Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 07/01/21. The contractual start date was in April 2009. The draft report began editorial review in May 2014 and was accepted for publication in September 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Helen Snooks is a member of the NIHR Journals Library Editorial Group.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Snooks et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Structure of this report
This study was a cluster randomised controlled trial (C-RCT) of a protocol for emergency ambulance paramedics to assess, and to refer to community-based care, older adults who had fallen and incorporated an economic evaluation and qualitative research.
The report begins with an overview of the literature and policy relating to older adults falling, avoidable conveyances to hospital, current paramedic practice, community falls services and the use of protocols for paramedics. We describe the underpinning theoretical framework for the intervention, clinical effectiveness and cost-effectiveness results and the qualitative findings.
We report a systematic review of the literature relating to interventions in the ambulance setting with older people who fall, and then describe the methods used to conduct the main C-RCT. We report the results of the trial, followed by results from the economic analysis and the qualitative components.
In the final chapter, we summarise and synthesise the findings from all three components of the study, the systematic review, C-RCT and qualitative study, providing interpretation in the light of other studies. We discuss the strengths and limitations of the research and generalisability to the NHS. The conclusions are followed by recommendations for future research.
Background
Falls in older people
Falls in older people are recognised as an important issue internationally,1,2 with high human costs, for the individual and their carers, and high organisational costs. It is estimated that around 30% of home-dwelling people aged ≥ 65 years fall every year,3–8 and the rate of falls is even higher among care home residents. 9 Studies suggest that falls in older people are the cause of 20–30% of mild to severe injuries and 10–15% of emergency department (ED) attendances in this group. 10,11 Falls in older people are often due to more than one underlying cause or risk factor; as the number of risk factors rises, so does the risk of falling. 12 Risk factors include muscle weakness, balance and gait, low blood pressure (or drop in blood pressure on assuming upright posture) and cognitive decline. The severity of fall-related complications increases with age. 13,14 Falls are a cause of substantial rates of mortality and morbidity, as well as considerable contributors to immobility. 8 Reduction in quality of life and physical activity leads to social isolation and functional deterioration with a high risk of resultant dependency and nursing home institutionalisation. 15–18 Recovery from fall injury is often delayed in older people, which increases the risk of subsequent falls. 8 Recurrent falls are associated with greater physician contact and functional decline. 19–21 An additional complication is post-fall anxiety, leading to a fear of falling, which in turn can further contribute to deconditioning and weakness and in the long run may actually increase risk of falls. 8
The About the National Health Interview Survey22 indicates that falls are the largest single cause of restricted activity days among older adults. Most people who fall do not seek any medical advice, and those who do are more likely to report to their general practitioner (GP). 23,24 The combination of high falls with a high susceptibility to injury makes a relatively mild fall dangerous. This is because of a high prevalence of clinical diseases such as osteoporosis and age-related changes, that is slowed protective reflexes. 8 In the UK, it has been estimated that falls account for 3% of total NHS service expenditure,10 with additional costs incurred by social care providers. 25 The prevention of falls in older people has been highlighted as a priority. 11,26
Although prevention appears effective,11 reducing falls and associated morbidity depends on early identification of people at high risk and delivery of interventions across traditional service boundaries;27 these priorities are now reflected in national and international guidelines. 28–30
Emergency department overcrowding and potentially avoidable attendances
Population growth, the increasing burden of chronic disease and population ageing, and the shortage of health-care workers are affecting health-care systems in many countries. 31 EDs are under considerable pressure and overcrowding is a significant international problem, with a negative impact on both patient care and providers. 32 Department of Health data33 show that from 2003/4 to 2012/3 the number of attendances in English NHS ED units increased by nearly 32% (from 16.5 million to 21.7 million), although the majority of the increase was in minor injuries units and walk-in centres. Many of the older people presenting to EDs have had a fall. 34 One study showed that older people presenting to EDs after a fall represented 20% of all attendances and 14% of all hospitalisations in people aged > 65 years,35 and the size of the problem is likely to be underestimated as falls are poorly defined, coded and recorded. 36
Older people can be kept for a longer time in the ED than younger adults because of difficulties in assessment and management, that is, they undergo more tests than younger adults, they are more likely to have cognitive limitations37 and potential underlying diseases or, if they have common diseases, atypical symptoms,38 and they are also more likely to be admitted than younger adults. 39 Pressures on acute services to discharge patients as soon as possible may mean that there is little focus on fall prevention interventions. 36 Older people taken to EDs following a fall are at high risk of falling again in the next year, with a 30% chance of sustaining fracture or dislocation. 35
It has been argued that many admissions of older people are avoidable, and that the demands placed on the hospital system may be relieved if alternatives can be found. 40 The 2006 White Paper Our Health, Our Care, Our Say set the direction on ‘improving patient experience and significantly reducing unnecessary admissions to hospital’,41 with paramedics and enhanced/senior paramedics to play a role in providing care at the scene. The National Medical Director of NHS England recently proposed key areas of change in the 2013 Keogh report Transforming Urgent and Emergency Care Services in England 2013. 42 The reports look at developing the ambulance service into a mobile urgent treatment service capable of treating more patients at the scene so they do not need to be conveyed to hospital to initiate care. The report highlights opportunities to shift care closer to home, stating that 40% of ED patients are discharged requiring no treatment, up to 1 million emergency admissions were avoidable in 2012 and up to 50% of calls could be managed at the scene.
Conveyance rate of older adults who fall
Although demand on UK ambulance services continues to increase steadily, a recent study found that only 10% of calls are life-threatening, and an estimated half of all emergency calls relate to patients who could be treated at home. 43
People aged ≥ 65 years commonly call an emergency ambulance (through the emergency services) following a fall. In London (UK), this group accounts for about 60,000 attendances (8% of emergency ambulance attendances) each year. 44 This is very similar to the proportion reported in an urban emergency medical services (EMS) system in the USA. 43
Non-conveyance to EDs is high in this group, at close to 40% in London,44 elsewhere in the UK45,46 and the USA. 43 In most cases (90%), patients who fall and are not conveyed to an ED have fallen in the home. 46 Non-conveyance of patients is recognised internationally as a safety and litigation risk. 47 In some UK ambulance services, performance targets are set for individual enhanced paramedics and paramedics regarding the percentage of patients they should leave at home, and the enhanced paramedic or paramedic decides who can be safely left at home. In 2011/12, the Department of Health, in conjunction with the College of Emergency Medicine, introduced eight accident and emergency (A&E) clinical quality indicators as part of the NHS Outcomes Framework. These became mandatory from 1 April 2011. Indicator 1 (ambulatory care) measures the proportion of patients who are able to be treated at home by improved pathways of care for patients to avoid hospital admission. 48
Little is known about how, in the absence of specific guidelines or training to leave older people who fall at home, paramedics make these decisions. A study acknowledged the pragmatic nature of negotiation with patients whether or not to go to hospital. 49 A UK study identified that the non-clinical factors affecting these decisions include experience and confidence of ambulance staff, time into the shift, presence of carers, quality of the accommodation, waiting times at the local ED and prior knowledge of the patient. 50
Ambulance services, with key stakeholders, have been required to develop alternative care pathways, some of which involve the direct referral of older patients who have fallen to primary51 or community services. 52 This is particularly relevant at a time when pressures on EDs give rise to safety concerns and challenges to demand management;53 general practice and wider community services are being required to support the ED directly in order to avoid secondary care, in a time of major system reorganisation. 54 Alternative care pathways (avoiding use of the ED) for ambulance clinicians have been incentivised through local targets in the Commissioning for Quality and Innovation payment framework. 55 This emphasis is likely to continue given the pressure on EDs.
The National Service Framework for Older People26 advocates that ambulance staff/clinicians refer to community-based care older people who have fallen, although this reflects consensus rather than research evidence. Previous studies in this setting have found that change in practice is difficult to achieve and new pathways of care are difficult to exploit. 56
Service models: community falls services
A range of different types of trial performed in community-dwelling individuals (someone who lives among the general population and is not living in an institution),57 care home residents and hospital patients has established the evidence base for falls interventions. 11 Recent clinical guidelines from the American Geriatrics Society, British Geriatrics Society and American Academy of Orthopaedic Surgeons panel on falls prevention29 have strongly advocated preventative approaches based on multidimensional risk factor assessment, exercise programmes (which include balance, strength and endurance training) and environmental assessment and modification. A 2004 meta-analysis demonstrated a 37% risk reduction in the monthly rate of falling for community-dwelling individuals when multifactorial intervention was implemented. 58 Falls clinics are one approach by which falls and injuries can be managed multifactorially. 59 A falls clinic is a space where older adults prone to falling can receive holistic support and treatment from nurses, physiotherapists and other health professionals. A recent randomised controlled trial (RCT) showed that the Chaos Falls Clinic in Finland is effective in preventing falls in home-dwelling people over 70 years of age at high risk of falling. 60 Patients in this trial were guided towards the falls clinic by regional health-care professionals (physicians, nurses or GPs), but relatives of patients could also contact the clinic for an assessment for eligibility.
A recent study found that referral to a community-based falls prevention of older people who had fallen and been left at home by their attending ambulance clinicians, service reduced further falls and improved clinical outcomes,61 and achieved cost-effectiveness. 62 Recent policy changes in the UK have encouraged the development and implementation of alternative models of care for the delivery by the ambulance service. The literature points to the development of extended skills paramedics in line with government policies and supported by protocols. The use of enhanced paramedics has the potential to reduce running costs of the service considerably, while improving quality and focus, although significant ‘one-off’ costs associated with training are also necessary. However, Newman63 noted, the ‘emphasis on the national standards plus local flexibility appeared to reflect supposed shifts in the role of state’ but more particularly presented a range of models which resulted in ‘confusing messages about the relationship between government, the professionals and the public’.
Theoretical underpinning for intervention
Explicit definition of the theoretical underpinning for an intervention to be evaluated is a necessary step in the process for developing both the intervention to be tested as well as the methods for its evaluation. The theoretical basis for the Support and Assessment for Fall Emergency Referrals (SAFER) 2 study intervention – the protocol for emergency ambulance paramedics to assess older patients attended for a fall, and allowing referral for those not needing immediate care at ED to a falls service for community-based care (see Appendix 1) – was built on work carried out previously by the research team and other published research in the two areas of emergency prehospital care paramedic practice and service delivery, and care of older people who fall.
The intervention is hypothesised to work by improving the decision-making of paramedics in terms of safe non-conveyance and referral to appropriate community-based services of older people who have had a fall. Through the protocol, pathway, training, support and feedback, the intervention provided a formalised framework for decision-making and referral for this patient group. This is hypothesised to make a difference by one or more of the following four mechanisms:
-
increasing paramedics’ clinical knowledge of how to make appropriate non-conveyance decisions
-
increasing paramedics’ knowledge of falls services and pathways for referral
-
increasing paramedics’ confidence about making a non-conveyance decision and reducing anxiety about risk
-
increasing awareness and likelihood that paramedics will consider non-conveyance and referral pathways as an option in appropriate cases.
For the intervention to make a difference to practice and to patient outcomes, a number of factors needed to be in place, including:
-
effective referral pathways, and sufficient capacity in falls teams to respond to referrals
-
training and support provided to paramedics that is appropriate and effective
-
motivation on the part of paramedics to use the new protocol and referral pathway, including them not finding it too onerous or time-consuming.
If improved decision-making can be achieved, based on our best knowledge, we can expect the following beneficial effects:61,62,64–66
-
better outcomes (fewer subsequent falls and emergency episodes; higher satisfaction with care) for patients, in particular for those who would have been left at home with no further care but who are now referred to falls services, and also for those who may have been taken to the ED unnecessarily, with related risks of inpatient admission and hospital-related adverse events (AEs)
-
reduced costs to the NHS and patients because of fewer initial ED episodes, inpatient admissions and subsequent falls and related care
-
improved paramedic skill sets, level of professionalisation and practitioner morale.
Uncertainties lie at the certain points on the required causal pathway in terms of the feasibility of implementation and uptake by paramedics; acceptability to patients of non-conveyance/referral; improvements to processes of care for patients; of any wider impact on the operation of the ambulance service, such as increased job cycle times; and of patient health outcomes, including their perception of their own health.
We designed the SAFER 2 trial to gather data about each of these elements of the pathway in order to assess not only outcomes but also processes that may lead to improved outcomes. Study objectives and outcomes reflect the theoretical underpinning and hypothesised causal pathway.
Research aim and objectives
Aim
To assess the benefits and costs to patients and the NHS of a complex intervention comprising education, clinical protocols and pathways enabling paramedics to assess older people who have fallen and refer them to community-based falls services when appropriate.
Objectives
-
To compare outcomes, processes and costs of care between intervention and control groups:
-
patient outcomes: rate and pattern of subsequent emergency health-care contacts or deaths, for any reason; health-related quality of life; psychological status, especially fear of falling; and change in place of residence
-
processes of care: pathway of care at index incident; subsequent health-care contacts; ambulance service operational indicators; and protocol compliance including clinical documentation
-
costs of care: provided by NHS and personal social services (PSS); incurred by patients or carers in seeking care.
-
-
To estimate wider system effects of the introduction of the intervention on ambulance service performance and costs.
-
To understand how patients experience the new health technology.
-
To identify factors which facilitate or hinder the use of the intervention.
-
To inform the development of methods for falls research especially outcome measures recommended for trials of interventions for older people who fall. 59
-
To carry out a systematic review on the implementation and impact of interventions by emergency medical staff who care for older people who fall.
Chapter 2 Systematic review of literature on effects of interventions by emergency medical staff for older people who fall
Abstract
Background
Since the publication of the National Service Framework for Older People 2001,26 the NHS has prioritised older people who fall. As the overall use of EDs increases, policy is shifting to encourage ambulances to convey fewer patients and refer them to other services, when appropriate.
Objective
To review evidence about effects of interventions within EMSs for older people who fall, which aim to reduce demand for EDs.
Method
We undertook a systematic search of 18 electronic databases. Studies were eligible for inclusion if they included empirical data on novel interventions by EMS in the community for older people who fall. We extracted outcomes, assessed studies for methodological quality and used narrative synthesis to analyse results.
Results
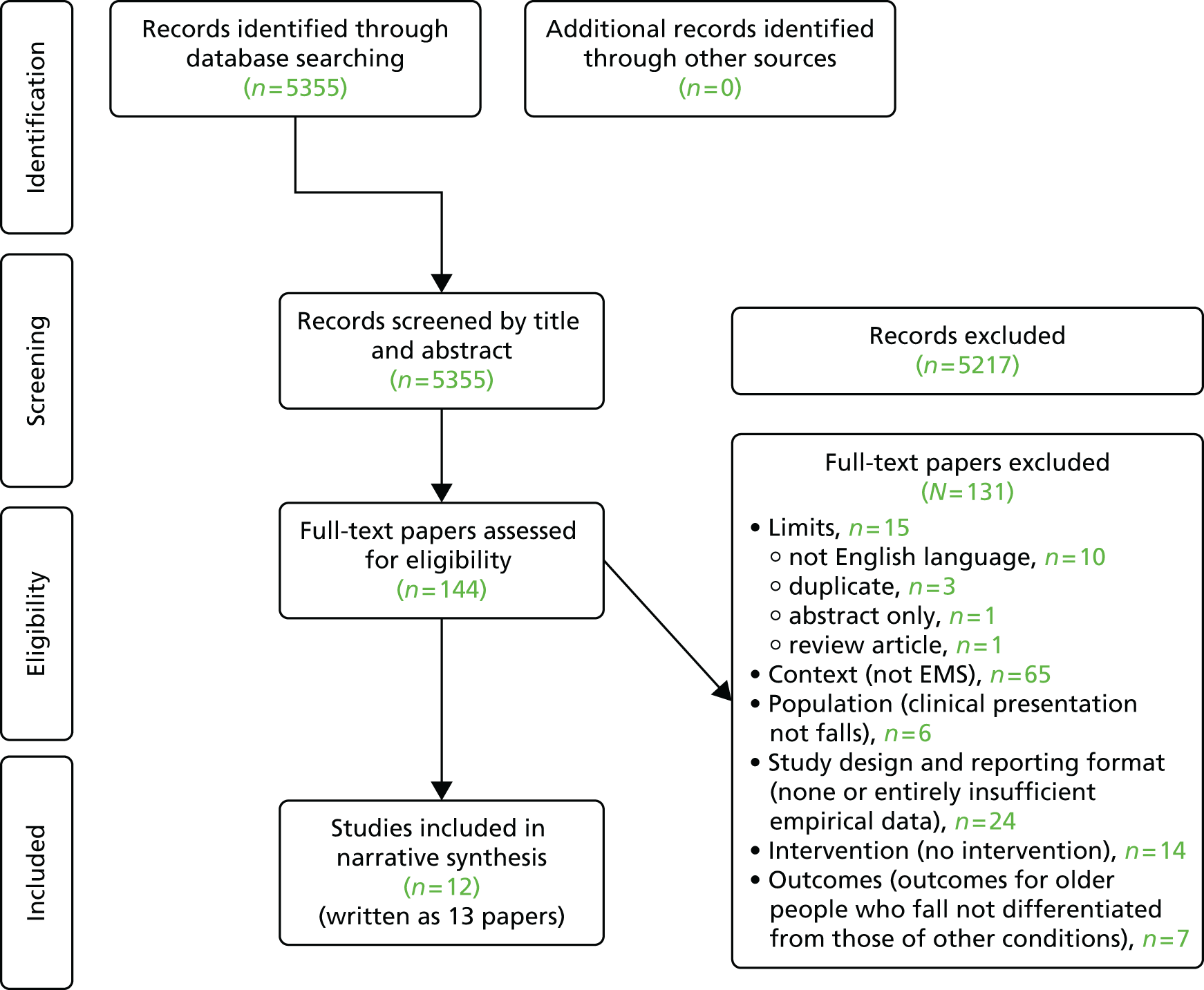
Of the 5355 articles identified, we selected 12 studies reported in 13 papers. Identified studies were excluded for the following main reasons: not English language, not EMS, not falls, no or entirely insufficient empirical data, no intervention or the outcomes of falls were not differentiated. The 13 papers reported data from 7411 participants: 7399 patients and 12 paramedics. Interventions fell into two groups: prospective screening on-scene or at the time of the emergency call and retrospective screening and referral to falls prevention.
Up to half of patients screened on-scene were conveyed to hospital, and referrals to falls services were low except when automatic (retrospectively). The majority of studies were judged to be of poor quality and data were heterogeneous, limiting opportunities for comparison and meta-analysis. Of the higher-quality studies, one trial reported a reduction in ED attendance and hospital admission and increased patient satisfaction; the other reported a reduction in ambulance calls over 12 months, with patients reporting fewer falls and increased confidence.
Discussion
Despite national policy to prevent falls and reduce use of emergency services, studies were few and evidence was mainly weak on effective ways to provide emergency care to older people who fall. When high-quality trial data were available, positive impact on patient and service outcomes was reported.
Study registration
This systematic review is registered on PROSPERO number CRD42013006418.
Introduction
This chapter presents a systematic review of the literature on the effects of novel interventions by EMSs for older people who fall. It describes the background and rationale for the review in the context of the SAFER 2 study, defines the methods used and presents findings to identify existing evidence and topics for further research.
Background and rationale for the review
Since the publication of the National Service Framework for Older People 2001,26 the NHS has prioritised older people who fall. These people have reduced quality of life and levels of physical activity, leading to social isolation and functional deterioration with high risk of increased dependency and institutionalisation. 15–17 Treatment of falls is a major and rising cost for health systems internationally. In the UK, falls cost the NHS more than £2.3B per annum,67 about 3% of total expenditure. 10 In the USA, costs will increase by almost 75% between 2010 and 202068 and in Australia by more than double between 2004 and 2021. 69 Older people who fall and need emergency attention make up a substantial part of the EMS workload. In London, for example, they generate over 60,000 attendances, about 8% of the workload. 44,51 International proportions are similar. 70 Standard paramedic practice is to assess injury and immediate care needs, move patients from where they have fallen and convey them to an ED unless they refuse. 71 In the face of rising ED attendances, policy is shifting to encourage emergency ambulance services to convey fewer patients to EDs in the UK and internationally. 40,72
Research has highlighted opportunities for alternative treatment for older people who fall that reflect their health status and risk. 43,46,73,74 Some older people who fall and call the emergency services can be identified in the ambulance call centre, allowing rapid and targeted alternative responses. 75 The cost of EMS attendance to older people who fall is high. 76 Innovative approaches are necessary and feasible,77,78 but evidence about cost-effectiveness of alternative treatment is needed. 76
A Cochrane review11 of 159 randomised trials of interventions to reduce incidence of falls among older people living in the community reported that exercise interventions reduce risk and rate of falls. However, very few studies reported interventions by EMS staff. 61,62,71,79 Gates et al. 65 found limited evidence supporting fall prevention programmes in EDs, primary care or the community but did not evaluate of any initiatives delivered by EMS. More recently a systematic review by Mikolaizak et al. 74 reported that one study found that 49% of non-transported patients who had fallen had unplanned health contact within 14 days;44 another study reported that 33% of such patients were admitted to hospital within 28 days;80 and two studies that found that attendance by specially trained paramedics reduced subsequent falls, hospital attendance and other AEs. 61,66,74 However, this review did not assess the quality of included studies or observe Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines,81 thus limiting interpretation of findings. None of these reviews considered issues affecting implementation of interventions for older people who fall, notably the views of EMS staff delivering care.
Methods
Protocol and registration
We registered this review with PROSPERO and the All Wales Systematic Review Register. We adhered to the guidance for reviews of health care by the Centre for Reviews and Dissemination82 and PRISMA. 81
Eligibility criteria
We defined inclusion and exclusion criteria in terms of the population, intervention, comparator, outcomes, context and study design (PICOCS) of included studies, which is an adaption of population, intervention, comparator, outcomes (PICO). The additional ‘C’ in the acronym recognises the importance of the context within which the intervention is delivered. 82,83
We included studies that evaluated interventions by EMS staff in the community to older people who had fallen and generated an emergency service call. We considered any treatment above the care routinely provided by a paramedic or other EMS staff. Table 1 shows our inclusion and exclusion criteria.
| PICOCS and limits | Inclusion | Exclusion |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Comparator | No comparator required since any study design included | |
| Outcome |
|
|
| Context |
|
|
| Study design and reporting format |
|
|
| Limits |
|
|
Sources and search strategy
We searched published and grey literature and reference lists of included studies. We searched the electronic databases listed in Table 2 during the first week of July 2013 using a search strategy focusing mainly on the target population and the setting of the intervention. We used medical subject headings (MeSHs) and keywords when available. Table 3 shows the search strategy for MEDLINE, the Allied and Complementary Medicine Database and Cumulative Index to Nursing and Allied Health Literature Plus.
| Type of literature | Data sources |
|---|---|
| Reviews | The Cochrane Library (Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, NHS Economic Evaluation Database, Cochrane Central Register of Controlled Trials and Cochrane Register of Methodological Reviews) |
| Reference lists of included articles | |
| General journal articles | AMED |
| ASSIA | |
| BNI | |
| CINAHL Plus | |
| EMBASE | |
| Internurse | |
| MEDLINE | |
| PsycINFO | |
| PubMed | |
| Scopus | |
| Reference lists of included articles | |
| Grey literature | The British Library |
| UK Institutional Repository Search | |
| GreyNet | |
| Conference Proceedings Citation Index (Web of Science) | |
| OpenGrey | |
| Zetoc | |
| Reference lists of included articles | |
| Journal citation reports | Web of Science |
| Search identification | Search terms | Search options |
|---|---|---|
| Limiters – English language | ||
| S22 | S4 AND S11 AND S20 | Search modes – Boolean/Phrase |
| S21 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 | Search modes – Boolean/Phrase |
| S20 | (MH ‘Ambulatory Care’) | Search modes – Boolean/Phrase |
| S19 | (MH ‘Ambulances’) | Search modes – Boolean/Phrase |
| S18 | (MH ‘Emergency Medical Services’) OR (MH ‘Emergency Medical Technicians’) | Search modes – Boolean/Phrase |
| S17 | urgent care | Search modes – Boolean/Phrase |
| S16 | emergency care | Search modes – Boolean/Phrase |
| S15 | pre hospital | Search modes – Boolean/Phrase |
| S14 | pre-hospital | Search modes – Boolean/Phrase |
| S13 | ambulance | Search modes – Boolean/Phrase |
| S12 | S6 OR S7 OR S8 OR S9 OR S10 | Search modes – Boolean/Phrase |
| S11 | age* | Search modes – Boolean/Phrase |
| S10 | (MH ‘Aged’) | Search modes – Boolean/Phrase |
| S9 | (MH ‘Health Services for the Aged’) | Search modes – Boolean/Phrase |
| S8 | (MH ‘Frail Elderly’) | Search modes – Boolean/Phrase |
| S7 | old* | Search modes – Boolean/Phrase |
| S6 | elder* | Search modes – Boolean/Phrase |
| S5 | S1 OR S2 OR S3 | Search modes – Boolean/Phrase |
| S4 | (MH ‘Accidental Falls’) | Search modes – Boolean/Phrase |
| S3 | trip* | Search modes – Boolean/Phrase |
| S2 | slip* | Search modes – Boolean/Phrase |
| S1 | fall* | Search modes – Boolean/Phrase |
Our search strategy focused on two elements of PICOCS:
-
population, using terms such as ‘aged’, ‘health services for the aged’, ‘frail elderly’, ‘age’, ‘accidental falls’, ‘trip’ and ‘slip’
-
context, using terms such as ‘emergency medical services’, ‘ambulatory care’, ‘ambulances’, ‘emergency medical technicians’, ‘urgent care’, ‘emergency care’ and ‘prehospital’.
The terms for each database varied slightly according to MeSH or other indexed terms. The key terms were included, as well as keywords in title, abstract or text.
The search strategy used in three of the databases (MEDLINE, EMBASE and PubMed) can be summarised as follows:
-
population, using the MeSH terms of ‘Aged’, ‘Health Services for the Aged’, Frail Elderly’, ‘Accidental Falls’ and the keywords of ‘age*’, ‘trip’ and ‘slip’
-
context, using the MeSH terms of ‘Emergency Medical Services’, ‘Ambulatory care’, ‘Ambulances’, ‘Emergency Medical Technicians’ and the keywords of ‘urgent care’, ‘emergency care’, ‘prehospital’, ‘pre-hospital’ and ‘emergency medical service*’
-
combination of elements, combining each of the population terms and each of the context terms with ‘OR’; and combing the population and the context terms with ‘AND’.
Study selection
We downloaded electronic search results into the EndNote bibliographic software (Thomson Reuters, CA, USA). One researcher (RC, MH or MK) screened the title, abstract and keywords of each study using the inclusion and exclusion criteria in Table 1. A second researcher, blind to the first researcher’s decision, screened 1 in 10 references, to ensure consistent decision-making. We resolved differences in discussion with the third researcher. We retrieved the full text of papers whose abstract met the inclusion criteria. We compared final recommendations and again achieved consensus on eligible studies in discussion with the third researcher.
Data extraction
We developed and piloted a data extraction framework reflecting the objectives of the review in line with guidance. 82 Two researchers independently extracted the following items:
-
year of publication, country of origin, setting, study design
-
aim or research question, outcome measure(s), method(s), study population, sample size
-
description of intervention
-
key findings.
When possible, we used the taxonomy developed by the Prevention of Falls Network Europe (ProFaNE),84 from the work of Hauer et al. ,85 to describe these data, thus increasing consistency of extraction across the included studies and opportunity for synthesis. The full data extraction table can be found in Appendix 2. We compared completed forms and agreed on content in discussion with the third researcher.
Assessment of the risk of bias (quality)
We assessed quality of included studies using checklists recommended by Centre for Reviews and Dissemination82 to inform comparisons and guide interpretation. 85 We identified these checklists as potentially suitable in the Centre for Reviews and Dissemination guidance. We used the Scottish Intercollegiate Guidelines Network checklist86 for all study methods except qualitative reports, for which we used the summary criteria of Walsh and Downe. 87 We assessed general methodological quality as high, acceptable or low, defined by Scottish Intercollegiate Guidelines Network86 thus:
-
high: almost all criteria met; low risk of bias; conclusions unlikely to change after further research
-
acceptable: most criteria met; some flaws with an associated risk of bias; conclusions may change after further research
-
low: either most criteria not met or clear flaws in study design; conclusions likely to change after further research.
Data synthesis
We assessed quantitative results for their potential to contribute to a meta-analysis. We used narrative synthesis to synthesise heterogeneous data. 88 We explored relationships within and between studies, seeking to explain similarities and differences between study findings.
Findings
Inclusion
We identified a total of 5355 references. Our review of titles and abstracts suggested that 138 articles might be eligible. After studying full texts, we confirmed that 13 papers61,62,66,80,89–97 reporting 12 studies met our inclusion criteria, as detailed in Figure 1. Table 4 summarises the 12 included studies; Tables 5 and 6 describe them in more detail and Table 7 assesses their quality. Appendix 3 lists excluded studies (at full-text screening stage) with reasons for exclusion.
FIGURE 1.
The PRISMA flow chart.
| First author | Year of publication | Country | Study design | Study population | Sample size | Description of intervention |
|---|---|---|---|---|---|---|
| Metcalfe89 | 2006 | UK | Cohort | Patients aged ≥ 65 years, but not transported | 49 | Provision of clinical assessment tool to paramedics with follow-up referral to rapid response team |
| Shah et al.90 | 2006 | USA | Cohort (with control group) | Patients aged ≥ 65 years | 258 | Screening tool used by paramedics |
| Mason et al.66 | 2007 | UK | C-RCT | Individuals aged > 60 years calling the emergency services and presenting with minor acute conditions in the scope of practice of the paramedic practitioner | 3018 | Assessment by a paramedic with an enhanced scope of practice in on-scene assessment, treatment and referral (paramedic practitioner) |
| Shandro et al.91 | 2007 | USA | Cohort | Patients aged ≥ 65 years, but not transported | Not reported | Paramedic referral to falls prevention |
| Gray and Walker80 | 2008 | UK | Cohort (with control group) | Patients aged ≥ 65 years | 233 attended by ECPs; 772 attended by ED | Provision of care by ECP (paramedic with further training) |
| Kue et al.92 | 2009 | USA | Retrospective cohort | Patients aged ≥ 60 years, but not transported | 721 | Paramedic referral to social services |
| aLogan et al.61 | 2010 | UK | RCT | Patients aged ≥ 60 years living in defined area, but not transported | 204 | Retrospective referral to falls prevention team following attendance by paramedic |
| aSach et al.62 | 2012 | UK | Cost-effectiveness | Patients aged ≥ 60 years and not transported | 157 | Retrospective referral to falls prevention service following attendance by paramedic |
| Shah et al.93 | 2010 | USA | Cohort | Patients aged ≥ 60 years | 814 | Provision of screening question to paramedics; follow-up referrals |
| Halter et al.94 | 2011 | UK | Qualitative | 12 ambulance staff who were trained in, and used the, clinical assessment tool | 12 paramedics | Provision of clinical assessment tool to paramedics |
| Hoyle et al.95 | 2012 | New Zealand | Retrospective cohort | Average age 62 years, but not all had suffered from falls | 131 | Provision of treatment protocols to ECPs |
| Studnek et al.96 | 2012 | USA | Retrospective cohort (with control group) | 911 callers to whom medical priority dispatch system sent ambulance | Phase 1, n = 160; phase 2, n = 101 | Triage led by despatch nurse |
| Comans et al.97 | 2013 | Australia | Cohort | Patients aged ≥ 65 years | 21 | Paramedic referral to falls prevention |
| Study | Number of patients screened using tool/total number of patients | Number of referrals/number of patients screened for referral (%) | Number of referrals accepted/number of patients referred (%) | Number conveyed to ED/number screened (% conveyed to ED) | Percentage admitted to hospital | Paramedics views of the intervention | Other outcomes |
|---|---|---|---|---|---|---|---|
| Metcalfe, 200689 | – | 53/89 (60%) | 51/53 (96.2%) | – | – | – | – |
| Shah et al., 200690 | 210/258 (79%, 95% CI 74% to 84%) | – | – | – | – | – | – |
| Mason et al., 200766 | – | – | – | ED attendance 0 to 28 days: intervention group, 62.6%; control group, 87.5% (p < 0.001) | Admittance to hospital 0 to 28 days: intervention group, 40.4%; control group, 46.4% (p < 0.001) | n/a | Total episode time: intervention group, 235 minutes; control group, 278 minutes (p < 0.001). Investigations received: intervention group, 49.7%; control group, 67.9% (p < 0.001). Treatment received: intervention group, 81.3%; control, group 72.8% (p < 0.001) |
| Shandro et al., 200791 | – | 17 (number screened not reported) | 11/17 (64.7%) | – | – | – | – |
| Gray and Walker, 200880 | – | – | – | 62/233 (27%) | 25% reduction in intervention group | – | – |
| Kue et al., 200992 | – | 7/721 (1%) | – | – | – | – | – |
| Shah et al., 201093 | 814 (total number not reported) | 124/814 (15%) | – | – | – | – | – |
| Halter et al., 201194 | – | – | – | – | – | Paramedics: reluctant to use novel intervention | – |
| Hoyle et al., 201295 | – | – | – | 44/131 (34%) | – | – | – |
| Studnek et al., 201296 | – | – | – | – | 9.3% reduction in intervention group | – | – |
| Comans et al., 201397 | – | 21/638 (3%) | 13/17 (76.5%) | – | – | – | – |
| Study | Further falls | EMS calls | Fear of falling | Costs and QALYs | Admission to hospital (outcome measure), (p-value) | Other outcomes (outcome measure: results) |
|---|---|---|---|---|---|---|
| Shah et al., 200690 | – | – | – | – | – | Discussion with physician to discuss risk of falls:a intervention, n = 8/82 (9.8%); control, n = 1/37 (2.7%); p = 0.30 Receipt of changes to home environment:a intervention, n = 12/82 (15%); control, n = 4/37 (11%); p = 0.91 Recollection of educational materials: n = 17/82 (21%); control not applicable |
| Mason et al., 200766 | – | – | – | – | See Table 5 | Subsequent unplanned contact with secondary care services (up to 28 days): intervention, 21.3%; control, 17.6% (p < 0.001) Worsening of physical health: intervention, 21.7%; control, 25.6%; p = 0.13 EQ-5D: no significant difference (p-value, NR) Mortality: no significant difference (p-value, NR) Patient satisfaction: very satisfied 85.5% intervention group vs. 73.8% control group; p < 0.001 |
| Gray and Walker, 200880 | – | – | – | – | Avoided admission rate: intervention group, 44%; control group, 52%; n = 1005; p = 0.05. 17% reduction at 28 days | – |
| Logan et al., 2010;61 Sach et al., 201262 | 55% reduction in intervention group (95% CI 42% to 65%; p < 0.001) | 40% reduction in intervention group, 95% CI 8% to 60%; p = 0.018) | 22% reduction in intervention group (95% CI 13% to 31%; p < 0.001) | Mean NHS and PSS costs: –£1551.00 less in intervention group (95% CI –£5932.00 less to £2829.00 more) Mean QALYs: 0.070 more in the intervention group (95% CI −0.010 to 0.150; p = 0.086) |
Number of hospital days: intervention group, 1257; control group, 1141; p = 0.70 | Nottingham extended activities of daily living scale medians: intervention group, n = 8; control group, n = 6; p < 0.001 |
| Comans et al., 201397 | – | – | – | – | – | Patients completing referral programme: 5/8 (62.5%) |
| Study | Internal validity score/total possible score (n n/a) | How well was the study done to minimise bias? | Particular limitations noted during quality appraisal |
|---|---|---|---|
| Controlled trials | |||
| Shah et al., 200690 | 4/5 (5 n/a) | Moderate quality | Potential bias from choosing intervention cluster from two without randomisation; cofounding not controlled for |
| Mason et al., 200766 | 8/9 (1 n/a) | High quality | Participants could not be blinded; as some outcomes were self-reported, there was potential for reporting bias; high level of attrition (50%) |
| aLogan et al., 201061 | 7/9 (1 n/a) | High quality | Participants could not be blinded |
| aSach et al., 201262 | 7/8 (1 n/a) | High quality | As outcomes were self-reported, there was potential for reporting bias |
| Qualitative study | |||
| Halter et al., 201194 | 10/12 (0 n/a) | High quality | Lacks detail about ethics, researchers and analysis |
| Cohort studies | |||
| Kue et al., 200992 | 3/7 (7 n/a) | Low quality | Data not presented clearly; limited by small study numbers and being in one site |
| Comans et al., 201397 | 5/11 (3 n/a) | Low quality | Very high attrition (75%); limited data used as the basis for evaluation |
| Hoyle et al., 201295 | 3/6 (8 n/a) | Low quality | Subjective assessment and possibly bias in dispatch, disparity in transportation rates; uncontrolled evaluation with limited follow-up data |
| Gray and Walker, 200880 | 3/10 (4 n/a) | Low quality | Nominally controlled but collected different data from intervention and control groups, limiting comparison |
| Studnek et al., 201296 | 4/8 (6 n/a) | Low quality | Nominally controlled but study sites changed between phases without relevant comparator/baseline data; very limited in terms of outcomes measured |
| Shandro et al., 200791 | 4/8 (6 n/a) | Low quality | Uncontrolled evaluation; very limited presentation of EMS-specific data and outcomes of care; number of exposed patients not stated |
| Shah et al., 201093 | 2/9 (5 n/a) | Low quality | Feasibility study without controls or patient outcome measures |
| Metcalfe, 200689 | 2/9 (5 n/a) | Low quality | Uncontrolled evaluation with poorly reported methods; authors’ conclusions do not match results |
Study characteristics
Of the 12 studies, six61,62,66,80,89,94 came from the UK, four90–93 came from the USA, one97 came from Australia and one95 came from New Zealand. Study designs comprised two RCTs61,66 (one of which61 published a separate paper evaluating cost-effectiveness element of the study),62 nine cohort studies (of which six did not include a comparator arm89,91–93,95,97 and three included intervention and control arms80,90,96) and one qualitative study. 94 Of the nine cohort studies, three were retrospective,92,95,96 five were prospective80,89–91,97 and one had both prospective (screening) and retrospective (referral) elements. 93 These study characteristics are summarised in Table 4.
The one-armed nature of six89,91–93,95,97 of the studies restricted them to reporting descriptive outcomes. All but Logan et al. 61 reported outcomes at the time of the intervention or soon after. The most common outcome measures were referrals made to a receiving unit or service,66,89,91–93,97 acceptance of referral by the patient66,89,91,92,97 and patient conveyance following attendance by EMSs. 66,80,95 Five studies reported follow-up outcomes for patients receiving a novel intervention (see Table 6). 61,66,80,90,97 Three66,80,90 used short follow-up periods (14 and 28 days) with limited inclusion of outcome measures in two,80,90 whereas another collected physical health, quality-of-life and mortality outcomes. 66 One written as two research papers reported outcomes over 12 months;61,62 but one did not report the period of follow-up. 97
Ten61,66,80,89,90,92,93,95–97 of these studies included a total of 7399 patients and the qualitative study interviewed 12 paramedics. 94 However, one study did not specify its sample size. 91
Methodological quality
The methodological quality of the studies was variable, but was generally weak (see Table 7). The controlled trials,61,66,90 economic evaluation62 and qualitative study94 were considered acceptable or high quality and scored highly for internal validity. The cohort studies were mostly of weak quality and did not report sufficient information to determine if their methods minimised risk of bias or confounding. Seven out of eight of the cohort studies80,89,90,92,93,96,97 failed to identify potential confounders in study design and analysis. Shah et al. 93 and Metcalfe89 did not provide a focused research question. Gray and Walker80 scored fairly low using the quality assessment tool, but reviewers defined this study as of acceptable quality as, compared with the other studies included in this review, it included a control arm, a clearly focused aim and clearly written methods and results sections. Kue et al. 92 did not define outcomes or reliably assess exposure. However, reviewers considered all studies that reported data that were directly relevant to this review, and all were included. 98 The full quality assessment for each included study is presented in Appendix 2, with a brief summary of the internal validity score, risk of bias and noted limitations given in Table 7.
Study findings
Interventions within ambulance services to treat older people who fall
The 12 evaluated interventions fell broadly into two main types; 10 encouraged EMS staff on-scene to adopt a new approach when making their initial assessment of the older person who had fallen;66,80,89–92,94,95,97 two did so retrospectively61,96 and one study93 did both through intervention on-scene by EMS staff and retrospective action by other staff. Of the others in the first group, eight used paramedics/paramedic practitioners to intervene at the time of attendance66,80,90–92,94,95,97 whereas the other did so within the despatch centre, also known as ambulance control. 96 The two other studies used individuals not participating in the initial EMS care retrospectively to screen patients for referral. 61,89
Seven interventions screened patients on-scene with a predefined tool to decide whether or not to make a referral with the option of referring to a community-based service,89–94,97 one used the expertise of health professionals other than paramedics to decide upon conveyance,96 three used paramedic practitioners trained to provide community-based clinical assessment for patients aged > 60 years,66,80,95 and one referred all eligible patients who were not conveyed following attendance by EMSs. 61 Screening tools ranged from a single question about the patient’s risk of falling,90 through several questions about eligibility for referral90–93,97 to a flow chart to guide the EMS staff through decision-making. 94 One study screened the patients off-scene, with a nurse who retrospectively screened ambulance service records to decide whether or not to refer patients to a community service. 89 Once the patient was successfully screened and a decision was made to refer the patient, the studies referred them to a falls prevention service,61,91,97 social services,66,92 the patient’s GP,66,90,94 district nurse,66 a rapid response service89 or a case management service. 93
Of the four66,80,95,96 studies not using predefined screening tools, but using the expertise of paramedic practitioners or health professionals other than paramedics, three assessed patients to decide whether to convey patients to hospital or to leave them at home;66,80,95 Mason et al. 66 used paramedic practitioners, and Gray and Walker80 and Hoyle et al. 95 both used emergency care practitioners (ECPs) on-scene, paramedics with extended skills but without specific screening questions or falls service referral routes. Studnek et al. 96 transferred patients with medical problems deemed of ‘low acuity’ to a nurse-led advice line while an ambulance was travelling to their location. The nurse provided advice on alternative modes of care or transportation. The ambulance response was stopped only if the patient requested it.
Effect of interventions by emergency medical services for older people who fall
The outcomes measures assessed by the included studies were heterogeneous. Only a minority of the studies followed up patient outcomes: five89,91–93,95 collected outcomes only from the initial contact with the patient, relating to the emergency service call itself or the ambulance service’s care of the patient on-scene; the remaining five reported outcomes after initial contact with the patient; and four66,80,90,97 studies reported both initial and subsequent outcomes. Among those reporting later outcomes, follow-up intervals were varied. Comans et al. 97 did not report this interval; two studies used periods of ≤ 1 month80,90 and the randomised trial assessed effectiveness and cost-effectiveness over 1 year. 61,62 To try to synthesise the effect of the novel interventions on patients, we stratify the findings of the included studies by the time point at which the outcome was collected.
Outcomes pertaining to initial patient contact
Referrals
The most widely reported outcome measure was numbers of patient referrals to a community service following screening prompted by a fall, as reported by five studies89,91–93,97 (Table 8). Referral rates were generally low (between 1% and 15% of screened patients). However, Metcalfe89 reported that 53 (60%) out of 89 patients screened by an experienced nurse within 24 hours of their fall were referred to a rapid response team or another appropriate service.
| Referral component | Study | ||||
|---|---|---|---|---|---|
| Kue et al., 200992 | Comans et al., 201397 | Shandro et al., 200791 | Shah et al., 201093 | Metcalfe, 200689 | |
| Intervention | Referral pathway from EMS to community service | ||||
| Outcome | Number of referrals | Number attempted to refer | Number of referrals | Number of patients referred because of falls | Number of referrals made for patients experiencing a fall |
| Number of referrals | 7 | 21 | 17 | 124 | 53 |
| Sample size (patients screened for referral) | 721 | 638 | Unknown | 814 | 89 |
| Percentage referred | 1 | 3 | Unknown | 15 | 60 |
Three studies89,91,97 reported numbers of patients accepting referrals (Table 9). The acceptance rate was high, reported by Comans et al. 97 and Shandro et al. 91 to be 76% and 65%, respectively. Metcalfe89 reported that just two patients (3.8%) refused the referral generated by the rapid response team, giving a 96% acceptance rate. Although we have presented these data together, it should be noted that these studies measured referral acceptance at different time points in the referral process, with Comans et al. 97 reporting patients who consented to the study and underwent initial assessments, Shandro et al. 91 assessing the number of patients enrolling on the programme, and Metcalfe89 assessing the number of patients who accepted referrals.
| Referral component | Study | ||
|---|---|---|---|
| Comans et al., 201397 | Shandro et al., 200791 | Metcalfe, 200689 | |
| Intervention | Referral pathway from EMS to community service | Provision of screening tool with referral to community service | |
| Outcome | Consented to study and underwent initial assessment | Number of enrolments on falls prevention programme from EMS referrals | Number patients accepting referrals |
| Data | 13 | 11 | 51 |
| Sample size (number of patients referred) | 17 | 17 | 53 |
| Percentage consented/accepted | 76.5 | 64.7 | 96.2 |
Referral mechanisms that required on-scene referrals by EMS staff91,92,97 were undertaken less frequently and had lower patient acceptance rate than retrospective referrals, which had high patient acceptance. 89 As all these studies were of low quality, however, findings are not robust.
Conveyance to emergency department
In three studies,66,80,95 ECPs or PPs (paramedics with enhanced training) took the decision to convey a patient to ED. ECPs or PPs did not use any additional decision-making tool above clinical judgement. Conveyance to the ED can only be reported here for two of the studies80,95 as the third study combined reporting of conveyance at the time (0 days) with conveyance at 28 days66 and was varied (Table 10).
| Referral component | Study | |
|---|---|---|
| Hoyle et al., 201295 | Gray and Walker, 200880 | |
| Intervention | Paramedics with extended training (with no referral pathway) | |
| Outcome | Percentage of patients transported to ED | Patients attending ED |
| Data | 44 | 62 |
| Sample size (number of patients screened/attended) | 131 | 233 |
| Percentage of patients transported to ED | 34 | 27 |
Admission to hospital
Two studies80,96 assessed whether or not patients who received a novel EMS intervention after making the emergency service call experienced reduced hospital admissions. Studnek et al. 96 found that hospital admissions fell from 35% (n = 56) to 25.7% (n = 26) when emergency service callers who had sustained a fall were screened to receive nurse-led telephone advice, in addition to a standard EMS attendance. Studnek et al. 96 did not calculate individual significant values for patients who had fallen, but found that, for all patients (with all possible medical complaints), there was a statistically significant difference in the proportion of patients discharged home following attendance at the ED (i.e. not admitted to hospital) compared with the control period (p = 0.03; CIs not reported). Gray and Walker80 assessed hospital admittance at 72 hours post EMS attendance. Admission rates decreased from 51% (n = 396) during the control period to 26% (n = 62) during the intervention period (significance levels not reported).
Outcomes collected following initial contact with patients
Five studies, written as six research papers,61,62,66,80,90,97 reported follow-up outcomes. Five reported the impact on subsequent falls and health service utilisation61,66,80,90,97 and one reported the impact on costs to the NHS. 62
Subsequent falls and use of health care
Logan et al. 61 reported that patients referred to a falls prevention team experienced 55% fewer falls over 12 months than the control group [95% confidence interval (CI) 0.35 to 0.58; p < 0.001]. Patients also had reduced fear of falling (assessed by the falls efficacy scale, mean difference –16.5, 95% CI –23.2 to –9.8; p < 0.001), were more active [assessed by the Barthel Activities of Daily Living Index, odds ratio (OR) 2.91, 95% CI 1.18 to 7.20]. There was also a significant reduction in emergency ambulance calls for falls over 12 months (effect size 0.60, 95% CI 0.40 to 0.92; p = 0.018).
Mason et al. 66 reported several patient outcomes with a significant difference for the intervention group (those attended by a paramedic practitioner): a 25% decrease in attendance at an emergency department at 0 and 28 days following the incident (relative risk 0.72, 95% CI 0.68 to 0.75; p < 0.001), a 6.1% decrease in hospital admission during the same period (relative risk 0.87, 95% CI 0.81 to 0.94; p < 0.001), an increase in subsequent unplanned contact with secondary care services (relative risk 0.1.21, 95% CI 1.06 to 1.38; p < 0.001), and an 11.7% increase in those reporting being ‘very satisfied with their care’ (relative risk 1.16, 95% CI 1.09 to 1.23; p < 0.001).
The other three studies80,90,97 reporting follow-up outcomes were cohort studies collecting outcome measures associated with specific aspects of the novel intervention. Shah et al. 90 assessed whether or not patients had discussed their risk of falls with their doctor and if they had received changes to their home environment. Although increased numbers of patients had these attributes in the intervention arm, the difference was not significant.
Gray and Walker80 reported a 17% reduction in admissions at 28 days following EMS attendance during the intervention period than in the control period when patients were attended by paramedics with usual training (reduction from 52% to 44%, n = 1005, df = 1; p = 0.05).
Comans et al. 97 reported the number of patients who completed the referral programme, with five patients who were referred to a falls prevention service completing the programme, out of the eight patients who initially enrolled on the programme.
Effect on cost
One paper62 found that the referral of patients who had been attended and left at home by EMS to a falls prevention service, carried out within a randomised trial,60 was cost-effective. The mean difference in NHS and PSS costs between the intervention and control groups was –£1551.00 per patient over 1 year (95% CI –£5932.00 to £2829.00). The mean difference in quality-adjusted life-years (QALYs) was 0.070 (95% CI −0.010 to 0.150) in favour of the intervention group.
What is the impact on and views of emergency medical services staff of interventions designed to improve the care of and outcomes for older people who fall?
Staff appeared reluctant to use new interventions to treat older people who fall, according to two studies. 94,97 Halter et al. 94 reported variable use of a clinical assessment tool to review whether to safely leave a patient at home or convey him or her to the ED. This qualitative study reported that paramedics were reluctant to use a systematic decision-making tool but instead relied on informal processes, showing the need for a consistent message and support for ambulance staff. Comans et al. 97 identified that repeated education sessions, good relations and regular contact between falls services and paramedics raised referral rates, but these were not sustained when awareness-raising ended.
Discussion
This systematic review identified limited and mainly weak evidence regarding the most effective ways to deliver alternative treatments to older people who fall. The 12 studies that were included in this review implemented variable novel interventions, limiting comparisons that can be made between studies. We classified the interventions within two groups: (1) on-scene screening during patient assessment or triage during the emergency service call to refer them to a community health service or hospital conveyance; or (2) retrospective screening and referral to a community health service.
The studies included in this review are heterogeneous in terms of interventions and outcomes, and, while this is a finding in itself, we have considered the studies to be similar enough, in a small research field, to analyse as a group because of the similarity of the context and patient group included in all the studies. We have not attempted meta-analysis for this reason, and it is the heterogeneity of outcome measures, and a lack of follow-up outcomes to assess the long-term effect of the novel interventions on patients, that means it is difficult to assess the impact of these interventions. The majority of outcome measures were descriptive, detailing the number of referrals that were made and the acceptance of these referrals to patients. Studies utilising these descriptive outcome measures identified that a low percentage of the overall number of screened patients were referred, except where the referral was made retrospectively externally to the ambulance service. Similarly, acceptance of the referral by patients increased when the referral was undertaken externally to the ambulance service. Although these outcome measures are useful for understanding the paramedics’ and patients’ adoption of the intervention, they do not allow understanding of the effect of the novel intervention on the patient.
Five studies, written as six research papers, undertook follow-up of patients beyond the initial contact with EMS,61,66,80,90,96 five of which undertook between-group analyses. They identified that, compared with the control groups, patients who were treated for a fall by EMS had fewer future falls, called the EMS less often and received cost-effective care when referred to a fall prevention service;61 were less likely to be admitted to hospital when being treated by a paramedic practitioner66 or ECP;80 and were more likely to discuss fall risk with their doctor when a referral was made. 90 The study not undertaking between-group analyses found that five out of eight patients who enrolled in a fall prevention programme completed it. 97
Emergency medical services staff’s views of the novel interventions were seldom reported; the one qualitative study included in this review concluded that EMS staff were reluctant to use formalised assessment techniques, instead relying on their usual decision-making process. 94 One study did not directly report paramedics’ views, but did suggest that use of the intervention increased with regular contact and good relations. 97 Although other included studies did not directly assess EMS staffs views of the novel interventions, the studies that reported referral rates reported a low percentage of referrals taking place. These findings highlight the difficultly of changing practice with EMS.
Assessment of study quality, using recommended tools, identified that the included papers were mostly poorly reported and overall quality of the evidence was not high. Most of the studies were single-arm cohort studies and many had methodological drawbacks leaving them open to bias. The majority of the included studies were single-group cohorts and only one RCT was identified. Seven of the included papers were deemed to be of low quality, two of acceptable quality and three of high quality.
Previous systematic reviews undertaken to assess the effect of referral mechanisms on patients who fall have found varying level of benefits for patients. A review looking to assess the effect of multidisciplinary falls prevention service treatment on patients referred from community settings found limited evidence to support a reduction in falls or fall- related injuries for referred patients. 65 Another review, undertaken to identify evidence regarding patients who are not conveyed following a fall, found that appropriate interventions can benefit patients who have fallen, including reducing AE and EMS calls. 74
The current review identified benefits within a minority of the included studies – one study reported significant decreases to future EMS attendances and hospital admissions when patients are referred retrospectively to a falls prevention service, while two studies described a reduction in admission to hospitals when patients are attended by an ECP. These positive findings on patient and service outcomes are, however, set in the context of the number of studies for which such outcomes are not explored and the low quality of the majority of the included studies.
High-quality evidence from well-designed and rigorously conducted research is needed to understand how effective services can be adopted and delivered which will provide appropriate and safe care for patients. Future research should focus on the ability of paramedics to make decisions regarding a patients’ conveyance, paramedics’ views of the intervention and the long-term health consequences for patients of such interventions.
Strengths and limitations of this review
We used a systematic process in line with good practice82,99 to identify international research and review reported data. In undertaking this review, we were unable either to consider papers in languages other than English or to request original data from study authors because of time constraints.
Heterogeneity of interventions and outcomes and low study quality mean data should be interpreted with caution. It also limits ability to generalise findings.
The quality assessment tools that were utilised were not tailored to single-group cohort studies. Therefore, many of the questions were not relevant to the majority of studies that were included in this review. Nevertheless, the inability to answer a question was regarded as a sign of low quality.
Review findings as context for Support and Assessment for Fall Emergency Referrals 2
The SAFER 2 trial selected the age of 65 years and older as its cut-off point for inclusion, as both the National Service Framework for Older People 200126 and the National Institute for Health and Care Excellence (NICE) guidelines for falls67 use this cut-off point, although they recognise this as an arbitrary point that varies in relevance to individual health and disability.
In the systematic review, however, we chose to also include studies that stated their lower age for inclusion to be 60 years, as we were aware from our reading on the topic that two61,66 UK trials had used this slightly lower age breakpoint.
Although we recognise that this might suggest that the cut-off point of ≥ 60 years of age could or should have been used for the SAFER 2 trial, we are reassured that our results are comparable when we look at the mean age of participants in the 10 of the 12 studies that provide us with this demographic information about participants:61,66,89–93,95–97 7 of these 10 studies report mean ages of participants in the ‘frail older people’ group, ranging from 77 to 83 years61,66,90–93,97 and one of the most common age group of participants as 80–89 years. 89 The two studies of exception were those where fall was one condition only amongst a range studied, and these reported average ages of 4796 and 62 years. 95 We therefore feel confident that the different lower age parameter for the systematic review and the trial did not impact on relevance of one to the other.
We suggest that the fact that this review found limited evidence on the topic of support and assessment for older people who fall and are attended by the emergency ambulance service, and even more limited evidence of high quality, is the context and justification for the SAFER 2 trial, the findings of which are now reported.
Chapter 3 Methods
Overview
The SAFER 2 study design comprised a C-RCT, with economic evaluation and qualitative component.
Aim
To assess the benefits and costs to patients and the NHS of a complex intervention comprising education, clinical protocols and pathways enabling paramedics to assess older people who have fallen and refer them to community-based falls services when appropriate.
Objectives
-
To compare outcomes, processes and costs of care between intervention and control groups:
-
patient outcomes: rate and pattern of subsequent emergency health-care contacts or deaths; health-related quality of life; falls efficacy (fear of falling); and change in place of residence
-
processes of care: pathway of care at index incident; subsequent health-care contacts; ambulance service operational indicators and protocol compliance including clinical documentation
-
costs of care.
-
-
To understand how patients experience the new health technology.
-
To identify factors which facilitate or hinder the use of the intervention.
-
To inform the development of methods for falls research.
Cluster randomised controlled trial
Trial design
The trial was conducted in geographically defined sites within three UK ambulance services. The unit of clustering at each site was an ambulance station. The clusters comprised the paramedics based at eligible stations who volunteered to participate in the trial. Once stations had been randomly allocated to intervention or control groups, participating paramedics based at those stations were asked to deliver care according to their group allocation, irrespective of their location on any particular shift.
We chose a cluster design, as opposed to a patient-level RCT, as the intervention included training and new assessment skills, and it would be impossible to switch on and off as would be required in a patient-level RCT. Other units of randomisation have been used in trials based in prehospital emergency care, with limited success. 100 We chose to randomly allocate stations in order to allow the hosting ambulance services to support change in practice for paramedics based at intervention stations while minimising contamination to practice by paramedics based at control stations.
Trial management
Following the Medical Research Council guidelines for good practice in clinical trials,101 the management structure for the trial (see Appendix 4) included an independent Trial Steering Committee (TSC) and Data Monitoring and Ethics Committee (DMEC), with an internal Trial Management Group (TMG), local implementation team (LIT) in each area, core research team, and task and finish groups for specific aspects of the trial such as data management. The TSC provided external oversight and advice to the chief investigator, the Health Technology Assessment (HTA) programme and the sponsor on all aspects. The DMEC had access to unblinded comparative data to monitor the data and make recommendations to the TSC if there were ethical or safety reasons why the trial should not continue. The TMG managed the trial at an overarching level. The LITs dealt with operational issues at each site and provided liaison opportunities between participating services. The core team that managed the trial at a day-to-day operational level was smaller and included the chief investigator, site principal investigators and researchers.
Setting
We undertook the trial in prehospital emergency care, with paramedics delivering the intervention in partnership with community-based falls services (known as falls prevention services). We selected sites within three ambulance services in England and Wales in which a falls service was available, but no process was in place for paramedics to make direct referrals from the scene of emergency service call attendances. Appendix 5 maps stations and hospitals with ED departments at each site.
Participants
Ambulance stations were eligible for inclusion in the study as a cluster if they were situated within a participating ambulance service and were a base for paramedics who regularly attended patients within a participating falls prevention service’s catchment area.
We invited paramedics based at selected ambulance stations to participate in the trial before allocating those stations randomly between intervention and control groups. Paramedics were approached via e-mail, letter and station posters and were asked to return a reply slip if they were interested in participating. Paramedics who volunteered to participate were given a £50.00 voucher.
Patients received either intervention or control group care, depending on the group allocation of the attending paramedic. During training, intervention paramedics were instructed to lead on care if there was also a control group paramedic on-scene, and these patients were included in the intervention group for analysis.
Inclusion criteria:
-
aged ≥ 65 years
-
resident in the catchment area of participating falls services
-
attended by a study paramedic following an emergency call to the ambulance service which was coded by a dispatcher as a fall without priority symptoms (Advanced Medical Priority Dispatch System Code 17)
-
first eligible call during the trial period.
Randomisation
Randomisation of stations to groups was carried out in accordance with principles related to cluster randomisation and blinding of analysis team, as outlined in the West Wales Organisation for Rigorous Trials in Health and social care (WWORTH) standard operating procedure (SOP) on randomisation. 102 The trial statistician (WYC) and manager (JP) undertook randomisation after recruitment of paramedics had closed, to avoid selection bias, using trial site, volume of calls, falls service and the number of participating paramedics as stratification variables.
Recruitment
Patients were identified as being potentially eligible for study inclusion from routine emergency service dispatch records through standardised queries written for each site. Site researchers confirmed eligibility of individual patients by retrieving corresponding patient report forms (PRFs), which are routinely completed by paramedics when they attend a patient. PRFs include patient identifiers and demographics; and operational, clinical assessment and treatment information.
In this cluster trial we did not ask paramedics to approach patients for consent to participate in the trial during the emergency episode. Instead, following identification of eligible patients as detailed in Participants, we sought consent from patients for follow-up through routine medical records and by postal questionnaire. Following considerable discussion with the Research Ethics Committee, our consent process included contacting patients by post and then, if necessary, by telephone or a home visit. Patients then had the opportunity to actively ‘consent’ or ‘decline consent’ (dissent). However, we were unable to contact some patients at all (no response by post or telephone). We had Health Research Authority Confidentiality Advisory Group (HRA CAG) permission to follow up this group anonymously (but they neither ‘consented’ nor ‘declined consent’). The group we analysed consisted of those who had consented and those who we could not contact (follow-up was through an anonymised route). Only those who had actively declined consent (dissented) were excluded from this group. The postal consent pack (see Appendix 6) included:
-
covering letter
-
consent form
-
patient information sheet
-
1-month questionnaire (see Appendix 7)
-
Freepost return envelope
-
£5.00 voucher, to thank participants for their time.
Interventions
Experimental: intervention group care
The core of the health technology we evaluated was a clinical protocol for the care of older people who have fallen, enabling emergency ambulance paramedics to assess and refer them to community-based falls services (see Appendix 1). During a workshop held to define the intervention, participants from across specialties and sites agreed common minimum standards for each component of the intervention, with flexibility allowed for local differences in processes such as referral and documentation. The complex intervention comprised the assessment protocol (the health technology being trialled) and six other components, as shown in Table 11. Local variations are shown in detail in Appendix 8.
| Component | Core minimum standard | Local variation permitted |
|---|---|---|
| Assessment protocol | Clinical protocol to guide paramedic through the decision-making process and assess the patient’s risk of further falls and safety for non-conveyance | Consent process for patient agreement to be referred to falls service |
| Protocol may be used as aide memoire or as a specific additional form to the PRF | ||
| Training | One full day, with training package including programme, written materials and DVD (see Appendix 9) | Background and role of trainers, including members of falls teams when possible |
| Referral pathway | A pathway to allow intervention paramedics to refer patients to a falls prevention service, including a system to allow auditing of receipt of referral forms | Method and process of referral, to minimise any delays on-scene |
| Participation of GP practices across falls servicea catchment area | ||
| Referral tool | A form recording information to be passed to the falls prevention service, including basic demographic, clinical and contact details | Other information included in referral form |
| Falls service response to referral | Telephone contact with patient, by professional with ability to recognise cases where urgent input is needed | Time frame for initial patient contact and assessment |
| Initial face-to-face multifactorial assessment; multidisciplinary assessment if appropriate | ||
| Falls service provision | NICE guidance-adherent service: multidisciplinary treatment delivered by team of appropriately qualified professionals (may include, e.g. equipment, balance training, medical review) | Details of service and patient intervention |
| Clinical and operational support | Clinical support debrief with ED every 2–4 weeks plus feedback on outcomes for individual patients referred to falls service | Exact method and means of clinical support and feedback |
Control group care
Control group paramedics did not receive training in the intervention. We asked paramedics based at control stations to continue their usual practice. Although we know that conveyance rates vary considerably among services, stations and paramedics, we did not seek to standardise practice, as we were unable to identify best practice. Current practice in the control group was therefore care as usual comprising assessment of injury or other condition requiring immediate care, assistance in moving and conveyance to ED unless the patient refused.
Outcomes
Outcome measures at 1 month and 6 months after the patient’s index incident were consistent with recommendations of ProFaNE. 103
Primary outcome
A composite outcome of subsequent emergency health-care contacts (in order of severity, i.e. death, emergency admissions, ED attendances or emergency service calls), summarised by:
-
proportion of patients who suffer these events
-
interval to first event
-
event rate.
Secondary outcomes
At index incident:
-
onward pathway of care (conveyed to the ED; referred to falls service; referred to other provider)
-
compliance with guidelines for ambulance service clinical documentation
-
durations of: ambulance service job cycle (from receipt of emergency service call to time that ambulance reports being free for next call); episode of care (from receipt of emergency service call to end of emergency episode, i.e. the patient is left at home, discharged from ED or admitted to hospital); or time to falls service response.
At 1 month and 6 months after patient’s index incident:
-
duration of subsequent inpatient episodes
-
subsequent reported fractures
-
health-related quality of life, as measured by the Short Form questionnaire-12 items (SF-12)104
-
patient satisfaction as measured by the Quality of Care Monitor105 and ‘fear of falling’ as measured by the modified Falls Efficacy Scale (mFES)106
-
self-reported further falls
-
costs of care to NHS and PSS
-
self-reported costs incurred by patients and carers.
Qualitative:
-
views of ambulance service paramedics, managers and partners on implementation of the intervention
-
experience and satisfaction of patients receiving the intervention.
Data collection
-
Ambulance service: routine clinical and operational management information about index and subsequent contacts from despatch records (completed by emergency service call takers) and PRFs completed by paramedics during or immediately after patient attendance.
-
Falls services: information about referrals and falls service response.
-
Participants (or their carers): questionnaire data, sent by post to eligible patients at 1 month (see Appendix 7) and those who consented to a further questionnaire at 6 months (see Appendix 10).
-
Health and Social Care Information Centre (HSCIC) (England) and National Welsh Informatics Service (Wales): routine data about ED attendances, hospital admissions and deaths for all matched study patients over the study period.
At all three sites, patients who dissented by any means were excluded from all data collection. For all other patients, we collected anonymised data on index and subsequent health-care contacts. Identifying information collected at ambulance and falls services was split from clinical information by our trial partners within the three ambulance services. In order to improve the matching rate achieved by National Welsh Informatics Service and HSCIC, our ambulance service partners used imperfect emergency service call information such as name, address and date of birth to look up NHS numbers. Once patients were matched, clinical outcome data were retrieved and transferred for analysis into the Secure Anonymised Information Linkage (SAIL) gateway when it was joined up with questionnaire data.
Data entry
The method of data entry varied by source and site. Ambulance service despatch data were downloaded electronically to study databases. There were two types of PRF: paper and electronic. Sites 2 and 3 used only paper forms and site 1 used a mix of paper and electronic forms. Paper forms were input into study databases manually by the study team, whereas electronic forms were input automatically after they were downloaded from a central server. Questionnaires were input into study databases using Teleform software version 10 (Cardiff Software, Sunnyvale, CA, USA). A quality assurance check was carried out on all manually entered data.
Blinding
Blinding was carried out when possible. Paramedics, trial managers and site researchers were not blinded, as they needed to know the allocation of participating ambulance stations for operational reasons. The trial statistician and all other TMG members were kept blind to allocations in order to eliminate reporting bias. This was undertaken by coding the allocated groups in order to prevent group identification. Blinding statisticians is a technique recognised, both by statisticians in general and by the WWORTH SOP on statistics,107 as best practice in statistical analysis. Even though the WWORTH SOP also requires that trials agree statistical analysis plans before starting analysis, these cannot cover all eventualities, with the result that unblinded statisticians could unconsciously take analytical decisions that favour intervention over control or vice versa. Unblinding occurred after completion of primary analyses.
Sample size and power
We estimated our trial sample size from our principal outcome: the proportion of participants who, within 6 months, die or contact emergency services. From previous trials of interventions for older people who have sustained a fall and presented for emergency treatment, summarised in a recent systematic review,108 we made the conservative estimate that trial patients had about a 50% chance of making another emergency contact or dying within 6 months. We judged that a change of 5% in this proportion could be clinically and economically important. In the absence of clustering, a sample size of 4190 evaluable participants would have yielded 90% power to detect a change of at least 5% (from 50% to ≤ 45% or ≥ 55%) when using a two-sided 5% significance level. As participants came from 25 clusters, we needed to adjust this sample size to allow for intracluster correlation (ICC). We estimated this ICC from the findings of the SAFER 1 trial,79 which evaluated the clinical effectiveness and cost-effectiveness of computerised clinical decision support software for use by paramedics when attending older adults who had a fall. The SAFER 1 trial estimated the ICC for the same outcome, but over 1 month rather than 6 months, as 0 when clustering participants by station (as in the SAFER 2 trial), but 0.005 when clustering participants by paramedic (as in the SAFER 1 trial). 79 To be conservative, we allowed for an ICC of 0.002 by increasing the target evaluable sample to 6290, namely 25 clusters × 251.6 participants per cluster. This sample would have more than 90% power to detect a change of 0.18 in the number of emergency contacts of 1.8 over 6 months, given a standard deviation (SD) of 1.5. Hence, the SAFER 2 trial was able to detect a difference of 1 emergency contact in 10 avoided (or induced) by the intervention.
We had originally postulated that patients recruited to the study would have a 40% chance of making an emergency contact or dying within 6 months and that the ICC could be as high as 0.03. Under those assumptions our target sample of 6290 would have yielded 80% power to detect a change of at least 10% (i.e. from 40% to ≤ 30% or ≥ 50%) when using a two-sided 5% significance level. When the SAFER 1 trial showed that the assumed ICC was unduly pessimistic, recruitment was progressing well. Therefore, rather than finish the trial early, we decided, with the approval of both TSC and DMEC, to be less conservative in assuming a worst ICC of 0.02, thus yielding enough power to detect a change of only 5% in the emergency contact rate, still a clinically important difference in the view of our advisers.
Statistical methods
The full analysis plan can be found in Appendix 11. Primary analysis was by ‘treatment allocated’. Analyses included logistic regression for binary outcomes; cross-tabulations and risk ratios for categorical outcomes; and survival analysis including Cox’s proportional hazards models for times to events. We used multilevel modelling to estimate (random) station effects and (fixed) group effects and analysed repeated observations as such.
Our principal outcome is made up of a hierarchy of events. We therefore undertook analysis incrementally: first, deaths; second, emergency admissions plus deaths; third, ED attendances plus admissions and deaths; and, finally, emergency service calls plus attendances, admissions and deaths. Although we originally planned to undertake analysis for all events and for those coded as a fall, in practice data quality across the levels precluded analysis of falls only. We have presented results as follows: the proportion of patients who called the emergency services, attended ED, were admitted or died; survival analysis of the time to the first subsequent emergency contact; the mean number of further emergency contacts adjusted for time at risk, excluding days in hospital or after death; and recurrent event analysis when feasible. We also examined the effect of the intervention on patient satisfaction, health-related quality of life and costs (as described under Economic evaluation).
Potential predictors of triage decisions include the distance between the site of the index event and the ED; patients’ age, sex and history of previous falls; type of presentation [specifically, a seasonality term capturing when, during the calendar year, the call was made, and an indicator of whether or not it was made out of (GP) hours]; and time since recruitment started (recruitment point). The list of adjusting factors (covariates) includes those suggested by the TSC and may be divided into three subsets: (1) group and site interactions, reflecting study design; (2) participant characteristics (age and gender); and (3) characteristics related to the timing and location of the index incident. We used the covariates in the analysis. It is possible that patients in the catchment area of one station may receive care for a subsequent event from a paramedic based at another station participating in the study but allocated to a different group. Nevertheless, analysis was still by treatment allocated. We have identified referrals made to falls services at subsequent emergency service call attendances and are able to use this for censored analysis in order to minimise contamination, but this is not included in the current report.
We proposed to identify any wider system effects, by comparing response times during the trial period across the study catchment area and surrounding areas with pretrial response times and response times elsewhere. This analysis would only be necessary if effects were found on ambulance operational performance indicators – job cycle time within the trial population.
To inform the development of outcome measures for falls research as recommended by ProFaNE,103 we compared SF-12 and derived Short Form questionnaire-6 Dimensions (SF-6D) scores with mFES scores to establish their construct validity. We also assessed their predictive validity by comparing scores with the number of further events and the time to the first subsequent event.
Missing data
We adopt a consistent approach to missing data relating to both clinical effectiveness and cost-effectiveness, except when individual outcome measures require some variation in that approach. For each variable, we consider the frequency of missing data; if there is no reason to suspect that data are not missing completely at random, we use appropriate imputation methods to mitigate the problem of missing data. Specifically, in addition to taking the SF-6D score as 0 when a participant is dead at the data collection point, we imputed missing values by regression (thus adjusting for other covariates) from all available values of that score at other data points.
Adverse events
As the study population had high mortality and morbidity, we did not routinely record or report AEs that were neither serious nor adverse reactions (ARs) in the sense of possibly being caused by the new clinical protocol for referring to falls services. The main potential AR is misdiagnosis, which could lead to an inappropriate pathway of care. As misdiagnosis is reliably identifiable only through patient complaints or coroner’s inquest, we focus on these, and treat them as serious ARs. Any patient complaint or coroner’s inquest at which the ambulance service was asked to supply information related to non-conveyance of a trial participant from the index incident triggered was investigated by the local principal investigator and chief investigator. We also investigated suspected ARs brought to our attention in any other way.
Death or emergency hospital admissions are serious adverse events (SAEs). As these form the primary outcome of this trial, and are not unusual or unexpected in the study population, we report them at the end of the trial. In particular, the imbalance between intervention and control groups in the occurrence of SAEs or serious ARs was the subject of statistical analysis at the end of the trial.
Economic evaluation
Aim
We undertook an economic evaluation alongside the RCT from the perspective of the UK NHS and PSS, in line with the approach recommended by NICE. Economic analysis estimated the costs of providing the intervention and the consequences of the scheme for the NHS and PSS in terms of inpatient admissions, ED attendances, GP consultations, out-of-hours GP contacts, NHS Direct contacts and use of social services.
Method
We estimated the costs of providing the new intervention by utilising data collected from financial reports and documents, relevant information logged as a part of routine practice and from resource utilisation recording sheets, together with reference to patient records and discussions with relevant finance staff. We collected data on participants’ use of health service and social services resources from paramedic records, routine hospital records and patient-completed questionnaires. We estimated NHS resource use from routine data including duration of ambulance job cycles and episodes of care; records of resource use; and patient records. We also estimated social services resource costs from discussion with relevant social services departments. Costs were then calculated using published unit costs such as the Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care 2013123 and NHS Reference Costs 2011–12. 109
Health-related quality-of-life outcome
The SF-6D scores (derived from SF-12 scores) were used to estimate the QALYs gained from the intervention and an incremental cost per QALY, applying appropriate threshold incremental cost-effectiveness ratios, such as the £20,000.00 and £30,000.00 per QALY thresholds used by NICE. These ratios were presented along with their associated cost-effectiveness acceptability curve.
Lost to follow-up/missing data
If a participant was dead at the data collection point, the SF-6D score was taken as 0. To avoid outliers, SF-6D and mFES scores were taken to be the minimum value observed for that measure in the relevant treatment group. The problem of missing data was addressed using an appropriate regression-based imputation approach, as reported earlier.
Discounting
As the outcomes were assessed at 1 month and 6 months, no discounting was employed.
Uncertainty
We addressed uncertainty by applying bootstrapping for cost-effectiveness acceptability curves and CIs. Sensitivity analyses were undertaken to assess the robustness of results to changes in the configuration of the intervention and other health service costs.
Qualitative methods
Aim
The qualitative component of the trial was designed to address the following two of the study objectives:
-
Gain an in-depth understanding of how the intervention is experienced by patients.
-
Understand how the intervention is delivered in practice, identifying factors which enable or hinder its use.
Participants
Patients
We undertook qualitative interviews with a sample of trial patients who had experienced a fall, were seen by an intervention paramedic and agreed to the interview. Patients were selected from all three study sites, with a target number of 20 from each site. A mix of patients was identified for interview: those who had been taken to ED; those who had been referred to a falls service; and those who were neither taken to the ED nor referred to a falls service.
All eligible patients who had been referred to a falls service were selected for interview. The other two patient groups (taken to ED and left at home without referral) were much larger; sampling was therefore carried out so that only every 10th sequential patient was selected for interview. The selected patients were then telephoned to arrange an interview. Whenever possible, this occurred 6–8 weeks after the index incident, although in practice some interviews took place up to 4 months after the index incident. A log of the interviews undertaken and the characteristics of the patient’s index incident (i.e. location, disposal, patient sex and patient age) was kept in order to ensure that all patient groups were interviewed.
Paramedics
We invited all intervention paramedics who volunteered to take part in the study to discuss their expectations and experiences of the intervention. Whenever possible, paramedics were invited to take part in a focus group,110 bringing together between four and eight of their peer group in a local venue within their ambulance service area. When paramedics were not available to take part in a focus group, we invited them to take part in a face-to-face interview.
We carried out interviews with paramedics before they started to carry out the intervention (pre trial but after having received the training) and after the patient recruitment phase (post trial).
Other stakeholders
In each study site, data were gathered after the end of the trial period from other relevant staff involved in delivering the intervention: training staff and management staff from the ambulance service, and those involved in managing and delivering the falls service. Participants were selected purposively and were invited to take part in focus groups; those who were not able to attend a focus group were invited to take part in an interview instead.
In each of site 2 and 3, one focus group was held of staff involved in delivering the falls service, and one of staff in the ambulance service with a training or supervisory role. In addition to this, in site 3 two one-to-one interviews were conducted with stakeholders who were not able to attend a focus group. In site 1, stakeholders took part in four one-to-one interviews, but no focus group.
Data collection
We interviewed patients and paramedics only in the intervention arm (not in the control group) because we were interested in how the intervention was used and experienced in practice, and the mechanisms by which it may or may not have worked.
Patient interviews
A schedule (see Appendix 12) for face-to-face, semistructured patient interviews was developed by the research team, drawing on the aims and objectives of the study, in order to explore:
-
patients’ experience of the ambulance service
-
patients’ experience of those seen by a falls service
-
patients’ health since fall
-
patients’ satisfaction with treatment.
Face-to-face semistructured interviews were conducted by experienced researchers from the study team (RA, RC, MK, LW). In some cases, a carer or other person who had been present at time of fall also took part in the interview or was present to support the participant. Interviews took place in patients’ own homes, and were recorded and later transcribed in full.
Paramedic focus groups and interviews
Data collection with paramedics took place at two points in the study:
-
at baseline, after paramedics had been trained in the SAFER 2 trial intervention but before they started using it in practice (see Appendix 13)
-
after the end of the patient recruitment period (see Appendix 14).
Separate topic guides were developed by the research team for each phase of data collection, drawing on the aims and objectives of the study. The topic guides were reviewed by members of the LITs, which included ambulance service personnel at different clinical, operational and management levels. The focus group topic guides were adapted for use in one-to-one interviews. The topic guide covered:
-
paramedics’ views and attitudes towards the new intervention
-
any preconceptions about the new way of working
-
factors which enabled the use of the new referral pathway
-
factors which hindered the use of the new referral pathway.
Each focus group was led by one researcher, with a second member of the team acting as support and taking notes to enable the linkage of texts to speakers, and noting other details, such as points of consensus or disagreement, issues that drew strong emotional responses such as anger, fear or anxiety. All focus groups and interviews, with the permission of participants, were recorded and transcribed in full.
Stakeholder focus groups and interviews
Topic guides (see Appendix 15) were developed by the research team for use with ambulance service personnel and wider stakeholders, and covered:
-
perception of how well the intervention worked
-
impact on the stakeholder’s organisation
-
cross-organisational working
-
views on the process of implementing the intervention.
Stakeholder focus groups took place before the main results of the trial were known. Each was led by one researcher, with a second member of the team acting as support and taking notes to enable the linkage of texts to speakers, and noting other details, such as points of consensus or disagreement, issues that drew strong emotional responses such as anger, fear or anxiety. Each interview was carried out face to face, and was conducted by one member of the research team. All focus groups and interviews, with the permission of participants, were recorded and transcribed in full.
Qualitative data management
As this was a team-based project involving collection of data in multiple sites, maintaining consistency in data collection and transcription was crucial. The co-ordinator set up a data management system consisting of instructions on converting raw data to computer files (in the form of a transcription protocol), on organising data storage and on data archiving steps and a data management checklist. The transcription protocol ensured that standard conventions were adopted throughout the transcription process, and that a standard presentation format was used. All transcripts were anonymised and stored securely. Transcripts of interviews with stakeholders were sent back to the participant for checking, to ensure that they were accurate.
Qualitative data analysis
The data were analysed thematically using a modified version of the framework analysis approach for applied policy research. 111 This is a systematic, dynamic and transparent method of analysis, which generates themes from the original accounts of participants. 112
Two separate analysis tasks were carried out: data from patient interviews were analysed to address objective 3; and data from focus groups and interviews with paramedics and stakeholders were analysed to address objective 4. Each task consisted of the following stages:
-
The transcripts were distributed for reading among members of the research team (RA, RC, SG, MK, AP, LW and AT, the patient representative) so that each had at least five to read, with each transcript being read by two people.
-
Each member of the research team made notes on themes and ideas, guided by the relevant study objective.
-
The research team met to discuss and agree a coding frame.
-
Two researchers independently coded up two transcripts each using the coding frame, discussed how well it worked, and then revised the coding frame. The final coding frames are shown in Appendix 16.
-
RA, RC, MK and AP used the revised coding frame on one transcript, then compared coding to check consistency.
-
Transcripts were then shared among RA, RC, MK and AP for coding. RA then entered all codes into an NVivo database (QSR International, Warrington, UK) (one database relating to objective 3 and one relating to objective 4).
-
RC, MK and AP met to discuss overall themes and findings relating to each objective, drawing on the NVivo database and the coding frame.
The qualitative findings in Chapter 6 present anonymised quotations from participants. In line with the guidance from Corden and Sainsbury,113 quotations have been used to present evidence, to support explanation of complex ideas, to provide illustration, and to deepen understanding, particularly when respondents had an emotional response. Although many quotations were selected to illustrate the majority view, some show exceptional viewpoints, as noted. In some cases, quotations were selected to illustrate complexity or ambiguity of perspective, as noted.
Involvement of service users
Involving service users in research is encouraged to improve relevance, quality and accountability of research. 114–117 The SAFER 2 trial followed the principles and procedures outlined in the WWORTH SOP for user inclusion118 to ensure that members of the public were actively involved throughout the research process. This SOP provided a starting point for developing a model of user involvement in the SAFER 2 trial. Moreover, the SAFER 2 trial aimed to address the challenges of involving older people, who are often in poor health because of their falls history or falls risk. The model took into account the multiple layers of a multisite trial and proposed three tiers of involvement in different forums at the strategic, site and local levels where overall or specific input could be made. We followed best practice guidance by involving two service users in each of the strategic trial committees. 114,119,120 We also involved service users at site (n = 3) and local levels (n = 18) of the trial to provide a range of forums and opportunities for involvement by older people with risk of falling. Our involvement model received the Involving People Award in 2014 as an example of best practice.
Strategic level
Two service user members were sought for each of the TMG, TSC and DMEC. These strategic level meetings involved trial co-applicants and independent members. They were responsible for trial oversight and took strategic level decisions.
Site level
Local implementation team meetings took place at each site to oversee the delivery of the trial, and service users were sought to participate in these. In addition, in each of the three sites a Service User Reference Group was formed to provide forums for service users to discuss and contribute to the study. They were co-ordinated by the site researchers and held meetings at universities and community venues. Membership, meeting arrangements and frequency varied, reflecting local interest and individual needs.
Local level
Service user representatives took part in task-and-finish groups to develop the patient questionnaire and associated paperwork and to find ways to improve questionnaire response rates. Finally, towards the end of the study period, service users took part in qualitative analysis meetings.
Service users were recruited by various routes:
-
previous experience of participating in research studies or membership of a standing user involvement group connected to a university
-
membership of a third-sector organisation bringing together members of the target population (e.g. the Princess Royal Trust for Carers)
-
Involving People Network providing links to service users
-
personal contact from the research team.
All service users contributing to the trial were provided with training and support (including expenses payments) in line with guidelines set by the public involvement organisation INVOLVE. 114
Through the methods adopted by the trial, service users were involved in a range of trial processes, including developing and planning research; overseeing the management of the trial; refining data collection methods; and contributing to analysis, particularly of the qualitative data. Appendix 17 is a case study from one of our service users about his involvement in the SAFER 2 trial.
Support and Assessment for Fall Emergency Referrals 2 trial progress
This section details the ‘story’ of the study, charting progress from the awarding of funding to the completion of the project, highlighting the main events leading to the successful completion of the study and events that led to unforeseen setbacks to the project timetable.
The SAFER 2 study received confirmation of funding from the HTA programme in January 2009. The trial ethics application was submitted to the Multicentre Research Ethics Committee for Wales in April 2009. This highlighted the proposed consent process (the same used in the SAFER 1 trial), in which patients were invited to ‘opt out’ if they did not wish to take part in the study. The committee approved this process subject to permission from the then National Information Governance Board Ethics and Confidentiality Committee (now the HRA CAG), as it would involve accessing patient information without their explicit written consent. The Ethics and Confidentiality Committee did not give approval on the basis an active opt-in consent process should be used. This decision had implications for the trial as it required potential participants to return signed consent forms, which would be likely to lead to a low inclusion rate with the more elderly, frail and vulnerable patients under-represented. After consultation with our research team members, we proposed an alternative process for recruitment, combining both informed consent (gained either postally or via telephone) and anonymous follow-up, initially via the SAIL system in Wales. Ethical approval was gained in February 2010, 11 months behind schedule. In 2012, a further application to the HRA CAG for anonymised follow-up of patients from England who had not declined consent (dissented) through the HSCIC was approved.
Alongside this, the study team needed to confirm the participation of ambulance and falls services; negotiation was required with service providers to agree arrangements for participation.
-
In site 1, two of the six falls prevention services declined to participate in the trial because of concerns with capacity.
-
In site 2, one of the two health boards implemented a ‘Frailty Programme’ during the same time period the trial was scheduled to run. Under the Frailty Programme, all older people who fell and called the emergency services were referred on to be seen at home immediately. This compromised the trial methods, as there would be no control group. Negotiations were ongoing for several months as to the best way to run the two programmes alongside each other, but the health board eventually decided to not participate in the study because of this conflict with local service developments.
-
Owing to delays setting up the study, the commencement of the SAFER 2 trial coincided with the ambulance service that contained site 3 introducing a financial reimbursement for referrals to GPs of people who had fallen. This was incompatible with the RCT design because of the elimination of the control group, which would lead to significant issues at this site. Following the chief investigator’s attendance at a senior-level strategic meeting, site 3 reaffirmed its commitment to full participation in the trial, with the GP referral programme introduced across the service except in the trial catchment area. Research and development (R&D) permissions were signed off, with a collaborator’s agreement in place.
Owing to risks around the participation of site 3 and falls services in the site 1 and site 2, in August 2010 we held discussions with a fourth ambulance service that expressed an interest in joining the trial. After a period of negotiation and consideration across local partner services, it decided that it could not participate in the trial at this time.
By early 2010, participating services were confirmed. In total, the study involved three ambulance services, with 26 NHS partners based within five comprehensive local research networks (CLRNs) and NHS trusts. Research governance processes commenced across the three trial sites, later than scheduled, in March 2010. Although English ambulance services, which each span several CLRNs, had a lead CLRN identified, at the time it was not clear how this process (i.e. research processes, cost attribution and support to carry out studies) worked for the participating acute trusts and primary care trusts (PCTs) in the trial areas. On advice from these organisations, principal investigators were identified and approached for sign-up at the 26 NHS organisations. Site-specific information forms were prepared, but these could neither be completed nor a formal sign-up of NHS organisations be achieved without agreement of the attribution of costs across the trial. Although NHS costs had been estimated at the outset of the planning process, these were affected by changes to the study design (in particular the recruitment and data retrieval processes) and lack of clarity about cost attribution. Discrepancies between CLRN and NHS research site views on cost attribution led to the set-up of a meeting with the Department of Health in May 2010, in which the attribution of costs was finally agreed.
Alongside the processing of research governance approvals, the study team were developing the SAFER 2 trial intervention. Undertaken using the Medical Research Council guidance,64 the intervention was established through the use of previous literature, a stakeholder workshop, modelling and patient involvement (see Appendix 8).
It was very difficult to predict how long it would take to complete R&D processes at global and local levels across the research sites. R&D approvals for all three sites (with the exception of some acute trusts in site 3, where full R&D approvals were not gained until March 2012) were finally gained in October 2010, allowing the trial to commence.
The delays outlined above had a knock-on effect on the overall timescale of the project. In mid-2010, we revised the project timetable, proposing that the full pilot with recruitment of patients for the study started in January 2011 followed by the main trial in February. Owing to the study team receiving additional data regarding the number of older fallers seen by paramedics, we reassessed the expected recruitment rate in order to meet recruitment targets, resulting in a proposed extension to the recruitment phase of 2 months (until the end of October 2011 instead of the end of August 2011).
As the trial gained momentum, we looked to recruit two new research support officers, funded through service support costs (CLRN/National Institute for Social Care and Health Research) to undertake administrative tasks associated with patient recruitment. These ambulance service-based roles (which were undertaken by paramedics in site 2 and site 3 and an administrative assistant within site 1) were key to paramedic recruitment, as our researchers had restricted access to ambulance stations and identifiable data. Full funding agreements had to be in place before the ambulance services would proceed with recruitment to these posts, which led to delays in advertising and filling them. Further delays occurred in site 3 because of issues releasing paramedic staff to undertake these roles. Inevitably, this had a knock-on effect on the paramedic recruitment schedule.
Paramedic recruitment to the trial commenced in November 2010 at the three trial sites. Recruitment of paramedics was initially slow; some showed unwillingness to be involved in the trial when there was a 50% chance of being randomly allocated to the control group. In December 2010, we received approval from the ethics committee to provide a £50.00 voucher to paramedics for taking part (in London the money was pooled into a station training budget); this allowed paramedic recruitment to increase.
Paramedic training was undertaken once stations (clusters) were randomly allocated to either control or intervention arms of the trial. Paramedics based at intervention stations underwent training delivered by ambulance service trainers, falls service representatives and the study team, using a cascade method originating with the training team who developed the clinical protocol. In early 2011, following the successful completion of paramedic training, patient recruitment commenced. Site 1 was first to start in March 2011, with sites 2 and 3 following in April and July, respectively.
Identification of eligible patients required a high level of resources. In two of the trial sites (1 and 2), PRFs containing patient details needed to confirm eligibility into the trial were particularly difficult to locate. These forms were completed by paramedics on-scene and were stored at ambulance stations before being centrally collated. Considerable effort was put into locating the forms, which were often difficult to locate because of the issues with data reliability. Ambulance service senior managers were aware of the issue and were helpful in terms of supporting the location and retrieval of the outstanding forms.
The study team wrote to patients to gain informed consent once study eligibility had been confirmed. Informed consent is particularly challenging in prehospital care research and in the SAFER 2 trial this was even more so as the participants were frail and elderly. Initially, patient consent rates were low, at around 10%. In August 2011, following a review of the consent procedures, the study team proposed an alteration to the consent process, including simplification of the consent form, sending of the questionnaire with the initial patient letter and inclusion of a £5.00 voucher to thank patients for their time spent considering the study. A substantial amendment was submitted to and approved by the Multicentre Research Ethics Committee, allowing the process to be altered. The consent rate to identifiable data follow-up increased to 30%. In early 2012, a front cover was added to the existing questionnaire to improve response rates.
In October 2011, the trial was temporarily suspended at site 1, because of internal governance concerns regarding the processes of verbal consent of patients over the telephone. As a consequence, we revised the way in which verbal consent was recorded across the trial. From the start of the patient recruitment phase, it was clear that fewer eligible patients were being attended by study paramedics within sites 2 and 3 than estimated from the pilot data received at the start of the study: this was mainly because of paramedics working outside the study catchment area. This, coupled with the previously mentioned issues around ethical approvals, information governance and R&D permissions, meant the study fell behind its recruitment schedule. Originally, patient recruitment was scheduled to finish in December 2011. In early 2012, the HTA funded an extension to the study, allowing patient recruitment to carry on until the end of June 2012.
Summary of changes to the project protocol
The following changes were made to the original protocol after it was funded:
-
The process for recruiting patients to the trial was amended following ethical approval from an opt-out process to an active opt-in consent process including follow-up telephone call.
-
Participating ambulance stations at the London site were changed from South to North Central London stations, following set-up of a falls service in the original proposed study area.
-
The paramedic recruitment process was amended to include a £50.00 voucher for those who volunteered.
-
The number of paramedics recruited at each site was updated to reflect actual numbers recruited, which were greater than originally stated.
-
The European Quality of Health-5 Dimensions (EQ-5D) was not used. In order to be consistent with outcome measures used on the SAFER 1 trial, we instead used the derived SF-6D.
-
Patient recruitment was further amended after the trial commenced to include a simpler process and the addition of a £5.00 voucher with the invitation pack. This was in order to improve response rates.
-
An anonymised data follow-up process for the two English sites was added.
-
We originally planned to compare test–retest reliability and responsiveness of the instruments, by sending a retest questionnaire to 100 randomly selected patients from each site. We did not proceed with this because of the evident difficulties our frail and elderly patients were experiencing completing essential study documentation.
-
Administration of the Patient Generated Index was also originally included as part of the qualitative patient interviews. Owing to time and resource pressures this was not carried out.
-
The study received two extensions. The first extended the study by 15 months, from 30 June 2012 to 30 September 2013. Owing to difficulties in gaining ethical permission at the commencement of the study, there had been a delay to the start, which had a knock-on effect to the rest of the trial. Recruitment was also slower than expected, and the extension allowed for us to reach our projected recruitment target. The second (unfunded) extension was for a further 4 months, to 31 January 2014. This was to allow time for full analysis of the data, following difficulties in retrieving anonymised outcome data.
Ethics and research governance
Ethical approval was obtained from the Research Ethics Committee for Wales, Information Governance approval from the National Information Governance Board, and NHS R&D approval from each participating health board, NHS trust and PCT.
Trial registration
The trial is registered as Current Controlled Trials ISRCTN60481756 and UKCRN 6801. The trial protocol has been published. 71
Chapter 4 Clinical effectiveness results
Participant flow
Between March 2011 and June 2012 a total of 5914 eligible patients were attended by 215 paramedics based at 25 ambulance stations across the three study sites [Consolidated Standards of Reporting Trials (CONSORT) flow chart in Figure 2; site CONSORT flow charts in Appendix 18]. Six of 31 eligible stations withdrew after randomisation but before the start of patient recruitment because of a conflicting ‘Frailty Programme’ intervention being introduced throughout one participating health board area at site 2. Participating paramedics based at 14 stations were randomly allocated to the intervention group and those based at the remaining 11 stations were randomly allocated to the control group. After 1210 (20%) dissenting patients were excluded, 4704 (80%) were available for follow-up: 2420 in the intervention group and 2284 in the control group. As all but 49 patients were subsequently matched at SAIL or HSCIC, we included 4655 patients in analysis of anonymised linked data primary outcome.
FIGURE 2.
Flow of clusters and individuals through RCT for all participants. Adapted from Snooks et al. 121 with permission from the American College of Emergency Physicians. Copyright © 2017 American College of Emergency Physicians. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).

Recruitment
Patients were recruited to the trial between 14 March 2011 and 30 June 2012. Start dates varied between March and July, as sites were ready to begin recruiting patients. All sites finished recruitment at the same time point (Table 12).
| Site | Recruitment period | ||
|---|---|---|---|
| Start | End | Length in days | |
| Site 1 | 14 March 2011 | 30 June 2012 | 475 |
| Site 2 | 4 April 2011 | 30 June 2012 | 454 |
| Site 3 | 6 July 2011 | 30 June 2012 | 361 |
We followed up patients for 6 months after the index incident.
Baseline characteristics
Individual patient level
Although we expected recruitment of patients to be similar across ambulance service sites, and similar numbers of ambulance stations participated in the trial at each site, recruitment of patients was much higher at site 1 as a result of several factors including:
-
longer recruitment period at site 1
-
operational practice which took paramedics out of the trial catchment area, particularly in site 3
-
loss of six stations and related paramedics at site 2.
There was also variation in recruitment between trial arms across sites, with a higher proportion of control group patients recruited at site 1 than at either site 2 or 3. There was very little difference between groups in age, overall or at any site. There were more women than men recruited to the trial, although the proportion of men was slightly higher in the intervention group than the control group, with about 3% more at each site and overall. There was little difference between trial arms in the proportion of calls made outside usual GP operating hours was similar between trial arms, distance to ED or time to recruitment (Table 13). There were some differences between sites, for example site 3 had a lower proportion of female patients, a lower proportion of calls made ‘out of hours’ and shorter distances to ED. This was our most urban site, which may have accounted for these differences in study population.
| Variables | Group | |
|---|---|---|
| Intervention | Control | |
| Individual variables | ||
| Number of participants | ||
| All sites | 2420 | 2284 |
| Site 1 | 1329 | 1352 |
| Site 2 | 544 | 436 |
| Site 3 | 547 | 496 |
| Age (years), mean (SD) [n] | ||
| All sites | 82.54 (7.97) [2414] | 82.14 (8.11) [2275] |
| Site 1 | 82.99 (7.81) [1329] | 82.57 (7.91) [1352] |
| Site 2 | 82.79 (7.97) [538] | 81.79 (8.60) [427] |
| Site 3 | 81.20 (8.21) [547] | 81.28 (8.16) [496] |
| Female, proportion (%) | ||
| All sites | 1480/2419 (61.2) | 1477/2284 (64.7) |
| Site 1 | 816/1329 (61.4) | 882/1352 (65.2) |
| Site 2 | 351/543 (64.6) | 292/436 (67.0) |
| Site 3 | 313/547 (57.2) | 303/496 (61.1) |
| Emergency service index call out of hours, proportion (%) | ||
| All sites | 1012/2419 (41.8) | 954/2282 (41.8) |
| Site 1 | 624/1328 (47.0) | 626/1352 (46.3) |
| Site 2 | 221/544 (40.5) | 174/436 (39.9) |
| Site 3 | 167/547 (30.5) | 154/494 (31.2) |
| Distance to ED (miles), mean (SD) [n] | ||
| All sites | 4.77 (3.43) [2406] | 4.65 (3.08) [2270] |
| Site 1 | 5.03 (3.09) [1329] | 5.04 (2.61) [1352] |
| Site 2 | 7.33 (3.38) [542] | 6.75 (3.65) [434] |
| Site 3 | 1.55 (0.74) [535] | 1.71 (0.72) [484] |
| Recruitment point (days), mean (SD) [n] | ||
| All sites | 221.8 (129.0) [2420] | 220.8 (129.2) [2284] |
| Site 1 | 239.4 (136.4) [1329] | 238.1 (132.9) [1352] |
| Site 2 | 217.4 (128.8) [544] | 227.0 (128.7) [436] |
| Site 3 | 183.4 (98.6) [547] | 168.3 (102.9) [496] |
| Cluster variables | ||
| Number of stations (number of paramedics) | ||
| All sites | 14 (105) | 11 (110) |
| Site 1 | 5 (39) | 4 (38) |
| Site 2 | 5 (26) | 4 (26) |
| Site 3 | 4 (40) | 3 (46) |
| Recruited paramedics per station, mean (SD) | ||
| All sites | 7.5 (5.185) | 10 (6.708) |
| Site 1 | 7.8 (4.97) | 9.5 (4.203) |
| Site 2 | 5.2 (3.033) | 6.5 (2.082) |
| Site 3 | 10 (7.348) | 15.33 (11.15) |
Cluster level
We randomly allocated one more station to the intervention group than the control group at each site. However, we recruited fewer paramedics recruited per station in the intervention arm than in the control arm at each site.
Numbers analysed
Table 14 shows questionnaire response rates for all 4704 eligible patients who did not dissent and for whom we sought to retrieve linked data outcomes. However, SAIL and HSCIC could not match the demographic data for 29 intervention patients (18 in site 1, 4 in site 2 and 7 in site 3) and 20 control patients (15 in site 1, 3 in site 2 and 2 in site 3). Therefore, we could not retrieve data on ED attendances, hospital admissions or death for these 49 patients.
| Variable | Group | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||||
| Site 1 | Site 2 | Site 3 | Total | Site 1 | Site 2 | Site 3 | Total | ||
| Total number of eligible participants | 1329 | 544 | 547 | 2420 | 1352 | 436 | 496 | 2284 | 4704 |
| No consent to 1-month questionnaire (before new consent process), n | 330 | 117 | n/a | 447 | 301 | 93 | n/a | 394 | 841 |
| Died within 1 month, n | 86 | 31 | 30 | 147 | 79 | 26 | 32 | 137 | 284 |
| Participants sent 1-month questionnaire, n | 913 | 396 | 517 | 1826 | 972 | 317 | 464 | 1753 | 3579 |
| Valid 1-month questionnaires returned, n | 322 | 191 | 155 | 668 | 337 | 162 | 140 | 639 | 1307 |
| 1-month questionnaire response rate, % | 35.3 | 48.2 | 30.0 | 36.6 | 34.7 | 51.1 | 30.2 | 36.5 | 36.5 |
| No consent to 6-month questionnaire, n | 759 | 299 | 313 | 1371 | 743 | 261 | 295 | 1299 | 2670 |
| Died within 6 months, n | 249 | 116 | 93 | 458 | 270 | 75 | 75 | 420 | 878 |
| Participants sent 6-month questionnaire, n | 321 | 129 | 141 | 591 | 339 | 100 | 126 | 565 | 1156 |
| Valid 6-month questionnaires returned, n | 172 | 79 | 104 | 355 | 185 | 62 | 76 | 323 | 678 |
| 6-month questionnaire response rate, % | 53.6 | 61.2 | 73.8 | 60.1 | 54.6 | 62.0 | 60.3 | 57.2 | 58.7 |
Accounting for people who did not consent to questionnaires and those who died within 1 month, the overall response rate was 36.5%. Although there was little difference between intervention and control groups, response rates ranged from 30.0% at site 3 to 49.5% at site 2.
At 6 months the overall response rate was 58.7% (60.1% in the intervention group and 57.2% in the control group). Again there was variation in response rate between sites from 54.1% at site 1 to 67.4% at site 3. Furthermore, in site 3, 73.8% of the intervention group returned a 6-month questionnaire compared with 60.3% of the control group.
Outcomes and estimation
We did not find any significant differences between groups in our composite primary outcome at 1 month or 6 months. One-third of patients had suffered a further emergency episode or death by 1 month, rising to over two-thirds by 6 months. When primary outcome components were analysed separately we found evidence of significantly lower demand in the intervention group. Tables 15 and 16 show fewer further emergency service calls at both 1 and 6 months, with differences largely consistent across sites, and some indication of fewer ED attendances at 6 months, albeit with significant variations across the three sites (Tables 17 and 18).
| Primary outcome | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|
| Intervention | Control | Estimate, p-value | 95% CI | Estimate | 95% CI | |
| Overall composite outcome | ||||||
| Proportion of patients with further emergency service call, ED attendance, emergency admission or death,c n/N (%) | 870/2391 (36.4) | 843/2264 (37.2) | OR = 0.956; p = 0.461 | 0.848 to 1.077 | 0.0009 | 0 to 0.0048 |
| Primary outcome components | ||||||
| Proportion of patients dying (any cause),d n/N (%) | 147/2391 (6.1) | 136/2264 (6.0) | OR = 0.994; p = 0.960 | 0.780 to 1.266 | 0 | n/a |
| Proportion with further emergency admission,e n/N (%) | 517/2391 (21.6) | 475/2264 (21.0) | OR = 1.039; p = 0.595 | 0.903 to 1.196 | 0.0019 | 0.0002 to 0.0060 |
| Proportion of patients with further ED attendance,f n/N (%) | 463/2391 (19.4) | 418/2264 (18.5) | OR = 1.067; p = 0.392 | 0.920 to 1.237 | 0.0070 | 0.0021 to 0.0151 |
| Further ED attendances per patient,g mean (SD) [n] | 0.2631 (0.6162) [2197] | 0.2609 (0.7954) [2093] | Λ = 1.104 (p = 0.219) | 0.943 to 1.293 | 0.0058 | 0.0017 to 0.0128 |
| Further ED attendances/patient/day at risk,h mean (SD) [n] | 0.0236 (0.1018) [2197] | 0.0223 (0.0833) [2093] | Δ = 0.0011; p = 0.710 | –0.0045 to 0.0066 | 0.0068 | 0.0020 to 0.0150 |
| ΔL = 0.0436; p = 0.413 | –0.0609 to 0.1481 | 0.0100 | 0.0035 to 0.0204 | |||
| Proportion of patients with further emergency service call,i n/N (%) | 442/2391 (18.5) | 493/2264 (21.8) | OR = 0.815; p = 0.006 | 0.705 to 0.943 | 0.0056 | 0.0018 to 0.0119 |
| Further emergency service calls per patient,j mean (SD) [n] | 0.2981 (0.7758) [2197] | 0.3378 (0.7823) [2093] | Λ = 0.883; p = 0.049 | 0.780 to 1.000 | 0.0038 | 0.0011 to 0.0086 |
| Further emergency service calls/patient/day at risk,k mean (SD) [n] | 0.0204 (0.0641) [2197] | 0.0245 (0.0814) [2093] | Δ = –0.0040; p = 0.071 | –0.0083 to 0.0003 | 0.0043 | 0.0011 to 0.0101 |
| ΔL = –0.1354; p = 0.013 | –0.2418 to –0.0290 | 0.0046 | 0.0013 to 0.0103 | |||
| Primary outcome | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|
| Intervention | Control | Estimate, p-value | 95% CI | Estimate | 95% CI | |
| Overall composite outcome | ||||||
| Proportion of patients with further emergency service call, ED attendance, emergency admission or death,c n/N (%) | 1701/2391 (71.1) | 1592/2264 (70.3) | OR = 1.018; p = 0.789 | 0.895 to 1.157 | 0 | n/a |
| Primary outcome components | ||||||
| Proportion of patients dying (any cause),d n/N (%) | 458/2391 (19.2) | 419/2264 (18.5) | OR = 1.187; p = 0.094 | 0.971 to 1.451 | 0 | n/a |
| Proportion with further emergency admission,e n/N (%) | 1153/2391 (48.2) | 1084/2264 (47.9) | OR = 1.001; p = 0.984 | 0.891 to 1.125 | 0.0052 | 0.0016 to 0.0113 |
| Proportion of patients with further ED attendance,f n/N (%) | 1079/2391 (45.1) | 1021/2264 (45.1) | OR = 0.999; p = 0.986 | 0.888 to 1.123 | 0.0191 | 0.0085 to 0.0342 |
| Further ED attendances per patient,g mean (SD) [n] | 0.844 (1.392) [2380] | 0.913 (2.738) [2257] | Λ = 0.810; p < 0.001 | 0.722 to 0.909 | 0.0144 | 0.0062 to 0.0261 |
| Further ED attendances/patient/day at risk,h mean (SD) [n] | 0.0169 (0.0907) [2380] | 0.0144 (0.0686) [2257] | Δ = 0.0025; p = 0.292 | –0.0021 to 0.0071 | 0.0041 | 0.0011 to 0.0098 |
| ΔL = –0.0163; p = 0.711 | –0.1024 to 0.0699 | 0.0264 | 0.0127 to 0.0451 | |||
| Proportion of patients with further emergency service call,i n/N (%) | 1046/2391 (43.7) | 1046/2264 (46.2) | OR = 0.899; p = 0.076 | 0.799 to 1.011 | 0.0030 | 0.0006 to 0.0079 |
| Further emergency service calls per patient,j mean (SD) [n] | 1.136 (2.506) [2380] | 1.251 (2.672) [2257] | Λ = 0.931; p = 0.076 | 0.860 to 1.007 | 0.0040 | 0.0012 to 0.0090 |
| Further emergency service calls/patient/day at risk,k mean (SD) [n] | 0.0125 (0.0363) [2380] | 0.0172 (0.0599) [2257] | Δ = –0.0045; p = 0.002 | –0.0073 to -0.0017 | 0.0029 | 0.0004 to 0.0069 |
| ΔL = –0.1183; p = 0.010 | –0.2079 to –0.0286 | 0.0036 | 0.0009 to 0.0086 | |||
| Primary outcomes | Site | Raw data | Site effectsa,b | ||
|---|---|---|---|---|---|
| Intervention | Control | Main | Interaction | ||
| Proportion of patients with further emergency service call, ED attendance, emergency admission or death, n/N (%) | Site 1 | 481/1311 (36.7) | 509/1337 (38.1) | OR = 1.136; p = 0.268 | OR = 1.091; p = 0.583 |
| Site 2 | 172/540 (31.9) | 152/433 (35.1) | n/a | OR = 0.864; p = 0.285 | |
| Site 3 | 217/540 (40.2) | 182/494 (36.8) | OR = 1.078; p = 0.582 | OR = 1.333; p = 0.125 | |
| Proportion of patients dying (any cause), n/N (%) | Site 1 | 86/1311 (6.6) | 79/1337 (5.9) | OR = 0.983; p = 0.941 | OR = 1.173; p = 0.616 |
| Site 2 | 31/540 (5.7) | 26/433 (6.0) | n/a | OR = 0.953; p = 0.862 | |
| Site 3 | 30/540 (5.6) | 31/494 (6.3) | OR = 1.048; p = 0.864 | OR = 0.922; p = 0.830 | |
| Proportion with further emergency admission, n/N (%) | Site 1 | 271/1311 (20.7) | 272/1337 (20.3) | OR = 1.001; p = 0.993 | OR = 1.091; p = 0.644 |
| Site 2 | 104/540 (19.3) | 88/433 (20.3) | n/a | OR = 0.935; p = 0.679 | |
| Site 3 | 142/540 (26.3) | 115/494 (23.3) | OR = 1.190; p = 0.278 | OR = 1.257; p = 0.291 | |
| Proportion of patients with further ED attendance, n/N (%) | Site 1 | 256/1311 (19.5) | 244/1337 (18.2) | OR = 1.311; p = 0.078 | OR = 1.080; p = 0.711 |
| Site 2 | 79/540 (14.5) | 63/433 (14.5) | n/a | OR = 1.006; p = 0.972 | |
| Site 3 | 128/540 (23.7) | 111/494 (22.5) | OR = 1.702; p = 0.002 | OR = 1.065; p = 0.788 | |
| Further ED attendances per patient, mean (SD) [n] | Site 1 | 0.2642 (0.6574) [1230] | 0.2337 (0.5449) [1258] | Λ = 1.224; p = 0.161 | Λ = 1.103; p = 0.613 |
| Site 2 | 0.2017 (0.5017) [466] | 0.1901 (0.4824) [384] | n/a | Λ = 1.014; p = 0.938 | |
| Site 3 | 0.3174 (0.6042) [501] | 0.3969 (1.374) [451] | Λ = 2.050; p < 0.001 | Λ = 0.777; p = 0.240 | |
| Further ED attendances/patient/day at risk, mean (SD) [n] | Site 1 | 0.0217 (0.0775) [1230] | 0.0201 (0.0753) [1258] | Δ = 0.0063; p = 0.245 | Δ = –0.0018; p = 0.811 |
| ΔL = 0.1933; p = 0.058 | ΔL = –0.2631; p = 0.851 | ||||
| Site 2 | 0.0172 (0.0611) [466] | 0.0138 (0.0661) [384] | n/a | Δ = 0.0034; p = 0.600 | |
| n/a | ΔL = 0.0803; p = 0.504 | ||||
| Site 3 | 0.0341 (0.1648) [501] | 0.0357 (0.1115) [451] | Δ = 0.0219; p = 0.001 | Δ = –0.0050; p = 0.572 | |
| ΔL = 0.4744; p < 0.001 | ΔL = –0.0955; p = 0.563 | ||||
| Proportion of patients with further emergency service call, n/N (%) | Site 1 | 257/1311 (19.6) | 320/1337 (23.9) | OR = 1.689; p < 0.001 | OR = 0.855; p = 0.442 |
| Site 2 | 78/540 (14.4) | 68/433 (15.7) | n/a | OR = 0.906; p = 0.585 | |
| Site 3 | 107/540 (19.8) | 105/494 (21.3) | OR = 1.449; p = 0.031 | OR = 1.010; p = 0.966 | |
| Further emergency service calls per patient, mean (SD) [n] | Site 1 | 0.3130 (0.8111) [1230] | 0.3831 (0.8763) [1258] | Λ = 1.682; p < 0.001 | Λ = 0.824; p = 0.278 |
| Site 2 | 0.2318 (0.6508) [466] | 0.2292 (0.5686) [384] | n/a | Λ = 0.987; p = 0.933 | |
| Site 3 | 0.3234 (0.7920) [501] | 0.3034 (0.6384) [451] | Λ = 1.311; p = 0.078 | Λ = 1.077; p = 0.721 | |
| Further emergency service calls/patient/day at risk, mean (SD) [n] | Site 1 | 0.0196 (0.0595) [1230] | 0.0247 (0.0728) [1258] | Δ = 0.0073; p = 0.088 | Δ = –0.0068; p = 0.241 |
| ΔL = 0.3538; p = 0.001 | ΔL = –0.2094; p = 0.142 | ||||
| Site 2 | 0.0191 (0.0642) [466] | 0.0174 (0.0733) [384] | n/a | Δ = 0.0017; p = 0.736 | |
| n/a | ΔL = 0.0196; p = 0.873 | ||||
| Site 3 | 0.0238 (0.0743) [501] | 0.0301 (0.1067) [450] | Δ = 0.0127; p = 0.012 | Δ = –0.0080; p = 0.248 | |
| ΔL = 0.2877; p = 0.020 | ΔL = –0.1077; p = 0.525 | ||||
| Primary outcomes | Site | Raw data | Site effectsa,b | ||
|---|---|---|---|---|---|
| Intervention | Control | Main | Interaction | ||
| Proportion of patients with further emergency service call, ED attendance, emergency admission or death, n/N (%) | Site 1 | 933/1310 (71.2) | 948/1337 (70.9) | OR = 1.214; p = 0.101 | OR = 0.918; p = 0.598 |
| Site 2 | 372/540 (68.9) | 289/433 (66.7) | n/a | OR = 1.103; p = 0.476 | |
| Site 3 | 396/540 (73.3) | 355/494 (71.9) | OR = 1.273; p = 0.092 | OR = 0.976; p = 0.901 | |
| Proportion of patients dying (any cause), n/N (%) | Site 1 | 249/1311 (19.0) | 270/1337 (20.2) | OR = 1.208; p = 0.190 | OR = 0.710; p = 0.073 |
| Site 2 | 116/540 (21.5) | 75/433 (17.3) | n/a | OR = 1.306; p = 0.105 | |
| Site 3 | 93/540 (17.2) | 74/494 (15.0) | OR = 0.841; p = 0.333 | OR = 0.904; p = 0.671 | |
| Proportion with further emergency admission, n/N (%) | Site 1 | 597/1311 (45.5) | 620/1337 (46.4) | OR = 0.953; p = 0.663 | OR = 0.959; p = 0.782 |
| Site 2 | 258/540 (47.8) | 206/433 (47.6) | n/a | OR = 1.008; p = 0.950 | |
| Site 3 | 298/540 (55.2) | 258/494 (52.2) | OR = 1.205; p = 0.158 | OR = 1.117; p = 0.537 | |
| Proportion of patients with further ED attendance, n/N (%) | Site 1 | 592/1311 (45.2) | 584/1337 (43.7) | OR = 1.235; p = 0.062 | OR = 1.170; p = 0.310 |
| Site 2 | 196/540 (36.3) | 167/433 (38.6) | n/a | OR = 0.908; p = 0.467 | |
| Site 3 | 291/540 (53.9) | 270/494 (54.7) | OR = 1.920; p < 0.001 | OR = 1.068; p = 0.717 | |
| Further ED attendances per patient, mean (SD) [n] | Site 1 | 0.813 (1.362) [1310] | 0.790 (1.355) [1336] | Λ = 1.172; p = 0.067 | Λ = 1.259; p = 0.055 |
| Site 2 | 0.561 (0.912) [535] | 0.678 (1.083) [429] | n/a | Λ = 0.820; p = 0.058 | |
| Site 3 | 1.204 (1.743) [535] | 1.453 (5.296) [492] | Λ = 2.163; p < 0.001 | Λ = 1.009; p = 0.945 | |
| Further ED attendances/patient/day at risk, mean (SD) [n] | Site 1 | 0.0155 (0.0859) [1310] | 0.0117 (0.0461) [1336] | Δ = –0.0036; p = 0.426 | Δ = 0.0046; p = 0.455 |
| ΔL = 0.1424; p = 0.086 | ΔL = 0.0942; p = 0.405 | ||||
| Site 2 | 0.0145 (0.1033) [535] | 0.0153 (0.1117) [429] | n/a | Δ = –0.0008; p = 0.874 | |
| n/a | ΔL = –0.0690; p = 0.477 | ||||
| Site 3 | 0.0231 (0.0886) [535] | 0.0209 (0.0701) [492] | Δ = 0.0056; p = 0.297 | Δ = 0.0030; p = 0.677 | |
| ΔL = 0.5620; p < 0.001 | ΔL = 0.0353; p = 0.793 | ||||
| Proportion of patients with further emergency service call, n/N (%) | Site 1 | 590/1311 (45.0) | 635/1337 (47.5) | OR = 1.413; p = 0.002 | OR = 0.763; p = 0.077 |
| Site 2 | 233/540 (43.1) | 169/433 (39.0) | n/a | OR = 1.186; p = 0.195 | |
| Site 3 | 223/540 (41.3) | 242/494 (49.0) | OR = 1.500; p = 0.002 | OR = 0.618; p = 0.008 | |
| Further emergency service calls per patient, mean (SD) [n] | Site 1 | 1.260 (2.917) [1310] | 1.412 (3.163) [1336] | Λ = 1.684; p < 0.001 | Λ = 0.883; p = 0.252 |
| Site 2 | 0.849 (1.497) [535] | 0.839 (1.456) [429] | n/a | Λ = 1.011; p = 0.910 | |
| Site 3 | 1.120 (2.183) [535] | 1.173 (1.882) [492] | Λ = 1.398; p < 0.001 | Λ = 0.944; p = 0.656 | |
| Further emergency service calls/patient/day at risk, mean (SD) [n] | Site 1 | 0.0118 (0.0308) [1310] | 0.0177 (0.0604) [1336] | Δ = 0.0038; p = 0.165 | Δ = –0.0045; p = 0.228 |
| ΔL = 0.2946; p = 0.001 | ΔL = –0.2524; p = 0.034 | ||||
| Site 2 | 0.0125 (0.0376) [535] | 0.0139 (0.0620) [429] | n/a | Δ = –0.0015; p = 0.646 | |
| n/a | ΔL = 0.1088; p = 0.286 | ||||
| Site 3 | 0.0144 (0.0460) [535] | 0.0184 (0.0565) [492] | Δ = 0.0045; p = 0.170 | Δ = –0.0025; p = 0.573 | |
| ΔL = 0.3329; p = 0.001 | ΔL = –0.3508; p = 0.013 | ||||
Table 19 shows that rate of conveyance to ED at the index incident was similar between groups overall and at each site, although the proportion conveyed varied considerably by site, from < 60% at site 1 to nearly 80% at site 2. Eight per cent of trial eligible patients were referred to falls services by their attending paramedic in the intervention arm, varying from 7.5% at site 1 to 9.7% at site 3. Very few patients were referred to falls services in the control group; the rate was 1% overall, but higher at site 3, where there was a service-wide initiative to increase referrals of this patient group. More patients were left at scene without referral for further care in the control group than in the intervention group, 30% versus 23% overall; a proportion which varied widely by site and was highest in the control group at site 1 (37%). Completion of clinical documentation was high across groups and sites with no clear difference between trial arms. We also found no differences in the operational indicators of duration of episode of care (time from emergency service call until patient’s emergency episode was complete) or job cycle (time from emergency service call until ambulance free).
| Secondary outcome | Site | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|---|
| Intervention (A) | Control (B) | Estimate, p-value | 95% CI | Estimate | 95% CI | ||
| Conveyed to ED,c,d n/N (%) | All | 1579/2420 (65.2) | 1431/2284 (62.7) | OR = 1.082; p = 0.205 | 0.958 to 1.223 | 0.0512 | 0.0266 to 0.0832 |
| Site 1 | 779/1329 (58.6) | 755/1352 (55.8) | |||||
| Site 2 | 426/544 (78.3) | 344/436 (78.9) | |||||
| Site 3 | 374/547 (68.4) | 332/496 (66.9) | |||||
| Referred to falls service by emergency service crew,c,e n/N (%) | All | 204/2420 (8.4) | 26/2284 (1.1) | OR = 51.730; p < 0.001 | 16.46 to 162.54 | 0.0400 | 0.0204 to 0.0652 |
| Site 1 | 100/1329 (7.5) | 3/1352 (0.2) | |||||
| Site 2 | 51/544 (9.4) | 0/436 (0) | |||||
| Site 3 | 53/547 (9.7) | 23/496 (4.6) | |||||
| Left at scene without referral,f n/N (%) | All | 547/2420 (22.6) | 692/2284 (30.3) | OR = 0.686; p < 0.001 | 0.600 to 0.784 | 0.0375 | 0.0195 to 0.0612 |
| Site 1 | 379/1329 (28.5) | 496/1352 (36.7) | |||||
| Site 2 | 72/544 (13.2) | 84/436 (19.3) | |||||
| Site 3 | 96/547 (17.6) | 112/496 (22.6) | |||||
| Key physiological indicators recorded at scene | |||||||
| Respiratory rate,g n/N (%) | All | 2318/2420 (95.8) | 2165/2284 (94.8) | OR = 1.278; p = 0.090 | 0.963 to 1.695 | 0.0449 | 0.0215 to 0.0764 |
| Site 1 | 1281/1329 (96.4) | 1288/1352 (95.3) | |||||
| Site 2 | 495/544 (91.0) | 386/436 (88.5) | |||||
| Site 3 | 542/547 (99.1) | 491/496 (99.0) | |||||
| Pulse rate,h n/N (%) | All | 2319/2420 (95.8) | 2173/2284 (95.1) | OR = 1.216; p = 0.186 | 0.910 to 1.624 | 0.0511 | 0.0254 to 0.0851 |
| Site 1 | 1296/1329 (97.5) | 1309/1352 (96.8) | |||||
| Site 2 | 489/544 (89.9) | 378/436 (86.5) | |||||
| Site 3 | 534/547 (97.6) | 486/496 (98.0) | |||||
| Level of consciousness,i n/N (%) | All | 2327/2420 (96.2) | 2189/2284 (95.8) | OR = 1.058; p = 0.704 | 0.790 to 1.418 | 0.0016 | 0.0001 to 0.0055 |
| Site 1 | 1262/1329 (95.0) | 1285/1352 (95.0) | |||||
| Site 2 | 533/544 (98.0) | 427/436 (97.9) | |||||
| Site 3 | 532/547 (97.3) | 477/496 (96.2) | |||||
| Length of episode of care (minutes),j mean (SD) [n] | All | 196.8 (153.9) [2410] | 192.8 (152.8) [2273] | Δ = 2.048; p = 0.645 | –6.68 to 10.77 | 0.0180 | 0.0074 to 0.0336 |
| Site 1 | 185.4 (130.9) [1328] | 181.8 (135.8) [1352] | |||||
| Site 2 | 205.4 (211.0) [540] | 209.1 (217.9) [431] | |||||
| Site 3 | 216.2 (135.5) [542] | 208.7 (122.4) [490] | |||||
| Length of job-cycle timek (minutes), mean (SD) [n] | All | 99.9 (41.9) [2416] | 97.8 (43.9) [2277] | Δ = 1.685; p = 0.174 | –0.746 to 4.117 | 0.0167 | 0.0070 to 0.0308 |
| Site 1 | 97.5 (41.4) [1328] | 97.2 (44.9) [1352] | |||||
| Site 2 | 108.8 (47.7) [543] | 102.2 (48.2) [435] | |||||
| Site 3 | 96.9 (35.0) [545] | 95.8 (36.3) [490] | |||||
No differences were found in the secondary outcomes of duration of inpatient stay, or self-reported quality of life or fall-related self-efficacy (fear of falling) at 1 month or 6 months (Tables 20 and 21). There was evidence of differences between groups in the proportion reporting further falls at 1 and 6 months: lower in the intervention group at 1 month, but higher at 6 months amid significant variations across sites. There were also significant differences between groups in the interpersonal aspect of patient satisfaction at 1 month arising from higher scores from intervention patients in site 2, but not in the technical aspect of patient satisfaction. There was evidence of a difference in the proportion of patients with further fractures at 6 months (but not at 1 month), with pronounced differences between groups across the three sites (approximately equal at site 1, higher in intervention patients in site 2 and lower in intervention patients at site 3).
| Secondary outcome | Site | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|---|
| Intervention (A) | Control (B) | Estimate, p-value | 95% CI | Estimate | 95% CI | ||
| Duration of subsequent inpatient episodes (nights in hospital, truncated) at 30 days,c mean (SD) [n] | All | 2.25 (6.14) [2391] | 2.10 (6.05) [2264] | Δ = 0.141; p = 0.426 | –0.207 to 0.490 | 0.0012 | 0.0001 to 0.0045 |
| Site 1 | 1.98 (5.64) [1311] | 1.97 (5.73) [1337] | |||||
| Site 2 | 2.51 (6.72) [540] | 2.42 (6.77) [433] | |||||
| Site 3 | 2.64 (6.67) [540] | 2.17 (6.20) [494] | |||||
| Proportion with further reported fractures,d n/N (%) | All | 98/2391 (4.1) | 91/2264 (4.0) | OR = 1.002; p = 0.987 | 0.744 to 1.351 | 0.0049 | 0.0013 to 0.0114 |
| Site 1 | 38/1311 (2.9) | 42/1337 (3.1) | |||||
| Site 2 | 41/540 (7.6) | 27/433 (6.2) | |||||
| Site 3 | 19/540 (3.5) | 22/494 (4.5) | |||||
| Self-reported outcomes | |||||||
| Quality of life SF-12 MCS,e mean (SD) [n] | All | 39.80 (12.47) [447] | 38.89 (12.16) [410] | Δ = 0.902; p = 0.282 | –0.744 to 2.547 | 0.0080 | 0.0004 to 0.0306 |
| Site 1 | 40.68 (12.85) [214] | 40.30 (13.04) [217] | |||||
| Site 2 | 37.76 (11.59) [126] | 35.63 (10.69) [104] | |||||
| Site 3 | 40.44 (12.53) [107] | 39.26 (10.88) [89] | |||||
| Quality of life SF-12 PCS,f mean (SD) [n] | All | 29.07 (9.97) [447] | 29.40 (10.28) [410] | Δ = –0.495; p = 0.472 | –1.847 to 0.856 | 0 | n/a |
| Site 1 | 28.92 (9.81) [214] | 29.62 (11.47) [217] | |||||
| Site 2 | 28.13 (9.66) [126] | 28.39 (7.99) [104] | |||||
| Site 3 | 30.47 (10.55) [107] | 30.03 (9.58) [89] | |||||
| Patient satisfaction QCM Technical,g mean (SD) [n] | All | 62.82 (7.98) [563] | 63.21 (8.16) [551] | Δ = –0.320; p = 0.506 | –1.265 to 0.625 | 0.0102 | 0.0018 to 0.0273 |
| Site 1 | 63.13 (7.45) [274] | 63.79 (7.97) [295] | |||||
| Site 2 | 61.37 (9.78) [163] | 61.64 (8.63) [137] | |||||
| Site 3 | 64.01 (6.07) [126] | 63.58 (7.91) [119] | |||||
| Patient satisfaction QCM Interpersonal,h mean (SD) [n] | All | 68.92 (8.66) [563] | 68.04 (9.12) [551] | Δ = 3.132; p < 0.001 | 1.587 to 4.678 | 0.0123 | 0.0017 to 0.0357 |
| Site 1 | 67.59 (9.63) [274] | 67.94 (9.93) [295] | |||||
| Site 2 | 71.18 (7.42) [163] | 68.25 (8.51) [137] | |||||
| Site 3 | 68.88 (7.28) [126] | 68.06 (7.68) [119] | |||||
| Fall-related self-efficacy (fear of falling),i mean (SD) [n] | All | 3.714 (3.040) [634] | 3.815 (3.117) [600] | Δ = –0.055; p = 0.743 | –0.385 to 0.275 | 0.0062 | 0.0004 to 0.0224 |
| Site 1 | 3.836 (3.103) [302] | 4.052 (3.273) [321] | |||||
| Site 2 | 3.148 (2.866) [182] | 3.194 (2.666) [151] | |||||
| Site 3 | 4.156 (3.035) [150] | 3.955 (3.133) [128] | |||||
| Proportion of patients who reported ≥ 1 further fall,j n/N (%) | All | 413/621 (66.5) | 409/589 (69.4) | OR = 0.723; p = 0.025 | 0.544 to 0.961 | 0.0102 | 0.0016 to 0.0285 |
| Site 1 | 211/296 (71.3) | 215/314 (68.5) | |||||
| Site 2 | 112/178 (62.9) | 105/149 (70.5) | |||||
| Site 3 | 90/147 (61.2) | 89/126 (70.6) | |||||
| Outcome | Site | Raw data | Adjusted comparisona,b | Estimate | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Intervention (A) | Control (B) | Estimate, p-value | 95% CI significance level | ||||
| Routine data outcomes | |||||||
| Duration of subsequent inpatient episodes (nights in hospital, truncated at 180 days),c mean (SD) [n] | All | 11.18 (22.80) [2391] | 11.62 (23.52) [2264] | Δ = –0.563; p = 0.403 | –1.884 to 0.757 | 0.0065 | 0.0021 to 0.0138 |
| Site 1 | 9.48 (19.29) [1311] | 9.95 (19.95) [1337] | |||||
| Site 2 | 14.48 (29.56) [540] | 14.75 (30.01) [433] | |||||
| Site 3 | 12.03 (22.52) [540] | 13.42 (25.53) [494] | |||||
| Proportion with further reported subsequent fractures,d n/N (%) | All | 228/2391 (9.5) | 222/2264 (9.8) | OR = 1.449; p = 0.015 | 1.076 to 1.952 | 0.0172 | 0.0073 to 0.0318 |
| Site 1 | 93/1311 (7.1) | 107/1337 (8.0) | |||||
| Site 2 | 92/540 (17.0) | 59/433 (13.6) | |||||
| Site 3 | 43/540 (8.0) | 56/494 (11.3) | |||||
| Self-reported outcomes | |||||||
| Quality of life SF-12 MCS,e mean (SD) [n] | All | 43.21 (12.57) [258] | 42.82 (12.28) [241] | Δ = 0.463; p = 0.677 | –1.717 to 2.643 | 0 | n/a |
| Site 1 | 44.00 (12.50) [127] | 43.45 (12.55) [144] | – | – | – | – | |
| Site 2 | 41.84 (12.42) [53] | 38.95 (12.77) [43] | |||||
| Site 3 | 42.84 (12.84) [78] | 44.24 (10.67) [54] | |||||
| Quality of life SF-12 PCS,f mean (SD) [n] | All | 30.44 (11.33) [258] | 31.88 (11.67) [241] | Δ = –1.300; p = 0.198 | –3.282 to 0.682 | 0 | n/a |
| Site 1 | 29.83 (11.29) [127] | 32.36 (11.72) [144] | |||||
| Site 2 | 31.61 (12.89) [53] | 30.77 (12.79) [43] | |||||
| Site 3 | 30.64 (10.31) [78] | 31.49 (10.70) [54] | |||||
| Fall-related self-efficacy (fear of falling),g mean score (SD) [n] | All | 4.547 (3.328) [341] | 4.792 (3.393) [310] | Δ = –0.230; p = 0.368 | –0.729 to 0.270 | 0.0018 | 0 to 0.0219 |
| Site 1 | 4.643 (3.402) [167] | 5.091 (3.477) [176] | |||||
| Site 2 | 4.217 (3.254) [72] | 4.010 (3.423) [60] | |||||
| Site 3 | 4.624 (3.273) [102] | 4.716 (3.090) [74] | |||||
| Proportion with change in place of residence,h n/N (%) | All | 32/319 (10.0) | 19/280 (6.8) | OR = 1.497; p = 0.183 | 0.826 to 2.713 | 0.0032 | 0 to 0.0235 |
| Site 1 | 15/156 (9.6) | 9/163 (5.5) | |||||
| Site 2 | 5/73 (6.8) | 4/50 (8.0) | |||||
| Site 3 | 12/90 (13.3) | 6/67 (9.0) | |||||
| Proportion of patients who reported ≥ 1 further fall,i n/N (%) | Site 1 | 110/159 (69.2) | 105/172 (61.0) | OR = 1.423; p = 0.134 | 0.897 to 2.258 | – | – |
| Site 2 | 44/74 (59.5) | 43/56 (76.8) | OR = 0.365; p = 0.019 | 0.157 to 0.848 | – | – | |
| Site 3 | 74/96 (77.1) | 44/68 (64.7) | OR = 1.835; p = 0.084 | 0.922 to 3.652 | – | – | |
Contamination
Table 22 shows the percentage of control patients subsequently attended within the trial period by a paramedic from the intervention group, < 5% at 1 month rising to about 15% at 6 months, with broadly similar rates at each site.
| Site | Count, n/N (%) | |
|---|---|---|
| Within 1 month | Within 6 months | |
| All | 98/2264 (4.3) | 356/2264 (15.7) |
| Site 1 | 59/1337 (4.4) | 224/1337 (16.8) |
| Site 2 | 15/433 (3.5) | 60/433 (13.9) |
| Site 3 | 24/494 (4.9) | 72/494 (14.6) |
Patients ineligible for referral to the falls service
A subgroup of participants in site 1 were registered at GP practices without agreement for referral of patients to falls services and were less able to benefit from the full SAFER 2 intervention. Appendix 19 therefore presents the main results after excluding these patients. Results in these tables are consistent with those presented in the preceding sections.
Patterns of referral to the falls service
Sixty per cent of designated intervention group paramedics referred trial eligible patients to a falls service (Table 23). Paramedics referred up to 11 patients, although most made referrals once or twice. Patient age, sex, distance to ED did not appear to influence referral (Table 24); however, patients were more likely to be referred to falls services out of hours and less likely to be referred at site 1 than at the other sites (Table 25).
| Number of referrals to falls servicea | Site 1 paramedics, n (%) | Site 2 paramedics, n (%) | Site 3 paramedics, n (%) | Total paramedics, n (%) |
|---|---|---|---|---|
| 0 | 13 (33.3) | 7 (26.9) | 21 (52.5) | 41 (39.0) |
| 1 | 8 (20.5) | 9 (34.6) | 8 (20.0) | 25 (23.8) |
| 2 | 6 (15.4) | 2 (7.7) | 6 (15.0) | 14 (13.3) |
| 3 | 1 (2.6) | 3 (11.5) | 0 (0.0) | 4 (3.8) |
| 4 | 0 (0.0) | 0 (0.0) | 4 (10.0) | 4 (3.8) |
| 5 | 2 (5.1) | 3 (11.5) | 1 (2.5) | 6 (5.7) |
| 6 | 5 (12.8) | 0 (0.0) | 0 (0.0) | 5 (4.8) |
| 7 | 2 (5.1) | 1 (3.8) | 0 (0.0) | 3 (2.9) |
| 8 | 1 (2.6) | 0 (0.0) | 0 (0.0) | 1 (0.9) |
| 9 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 10 | 0 (0.0) | 1 (3.8) | 0 (0.0) | 1 (0.9) |
| 11 | 1 (2.6) | 0 (0.0) | 0 (0.0) | 1 (0.9) |
| Total paramedics recruited to study | 39 | 26 | 40 | 105 |
| Characteristics | Referred patientsa | Not referred patients | ||
|---|---|---|---|---|
| n (%) | SD | n (%) | SD | |
| Mean age (years) | 83.88 | 7.15 | 82.14 | 8.11 |
| Men | 61 (35.1) | – | 807 (35.3) | – |
| Women | 113 (64.9) | – | 1477 (64.7) | – |
| Mean distance to nearest ED (miles) | 4.57 | 3.27 | 4.65 | 3.08 |
| Out of hours | 91 (52.3) | – | 954 (41.8) | – |
| Site 1 | 81(46.6) | – | 1352 (59.2) | – |
| Site 2 | 49 (28.2) | – | 436 (19.1) | – |
| Site 3 | 44 (25.3) | – | 496 (21.7) | – |
| Total | 174 | – | 2284 | – |
| Predictor | B | p-value | Exp(B) | 95% CI for Exp (B) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Site 1 | –0.448 | 0.015 | 0.639 | 0.446 | 0.917 |
| Site 3 | 0.204 | 0.389 | 1.226 | 0.771 | 1.951 |
| Gender | 0.101 | 0.487 | 1.107 | 0.832 | 1.472 |
| Age | 0.079 | 0.025 | 1.082 | 1.010 | 1.160 |
| Age2 | –1.702 | 0.085 | 0.182 | 0.026 | 1.264 |
| Distance to ED | –0.041 | 0.137 | 0.960 | 0.910 | 1.013 |
| Out of hours | 0.456 | 0.001 | 1.578 | 1.202 | 2.072 |
| Recruitment point | –0.217 | 0.426 | 0.805 | 0.472 | 1.373 |
| Seasonality | 0.187 | 0.067 | 1.206 | 0.987 | 1.474 |
| Constant | –3.586 | – | – | – | – |
For most patients left at the scene by intervention group paramedics without referral to a falls service, no reason was identified. At site 1, 231 patients were not eligible for referral because, although they lived in the study catchment area, they were not registered with participating GPs. Other reasons for non-referral included refusal, not appropriate for referral or information that the patient was already under the care of a falls team or other service (Table 26).
| Reason | All, n (%) | Site 1, n (%) | Site 2, n (%) | Site 3, n (%) |
|---|---|---|---|---|
| No reason identified | 377 (68.9) | 241 (63.6) | 60 (83.3) | 76 (79.2) |
| Not registered with an eligible GP | 68 (12.4) | 68 (17.9) | 0 (0) | 0 (0) |
| Recorded by paramedic as | ||||
| Not appropriate for referral | 38 (6.9) | 25 (6.6) | 4 (5.6) | 9 (9.4) |
| Refused referral | 31 (5.7) | 20 (5.3) | 6 (8.3) | 5 (5.2) |
| Care plan in place | 13 (2.4) | 6 (1.6) | 2 (2.8) | 5 (5.2) |
| Already under a falls team | 20 (3.7) | 19 (5.0) | 0 (0) | 1 (1.0) |
| Total | 547 | 379 | 72 | 96 |
Comparison of outcome measures
To meet our methodological objective we compared the performance of the generic SF-12 with the mFES (‘Fear of Falling’), a falls-specific outcome measure, in this population (Table 27 and Figures 3–6). The SF-12 mental component summary (MCS) and physical component summary (PCS) scores at 1 month both showed mean values at the lower end of the scale (lower scores indicate worse health), indicating mental and physical scores below the population norms. Similarly, the mFES at 1 month showed a clustering of scores at the lower end of the scale, indicating worse health. At 6 months, both scales again showed mean score values at the lower end of the scale, indicating worse health. There was, however, a small increase in MCS, PCS and mFES scores, indicating a slight improvement in patient-reported outcomes since the 1-month follow-up.
| Outcome measure | n a | Mean score | SD |
|---|---|---|---|
| 1 month | |||
| SF-12 MCS | 1160 | 43.84 | 9.36 |
| SF-12 PCS | 1160 | 35.03 | 8.01 |
| mFES | 1252 | 3.47 | 3.07 |
| 6 months | |||
| SF-12 MCS | 595 | 44.95 | 9.04 |
| SF-12 PCS | 595 | 38.23 | 7.72 |
| mFES | 663 | 4.55 | 3.45 |
FIGURE 3.
Short Form questionnaire-12 items PCS and mFES scores at 1 month: correlation = 0.546.
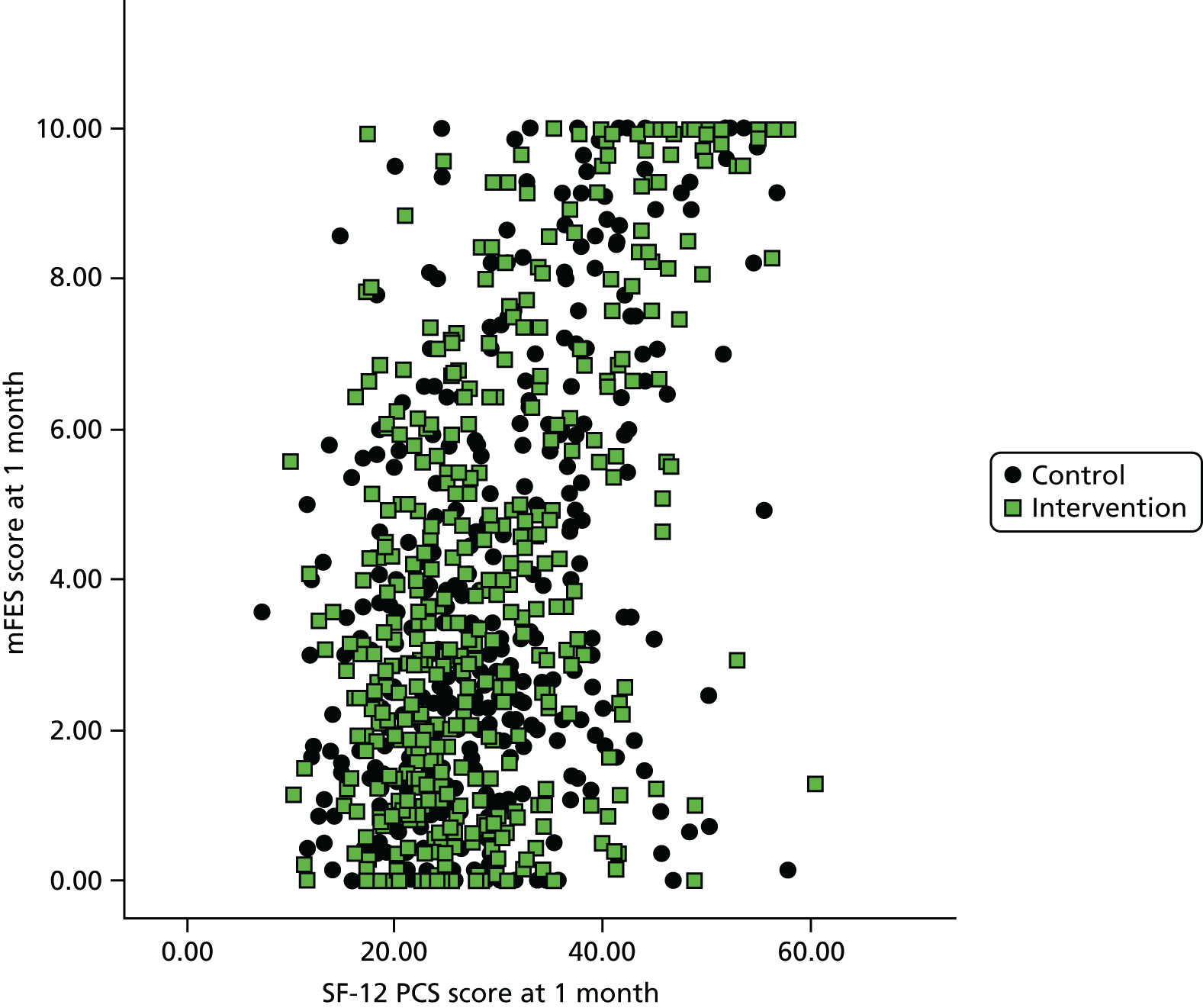
FIGURE 4.
Short Form questionnaire-12 items MCS and mFES scores at 1 month: correlation = 0.553.
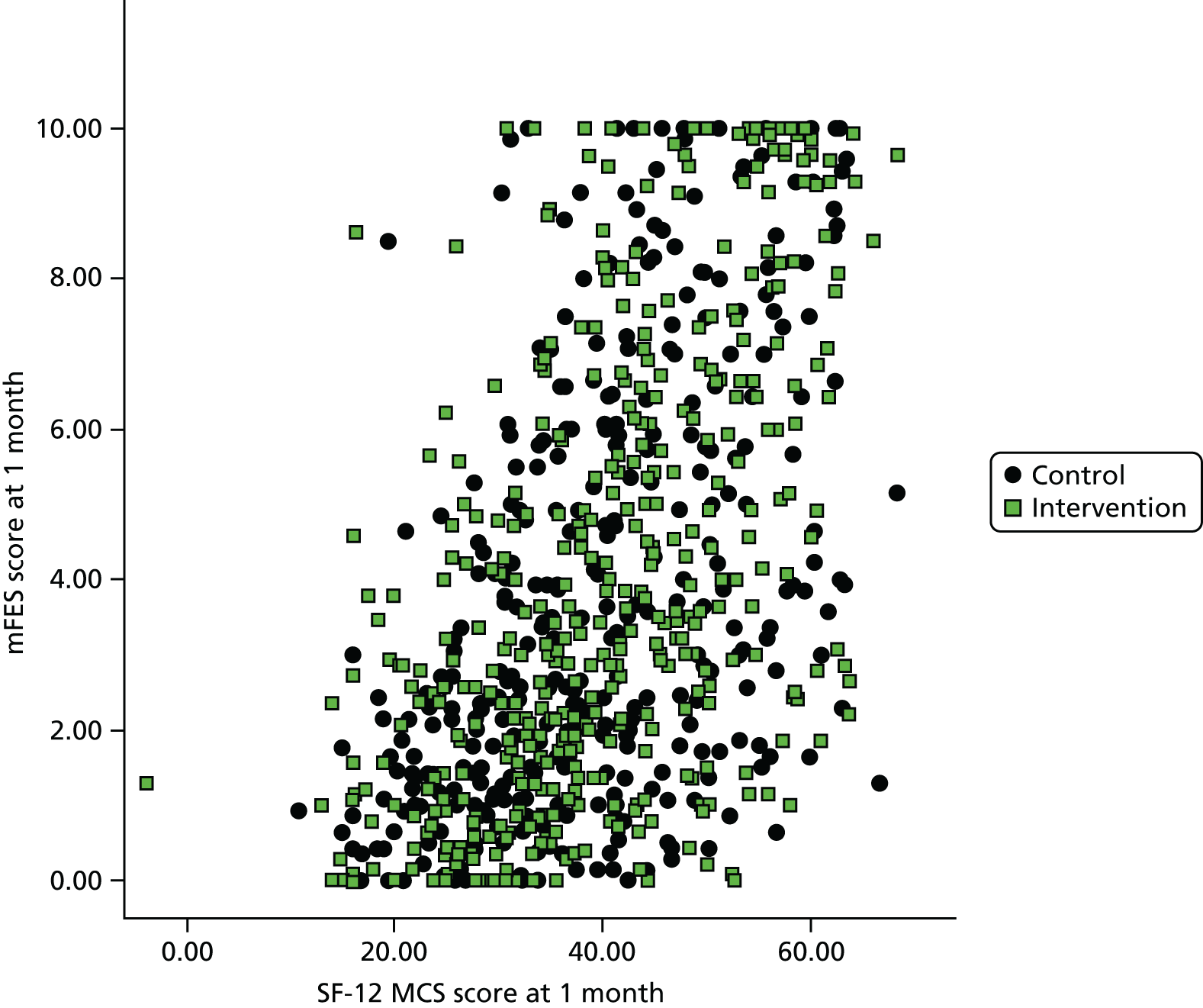
FIGURE 5.
Short Form questionnaire-12 items PCS and mFES scores at 6 months: correlation = 0.627.

FIGURE 6.
Short Form questionnaire-12 items MCS and mFES scores at 6 months: correlation = 0.547.
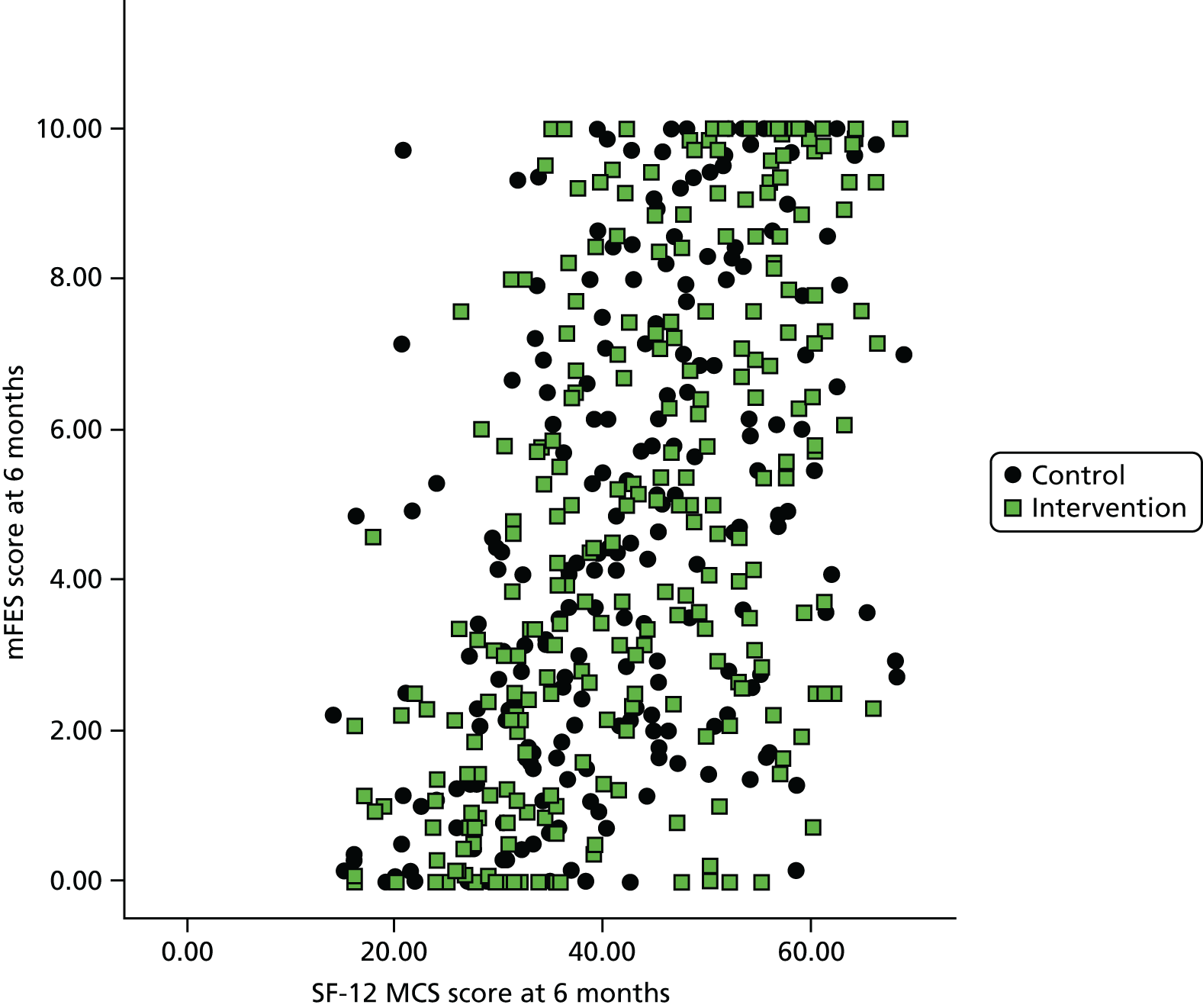
There was moderate correlation between the SF-12 MCS and PCS scores and the mFES scores at both 1 and 6 months (range 0.55–0.63). Unusually, there were significant floor and ceiling effects for the condition-specific measure, mFES, indicating less sensitivity to detect small changes in patient outcomes than the SF-12 disease-specific measure.
Analysis of non-response
We have not analysed dissenters, as the National Information Governance Board withdrew consent to use their data.
Questionnaire response rates for those who did not dissent did not vary between trial arms (Table 28). Responders were slightly younger and the significant difference in recruitment point shows that the response rate improved over the course of the trial.
| Variables | Responders to 1-month questionnaire | Non-responders to 1-month questionnaire | Adjusted comparison | |
|---|---|---|---|---|
| Estimate, p-value | 95% CI | |||
| Proportion in intervention group, n/N (%) | 668/1307 (51.1) | 1752/3397 (51.6) | OR = 0.982; p = 0.775 | 0.864 to 1.115 |
| Age (years), mean (SD) [n] | 81.33 (8.06) [1303] | 82.74 (8.00) [3384] | Δ = –1.408; p < 0.001 | –1.920 to –0.896 |
| Proportion of females, n/N (%) | 828/1307 (63.4) | 2129/3396 (62.7) | OR = 1.029; p = 0.675 | 0.901 to 1.174 |
| Proportion with index call out of hours, n/N (%) | 503/1305 (38.5) | 1462/3395 (43.1) | OR = 0.829; p = 0.005 | 0.728 to 0.945 |
| Distance to ED (miles), mean (SD) [n] | 4.87 (3.39) [1296] | 4.66 (3.22) [3380] | Δ = 0.209; p = 0.050 | 0.000 to 0.419 |
| Recruitment point (days), mean (SD) [n] | 246.1 (125.1) [1306] | 211.8 (129.4) [3396] | Δ = 34.30; p < 0.001 | 26.11 to 42.48 |
Harms
We defined a SAE as an emergency service call, ED attendance, emergency hospital admission or death identified as occurring within 2 days of the index incident. These are reported in Table 29. There is little difference in the rate of occurrence of these events between the intervention group and the control group, or in the total number of events between groups (n = 331 in intervention group vs. n = 334 in control group). During the trial there was no serious ARs in which a SAE was reported as possibly related to use of the intervention, including referral to a falls service.
| SAE | Intervention (N = 2420), n (%) | Control (N = 2284), n (%) | Total (N = 4704), n (%) |
|---|---|---|---|
| Emergency service call | 101 (4.2) | 117 (5.1) | 218 (4.6) |
| ED attendance | 78 (3.2) | 92 (4.0) | 170 (3.6) |
| Emergency admission | 133 (5.5) | 109 (4.8) | 242 (5.1) |
| Death | 19 (0.8) | 16 (0.7) | 35 (0.7) |
| Total | 331 (13.7) | 334 (14.6) | 665 (14.1) |
Chapter 5 Cost-effectiveness analysis
Results: summary of demographics
We included 4704 eligible participants in the analysis: 2681 from site 1, 980 from site 2 and 1043 from site 3. Of these, 2420 patients were randomly allocated to the intervention group and 2284 to the control group. Males accounted for 38.8% of the intervention group and 35.3% of the control group. The mean age was 82.5 years in the intervention group and 82.1 years in the control group.
Costs of Support and Assessment for Fall Emergency Referrals 2 trial intervention
The costs of the SAFER 2 trial intervention amounted to £41,854.00, which translates to a mean cost of £17.30 per eligible patient, as shown in Table 30. They include costs associated with training and implementation of the scheme, with a distinction made between costs associated with establishing the scheme (its ‘roll-out’ to other sites), which relate to development of the scheme and training in the respective sites, and the costs of enabling the delivery of the scheme in each area.
| Task | Site 1 | Site 2 | Site 3 | Data sources | Total | |||
|---|---|---|---|---|---|---|---|---|
| Basis of estimate | Actual cost | Basis of estimate | Actual cost | Basis of estimate | Actual cost | |||
| Central set-up costs | ||||||||
| Intervention meeting in Derby to define common core and local optional components of intervention | One meeting (5 hours) × five medical consultants at £50.00 per hour; three falls team leaders at £40.00 per hour; one nurse consultant at £40.00 per hour; one research champion (paramedic) at £26.00 per hour; one ECP at £32.25 per hour; two clinical trainers at £32.25 per hour; one clinical effectiveness manager at £32.25 per hour | £2825.00 | – | – | – | – | Ambulance service | £2825.00 |
| Intervention training subgroup to design DVD | Four meetings (1 hour each) + 1 day development work (7 hours) × one ECP at £32.25 per hour; one nurse consultant at £40.00 per hour | £795.00 | – | – | – | – | Ambulance service | £795.00 |
| Production of DVD for paramedic training | Falls specialists involvement 10 hours at £40.00 per hour | £400.00 | – | – | – | – | Ambulance service | £400.00 |
| Local set-up costs | ||||||||
| Training of clinical educators | One session (4 hours) × two trainers at O/T rates (£32.25 per hour) | £333.00 | Two sessions (including practice sessions) × one trainer at £187.50 daily rate | £375.00 | Two sessions × one trainer at £187.24 daily rate | £374.00 | Ambulance service | £1082.00 |
| Clinical educators provision of training to paramedics | Four sessions (4 hours) × two clinical educators at O/T rates (£32.25 per hour) | £1032.00 | Three sessions (7.5 hours each) × one trainer at £187.50 daily rate | £562.50 | Seven sessions (7.5 hours each) × two trainers at £187.24 daily rate | £2621.00 | Ambulance service | £4215.50 |
| Others provision of training to paramedics | Two sessions (4 hours) × one ECP at £32.25 per hour; one nurse consultant at £40.00 per hour | £578.00 | n/a | – | n/a | – | Ambulance service | £578.00 |
| Training of paramedics | 40 paramedics × 7.5 hours at £26.00 per hour (O/T included in the rate) Travel: 10 miles at £0.45 per mile |
£8175.00 | 26 paramedics × 1 day training (12-hour day) at daily rate £262.00 (O/T included in the rate) (1.5 ×) £21.83 Travel costs: 80 miles at £0.45 per mile |
£7748.00 | 40 paramedics × 8 hours session + extra O/T payment of 4 hours = 12 hours at £21.00 per hour Travel: 40 × two zone 1 + two tube ticket travel cards at £8.00 |
£10,400.00 | Ambulance service | £26,323.00 |
| Cost of catering for paramedic training | Four sessions × £25.00 per group per session | £100.00 | 26 paramedics at £5.00 meal allowance per head | £130.00 | 40 paramedics at £8.34 per head | £334.00 | Ambulance service | £564.00 |
| Falls service leads delivering training to paramedics | Four sessions (2 hours) × one falls service lead at £40.00 per hour Travel: £4.00 per session |
£336.00 | n/a | – | Four sessions (1 hour each) × one falls service lead at £15.60 hourly rate Travel: four × two zone 1 + two tube ticket travel cards at £8.00 |
£94.00 | Ambulance service | £430.00 |
| Partners and falls service set-up and implementation management costs | Six ambulance service-specific meetings (15 minutes each) × one operational support manager (£32.25 per hour); one head of audit and research (£49.90 per hour); one clinical tutor (£32.25 per hour); one lead nurse (£32.25 per hour). Two falls service meetings (60 minutes each) × three falls service team leader (£40.00 per hour). Two LIT meetings (15 minutes each) × AE consultant £50.00 per hour | £438.00 | Six LIT and other meetings (15 minutes to discuss referral pathway) × two clinical trainers at £21.00 per hour; four falls leads at £15.60; one emergency bed service manager at £21.90 per hour; one medical director at £48.90 per hour; one area operations manager at £30.00 per hour; one team leader at £18.30 per hour | £335.00 | Six LIT and other meetings (15 minutes to discuss referral pathway) × two clinical trainers at £21.00 per hour; four falls leads at £15.60; one emergency bed service manager at £21.90 per hour; one medical director at £48.90 per hour; one area operations manager at £30.00 per hour; one team leader at £18.30 per hour | £335.00 | Ambulance service | £1108.00 |
| Two operational support managers (£32.25 per hour); one head of audit and research; one clinical tutor (£32.25 per hour); one lead nurse (£32.25 per hour); three falls service team leader (£40.00 per hour) | ||||||||
| Delivery costs | ||||||||
| RSO/paramedic time providing feedback and clinical support to paramedics | 2 days per week at £14.70 per hour | £206.00 | 2 days per week × RSO day rate £187.50 | £375.00 | 2 days per week at RSO day rate £252.00 | £504.00 | Ambulance service | £1085.00 |
| Travel for ongoing clinical support | 20 miles per week in lease car | £303.00 | n/a | £0.00 | n/a | – | Ambulance service | £303.00 |
| Feedback forms from falls service to paramedics | 91 referrals × 30 minutes per referral undertaken by one falls therapist at £30.00 per hour | £1365.00 | n/a | – | 100 referrals (not all were eligible) × 30 minutes by falls therapist at £15.60 per hour | £780.00 | Ambulance service | £2145.00 |
| Total intervention costs | ||||||||
| Intervention costs total | £16,886.00 | Intervention costs total | £9525.50 | Intervention costs total | £15,442.00 | – | £41,854.00 | |
| Number of eligible patients | 1329 | Number of eligible patients | 544 | Number of eligible patients | 547 | – | 2420 | |
| Cost per eligible patient | £12.71 | Cost per eligible patient | £17.51 | Cost per eligible patient | £28.23 | – | £17.30 | |
Resource use
The costs of health care used by trial participants, in the care of trial paramedics, were derived by multiplying items of resource use by the published unit costs in Table 31.
| Health service resource | Average unit cost | Range of unit costs | Range of annualised equipment costs (3.5% discount) | Average annualised equipment cost (3.5% discount) | Source |
|---|---|---|---|---|---|
| Ambulance attendance (patient conveyed) | £230.00 | – | – | – | NHS Reference Costs 2012–13 122 |
| Ambulance attendance (patient not conveyed) | £174.00 | – | – | – | NHS Reference Costs 2012–13 122 |
| ED attendance cost | £115.00 | – | – | – | NHS Reference Costs 2012–13 122 |
| Non-elective inpatient long stay (4.0 days) | £2752.00 | £531.00–9657.00 | – | – | NHS Reference Costs 2012–13 122 |
| Non-elective inpatient long stay (excess days) | £230.00 | £67.00–556.00 | – | – | NHS Reference Costs 2012–13 122 |
| Non-elective inpatient short stay | £521.00 | £133.00 –1376.00 | – | – | NHS Reference Costs 2012–13 122 |
| Falls service referrals | £119.00 | – | – | – | NHS Reference Costs 2012–13 (from ‘Hospital at Home/Early Discharge Schemes’)122 |
| GP surgery visit (average 11.7 minutes) | £43.00 | – | – | – | PSSRU (2013)123 |
| GP telephone consultation (average 7.1 minutes) | £26.00 | – | – | – | PSSRU (2013)123 |
| GP home visit (average 23.4 minutes) | £110.00 | – | – | – | PSSRU (2013)123 |
| NHS Direct | £25.00 | – | – | – | BMA (2011)124 |
| Community nurse home visit (district nursing sister, district nurse) | £70.00 | – | – | – | PSSRU (2013)123 |
| Outpatient attendance (same as non-elective inpatient stay average short stay cost) | £467.00 | – | – | – | NHS Reference Costs 2012–13 122 |
| Nursing/residential care weekly (private) (average weekly cost) | £758.00 | – | – | – | PSSRU (2013)123 |
| Nursing/residential care weekly (local authority) (average weekly cost) | £796.00 | £415.00–1331.00 | – | – | PSSRU (2013)123 |
| Local authority day care (average cost) | £40.00 | – | – | – | PSSRU (2013)123 |
| Extra care package for older people (average weekly cost) | £428.00 | – | – | – | PSSRU (2013)123 |
| Adjustable shower stools and chairs | £81.00 | £14.00–148.00 | £1.80–18.00 | £9.90 | PSSRU (2013)123 |
| Perching stool with arms or back | £23.00 | – | £2.70 | £2.70 | PSSRU (2013)123 |
| Toilet frame and seat | £30.00 | – | £3.60 | £3.60 | PSSRU (2013)123 |
| Mobile shower chair | £55.00 | – | £6.60 | £6.60 | PSSRU (2013)123 |
| Bath step | £20.00 | – | £2.50 | £2.50 | PSSRU (2013)123 |
| Standard bath lift, two types | £317.00 | £303.00–330.00 | £36.00–40.00 | £38.00 | PSSRU (2013)123 |
| Linked bed raisers, pair | £32.00 | – | £3.80 | £3.80 | PSSRU (2013)123 |
| Adjustable trolley | £34.00 | – | £4.10 | £4.10 | PSSRU (2013)123 |
| High-back chair | £121.00 | – | £14.50 | £14.50 | PSSRU (2013)123 |
| Variety of indoor and outdoor grab rails | £47.00 | £3.40–91.00 | £0.40–11.00 | £5.70 | PSSRU (2013)123 |
| Walking sticks | £38.00 | £22.00–54.00 | £2.60–6.40 | £4.50 | PSSRU (2013)123 |
| Commodes | £57.00 | £29.00–85.00 | £3.40–10.30 | £6.85 | PSSRU (2013)123 |
| Wheelchair (per year) | £89.00 | – | – | – | PSSRU (2013)123 |
| Home care | £42.00 | – | – | – | PSSRU (2013)123 |
All but 49 patients were subsequently matched at SAIL or the HSCIC and, therefore, 4655 patients (2391 intervention, 2264 control) were included in the analysis of the anonymised linked data primary outcome. We combined two types of resource use. We calculated costs relating to emergency service calls, ED attendances and hospital stays for all matched participants, using routinely collected data for 1 month and 6 months following the index call, and then combined self-reported costs, obtained via questionnaires, over 1 and 6 months. Table 32 shows that the main differences at 6 months are in the mean costs of initial hospital stays (£2523.27 in the intervention group vs. £2329.79 for control), and of subsequent hospital stays (£3982.21 for intervention vs. £4111.10 for control). At 6 months, mean total costs were £7386.39 in the intervention group and £7301.31 in the control group. Consistent with the clinical effectiveness analysis in Chapter 4, there are statistically significant differences in the mean costs of subsequent emergency service calls over 1 month, and of ED attendances over 6 months. These may warrant further investigation, although such differences are generally obscured when aggregated with larger (but statistically non-significant) differences in other elements of resource use – notably, hospital stays (see Table 32 and its footnotes).
| Index | Intervention (n = 2391) | Control (n = 2264) | ||||
|---|---|---|---|---|---|---|
| Observed | Total cost | Mean cost (SD) | Observed | Total cost | Mean cost (SD) | |
| Routine data | ||||||
| Proportion conveyed at index emergency services call n/N (%) | 1562/2391(65.3%) | £503,506.00 | £210.58 (£26.66) | 1424/2264 (62.9%) | £473,680.00 | £209.22 (£27.06) |
| Proportion attending ED following index call n/N (%) | 1419/2391 (59.3%) | £163,185.00 | £68.25 (£56.50) | 1311/2264 (57.9%) | £150,765.00 | £66.59 (£56.79) |
| Proportion admitted to hospital following index call n/N (%) | 906/2391 (37.9%) | – | – | 843/2264 (37.2%) | – | – |
| Index hospital stays (nights in hospital, truncated at 1 month) | 12735 | £4,628,754.00 | £1935.91 (£3096.33) | 10857 | £4,057,019.00 | £1791.97 (£2954.50) |
| Index hospital stays (nights in hospital, truncated at 6 months) | 18068 | £6,033,134.00 | £2523.27 (£5221.25) | 15703 | £5,274,639.00 | £2329.79 (£4981.03) |
| Index falls service referrals | 204 | £24,276.00 | £10.15 (£33.25) | 26 | £3,094.00 | £1.37 (£12.68) |
| 1-month follow-up routine data | ||||||
| Subsequent emergency service callsa | 662 | £133,724.00 | £55.93 (£153.64) | 710 | £143,420.00 | £63.35 (£153.06) |
| Subsequent ED attendancesb | 591 | £67,965.00 | £28.43 (£68.94) | 552 | £63,480.00 | £28.04 (£88.41) |
| Subsequent hospital stays (nights in hospital, truncated at 1 month)c | 5375 | £2,287,737.00 | £956.81 (£2208.39) | 4758 | £2,042,487.00 | £902.16 (£2168.19) |
| 1-month follow-up self-reported questionnaire data | ||||||
| GP surgery visit | 331 | £14,233.00 | £21.50 (£53.51) | 359 | £15,437.00 | £24.20 (£58.99) |
| GP telephone consultation | 404 | £10,504.00 | £15.87 (£34.67) | 408 | £10,608.00 | £16.63 (£37.50) |
| GP home visit | 325 | £35,750.00 | £54.00 (£119.76) | 355 | £39,050.00 | £61.21 (£139.02) |
| NHS Direct | 169 | £4,225.00 | £6.38 (£26.20) | 158 | £3,950.00 | £6.19 (£26.45) |
| Community nurse (district nursing sister, district nurse) visit | 588 | £41,160.00 | £62.18 (£145.55) | 554 | £38,780.00 | £60.78 (£150.56) |
| Outpatients | 420 | £196,140.00 | £296.28 (£692.51) | 382 | £178,394.00 | £279.61 (£697.57) |
| Social service equipment (adjustable shower stools, walking frames, etc.) | – | £1,686.00 | £2.55 (£10.48) | – | £1,432.00 | £2.25 (£9.29) |
| Further home care/carer | – | £588.00 | £0.89 (£6.05) | – | £840.00 | £1.32 (£7.32) |
| Local authority day care/nursing/residential care weekly/extra care package for older people | – | £0.00 | £0.00 (£0.00) | – | £0 .00 | £0.00 (£0.00) |
| 1-month self-reported sub-total | 662 | £304,286.00 | £459.65 (£809.09) | 638 | £288,491.00 | £452.18 (£823.77) |
| 6-month follow-up routine data | ||||||
| Subsequent emergency services callsd | 2712 | £547,824.00 | £229.12 (£505.58) | 2825 | £570,650.00 | £252.05 (£539.13) |
| Subsequent ED attendancese | 2014 | £231,610.00 | £96.87 (£159.99) | 2063 | £237,245.00 | £104.79 (£314.41) |
| Subsequent hospital stays (nights in hospital, truncated at 6 months)f | 26739 | £9,521,458.00 | £3982.21 (£6840.75) | 26311 | £9,307,534.00 | £4111.10 (£6963.00) |
| 6-month follow-up self-reported questionnaire data | ||||||
| GP surgery visit | 682 | £29,326.00 | £83.55 (£175.15) | 602 | £25,886.00 | £80.14 (£161.92) |
| GP telephone consultation | 700 | £18,200.00 | £51.85 (£106.10) | 528 | £13,728.00 | £42.50 (£88.15) |
| GP home visit | 493 | £54,230.00 | £154.50 (£372.27) | 410 | £45,100.00 | £139.63 (£321.09) |
| NHS Direct | 393 | £9,825.00 | £27.99 (£93.32) | 270 | £6,750.00 | £20.90 (£73.78) |
| Community nurse (district nursing sister, district nurse) visit | 1100 | £77,000.00 | £219.37 (£418.91) | 1078 | £75,460.00 | £233.62 (£447.88) |
| Outpatients | 864 | £403,488.00 | £1149.54 (£2204.78) | 736 | £343,712.00 | £1064.12 (£2053.32) |
| Social service equipment (adjustable shower stools, walking frames, etc.) | – | £1,985.00 | £5.63 (£18.80) | – | £1,288.00 | £3.99 (£12.85) |
| Further home care/carer | – | £462.00 | £1.32 (£7.33) | – | £630.00 | £1.95 (£8.85) |
| 6-month self-reported subtotal | 351 | £594,506.20 | £1693.75 (£2759.19) | 323 | £512,553.95 | £1586.85 (£2527.89) |
| Intervention | 2391 | £41,352.00 | £17.30 (£0.00) | 2264 | £0.00 | £0.00 (£0.00) |
| Totals for 1 month | – | £8,154,797.55 | £3410.62 (£3597.28) | – | £7,222,436.70 | £3190.12 (£3526.34) |
| Totals for 6 months | – | £17,660,863.50 | £7386.39 (£8619.93) | – | £16,530,160.95 | £7301.31 (£8594.00) |
As questionnaire response rates were low at both 1 month and 6 months, self-reported resource use costs were used to impute unbiased estimates of such costs for all matched participants. Table 33 summarises all resource costs. Again using the linear modelling method outlined in Chapter 4, the estimated intervention effect (adjusted for statistically significant covariates) at 1 month is £190.24 (95% CI –£13.83 to £394.31; p = 0.068), and at 6 months is £24.20 (95% CI –£468.01 to £516.40; p = 0.923); see Table 33 and its footnotes.
| Index | Intervention (n = 2391) | Control (n = 2264) | ||
|---|---|---|---|---|
| Total cost | Mean cost | Total cost | Mean cost | |
| 1-month follow-up | ||||
| Cost of index call up to 1 month | £5,361,085 | £2,242.19 | £4,684,558 | £2,069.15 |
| Routine costs by 1 month | £2,489,426 | £1,041.17 | £2,249,387 | £993.55 |
| Self-reported costs at 1 month (imputed) | £1,091,880 | £456.66 | £1,022,581 | £451.67 |
| Total costs by 1 montha | £8,942,391 | £3,740.02 | £7,956,526 | £3,514.37 |
| 6-month follow-up | ||||
| Cost of index call up to 6 months | £6,765,465 | £2,829.55 | £5,902,178 | £2,606.97 |
| Routine costs by 6 months | £10,300,892 | £4,308.19 | £10,115,429 | £4,467.95 |
| Self-reported costs at 6 months (imputed) | £4,013,668 | £1,678.66 | £3,592,630 | £1,586.85 |
| Total costs by 6 monthsb | £21,080,025 | £8,816.41 | £19,610,237 | £8,661.77 |
Health-related quality of life
We estimated SF-6D utilities from questionnaires received at 1 and 6 months. However, the average proportion of missing data items was 5.5% at 1 month and 10.1% at 6 months; therefore, we imputed these missing items from the predicted SF-6D utilities adjusted for the number of reported deaths. The resulting imputed SF-6D utilities were higher in the control group at 6 months, although this did not achieve statistical significance. As the utilities were collected at 6 months, the QALYs gained by the intervention group was –0.0026 (95% CI –0.0066 to 0.0014), that is more QALYs were gained by the control group (Table 34).
| Index | Group | |||
|---|---|---|---|---|
| Intervention (A) | Control (B) | Adjusted comparison | 95% CI | |
| 1 month | ||||
| Derived SF-6D, mean (SD) [n] | 0.5565 (0.1264) [480] | 0.5547 (0.1278) [452] | Δ = –0.0011; p = 0.893 | –0.0173 to 0.0151 |
| 6 months | ||||
| Derived SF-6D, mean (SD) [n] | 0.5885 (0.1377) [280] | 0.5970 (0.1391) [257] | Δ = –0.0078; p = 0.509 | –0.0311 to 0.0155 |
| SF-6D (imputed), mean (SD) [n] | 0.4695 (0.2351) [2376] | 0.4838 (0.2376) [2249] | Δ = –0.0107; p = 0.114 | –0.0240 to 0.0026 |
| QALYs mean (SD) [n] | 0.2093 (0.0709) [2375] | 0.2133 (0.0713) [2245] | Δ = –0.0026; p = 0.202 | –0.0066 to 0.0014 |
Cost-effectiveness analysis
In summary, as there is no difference between groups in relation to resource use, the net cost of the intervention is £17.30. There is also no statistically significant difference in the number of QALYs generated between the two groups.
To test the extent to which this conclusion depends on the various assumptions we made, we conducted sensitivity analyses based on the upper and lower bounds of the 95% CI for both net cost (using the adjusted comparisons in Table 33) and net QALY (Table 35).
| Parameter | Incremental cost of intervention | Incremental QALY | Cost per QALY gained |
|---|---|---|---|
| Baseline (95% CI) | £17.30 (–£475.01 to £509.40) | –0.0026 (–0.0066 to 0.0014) | Usual care is dominant. North-west quadrant of cost-effectiveness plane |
| Upper 95% bound of net cost | £509 | – | £363,857. North-east quadrant of cost-effectiveness plane |
| Upper 95% bound of net QALY | – | 0.0014 | |
| Upper 95% bound of net cost | £509 | – | Usual care is dominant. North-west quadrant of cost-effectiveness |
| Lower 5% bound of net QALY | – | –0.0066 | |
| Lower 5% bound of net cost | –£475 | – | £71,971. South-west quadrant of cost-effectiveness plane |
| Lower 5% bound of net QALY | – | –0.0066 | |
| Lower 5% bound of net cost | –£475 | – | Intervention is dominant. South-east quadrant of cost-effectiveness plane |
| Upper 5% bound of net QALY | – | 0.0014 |
The sensitivity analysis highlights that the extent to which the SAFER 2 trial intervention can be regarded viewed as being cost-effective is inconclusive. This is further evidenced by the cost-effectiveness plane in Figure 7, generated from bootstrapping (5000 resamples). There is a net mean cost of £17.30, some clinically important statistically significant differences in the number of subsequent emergency service calls (at 1 month) and ED attendances (at 6 months), but no statistically significant difference in QALYs gained.
FIGURE 7.
Cost-effectiveness plane for the SAFER 2 trial intervention.
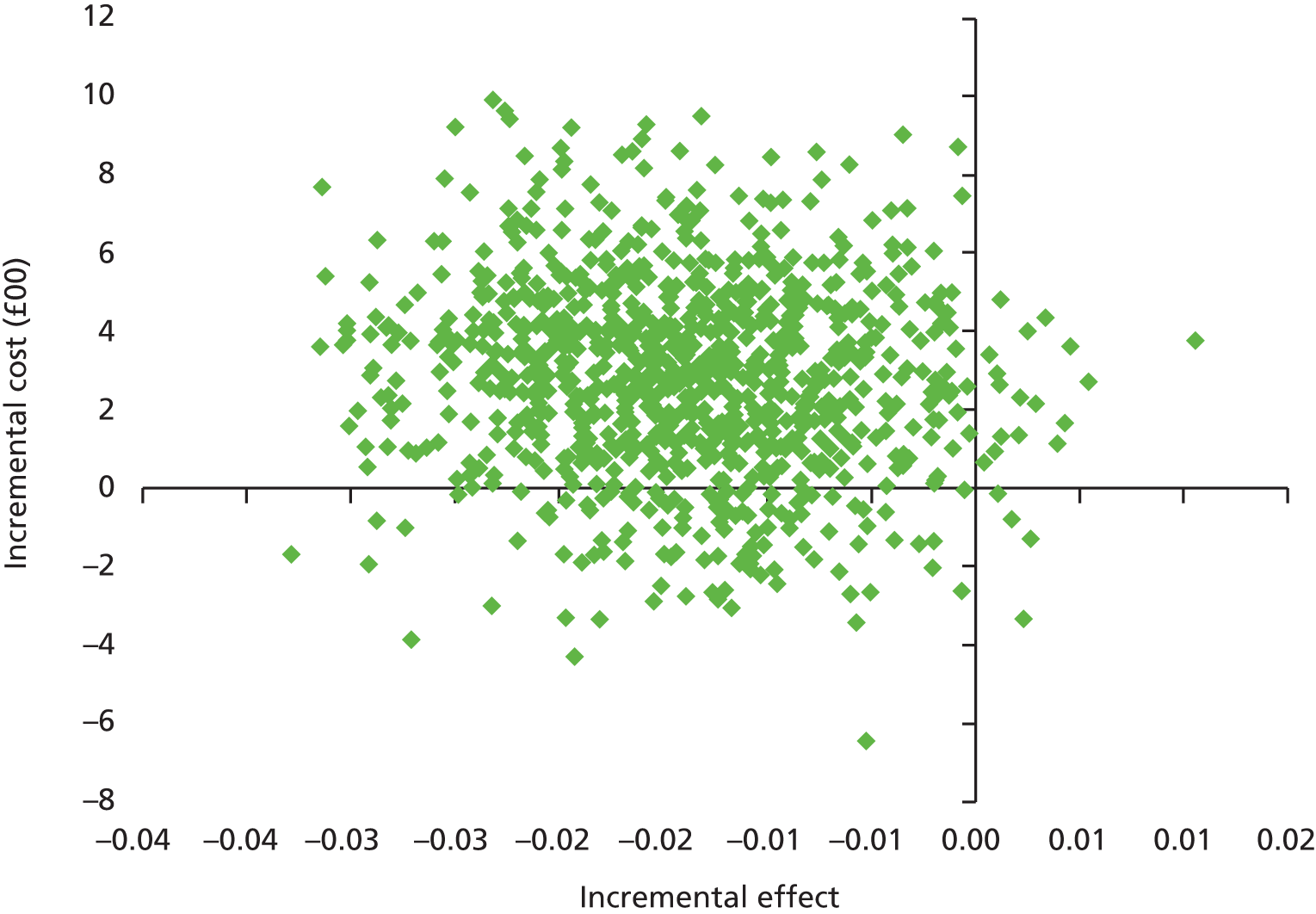
Conclusion
The relative cost-effectiveness of the SAFER 2 trial intervention is inconclusive, and further investigation is warranted to establish whether or not it represents value for money. It has resulted in important difference in the number of subsequent emergency service calls at 1 month and ED attendances at 6 months, but no difference between intervention and usual care in relation to QALYs gained.
Chapter 6 Qualitative results
Introduction
The qualitative component of the study was designed to find out how the intervention was experienced both by patients and by paramedics and other stakeholders involved in delivering it. In particular, it aimed to identify factors which facilitate or hinder use of the protocol and referral pathway. The SAFER 2 trial intervention was hypothesised to work by improving the decision-making of paramedics in terms of safe non-conveyance and referral of older people who have had a fall to appropriate community-based services, leading to better outcomes for patients, reduced costs and improved paramedic skill sets. Through the protocol, pathway, training, support and feedback, the intervention provided a formalised framework for decision-making and referral for this patient group, in comparison with the informal approaches that characterise existing practice. This is hypothesised to make a difference by one or more of the following four mechanisms:
-
increasing paramedics’ clinical knowledge of how to make appropriate non-conveyance decisions
-
increasing paramedics’ knowledge of falls services and pathways for referral
-
increasing paramedics’ confidence about making a non-conveyance decision and reducing anxiety about risk
-
increasing awareness of and likelihood that paramedics will consider non-conveyance and referral pathways as an option in appropriate cases.
In order for the intervention to make a difference to practice and to patient outcomes, a number of factors needed to be in place, including:
-
effective referral pathways, and sufficient capacity in falls teams to respond to referrals
-
training and support provided to paramedics that is appropriate and effective
-
motivation on the part of paramedics to use the new protocol and referral pathway.
The qualitative component of the study aimed to examine the perspective of paramedics and other clinical stakeholders on these hypothesised mechanisms and necessary factors. It also aimed to gather data from patients to assess whether or not they were satisfied with the new intervention and whether or not, if relevant, the referral pathways were effective.
To address how the intervention was experienced by patients, we interviewed 58 patients attended by paramedics trained in the use of the new protocol from across the three sites, of whom 36 had been transferred to hospital, 12 were referred to a falls service and 10 remained at home without a referral (Table 36). Full details of sampling and data collection processes are given in Chapter 4. In this chapter, respondents are identified by identification numbers: numbers beginning with 1 are from site 1, those beginning with 2 are from site 2, and those beginning with 3 are from site 3, then participants in each site are numbered sequentially in the order in which they were interviewed. An ‘H’ after the number indicates that the patient was transferred to hospital, an ‘F’ shows that the patient was referred to a falls service and an ‘N’ indicates that the patient had neither outcome and was simply left at home. Findings from all three sites are written up together, structured by theme, with variations between sites noted when relevant. In the majority of cases, the respondent is the patient. In 18 cases, a family member with caring responsibilities also took part in the interview; where relevant in the text, quotations from carers are indicated by a ‘c’ appended to the end of the patient identification number.
| Site | Transported to hospital | Referred to falls service | Neither transported nor referred | Total |
|---|---|---|---|---|
| Site 1 | 9 | 4 | 4 | 17 |
| Site 2 | 15 | 2 | 2 | 19 |
| Site 3 | 12 | 6 | 4 | 22 |
| Total | 36 | 12 | 10 | 58 |
As discussed in the qualitative data analysis section of Chapter 3, evidence is presented as anonymised quotations to support explanation of complex ideas, provide illustration and deepen understanding. Most quotations were selected to illustrate the majority view; however, some do convey exceptional viewpoints, as noted. In some cases, quotations were selected to illustrate complexity or ambiguity of perspective, as noted.
To address the experience of those delivering the intervention, we carried out focus groups and interviews with paramedics who were randomly allocated to the intervention group across the three sites at two time points: before the implementation of the intervention (24 paramedics) and after the completion of the live phase of the trial during which patients were recruited (25 paramedics). After the completion of the patient recruitment phase, we carried out focus groups and interviews with 31 stakeholders who had a role in delivering the intervention (e.g. ambulance service managers, training officers and staff of falls services). This chapter has been structured around themes related to the research questions and has been informed by the theoretical underpinning for the study. It brings together findings from the different staff groups and different sites, noting differences between sites when relevant. Table 37 summarises the paramedic and stakeholder focus groups and interviews that took place.
| Site | Data collection | Participants |
|---|---|---|
| Site 1 | Pretrial paramedic focus group | Four paramedics |
| Pretrial paramedic interviews | Two paramedics | |
| Post-trial paramedic focus group | Four paramedics | |
| Post-trial stakeholder focus group | Four stakeholders working for ambulance service: head of research and audit; research project manager; operational support manager; and clinical quality manager | |
| Post-trial stakeholder interviews | Four stakeholders: ambulance service clinical team leader; and three falls team leaders | |
| Site 2 | Pretrial paramedic focus group | Four paramedics |
| Post-trial paramedic focus group | Seven paramedics | |
| Post-trial stakeholder focus group 1 | Three stakeholders working for ambulance service: R&D manager; clinical effectiveness manager; and a research assistant | |
| Post-trial stakeholder focus group 2 | 13 stakeholders: community staff nurse; acute trust head of strategy; team leader; community deputy team leader; team leader; district nurse team leader; district nurse; team leader district nurse; district nurse; district nurse team leader; district nurse team leader; district nurse team leader; and community sister | |
| Site 3 | Pretrial paramedic focus group 1 | Six paramedics, one clinical tutor |
| Pretrial paramedic focus group 2 | Eight paramedics | |
| Post-trial paramedic focus group 1 | Seven paramedics | |
| Post-trial paramedic focus group 2 | Seven paramedics | |
| Post-trial stakeholder focus group 1 | Three stakeholders working for ambulance service: research manager; deputy information manager; and clinical tutor | |
| Post-trial stakeholder focus group 2 | Three stakeholders: senior ED clinical research nurse; falls co-ordinator and interim head of falls team; and falls lead physiotherapist | |
| Post-trial stakeholder interviews | Two stakeholders: ambulance service medical director and library housebound service manager |
How the intervention was experienced by patients
The fall in context
Every patient we interviewed described having a fall. Fifty-one respondents talked about the circumstances of the index incident and what they felt caused it. The majority (28) of the falls were described as taking place within the home, many of them trips and slips when moving around or using steps, and eight were cases of respondents sliding off chairs or the bed. A further 11 of the respondents described falls in the garden or outside the house, while hedge-trimming or watering plants, shovelling coal, putting the bins out, and so on. The remainder of the falls happened while the respondent was out and about. A minority of respondents described injuries resulting from the fall, ranging from fractures and being knocked unconscious to cuts and bruises.
Some falls were described as having a clear mechanical cause, such as 2–6H missing his footing on a stepladder while cutting the hedge. However, for many more, both inside and outside the home, the cause seemed unclear, as in the case of one respondent who fell in her kitchen:
All of a sudden, I never felt it, it just . . . just . . . like it just . . . my mind went blank. I just felt myself falling and when I looked around I was on the floor. So I thought to myself ‘silly bugger’.
3–21N
Many of the respondents explicitly stated that they did not know why they fell, while for a striking number the fall was something which ‘just’ happened: ‘my leg just gave way’ (1–1H); ‘I just dropped’ (1–7F); ‘I just slid down’ (1–2N), and so on.
Others seemed to be seeking an explanation for why they fell:
But you know being in the middle of the night, waking up out of a sleep, you’re not very steady, are you? I mean in the best of times.
3–9F
The falls happen like somebody’s switching off the light switch according to the doctor. It’s not a stumble or a trip, it–, this is just a fall which happens [clicks fingers], which is related to probably blood pressure or whatever. They are looking at the fact an epileptic fit may be involved here.
2–7H
In some cases this was expressed in terms of wanting to find an external cause for the fall:
But as I say the fact that I fell was simply something mechanical. I took a step back and I’d got a saucepan in one hand and a spoon in the other so I wasn’t holding onto things as I usually do. It’s the sort of thing that can happen to anybody, I think.
3–20N
Forty-three of the respondents described having had one or more previous falls, before the index incident, although not all of these incidents would have been attended by an ambulance. Some seemed habituated to falling:
Cause I’ve fell loads of times before.
1–11N
I have falls . . . I’m a faller.
3–18F
I can fall over at a drop of a hat, can’t I?
1–5H
However, while some of those who had previously fallen had said that they had managed to do so without damage, and without professional intervention to get back on their feet, for others there was past history of significant damage sustained in falling:
I said, ‘Oh my goodness, not again [wife’s name],’ ‘cause she’d broke the other hip 12 months ago.
1–4Hc
Thirteen of the respondents described having fallen again between the index incident and the interview. For the majority of them, this was a single fall, or a series of minor falls dismissed as ‘little trips’ (3–5H), but three described having had two or even three more major falls for which an ambulance had been called.
Patient experience of the ambulance service
Care
Respondents were asked to describe what happened when the paramedics arrived following the fall. In terms of immediate care or intervention, much of the largest group of responses (n = 29) concerned the patient being physically lifted, simply by hand, with the help of inflating equipment (n = 7) or in one case with the help of a towel. A small number of respondents compared the experience of being lifted by the paramedics with previous occasions when family, friends or neighbours had lifted them, sometimes resulting in hurt to themselves.
A minority of respondents described other forms of treatment administered by the paramedic, such as the dressing of wounds and the administration of pain relief, including morphine. In some cases, paramedics advised the patient to contact the GP for further care needs.
More generally, respondents talked about the way in which paramedics delivered care and built rapport with their patients. These comments were entirely positive across all three sites, and across all patient groups. The very process of examination and asking questions was described by some patients as having a positive effect:
I was very impressed, they gave me confidence, I felt safe with them, I felt they’d looked at what they needed to look at . . . yes they said to take painkillers and yes it was perfectly all right to have a drink because I might be a bit dehydrated by now and they said–, and I thought, yes now you’ve seen me I can do what I need to do.
1–6N
I thought they were very good. I mean they dealt with it efficiently, the questions gave me confidence . . . It was the confidence, you know you’re going to get a bit of pain but it’s the confidence they give you that you can work at it.
3–11H
Paramedics were described as treating respondents with respect, making them feel safe, and generally removing anxiety:
They put me at my ease lovely. I relaxed, I thought they were wonderful.
2–18H
Others used the words ‘fantastic’, ‘marvellous’, ‘efficient’, ‘caring’, ‘kindly’, ‘respectful’, ‘kind’, ‘nice’, ‘brilliant and a good laugh’ and ‘the nicest of all the public services’. This respondent reflected the overall tone of the interviews:
I can’t praise them enough.
2–16H
Assessment and examination
Respondents were asked to describe the processes of assessment and physical examination which they underwent after their fall. Recall of the details was frequently imprecise, not surprisingly, as the interviews were done some months after the incident, and stress or memory problems may have clouded their recall. Almost all showed patience with the assessment process and were positive in their reporting of it.
Respondents described in detail the various checks which paramedics went through:
They took me downstairs onto the ambulance and I was there for about half an hour. They were checking me over . . . and they were very very thorough and they were very good as well . . . Yes they checked my heart, blood pressure, they looked me over where I hurt myself and they were writing it all down which I suppose goes to the hospital. They written down all the drugs and they knew what they were.
3–16H
Thorough 100% medical . . . They phoned up the GP and checked my medication and took my blood pressure. They gave me a walking test and helped me . . . I was surprised at the thoroughness of the test. I just took it as the normal procedure.
3–7F
From what I can remember, she was as thorough as any doctor, with the things that she did, didn’t she?
1–14F
One respondent was pleased with the manner and confidence with which the paramedics went through the assessment, without referring to a ‘crib sheet’:
Oh, they were natural with it. They weren’t reading it up as we went, no . . . That would’ve affected my confidence if they had done.
1–10H
The only respondent who expressed reservations about the assessment and examination process was 1–6Hc, whose wife was attended after a fall:
Don’t get out to a patient’s house when everybody’s frustrated and uptight and everything about somebody being–, being very, very poorly and then start playing about with computers and, you know, this sort of this nonsense . . . Initially I get a little bit worked up about the fact that they ask so many what–, seems to me to be extraneous questions . . . But they seem to ask so many questions and you seem to be there forever and you think well, is all this relevant to taking somebody into hospital that’s sick? You ring an ambulance in the first place because you think it’s urgent that they need hospital attention, how can they burn all this time up?
1–6Hc
Those with previous experience of being attended by paramedics after a fall were asked to compare this experience (index incident) with any other falls. Three said they felt that the assessment as part of the SAFER 2 trial was more thorough, but the majority (n = 11) of respondents who made a comparison did not think there was a difference.
It was pretty much the same . . . Pretty consistent and they always use the same sort of procedures.
2–17H
Well I didn’t know they were following a new process, it seemed exactly the same as the last time they came.
3–19N
Decision-making
A minority of respondents described the process of decision-making which was informed by the assessment and examination. These descriptions were almost exclusively in terms of the decision about whether or not to attend hospital, rather than about referral to the falls team. One respondent, describing how a decision was reached by the lead paramedic, seemed very positive about the use of a decision-making tool:
And then eventually the young lady said, ‘I think you should go into hospital’, and . . . they took her by ambulance to the hospital. It was a very straight cut simple sort of uncomplicated affair. Much different to a lot of previous times we’ve called the ambulance.
1–4Hc
Not all the respondents were so clear about the process of reasoning which took place:
I didn’t know, they knew I had to get into hospital but I don’t think they knew what I had done, I’m not sure about this, not that they missed anything, but I’m not sure, but they certainly were very sure that I had to go to hospital.
3–9H
A few respondents described how the paramedics drew them into the decision-making process, offering them the choice of whether or not to go to hospital: some decided to stay home, while others chose to go in for additional examinations:
They gave me an option to go for a check-up in the hospital and I didn’t think it was necessary because the hospital would have just done the same treatment I received from the paramedics.
3–7F
I wanted to go, I wanted to make sure if there was anything broken they would fix it.
3–16H
A small number, although advised by paramedics to attend hospital, exercised their right to refuse, one of them in fairly strong terms:
They said it’s not just that we want you to go to hospital; we don’t know if a thorough enough examination has been done. We want to feel sure that everything has been done and we haven’t done it. PLEASE go. And I said ‘On my head be it, I won’t go and if anyone wants to know – you begged me to go . . . I don’t want to go to that bloody awful hospital.’
3–18F
But more common was a sense that the respondent put their confidence in the clinical skills and decision-making of paramedics:
I mean, you rely on their judgement, don’t you?
2–11H
Patient experience: those referred to a falls service
Twelve of the respondents had been identified as having been referred to a falls service by the attending ambulance crew. Respondents described being contacted within 2 weeks of referral at most, some within a week, and receiving a range of interventions, such as 6-week courses in falls avoidance at a day centre, home visits with exercise training, the installation of grab rails in the home, and equipment such as bed levers and perching stools.
Among the respondents who had been referred to the falls service and had received input, satisfaction was generally high:
Oh it’s the best thing that’s ever happened in my life.
1–8F
They’re tops. They really are. Not one of them you could fault. Very, very helpful . . . They’re marvellous people. And so patient with you.
1–12F
I had wonderful care from [local authority]. Absolutely remarkable.
3–4F
Being identified as suitable for a falls service did not necessarily equate to receiving the intervention. One respondent felt that the falls service offered nothing helpful, for another the intervention was stopped for medical reasons and a third was identified as suitable for referral to a falls service, but refused it altogether because:
I thought it was a waste of time really.
3–21N
Three respondents recorded as having been referred could not recall any contact, which may reveal a fault with the recording system or with the referral system.
Although respondents were forthcoming about their views on the falls services themselves, it was hard to disentangle any opinion on the process of being referred to the falls service as part of the SAFER 2 trial intervention. One respondent was unusual in commenting on this, indicating that she felt some confusion about the referral process:
Well, they just said to me when we–, ‘You know we have to refer you now to the falls team’ and so I said, ‘Right’. But I wondered what’s the falls team? What it was all about.
1–12F
More generally, it was not always clear whether the intervention the respondent was talking about was one which was delivered by a falls service associated with the SAFER 2 trial, or was actually a similar service delivered by another team or accessed through a different route. Respondents themselves were in some cases unclear about this:
Well, I feel as though, yes, I mean I got this appointment at the falls, although the doctor, obviously, did it, but I think it was through the SAFER 2 that they did it.
1–7F
Oh, sorry . . . I don’t know who arranged that then.
1–14F
Patient experience: those who attended hospital
Thirty-six of the respondents had been taken to hospital as part of the SAFER 2 trial. The care they received in hospital varied greatly, from being ‘sent home with some paracetamol’ (1–1H), to being admitted for surgery. Others were radiographed, stitched or were put in a cast, and a small number ended up with a lengthy stay in hospital.
The majority of respondents had a positive evaluation of their visit to hospital. Generally, this was expressed in terms of praise for the care provided by individual clinicians:
[The nurse] did fill me with confidence, you know, he was very, very good.
1–10H
The hospital staff, they were all absolutely wonderful, can’t rate them enough.
1–15H
They were very comforting, you know, they gave me confidence in them and they were thoughtful and kind and helpful. I can’t praise them enough, nor the nurse that did the stitching.
2–16H
But, yeah, the doctor was marvellous, the people who done the X-ray, great. No problems.
2–6H
Two respondents stated explicitly that the decision to go in to hospital had been the right one, the wife of 3–6Hc suggesting that it ‘saved your life’.
However, for some the experience of attending hospital proved to be very frustrating. 2–6H was radiographed for suspected broken ribs, although even after the radiograph, ‘they couldn’t say for sure if there was a break or not’. Another respondent was reported by a carer as receiving even less in the way of an intervention:
We went into [ED] in the [hospital], we were there till quarter to three when a doctor eventually came to see her. She had a quick look at her, asked me to get her off the bed and walk her, and because she walked, to take her home . . . not even an X-ray to see whether she had broken her leg.
2–3Hc
Other negative aspects of attending hospital reported by respondents included delays in handover and admission:
We were all lined up, it was like a production line, waiting to be handed over to the doctor.
2–10H
Another respondent mentioned the difficulty of getting only a one-way journey in the ambulance:
But, the only thing I have against all that, they’ll get you to the hospital but they don’t see about you getting home again.
1–1H
Patient health and quality of life since fall
Respondents were asked how their health had been since the fall, leading to extensive discussions not just of health, but also of mobility and quality of life. Some patients made a comparison between their current state and their prefall status, while others compared how they were at the time of the interview with their immediate post-fall status; a few talked through the whole sequence of fall and recovery. A great range of experience was described, across all three outcome groups, and all three study sites. It was not possible to discern a clear pattern of difference between the three outcome groups, except that the group of patients who had been taken to hospital, as might be expected, included some people with more significant injuries.
A minority of respondents had very positive stories of recovery after the fall. These were most striking in the case of people who had sustained fractures or other significant injury in the fall:
Getting better all the time.
2–10H
Mum is amazingly better. She walks around the whole house on her own. When she came back from hospital she was actually moved with a hoist, she had no movement whatsoever and that has changed dramatically.
2–17Hc
Among those who had been referred to a falls service, a minority described very clearly how the intervention they were receiving was supporting an improvement in their well-being:
And now with the exercises . . . they show you to do, which I keep doing. I mean I couldn’t have walked from here to the table at one time, now I can walk to the table . . . Walk round the house with confidence, you know . . . not frightened of falling.
1–12F
Well I’m walking better and I’m feeling better in myself because I’ve gotten over the fall. And I try to do little things. I haven’t quite got enough balance at the moment . . . and that’s what they’re trying to work on.
3–9F
Although there were positive stories of recovery, a larger number of respondents talked about the increased limitations they experienced since the fall. This was a case of adapting what they did, taking more care and keeping clear of risky places such as the garden:
I’ve been very careful . . . No I haven’t fallen since, I haven’t done any gardening though you see and I’ve only done very little housework so I’ve tended not to do anything where I might fall.
1–6N
For some, having to accept these limitations was distressing:
I haven’t been up that road on my own since that happened . . . I used to go out once a week. Yeah, I loved it. One leg wasn’t like 100% but I could do it. I can’t do it now, it breaks my heart . . . I definitely can’t walk like I used to.
2–4H
For many of the respondents, it was a loss of confidence and a fear of falling that prevented them from going out and about:
So I’ll freeze for fear of falling . . . Hoping to tell me legs where I want to go.
2–13H
No but I won’t go out in the street on my own. I can’t, I just can’t, I just freeze. I go to that door, I can’t even go out to the street door . . . Oh yeah. I used to go shopping and everything. I am frightened I am gonna fall.
3–7H
Some expanded on this theme, talking about the fall as something which had pushed them a little further along the inevitable journey into old age:
I have a loss of confidence, I am old but suddenly I feel much older. I feel a great sense of loss of freedom, of a loss of independence . . . Somebody said to me what do I most miss and I said ‘being out in the air’ I do stand at the back door, but I’m frightened of the stairs.
3–9H
I don’t get up around quite so much as I did. And it’s hard ‘cause I now, which I now, which I never felt before, feel old. I am a bit nervous about doing physical things and where I’m going and should I take my walking stick and things like that.
3–15H
I’m walking now and I start crying. Then they say why and I say all this things I don’t feel it before and it’s my age.
3–1N
A large proportion of the respondents described their health, following the fall, as much the same as before. However, many of these then went on to report pain, reduced mobility or lack of confidence since the fall, presumably because they were thinking of these as being distinct from health. For example, 2–15H reported his health as being ‘just the same’ since the fall but went on to describe having to take tablets for pain relief and now finding it hard to get up after sitting on the settee.
The patient in context: other health and social care provision
Nearly half of the respondents described the networks of health and social care provision which supported their lives, much of which had direct relevance to preventing falls or managing their impact.
The most commonly reported form of support was an emergency alarm (also known as a Lifeline or Linkline), mentioned by 12 respondents across all three study sites. These alarms feature a pendant carried around the neck, which the user presses to call for help after a fall. For some respondents, they featured as part of the story of the index incident; for others, they were mentioned more as a source of reassurance.
In all three areas, many respondents reported having previously been provided, through different routes, with the type of support offered by the falls services associated with the SAFER 2 trial intervention. This provision included the fitting of grab rails and other adaptations to the home, equipment such as commodes and walking frames, and physiotherapy. Routes to accessing services varied; for one respondent, the GP functioned as an effective gateway:
Well apparently if you fall more than a certain number of times in a year, it has to be reported which my GP did, so I had a occupational therapist came out to see me and a physiotherapist. And they sorted out all the things, the aids that they thought I would need, namely a trolley and the second hand rail on the stairs, and grip rails everywhere, which I’m thankful for.
1–5H
One respondent described how previous falls had acted as a trigger to push her up the waiting list:
Then when I had that fall, she got a bit worried so it moved up a bit to the next one, I moved up, and that’s how it’s been going on, moving up and moving up to the next one ‘til they found time to come down and assess me.
3–9F
An alternative route to provision was on hospital discharge, which was cited as a way of accessing both practical home care for a limited period, rehabilitation (described by one as ‘walking stick instructions’ 3–13H) and a range of useful equipment such as trolleys which contributes to falls prevention. These routes to access were not always straightforward, with two respondents describing having gone through the assessment process but then being found not eligible for support.
They did send an [occupational therapist] out to me, but she wasn’t very good, I didn’t end up getting anything . . . But my husband has–, well, we’ve been trying to get a rail for the bath for years, each time he’s had an assessment, but we never get it.
1–8F
Other respondents described other forms of health or social care that contributed to their well-being at home, including specialist falls clinic, foot clinic, pain clinic and visits from the district nurse. A small number of respondents described support which they paid for themselves, outside the range of public sector or third-sector provision. In two cases this was people employed to help with cleaning, laundry and gardening; in another three cases it was privately purchased equipment, such as a specialist bed, while two reported paying privately for physiotherapy.
How the intervention was delivered in practice: paramedic and stakeholder views
Paramedic and stakeholder expectations of the new intervention (pre trial)
Both paramedics and stakeholders expected significant usage of the new referral pathway. Paramedics thought that the new referral protocol would be utilised widely if it was simple to complete.
I do think it can’t be too difficult to do that referral, that’s going to be the biggy. It’s whether it takes an hour to sort something out. It needs to be a 5/10-minute phone call and ‘yeah, no problem’.
Site 1 paramedic
If you make it a 20-page document people are not going to go with it.
Site 3 paramedic
Paramedics believed that patient care would be improved through the intervention, through avoidance of ED and through referral to a falls prevention service.
Once they can determine why the patient’s having the falls, it could be just poor housing, rugs, things like that, slippers, could be medical, could be down to their medicines what they’re taking, . . . it’s got to build their confidence, it’s got to do.
Site 1 paramedic
Paramedics from all three study sites expected personal gains, including an increase in job satisfaction resulting from offering a more complete care intervention:
You feel like you’re finishing a job. You’re not leaving it half done. You know, it’s ‘Doris has fallen again, we’ll go back to her tomorrow’ [but] ‘Oh Doris is fallen, she’s being referred, someone is looking after her’.
Site 1 paramedic
You’ll feel like you’ve actually achieved something for the patient because you’re not actually just moving them along on a conveyer belt to hospital. You’ll feel that you’re actually benefiting them.
Site 3 paramedic
With the exception of one, paramedics believed that the intervention would increase time on-scene. Paramedics from sites 2 and 3 expressed anxiety on how the control room would respond to an increase in the time on-scene.
If you’re leaving people at home you need to do the checks to make sure they’re safe to stay, that’s the thing isn’t it, you can’t just do a quick blood pressure, a quick pulse . . . then go. You know, in the real world of course it isn’t like that and I think a lot of people up in like control, they think it is like that and it’s not . . .
Site 3 paramedic
The referral bit will take time. I don’t know how control will feel about that.
Site 2 paramedic
Despite paramedics’ worries, ambulance service managers in sites 1 and 3 did not feel that increases in time on-scene would be an issue.
I have no problem with paramedics spending an extra half an hour, three-quarters of an hour on-scene doing a thorough assessment that’s appropriate for the patient. And at the end of the day, the call cycle time will still be quicker than going into ED.
Site 1 stakeholder
I don’t necessarily think that time constraints on-scene would be a problem, I mean most paramedics are quite adamant that time on-scene is my time, I’m not going to get any pressure from, you know, control, if I’m with a patient then that’s the time that I need so I don’t think that that would have any impact on them referring or not referring.
Site 3 stakeholder
Concern was raised by falls team leaders at the number of referrals that would be received the trial, and the capacity of the services to deal with this, although one spoke of plans to bring in locum staff in order to cover increases in demand for their service.
Paramedics’ and other stakeholders’ experiences and views on context and existing practice
The majority of paramedics felt that current practice does not provide appropriate care to elderly patients who fall. Paramedics from all three of the ambulance services stated that current practice involved assessing patients for injuries, and depending on the outcome of the assessment and patient preference, conveying the patient to an ED, leaving the patient at home with no onward referral, or leaving the patient at home and referring to their GP. In two of the three sites (sites 1 and 3), there had been previous attempts to set up alternative pathways for elderly patients who had fallen, referring them to, for example, intermediate care teams, rapid response teams, district nurses and physiotherapy services, although these pathways had fallen out of use.
Overall, paramedics felt that they are able to make decisions regarding leaving patients at home and onward referrals, but they lack the referral pathways to properly undertake this. This was stated explicitly by a paramedic within site 1, with paramedics from sites 2 and 3 stating that they routinely make decisions regarding patient conveyance.
But this has been happening for years hasn’t it. We’ve never had anything put in place. I’d say we‘ve got more access to more places now than we’ve ever had, and it’s still not enough . . . because nine times out of 10 we know exactly what that patient needs, and we just can’t access it.
Site 1 paramedic
The process of deciding whether a patient stays at home or is referred to hospital is not always a straightforward one, and paramedics gave examples from existing practice where patients and paramedics disagreed. These were most striking in cases in which a patient wished to stay at home, but the paramedic felt, based on clinical assessment, that they should go to hospital; in these reported cases the paramedic’s view prevailed, in part because of anxieties about risk:
I had a lady the other day, she clearly needed to go in and she was arguing with us for half an hour. I think we just wore her down in the end, but she had to go.
Site 2 paramedic
You bully them, you do. You bully them to some extent ‘cause you think, I’m not risking it.
Site 2 paramedic
A number of paramedics discussed their anxieties about the risks of leaving a patient at home following a fall, worrying both about the patient, and about any comeback on the paramedic if it were to turn out to be the wrong decision:
I always think back at the end of the shift, oh God, I hope they’re all right.
Site 2 paramedic
At the back of our minds, it’s always gonna be . . . ‘am I gonna be wrong, am I gonna get in trouble’, you know, not that anybody wants to do anything wrong, not that we’d purposely do it. We’re always trying to do the right thing, but if you miss something for whatever reason, and we’re only human, . . . what are the ramifications gonna be?
Site 1 paramedic
Paramedics within sites 1 and 3 discussed the concept of ‘covering their backs’ when attending an elderly patient at home following a fall, in order to mitigate the risk of action against them if something were to go wrong. In some cases, this resulted in the patient being conveyed to hospital even if the paramedic could not see a clear clinical need:
Sometimes we convey the patient when quite clearly they didn’t need to go in. In essence you feel like you need to cover your own backside because nobody else will.
Site 3 paramedic
Referrals to GPs were seen as problematic in all three sites: paramedics were not confident that the GP would respond to a referral (owing to not realising the urgency or simply not receiving the referral) or that they would make an onward referral if appropriate:
They [GPs] just don’t seem to understand they have options as well, that they can refer people on. I just don’t trust the GP to make that choice, to know that there are more choices. It’s alright for us, we know we can refer onto social services . . .
Site 3 paramedic
Paramedics’ professional status was seen as an important factor in the ability of paramedics to consider alternatives to conveying patients to the ED. One paramedic appeared to express frustration that the potential of paramedics to act as the gateway to a range of care services was untapped:
I went to a fall, and there was a district nurse who turned up just after I got there, . . . and the questions she got asked, and the ease of [the district nurse] getting that person respite – I was just gobsmacked at how easy it was. All those questions I could have just easily done . . . I think that paramedics have generally been seen as just take them to hospital, they haven’t been seen as having any clue.
Site 1 paramedic
Pay, and the responsibilities attached to it, were mentioned by paramedics (although not managers) as an issue in sites 1 and 2:
Yeah, people are like, ‘Well I don’t get paid to [undertake additional decision-making to leave patients at home] so why should I do it?’ So then everybody goes to hospital, so then you’ve got an A&E then that is absolutely chocca full of people who could possibly have been treated elsewhere by a different pathway.
Site 2 paramedic
Experience of implementing the Support and Assessment for Fall Emergency Referrals 2 trial intervention
Post trial, paramedics and stakeholders reflected on the process of implementing SAFER 2 trial as part of the research study. Paramedics stated three main reasons for volunteering to take part in the study: persuasion by a colleague; opportunity for personal development and learning new skills; and dissatisfaction with existing practice, in terms of both the lack of referral options available and the frustration of multiple attendances to patients for falls.
And you’re taking somebody in and you know you’re going to be straight back out because, you know, so if there’s something that you can stop from going in so it’s not a . . . waste of resources.
Site 2 paramedic
In sites 2 and 3, parallel developments of other pathways, while the SAFER 2 trial was under development, were felt to have led to confusing messages for paramedics:
It made it quite complicated from a local point of view, so I had 30 paramedics who were trained as intervention paramedics and 60 who weren’t and trying to tell them, ‘No, you can’t choose the [SAFER 2] one yet,’ ‘Oh but we have seen adverts everywhere and we’re getting letters from operations directors saying we must refer patients,’ ‘Well no you can’t.’ So it was quite complicated getting the right message out to the right staff, I think we got there but it was quite challenging to do that.
Site 3 ambulance manager
In all three ambulance services, the majority of managers felt that implementation of the SAFER 2 trial intervention had an impact on their role and workload during the initial phases of the study, when paramedic training was being carried out, but less so in the latter parts of the study:
[My involvement] all seemed to be very front loaded and then I think I lost my way, if I’m perfectly honest with it, during the latter–, I’d still come to the meetings and stuff, but once the training was there and everything was set up, it was almost like, right, sort of sit back and watch what happens.
Site 1 manager
Factors which enabled/encouraged the use of the Support and Assessment for Fall Emergency Referrals 2 trial intervention
According to the paramedics, usage of the new referral pathway was encouraged by its simplicity.
Overall, paramedics were positive regarding the suitability of the training they received. One paramedic compared the benefits of the SAFER 2 trial training to previous training for novel ambulance service interventions, which (as at the other two sites as well) seemed to be limited to e-mail or notice board updates.
Well, there hasn’t been any training apart from this [the SAFER 2 trial training], . . . I mean this has been superb really, you know. You get to sit and relax and get trained on it but the new pathways are reading a piece of paper and acting on it. So, we’re not trained on it [previous pathways].
Site 1 paramedic
Only one stakeholder commented on the value of the SAFER 2 trial training, and in positive terms:
The [paramedics] have now had some training that’s been approved by some specialists so they feel very confident now at making those decisions with the backing of this triage tool.
Site 3 stakeholder
Paramedics in all three trial sites stated that they were aware of the clinical support available to them throughout the trial, although the majority did not actively seek clinical support at any point during the trial. Paramedics in all sites thought newsletters and e-mail updates were important to provide feedback and so maintain the motivation to refer:
[The newsletters were] a kind of confirmation that you are doing the right thing. I can’t remember any specific points but I remember one and I don’t know what it was, I can remember reading it and thinking, oh yeah, OK, I’m doing that so I’m doing the right thing.
Site 3 paramedic
Factors which hindered the use of the Support and Assessment for Fall Emergency Referrals 2 trial intervention
Both stakeholders and paramedics reported aspects of paramedic practice and the organisation of the ambulance service which hindered use of the SAFER 2 trial intervention. Paramedics from all three sites stated that taking a patient to the ED was often the easier option, especially when nearing the end of a shift.
You’ve got a lot of paramedics who, anything for an easy life – ‘I’ll go back take them to [ED] . . . Some of them want to do the best so they get off on time, or don’t have a late finish, or least path of resistance.
Site 1 paramedic
Time of day, coupled with the patient’s social situation, was mentioned by paramedics as affecting their ability to make a referral. Paramedics from all sites stated that they would feel uncomfortable leaving an elderly patient at home late at night without support, even if they were not injured. A small number of paramedics stated that a more immediate intervention than SAFER 2 trial was required by paramedics in order to assure confidence when leaving a patient at home.
I think if we had, as you said earlier, a direct phone number to a person that we knew was going to come out here in 2 or 3 hours, we’d maybe feel a little bit more confident to leave her there.
Site 2 paramedic
Paramedics said they often forgot to refer when on-scene, this being influenced by the time of day and the amount of time they had already been on the road.
At different times of the day . . . you’re more tired, so you do occasionally leave the scene and then think, ah, I haven’t done that [the SAFER 2 trial decision tool].
Site 2 paramedic
Ambulance service managers were aware of this, one suggesting that the use of the SAFER 2 trial declined over time:
I just feel that–, possibly ‘cause it’s over 12 months they did it– and . . . there wasn’t any other trigger mechanism to trigger them to participate actively, participate. And bit by bit, they started just to forget.
Site 1 clinical tutor
In contrast to examples described in Paramedics’ and other stakeholders’ experiences and views on context and existing practice of paramedics persuading patients that they needed to go to hospital, they also described examples of patients, or those who cared for them, putting pressure on paramedics for a hospital transfer, even where paramedics might propose that a patient be left at home with a referral to a falls team. Even though the SAFER 2 trial decision tool had been used, paramedics were frustrated in taking the recommended step to refer to a falls service:
You feel pressure. When you attend elderly fallers, you face pressure from the families, their next door neighbours, . . . generally speaking that patient will take the advice of their next door neighbour and they’ll go to the hospital. So we face a lot of pressures from around us to take them in. The family will say, ‘Oh, I’d prefer her to go in and see a doctor. I’d rather she went in and had an X-ray,’ even if you explain that they don’t X-ray people routinely. So there’s a lot of pressure around taking them in.
Site 2 paramedic
You’re dealing with a frail, elderly group and often with little support in the community . . . added to which I think there is still the ‘you call, we haul’ mentality . . . call for an ambulance, you expect to go to hospital, that’s what we’ll do then.
Site 3 stakeholder
Obtaining consent from patients to refer to the falls team was seen as an issue in all sites:
Patients didn’t want to be referred, we meet a lot of obstinate people who [laughs]–, ‘Get me off the floor, get me bed, I don’t want anything else from you and I’ll be calling you back tomorrow night’.
Site 3 paramedic
Paramedics and managers also reported that it could be difficult to ascertain from patients if they already have involvement from such a service, or from an equivalent service:
If you went to a couple of falls to the same person and in the meanwhile they’d had an intervention of some description from a falls team, they might not immediately recognise that as being the intervention . . . It’s really quite hard, I think.
Site 1 ambulance service manager
And we just feel, are you going on overkill almost, you know, if you start referring to another little team, you know, and they’ve already got this, that and the other coming in? You feel you’re just repeating things.
Site 1 paramedic
Paramedics reported particular issues to do with referrals of patients living in nursing homes, where the referral to the falls service could be seen by nursing home staff as threatening:
If you referred somebody in their own private address, it was welcomed because you explained the package . . . But in the nursing home environment, you felt as though you were actually putting them on the spot . . . they were being scrutinised because they weren’t providing the care or the facilities as what was available.
Site 2 paramedic
Paramedics in sites 1 and 2 saw lack of information regarding the role of the falls teams as an issue, specifically the time frames for initial contact and the interventions provided. Paramedics suggested that increased knowledge of the intervention would have positively influenced the number of referrals.
Evident across all interviews with ambulance service managers were some gaps in communication between them and the study paramedics. Although paramedics spoke of the importance of clinical support in the initial stages of a new pathway, most managers stated that they had not spoken directly to paramedics about the study and had not provided clinical support to study paramedics, with one manager in site 1 describing the difficulty of ‘catching’ a paramedic in order to discuss progress. Paramedics in all sites told a similar story.
[Asked if management were supportive of paramedics being involved in the trial] No one ever said anything.
Site 1 paramedic
I don’t think they [ambulance service managers] knew who was taking part and who wasn’t.
Site 2 paramedic
Impact of the Support and Assessment for Fall Emergency Referrals 2 trial intervention on paramedic practice
The Clinical Decision Flow Chart, used by paramedics on-scene, was felt to be a useful aide-memoire, but its impact on practice was variable. Paramedics from all three sites discussed a process of ‘settling in’ to the new assessment and referral process after their training. Many paramedics stated that it took time to get used to using the Clinical Decision Flow chart, but once they had, it was only used to remind them of specific details on-scene.
The more you used it, the less you needed to refer to it, or only certain points or anything. And if you weren’t sure about something then you’d–, oh, just let me go and check on that. So once you got used to it, as I say, it was very straightforward to use.
Site 2 paramedic
I found it useful as a memory jogger.
Site 3 paramedic
For those based in sites 1 and 3, the flow chart did not contain any new procedures that were not already undertaken on-scene, apart from the referral to the falls team:
I think it [the flow chart] just reinforced what we already know. I guess . . . we’re all used to dealing with falls.
Site 1 paramedic
In site 2, by contrast, the flow chart was felt to bring new assessment techniques into practice, to which paramedics responded positively:
I never did two blood pressures on people, when they were on the floor and when they got up. That didn’t cross my mind. So you know that was definitely a learning curve, so that’s given us extra skills.
Site 2 paramedic
Paramedics from all three sites felt that the SAFER 2 trial did not bring about significant changes in decision-making on-scene; paramedics felt that the decision to convey or leave a patient at home was a decision that they often made with some confidence but the new referral protocol ‘reinforced what they already knew’.
Paramedics in sites 1 and 2 stated that the SAFER 2 trial intervention increased their confidence to leave a patient at home through two mechanisms: the reassurance that the falls team will contact the patient and the confidence in the assessment of a patient who has fallen. Paramedics within site 3 only stated the former. Opinion of ambulance service managers was split between those who thought the confidence had increased, and those that believed that confidence was still an issue.
People are very confident, they are happy making those decisions [not to convey a patient to A&E] I’d say in general.
Site 3 manager
One of the things that we’ve highlighted as a possible reason [for not referring patients] is the lack of confidence, which is meaning that people aren’t leaving patients at home that could be possibly left at home.
Site 1 operational support manager
Paramedics from all three sites thought that the new pathway increased time on-scene, mainly through three mechanisms: increased time undertaking patient assessment, increased time recording patients’ assessment on PRF, and time spent on-scene making the referral to the falls team. Paramedics within site 3 discussed ‘welfare checks’ (a call from the control room to ensure the welfare of the paramedic after a certain period of non-communication), which the paramedics perceived as ‘hurry-up checks’. One paramedic realised a benefit to spending more time on-scene with the patient:
I think for the length of time that we would have been there before SAFER 2–, ‘cause you know, obviously when you actually do the referral it takes up to an hour, so then you get to see the patient sort of in their own environment and possibly doing things that you wouldn’t normally because you’d probably just take them down the hospital.
Site 3 paramedic
Impact of the new pathway on falls services
Falls service representatives from all three sites commented on the appropriateness of the referrals made from paramedics; the majority of patients were thought to have been referred appropriately, although one falls service representative suggested some were not:
. . . there were some who maybe should have gone into hospital and actually not being kept at home.
Site 3 stakeholder
Representatives stated that the referrals they received through the SAFER 2 trial were a mix of patients already known to the falls services, and patients of whom the falls services had not previously been aware. Falls service team leaders from sites 1 and 3 reported that the newly identified patients referred through the SAFER 2 trial were often more frail than those normally receiving treatment from falls teams; a number of patients referred had subsequent A&E attendances and emergency service calls between the referral being made and contact with the falls teams.
The impact of paramedic referrals on the falls service differed between trial sites. In site 2, falls service representatives reported the impact as substantial in terms of paperwork, time and difficulties with onward referral, although the assessment and onward referral process was not thought to be very different from normal practice.
It was a bit of a put off really, and I have to be honest, when the referral come through . . . you were sort of like dreading it a little bit.
Site 2 falls service representative
Representatives from sites 1 and 3, however, felt that the new referral pathway did not impact significantly upon the service, with representatives in site 3 commenting on the positive impact of the new pathway on their falls service.
I think the response time was quite interesting ‘cause ours was a community team, we had a response time and within 1 to 10 days or quicker . . . What SAFER 2 did was . . . it made us firm up a few systems in our single point of access to flag up these fallers, patients, with the SAFER 2 you know, they go on the top, they need to be prioritised so we had to do a bit of work around that which was I think good for the service to kick in a sort of more urgent response, which we hadn’t had before, we weren’t an urgent sort of rapid response team. But after SAFER 2 we had that ability.
Site 3 falls service representative
A number of representatives discussed receiving repeat referrals for the same patient; this was generally felt to be useful, helping to identify gaps in current patient care.
At a personal level, falls service representatives from sites 1 and 3 were positive about their involvement in the study, stating that it was ‘worthwhile’ and ‘enjoyable’. Despite the difficulties, representatives within site 2 were also positive regarding their involvement.
Keeping people well and healthy in their own homes for longer, so I’m glad we did take part. And I think it is something that, you know, the health board will look to develop further in future, but you know, we do need to make sure we get it right, and address some of the issues that you’ve all raised.
Site 2 falls service representative
Suggestions for modifications or developments of the Support and Assessment for Fall Emergency Referrals 2 trial intervention
Participants suggested modifications in four categories: the project set-up, training, patient assessment and referral processes/post referral. Suggested modifications differed by study site, reflecting the variety of issues experienced across the sites.
In sites 1 and 3, ambulance service managers suggested that key ambulance service staff should be involved as soon as possible in the set-up of a study, to make important decisions on behalf of the trust and to have input into the study design and data collection methods.
Falls service representatives from site 1 identified training as an issue, although their equivalents in the other two sites did not, perhaps reflecting the more limited involvement falls service representatives had in training in site 1. A falls service representative from site 1 suggested that training in the SAFER 2 trial should be carried out at regular intervals, in order to include and update more paramedics:
Going back to the training really and maybe just doing some supplementary training and . . . some scenarios with them . . . a quick half hour would have been enough just to say, ‘Thank you for your referrals, thank you for your interest’, . . . they could think of patients that they thought of, ‘oh yeah well I maybe could have referred that lady but she seemed quite fit . . . she seemed quite able but she’d had a couple of falls’.
Site 1 falls service representative
Paramedics in sites 2 and 3 felt that the clinical decision flow chart needed to be simplified, to include less routine information, and more about the causes of falls:
I think on the flow chart if you’re looking at possibly improving it maybe something a bit more . . . shorter version, maybe tick box type of thing.
Site 3 paramedic
On the flow chart, the current one, sometimes there was a bit too much information.
Site 2 paramedic
One site 3 paramedic felt that a smaller A5-sized flow chart would be better as it would to fit into paramedics’ pockets, to allow improved access on-scene. By contrast, other stakeholders across all sites did not comment on the flow chart being an issue.
Paramedics within both sites 1 and 3 felt that the decision to convey a patient would be easier to make if they had access to patients’ records on-scene.
A copy of what their blood pressure is normally like, their normal observations so then . . . we can see it’s . . . abnormal and then it’s going to help our decision-making whether we’re going to leave them or not.
Site 3 paramedic
In site 1, electronic patient report forms (ePRFs) were implemented during the study period, and ambulance service managers suggested that patient assessment could be improved if the ePRF included prompts to remind paramedics to consider a referral to the falls service. An assessment checklist on the ePRF was also considered beneficial by stakeholders.
. . . putting something on to the electronic Toughbook[® Panasonic, Newark, NJ, USA], create some sort of mandatory check. You know, . . . do not pass go unless you have notified the falls team, etc., whatever it might be, so there is some sort of check there built into the system and–, so it’s programmed and you’ve identified there’s a fall . . . for me, that way there, you will ensure that you’ve actually triggered the response that you want, to trigger it, it’s going to be referred.
Site 1 clinical trainer
Other suggested improvements included increasing the number of people on telephone lines receiving referrals, increasing the capacity to refer (suggested by a site 2 paramedic), and providing an information sheet to referred patients to help them understand ‘what will happen next’ (site 3 paramedic). Improvements to the feedback process were suggested by paramedics from all three study sites, and by stakeholders in site 1. Paramedics from sites 1 and 3 argued for prompt feedback following a falls service referral, while a paramedic from site 2 explained that confirmation that the patient received the intervention would increase their confidence in the referral process:
We weren’t sure what happened after we left. There was a presumption that they were going to be seen. It would have been nice to have some feedback to say that Doris has been seen yesterday and this has been done, so that you know it’s working rather than presuming it’s working.
Site 2 paramedic
Summary of qualitative findings
Patient experience
We used the qualitative phase of research to assess whether or not patients were satisfied with the new intervention and whether or not, if relevant, the referral pathways by which we had hypothesised that the SAFER 2 trial intervention would make a difference were effective.
Almost all the respondents were very satisfied with the processes of assessment and examination carried out by paramedics and tended to see them as part of a relationship based on empathy and care. The majority of those who were in a position to make a comparison between the SAFER 2 trial encounter with the ambulance service and a previous contact after a fall could not see much difference in the assessment and care delivered. When patients talked about having a say in decision-making, it was generally in terms of whether or not they would travel to hospital, not in terms of whether or not they wished to have contact with the falls service.
Even when patients were referred to the falls service, this did not necessarily lead to them receiving an intervention. Patients referred to falls services may in practice have come by many and various routes. Many of the patients in the SAFER 2 study were already tapping into a complex, and potentially confusing, network of community-based services, delivered by a range of providers (NHS, social services or third sector).
Although some patients reported good recovery after their fall, many had lasting ill-effects, with loss of confidence a major issue. Many worked out their own ways of reducing risk of a future fall, but at some cost to their quality of life.
For the vast majority of patients, the index incident was not the first fall they had experienced, although previous falls may not have resulted in contact with the ambulance service, and many went on to have a subsequent fall. Some seemed quite habituated to falling. Many falls were reported by patients as having an unspecified or unclear cause.
Paramedic and stakeholder experience
Through the qualitative component of the study, we aimed to examine the perspective of paramedics and other clinical stakeholders on the hypothesised mechanisms by which the SAFER 2 trial intervention was meant to work, that is, improving the decision-making of paramedics in terms of safe non-conveyance and referral of older people who have had a fall to appropriate community-based services, and necessary factors to allow this to happen.
The intervention was hypothesised to increase paramedics’ clinical knowledge of how to make appropriate non-conveyance decisions and their knowledge of falls services and pathways for referral. In sites 1 and 2 (but not site 3), paramedics reported that a lack of knowledge around the role of the falls team and the structure of their intervention limited their ability to refer.
It was also hypothesised that it would increase paramedics’ confidence about making a non-conveyance decision and reducing anxiety about risk and would increase the likelihood that paramedics will consider non-conveyance and referral pathways as an option in appropriate cases. There were mixed messages about whether or not confidence had been increased from both paramedics and managers. Paramedics emphasised that the decision-making process remained complex, with patients and carers having a voice which might contradict the paramedic and the protocol.
We also examined the three factors that we felt needed to be in place: effective referral pathways and sufficient capacity in falls teams; effective training and support for paramedics; and motivation on the part of paramedics to use the intervention. Before introduction of the intervention, falls service stakeholders also felt that the new pathway would impact upon their role greatly, although after the intervention stakeholders from two of the three sites reported no significant change to workload. Falls team managers in sites 1 and 2 stated that many referred patients declined the falls service intervention, although this was not mentioned as an issue at site 3. Paramedics in all three sites described reasons for not referring to falls services relating to patients’ social situation and patient autonomy.
After implementation, paramedics reported that support for implementing the new intervention (i.e. paramedic training, flow chart and clinical support) had a positive effect on their ability to refer and make decisions about patient conveyance. The structured training on the SAFER 2 trial was felt to be more helpful than previous, more informal, approaches to introducing innovations, especially in sites 1 and 2. In sites 1 and 2, the SAFER trial processes such as the get up and go test and taking sitting and standing blood pressures were new to paramedics, while paramedics in site 3 already undertook these.
In terms of motivation, before introduction of the intervention, paramedics generally saw it as an effective way to deal with elderly patients who fall, and potentially an improvement on current practice. Current practice was felt to be geared towards conveyance to hospital even when not appropriate for the patient, although paramedics from all sites stated that they routinely make the decision to leave a patient at home following a fall. Paramedics expected to make significant usage of the new referral pathway, resulting in increased time on-scene, but also personal gains in terms of their skills and job satisfaction.
Throughout the transcripts, there was a lack of evidence of paramedics and managers having ‘useful’ contact with each other. Paramedics from all three study sites stated that they had limited contact with their managers during the study period. This is reinforced by the fact that paramedics were ‘worried’ about increased times on-scene, but managers did not see this as an issue.
Suggested modifications differed by study site, reflecting the variety of issues experienced across the sites. Paramedics from all three sites agreed that a ‘simpler’ intervention would have sufficed, with a less detailed flow chart. This was not commented on by ambulance service managers.
Limitations of qualitative methods
Patient experience
The sampling of patients for the interviews was heavily skewed (36 out of 58) towards those who had been transported to hospital. This may have meant that the patients interviewed were more likely, on average, to have had a major fall, and/or were more likely to have wanted to be transported to hospital.
Some patients found it difficult to recall details of the index incident many months after the event. When patients had had a number of falls, it was not always entirely clear which fall they were recalling and describing in response to the interviewer’s questions.
It was hard to disentangle patients’ views on the SAFER 2 trial assessment protocol specifically from their views on the more general process of examination and assessment.
Paramedic and stakeholder experience
It proved difficult to interview an equivalent cross-section of ambulance service managers within each trust, which led to a small variation in the set of questions asked in each site.
Focus groups and interviews were undertaken at different times between May 2011 (pretrial focus groups) and March 2013 (post-trial focus groups). The time of year may have affected the responses provided by both stakeholders and paramedics, as service delivery pressures and priorities might have differed; therefore, it could possibly have affected the issues at the forefront of the interviewees’ minds.
Each site varied in the basic training provided to paramedics, the set-up of the service, service delivery pressures and priorities at the time of the study.
Chapter 7 Discussion, conclusions and recommendations
Summary of key findings
There is a limited evidence base on prehospital alternatives to conveyance to hospital for older people who fall. The systematic review included 12 papers, only two of which were RCTs. Studies were of variable quality, with the majority being rated as low quality. The review identified limited and weak evidence regarding the most effective ways to deliver alternative treatments to older people who fall. A minority of the included studies reported benefits: reductions in subsequent emergency calls and hospital admissions when patients who had been left at home by their attending ambulance crew were referred retrospectively to a falls prevention service or when patients were attended by a paramedic with additional skills (ECP). However, in the majority of studies such outcomes were not explored. The review concluded that high-quality evidence from well-designed and rigorously conducted research is needed to inform service delivery.
In our RCT, we did not find any differences between trial arms in the composite primary outcome. However, we found consistent evidence of a small reduction in subsequent emergency service calls, from 21.8% of participants in the control arm to 18.5% in the intervention arm at 1 month, and from 46.2% to 43.7% at 6 months. Six per cent of patients had died in each group by 1 month and 18% by 6 months. Nearly one-third of patients had suffered a further emergency episode or death by 1 month, rising to over two-thirds by 6 months. Referrals to falls services were low: 8% in the intervention group. Overall, and at each site, fewer patients were left at the scene without any referral for further care in the intervention group than in the control group. We did not find clear evidence of any differences in other secondary outcomes related to processes of care, further injuries or self-reported quality of life, satisfaction or fear of falling.
Uptake of the intervention was variable. Sixty per cent of intervention group paramedics made at least one referral, but most of these made only one or two in total.
The intervention cost £17.30 per patient and generated some clinically important, statistically significant differences in the number of subsequent emergency service calls (at 1 month) and ED attendances (at 6 months), but no statistically significant difference in QALYs gained.
Although the SAFER 2 trial intervention is relatively low cost, this was not offset over 6 months by reductions in health-care resource use, neither did it generate improved health-related quality of life among patients allocated at random to the intervention relative to those controls allocated to usual care.
Retrieval of anonymised linked data outcomes was highly successful in this ‘e-trial’, with analysable outcomes available for 80% of those eligible. Such a high rate of inclusion produces findings that are generalisable to the whole-study population. Further investigation and analysis of these trial findings is warranted to fully describe the benefits and risks of this new approach.
Through the qualitative component of the study, we examined the perspective of patients, paramedics and other clinical stakeholders to help us better understand how the SAFER 2 trial intervention might work. In terms of increasing paramedics’ clinical knowledge of how to make appropriate non-conveyance decisions, and their knowledge of falls services and pathways for referral, there were mixed messages, with paramedics in two sites reporting that a lack of knowledge around the role of the falls team and the structure of their intervention limited their ability to refer. Similarly, there were mixed messages in relation to the intervention’s role in increasing confidence to make non-conveyance decision and reducing in anxiety about risk. Paramedics emphasised that the decision-making process remained complex, with patients and carers having a voice which might contradict the paramedic and the protocol. Paramedics in all three sites described reasons for not referring to falls services relating to patients’ social situation and patient autonomy.
Patients and carers in the intervention arm were highly satisfied with the care received, although generally they did not notice differences in practice compared with previous contacts. Interviews with patients and carers revealed that the scope for the intervention to make a measurable impact is limited by a number of factors. For various reasons, the pathway may not have led to a falls service intervention. Many of the patients in the SAFER 2 study were already tapping into a complex, and potentially confusing, network of community-based services, delivered by a range of providers (NHS, social services or third sector). The index fall is not necessarily an isolated incident, but more often part of a bigger and more complex pattern of falling, so it may not be straightforward to restore confidence and mobility after a fall, even with an intervention.
Strengths and limitations
The SAFER 2 study was a large-scale, multicentre randomised trial in the challenging setting of prehospital emergency care. We met our recruitment target for this frail group and achieved, through retrieval of anonymised linked routine data outcomes, a very high rate of inclusion: we reported our primary outcome for 80% of eligible patients, a much higher proportion than usually achieved. 125 Completion of ‘designed data sets’ concerning compliance with treatment and trial protocols, including reasons for non-referral, was low. This may reflect the context; we carried out this trial in the emergency care environment in which crews are under pressure to not only meet the care needs of each patient they attend but also to meet operational requirements which largely consist of time-based performance standards. As a general rule in trials in this setting, including the SAFER 2 trial, we try to minimise the collection of any new data from practitioners and rely instead on routinely collected information. In this way we maximise the inclusion of patients and the completeness of key data items and minimise intrusion into the clinical and operational context of the trial. In the SAFER 2 trial our primary and many secondary outcomes were based on routinely collected clinical and operational information and the completeness of these data sets is very high. Data that relied on additional paperwork by crews or patients had low completion rates and a higher rate of missing data items.
With low ICC, there is little dilution from observed to effective sample sizes, so we can be confident in findings reported. Statistical analyses have attempted to assess the effect of the intervention while allowing for variations across the three sites; analyses with statistically significant interactions therefore require careful interpretation.
The SAFER 2 trial tested a complex intervention. We were able to clearly define the components of that intervention with our research and clinical partners across sites. We delineated each component, common minimum standards, and aspects that could vary locally. This allows our trial results to be transparent and repeatable, in a field in which interventions often lack clarity. 126
Some aspects of the trial limit the usefulness of the results, in particular the fact that the trial took place in a context of changing practice and competing service innovations to care for this patient group. At each trial site we lost geographical areas, GP practices, stations, paramedics and patients because of the changing environment in which the trial took place. In site 3, an alternative referral innovation was introduced service-wide, incentivised by local commissioners. In site 1, only some GP practices were able to access the falls service which was taking part in our study, and patients not registered to those practices were ineligible for the emergency service call referral; in addition, many patients who had fallen were diverted to a clinical desk in the ambulance control room for an alternative (non-paramedic) response. In site 2, a Frailty Programme was introduced in one of the initially participating health board areas, and, as a result, stations in this area were withdrawn from the trial. Six of 31 stations and 49 of 264 paramedics withdrew following randomisation, as presented in the CONSORT flow chart in Chapter 4. The withdrawal of stations was similar across trial arms, but withdrawal of paramedics was higher in the intervention arm. We do not know whether or not these withdrawals affected implementation of the intervention. Overall, we overcame these challenges which are perhaps inevitable in a pragmatic trial in a dynamic service environment. We completed the trial with balanced groups and achieved a sample size sufficient to detect important effects related to the intervention.
Uptake of the intervention was low, at 8% of patients in the intervention group. We do not know what the appropriate rate should be, as the protocol was intended to be applied across the spectrum of older people who had fallen, and many may have had a clinical need to be taken to the ED. Approximately one-quarter of patients were left at the scene of their call without a referral. Although this varied between groups and across sites, it is probably the best indication of the ‘pool’ of patients who might benefit from referral to a community-based service. The referral rate was variable between individual paramedics, with over one-third never making a referral at all during the study period. Referral rates did not vary by age, sex or distance to ED. Patients were less likely to be referred at site 1, although some patients were ineligible for the referral pathway at that site; and patients were more likely to be referred out of hours, but we do not have any further insight into why this was the case. In addition, we found no difference between trial arms on conveyance rate, suggesting that practice did not change significantly during the trial.
We recruited volunteer paramedics to participate in the trial, with the agreement of the three collaborating ambulance services. With slow recruitment we agreed to the introduction of £50.00 vouchers for each participating ambulance service, although, in practice, services used the payments in different ways. This reflects the practical considerations of carrying out multicentre experimental research in a live health service delivery environment. It does mean that the trial paramedics may not be representative of all paramedics and, therefore, we need to be cautious about interpretation of our findings.
It was not possible to undertake planned analyses of fall-related subsequent events, as data quality was found to be poor, with different codes and levels of completeness between hospitals and sites. It is well known that falls are poorly categorised, as, for example, slips, trips, stumbles or collapses, which is why we made the decision to analyse all events. Any effects on falls-related events would have also been evident in the all cause event proportions and rates, so this further exploration became less important once we had completed analysis of the primary outcome.
Implications (practice, policy and research)
With three participating ambulance services, 25 stations, > 200 paramedics and > 10 community-based falls services, and with outcomes available for 80% of eligible patients, we are confident that findings are generalisable to the UK setting and other similar health systems.
The SAFER 2 trial intervention was associated with a small reduction in the proportion of patients making further emergency service calls, and in the number of further calls made. However, this effect was not carried through to other parts of the emergency care system. There were no clear effects in secondary care, on ED attendances or emergency admissions. This finding is difficult to interpret, as we would have expected any difference in one part of the system to be reflected in other parts. It may be that patients in the intervention arm are more confident to self-manage if they fall again; however, the lack of impact at ED suggests that the effect may be restricted to those who were not conveyed to ED. Even a modest reduction in emergency service calls in this population is a success for the intervention in terms of prehospital care in which operational pressures are so high. Ambulance services may wish to implement this intervention in order to tackle rising demand but it will not make a huge difference to emergency service workload.
Uptake was lower than expected, with < 10% of trial eligible patients attended by intervention group paramedics referred to falls services. There may be several reasons for this, including a reluctance to change practice, a risk-averse climate within emergency prehospital care, patients who were unwilling to be referred or a lower than expected number of eligible older people who were not already under the care of a falls or similar frailty team. Some of these reasons reflect the population and context of the trial. Within the trial, all reasonable efforts were made to support a change in clinical practice; however, variability in referral rates suggests that uptake of the new referral pathway could have been higher. We do not know if higher use of the falls referral pathway would further reduce emergency service calls.
The smaller than expected effect may be because the pool of people who might benefit is smaller than previously expected, because preventative measures are more likely to be effective than an emergency intervention once a fall has occurred, or it may be because with many initiatives in place to target this group, there simply is little remaining scope for impact by emergency service paramedics. These results contrast with previous findings,61 perhaps because of the larger sample size and increased number of centres in the SAFER 2 trial.
Direct referral by ambulance crews to falls services is being implemented across the UK,78 alongside many other new clinical pathways. In terms of tackling rising demand and managing workload, particularly of patients who present repeatedly to the emergency service, we can be confident that direct referral is not going to revolutionise care. We have not found evidence of harm and have found evidence of limited benefit to patients and the NHS.
Conclusions and recommendations for research
The complex SAFER 2 trial intervention, with a protocol for paramedics to assess older people who had fallen and refer those without need for immediate clinical care to community-based falls services, was inexpensive and safe. We did not find any effect on our primary outcome, although, when broken down into its components, there was a small reduction in the occurrence and rate of further emergency service calls. We did not find any evidence of improved quality of life, although some aspects of satisfaction were higher in the intervention group. Referral to falls services was lower than expected and variable between paramedics, although fairly consistent between sites. Fewer patients were left at scene in the intervention group by their attending ambulance crews without ongoing care than in the control group; however, other processes of care were unaltered.
Retrieval of anonymised linked data outcomes was highly successful in this ‘e-trial’, with analysable outcomes available for 80% of those eligible. Such a high rate of inclusion produces findings that are generalisable to the whole study population.
In terms of research priorities:
-
Understanding implementation issues further is a research priority in this area for older people who fall and other groups for whom the default emergency service response is conveyance to hospital.
-
Further investigation and analysis of outcomes retrieved through anonymised data linkage is warranted to fully describe the benefits and risks of this new approach.
-
Further research regarding the performance of the SF-12 and the mFES for older people who fall is warranted, including:
-
exploring whether or not any differences exist in the either of the two scales between baseline and 6 months
-
comparing differences in outcomes between the intervention and the control sites at each time point
-
comparing the completion rates of the scales in the intervention and control sites
-
examining differences between scale scores in those patients who went on to have a further fall (using routine ED data)
-
examining whether or not either scale had any predictive ability in terms of predicting the likelihood of future falls.
-
In conclusion, the SAFER 2 trial findings indicate that ambulance services may introduce this new clinical pathway for patients without risk of harm, and with some limited impact on emergency service call workload. We did not find evidence of improved health outcomes for patients or reductions in emergency episodes across the NHS.
Acknowledgements
We would like to acknowledge and thank the following people who have contributed to the SAFER 2 study and the preparation of this report.
Bridie Evans (research officer), who contributed to the systematic review chapter and provided expertise on service user involvement throughout the trial.
Wai-Yee Cheung (senior lecturer in statistics and co-applicant), who contributed to the protocol development and provided statistical input to the early part of the trial, including randomisation.
Chris Garnsworthy (service user), who contributed to writing the Plain English summary and provided feedback about the results from a service user perspective.
Other acknowledgements
We would also like to thank the following people for their enthusiasm, support and hard work throughout the duration of the study.
To all the patients gave their time to complete questionnaires and interviews.
To all members of the falls services teams: Marie Ward; Kate Roberston; Jenny Fantom; Lyndsey Richardson; Lyn Messer; Paul Crank; Sonia Jones; Anna McCartney; and Rachel King.
To all the paramedics who participated, and to all the other ambulance service staff who supported the trial: Glyn Thomas; David Thomas; Caroline Hogan; Matthew Turner; Anne Spaight; Helen Stook; Sue Poucher; Joy Graves; Liz Team; Nadya Essam; Stacey Knowles; Michael Fuller; Darren Coxon; Martin Sheehan; Duncan Booth; Terry Doherty; Wendy Hazard; Melanie Edwards; and Jane Turner.
To National Institute for Social Care and Health Research, which provided invaluable support to the trial in Wales.
We thank the Trial Steering Committee members: Professor Chris Salisbury (chairperson), Chris Hartley-Sharpe, Greg Morgan, Dr Suzanne Wyatt; Professor Jonathan Benger and the Data Monitoring and Ethics committee members: Dr Kerenza Hood (chairperson), Dr Antony Bayer, Dr John Belcher and Colin Thomson.
To our colleagues at Swansea University, Moira Morgan, Anne Surman, Sherry Jenkins and Claire Evans, who have provided unfailing administrative support to the study.
To Rohan D’Silva and the Health Informatics Research Unit team.
Contributions of authors
Helen A Snooks (Professor of Health Services Research), chief investigator, led the development of the research question, study design, study implementation and report submission.
Rebecca Anthony (trial manager) managed all aspects of the conduct of the trial and supervised research staff, wrote the first draft of Chapter 1 and contributed to all other report chapters.
Robin Chatters (research associate), site researcher; managed day-to-day conduct of the trial at Nottingham site, wrote the first draft of Chapter 2 and contributed to all other report chapters.
Jeremy Dale (Professor of Primary Care), co-applicant, provided expertise in primary and emergency care research.
Rachael Fothergill (Head of Clinical Audit and Research), principal investigator, provided prehospital care research expertise.
Sarah Gaze (trial manager) managed all aspects of the conduct of the trial, supervised research staff and contributed to all report chapters.
Mary Halter (senior research fellow), co-applicant, acted as site academic lead, provided expertise in emergency prehospital care, care of older people who have fallen and local research management, and conducted the systematic review.
Ioan Humphreys (research officer) contributed to the economic analysis and wrote the first draft of Chapter 5.
Marina Koniotou (research officer) managed the day-to-day conduct of the trial at the London site and contributed to all report chapters.
Philippa Logan (Professor of Rehabilitation Research), co-applicant, provided expertise in falls prevention and research.
Ronan Lyons (Professor of Public Health), co-applicant, provided expertise in public health, emergency care, injury prevention and service evaluation (SAIL-linked data).
Suzanne Mason (Professor of Emergency Medicine), co-applicant, provided specialist advice related to emergency care research and supervision of site researcher.
Jon Nicholl (Professor of Health Services Research), co-applicant, provided expertise in health service research, HTA and emergency care.
Julie Peconi (trial manager), co-applicant, managed all aspects of the conduct of the trial and supervised research staff at the early stage of the trial.
Ceri Phillips (Professor of Health Economics), co-applicant, provided health economics expertise and analysis and led the economic analysis.
Judith Phillips (Professor of Gerontology), co-applicant, provided expertise in the social care and needs of older people and the design of the qualitative components of the trial.
Alison Porter (senior research officer) led the qualitative analysis, wrote Chapter 6 and contributed to all other report chapters.
A Niroshan Siriwardena (Professor of Primary and Pre-Hospital Health Care), principal investigator, gave advice related to development of protocol and training.
Graham Smith (service user), TMG member, gave advice throughout trial.
Alun Toghill (service user), TMG member, gave advice throughout trial.
Mushtaq Wani (consultant geriatrician), co-applicant, provided clinical expertise in the care of the elderly and falls.
Alan Watkins (senior statistician), provided analysis of trial data and wrote Chapter 4.
Richard Whitfield (development manager), principal investigator; provided prehospital care research expertise.
Lynsey Wilson (research assistant) managed day-to-day conduct of the trial at the Wales site.
Ian T Russell (Professor of Clinical Trials), co-applicant, gave methodological advice, gave mentorship of trials management, provided statistical analysis and contributed to all report chapters.
All authors contributed to the preparation of the final report and approved the final version.
Publications
Darnell G, Mason SM, Snooks H. Elderly falls: a national survey of UK ambulance services. Emerg Med J 2012;29:1009–10.
Snooks H, Anthony R, Chatters R, Cheung WY, Dale J, Donohoe R, et al. Support and assessment for fall emergency referrals (SAFER2) research protocol: Cluster randomised trial of the clinical and cost effectiveness of new protocols for emergency ambulance paramedics to assess and refer to appropriate community-based care. BMJ Open 2012;2:e002169.
Snooks HA, Anthony R, Chatters R, Dale J, Fothergill RT, Gaze S, et al. Paramedic assessment of older adults after falls, including community care referral pathway: cluster randomized trial [Published online ahead of print March 13 2017]. Ann Emerg Med 2017.
Data sharing statement
Data are stored within the Secure Anonymised Information Linkage (SAIL) databank at the Health Information Research Unit (HIRU) at Swansea University. All proposals to use SAIL data sets must comply with HIRU’s information governance policy.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Bergeron E, Clement J, Lavoie A, Ratte S, Bamvita JM, Aumont F, et al. A simple fall in the elderly: not so simple. J Trauma 2006;60:268-73. http://dx.doi.org/10.1097/01.ta.0000197651.00482.c5.
- Sikron F, Giveon A, Aharonson-Daniel L, Peleg K. My home is my castle! Or is it? Hospitalizations following home injury in Israel, 1997–2001. Isr Med Assoc J 2004;6:332-5.
- Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 1994;331:821-7. http://dx.doi.org/10.1056/NEJM199409293311301.
- Tinetti ME, Speechley M. Prevention of falls among the elderly. N Engl J Med 1989;320:1055-9. http://dx.doi.org/10.1056/NEJM198904203201606.
- Tinetti ME. Preventing falls in elderly persons. N Engl J Med 2003;348:42-9. http://dx.doi.org/10.1056/NEJMcp020719.
- Bergland A, Wyller TB. Risk factors for serious fall related injury in elderly women living at home. Inj Prev 2004;10:308-13. http://dx.doi.org/10.1136/ip.2003.004721.
- Gillespie L. Preventing falls in elderly people. BMJ 2004;328:653-4. http://dx.doi.org/10.1136/bmj.328.7441.653.
- Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 2006;35:ii37-ii41. http://dx.doi.org/10.1093/ageing/afl084.
- McKay C, Anderson KE. How to manage falls in community dwelling older adults: a review of the evidence. Postgrad Med J 2010;86:299-306. http://dx.doi.org/10.1136/pgmj.2009.093468.
- Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health 2003;57:740-4. http://dx.doi.org/10.1136/jech.57.9.740.
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community 2012. Cochrane Database System Rev 2012;9. http://dx.doi.org/10.1002/14651858.CD007146.pub3.
- NIH Senior Health . Falls and Older Adults. Causes and Risk Factors 2013. www.nihseniorhealth.gov/falls/causesandriskfactors/01.html (accessed 30 January 2013).
- O’Loughlin JL, Robitaille Y, Boivin J-F, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 1993;137:342-54.
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988;319:1701-7. http://dx.doi.org/10.1056/NEJM198812293192604.
- Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. BMJ 1993;307:1248-50. http://dx.doi.org/10.1136/bmj.307.6914.1248.
- Gibson MJ, Andres RO, Kennedy TE, Coppard LC. Kellog International Work Group on the Prevention of Falls by the Elderly. The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan Med Bull 1987;34:1-24.
- Tinetti ME. Factors associated with serious injury during falls by ambulatory nursing home residents. J Am Geriatr Soc 1987;35:644-8. http://dx.doi.org/10.1111/j.1532-5415.1987.tb04341.x.
- Keil DP, O’Sullivan P, Teno JM, Mor V. Health care utilization and functional status in the aged following a fall. Med Care 1991;29:221-8. http://dx.doi.org/10.1097/00005650-199103000-00004.
- Wolinsky FD, Johnson RJ, Fitzgerald JF. Falling, health status, and the use of health services by older adults. A prospective study. Med Care 1992;30:587-97. http://dx.doi.org/10.1097/00005650-199207000-00002.
- Tinetti ME, Williams CS. The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci 1998;53:M112-19. http://dx.doi.org/10.1093/gerona/53A.2.M112.
- Nevitt MC, Cummings SR, Kidd S, Black D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 1989;261:2663-8. http://dx.doi.org/10.1001/jama.1989.03420180087036.
- Centers for Disease Control and Prevention . About the National Health Interview Survey 2010. www.cdc.gov/nchs/nhis/about_nhis.htm (accessed 31 January 2014).
- Carr AJ, Higginson IJ. Are quality of life measures patient centred?. BMJ 2001;322:1357-60. http://dx.doi.org/10.1136/bmj.322.7298.1357.
- Graham HJ, Firth J. Home accidents in older people: role of primary health care team. BMJ 1992;305:30-2. http://dx.doi.org/10.1136/bmj.305.6844.30.
- Tian Y, Thompson J, Buck D, Sonola L. Exploring the System-wide Costs of Falls in Older People in Torbay. London: The King’s Fund; 2013.
- Department of Health . National Service Framework for Older People 2001 n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/198033/National_Service_Framework_for_Older_People.pdf (accessed 10 April 2014).
- Close JC. Interdisciplinary practice in the prevention of falls-a review of working models of care. Age Ageing 2001;30:8-12. http://dx.doi.org/10.1093/ageing/30.suppl_4.8.
- Aoyagi K, Ross PD, Davis JW, Wasnich RD, Hayashi T, Takemoto T. Falls among community-dwelling elderly in Japan. J Bone Miner Res 1998;13:1468-74. http://dx.doi.org/10.1359/jbmr.1998.13.9.1468.
- American Geriatric Society, American Academy of Geriatrics Society, Orthopaedic Surgeons Panel On Falls Prevention . Guideline for the prevention of falls in older persons. J Am Geriatr Soc 2001;49:664-72. http://dx.doi.org/10.1046/j.1532-5415.2001.49115.x.
- National Institute for Health and Care Excellence . Clinical Practice Guidelines for the Assessment and Prevention of Falls in Older People 2004 n.d. www.nice.org.uk/nicemedia/pdf/CG021fullguideline.pdf (accessed 17 April 2014).
- NHS Confederation . The Ambulance Service Network. A Vision for Emergency and Urgent Care: The Role of the Ambulance Services 2008 n.d. www.nhsconfed.org/Publications/Pages/Avisionfor.aspx (accessed 15 April 2014).
- Winkin V, Pinckaers V, D’Orio V, Ghuysen A. Overcrowding estimation in the emergency department: is the simplest score the best?. Crit Care 2013;17. http://dx.doi.org/10.1186/cc12196.
- The King’s Fund . Are Accident and Emergency Attendances Increasing 2013 n.d. www.kingsfund.org.uk/blog/2013/04/are-accident-and-emergency-attendances-increasing (accessed 15 April 2014).
- Close JC, Lord SR, Antonova EJ, Martin M, Lensberg B, Taylor M, et al. Older people presenting to the emergency department after a fall: a population with substantial recurrent healthcare use. Emerg Med J 2012;29:742-7. http://dx.doi.org/10.1136/emermed-2011-200380.
- Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet 1999;353:93-7. http://dx.doi.org/10.1016/S0140-6736(98)06119-4.
- Kawano T, Nishiyama K, Anan H, Tujimura Y. Direct relationship between aging and overcrowding in the ED, and a calculation formula for demand projection: a cross-sectional study. Emerg Med J 2014;31:19-23. http://dx.doi.org/10.1136/emermed-2012-202050.
- Result of Research of the Acceptance of the Medical Institution in Emergency Conveyance in 2009. Editor Communications Tokyo: The Fire Defense Agency; 2010.
- Bridges J. Listening Makes Sense: Understanding the Experiences of Older People and Relatives Using Urgent Care Services in England 2008. www.staff.city.ac.uk/~rbbc318/lms/resources/final_report.pdf (accessed 15 April 2014).
- Miller S. Unnecessary and Avoidable Hospital Admissions for Older People. Canberra, ACT: Department of Health and Ageing; 2003.
- Taking Healthcare to the Patient: Transforming NHS Ambulance Services. London: DH; 2005.
- Our Health, Our Care, Our Say. London: HMSO; 2006.
- Transforming Urgent and Emergency Care Services in England. Leeds: NHS England; 2013.
- Weiss SJ, Chong R, Ong M, Ernst AA, Balash M. Emergency medical services screening of elderly falls in the home. Prehosp Emerg Care 2003;7:79-84. http://dx.doi.org/10.1080/10903120390937148.
- Snooks HA, Halter M, Close JC, Cheung WY, Moore F, Roberts SE. Emergency care of older people who fall: a missed opportunity. Qual Saf Health Care 2006;15:390-2. http://dx.doi.org/10.1136/qshc.2006.018697.
- Marks PJ, Daniel TD, Afolabi O, Spiers G, Nguyen-Van-Tam JS. Emergency (999) calls to the ambulance service that do not result in the patient being transported to hospital: an epidemiological study. Emerg Med J 2002;19:449-52. http://dx.doi.org/10.1136/emj.19.5.449.
- Close JC, Halter M, Elrick A, Brain G, Swift CG. Falls in the older population: a pilot study to assess those attended by London ambulance service but not taken to A&E. Age Ageing 2002;31:488-9. http://dx.doi.org/10.1093/ageing/31.6.488.
- Goldberg RJ, Zautcke JL, Koenigsberg MD, Lee RW, Nagorka FW, Kling M, et al. A review of prehospital care litigation in a large metropolitan EMS system. Ann Emerg Med 1990;19:557-61. http://dx.doi.org/10.1016/S0196-0644(05)82189-4.
- Department of Health, College of Emergency Medicine . A&Amp;E Clinical Quality Indicators 2011 n.d. www.imperial.nhs.uk/patients/ourstandards/emergency-care-quality-indicators/index.htm (accessed 26 March 2014).
- Porter A, Snooks H, Youren A, Gaze S, Whitfield R, Rapport F, et al. ‘Should I stay or should I go?’ Deciding whether to go to hospital after a 999 call. J Health Serv Res Policy 2007;12:32-8. http://dx.doi.org/10.1258/135581907780318392.
- Snooks HA, Kearsley N, Dale J, Halter M, Redhead J, Foster J. Gaps between policy, protocols and practice: a qualitative study of the views and practice of emergency ambulance staff concerning the care of patients with non-urgent needs. Qual Saf Health Care 2005;14:251-7. http://dx.doi.org/10.1136/qshc.2004.012195.
- GP Newsletter February 2013 Edition 10 NHS 111 – Final Stages. London: London Ambulance Service NHS Trust; 2013.
- Falls Team Shortlisted for National Award. Nottingham: East Midlands Ambulance Service NHS Trust; 2013.
- Hassan T, McMillan P, Walsh C, Higginson I. The Drive for Quality. How to Achieve Safe, Sustainable Care in our Emergency Departments: System Benchmarks and Recommendations. London: The College of Emergency Medicine; 2013.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- NHS Institute for Innovation and Improvement . Commissioning for Quality and Innovation (CQUIN) Payment Framework 2006–2013 n.d. www.institute.nhs.uk/commissioning/pct_portal/cquin.html (accessed 16 April 2014).
- Cooper S, Barrett B, Black S, Evans C, Real C, Williams S, et al. The emerging role of the emergency care practitioner. Emerg Med J 2004;21:614-18. http://dx.doi.org/10.1136/emj.2003.011247.
- Anderson KN, Anderson LE, Glanze WD. Mosby’s Medical, Nursing, & Allied Health Dictionary. St. Louis, MO: Mosby-Year Book. Inc; 1994.
- Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.328.7441.680.
- Hill KD, Moore KJ, Dorevitch MI, Day LM. Effectiveness of falls clinics: an evaluation of outcomes and client adherence to recommended interventions. J Am Geriatr Soc 2008;56:600-8. http://dx.doi.org/10.1111/j.1532-5415.2007.01626.x.
- Palvanen M, Kannus P, Piirtola M, Niemi S, Parkkari J, Jarvinen M. Effectiveness of the Chaos Falls Clinic in preventing falls and injuries of home-dwelling older adults: a randomised controlled trial. Injury 2014;45:265-71. http://dx.doi.org/10.1016/j.injury.2013.03.010.
- Logan PA, Coupland CA, Gladman JR, Sahota O, Stoner-Hobbs V, Robertson K, et al. Community falls prevention for people who call an emergency ambulance after a fall: randomised controlled trial. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c2102.
- Sach TH, Logan PA, Coupland CA, Gladman JR, Sahota O, Stoner-Hobbs V, et al. Community falls prevention for people who call an emergency ambulance after a fall: an economic evaluation alongside a randomised controlled trial. Age Ageing 2012;41:635-41. http://dx.doi.org/10.1093/ageing/afs071.
- Newman J. Modernising Governance: New Labour, Policy and Society. London: Sage; 2001.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Gates S, Fisher JD, Cooke M, Carter Y, Lamb SE. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta-analysis. BMJ 2008;336:130-3. http://dx.doi.org/10.1136/bmj.39412.525243.BE.
- Mason S, Knowles E, Colwell B, Wardrope J, Dixon S, Gorringe R. Paramedic Practitioner Older People’s Support Trial (PPOPS): a cluster randomised controlled trial. BMJ 2007;335:919-25. http://dx.doi.org/10.1136/bmj.39343.649097.55.
- Falls: Assessment and Prevention of Falls in Older People. London: NICE; 2013.
- Centers for Disease Control and Prevention . Costs of Falls Among Older Adults 2013 n.d. www.cdc.gov/homeandrecreationalsafety/falls/fallcost.html (accessed 23 April 2014).
- Hendrie D, Hall SE, Arena G, Legge M. Health system costs of falls of older adults in Western Australia. Aust Health Rev 2004;28:363-73. http://dx.doi.org/10.1071/AH040363.
- Cone DC, Ahern J, Lee CH, Baker D, Murphy T, Bogucki S. A descriptive study of the ‘lift-assist’ call. Prehosp Emerg Care 2013;17:51-6. http://dx.doi.org/10.3109/10903127.2012.717168.
- Snooks H, Anthony R, Chatters R, Cheung W-Y, Dale J, Donohoe R, et al. Support and assessment for fall emergency referrals (SAFER 2) research protocol: cluster randomised trial of the clinical and cost effectiveness of new protocols for emergency ambulance paramedics to assess and refer to appropriate community-based care. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-002169.
- Darzi A. High Quality Care for All: NHS Next Stage Review Final Report. London: Department of Health; 2009.
- Tiedemann A, Mikolaizak AS, Sherrington C, Segin K, Lord SR, Close JC. Older fallers attended to by an ambulance but not transported to hospital: a vulnerable population at high risk of future falls. Aust N Z J Public Health 2013;37:179-85. http://dx.doi.org/10.1111/1753-6405.12037.
- Mikolaizak AS, Simpson PM, Tiedemann A, Lord SR, Close JC. Systematic review of non-transportation rates and outcomes for older people who have fallen after ambulance service call-out. Australas J Ageing 2013;32:147-57. http://dx.doi.org/10.1111/ajag.12023.
- Snooks H, Cheung WY, Gwini S, Humphreys I, Sánchez A, Siriwardena N. Can older people who fall be identified in the ambulance call centre to enable alternative responses or care pathways?. Emerg Med J 2011;28. http://dx.doi.org/10.1136/emj.2010.108605.15.
- Newton JL, Kyle P, Liversidge P, Robinson G, Wilton K, Reeve P. The costs of falls in the community to the North East Ambulance Service. Emerg Med J 2006;23:479-81. http://dx.doi.org/10.1136/emj.2005.028803.
- Mason S, Wardrope J, Perrin J. Developing a community paramedic practitioner intermediate care support scheme for older people with minor conditions. Emerg Med J 2003;20:196-8. http://dx.doi.org/10.1136/emj.20.2.196.
- Darnell G, Mason SM, Snooks H. Elderly falls: a national survey of UK ambulance services. Emerg Med J 2012;29:1009-10. http://dx.doi.org/10.1136/emermed-2011-200419.
- Snooks H, Cheung WY, Close J, Dale J, Gaze S, Humphreys I, et al. Support and Assessment for Fall Emergency Referrals (SAFER 1) trial protocol. Computerised on-scene decision support for emergency ambulance staff to assess and plan care for older people who have fallen: evaluation of costs and benefits using a pragmatic cluster randomised trial. BMC Emerg Med 2010;10. http://dx.doi.org/10.1186/1471-227X-10-2.
- Gray JT, Walker A. Avoiding admissions from the ambulance service: a review of elderly patients with falls and patients with breathing difficulties seen by emergency care practitioners in South Yorkshire. Emerg Med J 2008;25:168-71. http://dx.doi.org/10.1136/emj.2007.050732.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000097.
- University of York . Systematic Reviews CRD’s Guidance for Undertaking Reviews in Healthcare CRD 2009. www.york.ac.uk/inst/crd/pdf/Systematic_Reviews.pdf (accessed 23 April 2014).
- Petticrew S, Roberts H. Systematic Reviews in the Social Sciences, A Practical Guide. Oxford: Blackwell Publishing; 2006.
- Prevention of Falls Network Europe . Manual for the Fall Prevention Classification System 2007. www.profane.eu.org/documents/Falls_Taxonomy.pdf (accessed 23 April 2014).
- Hauer K, Lamb SE, Jorstad EC, Todd C, Becker C. Systematic review of definitions and methods of measuring falls in randomised controlled fall prevention trials. Age Ageing 2006;35:5-10. http://dx.doi.org/10.1093/ageing/afi218.
- Scottish Intercollegiate Guidelines Network . Sign 50 A Guideline Developer’s Handbook 2011 n.d. www.sign.ac.uk/pdf/sign50.pdf (accessed 23 April 2014).
- Walsh D, Downe S. Appraising the quality of qualitative research. Midwifery 2006;22:108-19. http://dx.doi.org/10.1016/j.midw.2005.05.004.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M. Guidance on the Conduct of Synthesis In Systematic Reviews 2006. www.lancaster.ac.uk/shm/research/nssr/research/dissemination/publications/NS_Synthesis_Guidance_v1.pdf (accessed 23 April 2014).
- Metcalfe J. Enhancing the care of older people in the community. Nurs Stand 2006;21:35-9. http://dx.doi.org/10.7748/ns2006.10.21.7.35.c6360.
- Shah MN, Clarkson L, Lerner EB, Fairbanks RJ, McCann R, Schneider SM. An emergency medical services program to promote the health of older adults. J Am Geriatr Soc 2006;54:956-62. http://dx.doi.org/10.1111/j.1532-5415.2006.00736.x.
- Shandro JR, Spain DA, Dicker RA. Recruitment strategies for a fall prevention program: if we build it, will they really come?. J Trauma 2007;63:142-6. http://dx.doi.org/10.1097/TA.0b013e318068428a.
- Kue R, Ramstrom E, Weisberg S, Restuccia M. Evaluation of an emergency medical services-based social services referral program for elderly patients. Prehosp Emerg Care 2009;13:273-9. http://dx.doi.org/10.1080/10903120802706179.
- Shah MN, Caprio TV, Swanson P, Rajasekaran K, Ellison JH, Smith K, et al. A novel emergency medical services-based program to identify and assist older adults in a rural community. J Am Geriatr Soc 2010;58:2205-11. http://dx.doi.org/10.1111/j.1532-5415.2010.03137.x.
- Halter M, Vernon S, Snooks H, Porter A, Close J, Moore F, et al. Complexity of the decision-making process of ambulance staff for assessment and referral of older people who have fallen: a qualitative study. Emerg Med J 2011;28:44-50. http://dx.doi.org/10.1136/emj.2009.079566.
- Hoyle S, Swain AH, Fake P, Larsen PD. Introduction of an extended care paramedic model in New Zealand. Emerg Med Australas 2012;24:652-6. http://dx.doi.org/10.1111/j.1742-6723.2012.01608.x.
- Studnek JR, Thestrup L, Blackwell T, Bagwell B. Utilization of prehospital dispatch protocols to identify low-acuity patients. Prehosp Emerg Care 2012;16:204-9. http://dx.doi.org/10.3109/10903127.2011.640415.
- Comans TA, Currin ML, Quinn J, Tippett V, Rogers A, Haines TP. Problems with a great idea: referral by prehospital emergency services to a community-based falls-prevention service. Inj Prev 2013;19:134-8. http://dx.doi.org/10.1136/injuryprev-2011-040076.
- Fitzpatrick-Lewis D, Ciliska D, Thomas H. The Methods for the Synthesis of Studies without Control Groups. Hamilton, ON: National Collaborating Centre for Methods and Tools; 2009.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011.
- Snooks H, Foster T, Nicholl J. Results of an evaluation of the effectiveness of triage and direct transportation to minor injuries units by ambulance crews. Emerg Med J 2004;21:105-11. http://dx.doi.org/10.1136/emj.2003.009050.
- Medical Research Council (MRC) . Good Clinical Practice In Clinical Trials 1998. www.mrc.ac.uk/Utilities/Documentrecord/index.htm?d=MRC002416 (accessed 14 May 2014).
- SOP24 Standard Operating Procedure for Randomisation. Swansea: Swansea University Medical School; 2012.
- Lamb SE, Jorstad-Stein EC, Hauer K, Becker C. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc 2005;53:1618-22. http://dx.doi.org/10.1111/j.1532-5415.2005.53455.x.
- Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. http://dx.doi.org/10.1097/00005650-199603000-00003.
- Carey RG, Seibert JH. A patient survey system to measure quality improvement: questionnaire reliability and validity. Med Care 1993;31:834-45. http://dx.doi.org/10.1097/00005650-199309000-00008.
- Hill KD, Schwarz JA, Kalogeropoulos AJ, Gibson SJ. Fear of falling revisited. Arch Phys Med Rehabil 1996;77:1025-9. http://dx.doi.org/10.1016/S0003-9993(96)90063-5.
- SOP28 Standard Operating Procedure for Statistics. Swansea: Swansea University Medical School; 2012.
- Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med 2002;39:238-47. http://dx.doi.org/10.1067/mem.2002.121523.
- NHS Reference Costs 2011–12. London: DH; 2012.
- Barbour RS. Are Focus Groups an Appropriate Tool for Studying Organisational Change. Developing Focus Group Research. London: Sage; 1999.
- Ritchie J, Spencer L, Huberman M, Miles M. The Qualitative Researcher’s Companion. London: Sage; 2002.
- Srivastava A, Thomson S. Framework analysis: a qualitative methodology for applied policy research. JOAAG 2009;4.
- Corden A, Sainsbury R. Using Verbatim Quotations in Reporting Qualitative Social Research: Researchers’ Views. York: Social Policy Research Unit, University of York; 2006.
- Briefing Notes for Researchers: Involving the Public in NHS, Public Health and Social Care Research. Eastleigh: INVOLVE; 2012.
- Boote J, Telford R, Cooper C. Consumer involvement in health research: a review and research agenda. Health Policy 2002;61:213-36. http://dx.doi.org/10.1016/S0168-8510(01)00214-7.
- Entwistle VA, Renfrew MJ, Yearley S, Forrester J, Lamont T. Lay perspectives: advantages for health research. BMJ 1998;316:463-6. http://dx.doi.org/10.1136/bmj.316.7129.463.
- Chalmers I. A guide to patient-led good controlled trials. Lancet 2000;356. http://dx.doi.org/10.1016/S0140-6736(05)73681-3.
- Evans BA, Bedson E, Bell P, Hutchings H, Lowes L, Rea D, et al. Involving service users in trials: developing a standard operating procedure. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-219.
- Boote J, Baird W, Sutton A. Public involvement in the design and conduct of clinical trials: a review. Int J Interdiscip Soc Sci 2011;5:91-111.
- INVOLVE . Public Involvement in Clinical Trials: Supplement to the Briefing Notes for Researchers 2012. www.nihr.ac.uk/get-involved/INVOLVEpublicinvolvementinclinicaltrialsBriefingnotes2012.pdf (accessed 23 February 2014).
- Snooks HA, Anthony R, Chatters R, Dale J, Fothergill RT, Gaze S, et al. Paramedic assessment of older adults after falls, including community care referral pathway: cluster randomized trial [Published online ahead of print March 13 2017]. Ann Emerg Med 2017. https://doi.org/10.1016/j.annemergmed.2017.01.006.
- NHS Reference Costs 2012–13. London: DH; 2013.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: PSSRU, University of Kent; 2013.
- Turner J, Snooks H, Youren A, Dixon S, Fall D, Gaze S, et al. The Costs and Benefits of Managing some Low Priority 999 Ambulance Calls by NHS Direct Nurse Advisers. Final Report to the Service Delivery and Organisation R&D Programme. Sheffield: ScHARR (School of Health and Related Research), Sheffield University; 2006.
- Fletcher B, Gheorghe A, Moore D, Wilson S, Damery S. Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2011-000496.
- Hawe P, Shiell A, Riley T, Gold L. Methods for exploring implementation variation and local context within a cluster randomised community intervention trial. J Epidemiol Community Health 2004;58:788-93. http://dx.doi.org/10.1136/jech.2003.014415.
Appendix 1 Support and Assessment for Fall Emergency Referrals 2 clinical decision protocol
Reprinted from Snooks et al. 121 with permission from the American College of Emergency Physicians. Copyright © 2017 American College of Emergency Physicians. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Appendix 2 Full data extraction and quality assessment tables
| Study (country) | Study design and purpose | Population characteristics | Intervention | Sample size | Outcome measure | Results |
|---|---|---|---|---|---|---|
| Metcalfe, 2006 (UK)89 | Cohort study to examine the benefit to patients of a single point of access to other services | Patients aged ≥ 65 years being attended by an emergency ambulance within the PCT area and being left at home | Clinical assessment tool and training to support ambulance staff. External agency undertook clinical triage for referral to a rapid response team and further onward referrals | n = 49 | Number of referrals made for patients experiencing a fall | n = 53 |
| Number of onward referrals and destination of referrals | n = 51: specialist nurse, n = 1; rapid response team, n = 17; community hospital, n = 1; geriatrician, n = 2; community physiotherapist, n = 4; GP, n = 9; district nurse, n = 8; community psychiatric nurse, n = 3; and social care, n = 6 | |||||
| Number patients refusing referrals | n = 2 | |||||
| Shah et al., 2006 (USA)90 | Cluster controlled trial to evaluate the effect of an EMS programme by screening at least 80% of community-dwelling older adults to identify those at risk for falls | Intervention group: residents aged ≥ 65 years (n = 1011 in 2000) Usual-care control group: residents aged ≥ 65 years (n = 720) Patients were excluded if they could not speak English, if they had been previously included in the study or if they were institutionalised (group home, nursing home or jail) |
EMTs provided with training, participating in a 90-minute case-based discussion on caring for older adults. Training on the screening programme was provided. EMTs instructed to screen community-dwelling patients during emergency responses to evaluate risk of falling. Instructional materials were given if the patient was considered to be at risk | n = 258 (total patients attended by EMTs for all conditions). n = 143 control | Patients’ risk status (falls) | Successful for screening for falls history n = 210/258 (79%, 95% CI 74% to 84%) |
| Recollection of educational materials | Poor recollection of falls brochure for intervention group, only n = 17 (21%) | |||||
| Recollection of discussions with physicians regarding risks | Infrequent discussions with PCPs about risks: intervention n = 8 (10%) and control n = 1 (3%), with no PCP visit in 35% intervention and 46% control cases | |||||
| Receipt of changes to the home environment | No difference in changes to prevent falls: intervention: n = 12/82 (15%), control: n = 4/37 (11%); p = 0.91 | |||||
| Mason et al., 2007 (UK)66 | C-RCT | Individuals aged 60 years and above calling the emergency services for a presenting complaint in the scope of practice of the paramedic practitioner | Paramedics with extended skills (paramedic practitioners) | n = 3018 | ED attendance 0 to 28 days | Intervention = 62.6%; control = 87.5% (p < 0.001) |
| Admittance to hospital 0 to 28 days | Intervention = 40.4%; control = 46.4% (p < 0.001) | |||||
| Total episode time | Intervention = 235 minutes; control = 278 minutes (p < 0.001) | |||||
| Investigations received | Intervention = 49.7%; control = 67.9% (p < 0.001) | |||||
| Treatment received | Intervention = 81.3%; control = 72.8% (p < 0.001) | |||||
| Shandro et al., 2007 (USA)91 | Cohort study to evaluate recruitment strategies and to outline challenges and solutions of the implementation of a fall prevention programme | Patients, who are living independently, were over 65 years of age and had an emergency service dispatch for a fall but were not transported to the ED | Provided with educated on the goals and design of a fall prevention programme. Voluntary referral mechanism for self-report or report of a medical provider for participants that had a recent fall and were able to participate in a home safety evaluation and strengthening programme | Eligible patient numbers not specified | Number of referrals by EMS staff | n = 17 referred to the prevention programme |
| Number of enrolments on falls prevention programme by EMS referrals | n = 11 (65%) enrolled onto the prevention programme | |||||
| Gray and Walker, 2008 (UK)80 | Time-series analysis cohort study with control arm to establish the impact of ECPs in terms of avoided admissions for falls | All patients aged ≥ 65 years who had called the emergency services after a fall and were seen by the ECP service; or who had attended ED following attendance by non-ECP ambulance personnel | ECP, with additional training, attending calls for conditions felt to benefit from ECP management | n = 233 ECP attended cases and n = 772 pre-intervention attended cases | % not conveyed following initial ECP attendance | Intervention arm: n = 171/233 (73%) |
| % avoiding admissions during pre-intervention period | Pre-intervention arm: n = 369/772 (48%) | |||||
| % ED attendance or hospital admission in 72 hours | Intervention arm: n = 21 further hospital attendances in 72 hours | |||||
| % ED attendance or hospital admission in 28 days | Intervention arm: n = 131 remained at home at 28 days (44% ED attendance/admission rate) Authors describe: ECPs reduce admissions by 17% at 28 days relative to the ED ‘initial contact’ figure (from 52% to 44%, n = 1005, df = 1, p = 0.05) |
|||||
| aKue et al., 2009 (USA)92 | Cohort study to describe the experience of implementing three referral programmes and to report frequencies of referrals made | Adults aged ≥ 60 years who called the emergency services in the city EMS area and were not conveyed | Paramedic in-service training; paramedic referrals to social services and retrospective EMS physician referral on chart review | n = 721 | Number of referrals for fall-related complaints | n = 32 |
| Number of acceptance of referral | n = 24 | |||||
| Logan et al., 2010 (UK)61 | RCT to evaluate whether or not a service to prevent falls in the community would reduce the rate of falls in older people who called the emergency services and were not taken to hospital | Adults aged ≥ 60 years living at home or in residential care in one of the PCT areas who were not taken to hospital | Retrospective identification of potential participants from ambulance service records. Use of a randomisation sequence, individualised multifactorial intervention programme following UK clinical fall guidelines | n = 204 (n = 102 in each group) | Died by 12-month follow-up | Control, n = 16; intervention, n = 14 (p = 0.74) |
| At least one falls-related fracture admitted to hospital | Control, n = 6; intervention, n = 3 (p = 0.35) | |||||
| Number of emergency ambulance calls received for falls over 12 months | Control, n = 365; intervention, n = 245 (p = 0.018) | |||||
| Number of days in hospital per year | Control, n = 1141; intervention, n = 1257 (p = 0.70) | |||||
| Total number of hospital admissions | Control, n = 99; intervention, n = 97 (p = 0.93) | |||||
| Median Falls Efficacy Scale (fear of falling) | Control, n = 76; intervention, n = 57 (p < 0.001) | |||||
| Median Nottingham Extended Activities of Daily Living score | Control, n = 6; intervention, n = 8 (p < 0.001) | |||||
| Median Barthel Index of Activities of Daily Living score | Control, n = 15; intervention, n = 15 (p = 0.021) | |||||
| Number with at least one fall during follow-up | Control, n = 96; intervention, n = 81; incidence rate ratio = 0.86 (p < 0.001) | |||||
| Median days to first fall incidence rate ratio, over 12 months (primary outcome) | Overall incidence of falls intervention group = 3.46 per person and control group 7.68; incidence rate ration 0.45 (95% CI 0.35 to 0.58; p < 0.001) | |||||
| Shah et al., 2010 (USA)93 | Cohort study to describe the development, implementation and, experience of a novel, community-based programme to identify rural-dwelling older adults with unmet medical and social needs | Community-dwelling older adults, aged 60 years and above, who accessed EMS for emergency care | EMS staff provided with training specific to geriatrics. The screening question looked at whether or not the patient had fallen in the previous year or if the EMS provider identified any falls risks in the home. Case managers intercepted the findings and contacted patients after 2 weeks to arrange a home visit | n = 814 (adults screened by EMS for falls) | Number of patients screened for falls | n = 814 |
| Number patients referred due to falls | n = 124 | |||||
| Number patients at risk of falls | n = 552 | |||||
| Halter et al., 2011 (UK)94 | Qualitative study to understand the decision-making processes of emergency ambulance staff dealing with older people who have fallen | 12 ambulance staff trained in, and used the, clinical assessment tool | Paramedics received 2-hour training session in the cause of falls, assessment of older person who has fallen and research methods. Paramedics completed clinical assessment tool for those patients who had a fall | 12 paramedics | Paramedics’ self-reported process of decision-making following 6 months use of the clinical assessment tool | Paramedics described the decision-making process as follows:
|
| Hoyle et al., 2012 (New Zealand)95 | To evaluate the first 1000 patients seen by emergency care paramedics | Average patient age of 62 years | Assessment by individual dispatchers to decide whether or not to send emergency care paramedic to patient. Emergency care paramedics followed clinical protocols that were specific to patient condition | n = 131 (number of falls out of the 1000 presentations attended by emergency care paramedics) | Patient disposition including ED and treated in community | 87 (66%) patients were treated in the community and 44 (34%) patients transported to ED |
| Reduced unnecessary transportation | 40% of patients transported; 74% of patients seen by standard ECPs were transported | |||||
| Sach et al., 2012 (UK)62 | Cost-effectiveness study to estimate the cost-effectiveness of a community falls prevention service compared with usual care, over the 12-month trial period | Patients aged ≥ 60 years, attended for a fall at home in four Nottinghamshire PCTs and were not transported to hospital | Participants in the intervention group were referred to a community falls prevention programme. Control group underwent normal care | n = 157 (82 intervention; 75 control) | Cost utility (QALY) | Mean difference in QALYs of 0.070, 95% CI −0.010 to 0.150; p = 0.086 |
| Cost-effectiveness (falls per patient) | Difference of mean number of falls per patient during 12 month follow-up period: –5.34, 95% CI −7.06 to −3.62; p < 0.001 | |||||
| Resource use (total NHS and social services resource use) | Mean difference: –£1551, 95% CI –£5932.00 to £2829.00 | |||||
| Studneck et al., 2012 (USA)96 | Cohort study to describe the experience of an EMS agency using the MPDS low-acuity omega protocol (omega = calls classified as not requiring immediate ambulance response or transport and appropriate transfer to an advice-line nurse) | Emergency service callers classified as low acuity by MPDS | Introduction of MPDS Omega responses assigned to patients deemed to be low acuity by MPDS including falls. Phase 1: triaged and ambulance dispatched. Phase 2: patients offered to speak to an advice-line nurse for secondary triage, with ambulance responses continued per standard protocol | Phase 1: fall, n = 160; phase 2 fall, n = 101 | % admitted to hospital | Phase 1, n = 56/160 (35%) hospital admission; phase 2, n = 66/101 (25.7%) hospital admission |
| % admitted to ICU | Phase 1, n = 3/160 (5.4%) ICU admission; phase 2, n = 0/101 ICU admission | |||||
| Comans et al., 2013 (Australia)97 | Cohort study to discuss the potential barriers and enablers of a collaborative approach between two health services and to compare referral pathways | Patients older than 65 years, living in the community; and had had a recent fall attended by a paramedic trained in the referral technique | Referral pathways were direct from a paramedic or self-referral after information provided by a paramedic. Participants received a falls assessment from the rehabilitation service with referral to an 8-week falls programme | n = 638 | Characteristics of referred patients (Baseline Frenchay Activities Index, Abbreviated Mental Test Score, EQ-5D and median falls in past 6 months showed) | No between-group descriptive differences |
| Strategies to improve referral rates | Repeated education sessions with officers; contact from rehabilitation service to confirm referral; rehabilitation observation days | |||||
| Number of participants referred | n = 21 | |||||
| Number of participants consented to referral | n = 17 | |||||
| Patients consented to study and initial assessment | n = 13 | |||||
| Patients enrolled onto programme | n = 8 | |||||
| Patients completed programme | n = 5 |
| Quality assessment | 1.1: clearly focused question | 1.2: comparable source populations | 1.3: participation rates stated | 1.4: outcome at time of enrolment taken into account | 1.5: percentage of participants dropping out | 1.6: comparison made between participants and those lost to follow-up | 1.7: outcomes clearly defined | 1.8: blinding | 1.9: if blinding not possible, recognition that exposure could influence outcome | 1.10: measure of assessment of exposure is reliable | 1.11: other sources cited to demonstrate outcome assessment is valid | 1.12: exposure level assessed more than once | 1.13: confounders identified and taken into account | 1.14: CIs provided | 2.1: how well was study done to minimise risk of bias? | 2.2: how strong is association between exposure and outcome? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| aMetcalfe, 200689 | No | n/a | n/a | No | 0% | n/a | Yes | n/a | No | Yes | n/a | No | No | No | Low | Weak |
| bShah et al., 200690 | Yes | Yes | Yes | n/a | 63% | No | Yes | No | Yes | Yes | n/a | n/a | No | Yes | Acceptable | Moderate |
| cShandro et al., 200791 | Yes | n/a | n/a | No | 35% | n/a | Yes | n/a | n/a | Yes | n/a | No | No | No | Low | Moderate |
| dGray and Walker, 200880 | Yes | Cannot say | No | No | n/a | n/a | Yes | n/a | No | Yes | n/a | n/a | No | No | Acceptable | Moderate |
| eKue et al., 200992 | Yes | n/a | n/a | Cannot say | 25% | n/a | No | n/a | n/a | Cannot say | n/a | n/a | Cannot say | Yes | Low | Weak |
| fShah et al., 201093 | No | n/a | n/a | No | Cannot say | n/a | Yes | n/a | n/a | Yes | n/a | No | No | No | Low | Strong |
| gHoyle et al., 201295 | Yes | n/a | n/a | n/a | n/a | n/a | Yes | n/a | n/a | Yes | n/a | n/a | Yes | No | Low | Moderate |
| hStudnek et al., 201296 | Yes | n/a | n/a | n/a | n/a | n/a | Yes | n/a | Yes | Yes | n/a | No | No | No | Low | Weak |
| iComans et al., 201397 | Yes | Yes | Yes | No | 75% | No | Yes | n/a | n/a | Yes | n/a | No | No | No | Low | Weak |
| Quality assessment | 1.1: the study addresses an appropriate and clearly focused question | 1.2: the assignment of subjects to treatment groups is randomised | 1.3: adequate concealment method used | 1.4: subjects and investigators are kept ‘blind’ to treatment allocation | 1.5: treatment and control groups similar at the start of the trial | 1.6: only difference between groups is treatment under investigation | 1.7: all relevant outcomes measured in a standard, valid and reliable way | 1.8: what percentage of the individuals or clusters recruited into each treatment arm of the study dropped | 1.9: all the subjects are analysed in the groups to which they were randomly allocated | 1.10: where the study is carried out at more than one site, results are comparable for all sites | 2.1: how well was the study done to minimise the risk of bias or confounding | 2.2: is the overall effect is due to the intervention |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| aLogan et al., 201061 | Yes | Yes | Yes | No (subjects were not blinded, but investigators were) | Yes | Yes | Yes | 6% | Yes | n/a | High | Yes |
| Mason et al., 200766 | Yes | Yes (by week) | Yes (forward roster concealed) | n/a | Yes | Yes | Yes | 27% | Yes | n/a | High quality | Yes |
| Quality assessment | 1.1: the study addresses an appropriate and clearly focused question | 1.2: the economic importance of the question is clear | 1.3: the choice of study design is justified | 1.4: all costs that are relevant from the viewpoint of the study are included and are measured and valued appropriately | 1.5: the outcome measures used to answer the question are relevant to that purpose and are measured and valued appropriately | 1.6: if discounting of future costs and outcomes is necessary, it’s been performed correctly | 1.7: assumptions are explicit, sensitivity analysis performed | 1.8: the decision rule explicit and comparisons made on the basis of incremental costs and outcomes | 1.9: the results provide information of relevance to policy makers | 2.1: how well was the study conducted | Are the results of this study directly applicable to the review question? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| aSach et al., 201262 | Yes | Yes | Yes | Yes | Yes | n/a | Yes | Yes | Yes | High quality | Yes |
| Quality assessment | Clear statement of, and rationale for, research questions/aims/purposes | Study thoroughly contextualised by existing literature | Method/design apparent, and consistent with research intent | Data collection strategy apparent and appropriate | Sample and sampling method appropriate | Analytical approach appropriate | Context described and taken into account of in interpretation | Clear audit trail given | Data used to support interpretation | Researcher reflexivity demonstrated | Demonstration of sensitivity to ethical concerns | Relevance and transferability evident |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Halter et al., 201194 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes |
Appendix 3 Excluded studies
The total number of excluded studies was 128; this excludes the three duplicate articles.
Limits (n = 12)
Not English (n = 10)
Asakawa Y, Takahashi R, Kagawa J. [Falling accidents among metropolitan elderly resulting in emergency ambulance transfer.] Nihon Ronen Igakkai Zasshi 2001;38:534–9.
Bauer C, Rietsch C, Groger I, Gassmann KG. [Mobility and safety for elderly (MoSi), a new intervention to improve mobility and gait in elderly people.] Z Gerontol Geriatr 2009;42:360–4.
Casas Herrero A, Martinez Velilla N, Alonso Renedo FJ. [Cognitive impairment and the risk of falling in the elderly.] Rev Esp Geriatr Gerontol 2011;46:311–18.
Casas-Herrero A, Izquierdo M. [Physical exercise as an efficient intervention in frail elderly persons.] An Sist Sanit Navar 2012;35:69–85.
Mamerow R. [Risk of accidental falls 2: and when it happens anyway.] Pflege Z 2003;56:268–9.
Niki R. [Critical appraisal of preventive care – from the perspective of health economics and policy.] Nihon Ronen Igakkai Zasshi 2012;49:54–7.
Pruckner S, Luiz T, Steinbach-Nordmann S, Nehmer J, Danner K, Madler C. [Emergency medicine – medicine for an ageing society. A contribution to the context of emergency missions for elderly people.] Anaesthesist 2008;57:391–6.
Rose DJ. [Preventing falls among older adults: no ‘one size suits all’ intervention strategy.] Rehabil Med 2011;15:37–49.
Szczerbinska K, Topor-Madry R. [The characteristics of falls based on the prospective registration in nursing home.] Przegl Lek 2011;68:576–84.
Yoshimoto Y. [The association between standardized incidence ratio of fall accidents with ambulance responses of elderly people and socio-economic status.] Nihon Koshu Eisei Zasshi 2011;58:183–9.
Abstract only (n = 1)
Snooks H, Cheung WY, Gwini S, Humphreys I, Sánchez A, Siriwardena N. Can older people who fall be identified in the ambulance call centre to enable alternative responses or care pathways? EMJ 2011;28:e1.
Review article (n = 1)
Mikolaizak AS, Simpson PM, Tiedemann A, Lord SR, Close JC. Systematic review of non-transportation rates and outcomes for older people who have fallen after ambulance service call-out. Australas J Ageing 2013;32:147–57.
Context (not emergency medical services) (n = 65)
Albert SM. Behavioral interventions to reduce risk of falls in nursing home residents. J Am Med Dir Assoc 2009;10:593–4.
Beswick A, Gooberman-Hill R, Smith A, Wylde V, Ebrahim S. Maintaining independence in older people. Rev Clin Gerontol 2010;20:128–53.
Bleijlevens MH, Hendriks MR, van Haastregt JC, van Rossum E, Kempen GI, Diederiks JP, et al. Process factors explaining the ineffectiveness of a multidisciplinary fall prevention programme: a process evaluation. BMC Public Health 2008;8:332.
Bouman A, van Rossum E, Evers S, Ambergen T, Kempen G, Knipschild P. Effects on health care use and associated cost of a home visiting program for older people with poor health status: a randomized clinical trial in the Netherlands. J Gerontol A Biol Sci Med Sci 2008;63:291–7.
Bradley SM. Falls in older adults. Mt Sinai J Med 2011;78:590–5.
Campbell AJ, Robertson MC. Reply. Age Ageing 2008;37:353.
Carpenter CR, Platts-Mills TF. Evolving prehospital, emergency department, and ‘inpatient’ management models for geriatric emergencies. Clin Geriatr Med 2013;29:31–47.
Carpenter CR, Shah MN, Hustey FM, Heard K, Gerson LW, Miller DK. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. J Gerontol A Biol Sci Med Sci 2011;66:775–83.
Catarina LN, Pereira V, Peter V, Fátima B. Role of physical activity in the prevention of falls and their consequences in the elderly. Eur Rev Aging Phys Act 2008;5:51–8.
Choi M, Hector M. Effectiveness of intervention programs in preventing falls: a systematic review of recent 10 years & meta-analysis. J Am Med Dir Assoc 2012;13:188(e13–21).
Cryer C. What Works to Prevent Accidental Injury Amongst Older People. Report to the Health Development Agency. Canterbury: University of Kent; 2001.
Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. Does a home-based strength and balance programme in people aged 80 years provide the best value for money to prevent falls? A systematic review of economic evaluations of falls prevention interventions. Br J Sports Med 2010;44:80–9.
Davison J, Marrinan S. Falls. Rev Clin Gerontol 2007;17:93–107.
Deasy C, Ryan D, O’Donnell C, Cusack S. The impact of a pre-hospital medical response unit on patient care & emergency department attendances. Irish Med J 2008;101:44–6.
Fairhall N, Sherrington C, Clemson L, Cameron ID. Do exercise interventions designed to prevent falls affect participation in life roles? A systematic review and meta-analysis. Age Ageing 2011;40:666–74.
Fitzharris MP, Day L, Lord SR, Gordon I, Fildes B. The Whitehorse No Falls trial: effects on fall rates and injurious fall rates. Age Ageing 2010;39:728–33.
Freiberger E, Haberle L, Spirduso WW, Zijlstra GA. Long-term effects of three multicomponent exercise interventions on physical performance and fall-related psychological outcomes in community-dwelling older adults: a randomized controlled trial. J Am Geriatr Soc 2012;60:437–46.
Frith J, Davison J. Falls. Rev Clin Gerontol 2013;23:101–17.
Ganz DA, Alkema GE, Wu S. It takes a village to prevent falls: reconceptualizing fall prevention and management for older adults. Inj Prev 2008;14:266–71.
Gates S, Fisher JD, Cooke M, Carter Y, Lamb SE. Multifactorial assessment and targeted intervention for preventing falls and injuries among older people in community and emergency care settings: systematic review and meta-analysis. BMJ 2008;336:130–3.
Gilbert T, Szczerbińska K, Ziere G, Ait S, Bonnefoy M, van der Velde N, et al. Management of falls: France, the Netherlands, Poland. Eur Geriatr Med 2012;3:246–53.
Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2009;2:CD007146.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9:CD007146.
Gunn H, Freeman J. Repeated falls: a key outcome or an adverse event? Physiother Res Int 2012;17:1–3.
Hendriks MR, Evers SM, Bleijlevens MH, van Haastregt JC, Crebolder HF, van Eijk JT. Cost-effectiveness of a multidisciplinary fall prevention program in community-dwelling elderly people: a randomized controlled trial. Int J Technol Assess Health Care 2008;24:193–202.
Holmes J, Bethel J. A different kind of care. Emerg Nurse 2007;15:8–12.
Holroyd-Leduc JM. Review: exercise interventions reduce falls in elderly people living in the community. Evid Based Med 2009;14:176.
Jenkyn KB, Hoch JS, Speechley M. How much are we willing to pay to prevent a fall? Cost-effectiveness of a multifactorial falls prevention program for community-dwelling older adults. Can J Aging 2012;31:121–37.
Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet 2005;366:1885–93.
Kurrle SE. Improving acute care services for older people. Med J Aust 2006;184:427–8.
Lamb SE. Multidisciplinary assessment of elderly people with a history of multiple falls reduces the risk of further falls. Aust J Physiother 2009;55:139.
Mayer D. Guidelines for care of the elderly. Ann Emerg Med 1998;32:115.
McClure RJ, Hughes K, Ren C, McKenzie K, Dietrich U, Vardon P, et al. The population approach to falls injury prevention in older people: findings of a two community trial. BMC Public Health 2010;10:79.
McKay C, Anderson KE. How to manage falls in community dwelling older adults: a review of the evidence. Postgrad Med J 2010;86:299–306.
Meier DE, Beresford L. Palliative care’s challenge: facilitating transitions of care. J Palliat Med 2008;11:416–21.
Meirink K. Guidelines for care of the elderly. Ann Emerg Med 1998;32:114–15.
Merrett A, Thomas P, Stephens A, Moghabghab R, Gruneir M. A collaborative approach to fall prevention. Can Nurse 2011;107:24–9.
Michael YL, Whitlock EP, Lin JS, Fu R, O’Connor EA, Gold R. Primary care-relevant interventions to prevent falling in older adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 2010;153:815–25.
Miller ET. Safe after 60. Rehabil Nurs 2011;36:2.
Murphy TE, Allore HG, Leo-Summers L, Carlin BP. Bayesian hierarchical modeling for a non-randomized, longitudinal fall prevention trial with spatially correlated observations. Stat Med 2011;30:522–30.
Norton R, Kobusingye O. Global health injuries. N Engl J Med 2013;368:1723–30.
Nowak A, Hubbard RE. Falls and frailty: lessons from complex systems. J R Soc Med 2009;102:98–102.
Odom JV, Odom CV, Leys MJ. Does improving vision reduce the risk of falls? A review. Insight 2011;4:92–9.
Oh DH, Park JE, Lee ES, Oh SW, Cho SI, Jang SN, et al. Intensive exercise reduces the fear of additional falls in elderly people: findings from the Korea falls prevention study. Korean J Intern Med 2012;27:417–25.
Oliver D. Development of services for older patients with falls and fractures in England: successes, failures, lessons and controversies. Arch Gerontol Geriatr 2009;49(Suppl. 2):S7–12.
Pan J-I, Yung C-J, Liang C-C, Lai L-F. An Intelligent Homecare Emergency Service System for Elder Falling. World Congress on Medical Physics and Biomedical Engineering 2006. New York, NY: Springer; 2007.
Peeters GM, Heymans MW, de Vries OJ, Bouter LM, Lips P, van Tulder MW. Multifactorial evaluation and treatment of persons with a high risk of recurrent falling was not cost-effective. Osteoporos Int 2011;22:2187–96.
Petridou ET, Manti EG, Ntinapogias AG, Negri E, Szczerbinska K. What works better for community-dwelling older people at risk to fall?: a meta-analysis of multifactorial versus physical exercise-alone interventions. J Aging Health 2009;21:713–29.
Quigley P. Prevention of fall-related injuries: a clinical research agenda 2009–2014. J Rehabil Res Dev 2009;46:vii–xii.
Rand D, Miller WC, Yiu J, Eng JJ. Interventions for addressing low balance confidence in older adults: a systematic review and meta-analysis. Age Ageing 2011;40:297–306.
Rose DJ, Hernandez D. The role of exercise in fall prevention for older adults. Clin Geriatr Med 2010;26:607–31.
Rose DJ. Preventing falls among older adults: no ‘one size suits all’ intervention strategy. J Rehabil Res Dev 2008;45:1153–66.
Salminen M, Vahlberg T, Kivela SL. The long-term effect of a multifactorial fall prevention programme on the incidence of falls requiring medical treatment. Public Health 2009;123:809–13.
Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing 2007;36:130–9.
Shah MN, Rajasekaran K, Sheahan WD, Wimbush T, Karuza J. The effect of the geriatrics education for emergency medical services training program in a rural community. J Am Geriatr Soc 2008;56:1134–9.
Shyu YI, Tsai WC, Chen MC, Liang J, Cheng HS, Wu CC, et al. Two-year effects of an interdisciplinary intervention on recovery following hip fracture in older Taiwanese with cognitive impairment. Int J Geriatr Psychiatry 2012;27:529–38.
Skelton D. Exercise and falls prevention in older people. CME Geriatric Medicine 2007;9:16–21.
Smulders E, Enkelaar L, Schoon Y, Geurts AC, van Schrojenstein Lantman-de Valk H, Weerdesteyn V. Falls prevention in persons with intellectual disabilities: development, implementation, and process evaluation of a tailored multifactorial fall risk assessment and intervention strategy. Res Dev Disabil 2013;34:2788–98.
Soriano G, Roman E, Cordoba J, Torrens M, Poca M, Torras X, et al. Cognitive dysfunction in cirrhosis is associated with falls: a prospective study. Hepatology 2012;55:1922–30.
Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Injury Prevention 2006;12:290–5.
Stewart J, McVittie C. Living with falls: house-bound older people’s experiences of health and community care. Eur J Ageing 2011;8:271–9.
Umegaki H, Suzuki Y, Yanagawa M, Nonogaki Z, Endo H. Falls in elderly at high risk of requiring care. Geriatr Gerontol Int 2012;12:147–8.
Vellas B, Villars H, Abellan G, Soto ME, Rolland Y, Guigoz Y, et al. Overview of the MNA – Its history and challenges. J Nutr Health Aging 2006;10:456–65.
Webster J, Courtney M, O’Rourke P, Marsh N, Gale C, Abbott B, et al. Should elderly patients be screened for their ‘falls risk’? Validity of the STRATIFY falls screening tool and predictors of falls in a large acute hospital. Age Ageing 2008;37:702–6.
Wu S, Keeler EB, Rubenstein LZ, Maglione MA, Shekelle PG. A cost-effectiveness analysis of a proposed national falls prevention program. Clin Geriatr Med 2010;26:751–66.
Population (clinical presentation not falls) (n = 6)
Augustine J. ‘He keeps falling out’ in the bathroom. Emerg Med Serv 2005;34:32.
Charney P, Sieber C, Cederholm T, Vellas B, Jensen G, Chumlea C, et al. Discussion. J Nutr Health Aging 2006;10:492–4.
Cooke M. Emergency care practitioners: a new safe effective role? Qual Saf Health Care 2006;15:387.
Rezende FM, Gaujac C, Rocha AC, Peres MP. A prospective study of dentoalveolar trauma at the Hospital das Clinicas, São Paulo University Medical School. Clinics 2007;62:133–8.
Shah MN, Lerner EB, Chiumento S, Davis EA. An evaluation of paramedics’ ability to screen older adults during emergency responses. Prehosp Emerg Care 2004;8:298–303.
Swain AH, Hoyle SR, Long AW. The changing face of prehospital care in New Zealand: the role of extended care paramedics. NZ Med J 2010;123:11–14.
Study design and reporting format (none or entirely insufficient empirical data) (n = 24)
Augustine JJ. No history, no meds. The challenges from an elderly woman’s fall just start with the broken hip. EMS Mag 2009;38:18–19.
Beghe C. Review: evidence from single studies shows that a few fall risk assessment tools can predict falls in elderly people. Evid Based Med 2007;12:186.
Brown K. Identifying patients at risk for falls. Intervention can improve outcomes and reduce repeat calls to 911. EMS Insider 2011;38:3–5.
Chase CA, Mann K, Wasek S, Arbesman M. Systematic review of the effect of home modification and fall prevention programs on falls and the performance of community-dwelling older adults. Am J Occup Ther 2012;66:284–91.
Clemson L. Prevention of falls in the community. BMJ 2010;340:c2244.
El Sanadi N. Geriatric injury prevention: a new role for EMS personnel? Emerg Med Serv 1996;25:51–3.
Emergency Department Management. Leverage front-line expertise to maximize trauma prevention efforts. ED Manag 2012;24:65–6.
Flavell E, Boyle M. Falls in the prehospital environment. J Paramedic Practice 2011;3:238–43.
Independent Nurse. Rapid community referral cuts falls. Independent Nurse 2010:4.
Lindstrom A. King County prevents falls. JEMS 2007;32:106.
Robitaille Y, Gauvin L. Fall prevention in older adults: towards an integrated population-based perspective. Inj Prev 2008;14:147–8.
Sadowski CA. Prevention of falls in older adults. Can Pharm J 2011;144:S17–18.
Scott T. Preventing emergency department admissions for older people. Br J Community Nurs 2011;16:392.
Shah MN, Rajasekaran K, Sheahan WD, Wimbush T, Karuza J. The effect of the geriatrics education for emergency medical services training program in a rural community. J Am Geriatr Soc 2008;56:1134–9.
Skelton DA, Hauer K, Lamb S. Re: ‘Falls definition validation’. Age Ageing 2007;36:111–12.
Snooks H, Cheung WY, Close J, Dale J, Gaze S, Humphreys I, et al. Support and Assessment for Fall Emergency Referrals (SAFER 1) trial protocol. Computerised on-scene decision support for emergency ambulance staff to assess and plan care for older people who have fallen: evaluation of costs and benefits using a pragmatic cluster randomised trial. BMC Emerg Med 2010;10:2.
Snooks H, Anthony R, Chatters R, Cheung W-Y, Dale J, Donohoe R, et al. Support and assessment for fall emergency referrals (SAFER 2) research protocol: cluster randomised trial of the clinical and cost effectiveness of new protocols for emergency ambulance paramedics to assess and refer to appropriate community-based care. BMJ Open 2012;2:6.
Snooks HA, Kingston MR, Anthony RE, Russell IT. New models of emergency prehospital care that avoid unnecessary conveyance to emergency department: translation of research evidence into practice? Sci World J 2013:182102.
Speechley M. Unintentional falls in older adults: a methodological historical review. Can J Aging 2011;30:21–32.
Spivack BS. Preventing falls: Direct intervention is needed. BMJ 2008;336:343.
Straus S. A 16-week tai chi programme prevented falls in healthy older adults. Evid Based Med 2008;13:54.
Udell J, Drahota A, Dean T, Sander R, Mackenzie H. Interventions for preventing falls in older people: an overview of Cochrane Reviews (Protocol). Cochrane Database Syst Rev 2011;4:CD009074.
van Hateren KJ, Kamper AM, Bilo HJ. Lack of evaluation of the effects of single preventive measures for falling. Arch Intern Med 201124;171:181–2.
Velhal G. Domestic accidents among the elderly. Ann Trop Med Public Health 2012;5:61–2.
Intervention (no intervention) (n = 14)
Close JC, Halter M, Elrick A, Brain G, Swift CG. Falls in the older population: a pilot study to assess those attended by London ambulance service but not taken to A&E. Age Ageing 2002;31:488–9.
Cone DC, Ahern J, Lee CH, Baker D, Murphy T, Bogucki S. A descriptive study of the ‘lift-assist’ call. Prehosp Emerg Care 2013;17:51–6.
Darnell G, Mason SM, Snooks H. Elderly falls: a national survey of UK ambulance services. Emerg Med J 2012;29:1009–10.
Dick T. Are you hip to this? Slip-and-fall injuries revisited. Emerg Med Serv 2003;32:32.
Halter M, Snooks H, Close J, Cheung WY, Moore F, Roberts SE. Emergency Care of Older People who fall: a missed opportunity. Emerg Med J 2006;23:321.
Newton JL, Kyle P, Liversidge P, Robinson G, Wilton K, Reeve P. The costs of falls in the community to the North East Ambulance Service. Emerg Med J 2006;23:479–81.
Page D. Is the lift worth it? New study concluded many lift-assist calls will result in callbacks. JEMS 2013;38:24–5.
Porter A, Snooks H, Youren A, Gaze S, Whitfield R, Rapport F, et al. ‘Covering our backs’: ambulance crews’ attitudes towards clinical documentation when emergency (999) patients are not conveyed to hospital. Emerg Med J 2008;25:292–5.
Snooks HA, Halter M, Close JC, Cheung WY, Moore F, Roberts SE. Emergency care of older people who fall: a missed opportunity. Qual Saf Health Care 2006;15:390–2.
Snooks H, Cheung WY, Gwini SM, Humphreys I, Sanchez A, Siriwardena N. Can older people who fall be identified in the ambulance call centre to enable alternative responses or care pathways? Emerg Med J 2011;28:e1.
Spaite DW, Criss EA, Valenzuela TD, Meislin HW, Ross J. Geriatric injury: an analysis of prehospital demographics, mechanisms & patterns. Ann Emerg Med 1990;19:1418–21.
Thomas SL, Muscatello DJ, Middleton PM, Zheng W. Characteristics of fall-related injuries attended by an ambulance in Sydney, Australia: a surveillance summary. NSW Public Health Bull 2011;22:49–54.
Tiedemann A, Mikolaizak AS, Sherrington C, Segin K, Lord SR, Close JC. Older fallers attended by an ambulance but not transported to hospital: a vulnerable population at high risk of future falls. Aust NZ J Public Health 2013;37:179–85.
Weiss SJ, Chong R, Ong M, Ernst AA, Balash M. Emergency medical services screening of elderly falls in the home. Prehosp Emerg Care 2003;7:79–84.
Outcomes (outcomes for older people who fall not differentiated from those of other conditions) (n = 7)
Dale J, Williams S, Foster T, Higgins J, Snooks H, Crouch R, et al. Safety of telephone consultation for ‘non-serious’ emergency ambulance service patients. Qual Saf Health Care 2004;13:363–73.
Larsson B, Sixt E. Via Senetutis. Proceedings of the 7th Congress of the EUGMS, Malaga, Spain. 28–30 September 2011. Eur Geriatr Med 2011;2:144–5.
Mason S, O’Keeffe C, Knowles E, Bradburn M, Campbell M, Coleman P, et al. A pragmatic quasi-experimental multi-site community intervention trial evaluating the impact of Emergency Care Practitioners in different UK health settings on patient pathways (NEECaP Trial). Emerg Med J 2012;29:47–53.
Mason S, Wardrope J, Perrin J. Developing a community paramedic practitioner intermediate care support scheme for older people with minor conditions. Emerg Med J 2003;20:196–8.
O’Hara R, O’Keeffe C, Mason S, Coster JE, Hutchinson A. Quality and safety of care provided by emergency care practitioners. Emerg Med J 2012;29:327–32.
Pointer JE, Levitt MA, Young JC, Promes SB, Messana BJ, Ader ME. Can paramedics using guidelines accurately triage patients? Ann Emerg Med 2001;38:268–77.
Schmidt T, Neely KW, Adams AL, Newgard CD, Wittwer L, Muhr M, et al. Is it possible to safely triage callers to EMS dispatch centers to alternative resources? Prehosp Emerg Care 2003;7:368–74.
Appendix 4 Support and Assessment for Fall Emergency Referrals 2 organisational flow chart
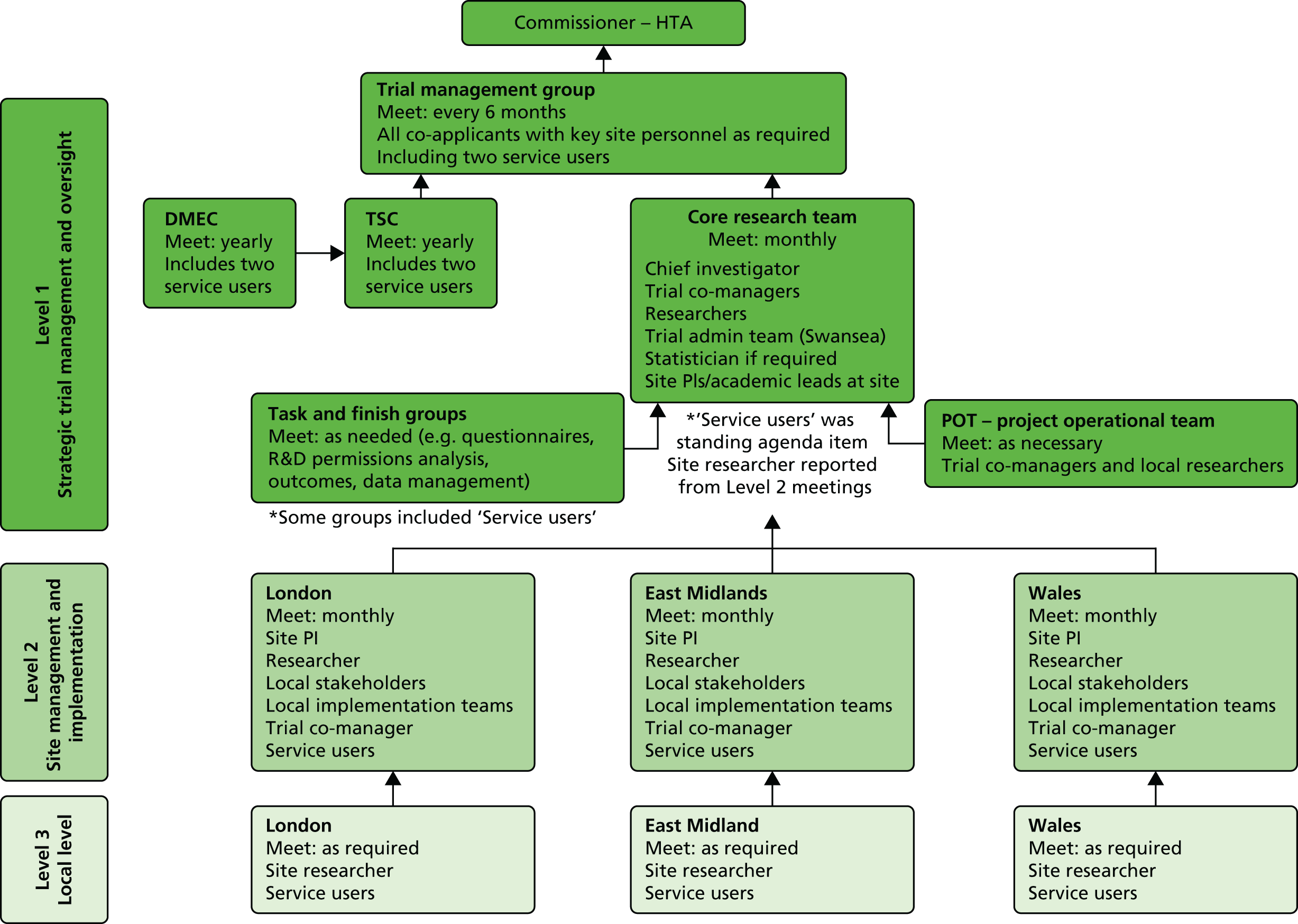
Appendix 5 Station location maps
Welsh Ambulance Services NHS Trust Ambulance Stations and Acute Trusts
London Ambulance Service Study Ambulance Stations and Acute Trusts
East Midlands Ambulance Service Study Ambulance Stations and Acute Trusts
Appendix 6 Support and Assessment for Fall Emergency Referrals 2 postal consent pack
Appendix 7 Support and Assessment for Fall Emergency Referrals 2 1-month questionnaire
Appendix 8 Final definition of the intervention
| Criterion | Core essential | To be agreed locally | East Midlands local agreement | London local agreement | Wales local agreement | Source |
|---|---|---|---|---|---|---|
| Training | Training to take the form of half- to 1-day face-to-face content followed up with home study DVD and competency assessment. Sheffield clinicians to train the trainers. Local ambulance service trainers to cascade training to paramedics. The core of the intervention is the paramedic protocol. Training will therefore be concerned with tailoring existing skills rather than providing education and training for new skills | Precise length and arrangements for face-to-face training and competency assessment. Processes for cascade training | No cascade training. Training form is variable, from group sessions with the Sheffield trainers to one-to-one sessions with the study research champion and research associate | Sheffield team will deliver training to assigned training officers and RSO at intervention stations. Training officers to deliver training to study paramedics across three sessions with one-to-one sessions if necessary | The RSO attended a train the trainer day with the Sheffield Training Team. Training was then cascaded through the RSO to groups of paramedics, with one-to-one sessions as necessary | As specified in original proposal. Discussed and modified at definitions meeting |
| Assessment tool | Two elements:
|
To be used as an aide memoire or a specific additional form to PRF. Consent process for patient agreement to be referred to falls service to be confirmed | The assessment tool is to be used as an aide memoire. Paramedics have also been given a list of GP surgeries that patients have to be registered to in order to be eligible for referral to falls service. Paramedics receive verbal consent from the patient for referral to the falls service | The assessment tool is to be used as an aide memoire. No further forms/documentation to be issued to paramedics. Patient’s consent verbally for referral to falls service | The assessment tool is to be used as an aide memoir with an accompanying Older Person who has Fallen Assessment Form which will log the outcome of the assessment. If the decision is made to refer the patient to the falls team, the patient will be informed; if referral is refused, this will be recorded on the PCR | As specified in original proposal. Discussed and modified at definitions meeting |
| Referral tool | Basic demographic, clinical and contact details to be completed in order to make referral to falls service | Specific tool to be agreed locally. Based on Welsh Ambulance Services NHS Trust form | Referral document produced in conjunction with EMAS, the falls services and the research team | Referral document produced in conjunction with the LAS EBS, the falls services and the research team | Referral document agreed locally with Welsh Ambulance Services NHS Trust, falls service and control room representatives | As specified in original proposal. Discussed and modified at definitions meeting |
| Process of referral | It is essential that there is some system in place to allow auditing of receipt of referral forms by falls service | The process and medium of referral from ambulance service to falls service to be agreed locally (referral via ambulance control, direct from scene or from station between jobs, by fax. or other route) | Referral made via control room via a specific telephone number (the ‘Safeguarding number’, as this line is also used for social services referrals). Referral taken by an emergency medical dispatcher (24/7). Project support officer collects referral forms from control room and faxes the referral to the appropriate falls service | Referral will be made through a single-point-of-access within LAS (the EBS desk). Access will be via assigned radio channel. EBS will fill out a referral proforma based on the information provided by the referring paramedic. EBS will call the appropriate falls service during office hours and will confirm receipt of referral and transfer proforma via fax | Control will be informed of the referral by the paramedic who will inform the falls service by faxing the locally agreed referral form to a single point-of-contact number. The referral form will record date and time referral received and the RSO will be informed by both control and the falls team | Discussed at final definitions meeting |
| Falls service response | Falls service to follow NICE guidance in terms of minimum follow-up of patient. Non-clinical assessment telephone contact with patient initially. Call to be made by a professional with the ability to recognise cases where more urgent input is needed and refer if necessary. Initial assessment of patient by an appropriately skilled and experienced individual health-care professional to take place following initial telephone contact. The timescale should fit with NICE guidance. Patient to be fed into an appropriate multifactorial intervention process following this assessment (based on NICE guidance) | Period of follow-up to be defined and agreed locally but should adhere to NICE guidance | Follow-up period variable depends on clinical need (which is recorded on the referral form). In all four of the locally participating falls services, the patient is called to book a home visit, the home visit is under taken, and then the patient is fed into the appropriate pathway. The patient is rung to assess clinical need and to arrange a home visit | Timescales agreed according to NICE guidance | Following referral, telephone contact is to be made by a district nurse within 72 hours and an in-home assessment will take place within 1 week | As specified in original proposal. Discussed and modified at definitions meeting |
| Falls service make-up | Appropriate skill set based on NICE criteria | Specific details of service and patient intervention to be recorded locally | The home visit is undertaken to assess which ‘treatment stream’ the patient is placed into; subsequent treatment is provided by occupational therapists, physiotherapists, and nurses. Some people may be referred to doctors, social workers, dieticians and psychologists | Specific details of service and patient intervention to be recorded by relevant falls service. Subsequent treatment is provided by occupational health, physiotherapists and rehabilitation | Within Wales, the Cwm Taf District Nursing Teams will be responsible for receiving the referral and making the initial phone call and assessment. Depending on assessment outcome, further services will be available to the patient. Further services include the intermediate care and rehabilitation service, The National Exercise Referral Scheme Falls Prevention Programme or GP | As specified in original proposal. Discussed and modified at definitions meeting |
| Clinical support/feedback loop | Clinical support debriefs with A&E every 2–4 weeks. Feedback loop between falls services and paramedics to report outcomes for individuals referred essential | Specific feedback mechanisms to be agreed locally | Paramedics able to call/e-mail research team to ask questions. Clinical or operational questions to be forwarded to an EMAS clinical tutor or research champion for answering. PRFs audited once a month to see if the correct path was followed. The Falls Services will complete a ‘data collection sheet’ for every patient referred – these are to be collected from the falls service, and ‘feedback information’ transferred to a ‘paramedic feedback sheet’ (i.e. referral date, date assessed and outcome of assessment). These details will be e-mailed to the referring paramedic | Details on referral rates and paramedic queries will be fed back to the study team at regular intervals and used for clinical feedback to participating paramedics. Where possible falls services to provide both short- and long-term patient outcomes for feedback. On-station clinical and operational support delivered through RSO (LAS paramedic on secondment to study) | A data collection and paramedic feedback form has been agreed locally which records the main outcomes of the initial assessment. Once the patient has been assessed the district nurse will send the feedback to each paramedic. To support paramedics clinically and operationally a support network has been put in place. This involved the main study team for general inquiries, the RSO for training and ongoing use of the decision tool and referral pathways and a clinical on calls system which is available to paramedics to address clinical queries. Paramedics use of the decision tool and referral pathways will be monitored by the research team paramedics contacted to discuss issues | As specified in original proposal. To be discussed and agreed |
Appendix 9 Support and Assessment for Fall Emergency Referrals 2 paramedic training session programme
Appendix 10 Support and Assessment for Fall Emergency Referrals 2 6-month questionnaire
Appendix 11 Support and Assessment for Fall Emergency Referrals 2 data analysis plan
Appendix 12 Patient semistructured interviews schedule
Patient experience (of ambulance service)
-
Can you tell me what happened when you fell and an ambulance was called?
Prompt:
Where did you fall?
How did you fall?
Were you hurt?
-
What did the ambulance crew do when they arrived?
-
Were you informed of what would happen next (e.g. referral to a falls service or taken to hospital)?
Prompt:
Did you understand what this would mean?
-
What did you feel about what they did?
Prompt:
At the time of fall and on reflection.
-
Have you fallen before and were you seen by an ambulance crew? (If answer is yes go to question 5a)
5a. In what ways was the assessment and treatment you received different from previously?
-
How did you feel about this decision?
Prompt:
Was it right for you and were you part of the decision?
Patient experience (of those seen by a falls service)
-
How long was it before someone from the falls service contacted you?
-
How did you feel about the amount of time it took before you were contacted?
-
What did the Falls Service offer you?
Prompt:
How did you feel about what they did?
Prompts:
Exercise Programme.
Prompt any of the following:
-
Home exercise programme to improve strength and balance.
-
One to one strength, balance and mobility training.
-
Referral to a balance group or other group.
-
Floor transfer practice.
Falls Prevention programme
Prompt:
Advice and education regarding how to reduce risk of falls, including pacing activity, sitting to put on trousers and shoes and appropriate footwear, etc.
Environmental adaptations or assistive devices
Prompt any of the following:
-
Walking aid provision such as walking frame, walking stick, wheelchair, etc. or any other devices such as pendant alarm, grab rails or anything else.
-
Advice on environmental adaptations and onward referrals to services to address issues such as loose rugs, wires, etc.
Occupational therapist
Prompt:
Occupational Therapy assessment of home environment, bed and toilet transfers and wheelchair suitability/or of ability to perform personal care (including dressing) and domestic tasks.
Physiotherapist
Prompt:
Physiotherapy assessment of strength, range of movement, balance and transfers.
Disability counsellor
Prompt:
To talk about feelings and problems in a supportive way.
Social services assessment
Prompt:
For a review of the adequacy of the care package or anything else.
Anything else
-
Could the service be improved in any way?
Prompt:
Were you happy with what they offered you and was there anything you were unhappy with?
Patient health (post fall)
-
Have you had a fall since?
-
In terms of your health, how is it different since your fall?
-
Since the fall have any areas of your life been affected?
Prompt:
Have any areas of your life improved?
Prompt:
Have any areas of your life got worse?
Patient satisfaction
-
This project is looking at helping ambulance paramedics decide the best treatment for you if you fall. At the time of your fall did you know they were following a new process for assessing elderly fallers and what do you think about this?
-
What did you think of the overall process?
-
How would you feel about being treated by the ambulance crew in this way in the future?
-
Is there anything else you would like to tell us relating to your fall and the attention you received?
Appendix 13 Support and Assessment for Fall Emergency Referrals 2 paramedic pretrial focus group interview schedule
Support and Assessment for Fall Emergency Referrals 2 paramedic pretrial focus group interview schedule
Thank you for taking part today. This session is to find out a bit more about your current practice and to get your thoughts and views on the new referral pathways proposed for the SAFER 2 trial.
Check that we have got the consent and demographic info forms completed.
Questions
What motivated you to get involved in the study?
Have there been any other ‘pathways of care’ or new ways of working introduced while you’ve been a paramedic?
Prompts:
-
How have new practices been introduced? What’s worked, what hasn’t?
-
Issues around changing practice – are there any pressures?
-
What are the attitudes towards new developments in the health service.
-
Differences between attitudes of paramedics and their managers.
-
Barriers and motivations to new developments?
-
Issues around using new developments.
-
Support for using new pathways/ways of working.
-
Operational impacts.
Do new pathways of care sometimes bring with them additional decision-making for paramedics?
Prompts:
-
Adapting to this.
-
Resistance?
-
Time to adopt new processes?
-
Levels/amount of training.
How do you deal with calls from older fallers at the moment?
Prompts:
-
Options available to the paramedic.
-
Links to other services to support older fallers.
-
Explore issues around deciding to leave at home or convey.
-
Any frustrations with the current system.
-
Risks with the current system – to patient.
-
Risks with the current system – to paramedic (confidence to leave patients at home).
Do you think that having access to a falls pathway will make a difference?
Prompts:
-
To the patient.
-
To you.
-
To the ambulance service.
-
Suitability of this patient group for the new care pathway.
And similarly, what are your expectations for this new pathway?
We asked at the beginning about your motivations for getting involved. We wondered what you thought your colleagues would make of you taking part in the study.
Prompts:
-
What could encourage more people to become involved?
Appendix 14 Support and Assessment for Fall Emergency Referrals 2 paramedic trial-end interview schedule
Thank you for taking part today. This session is to find out more about your involvement in the SAFER 2 study and experience of using the new protocol and to understand how you made your decisions on whether to convey patients to hospital, refer to a falls service or to leave the patient at home.
Your views, which will be kept confidential, will enable us to assess the benefit to patients of the ‘intervention’ and pathways to community-based falls services. We simply need to understand if it works and if it can improve patient outcomes in relation to injury, death and quality of life.
-
How did you find using the SAFER 2 trial flow chart in practice?
Prompts:
-
Which parts were useful and which were not, i.e. the ‘get up and go test’?
-
Did you need to make any additional decisions because patients did not fit into the protocol?
-
Did you keep a copy of the flow chart with you?
-
Did it make you feel more or less confident in your decision-making?
-
What were your expectations of the new way of working and were they met?
Prompts:
-
Increase your job satisfaction and/or confidence.
-
Aid your decision-making and assessments.
-
The idea of the flow chart was to make it safe to leave a patient at home with a referral to a falls service. We found this didn’t always happen and some patients were left at home without a referral – we’d like to find out what influenced your decision?
Prompts:
-
Meeting response times and/or last job or on-scene time.
-
Decision-making/confidence.
-
Patient preference.
-
Clinical judgement.
-
Familiarity with process.
-
Advising patients they did not need to go to hospital.
-
Patient already had a care package in place/or similar.
-
Something else.
-
How satisfied were you with the amount training you received?
Prompts:
-
Would you have liked to have received more or less training?
-
Was it informative enough – did you feel ready and confident to use the flow chart?
-
Did it enhance your clinical knowledge?
-
Was there any support available to you while you were taking part in the study?
Prompts:
-
Did anyone contact you by telephone or e-mail?
-
Did you feel well supported by ambulance service management and trainers?
-
What would you think if the initiative was introduced across the service?
Prompts:
-
Do you feel it would change your role at all or affect the way you work?
-
What factors would make it difficult and what could help the process?
-
When comparing the SAFER 2 trial to other similar studies, involving older fallers, it seems a higher proportion of patients were conveyed to hospital – we’d like to find out if the SAFER 2 trial changed the way you normally work?
Prompts
-
Did the intervention affect you decision-making?
-
Difficult/easier to assess this group of patients?
-
Did it make you convey patients more often or less often?
Appendix 15 Stakeholder trial-end interview schedules
Support and Assessment for Fall Emergency Referrals 2 ambulance personnel trial-end interview schedule
-
At the beginning of the study, what were your expectations of the SAFER 2 trial intervention and the new way of working?
Prompts:
-
Increase job satisfaction and/or confidence.
-
Aid decision-making and assessments.
-
Better patient care.
-
Increase workload/increased demand on service.
-
Increased efficiency/turnaround time.
-
How aware were they of the SAFER 2 trial and what it was meant to achieve?
-
In what ways did your involvement in the SAFER 2 trial impact on your role?
Prompts:
-
Time.
-
Advantages/Improvements.
-
Disadvantages/difficulties.
-
In what way do you think the SAFER 2 intervention has changed the way that colleagues within the organisation (paramedics, dispatch personnel) conduct their work?
Prompts:
-
Advantages.
-
Disadvantages.
-
More confident or less confident in decisions.
-
Make decisions in a different way.
-
Provides more protection.
-
Undermines/supports autonomy and clinical judgement.
-
What factors do you think had an effect on the extent to which the SAFER 2 trial was adopted within your organisation?
Prompts:
Factors within the organisation:
-
Time pressures.
-
Dispatch coding.
-
Beliefs.
-
Work habits.
Factors outside the organisation:
-
Other pathways or developments.
-
Patient choice.
-
Family of patients, etc.
-
Contact between roles (university, ambulance, falls).
-
Any other barriers.
-
We have found that some patients seen by an intervention paramedic were left at home without a referral. Why do you think this might have been?
Prompts:
-
Patient already had a care package in place/or similar.
-
Paramedics meeting response times and/or last job or on-scene time.
-
Paramedic decision-making/confidence.
-
Patient preference.
-
Clinical judgement.
-
Familiarity with process.
-
Advising patients they did not need to go to hospital.
-
Something else.
-
What would you think if the SAFER 2 trial was rolled out across a wider service area?
Prompts:
-
Good thing or not?
-
Advantages to patients/paramedics/organisation.
-
What factors would make it difficult and what could help the process?
-
Differences between a small scale trial and a big service change.
-
Boundary and equity issues i.e. thought it wasn’t fair that people living in some areas got the service and others didn’t.
-
Risk of duplication of initiatives.
-
Changes in work practices such as following new protocols/flow charts are an inevitable process.
-
Do you have any recommendations for how the process could be improved for future use?
-
Describe the SAFER 2 trial intervention using only one word?
-
Is there anything else about the study that you would like to say?
Support and Assessment for Fall Emergency Referrals 2 wider stakeholder trial-end focus group schedule
-
At the beginning of the study, what were your expectations of the SAFER 2 trial intervention and the new way of working?
Prompts:
-
Increase job satisfaction and/or confidence.
-
Aid decision-making and assessments.
-
Better patient care.
-
Increased workload/increased demand on services.
-
Increased efficiency/turnaround time.
-
Were your expectations met?
-
In what ways did your involvement in the SAFER 2 trial impact on your role?
Prompts:
-
Time?
-
Improvements/difficulties?
-
What factors do you think had an effect on the use of the SAFER 2 trial intervention within your organisation?
Prompts:
-
Internal communications/support.
-
Time pressures.
-
Problems referring patients onto further specialist assessment.
-
Beliefs/attitudes.
-
Expectations about role, clear or unclear.
-
Processes to be followed, clear or unclear.
-
What factors do you think had an effect on the use of the SAFER 2 trial intervention outside your organisation?
Prompts:
-
Other pathways or developments.
-
Other organisations/support.
-
Patient choice.
-
Family of patients, etc.
-
Contact between roles (university, ambulance, falls).
-
Have you had any feedback from service users about the SAFER 2 trial intervention?
Prompts:
-
Positive feedback.
-
Negative feedback.
-
What would you think if the new way of working was introduced across the service?
Prompts:
-
Good thing or not?
-
Advantages to patients/paramedics/organisation.
-
What factors would make it difficult and what could help the process?
-
Differences between a small scale trial and a big service change.
-
Boundary and equity issues i.e. thought it wasn’t fair that people living in some areas got the service and others didn’t.
-
Risk of duplication of initiatives.
-
Changes in work practices such as following new protocols/flow charts are an inevitable process.
-
Do you have any recommendations for how the process could be improved for future use?
-
Describe the SAFER 2 trial using only one word?
-
Is there anything else about the study that you would like to say?
Appendix 16 Support and Assessment for Fall Emergency Referrals 2 framework for analysis of interviews and focus groups
Support and Assessment for Fall Emergency Referrals 2 framework or analysis of interviews and focus groups with staff: including paramedics and staff of other relevant service areas
This analysis is of ‘before’ and ‘after’ data together.
-
Core coding.
-
Data source (code entire transcript to either subcode below).
-
– Interview.
-
– Focus group.
-
-
Site (code entire transcript to one of the subcodes below).
-
– London Ambulance Service.
-
– East Midlands Ambulance Service .
-
– Welsh Ambulance Services NHS Trust.
-
-
Role of speaker (each extract coded should also be crosscoded to one of the subcodes below).
-
– Paramedic.
-
– Other ambulance service staff.
-
– Falls service.
-
– Other.
-
-
-
Expectations of the SAFER 2 trial intervention (before).
-
Rate of referrals.
-
Monitoring/performance management function.
-
Better patient care.
-
Anticipated impact on process (paperwork/time at scene).
-
Anticipated impact on other services (e.g. falls service).
-
Unclear/uncertain expectations.
-
Other.
-
-
Implementation process for the SAFER 2 trial intervention (after).
-
Impact on workload and role – ambulance service.
-
Training and support.
-
Teamwork/networking/communication.
-
Other changes taking place at the same time.
-
Wider impact within ambulance service (e.g. raising awareness of falls as an issue).
-
Impact on workload and role – falls service/other (including comments on appropriateness of referrals).
-
Overall comments on the SAFER 2 trial intervention.
-
– Negative.
-
– Positive.
-
-
-
Referral practice post-implementation.
-
Reported reasons for not referring.
-
– Negative feedback.
-
– Taking easier option/embedded habits
-
– Difficulties with patient assessment.
-
– Time restrictions/end of shift.
-
-
Confidence in/anxiety about pathways and outcomes.
-
Suitability of patients for referral to falls service.
-
Referral to other services (including GPs).
-
Role of patient and family in decision-making.
-
Advice from/discussion with colleagues.
-
Other.
-
-
Tension between research and real world practice.
-
Motivation for involvement in research study or new innovation.
-
– Persuasion by an individual.
-
– Desire to improve service quality.
-
– Personal development and skills.
-
-
Factors discouraging involvement in research study.
-
Perspective on study as a contained piece of work (bounded area, end date, etc. plus comments about any problems with timetable).
-
Drive to recruit patients to target numbers.
-
Confusion/ambiguity around status and nature of research study (including references to other research studies in progress).
-
Future rollout.
-
Perceived benefits of study (e.g. evidence for commissioners).
-
Other.
-
-
Suggestions.
-
Follow-up/feedback on individual patients.
-
Adapting model (e.g. case finding of patients at lower risk levels, scaling up falls service, more links to other services).
-
Adapting the SAFER 2 trial process (e.g. putting a prompt on ePRF, devising flow chart, better communication).
-
Adapting implementation of trial (e.g. better communication about progress).
-
Other.
-
-
Existing practice re older fallers.
-
Decision-making.
-
Outcomes.
-
Perceived problems with existing practice.
-
Other.
-
-
Communication.
-
Previous experience of pathways and protocols.
-
Concerns, issues around pay, status, role, hours, breaks, etc.
Support and Assessment for Fall Emergency Referrals 2: framework for analysis of interviews with patients
-
Case coding for patient (note that the entire transcript will be coded to each of the nodes which start with 1).
-
Outcome of contact.
-
– Patient attended hospital as a result of index fall.
-
– Patient did not attend hospital as a result of index fall, referred to falls service.
-
– Patient did not attend hospital as a result of index fall, not referred to falls service.
-
-
Gender.
-
– Female.
-
– Male.
-
-
Site.
-
– London Ambulance Service.
-
– East Midlands Ambulance Service.
-
– Welsh Ambulance Services NHS Trust.
-
-
-
Other overall comments (these should be coded to specific points in the transcript).
-
Any evidence of/report of memory problems or confusion.
-
Nature/cause of fall.
-
Repeat falls.
-
– Previous fall(s) reported.
-
– Subsequent fall(s) reported.
-
-
Other medical conditions.
-
Description and nature of injury.
-
-
Patient perspective on ambulance service based on their contact at time of index fall.
-
Perspective on paramedics/ambulance technicians.
-
– Overall evaluation.
-
– Personal qualities – kindness/calm, etc.
-
– Impact on patient – maintaining dignity/minimising embarrassment/reassuring/asking rather than telling/explaining what’s going on, etc.
-
-
Perspective on other aspects of the ambulance service.
-
– Service overall – including waiting time.
-
– Despatch.
-
-
-
Process – when ambulance service attended patient for index fall.
-
Physical checks/examination.
-
Questions.
-
Lifting.
-
Social aspects – ‘having a laugh’/cup of tea/making lunch, etc.
-
Presence/role of family members/carers/others.
-
Patient’s reflection/comparison with any previous experience.
-
Paperwork/notes/records/communication.
-
-
Decision-making about transfer to hospital – when ambulance service attended patient for index fall.
-
Negotiation/paramedics offering choice.
-
Patients’ expressed will/autonomy.
-
Influences on patient’s decision-making.
-
-
Hospital attendance.
-
Experience of/perspective on attending hospital for index fall.
-
Experience of/perspective on past hospital attendance.
-
-
Experience of falls service.
-
Patient evaluation.
-
Confusion/ambiguity about role and contact.
-
-
Experience of other relevant health or support services.
-
Social care services (including voluntary sector).
-
Other health services.
-
Other or unclear.
-
Private health care/own resources.
-
-
Consequences of fall.
-
Overall impact on quality of life.
-
Impact on confidence/fear of falling.
-
Pain/other health consequences.
-
Appendix 17 Support and Assessment for Fall Emergency Referrals 2 Involving People case study
Appendix 18 Site Consolidated Standards of Reporting Trials flow charts
Site 1

Site 2

Site 3
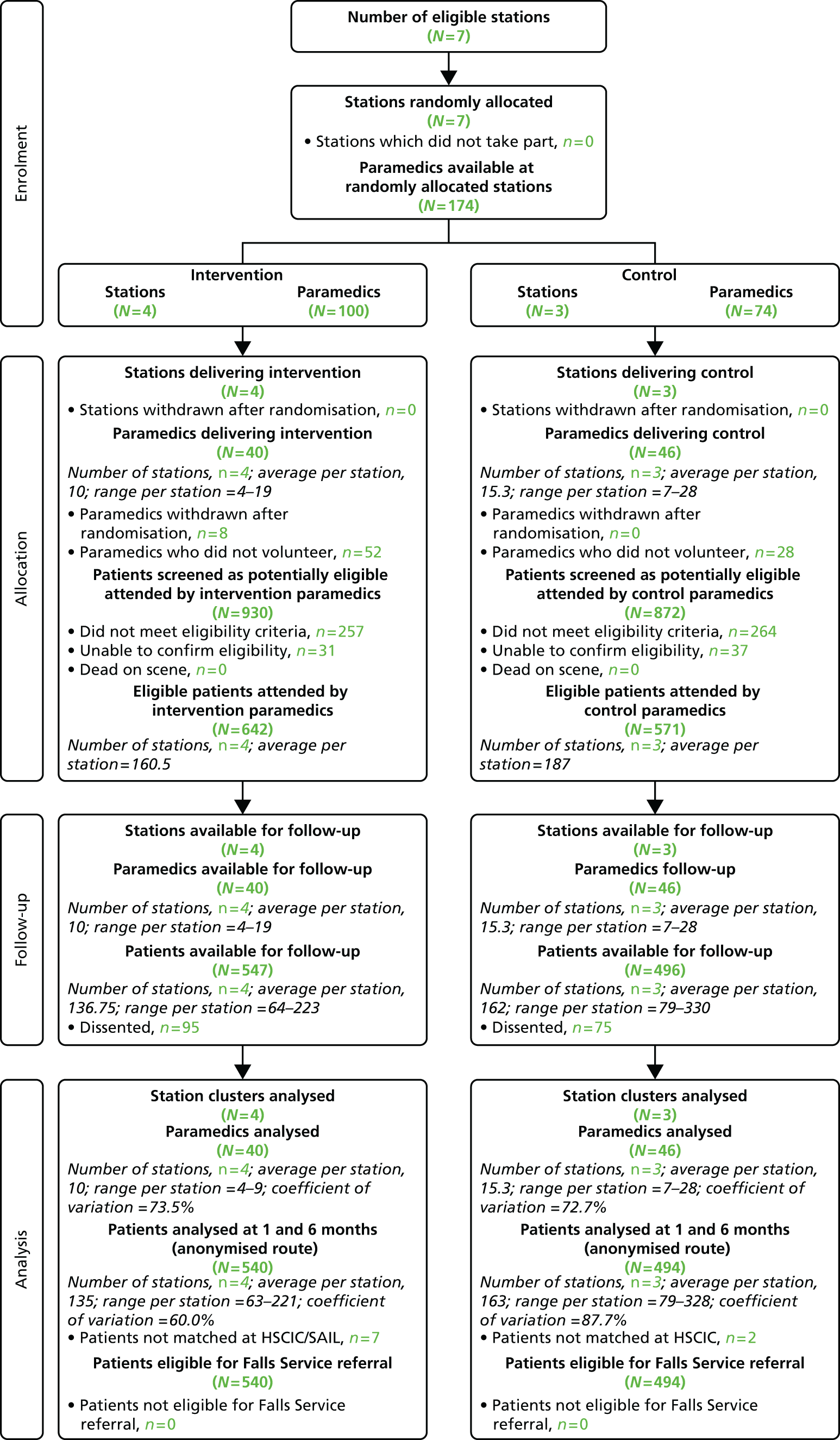
Appendix 19 Further clinical effectiveness results
Participant numbers and subgroups flow
As outlined in Chapter 4, a total of 5914 eligible patients were attended by 215 paramedics based at 31 ambulance stations across the three study sites. After dissenting patients were excluded, 80% (n = 4704) were available for follow-up: 2420 in the intervention group and 2284 in the control group. Various analyses in Chapter 4 exclude n = 49 participants not matched anonymously, as data on key components in the primary outcome were unavailable. A further subgroup of participants in site 1 were registered at a GP practice unable to refer patients to the falls referral service. In this appendix, we present the main results tables for the subgroup which also excludes these participants ineligible for a falls referral.
| Primary outcomes | Site | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Estimate, p-value | 95% CI | Estimate | 95% CI | ||
| Proportion of patients dying (any cause)c | All | 135/2161 (6.2%) | 119/1982 (6.1%) | OR = 1.011; p = 0.931 | 0.783 to 1.307 | 0 | n/a |
| Site 1 | 74/1081 (6.8%) | 62/1055 (5.9%) | |||||
| Site 2 | 31/540 (5.7%) | 26/433 (6.0%) | |||||
| Site 3 | 30/540 (5.6%) | 31/494 (6.3%) | |||||
| Proportion of patients with further emergency admission to hospital, or deathd | All | 561/2161 (26.0%) | 507/1982 (25.6%) | OR = 0.941; p = 0.430 | 0.808 to 1.095 | 0 | n/a |
| Site 1 | 278/1081 (25.7%) | 265/1055 (25.1%) | |||||
| Site 2 | 121/540 (22.4%) | 108/433 (24.9%) | |||||
| Site 3 | 162/540 (30.0%) | 134/494 (27.1%) | |||||
| Proportion of patients with further emergency event (ED attendance or emergency admission to hospital) or deathe | All | 673/2161 (31.1%) | 610/1982 (30.8%) | OR = 0.956; p = 0.534 | 0.828 to 1.103 | < 0.0001 | 0 to 0.0037 |
| Site 1 | 326/1081 (30.2%) | 320/1055 (30.3%) | |||||
| Site 2 | 157/540 (29.1%) | 135/433 (31.2%) | |||||
| Site 3 | 190/540 (35.2%) | 155/494 (31.4%) | |||||
| Proportion of patients with further emergency event (emergency service call, ED attendance, emergency admission to hospital) or deathf | All | 793/2161 (36.7%) | 743/1982 (37.5%) | OR = 0.895; p = 0.118 | 0.780 to 1.028 | 0.0021 | 0.0002 to 0.0071 |
| Site 1 | 404/1081 (37.4%) | 409/1055 (38.8%) | |||||
| Site 2 | 172/540 (31.9%) | 152/433 (35.1%) | |||||
| Site 3 | 217/540 (40.2%) | 182/494 (36.8%) | |||||
| Further emergency events per patient (emergency service call, ED attendance, admission to hospital) per day at risk,g mean (SD) [n] | All | 0.0780 (0.2254) [1979] | 0.0762 (0.2215) [1836] | Δ = 0.0032; p = 0.650 | –0.0107 to 0.0172 | 0.0023 | 0.0003 to 0.0070 |
| Site 1 | 0.0673 (0.1841) [1012] | 0.0688 (0.1959) [1001] | |||||
| Site 2 | 0.0755 (0.2066) [466] | 0.0675 (0.2021) [384] | ΔL = –0.0055; p = 0.943 | –0.1548 to 0.1438 | 0.0016 | 0.0001 to 0.0061 | |
| Site 3 | 0.1018 (0.3033) [501] | 0.1003 (0.2817) [451] | |||||
| Mean time to first event (days, truncated at 30),h mean (proportion truncated) | All | 22.48 (1368/2161) | 22.40 (1239/1982) | HR = 0.970; p = 0.557 | 0.878 to 1.073 | 0.0026 | 0.0004 to 0.0076 |
| Site 1 | 22.57 (677/1081) | 22.22 (646/1055) | |||||
| Site 2 | 23.22 (368/540) | 22.74 (281/433) | |||||
| Site 3 | 21.54 (323/540) | 22.49 (312/494) | |||||
| Primary outcomes | Site | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Estimate, p-value | 95% CI | Estimate | 95% CI | ||
| Proportion of patients dying (any cause) | All | 135/2161 (6.2%) | 119/1982 (6.0%) | OR = 1.011; p = 0.931 | 0.783 to 1.307 | 0 | n/a |
| Site 1 | 74/1081 (6.8%) | 62/1055 (5.9%) | |||||
| Site 2 | 31/540 (5.7%) | 26/433 (6.0%) | |||||
| Site 3 | 30/540 (5.6%) | 31/494 (6.3%) | |||||
| Proportion of patients with further emergency admission to hospitalc | All | 472/2161 (21.8%) | 425/1982 (21.4%) | OR = 1.024; p = 0.754 | 0.883 to 1.188 | 0.0012 | 0 to 0.0052 |
| Site 1 | 226/1081 (20.9%) | 222/1055 (21.0%) | |||||
| Site 2 | 104/540 (19.3%) | 88/433 (20.3%) | |||||
| Site 3 | 142/540 (26.3%) | 115/494 (23.3%) | |||||
| Proportion of patients with further ED attendanced | All | 419/2161 (19.4%) | 367/1982 (18.5%) | OR = 1.067; p = 0.420 | 0.912 to 1.248 | 0.0075 | 0.0024 to 0.0160 |
| Site 1 | 212/1081 (19.6%) | 193/1055 (18.3%) | |||||
| Site 2 | 79/540 (14.6%) | 63/433 (14.5%) | |||||
| Site 3 | 128/540 (23.7%) | 111/494 (22.5%) | |||||
| Further ED attendances per patient,e mean (SD) [n] | All | 0.2683 (0.6322) [1979] | 0.2609 (0.8087) [1836] | Λ = 0.839; p = 0.057 | 0.700 to 1.006 | 0.0052 | 0.0014 to 0.0120 |
| Site 1 | 0.2747 (0.6945) [1012] | 0.2268 (0.4995) [1001] | |||||
| Site 2 | 0.2017 (0.5017) [466] | 0.1901 (0.4824) [384] | |||||
| Site 3 | 0.3174 (0.6042) [501] | 0.3969 (1.3743) [451] | |||||
| Further ED attendances per patient per day at risk,f mean (SD) [n] | All | 0.0242 (0.1060) [1979] | 0.0219 (0.0816) [1836] | Δ = 0.0022; p = 0.483 | –0.0039 to 0.0082 | 0.0054 | 0.0013 to 0.0131 |
| Site 1 | 0.0225 (0.0821) [1012] | 0.0188 (0.0694) [1001] | |||||
| Site 2 | 0.0172 (0.0611) [466] | 0.0138 (0.0661) [384] | ΔL = 0.0486; p = 0.390 | –0.0623 to 0.1596 | 0.0099 | 0.0034 to 0.0204 | |
| Site 3 | 0.0341 (0.1648) [501] | 0.0357 (0.1115) [451] | |||||
| Proportion of patients with further emergency service callg | All | 401/2161 (18.6%) | 430/1982 (21.7%) | OR = 0.817; p = 0.010 | 0.700 to 0.953 | 0.0066 | 0.0021 to 0.0139 |
| Site 1 | 216/1081 (20.0%) | 257/1055 (24.4%) | |||||
| Site 2 | 78/540 (14.4%) | 68/433 (15.7%) | |||||
| Site 3 | 107/540 (19.8%) | 105/494 (21.3%) | |||||
| Further emergency service calls per patient,h mean (SD) [n] | All | 0.3032 (0.7931) [1979] | 0.3328 (0.7314) [1836] | Λ = 0.907; p = 0.143 | 0.795 to 1.034 | 0.0041 | 0.0011 to 0.0097 |
| Site 1 | 0.3261 (0.8500) [1012] | 0.3856 (0.8168) [1001] | |||||
| Site 2 | 0.2318 (0.6508) [466] | 0.2292 (0.5686) [384] | |||||
| Site 3 | 0.3234 (0.7920) [501] | 0.3038 (0.6384) [451] | |||||
| Further emergency service calls per patient per day at risk,i mean (SD) [n] | All | 0.0206 (0.0639) [1979] | 0.0245 (0.0823) [1836] | Δ = –0.0038; p = 0.100 | –0.0084 to 0.0007 | 0.0045 | 0.0011 to 0.0106 |
| Site 1 | 0.0198 (0.0580) [1012] | 0.0247 (0.0723) [1001] | |||||
| Site 2 | 0.0191 (0.0642) [466] | 0.0174 (0.0733) [384] | ΔL = –0.1261; p = 0.029 | –0.2391 to –0.0131 | 0.0051 | 0.0014 to 0.0116 | |
| Site 3 | 0.0238 (0.0743) [501] | 0.0301 (0.1066) [451] | |||||
| Primary outcomes | Site | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|---|
| Intervention (A) | Control (B) | Estimate, p-value | 95% CI | Estimate | 95% CI | ||
| Proportion of patients dying (any cause)c | All | 420/2161 (19.4%) | 362/1982 (18.3%) | OR = 1.199; p = 0.083 | 0.977 to 1.472 | 0 | n/a |
| Site 1 | 211/1081 (19.5%) | 213/1055 (20.2%) | |||||
| Site 2 | 116/540 (21.5%) | 75/433 (17.3%) | |||||
| Site 3 | 93/540 (17.2%) | 74/494 (15.0%) | |||||
| Proportion of patients with further emergency admission to hospital, or deathd | All | 1212/2161 (56.1%) | 1107/1982 (55.9%) | OR = 1.120; p = 0.147 | 0.961 to 1.305 | 0.0010 | 0 to 0.0050 |
| Site 1 | 576/1081 (53.3%) | 580/1055 (55.0%) | |||||
| Site 2 | 302/540 (55.9%) | 238/433 (55.0%) | |||||
| Site 3 | 334/540 (61.9%) | 289/494 (58.5%) | |||||
| Proportion of patients with further emergency event (ED attendance or emergency admission to hospital), or deathe | All | 1388/2161 (64.2%) | 1250/1982 (63.1%) | OR = 0.957; p = 0.532 | 0.834 to 1.098 | 0.0002 | 0 to 0.0038 |
| Site 1 | 664/1081 (61.4%) | 655/1055 (62.1%) | |||||
| Site 2 | 349/540 (64.6%) | 273/433 (63.0%) | |||||
| Site 3 | 375/540 (69.4%) | 322/494 (65.2%) | |||||
| Proportion of patients with further emergency event (emergency service call, ED attendance, emergency admission to hospital) or deathf | All | 1532/2161 (70.9%) | 1395/1982 (70.4%) | OR = 0.999; p = 0.990 | 0.872 to 1.144 | 0 | n/a |
| Site 1 | 764/1081 (70.7%) | 751/1055 (71.2%) | |||||
| Site 2 | 372/540 (68.9%) | 289/433 (66.7%) | |||||
| Site 3 | 396/540 (73.3%) | 355/494 (71.9%) | |||||
| Further emergency events per patient (emergency service call, ED attendance, admission to hospital) per day at risk,g mean (SD) [n] | All | 0.0477 (0.1552) [2150] | 0.0454 (0.1445) [1975] | Δ = 0.0024; p = 0.614 | –0.0068 to 0.0115 | 0.0016 | 0.0001 to 0.0057 |
| Site 1 | 0.0419 (0.1373) [1080] | 0.0398 (0.1025) [1054] | |||||
| Site 2 | 0.0464 (0.1577) [535] | 0.0438 (0.1806) [429] | ΔL = –0.0265; p = 0.647 | –0.1399 to 0.0869 | 0.0023 | 0.0002 to 0.0074 | |
| Site 3 | 0.0607 (0.1838) [535] | 0.0589 (0.1808) [492] | |||||
| Mean time to first event (days, truncated at 180),h mean (proportion truncated) | All | 84.36 (629/2161) | 84.54 (587/1982) | HR = 0.995; p = 0.903 | 0.926 to 1.071 | 0.0028 | 0.0004 to 0.0080 |
| Site 1 | 84.28 (317/1081) | 82.26 (304/1055) | |||||
| Site 2 | 90.69 (168/540) | 90.87 (144/433) | |||||
| Site 3 | 78.17 (144/540) | 83.88 (139/494) | |||||
| Primary outcomes | Site | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Estimate, p-value | 95% CI | Estimate | 95% CI | ||
| Proportion of patients dying (any cause) | All | 420/2161 (19.4%) | 362/1982 (18.3%) | OR = 1.199; p = 0.083 | 0.977 to 1.472 | 0 | n/a |
| Site 1 | 211/1081 (19.5%) | 213/1055 (20.2%) | |||||
| Site 2 | 116/540 (21.5%) | 75/433 (17.3%) | |||||
| Site 3 | 93/540 (17.2%) | 74/494 (15.0%) | |||||
| Proportion of patients with further emergency admission to hospitalc | All | 1039/2161 (48.1%) | 967/1982 (48.8%) | OR = 1.092; p = 0.252 | 0.940 to 1.269 | 0.0048 | 0.0013 to 0.0111 |
| Site 1 | 483/1081 (44.7%) | 503/1055 (47.7%) | |||||
| Site 2 | 258/540 (47.8%) | 206/433 (47.6%) | |||||
| Site 3 | 298/540 (55.2%) | 258/494 (52.2%) | |||||
| Proportion of patients with further ED attendanced | All | 961/2161 (44.5%) | 899/1982 (45.4%) | OR = 0.961; p = 0.535 | 0.849 to 1.089 | 0.0220 | 0.0099 to 0.0391 |
| Site 1 | 474/1081 (43.8%) | 462/1055 (43.8%) | |||||
| Site 2 | 196/540 (36.3%) | 167/433 (38.6%) | |||||
| Site 3 | 291/540 (53.9%) | 270/494 (54.7%) | |||||
| Further ED attendances per patient,e mean (SD) [n] | All | 0.843 (1.416) [2150] | 0.939 (2.886) [1975] | Λ = 0.809; p < 0.001 | 0.720 to 0.910 | 0.0133 | 0.0057 to 0.0246 |
| Site 1 | 0.804 (1.404) [1080] | 0.806 (1.375) [1054] | |||||
| Site 2 | 0.561 (0.912) [535] | 0.678 (1.083) [429] | |||||
| Site 3 | 1.204 (1.743) [535] | 1.453 (5.296) [492] | |||||
| Further ED attendances per patient per day at risk,f mean (SD) [n] | All | 0.0178 (0.0951) [2150] | 0.0142 (0.0673) [1975] | Δ = 0.0037; p = 0.157 | –0.0014 to 0.0087 | 0.0039 | 0.0009 to 0.0098 |
| Site 1 | 0.0168 (0.0940) [1080] | 0.0106 (0.0330) [1054] | |||||
| Site 2 | 0.0145 (0.1033) [535] | 0.0153 (0.1117) [429] | ΔL = –0.0354; p = 0.450 | –0.1272 to 0.0564 | 0.0277 | 0.0134 to 0.0475 | |
| Site 3 | 0.0231 (0.0886) [535] | 0.0209 (0.0701) [492] | |||||
| Proportion of patients with further emergency service callg | All | 940/2161 (43.5%) | 910/1982 (45.9%) | OR = 0.898; p = 0.092 | 0.792 to 1.018 | 0.0025 | 0.0004 to 0.0074 |
| Site 1 | 484/1081 (44.8%) | 499/1055 (47.3%) | |||||
| Site 2 | 233/540 (43.1%) | 169/433 (39.0%) | |||||
| Site 3 | 223/540 (41.3%) | 242/494 (49.0%) | |||||
| Further emergency service calls per patient,h mean (SD) [n] | All | 1.129 (2.560) [2150] | 1.250 (2.685) [1975] | Λ = 0.921; p = 0.055 | 0.846 to 1.002 | 0.0054 | 0.0017 to 0.0115 |
| Site 1 | 1.272 (3.086) [1080] | 1.453 (3.299) [1054] | |||||
| Site 2 | 0.849 (1.497) [535] | 0.839 (1.456) [429] | |||||
| Site 3 | 1.120 (2.183) [535] | 1.173 (1.881) [492] | |||||
| Further emergency service calls per patient per day at risk,i mean (SD) [n] | All | 0.0128 (0.0377) [2150] | 0.0166 (0.0541) [1975] | Δ = –0.0036 p = 0.010 | –0.0064 to –0.0009 | 0.0019 | 0.0005 to 0.0055 |
| Site 1 | 0.0122 (0.0328) [1080] | 0.0168 (0.0494) [1054] | |||||
| Site 2 | 0.0125 (0.0376) [535] | 0.0139 (0.0620) [429] | ΔL = –0.120; p = 0.014 | –0.2156 to –0.0246 | 0.0036 | 0.0008 to 0.0088 | |
| Site 3 | 0.0144 (0.0460) [535] | 0.0184 (0.0565) [492] | |||||
| Secondary outcomes | Site | Raw data | Adjusted comparisona,b | ICC | |||
|---|---|---|---|---|---|---|---|
| Intervention (A) | Control (B) | Estimate, p-value | 95% CI | Estimate | 95% CI | ||
| Duration of subsequent inpatient episodes: nights in hospital, truncated at 30 days,c mean (SD) [n] | All | 2.26 (6.14) [2161] | 2.16 (6.13) [1982] | Δ = 0.432; p = 0.061 | –0.019 to 0.884 | 0.0003 | 0 to 0.0031 |
| Site 1 | 1.95 (5.53) [1081] | 2.05 (5.81) [1055] | |||||
| Site 2 | 2.51 (6.72) [540] | 2.42 (6.77) [433] | |||||
| Site 3 | 2.64 (6.67) [540] | 2.17 (6.20) [494] | |||||
| Proportion with further reported injuries (fractures)d | All | 93/2161 (4.3%) | 81/1982 (4.1%) | OR = 1.043; p = 0.790 | 0.763 to 1.426 | 0.0048 | 0.0012 to 0.0113 |
| Site 1 | 33/1081 (3.1%) | 32/1055 (3.0%) | |||||
| Site 2 | 41/540 (7.6%) | 27/433 (6.2%) | |||||
| Site 3 | 19/540 (3.5%) | 22/494 (4.5%) | |||||
| Quality of life | |||||||
| SF-12 MCS,e mean (SD) [n] | All | 39.65 (12.46) [415] | 38.66 (12.04) [368] | Δ = 1.071; p = 0.220 | –0.642 to 2.784 | 0.0063 | 0.0002 to 0.0286 |
| Site 1 | 40.48 (12.92) [182] | 40.15 (13.04) [175] | |||||
| Site 2 | 37.76 (11.59) [126] | 35.63 (10.69) [104] | |||||
| Site 3 | 40.44 (12.53) [107] | 39.26 (10.88) [89] | |||||
| SF-12 PCS,f mean (SD) [n] | All | 29.14 (9.99) [415] | 29.41 (10.08) [368] | Δ = –0.424; p = 0.553 | –1.829 to 0.980 | 0 | n/a |
| Site 1 | 29.06 (9.85) [182] | 29.70 (11.36) [175] | |||||
| Site 2 | 28.13 (9.66) [126] | 28.39 (7.99) [104] | |||||
| Site 3 | 30.47 (10.55) [107] | 30.03 (9.58) [89] | |||||
| Derived SF-6D,g mean (SD) [n] | All | 0.5555 (0.1271) [444] | 0.5527 (0.1264) [406] | Δ = –0.0001; p = 0.994 | –0.0170 to 0.0168 | 0.0099 | 0.0011 to 0.0306 |
| Site 1 | 0.5597 (0.1260) [196] | 0.5658 (0.1338) [195] | |||||
| Site 2 | 0.5353 (0.1103) [134] | 0.5226 (0.1089) [114] | |||||
| Site 3 | 0.5719 (0.1443) [114] | 0.5620 (0.1254) [97] | |||||
| Patient satisfaction | |||||||
| QCM Technical,h mean (SD) [n] | All | 62.66 (8.10) [519] | 63.07 (8.37) [495] | Δ = –0.293; p = 0.572 | –1.310 to 0.725 | 0.0092 | 0.0013 to 0.0270 |
| Site 1 | 62.85 (7.63) [230] | 63.62 (8.38) [239] | |||||
| Site 2 | 61.37 (9.78) [163] | 61.64 (8.63) [137] | |||||
| Site 3 | 64.01 (6.07) [126] | 63.58 (7.91) [119] | |||||
| QCM Interpersonal,i mean (SD) [n] | All | 68.98 (8.78) [519] | 68.07 (9.22) [495] | Δ = 3.105; p < 0.001 | 1.522 to 4.689 | 0.0134 | 0.0020 to 0.0379 |
| Site 1 | 67.47 (10.03) [230] | 67.97 (10.29) [239] | |||||
| Site 2 | 71.18 (7.42) [163] | 68.25 (8.51) [137] | |||||
| Site 3 | 68.88 (7.28) [126] | 68.06 (7.68) [119] | |||||
| Fall-related self efficacy (fear of falling),j mean (SD) [n] | All | 3.676 (3.005) [585] | 3.734 (3.059) [535] | Δ = –0.010; p = 0.956 | –0.353 to 0.334 | 0.0081 | 0.0009 to 0.0254 |
| Site 1 | 3.772 (3.039) [253] | 3.942 (3.207) [256] | |||||
| Site 2 | 3.148 (2.866) [182] | 3.194 (2.666) [151] | |||||
| Site 3 | 4.156 (3.035) [150] | 3.955 (3.133) [128] | |||||
| Proportion of patients who reported one or more further fallk | All | 382/576 (66.3%) | 373/528 (70.6%) | OR = 0.682; p = 0.010 | 0.510 to 0.914 | 0.0141 | 0.0029 to 0.0356 |
| Site 1 | 180/251 (71.7%) | 179/253 (70.8%) | |||||
| Site 2 | 112/178 (62.9%) | 105/149 (70.5%) | |||||
| Site 3 | 90/147 (61.2%) | 89/126 (70.6%) | |||||
| Secondary outcomes | Site | Raw data | Adjusted comparisona,b | Estimate | 95% CI | ||
|---|---|---|---|---|---|---|---|
| Intervention (A) | Control (B) | Estimate, p-value | 95% CI | ||||
| Duration of subsequent inpatient episodes: nights in hospital, truncated at 180 days,c mean (SD) [n] | All | 11.18 (23.05) [2161] | 12.08 (23.52) [1982] | Δ = 1.334; p = 0.132 | –0.403 to 3.070 | 0.0061 | 0.0018 to 0.0135 |
| Site 1 | 9.11 (19.07) [1081] | 10.35 (20.41) [1055] | |||||
| Site 2 | 14.48 (29.56) [540] | 14.75 (30.01) [433] | |||||
| Site 3 | 12.03 (22.52) [540] | 13.42 (25.53) [494] | |||||
| Proportion with further reported subsequent injuries (fractures)d | All | 213/2161 (9.9%) | 195/1982 (9.8%) | OR = 1.200; p = 0.106 | 0.962 to 1.497 | 0.0166 | 0.0069 to 0.0309 |
| Site 1 | 78/1081 (7.2%) | 80/1055 (7.6%) | |||||
| Site 2 | 92/540 (17.0%) | 59/433 (13.6%) | |||||
| Site 3 | 43/540 (8.0%) | 56/494 (11.3%) | |||||
| Quality of life | |||||||
| SF-12 MCS,e mean (SD) [n] | All | 42.93 (12.44) [238] | 42.90 (12.02) [218] | Δ = 0.043; p = 0.970 | –2.203 to 2.290 | 0 | n/a |
| Site 1 | 43.52 (12.23) [107] | 43.71 (12.12) [121] | |||||
| Site 2 | 41.84 (12.42) [53] | 38.95 (12.77) [43] | |||||
| Site 3 | 42.84 (12.84) [78] | 44.24 (10.67) [54] | |||||
| SF-12 PCS,f mean (SD) [n] | All | 30.38 (11.31) [238] | 31.31 (11.24) [218] | Δ = –0.93; p = 0.368 | –2.961 to 1.099 | 0 | n/a |
| Site 1 | 29.57 (11.22) [107] | 31.42 (10.99) [121] | |||||
| Site 2 | 31.61 (12.89) [53] | 30.77 (12.79) [43] | |||||
| Site 3 | 30.64 (10.31) [78] | 31.49 (10.70) [54] | |||||
| Derived SF-6D,g mean (SD) [n] | All | 0.5865 (0.1368) [260] | 0.5933 (0.1349) [232] | Δ = –0.0069; p = 0.572 | –0.0308 to 0.0170 | 0 | n/a |
| Site 1 | 0.5842 (0.1395) [119] | 0.6055 (0.1387) [128] | |||||
| Site 2 | 0.5841 (0.1439) [57] | 0.5619 (0.1352) [47] | |||||
| Site 3 | 0.5913 (0.1292) [84] | 0.5916 (0.1236) [57] | |||||
| Fall-related self efficacy (Fear of falling),h mean (SD) [n] | All | 4.474 (3.295) [313] | 4.712 (3.345) [280] | Δ = –0.230; p = 0.328 | –0.776 to 0.260 | 0 | n/a |
| Site 1 | 4.497 (3.349) [139] | 4.999 (3.416) [146] | |||||
| Site 2 | 4.217 (3.254) [72] | 4.010 (3.423) [60] | |||||
| Site 3 | 4.624 (3.273) [102] | 4.716 (3.090) [74] | |||||
| Proportion with change in place of residence at 6 monthsi | All | 29/293 (9.9%) | 15/252 (6.0%) | OR = 1.719; p = 0.102 | 0.897 to 3.292 | 0.0102 | 0.0007 to 0.0368 |
| Site 1 | 12/130 (9.2%) | 5/135 (3.7%) | |||||
| Site 2 | 5/73 (6.8%) | 4/50 (8.0%) | |||||
| Site 3 | 12/90 (13.3%) | 6/67 (9.0%) | |||||
| Proportion of patients who reported one or more further fallj | All | 209/304 (68.8%) | 174/267 (65.2%) | OR = 0.418; p = 0.009 | 0.217 to 0.807 | 0.0171 | 0.0030 to 0.0457 |
| Site 1 | 91/134 (67.9%) | 87/143 (60.8%) | |||||
| Site 2 | 44/74 (59.5%) | 43/56 (76.8%) | |||||
| Site 3 | 74/96 (77.1%) | 44/68 (64.7%) | |||||
List of abbreviations
- A&E
- accident and emergency
- AE
- adverse event
- AR
- adverse reaction
- CI
- confidence interval
- CLRN
- comprehensive local research network
- CONSORT
- Consolidated Standards of Reporting Trials
- C-RCT
- cluster randomised controlled trial
- DMEC
- Data Monitoring and Ethics Committee
- ECP
- emergency care practitioner
- ED
- emergency department
- EMS
- emergency medical service
- ePRF
- electronic patient report form
- EQ-5D
- European Quality of Health-5 Dimensions
- GP
- general practitioner
- HRA CAG
- Health Research Authority Confidentiality Advisory Group
- HSCIC
- Health and Social Care Information Centre
- HTA
- Health Technology Assessment
- ICC
- intracluster correlation
- LIT
- local implementation team
- MCS
- mental component summary
- MeSH
- medical subject heading
- mFES
- modified Falls Efficacy Scale
- NICE
- National Institute for Health and Care Excellence
- OR
- odds ratio
- PCS
- physical component summary
- PCT
- primary care trust
- PICOCS
- population, intervention, comparator, outcomes, context and study design
- PRF
- patient report form
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- ProFaNE
- Prevention of Falls Network Europe
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- R&D
- research and development
- RCT
- randomised controlled trial
- SAE
- serious adverse event
- SAFER
- Support and Assessment for Fall Emergency Referrals study
- SAIL
- Secure Anonymised Information Linkage database
- SD
- standard deviation
- SF-12
- Short Form questionnaire-12 items
- SF-6D
- Short Form questionnaire-6 Dimensions
- SOP
- standard operating procedure
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
- WWORTH
- West Wales Organisation for Rigorous Trials in Health and social care