Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 06/05/01. The contractual start date was in December 2009. The draft report began editorial review in December 2015 and was accepted for publication in September 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Bernadka Dubicka is a member of the Health Technology Assessment Mental, Psychological and Occupational Health Panel and has received personal fees as a consultant to Lundbeck. She also has a licensed patent: there is a licence to Lundbeck to use brief psychosocial intervention in their current trial (future payment anticipated). Peter Fonagy is in receipt of a National Institute for Heath Research Senior Investigator Fellowship. Paul Wilkinson has received personal fees as a consultant to Lundbeck, a consultant to Takeda and a supervisor in interpersonal psychotherapy. He has also had non-financial support from the interpersonal psychotherapy UK Training Committee. Ian M Goodyer has received personal fees as a consultant to Lundbeck, is supported by a strategic award from the Wellcome Trust, research support from the Friends of Peterhouse and is senior scientific advisor to and chairperson of the Peter Cundill centre for research into mood disorders in young people, University of Toronto, ON, Canada. Raphael Kelvin has received personal fees as a consultant to Lundbeck.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Goodyer et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Some of the information in this report is based on Goodyer et al. 1 © The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY-NC-ND license.
Unipolar major depression in adolescents
Unipolar major depression is a significant mental illness affecting a substantial proportion of the adolescent population worldwide. 2 The disorder presents in episodes and the estimated 12-month period prevalence of major depression episodes in teenagers is 7.5%. Approximately twice as many girls as boys are affected and an estimated one in four cases experience a severe, impairing and clinically referable condition. 3,4 There is a growing concern based on longitudinal evidence that the consequences of some adolescent emergent major depression episodes include suicide, persistent and chronic mental health disorders, substance misuse, and failure to achieve both educationally and in the work place. 5 Furthermore, in adults there is evidence that a history of depression may interfere with treatment compliance and self-care in patients with type 2 diabetes and cardiovascular disease,6 which suggests that reducing incident risk for depression early in life may have wider physical health-care benefits for later in the life course. These medium- and long-term negative outcomes also come at great economic cost to the UK and other nations, including in the developing world where depression has been noted to be at least as disabling as any other chronic illness in adult life as urbanisation increases. 7,8 Therefore, clinical methods for the treatment of depressed adolescents must go beyond short-term remission of a single episode; objectives should include reducing the risks for diagnostic relapse and recurrence risk by lowering depressive symptoms before independent adult life.
The combined effect of a high level of emerging mental illness with long-term consequences for health, together with the increasing demands for treatment from adolescents and their parents/guardians, makes it imperative to provide effective interventions that can be implemented by developing the current mental health workforce. 9,10 From this policy perspective it is also essential to consider the extent to which any effective treatment is deliverable and affordable. Currently, the cost-effectiveness of treatments aimed at reducing recurrence risk by lowering depressive symptom rate and avoiding diagnostic relapse up to 18 months after entering treatment are not known.
Are there effective treatments for depressed adolescents?
Over the past 20 years there have been a series of important randomised controlled trials (RCTs) determining both the efficacy and clinical effectiveness of psychological and pharmacological treatments for depression in adolescents that result in remission in the short term, that is by 28 weeks. 11,12 Original guidance compiled in 2005 by the National Institute for Health and Care Excellence (NICE) for the treatment of a moderate to severe depression episode, referred to and treated in NHS Child and Adolescent Mental Health Services (CAMHS), advised the use of evidence-based psychological therapies, such as cognitive–behavioural therapy (CBT), as the first-line treatment, with selective serotonin reuptake inhibitor (SSRI) antidepressants constituting the pharmacological treatment of choice only if there was no satisfactory response. 13 The 2015 revisions now recommend that a SSRI may be used as a first-line treatment in combination with psychological therapy (individual CBT, interpersonal therapy, family therapy or psychodynamic psychotherapy) that runs for at least 3 months for a major depression episode, defined as five or more symptoms (of which one must be a depressed or irritable mood state of at least 2 weeks, most days of the week and most hours of the day) and associated with observable personal impairment. 14 However, the revised 2015 guidelines continue to warn against the use of SSRIs on their own. Furthermore, this revision applies only to patients with moderate to severe depression, defined as five or more symptoms associated with concurrent impairments in personal, social or educational life domains for longer than 2 weeks.
Research studies in adults have provided evidence for the clinical effectiveness of a number of psychological therapies for inducing clinical remission for adult patients suffering with a moderate to severe depression episode. These include CBT,15 interpersonal therapy, short-term psychoanalytic psychotherapy (STPP)16 and non-directive brief psychosocial interventions (BPIs). 17 Overall, psychological therapies appear to be effective in a broadly equivalent manner, although results vary with methods and measures. 18 Current evidence indicates that findings from adult patients cannot be assumed to reflect comparable efficacy or effectiveness for depressed adolescents. 19
Evidence to date from RCTs on adolescents suggest that CBT is not rapidly therapeutic in the acute phase of treatment. 11 Furthermore, in the short term, CBT may not provide added clinical value when patients are already receiving fluoxetine plus active specialist clinical care in a UK CAMHS setting. 12 There is relatively little evidence on the use of STPP with children or adolescents, although the one clinical trial with this population had encouraging outcomes. 20
Interpersonal psychotherapy is effective for adolescents with mild to moderate depression in the short term, but there is no evidence for efficacy in patients with moderate to severe depression episodes. However, interpersonal psychotherapy for adolescents (IPT-A) is not widely available on the NHS in the UK to treat depression in adolescents, although this problem is being addressed as part of the Improved Access to Psychological Therapies initiative of NHS England. 21 Relatively brief, problem-solving, approaches with a focus on promoting good interpersonal relationships may be of value in more severe forms of these illnesses but this remains to be fully evaluated. 22,23
Brief psychosocial intervention incorporates general principles from psychological therapies (e.g. agenda setting, problem-solving and facilitating relationships with peers, school and family). BPI has recently been formalised into a manual for systematic delivery within CAMHS clinics for the treatment of major depression aimed at inducing short-term remission. 24 A previous RCT reported that BPI combined with fluoxetine is as effective as BPI combined with fluoxetine and CBT in producing remission at 28 weeks of treatment. 12 It is not known if BPI alone is efficacious and clinically effective in the short term for patients suffering from a moderate to severe depression episode.
Only one study has tested the efficacy of psychological treatments against placebo and showed that time to remission is significantly quicker for SSRIs and SSRIs plus CBT against pill placebo. 11 All RCTs to 2016 have focused on establishing clinical effectiveness in reducing immediate symptoms and restoring personal functioning. 11,12,25 Although there is evidence for clinical effects, there is no evidence that any of the aforementioned treatments, individually or in combination, is efficacious in reducing recurrence risk by lowering depressive symptom rate or diminishing diagnostic relapse in the medium term (i.e. ≥ 1 year following intervention).
This lack of understanding about therapeutic effects on recurrence risk and clinical relapse is compounded by a remaining concern regarding the extent of the effectiveness of existing treatments and the natural history of these disorders. 4,5,26 RCT data to date have shown that, even when treatment is successfully delivered, a substantial number of depressed adolescents do not recover or they relapse following recovery. Thus, the proportion of depressed patients who meet the criteria for clinical remission did not rise above 70% by 28 weeks from the start of treatment. Indeed, in studies of moderate to severely depressed adolescents, one RCT in the UK reported that only 42% were very much or much improved by 12 weeks, rising to 53–61% by 28 weeks. 27 Of the remaining patients, a further 30% described themselves as no better or worse at 12 weeks, which fell to 18–24% by 28 weeks. 27 A recent meta-analysis noted that, compared with CBT alone, the combination of fluoxetine and CBT may produce greater improvement in psychosocial functions but no greater reduction in residual symptoms. 28 Even for successfully treated cases, there is a high relapse rate in the next 5–10 years. Overall, approximately 50–70% of patients attending a NHS CAMHS clinic may relapse in the 10 years between mid-adolescence and young adulthood, coinciding with some of the largest educational milestones and social changes they may face over their lifetime. 4,5,26
To date, there have been two naturalistic follow-up investigations of psychological treatment effects in the medium term (i.e. > 52 weeks) in depressed adolescents entered into RCTs. Both of these studies show that the likelihood of recurrence and relapse of diagnosis following successful treatment is substantial, occurring in 50–75% of treated patients, beginning within 1 year of clinical remission and being significantly higher in patients with recurrent versus single episodes. 29–31 These studies were, however, conducted with < 150 patients each and did not plan to investigate the relative effects of treatment in maintaining reduced depressive symptoms in the medium term.
There are no studies in the NHS that have investigated clinical effectiveness of specialist or general psychological treatments in reducing symptomatic recurrence risk or diminishing clinical diagnostic relapse of depression in the medium term up to 18 months following treatment. Therefore, it is unclear if there are superiority effects of one psychological treatment over another in reducing and maintaining lower depressive symptoms over time and, therefore, diminishing symptomatic recurrence risk.
Theoretically, psychodynamic practitioners suggest that potentially more enduring changes will be associated with this form of psychological treatment, as it aims to address and repair underlying mental models of interpersonal relationships that may be associated with the depressive symptoms. In a similar way, cognitive–behavioural therapists theoretically aim to teach new, more adaptive, methods of behaving and thinking, which should continue after therapy ends and, thus, reduce long-term relapse of disorder. These forms of therapy are therefore hypothesised to be more likely, if successful, to predict more enduring recovery than therapies simply addressing current symptom reduction, alleviating the impact of provoking life events and difficulties, providing psychoeducation and offering problem-solving advice.
Rationale for the current study
The current study was devised knowing that there is now a clear evidence base for implementing psychological treatments that are clinically effective for inducing short-term remission but whose efficacy for (1) reducing recurrence risk indexed by rising depressive symptoms in the medium term 18 months after treatment began or (2) preventing clinical diagnostic relapse after treatment is completed, remains unknown. The literature implicates a number of candidate specialist psychological treatments for putative effects on reducing recurrence risk and relapse rates, among which are CBT and STPP. Both treatments aim to reduce symptoms and future risk of relapse. Given clear-cut evidence that, in depressed adolescents, active psychological treatments are clinically more effective than no treatment, a pragmatic effectiveness superiority trial was conceived as the best design. The standard treatment chosen as the reference therapy was BPI, a relatively brief (i.e. maximum of 12 sessions) psychosocial approach to problem-solving, mental hygiene and well-being management with education about depressive illnesses. BPI was designed to be shorter than specialist psychological therapies and is aimed, theoretically, at gaining remission as quickly as possible from the depression episode. Therefore, the therapeutic protocol focuses on practical advice giving, psychoeducation about depression and how to manage daily life challenges.
Therefore, we designed a RCT to test the risk reduction effect of two specialist psychological treatments against a BPI primarily focused on short-term clinical remission. In each of the three arms of the RCT, SSRIs were available as a combination treatment option following the 2005 NICE guidelines. 13
The study must allow for the prescribing of SSRIs because short-term clinical effectiveness is also achievable with fluoxetine without the addition of a protocol driven psychological therapy. 11 However, as with psychological treatments, the contribution of SSRIs to reduce recurrence risk and relapse rate remains unknown. There is also evidence that cases which have been resistant to other antidepressant medication may show significant clinical improvement with a change to a different SSRI, if prescribed in conjunction with CBT. 25 This is the only published study25 of treatment resistance in depressed adolescents and suggests that medium-term treatment goals may be best achieved by combination therapies. This remains to be evaluated in a systematic RCT in which reduction in recurrence risk and relapse rates is the clinical outcome objective. Nevertheless, in the current study we judged it essential to abide by current NICE guidelines14 for the NHS and allow SSRI prescribing within each arm based on clinical judgement of psychological treatment progress.
Given the importance of cost-effectiveness and deliverability within the NHS, we also included an economic evaluation component to the trial. Results from a previous RCT conducted in the USA suggest that CBT alone is relatively expensive and cost-ineffective compared with a SSRI alone. 32 The same RCT demonstrated that fluoxetine alone was much more cost-effective than combined fluoxetine and CBT over 12 weeks. 32 In the UK, a RCT reported that adding CBT to an existing combination treatment of fluoxetine plus active specialist clinical care (the non-manualised forerunner of BPI) in a CAMHS setting was not cost-effective over 28 weeks. 33 Whether or not more expensive psychological treatments may become cost-effective in the medium term by diminishing the subsequent use of health, education and social services more than the use of a ‘treatment as usual’ or BPI protocol is not yet known.
For this study, clinic-referred depressed adolescents only were considered for recruitment. To make the results applicable to NHS CAMHS services, we included those with suicidal thoughts, psychotic behaviours and non-depression comorbid disorders. This is comparable to the Adolescent Depression Antidepressant and Psychotherapy Trial (ADAPT)12 but distinguishes both of these UK studies from the major study of adolescent depression [Treatment of Adolescent Study (TADS)11] in the USA, as suicidal and psychotic cases were excluded from TADS and participants were recruited by advertisement. 11,27,34
Participants were recruited from patients referred to routine NHS clinics. All trial participants were treated in standard clinical settings using NHS staff to deliver treatments under supervision. This maximised ecological validity and generalisability to NHS settings and was intended to assure commissioners and providers that the study results could inform routine NHS service design, delivery and implementation.
Unlike the UK ADAPT RCT,12 those who responded to an initial phase of BPI (2–3 weeks) and who therefore may have been close to remission or were especially responsive, were not excluded. This is because all participants were prescribed fluoxetine in ADAPT and it was in keeping with the clinical practice at the time of offering a BPI before patients were committed to a 6-month course of fluoxetine. At the time of starting Improving Mood with Psychoanalytic and Cognitive Behaviour Therapy (IMPACT), it was standard practice (in keeping with NICE guidelines) to start treatment with specific psychological therapy. In addition, unlike prior UK RCT studies,12,35 we added potential moderators of recurrence risk and relapse rates. These were individual differences in (1) self-reported rumination (persistently brooding or dwelling, often to the exclusion of other themes in the patient’s life)36,37 and (2) depressive thinking style (the extent to which patients with clinical depression may be characterised in terms of immaturity of the cognitive styles of self-criticism and perfectionism). 38–40
Aims and objectives
This superiority powered pragmatic effectiveness RCT was designed to determine whether or not psychological treatment delivered to adolescents with unipolar major depression would reduce the risk of recurrence through lowering depressive symptoms by 86 weeks post randomisation. As this was designed as a superiority effects trial, we tested whether or not, compared with a standard BPI, two specialist psychological treatments were more likely to result in lowering the rate of depressive symptoms from randomisation to 86 weeks after beginning treatment.
The primary objective contained two related questions. The first was to determine whether or not, in a specialist CAMHS setting, CBT and STPP were superior to a standardised BPI in reducing self-reported depressive symptoms over time. The second was to test if there were non-inferiority effects of CBT compared with STPP for lowering depressive symptoms by 86 weeks. The secondary hypothesis tested whether or not self-reported anxiety symptoms and research interviewer-evaluated psychosocial function were also significantly more likely to remain improved in those receiving STPP or CBT as opposed to BPI. An additional objective was to evaluate whether or not these specialist individual psychological treatments were more effective than standard BPI at reducing the clinical diagnostic rate for a major depression episode by 18 months after randomisation. However, the study was not powered to consider this outcome as a formal hypothesis.
Specific hypotheses
The hypotheses of the trial relate to the treatment effect in the post-treatment period (≥ 36 weeks).
The study had four primary hypotheses.
When comparing CBT with STPP:
-
CBT will show non-inferiority effects compared with STPP at 52 weeks
-
STPP will show superiority effects compared with CBT at 86 weeks
and when comparing CBT and STPP with BPI:
-
the specialist intensive interventions (CBT/STPP) will show superiority effects compared with BPI at 52 weeks
-
the specialist intensive interventions (CBT/STPP) will show superiority effects compared with BPI at 86 weeks.
This RCT tested a primary superiority clinical effectiveness hypothesis that, when compared with the reference BPI treatment:
-
STPP and CBT are both more clinically effective at maintaining a reduction in depressive symptoms at 52 and 86 weeks reassessment after randomisation.
The secondary hypothesis tested was:
-
STPP is superior in maintaining a reduction in depressive symptoms over the follow-up assessments (52 and 86 weeks) compared with CBT.
The RCT also tested an economic hypothesis to determine:
-
whether or not any additional costs of specialised treatments accrued by the end of treatment are justified by decreased use of resources (health, education and social care services, voluntary agencies) by 86 weeks of follow-up.
Chapter 2 Methods
The procedure for the study was to ascertain and recruit patients with an episode of Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV) major depression from routine NHS specialist CAMHS in three parts of the UK: East Anglia, North London and the north-west of England (Manchester and the Wirral).
East Anglia is a largely rural area of 3 million people, with four cities each containing approximately 100,000 people; North London is a densely populated urban sector of the metropolitan London region with around 4 million people; and north-west England is a region covering approximately 4 million people, of whom about 1 million are living in rural surroundings, with a further 3 million residing in the northern and central sectors of the large metropolitan area of the city of Manchester. Participants were recruited from 16 routine CAMHS clinics that agreed to participate from within these three regions.
The RCT was approved and monitored by the Multi-Centre Research Ethics Committee in Cambridgeshire. The sponsors were Cambridge and Peterborough NHS Foundation Trust, Cambridgeshire; Camden and Islington NHS Foundation Trust, North London; Cheshire and Wirral Partnership NHS Foundation Trust, Chester; and the Central Manchester University Hospital NHS Foundation Trust, Manchester. A scientific steering committee met every 6 months over the course of the RCT (chairperson: Professor Philip Cowen, University of Oxford; Professor Paul Stallard, University of Bath; Professor David Brent, University of Pittsburgh; and Professor Sabine Landau, King’s College London) and a Data Management Committee which also met every 6 months (chairperson: Professor Rona Campbell, University of Bristol; members: Dr Nicola Wiles, University of Bristol; and Professor Anna Marie Albano, Columbia University). The NHS Coordinating Centre for Health Technology Assessment audited accrual, progress and quality of the study throughout.
Participants and patient involvement
Patients from a prior treatment study provided advice on formulating the research question and evolving the BPI manual described in Chapter 3. Patients did not contribute to the recruitment procedure but those recruited provided ongoing feedback on the burden of assessment over the course of the study. This resulted in a 30–50% time reduction in the length of reassessment in the post-treatment follow-up phase. All participants and their families will receive a summary document of the main findings. Families will be informed that the full details of the study will also be posted on a weblink41 and be available through mandatory open access arrangements for published work under the auspices of the University of Cambridge, Cambridge, UK.
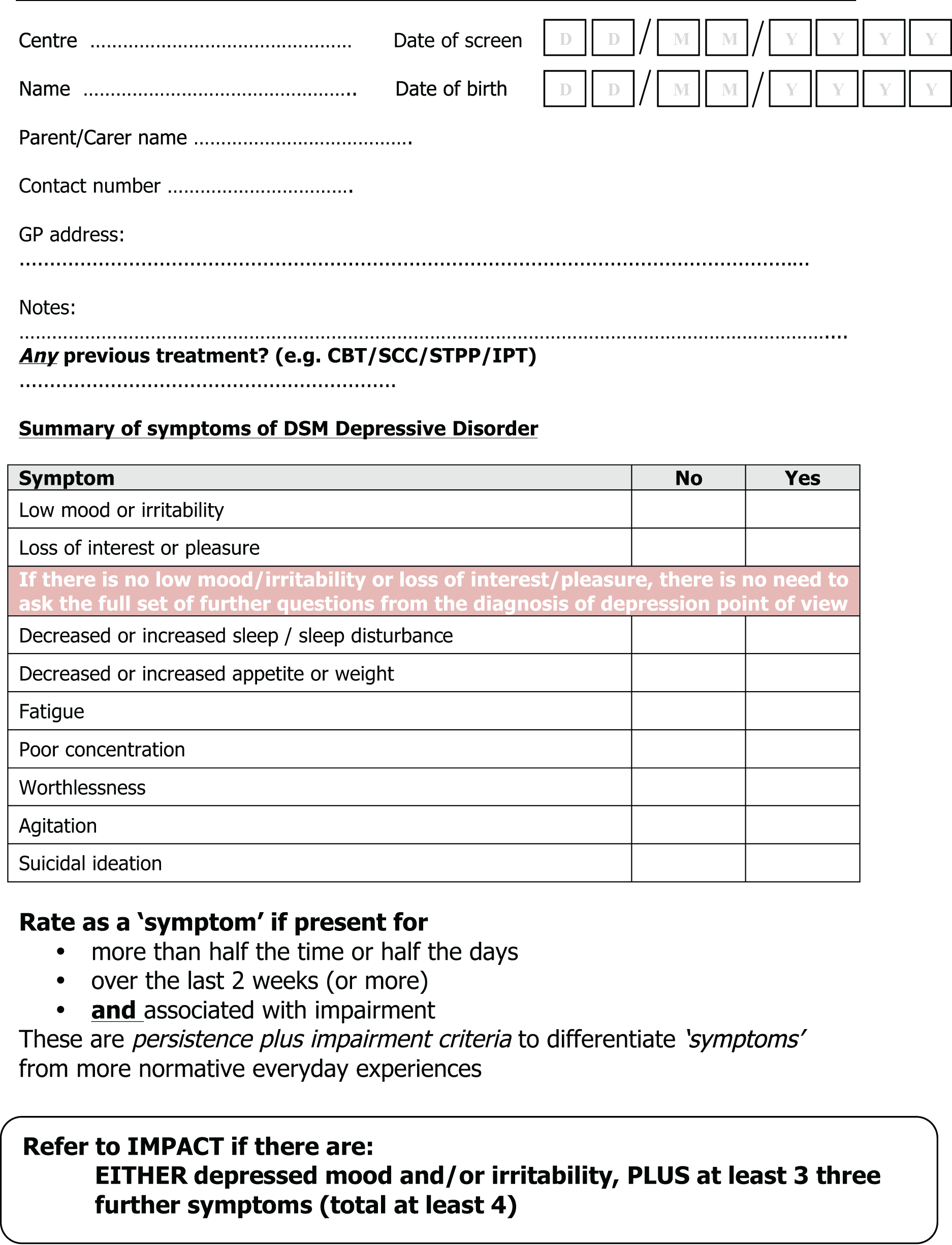
The research teams in each of the three regions contacted their regional clinics on a weekly basis to ascertain if there were any patients referred. The first point of contact was with clinical NHS staff who determined if their patient was in scope for the RCT. An initial screening checklist for major depression episode provided to the clinics by the research team and used to inform the research assessors of potential cases aided this clinical task (Figure 1).
FIGURE 1.
Screening to assess suitability for full assessment and recruitment.
Recruitment
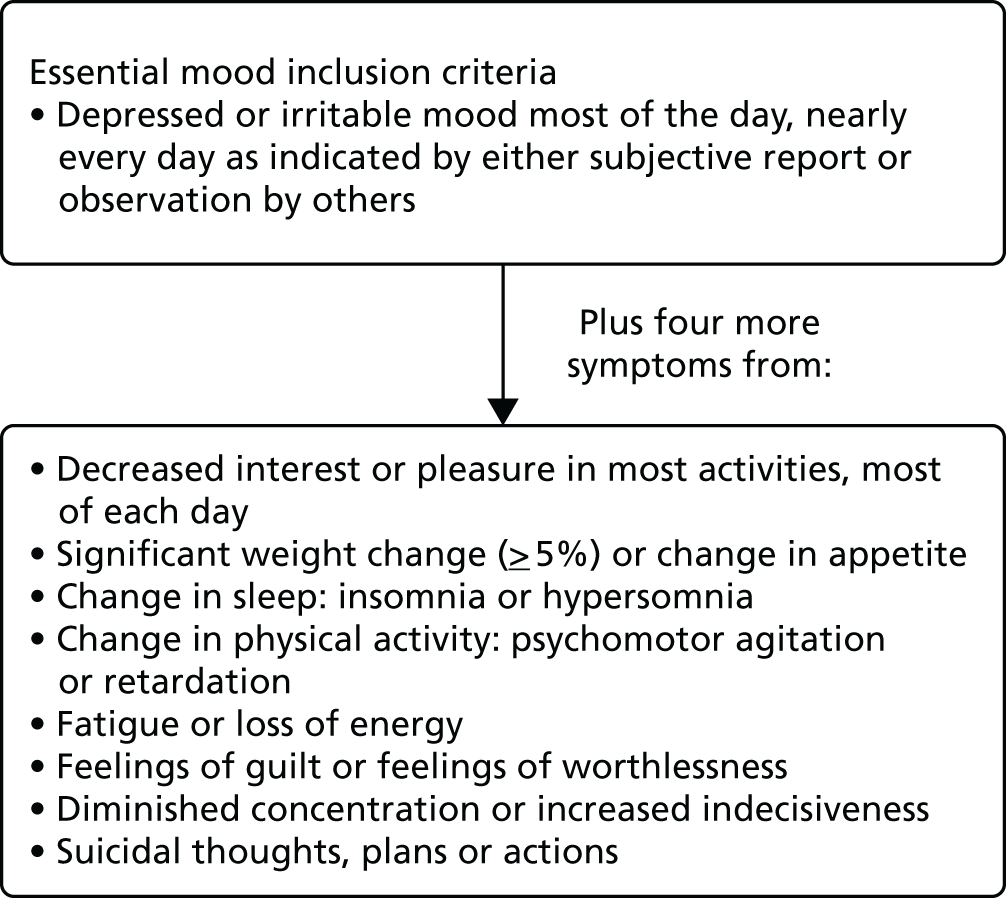
Participants were recruited if they met criteria for an episode of DSM-IV major depression and were aged between 11 and 17 years. This diagnosis is achieved by the presence of at least five symptoms, one of which must be a mood symptom present nearly every day and most of the day for at least 2 weeks, together with four others and accompanied by observable personal and/or social impairment. The criteria are shown in Figure 2. Mood change plus four other symptoms are required for the diagnosis.
FIGURE 2.
The DSM-IV criteria for major depression disorder.
Participants were recruited when clinical staff considered a patient to be depressed and requested that they completed the research checklist and asked them and their parents/guardians if they would consider taking part in a RCT investigating the extent to which treatment was able to lower recurrence risk and relapse rate. They were informed that the trial only included and compared treatments already known to contribute to producing clinical remission. If they expressed interest in the study, their contact details were passed to the research group and research staff contacted the patient with an expression of interest letter and a reply-paid envelope.
Inclusion criteria
-
Aged 11–17 years.
-
Current diagnostic episode of DSM-IV unipolar major depressive disorder (MDD).
Patients with suicidal intent, past or recent suicidal behaviour, psychotic symptoms or any comorbidity, other than those specifically defined in the exclusion criteria below, were included.
Patients who met the inclusion criteria but had started a SSRI within 1 month were included.
As part of the screening process prior to enrolment, individuals were asked if their current depressive illness was a first episode or a relapse.
Exclusion criteria
-
Generalised learning difficulties.
-
Pervasive developmental disorder.
-
Pregnancy.
-
Currently taking another medication that may interact with a SSRI and unable to stop this medication.
-
Substance abuse.
-
A primary diagnosis of bipolar type I, schizophrenia or eating disorders.
Individuals who had received a psychological therapy consistent with the trial protocol for CBT, STPP or BPI were excluded.
Overall, 470 individuals were recruited and provided written informed consent, as did their parents/guardians. Ethics approval was by the Cambridgeshire 2 Research Ethics Committee, Addenbrooke’s Hospital Cambridge, UK. Follow-up was undertaken with repeated reassessments at nominal points time periods set at 12, 36, 52 and 86 weeks after randomisation to evaluate recurrence of self-reported depressive symptoms and enable re-evaluation of clinical diagnosis of an episode of major depression.
Chapter 3 Measures
A multimethod measurement approach of current mental state and psychosocial impairment was used. Measures for the adolescent patients included a selected set of self-report measures on current moods, feelings and behaviours, an interviewer-based assessment of current and previous psychiatric disorder completed by patients and a parent/guardian, an assessment of suicidal behaviour and non-suicidal self-harm behaviours and, finally, self-reported assessment of current cognitive ruminations and depressive cognitive style. The purpose of these measures was to test the primary and secondary hypotheses and to examine whether or not there were any moderating cognitive processes influencing treatment response or outcome.
Psychopathology
Kiddie-Schedule for Affective Disorders and Schizophrenia Present and Lifetime
The Kiddie-Schedule for Affective Disorders and Schizophrenia Present and Lifetime (K-SADS-PL) version is a semistructured interview measure which was used to establish the presence of DSM-IV diagnoses at all research assessments (baseline, 6, 12, 36, 52 and 86 weeks). 42 Each symptom is rated on a 3-point scale: 1 = non-clinical, 2 = being subthreshold and 3 = being a clinically relevant symptom, with the additional option of rating 0 = no information given to make a rating. Only symptoms rated as 3 were taken as clinically significant and DSM-IV criteria were used to ascertain the presence of current and past major and subthreshold depression episodes. Patients and parents/guardians completed the measure and both interviews were used to construct a diagnosis based on positive symptom reporting from either respondent. Interinterviewer agreement on the presence or absence of diagnoses has previously been assessed as satisfactory in adolescents with current mental illness (kappa, range for all diagnoses 0.70–0.85). 43 The K-SADS-PL was also used to generate DSM-IV current comorbid diagnoses.
Reliability was assessed for Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS) depression diagnosis on 30 randomly selected cases. There was 100% agreement between two research assistants. For individual variables within K-SADS (660 items in total for 30 cases), there was agreement on 628 items and disagreement on the remaining 32 (5%).
Mood and Feelings Questionnaire
The Mood and Feelings Questionnaire (MFQ) is a 33-item self-report measure completed by the adolescent with current depressive symptoms present over the past 2 weeks and was administered at all research assessments. The instrument is designed to cover symptom areas specified in DSM-IV for an episode of MDD. 44,45 It has good test–retest reliability (Pearson’s r = 0.78)46 an α coefficient of 0.82 and discriminant validity for detecting an episode of major depression in clinical adolescent samples. 47 The MFQ is sensitive to change and can predict depression over time (weeks and months) in healthy adolescents with higher scores. 48,49 It is scored on a 3-point Likert scale of 0–2, giving a range of 0–66 and the higher the score, the greater the likelihood of increased number and severity of depressive symptoms.
Revised Children’s Manifest Anxiety Scale
This self-report questionnaire contains 28 items that measures current general anxiety, including physiological anxiety, worry/oversensitivity and social concerns. 50,51 Scoring is on a 4-point Likert scale and higher scores indicate greater levels of anxiety. 50,51 The internal reliability is good (Cronbach’s alpha < 0.80).
Short Leyton Obsessional Inventory
The short Leyton Obsessional Inventory (LOI) (child version) is an 11-item, self-report questionnaire for current symptoms of obsessive–compulsive disorder in children and adolescents. 52 Internal reliability of the scale is high for the short scale total (Cronbach’s alpha = 0.86). It is scored on a 4-point Likert scale and higher total sum scores indicate greater obsessional thinking and compulsive behaviour.
Behaviours checklist
The behaviours checklist is an 11-item self-reported checklist for symptoms of antisocial behaviour based on DSM-IV criteria for conduct and oppositional disorders. It is a self-report measure, scored on a 4-point Likert scale. 13
Columbia Suicide Severity Rating Scale
This instrument is designed to track suicidal adverse events across a treatment trial. 53 It is a prospective version of the system developed for the Food and Drug Administration of the USA54 as a way to get better safety monitoring and avoid inconclusive reporting of these events. Being feasible and of low burden (typical administration time 5 minutes), it assesses both behaviour and ideation and appropriately assesses and tracks all suicidal events. It uniquely addresses the need for a summary measure of suicidality. The Columbia Suicide Severity Rating Scale was administered in the form of an interviewer-led respondent-based semistructured interview, at all time points, alongside the K-SADS-PL.
The Risk-Taking and Self-Harming Inventory for Adolescents
This is based on existing instruments for assessing self-harm and risk-taking behaviour, and on clinical descriptions of these behaviours, using items that tap into these in both direct and indirect ways. 55 The 20 items range from milder behaviours, such as picking at wounds and pulling one’s hair out, to more serious self-harm, such as taking an overdose and attempting to commit suicide. Most items contain the word ‘intentionally’ or end with the phrase ‘to hurt or punish yourself’. The items are on a 4-point Likert scale, referring to lifelong history. The higher the score, the greater the general risk-taking and self-harm, and the two subscales (risk-taking and self-harm) can be scored separately. The instrument was administered at all time points.
Ruminative Responses Scale
The Ruminative Responses Scale (RRS) is a 39-item measure taken from the Nolen-Hoeksema’s Ruminative Depression Questionnaire. 36 It describes responses to low mood that are self-focused, symptom-focused and focused on the possible consequences and causes of the mood using a 4-point Likert scale. Rumination is a potential cognitive vulnerability factor for depressive symptoms among adolescents. 56 High rumination predicts onset of depressive disorder in healthy adolescents. 27,57 Preliminary data from the previous ADAPT RCT suggested that CBT may reduce rumination. Although this had no effect on depressive symptoms over 28 weeks, it may reduce relapse risk. 37
The Depressive Experience Questionnaire for Adolescents – Short Version
Adult patients with clinical depression may be characterised by putative cognitive style. 38–40 This cognitive style has been described generically as one of immaturity which is characterised by an excessive preoccupation with relatedness with others (principally focused on disappointment with relationships) and self-definition or identity (principally focused on self-criticism). In this study, relatedness and identity were measured by the short version of the Depressive Experiences Scale for Adolescents (DES-A). 58
The RRS and DES-A scales were completed prior to randomisation. The planned use was to determine individual differences in the baseline total score of the RRS and the subscale scores for relatedness and self-definition/criticism of the DES-A, and to test if they acted as potential moderators of treatment effects.
Health of the Nation Outcome Scales for Children and Adolescents
The Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA) is a routine outcome measurement tool that assesses the behaviours, impairments, symptoms and social functioning of children and adolescents with mental health problems. 12,59,60 It provides a global quantitative measure of an individual’s current mental health status. The instrument consists of 13 scales and each scale is interviewer-rated on a score between 0 and 4 (total range 0–52). The higher the sum and subscale scores, the greater the level of overall mental health problems within the adolescent. The measure is sensitive to change in mental state and psychosocial functioning over a brief (weeks and a few months) period. The measure was used at all time points as a semistructured interview with both subjects and parents/guardians. The planned use of the measures was as a correlate and adjunct to self-reported depression scores revealing the level of personal impairment for each patient over time.
Health economic measures
Child and Adolescent Service Use Schedule
Data on the use of all services included in the study were collected using the Child and Adolescent Service Use Schedule (CA-SUS), as previously used in the ADAPT. 33 Information about the study participants’ use of services was collected by an interviewer at baseline and at 6-, 12-, 36-, 52- and 86-week follow-up assessments with the adolescent and parents/guardians. At baseline, information covered the previous 3 months. At each of the follow-up interviews, service use since the previous interview was recorded; in this way, the entire period from baseline to final follow-up was covered. The CA-SUS asks participants for the number and duration of contacts with various services and professionals. At each treatment contact, BPI, STPP and CBT therapists recorded information on the details of the treatment session including the start and end time as well as attendance.
EuroQol-5 Dimensions
The EuroQol-5 Dimensions (EQ-5D) is a standardised instrument for use as a measure of health outcome. 61 Quality-adjusted life-years (QALYs) were calculated from EQ-5D scores taken at baseline, 6-, 12-, 36-, 52- and 86-week follow-up interviews. The EQ-5D is a non-disease-specific measure for describing and valuing health-related quality of life and it includes a rating of own health in five domains (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) plus a rating of own health by means of a visual analogue scale (a ‘thermometer’) (on a scale of 0–100). 62 A recent study provided initial evidence to support the relevance of the EQ-5D in adolescents with major depression63 and it was used successfully in a previous study of treatment for adolescent depression in the UK. 33 QALYs were calculated using the area under the curve approach after the health states from the EQ-5D were given a utility score using responses from a representative sample of adults in the UK. 64 It is assumed that changes in utility score over time followed a linear path. 65 QALYs in the second year were discounted at a rate of 3.5%, as recommended by NICE. 66
Chapter 4 Ascertainment
The trial recruited patients from three regional centres and utilised local CAMHS teams within those sites for trial recruitment. The local CAMHS teams (n = 15, five in each regional centre) were visited by principal investigators (PIs) based within their regional academic centre and had the study plan introduced to them. Three seminar days, one in each regional academic centre, were run to introduce the study design and planned recruitment procedures to clinical staff and service managers. NHS staff had the opportunity to inform the recruitment process by asking questions and seeking further information and clarification from the PIs about the science, the design and the objectives of the trial. Each clinic that was involved designated a clinical staff member to champion the study to other staff on a weekly basis to encourage recruitment invitations to patients. Clinical staff working within CAMHS conducted identification and initial screening of potential participants.
All study participants were identified from routine NHS (tier 3) referrals to the participating specialised (tier 3) CAMHS clinics. There were no recruitment strategies unique to the study and no use of advertisement. At the first assessment to CAMHS, the assessing clinicians were invited to complete a depression symptom screen designed to assist referral to IMPACT. Using a combination of routine clinical methods at first assessment, aided by a depression screen based on DSM-IV criteria, potential cases were identified as being within the scope of the study. The assessing clinicians informed the young person and their parents/guardians/carers about the trial and invited them to consider taking part. If an expression of interest to take part was obtained, then their details were passed to the research group. They were informed at this point that the study team would be in touch if they expressed an interest to participate. The potential participants were informed that recruitment was dependent on the research team assessments and whether or not the patient met the inclusion and exclusion criteria.
The participants and their parents/guardians were sent information sheets about the trial and a reply envelope indicating they had read the information and were willing to be contacted by a researcher who then scheduled an initial meeting during which the participants were invited to sign a consent form. In line with good clinical practice, young people under 16 years of age provided consent along with their parents/guardians, and those who did not wish to involve their parents/guardians or carers were encouraged to do so. Participants who were 16 or 17 years old, who met the criteria and had mental health capacity but did not want their parents/guardians or carers involved were included.
Two researchers working on parallel sessions administered all research baseline assessments to the young person and their parents/guardians/carers. After this, researchers confirmed whether or not the participants met the diagnostic and other entry criteria. When there was uncertainty, the parent/guardian/carer report, if available, was combined with the young person’s responses and, if still not clear, a consensus discussion was held with the local PI to establish eligibility. If they met criteria and gave consent, participants were randomised remotely into one of the treatment arms. The trial co-ordinator in each regional site then informed the young person and the referring clinic about the treatment allocation. Other researchers, some of whom conducted follow-up assessments, remained blind to treatment allocation. Following randomisation, trained and supervised CAMHS staff working in the participating clinics treated all patients in the trial.
The trial co-ordinator carried out treatment allocation using stochastic minimisation controlling for age, sex and self-reported depression sum score. The patients were followed up and reassessed at five planned time points from randomisation. The primary outcome was self-reported depression symptoms at the planned end point 86 weeks post randomisation (mean duration of last assessment for each arm = 95 weeks), which was at least 52 weeks after the end of treatment. The primary analysis was based on intention to treat.
The study sample recruitment procedure is shown in Figure 3.
FIGURE 3.
The CONSORT diagram of patient ascertainment for IMPACT. a, The primary hypothesis was analysed in 392 (84%) of 465 who were randomised, accepted treatment, and provided one or more self-reported depression symptom score over the 36-, 52- or 86-week assessment points. Five patients withdrew consent before starting treatment (n = 3 in the BPI group, n = 1 each in the CBT and STPP groups) and requested their data be deleted. Reproduced with permission from Goodyer et al. 1 © The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY-NC-ND license.
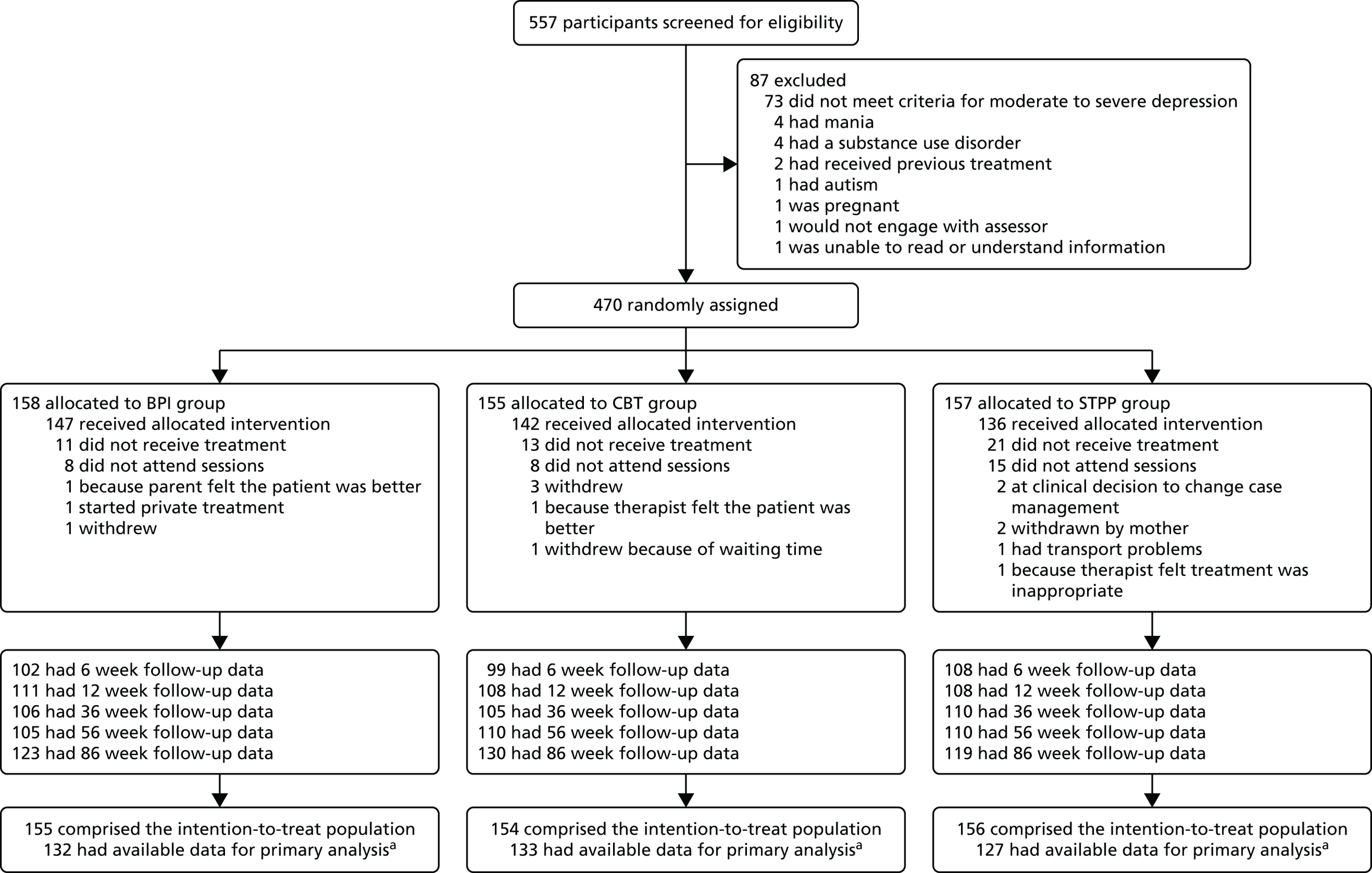
The patients approached were those considered by the CAMHS staff through routine clinical assessments to be clinically depressed. Therefore, those randomised are representative of the clinical populations at moderate to severe levels of severity attending these clinics.
The general levels of comorbidity, impairments and self-harm found in this study indicate comparability with previous studies12 for which depressed patients were recruited from general routine NHS CAMHS.
A total of 470 patients from 557 baseline assessments aged between 11 and 17 years were recruited and randomised. Of these, five subjects withdrew consent after baseline assessment and randomisation and have had their study records destroyed (two from North London and three from north-west England). There was no indication that this was related to treatment allocation. Out of the remaining 465 randomised patients, 185 (40%) were from East Anglia, 127 (27%) were from North London and 153 (33%) were from north-west England. Furthermore, a total of 348 patients (75%) were girls.
Chapter 5 Trial procedures
IMPACT compares three psychological interventions (STPP, CBT and BPI), which are delivered to treat an episode of DSM-IV major unipolar depression and to reduce the risks of recurrence of depression through reducing symptom levels over the follow-up period of 36–86 weeks.
After patient consent had been obtained and the baseline assessment had been carried out, a trial identifier was assigned. Treatment allocation was carried out by the trial co-ordinator using stochastic minimisation controlling for age (11–13 years, 14–15 years and 16–17 years), sex, self-reported depression sum score (≤ 29, 30–39, 40–49 and ≥ 50) and region (East Anglia, North London and north-west England). In view of the nature of the interventions, patients and clinicians were aware of treatment allocations. This was conducted by the trial co-ordinator using an online randomisation service (www.sealedenvelope.com). 67 Information about treatment allocation was forwarded to a clinic champion who ensured allocation of a therapist to the participants. To minimise bias, the outcome assessors were blind to treatment allocation and did not communicate with each other or with therapists about case assessments. All interviews were audiotaped and a random sample was rerated by independent raters. If blindness was broken, an alternative assessor carried out all subsequent assessments.
Planned interventions
IMPACT was a pragmatic superiority trial comparing the relative clinical effectiveness of three psychological treatments each with evidence of clinical efficacy being associated with clinical remission in the short term (i.e. 3–6 months). These treatments are available in CAMHS NHS practice, although distribution around the UK is not standardised. The three treatment approaches tested in this study were all manualised.
A duty of care by clinical staff to patients was observed in all clinical arms. This included parent/guardian support and engagement, explanation of treatment principles, maintenance and support of family during individual treatment, individual risk management strategies and contact with other agencies, if appropriate.
Comprehensive treatment protocols were developed for the trial and designed for delivery by practitioners working in routine NHS CAMHS settings. The rationale for using treatment manuals as guides to therapy is that manuals:
-
aid dissemination of treatment methods into clinical practice
-
help to standardise the intervention between therapists and across sites
-
form the basis for audio tape ratings of treatment adherence and differentiation; thus, ensuring that the interventions have been given properly in keeping with the trial protocol.
The three treatments differed in the total number of sessions they offered over the study period. The number of sessions offered for each treatment were as follows.
-
BPI: up to 12 sessions, consisting of up to eight individual and four family/parent/guardian sessions, to be delivered over 20 weeks.
-
STPP: up to 28 individual sessions plus up to seven parent/guardian sessions to be delivered over 30 weeks.
-
CBT: up to 20 individual sessions plus up to four family/parent/guardian sessions to be delivered over 30 weeks.
The treatments are described below.
Brief psychosocial intervention
Brief psychosocial intervention is a brief structured intervention for the treatment of moderate to severe unipolar major depression in adolescents. 68 The clinical care approach originally used in ADAPT was the basis for BPI used in this trial. 12,24,27 In ADAPT, the forerunner of BPI (described as non-manualised treatment as usual in CAMHS), together with 20–60 mg of fluoxetine daily, was as effective as treatment as usual + fluoxetine + CBT for moderate to severely depressed adolescents in routine NHS practice. 12,27 This clinical care was reformulated for the current study and formalised into a treatment manual. 24 Prescribing a SSRI is not a part of BPI per se but can be added and fully integrated if improvement is not judged to be occurring after 2–4 weeks, as per the NICE guidelines of 2005. 13
Meta-analytic studies of adolescent psychotherapies highlight the central therapeutic importance of care that is structured, evidence driven and founded on interpersonal effectiveness, warmth and trust. 69,70 The incorporation of collaborative care for depression in adults has been shown to provide added value for the treatment of depression in adults over and above psychological and/or medication treatments. 71,72
The BPI treatment manualised for this study emerged from the treatment as usual in ADAPT. The intervention is a treatment based on restructuring and codification of the principles and practices found in the domains of skilled assessment, listening, information-giving, advising, problem-solving, safety, caring and explaining about adolescent depression. The duration and number of treatment sessions in the BPI manual is based on clinical experience gained through ADAPT.
The BPI was delivered in this study as the standard control psychosocial intervention. Emphasis was placed on the importance of psychoeducation about depression and action-oriented, goal-focused, interpersonal activities as therapeutic strategies. Specific advice was given on improving and maintaining mental and physical hygiene, engaging in pleasurable activities, engaging with and maintaining school work and peer relations, and diminishing solitariness. BPI did not use cognitive or reflective analytic techniques. Therefore, there was no discussion of unconscious conflict and no deliberate effort to modify maladaptive models of attachment relationships. Neither was there any focus on changing cognitions and negative cognition-driven behaviours were not deconstructed. BPI consisted of up to 12 sessions, made up of up to eight individual and four family/parent/guardian sessions, delivered over 20 weeks. Liaison with external agencies and personnel (e.g. teachers, social care workers and peer groups) were commonly undertaken.
Case management in brief psychosocial intervention
As BPI case management has a rationale and relational framework, case management is founded on the three principles of:
-
interpersonal effectiveness
-
understanding of mental states
-
activation and problem-solving.
The case management process is integrated through the development of a formulation which is a general construct summarising the probable relationship between the three constructs above. The formulation is developed as a series of prospective working hypotheses that can be tested and evaluated against subsequent progress within the therapy. BPI is delivered within this framework in up to 12 sessions, consisting of up to eight individual and four family/parent/guardian sessions, over 20 weeks.
Therapy was delivered with the following strategies and principles being utilised throughout:
-
effective engagement, activation and problem-solving
-
diagnostic accuracy and mental state evaluation
-
sharing understanding and knowledge of the impairments and consequences of symptoms; the ‘lived experience’ including effects in other settings, such as school or peer relationships
-
attention to accuracy in conducting a risk assessment and its management
-
sharing aetiological description: defining risk and protective factors
-
a psychoeducative approach that at all points aims to help ‘activate’ and empower, including parents/guardians and family as necessary
-
an approach that includes understanding of the role of medication, its appropriate use and how it sits within the care package
-
a jointly agreed, collaboratively developed, and shared, management plan.
All of the above are delivered in a fashion that can help the child, young person and parents/guardians to manage and cope with their emotional expression.
Therapists, training and supervision
The BPI therapists in this study were drawn from a range of professional backgrounds, including mental health nursing, clinical psychology, psychiatry and mental health social work. However, the majority (> 80%) of therapists were psychiatrists in specialist CAMHS training as well as consultants. In IMPACT, clinicians had to have the following in order to be eligible for training as a BPI therapist:
-
a minimum of 6 months’ supervised or independent work in a multidisciplinary child and adolescent mental health setting
-
already established sufficient competence and skills to be allowed to undertake independent mental health assessment and treatment of adolescents with moderate to severe depression.
The BPI practitioners had basic training in BPI: reading of the manual, confirmation by the supervising clinician that they met the criteria to become a BPI therapist, attendance at a BPI training day, continued access to the BPI manual and ongoing supervision fitting in with usual local CAMHS NHS supervisory structures. The regional leads for BPI met and problem-solved supervisory issues in relation to BPI on a regular basis across the IMPACT period.
Short-term psychoanalytic psychotherapy
Psychoanalytic psychotherapy with children and young people is a well-established specialist treatment for emotional and developmental difficulties in childhood and adolescence, with an emerging evidence base. 73,74 It is one of several psychological therapies recommended by NICE as equally effective in the acute treatment of child and adolescent depression. 75 Its intellectual roots are drawn from psychoanalysis, child development, attachment theory and developmental psychopathology.
In this trial, all therapists were approved as psychoanalytically trained by the Association of Child Psychotherapists, UK. The STPP used shared therapeutic principles with time-limited psychodynamic work for adults with depression for which there is now a substantial evidence base. 73 It is a 28-session model, with parents/guardians or carers being offered up to seven additional sessions by a separate parent/guardian worker. STPP aims to elaborate and increase the coherence of the young person’s mental models of attachment relationships and thereby improve their capacity for affect regulation as well as the capacity for making and maintaining positive relationships with others. 76
The STPP method73,77 draws on a long history in the UK of psychoanalytic work with depressed children and young people,77,78 including an earlier clinical trial, in which STPP for children with depression demonstrated good outcomes. 35 As with the other manuals used in IMPACT, the STPP manual74 provided a guide to practice but not a recipe or a step-by-step guide, and drew on the existing skills and training of child and adolescent psychotherapists already working in the NHS.
The STPP method aims to elaborate and increase the coherence of the young person’s mental models of attachment relationships and thereby improve their capacity for affect regulation as well as the capacity for making and maintaining positive relationships with others. When treatment is successful, it should free the young person to engage in normal adolescent development including educational attainment and independent peer group development involving a degree of separation from their primary carers. 79
The techniques of child and adolescent psychotherapy are primarily based on close and detailed observation of the relationship the child or young person makes with their therapist. The therapist introduces the therapeutic task to the young person as one of understanding feelings and difficulties in their life. The therapist’s stance is non-judgemental and enquiring, and conveys the value of understanding; the aim is to put into words conscious and unconscious thoughts and feelings. Through actions and words, the therapist attempts to convey an openness to all forms of psychic experience – current preoccupations, memories, day dreams, nocturnal dreams and phantasies – but will be attuned specifically to evidence of unconscious phantasies which underlie the young person’s relationship to themself and others. This attentiveness to unconscious phenomena is specific to psychoanalytic psychotherapy and is related to the theoretical importance attributed to these deeper, less accessible, layers of the mind.
With all adolescents, most particularly those with difficult early years experiences, there is a need for the therapist to be in a state of mind characterised by availability to the reception of projected contents (anxieties, affects, uncertainties) of the adolescent’s mind. The patient’s experience of the therapist receiving, holding in mind and thinking about this projected material is a central feature of the therapy. The adolescents are helped to gain ownership of a previously disowned part of themselves and are strengthened by identification with another person (i.e. the therapist) who is experienced and capable of making meaning in this way and, thus, enabling more mature thinking to take place.
The STPP therapist and/or parent/guardian worker requires an alertness to the need, at times, for active communication and liaison with other significant individuals and agencies in the adolescent’s life. This may include external agencies such as school/college, youth and social services, and also mental health colleagues, including Child and Adolescent Psychiatrists, where there are issues about risk and a possible need for medication or hospitalisation. Prescribing a SSRI is not a part of STPP per se, but can be added and fully integrated if improvement is not seen after 2–4 weeks, as per the 2005 NICE guidelines. 13
Support for parents/guardians or carers, offered concurrently and in parallel with individual therapy for children and adolescents, is a well-established practice in the UK. There is some evidence that psychoanalytic therapy is more effective when undertaken with concurrent parent/guardian support work. 74 Parent/guardian support aims to help with parental anxieties and develop greater understanding about their relationship to their son or daughter. The duration of treatment and number of sessions prescribed is based on prior studies and clinical experience with adolescent patients.
Therapists, training and supervision
To be eligible to practise as a STPP therapist in IMPACT, the clinician had to have undertaken a 4-year postgraduate professional training, leading to membership of the Association of Child Psychotherapists or be a fourth year trainee member of the Association of Child Psychotherapists. In addition, those doing parent/guardian work had at least 6 months CAMHS experience following professional training in child psychotherapy, clinical or counselling psychology, child mental health nursing, family therapy or psychiatry.
The STPP training was designed and delivered on the basis that prospective STPP practitioners already have all the fundamental competencies and skills required to deliver all the components of STPP. Building on these existing skills, STPP training for IMPACT comprised reading of the STPP manual, confirmation by the clinician that they met the criteria to become a STPP therapist, and attendance at a STPP training day.
The STPP supervision by a consultant child and adolescent psychotherapist was provided as part of routine practice within the CAMHS team.
Cognitive–behavioural therapy
Cognitive–behavioural therapy in this trial is based on the classical form originally developed for adults with depression. This posits that emotional disorders are characterised by pervasive information processing biases which increase vulnerability to depression in the context of environmental stress, and which maintain and amplify core symptoms of depression including hopelessness, low mood and irritability. The focus of CBT is to identify the information processing biases that maintain depression and low mood and to amend these through a process of collaborative empiricism between the therapist and client.
Cognitive–behavioural therapy was adapted for this study to include parental involvement, a large focus on engagement and an emphasis on the use of behavioural techniques. 80,81 CBT included up to 20 sessions plus up to four parent sessions over 30 weeks. CBT therapists were routine CAMHS clinicians and were either clinical psychologists or other clinicians who had received post-qualification training in CBT. CBT emphasises ‘collaborative empiricism’, that is explicit, tangible and shared goals between the therapist and young person, and clear structured sessions. CBT links thoughts, feelings and behaviours, and the techniques include behavioural activation, identifying and challenging negative automatic thoughts, developing adaptive thoughts, and relapse prevention. Topics introduced within a therapy session are extended and supported outside the session by tasks completed by the client between sessions and reviewed at each subsequent session. CBT was delivered to the adolescent alone or to the young person and parents/guardians flexibly. A formulation was developed at the start of therapy, which included consideration of parental and family factors in the development and maintenance of depression. If it was considered relevant, the parents/guardians were involved in therapy sessions, by negotiation, to support the young person in treatment.
In this study, CBT was manualised and it incorporated adaptations for working with adolescents (as opposed to adults), including inclusion of simplified and age-appropriate cognitive techniques, as well as the flexibility to take a behavioural focus if cognitive work was considered too demanding for a young person. A number of additional amendments were made, including a greater focus on engagement in therapy, building the therapeutic alliance and working collaboratively with parents/guardians and schools. Parents/guardians were involved in treatment sessions as indicated by the formulation and the preferences of the family. There were no separate sessions for parents/guardians.
Treatment length for CBT was a maximum of 20 sessions, delivered weekly, tapering to every 2 weeks as needed for relapse prevention, plus up to four family/parent/guardian sessions. Sessions were structured with an agenda set by the therapist and young person at the start of every session and out-of-session assignments were agreed between the therapist and young person. Typically, early sessions (the first to fourth) focused on relationship building, understanding the young person’s current presentation and experience, and psychoeducation, including the CBT model. A provisional formulation of the young person’s difficulties, incorporating family history, key life events and transitions, recent stressors and coping strategies was developed with the young person (and parent/guardian when relevant). Subsequently the formulation guided treatment. This included using CBT techniques to treat non-depressive comorbid symptoms of anxiety, obsessions and compulsions and oppositional behaviours.
The mid-treatment phase focused on identifying and modifying the behavioural and cognitive processes that maintained depression and low mood for that young person. Behavioural work included activity scheduling, ratings of mastery and pleasure and reinforcement of engagement in activities. Cognitive work included identifying dysfunctional and unhelpful automatic thoughts and thought challenging using a range of techniques, including behavioural experiments. Modifications to the core CBT model, such as the use of mindfulness, were permitted depending on the individual formulation. The end of treatment was marked by a focus on relapse prevention. Typically this included a revisit to the formulation, identifying potential risk and vulnerability factors, problem-solving and building resilience. Prescribing a SSRI is not a part of CBT per se but can be added and fully integrated if improvement has not occurred after 2–4 weeks, as per the 2005 NICE guidelines. 13
Therapists, training and supervision
The CBT therapists were NHS staff from a range of professional backgrounds, including clinical and counselling psychology, nursing and occupational therapy. They delivered CBT for depression as part of their routine clinical practice in multidisciplinary CAMHS.
The CBT therapists had to have received specialist training in CBT, either as part of their core professional training (i.e. as a clinical psychologist) or as post-qualification training (i.e. as a nurse or occupational therapist). They were eligible to be IMPACT CBT therapists if they routinely used CBT in their NHS clinical work and if they could demonstrate some pre- or post-qualification training in CBT.
The CBT training was delivered as a 1-day workshop within services. It was designed as a top-up training for individuals who already had core CBT skills. The core features of the treatment manual were described and the practicalities and constraints of delivering CBT within the context of a research trial were discussed. All clinicians had copies of the CBT manual and familiarised themselves with it. Furthermore, CBT supervision was provided as part of routine practice within the CAMHS team.
Prescribing of fluoxetine during the trial
For all three arms, fluoxetine or another SSRI could be added if clinicians judged that combination therapy may accelerate the time to remission, following NICE guidelines for a major depression episode in adolescents. 13 A test dose of 10 mg was given for 48 hours, followed by 20 mg as a single dose. If there was no improvement within 2–4 weeks then the dose could be adjusted upwards to a maximum of 60 mg.
Chapter 6 Treatment fidelity and differentiation for each therapy modality
Establishing treatment differentiation between the three interventions, and treatment fidelity to each manualised intervention, are essential validity steps towards interpreting the effectiveness of different treatment approaches. This chapter provides results of the assessment of treatment fidelity based on measures of adherence to each protocol for each therapy and also to differentiation of therapies from each other.
Treatment fidelity refers to ‘the extent to which a therapist used interventions and approaches prescribed by the treatment manual, and avoided the use of intervention procedures proscribed by the manual’. 2 Therefore, fidelity in this study is not measuring the overall clinical competence of each therapist. The key task addressed is to answer the question ‘Did the therapy occur as intended by the manual?’ (treatment fidelity) and, in addition, ‘were each of the treatment arms sufficiently distinct from the others in regards to the techniques used?’ (treatment differentiation). Establishing fidelity to the manualised therapy, and differentiation between the treatment arms, are essential validity step towards interpreting the relative effectiveness of different treatment approaches, which is key to the primary and secondary objectives of this study.
The aim of the fidelity and differentiation study was therefore to assess:
-
the degree to which the therapists utilise prescribed or proscribed procedures, based on the treatment manual used in each arm of the study (‘treatment fidelity’)
-
whether or not treatments differed from each other along critical dimensions (‘treatment differentiation’).
Design
Two independent raters, blind to treatment allocation, rated each treatment session from the three treatment modalities using the Comparative Psychotherapy Process Scale (CPPS), which is a widely used measure of therapeutic techniques in psychodynamic therapies and CBTs. 82 These ratings were used to assess treatment fidelity for the CBT and STPP arms of the study and treatment differentiation between all three arms of the study. In addition, sessions from the BPI arm of the study were each rated by two raters, using a newly devised BPI fidelity measure in order to assess treatment fidelity to the BPI manual. Double ratings were used to check the reliability of each measure and improve the precision of the estimate for each tape.
Sample size
All therapists and young people in IMPACT agreed to their sessions being tape recorded for the purposes of the fidelity and differentiation analysis. Recorded sessions were categorised as either ‘early’ or ‘medium/late’ in therapy. A random sample of 232 tapes (76 CBT tapes, 81 STPP tapes and 75 BPI tapes) were selected and stratified by modality and timing (‘early’, i.e. the first third of therapy, or ‘medium/late’, i.e. the middle or last third of therapy), and were then rated on the measure of comparative (psychodynamic and cognitive–behavioural) techniques. The slight difference in the number of sessions rated by arms arose owing to the number of tapes available by treatment arm and site. As the comparative measure did not include the active features of BPI, the 75 BPI tapes were additionally rated on a treatment-specific measure.
Instruments
Comparative Psychotherapy Process Scale – External Rater form
The CPPS is a measure that assesses the degree to which a therapist uses techniques of psychodynamic interpersonal and/or cognitive–behavioural psychotherapy in an entire psychotherapy session. 82 Developed from an extensive empirical review of the comparative psychotherapy process literature,82 all items are rated on a 7-point Likert scale ranging from 0 (‘not at all characteristic’), 2 (‘somewhat characteristic’), 4 (‘characteristic’) to 6 (‘extremely characteristic’). The 20-item measure includes 10 psychodynamic interpersonal items and 10 cognitive–behavioural items, forming two distinct subscales. The psychometric properties of the CPPS have been well established in psychotherapy with adults. 82 Internal consistency of both scales has been good to excellent: Cronbach’s α of 0.82 to 0.92 for the psychodynamic interpersonal scale and 0.75 to 0.94 for the cognitive–behavioural scale. 82,83 Inter-rater reliability is reported as rating from good to excellent [intraclass correlation coefficient (ICC) 0.60–0.75]. 83,84
In the current study, the CPPS was used to assess treatment fidelity for the CBT and STPP arms of the study and to assess treatment differentiation between all three treatment modalities used in IMPACT. Overall, a CBT session was judged to be ‘adherent’ if the total mean score for items on the cognitive–behavioural subscale of the CPPS was ≥ 2, for which a mean score of 2 indicates that the use of cognitive–behavioural techniques was ‘somewhat characteristic’ of a session. A STPP therapy session was judged to be ‘adherent’ if the total mean score for items on the psychodynamic interpersonal subscale of the CPPS was ≥ 2, and a mean score of 2 indicates that the use of psychodynamic interpersonal techniques was ‘somewhat characteristic’ of a session.
The CPPS could not be used to rate treatment fidelity for BPI as it does not have a BPI subscale; however, it could be used to rate treatment differentiation between BPI and the other two therapies, as ratings of BPI sessions using the CPPS could be used to determine whether or not BPI clinicians were making use of techniques that were not part of the BPI manual but were associated with the specialist psychotherapies, whether psychodynamic (the psychodynamic interpersonal subscale) or cognitive–behavioural (the cognitive–behavioural subscale).
Raters were all postgraduate psychologists who were blind to treatment allocation. A total of seven raters went through approximately 30 hours of training on the measure until they were able to demonstrate a high level (> 80% for each pair of raters) of inter-rater reliability. Each session was listened to in its entirety, with the rater blind to treatment arm and then rated by the two judges independently.
Brief psychological intervention scale
The brief psychosocial intervention scale (BPI-S) is a new scale, developed specifically for use in this study to assess treatment fidelity to BPI. The 18 key components of the BPI manualised treatment were identified using expert consensus in the IMPACT team. A pilot investigation conducted by the BPI experts used a sample of five tapes to develop the fidelity scale. Following this phase, the measure was operationalised as an 8-item measure with three ‘core’ and five ‘general’ items, rated as a Likert scale (0 – no evidence, 1 – passing evidence, 2 – some evidence, 3 –clear evidence).
The three core items are (1) activation and problem-solving, (2) interpersonal effectiveness and (3) attention to mental state/current presentation or diagnosis. The five general items are (1) attention to vulnerability and protective factors, (2) psychoeducation, (3) setting case management within a BPI framework, (4) attending to the social context of the patient and (5) making an effort to help the patient manage their emotional expression. These eight items were chosen to (1) capture important treatment principles (relevance) based on the BPI manual and (2) cover all relevant treatment principles (comprehensiveness) as outlined in the BPI manual.
For each item, a score of ≥ 2 was considered an adequate level of fidelity. Overall, a BPI therapy session was judged to be ‘adherent’ if:
-
at least two out of three ‘core’ items were rated as ≥ 2 and
-
a total of at least four out of the eight items were rated as ≥ 2.
When this revised standard was applied to the five taped sessions previously rated, 100% agreement was obtained between the experts who rated four sessions as adherent and one session as not adherent.
Training for five independent raters was completed over 2 days. The raters were all trained in BPI and experienced senior clinicians with medical and psychiatric qualifications, and achieved high levels of inter-rater reliability (> 80%) by the end of the training. Feedback from the raters during the training process indicated high levels of face validity indicated by good comprehension of the BPI fidelity scale and an understanding of the rating measure and procedure. Each session was listened to in its entirety and then rated by the two judges independently, but raters were not blind to the treatment arm because BPI sessions only were rated using the BPI scale. The results of the reliability and validity analyses are given in Chapter 9.
Chapter 7 Moderation of treatment response
Little is understood regarding the factors that may influence treatment response in depressed adolescents. This study included two putative cognitive processes that the literature suggests may moderate therapeutic response to psychological treatments. These are as follows.
-
Individual differences in self-reported ruminative thinking while depressed. A ruminative response style is defined as persistently brooding or dwelling on current depressive thoughts and feelings, often to the exclusion of other themes in the patient’s life. 36,37
-
The quality of predominant depressive experiences which is defined as possessing a thinking style (dependent or self-critical) likely to predispose or be associated with depressive illness but not synonymous with a pattern of symptoms. 38
Ruminative response style
Rumination is the compulsively focused attention on the symptoms of one’s distress and on its possible causes and consequences as opposed to its solutions. 85 Rumination is similar to worry with the exception that rumination focuses on bad feelings and experiences from the past, whereas worry is concerned with potential bad events in the future. 86 Both rumination and worry are associated with clinical anxiety and depression. 86
Rumination has been widely studied as a cognitive vulnerability factor for depression but its measures have not been unified. 86 In the Response Styles Theory proposed by Nolen-Hoeksema,87 rumination is defined as ‘compulsively focused attention on the symptoms of one’s distress, and on its possible causes and consequences, as opposed to its solutions’. Because the Response Styles Theory has been empirically supported, this conceptual model of rumination is the most widely used.
Extensive research on the effects of rumination, or the tendency to self-reflect, shows that the negative form of rumination interferes with people’s ability to focus on problem-solving and results in dwelling on negative thoughts about past failures. 88 Evidence further suggests that the negative implications of rumination are due to cognitive biases, such as memory and attentional biases, which predispose ruminators to selectively devote attention to negative stimuli. 89 Such negative biases results in critical self-devaluing thinking and can be found in dysphoric adolescents with no history of depression but with a childhood temperamental style characterised by being easily distressed and fearful but likely to return to calm mood relatively rapidly. 90 Depressed adolescents who have high rumination scores are more likely to show persistent depression and demonstrate impairments in autobiographical memory retrieval. 91–93 Inducing ruminations in adolescents also results in increased depressive symptoms as there is a bias to ruminate on prior negative life events. 43,91,92
In this trial, self-reported rumination scores were measured by the ruminative responses styles questionnaire developed by Susan Nolen-Hoeksema and colleagues and validated independently. 94 The scale was completed prior to randomisation and the baseline raw sum score was planned (prior to analysis) to be tested as a potential moderator of treatment effects.
Hypothesis
Elevated RRS scores at baseline will be associated with the following:
-
lower treatment response in all arms and higher MFQ scores over the follow-up period of 36, 52 and 86 weeks
-
better treatment response in the CBT than the BPI and STPP arms.
Depressive experiences style
Both theoretical assumptions and empirical findings suggest that adult patients with clinical depression may be characterised in terms of immaturity of cognitive styles39,40,95,96 which manifest as excessive preoccupation with relatedness (principally focused on disappointment with relationships) and self-definition or identity (principally focused on self-criticism). Research has provided empirical evidence for the assumption that individuals with depression may be predominantly troubled by one of the following issues.
-
High concerns about the quality of interpersonal relatedness with feelings of emptiness and loneliness, and intense fears of being abandoned and left unprotected.
-
Possessing an extremely self-critical attitude together with feelings of worthlessness, guilt, failure and self-blame.
Two psychometrically relatively robust factors have been shown to emerge across a number of studies. 97 One factor, which may be termed dependent/relatedness is elevated by disruptions to rewarding affiliative interpersonal relationships. This is expressed primarily in dysphoric feelings following experiences characterised by personal loss, abandonment and being alone. The other is termed self-critical/identity and is elevated due to perceived personal failure and worthlessness. This is expressed in dysphoric feelings emerging in individuals who have a bias towards perfectionism but are vulnerable to criticism both from others and themselves.
Clinical evidence has accumulated on the difference in the responsiveness to different kinds of psychological treatment and their capacity to achieve therapeutic gain. Clinical research with depressed adult patients has indicated that elevated levels of the self-criticism factor at baseline are associated with poorer therapeutic outcome at termination of therapy and at the 3-month follow-up in brief treatments for depression. 96,98 In contrast, the dependent factor interfered with therapeutic progress primarily in the second half of the treatment process (in the last 8 weeks) by disrupting patients’ interpersonal relationships both within and external to the treatment process. 40,95
In this study, the short version of the DES-A (self-report) was used to measure relatedness and identity. 58 The scale was completed prior to randomisation and baseline subscale scores for relatedness and differentiation were tested as potential moderators of treatment effects.
We tested two hypotheses for the Depressive Experiences Questionnaire (DEQ) at baseline.
-
Elevated relatedness/dependent scores will be associated with a relatively better response in the STPP group than the BPI or CBT groups.
-
Elevated self-critical/identity scores will be associated with a relatively better response in the CBT group than the BPI or STPP groups.
The data analytic moderator strategy is described in Chapter 8 and the results are presented in Chapter 9.
Chapter 8 Statistical methods
This trial compares therapist-delivered treatments and, in order to be generalisable, the statistical models used to determine outcome include an estimate of between-therapist variations. 99 Personal characteristics and skills of individual therapists mean that the outcomes for different patients seen by one therapist (within-therapist variance) are likely to be more strongly correlated than outcomes of patients treated by different therapists using the same treatment approach (between-therapist variance). This is measured as intratherapist correlation coefficient (ITCC). If ITCC is not adjusted for, variance estimates will be too small, leading to type I error. Analysis of data from ADAPT gave an estimate of the ITCC after adjustment for baseline covariates of zero at 28 weeks for the self-reported level of recent (2 weeks) depressive symptoms, symptoms as measured by the MFQ. Given that estimates of ICC are imprecise, sample size and power estimation utilised ICC values of 0.025 and 0.05 as a sensitivity analysis. Methods for sample size calculation are described by Walwyn and Roberts. 100
ADAPT gave a standard deviation (SD) of the sum score of 14.6 at 28 weeks’ follow-up and correlation between baseline and follow-up of 0.41 for MFQ. We have assumed five points on the MFQ to be the minimum clinically important difference, which is justified in three ways:
-
This is approximately 25% of the change in the MFQ scale from baseline to 28 weeks observed in ADAPT.
-
It is also equivalent to a one-point improvement on five of the 33 items of the scale.
-
It is a standardised effect size of 0.34 (small to medium). 101
The primary analysis of the trial involved, first, a comparison of the two specialist treatments – CBT and STPP – and, second, a comparison of the two specialist treatments combined against BPI. A 2.5% two-sided significance level was therefore used for the sample size calculation. ADAPT had 92% follow-up at 28 weeks and so 90% follow-up was assumed. Statistical analysis was planned to adjust for baseline. Sample size calculation was adjusted for this assuming a correlation of 0.41 between baseline and follow-up, which was estimated from data in ADAPT.
In each of the three regional centres, six CAMHS units would be recruited with each unit having at least one therapist for the three treatment modalities being compared. The target patient recruitment for each clinic was 30 patients, giving 10 patients per treatment modality per clinic and a total sample size of 540. With these assumptions, the power for the comparison of CBT with STPP was 84% if the ICC was zero, 76% for an ICC of 0.025 and 69% if it was as large as 0.05. For the comparison of the specialist treatments (CBT and STPP) with BPI, the power was 93%, 88% and 82% for an ICC of 0.0, 0.025 or 0.05, respectively.
Data analytic strategy
Statistical analysis of the three randomised treatment groups was based on the intention-to-treat principle, subject to the availability of data. Statistical analyses were carried out using Stata® Release 13 (StataCorp LP, College Station, TX, USA).
Data cleaning of outcome and baseline data was conducted without the treatment group allocations in view. Many of the outcome measures were patient-completed or interviewer-rated psychometric instruments. When there were missing item-level data, these were imputed by replacing the missing item with the mean of the other available items for that occasion, provided that at least 50% of items had been completed (pro-rating).
To identify data errors prior to revealing treatment allocation, the trial research team reviewed the summary statistics of outcome data.
Analysis of the primary outcome measure and continuous secondary outcome measures
Characteristics of the study sample are reported using standard frequency measures and summary statistics. Preliminary inferential analysis investigated the pattern of missing outcome data comparing baseline characteristics of subjects with and without follow-up data using a logistic regression model.
Although time of assessment was scheduled at 6, 12, 36, 52 and 86 weeks, there was substantial variation in the timing of assessment compared with randomisation, leading to some overlap between assessment intervals of consecutive assessments. To prevent bias attributable to assessments being delayed, we have used time since randomisation as a continuous variable in a longitudinal mixed model rather than the notional assessment point. Random effects were included for between-subject variation in the intercept and time gradient of the subject. As there may be variations in patient outcomes, a between-therapists random-effect term was added to the models. When a participant’s therapist was not known or they received no therapy, the participant’s identifier code was used instead for the therapist code. Fixed covariates were included to model systematic differences due to treatment, the time with treatment interaction and prespecified participant characteristics at baseline (Table 1).
| Measure | Type of measure | Data collection method | Fixed covariates |
|---|---|---|---|
| Primary | |||
| MFQ | Continuous | Self-report | Baseline MFQ, LOI, ABQ scores, treatment allocation, region, sex, age at randomisation, comorbid behaviour disorder,a prescription of SSRI before trial entry |
| Secondary | |||
| RCMAS | Continuous | Self-report | Baseline RCMAS, LOI, ABQ scores, treatment allocation, region, sex, age at randomisation, comorbid behaviour disorder,a prescription of SSRI before trial entry |
| LOI | Continuous | Self-report | Baseline LOI, MFQ, ABQ scores, treatment allocation, region, sex, age at randomisation, comorbid behaviour disorder,a prescription of SSRI before trial entry |
| HoNOSCA | Continuous | Interview, rated | Baseline HoNOSCA, MFQ, LOI and ABQ scores, treatment allocation, region, sex, age at randomisation, comorbid behaviour disorder,a prescription of SSRI before trial entry |
| ABQ | Binary | Self-report | Baseline ABQ, plus MFQ score, treatment allocation, region, sex, age at randomisation, comorbid behaviour disorder,a prescription of SSRI before trial entry |
| K-SADS MDD | Binary | Interview, rated | See MFQ outcome above |
| MFQ score of ≥ 26 | Binary | Self-report | See MFQ outcome above |
Trial hypotheses (see Chapter 9, Assessment of clinical outcome) were related to the immediate post-treatment follow-up period and the longer-term follow-up. The model was therefore fitted to the post-treatment data (≥ 36 weeks) and the marginal effect of treatment was estimated at 52 and 86 weeks post randomisation. At each time point, two comparisons were made: STPP versus CBT, and CBT and STPP versus BPI. The sample size calculation used a significance level of 2.5% to allow for this multiplicity. A Bonferroni correction has not been applied to the p-values, but readers should use a 2.5% significance level to maintain the familywise 5% level at a particular point of assessment. As well as the marginal effects, the treatment effect and time with treatment interaction are also reported with accompanying inference based on a likelihood ratio test. For all models, time was centred by subtracting the overall (grand) mean of assessment times based on the available data for the particular analysis being undertaken. This makes the intercept interpretable when there is a treatment by time interaction.
When baseline scale covariate data were not obtained, simple imputation, which is based on multiple regression, was used as suggested by White and Thompson. 102 The following covariates were used: region, comorbid behaviour disorder (conduct disorder and/or oppositional defiant disorder), all anxiety disorders combined, SSRI prescription before trial entry (if missing assumed not to be prescribed), age at randomisation, sex and baseline severity MFQ score.
The proportion of the total variance caused by the therapist, which can be called the ITCC, varies with time owing to the random gradient term in the model. For comparative purposes, the ITCC was calculated as:
where σT2 is the between-therapist variance, σP2 is the patient-level random intercept variance and σE2 is the residual error variance. This estimates the ITCC at the grand mean centred time point.
A secondary analysis estimated the treatment effect over the treatment period based on data gathered before 36 weeks. This model did not include a time with treatment interaction as there was only the notional week 6 and 12 assessments to use as outcome data.
Analysis of the binary secondary outcome measures
The analysis of binary secondary end points, which included the Antisocial Behaviour Questionnaire (ABQ), MDD and MFQ sum scores of ≥ 26 were analysed using a longitudinal generalised estimating equation (GEE) model with robust standard errors. This model was fitted to post-treatment data (≥ 36 weeks) and the marginal differences in proportions were estimated for STPP versus CBT and for CBT plus STPP versus BPI at weeks 36, 52 and 86.
Planned subgroup analyses
This trial included an investigation of potential moderator effects on treatment response for the primary outcome before and after 36 weeks. The effect of moderators was tested by adding a moderator with treatment interaction into the main effects models for treatment. The moderator measures and their associated testable hypotheses are described in Chapter 7.
Economic evaluation method
Aim
The aim of the economic evaluation was to investigate the cost-effectiveness of psychological treatments for adolescent depression and, in particular, to determine whether or not the additional cost of the two specialised treatments, CBT and STPP, can be justified by improvements in effectiveness and/or decreased use of health and social care services compared with BPI by 86 weeks’ follow-up.
Perspective
The a priori perspective of the economic evaluation was societal, including the use of all health, social care, education and criminal justice sector resources plus family costs in the form of travel to trial intervention sessions and productivity losses of the primary carer resulting from their child’s illness. However, criminal justice and productivity losses were not found to be relevant to this population, being very low, and so were excluded from the analysis.
Method of economic evaluation
The primary economic analysis was a cost-effectiveness analysis with outcomes expressed as QALYs, as recommended by NICE. 66
Calculation of costs
The process of calculating costs was separated into the identification, measurement and valuation of relevant resources.
Identification of resources
Relevant resources were identified based on the results of previous studies in adolescent depression12 and discussions with study clinicians and patient representatives. Resource use was collected in the following domains.
Delivery of the brief psychosocial intervention, cognitive–behavioural therapy and short-term psychoanalytic psychotherapy interventions
Use of NHS secondary care services:
-
inpatient stays (mental health and all medical specialties)
-
outpatient appointments (mental health and all medical specialties)
-
accident and emergency attendances.
Use of NHS primary care services:
-
general practitioner (i.e. in surgery, at home and by telephone)
-
community nurse (e.g. practice nurse, district nurse, health visitor, midwife)
-
community paediatrician
-
community mental health service
-
community medical professional (e.g. physiotherapist)
-
school-based mental health and medical professionals.
Use of medication in the following areas:
-
antidepressants
-
sleeping tablets
-
mood stabilisers/antipsychotics.
Use of social care, education and voluntary sector services:
-
foster care and residential care
-
staffed accommodation, such as hostel
-
social worker
-
specialist education facilities
-
education psychologist
-
family support worker
-
youth worker
-
youth offending team worker.
Measurement of resources
Trial interventions
The trial therapists recorded details of attendance and non-attendance at treatment sessions, and duration of treatment sessions for each study participant throughout the trial.
Other health, social care, education and voluntary services
Data on use of all other services included in the study perspective were collected using the CA-SUS. 33 This was developed using data from several child and adolescent mental health trials and was further modified and successfully employed in a previous trial in adolescent depression. 33 The CA-SUS was completed with participants and family members in interview with a researcher at baseline and at the 6-, 12-, 36-, 52- and 86-week follow-up interviews. At baseline, information covered the previous 3 months. At each of the follow-up interviews, service use since the previous interview was recorded; in this way, the entire period from baseline to final follow-up was covered. The CA-SUS asks participants for the number and duration of contacts with various services and professionals.
Valuation of resources
To calculate the total cost of the resources used by each study participant, a unit cost was applied to each resource use item. All unit costs are for the financial year 2011/12 and are uprated, when necessary, using the Hospital and Community Health Services Index. 103 Costs in the second year were discounted at a rate of 3.5% as recommended by NICE. 66 All unit costs are summarised in Table 2.
| Service | Unit | Cost (£) |
|---|---|---|
| CBT | Per session | 71–111 |
| STPP | Per session | 64–190 |
| BPI | Per session | 58–171 |
| Medication | Per daily dose | Various |
| Inpatient | Per night | 495–632 |
| Outpatient | Per appointment | 30–624 |
| Accident and emergency | Per attendance | 131–155 |
| Ambulance | Per trip | 230 |
| GP surgery | Per minute of patient contact | 3.40 |
| GP home | Per home visit minute | 4.30 |
| GP telephone | Per minute of patient contact | 3.38 |
| Practice nurse | Per minute of face-to-face contact | 0.88 |
| District nurse, health visitor, midwife | Per home visit minute | 1.03 |
| CAMHS team | Per contact | 225 |
| Counsellor/therapist | Per minute of client contact | 1.08 |
| Social worker | Per minute | 3.43 |
| Support worker/youth worker | Per minute | 0.61 |
| Education psychologist | Per minute | 2.27 |
| Physiotherapist | Per contact | 80 |
| Speech and language therapist | Per contact | 88 |
| Dietitian | Per contact | 71 |
| Youth offending team worker | Per minute | 3.43 |
Trial treatments
Treatment sessions were costed on the basis of the profession and grade of the therapist that delivered each session for each trial participant, hence the range of unit costs detailed in Table 2. The length of the treatment sessions was extracted from the average duration of treatment recorded in the session record forms. The average duration of sessions was 45 minutes for BPI, 50 minutes for STPP and 55 minutes for CBT. For the base-case analysis, only the costs of the sessions that the young person attended were included. This assumption was employed because of an understanding that clinicians are usually able to do something else during the time freed up by missed appointments. In a sensitivity analysis, an estimate of the cost of the sessions that were offered but not attended was included. The data for this analysis came from the records held by the trial therapists and are the closest data to non-attendance available. The rate of non-attended sessions was included at 50% of the cost of a full session, which assumes professionals make some use of the time available, but not all.
Antidepressants and other medication
The total cost of antidepressants prescribed and other included medication costs was calculated using daily dose information and costs of the generic drug as listed in the British National Formulary. 104
Calculation of quality-adjusted life-years
The QALYs were calculated using the area under the curve approach after the health states from the EQ-5D (see Chapter 5 for details of method and evaluation) were converted into utility scores using responses from a representative sample of adults in the UK. 64 It was assumed that changes in utility score over time followed a linear path. 65 QALYs in the second year were discounted at a rate of 3.5%, as recommended by NICE,66 and all analyses were adjusted for baseline utility scores to take into consideration the impact any baseline differences will have on the area under the curve. 106
Data analysis
For base-case calculations, complete case analysis (excluding subjects with missing data) was used, with the impact of missing data explored in sensitivity analyses. All analyses were carried out on an intention to treat basis using Stata 11.1.
Resource use
Resource use by study participants is reported descriptively by randomised group at 86 weeks as mean use for the group as a whole and percentage of the group in contact with that service. No statistical comparisons between use of services were made to avoid problems associated with multiple testing and because the focus of the economic evaluation is on costs and cost-effectiveness.
Difference in costs and quality-adjusted life-years
A number of tests for differences in costs at 86 weeks between randomised groups were completed:
-
CBT versus BPI
-
STPP versus BPI
-
CBT versus STPP.
These were analysed using linear regression models with the following prespecified covariates: baseline costs (total cost over the previous 3 months), region (East Anglia, North London, north-west England), behavioural disorder at baseline (measured using the K-SADS-PL) and antidepressant use at baseline. The validity of the results was confirmed using bias-corrected, non-parametric bootstrapping (repeat resampling). 107 Despite the skewed nature of cost data, this approach is recommended to enable inferences to be made about the arithmetic mean. 108
Cost-effectiveness analyses
For the cost-effectiveness, analysis moves from considering differences in costs and outcomes in terms of statistical significance to analysing costs and outcomes together in a decision-making context. The cost-effectiveness analysis, undertaken using QALYs calculated from the EQ-5D measure of health-related quality of life, was completed for the following comparisons:
-
CBT versus BPI
-
STPP versus BPI
-
CBT versus STPP
-
CBT versus STPP versus BPI.
Initially, incremental cost-effectiveness ratios (ICERs) were calculated, which are the difference in mean cost divided by the difference in mean effect. 109 Because ICERs are calculated from four sample means and are therefore subject to statistical uncertainty, 5000 resamples (bootstrapping) from the cost and outcomes data were used to generate a distribution of mean costs and effects. 110 These distributions were plotted onto the cost-effectiveness plane for interpretation. Replications that fall in the south-west quadrant of the plane suggest that the intervention is less costly and less effective than the comparator, and those that fall in the south-east quadrant suggest that the intervention is less costly and more effective than the comparator. Replications in the north-west quadrant suggest the intervention is more costly and less effective than the comparator, while those in the north-east quadrant suggest the intervention is more costly and more effective than the comparator.
The bootstrapped distributions were also used to calculate the probability that each of the treatments is the optimal choice, subject to a range of possible maximum values (the ceiling ratio, λ) that a decision-maker might be willing to pay for a unit improvement in outcome. To explore the uncertainty that exists around estimates of mean costs and effects as a result of sampling variation and uncertainty regarding the maximum value of λ, cost-effectiveness acceptability curves (CEACs) are presented by plotting these probabilities for a range of possible values of the ceiling ratio (λ). 111 All analyses used baseline costs, region and behavioural disorder at baseline as covariates.
Sensitivity analyses
A number of sensitivity analyses were carried out to test the robustness of the assumptions made.
-
The cost of sessions offered, but not attended, was explored by increasing the cost from the assumption of zero applied in the main analysis (which assumes professionals are able to make use of the time available to undertake alternative tasks) to 50% of the cost of a session (which assumes professionals make some use of the time available, but not all). Data were calculated as the number of sessions offered minus the number of sessions attended, which may not be exactly equivalent to the number of those who did not attend, as sessions may have been offered but cancelled or rearranged. This analysis should therefore be interpreted with caution.
-
The impact of missing data was considered using multiple imputation of missing values.
-
Owing to the variation in the timing of follow-up, cost per week was calculated and analysed.
Chapter 9 Clinical Results
This chapter reports the characteristics of young people entering the trial, the details of trial therapies and medication received, the analysis of clinical outcomes and the moderator analyses, and summarises the data on adverse events. For clarity of exposition, some results are given in Appendix 1.
Characteristics of young people entering the trial
Between 29 June 2010 and 17 January 2013, a total of 557 participants had baseline assessments. Of these, 87 were excluded from the study (see Figure 3 for reasons for exclusion). The remaining 470 participants were randomised, of which five later withdrew consent (three BPI, one CBT and one STPP). Among the remaining 465 participants, 155, 154 and 156 were randomised to BPI, CBT and STPP, respectively. The East Anglia regional centre recruited the largest number of participants (40%, n = 185) followed by the north-west England centre (33%, n = 153) and the North London centre recruited the smallest number (27%, n = 127). Recruitment was from five CAMHS clinics each in East Anglia and North London, and from six clinics in north-west England.
Table 3 summarises the demographic and clinical characteristics of the three randomised groups at entry into the trial. The mean age of the sample was 15.6 years (SD 1.4 years). A total of 348 (75%) participants were female and 85% (382/450) were white. Based on those with SSRI prescription information, 20% were prescribed a SSRI prior to entry into the trial. The baseline characteristics of each treatment group are also presented in Table 3 and there were no marked differences between treatment groups. Note that baseline values of outcome measures are tabulated with the summaries of follow-up data in Table 12.
| Characteristic | Treatment group, frequency (%) | ||
|---|---|---|---|
| BPI (n = 155) | CBT (n = 154) | STPP (n = 156) | |
| Female | 115 (74) | 114 (74) | 119 (76) |
| Age (years) at entry | 15.6 (1.4)b | 15.6 (1.4)b | 15.6 (1.5)b |
| Whitec | 121 (82) | 131 (86) | 130 (86) |
| Regional centre | |||
| East Anglia | 61 (39) | 62 (40) | 62 (40) |
| North London | 43 (28) | 41 (27) | 43 (27) |
| North-west England | 51 (33) | 51 (33) | 51 (33) |
| SSRI prescribed before trial entryd | 29 (19) | 32 (21) | 28 (18) |
| Behavioural disorder | 20 (13) | 20 (13) | 16 (10) |
| Number of depressive symptoms | 8.4 (2.5)b | 8.7 (2.3)b | 8.3 (2.5)b |
Table 4 gives the prevalence of concurrent depressive symptoms from the K-SADS-PL. The most prevalent symptom was sleep disturbance (92%), followed by depressed mood (84%). The mean number of symptoms was 8.4 for the BPI group; 8.7 for CBT and 8.3 for STPP (see Table 3). Recent suicide attempts refer to current major depression episode. Lifetime suicide attempts refer to all lifetime except current episode.
| Depressive symptom | Treatment group, frequency (%) | |||
|---|---|---|---|---|
| BPI (n = 155) | CBT (n = 154) | STPP (n = 156) | Total (n = 465) | |
| 2 weeks prior to baseline assessment | ||||
| Sleep disturbance | 141 (91.0) | 141 (91.6) | 145 (92.9) | 427 (91.8) |
| Depressed mood | 131 (84.5) | 134 (87.0) | 125 (80.1) | 390 (83.9) |
| Disturbed concentration, inattention | 112 (72.3) | 119 (77.3) | 118 (75.6) | 349 (75.1) |
| Fatigue, lack of energy | 117 (75.5) | 113 (73.4) | 111 (71.2) | 341 (73.3) |
| Worthlessness | 108 (69.7) | 101 (65.6) | 105 (67.3) | 314 (67.5) |
| Anhedonia, apathy | 96 (61.9) | 104 (67.5) | 103 (66.0) | 303 (65.2) |
| Irritable, anger | 97 (62.6) | 104 (67.5) | 91 (58.3) | 292 (62.8) |
| Suicidal ideation | 95 (61.3) | 91 (59.1) | 97 (62.2) | 283 (60.9) |
| Decreased appetite | 71 (45.8) | 78 (50.6) | 71 (45.5) | 220 (47.3) |
| Hopelessness | 74 (47.7) | 66 (42.9) | 71 (45.5) | 211 (45.4) |
| Indecision | 47 (30.3) | 62 (40.3) | 51 (32.7) | 160 (34.4) |
| Guilt | 53 (34.2) | 51 (33.1) | 45 (28.8) | 149 (32.0) |
| Agitation | 43 (27.7) | 53 (34.4) | 50 (32.1) | 146 (31.4) |
| Psychomotor retardation | 37 (23.9) | 38 (24.7) | 36 (23.1) | 111 (23.9) |
| Weight loss | 29 (18.7) | 25 (16.2) | 23 (14.7) | 77 (16.6) |
| Increased appetite | 21 (13.5) | 23 (14.9) | 23 (14.7) | 67 (14.4) |
| Weight gain | 15 (9.7) | 12 (7.8) | 15 (9.6) | 42 (9.0) |
| Hallucinations | 12 (7.7) | 16 (10.4) | 6 (3.8) | 34 (7.3) |
| Delusions | 4 (2.6) | 5 (3.2) | 5 (3.2) | 14 (3.0) |
| Recent suicidal attempt | 3 (1.9) | 2 (1.3) | 7 (4.5) | 12 (2.6) |
| Lifetime suicidal attempt | 57 (36.8) | 48 (31.2) | 55 (35.3) | 160 (34.4) |
Table 5 gives a detailed breakdown of comorbid psychiatric diagnoses recorded in the baseline K-SADS-PL by treatment group. A total of 225 (48%) participants were concurrently comorbid for at least one other psychiatric disorder. Of these, 134 (29%) participants had one comorbidity and 60 (13%) participants had two comorbidities. The maximum number of comorbidities was five in the BPI group and four in the other two groups. Overall, the most frequent comorbid diagnoses were generalised anxiety disorder and social phobia. There were no marked differences between the three treatment groups in these characteristics.
| Comorbid diagnosis | Treatment group, frequency (%) | |||
|---|---|---|---|---|
| BPI (n = 155) | CBT (n = 154) | STPP (n = 156) | Total (n = 465) | |
| Generalised anxiety disorder | 34 (21.9) | 34 (22.1) | 31 (19.9) | 99 (21.3) |
| Social phobia | 19 (12.3) | 20 (13.0) | 22 (14.1) | 61 (13.1) |
| Oppositional defiant disorder | 14 (9.0) | 18 (11.7) | 12 (7.7) | 44 (9.5) |
| Specific phobia | 16 (10.3) | 13 (8.4) | 6 (3.8) | 35 (7.5) |
| Post-traumatic stress disorder | 6 (3.9) | 12 (7.8) | 14 (9.0) | 32 (6.9) |
| Separation anxiety disorder | 6 (3.9) | 9 (5.8) | 5 (3.2) | 20 (4.3) |
| Conduct disorder | 7 (4.5) | 2 (1.3) | 5 (3.2) | 14 (3.0) |
| Obsessive–compulsive disorder | 2 (1.3) | 5 (3.2) | 3 (1.9) | 10 (2.2) |
| Panic without agoraphobia | 2 (1.3) | 3 (1.9) | 2 (1.3) | 7 (1.5) |
| Agoraphobia | 3 (1.9) | 1 (0.6) | 3 (1.9) | 7 (1.5) |
| Alcohol abuse | 2 (1.3) | 2 (1.3) | 2 (1.3) | 6 (1.3) |
| Panic with agoraphobia | 2 (1.3) | 1 (0.6) | 2 (1.3) | 5 (1.1) |
| Attention deficit hyperactivity disorder | 2 (1.3) | 1 (0.6) | 1 (0.6) | 4 (0.9) |
| Bulimia nervosa | 0 (0) | 1 (0.6) | 2 (1.3) | 3 (0.6) |
| Substance abuse | 3 (1.9) | 0 (0) | 0 (0.0) | 3 (0.6) |
| Anorexia nervosa | 0 (0) | 0 (0) | 2 (1.3) | 2 (0.4) |
| Substance dependence | 1 (0.6) | 0 (0) | 1 (0.6) | 2 (0.4) |
| Enuresis | 1 (0.6) | 0 (0) | 1 (0.6) | 2 (0.4) |
| Alcohol dependence | 0 (0) | 0 (0) | 1 (0.6) | 1 (0.2) |
| Encopresis | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Non-suicidal self-injury
Recent non-suicidal self-injury during the current depression episode was reported by 85 (18.3%) patients and lifetime non-suicidal self-injury by 246 (52.9%) patients. The frequency of recent non-suicidal self-injury in the treatment groups was as follows: BPI (26 patients, 16.8%), CBT (25 patients, 16.2%) and STPP (34 patients, 21.8%). The frequency of lifetime non-suicidal self-injury in the treatment groups was as follows: BPI (87 patients, 56.1%), CBT (75 patients, 48.7%) and STPP (84 patients, 53.9%).
Trial treatments and medication
Uptake and duration of trial therapies
The number of patients recorded as having started trial therapy was 138 (89%) for BPI, 133 (86%) for CBT and 133 (85%) for STPP. Owing to differences in organisation and type of service, the time from randomisation to start of therapy could vary between treatments and regional centres. Figure 4 displays the time from randomisation until the start of therapy for the three trial interventions as a Kaplan–Meier plot. The longest time until the start of therapy was 36 weeks, which was for CBT. Forty-seven young people did not start therapy. There were no age differences between this subgroup and the remaining participants (no-therapy group: median age 15.58 years, range 11.30–17.90 years vs. therapy group: median age 15.86 years, range 12.74–17.99 years; Kruskal–Wallis rank test = 0.224). This no-therapy subgroup are censored at the longest recorded start time. When a Cox proportional hazards model was fitted to the time until start of therapy, with covariates including trial therapy and region, there was evidence of an interaction between region and trial therapy. Table 6 gives the median time to start of therapy by treatment and region, from which it is apparent that time until the start of BPI was rather shorter in North London than in other sites, and that time until the start of CBT was rather longer in East Anglia than in other sites. Table 6 also displays the median and mean number of sessions attended by participants in each treatment arm.
FIGURE 4.
Time from randomisation to start of trial therapy by group.
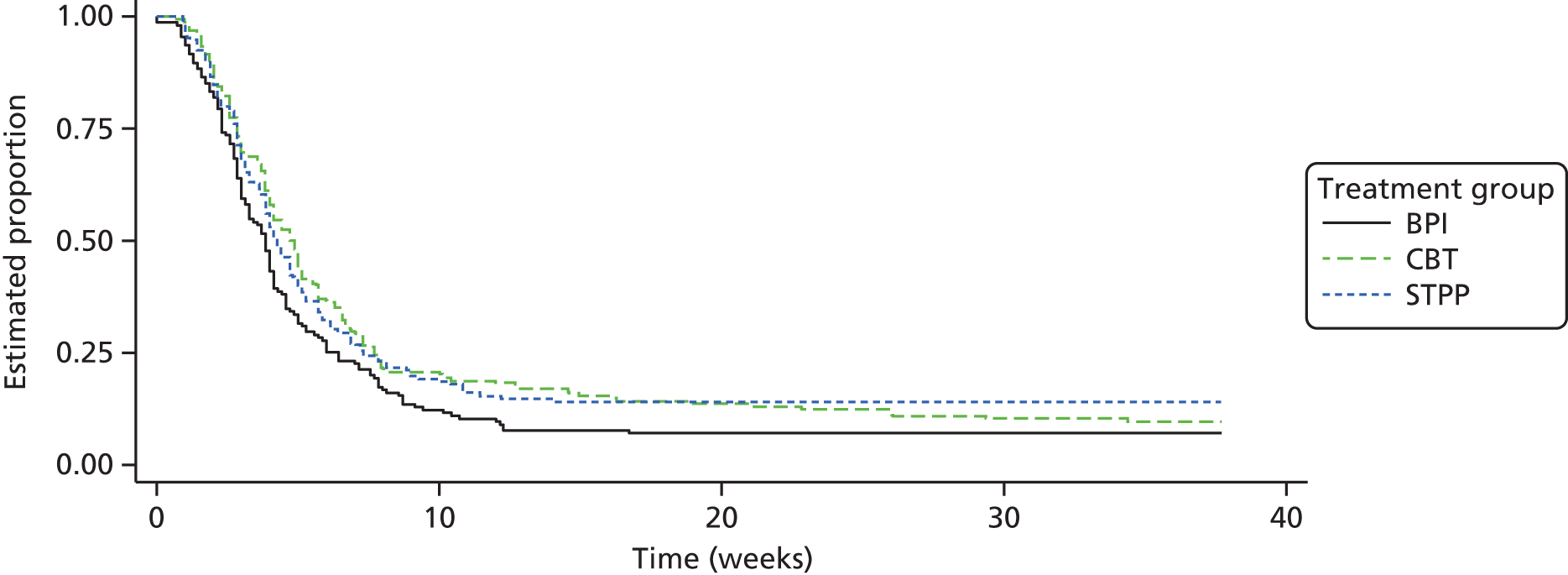
| Region | Treatment group, median (95% CI) | ||
|---|---|---|---|
| BPI | CBT | STPP | |
| East Anglia | 4.3 (3.3 to 5.6) | 7.3 (5.1 to 10.1) | 4.7 (3.9 to 5.7) |
| North London | 2.9 (2.0 to 3.7) | 4.0 (3.0 to 4.7) | 3.9 (2.7 to 4.4) |
| North-west England | 4.0 (3.1 to 4.6) | 4.0 (2.9 to 4.9) | 4.4 (3.1 to 6.1) |
Each of the three trial therapies recommended a number of treatment sessions (see Chapter 5). The number specified for each of the three trial interventions was 12 for BPI, 20 for CBT and 28 for STPP. Table 7 gives the number of clinical sessions attended by young people. Of those patients randomised to BPI, 17% (24/138) underwent more than the suggested 12 sessions. Of those randomised to CBT, 3% (5/133) underwent more than the recommended 20 sessions, and for those randomised to STPP, 2% (3/133) underwent more than the recommended 28 sessions. Table 7 also gives summary statistics for numbers of sessions received. Among patients who received therapy, those randomised to BPI had fewer sessions than those randomised to CBT or STPP (Kruskal–Wallis p < 0.001) and the median number of treatment sessions attended was six for BPI, eight for CBT and 11 for STPP. Fewer than half of all patients who received their randomised treatment attended more than half of the recommended number of sessions for that treatment modality.
| Number of sessions | Treatment group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| BPI | CBT | STPP | |||||||
| Frequency | % | Cumulative % | Frequency | % | Cumulative % | Frequency | % | Cumulative % | |
| Missing | 6 | 3.9 | – | 6 | 3.9 | – | 2 | 1.3 | – |
| 0 | 11 | 7.1 | 100.0 | 15 | 9.7 | 100.0 | 21 | 13.5 | 100.0 |
| 1 | 12 | 7.7 | 92.6 | 11 | 7.1 | 89.9 | 8 | 5.1 | 86.4 |
| 2 | 13 | 8.4 | 84.6 | 8 | 5.2 | 82.4 | 9 | 5.8 | 81.2 |
| 3 | 9 | 5.8 | 75.8 | 4 | 2.6 | 77.0 | 4 | 2.6 | 75.3 |
| 4 | 15 | 9.7 | 69.8 | 6 | 3.9 | 74.3 | 6 | 3.8 | 72.7 |
| 5 | 9 | 5.8 | 59.7 | 10 | 6.5 | 70.3 | 8 | 5.1 | 68.8 |
| 6 | 12 | 7.7 | 53.7 | 11 | 7.1 | 63.5 | 5 | 3.2 | 63.6 |
| 7 | 10 | 6.5 | 45.6 | 6 | 3.9 | 56.1 | 4 | 2.6 | 60.4 |
| 8 | 4 | 2.6 | 38.9 | 8 | 5.2 | 52.0 | 13 | 8.3 | 57.8 |
| 9 | 8 | 5.2 | 36.2 | 5 | 3.2 | 46.6 | 1 | 0.6 | 49.4 |
| 10 | 6 | 3.9 | 30.9 | 6 | 3.9 | 43.2 | 3 | 1.9 | 48.7 |
| 11 | 7 | 4.5 | 26.8 | 7 | 4.5 | 39.2 | 6 | 3.8 | 46.8 |
| 12 | 9 | 5.8 | 22.1 | 5 | 3.2 | 34.5 | 2 | 1.3 | 42.9 |
| 13 | 3 | 1.9 | 16.1 | 7 | 4.5 | 31.1 | 6 | 3.8 | 41.6 |
| 14 | 5 | 3.2 | 14.1 | 8 | 5.2 | 26.4 | 2 | 1.3 | 37.7 |
| 15 | 3 | 1.9 | 10.7 | 2 | 1.3 | 20.9 | 3 | 1.9 | 36.4 |
| 16 | 2 | 1.3 | 8.7 | 4 | 2.6 | 19.6 | 2 | 1.3 | 34.4 |
| 17 | 1 | 0.6 | 7.4 | 7 | 4.5 | 16.9 | 1 | 0.6 | 33.1 |
| 18 | 4 | 2.6 | 6.7 | 2 | 1.3 | 12.2 | – | – | 32.5 |
| 19 | 1 | 0.6 | 4.0 | 3 | 1.9 | 10.8 | 5 | 3.2 | 32.5 |
| 20 | 1 | 0.6 | 3.4 | 8 | 5.2 | 8.8 | 3 | 1.9 | 29.2 |
| 21 | 1 | 0.6 | 2.7 | 3 | 1.9 | 3.4 | 4 | 2.6 | 27.3 |
| 22 | – | – | 2.0 | 1 | 0.6 | 1.4 | 4 | 2.6 | 24.7 |
| 23 | 1 | 0.6 | 2.0 | – | – | 0.7 | 5 | 3.2 | 22.1 |
| 24 | – | – | 1.3 | 1 | 0.6 | 0.7 | 5 | 3.2 | 18.8 |
| 25 | – | – | 1.3 | – | – | 0.0 | 7 | 4.5 | 15.6 |
| 26 | – | – | 1.3 | – | – | 0.0 | 4 | 2.6 | 11.0 |
| 27 | -- | – | 1.3 | – | – | 0.0 | 4 | 2.6 | 8.4 |
| 28 | – | – | 1.3 | – | – | 0.0 | 6 | 3.8 | 5.8 |
| 29 | – | – | 1.3 | – | – | 0.0 | 1 | 0.6 | 1.9 |
| 33 | 1 | 0.6 | 1.3 | – | – | 0.0 | – | – | 1.3 |
| 39 | – | – | 0.7 | – | – | 0.0 | 1 | 0.6 | 1.3 |
| 42 | – | – | 0.7 | – | – | 0.0 | 1 | 0.6 | 0.6 |
| 43 | 1 | 0.6 | 0.7 | – | – | 0.0 | – | – | 0.0 |
| Total | 155 | 100 | 154 | 100 | 156 | 100.0 | |||
| Median (IQR)a | 6 | 4,11 | 9 | 5,14 | 11 | 5,23 | |||
A clinical estimate of adherence to therapy for each therapeutic modality was made by the lead clinical specialists for each trial treatment. As there is no prior scientific evidence, these operational definitions of minimum sufficient attendance were ‘best practice’ based and, therefore, cannot index a formal required therapeutic dose. They are given here for descriptive purposes only but may be hypothesis-forming for future reference.
Clinical adherence that might result in some therapeutic gain was defined by the lead therapeutic specialists in consultation with therapists in each treatment arm. The investigators agreed to set two sessions for BPI and five sessions for CBT and STPP as the minimum number of sessions likely to result in therapeutic gain. The proportion of patients in each treatment group attending what is estimated as inadequate or adequate number of sessions for putative clinical adherence is shown in Table 6. Conditional on attending at least one session, 17% (24/138) of patients exceeded the proscribed maximum number of sessions on BPI, compared with 4% (5/133) for CBT and 2% (3/133) for STPP. The number and per cent of sessions attended by treatment allocation is shown in Table 7.
Figure 5 displays the duration of trial therapy for those young people with a recorded start and completion date by treatment group. It was assumed that the duration of therapy was 1 day for young people attending just one therapy session. Summary statistics for the same data are given in Table 8. Average duration of therapy between treatment groups was quite similar and not significantly different (Kruskal–Wallis p = 0.238). However, the median duration of therapy was greater for STPP (30.1 weeks) than for either BPI (22.1 weeks) or CBT (23.1 weeks), which is illustrated in Figure 5. There is no noticeably greater variation in the length of therapy for BPI (SD 21.5 weeks) than for CBT (SD 17.7 weeks) and STPP (SD 16.8 weeks), which can be explained by rather more patients exceeding the suggested number of sessions for BPI (see Table 8).
FIGURE 5.
Duration of trial therapy by treatment group.

| Treatment group | Median | Maximum | Mean | SD | n |
|---|---|---|---|---|---|
| BPI | 22.1 | 111.9 | 27.5 | 21.5 | 130 |
| CBT | 23.1 | 99.6 | 24.9 | 17.7 | 130 |
| STPP | 30.1 | 97.0 | 27.9 | 16.8 | 131 |
All therapists delivering a trial therapy were given a trial therapist identifier. The therapist identifier was missing for 18 (12%) BPI trial treatments, 13 (9%) CBT trial treatments and 2 (1%) STPP trial treatments. A total of 63 therapists delivered BPI, 44 delivered CBT and 38 STPP. For all three modalities, the young person received their trial therapy from a single trial therapist. Figure 6 gives the distribution of the number of young people treated by each therapist for each treatment arm. The number of trial participants seen by a particular therapist ranged from 1 to 15. Forty BPI therapists treated only one young person in the trial, whereas the corresponding figures for CBT and STPP were 19 and 18, respectively. This difference in number of therapists per treatment group is due, in part, to the rather larger number of available BPI compared with CBT or STPP therapists within the 15 NHS CAMHS clinics.
FIGURE 6.
Frequency distribution of number of trial participants for each therapy modality seen by a trial therapist. (a) BPI; (b) CBT; and (c) STPP.



Fidelity and differentiation of trial therapies
Treatment fidelity
The reliability of the CPPS measure was obtained from each audio tape being rated by two separate raters on each subscale (cognitive–behavioural and psychodynamic interpersonal). The reliability was calculated with an ICC, which gave values of 0.78 for the cognitive–behavioural and 0.69 for the psychodynamic interpersonal subscale, respectively. The results were extrapolated using the Spearman–Brown formula to estimate the reliability of the two subscales across participants as follows:
where ICC is the ICC of the individual measures and m is the number of ratings that is used to calculate the mean or total for each person. In this case, m is 2 as we have two ratings of each tape, which gives results of 0.82 for the cognitive–behavioural and 0.80 for the psychodynamic interpersonal subscale, respectively. Table 9 summarises the ratings on the cognitive–behavioural and psychodynamic interpersonal subscales. Based on the CPPS ratings, 74% of the CBT sessions (56/76) had a score of ≥ 2 (‘somewhat characteristic’) on the cognitive–behavioural subscale and can therefore be considered adherent to the CBT treatment protocol. A total of 80% of the STPP sessions (65/81) had a score of ≥ 2 (‘somewhat characteristic’) on the psychodynamic interpersonal subscale and can therefore be considered adherent to the STPP protocol.
| Treatment group | CPPS subscale | n | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cognitive–behavioural | Psychodynamic interpersonal | ||||||||||||||
| Score of ≥ 2 | % | Mean | SD | Median | p25 | p75 | Score of ≥ 2 | % | Mean | SD | Median | p25 | p75 | ||
| BPI | 21 | 28.0 | 1.55 | 0.71 | 1.35 | 1 | 2.1 | 14 | 18.7 | 1.37 | 0.65 | 1.25 | 0.85 | 1.85 | 75 |
| CBT | 56 | 73.7 | 2.49 | 0.91 | 2.43 | 1.83 | 3 | 15 | 19.7 | 1.48 | 0.69 | 1.4 | 0.98 | 1.83 | 76 |
| STPP | 0 | 0 | 0.55 | 0.37 | 0.45 | 0.3 | 0.7 | 65 | 80.2 | 2.64 | 0.8 | 2.65 | 2.05 | 3.3 | 81 |
The kappa coefficient for the rating of adherence by the BPI-S was 0.51. Based on the BPI-S ratings, 81.3% of the BPI sessions (61/75) were rated as ≥ 2 on two out of three ‘core’ items and four out of eight items in total, and can therefore be considered adherent to the BPI protocol.
It should be kept in mind that the CPPS and BPI fidelity measures are not directly comparable, as each scale has its own criteria for assessing what signifies an ‘adherent’ treatment. Therefore, the results give an opportunity to compare levels of fidelity between STPP and CBT, but not a direct statistical comparison of the magnitude of fidelity between all three treatment arms.
Treatment differentiation
Table 9 gives the mean ratings for each of the three treatment arms on the CPPS subscales (psychodynamic interpersonal and cognitive–behavioural), showing the proportion of techniques associated with the other treatment arm that was used by BPI, CBT and STPP.
Figure 7 gives a box plot for the treatment differentiation score for each domain of the CPPS for the three treatments, and corresponding summary statistics are given in Table 12. This shows that all three treatment arms were significantly differentiated, based on blind double ratings of the CPPS. As predicted, the mean cognitive–behavioural subscale score was 1.91 higher for CBT than for STPP [95% confidence interval (CI) 1.73 to 2.09; p < 0.0001]. The mean psychodynamic interpersonal subscale score was 1.18 higher for STPP than for CBT (95% CI 1.01 to 1.3; p < 0.0001). BPI had a significantly lower cognitive–behavioural subscale mean than CBT (mean difference = –0.93, 95% CI –1.12 to – 0.75; p < 0.0001) and a significantly lower psychodynamic interpersonal subscale mean than STPP (mean difference = –1.30, 95% CI –1.48 to –1.11; p < 0.0001). In conclusion, ratings of the two CPPS subscales suggested that all three treatments were well differentiated.
FIGURE 7.
Treatment differentiation based on the CPPS. CB, cognitive–behavioural; PI, psychodynamic interpersonal.
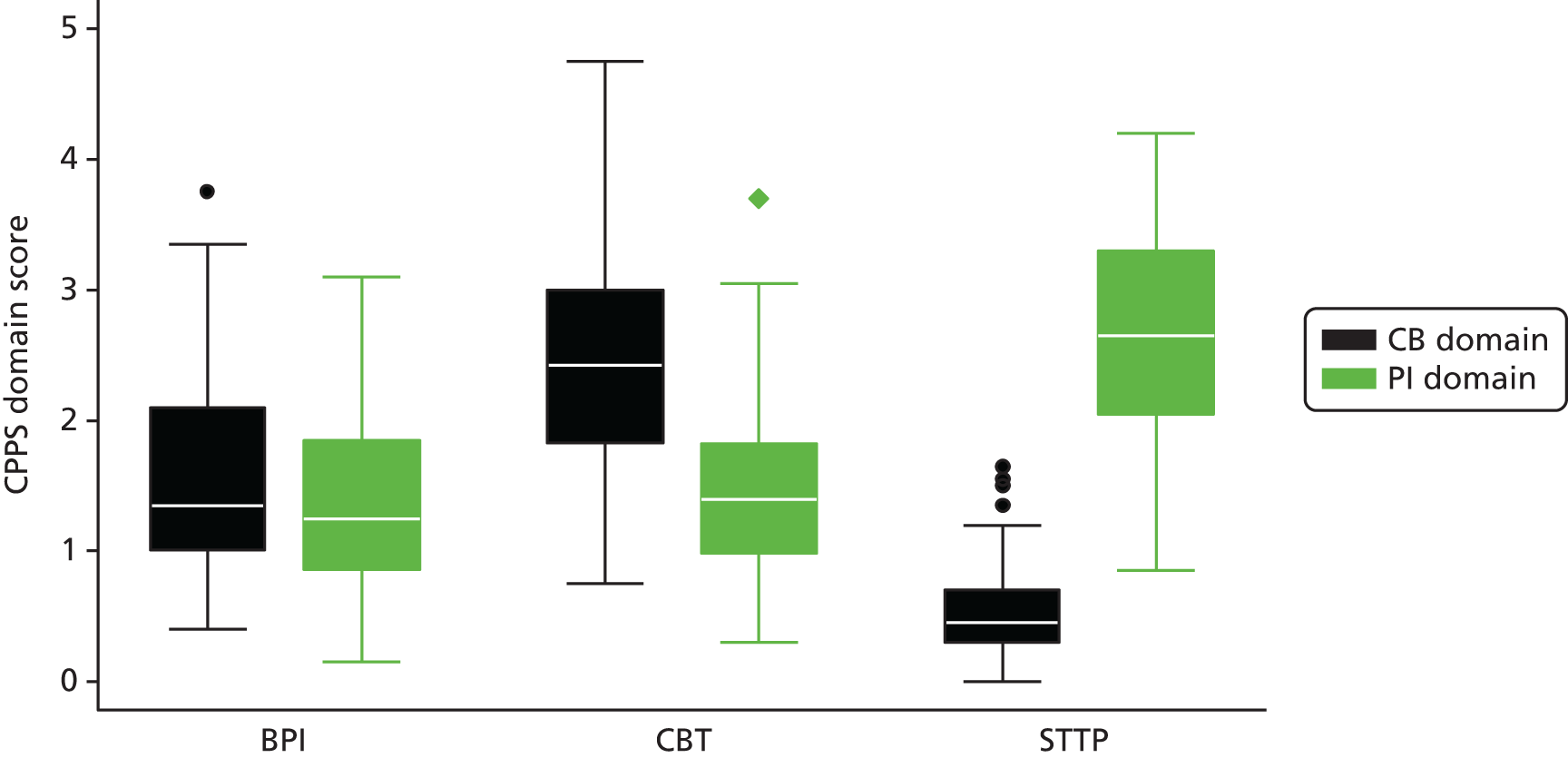
Conclusion of the treatment fidelity and differentiation analysis
This analysis, based on the blind double ratings of 232 tapes, stratified by modality and timing, aimed to evaluate treatment fidelity and differentiation within the study.
Fidelity ratings were conducted with good (for CPPS) to moderate (for BPI-S) intraclass correlations scores. Overall, there was a relatively high level of protocol fidelity by the therapists in each arm of the study, with 81.3% of sessions meeting the threshold of fidelity for BPI, compared with 80% for STPP and 74% for CBT. Previous studies (e.g. ADAPT) have reported mean scores for therapist fidelity and/or competence, but have not used predefined cut-off scores for fidelity. However, direct comparisons between the figures for BPI and the two specialist psychological therapies should be interpreted with caution, given that BPI sessions were assessed using a different measure to the CBT and STPP treatment arms. Unlike the CBT and STPP sessions, BPI sessions were not rated blindly for treatment fidelity and had lower levels of inter-rater reliability; therefore, findings regarding levels of fidelity to BPI must be interpreted with some caution.
In addition to demonstrating good levels of protocol fidelity, treatment differentiation was established between all three treatment arms. In line with our hypotheses regarding ratings on the CPPS, CBT sessions were significantly lower than STPP on the psychodynamic interpersonal subscale, STPP sessions were significantly lower than CBT on the cognitive–behavioural subscale, and BPI sessions were significantly lower than both STPP on the psychodynamic interpersonal subscale and CBT on the cognitive–behavioural subscale. This demonstrates that STPP and CBT sessions were significantly differentiated from each other and BPI sessions were significantly differentiated from both CBT and STPP.
Antidepressant medication
Table 10 shows the number and percentage of participants who were prescribed any antidepressant during treatment and follow-up, by arm, based on data provided by the health economic schedule CA-SUS. Receipt of antidepressant medication during treatment is a potential mediator of the outcome of psychological treatment. Overall, a similar proportion of young people in each arm were prescribed medication during the trial treatment period (< 36 weeks), suggesting that receipt of medication was independent of random allocation. There is therefore no reason to believe that medication during the therapy period would bias estimates of the treatment effect immediately post therapy, unless drug therapy interacted with therapeutic modality.
| Time period | Treatment group, frequency (%) | ||
|---|---|---|---|
| BPI | CBT | STPP | |
| < 36 weeks | n = 122 | n = 120 | n = 122 |
| Medication | |||
| Citalopram | 3 (2.5) | 5 (4.2) | 3 (2.5) |
| Fluoxetine | 29 (23.8) | 27 (22.5) | 23 (18.9) |
| Sertraline | 3 (2.5) | 3 (2.5) | 9 (7.4) |
| Any antidepressant | 34 (27.9) | 33 (27.5) | 32 (26.2) |
| Not receiving medication | 88 (72.1) | 87 (72.5) | 90 (73.8) |
| ≥ 36 weeks | n = 125 | n = 125 | n = 124 |
| Medication | |||
| Citalopram | 9 (7.2) | 9 (7.2) | 6 (4.8) |
| Fluoxetine | 36 (28.8) | 30 (24.0) | 24 (19.4) |
| Sertraline | 12 (9.6) | 5 (4.0) | 13 (10.5) |
| Any antidepressant | 50 (40.0) | 43 (34.4) | 43 (34.7) |
| Not receiving medication | 75 (60.0) | 82 (65.6) | 81 (65.3) |
| All follow-up | n = 137 | n = 137 | n = 137 |
| Any antidepressant | 56 (40.9) | 55 (40.1) | 50 (36.5) |
| Not receiving medication | 81 (59.1) | 82 (59.9) | 87 (63.5) |
During follow-up, the proportion of patients receiving any antidepressant medication increased from 27% in the treatment period to 34% for CBT, 35% for STPP and to 40% for BPI, although this difference between arms was not statistically significant (p = 0.584).
Assessment of clinical outcome
Table 11 gives the response rate for the primary outcome measure (MFQ) for each assessment. A total of 16 (10%) patients, 12 (8%) patients and 17 (11%) patients in the BPI, CBT and STPP groups, respectively, had no follow-up MFQ. The CBT group had the highest response rate of 80% at the 86-week assessment. To investigate baseline characteristics that might influence non-response, a logistic GEE model was fitted to an indicator variable of missing primary outcome data at each assessment (6–86 weeks) including the following covariates: randomisation, assessment number, age at randomisation, sex, region (East Anglia, North London, north-west England), baseline MFQ score, SSRI prescription before trial entry, behaviour disorder (a diagnosis of oppositional defiant disorder or conduct disorder), all anxiety disorders combined and a time by treatment by assessment interaction to investigate differential non-response. Two factors appeared to influence non-response: (1) regional centre with a higher response rate in the north-west England regional centre (p = 0.02) compared with East Anglia and (2) behaviour disorders at baseline with a lower response rate for subjects with conduct or oppositional defiant disorder (p = 0.004). Behavioural disorder was not in the original list of prespecified baseline covariates and so was added to all models to support the missing at random assumption for missing outcome data.
| Assessment number (week) | Treatment group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BPI (n = 155) | CBT (n = 154) | STPP (n = 156) | ||||||||||
| Response rate, frequency (%) | Time since randomisation (weeks) | Response rate, frequency (%) | Time since randomisation (weeks) | Response rate, frequency (%) | Time since randomisation (weeks) | |||||||
| Mean | Minimum | Maximum | Mean | Minimum | Maximum | Mean | Minimum | Maximum | ||||
| Baseline | 155 (100) | 154 (100) | 156 (100) | |||||||||
| 1 (6) | 99 (64) | 11.0 | 6 | 25 | 104 (68) | 12.3 | 7 | 41 | 107 (69) | 11.1 | 6 | 21 |
| 2 (12) | 112 (72) | 17.6 | 12 | 33 | 106 (69) | 19.0 | 11 | 38 | 108 (69) | 17.6 | 12 | 28 |
| 3 (36) | 105 (68) | 42.3 | 36 | 54 | 104 (68) | 42.9 | 35 | 63 | 109 (70) | 41.5 | 31 | 52 |
| 4 (52) | 105 (68) | 59.2 | 51 | 76 | 111 (72) | 60.3 | 48 | 92 | 110 (71) | 59.3 | 50 | 85 |
| 5 (86) | 116 (75) | 95.4 | 73 | 132 | 123 (80) | 94.9 | 82 | 147 | 114 (73) | 95.1 | 69 | 149 |
Table 12 gives summary statistics for the primary outcome measure MFQ and the secondary quantitative outcomes, which include Revised Children’s Manifest Anxiety Scale (RCMAS), LOI and ABQ, which are self-completed questionnaires. The HoNOSCA is interviewer rated.
| Outcome measure | Treatment group | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BPI (n = 155) | CBT (n = 154) | STPP (n = 156) | ||||||||||||||||
| Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | n | Mean | SD | Median | Minimum | Maximum | n | |
| Primary | ||||||||||||||||||
| MFQ | ||||||||||||||||||
| Baseline | 46.2 | 10.6 | 47 | 15 | 64 | 155 | 46.2 | 10.3 | 47 | 20 | 65 | 154 | 45.4 | 10.8 | 46 | 13 | 64 | 156 |
| 1 | 36.5 | 14.3 | 39 | 2 | 64 | 99 | 35.2 | 11.3 | 34.5 | 10 | 59 | 104 | 34.9 | 13.2 | 34 | 2 | 61 | 107 |
| 2 | 34.1 | 14.4 | 36 | 1 | 61 | 112 | 31.6 | 13.3 | 33 | 1 | 59 | 106 | 33.1 | 14.2 | 35.1 | 1 | 58 | 108 |
| 3 | 30.5 | 16.1 | 31 | 0 | 61 | 105 | 24.2 | 15.1 | 22.5 | 0 | 61 | 104 | 26.6 | 15.7 | 24 | 0 | 59 | 109 |
| 4 | 25.1 | 16.2 | 22.7 | 0 | 63 | 105 | 25.0 | 18.0 | 20.6 | 0 | 62 | 111 | 23.0 | 15.9 | 20 | 0 | 62.3 | 110 |
| 5 | 23.6 | 16.2 | 20.5 | 0 | 63 | 116 | 22.3 | 15.7 | 19 | 0 | 63 | 123 | 21.8 | 15.5 | 18.5 | 0 | 61 | 114 |
| Secondary | ||||||||||||||||||
| RCMAS | ||||||||||||||||||
| Baseline | 41.1 | 7.6 | 42 | 17 | 54 | 155 | 41.2 | 6.4 | 41 | 15 | 55 | 154 | 40.5 | 7.7 | 41.5 | 8 | 56 | 155 |
| 1 | 35.9 | 10.6 | 38.7 | 0 | 52 | 98 | 37.1 | 7.9 | 38.4 | 12 | 53 | 103 | 36.7 | 10.0 | 39 | 0 | 56 | 107 |
| 2 | 34.2 | 11.9 | 36.6 | 3 | 56 | 110 | 34.4 | 11.4 | 37 | 2 | 56 | 105 | 34.3 | 11.9 | 37 | 0 | 54 | 108 |
| 3 | 32.0 | 13.3 | 36 | 0 | 53 | 104 | 27.0 | 13.7 | 28 | 2 | 49 | 102 | 28.6 | 13.3 | 30 | 0 | 49 | 107 |
| 4 | 27.2 | 14.8 | 29 | 0 | 50 | 100 | 26.4 | 14.9 | 28 | 0 | 56 | 108 | 25.5 | 14.5 | 26.5 | 0 | 53 | 104 |
| 5 | 24.7 | 14.7 | 26 | 0 | 53 | 109 | 24.8 | 15.4 | 27 | 0 | 56 | 115 | 23.8 | 14.6 | 26.0 | 0 | 56 | 108 |
| LOI | ||||||||||||||||||
| Baseline | 10.0 | 5.3 | 9.9 | 0 | 22 | 155 | 10.8 | 5.4 | 10 | 0 | 22 | 152 | 9.2 | 5.0 | 8.9 | 0 | 22 | 154 |
| 1 | 7.8 | 5.4 | 7 | 0 | 22 | 98 | 7.6 | 5.0 | 7 | 0 | 22 | 102 | 7.6 | 5.0 | 6 | 0 | 21 | 107 |
| 2 | 6.6 | 5.6 | 5 | 0 | 22 | 111 | 6.7 | 5.2 | 6 | 0 | 22 | 104 | 7.3 | 5.1 | 7 | 0 | 22 | 107 |
| 3 | 6.3 | 5.4 | 5 | 0 | 19 | 103 | 4.8 | 4.8 | 4 | 0 | 21 | 101 | 5.2 | 4.9 | 4 | 0 | 21 | 107 |
| 4 | 5.6 | 5.8 | 4 | 0 | 22 | 99 | 5.1 | 5.5 | 3 | 0 | 22 | 107 | 4.9 | 4.7 | 4 | 0 | 18 | 102 |
| 5 | 5.0 | 5.4 | 3 | 0 | 22 | 107 | 4.9 | 5.0 | 3 | 0 | 21 | 115 | 4.0 | 4.6 | 3 | 0 | 22 | 106 |
| ABQ | ||||||||||||||||||
| Baseline | 3.5 | 3.4 | 3 | 0 | 18 | 155 | 3.1 | 2.8 | 2 | 0 | 14 | 152 | 3.3 | 3.3 | 3 | 0 | 18 | 154 |
| 1 | 2.5 | 2.5 | 2 | 0 | 11 | 98 | 1.9 | 2.1 | 1 | 0 | 10 | 102 | 2.1 | 2.6 | 1 | 0 | 13 | 107 |
| 2 | 2.3 | 2.9 | 1.1 | 0 | 17 | 111 | 1.7 | 2.7 | 1 | 0 | 15.4 | 104 | 1.5 | 2.3 | 0 | 0 | 12 | 107 |
| 3 | 1.8 | 2.5 | 1 | 0 | 16 | 103 | 1.0 | 1.5 | 0 | 0 | 7 | 101 | 1.4 | 2.0 | 1 | 0 | 9 | 107 |
| 4 | 1.1 | 1.6 | 0 | 0 | 8 | 99 | 1.4 | 2.7 | 0 | 0 | 16 | 107 | 1.1 | 2.5 | 0 | 0 | 22 | 102 |
| 5 | 0.8 | 1.4 | 0 | 0 | 7 | 107 | 1.2 | 2.2 | 0 | 0 | 13 | 115 | 0.9 | 1.5 | 0 | 0 | 8.8 | 106 |
| HoNOSCA | ||||||||||||||||||
| Baseline | 18.9 | 6.0 | 19 | 0 | 37.9 | 148 | 18.4 | 6.0 | 18 | 0 | 35 | 143 | 18.2 | 6.3 | 18 | 0 | 35.8 | 144 |
| 1 | 14.5 | 6.5 | 14 | 1 | 30 | 88 | 14.1 | 6.4 | 14 | 1 | 29 | 91 | 14.6 | 6.9 | 13 | 0 | 32.5 | 96 |
| 2 | 14.3 | 7.5 | 14 | 0 | 36.1 | 101 | 11.9 | 6.8 | 11 | 0 | 32 | 96 | 12.9 | 6.2 | 13 | 0 | 34.7 | 94 |
| 3 | 12.0 | 8.7 | 11 | 0 | 39 | 88 | 9.7 | 7.2 | 8 | 0 | 31 | 81 | 10.3 | 7.6 | 8 | 0 | 33.8 | 88 |
| 4 | 9.5 | 6.9 | 8.3 | 0 | 27.4 | 88 | 8.5 | 7.3 | 6 | 0 | 31.4 | 86 | 8.6 | 5.8 | 8 | 0 | 23.8 | 83 |
| 5 | 8.2 | 6.2 | 7 | 0 | 28.4 | 98 | 7.3 | 5.2 | 6 | 0 | 20.1 | 92 | 8.2 | 7.2 | 7 | 0 | 30 | 85 |
On initial inspection of the data, it was clear that the ABQ was highly skewed with the SD larger than the mean at many time points and medians of zero at weeks 52 and 86 for each group. Because of the substantial skewness, the decision was made to dichotomize this scale and compare the proportion of none zero scores. Further analysis of this scale is therefore presented with other binary outcome measures and results are shown in Table 15.
In Figure 8, the mean scores with 95% CIs are plotted against time since randomisation for the quantitative outcome measures. For all scales, lower scores represent a better outcome, hence a greater reduction in one treatment than another represents a beneficial effect. For all four measures, the profile of CBT and STPP is below that for BPI post randomisation across time points.
FIGURE 8.
Mean outcome by treatment group (95% CI). (a) MFQ; (b) RCMAS; (c) LOI; and (d) HoNOSCA.


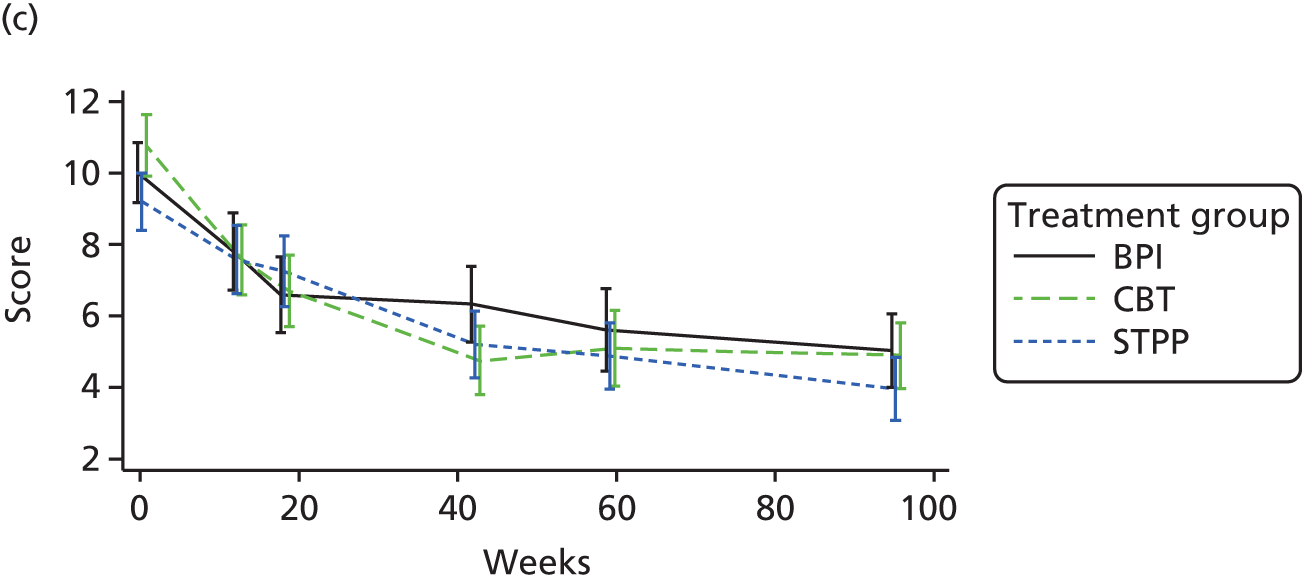

The hypotheses of the trial are regarding the treatment effect in the post-treatment period (≥ 36 weeks).
The study had four primary hypotheses.
When comparing CBT with STPP:
-
CBT will show non-inferiority effects compared with STPP at 52 weeks
-
STPP will show superiority effects compared with CBT at 86 weeks
and when comparing CBT and STPP with BPI:
-
the specialist intensive interventions (CBT/STPP) will show superiority effects compared with BPI at 52 weeks
-
the specialist intensive interventions (CBT/STPP) will show superiority effects compared with BPI at 86 weeks.
As described in Chapter 8, the mean differences were estimated at weeks 36, 52 and 86 post randomisation (1) between the two specialist psychological therapies (STPP vs. CBT = intensive therapies) and (2) between the two theory based treatments and BPI [(CBT or STPP) vs. BPI]. These mean differences were estimated using linear mixed-effects (LME) model fitted to post-treatment responses only (≥ 36 weeks from randomisation). As well as a main effect of treatment, a time by treatment interaction and other prespecified covariates were included in this model – details of which are given in the data analytic strategy (see Chapter 8).
Estimates of the time by treatment interaction from these models and the main effects of models are given in Appendix 1, Table 24. In total, 392 young people provided 1013 assessments of the primary outcome measure (MFQ), so the model includes 84% (392/465) of all participants contributing, on average, 2.6 assessments. To address the four hypotheses, the time point-specific treatment effect averaged over baseline covariates, sometimes called the marginal treatment effect, was estimated from the model including a time with treatment interaction. The mean differences between treatments at the three time points (36, 52 and 86 weeks post randomisation) are tabulated in Table 13. As higher scores reflect worse outcome for all scales, negative differences indicate a positive effect.
| Outcome measure | Time (weeks) | Treatment effect | 95% CI | p-valuea |
|---|---|---|---|---|
| Primary | ||||
| MFQ | ||||
| CBT – STPP | 36 | –0.179 | –4.088 to 3.731 | 0.929 |
| 52 | –0.307 | –3.774 to 3.161 | 0.862 | |
| 86 | –0.578 | –4.104 to 2.948 | 0.748 | |
| (CBT + STPP) – BPI | 36 | –3.234 | –6.611 to 0.143 | 0.061 |
| 52 | –2.806 | –5.790 to 0.177 | 0.065 | |
| 86 | –1.898 | –4.922 to 1.126 | 0.219 | |
| Secondary | ||||
| RCMAS | ||||
| CBT – STPP | 36 | –0.855 | –4.239 to 2.530 | 0.621 |
| 52 | –0.663 | –3.680 to 2.354 | 0.667 | |
| 86 | –0.254 | –3.489 to 2.980 | 0.878 | |
| (CBT + STPP) – BPI | 36 | –3.832 | –6.781 to –0.884 | 0.011 |
| 52 | –2.818 | –5.432 to –0.205 | 0.035 | |
| 86 | –0.663 | –3.460 to 2.134 | 0.642 | |
| LOI | ||||
| CBT – STPP | 36 | –0.816 | –1.972 to 0.341 | 0.167 |
| 52 | –0.574 | –1.601 to 0.452 | 0.273 | |
| 86 | –0.062 | –1.091 to 0.967 | 0.906 | |
| (CBT + STPP) – BPI | 36 | –1.249 | –2.258 to –0.240 | 0.015 |
| 52 | –1.120 | –2.010 to –0.231 | 0.014 | |
| 86 | –0.847 | –1.736 to 0.042 | 0.062 | |
| HoNOSCA | ||||
| CBT – STPP | 36 | –0.617 | –2.733 to 1.499 | 0.567 |
| 52 | –0.620 | –2.318 to 1.078 | 0.474 | |
| 86 | –0.626 | –2.066 to 0.814 | 0.394 | |
| (CBT + STPP) – BPI | 36 | –1.410 | –3.221 to 0.401 | 0.127 |
| 52 | –1.154 | –2.601 to 0.293 | 0.118 | |
| 86 | –0.611 | –1.819 to 0.598 | 0.322 | |
Presenting results chronologically, we first considered a secondary hypothesis concerning clinical outcome at 36 weeks, that is at the end of trial treatment phase. The difference between CBT and STPP was negative for the primary outcome (MFQ) and the secondary outcomes (RCMAS, LOI and HoNOSCA) (see Table 13). For MFQ, the differences showed a non-significant reduction of –0.18 (p = 0.929). For RCMAS, LOI and HoNOSCA the respected difference were also non-significant –0.86 (p = 0.621), –0.82 (p = 0.167) and –0.62 (p = 0.567), respectively. When the intensive treatment (CBT + STPP) was compared with BPI, the difference was –3.23 (95% CI –6.61 to 0.14; p = 0.061) for MFQ at 36 weeks. For both RCMAS and LOI, the reduction was statistically significant at a 2.5% level, suggesting benefit to the specialist psychological therapies at this time point on two of the secondary measures.
Moving to the hypothesis that CBT will show non-inferiority compared with STPP at 52 weeks (hypothesis 1), we need to consider the upper confidence limit of the difference in outcomes between CBT and STPP. For non-inferiority to be concluded, we need the upper limit to be smaller than a clinically important difference. For the purpose of the sample size calculation, this was assumed to be five points on the MFQ scale.
For all four measures in Table 13, the point estimate is negative and this represents a beneficial effect of CBT compared with STPP. For MFQ at 52 weeks, the treatment effect estimate is –0.307 (95% CI –3.774 to 3.161). As the upper limit (3.161) is less than a clinically important difference of 5 units, we can conclude that CBT is non-inferior to STPP at this time point. The corresponding upper limits for RCMAS, LOI and HoNOSCA were 2.354, 0.452 and 1.078, respectively, which would appear also to support the hypothesis of non-inferiority.
Consider now the hypothesis that STPP will show superiority effects compared with CBT at 86 weeks (hypothesis 2). Table 13 shows that the treatment effect for CBT compared with STPP is –0.578 (95% CI –4.100 to 2.950). With the point estimate representing a slight benefit for CBT compared with STPP, there is no evidence to support this hypothesis (p = 0.748). Similar conclusions can be drawn for RCMAS (p = 0.878), LOI (p = 0.906) and HoNOSCA (p = 0.394).
Hypotheses 3 and 4 consider superiority of the specialist psychological treatment compared with BPI at 52 and 86 weeks. At 52 weeks (hypothesis 3), the difference is –2.81 (95% CI –5.79 to 0.18; p = 0.065) for MFQ. Although this suggests that there is a benefit at this time point for the specialist psychological treatment, this difference is smaller than the 5-point difference hypothesised as clinically significant in the sample size calculation and is not statistically significant at a 2.5% level. Similar effects are observed for RCMAS (adjusted mean difference –2.81, 95% CI –5.43 to –0.21), LOI (adjusted mean difference –1.12, 95% CI –2.01 to –0.23) and HoNOSCA (adjusted mean difference –1.15, 95% CI –2.60 to 0.29), with the effect being close to the 2.5% level for RCMAS (p = 0.035) and statistically significant for LOI (p = 0.014), but less so for HoNOSCA (p = 0.118). At 86 weeks (hypothesis 4), the beneficial effect of the specialist psychological treatment compared with BPI is attenuated with the treatment effect for none of the four outcome measures being statistically significant at a 2.5% level.
The intraclass correlation coefficient (ICC) for therapists was estimated for the models by centring the time variable in the model. This gives the value of the ICC for the therapist at the mid-point of follow-up. The estimate of the ICC was found to be negligible (< 10–7) for all models.
Outcome data gathered prior to 36 weeks after randomisation (assessments 1 and 2) were also summarised in Table 12, but these data are not relevant to the hypotheses of this study. Inferential analyses of these data are included in the data analysis supplement (see Appendix 1, Table 25). When STPP was compared with CBT, there were no significant treatment effects for the primary outcome MFQ (p = 0.383), RCMAS (p = 0.681) or HoNOSCA (p = 0.398). Young people receiving STPP had a worse outcome on the LOI scale during this period (adjusted mean difference = 1.19, 95% CI 0.28 to 2.12; p = 0.011). When the two specialist psychological therapies were compared with BPI, there was no evidence of a treatment effect for MFQ (p = 0.382), RCMAS (p = 0.632) or HoNOSCA (p = 0.646), and the outcome for BPI lay between that for CBT (p = 0.309) and STPP (p = 0.120) (see Table 13).
The trial had two binary outcome measures: (1) presence of a MDD as determined by the K-SADS inventory and (2) threshold of primary outcome (MFQ score of > 25) indexing potential clinical caseness. 47,112 As mentioned above, the ABQ was dichotomised for the purpose of analysis owing to having a highly skewed distribution. The frequency distributions of these three measures by treatment and time point are given in Table 14. With a reduced rate representing benefit for all three scales, there was a similar pattern to that observed in the continuous scales (see Table 14), with CBT and STPP showing benefit at assessment 3 (36-week assessment). At assessment 5 (86-week assessment), there is some suggestion of a difference between groups but the pattern was not consistent across measures.
| Assessment | Treatment group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| BPI | CBT | STPP | |||||||
| Frequency | Total | % | Frequency | Total | % | Frequency | Total | % | |
| MDD (K-SADS positive or high clinical indication for MDD) | |||||||||
| 1 | 63 | 95 | 66.3 | 57 | 95 | 60.0 | 62 | 99 | 62.6 |
| 2 | 57 | 105 | 54.3 | 46 | 98 | 46.9 | 54 | 99 | 54.5 |
| 3 | 42 | 95 | 44.2 | 28 | 89 | 31.5 | 35 | 98 | 35.7 |
| 4 | 27 | 92 | 29.3 | 23 | 90 | 25.6 | 23 | 87 | 26.4 |
| 5 | 27 | 99 | 27.3 | 24 | 95 | 25.3 | 14 | 92 | 15.2 |
| MFQ score of > 25 | |||||||||
| Baseline | 149 | 155 | 96.1 | 148 | 154 | 96.1 | 148 | 156 | 94.9 |
| 1 | 74 | 99 | 74.7 | 82 | 104 | 78.8 | 82 | 107 | 76.6 |
| 2 | 82 | 112 | 73.2 | 73 | 106 | 68.9 | 75 | 108 | 69.4 |
| 3 | 66 | 105 | 62.9 | 48 | 104 | 46.2 | 53 | 109 | 48.6 |
| 4 | 48 | 105 | 45.7 | 47 | 111 | 42.3 | 41 | 110 | 37.3 |
| 5 | 48 | 116 | 41.4 | 45 | 123 | 36.6 | 40 | 114 | 35.1 |
| ABQ score of ≥ 1 | |||||||||
| Baseline | 121 | 155 | 78.1 | 124 | 152 | 81.6 | 128 | 154 | 83.1 |
| 1 | 75 | 98 | 76.5 | 71 | 102 | 69.6 | 73 | 107 | 68.2 |
| 2 | 78 | 111 | 70.3 | 57 | 104 | 54.8 | 52 | 107 | 48.6 |
| 3 | 62 | 103 | 60.2 | 45 | 101 | 44.6 | 55 | 107 | 51.4 |
| 4 | 47 | 99 | 47.5 | 43 | 107 | 40.2 | 41 | 102 | 40.2 |
| 5 | 39 | 107 | 36.4 | 49 | 115 | 42.6 | 43 | 106 | 40.6 |
A logistic GEE model was then fitted to all three outcomes for data gathered from week 36 onwards. This model was then used to estimate the difference in proportions at weeks 36, 52 and 86 averaged across covariates, that is the marginal difference in proportions between treatments. These differences with CIs are presented in Table 15.
| Outcome measure | Time (weeks) | Adjusted difference in proportions | 95% CI | p-value |
|---|---|---|---|---|
| MDD | ||||
| CBT – STPP | 36 | –0.064 | –0.206 to 0.078 | 0.375 |
| 52 | –0.018 | –0.120 to 0.084 | 0.727 | |
| 86 | 0.057 | –0.043 to 0.157 | 0.261 | |
| (CBT + STPP) – BPI | 36 | –0.043 | –0.160 to 0.073 | 0.465 |
| 52 | –0.053 | –0.142 to 0.035 | 0.239 | |
| 86 | –0.065 | –0.152 to 0.022 | 0.145 | |
| MFQ score of ≥ 26 | ||||
| CBT – STPP | 36 | 0.029 | –0.093 to 0.151 | 0.642 |
| 52 | 0.012 | –0.088 to 0.113 | 0.808 | |
| 86 | –0.022 | –0.125 to 0.081 | 0.677 | |
| (CBT + STPP) – BPI | 36 | –0.108 | –0.217 to 0.0005 | 0.051 |
| 52 | –0.102 | –0.193 to –0.011 | 0.028 | |
| 86 | –0.085 | –0.177 to 0.007 | 0.069 | |
| ABQ score of ≥ 1 | ||||
| CBT – STPP | 36 | –0.068 | –0.186 to 0.051 | 0.263 |
| 52 | –0.040 | –0.135 to 0.055 | 0.408 | |
| 86 | 0.018 | –0.083 to 0.120 | 0.725 | |
| (CBT + STPP) – BPI | 36 | –0.128 | –0.238 to –0.019 | 0.022 |
| 52 | –0.074 | –0.163 to 0.015 | 0.102 | |
| 86 | 0.040 | –0.051 to 0.131 | 0.389 | |
At 36 weeks, the adjusted difference of percentages in MDD between CBT and STPP was –6.4% (95% CI –20.6% to 7.8%; p = 0.375). The corresponding differences for the MFQ and ABQ thresholds at this time point were 2.9% (95% CI –9.3% to 15.1%; p = 0.642) and –6.8% (95% CI –18.6% to 5.1%; p = 0.263). Considering the hypothesis of non-inferiority of CBT compared with STPP at 52 weeks (hypothesis 1), for MDD the adjusted difference of proportions was –1.8% (95% CI –12.0% to 8.4%), for MFQ threshold it was 1.2% (95% CI –8.8% to 11.3%) and for ABQ threshold it was –4.0% (95% CI –13.5% to 5.5%). Although the adjusted differences are small, the CIs are quite wide and so the evidence to support non-inferiority is weak, indicating that these comparisons are under-powered. At 86 weeks (hypothesis 2), there was no evidence for MDD (p = 0.261), MFQ threshold (p = 0.6777) or ABQ (p = 0.725) of STPP being superior to CBT.
There were no significant differences for the comparison of the specialist psychological therapies against BPI at 36 weeks (p = 0.465), 52 weeks (hypothesis 3) (p = 0.239) or 86 weeks (hypothesis 4) (p = 0.145) for presence of a MDD.
As this is a pragmatic study with no control group, we compared the proportion in remission at 12 weeks with the proportion of remitted patients from the published TADS randomised to a pill placebo control group (n = 111) and also assessed at 12 weeks. 11 This comparison showed that there were 145 out of 305 (48%) patients in clinical remission at 12 weeks in this study compared with 37 out of 111 (33%) pill placebo patients in TADS. We also note that the treatment trial of resistant depression in adolescents reported that 61% of patients met the criteria for diagnostic remission by 72 weeks, compared with 78% who did so by the notional 86-week follow-up in this study. 25 Finally, these result show that 15 (11%) patients relapsed by end of study from the 140 in remission at the 36-week assessment. There were no significant differences in the proportion of relapsed cases between treatment arms [5/43 (11.6%) BPI; 8/49 (16.3%) CBT; 2/48 (4.2%) STPP; p = 0.149]; however, caution is required with these results. As the study was not powered for treatment group comparisons, there are missing interview data at each time point and the control comparison could be achieved at 12 weeks only.
The percentage of subjects with a MFQ score of > 25, the adjusted difference in proportions between intensive treatments and BPI was –10.8% (95% CI –21.7% to 0.05%; p = 0.051) at 36 weeks and –10.2% (95% CI –19.3% to –1.1%; p = 0.028) at 52 weeks (hypothesis 3). This reduced to a difference of –8.5% (–17.7% to 0.66%; p = 0.069) at 86 weeks (hypothesis 4). As this cut-off score is derived from MFQ, one would expect these differences to be broadly consistent with those for this scale (see Table 14).
For the threshold (ABQ score of > 0) the specialist psychological treatments were significantly improved at 36 weeks (adjusted difference –12.8%, 95% CI –23.8% to –1.9%; p = 0.022). There was no significant difference for 52 weeks (hypothesis 3) with p = 0.102, or for 86 weeks (hypothesis 4) with p = 0.389.
In summary, across both continuous and binary outcome measure we conclude that outcome for CBT and STPP were broadly similar at 52 weeks (hypothesis 1) and 86 weeks (hypothesis 2). Comparing the combined specialist psychological treatments with BPI, there was some suggestion that outcome was better at 52 weeks (hypothesis 3), although this effect may not be clinically important. What treatment effects there were appeared to have largely dissipated by 86 weeks (hypothesis 4).
Moderation of treatment effects
Moderator effects on the primary outcome were investigated by adding an interaction between the moderator variable and treatment allocation to the primary analysis model. Table 16 gives the estimates of the treatment by moderator effect for each of the moderator hypotheses proposed (see Chapter 7 for details of measures and Chapter 8 for analytic strategy and hypotheses). A negative estimate in this table indicates that a higher score of the moderator lowered the MFQ for the treatment relative to the comparator, that is an increase in the beneficial treatment effect.
| < 36 weeks | ≥ 36 weeks | |||||
|---|---|---|---|---|---|---|
| Effect | 95% CI | p-value | Effect | 95% CI | p-value | |
| DEQ dependency | ||||||
| STPP vs. (BPI + CBT) | –0.21 | –0.51 to 0.09 | 0.168 | 0.02 | –0.35 to 0.39 | 0.918 |
| STPP vs. BPI | –0.29 | –0.64 to 0.06 | –0.01 | –0.44 to 0.43 | ||
| STPP vs. CBT | –0.13 | –0.48 to 0.23 | 0.05 | –0.40 to 0.49 | ||
| DEQ self-criticism | ||||||
| CBT vs. (BPI + STPP) | –0.36 | –0.72 to 0.05 | 0.053 | –0.20 | –0.66 to 0.25 | 0.383 |
| CBT vs. BPI | –0.42 | –0.85 to 0.02 | –0.21 | –0.74 to 0.32 | ||
| CBT vs. STPP | –0.31 | –0.72 to 0.10 | –0.20 | –0.73 to 0.33 | ||
| Ruminative response scale | ||||||
| CBT vs. (BPI + STPP) | 0.04 | –0.14 to 0.22 | 0.671 | 0.004 | –0.23 to 0.23 | 0.975 |
| CBT vs. BPI | 0.02 | –0.18 to 0.22 | –0.06 | –0.31 to 0.19 | ||
| CBT vs. STPP | 0.07 | –0.14 to 0.28 | 0.08 | –0.18 to 0.35 | ||
First, we hypothesised that young people with elevated dependency subscale sum scores on the DEQ would have greater reduction in MFQ than those with lower scores if they received STPP rather than BPI or CBT treatment. Before 36 weeks, the direction of the effect was consistent with our hypothesis, but this was not statistically significant (p = 0.168). After 36 weeks there was clearly no evidence of an effect (p = 0.918).
Second, we hypothesised that young people with elevated self-critical subscale sum scores on the DEQ would have a better response than those with lower scores if they received CBT rather than either BPI or STPP treatment. The direction of the effect was consistent with our hypothesis both before and after 36 weeks. Before 36 weeks this was marginally statistically significant (p = 0.053), with the effect being much smaller after 36 weeks (p = 0.384).
Finally, we hypothesised that higher total scale scores for rumination response style of thinking when depressed (RRS) would show a better treatment response for CBT than for BPI or STPP treatment. There was little evidence of an effect either before (p = 0.671) or after (p = 0.976) 36 weeks. In this case, the direction of the effect was consistent with our hypothesis only when comparing CBT with BPI after 36 weeks.
In summary, there is some indication that CBT might be more beneficial for young people with elevated DEQ self-critical scores, but this effect was applied to the treatment period only, rather than a long-term benefit as evaluated in the follow-up phase.
Adverse events
We undertook a brief examination of potential side effects of psychological treatment defined using responses to a set of somatic items selected from existing self-report scales in the study. This provides a brief proxy measure of the potential for psychological treatment to have negative effects and we focused on physical symptoms only. A description of the items and the findings are given in Appendix 1.
Chapter 10 Economic evaluation results
Data completeness
At 86 weeks, full CA-SUS service use data were available for 94 participants (61%) in the CBT group, 91 (58%) in the STPP group and 92 (59%) in the BPI group, which was 60% of the total number randomised. Baseline demographic and clinical characteristics of cases with complete and missing service use data were compared using standard t-tests and analysis of variance, as appropriate, including age, sex, ethnicity, region and MFQ. No significant differences were identified.
Outliers
The cost data were examined to consider the impact of highly influential observations, defined by Weichle et al. 113 as those whose exclusion result in major changes in the results. Two observations were identified as above the 99th percentile for total costs, but only one of these would have increased parameter estimates by a factor of 1.4. Therefore, this one observation was removed from the main analysis as recommended. 113
Resource use
All resources used over the 86-week follow-up period are summarised by group in Table 21.
Trial treatment
For the sample of participants with full service use information, the average number of treatment sessions attended by the young people was 7.97 in the BPI group, 9.73 in the CBT group and 13.85 in the STPP group. The numbers differ slightly from those reported in Chapter 9 because they are the results for the subsample of participants for whom we had full service use data. On average, the number of sessions attended was lower than the number of sessions planned (BPI 12 sessions, CBT 20 sessions, STPP 28 sessions).
Other health and social services
Overall, there was little difference between randomised groups in levels of service use over the 86-week follow-up (Table 17). Levels of mental health admissions were low (< 2%) across all randomised groups. There were slight variations in non-mental health admissions, with 13% of the STPP group being admitted compared with 8% in the BPI group and 5% in the CBT group. Overall, up to one-fifth of participants had a non-mental health admission (BPI 23.40%, CBT 12.63% and STPP 19.57%).
| Type of service | Treatment group, mean, SD (%)a | ||
|---|---|---|---|
| BPI (n = 96) | CBT (n = 95) | STPP (n = 92) | |
| Treatment (sessions) | 7.97, 5.19 | 9.73, 6.54 | 13.85, 10.41 |
| Mental health inpatient (night) | 0.02, 0.20 (1.04) | 0.08, 0.72 (2.11) | 0.00, 0.00 (0) |
| Non-mental health inpatient (night) | 0.26, 1.06 (8.34) | 0.11, 0.57 (5.26) | 0.42, 1.54 (13.04) |
| Mental health outpatient (attendance) | 0.01, 0.10 (1.04) | 0.05, 0.51 (1.05) | 0.00, 0.00 (0) |
| Non-mental health outpatient (attendance) | 0.65, 1.83 (18.75) | 0.35, 1.19 (13.68) | 0.75, 1.90 (23.91) |
| Accident and emergency (attendance) | 0.45, 1.61 (22.91) | 0.14, 0.38 (12.63) | 0.35, 0.80 (19.57) |
| General practitioner (contact) | 2.79, 5.00 (66.67) | 2.40, 4.07 (71.58) | 2.60, 3.79 (64.13) |
| Community medical services (contact) | 0.12, 0.43 (8.33) | 0.09, 0.49 (5.26) | 0.37, 2.26 (4.35) |
| Community mental health services (contact) | 4.93, 11.12 (45.83) | 5.64, 14.08 (37.89) | 3.80, 10.85 (29.35) |
| Community social services (contact) | 1.33, 3.74 (20.83) | 0.95, 4.02 (11.58) | 6.88, 62.32 (14.13) |
| Education support services (contact) | 1.32, 5.18 (25.00) | 1.61, 6.90 (15.79) | 3.11, 11.00 (27.17) |
| Antidepressant medication | (30.77) | (28.57) | (31.73) |
| Other medication | (2.13) | (4.21) | (4.34) |
General practitioners were the most widely used service, accessed by 66%, 72% and 64% of participants in the BPI, CBT and STPP groups, respectively. Use of community mental health services, excluding the trial interventions, was highest in the BPI group (46% of BPI participants), compared with 38% and 29% of the CBT and STPP groups, respectively. Rates of social services contacts were also highest in the BPI group.
Antidepressant medication
Over the course of the study, patients were allowed to receive a SSRI in addition to psychological treatment if they met NICE guidelines13 for combined treatment to aid clinical remission by end of treatment. The proportion of participants prescribed antidepressant medication at any point over the 86-week follow-up was approximately 30% in each group.
Total cost
Treatment costs
On average, the cost of the trial interventions was lowest for CBT (£904.57) and highest for STPP (£1396.72), with BPI costing £1292.91. These differences reflect the variation in the number and duration of treatment sessions (reported in Table 21) and the cost of the professionals providing the therapy, summarised in Table 2.
Total costs over follow-up
The broadly similar levels of service use reported in Table 17 translated into similar total health, social care and education costs per participant over the 86-week follow-up across the three groups: £1368.04 in BPI, £1459.26 in CBT and £1668.51 in STPP. When the cost of the trial interventions was included, this generated total costs per participant over the 86-week follow-up of £2678.39 for the BPI, £2379.01 for CBT and £3081.70 for the STPP (Table 18).
| Type of cost | Treatment group, mean (SD) | ||
|---|---|---|---|
| BPI (n = 92) | CBT (n = 92) | STPP (n = 91) | |
| Health, social care and education costs | 1368.04 (1368.04) | 1459.26 (3481.02) | 1668.51 (3425.68) |
| Treatment costs | 1292.91 (1292.91) | 904.57 (607.25) | 1396.72 (1133.41) |
| Total costs | 2678.39 (2678.39) | 2379.01 (3643.85) | 3081.70 (3573.17) |
The results of the between-group comparisons, detailed in Table 19, show that there were no significant differences in costs between the groups. Bootstrapped CIs were similar to those calculated from the linear regression models so are not presented here.
| Treatment group comparisona | Coefficient | 95% CI | p-value |
|---|---|---|---|
| CBT vs. BPI (n = 180) | –338.54 | –1333.17 to 656.09 | 0.503 |
| STPP vs. BPI (n = 174) | 609.55 | –406.73 to 1625.83 | 0.238 |
| CBT vs. STPP (n = 178) | –709.23 | –1836.04 to 417.58 | 0.216 |
Outcomes
Health-related quality of life
The EQ-5D scores at baseline and all follow-up points are detailed in Table 20. Utility scores were generally higher in the CBT group than the BPI and STPP groups, and a higher score denotes higher levels of health-related quality of life. However, differences were small and at the 86-week follow-up, scores were marginally higher in the BPI group followed by the STPP group. The QALYs show very little between-group differences: CBT group 1.228 QALYs, STPP 1.246 QALYs and BPI group 1.241 QALYs. There were no significant between-group differences in QALYs, as shown in Table 21.
| Assessment point | n | Treatment group, mean (SD) | ||
|---|---|---|---|---|
| BPI | CBT | STPP | ||
| Baseline | 447 | 0.596 (0.275) | 0.578 (0.281) | 0.569 (0.258) |
| t1 (week 6) | 303 | 0.622 (0.278) | 0.685 (0.236) | 0.674 (0.275) |
| t2 (week 12) | 310 | 0.713 (0.236) | 0.714 (0.267) | 0.680 (0.259) |
| t3 (week 36) | 290 | 0.730 (0.262) | 0.797 (0.227) | 0.765 (0.233) |
| t4 (week 52) | 295 | 0.771 (0.227) | 0.803 (0.232) | 0.792 (0.257) |
| t5 (week 86) | 307 | 0.817 (0.228) | 0.780 (0.256) | 0.808 (0.240) |
| QALY | 294 | 1.241 (0.270) | 1.228 (0.304) | 1.246 (0.293) |
| Treatment group | Coefficient | 95% CI | p-value |
|---|---|---|---|
| CBT vs. BPI (n = 195) | –0.009 | –0.091 to 0.074 | 0.839 |
| STPP vs. BPI (n = 193) | 0.000 | –0.081 to 0.082 | 0.992 |
| CBT vs. STPP (n = 200) | –0.019 | –0.103 to 0.064 | 0.648 |
Cost-effectiveness analysis
Cognitive–behavioural therapy versus brief psychosocial intervention
For the CBT versus BPI comparison, CBT is less costly but slightly less effective in terms of QALYs than BPI. As a result, the replications produced in the scatterplot in Figure 9 are mainly in the south-west and south-east quadrants, reflecting lower costs in the CBT group (points below the x-axis) and the very small difference in outcomes between the two groups (points evenly spread across the y-axis). The CEAC in Figure 10 shows that for all levels of willingness to pay per QALY there is a higher probability that CBT is more cost-effective than BPI.
FIGURE 9.
Scatterplot of differences in costs vs. differences in QALYs for CBT vs. BPI.

FIGURE 10.
Cost-effectiveness acceptability curve showing the probability that CBT is cost-effective compared with BPI for different values at which a decision-maker might be willing to pay for improvements in QALYs.
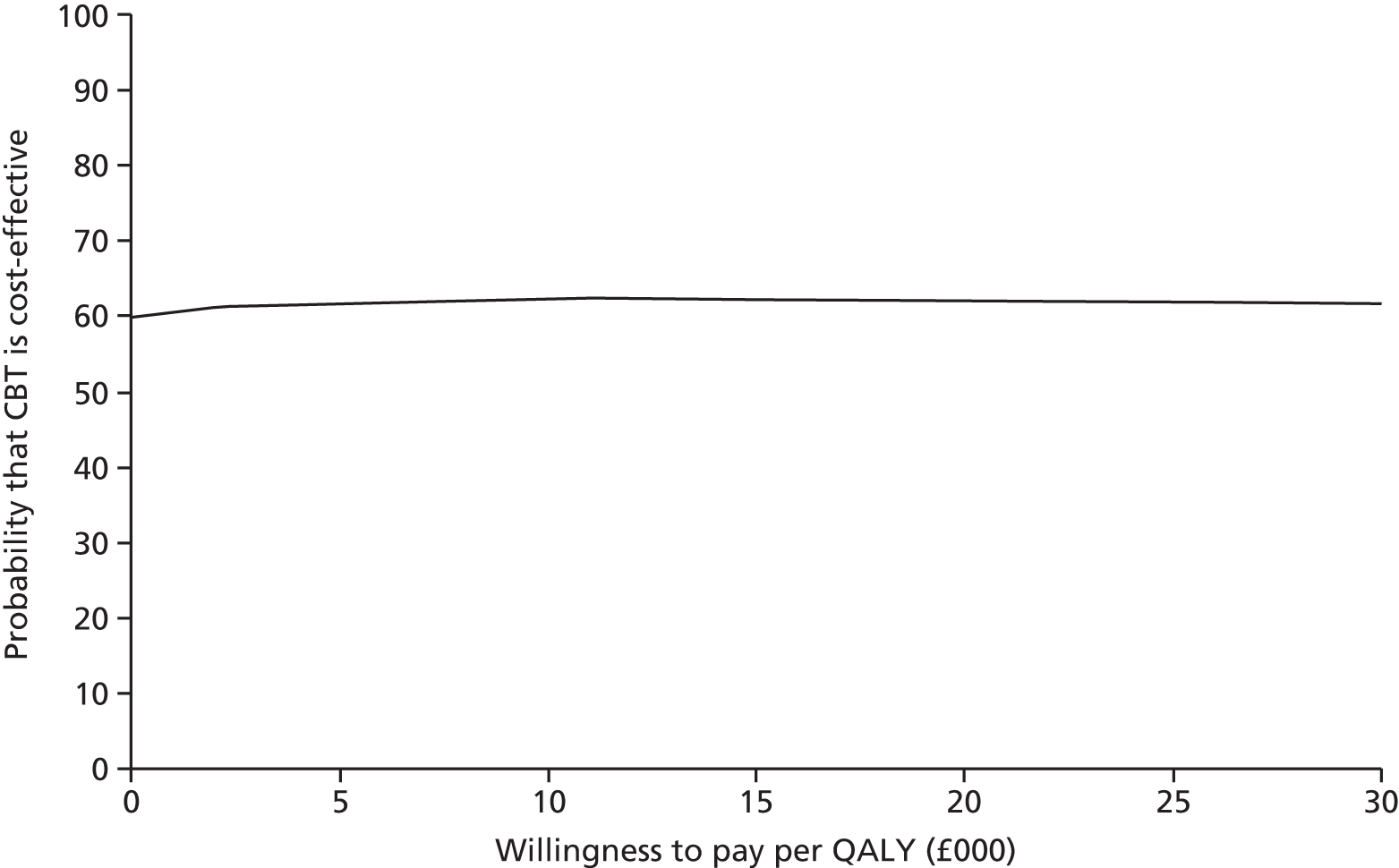
Short-term psychoanalytic psychotherapy versus brief psychosocial intervention
For the STPP versus BPI comparison, costs were, on average, £403 higher in the STPP group than in the BPI group and QALYs were equal. The bootstrapped replications for STPP versus BPI are shown in Figure 11. The majority are in the north-east and north-west quadrants, reflecting the higher costs in the STPP group (points above the x-axis). The CEAC in Figure 12 shows that there are no willingness-to-pay values for which the probability of STPP being cost-effective compared with BPI is > 23%, within the £20,000–30,000 ceiling level of willingness to pay that is considered acceptable by NICE. 66
FIGURE 11.
Scatterplot of differences in costs vs. differences in QALYs for STPP vs. BPI.
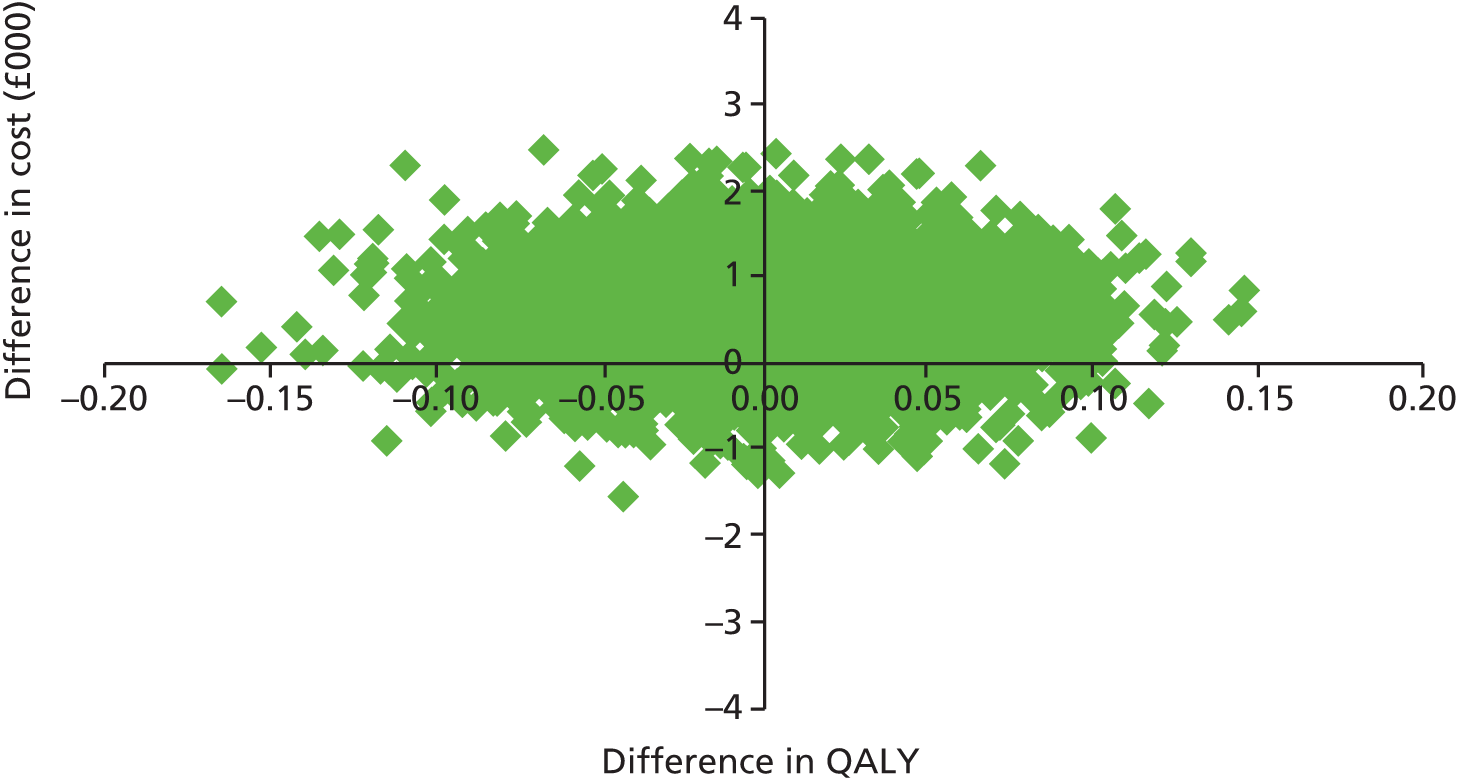
FIGURE 12.
Cost-effectiveness acceptability curve showing the probability that STPP is cost-effective compared with BPI for different values at which a decision-maker might be willing to pay for improvements in QALYs.

Cognitive–behavioural therapy versus short-term psychoanalytic psychotherapy
Comparing the two specialist psychological treatments, CBT and STPP, total costs per participant over the 86-week follow-up were, on average, £703 lower in the CBT group than in the STPP group and outcomes were 0.02 QALYs worse. As a result, the replications in the scatterplot in Figure 13 are mostly in the south-west quadrant. The CEAC shown in Figure 14 suggests that the probability that CBT is cost-effective compared with STPP for all willingness-to-pay values is > 50%.
FIGURE 13.
Scatterplot of differences in costs vs. differences in QALYs for CBT vs. STPP.
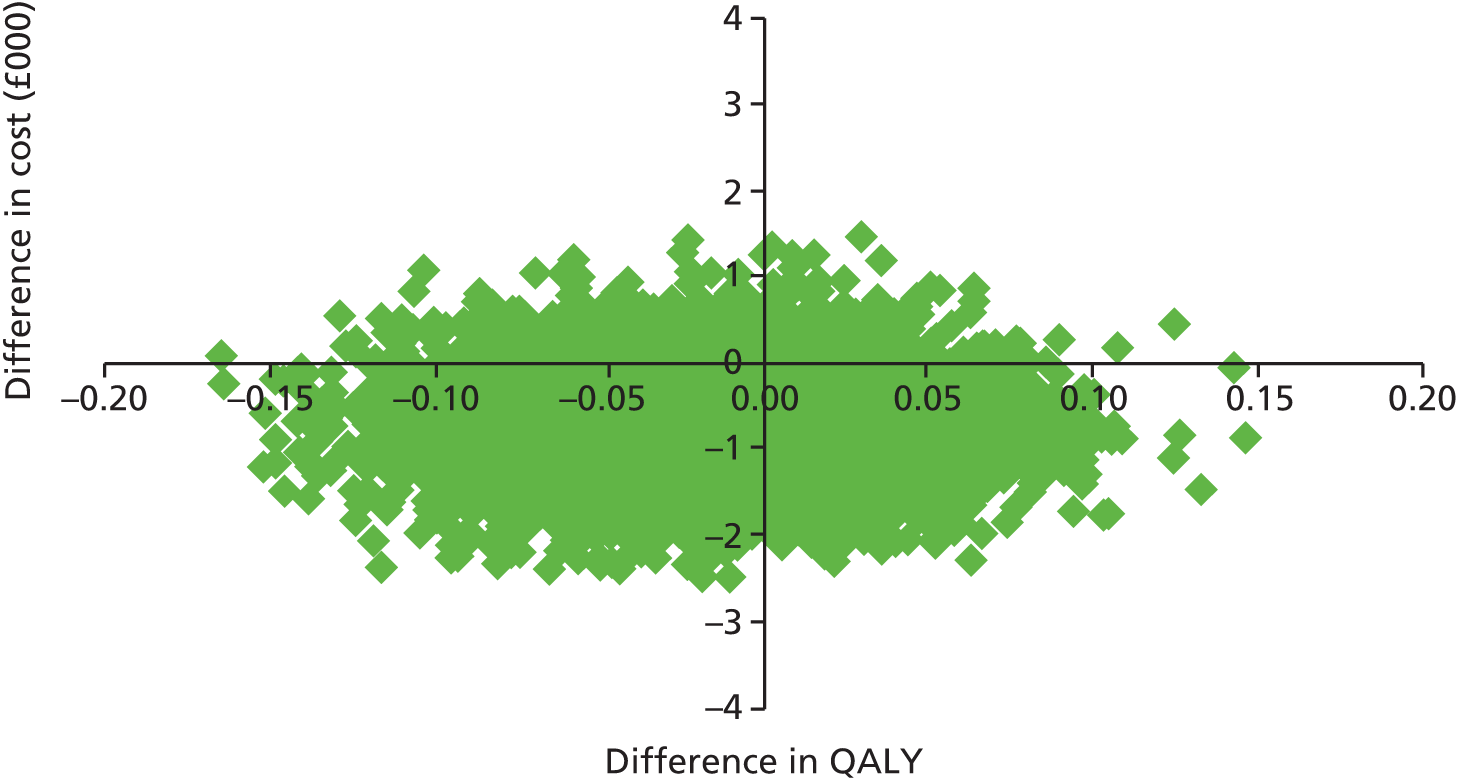
FIGURE 14.
Cost-effectiveness acceptability curve showing the probability that CBT is cost-effective compared with STPP for different values at which a decision-maker might be willing to pay for improvements in QALYs.

Cognitive–behavioural therapy versus short-term psychoanalytic psychotherapy versus brief psychosocial intervention
The three interventions were compared head to head in a three-way comparison. The CEACs in Figure 15 show that for all values at which a decision-maker might be willing to pay for a QALY, CBT has the largest probability of being cost-effective.
FIGURE 15.
Cost-effectiveness acceptability curve showing the probability that BPI, CBT and STPP are cost-effective for different values at which a decision-maker might be willing to pay for improvements in QALYs.
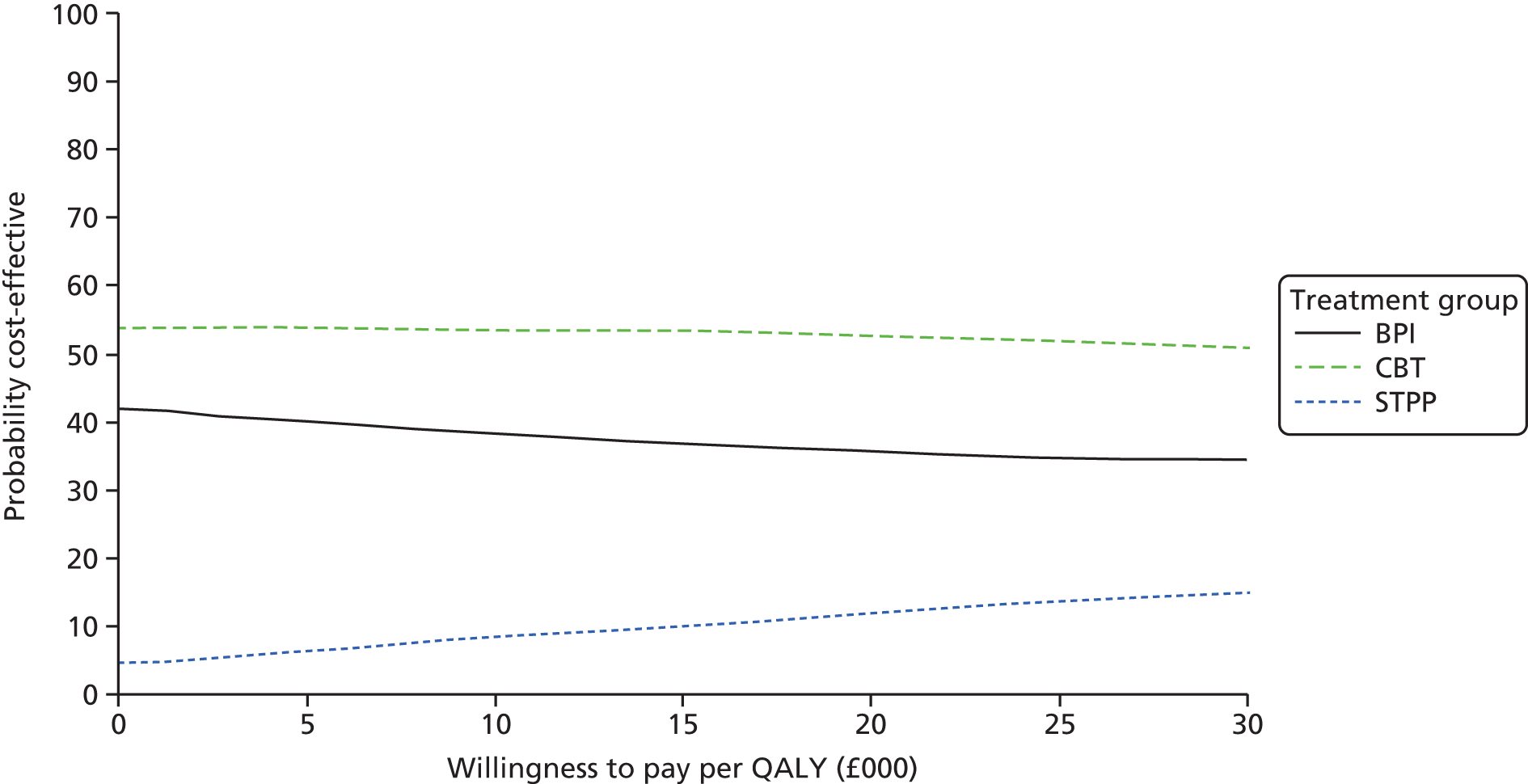
Sensitivity analysis
The results of the sensitivity analyses are detailed in Tables 22 and 23. Multiple imputation did not alter the direction of the differences in cost, nor did reanalysis using cost per week rather than cost over the entire follow-up period. Including an estimate of the cost of sessions that were scheduled but that the young person did not attend altered the order between the three interventions.
| Cost characteristic | Treatment group, mean (SD) | ||
|---|---|---|---|
| BPI | CBT | STPP | |
| Base-case analysis | 2678.39 (2881.89) | 2379.01 (3643.85) | 3081.70 (3573.17) |
| Non-attendance at 50% cost | 2907.30 (2939.08) | 3050.05 (5891.69) | 3364.14 (3563.08) |
| Multiple imputation | – (–) | – (–) | – (–) |
| Total cost per week | 28.76 (31.63) | 25.25 (38.35) | 32.42 (35.84) |
| Comparisona | Sensitivity analysis | Coefficient | 95% CI | p-value |
|---|---|---|---|---|
| CBT vs. BPI | Base case | –338.54 | –1333.17 to 656.09 | 0.503 |
| Non-attendance at 50% cost | 185.15 | –392.71 to 1657.16 | 0.225 | |
| Multiple imputation | –425.07 | –1384.58 to 534.43 | 0.381 | |
| Total cost per week | –3.95 | –14.58 to 6.68 | 0.464 | |
| STPP vs. BPI | Base case | 609.55 | –406.73 to 1625.83 | 0.238 |
| Non-attendance at 50% cost | 632.21 | –392.71 to 1657.16 | 0.225 | |
| Multiple imputation | 448.95 | –609.77 to 1507.66 | 0.399 | |
| Total cost per week | 6.12 | –4.47 to 16.72 | 0.256 | |
| CBT vs. STPP | Base case | –709.23 | –1836.04 to 417.58 | 0.216 |
| Non-attendance at 50% cost | –429.79 | –1955.24 to 1095.65 | 0.579 | |
| Multiple imputation | –891.47 | –1951.81 to 168.86 | 0.098 | |
| Total cost per week | –7.46 | –19.10 to 4.17 | 0.207 |
For the sample with full economic data, the average number of sessions that were offered but were not attended was three in the BPI group, 14 in the CBT group and six in the STPP group. The inclusion of the cost of these sessions (at 50% of the cost of a full session) resulted in the average cost of CBT (£3050) becoming more expensive than the BPI average cost (£2939), with STPP remaining the most costly group (average cost £3364). Although there are no statistically significant differences in cost between the groups, this change in direction has an impact on the cost-effectiveness analyses for the comparison of CBT and BPI, with CBT being dominated by BPI (costs higher and outcomes very slightly lower). Figure 16 shows the scatterplot for this comparison; the majority of the replications are in the north-east and north-west quadrants, denoting higher costs in the CBT group (points above the x-axis). The very similar outcomes mean that the CEAC in Figure 17 suggests that the probability that CBT is cost-effective compared with BPI is < 50% for all values at which a decision-maker might be willing to pay for a QALY. Figure 18 shows a head-to-head comparison of all three groups in terms of cost-effectiveness and including a cost for sessions missed. It demonstrates that there is a higher probability of BPI being cost-effective than CBT and STPP for all values of willingness to pay.
FIGURE 16.
Sensitivity analysis: scatterplot of differences in costs vs. differences in QALYs for CBT vs. BPI with non-attendance at 50% session cost.

FIGURE 17.
Sensitivity analysis: CEAC showing the probability that CBT is cost-effective compared with BPI for different values at which a decision-maker might be willing to pay for improvements in QALYs with non-attendance at 50% session cost.

FIGURE 18.
Sensitivity analysis: CEAC showing the probability that CBT, STPP and BPI are cost-effective for different values at which a decision-maker might be willing to pay for improvements in QALYs with non-attendance at 50% session cost.
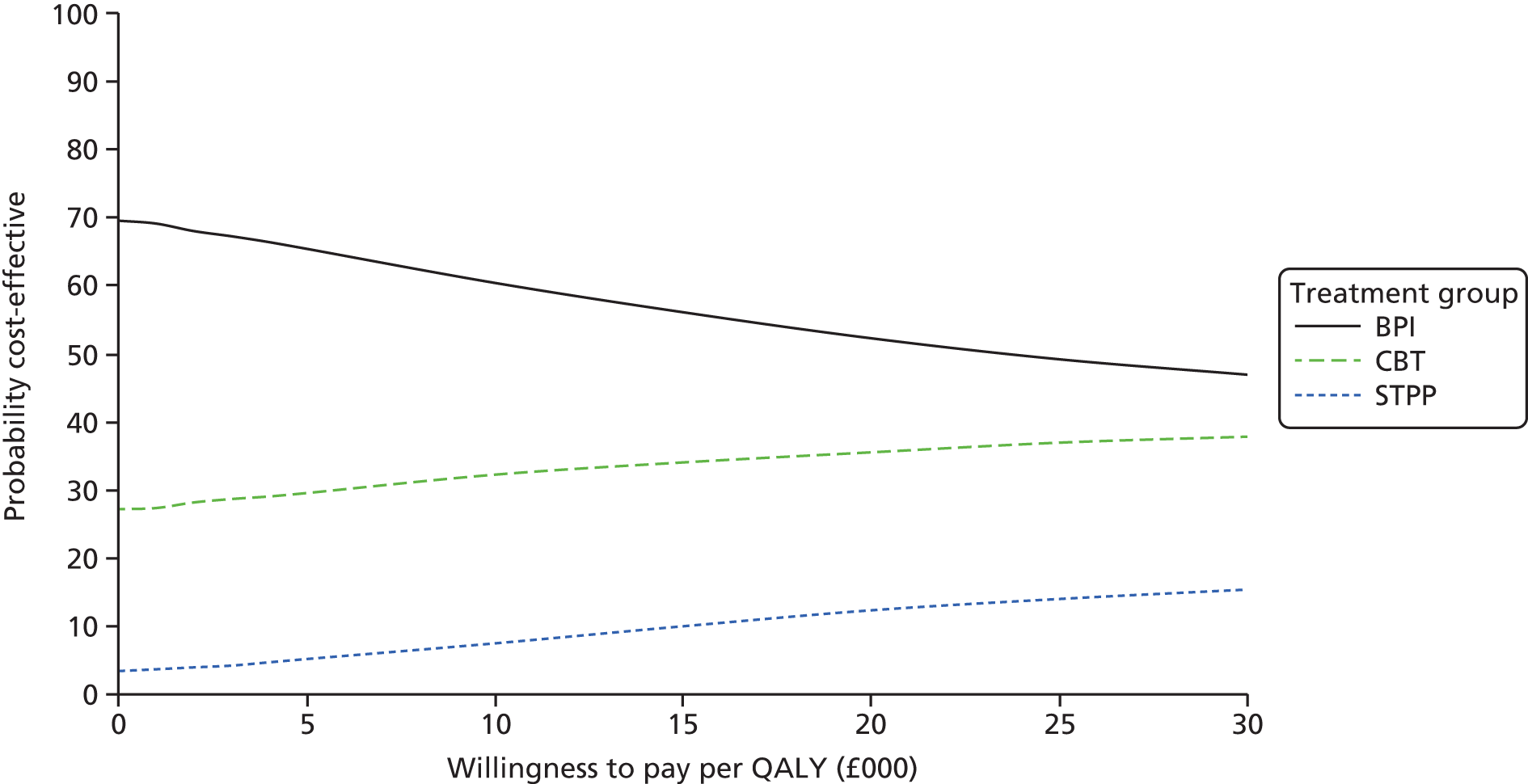
Chapter 11 Discussion
This RCT of the treatment of adolescents with unipolar major depression referred to routine CAMHS with DSM-IV MDD found no evidence for the superiority of two specialist psychological therapies, CBT or STPP, compared with a BPI for maintaining the reduction of self-reported depression symptoms observed at 36 weeks and reassessed over two follow-up assessments at 52 and 86 weeks after randomisation. All three treatment conditions were manualised. However, the duration of treatments in all three arms of the study was shorter than planned, with a median of between 6 and 11 sessions. There were no clear-cut indications that either specialist treatment was cheaper or more cost-effective than BPI. The average self-reported depression scores improved substantially from baseline to follow-up points across all three treatment groups. Whether or not this change can be causally attributed to the treatments cannot be determined because, for ethical reasons, there was no ‘no treatment’ control group.
Although this study provided a clear negative finding for its main hypothesis, there were results that – although were not definitive – are worth highlighting because further research may elucidate their potential importance for policy decisions and clinical practice. These refer to (1) the timing of the primary outcomes and outcomes other than depressive symptoms, (2) the economic analyses, (3) the new treatment, BPI, (4) the observed non-response to treatment and (5) the potential implications for clinical practice.
Timing of outcomes
The results showed a similar trend, seen across several symptom measures of depression, anxiety and obsessionality, for outcome scores in the specialist psychological treatment groups (CBT or STPP) to be somewhat lower than that of BPI at 52 weeks after randomisation, which was also seen at 36 weeks corresponding approximately to end of treatment. This is partly illustrated in Figure 7, showing the differences in individual scale scores for each treatment group. Although individual differences are not significantly different, there is a suggestion that the combined analysis (CBT or STPP) reveal that differences were close to statistical significance at the 2.5% level in Table 13. However, none of these mean differences was large and the clinical significance of somewhat lower sum scores seems uncertain. For example, the depression symptoms were significantly lower for the specialist treatment group with a mean difference of –3.28 at 36 weeks, –2.80 at 52 weeks and –1.98 at 86 weeks of follow-up assessment. Furthermore, although the mean difference is < 5 points on the MFQ, which we identified a priori as of clinical relevance, the confidence limits hint at patients showing greater individual differences in treatment response that may decline by 86 weeks.
Although multiple analyses across measures will tend to inflate type I errors, we note the consistency of the pattern of these results rather than the statistical or clinical significance of any one analysis. The average effect sizes across the four quantitative outcomes (see Table 13) were similar, ranging from 0.17 to 0.21 at 52 weeks. A slightly larger effect was observed at 36 weeks, ranging from 0.18 to 0.29. Equally, there was a consistent trend across these symptom measures for this difference to be much smaller and entirely non-significant by 86 weeks with effect sizes ranging from 0.04 to 0.17. The findings provide a pointer to the need for further research into timescales for symptomatic recovery from depression. The fall in symptoms deserves further investigation to establish whether or not it represents a meaningful difference in rate of recovery for some of those receiving specialist psychological treatments compared with BPI or, alternatively, that the observed difference in rate of recovery is not important. Reducing the period of time that an individual is suffering may be of value to them and their family. Further investigation may also reveal whether or not there are individual differences in the trajectory of symptomatic response to treatment and whether or not psychosocial adjustment correlates with or decouples from symptom change over time.
Economic analyses
On average, the observed cost of the trial treatments of those for which full data were available in the main analysis was lowest for CBT and highest for STPP. Although BPI was intended to be brief compared with both alternative treatments, in practice the average number of BPI treatment sessions attended was not substantially lower than in the CBT group (probably due to non-attendance of the planned longer-term therapies). Coupled with higher average therapist costs (as the majority of BPI was delivered by psychiatrists in specialist CAMHS training), BPI was estimated to cost somewhat more than CBT, although none of these differences was statistically significant. However, the inclusion of a cost for non-attendance reversed this finding, making CBT more expensive than BPI as a result of a larger difference between sessions offered and sessions attended. With a higher number of sessions attended per person, STPP remained the most expensive of the three treatments. Use of all other health and social services over the follow-up period was broadly similar, thus differences in total costs were primarily influenced by the cost of the trial treatments. In terms of cost-effectiveness, differences between groups were marginal and sensitive to the inclusion of the cost of sessions offered but not attended. Fewer therapy sessions attended could be taken either as an indicator of treatment effectiveness (fewer sessions needed before achieving a desired outcome) or as an indicator of lower treatment acceptability. Current results cannot in themselves clarify between these two alternatives or if both apply to different patients.
Brief psychosocial intervention
The protocol for high-quality active clinical care, referred to in this report as BPI, was developed for this study in order to ensure that the comparison condition was coherent and informed by all available research, and that it did not include active technical components of either CBT or STPP. As BPI was designed as a high-quality ‘active’ control condition, it was not evaluated against an intervention predicted to be less effective. This means that we cannot determine whether or not it was efficacious (as there is no passive control condition) or clinically effective in the absence of an appropriate clinical control group such as waiting list. However, as outcomes at 86 weeks in the BPI group were non-inferior to specialist therapies, BPI merits further consideration as a potential treatment. BPI was a multifaceted intervention with several elements (see Chapter 4 for details) that may have contributed to improvement in self-reported depression, including psychoeducation, support for increased activities, and attention to the young person’s family and school environment. It remains to be determined whether some or all of these elements may contribute to treatment effectiveness and also whether or not other components of BPI were important. For example, BPI may have been more tailored to variations in the young persons’ wishes or problems than the theory-based specialist treatments, which is consistent with evidence for advantages of personalised approaches to adolescent depression. 114
Treatment resistance and the maintenance of clinical high-risk status
A substantial proportion of patients (approximately 25%) continued to meet diagnostic criteria for unipolar major depression by 86 weeks. A further 15% reported depressive symptoms higher than the cut-off score (> 26) for potential cases. However, only 285 (60%) of the sample were available for full clinical assessment at this time point. This finding may suggest that, as there were no treatment group differences, there is a degree of treatment resistance or non-compliance in this cohort overall. Current therapeutic interventions used in this study appear to be potentially ineffective in a proportion of cases, an observation that resonates with prior trial findings on depressed adolescents. 11,12 This is a serious negative outcome that requires further investigation as providing potentially ineffective treatments to depressed adolescents is not good clinical practice. There is a marked lack of understanding regarding treatment failures and resistant depressions in this age range. There is a suggestion that more clinically severe presentations, the presence of suicidality and obsessive–compulsive disorder at presentation are associated with less treatment response by 28 weeks post randomisation. 115 Furthermore, the presence of non-suicidal self-injury at randomisation may be a predictor of increased suicidality and, therefore, a risk for treatment non-response. 116 These observations require replication and further investigation than they have received hitherto as identifying patients unlikely to respond to available therapies is an important clinical priority. The process of recovery may also be of interest. Numerous recent studies have identified rapid initial response to therapy (the first four or five sessions) as a critical indicator of ultimate benefit from therapy in adults. Further research with young people will be needed to investigate whether or not an early therapeutic response similarly indicates the absence of treatment resistance in a youth population.
Reducing depression symptom recurrence risk following treatment
Preventing clinical diagnostic relapse by maintaining low depressive symptoms is potentially of substantial clinical and cost value because even successfully treated adult patients may suffer, on average, between five and nine episodes over their life course at considerable personal and economic cost to both the individual and society. 2,117,118
The likelihood of relapse following successful treatment in depressed adolescents is also substantial, occurring in 50–75% of successfully treated patients. 29–31
These studies emphasise the potential value in lowering prospective diagnostic risk by reducing depressive symptoms in the medium term. Elevated symptom levels above the population norm predict the emergence of major depression in adolescents, correlate with persisting depressive disorders and predict relapse in adults with a history of depression. 93,119–122
Therefore, the current findings are encouraging as the lowered depressive symptoms by 86 weeks that is associated with these psychological treatments suggests progression towards prevention of diagnostic relapse for all three forms of interventions.
Strengths and limitations
This study had many strengths, including that participants were representative of depressed adolescents referred to a comprehensive health provision across diverse regions of the UK, that they all met research diagnostic criteria for DSM-IV MDD, that they were randomised remotely from the research team, and that reliable follow-up assessments were completed blind to treatment group assignment in > 75% of those randomised with no differences between the treatment groups. The most common reason for blindness break was the researcher being told by the respondent what treatment they were having. Breaks to blindness of treatment allocation were approximately 10–15% during the treatment phase but subsequently < 5% in the follow-up phase (36- to 86-week assessments). The sample size was greater than in any previous study and this is the first time, to our knowledge, that a trial of depressed adolescents has used follow-up as late as 86 weeks post randomisation as an end point of the trial. The participation rate was 84% for the primary outcome analysis, which is comparable to other studies in this field with similar duration of follow-up. Each of the three treatments was manualised, and fidelity and differentiation assessments demonstrated expected differences between them. Although there was a higher number of psychiatrists in specialist CAMHS training delivering the BPI treatment, overall clinicians who delivered each type of treatment were characteristic of those who deliver these treatments in routine clinical practice, which adds confidence to the findings.
There were limitations regarding the of outcome measures used. A decision had to be made between the research burden on vulnerable young people and the depth of information acquired. The relatively high level of consistency in trajectories between behavioural measures over the course of the study reassures us but acknowledges that functioning and adaptation was not as thoroughly assessed in the trial as symptomatology.
The use of a self-rated questionnaire has both advantages and disadvantages. We believe that, in the case of this study, the advantages offered were substantial. In particular, self-reporting reduced attrition rates over time as a significant number of participants did not want to attend follow-up face-to-face assessments beyond the treatment phase, but agreed to complete self-report questionnaires.
The overall trajectory of improvement seen with the self-report MFQ was similar to that seen with the interview-led HoNOSCA, suggesting multimodal measurement congruence between self-report and interviewer-led measures that focused on symptoms and their related functions, respectively. This was consistent with the findings published in ADAPT, for which self-reported depression and anxiety scores, together with research interview-led HoNOSCA and clinician-led clinical improvement ratings, were highly congruent in reporting responses to treatment. The multimodal measures used in this study (patient self-report, interviewer-led HoNOSCA and interviewer-led K-SADS together with self-report on depressive symptoms of anxiety, obsessive–compulsive and antisocial behaviour) provide a degree of acceptable validity and added value in measuring change over time in this treated cohort. However, this is limited in that there were no reliable and valid biomarkers of underlying pathophysiology available at the time of design or implementation of this study. Therefore, like all current treatment trial designs, we are limited to changes in the observed manifest symptoms following treatment. Advances in understanding aetiological and pathophysiological mechanisms for major depression are urgently required so that future treatment trials can determine their value in predicting treatment response and advance the need for more precision in determining what treatment works best for which patient.
The attendance rates through the trial are similar to previous findings in the UK ADAPT trial and not dissimilar to other large US trials, such as TORDIA (Treatment Of Resistant Depression In Adolescents). 25 The UK ADAPT and IMPACT trials were both pragmatic trials based in the NHS and the attendance rates reflect NHS service delivery and take-up rates by young people.
The inclusion of a manualised comparison condition, BPI, made it more likely that the quality of the treatment was similar across arms, enabled fidelity to be assessed and clarified the focus for supervision. It also ensured that the comparison condition did not include several of the significant features of STPP and CBT. The issue of overlap between therapies was evaluated with satisfactory findings from analysis of audio tapes, suggesting that the therapists were delivering treatment as per protocol and that these were substantially different between the three treatments. Nevertheless, it is acknowledged that some overlap in therapy processes may occur. In the absence of specific knowledge about the mechanisms of particular psychological treatment, it may be that there are commonalities that are shared and that exert sufficient clinical effects to diminish differences between specific treatment protocols in this study. In addition, BPI as an active manualised therapy does not constitute a low-level ‘treatment as usual’ concept. Further research on the mechanisms that lead to change when we expose depressed adolescents to psychological treatment is suggested for these results to disaggregate general from specific therapy effects.
Furthermore, we note the less than predicted attendance rates for each treatment arm. Understanding the precise relationships between duration of treatments, number of sessions attended and outcomes is an important topic for future studies. Finally, future studies should determine whether or not BPI may be of value in community child mental health settings, such as primary health care, schools and local authority services for adolescents, where depression is identified.
The economic results were limited by missing data, which were higher than for the primary clinical outcome measure (60%). However, multiple imputation of missing values did not change the results of the analysis, giving some confidence in the conclusions. The economic results, shown to be sensitive to the inclusion of the cost of participant non-attendance, are also limited by the reliance of this sensitivity analysis on accurate reporting by therapists. Data were calculated as the number of sessions offered minus the number of sessions attended. However, more detailed information (e.g. on whether sessions offered were cancelled or rearranged) was unavailable. These data are, therefore, a proxy for did not attend rates and so should be interpreted cautiously. The assessment of cost-effectiveness on the basis of the EQ-5D raises questions about the validity of the measure in an adolescent sample with depression. Although there is some evidence to support the use of the measure in this population,63 the evidence is relatively weak and further research into measures appropriate for young people with mental health problems is needed.
Summary of recommendations for future research
We may consider the following potential research questions on the basis of the findings reported above.
Determine the characteristics of depression prior to intervention that index the risk for non-response to treatment
The relatively high frequency of non-response to treatment raised questions about the possibility of identifying such individuals before the treatment begins, in the service of (1) offering alternatives or (2) prioritising other patients for these types of interventions. Delineating the antecedent factors that can identify treatment non-response is a key study to prevent application of non-therapeutic methods for individuals and to aid the development of new treatments for those likely to show persistent depression. Early minimal treatment response may be a similar key indicator of ultimate limited response.
Investigating the effectiveness of brief psychological interventions
These findings demonstrate the potential effectiveness of shorter-term therapy than currently prescribed for depressed patients. Further psychological therapy research should try and understand the minimum treatment period that is clinically effective in reducing symptoms by 50% and improving personal function.
A study to investigate treatment for cases resistant to first-line therapies
Designing and implementing an intervention study for treatment-resistant depressed adolescents to reduce adult service use and personal morbidity is a high priority, given the considerable prevalence of patients who fall into this group. In particular, it is interesting to ask if longer treatments or change of treatment following initial non-response may be the preferred pragmatic strategy.
Mechanisms of treatment response
The lack of substantial differences in outcomes suggests a potentially common neurocognitive basis for treatment response and maintenance of reduced depressive symptoms. Identifying these mechanisms could improve treatment outcomes by increasing the specificity of interventions. Revealing mechanisms that subserve treatment response should be a focus for further investigation using the methods of experimental medicine to identify the endophenotype for treatment success.
Person-centred treatment research
The comparable outcomes for different treatment modalities also suggests the desirability of a more person-centred approach to determine what treatment will work best for which patient. It is likely that current therapies are aimed at the ‘average’ patient, incorporating all techniques that are most likely to be effective for the largest range of participants. It is possible that, for each individual, only a particular aspect of each intervention was necessary. To make interventions more efficacious, revealing common therapeutic and more specific treatment factors using quantitative and qualitative person-centred analyses is called for.
Implementation in non-specialist settings and by less specialist staff
The findings relate to the specific environment of a specialist CAMHS clinic and relatively severely depressed adolescents. Whether or not any of these three therapies can be delivered with equal clinical effectiveness and cost-effectiveness by less highly qualified practitioners in non-specialist settings is an urgent research question. This is particularly clear in the case of BPI, but could also be relevant to the two theory driven modalities.
Conclusions
This RCT demonstrates no superiority for the specialist psychological therapies CBT and STPP compared with a high-quality active comparator, BPI, in maintaining the reduction of depressive symptoms after treatment through to 86 weeks post randomisation. All three treatments were associated with similar clinical effectiveness and cost-effectiveness and improved quality of life over the follow-up period.
Overall, these psychological treatments for unipolar major depression in adolescents differed markedly in theoretical and clinical approach but are associated with a similar degree of clinical improvement, cost-effectiveness and subsequent maintenance of lowered depressive symptoms. BPI offers an additional patient choice, alongside CBT and STPP, for depressed adolescents attending routine specialist CAMHS.
Acknowledgements
Contributions of authors
Ian M Goodyer (Professor of Child and Adolescent Psychiatry, University of Cambridge) designed the study, obtained the research funding and wrote papers arising from the study.
Shirley Reynolds (Professor of Evidence Based Psychological Therapies University of Reading) designed the CBT protocol, contributed to the study design including the fidelity and differentiation study and wrote papers arising from the study.
Barbara Barrett (Senior lecturer in Health Economics, King’s College London) undertook the health economics analysis and wrote the health economics chapter.
Sarah Byford (Professor of Health Economics, King’s College London) designed and undertook the health economics analysis, contributed to the grant application and wrote the health economics chapter.
Bernadka Dubicka (Consultant Psychiatrist and Lecturer, University of Manchester) contributed to measurement and study design and the BPI clinical protocol.
Jonathan Hill (Professor of Child and Adolescent Psychiatry, School of Psychology and Clinical Language Sciences, University of Reading) contributed to measurement, selection and study design while Professor of Child and Adolescent Psychiatry at the University of Manchester.
Fiona Holland (Research Associate in Statistics, University of Manchester) undertook data analysis.
Raphael Kelvin (Consultant Child and Adolescent Psychiatrist, Cambridge and Peterborough NHS Foundation Trust and Associate Lecturer, University of Cambridge) wrote the clinical manual and protocol for BPI, designed the fidelity and differentiation study and wrote papers arising from the study.
Nick Midgley (Child and Adolescent Psychotherapist, Anna Freud Centre and Lecturer at University College London) contributed to measurement and methods, contributed to writing the STPP protocol and manual, designed fidelity and differentiation study, and wrote papers arising from the study.
Chris Roberts (Professor of Biostatistics, University of Manchester) contributed to this grant application, designed the data analysis and wrote papers arising from the study.
Rob Senior (Senior Research Fellow, University College London, Medical Director and Honorary Consultant, Tavistock and Portman NHS Foundation Trust) contributed to study design and was the lead on recruitment in North London.
Mary Target (Professor of Psychoanalysis, University College London), contributed to the manual and clinical protocol of STPP, contributed to study design and wrote papers arising from the study.
Barry Widmer (Project Manager, University of Cambridge) designed the database and website, and managed the study.
Paul Wilkinson (University Lecturer, University of Cambridge) contributed to measures, contributed to writing of the BPI manual and wrote papers arising from the study.
Peter Fonagy (Freud Memorial Professor of Psychoanalysis, University College London) designed the study, obtained the research funding and wrote papers arising from the study.
We are grateful to the adolescent patients, former patients and their parents/guardians who actively contributed to the study design.
Publications
Goodyer IM, Tsancheva S, Byford S, Dubicka B, Hill J, Kelvin R, et al. Improving mood with psychoanalytic and cognitive therapies (IMPACT): a pragmatic effectiveness superiority trial to investigate whether specialised psychological treatment reduces the risk for relapse in adolescents with moderate to severe unipolar depression: study protocol for a randomised controlled trial. Trials 2011;12:175.
Goodyer IM, Reynolds S, Barrett B, Byford S, Dubicka B, Hill J, et al. Cognitive behavioural therapy and short-term psychoanalytical psychotherapy versus a brief psychosocial intervention in adolescents with unipolar major depressive disorder (IMPACT): a multicentre, pragmatic, observer-blind, randomised controlled superiority trial. Lancet Psychiatr 2017;4:109–19.
Data sharing statement
All trial data are held in a repository within the University of Cambridge. Access was made available following the publication of the main findings of the study in 2016. To obtain access please contact the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Goodyer IM, Reynolds S, Barrett B, Byford S, Dubicka B, Hill J, et al. Cognitive behavioural therapy and short-term psychoanalytical psychotherapy versus a brief psychosocial intervention in adolescents with unipolar major depressive disorder (IMPACT): a multicentre, pragmatic, observer-blind, randomised controlled superiority trial. Lancet Psychiatr 2017;4:109-19.
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013;382:1575-86. http://dx.doi.org/10.1016/S0140-6736(13)61611-6.
- Costello EJ, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression?. J Child Psychol Psychiatry 2006;47:1263-71. http://dx.doi.org/10.1111/j.1469-7610.2006.01682.x.
- Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey-adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 2015;54:37-44. http://dx.doi.org/10.1016/j.jaac.2014.10.010.
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry 2002;59:225-31. https://doi.org/10.1001/archpsyc.59.3.225.
- Kinley DJ, Lowry H, Katz C, Jacobi F, Jassal DS, Sareen J. Depression and anxiety disorders and the link to physician diagnosed cardiac disease and metabolic risk factors. Gen Hosp Psychiatry 2015;37:288-93. http://dx.doi.org/10.1016/j.genhosppsych.2015.03.022.
- Mokdad AH, Jaber S, Aziz MI, AlBuhairan F, AlGhaithi A, AlHamad NM, et al. The state of health in the Arab world, 1990-2010: an analysis of the burden of diseases, injuries, and risk factors. Lancet 2014;383:309-20. http://dx.doi.org/10.1016/S0140-6736(13)62189-3.
- Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2013;381:1987-2015. http://dx.doi.org/10.1016/S0140-6736(13)61097-1.
- Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry 2014;71:573-81. http://dx.doi.org/10.1001/jamapsychiatry.2014.16.
- Future in Mind. Promoting, Protecting and Improving our Children and Young People’s Mental Health and Wellbeing. London: NHS England Publication; 2015.
- March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA 2004;292:807-20. http://dx.doi.org/10.1001/jama.292.7.807.
- Goodyer I, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al. Selective serotonin reuptake inhibitors (SSRIs) and routine specialist care with and without cognitive behaviour therapy in adolescents with major depression: randomised controlled trial. BMJ 2007;335. http://dx.doi.org/10.1136/bmj.39224.494340.55.
- Depression in Children and Young People: Identification and Management in Primary, Community and Secondary Care. London: NICE; 2005.
- Depression in Children and Young People: Identification and Management in Primary, Community and Secondary Care – Update. London: NICE; 2015.
- Tolin DF. Is cognitive-behavioral therapy more effective than other therapies? A meta-analytic review. Clin Psychol Rev 2010;30:710-20. http://dx.doi.org/10.1016/j.cpr.2010.05.003.
- Driessen E, Cuijpers P, de Maat SC, Abbass AA, de Jonghe F, Dekker JJ. The efficacy of short-term psychodynamic psychotherapy for depression: a meta-analysis. Clin Psychol Review 2010;30:25-36. https://doi.org/10.1016/j.cpr.2009.08.010.
- Cuijpers P, Driessen E, Hollon SD, van Oppen P, Barth J, Andersson G. The efficacy of non-directive supportive therapy for adult depression: a meta-analysis. Clin Psychol Rev 2012;32:280-91. http://dx.doi.org/10.1016/j.cpr.2012.01.003.
- Barth J, Munder T, Gerger H, Nüesch E, Trelle S, Znoj H, et al. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: a network meta-analysis. PLOS Med 2013;10. http://dx.doi.org/10.1371/journal.pmed.1001454.
- Fonagy P, Cottrell D, Phillips J, Bevington D, Glaser D, Allison E. What Works for Whom? A Critical Review of Treatments for Children and Adolescents. New York, NY: Guilford Press; 2014.
- Palmer R, Nascimento LN, Fonagy P. The state of the evidence base for psychodynamic psychotherapy for children and adolescents. Child Adolesc Psychiatr Clin N Am 2013;22:149-214. http://dx.doi.org/10.1016/j.chc.2012.12.001.
- Fonagy P, Myles P, Pugh K, Shafran R, Kendall PC. Child and Adolescent Therapy: Dissemination and Implementation of Empirically Supported Treatment. Oxford: Oxford University Press; 2014.
- Mufson LH, Dorta KP, Olfson M, Weissman MM, Hoagwood K. Effectiveness research: transporting interpersonal psychotherapy for depressed adolescents (IPT-A) from the lab to school-based health clinics. Clin Child Fam Psychol Rev 2004;7:251-61. https://doi.org/10.1007/s10567-004-6089-6.
- Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 2004;61:577-84. http://dx.doi.org/10.1001/archpsyc.61.6.577.
- Kelvin R, Wilkinson P, Goodyer I, Birmaher B, Rey J. Treating Child and Adolescent Depression. Philadelphia, PA: Lippincott, Williams and Wilkins; 2009.
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA 2008;299:901-13. http://dx.doi.org/10.1001/jama.299.8.901.
- Dunn V, Goodyer IM. Longitudinal investigation into childhood- and adolescence-onset depression: psychiatric outcome in early adulthood. Br J Psychiatry 2006;188:216-22. http://dx.doi.org/10.1192/bjp.188.3.216.
- Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al. A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial. Health Technol Assess 2008;12. https://doi.org/10.3310/hta12140.
- Dubicka B, Elvins R, Roberts C, Chick G, Wilkinson P, Goodyer IM. Combined treatment with cognitive-behavioural therapy in adolescent depression: meta-analysis. Br J Psychiatry 2010;197:433-40. http://dx.doi.org/10.1192/bjp.bp.109.075853.
- Birmaher B, Brent DA, Kolko D, Baugher M, Bridge J, Holder D, et al. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Arch Gen Psychiatry 2000;57:29-36. https://doi.org/10.1001/archpsyc.57.1.29.
- Brenner SL, Burns BJ, Curry JF, Silva SG, Kratochvil CJ, Domino ME. Mental health service use among adolescents following participation in a randomized clinical trial for depression. J Clin Child Adolesc Psychology 2015;44:551-8. https://doi.org/10.1080/15374416.2014.881291.
- Burcusa SL, Iacono WG. Risk for recurrence in depression. Clin Psychol Rev 2007;27:959-85. http://dx.doi.org/10.1016/j.cpr.2007.02.005.
- Domino ME, Foster EM, Vitiello B, Kratochvil CJ, Burns BJ, Silva SG, et al. Relative cost-effectiveness of treatments for adolescent depression: 36-week results from the TADS randomized trial. J Am Acad Child Adolesc Psychiatry 2009;48:711-20. http://dx.doi.org/10.1097/CHI.0b013e3181a2b319.
- Byford S, Barrett B, Roberts C, Wilkinson P, Dubicka B, Kelvin RG, et al. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive behavioural therapy in adolescents with major depression. Br J Psychiatry 2007;191:521-7. http://dx.doi.org/10.1192/bjp.bp.107.038984.
- Goodyer IM, Tsancheva S, Byford S, Dubicka B, Hill J, Kelvin R, et al. Improving mood with psychoanalytic and cognitive therapies (IMPACT): a pragmatic effectiveness superiority trial to investigate whether specialised psychological treatment reduces the risk for relapse in adolescents with moderate to severe unipolar depression: study protocol for a randomised controlled trial. Trials 2011;12. http://dx.doi.org/10.1186/1745-6215-12-175.
- Trowell J, Joffe I, Campbell J, Clemente C, Almqvist F, Soininen M, et al. Childhood depression: a place for psychotherapy. An outcome study comparing individual psychodynamic psychotherapy and family therapy. Eu Child Adolesc Psychiatry 2007;16:157-67. https://doi.org/10.1007/s00787-006-0584-x.
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. J Abnorm Psychol 2000;109:504-11. https://doi.org/10.1037/0021-843X.109.3.504.
- Wilkinson PO, Goodyer IM. The effects of cognitive-behavioural therapy on mood-related ruminative response style in depressed adolescents. Child Adolesc Psychiatry Ment Health 2008;2. http://dx.doi.org/10.1186/1753-2000-2-3.
- Blatt SJ, Schaffer CE, Bers SA, Quinlan DM. Psychometric properties of the Depressive Experiences Questionnaire for adolescents. J Pers Assess 1992;59:82-98. http://dx.doi.org/10.1207/s15327752jpa5901_8.
- Hawley LL, Ho MH, Zuroff DC, Blatt SJ. The relationship of perfectionism, depression, and therapeutic alliance during treatment for depression: latent difference score analysis. J Consult Clin Psychol 2006;74:930-42. http://dx.doi.org/10.1037/0022-006X.74.5.930.
- Shahar G, Henrich CC, Winokur A, Blatt SJ, Kuperminc GP, Leadbeater BJ. Self-criticism and depressive symptomatology interact to predict middle school academic achievement. J Clin Psychol 2006;62:147-55. https://doi.org/10.1002/jclp.20210.
- University of Cambridge . Developmental Psychiatry, Department of Psychiatry n.d. dev.psychiatry.cam.ac.uk/projects (accessed January 2017).
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997;36:980-8. https://doi.org/10.1097/00004583-199707000-00021.
- Goodyer IM, Park RJ, Herbert J. Psychosocial and endocrine features of chronic first-episode major depression in 8-16 year olds. Biol Psychiatry 2001;50:351-7. https://doi.org/10.1016/S0006-3223(01)01120-9.
- Costello EJ, Angold A. Scales to assess child and adolescent depression: checklists, screens, and nets. J Am Acad Child Adolesc Psychiatry 1988;27:726-37. https://doi.org/10.1097/00004583-198811000-00011.
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, et al. The Great Smoky Mountains study of youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psych 1996;53:1129-36. https://doi.org/10.1001/archpsyc.1996.01830120067012.
- Wood A, Kroll L, Moore A, Harrington R. Properties of the mood and feelings questionnaire in adolescent psychiatric outpatients: a research note. J Child Psycho Psychiatry 1995;36:327-34.
- Kent L, Vostanis P, Feehan C. Detection of major and minor depression in children and adolescents: evaluation of the Mood and Feelings Questionnaire. J Child Psychol Psychiatry 1997;38:565-73. https://doi.org/10.1111/j.1469-7610.1997.tb01543.x.
- Goodyer IM, Herbert J, Secher SM, Pearson J. Short-term outcome of major depression: I. Comorbidity and severity at presentation as predictors of persistent disorder. J Am Acad Child Adolesc Psychiatry 1997;36:179-87. https://doi.org/10.1097/00004583-199702000-00008.
- Goodyer IM, Herbert J, Tamplin A. Psychoendocrine antecedents of persistent first-episode major depression in adolescents: a community-based longitudinal enquiry. Psychol Med 2003;33:601-10. https://doi.org/10.1017/S0033291702007286.
- Reynolds CR. Long-term stability of scores on the Revised-Children’s Manifest Anxiety Scale. Percept Mot Skills 1981;53. http://dx.doi.org/10.2466/pms.1981.53.3.702.
- Reynolds CR, Richmond BO. What I think and feel: a revised measure of children’s manifest anxiety. J Abn Child Psychology 1997;25:15-20. https://doi.org/10.1023/A:1025751206600.
- Bamber D, Tamplin A, Park RJ, Kyte ZA, Goodyer IM. Development of a short Leyton Obsessional Inventory for children and adolescents. J Am Acad Child Adolesc Psychiatry 2002;41:1246-52. https://doi.org/10.1097/00004583-200210000-00015.
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 2011;168:1266-77. http://dx.doi.org/10.1176/appi.ajp.2011.10111704.
- US Food and Drug Administration 2016. www.fda.gov/downloads/Drugs/Guidances (accessed July 2016).
- Vrouva I, Fonagy P, Fearon PR, Roussow T. The risk-taking and self-harm inventory for adolescents: development and psychometric evaluation. Psychol Assess 2010;22:852-65. http://dx.doi.org/10.1037/a0020583.
- Rood L, Roelofs J, Bögels SM, Nolen-Hoeksema S, Schouten E. The influence of emotion-focused rumination and distraction on depressive symptoms in non-clinical youth: a meta-analytic review. Clin Psychol Rev 2009;29:607-16. http://dx.doi.org/10.1016/j.cpr.2009.07.001.
- Wilkinson PO, Croudace TJ, Goodyer IM. Rumination, anxiety, depressive symptoms and subsequent depression in adolescents at risk for psychopathology: a longitudinal cohort study. BMC Psychiatry 2013;13. http://dx.doi.org/10.1186/1471-244X-13-250.
- Fichman L, Koestner R, Zuroff DC. Depressive styles in adolescents: assessment, relation to social functioning, and developmental trends. J Youth and Adolescents 1994;23:315-30. https://doi.org/10.1007/BF01536722.
- Gowers SG, Harrington RC, Whitton A, Beevor A, Lelliott P, Jezzard R, et al. Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA). Br J Psychiatry 1999;174:428-31. https://doi.org/10.1192/bjp.174.5.428.
- Gowers SG, Harrington RC, Whitton A, Lelliott P, Beevor A, Wing J, et al. Brief scale for measuring the outcomes of emotional and behavioural disorders in children. Health of the Nation Outcome Scales for children and Adolescents (HoNOSCA). Br J Psychiatry 1999;174:413-6. https://doi.org/10.1192/bjp.174.5.413.
- EuroQol Group . EQ-5D Products 2010. www.euroqol.org/eq-5d-products.html (accessed November 2016).
- Kind P, Spilker B. Quality of Life and Pharmacoeconomics. Philadelphia, PA: Lippincott-Raven; 1996.
- Byford S. The validity and responsiveness of the EQ-5D measure of health-related quality of life in an adolescent population with persistent major depression. J Ment Health 2013;22:101-10. http://dx.doi.org/10.3109/09638237.2013.779366.
- Dolan P, Gudex C, Kind P, Williams A. A Social Tariff for EuroQoL: Results From a UK General Population Survey. York: Centre for Health Economics, University of York; 1995.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Sealed Envelope . Randomisation and Online Databases for Clinical Trials n.d. www.sealedenvelope.com.
- Kelvin RG, Dubicka B, Wilkinson PO, Goodyer IM. Brief Psychosocial Intervention (BPI): A Specialist Clinical Care Treatment Manual For CAMHS Use. Cambridge: University of Cambridge; 2010.
- Weisz JR, Jensen-Doss A, Hawley KM. Evidence-based youth psychotherapies versus usual clinical care: a meta-analysis of direct comparisons. Am Psychol 2006;61:671-89. http://dx.doi.org/10.1037/0003-066X.61.7.671.
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: a meta-analysis. Psychol Bull 2008;132:132-49. http://dx.doi.org/10.1037/0033-2909.132.1.132.
- Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev 2012;10. http://dx.doi.org/10.1002/14651858.CD006525.pub2.
- Coventry PA, Hudson JL, Kontopantelis E, Archer J, Richards DA, Gilbody S, et al. Characteristics of effective collaborative care for treatment of depression: a systematic review and meta-regression of 74 randomised controlled trials. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0108114.
- Abbass AA, Rabung S, Leichsenring F, Refseth JS, Midgley N. Psychodynamic psychotherapy for children and adolescents: a meta-analysis of short-term psychodynamic models. J Am Acad Child Adolesc Psychiatry 2013;52:863-75. http://dx.doi.org/10.1016/j.jaac.2013.05.014.
- Midgley N, Kennedy E. Psychodynamic psychotherapy for children and adolescents: a critical review of the evidence base. J Child Psychol Psychiatry 2011;37:1-29. https://doi.org/10.1080/0075417x.2011.614738.
- Hopkins K, Crosland P, Elliott N, Bewley S. Clinical Guidelines Update Committee B . Diagnosis and management of depression in children and young people: summary of updated NICE guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h824.
- Target M, Fonagy P, Fonagy P. An Open Door Review of Outcome Studies in Psychoanalysis. London: International Psychoanalytical Association; 2002.
- Busch FMR, Shapiro T. The Treatment of Depression. Washington, DC: American Psychiatric Association; 2004.
- Midgley N, Cregeen S, Hughes C, Rustin M. Psychodynamic psychotherapy as treatment for depression in adolescence. Child Adolesc Psychiatr Clin N Am 2013;22:67-82. http://dx.doi.org/10.1016/j.chc.2012.08.004.
- Fonagy P, Target M. The history and current status of outcome research at the Anna Freud Centre. Psychoanal Study Child 2002;57:27-60.
- Spirito A, Esposito-Smythers C, Wolff J, Uhl K. Cognitive-behavioral therapy for adolescent depression and suicidality. Child Adolesc Psychiatr Clin N Am 2011;20:191-204. http://dx.doi.org/10.1016/j.chc.2011.01.012.
- Graham P, Reynolds S. Cognitive Behaviour Therapy for Children and Families. Cambridge: Cambridge University Press; 2015.
- Hilsenroth MJ, Blagys MD, Ackerman SJ, Bonge DR, Blais MA. Measuring psychodynamic-interpersonal and cognitive-behavioral techniques: development of the comparative psychotherapy process scale. Psychotherapy (Chic) 2005;42:340-56. https://doi.org/10.1037/0033-3204.42.3.340.
- Goldman R, Hilsenroth MJ, Gold J, Owen J. Psychotherapy integration and alliance: use of cognitive-behavioral techniques within a short-term psychodynamic treatment model. J Psychoth Integration 2013;23:373-85. https://doi.org/10.1037/a0034363.
- Stein MB, Pesale FP, Slavin JM, Hilsenroth MJ. A training outline for conducting psychotherapy process ratings: an example using therapist technique. Couns Psychoth Research 2010;10:50-9. https://doi.org/10.1080/14733140903229457.
- Nolen-Hoeksema SJ. High neuroticism and ruminative response style as predictors of change in depressive symptomatology. Cog Therap Research 1998;22:445-55. https://doi.org/10.1023/A:1018769531641.
- Smith JM, Alloy LB. A roadmap to rumination: a review of the definition, assessment, and conceptualization of this multifaceted construct. Clin Psychol Rev 2009;29:116-28. http://dx.doi.org/10.1016/j.cpr.2008.10.003.
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking Rumination. Perspect Psychol Sci 2008;3:400-24. http://dx.doi.org/10.1111/j.1745-6924.2008.00088.x.
- Lyubomirsky S, Kasri F, Zehm K. Dysphoric rumination impairs concentration on academic tasks. Cog Ther Research 2003;27:309-30. https://doi.org/10.1023/A:1023918517378.
- Joormann J, Dkane M, Gotlib IH. Adaptive and maladaptive components of rumination? Diagnostic specificity and relation to depressive biases. Behav Ther 2006;37:269-80. http://dx.doi.org/10.1016/j.beth.2006.01.002.
- Kelvin RG, Goodyer IM, Teasdale JD, Brechin D. Latent negative self-schema and high emotionality in well adolescents at risk for psychopathology. J Child Psychol Psychiatry 1999;40:959-68. https://doi.org/10.1111/1469-7610.00513.
- Park RJ, Goodyer IM, Teasdale JD. Effects of induced rumination and distraction on mood and overgeneral autobiographical memory in adolescent Major Depressive Disorder and controls. J Child Psychol Psychiatry 2004;45:996-1006. http://dx.doi.org/10.1111/j.1469-7610.2004.t01-1-00291.x.
- Park RJ, Goodyer IM, Teasdale JD. Categoric overgeneral autobiographical memory in adolescents with major depressive disorder. Psychol Med 2002;32:267-76. https://doi.org/10.1017/S0033291701005189.
- Goodyer IM, Herbert J, Tamplin A, Altham PM. First-episode major depression in adolescents. Affective, cognitive and endocrine characteristics of risk status and predictors of onset. Br J Psychiatry 2000;176:142-9. https://doi.org/10.1192/bjp.176.2.142.
- Kasch KL, Klein DN, Lara ME. A construct validation study of the Response Styles Questionnaire Rumination Scale in participants with a recent-onset major depressive episode. Psychol Assess 2001;13:375-83. https://doi.org/10.1037/1040-3590.13.3.375.
- Zuroff DC, Blatt SJ. The therapeutic relationship in the brief treatment of depression: contributions to clinical improvement and enhanced adaptive capacities. J Cons Clin Psychology 2006;74:130-40. https://doi.org/10.1037/0022-006X.74.1.130.
- Blatt SJ. Experiences of Depression: Theoretical, Clinical, and Research Perspectives. Washington, DC: American Psychological Association; 2004.
- Blatt SJ, Luyten P. A structural-developmental psychodynamic approach to psychopathology: two polarities of experience across the life span. Dev Psychopathol 2009;21:793-814. http://dx.doi.org/10.1017/S0954579409000431.
- Blatt SJ. The differential effect of psychotherapy and psychoanalysis with anaclitic and introjective patients: the Menninger Psychotherapy Research Project revisited. J Am Psychoanal Assoc 1992;40:691-724. https://doi.org/10.1177/000306519204000303.
- Roberts C. The implications of variation in outcome between health professionals for the design and analysis of randomized controlled trials. Stat Med 1999;18:2605-15. https://doi.org/10.1002/(SICI)1097-0258(19991015)18:19%3C2605::AID-SIM237%3E3.0.CO;2-N.
- Walwyn R, Roberts C. Therapist variation within randomised trials of psychotherapy: implications for precision, internal and external validity. Stat Methods Med Res 2010;19:291-315. http://dx.doi.org/10.1177/0962280209105017.
- Cohen J. Statistical Power Analyses For The Behavioural Sciences. Mahwah, NJ: Lawrence Erlbaum Associates; 1988.
- White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:993-1007. https://doi.org/10.1002/sim.1981.
- Curtis L. Unit Costs of Health and Social Care. Canterbury: Personal Social Services Research Unit, University of Kent; 2012.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2011.
- NHS Reference Costs 2011–12. London: HMSO; 2012.
- Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ 2004;13:1203-10. http://dx.doi.org/10.1002/hec.901.
- Efron B, Tibshirani R. An Introduction to the Bootstrap. New York, NY: Chapman and Hall; 1993.
- Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed?. BMJ 2000;320:1197-200. https://doi.org/10.1136/bmj.320.7243.1197.
- Drummond M, Sculpher M, Torrance GL, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8. http://dx.doi.org/10.1192/bjp.187.2.106.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. https://doi.org/10.1002/hec.635.
- Daviss WB, Birmaher B, Melhem NA, Axelson DA, Michaels SM, Brent DA. Criterion validity of the Mood and Feelings Questionnaire for depressive episodes in clinic and non-clinic subjects. J Child Psychol Psychiatry 2006;47:927-34. http://dx.doi.org/10.1111/j.1469-7610.2006.01646.x.
- Weichle T, Hynes DM, Durazo-Arvizu R, Tarlov E, Zhang Q. Impact of alternative approaches to assess outlying and influential observations on health care costs. Springerplus 2013;2. http://dx.doi.org/10.1186/2193-1801-2-614.
- Ng MY, Eckshtain D, Weisz JR. Assessing fit between evidence-based psychotherapies for youth depression and real-life coping in early adolescence. J Clin Child Adolesc Psychol 2015;53:1-17.
- Wilkinson P, Dubicka B, Kelvin R, Roberts C, Goodyer I. Treated depression in adolescents: predictors of outcome at 28 weeks. Br J Psychiatry 2009;194:334-41. http://dx.doi.org/10.1192/bjp.bp.108.052381.
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT). Am J Psychiatry 2011;168:495-501. http://dx.doi.org/10.1176/appi.ajp.2010.10050718.
- Kendler KS, Walters EE, Kessler RC. The prediction of length of major depressive episodes: results from an epidemiological sample of female twins. Psychol Med 1997;27:107-17. https://doi.org/10.1017/S0033291796003893.
- Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety 1998;7:3-14. https://doi.org/10.1002/(SICI)1520-6394(1998)7:1%3C3::AID-DA2%3E3.0.CO;2-F.
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, et al. Major depressive disorder: a prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse. J Affect Disord 1998;50:97-108. https://doi.org/10.1016/S0165-0327(98)00138-4.
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, et al. A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Arch Gen Psychiatry 1998;55:694-700. https://doi.org/10.1001/archpsyc.55.8.694.
- Maughan B, Collishaw S, Stringaris A. Depression in childhood and adolescence. J Can Acad Child Adolesc Psychiatry 2013;22:35-40.
- Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: age at onset, episode duration, and time to recurrence. J Am Acad Child Adolesc Psychiatry 1994;33:809-18. https://doi.org/10.1097/00004583-199407000-00006.
- Linden M. How to define, find and classify side effects in psychotherapy: from unwanted events to adverse treatment reactions. Clin Psychol Psychother 2013;20:286-96. http://dx.doi.org/10.1002/cpp.1765.
- Lilienfeld SO. Psychological treatments that cause harm. Perspect Psychol Sci 2007;2:53-70. http://dx.doi.org/10.1111/j.1745-6916.2007.00029.x.
Appendix 1 Data analysis supplement
| Outcome measure | Treatment effect | 95% CI | p-valuea | n (subjects, obs.) |
|---|---|---|---|---|
| Primary | ||||
| MFQ | ||||
| Time–treatment interaction | ||||
| STPP vs. CBT | 0.008 | –0.058 to 0.074 | 0.812 | (392, 1013) |
| CBT vs. BPI | 0.023 | –0.043 to 0.089 | ||
| STPP vs. BPI | 0.031 | –0.035 to 0.097 | ||
| (CBT + STPP) vs. BPI | 0.027 | –0.030 to 0.084 | 0.361 | |
| Treatment main effectb | ||||
| STPP vs. CBT | 0.411 | –2.901 to 3.723 | 0.808 | |
| CBT vs. BPI | –2.591 | –5.860 to 0.678 | ||
| STPP vs. BPI | –2.179 | –5.487 to 1.128 | ||
| (CBT + STPP) vs. BPI | –2.385 | –5.226 to 0.456 | 0.100 | |
| Secondary | ||||
| RCMAS | ||||
| Time–treatment interaction | ||||
| STPP vs. CBT | –0.012 | –0.732 to 0.049 | 0.701 | (383, 1013) |
| CBT vs. BPI | 0.069 | 0.007 to 0.131 | ||
| STPP vs. BPI | 0.057 | –0.005 to 0.120 | ||
| (CBT + STPP) vs. BPI | 0.063 | 0.009 to 0.117 | 0.022 | |
| Treatment main effectc | ||||
| STPP vs. CBT | 0.488 | –2.450 to 3.425 | 0.751 | |
| CBT vs. BPI | –2.140 | –5.052 to 0.772 | ||
| STPP vs. BPI | –1.652 | –4.601 to 1.297 | ||
| (CBT + STPP) vs. BPI | –1.896 | –4.432 to 0.640 | 0.116 | |
| LOI | ||||
| Time–treatment interaction | ||||
| STPP vs. CBT | –0.015 | –0.034 to 0.004 | 0.120 | (383, 957) |
| CBT vs. BPI | 0.016 | –0.004 to 0.035 | ||
| STPP vs. BPI | 0.0005 | –0.019 to 0.020 | ||
| (CBT + STPP) vs. BPI | 0.008 | –0.009 to 0.025 | 0.351 | |
| Treatment main effectb | ||||
| STPP vs. CBT | 0.318 | –0.659 to 1.295 | 0.527 | |
| CBT vs. BPI | –1.132 | –2.099 to –0.165 | ||
| STPP vs. BPI | –0.814 | –1.795 to 0.167 | ||
| (CBT + STPP) vs. BPI | –0.973 | –1.816 to –0.131 | 0.024 | |
| HoNOSCA | ||||
| Time–treatment interaction | ||||
| STPP vs. CBT | 0.0002 | –0.039 to 0.039 | 0.993 | (356, 796) |
| CBT vs. BPI | 0.016 | –0.022 to 0.054 | ||
| STPP vs. BPI | 0.016 | –0.023 to 0.055 | ||
| (CBT + STPP) vs. BPI | 0.016 | –0.017 to 0.049 | 0.348 | |
| Treatment main effectb | ||||
| STPP vs. CBT | 0.612 | –0.785 to 2.008 | 0.391 | |
| CBT vs. BPI | –1.055 | –2.414 to 0.303 | ||
| STPP vs. BPI | –0.444 | –1.820 to 0.932 | ||
| (CBT + STPP) vs. BPI | –0.749 | –1.925 to 0.426 | 0.207 | |
| Outcome measure | Treatment effect | 95% CI | p-valuea |
|---|---|---|---|
| Primary | |||
| MFQ | |||
| Treatment main effect | |||
| STPP vs. CBT | 1.215 | –1.511 to 3.941 | 0.383 |
| CBT vs. BPI | –1.662 | –4.381 to 1.056 | |
| STPP vs. BPI | –0.447 | –3.138 to 2.244 | |
| (CBT + STPP) vs. BPI | –1.055 | –3.391 to 1.282 | 0.382 |
| Secondary | |||
| RCMAS | |||
| Treatment main effect | |||
| STPP vs. CBT | 0.553 | –1.623 to 2.729 | 0.618 |
| CBT vs. BPI | 0.173 | –2.008 to 2.354 | |
| STPP vs. BPI | 0.726 | –1.421 to 2.873 | |
| (CBT + STPP) vs. BPI | 0.449 | –1.421 to 2.320 | 0.632 |
| LOI | |||
| Treatment main effectb | |||
| STPP vs. CBT | 1.199 | 0.278 to 2.120 | 0.011 |
| CBT vs. BPI | –0.478 | –1.401 to 0.444 | 0.309 |
| STPP vs. BPI | 0.721 | –0.187 to 1.628 | 0.120 |
| HoNOSCA | |||
| Treatment main effect | |||
| STPP vs. CBT | 0.623 | –0.821 to 2.068 | 0.398 |
| CBT vs. BPI | –0.608 | –2.045 to 0.828 | |
| STPP vs. BPI | 0.015 | –1.402 to 1.432 | |
| (CBT + STPP) vs. BPI | –0.297 | –1.528 to 0.934 | 0.646 |
| Outcome measure | Odds ratio | 95% CI | p-value | n (subjects, obs.) |
|---|---|---|---|---|
| MDD | ||||
| Time–treatment interaction | ||||
| STPP vs. CBT | 0.99 | 0.97 to 1.00 | 0.139 | (361, 837) |
| (CBT + STPP) vs. BPI | 1.00 | 0.98 to 1.01 | 0.572 | |
| MFQ score of ≥ 26 | ||||
| Time–treatment interaction | ||||
| STPP vs. CBT | 1.02 | 0.67 to 1.55 | 0.939 | (392, 1013) |
| (CBT + STPP) vs. BPI | 1.00 | 0.99 to 1.02 | 0.705 | |
| ABQ score of > 0 | ||||
| Time–treatment interaction | ||||
| STPP vs. CBT | 0.99 | 0.98 to 1.01 | 0.225 | (382, 947) |
| (CBT + STPP) vs. BPI | 1.02 | 1.00 to 1.03 | 0.009 | |
Adverse events
The five items from the RCMAS subscale (breathing problems, sleep disturbances, drowsy/tiredness, nausea and sweating) and one from the MFQ subscale (restless/overactive) were used to generate a physical adversity score ranging from 0–6, for which each item with a response of ‘never’ was assigned a zero score, otherwise, this was assigned a value of one. Pro-rating was used if one or two of the six items were missing using all the available data for the MFQ or RCMAS subscales, respectively. The summary statistics are shown in Table 27.
| Visit | Treatment group | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BPI | CBT | STPP | |||||||||||||
| Mean | SD | Median | Minimum | Maximum | Mean | SD | Median | Minimum | Maximum | Mean | SD | Median | Minimum | Maximum | |
| 0 | 5.0 | 1.1 | 5 | 1 | 6 | 5.1 | 1.0 | 5 | 2 | 6 | 5.0 | 1.1 | 5 | 2 | 6 |
| 1 | 4.4 | 1.5 | 5 | 0 | 6 | 4.6 | 1.3 | 5 | 2 | 6 | 4.4 | 1.5 | 5 | 0 | 6 |
| 2 | 4.2 | 1.6 | 4 | 0 | 6 | 4.0 | 1.5 | 4 | 0 | 6 | 4.2 | 1.6 | 4 | 0 | 6 |
| 3 | 4.1 | 1.6 | 4 | 0 | 6 | 3.6 | 1.6 | 4 | 0 | 6 | 3.6 | 1.7 | 4 | 0 | 6 |
| 4 | 3.5 | 1.8 | 3.5 | 0 | 6 | 3.5 | 1.9 | 4 | 0 | 6 | 3.2 | 1.9 | 3 | 0 | 6 |
| 5 | 3.3 | 1.8 | 3.5 | 0 | 6 | 3.4 | 1.9 | 4 | 0 | 6 | 3.2 | 1.8 | 3 | 0 | 6 |
Inspection of the data shows no observable differences between treatment groups over the course of the study. The decline in adverse event reporting over the five assessments is relatively consistent with a persistent lessening of positive responses from baseline recruitment to the end of follow-up.
Although the results show no treatment differences in somatic side effect profile, they are unlikely to provide a comprehensive estimate of psychological and social side effects or adverse effects that may accrue from psychological treatment of depressed adolescents. However, currently, there are no formally adopted methodologies for the measurement of such experiences, although the field is beginning to recognise the need for such methodologies. 123,124
List of abbreviations
- ABQ
- Antisocial Behaviour Questionnaire
- ADAPT
- Adolescent Depression Antidepressant and Psychotherapy Trial
- BPI
- brief psychosocial intervention
- BPI-S
- brief psychosocial intervention scale
- CA-SUS
- Child and Adolescent Service Use Schedule
- CAMHS
- Child and Adolescent Mental Health Services
- CBT
- cognitive–behavioural therapy
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CPPS
- Comparative Psychotherapy Process Scale
- DEQ
- Depressive Experiences Questionnaire
- DES-A
- Depressive Experiences Scale for Adolescents
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition
- EQ-5D
- EuroQol-5 Dimensions
- GEE
- generalised estimating equation
- HoNOSCA
- Health of the Nation Outcome Scales for Children and Adolescents
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- IMPACT
- Improving Mood with Psychoanalytic and Cognitive Behaviour Therapy
- ITCC
- intratherapist correlation coefficient
- K-SADS
- Kiddie-Schedule for Affective Disorders and Schizophrenia
- K-SADS-PL
- Kiddie-Schedule for Affective Disorders and Schizophrenia Present and Lifetime
- LME
- linear mixed effects
- LOI
- Leyton Obsessional Inventory
- MDD
- major depressive disorder
- MFQ
- Mood and Feelings Questionnaire
- NICE
- National Institute for Health and Care Excellence
- PI
- principal investigator
- QALY
- quality-adjusted life-year
- RCMAS
- Revised Children’s Manifest Anxiety Scale
- RCT
- randomised controlled trial
- RRS
- Ruminative Responses Scale
- SD
- standard deviation
- SSRI
- selective serotonin reuptake inhibitor
- STPP
- short-term psychoanalytic psychotherapy
- TADS
- Treatment of Adolescent Study