Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/93/01. The contractual start date was in May 2013. The draft report began editorial review in October 2015 and was accepted for publication in October 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
The Institute for Social Marketing is a member of the UK Centre for Tobacco and Alcohol Studies (UKCTAS; www.ukctas.ac.uk). Funding for UKCTAS from the British Heart Foundation, Cancer Research UK, the Economic and Social Research Council, the Medical Research Council and the National Institute for Health Research, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Bauld et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background and aims
This monograph reports the findings of the ‘Barriers to and facilitators of smoking cessation in pregnancy and following childbirth’ study. The study was funded to conduct evidence syntheses and primary qualitative research to enhance understanding of how these barriers and facilitators are perceived and experienced from the perspectives of women, their partners, family and friends, and health-care professionals (HPs). Through this enhanced understanding, the study provides a platform to inform recommendations for current practice and provide pointers for the design of future interventions with promise for improving smoking cessation in pregnancy and in the postpartum period.
This chapter describes the health implications and epidemiology of smoking in pregnancy, the importance of cessation and, hence, the rationale for conducting this study. The chapter concludes with the aims of the study.
Impact of smoking in pregnancy
Maternal smoking during pregnancy can cause substantial harm. 1,2 It increases the risk of miscarriage, premature birth, stillbirth and low birthweight. 3–7 Smoking during pregnancy also increases infant mortality by 40%8 and is estimated to account for 150 UK infant deaths each year. 9–12 Furthermore, 5% of all admissions to hospital in the first 8 months of life are attributable to smoking in pregnancy. 13 Children whose mothers smoked during pregnancy have twice the risk of being diagnosed with asthma,14 and bronchiolitis and other serious respiratory illnesses such as pneumonia are 25% more common than in children whose mothers did not smoke during pregnancy. 15 Prenatal smoking is also associated with an elevated risk of hyperactivity disorders and disruptive behaviour in children,16 and as having a detrimental effect on educational performance. 17 The risk of obesity and diabetes is also increased. 18
Maternal smoking in pregnancy also has significant implications for the NHS, as it impacts on limited health-care resources through the treatment of women for smoking-related illnesses and pregnancy complications, and the treatment of their infants for a range of smoking-related health problems. A 2010 study19 estimated the total extra annual NHS cost caused by smoking during pregnancy to be £8.1–64M for treating mothers and £12–23.5M for treating infants (aged 0–12 months).
Epidemiology of smoking in pregnancy
Accurate rates of smoking in pregnancy are difficult to obtain. Current monitoring practices, and thus smoking policy, are based on self-reported smoking rates that underestimate prevalence and overestimate quit rates in pregnancy. 20–22 Nonetheless, estimates show that one in four women smokes before or during her pregnancy and one in eight continues to smoke throughout. 23
In high-income countries, smoking in pregnancy is strongly associated with social disadvantage. 24 Compared with women in advantaged circumstances, women in disadvantaged circumstances are four times more likely to smoke prior to pregnancy and half as likely to quit during pregnancy. 25 Although rates of under-reporting may be similar across socioeconomic groups,26 reliance on self-reporting can result in twice as many undetected smokers in the most deprived areas as in the least deprived areas. 22,27
Social disadvantage also increases the chances of living with a partner who smokes,27,28 and the smoking status of partners and other household members is a predictor of maternal smoking habits before and during pregnancy,29,30 and of returning to smoking after birth. 27,31,32 Findings from the Millennium Cohort Study33 indicate that 70% of partners of women who smoked in pregnancy also smoked and that > 70% of these partners neither cut down nor quit. Underscoring the role of partners, maternal smoking in pregnancy is associated with difficulties in the relationship with the partner. 34 Social disadvantage is also associated with an elevated risk of mental illness; estimates suggest that approximately 50% of pregnant smokers have depression or another common mental disorder. 35 Given that around 80% of UK women have at least one baby,36 pregnancy is an opportunity to reach women who smoke and help them quit before their own health is permanently compromised. 37 Stopping during pregnancy also reduces the likelihood of a child growing up with parents who smoke and becoming a smoker him- or herself. 38
Smoking cessation in pregnancy
Reducing the numbers of women smoking in pregnancy is a policy priority in many countries. 39 In England, for example, the National Institute for Health and Care Excellence (NICE) in 2010 emphasised the importance of smoking cessation in pregnancy,40 and targets to reduce smoking in pregnancy have been introduced. Over the past decade there has been significant investment in providing tailored evidence-based smoking cessation services to support pregnant women who find it difficult to stop. 41 For example, NHS Stop Smoking Services (SSSs) in the UK offer behavioural support delivered by trained advisors, in clinic settings, in the home and by telephone, along with access to smoking cessation medications and nicotine replacement therapy (NRT) for smokers motivated to quit. Behavioural support helps pregnant women to stop smoking at least in the short term42 but only a small minority of women take up the offer of help during pregnancy or after childbirth; the majority of those making quit attempts therefore do so without professional assistance – and most will not succeed. 28 Among those women who do quit during pregnancy, nearly all wish to remain abstinent after the birth of their baby;43 however, the vast majority relapse within 12 months of the birth. 44,45 Much less is known about effective interventions to prevent postnatal relapse;45 behavioural support has not been shown to be effective for preventing postnatal relapse and is offered by only a minority of UK SSSs. 45 Smoking in pregnancy and postnatal relapse rates therefore remain high, particularly for women living in disadvantaged circumstances,46 suggesting that this group of smokers face particular social and economic barriers that may inhibit their ability to access support and/or to stop smoking. Understanding these barriers (and facilitators) offers scope for identifying other ways of reducing smoking in pregnancy and supporting women to remain abstinent after childbirth.
Rationale for conducting this study
Identifying and overcoming barriers to service access and, equally importantly, barriers to women’s motivation to try to stop smoking is challenging. Understanding what helps and hinders pregnant smokers in quitting and remaining abstinent post partum, from a range of perspectives, is essential if effective interventions are to be accessed by more women and if more women are to be supported to stop smoking.
Pregnant and postpartum women’s perspectives
Greater insight is required into how barriers to and facilitators of smoking cessation in pregnancy and after birth are perceived and experienced by women. To date, systematic reviews of qualitative studies involving pregnant women have had a broad focus on perceptions and experiences; barriers and facilitators may be identified but are not the primary concern. 47,48 For example, the systematic review by Flemming et al. 49 demonstrated how smoking in pregnancy was shaped by the contexts of women’s lives, including the embeddedness of smoking in their lives and the importance of it in the couple’s relationship. Although this review focused on studies of women’s experiences of smoking in pregnancy, it did not explicitly examine the barriers to and facilitators of smoking cessation faced by women while they are pregnant, and it also excluded papers that examined women’s experiences post partum.
Significant others’ perspectives
The smoking habits of women’s significant others (SOs) (i.e. partners, family and friends) are recognised as important barriers to sustained quitting,27,31,50 but these remain relatively under-researched in relation to smoking in pregnancy. Partners’ smoking status and attitudes to smoking cessation are identified as potentially important influences in a pregnant woman’s attempt to quit;30 for example, partners who try to quit at the same time as the pregnant woman can be seen as more supportive,51 whereas a partner’s failed quit attempt may reduce the chances of the woman succeeding. 52 Men may be less likely than their pregnant partners to receive advice to stop smoking from HPs and may be exposed to less pressure from friends and family to quit. 53 Further understanding of how SOs perceive the barriers to and facilitators of smoking cessation in pregnancy is needed, particularly from qualitative studies in which participants describe these issues in their own words.
Health-care professionals’ perspectives
The problems that women face in accessing effective support to stop smoking may involve structural, organisational and cultural barriers in the NHS or other services, rather than a reluctance or lack of knowledge among pregnant women. Recent studies in Scotland and England highlight a number of limitations to smokers being identified, referred and then supported to stop smoking. 54,55 For example, perceptions that HPs offered inconsistent advice on, and support for, quitting in pregnancy has emerged as a potential barrier. HPs themselves may fail to facilitate smoking cessation through, for example, midwives’ reluctance to ask about smoking, a lack of training in smoking cessation, organisational factors and HPs’ own smoking behaviour. 56 Fundamentally linked to the role of the HPs is the context in which services are delivered, the configuration and quality of which varies greatly throughout the country. To our knowledge, no review has been conducted of qualitative studies reporting HPs’ perceptions of the barriers and facilitators when addressing smoking in pregnancy. Given the pivotal role of many HPs involved in the care of women throughout their pregnancy, a better understanding is needed of the impact of the diversity of professional roles and practice, and how different organisational practices may both facilitate and create barriers to the delivery of cessation support that meets pregnant women’s preferences and needs.
Considering each of these three perspectives – pregnant and postpartum women, their SOs and HPs – the evidence suggests that a deeper understanding of what helps and hinders pregnant smokers to quit and remain abstinent post partum is needed; more specifically, how these barriers to and facilitators of smoking cessation are perceived and experienced by women and their families, and how they are accounted for by HPs in their approach to facilitating smoking cessation in pregnancy.
This study, therefore, takes into account the household and family context of smoking in pregnancy and compares and contrasts the views of women and their SOs with those of professionals involved in maternity and smoking cessation services. This is the first study in the UK to do this. By taking this more holistic approach, the study aims to both inform the delivery of existing interventions and serve as the foundation for the development of improved interventions to support pregnant women to quit.
Project aims
This study aims to explore and identify barriers to and facilitators of smoking cessation in pregnancy and post partum, and to explore the feasibility and acceptability of improved interventions to reach and support pregnant women to quit and remain abstinent. It builds on what is already known and explores, in more depth than in previous studies, what prevents, as well as facilitates, women quitting and how these factors can be used to improve existing interventions. The specific objectives of the study are to:
-
Briefly describe the current configuration of services within the UK and the available interventions to support pregnant women to quit smoking, to establish study context and inform the last objective in this list.
-
Examine existing qualitative literature on the barriers to and facilitators of smoking cessation in pregnancy and post partum from three perspectives (pregnant and postpartum women, the SOs of pregnant women and HPs who support pregnant women), building on a recently completed systematic review conducted by members of the study team. 25
-
Explore the views of pregnant women and women who have recently given birth regarding smoking, smoking cessation and interventions to support cessation with a specific focus on the barriers to and facilitators of smoking cessation in pregnancy and post partum. This will include women who have accessed support to stop and those who have not accessed such support.
-
Explore the views of the SOs of pregnant women regarding smoking, smoking cessation and interventions to support cessation, with a specific focus on the barriers to and facilitators of smoking cessation in pregnancy and post partum. This will examine, when relevant, their smoking as well as that of the woman.
-
Explore the views of HPs and advisors who support women to stop smoking regarding the barriers and facilitators related to their role to support smoking cessation in pregnancy and post partum, and their views on the barriers and facilitators facing pregnant women outside the health-care context. This group includes midwives and midwifery managers, health visitors, consultant obstetricians, general practitioners (GPs), and smoking cessation managers and advisors.
-
Make recommendations to inform proposals for interventions that could be tested to improve the current provision of interventions for pregnant women to stop smoking.
The study outcomes include barriers and facilitators that can contribute to changes in smoking behaviour during and immediately following pregnancy. A description of the barriers and facilitators from each of the participant groups in the study is developed. This is compared and contrasted with the barriers and facilitators identified through the three systematic reviews57–59 in a narrative synthesis to inform recommendations for changes to practice and proposals for future interventions.
Chapter 2 Research design and theoretical framework
This chapter presents an overview of the research design together with a description of the two study sites participating in the primary qualitative element of the research. It then describes the rationale for the choice of theoretical framework to represent the evidence on barriers to and facilitators of smoking cessation. The chapter concludes with an overview of the remaining chapters included in the report.
Research design
This was a mixed-methods study with three key elements:
-
element 1 – systematic reviews of qualitative studies covering three populations (pregnant and postpartum women, SOs of pregnant women and HPs)
-
element 2 – qualitative research with pregnant and postpartum women, their SOs and HPs at two study sites
-
element 3 – recommendations for new interventions for smoking cessation in pregnancy and postpartum abstinence to inform the development of proposals that can be tested in future research.
Before the main elements of the study were conducted, a brief mapping exercise was carried out to describe the available cessation interventions for pregnant women in the UK, including availability at each study site. This exercise was important to understand the framework within which interventions are delivered, and it is reported in Chapter 4. The catchment profile for each study site is outlined in Study sites.
Study sites
The qualitative interviews for element 2 took place in two NHS areas: one in Scotland (area A) and one in England (area B). Area A serves a mixed urban and rural population of around 850,000 people. It has an adult smoking rate of 20.5%, which is slightly lower than the Scottish average of 23.0%. 60 In area A, 17.3% of women smoke in pregnancy and 15.1% of women smoke post partum; both figures are a little lower than the Scottish averages of 20.0% and 16.9%, respectively, and are probably reflective of a slightly more affluent population than in Scotland as a whole. There is a very steep inequalities gradient, with approximately 6% of the most affluent quintile and 34% of the most deprived quintile of pregnant women smoking, an almost sixfold difference. SSSs are organised in area-based teams relating to the new Health and Social Care Partnership (Council) boundaries.
Area B also serves a mixed urban and rural population; it has around 796,000 people61 and is scattered over a wide geographical region, encompassing three principal urban centres as well as many small villages and market towns, where access to services, including smoking cessation services, may be an additional barrier to cessation. Levels of deprivation vary widely, with pockets of both affluence and high deprivation. In 2012, the region had an adult smoking rate of 18.9%, only slightly lower than the rate for England of 19.5%. 62 The prevalence of smoking in pregnancy (measured at time of delivery) in 2012–13 was 13.7%, ranging from 21.4% for women giving birth in areas of high deprivation to 10.8% for those in more affluent areas. 62 These figures may be compared with the national prevalence of 12.7% for smoking in pregnancy in 2012 and the national ambition of a smoking in pregnancy prevalence of ≤ 11% by the end of 2015. 63 The responsibility for commissioning SSSs recently transferred to local authorities, which have contracted a local provider to manage the service.
Theoretical framework
Our protocol64 identified the theory of planned behaviour (TPB)65 as an appropriate theoretical framework for the project. The TPB is a theoretical approach used in a number of other studies of smoking in pregnancy (e.g. Godin et al. ,66 de Vries and Backbier67 and Ben Natan et al. 68). It focuses on social–ecological framework (SEF) individual-level influences on behaviour (beliefs and intentions) alongside an appreciation of contextual factors, such as perceived social norms about smoking and the consideration that environmental and demographic influences on behaviour are mediated by individual-level influences.
However, the first stage of the project (the systematic reviews of qualitative studies57–59) made clear that environmental barriers and facilitators were key to understanding smoking cessation in pregnancy. These barriers and facilitators were embedded in the individual’s domestic, community and workplace settings and relationships.
Although individual-level factors were evident, they represented only one layer in a multitiered set of social factors that operated to promote or impede positive changes in smoking behaviour and, in the case of HPs, the provision of smoking cessation support. Both singly and together, the three systematic reviews57–59 pointed to the importance of a systems perspective that located the individual within their broader social environment (including the health-care environment). The initial stages of data analysis of the qualitative studies confirmed the importance of this wider perspective. Although the TPB incorporates context as an influence on behaviour, social psychological models are not focused on capturing the multifaceted and multilayered structure of the individual’s social environment. However, the evidence from the two major data sources for the project (the systematic reviews and primary studies) indicated that key barriers and facilitators resided in these environments. We therefore considered other frameworks that provided a more comprehensive description of the multitude of influences on behaviour than models such as the TPB. The capability, opportunity, motivation and behaviour (COM-B) model69 was one of those considered, as it parsimoniously specifies determinants of behaviour from 83 models of behaviour change70 and includes emphasis on environmental barriers to and facilitators of behaviour.
However, following an integrated review of the findings from the project’s systematic reviews and primary studies, the project team concluded that the evidence on barriers and facilitators was better represented by a framework that gave greater attention to the individual’s wider environment including its constituent domains and the interactions between them. Social–ecological perspectives (also called ecological systems perspectives) provide such a framework. With its origins in biology, the term ‘ecology’ refers to the inter-relations between organisms and their environments; social ecology focuses specifically on the social and institutional environments of which individuals are part. Similar to the TPB and COM-B models, SEFs are theory based, in this instance conceptualising behaviour as the outcome of an individual’s interactions with their environment. In consequence, SEFs typically locate the individual spatially in a set of concentric circles (or layers) ranging from micro to macro levels, with the circles/layers influencing behaviour synergistically.
Although the term may not be widely used within the health community, social–ecological approaches have long informed research and policy. 71–74 One influential example is Bronfenbrenner’s ecological framework. 75,76 Developed to highlight the influence on child development of environments external to the family, this model comprises a series of concentric layers, running from the ‘microsystem’ (the family), through the ‘mesosystem’ and ‘exosystem’ (e.g. the economy and welfare services) to the ‘macrosystem’ (e.g. the wider culture). Dahlgren and Whitehead’s ‘rainbow’ model of the social determinants of health77 provides a further example. In this widely used model,78–80 health is represented as the outcome of a set of interlocking factors, running from broad societal-level factors (described as ‘general socioeconomic, cultural and environmental conditions’) through both distal (‘living and working conditions’) and proximal (‘individual lifestyle factors’) determinants. 81
Social–ecological frameworks tend to be specific to the population and outcome of concern; those relating to child development75 are, therefore, likely to be different from those relating to adolescent smoking. 82 However, the frameworks conform to a common structure, with hierarchically ordered domains representing the interlocking influences on the outcome. The project’s overarching SEF is represented in Figure 1 and consists of the following factors:
-
individual characteristics, including knowledge and beliefs, mental health and well-being, and material circumstances
-
interpersonal factors, including relationships with SOs and health-care providers
-
community factors, including neighbourhood quality and local resources, cultural norms and social networks
-
organisational factors, including service provision, workplace resources, practices and regulations
-
societal factors, including the structure of the labour market, welfare systems and family policies.
FIGURE 1.
A SEF for smoking cessation in pregnancy: spheres of influence on barriers and facilitators.

A social–ecological perspective can be particularly helpful in the development of interventions. For example, it can inform approaches to improving health care by highlighting the importance of changes at multiple levels: individual, group, organisational and ‘larger system/environment’. 83 The perspective also provides a resource for health behaviour change interventions. As an example, the behaviour change wheel of Michie et al. 69 is structured around an understanding of behaviour as shaped by the interplay of individual-level and environmental factors. In particular, a SEF can help inform understandings of behaviour change through its recognition that:
-
multiple factors act as barriers to and facilitators of behaviour change; the approach therefore points to the importance of interventions (or packages of interventions) that address multiple levels simultaneously by, for example, integrating patient-focused interventions with ones that address barriers at the interpersonal, community and organisational levels82
-
the inter-relationships between an individual and their environment are dynamic and reciprocal, as individuals and environments change and influence each other73
-
positive changes in health behaviour are likely to require positive and sustained changes in the individual’s environment.
As detailed in Chapters 5–10, the significance and content of these domains varied among the three study populations of pregnant and postpartum women, their SOs and HPs. Thus, the organisational domain was a more important consideration for barriers and facilitators for service providers than for pregnant smokers and SOs, and, within this domain, workplace cultures and practices were more prominent as a barrier to quitting among SOs who smoke than among pregnant smokers.
The SEF, therefore, informed the analysis of primary data from this study and the synthesis of findings between the systematic reviews and interviews. In the concluding chapters of this report, we refer back to this framework and use it as a ‘lens’ through which to examine and explore our findings.
Report structure
The remainder of this report is structured as follows.
-
Chapter 3 details the methods used in the study.
-
Chapter 4 describes the available cessation interventions for pregnant women in the UK, including those available at each study site.
-
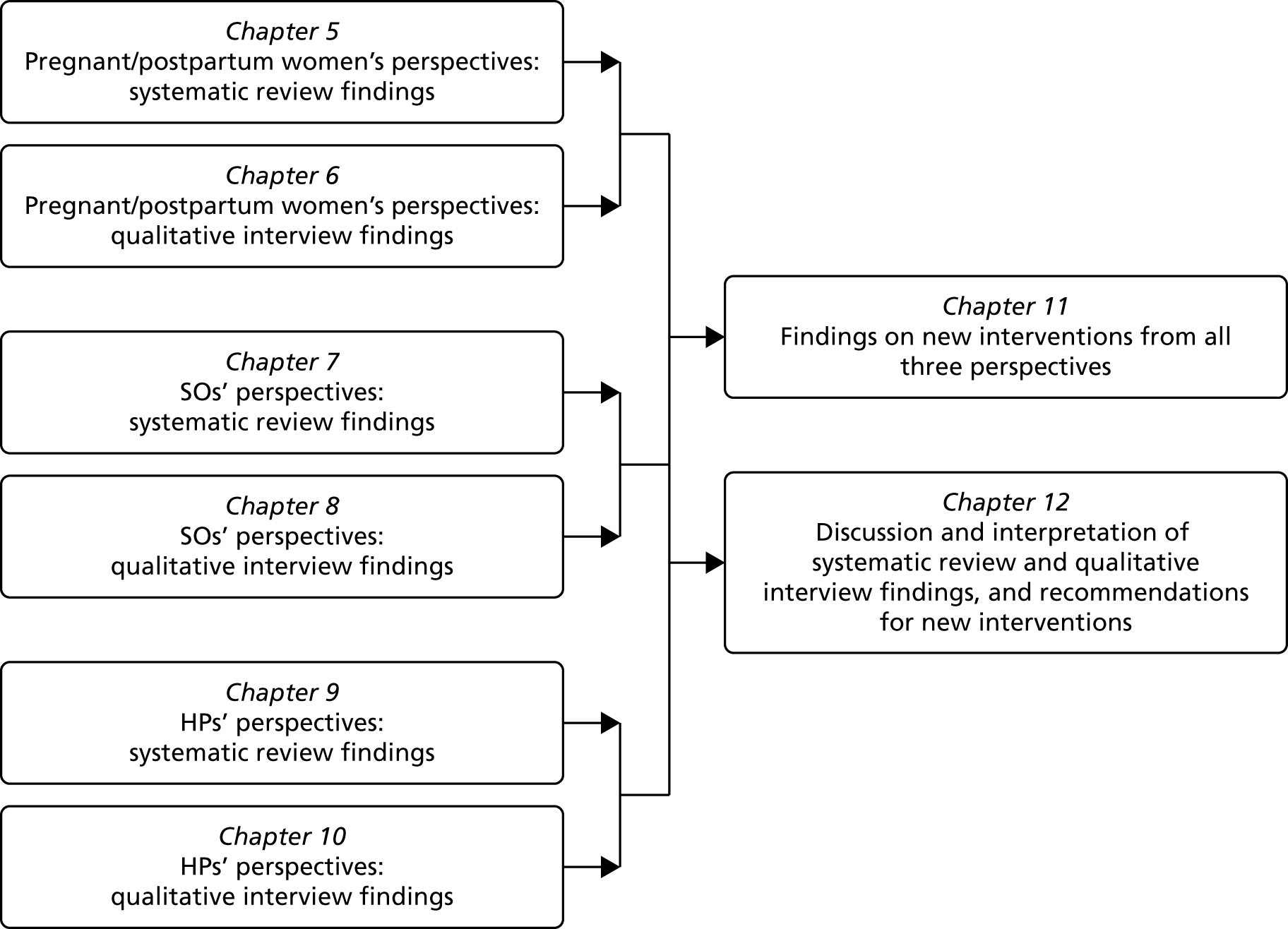
Chapters 5–10 present the findings of each of the systematic review and qualitative interview components of the study for each of the three populations of interest: pregnant and postpartum women, SOs and HPs (Figure 2). Each chapter concludes with a brief summary and discussion of the common themes emerging around smoking and smoking cessation, with concluding remarks in each of the qualitative chapters also taking into account the systematic review findings in the preceding chapter.
-
Chapter 11 presents findings for new interventions for smoking cessation in pregnancy and post partum as suggested by all three participant groups.
-
Chapter 12 presents an overall discussion of the findings from the systematic reviews and qualitative interviews, reflects on the differences between current and suggested interventions, draws out the implications for health care and makes recommendations for new interventions for smoking cessation in pregnancy and post partum that can be tested in future research.
FIGURE 2.
Chapter structure for findings and discussion of mixed-methods design components.
Chapter 3 Research methods
This chapter describes the methods used for the rapid mapping exercise of existing services for smoking cessation in pregnancy and each of the three key study components: systematic reviews, qualitative research and development of recommendations for new interventions. Any deviations from the original protocol study design are described throughout. The chapter concludes with details of the patient and public involvement in the study.
Rapid mapping exercise of existing services
The study team already had much of the information to feed into this exercise through their involvement in a range of ongoing research projects on smoking cessation in pregnancy, membership of key committees and networks, and extensive knowledge of the field. This information was supplemented with local details of services obtained from NHS colleagues who were coapplicants on the study, discussion with key management and commissioning staff at each study site, updates from relevant organisations such as Action on Smoking and Health (ASH), ASH Scotland, the National Centre for Smoking Cessation and Training, the Department of Health (DH) and the Scottish Government, and brief appraisal of studies under way testing new interventions for smoking cessation in pregnancy in the UK. A description of the available interventions and services was produced to inform the development of proposals for interventions that could be tested in future research.
Element 1: systematic reviews of qualitative research evidence
Three systematic reviews57–59 of the evidence relating to barriers to and facilitators of smoking cessation in pregnancy were conducted, building on the 2011 review for the DH on using qualitative research to inform interventions to reduce smoking in pregnancy in England. 25 The reviews covered three populations: (1) pregnant and postpartum women, (2) their SOs and (3) HPs with a role in supporting pregnant women to stop smoking.
Aims of the three reviews
-
To explore the barriers to and facilitators of smoking cessation experienced by women during pregnancy and post partum.
-
To explore the barriers to and facilitators of smoking cessation experienced by women’s SOs during pregnancy and post partum.
-
To explore HPs’ perceptions and experiences of the barriers to and facilitators of providing support for smoking cessation during pregnancy and post partum.
Approach to searching and data sources
For each review, we undertook comprehensive pre-planned searches that aimed to find all available studies. Search terms were developed in conjunction with an information specialist. A draft search strategy was developed for each review in the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and these were then adapted to run in MEDLINE, PsycINFO, Social Sciences Citation Index, the Economic and Social Research Council database and Google Scholar Advanced (GoogleTM, Mountain View, CA, USA), for both published and unpublished studies. In addition, a PubMed ‘ahead of print’ citation search identified papers yet to be indexed. We also used publication alerts to inform us of any papers published during the process of the review after the formal searches had been completed to ensure that the most up-to-date studies were included in the review. The reference lists of full-text papers were checked and consultation was undertaken with experts known to the project team, to identify papers not found through electronic searching. Details of the search strategies for each review are available in Appendix 1. Databases were searched from 1990 onwards for each review. As the reviews were undertaken sequentially, the end dates of searching varied as follows.
-
Review 1: May 2013 (from January 2012). For the period to December 2011, searches for studies relating to smoking during pregnancy and post partum had been undertaken for an earlier review. 49 The recently published (September 2015) thematic synthesis of qualitative data on postpartum smoking relapse is therefore not included in this review. 84
-
Review 2: January 2014.
-
Review 3: January 2015.
Inclusion criteria
Published and unpublished studies were eligible for inclusion if they:
-
were reported in English
-
used qualitative research methods
-
were conducted in a high-income country in which the stage of the cigarette smoking epidemic matched that reached in the UK (i.e. a strong association between social disadvantage and cigarette smoking).
Additional inclusion criteria relevant for each review were:
-
review 1 – studies investigating the barriers to and facilitators of smoking cessation that women experience during pregnancy and post partum
-
review 2 – studies investigating the views of women’s SOs of the barriers to and facilitators of smoking and smoking cessation in pregnancy and after childbirth
-
review 3 – studies investigating HPs’ experiences of the barriers to and facilitators of supporting smoking cessation during pregnancy and post partum.
Data extraction and quality appraisal
Relevant data were extracted from papers in each review (aim, type and number of participants, methodology used, methods of data collection, analysis and results). The data were extracted and checked by two reviewers. The papers were appraised for quality by two reviewers using an established checklist,85 with disagreements in scoring resolved by consensus. There was no a priori quality threshold for excluding papers; assessment was undertaken to ensure transparency in the process.
Synthesis methodology
All three reviews were undertaken using meta-ethnography. 86 Meta-ethnography is an interpretative approach to research synthesis that enables conceptual translation between different types of qualitative research. This approach consists of four iterative stages (Table 1). In each review, the following processes occurred: in phase 1, two reviewers read all papers in depth. Phase 2 involved the line-by-line coding of data (participant accounts and authors’ interpretations) in each paper relating to the focus of the review using ATLAS.ti 2010 software (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany).
| Phase of meta-ethnography | Processes involved |
|---|---|
| Phase 1: reading the studies | Studies read to develop an understanding of their position and context before being compared with others. Repeated rereading of studies to identify key findings |
| Phase 2: determining how the studies are related | Determining the relationships between individual studies by compiling a list of the key findings in each study and comparing them with those from other studies |
| Phase 3: translating the studies into one another | Determining the similarities and differences of key findings in one study with those in other studies and translating them into one another. The translations represent a reduced account of all studies (first level of synthesis) |
| Phase 4: synthesising translations | Identification of translations developed in phase 3 which encompass each other and can be further synthesised. Expressed as a ‘line of argument’ (second level of synthesis) |
The codes were then compared and grouped by the reviewers into broad areas of similarity through reciprocal translation analysis (phase 3) to generate a reduced set of codes (translations) about barriers and facilitators relevant to each review. Phase 4 focused on these translations; the reviewers examined and compared them to identify the ‘lines of argument’ emerging from the review.
Reporting
Reviews were reported in accordance with the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) statement,87 as recommended by the Equator Network for reporting syntheses of qualitative research (www.equator-network.org/reporting-guidelines/entreq/).
Element 2: qualitative research interviews and focus groups
This element of the research involved interviews with (1) pregnant women and women who had recently given birth, (2) their SOs and (3) HPs (e.g. midwives, health visitors, obstetricians, GPs) and SSS advisors with a role in caring for pregnant women. For the purposes of this report, further reference to HPs also includes SSS advisors. NHS ethics approval to conduct the research was received from South East Scotland Research Ethics Committee (REC) (reference 13/SS/0077).
Aims of the three qualitative studies
-
To explore the barriers to and facilitators of smoking cessation experienced by women during pregnancy and post partum, and elicit views on interventions to support cessation.
-
To explore the barriers to and facilitators of smoking cessation experienced by women’s SOs during pregnancy and post partum, and elicit views on interventions to support cessation.
-
To explore the perceptions and experiences of HPs with a role in supporting women to stop smoking regarding the barriers to and facilitators of providing support during pregnancy and post partum, elicit HPs’ views on the barriers to and facilitators of cessation experienced by women during pregnancy and post partum, and views on interventions to support cessation.
Inclusion and exclusion criteria
Eligibility criteria for participants in each group are listed in Table 2.
| Pregnant women | Pregnant women’s SOs | HPs |
|---|---|---|
| Aged ≥ 16 years | Aged ≥ 16 years | Aged ≥ 16 years |
| English speakinga | English speakinga | English speaking |
| Referred to NHS obstetrics services at study area A or B | Lives in same household as pregnant women or close friend/relative who spends at least 1 hour per week with pregnant woman | Significant role in the provision of care or smoking cessation support to pregnant women referred to NHS obstetric services at study area A or B |
| 6–15 weeks’ gestation at maternity booking | ||
| Self-reported smoker at maternity booking | Smoker or non-smoker | Smoker or non-smoker |
Sampling strategy
Purposive sampling was used to achieve maximum diversity within the recruited sample of pregnant women, their SOs and HPs. A sampling frame was used to obtain, as far as possible, a sample of pregnant women recruited for interview that took into account maternal age, that is 25% of the sample were to be aged < 25 years including two pregnant smokers aged < 20 years, and deprivation (i.e. 75% of sample from postcodes with the lowest Indices of Multiple Deprivation), and included both continuing smokers and quitters at around 20 weeks’ gestation. The professional sample was selected to reflect the perspectives of a range of professional groups on smoking cessation in pregnancy, and the various intervention options and opportunities available.
At the outset, the intention was to interview the following number of participants over the two study sites, as indicated in Figure 3: up to 40 pregnant women who were self-reported smokers at maternity booking, 20 of whom had stopped smoking by 20 weeks’ gestation and 20 of whom had not; 10 of these women a second time at up to 6 weeks after the birth of their babies; around 40–50 of these women’s SOs; and 40 HPs with a role in supporting pregnant women.
FIGURE 3.
Proposed participants for qualitative study at two study sites.
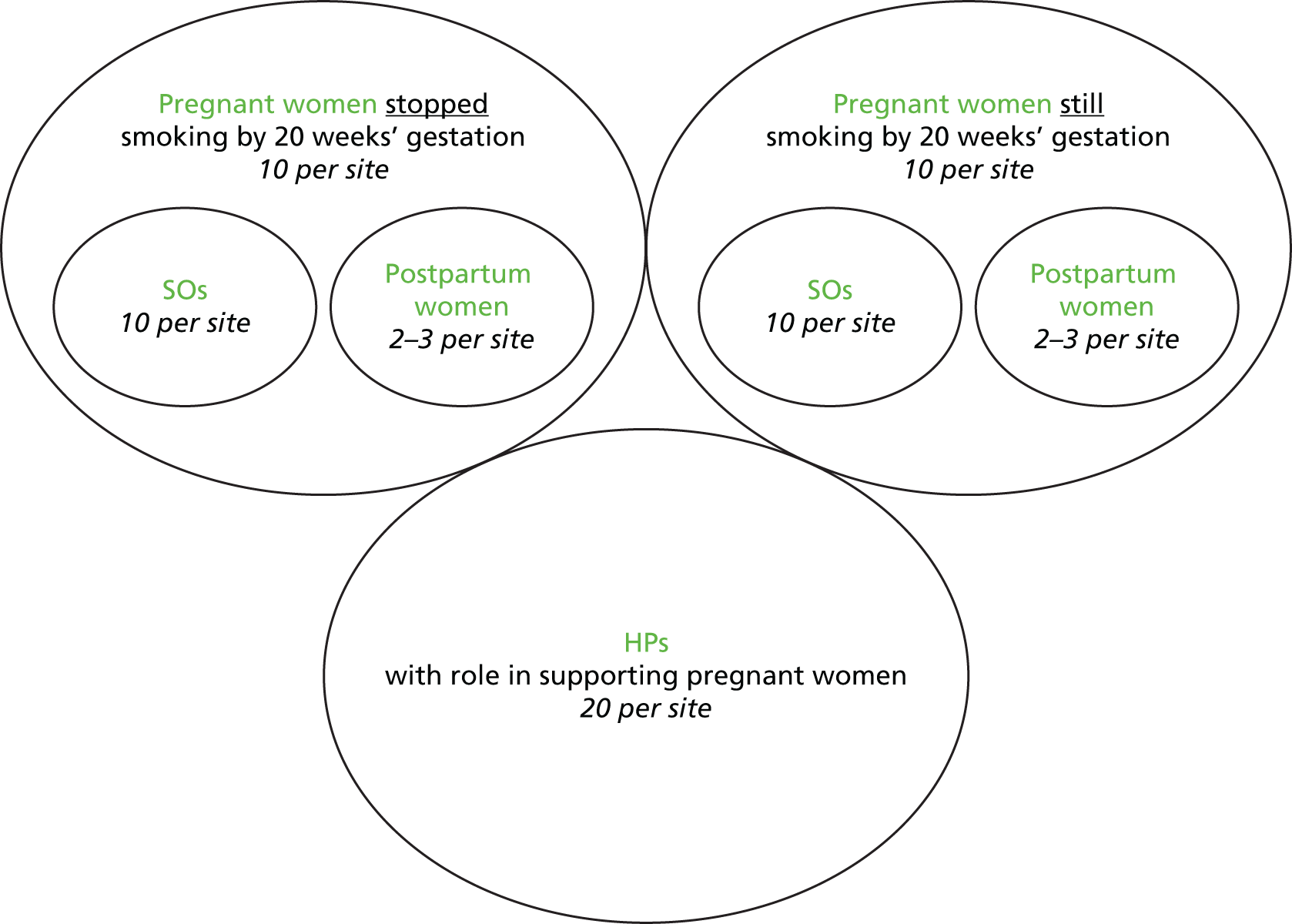
These targets were achieved, albeit by recruiting over a longer time period than planned, for pregnant women (9 months vs. the planned 5 months), postpartum women (7 months vs. the planned 4 months) and HPs (10 months vs. the planned 4 months). Interviews with HPs commenced earlier than planned (October 2013 rather than June 2014) because of delays in obtaining research and development (R&D) approvals to recruit pregnant women. In addition, for pragmatic reasons (i.e. when there was a significant number of relevant staff in similar roles, e.g. smoking cessation advisors and midwives) HPs (n = 26) participated in a focus group or a paired interview rather than an individual interview. Difficulties in recruiting women’s SOs, however, meant that the original target for this group of participants was unable to be reached despite an extended recruitment period (10 months vs. the planned 4 months). Further details of the changes made to recruitment approaches are described in Recruitment of participants.
A total of 121 individuals recruited from NHS study areas A and B participated (Table 3). A description of the characteristics of each group of participants is presented at the beginning of each of the qualitative findings chapters for pregnant and postpartum women (see Chapter 6), SOs (see Chapter 8) and HPs (see Chapter 10).
| Sample | Recruitment period | Area A | Area B | Total | Target |
|---|---|---|---|---|---|
| Pregnant women | November 2013–September 2014 | 21 | 20 | 41 | 40 |
| Number of whom were also interviewed post partum | June 2014–December 2014 | 5 | 5 | 10 | 10 |
| SOs | November 2013–September 2014 | 20 | 12 | 32 | 40–50 |
| HPs | October 2013–July 2014 | 26 | 22 | 48 | 40 |
Recruitment of participants
To encourage participation in the study, pregnant and postpartum women and SOs were offered a £15 Love2shop voucher as an incentive and as a way of thanking them for taking part in the study. No incentives were offered to HPs to participate in the study. SOs were also interviewed around the same time as the pregnant women rather than a few months later, as originally planned, following feedback from potential participants at the start of the study. Some interviews, however, still took place after the findings from the systematic review element of the study became available, thus allowing discussion of any new data emerging from the review to be incorporated into the interviews.
Pregnant and postpartum women
Pregnant women were recruited with the support of maternity services and/or SSS colleagues in each study site. Recruitment and consent processes differed between sites to fit around the structure of existing services.
In study area A, where pregnant smokers are routinely identified at maternity booking and referred (through an opt-out system) to the NHS SSS, recruitment was initiated by smoking cessation advisors. Women attending a face-to-face appointment with a smoking cessation advisor were informed about the study during this appointment. Those interested were given a study information sheet and permission was obtained for their contact details to be passed to the study team. Women who did not attend a face-to-face appointment were told about the study during routine telephone contact by the smoking cessation advisor. Those interested were sent a study information sheet by post. All women whose contact details were passed to the study team were called by a member of the local research team within an average of 14 days (range 2–43 days) of receiving the information sheet. At this call, the researcher explained the study, answered any questions that the woman had and obtained her verbal consent for participation. The research team remained in contact with those who consented through mobile phone text messaging until they were around 20 weeks pregnant, at which point they were contacted by the researcher to arrange an interview. A consent form was signed by the women prior to the interview commencing.
At study area B, self-reported smokers at the maternity booking appointment (at around 6–10 weeks’ gestation) were given a copy of the information sheet and asked to consider taking part in the study. At the dating or nuchal translucency scan that takes place at around 12 weeks’ gestation, they were invited to meet with the research midwife, who explained the study and discussed the information sheet. Women were invited to participate by the research midwife who also obtained written consent at that time from those who wished to be involved. Details of those consenting were entered into the participant database by the research midwife. At around 20 weeks’ gestation, the women were contacted by a member of the local research team to arrange a suitable interview date.
At the end of the interview in both study sites, women were asked if they would be willing for the researcher to contact them again around 4–6 weeks after having their baby to find out if they were smoking or not and, when appropriate, ask them to participate in a second interview. Of the 41 women interviewed while pregnant, all but one indicated that they would be willing to participate in a second interview. At the outset of the project, the intention was to purposively select women for a second interview depending on their smoking status when contacted in the postpartum period in order to gain a range of views based on diverse experiences. However, unexpected difficulties in contacting women again in the postpartum period, particularly in area A, meant that these criteria had to be modified. In area A, only half of the participants were able to be successfully contacted post partum, with only half of those contacted agreeing to participate; in total, therefore, five women were interviewed. In area B, the first five women we contacted postnatally agreed to participate. A further consent form was signed prior to the interview commencing.
Significant others
The recruitment of SOs to the study involved a number of different processes; most of these were influenced by recommendations from the REC that we not recruit SOs by the method of pregnant women asking their SOs to participate. Although this would have been the most straightforward recruitment approach, the REC felt that it might have caused tension or confrontation between women and their SOs if women had to ask these individuals to take part. Thus, we modified our approach in line with this.
At both sites, pregnant women were asked to simply pass on a brief information sheet to any of their SOs that they believed might be interested in taking part in an interview. This request was made either prior to the woman’s first interview [i.e. when arranging and confirming the first interview with the women (area A) or at the time of consent by the research midwife (area B)] or at the end of the woman’s first interview (both sites). The brief information sheet included a tear-off slip for SOs to complete and send to a member of the research team to indicate interest in the study. On receipt of this slip, a longer information sheet was sent to the individual, followed by a telephone call from a researcher to confirm participation and arrange an interview appointment. All SOs at both sites were asked to complete a consent form at the beginning of the interview.
It became clear during the course of fieldwork that the process recommended by the REC to recruit SOs was failing to produce the required number of participants, which prompted the research team to alter their approach. Attempts continued to attract participants using the brief information sheet/tear-off slip approach. At the same time, however, the study was also promoted to all SOs attending antenatal appointments with pregnant smokers rather than only the SOs of women who had agreed to take part in the study. This change was approved by the REC. This amendment to the recruitment process enabled the project team to attract further SOs to participate, although the original target set out in the protocol was still unable to be reached (32 of the target 40–48 SOs recruited). Nonetheless, the systematic review of qualitative studies of SOs (see Chapter 7) indicates that this qualitative study involving the 32 pregnant women’s SOs represents the largest UK study to date.
Health-care professionals
All professionals recruited to participate in the study had a role in supporting women during pregnancy. This included midwives and midwifery managers, health visitors, GPs, pharmacists, obstetricians, smoking cessation service managers and advisors. The recruitment of professionals was facilitated by study coapplicants and took place through the respective organisational structures. A multichannel approach to recruitment of HPs was applied, for example through team leaders, attendance at team meetings and use of e-mail invitations. Recruitment was further guided by the introduction of a target quota of HP ‘groups’ to be achieved over the two study sites, as detailed in Table 4. Nine more SSS advisors than planned were recruited to participate in the research primarily to accommodate as many individuals as possible from this key group.
| Professional group | Target | Actual |
|---|---|---|
| Midwives/midwifery managers | 18 | 17 |
| Health visitors | 4 | 4 |
| SSS advisors/managers | 10 | 19 |
| Obstetricians | 2 | 2 |
| GPs | 2 | 2 |
| Service commissioners | 2 | 2 |
| Community pharmacists | 2 | 2 |
| Total | 40 | 48 |
Information sheets regarding the study and taking part in an interview were provided to potential HPs before they agreed to participate, with written consent obtained prior to interviews commencing. The participants were given the opportunity to ask any questions about the study before the interviews commenced and were given assurances about confidentiality and anonymity of responses.
Interviews and focus groups
All interviews and focus groups were conducted by female researchers from the University of Stirling and University of York. At area A, two researchers (AF and JM) conducted the interviews with women and SOs. Nine of these interviews had two researchers present for the purposes of shadowing prior to maternity leave for one researcher (n = 4), observation of qualitative fieldwork by a visiting researcher from the University of Ireland, Galway (n = 3), and safety concerns about visiting some participants’ homes (n = 2). In all cases the second researcher did not participate in the interview process. JM completed approximately 10 interviews with women and partners and one focus group with HPs (smoking cessation advisors) before going on maternity leave in December 2013. Three project team members (LB, LS and JM) conducted the interviews and focus groups with HPs. At area B, one researcher (DM) conducted all of the individual and group interviews.
Interviewer descriptions
Allison Ford is a qualitative researcher specialising in sensitive topics. She has worked on numerous smoking-related studies conducting and analysing interviews and focus groups with young people, adults and professionals. She is in her mid-thirties with two young children and has never smoked.
Jennifer McKell is a researcher with several years’ experience in conducting qualitative research on topics relating to health and substance use. This has included interviewing pregnant smokers. She is in her early thirties and has never smoked. She was pregnant with her first child during the fieldwork stage of the study.
Dorothy McCaughan is a qualified registered nurse who has worked in a range of health-care contexts, both in the UK and overseas. She has extensive experience of conducting qualitative interviews, with both clinicians and recipients of health care, over a period of 20 years as an applied health services researcher. She is in her early sixties, has one son and has never smoked.
Lesley Sinclair is a researcher with > 15 years’ practical experience of co-ordinating health services research involving complex interventions for a variety of patient groups. She has worked in both NHS and university settings. In recent years her research has focused on smoking in pregnancy. She is in her late forties and has never smoked.
Linda Bauld is Professor of Health Policy at the University of Stirling and holds the Cancer Research UK(CRUK)/Bupa Chairperson in Behavioural Research for Cancer Prevention at CRUK. She chairs the multiagency Challenge Group on smoking in pregnancy in England and has 20 years’ experience in conducting applied public health research, including leading a number of studies on smoking in pregnancy. She is in her mid-forties, has two children and has never regularly smoked.
The interviews with pregnant and postpartum women and SOs mostly took place in the women’s or SOs’ homes or, less frequently, in a public place, such as a coffee shop, workplace or health centre. Women and their SOs were interviewed separately (the pregnant woman first), reflecting the intention to encourage greater openness, particularly regarding family and community norms and support viewed as probable barriers and facilitators. In the majority of cases, only the interviewee was present at interview; however, there were some instances in which other individuals, including children, were present, which could create a chaotic and noisy backdrop to the interview. In several instances there were also interruptions during the course of the interview, for example a telephone call or individuals turning up at the house. On occasion, interviews with participating women and their SOs were conducted in each other’s presence (n = 6), even when separate interviews had been explicitly requested beforehand. In a very few cases, SOs seemed unreceptive or were overtly disapproving of the pregnant woman being involved in a research interview.
Forty-four of the 48 HPs participated in a face-to-face interview/focus group in their workplace and four in area A participated in a telephone interview. Twenty-two professionals were interviewed individually and 26 took part in a focus group or paired interview (n = 22 in four groups and n = 4 in two paired interviews). Focus groups were conducted when there was a significant number of relevant staff in similar roles, for example smoking cessation advisors and midwives. At area A, three focus groups were conducted: one involving midwives (n = 4), another involving team leaders from the local SSS (n = 4) and a third involving facilitators from the local SSS (n = 10). One focus group was conducted in area B involving midwives (n = 4). In addition, two paired interviews were carried out across the two study sites: two midwives in area A and a SSS manager and an administrator in area B.
Interview format and duration
The format of all interviews and focus groups conducted was intentionally relaxed and informal, with the interviewer following a semistructured topic guide (see Appendix 2) to promote a conversational style. All interviews and focus groups were audio-recorded using a digital recorder.
The interviews with pregnant women ranged in duration from 25 minutes to 1 hour and 20 minutes, although most lasted between 40 and 50 minutes. Postpartum interviews tended to be shorter in duration, ranging from 17 minutes to just over 1 hour, with most lasting between 30 and 40 minutes. The shortest SO interview was 13 minutes and the longest was just under 1 hour; most interviews with this group were approximately 30 minutes long. The shorter duration of partner interviews was partially explained by fewer questions being involved, but also because most of these interviews were with men, who were briefer in their answers and/or who may have felt that some questions were not relevant to them (e.g. they were non-smokers), so questions relating to smoking were not relevant. The interviews with HPs (including smoking cessation advisors) ranged in duration from 17 minutes to 1 hour and 15 minutes. This large variation was a result of busy work schedules and limited time (i.e. interviews with GPs or obstetricians), or the extent to which smoking cessation was part of a professional’s role. The focus groups and paired interviews carried out lasted approximately 1 hour.
Transcription of interviews
All interviews and focus groups were transcribed verbatim. Some recordings were transcribed by a member of the research team but the majority were transcribed by professional transcribers regularly employed by the University of Stirling.
Development of topic guides
Prior to commencing interviews and focus groups with the three groups of participants, topic guides were prepared to support semistructured discussions. The guides (see Appendix 2) were informed by project team members’ previous and ongoing work relating to smoking in pregnancy, the theoretical framework used in the study and a mapping of current and new interventions in this area.
In the early stages of the study, project team members identified key themes (informed by the TPB) for inclusion in topic guides for each of the participant groups: smoking behaviour and quit attempts, beliefs and feelings about smoking in pregnancy, perceived barriers to and facilitators of smoking cessation in pregnancy, perceptions concerning the SSS, and views on available and in-development interventions for smoking cessation in pregnancy. These key themes were used as a basis for developing interview questions. The HPs’ topic guide was the first to be developed. This was initially produced by one member of the project team (FN) and reviewed by other members. Draft topic guides for interviews with pregnant women and SOs were then produced by another member of the project team (JM), taking account of relevant themes but also the style of the HPs topic guide. The draft topic guides were then reviewed by the wider project team for content, comprehensibility and ‘flow’ of questioning. A fourth topic guide was produced for interviews with postpartum women using a similar process of identifying relevant themes prior to refinement and modification.
Coding and analysis
Three separate groups within the project team analysed the data from the three different participant groups: pregnant and postpartum women (AF, JM and KA), SOs (JM, DE and KA) and HPs (FN, SH and LS). The analysis was guided by Braun and Clarke’s phases of thematic analysis88 and set within the interpretivist paradigm. This paradigm considers participant accounts elicited during research interactions as representing one of many possible ‘truths’ and recognises that interpretations of these interactions are influenced by the researchers’ knowledge, beliefs and values. For the analysis of the HPs focus group data, we did not analyse interactions or dynamics between participants (e.g. participants looking at each other, laughing at another participant’s comments, nodding), as these data were combined with individual interview data in which there were no interparticipant interactions. NVivo (version 10, QSR International, Warrington, UK) was used to facilitate the coding and analysis.
Coding frameworks were developed for each qualitative study separately using mind-mapping techniques. These frameworks were informed by the SEF. 74 The following process was repeated for each of the three qualitative studies: after familiarisation with the transcripts (i.e. reading and rereading), researchers independently microcoded several transcripts and all identified codes were categorised and inserted into one of the three SEF levels being examined, individual, interpersonal or organisational; after this researchers agreed on which codes to include in the draft framework, several further transcripts were coded and any new concepts (codes) that emerged were added.
The adequacy of the coding frameworks and consistency of coding between researchers was assessed using several methods. When dual coding was employed (i.e. 10 instances of dual coding for pregnant women’s transcripts and five for HPs transcripts), NVivo’s ‘coding stripes’ and/or coding consistency assessment query function was used to identify coding with potentially poor overlap (e.g. kappa coefficient < 0.7) that should be investigated. Although the coding consistency was acceptable for most codes, some codes had poor reliability having been applied inconsistently by the different researchers. These codes were discussed and resolved by making a number of minor changes to the coding framework, including the merging of some codes and changing of code labels and descriptions to maximise coherence and validity. For the SO transcripts, two researchers coded separate transcripts and then discussed the adequacy of the coding framework, including the addition or removal of certain codes.
Owing to similarities in the topics discussed and shared environments, the coding frameworks for interviews with postpartum women and SOs drew on the coding framework developed for pregnant women. A read-through of a sample of interviews from each of the study sites allowed further development in relation to key additions and omissions. The postpartum coding framework was particularly focused on any changes in perceptions, behaviour and support as the pregnancy progressed and once the baby was born. The SOs framework focused on participant’s relationships with the pregnant woman with reference to smoking and smoking cessation and perceptions of available support for cessation.
After all transcripts had been coded, the researchers read and reread the coded content, and summarised the key findings emerging from each code into higher-level categories. In line with ‘axial coding’,89 the researchers explored how the categories related to each other, leading to the emergence of preliminary themes. These themes were then refined through exploration and discussion of how well the preliminary themes mapped back onto the coded and raw data. Throughout this process, categories and themes were integrated into one of the three levels of the SEF being used to structure the codes, although interactions between categories and themes across these SEF levels were also examined. For all groups of participants, particular attention was paid throughout to similarities and differences in findings between research sites. In addition, similarities and differences in findings were examined between (1) women who had quit smoking and those who had continued to smoke through pregnancy, (2) partners and others with relationships with the pregnant women, and also SOs’ smoking status, and (3) the different groups of HPs, for example midwives, SSS advisors, etc. Once clear themes had been identified, these were named and described, accompanied by supporting quotations, as part of the process of writing up the findings. Supporting quotations were selected that generally expressed dominant views and demonstrated significant issues but also that reflected ‘deviant’ or ‘negative’ views. 90 As recommended when undertaking qualitative analysis,88 the process of analysis was recursive and often involved multiple iterations, particularly when identifying and refining themes from codes and categories.
Element 3: informing the development of proposals for future research
The final element of the study involved reviewing findings in order to identify (1) how existing services or interventions could be improved and (2) what new or modified interventions might be tested in the future. This was a relatively modest element of the study but drew on the two main data sources. The first was findings from the interviews in which participants were specifically asked for their views on whether or not particular new interventions already mentioned in the literature (e.g. financial incentives, social network interventions) might be of interest, or if there was anything else which might help women to stop smoking. These findings are outlined in each of the chapters that report the findings from the three groups of participants (pregnant and postpartum women, SOs and HPs) in the study. The second source of data for this final element of the research was team members’ related work. This had three main forms. First, the principal investigator (PI) served, during the lifetime of this study, as a member of the World Health Organization’s Guideline Development Group on smoking cessation during pregnancy. 39 This membership involved reviewing the wider international literature on cessation in pregnancy as part of the committee and from this promising future interventions were noted. Second, several members of the research team were involved in the Smoking in Pregnancy Challenge Group91 established in 2012 following a request from the DH to develop a smoking in pregnancy action plan for England. This plan was published in June 2013 with a commitment to meet annually to review progress. The 2015 review92 involved mapping existing gaps in the evidence base that were specifically relevant to services and interventions in England, and the findings from this have informed this report. Finally, the study team were involved in a number of other separately funded projects during the study period testing new interventions for smoking cessation in pregnancy that were either not available when the project began or not reported in the literature summarised in the three systematic reviews. 57–59 These projects are on the following topics: financial incentives for smoking cessation in pregnancy,93 self-help interventions using digital media94,95 (building on a previous systematic review by the authors96) and a scoping study on social network approaches to smoking cessation in pregnancy. Together, these data sources inform the concluding chapters of this report and have been synthesised with findings from interviews to highlight opportunities for future interventions and new research on this important topic.
Patient and public involvement
Patient and public involvement took place at all stages of the study via several mechanisms. At the research design stage, the proposal was discussed with the UK Centre for Tobacco and Alcohol Studies (UKCTAS) smokers’ panel, an established panel of 30 active smokers and individuals trying to quit, that meet regularly in the city of Bath, UK, to discuss smoking cessation research and policy initiatives. A member of the panel (Susanna Mountcastle), a smoker with two young children, also joined the study advisory group. During the set-up phase of the study, SM reviewed interview topic guides and patient information sheets. A participant representative from study area A also helped to pilot the interview topic guide for pregnant women.
Once the study was up and running, SM attended the advisory group meetings and, thus, contributed to the discussions and decisions made in relation to managing the study. SM also assisted in developing an alternative recruitment strategy for SOs when it became clear that the recruitment method specified in the protocol for this group of participants was not achieving the desired outcome. In addition, SM commented on interim and final results.
At the end of the study, findings were discussed with the UKCTAS smokers’ panel and their help was requested on approaches for disseminating findings and integration with policy. Four study participants (two from each study site) also provided feedback on a six-page summary of the findings (see Appendix 3) from the qualitative elements of the study.
Chapter 4 Current service provision to support pregnant women to quit smoking
This chapter describes the evolution of SSSs in the UK and more specifically the development of tailored provision for pregnant women. Support for pregnant women to stop smoking outside specialist SSSs is also described. The chapter concludes with a description of the structure and nature of support and services in the two study sites.
Development of Stop Smoking Services
A national network of SSSs was established in the UK following the publication of the 1998 White Paper Smoking Kills: A White Paper on Tobacco. 97 Initially piloted in deprived areas of England in 1999, SSSs were rolled out across the UK from 2000. The services were developed on the basis of national guidance issued by the DH that built on a review of the evidence of the effectiveness of smoking cessation interventions published in the journal Thorax. 98 This evidence emphasised the efficacy of intensive behavioural support (in groups or one to one) plus pharmacotherapy for smoking cessation. Services were established by primary care trusts and operated primarily in primary care settings delivering behavioural support and providing access to NRT and bupropion. From 2000 to 2004, a national evaluation of the services in England was conducted by members of our team. This reported in 2005 in a special issue of the journal Addiction. 99–101 The evaluation found that the services were effective in supporting smokers to quit in the short term (at 4 weeks)99 and the longer term (at 1 year),100 and were reaching smokers from more deprived groups. 101 A subsequent analysis by our team also found that they were making a contribution to reducing inequalities in health caused by smoking. 102
Since these studies were conducted, SSSs have continued to evolve, including offering more tailored support to priority groups including pregnant women, which we describe in Stop Smoking Services for pregnant women. The services overall have been affected by various financial and structural challenges. National developments including NICE guidance on services (published in 2008)103 have influenced what is available, and smoking cessation medications have also diversified, with new NRT products and the medication varenicline (not licensed for use in pregnancy but effective with the general adult population) providing additional options for smokers trying to stop.
One element that has changed in the past decade is the type and variety of behavioural support options available to smokers using the services; in particular, a heavier reliance on one-to-one support options in a far wider range of settings. Findings from our earlier research with the NHS SSS suggest that group interventions may be more effective in practice104 but that smokers, given a choice, will choose one-to-one support. Issues of perceived preference may have led to the dominance of one-to-one support in current services, although new forms of group counselling (such as ‘rolling groups’ that clients can join without having to wait for a new group to start) have emerged.
Another element that has evolved is who provides support to stop smoking. Before the services existed, this was primarily provided by doctors and nurses in primary care or hospitals with a few examples of specialist clinics. Currently, a wider variety of professionals are involved in delivering support; for example, community pharmacists can provide SSSs.
Following these changes, a second national study of effectiveness of the services in England was recently conducted and reported in 2015. 105,106 This study employed a similar research design to the 2005 research99–101 but involved more areas of the country and a larger sample of service clients. It found that overall abstinence rates from smoking had dropped from 15% to 8% at 52 weeks but that smokers who received the best combination of stop smoking medication and behavioural support delivered by trained specialists were two to three times more likely to quit than other clients. 105,106
Stop Smoking Services for pregnant women
The UK’s SSSs began to develop tailored provision for pregnant women from 2000. This involved the same combination of support developed for the general adult population (a combination of behavioural support and medication, in this case NRT, which is the only product licensed for use in pregnancy). In 2008, an observational audit of Scottish outcomes conducted by members of our research team suggested that delivering support through services developed solely for pregnant women may be more effective than supporting pregnant women through generic services, which support all smokers. 107 This involved smoking cessation advisors who had been specially trained to support pregnant women on a one-to-one basis, and to accurately convey the risks of smoking and help women to maintain their quit attempt through pregnancy and beyond. The Scottish audit found that there were five pregnancy specialist services across 10 hospitals/units (across five health boards) in which there are staff employed specifically to provide cessation support. These services, however, were often understaffed and overstretched. The remaining hospitals/units provide either ‘intermediate’ support services, that is, staff with a limited designated period for the provision of cessation support, or ‘generic’ support services in which any cessation support is not specific to pregnancy and is provided as part of community-based services. At the time of the audit’s publication, a number of services were in development.
In 2010, the first UK guidelines were released by NICE on how to stop smoking in pregnancy and following childbirth. 40 These guidelines made recommendations not only about which cessation interventions are effective for pregnant smokers, but also about ways in which health providers should try to identify and engage with pregnant women to offer them these interventions. One recommendation, for example, was that services should systematically introduce screening of exhaled carbon monoxide (CO) into routine care in order to identify pregnant smokers; the guidance also suggests that when a woman’s CO levels indicate that she is a smoker, she should be automatically offered NHS stop smoking support through an ‘opt-out’ referral pathway.
Following the release of this guidance, a national survey was conducted in England to determine how SSSs were delivering support to pregnant women. 41 It found that, in 2010–11, 55% of SSSs provided some support to pregnant women through specialist services (18% supported pregnant women only through specialist services and 37% supported them through a combination of generic and specialist services). A total of 76% of services in England had a specialist pregnancy advisor in post. Pregnant women were most commonly offered support in their home (72%), children’s centres (72%) and family doctor practices (71%). Most services offered behavioural support and either single (77%) or dual (86%) NRT. A number of services also offered relapse prevention support (65%), behavioural support only (62%) and financial incentives (35%). As an adjunct to routine support, 64% of services offered some form of self-help support (primarily a booklet/leaflet).
Other support for pregnant women to stop smoking
Support for pregnant women to stop smoking also exists outside specialist SSSs. A number of settings and HPs are involved, including the following.
-
General practitioner surgeries: GPs and other HPs sometimes offer brief advice and a prescription for NRT, although the provision of this is variable. For example, based on GP practice records between 2000 and 2009, it was estimated that 9% of pregnant smokers had been prescribed NRT. 108
-
Antenatal care: midwives are recommended to briefly discuss smoking at a woman’s booking visit and to follow this up at subsequent visits. International studies have found that midwives are more likely than GPs to advise women to cut down on smoking rather than abstain completely. For example, in one survey, only 11% of midwives said that they advised smoking clients to abstain completely, compared with 71% of GPs. In the UK, one survey found that only 31% of pregnant smokers reported being told by a midwife that they should stop smoking. Obstetricians and other antenatal HPs may also discuss smoking with clients and provide advice about cessation.
-
Telephone ‘quitlines’: pregnant women may choose to access support to stop smoking without seeing a HP, and telephone quitlines have been in place for a number of years in the UK to provide this kind of help. Examples include the NHS Smokefree helpline and telephone services offered by the baby charity Tommy’s and the National Childbirth Trust. These quitlines also make women aware that they can be prescribed NRT to help with their quit attempt and that in order to obtain this they need to see their GP or a NHS SSS, where more intensive behavioural support can also be provided.
-
Online resources: a variety of online resources also offer self-help options to women trying to stop smoking in pregnancy. For example, information is available through the ‘NHS Choices’ website and, for younger mothers, through Tommy’s ‘Baby be smokefree’ website. A number of other tailored websites exist in the UK and overseas, and increasingly research is being conducted on digital interventions for smoking cessation in pregnancy, including smoking cessation applications, text messaging and other new media forms of support. 91
Support to stop smoking in the two study sites
For women living in the two areas where this study was conducted, the structure and nature of support and services differed.
Area A had established smoking cessation support for pregnant women before the national SSS was established. From 1993, trained smoking cessation advisors, employed by a drug and alcohol service and linked to one maternity hospital in the centre of the area, were in post. These services were expanded to cover the whole area on a gradual basis when national funding for SSSs became available in Scotland from 2000. At the time of the study, a fairly comprehensive network of services was in place, involving a pathway from the identification of women who are smoking in pregnancy through to providing support to stop throughout the antenatal and into the postnatal period.
During the period when the study was beginning in 2013, the Scottish Government introduced a new maternity services framework as part of the Scottish Patient Safety Programme. 109 Known as the Maternity and Children Quality Improvement Collaborative, this included, among other priorities, a target to routinely refer 90% of women identified as smoking during pregnancy to SSSs. This target was to be met by offering a CO breath test to all women at maternity booking. Those whose CO test indicates a level of ≥ 4 parts per million (an appropriate cut-off point identified by members of our research team in a previous study42) or who self-report as smokers are automatically referred to their local smoking cessation service in the area. 42 All women are then contacted by the service and can choose to engage in a face-to-face appointment or to decline support. This opt-out referral pathway is consistent with NICE guidance and is intended to ensure that all pregnant smokers have the option of effective support to stop. 40
Local SSSs are organised into locality teams within area A. In most instances, pregnant women are seen by ‘generic’ advisors, that is trained smoking cessation staff who also treat other groups of smokers and not just pregnant women. Specialist guidance and training for these staff is provided by a senior smoking in pregnancy midwife. Women who choose to engage with the service are provided with one-to-one behavioural support by advisors and are offered NRT, with the vast majority of women choosing to use NRT, at least initially, in their quit attempt. Advisors also offer an option for pregnant women’s partners or other family members to attend behavioural support sessions with (or separately from) the pregnant woman if they also wish to stop. Behavioural support is available throughout pregnancy and, if women wish, after birth, with later appointments sometimes taking place by telephone rather than face to face. Quit dates and outcomes at 4 weeks post quit date are recorded by cessation advisors and entered into Scotland’s national SSS database held by the Information and Statistics Division of the Scottish Government.
Area B’s SSS was established from 2000 following the piloting of local services in neighbouring areas from 1999. From 2002, a part-time specialist smoking in pregnancy advisor was in post who had a remit of delivering tailored support to pregnant women in the locality. Additional funding for smoking cessation in pregnancy was allocated to midwives working in the acute trust who were provided with additional training to add smoking cessation to their role. Over the years, the team gradually expanded and at the time of the study a number of part-time smoking in pregnancy specialist advisors were in post, amounting to just under six whole-time equivalent posts. Structural changes took place within the NHS in England as the study was starting, with the SSS now commissioned by the local authority. However, the local acute trust employs the advisors, 75% of whom are allocated to a semirural area and 25% to the city within area B.
An important difference between areas A and B is the referral pathway to the SSS. At the time of the study, area B did not offer routine CO monitoring or opt-out referral to all women. One locality within the area was piloting CO monitoring and did try to refer all women if their CO reading indicated current smoking. In the remainder of the study area, however, CO monitoring was not routinely used so smoking status was based on whether or not women self-reported tobacco use to the midwife at maternity booking. If she did, then a referral was offered rather than being automatic as in area A. If the referral was accepted, women would be contacted by a smoking-in-pregnancy specialist who would agree to meet them face to face. The support offered from that point onwards was similar to that in area A, with behavioural support and NRT provided, although in this case primarily by a smoking-in-pregnancy specialist rather than generic advisors as in area A. Support commonly ran in 6- to 12-week blocks, although some women were seen for a longer period, including postnatally. As in area A, advisors tried to see women and partners together if the partner was smoking and agreed to access the service. Mothers or other family members could also be treated. Appointments often took place in children’s centres rather than in women’s homes or in clinics (homes and clinics being the main venue for support in area A). Additional telephone support was available to women who agreed to be contacted, and text messages were often used, particularly after an initial period involving face-to-face appointments. As in area A, the vast majority of service clients (around 80%) accepted the offer of NRT, which was dispensed by local pharmacists using a voucher scheme. Routine monitoring data were collected by advisors at the first appointment and smoking cessation outcomes reported at 4 weeks post quit date. These data were then submitted by locality to the Health and Social Care Information Centre (now known as NHS Digital) which reports on SSSs for England.
At the time of the study, electronic cigarette (e-cigarette) use was continuing to rise across the UK. Advisors in both areas indicated that some pregnant women they saw were using e-cigarettes as part of their quit attempt. However, owing to a lack of evidence on safety or efficacy during pregnancy and also the absence of any licensed e-cigarette product, advisors could not recommend or support e-cigarette use, although we did not identify any examples of use being explicitly discouraged. However, these products were not a major focus for the study and, thus, detailed information on their use by pregnant women was not collected during the study, although some women did mention them in interviews. Members of our team are now conducting a separate qualitative study with pregnant or recently pregnant women about their attitudes to e-cigarettes. This is funded by CRUK and should report in 2017.
Chapter 5 Findings of systematic review of pregnant and postpartum women’s perspectives and experiences of the barriers to and facilitators of smoking cessation
This systematic review has been published in the Journal of Advanced Nursing. Here we present the abstract of the paper. This abstract has been reproduced from the abstract © Flemming et al. 57 under the terms of the Creative Commons Licence 4.0 (CC BY); https://creativecommons.org/licenses/by/4.0/.
Aim
To explore the barriers to and facilitators of smoking cessation experienced by women during pregnancy and post partum by undertaking a synthesis of qualitative studies.
Background
The majority of pregnant women are aware that smoking in pregnancy compromises maternal and infant health. Despite this knowledge, quit rates among pregnant women remain low, particularly among women in disadvantaged circumstances; disadvantage also increases a woman’s chances of living with a partner who smokes and of returning to smoking after birth. A deeper understanding of what hinders and what helps pregnant smokers to quit and remain ex-smokers post partum is needed.
Design
A synthesis of qualitative research using meta-ethnography.
Data sources
Five electronic databases (searched January 1990–May 2013) were searched comprehensively, updating and extending the search for an earlier review to identify qualitative research related to the review’s aims.
Review methods
Following appraisal, 38 studies reported in 42 papers43,110–150 were included and synthesised following the principles of meta-ethnography. More than 1100 pregnant women were represented, the majority of whom were drawn from disadvantaged groups.
Results
Four factors were identified that acted as both barriers to and facilitators of women’s ability to quit smoking in pregnancy and post partum: psychological well-being, relationships with SO, changing connections with her baby through and after pregnancy, and appraisal of the risk of smoking.
Conclusion
The synthesis indicates that barriers and facilitators are not fixed and mutually exclusive categories; instead, they are factors with a latent capacity to help or hinder smoking cessation. For disadvantaged smokers, these factors are more often experienced as barriers to than facilitators of quitting.
Chapter 6 Findings from qualitative study of pregnant and postpartum women’s perspectives and experiences of the barriers to and facilitators of smoking cessation
This chapter presents the findings from the interviews undertaken with pregnant women and women who had recently given birth to explore their perspectives and experiences of the barriers to and facilitators of smoking cessation in pregnancy and post partum, and to elicit their views on existing services and interventions to support cessation.
Participant sample
Forty-one interviews were conducted with pregnant women across two research sites: area A (n = 21) and area B (n = 20). The mean age of participants was 26 years (Table 5). At interview, participants were on average 19 weeks pregnant and 15 (37%) said that they had stopped smoking. Differences in study recruitment procedures and referral pathways to the SSS at each site meant that all women in area A and 20% (n = 4) of women in area B had engaged with the SSS at the time of interview. Views regarding the SSS among women in area A are likely to represent those who experienced successful communication and took up SSS support. Ten of the pregnant women, five from each site, were also followed up in the postpartum period.
| Characteristic | Area A | Area B | Total |
|---|---|---|---|
| Age (years), mean (range) | 27 (18–42) | 25 (16–37) | 26 (16–42) |
| Aged < 25 years, n (%) | 7 (33) | 11 (55) | 18 (44) |
| Living in most deprived areas,a n (%) | 15 (71) | 5 (25) | 20 (49) |
| Gestation at interview (weeks), mean (range) | 19 (14–27) | 17 (12–29) | 20 (12–29) |
| Smoking at interview, n (%) | 11 (52) | 15 (75) | 26 (63) |
| Engaged with the SSS by time of interview, n (%) | 21 (100) | 4 (20) | 25 (61) |
Findings: pregnant women
A SEF-guided analysis of the interviews was undertaken (see Chapter 3, Coding and analysis). The findings of the interviews with pregnant women are presented through three of the SEF levels: individual, interpersonal and organisational. Most themes outlined acted as both barriers to and facilitators of positive behaviour change.
Postpartum interviews were analysed separately for changes in women’s perceptions since their first interview and to explore their experiences of smoking as their pregnancy progressed and after delivery.
Individual
An examination of women’s descriptions of their lives showed that many, in both research sites, lived in disadvantaged circumstances and faced a range of additional challenges associated with social disadvantage. Women described living in large households, not living with their current partner, being carers of children or parents in ill health, preparing to be single mothers, and being in financial insecurity with regard to welfare benefits and unstable jobs. Many described ongoing pregnancy and general health problems, including chronic conditions (depression, back pain, arthritis, asthma, diabetes). Smoking, a habit that was well established pre pregnancy, was described as a key part of their routines, as a break from work or family life, and as a way of coping with daily stress and boredom:
It’s just really hard, plus this wee one stresses you out sometimes and it’s like the only time I get like a 5-minute break sort of thing . . . I kind of look forward to that break.
Area A, pregnant woman 9, smoker
Most women said that they wanted to stop smoking in their pregnancy or remain abstinent after the birth. However, some, particularly in area B, said that they were satisfied with cutting down or continuing to smoke during the pregnancy. Risk perceptions and self-efficacy beliefs were key themes associated with smoking and smoking cessation.
Risk perceptions
All of the women acknowledged a potential risk to the baby from maternal smoking. However, although some gave detailed accounts of the risks, others expressed uncertainty about specific risks. Some admitted that they avoided thinking or learning about the risks, as these were unsettling:
I don’t [think of the risks] . . . I’ve tried to avoid all the stuff because I don’t really want to know. Yeah I have heard about, I think you can get breathing problems . . . and they can be small . . . but to be honest that’s about all I know . . . I’d prefer not to know.
Area B, pregnant woman 14, smoker
Although for some their assessment of risk was the primary motivating factor in wanting to stop smoking, others underplayed the risks. In a more extreme example, one woman considered any resulting health problems as ‘fixable’:
I know it is harmful from all the information that I’ve had . . . but most of it seems to be things that are fixable, and I don’t want that to sound nasty, but like having a small baby, the baby will grow, he can put on weight . . . and doctors are amazing now like . . . there’s more chance of the baby developing a cleft lip as well, that could be fixed with surgery.
Area A, pregnant woman 5, smoker
As a harm reduction strategy, some women described cutting down the number of cigarettes smoked, switching to lower-tar cigarettes and extinguishing cigarettes early. Cutting down was generally viewed as beneficial, although not as good as stopping smoking. A small number of women believed that HPs endorsed cutting down as an acceptable alternative to stopping smoking:
There is midwives that tell women ‘you know, just keep smoking. Don’t stress yourself out or the baby out . . . cut down but don’t completely stop’.
Area A, pregnant woman 18, non-smoker
Some described a desire to breastfeed as motivation for stopping smoking in pregnancy and post partum. However, women were generally uncertain of whether or not, and how, smoking could impact on breastfeeding, with an apparent lack of information given to women on this issue:
No I wouldn’t like [to continue smoking] . . . because I am going to breastfeed again . . . It wouldn’t be too good would it? I don’t know if it can go into the milk and baby is having its milk is there going to be a bad taste or, is nicotine going through my milk, I’ve no idea . . . I don’t know anything about it.
Area B, pregnant woman 19, smoker
Although there were varied views regarding the risk of smoking during pregnancy, all of the interviewees had a high sense of the risk to the baby from passive smoking post partum. Many considered this more harmful to the baby than smoking in pregnancy and described firm plans for not smoking around the baby after delivery:
I’d never smoke in the same house as my baby, I’d always go outside . . . it’s my choice me smoking when the baby is inside me, but it’s not the baby’s choice to be around the smoke.
Area B, pregnant woman 11, smoker
If you are smoking [in the car] and the children are there, yes fair enough you can open the window but you don’t actually realise how much of that is actually invisible and how much of that you know is going into the back obviously for them to breathe in, and you know you wouldn’t stick a pipe on the end of your exhaust pipe and stick that in the car because you know it’s going to harm them.
Area A, pregnant woman 10, smoker
Self-efficacy
Those who reported having stopped smoking at interview talked about having ‘focus’, resilience in the face of setbacks and triggers, ‘forcing’ themselves and having a strong desire to stop smoking for the baby and drawing on different strategies to help them. Their accounts reflected determination, confidence and willpower. In addition, some of those who quit reported less difficulty than expected to stop smoking, with several finding it ‘easy’. Pregnancy-related sickness had helped several women:
[Stopping smoking] was easier than I thought it would be, but . . . on a night when he’d go to bed that is when I’d crave it with a cup of tea and I just had to keep myself busy and go for a bath or something to take my mind off it.
Area B, pregnant woman 7, non-smoker
I found it quite easy to quit, once I had stopped being so ill, that is when my willpower kicked in.
Area A, pregnant woman 21, non-smoker
In contrast, women who were still smoking at interview spoke of the difficulty in stopping smoking, low desire or willpower to stop despite the potential harm to the baby, and half-hearted quit attempts. These accounts were characterised by self-doubt:
I knew I wasn’t going to put my mind to it . . . to try and stop smoking.
Area A, pregnant woman 2, smoker
Interpersonal
Relationships with partners
Women frequently reported that the ease with which they could stop smoking was influenced by their partner’s attitude towards smoking in pregnancy, whether or not their partner smoked and the support their partner offered:
If I’m home with my husband, he doesn’t smoke . . . so I suppose it’s not difficult at all. I don’t even think about it when I’m home, and I get on fine.
Area A, pregnant woman 14, non-smoker
I think it’s harder with you know [partner] smoking because if he goes for a cigarette then I will go with him for one.
Area B, pregnant woman 14, smoker
Most interviewees thought that their partners held negative attitudes towards smoking in pregnancy and would prefer them to stop smoking. Some women said their partners could be particularly vocal about this, often bringing up the health risks to the baby. Others felt that their partners avoided discussing smoking with them to avoid causing upset and additional stress:
He’s struggling to come to terms with me still smoking . . . He’s basically saying, you know, ‘I can’t believe you’re doing this to our unborn child’.
Area A, pregnant woman 8, smoker
Support from partners was acknowledged and appreciated; this included emotional support, such as providing encouragement and understanding, and practical support, such as not smoking around the woman, smoking outside the home, smoking less, providing lower-tar or fewer cigarettes and using distraction techniques to help with cravings. However, offering support could also draw attention to the woman’s efforts to abstain from smoking. Some women expressed frustration when partner support was lacking. Conversely, others said that they interpreted their partner’s support efforts as controlling and felt pushed into stopping smoking. In both circumstances, women described feeling demoralised:
I don’t want him to say ‘it’s OK’, you know, ‘you can just keep smoking’, but . . . the constant falling out and then it plays on my mind more through the week . . . it’s like, ‘does he even love me?’ you know ‘why is he threatening on leaving me when I’m 4 months pregnant?’. . . but that makes me want to stop less because I’m not doing it for him.
Area A, pregnant woman 8, smoker
Those with partners who smoked said that the most useful support in stopping smoking would be for their partner to stop at the same time. However, some women reported feeling that their pregnancy did not seem to motivate their partner to stop. Women reported annoyance at their partner for wanting them to stop smoking but not attempting to stop themselves:
I have to stop because I have someone growing inside of me. You [partner] think it’s all right for you because you have no-one growing inside of you. So I was kind of like envious, but annoyed with him because he didn’t seem to grasp that.
Area B, pregnant woman 5, non-smoker
Smoking was also regarded as a useful tool in maintaining a good relationship, encouraging spending time together and shared conversation. Women described how quit attempts could, therefore, negatively impact on relationships with partners because of nicotine cravings, stress, bickering, mood swings and spending less time together.
Relationships within wider social network
Many of the women interviewed described close relationships with other women who had smoked during pregnancy and felt that this influenced both their intent to stop smoking and their risk perceptions. Health problems observed in their partner’s, friends’ or family’s children that interviewees attributed to smoking in pregnancy could act as motivation for stopping smoking:
Without sounding cynical or stereotypical I find that more people that maybe smoke during the pregnancy, their children are maybe smaller, they are maybe premature, they might have slight difficulties.
Area A, pregnant woman 21, non-smoker
Conversely, many women recalled conversations with family and friends about babies born with no apparent ill-effects from maternal smoking, or health problems in babies born to those who did not smoke. These experiences were used by some women to refute the risks communicated by HPs and to make them feel better about smoking. Many described feeling a lack of external pressure to stop smoking, particularly from their mothers, who had often also smoked in pregnancy:
A few people have been quite nice about it, they’ve been like ‘oh, it doesn’t matter, I smoked all the way through mine’ and ‘I’ve got two beautiful perfectly healthy kids’. . . and ‘they smoked more than you’ that makes me feel a bit better.
Area A, pregnant woman 5, smoker
Children’s antismoking attitudes appeared to have a large influence on women’s views of smoking:
They all used to say to me ‘I don’t want you to die mum, that’s what they are doing to you, you are going to die if you smoke them’. . . it really upset me actually, my kid at 5 telling me that he doesn’t want me to die, it was heartbreaking yeah, so it’s like ‘I am stopping for you’.
Area B, pregnant woman 19, smoker
Organisational
Workplace
The workplace was reported to make quit attempts easier or more difficult depending on routines, job demands and level of stress. Some work environments were dominated by a smoking culture, in which smoking, taking breaks and socialising with colleagues were inter-related. Stopping smoking could have negative implications for all of these things:
When I’m at work I smoke a lot more, I think it’s just, it’s the only kind of break that I get sometimes . . . it gets me away from the customers when they’re annoying me.
Area A, pregnant woman 5, smoker
In work environments where employers had enacted policies or initiatives that actively discouraged smoking or promoted cessation, this could act as a facilitator of stopping:
It makes it easier because I’m doing an 8-hour shift on my own, so there’s like 9 hours where I’m not smoking.
Area A, pregnant woman 15, non-smoker
Health care
Influences on smoking in pregnancy within the health-care setting occurred through antenatal processes, protocols and relationships with HPs. As all women in area A had accessed the SSS and only four women in area B had accessed the SSS in their current pregnancy, the two locations are discussed separately when relevant.
Midwife’s role and relationship with pregnant woman
Smoking in pregnancy was reportedly raised by midwives at the booking appointment, usually around 8–12 weeks’ gestation. Interviewees described variation in the time devoted to the issue, with some feeling that discussions were rushed and included little detail about risks. Rather than offer cessation advice, the midwife’s role was perceived as one of gathering smoking status information and offering or making a referral to the SSS. Women expected smoking to be raised by their midwife and considered it part of the midwife’s job. Participants recalled that midwives would usually check whether or not the woman was smoking at subsequent appointments, although this was not always the case:
I think I tried to ask questions but she [midwife] kinda told me that she’s not a specialist . . . I did think my midwife would know – whether she’s a smoking specialist or not – she’d know what was dangerous and what wasn’t.
Area A, pregnant woman 7, smoker
Women often said that their midwife was ‘nice’ and ‘supportive’ and that they did not feel judged by them for smoking, even though they had expected to be. Participants said that midwives often reassured them about their smoking behaviour in early pregnancy or told them that they were doing well if they had cut down. Some women spoke about a mutual understanding with their midwife, particularly when there was a longer-term relationship because of previous pregnancies, in which the midwife was assumed to be aware of what the woman wanted to be told about her smoking behaviour. In addition, in area B, women more commonly described a lack of pressure in their midwife’s approach to smoking:
She said that she didn’t believe that she needed to sit and lecture me for a very long time and that I could approach the subject with her. She was very nice. And actually that was what I wanted, I didn’t want an overbearing lecture, there is enough things going on during pregnancy.
Area B, pregnant woman 9, smoker
Referral to a Stop Smoking Service
Within area A, women described a straightforward referral process, usually at the booking appointment. Once referred, women described receiving an initial telephone call from an advisor within a few days and having the first appointment within a week. Despite the opt-out pathway, some women saw referral as their choice, with their decision to engage with the SSS as voluntary. Others described being told by their midwife that they had to be referred. These perceptions had implications for how women viewed the referral, whether it was a positive start to stopping smoking or they felt forced into stopping without being ready:
I kind of felt like I was being forced into it a wee bit just because I wasn’t quite ready . . . I suppose if I hadn’t had went for it I’d have been still in the same position I was back then, so it did give me a bit of a boot.
Area A, pregnant woman 19, smoker
Although most women described being offered a referral to the SSS at booking, the referral process did not appear as smooth as in area A. Some women described waiting weeks for initial advisor contact. Some of those referred reported not receiving any SSS contact. Women said they were unlikely to chase referrals themselves; many spoke of a lack of confidence in making contact and telephone calls:
They probably did ring me and were quite reliable so I don’t really know because I’ve not heard from them in 4 or 5 months since I first was put forward . . . I don’t like talking on the phone so I very rarely ring out places . . . I wouldn’t like to ring them because I don’t really know much about it so I wouldn’t know what I was asking about.
Area B, pregnant woman 13, smoker
Reluctance to engage with the SSS sometimes appeared to be a result of a lack of knowledge about the service, such as the possibility of having home appointments, or because of a negative service image. Some women perceived attendance as causing additional stress and the possibility of being ‘lectured’ or judged by advisors. Women said they doubted that the support would be useful. Negative previous experience of SSS support in pregnancy had left some women unwilling to engage again. Others believed that they could stop smoking without SSS support:
If they could come at a time convenient that would be a lot more helpful and yeah it’s definitely something I’d be interested in doing.
Area B, pregnant woman 14, smoker
Because they are only going to sit there and say ‘this is why it’s not . . .’ I know it’s bad for you, it can cause you cancer, it makes you less healthy, what’s more to know?
Area B, pregnant woman 20, smoker
Carbon monoxide monitoring
Carbon monoxide monitoring served as a visual indicator of risk to the baby and helped women conceptualise the potential harm of smoking. In area A, where CO screening was compulsory at booking, those screened often described shock and feeling ‘bad’ or ‘embarrassed’ at seeing the result and could recall scores and indicator colours. Generally, CO testing was seen as helpful and a motivational tool, giving some insight into how smoking was directly affecting their baby:
I didn’t quite realise exactly how much CO’s going in . . . once I’d seen that . . . that’s when I tried as much as possible to stop.
Area A, pregnant woman 7, smoker
Repeatedly used, this was a tool which appeared to help women see the benefits of stopping smoking and aid encouragement, motivation and self-esteem:
It was a confidence boost, thinking ‘well that’s 2 weeks and it’s like, the nicotine, the [CO]’s out my body, what’s it going to be like at 4?’. So I go again tomorrow and I’m quite looking forward to going.
Area A, pregnant woman 12, non-smoker
Carbon monoxide screening helped some who had cut down to realise that their baby was still at risk. In addition, several women described how it had made them consider who was smoking around them and how this could impact on the baby. This was said to lead to partners or family members modifying their smoking behaviour:
When it goes up it’s horrible, but even if it only goes up a couple, my mum still smokes, so like if she is having a fag I don’t go near her any more, but she used to smoke in the house and now she doesn’t she smokes outside.
Area A, pregnant woman 17, non-smoker
Several women in area B who had not been CO screened indicated that they would be happy to be screened and would be interested in the reading, and felt that it would be a potentially helpful tool in stopping smoking:
I’d do it . . . you don’t think about how much is in one roll up or one cig[arette], you are just thinking that’s a cig, it can’t do much harm one on its own. Whereas if you are getting tested every time you go and see a midwife and say it gets higher or lower . . . then maybe you can nip it in the bud and maybe cut down or stop.
Area B, pregnant woman 6, smoker
Nicotine replacement therapy
Many interviewees commented that they had tried some form of NRT either during or outside pregnancy. Previous experiences could make women willing or unwilling to try particular types of NRT again. Perceptions of NRT were mixed but generally lozenges and chewing gum were viewed negatively. There were some positive accounts of using patches in pregnancy; some found that these were effective despite the discomfort they caused, but others discontinued their use because of skin reactions and burning and itching sensations. The weaker strength of the patches typically used in pregnancy was sometimes considered ineffective:
I swore by those, they were really good . . . you don’t even think about a fag when you are on a patch.
Area A, pregnant woman 17, non-smoker
The patches burnt, they didn’t agree with my skin . . . after a while I was taking them off which again, it doesn’t help trying to go cold turkey.
Area B, pregnant woman 10, smoker
Many, but not all, of those trying the inhalator gave positive accounts of how it had helped them to cut down or stop smoking. Some reported its usefulness in keeping hands occupied and continuing the hand-to-mouth action:
Definitely found it useful . . . I had a difficult call today . . . and I thought ‘oh no’, and I took a couple of draws and it just told my brain ‘all right, you’re feeling better now, you can get on with the job’, so that’s what I did . . . it’s like my security blanket.
Area A, pregnant woman 12, non-smoker
There was some concern over the safety of using NRT while pregnant, and several women said that they had sought clarification on this from HPs. Some of those who had stopped smoking felt that, although it was not ideal to be absorbing nicotine in pregnancy, it was much less harmful than smoking:
I made doubly sure. I was like ‘they are safe?’ and she goes, ‘I wouldn’t be prescribing them to you if they weren’t safe in pregnancy’.
Area B, pregnant woman 16, smoker
I think even [NRT] is bad because of the nicotine, but I think because the [CO] is worse, it is better to use that until you can actually do without anything.
Area A, pregnant woman 17, non-smoker
Cost was raised as a barrier to using NRT by several women in area B, suggesting that they were unaware of their entitlement to NRT free on prescription. In area A, women were more likely to speak of the advantage of getting NRT free on prescription.
Stop Smoking Services
For those who engaged with SSSs, perceptions on how helpful they found it were mixed. Overall, positive comments centred on the delivery of support, information and relationship with the cessation advisor. Negative responses generally focused on the inconvenience of attending appointments, unhelpful information and perceived pressure from the cessation advisor.
Offering flexibility so that women could choose their preferred support method appeared key to their engagement. Women saw lifestyle factors, such as work and child-care commitments, finances, lack of transport and health problems, as affecting their ability to engage and attend appointments. Home appointments were often said to be most convenient, offering privacy and comfort. However, prompt access to support through telephone calls and being able to change the level and delivery of support were also appreciated:
I know it sounds really horrible but I have been at work all day . . . I’ve just come home and you know it sounds really lazy and really bad but people are like that, I am like that . . . it’s more convenient for people to come and talk to you.
Area B, pregnant woman 5, non-smoker
Although there was criticism that attending meetings was inconvenient, most women felt that the one-to-one support they received, through a combination of face-to-face meetings, telephone calls and texts, was suitable, and they described being satisfied with the frequency of contact. Women generally presented negative views of group support, with many saying that they would be uncomfortable, shy or nervous in a group. Group sessions were seen as inflexible and inconvenient. Several women said that they would not engage with a SSS if only group support was offered:
I don’t think I’d ever go to the first meeting if it was a group one because I wouldn’t know what to expect and I would be a bit intimidated. I suffer quite a lot from anxiety.
Area B, pregnant woman 14, smoker
Women appeared most satisfied with cessation support when their advisor had provided practical advice such as new strategies for dealing with cravings or answering queries about NRT. However, some women said that they were not given any information that they did not already know, and at times the advice given by their cessation advisor could contradict that given by other HPs:
We talked about the things to stop me from smoking as well . . . like what to do instead of being in my routine, like maybe listening to music when I walk up to [partner’s house] . . . yeah it seemed helpful.
Area A, pregnant woman 4, smoker
The midwife tells you something completely different as to what the smoking woman tells me.
Area A, pregnant woman 15, non-smoker
There was a mixed response to the delivery of risk information by cessation advisors. Some women said that this information helped them better understand the risks and motivated them to stop smoking, although others said that they felt they were being ‘lectured’. Despite the delivery of risk information, some women reported that they were still uncertain of the harm because of the stories they were exposed to in their social networks.
Most of those who engaged with a SSS described their advisor as ‘friendly’, ‘lovely’ and ‘nice’, and women found the advisors encouraging, positive, interested, non-judgemental and reassuring after slip-ups. These viewpoints often contrasted with their stated prior expectations of the service. Continuity with one advisor was said to help foster positive relationships, and text messages and telephone calls were seen as useful to maintain the relationship and remind them of the advisor’s support. Women often spoke of advisors being quick to respond to calls or texts, flexible with appointments and inclusive of their families. Many women saw their advisor as being instrumental in their motivation to stop smoking:
So even just that wee text asking ‘did I get my prescription, is everything OK?’. It was good. It made me feel good about myself.
Area A, pregnant woman 5, smoker
She has been brilliant really . . . just knowing that I’ve got someone there to talk to. I had that momentum to keep going knowing that I had that kind of network with somebody.
Area B, pregnant woman 3, non-smoker
The advisor’s own smoking background seemed important to women. Ex-smokers were thought to have more empathy and understanding. This could help build rapport and respect. Negative accounts of the relationship often focused on the advisor’s approach, such as being ‘talked down to’ and the perception of pressure:
I did try, but the woman that they gave me, in one aspect she got on my nerves a bit because she would talk down at me because she had never been a smoker . . . I’d rather have someone that has smoked before, that has ripped their husband’s head off before while trying to stop than somebody who hasn’t.
Area B, pregnant woman 6, smoker
Findings: postpartum women
Ten interviewees were followed up 5–12 weeks after delivery to explore both their experiences as the pregnancy progressed and in the postpartum period, and if and how their perceptions had changed since their first interview. At follow-up interview, four women said that they were currently smoking; three of these reported smoking throughout their pregnancy and one, although abstaining from smoking for several weeks, had started again before the birth. The remaining six women reported as non-smokers, each having stopped smoking during pregnancy.
There was little change in interviewees’ perceptions and experiences of smoking between interviews. Similar barriers to and facilitators of smoking cessation in pregnancy at each level of the SEF, outlined in Findings: pregnant women, existed as the pregnancy progressed and during the postpartum period. However, the discussions at follow-up showed the increased importance of some of the themes at the individual, interpersonal and organisational levels.
Individual
Women reporting as non-smokers generally described finding it easy to stop smoking and remain abstinent. Some stated that protecting their baby from passive smoking had become a motivating factor for them after delivery. Others described how being able to purchase items for the baby using money saved from stopping smoking helped to keep them motivated. Several of these women said that they had not considered smoking because their lives were busy or stressful looking after a new baby. Others acknowledged that they had experienced a desire to smoke on occasion, usually at social events, but they had managed to resist:
I don’t have time [to smoke]. After the cleaning and looking after [baby] . . . I haven’t even thought about having a cigarette.
Area B, postpartum woman 3, non-smoker
When you are with other people that do [smoke], like at the wedding, everybody kept disappearing out for a cigarette and you are sitting there like that . . . and I think ‘why would you want to when you could think about what you could buy?’. Sometimes just going looking for something to focus on to buy him can be enough for me to think ‘well I can get him that if I don’t have them’.
Area A, postpartum woman 3, non-smoker
For the women who said that they had smoked throughout their pregnancy, refuting the risks of maternal smoking was a recurring theme. For example, one drew on her own children’s health as evidence of exaggeration of the risks. Another said that she found reassurance by receiving positive news from growth scans, relaxing her attitude towards smoking in pregnancy:
There is no proof I’d say because that’s me had two and they are both healthy, they have both been good weights, none of them were early and they’ve never had any problems.
Area A, postpartum woman 1, smoker
The motivation to quit was more at the start, and then as things progressed, it’s hard to explain, it was kind of like nothing had gone wrong; everything is fine, so what’s the point in torturing myself . . . it wasn’t ‘this baby is coming, I’ve got to stop’, it was kind of like ‘things are OK, I can get away with . . .’.
Area A, postpartum woman 2, smoker
All interviewees at follow-up were concerned about the effects of passive smoking on the baby and the baby’s exposure to toxins. Those who reported smoking described trying to minimise any risks by smoking outside the home, putting coats over their clothes or changing clothes, spraying toiletries, washing their hands and faces and using antibacterial gel:
We make sure that the living room door and the kitchen door are shut, but you can still you know put him in his cot, make sure he is safe and then we go out.
Area B, postpartum woman 5, smoker
I know when you are pregnant it goes into your blood seemingly, but when the baby is here, it’s a whole different . . . it seems worse to me . . . it seems to linger more, like on clothes and things like that . . . I wear a dressing gown when I am outside . . . wash my hands, use antibacterial . . . getting rid of as many toxins as we can.
Area A, postpartum woman 2, smoker
Interpersonal
The majority of interviewees described trying to influence some elements of the interpersonal environment. When visitors came to their homes it was usual for smokers to smoke outside. There appeared to be an implicit understanding that this is what people would do; several women mentioned that they had not needed to ask. Most women reported that when they visited friends or family members who were smokers these people usually went outside to smoke, either because this was where they usually smoked or because they had modified their behaviour because of the baby’s presence. In addition, a number of women said that should they ever be visiting people who continued to smoke inside with the baby present, they would leave:
Everyone smokes outside. That’s the rule . . . nobody’s ever asked . . . it’s just automatic that they go straight out.
Area B, postpartum woman 4, non-smoker
I say that to [partner] if we ever go to my mother’s and any of them are smoking we will just leave . . . We go to [visit sister-in-law] . . . she normally smokes in her kitchen, but she’s been going out the back since we’ve had the baby.
Area A, postpartum woman 3, smoker
The influence of partners came to the fore at follow-up. All of the women reporting as non-smokers said that their partners were also non-smokers, either because they had stopped smoking during the pregnancy or because they were former or never-smokers. The women whose partners had stopped smoking during pregnancy acknowledged that this was their main facilitator of success:
I would have struggled to stop [smoking if partner hadn’t stopped] because obviously I spend every minute of my life with him when he is not at work.
Area B, postpartum woman 3, non-smoker
[Partner] has helped me . . . when he quit as well I thought ‘oh well I definitely couldn’t go back to it because if I went back how much of a failure would I be when he smoked a lot more than me and he has really struggled to do it’.
Area A, postpartum woman 3, non-smoker
All but one of the women who said that they were smoking at postpartum interview had partners who also smoked. Their influence on the woman’s smoking was also shown:
I know for a fact [partner] will be a smoker for life . . . him still smoking is going to make it harder for me to quit one day.
Area A, postpartum woman 4, smoker
Organisational
Interviewees recalled little smoking-related discussion with HPs in the postpartum period. Some described being asked their smoking status by a midwife or a health visitor but then offered little support or encouragement to stop smoking if they said that they were smokers. Two of the women reporting as non-smokers said that they would have appreciated support after delivery to help them remain abstinent:
They sort of asked me if I was still smoking, that’s all they said to me. I think to be fair the midwives . . . they are busy.
Area B, postpartum woman 5, smoker
Maybe there should be a little note saying that they stopped smoking . . . like the health visitor never asked me if I needed patches or never asked me if I’d tried the chewing gum or like even just for someone to say, ‘listen if you need help, if you feel like that come to me’. . . it’s an ongoing thing, it’s always going to be there.
Area A, postpartum woman 5, non-smoker
Of the women who had accessed stop smoking support, those who said that they were smoking at follow-up generally reported more negative perceptions than those who stopped smoking during pregnancy. Three of those who reported smoking had engaged with a cessation advisor during pregnancy. After initial contact and meetings with an advisor, these women described subsequently avoiding the advisor’s telephone calls because they lacked motivation to stop smoking and, in one instance, were concerned over CO screening after relapsing. Two women said that, in hindsight, it would have been beneficial for them to maintain contact through face-to-face meetings, considered more helpful than telephone calls:
I do believe that if I had kept seeing her it might have given me that encouragement.
Area A, postpartum woman 4, smoker
She said ‘do you want to meet up again or do you want me to just phone you?’. And I think if I’d said to meet up again things might have . . . because you are face to face, whereas the phone calls were just ‘oh here we go’.
Area A, postpartum woman 2, smoker
Four of the women reporting as non-smokers had accessed the SSS. These women generally described positive experiences of the support, primarily because of the advisor–woman relationship but also because of NRT provision and CO screening. They felt that they could call on their advisor for support at any time, even after delivery, although nobody had done this:
She sent me a letter and said that if I am ever at that thinking point I’ve just to give her a call . . . she will help me through it whether that’s talking or offering some kind of help. I know that I could always call her.
Area A, postpartum woman 5, non-smoker
Discussion
Smoking and smoking cessation
Analysis of the qualitative interviews indicated that many different factors within women’s lives interacted to influence their smoking behaviour either positively or negatively. A SEF was used to unpick these factors into different levels of women’s environments: individual, interpersonal and organisational.
Overall, women’s perceptions and experiences were mixed, demonstrating that individual factors can act as barriers to or facilitators of smoking cessation depending on the context of women’s lives. However, there appeared a predominance of barriers at the individual level. Challenges related to a high incidence of disadvantaged circumstances and lack of self-belief in the ability to stop smoking made smoking cessation difficult for some women. Although all women acknowledged some potential harm from maternal smoking, risk perceptions were varied, with some women expressing uncertainty on this issue.
Women’s beliefs about smoking in pregnancy were greatly influenced by close relationships with family and friends at the interpersonal level. The accounts of women suggested that risk messages from their social networks often prevailed over information delivered by HPs, which women reported was received some way into the pregnancy (usually at booking, at around 8–12 weeks’ gestation) and described as inconsistent. Other women’s stories relating to smoking in pregnancy were often used to refute the risks of smoking. Among some women, however, these could also be used as motivation to stop smoking. It appeared women looked for, and received, reassurance that their choices around smoking were acceptable, especially from family and friends, but also from HPs, midwives in particular.
Women’s accounts also suggested that at the interpersonal level partners could significantly influence their smoking behaviour. Women described a high occurrence of partner support – emotional and practical. However, although this was generally appreciated, a partner’s smoking behaviour appeared to have a greater influence in facilitating smoking cessation or making it difficult for women to stop.
Within the organisational level women described how workplace routines, demands and relationships could make it easier or more challenging for them to stop smoking. Negative attitudes, expressed or perceived, from all those around them could lead to a defiant attitude in some women with regard to their smoking.
For the 10 women interviewed post partum, there was little change in their perceptions of the factors identified at the different levels of the SEF. However, the importance of some themes was shown at follow-up. There appeared to be a difference between those who accessed and kept attending stop smoking support and those who did not. Among those who stopped attending, there was a view that if they had maintained face-to-face contact with their advisor, this might have helped them to quit. In addition, post partum, the difference between the perceptions of risk from maternal smoking and the perceptions of risk from passive smoking came to the fore. Although risk perceptions of smoking in pregnancy were mixed, in the postpartum period all women were extremely concerned about their baby’s exposure to passive smoke and had detailed plans in place for minimising this. At follow-up, women described how the influence of their partner’s smoking status was crucial to their success or otherwise in stopping smoking and remaining abstinent. In the postpartum period, women also described an apparent lack of smoking-related discussion, advice and support by HPs.
Improvements to existing services/interventions
Factors emerging from the health-care setting were mostly helpful to women. Engagement with SSSs was key to women accessing support, although some described being discouraged by a negative service image. In this regard an opt-out referral pathway best facilitated women’s engagement. Although perceptions of SSSs were mixed, they did contribute to many women being successful in stopping smoking, although the study recruitment procedures likely influenced this finding. Women often described a positive relationship with their cessation advisor. This was a key feature in the continuity of stop smoking support and providing women with detailed information and advice. Women especially liked being offered flexibility in service delivery, home appointments and one-to-one support. There were mixed perceptions surrounding the use of NRT in pregnancy but some described successfully quitting using patches and the inhalator. CO screening was a powerful motivational tool for many women.
Chapter 7 Findings of systematic review of significant others’ perspectives and experiences of the barriers to and facilitators of smoking cessation
This systematic review has been published in BMC Public Health. Here we present the abstract of the paper. This abstract has been reproduced from the abstract © Flemming et al. 58 under the terms of the Creative Commons Licence 4.0 (CC BY) (https://creativecommons.org/licenses/by/4.0/).
Background
Smoking in pregnancy can cause substantial harm and, although many women quit, others continue to smoke throughout pregnancy. The role of partners is an important but relatively under-researched factor in relation to women’s smoking in pregnancy; partner’s smoking status and attitudes to smoking cessation are important influences in a pregnant women’s attempt to quit. Further understanding of how partners perceive the barriers to and facilitators of smoking cessation in pregnancy is needed, particularly from qualitative studies in which participants describe these issues in their own words.
Methods
A synthesis of qualitative research of partners’ views of smoking in pregnancy and post partum was conducted using meta-ethnography. Searches were undertaken from 1990 to January 2014 using terms for partner/household, pregnancy, post partum, smoking and qualitative in seven electronic databases. The review was reported in accordance with the ENTREQ statement. 87
Results
Nine studies reported in 14 papers were included,53,110,121,134,152–161 detailing the experience of 158 partners; the majority were interviewed during the postpartum period. Partners were all male, with a single exception. Socioeconomic measures indicated that most participants were socially disadvantaged. The synthesis identified recurring smoking-related perceptions and experiences that hindered (barriers) and encouraged (facilitators) partners to consider quitting during the woman’s pregnancy and into the postpartum period. These were represented in five lines of argument relating to smoking being an integral part of everyday life, becoming and being a father, the couple’s relationship, perceptions of the risks of smoking, and their harm reduction and quitting strategies.
Conclusions
The cluster of identified barriers to and facilitators of quitting offers pointers for policy and practice. The workplace emerges as an important space for and influence on partners’ smoking habits, suggesting alternative cessation intervention locations for future parents. Conversely, health and community settings are seen to offer little support to fathers. Interventions centred on valued personal traits, like willpower and autonomy, may have particular salience. The review points, too, to the potential for health information that directly addresses perceived weaknesses in official advice, for example around causal mechanisms and effects, and around the contrary evidence of healthy babies born to smokers.
Chapter 8 Findings from qualitative study of significant others’ perspectives and experiences of the barriers to and facilitators of smoking cessation in pregnancy
This chapter presents the findings from the interviews undertaken with pregnant women’s SOs to elicit their views of the barriers to and facilitators of smoking cessation in pregnancy and on existing services and interventions to support cessation.
Participant sample
Thirty-two interviews were conducted with SOs across the two sites: 20 in area A and 12 in area B. The majority of SOs were partners of pregnant women, but the sample also included three friends of pregnant women (two associated with the same woman), three mothers and one mother-in-law.
Findings
The findings from the qualitative study of SOs’ perspectives and experiences of the barriers to and facilitators of smoking cessation are presented across two of the SEF levels: interpersonal and organisational.
Interpersonal
At the interpersonal level, barriers and facilitators were identified in SOs’ own smoking behaviour, attitudes to smoking in pregnancy, relationships with pregnant women and the ways in which they attempted to support the pregnant women’s quit attempts. The influence of others within women’s wider social network was also shown. Mention of pregnant women’s physical environment, with specific regard to the smoking behaviour of others, is incorporated into discussion of interviews with reference to both interviewees and members of wider social networks.
Significant others
Smoking behaviour
About two-thirds of SOs were current, regular or habitual smokers (n = 20), although almost one-third were former smokers and some were using NRT or e-cigarettes to maintain a relatively recent quit. Four interviewees had never smoked or had only experimented with smoking in their youth. Interviewees typically smoked between 10 and 20 cigarettes per day and described having their first cigarette within minutes of waking (including former smokers prior to quitting). Manufactured cigarettes were most commonly smoked, with only a very small group using hand-rolled tobacco.
Smoking tended to be associated with individuals’ daily routines, such as after a meal, although interviewees also spoke of certain triggers for smoking such as socialising, stressful situations and inactivity (boredom). Most had started smoking in their early teens or before, which was generally perceived to be a result of peer influence and/or pressure. SOs who smoked often commented that they did not like smoking and would like to quit:
It’s a horrible habit, but, I don’t like it but it’s just something I’ve got so used to doing and it’s just like, well, I don’t need to but I want to, it’s mind over matter to be fair.
Area A, partner 44, smoker
Previous attempts to quit were frequently reported by SOs who smoked, with some reporting multiple attempts and the use of support aids, usually ‘patches’, to assist their attempts. Previous smoking abstinence following a quit ranged from, most commonly, a few days to months and occasionally years. Interviewees recognised significant benefits from quitting in relation to their own health, financial savings and improvements to the condition of their home environment, for example smell.
Regarding the current pregnancy, many described themselves as in the process of trying to stop and/or cutting down or having changed where they smoked, such as outside the home. Few reported having stopped altogether at the time of interview. Motivation for changes, including recent quit attempts, largely focused on a desire to help the pregnant woman stop smoking and/or to avoid exposing the baby to second-hand smoke (SHS) after birth but, interestingly, not on exposing the woman to SHS during pregnancy. Some of those who continued to smoke expressed an intention to stop by the time the baby was born:
I want to try again before the baby is here as well. I don’t want the baby smelling it off me and things eh, it’s not very nice.
Area A, mother 20, smoker
Although SOs made use of support aids to help them in their most recent quit attempt, some preferred to quit alone without any support:
I do have quite good willpower because when I went to stop I was going to try other things because I stopped previously, but in the end I thought well if I am going to do it I am just going to do it. Just get rid of it, I don’t want to be on anything else that costs more money; I am going to save the money, help my health so I just kicked it altogether.
Area B, partner 6, former smoker
Importance of smoking to relationship
The importance of smoking to relationships between SOs and pregnant women was not always stated overtly or apparently appreciated, but it was sometimes implicit in the way in which respondents spoke about smoking together:
A lot of the time we will have a cigarette together, say after tea [evening meal] we will go through and have a cup of tea and a fag and things like that. But as I say [pregnant woman] smokes more often than me. It’s now and again we will have cigarettes together but we don’t see it as a social aspect at all.
Area A, partner 53, smoker
Some characterised its importance to relationships in factual terms, for example as being part of a shared habit in which smoking could prompt the other’s decision to light up and in the joint concern of having sufficient cigarettes:
It was a part of the relationship because you would buy cigarettes for each other or you would, I would get a text saying get cigarettes on the way home, so yeah. And we both got into the habit of smoking in our flat as well which is quite a bad thing.
Area A, partner 51, former smoker using e-cigarette
Others appeared to relate to smoking in more emotional terms as an important part of spending time together and a means of communicating:
I think you talk a lot more when you are out having a cig[arette], so I think it’s good for communicating because you are both obviously smoking at the same time, so oh now I remember, before if you were just sat watching TV [television] or doing something else then it might not go through your head to remind each other what you have to do or everything you’ve got to tell them that happened during the day.
Area B, partner 2, former smoker
However, another group attached very little significance to smoking as part of their relationship, particularly in contexts in which smoking was not generally a shared activity:
. . . everybody in the house works different shifts and things, so I wouldn’t say it [smoking together] was something that we done, no.
Area A, mother 20, smoker
Attitudes towards smoking in pregnancy
Attitudes towards smoking in pregnancy were generally negative. Although levels of knowledge among SOs varied, most accepted that smoking during pregnancy was not good for the baby, linking it to, for example, lower birthweight and miscarriage:
Obviously the dangers are there, they are very real and they can be quite serious [smoking when pregnant].
Area B, partner 6, former smoker
Consequently, SOs of women who continued to smoke during their pregnancy tended to indicate a preference for the women to stop, whereas those associated with women who had quit said that they would have been unhappy had the women continued to smoke:
. . . if I could ask her to stop and she would stop I would be happy. I would probably prefer it if she didn’t.
Area A, partner 53, smoker
A minority of SOs, however, particularly those who continued to smoke, played down the health risks, suggesting that the effects were exaggerated, in many cases citing instances of healthy babies born to mothers who had smoked during pregnancy:
I don’t believe it is a bad thing [smoking during pregnancy], my parents smoked all the way through when I was . . . and [pregnant woman’s] mum, my other daughter, her mum smoked all the way through pregnancy . . . pretty much all the family smoked all the way through pregnancy, so it’s not something that I am totally against because it’s not harmed any of the kids up to now.
Area B, partner 5, smoker
Although most of those interviewed showed disapproval of smoking in pregnancy, for various reasons, this did not necessarily translate into SOs providing strong encouragement to, or putting pressure on, pregnant women to quit. Some interviewees mentioned sensitivities around raising smoking in pregnancy despite their fears about the possible risks. A key concern for some of those SOs who continued to smoke was the possible accusation of hypocrisy:
I feel like a hypocrite but it’s my grandchild you know, and, oh it’s crazy, but I wouldn’t have been happy with her [smoking] but I think it would have been in the back of my mind, that’s wrong, that’s wrong, but you cannae [cannot] help the way you think.
Area A, mother 20, smoker
There was also strong sympathy with the difficulties of giving up, particularly when smoking was considered important to coping with stress:
I really wish she wouldn’t, but she is really struggling to give up if you know what I mean. I know it’s damaging to the baby and stuff but I understand my wife, it’s really tough for her, especially with all the worry she is going through because we had a difficult pregnancy last time and then with the stillborn as well. I know it’s hard for her to give up but I really would like her to. It’s just one of those things you can’t get around.
Area A, partner 47, former smoker
Significant others were also concerned that raising the issue of smoking with pregnant women risked conflict, with some highlighting significant tension within relationships:
There’s no telling [pregnant woman] what to do . . . I mean if she wants to have a fag, she’ll have a fag . . . I’m just not going there, no.
Area A, partner 31, smoker
In addition, others appeared to adopt a passive, uncommitted stance to the pregnant women’s smoking, suggesting that stopping smoking was a personal decision for the woman:
Obviously health-wise for her and the baby and obviously having children as well, having other children it would be a good thing for them not to see and not to be around. But again if she wants to continue that is entirely her personal choice I think.
Area B, partner 6, former smoker
Nevertheless, there were some examples of SOs, mainly partners, who were actively encouraging pregnant women to quit or modify their smoking:
If I think she has already had sort of too many for a day or something or she is smoking too close together I will say to her ‘can’t you wait?’ sort of thing. She has cut down a lot. But I still think she is smoking too much.
Area A, partner 47, former smoker
Support for pregnant women
When pregnant women were attempting to quit smoking, most SOs appeared to recognise and acknowledge a need to be supportive. However, interviewee responses to providing support could vary. A common response was to try to avoid smoking in front of the pregnant woman so as not to provide temptation or make quitting more difficult:
. . . but it’s mostly, like I would just sneak out, like if she’s went in the shower I would just nip out quickly for a fag, or if she’s, well if she falls asleep I’ll go out for a fag and then in the morning like if she’s still sleeping after I’ve like had something to eat and that I’ll just go out for a quick fag.
Area A, partner 44, smoker
As in the previous quotation, often SOs attempted to support pregnant women by smoking outside the home, at open windows or in a specific room (usually the kitchen), and were also supportive of or applied these restrictions with regard to visitors. In some cases restrictions on smoking in the home were longstanding, which was often because of the presence of other children and their possible exposure to SHS. Few commented on smoking in cars, but those who did said that, similarly, they would avoid smoking there. Some were more directive in their efforts to support a quit attempt, for example, discouraging the purchase of, or withholding cigarettes:
Just basically told her to stop buying fags and that, and like, if she’s like, ‘I need a fag’, it would be, ‘Well no, you’re not having a fag, have a lozenge, you know, just take your mind off it, go for a shower or something so you’ve not got the temptation to go for a fag’. . .
Area A, partner 44, smoker
Others, particularly non-smokers, said that they provided positive encouragement or attempted to divert the pregnant woman’s attention by offering her alternatives to smoking:
I support her and we try to you know help her as much as we possibly can . . . just really to be encouraging and just to praise her you know and just be supportive and offer alternatives to the one, you know, if she gets stressed you know say, I don’t know let me give you a back massage or something like this you know just to, or just sit down and take deep breaths or whatever you know and just calm down really.
Area B, mother 8, non-smoker
A small group of SOs, especially partners, attempted to support the pregnant woman by deciding to quit smoking themselves, with some simultaneously receiving support from SSSs. SOs often recognised that by continuing to smoke they risked making it more difficult for the pregnant woman to quit:
This isn’t my first time I’ve tried it, I’ve tried so many times, this time my motivation was that if [pregnant woman] had to quit smoking then it wasn’t fair if I still smoked. And I was never going to smoke in her presence anyway, so it was a case of us stopping smoking at the same sort of time . . .
Area A, partner 51, former smoker using e-cigarette
Quitting together was also perceived to be beneficial in terms of providing mutual support:
. . . when both of us are maybe feeling a wee bit actual stressed or whatever we just actually try to talk about it, so just trying to find other ways to actually relieve that, and I think that’s probably the best bet, if you’re having a bad day, it’s probably best to talk about it rather that you just sitting there and just actually letting it build up and build up and think stuff it, I’m just actually going to have a cigarette . . . I think it’s the right time for both of us. If I didn’t have the support of [pregnant woman] I probably wouldn’t continue.
Area A, partner 24, former smoker using NRT
Although some interviewees jointly agreed to stop smoking, there were instances in which commitment to stopping within couples was mismatched, with one taking the lead over the other. Interestingly, this context could have different consequences, depending on the individuals involved. There was some indication that the absence of one’s smoking could encourage and support the other to quit, but also that a lack of commitment in one could undermine an initially successful quit in the other.
I think I went 3, just over 3 months without a cigarette at all . . . As I say I did it for a couple of months and then she just went, not that she wasn’t interested in giving up, but like I say I think you have to really got to want to, I don’t think she was that bothered about giving up so there is no, I suppose there is no point in me giving up because the point for me to give up to start with was for her benefit and she, if she didn’t want to give up smoking then I might as well start smoking again. So that’s probably 40 per cent, 50 per cent of the reason why I started again.
Area B, partner 3, smoker
In contrast, there were SOs whose approach to support was determined by the attitude of the pregnant woman, which could mean taking the woman’s decision to smoke as a cue that they could do so as well:
I’ll do anything I can to ensure the baby is healthy or happy or whatever as well as she would. So if she wanted to quit of course I would go along with her and support her. And if she wanted me to quit at the same time I would.
Area B, partner 11, smoker
Others, however, said that they would not be prepared to stop smoking in order to support their partner, or in the following case, their daughter:
. . . if she was to say to me now, ‘mum I really don’t want to smoke these two or three cigarettes will you stop with me?’, I’d be like ‘No, no’. But I would support her, I wouldn’t smoke around her you know, if she needed to let off steam she could let off steam. She could do whatever. But I would make it clear to her; ‘You don’t want to smoke that’s fine. I do. It’s my choice, it’s my body’. But she wouldn’t, she wouldn’t go against that either, she’d be like ‘Well, that’s up to you’.
Area B, mother 12, smoker
Wider social network
For many SOs, smoking was commonplace within their wider group, with almost everyone or a substantial proportion described as smokers:
Most . . . everyone apart from [pregnant woman’s brother] . . . apart from her brother because like my sister, her boyfriend smokes, my mum smokes, my niece and my nephew smokes in the house, I think a lot of people we know smoke, it seems to be the majority I know are smokers.
Area A, partner 53, smoker
Significant others recognised that smoking prevalence among the pregnant woman’s social circle could undermine quitting, although this was not true in all cases, as illustrated in the following quotation:
All her friends do [smoke] . . . And [pregnant woman’s father] smokes, her dad smokes . . . [But] it doesn’t affect her at all, do you know what, I look at her sometimes and I think how have you got so much willpower?
Area A, mother 12, smoker
In addition, there was a high level of awareness of other family members’ and friends’ quit attempts, including failed quits:
Her mother has tried stopping smoking before, and she is actually very religious and it’s part of her religion is that she shouldn’t be smoking. But no matter and honestly she is so devout she will not even touch bacon, but again trying to get her off the cigarettes it’s just, she just cannae [cannot] do it . . . Her sister has tried to stop smoking before and been successful but she is always going back . . .
Area A, partner 48, smoker
Significant others indicated that stopping smoking in pregnancy was generally preferred among members of the pregnant woman’s wider social network. However, reports of support for pregnant women among wider social networks with regard to quitting were mixed. Positive reports showed family members expressing approval of a decision to quit or cut down, and in some cases providing support aids (i.e. e-cigarettes):
My mum and dad have tried to support her, my dad when he was on the internet bought these things like e-cigarettes and stuff for her . . .
Area A, partner 47, former smoker
There were also reports of other family members encouraging partners of the pregnant woman to stop if they continued to smoke:
. . . then my mum found out, mum was kinda a bit iffy, you know, ‘Oh yes, you should quit’ you know, ‘You’re pregnant and that’, and then now that we’ve, you know, gradually cut down and that she’s not that (thingy) now you know, she’s still on to me, she’s not on at, about [pregnant woman]’s smoking, because [pregnant woman]’s basically quit . . .
Area A, partner 44, smoker
Furthermore, a common supportive response was to avoid smoking in front of the pregnant woman, and this could also be the case in others’ homes:
They have all, they are all really happy with her that she has stopped. They are all really chuffed for her. They have all been a great support, they have all been going out, not smoking around her as much, trying, if they want a cigarette they will actually leave their own house so it’s not like affecting her, so they have been good that way yes.
Area A, partner 52, smoker
In contrast, interviewees also felt that others’ responses to supporting the pregnant woman could be limited. SOs suggested that others may be supportive of a pregnant woman’s attempts to quit but not necessarily be willing to change their own behaviour. In particular, interviewees noted that some would continue to smoke in front of the pregnant woman in their own homes:
When we are at her mum’s house, her mum and her sister stay in the same house, and whenever we are there like I say we will go in the kitchen, but even if [pregnant woman] is not smoking another one of them will be smoking, so the kitchen is pretty smoke filled. So there is no kind of escaping it when you are in there.
Area A, partner 48, smoker
In addition, some SOs described friends and family as remaining relatively neutral or guarded, perhaps regarding the issue as sensitive and possibly offering support only when requested or when the mother-to-be had expressed a wish to stop:
To be honest I think [family would help] only if the pregnant woman was trying to stop, or had stopped.
Area A, partner 53, smoker
Organisational
At the organisational level, SOs identified barriers to and facilitators of smoking cessation for pregnant women in their contacts with statutory health-care services, encompassing initial discussion of smoking in pregnancy with HPs; the nature of the cessation support provided; CO monitoring; and the use of NRT.
Statutory smoking cessation support and services
Interviewees’ knowledge and understanding of the SSSs accessed by pregnant women, including referral, varied. Some knew little of the support women had received, whereas others, usually those who had attended appointments with HPs alongside the woman, could provide greater detail.
According to SOs, most referrals to stop smoking support for associated pregnant women were made by a midwife. Interviewees reported examples of midwives and GPs helping pregnant women to stop smoking, but accounts of cessation support provided by smoking cessation advisors were most common.
Prior to the current pregnancy, most SOs were aware of the availability of SSSs but knowledge of specialist services for pregnant women was more limited.
Health-care professionals raising the issue of smoking (brief advice)
Generally, most SOs were aware of HPs raising the issue of smoking in pregnancy because they had simultaneously attended health-care appointments with the pregnant woman (usually a midwife appointment). Most commonly, SOs reported one instance of smoking in pregnancy being raised by a midwife.
Significant others reported variation in the way that midwives had raised smoking in pregnancy with pregnant women. Although some had approached the issue directly and emphasised the importance of stopping smoking, other midwives had seemingly taken a more holistic approach:
So [pregnant woman] came out and she [midwife] was like right OK, have your cigarette, calm down, but she didn’t say to her you shouldn’t be doing that you know she took it from [pregnant woman]’s point of view as well and like just talked to her really. It’s like when you’ve had your cigarette just come back in you know and we will have a chat.
Area B, mother 12, smoker
Views on the approach taken by midwives to smoking varied among SOs. Some were unhappy with a candid approach that provided some pressure to stop, whereas others felt that this approach was most likely to be effective:
Yes, no beating around the bush, straight hard facts that’s what you need. I mean even if it shocks you the way she is saying it, it is going to sink in.
Area B, partner 7, non-smoker
Partners who witnessed discussions between the pregnant woman and HPs regarding smoking in pregnancy noted that the focus was on the woman’s behaviour. This was of little consequence to most but some felt that more attention could be paid to their role in supporting the woman, particularly in terms of information:
. . . when [pregnant woman] went to see the midwife it was the smoking cessation, all the leaflets were kind of aimed at [pregnant woman] but no, to let me know how I could support her, as much as I can: oh you are doing absolutely fantastic and that. What else could I do to support?
Area A, partner 50, non-smoker
Significant others were in general agreement about the appropriateness of HPs, particularly GPs and midwives, raising smoking in pregnancy with pregnant women because of those professionals’ roles in looking after the health of the pregnant woman and her baby:
Yes, because they’re [GP] there to keep the baby healthy as well as the mum.
Area A, friend 44 female, smoker
Brief advice was perceived to be helpful because it meant that information could be passed on about the associated risks and benefits of stopping. There was a sense, however, that brief advice from a HP would be insufficient to support a quit attempt:
I think it’s good because they get to understand and they get told it’s harmful and what you can do, but I don’t think that in itself is helpful in expecting to stop the smoking. It’s good to understand what it’s doing but it’s not good to help it stop because it’s nothing to help you stop.
Area A, friend 44 male, smoker
Similarly, some questioned whether or not midwives and GPs had sufficient specialist knowledge and skill as well as professional interest to raise smoking in pregnancy with pregnant women:
I don’t think it’s really the midwife’s position to talk more about it, unless she knows what’s she’s talking about it – like professionally knows what’s she’s talking about. Like to say, ‘Oh there’s somebody here that can help you with it’, and go into more detail, I think that’s what the midwife should really say as well.
Area A, partner 16, smoker
Stop smoking advice and support
Carbon monoxide monitoring
Significant others described witnessing and also undergoing CO monitoring while they attended midwifery (usually the booking appointment) and/or smoking cessation advisor appointments with pregnant women. Often interviewees noted that the pregnant woman had been shocked by the level of CO in her system. Such reactions were further intensified in situations when the HP demonstrated the CO levels of the fetus:
I think the last time [pregnant woman] blew into it she got a bit of a fright because I think she blew something like a 32 and the scale only goes up to 30. So she got a bit of a fright. And considering we had both pretty much had a cigarette at the same time going through. I blew I think it was eight and she blew 32. So then when she explained that 10 per cent of the baby’s blood was actually nicotine you seen the shock on her face.
Area A, partner 48, smoker
Significant others mentioned being similarly shocked or upset by their CO readings:
Shocking for me, it was really, really high . . . I think it was in the 30s.
Area A, partner 55, smoker
Interviewees demonstrated mixed views on CO monitoring. For those who viewed it positively, CO monitoring was helpful or useful in visualising the effects of smoking and providing motivation to quit and remain quit for pregnant women and others alike:
. . . sometimes if you can see or gauge it against that, a chart to say this is a danger level, you are smoking far too much, your [CO] is that. I quite liked that . . . so a visual representation is a good way of maybe prompting you to see or think about like this is bad, I need to stop.
Area A, partner 53, smoker
In contrast, some indicated reservations or scepticism regarding CO monitoring. Some questioned its reliability and there was also a suggestion that it could lead to complacency regarding the risks of smoking:
I just think she filled her head with, that it’s all right because she’s on the green, which it isn’t all right, because it’s still smoking, it’s still not good for you.
Area A, partner 17, smoker
Nature of support provided
Types of support received by pregnant women and mentioned by SOs included group and one-to-one support, sometimes involving home visits. SOs were generally very positive about the cessation support received by pregnant women. There was a lot of discussion of one-to-one support and particularly the personal support provided by HPs (i.e. smoking cessation advisors). Interviewees indicated an appreciation of the flexibility and responsiveness of the personal support provided by smoking cessation advisors:
. . . it’s not been every week but there has been a lot of contact between the two of them [pregnant woman and smoking cessation advisor] and then they have, if they can’t make it then they will speak on the phone and things like that, and if [pregnant woman] is feeling, I mean she hasn’t for weeks now but before if she felt like she was close to going and buying a packet she could phone [smoking cessation advisor] and she was always ready to talk to her and sort of give her encouragement and things. She couldn’t have done it without it.
Area A, mother 20, smoker
The benefits of one-to-one support were considered in comparison with group support. One-to-one support was experienced as, or was thought to be, preferable to group support, as it was perceived to provide more tailored support as well as greater privacy and convenience:
. . . some people might think I don’t know, they might feel embarrassed about going. Some people don’t do very well in group situations I guess. So yeah it’s nice that there is an option there and also I suppose if people are housebound and smoke, you know it’s always good to know that these people are willing to come out and support you, you know if you can’t go to them so I’d say that is a good thing yeah.
Area B, mother 8, non-smoker
However, SOs also recognised the benefits of receiving group support, highlighting this approach as providing individuals with opportunities to share experiences of quitting, including helpful tips and techniques, as well reassurance to others. Group support specifically for pregnant women was also seen to be beneficial:
Maybe wee get-togethers with other mothers or expectant mothers, wee coffee mornings or, where they can all, it’s back to this . . . so everybody can share their experiences at this coffee morning or whatever and I think that would be good.
Area A, partner 50, non-smoker
Nicotine replacement therapy
The use of NRT was frequently mentioned during interviews with SOs, particularly with regard to their or the pregnant woman’s experiences of current or previous quit attempts. SOs mentioned the use of patches, chewing gum, lozenges, inhalators and sprays, showing the extent to which they or the pregnant woman liked or found these effective, demonstrating very mixed experiences:
I think she found it alright, it was the new minty one, not the old minging [unpleasant] chewing gum so she found that a lot better.
Area A, partner 55, smoker
There was some awareness among SOs that not all forms of NRT were available for use by pregnant women and that there were limits on using these. This was perceived as a barrier to quitting for some, particularly when the pregnant woman was seen to be a heavy smoker:
. . . there are certain things that they can’t take to help them [pregnant women] stop whereas, so they would need advice about that. And so it is, you are treated different, even the patches, they don’t like giving them the stronger patches, so if you are a heavy smoker and you are pregnant, they lighter patches don’t really do you any good anyway so having the extra support to go through that would be helpful.
Area A, mother 20, smoker
There appeared to be little concern among SOs about the use of NRT in pregnancy, with most indicating that they believed NRT to be harmless or less harmful than continuing to smoke:
Well it is still putting nicotine into the system but it’s cutting out the rest of the chemicals and toxins out of the cigarettes so I think it’s a far better idea than smoking itself because yeah you are still getting nicotine, it’s not going to be great for the baby but it’s going to be a hell of a lot less harmful than the arsenic that is in cigarettes. It’s like two and a half thousand chemicals do you know what I mean. So if you can take two and a half thousand chemicals away and just give her the one then.
Area A, mother-in-law 47, non-smoker
Discussion
Smoking
Smoking or former experience of smoking was common among SOs; however, smoking itself was largely perceived as undesirable. Attitudes to smoking in pregnancy were even more stringent, with most SOs showing disapproval and a preference for women to quit during pregnancy. This largely remained the case, even when interviewees had experienced other women smoking during pregnancy with no apparent ill effects for the baby. SOs also expressed concern about exposing babies and children to SHS.
According to participants’ accounts, smoking appeared to have an important role within relationships between SOs and pregnant women, although this was not always acknowledged by interviewees themselves. Stopping smoking, however, was often recognised as a fraught issue for relationships, with SOs admitting to avoiding placing emphasis on women to stop, for fear of provoking tension or conflict within the relationship or putting women under excessive pressure.
Smoking cessation
Significant others and members of women’s wider social networks were generally supportive of pregnant women’s attempts to stop smoking and were often willing to change their behaviour to assist quit attempts including, most commonly, avoiding smoking in front of the pregnant woman. Others, particularly partners, had attempted to stop smoking at the same time as the pregnant woman, having recognised the potential negative influence of others’ smoking, and some were willing to attend SSS appointments simultaneously.
Significant others felt it was appropriate for generic HPs (i.e. midwives and GPs) to raise smoking in pregnancy with women but recognised the benefits of specialist cessation support, particularly when provided on a one-to-one basis. Interviewees relayed mixed experiences of NRT use from both their and the pregnant woman’s perspectives but appeared to have few or no concerns about its use during pregnancy. CO monitoring was generally considered to be a helpful motivational tool, although accounts cautioned against inappropriate interpretation of readings.
Improvements to existing services/interventions
Most SOs appeared largely satisfied with current interventions available to pregnant women in relation to smoking cessation. However, a minority suggested that brief advice provided by generic HPs and the range of NRT on offer for pregnant women may not necessarily be sufficient to support quit attempts. One possible improvement to services expressed by a similarly small group was for SSSs to pay more attention to and support the role of SOs, or more specifically partners, in supporting pregnant women’s quit attempts.
Chapter 9 Findings of systematic review of health-care professionals’ perspectives and experiences of the barriers to and facilitators of smoking cessation
This systematic review has been published in BMC Public Health. Here we present the abstract of the paper. This abstract has been reproduced from the abstract © Flemming et al. 59 under the terms of the Creative Commons Licence 4.0 (CC BY); https://creativecommons.org/licenses/by/4.0/.
Background
Reducing smoking in pregnancy is a policy priority in many countries and as a result there has been a rise in the development of services to help pregnant women to quit. A wide range of professionals are involved in providing these services, with midwives playing a particularly pivotal role. Understanding professionals’ experiences of providing smoking cessation support in pregnancy can help to inform the design of interventions as well as to improve routine care.
Methods
A synthesis of qualitative research of HPs’ perceptions of the barriers to and facilitators of providing smoking cessation advice to women in pregnancy and the postpartum period was conducted using meta-ethnography. Searches were undertaken from 1990 to January 2015 using terms for maternity HPs and smoking cessation advisors, pregnancy, post partum, smoking and qualitative in seven electronic databases. The review was reported in accordance with the ENTREQ statement. 87
Results
Eight studies reported in nine papers were included, reporting on the views of 190 HPs/key informants, including 85 midwives and health visitors. 113,133,162–168 The synthesis identified that both the professional role of participants and the organisational context in which they worked could act as either barriers to or facilitators of an individual’s ability to provide smoking cessation support to pregnant or postpartum women. Underpinning these factors was an acknowledgement that the association between maternal smoking and social disadvantage was a considerable barrier to addressing and supporting smoking cessation.
Conclusions
The review identifies a role for professional education, both pre qualification and in continuing professional development, that will enable individuals to provide smoking cessation support to pregnant women. Key to the success of this education is recognising the centrality of the professional–client/patient relationship in any interaction. The review also highlights a widespread professional perception of the barriers associated with helping women give up smoking in pregnancy, particularly for those in disadvantaged circumstances. Improving the quality and accessibility of evidence on effective health-care interventions, including evidence on ‘what works’ to support smoking cessation in disadvantaged groups, should therefore be a priority.
Chapter 10 Findings from qualitative study of health-care professionals’ perspectives and experiences of the barriers to and facilitators of smoking cessation
This chapter presents the findings from the interviews and focus groups undertaken with HPs to explore their views on the barriers to and facilitators of smoking cessation in pregnancy and post partum, and to elicit views on potential improvements to existing services and interventions. The chapter concludes with a brief discussion of the findings taking into account the systematic review findings in Chapter 9.
Participant sample
A total of 28 individual and group interviews were conducted with 48 professionals across the two study sites. The participants were midwives, health visitors, GPs, pharmacists, obstetricians, commissioners, SSS advisors and SSS administrators (Table 6) (for this chapter, all participants are referred to as HPs unless otherwise specified). Only one participant was male. There was a wide range of level of experience across all professional groups, ranging from several decades to newly qualified. Similarly, age ranged from the early twenties to mid-sixties. There were few current smokers but several professionals had smoked in the past.
| Professional group | Area A | Area B |
|---|---|---|
| SSS advisors/managers/administrators | 14 | 5 |
| Midwives | 7 | 9 |
| Midwifery managers | 0 | 1 |
| Health visitors | 2 | 2 |
| Obstetricians | 1 | 1 |
| GPs | 1 | 1 |
| Service commissioners | N/A | 2 |
| Community pharmacists | 1 | 1 |
| Total | 26 | 22 |
At the time of the study, area A operated an almost exclusive opt-out referral pathway from antenatal booking, meaning that those who were identified as smokers by either self-report or a CO breath test were referred to the SSS unless they declined. Area B had a mixture of opt-in and opt-out referral pathways, depending on the locality. The procedure for providing NRT pharmacy vouchers to pregnant smokers also differed between the two areas. When these differences are considered relevant to participant views, the locations are discussed separately.
Findings
The findings are divided into three out of the five main ‘levels’ of the SEF: organisational, interpersonal and individual. Although these levels are presented separately, some areas of overlap and interactions between the different levels emerged. These are described in Discussion.
Organisational
Overview
In both study sites, participants stated that the organisational support available for pregnant smokers was heavily influenced by external factors such as available funding and local and national health priorities. Several participants described multiple service and role reconfigurations that they believed had occurred in response to these issues. Some felt that frequent organisational changes had inhibited the ability of services to develop and embed a cohesive approach towards working with pregnant smokers, and that service quality had been compromised as a result:
. . . I think that the constant changes in commissioner, the constant changes in geography, well it doesn’t do anyone any favours, because you spend half your time trying to catch up to where you were, rather than actually developing the service . . .
Area B, commissioner 1
. . . our service has gone through sort of several sort of stages . . . so it’s just been we’ve not had a cohesive sort of run at how do we deal with pregnant woman.
Area A, SSS group 1
Although both study sites had various protocols to guide the support given to pregnant smokers, there were differences in how rigorously these were adhered to in practice. This was particularly notable when exploring referrals, CO monitoring and NRT prescribing. Organisational approaches towards smoking cessation training were also critiqued by participants.
Several SSS advisors felt that having more designated time available for telephone and text contact with pregnant smokers in between appointments and having greater opportunities for flexibility around appointment times and locations could all help to improve engagement. In addition, HPs and SSS advisors across both study sites felt that more staff members were needed for the specialist SSS pregnancy advisor role.
Referral
Most non-SSS HPs described their role with regard to smoking in pregnancy as one of raising the issue and referring pregnant smokers to SSSs rather than discussing smoking in depth themselves. Prompts in paperwork and clinical systems were considered useful cues that ‘allow for the conversation’ (area A, health visitor 1) on smoking and appeared to increase confidence in raising the issue. Views on the different referral pathways were mixed, particularly on opt-out pathways. Pharmacists largely described the opt-out process positively and as an opportunity for the women to receive specialist support with regular monitoring. When GPs and pharmacists were not required to refer, there was still a preference to do so, although some felt that choice was also important.
Among midwives, some were sceptical about the benefits of opt-out pathways and a few reported potential negative aspects. There were midwives from both areas who felt that it was not their role to refer women who, in their view, were not at the ‘right stage’ for stopping smoking, and others expressed discomfort at implementing the opt-out pathway if the pregnant smoker was reluctant:
Though I do offer everybody the chance to be referred to the smoking cessation person, but I don’t see it as my role to refer them if they are not at the stage when they are ready to stop smoking.
Area B, midwife 2
. . . if somebody says no I don’t want you to refer me, then I think that puts you in a really awkward situation.
Area A, midwife group 1
Other midwives, however, said that they were happy with the opt-out process and perceived it as simpler than opt-in for identifying referrals:
I think it’s good, it’s much better, before there didn’t seem to be an awful lot, so this is pretty straightforward, it’s easy enough to refer them, you know it’s just getting them to go I think that’s the thing.
Area A, midwife group 2
From the perspective of SSS advisors, views again were mixed. Several felt that the opt-out pathway clashed with the SSS philosophy of choice and suggested that it risked being coercive:
We are not here to tell people stop smoking. We are here to help people who have decided that they want to quit.
Area B, SSS advisor 2
And I think the fact that they are all referred it goes against the rest of our service because the majority of people who come to our service come voluntarily.
Area A, SSS group 2
I do worry that sometimes maybe midwives are putting girls under pressure to be referred, I don’t know if that’s the right thing or not.
Area B, SSS advisor 3
When opt-out referral was in place, several advisors noted that referral rates were lower than would be expected. Advisors also commented that referrals were at times poorly written or for women who appeared very uninterested in receiving support:
They tend to get referred, and this is just a problem for us internally, it’s often with very scant detail, it might only be a first name.
Area B, SSS administrator 1
. . . you know instantly they are going through the motions, they, the midwife is very enthusiastic about getting them referred, but that girl you can hear it in the voice and I would put money on her never turning up.
Area B, SSS advisor 3
In cases when pregnant smokers showed no interest in support, several advisors expressed frustrations with organisational requirements to continue pursuing contact and the negative impact on staff motivation:
Yeah, and it would be nice to say to us lot I’m not interested, but they just let you go through that process and you wait for them to come along and then you have got to chase them and you, they don’t answer their phone.
Area A, SSS group 2
However, the same advisors indicated that once positive telephone contact was achieved, it did seem to increase the likelihood of pregnant smokers attending a SSS appointment in person:
Now I have found that seems to work better, find out about other children, what are the kid’s names, are they working, are they, and then when I’ve got more information then perhaps they feel a wee bit more comfortable to think that they will turn up.
Area A, SSS group 2
Other advisors similarly reported that the opt-out referral pathway offered an effective way to engage women who might not otherwise have attended:
. . . there is always somebody that’s pleasantly surprised that we are that non-judgemental and we are there just to accept them kind of warts and all and we are there to help and support them.
Area A, SSS group 1
Carbon monoxide monitoring
Both study areas used CO monitoring at antenatal booking, with area A using it routinely and area B having more patchy coverage. In general, antenatal HPs with experience of conducting CO monitoring felt that it was acceptable to pregnant women and feasible to undertake as ‘it does only take seconds’ (area B, midwife group 1). CO monitoring was described as a useful visual tool and powerful motivator for quitting:
And it does give you that you know opportunity to speak to everybody about smoking and the people that do have a high reading, it’s re-emphasising the facts, the impact it can have on the baby and the pregnancy and I think it maybe makes them more inclined to maybe seek help.
Area B, midwife group 1
Very high CO readings were also seen to provide an opportunity to discuss topics such as stillbirth and cannabis use. Some also saw CO monitoring as an opportunity to establish whether or not a client is being honest:
. . . it kind of lets them see also that if they are just spinning you a yarn and they haven’t really stopped that you are seeing that.
Area A, midwife group 2
Repeated testing was described by some midwives as a positive way for pregnant smokers to see the benefits of their quitting or as a potential opportunity to highlight why cutting down does not necessarily reduce health risks. However, caution was expressed about ensuring that non-smokers are not repeatedly tested:
I wouldn’t want to push it on somebody who was a non-smoker so we have to identify who we are offering it to.
Area A, midwife group 1
Primarily, when CO monitoring was not practised routinely, some midwives expressed concerns about the time it would take and the potential impact on the HP’s relationship with pregnant smokers:
No, I don’t think they would have a problem doing it. I think they would think to themselves as I would, how the hell can I fit this into another thing to do?
Area B, midwife 1
I am not quite sure how I feel about doing it. I don’t know whether it might come across as a bit bullying by using them maybe. I don’t know. I don’t know enough about them.
Area B, midwife 3
From the perspective of SSS advisors, there were concerns in both areas that the approach used by midwives could have a significant impact, with the risk of an early loss of clients if CO readings were not properly explained. Improved training around CO monitoring was discussed as a way to help manage this issue, coupled with having information sheets or standardised text for midwives when carrying out the test.
Nicotine replacement therapy
Other than SSS advisors, most HPs seemed very cautious about the use of NRT (licensed for use in pregnancy across the UK) in pregnancy. A number of HPs indicated uncertainty about whether or not NRT was licenced in pregnancy; some felt that it was ‘probably not safe’ (area B, midwife 1) and others appeared to be misinformed:
I remember speaking to a like drug and therapeutics people about using it in pregnancy and he said well the manufacturers don’t want you to really, but it’s better than smoking.
Area B, GP 1
I know the patches aren’t licensed for use in pregnancy.
Area A, midwife group 2
Some SSS advisors themselves were also cautious about suggesting patches:
I mean usually you want them to like try an intermittent product first before going for a patch.
Area A, SSS group 2
Although advisors in area B could provide a pharmacy voucher for NRT at the initial appointment, advisors in area A explained that, owing to local policy, pregnant smokers accessing their service had to make a failed quit attempt without NRT before they were potentially eligible for NRT, if approved by the lead midwife. Several felt that this lengthy process could lead to disengagement among pregnant smokers, and some advisors described taking their own stance on what counted as a quit attempt in an effort to speed the process up:
. . . if they say you know I can’t even do an hour you think well there is no point in me making [them try without NRT].
Area A, SSS group 2
However, even with this liberal interpretation of a quit attempt, area A advisors stated that it took a minimum of 1 week from an initial appointment for pregnant smokers to receive a NRT voucher. Several advisors in area A felt that providing NRT sooner would increase the chances of pregnant smokers quitting successfully:
. . . I always thought if you could give them the patches straight away you would be halfway there.
Area A, SSS group 2
Training
Although most participants described having access to smoking cessation training, there did not appear to be any organisational requirements at either location for HPs to attend. The GP participants did not describe attending training themselves and the pharmacists described being encouraged rather than required to attend training, which was often delivered by the lead pharmacist, a midwife or pharmaceutical companies. One midwife mentioned having had a half-day on smoking as part of her midwifery training, and a few midwives and health visitors described receiving invitations for smoking cessation training (although it was not clear from whom). They again spoke about having a choice about attendance:
. . . we all get training invites but I suppose it’s up to us to then book ourselves on and I think it’s prioritising what training you need you know it’s really up to us to kind of keep ourselves up to date.
Area A, health visitor 2
For some, having the discretion to choose was seen positively, as it meant that they could focus on their areas of interest:
And it might be something that we do want, I am a smoker or you know and I want to do smoking cessation or I don’t feel that is my role, so it isn’t mandatory.
Area A, health visitor 2
However, others described either not knowing about or not feeling that they had training opportunities in smoking cessation, and this appeared to be connected to their reported lack of confidence in discussing smoking. A number of midwives and health visitors were also unable to recall having had any update training since starting their role. One midwife suggested that, if smoking cessation training was not mandatory, midwives might not think about proactively seeking opportunities to undertake it:
I don’t think people even think about going on [cessation training] but I could be wrong.
And how do you feel about that?
Well it’s awful isn’t it; I mean it doesn’t stop midwives if they see a course applying for it.
Area B, midwife 1
Several SSS advisors expressed concerns that, without adequate training, other HPs could give mixed messages about smoking in pregnancy or could fail to provide any information at all. These advisors speculated that the presence of multiple messages could result in pregnant smokers either adopting the views of family or partners over HPs, or pushing away guidance entirely:
. . . I think sometimes you know you get mixed messages from like their family, from their doctor, from the midwife and it’s, you know, who do they listen to really you know . . .
Area A, SSS group 2
If there is too much it makes it easier for them to push [the messages] away.
Area B, SSS administrator 1
Health-care practitioners and advisors also felt that improving staff knowledge about smoking in pregnancy would ensure that professionals gave a consistent message:
So it’s getting everyone on board at the hospital, your GP practice, your midwives, all HPs trained up to the same level, consistent messages and referrals into the specialist service.
Area B, commissioner 2
Interpersonal
Relationships with pregnant smokers
All HP groups saw positive relationships with pregnant smokers as important for facilitating discussions about smoking, and this was particularly emphasised by advisors, midwives and health visitors:
But the main bit, the key thing is first with the pregnant clients, developing that rapport with them and developing that strong relationship because it is a group that is a bit more sensitive and you have to approach more sensitively.
Area B, SSS advisor 1
. . . we can say I know you stopped smoking, but you can still smell cigarette smoke in the house, tell me what is going on and that’s where if you have actually built up a rapport with them they are going to me more truthful.
Area B, midwife 2
However, although seen as essential, having a positive relationship also seemed to hinder some HPs’ efforts to raise and explore the issue of smoking. Several HPs described an over-riding concern to not damage client relationships and were anxious to not sound judgemental for fear of clients disengaging. As such, HPs often took their cues from clients and would ‘back off’ if the client appeared annoyed or upset:
And if I start, if they see me as someone who is just going to nag them every time they come they might not want to come. So I think it’s about getting the balance right.
Area B, midwife 3
You both mentioned there about somebody who’s shutters might come down, how do you deal with that?
I’d probably back off a bit to be honest, because you kind of don’t want to ruin the relationship between you by kind of you know forcing it upon them . . .
Area A, midwife group 2
Concerns about relationships also seemed to affect how HPs delivered risk information and advice about cessation. For example, HPs often expressed a reluctance to link smoking with specific outcomes, such as miscarriage or stillbirth, and midwives generally were reluctant to emphasise the importance of quitting in pregnancy. Instead, they often used the language of choice and trying, and congratulated women who reported efforts to cut down. Post partum, HPs seemed to focus on protecting the baby from SHS rather than on advising the woman to quit.
As a consequence of this complex dynamic, some HPs admitted that information about risk was being lost, misunderstood or minimised by pregnant smokers:
. . . because nobody wants to say to women if you smoke your baby might die. What we say is if you smoke you will have a smaller baby and we’ve all done it . . . and actually that has been turned on its head and that’s been turned into a positive.
Area B, midwife 3
Commissioners also felt that many HPs were overly cautious about giving information about the consequences of smoking and providing firm advice to quit. They, and some SSS advisors, felt that pregnant smokers expected, and in some cases wanted, to hear a clear message about smoking in pregnancy:
I sometimes feel that we tread on eggshells a little bit, around, is it OK to bring it up . . . I’m not negating what midwives say about their relationships with pregnant mums, because they are the best ones to judge how it feels, but actually there is a reasonable amount of evidence base that says that they are expecting to be asked, women, it isn’t going to damage the relationship if you ask, or talk about smoking.
Area B, commissioner 1
Interservice relationships
The relationships between HPs and SSS staff appeared to have an important impact on the support that pregnant smokers received. In general, GPs and pharmacists described being satisfied with their relationship and level of contact with the SSSs. For midwives and health visitors, perceptions of the relationship with SSSs were more mixed, with some feeling positive about it and others describing limited or no contact with SSS staff. Meanwhile, although sympathetic to HPs’ workload demands, SSS advisors in both locations described frustrations that smoking was not given greater priority by antenatal HPs. However, some in area A speculated that this might change once opt-out referral was more embedded.
In instances when interservice communication was limited, willingness to refer and confidence in the feedback process appeared to be lacking from both perspectives:
Do you hear back when you refer people on, do you hear any more about how it’s gone along?
No, and that is frustrating too.
Would you like to?
Yes of course I would because if I am referring in and then it goes no further than that, that becomes a bit of a pointless process.
Area B, heath visitor 2
But they don’t really chase them up or follow them up to make sure that they’ve been to see us. I think if somebody doesn’t turn up and we phone the midwife and say could you just remind them, you often get yeah, yeah, yeah, oh well. You are pretty sure they don’t. So I don’t know how important it is for other people.
Area A, SSS group 2
Aware of this as a potential issue, commissioners expressed a keen wish to improve interagency working, and HPs in both locations felt that improved communication would benefit both the referral process and the support offered to pregnant smokers:
I think just developing relationships with the midwife team so that they can put a face to who they are referring people to and they can have confidence that we will chase the ladies up or that we will keep them in the loop.
Area A, SSS group 2
. . . it’s always very helpful when you know who is answering the phone to you, when you know the person who might be going out and delivering that service.
Area B, health visitor 2
Health-care practitioners and SSS staff suggested several approaches for improvements, including having update newsletters, opportunities to attend each other’s team meetings and increased guidance around local statistics, cessation rates and dealing with referrals.
Individual
Responsibility for addressing smoking
Individual HPs generally lacked confidence in discussing smoking in pregnancy and varied widely in the extent to which they saw addressing smoking as part of their role. The GPs and obstetricians in both areas felt that their role was to provide brief advice only and might raise smoking only if it was relevant to the appointment, feeling that midwives had more time and expertise to discuss smoking. In area B, where opt-in referral was more prominent, hospital midwives felt that community midwives were better placed to discuss smoking, although the community midwives often described feeling underskilled to explore smoking cessation in depth and might discuss smoking only briefly and if time allowed:
If we have time we will take the information, find one of the old forms that we have and contact the smoking cessation service. But most often we are asking the women to do that themselves, encouraging them to do it themselves.
Area B, midwife
In area A, where opt-out referral was in place, it seemed that midwives were more likely to prioritise smoking:
Do you see raising the issue around smoking . . . as part of your role?
Yeah.
Yeah, absolutely, you are a [HP] I mean at the end of the day you know obviously you are concerned for these women . . . But the big thing is the fetus.
Area A, midwives group 1
However, there were HPs in both areas, often those who were longer serving, or had either training or experience in smoking cessation, who described feeling strongly that smoking cessation was their responsibility:
It’s one of my things that I am quite keen to try and impact on and I feel frustrated that having been trained as a smoking cessation advisor it’s now not a commissioned part of my role.
Area B, health visitor 2
In some cases, the extent to which HPs prioritised smoking appeared to be connected with other external influences, such as the availability of NHS information or the political fashion at the time. Several HPs discussed the availability of guidance and leaflets for other health behaviours, including obesity, compared with that for smoking:
Now obesity is a big one . . . especially [area B] have had a new obesity guideline come in and leaflets. And that I think is one of the key sorts of things at the moment because it is one of the new things . . . and I would say that smoking is probably near the bottom.
Area B, midwife 4
Perception of barriers and facilitators faced by pregnant smokers
Participants suggested a number of factors that could act as both barriers and facilitators for pregnant smokers. In particular, the pregnant smoker’s age, whether or not she had other children, her understanding of the risks of smoking, her understanding of NRT, the role of her partner and family, and her own level of confidence and experience of quitting or witnessing others attempting to quit were all seen as potential barriers to or facilitators of quitting. Socioeconomic status and co-occurring issues such as depression were also raised as potential influential factors, as were practical issues such as proximity to support services and the availability of crèche facilities. Some HPs described physiological changes to nicotine metabolism in pregnancy as a potential barrier to quitting. Several HPs noted that pregnant smokers could experience multiple disadvantages and one commissioner described the cumulative effect that can occur:
Well, where do you start? They have, they have such chaotic lives, so women who smoke or continue to smoke during pregnancy often have, they are often young aren’t they, they perhaps have psychological problems, emotional problems, problems within the home such as like domestic abuse, you know they are living chaotic lives and giving up smoking is just their one thing that they think they have control over.
Area B, commissioner 2
Discussion
Health-care practitioners described a number of health-care-related factors that could affect a pregnant smoker’s ability to quit, both directly, through the advice or support provided, and indirectly, through care structure and environment. These operated and interacted across multiple levels.
Smoking
Health-care practitioners noted that alongside the psychological, physical and social environment of pregnant smokers, service and professional issues could have an important influence on smoking in pregnancy. Similar to the systematic review of HPs, a number of HPs in this study reported a lack of knowledge and confidence around raising and delivering information about smoking in pregnancy, and, particularly in opt-in areas, several felt that tackling smoking was not a routine part of their role. In both areas, smoking was frequently left for midwives to address. However, midwives, particularly in area B, often reported struggling to tackle smoking because of limited time, feeling undertrained and not having smoking as a priority in their work.
In terms of clinical paperwork, contrary to review findings, many participants in this study reported that prompts in clinical paperwork and systems positively facilitated the discussion of smoking. However, at a local level, shifting priorities in targeting risk factors or health behaviours in pregnancy appeared to affect the HPs’ perceptions of the importance of addressing smoking in pregnancy. Across all professional groups, smoking in pregnancy training opportunities appeared to be limited and, when available, were usually accessed only by self-motivated individuals. Although lack of training is a common theme in prior research, participants in this study reported that training issues were a potential cause of inconsistent messages provided by different HPs.
A central issue raised by HPs was the importance of the relationship developed with pregnant clients. As with the review, many HPs in this study were anxious about damaging relationships by discussing smoking and felt inhibited to discuss it as a result. This study extends the review findings by identifying how in some cases, protecting the client relationship appeared to be a factor in HPs downplaying the risks of prenatal smoking and failing to emphasise the importance of abstinence. In some cases, however, good rapport was described as enabling frank discussions about smoking behaviour and a minority believed that pregnant smokers expected and wanted to be told the risks. This reinforced the review’s conclusion that the professional’s relationship with the pregnant smoker can be both a barrier to and facilitator of addressing smoking.
Smoking cessation
New insights were generated about views of opt-out referral pathways combined with routine CO monitoring. Some midwives felt that opt-out referral pathways simplified referral and increased access to support, whereas others reported concerns about referring women who they felt were not at the ‘right stage’ to quit. Among SSS advisors, opt-out referral pathways were seen to increase client awareness about the SSSs, but some also discussed how the pathway clashed with their service philosophy of client choice. Other advisors expressed concerns that the information given to pregnant smokers around CO monitoring could lead to early dropout. These concerns about opt-out referral and client choice linked with the findings of the systematic review of HPs of the perceived importance of putting the woman at the centre of the decision to quit.
The relationship between HPs and SSS advisors was raised as a further important factor in smoking cessation work. In some cases, poor communication between antenatal HPs and SSS advisors was identified as contributing to deterioration in interservice relationships and mistrust. SSS advisors sometimes described frustrations with the reduction in quality of the referral information that they received from other HPs, although the HPs themselves sometimes felt that they lacked referral feedback from advisors. The quality of communication varied between sites, however, with some examples of effective relationships and efforts made to maintain good communication among both antenatal HPs and SSS advisors.
Aside from referral, HPs were very cautious about NRT use in pregnancy, despite near universal provision in the SSSs. This has been an enduring theme in prior research as identified by the systematic review of HPs. However, these findings identified additional barriers to NRT provision within SSSs, in which delays to provision were perceived as leading to disengagement among pregnant women.
Improvements to existing services/interventions
Several potential improvements were identified from this study’s findings. At an organisational level, improving existing paperwork to include more effective prompts and providing clear information for HPs regarding smoking could effectively elevate its perceived priority when it is inadequately addressed (contrary to local guidance). Several SSS advisors felt that having more designated time available for telephone and text contact with pregnant smokers between appointments and having greater opportunities for flexibility around appointment times and locations could all help to improve engagement. In addition, HPs and SSS advisors across both study sites felt that more staff members were needed for the specialist SSS pregnancy advisor role. Enabling staff members to be more fully involved in service development could potentially enable the service to make better use of staff expertise, increase staff buy-in and reduce the feeling among some staff that changes are imposed from elsewhere. Provision of NRT in a timely manner was also perceived to increase the chances of pregnant smokers quitting successfully.
At individual and interpersonal levels, improving communication pathways between HPs could lead to improvements in the referral process and greater trust between different professional groups; suggested approaches included having update newsletters, a presence at each other’s team meetings and increased guidance around local statistics, cessation rates and dealing with referrals. For HPs lacking confidence to conduct CO testing and/or deliver the opt-out pathway, providing mandatory training in this area could improve HPs’ confidence and equip them with the skills and knowledge to effectively raise smoking as a topic, provide very brief advice and implement the opt-out referral protocol. Improved communication together with the delivery of basic smoking cessation training for all HPs involved with pregnant smokers could then lead to greater consistency in health messages delivered to pregnant smokers.
Chapter 11 Perceptions of new interventions from three perspectives: pregnant and postpartum women, their significant others and health-care professionals
This final chapter focuses on ‘interventions’, setting out the views of pregnant women, SOs and HPs on these. The views of each group of participants are presented together for each suggested intervention. Not all groups of participants commented on every intervention.
Financial incentives
Pregnant women
The pregnant women interviewed had mixed perceptions on the use of financial incentives to encourage smoking cessation in pregnancy. Some had very positive views, suggesting ways in which incentives could work for them or other pregnant women. This was often seen in the context of the expense of having a baby. A number of women reported that incentives would be particularly motivating for those with financial concerns; the focus here was on being able to afford to buy things for the baby:
Yeah it probably would [help people to stop smoking] because to be fair you know, when you fall pregnant the first, I think your main worry is ‘how are you going to financially cope?’. So you know I suppose if you are getting a wee bit more of an incentive when it comes to a voucher, yeah it probably would, it would help.
Area A, pregnant woman 18, non-smoker
Offering a financial incentive was also seen by some as a useful motivational tool, one that could help pregnant women by having something to look forward to or being rewarded for their efforts. It was also considered useful in providing women with an extra reason to try to stop smoking; this could help those struggling to find motivation or willpower to stop smoking:
It would have given me more reason, more, I think it would have given me more willpower to stop.
Area B, pregnant woman 7, non-smoker
Negative perceptions focused more on moral arguments against using financial incentives rather than a perception that they would not be helpful to women. Some women likened it to ‘bribery’ or ‘blackmail’. Others said that the baby’s health should be motivation enough for stopping smoking in pregnancy. Other women were conflicted by the idea of incentives, on the one hand thinking it was a good idea but on the other hand concerned that it would lead to women being motivated by financial rather than health reasons:
I think it’s handy, because I know, even before you become pregnant, it’s, you struggle, everything’s so expensive nowadays, . . . it’s like, it’s handy because it means like, obviously you’ve got that wee bit more money to spend on your baby – or on other things that you need – but then at the same time . . . I don’t know, I think it feels a bit rude, ‘do this, and we’ll give you money’, I think it’s like a bit greedy.
Area A, pregnant woman 5, smoker
I don’t know, I think if you want to stop you should stop for your baby not for money. But then I am saying that and I am absolutely skint so it sounds like a great idea.
Area B, pregnant woman 14, smoker
Other negative perceptions focused on the possibility of gaming the financial payments, on uncertainty about the idea of incentives to help with smoking cessation and on remaining abstinent once the incentives ceased:
Yeah it would [help people to stop smoking], because a lot of people would do anything for money won’t they . . . but as soon as it stopped then they would go back on to smoking.
Area B, pregnant woman 8, smoker
Significant others
Significant others had mixed opinions on the idea of using financial incentives to encourage smoking cessation in pregnant women. Some interviewees perceived this idea positively, thinking that it could be helpful to pregnant women by providing them with a reward for stopping smoking. Others felt that using financial incentives would mainly attract, and therefore be most effective among, women on lower incomes, with some reporting that receiving shopping vouchers would be very helpful to women preparing for the arrival of a new baby:
I think that is a bloody good idea because again you can use the vouchers to go and get baby clothes and actually see the rewards and have the rewards there for it. I think that is, I think that is probably the best one I’ve heard actually.
Area A, partner 48, smoker
It might be for some people yeah, I think some people it could possibly work if they needed the money. For those that don’t need the money they would probably sit down and go, I don’t know, no sort of thing.
Area B, partner 5, smoker
A substantial proportion of SOs interviewed viewed the prospect of using financial incentives negatively, with some believing that it amounted to bribery. Others simply did not approve of paying pregnant women to stop smoking:
It’s more like bribery isn’t it; I think it should be a personal choice to be honest.
Area B, partner 5, smoker
I don’t see the point in paying someone for a bad habit, it would be like paying someone to stop taking drugs, you wouldn’t want to do that would you?
Area B, partner 2, non-smoker
Other interviewees reported reservations about using financial incentives to promote smoking cessation among pregnant women with a key concern relating to the extent of effectiveness. Some interviewees felt that offering a financial incentive would be insufficient to motivate and/or sustain smoking cessation, particularly once women were no longer receiving incentives, and one interviewee felt that willpower remained more important than the offer of financial incentives:
If somebody was offering you a few quid a month, and it helps you then all good, but I don’t see how a small financial reward could take away that craving. Because if somebody stops smoking what they gain in money from stopping smoking is far more than what they will be given. A bit sceptical but, for some, again if it works for a few people then that sort of thing.
Area A, partner 53, smoker
. . . well I suppose it would get, it would get more people to stop, but then again it’s like are they stopping to get something for it? Are they then going to get that and then go back to smoking? . . . it might not always work, but it might work sometimes I suppose.
Area B, partner 55, smoker
Those who had reservations about using financial incentives also reported concerns about the possibility of gaming the incentive, believing that some pregnant women would accept the incentive but continue to smoke:
I just think it might be, people might just be taking advantage of it saying, ‘Oh aye I’m stopping, I am stopping’, and with the money that they’re getting spending it on cigarettes . . . I think maybe some, some women might take it serious, but I don’t think every woman would.
Area A, partner 16, smoker
God can you imagine how many people will say that they smoke when they don’t, say they have stopped to get the money . . . Could you imagine though, 90%?
Area B, partner 9, smoker
In addition, SOs who reported the possibility of gaming the incentive among pregnant women, including most of those who perceived financial incentives to be useful to some, demonstrated limited confidence in CO monitoring:
That’s the only thing, like you could say to the women, ‘Right, do the CO thing in the morning, or in the afternoon’, but a’ she has to do is not have a cigarette for 2 and a half hours and it looks likes she’s stopped . . . have a shower before she goes, put clean clothes on and you would never know . . .
Area B, partner 16, smoker
Health-care professionals
Health-care professionals expressed mixed opinions on both the effectiveness of financial incentives in helping pregnant smokers to quit and how such incentives would be perceived by the general public. Some felt that financial incentives would be a positive way to increase engagement; others thought that they might help in the short term but not in the longer term, and still others felt that pregnant smokers should stop for their own benefit and not for financial incentives:
Well, about the financial benefit, if you are trying to target young people, yes the financial benefit will work, but once they have got a bit more money, they might just go back to it anyway after a while because they are like oh well I’ve got some money now, I am out with my friends and start smoking again. Because you haven’t got that real, I really, really want to stop smoking for me, not for the money, but for me.
Area A, SSS group 1
I just think they have got to want to do it for themselves and their baby and that money is maybe, it seems like a quick fix but it won’t necessarily work and it could be spent wrongly and the government is already short of money, the NHS is already short of money.
Area B, midwife 5
One GP expressed concerns that financial incentives could be counterproductive and could encourage people to relapse in order to get further incentives:
To pay people to stop? That just sounds horrendous, em [laughs] . . . you could, and I’m sure there’s, I’m sure it would work, whether or not that would have a lasting benefit, I would doubt because as soon as you’re not being paid anymore there’s no excuse and also it’s perhaps an incentive to start smoking again and get paid the next time, so I would worry about that.
Area A, GP 1
Alternative forms of incentive, such gym vouchers or relaxation classes, were seen as potentially helpful for increasing engagement among pregnant smokers. However, again, some expressed reservations, with particular concern about how these would be perceived by the public:
I don’t think it’s a great idea because I think you might get the, you know, the rest of the population’s back up.
Area A, midwife group 1
Although there were concerns about the perception of financial incentives, one HP also felt that uptake might not be that high and reflected on a conversation with a colleague in a neighbouring area, where incentives had not generated the interest expected:
I was speaking to the champion from [location] and she was saying we’ve been doing it. I said how do they afford that? I thought that women would snap your hand off, but she said no, the uptake actually was not very good. We know that a lot of smokers are in socially deprived circumstances, so you would think that a financial incentive – but I suppose it just proves the level of the addiction.
Area A, midwife group 1
Social media, smartphone applications and websites
Pregnant women
Some women did not have smartphones, had never downloaded smartphone applications and did not perceive these to be a helpful resource for stop smoking information or support. Other women, although aware of applications, were not interested in using them; either they preferred to get information from another source or they thought that the impetus for quitting had to come from the smoker rather than from an application:
I’m not really interested in all that kinda stuff, I’d prefer to talk to someone and get all my advice and all my help that way. Like, ‘cause as well as that, like the [applications] and stuff sometimes they don’t work and then it’s just, you have to download it all and, just hand me a bit of paper, it’s much easier . . . does that sound weird coming from a 23-year-old eh?
Area A, pregnant woman 5, smoker
On the other hand, some women had quite a positive attitude towards applications specifically for smoking cessation in pregnancy. Among women who were aware of, or had tried, applications for pregnancy or weight loss, there was discussion about the lack of a specific application for pregnant smokers or about smoking not being covered in the existing pregnancy applications:
. . . the only ones I have really downloaded are pregnancy ones so, but they don’t give you any advice. You know like the Mothercare one, I think it would be good if they did a you know are you a smoker part to their [application], I think that would be good because most women do download those ones. You get free money, vouchers and things. I am just doing that. So I think that would be a good way. I think they do a diet part to it . . . and things like that, but nothing for smokers.
Area B, pregnant woman 4, smoker
Attitudes towards general smoking applications that women either had used themselves or were aware of other people using were quite negative. The only type of smoking application that generated positive attitudes among the women was a money savings calculator; being able to visualise the money saved and watching the figure grow was quite powerful for some:
It says so far that’s £348.55, and 1049 fags is what I haven’t smoked . . . it tells you health, motivations, stuff like that. Yeah, how many different hours, yeah, look you see, coming up to 6 months, it tells you all the different things that are changing in your body over time. That’s quite good isn’t it?
Area B, pregnant woman 2, non-smoker
There were mixed views on the usefulness of the internet and websites. Some women were not aware of any online resources for smoking cessation in pregnancy. Others felt that having things online was not convenient and that social network websites were too ‘public’ for them; there was also the issue of credibility of information posted on websites. Conversely, a couple of woman described the internet as a useful and convenient source of information, and another described how online social network websites could be supportive. Some women also mentioned particular websites, the NHS and BabyCentre, that they had looked at for information:
I can look on the internet and stuff but then I don’t really, you know you don’t know what to trust and stuff on there so I prefer you know proper information . . .
Area B, pregnant woman 14, smoker
Significant others
Many SOs were either unaware of the existence of smoking cessation websites and applications for smartphones, or had never used them. A couple of respondents, however, described their actual experience of using smartphone applications for smoking cessation, one alongside their partner, and mentioned the interactivity, which they perceived as an expediter:
We both downloaded something about, you put in about how many cigarettes you smoke a day and how much they cost and the date and the sort of time that you gave up and then every day you can look and it tells you sort of how much you have saved, how much time you’ve saved. All that sort of stuff and then it’s got like milestones so you’ve not smoked 20 fags, you have not smoked a 100, you have saved 10 minutes of your life, and things that you can personalise and things that you can see that are relevant to yourself and it’s really good. And if you don’t look at it for a few days and you go back and you see how much money you have saved you know it’s a good incentive to do it.
Area B, partner 1, non-smoker
Some SOs believed that applications were a self-help approach that would not necessarily work for them but acknowledged that they could be useful for pregnant women. Others had more mixed views on both the usefulness and the effectiveness of applications. Lack of technical aptitude, however, was perceived by SOs as a barrier to their pregnant partners using applications or websites:
I think doing it more interactively is definitely a better way than charts and booklets and leaflets and stuff like that.
Area B, partner 3, smoker
I would say on a scale from 1 to 10 I’d say halfway, it’s really about the willpower you have got inside yourself really.
Area A, partner 52, smoker
For smokers in general, applications or websites were mostly perceived as a positive tool for cessation because of their accessibility and convenience, the availability of information and the ability to see others’ successes with applications on Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com):
I think that’s a better approach now, because I mean even, even the older generation now, my dad’s generation, I mean he has got a smartphone, my mum has got an iPad and an iPhone [Apple Inc., Cupertino, CA, USA], she uses her sat nav [satellite navigation] and all that and I think everybody uses it and it’s just a lot more modern, like you say it’s a quicker way, people text you or to have [applications].
Area B, partner 3, smoker
Some SOs gave their thoughts on the content of smoking cessation applications and websites, and made suggestions for improvement, including the development of an officially recognised application and the inclusion of stronger messages about harms:
I don’t like the word ‘official’, but if they created an official application that had all that kind of stuff and it was well made, because all the ones you can currently get are quite cheap and a bit rubbish, I mean they do the job, but if you could get something like that I think you would, you know you would get people more involved because it was more personal to them.
Area B, partner 1, non-smoker
Health-care professionals
Generally, HPs had fairly positive views on the usefulness of utilising websites such as Facebook or having a presence on Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com). Some felt that these tools would be appealing and accessible to people who had busy schedules or who experienced other social or physical barriers to accessing support:
. . . that’s how a lot of people live their lives now don’t they you know and if you have a Facebook group or whatever for stopping smoking in pregnancy, you would probably get a lot of helpful support and advice from other people going through the same thing . . . and it breaks down barriers of time commitments and so on.
Area B, GP 1
Facebook and texting seems to be the way to communicate.
Area B, midwife 3
However, issues were raised about Facebook, including concerns about confidentiality. SSS advisors explained that this was one reason why their service was not currently using Facebook. Some felt instead that having an increased community presence generally would help improve visibility, accessibility and convenience:
A couple of years ago we did a, I suppose it was kind of like a pop-up it was like a stall at the local market here . . . and it was testing people you know the sort of lung function for COPD [chronic obstructive pulmonary disease] they were doing a sort of mini spirometry thing, and you know we were inundated and people were so interested and that sort of oh I didn’t realise.
Area A, SSS group 1
Text messaging
Significant others
Only about one-third of SOs commented on the use of text messaging to support cessation, and responses were mixed. Approximately half of this group felt that text messaging could be supportive of cessation; for some this was because of accessibility and convenience, whereas for others text messaging was seen to provide more opportunities for support that was less intrusive than telephone calls from smoking cessation advisors:
Well yeah, that is quite good, like an instant support, yes, yes, yeah, something like that yeah just somebody or yeah, on hand just to when you are feeling like that yes, yes that would be more useful I would say, yes.
Area B, partner 8, non-smoker
One partner cautioned that text messaging could also be counterproductive if it was not used appropriately:
. . . as long as you don’t get a text through the day saying I hope you are doing well not smoking because then you will read that and go oh bloody hell smoking, if you had forgotten about it it’s just going to bring it back into your head again.
Area B, partner 2, non-smoker
The remainder of those commenting on text messaging included some who were less sure of its usefulness because texts could easily be ignored, and one partner who felt that it could simply be irritating:
I don’t think it would appeal to me. I think, I get sort of texts sometimes of even from like . . . I will get a text and I will see it’s from . . . and I just won’t want to read it and I think I have one from a few days ago and it’s still not read. I am not bothered, some people might.
Area B, partner 1, non-smoker
Health-care professionals
Text messaging was raised as a good way of keeping in contact with pregnant women, as it has benefits over traditional forms of communication. In particular, it was reported that pregnant smokers and families do not necessarily have landline telephones and, similarly, might not necessarily have enough credit on their mobile phones to be able to pick up voicemail messages:
A lot of people don’t have credit so if you leave an answering message they can never access the answer machine message. So the texting is very much the way to communicate.
Area B, midwife 3
Very few of our families have landlines now they have mobiles. And texting is the way they communicate with one another so often if I have got a hard-to-reach family, I am texting them rather than ringing through a landline.
Area B, health visitor 2
Text messaging was also seen as preferable to telephone calls, for example for cases when pregnant smokers feel uncomfortable talking on the telephone or feel anxious about having to make quick decisions:
In the last couple of years certainly texting is increasingly a communication tool, particularly with this client group and that is how they prefer to communicate. And I think sometimes when you get a phone call out of the blue or it’s not pre-arranged or you are not expecting it, you have to make a decision then and there whereas a text allows you that thinking time so you don’t have to respond straight away.
Area B, SSS administrator 1
Social or peer network interventions
Pregnant women
There were mixed opinions about social network interventions. Views tended to be more positive when women felt that they had already experienced this type of support from their partners, family and friends. More negative views expressed related to women’s perceptions of this type of intervention increasing pressure on them to quit:
Yes, I think it’s a good idea. [. . .] Because you will have more support around you not just like once a week. And you’d have each other for support so.
Area A, pregnant woman 1, smoker
It’s more pressurised though isn’t it . . . Like all together if it’s a big group, I can understand the ones that smoke sat in a group, yeah but if there is like the family members and everything else . . . it would be just pressure, because they are eager for mum to go and she didn’t actually really want to stop just like that, then it’s going to mean more pressure which is going to stop her from wanting to physically to do it.
Area B, pregnant woman 15, smoker
Suggestions for the format of social network support to overcome this potential for increased pressure included encouragement from the woman’s network rather than ‘nagging’ to quit smoking and conveying that it is very difficult to quit an addiction:
That would be actually good because, as I say my partner’s been supportive at times but other times we’ve been arguing and he was pushing me, so maybe if he went to groups like that maybe it would be easier for him to understand; it’s like being a drug addict, or any other addict, you know what I mean?
Area A, pregnant woman 14, non-smoker
Social network support, however, was most often thought to be suitable for other people but not these particular pregnant women or their friends and family, either as a result of typical family interaction or simply because cessation was a much more internalised process for that individual:
And I think if that was my family they would be like well you are the one who is pregnant, you are the one who is having a child, why should we stop? So I don’t think that anyone that I know would go to a group thing, but it might be alright for some people.
Area B, pregnant woman 7, non-smoker
Significant others
Significant others were generally positive about involving partners, family and friends in a scheme to support pregnant women to stop smoking and most said that they would be willing to participate if invited to do so. The main motivation for participation was to support the pregnant woman but some recognised that it could also help them or others who took part. A key reason for the usefulness of such a scheme was the opportunity for the pregnant woman to quit smoking alongside others, which was seen to make the experience easier. This was acknowledged by those SOs who were already trying to support the pregnant woman in this way:
I think it’s, well to me it’s better because there’s a group o’ you, like you and your friends, and it’s, it’s not directly one on one but it’s more than going to sit in a room full o’ people that you don’t know and just one person talking tae everyone.
And what else is helpful about that kind of support?
Like it’s individual as well, so if you’ve . . . if you’re needing like more or less support then you can ask.
Area B, friend 44, smoker
The idea of those closest to the pregnant women taking part in a scheme to aid cessation was perceived to provide a type of support that could not be provided either by HPs and/or by people who had already quit smoking or were in the process of quitting. SOs emphasised the benefit to women of being supported by those with long-standing relationships with them, thus offering greater familiarity and trust. One partner liked the idea of involving family in supporting cessation, as he felt that it was important that all those living in a household take responsibility for the baby’s health rather than only the pregnant woman, thereby minimising the risk of isolating the pregnant woman with related negative consequences:
I think that’s really good, because you are going to go through it together, you are going to have each other for support and it is somebody that you know and trust rather than somebody in an office with a bit of paper.
Area A, partner 48, smoker
I think that would be a lot better than like I say singling the pregnant woman out and saying you have got to give up smoking because you are the pregnant one. Because I think that makes them, there is a lot of them sort of rebel against that and so you know it’s not just me, why should I have to do it myself.
Area B, partner 3, smoker
In addition, when discussing this approach, a mother said that she felt that group support was preferable to individual support, which she believed placed too much pressure on an individual:
I think the support groups are really, really good, I think they are probably better than the one to ones . . . the bad thing about the one to one with [name 2] is a lot of the time you feel like, you are not getting picked on but it’s like the spotlight is on you, whereas when you are in a group, you are all in the same situation and you relate to each other and things, so.
Area B, mother 20, smoker
Some SOs reported that a family or social network approach would mean that those closest to and most keen to support the pregnant woman would be given the necessary information to help them provide the correct support. A mother-in-law spoke of how such a scheme could help close others to avoid well-meaning but unhelpful advice, and instead provide consistent and constructive support.
A minority of SOs were not supportive of the idea of a family or social network approach or questioned its effectiveness. A key theme within these responses was the belief that no amount of support from others would help a pregnant woman stop smoking if she did not want to stop or did not have the willpower to stop:
It’s all about the wanting to do it, willpower and then being able to do it . . . If people aren’t fully committed to wanting to stop they aren’t going to stop. They have got to want to.
Area B, partner 9, smoker
During discussions about social or peer network interventions, there was disagreement among interviewees about the smoking status and intentions of those who may take part to support the woman. Often interviewees assumed that those taking part in such an intervention would be smokers themselves or those who have had some success in quitting before. This raised concerns about the expectations that would be placed on SOs to stop smoking. Although simultaneous quitting or desire to quit was thought by some to be very important in this situation, others felt that SOs may be willing to take part to support the pregnant woman only if it did not also require them to stop or consider stopping; one partner wondered how this type of intervention would work if he were to take part and continue to smoke. Some interviewees appeared to indicate that non-smokers and even ex-smokers would not be interested in taking part:
I wouldn’t have thought they would be that keen on it no, because they wouldn’t really see that as their issue I don’t think. So as supportive as they are, I don’t think that they can offer any insight. Only my dad smokes so nobody else smokes so nobody else knows what it is like so it’s quite hard for them to sit through something without being sort of critical of us being smokers so they wouldn’t have any understanding I don’t think.
Area A, partner 51, non-smoker using e-cigarette
I would quite happily give [name 1] support if it helped her stop smoking . . . but then again she might just say right you can support me by stopping as well and then I’d be like oh well, but no the theory behind it, I would quite happily support her in anything she does so I’d be interested.
Area A, partner 53, smoker
Health-care professionals
Related to family interventions, some HPs felt that increasing service capacity for peer support could be beneficial. One midwife illustrated this by describing a time when she had witnessed a pregnant smoker talking in a group about her knowledge and experiences to others:
. . . she was pregnant, she was about 18. And she said this is what happens, this is why your baby gets more [CO], I know when I stop I am going to crave, when my pregnancy ends I am going to crave it more so I am prepared for that and she said all this. And I thought this is just brilliant. I thought this is better isn’t it because she is living it you know. And the girls all sat and listened actually.
Area B, midwife 3
One commissioner suggested that, for young pregnant smokers in particular, visiting formal services is quite an unnatural thing to do and suggested that peer support would improve people’s motivation to attend. However, some HPs were concerned that peer support could potentially feel stigmatising and that this might deter pregnant smokers from attending:
Sometimes I think it would be good if it was like a group, but maybe that’s sort of stigmatising that as well like oh gosh I am going to be the one in the pregnant smokers group.
Area A, midwife group 2
Increased support for families
Health-care professionals
Several HPs felt that increasing the capacity of SSSs to support families was important, with a number of advisors suggesting family therapy and providing more support for partners to stop. Some HPs emphasised that supporting mothers of pregnant smokers could also be particularly helpful, and one commissioner noted that although pregnant women’s mothers were not turned away from support, this was a less proactive part of the service than supporting partners to stop. One midwife summed it up by describing the potential ‘knock-on effect’ that could occur through offering more support to families:
I think families are definitely key but they are probably the hardest to reach you know, the pregnant woman has at least got some motivation that her family don’t always have . . . so maybe, maybe getting grandparents and fathers would have a knock-on effect.
Area A, midwife group 2
Although family interventions were seen as potentially positive, it was noted by some that they would probably be difficult to orchestrate, in terms of both family practicalities and service implications, as running a family intervention effectively would be time-consuming and resource heavy:
I mean I’ve seen mothers and daughters before together but it’s just again as you know if people can’t come at a certain time, getting them all in the one room for a start isn’t easy and then getting them all in one room and getting them all to agree to do that and stopping smoking is different matter. But yeah I think when it works it works really well.
Area A, SSS group 2
Some also reported that partners might not necessarily see quitting as their responsibility and as a consequence might not attend after the first one or two sessions:
I don’t think it would work, because I think that, when we talk about the people we’re dealing with, I often find that the mums will always buy into all the antenatal care, dads will come, there’s certain classes, they’ll come for labour, they’ll come to a token few, and that already shows you that they don’t see that part as being part o’ their responsibility, you know they see it as the women going to the classes, so I don’t know how you change the culture o’ that.
Area A, health visitor 1
One HP felt that more flexibility to visit families in their homes might help to alleviate some of these difficulties:
Maybe the service maybe needs to think more about going out to people’s homes all the time when families are around. Because as you say trying to get them when they are busy doing other things. You know if they are all home in the evening, Because we don’t actually really say to them oh we will come out to you, because you know we don’t have the facility to do that.
Area A, SSS group 2
Despite being seen as potentially beneficial, one HP noted that although families quitting together could motivate often each other, they could also cause a ‘domino effect’ (area A, SSS group 1) of relapses if somebody in the family intervention were to lapse:
They are just living the life that they live sort of thing, the sort of . . . and I went and there was the dog, there was the grandparents . . . home, but it was a really good experience, but they all fell like dominos, once one of them started.
Area A, SSS group 1
Electronic cigarettes
Pregnant women
Although e-cigarettes were not part of the pregnant women’s topic guide, some women talked about them, and their use was on the rise during the study period. Among those who raised the topic, e-cigarettes were viewed as a harm reduction tool that could potentially help women to stop smoking. There were comments relating to e-cigarette use both in and outside pregnancy. Some women described how family and friends had successfully stopped smoking using these devices. Others saw switching to e-cigarettes as not properly quitting smoking. Although there was interest in using e-cigarettes in pregnancy, generally women were uncertain about their safety. At the time of the study, midwives did not have any national guidance (either in England or in Scotland) regarding these devices. It was, therefore, not surprising that interviewees tended to follow their midwife’s advice that e-cigarettes should not be used in pregnancy:
[I tried] an e-cig[arette] which was really good . . . It’s good to have this you know the smoke coming out and going through all the motions, but I wasn’t allowed anything like that during pregnancy because they have not tested things like that properly yet.
Area A, pregnant woman 18, non-smoker
A few women had used e-cigarettes while pregnant. One woman had used a nicotine-free e-cigarette but had reverted to cigarettes after 2 days and was contemplating trying an e-cigarette with nicotine. Another woman had managed to quit for 2 weeks with an e-cigarette in a previous pregnancy. Previous experience, however, also resulted in some negative views on the effectiveness of e-cigarettes. A number of women considered them an expensive option:
I had one of them e-cig[arette] things you know the ones with the oil, and it lasted 3 weeks and then I got rid of it because it was rubbish to be fair. It was, you had to charge it all the time and then you had to buy the fluid and then it just ended up costing like the same amount as regular cigarettes. It was – there was no point.
Area B, pregnant woman 17, smoker
Significant others
Narratives surrounding e-cigarettes were mixed. Some SOs described their own positive experiences of using e-cigarettes. Others described other people’s successful use of e-cigarettes. Costs, flavourings and doing something with your hands were mentioned as benefits. As such, some of the SOs suggested them as an approach for their pregnant partners:
The e-cig[arette]s work . . . they are good, obviously they are not, well they say they are not harmful, it doesn’t smell, it doesn’t bother other people, you get the nicotine, you get the – I think the difference with the e-cig is that you actually get the sensation of smoking a cigarette so it’s a lot, a lot of it is psychological I am sure it is.
Area B, partner 9, smoker
E-cig [would be helpful to pregnant partner], yeah, they do work.
Area B, partner 9, smoker
Some respondents, however, described unsuccessful experiences of themselves or their pregnant partners using e-cigarettes or were cautious and felt uninformed:
Another way that I tried to support her was initially getting her some is it e-cigarettes? . . . But I think unfortunately the one we got, because I didn’t know there are different flavours and different strengths and everything, it made her feel a bit sick.
Area B, partner 8, mother, non-smoker
Specialist pregnancy versus generic cessation support
Pregnant women
Having access to specialist cessation support during pregnancy was important to women in area A. Advantages over generic support included greater understanding and knowledge about pregnancy-related issues and NRT, and more targeted risk information:
I think it is definitely good because then it, it makes you see it fae a different light . . . wi’ you being pregnant you’re limited to what you can get, so it is good tae[to] get the information on why you’re limited on that, and you know, and what can happen tae the child and how it affects the child and you know different things, because it’s just things that you don’t even think aboot[about], when you’re smoking you don’t even gi’e[give] it a thought about the baby tugging on the cord for 20 minutes.
Area A, pregnant woman 11, non-smoker
It was more difficult to know whether or not women in area B saw benefit in a specialist service, most probably because fewer participants had accessed the SSS. Among those who had not engaged with the SSS, there tended to be a negative view of smoking cessation services and women doubted that it would be of benefit to them:
I don’t think I would like that. I just think it’s, I work a lot as it is, so I am quite busy all the time, and I just think having to go to like a stop smoking, unless you are ready you know going to be willing to go . . . I don’t feel that service would help me.
Area B, pregnant woman 4, smoker
Significant others
All responses but one from SOs comparing dedicated SSSs for pregnant woman with generic SSSs were from area A. These SOs felt that a dedicated service for pregnant women was important in terms of pregnant women being able to obtain support specific to their situation, with some SOs relating this explicitly to harms to the baby. Others were less sure that the support should be different:
I think it probably would be more helpful if it was tailored more towards pregnant you know so that they could have their own, because you could obviously talk about different things and offer different things to what you would generally.
Area A, mother-in-law 47, non-smoker
Most of the SOs’ responses were positive towards the pregnant women receiving smoking cessation help. However, it was often unclear in their answers to the question whether or not this was comparing pregnancy-specific help with generic help or if it was comparing it with no help:
I think it is really important to be honest, because a lot of pregnant woman give up with that help. I think they would find it a lot harder if they didn’t have the help if you know what I mean.
Area A, partner 47, non-smoker
I think it’s a fantastic idea, I think it’s a really, really good idea, the person who came up with it needs a medal.
Area B, partner 7, non-smoker
Campaigns
Pregnant women
When interviewees were asked whether or not they could remember any mass media campaigns relevant to smoking in pregnancy, some women could not recall any, although there was some support for this idea:
I mean in pregnancy it should be on TV a lot more because they only advertise it on the smoking packets about the babies. In the adverts they only go on about it can give you lung cancer, not what it can do to your baby, so I think for pregnant women, smoking and drinking everything like that should be a bit more on TV, a bit more out there for them to see.
Area B, pregnant woman 12, non-smoker
Some women, however, could recall and clearly describe advertisements they had seen about passive smoking, either in the home or in the car. The influence of these was apparent when women described plans for not smoking around the baby after delivery. Women appeared to have a high sense of the risks from passive smoking and many considered it more harmful to the baby than smoking in pregnancy. Some women were encouraging of the use of repeated shock tactics in advertising, although one woman reported that she would just avoid exposure to such messages:
I’ve seen adverts, about, adverts where like you are smoking and the child is in the room and the smoke is going all around the child . . . I think they are good, they scare people don’t they, like I’d never, even if I was smoking now, which I am, but when the baby comes along like I’d never smoke in the same house as my baby, I’d always go outside because obviously that’s, it’s my choice me smoking when the baby is inside me, but it’s not the baby’s choice to be around the smoke do you know what I mean I would go outside and smoke.
Area B, pregnant woman 11, smoker
Many interviewees in area B recalled the ‘Stoptober’ stop smoking campaign. This is not surprising, as this campaign ran in England where area B was located but not in Scotland where area A was sited. Several described engaging with Stoptober and the campaign encouraging a quit attempt among themselves or their family members. However, there were mixed perceptions on the usefulness of information provided and whether or not it helped with smoking cessation:
I think they are pretty cool. For people who are trying to stop, that want, they have got that support as well as going to the doctors and stuff. . . . So that is quite cool to be involved in something like that.
Do you know anyone that has stopped smoking as a result of that? Stoptober?
No, I know people that have tried it, but have failed. . . . it would have been a bit of fun to be involved with that [if smoker at that time].
Area B, pregnant woman 12, non-smoker
Significant others
Many interviewees could not recall seeing or hearing smoking cessation campaigns on TV, radio or in printed media. However, of those who were aware of mass media campaigns, recall of the key narrative was quite detailed:
I remember seeing the adverts that were like pretty horrible . . . It was the one that really was pretty creepy, I think they were in the car and there was a wee baby in the back seat and the guy had the window open and it was like a snake or a hand . . . and it went up and round the bairn[baby], oh, it was horrible.
Area A, friend 44, smoker
However, in terms of a focus on the actual effects of smoking on babies, interviewees reported a lack of information:
There is not an awful lot of information out there about the effects of smoking on babies to be fair, I mean we have got four kids ourselves and there is not once that I’ve read a leaflet, seen an advert, anything about what affect it has on a baby, just the effects on the person who is smoking.
Area B, partner 10, non-smoker
When SOs were asked whether or not they thought campaigns would impact on their pregnant partner, responses were mixed. Some thought that campaigns could have a positive impact on a woman’s smoking, whereas others considered that there would be little or no impact. Responses were also mixed in terms of campaigns having an influence on the SO’s own smoking behaviours or on their encouragement/support of the pregnant woman:
No matter what actual advertisement you put on, if you actually want to stop, you’ll stop, if you don’t you won’t.
Area A, partner 24, non-smoker using NRT
You see the adverts ken[you know], like the smoke going into like the kids . . . Yeah it’s a bit mm, it makes you think . . . If you are sitting there around your kids and you are smoking and you see that advert you are kind of, you think well maybe not, so.
Area A, partner 55, smoker
Some SOs suggested that campaigns featuring shocking images, better tailored to the target audience and appearing at certain times of the day could enhance their impact:
I think for them to be successful they have got to be sort of really shocking or have a really powerful message so that that’s it you know I’ve seen it once, I am giving up.
Area A, partner 1, non-smoker
Health-care professionals
Several HPs felt that more government campaigns would increase people’s awareness about stopping smoking in pregnancy. Some referred to awareness campaigns about passive smoking to demonstrate their point that media can have a significant impact:
I think the impact of those sorts of campaigns and the advertising that we are seeing on telly about the impact on passive smoking on children, has changed parenting behaviour in terms of smoking over their children.
Area B, health visitor 2
It appeared, in some instances, that government campaigns made it easier for HPs to approach the issue of smoking in pregnancy and post partum:
Some o’ the government advertising, I really think it’s a very, very powerful, I would definitely say that my job became easier approaching smoking when the passive smoking adverts were on the TV . . .
Area A, health visitor 1
However, although previous campaigns had, from HPs’ recollections, tended to focus on postpartum risks, some felt that more campaigning around the risks of smoking during pregnancy was needed, including the use of ‘scare tactics’ advertising:
. . . they always talk about babies and children, maybe they need to do something advertising like a fetus you know.
Area A, midwife group 1
The TV advertisements, the packets, the notes on the packets of cigarettes, I think that maybe a scare tactic with regards to baby would be a good thing, because I am not sure that people really do you know . . .
Area B, midwife 5
Leaflets and posters
Pregnant women
Some of the women liked to hold on to leaflets, as a valuable reference source for themselves and others; for other interviewees, the leaflets held a more short-term value, read at the time but ultimately disposable:
The leaflets are good but once you’ve read the leaflet you chuck it out.
Area A, pregnant woman, non-smoker
Some of the women had good recall of the information contained in leaflets and had found the information useful and persuasive. One woman gave quite a detailed evaluation of a stop smoking leaflet she had been given, reporting it as too lengthy and quite technical, and suggesting that it could be better targeted to appeal to all age groups. Other women had similar suggestions:
I mean like certainly I think it’s just how they put it across I mean I think if I got an e-mail just with a big boring like 20-page essay, that’s not going to stick in my head. But if they maybe something like an e-mail with bullet points and interesting facts that would appeal to me.
Area B, pregnant woman 13, smoker
The main area identified for improvement related to the amount and type of smoking information provided in pregnancy, with some women wanting more written information and some wanting a stronger message about the harms to the baby to help motivate them to stop smoking:
Yeah, I think, I think if you shocked them more with what could happen to them while they are pregnant, then what could happen to the baby, then I think, you know just a picture of a pregnant tummy on the back of a cigarette packet is not beneficial. I think if the midwife was giving you leaflets with things in it saying this is what could happen, I think that would be quite good.
Area B, pregnant woman 4, smoker
For leaflets that women could pick up themselves (as opposed to being handed them or receiving them in the post), most women reported that these were available at their GP surgeries and hospitals, although not always to take away with them as some were displayed on the wall. Only a handful of women mentioned seeing posters displayed in their GP surgery, at the hospital and at the chemist:
. . . I think you need a bit more, you only get the occasional poster in a chemist or whatever if you are in there, it would be nice if you seen a wee bit more.
Area A, pregnant woman 18, non-smoker
Significant others
Significant others recalled that leaflets promoting smoking cessation and self-help to quit were usually seen, or handed out, only in primary and secondary health-care settings. The locations for signs, wall charts and posters were the same, although libraries were also mentioned:
Yes, I was aware and I think generally you see signs up in libraries; they are quite often in the doctor’s surgery as well so you know it’s quite prominent . . . as a non-smoker I mean I have noticed the availability of these posters and the courses and things available.
Area B, mother 8, non-smoker
Some SOs thought leaflets had been, or may be, useful to their pregnant partner or friend:
I think now with her being pregnant she might pick it up tae[to] help her stop smoking and what websites tae look at, but before she was pregnant I don’t think she would.
Area A, partner 16, smoker
She [pregnant partner] brought one leaflet with advice on it, how to stop smoking and why you should stop smoking and stuff like that . . . I think it was helpful aye because she read it and she obviously, once she read it she was kind of starting to cut down after she had read what obviously she read.
Area A, partner 46, non-smoker using e-cigarette
One respondent also spoke of how leaflets had been informative for him:
Well getting the reading from the [CO], the leaflets that tell you what’s in it, the carbon and all that, it’s, that put me off quite a lot. About what it can do to the baby when it’s inside you that put me off.
Area A, partner 52, smoker
However, respondents generally perceived leaflets as useful for some smokers to help them stop smoking but not for others. In addition, some were more negative in their assessment of leaflets; they were described as unhelpful, too time-consuming to read or something they would never read:
Em, well usually if I get a leaflet I just bin in, I didn’t [laughs], I never really read it like.
Area A, friend 44, smoker
Other intervention approaches
Significant others
Other types of interventions or approaches that SOs believed would help pregnant women who wanted to quit smoking included use of both graphic imagery to visualise the impact of smoking on the baby and graphic experiences presented by people with lung cancer or smoking-related illness.
Other suggestions offered by SOs included ensuring that pregnant women were well informed to allow them to reflect on a decision to quit, offering a range of alternative interventions and approaches to allow women to tailor support to their individual needs, providing mechanisms to enhance willpower, providing a healthy alternative/replacement to smoking and offering a range of alternative NRT formats compatible with morning sickness and hypnosis:
What will work for one person won’t necessarily work for another, so it just depends on the person [. . .] But if the support is there to sort of try these different things and they are offered these different things then they will find the one that will suit them so trial and error.
Area A, mother 20, smoker
So they are given a list of different options to fit in with their background and their ongoing troubles, and their lifestyles and they should make a choice whether they want to try one.
Area B, partner 10, non-smoker
Health-care professionals
Several HPs and advisors felt that targeting younger women before they become pregnant could be an important preventative intervention. HPs also suggested specific postnatal support, to reduce the risk of women resuming smoking after giving birth. In addition, several SSS advisors suggested that improving the physical space occupied by the SSS could help improve retention, by having more inviting premises in accessible locations. Overall, however, HPs emphasised the need to increase the number of specialist staff members able to deliver smoking cessation in pregnancy and the need to improve existing services through adequate funding and longer-term future planning.
Summary
A summary of interventions suggested and each group of participants’ views on these is given in Table 7.
| Intervention/approach | Participants’ views |
|---|---|
| Financial incentives | Pregnant women, SOs and HPs all had mixed perceptions on the use of financial incentives to encourage smoking cessation in pregnancy. Positive views focused on providing motivation for those with financial concerns with the emphasis on ability to buy things for baby, struggling with willpower to stop smoking and increasing engagement with SSSs. Negative perceptions focused more on moral arguments against using financial incentives and the extent of their effectiveness after they stopped |
| Social media, telephone applications and websites | Pregnant women had mixed views on applications and websites as resources for stop smoking information or support. A money savings calculator application generated the most positive attitudes from women and lack of a specific smartphone application for pregnant smokers or smoking being covered in existing applications was discussed. SOs were largely unaware of applications and websites for smoking cessation. HPs had fairly positive views on the usefulness of websites such as Facebook or Twitter, but had concerns regarding confidentiality |
| Text messaging | HPs perceived text messaging as a good way of keeping in contact with pregnant women, particularly those who did not have landline telephones or enough credit in mobile phones to pick up voicemail messages. SOs were less sure of the usefulness of this approach for pregnant women |
| Social or peer network interventions | HPs and SOs were generally positive about involving partners, family and friends in schemes to support pregnant women to stop smoking. A key reason for the usefulness of this approach was the opportunity for pregnant women to quit alongside others, facilitating an easier quitting experience. Pregnant women themselves had more mixed views about this type of intervention, with more positive perceptions stemming from previous experience of this type of support. Negative perceptions related to increased pressure to quit |
| Increased support for families | Many HPs felt that increasing capacity of SSSs to support families was important but acknowledged the practical difficulties and resource implications of family interventions |
| E-cigarettes | Although e-cigarettes were not part of the interview topic guides, some women and SOs talked about them; these were on the rise during the study period as a harm reduction tool that could potentially help women to stop smoking, but there was uncertainty about the safety of using them |
| Specialist pregnancy vs. generic support | Advantages of access to specialist cessation support during pregnancy were perceived to be a greater understanding and knowledge about pregnancy-related issues and NRT, and more targeted risk information |
| Campaigns | Pregnant women, SOs and HPs were generally supportive of advertising campaigns. The influence of advertisements relating to passive smoking was most apparent, with many considering it more harmful to the baby than smoking in pregnancy, which facilitated the ease of raising the issue for HPs. A lack of focus, however, on actual effects of maternal smoking on the fetus during pregnancy was emphasised |
| Leaflets and posters | Information leaflets were seen to be useful and persuasive; however, length and content of leaflets could be offputting, with little appeal to all age groups. The inclusion of stronger messages about harms was perceived to be helpful for motivation to stop smoking |
| Other intervention approaches | The use of graphic imagery to visualise the impact of smoking on the baby, offering a range of alternative interventions and NRT formats to allow women to tailor support to their individual needs, and providing mechanisms to enhance willpower were among the other interventions suggested by SOs. HPs suggested targeting younger women before they became pregnant, offering more relapse prevention support and having more inviting and accessible SSS premises |
Chapter 12 Discussion
The preceding chapters have set out the barriers to and facilitators of smoking cessation in pregnancy from the perspective of women themselves and of two groups that have a potentially important role to play in helping or hindering efforts to stop smoking: women’s partners or SOs, and HPs. Perspectives were drawn from three systematic reviews of the literature and interviews with each group in two study sites, one in England and one in Scotland. In addition, we sought the views of study participants regarding existing and new services and interventions, which are set out in Chapter 11.
This concluding chapter aims to synthesise our findings drawing on the theoretical framework for this study. This was the SEF described in Chapter 2. Here, we begin by reminding the reader of the key components of the SEF before moving on to discuss the findings within each ‘layer’ of the framework. Existing interventions are discussed as part of the organisational layer of the framework, with suggestions for future interventions, building on existing research, described in Future research and interventions.
Social–ecological framework
The SEF conceptualises behaviour as the outcome of an individual’s interactions with their environment. Although the term may be unfamiliar to the public health community, the underlying framework is not. It represents health and health behaviour as a series of interlocking layers running from micro to macro. Widely known examples of this framework include the model of the social determinants of health originally proposed by Dahlgren and Whitehead. 77
As outlined in Chapter 2, the following domains of influence on smoking and smoking cessation were identified:
-
individual characteristics, including knowledge and beliefs, mental health and well-being, and material circumstances
-
interpersonal factors, including relationships with SOs and HPs
-
community factors, including neighbourhood quality and local resources, cultural norms and social networks
-
organisational factors, including service provision, workplace resources, practices and regulations
-
societal factors, including the structure of the labour market, welfare systems and family policies.
In terms of the data collected, the individual, interpersonal and community domains were important and relevant to all three groups of study participants, and also came through strongly in the systematic reviews. 57–59 The organisational domain was also relevant to all three groups but was particularly salient when considering barriers and facilitators in terms of the relationship between pregnant women (and to a lesser extent their SOs) and HPs. Little information was available on higher-level societal influences (labour market, welfare systems and wider policies); such influences are hard to capture in studies in which the individual, rather than the wider system, is the focus of data collection and analysis. Not unexpectedly, these structural-level factors did not feature strongly in either the systematic reviews or the interviews. Instead, the data focused more on the views and perceptions of strangers or on health-care policy. Thus, we discuss the community and societal domains together, along with a synthesis of data relating to the other layers of the SEF. In our synthesis, we refer to evidence from the systematic reviews and our interviews together, aiming to integrate data from both within the SEF.
Individual characteristics
Through the systematic review and in the interviews in both study sites, women described the place that smoking had in their lives and identities. The first point to emphasise is that the vast majority of women in both elements of the study were living in disadvantaged circumstances and, in our interviews, they described some of the financial, housing or family issues they were facing. In addition, our interviews were conducted in the home and, thus, researchers saw for themselves that most women in the study had few resources; some were not working and had partners who were unemployed or, alternatively, they were single mothers. There were exceptions to this, but these day-to-day challenges influenced how women described their smoking and the place it had in their lives. These challenges are also reflected in the systematic review of women’s views but were perhaps even more stark in our interviews in a UK context, in which women in routine and manual occupational groups are six times more likely to smoke in pregnancy than professional or managerial women, and smoking in society is very closely associated with socioeconomic disadvantage. 91
With this context in mind, the women we interviewed, and also to some extent those included in the review, described smoking as conferring psychosocial benefits, in particular by providing a break and relieving stress in the context of disadvantaged or difficult circumstances. Beliefs about the risks of smoking during pregnancy were also a key theme in the review studies and interviews with the women and SOs.
Stress and enjoyment
In the studies included in the systematic review, across countries pregnant women described smoking as a resource for managing stress and suggested that attempting to quit could take away a stress management tool. 110–120 This is a consistent finding in the literature that has been described since members of our team first conducted research with disadvantaged women in the 1970s. 151
The importance of smoking to reduce stress was also described by partners and HPs. For partners, continuing to smoke themselves was described by some in the review studies as a mood management strategy and a ‘time out’. 121,152–155 Some review study participants cited stresses around their partner’s pregnancy, including her changes in mood, with smoking described as ‘. . . the excuse to get out of the house’. 154
Despite these accounts indicating that smoking helps to reduce and manage psychological stress, the wider literature provides more insight into the relationship between smoking and stress than in earlier studies. Some of the stress that women, or indeed partners, feel when trying to reduce their smoking or to stop smoking is likely to be a result of nicotine withdrawal, which creates cravings and feelings of anxiety. Pregnancy can, of course, exacerbate these feelings. However, it is known that adults who stop smoking are far more likely to report lower levels of stress, and that smoking cessation is beneficial for stress management and reduction. 169,170 It is important that this evidence is explained to women; however, it is also known that midwives and other HPs are not always aware of this evidence.
In the review women also talked about the enjoyment of smoking, as did partners who in a number of studies said they could not imagine their lives without cigarettes. 121,156–158 Enjoyment of smoking is often neglected in the smoking cessation literature but it is a key component of continued tobacco use and involves a wide range of factors, not just craving for nicotine. Women and partners in the review studies talked about the benefts of a smoking break by themselves or with others. 111,115,120,122–125 This was mirrored in our interviews. Smoking was a key part of daily routine, relieving boredom and providing a welcome pause and time away from other children, an unemployed partner or other members of the household. Smoking as a break in the workplace was also discussed and is described in Community influences supporting smoking cessation.
Beliefs and risks
Women’s (and partners’) beliefs about the risks of smoking were a central theme in this study. These beliefs could be modified or changed by interventions including contact with HPs and, in particular, SSSs. However, in the review studies and in our interviews, many of these beliefs stemmed from norms (discussed in Community and societal factors) or knowledge influenced by mass media campaigns or, arguably, earlier interventions including health information in childhood or early adulthood. Risk perceptions were often described as relating to smokers in the population, therefore a disembodied risk, rather than a personal one. Some women in the review studies questioned the applicability of these risks to them or even if these risks were ‘real’ at all. 113,115–117,126–128 In addition, the partner’s review illustrated a particular and widespread scepticism among those interviewed in the studies. They accepted there were some risks to smoking in pregnancy but felt that what was missing was more specific information on how smoking was damaging to the baby or indeed to themselves. 53,159,160 Partners in the review studies also felt that there were inconsistencies in government advice, and smoking partners had negative views about tobacco control policies.
In our own interviews with partners and SOs, there was a broader acceptance of the risks of smoking in pregnancy than reported in the review studies, perhaps reflecting more current knowledge and attitudes. Awareness of the links between smoking and lower birthweight and/or miscarriage, for example, was evident. However, even in our interviews, doubts were raised about the consistency, severity or magnitude of risks.
Beliefs about risks were shaped by personal experience. In the partners’ review, first-time fathers were more concerned than those who already had children, where the mother had smoked during her pregnancy and the baby appeared healthy. As outlined in Community and societal factors, for women, both their own experience and that of their mothers or other women in the community served to challenge HPs’ advice about the dangers of smoking or the benefits of quitting. Partners interviewed for our study also provided examples of healthy babies born to mothers who smoked, pointing out that known evidence on risks may not apply to all.
There was some distinction drawn, however, between risks in utero and once the baby was born, with pregnant women perceived by some to act as a ‘filter’ for the worst effects of smoking. In contrast to smoking in pregnancy, in which doubts were expressed about the risks to the unborn baby, there was an almost universal agreement among women and partners in both the systematic review studies57–59 and our interviews that babies should be protected from exposure to SHS. There was, therefore, widespread acceptance that exposing a baby or child to SHS was unacceptable. 53,121,152,154,157,159
Beliefs and cutting down
In our interviews with pregnant women in particular, interviewees described avoiding thinking or learning about the risks of smoking during pregnancy. For those who did engage with this evidence, a common response was to talk about the advantages of cutting down, which many perceived as conferring benefits. Some partners and SOs interviewed reported similar beliefs. In addition, a small number of women reported that they perceived that HPs encouraged cutting down.
The evidence on smoking reduction is now much clearer, including in pregnancy. Women who cut down without using NRT are more likely to engage in compensatory smoking, smoking more of each cigarette and taking longer and harder drags on each cigarette to get the nicotine they need. 171,172 This results in exposure to more toxins per cigarette, resulting in few, if any, health benefits to cutting down. 173 As with stress reduction, midwives and others may not know or understand this evidence, which may result in mixed messages being given to women. In contrast, research suggests that smoking reduction with NRT does not result in the same compensatory smoking and can also represent a step on the pathway to quitting. 174,175 Women who cut down their smoking in pregnancy should be supported to do so with NRT or other nicotine-containing devices, and the importance of stopping all tobacco use should be emphasised. 176
A finding of the review was that low birthweight was understood as a risk of smoking in pregnancy but also seen as an advantage, with a smaller baby perceived to make labour and delivery easier. 115,123,129,130 This view was still present in our interviews but from only a small number of women across both study sites, perhaps reflecting better current understanding, including via advice from HPs. This could be emphasised, however, in future training.
Identity
Women’s perceptions that smoking as a behaviour was part of their identity came through in the reviews of studies with women and also in our interviews with pregnant women and new mothers in both study sites, although not as prominently as in other qualitative research with non-pregnant populations who smoke. In terms of this discussion, it is perhaps best described as a set of beliefs that played a powerful role at different stages in women’s lives. Being pregnant represented a break for most women from the ‘acceptability’ of a smoker identity. This perception served as part of their motivation to stop or at least to try. Women interviewed in both sites, particularly those who managed to quit at least at some point during pregnancy, described willpower and determination as very important in the success of a quit attempt (reflecting any smoker’s experience of stopping), but with the added impetus of pregnancy-specific motivators as highly salient. Some of these motivators were tangible, such as nausea or changes in taste and smell, and others were sensed or perceived motivators, including the importance of stigma, which is discussed below in community and societal factors.
There were distinctions in smoking identity between being pregnant and having had the baby, and this emerged in both the reviews and in our interviews. During the postpartum period, women in the review studies in particular talked about ‘reclaiming’ part of their former self that they associated with smoking alongside specific more tangible benefits that they associated with tobacco use (e.g. weight control). Smoking cessation was perceived by some women as a temporary change undertaken for the baby in utero and while breastfeeding, particularly in the older studies in the reviews. 115,126,128,131 As such, any return to smoking in the postpartum period was seen as an assumed resumption and not a relapse.
In the systematic review, for men who contined to smoke, being a smoker was perceived as conveying autonomy and independence and a positive masculine identity. 121,155 Some men felt that they had a ‘right’ to smoke that was curtailed by tobacco control measures such as banning smoking in public places. 53 Some partners in the review studies talked about the fact that being forced to agree to quit could compromise parts of their (masculine) identity as well as causing tension or arguments. 152,155 However, a partner’s smoking identity could also be challenged by the fact that they were, or were about to become, a father. The review studies showed that some men recognised that their continued smoking would undermine their capacity to be a positive role model for their children and also, fundamentally, could harm their capacity to be around as their children grew up, given the real risks that continued smoking would pose to their life expectancy. 121,153,154,159,160
Interpersonal factors
A key focus of this study was how women’s interpersonal relationships acted as barriers to, or facilitators of, smoking cessation during pregnancy and in the postpartum period. The findings on this were detailed, although the results were not always the same between the studies in the systematic reviews and the interviews conducted in the two UK study sites. Our interview findings on the interpersonal element of the SEF are particularly important, as our study represents the largest to date that has interviewed the partners of pregnant women who smoke in the UK (we completed interviews with 25 partners and seven SOs).
Relationships with partners and SOs were central to how women experienced smoking, and their attempts to stop and maintain abstinence, and to avoid relapse. In both the systematic review studies and our interviews, examples of these relationships both facilitating and hindering smoking cessation came through clearly. Interpersonal relationships between pregnant women and HPs were also important; support from HPs was not just at an organisation level.
Support from partners and significant others
It was identified, in a number of studies included in the review, that partners helped to encourage and motivate women. There was a shared understanding that smoking cessation was not necessarily easy but it was important. 115,121,132 Some men who were smokers recognised that if they wanted their pregnant partner to stop, then they should attempt smoking cessation as well. 53 One study in the systematic review of partners explored this issue in depth and outlined how men proactively chose not to smoke around their partner in order to assist her quit attempt, and once the baby was born chose not to smoke around their children. 152 Men described undertaking activities together with their partner that involved not smoking and also offering praise and encouragement to women when they cut down or stopped. Men’s own attempts to quit, however, were often about being a good role model for their children and/or recognising the harm caused by SHS exposure, or at least its smell or even concerns about third-hand smoke on clothes or furnishings. 154
Partners who were non-smokers could serve as important supporters of a quit attempt. In the review of studies of partners’ views, just 10% were non-smokers, so few data were available on this aspect. This small group of men did find it challenging if their wives or girlfriends continued to smoke but also recognised that if they applied pressure on them to quit, it could in some circumstances ‘backfire’ and result in increased levels of smoking. 152
More information on non-smoking partners and SOs and their support in smoking cessation was available from our interviews, as just over one-third were ex-smokers or never-smokers. Particularly in discussing this with pregnant women, living with a non-smoking partner (or a mother who did not smoke) was perceived as helpful, normalising non-smoking in the household. In the few instances in which partners stopped alongside the pregnant woman, this was described as very helpful, a joint effort recognising the importance of the unborn child. Even the partners or SOs who were still smoking when interviewed reported actively trying to stop or cut down to support the pregnant woman and the unborn child. They talked about not wanting to be a ‘hypocrite’ for urging the pregnant woman to stop while not changing their own behaviour and therefore at least made attempts to stop, including some partners engaging with SSSs.
Barriers from partners and significant others
On the other hand, partners or SOs also acted as a barrier to smoking cessation during pregnancy. This finding was particularly prominent in the studies reviewed 112,128,133 but was also reported by some of our research participants. This negative influence operated in one of two ways. The first, and most common, was when the partner smoked and their continued smoking affected the couple’s interpersonal relationship in a variety of ways. The second was when the partner applied pressure on the woman to quit or maintain abstinence and this pressure had negative consequences.
In our interviews, women whose partners continued to smoke expressed disappointment or annoyance that either their partner had not tried or their attempts were unsuccessful, or their partner’s smoking behaviour somehow mattered less because they were not carrying a child. Women reported how some smoking partners blamed them for potential harm to the baby while simultaneously exposing them to SHS by continuing to smoke in their presence. They also expressed regret about a loss of shared rituals and time together that had been enjoyed when both smoked or at least when the woman was not trying to stop. Reported cravings, stress and mood swings combined with bickering and less time spent together could sometimes create a difficult situation.
In the review, women talked about partners who monitored their smoking, sometimes in ways that were controlling or abusive. 111,115,117,121,132,134,135 Examples of confrontation, removing cigarettes or withholding money were provided. 121,132,134 Some women who were struggling to quit felt forced to reduce their smoking or at least pretend to be doing so. Women and partners in the studies also expressed regret about the loss of a shared ritual and time together that smoking involved. 134,159 Unfortunately, however, the review also showed inconsistent or manipulative behaviour by some smoking partners, who might offer cigarettes during stressful times and then reprimand women for smoking on other occasions. 135
Support from health-care professionals
Although HPs’ roles in smoking cessation often operated at the organisational level, the qualitative data also highlight the importance of interpersonal relationships between women and midwives or doctors, for example in discussing smoking and supporting cessation.
In the reviews, women related how midwives, nurses or doctors treated them with respect and in this context they felt supported to talk about and try to change their smoking behaviour. HPs who were ‘facilitating’ were described as friendly, non-judgemental and applying a positive and systematic approach to supporting cessation. 115,116,122,123,136 In our interviews with women, there was a strong focus on the midwife or, for those who accessed cessation services, the SSS advisor. Women often described their midwife as supportive and reassuring, and they viewed this as an important and positive relationship. Overall, they did not feel pressurised by midwives in relation to smoking cessation.
In the review of HPs’ views, the value of a positive relationship with the pregnant women was also emphasised. A trusting relationship was described as a prerequisite to fulfilling their responsibilities to the woman and her baby, including around smoking cessation. 162 It was also considered important that, as HPs, they adopted positive and non-judgemental approaches, encouraging women to take small steps towards quitting, encouraging cutting down to quit and using positive messages around the health of the baby. There was also recognition in the review studies and interviews that HPs could take a more assertive position, drawing attention to the negative effects of smoking on the baby in pregnancy and regarding the risks of SHS after birth. 133,162–165 The systematic review of HPs found that professionals recognised the importance of involving women’s partners in smoking cessation advice but this type of engagement was described as difficult – perhaps more difficult in the review studies than in the experiences of partners and SOs interviewed for this study.
Community and societal factors
The influence of wider social networks in women’s communities and beyond emerged as an important theme in our reviews and interviews. There were both smoking and non-smoking norms that influenced pregnant women’s attempts to stop smoking and their success or relapse.
Community influences hindering smoking cessation
A prevalent theme to emerge from the reviews was that smoking was still considered a normal part of life for many in the communities where the studies took place. It was part of relationships in the home, workplace and community. 53,112,117,120,123,132 HPs widely understood that, despite their own role in promoting smoking cessation, they were pushing against community or societal (‘social determinants’) factors that influenced women’s smoking and that these factors could often outweigh any attempts they made to help women stop. 113,164–166 Risks of smoking in pregnancy were downplayed through the experience of others who had smoked during pregnancy but had healthy children, and stopping smoking was perceived (particularly in the studies in the systematic review of pregnant women) as severing important social connections. 111,137
The normalcy and commonplace nature of smoking in the local community was also mentioned by our interviewees, both pregnant women and SOs. Some listed those in their social network who smoked, often the majority. At least one partner mentioned that all of the pregnant woman’s friends smoked. Some examples of friends or family continuing to smoke in front of the pregnant woman were also given. There was a general recognition that these high smoking rates in the (often) disadvantaged communities where women lived made stopping more difficult.
Community influences or norms also undermined beliefs about the risks of smoking in pregnancy, as discussed above. In our interviews with pregnant women and some members of their social network (e.g. mothers or friends), the theme of previous healthy babies born to smoking mothers was also prevalent, and in some instances the pregnant woman herself had a mother who had smoked and she did not see this as having impacted on her own health in child- or adulthood. This ‘experiential’ evidence was presented to counter or refute the risks described by HPs. However, in the interviews a small number of women also provided concrete examples of when they thought that smoking had harmed the baby of family or friends, with miscarriage, low birthweight or asthma/respiratory conditions mentioned.
Norms also had a role to play in the smoking status of women after the baby was born. The accepted nature of smoking in some communities where the study took place did not extend to seeing women smoking during pregnancy (or when the pregnancy was visible) as ‘normal’. It was widely understood that it was not or at least should not be normal. However, returning to smoking after the baby was born was more acceptable in some cases; this was apparent in a number of interviews. In addition, in the review studies with pregnant women there was a widespread expectation – among women and their social networks – that they would resume smoking once the baby was born. 112,115,137,138
A final theme relating to community or societal views evident in the reviews (but not in the interviews) was that of status. Smoking was potentially a tool to conform to a desired female form in that it was also perceived as controlling weight gain. For younger women in particular, this was seen as particularly important in maintaining friendships and social standing. 123,124,129,130,136,139
Community influences supporting smoking cessation
Community influences also supported women’s efforts not to smoke, although less often than they supported continued smoking. In the reviews, smoking in pregnancy – and, to a lesser extent, resuming smoking post partum – aroused disapproval from some peers, particularly when the pregnancy was visible. 110,112,117,119,121,122,133,135 For some women, disapproval could facilitate positive changes in their smoking behaviour, although this was not the case for all. 112,115–117,121
The pregnant women interviewed in both study sites described negative views conveyed by colleagues or strangers. Some also talked about how these social norms had influenced their own negative view of women who continued to smoke during pregnancy prior to finding themselves in the same situation. Workplaces that were non-smoking could help women to stay away from cigarettes, although those working with other smokers found losing their cigarette break difficult, as discussed above regarding interpersonal relationships and continued smoking. This was also the case for partners, which was demonstrated in both the systematic review of partners’ views and the interviews with partners. 158 Recent research on smoking in pregnancy by members of the team showed the importance of avoiding time with other smokers as an important relapse prevention strategy, and this was a theme supported by the interviews in this study. 177
Organisational factors
Although a range of organisational factors can influence smoking behaviour, in this study this element of the SEF focused on the health-care setting and systems issues relating to how women and their partners interacted with processes to address smoking in pregnancy. Organisational factors that supported or hindered smoking cessation identified in the reviews and interviews are synthesised here, followed by a range of practical suggestions for improving the organisational context for smoking cessation drawn from the study interviews.
Organisational factors supporting smoking cessation
In the interviews, smoking was normally discussed with women by midwives (or in some cases their GP) early in pregnancy and in all cases at the booking appointment, no matter how briefly. In the interviews with women, partners and HPs, there was a general expectation that smoking would be raised, reflecting policy in both study sites and nationally in the UK. This expectation was helpful, and in general women understood that the midwife’s role in particular was to gather information and, where appropriate, refer on to a SSS.
In the review studies, in which 190 HPs’ views were included, and in the interviews with 48 professionals, supporting smoking cessation in pregnancy was widely recognised as needed and appropriate, but this could depend on the HP’s background and the organisational context in which they worked. The importance of training covering the risks of smoking, benefits of cessation and effective approaches to support cessation was emphasised, particularly in the HP systematic review. Preregistration education and postregistration professional development on these issues was described as very important but commonly insufficient.
Women who were struggling to stop smoking viewed advice on cutting down (vs. quitting) as useful and constructive. This was also evident in the review of pregnant women’s views, in which advice on cutting down was perceived as being understanding of difficult life circumstances and of the perceived stress that ‘abrupt’ stopping might cause. 116–119,123,124,127,136,140
The referral process from midwives or GPs to a SSS was a focus of the interviews and an important organisational element. Area A had an opt-out pathway and, despite some controversy about this (e.g. lack of choice), the women interviewed described this process as straightforward and not unexpected. In area B, the referral process was not opt-out and was more variable. As a result, in some cases those who accepted a referral waited for weeks for a SSS advisor to contact them. Some who thought they had been referred did not hear from the service, or had received an initial telephone call that had not been followed up.
Overall, CO testing at booking (in place in area A) and during appointments with SSS advisors (in both areas) were received positively by the women interviewed. Some expressed shock at seeing their high CO reading as a result of smoking, and in general this information was described as helpful. Seeing CO levels go down was motivating (e.g. described by one woman as ‘a confidence boost’) and advisors themselves (and others involved in CO testing, such as pharmacists) described CO monitoring as an important motivational tool.
In terms of experiences with SSSs, those women who accessed the services were, overall, positive in the interviews about what they had received. Chapter 6 provides detailed findings on the positive elements that will be of interest to SSS commissioners, managers and advisors working with pregnant women. To some extent this was also the case for partners and SOs in relation to their own smoking (see Chapter 8), particularly those who had contact with a SSS. This also came through in the interviews with women in the postpartum period, when they were able to reflect on what support they had received. For those that had been successful in quitting during pregnancy, SSS support had, in many cases, been key. SOs were generally also very positive about the cessation support received by pregnant women. Women and partners expressed preference for one-to-one support (often described as better than expecting women to attend groups) and particularly for the personal support provided by smoking cessation advisors. Partners and SOs indicated an appreciation of the flexibility and responsiveness of the personal support provided by smoking cessation advisors.
Nicotine replacement therapy was an additional element of the organisational context for smoking cessation, although, in the interviews, pregnant women’s perceptions of the value of NRT were mixed. In previous quit attempts (including pre pregnancy), NRT had not always worked. This was also the case for partners, some of whom described using NRT to stop, either successfully or, more commonly, in previous quit attempts that had not been sustained and had resulted in relapse. In the interviews, some women (and partners) reported that they were now using e-cigarettes which were, overall, described as helpful, although a lack of evidence about these devices was acknowledged.
Some women who were interviewed raised concerns about the safety of NRT in the context of a quit attempt, but these concerns had been allayed in some instances by HPs. However, no real evidence was found of partners or SOs expressing worry about NRT safety in pregnancy. The cost of NRT was a concern for some pregnant women, particularly in area B, which suggested that some were unaware that it was available free on prescription. In area A, women were positive about the offer of free NRT. In relation to individual NRT products, the nicotine inhalator was mentioned as helpful by some, particularly in offering a hand-to-mouth action similar to that provided by smoking.
Organisational factors hindering smoking cessation
In both the reviews and the interviews, the health-care context did not always help or promote cessation (or relapse prevention) to the extent that it might have done. Some of the barriers were attitudinal factors but this did vary between the review studies and the interviews, probably because some studies in the reviews were conducted some years ago or in other national contexts.
In the review of pregnant women’s views, although some HPs were described as facilitating quitting, most were seen as operating within systems that permitted ambivalent or negative views. Half-hearted support, combined with insufficient practical help and advice, was a barrier to quitting. 116,119,124,127,129,140 This was also apparent in the systematic review of HPs, in which some interviewees expressed a lack of confidence about what they could meaningfully do to help women quit. In those circumstances, promoting harm reduction (cutting down) was prominent and still practised. 162,164,165,167 There was less evidence found of promoting cutting down in the interviews we conducted with UK HPs, although some who were not trained smoking cessation advisors still regarded this as acceptable or helpful, or in some cases inevitable, particularly when dealing with women or families living in complex and disadvantaged circumstances.
In all of the evidence in the review, although the health-care system primarily aimed to support smoking cessation, there were also structural or systems factors that were seen as unhelpful. For HPs in the review, a lack of training was a barrier to providing smoking cessation in pregnancy, resulting in poor knowledge and skills, and lack of awareness of confidence around effective interventions, including the prescribing of NRT. Procedures and time pressures were also frequently cited, such as a lack of time during midwifery appointments to discuss smoking cessation.
There were also issues specific to SSSs or referrals to these services in the two UK study sites. These are described in detail from the HP perspective in Chapter 10. This included concerns about the viability and communication of routine CO screening and opt-out referral, the latter of which was operating fairly well in area A but was not universally in place in area B and so was still questioned. Communication problems or lack of information in referrals were mentioned by both SSS advisors and other HPs in both areas. As in the studies in the systematic review of HPs, problems around NRT provision during pregnancy were also raised by the professionals interviewed. Professionals who were not SSS advisors still expressed caution about the safety or benefits of NRT in pregnancy, despite it being available on prescription and almost universally provided by SSSs. From the perspective of the pregnant women interviewed, some issues raised that related to SSSs included women providing examples of not being offered home appointments and of negative experiences with some advisors who were viewed as judgemental, resulting in a declining of future appointments or a disinclination to engage.
Organisational factors were also key to the issue of addressing postpartum relapse. The systematic review of HPs showed that interviewees were very unsure about how they could prevent relapse, and in one study it was described as almost inevitable. 133 HPs correctly pointed out that the research evidence on how to support women to avoid relapse was very thin.
Improving the organisational context for smoking cessation
The studies included in our systematic reviews57–59 were from a range of countries and some were conducted one or two decades ago, so their relevance for informing current organisational practice in the UK may be limited. In contrast, the interviews with all three groups of participants (pregnant women, partners/SOs and HPs) provide practical suggestions for improving current provision. This concerns the organisational context for addressing smoking in pregnancy in general (i.e. contact with any HP the woman and/or SOs have) and more specifically for SSSs.
The interviews revealed an ongoing reluctance or concern among some HPs about discussing smoking and smoking cessation in detail with pregnant women because of the perception that it could damage a valuable relationship. This is a prevailing theme in the literature including in the systematic reviews. 57–59 It is somewhat dispiriting, therefore, that concern about the negative impact on the HP’s relationship with the pregnant smoker continues to persist when the risks of continued smoking in pregnancy and the benefits of cessation are so well established. Nevertheless, this concern remains, and it was evident in both study sites in the UK. On this topic, as outlined above, support and training for HPs are key, as are time and space during an appointment with a client/patient to raise and explore this important issue. It is also worth noting that, among midwives, there was some evidence that the introduction of an opt-out referral pathway to a SSS at maternity booking can help. The interview data indicated that midwives in area A, where this policy was in place, better understood smoking cessation as a priority and understood that there were steps in place for access to specialist support beyond the time they could afford during the appointment.
For HPs in general, other practical steps could be taken to improve how the issue of smoking cessation in pregnancy is managed. From the interviews, the most obvious is the importance of staff availability and capacity to deal with the many issues that they are responsible for, including advice on alcohol and weight management. There were also examples in both areas in which improving protocols to include more effective prompts, and providing clear information for HPs regarding smoking, could effectively elevate its perceived priority. This included clear information about NRT, greater confidence in which could be built among midwives, pharmacists and others by improving access to information about its safety in pregnancy. In addition, despite limited evidence of NRT’s effectiveness in clinical trials, its value in routine care could be useful, as illustrated by the positive outcomes for women who used it in both areas A and B (from the available routine SSS data from both areas).
Another practical step, among SSS staff in particular, is to enable staff members to be more fully involved in service development, potentially allowing the service to make better use of staff expertise, to increase staff buy-in and to reduce the feeling among some staff that changes are imposed from elsewhere. Other practical changes revealed in the interviews to improve the organisational context for smoking cessation in pregnancy were also important. Although the opt-out pathway was in place in area A, there were still reports that referrals could be low; however, it is important to note that, at the time of the research, this new process might not have been fully embedded. Delays in prescribing NRT (in the pathway between services and GPs) were also identified in both areas, and examples from elsewhere in the UK suggest that these can be addressed.
A very positive finding from this study was the value and, in most cases, reported acceptability of routine CO screening in pregnancy. This was useful both to identify pregnant smokers without stigma and as a motivational tool for those trying to quit. Routine CO monitoring is recommended in NICE guidance40 and other recent policy documents,91 and represents a valuable development in the UK’s approach to helping women stop smoking in pregnancy. The lack of reference to CO monitoring in the reviews reflects the relatively recent introduction of this tool.
A remaining unresolved area for service development is how to best support women not to relapse to smoking in the postpartum period. More research is needed that can inform practice, particularly to challenge women’s views that smoking cessation in pregnancy is only a temporary measure and that postpartum relapse is assumed. One potentially important finding from this study’s interviews with women post partum, however, was that those who had stopped attending cessation services and had relapsed to smoking would have tried again if they had managed to maintain face-to-face contact with an advisor. This may point to the potential for services to do more to help women regain confidence following a lapse, including increased efforts to keep in contact with women and offer alternative appointments or home visits for those who have relapsed.
Future research and interventions
All participants in the study were asked about whether or not there was ‘anything else’ or anything new that could help women who were struggling with smoking in pregnancy. A number of useful suggestions were made, as outlined in Chapter 11. We begin here by outlining general areas for improvement that could be explored in further research. We then go on to highlight three particular areas for future work that could build on existing systems and the work of SSSs: financial incentives, self-help approaches and social network interventions. Each of these is briefly discussed in turn and we highlight how recent research in the UK is improving our understanding of each.
Key overarching issues for future research
A somewhat disappointing finding from our interviews was that many of the barriers to smoking cessation in pregnancy identified in our systematic reviews remain and have not been addressed by existing services or interventions, or indeed by changes in social norms around smoking or support for pregnant women in general. Some of these merit exploration in further qualitative research for which the literature is still limited, for example around the role of partners in facilitating or hindering cessation in pregnancy. Others, however, should be the focus of empirical research designed to inform interventions or improve existing practice.
Identifying the best ways to enhance the motivation, capability and confidence of HPs around smoking cessation in pregnancy remains key. Some of the HPs we interviewed reported that they were not always confident about the best way to approach the issue, how to prioritise it above or alongside other aspects of maternal health, or what to recommend. This can potentially be addressed through the improved training of relevant groups and better access to evidence, such as on the benefits (or lack of) of cutting down or on the use of NRTs. Data are now available from two recent trials of NRT in pregnancy, one of which followed up infants of women using NRT for up to 2 years (to provide evidence on safety), and these results are possibly not well known. Likewise, two recent studies illustrating that routine CO screening and opt-out referral increases the number of pregnant women who stop smoking in the UK is important evidence to convey to HPs who are unsure about this type of system change (as observed in area B in our study).
Some pregnant women in our study reported that, although they were told about the risks of smoking in pregnancy, they were offered limited explanation of the mechanisms of harm or how smoking was harmful to the fetus and infant. Evidence on these issues exists, and further research could explore how best to convey this to HPs and, in turn, how they can develop the confidence to discuss it with pregnant women and others, including through the use of visual aids and tools.
Within existing interventions, concerns about weight both during pregnancy and, particularly, post partum need more attention and, potentially, further research. Women who smoke are aware that smoking helps them to stay slim (through both nicotine’s effects on metabolism and smoking instead of snacking) and that weight gain with smoking cessation is common. Although this is an issue for cessation interventions in general and is not limited to pregnancy, it merits further exploration, as it is a real and persistent barrier to cessation and a contributor to relapse.
Likewise, more research on relapse prevention is urgently required. We have already made this point elsewhere in this report, but the evidence base remains very poorly developed and, perhaps as a result, services and interventions are not well developed.
It is worth noting also that these gaps in research and priorities for improving practice are consistent with recent recommendations for improvement in this area published by the multiagency Smoking in Pregnancy Challenge Group cochaired by the PI of this study (along with the chief executive of a leading baby charity) and co-ordinated by ASH. The Challenge Group report from 201391 and its 2015 update92 should be consulted alongside the results of this study, as we believe that the two together provide important insights into how we can support pregnant women to stop smoking and reduce the harm that maternal smoking causes to mothers and children.
Financial incentives
In addition to priorities for research and improved practice discussed, newer approaches merit further study. The first of these is financial incentives. Adding financial incentives to behaviour change interventions and services is controversial, but in the context of this study it may be directly relevant to the SEF. Incentives arguably operate to modify some of the wider determinants of smoking and cessation, providing more money for the household and potentially easing income-related sources of individual and interpersonal stress. They provide women from smoking communities with an additional ‘reward’ for engaging in a behaviour change process that may be difficult to achieve. In the interviews, women, partners and HPs expressed an interest in this topic, although some were cautious about the acceptability of ‘paying’ women to stop smoking.
The study took place at a time when incentive schemes were in place in areas relatively near the study sites (one long-standing programme in Tayside in Scotland and a scheme established 3 years ago across the north-west of England). Participants had heard about these schemes either directly or in the media. In addition, while some of the postpartum interviews were taking place, members of our team published the world’s largest trial to date of incentives for smoking cessation in pregnancy, which built on earlier studies in the USA and involved a Phase II trial with just over 600 women in Glasgow93 that was extensively reported in the media at the time. Awareness of the principles of incentives, sometimes described as a ‘nudge’ intervention, was high.
Incentives are a valid and important area for future research. At the time of completing this report, members of our team had submitted funding proposals for a larger Phase III multicentre trial based on the earlier study and the majority of funding for this research has now been secured. This would combine cessation services support with incentives delivered at four time points during pregnancy, in the form of shopping vouchers up to a total value of £400. Results from the earlier trial supported those from US studies that showed that incentives were both clinically effective and cost-effective. 93,178 In fact, the Phase II trial showed that this combination of NHS support and vouchers resulted in biochemically validated abstinence rates from smoking at the end of pregnancy that were 2.5 times higher in the intervention group than in the control group. There is a need for a multicentre trial to test whether or not this can work as well in different health and social care settings and communities in the UK.
Self-help interventions
Interviewees also expressed an interest in new approaches to allow women and family members to ‘help themselves’ in the context of smoking cessation. On this topic, future interventions could focus on self-help approaches. A previous systematic review96 conducted by some members of the team found that self-help interventions for pregnant smokers almost doubled the odds of smoking cessation compared with usual care. Following this, we investigated the potential of using text messaging to deliver tailored self-help support to pregnant smokers,141 and designed and evaluated the feasibility and acceptability of an intervention using tailored written and text message support for pregnant smokers recruited via antenatal care (MiQuit). 179
In terms of current work, after refining the intervention and restricting delivery to tailored text message only, two parallel streams of evaluation research are being undertaken: evaluating the impact of MiQuit on smoking behaviour and assessing its uptake when offered for use in real-world contexts. For impact evaluation, a further trial of MiQuit [Coleman T, Naughton F, Cooper S, Sutton S, Parrott S, Hewitt C, et al. The MiQuit study: RCT and meta-analysis testing effectiveness and cost effectiveness of a tailored text message programme for smoking cessation in pregnancy (CRUK Population Research Committee)] is being undertaken. The results from this trial will then be combined with two previous trials in a pooled analysis to estimate the intervention effect on abstinence compared with a standard cessation leaflet comparison group. 94 For the uptake evaluation stream, we have assessed or are currently assessing smoking cessation in the following settings: (1) when promoted via a leaflet in maternity booking notes (without HP input),95 (2) when promoted by HPs via a leaflet in antenatal care, (3) when promoted on pregnancy test kits in 10 ASDA supermarkets180 (ASDA Stores Ltd, Leeds, UK) and (4) when promoted via paid for and free online advertising/links.
Formative work is soon to start to inform the design and development of a NRT adherence intervention for pregnant smokers provided with or using NRT, as part of a National Institute for Health Research (NIHR) Health Technology Assessment (HTA)-funded programme. A major component of this proposed intervention is likely to be delivered via digital self-help. Overall, therefore, self-help interventions represent an important area for further research on smoking cessation in pregnancy and may be promising for the future.
Social networks and other interventions
The findings of this study illustrate that smoking in pregnancy is heavily influenced not only by the individual characteristics of women but also by women’s interpersonal relationships and the communities they live in. It therefore seems a natural extension to suggest that services and interventions should also be rooted in, or at least take account of, this context. Good-quality behavioural support (of the type provided by trained advisors on smoking in pregnancy) should aim to include discussion of all these aspects with women and may involve practical help such as signposting to other local services that can assist with social or financial problems. Some services also actively aim to engage the pregnant woman’s partner or SOs (such as a parent or close friend) in the interventions offered, particularly if that individual also smokes; however, interventions that actively involve partners are underdeveloped in the UK and elsewhere. The women interviewed in this study still experienced support to stop smoking as an intervention focused on them rather than one involving their wider social network.
Valente181 described social network interventions as ‘purposeful efforts to use social networks or social network data to generate social influence and/or accelerate behaviour change among individuals, communities, organisations, or populations’. Studies that proactively involve social networks in smoking cessation have mainly centred on the general adult population182 and remain under-researched in pregnancy. Only five such studies were identified in the most recent Cochrane review183 of psychosocial interventions to support women to stop smoking in pregnancy. Evidence from this review suggested that social support interventions appeared effective when provided by peers (five studies: average risk ratio 1.49, 95% confidence interval 1.01 to 2.10), but the effect was unclear in a single trial of support provided by partners.
Determining precisely how a social network intervention for smoking cessation in pregnancy would be delivered and what it would involve is complicated. Identifying social network members and ascertaining whether or not and how they could support the pregnant woman who is smoking are not straightforward. For these reasons, some of the authors of this report have already undertaken a small feasibility study (funded by CRUK) that aims to address the following questions:
-
Can social networks be used to help pregnant women stop smoking? If yes, how can they be used, what support can they offer and how should they be supported?
-
What stage of pregnancy should the intervention be aimed at and should prevention of postpartum relapse be included or not?
-
How will social network members be defined, identified, approached and positively engaged (i.e. how can they be encouraged to take part)?
-
What will the intervention components be, and what level of resource will be required for a future pilot?
-
What are the barriers to using social networks for health behaviour change and how can they be overcome?
-
What capacity is there for social network approaches to be used to address other public health issues (obesity, alcohol consumption, diet and exercise)?
This study will report in 2017.
It is also worth noting that these suggestions for new interventions should sit alongside efforts to improve or further investigate what is already happening. We touch on this theme above, but it is clear that more research on the efficacy and safety of NRT in pregnancy is required that will help to improve the confidence of staff in prescribing NRT or providing information about these products to women. The awarded NIHR programme grant mentioned above includes a study that tests higher-dose (combination therapy) NRT with pregnant women (already used by some SSSs, as nicotine is metabolised more rapidly in pregnancy and standard doses do not have good evidence of efficacy) alongside the adherence research.
Finally, there is evidence that pregnant women who smoke are using e-cigarettes, which are currently the most popular aid to stopping smoking in the UK among the general adult population of smokers and are used in around one in three quit attempts. Members of the team have just completed a qualitative study of e-cigarette use among pregnant women in England and Scotland and are now beginning a UK-wide survey on this issue; both of these have been funded by CRUK. In addition, we are about to begin (with colleagues) a trial of e-cigarette use in pregnant women in England and Scotland, funded by NIHR HTA. Results from these new studies, along with studies under way in the USA, will provide much-needed evidence on e-cigarettes for smoking cessation among pregnant women.
Conclusions
This study examined the barriers to and facilitators of smoking cessation in pregnancy, drawing on systematic reviews57–59 of the international literature and qualitative research in one area in Scotland and another in England. We conclude this report by reflecting on some of the similarities and differences between the systematic reviews57–59 and our interviews, emphasising the strengths and limitations of the research and finally reflecting on how the theoretical framework we used may provide a useful platform for improving our understanding of current and future approaches to supporting women to stop smoking during pregnancy.
Systematic reviews and interviews
The contemporary accounts of women, their SOs and HPs in our interviews reflected themes that are prevalent in the international literature and were identified in our three systematic reviews. 57–59 Overall, there was a great deal of consistency between the systematic reviews and interviews, with some important exceptions.
Although the review studies were conducted in previous years and in both the UK and other countries, findings, particularly at the individual and interpersonal levels of the SEF, were similar between the review studies and our interviews. In high-income countries, there are marked socioeconomic inequalities in smoking in pregnancy and, therefore, it is not surprising that, for the most part, the role of disadvantage in women’s lives was relevant to their smoking. Women who smoke in pregnancy are more likely to have started in their early to mid-teens, to live in areas with many other smokers and to suffer financial hardship. These factors shaped the prevalent accounts from women and partners about smoking as a coping mechanism, a rare (and shared) break and pleasure. Any future interventions should acknowledge the context in which the majority of smoking in pregnancy occurs. These factors also influenced how HPs approached discussing smoking with pregnant women, often recognising the other difficulties they faced, prioritising developing a good relationship with their clients/patients and continuing to imply either directly or indirectly that cutting down was ‘good enough’. Women who managed to engage with SSS staff benefited from the staff’s knowledge and expertise in supporting women with challenging life circumstances and from techniques, tools and aids to promote complete abstinence from smoking as a realistic goal.
Areas in which the review findings differed from the interview findings were specific aspects of the influence of HPs, the viewing of cessation as a temporary change and risk perceptions. In the first area, the review found that women and partners often described HPs as ambivalent or negative about trying to stop smoking, perhaps reflecting previous social norms on smoking, less understanding of risks or local contexts in which cessation services were not in place. This perception was not prevalent in our interviews, but there were exceptions. Women expected to be asked about smoking and, for the most part, they were indeed asked and HPs aimed to be facilitative and understanding. In terms of SSS staff in particular, most women who accessed the services were positive about the support of their smoking cessation advisor.
Second, the reviews also indicated that cessation in pregnancy was widely regarded as a temporary change, with relapse post partum seen as largely inevitable. This may reflect different contexts and study populations from those in our study. The small number of women interviewed post partum cautions against firm conclusions being drawn. However, although relapse post partum was a theme in these interviews, women were clear that they wanted to remain non-smokers. It is also worth noting that we did not have any interviewees who had successfully stopped during pregnancy and who then started smoking again after birth. All of these non-smoking women expressed a strong desire to keep away from tobacco.
Finally, in the systematic review of pregnant women’s views, risk perceptions of smoking in pregnancy often operated as barriers to, rather than facilitators of, quitting. We certainly found some evidence of this in our interviews, not only with women but also with SOs. However, there were other examples of women who genuinely believed that smoking was harmful and who gave concrete instances of children they knew who had suffered ill effects, although these were few. Accurate perceptions of real harm did seem to help foster determination to quit, and this was also recognised by HPs, some of whom explicitly expressed the importance of being very truthful with women and family members regarding the potential impact of smoking in pregnancy.
Strengths and limitations of the research
This study had a number of strengths. These included the production of three new qualitative systematic reviews57–59 on topics of current importance for policy and practice. Qualitative reviews have a valuable role to play in drawing out key themes on topics of contemporary interest from the perspective of people’s lived experiences, providing a rich source of information that can capture common issues across time and different national and organisational contexts. We updated a previous systematic review, conducted by members of our team, that examined pregnant women’s views, and then carried out two new reviews on topics not previously examined systematically: SOs’ and HPs’ views on smoking and smoking cessation in pregnancy. The systematic review of partners and SOs was particularly useful, as it demonstrated the very considerable lack of evidence supporting the views of (primarily) male partners regarding smoking in pregnancy. In the systematic review of partners’ views, most of the studies were from Canada, with only one UK study included that involved only five male partners. By conducting interviews with many more male partners in our study (as well as mothers, friends and a mother-in-law of the pregnant women), we have significantly expanded the available qualitative literature on this topic.
A second strength of our study was the in-depth nature of the research we conducted with a reasonably large sample of pregnant women, their SOs and HPs. Each of these samples aimed to capture a range of individuals in different circumstances (i.e. by smoking status) and, for the HPs in particular, from a number of different occupations. Our interviews were, in many cases, long and detailed. They also aimed to provide constructive information on current and future services, and interventions to inform policy and practice in the UK context. A final strength was the detailed synthesis of findings between the systematic reviews and our qualitative data, examining areas of similarity and difference and structured around a theoretical model, the SEF, which provided a ‘lens’ through which to view and interpret our data.
In terms of limitations, the design of the research meant that our findings are grounded in qualitative studies; this enabled a sustained focus on perceived barriers and facilitators and not on outcomes relating to smoking or smoking cessation in pregnancy. Although the in-depth nature of the work is one of its strengths, it meant that sample sizes, both in the systematic reviews57–59 and in our primary studies, were smaller than those in quantitative studies, although they were still large for a qualitative study. Similar to other studies, we had particular difficulty recruiting partners and SOs in both sites (see Chapter 2), initially because of the requirements of the study set by the research ethics approval process and latterly simply as a result of men’s reluctance to be interviewed. We aimed to address this by alternative referral routes, again described in Chapter 2, but this did mean that some of the partners we interviewed in area A were not those of women in the study, limiting our ability to look at couples together during our data analysis.
An additional limitation relates to our study sites and how a combination of local service configuration and our recruitment processes may have produced a skewed sample. In both areas, we knew from previous experience that the best way to recruit research participants was to work with existing services and not try to disrupt or replicate local systems. We therefore tailored our approach to these established systems. In area B, members of our team were already working with a research midwife who had links to the maternity booking setting and therefore women could be recruited through that route. In area A this was not the case, but our team had an established relationship with the local SSS; this meant that we recruited women who already had some contact with the service, no matter how brief, building on the opt-out pathway in place in that site. In contrast, some women in area B had no contact with the SSS. Looking at our data now, we believe that this has resulted in a useful cross-section of views emerging in the findings across the two sites. However, it does mean that we have not captured the views of those women in area A who smoke or smoked and did not have any contact with the local SSS.
Further limitations relate to the methods used in some instances. We conducted one-to-one in-depth interviews with HPs, except for some smoking cessation service staff and midwives. In those instances, we chose to conduct a small number of focus groups, as we had a number of staff who were interested in participating, and conducting individual interviews with all of them would have been logistically challenging and time-consuming. We believe that the focus group discussions were useful and insightful, but it is possible that discussing the issues in a group meant that not all divergent views were captured. In addition, we chose from the outset not to follow up all pregnant women in the study postnatally but instead followed up only a subset of women who agreed to this at recruitment. This represented a good cross-section of women in different circumstances but means that we did not capture all women’s views in the postpartum period. These and other potential limitations should be kept in mind when reviewing our results.
Social–ecological framework
As we discussed in Chapter 2, in the initial months of this study we decided to draw on the SEF as a theoretical model for the research, as our initial scoping for the systematic reviews emphasised that environmental barriers and facilitators, operating at a range of interconnecting levels, were key to understanding smoking cessation in pregnancy. This approach has drawn attention to some overarching issues that have wider implications beyond our own study and are worth highlighting in the concluding paragraphs of this report. Two main issues emerge. The first is that it is helpful to locate interventions within the SEF and consider which aspects of the interventions offered address (or do not address) different elements of the framework. Different types of interventions will primarily operate at one or two levels but not all. For example, self-help materials or e-cigarettes are located at the individual level, family-based approaches are located at the community level and SSSs are located at the organisational level. The success of interventions at one level could be undermined by factors operating elsewhere in the framework; the assessment, measurement or attempted modification of these could be a viable area for research, and identifying the gaps could be constructive.
The second issue is that this framework recognises and encourages thinking beyond the individual domain. Most studies of behaviour change interventions, including smoking cessation studies, have a strong focus on the individual. Treatments, services or even policies are offered or introduced to smokers, and outcomes are then observed, most commonly in controlled studies in which one group receives one or more interventions and another receives something different. Even the ‘future interventions’ we identified in our study, and that we asked interviewees about, focus fairly heavily on the individual. Future research, and future service development, needs to go beyond a focus on the pregnant woman and her baby to wider networks and contexts. One approach may be to focus on thinking of organisations as particular settings for interventions, such as the workplace for pregnant women, their partners and SOs, and NHS settings for HPs.
Overall, our findings suggest that, to be effective in supporting smoking cessation in pregnancy, consideration needs to be given to all layers of the SEF and how they relate to individual women’s needs and experiences. Ideally, interventions, or connected sets of interventions, should simultaneously operate at multiple levels. This is challenging but provides a basis for thinking about how best to approach future studies on behaviour change in pregnancy and, indeed, during other stages of the life course and in different populations.
Acknowledgements
The study would not have been possible without the input of a number of colleagues.
We are very grateful to the NHS colleagues who assisted us with the proposal for this project and helped to make the study possible. These colleagues are Dr Dermot Gorman, Consultant in Public Health Medicine, from Area A, and Elizabeth Ross, Head of Midwifery at Area B.
In addition, we would not have been able to recruit study participants in either site without the considerable support and expertise provided by Helena Connelly and Anne Finnie from Area A, and Julie Howe and Bev Waterhouse from Area B.
Considerable thanks are also due to our study participants: the pregnant women who agreed to speak to us, along with the partners and SOs who gave up their time to be interviewed. Particular thanks go to the women who were interviewed twice: during their pregnancy and after the birth of their baby. Many HPs took time away from very busy schedules to also participate in one-to-one interviews or focus groups and this was very much appreciated. Some of our participants also gave feedback on our preliminary findings, which was invaluable.
The study was also discussed with the UKCTAS smoker’s panel and their contribution helped to inform the study.
In addition, we would like to thank:
-
our advisory group members – Professor Tim Coleman (chairperson), Cath Chamberlain, Brenda Friel and Susanna Mountcastle
-
Alex Bailey from NHS Lothian and Graeme Docherty from UKCTAS, who assisted with National Research Ethics Service applications, queries and amendments
-
local R&D leads who helped facilitate the research permissions for each site
-
our NIHR HTA project manager, Alexa Cross.
Finally, very many thanks to Carol Anne Greenan and Aileen Paton at the University of Stirling, who provided administrative support for the study and were tireless in their efforts to help us co-ordinate fieldwork, analysis, team meetings and the final report, and to Sally Stephenson, research group administrator at the University of York.
Ethics committee approvals
Full ethics approval for this study was obtained from South East Scotland REC 01.
Contributions of authors
All authors contributed to the interpretation of findings, writing and editing of the final report, and outputs from the study. More specifically:
Linda Bauld (Professor, Health Policy) was the PI with overall responsibility for the design, co-ordination and delivery of the study, and lead for the Scottish centre. Together with the coinvestigators, she conceived, designed and led the study, providing smoking cessation in pregnancy research expertise. She contributed to the systematic reviews, data collection in area A, and drafted and edited chapters of the final report including leading on the proposed future interventions for development, and contributed to all outputs from the study.
Hilary Graham (Professor, Health Sciences) was the co-PI for the study with responsibility for the study design and overseeing the researchers working on both the systematic reviews and qualitative data collection in England. Together with LB and KF she conceived and determined the methods for the review, screened the articles for inclusion and established the findings for the review. She provided input to the development of proposed interventions for future testing, led the development of the theoretical framework for the study, and drafted and edited sections of the final report.
Lesley Sinclair (Research Fellow, Trial/Project Management) was the project manager for the study. She co-ordinated the work of the team, managed the ethics and R&D approvals, facilitated recruitment at area A, conducted interviews with HPs in area A, contributed to the development of the coding framework for HP data, coded, analysed and synthesised HP interview data, compiled the final report, including drafting and editing chapters, and delivered presentations at national conferences.
Kate Flemming (Senior Lecturer, Systematic Reviews of Qualitative Research) was the lead for the three systematic reviews. She determined the methods for the reviews, reviewed the search strategies, screened the articles for inclusion, undertook data extraction, quality assessment and data synthesis, contributed to the design of the qualitative interview topic guides, drafted the review chapters of the report and presented at a national conference.
Felix Naughton (Senior Research Associate, Health Psychology) contributed psychology expertise in behaviour change theory to inform the study design and interpretation of data. He led the primary data collection element of the study for HPs, including design of the interview topic guide, development of the coding framework, coding, analysis, synthesis, interpretation of the HPs’ interview data and drafting of the qualitative HP chapter (see Chapter 10), presented at a national conference and provided input to all aspects of the project.
Allison Ford (Research Fellow, Qualitative Research) developed the topic guide for interviews with the postpartum women, conducted interviews with women and SOs at area A, developed the coding framework for both the pregnant and postpartum women’s data, and carried out the analysis, synthesis and reporting of these data, including drafting Chapter 6.
Jennifer McKell (Research Fellow, Qualitative Research) developed the interview topic guides for both the pregnant women and the SOs, conducted interviews with women, SOs and HPs at area A, developed the coding framework for the interview data for SOs and carried out the analysis, synthesis and reporting of these data, including drafting Chapter 8. She presented at a national conference.
Dorothy McCaughan (Research Fellow, Qualitative Research) contributed to the systematic review (screened the articles for inclusion, undertook data extraction and quality assessment, and established the findings of the review), contributed to the development of the interview topic guides, and organised and conducted all focus groups and interviews with women, partners/SOs and HPs at area B.
Sarah Hopewell (Research Assistant/SSS advisor, Health Psychology) contributed to the development of the coding framework for the HPs’ interview data and the coding, analysis, synthesis, interpretation and reporting of these data, including drafting the HP qualitative chapter (see Chapter 10).
Kathyrn Angus (Research Associate, Information Specialist) designed and undertook literature searches for the three systematic reviews, contributed to the coding, analysis and reporting of the pregnant women’s and SOs’ interview data, and proofread and managed the referencing for the final report.
Douglas Eadie (Senior Researcher, Qualitative Research) contributed to the coding, data analysis, synthesis and reporting of the SOs qualitative interviews.
David Tappin (Professor, Paediatrics and Trials in Children) provided clinical advice and smoking cessation in pregnancy expertise for the study design and conduct, and advised on all aspects of the study.
Publications
Flemming K, Graham H, McCaughan D, Angus K, Bauld L. The barriers and facilitators to smoking cessation experienced by women’s partners during pregnancy and the post-partum period: a systematic review of qualitative research. BMC Public Health 2015;15:849.
Flemming K, McCaughan D, Angus K, Graham H. Qualitative systematic review: barriers and facilitators to smoking cessation experienced by women in pregnancy and following childbirth. J Adv Nurs 2015;71:1210–26.
Flemming K, Graham H, McCaughan D, Angus K, Sinclair L, Bauld L. Health professionals’ perceptions of the barriers and facilitators to providing smoking cessation advice to women on pregnancy and during the post-partum period: a systematic review of qualitative research. BMC Public Health 2016;16:290.
Data sharing statement
Requests for access to data should be addressed to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Cnattingius S. The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res 2004;6:125-40. https://doi.org/10.1080/14622200410001669187.
- Castles A, Adams EK, Melvin CL, Kelsch C, Boulton ML. Effects of smoking during pregnancy. Five meta-analyses. Am J Prev Med 1999;16:208-15. https://doi.org/10.1016/S0749-3797(98)00089-0.
- Delpisheh A, Kelly Y, Rizwan S, Attia E, Drammond S, Brabin BJ. Population attributable risk for adverse pregnancy outcomes related to smoking in adolescents and adults. Public Health 2007;121:861-8. http://doi.org/10.1016/j.puhe.2007.03.015.
- Rogers JM. Tobacco and pregnancy: overview of exposures and effects. Birth Defects Res C Embryo Today 2008;84:1-15. http://dx.doi.org/10.1002/bdrc.20119.
- Salihu HM, Wilson RE. Epidemiology of prenatal smoking and perinatal outcomes. Early Hum Dev 2007;83:713-20. https://doi.org/10.1016/j.earlhumdev.2007.08.002.
- Hammoud AO, Bujold E, Sorokin Y, Schild C, Krapp M, Baumann P. Smoking in pregnancy revisited: findings from a large population-based study. Am J Obstet Gynecol 2005;192:1856-62. https://doi.org/10.1016/j.ajog.2004.12.057.
- Jaakkola JJ, Gissler M. Maternal smoking in pregnancy, fetal development, and childhood asthma. Am J Public Health 2004;94:136-40. https://doi.org/10.2105/AJPH.94.1.136.
- DH . Review of the Health Inequalities Infant Mortality PSA Target 2007. www.perinatal.nhs.uk/smoking/Health%20Inequalities%20report%202007.pdf (accessed 20 August 2015).
- Carpenter RG, Irgens LM, Blair PS, England PD, Fleming P, Huber J, et al. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet 2004;363:185-91. https://doi.org/10.1016/S0140-6736(03)15323-8.
- Mitchell EA, Milerad J. Smoking and Sudden Infant Death Syndrome. Background paper, WHO/NCD/TFI/99.11. Geneva: World Health Organization; 1999.
- Mitchell EA, Milerad J. Smoking and the sudden infant death syndrome. Rev Environ Health 2006;21:81-103. https://doi.org/10.1515/REVEH.2006.21.2.81.
- Centers for Disease Control and Prevention . Smoking-attributable mortality, years of potential life lost, and productivity losses – United States, 2000–2004. MMWR Morb Mortal Wkly Rep 2008;57:1226-8.
- Wisborg K, Henriksen TB, Obel C, Skajaa E, Ostergaard JR. Smoking during pregnancy and hospitalization of the child. Pediatrics 1999;104. https://doi.org/10.1542/peds.104.4.e46.
- Gilliland FD, Li YF, Peters JM. Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med 2001;163:429-36. http://dx.doi.org/10.1164/ajrccm.163.2.2006009.
- Jones LL, Hashim A, McKeever T, Cook DG, Britton J, Leonardi-Bee J. Parental and household smoking and the increased risk of bronchitis, bronchiolitis and other lower respiratory infections in infancy: systematic review and meta-analysis. Respir Res 2011;12. http://dx.doi.org/10.1186/1465-9921-12-5.
- Button TM, Maughan B, McGuffin P. The relationship of maternal smoking to psychological problems in the offspring. Early Hum Dev 2007;83:727-32. https://doi.org/10.1016/j.earlhumdev.2007.07.006.
- Batstra L, Hadders-Algra M, Neeleman J. Effect of antenatal exposure to maternal smoking on behavioural problems and academic achievement in childhood: prospective evidence from a Dutch birth cohort. Early Hum Dev 2003;75:21-33. https://doi.org/10.1016/j.earlhumdev.2003.09.001.
- Montgomery SM, Ekbom A. Smoking during pregnancy and diabetes mellitus in a British longitudinal birth cohort. BMJ 2002;324:26-7. https://doi.org/10.1136/bmj.324.7328.26.
- Godfrey C, Pickett K, Parrott S, Mdege N, Eapen P. Estimating the Costs to the NHS of Smoking in Pregnancy for Pregnant Women and Infants. Final Report. York: Public Health Research Consortium, University of York; 2010.
- Owen L, McNeill A. Saliva cotinine as indicator of cigarette smoking in pregnant women. Addiction 2001;96:1001-6. http://dx.doi.org/10.1080/09652140120053057.
- Moore L, Campbell R, Whelan A, Mills N, Lupton P, Misselbrook E, et al. Self help smoking cessation in pregnancy: cluster randomised controlled trial. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7377.1383.
- Shipton D, Tappin DM, Vadiveloo T, Crossley JA, Aitken DA, Chalmers J. Reliability of self reported smoking status by pregnant women for estimating smoking prevalence: a retrospective, cross sectional study. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b4347.
- Health and Social Care Information Centre . Infant Feeding Survey – UK, 2010: Early Results 2011. www.hscic.gov.uk/catalogue/PUB00648 (accessed 20 August 2015).
- Cnattingius S, Lambe M. Trends in smoking and overweight during pregnancy: prevalence, risks of pregnancy complications, and adverse pregnancy outcomes. Semin Perinatol 2002;26:286-95. https://doi.org/10.1053/sper.2002.34771.
- Graham H, Sowden A, Flemming K, Heirs M, Fox D. Using Qualitative Research to Inform Interventions to Reduce Smoking in Pregnancy in England: A Systematic Review of Qualitative Studies. York: Public Health Research Consortium; 2011.
- Vartiainen E, Seppälä T, Lillsunde P, Puska P. Validation of self reported smoking by serum cotinine measurement in a community-based study. J Epidemiol Community Health 2002;56:167-70. https://doi.org/10.1136/jech.56.3.167.
- Prady SL, Kiernan K, Bloor K, Pickett KE. Do risk factors for post-partum smoking relapse vary according to marital status?. Matern Child Health J 2012;16:1364-73. http://dx.doi.org/10.1007/s10995-011-0899-1.
- Graham H, Hawkins SS, Law C. Lifecourse influences on women’s smoking before, during and after pregnancy. Soc Sci Med 2010;70:582-7. http://dx.doi.org/10.1016/j.socscimed.2009.10.041.
- Hiscock R, Judge K, Bauld L. Social inequalities in quitting smoking: what factors mediate the relationship between socioeconomic position and smoking cessation?. J Public Health 2011;33:39-47. http://dx.doi.org/10.1093/pubmed/fdq097.
- Lu Y, Tong S, Oldenburg B. Determinants of smoking and cessation during and after pregnancy. Health Promot Int 2001;16:355-65. https://doi.org/10.1093/heapro/16.4.355.
- Letourneau AR, Sonja B, Mazure CM, O’Malley SS, James D, Colson ER. Timing and predictors of postpartum return to smoking in a group of inner-city women: an exploratory pilot study. Birth 2007;34:245-52. https://doi.org/10.1111/j.1523-536X.2007.00177.x.
- Ratner PA, Johnson JL, Bottorff JL, Dahinten S, Hall W. Twelve-month follow-up of a smoking relapse prevention intervention for postpartum women. Addict Behav 2000;25:81-92. https://doi.org/10.1016/S0306-4603(99)00033-7.
- Prady S, Graham H, Pickett K. Patterns of partnership smoking during pregnancy. J Epidemiol Community Health 2012;66. https://doi.org/10.1136/jech-2012-201753.130.
- Pickett KE, Wilkinson RG, Wakschlag LS. The psychosocial context of pregnancy smoking and quitting in the Millennium Cohort Study. J Epidemiol Community Health 2009;63:474-80. http://dx.doi.org/10.1136/jech.2008.082594.
- Goodwin RD, Keyes K, Simuro N. Mental disorders and nicotine dependence among pregnant women in the United States. Obstet Gynecol 2007;109:875-83. https://doi.org/10.1097/01.AOG.0000255979.62280.e6.
- Portani M, Whitworth S. A comparison of the characteristics of childless women and mothers in the ONS longitudinal study. Popul Trends 2009;136:10-2. https://doi.org/10.1057/pt.2009.15.
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.38142.554479.AE.
- Leonardi-Bee J, Jere ML, Britton J. Exposure to parental and sibling smoking and the risk of smoking uptake in childhood and adolescence: a systematic review and meta-analysis. Thorax 2011;66:847-55. http://dx.doi.org/10.1136/thx.2010.153379.
- WHO Recommendations for the Prevention and Management of Tobacco Use and Second-Hand Smoke Exposure in Pregnancy. Geneva: World Health Organization; 2013.
- Quitting Smoking in Pregnancy and Following Childbirth. London: NICE; 2010.
- Fahy SJ, Cooper S, Coleman T, Naughton F, Bauld L. Provision of smoking cessation support for pregnant women in England: results from an online survey of NHS Stop Smoking Services for pregnant women. BMC Health Serv Res 2014;14. http://dx.doi.org/10.1186/1472-6963-14-107.
- Bauld L, Hackshaw L, Ferguson J, Coleman T, Taylor G, Salway R. Implementation of routine biochemical validation and an ‘opt out’ referral pathway for smoking cessation in pregnancy. Addiction 2012;107:53-60. http://dx.doi.org/10.1111/j.1360-0443.2012.04086.x.
- Nichter M, Nichter M, Adrian S, Goldade K, Tesler L, Muramoto M. Smoking and harm-reduction efforts among postpartum women. Qual Health Res 2008;18:1184-94. http://dx.doi.org/10.1177/1049732308321738.
- McBride CM, Pirie PL, Curry SJ. Postpartum relapse to smoking: a prospective study. Health Educ Res 1992;7:381-90. https://doi.org/10.1093/her/7.3.381.
- Hajek P, Stead LF, West R, Jarvis M, Hartmann-Boyce J, Lancaster T. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev 2013;8. https://doi.org/10.1002/14651858.cd003999.pub4.
- NHS Digital . Chapter 11 Tables – Infant Feeding Survey 2010 n.d. http://data.gov.uk/dataset/infant-feeding-survey-2010 (accessed 22 August 2015).
- McDermott E, Graham H. Resilient young mothering: social inequalities, late modernity and the ‘problem’ of ‘teenage’ motherhood. J Youth Stud 2005;8:59-7. http://dx.doi.org/10.1080/13676260500063702.
- Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol 2005;58:1081-8. https://doi.org/10.1016/j.jclinepi.2005.09.002.
- Flemming K, Graham H, Heirs M, Fox D, Sowden A. Smoking in pregnancy: a systematic review of qualitative research of women who commence pregnancy as smokers. J Adv Nurs 2013;69:1023-36. http://dx.doi.org/10.1111/jan.12066.
- Van’t Hof SM, Wall MA, Dowler DW, Stark MJ. Randomised controlled trial of a postpartum relapse prevention intervention. Tob Control 2000;9:64-6. http://dx.doi.org/10.1136/tc.9.suppl_3.iii64.
- McBride CM, Baucom DH, Peterson BL, Pollak KI, Palmer C, Westman E, et al. Prenatal and postpartum smoking abstinence: a partner-assisted approach. Am J Prev Med 2004;27:232-8. http://dx.doi.org/10.1016/j.amepre.2004.06.005.
- Appleton PL, Pharoah POD. Partner smoking behaviour change is associated with women’s smoking reduction and cessation during pregnancy. Br J Health Psychol 1998;3:361-74. http://dx.doi.org/10.1111/j.2044-8287.1998.tb00580.x.
- Wakefield M, Reid Y, Roberts L, Mullins R, Gillies P. Smoking and smoking cessation among men whose partners are pregnant: a qualitative study. Soc Sci Med 1998;47:657-64. https://doi.org/10.1016/S0277-9536(98)00142-7.
- Tappin DM, MacAskill S, Bauld L, Eadie D, Shipton D, Galbraith L. Smoking prevalence and smoking cessation services for pregnant women in Scotland. Subst Abuse Treat Prev Policy 2010;5. http://dx.doi.org/10.1186/1747-597X-5-1.
- Fahy S, Cooper S, Bauld L. Smoking Cessation Support During Pregnancy: A National Audit of NHS Stop Smoking Services for Pregnant Women in England n.d. www.uknscc.org/uknscc2012_presentation_158.php (accessed 22 August 2015).
- Condliffe L, McEwen A, West R. The attitude of maternity staff to, and smoking cessation interventions with, childbearing women in London. Midwifery 2005;21:233-40. https://doi.org/10.1016/j.midw.2004.12.011.
- Flemming K, McCaughan D, Angus K, Graham H. Qualitative systematic review: barriers and facilitators to smoking cessation experienced by women in pregnancy and following childbirth. J Adv Nurs 2015;71:1210-26. http://dx.doi.org/10.1111/jan.12580.
- Flemming K, Graham H, McCaughan D, Angus K, Bauld L. The barriers and facilitators to smoking cessation experienced by women’s partners during pregnancy and the post-partum period: a systematic review of qualitative research. BMC Public Health 2015;15. http://dx.doi.org/10.1186/s12889-015-2163-x.
- Flemming K, Graham H, McCaughan D, Angus K, Sinclair L, Bauld L. Health professionals’ perceptions of the barriers and facilitators to providing smoking cessation advice to women in pregnancy and during the post-partum period: a systematic review of qualitative research. BMC Public Health 2016;16. http://dx.doi.org/10.1186/s12889-016-2961-9.
- Salomi Barkat S, Karanwal S, Lawder R, MacKinnon A, Stockton D, Moore F. ScotPHO Tobacco Profiles (Second Release) 2015. www.scotpho.org.uk/opt/Reports/scotpho-tobacco-profiles-secondrelease2015-overview-report.pdf (accessed 31 August 2015).
- Mid-2011 Population Estimates and Mid-2013 Population Estimates. Newport: ONS; 2014.
- Data from Integrated Household Survey: Smoking Prevalence Among Adults Aged 18+ by Region and Local Authority. January–December 2012. Newport: ONS; 2013.
- Health and Social Care Information Centre . Statistics on Women’s Smoking Status at Time of Delivery: England Quarter 4 – April 2013 to March 2014. Final Report 2014. www.hscic.gov.uk (accessed 2 September 2015).
- Bauld L, Graham H, Flemming K, Sinclair L, Naughton F, Tappin D, et al. Barriers and Facilitators to Smoking Cessation in Pregnancy and Following Childbirth: Literature Review and Qualitative Study: Study Protocol Version 2.0 29.04.2014 2014. https://njl-admin.nihr.ac.uk/document/download/2007181 (accessed 30 October 2015).
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- Godin G, Valois P, Lepage L, Desharnais R. Predictors of smoking behaviour: an application of Ajzen’s theory of planned behaviour. Br J Addict 1992;87:1335-43. https://doi.org/10.1111/j.1360-0443.1992.tb02742.x.
- de Vries H, Backbier E. Self-efficacy as an important determinant of quitting among pregnant women who smoke: the phi-pattern. Prev Med 1994;23:167-74. https://doi.org/10.1006/pmed.1994.1023.
- Ben Natan M, Golubev V, Shamrai V. Smoking during pregnancy: analysis of influencing factors using the theory of planned behaviour. Int Nurs Rev 2010;57:388-94. http://dx.doi.org/10.1111/j.1466-7657.2010.00807.x.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-42.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-37.
- Lalonde M. A New Perspective on the Health of Canadians: A Working Document. Ottawa, April 1974. Ottawa, ON: Minister of Supply and Services Canada; 1981.
- Blum HL. Planning for Health: Development and Application of Social Change Theory. New York, NY: Human Sciences Press; 1974.
- Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. Am Psychol 1992;47:6-22. https://doi.org/10.1037/0003-066X.47.1.6.
- Schneider M, Stokols D, Shumaker SA, Ockene JK, Riekert KA. The Handbook of Health Behavior Change. New York, NY: Springer; 2009.
- Bronfenbrenner U, Vasta R. Six Theories of Child Development: Revised Formulations and Current Issues. London: Jessica Kingsley Publishers; 1992.
- Bronfenbrenner U. Ecology of the family as a context for human development: research perspectives. Dev Psychol 1986;22. https://doi.org/10.1037/0012-1649.22.6.723.
- Dahlgren G, Whitehead M. Tackling Inequalities in Health: What Can We Learn From What Has Been Tried? 1993.
- Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Final Report of the CDSH. Geneva: World Health Organization; 2008.
- Whitehead M, Dahlgren G. Concepts and Principles for Tackling Social Inequities in Health: Levelling up Part 1. Copenhagen: World Health Organization Regional Office for Europe; 2006.
- Graham H. Health inequalities, social determinants and public health policy. Policy Polit 2009;37:463-79. https://doi.org/10.1332/030557309X445618.
- Dahlgren G, Whitehead M. Policies and Strategies to Promote Social Equity in Health. 1991.
- Corbett KK. Susceptibility of youth to tobacco: a social ecological framework for prevention. Respir Physiol 2001;128:103-18. https://doi.org/10.1016/S0034-5687(01)00269-9.
- Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q 2001;79:281-315. https://doi.org/10.1111/1468-0009.00206.
- Notley C, Blyth A, Craig J, Edwards A, Holland R. Postpartum smoking relapse – a thematic synthesis of qualitative studies. Addiction 2015;110:1712-23. http://dx.doi.org/10.1111/add.13062.
- Hawker S, Payne S, Kerr C, Hardey M, Powell J. Appraising the evidence: reviewing disparate data systematically. Qual Health Res 2002;12:1284-99. https://doi.org/10.1177/1049732302238251.
- Noblit GW, Hare RD. Meta-Ethnography: Synthesizing Qualitative Studies. Newbury Park, CA: Sage Publications Inc.; 1988.
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12. http://dx.doi.org/10.1186/1471-2288-12-181.
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitat Res Psychol 2006;3:77-101. https://dx.doi.org/10.1191/1478088706qp063oa.
- Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. London: Sage; 1998.
- Green J, Thorogood N. Qualitative Methods for Health Research. London: Sage Publications Inc.; 2014.
- Smoking Cessation in Pregnancy: A Call to Action. London: ASH; 2013.
- Smoking Cessation in Pregnancy: A Review of the Challenge. London: ASH; 2015.
- Tappin D, Bauld L, Purves D, Boyd K, Sinclair L, MacAskill S, et al. Financial incentives for smoking cessation in pregnancy: randomised controlled trial. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h134.
- Cooper S, Foster K, Naughton F, Leonardi-Bee J, Sutton S, Ussher M, et al. Pilot study to evaluate a tailored text message intervention for pregnant smokers (MiQuit): study protocol for a randomised controlled trial. Trials 2015;16. http://dx.doi.org/10.1186/s13063-014-0546-4.
- Naughton F, Cooper S, Bowker K, Sutton S, Leonardi-Bee J, Sloan M, et al. The adaption and uptake of a text message smoking cessation programme (MiQuit) for use in early antenatal care. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008871.
- Naughton F, Prevost AT, Sutton S. Self-help smoking cessation interventions in pregnancy: a systematic review and meta-analysis. Addiction 2008;103:566-79. http://dx.doi.org/10.1111/j.1360-0443.2008.02140.x.
- Smoking Kills: A White Paper on Tobacco. London: The Stationery Office; 1998.
- Raw M, McNeill A, West R. Smoking cessation guidelines for health professionals. A guide to effective smoking cessation interventions for the health care system. Thorax 1998;53:1-19. http://thorax.bmj.com/content/53/suppl_5/S1.
- Judge K, Bauld L, Chesterman J, Ferguson J. The English smoking treatment services: short-term outcomes. Addiction 2005;100:46-58. http://dx.doi.org/10.1111/j.1360-0443.2005.01027.x.
- Ferguson J, Bauld L, Chesterman J, Judge K. The English smoking treatment services: one-year outcomes. Addiction 2005;100:59-6. https://doi.org/10.1111/j.1360-0443.2005.01028.x.
- Chesterman J, Judge K, Bauld L, Ferguson J. How effective are the English smoking treatment services in reaching disadvantaged smokers?. Addiction 2005;100:36-45. https://doi.org/10.1111/j.1360-0443.2005.01026.x.
- Bauld L, Judge K, Platt S. Assessing the impact of smoking cessation services on reducing health inequalities in England: observational study. Tob Control 2007;16:400-4. https://doi.org/10.1136/tc.2007.021626.
- Stop Smoking Services. London: NICE; 2008.
- McEwen A, West R, McRobbie H. Effectiveness of specialist group treatment for smoking cessation vs. one-to-one treatment in primary care. Addict Behav 2006;31:1650-60. https://doi.org/10.1016/j.addbeh.2005.12.014.
- Dobbie F, Hiscock R, Leonardi-Bee J, Murray S, Shahab L, Aveyard P, et al. Evaluating long term outcomes of NHS Stop Smoking Services (ELONS). Health Technol Assess 2015;19. https://doi.org/10.3310/hta19950.
- Hiscock R, Murray S, Brose LS, McEwen A, Bee JL, Dobbie F, et al. Behavioural therapy for smoking cessation: the effectiveness of different intervention types for disadvantaged and affluent smokers. Addict Behav 2013;38:2787-96. http://dx.doi.org/10.1016/j.addbeh.2013.07.010.
- MacAskill S, Bauld L, Eadie D, Tappin D. Smoking Cessation Support in Pregnancy in Scotland. Glasgow: NHS Health Scotland; 2008.
- Dhalwani NN, Szatkowski L, Coleman T, Fiaschi L, Tata LJ. Prescribing of nicotine replacement therapy in and around pregnancy: a population-based study using primary care data. Br J Gen Pract 2014;64:e554-60. http://dx.doi.org/10.3399/bjgp14X681361.
- SPSP Maternity and Children: End of Phase Report. Edinburgh: Healthcare Improvement Scotland; 2016.
- Bull L, Burke R, Walsh S, Whitehead E. Social attitudes towards smoking in pregnancy in East Surrey: a qualitative study of smokers, former smokers and non-smokers. J Neonat Nurs 2007;13:100-6. https://doi.org/10.1016/j.jnn.2007.01.002.
- Cottrell L, Gibson M, Harris C, Rai A, Sobhan S, Berry T, et al. Examining smoking and cessation during pregnancy among an Appalachian sample: a preliminary view. Subst Abuse Treat Prev Policy 2007;2. https://doi.org/10.1186/1747-597X-2-14.
- Edwards N, Sims-Jones N. Smoking and smoking relapse during pregnancy and postpartum: results of a qualitative study. Birth 1998;25:94-100. https://doi.org/10.1046/j.1523-536x.1998.00094.x.
- Herberts C, Sykes C. Midwives’ perceptions of providing stop-smoking advice and pregnant smokers’ perceptions of stop-smoking services within the same deprived area of London. J Midwifery Womens Health 2012;57:67-73. http://dx.doi.org/10.1111/j.1542-2011.2011.00072.x.
- Howard LM, Bekele D, Rowe M, Demilew J, Bewley S, Marteau TM. Smoking cessation in pregnant women with mental disorders: a cohort and nested qualitative study. BJOG 2013;120:362-70. http://dx.doi.org/10.1111/1471-0528.12059.
- Kennison LH. Smoking and Pregnancy: Reconciling Incompatibilities 2003.
- Maclaine K, Clark JM. Women’s reasons for smoking in pregnancy. Nurs Times 1991;87:39-42.
- Nichter M, Nichter M, Muramoto M, Adrian S, Goldade K, Tesler L, et al. Smoking among low-income pregnant women: an ethnographic analysis. Health Educ Behav 2007;34:748-64. https://doi.org/10.1177/1090198106290397.
- Pletsch PK, Morgan S, Pieper AF. Context and beliefs about smoking and smoking cessation. MCN Am J Matern Child Nurs 2003;28:320-5. https://doi.org/10.1097/00005721-200309000-00012.
- Wigginton B, Lee C. A story of stigma: Australian women’s accounts of smoking during pregnancy. Crit Public Health 2013;23:466-81. https://doi.org/10.1080/09581596.2012.753408.
- Wood L, France K, Hunt K, Eades S, Slack-Smith L. Indigenous women and smoking during pregnancy: knowledge, cultural contexts and barriers to cessation. Soc Sci Med 2008;66:2378-89. http://dx.doi.org/10.1016/j.socscimed.2008.01.024.
- Bottorff JL, Kalaw C, Johnson JL, Stewart M, Greaves L, Carey J. Couple dynamics during women’s tobacco reduction in pregnancy and postpartum. Nicotine Tob Res 2006;8:499-50. https://doi.org/10.1080/14622200600789551.
- Arborelius E, Nyberg K. How should midwives discuss smoking behaviour in pregnancy with women of low educational attainment?. Midwifery 1997;13:210-15. https://doi.org/10.1016/S0266-6138(97)80008-3.
- Hotham ED, Atkinson ER, Gilbert AL. Focus groups with pregnant smokers: barriers to cessation, attitudes to nicotine patch use and perceptions of cessation counselling by care providers. Drug Alcohol Rev 2002;21:163-8. http://dx.doi.org/10.1080/09595230220139064.
- Lendahls L, Ohman L, Liljestrand J, Håkansson A. Women’s experiences of smoking during and after pregnancy as ascertained two to three years after birth. Midwifery 2002;18:214-22. https://doi.org/10.1054/midw.2002.0312.
- Psaros C, Pajolek H, Park ER. The role of negative affect management in postpartum relapse to smoking. Arch Womens Ment Health 2012;15:15-20. http://dx.doi.org/10.1007/s00737-011-0250-2.
- Abrahamsson A, Springett J, Karlsson L, Ottosson T. Making sense of the challenge of smoking cessation during pregnancy: a phenomenographic approach. Health Educ Res 2005;20:367-78. https://doi.org/10.1093/her/cyg127.
- Naughton F, Eborall H, Sutton S. Dissonance and disengagement in pregnant smokers: a qualitative study. J Smok Cessat 2013;8:24-32. http://dx.doi.org/10.1017/jsc.2013.4.
- Tod AM. Barriers to smoking cessation in pregnancy: a qualitative study. Br J Community Nurs 2003;8:56-64. http://dx.doi.org/10.12968/bjcn.2003.8.2.11088.
- Haslam C, Draper ES. A qualitative study of smoking during pregnancy. Psychol Health Med 2001;6:95-9. http://dx.doi.org/10.1080/713690228.
- Lawson EJ. The role of smoking in the lives of low-income pregnant adolescents: a field study. Adolescence 1994;29:61-79.
- Lowry RJ, Hardy S, Jordan C, Wayman G. Using social marketing to increase recruitment of pregnant smokers to smoking cessation service: a success story. Public Health 2004;118:239-43. http://dx.doi.org/10.1016/j.puhe.2003.09.010.
- Thompson KA, Parahoo KP, McCurry N, O’Doherty E, Doherty AM. Women’s perceptions of support from partners, family members and close friends for smoking cessation during pregnancy – combining quantitative and qualitative findings. Health Educ Res 2004;19:29-3. http://dx.doi.org/10.1093/her/cyg013.
- Borland T, Babayan A, Irfan S, Schwartz R. Exploring the adequacy of smoking cessation support for pregnant and postpartum women. BMC Public Health 2013;13. http://dx.doi.org/10.1186/1471-2458-13-472.
- Greaves L, Kalaw C, Bottorff JL. Case studies of power and control related to tobacco use during pregnancy. Womens Health Issues 2007;17:325-32. https://doi.org/10.1016/j.whi.2007.06.001.
- Ziebland S, Fuller A. Smoking cessation in pregnancy: what’s a man to do?. Health Educ J 2001;60:232-40. http://dx.doi.org/10.1177/001789690106000305.
- Dunn CL, Pirie PL, Lando HA. Attitudes and perceptions related to smoking among pregnant and postpartum women in a low-income, multiethnic setting. Am J Health Promot 1998;12:267-74. https://doi.org/10.4278/0890-1171-12.4.267.
- Nguyen SN, Von Kohorn I, Schulman-Green D, Colson ER. The importance of social networks on smoking: perspectives of women who quit smoking during pregnancy. Matern Child Health J 2012;16:1312-18. http://dx.doi.org/10.1007/s10995-011-0896-4.
- Bottorff JL, Johnson JL, Irwin LG, Ratner PA. Narratives of smoking relapse: the stories of postpartum women. Res Nurs Health 2000;23:126-34. https://doi.org/10.1002/(SICI)1098-240X(200004)23:2<126::AID-NUR5>3.0.CO;2-2.
- Wakefield M, Reid Y, Roberts L, Mullins R. Results of a qualitative study of smoking among pregnant adolescents. J Adolesc Health 1998;22:2-3. https://doi.org/10.1016/S1054-139X(97)00204-8.
- Haugland S, Haug K, Wold B. The pregnant smoker’s experience of ante-natal care – results from a qualitative study. Scand J Prim Health Care 1996;14:216-22. https://doi.org/10.3109/02813439608997088.
- Naughton F, Jamison J, Sutton S. Attitudes towards SMS text message smoking cessation support: a qualitative study of pregnant smokers. Health Educ Res 2013;28:911-22. http://dx.doi.org/10.1093/her/cyt057.
- Gaffney KF, Beckwitt AE, Friesen MA. Mothers’ reflections about infant irritability and postpartum tobacco use. Birth 2008;35:66-72. https://dx.doi.org/10.1111/j.1523-536X.2007.00212.x.
- Goldade K, Nichter M, Nichter M, Adrian S, Tesler L, Muramoto M. Breastfeeding and smoking among low-income women: results of a longitudinal qualitative study. Birth 2008;35:230-40. https://dx.doi.org/10.1111/j.1523-536X.2008.00244.x.
- Kennison LH. Smoking and pregnancy: reconciling incompatibilities. Holist Nurs Pract 2009;23:32-8. https://dx.doi.org/10.1097/01.HNP.0000343207.71957.e0.
- Lawson EJ. The Role of Smoking in the Lives of Low-Income Pregnant Adolescents 1993.
- Pletsch PK, Morgan S, Pieper AF. Context and beliefs about smoking and smoking cessation. MCN Am J Matern Child Nurs 2003;28:320-5. https://dx.doi.org/10.1080/07399330490458051.
- Quinn G, Ellison BB, Meade C, Roach CN, Lopez E, Albrecht T, et al. Adapting smoking relapse-prevention materials for pregnant and postpartum women: formative research. Matern Child Health J 2006;10:235-45. https://dx.doi.org/10.1007/s10995-005-0046-y.
- Ripley-Moffitt CE, Goldstein AO, Fang WL, Butzen AY, Walker S, Lohr JA. Safe babies: a qualitative analysis of the determinants of postpartum smoke-free and relapse states. Nicotine Tob Res 2008;10:1355-64. https://dx.doi.org/10.1080/14622200802238936.
- Taylor JA. Beliefs About NHS Stop Smoking Services and Nicotine Replacement Therapy in Pregnancy: Exploring the Potential Role of the Theory of Planned Behaviour in Promoting Uptake of Smoking Cessation Services 2010.
- Von Kohorn I, Nguyen SN, Schulman-Green D, Colson ER. A qualitative study of postpartum mothers’ intention to smoke. Birth 2012;39:65-6. https://dx.doi.org/10.1111/j.1523-536X.2011.00514.x.
- Graham H. Smoking in pregnancy: the attitudes of expectant mothers. Soc Sci Med 1976;10:399-405. https://doi.org/10.1016/0037-7856(76)90097-4.
- Gage JD. Male Partner Participation in Smoking Cessation of Women During Pregnancy 2005.
- Greaves L, Oliffe JL, Ponic P, Kelly MT, Bottorff JL. Unclean fathers, responsible men: smoking, stigma and fatherhood. Health Sociol Rev 2010;19:522-33. http://dx.doi.org/10.5172/hesr.2010.19.4.522.
- Kayser JW, Semenic S. Smoking motives, quitting motives, and opinions about smoking cessation support among expectant or new fathers. J Addict Nurs 2013;24:149-57. http://dx.doi.org/10.1097/JAN.0b013e3182a4caf1.
- Kwon JY, Oliffe JL, Bottorff JL, Kelly MT. Masculinity and fatherhood: new fathers’ perceptions of their female partners’ efforts to assist them to reduce or quit smoking. Am J Mens Health 2015;9:332-9. http://dx.doi.org/10.1177/1557988314545627.
- Bottorff JL, Radsma J, Kelly M, Oliffe JL. Fathers’ narratives of reducing and quitting smoking. Sociol Health Illn 2009;31:185-200. http://dx.doi.org/10.1111/j.1467-9566.2008.01126.x.
- Gould GS, Munn J, Avuri S, Hoff S, Cadet-James Y, McEwen A, et al. ‘Nobody smokes in the house if there’s a new baby in it’: aboriginal perspectives on tobacco smoking in pregnancy and in the household in regional NSW Australia. Women Birth 2013;26:246-53. http://dx.doi.org/10.1016/j.wombi.2013.08.006.
- Oliffe JL, Bottorff JL, Johnson JL, Kelly MT, Lebeau K. Fathers: locating smoking and masculinity in the postpartum. Qual Health Res 2010;20:330-9. http://dx.doi.org/10.1177/1049732309358326.
- Gage JD, Everett KD, Bullock L. A theoretical explanation of male partner participation in smoking cessation during the transition to fatherhood. J Smok Cessat 2011;6:89-96. http://dx.doi.org/10.1375/jsc.6.2.89.
- MacLean LM, Sims-Jones N, Hotte A, Edwards N. Perceived Partner Support and Teamwork: Living with Tobacco Use in Childbearing Families. Ottawa, ON: Community Health Research Unit, University of Ottawa; 2000.
- Bottorff JL, Oliffe J, Kalaw C, Carey J, Mroz L. Men’s constructions of smoking in the context of women’s tobacco reduction during pregnancy and postpartum. Soc Sci Med 2006;62:3096-108. https://doi.org/10.1016/j.socscimed.2005.11.058.
- Abrahamsson A, Springett J, Karlsson L, Håkansson A, Ottosson T. Some lessons from Swedish midwives’ experiences of approaching women smokers in antenatal care. Midwifery 2005;21:335-45. https://doi.org/10.1016/j.midw.2005.02.001.
- Herzig K, Huynh D, Gilbert P, Danley DW, Jackson R, Gerbert B. Comparing prenatal providers’ approaches to four different risks: alcohol, tobacco, drugs, and domestic violence. Women Health 2006;43:83-101. http://dx.doi.org/10.1300/J013v43n03_05.
- Aquilino ML, Goody CM, Lowe JB. WIC providers’ perspectives on offering smoking cessation interventions. MCN Am J Matern Child Nurs 2003;28:326-32. https://doi.org/10.1097/00005721-200309000-00013.
- McLeod D, Benn C, Pullon S, Viccars A, White S, Cookson T, et al. The midwife’s role in facilitating smoking behaviour change during pregnancy. Midwifery 2003;19:285-97. https://doi.org/10.1016/S0266-6138(03)00038-X.
- Bull L. Smoking cessation intervention with pregnant women and new parents (part 2): a focus group study of health visitors and midwives working in the UK. J Neonatal Nurs 2007;13:179-85. http://dx.doi.org/10.1016/j.jnn.2007.07.003.
- Herzig K, Danley D, Jackson R, Petersen R, Chamberlain L, Gerbert B. Seizing the 9-month moment: addressing behavioral risks in prenatal patients. Patient Educ Couns 2006;61:228-35. https://doi.org/10.1016/j.pec.2005.04.001.
- Ebert LM, Freeman L, Fahy K, van der Riet P. Midwives’ interactions with women who smoke in pregnancy. Br J Midwifery 2009;17:24-9. https://dx.doi.org/10.12968/bjom.2009.17.1.37651.
- Parrott AC. Smoking cessation leads to reduced stress, but why?. Int J Addict 1995;30:1509-16. https://doi.org/10.3109/10826089509055846.
- West R, Hajek P. What happens to anxiety levels on giving up smoking?. Am J Psychiatry 1997;154:1589-92. http://dx.doi.org/10.1176/ajp.154.11.1589.
- Strasser AA, Lerman C, Sanborn PM, Pickworth WB, Feldman EA. New lower nicotine cigarettes can produce compensatory smoking and increased carbon monoxide exposure. Drug Alcohol Depend 2007;86:294-300. https://doi.org/10.1016/j.drugalcdep.2006.06.017.
- Hatsukami DK, Le CT, Zhang Y, Joseph AM, Mooney ME, Carmella SG, et al. Toxicant exposure in cigarette reducers versus light smokers. Cancer Epidemiol Biomarkers Prev 2006;15:2355-8. https://doi.org/10.1158/1055-9965.EPI-06-0240.
- Hart C, Gruer L, Bauld L. Does smoking reduction in midlife reduce mortality risk? Results of 2 long-term prospective cohort studies of men and women in Scotland. Am J Epidemiol 2013;178:770-9. http://dx.doi.org/10.1093/aje/kwt038.
- Wennike P, Danielsson T, Landfeldt B, Westin A, Tønnesen P. Smoking reduction promotes smoking cessation: results from a double blind, randomized, placebo-controlled trial of nicotine gum with 2-year follow-up. Addiction 2003;98:1395-402. https://doi.org/10.1046/j.1360-0443.2003.00489.x.
- Smoking: Harm Reduction. London: NICE; 2013.
- Coleman T, Britton J, Thornton J. Nicotine replacement therapy in pregnancy. BMJ 2004;328:965-6. http://dx.doi.org/10.1136/bmj.328.7446.965.
- Naughton F, McEwen A, Sutton S. Use and effectiveness of lapse prevention strategies among pregnant smokers. J Health Psychol 2015;20:1427-33. http://dx.doi.org/10.1177/1359105313512878.
- Boyd KA, Briggs AH, Bauld L, Sinclair L, Tappin D. Are financial incentives cost-effective to support smoking cessation during pregnancy?. Addiction 2015;111:360-70. https://doi.org/10.1111/add.13160.
- Naughton F, Prevost AT, Gilbert H, Sutton S. Randomized controlled trial evaluation of a tailored leaflet and SMS text message self-help intervention for pregnant smokers (MiQuit). Nicotine Tob Res 2012;14:569-77. http://dx.doi.org/10.1093/ntr/ntr254.
- Hallsworth M, Chadborn T, Coleman T, Cooper S, Naughton F, Magee G. Smoking in Pregnancy MiQuit Project. London: Behavioural Insights Team; 2015.
- Valente TW. Network interventions. Science 2012;337:49-53. http://dx.doi.org/10.1126/science.1217330.
- Sterba KR, Rabius V, Carpenter MJ, Villars P, Wiatrek D, McAlister A. Dyadic efficacy for smoking cessation: preliminary assessment of a new instrument. Nicotine Tob Res 2011;13:194-201. http://dx.doi.org/10.1093/ntr/ntq236.
- Chamberlain C, O’Mara-Eves A, Oliver S, Caird JR, Perlen SM, Eades SJ, et al. Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev 2013;10. https://doi.org/10.1002/14651858.cd001055.pub4.
Appendix 1 Search strategies for systematic reviews
Example search strategies for the systematic review of pregnant women’s perspectives and experiences of the barriers to and facilitators of smoking cessation
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
Searched via EBSCOhost interface on 26 April 2013.
Limiters – published date: 20120101–20131231; English Language.
Notes: update of original Public Health Research Consortium (PHRC) review49 search strategy, minus the social disadvantage terms, limited to 2012–13 only.
| # | Query |
|---|---|
| S32 | S31 AND Limiters - Published Date from: 20120101-20131231 |
| S31 | S30 AND Limiters - English Language |
| S30 | S4 AND S12 AND S29 |
| S29 | S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 |
| S28 | TI ‘expectant mother*’ OR AB ‘expectant mother*’ |
| S27 | (MH ‘Expectant Mothers’) |
| S26 | TI (pregnant or pregnanc*) OR AB (pregnant or pregnanc*) |
| S25 | (MH ‘Breast Feeding’) |
| S24 | (MH ‘Postnatal Period+’) |
| S23 | (MH ‘Infant, Newborn’) |
| S22 | (MH ‘Analgesia, Obstetrical’) |
| S21 | (MH ‘Labor Pain’) |
| S20 | (MH ‘Prenatal Care’) |
| S19 | (MH ‘Perinatal Care’) |
| S18 | (MH ‘Prenatal Diagnosis+’) |
| S17 | (MH ‘Fetal Monitoring+’) |
| S16 | (MH ‘Fetus+’) |
| S15 | (MH ‘Maternal Health Services+’) |
| S14 | (MH ‘Pregnancy Complications+’) |
| S13 | (MH ‘Pregnancy+’) |
| S12 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 |
| S11 | (MH ‘Smoking/PC’) |
| S10 | (MH ‘Tobacco, Smokeless’) |
| S9 | (MH ‘Tobacco’) |
| S8 | (MH ‘Nicotine’) |
| S7 | (MH ‘Smoking Cessation Programs’) |
| S6 | (MM ‘Smoking’) |
| S5 | TI ((stop* or quit* or reduc* or give up or giving up) N2 (cigarette* or tobacco or smoking)) OR AB ((stop* or quit* or reduc* or give up or giving up) N2 (cigarette* or tobacco or smoking)) |
| S4 | S1 OR S2 OR S3 |
| S3 | qualitative |
| S2 | interview* or (MH ‘Interviews+’) |
| S1 | findings |
Social Sciences Citation Index
Searched via Web of Knowledge interface on 26 April 2013.
Databases = SSCI; timespan = 2012-01-01 – 2013-04-26; language = (English).
Notes: revised update of original PHRC review49 search strategy, minus the social disadvantage terms, limited to 2012–13 only.
| # | Query |
|---|---|
| #6 | (#5) AND Language=(English) |
| #5 | (#4) AND Language=(English) |
| #4 | #1 AND #2 AND #3 |
| #3 | TS=(pregnant or pregnanc* or ‘expectant mother*’) |
| #2 | TS=(cigarette* or tobacco or smok* or nicotine) |
| #1 | TS=(qualitative* or finding* or interview*) |
Economic and Social Research Council
Searched via www.esrc.ac.uk/search/advanced-search.aspx on 26 April 2013.
Notes: the Economic and Social Research Council website’s advanced search engine is configured to use the Porter Stemming plugin, which reduces search words down to their base word. Update of original PHRC review49 search strategy, minus the social disadvantage terms, no date limitation.
| All of these words: | AND | Any of these words: | |
|---|---|---|---|
| 1. | qualitative pregnant | cigarette tobacco smoker smoking nicotine | |
| 2. | interview pregnant | cigarette tobacco smoker smoking nicotine | |
| 3. | finding pregnant | cigarette tobacco smoker smoking nicotine | |
| 4. | qualitative pregnancy | cigarette tobacco smoker smoking nicotine | |
| 5. | interview pregnancy | cigarette tobacco smoker smoking nicotine | |
| 6. | finding pregnancy | cigarette tobacco smoker smoking nicotine | |
| 7. | qualitative expectant | cigarette tobacco smoker smoking nicotine | |
| 8. | interview expectant | cigarette tobacco smoker smoking nicotine | |
| 9. | finding expectant | cigarette tobacco smoker smoking nicotine |
PubMed (including MEDLINE)
Searched via the National Center for Biotechnology Information (NCBI) interface, on 9 May 2013.
Limited to Ahead of Print Citations.
Notes: update of original PHRC review49 search strategy, minus the social disadvantage terms.
| Search | Query |
|---|---|
| #5 | Search #4 AND pubstatusaheadofprint |
| #4 | Search ((#1) AND #2) AND #3 |
| #3 | Search ‘Pregnant Women’[mesh] OR ‘Breast Feeding’[mesh] OR ‘Postpartum Period’[mesh] OR ‘Infant, Newborn’[mesh] OR ‘Obstetric Surgical Procedures’[mesh] OR ‘Analgesia, Obstetrical’[mesh] OR ‘Labor Pain’[mesh] OR ‘Prenatal Care’[mesh] OR ‘Perinatal Care’[mesh] OR ‘Prenatal Diagnosis’[mesh] OR ‘Fetal Therapies’[mesh] OR ‘Fetal Monitoring’[mesh] OR ‘Fetus’[mesh] OR ‘Maternal Health Services’[mesh] OR ‘Pregnancy Complications’[mesh] OR ‘Pregnancy’[mesh] OR pregnant[tiab] OR pregnanc*[tiab] OR ‘expectant mother*’[tiab] |
| #2 | Search ‘Tobacco Smoke Pollution’[mesh] OR ‘Smoking/prevention and control’[Mesh] OR ‘Smoking/therapy’[Mesh] OR ‘Tobacco, Smokeless’[mesh] OR ‘Tobacco’[mesh] OR ‘Nicotine’[mesh] OR ‘Tobacco Use Disorder’[mesh] OR ‘Tobacco Use Cessation’[mesh] OR ‘Smoking Cessation’[mesh] OR ‘Smoking’[Majr] OR ((stop*[tiab] OR quit*[tiab] OR reduce*[tiab] OR reduct*[tiab] OR ‘give up’ [tiab] OR ‘giving up’ [tiab]) AND (cigarette*[tiab] OR tobacco[tiab] OR smoking[tiab])) |
| #1 | Search (findings OR qualitative OR interview* OR ‘Interviews as Topic’[mesh] OR ‘Interview, Psychological’[mesh]) |
Google Scholar
Searched via http://scholar.google.co.uk on 8 May 2013.
Limited to English language pages only and 2012–13 to capture ‘ahead of print’ but ‘published online’ articles excluding patents; cookies deleted between searches.
| All of these words | This exact phrase | Any of these words | |
|---|---|---|---|
| 1 | qualitative pregnant | published online | cigarette tobacco smoker smoking nicotine |
| 2 | interview pregnancy | published online | cigarette tobacco smoker smoking nicotine |
| 3 | qualitative ‘expectant’ | published online | cigarette tobacco smoker smoking nicotine |
| 4 | interview ‘expectant’ | published online | cigarette tobacco smoker smoking nicotine |
Example search strategies for the systematic review of significant others’ perspectives and experiences of the barriers to and facilitators of smoking cessation
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
Searched via EBSCOhost interface on 9 January 2014.
Limiters – published date: 19900101–20140131; English language.
| # | Query |
|---|---|
| S75 | S74 AND Limiters - Published Date: 19900101-20140131; English |
| S74 | S4 AND S11 AND S28 AND S73 |
| S73 | S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 |
| S72 | TI ((live OR living OR dwell* OR reside*OR stay* OR lodg* OR inhabit*) N1 together) OR AB (live OR living OR dwell* OR reside*OR stay* OR lodg* OR inhabit*) N1 together |
| S71 | TI (common N1 abode*) OR AB (common N1 abode*) |
| S70 | TI (acquaintance*) OR AB (acquaintance*) |
| S69 | TI (friend*) OR AB (friend*) |
| S68 | TI (visitor*) OR AB (visitor*) |
| S67 | TI (guest*) OR AB (guest*) |
| S66 | TI (flatmate* OR flat-mate* OR co-renter* OR corenter*OR roommate OR roommates OR room-mate OR room-mates OR lodger* OR tenant* OR landlord* OR land-lord*) OR AB (flatmate* OR flat-mate* OR co-renter* OR corenter*OR roommate* OR room-mate* OR lodger* OR tenant* OR landlord* OR land-lord*) |
| S65 | TI ((flat* OR apartment* OR room OR rooms OR house* OR home* OR accommodation) N1 shar*) OR AB ((flat* OR apartment* OR room OR rooms OR house* OR home* OR accommodation) N1 shar*) |
| S64 | TI (cohabit* OR co-habit*) OR AB (cohabit* OR co-habit*) |
| S63 | TI (relative OR relatives) OR AB (relative OR relatives) |
| S62 | TI (sibling*) OR AB (sibling*) |
| S61 | TI (child OR children*) OR AB (child OR children*) |
| S60 | TI (son OR sons OR daughter*) OR AB (son OR sons OR daughter*) |
| S59 | TI (family OR families OR familial) OR AB (family OR families OR familial) |
| S58 | TI (household*) OR AB (household*) |
| S57 | TI ((in OR common) N1 (law OR laws)) OR AB ((in OR common) N1 (law OR laws)) |
| S56 | TI (grand*) OR AB (grand*) |
| S55 | TI (step-*) OR AB (step-*) |
| S54 | TI (couple OR couples) OR AB (couple OR couples) |
| S53 | TI (significant N1 other*) OR AB (significant N1 other*) |
| S52 | TI (married OR marriage*) OR AB (married OR marriage*) |
| S51 | TI (partner*) OR AB (partner*) |
| S50 | TI (wife OR wives) OR AB (wife OR wives) |
| S49 | TI (husband*) OR AB (husband*) |
| S48 | TI (spous*) OR AB (spous*) |
| S47 | MH ‘Housing+’ |
| S46 | MH ‘Stepfamilies’ |
| S45 | MH ‘Spouses’ |
| S44 | MH ‘Significant Other’ |
| S43 | MH ‘Siblings’ |
| S42 | MH ‘Paternal Behavior’ |
| S41 | MH ‘Parenting’ |
| S40 | MH ‘Men’s Health’ |
| S39 | MH ‘Marriage’ |
| S38 | MH ‘Interpersonal Relations+’ |
| S37 | MH ‘Friendship’ |
| S36 | MH ‘Fathers+’ |
| S35 | MH ‘Father-Infant Relations’ |
| S34 | MH ‘Father-Child Relations’ |
| S33 | MH ‘Fatherhood’ |
| S32 | MH ‘Family+’ |
| S31 | MH ‘Extended Family+’ |
| S30 | TI (father*) OR AB (father*) |
| S29 | MH ‘Expectant Fathers’ |
| S28 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 |
| S27 | TI ‘expectant mother*’ OR AB ‘expectant mother*’ |
| S26 | (MH ‘Expectant Mothers’) |
| S25 | TI (pregnant or pregnanc*) OR AB (pregnant or pregnanc*) |
| S24 | (MH ‘Breast Feeding’) |
| S23 | (MH ‘Postnatal Period+’) |
| S22 | (MH ‘Infant, Newborn’) |
| S21 | (MH ‘Analgesia, Obstetrical’) |
| S20 | (MH ‘Labor Pain’) |
| S19 | (MH ‘Prenatal Care’) |
| S18 | (MH ‘Perinatal Care’) |
| S17 | (MH ‘Prenatal Diagnosis+’) |
| S16 | (MH ‘Fetal Monitoring+’) |
| S15 | (MH ‘Fetus+’) |
| S14 | (MH ‘Maternal Health Services+’) |
| S13 | (MH ‘Pregnancy Complications+’) |
| S12 | (MH ‘Pregnancy+’) |
| S11 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 |
| S10 | (MH ‘Tobacco, Smokeless’) |
| S9 | (MH ‘Tobacco’) |
| S8 | (MH ‘Nicotine’) |
| S7 | (MH ‘Smoking Cessation Programs’) |
| S6 | (MH ‘Smoking’) |
| S5 | TI ((stop* or quit* or reduc* or give up or giving up) N2 (cigarette* or tobacco or smoking)) OR AB ((stop* or quit* or reduc* or give up or giving up) N2 (cigarette* or tobacco or smoking)) |
| S4 | S1 OR S2 OR S3 |
| S3 | qualitative |
| S2 | interview* or (MH ‘Interviews+’) |
| S1 | findings |
PubMed (including MEDLINE)
Searched via NCBI interface on 10 January 2014.
Limited to Ahead of Print Citations and articles published in the last 2 months.
| Search | Query |
|---|---|
| #7 | #5 OR #6 |
| #6 | #4 AND (2013/11:2014 [edat] OR 2013/11:2014 [crdt] OR 2013/11:2014[dp]) |
| #5 | #4 AND pubstatusaheadofprint |
| #4 | #1 AND #2 AND #3 |
| #3 | ‘Pregnant Women’[mesh] OR ‘Breast Feeding’[mesh] OR ‘Postpartum Period’[mesh] OR ‘Infant, Newborn’[mesh] OR ‘Obstetric Surgical Procedures’[mesh] OR ‘Analgesia, Obstetrical’[mesh] OR ‘Labor Pain’[mesh] OR ‘Prenatal Care’[mesh] OR ‘Perinatal Care’[mesh] OR ‘Prenatal Diagnosis’[mesh] OR ‘Fetal Therapies’[mesh] OR ‘Fetal Monitoring’[mesh] OR ‘Fetus’[mesh] OR ‘Maternal Health Services’[mesh] OR ‘Pregnancy Complications’[mesh] OR ‘Pregnancy’[mesh] OR pregnant[tiab] OR pregnanc*[tiab] OR ‘expectant mother*’[tiab] |
| #2 | ‘Tobacco Smoke Pollution’[mesh] OR ‘Tobacco, Smokeless’[mesh] OR ‘Tobacco’[mesh] OR ‘Nicotine’[mesh] OR ‘Tobacco Use Disorder’[mesh] OR ‘Tobacco Use Cessation’[mesh] OR ‘Smoking Cessation’[mesh] OR ‘Smoking’[mesh] OR ((stop*[tiab] OR quit*[tiab] OR reduce*[tiab] OR reduct*[tiab] OR ‘give up’ [tiab] OR ‘giving up’ [tiab]) AND (cigarette*[tiab] OR tobacco[tiab] OR smoking[tiab])) |
| #1 | findings OR qualitative OR interview* OR ‘Interviews as Topic’[mesh] OR ‘Interview, Psychological’[mesh] |
Example search strategies for the systematic review of health-care practitioners’ perspectives and experiences of the barriers and facilitators to smoking cessation
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
Searched via EBSCOhost interface on 26 February 2014.
Limiters – published date: 19900101–20141231; English language.
| # | Query |
|---|---|
| S75 | S74 AND Limiters - Published Date: 19900101-20141231; English Language |
| S74 | S4 AND S11 AND S28 AND S73 |
| S73 | S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 |
| S72 | MH ‘Patient Education’ |
| S71 | MH ‘Research, Midwifery’ |
| S70 | MH ‘Practice Patterns’ |
| S69 | MH ‘Patient History Taking+’ |
| S68 | MH ‘Professional-Patient Relations’ |
| S67 | MH ‘Professional-Client Relations’ |
| S66 | MH ‘Professional-Family Relations’ |
| S65 | MH ‘Physician-Patient Relations’ |
| S64 | MH ‘Nurse-Patient Relations’ |
| S63 | MH ‘Community Role’ |
| S62 | MH ‘Professional Role’ |
| S61 | MH ‘Physician’s Role’ |
| S60 | MH ‘Nursing Role’ |
| S59 | MH ‘Employee Attitudes’ |
| S58 | MH ‘Midwife Attitudes’ |
| S57 | MH ‘Attitude of Health Personnel+’ |
| S56 | TI ((health OR ‘health care’ OR healthcare OR medical OR hospital) N2 (personnel OR worker# OR provider# OR employee# OR staff OR professional#)) OR AB ((health OR ‘health care’ OR healthcare OR medical OR hospital) N2 (personnel OR worker# OR provider# OR employee# OR staff OR professional#)) |
| S55 | (MH ‘Pharmacists’) OR (MH ‘Pharmacy Technicians’) OR (MH ‘Pharmacy Service+’) |
| S54 | TI (pharmacist# OR pharmacy OR pharmacies) OR AB (pharmacist# OR pharmacy OR pharmacies) |
| S53 | MH ‘Allied Health Personnel+’ |
| S52 | MH ‘Community Health Workers’ |
| S51 | MH ‘Community Health Nursing’ |
| S50 | MH ‘Home Health Aides’ |
| S49 | TI ((home OR health) N2 visit*) OR AB ((home OR health) N2 visit*) |
| S48 | MH ‘Physicians, Family’ |
| S47 | TI (GP# OR ‘general practitioner’ OR ‘general practitioners’) OR AB (GP# OR ‘general practitioner’ OR ‘general practitioners’) |
| S46 | TI (doctor# OR physician# OR clinician#) OR AB (doctor# OR physician# OR clinician#) |
| S45 | TI ((ante-natal OR antenatal) N1 (appointment# OR care OR service#)) OR AB ((ante-natal OR antenatal) N1 (appointment# OR care OR service#)) |
| S44 | TI (maternity N1 (care OR service#)) OR AB (maternity N1 (care OR service#)) |
| S43 | TI (consultant* N1 (obstetric* OR gyn#ecologic*)) OR AB (consultant* N1 (obstetric* OR gyn#ecologic*)) |
| S42 | MH ‘Obstetrics’ |
| S41 | TI (nursing N2 (staff OR personnel OR auxiliar*)) OR AB (nursing N2 (staff OR personnel OR auxiliar*)) |
| S40 | TI (nurse#) OR AB (nurse#) |
| S39 | (MH ‘Obstetric Nursing’) OR (MH ‘OB-GYN Nurse Practitioners’) |
| S38 | (MH ‘Pediatric Nursing’) OR (MH ‘Pediatric Nurse Practitioners’) |
| S37 | (MH ‘Family Nursing’) OR (MH ‘Family Nurse Practitioners’) |
| S36 | MH ‘Maternal-Child Nursing+’ |
| S35 | MH ‘Nurse Midwifery’ |
| S34 | MH ‘Midwives+’ |
| S33 | TI (midwi?e*) OR AB (midwi?e*) |
| S32 | TI ((train* OR service* OR support*) N2 cessation) OR AB ((train* OR service* OR support*) N2 cessation) |
| S31 | TI ((train* OR service* OR support*) N2 smoking) OR AB ((train* OR service* OR support*) N2 smoking) |
| S30 | TI ((advisor* OR assist* OR manager* OR professional* OR specialist*) N2 cessation) OR AB ((advisor* OR assist* OR manager* OR professional* OR specialist*) N2 cessation) |
| S29 | TI ((advisor* OR assist* OR manager* OR professional* OR specialist*) N2 smoking) OR AB ((advisor* OR assist* OR manager* OR professional* OR specialist*) N2 smoking) |
| S28 | S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 |
| S27 | TI ‘expectant mother*’ OR AB ‘expectant mother*’ |
| S26 | (MH ‘Expectant Mothers’) |
| S25 | TI (pregnant or pregnanc*) OR AB (pregnant or pregnanc*) |
| S24 | (MH ‘Breast Feeding’) |
| S23 | (MH ‘Postnatal Period+’) |
| S22 | (MH ‘Infant, Newborn’) |
| S21 | (MH ‘Analgesia, Obstetrical’) |
| S20 | (MH ‘Labor Pain’) |
| S19 | (MH ‘Prenatal Care’) |
| S18 | (MH ‘Perinatal Care’) |
| S17 | (MH ‘Prenatal Diagnosis+’) |
| S16 | (MH ‘Fetal Monitoring+’) |
| S15 | (MH ‘Fetus+’) |
| S14 | (MH ‘Maternal Health Services+’) |
| S13 | (MH ‘Pregnancy Complications+’) |
| S12 | (MH ‘Pregnancy+’) |
| S11 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 |
| S10 | (MH ‘Tobacco, Smokeless’) |
| S9 | (MH ‘Tobacco’) |
| S8 | (MH ‘Nicotine’) |
| S7 | (MH ‘Smoking Cessation Programs’) |
| S6 | (MH ‘Smoking’) |
| S5 | TI ((stop* or quit* or reduc* or give up or giving up) N2 (cigarette* or tobacco or smoking)) OR AB ((stop* or quit* or reduc* or give up or giving up) N2 (cigarette* or tobacco or smoking)) |
| S4 | S1 OR S2 OR S3 |
| S3 | qualitative |
| S2 | interview* or (MH ‘Interviews+’) |
| S1 | findings |
Social Sciences Citation Index
Searched via Web of Knowledge interface on 25 February 2014.
Databases = SSCI; timespan = 1990–2014; language = (English).
| # | Query |
|---|---|
| #21 | (#19 AND #3 AND #2 AND #1) AND LANGUAGE: (English) |
| #20 | (#19 AND #3 AND #2 AND #1) |
| #19 | #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 |
| #18 | TS=((health OR ‘health care’ OR healthcare OR medical OR hospital) NEAR/2 (personnel OR worker$ OR provider$ OR employee$ OR staff OR professional$)) |
| #17 | TS=(pharmacist$ OR pharmacy OR pharmacies) |
| #16 | TS=((home OR health) NEAR/2 visit*) |
| #15 | TS=(GP$ OR ‘general practitioner’ OR ‘general practitioners’) |
| #14 | TS=(doctor$ OR physician$ OR clinician$) |
| #13 | TS=((ante-natal OR antenatal) NEAR/1 (appointment$ OR care OR service$)) |
| #12 | TS=(maternity NEAR/1 (care OR service$)) |
| #11 | TS=(consultant* NEAR/1 (obstetric* OR gyn$ecologic*)) |
| #10 | TS=(nursing NEAR/2 (staff OR personnel OR auxiliar*)) |
| #9 | TS=(nurse$) |
| #8 | TS=(midwi?e*) |
| #7 | TS=((train* OR service* OR support*) NEAR/2 cessation) |
| #6 | TS=((train* OR service* OR support*) NEAR/2 smoking) |
| #5 | TS=((advisor* OR assist* OR manager* OR professional* OR specialist*) NEAR/2 cessation) |
| #4 | TS=((advisor* OR assist* OR manager* OR professional* OR specialist*) NEAR/2 smoking) |
| #3 | TS=(pregnant or pregnanc* or ‘expectant mother*’) |
| #2 | TS=(cigarette* or tobacco or smok* or nicotine) |
| #1 | TS=(qualitativ* or finding* or interview*) |
Appendix 2 Qualitative interview topic guides
Appendix 3 Patient and public involvement summary of findings
What helps or hinders women from stopping smoking in pregnancy and staying stopped?
Summary of the findings from three perspectives: pregnant women, their partners, family and friends and HPs.
Pregnant women’s perspective
Forty-one interviews were conducted with pregnant women. Participants were, on average, 26 years old and 19 weeks pregnant. Thirty-seven per cent said that they had stopped smoking. Interviews explored several topics, including women’s smoking behaviour, their thoughts about smoking in pregnancy, intentions to stop smoking, how midwives and other HPs discussed smoking, the smoking cessation support received and partner, family and friends’ smoking behaviour and attitudes. The main findings are presented in Table 8.
| Finding | Illustrative quotations from pregnant women |
|---|---|
| Women’s circumstances | |
| Many of the women faced challenges such as living in large households, not living with their current partner, being carers of children or parents in ill health, preparing to be single mothers and being in financial insecurity with regard to welfare benefits and unstable jobs. Many described ongoing pregnancy and general health problems. Smoking was a well-established part of their routines, and served as a break from work or family life, and a way of coping with daily stress and boredom | It’s just really hard, plus this wee one stresses you out sometimes and it’s like the only time I get like a 5-minute break sort of thing . . . I kind of look forward to that breakArea A, pregnant woman 9, smoker |
| Risk perceptions | |
| All women acknowledged a potential risk to the baby from maternal smoking. Although some gave detailed accounts of the risks, others expressed uncertainty about specific risks. Some women admitted that they avoided thinking or learning about the risks as they were unsettling, whereas for others their assessment of risk was the primary motivating factor in wanting to stop smoking | I don’t [think of the risks] . . . I’ve tried to avoid all the stuff because I don’t really want to know. I think you can get breathing problems . . . and they can be small . . . but to be honest that’s about all I know . . . I’d prefer not to knowArea B, pregnant woman 14, smoker |
| Self-belief and willpower | |
| Those who reported having stopped smoking talked about having ‘focus’, resilience in the face of setbacks and triggers, ‘forcing’ themselves and having a strong desire to stop smoking for the baby. Many reported less difficulty than expected to stop smoking. In contrast, women who were still smoking at interview spoke of the difficulty in stopping smoking, low desire or willpower to stop despite potential harm to the baby, and half-hearted quit attempts | On a night I’d crave it with a cup of tea and I just had to keep myself busy and go for a bath or something to take my mind off itArea B, pregnant woman 21, non-smokerI knew I wasn’t going to put my mind to it . . . to try and stop smokingArea A, pregnant woman 2, smoker |
| Influence of partners | |
| Women reported that their partner’s attitude towards smoking in pregnancy, whether or not their partner smoked and the support they offered, influenced the ease of stopping smoking | I think it’s harder with [partner] smoking because if he goes for a cigarette then I will go with him for oneArea B, pregnant woman 14, smoker |
| Influence of family and friends | |
| Many women recalled conversations with family and friends about babies born with no apparent ill effects from maternal smoking. These experiences were used by some women to refute the risks communicated by HPs and to make them feel better about smoking | A few people have been quite nice about it, they’ve been like ‘oh, it doesn’t matter, I smoked all the way through mine’ and ‘I’ve got two beautiful perfectly healthy kids’. . . and ‘they smoked more than you’ that makes me feel a bit betterArea A, pregnant woman 5, smoker |
| Workplace | |
| The workplace was reported to make quit attempts easier or more difficult depending on routines, job demands and level of stress. Some work environments were dominated by a smoking culture, in which smoking, taking breaks and socialising with colleagues were inter-related | At work I smoke a lot more, I think it’s just, it’s the only kind of break that I get sometimes . . . it gets me away from the customers when they’re annoying meArea A, pregnant woman 5, smoker |
| Midwife’s role and relationship with pregnant women | |
| Women said that smoking in pregnancy was raised by midwives at the booking appointment. They described variation in the time devoted to the issue, however, with some feeling discussions were rushed with little detail about risks. Women often said their midwife was ‘nice’, ‘supportive’ and non-judgemental. They also said that midwives often reassured them about their smoking behaviour in early pregnancy or told them that they were doing well if they had cut down. Some women described a lack of pressure in their midwife’s approach to smoking | I think I tried to ask questions but she [midwife] kinda told me that she’s not a specialist . . . I did think my midwife would know what was dangerous and what wasn’tArea A, pregnant woman 7, smokerShe said that she didn’t believe that she needed to sit and lecture me and that I could approach the subject with her . . . And actually that was what I wanted, I didn’t want an overbearing lecture, there is enough things going on during pregnancyArea B, pregnant woman 9, smoker |
| CO monitoring | |
| CO monitoring served as a visual indicator of risk to the baby and helped women understand the potential harm of smoking. Those screened often described shock and feeling ‘bad’ or ‘embarrassed’ at seeing the result. When repeatedly used, this was a tool that appeared to aid motivation and self-esteem | I didn’t realise exactly how much CO’s going in . . . once I’d seen that . . . I tried as much as possible to stopArea A, pregnant woman 7, smokerIt was a confidence boost, thinking ‘well that’s 2 weeks and it’s like, the nicotine, the carbon monoxide’s out my body, what’s it going to be like at 4?’Area A, pregnant woman 12, non-smoker |
| NRT | |
| Perceptions of NRT were mixed, but there were some positive accounts of using patches in pregnancy. Many of those trying the inhalator said it had helped them to cut down or stop smoking. There was some concern over the safety of using NRT while pregnant and several women had sought clarification from HPs | I swore by those, they were really good . . . you don’t even think about a fag when you are on a patchArea A, pregnant woman 17, non-smokerI was like ‘they are safe?’ and she goes, ‘I wouldn’t be prescribing them to you if they weren’t’Area B, pregnant woman 16, smoker |
| SSSs | |
| For those who engaged with the SSS, perceptions on how helpful they found it were mixed. Overall, positive comments centred on the delivery of support, information and relationship with the cessation advisor. Negative responses generally focused on the inconvenience of attending appointments, unhelpful information and perceived pressure from the cessation advisor | We talked about the things to stop me from smoking as well . . . like what to do instead of being in my routine, like maybe listening to music . . . yeah it seemed helpfulArea A, pregnant woman 4, smokerI did try, but the woman that they gave me, she got on my nerves a bit because she would talk down at me because she had never been a smokerArea B, pregnant woman 6, smoker |
Significant others’ perspective
Thirty-two SOs of pregnant women were interviewed, comprising 25 partners, three mothers, one mother-in-law and three friends (two associated with the same woman). Interviews covered SOs’ own smoking behaviour, the role of smoking within their relationship with the pregnant woman, their attitudes to smoking in pregnancy and details of the support they had given the woman in stopping smoking. SOs also discussed these topics in relation to members of the pregnant woman’s wider social network. Finally, interviewees were asked about cessation support for pregnant women from HPs, including views on HPs raising the issue of smoking in pregnancy, awareness of services and the nature of stop smoking support, CO monitoring and the use of NRT.
| Finding | Illustrative quotations from SOs |
|---|---|
| SOs’ smoking behaviour | |
| About two-thirds of SOs were current smokers and almost one-third were former smokers, some of whom were using NRT or e-cigarettes to maintain a recent quit attempt. Many of those who smoked said that they would prefer to quit and had often tried previously, sometimes on multiple occasions | It’s a horrible habit, but, I don’t like it but it’s just something I’ve got so used to doing and it’s just like, well, I don’t need to but I want to, it’s mind over matter to be fairArea B, partner 44, smoker |
| Importance of smoking to relationship | |
| The importance of smoking to relationships between SOs and pregnant women was not always stated or appreciated, but was sometimes implicit in the way in which respondents spoke about smoking together. SOs spoke in terms of a shared habit of smoking, as an important part of spending time together or a means of communicating | I think you talk a lot more when you are out having a cig[arette], so I think it’s good for communicating because you are both obviously smoking at the same time, so oh now I remember, before if you were just sat watching TV or doing something else then it might not go through your head to remind each other what you have to do or everything you’ve got to tell them that happened during the dayArea B, partner 2, former smoker |
| Attitudes to smoking in pregnancy | |
| Attitudes to smoking in pregnancy were generally negative reflecting general acceptance that smoking was bad for the baby and linked to low birthweight and miscarriage. However, not all SOs felt able to encourage quitting in pregnant women citing such reasons as fear of being accused of hypocrisy (when they continued to smoke), recognition of the role of smoking in the woman’s life, particularly as a coping mechanism, and the possible conflict such demands may cause | Obviously the dangers are there, they are very real and they can be quite serious [smoking when pregnant]Area B, partner 6, former smokerI feel like a hypocrite but it’s my grandchild you know, and, oh it’s crazy, but I wouldn’t have been happy with her [smoking] but I think it would have been in the back of my mind, that’s wrong, that’s wrong, but you cannae[cannot] help the way you thinkArea A, mother 20, smoker |
| Support for pregnant women | |
| Most recognised the need to support women in their attempts to quit smoking but the types of support provided by SOs varied. The most common response was to not smoke in front of the pregnant woman, mainly smoking outside the home. Some took the decision to quit at the same time as the woman, although with varying degrees of commitment and success | This isn’t my first time I’ve tried it, I’ve tried so many times, this time my motivation was that if [name 1] had to quit smoking then it wasn’t fair if I still smoked. And I was never going to smoke in her presence anyway, so it was a case of us stopping smoking at the same sort of time so yeahArea A, partner 51, former smoker using e-cigarette |
| Wider social network | |
| Smoking was similarly common among the pregnant woman’s wider social network with in many cases ‘everyone’ or a large proportion described as smokers. Family members and friends were also said to be supportive of quitting in pregnancy but again the picture was mixed in terms of providing support to the pregnant woman. Although some were willing to avoid smoking in the presence of the woman, in some cases even in their own home, others were described as continuing as normal | When we are at her mum’s house, her mum and her sister stay in the same house, and whenever we are there like I say we will go in the kitchen, but even if [name one] is not smoking another one of them will be smoking, so the kitchen is pretty smoke filled. So there is no kind of escaping it when you are in thereArea A, partner 48, smoker |
| HPs raising smoking in pregnancy (giving brief advice) | |
| SOs felt it was appropriate for HPs, especially midwives and GPs, to raise smoking in pregnancy with pregnant women given their role in looking after the woman and her baby. Brief advice provided by generic HPs was also perceived to be beneficial in terms of raising awareness of the risks of smoking and the benefits of stopping, although not necessarily in terms of providing sufficient support to quit | I think it’s good because they get to understand and they get told it’s harmful and what you can do, but I don’t think that in itself is helpful in expecting to stop the smoking. It’s good to understand what it’s doing but it’s not good to help it stop because it’s nothing to help you stopArea A, friend 44, smoker |
| Nature of stop smoking support | |
| In general, SOs were positive about the stop smoking support that pregnant women had received and revealed a particular appreciation for one-to-one support which was perceived to be flexible and responsive. There was less positivity about group support, although advocates indicated the advantage of members being able to share experiences and provide reassurance to others | . . . it’s not been every week but there has been a lot of contact between the two of them [pregnant woman and smoking cessation advisor] and then they have, if they can’t make it then they will speak on the phone and things like that, and if [name one] is feeling, I mean she hasn’t for weeks now but before if she felt like she was close to going and buying a packet she could phone [name 2] and she was always ready to talk to her and sort of give her encouragement and things. She couldn’t have done it without itArea A, mother 20, smoker |
| CO monitoring and use of NRT in pregnancy | |
| SOs largely recognised CO monitoring as a helpful motivational tool for pregnant women and other smokers alike. However, there were some that raised concern about the interpretation of readings. There appeared to be little concern about the use of NRT in pregnancy among SOs. However, some noted that the limited range of NRT available to pregnant women could be a barrier to quitting | I just think she filled her head with, that it’s all right because she’s on the green, which it isn’t all right, because it’s still smoking, it’s still not good for youArea A, partner 17, smoker. . . there are certain things that they can’t take to help them stop whereas, so they would need advice about that. And so it is, you are treated different, even the patches, they don’t like giving them the stronger patches, so if you are a heavy smoker and you are pregnant, they lighter patches don’t really do you any good anyway so having the extra support to go through that would be helpfulArea A, mother 20, smoker |
Health-care professionals’ perspective
Twenty-eight individual and group interviews were conducted with 48 HPs, including midwives, health visitors, GPs, pharmacists, obstetricians, commissioners, and SSS advisors and managers. Interviews explored several topics, including the support offered to pregnant smokers, referrals to SSSs, how midwives and health visitors discussed smoking, the use of CO breath test monitors and NRT, and ideas for improving services. The main findings are presented below.
| Finding | Illustrative quotations from HPs |
|---|---|
| Structure and set-up of services for pregnant women | |
| Most HPs interviewed felt that the services available for pregnant women could do more to support pregnant smokers. However, they often discussed how limited funding and changes to staff and service structures made it more difficult to offer that support. Participants also described how workload demands made it hard to cover everything in detail and that smoking sometimes got left out as a result of competing priorities | . . . our service has gone through sort of several sort of stages . . . so it’s just been we’ve not had a cohesive sort of run at how do we deal with pregnant womanArea A, SSS advisor from group 1 |
| Referral to stop smoking support | |
| Most midwives said their role was to refer pregnant smokers to SSSs for support. Some wanted to be more involved in smoking cessation work but most felt that support from the specialist SSS would be better. In some areas, midwives were required to refer all pregnant women identified as smokers to SSSs unless they opted out (‘opt-out’ referral), and some felt uncomfortable about this, feeling that it took away women’s choice. Others said ‘opt-out’ referral was a good idea and a way to encourage women to attend services. SSS advisors also had mixed views about ‘opt-out’ referrals, with some feeling that it should be the woman’s choice and others feeling that it was more important that pregnant smokers get referred for the support | Though I do offer everybody the chance to be referred to the smoking cessation person, but I don’t see it as my role to refer them if they are not at the stage when they are ready to stop smokingArea B, midwife 2We are not here to tell people stop smoking. We are here to help people who have decided that they want to quitArea B, SSS advisor 2. . . there is always somebody that’s pleasantly surprised that we are that non-judgemental and we are there just to accept them kind of warts and allArea A, SSS advisor from group 1 |
| Difficulty raising the issue and discussing risk | |
| Several HPs said they worried about upsetting clients and damaging client relationships by discussing the risks of smoking in pregnancy. They also worried about sounding judgemental and, as a result, sometimes avoided discussing risks in detail. Sometimes participants felt that other HPs had already discussed smoking and that they did not want to end up ‘lecturing’ women. However, some HPs said it was more important that pregnant smokers were made fully aware of the risks around smoking and also that pregnant smokers wanted to hear the risks | And if I start, if they see me as someone who is just going to nag them every time they come they might not want to comeArea B, midwife 3Actually there is a reasonable amount of evidence base that says that they are expecting to be asked, women, it isn’t going to damage the relationship if you ask, or talk about smokingArea B, commissioner 1 |
| CO monitoring | |
| Using CO breath monitors with pregnant smokers was seen as helpful to boost motivation around quitting and highlight risks from smoking in pregnancy. Some HPs worried about this upsetting pregnant women and causing them not to continue with support. Most, however, felt that it was a useful procedure | And it does give you that, you know, opportunity to speak to everybody about smoking and the people that do have a high reading, it’s re-emphasising the facts, the impact it can have on the baby and the pregnancyArea B, midwife from group 1 |
| NRT | |
| Some HPs were cautious about NRT and described that pregnant smokers could also be cautious or ‘put off’ using NRT once the risks and benefits had been explained to them. SSS advisor participants were generally positive about NRT and felt that it was helpful for pregnant smokers, especially if it could be quickly prescribed. Delays to NRT provision were seen as causing some women to lose motivation | . . . I always thought if you could give them the patches straightaway you would be halfway thereArea A, SSS advisor from group 2 |
| Training | |
| Apart from SSS advisors, most participants said that smoking in pregnancy training was not mandatory and several said that they would like more training. Some said that it was good that there was a choice, as it meant that staff could attend training that they felt was most important to them. Others, however, felt it was more important that all HPs be trained to the same level in smoking cessation, so that everyone gives the same message about smoking in pregnancy | . . . I think sometimes you know you get mixed messages from like their family, from their doctor, from the midwife and it’s, you know, who do they listen to really you know . . .Area A, SSS advisor from group 2 |
| Pregnant smoker’s environment | |
| Many HPs described difficulties that some pregnant smokers can face and spoke about how a difficult home life, living with smokers, being far away from services and having other emotional difficulties could all make it difficult to quit smoking in pregnancy. Several also noted that physical changes in pregnancy affect how the body processes nicotine, making it harder to stop | It’s harder to stop in pregnancy [. . .] we know it’s more difficult because of how the brain and the hormones affect the brain it’s harder to stopArea B, midwife from group 1 |
| Ways to improve the service | |
| Participants suggested several ways to improve support for pregnant smokers. This included having more staff to provide specialist support, more options for home visits and other flexible support, and more time set aside for telephone and text support. Other suggestions to improve support included use of social media such as Facebook and Twitter. In addition, participants felt that more interservice communication would be beneficial, as it would lead to services working together more effectively to support pregnant smokers | I think just developing relationships with the midwife team so that they can put a face to who they are referring people to and they can have confidence that we will chase the ladies up or that we will keep them in the loopArea A, SSS advisor from group 2 |
List of abbreviations
- ASH
- Action on Smoking and Health
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CO
- carbon monoxide
- COM-B
- capability, opportunity, motivation and behaviour
- CRUK
- Cancer Research UK
- DH
- Department of Health
- e-cigarette
- electronic cigarette
- ENTREQ
- Enhancing Transparency in Reporting the Synthesis of Qualitative Research
- GP
- general practitioner
- HP
- health-care professional
- HTA
- Health Technology Assessment
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NRT
- nicotine replacement therapy
- PI
- principal investigator
- R&D
- research and development
- REC
- Research Ethics Committee
- SEF
- social–ecological framework
- SHS
- second-hand smoke
- SO
- significant other
- SSS
- Stop Smoking Service
- TPB
- theory of planned behaviour
- TV
- television
- UKCTAS
- UK Centre for Tobacco and Alcohol Studies