Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 12/139/12. The contractual start date was in May 2014. The draft report began editorial review in February 2016 and was accepted for publication in November 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
John Norrie is a member of the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) Commissioning Board and the NIHR HTA and the Efficacy and Mechanism Evaluation Editorial Board. Linda Irvine was the Trial Manager on the NIHR Public Health Research funded study 11/3050/30 [Texting to Reduce Alcohol Misuse (TRAM): a multi-centre randomised controlled trial of a text message intervention to reduce binge drinking among disadvantaged men] while the current study was being conducted.
Disclaimers
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Crombie et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
This feasibility study was commissioned by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme. The remit was to develop an intervention to reduce alcohol consumption in obese men and to assess the feasibility of a trial investigating the effectiveness of an intervention. The intervention used the motivation of weight loss to promote moderated drinking. The commissioning brief is included at the end of the report (see Appendix 1). This chapter provides the scientific background and the aims and objectives of the study, and gives an overview of the study methods. It also outlines the structure of the report, as well as detailing ethics approval and modifications to the protocol.
Background
Heavy alcohol consumption by men who are obese increases their risk of death from liver disease 19-fold. 1 Having a raised body mass index (BMI) and consuming > 14 units of alcohol per week are both factors that independently increase the risk of liver disease. However, the combination of the two leads to a substantially greater risk. 1 The commissioning brief described this as the supra-additive effect of obesity and alcohol. The problem is compounded by the high prevalence of heavy drinking and of obesity. The English Health Survey 20122 found that 24% of men aged ≥16 years drank more than the then government-recommended 21 units per week. Data from 2011 revealed that 24% of men in England3 and 28% of men in Scotland4 were obese. Based on current trends, the UK government’s Foresight programme predicted an increase in the prevalence of obesity among men. 5 Furthermore, heavy alcohol consumption is associated with an increased risk of obesity. 6–8 Abdominal obesity is more common among men who drink beer. 9 Heavy drinking leads to overeating,10 thus increasing the potential for weight gain.
An intervention that could reduce both alcohol consumption and weight in obese men could make a significant contribution to improving public health. However, it is far from certain that obese men who drink heavily would engage in such an intervention. They may not regard their drinking as problematic and may not think it could contribute to weight gain. Many obese men want to lose weight, but are reluctant to try conventional weight loss approaches, because these are generally targeted at women. 11 Men are under-represented in weight loss interventions12 and attrition is high in weight loss studies. 13,14
Previous research has identified many features of an intervention that could make it attractive to potential male participants. Convenience and compatibility with a busy life are important,15–17 as is the use of community settings for intervention delivery. 18 The style and tone should be relaxed and friendly as opposed to strict and regimented. 16,17 The content should be personalised and accessible,15,18 but should be delivered in a matter-of-fact way. 18,19 The aim of the intervention should also be realistic and achievable. 17 The recently completed Football Fans in Training study20,21 provides an excellent example of an engaging community-based intervention that effectively changed behaviour. This previous research clarifies many of the requirements of an intervention for obese men. The present study aims to identify the specific content that would be required to change their drinking behaviour and to assess the feasibility of a trial to test the effectiveness of the intervention.
The feasibility study
This study aimed to develop a gender-specific extended alcohol intervention that could reduce alcohol consumption among obese men. The remit stated that it should use the motivation of weight loss to achieve this. The study also aimed to develop and test all the methods for a randomised controlled trial (RCT) of this intervention. Feasibility/pilot studies provide the opportunity to test and improve all study procedures. 22,23 Guidance from national funding bodies in the UK24 and Canada25 stress the need for these preliminary studies. The intention is to ensure that design weaknesses, technical problems and methodological flaws do not compromise the full RCT. 26
The challenges for this feasibility study arise from the nature of the study group and the design and delivery of the intervention. Identifying obese men who drink heavily could be difficult. Recruiting and retaining these men in the study would require a study design that elicits and sustains engagement. Part of the intervention was to be delivered by laypeople (study co-ordinators) whose training and support are crucial to the effective delivery of the intervention. Finally, sensitive process measures would be required to determine the fidelity of delivery and the extent to which there is engagement with the intervention.
The objectives for the feasibility study were:
-
to determine the best ways to recruit and retain obese men in a study aimed at reducing heavy drinking
-
to design an intervention that is an acceptable way to achieve a sustained reduction in alcohol consumption
-
to identify the content and timing of the delivery that is most likely to engage obese men in an intervention to reduce alcohol consumption
-
to develop high-quality training to enable the trained laypeople (study co-ordinators) to deliver their component of the intervention
-
to devise process measures to detect engagement with the steps on the causal model for behaviour change
-
to compile a manual of methods for participant recruitment, the training of lay staff and the design and delivery of the intervention.
The use of language
This study dealt with the issue of obesity but avoided the use of this term except in a few places. There were several reasons for avoiding the term obesity. People can be sensitive to terminology and do not like to be classified as ‘obese’. 16,27–29 Possibly the term is associated with pictures of extreme overweight seen in media images27 and would therefore appear inappropriate. This is supported by the finding that most men who are obese consider themselves to be overweight rather than obese, and some consider themselves to be of normal weight. 30 Obesity is considered a medical term that conveys society’s disapproval of overweight people. 28 Thus, the term very overweight was preferred to obese.
Study overview
This 21-month study was conducted in two phases. Phase 1 was to develop the recruitment strategy and the novel alcohol intervention. It was to comprise six focus groups with obese men aged 35–64 years, who would be recruited from a variety of community locations. In-depth interviews with six key stakeholders would also be conducted to help develop the strategy for the recruitment of participants.
Phase 2 was intended to recruit 60 men aged 35–64 years. Two complementary recruitment strategies were to be used. One would identify obese men from primary care records. The other would adopt a community outreach approach, time–space sampling (TSS), which was designed to identify hard-to-reach groups. 31 A key feature of the study is that trained laypeople would be involved in intervention delivery. The training programme used would be developed from the Department of Health manual,32 taking into account recent recommendations for training laypeople. 33 Each study co-ordinator would only deliver one type of intervention (either novel intervention or comparator) to prevent contamination across treatment arms.
The men in phase 2 would be randomised to a novel extended intervention group or a comparator group (a conventional alcohol brief intervention). The novel extended intervention would be informed by literature on changing health behaviours including recent systematic reviews34,35 and taxonomies of behaviour change techniques,36,37 including one specific to alcohol brief interventions. 38 The intervention would also draw on techniques developed for our successful NIHR feasibility study of a text message delivered intervention to reduce alcohol-related harm in disadvantaged men (project number 09/3001/09). 39 The comparator group was to receive a conventional brief alcohol intervention,40 which would be delivered in a face-to-face session by a trained layperson.
Ethics approval
The study received ethics approval from the East of Scotland Research Ethics Service REC2 on 28 May 2014 (reference 14/ES/0050).
Modifications to the initial protocol
Three changes were made to the intervention. One part of the intervention was to be a series of text messages encouraging behaviour change. A small number of text messages were to include images, which would extend the ideas conveyed in words. This approach was used successfully in a NIHR Public Health Research (PHR)-funded feasibility study (project number 09/3001/09). 39 However, unanticipated technical difficulties were recently encountered in the NIHR PHR-funded RCT (project number 11/3050/30). 41 Exploration of the problem suggests that changes in the commercial technology used to transmit images (Multimedia Messaging Service images), and variations in the systems used were the cause of the difficulties. Text messages that do not contain images are sent without problems. The proposal to use Short Message Service (SMS)-only messages was approved as a contract variation by NIHR HTA before the intervention was developed.
The second change to the intervention was the omission of a volitional help sheet which participants were to have been given at the end of their face-to-face session. This help sheet would have identified ways in which participants could cope with situations that might weaken their resolve to reduce their alcohol consumption. 42 However, a preliminary assessment of the face-to-face session showed that it would be best used to focus on increasing motivation to drink less. The next phase of the intervention, the text messages, would cover the specific techniques of goal-setting, action planning and relapse recovery. As the volitional help sheet is intended to assist in these steps, similar approaches were incorporated into the text messages.
The final change concerned measuring weight. The protocol stated that men would be asked to monitor and report their weight during the intervention phase. On reflection, the intervention period of 2 months was thought insufficient to achieve substantial change in weight. Worthwhile, but modest, reductions in alcohol consumption would yield small reductions in weight over such a short period. Thus, measuring weight loss might reduce rather that increase motivation to maintain reduced consumption. Consequently, the men were not asked to monitor their weight.
Conclusion
This study seeks to address an important public health problem. The approach that was taken was to develop each component of the feasibility study and then test its suitability. The intention was to create an initial robust design, then identify opportunities to improve it during the conduct of the feasibility study. Based on an evaluation of the success of the study, this report will make a recommendation on whether or not a full RCT is warranted. This will be based on technical feasibility and the likelihood of whether or not a meaningful answer will be supplied.
Structure of the report
Feasibility studies involve the development of study methods accompanied by a careful evaluation of whether or not each method achieves its objectives. This study comprises a series of substudies. For clarity, this report presents each substudy as a separate chapter, together with its methods and findings and a discussion of the implications. Thus, Chapters 2–11 describe these substudies. The final summary and conclusions chapter (see Chapter 12) summarises the findings from the separate chapters and highlights issues that involve a comparison of the findings from the separate chapters. It assesses whether or not the study objectives were met and makes recommendations for improvements to the design of the full RCT.
Chapter 2 Focus groups to explore drinking and losing weight
Introduction
The remit of this study stipulated that weight loss was to be used as a motivator to drink less among men who are obese and who drink heavily. The rationale for this is clear: alcohol is high in calories and drinking increases snacking and the consumption of high-calorie food. 43 However, the use of one behavioural outcome, weight loss, as the motivation to change a separate behaviour, alcohol consumption, is unusual. This approach is not one that has been well covered in the literature, so focus groups were conducted to explore it. Because the logic of the intervention, although compelling, is far from straightforward, the issue was approached indirectly. Initially, participants’ attitudes and motivation to drink less and to lose weight were explored separately. Once ideas on each topic had been reviewed, issues around using reduced alcohol consumption as a means of weight loss were discussed. The aim was to clarify opportunities and strategies for an intervention to promote reduced drinking and to identify potential barriers to engagement with the intervention.
Methods
Six focus groups were conducted with middle-aged men who drank regularly and were overweight. Socioeconomic status was measured using the Scottish Index of Multiple Deprivation (SIMD),44 which is similar to the English Index of Multiple Deprivation. 45 Systematic reviews have shown that the provision of monetary incentives can significantly increase recruitment to research studies. 46,47 Consequently, men who agreed to take part were given a £10 gift voucher and were reimbursed for their travel expenses.
Sampling and recruitment
Focus group participants (Table 1) were purposively sampled from a variety of venues likely to represent the diversity of the target population, ensuring variation in age and level of deprivation. 48
| Focus group | Recruited from | Venue for focus group | Number of participants | Age range of participants (years) |
|---|---|---|---|---|
| 1 | Community centre (job shop attendees) | Community centre | 6 | 51–62 |
| 2 | University (estates staff) | University staffroom | 4 | 48–67 |
| 3 | University (nursing students) | University meeting room | 3 | 33–57 |
| 4 | Golf club (club members) | Golf club | 3 | 39–64 |
| 5 | Sports centre (sport and leisure staff) | Sports centre | 4 | 42–62 |
| 6 | Amateur radio society and Rotary club (mixed group) | Hotel | 3 | 38–67 |
The venues comprised a community centre, two workplaces [a university (staff and students) and a sports centre], a golf club, an amateur radio society and a Rotary club. Twenty-three men who drank alcohol regularly and were overweight were recruited to the focus groups. The summary characteristics of the participants are shown in Table 2. The men spanned the age range 33–67 years, although most groups were within the narrower range of 39–62 years. Most of the men were married or lived with a partner and were in employment. The participants covered a wide range of socioeconomic statuses, measured by the SIMD44 and educational attainment.
| Factor | Number of participants (n = 23) |
|---|---|
| Participants’ age (years) | |
| 30–39 | 4 |
| 40–49 | 4 |
| 50–59 | 8 |
| 60–69 | 7 |
| Marital status | |
| Married/lives with a partner | 14 |
| Single | 7 |
| Separated/divorced | 1 |
| In a relationship | 1 |
| SIMD quintilea | |
| 1 (most disadvantaged) | 8 |
| 2 | 3 |
| 3 | 1 |
| 4 | 5 |
| 5 (least disadvantaged) | 5 |
| Employment status | |
| Employed | 16 |
| Unemployed | 6 |
| Other | 1 |
| Highest educational attainment | |
| University degree | 6 |
| Vocational qualification/further training | 8 |
| High school | 9 |
Data collection and analysis
Focus groups encourage interaction between participants49 and can result in increased disclosure,50 particularly when the participants are peers. 51 This is especially useful for exploring topics influenced in part by group norms and social expectations. 52 Alcohol intake in middle-aged men was expected to be one such topic. The topic guide explored three main topics: (1) reducing alcohol consumption, (2) losing weight and (3) potential intervention components. The first three focus groups explored benefits and barriers to drinking less and losing weight. To facilitate these discussions, participants were given cards and asked to write down their individual views on the benefits of drinking less, and then, on separate cards, to give their views on losing weight. There was no involvement of the researchers in these tasks. The cards were collected and used as a basis for discussion of the issues around drinking less and, after that, of losing weight. The comments on the cards were subsequently coded by two researchers (LI and IKC). The topic guide was revised following the first two focus groups to facilitate the further exploration of emerging issues. It was revised again following the third focus group as saturation had been reached in discussions of the benefits of reducing alcohol intake and weight. These were replaced with evaluations of activities that could be included in the intervention. The aim was to assess the ways in which participants responded to tasks such as calculating the units of alcohol they consumed in a week.
All participants were informed of the confidential nature of the research. All group sessions were audio-recorded and transcribed. An analysis of the transcripts was conducted by two members of the research team (KBC and AM) using a thematic approach. All data were coded by both analysts. Emerging findings were discussed with other members of the research team (IKC and LI). This encouraged the consideration of additional perspectives and interpretations. 53 Direct quotations are provided to illustrate the findings. 54
Results
The findings are organised by the three main sections of the topic guide: (1) reducing alcohol consumption, (2) being overweight and losing weight and (3) assessing intervention components.
Reducing alcohol consumption
The men in the focus groups were willing to discuss their alcohol intake. They talked openly and honestly about the amount of alcohol they consumed. Their drinks of choice varied and included different types of beer, cider, spirits, wine and cocktails. The environments in which they consumed alcohol were also diverse. Some men reported drinking mainly in their homes, others reported drinking mainly in public houses or clubs, and still others mentioned friends’ homes, golf clubs and social events.
Benefits of reducing alcohol consumption
The self-completed cards identified a wide range of potential benefits of reduced drinking (Table 3). Most frequent was the avoidance of the morning-after effects of drinking too much. However, long-term health, saving money and better relationships with family and friends were also common. Weight loss was seldom mentioned.
| Benefit | Frequency of reporting |
|---|---|
| Freedom from acute debilitating effects of alcohol | 29 |
| Mental well-being | 7 |
| Avoidance of hangover | 9 |
| More alert | 5 |
| Other (e.g. improved sleep, motivation, more energy) | 8 |
| Improved health | 15 |
| Financial | 11 |
| Improved relationships | 11 |
| Weight loss | 3 |
| Other (e.g. improved fitness, work opportunities) | 7 |
On completion of the task, the men were prompted to expand on the benefits they had identified from reducing their drinking. They often gave quite detailed personal benefits.
Hangover free
. . . enjoy your weekends more instead of having a hangover on the Saturday and the Sunday. Yes, just . . . more energy, and you’d get up and go and do stuff rather than just get up and feel bad for a few hours, and then maybe go out for a few hours and then come back.
Focus group 4, golf club members
. . . might be dinnertime before you come through the tunnel and be able to do anything, so that would give you . . . that’s time lost isn’t it, if you’re walking about in some sort of daze, with this hangover.
Focus group 2, estates staff
Health and weight
If I stop drink, better for my stomach, liver, everything.
Focus group 2, estates staff
Like I say, I think you get a lot of guys that have got big beer bellies, so that’s obviously not good for them, so the less you drink, especially if you’re drinking beer I would have thought, obviously you’re going to put on the weight if you’re standing propping up the bar every night.
Focus group 3, undergraduate nursing students
Financial
If you go to the pub you’re looking at two and a half, maybe three pound a pint, depends on where, so I would drink maybe five or six pints a night, so that’s . . . that’s 18 quid. That £18 can go towards maybe a pair of trainers, if you’ve got a family . . . you know what I mean?
Focus group 1, job shop attendees
If you want to buy yourself some clothes, or new trainers or shoes, whatever, yeah. That’s got to be better than just drinking it away.
Focus group 2, estates staff
Family
I suppose if you spend less time in the pub, you’re going to have more time for other things obviously. Spend time with your kids, spend time with your wife, spend time with the rest of your family, spend time doing things you like doing outside of alcohol I suppose, less in the pubs.
Focus group 2, estates staff
Career prospects
If you’re sober you’ve got a better chance of career prospects as well. They’ll say, ‘Well he seems alright, he does his work, and there’s them vacancies coming up, we’ll put him in for it’.
Focus group 1, job shop attendees
Barriers to reducing alcohol consumption
Some men thought that it would be difficult to reduce their alcohol consumption. Drinking was thought to form the basis of their social lives so that changes to customary drinking patterns would seriously affect friendships:
I think it’s hard to stop drinking because social life in this country is based around alcohol. I mean, you can’t go any place now, you can’t go to a disco, any place like that, without drink. Everybody drinks.
Focus group 2, estates staff
I couldn’t come down here with the guys, I couldn’t go to a Wednesday [usual drinking session] and sit down with orange juice.
Focus group 4, golf club members
It’s the only time I see my mates and that, they’ve got their own kids and families, and that, and the only time I really see them is in the pub. We don’t work together or anything like that, so if I didn’t meet them in the pub I would never see them.
Focus group 4, golf club members
The men also thought that peer pressure would make it difficult to reduce alcohol consumption. The importance of socialising when drinking may also lead to an expectation that everyone will drink and that not drinking or reducing drinking is abnormal:
Peer pressure . . . you might find yourself, you’re an oddball if you don’t drink. Social, mostly the pressure is social.
Focus group 2, estates staff
I think the biggest one, myself, would probably be socialising. Going out, you’ve got peer pressure to keep on drinking, this, that . . . your friends . . .
Focus group 6, amateur radio society and Rotary club members
Drinking as part of a celebration or through having nothing else to do were offered as reasons for continuing current drinking practices. These had less force than social factors but still contributed to the perceived difficulty of reducing alcohol consumption:
Even if there’s a thing going on, like a celebration or something, there’s always something going on isn’t there? You’ve got the Commonwealth Games haven’t you?
Focus group 1, job shop attendees
One of my mates will tell you, we would be in the local five nights a week . . . both single guys, just nothing else to do, ‘We’ll go for a pint, we’ll go for a pint’.
Focus group 3, undergraduate nursing students
Being overweight and losing weight
The men were also willing to discuss their weight and to classify themselves as overweight. (For the focus groups the term obesity was not used as men can find it stigmatising.) The self-completed cards identified several potential benefits of losing weight. These can be conveniently grouped into four categories covering health, physical functioning, mental and social well-being and body image (Table 4).
| Benefit | Frequency of reporting |
|---|---|
| Increased fitness/physical ability | 19 |
| Improved health | 18 |
| Mental/social well-being | 16 |
| Improved body image/appearance | 10 |
The subsequent discussion on weight centred around two inter-related subthemes: the limitations of being overweight and the benefits of losing weight. Being overweight is more than a measurement; its importance lies in its immediate impact on physical and emotional well-being. The men were remarkably frank in their assessment of excess weight on both their appearance and their capacity for physical activity. It is clear that their concerns were deeply felt because of the extent to which they adversely impacted on their lives:
Well you just get about . . . obviously if you’re overweight, not so much necessarily big, fat, but like you say you can’t get about so much, you’re out of breath or energy, doing whatever. Obviously . . . well that’s what I feel . . . I’ve got a bit of a fat stomach right, that’s obvious, but I feel it when I’m walking up big steep braes . . . my heart’s pounding, so obviously it’s affecting my health.
Focus group 2, estates staff
This might sound daft, but when the lifts are off at work, if we have to run up all those stairs, personally, I’m out of breath. And it’s got to be weight connected.
Focus group 2, estates staff
Self-image is strongly affected by being overweight, with most attention to stomach size:
I’d like to not have that . . . paunch . . . [his stomach] because I realise it’s bad for me, and especially at my age. And when I see it I’d rather not have it.
Focus group 6, amateur radio society and Rotary club members
I would like not to have that [his stomach], because like I said, it’s only there that it seems to manifest. Say, if you’re swimming . . . I’m like, ‘My arms are fine!’ And you’ve just got this thing there, and you’ve got your moobs and it’s . . . I’ve never had any problem putting fat on anywhere apart from a little bit in the moobs, but mainly in the gut. So I’ve never really care about how much I am on the scales, for me it’s a bit more aesthetic . . .
Focus group 3, undergraduate nursing students
And you don’t feel dressed, it doesn’t matter what you wear you look terrible in it, if you’ve overweight.
Focus group 2, estates staff
Yes, well obviously it’s not ideal wandering about with your stomach hanging out, it’s embarrassing . . . overhanging your jeans.
Focus group 2, estates staff
The men also identified the impact of losing weight on physical activity:
Yes, I would say if you’re more healthier and less overweight, you’re going to want to go out more aren’t you? More outgoing, definitely, but a walk through the park, go for walks in the countryside with the kids.
Focus group 1, job shop attendees
. . . just being able to do things without worrying about it, like . . . going hill climbing with your mates or whatever, and you just think, ‘Christ, that’s a bit of a bugger’, but you know you’re going to be able to do it if you’re fitter.
Focus group 3, undergraduate nursing students
Aye, it’s all walking . . . nearly every place. It’s a lot easier to walk [if you lose some weight].
Focus group 1, job shop attendees
Alcohol consumption and weight
When the link between alcohol consumption and weight was raised, the participants acknowledged that this existed, although they thought that many people would be unaware of it:
I think it’s getting people to recognise that the amount they’re drinking, contributes to, not only the risk of this, but also their weight as well. And I don’t think, necessarily, folk think that.
Focus group 5, sport and leisure staff
. . . but I don’t think a lot of folk . . . just talking . . . would associate that alcohol can also contribute to that [weight].
Focus group 5, sport and leisure staff
Many men believed that reducing alcohol intake would help with losing weight. Some of the men had experienced this for themselves, or had noticed an increase in their weight following an increase in their alcohol intake:
From my personal experience, I know it works. I lost a tremendous amount of weight, I lost 6 kilos . . . and largely because I’d stopped drinking . . . So, yeah, there’s no question, cutting out the alcohol makes a big difference.
Focus group 6, amateur radio society and Rotary club members
on times when I have stopped for a while, I have lost weight . . . So it definitely has an effect.
Focus group 1, job shop attendees
I’ve been putting on weight because of the fact I’m not working, you’re drinking more.
Focus group 1, job shop attendees
However, other men had experienced the opposite: an increase in their weight following a reduction in their alcohol consumption. They attributed this to eating as a replacement for drinking:
But I don’t think, now, stopping, made any difference to me. I didn’t lose any weight. I probably put on weight because I was just eating more.
Focus group 4, golf club members
It’s very strange because if I stop drink, I not lose the weight, I put on the weight. If I drink, I drink beer, beer has a lot of calories, one bottle about 300 calories.
Focus group 2, estates staff
Alcohol and eating
In laboratory studies, alcohol consumption has been shown to stimulate appetite. 55–57 The focus groups identified the ways in which this occurred: through increased consumption during and shortly after drinking sessions, by eating more the following day and in an apparent preference for less healthy foodstuffs:
Yes, because usually you’re really hungry after, it is . . . even if you’re sitting in the house . . . even like a packet of crisps, if you’re sitting and watching a film or something like that, a few beers, and a packet of crisps. It’s all tied in.
Focus group 2, estates staff
We used to call it the ‘whisky hunger’. You get the ‘whisky hunger’. And that’s been before time began! You’d get too drunk and then you’d want to eat something.
Focus group 2, estates staff
You leave the pub after four or five pints you go to the kebab shop . . .
Focus group 1, job shop attendees
But it’s true, like next Saturday we’ll be out on that night out, it’ll be a pretty heavy night, there’s a big crowd going, so we’ll all get up on Sunday, and I’ll eat junk all day. Crisps and stuff like that.
Focus group 4, golf club members
If you are drinking, you are going to eat the wrong stuff.
Focus group 6, amateur radio society and Rotary club members
. . . you’re not going to say, ‘I’m having a glass of wine, I’ll have a carrot!’
Focus group 6, amateur radio society and Rotary club members
And definitely, the next day, if you’ve over indulged, with the grease, just something to wrap it up and get yourself right. Like tomorrow I know I will be having a full breakfast, a full English, easily.
Focus group 3, undergraduate nursing students
Assessing intervention components
The focus groups also explored four potential activities to be undertaken as part of the intervention. These were measurement of alcohol consumption, the calculation of units of alcohol consumed, the calculation of calorie consumption from alcohol and a comparison of the calories in foodstuffs and in alcohol. These activities follow a logical sequence, as each builds on the previous one. The main reason for exploring these activities in the focus groups was to identify ways in which these activities could be used to help increase motivation to lose weight. They also provided estimates of the time taken for each task.
Measuring alcohol consumption
Alcohol consumption was to be measured using the Timeline Followback (TLFB) method,58 to obtain an accurate estimate of consumption. The men were provided with a calendar of the previous 28 days and were asked to write down how much alcohol they had consumed over that period. They were advised to start with regular drinking days (e.g. weekends), and then to add details of any special occasions or less usual drinking sessions. The time taken to perform this task ranged from 4 to 13 minutes. The completion of the drinking calendar highlighted how much alcohol was being consumed:
When you see it wrote down it actually makes you think, wait a minute, I’ve actually drunk that much.
Focus group 6, amateur radio society and Rotary club members
It’s certainly made me aware. I would say . . . I stopped drinking for a year actually, a couple of years ago, and I would say, now, and often do say, well I don’t drink anymore, but these figures would belie that. I don’t feel . . . I certainly don’t drink as much as I used to, but . . . it’s kind of shocking to me, to see how much I actually do drink. Just a large brandy, every couple of nights, maybe three nights in a row, it adds up, and it’s interesting to have to confront that.
Focus group 6, amateur radio society and Rotary club members
The calculation of unit consumption
From the 28-day calendar the men were asked to select a typical week. With the assistance of the researchers, a simple look-up table of units in common drinks and a calculator, the men calculated the number of units of alcohol consumed in their typical week. The calculation took between 2 and 5 minutes to perform. The men mentioned that totalling up the units they consumed was not something that they had done before:
I’ve never tallied it up before.
Focus group 4, golf club members
If you’re asked to do this, actually, it’s real though.
Focus group 4, golf club members
I’ve never actually dealt with them [units].
Focus group 6, amateur radio society and Rotary club members
The calculation of calorie consumption
Using a simple look-up table, the men were asked to calculate how many calories were in the drinks they had consumed in their typical drinking week. This process also took between 2 and 5 minutes. The men were surprised at the large number of calories from the alcohol that they had consumed:
You see I’d never given that a consideration, how much calories were in alcohol, I’d never even given that a thought.
Focus group 2, estates staff
I mean, as I say, I would never have guessed that a pint of beer had 180 calories, full stop!
Focus group 2, estates staff
It’s quite surprising, I’m surprised at this . . . the amount of calories in, especially, cider, which I drink, I’m quite amazed that that’s the highest of the lot to be quite honest.
Focus group 5, sport and leisure staff
Calorie equivalence of food and alcohol
The men were provided with information about the calorie equivalence of alcoholic drinks and certain foods. The hope was that the use of familiar foodstuffs would emphasise just how many calories alcohol contained. However, the key message they took from the information was that if they did not eat the foodstuff, they could drink more:
Six chicken nuggets, I’d rather have the five whiskies.
Focus group 4, golf club members
Instead of two packets of crisps, I could have two pints!
Focus group 4, golf club members
First reaction, is, ‘I don’t need the fish and chips, but five pints of lager sounds nice’.
Focus group 6, amateur radio society and Rotary club members
Discussion
These findings have important implications for the design of the intervention to reduce alcohol consumption in obese men aged 35–64 years. They identify potential levers for behaviour change that could support the study aim of using the benefits of weight loss to promote reduced drinking (Box 1). In addition, barriers to reduced drinking were identified and an approach that was thought to have promise had the potential to be counterproductive.
-
The men were surprised by how much they drank.
-
Few men monitored their alcohol consumption.
-
Many benefits of drinking less were identified.
-
Some disadvantages of drinking less were identified, particularly effects on social life.
-
The men were aware that drinking leads to:
-
increased snacking
-
additional meals
-
eating energy-dense foods.
-
-
The men were surprised by the calorie content of alcohol.
-
Being overweight, particularly having a protruding stomach, limits ability to be active and causes considerable embarrassment.
-
Many benefits of losing weight were identified. These could feature in the intervention, increasing the salience of these outcomes without risk of antagonising the men.
-
There were no disadvantages to losing weight.
-
Comparing the calorie content of alcohol and popular foodstuffs could lead to increased alcohol consumption.
The men identified many benefits of reducing drinking. Most prominent among these were the short-term consequences of heavy drinking, such as hangovers and loss of mental clarity. Although some longer-term health concerns were identified, they were much less commonly noted by the men. This finding not only identifies an important target for increasing motivation to drink less, but also provides one for maintenance of reduced drinking. Satisfaction with outcome is crucial for the maintenance of a new behaviour. 59,60 Benefits such as improved mental clarity are immediately appreciated, whereas many health benefits, such as avoiding diabetes or heart attack, will not be reaped for many years. Thus, the intervention could use the short-term benefits of reduced drinking to increase motivation, and then use the benefits obtained to promote maintenance.
The principal barrier to reduced drinking was the impact it would have on friends and social life. However, balanced against this was the finding that one benefit of reducing alcohol intake was a positive effect on relationships with family and friends. Thus, in the intervention, increasing the salience of the benefit could reduce or negate the impact of the barrier.
The calorie content of alcohol came as a surprise to many of the men. This makes it a high priority for inclusion in the intervention. The finding that drinking makes you eat more, and more unhealthily, is another important candidate for inclusion. The literature shows that moderate alcohol intake stimulates food consumption in the short term (within 1 hour). 55–57 Men also make unhealthier food choices when drinking. 43 Although this point did not feature on the self-completed cards, it emerged frequently in discussions and attracted no dissenting voices. Given the double benefit of less alcohol and fewer calories, the links between drinking alcohol and increased consumption of food should be emphasised in the intervention.
The way in which alcohol increases food consumption, particularly by snacking, was familiar to many men, although there was a perception that this effect was not widely known. This suggests that, although known, the effect has a low salience. This makes it an attractive target for intervention, as information about it may be readily accepted. One approach could be to ask men about their own experience, and then encourage them to reflect on what effect this has on their weight.
An unexpected finding was the hazard of describing calories in alcohol in terms of common food items. This was intended to be a simple method of conveying how many calories were in alcohol and it succeeded in that aim. However, the unintended consequence was that men could use the avoidance of high-calorie foodstuffs as an excuse to consume more alcohol; therefore, this topic should be avoided in the intervention.
Previous studies have shown that men care about body image61 and engage in negative body talk (making disparaging comments about their bodies). 62 Self-image and physical functioning are important motivators for weight loss. 18 These include the desire to improve appearance and physical attractiveness,63–65 but also to increase self-esteem and a sense of self-control. 63 A key finding from this study is that the men’s body image concerns were focused on the size and unsightliness of the stomach and the embarrassment that this causes. This presents an ideal lever to increase motivation to change, but it is one that needs to be handled sensitively. The implication that a participant is unattractive because of his shape could induce annoyance and rejection of the intervention. One way to overcome this would be to suggest that the men might recapture some of the vigour of their youth if they lost some weight.
The study also found that men were concerned about function, their ability to do everyday tasks, their engagement with their families and their ability to carry out work responsibilities. 66,67 Thus, another motivator for weight loss and/or reduced alcohol consumption found in this study is increasing effectiveness at work to become a greater asset to one’s workplace. 15 The men’s concerns about being able to function competently in society provide an opportunity to increase motivation to change, and have the benefit that, because they are conventional social obligations, they are likely to be readily accepted. Indeed, men may be more likely to welcome suggestions on how to increase their ability to meet these expectations.
In summary, the focus groups have identified opportunities for the development of an intervention to reduce drinking in a social group who have not been well studied: obese men who drink > 21 units of alcohol per week. These centre on improving physical, social and mental well-being by reducing alcohol consumption and losing weight. The proposed approach to weight loss, namely drinking less alcohol, offers benefits that are important to overweight men. The aim is to increase the salience of the benefits to increase motivation for change.
Chapter 3 The stakeholder interviews
Introduction
One element of the recruitment strategy proposed to use community outreach to identify eligible men. It would focus on venues that obese men were likely to frequent. To identify potential venues and the best ways to gain access to them, interviews were conducted with key stakeholders. These were individuals in managerial positions who frequently encounter men in the target group, and who could thus act as gatekeepers for recruitment of participants. Such individuals were also likely to have insight into the willingness of potential participants to discuss taking part in the study. The stakeholder interviews investigated opportunities for meeting with potential participants and possible venues for delivering the intervention.
Methods
Sampling and recruitment
Stakeholders were purposively sampled from a variety of venues that members of the target population were likely to attend either for work or for pleasure. Six interviews were conducted with stakeholders who were managers of venues in the local community, specifically a golf club, a community centre, a sports centre, an employment support service, a concert auditorium and a theatre.
Data collection and analysis
Data were collected from brief semistructured interviews. The stakeholders were told that the aim of the research was to encourage men to drink less and to lose weight. They were also told about the method of recruitment and that the intervention would be delivered by a face-to-face session followed by text messages. The interview schedule was structured around the issues of recruiting men for the study and delivering the face-to-face component of the intervention. All interviews were audio-recorded and transcribed. Thematic analysis was conducted by two members of the research team (KBC and AM).
Results
The interviews explored three main themes: (1) views on the research topic, (2) recruitment of participants and (3) venues for intervention delivery. The results are presented in these themes. No details of the stakeholders’ job titles or organisations are included, in order to protect their anonymity.
Views on the research topic
All of the stakeholders considered alcohol consumption and weight to be major public health issues. They believed that research exploring ways to reduce alcohol consumption in obese men aged 35–64 years would be challenging yet very worthwhile:
I think the aim is very worthy . . . if you’ve got some techniques that can pull out a bit more information around both alcohol consumption, levels of activity, that would be great, and certainly tying it into weight, that would be fantastic.
Stakeholder 6
It will be very challenging I should imagine! Because men don’t like to think they’re getting older either, so they don’t like to appreciate they need to drink less, so I think it will be very, very challenging . . . I think it’s hugely important . . .
Stakeholder 1
. . . you’ve got the social aspect, I think, of it, as well, and most of them will say to you that going for a drink is a social kind of thing to do. But then when it does start to over indulge . . . that’s where the weight comes in.
Stakeholder 3
Benefits to stakeholders
The stakeholders were willing to help to facilitate the research by assisting with the recruitment of participants and by providing venues for the delivery of the intervention sessions. The main reason for this positive response was that the aim dovetailed with their organisation’s philosophy and aims. Some commented that they saw it as part of their role and responsibility to their organisation’s staff and/or customers to provide access to health promotion initiatives:
It would be a positive for the workplace, so the aims of the study are brilliant, even as a standalone . . . in relation to work environment and management it would be useful, because obviously healthier members of staff are going to be more productive.
Stakeholder 2
Partly what we’re in the business of, is helping to improve people’s quality of life around physical activity and health . . . And the study seems to fit into that . . . So we were quite happy to support . . .
Stakeholder 6
I think it’s from the area that we work in, and what we see while we’re doing the work and the effects that alcohol and everything else has on the local community.
Stakeholder 3
I suppose because we’re interested in improving . . . anything that can improve people’s health and employment, and understanding, that’s why we’re interested in anything like that. Because it’s a whole . . . employment is a whole culmination of a lot of different things and employment and health is part of that . . . So yeah, if we can make people more aware of what’s going on, what’s surrounding them, what’s out there to help them, then that’s got to be better for us.
Stakeholder 5
Recruitment
All of the stakeholders indicated that men meeting the eligibility criteria of age 35–64 years and BMI of > 30 kg/m2 frequented their organisation either as members of staff or as customers. Some of the stakeholders were able to provide estimates of the numbers of such men. These numbers ranged from roughly 50 per week (community centre) to 200 members (golf club). No stakeholders were aware of the amount of alcohol consumed by the men meeting the eligibility criteria of age and BMI. The stakeholders were willing to identify opportunities for members of the research team to meet with potential participants and were happy to facilitate such meetings. In general they did not believe that men would be embarrassed about being approached to take part in a study on the topics of alcohol consumption and weight and they did not anticipate any adverse reactions from men approached:
We see a lot of people through the doors here, who need to take action. It’s in the press all the time isn’t it, how obesity is causing the NHS no end of grief, so from what’s coming in here, it’s not going to get any better.
Stakeholder 1
I know we have lots of candidates here!
Stakeholder 4
I would think if you send someone here on a Saturday afternoon, that’s a Saturday or a Sunday, or both preferably. If you want people who don’t know each other, come both days . . . I don’t think . . . you won’t get any abuse or adverse reactions, they’ll either say, no, or they’ll make a joke about it.
Stakeholder 4
I think once you can get them engaged, I think they’ll be OK. I think they’ll be . . . certainly on a one to one basis, we’re interviewing people pretty much all the time on a one to one, even quite disengaged people quite like speaking about themselves!
Stakeholder 5
. . . they wouldn’t think they were particularly overweight you know? But the bigger guys that we see in the main, I suppose, are usually quite jovial people, so I don’t think they would be too negative. But if they just went, ‘No’, that would be it, that’s it.
Stakeholder 1
Anticipated barriers to recruitment
The main barriers to recruitment were thought to be gaining access to individuals and reluctance because of the time it might take. The view was that people visit a location for a purpose and once that purpose is served they want to move on:
I know the initial barrier is actually accessing them, but it’s just . . . yes . . . I mean, we also have the Box Office, now whether it would be worth, sometimes, you being in there, for a couple of hours a day, you can’t guarantee who’s going to come in, but there are a certain level of people who come in who do need to look at their weight, men, you know?
Stakeholder 1
I suppose it’s just that thing of, ‘Do I want to actually participate in that?’ so it’s just time more than anything else. It depends on what they’re being required to do . . .
Stakeholder 2
I think there’s a general reluctance, and part of that is about . . . I think people who are coming into a sports centre, particularly . . . if it’s a winter sports centre or swimming pool, a lot of time they’re going there to do their activity and go away again. Particularly at lunch times or . . . they’re doing their five-a-side football, or their badminton, and they’re coming in, they’re doing their activity, getting changed and going away.
Stakeholder 3
Again, getting them at a time where it’s going to be suitable for them, and they’re going to feel like, ‘Yes, I want to’, that might be another barrier. But, I cannot think of anything else, any other barriers.
Stakeholder 6
Being aware of the potential barriers to recruitment led some stakeholders to try to identify potential solutions. It appeared that their enthusiasm for the research encouraged them to volunteer to assist in the process, often to make the first approach to potential participants:
I would say the easiest thing to do would be to use either myself or one of the administration assistants as a medium, just if you send . . . a similar e-mail to what you had sent to me, but maybe a bit more relevant to specifically what you need from them, we could pass it on, as basically an all-staff e-mail.
Stakeholder 2
If you e-mail me one [information sheet] for him, then I could just pass the e-mail on to him, and he can have a look at it, and then he can decide and get back in touch. But I’ll tell him to get back in touch and say, yes or no, just so that you know.
Stakeholder 1
I think it would be easier for us to facilitate that, but . . . , so giving us some information and we could go and set something up, to start off . . . try and get some staff’s interest.
Stakeholder 3
Venues for intervention delivery
Stakeholders were often positive about providing rooms within their organisations for the delivery of the face-to-face component of the intervention. Some were apologetic that a lack of space meant that they were unable to provide a room:
Yes, absolutely, you could do that in a number of ways. You could either do it on a general . . . setting up some sort of stall I suppose, in a reception area, whether it be here or elsewhere, or where we’ve got particular sessions that we know are attended by a number of people within that target group, you could come along and directly speak to them there.
Stakeholder 3
Yes, you could do it in here if you want. . . . This room’s only used once a month for a meeting, so . . . As long as you tell me, just give me a phone . . . As long as they know you’re coming, that’s fine, it’s not a problem.
Stakeholder 4
[Do you have a room that we could use?] Oh, there’s no problem with that, yes.
Stakeholder 1
Availability of rooms
The willingness to provide rooms was tempered in some cases by an awareness of the practical difficulty of accessing rooms. This was not meant as a barrier, but as advice on how best to ensure that rooms would be available:
Yes, we’ve got rooms and stuff that you can book, as long as it’s booked in advance, then normally we can.
Stakeholder 6
Yes, I think in principle, yes, it’s not a problem doing that. So if you’ve got a group of people who are using the [buildings mentioned], the principle is yes it’s not a problem, I think in practice it’s about finding the space at any particular time.
Stakeholder 3
And if you’re linking in with the time they’re in, then that’s fine. If you were coming into the factory and doing it there, then I imagine you’re more likely to get the factory willing to let you come in and spend whatever amount of time with each individual, rather than them having to go some place, because you’re not taking them away for any other time.
Stakeholder 5
Discussion and implications
These interviews have identified considerable enthusiasm among stakeholders for the study. Some of the stakeholders saw it as their role to provide access to health promotion for their members/customers/employees. Others did not see it as their role but still thought that weight and alcohol consumption were problems that needed to be addressed. Not only were they willing to provide access to potential participants, many could provide rooms for delivery of the face-to-face component of the intervention. This augurs well for recruitment.
The enthusiasm for the research is more than just altruism and a general willingness to help. It derives from a shared assessment of the scale of the public health problems posed by alcohol and by obesity. Furthermore, many of the organisations that were approached identified improving the health and well-being of their staff or their client group as a core value of their institution. This raises the possibility that, if the intervention proved effective, there could be opportunities for national roll-out through organisations that have similar core values. Naturally, there may be organisational obstacles that impede the progress of roll-out; however, the findings suggest that a possible approach could begin with discussions with senior staff in order to review shared values and the potential benefits arising from the intervention. This could lead to an evaluation of how the intervention could be implemented and an assessment of obstacles that would need to be overcome. A possible attraction for senior staff could be the low cost and time commitment of the intervention.
For the present study, the interviews have identified that although there may be many potential participants at some venues, accessing them may be difficult. Perceived lack of time may be the main issue. The stakeholders thought that the men would not be annoyed by being approached, although this falls some way short of being receptive to the invitation to participate in a research study. Another potential impediment is the preference of stakeholders to act as intermediaries in recruiting their staff. This could cause reluctance among staff to volunteer, as it could imply that they are overweight and drink too much.
In summary, these interviews have identified an unexpected enthusiasm for the research. This may extend to the provision of support for recruitment and of rooms for conducting face-to-face sessions. In addition, if managed sensitively, there may be opportunities for national roll-out of an effective intervention.
Chapter 4 Designing the intervention
Background
The remit for this study included the design of an intervention that used the motivation of weight loss to promote reduced drinking. The study focused on men who were obese (BMI of > 30 kg/m2) and who drank > 21 units of alcohol per week. These men are at a 19-fold increased risk of mortality from liver disease because alcohol and obesity have a supra-additive effect on risk. 1 The rationale for the intervention is that alcohol is high in calories, and therefore reducing alcohol consumption could have a similar effect to eating less, thus reducing both risk factors at once. However, the logic of the health promotion message is complex. It takes the form of: if you take this action (drink less) then, because of this fact (alcohol is high in calories), you will get this benefit (consume fewer calories) and achieve that outcome (lose weight). The challenge is to deliver this logic in a form that is understood and that engages middle-aged men. This may be difficult, as the target group comprises men who are not seeking help, who do not think they have a drinking problem and who may well believe that they drink moderately.
The intervention was planned to involve a face-to-face session at which BMI (height and weight) would be measured and alcohol consumption would be assessed. This session would be delivered by trained laypeople (study co-ordinators). It was to be followed by a series of text messages developed using the techniques established in our previous NIHR funded studies (NIHR PHR 09/3001/09,39 NIHR PHR 11/3050/3041). Together, these components would deliver a complete strategy for behaviour change. Both components of the intervention drew heavily on the elements of effective brief alcohol interventions described in systematic reviews34,68 and a review of reviews. 35
The intervention was to be based on the causal model for behaviour change specified in the protocol, with modifications made in light of the findings from the focus groups. The initial causal model for behaviour change was (1) generate interest in the study, (2) increase awareness of consumption levels that are defined as harmful, (3) identify motivational beliefs, (4) increase awareness of susceptibility to alcohol-related harm for men who are already obese, (5) increase motivation to lose weight by reducing alcohol consumption, (6) alter alcohol expectancies, (7) gain commitment to change, (8) develop goals, action plans and coping plans, (9) increase refusal skills, (10) implement strategies to prevent relapse and (11) reduce total alcohol consumption, which would in turn lead to weight loss.
This chapter describes the rationale for the activities, discussions and behaviour change techniques that were incorporated into the face-to-face session and the subsequent series of text messages. Initially, several questions were identified:
-
How should the causal model be modified by the focus group findings?
-
How should the intervention be divided between the face-to-face session and the text messages?
-
To what extent should the content of the text messages reinforce the face-to-face session?
Separate issues for the face-to-face session were how best to use the measurements of BMI and alcohol consumption in the intervention and what constraints would be imposed by the use of laypeople (study co-ordinators) to deliver the intervention. A further concern was how to design the intervention to overcome potential barriers to engagement and behaviour change.
Implications of the focus group analyses
The focus group analyses identified several opportunities to increase motivation to drink less. These included feedback of data on alcohol consumption, increasing the perceived relevance and importance of the benefits of reducing alcohol consumption, highlighting the benefits of weight loss, and feedback of data on calories consumed through alcohol. Feedback of data on alcohol consumption is a common component of alcohol brief interventions. 34,68 The focus groups confirmed that men in the target group (i.e. men who are overweight and regularly consume alcohol) are often surprised by how much alcohol they drink. As few men monitored their alcohol consumption, there could be value in encouraging this to provide motivation to drink less and to sustain reduced consumption. However, men also felt that the potentially detrimental effect on their social life would make them reluctant to drink less. This issue will need to be handled sensitively in the intervention. One approach would be to draw attention to the many social benefits of drinking less that the focus groups identified, such as improved relationships with family and friends.
The focus groups also confirmed that being overweight is recognised as a major problem, because of its adverse impact on self-image and on ability to carry out everyday activities. This is consistent with the findings of a recent NIHR HTA systematic review. 18 However, the focus groups also showed that the key issue was the so-called ‘beer belly’, as this caused embarrassment and made physical activities difficult. Engaging men with the benefits of losing this unsightly protuberance is a specific target for the intervention that could increase motivation to lose weight. Given that men volunteered no disadvantages of losing weight, suggestions of easily implemented techniques to lose this ‘beer belly’ should be well received.
A key finding from the focus groups was that men were aware that alcohol was associated with increased snacking. This effect of alcohol is well established in the literature,55–57 but it was unclear whether or not the men in this study would know about it. The finding that, when prompted, men agreed that they do eat more snacks when drinking could be used to increase motivation for reducing alcohol consumption. Thus, men would experience the dual benefits of reduced calorie consumption from both alcohol and food.
The focus groups confirmed that measuring alcohol consumption could provide useful data for behaviour change. The surprise expressed by men at their consumption could lead to a discussion of the benefits of changing behaviour. The measurements could easily be arranged in a sequence following the logic of the intervention. Initially, feedback on alcohol consumption could be used to develop a discussion of the benefits of drinking less, increasing motivation to reduce consumption. BMI could then be measured, leading to a discussion of the disadvantages of being overweight thereby increasing motivation to lose weight. Finally, the calories contained in alcohol could be calculated, personalising this by using the participant’s alcohol consumption. This could be supported by reviewing the ways in which alcohol stimulates appetite and leads to increased consumption of energy dense foods. Overall, the approach dissects the logic of the behaviour change strategy, illustrating each component with personal data and building simple steps into the complex argument. Crucially, motivation for action on each component should be gained before the next component is addressed.
The focus groups also provided approximate timings for making and discussing the measurements of alcohol consumption (10 minutes), calculating units in alcohol (5 minutes) and calories in alcohol (5 minutes).
The face-to-face session
The literature and the focus group findings identified ways in which measurements of alcohol consumption and BMI could be used to increase motivation to lose weight. As these measurements would be made in the face-to-face session, the most advantage would be gained by exploiting them as the data were obtained. Whether or not this session could also cover volitional components such as goal-setting and action planning would depend on the time available. The session was designed in a pragmatic way by exploring what could consistently be achieved for all participants.
The session had to be brief to be acceptable to participants who perceive that they have limited free time. 17 In the absence of direct information on what constituted brief, the arbitrary decision was taken to work initially with a 30-minute duration, although the exact length could subsequently be modified. Within this time, height and weight had to be measured, and the TLFB58 and baseline questionnaire had to be completed.
The other components of acceptability are the style and content of the session. Previous intervention studies have found that men appreciate a friendly, relaxed and non-directive approach20 and being given easily understood information. 18 The use of laypeople, who are likely to have an informal rather than professional style, could help achieve this.
A starting assumption was that participants will vary in their readiness to reduce their alcohol consumption. Thus, the intervention has to be appropriate for men who initially have no intention to change as well as those who are currently thinking about drinking less. The alternative would be to design a series of interventions tailored to individual motivation to change. This would create considerable logistical difficulties, as participants would have to be screened and stratified prior to intervention delivery and laypeople would have to be trained to deliver different versions of the intervention. The principle of having an intervention that could easily be rolled out nationally also militates against this approach.
Another constraint was that the face-to-face session component has to be delivered by laypeople. Although training would be given, there is a limit to the demands that can be placed on laypeople. The intention was to use some techniques from motivational interviewing (MI), but full training in MI would not be possible. The question then became how much training would they need to be able to deliver what could be covered in a reasonable time in the session. This was answered by reviewing how the alcohol and BMI measurements would be made and how they would be exploited.
Using participant data on alcohol consumption
The proposed method of measuring alcohol consumption was the TLFB. 58 Men could enter their alcohol consumption over the previous 28 days on a prepared calendar. They could then select a typical drinking week and, with help from the study co-ordinator, count the units consumed. This was intended to increase ownership of the result and preclude rejection on the grounds that the week was unusual. To do the calculation, a simple look-up table of units in common drinks could be provided. Any response to the total units consumed could be used to discuss feelings about current consumption and good and bad aspects of alcohol consumption, helping build motivation to change.
Using body mass index and weight loss
The decision to avoid the term obesity was taken at an early stage because the literature clearly shows that people do not like to be classified as ‘obese’. 16,27–29 Instead the term ‘very overweight’ was used. It was important to convey that the men had a BMI that placed them at the extreme end of the overweight spectrum. If the men could gain ownership of their high BMI by being involved in its calculation, this could form a useful part of the behaviour change strategy. To simplify the process, and to provide a visual representation of each man’s BMI, a graded height and weight chart from NHS Choices was used (with permission) (www.nhs.uk/livewell/loseweight/pages/height-weight-chart.aspx). 69 This plotted height against weight using brightly shaded bands to represent normal weight (yellow), overweight (orange), obese (dark orange) and very obese (red). The terms obese and very obese were replaced on the chart with a single label very overweight. Asking participants to plot their own height and weight on the chart allowed a discussion of reactions to being in the very overweight category and of the disadvantages of being so overweight.
Extending the use of the alcohol data
Alcohol is second only to fat in the calories it contains (7 calories per gram). As the units of alcohol consumed in a typical week would have already been obtained, there would be opportunity to calculate the calories in those units. Again, a simple look-up table of calories in common drinks could be provided. The focus groups showed that men were surprised by the calories they were consuming through alcohol. As well as highlighting the contribution of alcohol to weight gain, the calculation could provide the opportunity to explore other ways in which drinking leads to increased calorie consumption (e.g. through snacking and the use of drink mixers containing sugar).
Using interviewing skills from motivational interviewing
The tasks in the face-to-face session follow a common pattern: encouraging men to engage in an activity, developing a discussion around what men felt about the measurements and guiding them to reflect on the benefits of drinking less and/or losing weight. Performing these tasks would require the core interviewing skills from MI. They are identified by the acronym OARS: open questions, affirmation, reflective listening and summarising. 70 Open questions help to reassure participants and build their trust in the relationship. They also encourage participants to talk about themselves and to begin thinking about their behaviour. Affirmations are statements that recognise the participant’s achievements, increasing their confidence in their ability to change their lives. Reflective listening involves paraphrasing what the participant has said, to demonstrate that their views are being listened to. Reflections on the benefits of behaviour change can increase motivation to change. Summarising is a form of reflective listening that is particularly useful at transition points. In this study, it would be useful when moving from one activity to the next, for example when moving from discussing alcohol to measuring height and weight. It could also be used when closing the session.
Review of the session
The foregoing review clarified the ways in which the measurements of alcohol consumption and BMI could be used to increase motivation to lose weight and drink less. The outstanding issue was whether or not the session should be extended to cover volitional processes. This was decided by the available time. The session was intended to be brief, and so around 30 minutes was decided upon as an appropriate session length. Taking the measurements, doing the calculations and developing motivation to drink less and lose weight could take most if not all of this time. The focus groups showed that the measurements alone were likely to take about 15 minutes. The initial greeting and the closing of the session, together with the other discussions, would most likely occupy the remaining time. Thus, the decision was taken to restrict the session to increasing motivation to reduce drinking, allowing the subsequent text messages to complete the behaviour change process. Although it might have been possible to incorporate other components, such as goal-setting and action planning, this would not have been without risk. Covering a larger number of topics would mean that the time spent on each would be reduced. This could lead to a session that was hurried rather than relaxed, with limited time to explore motivational factors. Without sufficient motivation, the value of the extra topics might not be realised. Furthermore, if participants felt overwhelmed or rushed into decision-making, their motivation to change could be reduced. 71 Finally, the demands placed on the laypeople would be increased, possibly reducing both job satisfaction and the fidelity of delivery of the intervention.
Two potential levers for behaviour change were not included in the face-to-face session. First, information on the harms of drinking too much or of being very overweight was not mentioned unless asked for by the participant. This is consistent with our MI-based approach, and presenting information on risk could be counterproductive if unaccompanied by guidance on how to reduce that risk. Second, a comparison of the calorie content of specific foods (e.g. a hamburger) with that of alcoholic drinks was not presented. The focus groups found that men view such information as an invitation to substitute rather than reduce calories, for example ‘I won’t have the crisps so I can have another pint’, or taking it even further: ‘I don’t eat crisps so I can have a pint’.
Aims of the face-to-face session
The assessment of the opportunities and constraints of the face-to-face session has indicated that it should focus on increasing motivation (to reduce alcohol consumption and to lose weight). Furthermore, at the end of the session men should feel well disposed to the study so that they will be receptive to the text messages following the face-to-face session.
The specific objectives were to assist the participant in realising that:
-
he drinks more than he realises
-
he is very overweight
-
his drinking contributes to his being overweight
-
being overweight could affect his health
-
losing weight could bring him personal and social benefits.
The text messages
Background
A series of text messages was to be delivered by mobile phone over a 2-month period. Text message interventions are commonly used to modify other adverse health behaviours72,73 and to increase health-care uptake. 74,75 Recent systematic reviews have shown that text messages can successfully change behaviour. 76–78 This type of intervention is particularly well suited to middle-aged men because their ownership of mobile phones is high. 79
The behaviour change strategy was based on the Health Action Process Approach (HAPA). 80 The HAPA was chosen because it is supported by evidence and provides a useful framework to integrate effective behaviour change techniques and guide decisions on the sequences in which these techniques are delivered. The strategy also used techniques shown to be effective with obese adults. 81
A series of interactive text messages were designed using the successful approach developed for our NIHR PHR funded feasibility study (NIHR PHR 09/3001/09)39 and its subsequent RCT (NIHR PHR 11/3050/30). 41 In particular, the texts employed many of the devices used successfully to promote engagement with the intervention such as tailoring messages to the target group, use of humour, informal text style, questions to promote interactivity and sensitive timing of messages. Findings from the focus group analyses, particularly the dislike of protruding stomachs and the perceived benefits of drinking less and of losing weight, were incorporated into the texts.
The text messages were designed to reinforce the content of the face-to-face intervention and to extend the behaviour change strategy. The logical sequence of the text messages to encourage men to drink less is shown in Box 2. The early texts sought to establish rapport with the participants and increase motivation to drink less. Subsequent texts encouraged participants to set realistic goals to reduce consumption, implement a plan of action, monitor drinking behaviour, identify barriers and construct strategies to deal with these barriers. Texts would increase self-efficacy for maintenance of reduced drinking and participants would be encouraged to develop strategies for relapse prevention. 80 This interactive intervention delivered over an extended period is designed to encourage sustained behaviour change.
-
Friendly welcome and introduction.
-
Plant idea of drinking too much.
-
Illustrate contribution of alcohol to weight gain.
-
Increase motivation to lose weight.
-
Increase salience of the adverse effects of obesity.
-
-
Increase motivation to reduce drinking.
-
Salience of alcohol as cause of obesity.
-
-
Set goal for alcohol reduction.
-
Encourage action plans.
-
Increase action self-efficacy.
-
Empathise with lapses.
-
Increase recovery self-efficacy.
-
Positive reinforcement of success.
Promoting interactivity is a major feature of the intervention. Our previous research showed that when prompted, men respond enthusiastically and often give well-thought-out answers. 82 These answers can give insight into the impact of components of the behaviour change strategy. In this study, prompts and questions were used to elicit responses at all of the key steps in the strategy, particularly awareness of harms, benefits of reducing consumption, goal-setting, action planning, self-efficacy for change and relapse prevention.
The use of narrative
A narrative structure was used to provide coherence to the text messages and to illustrate the process of behaviour change. There are several advantages of using narrative. Information presented in a narrative format has more effect on knowledge, attitudes and intentions than the same information presented in a non-narrative format. 83 Narrative is particularly useful for changing perceived social norms and behavioural intentions. 84 It can ‘strengthen existing prosocial beliefs and behaviours as well as counteract unhealthy ones’. 85 Resistance to behaviour change is overcome because individuals are engaged with the narrative. 86
To be effective on behaviour change, the narrative and the characters in it have to engage the reader, a process which can be aided by making the protagonists culturally similar to the target audience. 87,88 The narrative also has to be plausible and internally consistent. 89 The depiction of a character who succeeds against the odds can boost motivation for personal goals. 90
A major benefit of the use of narrative is that characters can model the stages in the journey to behaviour change. For example, action planning to reduce alcohol consumption should specify when a new behaviour will be adopted, where it will be carried out and how it will be achieved. This was described in a text message, then illustrated in a subsequent message by a character going through the process of identifying the where, when and how. Similarly, relapse prevention was addressed in another text message. This allowed a character to explain why he had relapsed and why he was now determined to keep to his original plan to reduce his drinking. By creating sympathetic characters and fostering engagement with the narrative, this illustrative device may encourage participants to take active steps towards behaviour change.
The process of writing the text messages
The development of the text messages followed the four stages shown in Figure 1: (1) establishing the provisional structure, (2) drafting the text messages, (3) review and revision and (4) piloting and final revision. It began with an exposition of the behaviour change strategy, the construction of a narrative to depict the process of behaviour change and the creation of characters to give life to the narrative. This established a provisional structure within which the text messages could be written. In practice, there was much iteration in the writing process, with modifications made to the narrative, the characters and the texts as the structure and content of individual text messages was developed.
FIGURE 1.
Stages in the writing of the text messages.
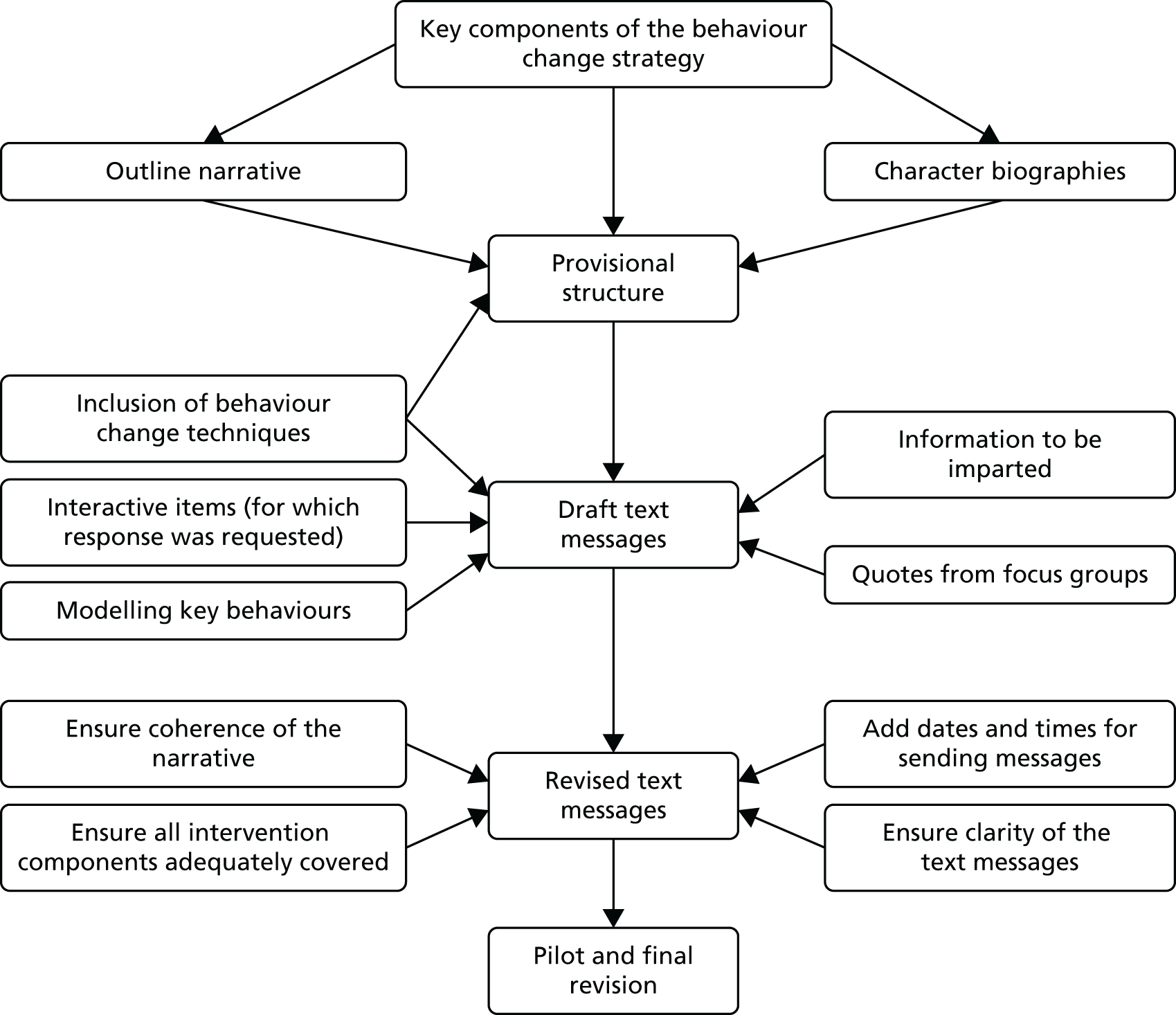
Establishing the provisional structure
The basis of the behaviour change strategy was the HAPA,80 a comprehensive model that allows integration of a range of evidence-based behaviour techniques. As with existing theories, the HAPA addresses pre-intentional motivational processes that lead to behavioural intentions. This model suggests the adoption, initiation, and maintenance of new health behaviour occurs as a process involving a motivational phase and a volitional phase. The volitional phase includes planning, action, and maintenance. Perceived self-efficacy has a crucial role in achieving success in all of the stages. The strategy also used successful approaches to changing health behaviours informed by recent systematic reviews34,35 and taxonomies of behaviour change techniques36,37 including a taxonomy specifically for interventions to reduce excessive alcohol consumption. 38 The intervention drew on experience from our NIHR feasibility study39 on ways to embed theory and behaviour change techniques into intervention design and delivery.
In this study, the narrative is relayed through the lead character and features several minor characters. The characters are diverse in socioeconomic status and amount of alcohol consumption. The linking theme is the five-a-side football team for which most characters used to play and some still do. This allows motivational themes to be developed, specifically:
-
awareness
-
of drinking heavily
-
of the calories in alcohol
-
of snacking when drinking
-
-
the discrepancy between desired and actual fitness, specifically being overweight
-
the contrast between fitness when young and present fitness
-
the contrast between the energy of the lead character’s children and his own fitness
-
the adverse impact of drinking and obesity on close personal relationships, particularly partner and children
-
the benefits of drinking less on fitness, personal relationships and finances
-
the importance of friendship and social support in behaviour change.
The narrative charts the journey of the central character (Mark) from the realisation that he is drinking heavily and is obese through his attempts to reduce his drinking, and culminates in his successful weight loss. It illustrates Mark’s growing realisation that his drinking is adversely affecting both his personal well-being and that of his family. This leads to a commitment to change in which the processes of goal-setting and action planning are modelled. In the interest of realism and relatability, Mark experiences relapses that are used to affirm commitment to goals and to model the development of relapse prevention strategies. The story concludes with Mark achieving his goal and enjoying the benefits of reduced alcohol consumption. Alongside this narrative, the minor characters highlight the adverse effects of heavy drinking and provide models of goal-setting and action planning.
Creating the text messages
The journey of the main character followed the sequence of behaviour change outlined in the HAPA. 80 Rendering this journey in text messages involved identifying the stages the character would progress through, for example, the attitudinal changes to be achieved, the key skills that were required to reduce alcohol consumption and the major barriers to behaviour change that had to be overcome. This was supported by exploring the information on alcohol and calories that would be needed. Pithy quotations from the focus groups were incorporated into the texts to illustrate stages of the behaviour change process. Texts were also written to allow characters to model behaviour change activities. Finally, some texts were written to ask questions that prompted responses. The resulting text messages were mapped onto the outline narrative, and identified which characters should be involved. The narrative and the character biographies were modified to enable all of the points to be covered.
Limiting the content of texts to a single message (160 characters) was often challenging. Scene setting and character development often required extended description. Initial drafts of texts often required more than 160 characters, for example a clear description of how to calculate BMI and the interactive texts that presented multiple-choice questions. To cope with this, long words were replaced by short ones and characters were given short names. Some components were delivered using a sequence of texts sent a few minutes apart; for example, for setting goals, the first text clarified the value of goals, the second explained the attributes of a strong goal and the third used a character to illustrate the process of setting of a goal.
The joint demands of covering the detailed behaviour change strategy, creating multifaceted characters and conveying the narrative would have required a large number of texts. Given the time period of 2 months specified in the protocol, not all items could be covered in as much detail as we might have wanted. Thus, the narrative was scaled back and the number of characters was reduced, transferring key attributes of excluded characters to retained ones. The amount of background information about alcohol and calories was also reduced. Finally, although the full behaviour change sequence was preserved, the extent of repetition and reinforcement was reduced. Extending the duration and number of text messages is recommended for the full RCT.
The first complete draft of the text messages was reviewed by the research team to check for coverage of essential behaviour change components. They also checked that the narrative was coherent, plausible and sufficiently interesting to retain attention. The input of individuals who had not been involved in the creation of the text messages was important. The language used was also assessed for suitability for the target group. As a result of this input, the narrative and the text messages were again modified. Finally, the text messages were piloted by asking user group representatives and the intervention group study co-ordinators to comment on printed versions of the text messages. This identified a few instances of lack of clarity and clumsy phrasing, which were subsequently improved.
Delivery of the interventions
The intervention was designed to be delivered by a face-to-face session followed by a series of text messages. The process of recruiting and training laypeople to deliver the face-to-face session is described in Chapter 6.
The text messages
Short Message Service text messages were sent by an automated computer system that was programmed to send text messages to mobile phones in a predetermined sequence. The system that proved to be successful for our NIHR-funded feasibility study39 was used with appropriate modifications. The exchange of text messages with the participants was via a secure server based within the Health Informatics Centre at the University of Dundee. Messages delivered to the participants appeared to originate from the project’s mobile phone, but the message content and participant’s address were assembled on the secure server and routed via the Joint Information Systems Committee funded Joint Academic Network to a UK-based mobile network service provider and thereby to the clients. All replies from the participants followed the reverse path. A commercial company, Textlocal (www.textlocal.com), provided the simplest solution compatible with providing effective communication between the participants and the project team.
The design and operation of the system to send the text messages was the responsibility of an experienced programmer and collaborator (CJ). To run, the system had to be supplied with the participant’s first name (or preferred name), mobile phone number and the start date for the sending of the messages. The start date was the first Monday after the participant had received the face-to-face intervention session.
The text delivery system allows for personalisation of messages. Placeholder types are defined that relate to the participants name, researcher contact and character names. The text service algorithm replaces any placeholders within the messages with the predefined fields at the point of sending. In this scenario based project, to avoid confusion between the participant’s name and the character names, alternative character names were also predefined and were adopted where there was a match with the participant’s name.
Monitoring delivery
Provision was made for monitoring the delivery of text messages, to identify possible interruptions in the service. The system sent out a daily status notification to alert the programmer to issues with the delivery of messages. Initial piloting identified most problems, such as the unexpected effects of the apostrophe. It was a special command character which caused problems for the delivery system.
Remote monitoring was also in place for undelivered messages. Rules were applied to the system to identify when five consecutive messages to a participant were recorded as undelivered. The research team were given access to the names of these participants, so that they could to contact them by another method (e-mail, landline or letter) to resolve the problem.
Monitoring replies
Responses were monitored on a daily basis for several reasons. Participants had been informed of their right to withdraw from the study and could do so at any time. Participants were also asked to notify the study team of a change to their phone number. In addition, many of the text messages prompted the participants to reply. Previous experience had also shown that a few participants report being in some distress or may request further support. All replies that raised concern were reviewed by the research team so that appropriate action could be taken. The replies were de-anonymised where necessary. A full audit of messages that were de-anonymised and the actions taken was stored.
Conclusions
A comprehensive and coherent behaviour change intervention was successfully developed. This required an explication of the theoretical processes of behaviour change, combined with a careful review of the opportunities and constraints of the study design and the modes of intervention delivery. The intervention followed the remit set by NIHR HTA, which provided a powerful underlying logic to behaviour change. The use of text messages enabled reinforcement of components of the face-to-face session.
The description of the intervention follows the Template for Intervention Description and Replication (TIDieR) checklist and guide items for the reporting of interventions. 91 Two items from the TIDieR checklist that are not presented here are covered in other chapters; see Chapter 6 for the training of the intervention provider and Chapters 9–11 for fidelity of delivery of the intervention.
The creation of the intervention was a lengthy process that required input from several members of the research team. The key to the design of the face-to-face session was the measurement of BMI (height and weight) and alcohol consumption. These will be the primary outcomes for the full RCT, so a function of the feasibility study was to ensure that participants were happy for the measurements to be taken and that both BMI and alcohol consumption could be accurately measured. They also provided personal data that could be fed back to participants, a key feature of many behaviour change interventions. 36,37 This provided the opportunity to develop discussions to increase motivation to change.
Text messages can offer several advantages. Modelling of behaviour change techniques by characters offers a potentially powerful method of reducing alcohol consumption. Direct quotations from focus groups provide concise, authentic phrases that convey lived experiences. It would be difficult to obtain this verisimilitude unless a highly skilled professional writer were employed. A longer narrative over 3–4 months might have been preferable. This would allow more development of the narrative and would provide additional time to deal more fully with relapse, recovery and maintenance of the new behaviour. The longer time frame would also give more opportunities for interactive texts. Nonetheless, despite this reservation the intervention delivers a detailed behaviour change strategy in an easily accessible format with content that has been carefully tailored for the target group.
Chapter 5 The control package
Introduction
The remit for this study required that the control group be given a conventional alcohol brief intervention. The one selected was from the Screening and Intervention Programme for Sensible drinking (SIPS)92 funded by the Department of Health. This programme tested three levels of intervention: a participant information leaflet, a brief advice session and an extended intervention involving lifestyle counselling. These interventions were tested in three linked studies: one conducted in primary care,93 one conducted in emergency departments94 and one conducted in a criminal justice setting. 95
The present study used the mid-level brief advice session, as it provides an attractive comparator containing the components of a conventional alcohol brief intervention. The SIPS website92 provides an outline of the brief advice session together with the materials used to train staff to deliver the session. These comprise the Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) slides that describe the aims of the session, a brief advice tool and a video demonstrating how to use the brief advice tool. Permission to use the SIPS materials was kindly granted by Professor C Drummond.
The SIPS brief advice session
The SIPS brief advice session involved giving participants feedback on their drinking. This was followed by a 5-minute session of structured advice using a brief advice tool as a prompt. An initial version was developed for the World Health Organization collaborative study on alcohol screening and brief intervention. 96,97 The version used in the SIPS trials93–95 is available on their website. 98 The revised tool presented the components of a conventional brief alcohol intervention in five diagrams and tables. It gave details of the health and social consequences of hazardous drinking, compared the participants’ alcohol consumption to that of the general population and identified the benefits of reduced drinking. Participants were then encouraged to make a plan to reduce their consumption and set a target for achieving the plan.
At the end of the brief advice session participants were given a 16-page participant information leaflet. 99 This gives information on the units of alcohol in common drinks and presents recommended drinking levels. It describes the short- and long-term risks of exceeding the recommended limits, including the social and psychological consequences of alcohol misuse. It invites readers to complete a quiz to identify whether or not they are drinking too much and gives guidance on how to seek help.
Training for the SIPS brief intervention
In the SIPS trials those delivering the brief advice (professional staff in health care and criminal justice) received a 1-hour training session. This showed them how to deliver the brief advice session in 5 minutes following a standard protocol using the structured advice tool as a prompt. Those delivering the intervention then engaged in a role play session delivering the intervention to a coworker. This was followed by feedback from the trainer.
Training for the control package in this study
This feasibility study planned to use laypeople (study co-ordinators) to deliver the face-to-face session. Furthermore, the session involved more than delivering the intervention; the baseline questionnaires had to be administered, and height and weight had to be measured. Thus, the training was extended to three 2-hour sessions followed by an assessment session and two pilot sessions with men from the target group. The training sessions comprised short, interactive lectures followed by supervised activities and role play with supportive feedback. The first session covered the background to the study, the completion of the questionnaires and the measurement of height and weight. The second session introduced the SIPS brief advice tool, demonstrated its use and allowed candidates to practice delivering it to each other. The final session allowed candidates to run through all the components of the control package. A full description of the design of the training is can be found in Chapter 6, Recruitment and training of the study co-ordinators.
Conclusions
The well-established SIPS alcohol brief intervention formed an ideal active control for this study. The availability of the SIPS training materials greatly aided the development of the training programme. The training for this study was longer than that given in the SIPS because of the additional demand made by this study.
Chapter 6 Recruitment and training of the study co-ordinators
Introduction
Study co-ordinators, trained laypeople, were used to deliver the face-to-face component of the intervention. The decision was based on two considerations: (1) engagement with the intervention and (2) implementation should the intervention prove to be effective. The study was conducted in the community and recruited men who were likely to think that their alcohol consumption was normal and did not cause them problems. Using authority figures such as experienced researchers could make it difficult to build rapport with the participants. In contrast, laypeople may be perceived as less intimidating by participants, leading to more engagement with the intervention. The other benefit is the potential for roll-out of the intervention, if it proves effective. If laypeople can be trained to deliver the intervention with high fidelity, this would be a low cost method for its widespread delivery.
This chapter describes the processes by which the laypeople (study co-ordinators) were identified, selected and trained. An overview of these processes is shown in Figure 2. The details of the methods used, and the rationale behind them, will enable replication elsewhere. In addition to this report, detailed manuals of study methods were produced. These manuals were provided to the study co-ordinators to aid intervention delivery. The manuals were given out and used during the training sessions.
FIGURE 2.
Overview of the recruitment of the study co-ordinators.

Recruitment strategy
The recruitment was designed to identify individuals with the aptitude for delivering an intervention that addressed potentially sensitive subjects (alcohol and obesity) in an empathic and supportive manner. The recruitment strategy comprised three stages:
-
clarifying the key characteristics and skills that were required
-
identifying the locations at which recruitment efforts could be focused
-
developing an extended selection process to identify individuals with key attributes.
Key characteristics
The role of the study co-ordinator was to put participants at ease; to measure alcohol consumption, height and weight; and to deliver the intervention or control package with high fidelity. Several essential characteristics were identified for use in selection of suitable individuals. These characteristics included fluency in English, previous experience of working with people, and excellent communication, organisation and interpersonal skills such as friendliness and approachability.
Recruitment
The recruitment strategy was developed from the methods established in a previous study (Dimova E, Swanson V, Melson A, Fraser T, Crombie I, McMahon S, Barbour R, Rice P, Irvine L. University of Dundee, 2017) and combined marketing approaches with direct contact with potential candidates. It targeted individuals who would have sufficient free time, particularly volunteers and part-time workers. Posters were placed at selected venues such as community centres, gyms, charity shops, job centres, libraries, supermarkets, sports centres and bus and train stations. The posts were also advertised on the intranets of the NHS and local universities. Direct contact was made with individuals attending sports centres, gyms and community centres as well as with charity shop workers.
All the marketing approaches provided an e-mail address and a telephone number to contact to obtain further information about the post and a copy of the application form. Completion of the form involved answering open questions to permit assessment of the quality of written English. It could be returned by either e-mail or post.
Selection
Three stages of selection were carried out: (1) assessment of the application form, (2) assessment at interview and (3) assessment during the training. Although six study co-ordinator posts were to be filled, twice that number were trained. Candidates were told that there would be a selection process at the end of the training. This enabled selection of the most able candidates and allowed for dropouts during selection and training. The selection criteria at each of the three stages are shown in Table 5. Briefly, the application form assessed motivation for applying, prior experience and communication skills. Individuals with previous experience of MI or behaviour change techniques were excluded. The feasibility study aimed to assess whether or not people with no previous experience could be trained to deliver a behaviour change intervention with high fidelity. The interview assessed the same items as the application stage, exploring them in greater detail. Applicants were asked how they would cope with challenging situations such as an unresponsive participant or an angry participant, and how they would manage conflicting priorities. To compensate them for their time all candidates were paid for attendance at training. Finally, at the end of the training period, candidates were assessed on their skills at delivering either the intervention or control package in role play, with the researchers acting as difficult participants.
| Selection criteria | Recruitment stages | ||
|---|---|---|---|
| Shortlisting | Individual interview | Extended training | |
| Fluent English | ✓ | ✓ | |
| Experience working with people | ✓ | ||
| Friendly and approachable | ✓ | ✓ | |
| Empathic | ✓ | ✓ | |
| Non-judgemental | ✓ | ✓ | ✓ |
| Available to attend training sessions | ✓ | ||
| Available over period of intervention | ✓ | ||
| No previous MI training | ✓ | ||
| No previous behaviour change experience | ✓ | ||
| Motivation to apply consistent with study ethos | ✓ | ✓ | |
| Communication skills | ✓ | ✓ | ✓ |
| Organisational skills | ✓ | ✓ | |
| Interpersonal skills | ✓ | ✓ | |
| Ability to stick to a brief | ✓ | ||
Randomisation of study co-ordinators
To prevent contamination of the control package by the intervention one and vice versa, co-ordinators were assigned to deliver either the intervention or the control package. The two groups were trained separately to ensure they were blind to treatment status (intervention or control). To achieve balance between co-ordinator characteristics in the two arms of the study, a formal randomisation process was used. The research team assessed individuals by age and sex, constructing matched pairs of co-ordinators. One member of each pair was then randomly assigned to one study arm, and the other assigned to the remaining arm. Randomisation occurred after the interview stage, at which point 12 candidates were selected for training, with equal numbers assigned to the intervention and control groups.
Training
The training was designed following a review of the tasks that the study co-ordinators had to perform. It took the form of short presentations followed by practical activities, role play and discussion sessions. The presentations explained the purpose behind each task and identified the knowledge and skills that would be required to perform it. The practical activities and role play gave the co-ordinators experience in carrying out the tasks, including coping with problems that might be encountered in practice. The subsequent discussions picked up on problems identified during role play and reviewed strategies that could be used to overcome them. The training focused on the tasks that had to be completed during the face-to-face session. Each component of the session was carefully reviewed to identify the knowledge and skills required to perform it.
The training was conducted in a relaxed atmosphere to encourage the candidates to ask questions and/or make comments at any point. All of the training sessions were attended by at least three members of the research team, who acted as participants in role play. After a welcome and introductions, candidates were invited to help themselves to coffee and sandwiches. Training began with an overview of the study aims and methods, identifying the key contribution of the study co-ordinators. It was conducted at a moderate pace in case candidates were not used to an educational environment. No pre-course reading was required, as many applicants had full-time jobs or other commitments, and it would have been unreasonable to expect them to spend much time reading the study documentation.
The training for both intervention and control study co-ordinators covered completion of a TLFB58 calendar of alcohol consumption, a baseline questionnaire (see Appendix 2) and the measurement of height and weight. The baseline questionnaire was to be self-completed by participants, and the study co-ordinators were trained to check for completeness and to probe for details about the brand of drink and the volume consumed. This was essential because many beers, lagers and spirits come in differing strengths and volumes. During the training sessions, study co-ordinators practised completing the questionnaire and checked pre-prepared poorly completed questionnaires. The training also allowed study co-ordinators to practise measuring height and weight, and provided them with advice from the research team on improving their technique.
The co-ordinators were encouraged to greet participants warmly, to thank them for attending and to conduct the session in a relaxed and friendly manner. They were encouraged to ensure that all of the information provided was understood and to respond fully to all questions asked.
Intervention study co-ordinators
The intervention co-ordinators attended four training sessions plus an assessment session at which the best-performing individuals were selected to deliver the intervention. The first session provided the study overview and gave experience in questionnaire completion, calculation of units and calories in alcohol and measuring height and weight. The second session was delivered by a psychologist trained in MI. It covered the core interviewing skills from MI, identified by the acronym OARS: open questions, affirmation, reflective listening and summarising. 70 The lecture describing these skills was followed by a demonstration of the techniques by two of the research team through role playing. The study co-ordinators then practised these techniques through role play with research team members (who used scenarios of compliant and difficult participants). The role play covered discussions of units of alcohol consumed, the plotting of height and weight on the NHS Choices BMI chart and discussion of calories in alcohol. The third session provided additional practice at taking all the required measurements and in fostering discussions with participants (role-playing researchers). The study co-ordinators’ manual for the intervention group was also given out. The final session also used role playing researchers to allow candidates to run through all aspects of the face-to-face session. Individual and group feedback was provided on all the activities carried out, and each session concluded with a review of the topics covered and the lessons learned.
Control study co-ordinators
The control group study co-ordinators attended three training sessions plus an assessment session. They were trained to deliver the established SIPS brief intervention. 93 The training for this was based on the training materials supplied by the SIPS team on their website. 98 The SIPS brief intervention is based on a leaflet that presents the components of a conventional brief intervention in five diagrams and tables. These were designed to require only a simple description by researchers and to be easily understood by participants. The leaflet includes (1) a table that indicates the risks from hazardous and harmful drinking, (2) a graph to show that the participant’s drinking places him at a higher risk of alcohol related harm than most people, (3) a list of the benefits of reduced drinking, (4) targets that the participants can aim for and (5) how to make a plan to reduce drinking.
As with the intervention study co-ordinators’ training, the first control session provided the study overview, and gave experience in completing the alcohol and demographic questionnaires and in measuring height and weight. The second session covered the sections of the SIPS leaflet. A presentation describing the contents of the leaflet was followed by a demonstration of how to deliver the brief intervention by two role-playing research staff. The study co-ordinators then practised delivering the intervention in role play. The final session gave practice in welcoming participants, running through the session activities and closing the meeting with participants. The control co-ordinators were given the study co-ordinators’ manual for the control group.
Preparation of the study co-ordinators’ manuals
Separate manuals were written to assist in the delivery of the intervention and control sessions. The manuals were prepared by creating an initial list of the tasks that were to be performed. These manuals were intended to be used during the sessions and had to be concise and user friendly. To achieve this, the manuals were laid out in short sections, one for each task, with numbered headings. Technical terms were avoided. Guidance on each task was written in the active voice, for example ‘ask for the participant’s permission to record the session’. Bullet lists were used when several items were needed for a task, and for complex tasks that involved a sequence of active voice statements. For those tasks for which participants would need some explanation, example scripts were given in text boxes. To enable the study co-ordinators to deal with unexpected events and to cope with questions from participants, a ‘What If?’ section provided guidance on how to respond.
A lone worker’s policy (see Appendix 3) was included in the manual. This explained why adherence to the policy was important and presented a flow diagram of the steps involved. Separate guidance, in numbered sections, gave the information necessary to carry out each step. All study materials, including questionnaires and participant information sheets, were also included. The manuals will be available from the corresponding author under terms of confidentiality.
Post-training evaluation
At the end of training all those attending (n = 9) completed a short questionnaire evaluating the components of the training (see Appendix 4). All attendees reported that the number of sessions and the pace of the sessions was just right. The following quotation is reflective of the responses:
Pace was good. Given enough time to take everything in.
Study co-ordinator 2
The content of the sessions was also thought to be about right, although one respondent thought that the addition of a short video would be helpful. The role play was particularly valued by all participants:
Always useful, allows errors to come out in a safe environment.
Study co-ordinator 1
The manual that was written to support the delivery of the control brief intervention was thought to contain all the necessary information and guidance and to be clearly presented. The examples provided in the manual of how to phrase introductions to sections and interpretation of data were also commended. One candidate suggested providing a checklist of activities for the face-to-face session, as it would provide a useful aide memoire. This was prepared and subsequently used in the delivery of sessions. In response to a question asking if the candidates had any additional comments the respondents expressed considerable support for the training: ‘it was a fabulous experience’ and ‘excellent training’.
Selection, distribution of study materials and piloting
Selection of the best candidates took place after an assessment session in which each study co-ordinator delivered the whole face-to-face session to a role-playing researcher. The choice of the most able co-ordinators was made by the research team, utilising notes from the training sessions as well as feedback from the assessment session. The six successful candidates attended a subsequent session at which mobile phones, audio-recorders, scales and stadiometers were distributed. Housekeeping matters (e.g. room booking, travel expenses, gift voucher distribution and completion of payment forms) were also explained.
Two pilot sessions were organised for each study co-ordinator. These involved men recruited from the community and were held at community venues, replicating study conditions. The sessions were audio-recorded and individual feedback was given. This was intended to promote confidence but also to ensure fidelity of delivery.
Study co-ordinator security
As the face-to-face sessions were conducted in the community, the importance of personal safety was stressed. A lone worker’s policy was developed from the Universities and Colleges Employers Association policy: Guidance on Health and Safety in Fieldwork,100 customising it to the study methods. Safety and risk were reviewed by the study team, and the co-ordinators were advised to avoid risky situations. Each co-ordinator was supplied with a mobile phone and a personal alarm. When arranging the face-to-face sessions, the co-ordinators were required to inform the study team of the date, time and venue. They were advised to terminate the session politely if they felt at risk, and to dial 999 if their safety was threatened. On completion of the session, a text message had to be sent to the main study phone, confirming that the co-ordinator had left the venue. If the text was not received within 10 minutes of the expected completion time, a sequence of attempts at contact would be made starting with the co-ordinator, followed by the venue and culminating with the police.
Results and discussion
In total, 45 individuals applied for the posts, after only 3 weeks of advertising. This was encouraging because the post offered only a few hours of work per week for a short time period (3 months). The advertising may have tapped into social networks, as some applicants reported that other people had told them about the job. In a future study, it could be helpful to encourage this process, possibly by including a statement on the poster such as ‘do you have a friend who might want this job?’.
Twenty-two applicants were selected for interview. Interviewing identified those who were ineligible because they had prior experience in behaviour change, because they had had strong views about alcohol or because they had limited experience in dealing with people. All of the candidates were content with the selection process that would take place at the end of training. Twelve suitable individuals were selected for training, although three of these subsequently withdrew for personal reasons prior to training.
The training programme was well received, and all those who attended the first session completed all training and evaluation. The methods for measuring height and weight were quickly acquired, but recording alcohol consumption accurately proved challenging. This occurred because of the large variety of drinks available, particularly those whose brand name is available in different volumes and strengths of alcohol. For example, cans of Stella Artois are available in 440 ml, 500 ml and pint (568 ml) sizes with strengths at 4.0% alcohol by volume (ABV) or 4.8% ABV. The study co-ordinators had to be prompted to probe participants for fuller details of drinks consumed. In further studies, additional training could be given to cope with the profusion of alcoholic drinks. A few of the potential control study co-ordinators struggled with interpreting the graph of the frequency distribution of alcohol consumption.
After several role-play sessions, with supportive feedback, the potential intervention study co-ordinators quickly learned MI-based skills. It is possible that the selection process had identified individuals for whom attentive listening and empathising were normal behaviours. Additionally, the amount of practice included in training would have improved their skills.
The delivery of training required the presence of at least three members of the research team at each session. Role playing was an essential part of the training, with members of the research team acting as amenable or recalcitrant participants. To meet the needs of study co-ordinators with full time jobs, these sessions were additional to the working day. In total, nine sessions were given (five intervention, four control), with at least three researchers attending each session. To ensure they were familiar with the materials used, the researchers were also involved in developing the training. Funding for the extra research staff should be included in any further studies.
The selection of six individuals to deliver the intervention and control sessions proved straightforward. Although based mainly on the evaluation session, in practice the researchers made notes during each training session. All of the decisions were unanimous, with remarkable consistency between performance during training and at the evaluation. However, it was thought useful to keep the evaluation session, as it provided a target for candidates to aim at and gave useful practice in delivering the session.
The pilot sessions conducted in community venues were essential. The study co-ordinators found these much less stressful than the assessment session and also benefited from the additional practice. Feedback based on the audio-recording of these sessions was intended to boost confidence as well as to tackle weaknesses. The most common problem was the one encountered in the training sessions: insufficient probing for detailed descriptions of drinks consumed.
In summary, able candidates for the study co-ordinator posts were successfully recruited and trained. Initial over-recruitment, to allow for withdrawals and the selection of the most able candidates, was essential. The extended selection process helped to identify those who could empathise with participants and who could master the components of the face-to-face session. The training was well received with 100% attendance at the sessions. Most of the necessary skills were mastered, although additional training should be introduced for measuring alcohol consumption.
Chapter 7 Recruitment of participants
Introduction
Recruitment to clinical trials is challenging, but recruitment to prevention trials is even more difficult. 101 This could be a particular problem in this study because alcohol consumption and obesity are sensitive subjects, and addressing both in the recruitment process could reduce participation rates. Thus, the study used two recruitment methods to ensure good coverage of obese men who drink heavily, one recruiting through primary care and the other by community outreach. In addition, information was gathered on the processes involved in recruitment to determine where challenges to recruitment lay.
Systematic reviews have shown that several techniques can increase recruitment in general population groups: repeated attempts at contact at different times on different days, financial incentives, personalised approaches, assurances of confidentiality, sponsorship by a prestigious body such as a university and minimising the length of questionnaires used. 46,47,102–107 These techniques were incorporated into the recruitment strategies.
Methods
Participants
Men aged 35–64 years who regularly consumed > 21 units of alcohol per week and were obese (BMI of > 30 kg/m2) were recruited. The exclusion criteria were (1) already attending alcohol problem services, (2) using weight management classes/services and (3) would not be contactable by mobile phone during the study period.
Overview of methods
Two recruitment strategies were employed. One used primary care registers and the other used a community outreach method, TSS. 31 The recruitment process involved several steps. Once potential participants had been identified, they were assessed for eligibility based on age, alcohol consumption and BMI (self-reported height and weight). Eligible men were then asked if they were interested in taking part and, if so, informed consent was obtained after the study was explained in detail. The men were then randomised to receive intervention or control packages.
Criteria for evaluating recruitment
As well as judging the success of the recruitment by achieving the target of 30 men by each method, criteria were set for the steps involved in each of the recruitment methods. The aim was to shed light on the feasibility and the workload of the methods, providing a fuller assessment of the success of the recruitment. Three criteria were set against which the success of each method could be judged.
The criteria for primary care registers were:
-
10% of men aged 35–64 are registered as being obese.
-
25% of men who are obese drink > 21 units of alcohol per week.
-
The proportion of eligible men (on obesity and drinking) who are recruited to the study is 50%.
The criteria for community outreach were:
-
Identify at least 15 venues at which men could be recruited.
-
Recruit no more than two men per visit (to avoid contamination).
-
Recruit at least one man per three visits to a venue.
Strategy 1: recruitment through primary care
Potential participants were identified from the practice lists of three general practices by staff from the Scottish Primary Care Research Network (SPCRN). The lists provided data on age, telephone numbers and BMI, enabling the selection of men aged 35–64 years with a BMI of > 30 kg/m2. Two hundred potential participants who met the age and BMI criteria were randomly selected by SPCRN staff from each practice list. After the potential participants were vetted, the general practitioner (GP) sent them a letter inviting them to take part (see Appendix 5). The letter was personalised, mentioned the University of Dundee and stated that a financial reward would be given. The accompanying participant information sheet (see Appendix 6) carried the university’s logo and stressed the confidentiality of the study. An opt-out strategy was used for recruitment: the men could return a pre-paid postcard stating that they did not wish to participate. The name, address and telephone number of those who did not decline to take part were provided to the researchers by the SPCRN staff. Contact with these individuals was made by telephone approximately 2 weeks after the GP letter was sent. Attempts at contact by telephone were made at different times of the day and on different days of the week to the men who had not opted out. Informed consent was then obtained from eligible individuals (see Screening questionnaire and informed consent).
Strategy 2: time–space sampling
A community outreach method, TSS,31 was used to recruit half of the study population. TSS recruits participants from a number of venues and involves sampling at different times of day and on different days of the week. The strategy was based on experience with previous studies (NIHR PHR 09/3001/09,39 NIHR PHR 11/3050/3041) and findings from the interviews with key stakeholders. This was augmented by fieldwork to identify appropriate venues and suitable times for recruitment. A variety of venues was explored for recruitment potential, including a town centre, workplaces, community groups, football grounds and golf clubs. Judgement was used in approaching men likely to be in the target age range (35–64 years) with a BMI of > 30 kg/m2. Once approached, the men were asked their age and about their alcohol consumption to confirm their eligibility. Eligible men were then given the participant information sheet (see Appendix 7) and a suitable time was arranged to contact them by telephone.
Screening questionnaire and informed consent
Potential participants identified by both methods were telephoned to administer the screening questionnaire. To assess their eligibility, their age, self-reported height and weight (to calculate BMI) and current weekly alcohol consumption were obtained. The researcher described the study to eligible individuals and answered any questions that arose. The details on the participant information sheet were explained, such as participants’ right to withdraw from the study at any time and the confidentiality of the data. Verbal consent was sought after potential participants confirmed that they had understood the contents of the participant information sheet. Those who agreed to participate were sent a text message which asked them to reply to the message if they wanted to take part in the study. This meant that potential participants had to indicate their consent to participate by taking the positive action of responding to a text message. During the screening interview, a consent form was completed by the researcher. When the responses to the consent text were received, the date and time of obtaining consent were recorded and the form was signed by the researcher. The responses to the consent text, which were captured by the computer program, were retained as proof of consent.
Financial incentives
All participants were told they would be given a £10 gift voucher for completing the baseline questionnaire and a £10 voucher for completing the outcome assessment. The men in the intervention group were also sent a £5 gift voucher every 2 weeks for the 8-week period of the delivery of the text messages.
Results
Recruitment began on 1 March 2015 and was completed on 2 June 2015. A total of 69 men were recruited, exceeding the target of 60.
Recruitment through primary care
Three GP practices kindly agreed to participate. SPCRN staff identified 5198 men aged 35–64 years, of whom 1022 (19.7%) were recorded with a BMI of > 30 kg/m2. A random sample of 200 men was taken from each general practice. GPs screened these samples to exclude men who should not be contacted. This removed 167 of the 600 men as a result of concerns about health, family problems or other issues. A further 14 men opted out after receiving a letter of invitation from their GP. This left 419 men to be contacted by telephone. Figure 3 shows the outcome after several attempts at contacting these 419 men. Nearly half (44%) were excluded because they did not meet the threshold of drinking > 21 units per week. Invalid telephone numbers and failure to achieve contact accounted for almost one-third (32%) of the men approached. Only 2% were ineligible because their BMI was ≤ 30 kg/m2. Thus, of the original 419 men, 283 (68%) were contactable. Of those contactable, 87 (31%) were eligible for the study. Of those eligible, 36 (41%) were screened, gave informed consent and were randomised.
FIGURE 3.
Flow diagram of GP recruitment.
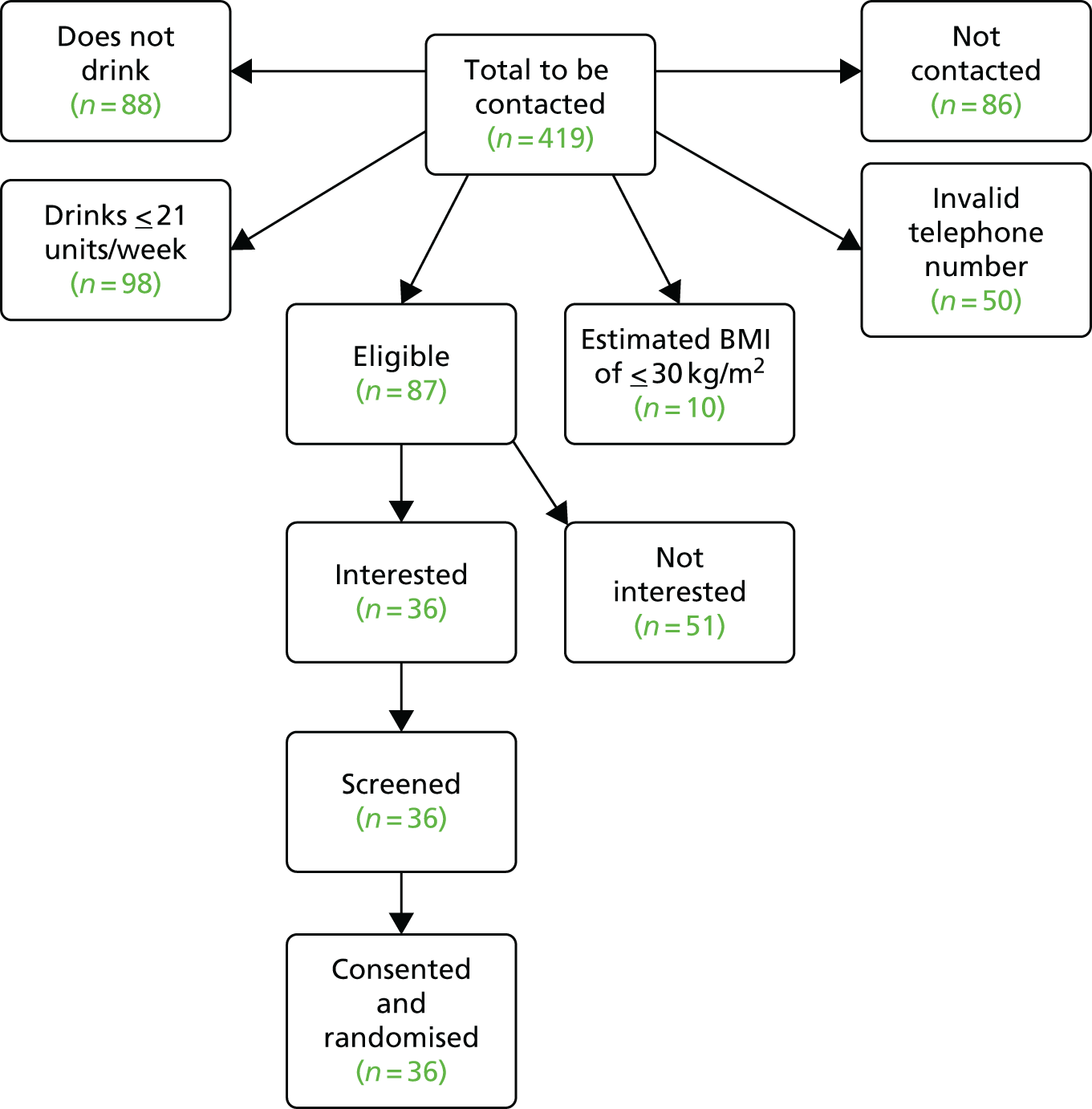
Assessment against pre-specified criteria
Of the 5198 men initially identified, 19.7% had a recorded BMI of > 30 kg/m2, exceeding the target of 10%. Of the 283 men contacted, 97 (34%) consumed > 21 units of alcohol per week, exceeding the target of 25%. However, if those who could not be contacted are included in the denominator, then only 21% met the consumption criterion. Only 36 of the 87 eligible men (41%) were recruited (i.e. gave consent and were randomised), falling short of the target of 50%. Applying the second and third criteria simultaneously to the 283 men contacted would predict that 35 men should be recruited, similar to the actual total of 36.
Lessons learned from primary care recruitment
-
GP records identify large numbers of men with a recorded BMI of > 30 kg/m2.
-
A high proportion of eligible men were recruited.
-
Repeated attempts at contact at different times of day are essential.
Recruitment through time–space sampling
Some 370 locations were visited to identify potential participants. These included all premises on 12 industrial estates (329 businesses), four large employers, two supermarkets, five taxi ranks, two golf clubs and two football matches. In addition, 28 visits were made to high streets and shopping centres. In total, 470 men were approached, yielding 33 men who were recruited and randomised. Thirteen men were recruited from public places such as the city centre and high streets, 10 were recruited from small businesses on industrial estates, seven were recruited from small businesses throughout the city, two were recruited from taxi ranks and one was recruited from a golf club.
The process of recruitment, from being approached to entry into the study, is shown in Figure 4. More than half (53%) of the men approached reported that they did not drink enough alcohol to be eligible for the study (i.e. they drank ≤ 21 units per week). A small number (18%) were outside the target age range. Thus, almost one-quarter (24%) of the men approached were eligible on age and alcohol consumption. Of those eligible, 50 men (45%) were interested. Some men were lost because they could not be contacted by subsequent telephone calls (n = 7), or they did not meet the obesity criterion at telephone screening (n = 10). Thus, 33 men were recruited.
FIGURE 4.
Flow diagram of TSS recruitment.

Assessment against pre-specified criteria
The target of identifying at least 15 locations suitable for recruitment was easily exceeded, as the fieldwork identified 370 venues where eligible men could be located. The target of not recruiting more than two men from each venue was met because of the profusion of venues available for recruitment. However, the target of one man recruited per three visits to venues was not met. Recruitment was challenging so that the ratio was 1 per 11 visits. (Note that a single visit to a high street or shopping centre involved 2 hours of walking up and down past many shops. It could be argued that this constitutes more than a single venue, making the ratio lower than 1 : 11.) The main finding is that a large number of venues need to be visited in order to recruit one participant.
Lessons learned from time–space sampling
-
Persistence, in the form of repeated efforts at different times and places, is the key to successful recruitment.
-
It is important to maintain high morale among research staff during periods of drought in recruitment.
-
Small businesses, particularly on industrial estates, are a source for recruitment.
-
Town centres, shopping centres and other areas with high footfall are productive venues.
-
Poor weather, especially cold, wind and rain, reduce footfall and hence recruitment.
-
Recruitment from large organisations tends to be poor. Commonly, a senior member of staff will offer to ask employees themselves, which is detrimental to recruitment for two reasons. First, that individual may not have sufficient information to be able to fully answer questions the employees may have. Second, being approached by a senior member of staff may deter men from volunteering because of reluctance to be viewed as eligible for an alcohol intervention. Thus, direct access to individuals is essential.
-
Leaving information such as participant information sheets at venues is ineffective. Few individuals have the enthusiasm to contact a university to offer to participate in research.
-
The opening remarks when approaching a potential participant are crucial.
-
Phrases that help initiate conversation include ‘Excuse me mate, would you happen to be in the age range 35–64?’ and ‘Excuse me, I’m from the University of Dundee, could you help me out?’.
-
Phrases that often elicit rejection include ‘Have you got a minute?’, ‘Can I have a moment of your time?’ and ‘Hi, just a quick question’.
-
-
Eligibility on age and alcohol consumption should be established at an early stage. Ineligible men can then be thanked, without need for a detailed explanation of the study.
-
The telephone call to complete the screening questionnaire and obtain informed consent should be conducted at the earliest time suitable to the participant.
Other lessons learned
-
The offer of gift vouchers for participation elicited little response. This is in contrast to our previous trial with disadvantaged men (NIHR PHR 11/3050/30),41 in which financial reward appeared very welcome. Possibly for more affluent men a larger sum would be required to compensate for the burden of study participation.
-
Success at recruitment increases with experience, by identifying which approaches work and which do not. Hence, recruitment will be slow initially, but rates will increase over time.
Discussion
The recruitment target of 60 men was met, although achieving this proved challenging. The recruitment methods met their prespecified criteria, except for the community outreach criterion of number of men per venue visited. Several factors contributed to the challenge of meeting the recruitment target. More men than expected reported that they did not drink. Survey data for 2013 showed that approximately 10% of men in the same age range claimed to be non-drinkers. 108 The higher frequency of non-drinkers approached (24%) could have occurred because the target group, obese men, may be more likely to be abstainers. Alternatively, some men may have reported abstinence as a method of declining to participate in the study.
Recruitment from primary care registers was a straightforward process that required repeated attempts at contact by telephone. However, recruitment through community outreach proved difficult. A direct comparison of the two methods might suggest that they were similarly effective: primary care registers yielded 36 recruits from 419 approached, while community outreach yielded 33 from 470 approached. However, the workload involved in making telephone calls to the men on primary care registers was substantially lower than that involved in visiting and exploring venues for the community outreach. The researcher who did the recruitment estimated that at least twice as much time was required for the community outreach. (The collection of such data was not part of the study design.)
The challenge of recruitment by community outreach arose partly because two entry criteria (BMI and alcohol consumption) were applied simultaneously, so that many men were automatically excluded. This contrasts with the primary care selection whereby all those approached had been pre-selected to meet the BMI criterion. Recruitment through community outreach suffered because only a small number of overweight men were identified at the venues visited. Inspection of the community venues during preliminary fieldwork suggested that more than a sufficient number of men should have been available, but few were available when it came to recruiting them. This may be an example of the operation of Lasagna’s law109 in a community setting.
A surprising finding was that attempts at recruitment through large institutions (such as businesses or the local authority) proved unsuccessful. Interviews with key stakeholders had identified considerable enthusiasm for the project and a willingness for their staff to become involved. This enthusiasm was still evident during the fieldwork, but the assistance took the form of circulating leaflets (the participant information sheet) or asking men to contact us. In the event, no men from large institutions volunteered for the study. It is possible that many men were willing, but they may have had reservations about the study, or may not have wanted senior colleagues to think that they were heavy drinkers. Some may have intended to volunteer but never did so. In some cases, these barriers might have been overcome by direct contact with the researcher. The concerns could be addressed by explaining the non-demanding, confidential and supportive nature of the study. In future, stakeholder interviews should explore this issue and seek approval for direct contact with the men. This would require identification of appropriate times for contacting individuals in these institutions.
An observation by the researcher doing the fieldwork was that the financial incentive offered for participation (£40) often elicited little or no response from potential participants. This is in contrast with a previous study with disadvantaged men, during which the researchers noted a marked increase in interest when the incentive was mentioned. It is possible that, in the present study, the incentive was too small to encourage men who were, on average, more affluent than the disadvantaged group. There is some evidence that higher financial incentives may be more effective for recruitment110 suggesting that for a full RCT a larger incentive might aid recruitment.
None of the men who were approached in community outreach was reluctant to discuss his alcohol consumption. In contrast, four of the men approached by letter from the general practice registers asked why they had been nominated for the study by their GP. Some were concerned that this implied that they had a drinking problem. The men were reassured when it was explained that the researchers had no information about their drinking. This suggests that a change should be made to the approach letter, highlighting the point that selection is not based on the individual’s alcohol consumption.
In summary, although recruitment proved challenging, the target was exceeded within the time period allocated. This indicates that a RCT would be feasible. A multicentre study could recruit 30–40 GP practices from which some 400–500 men could be recruited. If community outreach were employed, it would be best to select centres with large populations to provide sufficient venues for recruitment.
Chapter 8 Baseline findings
Introduction
The men who were recruited and randomised were invited to attend a face-to-face session with a study co-ordinator. This session enabled baseline data to be collected (height, weight and the previous 4 weeks’ alcohol consumption) and the face-to-face intervention or control treatment to be delivered. This chapter assesses how well these activities were conducted and presents the data on the demographic characteristics and alcohol consumption of the participants. It also evaluates the suitability of screening tools that were used to identify eligible participants.
Methods
Randomisation
Sixty-nine men were recruited and randomised to receive the intervention or control package. The randomisation was carried out using the secure remote web-based system provided by the Tayside Clinical Trials Unit. Randomisation was stratified by the recruitment method and restricted using block sizes of randomly varying lengths. The research assistant was given the randomisation codes so that men could be allocated to an appropriate study co-ordinator (intervention or control). The study co-ordinators were given the contact details of participants so that they could arrange their face-to-face sessions. These were held at venues and times convenient to the participants.
Baseline data collection
The study co-ordinators contacted participants by telephone to arrange a suitable time and venue for the session. The participants completed a baseline questionnaire at the face-to-face session (see Appendix 2). Sociodemographic data including education, employment, SIMD111 and marital status were collected. Weight was measured by Seca 813 medical scales (Seca United Kingdom, Birmingham, UK). The participants were asked to remove their shoes and any heavy outer garments (jackets or coats), and to take loose change and keys out of their pockets, before weighing. They were asked to stand, facing forwards, in the centre of the scales with their heels against the back edge of the scales.
Height was measured using a portable Seca 213 stadiometer with men in stockinged feet. The men were asked to stand up straight against the backboard with their body weight evenly distributed and both of their feet flat on the platform. They were positioned with their heels together and toes slightly apart, such that the back of the head, shoulder blades, buttocks and heels were in a straight line. The men were asked to look straight ahead and the stadiometer head piece was lowered to rest firmly on top of their head. The measurement was repeated and a third measurement was taken to resolve any discrepancy.
The alcohol TLFB questionnaire58 was used to measure alcohol consumption accurately over the previous 28 days. This will be used to derive the first primary outcome measure for the RCT, that is, weekly alcohol consumption. The Fast Alcohol Screening Test (FAST)112 was administered to identify hazardous drinkers. The Readiness Ruler113 was also used to identify intention to reduce alcohol consumption.
Piloting
Twelve men who met the study entry criteria (age, BMI and alcohol consumption) were recruited from the community. They were told that they would participate in the piloting of the study methods and would be asked to comment on them. Two men were allocated to each study co-ordinator, who organised the time and venue for the face-to-face session. The sessions were audio-recorded so that feedback could be given to the study co-ordinators. Opportunities were identified for increased use of MI techniques for intervention group co-ordinators, particularly open-ended questions and reflective listening. In addition, the study co-ordinators in both groups needed some encouragement to probe participants about alcohol consumption to identify all instances of drinking.
Results
The study co-ordinators made repeated efforts to contact the 69 men who had been randomised. The outcome of this is shown in Figure 5. Three men could not be contacted and four withdrew when contacted (three because of changed family circumstances and one due to ill-health). Four of these men were from the intervention group and three from the control group. The characteristics of the men who were not seen, based on information gained at the telephone screening contact, are shown in Table 6.
FIGURE 5.
Flow chart of conduct of the baseline interviews.

| Characteristic | Median | Range |
|---|---|---|
| Age (years) | 46 | 40–64 |
| Weekly alcohol consumption (units) | 35 | 24–94 |
| BMI [kg/m2 (self-reported)] | 32 | 30–48 |
| SIMD (deciles) | 4 | 1–8 |
Appointments were arranged for the remaining 62 men. All these men were willing to take part, but other priorities sometimes made this difficult. Eight men cancelled their appointments and one did not attend. Of these men, seven were seen at their first re-appointment. The two remaining men required several appointments because of cancellation or failure to attend before they were finally seen.
The face-to-face sessions were held in a variety of venues: the participant’s home (n = 31), a community centre (n = 14), the participant’s workplace (n = 10), a library (n = 5), a church (n = 1) and a yacht club (n = 1). In total, excluding homes and workplaces, nine different types of venue were used. All sessions were conducted without difficulty and all men agreed to the session being audio-recorded. The lone worker’s policy was consistently adhered to, but in the event no problems were encountered.
Characteristics at baseline
The baseline characteristics of the men who attended are shown in Table 7. They spanned the age range from 35 to 64 years and most were married (or living with a partner) and in employment. The men varied by deprivation level and educational attainment. There was little difference between intervention and control groups in the baseline characteristics.
| Factor | Control group (N = 31), n (%) | Intervention group (N = 31), n (%) | Total (N = 62), n (%) |
|---|---|---|---|
| Participants’ age (years) | |||
| 35–39 | 0 | 2 (6) | 2 (3) |
| 40–44 | 6 (19) | 2 (6) | 8 (13) |
| 45–49 | 9 (29) | 5 (16) | 14 (23) |
| 50–54 | 4 (13) | 8 (26) | 12 (19) |
| 55–59 | 9 (29) | 6 (19) | 15 (24) |
| 60–64 | 3 (10) | 8 (26) | 11 (18) |
| Marital status | |||
| Single | 4 (13) | 3 (10) | 7 (11) |
| Married/lives with a partner | 20 (65) | 24 (77) | 44 (71) |
| Separated/divorced | 5 (16) | 4 (13) | 9 (15) |
| In a relationship | 2 (6) | 0 | 2 (3) |
| SIMD quintile | |||
| 1 (most disadvantaged) | 10 (32) | 8 (26) | 18 (29) |
| 2 | 3 (10) | 6 (19) | 9 (15) |
| 3 | 3 (10) | 4 (13) | 7 (11) |
| 4 | 10 (32) | 6 (19) | 16 (26) |
| 5 (least disadvantaged) | 5 (16) | 7 (23) | 12 (19) |
| Employment status | |||
| Employed | 26 (84) | 22 (71) | 48 (77) |
| Unemployed | 5 (16) | 5 (16) | 10 (16) |
| Retired | 0 | 4 (13) | 4 (6) |
| Highest educational attainment | |||
| University degree | 3 (10) | 5 (16) | 8 (13) |
| Vocational qualification/further training | 7 (23) | 12 (39) | 19 (31) |
| High school | 21 (68) | 14 (45) | 35 (56) |
| BMI (kg/m2) | |||
| 29–34 | 16 (52) | 13 (42) | 29 (47) |
| 35–39 | 9 (29) | 13 (42) | 22 (35) |
| 40–44 | 6 (19) | 5 (16) | 11 (18) |
Almost all of the men (92%) were classified as hazardous drinkers using the FAST questionnaire (Table 8). The mean weekly consumption was 47 units per week, well above the inclusion criterion of > 21 units. There was also considerable variation in the amount consumed. Four men drank less than the entry criterion (> 21 units per week), although they had reported drinking more than this at screening. These men consumed between 14 and 19 units per week. The pattern of drinking varied among men, although most men drank on at least 10 days out of the 28-day period and almost half drank every second day. Nearly all men engaged in binge drinking (> 8 units in a session) and many did so regularly.
| Factor | Control group (N = 31), n (%) | Intervention group (N = 31), n (%) | Total (N = 62), n (%) |
|---|---|---|---|
| Hazardous drinkers (Positive FAST) | 30 (97) | 27 (87) | 57 (92) |
| Alcohol consumption | |||
| Mean weekly consumption [units (SD)] | 53.3 (40.7) | 41.1 (31.9) | 47.2 (36.8) |
| Total consumption in previous 28 days (units) | |||
| ≤ 84 | 4 (13) | 3 (10) | 7 (11) |
| 85–149 | 9 (29) | 17 (55) | 26 (42) |
| 150–199 | 5 (16) | 6 (19) | 11 (18) |
| 200–249 | 6 (19) | 2 (6) | 8 (13) |
| ≥ 250 | 7 (23) | 3 (10) | 10 (16) |
| Number of drinking days in previous 28 days | |||
| 0 | 0 | 0 | 0 |
| 1–4 | 2 (6) | 1 (3) | 3 (5) |
| 5–9 | 6 (19) | 6 (19) | 12 (19) |
| 10–14 | 10 (32) | 7 (23) | 17 (27) |
| 15–19 | 4 (13) | 9 (29) | 13 (21) |
| ≥ 20 | 9 (29) | 8 (26) | 17 (27) |
| Number of binge drinking days in previous 28 days (> 8 units in one session) | |||
| 0 | 1 (3) | 1 (3) | 2 (3) |
| 1–4 | 6 (19) | 6 (19) | 12 (19) |
| 5–9 | 9 (29) | 14 (45) | 23 (37) |
| 10–14 | 9 (29) | 3 (10) | 12 (19) |
| 15–19 | 4 (13) | 6 (19) | 10 (16) |
| ≥ 20 | 2 (6) | 1 (3) | 3 (5) |
There was a marked difference in drinking between intervention and control groups on several measures of alcohol consumption. The proportion of men who were drinking hazardously (FAST positive),112 the mean weekly consumption, the proportion of men who drank in excess of 50 units per week and the proportion of men who had at least 10 binge drinking days (in the previous 28 days) were all higher in the control group.
The mean BMI was 35.7 kg/m2, well above the inclusion criterion of 30 kg/m2, and a few men had a BMI of > 40 kg/m2 (Table 9). The mean BMI scores in the intervention and control groups were very similar.
| Factor | Control group (N = 31), n (%) | Intervention group (N = 31), n (%) | Total (N = 62), n (%) |
|---|---|---|---|
| Mean BMI, kg/m2 (SD) | 35.5 (3.9) | 35.9 (5.4) | 35.7 (4.7) |
| Distribution of BMI, kg/m2 | |||
| 29–34 | 16 (52) | 13 (42) | 29 (47) |
| 35–39 | 9 (29) | 13 (42) | 22 (35) |
| 40–44 | 6 (19) | 5 (16) | 11 (18) |
Assessment of initial screening for body mass index
The study focused on men with a BMI of > 30 kg/m2. However, the men were recruited on the basis of self-reported height and weight, raising the question of the accuracy of self-reported BMI. The mean BMI measured at baseline (35.7 kg/m2) was slightly higher than that self-reported (34.5 kg/m2). Only 10 men had a measured BMI that was lower than that reported at screening BMI. Furthermore, only two men had a measured BMI of < 30 kg/m2 (Table 10), and both were within 1 BMI unit of the threshold (29.06 kg/m2 and 29.27 kg/m2). Both of these men had been recruited by community outreach. Thus, having a self-reported BMI of ≥ 30 kg/m2 will almost always mean that the potential participant is eligible for the study.
| Method of recording BMI | Self-reported BMI (kg/m2) | |||
|---|---|---|---|---|
| < 30 | 30–34 | 35–39 | ≥ 40 | |
| Measured BMI (kg/m2) | ||||
| < 30 | 0 | 2 | 0 | 0 |
| 30–34 | 0 | 27 | 0 | 0 |
| 35–39 | 0 | 7 | 13 | 2 |
| ≥ 40 | 0 | 0 | 4 | 7 |
Frequency of obesity and heavy drinking
Over 50% of men had a BMI of ≥ 35 kg/m2, indicating a high level of risk. Comparing BMI and alcohol data of individual men identified that many men had very high values for both alcohol consumption and obesity (Table 11). More than 30% (n = 19) drank > 35 units per week and had a BMI of > 35 kg/m2. A further 35% (n = 22) had very high values of either alcohol or obesity. Almost all of the men (95%) were at a 19-fold increase in the risk of dying from liver disease (BMI of > 30 kg/m2 and > 14 units of alcohol per week). 1
| Alcohol consumption (units) | BMI (kg/m2), n | ||
|---|---|---|---|
| < 30 | 30–34 | ≥ 35 | |
| < 21 | 0 | 3 | 4 |
| 21–35 | 1 | 12 | 10 |
| > 35 | 1 | 12 | 19 |
The impact of recruitment method
Two recruitment methods were used: GP practice records and TSS. Each method seeks to provide a representative sample of the target population. A comparison of the men recruited by each method showed that they were very similar in terms of demographic characteristics (Table 12) and alcohol consumption (Table 13). The men recruited by TSS had lower mean BMI and lower mean alcohol consumption than the men recruited from GPs; however, the differences were small.
| Factor | GP (N = 32), n (%) | TSS (N = 30), n (%) | Total (N = 62), n (%) |
|---|---|---|---|
| Participants’ age (years) | |||
| 35–39 | 0 | 2 (7) | 2 (3) |
| 40–44 | 3 (9) | 5 (17) | 8 (13) |
| 45–49 | 9 (28) | 5 (17) | 14 (23) |
| 50–54 | 6 (19) | 6 (20) | 12 (19) |
| 55–59 | 7 (22) | 8 (27) | 15 (24) |
| 60–64 | 7 (22) | 4 (13) | 11 (18) |
| Marital status | |||
| Single | 4 (13) | 3 (10) | 7 (11) |
| Married/lives with a partner | 21 (66) | 23 (77) | 44 (71) |
| Separated/divorced | 6 (19) | 3 (10) | 9 (15) |
| In a relationship | 1 (3) | 1 (3) | 2 (3) |
| SIMD quintile | |||
| 1 (most disadvantaged) | 12 (38) | 6 (20) | 18 (29) |
| 2 | 7 (22) | 2 (7) | 9 (15) |
| 3 | 3 (9) | 4 (13) | 7 (11) |
| 4 | 6 (19) | 10 (33) | 16 (26) |
| 5 (least disadvantaged) | 4 (13) | 8 (27) | 12 (19) |
| Employment status | |||
| Employed | 25 (78) | 23 (77) | 48 (77) |
| Unemployed | 4 (13) | 6 (20) | 10 (16) |
| Retired | 3 (9) | 1 (3) | 4 (6) |
| Highest educational attainment | |||
| University degree | 5 (16) | 3 (10) | 8 (13) |
| Vocational qualification/further training | 7 (22) | 12 (40) | 19 (31) |
| High school | 20 (63) | 14 (47) | 35 (56) |
| BMI (kg/m2) | |||
| 29–34 | 12 (38) | 17 (57) | 29 (47) |
| 35–39 | 14 (44) | 8 (27) | 22 (35) |
| 40–44 | 6 (19) | 5 (17) | 11 (18) |
| Mean BMI (SD) | 36.5 (5.0) | 34.9 (4.2) | 35.7 (4.7) |
| Factor | GP (N = 32), n (%) | TSS (N = 30), n (%) | Total (N = 62), n (%) |
|---|---|---|---|
| Hazardous drinkers (Positive FAST) | 30 (94) | 27 (90) | 57 (92) |
| Alcohol consumption | |||
| Mean consumption in past 28 days [units (SD)] | 194.9 (173.9) | 182.2 (114.4) | 188.7 (147.1) |
| Mean weekly consumption [units (SD)] | 48.7 (43.5) | 45.6 (28.6) | 47.2 (36.8) |
| Total consumption in previous 28 days (units) | |||
| ≤ 84 | 3 (9) | 4 (13) | 7 (11) |
| 85–149 | 14 (44) | 12 (40) | 26 (42) |
| 150–199 | 7 (22) | 4 (13) | 11 (18) |
| 200–249 | 4 (13) | 4 (13) | 8 (13) |
| ≥ 250 | 4 (13) | 6 (20) | 10 (16) |
| Number of drinking days in previous 28 days | |||
| 0 | 0 | 0 | 0 |
| 1–4 | 2 (6) | 1 (3) | 3 (5) |
| 5–9 | 6 (19) | 6 (20) | 12 (19) |
| 10–14 | 10 (31) | 7 (23) | 17 (27) |
| 15–19 | 9 (28) | 4 (13) | 13 (21) |
| ≥ 20 | 5 (16) | 12 (40) | 17 (27) |
| Number of binge drinking days in previous 28 days (> 8 units in one session) | |||
| 0 | 1 (3) | 1 (3) | 2 (3) |
| 1–4 | 6 (19) | 6 (20) | 12 (19) |
| 5–9 | 14 (44) | 9 (30) | 23 (37) |
| 10–14 | 6 (19) | 6 (20) | 12 (19) |
| 15–19 | 4 (13) | 6 (20) | 10 (16) |
| ≥ 20 | 1 (3) | 2 (7) | 3 (5) |
Discussion
The assessment showed that the baseline interviews were successfully conducted and complete baseline data were obtained. Those recruited covered a wide range of age, education, alcohol consumption and BMI. The study found that screening, using self-reported BMI (height and weight) and alcohol consumption, identified eligible individuals. Many participants were found to be at very high risk of liver disease because of the combination of high BMI and alcohol consumption.
Almost all of the men (95%) were at a 19-fold increase in the risk of dying from liver disease1 (BMI of > 30 kg/m2 and > 14 units of alcohol per week). Many men recruited drank very heavily and were also severely obese, placing them at a very much higher risk of liver disease. The recruitment methods of this study can identify men who are in urgent need of intervention.
The two recruitment strategies were intended to produce representative samples of the target population, albeit using quite different methodologies. TSS is often used to recruit hard to reach individuals. 31 If there were sub-sections of the target group who were reluctant to participate, this community-based face-to-face method of recruitment might be more successful in recruiting them. In the event, the two strategies yielded almost identical samples. As the evaluation of the recruitment (see Chapter 7) showed that recruitment through GP registers was simpler and quicker, this method is recommended for the RCT.
The data showed a marked imbalance in alcohol consumption between intervention and control groups. This was a small study and a difference of this size could be due to random variation resulting from the small number of men randomised. This is recognised to occur frequently. 22 The intervention and control groups were balanced on demographic characteristics and BMI: imbalance on one factor would not be unexpected. Current guidance on feasibility studies highlights the limitation of feasibility studies because of their small sample size114 and the likelihood of imbalance at baseline. 25
Screening using self-reported values for alcohol and height and weight proved successful. Previous studies report that self-reported height and weight show a modest tendency to under-estimate weight and to overestimate height. 115 In this study three men were below the inclusion criterion for alcohol and obesity, but all were close to the threshold values. This places them at high risk of developing liver disease, as their risk is only slightly lower than men just above the threshold. In a RCT these men could be excluded for violating the protocol, although this would seem unjustified as they all have the potential to benefit from the intervention.
Two important and related findings were that organising the face-to-face sessions proved more difficult than expected and that, despite repeated efforts, appointments could not be made for some of the men who had been recruited. Some men did not answer their phones, meaning that several calls had to be made and reminder text messages had to be sent. Appointments were sometimes cancelled at short notice and alternative times had to be arranged. This caused some difficulty for the study co-ordinators and should be addressed in the training session for any future study. To minimise the loss of men from the study the study co-ordinators could be encouraged to arrange appointments as soon as possible after the screening interview.
Many different venues were used to hold the face-to-face sessions, and most often these were provided at low or no cost. The initial fieldwork to identify these venues was crucial to the success of this part of the study. The fieldwork would be essential for scaling up to a RCT. A surprising finding was that many of the men requested appointments at their own homes. It is possible that this was simply more convenient for the participants; however, it raises the issue of safety of the study co-ordinators as lone workers. A lone workers policy was successfully implemented, but this relied on the research team to monitor safety. A more formal arrangement with a commercial firm would be needed in a RCT.
The use of study co-ordinators made more demands on the research team than was expected. Distributing baseline questionnaires and collecting them on completion, obtaining and evaluating the audio-recordings of study sessions, and the provision of mentoring support and feedback all took time. Collection of data on this workload was not a planned part of the study, so exact figures are not available. However, it is likely these activities would add substantially to the cost of delivering the intervention and thus should be included in any cost-effectiveness study that accompanied a RCT.
In summary, the selection and recruitment methods were effective in identifying men who met the inclusion criteria. A delay between recruitment and baseline interview may have led some men to withdraw from the study. This delay should be minimised in future studies. The two recruitment methods gave similar samples, and so the easier and quicker GP register approach would be preferred. The recruitment methods of this study identified men who are at very high risk of liver disease. There is an urgent need for an intervention to reduce this risk in these men.
Chapter 9 Evaluation of the delivery of the face-to-face session
Introduction
A major concern for behaviour change interventions is implementation fidelity, that is, the extent to which the intervention is delivered as intended. 116–118 Three elements of implementation fidelity were particularly important for this study: adherence, that is, whether or not all components of the intervention were covered; competence, that is, whether or not the components were delivered to a high standard; and treatment differentiation, that is, the extent to which the intervention and control packages differ in their immediate impact on participants. Other important issues were the acceptability of the study to participants and whether or not participants were actively engaged with the intervention components. Methods to assess these items were developed and tested as part of this feasibility study. This chapter describes the findings from these evaluations.
Methods
At the end of the face-to-face session, just before they were given their gift voucher and travel expenses, the men were asked to complete an evaluation questionnaire (see Appendix 8). The questionnaire explored the process of arranging the session, the acceptability of the venue and the men’s experience of the session. It also explored the communication skills of the study co-ordinator, particularly sensitivity to the participants’ interests and feelings. Finally, it explored the men’s responses to the information given. After completing the questionnaire, participants placed it in an envelope, which was returned unopened to the research team.
The face-to-face sessions were audio-recorded to enable assessment of the study co-ordinators adherence to the set tasks and competence in performing them. Detailed instructions on the conduct of the tasks were given during the co-ordinator training, and these provided criteria to assess adherence to each task. Separate task lists were used for intervention and control study co-ordinators (see Appendix 9). Performance at these tasks was assessed by a research psychologist (ED) using the audio-recordings. To facilitate feedback to the study co-ordinators, comments on desired improvements were listed, together with comments giving positive feedback on tasks done well.
The intervention co-ordinators, who had been trained in some MI-based skills, were assessed on their competence using relevant items from the Behaviour Change Counselling Index (BECCI). 119 This was performed by a research psychologist (ED) using the audio-recordings. The items covered were: showing empathy, being sensitive to the participants’ views, asking open questions and summarising at the end of the session. Twenty per cent of recordings were reviewed independently by two researchers to ensure a standardised approach to coding.
Results
The questionnaire showed extremely high levels of approval of components of the study: organisation of the session (100%), acceptability of the venue (100%) and ability of the study co-ordinator to hold the participant’s interest (100%). The written comments from participants show that the sessions were run in a relaxed, friendly atmosphere and that the information provided was perceived as useful by both intervention and control participants (Box 3).
It was quick and easy.
Very relaxed easy pace.
The explanation to all the ins and outs of alcohol was explained really well.
Helpful and worthwhile.
I enjoyed the session, and I look forward to the follow-up in 5 months’ time.
Intervention group
Information and honesty.
Informal and informative, also non judgemental.
Friendly and relaxed.
Everything was sweet as a nut, lol.
Worthwhile session. Could be helpful for other overweight drinkers.
More interesting were the responses to the question about what was useful in the session. Some (35%) mentioned only that the information given was useful, but a slightly larger group (39%) said it was directly relevant to them, and a further 15% said that it identified the need for a change in their behaviour. Furthermore, there was a marked difference between the intervention and control group participants in what they found useful in the session. Although similar numbers mentioned alcohol (12 intervention, 8 control), substantially more men in the intervention group than in the control group mentioned the calories in alcohol (13 vs. 1).
The comments in response to a question about what was useful in the study shed light on the impact of the control and intervention packages. The intervention group comments identified information on risks of alcohol, on weight loss and the calories in alcohol (Box 4). In contrast, the control group focused exclusively on alcohol; its harms, the need to monitor consumption, the advisability of cutting back and goal-setting (Box 5). A feature common to both groups is the surprise men express when they reflect on their alcohol consumption. The intervention group also expressed surprise about their weight. This suggests active engagement with the activities of the face-to-face sessions, with a clear differentiation between intervention and control.
I guess it focused my attention on alcohol and my relation to it.
Yes, it opened your eyes to what you drink.
Yes, confirmation that I drink too much and I’m overweight.
Awareness of calories in alcohol
Yes, made aware of calories etc. in alcohol.
Yes. Better understanding of calories in wine!
Yes. Gotta shock how much calories I had in a week with alcohol.
Motivation to drink less/lose weight
Yes, now I really need to lose weight. Drinking less will help.
Yes found out my weight and height and how many calories I take per week.
It told me my weight might be creeping up and noticing my consumption would be good.
Handy to know that what I assume to be normal social drinking habits are considered by some to be excessive.
The session was very useful to me as it opened my eyes to the amount of alcohol I take.
Awareness of risks
Yes it made me aware of the health risks I may develop due to drinking.
Yes makes you realise how your drinking is affecting your life plus how much you really drink.
Monitoring/cutting down
Will keep a closer eye on how much I am drinking.
Yes – reinforced determination to cut down amount of drink and do more exercise.
Goals
Yes, information and goals.
Yes points out key areas I need to aim for and from a health point of view made me aware of areas to aim for.
Weight loss
Yes, discovered weight loss.
The audio-recordings of the sessions showed that adherence to all tasks was very high for all study co-ordinators; only one item was missed on a single occasion. For the intervention group study co-ordinators, competence was mostly satisfactory or better for all activities; typical evaluation comments given by the research psychologist are shown in Table 14. These identify that there was scope for improvement on some items, particularly probing about alcohol consumption, transition between activities and provision of summaries.
| Task | Examples of evaluation comments |
|---|---|
| Completion of questionnaire | Checked questionnaire when he’d finished then probed on type of and size of drinksTLFB explanation wasn’t very detailed |
| Calculation of participant’s typical alcohol consumption | Good involvement of participant in the calculation. Asked him how he feels about total units – goodReally good explanation of units |
| Discussion of pros and cons of the participant’s current alcohol intake | Good prompting by providing examples of cons (as participant didn’t mention any). Nicely linked to discussion of pros of reducing drinkingA lot of probing about the pros and cons of drinking. The man started talking about smoking, SC did well bringing him back to the discussion about alcohol. Good reflections |
| Measurement of height and weight | Asked permission to measure height and weightGave coherent instructions on how to stand on the stadiometer |
| Plotting of participant’s BMI | After the participant plotted his BMI and found out that he is overweight, SC remained silent for a few seconds before he asked: does this surprise you?Participant plotted his own height and weight – excellent |
| Calculation of the participant’s typical calorie consumption from alcohol | SC used participant’s surprise about his BMI to introduce calories -well doneAsked how he felt about his unit consumption. Acknowledged his reaction |
| Discussion of how alcohol can contribute to weight | Participant was familiar with the ways alcohol contributes to weight, so they didn’t discuss this. I think they should’ve discussed thisSC led the discussion well, mentioned reasons for eating more. Good discussion of participant’s experience |
| Finish | Didn’t ask for permission to summarise. But summarised wellReally good summary |
The audio-recordings revealed that the control group study co-ordinators also performed very well, with few activities that could be improved (Table 15). A direct comparison between intervention and control is not possible, as they performed different sets of tasks. For both groups of study co-ordinators, these comments enabled verbal feedback (by telephone) to be provided. This consisted of one or two supportive comments followed by discussion on improvements that could be made.
| Tasks | Examples of evaluation comments |
|---|---|
| Completion of questionnaire | Excellent explanation of the questionnaire and the TLFBExcellent. Excellent probing |
| Provision of information on risks of drinking and opportunity for participant to consider the risks | Explained the units in what he drinks very wellExcellent – SC reflected on the risks the participant had already mentioned |
| Comparison of participant’s drinking with general population | SC didn’t spend a lot of time explaining the graphExplained the graph and how his drinking compares with the rest of the population very well |
| Provision of information about benefits for reducing drinking | SC mentioned only one strategySC provided a coherent description of relevant benefits to reducing drinking |
| Provision of information about strategies for reducing drinking | SC gave examples, but not necessarily relevant to what he’d already saidReally good. The SC said ‘I’m not telling you to stop drinking but if you’re interested in cutting back, this is what you could do . . .’Excellent. SC acknowledged the fact that the participant is not interested in reducing drinking but provided the strategies |
| Provision of information about sensible drinking targets | Mentioned targets and explained possible ways to cut down but didn’t talk about specific strategies to achieve itExcellent |
| Measurement of participant’s height and weight | Didn’t hear instructions to take things out of pockets etc. before weighing but said it before taking the height measurement. Didn’t hear asking him to stand straight etc.Good instructions, measured height twice |
| Finish | Summarised what they did, but it was not personalisedExcellent, a very detailed summary, gave the opportunity to ask questions, explained what is going to happen next |
Assessment of MI-based skills (intervention group only) showed some variation across the items, although the lowest score was adequate (Table 16). The maximum possible score was 4.0. Scoring was high on some items, such as displaying empathy (3.62) and sensitivity to the participants’ concerns (3.59). The more challenging items were encouraging discussion of current drinking (2.9), and providing summaries at the end of the sessions (3.17). This pattern was seen for all intervention group study co-ordinators.
| Technique useda | Mean score (out of 4) |
|---|---|
| Sensitivity to talking about other issues | 3.66 |
| Encourages talking about drinking | 2.9 |
| Elicits how participant thinks and feels | 3.28 |
| Empathic listening statements | 3.62 |
| Summarises | 3.17 |
| Sensitive to participants’ concerns and understanding | 3.59 |
Discussion
The evaluation revealed very high levels of acceptability of the study methods. The participants found the face-to-face session relaxed and non-judgemental; they enjoyed it and felt they benefited from it. This might not have been expected in a study that addressed two potentially sensitive topics: heavy drinking and obesity. Furthermore, the evaluation showed that the intervention and control packages were delivered as intended and that there was a major difference between the immediate effects of the two packages.
The very high levels of satisfaction with the face-to-face session were probably partly due to social desirability bias. This results from the desire of participants to avoid embarrassment in the presence of the interviewer. 120 However, the nature of the face-to-face sessions could have upset the men. The intervention group were told that they were very overweight and that their alcohol consumption could contribute to weight gain. The control participants were told that that their drinking would harm their health and that they should drink less. As these men were not help-seeking and did not think they had an alcohol problem, it might be expected that some would object to what they were being told. Thus, the almost complete absence of any critical comments suggests that none of the components of the session caused annoyance.
Another factor that might explain the high acceptability of the face-to-face session could be the friendly and supportive style of the study co-ordinators. Sensitivity and the ability to empathise were key features of selection and training. The pace at which the face-to-face session was conducted could also have been important. The intervention sessions lasted on average 45 minutes, and the control 33 minutes. This provided ample time for participants to ask questions and to discuss their feelings about the information that was provided.
Finally, the setting in which the session was conducted and the use of laypeople as study co-ordinators could have contributed to an atmosphere of relaxed informality in which potentially critical statements were judged to be inoffensive. Although these are only possible explanations, it would seem best to replicate this approach in a RCT as, at the least, the methods did not cause offence.
The use of laypeople (study co-ordinators) to deliver the face-to-face session proved effective. The wide range of venues and appointment times requested by study participants were coped with by the use of three co-ordinators for each treatment arm. The study co-ordinators engaged with the whole process and appeared motivated by a desire to help people. They found that the participants were willing to openly discuss their drinking. The intervention group were also willing to discuss calories and being overweight (this topic was not covered in control group sessions).
The participant questionnaire highlighted differences between the intervention and control groups in what participants perceived to be useful about the session. As would be hoped, the intervention group commented on weight loss and calories in alcohol. In contrast, the control group mentioned only alcohol, except for one man who mentioned weight loss. This finding should be viewed cautiously, as it reflected perceptions directly at the end of a session. Nonetheless, what can be said is that there would be grounds for concern if differences between the intervention and control groups had not been found.
The intervention and control packages were delivered with high fidelity. The audio-recordings of the sessions showed that adherence to the tasks and activities in the session was very high. This probably reflects the highly structured nature of the session, in which there were set activities (measurements), each of which was followed by a discussion of the measurements made. The assessment of competence identified that three activities could be improved: probing of alcohol consumption, transition between sessions and summarising at the end of the session. To improve performance during the study, sensitive feedback was given on these activities. This began with positive statements on what was done well and led to guidance on what could be improved. In future studies, more attention could be given to the problematic activities during training.
The monitoring of adherence and competence identified opportunities to improve this process. Providing a rating score for each task (poor, acceptable, good) would simplify the provision of feedback to study co-ordinators. In addition, the score could be used in quantitative analyses to see if it influenced behaviour change.
The remit for this study required that the comparator was an active control, a conventional alcohol brief intervention. The control package was based on the brief intervention used in three trials in the SIPS, funded by the Department of Health. 93–95 The training in this study was expanded from the 1-hour session used in the SIPS to five 2-hour sessions (three teaching, one assessment and one pilot). This was partly because training was needed in the completion of the baseline questionnaires and in the measurement of height and weight. In the SIPS, the intervention session was intended to last 5 minutes, whereas in this study the average length was 33 minutes. The extra time was taken in collecting the baseline data, but also in discussing the participants’ responses to components of the control package. These differences mean that the findings from the SIPS studies are not directly comparable with this study.
In summary, the evaluation provides support for the acceptability and technical feasibility for this component of a full RCT. In particular, adherence to and competence at intervention delivery were high. Furthermore, the men in the two treatment arms differed in their responses to their interventions. This approach to assessing intervention fidelity could usefully be adopted in future studies.
Chapter 10 Outcome assessment
Introduction
The main purposes of the outcome assessment were to estimate the retention of participants, to assess the acceptability of the study methods and to measure the primary outcomes for a RCT. The protocol for the feasibility study identified the retention of study participants as a challenge. A recent systematic review has shown that men-only weight loss interventions have an average loss to follow-up of 22%. 121 A related concern is the acceptability of the study methods, as this could affect engagement with the intervention and retention in the study.
Methods
Participants were invited to attend a follow-up visit 5 months after the baseline session. They were sent a reminder letter and a text message 2 weeks before the intended date of interview. The letter also asked about the most suitable time to be contacted. The study co-ordinators were sent contact details of the men, together with the participants’ previous preferences for venue and time to be seen. Study co-ordinators were assigned participants whom they had not seen at baseline.
Questionnaire design
Primary outcomes for the full RCT, alcohol consumption and weight loss, were measured using the same techniques as in the baseline assessment. The alcohol TLFB questionnaire58 and the FAST112 were administered. The Readiness Ruler113 was also used to identify motivation to reduce alcohol consumption. Weight was measured using Seca 813 medical scales. Responses to selected items from the Drinking Refusal Self-efficacy Questionnaire122 were also collected.
Acceptability of the study methods was assessed by seven questions exploring what participants thought about taking part, including ways in which the study might be improved. Knowledge of alcohol units, BMI and calories in alcoholic drinks was assessed. Experience of attempting to reduce alcohol intake was explored across several questions about awareness of harms, plans to reduce drinking and perceived benefits of cutting down. The intervention group were also asked four questions about recall of the text messages they had been sent.
In preparation for a possible economic appraisal of the intervention in a RCT, two validated questionnaires were completed. One was the EuroQol-5 Dimensions (EQ-5D)™,123 a standardised tool for measuring health outcomes. The Short Service Use Questionnaire (courtesy of S Parrot at the Department of Health Sciences, University of York, York, UK) was used to monitor usage of health care, social care and criminal justice services. The whole questionnaire was tested by piloting on research staff, study co-ordinators and community volunteers.
Questionnaire administration
The outcome questionnaire was administered by the study co-ordinators. This ensured that participants gave complete answers to open-ended questions and avoided difficulties with literacy that were encountered at the baseline face-to-face session. The study co-ordinators attended two training sessions on the administration of the follow-up questionnaire (see Appendix 10). These outlined sections of the questionnaire and the reasons why each set of questions was being asked. The co-ordinators practised administering the questionnaire and received sensitive feedback on their performance. Many of the questions were open-ended and the co-ordinators were encouraged to record the specific responses. Each co-ordinator administered the questionnaire in two pilot sessions with community volunteers before the follow-up with participants began.
Evaluation of study co-ordinator experience
At the end of the follow-up sessions, the study co-ordinators were asked to complete a questionnaire exploring their experience of conducting the face-to-face interviews (see Appendix 11). The aim was to identify ways in which the training and the co-ordinators’ manual could be improved. Open questions were used.
Results
Of the 62 men who attended the baseline face-to-face session, 61 (98%) were interviewed at follow-up. However, only 59 men (95%) attended a session at which their weight was measured and questionnaires were completed. The other two men were interviewed by telephone, during which they gave a self-reported weight. Because 4 of the 59 men were difficult to contact, their session was conducted by a member of the research team and not by a study co-ordinator. The Consolidated Standards of Reporting Trials (CONSORT) flow diagram for enrolment, randomisation, follow-up and analysis can be found in Appendix 12.
Alcohol consumption reduced substantially from baseline in both the intervention and the control group (Table 17). The reduction in consumption was greater in the control group than in the intervention group. The control group had a higher consumption at baseline and, despite showing the greater reduction, had a higher consumption at follow-up. More men in the control group reduced their number of drinking days, whereas more men in the intervention group reduced their number of binge drinking days (> 8 units in one session).
| Factor | Control group (n = 30) | Intervention group (n = 31) | ||
|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |
| Mean weekly consumption [units (SD)] | 53.3 (41.4) | 38.4 (35.3) | 41.1 (31.9) | 30.8 (33.0) |
| Mean number of drinking days (SD) | 14.8 (7.5) | 11.8 (7.9) | 15.2 (6.3) | 13.2 (6.9) |
| Mean intake per drinking session [units (SD)] | 15.3 (7.9) | 13.2 (5.7) | 11.7 (7.7) | 9.2 (7.0) |
| Mean number of binge drinkinga days in previous 28 days | 9.77 (6.6) | 8.37 (6.8) | 8.65 (6.0) | 6.32 (5.8) |
The average weight of participants did not change between baseline and follow-up (Table 18). Over this period some men lost weight, some remained unchanged and some gained weight. The patterns were similar for intervention and control groups.
| Factor | Control group (n = 30) | Intervention group (n = 29) |
|---|---|---|
| Mean weight, kg (SD) | ||
| Baseline | 110.8 (12) | 110.9 (18) |
| Follow-up | 110.1 (11) | 111.3 (18) |
| Number of men making specified change in weight, kg (%) | ||
| Lost > 1 kg | 9 (30) | 6 (21) |
| Difference of ± 1 kg or less | 13 (43) | 11 (38) |
| Gained > 1 kg | 8 (27) | 12 (41) |
The elements of the FAST112 shed interesting light on the effects of drinking on the participants’ lives (Table 19). The men seldom experienced instances where they failed to remember a previous night’s drinking, and they only rarely failed to fulfil obligations because of drinking. Only a few men had been told that their drinking was a problem or that they should reduce their alcohol consumption.
| Factor | Control group (N = 30), n (%) | Intervention group (N = 31), n (%) |
|---|---|---|
| How often do you have 8 or more units of alcohol on one occasion? | ||
| Never | 0 | 2 (6) |
| Less than monthly | 1 (3) | 1 (3) |
| Monthly | 6 (20) | 4 (13) |
| Weekly | 21 (70) | 22 (71) |
| Daily or almost daily | 2 (7) | 2 (7) |
| How often since you began the study have you been unable to remember what happened the night before because you had been drinking? | ||
| Never | 22 (73) | 29 (94) |
| Less than monthly | 5 (17) | 2 (6) |
| Monthly | 3 (10) | 0 |
| Weekly | 0 | 0 |
| Daily or almost daily | 0 | 0 |
| How often since you began the study have you failed to do what was normally expected of you because of drinking? | ||
| Never | 21 (70) | 28 (90) |
| Less than monthly | 3 (10) | 2 (6) |
| Monthly | 4 (13) | 1 (3) |
| Weekly | 1 (3) | 0 |
| Daily or almost daily | 1 (3) | 0 |
| Since you began the study has a relative or friend, doctor or other health worker been concerned about your drinking or suggested that you cut down? | ||
| Never | 22 (73) | 26 (84) |
| Yes, on one occasion | 1 (3) | 3 (10) |
| Yes, on more than one occasion | 7 (23) | 2 (6) |
At follow-up, intentions and actions to reduce drinking were more frequent in the intervention group than the control group. More men in the intervention group had thought about reducing their drinking or made a plan to cut down (Table 20). Among those who tried to cut down, the main reason (n = 14) was long-term health benefits; money, short-term personal benefits and family concerns were seldom mentioned.
| Intention/action | Control group (n = 30) | Intervention group (n = 31) |
|---|---|---|
| Since the study began. . . | ||
| I have thought about cutting down | 16 | 22 |
| I have made a plan to cut down | 3 | 11 |
| I have tried to cut down | 9 | 19 |
| I have successfully cut down | 10 | 16 |
| I have made a plan to deal with difficult situations | 4 | 11 |
| I consider myself at risk from effects of alcohol | 7 | 9 |
The intervention group were also more likely to think that they had successfully cut down and to have made a plan to deal with difficult drinking situations. It is surprising that in spite of these reported intentions and actions, few men in either group considered themselves at risk of the harmful effects of alcohol. Furthermore, when asked in general terms about possible harms of drinking, the participants were able to identify many different harms (Table 21). The only notable difference between the treatment arms was that more men in the intervention group identified overweight/obesity as a consequence of drinking.
| Perceived harm | Control group (n = 30) | Intervention group (n = 31) |
|---|---|---|
| Short-term negatives (acute harms) | 19 | 20 |
| Long-term health problems | 18 | 21 |
| Money problems | 6 | 8 |
| Family problems | 5 | 4 |
| Overweight/obesity | 5 | 9 |
| Addiction/dependence | 2 | 3 |
| Losing job/license | 3 | 6 |
| Other | 0 | 1 |
The ability to refuse a drink in different scenarios was broadly similar in the intervention and control groups (Table 22). Possible exceptions were that more men in the intervention group strongly agreed that they could resist drinking while watching television and when friends were drinking. More notable is that half of participants did not think they could resist alcohol when drinking with friends.
| Refusal statement | Control group (N = 30), n (%) | Intervention group (N = 31), n (%) |
|---|---|---|
| Do you think you could resist alcohol when you are watching TV? | ||
| Strongly agree | 19 (63) | 25 (81) |
| Agree | 11 (37) | 4 (13) |
| Don’t know/disagree/strongly disagreea | 0 | 2 (6) |
| Do you think you could resist alcohol when someone offers you a drink | ||
| Strongly agree | 15 (50) | 16 (52) |
| Agree | 9 (30) | 12 (39) |
| Don’t know/disagree/strongly disagreea | 6 (20) | 3 (10) |
| Do you think you could resist alcohol when your friends are drinking? | ||
| Strongly agree | 7 (23) | 10 (32) |
| Agree | 7 (23) | 7 (23) |
| Don’t know/disagree/strongly disagreea | 16 (53) | 14 (45) |
| Do you think you could resist alcohol when you are bored? | ||
| Strongly agree | 17 (57) | 18 (58) |
| Agree | 8 (27) | 9 (29) |
| Don’t know/disagree/strongly disagreea | 5 (17) | 4 (13) |
In both the intervention and the control group, few men knew their BMI (Table 23). However, more men in the intervention group had counted the calories in the alcohol they consume. Almost all of the men in the study believed that their drinking contributed to their weight, with no difference between intervention and control.
| Factor | Control group (N = 30), n (%) | Intervention group (N = 31), n (%) |
|---|---|---|
| Number of men who report knowing their current BMI | 4 (13) | 4 (13) |
| Number who have counted the number of calories they consume from alcohol | ||
| Yes, before taking part in the study | 1 (3) | 2 (6) |
| Yes, since taking part in the study | 0 | 5 (16) |
| Both before and since taking part in the study | 2 (7) | 2 (6) |
| Number who believe that alcohol contributed to them becoming overweight | 24 (80) | 26 (84) |
Knowledge of the units of alcohol was assessed by asking the men to state the number of units in lager, wine and whisky. Because these drinks come in a range of strengths, the responses have been grouped, with one grouping covering the range of possible correct answers (i.e. 2.0–2.49 units for a pint of lager, 3.0–3.5 units for 250 ml of wine and 1.0–1.5 units for spirits). The results are broadly similar for the intervention and control groups (Figure 6). The men were mainly correct on the units in lager, but tended to either underestimate or overestimate the units in wine, and to overestimate the units in spirits.
FIGURE 6.
Participants’ estimates of the units in common types of drinks.
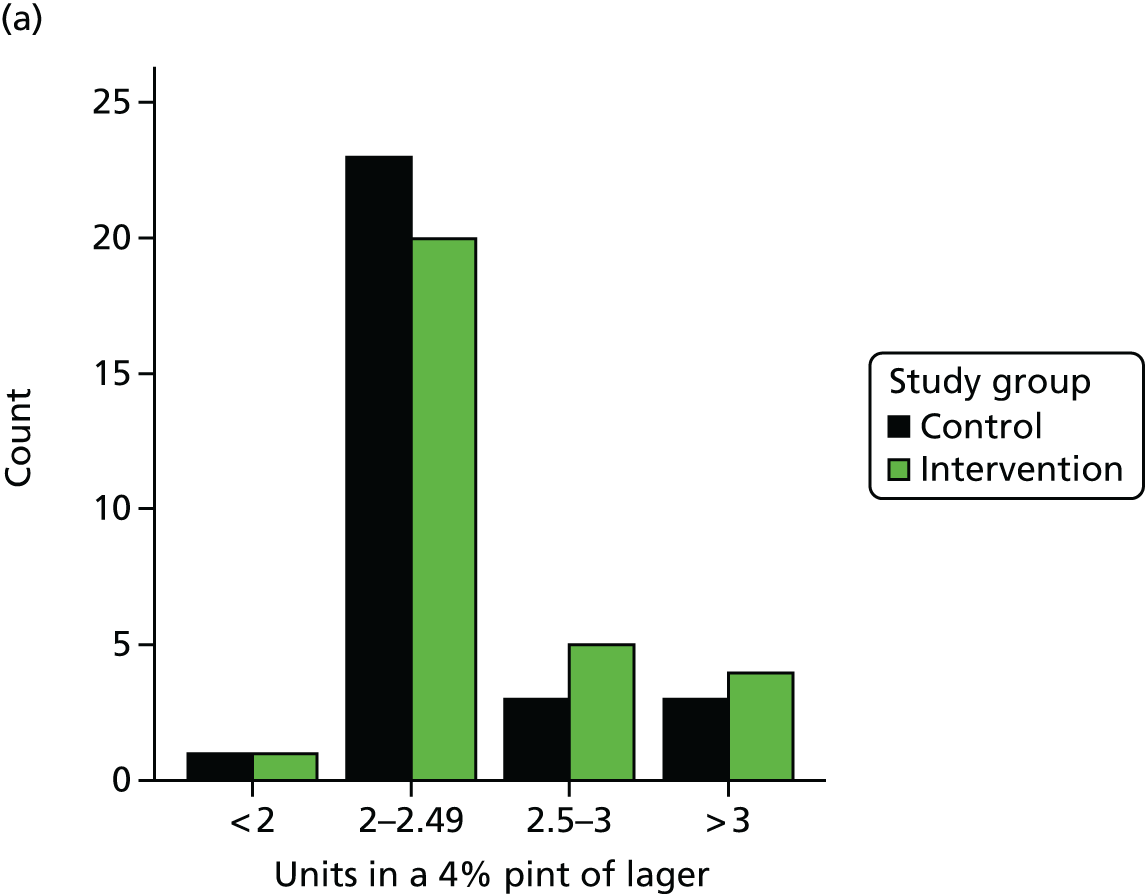


The question about the calories in common drinks was asked in the same way as the question about units in drinks. The correct answer for each type of drink fell in within a range: a pint of lager contains 150–249 kcal, a 250 ml glass of wine contains 150–249 kcal, and one measure of a spirit contains 50–99 kcal. The participants in both the intervention and the control group were more likely to be incorrect than correct, with a tendency to overestimate (Figure 7).
FIGURE 7.
Participants’ estimates of the calories in common types of drinks.
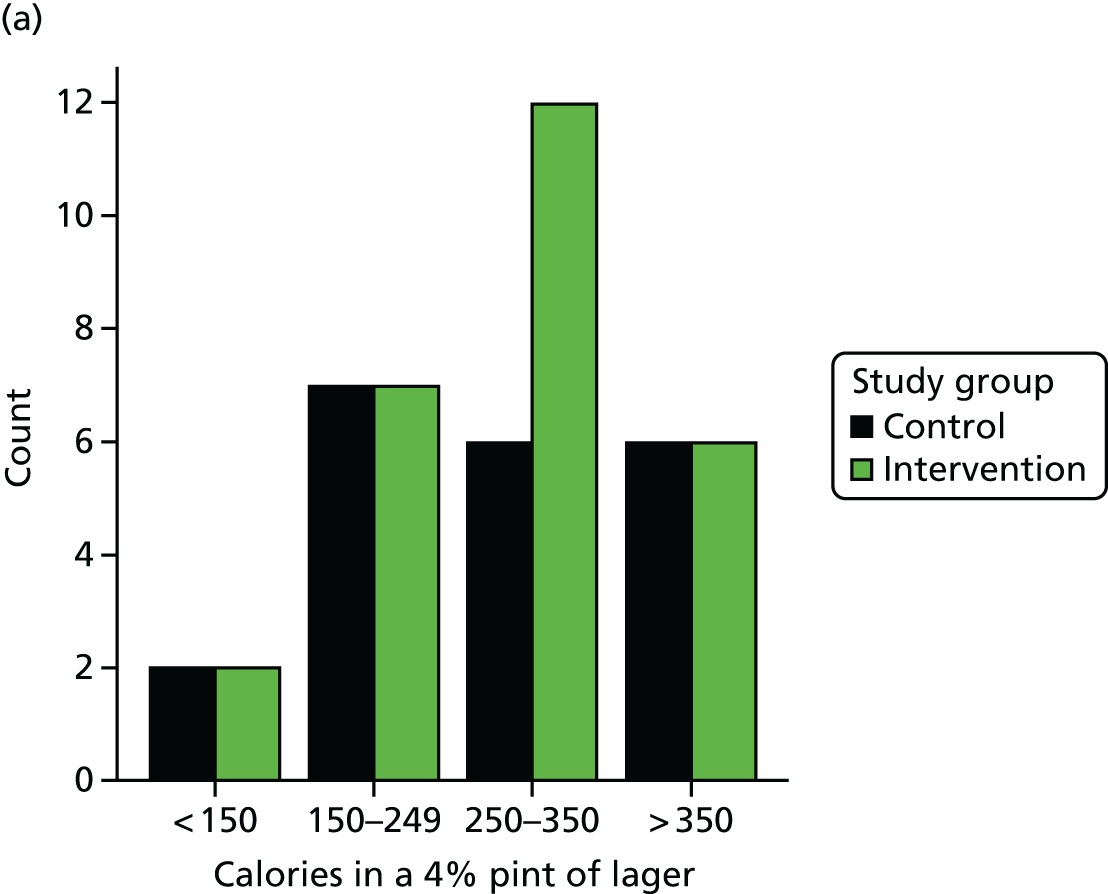
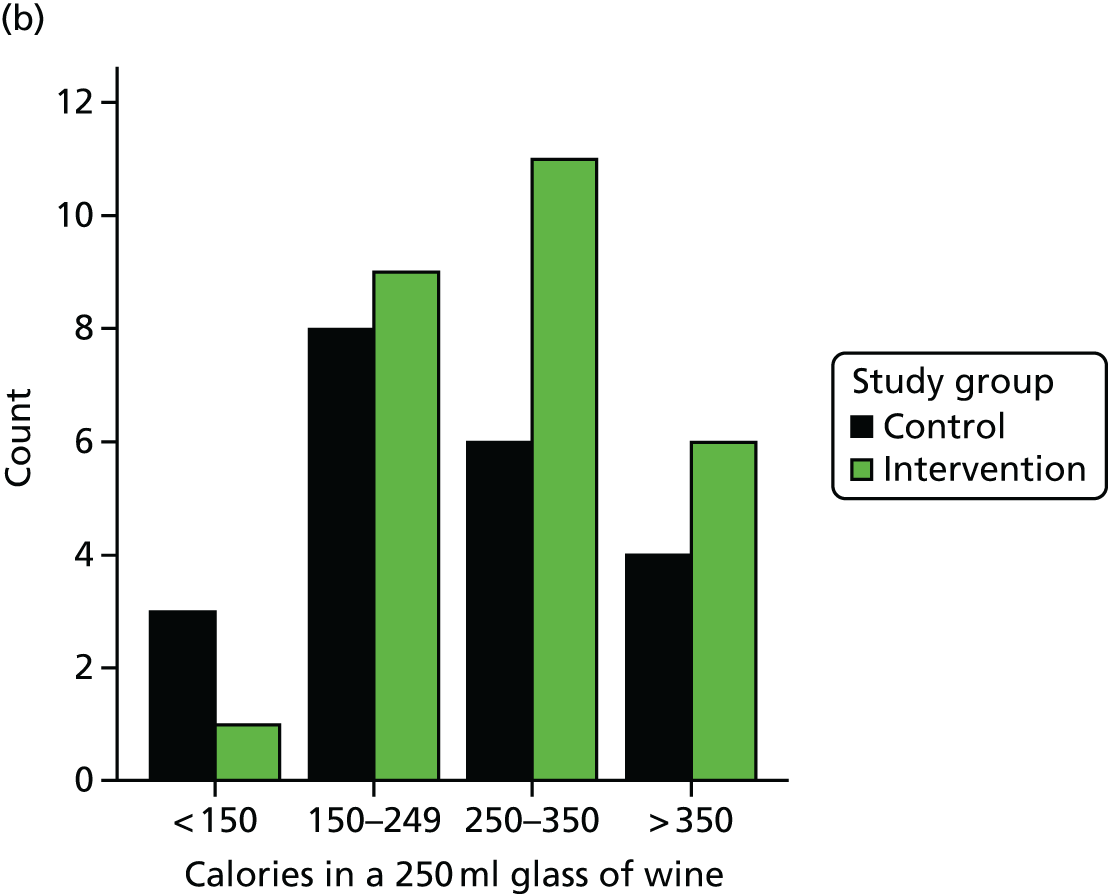

Acceptability of the study to participants
The acceptability of the study to participants was assessed using indirect questions such as whether or not they discussed the study with anyone and whether or not they would recommend the study to others (Table 24). The use of a direct question about acceptability was avoided, as some men may have chosen to give a polite rather than incisive answer. Acceptability ranged from 70% to 90%, depending on question phrasing, with acceptability levels being similar for intervention and control groups. The highest level of acceptability reported (90%) was for the perceived benefit of taking part in the study. Common specific benefits were increased awareness of personal alcohol consumption (n = 25) and having stopped or reduced drinking (n = 16). Most participants (> 80%) would recommend the study to others. The men were most likely to recommend the study to partners (n = 31) and to friends and colleagues (n = 22).
| Factor | Control group (N = 30), n (%) | Intervention group (N = 31), n (%) |
|---|---|---|
| Usefulness of the information given | ||
| Very useful | 10 (33) | 12 (39) |
| Useful | 17 (57) | 16 (52) |
| Don’t know | 2 (7) | 3 (10) |
| Not very useful | 1 (3) | 0 |
| Participant would recommend the study to others | 24 (80) | 26 (84) |
| Participant benefited from taking part | 23 (77) | 22 (71) |
| Participant discussed the study with other people? | 22 (73) | 23 (74) |
| Participant gave suggestions on how to improve the study | 14 (47) | 15 (48) |
The participants were told that this was a feasibility study and were asked for suggestions to improve it. The control group wanted more support in completing the TLFB (n = 6) and more information in the face-to-face session (n = 4). Overall, 15 men in the intervention group gave suggestions for improvement of the study. Most frequent was the request for alterations in the text messages (n = 9); some men wanted more humorous or hard-hitting texts, while others felt that the experiences of the characters in the text messages were not relevant to them. The men in the intervention group also requested more frequent meetings with a study co-ordinator (n = 6).
Preparation for an economic evaluation
Two standardised questionnaires were evaluated for usefulness in the economic evaluation that would accompany a RCT, one addressing quality of life (the EQ-5D)123 and the other the use of services (the Short Service Use Questionnaire). The EQ-5D showed that, although few men in either group had problems with self-care, usual activities, anxiety or depression, about one-third of men had problems with mobility and half reported pain or discomfort (Table 25).
| EQ-5D question | Control group (N = 30), n (%) | Intervention group (N = 31), n (%) |
|---|---|---|
| Number of participants reporting: | ||
| Problems with mobility | 11 (37) | 7 (23) |
| Problems with self-care | 1 (3) | 2 (6) |
| Problems doing usual activities | 5 (17) | 5 (16) |
| Feelings of pain or discomfort | 13 (43) | 17 (55) |
| Feelings of anxiety or depression | 7 (23) | 4 (13) |
| Reported overall health on a scale 0–100 | ||
| 0–50 | 3 (10) | 6 (19) |
| 51–60 | 4 (13) | 2 (6) |
| 61–70 | 7 (23) | 8 (26) |
| 71–80 | 12 (40) | 7 (23) |
| 81–90 | 4 (13) | 7 (23) |
| 91–100 | 0 | 1 (3) |
The responses to the service use questionnaire (Table 26) showed that the average number of contacts with the health-care system was very low. The data for contact with Social Services and Criminal Justice Services have not been shown as none of the participants had any contact with these services.
| Service use (in the past 6 months)a | All participants (N = 61), mean (median) |
|---|---|
| How many times have you visited an accident and emergency department as a patient? | 0.07 (0) |
| How many nights have you spent in hospital as a patient? | 0.02 (0) |
| How many times have you been admitted to hospital but not been kept in overnight? | 0.03 (0) |
| How many appointments have you had as an outpatient at the hospital? | 0.51 (0) |
| How many times have you visited a doctor at your GP practice? | 1.54 (1) |
| How many times has a doctor visited you at home? | 0 (0) |
| How many times have you visited the nurse at your GP practice? | 0.9 (1) |
| How many times has a nurse visited you at home? | 0.02 (0) |
| How many times have you received a prescription? | 2.84 (2) |
Comments from the study co-ordinators
The study co-ordinators appeared to have enjoyed their experience in the project and thought they had gained from it (Box 6). Some of the comments could prove useful for recruiting study co-ordinators for future studies. In addition, a few areas for improvement were identified, particularly guidance on dealing with extraneous noise in home settings. Furthermore, the suggestion that a checklist of the activities should be provided to supplement the manual has merit. Once study co-ordinators are familiar with the face-to-face session, they do not need the detailed content of the manual. The checklist, which was used as an aide memoire, was found to be helpful. The suggestion that less attention should be given to the measurement of height and weight should probably not be acted on. Although these activities seem straightforward, simple errors can creep in.
Confidence, learning and communication skills.
I have thoroughly enjoyed working on this study. It has been a great experience and has motivated me to do similar work in the future. I feel that my strength lies with communication.
It has benefited my personal development in communication and also in organisational skills.
Training
(Most helpful parts)
Role play. Obviously everything leading up to the role play also. But it is not until you do it yourself a few times that you feel comfortable and confident.
(Least helpful parts)
Possibly too long on weighing and measuring height.
Study co-ordinator manual
Was it helpful in preparing for sessions?
Initially very helpful but once I did a few I didn’t really read much of it.
Was it helpful in delivering the sessions?
Less helpful (a checklist is more practical)
Very helpful. Didn’t need all of it but the example script was invaluable!
Was anything missing from the manual?
Sometimes too much information can lead to overload, and for our roles probably wouldn’t be needed.
Could anything be explained more clearly?
What to do in participant’s own home, e.g. what to do if someone else is in the room or if the television is on.
Discussion
The follow-up analysis has shown that the rate of retention was very high, that the outcome data were collected and that the study methods were acceptable to participants.
Rates of retention are often poor in obesity trials. 124,125 Although rates across individual studies vary widely,126,127 reviews have found average retention rates of 70–80%. 121,128 A recent study of a mobile phone intervention in overweight adults had 68% retention. 129 The retention rate of 98% in this study may reflect the efforts made by the study co-ordinators and the research team to contact men. The goodwill that the participants felt towards the study could also have aided retention.
A reduction in alcohol consumption was seen in both intervention and control groups. This study used an active control – a conventional brief intervention – so a fall in consumption would be expected. However, the size of the reduction was greater in the control group than in the intervention group. Interpretation of this finding is difficult because consumption at baseline was much higher in the control group than the intervention group. Imbalance at baseline is recognised to occur in small studies, and current guidance is that such studies should not be used to estimate effectiveness. 22,25,114
Self-reported alcohol consumption amounts to only 40–60% of alcohol sold. Recent survey data from four English-speaking countries account for only 31–57.5% of alcohol actually sold. The under-reporting for Scotland is 54%. 130 One explanation for this is social desirability bias, in which individuals report drinking less to make a good impression. 131 The bias would need to increase greatly from baseline to follow-up to account for the observed falls in consumption. This seems unlikely.
The findings on the fall in alcohol consumption could also be explained by regression to the mean. 132 Some men could have consumed an unusually large amount of alcohol just before the baseline session, resulting in a high mean consumption. However, by the time of the follow-up session the participants could have been drinking more normal amounts, producing the observed fall in consumption. These findings illustrate why an adequately powered RCT is required to provide a reliable estimate of the effectiveness of the intervention.
No loss in weight was seen in either the intervention or control groups. Although alcohol consumption was reduced, a longer interval would be needed before weight loss would be observed. It is also possible that an extended intervention period would be helpful. Weight loss interventions are commonly delivered over a period of several months. 18 Extending the text messages would enable additional time to be given to relapse recovery and maintenance of the new behaviour.
The acceptability of the study methods was high when measured by several indirect questions. Participants reported that they found the information given useful, they discussed the study with family and friends and they would recommend it to others. Some men suggested improvements to the study, but these mainly consisted of a wish for more information or for more contact with study co-ordinators. The only critical comments were on the content of a few of the text messages that the intervention group received.
An important finding was that most participants did not view their drinking as harmful, despite being knowledgeable about the harms of alcohol. Possibly this sense of invulnerability occurred because few suffered from acute effects such as forgetting what had happened during the previous night’s drinking or being unable to perform usual activities because of alcohol. Thus, the men may think that these harms will affect only other drinkers. The challenge for an intervention is to increase the perceived relevance and importance of these harms. In a full RCT, more attention should be given to the increased risk of liver disease that results from being obese and drinking heavily. In addition, efforts should be made to increase perceived susceptibility to these risks.
Recall of the units of alcohol in common drinks was poor in both the intervention and the control groups. One explanation for this could be that men do not often think about their alcohol consumption in terms of units. There is evidence that people measure their consumption in drinks rather than in units133 and find the arithmetical difficulty of the calculation a deterrent to the use of units. 134 In the light of this, it is not surprising that there is poor retention of the detailed information given on one or two occasions. For the RCT, it would be better to focus on reducing the quantity of alcohol consumed. This would allow men to visualise their consumption in ways that are familiar to them.
A few men felt that one theme of the text messages, five-a-side football, was not relevant to them. This was used as a device to encourage men to reflect on the physical capabilities of their youth, so that recapturing some of that lost fitness could be used as a motive for losing weight. An alternative theme that would be relevant to all men could be climbing stairs or walking a road with a steep incline. These are activities that the men in this study recalled performing with ease in their youth that they perceived to be important and relevant to them in the present and future. This theme could be incorporated into the text messages for a RCT.
The questionnaires that would be used in an economic evaluation produced mixed findings. The quality of life instrument, EQ-5D,123 detected problems that could be associated with obesity, mobility problems and pain and discomfort. It would be useful for a RCT. The Short Service Use Questionnaire recorded very few contacts with police/criminal justice, social services and the health-care system. In any planned economic evaluation, consideration will need to be given to the fact that the baseline contacts with the health system and criminal justice system will be very low. Any benefit of reduced alcohol consumption and weight is most likely to be observed in the future rather than during the study period.
In summary, the follow-up analysis has demonstrated that a high retention rate can be achieved with the target group and that the outcome measures for a RCT can be measured. It has also shown that the study methods are acceptable to the participants. Several findings are consistent with the intended mode of action of the intervention. More men in the intervention group than the control group reported making a plan to reduce their drinking, succeeding in reducing their drinking, thinking that alcohol led to overweight/obesity and counting the calories in the alcohol they consumed. The analysis has also identified several ways in which the intervention could be strengthened, particularly by increasing the perceived risk of the harms of alcohol and by extending the intervention period.
Chapter 11 Evaluation of the text message intervention
Introduction
The intervention group received a series of 95 SMS messages that were delivered over a period of 8 weeks. The control group were sent four messages during these 8 weeks as a way of keeping in touch with participants and maximising retention in the study. The results in this chapter are based on the data from the 31 men in the intervention group.
The text messages were designed to promote interaction and increase engagement with the intervention. Some messages were intended to prompt a response, but participants could reply to any of the text messages they received. The responses from participants were anonymised and collated by the Health Informatics Centre at the University of Dundee. The computer package that delivered the messages also stored all text message responses received from participants electronically (see Chapter 4).
Methods
Fidelity of the delivery of the intervention was assessed by monitoring delivery of the text messages to the mobile phones of the participants. Engagement with the intervention was assessed by recording the frequency of responses from the participants during the intervention phase. Content analysis of the responses given provided a method to ascertain the nature of engagement with components of the behaviour change intervention.
Fidelity of delivery of the text messages
Short Message Service messages can be tracked to determine whether or not they were delivered to the recipient’s mobile phone. When the messages were not delivered, for example because the phone was switched off, the computer program resent the message for 24 hours. A message that was never delivered during this period was recorded as a delivery failure. The program would then send the next message in the sequence of 95 messages.
The delivery status of the SMS messages was recorded as delivered (the phone had reception and was switched on), undelivered (the phone was switched off or it had no signal for 24 hours) or no status returned. The program could not record whether or not messages delivered to the phones were opened by the recipient.
Content of the text message responses
The series of SMS messages that made up the intervention were based on the HAPA80 and incorporated behaviour change techniques. 38 Fourteen of the 95 messages requested a response to a specific question. The questions were crafted to reinforce key components of the intervention. Responses to a question confirmed that the participants had opened and read the message, understood the question, reflected on the content/context of the question and had given a considered response. Analysis of the content of the messages received from the intervention group participants permitted an assessment of the degree of engagement with the study and with the psychological constructs of the intervention.
The key steps in the behaviour change sequence were identified and addressed in the text message intervention (see Chapter 4). In order to assess engagement with these steps, text message questions were constructed to assess the following:
-
self-monitoring of alcohol consumption
-
awareness that heavy drinking encourages unhealthy eating
-
perceived benefits of drinking less
-
awareness of harmful effects of obesity
-
subjective norms (perception of significant others’ beliefs)
-
goal-setting and action planning
-
perceived benefits of changing current drinking pattern
-
coping planning
-
benefits enjoyed by drinking less.
Monitoring for adverse events
The anonymised responses from the participants were screened daily by a member of the research team. This was essential so that issues raised by the participants could be addressed quickly, for example a cry for help with an alcohol problem, a change of address or phone number, or a request to be withdrawn from the study.
Results
Fidelity of delivery of the text message intervention
The intervention package included 95 SMS text messages. Thus, a total of 2945 messages were sent to the 31 participants during the intervention period. Of these, 2887 messages (98%) were delivered to the participants’ telephones. The remaining 58 messages were recorded as undelivered (the phone was switched off or it had no signal for 24 hours). Twenty-two men failed to receive one or more messages. The number of undelivered messages per participant ranged from one to seven of the 95 sent, with a median two messages missed. None of the participants missed consecutive messages.
Responses to the text messages
Text message responses were received from all but two of the participants (94%). A total of 456 messages were received from the remaining 29 men (Figure 8). The number of responses per participant ranged from 0 to 41 (mean 14.7, median 12). More than 60% of the men responded more than 10 times. However, there was marked variation between participants. Four men responded more than 35 times, while seven responded on fewer than five occasions.
FIGURE 8.
Number of responses to text messages per participant. ID, identification.
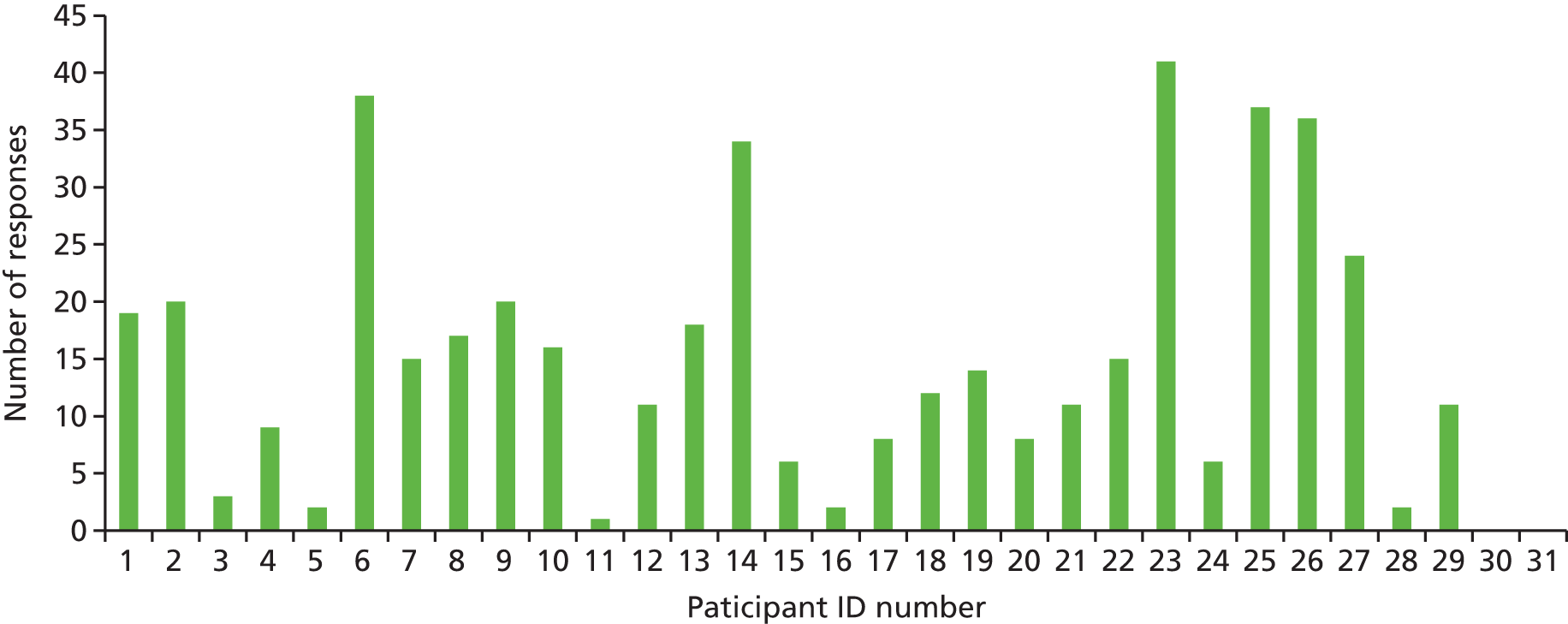
A total of 245 responses were received to the 14 text messages that prompted a response, giving a mean response of 17.5 per message (Figure 9). In addition, many of the participants responded to other text messages. Of the 81 messages which did not request a response, 40 received at least one reply. The mean response to these 81 messages was 2.6 responses per message.
FIGURE 9.
Number of replies to text messages that prompted a response.

Twenty-nine of the 31 participants responded to the text messages that asked questions (see Figure 9). More than 80% of the participants (25 men) answered the first and sixth questions. Overall, 10 of the 14 questions elicited responses from > 50% of participants. The first eight questions attracted ≥ 16 responses each, whereas four of the remaining questions attracted ≤ 13 responses. This may indicate that there was some attenuation during the second half of the intervention period. However, 20 men (65%) answered the penultimate question, indicating that interest was maintained throughout.
Content of the text messages
Engagement with the study and components of the intervention was assessed by reviewing the content of the responses received from the participants. Three questions (text numbers 4, 39 and 83; see Figure 9), provided multiple choice responses. These questions attracted a high number of responses. The remaining questions asked personal questions that required the participants to reflect on their position and give a considered answer. In general, a great deal of thought had gone into the responses. Many of the messages were longer than the 160 characters permitted in one text message. Illustrative responses are presented to specific text message questions, to demonstrate engagement with the components of the behaviour change strategy.
Self-monitoring of alcohol consumption
Early text messages suggested that the participants should try to keep track of how much they were drinking. A week into the intervention period, a text message asked: ‘Did you manage to count how much you drank over the week? Text me your answer please’ (text number 23).
More than half of the participants responded to this question. Some gave an exact amount, while others gave a self-assessed comment on their consumption. Some men were satisfied with their consumption but others realised that they were drinking too much:
5 pints And 7 nips I’ve done great this week.
Only 26 units :-(
Sorry but up to 12 gins 5 pints and 8 bottles of Heineken up to now still on it . . .
Too much again . . .
Awareness that heavy drinking encourages unhealthy eating
An important part of the intervention was to increase awareness of the connection between heavy drinking and unhealthy eating. At the beginning of the third week of the intervention period the men were asked: ‘Has your drinking ever influenced what you eat? Text me if you’ve noticed that it does’ (text number 29).
Twenty-three men responded to this question, and many recognised that they were inclined to eat more during or after a heavy drinking session:
Kebabs . . . beef curry fried rice . . . after a few pints . . .
Yes, sometimes if I have a drink I will eat crisps if at home or if I’m out will get a kebab or pizza. If not having a drink I probably wouldn’t even think about having extra to eat.
Yeh I make up for the lack of sweet things the night before by eating lots of cakes . . .
I eat a lot of junk food while having a can of beer in the house . . .
I don’t eat a lot when I’m drinking . . .
Perceived benefits of drinking less
The intervention was designed to encourage the participants to re-evaluate their current drinking habits. This was presented as a question to encourage men to consider the benefits of drinking less and commit their thoughts to words. The question on day 18 asked: ‘Can you think of any reasons why it might be a good idea for you to cut down a bit on your drinking? Please text me your answer’ (text number 33).
Twenty-one men responded to this question, indicating that they were well aware of the potential benefits of cutting down:
Get rid of the beer belly . . .
To stave off periods of gout, lose weight, feel generally healthier . . .
My weight diabetes sanity marriage . . .
Much easier to lose weight when not drinking. Also feel more clear headed and active. Earlier to rise in the morning, too.
I can think of many good reasons to cut down and even stop but that is something you would want to do . . .
Awareness of harmful effects of obesity
The intervention introduced the concept that reduced drinking could help with weight loss, and the problems associated with obesity were discussed. On day 20 the participants were asked: ‘Does being overweight affect anything you do? Please text me your answer’ (text number 36).
Participants clearly had experienced a range of problems, particularly with mobility:
Got asked to play five-a-side football a couple of weeks ago but for age and weight reasons I decided against it . . .
Being overweight causes any kind of serious exercise problems including those of a sexual nature.
I struggle on the golf course after 1st 9 . . .
No! Still able to do what needs done . . .
Yes stops me running around with my grandson . . .
One man put a great deal of thought into this question and identified many consequences of being overweight, which he related in three separate messages:
Yes. Doing up my shoe laces. Getting in and out the car. And more. I’ll text again when I think of more.
Stairs. Doing the paper work on the loo. Getting off the sofa.
. . . Yeah it doesn’t do wonders for the stud in me either. It’s also that alcohol breath that doesn’t do it for the wife . . .
Subjective norms
More than 3 weeks into the intervention period the participants were asked: ‘Can you think of someone who’d be happy if you drank a bit less? What would you hear them say? Please text me your answer’ (text number 42). This message was intended to encourage the men to identify people who would approve of their efforts to reduce consumption and would offer their support. Seventeen men responded, identifying a variety of friends and family, and reporting what their responses would be:
Probably my kids. They are adults and hardly drink at all. They would probably tell me I’ll live a bit longer if I cut back.
My wife. You’ve been drinking 4 times this week you’ll never see 60 if you keep that up . . .
My daughter and girlfriend they would say thank god I’ll save a fortune . . .
Yes the wife, told u that u would feel better about things . . .
My wife and my belly come to mind . . .
My daughter would be happier . . .
Goal-setting and action planning
Goal-setting and action planning facilitate behaviour change. Initially, the men were asked: ‘If you made a goal to cut down a bit on your drinking, what would it be? Text me your answer please’ (text number 50). Seventeen men responded with a variety of options, including avoiding opportunities for drinking and reducing the amount consumed in a session:
No drinking when football is on . . .
No drinking mid week would be a goal.
Two bottels [sic] of wine a week rather than three is a start . . .
Try to cut out Monday to Thursday when I usually have a couple of beers . . .
Having had a day to think about goals to reduce drinking, the men were then asked to consider making a plan to implement changes in order to achieve their goals. The men were sent a text message with information on how to go about making their own plans: ‘When you make a plan it always works better if you make sure you say: WHEN; WHERE; and HOW you will do it.’ This was followed by an invitation to make a plan of their own: ‘If you made a plan, what would it be? Text me your answer. Remember: WHEN; WHERE; HOW?’ (text number 56).
Thirteen men presented their plans, with some spelling out the when; where; and how of how it would be implemented. A common theme was simply an intention to purchase less alcohol:
When: weekends. Where: change buying habits. How: buy only one bottle of wine and maybe 2 beers for the whole weekend . . .
Buy less cans when I go to the shops just get 4 instead of 8 or 12 . . .
I’ve got a plan. Instead of buying 75cl bottles I’m going to buy 37.5’s instead. Just not sure when my next wine purchase will be!
No plan, just one bottle less this week . . .
This question attracted fewer responses than any of the previous questions. This may simply be a reflection of participants’ position. They may have considered making a goal (previous question), but not yet thought about how to achieve it.
Perceived benefits of changing current drinking pattern
To encourage the men to persevere with their new behaviour, they were asked to identify potential benefits they could enjoy: ‘Getting a result from changing things makes the effort involved worthwhile. What would make it worthwhile for you to cut back a bit? Please text me your answer’ (text number 63). More than 60% of the participants presented very personal benefits. This question intentionally did not specify what type of benefits they may feel, but almost all of the responses referred to the benefits of weight loss:
Weight loss would be great . . .
Getting my health back and getting back into my 32 jeans . . .
I can’t lose weight without limiting my alcohol intake. I need to lose weight for health reasons.
Feeling comfortable in summer clothes . . .
Having a few more pounds in my wallet rather than on my waistline . . .
If it meant not having to take high blood pressure medication every day.
My time with my family . . .
Coping planning
To encourage maintenance of their reduced drinking, participants were encouraged to think about strategies to deal with situations when they may find it difficult to avoid drinking. Thus, they were asked: ‘Thinking about tricky drinking situations, what could you do to help you to stick to your plan? Text me your answer’ (text number 76).
This question was relevant only to those who had already made a plan to cut down on their drinking. Thus, only nine men responded, but those who did had carefully considered strategies:
Limit time spent where alcohol is served reduce intake . . .
I would go to my workshop or gym and try to keep myself busy . . .
I need to avoid keeping alcohol in the house and only drink when out socialising.
If i go to a meeting or a funeral etc and i do not want to get involved i just take the car, no temptation.
Take enough money out for a few pints and leave the bank card at home . . .
Benefits of drinking less
Towards the end of the intervention period participants were invited to report any effects of reduced consumption: ‘If you have cut down on your drinking a bit, have you noticed any difference?’ (text number 85).
This question would only be relevant if the participant had indeed managed to reduce his drinking. Twelve men responded, the majority of whom had experienced benefits from reduced drinking. A few, however, reported that they had not:
Yes, feeling fresher in the mornings and getting into work sharp.
Yes I’ve made a big change to my drinking habits. Cut down tremendously and exceeded my goals by far. I haven’t lost any weight as yet and need to begin my fitness program. Starting to feel a bit better.
Not yet . . .
Responses to text messages that did not seek a response
Participants frequently responded to text messages, even when no question was asked. One message that attracted many responses was one which gave instructions on how to calculate BMI. This prompted a number of men to respond, some of whom had calculated their own BMI:
Oops I’m 34.9 lol . . .
With my calculations, I’m also obese but not like really obese, also just a few too many kilos . . .
I’m not overweight I’m just under height for my weight if I was 7 feet 5 inches I would be fine . . .
Bmi s[sic] . . . just confirm what you already know. Its do you have the will to do something about it . . .
Daily monitoring of text messages
In addition to responding to the content of the intervention, participants could send messages if they needed to get in touch with the research team. They had been asked to tell the study team about changes in address or telephone number, or if they wanted to withdraw from the study. Most importantly, they could report adverse events or any distress they were experiencing. Thus, anonymised responses from the participants were screened daily by a member of the research team. Text messages from four men required action to be taken. Three of the men were called to discuss the issues raised, and one was sent a text message. All four men continued to be part of the study.
One participant sent a message saying ‘Can you stop texting!’. He was subsequently called by a research assistant to discuss the problem and to determine whether or not he wanted to withdraw from the study. The participant reported that he felt he was receiving too many messages. However, following a discussion with the research assistant, the participant decided to remain in the study.
A message from one participant indicated that he was feeling very despondent. The trial manager called him immediately and established that he was now with a friend. He was encouraged to visit his GP the next day. This was followed up by another phone call 4 days later to ensure that the participant was feeling better.
Two consecutive messages from another participant revealed that he felt some of the messages were not relevant to him. A research assistant called to reassure him that although some messages may not be relevant, his input and contribution to the study was valued.
The fourth man sent a message giving details of hospital tests that he had undergone. This information was passed to the study co-ordinator who was scheduled to conduct the follow-up appointment. It was important that the study co-ordinator had the background information in case he discussed his health problems at the follow-up appointment.
Discussion
This feasibility study has shown that the target group, men who are obese and drink more than the recommended guidelines, engaged with the tailored, interactive intervention that was delivered by text message. The methods used for monitoring delivery of the messages and evaluating the participants’ responses showed that the men received the text messages, they opened and read them, they carefully considered the content of the messages, they engaged with the components of the behaviour change strategy and they took the time to respond to questions asked.
Fidelity of delivery is essential for the success of an intervention. 135 This study has shown that a text message intervention can be delivered with very high fidelity. Almost all of the messages (98%) were successfully delivered to the phones of the participants. The high volume of responses received from the men, more than 450 over a 2-month period, confirmed that the messages had been read and understood.
Comprehension of the intervention and ensuring that participants are able to perform the new skills taught are also important measures of fidelity. 136 By incorporating questions that addressed steps on the causal model to behaviour change, the study provided a method to assess both of these requirements. All of the responses indicated that the participants had understood the questions. Many responses were what would be expected if there was a high degree of engagement with the intervention. Clearly, some of the men were willing to act on the messages in ways that could lead to behaviour change. For example, a precursor to action to change behaviour for men in this study is the recognition that obesity is affecting them personally, and the realisation that reduced drinking could help to address this. For many men who identified potential benefits of reducing drinking, the reason was related to obesity, for example getting ‘rid of the beer belly’, losing weight, and avoiding gout and diabetes. This gave a clear indication that the men were engaging with the intervention. Later in the intervention period, the responses demonstrated that the men were able to use the behavioural skills demonstrated in the text messages for example goal-setting and action planning, and the cognitive skills taught such as preparing for risky drinking situations. For example, some men had considered and implemented strategies to avoid excessive drinking, including taking their car on nights out, finding alternative activities to those that involved drinking, and simply buying less alcohol.
The study has shown that interest was maintained throughout the intervention period. Some attenuation in the number of men responding to the later questions was observed. However, this was partially due to the nature of the questions posed during the last two weeks of the intervention. Some of the later questions were relevant only to those men who had already made changes, that is the questions asked about coping planning, strategies to maintain reduced drinking and about the benefits of reduced consumption. The intervention period of 8 weeks was possibly too short to guide participants through the complete behaviour change process. For a RCT, a longer period of at least 3 months would give participants a greater opportunity to work through the steps to behaviour change.
A major advantage of this intervention is that participants respond in real time. They can read and re-read the messages at a time that suits them, they can take time to consider the content and consider their response or reaction to the messages and, if they so wish, send a response back. These responses give an indication of the impact of components of the intervention as it happens. These steps form a valuable part of the intervention, as well as serving as a tool for process evaluation.
The final benefit of monitoring the text message responses was the opportunity to detect any dissatisfaction among the participants or adverse events. By reviewing the text messages every day, the research team were able to act on any problems swiftly and effectively. Monitoring responses is important for ethical reasons in research studies. However, for a substantive service delivered over a wide area, an alternative approach might be required to reduce the workload of monitoring.
Conclusions
The text message intervention was delivered with high fidelity to the target group. Content analysis has shown that the text messages were understood, and that the participants engaged with the intervention. Without suggestion, men identified losing weight as the main benefit of changing their current drinking pattern. The responses also demonstrated that the men were able to use the behavioural and cognitive skills demonstrated in the text messages, for example goal-setting and action planning. More text messages, delivered over a longer period, may be required to allow the participants more time to progress through the behaviour change process.
Chapter 12 Summary and conclusions
The feasibility study developed a novel intervention and tested all of the methods that would be required for a RCT. The question now is whether or not the methods were sufficiently robust to justify proceeding to a full RCT. This chapter summarises the main findings from each of the results chapters, pulling together relevant findings from several chapters. It provides a critical assessment of the methods on which a decision to proceed to a RCT could be based. It begins with an appraisal of whether or not the main study objectives were met, before summarising the key findings.
Extent to which the feasibility study objectives were achieved
The protocol identified six key objectives for this feasibility study. A brief assessment of the extent to which these objectives were met is given here.
Objective 1: to determine the best ways to recruit and retain obese men in a study aimed at reducing heavy drinking
The two methods of recruitment each exceeded their recruitment targets. However, only one method, recruitment through GP registers, met the pre-specified criteria of success. The other method, community outreach, failed on one criterion: the recruitment rate per venue visited. The two methods produced samples of men who were similar in demographic characteristics and alcohol consumption. As recruitment through GP registers identified a large pool of potential participants; this method would be preferred for a RCT. A high rate of follow-up (98%) was achieved, indicating that the strategies to promote retention were successful.
Objective 2: to design an intervention that is an acceptable way to achieve a sustained reduction in alcohol consumption
The intervention was based on formative research, public involvement and behaviour change theory, and incorporated a range of behaviour change techniques. It proved highly acceptable to study participants.
Objective 3: to identify the content and timing of the delivery that is most likely to engage obese men in an intervention to reduce alcohol consumption
Extensive process evaluation revealed that the intervention successfully engaged the participants. The positive responses to key components of the behaviour change strategy suggest that the intervention could be effective. The high retention rate in the study, 98%, suggests sustained engagement.
Objective 4: to develop high quality training to enable the laypeople to deliver their component of the intervention
The training programme was well received by study co-ordinators. Audio-recordings of face-to-face sessions showed that the study co-ordinators delivered the intervention with high fidelity.
Objective 5: to devise process measures to detect engagement with the steps on the causal model for behaviour change
Four methods of process evaluation were developed: audio-recordings of the baseline sessions, questionnaires following the baseline sessions, a questionnaire at the final outcome assessment sessions, and the responses participants sent to the text message component of the intervention. These showed engagement with the motivational and volitional components of the intervention. They also showed that men in the intervention group were much more likely to identify alcohol as a cause of increased weight and to view weight loss as a benefit of drinking less.
Objective 6: to compile a manual of methods for participant recruitment, training of lay staff, and design and delivery of the intervention
Three detailed manuals were written; one for the research team, and one each for the intervention and control study co-ordinators.
Patient and public involvement
This feasibility study has demonstrated the importance of involving members of the public in all stages of the design and conduct of research. Two user group representatives provided guidance on developing the recruitment strategy, the design of the intervention and the interpretation of the findings. The feasibility study involved focus groups that explored attitudes and beliefs about drinking and losing weight with men from the target group. This clarified opportunities to increase motivation to change behaviour and identified potential barriers to behaviour change. Their views shaped the content of the intervention. Laypeople also delivered the face-to-face component of the intervention. This helped the study participants, men who were confident that they did not have a problem with alcohol, to engage with an intervention designed to reduce their alcohol consumption. Key stakeholders, managers of local businesses and community groups, showed considerable enthusiasm and a willingness to be involved in research to improve public health. This has established a possible route for national roll-out of an effective intervention.
Discussing drinking and weight
Focus groups were held with men in the target group. These groups identified both levers and barriers to behaviour change. The men talked openly about their drinking and the benefits of losing weight. Thus, they would be receptive to an intervention that involved frank discussion of these topics. During the focus group discussions, the men described many benefits of losing weight, and identified no disadvantages to the prospect of weight loss. This suggests that the men might seriously consider guidance on how to reduce weight.
The main barrier to drinking less was the impact that the men perceived this would have on their social life. However, the men also thought that their relationships with close family and friends could improve if they drank less. The intervention could increase the salience of this benefit by capitalising on the surprise that men expressed when they calculated the amount of alcohol they consumed. The men could be encouraged to explore what benefits their close family would enjoy if they reduced their alcohol consumption.
The effect of alcohol on weight
The men in the focus groups required prompting to acknowledge the connection between alcohol consumption and being overweight; however, once prompted, they agreed that alcohol had an important effect. Prompting was also required to clarify the nature of the relationship, that drinking leads to increased snacking and additional late night meals. Again, the men were confident that this was a common phenomenon. In contrast, the men were unaware of, and expressed surprise at, the number of calories in alcohol. This suggests that men can readily appreciate the nature of the link between alcohol and weight. The intervention should reinforce this link and increase its salience to the participants.
The consequences of obesity
Men in the focus groups were concerned about the way they looked, to the extent that it caused embarrassment. Some men were also concerned about the ways in which excess weight limits carrying out usual activities such as climbing stairs and playing with their grandchildren. These factors could be used to increase motivation to lose weight.
The focus groups also clarified an acceptable style of delivery of components of the intervention. For example, information about the calorie content of alcohol could be conveyed as interesting and new. However, the benefits of drinking less were well known by the target group. Thus, the approach should be to increase the perceived personal relevance and importance of the benefits.
A counterproductive idea
Finally, the focus groups showed that an apparently attractive lever, illustrating the calories in alcohol by comparing them with the calories in common foodstuffs, could be counterproductive. Given the choice, the men were willing to forgo food in order to justify consuming alcohol containing the same number of calories as the forgone foodstuff.
Stakeholder interviews
Interviews with managers of venues in the local community identified a willingness to help with the recruitment of participants. The stakeholders requested direct involvement, by making contact with potential participants themselves. In the event, this appeared to act as a barrier, as no-one was recruited in this way. However, the enthusiasm for tackling obesity and alcohol consumption could offer a method for national roll-out of the intervention. Based on the findings of the present study, it would require prior negotiation to gain direct access to potential participants. This could be achieved if the initiative were part of a national campaign to tackle what the stakeholders perceive as major problems: heavy drinking and obesity.
Recruiting and training laypeople
The tailored recruitment strategy identified enthusiastic and empathic laypeople. Adequate training with continued mentoring equipped the laypeople to deliver the face-to-face component of the intervention. Each layperson delivered the intervention to an average of 10 people. The time required for training was of the same order as the time each layperson spent delivering the intervention. If the intervention were to be scaled up for a RCT or national roll-out, it could be more cost-effective to employ staff on half-time or full-time contracts. A comprehensive lone worker’s policy is necessary to ensure the safety of the laypeople doing the interviews.
Designing the intervention
The intervention was designed to follow the steps in the causal model to behaviour change. It was delivered in a face-to-face session followed by a series of text messages. The face-to-face session capitalised on the measurement of alcohol consumption and weight. Feedback of information on current behaviour is a common technique in alcohol brief interventions. Thus, the intervention gave men the opportunity to calculate for themselves the units of alcohol and the calories in the alcohol they consumed. They also plotted their height and weight on a BMI chart, revealing that they were in the upper extreme BMI category. Together, these measurements and calculations illustrated the intended logic of the intervention: reducing alcohol consumption could result in weight loss. This was reinforced by a discussion of the ways in which alcohol increased food intake (e.g. by increasing snacking) and the benefits that the men would enjoy if they lost weight.
The series of text messages was designed to strengthen the motivation engendered in the face-to-face session. More importantly, the text messages were intended to promote action to reduce alcohol consumption through goal-setting and action planning. Relapse recovery and maintenance of the new behaviour were also addressed. For a future trial, additional text messages should be written to reinforce maintenance of reduced drinking.
Recruitment of participants
In total, 69 men were recruited, exceeding the target of 60. Recruitment through GP registers identified a large pool of potential participants (men with a BMI of > 30 kg/m2), enabling recruitment to proceed smoothly. The high proportion of men who drank less than the entry criterion (> 21 units per week) was the main challenge in recruiting from the GP lists. Recruitment by community outreach was time-consuming because very few men were recruited from each venue visited. This resulted in a higher workload for community outreach than for recruitment through GP registers. Of the men approached in community outreach, a high proportion (49%) reported drinking < 21 units per week. The city centre was the most productive location for recruiting men by community outreach. Recruitment from large organisations was largely unsuccessful, and leaving Participant Information Sheets at potential venues for recruitment was ineffective.
Baseline findings
Baseline interviews were successfully conducted at a variety of community venues convenient to participants. Initial fieldwork is necessary to identify these locations. Many men requested visits at their homes. The participants covered a wide age range and the full spectrum of socioeconomic status.
The screening methods successfully identified men meeting the entry criteria on BMI and alcohol consumption. These methods could be used in a RCT. On average, the participants drank well above government guidelines and frequent binge drinking was common. The recruitment methods of this study identified men who have a 19-fold increased risk of dying from liver disease. There is an urgent need for an intervention to reduce this risk in these men.
Evaluation of the face-to-face sessions
The methods for assessing the fidelity of delivery of the face-to-face sessions were successful. They established that although the quality was high, there were areas for improvement, particularly in probing for details of alcohol consumption and summarising the content of the session. Individual feedback to study co-ordinators was well received. Mentoring the study co-ordinators and providing them with study materials was a time-consuming process.
The face-to-face session for the intervention group was restricted to increasing motivation to reduce alcohol consumption. This decision, taken when designing the intervention, proved to be sensible. The session was intended to last for about 30 minutes, but in the event the average duration was 45 minutes. Adding in volitional activities would have overburdened the session.
Fidelity of delivery of the text messages
Almost all of the text messages (98%) were delivered to the participants’ phones. As judged by the responses they made to these texts, the participants engaged enthusiastically with this phase of the intervention. The nature of their responses showed that the men had understood the text messages. They also showed that men responded as intended to key steps in the behaviour change sequence. Text messages provide a low-cost method of delivering an intervention over an extended period.
Responses to the text messages sent to the intervention group were monitored daily to determine if any action was required. In the event, four men (13%) were contacted because of concerns and all were resolved satisfactorily. It is important that all studies using text messages make provision for this monitoring.
Follow-up of participants
A very high follow-up rate was achieved (98%). Sessions were organised to be convenient for participants, in both location and timing. The sessions were run in a friendly, supportive manner, and participants’ questions and concerns were fully addressed. Several methods of contact (mobile phone, home telephone, postal address and e-mail address) were used to maximise follow-up. Text messages were sent to keep in touch during the follow-up period. Finally, the study co-ordinators and the research team made considerable efforts to arrange follow-up appointments. All these techniques could easily be replicated in a RCT; however, it is likely that the follow-up rate would be lower in a RCT because the follow-up period would be longer than that used in this feasibility study.
Outcome assessment
Two outcome measures that would be used in a RCT, alcohol consumption and weight, were successfully measured. The average weekly alcohol consumption remained high at follow-up (34.6 units) and most men continued to binge drink at least weekly. Both intervention and control groups identified a wide range of harms of alcohol. Despite this high consumption and knowledge of harms, most men (74%) believed they were at low risk of harm from alcohol. An explanation could be that their perceived lack of vulnerability was because they seldom suffered acute harms (e.g. hangovers) and made few visits to a GP or hospital. In a RCT, more attention should be given to increasing the perceived relevance of harms.
Weight did not change in either group, although alcohol consumption fell. However, given the short duration of follow-up, a large fall in weight was not expected. A longer period of follow-up would be required for a RCT.
In this study, the outcomes were assessed by the same set of study co-ordinators who did the baseline assessment. Although the study co-ordinators were blind to treatment group, it would be better for a RCT to have the outcomes assessed by an independent researcher.
Estimating effectiveness
The study did not attempt to estimate the effectiveness of the intervention. Current guidance on feasibility studies cautions against estimating effect sizes, as feasibility studies are under-powered and the estimates they provide are likely to be biased. In this study, there was an imbalance in alcohol consumption at baseline between the intervention and control groups, which confirms that an effect size should not be calculated. Instead, the study provided estimates of the variance of the primary outcome measures (alcohol consumption and weight), which could be used in the power calculation for a RCT.
Acceptability of the study
The study methods were found to be acceptable at baseline, with the face-to-face session being described as friendly, informative and worthwhile. The very high follow-up rate (98%) suggests that the men had participated enthusiastically and indicates that they were very willing to maintain their involvement. At follow-up, most men thought they had benefited from taking part, providing examples of awareness of their high alcohol consumption and their commitment to drinking less.
Economic evaluation
The quality of life instrument, the EQ-5D, detected problems that could be associated with obesity, specifically mobility problems, pain and discomfort. It would be useful for a RCT. However, the instrument used to detect usage of police/criminal justice, social services and the health-care system, the Short Service Use Questionnaire, recorded very few contacts. Nevertheless, it may be important to establish that this group of subjects is currently consuming few health-care resources. For that reason, the inclusion of this short resource questionnaire may be required. The design of the economic evaluation will need to consider that the benefits of reducing alcohol consumption and weight, in terms of improved quality of life and reduced resource consumption, are likely to occur some years after the delivery of the intervention. For this reason, any economic evaluation is likely to require an extensive modelling component based on surrogate endpoints included in the trial.
Conclusions
In summary, this feasibility study was conducted successfully. The focus groups made an important contribution to the design of the intervention. They provided a helpful way of testing intended components of behaviour change interventions, and thus we recommend that the use of focus groups should be standard practice in feasibility studies. The objectives for recruitment, retention and acceptability of the study methods were all met. An intervention that fully met the remit set by NIHR HTA was developed and delivered. The study showed that the men, who thought they were at low risk, were in fact at very high risk of liver disease. However, these men engaged enthusiastically with an intervention intended to change their behaviour. Furthermore, they responded as intended to the key steps in the behaviour change strategy. This suggests that an intervention targeted at these high men could be successful. There is an urgent need for an intervention to reduce the risk in these men. The feasibility study methods will enable a RCT to evaluate the effectiveness of the intervention to be carried out to a very high standard.
Modifications for a randomised controlled trial
A main purpose of feasibility studies is to identify improvements for RCTs. Although the methods of this study were shown to be robust, several opportunities for improvement were identified.
Recruitment of participants
-
Consider recruiting only from GP registers. The letter of invitation from the GP should emphasise that the nomination of the potential participant was unrelated to their alcohol consumption. It should also state that the person’s future care will not be influenced by whether or not they decide to participate.
-
A risk assessment should be carried for home visits by lone workers.
-
Consider a higher financial incentive for participants.
-
Consider lowering the entry criterion for alcohol consumption from > 21 units per week to > 14 units per week.
Employing study co-ordinators
-
Use quotations from previous study co-ordinators in marketing materials for the new co-ordinators.
-
Make allowance for the work of the research team in training and mentoring the study co-ordinators.
-
Include more training on the diversity of alcoholic beverages and the need to probe for details of these drinks.
-
Include payment for the time taken by study co-ordinators to organise the face-to-face sessions.
-
Encourage study co-ordinators to organise the face-to-face sessions within 2–3 days of being given the participant’s contact details.
-
Consider appointing study co-ordinators on a more substantive contract, for example, 0.5 full-time equivalent.
Face-to-face intervention session
-
Display normative data on alcohol to demonstrate to participants that their alcohol consumption is much greater than that of most men of their age.
-
Give more attention to the increased risk of liver disease that results from being obese and drinking heavily. In addition, efforts should be made to increase perceived susceptibility to these risks.
Text message intervention
-
Increase the period of time over which text messages are sent. This will allow participants to begin to lose weight and appreciate the benefits of weight loss.
-
Increase the number of text messages.
-
Strengthen the messages that deal with the contribution of alcohol to overweight.
-
Give increased prominence to the ‘beer belly’ as a motivator to drink less.
-
Increase the references to common activities that demonstrate the benefits of losing weight, such as climbing stairs and playing with grandchildren.
-
Encourage self-monitoring of weight loss.
Follow-up
-
Consider using an independent, blinded assessor to measure the study outcomes.
Economic evaluation
-
Incorporate extensive modelling using surrogate endpoints in the economic evaluation.
Acknowledgements
We are indebted to the men who participated so willingly in the study.
We are grateful to the following academics for allowing us to use their materials: Professor C Drummond for the use of the SIPS leaflet, Dr S Parrot for use of the Short Service Use Questionnaire and Dr E Robinson for the use of photographs of men with their BMI measurement.
We would like to thank the three general practices for helping us to recruit participants. Recruitment through general practice was co-ordinated through the SPCRN and we are grateful to Marie Pitkethley and Kim Stringer for the efforts they made to make this a success.
Recruitment by community outreach would not have been possible without the active support of many community groups that helped recruitment and provided venues for the conduct of the face-to-face sessions.
We would like to thank Katie Crandall for training in the use of techniques from Motivational Interviewing.
We would like to thank Phil and Niall (user group representatives) who attended steering group meetings and contributed to the study design and interpretation of the findings.
Finally, we would like to thank the members of the Trial Steering Committee – Professor Lawrie Elliott (chairperson), Dr Diane Dixon and Mr Graeme Haddow – for their support, guidance and encouragement.
Contributions of authors
Professor Iain K Crombie (Professor of Public Health) was the chief investigator for the study. He designed the study and supervised its conduct. He led the design of the intervention and the training programme for the study co-ordinators, contributed to the training of study co-ordinators, analysed the data and wrote the first draft of the final report.
Dr Kathryn B Cunningham (Research Assistant) recruited focus group participants and key stakeholders, conducted the focus groups and stakeholder interviews, led the analysis of the focus group data, assisted in the design of the intervention, recruited and led the training of the study co-ordinators. She wrote the first draft of the Study Manuals.
Dr Linda Irvine (Senior Research Fellow/Trials Manager) contributed to the study design, intervention development, training and supervision of the study co-ordinators, analysis of the data and the writing of the final report. She also wrote the text messages.
Professor Brian Williams (Director of the Nursing, Midwifery and Allied Health Professions Research Unit) contributed to the study design and the text message intervention.
Professor Falko F Sniehotta (Professor of Behavioural Medicine and Health Psychology) contributed to the study design, and provided guidance on the recruitment of participants and the writing of the Study Manuals.
Professor John Norrie [Professor of Clinical Trials and Biostatistics, Director, Centre for Healthcare Randomised Trials (CHaRT)] contributed to the study design.
Dr Ambrose Melson (Research Associate) contributed to the study design, conducted the focus groups and analysed the transcripts, and contributed to the design of the intervention.
Dr Claire Jones (Senior Software Engineer) was responsible for the web-based randomisation system and created, ran and monitored the message delivery system, the system for recording receipt of SMS texts and the mechanism for storing text message responses from participants.
Professor Andrew Briggs (Health Economist) advised on approaches to economic evaluation and suggested questionnaires that could be used.
Dr Peter M Rice (Consultant Psychiatrist) contributed to the study design, advised on alcohol questionnaires and alcohol related problems.
Dr Marcus Achison (Research Assistant) recruited participants from GP practices and by community outreach. He co-ordinated the allocation of participants to study co-ordinators at baseline and follow-up, and assisted in the supervision of the study co-ordinators.
Andrew McKenzie (Research Assistant) recruited participants by community outreach. He assisted with the training and supervision of the study co-ordinators and analysed the trial data.
Elena Dimova (Research Assistant) assisted with the design and delivery of the study co-ordinator training, contributed to the Study Manuals, assessed the audio-recordings of the intervention sessions and provided feedback to the study co-ordinators.
Dr Peter W Slane (GP) advised on recruitment methods and contributed to the study design.
All authors have contributed to the final report.
Data sharing statement
For research purposes, data can be obtained from the corresponding author: Professor Iain K Crombie, Division of Population Health Sciences, School of Medicine, University of Dundee, UK, i.k.crombie@dundee.ac.uk.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Hart CL, Morrison DS, Batty GD, Mitchell RJ, Davey Smith G. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c1240.
- Health Survey for England, 2012. Leeds: The Health and Social Care Information Centre; 2013.
- Statistics on Obesity, Physical Activity and Diet: England, 2011. Leeds: The Health and Social Care Information Centre, Lifestyles Statistics; 2011.
- Rutherford L, Sharp C, Bromley C. The Scottish Health Survey Volume 1: Adults. Edinburgh: The Scottish Government; 2012.
- Butland B, Jebb S, McPherson K, Thomas S, Mardell J, Parry V, et al. Foresight. Tackling Obesities: Future Choices – Project Report. London: Government Office for Science; 2007.
- Wannamethee SG, Shaper AG. Alcohol, body weight, and weight gain in middle-aged men. Am J Clin Nutr 2003;77:1312-17.
- Arif AA, Rohrer JE. Patterns of alcohol drinking and its association with obesity: data from the Third National Health and Nutrition Examination Survey, 1988–1994. BMC Public Health 2005;5. https://doi.org/10.1186/1471-2458-5-126.
- Traversy G, Chaput JP. Alcohol consumption and obesity: an update. Curr Obes Rep 2015;4:122-30. http://dx.doi.org/10.1007/s13679-014-0129-4.
- Bendsen NT, Christensen R, Bartels EM, Kok FJ, Sierksma A, Raben A, et al. Is beer consumption related to measures of abdominal and general obesity? A systematic review and meta-analysis. Nutr Rev 2013;71:67-8. http://dx.doi.org/10.1111/j.1753-4887.2012.00548.x.
- Lloyd-Richardson EE, Lucero ML, Dibello JR, Jacobson AE, Wing RR. The relationship between alcohol use, eating habits and weight change in college freshmen. Eat Behav 2008;9:504-8. http://dx.doi.org/10.1016/j.eatbeh.2008.06.005.
- Pallister C, Avery A, Stubbs J, Lavin J. Influence of Slimming World’s lifestyle programme on diet, activity behaviour and health of participants and their families. J Hum Nutr Diet 2009;22:351-8. https://doi.org/10.1111/j.1365-277X.2009.00959.x.
- Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity 2012;20:1234-9. http://dx.doi.org/10.1038/oby.2011.140.
- Sniehotta FF, Dombrowski SU, Avenell A, Johnston M, McDonald S, Murchie P, et al. Randomised controlled feasibility trial of an evidence-informed behavioural intervention for obese adults with additional risk factors. PLOS ONE 2011;6. http://dx.doi.org/10.1371/journal.pone.0023040.
- Douketis JD, Macie C, Thabane L, Williamson DF. Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. Int J Obes 2005;29:1153-67. https://doi.org/10.1038/sj.ijo.0802982.
- Sabinsky MS, Toft U, Raben A, Holm L. Overweight men’s motivations and perceived barriers towards weight loss. Eur J Clin Nutr 2007;61:526-31.
- Gray CM, Hunt K, Lorimer K, Anderson AS, Benzeval M, Wyke S. Words matter: a qualitative investigation of which weight status terms are acceptable and motivate weight loss when used by health professionals. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-513.
- Morgan PJ, Warren JM, Lubans DR, Collins CE, Callister R. Engaging men in weight loss: Experiences of men who participated in the male only SHED-IT pilot study. Obes Res Clin Pract 2011;5:e169-266. http://dx.doi.org/10.1016/j.orcp.2011.03.002.
- Robertson C, Archibald D, Avenell A, Douglas F, Hoddinott P, van Teijlingen E, et al. Systematic reviews of and integrated report on the quantitative, qualitative and economic evidence base for the management of obesity in men. Health Technol Assess 2014;18. http://dx.doi.org/10.3310/hta18350.
- Smith JA, Braunack-Mayer AJ, Wittert GA, Warin MJ. Qualities men value when communicating with general practitioners: implications for primary care settings. Med J Aust 2008;189:618-21.
- Gray CM, Hunt K, Mutrie N, Anderson AS, Leishman J, Dalgarno L, et al. Football Fans in Training: the development and optimization of an intervention delivered through professional sports clubs to help men lose weight, become more active and adopt healthier eating habits. BMC Public Health 2013;13. http://dx.doi.org/10.1186/1471-2458-13-232.
- Wyke S, Hunt K, Gray C, Fenwick E, Bunn C, Donnan PT, et al. Football Fans in Training (FFIT): a randomised controlled trial of a gender-sensitised weight loss and healthy living programme for men – end of study report. Public Health Res 2015;3.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. http://dx.doi.org/10.1111/j.2002.384.doc.x.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10. http://dx.doi.org/10.1186/1471-2288-10-67.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- Arnold DM, Burns KE, Adhikari NK, Kho ME, Meade MO, Cook DJ. McMaster Critical Care Interest Group . The design and interpretation of pilot trials in clinical research in critical care. Crit Care Med 2009;37:69-74. http://dx.doi.org/10.1097/CCM.0b013e3181920e33.
- Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med 2009;36:452-7. http://dx.doi.org/10.1016/j.amepre.2009.02.002.
- Obese and Fat are the Most Hurtful Words a Doctor Can Use. London: Weight Concern Press Release; 2008.
- Thomas SL, Hyde J, Karunaratne A, Herbert D, Komesaroff PA. Being ‘fat’ in today’s world: a qualitative study of the lived experiences of people with obesity in Australia. Health Expect 2008;11:321-30. http://dx.doi.org/10.1111/j.1369-7625.2008.00490.x.
- Wadden TA, Didie E. What’s in a name? Patients’ preferred terms for describing obesity. Obes Res 2003;11:1140-6. http://dx.doi.org/10.1038/oby.2003.155.
- Truesdale KP, Stevens J. Do the obese know they are obese?. N C Med J 2008;69:188-94.
- Semaan S. Time-space sampling and respondent-driven sampling with hard-to-reach populations. Methodological Innovations Online 2010;5:60-75. http://dx.doi.org/10.4256/mio.2010.0019.
- Michie S, Rumsey N, Fussell A, Hardeman W, Johnston M, . Improving Health: Changing Behaviour – NHS Health Trainer Handbook. London: Department of Health; 2008.
- Mathers J, Parry J. A Review of the Implementation of the National Health Trainer Service Initiative. Birmingham: School of Health and Population Sciences, University of Birmingham; 2014.
- Kaner EF, Dickinson HO, Beyer F, Pienaar E, Schlesinger C, Campbell F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev 2009;28:301-23. http://dx.doi.org/10.1111/j.1465-3362.2009.00071.x.
- O’Donnell A, Anderson P, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, et al. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol 2014;49:66-78. http://dx.doi.org/10.1093/alcalc/agt170.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. http://dx.doi.org/10.1007/s12160-013-9486-6.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. http://dx.doi.org/10.1037/0278-6133.27.3.379.
- Michie S, Whittington C, Hamoudi Z, Zarnani F, Tober G, West R. Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction 2012;107:1431-40. http://dx.doi.org/10.1111/j.1360-0443.2012.03845.x.
- Crombie IK, Falconer DW, Irvine L, Williams B, Ricketts IW, Humphris G, et al. Reducing alcohol-related harm in disadvantaged men: development and feasibility assessment of a brief intervention delivered by mobile telephone. Public Health Res 2013;1.
- Kaner E, Bland M, Cassidy P, Coulton S, Deluca P, Drummond C, et al. Screening and brief interventions for hazardous and harmful alcohol use in primary care: a cluster randomised controlled trial protocol. BMC Public Health 2009;9. https://doi.org/10.1186/1471-2458-9-287.
- Crombie IK, Irvine L, Williams B, Sniehotta FF, Petrie D, Jones C, et al. Texting to Reduce Alcohol Misuse (TRAM): a multi-centre randomised controlled trial of a text message intervention to reduce binge drinking among disadvantaged men. Public Health Res 2017.
- Armitage CJ, Arden MA. A volitional help sheet to reduce alcohol consumption in the general population: a field experiment. Prev Sci 2012;13:635-43. http://dx.doi.org/10.1007/s11121-012-0291-4.
- Breslow RA, Chen CM, Graubard BI, Jacobovits T, Kant AK. Diets of drinkers on drinking and nondrinking days: NHANES 2003-2008. Am J Clin Nutr 2013;97:1068-75. http://dx.doi.org/10.3945/ajcn.112.050161.
- Scottish Indices of Deprivation. Oxford: Department of Social Policy and Social Work, University of Oxford; 2003.
- The English Indices of Deprivation 2010. London: Neighbourhoods Statistical Release; 2011.
- Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009;3. https://doi.org/10.1002/14651858.mr000008.pub4.
- Watson JM, Torgerson DJ. Increasing recruitment to randomised trials: a review of randomised controlled trials. BMC Med Res Methodol 2006;6. https://doi.org/10.1186/1471-2288-6-34.
- Patton MQ. Qualitative Evaluation and Research Methods. Thousand Oaks, CA: Sage Publications, Inc.; 1990.
- Kitzinger J. The methodology of focus groups: the importance of interactions between research participants. Sociol Health Illn 1994;16:103-21.
- Morgan DL, Krueger RA, Morgan DL. Successful Focus Groups: Advancing the State of the Art. London: Sage; 1993.
- Farquhar C, Das R, Barbour R, Kitzinger J. Developing Focus Group Research: Politics, Theory and Practice. London: Sage; 1999.
- Bloor M, Frankland J, Thomas M, Robson K. Focus Groups in Social Research. London: Sage; 2001.
- Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inform 2004;22:63-75. https://doi.org/10.3233/EFI-2004-22201.
- Elliott R, Fischer CT, Rennie DL. Evolving guidelines for publication of qualitative research studies in psychology and related fields. Br J Clin Psychol 1999;38:215-29. https://doi.org/10.1348/014466599162782.
- Caton SJ, Ball M, Ahern A, Hetherington MM. Dose-dependent effects of alcohol on appetite and food intake. Physiol Behav 2004;81:51-8. http://dx.doi.org/10.1016/j.physbeh.2003.12.017.
- Caton SJ, Marks JE, Hetherington MM. Pleasure and alcohol: manipulating pleasantness and the acute effects of alcohol on food intake. Physiol Behav 2005;84:371-7. https://doi.org/10.1016/j.physbeh.2004.12.013.
- Hetherington MM, Cameron F, Wallis DJ, Pirie LM. Stimulation of appetite by alcohol. Physiol Behav 2001;74:283-9. https://doi.org/10.1016/S0031-9384(01)00598-4.
- Sobell L, Allen J, Wilson V. Assessing Alcohol Problems: A Guide for Clinicians and Researchers. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003.
- Baldwin AS, Rothman AJ, Hertel AW, Linde JA, Jeffery RW, Finch EA, et al. Specifying the determinants of the initiation and maintenance of behavior change: an examination of self-efficacy, satisfaction, and smoking cessation. Health Psychol 2006;25:626-34. https://doi.org/10.1037/0278-6133.25.5.626.
- Finch EA, Linde JA, Jeffery RW, Rothman AJ, King CM, Levy RL. The effects of outcome expectations and satisfaction on weight loss and maintenance: correlational and experimental analyses – a randomized trial. Health Psychol 2005;24:608-16. https://doi.org/10.1037/0278-6133.24.6.608.
- Gillon E, McPherson K, White A, Pettifer M. Hazardous Waist: Tackling Male Weight Problems. Oxford: Radcliffe Publishing; 2007.
- Sladek MR, Engeln R, Miller SA. Development and validation of the Male Body Talk Scale: a psychometric investigation. Body Image 2014;11:233-44. http://dx.doi.org/10.1016/j.bodyim.2014.02.005.
- Lewis S, Thomas SL, Hyde J, Castle DJ, Komesaroff PA. A qualitative investigation of obese men’s experiences with their weight. Am J Health Behav 2011;35:458-69. https://doi.org/10.5993/AJHB.35.4.8.
- Hankey CR, Leslie WS, Lean ME. Why lose weight? Reasons for seeking weight loss by overweight but otherwise healthy men. Int J Obes Relat Metab Disord 2002;26:880-2. http://dx.doi.org/10.1038/sj.ijo.0801999.
- Wolfe BL, Smith JE. Different strokes for different folks: why overweight men do not seek weight loss treatment. Eat Disord 2002;10:115-24. https://doi.org/10.1080/10640260290081687.
- Grogan S, Richards H. Body image focus groups with boys and men. Men Masc 2002;4:219-32.
- Watson J. Male Bodies. Health, Culture and Identity. Buckingham: Open University Press; 2000.
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, et al. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med 2012;157:645-54. https://doi.org/10.7326/0003-4819-157-9-201211060-00544.
- NHS Choices. Height/Weight Chart n.d. www.nhs.uk/livewell/loseweight/pages/height-weight-chart.aspx (accessed March 2017).
- Miller WR, Rollnick S. Motivational Interviewing. Helping People Change. New York, NY: The Guilford Press; 2013.
- Rains SA. The nature of psychological reactance revisited: a meta-analytic review. Hum Commun Res 2013;39:47-73. https://doi.org/10.1111/j.1468-2958.2012.01443.x.
- Vidrine DJ, Arduino RC, Lazev AB, Gritz ER. A randomized trial of a proactive cellular telephone intervention for smokers living with HIV/AIDS. AIDS 2006;20:253-60. http://dx.doi.org/10.1097/01.aids.0000198094.23691.58.
- Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control 2005;14:255-61. https://doi.org/10.1136/tc.2005.011577.
- Geraghty M, Glynn F, Amin M, Kinsella J. Patient mobile telephone ‘text’ reminder: a novel way to reduce non-attendance at the ENT out-patient clinic. J Laryngol Otol 2008;122:296-8. https://doi.org/10.1017/S0022215107007906.
- Franklin VL, Greene A, Waller A, Greene SA, Pagliari C. Patients’ engagement with ‘Sweet Talk’ – a text messaging support system for young people with diabetes. J Med Internet Res 2008;10. http://dx.doi.org/10.2196/jmir.962.
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56-69. http://dx.doi.org/10.1093/epirev/mxq004.
- Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med 2009;36:165-73. http://dx.doi.org/10.1016/j.amepre.2008.09.040.
- Whittaker R, Borland R, Bullen C, Lin RB, McRobbie H, Rodgers A. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev 2009;4. https://doi.org/10.1002/14651858.cd006611.pub2.
- Office for National Statistics . Mobile or Smartphone Users by Age Group, GB, 2012. FOI Request: Mobile and Smartphone Usage. Ref Number: 001478 2012.
- Schwarzer R. Modeling health behaviour change: how to predict and modify the adoption and maintenance of health behaviours. Appl Psychol 2008;57:1-29.
- Dombrowski SU, Sniehotta FF, Avenell A, Johnston M, MacLennan G, Araujo-Soares V. Identifying active ingredients in complex behavioural interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: a systematic review. Health Psychol Rev 2012;6:7-32.
- Irvine L, Falconer DW, Jones C, Ricketts IW, Williams B, Crombie IK. Can text messages reach the parts other process measures cannot reach: an evaluation of a behavior change intervention delivered by mobile phone?. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0052621.
- Murphy ST, Frank LB, Chatterjee JS, Baezconde-Garbanati L. Narrative versus nonnarrative: the role of identification, transportation and emotion in reducing health disparities. J Commun 2013;63:116-37. http://dx.doi.org/10.1111/jcom.12007.
- Moran MB, Murphy ST, Frank L, Baezconde-Garbanati L. The ability of narrative communication to address health-related social norms. Int Rev Soc Res 2013;3:131-49. https://doi.org/10.1515/irsr-2013-0014.
- Miller-Day M, Hecht ML. Narrative means to preventative ends: a narrative engagement framework for designing prevention interventions. Health Commun 2013;28:657-70. http://dx.doi.org/10.1080/10410236.2012.762861.
- Hinyard LJ, Kreuter MW. Using narrative communication as a tool for health behavior change: a conceptual, theoretical, and empirical overview. Health Educ Behav 2007;34:777-92. https://doi.org/10.1177/1090198106291963.
- Larkey LK, Hecht M. A model of effects of narrative as culture-centric health promotion. J Health Commun 2010;15:114-35. http://dx.doi.org/10.1080/10810730903528017.
- de Graaf A. The effectiveness of adaptation of the protagonist in narrative impact: similarity influences health beliefs through self-referencing. Hum Commun Res 2014;40:73-90.
- Cho H, Shen L, Wilson K. Perceived realism: dimensions and roles in narrative. Commun Res 2012;20:1-24.
- Prestin A. The pursuit of hopefulness: operationalizing hope in entertainment media narratives. Media Psychol 2013;16:318-46.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Br Med J 2014;348. https://doi.org/10.1136/bmj.g1687.
- Screening and Intervention Programme for Sensible drinking (SIPS) . Programme Summary n.d. www.sips.iop.kcl.ac.uk (accessed 24 February 2017).
- Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, et al. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.e8501.
- Drummond C, Deluca P, Coulton S, Bland M, Cassidy P, Crawford M, et al. The effectiveness of alcohol screening and brief intervention in emergency departments: a multicentre pragmatic cluster randomized controlled trial. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0099463.
- Newbury-Birch D, Coulton S, Bland M, Cassidy P, Dale V, Deluca P, et al. Alcohol screening and brief interventions for offenders in the probation setting (SIPS Trial): a pragmatic multicentre cluster randomized controlled trial. Alcohol Alcohol 2014;49:540-8. http://dx.doi.org/10.1093/alcalc/agu046.
- Wutzke SE, Shiell A, Gomel MK, Conigrave KM. Cost effectiveness of brief interventions for reducing alcohol consumption. Soc Sci Med 2001;52:863-70. https://doi.org/10.1016/S0277-9536(00)00189-1.
- Babor TF, Grant M. Programme on Substance Abuse: Project on Identification and Management of Alcohol-related Problems. Report on Phase II: An Randomized Clinical Trial of Brief Interventions in Primary Health Care. (WHO/PSA/91.5). Geneva: World Health Organization; 1992.
- Screening and Intervention Programme for Sensible drinking (SIPS) . Brief Advice Training n.d. www.sips.iop.kcl.ac.uk/ba.php (accessed March 2017).
- Screening and Intervention Programme for Sensible drinking (SIPS) . How Much Is Too Much? n.d. www.sips.iop.kcl.ac.uk/documents/gnr/dhpil.pdf (accessed March 2017).
- Guidance on Health and Safety in Fieldwork (Including Offsite Visits and Travel in the UK and Overseas). Eastbourne: USHA and UCEA; 2011.
- Cooper CL, Hind D, Duncan R, Walters S, Lartey A, Lee E, et al. A rapid review indicated higher recruitment rates in treatment trials than in prevention trials. J Clin Epidemiol 2015;68:347-54. http://dx.doi.org/10.1016/j.jclinepi.2014.10.007.
- Smith W, Chey T, Jalaludin B, Salkeld G, Capon T. Increasing response rates in telephone surveys: a randomized trial. J Public Health Med 1995;17:33-8.
- Treweek S, Mitchell E, Pitkethly M, Cook J, Kjeldstrøm M, Johansen M, et al. Strategies to improve recruitment to randomised controlled trials. Cochrane Database Syst Rev 2010;4. http://dx.doi.org/10.1002/14651858.MR000013.pub5.
- Nakash RA, Hutton JL, Jørstad-Stein EC, Gates S, Lamb SE. Maximising response to postal questionnaires – a systematic review of randomised trials in health research. BMC Med Res Methodol 2006;6. https://doi.org/10.1186/1471-2288-6-5.
- Edwards P, Cooper R, Roberts I, Frost C. Meta-analysis of randomised trials of monetary incentives and response to mailed questionnaires. J Epidemiol Community Health 2005;59:987-99. https://doi.org/10.1136/jech.2005.034397.
- McDonald PW. Population-based recruitment for quit-smoking programs: an analytic review of communication variables. Prev Med 1999;28:545-57. https://doi.org/10.1006/pmed.1998.0479.
- Harrison RA, Cock D. Increasing response to a postal survey of sedentary patients - a randomised controlled trial [ISRCTN45665423]. BMC Health Serv Res 2004;4. https://doi.org/10.1186/1472-6963-4-31.
- Bromley C, Dowling S, Gray L, Hughes T, Leyland AH, McNeill G, et al. The Scottish Health Survey 2013 Edition. Edinburgh: The Scottish Government Health Directorate; 2014.
- van der Wouden JC, Blankenstein AH, Huibers MJ, van der Windt DA, Stalman WA, Verhagen AP. Survey among 78 studies showed that Lasagna’s law holds in Dutch primary care research. J Clin Epidemiol 2007;60:819-24. https://doi.org/10.1016/j.jclinepi.2006.11.010.
- Hashemi A, You W, Boyle KJ, Parmeter CF, Kanninen B, Estabrooks PA. Identifying financial incentive designs to enhance participation in weight loss programs. J Obes Weight Loss Ther 2015;5. http://dx.doi.org/10.4172/2165-7904.1000247.
- Scottish Index of Multiple Deprivation 2004 Technical Report. Edinburgh: Scottish Executive; 2004.
- Manual for the Fast Alcohol Screening Test (FAST). London: Health Development Agency; 2002.
- Heather N, Smailes D, Cassidy P. Development of a Readiness Ruler for use with alcohol brief interventions. Drug Alcohol Depend 2008;98:235-40. http://dx.doi.org/10.1016/j.drugalcdep.2008.06.005.
- Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res 2011;45:626-9. http://dx.doi.org/10.1016/j.jpsychires.2010.10.008.
- Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obesity Rev 2007;8:307-26.
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci 2007;2. http://dx.doi.org/10.1186/1748-5908-2-40.
- Leeuw M, Goossens ME, de Vet HC, Vlaeyen JW. The fidelity of treatment delivery can be assessed in treatment outcome studies: a successful illustration from behavioral medicine. J Clin Epidemiol 2009;62:81-90. http://dx.doi.org/10.1016/j.jclinepi.2008.03.008.
- Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent 2011;71:S52-S63. http://dx.doi.org/10.1111/j.1752-7325.2011.00233.x.
- Lane C. The Behaviour Change Counselling Index (BECCI). Manual for Coding Behaviour Change Counselling. Cardiff: University of Wales College of Medicine; 2002.
- Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull 2007;133:859-83. https://doi.org/10.1037/0033-2909.133.5.859.
- Young MD, Morgan PJ, Plotnikoff RC, Callister R, Collins CE. Effectiveness of male-only weight loss and weight loss maintenance interventions: a systematic review with meta-analysis. Obes Rev 2012;13:393-408. http://dx.doi.org/10.1111/j.1467-789X.2011.00967.x.
- Oei TP, Young RS, Allen JP, Wilson VB. Assessing Alcohol Problems. A Guide for Clinicians and Researchers. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003.
- Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med 2001;33:337-43. https://doi.org/10.3109/07853890109002087.
- Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ Res 2005;20:439-47. https://doi.org/10.1093/her/cyg139.
- Yoong SL, Carey M, Sanson-Fisher R, Grady A. A systematic review of behavioural weight-loss interventions involving primary-care physicians in overweight and obese primary-care patients (1999–2011). Public Health Nutr 2013;16:2083-99. http://dx.doi.org/10.1017/S1368980012004375.
- Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev 2011;12:709-23. http://dx.doi.org/10.1111/j.1467-789X.2011.00892.x.
- Zheng Y, Klem ML, Sereika SM, Danford CA, Ewing LJ, Burke LE. Self-weighing in weight management: a systematic literature review. Obesity 2015;23:256-65. http://dx.doi.org/10.1002/oby.20946.
- Fabricatore AN, Wadden TA, Moore RH, Butryn ML, Gravallese EA, Erondu NE, et al. Attrition from randomized controlled trials of pharmacological weight loss agents: a systematic review and analysis. Obes Rev 2009;10:333-41. http://dx.doi.org/10.1111/j.1467-789X.2009.00567.x.
- Ni Mhurchu C, Whittaker R, McRobbie H, Ball K, Crawford D, Michie J, et al. Feasibility, acceptability and potential effectiveness of a mobile health (mHealth) weight management programme for New Zealand adults. BMC Obes 2014;1. http://dx.doi.org/10.1186/2052-9538-1-10.
- Beeston C, Reid G, Robinson M, Craig N, McCartney G, Graham L, et al. Monitoring and Evaluating Scotland’s Alcohol Strategy. Third Annual Report. Edinburgh: NHS Health Scotland; 2013.
- Davis CG, Thake J, Vilhena N. Social desirability biases in self-reported alcohol consumption and harms. Addict Behav 2010;35:302-11. http://dx.doi.org/10.1016/j.addbeh.2009.11.001.
- Bland JM, Altman DG. Regression towards the mean. BMJ 1994;308. https://doi.org/10.1136/bmj.308.6942.1499.
- Lovatt M, Eadie D, Meier PS, Li J, Bauld L, Hastings G, et al. Lay epidemiology and the interpretation of low-risk drinking guidelines by adults in the United Kingdom. Addiction 2015;110:1912-19. http://dx.doi.org/10.1111/add.13072.
- Kerr WC, Stockwell T. Understanding standard drinks and drinking guidelines. Drug Alcohol Rev 2012;31:200-5. http://dx.doi.org/10.1111/j.1465-3362.2011.00374.x.
- Steckler A, Linnan L. Process Evaluation for Public Health Interventions and Research. San Francisco, CA: Jossey Bass; 2002.
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change consortium. Health Psychol 2004;23:443-51.
- Fast Alcohol Screening Test (FAST) n.d. www.effectivepi.co.uk/files/FAST%20&%20other%20AUDIT%20questions_EPI%20version%20Mar%2009.pdf (accessed March 2017).
- Personal Well-being Survey User Guide: 2013-2014 Dataset. ONS: South Wales; 2014.
Appendix 1 Commissioning brief from National Institute for Health Research Health Technology Assessment
Appendix 2 Baseline questionnaire
Appendix 3 Lone worker’s policy
Appendix 4 Study co-ordinator evaluation
Appendix 5 General practitioner letter of invitation
Appendix 6 Participant information sheet: general practitioner
Appendix 7 Participant information sheet: time–space sampling
Appendix 8 Participant evaluation form
Appendix 9 Key tasks and activities for the study co-ordinators
Control group
-
Introduction.
-
Completion of questionnaire.
-
Demographics.
-
TLFB.
-
FAST.
-
-
Provision of information on risks of drinking.
-
Opportunity for participant to consider the risks.
-
Comparison of participant’s drinking with general population.
-
Provision of information about benefits of reducing drinking.
-
Provision of information about strategies for reducing drinking.
-
Provision of information about sensible drinking targets.
-
Provision of ‘How much is too much?’ leaflet.
-
Measurement of participant’s height and weight.
-
Finish.
Intervention group
-
Introduction.
-
Completion of questionnaire.
-
Demographics.
-
TLFB.
-
FAST.
-
-
Calculation of participant’s typical alcohol consumption.
-
Discussion of pros and cons of the participant’s current alcohol intake.
-
Discussion of pros of the participant reducing alcohol consumption.
-
Measurement of height and weight.
-
Charting of participant’s BMI.
-
Calculation of the participant’s typical calorie consumption from alcohol.
-
Discussion of how alcohol can contribute to weight.
-
Finish.
Appendix 10 Follow-up questionnaire
Appendix 11 Study co-ordinator end-of-study evaluation
Appendix 12 The CONSORT flow diagram
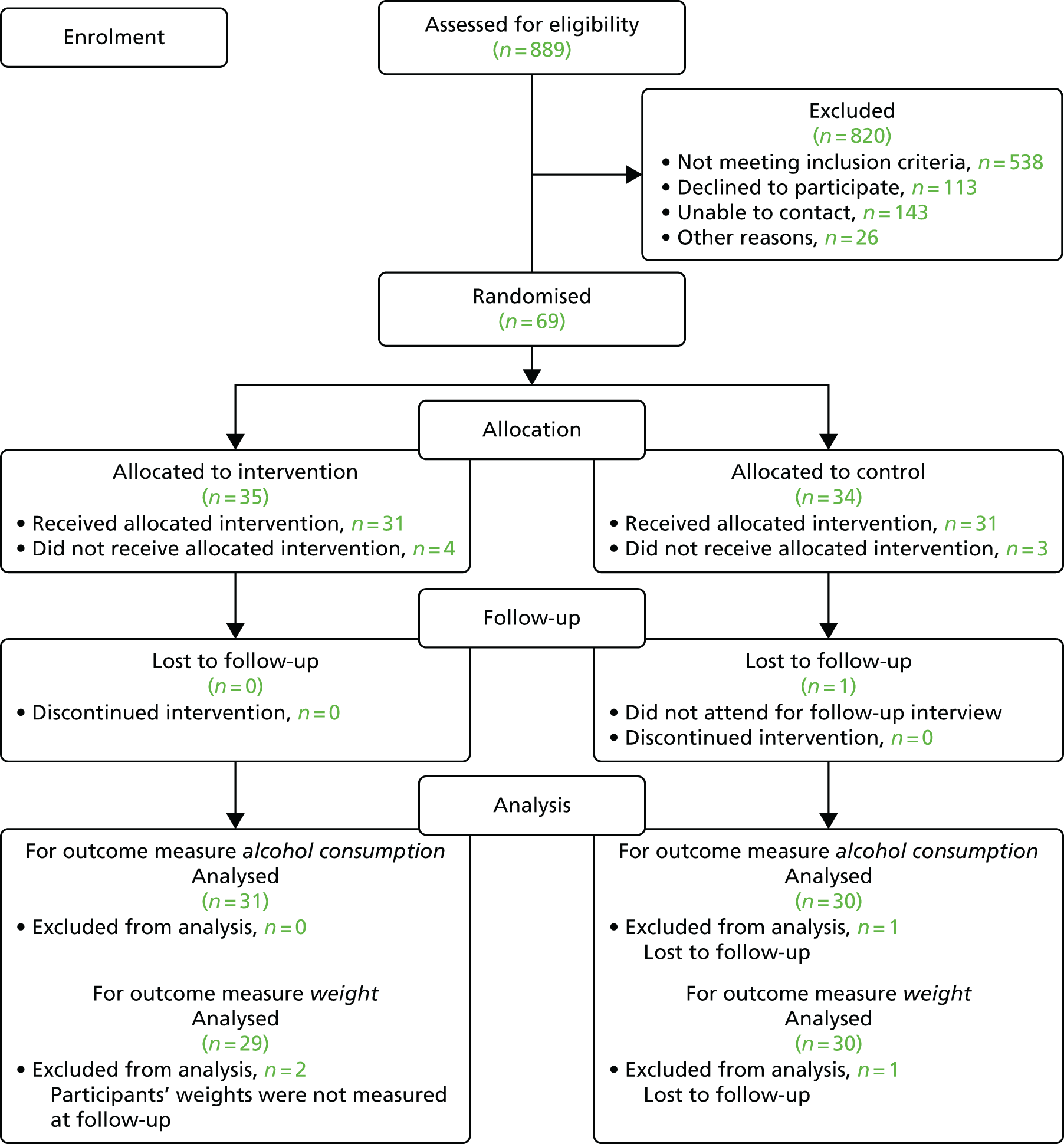
List of abbreviations
- ABV
- alcohol by volume
- BECCI
- Behaviour Change Counselling Index
- BMI
- body mass index
- CONSORT
- Consolidated Standards of Reporting Trials
- EQ-5D
- EuroQol-5 Dimensions
- FAST
- Fast Alcohol Screening Test
- GP
- general practitioner
- HAPA
- Health Action Process Approach
- HTA
- Health Technology Assessment
- MI
- motivational interviewing
- NIHR
- National Institute for Health Research
- OARS
- open questions, affirmation, reflective listening and summarising
- PHR
- Public Health Research
- RCT
- randomised controlled trial
- SIMD
- Scottish Index of Multiple Deprivation
- SIPS
- Screening and Intervention Programme for Sensible drinking
- SMS
- Short Message Service
- SPCRN
- Scottish Primary Care Research Network
- TIDieR
- Template for Intervention Description and Replication
- TLFB
- Timeline Followback
- TSS
- time–space sampling