Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 13/75/01. The contractual start date was in September 2014. The draft report began editorial review in February 2016 and was accepted for publication in December 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Claire Goodman is a National Institute for Health Research Senior Investigator. Rowan Harwood is a member of the Health Technology Assessment Primary Care, Community and Preventive Interventions Panel. Jo Rycroft-Malone is Programme Director and Chairperson of the Health Services and Delivery Research Commissioning Board.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Goodman et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Being incontinent of faeces is distressing for any adult to experience. Adults who are unable to care for themselves, such those with dementia, must rely on others to provide care for them. In group residential settings such as care homes, preventing and managing faecal incontinence (FI) is a significant and persistent challenge for staff and visiting clinicians.
This realist synthesis draws together evidence from different strands of research to inform interventions that address the realities of working in and across complex overlapping systems of care. For example, we sought evidence on the physiology and management of FI and urinary incontinence (UI) in ageing populations and those living with dementia in care homes, and the relative availability, acceptability and efficacy of different types of incontinence products. We also included experiential evidence on living with dementia and incontinence from the perspectives of people with dementia and their paid and unpaid carers. Realist methodology enables us to deconstruct the component theories of different FI-related interventions and to consider relevant contextual data to test the applicability of different approaches for this population and setting.
Aim and objectives
The aim of this review is to provide a theoretical explanation of how different interventions support (or do not support) the reduction and management of FI in people with advanced dementia living in care homes.
The objectives are:
-
to identify which interventions could potentially be effective, how they work, on what range of outcomes (i.e. organisational, resource use and patient’s level of care) and for whom (or why they do not work);
-
to establish what evidence there is on the relative feasibility and (when appropriate) cost of interventions to manage FI.
Background
Care homes
In England, there are approximately 17,500 care homes that are home to about 487,000 older people, the majority of whom are women aged ≥ 80 years. 1 Care homes are the main providers of long-term care for older people in the UK, and there are approximately three times as many beds in the care home sector as there are NHS hospital beds. 2 The terms ‘care home’ and ‘long-term care’ refer to residential care provided to older people who require help with personal care and cannot be supported in their own home because of frailty, lack of mental capacity and/or functional limitations. The terms include homes that have on-site nursing provision and those that do not. In this report, the phrases ‘long-term care’ and ‘care home’ are used interchangeably. In the UK, care homes are run by both for-profit and not-for-profit provider organisations. The care home sector is diverse, varying in size, ownership, funding sources, focus, education of the workforce and organisational culture. 3 This variability in provision has implications for the way in which interventions to support continence care are understood and implemented, for example the presence or absence of on-site nurses, topic expertise in the workforce, organisational structure, funding and staffing.
Care home residents rely on primary health-care professionals, and general practitioners (GPs) in particular, for access to medical care and referral to specialist services, including continence services. 4–7 Public funding for care varies by region,8 and a recent review of health service provision to care homes9 concluded that access to specialist services is unpredictable and inequitable.
Residents living with dementia
Almost all care home residents have three or more health conditions, with 80% living with dementia, one-third of whom may be at the advanced stage of the disease, although a diagnosis is not always documented. 7,10 In clinical practice, severe or advanced dementia is variably defined but usually includes almost complete loss of memory and recognition, severe dependency in everyday activities, poor or absent communication, incontinence and poor mobility, and often swallowing difficulty and weight loss. 11 Reisberg et al.,11 in their review of severe dementia and how the stages of dementia are assessed, define the phase of severe dementia as that time when:
. . . the cognitive deficits are of sufficient magnitude as to compromise an otherwise healthy person’s capacities to independently perform basic activities of daily life such as dressing, bathing and toileting.
p. 8311
Care homes have been crucial in the service response to the rapidly increasing number of people with dementia who need this kind of continuous care and support.
Faecal incontinence prevalence, evidence, guidance and impact on residents and staff
Faecal incontinence is the involuntary loss of liquid or solid stool that is a social or personal hygiene problem. 12 The prevalence of FI in people aged > 80 years is estimated to range from 12% to 22%. 13,14 Epidemiological studies have identified dementia as an independent risk factor for FI,15–17 and a study of primary care patients found FI to be four times higher in people with dementia than in a matched community-dwelling sample with FI but without a diagnosis of dementia. 18 Studies suggest that the prevalence of FI in care homes is between 30% and 50%. 15,19–23 The level of variation is believed to reflect differences in care and the way in which continence is defined (by frequency, amount and detection method) as well as the individual characteristics of older people. It is unclear how dementia has an impact on a person’s gut and anal sphincter, but there is a widely held, albeit untested, view that eventually everyone with dementia will become incontinent if they live long enough. 11
The evidence about the prevention and treatment of FI in care homes is variable. Although there is evidence about risk factors and associations, there are few intervention studies. Research on continence care in care homes tends to focus on UI. 24–27 It is also important to understand the ways in which public funding is deployed for continence care in care home settings and any consequences for FI management at the individual and organisational levels.
The most recent Cochrane systematic reviews of interventions for the prevention and treatment of FI found no randomised controlled trials (RCTs) focusing specifically on people living with dementia (PLWD) in care homes. 28–30 Care home residents can experience dermatitis, discomfort, delirium and unplanned hospital admissions secondary to FI. 31,32 FI frequency is strongly linked to negative impact on quality of life. 33–37 It affects opportunities for social interaction and stimulation and can compound the isolation created by living with dementia. 38 Dealing with FI may also affect care home staff turnover and morale in a workforce that is already low paid and receives little clinical support. 39 The effectiveness of programmes to address the known problems of FI in care homes is, therefore, contingent not only on specific bowel-focused interventions, but also on contextually situated decision-making. 40 Interventions designed to improve FI for PLWD in care homes will perforce be multicomponent, shaped by the choices and behaviours of those delivering and receiving the care, and be characterised by a context-dependent effectiveness.
National and international guidelines33,41 emphasise that all patients with FI should be assessed for treatable causes, regardless of their cognitive status. Particularly relevant to care home residents living with dementia are overflow from faecal impaction and FI from loose stools, both of which can be assessed and managed in the care home setting. Treating constipation has been found to be effective in improving overflow FI and reducing staff workload (based on soiled laundry counts) by 42% in those with effective bowel clearance. 42 Loose stool may be a result of reversible causes, such as dietary intolerances, medication side effects including laxative use,21,43 and antibiotic-related diarrhoea. 44 For patients living with dementia who lack cortical control of the defaecation process, and who void a formed stool following mass peristaltic movements, prompted or scheduled toileting (preferably after meals) can increase the number of dependently continent bowel movements. 45,46
In 2012, a specific care home continence audit, educational and care planning tool was piloted in the UK. This highlighted some of the process and organisational problems that can be barriers to implementing FI programmes. 47 Ageism, lack of training, pad restrictions due to cost control and poorly integrated services were identified as likely contributors to low standards of care for FI. A review of local continence guidelines in England48 revealed a paucity of dementia-specific information.
There is, however, an extensive, more general care home and dementia-specific research literature, including intervention research, on the impact of the leadership, culture of care and care home routines on residents’ health and well-being. 49 Care home studies that are relevant but do not focus specifically on FI include those on nutrition and hydration,50 patterns of meal times,51 medication use52,53 and activities of daily living. 54,55
Some studies based in care homes can also offer transferable learning about how interventions are developed and implemented. For example, research to support people living with depression or identify residents at risk of unplanned hospital admission has moved towards advocating interventions targeted at specific subgroups rather than care home-wide strategies. 56 Others query the sustainability of interventions that were not developed in collaboration with staff and in consultation with residents or their representatives, and how to maintain clinician involvement. 6,57,58 It is the complexity of the relationships between evidence use, care experiences, quality of life and overall standards within care homes that pose particular challenges for intervention studies. 59
We now turn to report the methods of the realist synthesis.
Chapter 2 Methods
Rationale for using a realist review
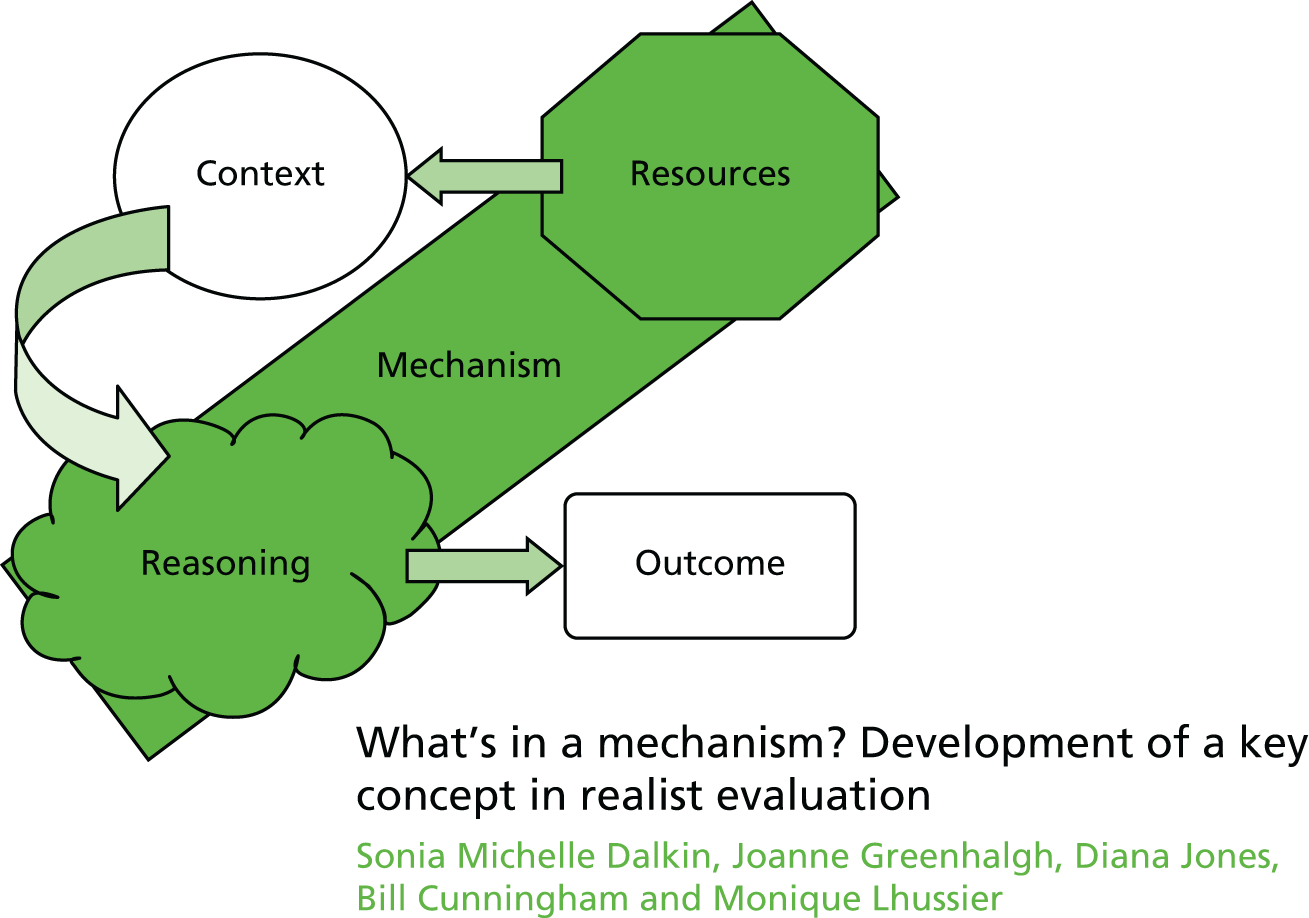
The rationale for using a realist synthesis approach is twofold: (1) the absence of evidence of what is effective in the reduction and management of FI in care homes and (2) a recognition that future interventions designed to address FI in PLWD will need to be multicomponent, depending on the behaviours and choices of those delivering and receiving the care. Realist review is a theory-driven interpretive approach to evidence synthesis. 60–62 It assumes that there is more to reality than the way in which it is socially constructed. There is an external reality or world that can be observed and measured; however, how this reality is articulated and responded to is constantly being shaped by individuals’ perceptions and reasoning and/or dominant social and cultural mores. It is this constant interaction that creates particular responses that lead to observed outcomes. 63 Realist synthesis, therefore, endeavours to go beyond lists of barriers to and enablers of care to unpack the ‘black box’ of how interventions to reduce and manage FI work. The often repeated statement used to explain the focus and purpose of realist synthesis is that it makes explicit ‘what works, for whom, in what circumstances?’. It uses a theory-driven approach to articulate how particular contexts (C) or resources, have prompted certain mechanisms (M) or responses by those providing and receiving care to lead to the observed outcomes (O). The underlying premise is that the observed ‘demi-regular patterns’ of interactions between the components that make up complex interventions in the evidence reviewed can be explained through theoretical propositions. The iterative process of the review tests those theories that are thought to work against the observations reported in the evidence included in the syntheses. 64 This enables us to take account of a broad evidence base as well as the experiential and clinical knowledge that relates to the physiology and management of FI in older people, and specifically in older people with advanced dementia living in long-term care. It will also help us to take account of the heterogeneity of care home provision in the UK (Box 1).
-
Context (C): that is, the ‘backdrop’ conditions (which may change over time), for example provision of training in FI continence care, residents’ level of nutrition and hydration and cost of continence aids. Context can be broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism.
-
Mechanism (M): a mechanism is the generative force that leads to outcomes. Often denotes the reasoning (cognitive or emotional) of the various ‘actors’, that is, care home staff, residents, relatives and health-care professionals. Mechanisms are linked to, but are not the same as, the strategies of a service. Identifying the mechanisms goes beyond describing ‘what happened’ to theorising ‘why it happened, for whom and under what circumstances’.
-
Outcomes (O): intervention outcomes, for example reduction in episodes of FI, resident distress and costs and increase in staff confidence.
-
Programme theory: those ideas about what needs to be changed or improved in how FI is reduced and managed in care homes for PLWD, what needs to be in place to achieve an improvement and how this is believed to work. It specifies what is being investigated and the elements and scope of the review.
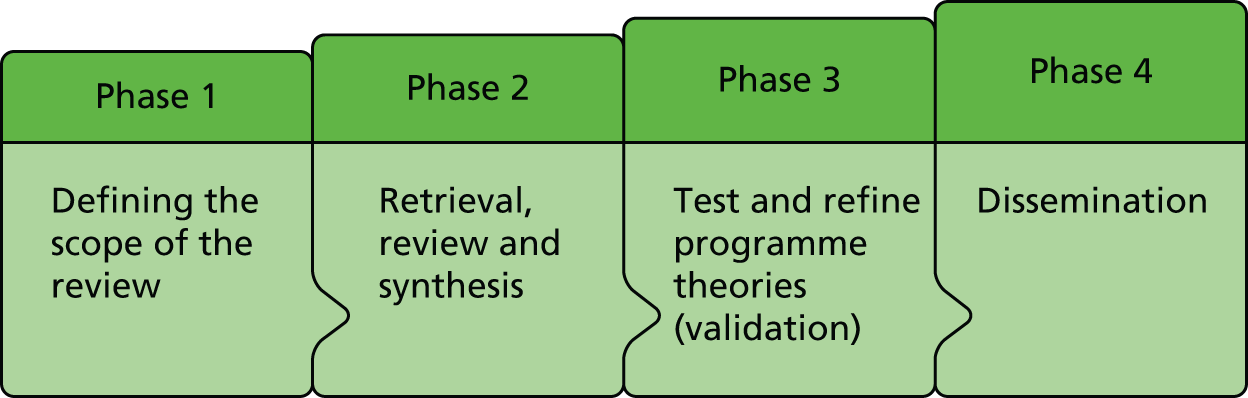
A realist review does not follow a neat linear process, although it does have distinct phases summarised in Figure 1. This process was specified in the review protocol. 65
FIGURE 1.
Four-phased approach to the synthesis.
It is an assumption that mechanisms will only activate in the right conditions, providing a context + mechanism = outcome formula. Explicit disaggregation of resources as a component of a context helps to be more explicit about the aspects of an intervention that trigger different responses. We have characterised this as context (intervention)–mechanism–outcome (C–M–O) and used this approach in our analysis of the evidence.
Changes from the submitted protocol in the review process
A realist review is an iterative process, and adjustments are made to the review protocol in the light of emerging or new lines of enquiry. Changes to the protocol submitted to the funder are outlined in Table 1.
| Protocol | Change | Agreed |
|---|---|---|
| Target population: people with advanced dementia in care homes | We dropped the term ‘advanced’ from the synthesis title. ‘Advanced’ dementia was considered too narrow and not clearly defined as a concept in the literature | Study Steering Committee December 2014 |
| Focus on FI only | Consider FI in the context of double incontinence as FI alone accounts for only a small proportion of residents living with FI | Core team |
| Timing of searches: protocol proposes a final search strategy will be developed after phases 1 and 2 | Searches carried out in phases 1, 2 and 3. Scoping searches in phase 1, main searches in phase 2 and follow-up searches in phase 3 | Core team |
| Health Technology Assessment protocol suggests we will look at research with older people with dementia living at home or in hospital | Although wider literature is not ignored we retained a focus on care home research. Context of care for people living at home or in hospital is very different in terms of resources and practitioners involved in providing care | Core team |
| Timings of stakeholder input: phase 4 – consensus meeting in London with online link | The consensus meeting was held as part of a meeting of the National Care Home Research and Development Forum. There was insufficient time to complete the synthesis and organise a standalone consensus meeting with online link | Study Steering Committee September 2015 |
Phase 1: defining the scope of the realist synthesis – concept mining and theory development
Concept and theory development by the team
A realist synthesis often uses input from content experts to help develop programme theories. In this project our Research Management Team (RMT) and Study Steering Committee (SSC) included many of the national experts in the field of continence care and care home research in the UK (see Appendix 1). The first RMT meeting in September 2014 included an open discussion by the team in which they were asked to draw on their expertise to articulate:
-
the dominant approaches and assumptions that informed current thinking about what supported (and how) the reduction and management of FI
-
important outcomes and how impact was measured.
The full notes from this meeting are included in Appendix 2. After the meeting all RMT members were asked to send relevant reviews, papers or guidelines that had been referred to at the meeting to the core team. The early progress was reported to the SSC in November 2014.
Scoping interviews
To complement the expertise provided by the team we interviewed key stakeholders. They were identified through the clinical and research networks of the RMT, and five key groups were identified and approached to inform the scoping process (Table 2).
| Target stakeholder group | Rationale |
|---|---|
| Providers of care | |
| Care home managers from different provider organisations identified through representative organisations and charities [My Home Life, Enabling Research in Care Homes (ENRICH) and Alzheimer’s Society] | Care home managers know and understand organisational processes, protocols and ‘industry’ best practice and are aware of how well all these rules and guidelines are applied within the care homes in which they work. In addition, they will be aware of factors that inhibit or facilitate the implementation of the rules and guidelines |
| Care home staff | Distinct from managers, care home staff understand actual practice and therefore provide an invaluable insight into how continence care is managed |
| Recipients of care | |
| User representatives (identified through the resident and relatives representatives of the Bladder and Bowel Foundation and family carers with experience of caring for a relative living with FI in a care home) | Resident representatives were chosen to give the closest possible approximation of residents’ own opinions of continence care |
| Academics and practice educators with an interest in care homes | |
| A meeting of the National Care Home Research and Development Forum | To ensure we are up to date with the most relevant current research, particularly work that may not yet be published |
| Clinicians with a special interest in FI | |
| Special interest group on continence of the British Geriatrics Society | To gain the perspective of clinicians and other specialists who have an interest in continence management for older people generally |
| Continence specialists, commissioners and providers of continence services | |
| Continence specialists, commissioners and providers of continence services identified through NHS trusts, providing and professional associations and charities | To gain the perspective of continence nurses and community providers who are likely to provide advice and services into care homes |
Interviews
Interviews were conducted either one to one or in a group by Claire Goodman, Marina Buswell and Bridget Russell. All interviews were face to face. Interviews were recorded, when possible, and transcribed. A set of interview prompts was developed and tailored to reflect the focus and expertise of each group. We wanted to explore:
-
participants’ experience of working with and for people with dementia and FI in care homes
-
estimates of how severe FI is in care home residents
-
why they think FI occurs
-
what good continence care looks like and what is necessary to achieve that and why
-
who needs to be involved in providing and reviewing care
-
how having dementia specifically affects continence care, assessment and decision-making, and what needs to be in place to address the effects of dementia
-
how they would define success from the perspective of the resident, the care home staff, visiting clinicians and family carers
-
when and why the decision would be made to use pads.
All participants highlighted the importance of person-centred care. The interviewers sought to understand how this approach to care was articulated in the assessment, care and review of continence care provided in care homes. In many of the interviews the prompts led to narratives of success and failure with particular residents; these examples demonstrated the participant’s understanding of what needed to be done and what good care looks like.
Continence specialists
Interviews were completed at the continence specialists’ place of work. We approached three continence specialist teams but were able to access only one team and interviewed three nurses who visited care homes. This was supplemented with a group discussion with members of the British Geriatrics Society (BGS) continence special interest group, which included physicians and nurses.
Interviews with care home managers and care home staff
We recruited care home managers through two care home provider organisations, one not for profit and one commercial chain. Meetings were organised by the two care home organisations on our behalf and held on their premises.
Care home staff involved in providing direct care to residents were recruited through contacts with local care homes (which were not part of the care home chain that managers were recruited from) and via the networks of the RMT. We recruited seven care home staff, one of whom was a senior care worker. Two of the participants worked nightshifts in separate care homes and were interviewed face to face. The remaining five worked in the same care home and were able to participate in a focus group discussion. Questions focused on their experiences of providing care, how they defined good care, what they thought about how a person’s dementia affected their ability to provide continence care and what was important to enable them to achieve that.
Interviews with family members of residents with dementia and experienced faecal incontinence
In phase 1, we attempted to recruit family members who had experience of supporting a relative with FI and dementia through relevant charities [a local branch of the Alzheimer’s Society and the Bladder and Bowel Foundation (BBF)]. Despite several attempts, these approaches were unsuccessful. An invitation through a local care home provider to invite participants yielded three expressions of interest; two of these people participated in a group interview. An analysis of the phase 1 interviews was undertaken thematically using the prompts as the organising framework, and the findings from this were fed into the RMT deliberations and workshop.
In phase 3, to identify people with personal experience of FI and dementia through caring, we renewed our request for help to the BBF. This time the BBF supported a mail-out to their members that elicited responses from interested relatives (see Appendix 3).
To ensure transparency of approach and an audit trail, focus group discussions and interviews were recorded and transcribed. Structured field notes were kept about which sources of evidence and experiential knowledge may be linked to which strands of theoretical development.
Literature scoping: phase 1
Search methods
We conducted four separate searches. The initial search built on literature identified as relevant at the first RMT meeting. This focused on evidence on continence-related research in care homes, dementia and continence, older people and continence, implementation research in care homes and person-centred care. A second search was then conducted that was designed to identify papers on FI and care homes and incontinence pads (see Appendix 4).
The scoping interviews with geriatricians at the BGS highlighted the link between diet and hydration and good bowel health, and a further search was conducted to capture literature on interventions to promote nutrition and hydration (eating and drinking) for PLWD in care homes. This search was conducted to test whether or not this body of work included outcomes related to continence and FI. After the second SSC meeting in November 2014, a decision was made to scope the learning disability literature for continence-related research.
Selection and appraisal of documents: phase 1
Frances Bunn, Claire Goodman and Bridget Russell carried out the first searches and selected studies for initial inclusion based on the broad themes outlined by the RMT. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram was produced, although as the review progressed it did not capture the iterative process of searching, selecting and appraisal of documents for this process (ultimately replaced by a flow diagram; Figure 2). A summary of this scoping search was presented to the RMT in January 2015.
FIGURE 2.
Document flow and review of progress: conceptual diagram. CH, care home; PCC, patient-centred care.

Data extraction: phase 1
A narrative process rather than a formal data extraction was used to produce the first scoping summary (see Appendix 2). In phase 1, however, we began to develop a data extraction process that captured our thinking about the putative theories and context–mechanism–outcomes (C–M–Os) of interest (see Phase 1: defining the scope of the realist synthesis – concept mining and theory development, and Prototype data extraction form).
Analysis and synthesis processes: phase 1 (concept mining and theory development)
Meetings
Team meetings formed an essential and productive part of the analysis and synthesis process. Formal meetings of the SSC and RMT were recorded and detailed meeting notes were made. Informal team meetings of the smaller core team (FB, MB, CG and BRu) were not recorded but notes and actions of these meetings were kept in log books (see Log books).
Log books
Log books were used as project notebooks to record when and how important decisions, thinking, sourcing of papers or documents and actions occurred. They provided a useful source of ‘raw’ data and reference points for analysis, and included notes about key papers that informed a shift in thinking and synthesis. These became the structured field notes on suggestions and decision-making processes about which sources of evidence were linked to which strands of theoretical development.
‘If . . . then’ statements
At the end of the RMT meeting in January 2015, a series of ‘if . . . then’ statements were tabled that drew on the interview and scoping data. ‘If . . . then’ statements are the identification of an intervention/activity linked to outcome(s) and contain reference to contexts and mechanisms (although these may not be very explicit at this stage) and/or barriers and enablers (which can be both mechanism and context). 66 Although we did not use logic models, the ‘if . . . then’ statement route of thinking logically and working back from outcomes provided a helpful way of structuring our thinking. It also helped to focus the process of taking ideas and assumptions about how interventions work and testing them against the evidence we found (see Appendix 5).
Prototype data extraction form
Early data extraction was carried out in parallel with development of ‘if . . . then’ statements and developing a framework using diagrams and mind mapping. At this point, the data extraction process was more a matter of concept mining. We developed a table in Microsoft Excel® 2013 (Microsoft Corporation, Redmond, WA, USA) and used headings that drew on findings from the early scoping and discussions within the team. This form was piloted on five initial papers recognised as important in FI and care home research and then refined further.
Diagrams and concept mapping
The diagrams and concept mapping captured a summary of evidence and thinking, overarching themes, likely barriers, enablers, contexts and outcomes. This was the basis for conversations about possible interactions and the identification of areas for which there was consensus about what ‘good FI care’ may look like for PLWD in care homes. We also used flip charts to map possible C–M–O configurations and these helped in the development of the data extraction form.
Narratives
Narratives were an important tool for making thought processes explicit and facilitating theory development. We used two main formats for narratives.
In the first, we created detailed narratives around specific research areas, for example a historical narrative of prompted voiding (PV) studies and care home research, or a summary of guidelines and reviews relevant to continence care in older people. While we were ‘data extracting’ individual sources, our core team discussions started to cluster around themes and particular areas and programmes of research.
The second format was ‘working paper’ narratives, which were presented to the wider team to ensure that everyone could keep up to date with methods, results, idea flows and theory development between meetings. In a realist review it is not possible for the process to be completely transparent. However, capturing our narrative thinking in this way should help others to understand and critically evaluate how we have come to our conclusions. It also meant that the process for developing theory could be understood, and challenged, by the research team, the SSC and our stakeholders. Pearson et al. 66,67 have commented on how little information is available about how the realist review process is enacted; these working papers helped to make explicit our thinking and decision-making.
Phase 2: retrieval, review and synthesis
Searching processes: phase 2
In March 2015 the scoping searches conducted in phase 1 were refined and expanded to include additional evidence sources (see Appendix 4). The RMT agreed that literature regarding facilities other than care homes was unlikely to add to what had already been obtained; however, relevant UI literature and care home studies with transferable methods and similar aims were to be included.
We included studies of any design including RCTs, controlled studies, effectiveness studies, uncontrolled studies, interrupted time-series studies, cost-effectiveness studies, process evaluations, surveys and qualitative studies of participants’ views and experiences of interventions. We also included unpublished and grey literature, such as policy documents and information about locally implemented continence programmes or proceedings, which could provide a model for future practice or merit future evaluation.
The search was limited to papers published between 1990 and 2014, although we did include seminal papers from earlier, such as the work of Tobin and Brocklehurst,68 and those identified from lateral searches. There were several reasons for this time limit. Health-care research in care homes is a relatively recent phenomenon. Gordon et al. 69 identified that of 292 RCTs conducted in care homes between 1974 and 2009, half had been published after 2003. Dementia research has been significantly influenced by the work of Kitwood,70 whose seminal work was first published in 1990. Furthermore, the organisation and funding of care homes was radically altered in 1993 by the implementation of the 1990 National Health Service and Community Care Act. 71 This led to progressive changes in the overall size, ownership and structure of the sector. The increased emphasis on domiciliary care has also meant that the level of dependency and frailty of older people now admitted to long-term care has increased. 72
Previous dementia reviews undertaken by members of the project team73,74 have highlighted the importance of lateral searching for identifying studies for dementia-related reviews. Therefore, in addition to the above electronic database searches, we undertook the following lateral searches:
-
checking of reference lists from primary studies and relevant systematic reviews (snowballing)75
-
citation searches using the ‘cited by’ option on Web of Science, Google Scholar and Scopus and the ‘related articles’ option on PubMed and Web of Science (‘lateral searching’)
-
contact with experts and those with an interest in dementia, care homes and FI to uncover grey literature (e.g. National Library for Health Later Life Specialist Library, Alzheimer’s Society, Royal College of Physicians, Royal College of Nursing and The Queen’s Nursing Institute)
-
contact with disease-specific charities and user groups, residents and relatives associations
-
internet searches for grey literature and searches for continence-related evaluations or intervention research that makes specific reference to FI and/or people with a dementia diagnosis, national inspection and regulation quality reports by the UK regulator (Care Quality Commission and predecessors).
Four overlapping searches were completed that built on and expanded the search completed in phase 1 (see Appendix 4).
-
Searches 1a and 1b searched for evidence on care home research, either continence or FI related, that included PLWD, and care home research covering implementation or patient-centred care (PCC) that included people with dementia.
-
Search 2 focused on continence literature in care homes that may be about factors associated with FI, such as the use of incontinence pads or constipation.
-
Search 3 focused on research in care homes for people with dementia that concerned nutrition and/or hydration in the care home population. We were interested both in whether or not this research mentioned outcomes relevant to FI or continence generally and in discussion about how eating and drinking interventions may be implemented.
-
Search 4 focused on literature on continence care for people with learning disabilities living in residential care.
As the review progressed, and particularly the idea of needing to fit into care home routines, wider literature that discussed the impact of care home routines and working practices was consulted by team members (see note on bias in Strengths and limitations of the review). Further papers, professional journals and books were identified through lateral searches, alerts from professional networks, recommendations from the SSC and conference abstracts.
Theory development: phase 2
In parallel with the second phase of literature searching just described, mid-range theories were developed. This process is represented in Figure 2 and the results of theory development are described in the results. Six mid-range theories or ‘theory areas’ were developed and assessed against the selected literature using the data extraction process described in Data extraction: phase 2.
Selection and appraisal of documents: phase 2
Management of references
Search results from electronic databases were imported into EndNote bibliographic reference management software (Thomson Reuters, CA, USA) and, when possible, duplicates were deleted. Documents from other sources were manually recorded in the same EndNote library. At least two reviewers (BRu, MB, CG and FB) independently screened titles and abstracts to identify potentially relevant documents to be retrieved and assessed. Disagreements were resolved by discussion. To enable us to keep track of the large body of literature and the changing ‘inclusion’ criteria as the mid-range theories emerged, decisions made at different points in time were recorded in the EndNote record for each paper.
Although literature was considered for inclusion in terms of its relevance to the UK care home sector, the nature of a realist review meant a linear included/excluded paradigm was not wholly appropriate. Instead the team regularly revisited the literature to assess whether or not, in the light of evolving theory development, previously ‘excluded’ sources may in fact be relevant.
Data extraction: phase 2
The second phase of data extraction took place from July 2015 to October 2015.
Development of data analysis and synthesis form
We developed a prototype data analysis and synthesis form (DASF) tailored to reflect the phase 1 findings; this reflected the six mid-range theories which were to be tested. All RMT members completed data extraction on at least two of three papers, with all papers and other sources of evidence (e.g. books and professional papers) being reviewed by at least two members of the team. Most of the reviewing was completed by the core team (MB, BRu, CG and FB).
It should be noted that ‘data’ in a realist sense are not just restricted to the study results or outcomes measured. Author explanations and discussions can provide a rich source of ‘data’, and so these were included in the DASF. Box 2 summarises the six sections of the DASF.
Section 1: relevance is when the source is assessed against the theories being tested, which were restated briefly (theories 1–6) within the form to keep focus.
Section 2: interpretation of meaning. Here, an attempt is made to explicitly identify C–M–Os in the relevant text.
Section 3: judgements about C–M–O configurations. Once C–M–Os are identified, they need to be ‘configured.’ This is what takes us from a simplistic understanding of ‘barriers and enablers’ to a richer description in which we try and understand which context–resource combinations trigger which mechanisms, resulting in different outcomes (intended or unintended).
Section 4: judgements about mid-range theory. Here we attempt to complete the analysis circle. Taking sections of the text and assessing them as relevant, unpicking with respect to C–M–O configurations then referring those C–M–O configurations back to the proposed mid-range theories.
Section 5: rigour. This is the realist ‘quality assessment’ and is not conceptualised in the same way as in a systematic review. It is an assessment based on the weight that should be given to the C–M–O configurations found within the source, dependent on the quality of the study and also the richness of the explanations.
Section 6: population. This section keeps a focus on which groups the source is addressing so that an assessment can be made of how transferable the C–M–O configurations would be to our population of older people with dementia living in care homes.
The ‘questions raised not captured elsewhere’ and ‘notes’ sections are included to try to keep a track of all thinking and for future reference in combined synthesis meetings.
Three exemplar DASFs are given in Appendix 6.
Synthesis
The process of synthesising the data from the individual DASFs included:
-
the organisation of extracted information into evidence tables representing the different groups of literature (i.e. care home interventions, FI and UI and person-centred care)
-
theming across the evidence tables in relation to the C–M–Os and emerging patterns of association seeking confirming and disconfirming evidence
-
linking these observed demi-regularities (patterns) to develop hypotheses.
Integral to this process were cross-team discussions about the integrity of each theory and the competing accounts of why interventions did or did not work. This included a consideration of the unintended consequences of some approaches to continence care: what appeared to be true regardless of setting (e.g. by national care system or presence or absence of clinical staff), what was a setting-specific outcome, what were intermediate outcomes (e.g. changes in staff behaviour and knowledge) and what was a FI-specific outcome (e.g. reduced episodes of FI).
The findings were discussed by the core team and with some members of the wider team. In addition, a full draft was circulated to the team for detailed comment. Time constraints meant that it was not possible to hold a second workshop with the RMT as originally planned. Moreover, the team considered that at this stage it was more important to focus on presenting and discussing the findings and resultant hypotheses with the stakeholder groups. Initially, we had proposed that these would be presented to the stakeholders as a series of C–M–O links and the characteristics of the evidence underpinning them. The nature of the evidence (and lack thereof) ultimately led the team to focus on the development of programme theory that posited the likely C–M–O configurations that would lead to improved continence care.
Phases 3 and 4: test and refine programme theories (validation) and develop actionable recommendations and evidence-informed framework
To enhance the trustworthiness of the resultant hypotheses and to develop a final review narrative to address what is necessary for the effective implementation of programmes to manage FI in care homes, we reviewed the hypotheses and supporting evidence through consultation with the SSC and interviews with stakeholder groups, some of whom had participated in the scoping. Findings were presented to:
-
the continence specialist interest group at the BGS who had participated in the phase 1 interviews; approximately 60 delegates attended the conference on 6 November 2015 – 11 provided active feedback and comment during the discussion and six did so during the lunch break, and comments from four other speakers provided support for aspects of the emergent findings;
-
members of the BBF who had personal experience through their caring roles of living with FI and dementia;
-
a meeting of the National Care home Research and Development Forum (1 January 2015);
-
organised meetings in two separate care homes with staff involved in providing direct care from one of the care home organisations that had participated in phase 1 (9 December 2015).
Discussion focused on stakeholders’ views on the resonance and significance of the programme theory and the suggested C–M–O threads from both a practice and a service user perspective. In addition, there was an invited presentation at an Evidence Synthesis Network [hosted by National Institute for Health and Care Excellence (NICE) and the University of Manchester] workshop on realist methodology held on 17 November 2015. The presentation using the Faecal INcontinence in people with advanced dementia resident in Care Homes (FINCH) study and its findings was an exemplar of how the programme theory was developed and tested, focusing on how we differentiated between contexts and outcomes in the evidence reviewed.
Ongoing dissemination work on the FINCH study was planned through seminars and a plan for publications and briefings in association with the care home manager member of the RMT and the SSC.
Public and patient involvement
The proposal was circulated and discussed with members of the public and patient involvement group at the University of Hertfordshire and amended accordingly. In addition to public and patient involvement representation on the SSC (Paul Millac), engagement with user and patient representative groups was key to stages 1 and 3 of the synthesis. There was public and patient involvement in the National Care Home Research and Development Forum meeting, during which emergent findings were discussed.
It was not possible to involve residents with dementia and experience of FI in the study. Karen Cummings and Victoria Elliot of the Orders of St John Care Trust care home group provided input to the RMT and SSC as individuals with direct experience of providing and managing continence care in care homes.
Chapter 3 Results
Document flow diagram
The document flow and review progress conceptual diagram (see Figure 2) shows the iterative nature of realist searching and concurrent theory development and synthesis over phases 1 and 2.
Phase 1: concept mining and theory development
Scoping: phase 1
Scoping meetings
After the first RMT meeting, the wide-ranging discussions were organised and structured under three main headings that reflected the idea that FI is affected by biomedical, psychosocial and wider organisational factors: (1) bowel-related causes of FI, (2) the physical, social and cultural environmental impact on FI and (3) how FI is defined, recognised and managed in a care home setting for PLWD.
Three clear themes emerged from the discussions as key to understanding what supported or inhibited practices that in turn supported or inhibited the reduction and management of FI:
-
the ‘normalisation’ of incontinence and pad use in long-term care settings
-
theories of learning and groups in long-term care settings
-
interprofessional working, staff turnover and workforce capacity, and the role of the regulator.
The commissioning brief had specified that people with advanced dementia in care homes should be the focus of the review. Based on the first cut of the literature, and on previous experience of working and completing research in care homes, the RMT argued that this was an unhelpful distinction. Changes in functional performance and activities of daily living skills characterise the dementia trajectory. There are tools that measure these changes. 11 Many care home residents, however, do not have a formal dementia diagnosis, and living with mild to moderate dementia can still have a major impact on an individual’s ability to recognise the need to eliminate, recognise the toilet, undress or respond to prompts to use the toilet. The SSC agreed that dementia should replace ‘advanced dementia’ as the search term for the reviews.
Scoping interviews
Details of the participants of the scoping interviews are given in Table 3.
| Stakeholder group | Details |
|---|---|
| Carers of people with dementia resident in care homes who have FI (n = 2) | Interview in one of the participants’ homes with the spouses of two residents living in a local care home. Both residents had dementia and one resident had almost constant UI; neither was represented by their carer as having FI, apart from what were described as accidents from difficulties getting undressed, finding the toilet or staff not being present to help their relative |
| Geriatricians with interest in incontinence and continence specialists (n = 15) | A focus group was held at the 2014 BGS Bladder and Bowel Conference. Fifteen delegates participated. They were geriatricians at registrar and consultant grade and continence nurse specialists |
| Interview with three continence specialist nurses who provided support to their local care homes in the west of England (n = 3) | Part of their service provided continence assessment and support to the local care homes |
| Care home managers (n = 17) | Two focus groups were held with care home managers from two care home provider organisations that included care homes with and without on-site nursing (n = 5 and n = 12, respectively) |
| Direct care staff (n = 7) | Two care workers known to a member of the RMT were interviewed separately. Both worked night shifts in two different care homes. Both had > 6 years’ experience of working in care homes Focus group with four care staff and one senior care worker of a local care home without on-site nursing |
All participants in the scoping interviews highlighted the importance of knowing the resident and how distressing FI could be for both residents and staff. There were differences in emphasis between the stakeholder groups; for example, person-centred care was central to one group but secondary to a knowledge of the causes of FI or being able to provide care using the resources of the care home. Unsurprisingly, participants’ views reflected their training, background and personal experiences of care.
Clinicians from the BGS group and the continence services believed that care home managers and senior care staff did not know what causes FI in older people. They highlighted limited knowledge about the impact of polypharmacy, misuse of laxatives, failures to address resident dehydration and diet that lacked fibre, and about how to assess whether or not someone was constipated. This lack of knowledge was seen as being compounded by the inappropriate use of pads.
Staff can’t do the right thing if they lack the information, knowledge, skills. From understanding the causes of FI and how to address them to knowing which size of pad to use for which person [when pads have to be used]. If pads must be used getting the right size and design make all the difference in terms of comfort and confidence for the wearer.
Continence nurse specialist
In contrast, group discussions with the two groups of care home managers and, to a lesser extent, those involved in providing direct care to residents provided a counter narrative. The care home managers were able to discuss the multiple causes of FI, the role of constipation in FI and the importance of hydration, nutrition, physical activity and person-centred care. Managers emphasised the value of reinforcing with staff the need for empathy and reflection in how they approached the care of the resident. In one example, a manager overheard a carer telling a resident who had asked to be taken to the toilet to relieve themselves in their pad instead. In another example, when a resident asked if she could be taken to the toilet, the carer asked if she could wait until after breakfast. These examples of bad practice were used to illustrate the importance of learning ‘on the job’ and of the managers’ role in reinforcing what good, and bad, care looks like.
Care home managers viewed person-centred care in a communal environment as important but difficult to implement or apply to the specific continence needs of residents. They recognised, from a person-centred care perspective, that certain behaviours such as repetitive vocalisation (e.g. calling for the toilet), constantly visiting the toilet or refusing to go to the toilet may arise because a person is communicating an unmet need. This was often difficult for care home staff to interpret. The care home managers suggested that their staff would all err on the side of caution and always respond on request, but that this was not always possible when the care home was short of staff or reliant on agency staff. Similarly, when residents resisted being taken to the toilet by staff and became distressed, staff members did not want to be seen to be forcing someone to do something or to go against their wishes. Staff involved in direct care emphasised the importance of residents’ cleanliness and comfort; their job was to change pads and to make sure that people who could go to the toilet were helped to do so and had enough time when there. This work was described as ‘common sense’.
There was no consensus when those in the groups were asked how long they might persevere with trying to help someone to become continent. There was little evidence from the within-group conversations to suggest that participants would persevere with a toileting regime for longer than 4 weeks. Direct care staff saw the value of regular toileting but described their work more in terms of ensuring dignity and comfort. A continence assessment when someone entered a care home was more about ensuring that the care home could access pads than informing decisions about how to support continence.
The interpretation of resident choice around toileting, and whether or not to persevere, was an issue raised by the two relatives who were interviewed. One woman saw this as evidence of lack of training in how to respond to PLWD. She thought that those staff members who were less qualified or less experienced in working with PLWD were more likely to accept a resident’s refusal to go to the toilet. More skilled staff were more likely to try other strategies to encourage residents to walk and use the toilet. She could differentiate between staff who were thoughtful and understood her husband and his needs and those who were less able to find alternative ways of engaging with her husband when his dementia affected his ability to respond. In the following quotations, text marked in bold highlights what the research team identified as being significant for understanding the processes of care.
There is a difference in knowledge [about dementia] needed for people at the different stages of the disease, there was one carer [name] who was very good at caring for my husband when he was able to have a conversation but who then did not have the skills to engage with him now that there is very little response. In contrast [name] does have these skills, I can trust him to be caring to be able to get my husband up and about.
Wife of resident in care home
Both relatives highlighted practical issues of location of toilets and difficulties that their relatives had with clothing and recognising when they needed to eliminate:
I don’t know if he is incontinent or if it is just about getting to the toilet. They have put a picture on his toilet. I bought him pull-up trousers but they have disappeared. I don’t know how severe his incontinence is, though he is weeing everywhere and that is partly the dementia and partly not thinking far enough ahead and being able to manage the trousers.
Wife [2] of resident in care home
The erratic level of clinical support that the care home received was also seen as contributing to problems of assessment and management, and this was not specific to their relatives’ incontinence but was seen as an important contextual factor. One relative referred to 14 GPs from one practice who visited the care home as ‘a fleet of GPs’ who did not know much about frailty or dementia.
We found it useful to summarise these discussions with stakeholders by interventions thought likely to be helpful, elements of intervention, outcome, enablers and inhibitors (Table 4). The data from the interviews ensured that we had considered the different perspectives of how good continence care is achieved. They also informed, along with the scoping of the literature, the development of the programme theories.
| Resource/context | Response/mechanism | Reported outcomes | Enablers | Inhibitors |
|---|---|---|---|---|
| Family carers of people with dementia resident in care homes that have FI | ||||
|
|
|
|
|
| Geriatricians with specialist interest in continence | ||||
|
|
|
|
|
| Continence specialists | ||||
|
|
|
|
|
| Care home managers | ||||
|
|
|
|
|
| Direct care staff (including night shifts) (n = 6) | ||||
|
|
|
|
|
Literature scoping: phase 1
Search results
The first electronic search focused on incontinence and care homes, person-centred care and implementation in care homes. This resulted in > 1000 hits, of which 75 were deemed potentially relevant. These were then reduced to 31 priority records for in-depth review. Additional searches around FI and the use of pads, nutrition and hydration (systematic reviews only) and learning disability resulted in 193, 10 and 20 records, respectively (see Figure 2 and Appendix 4). These, along with some papers from lateral searches, informed the first overview presented for discussion to the SSC and the RMT.
Scoping summary
The literature was summarised for the RMT into four broad topic areas:
-
biomedical approaches to the assessment and management of FI
-
person-centred care
-
care home implementation
-
nutrition and dementia in care homes (reviews only).
For each area, a summary was provided of the interventions, the outcomes measured and the reported barriers and enablers (see Appendix 2).
Analysis and synthesis processes: phase 1 (concept mining and theory development)
The RMT meeting in January 2015 mapped the findings (literature scoping and stakeholder scoping) to a framework that considered the different types of FI, as defined by the work of Saga,76 that reflected a trajectory from continence to incontinence. Initially, it helped to conceptualise whether or not a particular type of FI intervention/approach would be more amenable to management (i.e. it may be time limited or could be treated and reduced) or to containment (treatment not possible).
‘If . . . then’ statements
A set of ‘if . . . then’ statements were produced ahead of the May RMT meeting based on earlier discussions and iterations. They were divided into:
-
‘What to do?’ – intervention/management to address review objective 1.
-
‘How to do it?’ – implementation, sustainability and feasibility to address review objectives 2 and 3.
‘How to do it?’ was further split into the ‘level’ of the intervention, staff, care home and wider organisational/policy, to ensure that the different audiences for the review findings were kept in mind. Table 5 gives some examples of these statements and a fuller version with more statements and cross-referencing to the literature is included in Appendices 2 and 3.
| If | Then |
|---|---|
| What to do | |
| If FI is not ‘curable’ (neurogenic disinhibition/dementia-caused/anorectal dysfunction/dyssynergia) | Then appropriate containment is required, which may be timed toileting/PV, bowel regime or use of most appropriate pads |
| If a person has regular bowel movements and responds well to being taken to the toilet | Then PV will reduce FI episodes |
| If FI is a result of functional reasons (access and ability to get to the toilet) | Then a suitably adapted environment and staff on hand to assist as needed will reduce FI episodes |
| How to do it | |
| Staff level | |
| If staff have more time with residents and opportunity to know and document what is normal for them | Then they will deliver better continence care and FI will reduce |
| If staff have specialist dementia and FI training/knowledge | Then they will deliver better continence care and FI will reduce |
| Care home level | |
| If staff experience a supportive working environment | Then residents will experience less FI and be more content |
| If it is considered normal that all residents are in pads | Then FI will not improve |
| Wider organisational/policy level | |
| If provision of pads is dependent on assessment protocols | Then FI will be overdiagnosed and managed with pads |
| If care homes were performance managed on FI | Then practitioners would be more aware and there would be less FI (or FI would be recorded more accurately) |
The statements aimed to capture the range of possible theories/contexts/mechanisms suggested by all of our stakeholders and the literature viewed to date. We included a section for enablers and barriers if we felt that they were cross-cutting or not fully captured in the statements.
The RMT were asked if these ‘if . . . then’ statements:
-
covered outcomes sufficiently, for example comfort, minimisation of distress, reduction of FI episodes, reduction of FI (incidence vs. prevalence) resource use, restoring normal bowel function and staff outcomes
-
fitted with professional understanding of how continence is defined and understood, for example the International Continence Society paradigm, independent continence, dependent continence and containment
-
addressed dementia factors well enough
-
could be collapsed further.
Prototype data extraction form
We piloted the phase 1 data extraction form with five papers. This resulted in the addition of 10 new fields, most of which annotated additional possible outcomes from FI-related interventions. The different literature sources consulted in the scoping included research on continence care in care homes, person-centred care and psychosocial interventions in care homes and related FI- or dementia-specific studies. The data extraction form fields of particular interest at this point in the study were the implicit or explicit study hypotheses about what was likely to support good (continence) care for care home residents.
Discussions among the core team about the original data extraction form, the ‘if . . . then’ statements and the flip chart diagrams and mapping we had produced were pulled together in a conceptual diagram77 that mapped outcomes, contexts, barriers and enablers (Figure 3).
FIGURE 3.
Conceptual diagram mapping outcomes, contexts, barriers and enablers.

Narratives
General narratives were written that kept the team up to date on the flow of ideas. As working papers for the team, they did not have a clear distinction between methods, results and discussion. These are all held together in a narrative format (see Appendix 2).
-
FINCH working paper: presented to the RMT in May 2015.
-
Flow of ideas from the six theory areas emerging from the RMT in May 2015: sent to RMT members in August 2015 to help with data extraction.
-
FINCH ideas flow paper; presented to the SSC in September 2015.
These narratives suggested that we return to thinking about dementia. The following excerpt summarises our thinking:
We are concerned that we lose the focus on (advanced) dementia as in so much of the evidence this is not described in particular detail and because it is care homes there is an implicit (correct) assumption that most residents have a degree of cognitive impairment. We suggest that we need to always keep dementia as a context with the other contexts and so always think, ‘with these contexts, this mechanism triggers such and such; how does dementia affect that?’ (However, going back to Kitwood dementia in itself isn’t the context, because when you’ve met one person with dementia, you’ve met one person with dementia . . .) Should we be listing some of the behaviours and morbidities and psychological symptoms of dementias as contexts?
Log book notes RMT meeting May 2015
The narratives took a historical view of the literature in the sense of understanding how research in continence, particularly FI, has developed over time and, similarly, how research in care homes has developed.
There were two main strands to these narratives. The first was to understand how best practice in the treatment and management of FI, when relevant to older PLWD, is articulated in professional guidance and reviews. The second was to identify the potential for transferable learning from research with older PLWD in care homes, but that was not continence specific.
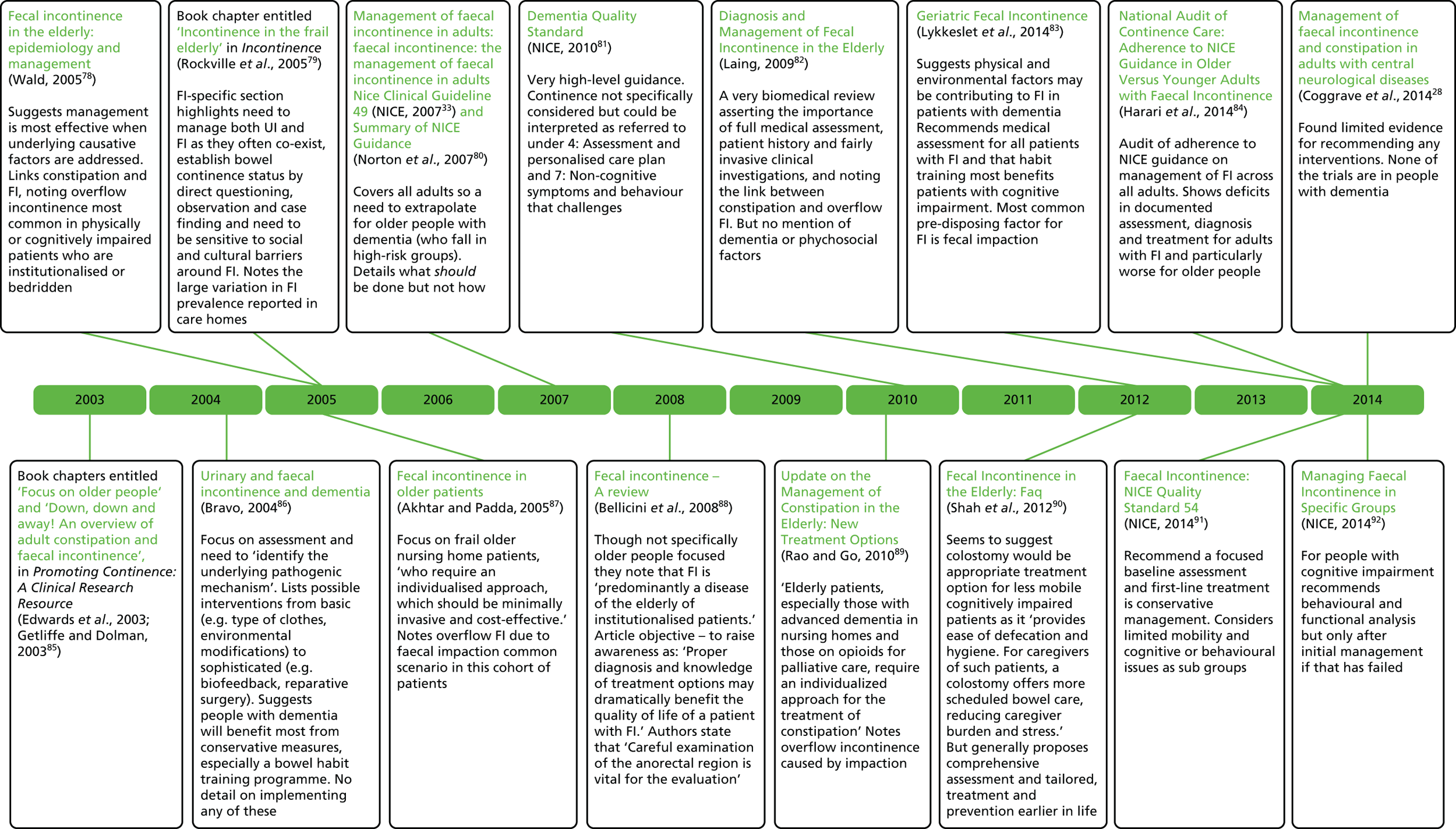
The first strand summarises the guidance and review articles relevant to the management of FI in older people living in care homes/long-term care. This is presented in a timeline format (Figure 4) and demonstrates how thinking about FI is discussed for health-care professionals and where the sources of evidence and guidance are located. The importance attributed to assessment and the diagnosis of faecal impaction is emphasised. There is limited acknowledgement or guidance about how to implement this essentially biomedical guidance (e.g. careful examination of the anorectal region is recommended) in settings with limited access to clinicians and lack of discussion about how to implement assessment or treatment options for PLWD. A strong theme that emerges is the belief that direct clinical assessment is essential but that there is little direction on how this could be achieved, particularly in care home settings for PLWD.
FIGURE 4.
Timeline of guidance and review articles relevant to the management of FI in older people in care homes/long-term care.
The second strand considers the potential for transferable learning. Essentially, there is a body of continence research in US nursing homes (some of which is focused on FI) by Ouslander et al. ,45,93,94 Leung et al. ,95,96 Levy-Storms et al. ,97 Rahman et al. 98,99 and Schnelle et al.,100–106 but there is little consideration of the impact of dementia on continence or implementing the interventions (based around PV). There is also a body of literature on the non-pharmacological approaches to the reduction and management of behavioural and psychological symptoms of dementia (BPSD) in UK care homes by Ballard et al. ,107 Fossey et al. ,108,109 Lawrence et al. 110,111 and Whitaker et al. 112,113 We theorised parallels between the experience of FI and BPSD and the use of ‘containment’ as the predominant but not ideal approach to management:
-
There is stigma and revulsion at FI and BPSD.
-
Containment is the ‘easier’ option (either pads or antipsychotics).
-
Alternatives to this option (PV for FI and psychosocial interventions for BPSD) are difficult to implement and need to draw on the assumptions of individualised care and person-centred approaches.
Figure 5 demonstrates how both these programmes of work have developed over time from a specific intervention through multicomponent intervention trials to more detailed work around implementation in the care home/nursing home setting. The continence studies give specific results around FI and the BPSD studies on working with PLWD. The learning from these programmes of work suggests that training, learning, mentoring and post-training support are important contexts but do not, of themselves, lead to staff engagement and motivation to change practice or care routines.
FIGURE 5.
Schematic showing of the development over time in two research groups of a common understanding of the need for multicomponent interventions and the complexity of implementing new practices in care homes. QoL, quality of life.

In addition, the recent work on the prevalence and management of FI in Norwegian nursing homes76 confirmed earlier discussions by the RMT that double incontinence is more prevalent than FI alone and that double incontinence is associated with more cognitive impairment.
Outcomes
We categorised outcomes identified in the phase 1 scoping work as resident, staff or organisational outcomes. These outcomes were identified from the phase 1 stakeholder input (interviews, focus groups and RMT and SSC discussions) and from the continence, PCC and care home implementation literature reviewed in phase 1. This is summarised in Table 6, which clearly shows the different outcomes prioritised between the different research perspectives. Particularly notable are the gaps between the resident outcomes in the continence literature (which has more of a biomedical focus) and the PCC and care home intervention literature (which has more of a quality-of-life focus). Distress and improvement in symptoms are noted in both.
| Resident outcomes | Staff outcomes | Organisation outcomes |
|---|---|---|
| Outcomes proposed by stakeholders | ||
|
|
|
| Outcomes from the continence literature | ||
|
|
|
| Outcomes from the PCC literature | ||
|
|
|
| Outcomes from the care home implementation literature | ||
|
|
|
Outcomes identified by stakeholders and not explicit in the research literature include resident outcomes of comfort and dignity, staff outcomes of change in attitude and work satisfaction, organisational outcomes of workforce turnover and organisational reputation. These staff and resident outcomes identified by stakeholders as important for PLWD in care homes who experience FI are more aligned to the outcomes measured in dementia care and care home implementation studies.
Cost outcomes are not well defined by studies or stakeholders. Resource use is broad and not care home specific (staff, buildings, laundry, continence aids and prescribing).
The use of pads to manage FI is the most common continence aid used in care homes. The following provides an account of the literature on this topic and related outcomes; however, we did not extract data from the majority of the literature. There was insufficient detail to test our programme theories in the evidence reviewed. The impact of a person’s dementia, the level of staff preparedness and how use was linked to clinical assessment were not discussed.
Literature on use of continence aids for care home residents
The initial searches identified only one study on the use of pads. This study114 focused on the incorporation of a pocket with wipes in the design of the pads. It tested how this design change affected pad changes, and how staff used the equipment/resources available.
A further scoping by Mandy Fader considered a wider literature on absorbent pads and products (colloquially known as ‘pads’) that was not necessarily dementia or care home specific. This literature on the management of FI with products can be broadly divided into three areas:
-
management of FI with absorbent products
-
incontinence-associated dermatitis and development of pressure ulcers
-
management of FI with mechanical devices.
Management of faecal incontinence with absorbent products
Very few studies have compared the different designs of absorbent products for FI, and the emphasis has been mainly on testing pads with patients with UI. It is recognised that different absorbent designs are more or less likely to be effective and acceptable, depending on patient attributes (e.g. ability to stand, ability to toilet independently and sex) and preferences. 115–120 However, these attributes and preferences do not consider issues directly related to how dementia affects the person’s continence. These designs may also be cost-effective in different settings [e.g. day vs. night and easier to use or change than others (by carers and residents)]. A putative C–M–O configuration from this would, therefore, suggest that a patient decision-making tool (resource) may be valuable in determining which products to use for a particular patient, taking into account when it is to be used (C) and how easy users (carers or residents) find it to use (C) because it could trigger regular toileting ‘being less of a practical difficulty’ (M) and thus FI may be reduced – even if pads are being worn (O).
Incontinence-associated dermatitis
There is a considerable body of literature from baby and adult nappy studies that shows the effect of urine and/or faeces on skin health and describes the processes that lead to dermatitis and to pressure ulcers. 121–124 There is some evidence that liquid stool or a combination of urine and faeces provide the most damaging skin environment. A further body of literature focuses on skin protection and skin cleansing as methods of avoiding skin damage. Hypothetically, the management of UI (e.g. the use of a catheter or penile sheath) separately from FI (mechanical device or absorbent pad) may reduce incontinence-associated dermatitis. However, this is an option for women only if a urinary catheter is used, and this is not recommended for long-term use. Neither does this management option really take any account of the acceptability of these sorts of options for people with dementia. 114
Management of faecal incontinence with mechanical devices
A Cochrane review on anal plugs and a literature on the use of catheter/tube devices to drain liquid stool. 125–131 The studies included mainly reported on dependent bed-bound patients in intensive care units who had a urinary catheter, and are, therefore, not relevant to care home settings. Studies reported risks and some major adverse events (e.g. haemorrhage132,133) related to the use of some mechanical devices. Moreover, there are consent and ethical issues related to the use of these devices. It is, therefore, unlikely that mechanical devices would play a major role in the management of FI in care homes.
Tables 7–9 summarise the evidence on absorbent designs that is relevant to the review and the limited sources of evidence that address the needs of PLWD and FI resident in care homes.
| Reference | Main subject areas |
|---|---|
| Fader et al., 2008115 | Research evidence of absorbents’ design features and their suitability/popularity among different types of incontinence and users |
| Fader et al., 2010116 | Literature review of current product design for FI/UI. Need for different designs to accommodate variety of needs |
| Bliss and Savik, 2008119 | Use of a small absorbent dressing to contain FI |
| Bliss et al., 2011118 | Survey of the use of absorbents by community-living elderly. Preferences for design of products for FI |
| Beguin et al., 2010120 | Described and tested pads that create an acidic surface and breathable side panels to reduce skin moisture and damage |
| Reference | Main subject areas |
|---|---|
| Shigeta et al., 2009122 | Research study showed association between diarrhoea and contact dermatitis |
| Shigeta et al., 2010121 | Research study in nursing homes found skin hydration and pH higher in residents with faecal and double incontinence |
| Rohwer et al., 2013123 | Found an association between dermatitis and FI. Community-based study |
| Beeckman et al., 2014124 | Found double incontinence to be a significant predictor of pressure ulcers |
| Reference | Main subject areas |
|---|---|
| Denat and Khorshid, 2011125 | Use of perianal pouch for bed-ridden patients |
| Jones et al., 2011126 | Description of rectal catheter for the containment of faeces and Clostridium difficile |
| Allymamod and Chamanga, 2014131 | Used faecal collecting device for bed-bound community patients. Used fewer sacral wound dressing changes, increased comfort and fewer nurse visits |
| Mulhall and Jindal, 2013132 | Case study of gastrointestinal haemorrhage as a result of using a faecal management system |
| Shaker et al., 2014133 | Case study of rectal ulceration as a result of using a faecal management system |
At the end of phase 1 (see Figure 2), we had established how effective reduction and management of FI for PLWD is represented in the literature and the range of outcomes that are used to measure this. Practitioner accounts, professional literature and discussions with stakeholders raised issues around the specific problems of PLWD and what supports or inhibits implementation of best practice in care home settings.
The scoping work led us to clarify and expand our definitions of dementia and continence for PLWD in care homes.
Definitions
Dementia
The International Classification of Diseases, Tenth Edition (ICD-10),134 defines dementia as a disorder with deterioration in both memory and thinking that is sufficient to impair personal activities of daily living. The definition requires that the patient have deficits in thinking and reasoning in addition to memory disturbance. The Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition135 (DSM-IV) defines dementia as a syndrome characterised by the development of multiple cognitive deficits including memory impairment and at least one of the following cognitive disturbances: aphasia, apraxia, agnosia and a disturbance in executive functioning. The deficits must be sufficiently severe to cause impairment in occupational or social functioning and must represent a decline from a previously higher level of functioning. The lack of continence studies addressing dementia and an inconsistency in how dementia is assessed and recorded for care home residents, coupled with the lack of consensus on how to define advanced dementia in relation to continence care, meant that the working definition of advanced dementia was loosely defined and sometimes had to be inferred when undertaking the review.
Continence
The protocol definition and starting point of the review was ‘leakage of solid or liquid stool that is a social or hygienic problem’;41 the sense that it can be a ‘social or hygienic’ problem did not capture the behavioural aspects of FI that had been raised in scoping.
The scoping of the literature identified two ways of defining and categorising different types of continence for older people with dementia and, specifically, FI. Saga76 provides a list of clinical or physiological causes that identifies dementia-related incontinence as a particular cause of FI. Stokes,136 in contrast, sees incontinence and specifically FI as a single factor (of nine causes or contexts) for ‘toileting difficulties’ (Table 10).
| Definitions of FI (Saga 201476) | Definitions of toileting difficulties (Stokes 2013136) |
|---|---|
|
|
Stokes’ definition of incontinence has an emphasis on behavioural issues that arise from living with dementia: ‘The voiding of urine or faeces, either following an unsuccessful effort, or with no apparent attempt to employ an acceptable facility (e.g. toilet, commode, urine bottle)’. Examples of behavioural incontinence (or toileting difficulties) include:
-
parcelling (e.g. wrapping and concealing the evidence in drawers or cupboards)
-
wetting or soiling clothes – while sitting or lying in bed (passive)
-
wetting or soiling clothes – while standing/walking (active)
-
using an inappropriate receptacle (e.g. bin, fire bucket or sink)
-
urinating against a wall or radiator
-
smearing.
Drawing on person-centred care approaches, Stokes136 posits a theory of a pathway to successful toileting in PLWD. This includes:
-
recognising the need to initiate and postponing within limits the act of voiding (failure = incontinence)
-
being motivated to use the toilet
-
possessing the physical strength and steadiness to stand
-
possessing the mobility and confidence to cover the distance to the toilet and overcome any obstacles along the way (e.g. floor coverings, stairs or outstretched legs of others)
-
maintaining goal-oriented behaviour
-
being able to locate the toilet (or acceptable alternative)
-
perceiving and experiencing the toilet as accessible, safe, hygienic and private
-
possessing the dexterity and co-ordination to adjust clothing
-
initiating the act of voiding.
Faecal incontinence in this definition is recognised as having multiple causes that may include constipation, cortical atrophy, neuropsychological, sensory disability, physical disability (mobility and dexterity), medication effects (sedatives, antidepressants and diuretics) and psychological factors (personality, habits, life experience and mood). All of these can be compounded by the built environment, for example distance to the toilets, obstacles, visual access, signage, and the actions and attitudes of others.
Phase 2: theory development, review and synthesis
This section describes the development of the six theory areas tested against the evidence in this review, provides an overview of the sources of evidence and a review of the type of evidence, and an analysis and synthesis of the evidence by theory area, finishing with a concluding synthesis across all the areas.
Theory development
Initially, the ideas presented in phase 1 (as narratives, barriers and enablers, ‘if . . . then’ statements, diagrams and concept mapping) were presented to the research team in linked statements as the factors that were recognised as important when supporting care home residents living with dementia and FI (Box 3).
Interventions to reduce and manage well FI in people with dementia living in care homes need to establish a common understanding of the potential for recovery, reduction and management of FI, for example through training (person-centred care and FI knowledge), support . . . supported by structured assessment (including digital rectal examination when appropriate) and access to clinicians, for example GPs, geriatricians or continence specialists with adequate staff ratios and toilet facilities to develop interventions that reflect the degree of cognitive and physical capacity of the resident (personalised care plans), for example PV, nutrition, hydration, exercise, appropriate medication and appropriate pads that can be introduced as part of the everyday work pattern of the care home, for example care home regimes that incorporate time to assess, prevent and ‘toilet’ and allow for adapted environment.
These linked statements provided an overview of the issues rather than the specifics of how the reduction and management of FI in PLWD resident in care homes may be achieved. It did not address the detail of the process of care or the insights gained from scoping interviews as to the ways in which care staff, clinicians and managers are constantly negotiating the trade-offs between different resident, care home and staff priorities. Neither did they address the links between constipation, faecal impaction and its assessment and management in the care home.
The core team took this feedback and developed a set of six potential mid-range theories and their possible C–M–Os. The purpose was to make explicit certain underlying assumptions and look for confirming or disconfirming evidence in the literature.
These assumptions, the ideas people have about what is most important or would really make all the difference, are listed below as six statements:
Well really the most important thing to address is . . .
. . . making sure people get a proper assessment by a clinician.
. . . staff training.
. . . constipation and impaction.
. . . implementing person-centred care.
. . . the nihilism of staff, the fact that many believe incontinence is inevitable.
. . . how FI care fits with the everyday workflow and patterns of the care home.
These are expanded in Box 4 into mid-range theories with potential C–M–Os.
This area reflects the assumptions and training of clinicians (i.e. doctors, nurses and allied health professionals).
Clinician-led assessment and ongoing support and review (C) informed by the use of jointly agreed approaches (C) to the promotion of continence and alternatives to the use of pads will achieve observable improvements in continence and resident well-being (O).
The assumption is that the involvement of clinicians is key because care home staff do not have the authority or expertise (C) to be able to complete an assessment, particularly digital rectal examination, diagnosis of diarrhoea or drug review. When clinicians take a lead, care staff are confident (M) to accept (M) the delegated responsibility of assessment and management and the shared communication and review of residents increases staff awareness and involvement in continence care (M). Care home staff observe and document changes in the resident and this is fed back into the assessment/review process and this reinforces (M) practices that support effective continence care (O).
Ongoing teaching and feedback for staff that involves care home staff in planning, action, review and implementation [e.g. Plan Do Study Act (PDSA)] will achieve positive continence-related outcomesThis expresses the viewpoint that giving staff access to the appropriate training, education and facilitation will result in a change in practice (C). The mechanisms are that knowledge feedback and review (C) triggers changes in how staff recognise and interpret (M) residents’ continence needs, their confidence (M) and how they work. The assumption is that this will lead to improved continence care (O). This theory is important to consider as so many care home interventions employ a training/education/facilitation approach.
Dealing properly with constipation in older people with dementia in care homes will ameliorate a significant proportion of faecal incontinence as it is laxative induced or overflow faecal incontinence due to constipation and impactionThis area posits that a focus on the recognition, treatment and management of constipation (C) will prompt (M) staff to review residents’ medication management, fluid and nutrition intake, bowel function and activities (C) that reduce the risk of constipation, such as exercise, communication strategies that encourage (M) the resident to ask to be willing to engage and regular toileting leading to appropriate containment and reduction of FI and resident discomfort and pain (O).
Interventions that take account of the history, preferences and wishes of the person together with acknowledgement of the degree of cognitive and physical capacity of the resident (individualised care) will reduce faecal incontinenceThis area encapsulates the PCC approach to care. It assumes that if the resident, their history, their normal bowel patterns and their signals for needing the toilet are known (C) and staff are able to document and review in collaboration with a clinician assessment and family input (C) this means staff conceptualise continence care as unique to the individual resident (M) with the result that there is more dependent continence rather than FI (and UI) as well as outcomes that are consistent with the minimisation of distress and promotion of comfort (O).
Establish a common understanding of the potential for recovery, reduction and management of faecal incontinence for people with dementia will result in attempts to reduce faecal incontinenceThis area addresses and seeks to militate against beliefs of therapeutic nihilism, as proposed by Kitwood,137 that is, the belief that nothing can be done and therefore nothing should be attempted. In its place a belief and value system is advanced about the residents’ potential to maintain or improve functional abilities even when the trajectory is one of deterioration (expressed in staff training, documentation, language of care and handover) (C), and that it is possible to ameliorate FI in residents living with dementia, will mean that staff will be willing to engage and learn about what is causing the FI and attempt interventions (M) to promote continence and the management of FI are put in place (O).
Making faecal incontinence care integral to the everyday work pattern and environment (i.e. ‘fit’) will reduce faecal incontinenceThis argues that even if staff know about managing FI (C) and know about person-centred care practices for people with dementia (C), their capacity (C) to implement them will depend on how it fits (M) with the everyday work pattern and environment. A number of different contexts (knowledge of FI, knowing the person, appropriate staffing levels, availability of clinical expert input – geriatricians/GPs/continence nurses, belief continence can be improved and physical environment) will trigger ‘doing the right thing’ (M) and result in less FI and, most likely, dependent continence (O). These contexts may trigger other mechanisms, such as ‘risk aversion’ and ‘pre-emptive pad use’ that will not result in the desired outcomes. This area incorporates the ideas of staff balancing, juggling and making ‘trade-offs’ in their everyday practice.
Sources of evidence and review
As described in Chapter 2, 62 sources were selected, and DASFs were completed for each one. Box 5 gives an overview of the literature based on the research area they are from and the type of literature (e.g. intervention study, observational study, policy document). Appendix 7 gives greater details, including country, setting, methods, study outcomes and which of the six theory areas they relate to.
Two intervention studies (one crossover RCT) from the 1990s about environmental effects on incontinence problems in Alzheimer’s patients living in a specialist care facility and a book for direct care staff of people who have dementia and are resident in care homes with a section specifically addressing continence care.
Continence: urinary incontinence – those addressing continence care in a care home setting but not dementia or FI – 21 sources (see Table 33, Appendix 7)Sources from 1989 to 2015 focusing on UI management and treatment. There were nine intervention studies (one RCT) and eleven observational studies, of which four were qualitative interview studies, and a review. The earlier studies are intervention, the later studies observational with the most recent (2014) intervention study actually about the training intervention needed to implement a PV programme.
Continence: faecal incontinence – those addressing continence care and FI and/or bowel health (so also covering constipation) in a care home setting but not dementia – 15 sources (see Table 34, Appendix 7)Sources from 1986 to 2015 focusing on FI, bowel problems (including constipation) and diarrhoea in care homes. Five intervention studies (one RCT), seven observational studies and three reviews.
Dementia: care homes – those addressing care or interventions specifically for people with dementia but not continence interventions, in care home settings – 12 sources (see Table 35, Appendix 7)Sources from 2003 to 2015 covering psychosocial interventions, morning care, bathing, eating and drinking and person-centred care interventions. Seven intervention studies (three cluster RCTs and one RCT), four reviews and an observational study.
Implementation: those addressing ‘implementation’ of interventions in a care home setting – seven sources (see Table 36, Appendix 7)Sources from 2000 to 2015 covering implementation in care home settings. Three were intervention studies, two were observational studies, one was a review and one was a book.
Novel interventions: those addressing specific novel interventions to manage continence/bowel health in a care home context – four sources (see Table 37, Appendix 7)Studies from 2000 to 2013 that address residents in care homes with dementia or make reference to the application to the person with dementia. There were four intervention studies (one RCT).
The sources included eight RCTs: quality assessments were completed for each of these using a modified version of the Cochrane risk-of-bias tool. Three were assessed as having low risk of bias and the remaining five had a moderate-to-high risk of bias (see Appendix 8).
Analysis and synthesis
Once completed, the 62 DASFs contained notes of whether or not the source had relevant evidence to the six theory areas (either confirming or disconfirming). They also had multiple C–M–O configurations specific to the evidence source. This process of reflecting on the strength of the evidence to support the initial assumptions and theory areas, producing very specific C–M–O configurations, led us to an articulation of the possible programme theories and underlying C–M–O configurations at work.
We present the findings by theory area in the order that gives the best narrative flow (different from the list in the DASFs, which was given in no particular order of significance).
Theory area: clinician-led support and review
Sixteen of the 62 sources had evidence that was relevant to this area. Eleven gave rich and detailed descriptions and are discussed in Appendix 8. The evidence from the studies reviewed for this set of C–M–O configurations (Table 11) suggests that clinician assessment and review is important. There is some indication that when clinicians (specifically geriatricians in the research cited) apportion time and energy to working with care homes,68,106,138,139 they drive improvements in the presence and management of FI. We found no evidence for the contexts and mechanisms proposed but this was mainly because the papers did not give enough detail to assess them.
| Resources | Contexts | Mechanisms | Outcomes |
|---|---|---|---|
|
|
|
|
The seminal text by Tobin and Brocklehurst68 demonstrated that a geriatrician completing an assessment including digital rectal examination and giving clear directions to GPs and district nurses can achieve compliance with the prescribed treatment (e.g. management of constipation) in two-thirds of residents. Key to this process was the engagement of other visiting clinicians and the heightened attention on residents’ continence that arose from the extra resource generated by the intervention. This paper was a source document for many subsequent publications of evidence that clinician-led assessment is an important contextual factor in the reduction and management of FI.
We found no studies on the role of clinical assessment and review for the management of UI or FI for older PLWD in care homes. Indeed, in the discussion of their findings in a study investigating factors contributing to FI in older people, Akpan et al. 140 suggest that the ‘simple measures’ used by Tobin and Brocklehurst68 no longer apply in care home populations:
In their landmark paper, Tobin and Brocklehurst (1986) demonstrated the potential for improvement in the care home sector using simple measures. These included daily enemas followed by lactulose and weekly enema for those with faecal loading and codeine phosphate daily with twice weekly enemas for those with anorectal incontinence. The FI did not resolve in any of the nursing home subjects in the current study. This issue needs to be considered in future work as either the original study does not apply to the current nursing home population, or the findings are not being implemented, or both.
p. 143140
The only study that looked at the role of clinician assessment for FI in care homes is 30 years old and was of a population that was younger, less frail and less cognitively impaired than the care home populations of today. 141 A more current finding around clinician assessment and involvement in the support of care home residents is from a paper on antibiotic prescribing and associated diarrhoea. 142 Three-quarters of the 274 residents in the study were prescribed antibiotic during the 16-month study period and 43.5% of residents had had at least one episode of antibiotic-associated diarrhoea. Residents in care homes were more likely to be prescribed antibiotics if they were resident in a care home with on-site nursing (a nursing home) or if they routinely used incontinence pads. The authors suggest that the potential benefits of antibiotics should be considered against the possible side effects of diarrhoea. For the purposes of this review, the paper highlights the unintended consequences of clinician involvement leading to what could be wrongly construed as FI.
Most of the review articles and guidelines describe prevalence and aetiology of FI in older people and recommended treatment options (see Figure 4). Reviews and guidelines highlight the importance of taking patient history, including direct questioning, because of the social stigma associated with FI:
Many patients feel too embarrassed to volunteer information about FI . . . Therefore a high index of suspicion and low threshold for directed history from patients and caregivers, and a careful physical examination, are the keys to early diagnosis and adequate management of this embarrassing medical and social problem.
p. 5887
Physical examination and available diagnostic tests are described and the high prevalence of FI in physically and cognitively impaired patients is noted but advice or details on how to take a history and complete examinations in patients with dementia are not provided. The difficulties of achieving the ideal level of investigation and assessment, especially in long-term care facilities, is noted by some of the authors. The descriptions of conservative treatment options, however, mask the complexity of delivery and provide minimal detail about what needs to be done to achieve what are described as ‘simple measures’. For example:
Older persons with dementia may simply need to be directed to the toilet or reminded of such use at regular intervals. Physical limitations and obstacles in the environment need to be addressed if they are contributing to the incontinence, as they can often be overcome by simple measures, such as easier access to toileting facilities and assistance for those who require it with their activities of daily living.
p. 579143
And:
A custom-tailored approach is required with judicious use of compassionate nursing care, relief and prevention of constipation, programmed toileting, exercise, pharmacological and behavioural therapy, and surgical intervention, as indicated (though it is noted earlier in the piece that, ‘Frail older patients with advanced dementia and inability to cooperate are not good surgical candidates. FI in these patients may be managed by planned and alternate use of constipating agents and laxatives’).
p. 54–6087
The NICE guidance for specific groups92 suggests that a behavioural and functional analysis should take place if the initial assessment and management of FI has not worked. Although part of the recommended initial assessment is a cognitive assessment, the guidance does not provide guidance about what should be done if the person is found to have significant cognitive impairment.
In addition, in their conclusions from a 2013 review of the ‘factors with the management of incontinence and promotion of continence in older people in care homes’, Roe et al. 27 show that the belief in the importance of full clinical assessment is common. When discussing what is needed to avoid incontinence dermatitis and promote good skin care in people with UI and FI, they state that ‘this will undoubtedly involve a multidisciplinary approach with full clinical assessment of incontinence’ (emphasis added).
Another source relevant to this theory area was a paper looking at the ethical challenges associated with providing continence care in Australian care homes,144 which cited a lack of access to registered nurses (RNs) for the direct care staff as a barrier to good care, ‘. . . and RNs were not always physically present at facilities causing participants to express they felt alone and unsupported’. In addition, the 2007 audit of continence care145 observes that care homes simply enact a management plan from prior assessment of FI and that assessment of FI in this setting is inadequate.
Also relevant to this theory area is the US programme of nursing home studies led by Schnelle and Ouslander (Figure 6). These authors have been investigating interventions to improve continence for people living in nursing homes since the 1980s and were considered in respect to this theory area because the prompted toileting intervention is promoted by clinicians and involves a certain level of assessment and review. Over the course of their studies there has been a shift in thinking, moving from the implementation of strategies that address one aspect of continence care to multicomponent interventions that include staff training courses designed to accommodate workplace demands on care home staff time and availability. Although clinician-led, the studies do not investigate clinician assessment and review.
FIGURE 6.
Timeline highlighting the key Schnelle group of studies of interventions to improve continence in nursing home residents, showing the alteration in focus from single to multicomponent interventions.

Continence management specifically related to PLWD is not directly investigated in this programme of studies by Schnelle and Ouslander; however, the authors recognise that dementia increases the probability that people living in nursing homes will develop incontinence. The studies do not explain how the increasingly complex interventions are thought to work or for whom they are thought to work for, but they do signal a recognition of the multicomponent nature of continence interventions and their reliance on staff engagement as a key mechanism of interest. In addition, as noted in the introduction to this report, these authors recognise the particular benefits of prompted toileting for people with dementia ‘who lack cortical control of the defaecation process, and therefore tend to void formed stool following mass peristaltic movements’. 45
One of the early RCTs conducted by Ouslander et al. 45 epitomised their approach to improving urinary and faecal continence. The intervention involved 2-hourly toileting conducted by researchers for 12 hours each day; randomisation was on a unit-by-unit basis. The research team interviewed staff to ascertain the residents’ normal toileting patterns and collected baseline data about wetness and soiling for 3 days. The intervention was continued 5 days per week for 9 or 10 weeks. Of the 165 residents who participated in the study, 77 (46%) responded well to the PV to improve UI. Although the study was designed primarily as an intervention for UI, overall there was a statistically significant improvement in the number of continent bowel movements and an overall increase in the frequency of bowel movements after the initial 7- to 10-day period. The authors suggested that this could be a result of the marked increase in mobility of the residents because of the intervention, and that the residents were offered fluids with each prompt and so faecal impactions may have been resolved. There was no alteration in laxative use by residents.
Although none of the studies was designed to assess the impact of the intervention in relation to the functional abilities of the person living with dementia, it is interesting to note the researchers’ observations in one of the early studies of PV and their observation about the difficulties of documenting improvements in quality of life:45
Particularly noteworthy that some residents whose urinary incontinence did not respond well to prompted voiding had improvement in their bowel continence. This suggests that some type of prompted toileting program may be of benefit even for those residents whose urinary incontinence does not markedly improve, especially since faecal incontinence is highly associated with the development of pressure sores and is extremely unpleasant for nursing home residents as well as caregivers. Given the reported distress of constipation in older adults, the increase in bowel movements we noted with prompted voiding may also contribute to an improved quality of life for some nursing home residents, though such improvements in quality of life are difficult to document among cognitively impaired incontinent nursing home residents.
Chassagne et al. 45
One of the later multicomponent studies102 was carried out in a nursing home environment in which a high proportion of people had dementia [intervention group, Mini Mental State Examination (MMSE) 12.9 ± 8.4; control group, MMSE 9.6 ± 8.4]. They found that PV seemed to particularly benefit some residents with cognitive impairment:
A result not previously reported was that subjects with more cognitive impairment were most responsive to prompted voiding. This finding is important because NHs [nursing homes] often exclude residents from programs because of dementia or other vague cognitive impairment criteria. It has been argued that such exclusions are not valid, and the findings from this study support this conclusion.
p. 1508102
In 2008, a review article of studies that implemented PV or scheduled toileting was conducted, with a particular focus on studies that also included a physical activity programme. 96 In the review, the most significant fall in FI was achieved by the intervention that combined PV with a programme of exercise and fluid intake. 147 As already noted, the improvement in bowel movements in relation to the intensity of the intervention was disappointing. The authors suggested this may have been because of a high prevalence of sphincter dyssynergia in nursing home residents with FI; however, we were unable to find any evidence that tested this.
After 2008, the Schnelle and Ouslander studies take one of two paths. One path continues to investigate and refine the elements of multicomponent interventions that involve residents directly, for example Schnelle et al. 102 The second begins to address the issue of implementation by creating staff training interventions. 98,99,146 These interventions are multicomponent and involve staff learning how to assess residents and implement the programme of PV, exercise and dietary and fluid intake. Staff were also given support and feedback during the implementation process to consolidate their learning and adjust the programme with regard to local factors. This leads into the second programme theory, in which the focus shifts to working with care home staff by providing ongoing teaching, review and feedback on residents’ FI-related outcomes.
Theory area: ongoing teaching and feedback for staff on the assessment and management of faecal incontinence
Linked to the arguments about the importance of clinician assessment is the assumption that giving staff access to the appropriate training, education and facilitation will result in a change in practice. In addition, the assumption is that feedback and review of learning will change the working practices of care home staff. This area is important to consider, as so many care home interventions employ a training, education or facilitation approach (Table 12).
| Resources | Contexts | Mechanisms | Outcomes |
|---|---|---|---|
|
|
|
|
Sixteen of the 62 sources had evidence relevant to this area, and six are discussed in detail in Appendix 7. Two were from the US nursing home PV group of studies,98,99 investigating training as a means of implementing PV. Three sources (two of which were reviews) were from the reducing antipsychotic prescribing and implementing psychosocial interventions fields of research in care homes. 108,111,148 A very recent pilot study directly addressed the ‘feasibility, acceptability and adherence of two educational programs for care staff concerning nursing home patients’ FI’. 149 The evidence suggests that although education, training and feedback are all important resources for implementing good practice in care, the setting in which they are delivered and how they are delivered are key. Therefore, the proposed C–M–O configuration stated is dependent on other important elements, such as how it actually fits with existing care home practices. These findings are discussed later.
Two studies used distance learning course work and coaching with staff from 48 nursing homes98 and webinars with seven nursing homes99 to support the implementation of PV programmes. They had limited success: the 2012 study had a one-third attrition and incomplete implementation of the programme at 7–8 months. There was a significant improvement in the knowledge of those who completed the course. The study provides insufficient detail to understand what elements of the training (what works) were working for which particular care homes (for whom) and what particular contexts were important (in what circumstances). The webinar-based training course99 introduced each step/concept (of PV) with gaps of between 1 and 4 weeks (C). The time scale of the training gave staff the opportunity to absorb and try their new knowledge and skills (M). In this study, the researchers changed the timings of some of the webinars based on feedback from the nursing homes. However, the context factor of ‘time to do training’ did not clearly link through to outcomes. The variability in length, intensity and content meant that it was difficult to disaggregate what aspects of the interventions did or did not influence staff uptake and utilisation of the programmes offered.
A similar picture emerged from studies investigating the implementation of psychosocial interventions in care homes as a response to the drive to reduce antipsychotic prescribing. The 2012 systematic review of psychosocial interventions111 raised a number of important contexts and mechanisms for other theory areas; however, specifically in relation to training and education, the authors noted that ‘training and mentoring programmes can require a substantial time commitment’, supporting the context that time allocated for training is as important as the content. A more recent qualitative study by the same group of authors110 with the objective ‘to contribute to an optimised training programme for care staff that supports the implementation of evidence-based psychosocial interventions in long-term care’ had richer descriptions and so enabled some C–M–O configurations to be drawn from their findings (Table 13).
| Resource/intervention | Context | Mechanism | Outcome |
|---|---|---|---|
|
|
|
|
Their results suggest that it is not simply having enough time to attend training that is a key context nor are the mechanisms for successful implementation the staff responses to having knowledge and skills. Rather, the shared understanding and enhanced status of the work leads to intermediate outcomes of better communication and staff feeling more valued.
Boersma et al.,148 in a review of psychosocial interventions in residential dementia care, found that, despite increases in staff knowledge, about half of the included studies demonstrated an improvement in staff attitudes and/or behaviour after training. Thus, the proposal that increase in knowledge will result in improved practice is only partially supported. It is possible to change staff behaviours through training but either knowledge did not increase or there are additional factors involved for which knowledge may be a necessary but not sufficient condition for behaviour change.
The hypothesis of the small but ambitious pilot study in 2015 by Blekken et al. 149 is ‘that faecal incontinence can be prevented, cured, or ameliorated by offering care staff knowledge of best practice’. The findings from this small study were equivocal. The authors had difficulty recruiting nursing homes and reported limited impact, and changes to the rates of FI were not sustained. The study-specific C–M–O configurations developed from this paper are given in Table 14.
| Resource/intervention | Context | Mechanism | Outcome |
|---|---|---|---|
|
|
|
|
In the discussion the authors suggest ‘for the main study, empowering RNs in the nursing role and helping them find ways to best organize the work on their own unit and give feedback to the rest of the care staff will be important’. This suggests that even the multicomponent training, which also included the recruitment of a local opinion leader and educational outreach visits, is unlikely to be sufficient. The evidence from this small study suggests that it could be important to look at the division of labour and status of different types of work in this residential setting.
The evidence from this review suggests that offering more training for care staff on FI with structured guidelines and a facilitator will not lead to better management or reduction of FI if it does not account for the work pressures of the care home.
Theory area: knowledge about the management of constipation for older people with dementia
A related proposition from the scoping work was that a focus on one particular aspect of bowel-related continence care, the management of constipation, could lead to improved outcomes for older PLWD (Table 15). This theory area overlaps with the clinician-led support and review theory area. The key difference is the argument that a focus on management of constipation, as a significant contributory factor of FI, would then trigger both a prioritisation of clinical assessment and medication review and those activities that supported bowel health, such as promotion of physical activity and improved nutrition and hydration.
| Resource | Context | Mechanism | Outcome |
|---|---|---|---|
|
|
|
|
The scoping phase identified two studies for which evidence pointed towards the need to deal with constipation to reduce FI. In addition, expert opinion from clinicians in our stakeholder interviews suggested that dealing with constipation could make a significant contribution to addressing FI-related problems. A controlled trial42 specifically asking if the treatment of constipation would improve FI in institutionalised elderly patients concluded that ‘when long-lasting and complete rectal emptying is achieved by laxatives, the number of episodes of faecal incontinence as well as the workload for caregivers is reduced’. Another study of 14 cases of faecal smearing (scatolia) as a dementia-specific characteristic of FI in older people with dementia found that all 14 people were constipated. 150
Twelve of the 62 sources had evidence relevant to this with six providing a particular contribution to theory testing. Two were from the Ouslander and Schnelle group of studies (see Figure 6). A 1996 study45 found that PV resulted in an increase in continent bowel movements and the authors proposed that ‘as the residents began to be toileted, moved and offered fluids, these [rectal] impactions may have been resolved, resulting in an increase in bowel movement frequency’.
A later paper, however, by Leung and Schnelle,96 discusses the use of softeners and laxatives as prophylactic treatment against constipation and impaction. The authors warn:
. . . in the presence of impaired sphincter function and decreased rectal sensation, the fluidity of the stool induced by the use of laxatives and stool softeners administered to prevent constipation and impaction may in fact predispose the nursing home residents to manifest FI.
p. 696
There were three studies (four papers)76,151–153 with a constipation focus that were included for data analysis and synthesis. The first paper151 about laxative use (and therefore constipation) noted the effect of ‘care home characteristics’ on the use of laxatives:
. . . our findings show that differences in laxative use exist between care homes beyond those accounted for by resident characteristics.
Gage et al. 151
A paper from the same study58 suggested that a change in pro re nata prescribing (and not clinician or carer assessment or practice), in other words the organisation of care, could explain these differences:
The review of residents’ notes did not identify an increase in bowel care-related planning in the intervention care homes. Nor did the benchmarking intervention prompt a review of laxative prescribing by district nurses. The reduction in laxative-induced diarrhoea was due to a change in the care home practice of routinely dispensing laxatives that had been prescribed pro re nata (PRN).
p. 58658
Dementia was a risk factor for laxative use, raising the possibility that linking dementia care with a focus on the management of constipation could lead to unintended consequences, such as an overuse of laxatives.
The second paper152 examined the effectiveness of a training and education intervention for constipation management across four different long-term care settings; it was one of the few studies that considered the experience and prior training of staff involved. The main outcome measures used in the assessment were staff knowledge and laxative use. Staff knowledge on constipation improved. There was some change in laxative prescribing but not in the care of the elderly (care home) setting, and the study did not provide information on resident diagnosis or characteristics. Both studies suggested that the education and training of care staff or visiting health-care professionals on constipation, apart from highlighting the possibilities of laxative-induced diarrhoea, were not likely to achieve improved FI-related outcomes.
The Saga-led studies76,153 on FI in care homes suggest that focusing on one aspect of continence can result in unintended consequences. Activities that would support good bowel care were superseded by a preoccupation of the nursing staff with a person’s bowel being empty. As this extended quotation demonstrates, it was a poor compromise:
. . . the findings were that constipation was the primary concern of registered nurses. To empty the patients’ bowels was the aim of preventive tasks and nursing intervention. Although some preventive measures were taken, faecal incontinence was mainly treated passively with diapers; which in turn likely compromised the patient’s need for well-being and dignity . . . FI and diarrhoea were not recognized as significant problems by the registered nurses, despite high prevalence of both. . . . Instead, due to hindering factors for good bowel care related to a challenging patient group, patient and family experience, physical and organizational working conditions and professional challenges within the nursing group, the registered nurses are compromising, making emptying of the patients’ bowels the most important task. This study shows that to improve bowel care among nursing home patients, structural changes founded in nursing management are necessary . . . To bridge the gap between patient needs and available resources, nurses are continuously making compromises, of which one outcome is exclusive focus on emptying the patients’ bowels rather than maintaining continence and good bowel care.
p. 9176
A preoccupation with one element of bowel care (an empty bowel) meant that staff did not consider pad use or episodes of FI as areas in which there was potential for change. This highlights the association between institutional and wider policies that improve one circumstance to the detriment of others. Table 16 summarises as C–M–O configurations the intended and unintended consequences of focusing on constipation.
| Resource | Context | Mechanism | Outcome |
|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
This would suggest that focusing on the management of constipation to the extent that ‘emptying the bowels’ becomes the priority works against the ongoing assessment and review of residents’ care or staff beliefs that it is possible to improve outcomes. A mechanism that this approach lacks is one that connects new knowledge (the management of constipation) with the benefits for the resident, did they feel better and were they continent, as well as the wider concerns and activities of the care home. A doctoral thesis on care staff and care home working154 highlighted how a focus on one activity (in this case person-centred care at meal times to support resident choice and participation) had unintended consequences for the rest of the care home staff’s workload. The result was that they rushed other aspects of care in order to meet the expectations of what should happen at meal times:
The official understanding of the mealtime standards is that they produce pleasant dining experiences. However, what the regulatory pleasant dining experience accomplished in the staff and resident routines was a process of hurried practices that precluded possibilities for workers and residents to amble. The staff had to rush to complete their personal care work in order to get to the dining room.
p. 133154
There were two small care home studies that tested the feasibility of novel interventions for addressing constipation using transcutaneous posterior tibial nerve stimulation155 and mechanical vibration to provide abdominal massage. 156 Neither included PLWD and it was unclear who, apart from the research team, were involved and how the interventions could be implemented by care home staff for PLWD.
The conclusion from considering this theory area is that, although dealing with constipation may be important, an excessive focus on one specific factor (constipation) could have unintended consequences such as the overuse of laxatives and other areas of important care work and activities to promote bowel health being given lower priority. A focus on treating constipation without considering the individual needs of the person could have negative care outcomes. The next theory area then draws on the theory that the implementation and process of PCC will be key.
Theory area: interventions that reflect degree of cognitive and physical capacity of resident – personalised care planning
This theory area encapsulates the PCC approach to care in that knowing the person’s needs, wants and abilities, specifically in relation to toileting and continence, will reduce reversible FI. It links to a broader understanding of FI in PLWD as one aspect of toileting behaviours. It recognises that the personality of PLWD is increasingly concealed. 157 It is therefore important to prioritise the relationship as much as the care tasks. It is the personalisation of the person’s continence care and their environment and interpretation of behaviour from the person’s viewpoint that takes precedence (Table 17).
| Range of activities | Contexts | Mechanisms | Outcomes |
|---|---|---|---|
|
|
|
|
We found very little person-centred care literature that addresses continence or discussion in the wider continence literature of what a person-centred approach might involve.
There were only two studies that designed dementia-specific continence interventions158,159 and these were conducted in the early 1990s in an Alzheimer’s disease unit. Another study,160 from 1989, considered how the signs and symptoms of dementia affected nursing home residents’ ability to engage with interventions to reduce and manage UI. Of the 43 studies that addressed continence care in some form, only 20 included PLWD, and 16 of those had an assessment of some form for dementia. However, as noted above, only one considered the impact of dementia on the uptake of the intervention. Table 18 summarises the 20 studies and how dementia was measured and considered. It is striking that, apart from the acknowledgement that dementia is a risk factor for FI and that this increases with immobility, only three studies specifically address dementia behaviours and FI with the continence intervention. 17,68,140
| Title and authors (year) | Dementia measure? | Risk factor | Functioning | Behaviour | Other information | Comments |
|---|---|---|---|---|---|---|
| Faecal incontinence in residential homes for the elderly: prevalence, aetiology and management. Tobin and Brocklehurst (1986)68 | 91% of participants had mental test scores of ≤ 6 suggesting dementia | Dementia as a risk factor for faecal impaction, explained as neglect of the ‘call to stool’ | The study implements a controlled trial comparing the continence outcomes for the treatment group, assessment with treatment recommendations and the control group, no assessment or recommendations | Results disaggregated by condition and dementia score | ||
| A clinical trial of behavioural therapy to reduce urinary incontinence in nursing homes. Hu et al. (1989)160 | MMSE scores for each participant | ADL score for each participant (inclusion criteria were female, age ≥ 65 years and ability to use the toilet and to recognise own name) | The programme aimed to raise residents’ awareness of the need to void urine and encourage them to seek help if necessary. It was implemented and maintained 7 days a week (waking hours only) for 3 months. Improvements in the intervention group were sustained at 22-week follow-up. Note that only female participants and UI were included | The researchers conducted an a priori power calculation and gathered data from the required number of participants. Results were disaggregated by MMSE scores within each condition | ||
| A staff management system for maintaining improvements in continence with elderly nursing home residents. Burgio et al. (1990)161 | MMSE scores stated for all four participants | All participants are described as ‘non-ambulatory’ | One (out of four) participants is described as non-compliant during toileting assistance | A US study, the intervention focused on monitoring staff actions in respect of continence checks and toileting and on the usefulness of performance feedback for staff | Results not disaggregated by severity of dementia | |
| Behavioural treatment of incontinence in the long-term care setting. Engel et al. (1990)162 | Mean MMSE score for all 62 residents included in the study was 14.3 | No mention of physical abilities. Depression levels among the group were described as below the national (US) average for the age range | A US study, the intervention focused on monitoring staff actions in respect of continence checks and toileting and on the usefulness of performance feedback for staff | Results not disaggregated by severity of dementia | ||
| Environmental effects on incontinence problems in Alzheimer’s disease patients. Namazi et al. (1991)158 | Probable Alzheimer’s disease, CDR scores given for 14 out of 17 participants | Being able to see the toilet facilities and using them | Intervention, using observational pre- and post-test data collection | Results not disaggregated by severity of dementia | ||
| Physical environmental cues to reduce the problems of incontinence in Alzheimer’s disease units. Namazi et al. (1991)159 | Probable Alzheimer’s disease | Clear signage facilitates toilet use | Intervention, observational pre and post test | Severity of dementia not mentioned | ||
| Effects of prompted voiding on fecal continence among nursing home residents. Ouslander et al. (1996)45 | Mean MMSE score of 12.4 | 55% required assistance with mobility | Residents with behavioural issues, for example aggression, were excluded | The intervention was carried out entirely by research staff | The results are not disaggregated by dementia score | |
| Risk factors for fecal incontinence in a nursing home population. Johanson et al. (1997)17 | Dementia was established based on each individual’s orientation to person, place and time | Yes, dementia as a risk factor for incontinence is a finding | The degree of mobility was categorised by a resident’s ability to walk without assistance, using a walker, or confinement to a wheelchair or to bed | Data collection from 388 participants | The results are not disaggregated by dementia score | |
| Continent or incontinent? That is the question. Taunton et al. (2005)163 | More of the participating residents at site 3 were moderately or severely cognitively impaired than at site 1 or 2 | More of the participating residents at site 3 were constantly incontinent than at site 1 or 2 | A US study; 17 residents participated across three care homes, no information about numbers at individual sites | No information is given about the measure used to assess cognitive impairment | ||
| Privacy for defaecation and fecal incontinence in older adults. Akpan et al. (2006)164 | MMSE scores ranging from 19.5 to 30 | This study is not care home specific | The results are not disaggregated by MMSE scores; however, people living at home had fewest problems with privacy and highest MMSE scores (29–30) compared with those living in nursing homes who had the greatest problems with privacy and the lowest MMSE scores (19.5–27.5) | |||
| Factors contributing to fecal incontinence in older people and outcome of routine management in home, hospital and nursing home settings. Akpan et al. (2007)140 | MMSE scores ranging from 19.5 to 30 | Yes, ‘impaired cognitive function’ as a risk factor for FI is a finding | This study compares risk factors for FI among older adults across a variety of accommodation, own home, acute care and long-term care | |||
| Smart wireless continence management system for persons with dementia. Wai et al. (2008)165 | Single participant with ‘mild to moderate’ dementia and UI | Unsteady gait | Changes to involution | A sensor inserted into an incontinence pad sent a wireless signal to inform staff of a wetness episode | During a one week trial the system functioned well with no false alarms | |
| Laxative use in care homes. Gage et al. (2010)151 | From records 50% of participants had a diagnosis of dementia | Yes | ADL scores 24% severe, 20% moderate and 56% low | A UK study investigating the use of laxatives for older people resident in care homes | Dementia diagnosis was a statistically significant predictor of laxative use, after no. of medications, length of stay in care home and sex | |
| A controlled trial of an intervention to improve urinary and fecal incontinence and constipation. Schnelle et al. (2010)102 | Mean 9.6 (intervention), 12.9 (control) | Yes | Site to stand measure and measure of walking distance | A US study of six nursing homes. A 12-week intervention that combined prompted voiding, increased food and fluid intake with increased physical activity. Used a monitoring device worn for 8 hours on 2 consecutive days | Multicomponent intervention, people with more cognitive impairment responded to prompted voiding and prompted fluid and nutritional intake. FI episodes did not change but appropriateness and frequency of bowel movements improved | |
| Can district nurses and care home staff improve bowel care for older people using a clinical benchmarking tool? Goodman (2013)166 | Records were available for 40% of residents, of those 50% had a diagnosis of dementia | This study states that incontinence is not an inevitable result of dementia | ||||
| What characteristics predispose to continence in nursing home residents?: a population-based cross-sectional study. Saga (2015)167 | Cognitive impairment question ‘. . . is the resident aware of the current time, place and situation? – yes/no’ | Double incontinence was strongly correlated with cognitive impairment | ADL measured on the Barthel index | A Norwegian study. Nurses completed anonymous questionnaires about the continence of residents of nursing homes in a particular municipality | ||
| Ethical challenges associated with providing continence care in residential aged care facilities: findings from a grounded theory study. Ostaszkiewicz et al. (2014)144 | Dementia mentioned as an unpredictable factor complicating factor for continence care | Australian grounded theory observational study, focusing on the difficulties/dilemmas faced by staff who give continence care to older people in care homes | Staff have to make spur of the moment decisions about the best course of action in a given situation, for example allow a frail resident to walk to the toilet or try to restrain them to prevent a possible fall | |||
| Bowel problem management among nursing home residents: a mixed methods study. Saga et al. (2014)153 | Staff completed questionnaire asked about cognitive impairment (questions not available in English) | Yes, but not solely | Individual ADL scores obtained | The results are not disaggregated by cognitive impairment score | ||
| Incontinence care in nursing homes: a cross-sectional study. Mandl et al. (2015)168 | Dementia was diagnosed from International Classification of Diseases, Tenth Edition134 (ICD-10) scores | Yes, but within a complex and dynamic relationship | Austrian study, interview and questionnaire data gathered from or for 1302 care home residents | A qualitative study to gauge the type and standard of continence care | ||
| Feasibility, acceptability, and adherence of two educational programs for care staff concerning nursing home patients’ fecal incontinence: a pilot study preceding a cluster-randomized controlled trial. Blekken et al. (2015)149 | Approximately 80% of residents in the study had some degree of CI | Yes | Mean ADL score for entire sample | This was a pilot feasibility study. The focus was on staff knowledge increase and the use of that knowledge in practice |
The scoping, however, and the work of Stokes136 had suggested that approaches that recognised and addressed the personal history of PLWD were more likely to achieve improved toileting outcomes. The only paper169 that used a so-called personhood-centred care process to continence care in care homes and that included PLWD specifically excluded participants with FI. It developed as a standardised package of care for each resident, many of whom had dementia, and included changes to diet, fluids, physical mobilisation, toileting, massage, attention to environment and use of laxatives/manual evacuation. Results were promising in terms of reduction in constipation and in use of bowel-related interventions. The mechanism of interest (Table 19) may have been that staff were more likely to promote bowel health when the individual needs of the resident were systematically considered and linked to a standardised checklist. The study was small, and did not explain how the personalisation was achieved specifically in response to the person’s dementia.
| Resource/intervention | Context | Mechanism | Outcome |
|---|---|---|---|
| Education to individualise giving of laxatives, enemas and manuals Structured input for residents Structured approach to care planning |
Patient-centred care assessments. Care package of changes for each resident regarding diet, fluids, physical mobilisation, toileting, massage, attention to environment and use of laxatives/manual evacuation combined with nursing assessments | Staff more likely to act to promote bowel health | Reduced number of bowel-related interventions; reduction in number of patients with constipation |
To understand and test a theory of how personalised care, and specifically PCC approaches, could lead to improved outcomes, we searched a wider non-continence-specific literature. Thirty of the 62 sources had evidence relevant to this area; 15 had rich enough detail to inform theory and are discussed in Appendix 8.
The scoping established that although there was an extensive literature on person-centred care in care homes, very little of it provided detail about how it should be delivered and the kind of outcomes that were likely to be achieved. Work by Edvardsson et al. 157 suggested that a key contextual influence on how PCC is implemented is whether or not the people providing care have the authority and organisational permission to work in this way and this informed how we interrogated the wider care home literature on person-centred care.
Our synthesis and review reinforced these findings. Addressing person-centred care, Ericson-Lidman et al. 170 conducted a small-scale interview study among staff (n = 12) at one residential aged care home in Sweden. They found that the concept of person-centred care was poorly defined and there was a lack of staff understanding and little managerial support. These variables led to individual staff interpretations of person-centred care and contradictory responses to a given situation. The need to understand the detail of what constitutes person-centred care activities as they relate to continence and practice in the care home is illustrated by the work on the implementation of psychosocial interventions in English care homes of Lawrence et al. 110 They found that when emotional bonds between carers and residents are discouraged by managers, staff burnout occurs more frequently, leading to absence and higher staff turnover. However, when chatting and forming bonds with residents is valued, staff develop a person-centred working style and focus on residents as individuals with differing needs and preferences, rather than taking a task-oriented approach. 110
Three non-continence interventions that provided detailed accounts of using a person-centred care approach in care homes were identified. These focused on using PCC as an alternative to antipsychotic prescribing,108 the use of PCC compared with other approaches171 to reduce resident agitation and distress and interventions that are designed to minimise resistance to care when bathing residents with dementia. 172–174 One study,173 which aimed to improve morning care with an individualised abilities-focused approach, found no change in resident behaviour. This intervention included a one-off training session for staff but this was not developed in partnership with the care staff and did not appear to include facilitation.
Two US studies172,174 address bathing people with dementia living in care homes, activities that offer transferable learning for toileting and maintaining a person’s skin integrity. This intervention links the assumptions of PCC by attending to the relationship and interaction with the resident; using techniques that support enhanced communication and interpersonal skills; and adapting the physical environment and bathing procedures to decrease distress and discomfort. Both research teams considered the causes of resident distress and have developed alternative ways of bathing that achieve the dual aims of cleanliness and minimising distress. The evaluation by Gozalo et al. 174 demonstrated reduced distress, agitation and calling out. It was also noted that there was less distress and staff were able to bathe residents more quickly. 172 Both note that ‘organisational factors’172 and ‘facility-wide culture change’174 are important. These studies offered a dementia-focused theory of engagement that was practice-specific and detailed, although they did not unpick organisational-level factors.
Theoretically, the ability of an intervention to involve particular care home staff (C), the provision of education and training (C) that encourages staff to recognise the person with dementia’s situation and acknowledges the difficulties staff face providing care (C) could lead to staff developing empathy (M) for residents’ feelings, believing that change is both possible (M) and worthwhile (M) with the result that residents will be less agitated or distressed (O). A recognition of the care home environment, and its related challenges for the workforce and their ability or authority to change practice, is as important as understanding the person with dementia’s needs and how they might interpret the intentions and actions of staff.
Whitaker et al. 113 conducted a review of what needs to be in place for psychosocial interventions, such as PCC, to work in care homes. The following quotation shows how they articulate these main findings:
. . . a number of key issues that, if addressed, would help to enable the widespread implementation of psychosocial interventions in care homes. This includes the importance of providing individualised interventions that are tailored to the person’s preferences and abilities and of obtaining the full support of care staff. [our emphasis] Staff members enable access to psychosocial interventions and provide essential encouragement and reassurance. Yet it is apparent that pressures on staff time, an associated focus on ‘priority needs’ and a preoccupation with risk present enduring barriers to implementation . . . Too often staff members are reluctant participants in dementia care training . . . It is essential to demonstrate that psychosocial interventions are a valuable option. Collaborative approaches that acknowledge staff perspectives and expertise from the outset offer an important method of engagement. This involves listening to any preferences or concerns that staff members have about the intervention in question. Finally, it is essential to obtain the full support of managers given their role in facilitating interventions and effecting cultural change within the home.
p. 348111
Whitaker et al. 113 go on to highlight the need to consider the resources and time available to the staff to allow them to modify work schedules and mentor staff. Activities, such as role-play, videos and vignettes, life review work or music events with PLWD, in other words activities that encouraged the mechanism of empathy, can help staff to see beyond the symptoms of dementia, to broaden their conceptualisation of the caregiving role and to reflect on their practice.
One Australian study144 illustrated the tension that care home staff may experience when asked to implement PCC if the goal of care does not fit with the priority of the care home, for example if the need for residents to appear clean and well groomed is given priority over person-centred care. In addition, if care home staff have ‘inadequate information about resident’s care needs’ on which to base their responses, the possibilities for delivering person-centred care are diminished.
An observational study on intimate continence care from the learning disability literature175 demonstrates the loss of dignity that can occur when the principles of person-centred care are not applied and when bathroom facilities and toileting support do not consider the needs of the resident (Table 20). When staff focus on a task and fail to view a resident as a person, indignities and mistreatment can occur. For example, seating a resident on the toilet for other aspects of care can cause confusing associations with the toilet and possibly contribute to incontinence. The following summarises the C–M–O configurations that were evident in this study. It was the only study that considered the adverse outcomes when continence care is rushed, no attention is given to a person’s preferences and continence care is subsumed in other activities.
| Resource/intervention | Context | Mechanism | Outcome (negative) |
|---|---|---|---|
| Being helped to use the toilet | Staff rushed to get the job done | ‘Task-oriented’ approach | Left naked while sitting on toilet |
| Dependent continence: the person has to be helped to use the toilet | Staff believe that it does not matter if person is naked | Objectification of the person | |
| Using the toilet as a seat for other aspects of care | Service user not given opportunity to urinate or defaecate privately | Triggers confusion in associating the toilet with urinating and defaecating | Could contribute to incontinence |
| Dependent continence: the person has to be helped to use the toilet | Staff indifferent, ‘can’t be bothered’ Person unable to communicate their needs. Staff do not try to find what is wanted |
Triggers the person being left waiting when they need to go to the toilet | Incontinent episode |
| Shared bathroom facilities | Triggers less privacy for defaecation | Person may be disturbed (intrusion) while using the toilet |
Using external experts, keeping staff up to date and encouraging a group understanding of PCC have value, but to achieve outcomes, such as reduced resident distress, using a more reflective personalised approach requires both empathy and the time to address the workplace challenges. For PCC approaches to be relevant they need to be discussed in relation to continence-specific activities. The evidence suggests that PCC approaches constitute a contextual factor that needs to be in place to support continence care for older PLWD experiencing FI.
Addressing the environment to promote continence for someone living with dementia as an example of personalised care
The environment (building, signage and adaptations) and factors that facilitate people with cognitive impairment to get to the toilet and use the toilet appropriately and on time (mobility, visibility, suitable clothing and staff time) was identified in scoping as a likely important factor in helping to reduce FI. One of the stakeholders interviewed in phase 1 suggested that the most effective intervention for someone living with dementia was proximity to toilet and the ability to recognise it. We found two research papers on this topic, both from 1991. 158,159 In one small study158 (14 participants, random allocation, crossover design and 9-day intervention) removing the visual barrier to the toilet in patients’ rooms (taking away screens and visual barriers so that toilets were constantly visible) resulted in an eightfold increase in toilet use, but this may have also had the unintended consequence of causing potentially pathological frequency (every 9.8 minutes on average). Researchers placed tape on toilet seats and used detached tape to indicate toilet use. However, researchers could not tell if residents actually urinated or defaecated, or simply sat then flushed. 158 The second study159 evaluated the use of improved signposting to the toilet in a dementia specialist aged care facility in the USA. Pre- and post-observational data were collected on 44 residents. A number of different signs were trialled: using bright colours, using pictures, using the word ‘toilet’ rather than ‘restroom’ and placing arrows on the floor for use by patients with advanced dementia who look at the floor while walking. The overall conclusion was that visual cues increased visits to the toilet but did not necessarily result in appropriate toilet use. This study indicated that the best results for getting residents to use a publicly available toilet on their unit were obtained by adding the word ‘toilet’ to an arrow on the floor that pointed to the toilet. Placing a graphic depicting a toilet at eye level on the toilet door was also effective but not as effective as the arrow on the floor. These two small studies were carried out in a specialist purpose-built dementia care facility that had circular paths for wandering, an activities programme and a culture that enhanced PCC and resident autonomy and dignity in place. The studies provided some evidence that appropriate visual cues can encourage toilet visits for older PLWD in aged care facilities but that this may not translate into appropriate toilet use (Table 21). Finding the toilet may be a necessary but not a sufficient criterion.
| Resource | Context | Mechanism | Outcome |
|---|---|---|---|
| Visual cues for the toilet – in person’s own room toilet left visible, in communal settings, ‘toilet’ label, picture of toilet and wayfinding arrows on floor | A setting where it is possible to implement these cues (floor arrows may not be possible in all settings) A level of physical mobility in the individual to get to the toilet |
Resident recognises where there is a toilet | More visits to the toilet room (this may then be a resource/context for appropriate use but additional resources or contexts will be needed to trigger that) |
One case study165 on the use of a wireless wetness sensor and system for people living with dementia suggested that this system could be used to implement ‘personalised continence management’ by identifying individual toileting needs. However, this was not explained or developed, and the authors recognised that the requirement for staff to carry out a number of tasks to implement the system proved to be a barrier to the system working correctly.
We found no further published research evidence on environmental cues or technological aids to promote continence in older PLWD, apart from one report in which a urinal had been placed in a resident’s room as previously he had been urinating against the wall. 176 What is interesting is that these ideas have worked their way into recommendations, for example in The King’s Fund tool ‘Is your care home dementia friendly? EHE Environmental Assessment Tool’177 and a Nursing Times article ‘Maintaining continence in people with dementia’178 (not care home specific), despite a lack of robust or recent studies in UK care home contexts.
Theory area: establish a common understanding of the potential for recovery, reduction and management of faecal incontinence for people with dementia
This theory area posits that nihilism, a belief that nothing can be done for a person with dementia with FI, influences care choices by staff in care homes. It links to the theory areas that advocate the importance of education and person-centred care to influence staff attitudes and behaviours. The example from the Medway community health-care leaflet, ‘A guide for staff in care homes’,179 clearly states that care home staff can make a difference. The wording of the leaflet suggests that the authors believe that nihilistic attitudes persist and that staff education is needed to counter these views.
Incontinence is not the resident’s fault. It is not a normal part of ageing. The resident is not bad or lazy, he or she has a health or mobility problem and you can help.
The leaflet continues:
You are Key – Incontinence can be improved provided residents get the right care. You are an important part of the team that will make treatment or management work.
The theory area is a response to the idea that nihilism persists, and a possible C–M–O configuration shows how it could be considered the mechanism for other theory areas (Table 22).
| Resource | Context | Mechanism | Outcome |
|---|---|---|---|
| Education for staff that incontinence is not an inevitable part of dementia and ageing Person-centred care approaches across the care home |
Use of assessment tools and referral to clinicians Review of residents’ progress |
Belief in the residents’ potential to maintain or improve functional abilities even when the trajectory is one of deterioration | Staff engage and learn about what is causing the FI and attempt interventions to promote continence and the management of FI |
Twenty-two documents from the 62 sources are noted as contributing to this theory area; however, all are also associated with the theory areas around clinician-led assessment and review, ongoing teaching, review and feedback and PCC approaches.
This suggests that what is being identified is a mechanism by which other approaches could be seen to be enacted. For example, a study in Norwegian nursing homes153 found that RNs held mixed views about FI. Some RNs said residents did not care about being faecally incontinent, although others felt that residents experienced shame or anxiety about FI accidents. One RN viewed FI accidents as attention seeking and another RN suggested that agitated, restless or jumpy residents are often that way because they are constipated. Some residents wore pads for safety, whereas others were ashamed to wear pads. Residents were reluctant to talk about bowels with their families, who were also reluctant to discuss this topic. This evidence suggests that FI care would benefit from an intervention addressing nihilist assumptions about the value of assessment and toileting interventions.
The ‘bathing without a battle’ intervention174 included residents with moderate and severe dementia and used a ‘train the trainer’ model, with cascade training and inclusion of new staff. Trainers were RNs or senior certified nursing assistants. Few details are given about the intervention but it appears to describe a person-centred approach, including enhanced communication, respect for resident preferences, a view of distress as the manifestation of unmet need and a belief in the need to maximise comfort. The implicit mechanism is that it works through shared understanding but this is not something that is measured.
Thus, this area is kept as a potential mechanism; although most of the evidence is implicit, either nihilism or lack of shared understanding is a mechanism that blocks the success of interventions or uptake of learning.
Theory area: integral to the everyday work pattern and environment, ‘fit’
Forty of the 62 sources are noted as having some bearing on this theory. The literature on the other programme theories had underlined the need for new approaches to care to fit within existing structures of authority and working practices in the care home (these are not directly measured but rather are the observations by the study authors in the discussion sections).
The evidence supporting this mid-range theory was apparent when we considered the recurring narratives from care home research that have been previously discussed. The accounts reviewed demonstrated that for staff to believe that change was possible, enough time, encouragement and support were required within the workplace. Rovner et al. 180 described the requirement for physicians to complete documentation and to be involved in ongoing discussion with staff as the potential reason that their intervention had been sustained (for 9 months after the end of the study period). It made the intervention a work priority for all the staff, and the ongoing involvement of the clinician endorsed the activity.
Saga76 and Saga et al. 153 noted that the resident’s need for assistance was a trigger or ‘protective’ factor for FI, with staff being more proactive in supporting the achievement of dependent continence:
In addition, patients who needed some help in transfer from bed to chair was a protective factor for FI, indicating that patients who needed this kind of care had a relation to the nursing staff, which in turn released a certain kind of assistance compared to patients who were independent in transfer from bed to chair. The registered nurses in the focus group interview described patients who toileted independently as a challenge for the nursing home staff, due to problems regarding observation and monitoring of bowel function. This indicates that there is a potential for improvement regarding FI care despite the challenging characteristics of this patient group.
p. 90153
As noted, in one of the later multicomponent studies101 on PV, people with cognitive impairment responded particularly well to the intervention. The suggestion is that older PLWD can benefit from toileting assistance and prompting and the presence of a dementia diagnosis should not prevent them being offered this assistance. This also resonates with the perspective of one of the direct care staff who we spoke to, who felt very strongly that everyone has the right (their emphasis) to be taken to the toilet, with the suggestion that there is ‘always time’ to help someone to the toilet. Table 23 shows a potential C–M–O configuration developed from these insights.
| Resource | Context | Mechanism | Outcome |
|---|---|---|---|
| 2-hourly toileting Assistance with getting to the toilet and extra staff to support the intervention |
Dementia is a risk factor for FI PLWD need help to recognise or communicate their need to go to the toilet to defaecate Residents’ dementia/health, limits their mobility |
Staff incorporate a routine of toileting into the residents’ day and their work because they are routinely involved in providing regular physical care Residents learn a routine |
Continent bowel movements Reduction in constipation |
The ability to incorporate an intervention into the work pattern of the care home was important. A study investigating the effects of better urinary and faecal continence on skin integrity46 included exercise as a planned component of the intervention. It was hypothesised that exercise and PV together would reduce the incidence of both UI and FI, thus improving skin health. The intervention improved continence for many of the residents, although the outcomes for skin health were less clear. The authors suggest that following the protocol 7 days a week may make a more measurable improvement to skin health but noted that nursing home staff would have difficulty implementing the intervention for all residents with UI or FI.
At a similar time (1990) as the early Ouslander and Schnelle studies,138,139 another group of researchers, Burgio et al. 161 and Engel et al. ,162 who had been studying behavioural treatments for UI and FI for ‘the past 20 years’ concluded ‘the only two mechanisms by which toileting programs are likely to succeed: one is by increasing the number of trained personnel and the other is by redistributing staff time . . .’. 162 This indicates that this theory area is not new but we suggest has not been previously explored to such depth or acted on.
Two systematic reviews, one on implementing psychosocial interventions in care homes for people with dementia111 and the other on interventions in care homes to reduce inappropriate antipsychotic prescribing for people with dementia,181 draw out some of the theories of why or why not interventions may be working. The staff’s ability to ‘juggle’ competing demands was an important factor or mechanism in whether or not outcomes were achieved:
The overall picture is one in which it would seem that the current guidelines to limit antipsychotic prescribing are difficult to implement in the day-to-day reality of practice, whilst juggling (our emphasis) ethical concerns, staffing levels, staff competence with non-pharmacological alternatives, and the wishes of distressed relatives and carers.
p. 716181
Some of the C–M–O configurations we identified from this and findings from the studies reviewed are given in Table 24. They illustrate that how staff interpret their (invariably) task-based work is framed by the organisation and management support received, the recognition of the skills required and the value placed on these activities. This may be further influenced by family or regulators’ demands and expectations.
| Resource/intervention | Context | Mechanism | Outcome |
|---|---|---|---|
| Opportunity to talk to residents during personal care | Seen by management as time-wasting (within the pressures) | Triggers task-oriented approach to care and less communication with residents | Tasks completed as quickly as possible |
| Opportunity to talk to residents during personal care | Reinforced as invaluable opportunity to interact (within the time pressures) | Time is made available to implement ‘person-centred’ approach to care | Staff to focus on individual needs |
| Training programme (in psychosocial interventions) | Delivered to all staff and family members | A shared understanding about behaviours that challenge | All staff groups and family work together and communicate well about the care of the resident |
| Care home routines | Dominance of regulatory model | Triggers prioritisation of routines | Task-oriented care |
| Training programme (in psychosocial interventions) | Training teams promote the visibility of staff achievements and skills within the training | Status and importance of care assistant’s work recognised among families, managers and commissioners | Staff feel more valued |
| Evaluation of the training programme (in psychosocial interventions) by researchers shows the benefits to resident care | The research is tailored to the working practices of the care home | Managers and commissioners believe in benefits of this approach to care and that it is possible to achieve change | More resources committed to psychosocial interventions |
| Attachments between care staff and residents | Discouraged by management: lack of support | Triggers emotional burnout | Staff sickness/absence/turnover |
| Attachments between care staff and residents | Encouraged by management (plus peer support/cohesive team) | Triggers good relationships and empathy between staff and residents | Easier to implement psychosocial interventions |
The idea that leadership and management support are the contextual factors that trigger change are challenged by Killet et al. 182 in their analysis of care home culture. They contest assumptions that achieving improved care requires a clear leader, robust organisational values or staff who are properly trained. They argue, similarly to Thompson Coon et al. , that it is a fluid process subject to fluctuating demands:
Rather, it is necessary to find ways of resolving the everyday demands of practice in ways that are consistent with espoused values. It is through this everyday practice that assumptions continuously evolve, either consistent with or divergent from, espoused values. . . . For managers and leaders, the implications are that there is a need to be engaged with ongoing problem solving in practice. Managers need to be aware of day-to-day problems and how staff deal with these. They need to help to find solutions that explicitly fit with the espoused values of the organisation.
p. 185182
This evidence then led the research team to consider the way in which continence care is represented in the literature as one of the everyday demands of practice and as part of the provision of intimate and personal care by care home staff. A grounded theory study of the work of nurses and care staff in residential settings144 describes continence care as an activity that is locally produced and, specifically when considering the work of continence care in long-term care settings, as ‘caring against the odds’.
A particularly interesting conceptualisation of this comes from the some of same authors who were considering an abilities approach to morning care. 183 They proposed a mid-range theory of how care workers (personal support workers) practise through ‘figuring it out in the moment’. 184 They used it to explain how unregulated care providers (i.e. frontline care staff) in a Canadian context in dementia care settings practise in the context of ‘unpredictability, variability and personal threat’. They proposed that although there is knowledge and evidence of what the best dementia care practices are, there is an absence of knowledge as to how best to promote these in care homes (Figure 7).
FIGURE 7.
Summary of ‘figuring it out in the moment’ mid-range theory (by Janes et al. 184). The emergent theory of figuring it out in the moment explicates the process by which unregulated care providers make decisions about, and act on, knowledge related to person-centred care and how contextual, individual and relational factors may influence these efforts. C, contextual; I, individual; R, relational.
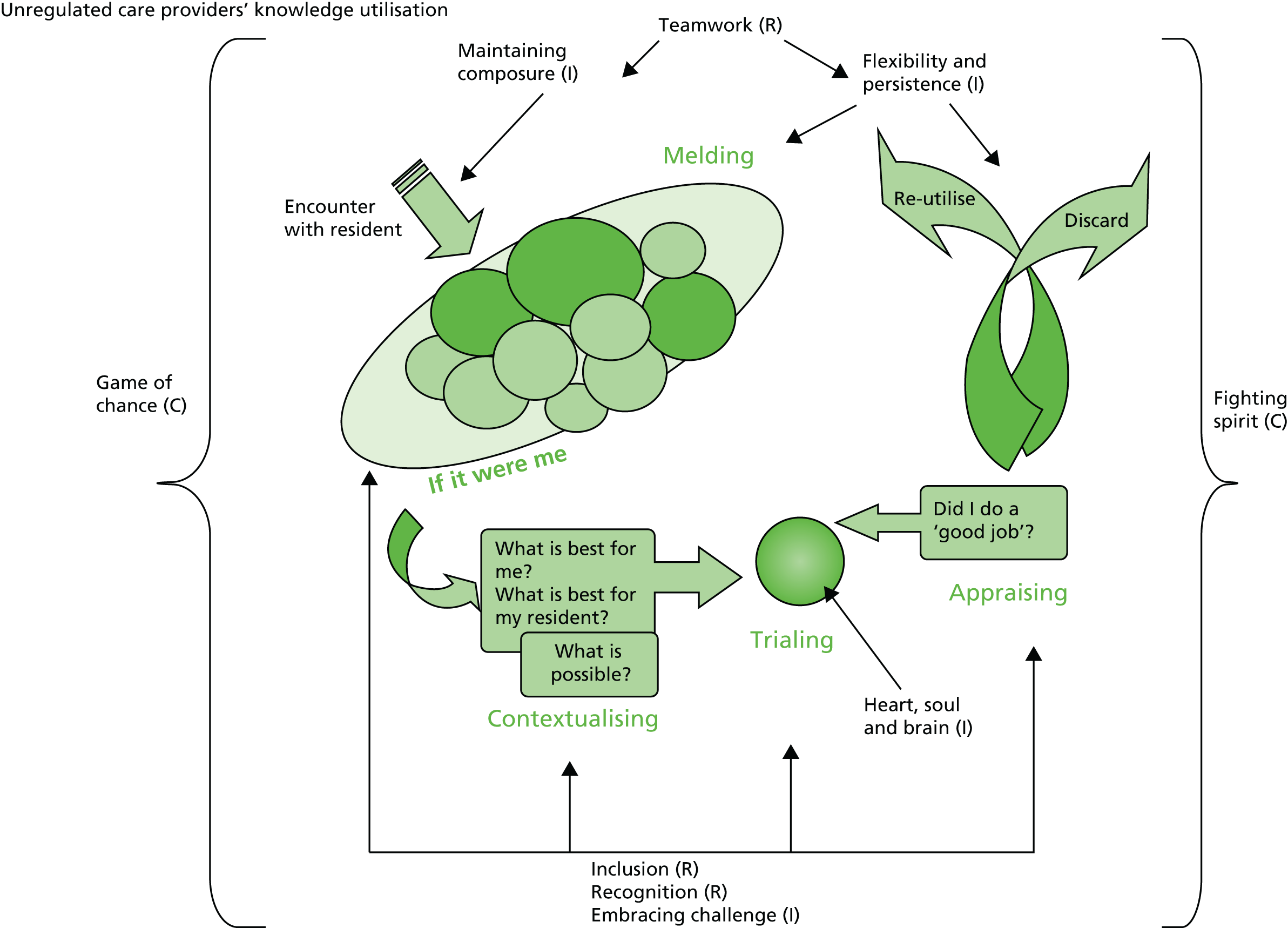
This literature stressed the significance of being able to acknowledge the (changing) difficulties and challenges of an unpredictable work environment. An Australian144 study on continence care in care homes:
. . . revealed broader contextual conditions that influenced the overall context of care, and not just continence care. Specifically, the findings revealed a basic social problem that was characterised by multiple constraints to residents’ day-to-day care, and which caused residential aged care staff to be in a situation in which they were ‘caring against the odds’. ‘Caring against the odds’ was characterised by four major subcategories: (1) working in a highly regulated work environment; (2) encountering ethically challenging situations; (3) working with highly dependent residents; and (4) a devalued role.
p. 5144
It was the idea of the devalued role (a lack of value attributed to continence care and toileting) that led the research team to revisit issues raised in phase 1 regarding the way in which continence care is aligned with the personal care of the resident: work that is invariably the least valued and undertaken by the most junior and least qualified staff in a care home.
Synthesis: continence care as intimate care of people living with dementia
Research that is not specifically about FI or continence but does address the personal care of older PLWD in care homes reframes continence care as an intimate care activity that requires particular skills to avoid causing distress to PLWD. In this research and practice literature, continence care is seen as complex care completed as part of life in a care home and as part of a more embedded relationship between care home staff (as well as residents). 185 However, because of its association with excrement and pollution, this care is often stigmatised.
Twigg186 provided an analysis on how care staff manage the body and bodily fluids in their everyday encounters and considered how they negotiate nakedness and touch, manage dirt and disgust, and balance intimacy and distance. All of which is relevant to how continence care and the reduction and containment of FI are valued and organised within a care home. Twigg argues that the way in which care work as ‘bodywork’ is represented then influences whether or not it is acknowledged by staff and their organisation as work that requires specific skills and is important. The continence research reviewed here focused on management and education and did not discuss bodywork. Twigg characterises this as a ‘zone of silence’ and argues that care workers do not receive help or guidance on such practices. Kelly187 considered bodywork in dementia care at the micro level of care and suggested activities that encourage empathy when care home staff:
. . . see beyond the distasteful nature of their work and the perceived differentness of their patients to working to identify with aspects of their patients’ selfhood that are common to them (whether it be the commonality of having a body, sharing gender, sharing roles of being someone’s son or daughter, the commonality of experiencing pain or fear, or needing to have social contact).
p. 1086
She argued these could transform bodywork from a task that is distasteful to the care worker to one in which respectful care dignifies both the care worker and the care recipient. It is an argument that seeks to apply an understanding of PCC in specific staff–resident encounters.
We considered evidence, therefore, on how care home staff provided intimate personal care for PLWD and the learning this offers about what factors are likely to support improvements in the management and reduction of FI. There was only one source that addressed how to encourage someone with dementia to use a toilet who may not understand what is expected and who may resist staff prompts and encouragement.
Dementia Care: A Practical Photographic Guide185 is a book that describes the practical learning from an Australian study looking at resistance to care in older PLWD who are living in residential aged care facilities. It is written as a practical guide for frontline care staff. The authors give detailed descriptions of behaviours that care workers may encounter in taking someone with dementia to the toilet or changing incontinence pads. They describe reasons for these and appropriate caring measures, with photographic illustrations to communicate and alleviate distress. The book does not specifically address FI but lists factors that contribute to incontinence. Similar to the work by Stokes,136 it places continence care as one aspect of personal and intimate care activities that need to take account not only of cognitive decline but also of reduced mobility and sensory changes.
The range of approaches used to improve FI in PLWD in care homes are elaborated into a programme theory of continence care for this population and setting (Figure 8). The different coloured pathways demonstrate some (but not all) of the different ways that the proposed links between resources/contexts and mechanisms can lead to intermediate outcomes, which can generate a further response or mechanism that supports continence-specific outcomes for residents and staff. Based on the evidence reviewed, it sets out:
-
The resources (white boxes) that need to be in place (resident assessment, knowledge of causes of FI, clinician support, skills in person-centred care applied to continence care). These inform the contexts or ‘backdrop’ conditions that trigger or modify the behaviour of a mechanism, that is, provision of training and support for care home staff in dementia-specific skills for continence care, care home and clinician endorsement that gives staff authority to act of their knowledge (dark-green boxes).
-
The mechanisms (light-green circles) that are the generative force that leads to outcomes. Specifically, these propose the reasoning and responses of care home staff and residents that arise from the interplay of the identified contexts. For example, residents with dementia no longer feeling threatened or distressed by prompted toileting interventions arises from staff having the authority and skills to apply person-centred care approaches to continence care based on a conviction that improvements are possible and this is valuable work.
-
Intermediate outcomes (grey boxes) changed are staff behaviours and organisation of personal care work, increased use of resources (staff time and training) for continence care, staff attitudes and ongoing assessment and review. This in turn provides feedback and a mechanism that is expressed as staff confidence in their skills and prioritising personal care as skilled work, that is, the generative force to achieve and sustain continence-specific changes in residents’ experiences, staff satisfaction and appropriate use of medication and pads.
FIGURE 8.
Programme theory for the reduction and management of FI in PLWD in care homes.

Phase 3: test and refine programme theories (validation)
In the final phase of the review we tested the emergent findings with stakeholders, many of whom had participated in the earlier scoping work. Participants included the SSC members and those with direct experience of commissioning and providing care in care home settings, clinical expertise in continence care for PLWD and researching continence and health care in care homes. We were also able to recruit additional family carers who had supported relatives living with FI through the BBF.
There were also opportunistic conversations about the methods and findings with one US researcher (Ouslander) at the Nursing Home Research International Working Group Meeting December 2015 and other conversations following a presentation on the FINCH realist methodology at the University of Manchester’s Evidence Synthesis Network.
Findings were presented as summary documents, presentations at scheduled professional meetings (the BGS special interest group on 6 November 2015 and the National Care Home Research and Development Forum on 1 December 2015) and scheduled conversations and interviews with care home staff and relatives.
Summary Study Steering Committee (September 2015)
The emergent findings were presented to the SSC. This presentation outlined the six theory areas, the theory areas deemed most promising, the historical perspective of studies in care homes and the parallels in methodology between the US programme of work,45,46,95,98,102,106,188 and the work by Fossey et al. 110,111 and Lawrence et al. 95,96 on antipsychotic prescribing reduction in the UK.
The key points endorsed by the SSC and what should be emphasised in the findings and discussion were:
-
the lack of connection observed between continence research and dementia care, that is, the finding that the continence literature does not investigate dementia and FI beyond considering dementia as a risk factor for FI. Issues are considered in isolation
-
the fact that the work of Stokes136 on toileting problems and person-centred care was useful but needs to be operationalised in terms of the particular challenges that arise around resistance to care and helping someone living with dementia use the toilet and other continence aids
-
the lack of evidence about the extra hours and resource required for toileting interventions and how this informs care home business models
-
that the wider care home research literature confirms that care home working is often organised according to tasks that need to be completed.
British Geriatrics Society Special Interest Group Bladder and Bowel Conference (November 2015)
Participants included geriatricians, urologists and gastroenterologists, specialist continence nurses, continence service managers, medical students and researchers specialising in various aspects of continence and Parkinson’s disease. Twenty participants took part in the discussion that followed the presentation of emergent findings from the FINCH study (see Appendix 9). Particular emphasis was given to the evidence about care, home staff’s understanding of intimate care, especially toileting, and their responsibilities in that respect, the challenges encountered by a person living with dementia when using the toilet or continence aids and the integration of person-centred care with clinician-led continence assessment and review when addressing the secondary causes of FI.
Questions and comments on the findings from delegates fell into three themes, the ‘journey to incontinence’, the location of training and staff involvement in designing and planning training.
-
The journey to incontinence: incontinence, as in a person starting to use pads, often begins during a stay in hospital but research seldom considers this.
-
The location of training: specialist continence nurses know that training for care workers needs to be in-house to minimise the need for agency cover. However, translating this into practice is difficult and involves agreement from trust managers, care home providers, etc. Related to this point is the issue of staff turnover with the consequent loss of expertise.
-
Staff involvement in designing and planning training: there was interest and support for the idea that care home staff could and should be involved in the choice, planning and design of training programmes. This could help to maximise their engagement with continence care and improve the chances of integrating this aspect of care work into everyday practice.
Specific points made that were relevant to the findings, identified gaps or need for future research, were:
-
Nihilism and the normalisation of incontinence and pad use are linked to lack of knowledge of what is achievable, stigma of incontinence for older people and those providing continence care.
-
It is important not to underestimate the importance of access to a continence specialist in maintaining the dignity of older people with continence problems and to give value to this work.
-
The need to expand how FI and continence care were defined for this population was strongly supported. One participant characterised ‘continence care’ as knowing what a person wants and understanding how they understood continence before they lost capacity.
-
One issue that was not raised by the findings was the problem of multiple referral pathways and crossover between nurses in different disciplines who may be covering aspects of the same service provided to the care home.
-
More work is needed to understand who takes responsibility for continence care and how care home staff access that support.
-
Physical health influences how the dementia trajectory is experienced, and maintaining mobility and physical functioning is important for good continence outcomes. Linked to the findings about the need to assess a person living with dementia’s functional abilities to plan continence care are other issues, such as visual acuity, that are not dementia specific.
-
How can medical staff generally improve the relationship between care homes and primary or secondary medical care facilities? Do these findings suggest there is a need to align care home and NHS policies, Care Quality Commission and Quality and Outcomes Framework requirements and the approach strategies of individual clinicians and care home managers?
Account of National Care Home Research Forum feedback session
The FINCH core team presented the emerging findings at the National Care Home Research and Development forum on 1 December 2015. There were 30 participants from across charitable, professional and voluntary organisations (including care providers), the NHS, local authority, police, universities and one carer representative (see Appendix 9). The FINCH presentation was one of four.
The other three presentations focused on:
-
person-centred care and the role of the RN
-
NHS provision to care homes: findings from a NIHR-funded care home study.
-
The introduction of vanguard sites (Department of Health-integrated care initiatives that include six sites that are working with care homes).
Three main discussion areas from the audience were particularly relevant to the FINCH findings: the role of the occupational therapist, predictable conflict in vulnerable adults and the need for time for reflection and sharing in practice.
Occupational therapists: environmental assessment and sense of ‘it’s obvious’
One participant commented that the involvement of occupational therapists could address some of the dementia-specific issues that the review had identified. She commented that occupational therapists ‘just know what to do’ and gave an example of a person who moved into a care home and the occupational therapist suggested moving the bed to match the layout in their home so they could be easily oriented to the bathroom. This raised the question of whether or not this perspective is missing from the review and even from the range of professional input that care homes receive for continence care.
Predictable conflict
One participant from a local mental health trust mentioned that most predictable conflict in care of adults who have dementia or learning disabilities is around personal and intimate care. This view supported our framing of the issue of FI as linked to skills in providing intimate and personal care.
Time for reflection and sharing
A modern matron at the local mental health trust suggested that individualised care requires time for the direct care staff to reflect on and share practice. In response to this another participant suggested that encouraging nurses to write up what they do in practice and what they find is working would be a way of sharing evidence of what works. This supported findings from this review that time for reflection and sharing practice improves care and suggests that case study research could be a potential way forward for understanding FI reduction and management in care homes.
The consensus from the discussion was that the findings resonated with participants’ knowledge and experience.
Individuals with experience of caring for people with dementia and faecal incontinence
The BBF contacted 49 members who care for someone with both FI and dementia, and three responses were received. Interested participants received information about the study and confirmed participation. Two completed a telephone interview and one a combined e-mail exchange and a telephone interview. These participants were eloquent about the experience of FI both from the perspective of the person living with dementia and those caring for them.
Accounts from the carers reinforced the dementia-specific issues identified in the review that can arise relating to FI. These were resistance to using pads or going into unfamiliar toilets, going to the toilet every few minutes, usually without success, and irritability when there is a need to be cleaned or showered. Constipation was recognised as linked to FI and faecal smearing, and one carer commented on the delay in this being recognised by nursing staff. The difficulties of keeping both the person and the environment clean were described by two participants as exhausting and as being not understood by visiting professionals. Attempts to secure help in this process was characterised by one carer as similar to trying to walk ‘through a brick wall’.
Participants highlighted three areas of concern that had been identified in phase 1 but phase 2 had not touched on. These were cross-infection and contamination secondary to FI, how it is possible to know when a person with dementia has no awareness of the need to defaecate and the provision of pads in relation to the severity of the FI. In a situation when there was no sphincter control, one daughter highlighted that the pads provided were ‘inadequate in number and usefulness’.
In relation to the findings on the impact of dementia on how continence care is understood, one woman stated:
I do think that you [the FINCH study] are on the right lines. In my experience, relatives and carers have a role in assist the professionals within a care home. For example, they can spot and report on signs that their relative is developing constipation. My mother’s incontinence has been much better managed in a dementia unit than it was in the community, where, we as relatives were literally left mopping up the shit. We certainly experienced the cruel division of patient care funding between NHS and social care.
Family carer, from an e-mail
Care home managers and care home staff
Two care homes were visited and conversations had with three care home managers and two frontline staff. Discussions focused on the findings about what supported the provision of personal care as part of continence care. One manager stated that maintaining continence was considered important in most units of her care home, with staff assisting residents to the toilet and paying attention to hydration, nutrition and mobility. She stressed, however, that there was a difference between residents in the residential units and those in the nursing units and suggested the review should consider this. In the nursing unit she thought that staff would be less likely to persevere with toileting regimes because these residents were frailer and, she thought, less likely to benefit.
One care home manager had support from a continence specialist nurse and two did not (although one was a home with on-site nursing). One care home (nursing home) manager echoed the finding from phase 1 and restated that the continence service assessment was done ‘mainly to get pads’; this same manager described how they used regular toileting to give people the opportunity to go on the toilet or commode. Although ideally residents would be taken to the toilet when they communicated the need, regular toileting on waking, before meals and before bed was easier to incorporate into routines. Care home staff providing personal care agreed that providing assistance with toileting and changing pads was a large part of their daily work. They did not think that they had met a continence nurse. One described how they recognised the value of trying to learn residents’ preferences and ‘ways of doing things’ to try to make the process as easy as possible for the resident and the staff. This, they acknowledged, was not documented or discussed more widely in the care home.
Summary
The validation phase endorsed the review findings on how understanding of FI has developed over time, factors that influence whether or not someone has FI, and the knowledge that clinicians and care home staff need. Two key emergent findings were seen as important: (1) the need to link continence expertise with expertise in dementia care to provide care that recognises and accommodates the functional abilities of PLWD and (2) that future research and practice should consider the links between personal intimate care activities and continence care in the care home were recognised as having potential and being worth further investigation.
Gaps and issues that were only partially considered and that could benefit from being revisited were cross-infection and contamination secondary to FI, the role of occupational therapists in care homes and the time and resources that providing FI-related care requires. Further work was thought to be needed to help staff to differentiate between residents living with dementia who could benefit from proactive care and those for whom pads were the most appropriate response and for whom assessment frameworks could allocate pads based on residents’ need.
Chapter 4 Discussion
Key points
-
The review has provided a comprehensive account of what approaches contribute to the reduction and management of FI, their underlying theoretical assumptions and the evidence that supports or negates these approaches.
-
Dementia is a risk factor for FI. Residents living with dementia in a care home are more likely to be doubly incontinent than have episodes of only FI.
-
There are gaps in the evidence about both the ways in which having dementia impacts on a person’s ability to engage with and benefit from different continence interventions and the dementia-specific skills that staff may require to provide continence care.
-
Understanding how research on FI in care homes has developed over time demonstrates both the increasing methodological sophistication and complexity of interventions also the limitations of interventions designed without the involvement of care home staff.
-
There is a split in the literature between a clinical approach and functional approach to the reduction and management of FI in care homes, which is artificial in practice and consequently unhelpful. Clinical assessment, knowledge of the causes of FI, including nutrition, hydration constipation and pharmacological, and behavioural therapy are necessary but not sufficient to achieve change.
-
Future continence interventions should consider how the proposed activity fits with the ways in which care home staff and their managers recognise, organise and value the intimate personal care they provide to older PLWD.
The realist review synthesis
The impetus for using a realist approach was the recognition that the current evidence about FI in care homes is mixed, with some good evidence on risk factors and associations but few intervention studies. It is an area of dementia care that, despite the advent of person-centred approaches in long-term care and detailed understanding of contributory factors to FI, is resistant to change. Prevalence rates for double incontinence in people with dementia are similar across Europe and North America. 168 The audiences for this work are those who provide, design, commission and research continence care for PLWD resident in care homes who are seeking to reduce and manage the impact of FI on residents’ quality of care and life, staff working and resource use.
The scoping and the detailed review of 62 papers demonstrated that most of the evidence and linked guidance did not consider how living with dementia impinged on continence-related activities. Dementia is characterised by a gradual but often unpredictable decline in cognition, behaviour and function and around 70% of care home residents in the UK have dementia or significant memory problems. 189 Cognitive function is not confined to memory, it includes language, perception, creativity and social activity190 and the ability to perform activities of daily living, and it deteriorates differently for different activities, with toileting activities often less impaired across the different dementia stages. 191 Documentation of daily functioning has the potential to enable FI-related interventions to be tailored to the person’s retained abilities, needs and preferences. There was no evidence, in the literature reviewed, that studies differentiated between the functional abilities of residents with dementia and how the severity of their dementia or any other comorbid conditions, such as limited visual acuity or arthritis, affected their ability to benefit from particular interventions.
Scores to assess cognitive ability or functional milestones that mark the progression and severity of dementia were used in some studies but the information was not used to interpret the appropriateness of the intervention for people with different abilities and symptoms secondary to living with dementia. The extent to which a person’s ability to locate, recognise and use a toilet, interpret the need to eliminate or recognise and accept continence aids affects the uptake of an intervention was also not documented. The majority of the research that identified dementia as a risk factor for FI required staff to act on a residents’ behalf to achieve continence or containment using regular toileting schemes or reminders. They did not, however, then disaggregate their results by the severity of the dementia and how that affected the person’s ability to engage with or sustain the intervention. This constrained our ability to answer what kind of continence interventions are suitable for what kind of resident living with dementia. The definition of behavioural incontinence from Stokes,136 as the voiding of urine or faeces either following an unsuccessful effort, or with no apparent attempt to employ an acceptable facility (e.g. toilet, commode or urine bottle), expanded our starting definition of leakage of solid or liquid stool which is a social or hygienic problem. 41 It drew attention from the outset to the need to consider continence and how it is linked to a person with dementia’s ability to perform activities of daily living.
There was evidence of improvement and increasing sophistication in the methodological development and refinement of continence research in care homes over time, with much of the research focused on UI rather than FI or even double incontinence. This evolution in complexity of design was mirrored in other studies focused on PLWD in care homes. In the last 20 years interventions have developed from the application of toileting programmes that utilised research staff as the care providers to multicomponent interventions. These involve care home staff in education and training programmes (both in-house and accredited) that are informed by person-centred care approaches, clinician-led review and ongoing facilitation. This shift in approach reflects a growing understanding of what needs to be in place to achieve knowledge transfer and context-specific interventions. 192
Research on continence that was care home specific demonstrated that there was limited value for people with dementia in focusing solely on FI or on one possible cause, for example constipation. 153 The majority of people with FI will also have UI, that is, double incontinence. The minority of residents with FI alone may be a group who are more likely to benefit from interventions that address symptoms of FI as indicative of underlying physical problems or as a consequence of medication mismanagement (e.g. antibiotic prescribing or inappropriate use of laxatives). There is evidence to suggest that there is a subgroup of residents that fit this category. 142 In the scoping and the professional literature reviewed, there were statements that some people with dementia (because of its severity or how it affects sphincter control, or through comorbidities) will not benefit from prompted toileting and interventions that promote bowel health. We were unable to find evidence that could provide guidance on how this could be assessed or how long interventions to promote continence should persist.
We identified six broad theory areas from the phase 1 scoping:
-
clinician-led support and review
-
ongoing teaching and feedback for staff on the assessment and management of FI
-
knowledge about the management of constipation for older people with dementia
-
interventions that reflect degree of cognitive and physical capacity of resident – personalised care planning
-
the need to establish a common understanding of the potential for recovery, reduction and management of FI for people with dementia
-
integration into the everyday work pattern and environment, ‘fit’.
We tested different C–M–O configurations. The programme theory that showed the most promise explained how and why care home staff work to support residents’ continence. In other words, how an intervention fits with the everyday care work of the care home and the ability of staff to incorporate person-centred care practices into the intimate work of toileting and bathing. The concept of ‘fit’ refers to an understanding of what can support or inhibit good practice for PLWD and experiencing FI within the care home environment. It challenges the artificial split in the literature between a clinical approach and a functional approach to the reduction and management of FI in care homes. Clinical assessment, knowledge of the causes of FI, including nutrition, hydration, constipation and pharmacological, and behavioural therapy are necessary but not sufficient. They are all required as a resource for change but the evidence reviewed suggests that this will be acted on only when the activities that arise from this knowledge align with how staff understand their priorities for care and risk and when they have the authority or permission to act on their knowledge.
The value placed on providing intimate and personal care, making the link between person-centred care and intimate and personal care, the management and avoidance of risk and meeting regulatory requirements are all important contextual factors that all have the potential to give staff the impetus (or not) to use their knowledge and skills to reduce and manage FI. Key to the reduction and management of FI in care homes is a reframing of intimate and personal care activities. What was represented as routine tasks becomes recognised as skilled work that supports resident choice, dignity and ultimately a reduction or appropriate management of FI. This could be achieved through feedback to care staff that their knowledge of, and empathy with, the resident has the potential to change outcomes. This needs to be accompanied by senior support from a clinician or facilitator to address problems encountered and input into care planning and care decisions. Evidence that supported this came from the learning disability literature on intimate care, how the culture of care and espoused values are negotiated in care homes175,182 and intervention research to promote person-centred care. 108,193,194 This was reinforced by studies with negative outcomes from research that treated training, education and continence interventions in care homes as discrete activities, developed in isolation from other care home work, or that did not give staff the authority or permission to act on their knowledge. 144,145,148,163,164,176 There was also evidence that perverse incentives that were more concerned about risk both to residents and to the organisation could lead to routinised use of pads and worked against staff reviewing residents’ personal care needs195 and care home staff acting on their knowledge. 196 A recent paper from Canada,197 identified since the searches, reported that health-care workers often rush essential care, such as toileting and talking to the resident, but that staff who work in care home settings that offer opportunities to reflect and discuss best practice appear to be able to give more time to these essential activities.
Education and support of care home staff in person-centred care approaches were key contextual factors that help staff to be ready to engage with residents’ continence needs. To achieve a change in practice, however, it is also important that the problems of providing external clinician support (whether that be GP, continence advisor, district nurse or specialist clinician) within a care home are addressed. Then, clinicians working with key staff members can combine their expertise in continence care with care home staff’s experiential knowledge of the activities of residents who have dementia and preferences around personal care, toileting and continence aids. 109,193 Related evidence from North America on how staff can be supported to address resistance to care offers a way forward for how continence interventions can be developed and trialled. 172 In interviews care home staff suggested that they could differentiate between residents who are more or less likely to benefit from specific continence interventions (such as regular toileting) based on their assessment of their functional abilities, activities residents find distressing or the level of overall frailty. We identified one book185 that provided detailed accounts of how care home staff can help someone with dementia use the toilet (positioning and orienting the person to place and purpose) and one example of local continence guidelines for nurses working in care homes. Stakeholder interviews had also suggested that signage and location of toilets in the care home were important contextual factors in supporting PLWD to reduce and manage FI. We found only one study159 that considered this in any detail and evidence on care home design provided insufficient detail. These gaps in the range and quality of the evidence have implications for what it is possible to say about what interventions or approaches need to include to achieve improvements in the reduction and management of FI for PLWD in care homes.
Future interventions need to include an assessment of if and how the care home context and the intervention approach enables care staff to tailor continence assessment work as part of their everyday practice. The starting point must be that frontline staff know that FI is not an inevitable consequence of ageing or dementia and that they have enough authority or permission (through either peer support or role) to implement what they have been taught is best practice in the delivery of personal care. This also requires that staff have the capacity and skills to address and meaningfully reduce the impact of behaviours that are associated with dementia (e.g. resistance to care). The evidence reviewed (that was continence specific and those studies that addressed wider issues of care for people with dementia in care homes), it was interventions that validated personal care work. Engaging with how and why staff deliver care, the care home-specific problems encountered, and encouraging staff to engage with the experience of being a resident in a care home, have the potential to encourage staff empathy with the resident. A recent report on the implementation into care homes of research findings on reducing antipsychotic prescribing107 used dementia care coaches to teach a 9-month education and supervision programme for care home staff. According to the report, it was possible to increase staff knowledge, but implementation of the programme and improvement of resident outcomes were contingent on other contextual factors, such as staff having sufficient time, role clarity and ongoing management support. 198 A 2010 Health Technology Assessment systematic review199 of the links between human resource management practices and performance are identified some potentially effective practices for both health and non-health areas: practices that enhance employee autonomy and control, involve employees in the design and implementation of changes and recognising the importance of feedback. These resonate strongly with the findings from this synthesis.
Strengths and limitations of the review
This realist synthesis provides a comprehensive account of how research in this field has changed over time and what influences, supports and inhibits practices that promote the uptake of clinical guidance and the reduction and management of FI in PLWD in care homes. It also challenges certain assumptions about effective continence care and the unintended consequences of some interventions, such as an overemphasis on the management of constipation. This provides a robust platform for future research.
The realist approach enabled us to consider activities to reduce and manage FI as social interventions within a complex system of care that are reliant on a number of factors to achieve implementation. By drawing on a range of sources that offered transferable learning about what supports effective working with people who have limited cognitive understanding, it provides a theory-driven understanding of the conditions influencing how care home staff understand continence care and the conditions under which improvement is likely to be successful.
Included papers ranged from summary accounts of how change was achieved in care home settings to those that applied careful analysis and provided detailed presentation of findings. Papers were not excluded based on study design or level of detail/evidence provided; however, we were constrained by the limited amount of UK-based evidence. There were few resources to draw on that meant we could test links between a resident’s previous experience of FI, particularly in a hospital, prior to admission to a care home or about the impact of FI on unplanned hospital admissions. There were, however, key source papers and programmes of work,45,76,94,97,99–101,103,104,106,108–111,144,149,153,193,196,200–207 whose accounts of original research provided sufficient detail about what had and had not worked. These became the reference points for the testing and refinement of our theories. There were some novel interventions that offered a potential way forward, for example transcutaneous posterior tibial nerve stimulation,155,156,165,208 but the studies were small, provided insufficient detail or excluded people with dementia. The lack of an explicit articulation of theory or discussion of the theoretical underpinnings in much of the evidence reviewed is, however, a limitation and may mean that our interpretation of how and why certain interventions were developed is open to challenges of bias. To mitigate this possibility, we have at every point provided a detailed and transparent account of how and why we reviewed the evidence and the judgements made in order to test the programme theories and answer the review questions. The feedback and discussion of findings with our stakeholders also provided the opportunity for challenge.
The evidence on how the care home context at individual-service and funding levels affect residents’ outcomes is rapidly changing and we were able to address this only in part. The use of context assessment tools209 offers the opportunity to provide a more fine-grained account of what resources (e.g. location of management and internal hierarchies in the care home) need to be in place for continence interventions to be implemented. The ambition of the synthesis and testing of six theory areas meant that it was not possible within the resources of the review to pursue this in any depth.
Discussion of the findings with family carers highlighted that the review had not addressed the amount of time and resources given to cleaning up after episodes of FI, how emotionally and physically draining this work was or concerns about cross-infection arising from, for example, smearing and parcelling of faeces. It is a limitation that we were not able to involve family carers and residents living with FI and dementia in the discussions of the findings.
Writing on societal responses to excreta, the associated stigma and fears of contamination and cross-infection210,211 were recognised in the scoping work. The evidence included in the synthesis acknowledged this inasmuch it recognised the low priority placed on personal and continence care. It may be that more detailed accounts of dealing with risks of cross-infection or countering reactions of disgust and fear of contamination are based on textbooks, as exemplified by the one book that was included. 185 This text gave very specific guidance on toileting when supporting PLWD.
It is a further limitation that this review was not able to address how the use of continence aids could ameliorate the impact of FI or the relative costs of different approaches. We were also unable to provide any commentary based on the evidence reviewed on how the presence or absence of nursing staff in the care home or access to particular clinicians will have an impact on FI-related outcomes. Others have argued that, to protect and promote high standards of individual person-centred care and ensure quality, it may be important to rediscover ‘embodied practice’ as a core activity of nursing care. Meeting essential needs relating to hydration, skin care and toileting constitute ‘embodied practice’ and the basis of promoting and maintaining continence in care home residents. 212 This could be a fruitful area for future work, but our inability to substantiate this belief is indicative, we believe, of the lack of research in care homes on both how the qualifications, experiences and skills of the workforce influence resident outcomes and the detail (rather than the organisation) of how care is provided to PLWD. 141
Chapter 5 Conclusion
Continence care is personal and intimate care. The programme theory developed from this synthesis articulates why interventions to reduce FI in older people with dementia resident in care homes have had limited impact. It recognises continence care as part of the everyday work of the care home and articulates the need to incorporate principles of person-centred care with the specifics of taking someone to the toilet or washing them. Only when the education, training, facilitation and positive feedback that care staff receive lead to staff valuing their personal care work with PLWD, and having the skills to tailor practice accordingly, will continence care improve. We argue that these contexts can combine to create a conviction in staff that they are ‘doing the right thing’ in persevering with regular toileting and an ongoing assessment and review of what is likely to support the reduction and management of FI.
This realist synthesis has provided an account of significant gaps in evidence. Very little is known about how a person’s functional abilities or the behavioural symptoms of dementia affect outcomes from strategies to prevent or reduce FI. Neither is there any discussion or acknowledgement in the empirical literature that there are practical dementia-specific skills that staff need in order to support continence care for PLWD. Future work should take account of how having dementia affects a resident’s ability to benefit from different interventions and work with care home staff to find ways that continence care as an aspect of personal care can be prioritised and valued.
Implications for practice
There is a need to reframe continence care as integral to intimate and personal care work for older people with dementia.
-
Personal and intimate care requires a set of skills that can ensure care is personalised and responsive to the resident’s preferences and needs. These need to be formalised in job descriptions, taught to those who give this care (junior/inexperienced staff) and valued and supported by senior staff.
-
Staff also need to have dementia care skills so that they can assess and address how a person’s dementia affects, in particular, their ability to be continent, communicate their need for the toilet, and recognise and remember how to use a toilet, and so that residents’ distress is minimised when they receive intimate care.
-
We do not currently know enough about how dementia affects FI outcomes and that makes it difficult to identify strategies that will improve incontinence. However, we do know that some simple strategies are likely to work and these include:
-
– practical training on how to support a person with dementia to continue to use the toilet
-
– implementation of prompted toileting (when appropriate)
-
– appropriate diet, fluid intake and increased mobility – taking into account personal preferences and the support of activities in the home.
-
-
The normalisation of the use of pads needs to be acknowledged as an undesirable method used to manage the competing demands of care home staff and this practice is likely to reflect a lack of skills.
-
Visiting clinicians have a role in valuing the personal and intimate care work of unqualified and junior staff and providing ongoing support and reinforcement of good practice and education.
-
Care home staff across different disciplines and grades need to have the opportunity to reflect on practice and learn from each other about how to promote continence. When reflective practice is already part of care home practice, continence, FI, intimate and personal care, and dementia care should be explicitly linked.
-
Planning for care-home-based interventions to improve continence needs to explicitly address residents’ functional limitations (both physical and cognitive) and how these will be addressed with the available staffing and resources.
-
There is good evidence that appropriate diet, fluid intake and increased mobility help as part of improving FI. How these are introduced should incorporate both the preferences of the person with dementia and consideration of how the activities and routines of the care home support this.
-
An overemphasis on constipation as a major cause of FI can have the unintended consequence of staff focusing solely on the assessment and management of constipation at the expense of person-centred approaches that take account of the person’s dementia and personal history.
Research recommendations
Any future technology assessment should address or incorporate the following:
-
research on how care home staff understand continence care, the particular challenges they encounter and skills they need when providing care to people with dementia and UI and FI
-
interventions that test person-centred approaches to address resistance to care when providing intimate care and activities, such as prompted toileting
-
the ways in which a person’s dementia, pre-care-home history and ability to perform activities of daily living affect the uptake and implementation of interventions designed to reduce and manage double incontinence or FI
-
interventions on environmental design and adaptation and therapy-led intervention that support people with dementia to maintain abilities to achieve independent and dependent continence
-
interventions to reduce and manage double incontinence or FI that consider approaches that support co-design between clinicians and care home staff of continence interventions paying specific attention to how the intervention can be incorporated into the workflow and priorities of the care home and address how intimate and personal care is represented as continence care work
-
the role of constipation or impaction in the aetiology of FI and the relative efficacy of constipation-specific interventions over time
-
the costs of providing continence care in care homes, particularly staffing resources used. Even if full economic assessment is not carried out, detail about staff skill-mix, time and resources should be included in all studies.
Acknowledgements
The team would like thank all the practitioners and family members of people who contributed to this study: Geraint Collingridge at the BGS Continence special interest group, Robert Dixon of the BBF, Helene Stewart of the Healthcare Management Trust, Kevin Hall of the Order of St John Care Trust and Quantum Care for supporting access to relevant stakeholders.
Lindsey Parker is thanked for her administrative support throughout the project.
Contributions of authors
Claire Goodman (Professor in Health Care Research, Principal Investigator) led the design of the project, oversaw the project, conducted some data extraction, contributed sections of the report and led the writing of the final draft.
Christine Norton (Florence Nightingale Foundation, Chairperson in Clinical Nursing Practice Research) contributed to project design, provided expertise on the management of FI, conducted some data extraction, participated in project workshops and contributed to revised drafts of the report.
Marina Buswell (Research Fellow) led the realist synthesis, reviewer, data extraction, co-ordinated the writing of the report, wrote and revised sections and commented on the final draft.
Bridget Russell (Research Assistant) co-ordinated day-to-day running of the project, reviewed all papers with Marina Buswell, performed data extraction, wrote and revised sections of the report, contributed to revisions and commented on the final report.
Danielle Harari (Consultant Physician in Geriatric Medicine) contributed to project design, provided expertise on continence management in care homes, undertook some data extraction, participated in project workshops and commented on final report drafts.
Rowan Harwood (Professor of Geriatric Medicine) contributed to project design, provided expertise on the ethical and clinical challenges of providing care for frail older people, completed some data extraction, participated in project workshops and commented on drafts of the final report.
Brenda Roe (Professor of Health Research) contributed to project design, provided methodological and public and patient involvement expertise, completed some data extraction, participated in project workshops and commented on drafts of the final report.
Jo Rycroft-Malone (Pro-Vice Chancellor Research and Impact) contributed to project design and use of realist methodology, participated in project workshops and commented on drafts of the final report.
Vari M Drennan (Professor of Health Care and Policy Research) contributed to project design, advised on dementia and continence research, conducted some data extraction, participated in project workshops and commented on revised drafts of the report.
Mandy Fader (Professor of Continence Technology) contributed to project design, completed data extraction, wrote the review of the literature on the use of continence aids and commented on revised drafts of the report.
Michelle Maden (Independent Clinical Information Specialist) led database searches for phase two of the synthesis and commented on a final draft of the report.
Karen Cummings (Care Home Manager) advised on continence management in care homes, advised on stakeholder interviews and scoping, and commented on emergent findings and implications for practice.
Frances Bunn (Reader in Evidence Based Health Care) contributed to project design, led search strategies and the scoping phases of the project, completed some data extraction and commented on the final draft of the report.
The final report and any errors remain the responsibility of the University of Hertfordshire. Professor Claire Goodman is guarantor.
Data sharing statement
Requests for access to data should be addressed to Professor Claire Goodman.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- The Adult Social Care Market and the Quality of Services. Newcastle upon Tyne: Care Quality Commission; 2010.
- A Vision for Care Fit for the Twenty-First Century. London: Demos; 2014.
- Care of Elderly People Market Survey 2012/13. London: Laing and Buisson; 2013.
- Glendinning C, Jacobs S, Alborz A, Hann M. A survey of access to medical services in nursing and residential homes in England. Br J Gen Pract 2002;52:545-8.
- Davies SL, Goodman C, Bunn F, Victor C, Dickinson A, Iliffe S, et al. A systematic review of integrated working between care homes and health care services. BMC Health Serv Res 2011;11. http://dx.doi.org/10.1186/1472-6963-11-320.
- Quest for Quality: A Joint Working Party Inquiry into the Quality of Healthcare Support for Older People in Care Homes. London: BGS; 2011.
- Gordon AL, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman JR. Health status of UK care home residents: a cohort study. Age Ageing 2014;43:97-103. http://dx.doi.org/10.1093/ageing/aft077.
- Humphries R. Paying for Social Care: Beyond Dilnot. London: The King’s Fund; 2013.
- Iliffe S, Davies SL, Gordon AL, Schneider J, Dening T, Bowman C, et al. Provision of NHS generalist and specialist services to care homes in England: review of surveys. Prim Health Care Res Dev 2016;17:122-37. https://doi.org/10.1017/S1463423615000250.
- Dementia 2014 Report Statistics. London: Alzheimer’s Society; 2014.
- Reisberg B, Wegiel J, Franssen E, Kadiyala S, Auer S, Souren L, et al. Severe Dementia. Chichester: Wiley; 2006.
- Norton C, Whitehead WE, Bliss DZ, Harari D, Lang J. Conservative Management of Fecal Incontinence in Adults Committee of the International Consultation on Incontinence. Management of fecal incontinence in adults. Neurourol Urodyn 2010;29:199-206. http://dx.doi.org/10.1002/nau.20803.
- Harari D, Fillit HM, Rockwood K, Woodhouse K. Brocklehurst’s Textbook of Geriatric Medicine. Philadelphia, PA: Saunders Elsevier; 2014.
- Harari D. Faecal incontinence in older people. Rev Clin Gerontol 2009;19. https://doi.org/10.1017/S0959259809990153.
- Chassagne P, Landrin I, Neveu C, Czernichow P, Bouaniche M, Doucet J, et al. Fecal incontinence in the institutionalized elderly: incidence, risk factors, and prognosis. Am J Med 1999;106:185-90. https://doi.org/10.1016/S0002-9343(98)00407-0.
- Nakanishi N, Tatara K, Naramura H, Fujiwara H, Takashima Y, Fukuda H. Urinary and fecal incontinence in a community-residing older population in Japan. J Am Geriatr Soc 1997;45:215-19. https://doi.org/10.1111/j.1532-5415.1997.tb04511.x.
- Johanson JF, Irizarry F, Doughty A. Risk factors for fecal incontinence in a nursing home population. J Clin Gastroenterol 1997;24:156-60. https://doi.org/10.1097/00004836-199704000-00007.
- Grant RL, Drennan VM, Rait G, Petersen I, Iliffe S. First diagnosis and management of incontinence in older people with and without dementia in primary care: a cohort study using The Health Improvement Network primary care database. PLOS Med 2013;10. https://doi.org/10.1371/journal.pmed.1001505.
- Borrie MJ, Davidson HA. Incontinence in institutions: costs and contributing factors. CMAJ 1992;147:322-8.
- Nelson R, Furner S, Jesudason V. Fecal incontinence in Wisconsin nursing homes: prevalence and associations. Dis Colon Rectum 1998;41:1226-9. https://doi.org/10.1007/BF02258218.
- Brocklehurst JC, Brocklehurst J. Promoting Continence: Clinical Audit Scheme for the Management of Urinary and Faecal Incontinence. London: Royal College of Physicians of London, Research Unit; 1998.
- Harrington C, Carrillo H, Garfield R. Nursing Facilities, Staffing, Residents and Facility Deficiencies, 2005 through 2010. San Francisco, CA: University of California; 2011.
- Rodriguez NA, Sackley CM, Badger FJ. Exploring the facets of continence care: a continence survey of care homes for older people in Birmingham. J Clin Nurs 2007;16:954-62. https://doi.org/10.1111/j.1365-2702.2006.01759.x.
- Flanagan L, Roe B, Jack B, Barrett J, Chung A, Shaw C, et al. Systematic review of care intervention studies for the management of incontinence and promotion of continence in older people in care homes with urinary incontinence as the primary focus (1966–2010). Geriatr Gerontol Int 2012;12:600-11. https://doi.org/10.1111/j.1447-0594.2012.00875.x.
- Flanagan L, Roe B, Jack B, Shaw C, Williams KS, Chung A, et al. Factors with the management of incontinence and promotion of continence in older people in care homes. J Adv Nurs 2014;70:476-96. http://dx.doi.org/10.1111/jan.12220.
- Roe B, Flanagan L, Jack B, Barrett J, Chung A, Shaw C, et al. Systematic review of the management of incontinence and promotion of continence in older people in care homes: descriptive studies with urinary incontinence as primary focus. J Adv Nurs 2011;67:228-50. http://dx.doi.org/10.1111/j.1365-2648.2010.05481.x.
- Roe B, Flanagan L, Jack B, Shaw C, Williams K, Chung A, et al. Systematic review of descriptive studies that investigated associated factors with the management of incontinence in older people in care homes. Int J Older People Nurs 2013;8:29-4. http://dx.doi.org/10.1111/j.1748-3743.2011.00300.x.
- Coggrave M, Norton C, Cody JD. Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database Syst Rev 2014;1. https://doi.org/10.1002/14651858.cd002115.pub5.
- Maeda Y, Laurberg S, Norton C. Perianal injectable bulking agents as treatment for faecal incontinence in adults. Cochrane Database Syst Rev 2010;5. https://doi.org/10.1002/14651858.cd007959.pub2.
- Norton C, Cody JD. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults (Review). Cochrane Database Syst Rev 2012;7. https://doi.org/10.1002/14651858.cd002111.pub3.
- Morley JE, Steinberg KE. Diarrhea in long-term care: a messy problem. J Am Med Dir Assoc 2009;10:213-17. http://dx.doi.org/10.1016/j.jamda.2009.01.007.
- Gray M, Beeckman D, Bliss DZ, Fader M, Logan S, Junkin J, et al. Incontinence-associated dermatitis: a comprehensive review and update. J Wound Ostomy Continence Nurs 2012;39:61-74. http://dx.doi.org/10.1097/WON.0b013e31823fe246.
- Faecal Incontinence: The Management of Faecal Incontinence in Adults – Methods, Evidence and Guidance. London: National Collaborating Centre for Acute Care; 2007.
- Markland AD, Goode PS, Burgio KL, Redden DT, Richter HE, Sawyer P, et al. Incidence and risk factors for fecal incontinence in black and white older adults: a population-based study. J Am Geriatr Soc 2010;58:1341-6. http://dx.doi.org/10.1111/j.1532-5415.2010.02908.x.
- Perry S, Shaw C, McGrother C, Matthews RJ, Assassa RP, Dallosso H, et al. Prevalence of faecal incontinence in adults aged 40 years or more living in the community. Gut 2002;50:480-4. https://doi.org/10.1136/gut.50.4.480.
- Bharucha AE, Zinsmeister AR, Locke GR, Seide BM, McKeon K, Schleck CD, et al. Risk factors for fecal incontinence: a population-based study in women. Am J Gastroenterol 2006;101:1305-12. https://doi.org/10.1111/j.1572-0241.2006.00553.x.
- Bharucha AE, Zinsmeister AR, Locke GR, Seide BM, McKeon K, Schleck CD, et al. Prevalence and burden of fecal incontinence: a population-based study in women. Gastroenterology 2005;129:42-9. https://doi.org/10.1053/j.gastro.2005.04.006.
- Drennan VM, Cole L, Iliffe S. A taboo within a stigma? A qualitative study of managing incontinence with people with dementia living at home. BMC Geriatr 2011;11. http://dx.doi.org/10.1186/1471-2318-11-75.
- Hussein S, Manthorpe J. Structural marginalisation among the long-term care workforce in England: evidence from mixed-effect models of national pay data. Aging Soc 2014;34:21-4. https://doi.org/10.1017/S0144686X12000785.
- Rycroft-Malone J. Evidence-informed practice: from individual to context. J Nurs Manag 2008;16:404-8. http://dx.doi.org/10.1111/j.1365-2834.2008.00859.x.
- Norton C, Whitehead W, Abrams, Cardozo L, Khoury S, Wein A. Incontinence. Paris: Health Publication Ltd; 2009.
- Chassagne P, Jego A, Gloc P, Capet C, Trivalle C, Doucet J, et al. Does treatment of constipation improve faecal incontinence in institutionalized elderly patients?. Age Ageing 2000;29:159-64. https://doi.org/10.1093/ageing/29.2.159.
- Goodman C, Davies S, Norton C, Leyshon S, Gage H, Fader M. Can Clinical Benchmarking Improve Bowel Care in Care Homes for Older People 2007.
- Tal S, Gurevich A, Guller V, Gurevich I, Berger D, Levi S. Risk factors for recurrence of Clostridium difficile-associated diarrhea in the elderly. Scand J Infect Dis 2002;34:594-7. https://doi.org/10.1080/00365540210147525.
- Ouslander JG, Simmons S, Schnelle J, Uman G, Fingold S. Effects of prompted voiding on fecal continence among nursing home residents. J Am Geriatr Soc 1996;44:424-8. https://doi.org/10.1111/j.1532-5415.1996.tb06415.x.
- Bates-Jensen BM, Alessi CA, Al-Samarrai NR, Schnelle JF. The effects of an exercise and incontinence intervention on skin health outcomes in nursing home residents. J Am Geriatr Soc 2003;51:348-55. https://doi.org/10.1046/j.1532-5415.2003.51108.x.
- Harari D, Husk J, Lowe D, Lourtie J. National Audit of Continence Care (NACC): Pilot Audit Evaluation Report. London: Royal College of Physicians; 2012.
- Drennan VM, Norrie C, Cole L, Donovan S. Addressing incontinence for people with dementia living at home: a documentary analysis of local English community nursing service continence policies and clinical guidance. J Clin Nurs 2013;22:339-46. https://doi.org/10.1111/j.1365-2702.2012.04125.x.
- Froggatt K, Davies S, Meyer J. Understanding Care Homes: A Research and Development Perspective. London: Jessica Kingsley Publishers; 2009.
- Kenkmann A, Price GM, Bolton J, Hooper L. Health, wellbeing and nutritional status of older people living in UK care homes: an exploratory evaluation of changes in food and drink provision. BMC Geriatr 2010;10. http://dx.doi.org/10.1186/1471-2318-10-28.
- Abbott RA, Whear R, Thompson-Coon J, Ukoumunne OC, Rogers M, Bethel A, et al. Effectiveness of mealtime interventions on nutritional outcomes for the elderly living in residential care: a systematic review and meta-analysis. Ageing Res Rev 2013;12:967-81. http://dx.doi.org/10.1016/j.arr.2013.06.002.
- Alldred DP, Barber N, Buckle P, Carpenter J, Dean-Franklin B, Dickinson R, et al. Care Home Use of Medicines Study (CHUMS). Medication Errors in Nursing and Residential Care Homes: Prevalence, Consequences, Causes and Solutions 2009:1-309.
- Parsons C, Johnston S, Mathie E, Baron N, Machen I, Amador S, et al. Potentially inappropriate prescribing in older people with dementia in care homes: a retrospective analysis. Drugs Aging 2012;29:143-55. http://dx.doi.org/10.2165/11598560-000000000-00000.
- Sackley C, Wade DT, Mant D, Atkinson JC, Yudkin P, Cardoso K, et al. Cluster randomized pilot controlled trial of an occupational therapy intervention for residents with stroke in UK care homes. Stroke 2006;37:2336-41. https://doi.org/10.1161/01.STR.0000237124.20596.92.
- Sackley CM, van den Berg ME, Lett K, Patel S, Hollands K, Wright C, et al. Effects of a physiotherapy and occupational therapy intervention on mobility and activity in care home residents: a cluster randomised controlled trial. BMJ 2009;339. https://doi.org/10.1136/bmj.b3123.
- Underwood M, Lamb SE, Eldridge S, Sheehan B, Slowther A, Spencer A, et al. Exercise for depression in care home residents: a randomised controlled trial with cost-effectiveness analysis (OPERA). Lancet 2013;381. http://dx.doi.org/10.3310/hta17180.
- Goodman C, Davies SL, Gordon AL, Meyer J, Dening T, Gladman JR, et al. Relationships, expertise, incentives, and governance: supporting care home residents’ access to health care. An interview study from England. J Am Med Dir Assoc 2015;16:427-32. http://dx.doi.org/10.1016/j.jamda.2015.01.072.
- Goodman C, Davies SL, Dickinson A, Gage H, Froggatt K, Morbey H, et al. A Study to Develop Integrated Working between Primary Health Care Services and Care Homes. Southampton: NIHR; 2013.
- Tolson D, Morley JE, Rolland Y, Vellas B. Advancing nursing home practice: the International Association of Geriatrics and Gerontology Recommendations. Geriatr Nurs 2011;32:195-7. http://dx.doi.org/10.1016/j.gerinurse.2011.03.001.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. J Adv Nurs 2013;69:1005-22. http://dx.doi.org/10.1111/jan.12095.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-21.
- Pawson R. Evidence-Based Policy: A Realist Perspective 2006. https://doi.org/10.4135/9781849209120.
- Pawson R, Greenhalgh J, Brennan C, Glidewell E. Do reviews of healthcare interventions teach us how to improve healthcare systems?. Soc Sci Med 2014;114:129-37. http://dx.doi.org/10.1016/j.socscimed.2014.05.032.
- Shepperd S, Lewin S, Straus S, Clarke M, Eccles MP, Fitzpatrick R, et al. Can we systematically review studies that evaluate complex interventions?. PLOS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000086.
- Goodman C, Dening T, Gordon AL, Davies SL, Meyer J, Martin FC, et al. Effective health care for older people living and dying in care homes: a realist review. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1493-4.
- Pearson C, Hunt H, Cooper C, Sheppard S, Pawson R, Anderson R. Intermediate Care: A Realist Review and Conceptual Framework. London: National Institute for Health Research; 2013.
- Pearson M, Hunt H, Cooper C, Shepperd S, Pawson R, Anderson R. Providing effective and preferred care closer to home: a realist review of intermediate care. Health Soc Care Community 2015;23:577-93. http://dx.doi.org/10.1111/hsc.12183.
- Tobin GW, Brocklehurst JC. Faecal incontinence in residential homes for the elderly: prevalence, aetiology and management. Age Ageing 1986;15:41-6. https://doi.org/10.1093/ageing/15.1.41.
- Gordon AL, Logan PA, Jones RG, Forrester-Paton C, Mamo JP, Gladman JR. Medical Crises in Older People Study Group . A systematic mapping review of randomized controlled trials (RCTs) in care homes. BMC Geriatr 2012;12. http://dx.doi.org/10.1186/1471-2318-12-31.
- Kitwood T. The dialectics of dementia: with particular reference to Alzheimer’s disease. Aging Soc 1990;10:177-96. https://doi.org/10.1017/S0144686X00008060.
- National Health Service and Community Care Act. London: The Stationery Office; 1990.
- Andrews GJ, Phillips DR. Changing local geographies of private residential care for older people 1983–1999: lessons for social policy in England and Wales. Soc Sci Med 2002;55:63-78. https://doi.org/10.1016/S0277-9536(01)00207-6.
- Bunn F, Goodman C, Sworn K, Rait G, Brayne C, Robinson L, et al. Psychosocial factors that shape patient and carer experiences of dementia diagnosis and treatment: a systematic review of qualitative studies. PLOS Med 2012;9. https://doi.org/10.1371/journal.pmed.1001331.
- Trivedi D, Goodman C, Gage H, Baron N, Scheibl F, Iliffe S, et al. The effectiveness of inter-professional working for older people living in the community: a systematic review. Health Soc Care Community 2013;21:113-28. http://dx.doi.org/10.1111/j.1365-2524.2012.01067.x.
- Dixon-Woods M, Cavers D, Agarwai S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6. https://doi.org/10.1186/1471-2288-6-35.
- Saga S. Understanding Faecal Incontinence in Nursing Home Patients: Epidemiology and Nurses’ Management 2014.
- Yen IH, Fandel Flood J, Thompson H, Anderson LA, Wong G. How design of places promotes or inhibits mobility of older adults: realist synthesis of 20 years of research. J Aging Health 2014;26:1340-72. http://dx.doi.org/10.1177/0898264314527610.
- Wald A. Faecal incontinence in the elderly: epidemiology and management. Drugs Aging 2005;22:131-9. https://doi.org/10.2165/00002512-200522020-00004.
- Rockville MD, Fonda D, DuBeau CE, Harari D, Oulsander JG, Palmer M, et al. Incontinence. Monaco: Health Publication Ltd; 2005.
- Norton C, Thomas L, Hill J. Management of faecal incontinence in adults: summary of NICE guidance. BMJ 2007;334:1370-1. https://doi.org/10.1136/bmj.39231.633275.AD.
- Dementia Quality Standard. Manchester: NICE; 2010.
- Laing JT. Diagnosis and mangement of fecal incontinence in the eldery. Incont Pelvic Floor Dysfunct 2009;3:65-8.
- Lykkeslet E, Gjengedal E, Skrondal T, Storjord MB. Sensory stimulation – a way of creating mutual relations in dementia care. Int J Qual Stud Health Well-Being 2014;9. https://doi.org/10.3402/qhw.v9.23888.
- Harari D, Husk J, Lowe D, Wagg A. National audit of continence care: adherence to National Institute for Health and Clinical Excellence (NICE) guidance in older versus younger adults with faecal incontinence. Age Ageing 2014;43:785-93. https://doi.org/10.1093/ageing/afu056.
- Edwards C, Dolman M, Horton N, Getliffe K, Dolman M. Promoting Continence: A Clinical Research Resource. Edinburgh: Balliere Tindall; 2003.
- Bravo CV. Urinary and faecal incontinence and dementia. Reviews Clin Gerontol 2004;14:129-36. https://doi.org/10.1017/S0959259804001388.
- Akhtar AJ, Padda M. Fecal incontinence in older patients. J Am Med Dir Assoc 2005;6:54-60. https://doi.org/10.1016/j.jamda.2004.12.012.
- Bellicini N, Molloy PJ, Caushaj P, Kozlowski P. Fecal incontinence: a review. Dig Dis Sci 2008;53:41-6. https://doi.org/10.1007/s10620-007-9819-z.
- Rao SS, Go JT. Update on the management of constipation in the elderly: new treatment options. Clin Interv Aging 2010;5:163-71. https://doi.org/10.2147/CIA.S8100.
- Shah BJ, Chokhavatia S, Rose S. Fecal incontinence in the elderly: FAQ. Am J Gastroenterol 2012;107:1635-46. https://doi.org/10.1038/ajg.2012.284.
- Faecal Incontinence: NICE Quality Standard 54. Manchester: NICE; 2014.
- Managing Faecal Incontinence in Specific Groups. Manchester: NICE; 2014.
- Ouslander JG, AI-Samarrai N, Schnelle JF. Prompted voiding for night time incontinence in nursing homes: is it effective?. J Am Geriatr Soc 2001;49:706-9. https://doi.org/10.1046/j.1532-5415.2001.49145.x.
- Ouslander JG, Griffiths PC, McConnell E, Riolo L, Kutner M, Schnelle J. Functional incidental training: a randomized, controlled, crossover trial in Veterans Affairs nursing homes. J Am Geriatr Soc 2005;53:1091-100. https://doi.org/10.1111/j.1532-5415.2005.53359.x.
- Leung AW, Karyotakis NC, Rahman HU, Marshall CE, Brazier JM, Rosenthal MJ. Fecal incontinence in a nursing home and an ambulatory population. Gastroenterology 1998;114. https://doi.org/10.1016/s0016-5085(98)83218-6.
- Leung FW, Schnelle JF. Urinary and fecal incontinence in nursing home residents. Gastroenterol Clin North Am 2008;37:697-70. http://dx.doi.org/10.1016/j.gtc.2008.06.005.
- Levy-Storms L, Schnelle JF, Simmons SF. What do family members notice following an intervention to improve mobility and incontinence care for nursing home residents? An analysis of open-ended comments. Gerontologist 2007;47:14-20. https://doi.org/10.1093/geront/47.1.14.
- Rahman AN, Schnelle JF, Applebaum R, Lindabury K, Simmons S. Distance coursework and coaching to improve nursing home incontinence care: lessons learned. J Am Geriatr Soc 2012;60:1157-64. http://dx.doi.org/10.1111/j.1532-5415.2012.03939.x.
- Rahman AN, Schnelle JF, Osterweil D. Implementing toileting trials in nursing homes: evaluation of a dissemination strategy. Geriatr Nurs 2014;35:283-9. https://doi.org/10.1016/j.gerinurse.2014.03.002.
- Schnelle JF, Alessi CA, Simmons SF, Al-Samarrai NR, Beck JC, Ouslander JG. Translating clinical research into practice: a randomized controlled trial of exercise and incontinence care with nursing home residents. J Am Geriatr Soc 2002;50:1476-83. https://doi.org/10.1046/j.1532-5415.2002.50401.x.
- Schnelle JF, Leung FW. Urinary and fecal incontinence in nursing homes. Gastroenterology 2004;126:41-7. https://doi.org/10.1053/j.gastro.2003.10.017.
- Schnelle JF, Leung FW, Rao SS, Beuscher L, Keeler E, Clift JW, et al. A controlled trial of an intervention to improve urinary and fecal incontinence and constipation. J Am Geriatr Soc 2010;58:1504-11. http://dx.doi.org/10.1111/j.1532-5415.2010.02978.x.
- Schnelle JF, MacRae PG, Ouslander JG, Simmons SF, Nitta M. Functional incidental training, mobility performance and incontinence care with nursing home residents. J Am Geriatr Soc 1995;43:1356-62. https://doi.org/10.1111/j.1532-5415.1995.tb06614.x.
- Schnelle JF, Newman D, White M, Abbey J, Wallston KA, Fogarty T, et al. Maintaining continence in nursing home residents through the application of industrial quality control. Gerontologist 1993;33:114-21. https://doi.org/10.1093/geront/33.1.114.
- Schnelle JF, Simmons SF, Beuscher L, Peterson EN, Habermann R, Leung F. Prevalence of constipation symptoms in fecally incontinent nursing home residents. J Am Geriatr Soc 2009;57:647-52. http://dx.doi.org/10.1111/j.1532-5415.2009.02215.x.
- Schnelle JF, Traughber B, Sowell VA, Newman DR, Petrilli CO, Ory M. Prompted voiding treatment of urinary incontinence in nursing home patients: a behavior management approach for nursing home staff. J Am Geriatr Soc 1989;37:1051-7. https://doi.org/10.1111/j.1532-5415.1989.tb06919.x.
- Ballard C, O’Brien J, James I, Mynt P, Lana M, Potkins D, et al. Quality of life for people with dementia living in residential and nursing home care: the impact of performance on activities of daily living, behavioral and psychological symptoms, language skills, and psychotropic drugs. Int Psychogeriatr 2001;13:93-106. https://doi.org/10.1017/S1041610201007499.
- Fossey J, Ballard C, Juszczak E, James I, Alder N, Jacoby R, et al. Effect of enhanced psychosocial care on antipsychotic use in nursing home residents with severe dementia: cluster randomised trial. BMJ 2006;332:756-61. https://doi.org/10.1136/bmj.38782.575868.7C.
- Fossey J, Masson S, Stafford J, Lawrence V, Corbett A, Ballard C. The disconnect between evidence and practice: a systematic review of person-centred interventions and training manuals for care home staff working with people with dementia. Int J Geriatr Psychiatry 2014;29:797-80. https://doi.org/10.1002/gps.4072.
- Lawrence V, Fossey J, Ballard C, Ferreira N, Murray J. Helping staff to implement psychosocial interventions in care homes: augmenting existing practices and meeting needs for support. Int J Geriatr Psychiatry 2015;31:284-93. http://dx.doi.org/10.1002/gps.4322.
- Lawrence V, Fossey J, Ballard C, Moniz-Cook E, Murray J. Improving quality of life for people with dementia in care homes: making psychosocial interventions work. Br J Psychiatry 2012;201:344-51. http://dx.doi.org/10.1192/bjp.bp.111.101402.
- Whitaker R, Ballard C, Stafford J, Orrell M, Moniz-Cook E, Woods RT, et al. Feasibility study of an optimised person-centred intervention to improve mental health and reduce antipsychotics amongst people with dementia in care homes: study protocol for a randomised controlled trial. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-13.
- Whitaker R, Fossey J, Ballard C, Orrell M, Moniz-Cook E, Woods RT, et al. Improving Well-being and Health for People with Dementia (WHELD): study protocol for a randomised controlled trial. Trials 2014;15. http://dx.doi.org/10.1186/1745-6215-15-284.
- Al-Samarrai NR, Uman GC, Al-Samarrai T, Alessi CA. Introducing a new incontinence management system for nursing home residents. J Am Med Dir Assoc 2007;8:253-61. https://doi.org/10.1016/j.jamda.2006.10.001.
- Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al. Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product designs. Health Technol Assess 2008;12. https://doi.org/10.3310/hta12290.
- Fader M, Bliss D, Cottenden A, Moore K, Norton C. Continence products: research priorities to improve the lives of people with urinary and/or fecal leakage. Neurourol Urodyn 2010;29:640-4. http://dx.doi.org/10.1002/nau.20918.
- Bliss DZ, Fischer LR, Savik K. Managing fecal incontinence: self-care practices of older adults. J Gerontol Nurs 2005;31:35-44. https://doi.org/10.3928/0098-9134-20050701-08.
- Bliss DZ, Lewis J, Hasselman K, Savik K, Lowry A, Whitebird R. Use and evaluation of disposable absorbent products for managing fecal incontinence by community-living people. J Wound Ostomy Continence Nurs 2011;38:289-97. http://dx.doi.org/10.1097/WON.0b013e31821530ca.
- Bliss DZ, Savik K. Use of an absorbent dressing specifically for fecal incontinence. J Wound Ostomy Continence Nurs 2008;35:221-8. http://dx.doi.org/10.1097/01.WON.0000313647.44870.9a.
- Beguin AM, Malaquin-Pavan E, Guihaire C, Hallet-Lezy AM, Souchon S, Homann V, et al. Improving diaper design to address incontinence associated dermatitis. BMC Geriatr 2010;10. http://dx.doi.org/10.1186/1471-2318-10-86.
- Shigeta Y, Nakagami G, Sanada H, Konya C, Sugama J. Factors influencing intact skin in women with incontinence using absorbent products: results of a cross-sectional, comparative study. Ostomy Wound Manage 2010;56:26-8.
- Shigeta Y, Nakagami G, Sanada H, Oba M, Fujikawa J, Konya C, et al. Exploring the relationship between skin property and absorbent pad environment. J Clin Nurs 2009;18:1607-16. http://dx.doi.org/10.1111/j.1365-2702.2008.02606.x.
- Rohwer K, Bliss DZ, Savik K. Incontinence-associated dermatitis in community-dwelling individuals with fecal incontinence. J Wound Ostomy Continence Nurs 2013;40:181-4. https://doi.org/10.1097/WON.0b013e31827e8b3d.
- Beeckman D, Van Lancker A, Van Hecke A, Verhaeghe S. A systematic review and meta-analysis of incontinence-associated dermatitis, incontinence, and moisture as risk factors for pressure ulcer development. Res Nurs Health 2014;37:204-18. https://doi.org/10.1002/nur.21593.
- Denat Y, Khorshid L. The effect of 2 different care products on incontinence-associated dermatitis in patients with fecal incontinence. J Wound Ostomy Continence Nurs 2011;38:171-6. http://dx.doi.org/10.1097/WON.0b013e31820af24e.
- Jones SW, Towers V, Welsby S, Wishin J, Bowler P. Clostridium difficile containment properties of a fecal management system: an in vitro investigation. Ostomy Wound Manage 2011;57:38-49.
- Jones T, Springfield T, Brudwick M, Ladd A. Fecal ostomies: practical management for the home health clinician. Home Healthc Nurse 2011;29:306-17. http://dx.doi.org/10.1097/NHH.0b013e3182173a89.
- Pittman J, Beeson T, Terry C, Kessler W, Kirk L. Methods of bowel management in critical care: a randomized controlled trial. J Wound Ostomy Continence Nurs 2012;39:633-9. http://dx.doi.org/10.1097/WON.0b013e31826a4b9c.
- Langill M, Yan S, Kommala D, Michenko M. A budget impact analysis comparing use of a modern fecal management system to traditional fecal management methods in two Canadian hospitals. Ostomy Wound Manage 2012;58.
- Whiteley I, Sinclair G. Faecal management systems for disabling incontinence or wounds. Br J Nurs 2014;23:881-5. http://dx.doi.org/10.12968/bjon.2014.23.16.881.
- Allymamod A, Chamanga ET. The use of a faecal management system in sacral pressure ulcer care. J Community Nurs 2014;28:29-35.
- Mulhall AM, Jindal SK. Massive gastrointestinal hemorrhage as a complication of the Flexi-Seal fecal management system. Am J Crit Care 2013;22:537-43. http://dx.doi.org/10.4037/ajcc2013499.
- Shaker H, Maile EJ, Telford KJ. Complete circumferential rectal ulceration and haemorrhage secondary to the use of a faecal management system. Therap Adv Gastroenterol 2014;7:51-5. https://doi.org/10.1177/1756283X13501947.
- International Statistical Classification of Diseases and Related Health Problems. Geneva: World Health Organization; 2016.
- Diagnostic and Statistical Manual of Mental Disorders. Arlington County, VA: American Psychiatric Association; 2000.
- Stokes G. Toileting difficulties or incontinence? Changing the landscape of dementia care. British Geriatrics Society Bladder and Bowel Conference. London: BGS; 2013.
- Kitwood T. Towards a theory of dementia care: the interpersonal process. Aging Soc 2008;13. https://doi.org/10.1017/S0144686X00000647.
- Ouslander JG, Blaustein J, Connor A, Pitt A. Habit training and oxybutynin for incontinence in nursing home patients: a placebo-controlled trial. J Am Geriatr Soc 1988;36:40-6. https://doi.org/10.1111/j.1532-5415.1988.tb03432.x.
- Schnelle JF, Sowell VA, Hu TW, Traughber B. Reduction of urinary incontinence in nursing homes: does it reduce or increase costs?. J Am Geriatr Soc 1988;36:34-9. https://doi.org/10.1111/j.1532-5415.1988.tb03431.x.
- Akpan A, Gosney MA, Barrett J. Factors contributing to fecal incontinence in older people and outcome of routine management in home, hospital and nursing home settings. Clin Interv Aging 2007;2:139-45. https://doi.org/10.2147/ciia.2007.2.1.139.
- Goodman C, Gordon AL, Martin F, Davies SL, Iliffe S, Bowman C, et al. Effective health care for older people resident in care homes: the optimal study protocol for realist review. Syst Rev 2014;3. http://dx.doi.org/10.1186/2046-4053-3-49.
- Gillespie D, Hood K, Bayer A, Carter B, Duncan D, Espinasse A, et al. Antibiotic prescribing and associated diarrhoea: a prospective cohort study of care home residents. Age Ageing 2015;44:853-60. http://dx.doi.org/10.1093/ageing/afv072.
- Tariq SH. Geriatric fecal incontinence. Clin Geriatr Med 2004;20:571-87. http://dx.doi.org/10.1016/j.cger.2004.04.010.
- Ostaszkiewicz J, O’Connell B, Dunning T. Ethical challenges associated with providing continence care in residential aged care facilities: findings from a grounded theory study. ANZCJ 2014;20:179-86.
- Potter J, Peel P, Mian S, Lowe D, Irwin P, Pearson M, et al. National audit of continence care for older people: management of faecal incontinence. Age Ageing 2007;36:268-73. https://doi.org/10.1093/ageing/afm004.
- Rahman AN, Schnelle JF, Yamashita T, Patry G, Prasauskas R. Distance learning: a strategy for improving incontinence care in nursing homes. Gerontologist 2010;50:121-32. http://dx.doi.org/10.1093/geront/gnp126.
- Schnelle JF, Kapur K, Alessi C, Osterweil D, Beck JG, Al-Samarrai NR, et al. Does an exercise and incontinence intervention save healthcare costs in a nursing home population?. J Am Geriatr Soc 2003;51:161-8. https://doi.org/10.1046/j.1532-5415.2003.51053.x.
- Boersma P, van Weert JC, Lakerveld J, Dröes RM. The art of successful implementation of psychosocial interventions in residential dementia care: a systematic review of the literature based on the RE-AIM framework. Int Psychogeriatr 2015;27:19-35. https://doi.org/10.1017/S1041610214001409.
- Blekken LE, Nakrem S, Gjeilo KH, Norton C, Mørkved S, Vinsnes AG. Feasibility, acceptability, and adherence of two educational programs for care staff concerning nursing home patients’ fecal incontinence: a pilot study preceding a cluster-randomized controlled trial. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0263-8.
- Begg AH, McDonald C. Scatolia in elderly people with dementia. Int J Geriatr Psychiatry 1989;4:53-4. https://doi.org/10.1002/gps.930040112.
- Gage H, Goodman C, Davies SL, Norton C, Fader M, Wells M, et al. Laxative use in care homes. J Adv Nurs 2010;66:1266-72. http://dx.doi.org/10.1111/j.1365-2648.2010.05297.x.
- Grainger M, Castledine G, Wood N, Dilley C. Researching the management of constipation in long-term care. Part 2. Br J Nurs 2007;16:1212-17. http://dx.doi.org/10.12968/bjon.2007.16.19.27361.
- Saga S, Seim A, Mørkved S, Norton C, Vinsnes AG. Bowel problem management among nursing home residents: a mixed methods study. BMC Nurs 2014;13. http://dx.doi.org/10.1186/s12912-014-0035-9.
- Benjamin K, Rankin J, Edwards N, Ploeg J, Legault F. The social organization of a sedentary life for residents in long-term care. Nurs Inq 2016;23:128-37. https://doi.org/10.1111/nin.12120.
- Booth J, Hagen S, McClurg D, Norton C, MacInnes C, Collins B, et al. A feasibility study of transcutaneous posterior tibial nerve stimulation for bladder and bowel dysfunction in elderly adults in residential care. J Am Med Dir Assoc 2013;14:270-4. http://dx.doi.org/10.1016/j.jamda.2012.10.021.
- Mimidis K, Galinsky D, Rimon E, Papadopoulos V, Zicherman Y, Oreopoulos D. Use of a device that applies external kneading-like force on the abdomen for treatment of constipation. World J Gastroenterol 2005;11:1971-5. https://doi.org/10.3748/wjg.v11.i13.1971.
- Edvardsson D, Winblad B, Sandman PO. Person-centred care of people with severe Alzheimer’s disease: current status and ways forward. Lancet Neurol 2008;7:362-7. http://dx.doi.org/10.1016/S1474-4422(08)70063-2.
- Namazi KH, DiNatale Johnson B. Environmental effects on incontinence problems in Alzheimer’s disease patients. AJADD 1991;6:16-21. https://doi.org/10.1177/153331759100600604.
- Namazi KH, DiNatale Johnson B. Physical environmental cues to reduce the problem of incontinence in Alzheimer’s disease units. AJADD 1991;6:22-8. https://doi.org/10.1177/153331759100600605.
- Hu TW, Igou JF, Kaltreider DL, Yu LC, Rohner TJ, Dennis PJ, et al. A clinical trial of behavioral therapy to improve urinary incontinence in nursing homes. JAMA 1989;261:2656-62. https://doi.org/10.1001/jama.1989.03420180080035.
- Burgio LD, Engel BT, Hawkins A, McCormick KA, Scheve AS, Jones LT. A staff management system for maintaining improvements in continence with elderly nursing home residents. J Appl Behav Anal 1990;23:111-18. https://doi.org/10.1901/jaba.1990.23-111.
- Engel BT, Burgio LD, McCormick KA, Hawkins AM, Scheve AA, Leahy E. Behavioral treatment of incontinence in the long-term care setting. J Am Geriatr Soc 1990;38:361-3. https://doi.org/10.1111/j.1532-5415.1990.tb03522.x.
- Taunton RL, Swagerty DL, Lasseter JA, Lee RH. Continent or incontinent? That is the question. J Gerontol Nurs 2005;31:36-44. https://doi.org/10.3928/0098-9134-20050901-08.
- Akpan A, Gosney MA, Barrett J. Privacy for defecation and fecal incontinence in older adults. J Wound Ostomy Continence Nurs 2006;33:536-40. https://doi.org/10.1097/00152192-200609000-00012.
- Wai AA, Fook VF, Jayachandran M, Biswas J, Nugent C, Mulvenna M, et al. Smart wireless continence management system for persons with dementia. Telemed J E Health 2008;14:825-32. http://dx.doi.org/10.1089/tmj.2008.0084.
- Goodman C, Davies SL, Norton C, Fader M, Morris J, Wells M, et al. Can district nurses and care home staff improve bowel care for older people using a clinical benchmarking tool?. Br J Community Nurs 2013;18:580-7. https://doi.org/10.12968/bjcn.2013.18.12.580.
- Saga S, Vinsnes AG, Mørkved S, Norton C, Seim A. What characteristics predispose to continence in nursing home residents? A population-based cross-sectional study. Neurourol Urodyn 2015;34:362-7. https://doi.org/10.1002/nau.22563.
- Mandl M, Halfens RJ, Lohrmann C. Incontinence care in nursing homes: a cross-sectional study. J Adv Nurs 2015;71:2142-52. http://dx.doi.org/10.1111/jan.12676.
- Palese A, Granzotto D, Broll MG, Carlesso N. From health organization-centred standardization work process to a personhood-centred care process in an Italian nursing home: effectiveness on bowel elimination model. Int J Older People Nurs 2010;5:179-87. https://doi.org/10.1111/j.1748-3743.2010.00220.x.
- Ericson-Lidman E, Larsson LL, Norberg A. Caring for people with dementia disease (DD) and working in a private not-for-profit residential care facility for people with DD. Scand J Caring Sci 2014;28:337-46. http://dx.doi.org/10.1111/scs.12063.
- Chenoweth L, Forbes I, Fleming R, King MT, Stein-Parbury J, Luscombe G, et al. PerCEN: a cluster randomized controlled trial of person-centered residential care and environment for people with dementia. Int Psychogeriatr 2014;26:1147-60. https://doi.org/10.1017/S1041610214000398.
- Hoeffer B, Talerico KA, Rasin J, Mitchell CM, Stewart BJ, McKenzie D, et al. Assisting cognitively impaired nursing home residents with bathing: effects of two bathing interventions on caregiving. Gerontologist 2006;46:524-32. https://doi.org/10.1093/geront/46.4.524.
- Sidani S, Streiner D, Leclerc C. Evaluating the effectiveness of the abilities-focused approach to morning care of people with dementia. Int J Older People Nurs 2012;7:37-45. http://dx.doi.org/10.1111/j.1748-3743.2011.00273.x.
- Gozalo P, Prakash S, Qato DM, Sloane PD, Mor V. Effect of the bathing without a battle training intervention on bathing-associated physical and verbal outcomes in nursing home residents with dementia: a randomized crossover diffusion study. J Am Geriatr Soc 2014;62:797-804. http://dx.doi.org/10.1111/jgs.12777.
- Clark J. Providing intimate continence care for people with learning disabilities. Nurs Times 2009;105:26-8.
- Heckenberg G. Improving and ensuring best practice continence management in residential aged care. Int J Evid Based Healthc 2008;6:260-9. http://dx.doi.org/10.1111/j.1744-1609.2008.00087.x.
- Is Your Care Home Dementia Friendly?. London: The King’s Fund; 2014.
- Andrews J. Maintaining continence in people with dementia. Nurs Times 2013;109:20-1.
- Medway Community Healthcare . A Guide for Staff in Care Homes: Leaflet MCH293 n.d. www.medwaycommunityhealthcare.nhs.uk/uploads/documents/leaflets/continence-care/continence-care-a-guide-for-staff-in-care-homes-mch293.pdf (accessed 21 July 2017).
- Rovner BW, Steele CD, Shmuely Y, Folstein MF. A randomized trial of dementia care in nursing homes. J Am Geriatr Soc 1996;44:7-13. https://doi.org/10.1111/j.1532-5415.1996.tb05631.x.
- Thompson Coon J, Abbott R, Rogers M, Whear R, Pearson S, Lang I, et al. Interventions to reduce inappropriate prescribing of antipsychotic medications in people with dementia resident in care homes: a systematic review. J Am Med Dir Assoc 2014;15:706-18. https://doi.org/10.1016/j.jamda.2014.06.012.
- Killett A, Burns D, Kelly F, Brooker D, Bowes A, La Fontaine J, et al. Digging deep: how organisational culture affects care home residents’ experiences. Aging Soc 2014:1-29.
- Sidani S, Leclerc C, Streiner D. Implementation of the abilities-focused approach to morning care of people with dementia by nursing staff. Int J Older People Nurs 2009;4:48-56. https://doi.org/10.1111/j.1748-3743.2008.00154.x.
- Janes N, Sidani S, Cott C, Rappolt S. Figuring it out in the moment: a theory of unregulated care providers’ knowledge utilization in dementia care settings. Worldviews Evid Based Nurs 2008;5:13-24. http://dx.doi.org/10.1111/j.1741-6787.2008.00114.x.
- Grealy J, McMullen H, Grealy J. Dementia Care: A Practical Photographic Guide. Oxford: Blackwell Publishing; 2005.
- Twigg J. Carework as a form of bodywork. Aging Soc 2000;20:389-411. https://doi.org/10.1017/S0144686X99007801.
- Kelly F. Bodywork in dementia care: recognising the commonalities of selfhood to facilitate respectful care in institutional settings. Aging Soc 2014;34:1073-90. https://doi.org/10.1017/S0144686X13000093.
- Simmons SF, Schnelle JF. Effects of an exercise and scheduled-toileting intervention on appetite and constipation in nursing home residents. J Nutr Health Aging 2004;8:116-21.
- Prince M, Knapp M, Guerchet M, McCrone P, Prina P, Comas-Herrera A, et al. Dementia UK: Update. London: Alzheimer’s Society; 2014.
- Rossor M, Knapp M. Can we model a cognitive footprint of interventions and policies to help to meet the global challenge of dementia?. Lancet 2015;386:1008-10. http://dx.doi.org/10.1016/S0140-6736(15)60248-3.
- Giebel CM, Sutcliffe C, Challis D. Activities of daily living and quality of life across different stages of dementia: a UK study. Aging Ment Health 2015;19:63-71. http://dx.doi.org/10.1080/13607863.2014.915920.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Stein-Padbury J, Chenoweth L, Jeon YH, Brodaty H, Haas M, Normon R. Implementing person-centered care in residential dementia care. Clin Gerontol 2012;35:404-24. https://doi.org/10.1080/07317115.2012.702654.
- Chenoweth L, King MT, Jeon YH, Brodaty H, Stein-Parbury J, Norman R, et al. Caring for Aged Dementia Care Resident Study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: a cluster-randomised trial. Lancet Neurol 2009;8:317-25. http://dx.doi.org/10.1016/S1474-4422(09)70045-6.
- Schnelle JF, Newman DR, Fogarty TE, Wallston K, Ory M. Assessment and quality control of incontinence care in long-term nursing facilities. J Am Geriatr Soc 1991;39:165-71. https://doi.org/10.1111/j.1532-5415.1991.tb01620.x.
- Ostaszkiewicz J, O’Connell B, Dunning T. Fear and overprotection in Australian residential aged-care facilities: the inadvertent impact of regulation on quality continence care. Australas J Ageing 2016;35:119-26. http://dx.doi.org/10.1111/ajag.12218.
- Knopp-Sihota JA, Niehaus L, Squires JE, Norton PG, Estabrooks CA. Factors associated with rushed and missed resident care in western Canadian nursing homes: a cross-sectional survey of health care aides. J Clin Nurs 2015;24:2815-25. http://dx.doi.org/10.1111/jocn.12887.
- Brooker D, Latham I, Jacobson N, Perry W, Evons S. ‘FITS into Practice’ Developing Dementia Specialist Care Homes Summary Report. London: Alzheimer’s Society; 2014.
- Patterson M, Rick J, Wood S, Carroll C, Belains S, Booth A. Systematic review of the links between human resource management practices and performance. Health Technol Assess 2010;14. https://doi.org/10.3310/hta14510.
- Schnelle JF, Traughber B, Morgan DB, Embry JE, Binion AF, Coleman A. Management of geriatric incontinence in nursing homes. J Appl Behav Anal 1983;16:235-41. http://dx.doi.org/10.1901/jaba.1983.16-235.
- Ostaszkiewicz J. A clinical nursing leadership model for enhancing continence care for older adults in a subacute inpatient care setting. J Wound Ostomy Continence Nurs 2006;33:624-29. https://doi.org/10.1097/00152192-200611000-00006.
- Ostaszkiewicz J, Johnson L, Roe B. Timed voiding for urinary incontinence in adults. Cochrane Database Syst Rev 2004;4.
- Ostaszkiewicz J, Johnston L, Roe B. Timed voiding for the management of urinary incontinence in adults. Cochrane Database Syst Rev 2004;1. https://doi.org/10.1002/14651858.cd002802.pub2.
- Ostaszkiewicz J, O’Connell B, Dunning T. Sociological responses to personal and continence care in residential aged care facilities. ANZCJ 2013;19:110-11.
- Ostaszkiewicz J, Roe B, Johnston L. Effects of timed voiding for the management of urinary incontinence in adults: systematic review. J Adv Nurs 2005;52:420-31. https://doi.org/10.1111/j.1365-2648.2005.03608.x.
- O’Connell B, Ostaszkiewicz J, Hawkins M. A suite of evidence-based continence assessment tools for residential aged care. Australas J Ageing 2011;30:27-32. http://dx.doi.org/10.1111/j.1741-6612.2010.00449.x.
- Saga S, Vinsnes AG, Mørkved S, Norton C, Seim A. Prevalence and correlates of fecal incontinence among nursing home residents: a population-based cross-sectional study. BMC Geriatr 2013;13. http://dx.doi.org/10.1186/1471-2318-13-87.
- Haig L. The Effect of Vibration Therapy on Bowel Stimulation in Elderly Patients With Dementia – A Pilot Study 2000. www.isrctn.com/ISRCTN93377248 (accessed 21 July 2017).
- Estabrooks CA, Squires JE, Hayduk LA, Cummings GG, Norton PG. Advancing the argument for validity of the Alberta Context Tool with healthcare aides in residential long-term care. BMC Med Res Methodol 2011;11. http://dx.doi.org/10.1186/1471-2288-11-107.
- Douglas M. Purity and Danger: An Analysis of Concepts of Pollution and Taboo. London: Routledge; 2003.
- Miller WI. The Anatomy of Disgust. Cambridge, MA: Harvard University Press; 1998.
- Roe B, Flanagan L, Maden M. Systematic review of systematic reviews for the management of urinary incontinence and promotion of continence using conservative behavioural approaches in older people in care homes. J Adv Nurs 2015;71:1464-83. https://doi.org/10.1111/jan.12613.
- Mathis S, Ehlman K, Dugger BR, Harrawood A, Kraft CM. Bladder buzz: the effect of a 6-week evidence-based staff education program on knowledge and attitudes regarding urinary incontinence in a nursing home. J Contin Educ Nurs 2013;44:498-506. https://doi.org/10.3928/00220124-20130903-78.
- Sjogren K, Lindkvist M, Sandman PO, Zingmark K, Edvardsson D. Person-centredness and its association with resident well-being in dementia care units. J Adv Nurs 2013;69:2196-205. https://doi.org/10.1111/jan.12085.
- Rosvik J, Kirkevold M, Engedal K, Brooker D, Kirkevold O. A model for using the VIPS framework for person-centred care for persons with dementia in nursing homes: a qualitative evaluative study. Int J Older People Nurs 2011;6:227-36. https://doi.org/10.1111/j.1748-3743.2011.00290.x.
- Brooker DJ, Surr C. Dementia Care Mapping (DCM): initial validation of DCM 8 in UK field trials. Int J Geriatr Psychiatry 2006;21:1018-25. https://doi.org/10.1002/gps.1600.
- Woolley RJ, Young JB, Green JR, Brooker DJ. The feasibility of care mapping to improve care for physically ill older people in hospital. Age Ageing 2008;37:390-5. https://doi.org/10.1093/ageing/afn055.
- Rokstad AM, Vatne S, Engedal K, Selbaek G. The role of leadership in the implementation of person-centred care using Dementia Care Mapping: a study in three nursing homes. J Nurs Manag 2015;23:15-26.
- Willemse BM, De Jonge J, Smit D, Visser Q, Depla MF, Pot AM. Staff’s person-centredness in dementia care in relation to job characteristics and job-related well-being: a cross-sectional survey in nursing homes. J Adv Nurs 2014;71:404-16. https://doi.org/10.1111/jan.12505.
- Board M, Heaslip V, Fuggle K, Gallagher J, Wilson J. How education can improve care for residents with dementia. Nurs Older People 2012;24:29-31. https://doi.org/10.7748/nop2012.06.24.5.29.c9116.
- Rosvik J, Engedal K, Kirkevold O. Factors to make the VIPS practice model more effective in the treatment of neuropsychiatric symptoms in nursing home residents with dementia. Dement Geriatr Cogn Disord 2014;37:335-46. https://doi.org/10.1159/000357773.
- Temkin-Greener H, Cai S, Zheng NT, Zhao H, Mukamel DB. Nursing home work environment and the risk of pressure ulcers and incontinence. Health Serv Res 2012;47:1179-200. https://doi.org/10.1111/j.1475-6773.2011.01353.x.
- Sackley CM, Rodriguez NA, Berg M, Badger F, Wright C, Besemer J, et al. A phase II exploratory cluster randomized controlled trial of a group mobility training and staff education intervention to promote urinary continence in UK care homes. Clinical Rehabilitation 2008. http://cre.sagepub.com/content/22/8/714.full.pdf.
- Ryden MB, Gross CR, Savik K, Krichbaum K, Snyder M, Pearson V, et al. Value-added outcomes: the use of advanced practice nurses in long-term care facilities. Gerontologist 2000;40:654-62. https://doi.org/10.1093/geront/40.6.654.
- Bunn F, Burn AM, Goodman C, Rait G, Norton S, Robinson L, et al. Comorbidity and dementia: a scoping review of the literature. BMC Med 2014;12:1-15. https://doi.org/10.1186/s12916-014-0192-4.
- Jackson J, Currie K, Graham C, Robb Y. The effectiveness of interventions to reduce undernutrition and promote eating in older adults with dementia: a systematic review. JBI Lib System Rev 2011;9:1509-49. https://doi.org/10.11124/01938924-201109370-00001.
- Liu JY, Lai C. Implementation of observational pain management protocol to improve pain management for long-term institutionalized older care residents with dementia: study protocol for a cluster-randomized controlled trial. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-78.
- Abdelhamid A, Bunn D, Dickinson A, Killett A, Poland F, Potter J, et al. Effectiveness of interventions to improve, maintain or facilitate oral food and/or drink intake in people with dementia: systematic review. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-S2-P1.
- Wagg A, Peel P, Lowe D, Potter J. National Audit of Continence Care for Older People. London: Royal College of Physicians; 2006.
- Rao SS. Diagnosis and management of fecal incontinence. American College of Gastroenterology Practice Parameters Committee. Am J Gastroenterol 2004;99:1585-604. https://doi.org/10.1111/j.1572-0241.2004.40105.x.
- Commissioning Guide: Faecal Incontinence. London: Royal College of Surgeons; 2014.
- Harari D, Rogers J, Eustice S, Colley W. Continence Care Services: England 2013. London: Parliament; 2013.
- Specialised Care for Faecal Incontinence. Manchester: NICE; 2012.
- Faecal-Incontinence Overview. Manchester: NICE; 2014.
- Managing Faecal Incontinence. Manchester: NICE; 2014.
- McCormack B, McCance TV. Development of a framework for person-centred nursing. J Adv Nurs 2006;56:472-9. https://doi.org/10.1111/j.1365-2648.2006.04042.x.
- Rokstad AM, Rosvik J, Kirkevold O, Selbaek G, Saltyte Benth J, Engedal K. The effect of person-centred dementia care to prevent agitation and other neuropsychiatric symptoms and enhance quality of life in nursing home patients: a 10-month randomized controlled trial. Dement Geriatr Cogn Disord 2013;36:340-53. https://doi.org/10.1159/000354366.
- Kinley J, Stone L, Dewey M, Levy J, Stewart R, McCrone P, et al. The effect of using high facilitation when implementing the Gold Standards Framework in Care Homes programme: a cluster randomised controlled trial. Palliat Med 2014;28:1099-109. https://doi.org/10.1177/0269216314539785.
- Arvanitakis M, Coppens P, Doughan L, Van Gossum A. Nutrition in care homes and home care: recommendations – a summary based on the report approved by the Council of Europe. Clin Nutr 2009;28:492-6. https://doi.org/10.1016/j.clnu.2009.07.011.
- Emmel N. RAMESES Discussion Group RAMESES@JISCMAIL.AC.UK Archive n.d. www.jiscmail.ac.uk/cgi-bin/webadmin?A2=RAMESES;d9a14671.1507 (accessed 21 July 2017).
- McCance T, Gribben B, McCormack B, Laird E. Promoting person-centred practice within acute care: the impact of culture and context on a facilitated practice development programme. Int Pract Dev J 2013;3.
- Wong G, Greenhalgh T, Westhrop G, Pawson R. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: the RAMESES (Realist And Meta-narrative Evidence Syntheses: Evolving Standards) project. Health Serv Deliv Res 2014;2.
- Bunn DK, Abdelhamid A, Copley M, Cowap V, Dickinson A, Howe A, et al. Effectiveness of interventions to indirectly support food and drink intake in people with dementia: Eating and Drinking Well IN dementiA (EDWINA) systematic review. BMC Geriatr 2016;16.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. http://dx.doi.org/10.1186/s13012-015-0237-x.
- Burgio LD, McCormick KA, Scheve AS, Engel BT, Hawkins A, Leahy E. The effects of changing prompted voiding schedules in the treatment of incontinence in nursing home residents. J Am Geriatr Soc 1994;42:315-20. https://doi.org/10.1111/j.1532-5415.1994.tb01758.x.
- Simmons SF, Ouslander JG. Resident and family satisfaction with incontinence and mobility care: sensitivity to intervention effects?. Gerontologist 2005;45:318-26. https://doi.org/10.1093/geront/45.3.318.
- Wright J, McCormack B, Coffey A, McCarthy G. Developing a tool to assess person-centred continence care. Nurs Older People 2006;18:23-9.
- Goodman C, Davies SL, Norton C, Fader M, Morris J, Wells M, et al. Can district nurses and care home staff improve bowel care for older people using a clinical benchmarking tool?. Br J Community Nurs 2013;18:580-8. http://dx.doi.org/10.12968/bjcn.2013.18.12.580.
- Leung FW, Rao SS. Fecal incontinence in the elderly. Gastroenterol Clin North Am 2009;38:503-11. https://doi.org/10.1016/j.gtc.2009.06.007.
- Rapp MA, Mell T, Majic T, Treusch Y, Nordheim J, Niemann-Mirmehdi M, et al. Agitation in nursing home residents with dementia (VIDEANT trial): effects of a cluster-randomized, controlled, guideline implementation trial. J Am Med Dir Assoc 2013;14:690-5. https://doi.org/10.1016/j.jamda.2013.05.017.
- Watson R, Manthorpe J, Stimpson A. Learning from carers’ experiences: helping older people with dementia to eat and drink. Nurs Older People 2003;14:23-7. https://doi.org/10.7748/nop2003.02.14.10.23.c2200.
- Robinson SB, Rosher RB. Can a beverage cart help improve hydration?. Geriatr Nurs 2002;23:208-11. https://doi.org/10.1067/mgn.2002.126967.
- Levenson SA, Morley JE. Evidence rocks in long-term care, but does it roll?. J Am Med Dir Assoc 2007;8:493-501. https://doi.org/10.1016/j.jamda.2007.07.003.
- Cambridge P, Carnaby S, Cambridge P. Intimate and Personal Care with People with Learning Disabilities. London: Jessica Kingsley Publishers; 2006.
Appendix 1 Research Management Team and Study Steering Committee expertise
| RMT (alphabetically listed) | |
|---|---|
| Frances Bunn (FB), Marina Buswell (MB), Karen Cummings (KC), Vari Drennan (VMD), Mandy Fader (MF), Claire Goodman (CG), Dannielle Harari (DH), Rowan Harwood (RH), Michelle Maden (MM), Christine Norton (CN), Brenda Roe (BRo), Bridget Russell (BRu), Jo Rycroft-Malone (JRM) | |
| SSC | |
| Geoff Wong (GW; chairperson), Francine Cheater (FC), Alan Cottenden (AC), Victoria Elliott (VE), Paul Millac (PM), Jo Moriarty (JM), Tom Owen (TO), Greta Rait (GR) and Liz Sampson (LS) | |
| Areas of expertisea | |
| Research and practitioner experience in the organisation and delivery of care to residents in care homes | CG, KC, JRM, DH, RH, VE, JM, TO, LS |
| Clinical and research expertise in the support of people with dementia with continence-related problems | RH, VMD, DH, PM, FC, GR |
| Clinical and research expertise in incontinence in older people resident in care homes | DH, CG, BRo |
| Research and clinical expertise in the causes, treatment and management of UI and FI | CN, BRo, FC |
| Research on interventions to promote faecal continence | CN, DH |
| Continence research in long-term care settings | BRo, JRM, CG, MF, DH |
| Delivery of continence services to people with dementia and dementia-sensitive care | DH, RH, VMD, JRM, FB, CN, KC, PM |
| Commissioning and service provision to people with dementia | FB, VMD, CG, VE, TO, JM, GR |
| Research expertise in the science of containment, continence aids and equipment | MF, VMD, AC |
| Practice development in care home settings | CG, JRM, BRo, TO, VE |
| NICE and international guidelines and professional guidelines for continence care for people with dementia | CN, DH, VMD, BRo, FC, AC |
| Integrated working between health care and care homes | CG, TO, JM, LS, GR |
| Practice and research expertise on the social care workforce | KC, JM, VE, TO |
| Methodology expertise in realist approaches to evidence synthesis, particularly in the care of people with dementia | JRM, FB, MM, GW |
Appendix 2 Meeting notes and ideas flow from the Research Management Team and Study Steering Committee meetings
This provides a narrative of the discussions between the RMT members over the course of the realist synthesis.
FIGURE 9.
Flow chart of study selection process and progress: version 2 revised for January 2015 RMT meeting. a, Addressing one or more of continence care, implementation in care homes and person-centred care; b, second scoping onwards – adds new information.
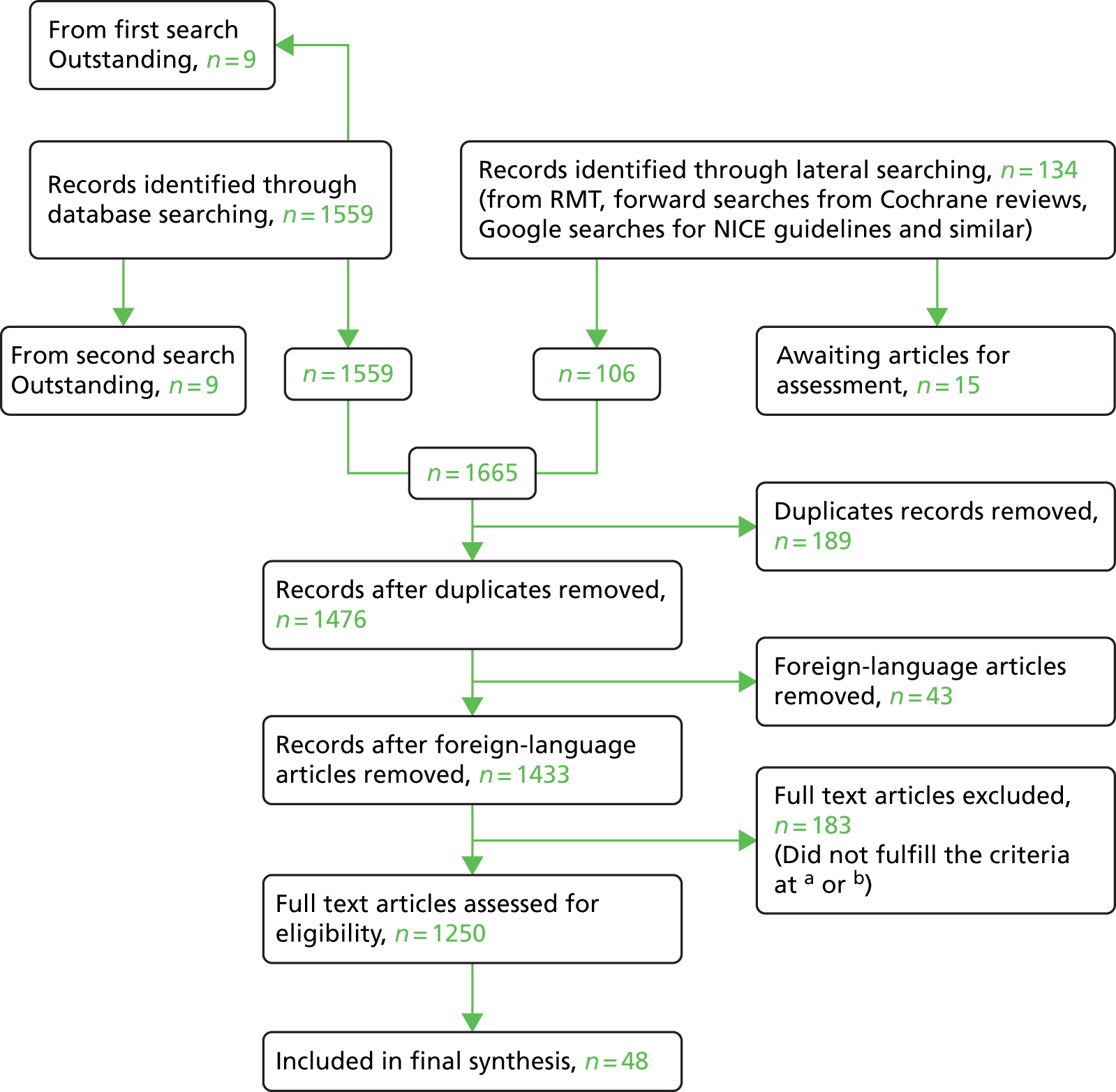
Summary of scoping findings
| Research area | Elements of interventions | Outcomes | Barriers and enablers |
|---|---|---|---|
| Biomedical approaches to the assessment and management of FI (Akhtar and Padda, 2005;87 Booth et al., 2013;155 Whitaker et al., 2013;112 Fader et al., 2008;115 Bellicini et al., 2008;88 Coggrave et al., 2014;28 Flanagan et al., 2014;25 Flanagan et al., 2012;24 Harari et al., 2012;47 Mathis et al., 2013;213 Wald, 200578) |
|
|
|
| Person-centred care (Sjogren et al., 2013;214 Chenoweth et al., 2009;194 Rosvik et al., 2011;215 Brooker and Surr, 2006;216 Woolley et al., 2008;217 Mathis et al., 2013;213 Rokstad et al., 2015;218 Willemse et al., 2014)219 |
|
|
|
| Care home implementation (Al-Samarrai et al., 2007;114 Board et al., 2012;220 Mathis et al., 2013;213 Rosvik et al., 2014;221 Booth et al., 2013;155 Temkin-Greener et al., 2012;222 Andrews, 2013;178 Flanagan et al., 2013;25 Flanagan et al., 2012;24 Fossey et al., 2014;109 Heckenberg, 2008;176 Rahman et al., 2012;98 Sackley et al., 2008;223 Rokstad et al., 2015;218 Ryden et al., 2000224) |
|
|
|
| Nutrition and dementia/care homes (reviews only) Abbott et al., 2013;51 Bunn et al., 2014;225 Jackson et al., 2011;226 Liu et al., 2014;227 Abdelhamid, 2014228 (protocol only) |
|
|
|
FIGURE 10.
Summary of barriers to and enablers of the reduction and management of FI.

Overview narrative: faecal incontinence in people with dementia and/or resident in care homes
An audit of continence care in 2006229 for older people in England found that assessment was not carried out either routinely or reliably. Subsequent guidelines from NICE and other sources make specific recommendations regarding the initial assessment, treatment and continuing assessment of FI in the general population. Baseline assessment should include clinical assessment, functional assessment and patient-reported bowel function history. 33,230–232 NICE recommends treatment pathways depending upon the outcome of the initial assessment. 33,92 The assessment and recommendations take into account neurological problems, diet and nutrition, mobility and exercise, gut motility and physiological problems, drugs and drug interactions, comorbidities, cognitive and behavioural issues and learning disabilities. 33,92,233 Best practice guidelines and findings from continence audits25,33,88,114,178,234 agree that there are key activities that contribute to optimal care of people with FI. These include careful assessment of the individual using a structured approach to inform care planning (e.g. assessment of functional and cognitive ability, previous medical history, comorbidities and, when appropriate, use of radiography and anorectal test). 33,78,87,230,231,234,235 It is also important to discount avoidable causal factors relating to medication, poor nutrition and hydration and inadequate signage. 87,220
It is recognised that it is not possible to discuss FI without addressing constipation and that often there is interplay between FI, constipation and UI. Interventions in the research reviewed to date include, staff training, education and workforce cohesion and job satisfaction,213,222 interventions that improve functional ability,96 tibial nerve stimulation,155 medication review,28,112 and environmental and system changes that make it easier for residents to use toilets and to remove clothing. 115,178,220
Person-centred care for people with dementia living in care homes
Research highlights the influence of Kitwood137 and McCormack and McCance236 in the development of the theory and practice-based approaches to person-centred care. There is a wide range of approaches to person-centred care, the minority of which have an evidence base. Dementia care mapping216,217,237 is a particular approach that is reported to be time-consuming and expensive compared with other forms of PCC but achieves equivalent or improved outcomes for residents in care homes. 216 The majority of person-centred care research among PLWD in care homes focuses on outcomes, such as quality of life, activities of daily living and behavioural symptoms such as agitation. 112,214,215,221
There is some survey work that links person-centred approaches to job satisfaction (Willemse et al. , 2014219). The demand–control–support model was the theoretical framework used to design the study. The demand–control–support model assumes that the most adverse outcomes (e.g. stress, dissatisfaction) are expected in jobs with high levels of demands and low levels of control and/or social support. The study on PCC surveyed 1147 care home staff (59% response rate) and found that person-centred staff members feel more satisfied and competent to perform their job but are also more likely to become emotionally exhausted. Authors suggested that to achieve PCC, care home staff need to have decision authority and; feel supported by the organisation and their manager or supervisor in particular.
Implementation in care homes
This work overlaps in approach and assumptions with person-centred care research in care homes. Research on implementation points to the use of multicomponent interventions that involve care home staff in the planning and provision of changes in care,215,221 the use of facilitators and specific interventions designed to improve resident outcomes (e.g. functional ability, bowel and urinary continence, reduced use of antipsychotics). 112,155,221
Al-Samarrai et al. 114 trialled a new pad with integrated wipes and found little difference regarding the time needed to conduct incontinence care or how correct skin cleansing was done, but care assistants had fewer interruptions and perceived it as better. Fossey et al. 109 emphasise the disconnect between person-centred interventions training, which is routinely available, and the evidence base that would support their benefit, suggesting that there is a need to move to a set of standards in which evaluation of the benefits of training is part of the accreditation process. This review raises questions about how to gauge the participatory nature of the staff training aspect of interventions.
A National Audit of Continence Care47 found that NICE standards were less well adhered to in older people than in younger people, with deficits in documented assessment, diagnosis, treatment and patient communication. Improvements in some aspects of care for older people in hospitals were seen when compared with the previous audit results, suggesting that an ongoing National Audit of Continence Care with linked information resources is useful as both a monitor of and an agent for change. The authors suggest that ageism, a lack of training and poorly integrated services are likely to contribute to lower standards of care in older people. A UK care home survey found that trained staff cited advanced age as the main cause of incontinence. 145
An Australian study176 implemented a new audit and assessment tool in care homes leading to personalised PV schedules for residents. Some resistance to the intervention by staff indicated the drawbacks of being driven by an audit tool to which staff gave no prior input. It also suggests a resistance to documentation to drive change. Rahman et al. 98 experienced something similar: they conducted a distance training programme (six or eight teleconferences of 40–90 minutes’ duration) for nurses (not nursing assistants) to improve UI outcomes among care home residents. The learning did not lead to complete implementation of the strategies at 7- or 8-month follow-up and 33% of staff dropped out before the training was complete.
The style of leadership is a possible barrier to or facilitator of successful implementation and may influence outcomes. Rokstad et al. 237 reported that professional leadership facilitated staff engagement with PCC awareness and practice, whereas market approach and traditional approach did not give a clear vision or commitment to professional development. This was a small study (only three care homes participated), but it addresses how leadership style influences uptake of PCC and also draws a link with outcomes and funding and care home organisation. These issues are echoed by Temkin-Greener et al. 222
Another approach to implementation of new practices in care homes is the use of specialists who visit to assess residents or train staff. Ryden et al. 224 evaluated the usefulness of advanced practice nurses using scientifically based clinical protocols when working with newly admitted residents and staff. They aimed to improve resident outcomes related to four clinical problems: incontinence, pressure ulcers, depression and aggressive behaviour. Of the four outcomes, only the incidence and severity of pressure ulcers improved under the new practices compared with usual care. However, the authors believe that in other areas problems were stabilised and prevented from worsening.
[Note the discussion in the wider implementation literature about the role and type of facilitation and how that influences whether or not staff engage with a programme. One end-of-life care study talks about facilitation that focuses on being present (Kinley et al. , 2014238).]
Nutrition and dementia/care homes (followed up in response to stakeholder comments)
Older adults with dementia are at risk of poor food intake, malnutrition and dehydration. They may have difficulties with eating and drinking for several reasons: they may experience deterioration in motor and cognitive skills making eating difficult, they may forget to eat, fail to recognise food or they may suffer from dysphagia. 226 There may also be organisational and institutional factors related to care homes that make eating and drinking difficult for people with dementia: for example, lack of awareness of the nutritional needs of older people, lack of time to help residents, inappropriate organisation and atmosphere during meal times and absence of protocols for nutritional monitoring and support. 239 Dehydration and poor food intake may in turn impact on bowel function leading to constipation and FI.
Four relevant reviews51,225–227 and one review protocol228 were found. Three reviews were focused on PLWD226–228 and two on people in long-term care. 51,227 Two reviews looked at mealtime,225 interventions. 51 The primary outcomes in all reviews were fluid or food intake or body weight. Only one review225 included constipation as an outcome and none included FI.
A review on interventions to reduce undernutrition and promote healthy eating in older adults with dementia included studies involving adults over the age of 60 years with dementia in any care setting. 226 The review included 11 studies (only one of which was a RCT). They found moderate evidence to suggest that the following interventions could lead to improvements in dietary intake and/or nutritional status:
-
education of health-care staff
-
simple environmental manipulations, such as the use of high-contrast tableware or small dining rooms
-
the introduction of something of interest such as an aquarium or background music or the provision of feeding assistance
-
provision of enhanced menus
-
use of a decentralised food service
-
enhanced nutritional screening combined with increased dietetic time.
Interventions to reduce dehydration
A review including 23 studies looked at interventions to increase fluid intake and reduce dehydration in older people in long-term care. 225 The evidence base was weak but there were a number of interventions that looked promising. This included greater choice and availability of beverages, increased staff awareness, increased staff assistance with drinking and toileting and assessment. Evidence on modifications to dining environments was inconclusive.
Meal time practices
One meta-analysis51 found inconsistent evidence of effects on body weight of changes to food service, food improvement interventions or alterations to dining environment. Findings from observational studies within these intervention types were mixed but generally positive. A narrative review227 reported that nutritional supplements showed moderate evidence to increase food intake, body weight and body mass index. Training/education programmes demonstrated moderate evidence to increase eating time and decrease feeding difficulty. Both training/education programmes and feeding assistance were insufficient to increase food intake. Environment/routine modification indicated low evidence to increase food intake and insufficient evidence to decrease agitation. Evidence was sparse on nutritional status, eating ability, behaviour disturbance, behavioural and cognitive function or level of dependence.
Flow of ideas from the six theory areas emerging from the May Research Management Team meeting
After the May RMT meeting we came away with six theory areas to pursue, these were developed from the literature assessed so far and the expert input from the team through discussion at the meeting.
Initial mid-range theories
These six areas are as follows.
-
Integral to the everyday work pattern and environment: this mid-range theory understands that even if staff know about managing FI and know about person-centred care practices for people with dementia, their ability to implement them will depend on how it fits with the everyday work pattern and environment. A number of different contexts [knowledge of FI, knowing the person, appropriate staffing levels, availability of clinical expert input (geriatricians/GPs/continence nurses), belief that continence can be improved, physical environment] will trigger ‘doing the right thing’ (mechanism) and result in less FI (and UI) and, most likely, in dependent continence. Obviously, these contexts may trigger other mechanisms, such as ‘risk aversion’ or ‘pre-emptive pad use’, that will not result in the desired outcomes. These ideas of staff balancing/juggling/making ‘trade-offs’ in their everyday practice were put forward at the RMT.
Claire found through lateral searching a paper (in another study) and the mid-range theory of ‘Figuring it out in the moment’ seems to neatly encapsulate our theory area 1. 184 Having just read the RAMESES240 discussion about grounded theory being ‘flat’ need to consider that we articulate how this could work as a C–M–O for continence care.
-
Interventions that reflect the degree of cognitive and physical capacity of the resident (personalised care): this mid-range theory very much encapsulates the PCC approach to care. It assumes that if the resident, their history, their normal bowel patterns and their signals for needing the toilet are known, and staff are able to document and review in collaboration with a clinician assessment and family input, this triggers personalised care (mechanism) resulting in more dependent continence rather than FI (and UI) as well as outcomes consistent with the minimisation of distress and promotion of comfort.
Possible mid-range theory person-centred practice framework241 could be adapted . . . (although it’s a bit motherhood and apple pie esque) and again ‘flat’.
-
Clinician-led support, assessment and review: this mid-range theory is very much proposed by clinicians. Clinician-led assessment and ongoing support and review, informed by the use of jointly agreed approaches to the promotion of continence and alternatives to the use of pads, will achieve observable improvements in continence and resident well-being. The assumption is that the involvement of clinicians is key because care home staff do not have the authority or expertise to be able to complete an assessment, particularly digital rectal examination, and therefore clinicians take a lead and care staff respond through a delegated responsibility and mutual communication (mechanism) and, because of the joint approaches, what care staff observe in the resident gets fed back into the assessment/review process so the interventions needed are always appropriate and improvement in faecal continence is seen.
We have not come across any similar published mid-range theories (yet).
-
Establish a common understanding of the potential for recovery, reduction and management of FI for people with dementia: an underlying belief and explicit goals (expressed in staff training, documentation and handover) that it is possible to ameliorate FI in residents living with dementia will mean that attempts are made to understand what is causing the FI and interventions to promote continence and the management of FI are put in place.
No expressed similar mid-range theories in literature were found. This mid-range theory addresses the idea that there is a nihilism in care home care.
-
Ongoing teaching, review and feedback for staff that involves care home staff in planning, action, review and implementation (e.g. Plan Do Study Act) will achieve positive continence-related outcomes: this mid-range theory expresses the viewpoint that giving staff access to the appropriate training, education and facilitation will result in a change in practice. The mechanism is that knowledge, feedback and review trigger changes in how people work.
This mid-range theory is important to consider as so many care home interventions employ a training/education/facilitation approach.
-
Dealing properly with constipation in older people with dementia in care homes will ameliorate a significant proportion of FI because some FI is laxative-induced or overflow FI due to constipation and impaction: this mid-range theory addresses the issue that a focus on constipation can lead to unintended consequences of FI if it is not carried out properly. It looks at the link between FI and constipation.
FIGURE 11.
Patient-centred care framework.
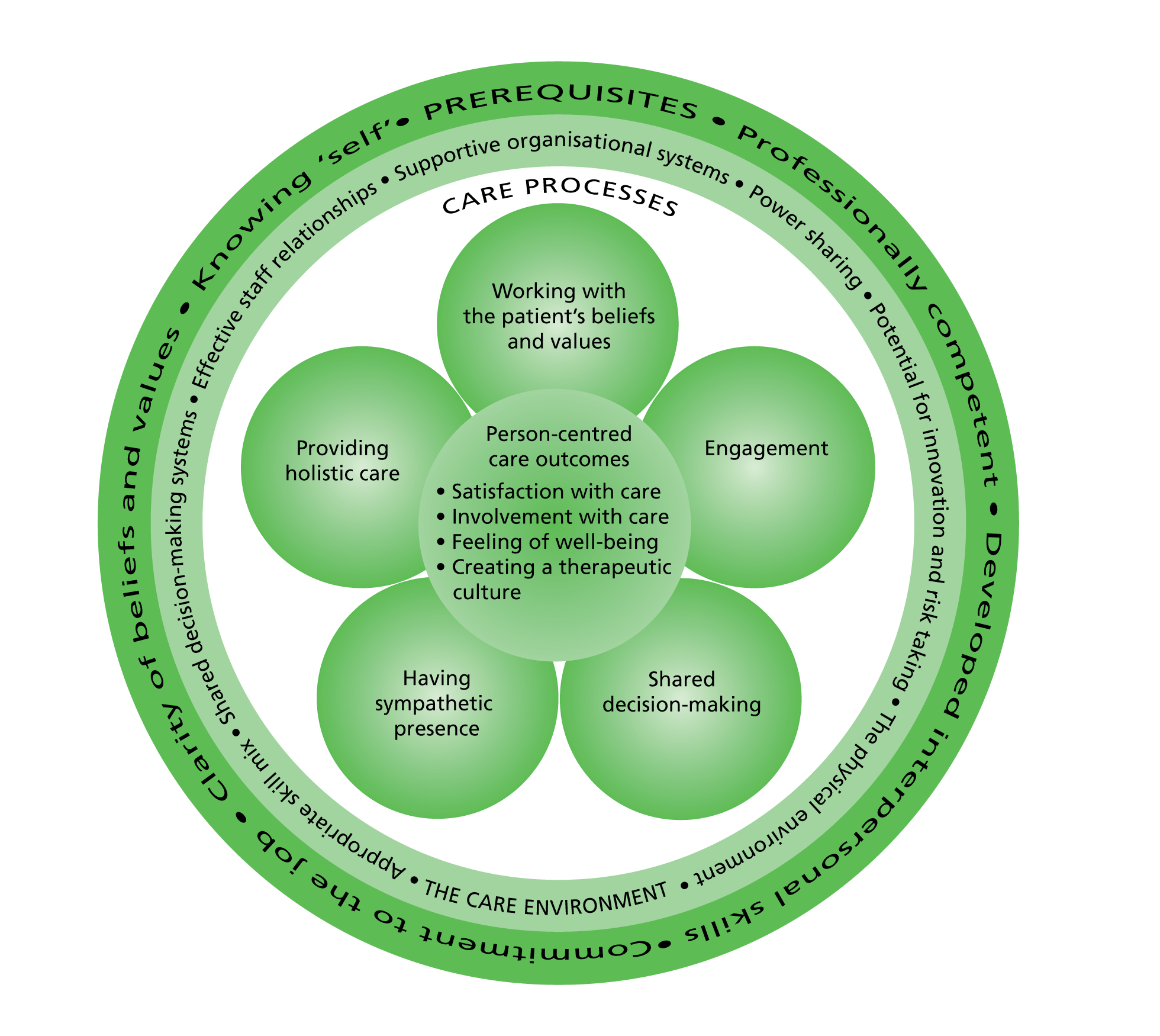
‘Data’ extraction and narrative summaries
We started two parallel processes, (1) data extraction using a modified version of Geoff Wong’s analysis and synthesis form and (2) narrative summaries around grouped papers/evidence. 242
Although we had looked already at 30 or so papers, we started to revisit these in the light of our working mid-range theories and with a better understanding of how to pick out C–M–O configurations. The forms contained the following fields:
-
Relevance
-
Are the contents of a section of text within an included document referring to data that may be relevant to our mid-range theories? Which ones?
-
-
Interpretation of meaning:
-
If it is relevant, do the contents of a section of text provide data that may be interpreted as being a context, mechanism (resource/response) or outcome?
-
-
Judgements about C–M–O configurations
-
What is the C–M–O configuration (partial or complete) for the data?
-
-
Judgements about mid-range theory
-
How does this (full or partial) C–M–O configuration relate to the mid-range theory?
-
Within this same document, are there data that inform how the C–M–O configurations relate to the mid-range theory?
-
If not, are these data in other documents? Which ones?
-
In the light of this C–M–O configuration and any supporting data, does the mid-range theory need to be changed?
-
-
Rigour
-
Are the data sufficiently trustworthy and rigorous to warrant making changes to the C–M–O configurations?
-
Are the data sufficiently trustworthy and rigorous to warrant making changes to the mid-range theory?
-
-
Has this process made you think of any potentially relevant literature? Please note it here.
-
Questions raised not captured elsewhere
We have written narrative summaries of areas of the literature that may include reference to a number of the mid-range theories but are useful to look at as a whole because of the particular lens they bring to the issues.
We started with the two bodies of work directly related to continence, particularly FI, in older people living in care homes:
-
A summary of the studies produced by USA-based researchers working with John Schnelle at the Vanderbilt University, Nashville (BRu).
-
Saga thesis and papers summary and emerging theories and C–M–Os (MB).
We considered the body of clinician reviews and guidance on FI in the peer-reviewed journal literature (MB).
Then looking at a relevant body of work in older people with dementia living in care homes:
-
Summary of studies on interventions to reduce antipsychotic prescribing in care homes and the implementation of psychosocial interventions and emerging theories and C–M–Os (MB).
Finally looking at guidance:
-
Summary of NICE continence care and NICE dementia care guidelines, and implicit theories and C–M–Os (BRu).
We also wrote up the narratives around:
-
Why it is important we consider double incontinence rather than FI alone (MB).
-
Evidence that training, learning, mentoring and post-training support (Theory area 5) are contexts not mechanisms (BRu) – acknowledging we have reached ‘saturation’ in this theory area and will now discard it.
Next steps
Following from our look at NICE guidance and ‘expert’ clinician reviews/guidance in journals, and a push from a realist researcher that we need to be looking more at the ‘grey’ literature and finding out what is happening on the ground, we are going to search for guidance and guidelines that care home staff may have access to, for example:
-
search for localised continence guidance for care homes that might be produced by local continence services (google and e-mail to service leads – if we can get a list)
-
look at the Royal College of Nursing continence care in care homes framework and look for similar from other national bodies (e.g. Association for Continence Advice)
-
look at the professional journals one might find in care homes, for example The Journal of Dementia Care and Caring Times and seek articles on managing FI.
The idea here is that we are looking at how management of FI is being interpreted from high-level guidance to the next level, practice guidance.
There is still a ‘long list’ of ‘not yet excluded’ papers from the systematic searching and our work to date will now influence how we select which papers we should look at in more detail (use the DASF).
Nutrition papers: rather than looking at these from the perspective as how nutrition impacts on bowel health in people with dementia living in care homes we will interrogate with respect to the five remaining theory areas, particularly thinking what interventions to improve eating and drinking in people with dementia in care homes have worked and why? [Eating and Drinking Well IN Dementia (EDWINA) study relevant here. 243]
Implementation in care homes research: we are looking for anything new in this research and particularly keen to look at interventions based on PCC (theory area 2), addressing nihilism (theory area 4) and clinician-led review (theory area 3) as evidence in these areas does not feel like it has reached saturation [unlike teaching and learning (theory area 5)]. [Optimal NHS service delivery to care homes: a realist evaluation of the features and mechanisms that support effective working for the continuing care of older people in residential settings (OPTIMAL) study particularly relevant here. 57]
Constipation literature: because this is coming across as important somehow, perhaps there has been an unintended consequence of a focus on constipation over bowel health in general such that ‘emptying of the bowels at all costs’ has been a focus. We need to interrogate the literature with respect to the five remaining theory areas.
Dementia friendly/person-centred care in care homes: to really try to find some C–M–Os, particularly mechanisms, in the literature we have in our systematic searches.
Which mid-range theory?
At this point in time the most promising theory is 1 – fit and doing the right thing. Education, training and facilitation (theory area 5) appears to be context and PCC approaches (theory area 2) looks as though it may also be context – both necessary but not sufficient. Theory areas 3, 4 and 6 still need more unpicking.
Worries . . .
That we lose the focus on (advanced) dementia. Perhaps we need to always keep dementia as a context with the other contexts and so always think, ‘with these contexts, this mechanism triggers such and such; how does dementia affect that?’ (However, going back to Kitwood,137 dementia in itself is not the context, because when you have met one person with dementia, you have met one person with dementia . . .) Should we be listing some of the behaviours and morbidities and psychological symptoms of dementias as contexts?
Presentation and discussion points produced for the May 2015 Research Management Team meeting
Appendix 3 Bladder and Bowel Foundation stakeholder information
Appendix 4 Searches
Original searches Faecal INcontinence in people with advanced dementia resident in Care Homes study
Search 1 (PubMed and The Cochrane Library, 24 September 2014)
(((((‘incontinence’[Title/Abstract]) OR ‘continence’) AND ‘dementia’ OR alzheimer*)) OR (((‘care home’) OR ‘nursing home’) AND ‘incontinence’)) OR (((‘care home’) AND ‘implementation’) OR ‘person centred’) No limits.
Search 2 (PubMed only, 15 October 2014)
(faecal OR fecal OR constipation OR constipated OR pads OR diapers OR skin cleansing[Title/Abstract]) AND care home or nursing home.
Restricted to following article types:
-
clinical trial
-
comparative study
-
controlled clinical trial
-
randomised controlled trial
-
English abstract
-
multicentre study
-
review
-
systematic review.
Search 3 (PubMed and The Cochrane Library, 7 January 2015)
(nutrition OR eating OR drinking OR hydration OR dehydration) AND (dementia OR nursing home OR care home).
Restricted to reviews only.
Search 4 (PubMed, 16 December 2014)
( TITLE-ABS-KEY ( ( learning disability ) ) AND TITLE-ABS-KEY ( continen* ) OR TITLE-ABS-KEY ( incontinen* ) OR
TITLE-ABS-KEY ( ( continence intervention ) ) AND
TITLE-ABS-KEY ( care OR resident* ) )
PUBYEAR > 1989
Lateral searching includes keyword searches on Google, citation searching and checking reference lists.
Search 3 was developed after the focus group with geriatricians and search 4 was suggested at the SSC meeting. The search terms used in search 4 are probably the weakest (Marina Buswell conducted that search, Frances conducted the first three); only 54 articles were returned, of which nine are relevant to a greater or lesser extent.
Faecal INcontinence in people with advanced dementia resident in Care Homes study search protocol March 2015
The following databases were searched from their inception to 14 March 2015 via NICE Evidence (www.evidence.nhs.uk): MEDLINE (1946–), EMBASE (1980–), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1981–), PsycINFO (1806–), Joanna Briggs Database of Systematic Reviews and Intervention Reports and The Cochrane Library, which consists of The Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, The Cochrane Controlled Trials Register, NHS Economic Evaluation Database and the Health Technology Assessment database. Searches were limited to English-language publications.
| Databases | Date searched | Platform/version/URL | Total number retrieved |
|---|---|---|---|
| MEDLINE | 20 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 14 |
| EMBASE | 20 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 17 |
| CINAHL | 20 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 9 |
| PsycINFO | 20 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 5 |
| The Cochrane Library | 20 March 2014 | Wiley InterScience, www.cochranelibrary.com | CDSR, 1; other reviews, 1; trials, 10 |
| Joanna Briggs Database of Systematic Reviews and Intervention Reports | 20 March 2014 | http://joannabriggslibrary.org/index.php/jbisrir/search/search | 0 |
| Search strategies | |||
| MEDLINE (via Ovid) | |||
| 1. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (44,722) | |||
| 2. exp *DEMENTIA/ (100,534) | |||
| 3. exp *ALZHEIMER DISEASE/ (54,989) | |||
| 4. (dementia OR alzheimer*).ti (76,123) | |||
| 5. 2 OR 3 OR 4 (109,881) | |||
| 6. 1 AND 5 (3073) | |||
| 7. exp *FECAL INCONTINENCE/ (5210) | |||
| 8. (incontinen* OR continen*).ti (23,590) | |||
| 9. 7 OR 8 (25,338) | |||
| 10. 6 AND 9 (16) | |||
| 11. 10 [Limit to: English Language] (14) | |||
| CINAHL | |||
| 38. exp NURSING HOMES/ (17,085) | |||
| 39. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (30,679) | |||
| 40. 38 OR 39 (39,489) | |||
| 41. exp *DEMENTIA/ (26,851) | |||
| 42. dementia.ti (14,291) | |||
| 43. exp *ALZHEIMER’S DISEASE/ (10,909) | |||
| 44. alzheimer*.ti (8935) | |||
| 45. 41 OR 42 OR 43 OR 44 (29,501) | |||
| 46. 40 AND 45 (2880) | |||
| 47. exp *FECAL INCONTINENCE/ (1096) | |||
| 48. (incontinen* OR continen*).ti (6836) | |||
| 49. 47 OR 48 (7209) | |||
| 50. 46 AND 49 (9) | |||
| 51. 50 [Limit to: (Language English)] (9) | |||
| EMBASE (via HDAS) | |||
| 18. exp NURSING HOME/ (40,123) | |||
| 19. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (53,027) | |||
| 20. 18 OR 19 (71,535) | |||
| 21. exp *ALZHEIMER DISEASE/ (78,504) | |||
| 22. alzheimer*.ti (62,586) | |||
| 23. exp *DEMENTIA/ (151,171) | |||
| 24. dementia.ti (41,211) | |||
| 25. 21 OR 22 OR 23 OR 24 (155,959) | |||
| 26. 20 AND 25 (4872) | |||
| 27. exp *FECES INCONTINENCE/ (6308) | |||
| 28. (incontinen* OR continen*).ti (29,701) | |||
| 29. 27 OR 28 (31,664) | |||
| 30. 26 AND 29 (20) | |||
| 31. 30 [Limit to: English Language] (17) | |||
| PsycINFO | |||
| 60. exp NURSING HOMES/ (6925) | |||
| 61. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (15,994) | |||
| 62. 60 OR 61 (16,898) | |||
| 63. exp *DEMENTIA/ (50,682) | |||
| 64. dementia.ti (21,055) | |||
| 65. exp *ALZHEIMER’S DISEASE/ (30,301) | |||
| 66. alzheimer*.ti (23,257) | |||
| 67. 63 OR 64 OR 65 OR 66 (53,166) | |||
| 68. exp *FECAL INCONTINENCE/ (491) | |||
| 69. (incontinen* OR continen*).ti (910) | |||
| 70. 68 OR 69 (1312) | |||
| 71. 62 AND 67 AND 70 (5) | |||
| 72. 71 [Limit to: English Language] (5) | |||
| The Cochrane Library | |||
| care NEAR/3 home* or nursing NEAR/3 home* or residential NEAR/3 home* in Title, Abstract, Keywords and dementia or alzheimer* in Title, Abstract, Keywords and continen* or incontinen* in Title, Abstract, Keywords | |||
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | |||
| (care or resident* or nursing) AND (home*) AND (dementia OR alzheimer*) AND (incontinen* or continen*) | |||
| Databases | Date searched | Platform/version/URL | Total number retrieved |
|---|---|---|---|
| EMBASE | 20 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 38 |
| CINAHL | 20 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 50 |
| PsycINFO | 20 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 28 |
| The Cochrane Library | 20 March 2014 | Wiley InterScience, http://www.cochranelibrary.com/ | Other reviews, 2; trials, 59 |
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | 20 March 2014 | http://joannabriggslibrary.org/index.php/jbisrir/search/search | 7 |
| Search strategies | |||
| MEDLINE (via Ovid) | |||
| 1. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (44,722) | |||
| 2. exp *DEMENTIA/ (100,534) | |||
| 3. exp *ALZHEIMER DISEASE/ (54,989) | |||
| 4. (dementia OR alzheimer*).ti (76,123) | |||
| 5. 2 OR 3 OR 4 (109,881) | |||
| 6. 1 AND 5 (3073) | |||
| 7. exp PATIENT-CENTERED CARE/ [Limit to: English Language] (11,074) | |||
| 8. exp HEALTH PLAN IMPLEMENTATION/ [Limit to: English Language] (3590) | |||
| 9. ((‘patient centre*’ OR ‘person centre*’ OR ‘patient center*’ OR ‘person center*’)).ti; [Limit to: English Language] (3438) | |||
| 10. implementation.ti [Limit to: English Language] (18,043) | |||
| 11. 7 OR 8 OR 9 OR 10; [Limit to: English Language] (32,795) | |||
| 12. 6 AND 11[Limit to: English Language] (62) | |||
| CINAHL | |||
| 38. exp NURSING HOMES/ (17,085) | |||
| 39. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (30,679) | |||
| 40. 38 OR 39 (39,489) | |||
| 41. exp *DEMENTIA/ (26,851) | |||
| 42. dementia.ti; (14,291) | |||
| 43. exp *ALZHEIMER’S DISEASE/ (10,909) | |||
| 45. alzheimer*.ti (8935) | |||
| 46. 41 OR 42 OR 43 OR 45 (29,501) | |||
| 47. 40 AND 46 (2880) | |||
| 48. ((‘patient centre*’ OR ‘person centre*’ OR ‘patient center*’ OR ‘person center*’)).ti (2428) | |||
| 49. implementation.ti [Limit to: (Language English)] (8188) | |||
| 50. 48 OR 49 [Limit to: (Language English)] (10,578) | |||
| 51. 50 AND 47 [Limit to: (Language English)] (50) | |||
| EMBASE (via HDAS) | |||
| 18. exp NURSING HOME/ (40,123) | |||
| 19. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (53,027) | |||
| 20. 18 OR 19 (71,535) | |||
| 21. exp *ALZHEIMER DISEASE/ (78,504) | |||
| 22. alzheimer*.ti (62,586) | |||
| 23. exp *DEMENTIA/ (151,171) | |||
| 24. dementia.ti (41,211) | |||
| 25. 21 OR 22 OR 23 OR 24 (155,959) | |||
| 26. 20 AND 25 (4872) | |||
| 27. ((‘patient centre*’ OR ‘person centre*’ OR ‘patient center*’ OR ‘person center*’)).ti (4062) | |||
| 28. implementation.ti [Limit to: (Language English)] (22,839) | |||
| 29. 27 OR 28 [Limit to: (Language English)] (26,668) | |||
| 30. 26 AND 29 [Limit to: (Language English)] (38) | |||
| PsycINFO | |||
| 60. exp NURSING HOMES/ (6925) | |||
| 61. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (15,994) | |||
| 62. 60 OR 61 (16,898) | |||
| 63. exp *DEMENTIA/ (50,682) | |||
| 64. dementia.ti (21,055) | |||
| 65. exp *ALZHEIMER’S DISEASE/ (30,301) | |||
| 66. alzheimer*.ti (23,257) | |||
| 67. 63 OR 64 OR 65 OR 66 (53,166) | |||
| 68. ((‘patient centre*’ OR ‘person centre*’ OR ‘patient center*’ OR ‘person center*’)).ti (1791) | |||
| 69. implementation.ti [Limit to: (Language English)] (7553) | |||
| 70. 68 OR 69 [Limit to: (Language English)] (9251) | |||
| 71. 62 AND 67 AND 70 [Limit to: (Language English)] (28) | |||
| The Cochrane Library | |||
| care NEAR/3 home* or nursing NEAR/3 home* or residential NEAR/3 home* in Title, Abstract, Keywords and ‘patient centre*’ OR ‘person centre*’ OR ‘patient center*’ OR ‘person center*’ OR implementation in Title, Abstract, Keywords and dementia or alzheimer* in Title, Abstract, Keywords | |||
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | |||
| (care or resident* or nursing) AND (home*) AND (dementia OR alzheimer*) AND (‘patient centre*’ OR ‘person centre*’ OR ‘patient center*’ OR ‘person center’) | |||
| Databases | Date searched | Platform/version/URL | Total number retrieved |
|---|---|---|---|
| MEDLINE | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 61 |
| EMBASE | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 77 |
| CINAHL | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 21 |
| PsycINFO | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 4 |
| The Cochrane Library | 14 March 2014 | Wiley InterScience, www.cochranelibrary.com | CDSR, 4; trials, 30; NHS EED, 1 |
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | 14 March 2014 | http://joannabriggslibrary.org/index.php/jbisrir/search/search | 2 |
| Search strategies | |||
| MEDLINE (via Ovid) | |||
| 1. exp *FECAL INCONTINENCE/ (5210) | |||
| 2. (faecal OR fecal).ti (13,961) | |||
| 3. constipat*.ti (5094) | |||
| 4. (pad OR pads).ti (2986) | |||
| 5. (diaper OR diaper*).ti (648) | |||
| 6. (skin adj3 cleans*).ti (133) | |||
| 7. exp *CONSTIPATION/ (6781) | |||
| 8. exp *INCONTINENCE PADS/ (197) | |||
| 9. 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 (27,779) | |||
| 10. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (44,722) | |||
| 11. 9 AND 10 (200) | |||
| 12. 11 [Limit to: (Publication Types Clinical Trial, All or Comparative Study or Meta Analysis or Randomized Controlled Trial or Systematic Reviews)] (65) | |||
| 13. 12 [Limit to: English Language and (Publication Types Clinical Trial, All or Comparative Study or Meta Analysis or Randomized Controlled Trial or Systematic Reviews)] (61) | |||
| CINAHL | |||
| 14. exp FECAL INCONTINENCE/ (1691) | |||
| 15. exp *CONSTIPATION/ (1693) | |||
| 16. exp *INCONTINENCE AIDS/ (397) | |||
| 18. constipat*.ti (1352) | |||
| 19. (pad OR pads).ti (610) | |||
| 20. (diaper OR diaper*).ti (194) | |||
| 21. (skin adj3 cleans*).ti (41) | |||
| 22. 14 OR 15 OR 16 OR 18 OR 19 OR 20 OR 21 (4511) | |||
| 23. exp NURSING HOMES/ (17,085) | |||
| 24. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (30,679) | |||
| 25. 23 OR 24 (39,489) | |||
| 26. 22 AND 25 (140) | |||
| 27. exp COMPARATIVE STUDIES/ (71,833) | |||
| 28. 26 AND 27 (11) | |||
| 29. 28 [Limit to: (Language English)] (11) | |||
| 30. 26 [Limit to: (Publication Type Clinical Trial or Review or Systematic Review) and (Language English)] (21) | |||
| 31. 29 OR 30 [Limit to: (Language English) and (Publication Type Clinical Trial or Review or Systematic Review)] (21) | |||
| PsycINFO | |||
| 59. exp NURSING HOMES/ (6925) | |||
| 60. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (15,994) | |||
| 61. exp *FECAL INCONTINENCE/ (491) | |||
| 62. exp *CONSTIPATION/ (227) | |||
| 63. constipat*.ti (195) | |||
| 64. (pad OR pads).ti (107) | |||
| 65. (diaper OR diaper*).ti (25) | |||
| 66. (skin adj3 cleans*).ti (1) | |||
| 67. 59 OR 60 (16,898) | |||
| 68. 61 OR 62 OR 63 OR 64 OR 65 OR 66 (860) | |||
| 69. 67 AND 68 (17) | |||
| 70. exp CLINICAL TRIALS/ (8445) | |||
| 71. exp LITERATURE REVIEW/ (22,062) | |||
| 72. exp META ANALYSIS/ (3583) | |||
| 73. review.ti,ab (290,503) | |||
| 74. trial.ti,ab (73,327) | |||
| 75. comparative.ti,ab (43,190) | |||
| 76. 70 OR 71 OR 72 OR 73 OR 74 OR 75 (416,228) | |||
| 77. 69 AND 76 (4) | |||
| EMBASE (via HDAS) | |||
| 32. exp NURSING HOME/ (40,123) | |||
| 33. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (53,027) | |||
| 34. 32 OR 33 (71,535) | |||
| 35. exp *FECES INCONTINENCE/ (6308) | |||
| 36. exp *CONSTIPATION/ (10,279) | |||
| 37. exp *DIAPER/ (358) | |||
| 38. constipat*.ti (7012) | |||
| 39. (pad OR pads).ti (3418) | |||
| 40. (diaper OR diaper*).ti (788) | |||
| 41. (skin adj3 cleans*).ti (164) | |||
| 42. 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 (20,876) | |||
| 43. exp RANDOMIZED CONTROLLED TRIAL/ (362,270) | |||
| 44. exp REVIEW/ (1,998,667) | |||
| 45. exp COMPARATIVE STUDY/ (994,296) | |||
| 46. exp ‘CLINICAL TRIAL (TOPIC)’/ (135,700) | |||
| 47. 43 OR 44 OR 45 OR 46 (3,308,424) | |||
| 48. 42 AND 47 (4120) | |||
| 49. 34 AND 48 (80) | |||
| 50. 49 [Limit to: English Language] (77) | |||
| The Cochrane Library | |||
| care NEAR/3 home* or nursing NEAR/3 home* or residential NEAR/3 home* in Title, Abstract, Keywords and faecal or fecal or constipat* or pad or pads or diaper* or skin NEAR/3 cleans* in Title | |||
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | |||
| (care or resident* or nursing) AND (home*) AND (faecal or fecal or constipat* or pad or pads or diaper* or ‘skin cleansing’ | |||
| Databases | Date searched | Platform/version/URL | Total number retrieved |
|---|---|---|---|
| MEDLINE | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 45 |
| EMBASE | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 53 |
| CINAHL | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 33 |
| PsycINFO | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 4 |
| The Cochrane Library | 14 March 2014 | Wiley InterScience, www.cochranelibrary.com | CDSR, 7; other reviews, 6 |
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | 14 March 2014 | http://joannabriggslibrary.org/index.php/jbisrir/search/search | 0 |
| Search strategies | |||
| MEDLINE (via Ovid) | |||
| 37. exp *NUTRITION THERAPY/ (48,090) | |||
| 38. exp *EATING/ (22,580) | |||
| 39. exp *DRINKING/ (4081) | |||
| 40. exp *DEHYDRATION/ (5189) | |||
| 41. (eating OR drinking OR hydration OR dehydration OR nutrition).ti (92,160) | |||
| 42. 37 OR 38 OR 39 OR 40 OR 41 (149,929) | |||
| 43. (nursing adj3 home* OR care adj3 home* OR residential adj3 home*).ti,ab (45,374) | |||
| 44. dementia.ti,ab (69,692) | |||
| 45. exp *DEMENTIA/ [Limit to: English Language] (89,144) | |||
| 46. 43 OR 44 OR 45 [Limit to: English Language] (148,676) | |||
| 47. 42 AND 46 [Limit to: English Language] (1131) | |||
| 48. 47 [Limit to: English Language and (Publication Types Systematic Reviews)] (45) | |||
| CINAHL | |||
| 1. exp *NUTRITION/ (41,036) | |||
| 2. exp *EATING/ (954) | |||
| 3. (eating OR drinking).ti,ab (23,298) | |||
| 4. hydration.ti,ab (1873) | |||
| 5. exp *DEHYDRATION/ (1034) | |||
| 6. dehydration.ti,ab (1612) | |||
| 7. 1 OR 2 OR 3 OR 4 OR 5 OR 6 (65,176) | |||
| 8. exp NURSING HOMES/ (17,085) | |||
| 9. (nursing adj3 home* OR care adj3 home* OR residential adj3 home*).ti,ab (31,015) | |||
| 10. exp *DEMENTIA/ (26,851) | |||
| 11. dementia.ti,ab (20,909) | |||
| 12. 8 OR 9 OR 10 OR 11 (68,654) | |||
| 13. 7 AND 12 (1192) | |||
| 14. 13 [Limit to: (Publication Type Systematic Review) and (Language English)] (33) | |||
| PsycINFO | |||
| 50. exp NURSING HOMES/ (6925) | |||
| 51. exp *DEMENTIA/ (50,682) | |||
| 52. (nursing adj3 home* OR care adj3 home* OR residential adj3 home*).ti,ab (16,610) | |||
| 53. dementia.ti,ab (45,241) | |||
| 54. 50 OR 51 OR 52 OR 53 (78,838) | |||
| 55. exp *NUTRITION/ (5538) | |||
| 56. exp *DEHYDRATION/ (170) | |||
| 57. (nutrition OR drinking OR eating OR dehydration OR hydration).ti (27,860) | |||
| 58. 55 OR 56 OR 57 (31,210) | |||
| 59. 54 AND 58 (288) | |||
| 60. 59 [Limit to: English Language and (Document Types Reviews)] (4) | |||
| 61. ‘systematic review’.ti,ab (11,051) | |||
| 62. 59 AND 61 (4) | |||
| 63. 62 [Limit to: English Language] (4) | |||
| EMBASE (via HDAS) | |||
| 16. exp NURSING HOME/ (40,123) | |||
| 17. (care adj3 home* OR residental adj3 home* OR nursing adj3 home*).ti,ab (53,027) | |||
| 18. exp *DEMENTIA/ (151,171) | |||
| 19. dementia.ti,ab (94,494) | |||
| 20. 16 OR 17 OR 18 OR 19 (251,499) | |||
| 21. exp *NUTRITION/ (693,357) | |||
| 22. exp *EATING/ (5917) | |||
| 23. exp *DRINKING/ (4474) | |||
| 24. exp *HYDRATION/ (3135) | |||
| 25. exp *DEHYDRATION/ (6158) | |||
| 26. (eating OR drinking OR hydration OR dehydration OR nutrition).ti (9040) | |||
| 27. 21 OR 22 OR 23 OR 24 OR 25 OR 26 (701,547) | |||
| 28. 20 AND 27 (4027) | |||
| 29. 28 [Limit to: English Language and (Publication Types Review)] (416) | |||
| 30. exp SYSTEMATIC REVIEW/ (86,062) | |||
| 31. 29 AND 30 (54) | |||
| 32. 31 [Limit to: English Language] (53) | |||
| The Cochrane Library | |||
| care NEAR/3 home* or nursing NEAR/3 home* or residential NEAR/3 home* in Title, Abstract, Keywords and eating OR drinking OR hydration OR dehydration OR nutrition in Title, Abstract, Keywords | |||
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | |||
| (care or resident* or nursing) AND (home*) AND (eating OR drinking OR hydration OR dehydration OR nutrition) | |||
| Databases | Date searched | Platform/version/URL | Total number of retrieved |
|---|---|---|---|
| MEDLINE | 13 March 2014 | OVID | 10 |
| EMBASE | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 6 |
| CINAHL | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 13 |
| PsycINFO | 13 March 2014 | HDAS NHS Evidence, www.evidence.nhs.uk | 10 |
| The Cochrane Library | 14 March 2014 | Wiley InterScience, www.cochranelibrary.com/ | 0 |
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | 14 March 2014 | http://joannabriggslibrary.org/index.php/jbisrir/search/search | 0 |
| Search strategies | |||
| MEDLINE (via Ovid) | |||
| 1. exp Learning Disorders/ (19,223) | |||
| 2. ‘learning disabilit*’.mp. (5865) | |||
| 3. ‘learning disorder*’.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] (13,073) | |||
| 4. 1 or 2 or 3 (21,647) | |||
| 5. exp Fecal Incontinence/ (8044) | |||
| 6. continen*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] (142,781) | |||
| 7. incontinen*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] (45,408) | |||
| 8. 5 or 6 or 7 (179,294) | |||
| 9. 4 and 8 (188) | |||
| 10. (nursing adj3 home*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] (45,216) | |||
| 11. (resident* adj3 home*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] (7228) | |||
| 12. (care adj3 home*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] (47,142) | |||
| 13. *’Nursing Homes’/ (20,108) | |||
| 14. 10 or 11 or 12 or 13 (85,300) | |||
| 15. 9 and 14 (10) | |||
| EMBASE (via HDAS) | |||
| 38. exp LEARNING DISORDER/ (26,204) | |||
| 39. ‘learning disabilit*’.ti,ab (7723) | |||
| 40. ‘learning disorder*’.ti,ab (1156) | |||
| 41. 38 OR 39 OR 40 (28,159) | |||
| 42. exp FECES INCONTINENCE/ (14,549) | |||
| 43. continen*.ti,ab (37,277) | |||
| 44. incontinen*.ti,ab (53,215) | |||
| 45. 42 OR 43 OR 44 (85,516) | |||
| 46. 41 AND 45 (121) | |||
| 47. exp NURSING HOME/ (40,123) | |||
| 48. (nursing adj3 home*).ti,ab (30,227) | |||
| 49. (care adj3 home*).ti,ab (28,218) | |||
| 50. (resident* adj3 home*).ti,ab (9390) | |||
| 51. 47 OR 48 OR 49 OR 50 (72,968) | |||
| 52. 46 AND 51 (6) | |||
| 53. 52 [Limit to: English Language] (6) | |||
| CINAHL (via HDAS) | |||
| 12. exp LEARNING DISORDERS/ (5754) | |||
| 13. ‘learning disabilit*’.ti,ab (4999) | |||
| 14. ‘learning disorder*’.ti,ab (138) | |||
| 15. 12 OR 13 OR 14 (9056) | |||
| 16. exp FECAL INCONTINENCE/ (1691) | |||
| 17. continen*.ti,ab (4221) | |||
| 18. incontinen*.ti,ab (6962) | |||
| 19. 16 OR 17 OR 18 (10,816) | |||
| 20. 15 AND 19 (39) | |||
| 21. exp NURSING HOMES/ (17,085) | |||
| 22. (nursing adj3 home*).ti,ab (14,926) | |||
| 23. (care adj3 home*).ti,ab (19,457) | |||
| 24. (resident* adj3 home*).ti,ab (5369) | |||
| 25. 21 OR 22 OR 23 OR 24 (40,016) | |||
| 27. 20 AND 25 (13) | |||
| PsychInfo (via HDAS) | |||
| 25. exp LEARNING DISABILITIES/ (24,600) | |||
| 26. ‘learning disabilit*’.ti,ab (14,432) | |||
| 27. ‘learning disorder*’.ti,ab (1317) | |||
| 28. 25 OR 26 OR 27; (29,137) | |||
| 29. exp FECAL INCONTINENCE/ (565) | |||
| 30. continen*.ti,ab (3442) | |||
| 31. incontinen*.ti,ab (2109) | |||
| 32. 29 OR 30 OR 31 (5700) | |||
| 33. 28 AND 32 (35) | |||
| 34. exp NURSING HOMES/ (6925) | |||
| 35. (nursing adj3 home*).ti,ab (9504) | |||
| 36. (care adj3 home*).ti,ab (8181) | |||
| 37. (resident* adj3 home*).ti,ab (4613) | |||
| 38. 34 OR 35 OR 36 OR 37 (17,941) | |||
| 39. 33 AND 38 (10) | |||
| The Cochrane Library | |||
| ‘learning disabilit*’ or ‘learning disorder*’ in Title, Abstract, Keywords and continen* or incontinen* in Title, Abstract, Keywords and faecal or fecal in Title, Abstract, Keywords and care or residen* in Title, Abstract, Keywords | |||
| Joanna Briggs Database of Systematic Reviews and Implementation Reports | |||
| (‘learning disabilit*’or ‘learning disorder*’) AND (continen* or incontinen*) | |||
Appendix 5 ‘If . . . then’ statements
| What to do | |||
|---|---|---|---|
| Number | If | Then | Cross-reference and comments |
| 1 | If a person with dementia has FI | then assessment, including digital rectal examination, must be undertaken to ascertain the reasons | Akhtar and Padda (2005)87 – yes, assessment means problems that can be immediately ascertained and addressed, then dementia issues can be addressed Andrews (2013),178 Booth et al. (2013)155 – partial support, assessment to decide if this particular treatment would be suitable Fossey et al. (2014)109 – yes, necessity of biomedical approaches acknowledged BUT importance of empathy also acknowledged Willemse et al. (2014)219 – yes, breaks PCC in five aspects, attachment, comfort, identity, inclusion and occupation, which can act to improve or lower mood Akpan et al. (2007)140 – biomedical, advocates assessment as central to resolving FI Bellicini et al. (2008)88 – all about the doctor’s role, assessment and diagnosis are paramount |
| 2 | If FI is not ‘curable’ (neurogenic disinhibition/dementia-caused/anorectal dysfunction/dyssynergia) | then appropriate containment is required, which may be timed toileting/PV, bowel regime or use of most appropriate pads | Bellicini et al. (2008)88 – assessment for people living in nursing homes, with relevant treatment options for each ‘cause’ of FI including containment for non-curable FI Fader et al., (2008)115 – examines various pad options and discusses their efficacy in different circumstances Al-Samarrai et al. (2007)114 – trial of new equipment and protocol for pad changing Akhtar and Padda (2005)87 – yes, refers to faecal management system Al-Samarrai et al. (2007)114 – method of containment not mentioned elsewhere |
| 3 | If a person has regular bowel movements and responds well to being taken to the toilet | then PV will reduce FI episodes | Akhtar and Padda (2005)87 – biomedical review of current knowledge, does not mention PV but recommends maintaining greatest activity level possible, upright stance reduces FI Andrews (2013)178 – yes, watch usual patterns and offer discreet encouragement to use the toilet |
| 4 | If FI is a result of faecal impaction | then appropriate combination of laxatives, rectal intervention (and appropriate diet, movement, drinks?) will restore normal bowel function | Bellicini et al. (2008)88 – see points 1 and 2 Akpan et al. (2007)140 – see point 1, observes/analyses various medical interventions Akhtar and Padda (2005)87 – see point 3 |
Marina Buswell
Bridget Russell
Both
| What to do | |||
|---|---|---|---|
| Number | If | Then | Cross-reference and comments |
| 5 | If FI is a result of diarrhoea | then medical referral is required for diagnosis and specific treatment to treat/reduce the FI | Bellicini et al. (2008)88 – taken as read that a doctor will assess Akpan et al. (2007)140 – as for Bellicini Akhtar and Padda (2005)87 – as for Bellicini |
| 6 | If FI is a result of functional reasons (access and ability to get to the toilet) | then a suitably adapted environment and staff on hand to assist as needed will reduce FI episodes | Akpan et al. (2007)140 – partial support, functional disability was observed as a significant contributor to incidence of FI but no solution was suggested Akhtar and Padda (2005)87 – see point 3 Andrews (2013)178 – yes, advocates appropriate signage, lighting, non-reflective surfaces, visual clues to indicate a toilet, avoiding such clues in other places |
| 7 | If FI is comorbidity related | then the comorbidity (stroke/diabetes/medication, etc.) must first be addressed to see if that ‘cures’ the FI | Bellicini et al. (2008),88 Akpan et al. (2007)140 and Akhtar and Padda (2005)87 – all three papers address/advocate this point Andrews (2013)178 – yes, initial assessment of underlying causes important |
| How to do it | |||
| Staff level | |||
| 8 | If full, proper and complete assessment and management is to be implemented | then trained, confident staff are needed with sufficient resources and access to expert support | Andrews (2013)178 – partial support, agrees with the sentiment but offers no suggestions for implementation Fossey et al. (2014)109 – partial support, using manuals to drive care (PCC for reduction of antipsychotic meds and agitation) |
| 9 | If staff are trained in PCC | then they will deliver better continence care and FI will reduce | Willemse et al. (2014)219 – partial support, DCM improved some aspects of psychosocial functioning. Or PCC may help in recognising discomfort; elements of identity and inclusion if addressed have positive effect on mood and engagement and could also be included in FI management Fossey et al. (2006),108 Fossey et al. (2014)109 – partial support, staff sensitivity contributes to reduced neuroleptic prescribing (2006) and quality of life can be improved by implementing and maintaining PCC (2014). Or, no PCC alone does not improve care of specific condition but is an enabling component in a training and support package (2006), no, training in PCC alone is not the answer, although may be an important component (2014) Chenoweth et al. (2009)194 – not directly relevant, PCC/DCM reduce agitation in people with dementia |
Marina Buswell
Bridget Russell
Both
| How to do it | |||
|---|---|---|---|
| Staff level | |||
| Number | If | Then | Cross-reference and comments |
| 10 | If staff have more time with residents and opportunity to know and document what is normal for them | then they will deliver better continence care and FI will reduce | Akpan et al. (2007)140 – yes, residents who can ask for help and have some degree of mobility can successfully manage toileting Schnelle et al. (2010)102 – yes, intervention was delivered by researchers, effectively increasing the number of care staff and the ability of the workforce to accommodate residents’ requirements |
| 11 | If staff have specialist dementia and FI training/knowledge | then they will deliver better continence care and FI will reduce | Schnelle et al. (2010)102 – partial support, researchers had training/knowledge to deliver better continence care Rahman et al. (2012),98 Rahman et al. (2014)99 – distance learning while staff implement a continence intervention may enhance the implementation (2012) and staff knowledge/training to assess residents can reduce episodes of incontinence (2014) |
| 12 | If staff have more autonomy over how to they deliver continence care | then FI will reduce | From CG, FB, MB and BRu discussions |
| Care home level | |||
| 13 | If the physical environment of the care home is ‘dementia friendly’ (signage, layout, etc.) | then there will be less episodes of FI and more content residents | From stakeholder interviews and RMT discussions |
| 14 | If staff experience a supportive working environment | then residents will experience less FI and be more content | Andrews (2013)178 – yes, maintaining pride in work (workforce), positive and practised. Implicit that a good team ‘atmosphere’ helps |
| 15 | If training interventions to improve FI for people with dementia are to work | then they need to be evidence based (what to do? If . . . thens . . .) and delivered on-site over a prolonged period (≥ 4 months) with ongoing supervision and support (e.g. distance coaching) | Roe et al. (2011)26 – partial support, review found if FI interventions are to work comprehensive evidence base is needed Fossey et al. (2014)109 – yes, evidence of PCC effectiveness is scarce but training must last 4 months plus to cause permanent change Schnelle et al. (2010)102 – yes, intervention was evidence based, worked while the researchers were present to deliver it |
| 16 | If it is considered normal that all residents are in pads | then FI will not improve | Roe et al. (2011)26 – yes, use of incontinence pads and toileting programmes comprised the most common management approaches. No studies attempted to maintain continence of residents in care homes |
| How to do it | |||
| Wider organisational/policy level | |||
| No. | If | Then | Cross-reference and comments |
| 17 | If assessment is only carried out on admission | then FI will be poorly diagnosed and managed (really want the opposite positive statement) | From stakeholder interviews and RMT discussions |
| 18 | If provision of pads is dependent on assessment protocols | then FI will be over diagnosed and managed with pads | From stakeholder interviews and RMT discussions |
| 19 | If the restrictions on the provision of pads can be taken out of the relationship between continence services and care homes | then there will be reduction and better management of FI as a diagnosis of FI (or incontinence) will not influence pad provision | From stakeholder interviews and RMT discussions |
| 20 | If care homes were performance managed on FI | then there would be less FI (or just recorded, perverse incentives, Regulation Theory?) | From stakeholder interviews and RMT discussions |
| Enablers | |||
| a | Maintaining pride in work (workforce), positive and practised. Implicit that a good team ‘atmosphere’ helps | Andrews (2013)178 | |
| b | Well adapted physical environment | Fossey et al. (2014)109 | |
| c | Staff knowledge of FI and dementia | ||
| d | Staffing numbers/skill mix | From stakeholder interviews and RMT discussions | |
| e | PCC | ||
| f | Social learning/group learning (or is it a mechanism?) | From stakeholder interviews and RMT discussions | |
| Barriers | |||
| i | Choosing the ‘wrong’ training intervention that is not effective in changing practice | Fossey et al. (2014)109 | |
| ii | Social embarrassment, therefore diagnosed late | Akhtar and Padda (2005)87 | |
| iii | Fear of overstepping re safeguarding, best interests (e.g. not doing digital examination, not taking to toilet for fear of falling) | From stakeholder interviews and RMT discussions | |
| iv | Restrictions on access to pads (needing to game the system and label people incontinent) | From stakeholder interviews and RMT discussions | |
| v | Assessment on arrival as only assessment | From stakeholder interviews and RMT discussions | |
Appendix 6 Development of the data extraction form
Faecal INcontinence in people with advanced dementia resident in Care Homes study version 3: information to include on data extraction form – initial scoping/theory elicitation
Data extraction form for phase 2: three exemplar data extraction forms
Example data extraction form 1
| Theory areas | |||
|---|---|---|---|
|
|||
| Source (reference) | |||
| Stein-Parbury J, Chenoweth L, Jeon YH, Brodaty H, Haas M, Norman R. Implementing person-centered care in residential dementia care. Clin Gerontol 2012;35:404–425193 | |||
| Author lens (e.g. geriatrician, nurse, care home researcher) | |||
| Written by the nurse who worked on the CADRES trial, this paper is an account of the process of implementation and how the care home staff were prepared and supported to participate | |||
| 1. Relevance: are the contents of a section of text within an included document referring to data that may be relevant to our mid-range theories? Which ones? | |||
| The contents are very relevant and provide detail about theories 1, 2, 4, 5 and transferable learning about 6 (this is focusing on reducing distress not improving continence) | |||
| How does it fit with everyday work? (Theory 1) | |||
| Worked with care home staff who were designated as champions by their managers and had the authority to institute change, the learning was experiential ‘numerous role play activities based on participants’ care experiences’ (p. 409). The training acknowledged the difficulties and challenges of working in a care home. Acknowledged and incorporated staff’s own feelings and difficulties and encouraged shared learning. ’Participants expressed uncertainty about how they were going to implement PCC in their care settings . . . as they recognised that changes such as relinquishing a priority to complete tasks within a rigid time frame were necessary to achieve successful implementation . . .’ (p. 409), had authority to implement change from manager (p. 419) | |||
| PCC (Theory 2) | |||
| Training started with a true/false activities about dementia, for example ‘people with dementia lose their ability to communicate’ (p. 409) The course was based on the assumption that the personhood of the person can be fostered and nurtured through interpersonal interactions, ‘most importantly the activity highlighted that the disabling effects of dementia could be exacerbated by how the person with dementia is treated within the psycho-social world’ (p. 409). Emphasis on discovering the meaning of behaviour and training in empathy asking care workers how they would feel in similar situations gave skills in engagement not distraction | |||
| Clinician-led support, assessment and review (Theory 3) | |||
| Two-day training course off site with two care workers from the care homes, facilitated by the author who also provided two site visits and telephone support. Stated that site visits essential to move from theoretical learning to practice. Visits lasted an average of 6 hours and worked with reference to specific residents | |||
| Establish common understanding of potential for reduction and management of FI (Theory 4) | |||
| Yes there was a focus on the fact that people with dementia can still communicate | |||
| Ongoing teaching, review and feedback (Theory 5) | |||
| Overlaps with 3 | |||
| Dealing with constipation (Theory 6) | |||
| Inasmuch it focused on specific activities and specific residents | |||
| 2. Interpretation of meaning: if it is relevant, do the contents of a section of text provide data that may be interpreted as being context, mechanism (resource/response) or outcome? | |||
| Care home staff when supported by a clinician (C) to change practice by their manager (C) with an intervention that models good practice (M), encouraging empathy with the person with dementia (M) that is achievable within a care home (C) and focuses on specific residents (C) can support change in practice and resident agitation | |||
| 3. Judgements about C–M–O configurations: what is the C–M–O configuration (partial or complete) for the data? | |||
| Resource/intervention | Context | Mechanism | Outcome |
| Teaching on PCC | Provided in care homes and off site with designated staff who have the authority to change (p. 419) | Experiential learning that acknowledges staff feelings | Change in staff behaviour |
| Acknowledgement that there are competing priorities | Modelling of best practice and helps staff to work through change process | Improved resident behaviour | |
| Targets specific residents | |||
| 4. Judgements about mid-range theory | |||
|
|||
| It supports the theory about fit with the care home and the need to have as a starting point an understanding and empathy for people with dementia | |||
| 5. Rigour | |||
|
|||
| A good and full description but it is interesting that the author provides detail about how much trouble was given to ensure that the intervention was suited to the care home, that it was targeted on particular residents and that they had the necessary managerial support to achieve change BUT the conclusion is all about the importance of teaching empathy. I would not have seen the teaching of empathy as the generative force | |||
| 6. Population | |||
|
|||
| Questions raised not captured elsewhere | |||
| The focus of the training and the support was on specific residents this was not an intervention that tried to use the principles of PCC for all the residents in the care home, worked on 29 of 77 residents It also emphasised experiential learning and training that encouraged empathy and identification with the person with dementia |
|||
| Notes | |||
Example data extraction form 2
| Theory areas | |||
|---|---|---|---|
|
|||
| Source (reference) | |||
| Ostaszkiewicz J, O’Connell B, Dunning T. Ethical challenges associated with providing continence care in residential aged care facilities: findings from a grounded theory study. A N Z C J 2014;179–186144 | |||
| Author lens: (e.g. geriatrician, nurse, care home researcher) | |||
| Ostaszkiewicz – research and practice interests in the management of incontinence in frail older adults O’Connell – researching into fall prevention, care of older people, continence care, risk management and carer needs Dunning – research and practice in diabetes care |
|||
| 1. Relevance: are the contents of a section of text within an included document referring to data that may be relevant to our mid-range theories? Which ones? | |||
| How does it fit with everyday work? (Theory 1) | |||
| Results, p. 181 – overall grounded theory around ‘caring against the odds’ and ‘weathering constraints’ describe problems staff encounter trying to provide continence care and how they respond to these problems. The descriptive lists of barriers provide useful contexts and the explanations of staff responses and some possible mechanisms. p. 181, second column, paragraph 1 describes how staff ‘found it difficult to uphold residents’ rights because they needed to grapple with multiple, competing and conflicting expectations about residents’ care needs,’ p. 182, second column, ‘Workforce constraints’ descriptions of low staffing levels resulting in compromised care p. 183 section, ‘An unpredictable work environment’ p. 184, ‘Conditioning strategies’ the techniques to persuade (even continent) residents to wear pads – is it because they do not believe resident could be continent [Theory 4], or because they do not think they have enough resources to enable the resident to be continent? |
|||
| PCC (Theory 2) | |||
| Perhaps a converse to PCC is the finding that the main outcome of care is that ‘residents had to appear to be clean and well groomed’ (p. 181, results) p. 182, second column, section ‘Inadequate information about resident’s care needs’ a description of where staff find it difficult to know individual care needs p. 185, first column, description of ignoring resident wishes to provide continence care – changing pads – because of alternative options of care A sense that PCC may not fully encompass continence care |
|||
| Clinician-led support, assessment and review (Theory 3) | |||
| Lack of access to RNs is cited as a barrier to good care (p. 182, second column, third paragraph) ‘. . . and RNs were not always physically present at facilities causing participants to express they felt alone and unsupported’ | |||
| Establish common understanding of potential for reduction and management of FI (Theory 4) | |||
| Evidence for the nihilism side of this theory – that pad use is encouraged and normalised. p. 184 ‘Conditioning strategies’ the techniques to persuade (even continent) residents to wear pads – is it because they don’t believe resident could be continent, or because they don’t think they have enough resources to enable the resident to be continent? | |||
| Ongoing teaching, review and feedback (Theory 5) | |||
| Education and training in continence care not cited at all – only the low educational level of the staff (‘workforce constraints’) providing care and a sentence in the discussion from the authors perspective that ‘staff should be empowered with the knowledge and skill not only to manage the resident’s responses but, more importantly, prevent the situation from escalating into a struggle for power and control’ (p. 185, second column, first paragraph) | |||
| Dealing with constipation (Theory 6) | |||
| Constipation is not discussed (perhaps because it does not interfere with cleanliness? – is it a form of containment?) | |||
| 2. Interpretation of meaning: if it is relevant, do the contents of a section of text provide data that may be interpreted as being context, mechanism (resource/response) or outcome? | |||
| This is not an intervention study but an observational study. However, it provides a number of: Contexts – highly regulated work environment, residents with high levels of dependence, devalued role, workforce constraints, inadequate information about resident care needs, unpredictable work environment, multiple and conflicting expectations about residents’ care needs, risk of falls, staggered shift start times, RN’s role more managerial and less hands on, resident does not want help Resources – pads available, care staff Mechanisms – attempting to accommodate the context of care, adopting self-protective distancing strategies Outcomes – pad use normalised, some levels and types of incontinence are tolerated, residents need to appear clean and well-groomed, staff do not know resident care needs |
|||
| 3. Judgements about C–M–O configurations: what is the C–M–O configuration (partial or complete) for the data? | |||
| Resource/intervention | Context | Mechanism | Outcome |
| Pads | Not enough time to take residents to toilet | Use of pads promoted as precautionary measure | Most residents in pads (and therefore ‘clean and well-groomed residents’) |
| Residents with high levels of dependence, unpredictable work environment, not enough time to meet all residents’ needs (one person is in the shower, someone else needs to go to the toilet urgently) | Use of pads promoted as precautionary measure | Some levels and types of incontinence are tolerated (contained incontinence) | |
| Staggered shift patterns, resident care needs not properly documented | Key information about the resident is passed by word of mouth so it is often not communicated to staff delivering care | Staff do not know what the resident’s care needs are | |
| Resident does not want help to go to the toilet | Pressure from staff to wear pads and avoid ‘dangerous’ activity – going to toilet unaided | Residents become compliant in wearing pads and accept incontinence | |
| Resident does not want to wear pads | Conditioning strategies are used to get resident into pads (everyone else uses them, slowly using bigger pads/underwear style pads) | Residents become compliant in wearing pads and accept incontinence | |
| Highly regulated work environment | Devalued role (care staff), RN’s role moved to managerial and less hands on | Prioritise cleanliness over other aspects of care (p. 181) | Residents clean and well-groomed (but not continent, or even comfortable) Could we argue constipation is a form of containment? |
| 4. Judgements about mid-range theory | |||
|
|||
| Mostly relates to Theory 1 particularly juggling competing needs and priorities. Sociological responses to personal and continence care in residential aged care facilities: Ostaszkiewicz J, O’Connell B and Dunning T School of Nursing and Midwifery, Deakin University, Melbourne,VIC, Australia particular quotation in this paper about staff approaches to continence care and ‘Nurses and PCAs described being undervalued, disempowered, subordinate, marginalised, contaminated and limited to “just doing dirty work”, “just doing the wees and poos”, or limited to “helping residents get ready for lifestyle staff”. In addition to believing their work was underappreciated, they felt other people had very little understanding about the work they actually performed on an everyday basis.’ In theory 1 about fit but also encapsulating PCC approaches the idea that continence is not part of the ‘lifestyle staff’ work assuming this is the singing, art, jigsaw, memories, etc., type therapy staff so continence (or incontinence) care is fitted in before that |
|||
| 5. Rigour | |||
|
|||
| Convenience sample of six RNs, six enrolled nurses and six PCAs who heard about research at professional forum, from colleague or at undergrad info session – possible bias in sample in that they are people interested in this area so perhaps have more knowledge? Therefore findings suggest an awareness that they know they should be doing alternatives and are constrained The observational data helps to counterbalance this bias by observing even the non-‘keeny beany’ staff These data are supporting, not changing the mid-range theory 1 |
|||
| 6. Population | |||
| Characteristics of residents not described rather that of the staff and homes Six RNs, six enrolled nurses and six PCAs. Four of the RNs worked as directors of nursing, two were clinical nurse educators. Five out of six RNs had postgraduate qualifications. One enrolled nurse and two PCAs enrolled on a nursing degree programme Two purposively selected homes: one 75-bed, not-for-profit home and one private, 50-bed, for-profit home RACFs had a resident population with ‘a large number of highly dependent residents’ and ‘included, but was not limited to, individuals with dementia’ |
|||
| Questions raised not captured elsewhere | |||
| This paper does not describe or elaborate on any observed differences between the two homes observed | |||
| Notes | |||
| Reference 5: www.continence.org.au/resources.php/01tG0000002pcRqIAI/deloitte-access-economics-report-the-economic-impact-of-incontinence-in-australia Contains prevalence data on continence in Australian care homes. Note Deloitte say it’s use is ONLY for the continence society of Australia Comments from the author about (p. 185, second column) ‘education programmes need to prepare RACF staff with the knowledge and skill to interpret and respond sensitively to residents’ emotional responses to incontinence’ are slightly at odds with the final conclusions that ‘underlying structural factors’ need to be addressed. Again the fall back on education and training can be seen – even though the evidence points to these ‘structural factors’ and to give credit these are suggested as the area for focus. However, there is a risk of bias because it is the ‘keen’ staff interviewed one could argue they would say – we know what we should be doing but we just cannot fit it into our work UI and FI dealt with as one – incontinence. Distinction comes with cleanliness. So containment acceptable |
|||
Example data extraction form 3
| Theory areas | |||
|---|---|---|---|
|
|||
| Source (reference) | |||
| Lawrence V, Fossey J, Ballard C, Ferreira N, Murray J. Helping staff to implement psychosocial interventions in care homes: augmenting existing practices and meeting needs for support. Int J Geriatr Psychiatry 2015110 | |||
| Author lens (e.g. geriatrician, nurse, care home researcher) | |||
| Lawrence – Lecturer in Qualitative Social Sciences Fossey – Associate Director of Psychological Services Oxford Health NHS Foundation Trust, Clinical Research Fellow, Department of Psychiatry Ballard – Professor of Age Related Diseases, Co-Director of the Biomedical Research Unit for Dementia at the Institute of Psychiatry Ferreira Murray |
|||
| 1. Relevance: are the contents of a section of text within an included document referring to data that might be relevant to our mid-range theories? Which ones? | |||
| How does it fit with everyday work? (Theory 1) | |||
| ‘Whole home’ issues, time pressures, understaffing and care staff feeling undervalued | |||
| PCC (Theory 2) | |||
| Relationships with residents underpins positive working practices (p. 5), having opportunity to talk to older people, enduring dominance of medical model and tendency to prioritise routines (p. 6 – provision of PCC) | |||
| Clinician-led support, assessment and review (Theory 3) | |||
| – | |||
| Establish common understanding of potential for reduction and management of FI (Theory 4) | |||
| – the common understanding part of this theory. Staff suggest involving family members in the training would help implementation (table 1 2b, p. 5, relationships with relatives) | |||
| Ongoing teaching, review and feedback (Theory 5) | |||
| – | |||
| Dealing with constipation (Theory 6) | |||
| – | |||
| 2. Interpretation of meaning: if it is relevant, do the contents of a section of text provide data that may be interpreted as being context, mechanism (resource/response) or outcome? | |||
| The three emerging themes identified are (are these contexts? – have tried to unpick C–M–O configurations below); Undervalued and understaffed Centrality of relationships Existing practices and desire for support |
|||
| 3. Judgements about C–M–O configurations: what is the C–M–O configuration (partial or complete) for the data? | |||
| Resource/intervention | Context | Mechanism | Outcome |
| Opportunity to talk to residents during personal care | Seen as time-wasting or ‘dossing’ (within the time pressures) | Triggers task-oriented approach to care and less communication with residents | Tasks completed as quickly as possible |
| Opportunity to talk to residents during personal care | Seen as invaluable opportunity to interact (within the time pressures) | Triggers more ‘person-centred’ approach to care | Allows staff to focus on individual needs |
| Training programme (in psychosocial interventions) | Delivered to all staff AND family members | Triggers a shared understanding about challenging behaviours | All staff groups and family work together and communicate well about the care of the resident |
| Care home routines | Dominance of medical model | Triggers prioritisation of routines | Task-oriented care |
| Medication reviews (annual, biannual) | Prescribing clinicians do not take staff views into account | Care staff feel undervalued/disengaged? | Staff stress? |
| Training programme (in psychosocial interventions) | Training teams promote the visibility of staff achievements and skills within the training | Triggers enhanced status of care assistants among families, managers and commissioners | Staff feel more valued |
| Evaluation of the training programme (in psychosocial interventions) by researchers shows the benefits to resident care | The research is taking place in their care home | Triggers managers and commissioners to believe in benefits of this approach to care | More resources committed to psychosocial interventions |
| Attachments between care staff and residents | Discouraged by management – lack of support | Triggers staff burnout emotionally | Staff sickness/absence/turnover |
| Attachments between care staff and residents | Encouraged by management with appropriate support (peer support/cohesive team) | Triggers good relationships and understanding between staff and residents | Easier to implement psychosocial interventions |
| 4. Judgements about mid-range theory | |||
|
|||
| The C–M–O configurations are propositions from the qualitative focus groups and are not tested It is not quite clear where the issue about staff feeling undervalued falls in our theory areas. It possibly falls between 1, 2 and 4. The overall results suggest that interventions need to account for ‘whole home’ issues and staff desired the authority to implement the interventions more widely, concurs with the ‘fit’ and ‘doing the right thing’ idea in theory 1 |
|||
| 5. Rigour | |||
|
|||
| Large study for a qualitative study Setting London and the south-east of England only Study themes are from focus groups where staff are proposing what they believe will help successfully implement psychosocial interventions and what barriers may be. They are not tested empirically |
|||
| 6. Population | |||
| Cluster RCT: 16 care homes in London, Oxfordshire and Buckinghamshire Eight convenience sample of local care homes Eight randomly selected care homes from south-east England rated as adequate or better on Care Quality Commission register Eight based in large city, eight in small towns or rural Three government funded, nine private, four voluntary/charity 119 participants: Focus groups (of 8–10 people) 53 care assistants (45%), 30 senior care assistants (25%), 13 activity therapists (11%), six RNs (6%), five deputy managers (4%), two managers (2%), 10 other staff (8%) |
|||
| Questions raised not captured elsewhere | |||
| The theme about staff feeling undervalued is not quite picked up in our theories – but maybe it is a context? | |||
| Notes | |||
Appendix 7 Included sources of evidence
| Source | Search source | Setting | Country | Study type/methods | Process information – level of detail | Study outcome focus | Theoriesa | Outcome(s) measured | Outcome(s) discussed but not measured | Outcome(s) mapped |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention studies | ||||||||||
| Environmental effects on incontinence problems in Alzheimer’s disease patients (Namazi et al., 1991158) | First search | NH | USA | Intervention: repeated measures; pre- and post-intervention comparison. Two conditions toilet clearly visible or hidden | Very clear and detailed description of the two conditions and the data collection method | Residents, continence | 1 | Observational data regarding residents’ abilities to find the toilet depending on whether it was visible or concealed | Higher numbers of ‘clean up’ calls convinced staff that concealed toilets increased the number of incontinent episodes | Continence |
| Physical environmental cues to reduce the problem of incontinence in Alzheimer’s disease units (Namazi et al., 1991159) | First search | NH | USA | Intervention: a variety of signage was presented to gauge which gave residents the most help in finding the toilet | It is unclear how the sign colours were rotated between areas of the building. ‘The color of the signs was changed on a daily basis but remained the same on each wing of the building’, p. 25. Other aspects of the methodology are clear and detailed | Residents, continence | 1, (2) | Observational data regarding residents’ abilities to navigate to the toilet using a variety of different signs | Entering the bathroom did not always result in use of the toilet | Continence |
| Learning resource | ||||||||||
| Maintaining continence in people with dementia (Andrews, 2013178) | Second search | N/A | UK | Knowledge dissemination | N/A | Incontinence management | 2, 3, (4) | N/A | Dignity, family/carer burden | |
| Title | Search source | Setting | Country | Study type/methods | Process information – level of detail | Study outcome focus | Theoriesa | Outcome(s) measured | Outcome(s) discussed but not measured | Outcome(s) mapped |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention studies | ||||||||||
| A staff management system for maintaining improvements in continence with elderly nursing home residents (Burgio et al., 1990161) | First search | NH | USA | Intervention: monitoring and feedback for staff regarding continence checks and care for residents | Relevant demographic information for residents and staff is given. There is information about the time given to training and what staff were expected to do but no examples of how they were expected to do it | Staff | 1, 5 | Wetness/dryness, adherence to PV programme | 0 | Continence |
| The effects of changing prompted voiding schedules in the treatment of incontinence in nursing home residents (Burgio, 1994)245 | Lateral searches | NH | USA | Intervention (information from abstract, full text unavailable): a comparison of four PV schedules for UI, including 2- and 3-hourly PV, participants assigned to groups based on assessment of clinical criteria | Full text not available | Resident | Wetness/dryness, adherence to PV programme | 0 | Continence | |
| Behavioural Treatment of incontinence in the long-term care setting (Engel et al., 1990162) | Second search | NH | USA | Intervention: monitoring and feedback for staff regarding continence checks and care for residents | The mean age and broad descriptive demographic details are given for the care staff. There are no details of how the PV intervention should be implemented, the three levels of feedback are described. Mean age, percentage of female residents and MMSE score are given for the residents | Staff | (4 – UI), 5 | Dryness (pants/pads check), implementation of toileting programme | Reference to cost per wet episode for nursing resources | Continence |
| Distance coursework and coaching to improve nursing home incontinence care: lessons learned (Rahman et al., 201298) | Second search | NH | USA | Intervention: a distance learning programme for staff to improve continence care | Describes in detail the course delivery, personal motivation (Continuing Professional Development credits), assignments to be completed and contact between the facilitator and site liaison between teaching sessions. Course content is presented in a table, session by session | Staff | 1, 5 | Descriptive and comparative data for the two courses were collected using a resident assessment form to evaluate implementation of new practices, pre- and post-training quizzes, a course evaluation survey and a supervisor’s report | 0 | Increased knowledge about continence |
| Implementing toileting trials in nursing homes: evaluation of a dissemination strategy (Rahman et al., 201499) | Second search | NH | USA | Intervention: staff webinar training to implement toileting in NHs | Describes in detail the course delivery, personal motivation (Continuing Professional Development credits), assignments to be completed and contact between the facilitator and site liaison between teaching sessions | Staff | 1, 3, 5 | Data were collected using a course evaluation and implementation survey. Of particular interest was whether or not the course design prompted NH staff to implement the recommended protocol and whether or not participants preferred this course design to other models | Staff preferences regarding the design of the course | Increased knowledge about continence |
| Researching the management of constipation in long-term care. Part 2 (Grainger et al., 2007152) | Second search | CH | UK | Action research – observation leading to intervention with pre- and post-intervention data collection. The study aimed to improve constipation care in long-term care settings through staff education | Gives brief explanation of action research methodology, describes purpose and content of staff training and introduction of specialist link nurses to each site. Data were collected via staff and resident questionnaires at baseline and 6 weeks’ post training | Staff | (1), 5 – weak | Mean number of laxative doses, pre- and post-intervention staff questionnaire | Cost savings because of reduction in laxative use | Resource use: laxatives, increased knowledge about continence (constipation) |
| What do family members notice following an intervention to improve mobility and incontinence care for nursing home residents? An analysis of open-ended comments (Levy-Storms et al., 200797) | Second search | NH | USA | Intervention: controlled trial of PV and mobility training for residents by researchers, between subjects design with pre and post intervention comparisons | Methods are described briefly referring to studies that give more detail (Schnelle et al., 2002100; Simmons and Ouslander, 2005246). Data were collected via interviews with family members of residents at baseline and post intervention | Residents | 1 | Observational data gathered from family members of NH residents regarding continence and mobility in respect of a researcher-led intervention to improve both functions | Family members are reluctant to make judgements on behalf of the residents for certain quality-of-life aspects of continence and mobility care | Continence |
| Improving and ensuring best practice continence management in residential aged care (Heckenberg, 2008176) | Second search | RC | Australia | Intervention: staff training was given to improve adherence to continence care standards | Setting is described including divisions representing resident dependency levels. Audit of ‘current’ practice is described. Various specific or individualised interventions are described. Data collection for changes in practice pre to post intervention is via CH documentation/records. For individualised/specific interventions data are observational | Staff | 1 | Compliance with audit criteria | Increased staff awareness of continence management. Improved efficiency in toileting residents because of ‘calmer atmosphere’ as a result of extra activities being provided for residents in the dementia-specific area | Increased knowledge about continence, change in attitudes to ageing and dementia |
| A clinical trial of behavioural therapy to reduce urinary incontinence in nursing homes (Hu et al., 1989160) | First search | NH | USA | Intervention: controlled test to raise residents’ awareness of the need to void urine (all female sample) | Sample, selection process, baseline assessment and PV intervention described in detail. Data regarding frequency of UI were collected at baseline during and post intervention | Residents | 1 | Number of incontinent episodes pre and post intervention and by comparison with a usual care control group | 0 | Continence |
| Observational studies | ||||||||||
| Developing a tool to assess person-centred continence care (Wright, 2006247) | Third search (MM) | Rehabilitation units | Ireland | Observational: the aim of the research was to investigate the influences of contextual factors on staff capacity to give patient-centred continence care | The Promoting Action on Research Implementation in Health Services (PARIHS) framework is described in some detail, examples of relevant continua from the framework are given in a table. Data collection is via continence measures, audit, questionnaires, focus groups and observation | Staff | Continence facilities audit of staff continence knowledge, staff practice, leadership | 0 | Continence, increased knowledge about continence | |
| Nursing home work environment and the risk of pressure ulcers and incontinence (Temkin-Greener et al., 2012222) | Second search | NH | USA | Observational: from US minimum data set | ‘Staff cohesion’ is defined for the purposes of the study. Data are drawn from a minimum data set and questionnaires from staff at corresponding NHs | Staff | 1, (4), 5 mentioned | Pressure ulcers, incontinence | 0 | Continence, skin integrity |
| Continent or incontinent? That is the question (Taunton et al., 2005163) | Second search | NH | USA | Observational: the study investigated staff knowledge and implementation of continence care guidelines and standards | Protocol for observation is described in full. Data collection is via semistructured interviews with staff, residents or resident representatives | Staff | 1, 4 | Definitions of incontinence, basic care for incontinence programmes to improve incontinence, preparation of staff to care for incontinent residents, staff knowledge about continence care, staff attitudes towards continence care | Skin integrity, dignity (implicit) | Increased knowledge about incontinence, (change in) attitudes towards ageing (and dementia) |
| What characteristics predispose to continence in nursing home residents? A population-based cross-sectional study (Saga, 2014167) | Team (CN) | NH | Norway | Observational: staff completed questionnaires regarding the continence of residents | Detailed description is given of questionnaire data collection completed by staff on behalf of residents | Residents | 1, 3, 4, 6 | Continence | 0 | Continence |
| From health organization-centred standardization work process to a personhood-centred care process in an Italian nursing home: effectiveness on bowel elimination model (Palese et al., 2010169) | Second search | NH | Italy | Observation/intervention: crossover design. The study aimed to alter bowel care from a task-centred approach to a PCC approach (mobility, nutrition/hydration, maintenance of toilet facilities) | Detailed descriptions of initial assessment phase, intervention development and implementation and evaluation are given | Staff | 1, 2, 5, (6) | Constipation, spontaneous evacuations, numbers of ‘invasive practices’ | Capability of nurses to lead change, resource use: nurse time | Resource use: laxatives |
| Ethical challenges associated with providing continence care in residential aged care facilities: findings from a grounded theory study (Ostaszkiewicz et al., 2014144) | Lateral searches | RC | Australia | Qualitative: from a subset of data investigating how continence needs are determined and delivered; this study focused on the ethical problems of giving continence care | Details are given of the observational methods and data collected, examples of staff interview questions are not given but examples of common responses are quoted | Staff | 1, 2, 4, 4 | Staff experiences | Cleanliness – keeping residents clean | Confidence, work satisfaction |
| Fear and overprotection in Australian residential aged care facilities: the inadvertent impact of regulation on quality continence care (Ostaszkiewicz et al., 2016196) | Lateral searches | RC | Australia | Observational (information from PhD thesis – same data set): interviews with Australian CH staff investigating the barriers to and enablers of good continence care produced by the funding system | Article unpublished, first author provided the text of her thesis, which contains the same data. Quotations are given from staff interviews regarding the difficulties of completing the required documentation and complying with regulations of care | Staff | 1, 1, 2, 4 | Adherence to standards and protocols and completing documentation and assessments | Cleanliness – keeping residents clean | None |
| Sociological responses to personal and continence care in residential aged care facilities (Ostaszkiewicz et al., 2013204) | Lateral searches | RC | Australia | Qualitative: interviews with care staff investigating their feelings about dealing with continence care on a daily basis | Conference abstract. Data are from six staff interviews, no further details | Staff | 1, 2 | Staff attitudes and behaviours | Residents’ dignity | Confidence (implicit), work satisfaction (implicit) |
| Incontinence care in nursing homes: a cross-sectional study (Mandl et al., 2015168) | Second search | NH | Austria | Qualitative: interview and questionnaire data collection from 1302 CH residents or their representatives concerning continence care | Data are taken from a minimum data set and assessment of each resident is done independently by two nurses. Tables give details of continence issues/treatments and comorbidities | Residents | 1 | Incontinence, availability of specialised continence nurses, availability of information brochures, use of nursing interventions, for example pads, pelvic floor training, timed toileting | Knowledge and attitudes about continence and ageing | Incontinence, resource use (pads, toileting, etc.) but not costed |
| Laxative use in care homes (Gage et al., 2010151) | First search and team (CG) | CH | UK | Observational: investigating the use of laxatives for older people resident in CHs | Data were collected from patient records, details are given of each variable or demographic item utilised | Continence | (1), 3 | Laxative use | 0 | Resource use: laxatives |
| Providing intimate continence care for people with learning disabilities (Clark, 2009175) | Second search | CH | UK | Observational: the study investigated the intimate and personal care experiences of six people with learning disabilities | Some details of observational protocol are given, number and duration of observations is not included | Residents with learning disabilities | 1, 2 | Promotion of continence Respect for service users’ privacy and dignity |
0 | Dignity |
| Reviews | ||||||||||
| Factors with the management of incontinence and promotion of continence in older people in care homes (Flanagan et al., 201425) | First search and team (BRo) | Systematic review and narrative summary of intervention studies with urinary continence as the primary outcome | Full details of search, inclusion and exclusion criteria are given | N/A | Review, 1, 3 | |||||
| Title | Search source | Setting | Country | Study type/methods | Process information – level of detail | Study outcome focus | Theoriesa | Outcome(s) measured | Outcome(s) discussed but not measured | Outcome(s) mapped |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention studies | ||||||||||
| Feasibility, acceptability and adherence of two educational programs for care; staff concerning nursing home patients’ fecal incontinence: a pilot study preceding a cluster-randomized Controlled Trial (Blekken et al., 2015149) | Second search (protocol) and team (CN) | NH | Norway | Intervention: staff training, quantitative and qualitative analyses. Study hypothesis: FI can be prevented/cured/ameliorated by offering care staff knowledge of best practice. An RCT was used to assess the effect of two educational programmes for care staff | Protocol describes the intended methods, setting, intervention, sample size/demographics, data collection, etc. | Staff | Protocol, assumes 4, 5 | Frequency of FI among patients, change in knowledge among RNs, change in behaviour among care staff | Work satisfaction and confidence – indirectly in discussion about the unclear role of the RN | Continence, increased knowledge about continence |
| Can district nurses and care home staff improve bowel care for older people using a clinical benchmarking tool? (Goodman, 2013248) | Third search (MM) | CH | UK | Intervention: quasi-experimental trial of a benchmarking tool to facilitate individualised planning of bowel care by district nurses and CH staff for residents | Describes quasi-experimental design, staff and resident sample sizes/characteristics, intervention and data collection at baseline and follow-up | Staff | 1, 2, 4, 5 | Staff resources, bowel patterns, working relationships, changes in working practices | 0 | Resource use: staff |
| A controlled trial of an intervention to improve urinary and fecal incontinence and constipation (Schnelle et al., 2010102) | Second search | NH | USA | Intervention: controlled trial of toileting assistance, exercise and 2-hourly snacks and drinks | Describes the sample size and characteristics, inclusion and exclusion criteria, baseline and follow-up assessments and details of the intervention | Resident | 2, 4, 6 | Frequency of UI and FI and rate of appropriate toileting as determined by direct checks from research staff, anorectal assessments were completed on a subset of 29 residents | ‘[Residents] with more cognitive impairment were most responsive to prompted voiding. It is likely that the inability of cognitively impaired people to self-initiate behaviours . . . influence the problems more than with other residents. Prompting protocols compensate for these self-initiation problems . . .’ | Continence |
| Effects of prompted voiding on fecal continence among nursing home residents (Ouslander et al., 199645) | First search | NH | USA | Intervention: controlled PV intervention, the intervention was adapted for some residents who did not respond to PV alone – 2-hourly PV with oxybutynin, 3 days of hourly PV then 2-hourly PV or low-intensity exercise and 2-hourly PV | Describes the sample size and characteristics, inclusion and exclusion criteria, baseline and follow-up assessments and details of the intervention | Continence | 2 | Hourly checks for urination and defaecation for 3 days at baseline, 3 days during the intervention and 3 days at the 10-week follow-up | ‘. . . prompted voiding has significant and potentially clinically important effects on the proportion of bowel movements that are continent and on the frequency of incontinent bowel movements among those residents whose urinary incontinence responds well to this intervention’ | Continence |
| Faecal incontinence in residential homes for the elderly: prevalence, aetiology and management (Tobin and Brocklehurst, 198668) | First search | CH | UK | Intervention: controlled study of assessment for the causes of FI | Describes sample size, inclusion and exclusion criteria, baseline testing, intervention and outcomes | Continence | 3, (4) | FI | Staff attitudes (nihlism), increased knowledge about continence, use of health services | Continence |
| Observational studies | ||||||||||
| Antibiotic prescribing and associated diarrhoea: a prospective cohort study of care home residents (Gillespie et al., 2015142) | Lateral searches | CH | UK | Observation: 12-month prospective cohort study of antibiotic prescribing and associated diarrhoea in CHs in south Wales | Data sources, inclusion and exclusion criteria are listed, sample size and characteristics are given | Continence | 1, 2, 3 | Antibiotic-associated diarrhoea | 0 | None |
| Bowel problem management among nursing home residents: a mixed methods study (Saga et al., 2014153) | Second search and team (CN) | NH | Norway | Mixed methods: quantitative analysis of 980 questionnaires and qualitative analysis of focus group data with eight nurses | Describes sample size and characteristics (table 1), no information about the development of the staff completed questionnaire | Continence | 2, 4, 4 | Pad use, toileting schedule, laxative use, enemas, dietary interventions | Ability to find toilet, ability to communicate continence needs | Resource use: pads, laxatives, other interventions |
| Understanding faecal incontinence in nursing home patients: epidemiology and nurses’ management – conclusions and discussion (Saga, 201476) | Team (CN) | NH | Norway | Qualititive (PhD thesis): assessment of the magnitude and mechanisms behind FI among nursing home patients | Thesis – includes a literature review and mixed-methods study describing setting, participants, measures and data collection including focus group | Continence | 2, 4 | Pad use, toileting schedule, laxative use, enemas, dietary interventions | Ability to find toilet, ability to communicate continence needs | Resource use: pads, laxatives, other interventions |
| National audit of continence care for older people: management of faecal incontinence (Potter et al., 2007145) | Second search | CH | UK | Audit of the requirement for integrated continence services contained within the National Service Framework for Older People | Site recruitment and data sources are described, sample sizes – both patient numbers and site types and numbers – are given | Continence | 1, 3 | Documentation of continence care: resources, management, practice | 0 | None |
| Factors contributing to fecal incontinence in older people and outcome of routine management in home, hospital and nursing home settings (Akpan et al. 2007140) | Second search | NH | UK | Qualitative: questionnaire data from 120 people aged > 65 years with FI investigating the effect of FI on privacy during defaecation | Recruitment, sample size and assessments are described | Resident | 1, 3 | FI, faecal loading, functional disability, cognitive impairment, loose stools, anorectal incontinence, comorbidity | 0 | Continence |
| Privacy for defaecation and fecal incontinence in older adults (Akpan et al., 2006164) | Second search | NH | UK | Qualitative: questionnaire data from 120 people aged > 65 years with FI investigating the effect of FI on privacy during defaecation | Recruitment, sample size and assessments are described | Resident | 2 | Privacy while defaecating, awareness of leakage, ability of resident to clean themselves, access to patient information leaflets about FI | 0 | Dignity (implicit – associated with privacy) |
| Risk factors for fecal incontinence in a nursing home population (Johanson et al., 199717) | First search | NH | USA | Qualitative: questionnaire data were collected from residents or their representatives regarding continence to investigate the risk factors for NH residents | Recruitment, sample size and data collection methods are reported | Continence | 6 | FI | Recognition/use of toilet | Continence |
| Reviews | ||||||||||
| Fecal incontinence in the elderly (Leung, 2009249) | Second search | Clinical knowledge review | Knowledge review | Continence | 3, 6 | |||||
| Urinary and fecal incontinence in nursing home residents (Leung and Schnelle, 200896) | Second search | Review of PV intervention studies | Knowledge review | Continence | 1, 2, 6 | |||||
| Fecal incontinence in older patients (Akhtar and Padda, 200587) | Second search | Clinical knowledge review | Knowledge review | Continence | 2, 3, 4, 6 | |||||
| Title | Search source | Setting | Country | Study type/methods | Process information – level of detail | Study outcome focus | Theoriesa | Outcome(s) measured | Outcome(s) discussed but not measured | Outcome(s) mapped |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention studies | ||||||||||
| Effect of the bathing without a battle training intervention on bathing-associated physical and verbal outcomes in nursing home residents with dementia: a randomised crossover diffusion study (Gozalo et al., 2014174) | Second search | NH | USA | Intervention: staff training to deliver PCC-based bathing care | Describes resident sample size and characteristics, no data are given for care worker sample, intervention is described, methodology/delivery of staff training are not | Resident | 2, 4 – implemented through 2 and 5 | Rates of verbal and physical aggression, bath duration, bath modality, antipsychotic medication use | Resource use: suggestion that low cost of training and less time required to bathe residents would be resource saving | Minimisation of distress, increased knowledge about dementia |
| Agitation in nursing home residents with dementia (VIDEANT trial): effects of a cluster-randomised, controlled, guideline implementation trial (Rapp, 2013250) | Lateral searches | NH | Germany | Intervention: controlled investigation of the impact of guideline-based interventions on agitation and psychotropic prescriptions, focusing on implementation of physical and activity-based therapy interventions. Outcome measures were agitation (CMAI scores) and neuroleptic prescribing | Resident sample, selection, baseline and follow-up assessment are described, staff training and multiple interventions are described, no sample data for staff are reported | Resident | 2, 2 | Agitation (CMAI) and number of neuroleptics, antidepressants and cholinesterase inhibitors prescribed | 0 | Minimisation of distress |
| Implementing person-centered care in residential dementia care (Stein-Padbury et al., 2012193) | Lateral searches | RC | Australia | Methodological article relating to PCC for PLWD in CHs, as implemented in Chenoweth et al. (2009)194 | Resident sample size and recruitment are described, staff training is described in detail with examples | Resident | 1, 2, 3, 4, 5 –associated with 3 | Learning outcomes from PCC training | Changes to work schedules ‘culture change’ | Increased knowledge about dementia |
| Implementation of the abilities-focused approach to morning care of people with dementia by nursing staff (Sidani et al., 2009183) | Lateral searches | RC | Canada | Intervention/observation: staff training and implementation of abilities focused morning care, for PLWD in NHs. Data collection was observational pre- and post-intervention | Describes characteristics of sites and staff, briefly describes the intervention/training | Resident | 1, 2 | Agitation participation in morning care physical functioning psychosocial functioning | Modification of education programme to fit with day-to-day practice staff turnover | Minimisation of distress |
| Caring for aged dementia care resident study (CADRES) of person-centred care, dementia-care mapping, and usual care in dementia: a cluster-randomised trial (Chenoweth et al., 2009194) | Second search | RC | Australia | Intervention: controlled trial of Person Centered Care (PPC), DCM and usual care. The primary outcome was agitation (CMAI scores). Secondary outcomes included hallucinations, neuropsychological status, QoL, falls and cost of treatment. Outcome measures were assessed before and directly after intervention period and at 4-month follow-up | Describes resident sample and randomisation (figure 1), describes training interventions in detail and reports measures for baseline and follow-up assessment | Resident | 1, 1, 2 | Agitation, neuropsychiatric inventory, QoL incidents, falls, antipsychotic-drug doses, benzodiazepine drug doses, intervention cost | 0 | Minimisation of distress, costs |
| Assisting cognitively impaired nursing home residents with bathing: effects of two bathing interventions on caregiving (Hoeffer et al., 2006172) | Third search (MM) | NH | USA | Intervention: crossover design RCT implementing a PCC approach and two new bathing techniques to reduce agitation in PLWD in NHs. Data collection was self-report by care workers at baseline T1 (regarding technique 1) and T2 (regarding technique 2) | Both staff and resident samples are described in detail; methodology, staff training and assessment at three time points and between groups are reported. Data collection methods are described | Staff | 1, 2, 4 – not FI but common understanding of resident experience of bathing | Gentleness and verbal support measured using Caregiver Bathing Behaviour Rating Scale | 0 | Confidence, minimisation of distress |
| Effect of enhanced psychosocial care on antipsychotic use in nursing home residents with severe dementia: cluster randomised trial (Fossey, 2006108) | First search | NH | UK | Intervention: a controlled trial of training and support for staff (driven by policy requirements) over 10 months, to implement and maintain non-pharmaceutical alternatives to neuroleptic drugs to address BPSD | Resident sample characteristics (table 1); randomisation and assessment at baseline and follow-up and staff training and supervision are described in great detail | Resident | 1, 2, 3, 5 | Proportion of residents prescribed neuroleptics, proportion of residents taking other psychotropic drugs Falls Mean level of agitation and disruptive behaviour QoL |
0 | Minimisation of distress, resource use: psychotropic drugs prescribed |
| Observational studies | ||||||||||
| Caring for people with dementia disease (DD) and working in a private not-for-profit residential care facility for people with DD (Ericson-Lidman et al., 2014170) | Second search | RC | Sweden | Qualitative: interviews with staff to investigate staff understanding of their role (one CH) | Staff sample is described; some information about residents is given; data collection method is reported | Staff | 1, 2, 2, 5 | Staff perceptions of caring for older people with dementia | 0 | Confidence, work satisfaction |
| Reviews | ||||||||||
| The art of successful implementation of psychosocial interventions in residential dementia care: a systematic review of the literature based on the RE-AIM framework (Boersma et al., 2015148) | Lateral searches | Systematic review of psychosocial intervention implementations for PLWD in residential care | Search strategy and terms are reported; review procedure and data extraction are reported in detail | Staff | Review, 1, 2, 4, 5 | |||||
| Interventions to reduce inappropriate prescribing of antipsychotic medications in people with dementia resident in care homes: a systematic review (Thompson-Coon et al., 2014181) | Lateral searches | Systematic review of interventions to reduce antipsychotic prescribing for PLWD in CHs | Search strategy and terms, study selection, data extraction and synthesis are reported | Resident | Review of antipsychotic prescribing studies | |||||
| Improving quality of life for people with dementia in care homes: making psychosocial interventions work (Lawrence et al., 2012111) | Lateral searches | Systematic review and meta-analysis of qualitative research investigating improving QoL for PLWD in CHs | Search terms and strategy not stated, identification and selection of papers, quality appraisal and data extraction and synthesis are described in detail | Resident | Review 1, 2 | |||||
| Learning from carers’ experiences: helping older people with dementia to eat and drink (Watson, 2003251) | Second search | CH | UK | Knowledge dissemination/training material | Learning resource | |||||
| Title | Search source | Setting | Country | Study type/methods | Process information – level of detail | Study outcome focus | Theoriesa | Outcome(s) measured | Outcome(s) discussed but not measured | Outcome(s) mapped |
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention studies | ||||||||||
| The effect of using high facilitation when implementing the gold standards framework in care homes programme: a cluster randomised controlled trial (Kinley, 2014238) | Second search | CH | UK | Intervention: controlled trial making use of experts to implement Gold Standards Framework for end-of-life care | Detailed resident characteristics are given, no staff sample data are reported, site randomisation and staff training/interventions are described in detail | Staff | 1, 1, 3, 5, 6 – in a limited capacity | The number of resident deaths occurring in the CH vs. in hospital relative to the type of staff training given to assist with implementing the ‘Gold Standards Framework for Care Homes’ | ‘. . . facilitation of the programme is variable and is dependent on local initiatives’ | Staff knowledge and skills |
| Can a beverage cart help improve hydration? (Robinson, 2002252) | Team (FB) | NH | USA | Intervention: offering extra drinks mid-morning and mid-afternoon to improve hydration for residents of CHs (extra staff were employed to deliver the intervention including the social aspect of engaging residents interest, the trolley, cups, etc., were colourful) | Resident sample size, recruitment and characteristics are reported; the intervention and methodology are described in detail | Resident | 1, 2, 3, (4, 5), 6 | Data were collected weekly for the following: hydration, number of bowel movements, laxative use, enemas and falls; changes in mental status, urinary and respiratory tract infections; for 2 weeks prior to intervention, 5 weeks during intervention and 2 weeks post intervention | Improvement in residents’ affect because of expecting the arrival of the drinks trolley | Continence |
| Value-added outcomes: the use of advanced practice nurses in long-term care facilities (Ryden et al., 2000224) | Second search | NH | USA | Intervention: specialist nurses working with staff and residents to improve continence for CH residents | Resident sample size and allocation protocol are described, assessment at baseline and at two other time points is described | Continence | (2), 3, 4, 5 | Changes to status of incontinence, pressure ulcers and aggressive behaviour, and mean composite trajectory score | Significantly less deterioration in affect was noted in cognitively impaired residents in the treatment group | Continence, skin integrity |
| Observational studies | ||||||||||
| Helping staff to implement psychosocial interventions in care homes: augmenting existing practices and meeting needs for support (Lawrence et al., 2015110) | Lateral searches | CH | UK | Qualitative: interview focus group study, gathering opinions and insights from CH staff about PCC and non-pharmacological interventions for BPSD | Basic characteristics of the staff sample are reported | Staff | 1, 1, 2, 2, 4 | Lack of recognition of care staff Lack of resources, relationships |
Lack of resources | Increased knowledge about dementia, confidence, work satisfaction, resource use (discussed not measured) |
| Digging deep: how organisational culture affects care home residents’ experiences (Killett et al., 2014182) | Lateral searches | CH | UK | Qualitative: case studies of 11 CHs investigating the elements of organisational culture that influence quality of care | Through observation and staff interviews interactions between elements of organisational culture are examined including impact on care | Staff | 1, 1, 2, 2, (4) | The effects of differing cultural beliefs/attitudes on care outcomes | PCC | |
| Reviews | ||||||||||
| Evidence rocks in long-term care, but does it roll? (Levenson, 2007253) | Second search | Review of evidence for getting research findings into practice in long-term care for older people | Knowledge review | Resident | 1, (3, 6) | |||||
| Books | ||||||||||
| Developing policies, procedures and guidelines for intimate and personal care in services for people with learning disabilities (Cambridge, 2006254) | Second search | UK | Book for professionals; not a study. Knowledge summary and dissemination | Book | Resident | 1 | ||||
| Title | Authors | Setting | Country | Study type/methods | Process information – level of detail | Study outcome focus | Theoriesa | Outcome(s) measured | Outcome(s) discussed but not measured | Outcome(s) mapped |
|---|---|---|---|---|---|---|---|---|---|---|
| A feasibility study of transcutaneous posterior tibial nerve stimulation for bladder and bowel dysfunction in elderly adults in residential care (Booth et al., 2013155) | Second search | CH | UK | Intervention: feasibility study of transcutaneous posterior tibial nerve stimulation for bladder and bowel dysfunction in CH residents | Resident sample size, inclusion and exclusion criteria, randomisation and intervention are described | Continence | (3, 6) | UI symptoms Bowel symptoms |
Continence | |
| Smart wireless continence management system for persons with dementia (Wai et al., 2008165) | Second search | NH | Singapore | Intervention: single participant, sensor inserted into incontinence pad to inform staff when the resident has had a wetness episode | Characteristics of single participant reported, very detailed description of the intervention given | Continence | (1), 2 partial | Wetness episodes, wetness checks, wetness detection, nappy changes | Caregiver understanding/acceptance of intervention, fidelity to trial protocol, positioning of wetness sensor | Minimisation of leakage |
| Use of a device that applies external kneading-like force on the abdomen for treatment of constipation (Mimidis et al., 2005156) | Second search | NH | Greece/Israel | Intervention: use of a device that applies a kneading force to the abdomen to treat constipation | Basic demographic data are given for resident sample, intervention and data collection are described | Continence | 6 | Bowel movement rate, stool volume and consistency | Continence (constipation relief) | |
| The effect of vibration therapy on bowel stimulation in elderly patients with dementia – a pilot study (Haig, 2000208) | Second search | UK | Intervention | Article unavailable | Continence | Frequency of bowel movement enema/laxative use recording of adverse events. Note that we were not able to source the paper |
Appendix 8 Quality assessment of included randomised controlled trials
Faecal INcontinence in people with advanced dementia resident in Care Homes study: assessment of randomised controlled trials – modified version of Cochrane risk-of-bias tool
Assessed on the following:
-
percentage of those eligible who took part
-
random sequence generation
-
allocation concealment
-
blinding of outcome assessment
-
incomplete outcome assessment (attrition and exclusion).
Each criteria is assessed as DONE (signifies low risk of bias), NOT DONE or NOT REPORTED/NOT CLEAR (signify high risk of bias). Then there is an overall judgement of the quality of the study (high, low or moderate risk of bias).
| Reference and type of study | Quality/rigour | Main results | Notes |
|---|---|---|---|
| Booth et al., 2013;155 RCT |
|
UI symptoms: +, significant improvement in intervention group, p < 0.001 Bowel symptoms: no significant change |
Older people living in care homes or sheltered housing with bothersome bladder and/or bowel dysfunction. 50% UI predominant problem, 7% FI and 43% both bladder and bowel problems (bowel mainly constipation not FI) Excluded people with moderate or severe cognitive impairment Outcomes: ICIQ-SF bowel questions and American Urological Association Symptom Index |
| Chenoweth et al., 2009;194 cluster RCT |
|
Agitation: +, significantly lower in sites providing DCM (mean CMAI difference 10.9 points, 95% CI 0.7 to 21.2) and PCC (13.6, 95% CI 3.3 to 23.9) Psychiatric symptoms: –, significant trend over time in PCC sites, p = 0.04 Quality of life (measured by QUALID): no significant effect Falls: –, proportion of residents experiencing falls decreased (pre to post) with DCM but increased with PCC and usual care. Fewer falls with DCM than TAU (p = 0.02) but more falls in PCC than TAU (p = 0.03) |
Included people with dementia over the age of 60 (excluded those with serious comorbidities or receiving palliative care) Intervention was implemented by the researchers |
| Fossey et al., 2006;108 cluster RCT |
|
Proportion of residents prescribed neuroleptics: –, 23% in intervention homes vs. 42% in control homes: average reduction of 19.1% (95% CI 0.5% to 37.7%) Proportion of residents taking other psychotropic drugs: 63% in intervention group vs. 57% in control group, –, a non-significant difference (5.9%, –27.2% to 15.5%) Falls: –, no significant differences Mean level of agitation and disruptive behaviour (CMAI): –, no significant differences in agitation (MD 0.3, –8.3 to 8.9) or aggression (average difference 1.6%, –12.7% to 15.8%) Quality of life: –, no significant differences |
12 specialist nursing homes for people with dementia Follow-up at 12 months |
| Hoeffer et al., 2006;172 RCT |
High risk of bias |
Gentleness and verbal support measured using Caregiver Bathing Behaviour Rating Scale: –, found improvements on gentleness, verbal support, confidence and ease but not on hassle | Aim: to test the efficacy of two bathing interventions, PCC vs. standard care and the impact on caregiving behaviour for people with dementia Assessment at baseline, 3 weeks and 6 weeks Three groups: (1) PCC showering, then towel bathing; (2) towel bathing then showering; and (3) TAU Collected observational data |
| Hu et al., 1989;160 RCT |
|
Frequency UI: –, by 6 weeks the change in the number of wet episodes became statistically significant for the intervention group, p < 0.01. Reduction of about 0.4 episodes a day, by 7–9 weeks a reduction of 0.5 episodes a day and by 10–12 weeks a reduction of 0.6 per day. During 6-month follow-up improvement was maintained at 0.5 episodes per day | Baseline observations for 3 weeks Standardised hourly checking of wet episodes (14 times a day between 7 a.m. and 9 p.m.) Intervention group – more frequent self-initiated requests for help Those with higher MMSE scores had a better chance to improve (might tie in to the point above about self-initiated requests) – may be less useful for people with severe dementia |
| Namazi, 1991;159 crossover RCT |
|
Toilet use: –, greater when toilet visible | Concealed and visible conditions for toilet use for PLWD in long-term care. Early- and middle-stage dementia Closed curtain vs. open curtain Tape applied to toilet handle and broken tape taken to mean toilet had been used and flushed |
| Rapp, 2013;251 cluster RCT |
Moderate risk of bias |
Agitation: + (assessed using CMAI), significant change in score in intervention compared with control adjusted MD 6.24, 95% CI 2.03 to 14.14 Psychotropic prescribing: +, significant decrease |
Nursing home residents with dementia |
| Schnelle et al., 2010;102 RCT |
|
Frequency UI: +, p < 0.05 Rate of appropriate toileting UI: +, p < 0.88 Significant interaction between MMSE and treatment with those with higher MMSE scores responding less well to treatment, p = 0.05 Frequency FI: no significant effect when all participants included Rate of appropriate toileting FI: 52% difference in favour of intervention group. Participants with lower MMSE scores responded better to treatment |
FI and UI ascertained by 2-hourly checks over a period of 10 days: % of checks in which participant had UI or FI was calculated Appropriate toileting calculated by dividing n of voids in the toilet by total n of voids Duration of intervention: 12 weeks 45% of participants had no bowel movement |
Appendix 9 Presentation to stakeholders
Glossary
Realist methodology-specific definitions
See also Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. Research Methods Programme Methods Paper 2/2004. Manchester: Economic and Social Research Council Research Methods Programme, University of Manchester; 2004.
- Context
- The ‘backdrop’ conditions (which may change over time), for example the provision of training in faecal incontinence continence care, residents’ level of nutrition and hydration, and the cost of continence aids. Context can be broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism.
- Mechanism
- The generative force that leads to outcomes. Often denotes the reasoning (cognitive or emotional) and responses of the various ‘actors’, that is, care home staff, residents, relatives and health-care professionals. Mechanisms are linked to, but are not the same as, the strategies of a service. Identifying the mechanisms goes beyond describing ‘what happened’ to theorising ‘why it happened, for whom and under what circumstances’.
- Mid-range theory
- Delimited in its area of application, intermediate between a working hypotheses for testing and an all-inclusive grand theory about how to improve continence care.
- Outcome
- Intervention outcomes, for example a reduction in episodes of faecal incontinence, resident distress and costs and an increase in staff confidence.
- Programme theory
- Practical and specific to each programme or intervention, a programme theory specifies the components of a programme (or intervention) intended to mitigate or resolve the problem and the expected outcomes. It is explicit about the rationale and assumptions about mechanisms that link a programme’s processes and inputs to outcomes – and specifies the conditions (or context) necessary for change. For the purposes of this synthesis, the six programme theories draw on both explicit accounts of how continence interventions are believed to work and an interpretation by the research team, derived from the interviews and scoping work, of what needs to be in place for effective working.
Setting-specific definitions
The following are the definitions of a number of terms that are often used interchangeably. In this report, ‘care home’ is used as the overarching term for all residential care for older people with on-site care services. The key difference between settings is whether or not they have on-site nursing provision.
- Care home
- A residential setting where a number of older people live and have access to on-site care services, for example meals and personal care (such as help with washing and eating). Care homes may also provide nursing care. A home registered as a care home will provide personal care only (help with washing, dressing and giving medication) and/or care with on-site nursing. Colloquially, a care home is often called a residential care home or a nursing home. Some care homes are officially recognised as specialist providers, for example in dementia or palliative care.
- Long-term care facility
- The definition of a long-term care facility is synonymous with that of a care home or residential aged care facility; a long-term care facility is a residential setting that provides on-site care of services designed to meet a person’s health or personal care needs for a short or long period of time.
- Nursing home
- The same as a care home; however, it will also have registered nurses who can provide care for more complex health needs. Homes registered for nursing care may accept people who have only personal care needs but who may need nursing care in the future.
- Residential aged care facilities
- A term used in Australia to describe facilities for older people that offer personal and/or nursing care as well as accommodation. It is synonymous with a care home in a UK context.
Continence-specific definitions
- Constipation
- Infrequent, and frequently incomplete, bowel movements that are associated with hard stools, that is, being unable to have a bowel movement easily.
- Containment (or contained incontinence)
- Urine or faeces contained with appropriate pads or appliances.
- Continence
- The ability to control the bladder and bowels.
- Dependent continence (or controlled continence)
- Incontinence that occurs when receiving help getting to, using or being prompted to use a toilet facility.
- Digital rectal examination
- The manual examination of a person’s rectum and anus by a trained clinician/practitioner.
- Double incontinence
- Incontinence of both urine and faeces.
- Faecal impaction
- A solid, immobile bulk of faeces that can develop in the rectum as a result of chronic constipation.
- Faecal incontinence
- The leakage of solid or liquid stool that is a social or hygiene problem. Note that the definition of faecal incontinence is expanded and refined as part of this study.
- Faecal loading
- A large volume of stool, of any consistency, in the rectum.
- Incontinence
- The lack of ability to control the bladder and bowels, that is, when a person is wet or soiled of urine or faeces.
- Independent continence
- Unconditional continence not requiring medication, ongoing behavioural approaches or assistance of any sort to achieve this situation.
- Urinary incontinence
- Involuntary or accidental loss of urine that is a social or personal hygiene problem.
Realist methodology-specific definitions
See also Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction. Research Methods Programme Methods Paper 2/2004. Manchester: Economic and Social Research Council Research Methods Programme, University of Manchester; 2004.
- Context
- The ‘backdrop’ conditions (which may change over time), for example the provision of training in faecal incontinence continence care, residents’ level of nutrition and hydration, and the cost of continence aids. Context can be broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism.
- Mechanism
- The generative force that leads to outcomes. Often denotes the reasoning (cognitive or emotional) and responses of the various ‘actors’, that is, care home staff, residents, relatives and health-care professionals. Mechanisms are linked to, but are not the same as, the strategies of a service. Identifying the mechanisms goes beyond describing ‘what happened’ to theorising ‘why it happened, for whom and under what circumstances’.
- Mid-range theory
- Delimited in its area of application, intermediate between a working hypotheses for testing and an all-inclusive grand theory about how to improve continence care.
- Outcome
- Intervention outcomes, for example a reduction in episodes of faecal incontinence, resident distress and costs and an increase in staff confidence.
- Programme theory
- Practical and specific to each programme or intervention, a programme theory specifies the components of a programme (or intervention) intended to mitigate or resolve the problem and the expected outcomes. It is explicit about the rationale and assumptions about mechanisms that link a programme’s processes and inputs to outcomes – and specifies the conditions (or context) necessary for change. For the purposes of this synthesis, the six programme theories draw on both explicit accounts of how continence interventions are believed to work and an interpretation by the research team, derived from the interviews and scoping work, of what needs to be in place for effective working.
Setting-specific definitions
The following are the definitions of a number of terms that are often used interchangeably. In this report, ‘care home’ is used as the overarching term for all residential care for older people with on-site care services. The key difference between settings is whether or not they have on-site nursing provision.
- Care home
- A residential setting where a number of older people live and have access to on-site care services, for example meals and personal care (such as help with washing and eating). Care homes may also provide nursing care. A home registered as a care home will provide personal care only (help with washing, dressing and giving medication) and/or care with on-site nursing. Colloquially, a care home is often called a residential care home or a nursing home. Some care homes are officially recognised as specialist providers, for example in dementia or palliative care.
- Long-term care facility
- The definition of a long-term care facility is synonymous with that of a care home or residential aged care facility; a long-term care facility is a residential setting that provides on-site care of services designed to meet a person’s health or personal care needs for a short or long period of time.
- Nursing home
- The same as a care home; however, it will also have registered nurses who can provide care for more complex health needs. Homes registered for nursing care may accept people who have only personal care needs but who may need nursing care in the future.
- Residential aged care facilities
- A term used in Australia to describe facilities for older people that offer personal and/or nursing care as well as accommodation. It is synonymous with a care home in a UK context.
Continence-specific definitions
- Constipation
- Infrequent, and frequently incomplete, bowel movements that are associated with hard stools, that is, being unable to have a bowel movement easily.
- Containment (or contained incontinence)
- Urine or faeces contained with appropriate pads or appliances.
- Continence
- The ability to control the bladder and bowels.
- Dependent continence (or controlled continence)
- Incontinence that occurs when receiving help getting to, using or being prompted to use a toilet facility.
- Digital rectal examination
- The manual examination of a person’s rectum and anus by a trained clinician/practitioner.
- Double incontinence
- Incontinence of both urine and faeces.
- Faecal impaction
- A solid, immobile bulk of faeces that can develop in the rectum as a result of chronic constipation.
- Faecal incontinence
- The leakage of solid or liquid stool that is a social or hygiene problem. Note that the definition of faecal incontinence is expanded and refined as part of this study.
- Faecal loading
- A large volume of stool, of any consistency, in the rectum.
- Incontinence
- The lack of ability to control the bladder and bowels, that is, when a person is wet or soiled of urine or faeces.
- Independent continence
- Unconditional continence not requiring medication, ongoing behavioural approaches or assistance of any sort to achieve this situation.
- Urinary incontinence
- Involuntary or accidental loss of urine that is a social or personal hygiene problem.
List of abbreviations
- BBF
- Bladder and Bowel Foundation
- BGS
- British Geriatrics Society
- BPSD
- behavioural and psychological symptoms of dementia
- C–M–O
- context–mechanism–outcome
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- DASF
- data analysis and synthesis form
- FI
- faecal incontinence
- FINCH
- Faecal INcontinence in people with advanced dementia resident in Care Homes
- GP
- general practitioner
- MMSE
- Mini-Mental State Examination
- NICE
- National Institute for Health and Care Excellence
- PCC
- patient-centred care
- PLWD
- people living with dementia
- PV
- prompted voiding
- RCT
- randomised controlled trial
- RMT
- Research Management Team
- RN
- registered nurse
- SSC
- Study Steering Committee
- UI
- urinary incontinence