at baseline 95% were on antihypertensive medications (81% on angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin-receptor blockers (ARBs); 65% on beta-blockers; 33% on calcium channel blockers). Seventy-seven per cent were on statins, 9% on fibrates and 4% on ezetimibe. Forty-three per cent were on diuretics, unspecified, but loop diuretics are not recommended for use with canagliflozin and dapagliflozin.
A range of subgroups was specified in the protocol. 137 The results were analysed by staff from Boehringer Ingelheim, who co-funded it with Eli Lilly. The two empagliflozin groups were pooled for the analysis, because event rates were almost identical (CVD deaths 3.8% with 10 mg and 3.5% with 25 mg). When the main outcomes were assessed for the 10- and 25-mg empagliflozin groups separately, the differences were not significantly different from the placebo group.
The primary outcome was a composite of death from a cardiovascular cause, non-fatal MI and non-fatal stroke. The primary outcome occurred in 10.5% of people on empagliflozin and in 12.1% of those on placebo, giving a hazard ratio (HR) 0.86 (95% CI 0.74 to 0.99). Table 6 shows some of the outcomes.
| Results | Placebo | Empagliflozin |
|---|---|---|
| No. of patients | 2333 | 4687 |
| All-cause mortality | 8.3% | 5.7% |
| Cardiovascular mortality | 5.9% | 3.7% |
| Non-cardiovascular mortality | 2.4% | 2.0% |
| Primary composite outcome | 12.1% | 10.5% |
| MI | ||
| Non-fatal | 5.2% | 4.5% |
| Fatal | 0.2% | 0.3% |
| Silent | 1.2% | 1.6% |
| Stroke | 3.0% | 3.5% |
| Fatal | 0.4% | 0.3% |
| Non-fatal | 2.6% | 3.2% |
| Hospital admission | ||
| Heart failure | 4.1% | 2.7% |
| Unstable angina | 2.8% | 2.8% |
| UTIs | 18.1% | 18.0% |
| GTIs | 1.8% | 6.4% |
| DKA | 1 event | 4 events |
The DKA rate in the empagliflozin was double that in the placebo group, but the excess risk was only about 1 in 1500 per year, and numbers were very small.
The proportion of fatal to non-fatal MIs looks odd – 5 deaths out of 126 MIs. Similarly, of 69 strokes, only nine were fatal. This raises the question of where the 137 cardiovascular deaths come from.
Supplementary table S5 reports 11 deaths from acute MI in the placebo group and 15 in the pooled empagliflozin group, but these figures do not match those in table 1 in the main paper. The figures for fatal stroke also differ between main text and supplement, 11 versus 9 for placebo, 16 versus 14 for empagliflozin.
Supplementary table S5 gives cardiovascular deaths reproduced in Table 7.
| Cause | Placebo (%) | Empagliflozin (%) | Difference (%) |
|---|---|---|---|
| Sudden death | 1.6 | 1.1 | 0.5 |
| Heart failure | 0.8 | 0.2 | 0.6 |
| Acute MI | 0.5 | 0.3 | 0.2 |
| Stroke | 0.5 | 0.3 | 0.2 |
| Cardiogenic shock | 0.1 | 0.1 | 0 |
| Other cardiovascular deaths | 2.4 | 1.6 | 0.8 |
Total mortality was 8.3% in the placebo group and 5.7% in the pooled empagliflozin, a difference of 2.6%.
The ill-defined ‘other cardiovascular deaths’ constitute 41% and 44% of all cardiovascular deaths for placebo and empagliflozin, respectively, and they account for 29% and 28% of all deaths, respectively. Three causes account for 83% of the observed difference in mortality: sudden death, heart failure and ‘other cardiovascular deaths’.
The totals of proportions having the individual events in the composite primary outcomes exceeds the primary outcome proportion, presumably because some patients had more than one event.
The Kaplan–Meier curves diverge after about 2 months, with curious accelerations in the placebo group curves after 42 months.
How were these cardiovascular benefits achieved?
Glycated haemoglobin was 0.57% lower in the empagliflozin group than the placebo arm at week 12, but steadily narrowed thereafter to 0.35% at week 206. Given the weak relationship between glycaemic control and CVD,68 this difference seems unlikely to have caused the difference.
Systolic blood pressure fell by about 5.5 mmHg in the empagliflozin group and by about 2 mmHg in the placebo group by week 16, but the difference between the empagliflozin and placebo groups narrowed thereafter to about 2 mmHg. There was no difference in BP lowering between doses. Diastolic blood pressure (DBP) fell by about 2.5 mmHg in all three arms. By 206 weeks, there was no difference in DBP between empagliflozin and placebo groups.
For some complications of diabetes, BP control is as important as glycaemic control, as was shown by the UKPDS study, where ‘tight’ BP control (with a mean BP of 144/82 mmHg, it was not really tight) reduced overall mortality by 32% (RR 0.68, 95% CI 0.49 to 0.94). 138
Weight was reduced by 2 kg in the empagliflozin group and by 1.2 kg in the placebo group.
Changes in lipids were small. On empagliflozin 25 mg, LDL-C rose (placebo adjusted) from baseline 2.2 mmol/l to about 2.3 by 12 months, stayed there until about 136 weeks then fell to about 2.21 mmol/l, just below the placebo level. On empagliflozin 25 mg, HDL-C rose by about 0.05 mmol/l then fell slightly. The placebo level rose by about 0.01 mmol/l. (Figures derived from graph – data not provided in text.) The baseline TC/high-density lipoprotein (HDL) ratio was 3.5, perhaps because so many were on statins and other lipid-lowering drugs. These lipid changes seem insufficient to explain the mortality results.
However, the combination of factors might have more effect than the individual ones, and the reduction in BP, though small, is similar to that seen in the Heart Outcomes Prevention Evaluation (HOPE) trial,139 in which a reduction of 2–4 mmHg in BP from ramipril (an ACEI) was thought by the HOPE authors to be sufficient to explain about one-quarter of the observed 25% reduction in cardiovascular events, in another high-risk group with vascular disease and/or diabetes.
Discontinuation rates from study drugs due to adverse events are reported as 19.4% for placebo and 17.3% for empagliflozin in the paper but as 13.0% and 11.5% in appendix H.
Subgroup analysis for the primary composite outcome shows:
-
Statistically significant benefit in Asians (a mixed group, with about 44% from North East Asia) but not in white people, though death from cardiovascular causes is significantly reduced in white people. This implies that white people gained less for non-fatal MI and stroke. The Asian group is rather heterogeneous and no details are given of risks in East Asians versus South Asians. There are differences in the balance of insulin deficiency and insulin resistance.
-
Statistically significant benefit in those with baseline HbA1c under 8.5% but not in those above that.
-
Statistically significant benefit in those with BMI of < 30 kg/m2 but not in those above that level.
-
Statistically significant benefit in those on insulin but not in those on non-insulin regimens; 51% in both groups were on insulin.
-
Greater benefit in those aged over 65 years.
In a number of subgroups, reductions in cardiovascular death were statistically significant when reductions in the primary outcome were not. To recall, the primary outcome was cardiovascular death, non-fatal MI and non-fatal stroke. Of 282 primary outcome events in the placebo group, 49% were cardiovascular deaths. Of 490 primary outcome events in the empagliflozin groups, 35% were cardiovascular deaths. So a greater proportion of events in the empagliflozin group was of non-fatal events. The fact that in some subgroups, cardiovascular death rates are significantly different when the composite primary outcome is not, is explained by a lack of any statistically significant differences in non-fatal MI and non-fatal stroke.
Non-fatal MI was diagnosed on the basis of symptoms plus one or more of:
-
troponin or creatine kinase-MB
-
ECG changes
-
imaging of new non-viable or non-motile myocardium.
This study has attracted worldwide interest. It contrasts with the equivalent studies with the DPP-4 inhibitors, which did not show any reduction in cardiovascular outcomes. They were:
-
SAVOUR for saxagliptin (The Saxagliptin assessment Of Vascular Outcomes Recorded in patients with diabetes mellitus). 140
-
EXAMINE for alogliptin (Examination of cardiovascular outcomes with alogliptin versus standard of care in patients with type 2 diabetes mellitus and acute coronary syndrome). 141
-
TECOS for sitagliptin (Trial Evaluating Cardiovascular Outcomes with Sitagliptin). 142
There was no difference in cardiovascular outcomes in SAVOUR except that more patients on saxagliptin than on placebo (3.5% vs. 2.8%: HR 1.27, 95% CI 1.07 to 1.51) were admitted to hospital with heart failure.
The findings in EXAMINE were similar – no difference in end points – except an increase in heart failure in a subgroup analysis of patients with no heart failure at baseline (2.2% on alogliptin, 1.3% on placebo; HR 1.76, 95% CI 1.07 to 2.90).
The TECOS results were again similar – no differences in a composite primary end point of cardiovascular death, non-fatal MI and non-fatal stroke nor in other end points including hospital admission for heart failure and death from any cause.
These results were seen as providing reassurance, in the wake of the rosiglitazone story with an increase in cardiovascular events. 143 They could also be seen as disappointing in that they did not reduce the most important complication of diabetes, the excess of CVD. However, as has been pointed out by Hirshberg and Katz,144 these trials ran for only a few years and showed only small changes in HbA1c (reductions of 0.27–0.36% compared with placebo), so reducing the chance of showing reductions in cardiovascular events.
The subgroup analyses in EMPA-REG OUTCOME (Empagliflozin Cardiovascular Outcome Event Trial in Type 2 diabetes Mellitus Patients) trial are interesting. 136 Younger, lighter, better-controlled patients did better, as did the Asian group. There could be overlapping features here in that the East Asians tend to be lighter. Further details will no doubt be released but with such a very large study, further analysis is bound to take time.
The differences observed do not seem sufficient to justify the very optimistic media coverage, such as reports that ‘Lilly’s Jardiance diabetes pill could be a $6 billion-a-year blockbuster’. 145
It is worth noting that the EMPA-REG OUTCOME trial136 involved patients at high cardiovascular risk who had had diabetes for many years and who were on complex regimens for their diabetes. The results are not applicable to people starting monotherapy with empagliflozin.
Chapter 3 Network meta-analysis of sodium–glucose co-transporter 2 inhibitors and comparators in monotherapy
One question is whether or not all of the three flozins in this appraisal should be regarded as equally potent. In addition to the SGLT2 transport system in the kidney, there is also a related transport system in the gut, SGLT1. Most SGLT2 inhibitors appear to be highly selective, with no significant effect on SGLT1, but one of the class, canagliflozin, does affect SGLT1, and it has been suggested by Polidori et al. 53 that canagliflozin may reduce blood glucose by a dual action in both gut and kidney. However, that suggestion followed a very short-term study of canagliflozin in healthy individuals, and the gut effect was seen only with higher doses, such as 300 mg, and not with the 100-mg dose.
A study by Stein et al. 54 from Janssen Research and Development looked at the SGLT1 effect in people with type 2 diabetes and found that canagliflozin 300 mg, but not 150 mg, reduced postprandial PG, by about 0.5 mmol/l (from graph) for about 2 hours after administration, as it depends on an intestinal drug action not a systemic one. Hence this reduction would occur only after the single daily dose.
If the SGLT1 effect is clinically significant in people with type 2 diabetes then one might expect canagliflozin 300 mg to be more potent in reducing HbA1c levels than SGLT2 inhibitors without the SGTL1 effect.
The CANTATA-M study 201384 did not report weight SDs for the two doses of canagliflozin so this study could not be included in weight comparison. The weight data for canagliflozin 100 mg comes from the Inagaki 2014 study,76 in which the 100- and 200-mg doses of canagliflozin were used. We excluded the 200-mg dose as this is not a standard dose.
For assessing the relative merits of the SGLT2 inhibitors in monotherapy, the first comparison is amongst the usual starting doses: canagliflozin 100 mg, dapagliflozin 10 mg and empagliflozin 10 mg. By including empagliflozin 25 mg and canagliflozin 300 mg, we can assess the effect of increasing the doses. However, a caveat is necessary. The empagliflozin 25 mg and canagliflozin 300 mg are used in people who can tolerate the starting dose, but have an insufficient HbA1c response. Such patients may not respond as well to SGLT2 inhibition as the average patient, and the effect of increasing the doses may be less than that seen in the trials.
The aim of our NMA was not only to compare canagliflozin, empagliflozin and dapagliflozin, but also to assess their effects relative to active comparators.
Methods
Selection of trials
We applied the following selection criteria:
-
Trials of 24–26 weeks, starting with placebo as the common comparator.
-
Trials only of selected drugs. For example, we did not include all sulfonylureas but focused on gliclazide, which should be the sulfonylurea for comparison in trials of newer agents. 26 We did not include all DPP-4 inhibitors, originally intending to focus on sitagliptin.
-
Baseline HbA1c of 7.5% or more, based on the NICE guideline for treatment intensification. 8 There are some RCTs in patients with lower baseline HbA1c values, but they have less scope for lowering HbA1c.
-
Dropout rates of no more than 20%.
However, the first of these criteria had to be relaxed in order to include gliclazide, as we found no trials of gliclazide against placebo. We had to indirectly link gliclazide with placebo via linagliptin and pioglitazone. All of the other drugs included had trials against placebo. Unfortunately, we found no satisfactory trials of repaglinide for inclusion.
We searched the lists of trials used for the NICE guideline group on type 2 diabetes, but carried out additional searches specifically for gliclazide trials, as the guideline group pooled trials of sulfonylureas.
Evidence on repaglinide
The annex to the NICE guideline CG87 lists seven studies on repaglinide but only three gave 24-week data. 16
Abbatecola et al. 146 report a randomised trial comparing repaglinide and glibenclamide. The main outcome measure was cognitive function, with the hypothesis being the tighter control of postprandial PG would reduce cognitive decline, in patients aged 60–78 years, mean age 74 years. [Note that according to the British National Formulary (BNF), repaglinide is ‘not recommended’ in people over 75 years. 147]
The baseline HbA1c in patients in this trial was quite low – 7.25%. So it is an exclusion for our purposes. The final HbA1c is not given in the text, but from the graph is about 6.6% with no difference between the drugs.
In the Jovanovic 2000 trial,148 patients were randomised to placebo, and repaglinide 1 mg or 4 mg daily. Under 30% of patients were drug naive, and 10% had been on two glucose-lowering drugs. Baseline HbA1c was 8.6% in the placebo group and rose to 10% at 24 weeks. In those who had been on previous combination treatment, HbA1c rose by 1.8% on placebo, and fell by inconsequential 0.07% and 0.05% on repaglinide 1 mg and 4 mg. Dropout rates were very high – 60% in the placebo group, of which half had to start rescue treatment, and 23% and 31% in the repaglinide groups. Given that 70% had been on prior drug therapy, the high proportion in the placebo group requiring rescue treatment is not surprising, but it devalues any conclusions drawn from this study.
The third 24-week study used by NICE was by Saleem et al. 149 from Lahore. This compared the effects on HbA1c of repaglinide and glibenclamide. It says that 50 patients were ‘randomly selected’ for each group but gives no details of how this was done, or on allocation concealment. Blinding was not feasible because of different dosing frequencies – once or twice daily for glibenclamide, preprandially up to three times a day for repaglinide. No patients are reported to have dropped out. The recruitment period in this study (March 2006 to March 2007) overlaps with that for another paper by the same group (Shah et al. 2011150), which reports only PG, in 200 patients. The changes in fasting plasma glucose (FPG) and 2-hour PG are almost identical in the two studies. 149,150 The Shah paper150 has no HbA1c data. Saleem et al. 2011149 report a reduction by 24 weeks in HbA1c of 0.6% on repaglinide and 0.4% on glibenclamide. The final repaglinide dose was 4.27 mg daily, and the final glibenclamide dose was 8.8 mg (identical to the Shah et al. article150). The Shah article150 states that dosages were reported as being adjusted based on glucose levels, so it is not clear why the final glucose levels are so different, with a reduction in FPG in the repaglinide group which is almost double that in the glibenclamide group. No details of source of funding are given. We think that the patients in the Saleem study149 may be a subset of those in the Shah study. 150
We also note the trial by Jibran et al. 151 This paper is very similar to the Saleem et al. 2011149 paper, but has no authors in common. The numbers of patients are the same, and values for baseline age, weight and BMI have identical means and SDs. The result tables are identical in means and SDs. Much of the text is the same. The patients are said to have been recruited in different time periods.
Glibenclamide is a first-generation SU and was not included in our NMA, so the Saleem149/Jibran151 and Abbatecola146 trials are not included.
The NICE guideline group also considered evidence on repaglinide at 12 months, from four trials. These included the Abbatecola and Saleem trials146,149 mentioned above, and two better-quality ones by Derosa et al. 152 and Marbury et al. 153 The Derosa trial152 compared repaglinide with glimepiride, in patients with mean HbA1c of 8.0%, and showed a reduction of 1.2% at 12 months. We use the effect sizes from this study in our modelling, for changes in HbA1c, SBP and weight. However, we prefer gliclazide to glimepiride, so the Derosa trial152 is not included in our NMA. The Marbury trial153 recruited both patients who had never had any glucose-lowering drugs (13%) and those who had previously been treated with sulfonylureas and other drugs (87%). The reduction in HbA1c was much greater in the pharmacotherapy-naive group – 1.3% at 12 months, similar to the Derosa152 results. In previously treated patients, the HbA1c actually rose by 0.3%. Mean baseline HbA1c was quite high at 8.7% so the results may be less applicable to patients treated according to the NICE guidelines with close monitoring and prompt intensification when HbA1c exceeded 7.5%. The sulfonylurea comparator was glibenclamide, so the trial is not used in our NMA.
The network diagram is shown in Figure 2. The included trials are listed in Table 8.
FIGURE 2.
Network meta-analysis diagram. b.i.d., twice daily.
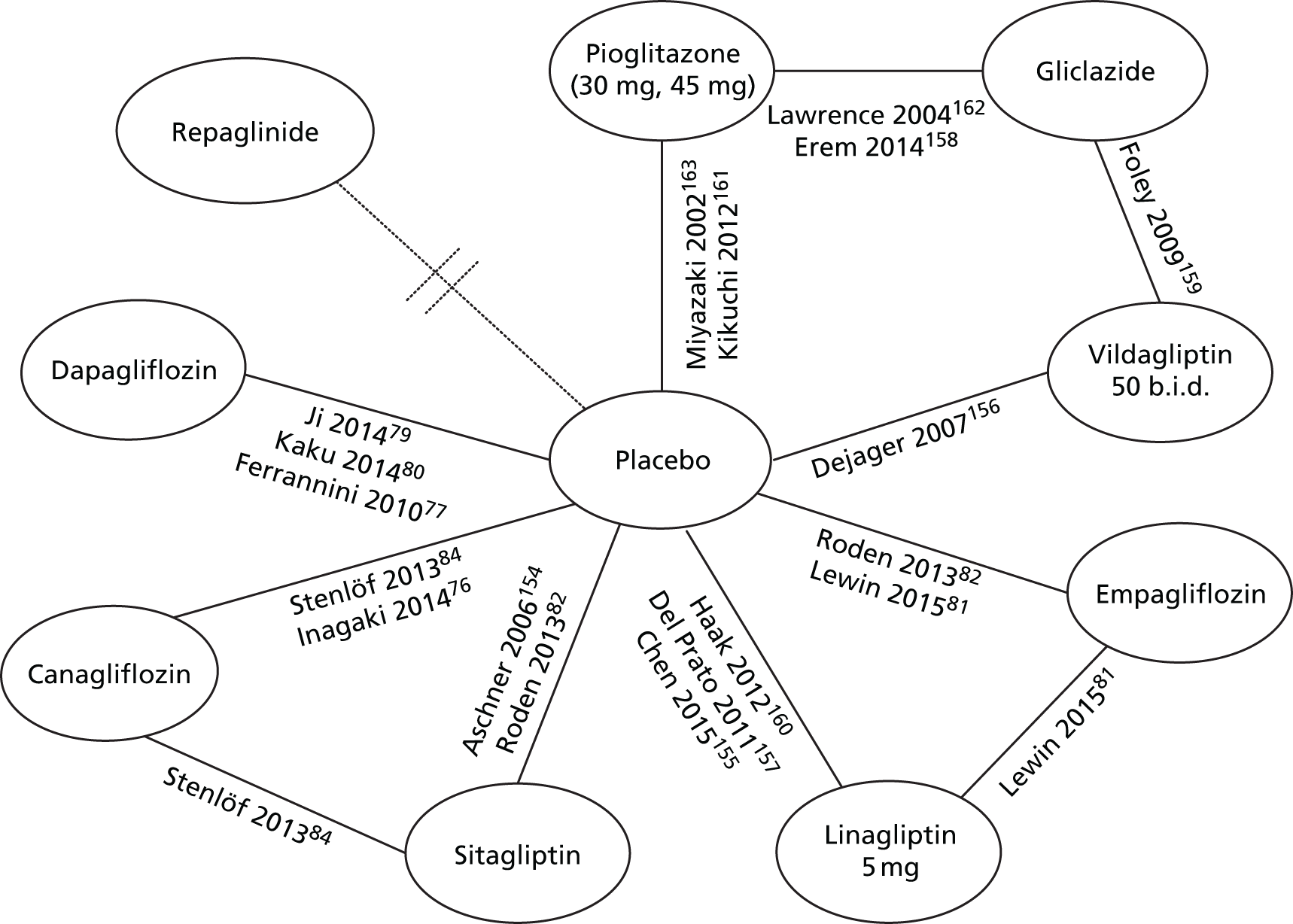
| Trial | Drug | Comparator | Notes |
|---|---|---|---|
| Inclusions | |||
| Aschner 2006154 | Sitagliptin 100 mg | Placebo | |
| Chen 2015155 | Linagliptin | Placebo | |
| Dejager 2007156 | Vildagliptin | Placebo | |
| Del Prato 2011157 | Linagliptin | Placebo | |
| Erem 2014158 | Pioglitazone | Gliclazide | |
| Ferranini 201077 | Dapagliflozin | Placebo | |
| Foley 2009159 | Gliclazide | Vildagliptin | |
| Haak 2012160 | Linagliptin | Placebo | |
| Inagaki 201476 | Canagliflozin 100 mg | Placebo | |
| Ji 201479 | Dapagliflozin | Placebo | |
| Kaku 201480 | Dapagliflozin | Placebo | |
| Kikuchi 2012161 | Pioglitazone | Placebo | |
| Lawrence 2004162 | Pioglitazone | Gliclazide | |
| Lewin 201581 | Empagliflozin | Placebo | Linagliptin |
| Miyazaki 2002163 | Pioglitazone | Placebo | |
| Roden 201383 | Empagliflozin | Placebo | Sitagliptin |
| Stenlöf 201384 | Canagliflozin 100 and 300 mg | Placebo | Sitagliptin in extension |
Summary measures
The primary measures of treatment effect were the mean differences (MDs) in change from baseline for HbA1c, weight gain and SBP. A negative value indicates improvement in the outcome. In the case of missing values for SD of change from baseline values, the SD was imputed as described in detail in the Cochrane Handbook. 75 In brief, we assumed a correlation of r = 0.5 between baseline and follow-up to estimate SD for change from baseline.
Data synthesis and model implementation
We used a Bayesian NMA method to analyse all the data, preserving randomised treatment effects within trials and accounting for correlation between comparisons with three arms or four arms using the freely available software, WinBUGS 1.4.3 (MRC Biostatistics Unit, Cambridge, UK). The statistical heterogeneity in treatment effect estimates was estimated using between-study variance (i.e. square root of the SD of underlying effects across trials) with 95% CrI. 164 To estimate inconsistency in the networks of evidence, we calculated the difference between indirect and direct estimates whenever indirect estimates could be constructed with a single common comparator. 164 Inconsistency was defined as disagreement between direct and indirect evidence with a 95% CrI excluding 0 for MD. 165 The model convergence was assessed using trace plots and the Brooks–Gelman–Rubin statistic. 166 The analysis was undertaken using two Markov chains, which were run simultaneously. The model was found to be converging adequately after 20,000 samples for both chains. We ran the model further using 70,000 samples and the results presented in the paper are based on these samples as we discarded the first 20,000 samples.
We used both the fixed- and random-effects models. The Bayesian deviance information criterion (DIC) was used to compare the two models to see which was appropriate to compare treatment effects. The DIC measures the fit of the model while penalising it for the number of effective parameters. The model with the lowest DIC value was considered as the most appropriate NMA model. Based on DIC values obtained from the two models and also because of small number of studies available for the NMA, a fixed-effects model was chosen. Owing to small number of studies, it would have been difficult to estimate between studies variance if a random-effects model was implemented.
All results are reported as posterior medians of MDs with corresponding 95% CrIs. CrIs are the Bayesian equivalent of classic CIs. A 95% CrI can be interpreted as there being a 95% probability that the parameter takes a value in the specified range. Drugs were not ranked, but were considered in terms of effect sizes and uncertainties.
Results
Glycated haemoglobin (haemoglobin A1c)
Networks of eligible comparisons for HbA1c are provided in Figure 3, showing predominantly pairwise comparisons of drugs with placebo. There were eleven comparisons (ten drugs plus placebo).
FIGURE 3.
Network plot: HbA1c.

Figure 4 and Table 9 display a caterpillar plot of the MD and 95% CrIs for all comparisons for mean change in HbA1c (at 24 weeks) from baseline. All SGLT2 inhibitors were significantly more effective than placebo in reducing mean change in HbA1c from baseline, with the reduction ranging from –1.19% to –0.59%. Canagliflozin 100 mg and 300 mg and pioglitazone were significantly more effective in reducing mean change in HbA1c from baseline than linagliptin 5 mg, dapagliflozin 10 mg and vildagliptin 50 mg. The reductions in HbA1c from baseline were similar for linagliptin 5 mg and dapagliflozin 10 mg. The between-study variance was small, suggesting no heterogeneity, but the CrIs were wide, which reflects the small number of studies available for pairwise comparisons. Analyses based on direct versus indirect comparisons showed no evidence of inconsistency between direct and indirect evidence in the network for HbA1c.
FIGURE 4.
Pairwise comparisons of all drugs for HbA1c.
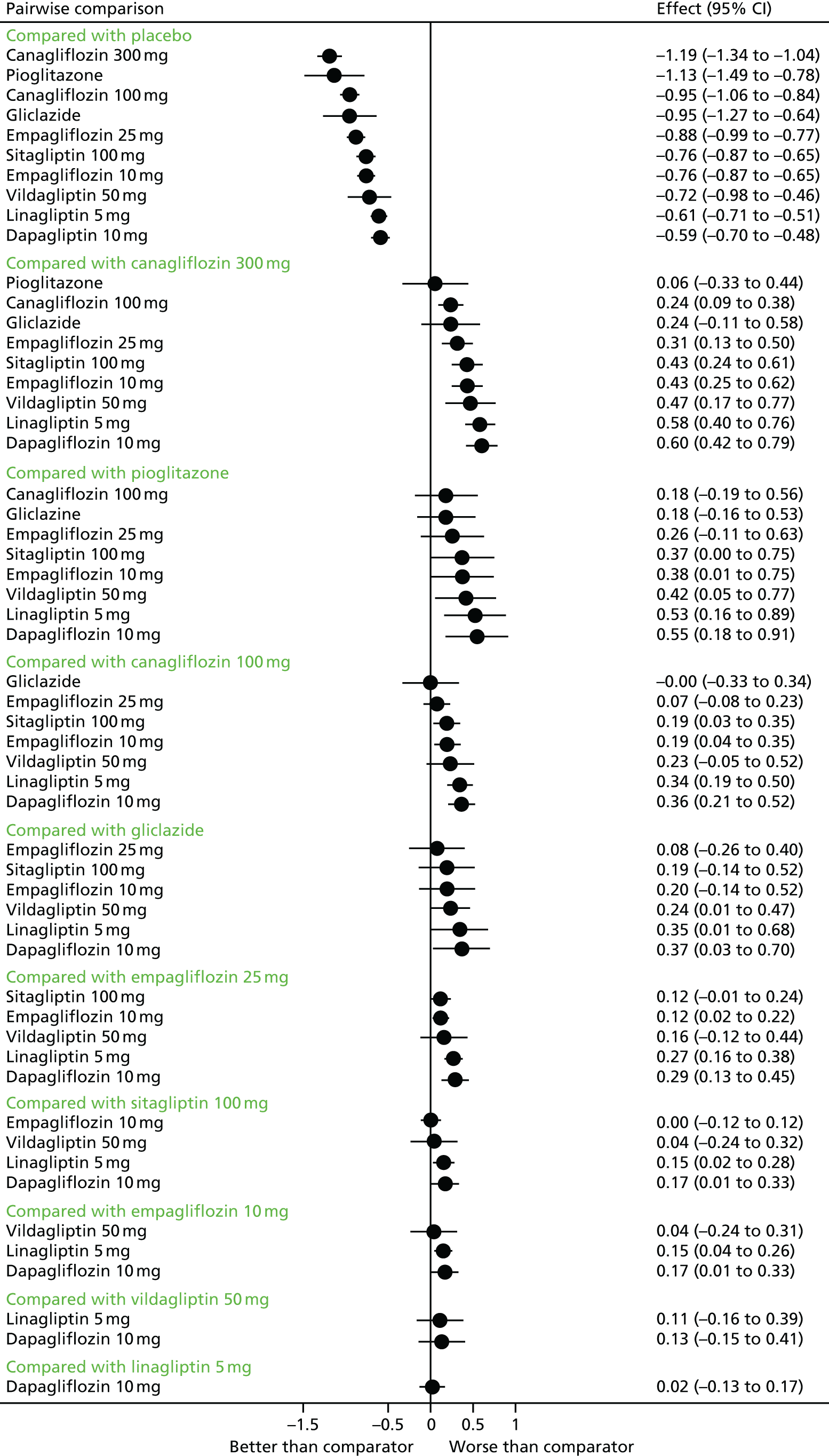
| Pairwise comparison | MD (95% CrIs) |
|---|---|
| Compared with placebo | |
| Canagliflozin 300 mg | –1.19 (–1.34 to –1.04) |
| Pioglitazone | –1.13 (–1.49 to –0.78) |
| Canagliflozin 100 mg | –0.95 (–1.06 to –0.84) |
| Gliclazide | –0.95 (–1.27 to –0.64) |
| Empagliflozin 25 mg | –0.88 (–0.99 to –0.77) |
| Sitagliptin 100 mg | –0.76 (–0.87 to –0.65) |
| Empagliflozin 10 mg | –0.76 (–0.87 to –0.65) |
| Vildagliptin 50 mg | –0.72 (–0.98 to –0.46) |
| Linagliptin 5 mg | –0.61 (–0.71 to –0.51) |
| Dapagliflozin 10 mg | –0.59 (–0.70 to –0.48) |
| Compared with canagliflozin 300 mg | |
| Pioglitazone | 0.06 (–0.33 to 0.44) |
| Canagliflozin 100 mg | 0.24 (0.09 to 0.38) |
| Gliclazide | 0.24 (–0.11 to 0.58) |
| Empagliflozin 25 mg | 0.31 (0.13 to 0.50) |
| Sitagliptin 100 mg | 0.43 (0.24 to 0.61) |
| Empagliflozin 10 mg | 0.43 (0.25 to 0.62) |
| Vildagliptin 50 mg | 0.47 (0.17 to 0.77) |
| Linagliptin 5 mg | 0.58 (0.40 to 0.76) |
| Dapagliflozin 10 mg | 0.60 (0.42 to 0.79) |
| Compared with pioglitazone | |
| Canagliflozin 100 mg | 0.18 (–0.19 to 0.56) |
| Gliclazide | 0.18 (–0.16 to 0.53) |
| Empagliflozin 25 mg | 0.26 (–0.11 to 0.63) |
| Sitagliptin 100 mg | 0.37 (0.00 to 0.75) |
| Empagliflozin 10 mg | 0.38 (0.01 to 0.75) |
| Vildagliptin 50 mg | 0.42 (0.05 to 0.77) |
| Linagliptin 5 mg | 0.53 (0.16 to 0.89) |
| Dapagliflozin 10 mg | 0.55 (0.18 to 0.91) |
| Compared with canagliflozin 100 mg | |
| Gliclazide | –0.00 (–0.33 to 0.34) |
| Empagliflozin 25 mg | 0.07 (–0.08 to 0.23) |
| Sitagliptin 100 mg | 0.19 (0.03 to 0.35) |
| Empagliflozin 10 mg | 0.19 (0.04 to 0.35) |
| Vildagliptin 50 mg | 0.23 (–0.05 to 0.52) |
| Linagliptin 5 mg | 0.34 (0.19 to 0.50) |
| Dapagliflozin 10 mg | 0.36 (0.21 to 0.52) |
| Compared with gliclazide | |
| Empagliflozin 25 mg | 0.08 (–0.26 to 0.40) |
| Sitagliptin 100 mg | 0.19 (–0.14 to 0.52) |
| Empagliflozin 10 mg | 0.20 (–0.14 to 0.52) |
| Vildagliptin 50 mg | 0.24 (0.01 to 0.47) |
| Linagliptin 5 mg | 0.35 (0.01 to 0.68) |
| Dapagliflozin 10 mg | 0.37 (0.03 to 0.70) |
| Compared with empagliflozin 25 mg | |
| Sitagliptin 100 mg | 0.12 (–0.01 to 0.24) |
| Empagliflozin 10 mg | 0.12 (0.02 to 0.22) |
| Vildagliptin 50 mg | 0.16 (–0.12 to 0.44) |
| Linagliptin 5 mg | 0.27 (0.16 to 0.38) |
| Dapagliflozin 10 mg | 0.29 (0.13 to 0.45) |
| Compared with sitagliptin 100 mg | |
| Empagliflozin 10 mg | 0.00 (–0.12 to 0.12) |
| Vildagliptin 50 mg | 0.04 (–0.24 to 0.32) |
| Linagliptin 5 mg | 0.15 (0.02 to 0.28) |
| Dapagliflozin 10 mg | 0.17 (0.01 to 0.33) |
| Compared with empagliflozin 10 mg | |
| Vildagliptin 50 mg | 0.04 (–0.24 to 0.31) |
| Linagliptin 5 mg | 0.15 (0.04 to 0.26) |
| Dapagliflozin 10 mg | 0.17 (0.01 to 0.33) |
| Compared with vildagliptin 50 mg | |
| Linagliptin 5 mg | 0.11 (–0.16 to 0.39) |
| Dapagliflozin 10 mg | 0.13 (–0.15 to 0.41) |
| Compared with linagliptin 5 mg | |
| Dapagliflozin 10 mg | 0.02 (–0.13 to 0.17) |
Weight gain
Networks of eligible comparisons for the weight gain are provided in Figure 5, showing predominantly pairwise comparisons of drugs with placebo. There were 11 comparisons (10 active drugs plus placebo).
FIGURE 5.
Network plot: weight gain.

Figure 6 and Table 10 display a caterpillar plot of the MD and 95% CrIs for all comparisons for mean change in weight gain from baseline. Sitagliptin 100 mg, vildagliptin 50 mg, gliclazide and pioglitazone were associated with significant weight gain compared with placebo, with the weight gain ranging from 0.74 kg to as much as 3.79 kg. Compared with placebo, canagliflozin 300 mg, canagliflozin 100 mg, empagliflozin 25 mg, empagliflozin 10 mg and dapagliflozin 10 mg were associated with significant weight loss, ranging from –2.91 kg to –1.58 kg. Compared with all other drugs in the network, canagliflozin 300 mg was associated with significant weight reduction. The between-study variance was small, suggesting no heterogeneity, but the CrIs were wide, which reflects the small number of studies available for pairwise comparisons. Analyses based on direct versus indirect comparisons showed no evidence of inconsistency between direct and indirect evidence in the network for weight gain.
FIGURE 6.
Pairwise comparisons for weight gain.

| Pairwise comparison | MD (95% CrIs) |
|---|---|
| Compared with placebo | |
| Canagliflozin 300 mg | –2.91 (–3.22 to –2.59) |
| Canagliflozin 100 mg | –2.02 (–2.41 to –1.65) |
| Empagliflozin 25 mg | –1.89 (–2.29 to –1.49) |
| Empagliflozin 10 mg | –1.74 (–2.15 to –1.33) |
| Dapagliflozin 10 mg | –1.58 (–2.01 to –1.14) |
| Linagliptin 5 mg | 0.31 (–0.17 to 0.79) |
| Sitagliptin 100 mg | 0.74 (0.39 to 1.10) |
| Vildagliptin 50 mg | 1.16 (0.07 to 2.26) |
| Gliclazide | 1.97 (0.76 to 3.20) |
| Pioglitazone | 3.80 (3.20 to 4.40) |
| Compared with canagliflozin 300 mg | |
| Canagliflozin 100 mg | 0.88 (0.57 to 1.21) |
| Empagliflozin 25 mg | 1.02 (0.51 to 1.54) |
| Empagliflozin 10 mg | 1.17 (0.67 to 1.70) |
| Dapagliflozin 10 mg | 1.33 (0.80 to 1.86) |
| Linagliptin 5 mg | 3.21 (2.64 to 3.79) |
| Sitagliptin 100 mg | 3.65 (3.18 to 4.12) |
| Vildagliptin 50 mg | 4.06 (2.92 to 5.21) |
| Gliclazide | 4.88 (3.63 to 6.15) |
| Pioglitazone | 6.71 (6.03 to 7.38) |
| Compared with canagliflozin 100 mg | |
| Empagliflozin 25 mg | 0.14 (–0.42 to 0.69) |
| Empagliflozin 10 mg | 0.28 (–0.26 to 0.85) |
| Dapagliflozin 10 mg | 0.45 (–0.12 to 1.02) |
| Linagliptin 5 mg | 2.33 (1.73 to 2.95) |
| Sitagliptin 100 mg | 2.76 (2.25 to 3.30) |
| Vildagliptin 50 mg | 3.18 (2.02 to 4.35) |
| Gliclazide | 3.99 (2.72 to 5.28) |
| Pioglitazone | 5.82 (5.12 to 6.53) |
| Compared with empagliflozin 25 mg | |
| Empagliflozin 10 mg | 0.15 (–0.27 to 0.57) |
| Dapagliflozin 10 mg | 0.31 (–0.27 to 0.92) |
| Linagliptin 5 mg | 2.20 (1.62 to 2.77) |
| Sitagliptin 100 mg | 2.63 (2.21 to 3.06) |
| Vildagliptin 50 mg | 3.05 (1.89 to 4.20) |
| Gliclazide | 3.86 (2.58 to 5.14) |
| Pioglitazone | 5.69 (4.95 to 6.41) |
| Compared with empagliflozin 10 mg | |
| Dapagliflozin 10 mg | 0.16 (–0.45 to 0.76) |
| Linagliptin 5 mg | 2.05 (1.48 to 2.62) |
| Sitagliptin 100 mg | 2.48 (2.06 to 2.91) |
| Vildagliptin 50 mg | 2.90 (1.72 to 4.06) |
| Gliclazide | 3.71 (2.44 to 4.98) |
| Pioglitazone | 5.54 (4.81 to 6.26) |
| Compared with dapagliflozin 10 mg | |
| Linagliptin 5 mg | 1.89 (1.23 to 2.53) |
| Sitagliptin 100 mg | 2.32 (1.74 to 2.88) |
| Vildagliptin 50 mg | 2.74 (1.56 to 3.92) |
| Gliclazide | 3.54 (2.24 to 4.86) |
| Pioglitazone | 5.38 (4.64 to 6.11) |
| Compared with linagliptin 5 mg | |
| Sitagliptin 100 mg | 0.43 (–0.14 to 1.00) |
| Vildagliptin 50 mg | 0.85 (–0.36 to 2.05) |
| Gliclazide | 1.66 (0.33 to 2.98) |
| Pioglitazone | 3.49 (2.74 to 4.25) |
| Compared with sitagliptin 100 mg | |
| Vildagliptin 50 mg | 0.41 (–0.73 to 1.59) |
| Gliclazide | 1.22 (–0.04 to 2.50) |
| Pioglitazone | 3.06 (2.37 to 3.75) |
| Compared with vildagliptin 50 mg | |
| Gliclazide | 0.81 (0.27 to 1.36) |
| Pioglitazone | 2.65 (1.38 to 3.87) |
| Compared with gliclazide | |
| Pioglitazone | 1.83 (0.45 to 3.17) |
Systolic blood pressure
Networks of eligible comparisons for the SBP are shown in Figure 7, showing predominantly pairwise comparisons of drugs with placebo. There were seven comparisons.
FIGURE 7.
Network plot: SBP.

Figure 8 and Table 11 display a caterpillar plot of the MD and 95% CrIs for all comparisons for mean change in SBP from baseline. Canagliflozin 100 mg and 300 mg, empagliflozin 25 mg, dapagliflozin 10 mg and empagliflozin 10 mg were significantly more effective in reducing mean change in SBP from baseline compared with placebo and sitagliptin 100 mg. Canagliflozin 300 mg gave the largest reduction in mean change in SBP from baseline compared with placebo (–5.65 mmHg). The between-study variance was small, suggesting no heterogeneity, but the CrIs were wide, which reflects the small number of studies available for pairwise comparisons. Analyses based on direct versus indirect comparisons showed no evidence of inconsistency between direct and indirect evidence in the network for SBP.
FIGURE 8.
Pairwise comparisons for SBP.

| Pairwise comparison | MD (95% CrIs) |
|---|---|
| Compared with placebo | |
| Canagliflozin 300 mg | –5.65 (–7.77 to –3.53) |
| Canagliflozin 100 mg | –4.24 (–6.01 to –2.44) |
| Empagliflozin 25 mg | –3.38 (–5.67 to –1.11) |
| Dapagliflozin 10 mg | –2.73 (–4.77 to –0.74) |
| Empagliflozin 10 mg | –2.59 (–4.88 to –0.33) |
| Sitagliptin 100 mg | 0.80 (–1.47 to 3.11) |
| Compared with canagliflozin 300 mg | |
| Canagliflozin 100 mg | 1.44 (–0.62 to 3.54) |
| Empagliflozin 25 mg | 2.27 (–0.85 to 5.42) |
| Dapagliflozin 10 mg | 2.92 (0.03 to 5.85) |
| Empagliflozin 10 mg | 3.09 (–0.07 to 6.25) |
| Sitagliptin 100 mg | 6.45 (3.36 to 9.59) |
| Compared with canagliflozin 100 mg | |
| Empagliflozin 25 mg | 0.83 (–2.07 to 3.72) |
| Dapagliflozin 10 mg | 1.48 (–1.18 to 4.22) |
| Empagliflozin 10 mg | 1.64 (–1.30 to 4.53) |
| Sitagliptin 100 mg | 5.01 (2.15 to 7.89) |
| Compared with empagliflozin 25 mg | |
| Dapagliflozin 10 mg | 0.66 (–2.35 to 3.69) |
| Empagliflozin 10 mg | 0.79 (–1.50 to 3.04) |
| Sitagliptin 100 mg | 4.20 (1.94 to 6.50) |
| Compared with dapagliflozin 10 mg | |
| Empagliflozin 10 mg | 0.16 (–2.95 to 3.12) |
| Sitagliptin 100 mg | 3.54 (0.53 to 6.55) |
| Compared with empagliflozin 10 mg | |
| Sitagliptin 100 mg | 3.40 (1.13 to 5.66) |
One question was whether or not canagliflozin is more potent than other SGLT2 inhibitors, due to its dual effect on SGLT2 and SGLT1 receptors. In monotherapy, both doses of canagliflozin lowered HbA1c slightly more than both doses of empagliflozin, which does not have a significant effect on SGLT1 receptors. Nor does canagliflozin 100 mg. This suggests that the SGLT1 effect does not explain all the differences in HbA1c results. It may explain some of the difference between the two doses of canagliflozin, or it may not be clinically significant.
However, irrespective of the mechanism, one finding is that canagliflozin 300 mg does have a greater effect on HbA1c than dapagliflozin and empagliflozin. Indeed, the 100-mg dose also has a clinically significantly greater reduction in HbA1c than dapagliflozin 10 mg (but see caveats to follow).
Table 12 compares the effects and AEs of the two doses of canagliflozin, with effects taken from our NMA and AEs from the published studies. Effects are compared with placebo. However, we do not know whether the reduction seen with canagliflozin 300 mg in the trials would be as great in patients who responded insufficiently to the 100-mg dose.
| Effect | Canagliflozin | Difference | |
|---|---|---|---|
| 100 mg | 300 mg | ||
| HbA1c reduction | 0.95% | 1.19% | 0.26% |
| Weight reduction | 2.02 kg | 2.91 kg | 0.89 kg |
| SBP reduction | 4.2 mmHg | 5.7 mmHg | 1.5 mmHg |
| UTIs by 12 months | 8.2% | 7.1% | No significant difference |
| GTIs by 12 months | 9.2% | 9.1% | |
| Volume depletion AEs | 1.5% | 2.0% | |
| Diuresis AEs | 4.6% | 7.6% | |
| Reported hypoglycaemia by 12 months | 5.1% | 3.6% | Placebo rate 2.6% |
If in patients in whom a SGLT2 inhibitor is considered the appropriate choice, it is considered worth trying canagliflozin 300 mg if the 100-mg dose does not have enough effect; it would be logical to also try canagliflozin 300 mg if dapagliflozin or empagliflozin are insufficiently effective. The licence implies that they would have to switch to canagliflozin 100 mg first, if only briefly. However, the same caveat would apply – the HbA1c reduction seen with canagliflozin 300 mg might be less amongst patients who have not responded sufficiently to starting doses.
Table 13 shows that the differences in effects of the two empagliflozin doses are slight, using figures from the Roden and Lewin trials. 81–83
| Effect | Empagliflozin | Difference | |
|---|---|---|---|
| 10 mg | 25 mg | ||
| HbA1c reduction | 0.66% and 0.83% | 0.78% and 0.95% | 0.12% |
| Weight reduction | 2.2 and 2.3 kg | 2.4 and 2.5 kg | 0.2 kg |
| SBP reduction | 2.1 mmHg | 3.7 mmHg | 1.6 mmHg |
| UTIs by 12 months | 16.3% | 10.4% | 5.9% in favour of 25 mg |
| GTIs by 12 months | 5.2% | 4.4% | 0.8% |
Again, a caveat is required. Those who do not respond to empagliflozin 10 mg may not achieve as great a reduction in HbA1c after increasing to 25 mg daily, as in Table 13. The differences are, in any case, mostly not clinically meaningful.
In the NMA reported here, dapagliflozin reduced HbA1c significantly less than canagliflozin 100 mg, but it should be noted that the Kaku 2014 trial80 of dapagliflozin recruited patients with mean baseline HbA1c of 7.5%, whereas most trials had baseline HbA1c of around 8%. To summarise, the placebo-adjusted HbA1c reductions in the trials at 24–26 weeks were, for the starting dosages:
-
canagliflozin 100 mg:
-
dapagliflozin 10 mg:
-
empagliflozin 10 mg:
Hence the Kaku trial,80 while qualifying for our NMA based on the baseline HbA1c of 7.5%, will be reducing the mean effect of dapagliflozin.
When interpreting weight changes, the baseline BMIs need to be considered. The trials in China and Japan recruited people with BMIs in the 25- to 26-kg/m2 range, whereas the European trials had mean BMIs ranging from 28 to almost 34 kg/m2. The pattern of type 2 diabetes differs in East Asians, with lower BMI and a more insulin-secretory defect. 167 This does not apply to South Asians (Indian subcontinent) in whom insulin resistance is more important.
Another factor to be considered in interpretation is that in the dapagliflozin trials, HbA1c fell in the placebo groups, by 0.29%, and by 0.23% in the Ji79 and Ferrannini77 trials. In the Ferrannini trial,77 weight fell significantly, by 2.2 kg. In the placebo groups in the canagliflozin trials, HbA1c rose by 0.29% (Inagaki76) and 0.14% (Stenlöf, CANTATA-M84). Ferranini et al. 77 (and the AstraZeneca submission, which talks of a ‘motivated placebo group’ on p. 58) suggested that the reduction in HbA1c in the placebo group might have been due to improved adherence to lifestyle advice in that group, but as the placebo tablets matched the dapagliflozin ones, this seems unlikely.
Problems with evidence and effect sizes for modelling
This review has encountered a number of problems.
Many trials provided data on only some of the variables which are used in the UKPDS Outcomes Model. For example, SBP changes were often not reported. This applied more to older trials of comparators than to the more recent trials of the SGLT2 inhibitors.
Some trials provided no data with which to calculate TC/HDL ratios. However, a more important problem is that when TC levels were reported, they were often high, giving quite high TC/HDL–C ratios. It is likely that greater use of statins renders such data obsolete. For our modelling, we will assume that all general practitioners (GPs) and diabetologists follow NICE guidance and are using atorvastatin 20 mg for primary prevention in all people with type 2 diabetes. This will produce a TC/HDL ratio of about 3.0.
Another problem is with effect sizes after intensifications. For example, there are reviews of the effects on HbA1c and weight of sulfonylureas when added to monotherapy, but the bulk of evidence is addition to metformin monotherapy. The weight gain after adding gliclazide to a SGLT2 inhibitor may be different – it may only restore weight to the baseline before weight loss on the flozin. And the weight gain after adding gliclazide to pioglitazone may be less because pioglitazone itself causes weight gain.
In passing, it is worth noting that the weight gains in trials may be greater than in routine primary care. De Fine Olivarius et al. 168 reported that 330 patients did not gain weight after starting on sulfonylureas. They make the point that most patients with type 2 diabetes are treated in primary care and are seldom recruited to trials, and that trials may therefore not be generalisable to all patients.
As regards reductions in adding sulfonylurea to monotherapy, some reviews report that adding a sulfonylurea to metformin results in a reduction in HbA1c of around 1%. However, the size of the reduction will depend on the HbA1c level on metformin alone. Genuth169 quotes a reduction of 1% from a baseline of 8.3%. This may be a bigger reduction than would be seen in people who have just crept over the NICE switching threshold of 7.5%.
In the same review, Genuth169 reports that pioglitazone added to metformin reduces HbA1c by 1.0%, and a DPP-4 inhibitor does so by 0.7%.
Hirst et al. 170 produced a good-quality systematic review and meta-analysis in which they examined reductions in HbA1c after starting sulfonylureas in dual therapy. Sulfonylureas (glibenclamide, glipizide and glimepiride) reduced HbA1c by 0.95% on average but with considerable heterogeneity – reductions ranged from 0.47% to 1.3%. They found little variation in HbA1c reductions by baseline HbA1c but most of those baselines were well above 8%, ranging from 7.5% to 9.5%. The only trial with baseline HbA1c under 8.4%, had starting HbA1c of 7.5%, and that was the trial by Feinglos et al. ,171 which showed a reduction of only 0.47%. This trial171 is closest to what we would expect in care as recommended by the NICE guideline,8 and with baseline HbA1c of 7.5%, the reduction in HbA1c of 0.47% would be sufficient to improve HbA1c to around 7.0% and would be seen as a reasonable result.
One problem with the review by Hirst et al. 170 was that most trials were short term. A very useful observational study by Cook et al. 172 used data on 2220 patients from the UK General Practice Research Database (GPRD) to study glycaemic control over time after a sulfonylurea was added to metformin, because of poor glycaemic control, with median HbA1c of 8.8%. There was a prompt reduction to median of 7.3% after 6 months of sulfonylurea, but thereafter, HbA1c started rising again, by 0.32% between months 6 and 12. Half of the patients had HbA1c of 8.0% or over by 1 year of starting sulfonylureas.
Cook et al. 172 also noted that intensification of treatment was often delayed until HbA1c is over 9%. However, their data were from 1998 to 2004 and may no longer apply. Nevertheless, the large drops often reported after sulfonylureas are started may be because of very poor control, and we should not expect such large reductions in HbA1c in carefully monitored patients who have only recently gone above the NICE switching threshold of 7.5%.
In a trial comparing dapagliflozin with glipizide as add-ons to metformin, and with baseline HbA1c of about 7.7%, the reductions in HbA1c by week 52 were 0.50% on dapagliflozin and 0.48% on glipizide. 173
The durability issue with sulfonylureas has been reported by several studies, of which the best known may be the ADOPT (A Diabetes Outcome Progression Trial) trial174 in which time to monotherapy failure was longer with rosiglitazone and metformin than with glibenclamide, with 34% of the glibenclamide patients needing additional treatment by 5 years compared with only 15% of those on rosiglitazone.
Del Prato et al. 173 looked at duration of effect of dapagliflozin and glipizide in dual therapy when added to metformin. HbA1c fell more rapidly, and further on glipizide, but then rose again more quickly. So at about 12 weeks, the falls were (from graph) about 0.8% on glipizide and 0.5% on dapagliflozin, but by 52 weeks the curves had met at reductions of about 0.5%, though about 20% of patients were absent by that time point. After 52 weeks, HbA1c rose on both drugs, but more on glipizide, with a gap of 0.30% by 208 months. However, the numbers by that time point were low – 20% of the dapagliflozin group and 18% of the glipizide group. The reductions were due to patients starting rescue therapy after HbA1c rose. Rescue was mandatory once HbA1c reached 8.0% or more, and was at the investigator’s discretion between 7.0% and 8.0%. So similar proportions in each group had to move to rescue therapy, implying no difference in durability.
There is a 2015 abstract by Bacon et al. 175 from Janssen, comparing time until insulin is started between canagliflozin and dapagliflozin, when used in dual or triple therapy. It also used the ECHO-T2DM (Economic and Health Outcomes Model for Type 2 Diabetes Mellitus) model. In triple therapy, the authors report insulin being started on average at 5.1 years with canagliflozin (starting with 100 mg daily and increasing as required to 300 mg) compared with 3.3 years with dapagliflozin. Insulin was started when HbA1c exceeded 7.5%.
For the effects of adding sitagliptin we have two useful trials with HbA1c baseline 7.7% and 7.8%, which reported reductions in HbA1c of 0.67% and 0.79% (Scott 2007,176 Nauck 2007177) giving a mean of 0.73%.
A recent report from the Canadian Agency for Drugs and Technologies in Health (CADTH) (see appendix of CADTH report)178 concludes that pioglitazone added to monotherapy reduces HbA1c by 0.78%. It also gives the reduction with DPP-4 inhibitors as a mean of 0.7%.
At intensification to triple therapy, one option would be to introduce a long-acting (LA) GLP-1 analogue. NICE has so far approved only exenatide LA for this purpose, but there are now other drugs in this group, including dulaglutide and albiglutide. 179
In the DURATION-1 (Diabetes Therapy Utilisation: Researching Changes in A1C, Weight and Other Factors Through Intervention with Exenatide Once Weekly) trial, Drucker et al. 180 compared exenatide LA with the short-acting, twice-daily form. Patients were on a mixture of baseline treatments with only 38% on dual therapy. However, reductions in HbA1c were reported to be similar across baseline treatment groups. On exenatide LA, HbA1c fell by 1.9% from a baseline of 8.3%, with 60% of patients getting HbA1c under 6.5%. The advantages of using a GLP-1 analogue, compared with insulin, are the once-weekly injection, weight loss (in DURATION 1 weight fell by 3.7 kg on exenatide LA), a low risk of hypoglycaemia (there were no severe hypoglycaemia in DURATION 1 and minor hypoglycaemia was seen only in patients on sulfonylurea) and some reduction in SBP (4.7 mmHg). Another advantage of adding a GLP-1 analogue to treatment with a SGLT2 inhibitor is that the latter increases plasma glucagon levels, which would be suppressed by the former, though if triple therapy includes a sulfonylurea such as gliclazide, glucagon secretion may already be suppressed. 181
Chapter 4 Clinical effectiveness aspects of the submissions from the manufacturers
Three submissions were received, from:
-
Janssen for canagliflozin
-
AstraZeneca for dapagliflozin
-
Boehringer Ingelheim for empagliflozin.
The submissions had three main sections:
-
a review of the evidence on clinical effectiveness and safety
-
a NMA comparing SGLT2 inhibitors with comparators
-
cost-effectiveness analysis.
Clinical effectiveness
As regards clinical effectiveness, the evidence provided by the manufacturers was very similar to that presented earlier in this report. The same trials were presented. The submissions were of good quality and we have very few comments.
The Janssen submission included 52-week results from an extension to the CANTATA-M study,92 which we omitted because there was no comparison group. In brief, the 52-week data showed that the reductions in HbA1c were largely maintained (reductions on 100 mg 0.91% at 26 weeks and 0.81% at 52 weeks; reductions on 300 mg 1.16% at 26 weeks and 1.11% at 52 weeks). However, a little more weight was lost by 52 weeks.
The Boehringer submission included data from a 76-week extension study, which had been published in abstract form only. 82 Almost 40% of patients dropped out, leading to extensive use of last observation carried forward (LOCF), which is not a reliable method because people do not drop out at random. It is likely that those who stayed in were doing better than those who dropped out.
The Boehringer submission made a useful point about adherence to therapy. This would apply not just to diabetes medications: people with diabetes tend to have comorbidities such as hypertension and osteoarthritis (due to excess weight) and so may be on other medications for other conditions. Donnan et al. 182 reported that the more medications were prescribed and the more complex the regimen, the poorer the compliance. Eli Lilly now market a combination tablet with empagliflozin and linagliptin.
One omission from the AstraZeneca submission was any mention of cancer risk. The FDA were concerned about breast, prostate and bladder cancer, even though in none of these cases was the risk statistically significantly raised. 183 In the trials, there were nine cases of bladder cancer amongst 5501 subjects in the dapagliflozin group versus one amongst 3516 in the placebo arms. Some of these cancers appeared too soon after the patients started dapagliflozin for credible causality, and all but one of the patients had had microscopic haematuria, suggestive of bladder pathology, before starting the drug or within 6 months of doing so. 184 One hypothesis is that an increased UTI rate in patients on dapagliflozin leads to increased testing or urine and hence of detection of bladder tumours, but 7 of the 10 patients diagnosed with bladder cancer had not had UTIs. 184
Breast cancer was observed in nine patients (0.04% of female patients) in the dapagliflozin arms but in none of the placebo groups. However, two cases were diagnosed within 6 weeks of starting dapagliflozin so were certainly not due to the drug.
There were 10 cases of prostate cancer in the dapagliflozin arms (0.34%) versus three cases in the placebo arms (0.16%).
Some cancers, albeit less common ones, were less common (though 95% CIs overlapped with no difference) in the dapagliflozin groups, and overall there was no difference in rates for all cancers.
It is difficult to explain the differences in bladder and breast cancer, but it seems unlikely that dapagliflozin is the cause.
Network meta-analyses
There were marked differences amongst the NMAs. For example, the AstraZeneca meta-analysis included seven trials of sulfonylureas, with five trials involving glibenclamide. The Janssen meta-analysis included nine trials of sulfonylureas, with five trials comparing glibenclamide with other sulfonylureas and two of glibenclamide against pioglitazone. Only one trial was in both NMAs.
The Boehringer NMA included 22 trials involving sulfonylureas: glibenclamide, seven; glimepiride, six; gliclazide, six; glipizide three; and tolbutamide, one.
Of the seven sulfonylurea trials in the AstraZeneca NMA, four were also in the Boehringer NMA. Of the nine sulfonylurea trials in the Janssen NMA, three were also in the Boehringer NMA. Only one trial was in all three of the manufacturers’ NMAs.
AstraZeneca
The AstraZeneca NMA starts with a major assumption with which the AG disagrees, which is that the classes of drugs (sulfonylureas, TZDs, DPP-4 inhibitors and SLT2 inhibitors) can be grouped. In the case of the TZDs, this does not matter because all of the trials cited include pioglitazone. However, our view is that the sulfonylureas have different effects, and that gliclazide is the sulfonylurea of choice, as explained in Chapter 1.
We also disagree with the assumption by AstraZeneca that when monotherapy fails, NPH insulin would be started. This seems strange when there is such a range of oral medications that can be tried. We note that a recommendation to introduce insulin as a second drug was one option in the consensus statement by a group on behalf of the ADA and the European Association for the Study of Diabetes in 2006. 185 However, this consensus was strongly criticised by a larger group of experts as being based more on opinion than evidence. 186
One problem with the AstraZeneca NMA is the data reported in the forest plot (figure 4.6) for the pooled sulfonylureas, which include glibenclamide, glimepride, glipizide and one gliclazide trial. The net effect size in HbA1c lowering is 0.12%, which is unusually low. Two trials provide 85% of the weight in this meta-analysis, Rosenstock 2013187 and Shihara 2011. 188 In the forest plot for the Shihara trial,188 glimepiride is shown as reducing HbA1c by 0.10%, and in the Rosenstock trial187 glipizide is shown as increasing HbA1c by 0.03%. These results are not credible.
In the Rosenstock trial,187 about half of the patients left the trial before conclusion, with 21.5% of the glipizide group doing so because they needed additional ‘rescue’ treatment because of hyperglycaemia. About half of the recruits had been on glucose-lowering drugs before entry, and had a 4-week washout period. However, the primary analysis included the rescued patients and this is reflected in the one of the analyses, which reported a 0.09% reduction in HbA1c. (It is not clear where the rise of 0.03% in the AstraZeneca forest plot comes from.) The baseline HbA1c in the glipizide group was 7.45%, and 33% had baseline HbA1c of 7.0% or less. So a large reduction in HbA1c would not be expected. However, if the rescue group is removed, those completing the trial had mean reduction in HbA1c of 0.31% (from text) or about 0.5% (from graph).
The Shihara 2011 trial188 compared glimepiride and pioglitazone monotherapy in drug-naive Japanese patients. Baseline HbA1c was 7.8% in the glimepiride group and it fell to 6.8% by 6 months (from graph – reduction of 6.9% in text at 3 months). It is not clear where the 0.1% figure used in the AstraZeneca meta-analysis comes from, though we note that the HbA1c difference between glimepiride and pioglitazone at 3 months as 0.1%.
One other sulfonylurea trial in the forest plot is shown as having a very small reduction in HbA1c. This is Erem 2014,158 which was used in the AG NMA. The AstraZeneca forest plot reports a reduction in HbA1c of 0.14% compared with placebo. There was no placebo group in Erem 2014158 which compared gliclazide with pioglitazone and metformin. The HbA1c was reduced from 8.26% at baseline in the gliclazide group to 6.92% at 6 months, so a more credible reduction against placebo might have been to use the 1.34% before-and-after figure.
Given that these Rosenstock187 and Shihara188 trials dominate the meta-analysis, the sulfonylurea section of it is not credible. It contains eight trials but the others are smaller and carry less weight. Apart from the Erem trial,158 their HbA1c results in the other five are as expected from sulfonylureas, showing reductions ranging from 0.6% to 1.8%.
However, these problems may just affect the forest plot. In appendix 8.9, the reduction attributed to glipizide in the Rosenstock trial187 is 0.23%, still smaller than usual but more credible. The reduction stated in this table for glimepiride in the Shihara trial188 is 1.0%. In addition, the caterpillar figure 8.9 in the appendices looks reasonable and is followed by a reported difference for sulfonylureas versus placebo of 0.80% in table 8.21.
Table 4.4 in the AstraZeneca NMA gives a reduction in HbA1c of 0.99% with sulfonylureas, compared with placebo. In the modelling a figure of –0.95% is used, which corresponds with both of the submitted AstraZeneca models and table 5.3 of their submission. So the forest plot figures are a minor mishap that does not affect the AZ modelling.
Review of statistical methods
The AstraZeneca submission estimated both fixed- and random-effects meta-analyses for the continuous and count-based outcome measures. It used the DIC to assess model fit, with at least a 3-point change signifying an improved model. Also, the manufacturer submission (MS) compared the posterior distribution of between-study SDs with the prior distributions to assess whether or not it was updated by the available evidence (i.e. the additional information had had an effect). Random-effects models were fitted first, as they were considered a priori as the appropriate model. Fixed-effects models were selected only if they significantly improved model fit as demonstrated by DIC and changes to the posterior distribution of between-study SDs. Clinical and statistical heterogeneity were assessed through an evaluation of sources and the I2-statistic for pairwise comparisons, respectively. Heterogeneity was examined through a sensitivity analysis using meta-regression to adjust for the effects of baseline HbA1c. Consistency was also assessed through a comparison of the direct and indirect evidence using pairwise meta-analyses of the active treatments versus placebo for the outcome of HbA1c only. The overall modelling strategy used in the MS seemed appropriate.
AstraZeneca undertook Bayesian Markov chain Monte Carlo (MCMC) NMAs for continuous and count-based outcome measures. It specifies that vague priors were used for unknown parameters; however, no details were provided as to the distributions or link functions used in the models. Vague priors are usually specified; however, there are occasions when other priors should be assessed to establish the possible effects on the posterior estimates [e.g. binomial model with a logit link function or a rate model with log link function (when a uniform prior is used for the SD) or when data are sparse and the model fails to converge (when vague gamma priors are used for precision)]. No sensitivity analyses assessing the effects of different distributions, link functions or priors were presented. As the treatments considered in the NMAs were assessed by class, this may be less of a concern. The MS reports that MCMC models were run using three chains starting from different values of the unknown parameters, used a burn-in of ≥ 20,000 iterations, an update of ≥ 100,000 iterations and a parameter thin of 10. Convergence was assessed using history plots of the chains for the relevant parameters (overlapping histories indicating convergence) and a Monte Carlo error for each parameter (error of ≤ 5% of posterior SD indicating convergence). No assessment is reported regarding the influence of autocorrelation. The approach taken in the MS to MCMC models appears appropriate.
The MS reports NMAs on classes of treatments (i.e. SGLT2s, DPP-4s, SUs, TZDs) rather than comparing individual treatments. Such ‘lumping’ of evidence is a concern as regards the assumption of consistency, leading to heterogeneity, difficulties in interpreting results and potential conflict between the direct and indirect evidence. The MS states that the rationale for considering the treatments as a class was due to the limited evidence base for some treatments; that previous NICE CGs had indicated that they could be considered as a class; and that heterogeneity among some individual studies in terms of study characteristics within a class of treatments meant that comparison of individual studies may be affected by a risk of bias. The MS should have considered a NMA of individual treatments as well as presenting one of class effects. This would have shown results similar to the AG NMA, when dapagliflozin has slightly less effect than empagliflozin 10 mg and canagliflozin 100 mg, the other starting doses. Although it is not clear which treatment was the reference treatment in the NMAs, results are presented for comparisons of the treatment classes with both placebo and SGLT2 only.
Continuous outcomes of mean change from baseline in HbA1c, weight and SBP (MD scale) and count-based outcomes of proportion of patients experiencing hypoglycaemia (odds ratios) were used in the NMA. Although data for the continuous outcomes were for ITT populations using LOCF, any missing data were based on estimates from the primary study. Data time points ranged from 18 to 30 weeks.
Comparison of the baseline characteristics of the 32 studies showed variability. Although the MS stated that the trials were generally similar in baseline characteristics, it identified that nine RCTs were conducted only in Asian patients, one RCT had a higher mean age, one RCT had a higher mean baseline HbA1c, eight RCTs had higher mean baseline weights and that average duration of diabetes and baseline BMI varied. It should be noted that the included studies were conducted between 1994 and 2014 and study duration ranged from 18 to 102 weeks. Although the effects of baseline HbA1c was assessed through meta-regression and those associated with the Asian-only studies through exclusion of the studies in a sensitivity analysis, possible heterogeneity associated with the other factors was not considered further.
The MS presents network diagrams of the decision space for the classes of treatment. The number of RCTs linking each treatment class is not clear, and subsequent forest plots are presented for comparisons with placebo only. It is difficult to judge whether or not sparse evidence networks or zero values were a concern, although the ‘lumping’ of evidence into treatment classes may well have overcome this issue. It is also unclear which treatment was used as the reference treatment.
The MS clearly specified the approach it had taken to the majority of the elements of its NMAs. It lacked details concerning the prior distributions and link functions used; its assessment of autocorrelation in MCMC models; and sensitivity analyses concerning the elements of the models themselves (e.g. prior distributions, link functions and priors for parameters). Although it assessed some possible causes of heterogeneity, others were not considered (e.g. participant characteristics, length of study follow-up). It appropriately examined consistency of the outcomes from the NMAs. The MS identified several limitations underlying its analysis, including high placebo effects associated with the assessment of body weight in a dapagliflozin monotherapy study and a study focusing on Asian patients; a lack of evidence on specific patient groups (i.e. metformin intolerant); limited duration of follow-up; different definitions of hypoglycaemia; and inconsistent reporting of safety outcomes. However, the key limitation that affects the NMA is the lack of evidence on individual treatments. As a result, the MS ‘lumps’ together the evidence by treatment class. This can cause concerns with regards to the assumption of consistency, and lead to heterogeneity, difficulties in interpreting results and potential conflict between the direct and indirect evidence.
Boehringer Ingelheim
The Boehringer NMA is shaded as confidential. It was very complex and included 37 studies, including some that the AG rejected for our NMA. All of the sulfonylureas trials were pooled into one node, which we think is undesirable, given the mix of drugs from tolbutamide to gliclazide. The NMA includes both the Saleem 2011149 and Jibran 2006151 papers with their striking similarities.
Janssen
The Janssen NMA included 40 studies, including some that the AG did not think relevant, such as dapagliflozin 5 mg. It included four DPP-4 inhibitors and four sulfonylureas. It did not include repaglinide but this was included in a sensitivity analysis.
Review of statistical methods
A Bayesian hierarchical model was used for the Janssen NMA. Although not explicitly stated, it is evident that both fixed- and random-effects models were estimated. No analysis was undertaken of possible effect modifiers using meta-regression; instead, sensitivity analyses excluded trials with different characteristics. The MS used the DIC to assess the goodness of fit of the models, selecting the model with the lowest DIC as the most appropriate. A threshold of 3 points on the DIC is used to judge significant change. Where a random-effects model was selected as the base-case analysis, a fixed-effects model was estimated in a sensitivity analysis. Given other statements in the MS, it is assumed that random-effects models may have also been estimated as a sensitivity analysis when a fixed-effects model was the base case. When trials had multiple arms, the MS correctly made adjustments to the statistical approach to account for the correlation between treatment effects from the same trials. The approach taken was based on a conditional distribution formulation of the multivariate normal distribution. The influence of heterogeneity was assessed through an analysis of the direct pairwise comparison of treatments using Cochran’s Q test (p = 0.1), I2-statistic (threshold > 50%), comparisons using forest plots and comparison of the characteristics of the trials. Consistency of the direct and indirect evidence was compared using the difference in the respective point estimates and their p-values, testing whether they differed statistically significantly from zero. As well as producing point estimates (and CrIs) of the MD and odds ratios, the MS ranked the probability of the different treatments as being the most effective based on the Surface Under the Cumulative Ranking (SUCRA). SUCRA produces probabilities that range from 100%, showing the treatment ranks first, to 0%, which shows it ranks last. These rankings formed the basis of the comparison of the different treatments, along with an assessment of the probability that canagliflozin performed better than the other treatments. The comparative ranks were interpreted on the basis that a treatment with > 70% was judged the best, between 30% and 70% no difference between treatments, and < 30% the alternative treatment was considered best. Although the analysis lacked an assessment of heterogeneity through meta-regression, the overall modelling strategy used in the MS appeared appropriate.
For the NMAs of continuous outcomes, the MS correctly assumed that a Normal distribution and identity link function should be used. Similarly, for binary outcomes, the MS appropriately selected a binomial distribution and logit link function. The MS states that it uses non-informative priors for unknown parameters. Priors for the Normal distributions for treatment effects (0, 104) and the uniform distributions for between-trial SDs (binary outcomes range (0,2); continuous outcomes range based on outcome scale with assessment of posterior distribution to select prior distribution) were specified. Although the priors are considered suitable, issues concerning sparse data may require other priors to be considered, particularly if the model fails to converge. Although not specifically stated in the MS, this issue appears to have been considered as a sensitivity analysis on the prior distributions for between-trial precision uses a gamma distribution (0.001, 0.001) for the random-effects model. No other prior distributions appear to have been examined in sensitivity analyses.
The NMAs used MCMC simulation in WinBUGS, running three chains with different starting values. It assessed convergence through history and Gelman–Rubin plots, although these are not presented. Fixed-effects NMAs used a burn-in of 20,000 iterations, which were discarded, and a further 20,000 iterations to monitor the parameters. Random-effects NMAs used a burn-in of 100,000 iterations (which were discarded) and monitored parameters for a further 100,000 iterations. Where convergence was not achieved, iterations were increased (numbers of iterations used not stated).
Treatments included in the NMA had to be in common use in the UK. The NMAs assessed both treatment- and dose-specific outcomes in the classes of SGLT2, TZD and DPP-4, with those for sulfonylurea pooled to reflect dose adjustments on a per-patient basis. The MS appropriately selected placebo as the reference treatment for all of the evidence network diagrams; however, all results were compared with canagliflozin. No comparisons were made between the other active treatments, which may reflect the sparse nature of the evidence.
Continuous outcomes measured the change from baseline in each treatment arm for HbA1c, FPG, weight, BMI and SBP. If data were missing, values were estimated as the difference between the final value and the value at baseline, with the variance calculated using an approach recommended by the NICE Decision Support Unit. Sensitivity analyses were conducted on the approach to estimating the variance of the mean change (i.e. within-patient correlation varied from base case of 0.5 to 0.7). Binary outcomes used the number of events and total patients in each treatment arm for calculating the proportion of patients reaching HbA1c of < 7%, proportion of patients with one or more hypoglycaemic events and proportion of patients reaching HbA1c of < 6.5%. Handling of missing data from binary outcomes is not discussed. Outcomes were assessed at 26 weeks ± 4 weeks, with a sensitivity analysis of 26 weeks ± 10 weeks. This variation may have led to heterogeneity in the outcomes reported, although the MS states that these were based on expert clinical opinion. Additional sensitivity analyses were also conducted including studies reporting outcomes from 16 to 21 weeks and/or 31–36 weeks.
There appeared to be some heterogeneity in the participant characteristics. Patients in the included studies ranged in age from 48 to 72 years; the proportion of males from 11% to 80%; the proportion who were white from 6% to 80%; and, in duration of their diabetes 1.1 years to 13 years. In many instances studies did not report the characteristics of their participant populations. As a result, heterogeneity was identified in the NMAs and sensitivity analyses were undertaken.
The MS presented evidence networks for the different comparisons undertaken. It was evident from the network diagrams that some of the treatments were in parts of the network that were unconnected, and these were excluded from the analyses. Other parts of the evidence networks were sparsely populated with only one trial. Such limited data may have resulted in posterior distributions of the SDs that included extreme values and the possibility of non-convergence of the model. This increased the uncertainty around the outcome of the NMAs. Trials including binary outcomes were affected by zero events. Where this occurred, the MS appropriately used a continuity correction (0.5 added to all cells counts of studies with at least one arm with a zero). Trials with no event in any arm or that were considered to affect convergence (basis of exclusion not stated) were excluded from the analysis.
The trials included in the evidence network were assessed through sensitivity analyses that excluded trials considered a source of heterogeneity or inconsistency; identified as lower quality (not double blind), where it was unclear if it assessed monotherapies; assessed a single ethnic group; or published in a non-peer reviewed journal or as part of a regulatory process. Further sensitivity analyses were conducted, which included an unpublished trial (DIA3011) assessing canagliflozin 100 mg and canagliflozin 300 mg, and repaglinide trials that included metformin and sulfonylurea.
The MS clearly outlined the key aspects of the NMAs. It estimated fixed- and random-effects Bayesian hierarchical models using MCMC simulation in WinBUGS, evaluating the fit of the models through DIC. Prior distributions and values were correctly assumed, with an alternative assessed through sensitivity analysis to examine the effects of sparse data. The MS discussed the simulation process in terms of chains run, iterations for burn-in and monitoring parameters, and the process for assessing convergence. The analysis also assessed heterogeneity, inconsistency between direct and indirect meta-analyses, and made adjustments for multiple treatment arms. The NMAs presented point estimates and CrIs for outcomes, and ranked treatments as to which performed the best. Treatments were compared with canagliflozin, with no comparisons of the other active treatments. Missing data were appropriately estimated for continuous measures; however, there is no discussion of missing data for binary outcomes. Outcomes were assessed at 26 weeks ± 4 weeks, with a sensitivity analysis at 26 weeks ± 10 weeks, which may have resulted in some heterogeneity. It was evident that the network was sparsely populated in certain comparisons and that there were zero values for binary outcomes. Although the zero values were handled appropriately through a continuity correction, the effects of sparse data for the continuous variables may lead to increased uncertainty around the estimates. The MS produced a range of sensitivity analyses to explore the robustness of the models. Overall, the methods used in the NMAs appeared appropriate and identified most limitations in the evidence. The sparse evidence base may influence the outcomes produced.
Comments
Despite the different approaches and inclusions, some findings from the different meta-analyses were similar. For example, the differences in effect sizes of HbA1c of canagliflozin 100 mg and dapagliflozin 10 mg were reported as 0.33% (Janssen), 0.365% (Boehringer) and 0.36% (AG).
There appears to be a systematic difference between results of the AG NMA and the Boehringer NMA, with effects on HbA1c being higher in the latter, with the AG results being closer to the trial results. The Janssen figures are similar to the AG ones. This is shown in Table 14.
| Drug | Janssena | AG | Trial |
|---|---|---|---|
| Dapagliflozin 10 mg | 0.64 | 0.59 | 0.66 (Ferrannini 201077) |
| Empagliflozin 10 mg | 0.74 | 0.76 | 0.74 (Roden 201482) |
| Empagliflozin 25 mg | 0.85 | 0.88 | 0.86 (Roden 201482) |
| Canagliflozin 100 mg | 0.97 | 0.95 | 0.91 (CANTATA-M 201384) |
| Canagliflozin 300 mg | 1.20 | 1.19 | 1.17 (CANTATA-M 210384) |
However, the relative differences between drugs are similar, and those are what matter in the modelling.
Chapter 5 Cost-effectiveness
Approach to modelling
There are several issues to consider in choosing sequences, including:
-
The assumption that in most patients, the condition will progress, requiring intensification of therapy by adding a second glucose-lowering agent – dual therapy – and, later, one or more others.
-
Whether or not the second drug should vary according to what the first was. For example, after a flozin as first drug, the choice of second drug includes sulfonylureas, gliptins and pioglitazone.
-
Whether or not these drugs could also come in at later stages. For example, if dual therapy with canagliflozin and gliclazide is failing, one option might be to add sitagliptin. Others include pioglitazone, insulin and a GLP-1 analogue.
-
We assume that if intensification to dual therapy is required, the doses of empagliflozin and canagliflozin will already have been raised to 25 mg and 300 mg, respectively.
These options could create a need for a very large number of pathways which is beyond the scope of this report. We also need to keep regimens after monotherapy as similar as possible in order to focus on the differences arising from the initial monotherapy.
Dual therapy
The NICE guideline on type 2 diabetes envisages, for patients who cannot take metformin, dual therapy with one of the following combinations:
-
pioglitazone and a sulfonylurea
-
pioglitazone and a gliptin
-
sulfonylurea and a gliptin.
In the interest of simplicity, we have chosen the sulfonylurea as the second drug, except after gliclazide monotherapy, when we use pioglitazone. The sulfonylurea was preferred to pioglitazone because of the latter’s safety record. Pioglitazone is preferred to a DPP-4 inhibitor only on cost grounds.
We have assumed that patients are at the maximum tolerated dose of each monotherapy drug before moving to dual therapy.
Triple therapy
Moving to triple therapy is more complicated, as after some of the dual regimens, pioglitazone and a gliptin are still available, and the GLP-1 analogues and insulin enter the frame. It is not possible to review all options.
At this stage, the NICE guideline recommends that insulin-based treatment should be considered. 16
In the interests of simplicity, our base case is therefore to bring in NPH insulin for triple therapy. We therefore have sequences as follow:
-
empagliflozin 25 mg → empagliflozin + gliclazide → empagliflozin + gliclazide + NPH insulin
-
canagliflozin 300 mg → canagliflozin + gliclazide → canagliflozin + gliclazide + NPH
-
dapagliflozin 10 mg → dapagliflozin + gliclazide → dapagliflozin + gliclazide + NPH
-
sitagliptin 100 mg → sitagliptin + gliclazide → sitagliptin + gliclazide + NPH
-
pioglitazone 45 mg → pioglitazone + gliclazide → pioglitazone + gliclazide + NPH
-
gliclazide → gliclazide + pioglitazone → gliclazide + pioglitazone + NPH.
Some patients will progress to needing short-acting insulin to control blood glucose after meals. We assume that once patients move to a basal-bolus insulin regimen, the sulfonylurea will be stopped.
Note that we have not introduced any of the flozins beyond monotherapy, as those situations were dealt with in the three single technology appraisals (STAs).
An alternative to bringing in insulin as third drug, is to consider the GLP-1 analogues. These are simpler for patients to manage, involving a once-a-week injection, and a low risk of hypoglycaemia.
The National Institute for Health and Care Excellence has adopted a very restrictive position on the GLP-1 analogues, based on a minimum BMI, and stopping rules requiring both a 1% reduction in HbA1c and 3% weight loss, but that was not based on any cost-effectiveness analysis and is due for review.
Only one long-acting GLP-1 analogue has been appraised by NICE – long-acting exenatide. If we bring that in as a third drug, basal insulin would be the fourth drug, with sequences as follow:
-
empagliflozin 25 mg → empagliflozin + gliclazide → empagliflozin + gliclazide + exenatide LA → empagliflozin + gliclazide + exenatide + NPH insulin
-
canagliflozin 300 mg → canagliflozin + gliclazide → canagliflozin + gliclazide + exenatide LA → canagliflozin + gliclazide + exenatide + NPH
-
dapagliflozin → dapagliflozin + gliclazide → dapagliflozin + gliclazide + exenatide LA → dapagliflozin + gliclazide + exenatide + NPH
-
sitagliptin 100 mg → sitagliptin + gliclazide → sitagliptin + gliclazide + exenatide LA → sitagliptin + gliclazide + exenatide + NPH
-
pioglitazone 45 mg → pioglitazone + gliclazide → pioglitazone + gliclazide + exenatide LA → pioglitazone + gliclazide + exenatide + NPH.
One problem with deriving effect sizes for modelling is that most trials recruit patients with rather poorer control than would be expected amongst patients who are being followed up according to NICE type 2 guidelines that recommend measuring HbA1c at 3–6 monthly intervals until HbA1c is stable (and presumably satisfactory).
So if the above guideline is being followed, patients whose HbA1c rises above the 7.5% intensification threshold, should have that detected within a few months, before it has gone much higher. Their HbA1c levels might be in the 7.5–8.0% range. Whereas most trials of intensification to dual or triple therapy recruit patients with much higher HbA1c, often in the 8.7–9.05% range but sometimes well over 9%.
The importance of this is that reductions in HbA1c tend to be larger when baseline HbA1c is higher. So the effect sizes in HbA1c seen in most trials will be larger than expected in management of type 2 diabetes according to the NICE guideline, with close monitoring and prompt intensification.
So we need to be selective in the trials from which we extract data, rather than using effect sizes from broad-spectrum meta-analysis.
The generalisability of trials to routine care has been examined by Thomsen et al. 7 in Denmark. They looked at the effects of adding a second drug to metformin in a large population-based cohort, and concluded that the results were similar to those seen in the trials. The mean HbA1c at intensification was 8.0%. They observed reductions in median HbA1c of 1.2% with sulfonylureas, 0.8% with DPP-4 inhibitors, 1.3% with GLP-1 receptor agonists and 2.4% with insulin. However, these differences reflect different baseline HbA1c levels, notably 9.5–10% amongst those who started insulin. Despite intensification, 41% had not achieved HbA1c < 7.5% 6 months later.
Thomsen et al. 7 also noted that the threshold for intensification had fallen over the years, from about 8.8% in 2000–3 to about 8.1% in 2010–12 (estimated from graph in supplementary material; figure 3). If this has also occurred in the UK, it reinforces the need to be selective in extracting effect sizes for modelling. In past studies, patients with type 2 diabetes were often left poorly controlled for several years before intensification,189,190 but this may be happening less nowadays, with improved control promoted by the Quality Outcomes Framework of payments to general practices for demonstrating performance against HbA1c control indicators,191 including DM007 for the HbA1c indicator. The three bands are now 59, 64 and 75 mmol/mol. All of them (not just the tightest) probably encourage initiation of insulin in practice.
Assessment Group cost-effectiveness literature review
Only one paper192 was identified that addressed the cost-effectiveness of flozin monotherapy in the patient group under consideration. Neslusan et al.,192 available only in abstract, used the ECHO-T2DM model to compare the cost-effectiveness of monotherapy canagliflozin 100 mg and canagliflozin 300 mg with lifestyle management within the USA. Patients could intensify to sulfonylurea and then on to insulin, both apparently with an 8.0% intensification threshold. By the 10th year the use of canagliflozin had delayed the intensification to insulin such that 27% of the canagliflozin-100 mg group and 19% of the canagliflozin-300 mg group were receiving insulin compared with 66% of those who started with lifestyle management. Canagliflozin was reported to lower total costs and result in improved QoL over a 30-year time horizon, and so dominated lifestyle management.
United Kingdom Prospective Diabetes Study and the United Kingdom Prospective Diabetes Study Outcomes Models
By way of background, for much cost-effectiveness modelling in type 2 diabetes the results of the UKPDS have been used. Until recently the main UKPDS publication relevant to cost-effectiveness modelling was the UKPDS68. 193 This outlines a number of equations for estimating the progression of the risk factors of HbA1c, SBP, TC/HDL and smoking status through time. Given the evolution of these risk factors, the UKPDS68193 also specifies a number of equations that calculate the annual risk of experiencing first ‘events’, these events being the macrovascular complications of diabetes, such as stroke, and the microvascular complications of diabetes, such as blindness. The UKPDS68193 also permits the calculation of annual probabilities of death. The UKPDS68193 was used by Oxford University to develop an electronic cost-effectiveness model, the UKPDS Outcomes Model v1 (OM1).
There are 10 equations:
-
equation 1: ischaemic heart disease (IHD)
-
equation 2: MI
-
equation 3: CHF
-
equation 4: stroke
-
equation 5: amputation
-
equation 6: blindness
-
equation 7: renal failure
-
equation 8: event mortality
-
equation 9: diabetes-related mortality
-
equation 10: other mortality.
The UKPDS68193 has recently been partially updated by the UKPDS82,194 the latter incorporating longer follow-up data of the UKPDS. This provides an alternative set of equations to estimate the probability of events and deaths, and also permits the estimation of the probability of some second events: MI, stroke and amputation. Oxford University has developed an updated electronic model, the UKPDS Outcomes Model v2 (OM2). As far as the AG is aware, this currently relies upon the UKPDS68193 for the evolution of the risk factors and the UKPDS82 for the probabilities of events and deaths. The AG has not had access to the OM2 during the course of the assessment.
The UKPDS82194 provides the following table (Table 15) to outline the differences in the predicted number of events at 10 years for patients of different ages.
| Event | 50–54 years | 60–64 years | 70–74 years | All ages | ||||
|---|---|---|---|---|---|---|---|---|
| OM1 | OM2 | OM1 | OM2 | OM1 | OM2 | OM1 | OM2 | |
| First MI | 14.9 | 7.5 | 22.5 | 10.3 | 29.6 | 13.3 | 21 | 9.9 |
| Second MI | n/a | 0.9 | n/a | 1.0 | n/a | 1.1 | n/a | 1.0 |
| Ulcer | n/a | 1.5 | n/a | 1.9 | n/a | 2.2 | n/a | 1.8 |
| Blindness | 2.2 | 2.2 | 3.5 | 3.1 | 4.9 | 4.0 | 3.3 | 2.9 |
| IHD | 8.6 | 6.9 | 10.3 | 8.3 | 10.5 | 9.0 | 9.5 | 7.8 |
| First stroke | 3.3 | 3.3 | 7.9 | 6.4 | 14.2 | 10.7 | 7.6 | 6.2 |
| Second stroke | n/a | 0.3 | n/a | 0.7 | n/a | 1.5 | n/a | 0.7 |
| Renal failure | 0.9 | 0.3 | 1.4 | 0.6 | 1.6 | 0.8 | 1.3 | 0.5 |
| First amputation | 1.7 | 1.3 | 2.0 | 1.6 | 1.7 | 1.8 | 1.8 | 1.5 |
| Second amputation | n/a | 0.4 | n/a | 0.6 | n/a | 0.4 | n/a | 0.4 |
| Heart failure | 3.0 | 2.5 | 5.9 | 4.3 | 9.9 | 6.4 | 5.7 | 4.0 |
| Death | 14.5 | 11.1 | 32.1 | 22.3 | 58.8 | 43.3 | 31.6 | 22.5 |
Ischaemic heart disease includes angina and consequences of procedures to relieve it, such as angioplasty and coronary artery bypass grafting.
The OM1 predicts roughly double the number of MIs over 10 years, and the rates of IHD are also noticeably higher. Possibly mainly as a consequence of the higher rate of MI predicted by the OM1, the 10-year death rate predicted by the OM1 is also noticeably higher. The OM1 will tend to over-predict event rates compared with the OM2. The OM1 is now likely to overstate the benefits and cost savings arising from any avoidance of the complications of diabetes that are associated with the more effective treatment.
It is anticipated that the longer follow-up data of the UKPDS associated with the UKPDS82194 will result in additional publications, one of which will update the evolution of the risk factors. The costs associated with events have already been updated, the UKPDS84195 being an update of the UKPDS65. 196 The QoL estimates have also been updated in Alva et al. 197 But the format of the analysis of Alva et al. 197 is less closely aligned with the events of the UKPDS84195 when compared with the alignment of the QoL estimates of the UKPDS62198 with the events of the UKPDS68. 193
Company submissions
There are three company submissions:
-
Boehringer Ingelheim for empagliflozin
-
AstraZeneca for dapagliflozin
-
Janssen for canagliflozin.
An overarching summary of the companies’ and the AG’s modelling assumptions, inputs and results is presented at the end of the economics section, permitting an easy read across. Readers may wish to work through this overarching summary first, before turning to the more detailed summaries presented below for more clarity around specific points of the individual modelling exercises.
All of the submissions contain modelling exercises with long-term time horizons of around 40 years, which for the majority of patients will be a lifetime horizon. They all undertake a cost–utility analysis using the appropriate perspectives of the NHS and Personal Social Services (PSS) for costs and the patient for benefits, and discount costs and benefits at 3.5%.
Boehringer Ingelheim designed a front end to the UKPDS OM1 model. The Boehringer Ingelheim submission has a great deal in common with the modelling of recent NICE CGs for type 2 diabetes, and the AG modelling for the current assessment, both of which design a front end to the UKPDS OM1.
AstraZeneca uses the Cardiff Diabetes Model (CDM), which uses many of the UKPDS68193 equations and so has much in common with the UKPDS OM1 model, but updates the calculation of the probabilities of having an event to use the UKPDS82,194 which is the basis of the OM2.
Janssen differs from AstraZeneca and Boehringer Ingelheim in using the ECHO-T2DM model. Its base case has assumptions that differ quite noticeably from those of the other two submissions. There is also relatively little detail in the Janssen submission, with most of the detail being contained in the appendices to the submission and the submitted electronic copy of the model.
In light of the above, the review of the company submissions below provides a reasonably in depth review of the Janssen modelling. This is followed by shorter reviews of the Boehringer Ingelheim and the AstraZeneca modellings, which are more in line with the AG modelling.
Janssen economic modelling
The ECHO-T2DM model is an individual patient simulation model developed by staff of the Swedish Institute for Health Economics. It has been routinely submitted to the Mount (Mt) Hood Challenges. The Mt Hood Challenges are intermittent events at which the main diabetes models are challenged to use a set of real-world clinical inputs to predict the longer-term incidences of the various complications of diabetes without having access to the actual longer-term incidences of the various complications. Their predictions are then compared with the actuals. But the ECHO-T2DM submissions to the Mt Hood Challenges were probably with different assumptions than those used for the Janssen submission, in particular with regard to the evolution of HbA1c.
The model was run with a 40-year time horizon and a cycle length of 1 year. Costs and benefits were discounted at 3.5%. The perspective was that of the patient for health impacts and of the NHS/PSS for costs.
One thousand probabilistic sensitivity analysis (PSA) iterations were run for the base case, with each PSA iteration modelling 2000 patients. It appears that each patient was run through the model only once, with no internal loops to reduce Monte Carlo error. For the scenario analyses the number of patients was reduced to 1500. The submission did not present any analysis of model convergence over the number of patients modelled. It appears that only results of analyses performing the 1000 PSA iterations were presented and that no deterministic analyses, that is analyses with no sampling of second order uncertainty, were undertaken. This could have permitted more than 2,000 patients to be simulated and some analysis of convergence of results as patient numbers were increased to be presented.
The model simulates the evolution of the severity of the microvascular complications of diabetes, based mainly upon Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) data:
-
retinopathy
-
CKD
-
neuropathy, this also encompassing PVD.
Chronic kidney disease health states range from stage 1 with an eGFR of > 90 ml/minute/1.73 m2 to end-stage renal disease (ESRD) with an eGFR of < 15 ml/minute/1.73 m2 for over 1 year.
The appendices to the Janssen submission state that four macrovascular complications are included:
-
IHD
-
MI
-
stroke
-
CHF.
The model also incorporates:
-
patient weight
-
severe hypoglycaemia
-
non-severe hypoglycaemia
-
UTIs
-
GTIs
-
peripheral oedema
-
discontinuations.
Patient characteristics
Patient characteristics at baseline were drawn from a pooled analysis of the CANTATA-M84,92 and Japanese canagliflozin76 studies, resulting in baseline estimates of 56 years of age, 52% male, 8.016% HbA1c, 128 mmHg SBP, 29.7 kg/m2 BMI, 200 mg/dl TC, 118 mg/dl LDL, 48 mg/dl HDL, 175 mg/dl triglycerides and a mean eGFR of 86 ml/minute/1.73 m2. Note that the inclusion of the Japanese study76 pulls down the mean BMI because the mean BMI was 25.6 kg/m2. Those in CANTATA-M84,92 had a higher BMI, mean 31.6 kg/m2.
Based upon the submitted electronic model input sheets, the mean disease duration was 4.6 years, and was assumed to range uniformly between 0 years and 9.2 years. The proportion of patients with background diabetic retinopathy (BDR) was 0.7%; microalbuminuria, 0.1%; and symptomatic neuropathy, 1.5%. The proportion of patients with IHD was 1.2%, MI 0.8%, stroke 0.1% and amputation 0.1%. The other complication rates were zero.
Sequences modelled and treatment effectiveness
The Janssen submission modelled the following treatment sequences (Table 16).
| Monotherapy | Intensification | |||
|---|---|---|---|---|
| First | Second | Third | Fourth | |
| Flozin | Flozin + SU | NPH insulin | NPH + aspart (insulin) | None |
| Pioglitazone | Pioglitazone + SU | NPH insulin | NPH + aspart | None |
| Gliclazide | Sitagliptin + SU | NPH insulin | NPH + aspart | None |
| Sitagliptin | Sitagliptin + SU | NPH insulin | NPH + aspart | None |
| Repaglinide | Pioglitazone | Pioglitazone + SU | NPH insulin | NPH + aspart |
Repaglinide was included only as a scenario analysis. For canagliflozin 100 mg it appears that two arms were modelled: one that intensified by adding gliclazide. The other was classed as confidential. But the Janssen submission is slightly ambiguous about this.
Clinical effectiveness estimates for the monotherapies were mainly drawn from the 26-week NMA, though infection rates were drawn from the canagliflozin trials, with the flozins being assumed to have the same rate as canagliflozin 100 mg and the other comparators the same rate as the placebo arm. Based upon the electronic input sheets submitted by Janssen and the model having an annual cycle, the 26-week estimates were assumed to apply at the end of the first cycle. Note also that the estimates of the electronic input sheets are stated as being relative to placebo, and that there does not appear to be a placebo effect within the electronic input sheets. As a consequence, it appears that the treatment effects relative to placebo rather than the absolute treatment effects have been applied within the Janssen modelling.
The appendices to the submission present two NMAs: with and without repaglinide. The central estimates of these appear to the AG to be virtually identical, with the exception of the rates of severe and non-severe hypoglycaemic events for pioglitazone and sitagliptin. Why these should differ between the two analyses is not clear (Table 17).
| Variable | Drug and dose | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Canagliflozin | Dapagliflozin | Empagliflozin | Gliclazide | Pioglitazone | Sitagliptin | Repaglinide | |||
| 100 mg | 300 mg | 10 mg | 10 mg | 25 mg | 160 mg | 30 mg | 100 mg | 2 mg | |
| HbA1c | –0.97 | –1.2 | –0.64 | –0.73 | –0.85 | –0.59 | –0.78 | –0.72 | –1.28 |
| SBP | –3.71 | –5.41 | –3.21 | –2.60 | –3.40 | 0.191 | 0.880 | 0.800 | 0.191 |
| BMI | –0.85 | –1.21 | –0.57 | –0.61 | –0.65 | 0.220 | 0.833 | 0.293 | 0.220 |
| TC | 4.512 | 7.544 | 4.512 | 4.512 | 4.512 | – | – | – | – |
| LDL | 1.655 | 6.156 | 1.655 | 1.655 | 1.655 | – | – | – | – |
| HDL | 3.447 | 3.236 | 3.447 | 3.447 | 3.447 | – | – | – | – |
| Triglycerides | –25.0 | –24.0 | –25.0 | –25.0 | –25.0 | – | – | – | – |
| AEs | |||||||||
| Female GTI | 0.208 | 0.161 | 0.208 | 0.208 | 0.208 | 0.065 | 0.065 | 0.065 | 0.065 |
| Male GTI | 0.047 | 0.165 | 0.047 | 0.047 | 0.047 | 0.015 | 0.015 | 0.015 | 0.015 |
| Upper UTI | 0.008 | 0.000 | 0.008 | 0.008 | 0.008 | 0.000 | 0.000 | 0.000 | 0.000 |
| Lower UTI | 0.107 | 0.109 | 0.107 | 0.107 | 0.107 | 0.071 | 0.071 | 0.071 | 0.071 |
| Severe hypoglycaemia | 0.008 | 0.000 | 0.003 | 0.008 | 0.008 | 0.034 | 0.002 | 0.002 | 0.010 |
| Non-severe hypoglycaemia | 0.046 | 0.065 | 0.057 | 0.046 | 0.046 | 0.508 | 0.027 | 0.031 | 0.156 |
| First-year discontinuation | 0.025 | 0.020 | 0.025 | 0.025 | 0.025 | 0.011 | 0.011 | 0.011 | 0.011 |
| Peripheral oedema | |||||||||
| Year 1 | 0.119 | 0.119 | 0.119 | 0.119 | 0.119 | 0.119 | 0.254 | 0.119 | 0.119 |
| Subsequent | 0.058 | 0.058 | 0.058 | 0.058 | 0.058 | 0.058 | 0.085 | 0.058 | 0.058 |
As already noted, the definition of hypoglycaemia used a cut-off of below 4.0 mmol/l, which is above the foot of the normal range of 3.5 mmol/l.
The submission appears to state that when a patient intensified by adding another therapy that the clinical effectiveness estimates of that therapy were applied. When a patient intensified therapy by switching to another therapy, rebound was assumed with the clinical effectiveness estimates of the initial therapy being removed prior to applying the clinical effectiveness estimates of the therapy to which the patient was switching. Rebound consequently appears to be to take the patients back to their baseline values for the risk factors. And the clinical effectiveness of a treatment was assumed to be the same whether it was being used as a monotherapy or was being added to other therapies.
At the progression to insulin the clinical effectiveness estimates in Table 18 were applied, the values being taken from the copy of the electronic model input sheet that was submitted. The source of these estimates was not clear to the AG.
| Variable | Drug | |
|---|---|---|
| NPH | Aspart | |
| HbA1c | –0.9 | –1.509 |
| SBP | – | – |
| BMI | 0.496 | 1.009 |
| TC | – | – |
| LDL | – | – |
| HDL | – | – |
| Triglycerides | – | – |
| AEs | ||
| Severe hypoglycaemia | 0.0049 | 0.04 |
| Non-severe hypoglycaemia | 0.67 | 44.95 |
Treatment intensification and discontinuation
Treatment intensification occurred if the patient breached the 7.5% HbA1c treatment intensification threshold. Some details in the Janssen submission were classed as confidential and cannot be replicated here.
A key issue is whether or not the subset of patients who do poorly when treated with canagliflozin 100 mg will, when they switch to canagliflozin 300 mg, experience the same peak HbA1c effect as estimated from the entire patient group in the trial, which was randomised to canagliflozin 300 mg from the start.
Patients could also discontinue their current treatment because of adverse events and contraindications. It is unclear to the AG whether those discontinuing one treatment were assumed to intensify to monotherapy with another agent or to dual therapy with another agent.
The submission states that the treatment effects associated with discontinuations were immediately reversed at discontinuation. If treatment effects were limited to, for example, one-off reductions in HbA1c it is easy to see how this treatment effect could be reversed and rebound could occur. But treatment effects are not limited to one-off effects. The evolution of HbA1c after the initial one-off effect is also treatment specific so has to be counted as a treatment effect. The AG assumption is that rebound was to baseline values, but this is not unambiguous and may have been treated differently for different risk factors, for example HbA1c and weight.
The Janssen submission is ambiguous about whether or not the model handles treatment intensifications and treatment discontinuations in the same manner. It is important to know whether or not rebound also occurs when treatments are withdrawn at treatment intensification, particularly for the intensification from repaglinide to pioglitazone, and for the intensification to insulin when patients are assumed to discontinue their oral therapies. Appendix 4 to the main submission states that:
Treatment intensification algorithms triggered when biomarker threshold levels are exceeded determine AHA and concomitant medication use (i.e. anti-hypertensive, dyslipidaemia) over time. Each drug (or drug combination) is described by a profile that includes price, initial treatment effects, bio-marker evolution, ‘rebound’ effects applied upon discontinuation, AE rates, non-compliance rates, contraindications, and disutility (if any). A treatment sequence of rescue medications can be specified by the user, including at least one line of rescue insulin therapy. Agents can be continued or discontinued at bio-marker failure (HbA1c for AHA, SBP for anti-hypertensive agents, and any of the cholesterol components for anti-dyslipidaemia agents).
To the AG, this suggests the intensifications, or discontinuation at biomarker failure of HbA1c in the above, may be treated in the same manner as discontinuations and treatment switches, and have rebound applied if specified by the user.
This raises the possibility of repaglinide rebounding at treatment failure, so adding 1.28% to the then current 7.5% patient HbA1c. Intensifications to pioglitazone with its –0.78% effect and then the subsequent intensification to add gliclazide and its effect of –0.59% may not reverse this rebound, given the incorporation of annual drift. If this applied, patients on repaglinide could spend little to no time on subsequent oral intensifications before intensifying to insulin. But the AG assumption is that rebound is to the baseline value rather than to the baseline value plus annual drift, and that this rebound applies to all of the risk factors and not just HbA1c.
It is not obviously reasonable to assume that there will be rebound when patients start insulin. The clinical effectiveness estimates for insulin may reflect the overall effect of a switch to insulin including any discontinuations of existing therapy.
Glycated haemoglobin evolution
A major difference in assumptions in the Janssen submission compared with the other submissions and the AG modelling is that rather than apply the UKPDS68193 equation to evolve HbA1c, treatment-specific linear evolutions were assumed. The argument for this is that though most NICE assessments in diabetes have used the UKPDS68193 equations to evolve HbA1c, these evolutions encompass treatment intensifications. As a consequence, if treatment effects are being associated with treatment intensifications in the modelling, using the UKPDS68193 evolution will tend to double count these treatment effects.
The values of these for the monotherapies were based upon values taken from the ADOPT trial as reported in Kahn et al. 174 The majority of the monotherapies under consideration were not used in the ADOPT trial, which used rosiglitazone, metformin and glyburide (the North American name for glibenclamide). Janssen assumes that values from treatments within the ADOPT trial apply to the monotherapies under consideration in Table 19.
| Monotherapy | ADOPT equivalent | Annual HbA1c drift (%) |
|---|---|---|
| Flozin | Metformin | 0.14 |
| DPP-4: sitagliptin | Metformin | 0.14 |
| SU: gliclazide | SU: glyburide | 0.24 |
| Repaglinide | SU: glyburide | 0.24 |
| Pioglitazone | Rosiglitazone | 0.07 |
Applying the glibenclamide progression rate to gliclazide may be pessimistic given the 6-year difference in start of insulin on gliclazide and glibenclamide, in favour of gliclazide. 17
Given the annual rates of drift and the initial HbA1c treatment effects estimated in the NMA, it is apparent that the annual rates of drift are likely to be as, if not more, important than the HbA1c treatment effects estimated in the NMA. Owing to the NMA estimating HbA1c from 24-week data, half the annual drift is added to the estimated treatment effect to provide the 52-week estimate.
At intensification, if another treatment is added the annual rate of HbA1c drift is assumed to be the average of the HbA1c annual drifts of the two treatments being used as dual therapy (Table 20).
| Dual therapy | Annual HbA1c drift (%) |
|---|---|
| Flozin + sulfonylurea | 0.19 |
| DPP-4 + SU | 0.19 |
| Pioglitazone + SU | 0.16 |
For those intensifying to insulin, Janssen derives an annual rate of drift of 0.15% from the UKPDS82. 194
The impact of these different annual drifts in HbA1c is applied in tandem with the initial treatment effects. For instance, at the central Janssen treatment effect estimates and a baseline value for HbA1c of 8.0% it appears that for those who do not discontinue for other reasons the following evolutions are implied up to the point at which HbA1c rises above 7.5% and treatment is intensified (Figure 9).
FIGURE 9.
Janssen modelled HbA1c drift by treatment at central values.
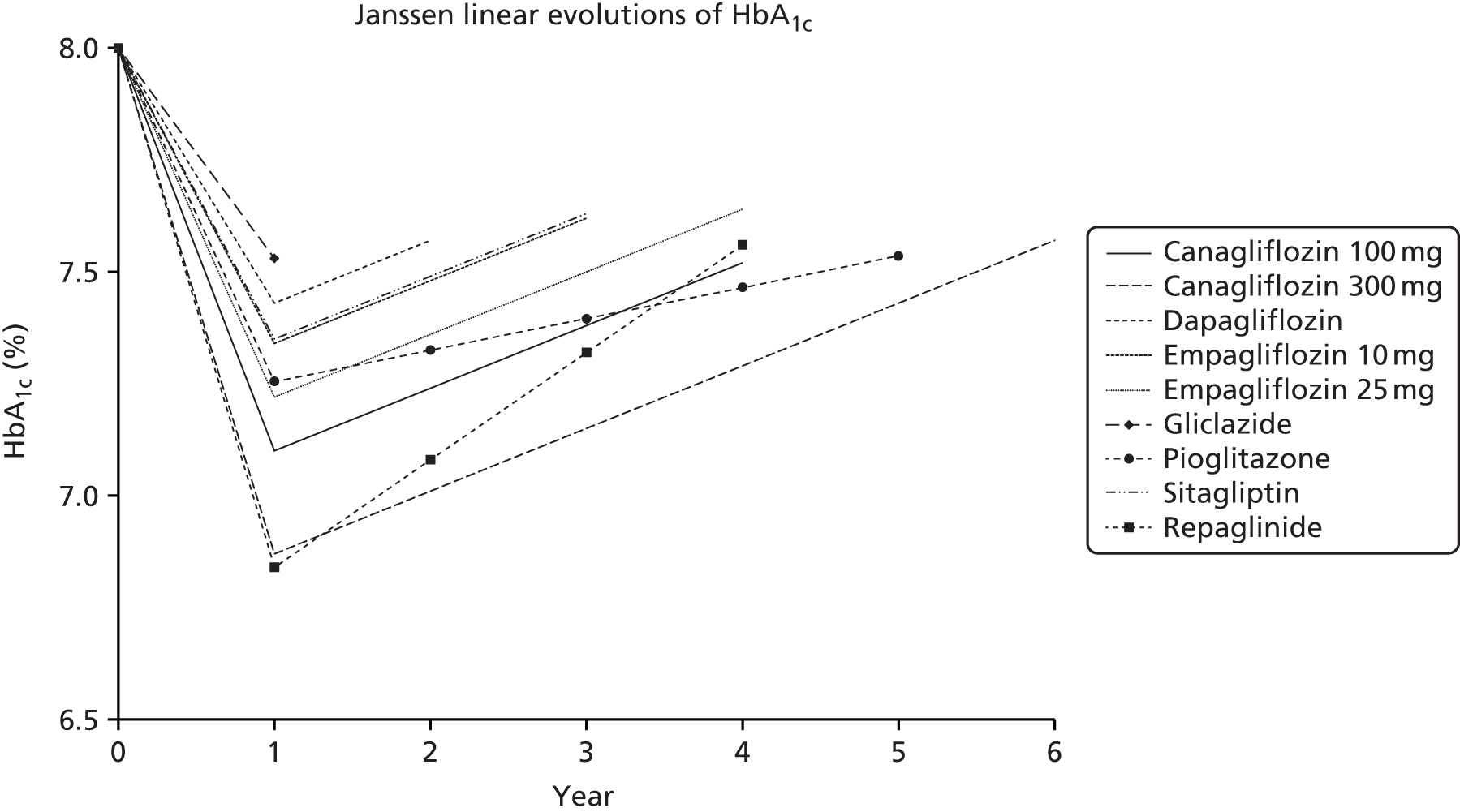
Immediately apparent is that for gliclazide (the topmost line) the treatment effect of –0.59% when coupled with half of the annual drift, that is an increase of 0.12%, means that the patient is above 7.5% at the end of the first cycle.
Turning to canagliflozin 100 mg (the solid line), despite its initial treatment effect of –0.97% being somewhat less than the –1.28% of repaglinide, they both breach the 7.5% HbA1c intensification threshold at the fourth year due to the differences in annual drift. The slower drift for canagliflozin 300 mg also means that despite an initial treatment effect of –1.20% it breaches the 7.5% HbA1c intensification threshold by 6 years.
Thereafter, it should be borne in mind that repaglinide is assumed to be replaced by pioglitazone. Owing to the withdrawal of treatment the AG reading of the Janssen submission is that in the model this causes the HbA1c to rebound to the original baseline value of 8.016%, and not to have the full rebound of the repaglinide 1.28% treatment effect applied. The –0.59% pioglitazone effect is then applied with the pioglitazone-specific HbA1c rate of drift applied, with a further intensification to pioglitazone plus SU after this. In other words, in the repaglinide arm there is the initial repaglinide evolution of HbA1c in the above example for 4 years, which is then followed by exactly the same HbA1c evolution as in the pioglitazone arm, only with this being lagged by 4 years.
The same annual drifts apply for empagliflozin, dapagliflozin and sitagliptin as for canagliflozin. They also intensify by adding gliclazide, and then on to insulin. Again, ignoring discontinuations for other reasons, the linear evolution of HbA1c means that any difference in the timings of the first intensification is also reflected in the timings of the intensification to insulin. It appears that the assumption of a linear evolution of HbA1c will maintain absolute differences in HbA1c between treatments, at least until the patient intensifies to insulin. Upon intensification to insulin it appears that the ECHO-T2DM model applies the linear evolution for HbA1c, but then permits the patient to increase his/her insulin dose in order to stabilise his/her HbA1c. The Janssen submission is not particularly clear on this point, but it appears that this means that HbA1c may eventually converge between treatments once the patient has started insulin.
Pioglitazone benefits from a slower annual rate of drift, and continues to derive some benefit from this source even after the intensification of adding gliclazide. At central parameter values and again ignoring discontinuations it will have a permanent HbA1c benefit over all the other comparators with the possible exception of canagliflozin 300 mg.
Reconciling the above with the evolutions of HbA1c reported in the Janssen submission is difficult, given the annual cycle of the model. But it should be borne in mind that the Janssen curves are averaged over a large number of patients and PSA iterations, and include the effects of discontinuations for other reasons (Figure 10).
FIGURE 10.
Janssen figure 13: submission reported evolutions of HbA1c.
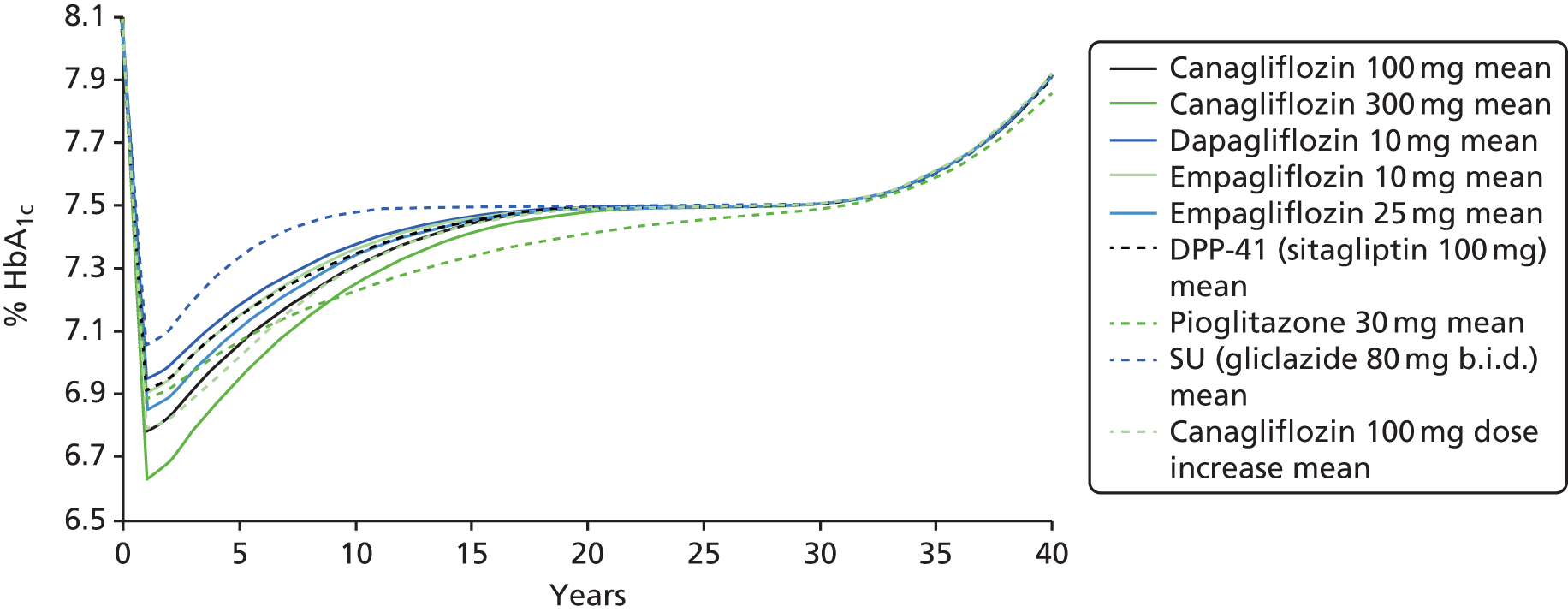
For instance, the mean first year effect for the gliclazide arm as shown by the topmost curve is around a 0.95% reduction in HbA1c, which is somewhat greater than the –0.59% mean estimate for gliclazide. Those discontinuing for reasons other than HbA1c apparently in effect switch to pioglitazone, the estimate for which is –0.78%. Similarly, the reduction of around 1.4% in HbA1c for canagliflozin 300 mg, as shown by the bottom curve, is also difficult to reconcile with its central estimate of –1.20%. Perhaps both discontinuations and their treatment effects and intensifications and their treatment effects are included in the year 1 estimates, though this timing could be questionable given the annual cycle of the model. It remains difficult to reconcile the above with the central estimates for treatment effectiveness.
At central estimates around one-third of the canagliflozin 300 mg patients would be required to not receive a boost of the –0.59% estimate for the intensification to gliclazide to achieve the reduction of 1.4% shown in the above figure. This also requires that none discontinue, rebound and receive a lesser treatment effect from whatever alternative to which they switch. Any discontinuations in the canagliflozin 300-mg arm would seem to require an even larger boost to the 1.2% canagliflozin 300-mg treatment effect among those not discontinuing if the reduction of around 1.4% is to be arrived at.
Even with the effects of second-order sampling, it is not clear to the AG how the above central estimates for the evolutions of HbA1c have been arrived at. Perhaps there are additional placebo treatment effects in addition to the treatment effects relative to placebo and the AG has not managed to identify these. In light of the above, while having read the Janssen submission and its appendices, the AG does not really understand how the model is implementing the changes in HbA1c and how the central estimate for canagliflozin 300 mg is to reduce the patient HBA1c, on average, from 8.016% at baseline to around 6.63% at 1 year: a reduction of around 1.4%.
The above figure also sees the HbA1c values converge between the arms. Janssen states that this is ‘Because of differences in the timing of requirements for rescue medication, HbA1c, SBP, and lipid curves tend to converge as patients with higher values benefit from treatment-related improvements earlier’. To the AG this does not obviously explain the convergence, or why the curve for gliclazide converges by essentially having zero increase from the tenth to the thirtieth year. A possible explanation might be the intensification to insulin with patients then being permitted to increase their insulin dose in order to stabilise their HbA1c.
The argument that the UKPDS68 equation 11193 includes the effects of treatment intensifications does have some force. But it should be borne in mind that the UKPDS68 equation 11193 explicitly includes a parameter for whether or not the patient is in his/her second year of diagnosis. This could be viewed as a proxy for the clinical effectiveness of the first treatment for diabetes being introduced, though the second year of diagnosis might be a little early for some patients. As a consequence, modelling could as an alternative apply treatment-specific effects and still apply the UKPDS68 equation 11193 thereafter, only ignoring the parameter related to whether or not the patient is in his/her second year. For the patient baseline characteristics outlined in the Janssen submission, the annual increases implied by the UKPDS68 equation 11193 in the years shortly after the second year are around 0.18%, which is broadly central to the rates Janssen takes from the ADOPT study as reported in Kahn et al. 174 This may be preferable to extrapolating linear rates from the ADOPT trial, particularly as these rates are being applied to treatments which were not used in the ADOPT trial, and to periods beyond the 5-year follow-up of the ADOPT trial, and with some distinctly ad hoc averaging for the rates for dual therapy.
The AG has some sympathy with the argument that HbA1c drift may initially be treatment specific. A linear evolution might even be the most reasonable functional form, particularly given the coefficients reported by Kahn et al. 174 But the AG does not view it as reasonable to assume a linear evolution of HbA1c throughout and that there will be no convergence between treatments, or at least none until a patient starts insulin therapy. This may artificially preserve differences between treatments, when the UKPDS68193 evolution clearly implies a convergence. The AG is also uncomfortable with the assumed linear rates of drift that have been imputed from Kahn et al. ,174 given that none of the monotherapies under consideration was studied by Kahn et al.
A scenario analysis where the model applies the UKPDS68193 evolution of HbA1c was presented.
Evolution of other risk factors
Linear drifts were also assumed for the other biomarkers but these were not differentiated by treatment: 0.30 mmHg for SBP, 0.03 mg/dl for lipids resulting in a flat TC/HDL evolution. These annual rates of drift were apparently derived from the UKPDS. The UKPDS was conducted largely before the use of statins, and it can be argued that alternative evolutions to those of the UKPDS are now appropriate. But given that the annual rates of drift were apparently derived from the UKPDS, it is unclear to the AG why the equations of the UKPDS68193 were not applied.
For a patient’s SBP, the common annual rate of drift will tend to maintain the absolute differences between the arms. As far as the AG can ascertain, it also appears that unlike HbA1c this absolute difference for SBP will be maintained even after insulin therapy has been started.
Weight was associated with an annual gain of 0.1 kg. Table 12 of the submission states that weight drifts upwards but there is no suggestion of a base-case assumption of convergence; table 13 goes on to suggest that for the base case the patient’s weight was assumed to converge at treatment discontinuation, with this being in line with figure 26 of the appendix. If this convergence applied, it is unclear whether it was at the first intensification or was when the oral therapies were being discontinued and the patient switched to insulin. A scenario analysis of a slower convergence over 2 years after treatment discontinuation was also presented.
Treatment discontinuation: renal impairment
In accordance with the canagliflozin Summary of Product Characteristics (SmPC), canagliflozin 100 mg was modelled as being discontinued if the eGFR fell below 45 ml/minute/1.73 m2; canagliflozin 300 mg was modelled as being discontinued if the eGFR fell below 60 ml/minute/1.73 m2. The SmPC states that if the eGFR falls below 60 ml/minute/1.73 m2 the patient should have his/her dose adjusted to 100 mg. Those intensifying from canagliflozin 100 mg to canagliflozin 300 mg would have already failed on canagliflozin 100 mg. The licence states that canagliflozin 100 mg should always be used before canagliflozin 300 mg. So dose reduction may be of limited relevance and discontinuation of canagliflozin 300 mg may be the appropriate assumption.
Empagliflozin has similar restrictions in its SmPC, with it being possible to increase the dose from 10 mg to 25 mg if the eGFR is more than 60 ml/minute/1.73 m2. If the eGFR falls below 60 ml/minute/1.73 m2 the patient should have his/her dose adjusted to 10 mg, and if the eGFR falls below 45 ml/minute/1.73 m2 the patient should discontinue empagliflozin.
The dapagliflozin SmPC has slightly different restrictions and is not recommended for patients with an eGFR of less than 60 ml/minute/1.73 m2.
The sitagliptin SmPC does make the administered dose depend on renal impairment, requiring it to be reduced to 50 mg in those with moderate renal impairment, and 25 mg in those with severe renal impairment. But discontinuation does not appear to be required.
As far as the AG can see the submission does not state what assumptions, if any, have been made about discontinuing empagliflozin and dapagliflozin based upon the patient’s eGFR. Table 12 of the submission is explicit in its consideration of the canagliflozin SmPC for discontinuations related to renal impairment and to the pioglitazone SmPC for discontinuations related to CHF, but makes no reference to the empagliflozin SmPC or the dapagliflozin SmPC. Appendix 4 of the submission mentions that empagliflozin and dapagliflozin also have treatment rules based upon eGFR. The input sheets to the electronic model suggest that empagliflozin 10 mg, empagliflozin 25 mg and dapagliflozin are assumed to be discontinued as per canagliflozin: if the eGFR drops below 60 ml/minute/1.73 m2. This appears to be incorrect for empagliflozin 10 mg, and illogical for empagliflozin 25 mg.
The use of the ECHO-T2DM model was, in part, justified by Janssen on grounds of the need to properly account for discontinuations due to renal impairment. In light of this, a scenario analysis that does not apply these discontinuations would have been useful in order to assess the importance of attempting to model this.
Treatment discontinuations: adverse events
Patients could discontinue treatments as a result of adverse events. It is not clear to the AG what was assumed to happen to these patients. They may have discontinued their current treatment and switched to whatever is next in the sequence, for example from flozins to SU and then on to NPH insulin, or they may switch to an alternative monotherapy, or they may have switched to an alternative dual therapy.
Hypoglycaemic events
Hypoglycaemia event rates were derived from the pooled 26-week data of the two canagliflozin trials. The NMA 26-week data provided the estimates for the other comparators with the exception of gliclazide. No hypoglycaemia rates were available for gliclazide, and, as a consequence, rates for glimepiride were adjusted by relative risks of 0.43 for symptomatic hypoglycaemia and 0.45 for severe hypoglycaemia. The AG is unclear whether or not these rates were adjusted to be annual rates and so to be in line with the annual model cycle.
Hypoglycaemia event rates were further modified by increasing the risk of hypoglycaemia for low HbA1c values. The relationship underlying this was based upon a large data set of the Diabetes Control and Complications Trial (DCCT) study among patients with type 1 diabetes. A 1% drop in HbA1c below the mean value of the clinical study was associated with an increased hazard of hypoglycaemia of 1.43. However, patients in the DCCT intensive arm were on either MDI or continuous subcutaneous insulin infusion (CSII) via insulin pumps.
Adverse events
The UTI and GTI event rates were derived from the pooled 26-week data of the two canagliflozin trials. The AG is unclear whether or not these rates were adjusted to be annual rates and so to be in line with the annual model cycle. The other flozins were assumed to have the same rates as canagliflozin 100 mg, with the other comparators being assumed to have the same rate as the pooled placebo arms of the canagliflozin trials.
Quality of life
A systematic literature review was conducted, with Janssen preferring the CODE-2 (Cost of Diabetes in Europe–Type 2) data of Bagust and Beale199 over the UKPDS62198 as a result of it providing greater richness for the microvascular complications. Bagust and Beale199 is also the source for the QoL coefficient for BMI.
Janssen reports that no appropriate studies were identified for adverse events, and as a consequence a time trade-off (TTO) study among 100 members of the UK general public was conducted to determine the QoL impacts from UTIs and GTIs. This TTO study also explored hypoglycaemia, GI symptoms and hypovolaemic events, but the estimates for these were disregarded (Table 21).
| Condition | Mean | SD | Disutility |
|---|---|---|---|
| Type 2 diabetes | 0.92 | 0.10 | – |
| and mild/moderate UTIs | 0.83 | 0.14 | 0.09 |
| and severe UTIs | 0.73 | 0.20 | 0.19 |
| and mycotic infection | 0.67 | 0.26 | 0.25 |
| and moderate hypoglycaemia | 0.81 | 0.19 | 0.11 |
| and severe hypoglycaemia | 0.77 | 0.21 | 0.15 |
| and fear of hypoglycaemia | 0.77 | 0.17 | 0.15 |
| and GI symptoms | 0.68 | 0.24 | 0.24 |
| and hypovolaemic events | 0.84 | 0.14 | 0.08 |
Based upon the references cited, these values apparently contributed to a regression analysis, which arrived at the final QALY decrements. Unfortunately, the AG has not been able to source this regression analysis.
The health state descriptors suggest that the estimates relate to ongoing infection and are not time limited, as is appropriate in a TTO study, but this implies that event health states need to be adjusted by the average duration of UTIs and GTIs, as occurs in the Janssen submission. The method of this adjustment does not appear to have been presented. At mean values, 1 week of a moderate UTI would roughly correspond with a –0.0012 QALY decrement; 2 weeks of a severe UTI would roughly correspond with a –0.0073 QALY decrement; and 1 week of a mycotic infection would roughly correspond with a –0.0046 QALY decrement.
The QoL values applied for the baseline characteristics and microvascular complications are presented in Table 22. Those for macrovascular complications, obesity, hypoglycaemic events and adverse events are presented in the overarching summary comparison of the companies’ and AG’s inputs (see Table 22).
| State | QoL | Source |
|---|---|---|
| Baseline | 1.027 | CODE 2 |
| Patient characteristics | ||
| Age (per 10 years) | –0.0235 | CODE 2 |
| Female | –0.0930 | |
| Duration of type 2 diabetes (per 10 years) | –0.0163 | |
| Microvascular complications | ||
| Retinopathy (BDR, MO, PDR and combinations) | 0.000 | CODE 2 |
| Blindness (one or both eyes, including combinations) | –0.057 | |
| Gross proteinuria | –0.048 | |
| ESRD | –0.175 | |
| Symptomatic neuropathy | –0.084 | |
| PVD | –0.061 | |
| Symptomatic neuropathy and PVD | –0.085 | |
| Diabetic foot ulcer | –0.170 | |
| One lower-extremity amputation | –0.272 | |
| Two lower-extremity amputations | –0.272 | |
Costs
Direct drug costs were sourced from BNF 69147 and are not presented here for reasons of space. Note that the Janssen analysis, in common with the other company analyses, applies the £608 cost for canagliflozin 300 mg as a result of the submission predating the equalisation of the canagliflozin list prices at the canagliflozin 100 mg list price of £477.
The costs of blindness, IHD, MI, CHF and stroke were derived from the UKPDS84195 but are not presented here again for reasons of space. Similar costs are presented within the section on the AG modelling. A variety of other costs are sourced from a variety of NICE guidelines and other sources. Again, for reasons of space, and because they have very little impact upon the modelling, these are not presented here. A full table of event costs is presented in the appendices of the Janssen submission in table 33, starting on p. 69. Costs are also summarised in the overarching comparison of the companies and AG modelling exercises.
Adverse event costs are given in Table 23.
| Adverse event | Cost (£) | Description and reference |
|---|---|---|
| Non-severe hypoglycaemic event | 0.00 | Assumption |
| Severe hypoglycaemic event | 380.00 | Value taken from NICE draft CG |
| Lower UTIs (male) | 93.01 | One GP visit plus trimethoprim 200 mg twice daily |
| Lower UTIs (female) | 47.01 | One GP visit plus trimethoprim 200 mg twice daily |
| Upper UTIs (male) | 94.02 | Two GP visits plus trimethoprim 200 mg twice daily |
| Upper UTIs (female) | 94.02 | Two GP visits plus trimethoprim 200 mg twice daily |
| GTI (male) | 52.86 | One GP visit plus fluconazole for 7 days |
| GTI (female) | 49.45 | One GP visit plus one 500 mg clotrimazole pessary |
Some additional costs for GTIs might be anticipated if a patient’s partner is also treated.
Results
The QALY losses in the model are presented in tables 42 and 43 of the appendices, which are summarised in Table 24. The AG interpretation of this is that canagliflozin 100 mg has been taken as the reference for survival with the absolute QALY losses associated with the various events also being presented. The net absolute QALY difference between canagliflozin 100 mg and each of the comparators is then presented, with the percentage contribution of the various events to this net QALY effect being presented alongside. As the complications of diabetes other than neuropathy make little contribution to this, they have been grouped together for reasons of space.
| Drug | Loss | Survival | Hypoglycaemia | AEs | Weight | Neuropathy | Other |
|---|---|---|---|---|---|---|---|
| Canagliflozin 100 mg | 1.258 | – | 0.213 | 0.015 | 0.553 | 0.358 | 0.119 |
| Absolute QALY differences relative to canagliflozin 100 mg, and proportionate contribution by source | |||||||
| Canagliflozin 300 mg | +0.044 | 38% | 11% | 1% | 42% | 5% | 3% |
| Canagliflozin 100/300 mg | +0.012 | 49% | 12% | 1% | 36% | 2% | 0% |
| Dapagliflozin | –0.033 | 26% | 7% | 1% | 51% | 9% | 6% |
| Empagliflozin 10 mg | –0.029 | 28% | 6% | 1% | 49% | 10% | 6% |
| Empagliflozin 25 mg | –0.015 | 7% | 8% | 1% | 70% | 8% | 6% |
| Pioglitazone | –0.041 | 27% | 33% | 0% | 36% | 1% | 4% |
| Gliclazide | –0.090 | 27% | 19% | 2% | 40% | 8% | 5% |
| Sitagliptin | –0.058 | 23% | 2% | 3% | 62% | 4% | 5% |
The above shows that within the modelling survival differences account for a reasonable proportion of the estimated differences in mean QALYs between the comparators: about one-quarter for the non-canagliflozin comparators. But the direct QoL impacts of weight, hypoglycaemia and, to a lesser extent, neuropathy account for the majority of the differences. The QALY losses from the other complications of diabetes are relatively insignificant. A similar analysis can be presented for the cost differences (Table 25).
| Drug | Total | Oral treatment | Insulin | Hypoglycaemia | AEs | Neuropathy | Other |
|---|---|---|---|---|---|---|---|
| Canagliflozin 100 mg | £23,525 | £3190 | £5604 | £142 | £179 | £6350 | £8060 |
| Absolute cost differences relative to canagliflozin 100 mg, and proportionate contribution by source | |||||||
| Canagliflozin 300 mg | £777 | 73% | 21% | 1% | 0% | 2% | 3% |
| Canagliflozin 100/300 mg | £144 | 61% | 33% | 0% | 0% | 0% | 4% |
| Dapagliflozin | £69 | 46% | 45% | 1% | 0% | 2% | 5% |
| Empagliflozin 10 mg | £55 | 47% | 44% | 0% | 0% | 3% | 6% |
| Empagliflozin 25 mg | £3 | 49% | 43% | 0% | 1% | 3% | 5% |
| Pioglitazone | –£3261 | 68% | 23% | 1% | 1% | 1% | 7% |
| Gliclazide | –£305 | 53% | 39% | 0% | 1% | 2% | 4% |
| Sitagliptin | –£82 | 49% | 30% | 1% | 3% | 2% | 14% |
As can be seen from Table 25, the main differences in cost arise from different treatment costs for both the oral drugs and insulin, with these being in part driven by the survival differences alluded to above. The only real exceptions to this are for the comparison with pioglitazone, for which an additional £156 treatment cost for CHF is anticipated compared with canagliflozin 100 mg.
Ranking treatments in order of increasing total costs, the Janssen base-case cost-effectiveness results are shown in Table 26. Note that the following table presents the ICERs relative to the cheapest comparator among those being considered. Not all of these ICERs are presented by Janssen, with some having been derived by the AG, so are subject to rounding errors (see Table 26).
| Drug | Cost (£) | QALY | vs. Pioglitazone | vs. Gliclazide | vs. Sitagliptin | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Δ£ | ΔQALY | ICER (£) | Δ£ | ΔQALY | ICER (£) | Δ£ | ΔQALY | ICER (£) | |||
| Pioglitazone | 20,264 | 9.998 | |||||||||
| Gliclazide | 23,220 | 9.949 | 2956 | –0.049 | Dom | ||||||
| Sitagliptin | 23,443 | 9.981 | 3179 | –0.017 | Dom | 223 | 0.032 | 6969 | |||
| Canagliflozin 100 mg | 23,525 | 10.039 | 3261 | 0.041 | 79,537 | 305 | 0.090 | 3377 | 82 | 0.058 | 1414 |
| Empagliflozin 25 mg | 23,528 | 10.024 | 3264 | 0.026 | 125,538 | 308 | 0.075 | 4107 | 85 | 0.043 | 1977 |
| Empagliflozin 10 mg | 23,580 | 10.010 | 3316 | 0.012 | 276,333 | 360 | 0.061 | 5902 | 137 | 0.029 | 4724 |
| Dapagliflozin | 23,594 | 10.006 | 3330 | 0.008 | 416,250 | 374 | 0.057 | 6561 | 151 | 0.025 | 6040 |
| Canagliflozin 100/300 mg | 23,669 | 10.051 | 3405 | 0.053 | 64,245 | 449 | 0.102 | 4402 | 226 | 0.070 | 3229 |
| Canagliflozin 300 mg | 24,302 | 10.083 | 4038 | 0.085 | 47,456 | 1082 | 0.134 | 8075 | 859 | 0.102 | 8422 |
Pioglitazone is the cheapest owing to its acquisition cost. As a consequence, although other treatments are estimated to be more effective compared with pioglitazone their cost-effectiveness is poor. Both gliclazide and sitagliptin are estimated to be dominated by it. Sitagliptin being dominated by pioglitazone may be due to its assumed faster rate of HbA1c drift. Canagliflozin 100 mg is estimated to have an ICER of £79,537 per QALY compared with pioglitazone. Canagliflozin 100 mg also provides more QALYs at a cheaper cost than empagliflozin and dapagliflozin, so dominating them. Canagliflozin 100 mg followed by canagliflozin 300 mg has a better cost-effectiveness against pioglitazone than canagliflozin 100 mg, so extendedly dominates canagliflozin 100 mg. But it is, in turn, extendedly dominated by canagliflozin 300 mg, which is estimated to have a cost-effectiveness compared with pioglitazone of £47,456 per QALY.
The cost-effectiveness of sitagliptin and the flozins is estimated to be more reasonable when compared with gliclazide. But canagliflozin 100 mg extendedly dominates sitagliptin and dominates empagliflozin and dapagliflozin.
Across the nine comparators, the probabilistic modelling suggested that if the willingness to pay is zero, pioglitazone has a 100% probability of being the most cost-effective treatment. This probability declined as the willingness to pay increased, until at around a willingness to pay of £55,000 it ceased to have the highest probability of being the most cost-effective treatment. At this point canagliflozin 300 mg overtook it, with a probability of being the most cost-effective of around 25%.
At high willingness-to-pay values of £200,000 per QALY it appears that the probabilities of being the most cost-effective have stabilised. Canagliflozin 300 mg remains the highest with a probability of around 33%.
The others increase their probabilities as the willingness to pay rises, but still converge only to values under 20%, with the values for empagliflozin 10 mg, dapagliflozin 10 mg, sitagliptin 100 mg and gliclazide never rising above 10%.
Sensitivity analyses
The univariate sensitivity analyses presented by Janssen vary parameters by an arbitrary ±20% and are consequently of limited interest. Full results of these are presented in tables 46–48 of the appendices to the submission. The main result of interest is that the modelling is sensitive to the annual rate of HbA1c drift that is assumed for canagliflozin: deterministic sensitivity analyses (DSAs) number 6 lower value and upper value (6L and 6U), which, respectively, decrease and increase the base case 0.14% annual rate of drift by 20%. The cost-effectiveness estimates under DSA 6L and DSA 6U for canagliflozin 100 mg compared with:
-
pioglitazone are £45,862 per QALY and £211,000 per QALY, respectively
-
gliclazide are £593 per QALY and £8751 per QALY, respectively
-
sitagliptin are dominance and £8528 per QALY, respectively.
In the opinion of the AG these changes are likely to be due more to the time spent on therapy and its immediate effects upon treatment cost, weight, adverse events and hypoglycaemia than to any changes in the modelled complications of diabetes. An exception to this might be the modelled rates of neuropathy.
Scenario analyses
A range of scenario analyses as summarised in table 13 on p. 52 of the Janssen submission is presented, with summary results for all of these in tables 19 and 20 of the Janssen submission. The main points of interest identified by the AG are summarised below.
For the comparison with empagliflozin and dapagliflozin the main scenario analyses of interest are those that:
-
revise the patient characteristics at baseline from those that Janssen pools from its trials to those of The Health Improvement Network (THIN) database, which is the database that underlies the patient characteristics of the modelling for the draft NICE CG: Sc5. The THIN database has anonymised patient data from 562 general practices covering 6.2% of the population. 200
-
apply the UKPDS68193 HbA1c evolution equation and UKPDS62198 QoL values, while also assuming that patients can intensify to NPH insulin but not to basal-bolus insulin: Sc6; and,
-
apply the UKPDS68193 HbA1c evolution equation: Sc14.
These scenario analyses remove the dominance of canagliflozin 100 mg over empagliflozin and dapagliflozin with the cost-effectiveness estimates typically changing to lie between £5000 and £10,000 per QALY.
Scenario analysis 14 is rather more dramatic in terms of the cost-effectiveness estimates. But it would probably be more accurate to describe it as showing broad clinical equivalence, but additional costs from canagliflozin compared with dapagliflozin, empagliflozin 10 mg and empagliflozin 25 mg of £198, £150 and £65, respectively.
Including repaglinide: scenario 1
The analysis that includes repaglinide differs little from the base-case analysis, but with repaglinide being estimated to have total costs of £22,170 and total QALYs of 9.967. As a consequence it is dominated by pioglitazone. If pioglitazone is excluded from this analysis gliclazide is still dominated, only now by sitagliptin. Sitagliptin with a cost-effectiveness of £79,400 per QALY compared with repaglinide is, in turn, extendedly dominated by canagliflozin 100 mg, which has a cost-effectiveness of £21,050 per QALY compared with repaglinide. Empagliflozin and dapagliflozin remain dominated by canagliflozin 100 mg. Canagliflozin 100 mg followed by canagliflozin 300 mg has a cost-effectiveness estimate compared with repaglinide of £20,816 per QALY, which is, again, extendedly dominated by canagliflozin 300 mg, which has a cost-effectiveness of £20,200 per QALY compared with repaglinide.
Same annual glycated haemoglobin drift across the monotherapies: scenario 2
Unfortunately, table 50 of the Janssen submission appendices does not provide the estimates for the canagliflozin 300-mg arm. But the estimates for canagliflozin 100 mg and canagliflozin 100/300 mg are extremely similar to those of the base case, and, as a consequence, the AG has used the estimates of the base case for canagliflozin 300 mg for Table 27. The reported ICERs are all compared with repaglinide (see Table 27).
| Drug | Cost (£) | QALY | ICER |
|---|---|---|---|
| Repaglinide | 20,982 | 10.03 | |
| Pioglitazone | 21,485 | 9.95 | Dom |
| Gliclazide | 22,589 | 10.01 | Dom |
| Sitagliptin | 23,615 | 9.99 | Dom |
| Canagliflozin 100 mg | 23,732 | 10.05 | £137,500 |
| Empagliflozin 25 mg | 23,732 | 10.03 | Dom |
| Empagliflozin 10 mg | 23,739 | 10.02 | Dom |
| Dapagliflozin | 23,786 | 10.02 | Dom |
| Canagliflozin 100/300 mg | 23,853 | 10.06 | £95,700 |
| Canagliflozin 300 | 24,594 | 10.09 | £63,368 |
If the annual HbA1c drift across the monotherapies is set equal to that of canagliflozin 100 mg, this somewhat worsens the cost-effectiveness of pioglitazone to the extent that it is now dominated by repaglinide. The cost-effectiveness estimate for canagliflozin 100 mg compared with pioglitazone improves to £24,233 per QALY.
Assuming the same annual rate of HbA1c drift across the comparators improves the cost-effectiveness of repaglinide and somewhat worsens the cost-effectiveness estimates for canagliflozin compared with repaglinide. But the cost-effectiveness estimate for canagliflozin compared with pioglitazone improves.
Lower body mass index disutility: scenario 4
Revising the disutility per BMI point from 0.0061 to 0.0038 has quite a large impact upon some results, as would be anticipated. The cost-effectiveness estimate for canagliflozin 100 mg compared with pioglitazone worsens to £146,000 per QALY and compared with repaglinide to £26,378 per QALY. The other cost-effectiveness estimates are not particularly affected. Canagliflozin 100 mg is still estimated to dominate the other flozins.
UKPDS68 glycated haemoglobin evolution coupled with UKPDS62 quality of life: scenario 6
This scenario applied the UKPDS68193 HbA1c evolution and some of the UKPDS62198 QoL values. It also assumed that there was no intensification to basal-bolus insulin. The rationale for these grouped changes is not obvious, and as a consequence the AG prefers scenario analysis 14.
UKPDS glycated haemoglobin evolution: scenario 14
Applying the UKPDS HbA1c evolution isolates the effects of this compared with scenario 6. The full results for this scenario do not appear to be reported in the Janssen appendices. As already reported above, for the comparisons with the other flozins there is broad clinical equivalence but there are additional costs from canagliflozin 100 mg compared with dapagliflozin, empagliflozin 10 mg and empagliflozin 25 mg of £198, £150 and £65, respectively. Similarly, there is broad clinical equivalence with gliclazide but a rather larger incremental cost of £744. The cost-effectiveness of canagliflozin 100 mg compared with pioglitazone improves somewhat to £31,945 per QALY.
The assumptions around the evolution of HbA1c are clearly central to the Janssen modelling. In the opinion of the AG this is not due to the complications of diabetes being modelled as changing. In the opinion of the AG it is likely to be mainly due to the amount of time a patient is modelled as spending on the various oral therapies changing. This primarily affects the direct drug costs of treatment, patients’ weights, hypoglycaemia and adverse events.
AstraZeneca economic modelling
The CDM is an individual patient-level model that has been used for previous NICE assessments. It has been routinely submitted to the Mt Hood Challenges. But these submissions to the Mt Hood Challenges were with different assumptions than those used for the AstraZeneca submission.
The modelling of the complications of diabetes within the CDM was previously largely based upon the UKPDS68193 risk equations, these being the basis of the UKPDS OM1 model. For the AstraZeneca submission, the CDM modelling of the complications of diabetes has been updated to use the UKPDS82194 risk equations, these being the basis of the UKPDS OM2 model. Note that for the probabilistic modelling the UKPDS researchers have made available the 1000 bootstraps of the equations underlying the UKPDS OM1 model to the Mt Hood Challenge modellers. As far as the AG is aware, the corollary of these has not been made available for the equations underlying the UKPDS OM2 model. As a consequence, it is not clear how the CDM of the AstraZeneca submission has implemented the probabilistic modelling.
During the STA of dapagliflozin the ERG noted various errors in the CDM implementation formulae for the evolution of the risk factors, which were subsequently corrected during the course of the STA. The AG assumption is that within the AstraZeneca submission these errors have been corrected.
The model was run with a 40-year time horizon and a cycle length of 6 months. Costs and benefits were discounted at 3.5%. The perspective was that of the patient for health impacts and of the NHS/PSS for costs.
It appears that for a deterministic model run 30,000 patients were run. It appears that each patient was run through the model only once, with no internal loops to reduce Monte Carlo error. Probabilistic modelling was based upon 1000 PSA iterations, each with 30,000 patients being simulated. The submission did not present any analysis of model convergence over the number of patients modelled. The CDM permits only pairwise comparisons. As a consequence, the uncertainty around the cost-effectiveness estimates is not presented across all of the comparators, but only in a pairwise fashion.
The AstraZeneca submission notes that among those receiving monotherapy, among the comparators within the NICE scope, sulfonylurea has the largest market share of 80%. The gliptins share is stated as being 13%, followed by 4% for the glitazones. AstraZeneca argues that the main comparator for the flozins will be the gliptins, which, if true, would justify the concentration upon pairwise comparisons.
The CDM models the incidence of the following microvascular complications:
-
amputation
-
nephropathy
-
blindness.
Four macrovascular complications are included:
-
IHD
-
MI
-
stroke, and
-
CHF.
The model also incorporates:
-
patient weight
-
severe hypoglycaemia
-
UTIs
-
GTI, and
-
discontinuations.
Patient characteristics
Patient characteristics at baseline were mainly drawn from the NMA, resulting in baseline estimates of 55 years of age, 54.6% male, 7.5% HbA1c due to NICE CGs, though the NMA mean of 8.2% was used as a scenario analysis, 128.3 mmHg SBP, 195 mg/dl TC, 46 mg/dl HDL and a weight of 80 kg.
The submission does not appear to state what the baseline prevalence of the complications of diabetes was. The submitted electronic model sets these to zero.
Sequences modelled and treatment effectiveness
The comparators were grouped into their class as per the AstraZeneca NMA, for example the cost-effectiveness of flozins as a group was estimated compared with the gliptins as a group. Note that of the glitazones only pioglitazone was considered, rather than a class effect being applied. Repaglinide was not considered as a comparator owing to a lack of evidence.
AstraZeneca argues that allowing the intensifications to differ between the arms would not permit a fair assessment of the cost-effectiveness of alternative monotherapies, but would rather be a comparison of the cost-effectiveness of alternative treatment sequences. Consequently, the AstraZeneca submission modelled the following treatment sequences despite this not reflecting UK clinical practice (Table 28).
| Monotherapy | Intensification | |
|---|---|---|
| First | Second | |
| Flozin | NPH insulin | Intensified NPH |
| Gliptin | NPH insulin | Intensified NPH |
| Pioglitazone | NPH insulin | Intensified NPH |
| Sulfonylurea | NPH insulin | Intensified NPH |
Intensified insulin was assumed to involve a 50% dose escalation.
Clinical effectiveness estimates for the monotherapies were drawn mainly from the 24-week NMA. Infection rates were not meta-analysed, but were drawn from a weighted pooled mean of incidence data at 24 weeks from the papers included in the NMA. Clinical effectiveness estimates for insulin were drawn from Monami et al. 201 for NPH and from Waugh et al. 202 for intensified NPH (Table 29). (The AG does not know how these figures for ‘intensified NPH’ were obtained. Usually if NPH was insufficient, short-acting insulin would be added at mealtimes.)
| Drug | Flozin | Gliptin | Pioglitazone | SU | NPH | Intensified NPH |
|---|---|---|---|---|---|---|
| HbA1c | –0.74 | –0.64 | –0.90 | –0.95 | –1.10 | –1.11 |
| SBP | –5.87 | –1.53 | –1.31 | –0.65 | – | – |
| Weight (kg) | –2.81 | –0.13 | 2.61 | 0.07 | 1.08 | 1.90 |
| AEs | ||||||
| UTI | 0.092 | 0.022 | 0.153 | – | – | – |
| GTI | 0.074 | 0.002 | – | – | – | – |
| Severe hypoglycaemia | 0.010 | 0.016 | 0.024 | 0.055 | 0.0004 | 0.0136 |
| Non-severe hypoglycaemia | – | – | – | – | 0.0104 | 0.6024 |
| First-cycle discontinuation | 0.034 | 0.039 | 0.177 | 0.061 | – | – |
Treatment intensifications and discontinuations
A patient is modelled as intensifying treatment, first to NPH and then to intensified NPH, when their HbA1c breaches the 7.5% intensification threshold. The AG assumption is that the monotherapies are withdrawn at treatment intensification, but this is not explicit within the AstraZeneca submission.
Patients may also discontinue due to adverse events. The AG was unable to identify what was assumed for these patients: whether they switched to an alternative monotherapy and, if so, which, or they intensified to NPH insulin.
Glycated haemoglobin evolution
In common with the AG modelling, the evolution of HbA1c is based upon equation 11 of the UKPDS68. 193 Treatment intensification occurs if a patient’s HbA1c breaches the 7.5% intensification threshold. This leads to a sawtooth evolution of HbA1c, as described in more detail in the section on the AG modelling.
Evolution of other risk factors
The evolution of SBP and the TC/HDL ratio was also based upon equations 12 and 13 of the UKPDS68. 193 The section on the AG modelling describes this in some detail so it is not further described here.
Weight loss with the flozins is assumed to be maintained for 2 years, after which it is assumed that patients rebound to their starting weight. A similar assumption appears to have been made for the gliptins, though the weight loss is maintained for only 1 year. The weight increases associated with the other treatments are assumed to be retained. Weight is also assumed to increase by 0.1 kg annually.
Quality of life
The QoL for a patient without any complications is a function of patient age, as drawn from analysis of EuroQol-5 Dimensions (EQ-5D) data from the Health Survey for England 2003:203
This results in a baseline QoL of 0.882, with this slowly declining over time.
Quality-of-life decrements associated with the complications of diabetes were drawn from the UKPDS62198 with the exception of that for ESRD, which was drawn from the standard UKPDS OM1 source. QoL decrements for hypoglycaemic events were drawn from Currie et al. 204 but note that it appears that the coefficient for symptomatic event was applied to the number of symptomatic events rather than to their logarithm. The QoL impacts of increasing BMI was drawn from Bagust and Beale. 199 These sources and values are all as per the AG modelling, so are not tabulated here for reasons of space.
Note that the submission suggests that the BMI disutility is applied for all BMI changes and is not limited in its effects to changes in BMI when the patient BMI is greater than 25 kg/m2. If this applies it may have biased the analysis in favour of the flozins by valuing reductions on patients’ BMI among those with a BMI of less than 25 kg/m2. But given the mean BMI at baseline of 29.2 kg/m2 this may not be a particular concern.
A systematic literature review was conducted for UTI and GTI QoL decrements. For UTIs the average of the values of Barry et al. 205 of –0.3732 for pyelonephritis and of –0.2894 for dysuria appears to have been coupled with an assumed duration of around 3 days to yield a QALY decrement of –0.00283 per UTI. Apparently no values were found for GTIs and, as a consequence, these had the same disutility applied.
Costs
The direct drug costs were sourced from the BNF 69. 147 For both the flozins and the gliptins, weighted average costs based upon their UK market share were used. This resulted in a mean annual flozin cost of £482 and a mean annual gliptin cost of £429. The annual cost of pioglitazone was £19 and the annual sulfonylurea cost was based upon gliclazide at an annual cost of £66. The cost of gliclazide suggests to the AG that MR gliclazide has been assumed, as the standard version would be around half of the cost that was applied.
The costs of the complications of diabetes in the first year and for subsequent years for blindness and amputation were based upon the UKPDS84. 195 This is the same source as the AG, though the AG arrives at somewhat lower values. There may be a suggestion that indexation by AstraZeneca was based on 2007 prices, when the UKPDS84195 is in 2012 prices. But the source of the discrepancies is unclear.
The AG calculations suggest that the UKPDS84195 average inpatient costs and outpatient costs for those without any of the modelled complications have not been included within the AstraZeneca modelling. If this is the case it would be a quite serious omission, and would tend to bias the analysis in favour of the more effective treatment.
AstraZeneca may have used the UKPDS84195 bespoke costing template to derive costs for a representative baseline patient, but this seems unlikely to be the source of the discrepancies between AstraZeneca and the AG. The AstraZeneca mean age at baseline is 55 years, whereas the AG, in order to be able to implement the costs probabilistically, has taken the costs example of the UKPDS82194 for a 60-year-old man. Costs are typically increasing with age in the UKPDS84. 195
Table 5.10 of the AstraZeneca submission also does not include a cost for fatal IHD events despite these being within the UKPDS84195 and seeming to be associated with deaths in the UKPDS82194 and the UKPDS OM2. The UKPDS65,196 which goes along with the UKPDS68193 and the UKPDS OM1, does not itemise a cost for fatal IHD events. But the AG understanding is that the AstraZeneca CDM modelling is based upon the UKPDS82194 and, as a consequence, does not understand why fatal IHD events have had a zero cost assigned.
For reasons that are unclear, AstraZeneca chose to revert to the costs of the UKPDS65196 for the ongoing costs among those with a history of IHD, CHF and stroke, and probably MI as well. This seems peculiar to the AG, given that the UKPDS82194 and the UKPDS65196 are very similar in their format, with the UKPDS82194 also presenting cost estimates for those with a history of IHD, CHF, stroke and MI.
End-stage renal disease was costed using the estimate of Baboolal et al. 206 for continuous ambulatory peritoneal dialysis. Previous NICE assessments have also used this reference, though have also tended to use the higher cost estimates within Baboolal et al. 206 for hospital haemodialysis. AstraZeneca argued that the use of the peritoneal dialysis cost was conservative.
Severe hypoglycaemia was costed using the Hammer et al. (2009) reference,207 which is the reference used for the AG modelling. UTIs and GTIs were assumed to involve one GP appointment, costed at £46 using the Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care 2014208 (Table 30).
| Event | First year | Subsequent years | |
|---|---|---|---|
| Fatal | Non-fatal | ||
| IHD | 12,762 | 1395 | |
| MI | 2605 | 7938 | 2177 |
| CHF | 5180 | 1656 | |
| Stroke | 5188 | 11,450 | 1378 |
| Amputation | 13,499 | 4618 | |
| Blindness | 6502 | 2307 | |
| ESRD (including dialysis) | 18,776 | 18,776 | |
| Severe hypoglycaemia | 424 | 424 | |
| UTI | 46 | 46 | |
| GTI | 46 | 46 | |
Results
The CDM modelling for the base-case results is shown in Table 31. The AG assumption is that this is based upon deterministic modelling, that is with no second order sampling.
| Costs | Flozins | Gliptins | Net | Pioglitazone | Net | SU | Net |
|---|---|---|---|---|---|---|---|
| Drug | £5638 | £5449 | £190 | £4066 | £1572 | £4128 | £1510 |
| Macrovascular complications | £9179 | £9251 | –£72 | £9319 | –£140 | £9226 | –£47 |
| Microvascular complications | £12,924 | £12,938 | –£14 | £12,433 | £491 | £12,935 | –£11 |
| Hypoglycaemia | £175 | £184 | –£9 | £197 | –£22 | £244 | –£69 |
| Other AE | £63 | £51 | £12 | £53 | £10 | £49 | £14 |
| Total | £27,979 | £27,873 | £106 | £26,067 | £1912 | £26,582 | £1397 |
| QALYs | 13.206 | 13.188 | 0.018 | 13.111 | 0.095 | 13.179 | 0.027 |
| ICER | £5904 | £20,089 | £52,047 |
Within the pairwise comparisons, compared with the sulfonylureas the flozins offer some additional benefit of 0.027 QALYs, but there are reasonable additional costs of £1397 associated with this resulting in a cost-effectiveness estimate of £52,047 per QALY.
The gains from the flozins compared with pioglitazone are larger at 0.095 QALYs, which may be sufficient to justify the additional cost of £1912, which results in a cost-effectiveness estimate of £20,089 per QALY.
When compared with the gliptins, the flozins provide only a small additional gain of 0.018 QALYs, but this is also at a relatively modest additional £106 cost, which results in a cost-effectiveness estimate of £5904 per QALY.
The probabilistic pairwise modelling suggests that the flozins have a probability of being cost-effective (using the NICE threshold of £30,000 per QALY) compared with the gliptin of 66%, compared with pioglitazone of 51% and compared with the sulfonylureas of 13%.
Ranking results in order of increasing cost are provided in Table 32.
| Drug | Cost (£) | Net (£) | QALY | Net | ICER (£) |
|---|---|---|---|---|---|
| Pioglitazone | 26,067 | 13.111 | |||
| SU | 26,582 | 515 | 13.179 | 0.068 | 7574 |
| Gliptins | 27,873 | 1291 | 13.188 | 0.009 | 143,444 |
| Flozins | 27,979 | 106 | 13.206 | 0.018 | 5904 |
As would be anticipated from the pairwise comparisons, it appears that the sulfonylureas have an acceptable cost-effectiveness compared with pioglitazone of £7574 per QALY. The gliptins offer minimal patient benefit compared with the sulfonylureas, 0.009 QALYs or the equivalent of around an additional 4 days’ survival, but with a reasonable increase in costs of £1291 and a cost-effectiveness estimate of £143,000 per QALY. As already noted, the flozins cost-effectiveness estimate compared with the gliptins is good at £5904 per QALY, but is poor against the sulfonylureas at £52,047 per QALY.
A variety of univariate sensitivity analyses were presented, which varied the clinical effectiveness estimates to their upper and lower CI limits, the disutilities for BMI changes to their upper and lower CI limits; the disutilities for complications by ±10%; and the total non-drug costs by ±25%.
Only the changes to the BMI disutility had any marked impact, with these impacts being mainly for the comparisons with pioglitazone and sulfonylurea. The lower confidence limit for the disutility of weight gains improved the cost-effectiveness estimate compared with pioglitazone from £20,089 per QALY to £14,626 per QALY, whereas the upper confidence limit worsened it to £32,065 per QALY. The lower confidence limit for the utility of weight losses worsened the cost-effectiveness compared with the sulfonylureas from £52,047 per QALY to £62,810 per QALY, whereas the upper confidence limit improved it to £4434 per QALY.
Owing to the CDM of AstraZeneca modelling only pairwise comparisons, the probabilistic modelling is presented only for the pairwise comparisons.
Compared with the gliptins, at willingness-to-pay values of £0, £20,000 and £30,000 per QALY the flozins are estimated to have a probability of being the most cost-effective of around 42%, 65% and 68%, with the cost-effectiveness acceptability curve (CEAC) converging to a little over 70% at high willingness-to-pay values.
Compared with pioglitazone, at willingness-to-pay values of £0, £20,000 and £30,000 per QALY the flozins are estimated to have a probability of being the most cost-effective of around 0%, 50% and 80%, with the CEAC converging to a little over 95% at high willingness-to-pay values.
Compared with sulfonylurea, at willingness-to-pay values of £0, £20,000 and £30,000 per QALY the flozins are estimated to have a probability of being the most cost-effective of around 0%, 12% and 26%, with the CEAC still slowly increasing to a little over 60% at a willingness to pay of £100,000 per QALY.
Scenario analyses
A range of scenario analyses were undertaken, mainly varying the HbA1c values at baseline and HbA1c thresholds for intensifying treatment, altering the assumptions around maintenance of weight effects and the drug costs that were applied (Table 33).
| Scenario | vs. Gliptins | vs. Pioglitazone | vs. SUs | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Δ£ | ΔQALY | ICER | Δ£ | ΔQALY | ICER | Δ£ | ΔQALY | ICER | |
| HbA1c baseline 7.5%, threshold 8.0% | £225 | 0.021 | £10,799 | £3059 | 0.106 | £28,970 | £2335 | 0.037 | £63,783 |
| HbA1c baseline 8.19%, threshold 8.19% | £198 | 0.023 | £8694 | £3327 | 0.101 | £32,982 | £1846 | 0.021 | £88,934 |
| HbA1c baseline 7.5%, threshold 7.5%, 8.0% | £100 | 0.020 | £4977 | £1902 | 0.101 | £18,884 | £1382 | 0.026 | £53,057 |
| Flozin weight maintenance 1 year | £22 | 0.014 | £1583 | £1828 | 0.091 | £20,077 | £1313 | 0.023 | £57,839 |
| Comparator weight maintenance 2 years | £115 | 0.014 | £8137 | £1913 | 0.101 | £19,032 | £1435 | 0.028 | £51,166 |
| Flozin and pioglitazone weight convergence at final switch | – | – | – | £1818 | 0.048 | £38,199 | – | – | – |
| No discontinuations | £69 | 0.023 | £3035 | NA | NA | NA | £1431 | 0.028 | £51,718 |
| No AE disutility | £106 | 0.019 | £5685 | NA | NA | NA | £1397 | 0.028 | £50,456 |
| Canagliflozin 100 mg and 300 market share 10% | £137 | 0.018 | £7585 | £1943 | 0.095 | £20,407 | £1427 | 0.027 | £53,176 |
| Sitagliptin price | £90 | 0.018 | £4996 | – | – | – | – | – | – |
| Alogliptin price | £410 | 0.018 | £22,756 | – | – | – | – | – | – |
| 20-year time horizon | £100 | 0.020 | £5093 | £1841 | 0.089 | £20,611 | £1399 | 0.028 | £49,275 |
The scenario analyses around adverse events and discontinuations for the comparison with pioglitazone were reported as having the same values as the corresponding analyses for sitagliptin, so appear to be typographical errors.
Less stringent thresholds for intensification of therapy tended to worsen the cost-effectiveness estimates. This seems likely to be mainly due to patients remaining on their monotherapy for longer and the associated increase in the direct drug costs, and not due to differences in the modelled complications of diabetes.
Weight convergence between the flozins and pioglitazone somewhat worsens the cost-effectiveness estimate, because of this removing the weight gains associated with pioglitazone. Note that this convergence is imposed only at around the seventh or eighth year of the modelling.
Results compared with the gliptins are not particularly sensitive to whether the sitagliptin price is applied rather than the gliptins’ prices weighted by their market shares, due to AstraZeneca estimating sitagliptin to have a market share of the gliptin monotherapy of 56% with the similarly prices saxagliptin and linagliptin having market shares of 16% and 25%, respectively. Alogliptin is notably cheaper but is estimated to have less than a 1% market share.
Boehringer Ingelheim economic modelling
Boehringer Ingelheim presented the results of two modelling exercises: model A and model B. However, much of their NMA and cost-effectiveness analysis was classed as confidential, so what follows is mainly methods with no results.
Model A simulated the effects of 1 year of treatment. Thereafter, the path of the patient was determined by the UKPDS OM1. This appears to have limited the direct treatment effects for elements such as treatment cost and the direct treatment effects upon adverse events and the QoL impact of weight changes to 1 year’s duration. At the end of the first year the AG assumption is that the treatment effects upon HbA1c, SBP, the TC/HDL ratio and weight were fed into the UKPDS OM1 to model the lifetime impact of the monotherapy. But the AG has not been able to identify how the model A does this and this assumption is based upon the written Boehringer Ingelheim submission, which states that ‘Model A . . . approach . . . patients undergo different comparator therapies for a year . . . the UKPDS model then undergoes a full 40 year . . . run’.
The AG understanding, which may not be correct, is that, in effect, this assumed that the patient remained on the monotherapy for the patient lifetime. And that it also assumed that the direct treatment costs, adverse events and direct QoL impacts from weight changes would apply only during the first year.
Model B was somewhat more involved, and took a similar modelling approach to that of the modelling for the draft NICE CG for type 2 diabetes and the AG modelling for the current assessment. A Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) front end was designed for the UKPDS OM1, which modelled the initial treatment effects and then used the UKPDS risk equations to model the evolution of the risk factors and the complications of diabetes. When patients’ HbA1c breached the 7.5% intensification threshold they could first intensify by adding another oral drug, with a second intensification to NPH insulin also being possible. The survival curve of the OM1 coupled with the timing of intensifications permitted model B to calculate treatment-specific treatment costs, adverse event rates and QoL impacts from weight changes to add to the outputs of the OM1 model.
Boehringer Ingelheim noted that model B ran the OM1 1 year at a time, and that this can lead to an underestimation of the total costs and total QALYs over the 40-year time horizon. Boehringer Ingelheim suggested that this will tend to have underestimated the cost-effectiveness of empagliflozin. Note that the AG approach was to run the OM1 model over the 40-year time horizon for each patient simulated.
Patient characteristics
Patient characteristics were drawn from patients within the Clinical Practice Research Datalink (CPRD). This identified 9211 UK patients who started their first oral antidiabetic treatment in 2014. Although not all of the codes used for the search appear to have been specific to type 2 diabetes, for example diabetes mellitus, the minimum age at diagnosis was 23 years, with a mean of 60 years and a SD of 12 years, and the requirement to be starting an oral therapy should have restricted the sample to patients with type 2 diabetes.
The average duration of diabetes was 2.9 years, 57% being male. The mean HbA1c was 8.49%, SBP 134 mmHg, HDL 1.2 mmol/l and LDL 4.0 mmol/l. The mean BMI was 31 kg/m2.
The presence of existing complications was included: 6.63% for atrial fibrillation, 3.18% for PVD, 2.21% for MI, 1.92% for CHF, 1.62% for stroke, 6.13% for IHD, 0.29% for amputation, 0.23% for blindness and 0.05% for renal failure.
Sequences modelled and treatment effectiveness
Model A considers only the first year of treatment with monotherapy and then adds the UKPDS costs and complications to this.
Model B considers the treatment sequences in Tables 34 and 35 with patients intensifying to the next line of therapy when their HbA1c breaches the 7.5% intensification threshold.
| Monotherapy | Intensification | |
|---|---|---|
| First | Second | |
| Repaglinide 1 mg | + Gliclazide | + NPH insulin |
| Gliclazide | + Sitagliptin | |
| Pioglitazone 45 mg | + Gliclazide | |
| Sitagliptin 100 mg | + Gliclazide | |
| Empagliflozin 10 mg | + Gliclazide | |
| Empagliflozin 25 mg | + Gliclazide | |
| Monotherapy | Intensification | |
|---|---|---|
| First | Second | |
| Dapagliflozin 5 mg | + Gliclazide | + NPH insulin |
| Dapagliflozin 10 mg | + Gliclazide | |
| Canagliflozin 100 mg | + Gliclazide | |
| Canagliflozin 300 mg | + Gliclazide | |
| Empagliflozin 10 mg | + Gliclazide | |
| Empagliflozin 25 mg | + Gliclazide | |
Pioglitazone 45 mg was chosen because of it being the most commonly prescribed dose. The differences in cost between pioglitazone 30 mg and pioglitazone 45 mg are minimal.
Note that if repaglinide was insufficient, it would be replaced, as for dual use it is licensed only with metformin. So it would not be logical to add gliclazide to repaglinide since they act largely on the same receptors. Note also that 1 mg is a small dose of repaglinide.
Clinical effectiveness data were based upon 52-week data where available, though this was apparently not available for canagliflozin or dapagliflozin. Sitagliptin clinical effectiveness estimates were apparently based upon 24-week data, though the submission does not state that 52-week data were not available. The effect upon SBP and rates of UTIs were also based upon 24-week data because of 52-week data not being available.
Hypoglycaemia rates were based upon the sulfonylurea 16.4% annual rate from the NMA (for pooled sulfonylureas) coupled with odds ratios for each of the comparators against sulfonylurea. A ratio of non-severe to severe hypoglycaemia event rate of 17.2 was based upon the 0.009 annual rate of severe hypoglycaemia event rates of Leese et al.,18 coupled with the overall rates of hypoglycaemia in the NMA.
Urinary tract infection event rates were based upon the annual placebo rates of 3.5% from the NMA coupled with odds ratios for each of the comparators.
Treatment intensifications and discontinuations
Within model A there are no treatment intensifications. Treatment with the monotherapies is for 1 year only, after which it appears that the UKPDS OM1 model is appended to this.
Within model B, treatment is intensified when a patient is modelled as breaching the 7.5% HbA1c threshold.
It appears that discontinuations of therapy for reasons other than breaching the HbA1c threshold of 7.5% have not been modelled.
Glycated haemoglobin evolution
The evolution of HbA1c is based upon equation 11 of the UKPDS68. 193
Within model A it appears that the patient’s baseline HbA1c has the treatment effect of the initial monotherapy applied, with the UKPDS OM1 and hence relevant equation of the UKPDS68193 being used to model its evolution thereafter. But, as stated in the introduction, the AG has not been able to identify how model A interacts with the UKPDS OM1.
Within model B it appears that the patient’s baseline HbA1c has the treatment effect of the initial monotherapy applied. Equation 11 of the UKPDS68193 is then used to model the evolution of the patient’s HbA1c until it breaches the 7.5% intensification threshold, at which point the treatment effect of the first intensification is applied. Equation 11 of the UKPDS68193 is then applied until the second intensification occurs with the associated treatment effect. HbA1c is then modelled as progressing as per equation 11 of the UKPDS68. 193
Evolution of the other risk factors
The evolution of SBP and the TC/HDL is based on the UKPDS OM1 and hence on the relevant equation of the UKPDS68. 193
Within model A, it appears that the patient’s baseline SBP had the treatment effect of the initial therapy applied, with equation 12 of the UKPDS68193 being used to model its evolution thereafter. For the TC/HDL ratio, as a result of there being no treatment effects estimated, it appears that equation 13 of the UKPDS68193 was used to model the evolution throughout. But, again, as stated in the introduction, the AG has not been able to identify how model A interacts with the UKPDS OM1.
Within model A the direct impacts of weight changes upon QoL were evaluated only during the first year. For the UKPDS modelling it appears that weight losses were assumed to rebound to baseline after 1 year, whereas weight gains were assumed to remain indefinitely.
Within model B it appears that the patient’s baseline SBP had the treatment effect of the initial therapy applied, with equation 12 of the UKPDS68193 being used to model its evolution except for when a treatment intensification took place at which point the treatment effect of the intensification was applied. For the TC/HDL ratio, as a result of there being no treatment effects estimated, it appears that equation 13 of the UKPDS68193 was used to model the evolution throughout.
Within model B, weight losses from treatment were assumed to apply at 52 weeks and then to rebound to baseline at 104 weeks. Weight gains from treatment were assumed to be maintained indefinitely. A 0.1-kg annual weight gain from natural history was also applied.
Quality of life
The QoL at baseline and the QoL decrements associated with the complications of diabetes were drawn from the recent paper by Alva et al. ,197 which reanalysed the updated UKPDS data set and in some sense updated the values of the UKPDS62,198 which is the paper that the AG modelling relies upon. The values and a commentary upon this are presented later in the comparison of modelling inputs used by the companies and the AG.
In common with the other companies, the QoL impact of hypoglycaemic events was drawn from Currie et al. 204 Similarly, the QoL decrement of –0.0061 per BMI point above 25 kg/m2 was drawn from Bagust and Beale. 199
The QoL decrement of –0.00283 per UTI was based upon the estimates of Barry et al. 205
Costs
Treatment costs were based upon the March 2015 Monthly Index of Medical Specialities (MIMS).
The costs of diabetes without complications and the costs of the complications of diabetes were taken from the UKPDS84. 195 Boehringer Ingelheim appears to have applied only the inpatient costs of the UKPDS84195 and ignored the outpatient costs.
A cost of £380 per severe hypoglycaemic event was drawn from the draft NICE CG for type 2 diabetes, which is similar to that of the other company submissions and AG value.
Urinary tract infections were associated with a £36 cost, based upon the ERG report52 for the previous STA of dapagliflozin for type 2 diabetes combination therapy.
Note that the UKPDS costs of model B that are reported in Tables 36 and 37 are around half of those of model A. The reason for these discrepancies is far from obvious.
| Effect | Table 71 | Table 72 | ||||
|---|---|---|---|---|---|---|
| UKPDS | Tx | Severe hypoglycaemia | UTI | Total | Total | |
| Empagliflozin 25 mg | 7774 | 3890 | 108 | 13 | 11,785 | 11,664 |
| Empagliflozin 10 mg | 7772 | 3894 | 214 | 26 | 11,907 | 11,667 |
| Pioglitazone 45 mg | 7836 | 994 | 311 | 38 | 9180 | 8830 |
| Repaglinide 1 mg | 7816 | 1649 | 463 | 50 | 9978 | 9465 |
| Sitagliptin 100 mg | 7809 | 3525 | 578 | 61 | 11,972 | 11,334 |
| Gliclazide | 7819 | 2538 | 666 | 77 | 11,100 | 10,357 |
| Drug | Table 71 | Table 72 | ||||
|---|---|---|---|---|---|---|
| UKPDS | Tx | Severe hypoglycaemia | UTI | Total | Total | |
| Empagliflozin 25 mg | 7769 | 3811 | 120 | 13 | 11,713 | 11,580 |
| Empagliflozin 10 mg | 7773 | 3830 | 236 | 26 | 11,864 | 11,602 |
| Canagliflozin 300 mg | 7752 | 4753 | 346 | 40 | 12,891 | 12,504 |
| Canagliflozin 100 mg | 7764 | 3772 | 475 | 57 | 12,068 | 11,536 |
| Dapagliflozin 10 mg | 7776 | 3758 | 597 | 72 | 12,204 | 11,534 |
| Dapagliflozin 5 mg | 7771 | 3806 | 712 | 91 | 12,380 | 11,577 |
Assessment Group economic modelling
Model
The protocol specified that either the UKPDS OM1 or the UKPDS OM2 would be used by the AG. For some of its outputs the OM1 is quite different from the OM2 in its predictions. But the OM2 was not made available to the AG in time for the assessment and so, as specified in the protocol, the OM1 has been used.
As already noted, the OM1 predicts roughly double the number of MIs over 10 years, and the rates of IHD are also noticeably higher than those of the OM2. The 10-year mortality is also higher with the OM1. Compared with the OM2, the OM1 will tend to overpredict event rates and so overstate the benefits and cost savings arising from any avoidance of the complications of diabetes that are associated with the more effective treatment. Being more recent and more reflective of current practice, the OM2 would consequently have been much preferable had it been available to the AG.
The OM1 was used for the modelling that underlies the NICE CG for diabetes. During its development the Guideline Development Group (GDG) reviewed in detail 10 type 2 diabetes cost-effectiveness models. These included the JADE209 and CORE210 models, but not the ECHO-T2DM model. Based upon validation and consistency with the NICE reference case, the GDG very much preferred the OM1, in no small part because of it being based upon a single RCT rather than drawing a range of modelling inputs from disparate sources.
The AG has developed a front and back end to the OM1. Briefly, for each patient and treatment strategy that is simulated the AG front end models the patient’s progression from monotherapy through the various treatment intensifications over a 40-year time horizon in annual cycles. This, in turn, introduces the patient’s evolutions of HbA1c, SBP, TC/HDL, BMI, hypoglycaemia event rates, adverse events and treatment costs. The evolutions of the patient’s HbA1c, SBP and TC/HDL are then fed into the OM1, which models the complications of diabetes and patient lifespan, and outputs the costs and QoL impacts of living with diabetes and the patient’s survival curve. The AG back end takes the OM1 survival curve and uses this to condition the evolutions of the patient’s BMI, hypoglycaemia event rates, adverse events and treatment costs. The cost and QoL impacts of these are then summed with the cost and QoL impacts outputted by the OM1.
In slightly more detail, patients start on monotherapy but intensify their treatment if their HbA1c is modelled as breaching the 7.5% threshold. Intensifications typically add another treatment to a patient’s existing treatment(s). This permits treatment sequences to be modelled, starting with monotherapy but with subsequent treatment intensifications, these intensifications eventually leading to first basal insulin and then basal-bolus insulin. Each treatment within a sequence is associated with treatment costs, weight changes, hypoglycaemic events and adverse events. The AG modelling also permits treatments to be associated with a discontinuation rate in their first year, with patients who discontinue being assumed to switch to another treatment at the same line of therapy.
For each patient who is modelled, the modelled treatment sequences lead to a modelled evolution of HbA1c, SBP and TC/HDL ratio. These, together with the patient’s baseline characteristics, are fed into the OM1. The OM1 then models the rates of the complications of diabetes, such as CHF, and the patient survival, which results in estimates for the discounted costs and QALY impacts of the complications of diabetes over the modelled lifetime of the patient. A survival curve is also drawn from the OM1 model. Owing to the model being an individual patient simulation, any given patient is run through the model many times, say 1000 inner loops, in order to reduce Monte Carlo sampling error. In effect this is the same as running a cohort of 1000 identical patients through the model. The OM1 survival curve is the proportion of this cohort, or 1000 inner loops, that is modelled as surviving. This survival curve conditions the AG front end evolutions of treatment sequences and the cost and QALY impacts of their treatment costs, weight changes, hypoglycaemic events and adverse events.
For the deterministic model run, the OM1 correctly outputs the relevant survival curve. Unfortunately, for the PSA iterations it appears that the OM1 does not output the relevant survival curve. As a consequence, the relevant survival curve has had to be imputed from the OM1 annual discounted QALY estimates by an initial run of the model with the baseline QoL set equal to unity and the QoL decrements of the complications all set to zero. The resulting annual discounted QALYs were then undiscounted to arrive at the patient-specific survival curve. (For the PSA each patient was run with 100 inner loops, and, as a consequence, the imputed survival curve had a granularity of 1%.) But this also meant that the PSA had to run the OM1 model twice for each strategy for a given patient, for a given PSA iteration. This also required that the same random number seed be used for each of these model runs in order for the imputed survival curve to be consistent with the second run of the model that estimated the strategy’s costs and benefits. The OM1 permits the random number seed to be only 1 of 100 values. The AG model randomly assigned this value during the PSA, keeping this value constant between the two model runs for a given patient, for a given PSA iteration. Having to run the model twice for a given patient for a given PSA iteration also significantly increased the time it took to run the PSA.
An element that the OM1 cannot address is the requirement for patients receiving a flozin to have their dose of it reduced or discontinued based upon renal function and eGFR rates. Although the AG has a number of issues with the Janssen modelling, the use of the ECHO-T2DM model did permit this to be explored, though the AG has not reviewed the implementation of this in any detail. It would be interesting to know the impact that turning off these discontinuations would have upon the cost-effectiveness estimates of the Janssen modelling. If this is significant enough to affect the conclusions that would be drawn from the Janssen modelling it could suggest additional modelling uncertainty from the AG use of the OM1.
The AG visual basic modelling has the advantage of permitting up to 12 treatment strategies to be simultaneously compared with one another, with the correlation between treatments’ effects being properly taken into account. Each PSA iteration also uses the same set of parameter values and random number seed across all of the treatment strategies being modelled. This, in turn, permits the correct characterisation of uncertainty within the probabilistic modelling.
Model runs
The NICE CG group for type 2 diabetes concluded after a number of model runs that with a patient cohort of 35,000 or more there was little to be gained from running more than 100 inner loops to reduce Monte Carlo sampling error. As a consequence, probabilistic results were based upon 1000 PSA iterations, each with a patient cohort of 50,000 with 100 inner loops. For deterministic model runs, that is those without any second order sampling, the modelling for the CG increased the number of inner loops to 1000, as recommended within the OM1 manual.
The AG has adopted the same approach.
Probabilistic sampling
The risk factor evolution parameters of equations 11–13 of the UKPDS68193 were received as 1000 bootstrap samples from the UKPDS group (Professor Alastair Gray, University of Oxford, June 2015, personal communication). The UKPDS OM1 also permits only 1000 bootstraps.
The other parameters within the modelling were sampled by the AG. Clinical effectiveness was sampled within the NMA, with this outputting 10,000 look-up values for the various clinical effectiveness parameters. But as a result of the OM1 permitting only 1000 bootstraps and the time taken to run the PSA, a subset of 1000 was sampled from the 10,000 look-up values of the NMA. It was checked that these subsets had means that were similar to the central estimates of the NMA.
Other parameters were sampled by the AG using the distributions outlined below.
Patient characteristics at baseline
The patient characteristics at baseline are taken from the draft NICE CG for diabetes. This undertook extensive analysis of the THIN database, supported by some additional data from the Health Survey for England (Table 38).
| Risk factors | |
|---|---|
| Age | 59.8 years |
| Duration of diabetes | 2.0 years |
| Male | 57% |
| BMI | 31.9 kg/m2 |
| HbA1c | 8.40% |
| SBP | 137.5 mmHg |
| TC | 4.96 mmol/l |
| HDL | 1.18 mmol/l |
| Complication rates (%) | |
| Current smoker | 18.1 |
| Past smoker | 34.0 |
| Atrial fibrillation | 0.81 |
| PVD | 0.51 |
| MI | 0.80 |
| CHF | 0.50 |
| Stroke | 0.50 |
| IHD | 2.70 |
| Amputation | 0.10 |
| Blindness | 0.40 |
| Renal failure | 0.20 |
These were sampled once for the modelling using the full variance–covariance between the characteristics, as per the modelling for the current draft NICE CG for diabetes.
The AG has adopted these values with the exception of the baseline the baseline TC/HDL ratio. TC/HDL has been assumed to be 3.0 owing to NICE guidelines on atorvastatin use in people with diabetes. This change in therapy may be partly the cause of the differences between the OM1 and the OM2. A scenario analysis applies the values of the NICE CG and evolves these according to the UKPDS68193 equation 13.
AstraZeneca argued that the baseline HbA1c should be 7.5% in order to be in line with NICE guidelines. But the patients modelled are starting their first drug treatment after, on average, having been diagnosed with diabetes for 2.0 years. The mean HbA1c at diagnosis was estimated to be 8.2%. It seems unlikely that most patients will have successfully controlled their diabetes through diet and exercise and got below 7.5% if they were above it at diagnosis, only to subsequently lose this control. As a consequence, the base case will apply the baseline HbA1c values as estimated within the draft NICE CG. A scenario analysis applies a common 7.5% HbA1c at baseline across the 50,000 patients simulated.
Sequences modelled
As outlined in the assessment protocol, in line with NICE guidelines patients will intensify their treatment if their HbA1c breaches the 7.5% intensification threshold. As a consequence, the modelling needs to take into account the clinical effects and costs of these intensifications. Based upon expert opinion the AG has modelled the treatment sequences in Table 39.
| Monotherapy | Intensification | ||
|---|---|---|---|
| First | Second | Third | |
| Repaglinide | – Repaglinide | + NPH insulin | – Gliclazide |
| + Pioglitazone | + Bolus insulin | ||
| + Gliclazide | |||
| Gliclazide | + Pioglitazone | + NPH insulin | – Gliclazide |
| + Bolus insulin | |||
| Pioglitazone | + Gliclazide | + NPH insulin | – Gliclazide |
| + Bolus insulin | |||
| Sitagliptin | + Gliclazide | + NPH insulin | – Gliclazide |
| + Bolus insulin | |||
| Dapagliflozin | + Gliclazide | + NPH insulin | – Gliclazide |
| + Bolus insulin | |||
| Empagliflozin | + Gliclazide | + NPH insulin | – Gliclazide |
| + Bolus insulin | |||
| Canagliflozin 100 mg | + Gliclazide | + NPH insulin | – Gliclazide |
| + Bolus insulin | |||
Clinical effectiveness
The clinical effectiveness estimates are drawn from the Warwick AG NMA as presented in the clinical effectiveness section and from a review of the literature. Events rates are annual unless otherwise stated (Tables 40 and 41).
| Variable | Gliclazide | Pioglitazone | Repaglinide | Sitagliptin | ||||
|---|---|---|---|---|---|---|---|---|
| µ | SE | µ | SE | µ | SE | µ | SE | |
| HbA1c | –1.301 | 0.014 | –1.200 | 0.011 | –1.200 | 0.360 | –0.723 | 0.019 |
| SBP | –0.600 | 0.520 | –1.400 | 0.500 | –1.000 | 0.000 | 0.394 | 0.048 |
| Weight | 1.397 | 0.013 | 2.962 | 0.009 | 0.100 | 0.670 | –0.003 | 0.275 |
| Severe hypoglycaemia | 0.10% | 0.04% | 0.00% | 0.00% | 2.00% | 0.70% | 0.00% | 0.00% |
| Symptomatic hypoglycaemia | 1.30% | 0.40% | 0.00% | 0.00% | 13.00% | 1.70% | 0.00% | 0.00% |
| UTI | 4.00% | 1.00% | 4.00% | 1.00% | 4.00% | 1.00% | 4.00% | 1.00% |
| GTI | 1.00% | 0.49% | 1.00% | 0.49% | 1.00% | 0.49% | 1.00% | 0.49% |
| Discontinuation | 3.30% | 0.82% | 9.00% | 0.74% | 5.00% | 3.00% | 4.00% | 1.30% |
| Variable | Dapagliflozin 10 mg | Empagliflozin 25 mg | Canagliflozin 300 mg | |||
|---|---|---|---|---|---|---|
| µ | SE | µ | SE | µ | SE | |
| HbA1c | –0.704 | 0.016 | –0.870 | 0.016 | –1.153 | 0.032 |
| SBP | –2.931 | 0.024 | –3.743 | 0.054 | –1.338 | 0.048 |
| Weight | –2.457 | 0.006 | –2.471 | 0.008 | –3.577 | 0.012 |
| Severe hypoglycaemia | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% |
| Symptomatic hypoglycaemia | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% | 0.00% |
| UTI | 5.50% | 1.97% | 5.40% | 1.50% | 6.60% | 1.80% |
| GTI | 4.50% | 1.80% | 3.60% | 0.64% | 5.00% | 2.00% |
| Discontinuation | 3.00% | 1.50% | 1.80% | 0.91% | 2.00% | 1.00% |
For the flozins the UTI rates and GTI rates are half-yearly.
For the intensifications, because of a lack of data the addition of a treatment is assumed to have the same clinical effectiveness regardless of what it is being added to (Tables 42 and 43).
| Variable | + Pioglitazone | + Gliclazide | – Repaglinide, + gliclazide, + pioglitazone | |||
|---|---|---|---|---|---|---|
| µ | SE | µ | SE | µ | SE | |
| HbA1c | –1.200 | 0.011 | –1.010 | 0.011 | –1.200 | 0.011 |
| SBP | –1.400 | 0.500 | –0.600 | 0.520 | –1.400 | 0.500 |
| Weight | 2.800 | 0.160 | 1.300 | 0.070 | 2.800 | 0.160 |
| Severe hypoglycaemia | 0.00% | 0.00% | 0.00% | 0.00% | 0.10% | 0.18% |
| Symptomatic hypoglycaemia | 10.70% | 1.80% | 11.20% | 2.10% | 10.70% | 1.80% |
| GMI | 4.0% | 1.0% | 4.0% | 1.0% | 4.0% | 1.0% |
| UTI | 1.0% | 0.5% | 1.0% | 0.5% | 1.0% | 0.5% |
| Variable | + NPH | + Bolus | ||
|---|---|---|---|---|
| µ | SE | µ | SE | |
| HbA1c | –1.200 | 0.300 | –0.660 | 0.060 |
| SBP | –0.500 | 1.200 | 0.000 | 0.000 |
| Weight | 3.600 | 0.500 | 0.800 | 0.200 |
| Severe hypoglycaemia | 0.40% | 0.17% | 0.7% | 0.5% |
| Symptomatic hypoglycaemia | 14.0% | 5.1% | 38.0% | 2.9% |
| UTI | 0.0% | 0.0% | 6.0% | 1.4% |
| GTI | 0.0% | 0.0% | 0.0% | 0.0% |
Adjusting the glycated haemoglobin effect for a patient’s baseline glycated haemoglobin
The NICE CG modelling estimated two alternative models for the change at 1 year in HbA1c. The first corresponded to the base-case approach of the AG, though metformin was the reference treatment in the NICE CG NMA rather than placebo, as in the AG NMA.
-
Estimate a reference treatment’s absolute change in HbA1c from baseline, t0, to the end of the first cycle, t1: Δabs.
-
Estimate the difference between the reference treatment and the other treatments at the end of the first cycle: ΔTxrel.
-
H1 = H0 + Δabs + ΔTxrel.
For instance, suppose that the change between t0 and t1 for metformin Δabs = –1.49 and that the difference between metformin and canagliflozin at t1 was ΔTxrel = –0.51. A patient with a baseline H0 = 9.00 would be estimated to have H1 = 9.00 – 1.49 – 0.51 = 7.00, whereas a patient with a baseline H0 = 7.00 would be estimated to have H1 = 7.00 – 1.49 – 0.51 = 5.00.
But a strong correlation was observed between the trials’ metformin absolute effect between t0 and t1 and their mean baseline HbA1c. As a consequence the NICE CG explored adding an additional term to Δabs to make the change also a function of the baseline HbA1c, H0. This led to the following adjusted model for the HbA1c at the end of the first cycle:
with ΔTxrel being taken from the NICE CG NMA.
The Δabs and β were not estimated during the NMA, but were separately estimated using the same data for metformin as was used in the NMA. The adjusted model simplifies to the unadjusted model by setting β = 0. This resulted in the following coefficients (Table 44), and the following unadjusted and adjusted treatment effects for metformin (Figure 11).
| Variable | Unadjusted (95% CrI) | Adjusted (95% CrI) |
|---|---|---|
| Δabs | –1.49 (–2.16 to –0.90) | –0.78 (–1.65 to 0.03) |
| β | – | –0.50 (–0.78 to –0.21) |
FIGURE 11.
National Institute for Health and Care Excellence CG adjustment to reference treatment HbA1c effect by baseline HbA1c.

In essence, the adjusted function adds the difference between the two intercepts –1.49 and –0.78, or a constant 0.71, and the β (H0 –7.5) to the unadjusted H1. In other words for a given baseline H0, the H1 of the adjusted function is a constant difference from the H1 of the unadjusted function, regardless of the treatment effect relative to metformin ΔTxrel. As β = –0.50 is negative, the reduction in HbA1c between t0 and t1 is larger for those with a high baseline H0. The application of the adjusted function means that more patients will see a treatment reduce their HbA1c to below the NICE treatment intensification threshold of 7.5%. It also prevents patients with a low baseline H0 being modelled as falling to perhaps unrealistically low values of HbA1c.
The adjusted function was preferred for the NICE CG because of a superior information criterion and because the influence of β was judged to be significant with its 95% CrI all lying below zero.
For the patient with a baseline H0 = 9.00, the adjusted model estimates that under canagliflozin his/her H1 = 9.00 – 0.78 – 0.50 × (9.00 – 7.50) – 0.51 = 6.96 in contrast to the estimate of H1 = 7.00 of the unadjusted model. Similarly, for the patient with a baseline H0 = 7. 00, the adjusted model estimates that under canagliflozin their H1 = 7.00 – 0.78 – 0.50 × (7.00 – 7.50) – 0.51 = 5.96 in contrast with the estimate of H1 = 5.00 of the unadjusted model.
The NICE CG function is for metformin monotherapy. It was also estimated using a very different data set than the current AG NMA. Any read across from it to the current assessment is consequently almost submerged in caveats. But if a hypothetical placebo in the monotherapy metformin trials would have a reasonably constant relative effect, Txrel, at t1 compared with metformin, and this placebo effect could reasonably be read across to the current patient group, it would be reasonable to explore the impact of the above relationship in the current assessment. For a deterministic analysis this simply requires 0.71 – 0.50 (H0 – 7.5) to be added to the overall unadjusted H1 treatment effect estimated for each of the active treatments within the AG NMA. This will be explored as a scenario analysis.
Treatment discontinuations
Those discontinuing in the first year for reasons other than their HbA1c not falling below the 7.5% threshold are assumed to switch to another monotherapy:
-
From:
-
flozins to gliclazide
-
sitagliptin to gliclazide
-
pioglitazone to gliclazide
-
gliclazide to pioglitazone
-
repaglinide to pioglitazone.
-
Note that those discontinuing are in effect assumed to switch to the alternative monotherapy, and its associated subsequent sequence of treatments. These sequences were retained in part due to data availability and in part due to a desire not to introduce new sequences with a different number of possible intensification steps.
But these subsequent sequences may also contain the treatment that the patient was intolerant of as a monotherapy. This affects only those discontinuing from pioglitazone and those discontinuing from gliclazide. In light of this, a scenario analysis will be undertaken, whereby, among those discontinuing and switching treatment, the intensification step to a treatment, to which the patient was intolerant as a monotherapy, is omitted.
The modelling of the evolution of the risk factors
For HbA1c the base case applies the treatment effect in the first year of therapy. HbA1c is then evolved according to the UKPDS68193 equation 11. But this is with the proviso of the UKPDS68193 equation 11 parameter for a patient being in their second year at diagnosis not being applied. Given the average patient duration of 2 years since diagnosis, the AG is of the opinion that including the UKPDS68193 equation 11 parameter for a patient being in their second year since diagnosis would tend to double count the treatment effect of starting a monotherapy. HbA1c is evolved according to the UKPDS68193 equation 11 until the treatment intensification threshold of 7.5% is breached.
At this point, the patient intensifies treatment and receives the associated treatment effect. HbA1c is then once more evolved according to the UKPDS68193 equation 11 until the treatment intensification threshold of 7.5% is breached, at which point another treatment intensification occurs. When the patient is on the last line of treatment, HbA1c evolves according to the UKPDS68193 equation 11 with no further treatment intensifications.
Should a patient discontinue and move on to an alternative treatment at the same line of therapy, the treatment effect of the first line of therapy of the first year is removed, 1 year’s evolution according to the UKPDS68193 equation 11 added, and the treatment effect of the alternative treatment applied.
The paragraphs that follow are purely for illustration. The data are hypothetical and bear no relation to the actual inputs used in the AG modelling.
Figure 12a shows how this results in a sawtooth evolution of HbA1c. It applies to a patient aged 40 years with a current baseline HbA1c of 7.6%, who at diagnosis was aged 30 years and had a HbA1c of 7.0%. It assumes four strategies, with initial reductions in HbA1c of 1.8%, 1.6%, 1.4% and 1.2% for strategies 1–4, respectively. It also assumes that two further treatment intensifications are possible, these having the reductions in HbA1c of 2.0% and 1.5% across the four strategies.
The modelled evolution of strategies 2–4 are very similar, with the first treatment intensification at year 6. The slightly greater initial reduction in HbA1c of strategy 1 is sufficient for HbA1c not to breach the treatment intensification threshold of 7.5% until 1 year later, and, as a consequence, the first treatment intensification does not occur until year 7.
Figure 12b illustrates how a discontinuation could affect the modelled evolution of HbA1c for strategy 1. This still assumes a reduction in HbA1c from the original treatment of 1.8%, but from the alternative treatment that the patient discontinues, a reduction of only 0.5%. As before, this also assumes that two further treatment intensifications are possible, with reductions in HbA1c of –2.0% and –1.5% in the sequence to which the patient has discontinued.
In light of the Janssen submission, the model has been constructed to permit a scenario analysis of HbA1c having a linear increase and for the annual rate of increase to be treatment specific. The following illustrates the same initial treatment effects for strategies 1–4, but for the annual linear increase while on first-line treatment to be 0.1%, 0.2%, 0.3% and 0.4%, respectively. For those discontinuing from strategy 1, the annual linear increase while on the first-line treatment is assumed to be 0.05%. Subsequent to treatment intensification, the evolution of HbA1c is assumed to revert to the UKPDS68193 equation 11, but the model has the facility to impose treatment-specific annual linear increases in HbA1c at any or all treatment lines (Figure 13).
FIGURE 13.
Example of the modelled evolution of HbA1c: linear evolution.
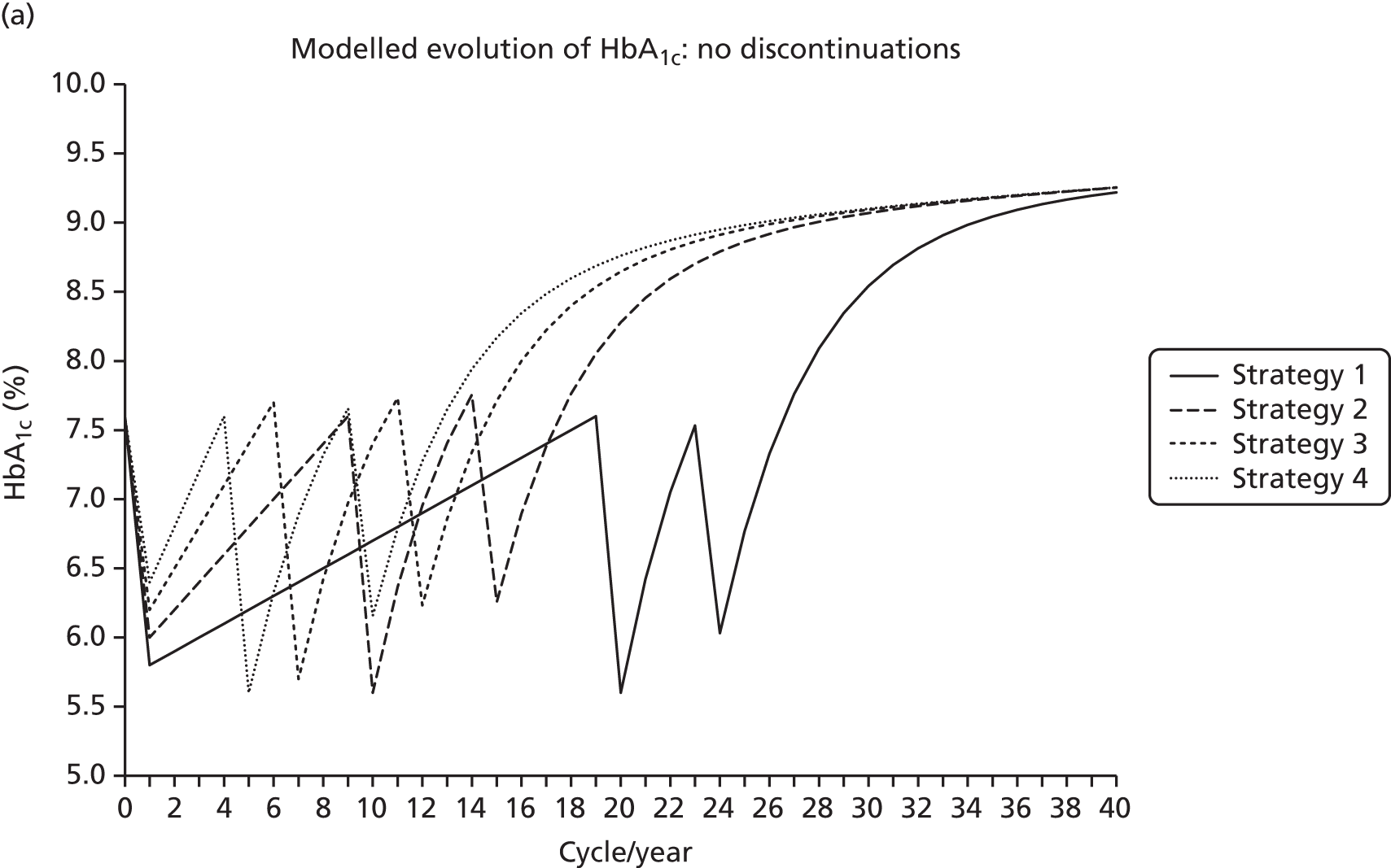

A similar approach is taken for the modelling of the evolution of SBP and can be for the TC/HDL ratio, though the base case holds the TC/HDL ratio constant at 3.0. The UKPDS68193 specifies equations 12 and 13, respectively. Treatment intensifications are still determined by the modelled HbA1c.
Figure 14 illustrates the modelled evolution of SBP for the same patient as before, with HbA1c being modelled to evolve according to the UKPDS68193 equation 11, with a SBP at baseline of 130 mmHg and at diagnosis of 120 mmHg. It assumes initial treatment effects of –20 mmHg, –15 mmHg, –10 mmHg and –5 mmHg for strategies 1–4, respectively. The intensifications result in treatment effects of –15 mmHg and –10 mmHg. For the patient modelled as discontinuing during strategy 1, the alternative treatment effect is –5 mmHg.
FIGURE 14.
Example of the modelled evolution of SBP.


Figure 15 illustrates the UKPDS modelled evolution of the TC/HDL ratio for the same patient as before, with HbA1c being modelled to evolve according to the UKPDS68193 equation 11, with a TC/HDL ratio at baseline of 4.0 and a ratio at diagnosis of 3.5. It assumes initial treatment effects of –1.0, –0.8, –0.6 and –0.4 for strategies 1–4 respectively. The intensifications result in treatment effects of –0.8 and –0.6. For the patient modelled as discontinuing during strategy 1, the alternative treatment effect is –0.4.
FIGURE 15.
Example of the modelled evolution of the TC/HDL ratio.
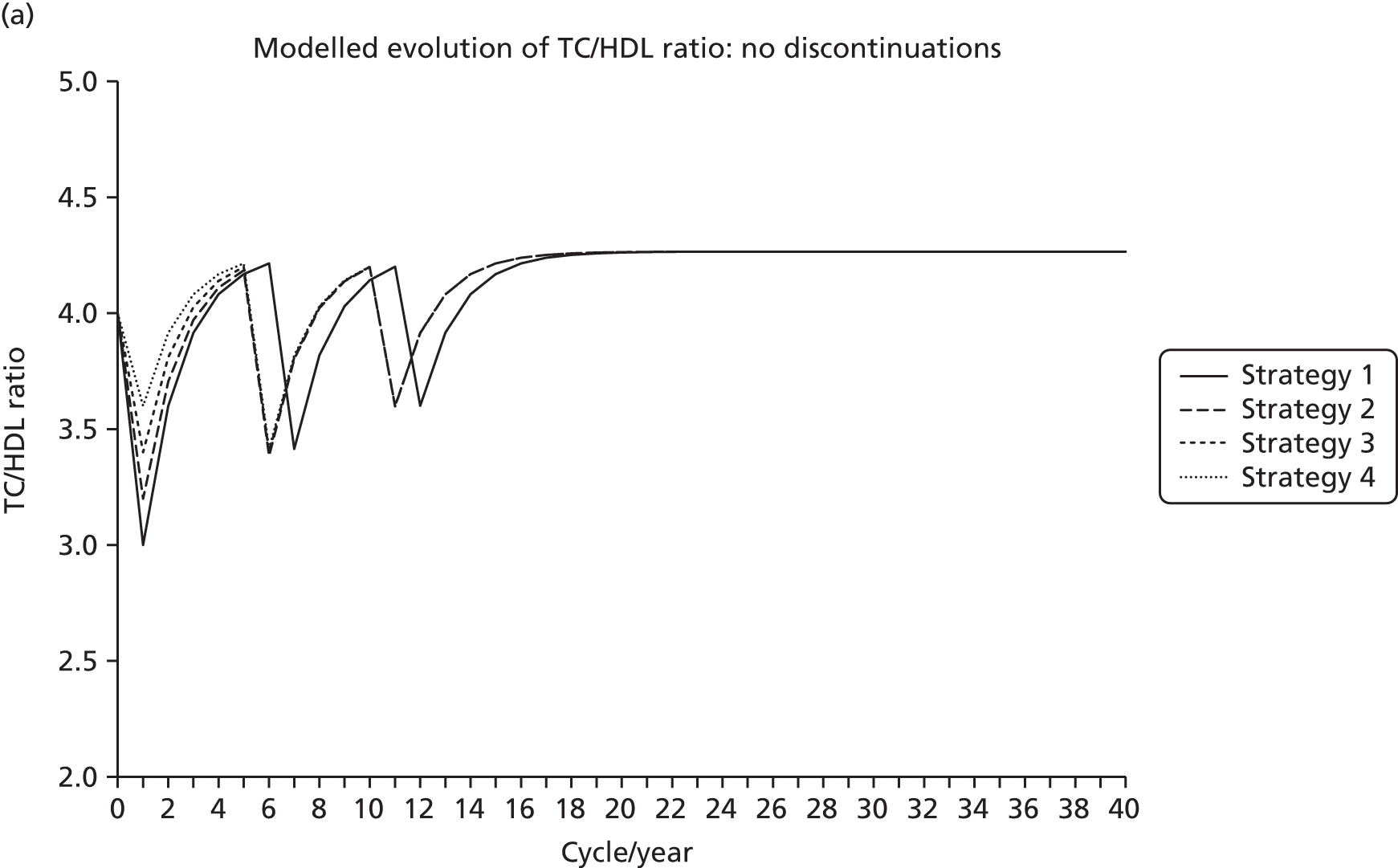

The modelled evolution of HBA1c, SBP and the TC/HDL ratio for a range of inputted patient characteristics was cross-checked with that modelled by the UKPDS OM1 at central UKPDS68193 parameter values. The modelled evolutions values were typically around 99.99% of the values simulated by the UKPDS OM1 model.
The evolution of the patient BMI is based upon a mean annual increase in weight of 0.1 kg, as has typically been used in previous NICE assessments of treatments for diabetes, and is apparently originally sourced from the 2006 NICE CG on obesity. 211 Over the course of NICE assessments and guidelines development for treatments for type 2 diabetes, quite a lot of discussion has focused upon what is reasonable to assume about the duration of weight effects. There has been some argument that initial weight losses associated with treatment may tend to be transient, whereas initial weight gains associated with treatment may tend to be more permanent. In light of this, five scenarios are modelled:
-
treatment weight changes maintained, with no rebound to natural history
-
treatment weight gains maintained, weight losses rebound to natural history after 1 year
-
treatment weight gains maintained, weight losses rebound to natural history at intensification
-
treatment weight changes rebound to natural history after 1 year
-
treatment weight changes rebound to natural history at intensification.
Figures 16 and 17 illustrate weight changes being maintained for a patient of 85 kg at baseline. Initial hypothetical treatment effects are 5 kg, –5 kg, 10 kg and –4 kg for strategies 1–4, respectively. The intensifications result in treatment effects of 3 kg and 7 kg. For the patient modelled as discontinuing during strategy 1, the alternative treatment effect is 4 kg, with the additional weight gains in the alternative sequence thereafter being assumed to be the same as in the original sequence.
FIGURE 16.
Example of the modelled evolution of patient weight: no rebound.

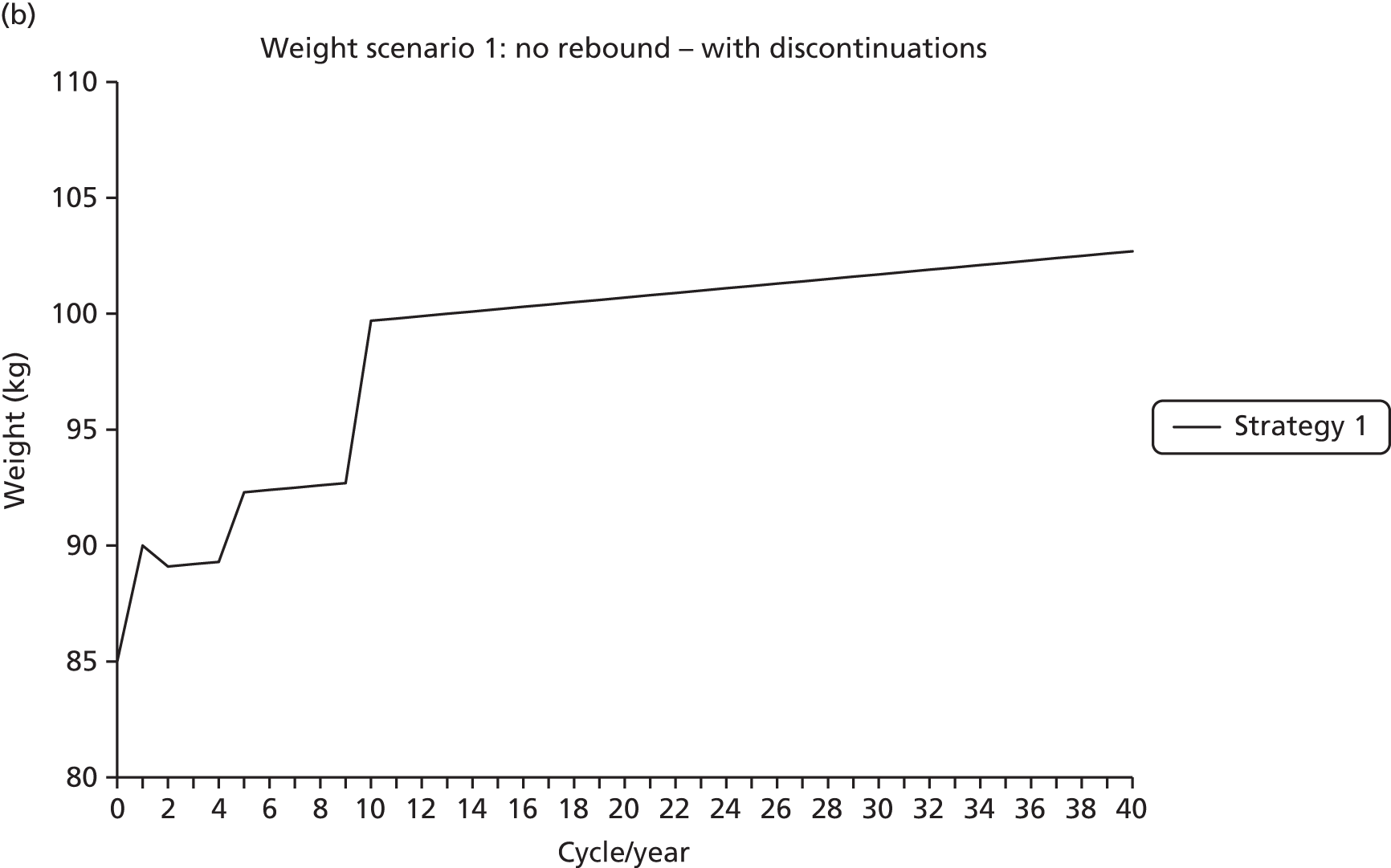
The above is largely self-explanatory. Within the evolution of weight for the patient under strategy 1 who discontinues, there is a drop in weight between year 1 and year 2. This arises as a result of the patient being assumed to come off his/her original treatment, which would have increased his/her weight by 5 kg and to move on to the alternative treatment which increases his/her weight by only 4 kg. Quite when the patient would discontinue, and, as a consequence, quite what the balance would be, in practice, between the 5-kg increase and the 4-kg increase during the first line of treatment, is a moot point.
FIGURE 17.
Example of the modelled evolution of patient weight: rebound scenarios. Tx, treatment.

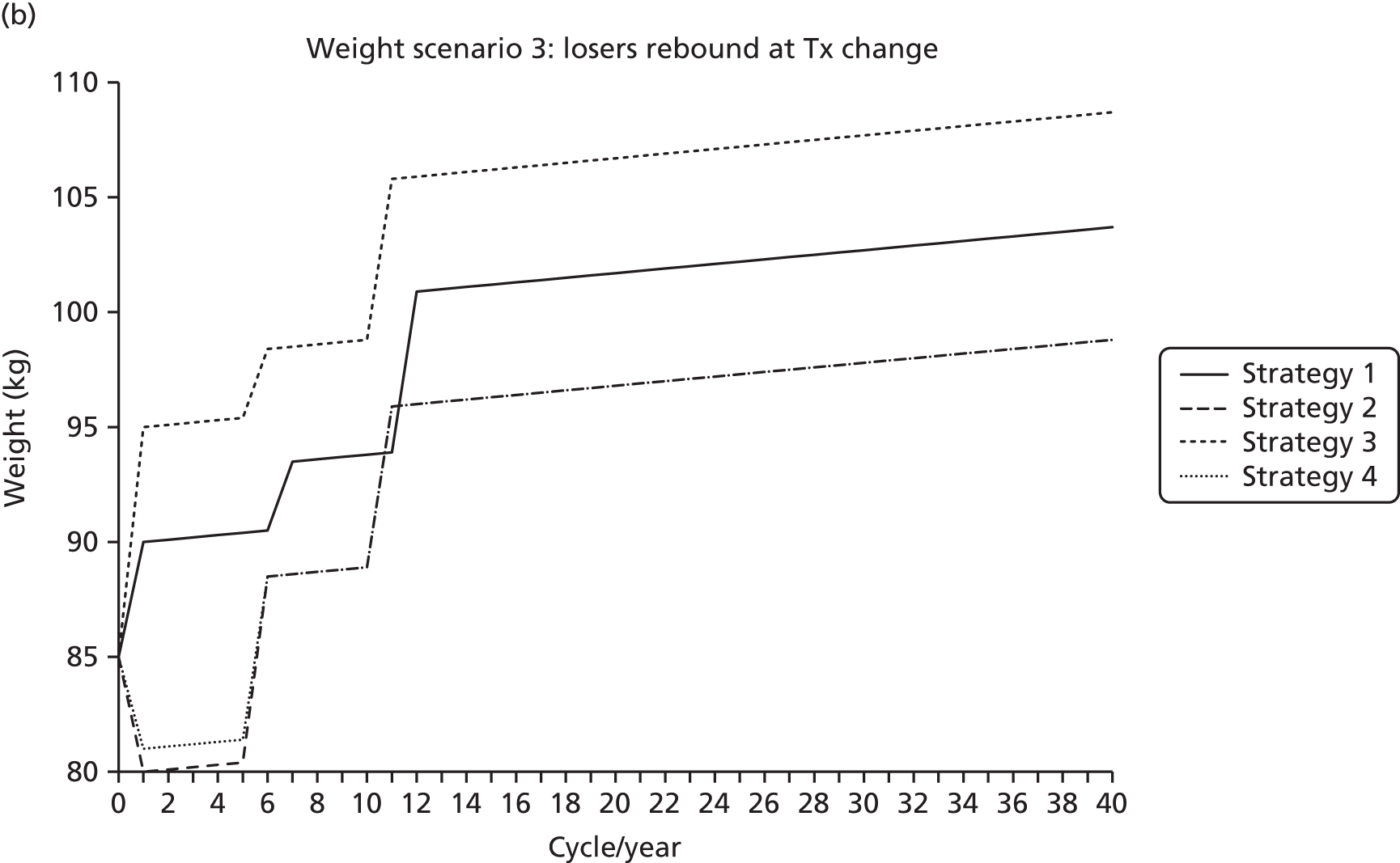

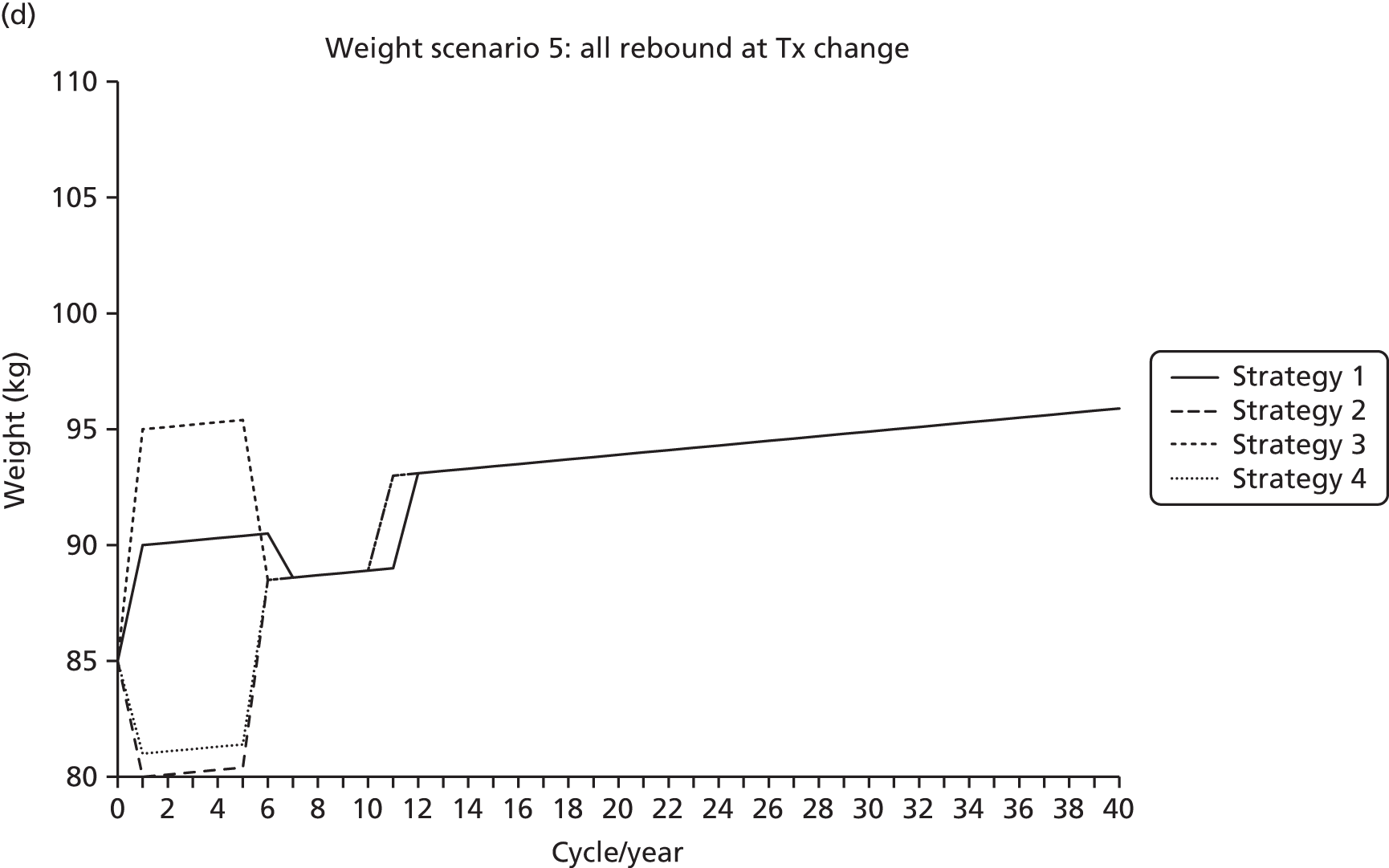
Body mass index scenarios 2 and 3, which have weight losses rebounding to natural history, do not affect strategies 1 and 2, as they incur only weight gains.
Body mass index scenario 2 sees weight losses rebound to natural history after 1 year. So at year 2 both strategies 2 and 4 have rebounded to natural history and 85.2-kg weight. Thereafter, they follow the same weight profile, as their treatment intensifications also occur at the same time: years 6 and 11.
Body mass index scenario 3 sees weight losses rebound to natural history at treatment intensification. To model this, the rebound to natural history that would have applied in the previous year is first calculated – 85.5 kg – to which the intensification treatment effect of 3.0 kg is added to give a weight of 88.5 kg at year 6. An alternative way of looking at this is to view the intensification treatment effect of 3.0 kg being composed of two parts: 0.1 kg for natural history and 2.9 kg for additional treatment effect.
Body mass index scenario 4 sees all weight changes rebound to natural history after 1 year. The figure is largely self-explanatory, with all initial treatment effects being removed at year 2. Thereafter, strategies 2–4 intensify treatment at years 6 and 11, and see the weight gains associated with intensifications rebound to natural history at years 7 and 12. Strategy 1 intensifies later at years 7 and 12, hence the later rebounds to natural history.
Body mass index scenario 5 sees all weight changes rebound to natural history at treatment change. Strategies 2–4 intensify treatment at years 6 and 11, so rebound to natural history the following year. But the weight gains associated with the intensifications are then added to where the patients rebound. As a result, after the first intensification at year 6 the patient weight is 88.5 kg for strategies 2–4. For strategy 1 the intensification is 1 year later, with it joining the other strategies at a weight of 88.6 kg in year 7. Much the same happens at the subsequent intensification.
Note that the BMI scenarios 4 and 5 may be felt to be literally unrealistic, with weight gains rebounding to natural history after 1 year or at the next treatment change. But they may be better thought of as causing weight to converge between strategies either after 1 year or at treatment change. In terms of the modelling of the impact of BMI upon QoL this will not be exactly arithmetically correct because of the floor of 25 kg/m2 on the BMI QoL coefficient of –0.0061. Given the baseline BMI of 31.6 kg/m2 (SD 6.0 kg/m2), around 13% of patients are modelled as having a BMI of less than 25 kg/m2. For some of these patients, the rebounds of scenarios 4 and 5 may not be exactly equivalent in their QoL impacts to weight converging between the strategies by some other means, for example at the value of strategy with the higher BMI. But the AG is of the opinion that any differences are likely to be minor.
Note that there is a minor error within the implementation of weight in the AG modelling. The UKPDS68193 requires that the BMI at diagnosis is used and this has been implemented correctly. But the AG modelling assumes that the BMI at diagnosis also applies at baseline. It can be argued that the BMI at baseline should be the BMI at diagnosis plus the natural history increase that would be implied by the duration at baseline. But as the mean duration of diabetes at baseline is estimated to be 2.0 years, and that this adjustment would affect results for only the subset of patients during the cycles they bordered, the 25 kg/m2 threshold, this error will have negligible effects upon net results.
Diabetic ketoacidosis
There has been some suggestion that the flozins may increase the risk of DKA. But rates are low in absolute terms, with the EMA reporting 101 cases over about 500,000 patient-years of flozins use.
The Diabetics With Eating Disorders surveyed England’s primary care trusts (PCTs) in 2010. 212 Among the 45 PCTs that responded, the mean cost per DKA event was £1438, or £1552 in 2014 prices. But given an event rate of 1 per 5000 patient-years, the average increase in costs associated with this is minimal: around 30p per year of treatment. The typical duration of DKA events is also quite short, certainly less than 1 week, though there may be recurrence. But even with quite a large QoL decrement, given the absolute event rate and the short duration any overall average QALY impact will also be minimal.
There remains the possibility of an increased mortality with DKA among those with type 2 diabetes. This could have more of an impact upon the modelled average QALY in the flozin arms. But there is no simple means of incorporating this mortality into the OM1 modelling, this being a black box to the AG.
For the above reasons, DKA has not been incorporated into the economic modelling.
Quality of life: diabetes and the complications of diabetes
Given the use of the OM1 model, the AG draws the QoL value for those without any complications and QoL impacts for the complications of diabetes from the UKPDS62198 (Table 45). A value for renal failure is not given in the UKPDS62198 and, as a consequence, the AG has used the OM1 default value of –0.263 as drawn from Kiberd and Jindal. 213
| Complication | Mean | SE | Distribution |
|---|---|---|---|
| No complications | 0.785 | 0.005 | Beta |
| MI | –0.055 | 0.006 | Log-normal |
| IHD | –0.090 | 0.018 | Log-normal |
| Stroke | –0.164 | 0.030 | Log-normal |
| CHF | –0.108 | 0.031 | Log-normal |
| Amputation | –0.280 | 0.056 | Log-normal |
| Blindness | –0.074 | 0.033 | Log-normal |
| Renal failure | –0.263 | 0.020 | Log-normal |
Quality of life: weight
In common with most NICE assessments of treatment for type 2 diabetes and the draft NICE type 2 diabetes CG, the AG applies the utility decrement of –0.0061 (SE 0.001) of Bagust and Beale. 199 Within Bagust and Beale,199 this decrement applies if the patient BMI is above 25 kg/m2.
The mean BMI within the UKPDS RCT was 27.7 kg/m2, and it is from here that the mean baseline utility of 0.785 is drawn. As a consequence, as the modelling applies the –0.0061 QoL decrement when the patient BMI rises above 25 kg/m2, it can be argued that the baseline utility of 0.785 should have 0.0061 × 2.7 = 0.0165 added to it. This modification is adopted for the AG base case.
Quality of life: treatment discontinuations
Treatment discontinuations were assigned a QALY decrement associated with nausea as drawn from Matza et al. 214 The with- and without-nausea QoL values of 0.85 and 0.89 were taken to apply yielding a mean decrement of 0.04, which the GDG thought a 6-week duration would be most reasonable estimate, this yielding a mean QALY decrement of –0.00462.
Quality of life: adverse events
The 2012 NICE CG on infection, CG139,215 undertook a systematic review of the literature for studies of the QoL impacts of symptomatic UTIs. This identified 11 studies, but a number of these are of limited relevance to the current assessment because, for example, being among patients with spinal cord injuries. Of the 11 studies, five appear most relevant to the current assessment.
Clinical guideline 139215 also undertook economic modelling of treatments for UTIs. But as a result of the available clinical effectiveness estimates being largely limited to those with spinal cord injury, the QoL values applied are of limited relevance to the current assessment. This modelling also considered progression from symptomatic UTIs through to first-line drug resistance and multidrug resistance, with these causing increased costs and mortality.
The AG modelling for the current assessment only considers the QoL and cost impacts of treating UTIs and GTIs, with the assumption that none will progress to a more serious condition. So there are caveats around these estimates, and for a given set of inputs they could be seen as being biased and on the low side.
Barry et al. 205 used the Index of Wellbeing (IWB) to estimate QoL among young women with UTIs. The IWB is a generic QoL instrument. The mapping function from the IWB to QoL values was apparently based upon 62 American nurses and non-medical graduate students ranking health states on a 16-point scale. Barry et al. 205 report that the IWB includes hospitalisation, self-care and ambulatory status, and permits the inclusion of the following symptoms: pain; bleeding; itching discharge from sexual organs; painful burning or frequent urination; burning or itching rash on large areas of the body; taking medication; fever or chills with aching all over; and pain in the chest, stomach, sides, back or hips. But Barry et al. 205 do not describe quite how the QoL values for the health states for their model have been derived. It appears to be based upon an index patient with a set of symptoms; that is expert opinion linked to the IWB. They estimated disutilities of 0.3732 for pyelonephritis, and 0.2894 for vaginitis and persistent dysuria. Their duration was estimated to be 10 days, 5 days and 5 days, respectively.
Gold et al. 216 catalogued 130 health states using the Health and Activity Limitation Index (HALex), with the score being based upon the answers to two questions of the US National Health Interview Survey. A multiattribute utility model resulted in QoL estimates of 1.00 for perfect health, and 0.73 for bladder infection and 0.66 for kidney infection. The derivation of these weights is not particularly clear within the paper.
Ackerman et al. 217 used the standard gamble to estimate QoL values among 13 men with moderate to severe benign prostatic hyperplasia. A variety of health states were described, with the QoL impacts of severe UTIs being estimated among these. The six risk-averse men reported an average value of 0.972 for a severe UTI, whereas the seven non-risk-averse men reported an average value of 0.893. Over the 13 respondents this suggests an average disutility per severe UTI of 0.071.
Ellis and Verma218 measured the impact of UTIs among 118 otherwise healthy Canadian women through a case-controlled analysis using the Short Form questionnaire-36 items (SF-36) with a recall period of 1 day. The mapping from the SF-36 to the EQ-5D QoL values based upon the algorithm of Ara and Brazier219 appears to have been undertaken by the NICE CG, as Ellis and Verma218 report only the mean values for the eight main elements of the SF-36. This resulted in those with no UTI having a mean QoL of 0.922 compared with 0.724 for those with a UTI.
Ernst et al. 220 used the Quality of Wellbeing (QWB) to estimate the QoL among 146 American women who were diagnosed with acute cystitis, and the effect of treatment upon QoL. Those with type 2 diabetes were excluded from the study. The QWB was administered 3, 7, 14 and 28 days after the initial visit. The QoL at baseline was 0.68 (SD 0.03) compared with 0.81 (SD 0.11) at the 28-day point. QoL among those cured compared with those not cured was statistically significantly different at the 5% level at days 3, 7 and 14, with respective QWB scores of 0.77 vs. 0.72, 0.82 vs. 0.71 and 0.83 vs. 0.76 (Table 46).
| Source | Barry 1997205 | Gold 1998216 | Ackerman 2000217 | Ellis and Verma 2000218 | Ernst 2005220 | ||
| Year | 1997 | 1998 | 2000 | 2000 | 2005 | ||
| Country | USA | USA | USA | Canada | USA | ||
| N | NA | NA | 13 men | 118 women | 146 women | ||
| Method | IWB | HALex | SG | SF-36 | QWB | ||
| Condition | Pyelonephritis | Vaginitis/dysuria | Bladder | Kidney | UTIs | UTIs | Cystitis |
| Disutility | 0.3732 | 0.2894 | 0.27 | 0.33 | 0.028–0.107 | 0.198 | 0.05–0.13 |
Of the above papers, Ackerman et al. 217 could be argued as coming closest to the NICE reference case. But the usefulness of these estimates is compromised by the small sample size. As a consequence, the AG will use the results of the Janssen TTO study for the base case of QoL impact of –0.19 for a UTI and –0.25 for a GTI. Nicolle et al. 98 estimated median durations of UTIs of between 11.0 days and 12.5 days, and, as a consequence, the base case will assume 2 weeks’ average duration.
Quality of life: hypoglycaemia
Following the lead of the draft NICE CG for type 2 diabetes, the source for the base case for the QoL decrements associated with hypoglycaemia events will be Currie et al. 204 This used two separate 3-month recall surveys among patients with diabetes (n = 408 and n = 897), undertaken at different time points, though 145 patients responded to both surveys.
The first survey was used to estimate a relationship between a patient’s score on the Hypoglycaemic Fear Survey (HFS) and the number of non-severe and severe hypoglycaemic episodes with coefficients of 1.773 (SE 0.230) and 5.881 (SE 1.553), respectively. The second survey was used to estimate the relationship between the HFS and the EQ-5D QoL with a coefficient of –0.008 (SE 0.001).
Given the 3-month recall period, the mapping between non-severe hypoglycaemia event rates and the patient’s score on the HFS requires that rates be converted to 3-monthly rates before the 1.773 HFS coefficient can be applied to arrive at the correct QALY decrement.
The authors of the draft NICE CG for type 2 diabetes also point out that the table 4 coefficient of Currie et al. 204 for non-severe hypoglycaemia events is based upon the natural logarithm of the event rate rather than the event rate. As such it is non-linear. To account for this the AG has followed the method of the authors of the draft NICE CG for type 2 diabetes and applied a Poisson distribution to give the spread of possible patient event rates prior to applying the coefficients of Currie et al. 204
The 5.881 HFS coefficient of table 4 of Currie et al. 204 for severe hypoglycaemic events was derived on a dichotomous basis, equal to 1 if there were any events reported during the previous 3 months and equal to 0 if there were none reported. The draft NICE CG gives a quite complicated formula for accounting for this using a binomial distribution, but this apparently simplifies to the quarterly probability times the utility decrement (Gabriel Rogers, NICE, 17 August 2015, personal communication).
Table 47 presents a range of estimates based upon this method.
| Scenario | Severe | Non-severe | |||||
|---|---|---|---|---|---|---|---|
| Annual | 1.00 | 10 | 20 | 30 | 40 | 50 | 60 |
| Quarterly | 0.22 | 2.50 | 5.00 | 7.50 | 10.00 | 12.50 | 15.00 |
| HFS | 1.30 | 1.39 | 2.65 | 3.44 | 3.98 | 4.40 | 4.74 |
| Annual QALY loss | –0.010 | –0.011 | –0.021 | –0.032 | –0.035 | –0.038 | –0.040 |
But the values of Currie et al. 204 come with some major caveats. As Currie et al. 204 note regarding the two data sources, ‘These studies were commissioned by the pharmaceutical industry to inform drug developments around new treatments for diabetes that were found to reduce the frequency of hypoglycaemia’. The paper authorship also includes staff of Novo Nordisk and Sanofi-Aventis.
The values are based on results from two surveys, with a response rate of 31%. The hypoglycaemic episodes were recent events and perhaps therefore fresh in the memory. Forty-five per cent of respondents were on insulin. Respondents might have been more likely to have been concerned about hypoglycaemia than non-respondents.
Around one-third of respondents had type 1 diabetes mellitus (T1DM) with around two-thirds of respondents having type 2 diabetes. Quite what covariates were considered and quite how the paper arrived at the final regressions is not entirely explicit. Patient data from the first survey were removed if the patient also responded to the second survey, reducing the sample to 57% of the original, though the reasons for this and impacts of doing so are not clear. Similarly, the grouping of complications was also possibly subjective.
The 5.881 coefficient for severe hypoglycaemia episodes was also based on whether patients had had any severe hypoglycaemia events during the recall period. If, within this group, the mean number of severe hypoglycaemic episodes was more than one, it seems likely that the coefficient somewhat overestimates the impact of having one severe hypoglycaemia events within a quarter.
The patient number and demographics reported by Currie et al. 204 for the first survey are based upon the full 408 patients of this survey. But for the analysis, 175 of these patients were excluded because of also being in the second survey. As a consequence the demographics and events rates that were used when analysing the data subset of the first survey cannot be determined.
For the full 408 patients of the first survey, only 2.3% (n = 9) reported experiencing at least one severe hypoglycaemic event during the previous 3 months. This was somewhat less than the 8.6% (n = 77) proportion who reported experiencing at least one severe hypoglycaemic event during the previous 3 months in the second survey.
For severe hypoglycaemic event rates, Currie et al. 204 state that within the surveys ‘very few people > 1 event’ and they report a mean rate of ‘1.47 events per patient-year’. It seems likely that this mean rate was the average across the two surveys. It would have been useful to have known the mean rate for each survey, and for the small subset of the first survey that was actually analysed.
The relationship between having experienced at least one severe hypoglycaemic event in the last 3 months and the HFS index, that is the 5.881 coefficient, consequently appears to have been based upon, at most, nine patients reporting. The restriction of the subset analysed to 57% of the total sample of the first survey suggests that this number is likely to have been somewhat less than nine patients. This gives rise to the possibility of an outlier patient within this small subset having an unreasonable impact upon results. The construction of the subset was at investigator discretion.
The AG cannot further interrogate the data underlying the estimates of Currie et al.,204 and it is possible that they may be overestimates. Note that in common with previous analyses, the method of the table above in effect assumes that a patient experiences at most one severe hypoglycaemic event per quarter. There may be an argument for dividing the QALY decrement associated with severe hypoglycaemic events by 1.47, the mean event rate reported in Currie et al. 204
Costs: direct drug costs
Treatment costs are based upon the NHS drug tariff, and upon list prices for which there are no entries in the NHS drug tariff. Daily doses are assumed to be 60 mg for gliclazide MR, 45 mg for pioglitazone, 6.0 mg for repaglinide, 100 mg for sitagliptin, 10 mg for dapagliflozin, 25 mg for empagliflozin and 300 mg for canagliflozin. Insulins costs are based upon a requirement of 0.3 IU/kg when starting NPH, with this rising to 0.55 IU/kg when adding bolus which itself is required at 0.2 IU/kg.
The AG expert opinion also suggests that those receiving pioglitazone should have their BNP measured, perhaps initially 6-monthly but annually thereafter. A marginal cost of £21 has been taken from Craig et al. 45 and inflated to 2014 prices using a 1.25 multiplier from the PSSRU Unit Costs of Health and Social Care index. This has also been assumed to require a dedicated GP appointment, costed at £46 using the PSSRU Unit Costs of Health and Social Care 2014. 208
This results in the following treatment costs for the oral therapies (Table 48).
| Strategy | Monotherapy | Cost | First intensification | Cost | Second intensification | Cost | Third intensification | Cost |
|---|---|---|---|---|---|---|---|---|
| S1 | Empagliflozin | 476.98 | Gliclazide MR | 62.18 | Gliclazide MR | 62.18 | ||
| Empagliflozin | 476.98 | Empagliflozin | 476.98 | Empagliflozin | 476.98 | |||
| INS | 140.38 | Int. INS | 351.36 | |||||
| SMBG | 51.09 | SMBG | 119.54 | |||||
| S1 total cost | 476.98 | 539.16 | 730.63 | 947.88 | ||||
| S2 | Canagliflozin | 476.93 | Gliclazide MR | 62.18 | Gliclazide MR | 62.18 | ||
| Canagliflozin | 476.93 | Canagliflozin | 476.93 | Canagliflozin | 476.93 | |||
| INS | 140.38 | Int. INS | 351.36 | |||||
| SMBG | 51.09 | SMBG | 119.54 | |||||
| S2 total cost | 476.93 | 539.11 | 730.58 | 947.83 | ||||
| S3 | Dapagliflozin | 476.98 | Gliclazide MR | 62.18 | Gliclazide MR | 62.18 | ||
| Dapagliflozin | 476.98 | Dapagliflozin | 476.98 | Dapagliflozin | 476.98 | |||
| INS | 140.38 | Int. INS | 351.36 | |||||
| SMBG | 51.09 | SMBG | 119.54 | |||||
| S3 total cost | 476.98 | 539.16 | 730.63 | 947.88 | ||||
| S4 | Sitagliptin | 433.57 | Gliclazide MR | 62.18 | gliclazide MR | 62.18 | ||
| Sitagliptin | 433.57 | Sitagliptin | 433.57 | Sitagliptin | 433.57 | |||
| INS | 140.38 | Int. INS | 351.36 | |||||
| SMBG | 51.09 | SMBG | 119.54 | |||||
| S4 total cost | 433.57 | 495.75 | 687.22 | 904.47 | ||||
| S5 | Pioglitazone | 93.25 | Gliclazide MR | 62.18 | Gliclazide MR | 62.18 | ||
| Pioglitazone | 93.25 | Pioglitazone | 93.25 | Pioglitazone | 93.25 | |||
| INS | 140.38 | Int. INS | 351.36 | |||||
| SMBG | 51.09 | SMBG | 119.54 | |||||
| S5 total cost | 93.25 | 155.43 | 346.90 | 564.15 | ||||
| S6 | Gliclazide MR | 62.18 | Gliclazide MR | 62.18 | Gliclazide MR | 62.18 | ||
| Pioglitazone | 93.25 | Pioglitazone | 93.25 | Pioglitazone | 93.25 | |||
| INS | 140.38 | Int. INS | 351.36 | |||||
| SMBG | 51.09 | SMBG | 119.54 | |||||
| S6 total cost | 62.18 | 155.43 | 346.90 | 564.15 | ||||
| S7 | Repaglinide | 71.91 | Gliclazide MR | 62.18 | Gliclazide MR | 62.18 | ||
| Pioglitazone | 93.25 | Pioglitazone | 93.25 | Pioglitazone | 93.25 | |||
| INS | 140.38 | Int. INS | 351.36 | |||||
| SMBG | 51.09 | SMBG | 119.54 | |||||
| S7 total cost | 71.91 | 155.43 | 346.90 | 564.15 | ||||
The AG modelled sequences differ from those of the company submissions in that patients add NPH insulin rather than switch to it and as a consequence the cost differences between the sequences are maintained over the horizon of the modelling. In light of this, a scenario analysis is undertaken, which withdraws the initial monotherapies when patients switch to NPH insulin. Note that this affects only the direct drug costs and not the clinical effectiveness estimates.
Costs: treatment intensifications and switches
Treatment intensifications due to breaching the 7.5% HbA1c threshold and treatment switches due to intolerance are assumed to involve one 12-minute GP appointment. This is costed using the PSSRU Unit Costs of Health and Social Care 2014 at £46. 208
Costs: adverse events
The AG treatment assumptions are broadly in line with those of the Janssen submission (Table 49), with this resource use being confirmed by AG expert opinion. Medication for UTIs is assumed to be 7 days of trimethoprim 200 mg twice daily, for male GTIs fluconazole 200 mg and female GTIs three 200-mg clotrizamole pessaries (see Table 49).
| Infection | GP visits | Unit cost (£) | Cost (£) | Drug tariff (£) | Cost/day (£) | Days | Cost (£) | Total cost (£) |
|---|---|---|---|---|---|---|---|---|
| UTI | ||||||||
| Male | 2 | 46 | 92 | 1.87 | 0.62 | 7 | 4.36 | 96 |
| Female | 1 | 46 | 46 | 1.87 | 0.62 | 7 | 4.36 | 50 |
| Total UTI cost | 73 | |||||||
| GTI | ||||||||
| Male | 1 | 46 | 46 | 6.23 | 0.89 | 7 | 6.23 | 52 |
| Female | 1 | 46 | 46 | 3.10 | – | – | 3.10 | 49 |
| Total GTI cost | 51 | |||||||
These costs are largely based upon assumption and have consequently been treated deterministically within the probabilistic modelling.
Costs: hypoglycaemic events
The AG have followed the draft NICE CG when costing severe hypoglycaemic events.
Hammer et al. ,207 in an industry-sponsored study, surveyed 147 UK patients with type 2 diabetes using insulin, with 19 reporting at least one severe hypoglycaemic episode in the previous year, with 10 of these being treated by the NHS. Hammer et al. 207 acknowledge the non-random selection of their patient sample, but provide few details about it other than to note that it was predominantly through health-care professionals. Patients were surveyed using a structured questionnaire about the resource use associated with their events.
Patients were divided into three groups: those who had their severe hypoglycaemic event treated by family members; by medical practitioners in the community; and, in hospital. The mean direct costs by type, in 2007 prices, were £33 for those treated by family members, due to NHS follow-up costs; £231 for those treated by the NHS in the community; and £862 for those treated in hospital. Owing to the non-random sample selection, there is no definitive means to translate these into a weighted average cost. But the GDG of the draft NICE CG was reportedly happy to use the sample proportion treated by family members (9/19), coupled with an assumption that, of the remainder, 65% would be treated in hospital.
This results in a mean cost per severe hypoglycaemic event of £353 in 2007 prices, which, when uplifted by a 1.16 multiplier from the PSSRU Unit Costs of Health and Social Care 2014,208 results in an estimate of £411.
Costs: diabetes and the complications of diabetes
The costs of diabetes and the complications of diabetes are taken from the UKPDS84195 tables, and uprated for inflation using a multiplier of 1.03 from the PSSRU Hospital and Community Health Services index208 (Table 50).
| Event | Inpatient costs (£) | Outpatient costs (£) | Total, mean (£) | ||||
|---|---|---|---|---|---|---|---|
| Mean | SE | Distribution | Mean | SE | Distribution | ||
| No event | 472 | 33 | Gamma | 547 | 23 | Gamma | 1019 |
| Event year | |||||||
| Fatal MI | 1564 | 531 | Gamma | 1564 | |||
| Fatal IHD | 3873 | 1250 | Gamma | 3873 | |||
| Fatal stroke | 4066 | 1158 | Gamma | 4066 | |||
| MI | 6560 | 1062 | Gamma | 990 | 95 | Gamma | 7550 |
| IHD | 10,044 | 1484 | Gamma | 888 | 78 | Gamma | 10,932 |
| Stroke | 6998 | 1685 | Gamma | 1122 | 191 | Gamma | 8120 |
| Heart failure | 3281 | 846 | Gamma | 1007 | 167 | Gamma | 4288 |
| Amputation | 9816 | 1849 | Gamma | 2775 | 713 | Gamma | 12,592 |
| Blindness in one eye | 1393 | 588 | Gamma | 1841 | 571 | Gamma | 3234 |
| Subsequent years | |||||||
| MI | 1187 | 158 | Gamma | 690 | 49 | Gamma | 1877 |
| IHD | 1249 | 153 | Gamma | 673 | 42 | Gamma | 1922 |
| Stroke | 1157 | 234 | Gamma | 777 | 89 | Gamma | 1934 |
| Heart failure | 1515 | 347 | Gamma | 1001 | 98 | Gamma | 2515 |
| Amputation | 1843 | 494 | Gamma | 1657 | 242 | Gamma | 3499 |
| Blindness in one eye | 466 | 99 | Gamma | 759 | 89 | Gamma | 1225 |
It should be noted that these costs are for a representative 60-year-old male patient, and are for a patient with only one complication. Costs are to a degree a function of age. There are interactions between complications within the UKPDS82,194 which mean that those with more than one complication do not necessarily incur a simple sum of the individual complication costs. Only one set of the costs of complications can be fed into the OM1. As a consequence, it has not been possible to take these effects into account, but they are not particularly marked.
The UKPDS84195 does not provide a costing for renal disease. In common with the draft NICE CG for diabetes, these have been drawn from Lamping et al. 221 with the inpatient cost in 1996 prices of £20,802 (SE £613) being uprated for inflation using a multiplier of 1.75 from the PSSRU HCSC index.
Assessment Group sensitivity analyses
All scenario analyses have been run deterministically with a cohort of 50,000 patients and 1000 inner loops to reduce Monte Carlo error. The sensitivity analyses around the –0.0061 QoL decrement per BMI point above 25 kg/m2 and the rebound of treatments’ effect upon weight are presented for all analyses:
-
BMI 1 Natural history progression with no rebound
-
BMI 2 Natural history progression with weight losses rebounding after 1 year
-
BMI 3 Natural history progression with weight losses rebounding at treatment change
-
BMI 4 Natural history progression with weight rebounding after 1 year
-
BMI 5 Natural history progression with weight rebounding at treatment change.
The AG has also undertaken the following sensitivity analyses.
-
SA01 At the third intensification patients switch to insulin plus gliclazide, and cease their other treatments.
-
SA02 Applying the UTI and GTI rates to all cycles of the model.
-
SA03 Assuming that all patients when starting monotherapy have a HbA1c of 7.5%.
-
SA04 Adjusting the HbA1c treatment effect for patients’ baseline HbA1c values as in the NICE CG.
-
SA05 Not applying the discontinuation rates.
-
SA06 Applying the NICE CG baseline TC/HDL values and the UKPDS68193 TC/HDL progression.
-
SA07 Applying the UKPDS68193 year 2 parameter for the evolution of HbA1c.
-
SA08 Intensifying when adding gliclazide having a –0.47% HbA1c effect.
-
SA09 Applying the Janssen linear evolutions of HbA1c for all treatments.
-
SA10 Assuming that those discontinuing from a treatment omit any subsequent intensification step that reapplies this treatment.
-
SA11 SA01 and SA08 combined.
Assessment Group base-case results
The disaggregate costs of the base case provided in Table 51.
| Quantity | Empagliflozin 25 mg | Canagliflozin 300 mg | Dapagliflozin 10 mg | Sitagliptin 100 mg | Pioglitazone | Gliclazide | Repaglinide |
|---|---|---|---|---|---|---|---|
| OM1 costs | 22,880 | 22,925 | 22,926 | 23,039 | 22,905 | 22,876 | 22,871 |
| Tx costs | 9768 | 9624 | 9811 | 9199 | 4521 | 4323 | 4401 |
| Tx change | 95 | 92 | 96 | 96 | 94 | 91 | 92 |
| Hypoglycaemic episodes | 20 | 20 | 21 | 21 | 19 | 20 | 46 |
| UTI | 8 | 10 | 8 | 3 | 3 | 3 | 3 |
| GTI | 4 | 5 | 5 | 1 | 1 | 1 | 1 |
| Total costs | £32,775 | £32,676 | £32,866 | £32,358 | £27,543 | £27,314 | £27,413 |
The UKPDS costs for all the flozins are similar, with slightly lower costs than sitagliptin due, in part, to the latter having little impact upon SBP, whereas the flozins reduce it.
Pioglitazone, gliclazide and repaglinide are estimated to have similar or slightly lower UKPDS OM1 costs than the flozins, which is in line with the estimates of them having slightly larger effects upon HbA1c.
Treatment costs are the main source of the differences in costs, as would be anticipated. The flozins are of similar cost, but canagliflozin is a reasonable amount cheaper. This arises due to the greater HbA1c effect of canagliflozin meaning that patients will tend to intensify to the more expensive subsequent lines of treatment slightly later.
For the base case, with the exception of repaglinide, and to a lesser extent gliclazide, patients remain on their initial monotherapy throughout, adding treatments to it when they intensify. As a consequence, the annual treatment costs difference between sitagliptin and the flozins is maintained over the time horizon of the model and the sitagliptin treatment costs are noticeably lower than those of the flozins. This outweighs the slightly higher UKPDS OM1 costs for sitagliptin, and its total costs are a reasonable amount less than those of the flozins.
Pioglitazone, gliclazide and repaglinide treatment costs are considerably lower than those of the flozins and sitagliptin. Treatment costs cause the total costs of pioglitazone, gliclazide and repaglinide to be considerably less than those of the flozins and sitagliptin.
The disaggregate QoL impacts of the base case provided in Table 52. Within this, the total QALYs estimated under the UKPDS OM1 model and those associated with treatment switching, hypoglycaemic events and UTIs and GTIs, are summed to give a subtotal. This subtotal corresponds to the sensitivity analysis of assuming that a patent’s BMI has no impact upon the patient’s QoL. The QALY impacts from assuming a –0.0061 QoL decrement for each BMI point above 25 kg/m2 are then presented for each of the five weight progression scenarios that are modelled (see Table 52).
| Quantity | Empagliflozin 25 mg | Canagliflozin 300 mg | Dapagliflozin 10 mg | Sitagliptin 100 mg | Pioglitazone | Gliclazide | Repaglinide |
|---|---|---|---|---|---|---|---|
| OM1 QALYs | 10.380 | 10.382 | 10.369 | 10.355 | 10.385 | 10.393 | 10.390 |
| Tx switch | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Hypoglycaemic episodes | –0.001 | –0.000 | –0.000 | –0.000 | –0.000 | –0.000 | –0.001 |
| UTI and GTI | –0.001 | –0.002 | –0.002 | –0.000 | –0.000 | –0.000 | –0.000 |
| Subtotal | 10.378 | 10.380 | 10.367 | 10.355 | 10.384 | 10.392 | 10.389 |
| BMI 1 | –0.631 | –0.600 | –0.633 | –0.697 | –0.772 | –0.759 | –0.726 |
| BMI 2 | –0.694 | –0.689 | –0.696 | –0.700 | –0.772 | –0.759 | –0.726 |
| BMI 3 | –0.684 | –0.673 | –0.686 | –0.699 | –0.772 | –0.759 | –0.726 |
| BMI 4 | –0.612 | –0.610 | –0.612 | –0.616 | –0.622 | –0.622 | –0.619 |
| BMI 5 | –0.622 | –0.613 | –0.623 | –0.636 | –0.656 | –0.653 | –0.645 |
The QALY estimates are driven by the UKPDS OM1 outputs, and the BMI QoL decrements if these are applied. The other elements have little impact, though it should be borne in mind that the base case applies the UTI rates and GTI rates only during the first year.
The QALY losses associated with the –0.0061 QoL decrement for each BMI point above 25 kg/m2 may appear large, at around 6% of the total QALYs. But the baseline QoL of 0.801 in the absence of complications, the QoL impacts of complications and the baseline mean BMI of 31.9 kg/m2 should be borne in mind. The baseline mean BMI of 31.9 kg/m2, when coupled with the –0.0061 QoL decrement per BMI point above 25 kg/m2, reduces the baseline QoL of 0.801 in the absence of complications by around 4.5% by itself.
A summary of the total costs and QALYs with treatments ranked from the least expensive to the most expensive is presented in Table 53.
| Treatment | Total costs (£) | Total QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 27,314 | 10.392 | 9.633 | 9.633 | 9.633 | 9.771 | 9.739 |
| Repaglinide | 27,413 | 10.389 | 9.663 | 9.663 | 9.663 | 9.770 | 9.744 |
| Pioglitazone | 27,543 | 10.384 | 9.612 | 9.612 | 9.612 | 9.762 | 9.728 |
| Sitagliptin 100 mg | 32,358 | 10.355 | 9.657 | 9.655 | 9.655 | 9.739 | 9.719 |
| Canagliflozin 300 mg | 32,676 | 10.380 | 9.780 | 9.691 | 9.707 | 9.770 | 9.767 |
| Empagliflozin 25 mg | 32,775 | 10.378 | 9.747 | 9.683 | 9.694 | 9.766 | 9.756 |
| Dapagliflozin 10 mg | 32,866 | 10.367 | 9.734 | 9.671 | 9.681 | 9.756 | 9.745 |
These quantities can be subtracted from one another to present how much more costly and effective each treatment is compared with the least costly treatment (Table 54).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | – | – | – | – | – | – | – |
| Repaglinide | 100 | –0.003 | 0.030 | 0.030 | 0.030 | –0.001 | 0.005 |
| Pioglitazone | 230 | –0.008 | –0.021 | –0.021 | –0.021 | –0.008 | –0.011 |
| Sitagliptin 100 mg | 5045 | –0.037 | 0.024 | 0.022 | 0.022 | –0.031 | –0.020 |
| Canagliflozin 300 mg | 5362 | –0.012 | 0.147 | 0.057 | 0.074 | 0.000 | 0.028 |
| Empagliflozin 25 mg | 5461 | –0.015 | 0.113 | 0.050 | 0.061 | –0.005 | 0.017 |
| Dapagliflozin 10 mg | 5553 | –0.025 | 0.101 | 0.038 | 0.048 | –0.015 | 0.006 |
There is a large step in total costs when moving from pioglitazone to sitagliptin driven by treatment costs. There is a reasonable step in total costs when moving from sitagliptin to canagliflozin.
Pioglitazone is estimated to be both more costly and less effective than repaglinide under all of the BMI scenarios. Similarly, empagliflozin and dapagliflozin are estimated to be more costly and less effective than canagliflozin under all BMI scenarios, though the differences are not particularly large. This dominance is reflected in the estimates of cost-effectiveness as tabulated (Table 55). Note that the following ICERs are not relative to the least costly treatment, but are relative to the next least-costly treatment that is not dominated. In other words for BMI 1 the cost-effectiveness of repaglinide compared with gliclazide is £3331 per QALY and the cost-effectiveness of canagliflozin relative to repaglinide is £44,994 per QALY.
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Gliclazide | – | – | – | – | – | – |
| Repaglinide | Dom | 3331 | 3331 | 3331 | Dom | 18,507 |
| Pioglitazone | Dom | Dom | Dom | Dom | Dom | Dom |
| Sitagliptin 100 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Canagliflozin 300 mg | Dom | 44,994 | 192,000 | 119,000 | Dom | 235,000 |
| Empagliflozin 25 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Dapagliflozin 10 mg | Dom | Dom | Dom | Dom | Dom | Dom |
If the effects of BMI upon QoL are ignored or assumed not to apply then gliclazide is estimated to be both the cheapest and the most effective treatment. It is cheaper than sitagliptin and the flozins by quite a large amount, though the differences in the total lifetime QALYs are less marked.
For the scenarios of BMI progressing with natural history and the –0.0061 BMI QoL impact applying, if there is no rebound of treatment weight effects or only weight losses rebound the weight gain associated with gliclazide reduces its relative effectiveness. The smaller weight gain associated with repaglinide means that it is estimated to have a cost-effectiveness of £3331 per QALY compared with repaglinide under these scenarios.
The scenarios of both weight gains and weight losses rebounding may be felt to be unrealistic. But these are better seen as scenarios that explore when weight might tend to converge between the alternative treatments. If this happens after only 1 year the differences in weight between gliclazide and repaglinide are not maintained long enough for the BMI QALY effects to outweigh the QALYs estimated under the UKPDS OM1 and repaglinide remains dominated. Maintaining the difference for a longer period up until treatment change is sufficient for repaglinide to confer more QALYs and yields a cost-effectiveness estimate of £18,507 per QALY.
Pioglitazone is estimated to yield slightly fewer QALYs under the UKPDS OM1 than gliclazide, and its larger weight gain than gliclazide further hampers it. It remains dominated by gliclazide under all scenarios. But this should not obscure the fact that the UKPDS OM1 estimates pioglitazone to be more effective than sitagliptin and marginally more effective than the flozins. Pioglitazone is also considerably cheaper than sitagliptin and the flozins. Without the QoL impacts of weight changes pioglitazone is formally estimated to dominate sitagliptin and the flozins. Even with the QoL impacts of weight changes the cost-effectiveness estimates for sitagliptin and the flozins compared with pioglitazone are poor and well above conventional thresholds. Only canagliflozin and empagliflozin show any reasonable cost-effectiveness estimates compared with pioglitazone, and these occur only if treatment weight changes and the resulting differences in weight between treatments are assumed to be maintained over the patient lifetime. The BMI 1 scenario results in cost-effectiveness estimates for canagliflozin and empagliflozin compared with pioglitazone of £30,537 per QALY and £38,889 per QALY, respectively.
The UKPDS OM1 estimates sitagliptin to be slightly less effective than gliclazide. Being weight neutral, its weight profile is superior to gliclazide, but this is insufficient to render it cost-effective at conventional thresholds under any of the BMI scenarios when compared with gliclazide. Sitagliptin is dominated by gliclazide if there are no direct QoL impacts from weight, and for the BMI scenarios 4 and 5. For the BMI scenarios 1–3 the cost-effectiveness estimates for sitagliptin compared with gliclazide are £207,000, £231,000 and £227,000 per QALY.
The UKPDS OM1 estimates canagliflozin to be slightly less effective than both gliclazide and repaglinide. Its superior weight profile means that applying the –0.0061 QoL impact per BMI point, canagliflozin is estimated to provide more benefits than both gliclazide and repaglinide, except for the scenario of all weight changes rebounding after 1 year. The cost-effectiveness of canagliflozin compared with repaglinide is £44,994 per QALY if weight changes are maintained indefinitely. But for the other scenarios the cost-effectiveness estimates are well into six figures.
If the main comparator of the flozins is sitagliptin, this eliminates the much less costly alternatives. The net quantities relative to sitagliptin are provided in Table 56.
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Sitagliptin 100 mg | – | – | – | – | – | – | – |
| Canagliflozin 300 mg | 318 | 0.025 | 0.123 | 0.036 | 0.052 | 0.031 | 0.048 |
| Empagliflozin 25 mg | 416 | 0.023 | 0.089 | 0.028 | 0.038 | 0.026 | 0.037 |
| Dapagliflozin 10 mg | 508 | 0.013 | 0.077 | 0.017 | 0.026 | 0.017 | 0.026 |
The cost-effectiveness estimates for the flozins compared with sitagliptin is outlined in Table 57.
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 12,623 | 2590 | 8913 | 6111 | 10,256 | 6627 |
| Empagliflozin 25 mg | 18,341 | 4676 | 14,716 | 10,841 | 15,734 | 11,300 |
| Dapagliflozin 10 mg | 40,383 | 6632 | 30,710 | 19,787 | 30,487 | 19,679 |
Even without their superior weight profiles, canagliflozin and empagliflozin are estimated to have reasonable cost-effectiveness estimates compared with sitagliptin of £12,623 per QALY and £18,341 per QALY, respectively. Factoring in the weight profiles, and assuming that the –0.0061 QoL decrement applies, improves these cost-effectiveness estimates. The picture for dapagliflozin is more mixed, in part due to the estimate of its impact upon HbA1c being similar to that of sitagliptin.
The central cost-effectiveness estimates of the probabilistic modelling are much the same as the corresponding deterministic estimates. Given previous assessments in the area, the likelihood of different treatments being cost-effective are presented for only the BMI 2 and BMI 3 scenarios. The full results of the probabilistic modelling are presented in Appendix 7.
For the BMI 2 scenario, if all comparators are included the probabilities of the flozins being cost-effective are zero for willingness-to-pay values up to £50,000 per QALY. If the flozins are compared only with sitagliptin, at a willingness to pay of £20,000 per QALY canagliflozin 300 mg is estimated to have the highest likelihood of being cost-effective at 61%, followed by empagliflozin 25 mg at 24%, sitagliptin at 11% and dapagliflozin 10 mg at 4%. Increasing the willingness to pay to £30,000 per QALY revises these probabilities to 64% for canagliflozin 300 mg, 27% for empagliflozin 25 mg, 5% for sitagliptin and 4% for dapagliflozin.
For the BMI 3 scenario, if all comparators are included again up to a willingness to pay of £50,000 per QALY there is effectively no probability of the flozins being cost-effective, though canagliflozin 300 mg is estimated to have a 2% probability of being cost-effective at a willingness to pay of £50,000 per QALY. If the flozins are compared only with sitagliptin then canagliflozin 300 mg is estimated to have the highest likelihood of being cost-effective at 74%, followed by empagliflozin 25 mg at 19%, sitagliptin at 3% and dapagliflozin 10 mg at 3%. Increasing the willingness to pay to £30,000 per QALY revises these probabilities to 77% for canagliflozin 300 mg, 20% for empagliflozin 25 mg, 1% for sitagliptin and 3% for dapagliflozin.
Assessment Group sensitivity analyses results
SA01: Patients switch to insulin plus gliclazide and drop other therapies
Applying the same cost for the insulin-containing regimes across the treatment arms results in the flozins changing their ordering when ranked by increasing total cost. Canagliflozin 300 mg is now slightly more expensive than the other flozins. This is probably due to the larger HbA1c effect of canagliflozin meaning that patients, on average, switch to insulin slightly later than the other flozins (Table 58).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 26,628 | 10.392 | 9.633 | 9.633 | 9.633 | 9.771 | 9.739 |
| Repaglinide | 26,719 | 10.389 | 9.663 | 9.663 | 9.663 | 9.770 | 9.744 |
| Pioglitazone | 26,835 | 10.384 | 9.612 | 9.612 | 9.612 | 9.762 | 9.728 |
| Sitagliptin 100 mg | 28,875 | 10.355 | 9.657 | 9.655 | 9.655 | 9.739 | 9.719 |
| Empagliflozin 25 mg | 28,990 | 10.378 | 9.747 | 9.683 | 9.694 | 9.766 | 9.756 |
| Dapagliflozin 10 mg | 29,010 | 10.367 | 9.734 | 9.671 | 9.681 | 9.756 | 9.745 |
| Canagliflozin 300 mg | 29,040 | 10.380 | 9.780 | 9.691 | 9.707 | 9.770 | 9.767 |
Total costs have fallen. As would be expected they have fallen furthest for the flozins and by almost as much for sitagliptin when compared with the base case (Table 59). As only the treatment costs are changing, there is no difference in QALYs.
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | –685 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Repaglinide | –694 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Pioglitazone | –709 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Sitagliptin 100 mg | –3483 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Empagliflozin 25 mg | –3785 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Dapagliflozin 10 mg | –3856 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Canagliflozin 300 mg | –3635 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
Owing to the reordering of the treatments by total costs, empagliflozin is no longer dominated (Table 60).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Gliclazide | – | – | – | – | – | – |
| Repaglinide | Dom | 3026 | 3026 | 3026 | Dom | 16,814 |
| Pioglitazone | Dom | Dom | Dom | Dom | Dom | Dom |
| Sitagliptin 100 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Empagliflozin 25 mg | Dom | 27,230 | 112,991 | 74,209 | Dom | 201,000 |
| Dapagliflozin 10 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Canagliflozin 300 mg | Dom | 1504 | 6882 | 3722 | Dom | 4559 |
The cost-effectiveness of repaglinide compared with gliclazide improves slightly for the BMI 1–3 scenarios to £3026 per QALY and for the BMI 5 scenario to £16,814 per QALY.
The flozins remain dominated if there are no direct QoL impacts from weight changes. For the BMI scenarios 1–3 the cost-effectiveness of empagliflozin compared with repaglinide is £27,230 per QALY, £113,000 per QALY and £74,209 per QALY, respectively, whereas for the BMI scenario 5 it is £201,000 per QALY. But these cost-effectiveness estimates for empagliflozin are extendedly dominated by canagliflozin, which has cost-effectiveness estimates compared with repaglinide of £19,850 per QALY, £84,634 per QALY and £52,571 per QALY for the BMI scenarios 1–3, and £104,000 per QALY for the BMI scenario 5.
For the cost-effectiveness of the flozins compared with sitagliptin the estimates improve quite considerably because of the greater cost reductions for the flozins (Table 61).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 6567 | 1347 | 4637 | 3179 | 5335 | 3447 |
| Empagliflozin 25 mg | 5054 | 1288 | 4055 | 2987 | 4335 | 3114 |
| Dapagliflozin 10 mg | 10,739 | 1764 | 8166 | 5262 | 8107 | 5233 |
SA02: Urinary tract infection and genital tract infection rates applied to all model cycles
If the UTI and GTI rates are applied to all model cycles this has a slightly larger impact upon the flozins than the other treatments. Compared with the values of the base case the following changes occur (Table 62).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 65 | –0.007 | –0.007 | –0.007 | –0.007 | –0.007 | –0.007 |
| Repaglinide | 65 | –0.007 | –0.007 | –0.007 | –0.007 | –0.007 | –0.007 |
| Pioglitazone | 66 | –0.007 | –0.007 | –0.007 | –0.007 | –0.007 | –0.007 |
| Sitagliptin 100 mg | 68 | –0.007 | –0.007 | –0.007 | –0.007 | –0.007 | –0.007 |
| Canagliflozin 300 mg | 93 | –0.010 | –0.010 | –0.010 | –0.010 | –0.010 | –0.010 |
| Empagliflozin 25 mg | 84 | –0.009 | –0.009 | –0.009 | –0.009 | –0.009 | –0.009 |
| Dapagliflozin 10 mg | 86 | –0.009 | –0.009 | –0.009 | –0.009 | –0.009 | –0.009 |
The pattern of dominated strategies is as for the base case. Given the similarity of changes for both gliclazide and repaglinide the cost-effectiveness estimates for repaglinide compared with gliclazide are little different from those of the base case.
Owing to the flozins being slightly worse affected by this, the cost-effectiveness estimates for canagliflozin compared with repaglinide for BMI scenarios 1–3 and 5 worsen slightly to £46,721 per QALY, £223,000 per QALY, £131,000 per QALY and £283,000 per QALY, respectively. There is also some worsening in the cost-effectiveness estimates for the flozins compared with sitagliptin (Table 63).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 15,805 | 2875 | 10,656 | 7065 | 12,465 | 7709 |
| Empagliflozin 25 mg | 21,167 | 4987 | 16,622 | 11,973 | 17,878 | 12,513 |
| Dapagliflozin 10 mg | 52,010 | 7093 | 37,364 | 22,660 | 37,046 | 22,523 |
SA03: A common baseline HbA1c of 7.5%
The common baseline HbA1c of 7.5% does not change the ordering of treatments by their total costs, with the aggregate outcomes being as shown in Table 64.
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 26,593 | 10.432 | 9.687 | 9.687 | 9.687 | 9.810 | 9.776 |
| Repaglinide | 26,710 | 10.429 | 9.717 | 9.717 | 9.717 | 9.810 | 9.784 |
| Pioglitazone | 26,814 | 10.425 | 9.665 | 9.665 | 9.665 | 9.802 | 9.763 |
| Sitagliptin 100 mg | 31,501 | 10.404 | 9.716 | 9.714 | 9.714 | 9.787 | 9.767 |
| Canagliflozin 300 mg | 31,925 | 10.421 | 9.831 | 9.742 | 9.766 | 9.810 | 9.815 |
| Empagliflozin 25 mg | 32,003 | 10.420 | 9.800 | 9.737 | 9.752 | 9.808 | 9.803 |
| Dapagliflozin 10 mg | 32,044 | 10.414 | 9.789 | 9.728 | 9.742 | 9.801 | 9.794 |
Total costs have fallen and the total QALYs have increased compared with the base case as outlined in Table 65.
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | –721 | 0.040 | 0.054 | 0.054 | 0.054 | 0.039 | 0.037 |
| Repaglinide | –703 | 0.041 | 0.054 | 0.054 | 0.054 | 0.040 | 0.040 |
| Pioglitazone | –730 | 0.041 | 0.053 | 0.053 | 0.053 | 0.040 | 0.035 |
| Sitagliptin 100 mg | –858 | 0.049 | 0.059 | 0.059 | 0.059 | 0.048 | 0.048 |
| Canagliflozin 300 mg | –751 | 0.041 | 0.050 | 0.052 | 0.059 | 0.040 | 0.048 |
| Empagliflozin 25 mg | –772 | 0.043 | 0.053 | 0.054 | 0.058 | 0.042 | 0.047 |
| Dapagliflozin 10 | –822 | 0.046 | 0.055 | 0.057 | 0.061 | 0.045 | 0.049 |
Although the effects are reasonably similar across all the treatments, they appear to be larger for sitagliptin and in some instances for the flozins too. Whereas the differences in total QALYs are sometimes slight for sitagliptin compared with the cheaper alternatives, there is always a cheaper alternative that offers slightly more QALYs. The cost differences remain large and as a consequence sitagliptin remains dominated.
For BMI scenarios 1–3 the cost-effectiveness of repaglinide compared with gliclazide rises slightly to £3911 per QALY. For BMI scenarios 1–3 and 5 the cost-effectiveness of canagliflozin worsen slightly to £45,968, £207,000, £107,000 and £173,000, respectively.
For the cost-effectiveness of the flozins compared with sitagliptin the estimates worsen as a result of the relative improvement of sitagliptin (Table 66).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 24,939 | 3717 | 14,961 | 8237 | 18,309 | 8880 |
| Empagliflozin 25 mg | 30,150 | 6042 | 21,643 | 13,310 | 24,300 | 13,972 |
| Dapagliflozin 10 mg | 54,863 | 7442 | 38,256 | 19,902 | 38,725 | 20,011 |
SA04: Initial glycated haemoglobin treatment effect a function of baseline glycated haemoglobin
If the monotherapies’ treatment effects upon HbA1c are made a function of patients’ baseline HbA1c, as derived from the NICE CG modelling, which implies a larger effect for those with a higher baseline value, the following applies (Table 67).
| Treatment | Costs (£) | QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 27,410 | 10.393 | 9.629 | 9.629 | 9.629 | 9.771 | 9.738 |
| Repaglinide | 27,518 | 10.389 | 9.658 | 9.658 | 9.658 | 9.770 | 9.741 |
| Pioglitazone | 27,650 | 10.384 | 9.608 | 9.608 | 9.608 | 9.762 | 9.729 |
| Sitagliptin 100 mg | 32,588 | 10.358 | 9.654 | 9.651 | 9.652 | 9.742 | 9.718 |
| Canagliflozin 300 mg | 32,782 | 10.381 | 9.777 | 9.687 | 9.700 | 9.771 | 9.760 |
| Empagliflozin 25 mg | 32,953 | 10.380 | 9.744 | 9.680 | 9.687 | 9.768 | 9.751 |
| Dapagliflozin 10 mg | 33,100 | 10.371 | 9.732 | 9.669 | 9.674 | 9.759 | 9.740 |
And the following changes from the baseline values (Table 68):
| Treatment | Costs (£) | QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 97 | 0.001 | –0.004 | –0.004 | –0.004 | 0.001 | –0.001 |
| Repaglinide | 105 | 0.000 | –0.005 | –0.005 | –0.005 | 0.000 | –0.003 |
| Pioglitazone | 106 | 0.000 | –0.004 | –0.004 | –0.004 | 0.000 | 0.001 |
| Sitagliptin 100 mg | 230 | 0.003 | –0.003 | –0.004 | –0.004 | 0.002 | –0.001 |
| Canagliflozin 300 mg | 106 | 0.001 | –0.003 | –0.003 | –0.008 | 0.001 | –0.006 |
| Empagliflozin 25 mg | 179 | 0.003 | –0.003 | –0.003 | –0.007 | 0.002 | –0.005 |
| Dapagliflozin 10 mg | 234 | 0.004 | –0.002 | –0.003 | –0.007 | 0.003 | –0.004 |
This does not change the treatments that are modelled as being dominated. The cost-effectiveness estimates for repaglinide compared with gliclazide are little changed at £3747 per QALY for the BMI scenarios 1–3 but the cost-effectiveness estimate for the BMI scenario 5 worsens to £34,225 per QALY due to the similarity in effectiveness between the two treatments.
For the BMI scenarios 1–3 and 5 the cost-effectiveness estimates for canagliflozin compared with repaglinide are broadly similar to those of the base case at £44,115 per QALY, £179,000 per QALY, £127,000 per QALY, and £272,000 per QALY, respectively.
The cost-effectiveness estimates for the flozins compared with sitagliptin are typically slightly better than those of the base case (Table 69).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 8314 | 1570 | 5367 | 4037 | 6636 | 4570 |
| Empagliflozin 25 mg | 16,222 | 4063 | 12,671 | 10,411 | 13,894 | 11,064 |
| Dapagliflozin 10 mg | 37,733 | 6582 | 29,767 | 23,093 | 29,242 | 22,808 |
SA05: No discontinuation rates
Not applying the treatment discontinuation rates results in the following (Tables 70 and 71).
| Treatment | Costs (£) | QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 27,320 | 10.393 | 9.634 | 9.634 | 9.634 | 9.771 | 9.739 |
| Repaglinide | 27,421 | 10.389 | 9.665 | 9.665 | 9.665 | 9.770 | 9.745 |
| Pioglitazone | 27,571 | 10.383 | 9.610 | 9.610 | 9.610 | 9.761 | 9.727 |
| Sitagliptin 100 mg | 32,456 | 10.354 | 9.658 | 9.655 | 9.656 | 9.739 | 9.718 |
| Canagliflozin 300 mg | 32,735 | 10.379 | 9.781 | 9.690 | 9.707 | 9.769 | 9.766 |
| Empagliflozin 25 mg | 32,826 | 10.377 | 9.747 | 9.683 | 9.694 | 9.765 | 9.755 |
| Dapagliflozin 10 mg | 32,944 | 10.367 | 9.735 | 9.671 | 9.681 | 9.755 | 9.744 |
| Treatment | Costs (£) | QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 6 | 0.000 | 0.001 | 0.001 | 0.001 | 0.000 | 0.000 |
| Repaglinide | 7 | 0.000 | 0.002 | 0.002 | 0.002 | 0.000 | 0.001 |
| Pioglitazone | 28 | –0.001 | –0.002 | –0.002 | –0.002 | –0.001 | –0.001 |
| Sitagliptin 100 mg | 98 | –0.001 | 0.000 | 0.000 | 0.000 | –0.001 | 0.000 |
| Canagliflozin 300 mg | 59 | –0.001 | 0.001 | 0.000 | 0.000 | –0.001 | 0.000 |
| Empagliflozin 25 mg | 52 | 0.000 | 0.001 | 0.000 | 0.000 | 0.000 | 0.000 |
| Dapagliflozin 10 mg | 78 | –0.001 | 0.001 | 0.000 | 0.000 | –0.001 | 0.000 |
Repaglinide increases in cost slightly, but the small increases in the total QALYs are proportionally slightly greater and there is a minor improvement in the cost-effectiveness estimates for repaglinide compared with gliclazide compared with those of the base case for the BMI scenarios 1–3 and 5.
The costs for sitagliptin and the flozins increase slightly with minimal impact upon the total QALYs associated with them. Compared with the cost-effectiveness estimate of the base case, the cost-effectiveness estimates for canagliflozin compared with repaglinide for the BMI scenarios 1–3 and 5 worsen slightly, but the effect is small.
SA06: National Institute for Health and Care clinical guideline baseline TC/HDL values and UKPDS68 progression
If the NICE CG baseline TC/HDL values are applied and the TC/HDL ratio is evolved as per the UKPDS68193 equation 13 the patient outcomes worsen and costs rise, as shown in Tables 72 and 73.
| Treatment | Costs (£) | QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 27,783 | 10.006 | 9.273 | 9.273 | 9.273 | 9.404 | 9.373 |
| Repaglinide | 27,884 | 10.003 | 9.302 | 9.302 | 9.302 | 9.404 | 9.379 |
| Pioglitazone | 27,996 | 9.997 | 9.251 | 9.251 | 9.251 | 9.394 | 9.361 |
| Sitagliptin 100 mg | 32,676 | 9.963 | 9.289 | 9.287 | 9.287 | 9.367 | 9.348 |
| Canagliflozin 300 mg | 32,968 | 9.990 | 9.411 | 9.325 | 9.341 | 9.400 | 9.398 |
| Empagliflozin 25 mg | 33,057 | 9.989 | 9.379 | 9.318 | 9.329 | 9.397 | 9.387 |
| Dapagliflozin 10 mg | 33,154 | 9.977 | 9.366 | 9.305 | 9.315 | 9.385 | 9.375 |
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 469 | –0.386 | –0.361 | –0.361 | –0.361 | –0.367 | –0.366 |
| Repaglinide | 470 | –0.386 | –0.361 | –0.361 | –0.361 | –0.366 | –0.365 |
| Pioglitazone | 452 | –0.388 | –0.362 | –0.362 | –0.362 | –0.368 | –0.367 |
| Sitagliptin 100 mg | 318 | –0.392 | –0.368 | –0.368 | –0.368 | –0.372 | –0.371 |
| Canagliflozin 300 mg | 292 | –0.390 | –0.369 | –0.366 | –0.366 | –0.370 | –0.369 |
| Empagliflozin 25 mg | 283 | –0.389 | –0.367 | –0.365 | –0.365 | –0.369 | –0.368 |
| Dapagliflozin 10 mg | 288 | –0.390 | –0.369 | –0.366 | –0.366 | –0.370 | –0.370 |
The cost-effectiveness estimates for repaglinide compared with gliclazide are little different from those of the base case.
The cost-effectiveness estimates for canagliflozin compared with repaglinide for the BMI scenarios 1–3 and 5, of £46,562 per QALY, £129,000 per QALY, £223,000 per QALY and £272,000 per QALY respectively, are broadly similar to those of the base case.
The cost-effectiveness estimates of the flozins compared with sitagliptin show some improvements compared with the base-case estimates (Table 74).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 10,601 | 2403 | 7748 | 5420 | 8807 | 5845 |
| Empagliflozin 25 mg | 14,657 | 4237 | 12,152 | 9208 | 12,873 | 9552 |
| Dapagliflozin 10 mg | 33,394 | 6284 | 26,373 | 17,585 | 26,173 | 17,486 |
SA07: Applying the UKPDS68 year 2 parameter for the evolution of glycated haemoglobin
Applying the UKPDS68193 year 2 parameter of equation 11 for the evolution of HbA1c has little impact upon results compared with the base case in absolute terms (Table 75).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | –7 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 |
| Repaglinide | 3 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 |
| Pioglitazone | –4 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Sitagliptin 100 mg | –5 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 |
| Canagliflozin 300 mg | –16 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Empagliflozin 25 mg | –12 | 0.000 | 0.000 | 0.000 | 0.001 | 0.000 | 0.000 |
| Dapagliflozin 10 mg | –8 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 |
The cost-effectiveness estimates for the treatments that are not dominated are little different from those of the base case. The cost-effectiveness estimates compared with sitagliptin are similar to those of the base case (Table 76).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 12,919 | 2527 | 8936 | 6036 | 10,356 | 6563 |
| Empagliflozin 25 mg | 18,616 | 4635 | 14,818 | 10,825 | 15,879 | 11,294 |
| Dapagliflozin 10 mg | 41,268 | 6630 | 31,255 | 19,911 | 31,026 | 19,801 |
SA08: Intensifying by adding gliclazide has a –0.47% glycated haemoglobin reduction
If the intensification of adding gliclazide to a monotherapy results in only a –0.47% reduction in HbA1c, then this has very little impact upon those who had gliclazide and repaglinide monotherapy, as a result of this affecting only the small percentage who discontinue because of adverse events. But the impact upon the other treatments is quite marked. For these, the change affects the vast majority of patients. They have an overall smaller clinical effect applied, which is, in itself, harmful, and will also tend to progress through to insulin more quickly than the base case (Table 77).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 27,320 | 10.393 | 9.634 | 9.634 | 9.634 | 9.771 | 9.739 |
| Repaglinide | 27,421 | 10.389 | 9.665 | 9.665 | 9.665 | 9.770 | 9.745 |
| Pioglitazone | 27,571 | 10.383 | 9.610 | 9.610 | 9.610 | 9.761 | 9.727 |
| Sitagliptin 100 mg | 32,456 | 10.354 | 9.658 | 9.655 | 9.656 | 9.739 | 9.718 |
| Canagliflozin 300 mg | 32,735 | 10.379 | 9.781 | 9.690 | 9.707 | 9.769 | 9.766 |
| Empagliflozin 25 mg | 32,826 | 10.377 | 9.747 | 9.683 | 9.694 | 9.765 | 9.755 |
| Dapagliflozin 10 mg | 32,944 | 10.367 | 9.735 | 9.671 | 9.681 | 9.755 | 9.744 |
This results in the following differences in costs and QALYs compared with the base case (Table 78).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 5 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Repaglinide | 13 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Pioglitazone | 273 | –0.016 | –0.020 | –0.020 | –0.020 | –0.016 | –0.016 |
| Sitagliptin 100 mg | 299 | –0.019 | –0.023 | –0.023 | –0.023 | –0.018 | –0.018 |
| Canagliflozin 300 mg | 266 | –0.018 | –0.023 | –0.023 | –0.023 | –0.018 | –0.018 |
| Empagliflozin 25 mg | 281 | –0.018 | –0.022 | –0.022 | –0.022 | –0.018 | –0.017 |
| Dapagliflozin 10 mg | 286 | –0.020 | –0.024 | –0.024 | –0.024 | –0.020 | –0.019 |
And the following cost-effectiveness estimates (Table 79).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Gliclazide | – | – | – | – | – | – |
| Repaglinide | Dom | 3604 | 3604 | 3604 | Dom | 19,784 |
| Pioglitazone | Dom | Dom | Dom | Dom | Dom | Dom |
| Sitagliptin 100 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Canagliflozin 300 mg | Dom | 58,292 | 1.1M | £254,000 | Dom | £1.1M |
| Empagliflozin 25 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Dapagliflozin 10 mg | Dom | Dom | Dom | Dom | Dom | Dom |
If second-line gliclazide is less effective, and crucially is less effective than the second-line pioglitazone in the gliclazide and repaglinide arms, this considerably worsens the cost-effectiveness estimates for the flozins compared with gliclazide and repaglinide. It also worsens their cost-effectiveness estimates compared with pioglitazone.
For the comparisons with sitagliptin the cost-effectiveness estimates for the flozins are provided in Table 80.
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 11,125 | 2311 | 7903 | 5435 | 9065 | 5909 |
| Empagliflozin 25 mg | 17,003 | 4442 | 13,784 | 10,214 | 14,676 | 10,638 |
| Dapagliflozin 10 | 43,173 | 6551 | 32,025 | 20,133 | 31,759 | 19,999 |
The flozins continue to show reasonable cost-effectiveness estimates compared with sitagliptin, though, again, the picture is more mixed for dapagliflozin.
SA09: Applying the Janssen linear evolutions of glycated haemoglobin
Applying the Janssen linear evolutions for treatments causes pioglitazone to become the cheapest as shown in Table 81.
| Treatment | Costs (£) | QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Pioglitazone | 25,818 | 10.486 | 9.740 | 9.740 | 9.740 | 9.861 | 9.811 |
| Gliclazide | 25,986 | 10.476 | 9.734 | 9.734 | 9.734 | 9.852 | 9.807 |
| Repaglinide | 26,139 | 10.470 | 9.761 | 9.761 | 9.761 | 9.849 | 9.812 |
| Sitagliptin 100 mg | 31,303 | 10.426 | 9.741 | 9.738 | 9.739 | 9.808 | 9.782 |
| Canagliflozin 300 mg | 31,385 | 10.465 | 9.882 | 9.793 | 9.821 | 9.853 | 9.857 |
| Empagliflozin 25 mg | 31,643 | 10.453 | 9.836 | 9.773 | 9.790 | 9.840 | 9.831 |
| Dapagliflozin 10 mg | 31,836 | 10.438 | 9.817 | 9.754 | 9.769 | 9.825 | 9.813 |
Compared with the base case, costs have fallen considerably for all treatments, and total QALYs have risen (Table 82).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Pioglitazone | –1725 | 0.101 | 0.128 | 0.128 | 0.128 | 0.099 | 0.082 |
| Gliclazide | –1328 | 0.084 | 0.101 | 0.101 | 0.101 | 0.082 | 0.069 |
| Repaglinide | –1275 | 0.081 | 0.098 | 0.098 | 0.098 | 0.079 | 0.067 |
| Sitagliptin 100 mg | –1055 | 0.071 | 0.083 | 0.083 | 0.083 | 0.069 | 0.063 |
| Canagliflozin 300 mg | –1291 | 0.085 | 0.102 | 0.102 | 0.114 | 0.083 | 0.091 |
| Empagliflozin 25 mg | –1131 | 0.076 | 0.090 | 0.090 | 0.096 | 0.074 | 0.075 |
| Dapagliflozin 10 mg | –1030 | 0.071 | 0.083 | 0.083 | 0.088 | 0.069 | 0.068 |
Gliclazide is now dominated by pioglitazone, though the pattern of dominance of the base case has not otherwise changed.
The cost-effectiveness estimates for repaglinide compared with pioglitazone are somewhat worse than the corollaries for repaglinide compared with gliclazide of the base case. The cost-effectiveness estimates for canagliflozin compared with repaglinide are surprisingly similar, though the estimates for BMI scenario 5, and to a lesser extent scenario 3, have improved (Table 83).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Pioglitazone | – | – | – | – | – | – |
| Gliclazide | Dom | Dom | Dom | Dom | Dom | Dom |
| Repaglinide | Dom | 15,633 | 15,633 | 15,633 | Dom | 343,000 |
| Sitagliptin 100 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Canagliflozin 300 mg | Dom | 43,246 | 163,000 | 86,862 | Dom | 115,000 |
| Empagliflozin 25 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Dapagliflozin 10 | Dom | Dom | Dom | Dom | Dom | Dom |
Despite the quite radical change in the evolution of HbA1c, the cost-effectiveness estimates for the flozins compared with sitagliptin are not radically different from those of the base case, but have improved somewhat for canagliflozin and empagliflozin (Table 84). The picture for dapagliflozin remains mixed.
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 11,125 | 2311 | 7903 | 5435 | 9065 | 5909 |
| Empagliflozin 25 mg | 17,003 | 4442 | 13,784 | 10,214 | 14,676 | 10,638 |
| Dapagliflozin 10 mg | 43,173 | 6551 | 32,025 | 20,133 | 31,759 | 19,999 |
SA10: Those discontinuing a treatment omit the intensification step that applies this treatment
This sensitivity analysis has little impact upon results and does not affect the ordering of treatments by their total costs. The pattern of dominated treatments is also not affected.
The cost-effectiveness of repaglinide compared with gliclazide is estimated to improve for the BMI scenarios 1–3 to £2744 per QALY, and for BMI scenario 5 to £14,190 per QALY.
The cost-effectiveness estimates of canagliflozin compared with repaglinide are little affected, being £45,679 per QALY, £206,000 per QALY, £124,000 per QALY and £257 per QALY for the BMI scenarios 1–3 and 5, respectively.
The cost-effectiveness estimates for the flozins compared with sitagliptin are essentially those of the base case.
SA11: SA01 and SA08 combined
If intensifying from monotherapy, by adding gliclazide only, results in a –0.47% reduction in patients HbA1c, and, when switching to insulin, patients receive only insulin and gliclazide, the combined effects of this are as shown in Table 85. As for SA01, canagliflozin is now estimated to be the most expensive treatment (see Table 85).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 26,631 | 10.392 | 9.633 | 9.633 | 9.633 | 9.770 | 9.739 |
| Repaglinide | 26,730 | 10.389 | 9.663 | 9.663 | 9.663 | 9.770 | 9.744 |
| Pioglitazone | 27,054 | 10.368 | 9.592 | 9.592 | 9.592 | 9.746 | 9.713 |
| Sitagliptin 100 mg | 28,922 | 10.336 | 9.634 | 9.632 | 9.632 | 9.721 | 9.701 |
| Empagliflozin 25 mg | 28,988 | 10.359 | 9.724 | 9.661 | 9.671 | 9.748 | 9.738 |
| Dapagliflozin 10 mg | 29,018 | 10.347 | 9.710 | 9.647 | 9.657 | 9.736 | 9.726 |
| Canagliflozin 300 mg | 29,022 | 10.361 | 9.758 | 9.668 | 9.685 | 9.752 | 9.749 |
The pattern of changes in cost is much as per SA01, whereas the pattern of changes in QALYs is as per SA08 (Table 86).
| Treatment | Net costs (£) | Net QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | –682 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Repaglinide | –684 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Pioglitazone | –489 | –0.016 | –0.020 | –0.020 | –0.020 | –0.016 | –0.016 |
| Sitagliptin 100 mg | –3437 | –0.019 | –0.023 | –0.023 | –0.023 | –0.018 | –0.018 |
| Empagliflozin 25 mg | –3787 | –0.018 | –0.022 | –0.022 | –0.022 | –0.018 | –0.017 |
| Dapagliflozin 10 mg | –3848 | –0.020 | –0.024 | –0.024 | –0.024 | –0.020 | –0.019 |
| Canagliflozin 300 mg | –3654 | –0.018 | –0.023 | –0.023 | –0.023 | –0.018 | –0.018 |
Owing to the reordering of the treatments by total costs, empagliflozin is no longer dominated.
Note that the erratic pattern for canagliflozin as the BMI scenarios are worked across is due to it being compared with empagliflozin for the BMI scenarios 1, 3 and 5, but to repaglinide for the BMI scenarios 2 and 4 (Table 87).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Gliclazide | – | – | – | – | – | – |
| Repaglinide | Dom | 3278 | 3278 | 3278 | Dom | 17,994 |
| Pioglitazone | Dom | Dom | Dom | Dom | Dom | Dom |
| Sitagliptin 100 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Empagliflozin 25 mg | Dom | 36,837 | Dom | 268,000 | Dom | Dom |
| Dapagliflozin 10 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Canagliflozin 300 mg | Dom | 1030 | 460,000 | 2581 | Dom | 470,000 |
The flozins remain dominated if there are no direct QoL impacts from weight changes. For the BMI scenarios 1 and 3 the cost-effectiveness of empagliflozin compared with repaglinide is £36,837 per QALY and £268,000 per QALY, respectively. But these cost-effectiveness estimates for empagliflozin are extendedly dominated by canagliflozin, which has cost-effectiveness estimates compared with repaglinide of £24,226 per QALY and £105,000 per QALY, respectively, for the BMI scenarios 1 and 3.
For the cost-effectiveness of the flozins compared with sitagliptin the estimates improve quite considerably because of the greater cost reductions for the flozins and sitagliptin seeing similar falls in total QALYs as the flozins (Table 88).
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 3927 | 816 | 2789 | 1918 | 3199 | 2085 |
| Empagliflozin 25 mg | 2818 | 736 | 2285 | 1693 | 2432 | 1763 |
| Dapagliflozin 10 mg | 8399 | 1274 | 6230 | 3917 | 6178 | 3891 |
Canagliflozin 300 mg systolic blood pressure effect
The AG cost-effectiveness modelling provided to NICE relied upon the results of the AG NMA, which had an incorrect figure of 0.5 mmHg for canagliflozin, whereas the correct figure was 5 mmHg. Correcting this, a revised estimate for the SBP effect of canagliflozin 300 mg improves its net cost and QALY estimates as shown in Table 89 for the pairwise comparisons with gliclazide, pioglitazone and sitagliptin.
| Comparison | Net cost (£) | No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 |
|---|---|---|---|---|---|---|---|
| vs. Gliclazide | 5224 | 0.005 | 0.163 | 0.074 | 0.090 | 0.016 | 0.044 |
| vs. Pioglitazone | 4991 | 0.013 | 0.185 | 0.095 | 0.112 | 0.025 | 0.055 |
| vs. Sitagliptin | 187 | 0.042 | 0.139 | 0.052 | 0.068 | 0.048 | 0.064 |
These changes, in turn, yield the following cost-effectiveness estimates in Table 90.
| Comparison | No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 |
|---|---|---|---|---|---|---|
| vs. Gliclazide | 1.1M | 32,015 | 71,038 | 57,865 | 330,000 | 118,000 |
| vs. Pioglitazone | 385,000 | 27,003 | 52,432 | 44,590 | 201,000 | 90,653 |
| vs. Sitagliptin | 4401 | 1341 | 3586 | 2729 | 3929 | 2896 |
Summary of the Assessment Group modelling
The AG modelling base case estimates that the lifetime QALYs arising from diabetes, its complications and adverse events are highest for gliclazide at 10.392 QALYs, with repaglinide having a similar estimate of 10.389 QALYs. Pioglitazone accrues slightly fewer at 10.384 QALYs. The flozins lie a little below this, with canagliflozin being estimated to yield 10.380 QALYs, empagliflozin 10.378 QALYs and dapagliflozin 10.367 QALYS. Sitagliptin fares worse at 10.355 QALYs. Gliclazide is estimated to be superior to the flozins by 0.012 QALYs compared with canagliflozin, 0.015 QALYs compared with empagliflozin, and 0.025 QALYs compared with dapagliflozin. Adverse events contribute relatively little to these estimates, and even less to the estimates of the differences between treatments. To place these amounts in context, at the baseline QoL of 0.801 they would be equivalent to survival gains of around 6 days compared with canagliflozin, 7 days compared with empagliflozin and 11 days compared with dapagliflozin.
But these amounts ignore the direct QoL effects of weight changes. The flozins have a superior weight profile, with canagliflozin providing the largest weight losses. If the monotherapy weight changes are retained over the patient lifetime then canagliflozin is estimated to yield an additional 0.147 QALYs compared with gliclazide: equivalent to 67 days’ additional survival at the baseline QoL of 0.801. These gains are reduced if it is assumed that weight losses rebound after 1 year to only 0.057 QALYs, and rebound at treatment change to 0.074 QALYs.
The flozins and, to a slightly lesser extent sitagliptin, are estimated to be considerably more expensive than gliclazide, repaglinide and pioglitazone, with the increases in lifetime costs ranging between £5000 and £5500.
In light of the above, if there are no direct QoL effects from weight changes, the flozins are estimated to be dominated. But if there are direct QoL impacts from weight changes, and the monotherapy weight changes persist throughout the patient lifetime, the flozins are no longer dominated. Repaglinide remains more expensive than gliclazide, but now yields slightly more QALYs and has a cost-effectiveness estimate compared with gliclazide of £3331 per QALY. Canagliflozin has a cost-effectiveness estimate of £44,994 per QALY compared with repaglinide. Although canagliflozin formally dominates the other flozins, the cost-effectiveness estimates for empagliflozin and for dapagliflozin compared with gliclazide are £48,169 per QALY and £55,000 per QALY, respectively.
It may be unrealistic to expect the monotherapies’ weight changes, and the differences they imply between treatments, to persist indefinitely. If weight losses rebound after 1 year the cost-effectiveness of canagliflozin compared with repaglinide worsens considerably to £192,000 per QALY; if they persist until treatment intensification then the cost-effectiveness estimate for canagliflozin compared with repaglinide worsens to £119,000 per QALY.
The companies argue that the main comparator for the flozins is sitagliptin. The flozins are estimated to provide slightly greater total QALYs from the modelling of diabetes, its complications and the adverse events associated with treatments. The flozins are also associated with somewhat larger weight losses than sitagliptin, which is broadly weight neutral. Total costs are higher than sitagliptin by £318 for canagliflozin, £416 for empagliflozin and £508 for dapagliflozin. Even without the direct QoL effects of weight changes, canagliflozin has a reasonable cost-effectiveness compared with sitagliptin of £12,623 per QALY, as does empagliflozin at £18,341 per QALY. Dapagliflozin fares worse with a cost-effectiveness estimate of £40,383 per QALY.
With the direct QoL effects of weight changes and weight changes being assumed to persist over the patient lifetime the cost-effectiveness of the flozins compared with sitagliptin improves considerably. Canagliflozin has an estimate of £2590 per QALY, empagliflozin has an estimate of £4676 per QALY and dapagliflozin has an estimate of £6632 per QALY. If weight changes are assumed to rebound either after 1 year or at treatment change, the cost-effectiveness estimates for the flozins generally remain within conventional thresholds. The exception to this is dapagliflozin, for which if weight rebounds after 1 year the cost-effectiveness estimates go slightly above the £30,000 threshold.
A key difference between the AG modelling and that of the companies is that the AG has assumed that patients remain on their monotherapy and add treatments to it. When patients intensify to insulin, they do so by adding it to their existing regime, for example they intensify from canagliflozin plus gliclazide to canagliflozin plus gliclazide plus insulin. Retaining the original monotherapy increases the total costs, and, in particular, increases the total cost for the flozins and, to a slightly lesser extent, sitagliptin. If it is assumed that the monotherapies are discontinued when the patients intensify to insulin then the net costs fall to be within the range of £2362–2412 for the flozins and to £2247 for sitagliptin.
The flozins remain dominated if the direct QoL impact of weight changes are not included, but applying them, and assuming that weight changes persist indefinitely, improves the cost-effectiveness estimates for the flozins compared with repaglinide to £19,850 per QALY for canagliflozin, £27,230 per QALY for empagliflozin and £32,288 per QALY for dapagliflozin. Weight losses rebounding after 1 year cause these estimates to worsen to £84,634 per QALY, £112,000 per QALY and £274,000 per QALY, respectively, whereas weight losses rebounding at change of treatment cause these estimates to worsen to £52,571 per QALY, £74,209 per QALY and £128k per QALY, respectively.
This sensitivity analysis also sees the flozins being estimated to be cost-effective relative to sitagliptin under all of the weight-change scenarios including that of no direct QoL impact from weight changes.
The base case applied the baseline HbA1c values for those starting a monotherapy of the NICE CG, which had a mean of 8.4% (SD 1.8%). This differs from some of the companies’ modelling, which assumed a common baseline HbA1c of 7.5%. As would be expected, this both improved patient outcomes and lowered total costs. It did not alter the patterns of dominance, and, although the cost-effectiveness estimates for the flozins compared with repaglinide worsened, the effect was not major.
Of more interest was that the cost-effectiveness estimates of the flozins compared with sitagliptin worsened. With no direct QoL impacts from weight these worsened to £24,939 per QALY for canagliflozin, £30,150 per QALY for empagliflozin and £54,863 per QALY for dapagliflozin. With the monotherapy BMI effects persisting for the patient lifetime, these cost-effectiveness estimates improve to £3717 per QALY, £6042 per QALY and £7442 per QALY, respectively. Weight loss rebound after 1 year reduces the improvements to £14,961 per QALY, £21,643 per QALY and £38,256 per QALY, whereas weight loss rebound at treatment change reduces the improvements to £8237 per QALY, £13,310 per QALY, and £19,902 per QALY, respectively.
Making the HbA1c treatment effect a function of patients’ baseline HbA1c had little practical impact upon the cost-effectiveness estimates for the flozins compared with gliclazide, repaglinide and pioglitazone. But it improved the cost-effectiveness estimates for canagliflozin compared with sitagliptin by around one-third. The impact for empagliflozin is less, and there was little impact for dapagliflozin. This is as would be expected, given the greater HbA1c effect for canagliflozin compared with sitagliptin, the slightly greater effect for empagliflozin, and broad equivalence between dapagliflozin and sitagliptin.
Janssen applied linear evolutions of HbA1c with the annual rate of change being treatment specific. Applying the same annual rates of change within the AG modelling reduced total costs and increased total QALYs quite considerably. It also caused pioglitazone to be estimated as the cheapest treatment, with it dominating gliclazide. Pioglitazone also dominated repaglinide if there were no direct QoL impacts from weight changes. Including these with no rebound for weight gains caused the cost-effectiveness of repaglinide compared with pioglitazone to improve to £15,633 per QALY. The pattern of dominance was not otherwise altered.
The linear HbA1c evolutions still saw the flozins dominated unless there were direct QoL impacts from weight changes. Given these, the cost-effectiveness estimates for canagliflozin compared with repaglinide were surprisingly similar to those of the base case, though the higher cost-effectiveness estimates varied more because of the divisions by small net QALY gains.
Assuming that adding gliclazide at the first intensification causes only a –0.47% reduction in HbA1c compared with the –1.01% reduction of the base case has little to no impact for gliclazide and repaglinide, as patients will not use this intensification. But it increases costs and reduces QALYs in the other arms, so worsening the cost-effectiveness estimates for the flozins. The cost-effectiveness estimates for the flozins compared with sitagliptin are not particularly affected, though those for dapagliflozin do worsen slightly.
Assuming that the UTI and GTI rates apply throughout the modelling, rather than just for the first cycle, has little practical impact upon results.
Summary: a comparison of the modelling exercises’ assumptions and inputs
National Institute for Health and Care Excellence checklist
The modelling exercises and their data sources can be assessed against the NICE reference case checklist (Table 91).
| Factor | Janssen | AstraZeneca | Boehringer Ingelheim | AG | |
|---|---|---|---|---|---|
| Comparator(s) | The individual flozins were assessed alongside sitagliptin 100 mg, pioglitazone and SU | The flozins were grouped into a class effect, as are the gliptins, with pioglitazone and SU also being considered | The main analysis compared empagliflozin 10 mg, empagliflozin 25 mg, sitagliptin 100 mg, pioglitazone, SU and repaglinide | Canagliflozin 100 mg, dapagliflozin 10 mg, empagliflozin 10 mg, empagliflozin 25 mg, sitagliptin 100 mg, pioglitazone and SU | |
| Patient group | Adult patients with type 2 diabetes, unable to take metformin starting monotherapy | ||||
| Perspective: costs | NHS and PSS | ||||
| Perspective: benefits | patient | ||||
| Analysis | Cost utility | ||||
| Time horizon | 40 years | ||||
| Clinical evidence | Own NMA | Own NMA | Own NMA | Own NMA | |
| Outcome measure | QALYs | ||||
| Health states generic QoL | Other than UTIs and GTIs | Yes, EQ-5D | Yes, EQ-5D | Yes, EQ-5D | Yes, EQ-5D |
| UTIs and GTIs | No | IWB | IWB | No | |
| Benefit valuation | Other than UTIs and GTIs | TTO | TTO | TTO | TTO |
| UTIs and GTIs | Janssen TTO | Ranking scale | Ranking scale | Janssen TTO | |
| Health-related QoL preference data | Other than UTIs and GTIs | UK tariff | UK tariff | UK tariff | UK tariff |
| UTIs and GTIs | 100 UK Public | 62 US PubMed search | 62 US PubMed search | 100 UK Public | |
| Discount rates | 3.5% for both costs and benefits | ||||
| Equity | Equal QALY regardless of patient characteristics | ||||
| Probabilistic modelling | Yes | Yes | No (model B) | Yes | |
| Sensitivity analyses | Yes | Yes | No | Yes | |
Modelling assumptions
In terms of the main assumptions and data sources, the companies and the AG have used the assumptions in Table 92. These represent a simplification. For instance, the Janssen submission has a large number of health states associated with eGFR levels, which also have ongoing costs associated with them. These are not sourced from the UKPDS84. 195 The ECHO-T2DM model used by Janssen has been submitted to the Mt Hood Challenges. But the Janssen implementation of the ECHO-T2DM and base-case assumptions is likely to have differed quite considerably from that submitted to the Mt Hood Challenges.
| Variable | Janssen | AstraZeneca | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| HbA1c | Linear | UKPDS68193 | UKPDS68193 | UKPDS68193 |
| SBP | Linear | UKPDS68193 | UKPDS68193 | UKPDS68193 |
| TC/HDL | Linear | UKPDS68193 | UKPDS68193 | UKPDS68193 |
| Weight | Linear | Linear | Linear | Linear |
| Complications modelling | Variety | UKPDS82194 | UKPDS68193 | UKPDS68193 |
| QoL main source | CODE-2 | UKPDS62198 | Alva 2014197 | UKPDS62198 |
| Costs main source | UKPDS84195 | UKPDS65196/84195 | UKPDS84195 | UKPDS84195 |
But Table 92 does help highlight the main differences between the submissions and the AG modelling. Janssen is the outlier in terms of its approach, both in terms of the modelling of its complications and its assumptions about the linearity of the evolution of HbA1c and SBP. AstraZeneca and Boehringer Ingelheim use the UKPDS68193 to model the evolution of HbA1c, SBP and the TC/HDL ratio. The AG does as well with the exception of the TC/HDL ratio which is assumed to be constant for the base case, but is evolved using the UKPDS68193 in a sensitivity analysis. Janssen argues that the evolutions of the UKPDS include the effects of treatment intensifications so cannot be used when the modelling is separately accounting for the treatment intensifications. There is some force to this argument. But it then has to be asked whether or not the alternative of linear evolutions is preferable. The treatment-specific linear evolutions of HbA1c within the Janssen submission are not obviously related to the treatments under consideration. There are also concerns with linear evolutions maintaining absolute differences indefinitely when the UKPDS clearly suggests convergence.
As already discussed, the UKPDS OM2, which is based upon the UKPDS82,194 was not available to the AG. As a consequence, in line with the modelling of Boehringer Ingelheim, the older OM1 was used to model the complications of diabetes, this being based upon the UKPDS68. 193 The AstraZeneca modelling was based upon the UKPDS68193 for the evolution of the risk factors, and the UKPDS82194 for the calculation of event probabilities, as implemented within the CDM. As far as the AG is aware, this version of the CDM has not been previously used; submitted to the Mt Hood Challenges; and independently interrogated or validated.
A concern with the Janssen and the AstraZeneca models is that there has been little presented on model convergence. The AG has relied upon the work of the draft NICE CG for diabetes, which resulted in deterministic model runs having 50,000 patients simulated with 1000 inner loops for each patient to reduce the Monte Carlo error. The draft NICE CG for diabetes could be read as suggesting that only 100 inner loops are necessary for convergence, but even this seems to be somewhat more model runs that any of the company submissions. As a consequence, the AG is uncertain whether the company models have reliably converged. Boehringer Ingelheim did present some work on convergence and concluded that results of the OM1 stabilised after 1000 inner loops for each patient had been run, choosing to run the model with 10,000 inner loops though only for 9211 patients so around 92 million model runs: approximately double the 50 million of the AG.
Monotherapies modelled and sequences compared
The companies and the AG considered the following monotherapies (Table 93).
| Janssen | AstraZeneca | Boehringer Ingelheim | AG | |
|---|---|---|---|---|
| Base analysis | Base analysis | 24-week analysis | 52-week analysis | Base analysis |
| Flozin | ||||
| Canagliflozin 100 mg | Canagliflozin 100 mg | |||
| Canagliflozin 300 mg | Canagliflozin 300 mg | Canagliflozin 300 mg | ||
| Dapagliflozin 5 mg | ||||
| Dapagliflozin 10 mg | Dapagliflozin 10 mg | Dapagliflozin 10 mg | ||
| Empagliflozin 10 mg | Empagliflozin 10 mg | Empagliflozin 10 mg | ||
| Empagliflozin 25 mg | Empagliflozin 25 mg | Empagliflozin 25 mg | Empagliflozin 25 mg | |
| Gliptin | ||||
| Sitagliptin 100 mg | Sitagliptin 100 mg | Sitagliptin 100 mg | ||
| Pioglitazone | Pioglitazone | Pioglitazone | Pioglitazone | |
| Sulfonylurea | Sulfonylurea | Sulfonylurea | Gliclazide | |
| Repaglinide | Repaglinide | |||
Note that Janssen considered repaglinide in a scenario analysis.
AstraZeneca pooled the flozins into a single-treatment group, with pooled treatment effect estimates and weighted average direct drug costs. The gliptins were similarly pooled.
The following treatment intensifications were assumed for the base cases, with treatment intensifications occurring when a patient’s HbA1c was modelled as breaching the 7.5% intensification threshold (Table 94).
| Intensification | Janssen | AstraZeneca | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| First | + Gliclazide | Switch to NPH | + SU; or + sitagliptin | –Repaglinide, + pioglitazone; and/or + gliclazide |
| Second | Switch to NPH | Intensify NPH | Switch to NPH | + NPH |
| Third | + Aspart | None | None | –Gliclazide, + bolus |
Within the Boehringer Ingelheim submission all but gliclazide had a first intensification of adding gliclazide to the existing monotherapy. Those on gliclazide monotherapy had a first intensification of adding sitagliptin.
Similarly, for the first intensification within the AG modelling all but gliclazide added gliclazide to the existing monotherapy. Those on gliclazide monotherapy had a first intensification of adding pioglitazone. The repaglinide monotherapy arm stands out, having repaglinide withdrawn and both pioglitazone and gliclazide added. For the second intensification all strategies intensify by adding NPH insulin. The third intensification adds bolus insulin and withdraws gliclazide.
The AG modelled sequences differ from those of the company submissions in that patients add NPH insulin rather than switch to it. The retention of the monotherapies in the AG triple therapy combinations with gliclazide and NPH means that the differences in costs between the monotherapies are retained throughout the AG base-case modelling. In light of this, a scenario analysis was undertaken, which withdraws the initial monotherapies when patients now, in effect, switch to NPH insulin, although this affected only the direct drug costs and not the clinical effectiveness estimates.
Patient characteristics and complications prevalences at baseline
The patient baseline characteristics are shown in Table 95.
| Variable | Janssen | AstraZeneca | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| Source | Canagliflozin trials | NMA | CPRD | THIN/Health Survey for England |
| Age, years | 56.2 | 55.0 | 63.1 | 59.8 |
| Duration diabetes, years | 4.7 | 3.6 | 2.9 | 2.0 |
| Male, % | 53 | 55 | 57 | 57 |
| BMI, kg/m2 | 29.7 | 28.9 | 31.1 | 31.9 |
| Male | – | 31.0 | – | |
| Female | – | 32.0 | – | |
| HbA1c, % | 8.02 | 7.50 | 8.49 | 8.40 |
| SBP, mmHg | 127.7 | 128.3 | 134.7 | 137.5 |
| TC, mmol/l | 5.17 | 5.07 | – | 4.96 |
| HDL, mmol/l | 1.25 | 1.20 | 1.20 | 1.18 |
| LDL, mmol/l | 3.06 | 3.32 | 4.02 | – |
| Current smoker, % | 9.0 | 36.90 | 16.7 | 18.1 |
| Past smoker, % | – | – | 36.5 | 34.0 |
Note that the baseline HbA1c of 7.5% of AstraZeneca is based upon the treatment intensification threshold rather than the AstraZeneca NMA, which had a mean of 8.2%. The AstraZeneca proportion of patients who smoke has been taken from the electronic model, where it is ambiguous whether this is the proportion at diagnosis, the proportion at baseline, or both.
The mean baseline age differs quite a lot across the companies’ and AG’s estimates, with the AG’s estimate lying somewhere in the middle. Baseline age is likely to affect results, as this determines the amount of time left for the longer-term impacts of clinical effects to be realised. Perhaps more pertinently, it will also affect the amount of time that the direct QoL impacts of weight changes apply if weight changes are modelled as being maintained into the long term.
The proportion modelled as smoking is unclear within the Janssen submission, but it seems likely to have been somewhat lower than the other exercises; within the AstraZeneca submission it is somewhat higher, though there is some ambiguity about this. The AG assumption, given the electronic copy of the CDM that was submitted, is that the 36.9% is the proportion at both diagnosis and at baseline, as only one value for smoking could be found.
The prevalences of the complications of diabetes at baseline were as shown in Table 96.
| Complication | Janssen | AstraZeneca | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| Atrial fibrillation | – | 0.00 | 6.63 | 0.81 |
| PVD | 0.00 | 0.00 | 3.18 | 0.51 |
| MI | 0.80 | 0.00 | 2.21 | 0.80 |
| CHF | 0.00 | 0.00 | 1.92 | 0.50 |
| Stroke | 0.10 | 0.00 | 1.62 | 0.50 |
| IHD | 1.20 | 0.00 | 6.13 | 2.70 |
| Amputation | 0.10 | 0.00 | 0.29 | 0.10 |
| Blindness | 0.00 | 0.00 | 0.23 | 0.40 |
| Renal failure | 0.00 | 0.00 | 0.05 | 0.20 |
Given the recentness of the diagnosis of diabetes, the companies and the AG all suggest low prevalences of complications at baseline. But AstraZeneca assumes these to be zero. As the CDM models the instances of initial events, and some secondary events, this will slightly bias the analysis of AstraZeneca towards the more effective treatment.
Again, the above does some disservice to the Janssen submission, which modelled a range of other microvascular conditions.
Clinical effectiveness estimates
The main clinical effect estimates are as shown in Tables 97–99. The Janssen NMA is for BMI rather than for weight in kilograms. To aid comparison with the other estimates, the Janssen estimates have been converted to kilograms, assuming a patient weight of 85 kg and a patient BMI of 30 kg/m2. The Janssen BMI estimates are presented within parentheses (see Table 99). No Boehringer Ingelheim figures are shown because they classed their NMA as confidential.
| Treatment | Janssen | AstraZeneca | AG |
|---|---|---|---|
| Base | Base | Base | |
| Flozins pooled | – 0.74 | ||
| Canagliflozin 100 mg | – 0.97 | ||
| Canagliflozin 300 mg | – 1.20 | – 1.153 | |
| Dapagliflozin 5 mg | |||
| Dapagliflozin 10 mg | – 0.64 | – 0.704 | |
| Empagliflozin 10 mg | – 0.73 | ||
| Empagliflozin 25 mg | – 0.85 | – 0.870 | |
| Gliptins pooled | – 0.64 | ||
| Sitagliptin 100 mg | – 0.72 | – 0.723 | |
| Pioglitazone | – 0.78 | – 0.90 | – 1.200 |
| Sulfonylurea | – 0.59 | – 0.95 | – 1.301 |
| Repaglinide | – 1.28 | – 1.200 |
| Treatment | Janssen | AstraZeneca | AG |
|---|---|---|---|
| Base | Base | Base | |
| Flozins pooled | –5.87 | ||
| Canagliflozin 100 mg | –3.71 | –4.2 | |
| Canagliflozin 300 mg | –5.41 | –5.7 | |
| Dapagliflozin 5 mg | |||
| Dapagliflozin 10 mg | –3.21 | –2.931 | |
| Empagliflozin 10 mg | –2.60 | ||
| Empagliflozin 25 mg | –3.40 | –3.743 | |
| Gliptins pooled | –1.53 | ||
| Sitagliptin 100 mg | +0.80 | +0.394 | |
| Pioglitazone | +0.88 | –1.31 | –1.400 |
| Sulfonylurea | +0.19 | –0.65 | –0.600 |
| Repaglinide | +0.19 | –1.000 |
| Treatment | Janssen | AstraZeneca | AG |
|---|---|---|---|
| Base (BMI) | Base | Base | |
| Flozins pooled | – 2.81 | ||
| Canagliflozin 100 mg | –2.40 (–0.85) | ||
| Canagliflozin 300 mg | –3.42 (–1.21) | –3.577 | |
| Dapagliflozin 5 mg | |||
| Dapagliflozin 10 mg | –1.61 (–0.57) | –2.457 | |
| Empagliflozin 10 mg | –1.72 (–0.61) | ||
| Empagliflozin 25 mg | –1.84 (–0.65) | –2.471 | |
| Gliptins pooled | –0.13 | ||
| Sitagliptin 100 mg | +0.82 (+0.29) | –0.003 | |
| Pioglitazone | +2.35 (+0.83) | +2.61 | +2.962 |
| Sulfonylurea | +0.62 (+0.22) | +0.07 | +1.397 |
| Repaglinide | +0.62 (+0.22) | +0.100* |
The estimates for the HbA1c changes are broadly in line for the flozins and sitagliptin. Among the flozins, all sources that provide individual estimates suggest that canagliflozin 300 mg provides that largest reduction, though the practical clinical differences between these estimates is a moot point. The AG estimates for pioglitazone and sulfonylurea are larger than those of the companies – to the extent that these are estimated to be more effective than canagliflozin 300 mg (see Table 97).
Table 98 shows SBP estimates.
Although not perfectly aligned, the estimates of weight changes are similar across the sources. The AG suggests slightly larger reductions in weight than the companies’ estimates for dapagliflozin 10 mg and empagliflozin 25 mg, with the AG also suggesting that sitagliptin is broadly weight neutral.
Quality-of-life values
Turning to the main QoL values, these are as follows, though again the presentation is slightly biased against the Janssen submission because of the number of health states within the ECHO-T2DM model and these not being particularly aligned with those of the other modelling (Table 100).
| Health state | Janssen | AstraZeneca | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| No complications | 0.843 | 0.882 | 0.720 | 0.801 |
| MI year | –0.028 | –0.055 | –0.065 | –0.055 |
| MI history | –0.028 | –0.055 | 0.008 | –0.055 |
| IHD | –0.028 | –0.090 | –0.028 | –0.090 |
| Stroke | –0.115 | –0.164 | –0.165 | –0.164 |
| CHF | –0.028 | –0.108 | –0.101 | –0.108 |
| Amputation | –0.272 | –0.280 | –0.172 | –0.280 |
| Blindness | –0.057 | –0.074 | 0.033 | –0.074 |
| ESRD | –0.175 | –0.263 | –0.263 | –0.263 |
| Per BMI > 25 kg/m2 | –0.0061 | –0.0061 | –0.0061 | –0.0061 |
| Severe hypoglycaemia | –0.0470 | –0.0470 | –0.0470 | –0.0470 |
| Non-severe hypoglycaemia | –0.0142 | –0.0142 | –0.0142 | –0.0142 |
| UTI (QALY) | –0.0043 | –0.0028 | –0.0028 | –0.0073 |
| GTI (QALY) | –0.0046 | –0.0028 | – | –0.0096 |
Janssen is unusual in selecting the CODE-2 data set as its main source of QoL estimates. But this is a respected publication, and, as Janssen is using the ECHO-T2DM model, the health states of their model are not so obviously aligned with the health states of the UKPDS OM1 and UKPDS OM2 for which UKPDS QoL estimates are available. AstraZeneca, Boehringer Ingelheim and the AG all use models based upon the UKPDS, and, as a consequence, QoL estimates from the UKPDS are a natural choice.
For QoL, Boehringer Ingelheim draws most of its values from the fixed-effects estimates of Alva et al. (2014),197 which is an analysis of the updated UKPDS data set with Alva et al. 197 expressing a clear preference for the fixed-effects estimates over their ordinary least squares (OLS) estimates. This explicitly analyses the data longitudinally in order to estimate the QoL pre and post and event and the impact of events upon an individual, rather than comparing patients cross-sectionally. This has obvious attractions, but there may be some difficulty when applying these estimates in that the coefficients for blindness and a history of MI are positive. Within Alva et al.,197 these coefficients and that for IHD are not statistically significant, so it could be argued that these could or should be set to zero. But if these are set to zero, it would obviously be preferable for the coefficients to have been further explored or excluded within the analysis of Alva et al.,197 in order to explore the impact that this would have upon the estimates of the other coefficients. But, given its choice of Alva et al. 197 as the source of its QoL estimates, this option was not available to Boehringer Ingelheim.
The AG is not as familiar with the Alva et al. 197 estimates as with those from the UKPDS62. 198 It seems likely that there is an age effect within the estimates of Alva et al. 197 as well, due to the mean age at completion of the first questionnaire being 62 compared with a mean age of 71 years for the seventh, coupled with negative and statistically significant coefficients for the questionnaires. Whether it is reasonable to apply the mean value of the EQ-5D in the absence of complications of 0.72 or it would be better to estimate it from the fixed-effects model is a moot point, but it can be noted that the constant for the fixed-effects model was somewhat higher at 0.807. But the values of Alva et al. 197 are reasonable to apply.
All of the analyses have used the CODE-2 QoL decrement for BMI above 25 kg/m2. AstraZeneca may not have restricted this to when the patient BMI is above 25 kg/m2, but, given baseline BMIs, the impact of this will not have been large. All of the analyses also rely upon the estimates of Currie et al. (2006)204 for the QoL impacts of hypoglycaemic events, though again it appears that AstraZeneca may have applied the coefficient for non-severe hypoglycaemia to the event rate rather than to its logarithm.
And all analyses apply fairly similar absolute QALY decrements per UTI and per GTI: they are small. Those of the AG are slightly higher, this probably being due to the assumption of 2 weeks’ duration as drawn from Nicolle et al. (2014)98 who estimated median durations of UTIs of between 11.0 days and 12.5 days.
Costs
Turning to the main costs, these are as follows, though again the presentation is slightly biased against the Janssen submission. The Janssen submission has a number of health states associated with a patient’s eGFR and the cost in the absence of complications will not have been zero. But it is difficult to identify quite what the cost in the absence of complications was. In the opinion of the AG, it is likely to have been quite small (Table 101).
| Drug | Janssen | AZ | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| Empagliflozin 10 mg | 477.30 | 476.98 | 477.98 | 476.98 |
| Empagliflozin 25 mg | 477.30 | 476.98 | 477.98 | 476.98 |
| Dapagliflozin 5 mg | – | – | 477.98 | – |
| Dapagliflozin 10 mg | 477.30 | 476.92 | 477.98 | 476.98 |
| Canagliflozin 100 mg | 477.26 | 476.93 | 477.98 | 476.93 |
| Canagliflozin 300 mg | 608.63 | 608.21 | 476.93 | |
| Flozin average | – | 481.79 | – | – |
| SU (gliclazide MR) | 25.81 | 65.70 | 68.36 | 62.18 |
| Pioglitazone | 20.48 | 19.03 | 24.25 | 20.99 |
| Repaglinide 6 mg | 71.10 | – | 93.40 | 71.91 |
| Sitagliptin 100 mg | 433.86 | 433.57 | 433.86 | 433.57 |
| Gliptin average | – | 429.13 | – | – |
It seems likely that Janssen assumed the costs for gliclazide rather than the costs for gliclazide MR. The company submissions also predated the recent change to the canagliflozin 300 mg cost.
Note that the AG adds an additional £72.26 to the cost of pioglitazone for BNP monitoring: £26.26 for the test itself and £46.00 for a dedicated GP appointment (Tables 102 and 103).
| Event | Janssen | AstraZeneca | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| No complications | 0 | 0 | 459 | 1019 |
| Complications first year | ||||
| Fatal MI | 1566 | 2605 | 1521 | 1564 |
| Fatal IHD | 3818 | 0 | 3766 | 3873 |
| Fatal stroke | 4255 | 5188 | 3954 | 4066 |
| Fatal CHF | 3366 | 0 | 3191 | NA |
| Non-fatal MI | 6665 | 7938 | 6379 | 7550 |
| Non-fatal IHD | 10,116 | 12,762 | 9767 | 10,932 |
| Non-fatal stroke | 7247 | 11,450 | 6805 | 8120 |
| Non-fatal CHF | 3337 | 5180 | 3191 | 4288 |
| Amputation | 11,810 | 13,499 | 9546 | 12,592 |
| Blindness | 2260 | 6502 | 1355 | 3234 |
| ESRD | 26,297 | 18,776 | 35,715 | 36,801 |
| Event | Janssen | AstraZeneca | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| MI | 875 | 2177 | 1154 | 1877 |
| IHD | 920 | 1395 | 1215 | 1922 |
| Stroke | 934 | 1378 | 1125 | 1934 |
| CHF | 1527 | 1656 | 1473 | 2515 |
| Amputation | 2531 | 4618 | 1792 | 3499 |
| Blindness | 215 | 2307 | 453 | 1225 |
| ESRD | 26,152 | 18,776 | 35,631 | 36,801 |
For Janssen the first-year costs of events appear to be broadly in line with those of the AG. But the costs for those with a history of events are somewhat lower. It appears that these costs may not have included the outpatient costs.
For AstraZeneca the costs of all events are somewhat higher than those of the AG. The AG cannot definitively identify the source of these discrepancies, and any error may well be on the side of the AG. But it seems possible that AstraZeneca may have indexed the UKPDS84195 costs from 2007 rather than from 2012. AstraZeneca also assumed zero costs in the absence of complications, which is not in line with the UKPDS84. 195 This will have tended to exaggerate the differences between treatments’ total costs.
Boehringer Ingelheim appear to have applied only the inpatient costs of the UKPDS84,195 and to have ignored the outpatient costs (Table 104).
| Adverse event | Janssen | AstraZeneca | Boehringer Ingelheim | AG |
|---|---|---|---|---|
| Severe hypoglycaemia | 380 | 424 | 380 | 411 |
| Non-severe hypoglycaemia | 0 | 0 | 0 | 0 |
| UTI | 82 | 46 | 36 | 73 |
| GTI | 51 | 46 | NA | 51 |
In the above presentation the Janssen costs for UTIs are a simple mean of the Janssen costs of upper UTIs and lower UTIs, but the Janssen modelling explicitly accounts for this.
Summary and conclusions: a comparison of the modelling exercises’ results
All of the company submissions apply the old £608 annual cost for canagliflozin 300 mg, rather than the recently revised list price that equalises this with the £477 annual canagliflozin 100 mg. As a consequence, the summary of cost-effectiveness results of the companies concentrates upon the canagliflozin 100 mg results.
Owing in part to the assumed slow rate of HbA1c drift for pioglitazone, Janssen estimates that it has the lowest total costs of £20,264 and yields and average 9.998 QALYs. Gliclazide is estimated to be somewhat more expensive than pioglitazone with total costs of £2956 and to yield 9.949 QALYs so is dominated by pioglitazone. Sitagliptin is also more expensive with a total cost of £23,442 and yields a total of 9.981 per QALY so is dominated by pioglitazone, though has a cost-effectiveness estimate compared with gliclazide of £6969 per QALY.
Janssen estimates that canagliflozin 100 mg has total costs of £23,525 and yields 10.039 QALYs, which implies a cost-effectiveness estimate of £79,537 per QALY compared with pioglitazone. The cost-effectiveness estimate compared with gliclazide is £3377 per QALY, this being largely due to the higher costs in the gliclazide arm compared with pioglitazone. Canagliflozin 100 mg is estimated to dominate empagliflozin 10 mg, empagliflozin 25 mg and dapagliflozin 10 mg.
The Janssen cost-effectiveness estimates for the flozins compared with sitagliptin are £1414 per QALY for canagliflozin 100 mg, £1977 per QALY for empagliflozin 25 mg, £4724 per QALY for empagliflozin 10 mg, and £6040 per QALY for sitagliptin.
If that annual rate of increase in HbA1c is equalised between the treatments and repaglinide is included as a comparator, it appears that this worsens the cost-effectiveness estimate for canagliflozin compared with repaglinide to £189,000 per QALY. The cost-effectiveness estimates for canagliflozin 100 mg compared with gliclazide and sitagliptin worsen to £21,580 per QALY and £21,470 per QALY, respectively. Applying the UKPDS68193 evolution of HbA1c results in broad clinical equivalence between canagliflozin 100 mg and gliclazide, but the costs of canagliflozin 100 mg are £744 greater.
AstraZeneca pooled the flozins into a class effect. Given this pioglitazone was estimated to be the least costly with total costs of £26,067 and to yield 13.111 QALYs. The sulfonylureas were estimated to have a total cost of £26,582 so £515 higher than pioglitazone, and to yield 13.179 QALYs so have a cost-effectiveness estimate of £7574 per QALY compared with pioglitazone. The gliptins were estimated to have a total cost of £27,873 and to yield 13.188 QALYs or only 0.009 QALYs more than the sulfonylureas, hence have a cost-effectiveness compared with the sulfonylureas of £143,000 per QALY. The flozins were only £106 more expensive than the gliptins and yielded an additional 0.018 QALYs, so had a cost-effectiveness compared with the gliptins of £5904 per QALY. But the flozins cost-effectiveness compared with the sulfonylureas was poor, at £52,047 per QALY.
AstraZeneca sensitivity analyses showed results were sensitive to the HbA1c intensification threshold and to the assumptions around the evolution of weight.
The AG modelling suggests that gliclazide is the least expensive, with total costs of £27,314. Repaglinide and pioglitazone have similar total costs of £27,413 and £27,543, respectively. The increased costs for pioglitazone are due in part to the AG including a £72 allowance for annual BNP monitoring. Costs increase quite markedly with sitagliptin at a total cost of £32,358, and increase further with the flozins being clustered between £32,676 and £32,866. Sitagliptin is estimated to be £5045 more expensive than gliclazide, and the flozins between £5362 and £5553 more expensive than gliclazide.
If there are no direct QoL impacts from weight changes, gliclazide is estimated to yield 10.392 QALYs. This is the highest total QALYs for this scenario and, as a consequence, gliclazide dominates all of the other treatments.
Including direct QoL impacts from weight changes and assuming that the weight changes associated with the monotherapies persist indefinitely results in repaglinide now being superior to gliclazide by 0.030 QALYs and so having a cost-effectiveness estimate of £3331 per QALY. Repaglinide formally dominates pioglitazone and sitagliptin, but canagliflozin yields an additional 0.177 QALYs at an additional cost of £5262 so has a cost-effectiveness estimate of £44,994 per QALY compared with repaglinide. If weight losses associated with treatment tend to rebound at either 1 year or at treatment intensification the cost-effectiveness estimate for canagliflozin compared with repaglinide worsens to £192,000 per QALY and £119,000 per QALY, respectively.
Canagliflozin is estimated to be around £100 less expensive than empagliflozin and £200 less expensive than dapagliflozin. With no direct QoL effects from weight changes it is estimated to be marginally more effective than empagliflozin by 0.002 QALYs and 0.013 QALYs more effective than dapagliflozin. Including the effects of weight upon QoL increases these net gains to 0.034 QALYs and 0.046 QALYs if weight changes persist indefinitely. If they rebound after 1 year these gains fall to 0.007 QALYs and 0.019 QALYs, whereas if they rebound at treatment change they fall to 0.014 QALYs and 0.026 QALYs.
Both canagliflozin and empagliflozin have reasonable cost-effectiveness estimates compared with sitagliptin of £12,623 per QALY and £18,341 per QALY even if there are no QoL impacts from weight changes. Including these effects improves their cost-effectiveness estimates compared with sitagliptin.
Dapagliflozin fares slightly worse compared with sitagliptin. It costs an additional £508 but yields only an additional 0.013 QALYs if there are no direct QoL impacts from weight changes, so has a cost-effectiveness estimate of £40,383 per QALY compared with sitagliptin. This improves to £6632 per QALY if weight changes have a QoL impact and are assumed to persist indefinitely. If they only persist for 1 year the cost-effectiveness estimate worsens to a little over £30,000 per QALY, but if they persist until treatment change the cost-effectiveness estimate worsens but only to a little under £20,000 per QALY.
The AG results showed some sensitivity to whether patients add insulin to their existing treatments or switch to it, the application of a common 7.5% HbA1c baseline and applying a reduced –0.47% HbA1c effect for gliclazide as recently reviewed above.
Chapter 6 Discussion and research needs
Principal findings
The key findings are:
-
Canagliflozin, dapagliflozin and empagliflozin are clinically effective in improving glycaemic control when used in monotherapy.
-
They also provide modest reductions in SBP and promote weight loss.
-
The main AEs are urinary tract and genital area infections.
-
There are concerns following reports of DKA and bone loss. DKA appears rare – about 1 per 3000 patient-years. Fractures were not increased after 3 years of empagliflozin treatment in the empagliflozin outcomes trial.
-
The AG modelling results suggest that dapagliflozin, canagliflozin and empagliflozin are not cost-effective compared with gliclazide or pioglitazone, nor probably to repaglinide, though the evidence base for repaglinide is poorer.
-
However, if patients cannot take one of the older drugs, both canagliflozin and dapagliflozin are cost-effective compared with sitagliptin.
-
Dapagliflozin is cost-effective compared with sitagliptin if direct utility gains from weight loss are accepted.
Limitations
-
There are no head-to-head comparisons amongst the flozins so relative effects have to be drawn from NMAs. In these there is a problem because in some dapagliflozin trials HbA1c improved in the placebo groups, reducing the placebo-adjusted improvement after dapagliflozin treatment. In the canagliflozin trials, HbA1c rose in placebo groups.
-
Patients in one dapagliflozin trial had a low baseline HbA1c, and hence less chance of a large reduction.
-
Patients randomised to 300 mg of canagliflozin, started on that dose. In routine care adhering to the licence, patients would start on 100 mg and change to the higher dose only if it was insufficiently effective. Those who do not respond well to 100 mg may have a lower effect from 300 mg than the trial patients did.
-
The above features would make it unwise to conclude that any one flozin is better than the others.
-
Some trials were conducted in East Asian populations with a much lower baseline BMI than in European populations.
-
In the trials, HbA1c was usually above 8%. The higher the baseline HbA1c, the greater the likely reduction. Their results may not apply if the NICE guidelines are followed, with close monitoring of glycaemic control and prompt intervention once HbA1c rises above 7.5%.
-
Cost-effectiveness analysis requires extrapolating from short-term results to long-term outcomes.
-
Some QALY differences were very small, making ICERs unstable.
Other options
The NICE scope did not include all possible comparators. Five not included were:
-
intensive lifestyle interventions
-
bariatric surgery, which is covered by other guidance
-
early intensive treatment
-
very-low-calorie diets
-
other non-pharmacological interventions.
Intensive lifestyle interventions
The work of Aas et al. 222 has been reported in previous reviews for NICE. Aas et al. 222 carried out a trial in 38 diabetic subjects poorly controlled (HbA1c 8–10.5%; mean 9.0%) on oral drugs and being considered for insulin treatment. They were randomised to insulin treatment or to an intensive lifestyle intervention based on exercise and diet, or both. After 12 months, HbA1c improved by 1.2% in the lifestyle arm and by 1.5% in the insulin (NPH twice daily, with short-acting at mealtimes if required) arm. Weight fell by 3 kg in the lifestyle arm, but rose 4.9 kg in the insulin arm. The lifestyle intervention comprised 14 sessions of dietary advice, two individual sessions and 1 hour of exercise of moderate intensity twice a week, including group aerobics, walking and swimming. Unfortunately, a year after the intervention had finished, HbA1c and weight rose again in the lifestyle group.
Coppell et al. from Otago223 carried out a randomised trial of an intensive nutritional intervention (seven individual sessions with a dietitian, one group session and telephone calls) compared with standard care (GP or hospital clinic). After 6 months, the intensive group recorded reductions in HbA1c (0.5%), weight (2.1 kg), waist circumferences (3.5 cm), SBP (4.1 mmHg) and TC (0.24 mmol/l), whereas HDL-C was unchanged. The control group showed little change and none in HbA1c.
Bariatric surgery
The NICE guidance on bariatric surgery224 includes a section specific to type 2 diabetes, reproduced in Box 4.
1.11.1 Offer an expedited assessment for bariatric surgery to people with a BMI of 35 or over who have recent-onset type 2 diabetes as long as they are also receiving or will receive assessment in a tier 3 service (or equivalent).
1.11.2 Consider an assessment for bariatric surgery for people with a BMI of 30–34.9 who have recent-onset type 2 diabetes as long as they are also receiving or will receive assessment in a tier 3 service (or equivalent).
1.11.3 Consider an assessment for bariatric surgery for people of Asian family origin who have recent-onset type 2 diabetes at a lower BMI than other populations (see recommendation 1.2.8) as long as they are also receiving or will receive assessment in a tier 3 service (or equivalent).
Early intensive treatment
The use of intensive treatment at diagnosis was first reported by a Chinese study in 2004. 225 Two weeks of intensive insulin treatment (with CSII) improved beta cell function, after which 47% remained well controlled on diet alone for 12 months and 42% for 2 years. A later trial randomised 410 Chinese patients to intensive insulin or oral agents (metformin or gliclazide, or both). Once patients had been normoglycaemic for 2 weeks, the drugs were stopped. After insulin, 51% of the CSII group and 45% of the MDI group remained in good glycaemic control a year later, compared with 27% of those on oral agents, suggesting that how the normoglycaemia is achieved is important (Yang and Weng226).
A systematic review published in 2013 by Kramer et al. 227 found seven studies of short-term intensive insulin therapy at diagnosis of type 2 diabetes. Two were RCTs and five were case series from China. When considering data from China, we need to bear in mind that Chinese people with type 2 diabetes have a more insulin-deficient, and less insulin-resistant, pattern.
Two small studies in white populations were not included in the Kramer review. Ilkova et al. 228 from Turkey and Israel treated 13 patients with newly diagnosed type 2 diabetes not responding to 3–6 weeks of diet and physical activity with CSII for 2 weeks. Most (9/13) responded and three had 3–5 years’ remission of diabetes. In five patients control deteriorated after 9–36 months but good control was restored after a second fortnight of CSII. Ryan229 in Canada treated 16 people newly diagnosed with type 2 diabetes with MDI for 2–3 weeks, and a year later seven people were on no glucose-lowering agents.
Introducing metformin earlier after diagnosis has been advocated by Brown et al. 230 They noted that in a cohort of 1799 patients that had metformin as first ever glucose-lowering drug, those who started it less than 3 months after diagnosis of diabetes had a lower failure rate (12.2% a year) than those who started metformin 12 or more months after diagnosis (about 20% a year).
Another form of early intensive treatment is triple therapy from diagnosis. Abdul-Ghani et al. 231 report the results of the EDICT (Efficacy and Durability of Initial Combination Therapy for type 2 diabetes) in which patients were treated from diagnosis with metformin, pioglitazone and exenatide, and compared with a control arm that had a more standard approach of starting with metformin followed by addition of sulfonylurea then glargine as required. The hypothesis behind the trial combination was to have a combination of drugs to improve both insulin secretion and sensitivity. The triple therapy group had lower HbA1c (by 0.55%), far less hypoglycaemia, and 1.2-kg weight loss compared with 4-kg gain on the standard sequence.
Very-low-calorie diets
Taylor et al. 232 from Newcastle have challenged the consensus that diabetes is a progressive irreversible disease, by showing that very-low-calorie diets (600 kcal/day for 8 weeks) can reverse type 2 diabetes by restoring beta cell function and hepatic insulin sensitivity. They did this first for relatively recent-onset cases in the Counterpoint Study,233 but then showed that about half of people with long-standing diabetes could return to normal glucose levels and stop their glucose-lowering medications. This was achieved by weight loss averaging 14–15 kg. The 8-week time period was too short to show full effect on HbA1c but even by then it fell by 1.15 in the short duration group and by an average of 0.6% in the long-duration group. Steven and Taylor (2015)232 report that e-mail feedback from people who lost weight and kept it off have continued to have normal glucose levels for up to 3 years, so far. So it appears that as long as weight loss is maintained, they remain non-diabetic.
Non-pharmacological interventions
A very large number of trials reporting effects of different drugs are mentioned in this report and the industry submissions. Research into the management of type 2 diabetes is very pharmacocentric, partly because the manufacturers of the drug have to carry out such trials for licensing purposes. There is no such pressure on developers of lifestyle interventions, nor guaranteed funding.
However, lifestyle interventions should also be considered. Type 2 diabetes is strongly associated with overweight and obesity, and physical inactivity, and lifestyle change can be effective.
The problem with lifestyle interventions is adherence. A previous health technology assessment on prevention of diabetes in people with impaired glucose tolerance noted the tendency for gains after lifestyle interventions to be lost once the intervention was stopped, with the exception of the Finnish Diabetes Prevention Study234 in which the intervention continued for 4 years.
However, ways of improving adherence have been researched. Perri et al. 235 randomised 379 adults to walking at different speeds, and found that increasing the frequency of exercise achieved better adherence than increasing the intensity. Their study was prompted by awareness of a public perception that health benefits would be achieved only by frequent high-intensity exercise.
Hansen et al. 236 from Belgium and the Netherlands also reported that prolonged low-to-moderate exercise was almost as effective as more intense exercise. Their participants had three sessions a week of supervised walking, cycling or cross-country ski-type exercise for 6 months. In the moderate intensity group, HbA1c fell from 7.4% at baseline to 7.2% at 6 months. There were modest improvements in weight (91.1 kg) and TC. The higher-intensity group did better, with HbA1c reduction of 0.5% and weight loss of 1.8 kg. The authors note that participants are more likely to drop out of high-intensity physical activity, partly because people with long-standing type diabetes often have comorbidities that restrict such exercise.
Walking supported by pedometer use has been reported to be effective in a 12-month trial from Leicester. 237 However, arguments to the contrary have appeared in recent years, suggesting that short-duration, high-intensity exercise may be effective, with the brevity improving adherence. 238
Snowling and Hopkins239 carried out a meta-analysis of the effects of different forms of exercise (aerobic, resistance, mixed) in type 2 diabetes. They reported an improvement in HbA1c of 0.8%, which is as great as many drugs achieve.
A full review of the benefits of physical activity in type 2 diabetes is beyond the scope of this report. Reviews of exercise therapy in type 2 diabetes and the mechanisms are provided by Praet and van Loon240 and Zanuso et al. 241
The NICE Public Health Guidance on weight management242 noted that even modest weight loss could be cost-effective if sufficient and maintained. An Australian review of six interventions to promote physical activity also concluded that most would be cost-effective. 243
A review by Fujioka244 also concluded that in type 2 diabetes, weight loss of 1–4 kg improved metabolic control and cardiovascular risk, though greater weight loss achieved greater benefit. Wing et al. 245 reported from the Look AHEAD trial (Action for Health in Diabetes) that modest weight loss (5–10% body weight, 7.25 kg) improved glycaemic control (HbA1c reduced by 0.5%), BP (6 mmHg) and HDL-C, but even minor weight loss (2–5%) showed some benefit (HbA1c reduced by about 0.25%, SBP by about 4 mmHg).
A full review of the benefits of weight loss in type 2 diabetes is outwith the scope of the this report, and others have reviewed the subject. 246 The cost-effectiveness of lifestyle interventions was reviewed by Jacobs-van der Bruggen et al.,247 who concluded that short-term results showed that they were cost-effective. However, they noted a lack of long-term maintenance of benefit.
In summary, there is a range of effective lifestyle interventions, but the main problems are adherence and long-term maintenance.
Research needs
The clinical effectiveness of the SGLT2 inhibitors for at least 2 years is not in doubt, and we now need data on long-term effectiveness and safety. The empagliflozin cardiovascular outcomes trial136 has reported, though some clarifications are required. The equivalent studies for canagliflozin [CANVAS129 (CANagliflozin cardioVascular Assessment Study)] and dapagliflozin [DECLARE130 (Multicenter Trial to Evaluate the Effect of Dapagliflozin on the Incidence of Cardiovascular Events)] are under way. Continued monitoring for DKA and fractures is required.
One of the anonymous National Institute for Health Research referees suggested two subgroups for which research is required.
-
The first is individuals with type 2 diabetes diagnosed at < 40 years old. This population of type 2 diabetes is rising very quickly. Phenotypically, they are different from the conventional ‘late-onset’ type 2 diabetes, because they are associated with more aggressive CVD; they are hypertensive, obese and insulin resistant; and they are at risk of progression of diabetic nephropathy.
-
The second is elderly patients with type 2 diabetes. Elderly patients are more at risk of fractures, hypoglycaemia and falls. This may be relevant when comparing different glucose-lowering therapies, because of recognised side effects of currently available agents.
The first trials of the SGLT2 in type 1 diabetes are emerging, and because of their insulin-independent mode of action, they would be expected to be useful there. However, the DKA risk would be more of a concern than in type 2 diabetes.
Conclusions
The SGLT2 inhibitors are effective in improving glycaemic control, promoting weight loss and reducing BP – the first oral drugs for diabetes to do so. Their safety record remains to be established, but the only common AEs are small increases in the frequency of urinary and GTIs, seldom serious. However, they are much more expensive than older drugs such as gliclazide and pioglitazone.
Acknowledgements
We thank Emma Loveman for checking data extractions. The authors are indebted to Gabriel Rogers and Steven Ward who provided advice on the economics and without whom the probabilistic modelling would not have been possible.
Norman Waugh is guarantor for this report.
Contributions of authors
Pamela Royle did literature searches, generated the list of references, and edited and formatted the final report.
Christine Clar, Rachel Court, Bee Kang Tan and Saran Shantikumar extracted data from the trials in Chapter 2. Christine Clar drafted the clinical effectiveness section. Bee Kang Tan drafted the section on UTIs and GTIs.
Christine Clar and Jill Colquitt extracted data for the NMA, which was carried out by Olakan Uthman.
Andrew Clegg provided a technical critique of the methods of the manufacturers’ NMAs.
Rhona Johnston and Ewen Cummins wrote additions to the UKPDS Outcomes Model and carried out the economic modelling.
Norman Waugh drafted Chapters 1 and 6, wrote various other sections, and edited the final report.
David McGrane, J Paul O’Hare and Tim Holt provided clinical advice.
Data sharing statement
There are no further data to share.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Public Health England . Diabetes Prevalence Model (APHO) 2014. www.yhpho.org.uk/resource/view.aspx?RID=81090 (accessed 4 September 2015).
- Hex N, Bartlett C, Wright D, Taylor M, Varley D. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs. Diabet Med 2012;29:855-62. https://doi.org/10.1111/j.1464-5491.2012.03698.x.
- Health and Social Care Information Centre . Prescribing for Diabetes: England 2005–06 to 2013–14 2014. www.hscic.gov.uk/catalogue/PUB14681/pres-diab-eng-200506-201314-rep.pdf (accessed 4 September 2014).
- UK Prospective Diabetes Study (UKPDS) Group . UK Prospective Diabetes Study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes 1995;44:1249-58. https://doi.org/10.2337/diab.44.11.1249.
- Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA 1999;281:2005-12. https://doi.org/10.1001/jama.281.21.2005.
- Hippisley-Cox J, Pringle M. Prevalence, care, and outcomes for patients with diet-controlled diabetes in general practice: cross sectional survey. Lancet 2004;364:423-8. http://dx.doi.org/10.1016/S0140-6736(04)16765-2.
- Thomsen RW, Baggesen LM, Søgaard M, Pedersen L, Nørrelund H, Buhl ES, et al. Early glycaemic control in metformin users receiving their first add-on therapy: a population-based study of 4,734 people with type 2 diabetes. Diabetologia 2015;58:2247-53. http://dx.doi.org/10.1007/s00125-015-3698-1.
- National Institute for Health and Care Excellence (NICE) . Type 2 Diabetes: The Management of Type 2 Diabetes 2009. www.nice.org.uk/guidance/cg87 (accessed September 2015).
- National Institute for Health and Care Excellence (NICE) . Dapagliflozin in Combination Therapy for Treating Type 2 Diabetes 2013. www.nice.org.uk/guidance/ta288 (accessed 29 September 2015).
- National Institute for Health and Care Excellence (NICE) . Canagliflozin in Combination Therapy for Treating Type 2 Diabetes 2014. www.nice.org.uk/guidance/ta315 (accessed 29 September 2015).
- National Institute for Health and Care Excellence (NICE) . Empagliflozin in Combination Therapy for Treating Type 2 Diabetes 2015. www.nice.org.uk/guidance/ta336 (accessed 29 September 2015).
- European Medicines Agency (EMA) . Trulicity (dulaglutide): Summary of Product Characteristics 2014. www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002825/WC500179470.pdf (accessed 29 July 2015).
- European Medicines Agency (EMA) . Eperzan (albiglutide): Summary of Product Characteristics 2014. www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002735/WC500165117.pdf (accessed 29 September 2015).
- Robinson LE, Holt TA, Rees K, Randeva HS, O’Hare JP. Effects of exenatide and liraglutide on heart rate, blood pressure and body weight: systematic review and meta-analysis. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-001986.
- Black C, Donnelly P, McIntyre L, Royle PL, Shepherd JP, Thomas S. Meglitinide analogues for type 2 diabetes mellitus. Cochrane Database Syst Rev 2007;2. https://doi.org/10.1002/14651858.cd004654.pub2.
- National Institute for Health and Care Excellence (NICE) . Type 2 Diabetes in Adults: Management 2015. www.nice.org.uk/guidance/ng28 (accessed January 2016).
- Satoh J, Takahashi K, Takizawa Y, Ishihara H, Hirai M, Katagiri H, et al. Secondary sulfonylurea failure: comparison of period until insulin treatment between diabetic patients treated with gliclazide and glibenclamide. Diabetes Res Clin Pract 2005;70:291-7. http://dx.doi.org/10.1016/j.diabres.2005.04.002.
- Leese GP, Wang J, Broomhall J, Kelly P, Marsden A, Morrison W, et al. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Diabetes Care 2003;26:1176-80. https://doi.org/10.2337/diacare.26.4.1176.
- Schopman JE, Simon AC, Hoefnagel SJ, Hoekstra JB, Scholten RJ, Holleman F. The incidence of mild and severe hypoglycaemia in patients with type 2 diabetes mellitus treated with sulfonylureas: a systematic review and meta-analysis. Diabetes Metab Res Rev 2014;30:11-22. http://dx.doi.org/10.1002/dmrr.2470.
- Monami M, Dicembrini I, Kundisova L, Zannoni S, Nreu B, Mannucci E. A meta-analysis of the hypoglycaemic risk in randomized controlled trials with sulphonylureas in patients with type 2 diabetes. Diabetes Obes Metab 2014;16:833-40. http://dx.doi.org/10.1111/dom.12287.
- Schernthaner G, Grimaldi A, Di Mario U, Drzewoski J, Kempler P, Kvapil M, et al. GUIDE study: double-blind comparison of once-daily gliclazide MR and glimepiride in type 2 diabetic patients. Eur J Clin Invest 2004;34:535-42. http://dx.doi.org/10.1111/j.1365-2362.2004.01381.x.
- Gerstein HC, Bosch J, Dagenais GR, Díaz R, Jung H, Maggioni AP, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med 2012;367:319-28. http://dx.doi.org/10.1056/NEJMoa1203858.
- Zoungas S, Chalmers J, Kengne AP, Pillai A, Billot L, de Galan B, et al. The efficacy of lowering glycated haemoglobin with a gliclazide modified release-based intensive glucose lowering regimen in the ADVANCE trial. Diabetes Res Clin Pract 2010;89:126-33. http://dx.doi.org/10.1016/j.diabres.2010.05.012.
- UK Hypoglycaemia Study Group . Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia 2007;50:1140-7. https://doi.org/10.1007/s00125-007-0599-y.
- Landman GW, de Bock GH, van Hateren KJ, van Dijk PR, Groenier KH, Gans RO, et al. Safety and efficacy of gliclazide as treatment for type 2 diabetes: a systematic review and meta-analysis of randomized trials. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0082880.
- Schrijnders D, Houweling ST, Landman GW. Comment on Genuth. Should sulfonylureas remain an acceptable first-line add-on to metformin therapy in patients with type 2 diabetes? No, it’s time to move on!. Diabetes Care 2015;38:170-5. https://doi.org/10.2337/dc15-0293.
- Simpson SH, Lee J, Choi S, Vandermeer B, Abdelmoneim AS, Featherstone TR. Mortality risk among sulfonylureas: a systematic review and network meta-analysis. Lancet Diabetes Endocrinol 2015;3:43-51. http://dx.doi.org/10.1016/S2213-8587(14)70213-X.
- Schramm TK, Gislason GH, Vaag A, Rasmussen JN, Folke F, Hansen ML, et al. Mortality and cardiovascular risk associated with different insulin secretagogues compared with metformin in type 2 diabetes, with or without a previous myocardial infarction: a nationwide study. Eur Heart J 2011;32:1900-8. http://dx.doi.org/10.1093/eurheartj/ehr077.
- Scottish Intercollegiate Guidelines Network (SIGN) . Management of Diabetes 2010. www.sign.ac.uk/guidelines/fulltext/116/index.html (accessed 4 September 2015).
- American Diabetes Association (ADA) . (7) Approaches to glycemic treatment. Diabetes Care 2015;38:41-8. https://doi.org/10.2337/dc15-S010.
- Drouin P. Diamicron MR once daily is effective and well tolerated in type 2 diabetes: a double-blind, randomized, multinational study. J Diabetes Complicat 2000;14:185-91. https://doi.org/10.1016/S1056-8727(00)00086-6.
- Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1.9 million people. Lancet Diabetes Endocrinol 2015;3:105-13. https://doi.org/10.1016/S2213-8587(14)70219-0.
- Idris I, Warren G, Donnelly R. Association between thiazolidinedione treatment and risk of macular edema among patients with type 2 diabetes. Arch Intern Med 2012;172:1005-11. https://doi.org/10.1001/archinternmed.2012.1938.
- Tzoulaki I, Molokhia M, Curcin V, Little MP, Millett CJ, Ng A, et al. Risk of cardiovascular disease and all cause mortality among patients with type 2 diabetes prescribed oral antidiabetes drugs: retrospective cohort study using UK General Practice Research Database. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b4731.
- Colhoun HM, Livingstone SJ, Looker HC, Morris AD, Wild SH, Lindsay RS, et al. Hospitalised hip fracture risk with rosiglitazone and pioglitazone use compared with other glucose-lowering drugs. Diabetologia 2012;55:2929-37. http://dx.doi.org/10.1007/s00125-012-2668-0.
- Azoulay L, Yin H, Filion KB, Assayag J, Majdan A, Pollak MN, et al. The use of pioglitazone and the risk of bladder cancer in people with type 2 diabetes: nested case-control study. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e3645.
- Neumann A, Weill A, Ricordeau P, Fagot JP, Alla F, Allemand H. Pioglitazone and risk of bladder cancer among diabetic patients in France: a population-based cohort study. Diabetologia 2012;55:1953-62. http://dx.doi.org/10.1007/s00125-012-2538-9.
- Lewis JD, Habel LA, Quesenberry CP, Strom BL, Peng T, Hedderson MM, et al. Pioglitazone use and risk of bladder cancer and other common cancers in persons with diabetes. JAMA 2015;314:265-77. http://dx.doi.org/10.1001/jama.2015.7996.
- Ryder RE. Pioglitazone has a dubious bladder cancer risk but an undoubted cardiovascular benefit. Diabet Med 2015;32:305-13. http://dx.doi.org/10.1111/dme.12627.
- Gale EA. Pioglitazone: are rumours of its death exaggerated?. Diabet Med 2015;32:431-7. http://dx.doi.org/10.1111/dme.12708.
- Levin D, Bell S, Sund R, Hartikainen SA, Tuomilehto J, Pukkala E, et al. Pioglitazone and bladder cancer risk: a multipopulation pooled, cumulative exposure analysis. Diabetologia 2015;58:493-504. http://dx.doi.org/10.1007/s00125-014-3456-9.
- Zhu Z, Wang X, Shen Z, Lu Y, Zhong S, Xu C. Risk of bladder cancer in patients with diabetes mellitus: an updated meta-analysis of 36 observational studies. BMC Cancer 2013;13. http://dx.doi.org/10.1186/1471-2407-13-310.
- European Medicines Agency (EMA) . European Medicines Agency Clarifies Opinion on Pioglitazone and the Risk of Bladder Cancer 2011. www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2011/10/news_detail_001368.jsp&mid=WC0b01ac058004d5c1 (accessed 4 September 2015).
- Medicines and Healthcare products Regulatory Agency (MHRA) . Pioglitazone: Risk of Bladder Cancer 2011. www.gov.uk/drug-safety-update/pioglitazone-risk-of-bladder-cancer (accessed 4 September 2015).
- Craig J, Bradbury I, Cummins E, Downie S, Foster L, Stout A. The Use of B-Type Natriuretic Peptides (BNP and NT-ProBNP) in the Investigation of Patients With Suspected Heart Failure 2005. www.healthcareimprovementscotland.org/previous_resources/hta_report/hta_6.aspx (accessed 9 September 2015).
- Hansen L, Ekstrom CT, Tabanera YPR, Anant M, Wassermann K, Reinhardt RR. The Pro12Ala variant of the PPARG gene is a risk factor for peroxisome proliferator-activated receptor-gamma/alpha agonist-induced edema in type 2 diabetic patients. J Clin Endocrinol Metab 2006;91:3446-50. https://doi.org/10.1210/jc.2006-0590.
- Shyangdan D, Clar C, Ghouri N, Henderson R, Gurung T, Preiss D, et al. Insulin sensitisers in the treatment of non-alcoholic fatty liver disease: a systematic review. Health Technol Assess 2011;15. http://dx.doi.org/10.3310/hta15380.
- Santer R, Kinner M, Lassen CL, Schneppenheim R, Eggert P, Bald M, et al. Molecular analysis of the SGLT2 gene in patients with renal glucosuria. J Am Soc Nephrol 2003;14:2873-82. https://doi.org/10.1097/01.ASN.0000092790.89332.D2.
- Hanefeld M, Forst T. Dapagliflozin, an SGLT2 inhibitor, for diabetes. Lancet 2010;375:2196-8. http://dx.doi.org/10.1016/S0140-6736(10)60749-0.
- Komoroski B, Vachharajani N, Boulton D, Kornhauser D, Geraldes M, Li L, et al. Dapagliflozin, a novel SGLT2 inhibitor, induces dose-dependent glucosuria in healthy subjects. Clin Pharmacol Ther 2009;85:520-6. http://dx.doi.org/10.1038/clpt.2008.251.
- Liu JJ, Lee T, DeFronzo RA. Why Do SGLT2 inhibitors inhibit only 30-50% of renal glucose reabsorption in humans?. Diabetes 2012;61:2199-204. http://dx.doi.org/10.2337/db12-0052.
- Komoroski B, Vachharajani N, Feng Y, Li L, Kornhauser D, Pfister M. Dapagliflozin, a novel, selective SGLT2 inhibitor, improved glycemic control over 2 weeks in patients with type 2 diabetes mellitus. Clin Pharmacol Ther 2009;85:513-19. http://dx.doi.org/10.1038/clpt.2008.250.
- Polidori D, Sha S, Mudaliar S, Ciaraldi TP, Ghosh A, Vaccaro N, et al. Canagliflozin lowers postprandial glucose and insulin by delaying intestinal glucose absorption in addition to increasing urinary glucose excretion: results of a randomized, placebo-controlled study. Diabetes Care 2013;36:2154-61. http://dx.doi.org/10.2337/dc12-2391.
- Stein P, Berg JK, Morrow L, Polidori D, Artis E, Rusch S, et al. Canagliflozin, a sodium glucose co-transporter 2 inhibitor, reduces post-meal glucose excursion in patients with type 2 diabetes by a non-renal mechanism: results of a randomized trial. Metab Clin Exp 2014;63:1296-303. http://dx.doi.org/10.1016/j.metabol.2014.07.003.
- Baker WL, Smyth LR, Riche DM, Bourret EM, Chamberlin KW, White WB. Effects of sodium-glucose co-transporter 2 inhibitors on blood pressure: a systematic review and meta-analysis. J Am Soc Hypertens 2014;8:262-75.e9. http://dx.doi.org/10.1016/j.jash.2014.01.007.
- NHS Business Services Authority . Electronic Drug Tariff 2015. www.nhsbsa.nhs.uk/PrescriptionServices/4940.aspx (accessed 4 September 2015).
- National Institute for Health and Care Excellence (NICE) . Canagliflozin, Dapagliflozin and Empagliflozin Monotherapy for Treating Type 2 Diabetes. Final Scope 2015. www.nice.org.uk/guidance/TA390/documents/diabetes-type-2-canagliflozin-dapagliflozin-and-empagliflozin-monotherapy-id756-final-scope2 (accessed April 2015).
- Bailey CJ, Turner RC. Metformin. N Engl J Med 1996;334:574-9. http://dx.doi.org/10.1056/NEJM199602293340906.
- Garber AJ, Duncan TG, Goodman AM, Mills DJ, Rohlf JL. Efficacy of metformin in type II diabetes: results of a double-blind, placebo-controlled, dose-response trial. Am J Med 1997;103:491-7. https://doi.org/10.1016/S0002-9343(97)00254-4.
- DeFronzo RA, Goodman AM. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. The Multicenter Metformin Study Group. N Engl J Med 1995;333:541-9. http://dx.doi.org/10.1056/NEJM199508313330902.
- Blonde L, Dailey GE, Jabbour SA, Reasner CA, Mills DJ. Gastrointestinal tolerability of extended-release metformin tablets compared to immediate-release metformin tablets: results of a retrospective cohort study. Curr Med Res Opin 2004;20:565-72. http://dx.doi.org/10.1185/030079904125003278.
- Scarpello JH. Improving survival with metformin: the evidence base today. Diabetes Metab 2003;29:36-43.
- Scarpello JH, Hodgson E, Howlett HC. Effect of metformin on bile salt circulation and intestinal motility in type 2 diabetes mellitus. Diabet Med 1998;15:651-6. http://dx.doi.org/10.1002/(SICI)1096-9136(199808)15:8%3C651::AID-DIA628%3E3.0.CO;2-A.
- Emslie-Smith AM, Boyle DI, Evans JM, Sullivan F, Morris AD. DARTS/MEMO Collaboration . Contraindications to metformin therapy in patients with Type 2 diabetes: a population-based study of adherence to prescribing guidelines. Diabet Med 2001;18:483-8. https://doi.org/10.1046/j.1464-5491.2001.00509.x.
- Salpeter SR, Greyber E, Pasternak GA, Salpeter EE. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev 2010;4. http://dx.doi.org/10.1002/14651858.CD002967.pub4.
- Okayasu S, Kitaichi K, Hori A, Suwa T, Horikawa Y, Yamamoto M, et al. The evaluation of risk factors associated with adverse drug reactions by metformin in type 2 diabetes mellitus. Biol Pharm Bull 2012;35:933-7. https://doi.org/10.1248/bpb.35.933.
- American Diabetes Association (ADA) . (6) Glycemic targets. Diabetes Care 2015;38:33-40. https://doi.org/10.2337/dc15-S009.
- Hemmingsen B, Lund SS, Gluud C, Vaag A, Almdal T, Hemmingsen C, et al. Intensive glycaemic control for patients with type 2 diabetes: systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d6898.
- UK Prospective Diabetes Study (UKPDS) Group . Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837-53. https://doi.org/10.1016/S0140-6736(98)07019-6.
- Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359:1577-89. http://dx.doi.org/10.1056/NEJMoa0806470.
- Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, Buse JB, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545-59. http://dx.doi.org/10.1056/NEJMoa0802743.
- Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560-72. http://dx.doi.org/10.1056/NEJMoa0802987.
- Boussageon R, Bejan-Angoulvan T, Saadatian-Elahi M, Lafont S, Bergeonneau C, Kassaï B, et al. Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d4169.
- Vijan S, Sussman JB, Yudkin JS, Hayward RA. Effect of patients’ risks and preferences on health gains with plasma glucose level lowering in type 2 diabetes mellitus. JAMA Intern Med 2014;174:1227-34. http://dx.doi.org/10.1001/jamainternmed.2014.2894.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions 2011. http://handbook.cochrane.org/ (accessed 24 September 2105).
- Inagaki N, Kondo K, Yoshinari T, Takahashi N, Susuta Y, Kuki H. Efficacy and safety of canagliflozin monotherapy in Japanese patients with type 2 diabetes inadequately controlled with diet and exercise: a 24-week, randomized, double-blind, placebo-controlled, Phase III study. Expert Opin Pharmacother 2014;15:1501-15. http://dx.doi.org/10.1517/14656566.2014.935764.
- Ferrannini E, Ramos SJ, Salsali A, Tang W, List JF. Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes Care 2010;33:2217-24. http://dx.doi.org/10.2337/dc10-0612.
- Bailey CJ, Morales Villegas EC, Woo V, Tang W, Ptaszynska A, List JF. Efficacy and safety of dapagliflozin monotherapy in people with Type 2 diabetes: a randomized double-blind placebo-controlled 102-week trial. Diabet Med 2015;32:531-41. http://dx.doi.org/10.1111/dme.12624.
- Ji L, Ma J, Li H, Mansfield TA, T’joen CL, Iqbal N, et al. Dapagliflozin as monotherapy in drug-naive Asian patients with type 2 diabetes mellitus: a randomized, blinded, prospective phase III study. Clin Ther 2014;36:84-100. http://dx.doi.org/10.1016/j.clinthera.2013.11.002.
- Kaku K, Kiyosue A, Inoue S, Ueda N, Tokudome T, Yang J, et al. Efficacy and safety of dapagliflozin monotherapy in Japanese patients with type 2 diabetes inadequately controlled by diet and exercise. Diabetes Obes Metab 2014;16:1102-10. http://dx.doi.org/10.1111/dom.12325.
- Lewin A, DeFronzo RA, Patel S, Liu D, Kaste R, Woerle HJ, et al. Initial combination of empagliflozin and linagliptin in subjects with type 2 diabetes. Diabetes Care 2015;38:394-402. http://dx.doi.org/10.2337/dc14-2365.
- Roden M, Weng J, Merker L, Christiansen AV, Roux F, Salsali A, et al. Empagliflozin (EMPA) monotherapy for >76 weeks in drug-naive patients with type 2 diabetes (type 2 diabetes). Diabetes 2014;63.
- Roden M, Weng J, Eilbracht J, Delafont B, Kim G, Woerle HJ, et al. EMPA-REGMONO trial investigators . Empagliflozin monotherapy with sitagliptin as an active comparator in patients with type 2 diabetes: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol 2013;1:208-19. http://dx.doi.org/10.1016/S2213-8587(13)70084-6.
- Stenlöf K, Cefalu WT, Kim KA, Alba M, Usiskin K, Tong C, et al. Efficacy and safety of canagliflozin monotherapy in subjects with type 2 diabetes mellitus inadequately controlled with diet and exercise. Diabetes Obes Metab 2013;15:372-82. http://dx.doi.org/10.1111/dom.12054.
- Rajeev SP, Cuthbertson DJ, Wilding JP. Energy balance and metabolic changes with SGLT2 inhibition. Diabetes Obes Metab 2016;18:125-34. https://doi.org/10.1111/dom.12578.
- Ferrannini G, Hach T, Crowe S, Sanghvi A, Hall KD, Ferrannini E. Energy Balance after sodium-glucose cotransporter 2 inhibition. Diabetes Care 2015;38:1730-5. http://dx.doi.org/10.2337/dc15-0355.
- Amiel SA. It’s all in the name: what exactly is hypoglycemia?. Diabetic Hypoglycemia 2013;5:15-8.
- Plowman R, Graves N, Esquivel J, Roberts JA. An economic model to assess the cost and benefits of the routine use of silver alloy coated urinary catheters to reduce the risk of urinary tract infections in catheterized patients. J Hosp Infect 2001;48:33-42. http://dx.doi.org/10.1053/jhin.2001.0938.
- Geerlings S, Fonseca V, Castro-Diaz D, List J, Parikh S. Genital and urinary tract infections in diabetes: impact of pharmacologically-induced glucosuria. Diabetes Res Clin Pract 2014;103:373-81. http://dx.doi.org/10.1016/j.diabres.2013.12.052.
- Nyirjesy P, Sobel JD. Genital mycotic infections in patients with diabetes. Postgrad Med 2013;125:33-46. http://dx.doi.org/10.3810/pgm.2013.05.2650.
- Grandy S, Fox KM, Hardy E. Prevalence and recurrence of urinary tract and genital infections among adults with and without type 2 diabetes mellitus in the general population: a longitudinal cohort study. J Diab Res Clin Met 2013;2. https://doi.org/10.7243/2050-0866-2-5.
- Stenlöf K, Cefalu WT, Kim KA, Jodar E, Alba M, Edwards R, et al. Long-term efficacy and safety of canagliflozin monotherapy in patients with type 2 diabetes inadequately controlled with diet and exercise: findings from the 52-week CANTATA-M study. Curr Med Res Opin 2014;30:163-75. http://dx.doi.org/10.1185/03007995.2013.850066.
- Lavalle-González FJ, Januszewicz A, Davidson J, Tong C, Qiu R, Canovatchel W, et al. Efficacy and safety of canagliflozin compared with placebo and sitagliptin in patients with type 2 diabetes on background metformin monotherapy: a randomised trial. Diabetologia 2013;56:2582-92. http://dx.doi.org/10.1007/s00125-013-3039-1.
- Inagaki N, Kondo K, Yoshinari T, Kuki H. Efficacy and safety of canagliflozin alone or as add-on to other oral antihyperglycemic drugs in Japanese patients with type 2 diabetes: a 52-week open-label study. J Diabetes Investig 2015;6:210-18. http://dx.doi.org/10.1111/jdi.12266.
- Leiter LA, Yoon KH, Arias P, Langslet G, Xie J, Balis DA, et al. Canagliflozin provides durable glycemic improvements and body weight reduction over 104 weeks versus glimepiride in patients with type 2 diabetes on metformin: a randomized, double-blind, phase 3 study. Diabetes Care 2015;38:355-64. http://dx.doi.org/10.2337/dc13-2762.
- Neal B, Perkovic V, de Zeeuw D, Mahaffey KW, Fulcher G, Ways K, et al. Efficacy and safety of canagliflozin, an inhibitor of sodium-glucose cotransporter 2, when used in conjunction with insulin therapy in patients with type 2 diabetes. Diabetes Care 2015;38:403-11. http://dx.doi.org/10.2337/dc14-1237.
- Davies M, Kushner P, Vijapurkar U, Meininger G. Incidence of genital mycotic infections decreases over time in older patients with type 2 diabetes mellitus treated with canagliflozin. J Gen Intern Med 2015;30:S61-2.
- Nicolle LE, Capuano G, Fung A, Usiskin K. Urinary tract infection in randomized phase III studies of canagliflozin, a sodium glucose co-transporter 2 inhibitor. Postgrad Med 2014;126:7-17. http://dx.doi.org/10.3810/pgm.2014.01.2720.
- Nyirjesy P, Sobel JD, Fung A, Mayer C, Capuano G, Ways K, et al. Genital mycotic infections with canagliflozin, a sodium glucose co-transporter 2 inhibitor, in patients with type 2 diabetes mellitus: a pooled analysis of clinical studies. Curr Med Res Opin 2014;30:1109-19. http://dx.doi.org/10.1185/03007995.2014.890925.
- Bailey CJ, Gross JL, Hennicken D, Iqbal N, Mansfield TA, List JF. Dapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trial. BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-43.
- Johnsson KM, Ptaszynska A, Schmitz B, Sugg J, Parikh SJ, List JF. Urinary tract infections in patients with diabetes treated with dapagliflozin. J Diabetes Complications 2013;27:473-8.
- Kaku K, Maegawa H, Tanizawa Y, Kiyosue A, Ide Y, Tokudome T, et al. Dapagliflozin as monotherapy or combination therapy in Japanese patients with type 2 diabetes: an open-label study. Diabetes Ther 2014;5:415-33. http://dx.doi.org/10.1007/s13300-014-0086-7.
- Bailey CJ, Gross JL, Pieters A, Bastien A, List JF. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial. Lancet 2010;375:2223-33. http://dx.doi.org/10.1016/S0140-6736(10)60407-2.
- Matthaei S, Bowering K, Rohwedder K, Grohl A, Parikh S. Study 05 Group . Dapagliflozin improves glycemic control and reduces body weight as add-on therapy to metformin plus sulfonylurea: a 24-week randomized, double-blind clinical trial. Diabetes Care 2015;38:365-72. http://dx.doi.org/10.2337/dc14-0666.
- Rosenstock J, Hansen L, Zee P, Li Y, Cook W, Hirshberg B, et al. Dual add-on therapy in type 2 diabetes poorly controlled with metformin monotherapy: a randomized double-blind trial of saxagliptin plus dapagliflozin addition versus single addition of saxagliptin or dapagliflozin to metformin. Diabetes Care 2015;38:376-83. http://dx.doi.org/10.2337/dc14-1142.
- Ptaszynska A, Johnsson KM, Parikh SJ, de Bruin TW, Apanovitch AM, List JF. Safety profile of dapagliflozin for type 2 diabetes: pooled analysis of clinical studies for overall safety and rare events. Drug Saf 2014;37:815-29. http://dx.doi.org/10.1007/s40264-014-0213-4.
- Roden M, Weng J, Eilbracht J, Delafont B, Kim G, Woerle HJ, et al. Empagliflozin monotherapy improves glucose control in drug-naive patients with type 2 diabetes (type 2 diabetes). Diabetes 2013;62.
- Barnett AH, Mithal A, Manassie J, Jones R, Rattunde H, Woerle HJ, et al. EMPA-REG RENAL trial investigators . Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 2014;2:369-84. http://dx.doi.org/10.1016/S2213-8587(13)70208-0.
- DeFronzo RA, Lewin A, Patel S, Liu D, Kaste R, Woerle HJ, et al. Combination of empagliflozin and linagliptin as second-line therapy in subjects with type 2 diabetes inadequately controlled on metformin. Diabetes Care 2015;38:384-93. http://dx.doi.org/10.2337/dc14-2364.
- Rosenstock J, Jelaska A, Frappin G, Salsali A, Kim G, Woerle HJ, et al. EMPA-REG MDI Trial Investigators . Improved glucose control with weight loss, lower insulin doses, and no increased hypoglycemia with empagliflozin added to titrated multiple daily injections of insulin in obese inadequately controlled type 2 diabetes. Diabetes Care 2014;37:1815-23. http://dx.doi.org/10.2337/dc13-3055.
- Rosenstock J, Jelaska A, Zeller C, Kim G, Broedl UC, Woerle HJ. EMPA-REG BASALTM trial investigators . Impact of empagliflozin added on to basal insulin in type 2 diabetes inadequately controlled on basal insulin: a 78-week randomized, double-blind, placebo-controlled trial. Diabetes Obes Metab 2015;17:936-48. http://dx.doi.org/10.1111/dom.12503.
- Häring HU, Merker L, Seewaldt-Becker E, Weimer M, Meinicke T, Woerle HJ, et al. EMPA-REG METSU Trial Investigators . Empagliflozin as add-on to metformin plus sulfonylurea in patients with type 2 diabetes: a 24-week, randomized, double-blind, placebo-controlled trial. Diabetes Care 2013;36:3396-404. http://dx.doi.org/10.2337/dc12-2673.
- Häring HU, Merker L, Seewaldt-Becker E, Weimer M, Meinicke T, Broedl UC, et al. EMPA-REG MET Trial Investigators . Empagliflozin as add-on to metformin in patients with type 2 diabetes: a 24-week, randomized, double-blind, placebo-controlled trial. Diabetes Care 2014;37:1650-9. http://dx.doi.org/10.2337/dc13-2105.
- Haring HU, Merker L, Christiansen AV, Roux F, Salsali A, Kim G, et al. Empagliflozin (EMPA) for >76 weeks as add-on to metformin plus sulfonylurea (SU) in patients with type 2 diabetes (type 2 diabetes). Diabetes 2014;63.
- Merker L, Haring HU, Christiansen AV, Roux F, Salsali A, Kim G, et al. Empagliflozin as add-on to metformin in people with Type 2 diabetes. Diabet. Med 2015;32:1555-67. https://doi.org/10.1111/dme.12814.
- Ridderstråle M, Andersen KR, Zeller C, Kim G, Woerle HJ, Broedl UC. EMPA-REG H2H-SU trial investigators . Comparison of empagliflozin and glimepiride as add-on to metformin in patients with type 2 diabetes: a 104-week randomised, active-controlled, double-blind, phase 3 trial. Lancet Diabetes Endocrinol 2014;2:691-700. http://dx.doi.org/10.1016/S2213-8587(14)70120-2.
- Kovacs CS, Seshiah V, Swallow R, Jones R, Rattunde H, Woerle HJ, et al. EMPA-REG PIO™ trial investigators . Empagliflozin improves glycaemic and weight control as add-on therapy to pioglitazone or pioglitazone plus metformin in patients with type 2 diabetes: a 24-week, randomized, placebo-controlled trial. Diabetes Obes Metab 2014;16:147-58. http://dx.doi.org/10.1111/dom.12188.
- Kovacs CS, Seshiah V, Merker L, Christiansen AV, Roux F, Salsali A, et al. Empagliflozin as Add-on Therapy to Pioglitazone With or Without Metformin in Patients With Type 2 Diabetes Mellitus. Clin Ther 2015;37:1773-88.e1. http://dx.doi.org/10.1016/j.clinthera.2015.05.511.
- Nauck MA, Del Prato S, Meier JJ, Duran-Garcia S, Rohwedder K, Elze M, et al. Dapagliflozin versus glipizide as add-on therapy in patients with type 2 diabetes who have inadequate glycemic control with metformin: a randomized, 52-week, double-blind, active-controlled noninferiority trial. Diabetes Care 2011;34:2015-22. https://doi.org/10.2337/dc11-0606.
- Gangal NS, Kelton C, Heaton PC. Urinary tract infection among the SGLT 2 Inhibitors: a meta-Analysis of 19 randomized controlled trials. Value Health 2015;18. https://doi.org/10.1016/j.jval.2015.03.308.
- European Medicines Agency (EMA) . Review of Diabetes Medicines Called SGLT2 Inhibitors Started 2015. www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/SGLT2_inhibitors/human_referral_prac_000052.jsp&mid=WC0b01ac05805c516f (accessed 4 September 2015).
- US Food and Drug Administration (FDA) . FDA Drug Safety Communication: FDA Warns That SGLT2 Inhibitors for Diabetes May Result in a Serious Condition of Too Much Acid in the Blood 2015. www.fda.gov/drugs/drugsafety/ucm446845.htm (accessed 4 September 2015).
- Erondu N, Desai M, Ways K, Meininger G. Diabetic Ketoacidosis and Related Events in the Canagliflozin Type 2 Diabetes Clinical Program. Diabetes Care 2015;38:1680-6. http://dx.doi.org/10.2337/dc15-1251.
- Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care 2015;38:1638-42. https://doi.org/10.2337/dc15-1380.
- Srivali N, Thongprayoon C, Cheungpasitporn W, Ungprasert P. Acute pancreatitis in the use of canagliflozin: a rare side-effect of the novel therapy for type 2 diabetes mellitus. J Basic Clin Pharm 2015;6:101-2. http://dx.doi.org/10.4103/0976-0105.160753.
- Kaur A, Winters SJ. Severe hypercalcemia and hypernatremia in a patient treated with canagliflozin. Endocrinol Diabetes Metab Case Rep 2015. http://dx.doi.org/10.1530/EDM-15-0042.
- US Food and Drug Administration (FDA) . MedWatch: The FDA Safety Information and Adverse Event Reporting Program 2015. www.fda.gov/Drugs/DrugSafety/ucm459579.htm (accessed 4 September 2015).
- Wilding JP. The role of the kidneys in glucose homeostasis in type 2 diabetes: clinical implications and therapeutic significance through sodium glucose co-transporter 2 inhibitors. Metab Clin Exp 2014;63:1228-37. http://dx.doi.org/10.1016/j.metabol.2014.06.018.
- Janssen Research & Development LLC . CANVAS – CANagliflozin CardioVascular Assessment Study 2015. https://clinicaltrials.gov/ct2/show/NCT01032629 (accessed 4 September 2015).
- AstraZeneca . Multicenter Trial to Evaluate the Effect of Dapagliflozin on the Incidence of Cardiovascular Events (DECLARE-TIMI58) 2015. https://clinicaltrials.gov/ct2/show/NCT01730534 (accessed 4 September 2015).
- Tahrani AA, Barnett AH, Bailey CJ. SGLT inhibitors in management of diabetes. Lancet Diabetes Endocrinol 2013;1:140-51. http://dx.doi.org/10.1016/S2213-8587(13)70050-0.
- US Food and Drug Administration (FDA) . FDA Drug Safety Communication: FDA Revises Label of Diabetes Drug Canagliflozin (Invokana, Invokamet) to Include Updates on Bone Fracture Risk and New Information on Decreased Bone Mineral Density 2015. www.fda.gov/Drugs/DrugSafety/ucm461449.htm (accessed 27 September 2015).
- Kohan DE, Fioretto P, Tang W, List JF. Long-term study of patients with type 2 diabetes and moderate renal impairment shows that dapagliflozin reduces weight and blood pressure but does not improve glycemic control. Kidney Int 2014;85:962-71. https://doi.org/10.1038/ki.2013.356.
- Kwon H. US Food and Drug Administration (FDA) . Canagliflozin: Clinical Efficacy and Safety 2013. www.fda.gov/downloads/advisorycommittees/committeesmeetingmaterials/drugs/endocrinologicandmetabolicdrugsadvisorycommittee/ucm336234.pdf (accessed August 2005).
- Taylor SI, Blau JE, Rother KI. SGLT2 Inhibitors may predispose to ketoacidosis. J Clin Endocrinol Metab 2015;100:2849-52. http://dx.doi.org/10.1210/jc.2015-1884.
- Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117-28. http://dx.doi.org/10.1056/NEJMoa1504720.
- Zinman B, Inzucchi SE, Lachin JM, Wanner C, Ferrari R, Fitchett D, et al. Rationale, design, and baseline characteristics of a randomized, placebo-controlled cardiovascular outcome trial of empagliflozin (EMPA-REG OUTCOME™). Cardiovasc Diabetol 2014;13. http://dx.doi.org/10.1186/1475-2840-13-102.
- UK Prospective Diabetes Study (UKPDS) Group . Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703-13. https://doi.org/10.1136/bmj.317.7160.703.
- Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000;342:145-53. http://dx.doi.org/10.1056/NEJM200001203420301.
- Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 2013;369:1317-26. http://dx.doi.org/10.1056/NEJMoa1307684.
- White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med 2013;369:1327-35. http://dx.doi.org/10.1056/NEJMoa1305889.
- Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015;373:232-42. http://dx.doi.org/10.1056/NEJMoa1501352.
- Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med 2007;356:2457-71. http://dx.doi.org/10.1056/NEJMoa072761.
- Hirshberg B, Katz A. Insights from cardiovascular outcome trials with novel antidiabetes agents: what have we learned? An industry perspective. Curr Diab Rep 2015;15. http://dx.doi.org/10.1007/s11892-015-0663-9.
- Indianapolis Business Journal . Analyst: Lilly’s Jardiance Diabetes Pill Could Be a $6 Billion-a-Year Blockbuster 2015. www.ibj.com/blogs/12-the-dose/post/54957-analyst-lillys-jardiance-diabetes-pill-could-be-a-6-billion-a-year-blockbuster (accessed 25 September 2015).
- Abbatecola AM, Rizzo MR, Barbieri M, Grella R, Arciello A, Laieta MT, et al. Postprandial plasma glucose excursions and cognitive functioning in aged type 2 diabetics. Neurology 2006;67:235-40. http://dx.doi.org/10.1212/01.wnl.0000224760.22802.e8.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; n.d.
- Jovanovic L, Dailey G, Huang WC, Strange P, Goldstein BJ. Repaglinide in type 2 diabetes: a 24-week, fixed-dose efficacy and safety study. J Clin Pharmacol 2000;40:49-57. https://doi.org/10.1177/00912700022008694.
- Saleem K, Yasin MA, Asrar A, Qamar S. Comparison of repaglinide with glibenclamide in the reduction of 13 HbA1C of type 2 diabetic patients. Pak J Med Health Sci 2011;5:23-6.
- Shah ZH, Saleem K, Mahboob F, Jibran R. A comparative study of repaglinide and glibenclamide in type 2 diabetic patients. Pak J Med Health Sci 2011;5:476-9.
- Jibran R, Suliman M, Qureshi F, Ahmed M. Safety and efficacy of repaglinide compared with glibenclamide in the management of type 2 diabetic Pakistani patients. Pak J Med Sci 2006;22:385-90.
- Derosa G, Mugellini A, Ciccarelli L, Crescenzi G, Fogari R. Comparison between repaglinide and glimepiride in patients with type 2 diabetes mellitus: a one-year, randomized, double-blind assessment of metabolic parameters and cardiovascular risk factors. Clin Ther 2003;25:472-84. https://doi.org/10.1016/S0149-2918(03)80090-5.
- Marbury T, Huang WC, Strange P, Lebovitz H. Repaglinide versus glyburide: a one-year comparison trial. Diabetes Res Clin Pract 1999;43:155-66. https://doi.org/10.1016/S0168-8227(99)00002-9.
- Aschner P, Kipnes MS, Lunceford JK, Sanchez M, Mickel C, Williams-Herman DE. Sitagliptin Study 021 Group . Effect of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care 2006;29:2632-7. http://dx.doi.org/10.2337/dc06-0703.
- Chen Y, Ning G, Wang C, Gong Y, Patel S, Zhang C, et al. Efficacy and safety of linagliptin monotherapy in Asian patients with inadequately controlled type 2 diabetes mellitus: a multinational, 24-week, randomized, clinical trial. J Diabetes Investig 2015;6:692-8. http://dx.doi.org/10.1111/jdi.12346.
- Dejager S, Razac S, Foley JE, Schweizer A. Vildagliptin in drug-naïve patients with type 2 diabetes: a 24-week, double-blind, randomized, placebo-controlled, multiple-dose study. Horm Metab Res 2007;39:218-23. https://doi.org/10.1055/s-2007-970422.
- Del Prato S, Barnett AH, Huisman H, Neubacher D, Woerle HJ, Dugi KA. Effect of linagliptin monotherapy on glycaemic control and markers of β-cell function in patients with inadequately controlled type 2 diabetes: a randomized controlled trial. Diabetes Obes Metab 2011;13:258-67. http://dx.doi.org/10.1111/j.1463-1326.2010.01350.x.
- Erem C, Ozbas HM, Nuhoglu I, Deger O, Civan N, Ersoz HO. Comparison of effects of gliclazide, metformin and pioglitazone monotherapies on glycemic control and cardiovascular risk factors in patients with newly diagnosed uncontrolled type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes 2014;122:295-302. http://dx.doi.org/10.1055/s-0034-1370989.
- Foley JE, Sreenan S. Efficacy and safety comparison between the DPP-4 inhibitor vildagliptin and the sulfonylurea gliclazide after two years of monotherapy in drug-naïve patients with type 2 diabetes. Horm Metab Res 2009;41:905-9. http://dx.doi.org/10.1055/s-0029-1234042.
- Haak T, Meinicke T, Jones R, Weber S, von Eynatten M, Woerle HJ. Initial combination of linagliptin and metformin improves glycaemic control in type 2 diabetes: a randomized, double-blind, placebo-controlled study. Diabetes Obes Metab 2012;14:565-74. http://dx.doi.org/10.1111/j.1463-1326.2012.01590.x.
- Kikuchi M, Kaku K, Odawara M, Momomura S, Ishii R. Efficacy and tolerability of rosiglitazone and pioglitazone in drug-naïve Japanese patients with type 2 diabetes mellitus: a double-blind, 28 weeks’ treatment, comparative study. Curr Med Res Opin 2012;28:1007-16. http://dx.doi.org/10.1185/03007995.2012.694361.
- Lawrence JM, Reid J, Taylor GJ, Stirling C, Reckless JP. Favorable effects of pioglitazone and metformin compared with gliclazide on lipoprotein subfractions in overweight patients with early type 2 diabetes. Diabetes Care 2004;27:41-6. https://doi.org/10.2337/diacare.27.1.41.
- Miyazaki Y, Matsuda M, DeFronzo RA. Dose-response effect of pioglitazone on insulin sensitivity and insulin secretion in type 2 diabetes. Diabetes Care 2002;25:517-23.
- Veroniki AA, Vasiliadis HS, Higgins JP, Salanti G. Evaluation of inconsistency in networks of interventions. Int J Epidemiol 2013;42:332-45. http://dx.doi.org/10.1093/ije/dys222.
- Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med 2010;29:932-44. http://dx.doi.org/10.1002/sim.3767.
- Brooks SP, Gelman A. Alternative methods for monitoring convergence of iterative simulations. J Comp Graph Stat 1998;7:434-5.
- Kim YG, Hahn S, Oh TJ, Kwak SH, Park KS, Cho YM. Differences in the glucose-lowering efficacy of dipeptidyl peptidase-4 inhibitors between Asians and non-Asians: a systematic review and meta-analysis. Diabetologia 2013;56:696-708. http://dx.doi.org/10.1007/s00125-012-2827-3.
- De Fine Olivarius N, Andreasen AH, Siersma V, Richelsen B, Beck-Nielsen H. Changes in patient weight and the impact of antidiabetic therapy during the first 5 years after diagnosis of diabetes mellitus. Diabetologia 2006;49:2058-67. https://doi.org/10.1007/s00125-006-0328-y.
- Genuth S. Response to comment on Genuth. Should sulfonylureas remain an acceptable first-line add-on to metformin therapy in patients with type 2 diabetes? No, it’s time to move on! Diabetes Care 2015;38:170–5. Diabetes Care 2015;38. http://dx.doi.org/10.2337/dc15-0519.
- Hirst JA, Farmer AJ, Dyar A, Lung TW, Stevens RJ. Estimating the effect of sulfonylurea on HbA1c in diabetes: a systematic review and meta-analysis. Diabetologia 2013;56:973-84. http://dx.doi.org/10.1007/s00125-013-2856-6.
- Feinglos M, Dailey G, Cefalu W, Osei K, Tayek J, Canovatchel W, et al. Effect on glycemic control of the addition of 2.5 mg glipizide GITS to metformin in patients with T2DM. Diabetes Res Clin Pract 2005;68:167-75. http://dx.doi.org/10.1016/j.diabres.2004.09.002.
- Cook MN, Girman CJ, Stein PP, Alexander CM, Holman RR. Glycemic control continues to deteriorate after sulfonylureas are added to metformin among patients with type 2 diabetes. Diabetes Care 2005;28:995-1000. https://doi.org/10.2337/diacare.28.5.995.
- Del Prato S, Nauck M, Durán-Garcia S, Maffei L, Rohwedder K, Theuerkauf A, et al. Long-term glycaemic response and tolerability of dapagliflozin versus a sulphonylurea as add-on therapy to metformin in patients with type 2 diabetes: 4-year data. Diabetes Obes Metab 2015;17:581-90. http://dx.doi.org/10.1111/dom.12459.
- Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med 2006;355:2427-43. http://dx.doi.org/10.1056/NEJMoa066224.
- Bacon T, Willis M, Johansen P, Neslusan C. Time until insulin initiation for canagliflozin (CANA) versus dapagliflozin (DAPA) in dual and triple therapy for type 2 diabetes mellitus (T2DM) in Ireland. Value Health 2015;18. https://doi.org/10.1016/j.jval.2015.03.324.
- Scott R, Loeys T, Davies MJ, Engel SS. Efficacy and safety of sitagliptin when added to ongoing metformin therapy in patients with type 2 diabetes. Diabetes Obes Metab 2008;10:959-69. https://doi.org/10.1111/j.1463-1326.2007.00839.x.
- Nauck MA, Meininger G, Sheng D, Terranella L, Stein PP. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, in patients with type 2 diabetes inadequately controlled on metformin alone: a randomized, double-blind, non-inferiority trial. Diabetes Obes Metab 2007;9:194-205. https://doi.org/10.1111/j.1463-1326.2006.00704.x.
- Canadian Agency for Drugs and Technologies in Health (CADTH) . Second- and Third-Line Pharmacotherapy for Type 2 Diabetes 2013. www.ncbi.nlm.nih.gov/pubmedhealth/PMH0061000 (accessed 7 September 2015).
- National Institute for Health and Care Excellence (NICE) . Exenatide Prolonged-Release Suspension for Injection in Combination With Oral Antidiabetic Therapy for the Treatment of Type 2 Diabetes 2012. www.nice.org.uk/guidance/ta248 (accessed August 2015).
- Drucker DJ, Buse JB, Taylor K, Kendall DM, Trautmann M, Zhuang D, et al. DURATION-1 Study Group . Exenatide once weekly versus twice daily for the treatment of type 2 diabetes: a randomised, open-label, non-inferiority study. Lancet 2008;372:1240-50. http://dx.doi.org/10.1016/S0140-6736(08)61206-4.
- Hattersley AT, Thorens B. Type 2 diabetes, SGLT2 inhibitors, and glucose secretion. N Engl J Med 2015;373:974-6. http://dx.doi.org/10.1056/NEJMcibr1506573.
- Donnan PT, MacDonald TM, Morris AD. Adherence to prescribed oral hypoglycaemic medication in a population of patients with type 2 diabetes: a retrospective cohort study. Diabet Med 2002;19:279-84. https://doi.org/10.1046/j.1464-5491.2002.00689.x.
- US Food and Drug Administration (FDA) . NDA 202293 Dapagliflozin Tablets, 5 and 10 mg 2011. www.fda.gov/DOWNLOADS/ADVISORYCOMMITTEES/COMMITTEESMEETINGMATERIALS/DRUGS/ENDOCRINOLOGICANDMETABOLICDRUGSADVISORYCOMMITTEE/UCM262994.PDF (accessed 2 October 2015).
- Ptaszynska A, Cohen SM, Messing EM, Reilly TP, Johnsson E, Johnsson K. Assessing Bladder Cancer Risk in Type 2 Diabetes Clinical Trials: the Dapagliflozin Drug Development Program as a ‘case study’. Diabetes Ther 2015;6:357-75. http://dx.doi.org/10.1007/s13300-015-0128-9.
- Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, et al. American Diabetes Association (ADA) . Medical management of hyperglycaemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia 2009;52:17-30. http://dx.doi.org/10.1007/s00125-008-1157-y.
- Schernthaner G, Barnett AH, Betteridge DJ, Carmena R, Ceriello A, Charbonnel B, et al. Is the ADA/EASD algorithm for the management of type 2 diabetes (January 2009) based on evidence or opinion? A critical analysis. Diabetologia 2010;53:1258-69. http://dx.doi.org/10.1007/s00125-010-1702-3.
- Rosenstock J, Wilson C, Fleck P. Alogliptin versus glipizide monotherapy in elderly type 2 diabetes mellitus patients with mild hyperglycaemia: a prospective, double-blind, randomized, 1-year study. Diabetes Obes Metab 2013;15:906-14. http://dx.doi.org/10.1111/dom.12102.
- Shihara N, Kitaoka M, Inagaki N, Kadowaki T, Koumoto S, Satoh J, et al. Randomized controlled trial of single-agent glimepiride and pioglitazone in Japanese patients with type 2 diabetes: a comparative study. J Diabetes Investig 2011;2:391-8. http://dx.doi.org/10.1111/j.2040-1124.2011.00115.x.
- Calvert MJ, McManus RJ, Freemantle N. Management of type 2 diabetes with multiple oral hypoglycaemic agents or insulin in primary care: retrospective cohort study. Br J Gen Pract 2007;57:455-60.
- Rubino A, McQuay LJ, Gough SC, Kvasz M, Tennis P. Delayed initiation of subcutaneous insulin therapy after failure of oral glucose-lowering agents in patients with type 2 diabetes: a population-based analysis in the UK. Diabet Med 2007;24:1412-18. http://dx.doi.org/10.1111/j.1464-5491.2007.02279.x.
- Health and Social Care Information Centre . Quality and Outcomes Framework (QOF) 2015. http://qof.hscic.gov.uk/ (accessed 27 September 2015).
- Neslusan C, Johansen P, Willis M, Martin S. A health economic analysis of the long-term benefits and associated cost offsets of canagliflozin monotherapy in the U.S. Diabetes 2013;62.
- Clarke PM, Gray AM, Briggs A, Farmer AJ, Fenn P, Stevens RJ, et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia 2004;47:1747-59. https://doi.org/10.1007/s00125-004-1527-z.
- Hayes AJ, Leal J, Gray AM, Holman RR, Clarke PM. UKPDS Outcomes Model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study: UKPDS 82. Diabetologia 2013;56:1925-33. http://dx.doi.org/10.1007/s00125-013-2940-y.
- Alva ML, Gray A, Mihaylova B, Leal J, Holman RR. The impact of diabetes-related complications on healthcare costs: new results from the UKPDS (UKPDS 84). Diabet Med 2015;32:459-66. http://dx.doi.org/10.1111/dme.12647.
- Clarke P, Gray A, Legood R, Briggs A, Holman R. The impact of diabetes-related complications on healthcare costs: results from the United Kingdom Prospective Diabetes Study (UKPDS study no. 65). Diabet Med 2003;20:442-50. https://doi.org/10.1046/j.1464-5491.2003.00972.x.
- Alva M, Gray A, Mihaylova B, Clarke P. The effect of diabetes complications on health-related quality of life: the importance of longitudinal data to address patient heterogeneity. Health Econ 2014;23:487-500. http://dx.doi.org/10.1002/hec.2930.
- Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Making 2002;22:340-9. https://doi.org/10.1177/027298902400448902.
- Bagust A, Beale S. Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Econ 2005;14:217-30. http://dx.doi.org/10.1002/hec.910.
- University College London . THIN Database n.d. www.ucl.ac.uk/pcph/research-groups-themes/thin-pub/database (accessed 2 December 2016).
- Monami M, Marchionni N, Mannucci E. Long-acting insulin analogues vs. NPH human insulin in type 1 diabetes. A meta-analysis. Diabetes Obes Metab 2009;11:372-8. http://dx.doi.org/10.1111/j.1463-1326.2008.00976.x.
- Waugh N, Cummins E, Royle P, Clar C, Marien M, Richter B, et al. Newer agents for blood glucose control in type 2 diabetes: systematic review and economic evaluation. Health Technol Assess 2010;14. http://dx.doi.org/10.3310/hta14360.
- Department of Health (DH) . Health Survey for England 2003 2004. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/publicationsandstatistics/publications/publicationsstatistics/dh_4098712 (accessed 1 October 2015).
- Currie CJ, Morgan CL, Poole CD, Sharplin P, Lammert M, McEwan P. Multivariate models of health-related utility and the fear of hypoglycaemia in people with diabetes. Curr Med Res Opin 2006;22:1523-34. https://doi.org/10.1185/030079906X115757.
- Barry HC, Ebell MH, Hickner J. Evaluation of suspected urinary tract infection in ambulatory women: a cost-utility analysis of office-based strategies. J Fam Pract 1997;44:49-60.
- Baboolal K, McEwan P, Sondhi S, Spiewanowski P, Wechowski J, Wilson K. The cost of renal dialysis in a UK setting: a multicentre study. Nephrol Dial Transplant 2008;23:1982-9. http://dx.doi.org/10.1093/ndt/gfm870.
- Hammer M, Lammert M, Mejías SM, Kern W, Frier BM. Costs of managing severe hypoglycaemia in three European countries. J Med Econ 2009;12:281-90. http://dx.doi.org/10.3111/13696990903336597.
- Curtis L. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2014.
- Chen J, Alemao E, Yin D, Cook J. Development of a diabetes treatment simulation model: with application to assessing alternative treatment intensification strategies on survival and diabetes-related complications. Diabetes Obes Metab 2008;10:33-42. https://doi.org/10.1111/j.1463-1326.2008.00885.x.
- Palmer AJ, Roze S, Valentine WJ, Minshall ME, Foos V, Lurati FM. The CORE Diabetes Model: Projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin 2004;20:5-26. https://doi.org/10.1185/030079904X1980.
- National Institute for Health and Care Excellence (NICE) . Obesity Prevention 2006. www.nice.org.uk/guidance/cg43 (accessed 1 August 2015).
- Diabetics With Eating Disorders (DWED) . Diabetes and DKA in England’s Primary Care Trusts 2010. http://dwed.org.uk/sites/default/files/DwedReportDKAPCT.pdf (accessed 20 September 2015).
- Kiberd BA, Jindal KK. Screening to prevent renal failure in insulin dependent diabetic patients: an economic evaluation. BMJ 1995;311:1595-9. https://doi.org/10.1136/bmj.311.7020.1595.
- Matza LS, Boye KS, Yurgin N, Brewster-Jordan J, Mannix S, Shorr JM, et al. Utilities and disutilities for type 2 diabetes treatment-related attributes. Qual Life Res 2007;16:1251-65. https://doi.org/10.1007/s11136-007-9226-0.
- National Institute for Health and Care Excellence (NICE) . Infection: Prevention and Control of Healthcare-Associated Infections in Primary and Community Care 2012. www.nice.org.uk/guidance/cg139/documents (accessed 21 September 2015).
- Gold MR, Franks P, McCoy KI, Fryback DG. Toward consistency in cost-utility analyses: using national measures to create condition-specific values. Med Care 1998;36:778-92. https://doi.org/10.1097/00005650-199806000-00002.
- Ackerman SJ, Rein AL, Blute M, Beusterien K, Sullivan EM, Tanio CP, et al. Cost effectiveness of microwave thermotherapy in patients with benign prostatic hyperplasia: part I-methods. Urology 2000;56:972-80. https://doi.org/10.1016/S0090-4295(00)00828-1.
- Ellis AK, Verma S. Quality of life in women with urinary tract infections: is benign disease a misnomer?. J Am Board Fam Pract 2000;13:392-7. https://doi.org/10.3122/15572625-13-6-392.
- Ara R, Brazier J. Deriving an algorithm to convert the eight mean SF-36 dimension scores into a mean EQ-5D preference-based score from published studies (where patient level data are not available). Value Health 2008;11:1131-43. http://dx.doi.org/10.1111/j.1524-4733.2008.00352.x.
- Ernst EJ, Ernst ME, Hoehns JD, Bergus GR. Women’s quality of life is decreased by acute cystitis and antibiotic adverse effects associated with treatment. Health Qual Life Outcomes 2005;3. http://dx.doi.org/10.1186/1477-7525-3-45.
- Lamping DL, Constantinovici N, Roderick P, Normand C, Henderson L, Harris S, et al. Clinical outcomes, quality of life, and costs in the North Thames Dialysis Study of elderly people on dialysis: a prospective cohort study. Lancet 2000;356:1543-50. https://doi.org/10.1016/S0140-6736(00)03123-8.
- Aas AM, Bergstad I, Thorsby PM, Johannesen O, Solberg M, Birkeland KI. An intensified lifestyle intervention programme may be superior to insulin treatment in poorly controlled type 2 diabetic patients on oral hypoglycaemic agents: results of a feasibility study. Diabet Med 2005;22:316-22. http://dx.doi.org/10.1111/j.1464-5491.2005.01421.x.
- Coppell KJ, Kataoka M, Williams SM, Chisholm AW, Vorgers SM, Mann JI. Nutritional intervention in patients with type 2 diabetes who are hyperglycaemic despite optimised drug treatment – Lifestyle Over and Above Drugs in Diabetes (LOADD) study: randomised controlled trial. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c3337.
- National Institute for Health and Care Excellence (NICE) . Obesity: Identification, Assessment and Management of Overweight and Obesity in ChIldren, Young People and Adults n.d. www.nice.org.uk/guidance/cg189 (accessed 2 October 2015).
- Li Y, Xu W, Liao Z, Yao B, Chen X, Huang Z, et al. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients is associated with improvement of beta-cell function. Diabetes Care 2004;27:2597-602. https://doi.org/10.2337/diacare.27.11.2597.
- Yang W, Weng J. Early therapy for type 2 diabetes in China. Lancet Diabetes Endocrinol 2014;2:992-1002. http://dx.doi.org/10.1016/S2213-8587(14)70136-6.
- Kramer CK, Zinman B, Retnakaran R. Short-term intensive insulin therapy in type 2 diabetes mellitus: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2013;1:28-34. http://dx.doi.org/10.1016/S2213-8587(13)70006-8.
- Ilkova H, Glaser B, Tunçkale A, Bagriaçik N, Cerasi E. Induction of long-term glycemic control in newly diagnosed type 2 diabetic patients by transient intensive insulin treatment. Diabetes Care 1997;20:1353-6. https://doi.org/10.2337/diacare.20.9.1353.
- Ryan EA, Imes S, Wallace C. Short-term intensive insulin therapy in newly diagnosed type 2 diabetes. Diabetes Care 2004;27:1028-32. https://doi.org/10.2337/diacare.27.5.1028.
- Brown JB, Conner C, Nichols GA. Secondary failure of metformin monotherapy in clinical practice. Diabetes Care 2010;33:501-6. http://dx.doi.org/10.2337/dc09-1749.
- Abdul-Ghani MA, Puckett C, Triplitt C, Maggs D, Adams J, Cersosimo E, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT): a randomized trial. Diabetes Obes Metab 2015;17:268-75. http://dx.doi.org/10.1111/dom.12417.
- Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 2011;54:2506-14. http://dx.doi.org/10.1007/s00125-011-2204-7.
- Steven S, Taylor R. Restoring normoglycaemia by use of a very low calorie diet in long- and short-duration type 2 diabetes. Diabet Med 2015;32:1149-55. http://dx.doi.org/10.1111/dme.12722.
- Gillett M, Royle P, Snaith A, Scotland G, Poobalan A, Imamura M, et al. Non-pharmacological interventions to reduce the risk of diabetes in people with impaired glucose regulation: a systematic review and economic evaluation. Health Technol Assess 2012;16. http://dx.doi.org/10.3310/hta16330.
- Perri MG, Anton SD, Durning PE, Ketterson TU, Sydeman SJ, Berlant NE, et al. Adherence to exercise prescriptions: effects of prescribing moderate versus higher levels of intensity and frequency. Health Psychol 2002;21:452-8. https://doi.org/10.1037/0278-6133.21.5.452.
- Hansen D, Dendale P, Jonkers RA, Beelen M, Manders RJ, Corluy L, et al. Continuous low- to moderate-intensity exercise training is as effective as moderate- to high-intensity exercise training at lowering blood HbA(1c) in obese type 2 diabetes patients. Diabetologia 2009;52:1789-97. http://dx.doi.org/10.1007/s00125-009-1354-3.
- Yates T, Davies M, Gorely T, Bull F, Khunti K. Effectiveness of a pragmatic education program designed to promote walking activity in individuals with impaired glucose tolerance: a randomized controlled trial. Diabetes Care 2009;32:1404-10. http://dx.doi.org/10.2337/dc09-0130.
- Hawley JA, Gibala MJ. Exercise intensity and insulin sensitivity: how low can you go?. Diabetologia 2009;52:1709-13. http://dx.doi.org/10.1007/s00125-009-1425-5.
- Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care 2006;29:2518-27. https://doi.org/10.2337/dc06-1317.
- Praet SF, van Loon LJ. Exercise therapy in type 2 diabetes. Acta Diabetol 2009;46:263-78. http://dx.doi.org/10.1007/s00592-009-0129-0.
- Zanuso S, Jimenez A, Pugliese G, Corigliano G, Balducci S. Exercise for the management of type 2 diabetes: a review of the evidence. Acta Diabetol 2010;47:15-22. http://dx.doi.org/10.1007/s00592-009-0126-3.
- National Institute for Health and Care Excellence (NICE) . Weight Management: Lifestyle Services for Overweight or Obese Adults 2014. www.nice.org.uk/guidance/ph53 (accessed 2 October 2015).
- Cobiac LJ, Vos T, Barendregt JJ. Cost-effectiveness of interventions to promote physical activity: a modelling study. PLOS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000110.
- Fujioka K. Benefits of moderate weight loss in patients with type 2 diabetes. Diabetes Obes Metab 2010;12:186-94. http://dx.doi.org/10.1111/j.1463-1326.2009.01155.x.
- Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011;34:1481-6. http://dx.doi.org/10.2337/dc10-2415.
- Anderson JW, Kendall CW, Jenkins DJ. Importance of weight management in type 2 diabetes: review with meta-analysis of clinical studies. J Am Coll Nutr 2003;22:331-9. https://doi.org/10.1080/07315724.2003.10719316.
- Jacobs-van der Bruggen MA, van Baal PH, Hoogenveen RT, Feenstra TL, Briggs AH, Lawson K, et al. Cost-effectiveness of lifestyle modification in diabetic patients. Diabetes Care 2009;32:1453-8. http://dx.doi.org/10.2337/dc09-0363.
- Bailey CJ, Iqbal N, T’joen C, List JF. Dapagliflozin monotherapy in drug-naïve patients with diabetes: a randomized-controlled trial of low-dose range. Diabetes Obes Metab 2012;14:951-9. http://dx.doi.org/10.1111/j.1463-1326.2012.01659.x.
- Berhan A, Barker A. Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord 2013;13. http://dx.doi.org/10.1186/1472-6823-13-58.
- Blüher M, Schweizer A, Bader G, Foley JE. Changes in body weight after 24 weeks of vildagliptin therapy as a function of fasting glucose levels in patients with type 2 diabetes. Vasc Health Risk Manag 2014;10:661-4. http://dx.doi.org/10.2147/VHRM.S73608.
- Brand T, Macha S, Mattheus M, Pinnetti S, Woerle HJ. Pharmacokinetics of empagliflozin, a sodium glucose cotransporter-2 (SGLT-2) inhibitor, coadministered with sitagliptin in healthy volunteers. Adv Ther 2012;29:889-99. http://dx.doi.org/10.1007/s12325-012-0055-3.
- Escudero Vilaplana B, Almodóvar Carretón MJ, Herrero Hernández S. Dapagliflozin, a novel oral antidiabetic with an uncertain future. Farm Hosp 2014;38:468-74. http://dx.doi.org/10.7399/fh.2014.38.6.7963.
- Ferrannini E, Berk A, Hantel S, Pinnetti S, Hach T, Woerle HJ, et al. Long-term safety and efficacy of empagliflozin, sitagliptin, and metformin: an active-controlled, parallel-group, randomized, 78-week open-label extension study in patients with type 2 diabetes. Diabetes Care 2013;36:4015-21. http://dx.doi.org/10.2337/dc13-0663.
- Goring S, Hawkins N, Wygant G, Roudaut M, Townsend R, Wood I, et al. Dapagliflozin compared with other oral anti-diabetes treatments when added to metformin monotherapy: a systematic review and network meta-analysis. Diabetes Obes Metab 2014;16:433-42. http://dx.doi.org/10.1111/dom.12239.
- Henry RR, Murray AV, Marmolejo MH, Hennicken D, Ptaszynska A, List JF. Dapagliflozin, metformin XR, or both: initial pharmacotherapy for type 2 diabetes, a randomised controlled trial. Int J Clin Pract 2012;66:446-56. http://dx.doi.org/10.1111/j.1742-1241.2012.02911.x.
- Hussey EK, Kapur A, O’Connor-Semmes R, Tao W, Rafferty B, Polli JW, et al. Safety, pharmacokinetics and pharmacodynamics of remogliflozin etabonate, a novel SGLT2 inhibitor, and metformin when co-administered in subjects with type 2 diabetes mellitus. BMC Pharmacol Toxicol 2013;14. http://dx.doi.org/10.1186/2050-6511-14-25.
- Johnsson KM, Ptaszynska A, Schmitz B, Sugg J, Parikh SJ, List JF. Vulvovaginitis and balanitis in patients with diabetes treated with dapagliflozin. J Diabetes Complicat 2013;27:479-84. http://dx.doi.org/10.1016/j.jdiacomp.2013.04.012.
- Kadowaki T, Haneda M, Inagaki N, Terauchi Y, Taniguchi A, Koiwai K, et al. Empagliflozin monotherapy in Japanese patients with type 2 diabetes mellitus: a randomized, 12-week, double-blind, placebo-controlled, phase II trial. Adv Ther 2014;31:621-38. http://dx.doi.org/10.1007/s12325-014-0126-8.
- Kaku K, Watada H, Iwamoto Y, Utsunomiya K, Terauchi Y, Tobe K, et al. Efficacy and safety of monotherapy with the novel sodium/glucose cotransporter-2 inhibitor tofogliflozin in Japanese patients with type 2 diabetes mellitus: a combined Phase 2 and 3 randomized, placebo-controlled, double-blind, parallel-group comparative study. Cardiovasc Diabetol 2014;13. http://dx.doi.org/10.1186/1475-2840-13-65.
- Lutz SZ, Staiger H, Fritsche A, Häring HU. Antihyperglycaemic therapies and cancer risk. Diab Vasc Dis Res 2014;11:371-89. http://dx.doi.org/10.1177/1479164114549553.
- Matthaei S. Canagliflozin monotherapy: clinical study data in type 2 diabetes mellitus. Dtsch Med Wochenschr 2014;139:59-64. https://doi.org/10.1055/s-0033-1359992.
- Nauck M, del Prato S, Meier JJ, Durán-García S, Rohwedder K, Elze M, et al. Dapagliflozin versus glipizide as add-on therapy in patients with type 2 diabetes who have inadequate glycemic control with metformin. Dtsch Med Wochenschr 2013;138:6-15. http://dx.doi.org/10.1055/s-0032-1305283.
- Orme M, Fenici P, Lomon ID, Wygant G, Townsend R, Roudaut M. A systematic review and mixed-treatment comparison of dapagliflozin with existing anti-diabetes treatments for those with type 2 diabetes mellitus inadequately controlled by sulfonylurea monotherapy. Diabetol Metab Syndr 2014;6. http://dx.doi.org/10.1186/1758-5996-6-73.
- Pafili K, Papanas N. Tofogliflozin: the road goes ever on. Expert Opin Pharmacother 2014;15:1197-201. http://dx.doi.org/10.1517/14656566.2014.916278.
- Phung OJ, Sobieraj DM, Engel SS, Rajpathak SN. Early combination therapy for the treatment of type 2 diabetes mellitus: systematic review and meta-analysis. Diabetes Obes Metab 2014;16:410-17. http://dx.doi.org/10.1111/dom.12233.
- Plosker GL. Dapagliflozin: a review of its use in type 2 diabetes mellitus. Drugs 2012;72:2289-312. http://dx.doi.org/10.2165/11209910-000000000-00000.
- Plosker GL. Canagliflozin: a review of its use in patients with type 2 diabetes mellitus. Drugs 2014;74:807-24. http://dx.doi.org/10.1007/s40265-014-0225-5.
- Polidori D, Mari A, Ferrannini E. Canagliflozin, a sodium glucose co-transporter 2 inhibitor, improves model-based indices of beta cell function in patients with type 2 diabetes. Diabetologia 2014;57:891-90. http://dx.doi.org/10.1007/s00125-014-3196-x.
- Raskin P. Sodium-glucose cotransporter inhibition: therapeutic potential for the treatment of type 2 diabetes mellitus. Diabetes Metab Res Rev 2013;29:347-56. https://doi.org/10.1002/dmrr.2403.
- Rosenstock J, Aggarwal N, Polidori D, Zhao Y, Arbit D, Usiskin K, et al. Dose-ranging effects of canagliflozin, a sodium-glucose cotransporter 2 inhibitor, as add-on to metformin in subjects with type 2 diabetes. Diabetes Care 2012;35:1232-8. http://dx.doi.org/10.2337/dc11-1926.
- Rosenstock J, Vico M, Wei L, Salsali A, List JF. Effects of dapagliflozin, an SGLT2 inhibitor, on HbA(1c), body weight, and hypoglycemia risk in patients with type 2 diabetes inadequately controlled on pioglitazone monotherapy. Diabetes Care 2012;35:1473-8. http://dx.doi.org/10.2337/dc11-1693.
- Rosenstock J, Seman LJ, Jelaska A, Hantel S, Pinnetti S, Hach T, et al. Efficacy and safety of empagliflozin, a sodium glucose cotransporter 2 (SGLT2) inhibitor, as add-on to metformin in type 2 diabetes with mild hyperglycaemia. Diabetes Obes Metab 2013;15:1154-60. http://dx.doi.org/10.1111/dom.12185.
- Scheen AJ. Pharmacodynamics, efficacy and safety of sodium-glucose co-transporter type 2 (SGLT2) inhibitors for the treatment of type 2 diabetes mellitus. Drugs 2015;75:33-59. http://dx.doi.org/10.1007/s40265-014-0337-y.
- Seino Y, Sasaki T, Fukatsu A, Sakai S, Samukawa Y. Efficacy and safety of luseogliflozin monotherapy in Japanese patients with type 2 diabetes mellitus: a 12-week, randomized, placebo-controlled, phase II study. Curr Med Res Opin 2014;30:1219-30. https://doi.org/10.1185/03007995.2014.901943.
- Seino Y, Sasaki T, Fukatsu A, Ubukata M, Sakai S, Samukawa Y. Efficacy and safety of luseogliflozin as monotherapy in Japanese patients with type 2 diabetes mellitus: a randomized, double-blind, placebo-controlled, phase 3 study. Curr Med Res Opin 2014;30:1245-55. http://dx.doi.org/10.1185/03007995.2014.912983.
- Seino Y, Sasaki T, Fukatsu A, Ubukata M, Sakai S, Samukawa Y. Dose-finding study of luseogliflozin in Japanese patients with type 2 diabetes mellitus: a 12-week, randomized, double-blind, placebo-controlled, phase II study. Curr Med Res Opin 2014;30:1231-44. http://dx.doi.org/10.1185/03007995.2014.909390.
- Strojek K, Yoon KH, Hruba V, Elze M, Langkilde AM, Parikh S. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride: a randomized, 24-week, double-blind, placebo-controlled trial. Diabetes Obes Metab 2011;13:928-38. https://doi.org/10.1111/j.1463-1326.2011.01434.x.
- Strojek K, Yoon KH, Hruba V, Elze M, Langkilde AM, Parikh S. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride. Dtsch Med Wochenschr 2013;138:16-2. http://dx.doi.org/10.1055/s-0032-1305277.
- Strojek K, Yoon KH, Hruba V, Sugg J, Langkilde AM, Parikh S. Dapagliflozin added to glimepiride in patients with type 2 diabetes mellitus sustains glycemic control and weight loss over 48 weeks: a randomized, double-blind, parallel-group, placebo-controlled trial. Diabetes Ther 2014;5:267-83. http://dx.doi.org/10.1007/s13300-014-0072-0.
- Usiskin K, Kline I, Fung A, Mayer C, Meininger G. Safety and tolerability of canagliflozin in patients with type 2 diabetes mellitus: pooled analysis of phase 3 study results. Postgrad Med 2014;126:16-34. http://dx.doi.org/10.3810/pgm.2014.05.2753.
- Wilding JP, Ferrannini E, Fonseca VA, Wilpshaar W, Dhanjal P, Houzer A. Efficacy and safety of ipragliflozin in patients with type 2 diabetes inadequately controlled on metformin: a dose-finding study. Diabetes Obes Metab 2013;15:403-9. http://dx.doi.org/10.1111/dom.12038.
- Yang XP, Lai D, Zhong XY, Shen HP, Huang YL. Efficacy and safety of canagliflozin in subjects with type 2 diabetes: systematic review and meta-analysis. Eur J Clin Pharmacol 2014;70:1149-58. http://dx.doi.org/10.1007/s00228-014-1730-x.
- Zambrowicz B, Ding ZM, Ogbaa I, Frazier K, Banks P, Turnage A, et al. Effects of LX4211, a dual SGLT1/SGLT2 inhibitor, plus sitagliptin on postprandial active GLP-1 and glycemic control in type 2 diabetes. Clin Ther 2013;35:273-85.e7. http://dx.doi.org/10.1016/j.clinthera.2013.01.010.
- Zhang M, Zhang L, Wu B, Song H, An Z, Li S. Dapagliflozin treatment for type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Metab Res Rev 2014;30:204-21. https://doi.org/10.1002/dmrr.2479.
- Aronoff S, Rosenblatt S, Braithwaite S, Egan JW, Mathisen AL, Schneider RL. Pioglitazone hydrochloride monotherapy improves glycemic control in the treatment of patients with type 2 diabetes: a 6-month randomized placebo-controlled dose-response study. The Pioglitazone 001 Study Group. Diabetes Care 2000;23:1605-11. https://doi.org/10.2337/diacare.23.11.1605.
- Barnett AH, Patel S, Harper R, Toorawa R, Thiemann S, von Eynatten M, et al. Linagliptin monotherapy in type 2 diabetes patients for whom metformin is inappropriate: an 18-week randomized, double-blind, placebo-controlled phase III trial with a 34-week active-controlled extension. Diabetes Obes Metab 2012;14:1145-54. http://dx.doi.org/10.1111/dom.12011.
- Barzilai N, Guo H, Mahoney EM, Caporossi S, Golm GT, Langdon RB, et al. Efficacy and tolerability of sitagliptin monotherapy in elderly patients with type 2 diabetes: a randomized, double-blind, placebo-controlled trial. Curr Med Res Opin 2011;27:1049-58. http://dx.doi.org/10.1185/03007995.2011.568059.
- Chou HS, Truitt KE, Moberly JB, Merante D, Choi Y, Mun Y, et al. A 26-week, placebo- and pioglitazone-controlled monotherapy study of rivoglitazone in subjects with type 2 diabetes mellitus. Diabetes Obes Metab 2012;14:1000-9. http://dx.doi.org/10.1111/j.1463-1326.2012.01631.x.
- Goldstein BJ, Feinglos MN, Lunceford JK, Johnson J, Williams-Herman DE. Sitagliptin 036 Study Group . Effect of initial combination therapy with sitagliptin, a dipeptidyl peptidase-4 inhibitor, and metformin on glycemic control in patients with type 2 diabetes. Diabetes Care 2007;30:1979-87. http://dx.doi.org/10.2337/dc07-0627.
- Kamel AN, Cetinarslan B, Uysal AR, Baskal N, Corapcioglu D, Tonyukuk V. Efficacy of monotherapy with acarbose, glibenclamide, gliclazide, metformin or placebo in NIDDM patients. Diabetologia 1997;40.
- Mohan V, Yang W, Son HY, Xu L, Noble L, Langdon RB, et al. Efficacy and safety of sitagliptin in the treatment of patients with type 2 diabetes in China, India, and Korea. Diabetes Res Clin Pract 2009;83:106-16. http://dx.doi.org/10.1016/j.diabres.2008.10.009.
- Moses R, Slobodniuk R, Boyages S, Colagiuri S, Kidson W, Carter J, et al. Effect of repaglinide addition to metformin monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care 1999;22:119-24. https://doi.org/10.2337/diacare.22.1.119.
- Moses RG, Gomis R, Frandsen KB, Schlienger JL, Dedov I. Flexible meal-related dosing with repaglinide facilitates glycemic control in therapy-naive type 2 diabetes. Diabetes Care 2001;24:11-5. https://doi.org/10.2337/diacare.24.1.11.
- Raz I, Hanefeld M, Xu L, Caria C, Williams-Herman D, Khatami H. Sitagliptin Study 023 Group . Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy in patients with type 2 diabetes mellitus. Diabetologia 2006;49:2564-71. https://doi.org/10.1007/s00125-006-0416-z.
- Scherbaum WA, Göke B. German Pioglitazone Study Group . Metabolic efficacy and safety of once-daily pioglitazone monotherapy in patients with type 2 diabetes: a double-blind, placebo-controlled study. Horm Metab Res 2002;34:589-95. http://dx.doi.org/10.1055/s-2002-35421.
Appendix 1 Search strategy
Clinical effectiveness searches
Searches for journal articles
Search strategy for Ovid MEDLINE (1946–February 16, 2015) and Ovid EMBASE (1974–February 16 2015)
-
(empagliflozin or canagliflozin or dapagliflozin or sodium glucose cotransporter 2 inhibitor* or sodium glucose co-transporter 2 inhibitor* or SGLT2 inhibitor* or SGLT-2 inhibitor*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
randomized controlled trial.pt.
-
random*.tw.
-
2 or 3
-
1 and 4
164 retrieved in MEDLINE and 239 in EMBASE.
There were no restrictions by language.
Weekly auto-alerts of both searches were then run from February 2015 until the end of August 2015 in MEDLINE, EMBASE and PubMed to check for newly emerging studies.
A total of 403 records were downloaded into EndNote, and after removal of duplicates, 246 unique records remained, of which 195 were excluded on the basis of title and abstract on the first screening. The full text of the 51 records remaining was obtained and a second screening was performed. Seven trials (eight full-text articles) were included in clinical effectiveness.
Appendix 2 gives reasons for exclusion for full-text studies.
Search for meeting abstracts
Search strategy for Ovid EMBASE (1947 to 2015 Week 12)
-
(empagliflozin or canagliflozin or dapagliflozin).m_titl.
-
conference.pt.
-
1 and 2
400 retrieved.
Search strategy for Web of Science Core Collection (from inception to February 2015)
TITLE field: (empagliflozin or canagliflozin or dapagliflozin); Refined by: Document Types: (MEETING ABSTRACT)
239 retrieved.
A total of 636 meeting abstracts were downloaded into EndNote (version 7; Thomson Reuters, CA, USA) and, after removing duplicates, there were 372 unique records. These were screened on the basis of title (and abstract if available) and 46 were selected for further scrutiny, of which one was selected for inclusion.
Cost-effectiveness searches
Ovid MEDLINE (1946 to July Week 1 2015, Ovid MEDLINE® In-Process & Other Non-Indexed Citations July 13, 2015)
-
exp Economics/
-
exp “Costs and Cost Analysis”/
-
Health Status/
-
exp “Quality of Life”/
-
exp Quality-Adjusted Life Years/
-
(pharmacoeconomic* or pharmaco-economic* or economic* or cost*).tw.
-
(health state* or health status).tw.
-
(qaly* or ICER* or utilit* or EQ5D or EQ-5D or euroqol or euro-qol or SF-36 or SF36 or SF-6D or SF-6D or SF6D or HUI).tw.
-
(markov or time trade off or TTO or standard gamble or hrql or hrqol or disabilit* or disutilit*).tw.
-
(quality adj2 life).tw.
-
(decision adj2 model).tw.
-
(visual analog* scale* or discrete choice experiment* or health* year* equivalen* or (willing* adj2 pay)).tw.
-
“resource use”.tw.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13
-
(empagliflozin or canagliflozin or dapagliflozin).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
(sodium glucose cotransporter 2 or sodium glucose co-transporter 2 or SGLT2* or SGLT-2*).m_titl.
-
15 or 16
-
14 and 17
29 retrieved.
Ovid EMBASE 1974 to 2015 July 13
-
exp health economics/
-
exp health status/
-
exp “quality of life”/
-
exp quality adjusted life year/
-
(pharmacoeconomic* or pharmaco-economic* or economic* or cost*).tw.
-
(health state* or health status).tw.
-
(qaly* or ICER* or utilit* or EQ5D or EQ-5D or euroqol or euro-qol or short-form or SF-12 or SF12 or SF-36 or SF36 or SF-6D or SF6D or HUI).tw.
-
(markov or time trade off or TTO or standard gamble or hrql or hrqol or disabilit* or disutilit* or net benefit or contingent valuation).tw.
-
(quality adj2 life).tw.
-
(decision adj2 model).tw.
-
(visual analog* scale* or discrete choice experiment* or health* year* equivalen* or (willing* adj2 pay)).tw.
-
(resource* or quality of well-being or qwb).tw.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
-
(empagliflozin or canagliflozin or dapagliflozin).mp.
-
(sodium glucose cotransporter 2 or sodium glucose co-transporter 2 or SGLT2* or SGLT-2*).m_titl.
-
14 or 15
-
13 and 16
-
(monotherap* or placebo).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
17 and 18
136 retrieved.
The Cochrane Library: NHS Economic Evaluation Database in July 2015
-
(empagliflozin or canagliflozin or dapagliflozin) in Title, Abstract or Keywords
2 retrieved.
The EndNote database had 167 references. Retained 43 for a second viewing; the full text of six were retrieved.
Searches for trials of gliclazide in monotherapy lasting 24–26 weeks, versus placebo
Search strategy in Ovid MEDLINE (1946–April 7 2005)
-
gliclazide.mp. or exp Gliclazide/
-
randomized controlled trial.pt.
-
1 and 2
142 retrieved.
Search strategy in Ovid EMBASE
-
gliclazide.mp. or gliclazide/
-
(placebo or monotherapy).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
-
1 and 2
-
random*.mp.
-
3 and 4
-
randomized controlled trial/
-
5 and 6
153 retrieved.
In total, 295 in EndNote; 230 after removing duplicates; 138 selected in first screening and 58 in the second screening of 11 full text requested.
Searches for systematic reviews of sulfonylureas and gliclazide
Search strategy for Ovid MEDLINE 1946 – April 7 – then updated September Week 1, 2015
-
(sulfonylurea* or sulphonylurea* or gliclazide).tw.
-
meta-analysis.pt.
-
(systematic review or meta-analysis).tw.
-
2 or 3
-
1 and 4
143 retrieved.
Ovid EMBASE 1974 – September 14, 2015
-
(sulfonylurea* or sulphonylurea* or gliclazide).tw.
-
(systematic review or meta-analysis).tw.
-
1 and 2
263 retrieved.
Total of 406 combined; after removal of duplicates it was 301. After a first screening, 34 were selected for a second screening and 15 full text were selected.
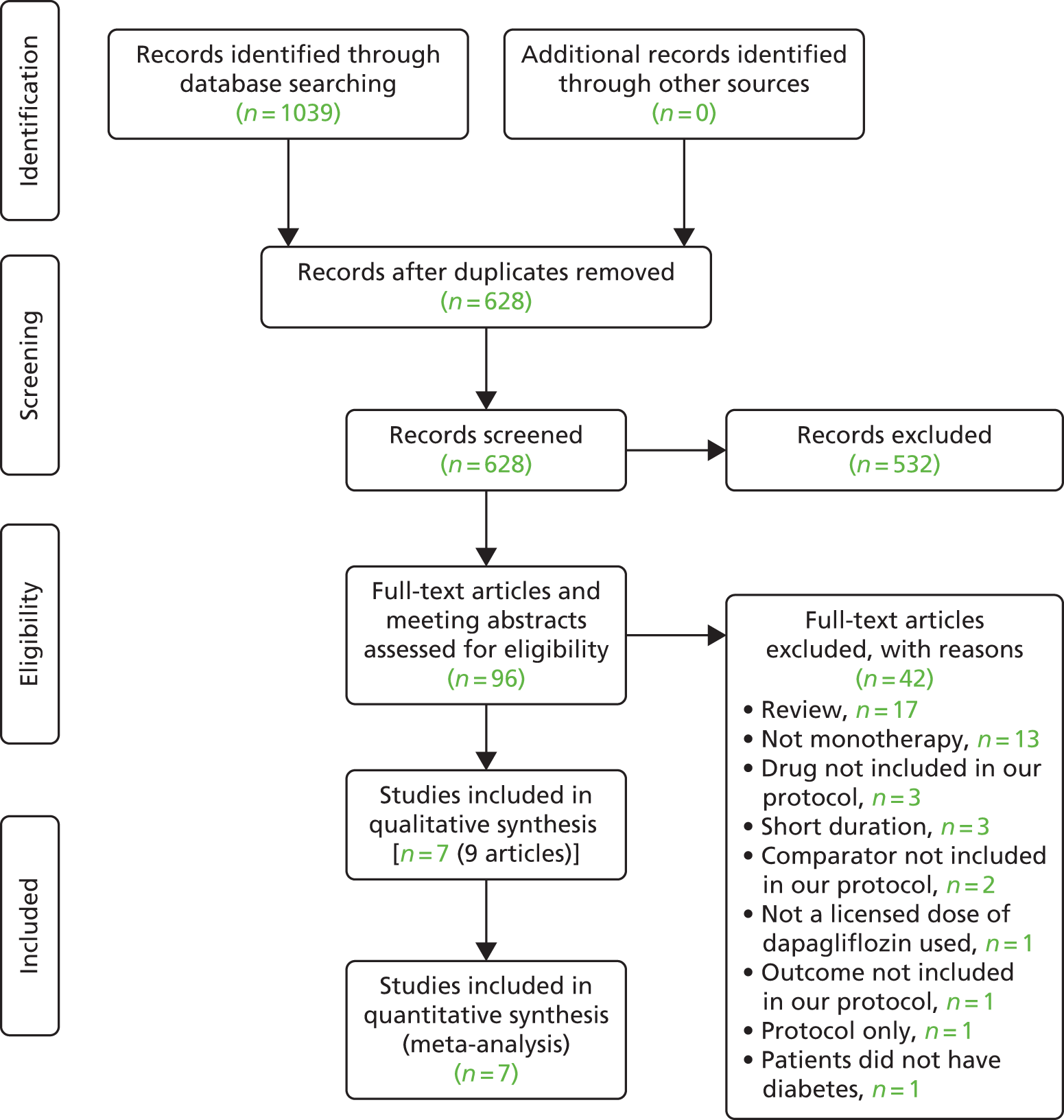
Appendix 2 Reasons for exclusions
| Study ID | Reason for exclusion |
|---|---|
| Bailey 2012248 | Not a licensed dose of dapagliflozina used |
| Berhan 2013249 | Review |
| Bluher 2014250 | Review |
| Brand 2012251 | Patients did not have diabetes |
| Escudero Vilaplana 2014252 | Review |
| Ferrannini 2013253 | Not monotherapy |
| Goring 2014254 | Not monotherapy |
| Henry 2012255 | Comparator not included in our protocol |
| Hussey 2013256 | Short duration |
| Johnsson 2013101 | Review |
| Johnsson 2013257 | Review |
| Kadowaki 2014258 | Short duration |
| Kaku 2014259 | Comparator not included in our protocol |
| Lavalle-Gonzalez 201393 | Not monotherapy |
| Lutz 2014260 | Review |
| Matthaei 2014261 | Review |
| Nauck 2011119 | Not monotherapy |
| Nauck 2013262 | Not monotherapy |
| Orme 2014263 | Not monotherapy |
| Pafili 2014264 | Review |
| Phung 2014265 | Review |
| Plosker 2012266 | Review |
| Plosker 2014267 | Review |
| Polidori 2014268 | Outcome not included in our protocol |
| Raskin 2013269 | Review |
| Rosenstock 2012270 | Not monotherapy |
| Rosenstock 2012271 | Not monotherapy |
| Rosenstock 2013272 | Not monotherapy |
| Scheen 2015273 | Review |
| Seino 2014274 | Drug not included in our protocol |
| Seino 2014275 | Drug not included in our protocol |
| Seino 2014276 | Drug not included in our protocol |
| Strojek 2011277 | Not monotherapy |
| Strojek 2013278 | Not monotherapy |
| Strojek 2014279 | Not monotherapy |
| Tahrani 2013131 | Review |
| Usiskin 2014280 | Review |
| Wilding 2013281 | Not monotherapy |
| Yang 2014282 | Review |
| Zambrowicz 2013283 | Short duration |
| Zhang 2014284 | Review |
| Zinman 2014137 | Protocol only |
Appendix 3 Study characteristics
| Study | Participants and baseline data | Intervention/outcomes |
|---|---|---|
| Canagliflozin (Invokana, Janssen, High Wycombe, UK) | ||
| CANTATA-M (Stenlöf 2013)84 Setting: multicentre (n = NR); 17 countries (USA, Austria, Colombia, Estonia, Guatemala, Iceland, India, Korea, Republic of, Lithuania, Malaysia, Mexico, Philippines, Poland, Puerto Rico, Romania, South Africa, Spain and Sweden) Design: phase III RCT, double-blind, placebo controlled Duration: 26 weeks Extension: 26-week extension, replacing placebo with sitagliptin Sponsor: Janssen Research & Development, LLC |
N: 584 (172/195 completers in the cana100 group, 175/197 in the cana300 group, 160/192 in the placebo group; 152/170 completed extension in cana100 group, 165/170 in cana300 group, 135/155 in placebo group); 91 in the high-glycaemic substudy (40/47 completers in the cana100 group, 40/44 in the cana300 group) Inclusion criteria: age 18–80 years, type 2 diabetes inadequately controlled with diet and exercise or on AHAs, who underwent washout of the agent; HbA1c for participants not on AHAs ≥ 7.0% to ≤ 10.0%; HbA1c for participants on AHA monotherapy or SU plus metformin ≥ 6.5% and ≤ 9.5% at screening and ≥ 7.0% and ≤ 10% and FPG < 15 mmol/l at –2 weeks; substudy conducted for participants with HbA1c > 10.0% and ≤ 12.0% at screening or –1 weeks and FPG ≤ 19.4 mmol/l at –1 weeks Exclusion criteria: repeated FPG repeatedly > 15.0 mmol/l during pretreatment (or > 19.4 mmol/l for the high-glycaemic substudy); history of type 1 diabetes, hereditary glucose/galactose malabsorption, primary renal glucosuria or CVD; treatment with a PPARGagonist, insulin, another SGLT2 inhibitor or any other AHA except as specified in the inclusion criteria within 12 weeks before screening; eGFR < 50 ml/minute/1.73 m2 at screening Age (years): cana100: 55.1 (SD 10.8); cana300: 55.3 (SD 10.2); placebo: 55.7 (SD 10.9); cana100 high HbA1c: 49.7 (SD 11.1); cana300 high HbA1c: 48.8 (SD 10.8) Sex (% women): cana100: 58.5%; cana300: 54.8%; placebo: 54.2%; cana100 high HbA1c: 51.1%; cana300 high HbA1c: 56% Ethnicity: cana100: 63.6% White, 9.2% Black, 13.8% Asian, 13.3% other; cana300: 69.5% White, 7.1% Black, 14.7% Asian, 8.6% other; placebo: 69.8% White, 4.7% Black, 15.1% Asian, 10.4% other; cana100 high HbA1c: 53.2% White, 6.4% Black, 23.4% Asian, 17.0% other; cana300 high HbA1c: 68.2% White, 2.3% Black, 15.9% Asian, 13.6% other Diabetes duration (years): cana100: 4.5 (SD 4.4); cana300: 4.3 (SD 4.7); placebo: 4.2 (SD 4.1); cana100 high HbA1c: 4.6 (SD 4.6); cana300 high HbA1c: 5.2 (SD 4.8) HbA1c (%): cana100: 8.1 (SD 1.0); cana300: 8.0 (SD 1.0); placebo: 8.0 (SD 1.0; cana100 high HbA1c: 10.6 (SD 0.9); cana300 high HbA1c: 10.6 (SD 0.6) BMI (kg/m2): cana100: 31.3 (SD 6.6); cana300: 31.7 (SD 6.0); placebo: 31.8 (SD 6.2); cana100 high HbA1c: 30.4 (SD 7.1); cana300 high HbA1c: 30.5 (SD 5.5) Baseline medication: patients on AHA at screening: cana100: 48.2%; cana300: 48.2%; placebo: 47.9%; cana100 high HbA1c: 23.4%; cana300 high HbA1c: 22.7% |
Intervention cana100 (n = 195): 100 mg/day canagliflozin cana300 (n = 197): 300 mg/day canagliflozin cana100 high HbA1c (n = 47): 100 mg/day canagliflozin in participants with HbA1c > 10.0% and ≤ 12.0% cana300 high HbA1c (n = 44): 300 mg/day canagliflozin in participants with HbA1c > 10.0% and ≤ 12.0% Control (n = 192): placebo Run-in: 8 weeks and diet and exercise and washout period for participants on AHA, followed by a 2-week single-blind placebo run-in period; participants not on AHA directly entered the 2-week placebo run-in period; participants in the high-glycaemic substudy entered a 1-week, single-blind placebo run-in period Extension: after 26 weeks, the placebo group received double-blind sitagliptin (100 mg/day) All groups: rescue therapy with metformin was initiated if FPG was > 15.0 mmol/l after day 1 to week 6, > 13.3 mmol/l after week 6 to week 12 and > 11.1 mmol/l after week 12 to week 26; HbA1c > 8% after week 26 Outcomes Primary outcome: change in HbA1c from baseline to week 26 Secondary outcomes: proportion achieving HbA1c < 7.0%, FPG, 2-hour postprandial glucose, HOMA, SBP, HDL-C, triglycerides, body weight Other outcomes: LDL-C, non-HDL-C, apolipoprotein B, DBP, safety assessments (including laboratory, vital signs, hypoglycaemia) Note: the main outcomes for the extension period were reported only for the canagliflozin groups (not considered in the data extraction); safety parameters for all groups |
| Inagaki 201476 Setting: multicentre (n = 31); Japan Design: phase III RCT, double blind, parallel group, placebo controlled Duration: 24 weeks Follow-up: 2 weeks’ post-intervention follow-up Sponsors: Mitsubishi, Tanabe Pharma Corp |
N: 183 in relevant comparison groups (84/90 completers in the cana100 group, 74/93 in the placebo group) Inclusion criteria: age ≥ 20 years, type 2 diabetes mellitus diagnosed ≥ 3 months before run-in, HbA1c 7.0% to 10%, on diet and exercise therapy for ≥ 55 days; patients on antihyperglycaemic treatment had to start a washout period of ≥ 55 days before starting run-in Exclusion criteria: non-type 2 diabetes, current or history of severe diabetic complications, FPG > 270 mg/dl, indication for insulin therapy, hereditary glucose/galactose malabsorption or renal glycosuria, inadequately controlled thyroid abnormality, anorexia or bulimia, current or history of urinary tract/genital infection < 1 year before run-in, triglyceride ≥ 6.72 mmol/l, BP ≥ 160/≥ 100 mmHg during run-in or patients with known hypertension immediately requiring the addition/modification of antihypertensive therapy, heart disease, serious liver disease, serious kidney disease, eGFR < 50 ml/minute/1.73 m2; urinary albumin/creatinine ratio ≥ 300 mg/g creatinine, history of malignancy, neuropsychiatric disorder likely to hinder study evaluations; history of drug-related shock or anaphylactic symptoms; unwilling to use contraception; pregnant or breast feeding women, prior use of canagliflozin Age (years): cana100: 58.4 (SD 10.4); placebo: 58.2 (SD 11.0) Sex (% women): cana100: 34.4%; placebo: 35.5% Ethnicity: 100% Japanese Diabetes duration (years): cana100: 4.72 (SD 4.59); placebo: 5.63 (SD 5.76) HbA1c (%): cana100: 7.98 (SD 0.73); placebo: 8.04 (SD 0.70) BMI (kg/m2): cana100: 25.59 (SD 4.20); placebo: 25.85 (SD 4.39) Comorbidities: NR Baseline medication: cana100: 22.2% previously on OADs; placebo: 25.8% previously on OADs |
Intervention cana100 (n = 90): 100 mg/day canagliflozin, once daily before breakfast Control (n = 93): placebo, once daily Note: the trial also included a 200-mg group, this was not considered here Run-in: 4-week, single-blind placebo lead-in All groups: patients were instructed to continue diet and exercise therapy as before Outcomes Primary outcome: change in HbA1c from baseline to week 24 Secondary outcomes: FPG, body weight, proportion achieving HbA1c < 7%, 2-hour postprandial glucose, waist circumference, lipids, BP, HOMA, proinsulin, C-peptide Other outcomes: safety assessments (including laboratory, vital signs, hypoglycaemia) |
| Study | Participants and baseline data | Intervention/outcomes |
|---|---|---|
| Dapagliflozin (Farxiga, Bristol-Myers Squibb, Luton, UK) | ||
| Ferrannini 2010/Bailey 201577,78 Setting: multicentre (n = 85); USA, Canada, Mexico and Russia Design: phase III RCT, double blind, parallel group, placebo controlled Duration: 24 weeks Extension: 78 weeks (Bailey 201578), double-blind Sponsors: Bristol-Myers Squibb; AstraZeneca |
N: 260 in relevant comparison groups (156/185 completers in the dapa10 groups, 63/75 in the placebo group; 42/56 completed extension in dapa10 AM group, 42/62 in placebo group) Inclusion criteria: age 18–77 years, type 2 diabetes mellitus inadequately controlled with diet and exercise, naive to treatment, BMI ≤ 45 kg/m2, fasting C-peptide ≥ 1.0 ng/ml Exclusion criteria: type 1 diabetes, serum creatinine ≥ 133 µmol/l (men) or ≥ 124 µmol/l (women), urine albumin/creatinine ratio > 200 mg/mmol, aspartate transaminase and/or alanine transaminase > 3 times the upper limits of normal, creatine kinase ≥ 3 times the upper limit of normal, symptoms of severely uncontrolled diabetes (including marked polyuria and polydipsia with > 10% weight loss during last 3 months before enrolment); significant renal, hepatic, haematological, oncological, endocrine, psychiatric, or rheumatic diseases, cardiovascular event within 6 months of enrolment, severe uncontrolled BP (systolic ≥ 180 mmHg and/or diastolic ≥ 110 mmHg) Age (years): dapa10 AM: 50.6 (SD 10.0); dapa10 PM: 50.7 (SD 9.7); dapa10 high HbA1c: 47.9 (SD 12.1); placebo: 52.7 (SD 10.3) Sex (% women): dapa10 AM: 51.4%; dapa10 PM: 48.7%; dapa10 high HbA1c: 41.0%; placebo: 58.7% Ethnicity: dapa10 AM: 90% White, 2.9% Black, 4.3% Asian, 2.9% other; placebo: 94.7% White, 2.7% Black, 2.7% Asian Diabetes duration (years, median, IQR): dapa10 AM: 0.45 (0.1–3.4); dapa10 PM: 0.40 (0.1–2.45); dapa10 high HbA1c: 1.4 (0.2–3.5); placebo: 0.5 (0.1–3.4) HbA1c (%): dapa10 AM: 8.01 (SD 0.96); dapa10 PM: 7.99 (SD 1.05); dapa10 high HbA1c: 10.73 (SD 0.85); placebo: 7.84 (SD 0.87) BMI (kg/m2): dapa10 AM: 33.6 (SD 5.4); dapa10 PM: 33.3 (SD 5.6); dapa10 high HbA1c: 31.1 (SD 5.9; placebo: 32.3 (SD 5.5) Comorbidities: dapa10 AM: 1.4% diabetic neuropathy, 1.4% microalbuminuria, 41.4% hypertension; placebo: 8% diabetic neuropathy, 1.3% diabetic neuropathy, 1.3% microalbuminuria, 52% hypertension Baseline medication: no OAD; dapa10 AM: 41.4% on antihypertensives; placebo: 41.3% on antihypertensives |
Intervention
Note: the trial also included 2.5- and 5-mg groups – these were not considered here Run-in: 2-week diet/exercise placebo lead-in (1 week for patients with HbA1c 10.1–12.0%) Extension: after 24 weeks, the placebo group received low-dose metformin (500 mg/day) and the dapa groups received matching placebo; results only reported for main dapa AM groups vs. placebo All groups: if fasting FPG was > 270 mg/dl at week 4, > 240 mg/dl at week 8 or > 200 mg/dl at weeks 12 to 24, patients were eligible for open-label rescue medication (500 mg metformin, titrated as needed up to 2000 mg); patients with HbA1c > 8.0% for 12 weeks despite maximum tolerated metformin dose were discontinued; the strategy for rescue medication based on HbA1c was continued during the extension period. Patients received diet/exercise counselling according to ADA recommendations throughout the study Outcomes Primary outcome: change from baseline in HbA1c at week 24 in the dapa10 AM group Secondary outcomes: FPG, body weight Other outcomes: safety assessments and adverse events (including laboratory, vital signs, urinary tract and genital infections, hypoglycaemia) |
| Ji 201479 Setting: multicentre (n = 40); China, Korea, Taiwan and India Design: phase III RCT, double-blind, parallel group, placebo controlled Duration: 24 weeks Follow-up: 28 days post intervention (not reported) Sponsors: Bristol-Myers Squibb; AstraZeneca |
N: 265 in relevant comparison groups (117/133 completers in the dapa10 group, 113/132 in the placebo group) Inclusion criteria: aged ≥ 18 years, inadequately controlled type 2 diabetes mellitus (HbA1c ≥ 7.5% and ≤ 10.5% at enrolment and ≥ 7.0% and ≤ 10.5% during lead-in), drug naive, BMI ≤ 45 kg/m2, C-peptide ≥ 1.0 ng/ml Exclusion criteria: aspartate aminotransferase and/or alanine aminotransferase levels > 3 times upper limit of normal, serum total bilirubin > 34.2 µmol/l, serum creatinine ≥ 132.6 µmol/l for men or ≥ 123.8 µmol/l for women, haemoglobin ≤ 110 g/l for men and ≤ 100 g/l for women, creatine kinase ≥ 3 times the upper limit of normal, urine albumin/creatinine ratio > 1800 mg/g, severe hypertriglyceridaemia (triglyceride > 9.3 mmol/l), urinary excretion of N-acetyl-β-d-glucosaminidase > 84 µmol/hour per millimole of creatinine, urinary excretion of α1 microglobulin > 28 mg/g creatinine, parathyroid hormone value > 1.5 times the upper limit of normal, calcium or serum phosphate values outside the normal reference range, abnormal free thyroxine levels, positive hepatitis B surface antigen or positive anti-hepatitis C antibodies; currently unstable or serious vascular, renal, hepatic, haematological, oncologic, endocrine, psychiatric, or rheumatic diseases Age (years): dapa10: 51.2 (SD 9.9); placebo: 49.9 (SD 10.9) Sex (% women): dapa10: 35.3%; placebo: 34.1% Ethnicity: dapa10: 88.7% Chinese, 6.8% Asian Indian, 3.8% Korean, 0.8% other Asian; placebo: 88.6% Chinese, 6.1% Asian Indian, 3.8% Korean, 0.8% Japanese, 0.8% other Asian Diabetes duration (years): dapa10: 1.67 (SD 2.8) (range 0–13); placebo: 1.3 (SD 2.0) (range 0–9.9) HbA1c (%): dapa10: 8.28 (SD 0.95); placebo: 8.35 (SD 0.95) BMI (kg/m2): dapa10: 25.76 (SD 3.43); placebo: 25.93 (SD 3.64) Comorbidities: dapa10: 42.9% history of dyslipidaemia, 37.6% history of hypertension; placebo: 40.2% history of dyslipidaemia, 40.9% history of hypertension Baseline medication: no OAD; others not reported |
Intervention
Run-in: 6-week single-blind placebo run-in with diet and exercise counselling consistent with China Diabetes Society recommendations All groups: open-label rescue therapy with metformin (500 mg daily, titrated to 2000 mg if necessary) could be given if glycaemic control was inadequate (during weeks 4–12, FPG > 13.3 mmol/l; during weeks 12–24, FPG level > 11.1 mmol/l); patients with FPG values consistently greater than protocol-specified values for 12 weeks despite a maximum tolerated dose of metformin were discontinued from the study Outcomes Primary outcome: change in HbA1c from baseline to week 24 Secondary outcomes: FPG, 2-hour postprandial glucose, proportion achieving HbA1c < 7%, body weight Other outcomes: beta cell function and insulin resistance, waist circumference, lipids, proportion of patients with ≥ 3% or ≥ 5% reduction in total weight, fasting urinary glucose/creatinine ratio, safety and tolerability (including laboratory, vital signs, hypoglycaemia) |
| Kaku 201480 Setting: multicentre (n = NR); Japan Design: phase III RCT, double blind, parallel group, placebo controlled Duration: 24 weeks Follow-up: 3-week post-intervention follow-up Sponsors: Bristol-Myers Squibb, AstraZeneca |
N: 175 in relevant comparison groups (79/88 completers in the dapa10 group, 79/87 in the placebo group) Inclusion criteria: age ≥ 20 years, type 2 diabetes mellitus inadequately controlled with diet and exercise, naive to drug treatment or on antihyperglycaemic treatment (the latter underwent a washout period before study began), HbA1c ≥ 6.5% and ≤ 10% for drug-naive patients and ≤ 8% for patients on ongoing treatment Exclusion criteria: type 1 diabetes, FPG > 13.3 mmol/l, creatinine kinase > 3 times upper limit of normal, eGFR < 45 ml/minute or serum creatinine > 133 µmol/l for men and > 124 µmol/l for women; severe hepatic insufficiency and/or significant abnormal liver function (aspartate aminotransferase > 3 times upper limit of normal and/or alanine aminotransferase > 3 times upper limit of normal; New York Heart Association class IV CHF; unstable or acute CHF; treatment with TZDs < 6 months before enrolment; pregnant or breastfeeding women Age (years): dapa10: 57.5 (SD 9.3); placebo: 60.4 (SD 9.7) Sex (% women): dapa10: 39.8%; placebo: 40.2% Ethnicity: 100% Japanese Diabetes duration (years): dapa10: 4.93 (SD 4.52); placebo: 5.29 (SD 6.17) HbA1c (%): dapa10: 7.46 (SD 0.61) (21.6% < 7%); placebo: 7.50 (SD 0.63) (24.1% < 7%) BMI (kg/m2): dapa10: 26.06 (SD 4.52); placebo: 25.22 (SD 4.39) Comorbidities: dapa10: 50% history of CVD, 40.9% hypertension only; placebo: 42.5% history of CVD, 35.6% hypertension only, 2.3% CHF; most patients in both groups had mild to moderate renal impairment (69% stage 1 or mild CKD, 28% stage 2 or moderate CKD) Baseline medication: NR |
Intervention
Run-in: 2-week screening period and 4-week single-blind placebo lead-in Follow-up: post-intervention follow-up mainly used for safety monitoring – no further results reported All groups: no further information Outcomes Primary outcome: change in HbA1c from baseline to week 24 Secondary outcomes: FPG, body weight Other outcomes: body weight in patients with BMI ≥ 25 kg/m2, fasting insulin and C-peptide, SBP, blood lipids, proportion achieving HbA1c < 7%; safety assessments (including laboratory, vital signs, hypoglycaemia) |
| Empagliflozin (Jardiance, Boehringer Ingelheim, Ingelheim, Germany/Eli Lilly and Company, Indianapolis, IN, USA) | ||
| Lewin 201581 Setting: multicentre (n = 197); 22 countries (no UK sites) Design: phase III RCT, double blind, parallel group Duration: 52 weeks, primary end point at 24 weeks Follow-up: follow-up visit 4 weeks after the last dose of study drug Sponsors: Boehringer Ingelheim; Eli Lilly |
N: 404 in relevant comparison groups (398 with on treatment measurements) (114/133 completers in the empa25 group, 110/132 in the empa10 group, 116/133 in the lina5 group) Inclusion criteria: age ≥ 18 years, type 2 diabetes mellitus inadequately controlled with diet and exercise, no therapy with OAD, GLP1-analogue or insulin for ≥ 12 weeks prior to randomisation, BMI ≤ 45 kg/m2, HbA1c > 7% and ≤ 10.5% Exclusion criteria: uncontrolled hyperglycaemia (FPG > 13.3. mmol/l); eGFR < 60 ml/minute/1.73 m2; acute coronary syndrome, stroke, or transient ischaemic attack within 3 months prior to consent; bariatric surgery in the past 2 years; treatment with anti-obesity drugs within 3 months prior to consent Age (years): empa25: 56.0 (SD 9.3); empa10: 53.9 (SD 10.5); lina5: 53.8 (SD 11.5) Sex (% women): empa25: 42.1%; empa10: 51.5%; lina5: 43.6% Ethnicity: empa25: 69.9% White, 14.3% Asian, 15.8% other; empa10: 75.0% White, 9.8% Asian, 15.2% other; lina5: 77.4% White, 12.8% Asian, 9.8% other; Asians were from Malaysia, the Philippines, Taiwan; no South Asian recruits; other mainly Hispanic Diabetes duration (time since diagnosis): empa25: 36.1% ≤ 1 year, 36.1% > 1–5 years, 18.8% > 5–10 years, 9.0% > 10 years; empa10: 32.6% ≤ 1 year, 45.5% > 1–5 years, 11.4% > 5–10 years, 10.6% > 10 years; lina5: 37.6% ≤ 1 year, 42.9% > 1–5 years, 16.5% > 5–10 years, 3.0% > 10 years HbA1c (%): empa25: 7.99 (SD 0.97 (27.1% ≥ 8.5%); empa10: 8.05 (SD 1.03 (28.8% ≥ 8.5%); lina5: 8.05 (SD 0.89 (25.6% ≥ 8.5%) BMI (kg/m2): empa25: 31.2 (SD 5.7); empa10: 31.5 (SD 5.7); lina5: 31.9 (SD 5.9) Comorbidities: empa25: n = 20 (15%) microalbuminuria, n = 0 macroalbuminuria; empa10: n = 21 (16%) microalbuminuria, n = 3 (2%) macroalbuminuria; lina5: n = 16 (12%) microalbuminuria, n = 2 (1.5%) macroalbuminuria Baseline medication: no antihyperglycaemic medication |
Intervention
Run-in: 2-week placebo run-in All groups: rescue medication initiated if blood glucose > 240 mg/dl after overnight fast between weeks 1 and 12, blood glucose > 200 mg/dl after overnight fast between weeks 12 and 24, or blood glucose > 180 mg/dl or HbA1c > 8% after overnight fast between weeks 24 and 52 (initiation, choice and dosage of rescue medication at the discretion of the investigator but use of DPP-4 inhibitors, GLP-1 analogues, SGLT2 inhibitors not permitted); in cases of hypoglycaemia, rescue medication was to be reduced in dose or discontinued; if hyper- or hypoglycaemia could not be controlled, participant was discontinued from the trial Outcomes Primary outcome: change in HbA1c from baseline to week 24 Secondary outcomes: FPG, body weight, proportion achieving HbA1c < 7% (of participants with HbA1c ≥ 7%) Other outcomes: SBP, DBP, blood lipids, safety assessments (including laboratory, vital signs, hypoglycaemia) |
| Roden 2013/1482,83 Setting: multicentre (n = 124); nine countries (Belgium, Canada, China, Germany, India, Ireland, Japan, Switzerland and USA) Design: phase III RCT, placebo controlled, double blind, parallel group Duration: 24 weeks Extension: 76-week extension trial Sponsors: Boehringer Ingelheim and Eli Lilly |
N: 986 (899 randomised, 87 in open-label empagliflozin) in relevant comparison groups (187/228 completed control, 206/224 completed empa10, 204/224 completed empa25, 206/223 completed sita100, 78/87 completed empa25open) Inclusion criteria: previously untreated type 2 diabetes (no oral or injected anti-diabetes treatment for 12 weeks before randomisation or start of open-label treatment), aged ≥ 18 years (≥ 20 years in Japan, 18–65 years in India), BMI ≤ 45 kg/m2, and insufficient glycaemic control despite diet/exercise regimen [HbA1c 7.0–10.0% (or 7.0–9.0% in Germany)] at screening for patients eligible for randomised treatment, or > 10.0% for those eligible for the open-label treatment group (this arm not included in Germany or Ireland) Exclusion criteria: uncontrolled hyperglycaemia (PG > 13.3 mmol/l after overnight fast during placebo run-in phase and confirmed by second measurement), eGFR (estimated using modification of diet in renal disease equation) < 50 ml/minute/1.73m2 (or < 60 ml/minute/1.73 m2 in China), any contraindications to sitagliptin according to local label, treatment with anti-obesity drugs within 3 months before informed consent, treatment with systemic steroids at time of informed consent, change in thyroid hormone dose within 6 weeks before informed consent, any uncontrolled endocrine disorder apart from type 2 diabetes Age (years): empa10: 56.2 (SD 11.6), empa25: 53.8 (SD 11.6), sita100: 55.1 (SD 9.9), empa25open: 50.2 (SD 11.3), placebo: 54.9 (SD 10.9) Sex (% women): empa10: 37%, empa25: 35%, sita100: 37%, empa25open: 26%, placebo: 46% Ethnicity: empa10: 64% Asian, 34% White, 1% Black/African American, < 1% Hawaiian/Pacific Islander; empa25: 64% Asian, 33% White, 3% Black/African American; sita100: 64% Asian, 34% White, 1% Black/African American, < 1% American Indian/Alaska Native; empa25open: 61% Asian, 33% White, 2% Black/African American, 2% American Indian/Alaska Native, 1% information not available, placebo: 64% Asian, 33% White, 3% Black/African American Diabetes duration: empa10: 39% ≤ 1 year, 41% 1–5 years, 13% 5–10 years, 7% > 10 years; empa25: 41% ≤ 1 year, 37% 1–5 years, 17% 5–10 years, 6% > 10 years; sita100: 42% ≤ 1 year, 39% 1–5 years, 14% 5–10 years, 5% > 10 years; empa25open: 52% ≤ 1 year, 25% 1–5 years, 14% 5–10 years, 8% > 10 years; placebo: 32% ≤ 1 year, 46% 1–5 years, 15% 5–10 years, 8% > 10 years HbA1c (%): empa10: 7.87 (SD 0.88), empa25: 7.86 (SD 0.85), sita100: 7.85 (SD 0.79), empa25open: 11.50 (SD 1.39), placebo: 7.91 (SD 0.78) BMI (kg/m2): empa10: 28.3 (SD 5.5), empa25: 28.2 (SD 5.5), sita100: 28.2 (SD 5.2), empa25open: 28.2 (SD 5.5), placebo: 28.7 (SD 6.2) Baseline medication: no oral/injectable anti-diabetic drug |
Intervention
Extension: 68.4% of the 899 patients continued in a double-blind extension (numbers in each group not given) for ≥ 52 weeks All groups: All received diet/exercise counselling according to local recommendations; rescue medication was started at FPG > 13.3 mmol/l between weeks 1 and 12 or FPG > 11.1 mmol/l between weeks 12 and 24 (drug of choice at the discretion of the investigator, but GLP-1 agonists and DPP-4 inhibitors were not permitted) Outcomes Primary outcome: change from baseline HbA1c at week 24 Secondary outcomes: weight, systolic and DBP Other outcomes: percentage achieving HbA1c < 7.0% (of those with HbA1c > 7.0% at baseline), FPG, percentage with > 5.0% reduction in body weight, waist circumference, percentage of patients with previously uncontrolled hypertension who achieved controlled BP (< 130 mmHg systolic, < 80 mmHg diastolic); use of rescue therapy, safety end points (vital signs, clinical laboratory parameters, adverse events, e.g. hypoglycaemic episodes, urinary tract and genital infections) |
Appendix 4 Quality assessment
Rate as: adequate, inadequate, unclear, not reported.
| Trial | Method of randomisation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | ITT analysis | Selective reporting | Similarity at baseline | Other (e.g. power analysis) | Overall |
|---|---|---|---|---|---|---|---|---|---|---|
| Canagliflozin | ||||||||||
| CANTATA-M (Stenlöf 2013) 84 | Unclear Method not reported; Randomisation stratified by previous AHA use |
NR | Adequate Double blind |
NR | Adequate (main analysis) 11.8% discontinuation in cana100 group, 11.2% in cana300 group, 16.7% in placebo group |
Adequate ITT for all patients receiving at least one dose of study drug; LOCF for missing data |
Partial Some data shown only in graphs with no numeric values given |
Adequate For main study |
Adequate 90% power to detect a difference in HbA1c with 85 participants per group |
5/9 adequate |
| Inagaki 2014 76 | Adequate Block randomisation (block size of 6 and 97 blocks); randomisation code list prepared by investigational product allocation manager and maintained until code was broken |
Adequate Randomisation code not broken until data entry had been completed or unless needed in an emergency |
Adequate Double blind |
Adequate Code not broken until data entry completed |
Imbalance 6.7% discontinuation in cana100 group, 20.4% in placebo group; reasons given |
Adequate Efficacy analyses performed in the full analysis set of patients receiving at least one dose of study drug, except patients who did not have any efficacy data after administration of drug; LOCF for missing data |
Adequate All outcomes reported as indicated in the methods section |
Adequate Some difference between groups were noted regarding sex and GFR, but this seemed to apply mainly to the 200-mg canagliflozin group |
Adequate 95% power to detect a difference in HbA1c with 80 participants per group |
8/9 adequate |
| Dapagliflozin | ||||||||||
| Ferrannini 2010/Bailey 2015 77 , 78 | Adequate ‘Computer-generated randomisation by an interactive voice response system, stratified by site in blocks of 7’ |
Adequate ‘Randomisation codes kept centrally at Bristol-Myers Squibb’ |
Adequate ‘Investigators, other clinical staff and participants blinded to treatment allocation during the 24-week initial and 78-week extension periods’ |
Adequate See previous |
Adequate 15.7% discontinuation in dapa10 groups, 16% in placebo group; 60% completed extension in dapa10 AM group, 56% in placebo group; reasons given |
Unclear States that analyses were based on all participants taking at least one dose of medication, but main follow-up data appear to be based on fewer participants? |
Adequate All outcomes reported as indicated in the methods section |
Adequate Between dapa10 AM/PM groups and placebo, the dapa10 high HbA1c group had a longer diabetes duration (other than a higher HbA1c) |
Adequate 90% power to detect a difference in HbA1c with 67 participants per group (primary end point) |
8/9 adequate (main analysis) |
| Ji 2014 79 | Adequate Participants were ‘randomised sequentially by using an interactive voice response system in a blinded manner’ |
Adequate See previous |
Adequate ‘Patients, investigators and the sponsors were blinded to the treatment group’ |
Adequate See previous |
Adequate 12.0% discontinuation in dapa10 group, 14.4% in placebo group; reasons given |
Adequate ‘Patients randomised to treatment who received at least 1 dose of double-blind study medication and had both a baseline and post-baseline measurement were included in the efficacy analyses; patients who received at least 1 dose of double-blind study medication were included in the safety analyses’ |
Adequate All outcomes reported as indicated in the methods section |
Adequate Stated that demographic and baseline characteristics were similar between groups |
Adequate 97% power to detect a difference in HbA1c with 120 participants per group |
9/9 adequate |
| Kaku 2014 80 | NR | NR | Adequate ‘Double-blind’ |
NR | Adequate 10.2% discontinuation in dapa10 group, 9.2% in placebo group; reasons given |
Adequate ‘Efficacy data were analysed with a full analysis set of individuals who took at least one dose of study medication’ |
Adequate All outcomes reported as indicated in the methods section |
Adequate Stated that demographic and baseline characteristics were similar between groups |
Adequate 90% power to detect a difference in HbA1c with 85 participants per group |
6/9 adequate |
| Empagliflozin | ||||||||||
| Lewin 2015 81 | Adequate Third-party interactive voice and web response system; stratified by baseline HbA1c, eGFR and region |
NR | Adequate ‘Double-blind’ |
NR | Adequate 17% discontinuation in the empa25 group, 19.4% in the empa10 group, 15.6% in the lina5 group |
Adequate Efficacy data were analysed with a full analysis set of individuals who took at least one dose of study medication and had at least one on treatment HbA1c value; missing values imputed using LOCF |
Adequate Some data shown on only one graph with no numeric values given |
Adequate Stated that baseline characteristics were balanced between groups |
Unclear 89% power to detect a difference in HbA1c with 133 participants per group; slightly underpowered after dropouts |
6/9 adequate |
| Roden 2013 83 | Adequate Computer-generated random sequence in block sizes of four, stratified by region (Asia, Europe, North America), HbA1c at screening (< 8.5%, ≥ 8.5%) and eGFR (≥ 90, 60–89, 50–59 ml/minute) |
Adequate Study sponsor allocated participants using an interactive voice and internet-based response system |
Adequate ‘Patients, investigator and individuals involved in the analysis of trial data were masked to treatment assignment’ |
Adequate See previous |
Adequate (all < 20%) Discontinuation rates: 18% control, 8% empa10, 9% empa25, 8% sita100, 10% empa25open; reasons given |
Adequate Efficacy data were analysed with a full analysis set of individuals who took at least one dose of study medication; missing values imputed using LOCF |
Adequate All outcomes reported as indicated in the methods section |
Adequate Between empa10, empa25, sita100 and control groups; empa25open had greater proportion of participants at ≤ 1 year |
Adequate 95% power to detect a difference in HbA1c with 180 participants per group (primary end point) |
9/9 adequate |
Appendix 5 Cochrane risk of bias table: EMPA-REG OUTCOME
Overall, the trial scores well, and it is likely that the unclear items are just failure to report the processes rather than causing a high risk of bias.
| Entry | Judgement | Support for judgement |
|---|---|---|
| Random sequence generation (selection bias) | Low risk | Computerised randomisation |
| Allocation concealment (selection bias) | Low risk | Paper reports that a computerised randomisation system was used |
| Blinding of participants and personnel (performance bias) | Unclear | No information on appearance of placebo and empagliflozin tablets |
| Blinding of outcome assessment (detection bias) (patient-reported outcomes) | Unclear | Paper says ‘All CV outcome events and deaths are being prospectively adjudicated by the Clinical Events Committee (one for cardiac events and one for neurological events), as recommended in FDA guidelines’ but gives no detail as to whether or not the assessors are blinded to allocation |
| Blinding of outcome assessment (detection bias) (mortality) | Unclear | As above. But death from any cause 8.3% in placebo group and 5.7% in empagliflozin group |
| Incomplete outcome data addressed (attrition bias) [short-term outcomes (2–6 weeks)] | NA | Outcomes long term |
| Incomplete outcome data addressed (attrition bias) [longer-term outcomes (> 6 weeks)] | Low risk | Very good retention of participants, with around 97% completing the study |
| Selective reporting (reporting bias) | Low risk |
Appendix 6 Trials excluded in network meta-analysis
| Trial | Drug | Comparator | Notes |
|---|---|---|---|
| Abbatecola 2006146 | Repaglinide | Glibenclamide | Baseline HbA1c 7.2% |
| Aronoff 2000285 | Pioglitazone | Placebo | High dropout rate and mean baseline HbA1c high |
| Barnett 2012286 | Linagliptin | Placebo then glimepiride | 18 weeks vs. placebo |
| Barzilai 2011287 | Sitagliptin 50 or 100a | Placebo | High dropout rate. Some not new to drug treatment. Mixed doses according to renal function |
| Chou 2012288 | Pioglitazone | Placebo | Dropout rate |
| Goldstein 2007289 | Sitagliptin | Placebo | High dropout rate and entry HbA1c up to 11% |
| Jovanovic 2000148 | Repaglinide | Placebo | High dropout rate |
| Kamel 1997290 | Glibenclamide, gliclazide, metformin, acarbose | Placebo | Abstract only, and only 43 patients across five arms |
| Mohan 2009291 | Sitagliptin | Placebo | Only 18 weeks |
| Moses 1999292 | Repaglinide with/without metformin | Metformin | All failed on metformin monotherapy and 25% HbA1c > 9% Duration |
| Moses 2001293 | Repaglinide | Placebo | 16 weeks |
| Raz 2006294 | Sitagliptin | Placebo | Only 18 weeks |
| Saleem 2011,149 Shah 2011,150 Jibran 2006151 | Repaglinide | Glibenclamide | Wrong comparator and quality issues. The Jibran 2006151 and Saleem 2011149 papers are very similar but have no authors in common. They are reported to be from different time periods but almost all figures are identical |
| Scherbaum 2002295 | Pioglitazone | Placebo | Dropout rate |
Appendix 7 Probabilistic modelling
The model was run probabilistically over 996 iterations for each of the BMI scenarios:
-
No BMI direct effect upon QoL
-
BMI 1: natural history progression with no rebound
-
BMI 2: natural history progression with weight losses rebounding after 1 year
-
BMI 3: natural history progression with weight losses rebounding at treatment change
-
BMI 4: natural history progression with weight rebounding after 1 year
-
BMI 5: natural history progression with weight rebounding at treatment change.
The central estimates for these are as shown in Tables 105 and 106.
| Drug | Costs (£) | No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 |
|---|---|---|---|---|---|---|---|
| Gliclazide | 28,222 | 10.649 | 9.850 | 9.850 | 9.850 | 9.996 | 9.963 |
| Repaglinide | 28,338 | 10.645 | 9.880 | 9.873 | 9.875 | 9.995 | 9.968 |
| Pioglitazone | 28,456 | 10.640 | 9.827 | 9.827 | 9.827 | 9.987 | 9.952 |
| Sitagliptin | 33,472 | 10.612 | 9.878 | 9.874 | 9.874 | 9.966 | 9.944 |
| Canagliflozin | 33,813 | 10.635 | 10.005 | 9.909 | 9.927 | 9.995 | 9.991 |
| Empagliflozin | 33,922 | 10.634 | 9.972 | 9.903 | 9.915 | 9.992 | 9.982 |
| Dapagliflozin | 34,023 | 10.624 | 9.956 | 9.891 | 9.900 | 9.981 | 9.969 |
This suggests the following cost-effectiveness estimates.
| Drug | No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 |
|---|---|---|---|---|---|---|
| Gliclazide | – | – | – | – | – | – |
| Repaglinide | Dom | £3858 | £4949 | £4708 | Dom | £22,679 |
| Pioglitazone | Dom | Dom | Dom | Dom | Dom | Dom |
| Sitagliptin | Dom | Dom | £34M | Dom | Dom | Dom |
| Canagliflozin | Dom | £43,952 | £9583 | £105,000 | Dom | £242,000 |
| Empagliflozin | Dom | Dom | Dom | Dom | Dom | Dom |
| Dapagliflozin | Dom | Dom | Dom | Dom | Dom | Dom |
The patterns of dominance are the same across the deterministic results with the exception of the BMI scenario 2 in which sitagliptin is no longer inferior to repaglinide, but is now slightly superior to it. This results in a cost-effectiveness estimate for sitagliptin compared with repaglinide of £34M per QALY. But, given a cost-effectiveness estimate for canagliflozin compared with repaglinide of £153,000 per QALY, sitagliptin is extendedly dominated.
The cost-effectiveness estimates for repaglinide compared with gliclazide of £3858 per QALY, £4949 per QALY and £4708 per QALY for BMI scenarios 1–3, and £22,679 per QALY for the BMI scenario 5 are reasonably similar to the £3331 per QALY for BMI scenarios 1–3 and £18,507 per QALY for BMI scenario 5 of the deterministic analysis. In the opinion of the AG, the differences between the probabilistic analyses and the deterministic analyses are unlikely to be the result differences in the simulated complications of diabetes, hypoglycaemic events and adverse events. The most likely explanation is that the sampling of weight changes results in around 40% of the PSA iterations for repaglinide having a weight loss, but 0% of the PSA iterations for gliclazide. Apart from the scenario of weight changes having no impact upon QoL, these repaglinide weight losses rebound under the various BMI scenarios. For the 40% of iterations with a repaglinide weight loss the cost-effectiveness estimate for repaglinide compared with gliclazide worsens. As a consequence, the central estimate for the cost-effectiveness estimate for repaglinide compared with gliclazide worsens.
The cost-effectiveness estimates for canagliflozin compared with repaglinide are similar to those of the deterministic model, though for the BMI scenario 2 it has improved from the £192,000 per QALY of the deterministic modelling to £153,000 per QALY. The issue around 40% of repaglinide iterations being associated with weight losses appears to have less of an impact due to the larger absolute QALY differences between canagliflozin and repaglinide compared with the differences between repaglinide and gliclazide.
The probabilistic cost-effectiveness estimates of the individual flozins compared with sitagliptin are shown in Table 107.
| Drug | No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 |
|---|---|---|---|---|---|---|
| Sitagliptin | – | – | – | – | – | – |
| Canagliflozin | 14,714 | 2704 | 9583 | 6532 | 11,685 | 7305 |
| Empagliflozin | 20,040 | 4795 | 15,051 | 11,168 | 17,021 | 12,048 |
| Dapagliflozin | 47,766 | 7110 | 32,372 | 21,194 | 35,379 | 22,208 |
The probabilistic central estimates for the cost-effectiveness of the flozins compared with sitagliptin are much as per the deterministic estimates. Although those for dapagliflozin have worsened slightly, they are qualitatively the same.
In the figures that follow, the ordering of the legends helps to identify the curves. The topmost curve in the legend is the curve of the treatment which is the most likely to be cost-effective at a willingness to pay of £0 per QALY, that is at the vertical axis. As the willingness to pay is £0 per QALY only costs are of interest, so this point depicts which treatment has the highest likelihood of being cost saving. The curve below this in the legend is the curve for the treatment that, as the willingness to pay is increased, next becomes the most likely to be cost-effective. And so on down the legend until the frontier is specified. The curves within the legend that lie below the entry for the frontier in the legend are those that do not achieve the frontier at any willingness to pay in the range of £0–50,000 per QALY. When a curve is mentioned in the legend but is not visible in the figure it coincides with the horizontal axis, that is estimated to have no probability of being cost-effective over the willingness-to-pay range of £0–50,000 per QALY.
Also note that the frontier has been arbitrarily lifted by 0.5% in all figures so that it does not overlay the treatment curve to which it corresponds in order to ease identification of the relevant treatment curve.
Scenario: no body mass index – body mass index has no impact upon QoL
FIGURE 18.
Body mass index no QoL effect: cost-effectiveness acceptability frontier (CEAF) across all comparators.

| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) | Pioglitazone (%) | Gliclazide (%) | Repaglinide (%) |
|---|---|---|---|---|---|---|---|
| 0 | 0 | 0 | 0 | 0 | 2 | 66 | 31 |
| 10,000 | 0 | 0 | 0 | 0 | 4 | 61 | 35 |
| 20,000 | 0 | 0 | 0 | 0 | 5 | 59 | 36 |
| 30,000 | 0 | 0 | 0 | 0 | 5 | 58 | 37 |
| 40,000 | 0 | 0 | 0 | 0 | 6 | 56 | 38 |
| 50,000 | 0 | 0 | 0 | 0 | 6 | 55 | 39 |
The probabilistic analysis suggests that the flozins and sitagliptin have no real probability of being cost-effective. The main uncertainty is around whether glicalazide or repaglinide is the most cost-effective, with it becoming more finely balanced between the two as the willingness to pay approaches £50,000 per QALY.
FIGURE 19.
Body mass index no QoL effect: acceptability frontier for flozins and sitagliptin.
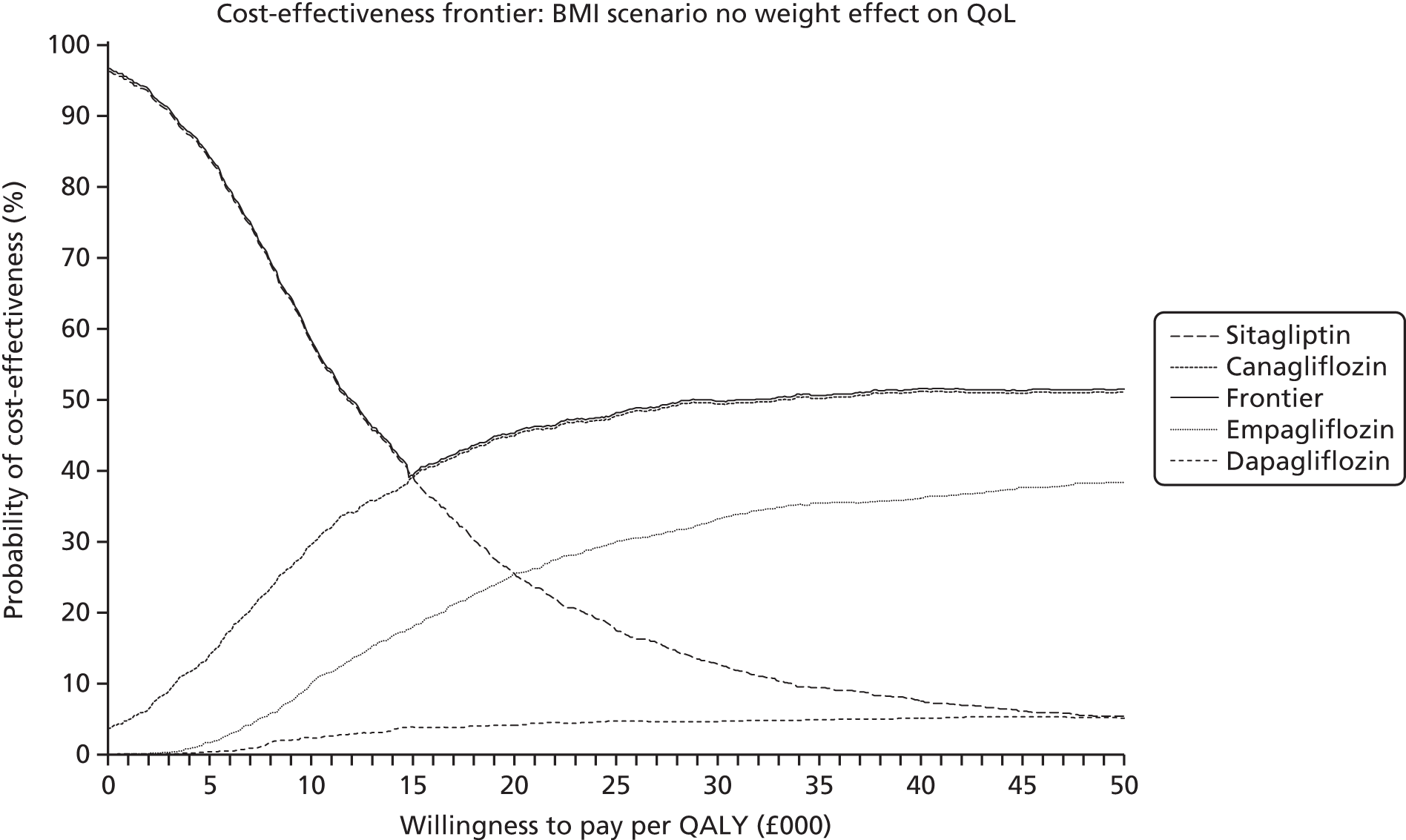
| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) |
|---|---|---|---|---|
| 0 | 0 | 4 | 0 | 96 |
| 10,000 | 10 | 30 | 2 | 58 |
| 20,000 | 26 | 45 | 4 | 26 |
| 30,000 | 33 | 49 | 5 | 13 |
| 40,000 | 36 | 51 | 5 | 8 |
| 50,000 | 38 | 51 | 5 | 5 |
At low values of willingness to pay, the additional cost of the flozins is not warranted. Sitagliptin is estimated to be the most likely to be cost-effective up to a willingness to pay of around £15,000. Thereafter, canagliflozin becomes the most likely to be cost-effective, though the probability of empagliflozin being the most cost-effective is not that far behind. Dapagliflozin fares worse, with there being little likelihood of it being the most cost-effective at any willingness-to-pay value.
Scenario: body mass index 1 – body mass index changes retained indefinitely
FIGURE 20.
Body mass index scenario 1: cost-effectiveness acceptability frontier (CEAF) across all comparators.
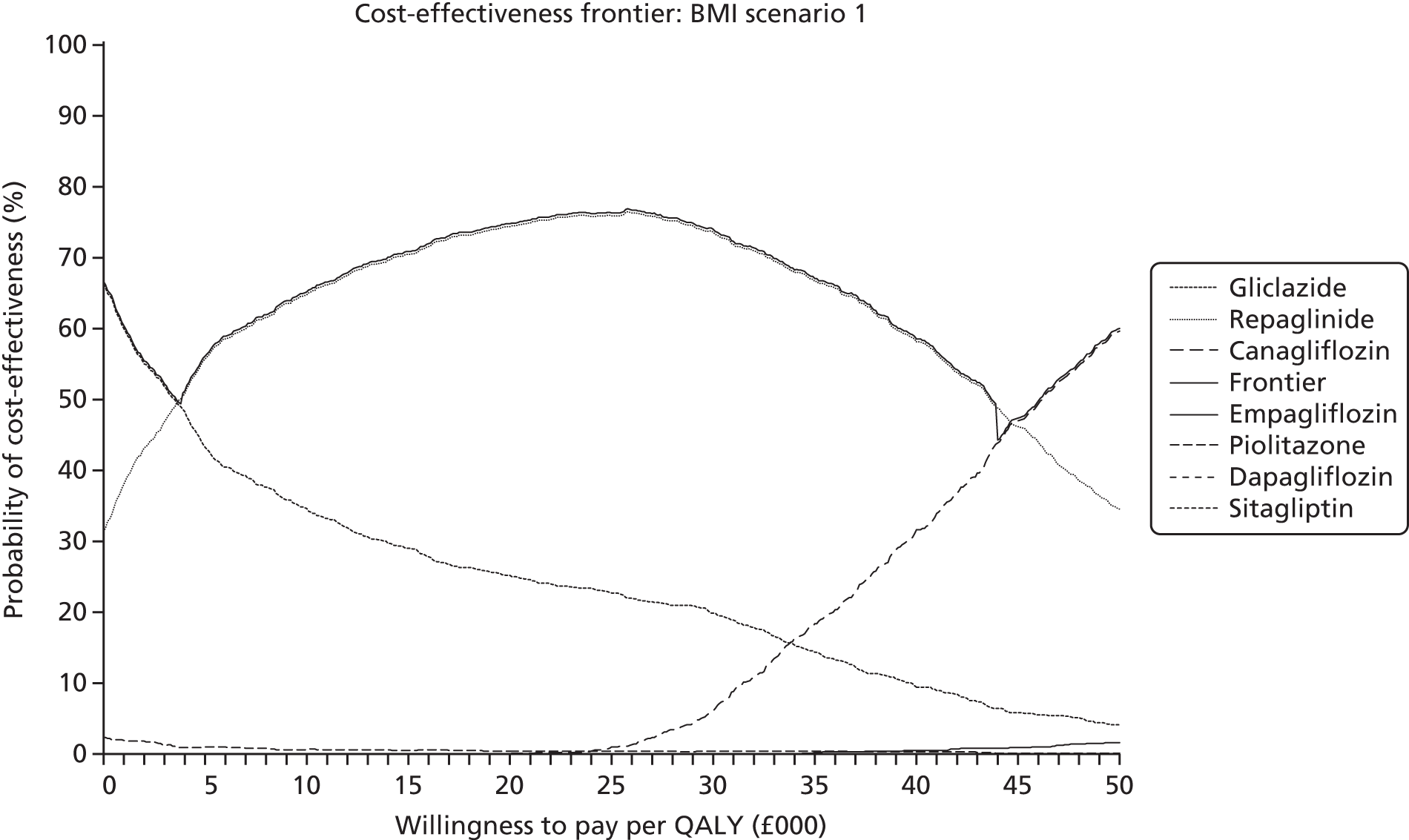
| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) | Pioglitazone (%) | Gliclazide (%) | Repaglinide (%) |
|---|---|---|---|---|---|---|---|
| 0 | 0 | 0 | 0 | 0 | 2 | 66 | 31 |
| 10,000 | 0 | 0 | 0 | 0 | 1 | 35 | 65 |
| 20,000 | 0 | 0 | 0 | 0 | 0 | 25 | 74 |
| 30,000 | 0 | 6 | 0 | 0 | 0 | 20 | 74 |
| 40,000 | 1 | 32 | 0 | 0 | 0 | 9 | 58 |
| 50,000 | 2 | 60 | 0 | 0 | 0 | 4 | 35 |
With weight changes being retained indefinitely, gliclazide is soon overtaken by repaglinide due to the greater weight gain with gliclazide. But canagliflozin is associated with the largest weight losses of the treatments. As the willingness to pay rises to around £45,000 per QALY, canagliflozin has the highest likelihood of being cost-effective. This £45,000 per QALY is broadly in line with the cost-effectiveness estimate for canagliflozin of both the deterministic and the probabilistic modelling.
FIGURE 21.
Body mass index scenario 1: cost-effectiveness acceptability frontier (CEAF) for flozins and sitagliptin.
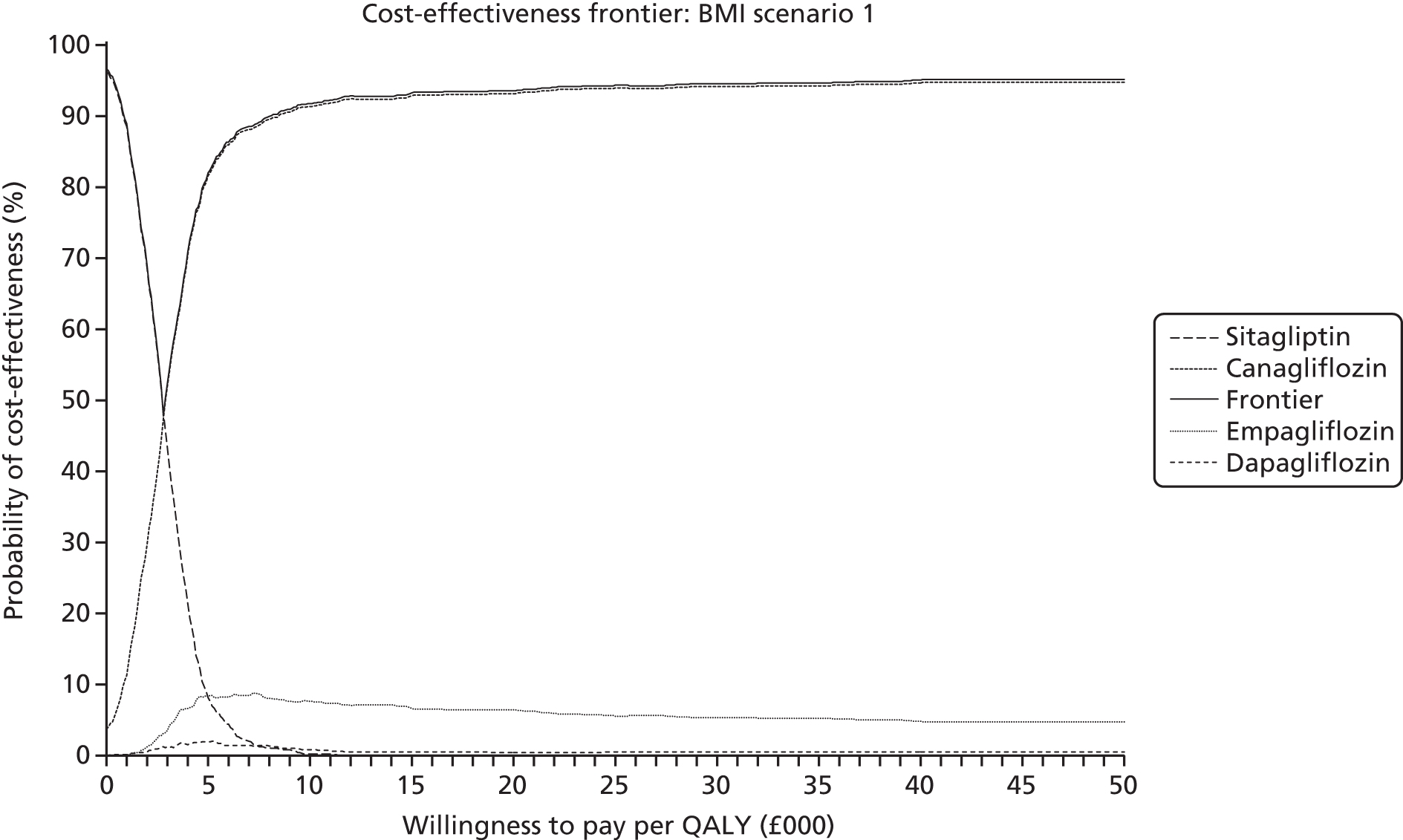
| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) |
|---|---|---|---|---|
| 0 | 0 | 4 | 0 | 96 |
| 10,000 | 8 | 91 | 1 | 0 |
| 20,000 | 6 | 93 | 0 | 0 |
| 30,000 | 5 | 94 | 1 | 0 |
| 40,000 | 5 | 95 | 1 | 0 |
| 50,000 | 5 | 95 | 1 | 0 |
Given the greater weight changes associated with canagliflozin, if weight changes are retained indefinitely canagliflozin is estimated to have the greatest likelihood of being cost-effective at all but low willingness to pay values and there is little uncertainty around this.
Scenario: body mass index 2 – body mass index weight loss rebounds after 1 year
FIGURE 22.
Body mass index scenario 2: cost-effectiveness acceptability frontier (CEAF) across all comparators.
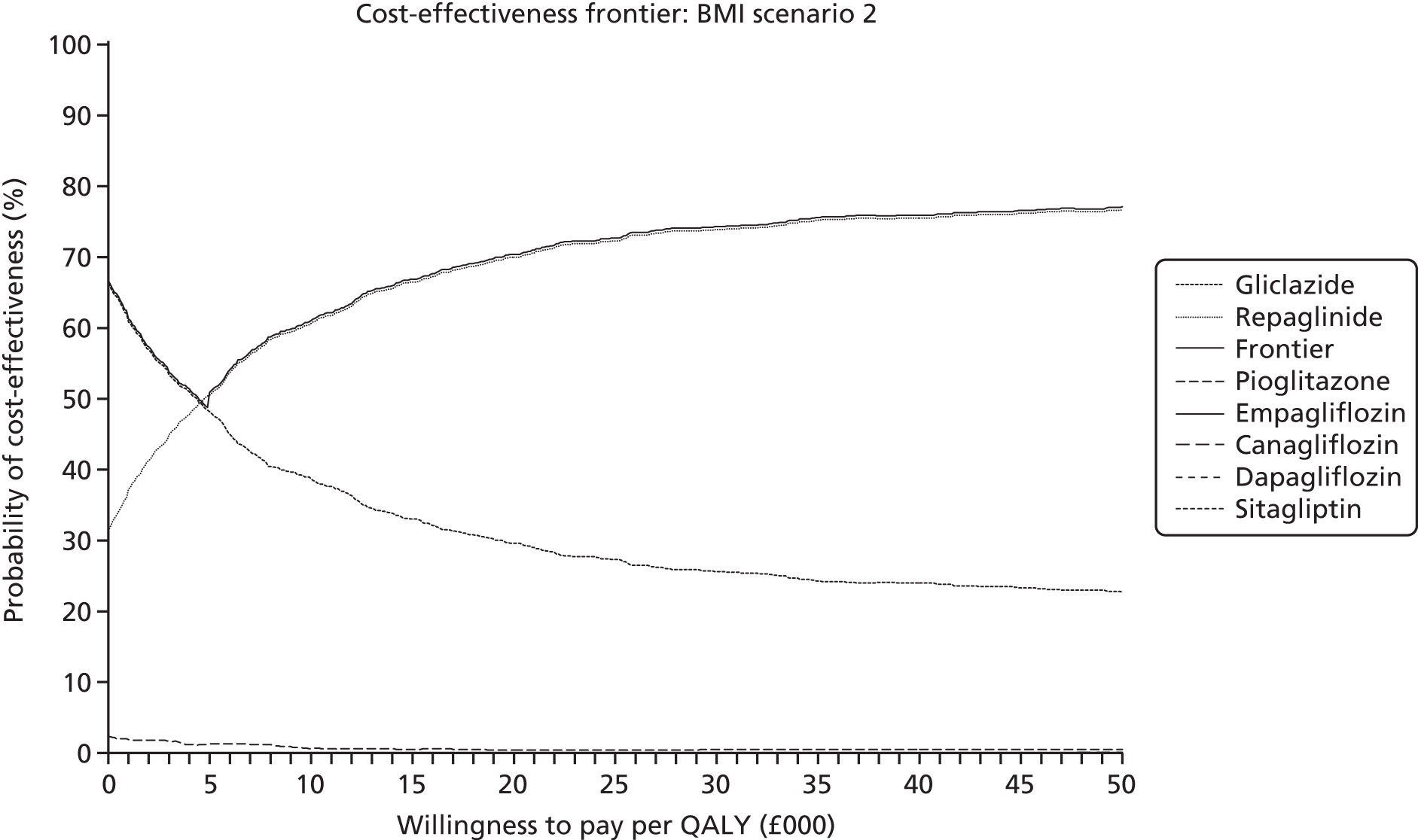
| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) | Pioglitazone (%) | Gliclazide (%) | Repaglinide (%) |
|---|---|---|---|---|---|---|---|
| 0 | 0 | 0 | 0 | 0 | 2 | 66 | 31 |
| 10,000 | 0 | 0 | 0 | 0 | 1 | 39 | 61 |
| 20,000 | 0 | 0 | 0 | 0 | 0 | 30 | 70 |
| 30,000 | 0 | 0 | 0 | 0 | 1 | 26 | 74 |
| 40,000 | 0 | 0 | 0 | 0 | 1 | 24 | 76 |
| 50,000 | 0 | 0 | 0 | 0 | 1 | 23 | 77 |
If weight changes are only retained for 1 year compared with them being retained indefinitely there is little impact upon where gliclazide and repaglinide cross over. The main impact is that canagliflozin no longer shows a probability of being cost-effective as the willingness to pay increases further towards £50,000 per QALY.
FIGURE 23.
Body mass index scenario 2: cost-effectiveness acceptability frontier (CEAF) for flozins and sitagliptin.

| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) |
|---|---|---|---|---|
| 0 | 0 | 4 | 0 | 96 |
| 10,000 | 12 | 43 | 2 | 43 |
| 20,000 | 24 | 61 | 4 | 11 |
| 30,000 | 27 | 64 | 4 | 5 |
| 40,000 | 28 | 65 | 4 | 3 |
| 50,000 | 29 | 64 | 4 | 2 |
Compared with the scenario of weight changes being retained indefinitely, the shorter retention of the larger weight gain from canagliflozin compared with empagliflozin means that there is greater uncertainty as to which is the most cost-effective treatment. At a willingness to pay of £30,000 per QALY, the probability of canagliflozin being the most cost-effective treatment is now only double that of empagliflozin.
Scenario: body mass index 3 – body mass index weight loss rebounds at treatment change
FIGURE 24.
Body mass index scenario 3: cost-effectiveness acceptability frontier (CEAF) across all comparators.

| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) | Pioglitazone (%) | Gliclazide (%) | Repaglinide (%) |
|---|---|---|---|---|---|---|---|
| 0 | 0 | 0 | 0 | 0 | 2 | 66 | 31 |
| 10,000 | 0 | 0 | 0 | 0 | 1 | 38 | 61 |
| 20,000 | 0 | 0 | 0 | 0 | 0 | 29 | 71 |
| 30,000 | 0 | 0 | 0 | 0 | 1 | 25 | 75 |
| 40,000 | 0 | 0 | 0 | 0 | 1 | 23 | 76 |
| 50,000 | 0 | 2 | 0 | 0 | 1 | 21 | 77 |
The scenario of weight losses rebounding at treatment change is a half-way house. But this half-way house is still insufficient for canagliflozin to be modelled as having any real probability of being the most cost-effective treatment. This requires weight changes to be modelled as being retained indefinitely.
FIGURE 25.
Body mass index scenario 3: cost-effectiveness acceptability frontier (CEAF) for flozins and sitagliptin.
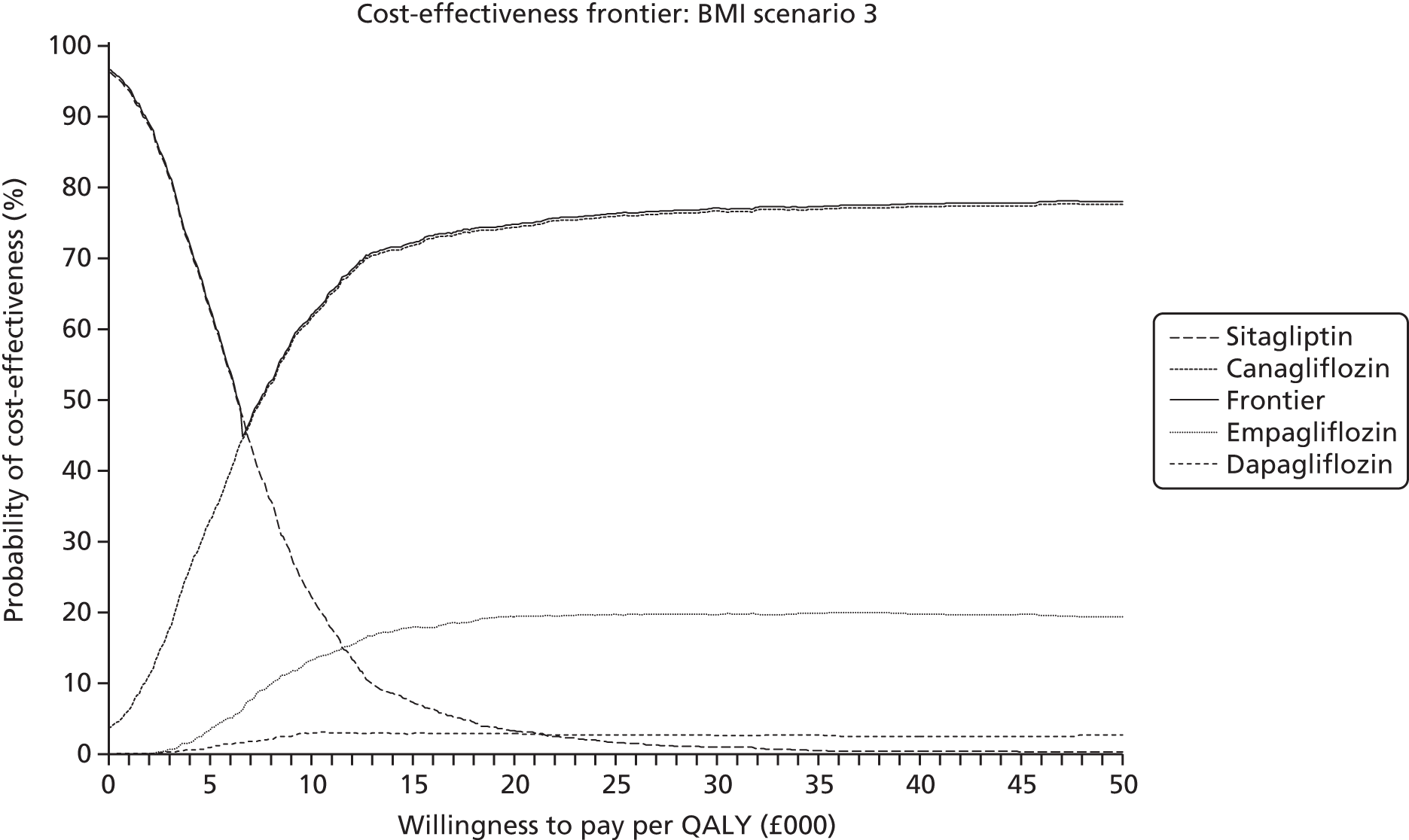
| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) |
|---|---|---|---|---|
| 0 | 0 | 4 | 0 | 96 |
| 10,000 | 13 | 62 | 3 | 22 |
| 20,000 | 19 | 74 | 3 | 3 |
| 30,000 | 20 | 77 | 3 | 1 |
| 40,000 | 20 | 77 | 3 | 0 |
| 50,000 | 19 | 78 | 3 | 0 |
The longer retention of weight changes compared with BMI scenario 2 means that the greater weight loss with canagliflozin compared with empagliflozin increases the likelihood of canagliflozin being the most cost-effective and reduces that of empagliflozin.
Scenario: body mass index 4 – body mass index weight changes rebound after 1 year
FIGURE 26.
Body mass index scenario 4: cost-effectiveness acceptability frontier (CEAF) across all comparators.
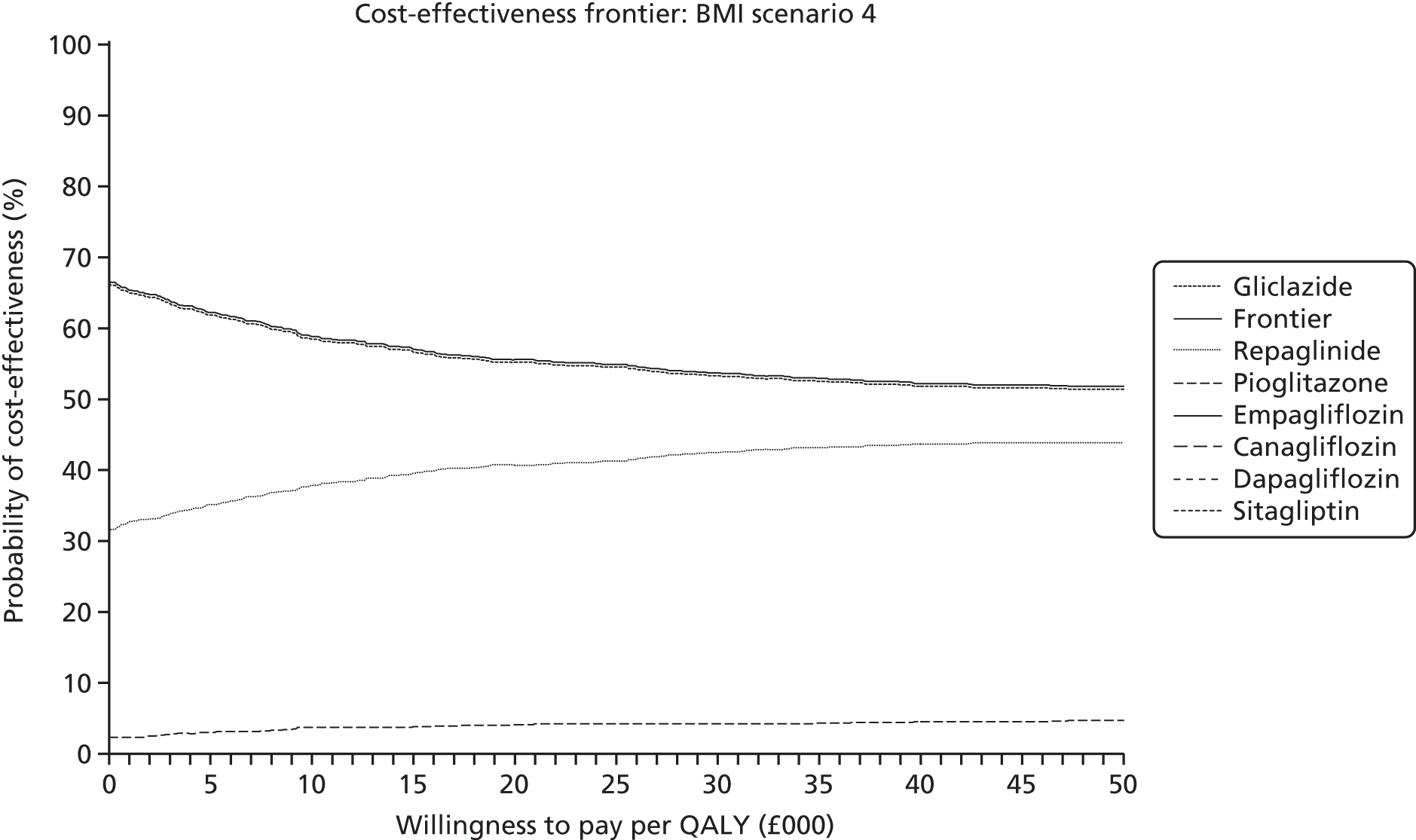
| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) | Pioglitazone (%) | Gliclazide (%) | Repaglinide (%) |
|---|---|---|---|---|---|---|---|
| 0 | 0 | 0 | 0 | 0 | 2 | 66 | 31 |
| 10,000 | 0 | 0 | 0 | 0 | 4 | 58 | 38 |
| 20,000 | 0 | 0 | 0 | 0 | 4 | 55 | 41 |
| 30,000 | 0 | 0 | 0 | 0 | 4 | 53 | 42 |
| 40,000 | 0 | 0 | 0 | 0 | 5 | 52 | 44 |
| 50,000 | 0 | 0 | 0 | 0 | 5 | 51 | 44 |
As would be expected given the short duration of weight changes, the cost-effectiveness acceptability frontier (CEAF) is little different from that of the scenario where BMI has no impact upon QoL, though by a willingness to pay of £50,000 per QALY the curves for gliclazide and repaglinide show a slightly greater convergence.
FIGURE 27.
Body mass index scenario 4: CEAF for flozins and sitagliptin.

| WTP | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) |
|---|---|---|---|---|
| 0 | 0 | 4 | 0 | 96 |
| 10,000 | 11 | 36 | 2 | 51 |
| 20,000 | 24 | 55 | 4 | 17 |
| 30,000 | 30 | 58 | 4 | 7 |
| 40,000 | 33 | 59 | 4 | 4 |
| 50,000 | 34 | 59 | 5 | 3 |
Comparing weight changes being retained for 1 year to weight changes having no direct QoL impact, the difference between the probability of canagliflozin being the most cost compared with that of empagliflozin is slightly greater. This increases as the willingness to pay increases.
Scenario: body mass index 5 – body mass index weight changes rebound at treatment change
FIGURE 28.
Body mass index scenario 5: CEAF across all comparators.
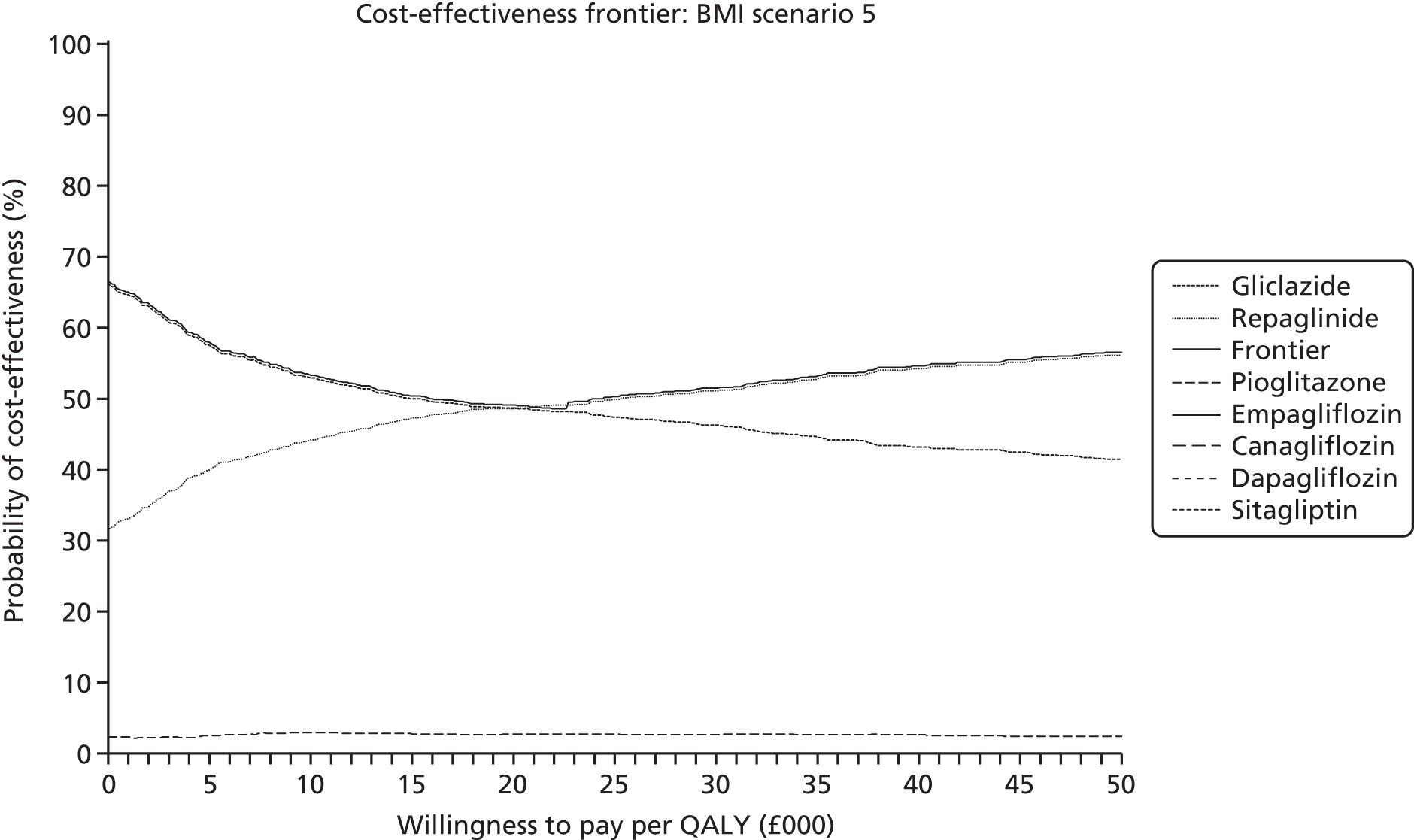
| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) | Pioglitazone (%) | Gliclazide (%) | Repaglinide (%) |
|---|---|---|---|---|---|---|---|
| 0 | 0 | 0 | 0 | 0 | 2 | 66 | 31 |
| 10,000 | 0 | 0 | 0 | 0 | 3 | 53 | 44 |
| 20,000 | 0 | 0 | 0 | 0 | 3 | 49 | 49 |
| 30,000 | 0 | 0 | 0 | 0 | 3 | 46 | 51 |
| 40,000 | 0 | 0 | 0 | 0 | 3 | 43 | 54 |
| 50,000 | 0 | 0 | 0 | 0 | 2 | 41 | 56 |
If weight changes are retained until treatment change the probabilities of being the most cost-effective for gliclazide and for repaglinide are roughly equal at a willingness to pay of £20,000 per QALY, and have diverged only slightly at a willingness to pay of £30,000 per QALY.
FIGURE 29.
Body mass index scenario 5: CEAF for flozins and sitagliptin.

| WTP (£) | Empagliflozin (%) | Canagliflozin (%) | Dapagliflozin (%) | Sitagliptin (%) |
|---|---|---|---|---|
| 0 | 0 | 4 | 0 | 96 |
| 10,000 | 13 | 57 | 3 | 27 |
| 20,000 | 21 | 72 | 3 | 4 |
| 30,000 | 23 | 73 | 3 | 1 |
| 40,000 | 22 | 74 | 3 | 0 |
| 50,000 | 23 | 74 | 3 | 0 |
Sitagliptin and canagliflozin have the highest estimates for their probabilities of being cost-effective, with canagliflozin having the highest estimate at conventional NICE willingness to pay thresholds. Empagliflozin has some probability of being cost-effective but it is only around one-third of that of canagliflozin.
Erratum
The AG modelling did not apply a baseline prevalence of 2.7% IHD. Applying the 2.7% baseline IHD prevalence results in very small differences, as outlined in Tables 120–122.
| Treatment | Total costs (£) | Total QALYs | |||||
|---|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | ||
| Gliclazide | 27,600 | 10.376 | 9.618 | 9.618 | 9.618 | 9.755 | 9.723 |
| Repaglinide | 27,704 | 10.374 | 9.649 | 9.649 | 9.649 | 9.755 | 9.730 |
| Pioglitazone | 27,827 | 10.367 | 9.596 | 9.596 | 9.596 | 9.746 | 9.712 |
| Sitagliptin 100 mg | 32,631 | 10.337 | 9.641 | 9.638 | 9.639 | 9.723 | 9.702 |
| Canagliflozin 300 mg | 32,933 | 10.362 | 9.763 | 9.674 | 9.691 | 9.753 | 9.750 |
| Empagliflozin 25 mg | 33,031 | 10.360 | 9.730 | 9.667 | 9.678 | 9.749 | 9.739 |
| Dapagliflozin 10 mg | 33,136 | 10.350 | 9.718 | 9.656 | 9.665 | 9.740 | 9.729 |
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Gliclazide | – | – | – | – | – | – |
| Repaglinide | Dom | 3388 | 3388 | 3388 | 434,000 | 16,413 |
| Pioglitazone | Dom | Dom | Dom | Dom | Dom | Dom |
| Sitagliptin 100 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Canagliflozin 300 mg | Dom | 45,641 | 207,000 | 124,000 | Dom | 259,000 |
| Empagliflozin 25 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Dapagliflozin 10 mg | Dom | Dom | Dom | Dom | Dom | Dom |
| Treatment | ICERs (£) | |||||
|---|---|---|---|---|---|---|
| No BMI | BMI 1 | BMI 2 | BMI 3 | BMI 4 | BMI 5 | |
| Canagliflozin 300 mg | 12,034 | 2467 | 8494 | 5820 | 9777 | 6312 |
| Empagliflozin 25 mg | 17,278 | 4471 | 13,917 | 10,294 | 14,864 | 10,724 |
| Dapagliflozin 10 mg | 37,871 | 6542 | 29,341 | 19,172 | 29,116 | 19,062 |
The pattern of dominance is unchanged compared with the base case of the AG report, with the exception of the BMI scenario 4, in which repaglinide has changed from being modelled as being marginally inferior to being marginally superior compared with gliclazide.
The cost-effectiveness estimates for canagliflozin compared with repaglinide are essentially the same as those of the AG report base case, though those in six figures show greater absolute changes due to the very small divisor.
The cost-effectiveness estimates for the flozins compared with sitagliptin are similarly close to those of the AG report base case, though those for the scenario of weight having no direct QoL impact show some improvement for empagliflozin and dapagliflozin. There has been a marginal improvement in those for dapagliflozin, such that the cost-effectiveness ratios that were previously estimated as being slightly above £30,000 per QALY are now slightly below £30,000 per QALY.
List of abbreviations
- ACCORD
- Action to Control Cardiovascular Risk in Diabetes
- ACEI
- angiotensin-converting enzyme inhibitor
- ADA
- American Diabetes Association
- ADOPT
- A Diabetes Outcome Progression Trial
- ADVANCE
- Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation
- AE
- adverse effect
- AG
- Assessment Group
- AHA
- antihyperglycaemic agent
- ARB
- angiotensin-receptor blocker
- BDR
- background diabetic retinopathy
- BMI
- body mass index
- BNF
- British National Formulary
- BNP
- B-type natriuretic peptide
- BP
- blood pressure
- CADTH
- Canadian Agency for Drugs and Technologies in Health
- CANTATA-M
- CANagliflozin Treatment and Trial Analysis – Monotherapy
- CDM
- Cardiff Diabetes Model
- CEAC
- cost-effectiveness acceptability curve
- CEAF
- cost-effectiveness acceptability frontier
- CG
- clinical guideline
- CHF
- congestive heart failure
- CI
- confidence interval
- CKD
- chronic kidney disease
- CODE-2
- Cost of Diabetes in Europe–Type 2
- CPRD
- Clinical Practice Research Datalink
- CrI
- credible interval
- CSII
- continuous subcutaneous insulin infusion
- CVD
- cardiovascular disease
- DBP
- diastolic blood pressure
- DCCT
- Diabetes Control and Complications Trial
- DIC
- deviance information criterion
- DKA
- diabetic ketoacidosis
- DPP-4
- dipeptidyl peptidase-4
- DSA
- deterministic sensitivity analysis
- DURATION-1
- Diabetes Therapy Utilisation: Researching Changes in A1C, Weight and Other Factors Through Intervention with Exenatide Once Weekly
- ECHO-T2DM
- Economic and Health Outcomes Model for Type 2 Diabetes Mellitus
- EDICT
- Efficacy and Durability of Initial Combination Therapy for Type 2 diabetes
- eGFR
- estimated glomerular filtration rate
- EMA
- European Medicines Agency
- EMPA-REG BASAL
- Impact of empagliflozin added on to basal insulin in type 2 diabetes inadequately controlled on basal insulin
- EMPA-REG METSU
- Empagliflozin as add-on to metformin plus sulfonylurea in patients with type 2 diabetes
- EMPA-REG OUTCOME
- Empagliflozin Cardiovascular Outcome Event Trial in Type 2 diabetes Mellitus Patients
- EMPA-REG RENAL
- Efficacy and Safety of Empagliflozin in Patients With Type 2 diabetes and Renal Impairment
- EQ-5D
- EuroQol-5 Dimensions
- ERG
- Evidence Review Group
- ESRD
- end-stage renal disease
- FDA
- Food and Drug Administration
- FPG
- fasting plasma glucose
- GDG
- Guideline Development Group
- GFR
- glomerular filtration rate
- GI
- gastrointestinal
- GLP-1
- glucagon-like peptide-1
- GP
- general practitioner
- GPRD
- General Practice Research Database
- GTI
- genital tract infection
- GUIDE
- GlUcose control In type 2 diabetes: Diamicron MR vs. glimEpiride
- HALex
- Health and Activity Limitation Index
- HbA1c
- glycated haemoglobin (A1c)
- HDL
- high-density lipoprotein
- HDL-C
- high-density lipoprotein cholesterol
- HFS
- Hypoglycaemic Fear Survey
- HOPE
- Heart Outcomes Prevention Evaluation Study
- HR
- hazard ratio
- ICERs
- incremental cost-effectiveness ratio
- IHD
- ischaemic heart disease
- IQR
- interquartile range
- ITT
- intention to treat
- IWB
- Index of Wellbeing
- LA
- long acting
- LDL
- low-density lipoprotein
- LDL-C
- low-density lipoprotein cholesterol
- LOCF
- last observation carried forward
- MCMC
- Markov chain Monte Carlo
- MD
- mean difference
- MDI
- multiple daily injections
- MHRA
- Medicines & Healthcare products Regulatory Agency
- MI
- myocardial infarction
- MO
- macular oedema
- MR
- modified release
- MS
- manufacturer submission
- Mt
- Mount
- NAFLD
- non-alcoholic fatty liver disease
- NICE
- National Institute for Health and Care Excellence
- NMA
- network meta-analysis
- NPH
- neutral protamine Hagedorn
- OLS
- ordinary least squares
- OM1
- UKPDS Outcomes Model v1
- OM2
- UKPDS Outcomes Model v2
- PCT
- primary care trust
- PDR
- proliferative diabetic retinopathy
- PG
- plasma glucose
- PPARG
- peroxisome proliferator-activated receptor gamma
- PROactive
- PROspective pioglitAzone Clinical Trial In macroVascular Events
- PSA
- probabilistic sensitivity analysis
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- PVD
- peripheral vascular disease
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- QWB
- Quality of Wellbeing
- RCT
- randomised controlled trial
- RR
- risk ratio
- SBP
- systolic blood pressure
- SD
- standard deviation
- SE
- standard error
- SF-36
- Short Form questionnaire-36 items
- SGLT1
- sodium–glucose co-transporter 1
- SGLT2
- sodium–glucose co-transporter 2
- SIGN
- Scottish Intercollegiate Guidelines Network
- SLC5A2
- solute carrier family 5 (sodium–glucose co-transporter), member 2
- SMBG
- self-monitoring of blood glucose
- SmPC
- Summary of Product Characteristics
- STA
- single technology appraisal
- SU
- sulphonylurea or sulfonylurea
- SUCRA
- Surface Under the Cumulative Ranking
- T1DM
- type 1 diabetes mellitus
- TC
- total cholesterol
- THIN
- The Health Improvement Network
- TTO
- time trade-off
- TZD
- thiazolidinedione
- UKPDS
- United Kingdom Prospective Diabetes Study
- UTI
- urinary tract infection
- WESDR
- Wisconsin Epidemiologic Study of Diabetic Retinopathy
- YHPHO
- York and Humber Public Health Observatory