Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/33/03. The contractual start date was in November 2012. The draft report began editorial review in February 2016 and was accepted for publication in August 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Joanna M Charles and Rhiannon T Edwards declare grants from Public Health Wales outside the submitted work. Clare Wilkinson is the chairperson of the Health Technology Assessment programme Commissioning Panel – Primary Care Community Preventive Interventions.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Williams et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Proximal femoral fracture, more commonly referred to as hip fracture, is a common major health problem in old age. It refers to a fracture in the area between the femoral head and 5 cm distal to the lesser trochanter. These fractures are further subdivided into those proximal to the insertion of the joint capsule, termed intracapsular, subcapital or femoral neck fractures, and those distal to the joint capsule, termed extracapsular, which can be split further into trochanteric and subtrochanteric fractures. The total number of patients entered into the National Hip Fracture Database in England, Wales and Northern Ireland in 2012/13 was 61,5081 and, as the population ages, the number of elderly people falling and fracturing their hips is projected to increase further. Hip fracture is strongly associated with decreased bone mineral density, increased age, prior fragility fracture, cognitive impairment, other health problems, undernutrition, frailty, poor physical functioning, vision problems and weight loss. 2 Mortality is high, with 25% of patients dying within the following 12 months. A review of the long-term disability associated with proximal femoral fracture found that 29% of patients did not regain their level of functioning after 1 year in terms of restrictions in activities of daily living (ADL). 3 Many who were living independently before their fracture lose their independence afterwards and so a large cost burden on society is imposed, amounting to about £2B per year. 4 Particularly frail individuals may go on to have a further proximal femoral fracture, resulting in additional disability and death. Risk factors for subsequent fracture include older age, cognitive impairment, lower bone mass, impaired depth perception, impaired mobility, previous falls, dizziness and poor self-perceived health. 5
Three phases of recovery from proximal femoral fracture have been proposed. 6 The first phase occurs in hospital, with the patient recovering from injury and surgery and becoming safe to discharge. The second phase consists of rehabilitation, either in an institution or at home. The final phase is the enduring stage in which patients use their own previous health belief strategies to determine if and when they have recovered. The National Institute for Health and Care Excellence (NICE) has issued guidelines for the management of hip fracture. 7 As well as prompt surgical treatment, the guidelines recommend that associated medical needs are assessed promptly by a physician specialised in caring for this patient group, who can also identify goals for a programme of multidisciplinary rehabilitation. Such rehabilitation starts while in hospital during post-operative recovery and continues in the community following hospital discharge. Patients should be offered physiotherapy assessment and mobilisation on the day after surgery unless medically or surgically contraindicated. They should be offered mobilisation at least once a day and receive regular physiotherapy. They should receive a formal hip fracture programme that includes all of the following: orthogeriatric assessment, rapid optimisation of fitness for surgery, early identification of individual goals for multidisciplinary rehabilitation to recover mobility and independence and, to facilitate return to pre-fracture residence and long-term well-being, continued co-ordinated orthogeriatric and multidisciplinary review, and communication with the primary care team. Patients with cognitive impairment should be actively sought and offered individualised care to minimise delirium and maximise independence.
Rehabilitation has the potential to maximise recovery, enhance quality of life and maintain independence, but what is the evidence in this patient group? There have been three relevant Cochrane systematic reviews. 8–10 A review of multidisciplinary rehabilitation for older people with hip fractures identified 13 randomised controlled trials (RCTs) involving 2498 older patients who received rehabilitation interventions following hip fracture surgery. 8 The majority of participants in these RCTs were women, with a mean age of 78–84 years. There was substantial clinical heterogeneity in the trial populations and the trial interventions. Inpatient rehabilitation was examined in 11 RCTs. In six of these trials patients either were transferred to a geriatric orthopaedic rehabilitation unit (intervention group) or received usual care from the orthopaedic team (control group). The main component of the intervention was close co-operation between geriatricians and orthopaedic surgeons in the medical care of patients, together with multidisciplinary teamwork from allied health professionals. Four inpatient RCTs compared a more intensive rehabilitation programme with usual rehabilitation care. The intervention consisted of early assessment by a rehabilitation physician or geriatrician, an emphasis on re-establishing physical independence and discharge planning. One RCT compared multidisciplinary rehabilitation in a geriatric ward with care in local community hospitals supervised by general practitioners (GPs). Two RCTs examined home-based rehabilitation. One RCT compared discharge home after 48 hours to home-based interdisciplinary rehabilitation with usual hospital-based interdisciplinary rehabilitation. The home-based intervention concentrated on early resumption of self-care and domestic activities. The other RCT compared intensive home-based rehabilitation (six weekly visits) with less intensive home-based rehabilitation (three or fewer weekly visits). A meta-analysis of eight RCTs examining multidisciplinary inpatient rehabilitation combined death and deterioration as ‘poor outcome’ and showed a non-statistically significant tendency in favour of the intervention at long-term follow-up [risk ratio 0.89, 95% confidence interval (CI) 0.78 to 1.01]. All 11 RCTs of inpatient rehabilitation reported mortality and a meta-analysis found no statistically significant difference (risk ratio 0.90, 95% CI 0.76 to 1.07) between the groups. Hospital readmissions were reported in six RCTs but did not differ significantly between the groups (risk ratio 0.99, 95% CI 0.82 to 1.19). Individual RCTs found better results in the intervention group than the control group for ADL. There was much heterogeneity in the data for length of hospital admission and costs. Carer burden was not increased by the intervention in three RCTs. The RCT comparing home-based rehabilitation with inpatient care found a marginal improvement in function for patients and a clinically significant reduction in burden for carers in the intervention group. The RCT examining different intensities of home-based rehabilitation found no difference between the groups. Overall, the review concluded that the results were inconclusive and that more RCTs examining clinical effectiveness and cost-effectiveness were needed.
A systematic review of mobilisation strategies9 identified 19 small RCTs and quasi-RCTs involving 1589 participants. Twelve of these examined early mobilisation strategies following surgery. Single trials found improvements in mobility from an early weight-bearing programme, quadriceps muscle strengthening and pain-relieving electrical stimulation. Single trials did not find a significant improvement in mobility following treadmill gait retraining, a 12-week resistance training programme and a 16-week programme of weight-bearing exercise. There were contradictory results from an early ambulation intervention. One trial that was 40 years old did not find any significant differences between starting weight bearing at 2 weeks or starting weight bearing at 12 weeks. Two trials evaluated more intensive physiotherapy, with one finding no differences between the intervention group and the control group and one reporting a higher dropout rate in the intervention group. Two trials tested electrical stimulation of the quadriceps. In one of the trials this was poorly tolerated and ineffective, whereas in the other it was well tolerated and improved mobility. Seven trials examined community interventions following hospital discharge. Two trials found that exercise interventions started soon after discharge were effective. One of these compared 12 weeks of intensive physical training with placebo motor activities; the other compared a home-based physical therapy programme with unsupervised home exercises. Five trials began after usual physical therapy care had been completed and compared an extra physical training intervention with no or a low-intensity intervention. The results of these trials were mixed. One trial found increased activity levels after 1 year of exercises led by a personal trainer. One trial found improved outcome after 6 months of intensive physical training, whereas another trial found no significant effects of 12 weeks of home-based resistance or aerobic training. One trial found improved outcome after practice of home-based exercises started at 22 weeks, whereas another trial found that home-based weight-bearing exercises started at 7 months were ineffective. In conclusion, it was possible to enhance mobility after hip fracture, but the best method to achieve this was unclear. There was insufficient evidence to determine the effects of any particular mobilisation strategy.
Psychological factors such as fear of falling, perceived control and coping strategies have been identified as influencing recovery following hip fracture. 11–14 Fear of falling is present in at least half of patients following hip fracture. It is associated with loss of mobility, institutionalisation and mortality and is related to less time spent on exercise and an increase in falls. 14 Psychosocial factors associated with healthy ageing are protective, such as being married, living in present accommodation for at least 5 years, having private health insurance, using proactive coping strategies, having a high level of life satisfaction and engagement in social activities. 15 A systematic review of rehabilitation for improving physical and psychosocial functioning after hip fracture identified nine small RCTs involving 1400 patients. 10 The trials were clinically heterogeneous and involved different interventions, providers, settings and outcomes. Three RCTs examined inpatient interventions: reorientation measures, intensive occupational therapy and cognitive–behavioural therapy. These trials found no significant differences in outcomes between the intervention group and the control group. Two RCTs examined nurse specialist care carried out mostly or completely after hospital discharge, with one finding a short-term reduction in ‘poor outcome’ in the intervention group and the other finding no differences between the groups. Two RCTs examined educational and motivational coaching. One trial in hospital found that educational and motivational coaching had no effect on function or mortality at 6 months; the other trial, which started at home after discharge from rehabilitation, found that coaching improved self-efficacy at 6 months, but not when combined with exercise. Two RCTs starting several weeks after hip fracture found no effect on outcomes of home rehabilitation and a group learning programme. Further research on psychosocial interventions was recommended.
Patients with cognitive impairment make up a large proportion of patients presenting with a hip fracture and several studies have shown a worse outcome for cognitively impaired patients following hip fracture. 16 Indeed, patients with cognitive impairment were either excluded from or not commented on in 60% of hip fracture studies reviewed for the NICE guidelines. 7 However, a systematic review of rehabilitation in patients with dementia following hip fracture found that those with mild to moderate dementia showed similar relative gains in function to those without dementia. 17 In addition, hip fracture patients with cognitive impairment are at increased risk of delirium, medical complications, death, prolonged stay and loss of independence. According to the NICE guidelines on delirium,18 patients with memory problems are known to benefit from comprehensive geriatric assessment and targeted intervention to reduce the risk of delirium.
The NICE clinical practice guideline for the assessment and prevention of falls in older people19 is relevant for the secondary prevention of falling in hip fracture patients. The guidelines recommend that older people with recurrent falls should be considered for an individualised multifactorial intervention programme including strength and balance training, home hazard assessment and intervention, vision assessment and referral and medication review with modification and withdrawal of psychotropic medication. Following treatment for an injurious fall, such as a hip fracture, older people should be offered a multidisciplinary assessment to identify and address future risks and individualised intervention to promote independence and improve physical and psychological function.
In conclusion, previous systematic reviews have not found sufficient evidence that multidisciplinary rehabilitation programmes have demonstrated overall effectiveness or cost-effectiveness. Individual components of such packages show promise, but it needs to be determined which components work for which patient group in which circumstances. Guidelines have stated that rehabilitation programmes may be effective but that more research is needed.
Study objectives
Phase I: developing the intervention
-
To undertake a realist review to identify the important components of a multidisciplinary rehabilitation programme following surgical treatment for hip fracture in older people and to understand the mechanism, context and outcome of successful interventions.
-
To assess the current provision of rehabilitation programmes following hip fracture surgery in the NHS throughout the UK.
-
To assess the views of patients, their carers and health professionals in multidisciplinary rehabilitation teams on the rehabilitation that they received or provided following surgical repair of a proximal hip fracture; how programmes could be improved; and the findings from the realist review and survey.
-
To design a rehabilitation programme based on the findings from the realist review, survey and focus groups.
Phase II: feasibility study
-
To assess the feasibility of a future definitive RCT by assessing the number of eligible patients, monitoring recruitment and retention rates and exploring the willingness of patients to be randomised and the willingness of patients and carers to complete process and outcome measures.
-
To produce means and standard deviations (SDs) of the quantitative measures so that effect sizes can be calculated for planning the future RCT.
-
To assess the acceptability of, and compliance with, the rehabilitation programme among patients, carers and clinicians and the fidelity of its delivery and to identify any adverse events (AEs).
-
To explore the methodological issues associated with conducting an economic evaluation alongside a future RCT.
Study design
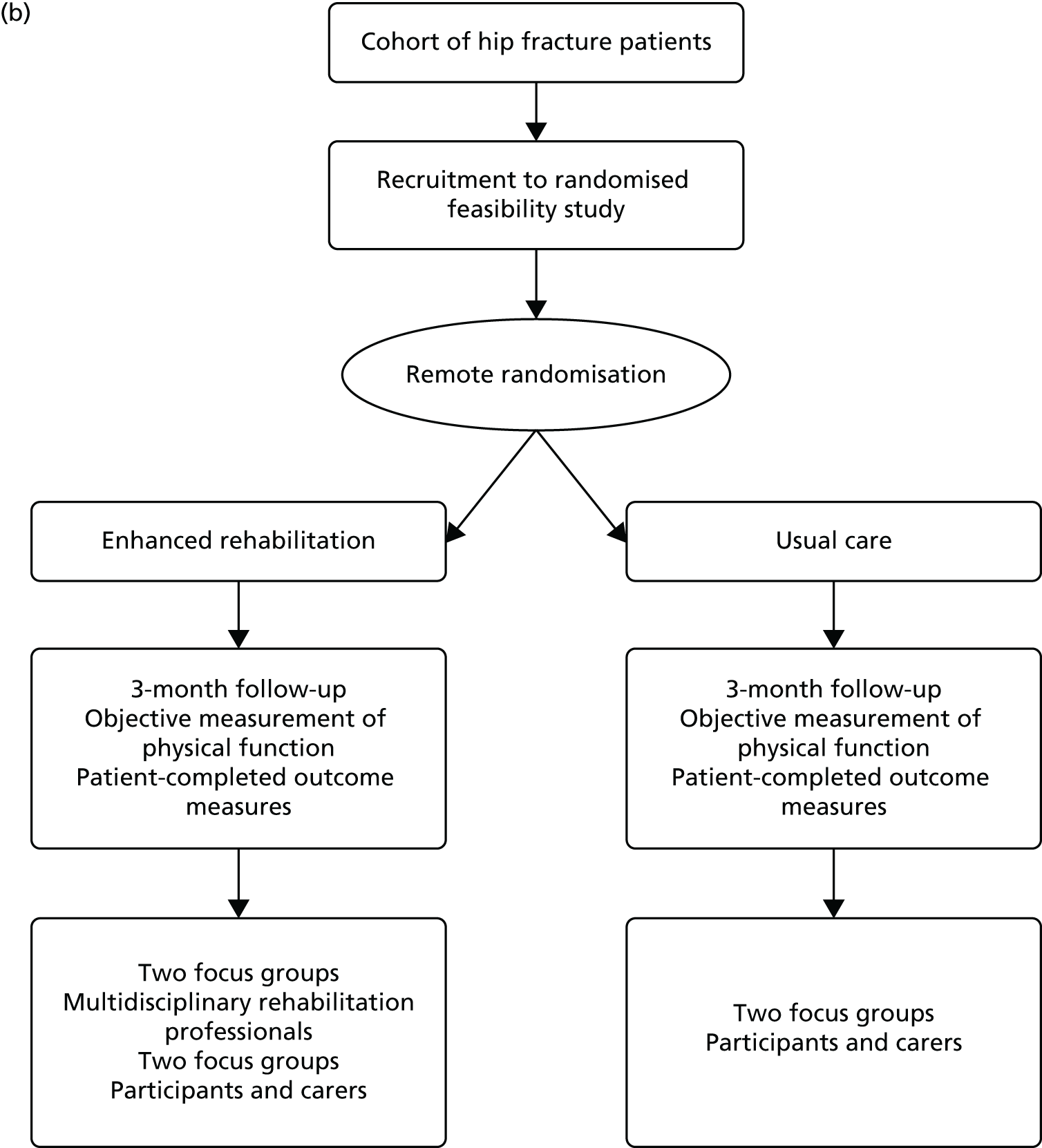
This was a preliminary study to complete the first two stages of the Medical Research Council’s framework for the development of complex interventions. 20 In the first stage a realist literature review was used to identify the relevant existing evidence base and a coherent theoretical basis for the rehabilitation intervention was developed. The literature review incorporated the principles of realist synthesis to identify the implicit or explicit theories that explain the mechanisms of interventions (how they are expected to work and why they work or did not work). 12–15 A survey of current services determined usual practice and was an additional source of relevant theories that contributed to the realist synthesis review. Focus groups with multidisciplinary rehabilitation teams, as well as hip fracture patients and their carers, informed the design of a complex multicomponent community-based rehabilitation programme (Figure 1a). The second stage assessed the feasibility of the new rehabilitation programme and consisted of a randomised feasibility study to assess recruitment and retention rates, the acceptability of randomisation and the change in outcome measure scores for a sample size calculation for a future definitive trial. A cohort study of all hip fracture patients admitted to the three acute hospitals in the Betsi Cadwaladr University Health Board (BCUHB), North Wales, over a 6-month period allowed us to assess the representativeness of our recruited population. The acceptability and feasibility of the new rehabilitation programme was assessed further using focus groups with multidisciplinary rehabilitation team members and hip fracture patients and their carers (see Figure 1b).
FIGURE 1.
Study flow chart: (a) Phase I – developing the new rehabilitation intervention; and (b) Phase II – cohort and feasibility study.

Chapter 2 Developing a community-based multidisciplinary rehabilitation package for hip fracture patients using realist review methods: Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR)
Background
Previous systematic reviews3,9,10,21–38 have found insufficient evidence for the overall effectiveness or cost-effectiveness of multidisciplinary rehabilitation programmes following proximal femoral fracture. However, the recommendations made by such reviews, as well as existing guidelines, suggest that individual components show promise but it needs to be determined which components work for which patient groups in which circumstances. The hip fracture population is heterogeneous and the important contextual factors need to be determined. NICE guidelines7 for the management of hip fracture relevant to rehabilitation interventions recommend the following research:
What is the clinical and cost-effectiveness of additional intensive physiotherapy or occupational therapy (for example, resistance training) after hip fracture? The rapid restoration of physical and self-care functions and the maintenance of independent living are important goals. Approaches worthy of future development and investigation include progressive resistance training, progressive balance and gait training, supported treadmill gait re-training, dual task training and Activities of Daily Living training.
National Institute for Health and Care Excellence’s publication entitled Hip Fracture: Management. Available from www.nice.org.uk/guidance/cg124. 7 NICE guidance is prepared for the National Health Service in England, and is subject to regular review and may be updated or withdrawn. NICE has not checked the use of its content in this publication to confirm that it accurately reflects the NICE publication from which it is taken. The information provided by NICE was accurate at the time this publication was issued
Rationale for the review
This realist review, along with a national UK survey of current rehabilitation practice and focus groups with patients, carers and multidisciplinary rehabilitation teams, was performed to inform the development of an enhanced rehabilitation programme following proximal femoral fracture.
Objectives and focus of the review
The main objective of this review was to identify the important components of a multidisciplinary rehabilitation programme following surgical treatment for hip fracture in older people, in particular to distil and understand the evidence relating to how successful interventions work, in which setting and context, for which outcome and in which group of patients.
Research questions
-
What community-based multidisciplinary rehabilitation programmes have been developed and what were their main aims (intended outcomes)?
-
What were the mechanisms by which community-based rehabilitation of hip fracture patients is believed to result in its intended outcomes?
-
What are the identified contexts that determine whether different mechanisms yield intended outcomes?
Given the evidence in response to questions 1–3 we also drew conclusions regarding the following questions.
-
In what circumstances are the rehabilitation programmes likely to be clinically effective and cost-effective if implemented in the NHS?
-
In what circumstances and with which combination of mechanisms and contexts are the rehabilitation programmes likely to generate unintended effects or costs?
Methods
Rationale for using realist synthesis
A realist review was undertaken to identify suitable components for an enhanced multidisciplinary rehabilitation programme following proximal femoral fracture. Such rehabilitation programmes are complex interventions because they are multifaceted and interact in complex ways with many contextual factors39 (see Appendix 1). Compared with systematic reviews, realist reviews aim to build a deeper understanding of the mechanisms behind an intervention and to identify ‘what works, for whom, in what circumstances and why’. 39,40 Whereas conventional systematic reviews judge the overall effectiveness of an intervention and pay less attention to context, realist reviews attempt to explain mechanisms by which interventions produce different patterns of outcomes according to different contextual factors (see Appendix 2). The realist review was conducted by a researcher experienced in large-scale systematic reviews, traditional and network meta-analyses, large-scale database analyses and mixed-method process evaluations of policy or intervention trials, supported by team members with expertise in realist review and realist evaluation methodology.
Realist reviews use a theory-driven approach with a philosophy of realism and adopt an explanatory rather than a judgemental approach to evidence synthesis. 40 They seek to produce more transferable findings by taking into account, for example, the heterogeneous nature of rehabilitation programmes and the heterogeneous hip fracture population. The findings are then formulated into statements, the ‘programme theories’, which are propositions for how a programme is considered to produce intended outcomes. They can be generated from various sources of evidence such as the literature, discussions with experts and, as in our study, a survey of current practice (see Chapter 4) and focus groups with patients, carers and rehabilitation professionals (see Chapter 5). During the review process, these intermediate theories are tested, rejected or developed into the final programme theories to make recommendations for future practice, policy and research. We used the guidelines developed by the RAMESES (Realist And Meta-narrative Evidence Syntheses: Evolving Standards) collaboration41,42 (see Appendix 3) to report our methods and findings.
Extending the realist review to include any economic evidence allows the consideration of behavioural economic theories relating to factors such as welfare judgements,43 expected utility gains44 and choice architecture. 45 Additional costs may be accrued when modifying the setting in which the rehabilitation takes place (e.g. home based vs. hospital based) or the delivery team responsible for the rehabilitation programme (e.g. multidisciplinary vs. a single practitioner). The intervention itself could accrue additional costs, for example through additional training required by practitioners, additional time required by practitioners to deliver the rehabilitation programme and additional technology or equipment required for the rehabilitation programme (e.g. instruction packs for exercises). However, we recognised that the literature may not be rich enough to provide understanding of all behavioural economic factors in this field.
Scoping the literature
A scoping search of the literature was carried out in MEDLINE, EMBASE and PubMed for relevant systematic reviews concerning multidisciplinary rehabilitation following hip fracture and stroke and in the frail elderly using the broad search terms ‘rehabilitation’, ‘frail’, ‘elderly’, ‘stroke’, ‘hip/femur fracture’. The reviews identified3,5,9,10,14,17,21–38,46–60 and their reference lists were the starting point for identifying both the implicit and the explicit theories behind the success or failure of rehabilitation programmes or their components. Existing UK and international guidelines were also searched for additional contributions to theory development.
Immersion in the literature to develop initial theory areas
Initial immersion in the rehabilitation literature sought to identify an initial list of relevant intermediate programme theories. We scanned relevant primary studies and other linked papers with a strong theoretical content identified from the reference lists of the included reviews. This process helped to map out important areas and research gaps in the literature, resulting in a list of unanswered questions under different domains related to receivers (patients), deliverers (health-care and rehabilitation teams), programmes (rehabilitation) and settings or systems (hospital, community, etc.) used to deliver such rehabilitation programmes (see Appendix 4).
Developing and refining the intermediate programme theories in interactive workshops
These lists of questions were formulated into statements (see Appendix 5) to signify how the different domains of a programme interact and might affect all of the agencies (stakeholders) involved. These intermediate programme theories were refined during discussions between members of the evaluation team and with other researchers engaged in similar realist evaluations (at two realist evaluation workshops in the School of Healthcare Sciences, Bangor University, convened by one of the senior researchers, JR-M). To keep track of these emerging programme theories a table was constructed in which the theories could be recorded, cross-referenced and commented on. Feedback from the workshops was integrated into this table.
The list of questions enabled the building of context, mechanism and outcome (CMO) configurations that formed the basis of the development of the final programme theories of how complex programmes (systems) work in certain contexts to produce intended (or unintended) outcomes. The initial list of these CMO configurations is presented in Appendix 6; again, this was refined iteratively in team meetings.
Feedback from patient/carer interviews and the health professional survey
Results from the survey of health professionals (see Chapter 4) and focus groups with patients, carers and rehabilitation professionals (see Chapter 5) were also used to refine these programme theories. These refined theories were incorporated into the review as it progressed. Findings from the health professional survey that contributed to theory development included the importance of tailoring, the importance of feedback mechanisms and variation in the delivery of rehabilitation in different areas based on the availability of staff and facilities (see Chapter 4). The focus groups with patients and their carers highlighted unmet information needs with regard to the process of recovery, the availability of services that patients are entitled to access but which they are not necessarily aware of and geographical variation in the provision of services (see Chapter 5).
Developing programme theories
As already described, the summary of findings from our initial immersion in the literature, feedback from meetings and workshops (from experts in health psychology, rehabilitation and implementation research) and the findings from the patient/carer focus groups and health professional survey were integrated into our candidate programme theories. The emergent list of intermediate working theories was used as the basis for the development of bespoke data extraction forms.
Developing bespoke data extraction forms
Two sets of bespoke data extraction forms were developed using a Microsoft Access® database (2013; Microsoft Corporation, Redmond, WA, USA) to extract data from both comparative studies (RCTs/quasi-RCTs/non-RCTs, comparative cohort and case–control studies) and non-comparative studies (qualitative studies involving patients or health professionals, service evaluations, routinely collected database studies). The data extraction form for comparative studies (see Tables 37 and 38) was designed to collect data from each study on study characteristics (design, sample type, sample size), the intervention/programme and the control, process details (fidelity of the intervention, dosage), contextual factors in the study setting, outcomes collected and theories or mechanisms postulated by the authors to explain the results. The data extraction form for non-comparative studies (see Table 39) was designed to collect data on study characteristics, research methods, the theoretical approach, the sample type, the intervention/programme and the method of analysis as well as evidence to test the programme theories.
The forms were used in two stages to extract data from included studies and test the intermediate and final programme theories. The first set of forms was used to populate the initial themes with evidence from effective (or ineffective) components of rehabilitation programmes and how these interacted with outcomes in given contexts. These themes were then refined into statements, which led to the development of intermediate programme theories. The second set of forms was used to test these theories and adjudicate between competing theories (see Table 40).
Literature search
The literature search strategy used in the NICE guideline review of multidisciplinary rehabilitation programmes for hip fracture7 was adapted to encompass all of the theory areas of the first phase of the review process. No filters for study design were applied so that all study designs such as RCTs and non-RCTs and observational, economic and qualitative studies could be included. Full details of the search strategies for the major electronic databases are reported in Appendix 8.
The following databases were searched from inception to February 2013 for published, semi published and grey literature:
-
MEDLINE
-
MEDLINE In-Process & Other Non-Indexed Citations
-
OLDMEDLINE
-
EMBASE
-
Cumulative Index to Nursing and Allied Health Literature
-
Allied and Complementary Medicine Database
-
British Nursing Index
-
Health Management Information Consortium
-
PsycINFO
-
Cochrane Central Register of Controlled Trials
-
Database of Abstracts of Reviews of Effects
-
Cochrane Database of Systematic Reviews
-
Health Technology Assessment database
-
NHS Economic Evaluation Database
-
Science Citation Index
-
Social Science Citation Index
-
Index to Scientific & Technical Proceedings
-
Physiotherapy Evidence Database
-
Biosciences Information Service
-
System for Information on Grey Literature in Europe
-
ProQuest Dissertations & Theses database.
Identified references were deduplicated and transferred to bibliographic software (EndNote X5; Thomson Reuters, CA, USA) to facilitate assessment for inclusion and the categorisation of relevant studies. Multiple publications arising from the same study were identified, grouped together and represented by a single reference.
Realist review involves iterative and purposive literature searching39,41 and so citations were tracked (forwards and backwards) and internet search engines, such as Google Scholar (Google Inc., Mountain View, CA, USA), and individual publisher websites were used to identify additional evidence as the review progressed and new ideas emerged. The reference lists of previous systematic reviews and included studies were also screened to identify relevant studies. Using this method, no attempt was made to include every relevant study but materials were retrieved purposively to answer specific questions or test-specific theories. The process stopped when sufficient evidence had been collected to answer these questions or test the theories. Conversely, if a new question arose, it triggered further literature searching to answer the question posed and to determine its fit within existing theory or whether or not a new theory needed to be formulated.
Screening of references for relevance
A working definition of multidisciplinary rehabilitation to be used for screening sources of evidence (Table 1) was adapted from a review of intermediate care services;61,62 the working definition in this review had been adapted, in turn, from Godfrey et al. 63
| Component | Definition |
|---|---|
| Purpose | Supports re-enablement of the frail elderly following proximal hip fracture to achieve their functional potential and maintain independent living when possible |
| Functions | A bridge between (a) the hospital and the community and between (b) different health-care sectors and personal social care |
| Views people holistically | |
| Time limited | |
| Structure | Teams based in hospitals or the community or across both sectors |
| Content | Treatment and therapy (to increase strength, confidence, ADL and functional abilities) |
| Psychological, practical and social support | |
| Support/training to develop skills and strategies | |
| Delivery | Care delivered by a multidisciplinary team or teams |
This definition was used when screening the titles and abstracts of identified studies in the EndNote library for relevance. Screening was carried out independently by separate reviewers and discrepancies were resolved after discussion. In addition, potentially relevant studies were categorised according to study type: systematic review, RCT or non-RCT, observational study, economic evaluation or qualitative study. There were no language restrictions and non-English publications were translated whenever possible using Google Translate (Google Inc., Mountain View, CA, USA) or by other research colleagues who could speak the relevant language.
Participants of interest were elderly adults with proximal hip fracture. The intervention of interest was multidisciplinary rehabilitation following proximal hip fracture. The outcomes of interest were mortality, pain, functional status, quality of life, health utility, health service use, costs and patients’ experiences.
Literature identified in the initial search was screened in two stages for both behavioural economic evidence and evidence of economic evaluation (e.g. cost analysis, cost-effectiveness analysis, cost–benefit analysis, cost–utility analysis). Screening for economic studies at the title and abstract stage was conducted by the four main reviewers. Potential economic studies identified in the initial search were then screened by two experienced health economists, who excluded studies based on the following criteria:
-
clearly falls outside the definition of multidisciplinary rehabilitation for hip fracture (see Table 1)
-
clearly is not an economic evaluation or comparative cost study or does not include behavioural economic theory
-
does not involve services users who belong to our service user group of interest.
The detailed screening process for economic evidence and the study flow chart are presented in Chapter 3.
Conceptual categorisation of screened relevant references
Potentially relevant references were conceptually categorised as ‘rich’, ‘thick’ or ‘thin’ based on the criteria described by Ritzer64 and Roen et al. 65 and as used in a recent review of intermediate care. 61 This process made the database manageable and enabled information to be gleaned from the most appropriate studies for theory building and testing. A detailed description of the criteria used for this purpose is provided in Appendix 9.
Inclusion and exclusion of studies
Study design
All types of studies that presented explicit theories about the success or failure of an intervention in certain contexts or which had implicit information that could be used to confirm or refute a theory were included. Study designs included RCTs, quasi-RCTs, non-RCTs, cohort studies (with concurrent or historical control subjects), case–control studies, before-and-after studies, qualitative studies and full economic evaluations, as defined by Drummond et al. 66 The Cochrane Handbook for Systematic Reviews of Interventions67 provided context related to the strength of evidence.
Patient population
Studies were included involving older adults who had fractured their hip, undergone surgery and received rehabilitation afterwards.
Interventions
Studies were included looking at any intervention or initiative (policy, process, etc.) used as part of a rehabilitation package following hip fracture surgery and delivered in any setting.
Outcomes
All relevant patient-based outcomes, such as pain, disability, functional status, adverse effects, health status, quality of life, health service use and costs, were considered.
Selection and appraisal of documents
After the initial screening and conceptual categorisation of the references in the EndNote library, potentially relevant studies were exported into a separate library for full document retrieval. Study inclusion criteria were applied to these retrieved documents by two reviewers independently and conflicts were resolved by discussion or after consulting a third reviewer. A list of all studies to be included was prepared for data extraction.
Data extraction
Data were extracted by one reviewer and checked for accuracy by a second. Inconsistencies or disagreements were resolved by mutual discussion and checking against the source study.
Comparative effectiveness studies
Data were extracted in the following domains.
-
Study characteristics. Author, year, location and country, setting, design, sample type, sample size, study population, conceptual categorisation.
-
Intervention characteristics. Description of the intervention and control, process details (fidelity of the intervention, dosage), duration of follow-up, any variations in intervention delivery other than those originally planned.
-
Theoretical underpinning. Explicit theories or mechanisms postulated by the authors to explain the results and/or implicit theories derived from the introduction or discussion of the study; contextual factors in the study setting.
-
Outcome measures. We did not extract final mean scores or mean change scores or their distributions because the purpose of the review was not to quantify the strength of effects but to develop an explanation for these effects. The direction of effect was described using the following symbols: ++, intervention effect statistically significant; ==, no statistically significant difference between the intervention and the control; –, control better than the intervention.
Qualitative studies
Data were extracted in the following domains.
-
Study characteristics. Author, year, location and country, setting, design, sample type, sample size, study population, conceptual categorisation, related effectiveness studies.
-
Qualitative methods. Sampling technique, theoretical approach, method of data analysis.
-
Theoretical underpinning. Explicit theories or mechanisms postulated by the authors to explain the results or implicit theories derived from the introduction or discussion of the study; contextual factors in the study setting.
-
Evidence for theory testing or explanation building. Explanations gleaned from qualitative accounts as evidence to test the programme theories.
Quality assessment
Study quality was assessed using the Mixed Methods Appraisal Tool for mixed studies reviews,68 which can be used across different study designs (qualitative studies, trials, observational studies). The purpose of appraising the ‘quality’ of studies was to assist in the judgement of the relevance and rigour of different evidence from a ‘fitness for purpose’ perspective as opposed to scoring the studies for acceptance or rejection.
Data synthesis
The data from the quantitative, comparative effectiveness and qualitative studies were synthesised separately.
The data from the effectiveness studies were exported into structured tables to show the strength and direction of the treatment effects. Outcomes reported in the included studies were broadly categorised into four domains: physical/physiological, psychological, health service utilisation and AEs. These were subcategorised further under the following headings (the outcome measure instruments used are listed in Appendices 10 and 11):
-
physical/physiological
-
ADL
-
composite scores
-
favourable clinical outcome
-
functional recovery
-
-
exercise behaviour
-
quality of life
-
function
-
physical function
-
mobility
-
functional recovery
-
balance
-
-
physiological measurements/muscle strength
-
-
psychosocial
-
patient satisfaction
-
carer satisfaction
-
cognitive function/dementia
-
depression
-
fear of falling
-
psychological morbidity
-
self-efficacy/falls efficacy
-
socialisation
-
social support
-
-
health service use
-
physical/occupational therapy sessions
-
discharge destination/new nursing home admissions
-
falls and hospital readmissions
-
health-care utilisation
-
length of hospital stay
-
severity of illness/disease burden
-
-
AEs
-
malnourishment
-
morbidity rate
-
mortality rate
-
pain
-
rate of (repeat) falls.
-
The rehabilitation settings where the programmes were delivered varied from the acute hospital setting to the community setting and were categorised as below:
-
acute hospital
-
inpatient
-
specialised orthopaedic ward
-
specialised orthogeriatric ward
-
-
outpatient
-
general outpatient rehabilitation unit
-
specialised orthogeriatric outpatient rehabilitation unit
-
-
rehabilitation unit
-
general elderly rehabilitation unit
-
specialised orthogeriatric rehabilitation unit
-
-
-
community
-
place of residence
-
nursing, care or residential home
-
specialised nursing home rehabilitation unit
-
community hospital
-
community rehabilitation centre.
-
Testing the theories with quantitative and qualitative evidence
Data from each individual study were examined in terms of the identified programme theories and the interaction between mechanisms, context and outcomes. Next, the data across the different studies were examined to detect patterns and themes for each theory in turn. Separate fields were created in the Microsoft Access database to capture these interactions as well as raw statement data from the included studies to support reviewers’ reflections. Data synthesis involved individual reflection and team discussions to question the integrity of each theory, adjudicate between competing theories, consider the same theory in comparative settings and compare the theory with actual practice. When candidate theories failed to explain the data, new theories were sought from included studies or from the wider rehabilitation literature, such as studies of rehabilitation following stroke or following inpatient admission after being unable to stand. The narrative of the review was guided by the final theories that emerged from this process. The literature analysis relating to each identified theory is presented in detail, followed by a data summary to show the relationships between data themes and the theories in the final synthesis. Extracts were taken from participant quotations (patient, carer or health professional) reported in the included qualitative studies and used as evidence to support subthemes of the main theories. This is an established method used in a recently reported review of intermediate services61 to incorporate and integrate the theoretical perspectives from qualitative evidence into quantitative evidence.
Results
Results of the initial scoping review
The scoping search for systematic reviews and other reviews as well as guidelines relating to the rehabilitation of older frail populations identified 39 reviews, both Cochrane reviews9,10,27,33,37,49 and other traditional systematic reviews. 3,5,14,17,21–26,28–32,34–36,38,46–48,50–60 The majority of the reviews were related to hip fracture rehabilitation,3,5,9,10,14,17,21–24,26,27,29,30,32–36,49,51–57,59,60 but a few also included rehabilitation for stroke as well as for other conditions in older frail populations needing continuous care. 24,25,28,31,37,46–48,50,58 A few conceptually rich and theoretically sound primary studies from the reference lists of these reviews were also obtained. 69–73 The search also identified five sets of guidelines, from the UK [NICE,7 Scottish Intercollegiate Guidelines Network (SIGN)74], USA,75 Canada76 and Australia and New Zealand. 77
Study flow diagram for the realist review
The electronic searches identified 19,646 references, with a further 24 references identified by hand searching. Deduplication resulted in 12,278 unique references that were screened for relevance by two independent reviewers. The full texts of 610 references were obtained and, after collating multiple publications, 128 studies were included in the review12,13,69,72,78–201 (Figure 2; see Appendix 12 for the total number of references retrieved from each electronic database).
FIGURE 2.
Realist and economic review flow chart.
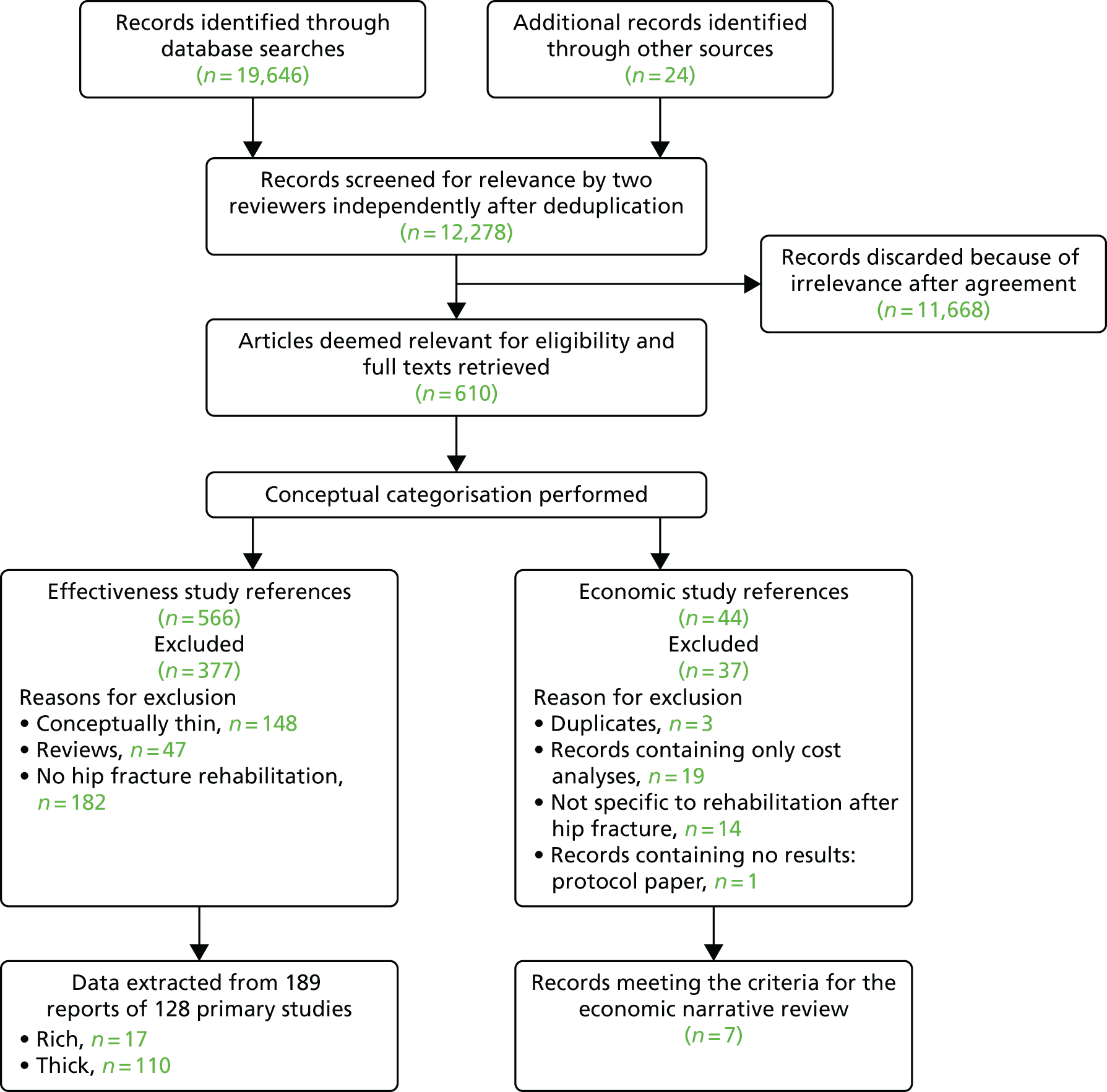
Study characteristics
Of the 128 primary studies included in the review, 17 were conceptually rich13,69,72,78–80,83,86,89,106,107,124,131,165,176,193,197 and 111 were conceptually thick12,81,82,84,85,87,88,90–105,108–123,125–130,132–164,166–175,177–192,194–196,198–201 (see Appendix 13). Thin sources were screened but were not included in the review for data extraction (see Appendix 14). A list of studies excluded from the review with reasons can be found in Appendix 15. Appendices 16–18 present the raw data tables describing the general characteristics of the included studies, the populations of interest, the treatment categories with characteristics of the interventions and the strengths, limitations and conclusions as presented by authors, respectively. These data are described briefly in the following sections according to the types of research methods used.
Summary of participant characteristics
The number of patients/participants included in the studies ranged from 1 to 2762. The review included a total of 22,443 patients and 97 health professionals. In total, 6282 (range 90–401) patients participated in RCTs,12,69,78,80,87,90–126,128–130,197,199 276 (range 24–95) patients participated in quasi-RCTs,83,131–133 116 (range 20–30) patients participated in non-RCTs,79,134–137 3044 (range 1–919) patients participated in historical cohort studies,13,157–165,170,173,178 7136 (range 18–946) patients participated in concurrent cohort studies,81,138–152,169,177,179,181,182,184,187,188,190–193,196,200,201 1697 (range 3–764) patients participated in controlled before-and-after studies,85,153–156,180,186,195 45 patients participated in mixed-method studies,84,89 3243 (range 130–2762) patients participated in database analyses166–168 and 521 (range 12–222) patients/health professionals participated in qualitative studies,72,82,86,88,127,174–176,183,185,189,198 with two studies involving health professionals (n = 97) rather than patients. 176,198 Two studies used administrative/work process data and did not include any patient data. 171,172
The majority of the studies included patients aged ≥ 65 years. 79,80,82–86,88,90–93,95,97,99–102,105,107,109,111,113,115,116,120,121,124–127,131,135,138–148,151,153,155–157,160,162,163,165,166,175,178–180,182–184,189–191,199,201 Six studies included adults of any age with a hip fracture and undergoing rehabilitation;78,112,167,174,185,186 two of these included carers174 or health professionals. 185 Eight studies included patients aged ≥ 50 years;87,98,103,118,173,187,188,192 18 studies included patients aged ≥ 60 years;12,89,96,104,114,117,119,122,132,133,149,154,164,193–197 19 studies included patients aged ≥ 70 years;69,72,79,88,106,108,110,111,116,120,131,136,143,148,150,161,180,183,184 and seven studies included patients aged ≥ 80 years. 13,81,123,134,137,152,178 The age of the included participants could not be determined from the study reports for four studies. 171,172,181,200 Sixteen studies included only female participants69,79,80,102,104,123,126,147,156,158,165,174,180,183,185,191 and one included only male participants. 159 The rest included participants of both genders but the majority of studies included a greater proportion of women.
The majority of studies excluded patients who had a cognitive impairment or dementia or who lacked mental capacity to give informed consent;12,13,69,72,78–100,102–109,111–118,120–122,124–138,140,142–151,153–156,158–169,171–181,183,185–201 11 studies included such patients,101,110,119,123,139,141,152,157,170,182,184 with one study stating that such patients would be included only if suitable carers ready to participate in the study were identified. 119 The majority of the studies included participants who were mobile and living independently in their own home or in a care home before their hip fracture. 12,69,72,79–86,88–90,92–114,116–119,121,123,124,126–130,132–136,138,139,143,145–149,153,156–158,161,165,166,168,169,171,175–177,179,180,183–186,191,193,194,196,197,199,201 Only seven studies included patients with a medical or psychological comorbidity;123,139,145,157,158,184,193 the majority of studies excluded such patients, especially when exercise would have been contraindicated. Only two studies included patients who had a history of a previous fracture. 175,184
The majority of the studies were carried out in English-speaking countries and involved mainly white Caucasian populations. Three Swedish studies,90,99,127 two Taiwanese studies,119,196 one German study93 and one Danish study84 included only patients who could speak, read and write in these languages, with other patients excluded.
Summary of interventional studies
Forty-eight of the studies were RCTs,12,69,78,80,87,90–126,128–130,191,197,199 with 10 from Australia,87,94,95,110,112,117,118,123,125,129 nine from the USA,69,80,91,92,107,113,121,126,191 six from the UK,12,102,109,115,128,197 four each from Sweden90,98,99,120 and Taiwan,95,105,119,122 two each from Canada,108,111 Norway,116,199 Finland,101,114 Hong Kong103,106 and Switzerland,93,96 and one each from Denmark,104 Belgium,97 Italy,78 Spain124 and Germany. 130 Only seven studies69,78,80,106,107,124,197 were categorised as being conceptually rich.
Four of the studies were quasi-RCTs83,131–133 and five were non-RCTs,79,134–137 with two each from Canada134,135 and the USA,79,83 and one each from Israel,131 Japan,137 Italy,133 South Africa136 and Taiwan. 132 Three of these studies were categorised as being conceptually rich. 79,83,131
Thirty-two of the studies were concurrent cohort studies,81,138–152,169,177,179,181,182,184,187,188,190,192–194,196,200,201 with nine from the USA,81,142,146,147,149,181,191,192,194 four each from Italy,141,143,177,182 Israel138,148,179,201 and Sweden,139,187,188,193 two each from the UK,150,200 the Netherlands,140,144 Taiwan190,196 and Germany,151,152 and one each from Norway,145 France184 and Canada. 169 None of these studies was categorised as being conceptually rich.
Eight of the studies were controlled before-and-after studies,85,153–156,180,186,195 with two each from the USA153,156 and the UK,85,155 and one each from Canada,195 Denmark,154 Sweden180 and the Netherlands. 186 None of these studies was categorised as being conceptually rich.
Thirteen of the studies were historical cohort studies,13,157–165,170,173,178 with three from the USA,159,165,173 two from the UK,13,158 and one each from Australia,161 Austria,178 Canada,157 Germany,163 Israel,162 Italy,170 Japan164 and Sweden. 160 None of these studies was categorised as being conceptually rich.
Among the non-comparative interventional studies there were two mixed-method studies,84,89 one each from the USA89 and Denmark. 84 One study from Finland166 reported a cross-sectional analysis of pre-trial data, two studies from the USA167,168 reported a hospital database analysis and another study from the USA reported longitudinal data from a survey. One study from Australia169 reported before-and-after outcome data for a cohort who underwent an intensive rehabilitation programme in the acute hospital. There were also two case report studies:13,170 one from Italy170 and one from the UK. 13 Two mixed-method studies84,89 and a case series81 were categorised as being conceptually rich.
Summary of non-interventional studies
Non-interventional studies did not use any intervention or treatment to affect the outcomes but were useful for their conceptual input to the theoretical framework and provided explanations for elements of the proposed theories. Two studies, one from the USA171 and one from Canada,172 reported service and work process restructuring. One study from Australia161 utilised hospital data on hip fracture patients 4 months post surgery who had been successfully rehabilitated into the community. These patients were divided into fallers or non-fallers after their rehabilitation. None of these studies was categorised as being conceptually rich.
Twelve of the studies were qualitative studies,72,82,86,88,127,174–176,183,185,189,198 with three each from the UK86,176,198 and USA,72,174,183 two from Sweden88,127 and one each from Australia,185 Canada,175 China189 and Taiwan. 82 Six of these studies72,86,127,175,183,189 interviewed hip fracture patients after discharge about their experiences of the whole process and the rehabilitation that they went through. Two of the studies176,198 interviewed health professionals providing rehabilitation services regarding their experiences about such provision as well as any issues encountered that might be amenable to service improvement. Three of these studies were categorised as being conceptually rich. 72,86,176
Summary of the study settings
Twenty-two of the included studies69,72,82,92,107,114,115,117,118,121,122,125–127,135,142,156,161,163,165,174,201 were conducted in the community after the patients had been discharged from the acute or community hospital to either their pre-fracture place of residence or a care home. Sixty-seven studies12,13,78–80,83,87–89,93,96–98,100–102,104,106,108,111,112,116,119,124,129,132,134,137–141,146,148,152,157–160,162,164,166–173,175–187,194,195,197,198,200 were conducted while patients were still in the acute hospital following surgery. In 39 studies the intervention started in the acute hospital but continued in the community following discharge. 81,84–86,90,91,94,95,99,103,105,109,110,113,120,123,128,130,131,133,136,143–145,147,149–151,153–155,188–193,196,199
Overview of the rehabilitation programmes
Appendix 17 summarises the interventions and comparators as described in the included studies.
Physical activity components of the rehabilitation programmes
Fifty-two of the included studies reported some form of physical intervention69,78–81,83,87,91–93,96,98,99,103,104,107–110,112–115,117,118,121,122,126,130,131,134,136,148,151,153,154,156,158,162,164,169,170,177,180–182,186,187,191,192,194,199 and seven also included a psychological component. 78–80,91,148,180,191 Twenty studies compared intensive physical exercise with less intensive physical activity or an inactive control. 69,78,80,83,91–93,104,107–110,113,114,117,118,122,126,130,169 Twenty-four studies compared supervised programmes with conventional programmes that either did not include supervision as part of the programme or included only minimal supervision to ensure patient safety. 69,80,83,87,91–93,104,107–110,112–114,126,131,136,151,153,180,186,191,199 Nine studies compared specifically tailored programmes with generic rehabilitation programmes. 69,79,80,83,99,109,113–115
Psychological components of the rehabilitation programmes
Fourteen studies reported using a psychological intervention in isolation12,106,137,141,171,197,201 or as part of a comprehensive rehabilitation programme along with physical components. 78–80,91,148,180,191 Three of these studies141,171,191 did not report any outcome data but were utilised mainly for theory explanation.
Place of rehabilitation
Twenty-six studies compared different rehabilitation settings. 81,97,101,103,112,120,125,128,131,133,135,143,145–147,149,151,152,154,160,161,179,188,195,200,201 Ten of these studies compared some form of community (own home or care home) rehabilitation with hospital-based rehabilitation,101,103,125,128,131,133,135,143,145,160 with one comparing hospital plus home rehabilitation with hospital rehabilitation only. 133 Eight studies97,112,120,146,149,151,152,200 compared hospital-based rehabilitation with usual care, no post-discharge care or rehabilitation in nursing facilities. Other studies did not compare rehabilitation settings per se but included comparisons based on patients’ characteristics, such as fallers compared with non-fallers,161 very old patients compared with younger patients201 and treated in a cognitive specialised rehabilitation unit compared with treated in a non-cognitive specialised rehabilitation unit. 152 One study compared the discharge practices of four hospitals after inpatient rehabilitation. 147
Process or system improvement
Twenty-nine studies investigated the effects of improvement or change in existing health-care rehabilitation structures. 69,83,94,95,98,100,102,105,111,116,117,119,120,123,124,127,128,132,138–140,144,150,155,157,159,163,167,184 Seventeen studies compared the development of multidisciplinary co-ordination programmes with usual care or another existing programme. 69,83,98,102,111,117,119,120,123,124,127,132,144,155,157,159,184 There was large variation in these programmes from different health-care systems, but common features included comprehensive geriatric assessment both pre and post surgery, assessment of patient needs and assignment of appropriate health-care staff to address those needs, regular multidisciplinary meetings to discuss progress and care pathways that continue into the community after discharge. Usual or conventional care varied greatly among the studies, ranging from simple control of post-operative symptoms117 to comprehensive assessment. 69,83,120
Eight studies reported on structured discharge planning from hospital to the community based on patients’ abilities, the extent of support needed and the availability of support from family or friends during the recovery period. 94,95,100,105,128,139,140,150 Six studies compared the early discharge of patients to their own home with usual discharge,94,95,100,128,140,150 one study compared early discharge to a rehabilitation unit of a community hospital with early discharge home139 and one study compared early discharge to the rehabilitation ward of a nursing home with conventional (delayed) discharge to the same ward. 105
Four studies reported the implementation of new ward protocols. 116,138,163,167 One study compared a newly commissioned orthogeriatric ward with a traditional orthopaedic ward116 and another study compared comprehensive geriatric assessment with usual care. 138 The other two studies were non-interventional improvement reports that utilised routinely collected hospital data in their analyses. 163,167 One did not report any patient-related outcomes but was useful for theory development. 163
Summary of outcomes
Outcomes data were extracted from 70 of the included studies. 12,69,78,80,81,83,87,90–93,95–97,100–103,105–111,114,115,117–124,130–133,135–140,143,144,146–149,151–158,160–162,167,169,184,192,195,199–201 Sixty-five of these studies reported physical or physiological outcomes,12,69,78,80,81,83,87,90–93,95,97,100,102,103,105–111,114,115,117–124,130–133,135–140,143,144,146–149,151–157,161,162,167,169,184,192,195,199,201 22 reported psychological or social outcomes,69,80,81,83,90,95,105,106,110,115,117–119,121,130,136–138,143,151,161,169 26 reported health service utilisation83,87,90,93,97,100–102,105,111,119,120,124,138,140,143,147,148,152,154,155,157,158,160,200,201 and 16 reported AEs93,96,97,100,101,110,111,119,124,133,137,144,148,154,155,162 as their main outcomes.
The rest of the included studies13,72,79,82,84–86,88,89,94,98,99,104,112,113,116,125–129,134,141,142,145,150,159,163–166,168,170–183,185–191,193,194,196–198 mainly contributed to theory building and explanation.
The directions of effect at various follow-up points are presented in structured tables in Appendix 19. The outcomes reported are discussed further when appropriate in the following discussion of the evidence for the final programme theories.
Study quality assessment
The results of the quality assessment are presented in Appendix 20.
Final working theory
Based on the characteristics of the individual components of rehabilitation programmes, and after discussions in the interactive workshops, an overarching working theory was developed as follows: successful rehabilitation after fractured neck of femur will be dependent on the characteristics and delivery of the intervention, the co-ordination and approach of the multidisciplinary team, the fit of the multidisciplinary team with the characteristics of the patient and the types of setting in which rehabilitation will be delivered.
This was then described in its CMO configuration in terms of the realist review approach as follows: in the context of patients with a great range and variety of pre-fracture physical and mental health comorbidities affecting their ability to meet rehabilitation goals (C), a tailored (M) intervention incorporating increased quality and amount of practice of exercise and ADL (M) in addition to usual rehabilitation leads to better confidence, mood, self-efficacy, function and mobility and a reduced fear of falling (O).
This overarching theory was then broken down into three component programme theories, which are described in the following sections.
Programme theory 1: improve patient engagement by tailoring the intervention according to individual needs and preferences
Proximal hip fracture patients presenting with a range of pre-fracture physical and mental functioning and a variety of comorbidities (C) need a rehabilitation programme that is tailored to individual needs (M) to achieve appropriate outcomes such as improved physical functioning, greater mobility, reduced disability and independent living (O).
Tailoring of rehabilitation activities involved the interplay of many factors encompassing the patient, the health-care professional and the environment in which the rehabilitation took place. The main theme revolved around making rehabilitation planning patient centred and contextualising what is important for patients so that this can be incorporated into their care plan, allowing a better chance of engaging patients in their recovery.
Assessment of patients’ pre-fracture function, cognitive status and comorbidities
Common sequelae of hip fracture included physical limitations,202,203 dependency in daily activities,151 social restrictions,11 malnutrition144 and depression. 196,204,205 Assessing patients’ pre-fracture level of functioning, their cognitive status and any existing comorbid conditions allowed health professionals to formulate a plan including short- and long-term goals of rehabilitation. This was important for planning the mix of skills needed to address patients’ rehabilitation needs90 and for deciding the most appropriate setting for programme delivery. It was also important for addressing other social needs,193 especially in the presence of cognitive impairment,184 with appropriate adjustment of programme delivery. These programmes needed to take into account the constraints of existing resources, which may result in the setting of revised goals. Orthogeriatric models of patient care provided good examples of comprehensive multidisciplinary assessment delivered while patients were still in hospital. 138 Addressing comorbid conditions by early geriatric intervention so that patients could participate in the subsequent rehabilitation programme led to improved function,120,138 discharge to the place of pre-fracture residence120 and a shorter length of hospital stay. 120,138
Several studies stressed that health professionals needed to know about patients’ situation, their personality and any physical or mental conditions78 to enable rehabilitation interventions to be adapted to enhance recovery. 90,163,187 Rehabilitation programmes often involved the execution and performance of new tasks after learning new skills and this could be accomplished only if patients had the capability to go through such steps. Assessment of patients’ capabilities enabled health-care professionals to design rehabilitation activities that best suited individual need, rather than using an untailored generic programme. 116 Self-efficacy, which is an important tenet of social cognitive theory, is the belief in one’s ability to successfully complete tasks, reach goals and face challenges. 69,71,73 This influences the activities that a person engages in and his or her perseverance in the face of difficulties:206
I was just determined to do them [exercises], and I was determined to walk. I was determined to do everything for myself that I could. I just knew that it was the best way to get well.
Female patient72
Fracture or surgery-related complications such as pain, or comorbid conditions, can be perceived by patients as barriers to recovery, but it was not clear whether medical contraindications arising from these complications or patients’ own self-imposed restrictions led to an inability to actively engage in rehabilitation. 207 The factors that are amenable to correction144,208,209 and those that are not should be recognised at the start of any rehabilitation programme so that proper resources can be identified and expectations adjusted when chances of improvement are minimal. 179 Health professionals could then implement interventions to effectively motivate individuals who may not have been self-directed or determined to exercise,72 especially when patients develop a sense of losing control86 and become passive receivers of a service rather than actively seeking help. Cultural factors needed to be taken into account as well, so that clinicians could determine how they could best foster social support to help older patients maintain a positive sense of self. This was achieved through engaging them in conversations to promote independence82 and by involving family members, locating needed resources and providing tailored information and education about the injury and the recovery process. 86
Patients’ experience gained through the hospital stay could be incorporated into their rehabilitation plan. For example, seeing people who were more poorly and who had more disabilities than they did allowed patients to reflect that their own situation could be worse. 90,210
I feel, now that I’ve come home [from hospital], that I have a lot to be thankful for. I’m not in a wheelchair or anything like that. I’ve been much, much more humble!
Female patient90
Positive experiences of help during their illness, as well as kind and competent treatment, helped develop such perspectives. 90,210 Such patients would then become advocates of health professionals, recommending and encouraging rehabilitation in other patients:
Listen to the advice from medical staff such as doctors, therapists, and nurses . . . Do a lot of physical and occupational therapy even if it’s painful!
Young and Resnick207
Collaborative decision-making
Collaborative decision-making between patients, their carers and health-care providers was important for deciding on an optimum plan for recovery and rehabilitation. This included the consideration of patients’ psychological make-up and their built environment, the configuration of local health services in the context of programme delivery, system constraints and the tension between health professionals’ and patients’ preferences and perceptions about the appropriate short-term and long-term goals of rehabilitation. 211,212 Inadequate involvement of patients and their carers in the decision-making process could potentially lead to barriers with regard to patients’ ability to cope with multiple issues surrounding their ill health212 and an inability of the rehabilitation programme to realise its full potential in their recovery. Collaborative decision-making involved multiple facets, which are discussed in the following sections.
Setting and agreeing goals of rehabilitation
Setting rehabilitation goals early on, such as returning home, regaining or maintaining pre-fracture function and independence or ambulation without assistance, facilitated the recovery process, as did intermediate goals such as the number of minutes exercised per day:207
The trainer told me that if I stop exercising I would be back to where I started in two weeks. I thought, I have gotten to this point I can’t quit. They said no, no you can’t! You tell yourself you have to keep it up.
Female patient72
Agreeing the goals of rehabilitation was not always straightforward, as goals that were considered appropriate by the health professional sometimes did not align with goals of the patient, resulting in a mismatch between their conceptions of short- and long-term rehabilitation goals. 211,213 Health professionals usually suggested the suitability of a setting based on a set of physical function goals to be achieved within a specific time period, whereas patients viewed the suitability of the setting in the context of their overall well-being, of which long-term physical functional improvement was only a part. 211,213,214 If such objectives were prescribed authoritatively at this time of vulnerability,211,212 patients felt forced to accept something that they did not understand, leading to them disengaging and becoming passive recipients of a service, rather than having ownership of their recovery. 214–216
Similarly, setting goals was sometimes felt by health professionals to be a constraint on their time,176 leading to low levels of communication and negotiation and resulting in a failure to engage patients and achieve desirable outcomes. Interprofessional disagreements concerning what goals were appropriate also resulted in patients’ issues not being addressed appropriately,176 for example when hospital staff did not understand how community services worked and discharged patients quickly without adequate assessment. 217 When a programme incorporated detailed discussion of and agreement on the intended goals with patients and their family or carers and then tailored programmes towards these goals in the context of locally existing health and social care systems, there was more chance of engaging patients and achieving the desired functional outcomes. 83
Agreeing the place of rehabilitation
The most appropriate setting for rehabilitation needed to be agreed between patients and their family and carers, according to patients’ needs and abilities. 95,139,218 Often patients and health professionals held differing views about the most suitable location, especially when patients had other comorbid conditions and felt vulnerable. 214 Health professionals sometimes had to make decisions based on available resources and established systems. 217 Patients’ sense of vulnerability as well as their inability to comprehend the complexities and demands posed by home-based care,216 especially when support from friends and family was limited or not available, led to them preferring a hospital setting where they felt safer. 214,217 In addition, patients feared being a burden on family and carers219 and were anxious about their ability to manage at home. 95 Given the choice, patients and their carers preferred a longer hospital stay to home rehabilitation, particularly those living alone, as they feared that they would be left on their own and would be socially isolated. 193,214 When patients were discharged home, tailored support for them and their family could help them retain control. 86,216
Home rehabilitation also had the disadvantage that equipment and facilities were limited. In addition, in rural areas, health professionals felt that their time was not being utilised efficiently because a lot of time was spent travelling. In such situations, co-ordination between social care staff and rehabilitation professionals was very important. Home rehabilitation was not necessarily cheaper. A Dutch study found that, although moving rehabilitation from the acute hospital to the community freed up much-needed hospital beds, it did not result in reduced overall costs as costs were simply transferred from the hospital to the community. 140
In the presence of minimal support patients felt abandoned, unsure of what to do and unable to achieve the full potential of a rehabilitation programme, leading to further restrictions in functioning and deterioration in quality of life:
It’s a problem when you can’t manage on your own . . . I think about my finances and about how many payment reminders are going to come . . . they have to be paid . . . I have to pay the rent. Of course you think about whether there’s anybody that can help with that!
Female patient90
In contrast, because of the drive to discharge patients more quickly, together with some evidence that home rehabilitation with appropriate support can have positive outcomes,86,95 health professionals preferred home rehabilitation. Educating providers, patients and carers about accelerated discharge and home-based rehabilitation for those with the fewest disabilities could result in improvements in independence and confidence to perform day-to-day activities. 86,220 Apart from providing cost savings, home rehabilitation was viewed as providing a familiar place to patients where they could feel comfortable carrying out the agreed activities at their own pace and in their own time. Although some studies found that patients could feel comfortable with home rehabilitation, as long as they received continuous support to see them through this transitional period of functional recovery, other studies identified feelings of worry and fear about how to deal with the aftermath of injury and the recovery process, especially if services stopped abruptly rather than there being a managed and tapered withdrawal. 217 Some patients found the hospital environment intimidating and depressing and wanted to be discharged early with the understanding that they would be better cared for at home. Such people tended to be otherwise medically fit or to have a good level of support from family and friends.
Provision of enhanced formal (professional/social services) and informal (family/friends/carers) social support
Most patients regarded support and encouragement from family, friends and carers165 as being essential to recovery, allowing them to maintain an optimistic attitude during rehabilitation:
The help, encouragement, and support that I got from my family and friends are essential . . . People around me lifted up my spirit.
Female patient207
Some patients had difficulty engaging with complex collaborative decision-making because of unfavourable professional customs and configurations of local services; increased vulnerability arising from distress, anxiety and fear; existing or future comorbid medical conditions; a rapid decline in physical ability or mental capacity; or the loss or unavailability of close family or friends. These issues could coexist with poor coping strategies, such as distancing and avoiding seeking help from support networks. 165 In such cases patients would need extra support and help. 72,165
Motivating and facilitating practice and adherence to exercise and activities of daily living
Adjustments in family relations and renegotiation of day-to-day tasks were essential to cope with the difficulties posed by the altered physical reality following hip fracture and surgery. This entailed patients reassessing their own capabilities, and how to seek help without becoming dependent on others, while maintaining their own self-respect. 90 Many patients relied on members of their social support system for physical care, necessary information and psychological support and to act as an intermediary between them and the health-care system during the recovery process. 221 An evaluation of a randomised trial of a combined physical activity and psychological intervention showed that social support, verbal encouragement and feedback through the family provided a sense of security and motivation during exercise sessions:69,72
I have two sons, one especially who is very athletic. He calls me twice a week to prod me along. He wants me to try getting up out of the chair without holding on. He does push to keep me exercising!
Female patient72
Professional, social and family support was even more important when formal social support networks did not exist. Other sources of support included religious institutions and volunteer organisations, but family support was regarded as the most important for maintaining independence. 82
When cognitive impairment was a comorbidity, special arrangements and tailored interventions could be used to help patients adhere to rehabilitation programmes. 69,78,184 Active engagement of family members and carers to facilitate the regular rehabilitation activities was mandatory in such situations to ensure participation and adherence in the initial few months post fracture. 69
Improving health perceptions
Social support, defined as the number of contacts that patients made outside their home, had a positive effect on outcomes, particularly in those with a low level of social support at baseline. 157 A lingering sense of insecurity and a reduced hope of recovery could persist for up to a year after hip fracture. 210 This was the time when patients needed more support to come to terms with their changed reality. 157,163,204 This support could help engage patients in their rehabilitation activities; otherwise, they may withdraw from all social activities, leading to them becoming inactive and isolated and their condition worsening. 90
When hip fracture was seen as part of the normal ageing process it could deter people from actively participating in a rehabilitation programme because of the perceived bleak outlook. 90 Such feelings resulted in a further loss of confidence and self-efficacy and an increased risk of falls13 and a lack of engagement with intensive physical therapy despite proper supervision and support. 90,222 Finally, the experience of strangers offering help or finding new friends while in hospital could be a positive influence on patients’ personal and social life.
And the contact, so to speak, with the world around you has become a lot softer . . . I didn’t believe that there was such kindness and consideration in people that there really is.
Female patient90
Addressing outcome expectations
Limited expectations of outcome could interfere with rehabilitation programmes, such as a belief by patients that once they had attained their previous mobility they did not need to continue to exercise:
I feel much better. My hip is doing better, and I didn’t think I needed to do it anymore.
Female patient72
Some patients thought that returning to their previous state was nearly impossible and that they would have to accept having a disability because, in their view, it was impossible to influence the recovery process. Patients felt that they needed to slow down the pace of their life and come to terms with the new reality. 210 Some considered the hip fracture to be a sign of forthcoming death, leading to a sense of hopelessness. 90
So [sigh], I have to accept that I’ve reached the age when people break their hip. Since, I’ve always thought that it’s only old people. I’m not that old. [Interviewer: What does it mean to reach that age, do you think?] That I only have a short time left to live.
Gender of patient unspecified90
At the other end of the spectrum, some patients had unrealistic expectations of recovering fully to their pre-fracture level, hence the need to discuss at the outset the factors that may affect rehabilitation outcomes that are not amenable to correction. 179
Addressing information needs
Patients fracturing their hip usually had unmet information/education needs regarding their injury, the recovery process,207 sources of help and support, the number and extent of exercises to carry out at particular points during their recovery and how to adjust to the new reality of a changed body. 90 For example, one study showed that patients who were informed about restricting their movement post surgery to prevent damage to their joint replacement felt uncertain about when to start exercising and how much exercise to do:
It’s about bending over . . . Because I don’t know how much I’m allowed to do . . . They said that I shouldn’t bend over. But I don’t know for how long . . . I shouldn’t bend down or bend over and I shouldn’t lift my left leg too much . . . Until it had healed.
Female patient90
A rehabilitation programme73 that used written materials as reminders to continue exercising safely was shown to be acceptable to participants and kept them motivated and reassured about the safety and effectiveness of the programme, with the majority of patients commending its simplicity and ease of use. 72 Similarly, visual cues in the booklets helped patients to remember to exercise:
Having the booklet with the exercise helped. I would open that up and do them; I plan to continue to keep a calendar and write it down when I exercise. If I don’t write it down I know I can let something slide for a couple of days.
Female patient72
Summary of programme theory 1
A summary of programme theory 1 is provided in Box 1.
Elderly proximal hip fracture patients presenting with a range of pre-fracture physical and mental functioning and a variety of comorbidities (C) need a rehabilitation programme that is tailored to individual needs (M) to achieve appropriate outcomes such as improved physical functioning, greater mobility, reduced disability and independent living (O). Important components include:
-
detailed assessment of patients’ pre-fracture level of functioning, current cognitive status and other comorbid conditions
-
collaborative decision-making through discussion and agreement with patients, their family and carers regarding –
-
realistic and achievable, but modifiable, short-term and longer-term goals of rehabilitation
-
the most appropriate setting for rehabilitation suited to patients’ needs and abilities
-
adaptation of the physical environment to facilitate day-to-day activities
-
-
provision of enhanced support through active engagement of carers and rehabilitation professionals to –
-
motivate patients and facilitate the regular practice of exercises and ADLs
-
improve health perceptions
-
address/adjust outcome expectations
-
address information needs.
-
Programme theory 2: reducing the fear of falling and improving self-efficacy to exercise and carry out activities of daily living
Proximal hip fracture results in poor physical functioning, fear of falling, low mood and lack of self-efficacy (C), requiring improved quality and an increased amount of practice of physical exercises, ADL and psychological tasks (M) to gain mastery and control to improve confidence, mobility and physical functioning (O).
Professional coaching, verbal encouragement and support to enhance mastery
Hip fracture changed how patients felt about their bodies, leading to feelings of discomfort and insecurity and restrictions in mobility. Uncertainty about the extent to which they could move around safely made patients cautious and unclear about what their body could tolerate. 90 Professional support, guiding patients about how and when to exercise and what types of exercise to perform, was considered very helpful, with patients describing it as a ‘recipe’ to help them continue to exercise on their own. Repeated encouragement to exercise to achieve individually set goals, and regular review of progress towards these goals led to a perception of being cared for, which encouraged patients to continue practising independently. 72 This support appeared to have a positive effect in hip fracture patients on both the initiation and the maintenance of exercise and physical activities,72 similar to the positive effects seen in other older non-hip fracture populations:223,224
They [the trainers] encouraged me. They taught me about the benefits of exercise and encouraged me to do it. I wasn’t too interested in the beginning but they helped me believe that it was important.
Female patient72
One aspect of coaching patients was to assess their capabilities and perceptions about the complexities of the rehabilitation package and their ability to follow it through. The stepped approach, progressing from simple to more challenging exercise against resistance, allowed patient to adjust and learn as they went along; otherwise, the challenge could be too demanding, leading to withdrawal from the programme. 72 Self-efficacy could be enhanced and maintained by attaining small successes and step-by-step mastery of skills and tasks.
Supervision to increase the quality and quantity of practice of exercises and activities of daily living to regain confidence and strength
When designing a rehabilitation plan, health professionals needed to consider the physical injury causing the disability, and the psychological issues arising as a result, to enable patients to leave the house and socialise. 210 Fear of falling was one of the biggest factors hindering patients’ willingness to engage in physical activities independently. 90 Practising the prescribed exercises under supervision of a trainer helped patients gain confidence so that they could continue practising alone:72,210
It’s up to each and everyone, I think. If the doctor has done his part, and the health services have done theirs, then it’s up to the patient to make the best of it . . . To get started, and as fast as possible. Definitely!
Female patient210
Patients who started physiotherapy in hospital or in a skilled nursing facility as soon as possible after hip fracture surgery were more likely to return to the community than those who did not, even after adjusting for demographic characteristics and comorbid illness. 192 Similarly, greater participation in the therapy sessions led to better functional recovery in the short and medium term. 194
High-intensity physical exercise programmes could be delivered to older people in their own homes,143 to those who were dependent on others for their daily activities110 or to residents of care facilities, regardless of their cognitive function. 197,225 Increased dose and frequency of exercise had better outcomes for walking, physical performance, mobility, balance, co-ordinated stability and falls efficacy, including for those with cognitive impairment. 110
Patients gained confidence from repeated, supervised practice of prolonged exercise sessions,72,207 recognition of the resulting positive outcomes, verbal encouragement from the supervising professionals72 and modelling exercises,226 in which the professionals performed the exercise with the participants, all of which increased their self-efficacy and willingness to engage in the exercise programme.
Patients usually preferred an extended duration of rehabilitation, especially physiotherapy sessions,198 together with nursing care at home in conjunction with improved social services to facilitate the recovery process. 207 Extending multicomponent rehabilitation beyond the usual 6 weeks of therapy, either at home121 or in hospital,92,187 was also shown to have positive outcomes. This was important because fear of falling could recur after a period of 6–12 months, which could restrict the practice of activities, leading to a failure to achieve the full potential of rehabilitation. 69 Similarly, pain during these later stages could lead to restrictions in activities. 227 In the majority of cases, after excluding a problem with the implant or other bone-related disorders, simple reassurance to keep exercising safely was sometimes all that was required. 69 The increased cost of extended therapy services or exercise programmes in the community could be mitigated by using therapy assistants who work under the supervision of trained therapists. 226
Addressing psychological concerns and needs to enhance participation and adherence
Psychological factors228 that determine a person’s capacity to cope with stressful life changes include self-efficacy (i.e. people’s belief about their capacity),206 locus of control (i.e. where individuals conceptually place responsibility, choice and control for events in their lives)229 and positive attitude (i.e. sense of optimism). 230 Patients with high positive affect had a more rapid physical recovery after hip fracture than those with a low positive affect or depression. 142 Patients’ own determination to regain function motivated them to exercise and get involved with physical activities. Patient beliefs such as ‘my determination to walk again,’ ‘my mental attitude – never give up’ and ‘my determination to learn and improve’ helped them during their entire recovery process. 207
Barriers to adherence such as unpleasant sensations, shortness of breath, fatigue and, most importantly, fear of falling lead to non-participation and non-adherence to proposed exercise programmes. An understanding of the factors influencing exercise behaviour during the early post-hip fracture period and consideration of the factors that influence adherence to exercise over time were found to be important for increasing the time spent in exercise and overall physical activity to ensure optimal recovery. 69 Rehabilitation programmes need to take into account the fact that adherence needs longer-term support. The social encounter and reinforcement aspects of health professional support encouraged patients’ adherence to exercise programmes and the transition to independent management of their rehabilitation. 69 One aspect that required attention was that some patients who recovered quickly discontinued exercising, thinking that they no longer needed to do so. Observing or expecting such responses during regular visits allowed the supporting health professionals to reinforce the importance of long-term adherence. 72
Symptoms of depression after a hip fracture tended to improve over time, along with the alleviation of pain and fear of falling, after proper treatment and support. Persistent fear of falling needed to be resolved with aggressive strategies. 85 The full potential of rehabilitation could be attained only if adherence to exercise was improved by optimising self-efficacy related to exercise,69 as self-efficacy was one of the most important single variables that consistently directly influenced exercise behaviour. 69 Controlling anxiety symptoms related to the injury and allaying future concerns were very important for the successful participation of patients in their rehabilitation programme. The relief of such symptoms, for example by the practice of relaxation techniques, led to successful participation in the rehabilitation programme. 13 One issue that the supervising health professionals needed to take into account was that self-efficacy tended to diminish when patients first encountered an exercise professional (i.e. exercise trainer), because he or she helped them to recognise the true extent of their poor physical functioning, with a consequent decrease in confidence. This decline could occur after exposure to a new exercise programme, after a change in their clinical condition or ability, after a reduction in participation in exercise classes, in encounters with the trainer if in the home setting or when the exercise programme became progressively more challenging. 231
A mechanism whereby patients could organise their exercise schedule to suit a particular time of the day helped them stick to their plan and regularise their practice of the tasks suggested by their supervising health professional. 72 The support offered by the trainer was seen as an additional source of motivation in the sense that patients reciprocated the kindness that they received from the trainer by being determined to do what the trainer advised:
I wanted to be able to tell her I was doing them [the exercises].
I just liked her so much as a person.
I wanted to do what she wanted me to.
Multiple patients72
Summary of programme theory 2
A summary of programme theory 2 is provided in Box 2.
Proximal hip fracture results in poor physical functioning, fear of falling, low mood and lack of self-efficacy (C) requiring improved quality and an increased amount of practice of physical exercises, ADL and psychological tasks (M) to gain mastery and control to improve confidence, mobility and physical functioning (O).
Enhancing the practice and quality of exercise and ADL has both physical and psychological components:
-
the provision of coaching by health professionals to enhance practice skills and mastery to improve confidence for the transition to independent and unsupervised practice
-
the provision of supervision by physiotherapists/occupational therapists to increase the duration/frequency and improve the quality and quantity of exercises such as strength, balance, reverse and gait training as well as ADL sessions
-
adaptation of the physical environment for the safe practice of exercises and ADL
-
addressing psychological concerns and needs to improve mood and reduce depression
-
improving motivation to practise the exercises and ADL by
-
setting appropriate, realistic practice goals and collaboratively working towards these
-
developing mechanisms of monitoring of and/or feedback (self and/or health professional) about progress through the programme.
-
Programme theory 3: co-ordination of services and sectors delivering rehabilitation
The diversity of services provided by different disciplines across sectors from a variety of funders (C) requires co-ordinated provision of multidisciplinary rehabilitation programmes (M) to deliver appropriate physical, functional and psychological interventions to patients in a timely manner (O).
Multidisciplinary co-ordination
Rehabilitation should start as soon as possible after hip fracture repair and continue into the community after discharge. 7 As hip fracture patients usually had multiple comorbidities,159 a multidisciplinary approach had a greater chance of success and produced better functional and psychological outcomes. 119,120,232–236 Acute health care usually focused on treating the acute injury and did not account for the psychological distress that ensued after the hip fracture. Hence, a rehabilitation programme needed to take into account this profound psychological and social impact, which could be addressed by including multiprofessional contacts to support the recuperation of elderly patients from their injury during rehabilitation after hospital discharge. 90
Patients valued the help and support that they received from health-care teams during their recovery and regarded this as the single most important factor in their recovery. The frequent interactions with their care staff were described as having a medicinal effect; care staff were described as ‘very good doctors’ or ‘good surgeons’ and patients talked about receiving ‘correct’ or ‘professional’ care from their rehabilitation providers. Patients developed perceptions about health professionals’ skills and evaluated these based on successful outcomes or usefulness of the information that they received to facilitate recovery. Hence, communication and a positive attitude displayed by the health professionals appeared important to participants. 176
Linking different health-care and rehabilitation organisations together should enable programmes not only to help heal fractured bones but also to repair the resulting social and existential cracks. 207 Health professionals valued a system with integrated services in which the roles of different professionals were clearly defined to ensure continuity of care:176
If you compare some of the patients with other problems you notice much more with the new ICPs [integrated care pathways] that things are done much more thoroughly and that people do work together better than if a patient came in with a different problem. I do not think it’s degrading. It is a good checklist.
Staff nurse176
Service improvement/restructuring
Verbal and written miscommunication (paper or electronic) led to delays in patient care, through uncertainty in clinical decision-making and in managing resources by managers. Lack of professional interpersonal communication appeared to be the main underlying cause:
To a greater extent I have to go looking for the information . . . It is not like people will call me and say the OT [occupational therapist] did the home visit and this was the result . . . We are the ones who have to wait basically until everyone else has their stuff done before we can really do our part . . . and yet they don’t really tell me that they are done . . . and if I don’t come regularly looking to find that out then I wouldn’t know.
Care manager176
Multidisciplinary care pathways have improved patient care and functional outcomes46,102,155,237 and quality of life144 and reduced morbidity or mortality,124,159 but their successful execution requires the completion of successive steps by a chain of professionals. Non-completion or partial completion of tasks in the pathway led to delays in patient care and the risk of litigation. The integrated care pathways appeared to exacerbate rather than reduce interprofessional conflicts because of increasing awareness of health professionals about why discharge delays occurred. Integrated care pathways also challenged professional boundaries and identities:
It has highlighted areas that are lacking . . . areas where we can improve and areas that people actually haven’t paid attention to . . . The OTs [occupational therapists] they were frustrating because there was . . . there is such a barrier there and whenever anything is questioned what is written – you can’t get through but I think that is more deep seated than just this ICP [integrated care pathway].
Staff nurse176
Cross-fertilisation of ideas, team-building meetings, sharing office space and strategies to enhance formal and informal communication all seemed to allay such anxieties and facilitated the change process through iterative discussions regarding both the content and the process of care, resulting in consolidated, patient-oriented service provision. 172
One of the issues related to the integrated care pathways was that they involved completing a large number of forms, which distracted staff from paying attention to the patients. The perceived need to get the work done led to complaints of being rushed and that they had to approach their work as a series of tasks to be achieved in a set time. This also led to interprofessional tension as everyone was trying to complete their own tasks rather than working towards the overall welfare of patients:
Therapists and nurses have a different agenda in the morning. The nurses are wanting to get people up and dressed quickly and have their breakfast . . . A lot of nurses get peeved because we are expected to do physio and OT [occupational therapy], but they won’t put patients on the toilet, which is all part of physio and OT. They’ll shout for an auxiliary or one of us.
Staff nurse198
Discharge planning
Demand pressures in health-care systems have led to the earlier discharge of patients with hip fracture,128 with a consequence that patients are leaving hospitals sicker and community care has struggled to cope with demand. Standardised care pathways designed and rolled out to meet these demands have shown inconsistent results for patient benefit and functional improvements. 23,121,128,157,238,239 When they were reported to improve patients’ functional outcomes46,95,100,102,140,155,218,237 or quality of life,100,144 or to reduce morbidity or mortality,100,124 the trade-off was usually a longer hospital stay, leading to increased cost and resource implications. 124,155 One element that was important in attaining better outcomes was discharge planning that took into account patients’ self-care information and education needs. 105 There were reservations among some professionals regarding the usefulness of multidisciplinary care pathways, as these were seen as very prescriptive and as regarding patients as checklists. They disregarded the human factor that health professionals should use when caring for patients. Multidisciplinary care pathways took up more of their time so that they spent less time with their patients, and they also did not allow health professionals to tailor interventions:
I think that those ICPs [integrated care pathways] treat you like you are a bit thick so . . . you don’t need to show initiative. They are so regimented.
Staff nurse176
Hence, careful assessment of selected subgroups of patients (e.g. patients who were independent pre fracture) who are most likely to benefit from standardised rather than individualised care95,140,218 needs to be undertaken if the potential of such systems is to be harnessed. 101,111,150,157 A more efficient and effective system that is well co-ordinated with more resources allocated in the community may help address this challenge172 and may add to the long-term health and economic benefits to both the patients and the health-care system. 232
There was evidence that functional outcomes were better the earlier that rehabilitation started,167 with a shorter hospital stay. 129 Discharging patients early without assessing their rehabilitation needs may lead to a delay in patients accessing health and social services, resulting in worse outcomes with increased consumption of such services155,172 and longer rehabilitation times. 218 This may merely shift the cost from hospitals to the community. 140 Targeted integrated care pathways could help offset costs by providing savings to social services once health and social services were unified,155 along with improving patient functional outcomes. 95,218
Summary of programme theory 3
A summary of programme theory 3 is provided in Box 3.
The diversity of services provided by different disciplines across sectors from a variety of funders (C) requires co-ordinated provision of multidisciplinary rehabilitation programmes (M) to deliver appropriate physical, functional and psychological interventions to patients in a timely manner (O).
This requires:
-
multidisciplinary co-ordination of care from the acute hospital into the community
-
improved communication between rehabilitation professionals
-
careful discharge planning.
Discussion
Summary of findings
Three programme theories arose from this realist review that appeared to put patients at the heart of rehabilitative care and improve outcomes. These were:
-
tailoring the intervention according to patients’ individual needs and preferences to improve patient engagement
-
reducing fear of falling and improving self-efficacy to exercise and perform ADL through increased quality and frequency of the practice of exercises and daily tasks under supervision
-
the co-ordination of services and sectors delivering the rehabilitation.
Strengths and limitations
This was a realist rather than a systematic review of multidisciplinary rehabilitation following hip fracture aimed at synthesising evidence to develop an enhanced rehabilitation package for such patients. To our knowledge, this is the first realist review that has attempted to build an explanatory account about the effectiveness of different components of rehabilitation interventions following hip fracture in the context of what works for whom and under what circumstances. 39,40 As such, we did not attempt to summarise all of the evidence and judge whether or not rehabilitation programmes were effective, but rather we attempted to build an explanatory account of the mechanisms behind their effectiveness and to establish which components were effective in certain circumstances and contexts.
No studies were excluded based on a particular outcome and data for all reported outcomes were extracted. Particular caution needs to be exercised when the included studies have used non-validated measures or measures have been combined to give a cumulative outcome, such as combining numbers of readmissions and deaths into a single outcome designated as ‘poor outcome’. 26 About 35 outcomes using 152 outcome measure instruments were recorded (see Appendices 10 and 11). Such a variety of outcomes in hip fracture rehabilitation studies has been reported by the majority of reviews3,21 explored during theory-building and scoping searches. This applies to both long-term3 and short-term14 disability arising as a result of hip fracture. This was recognised as a limitation of traditional review methods, as were the myriad of treatment strategies used and inconsistent reporting,9,10,23,24,47,50 which made comparisons across studies difficult and led to inconclusive results. 3,8–10,21,23–25,28,29,47,49,50,240,241 These issues also led to difficulties in replicating intervention designs in different health-care systems as well as in drawing evidence-based conclusions about best practice. 10,24 Successfully combining a few commonly reported outcomes to estimate the long-term health outcomes of rehabilitation programmes10 could help to more accurately estimate the comorbid disease burden, which may benefit from longer-term rehabilitation and falls prevention programmes, leading to health gains and reduced costs in the long term. 3
It is acknowledged that the pragmatic method of reviewing the literature and synthesising the evidence may be difficult to replicate and that another team carrying out a similar review may reach different conclusions. This review has attempted to be as inclusive as possible and incorporate evidence from multiple sources and study types, which helped to provide context to the findings of the comparative studies. The use of a specific definition of rehabilitation programmes and categorising sources of evidence according to their conceptual richness might have resulted in some relevant studies being missed or excluded. However, this was mitigated by the comprehensive electronic literature searches, complemented by manual citation tracking.
The process of identifying and formulating programme theories was challenging, particularly when some studies did not explicitly state how the intervention being tested was developed or the content and operation of services in the context of that particular intervention. This similar issue has been highlighted in a recent review of intermediate care services, which recommended that the research community provide more information about ‘how’ and ‘why’ the interventions/services being evaluated were developed and delivered. 62
Comparison with previous literature
As discussed in the previous section, a realist approach was used to tease out which components of rehabilitation programmes were useful and which were not,10,23 rather than summarising overall effectiveness as in previous systematic reviews. It also addressed some of the gaps in hip fracture rehabilitation, such as the lack of interventions that enhance self-efficacy24,169,242,243 and address postural balance and fear of falling,14,21,24,169 the exclusion of moderately cognitively impaired patients,10,16,17,24,36,57,244 the short-term provision of rehabilitation services10,244 and the lack of reporting of carer outcomes. 10
Self-efficacy to exercise has long been recognised as an important mediator for regaining confidence in daily activities and function and overcoming the fear of falling, to enable an increase in the practice of physical activities and exercise. 14,69,72,227,245 But such potential has not been realised fully in rehabilitation interventions, especially once patients have been discharged from the acute hospital. 157,169,242,246 Targeted information provision and education,246 skills enhancement,227 addressing and accommodating user needs and views214 and social and peer support are important to improve motivation and engagement and help patients regain control and confidence after the medical and psychological crisis presented by hip fracture. 227 A rehabilitation intervention model addressing both psychological and physical needs may be an answer to this dilemma, as such strategies in isolation have minimal positive effects on outcomes. 10,73,91 This has been successfully shown in the rehabilitation of patients with stroke247 and other conditions. 61,62,214 This review identified that mutual aid and social support,246 combined with the development of practical skills through supervised practice and exercise,243,248 have the potential to improve quality of life and reduce the rates of rehospitalisation and long-term institutionalisation. This is mediated by building confidence, cognitive understanding and practical skills.
Recent drives to both improve patient outcomes following hip fracture and reduce costs through effective rehabilitation programmes have highlighted the importance of tailoring specific rehabilitation packages according to individual patient needs rather than following set programmes that do not take into account patients’ circumstances. 227 Such tailoring activity involves multidisciplinary team decision-making in consultation with the patient and his or her carers about the appropriate timing and place of such activities. The timing of different interventions is important, as some intervention activities appear to produce better outcomes if introduced at certain time points and in appropriate settings. For example:
-
coaching may have a minimal effect if started immediately after surgery in hospital91 but has been shown to enhance patients’ self-efficacy, skills and mastery to perform exercises independently if provided in the community soon after discharge36,69,72,73,244,245,249
-
occupational therapy and interventions for fear of falling in the acute hospital have a minimal effect99,245 but appear to be effective when provided at patients’ usual place of residence,244,245,250 probably because patients start ambulating either independently or with help and can appreciate that the occupational therapy supervision aims to make the environment safe for them to practise exercises and ADL28
-
supervised physical training and earlier mobilisation in rehabilitation programmes during the acute hospital stay,36 and strength and progressive resistance training later in the programmes, either during or after discharge, appear to improve outcomes,25,36,57,251 as earlier commencement of intensive physical therapy may act as a hindrance and there is a danger of patients becoming disengaged or dropping out of programmes9 because of the challenging nature of the tasks
-
falls prevention programme training combined with supervised exercise to improve self-efficacy and regain confidence,36 but only after patients have restarted walking. 5,9
Similarly, no single pathway provides the answers to all patient issues because of the complexity of comorbidities with which hip fracture patients can present. 8,29,49,240 Geriatric orthopaedic rehabilitation units are likely not to be cost-effective but can be beneficial for frailer patients to reduce complication rates, readmissions, nursing home placements and in-hospital deaths; however, they showed little effect on the rate of death post discharge, in both the short term and the long term. 29 Similarly, geriatric hip fracture programmes and early supported discharge can be cost-effective if offered to suitable patients, as they appear to reduce the length of hospital stay in such groups. 47,252 If they are offered to all patients without distinction, however, they will simply transfer the cost from the hospital to the community, as some patients may need prolonged care in the community. 140 Multidisciplinary co-ordination would play an important role in such instances to determine the appropriate skills mix of rehabilitation professionals during a patient’s inpatient rehabilitation and discharge planning8,49,240 as well as rehabilitation beyond the acute care setting and into the community. 252 Such rehabilitation programmes would need to be flexible with a mix of components to respond and adapt to individual patient needs and requirements.
Implications for practice, policy and research
In the early post-operative period, patients’ needs and wishes should be used to tailor the rehabilitation package (the timing of delivery of certain components of the programme, the skills mix of rehabilitation professionals needed, the appropriate place and support element built into the programme) to allow it to produce positive outcomes and be cost-effective in the long term.
Rehabilitation programmes need to take into account the longer-term needs of patients to reduce the detrimental sequelae that follow, for example fear of falling again leading to movement restriction, reduced participation in physical activities and ADL, reduced function leading to disability and dependence and psychological issues leading to isolation and reduced quality of life.
Rehabilitation programmes should have elements of support, supervision and coaching to help patients regain lost confidence and realise the importance of the enhanced practice of physical activities and ADL for improving function and reducing disability.
Realist review methodology provides a flexible and pragmatic way of developing complex intervention such as rehabilitation programmes for hip fractures through an explanatory building exercise and teasing out individual and effective components of such programmes.
The programme theories that emerged from this realist review were combined with the findings of the survey of therapy professionals (see Chapter 4) and the patient/carer focus groups (see Chapter 5) to develop the rehabilitation package (see Chapter 6) to be tested in a feasibility study (see Chapter 7).
Chapter 3 Health economics systematic review
Introduction
There is only limited evidence for the cost-effectiveness of multidisciplinary rehabilitation for hip fracture. Handoll et al. 8 conducted a Cochrane review of the clinical effectiveness and cost-effectiveness of multidisciplinary rehabilitation for older people with hip fractures, in either inpatient or ambulatory care settings. The comparison was between multidisciplinary rehabilitation delivered by a multidisciplinary team, supervised by a geriatrician or rehabilitation physician/clinician, and usual care (control group). Programmes were provided in an inpatient or an ambulatory setting (or both). Ambulatory settings consisted of home, outpatient department or day hospital locations. Usual care for the control group consisted of usual orthopaedic or medical care or a rehabilitation programme of lesser intensity or with different components of the intervention under study. Multidisciplinary rehabilitation was reviewed as an overall intervention rather than individual components of interventions being evaluated. Four cost-analysis studies were identified. 8,238,253–255 One study found that costs were significantly reduced in the intervention group compared with the control group,253 whereas the other studies reported higher costs for the intervention group. Handoll et al. 8 concluded that, although there was no conclusive evidence of the clinical effectiveness and cost-effectiveness of multidisciplinary inpatient rehabilitation following hip fracture surgery in older people, there was a trend towards effectiveness for all of the main outcomes assessed. They also reiterated the need for future trials to establish both the clinical effectiveness and the cost-effectiveness of multidisciplinary rehabilitation.
The lack of cost-effectiveness evidence was highlighted by NICE7 in its guidance on the management of hip fracture in adults. No published economic studies on hospital-based multidisciplinary rehabilitation for hip fracture compared with usual care were found by NICE. Five studies of community-based multidisciplinary rehabilitation compared with usual care were found;7,140,256–259 however, two of these studies were excluded. 140,256 The study by Coast et al. 256 was excluded as it included a mixed population and only 31% of the sample were hip fracture patients. The study by Van Balen et al. 140 was excluded as patients in the sample were discharged to a nursing home and not their own home. Because of the limited amount of published evidence, NICE conducted decision-analytical modelling to accompany the guidance. This original analysis determined the cost-effectiveness of a hip fracture programme (formal ‘orthogeriatric’ care, with the geriatric medical team contributing to joint pre-operative patient assessment and increasingly taking the lead in post-operative medical care, multidisciplinary rehabilitation and discharge planning) compared with a geriatric orthopaedic rehabilitation unit (a separate geriatrician-led trauma ward). The extent of surgical input varied depending on how early patients were moved from the acute trauma ward. The extent of surgical input also varied depending on how early patients were moved from a mixed assessment and rehabilitation unit (a rehabilitation unit able to accept patients with a variety of medical, surgical and orthopaedic conditions) compared with usual inpatient rehabilitation (usual care). The analysis revealed the hip fracture programme to be the dominant strategy (less costly and more effective than a geriatric orthopaedic rehabilitation unit/mixed assessment and rehabilitation unit and usual care). However, the guidance stated that this evidence had minor limitations with regard to direct applicability. In particular, the results were sensitive to the proportion of patients returning home after rehabilitation. If the probability of patients returning home was increased from 79% in the base case to 83% for a geriatric orthopaedic rehabilitation unit/mixed assessment programme, then the geriatric orthopaedic rehabilitation unit care option would be considered the optimal strategy. With regard to community-based rehabilitation, the decision-analytic model showed that community multidisciplinary rehabilitation was cost-effective. However, this finding was sensitive to variations in the length of stay, both in hospital and at home. The model has limitations, most notably that the clinical evidence for the model’s parameters came from a single RCT conducted in Australia. The follow-up period was also limited to 4 months, with no information regarding the impact of community multidisciplinary rehabilitation available after that time point.
In summary, the economic evidence highlighted in previous systematic reviews was sparse. There was a need to perform an up-to-date systematic review of the economic evidence relating to multidisciplinary rehabilitation for hip fracture.
Objective
To conduct a systematic review of the available evidence assessing the cost-effectiveness of multidisciplinary rehabilitation for proximal femoral fracture in the older adult population.
Methods
Details of the search strategy are provided in Chapter 2. This search did not contain study design filters as the reviewers were interested in different types of study: RCTs and non-RCTs and observational, economic and qualitative studies. The population cohort of interest was elderly adults with proximal hip fracture. The intervention of interest was multidisciplinary rehabilitation. The comparator was also reported (when stated). Outcomes of interest were mortality, pain, functional status, quality of life, health utility, health service use and costs. The search strategy was applied to 21 databases, including NHS EED (see Chapter 2 for further details).
The inclusion criteria were as follows:
-
studies that contained a full economic evaluation, defined as an economic analysis that synthesised both costs and outcomes, for example cost–utility analyses, cost–benefit analyses and cost-effectiveness analyses
-
studies that included behavioural economic theory, for example welfare judgements,43 expected utility gains44 and choice architecture45
-
studies that clearly fall inside our definition of multidisciplinary rehabilitation for hip fracture (see definition in Chapter 2).
We removed duplicated abstracts and transferred all references to bibliographic software (EndNote) to facilitate the assessment of inclusion and the categorisation of relevant studies. The literature was screened for evidence of economic evaluation in two stages. Screening for economic studies at the title and abstract stage was conducted by the four main reviewers. Potential economic studies identified in the initial search were then screened by two experienced health economists according to the inclusion criteria above. Discrepancies were resolved through discussion. A set of bespoke data extraction forms was created using a Microsoft Access database. The data extraction forms for economic evidence included the following fields:
-
study characteristics – authors, publication year, region/city, patient group (including number of participants), type of rehabilitation programme (brief description), rehabilitation setting (e.g. home, hospital or clinic)
-
study methods – type of economic evaluation (e.g. cost-effectiveness analysis), outcome measure assessed [e.g. quality-adjusted life-years (QALYs)], comparator measure, perspective of analysis, types of costs measured, cost year, time horizon and discounting, sensitivity analysis
-
study results – mean cost of intervention and mean cost of comparator, incremental cost, incremental effectiveness, incremental cost-effectiveness ratio (ICER) (if available).
Data extraction
Data were extracted by one reviewer and checked for accuracy by a second. Inconsistencies and disagreements were resolved by discussion after checking against the source study.
Quality assessment
Study quality was assessed using the checklist for economic evaluations of Drummond et al. 66
Evidence synthesis
The economic outcome data were exported into structured tables. Unfortunately, there was insufficient homogeneity between studies to allow for meta-analysis and therefore a narrative review of the findings is presented.
The method of interrogation used to appraise the included papers was to explore the study setting (country), year of publication, perspective of measurement for cost and benefits, type of study, comparator, range of costs and benefits measured, source of unit costs, year of unit costs and currency. We also assessed whether discounting of costs or benefits took place, whether or not sensitivity analysis was undertaken, the extent to which the results were compared with the results of other studies and, finally, whether or not the results were argued to be generalisable to other settings.
Results
From the results of the original systematic review search (see Chapter 2), 44 papers were identified as being economic studies. Seven studies met the inclusion criteria for the review. 253,254,260–264 Of the 37 excluded papers, three were duplicates of other papers, one was a protocol paper and contained no results, 19 were cost-analysis papers and 14 papers were not specific to rehabilitation following hip fracture (typically papers on post-surgery costs or osteoporosis- or osteoarthritis-specific papers) (see Appendix 15). The flow diagram in Figure 3 illustrates the process of the identification of economic evidence from the wider systematic review process.
FIGURE 3.
Flow chart outlining the selection process for economic studies.

Of the seven included papers, three were classified as cost-effectiveness analyses,253,260,261 two as cost–benefit analyses254,262 and two as cost-minimisation analyses. 263,264 These seven papers not only used different methods of economic analysis, but also assessed different rehabilitation pathways, interventions and settings. It was therefore not possible to synthesise the results, and a narrative review of the findings is presented. The included papers are presented by type of economic evaluation conducted in reverse chronological order, that is, with the most recent studies described first. Table 2 provides a summary of all seven included studies.
| Characteristic | Olsson 2009260 | Kramer 1997261 | Cameron 1994253 | Ruchlin 2001262 | Fordham 1986254 | Polder 2003263 | Elliot 1996264 |
|---|---|---|---|---|---|---|---|
| Country | Sweden | USA | Australia | USA | UK | The Netherlands | New Zealand |
| Patient group (number in sample) | Patients aged ≥ 65 years admitted for a hip fracture and living independently (ICP, n = 56; usual care, n = 56) | Elderly hip fracture patients and stroke patients admitted to 92 hospital-based units across 17 states in the USA (518 hip fracture patients and 485 stroke patients) | Elderly patients with proximal femur fracture (accelerated rehabilitation intervention, n = 127; conventional rehabilitation, n = 125) | Patients aged > 64 years who had been admitted for hip fracture (patient education self-efficacy video and high-intensity strength intervention, n = 59; usual care, n = 55) | Women aged > 65 years with a fractured neck of femur (new joint management system, n = 50; single specialty orthopaedic management system, n = 58) | Patients with a fresh hip fracture admitted to a general hospital in Rotterdam, the Netherlands (early discharge, n = 106; conventional discharge, n = 102) | Patients aged 65 years with a femoral fracture admitted to an acute orthopaedic ward (geriatrician assessment, n = 61; standard care, n = 57) |
| Type of rehabilitation programme and setting | Individualised hip fracture rehabilitation pathway (the ICP) as part of inpatient hospital rehabilitation | Patients were randomly assigned to the following different rehabilitation settings: traditional nursing home, subacute nursing home, rehabilitation hospital | Accelerated rehabilitation intervention with a focus on early mobilisation, retraining of physical independence and detailed discharge planning delivered in a general hospital | Patient education self-efficacy video and high-intensity strength intervention delivered in hospitals | The joint management system consisted of joint geriatric and orthopaedic management including early post-admission assessment, joint weekly bedside consultation, joint consultant decision-making with regard to the rehabilitation programme, any ward/hospital transfers and discharge | Early discharge programme as part of the hospital care pathway | Geriatrician assessment |
| Type of economic evaluation | Cost-effectiveness analysis | Cost-effectiveness analysis | Cost-effectiveness analysis | Cost–benefit analysis | Cost–benefit analysis | Cost-minimisation analysis | Cost-minimisation analysis |
| Outcome measure assessed | Successfully rehabilitated participants based on comparing patients self-estimated pre-fracture ADL level with their actual ADL level at discharge | Recovery of patients’ premorbid levels of ADL 6 months post admission | The two rehabilitation interventions were assessed by comparing patients’ pre-fracture and post-rehabilitation physical independence, using the Barthel Index of Activities of Daily Living265 | The physical role limitation, physical functioning and social functioning components of the SF-36266 were assessed at baseline and at 6 months’ follow-up for the intervention and control groups | The different management systems were assessed based on the average cost of hospital stay per patient, length of stay per patient, ADL, prognosis and place of discharge | The effects of the two discharge programmes were assessed by comparing patients’ functional outcome and cognitive status using the RAP267 and the MMSE268 | The length of stay, cost of care and discharge destination were compared for each group |
| Perspective of analysis | Hospital perspective | Hospital perspective | Hospital and community perspective | Societal perspective | Hospital perspective | Societal perspective | Hospital perspective |
| Types of costs measured | Direct hospital costs, treatment costs (e.g. surgery, post-operative care) and hotel costs (salaries, drugs, food, accommodation, administration) | Direct health service costs such as Medicare-reimbursed costs | Direct hospital costs – inpatient surgical and post-surgical care, readmissions; community costs – community support services and institutional care | Direct medical costs including costs of outpatient and inpatient care, emergency care, acute hospital care, post-hospital rehabilitation in a long-term care facility, nursing home care, physical and occupational therapy, visiting nurse care and prescription drugs. Community care-based costs including costs of home assistance, transportation costs and informal care provided by family and/or friends | Direct hospital costs, number of bed-days utilised and staff inputs into rehabilitation (e.g. physiotherapists’ and occupational therapists’ time) | Costs included manpower, equipment, materials, housing and overheads, all medical costs and patient-borne costs, including those borne by families (e.g. travelling) | Direct hospital costs such as surgery and post-operative care costs |
| Currency and cost year | Swedish crowns were converted to euros using the annual average exchange rate for cost year 2004 (9.1268 SEK per €) | US dollars (cost year not reported) | Australian dollars (cost year 1990) | US dollars (cost year 1995) | UK pounds sterling (cost year 1985) | Euros (cost year 1998) | New Zealand dollars (cost year 1993) |
| Discounting and sensitivity analysis | Discounting of costs and benefits was not conducted. Sensitivity analysis was not reported | Costs were not discounted as the study follow-up period was < 1 year. No sensitivity analysis was conducted | Discounting of costs and benefits was not reported; however, the study follow-up period was < 1 year. Sensitivity analysis was conducted modifying the hospitalisation duration and varying the rates of recovery for the two types of rehabilitation | A discount rate of 3% was applied. Sensitivity analyses were conducted varying the unit cost of staff wages and varying the discount rate from 3% to 5% | Discounting of costs and benefits was not reported | Discounting was not applied as the costs of the interventions fell within a 1-year time horizon. No sensitivity analysis was reported | Discounting was not applied as the costs fell within a 1-year time horizon. Sensitivity analysis was not conducted |
| Mean cost of the intervention | The ICP cost €14,535, including development costs | Not reported | The total cost of accelerated rehabilitation was AUS$10,600 (this included an additional AUS$10 per patient for an extra 30 minutes of nursing support or allied health professional support per day and AUS$25 per day for physician costs) and the cost of conventional rehabilitation programmes was AUS$12,800 | The cost of the intervention was US$13,842 per patient (SD US$11,941) and the cost of usual care was US$17,139 (SD US$21,577) | The joint management system cost £151.20 per patient and the single specialty (control) system cost £55.10 | Not reported | The cost per case on the intervention ward was NZ$9400 (95% CI NZ$8300 to NZ$10,500) and on the control ward was NZ$11,500 (95% CI NZ$9900 to NZ$13,200) |
| Findings | The ICP produced 36 successfully rehabilitated participants at a cost of €534,249, whereas usual care produced 27 successfully rehabilitated participants at a cost of €861,532. This was a cost of €14,840 per successfully rehabilitated participant (classed as having an ADL level of A–C) and a failure rate of 25% in the ICP group compared with a cost of €31,908 per successfully rehabilitated participant and a failure rate of 45% in the usual care group | Medicare costs were greater (p < 0.001) for hospital patients than for subacute nursing home patients. The costs of subacute nursing home patients were greater (p = 0.009) than the costs of traditional nursing home patients | Cost-effectiveness ratios were calculated based on 50% of patients recovering in the accelerated rehabilitation group and 41% recovering in the conventional rehabilitation group. The cost per recovered patient was AUS$21,240 in the accelerated rehabilitation group and AUS$31,190 in the conventional rehabilitation group | The change between baseline and 6 months in the physical role limitation component was significantly higher for the intervention group (66.1) than for the control group (38.9) (p = 0.02). The change in physical functioning score was 46.3 for the intervention group and 38.9 for the control group (p > 0.05). The change in social functioning score was 44.2 for the intervention group and 39.4 for the control group (p > 0.05) | The mean length of stay was 56 days for the intervention group and 44 days for the control group. There were no savings in terms of bed-days used between strategies. There were no statistically significant differences between the groups for ADL, prognosis and place of discharge | 4 months after hip fracture, the RAP score was 14.9 for the early discharge group and 14.5 for the conventional discharge group (based on a possible score of 0–36). The MMSE score was 20.6 for the early discharge group and 20.8 for the conventional discharge group (based on a possible score of 0–29). Early discharged patients stayed an average of 13.5 days fewer in hospital than conventionally discharged patients, although this difference was not statistically significant. Average costs during the 4 months after hip fracture were €14,281 for early discharged patients and €15,338 for conventionally discharged patients, although this difference was not statistically significant | The total mean length of stay was 20.7 days (95% CI 17.4 to 23.9 days) for the intervention group and 26.3 days (95% CI 21.2 to 31.4 days) for the non-intervention group. The mean length of stay in the rehabilitation ward was 12.7 days (95% CI 9.0 to 16.3 days) for the intervention group and 18.9 days (95% CI 13.6 to 24.2 days) for the non-intervention group. The proportion of patients discharged to a higher level of care (i.e. more nursing intensive) was 11% and 23% for the intervention and non-intervention groups, respectively |
| Conclusions | ICP was less costly and more effective than usual care, and the application of patient-centred care appears to enhance both rehabilitation outcomes and cost-effectiveness | Enhanced health outcomes were obtained with higher costs for elderly patients treated for stroke in rehabilitation hospitals. However, patients treated for hip fracture did not achieve enhanced outcomes | Accelerated rehabilitation was more cost-effective than conventional rehabilitation in treating proximal femur fracture | The intervention resulted in significant improvements in the physical role limitation component compared with standard post-operative care. The economic benefits of the intervention exceeded the costs | Geriatric–orthopaedic collaborations should take particular care in assessing the impact on hospitals of length of hospital stay and personal benefits to patients | Early discharge of hip fracture patients from hospital led to a limited non-significant reduction in total costs | The intervention led to a shorter hospital stay and reduced hospital costs without the need for increased patient dependency |
Cost-effectiveness studies
Three cost-effectiveness analyses were identified in the review.
Olsson et al. 260 conducted a cost-effectiveness analysis of an individualised hip fracture rehabilitation pathway, the integrated care pathway (n = 56), compared with usual care (n = 56) in a Swedish hospital, with a focus on motivation, prerequisites for rehabilitation and early first ambulation. Patients aged ≥ 65 years, admitted for a hip fracture and living independently, participated in the study. In the analysis, a hospital perspective was used and only direct hospital costs were considered. Costs were collected over an 18-month period during 2003–5 from the hospital’s financial database (cost year 2004). Costs were not discounted as the study follow-up period was < 1 year and loss in productivity costs were not calculated because of the age of the participants (mean age 84 years). Costs were converted from Swedish crowns to euros using the annual average exchange rate for 2004 (9.1268 SEK per €). Direct hospital costs included treatment costs (e.g. surgery, post-operative care) and hotel costs (salaries, drugs, food, accommodation, administration). The effects of the integrated care pathway and usual care were assessed by comparing participants’ self-estimated pre-fracture ADL level with their actual ADL level at discharge using a tool developed by Katz et al. 269 This tool used a hierarchical scale with steps ranging from A (completely independent) to G (completely dependent). The integrated care pathway produced 36 successfully rehabilitated participants at a cost of €534,249, whereas usual care produced 27 successfully rehabilitated participants at a cost of €861,532. Olsson et al. 260 calculated an ICER of €14,840 per successfully rehabilitated participant (classed as an ADL level of A–C) and a failure rate of 25% in the integrated care pathway group, and an ICER of €31,908 per successfully rehabilitated participant and a failure rate of 45% in the usual care group. No sensitivity analysis was reported. The authors concluded that the integrated care pathway was less costly and more effective than usual care, and that the application of patient-centred care appears to enhance both rehabilitation outcomes and cost-effectiveness. They stated that it was difficult to compare costs and outcomes for a group of patients such as hip fracture patients because of individual variability within the sample and the differing organisational structures of health care between countries. Concerning the generalisability of the results, they acknowledged that the sample size was small but argued that the statistically significant improvements in levels of ADL were likely to remain statistically significant in a larger sample.
Kramer et al. 261 conducted a cost-effectiveness analysis of different rehabilitation settings with 518 randomly selected elderly hip fracture patients and 485 stroke patients admitted between November 1991 and February 1994 from 92 hospital-based units across 17 states in the USA. The patients were randomly assigned to the following different rehabilitation settings: (1) traditional nursing home, (2) subacute nursing home and (3) rehabilitation hospital. A hospital perspective was used and only direct hospital costs were considered. Service use information was collected from admission until 6 months post admission from Medicaid forms. Costs were presented in US dollars (cost year not reported). Costs were not discounted as the study follow-up period was < 1 year. Direct health service costs were considered, such as Medicare-reimbursed costs. The outcomes of treatment in these settings were assessed in terms of the recovery of patients to premorbid levels of ADL 6 months post admission. This study assessed five ADL: bathing, dressing, toileting, transferring out of bed and walking 20 feet. Analysis was conducted for completers only. Hip fracture patients admitted to rehabilitation hospitals did not differ from patients admitted to nursing homes in terms of returning to the community [adjusted odds ratio (OR) 1.3, 95% CI 0.6 to 2.6] or the number of ADL recovered to premorbid levels (difference 0.09 ADL, 95% CI 0.27 to 0.44 ADL). There was no difference in return to the community between patients admitted to subacute nursing homes and patients admitted to traditional nursing homes (adjusted OR 1.6, 95% CI 0.7 to 3.6). Medicare costs were greater (p < 0.001) for rehabilitation hospital patients than for subacute nursing home patients. The costs of subacute nursing home patients were greater (p = 0.009) than those for traditional nursing home patients. No sensitivity analysis was conducted. The authors concluded that enhanced health outcomes were obtained at higher costs. Enhanced outcomes were obtained with higher costs for elderly patients treated for stroke in rehabilitation hospitals. However, patients treated for hip fracture did not achieve enhanced outcomes. The authors did not state if the results of the study were generalisable to other settings and did not compare the results with the results of other studies.
Cameron et al. 253 conducted a cost-effectiveness analysis of an accelerated rehabilitation intervention (n = 127) compared with conventional rehabilitation (control group) (n = 125) for elderly patients with proximal femur fracture in an Australian general hospital between 1989 and 1990. Patients in the accelerated rehabilitation group received earlier assessment of rehabilitation goals, early commencement of rehabilitation (usually within 24 hours of surgery), early mobilisation, retraining of physical independence, closer family caregiver contact and detailed discharge planning combined with elements of geriatric assessment. The control group received conventional rehabilitation (a variety of rehabilitation programmes depending on functional status following surgery). Forty-five control group participants received interdisciplinary rehabilitation (equivalent to orthogeriatric care), 23 participants received little formal rehabilitation as they had limited disability and were discharged directly home, 12 patients were discharged to a nursing home before they could return to their own home because of poor prognosis and 45 patients were transferred back to their nursing home on discharge. Costs were considered from a hospital and community perspective. Direct hospital costs included the costs of inpatient surgical and post-surgical care, readmissions, community support services and institutional care. No family costs of rehabilitation were considered. Costs post hospital discharge were calculated and included the costs of follow-up treatment, changes in residential care and home support services. Service use was collected from admission, with a 4-month post-operative follow-up. Unit costs were gathered from published data, local service providers or government subsidies for residential care. Costs were presented in Australian dollars (cost year 1990). Discounting of costs and benefits was not reported; however, the study follow-up period was < 1 year. The effects of the two rehabilitation interventions were assessed by comparing patients’ pre-fracture and post-rehabilitation physical independence, using the Barthel Index of Activities of Daily Living. 265 This index, which is a standard, validated method of measuring physical independence levels, was administered by a trained research nurse during admission and again 4 months after fracture. A recovered patient is a patient who has returned to disability-free living, defined as requiring no or limited assistance in ADLs and characteristically having a score of ≥ 80 on the index. If a patient had significant disability prior to fracture (classed as scoring < 80 on the index) then recovery was defined as regaining the premorbid level of physical independence. In the accelerated rehabilitation group, 63 of the 127 patients (49.6%) met the criteria for recovery, whereas in the conventional care group, 52 of the 125 (41.6%) patients met the criteria for recovery; this difference was not statistically significant. The total cost of accelerated rehabilitation was AUS$10,600 (this included an additional AUS$10 per patient for an extra 30 minutes of nursing support or allied health professional support per day and AUS$25 per day for physician costs) and of the conventional rehabilitation programmes was AUS$12,800. Cost-effectiveness ratios were calculated as the total direct cost per recovered patient of accelerated rehabilitation and conventional care, based on 50% of patients recovering in the accelerated rehabilitation group and 41% of patients recovering in the conventional rehabilitation group (difference of 9%, 95% CI –3% to 21%). The cost per recovered patient was AUS$21,240 in the accelerated rehabilitation group and AUS$31,190 in the conventional rehabilitation group. When only the costs after surgery were considered, the cost-effectiveness ratios produced a cost per recovered patient of AUS$15,290 in the accelerated rehabilitation group and AUS$25,250 in the conventional rehabilitation group. Sensitivity analysis was conducted modifying the duration of hospitalisation and varying the rates of recovery for the two types of rehabilitation. The sensitivity analysis demonstrated that patients in the accelerated group needed to be hospitalised for approximately 1.5–2 days fewer than patients in the conventional care group for the intervention to start generating cost savings. Given the reduction in length of stay achieved by accelerated rehabilitation, accelerated rehabilitation patients could receive treatment costing up to 40% more per bed-days than conventional care patients and still generate savings in gross costs. If the criterion for recovery changed from a Barthel Index score of 80 to a score of ≥ 90, no differences were found in the relative costs of the two rehabilitation programmes; the cost per recovered patient in each of the two rehabilitation programmes increased by approximately 20%. The authors concluded that accelerated rehabilitation was more cost-effective than conventional rehabilitation in treating proximal femur fracture. They did not state if their results were generalisable to other settings and did not compare their results with the results of other studies.
Cost–benefit analysis
Two cost–benefit analyses were identified in the review.
Ruchlin et al. 262 conducted a cost–benefit analysis of a patient education and high-intensity strength intervention to improve rehabilitation after hip fracture compared with standard post-operative care (control condition). In total, 114 patients aged > 64 years who had been admitted for a hip fracture to the New York Hospital, the Hospital for Special Surgery or the New York Hospital – Queens received either the patient education self-efficacy video and high-intensity strength intervention (n = 59) or usual care (n = 55). Costs were collected from a societal perspective and included direct medical costs and non-medical costs (e.g. costs of community-based care). Direct medical costs included the costs of outpatient and inpatient care, emergency care, acute hospital care, post-hospital rehabilitation in a long-term care facility, nursing home care, physical and occupational therapy, visiting nurse care and prescription drugs. Community care-based costs included the costs of home assistance, transportation and informal care provided by family and/or friends. Service use was collected via self-reported service utilisation questionnaires administered by telephone interview to patients. Medicare reimbursement rates were used to provide the unit costs of direct and community care. Service use data were collected until 18 months post fracture. Costs were presented in US dollars (cost year 1995). As data were collected until 18 months post fracture, a discount rate of 3% was applied. Physical role limitation, physical functioning and social functioning components of the Short Form questionnaire-36 items (SF-36)266 were assessed at baseline and 6 months’ follow-up for the intervention and control groups. The protocol stated that each patient in the intervention group should receive 16 strength training sessions; however, only 35 of the 59 intervention patients (59.3%) received any strength training. The video was seen by 42 of the intervention patients (71.2%) and 24 of the intervention patients (40.7%) had at least one contact with a peer advocate. The change between baseline and 6 months in the physical role limitation component was significantly higher for the intervention group (66.1) than for the control group (38.9) (p = 0.02). The change in physical functioning score was 46.3 for the intervention group and 38.9 for the control group (p > 0.05). The change in social functioning score was 44.2 for the intervention group and 39.4 for the control group (p > 0.05). The cost of the intervention was US$13,842 per patient (SD US$11,941) and the cost of usual care was US$17,139 (SD US$21,577) per patient. The total intervention cost was US$42,593. The total saving for the intervention compared with usual care was US$194,527 (US$66,799 in direct medical savings and US$127,725 in non-medical savings). The cost–benefit ratio was 4.57, higher than the threshold of 1.0, and the net present value of the intervention was US$151,934. Sensitivity analyses were conducted varying the unit cost applied to staff wages from the federal minimum wage (US$4.25 per hour) to market wages (US$11.50 per hour). When the 3% discount rate was maintained and the higher market wage was applied (US$11.50 per hour), the total saving for the intervention compared with usual care was US$226,661 (US$66,799 in direct medical savings and US$159,856 in non-medical savings). The cost–benefit ratio was 5.32, with a net present value of US$184,068. In addition, as part of the sensitivity analysis a 5% discount rate was applied to test the robustness of the findings. When applying the 5% discount rate to the estimates using the federal minimum wage value (US$4.25 per hour) to calculate wage costs, the total saving for the intervention compared with usual care was US$193,567 (US$66,746 in direct medical savings and US$126,809 in non-medical savings). The cost–benefit ratio was 4.54, with a net present value of US$150,974. When the 5% discount rate was applied to the estimates using the market wage value (US$11.50 per hour) to calculate wage costs, the total saving for the intervention compared with usual care was US$225,660 (US$66,746 in direct medical savings and US$158,898 in non-medical savings). The cost–benefit ratio was 5.30, with a net present value of US$183,067. The authors concluded that the intervention results in significant improvements in the physical role limitation component compared with usual care. The economic benefits of the intervention exceeded its costs. The authors did not state if the results of the study were generalisable to other settings and did not compare their results with the results of other studies.
Fordham et al. 254 conducted a cost–benefit analysis of a new joint management system compared with a single specialty orthopaedic management system (standard care). In total, 108 women aged > 65 years with a fractured neck of femur were randomly assigned to either the new joint management system (n = 50) or the single specialty orthopaedic management system (n = 58) in Huddersfield, UK. The joint management system consisted of joint geriatric and orthopaedic management including early post-admission assessment, joint weekly bedside consultations, joint consultant decision-making with regard to the rehabilitation programme and any ward/hospital transfers and discharge. Standard care patients were treated solely by an orthopaedic consultant, with advice from a geriatrician when necessary. Costs were collected from a hospital perspective and only direct hospital costs were considered. Service use was collected from hospital records using a specially designed patient profile data collection form, from admission up to and including discharge, at fixed intervals. Sources of unit costs were not reported in the paper. Costs were presented in UK pounds sterling (cost year 1985). Discounting of costs and benefits was not reported. Costs taken into consideration included the cost of the bed-days utilised and staff inputs into rehabilitation, for example physiotherapists’ and occupational therapists’ time. Additional costs for the joint management system were considered and included the costs of extra geriatrician input, medical travel and ambulance transfer. Costs were not discounted as the study follow-up period was < 1 year. The different management systems were assessed based on the average cost of the hospital stay per patient, the length of stay per patient, ADL, prognosis and place of discharge. Measures were taken at fixed intervals during the study: at admission, during the fourth week of hospitalisation and at discharge. ADL, prognosis and place of discharge were assessed against a classification system devised by the research team rather than a standardised system. The mean length of stay was 56 days for the intervention group and 44 days for the control group. The study showed no savings in terms of bed-days used. There were no statistically significant differences between groups for ADL, prognosis and place of discharge. The joint management system cost £151.20 per patient and the single specialty (control) system cost £55.10 per patient. Joint management was £96 more expensive per patient than single specialty management. In relation to total costs, this represented a 3.6% increase, which was quite small in proportion to the total hospital costs. No sensitivity analysis was reported. The authors concluded that future geriatric–orthopaedic collaborations should take particular care in assessing the impact on length of hospital stay and personal benefits to patients. They also stated that costs could have been reduced further if arrangements for joint management had been based at a single site, as travel between sites was a major source of additional costs. In this case, the costs of the joint management would have been only 2% more expensive. The authors advised caution when generalising the results of this study to other settings because of the small sample size and did not compare the results with those of other studies.
Cost-minimisation analysis
Two cost-minimisation analyses were identified in the review.
Polder et al. 263 conducted a cost-minimisation analysis of two discharge programmes in 208 patients with a fresh hip fracture between October 1996 and October 1998 in a general hospital in Rotterdam, the Netherlands. The two discharge programmes were classed as conventional discharge (n = 102) and early discharge (n = 106). Conventional discharge patients stayed in hospital longer for rehabilitation than early discharge patients. The treatment consisted of physical therapy, which was administered twice per day by the hospital’s physiotherapists under the supervision of ward physicians. Early discharge was implemented by a discharge protocol that started 5 days post-operatively. Administrative procedures were accelerated and the number of available beds on the rehabilitation ward was increased. Physiotherapists, occupational therapists and social workers were involved in the rehabilitation process and were supervised by a physician trained in geriatric medicine. Costs were considered from a societal perspective and included the costs of manpower, equipment, materials, housing and overheads, all medical costs and patient-borne costs including those borne by families (e.g. for travelling). Service use was gathered through interviews, including with family members to gather any family-borne costs, and from hospital records. The costs were divided into seven categories: (1) preadmission, (2) from admission to day 5 after hip fracture, (3) from day 6 after fracture until discharge, (4) nursing home, (5) care home, (6) own home and (7) readmission to hospital or nursing home. This resulted in a calculation of the total average cost per day for each patient. Service use was estimated for a 7-month period (3 months pre-operatively and 4 months post-operatively) and unit costs were gathered from hospital financial records. Costs were presented in euros (cost year 1998). Discounting was not applied as the costs of the interventions fell within a 1-year time horizon. The effects of the two discharge programmes were assessed by comparing patients’ functional outcome and cognitive status using the Rehabilitation Activities Profile (RAP)267 and the Mini Mental State Examination (MMSE). 268 The RAP is based on the International Classification of Impairments, Disabilities and Handicaps and measures disabilities in communication, mobility and personal care. Four months after hip fracture, the RAP score was 14.9 for the early discharge group and 14.5 for the conventional discharge group (based on a possible score of 0–36). The MMSE score was 20.6 for the early discharge group and 20.8 for the conventional discharge group (based on a possible score of 0–29). Early discharged patients stayed an average of 13.5 days less in hospital than conventionally discharged patients, although this difference was not statistically significant. Average costs during the 4 months after hip fracture were €14,281 for early discharged patients and €15,338 for conventionally discharged patients, although this difference was not statistically significant. No sensitivity analysis was reported. The authors concluded that early discharge of hip fracture patients from hospital led to a limited non-significant reduction in total costs. Although the reduction in hospital stay for the early discharge programme was larger than that reported in Australian studies by Cameron et al. ,253 Farnworth et al. 247 and Sikorsky and Senior,270 significant cost-savings were not observed. The authors advised caution when generalising the results of this study to other settings because of the small sample size.
Elliot et al. 264 conducted a cost-minimisation analysis in Christchurch, New Zealand, of geriatrician assessment (n = 61) of patients aged 65 years with a femoral fracture admitted to an acute orthopaedic ward compared with standard care (n = 57), whereby geriatrician input was given only following a request from the orthopaedic medical staff. Costs were considered from a hospital perspective, with direct hospital costs calculated (e.g. surgery, post-operative care). Service use was estimated from admission to discharge from the hospital, gathered from hospital data. Unit costs were obtained from hospital financial records. Costs were presented in New Zealand dollars (cost year 1993). Discounting was not applied as the costs fell within a 1-year time horizon. The total mean length of stay was 20.7 days (95% CI 17.4 to 23.9 days) for the intervention group and 26.3 days for the non-intervention group (95% CI 21.2 to 31.4 days). The mean length of stay in the rehabilitation ward was 12.7 days (95% CI 9.0 to 16.3 days) for the intervention group and 18.9 days (95% CI 13.6 to 24.2 days) for the non-intervention group. The proportion of patients discharged to a higher level of care (i.e. more nursing intensive) was 11% and 23% for the intervention and non-intervention groups, respectively. The length of stay, cost of care and discharge destination were compared for each group. The cost per case on the intervention ward was NZ$9400 (95% CI NZ$8300 to NZ$10,500) and on the control ward was NZ$11,500 (95% CI NZ$9900 to NZ$13,200). No sensitivity analysis was conducted. The authors concluded that the intervention led to a shorter hospital stay and reduced hospital costs, without the need for increased patient dependency. These results agree with other findings that geriatricians provide additional health benefit, either at a lower cost or at an equal cost to that of conventional care. Because of the small sample size, caution is needed when generalising the results of this study to other settings.
Quality assessment
Table 3 provides the results of the quality assessment of the included economic studies using the checklist of Drummond et al. 66
| Checklist question | Olsson 2009260 | Kramer 1997261 | Cameron 1994253 | Ruchlin 2001262 | Fordham 1986254 | Polder 2003263 | Elliot 1996264 |
|---|---|---|---|---|---|---|---|
| Was a well-defined question posed in an answerable form? | Yes, the analysis assessed the costs and effects of an individualised hip fracture rehabilitation pathway, the ICP, compared with usual care | Yes, the analysis assessed the costs and effects of different rehabilitation settings for elderly patients admitted for hip fracture and stroke | Yes, the analysis assessed the costs and effects of an accelerated rehabilitation intervention compared with conventional rehabilitation | Yes, the analysis assessed the costs and benefits of a patient education and high-intensity strength intervention compared with standard post-operative care | Yes, the analysis assessed the costs and benefits of a new joint management system compared with a single specialty orthopaedic management system (standard care) | Yes, the analysis assessed two discharge programmes using cost-minimisation analysis | Yes, the analysis assessed geriatrician assessment compared with standard care, in which geriatrician input was given only following a request from the orthopaedic medical staff, using cost-minimisation analysis |
| Was a comprehensive description of the competing alternatives given? | The intervention was well described; however, no description was provided of usual care | Minimal descriptions were provided for the different settings | Both the intervention and the control conditions were well described | The intervention was well described; however, no description was provided of usual care | Both the intervention and the control conditions were well described | Both the intervention and the control conditions were well described | A limited description was given for both the intervention and the control conditions |
| Was the effectiveness of the programmes or services established? | Yes, the effects of the ICP and usual care pathways were assessed by comparing patients’ self-estimated pre-fracture ADL level with their actual ADL level at discharge using a tool developed by Katz et al.269 | Yes, the effects of treatment settings were assessed in terms of the recovery of patients to premorbid ADL levels at 6 months post admission. In this study, five ADLs were assessed: bathing, dressing, toileting, transferring out of bed and walking 20 feet | Yes, the effects of the accelerated rehabilitation intervention and conventional rehabilitation were assessed by comparing patients’ pre-fracture and post-rehabilitation physical independence using the Barthel Index of ADL265 | Yes, physical role limitation, physical functioning and social functioning components of the SF-36266 were assessed at baseline and at 6 months’ follow-up | Yes, the different management systems were assessed based on the average cost of the hospital stay per patient, length of stay per patient, ADL, prognosis and place of discharge | Yes, the effects of the two discharge programmes were assessed by comparing patients’ functional outcome and cognitive status using the RAP267 and the MMSE268 | Yes, the effects of the two assessment packages were assessed by comparing length of stay, cost of care and discharge destination |
| Were all of the important and relevant costs and consequences for each alternative identified? | Only direct hospital costs were considered in the analysis, such as treatment costs (e.g. surgery, post-operative care) and hotel costs (salaries, drugs, food, accommodation, administration) | Only direct hospital costs were considered in the analysis | Direct hospital costs included the costs of inpatient surgical and post-surgical care, readmissions, community support services and institutional care | Direct medical costs and non-medical costs (e.g. community-based care) were considered in the analysis | Only direct hospital costs were considered in the analysis | A wide range of costs was considered including the costs of manpower, equipment, materials, housing and overheads, all medical costs and patient-borne costs including those borne by families (e.g. for travelling) | Only direct hospital costs (e.g. surgery, post-operative care) were considered in the analysis |
| Were costs and consequences measured accurately in appropriate physical units? | The costs and consequences were measured appropriately given the aim of the analysis | The costs and consequences were measured appropriately given the aim of the analysis | The costs and consequences were measured appropriately given the aim of the analysis | The costs and consequences were measured appropriately given the aim of the analysis | The costs and consequences were measured appropriately given the aim of the analysis | The costs and consequences were measured appropriately given the aim of the analysis | The costs and consequences were measured appropriately given the aim of the analysis |
| Were costs and consequences valued credibly? | Costs and consequences were clearly identified and appropriate for the research question | Costs and consequences were clearly identified and appropriate for the research question | Costs and consequences were clearly identified and appropriate for the research question | Costs and consequences were clearly identified and appropriate for the research question | Costs and consequences were clearly identified and appropriate for the research question | Costs and consequences were clearly identified and appropriate for the research question | Costs and consequences were clearly identified and appropriate for the research question |
| Were costs and consequences adjusted for differential timing? | No, costs were not discounted as the study follow-up period was < 1 year | Costs were not discounted as the study follow-up period was < 1 year | Discounting of costs and benefits was not reported; however, the study follow-up period was < 1 year | A discount rate of 3% was applied | Costs were not discounted as the study follow-up period was < 1 year | Discounting was not applied as the costs of the interventions fell within a 1-year time horizon | Discounting was not applied as the costs fell within a 1-year time horizon |
| Was an incremental analysis of the costs and consequences of alternatives performed? | Yes, ICERs were calculated per successfully rehabilitated participant (classed as having an ADL score of A–C) | No, as no intervention was proven to be cost-effective. Enhanced health outcomes were obtained with higher costs for patients admitted for stroke | Cost-effectiveness ratios were calculated as the total direct cost per recovered patient of accelerated rehabilitation and conventional care | A cost–benefit analysis was conducted based on the physical role limitation, physical functioning and social functioning components of the SF-36266 | A cost–benefit analysis was conducted based on the average cost of the hospital stay per patient, length of stay per patient, ADL, prognosis and place of discharge | A cost-minimisation analysis was conducted based on patients’ functional outcome and cognitive status using the RAP267 and the MMSE268 | A cost-minimisation analysis was conducted based on length of stay, cost of care and discharge destination |
| Was allowance made for uncertainty in the establishments of costs and consequences? | No sensitivity analysis was reported | No sensitivity analysis was conducted | Sensitivity analysis was conducted modifying the duration of hospitalisation and varying the rates of recovery for the two types of rehabilitation | Sensitivity analyses were conducted varying the unit cost of staff wages and varying the discount rate from 3% to 5% | No sensitivity analysis was reported | No sensitivity analysis was reported | No sensitivity analysis was conducted |
| Did the presentation and discussion of the study results include all issues of concern to users? | The authors concluded that the ICP was less costly and more effective than usual care. Concerning the generalisability of the results, they acknowledged that the sample size was small but argued that the statistically significant improvements in levels of ADL were likely to remain statistically significant in a larger sample | The authors did not state if the results of the study were generalisable to other settings and did not compare their results with the results of other studies | The authors concluded that accelerated rehabilitation was more cost-effective than conventional rehabilitation in treating proximal femur fracture. They did not state if the results were generalisable to other settings and did not compare their results with the results of other studies | The economic benefits of the intervention exceeded its costs. The authors did not state whether the results of the study were generalisable to other settings and did not compare the results with the results of other studies | There were no savings in bed-days used despite similar levels of ADL and places of discharge in the two groups. The authors advised caution when generalising the results of the study to other settings because of its small sample size and did not compare the results with the results of other studies | The authors concluded that early discharge of hip fracture patients from hospital led to a limited non-significant reduction in total costs. Although the reduction in hospital stay in the early discharge programme was larger than those reported in Australian studies conducted by Cameron et al.,253 Farnworth et al.247 and Sikorsky and Senior,270 the authors did not observe significant cost-savings. They advised caution when generalising the results of this study to other settings because of the small sample size | The authors concluded that the intervention led to a shorter hospital stay and reduced hospital costs, without the need for increased patient dependency. Because of the small sample size, the results of this study should be generalised to other settings with caution |
Discussion
The review identified seven economic evaluations: three cost-effectiveness analyses,253,260,261 two cost–benefit analyses254,262 and two cost-minimisation analyses. 263,264 The year of publication ranged from 1986 to 2009. The studies were conducted in Australia, New Zealand, the Netherlands, Sweden, the UK and the USA. The majority of the studies calculated costs from a hospital perspective, considering direct hospital costs only, such as the costs of treatment, medication and care. 254,260,261,264
Summary of findings
Two out of the three cost-effectiveness studies found that rehabilitation pathways were cost-effective. Olsson et al. 260 demonstrated that an integrated care pathway with a focus on motivation for rehabilitation and early first ambulation was less costly and more effective than a usual care pathway. The application of patient-centred care appeared to enhance both rehabilitation outcomes and cost-effectiveness in a Swedish hospital. Cameron et al. 253 found that an accelerated rehabilitation intervention using early assessment, early mobilisation, physical independence and detailed discharge planning was more cost-effective than conventional rehabilitation in treating proximal femur fracture in an Australian general hospital. On the other hand, Kramer et al. 261 conducted a cost-effectiveness analysis of different rehabilitation settings and found that enhanced health outcomes were obtained with higher costs for patients admitted with stroke and that therefore the intervention could not be considered cost-effective. Of the two cost–benefit analyses, only one found that the benefits of the intervention outweighed the costs. Ruchlin et al. 262 found that a patient education and high-intensity strength intervention to improve rehabilitation after hip fracture resulted in significant improvements in physical role limitation compared with standard post-operative care and that these benefits exceeded the costs. Fordham et al. 254 found that the number of bed-days and the costs increased for the intervention group compared with the control group. Both Polder et al. 263 and Elliot et al. 264 revealed that the interventions under study reduced costs without reducing outcomes compared with usual care, thus demonstrating that the interventions could be lower-cost alternatives to regular practice.
Strengths and limitations
Many of these studies had small sample sizes. This is common in economic analyses as the power calculations of most studies are based on detecting differences in clinical outcomes. 271 A small sample size can lead to difficulties in detecting differences between groups and to the misinterpretation of results.
Other potential biases were also noted. In the study by Cameron et al. ,253 both the control group and the intervention group were treated on the same ward by the same practitioners, with a potential for cross-contamination of those in the control group if they overheard advice from the practitioners or received elements of the intervention by mistake. Polder et al. 263 found that health-care costs in the study shifted from hospitals to nursing homes, highlighting the importance of a detailed cost analysis based on real resource use to detect whether there are true cost-savings or just redistribution of costs. Polder et al. 263 also found that costs increased for individuals with comorbidities and impaired cognitive status and for the oldest members of the sample. Elliot et al. 264 did not report their recruitment process; however, in their discussion they highlighted the potential for bias, in particular in patients who were allocated to the treatment ward based on staff judgements that they would benefit more from the intervention than from usual care.
The studies were carried out in different countries, making cost and care pathway comparisons difficult. In particular, there was a lack of UK evidence; of the seven economic studies identified, only one came from the UK. Three methods of economic evaluation were identified in the included studies: cost-effectiveness analysis, cost–benefit analysis and cost-minimisation analysis. Each of these methods uses different techniques to value and compare the costs and effects of an intervention. Each study compared a different rehabilitation pathway, intervention or setting, making comparisons difficult, although Olsson et al. 260 and Cameron et al. 253 both championed patient-centred approaches to rehabilitation such as early assessment and early ambulation/mobilisation. There was also a lack of recent economic evaluations; the latest evaluation included in the review was published in 2009.
Another limitation noted was the lack of detail when describing how the costs of the interventions were calculated to help determine exactly what costs were included in the analyses. As shown in Table 3, the majority of studies stated that only direct hospital costs were considered. Certain studies gave examples of these costs, but this was not consistent across the included studies. Although Olsson et al. 260 showed that the integrated care pathway was cost-effective in a Swedish hospital, they did not state if the costs of the integrated care pathway, including any development costs, were included with the direct hospital costs, such as treatment and hotel costs, in the cost-effectiveness ratio. Kramer et al. 261 provided a limited explanation of how the cost data were handled and no price year was reported in the paper. A more detailed description of how costs were collected and used for the purpose of the analyses would have been useful.
Implications for practice and future research
This review is in agreement with the NICE hip fracture guidance7 and the Cochrane review by Handoll et al. 8 in finding that there is a limited evidence base for multidisciplinary hip fracture rehabilitation, particularly from UK settings. Five of the seven interventions studied were shown to be a good use of resources, using cost-effectiveness, cost–benefit or cost-minimisation analysis. However, the range of methods used and the range of interventions studied did not allow us to make firm conclusions about any one type of rehabilitation intervention. Despite this, two of the cost-effectiveness analyses showed that patient-centred approaches to rehabilitation were a good use of hospital resources. However, more economic evidence is needed, particularly from the UK.
Chapter 4 Survey of hip fracture centres, physiotherapists and occupational therapists
Introduction
The second component of Phase I (developing the multidisciplinary rehabilitation programme) was a survey of current UK NHS hip fracture physical rehabilitation services to determine usual practice and identify components of good practice. As we aimed to develop an intervention targeting the physical rehabilitation of patients and their engagement in the practice of physical exercises, we focused this survey on physiotherapy and occupational therapy services.
Aim
To investigate and describe current UK NHS hip fracture physical rehabilitation service provision for patients aged ≥ 65 years in both acute and community settings who have had dynamic hip screw or hemiarthroplasty surgery for proximal hip fracture.
Objectives
To describe the variability in current practice and service provision, and obtain examples of good practice and respondents’ views on how provision could be improved.
Methods
We conducted a UK-wide web-based survey of physiotherapists, occupational therapists and hip fracture centre therapy service managers working in the rehabilitation of patients aged ≥ 65 years who have had surgery for proximal hip fracture. We chose to focus on patients who had a dynamic hip screw or hemiarthroplasty, as both of these operations enable immediate weight-bearing rehabilitation.
Questionnaire design and pilot
National Institute for Health and Care Excellence guidance on hip fracture rehabilitation7 was used as the starting point for developing the survey questions because it outlines best practice recommendations based on current evidence. The particular recommendations were those pertaining to rehabilitation:
-
orthogeriatric assessment
-
early mobilisation and physiotherapy
-
early assessment of cognition
-
early identification of individual goals for multidisciplinary rehabilitation to recover mobility and independence
-
facilitate return to pre-fracture residence and long-term well-being
-
ongoing multidisciplinary team co-ordination and review
-
liaison or integration with related services, particularly mental health, falls prevention, bone health, primary care and social services
-
offer patients (or, as appropriate, carers and/or family members) information about treatment and care.
The questions were designed to provide descriptive data on how these recommendations may have been operationalised in clinical practice and service organisation. In addition, patient mood,11 self-efficacy13,272 (defined as a belief in one’s ability to organise and carry out/execute a general or specific action273) and fear of falling12 have been shown to impact on rehabilitation outcomes following hip fracture as well as elective hip surgery and so we also asked all respondents whether or not these were routinely assessed and, if so, what measures were used. We also asked respondents for their views of good practice and where improvements could be made.
Most elements of rehabilitation that this project focused on were delivered by both physiotherapists and occupational therapists across different health-care settings and so we chose to survey these professions from both the clinical and the service management perspectives. As a result, three versions of the survey were developed to address the different professional roles of potential respondents: one for physiotherapists (see Appendix 21), one for occupational therapists (see Appendix 22) and one for hip fracture centre therapy service managers (see Appendix 23). The therapist versions were further subdivided by type of health-care setting, that is, for those working in acute hospitals, community hospitals or similar community inpatient facilities and community-based teams providing services to patients in their own homes, including care/nursing homes.
By combining the answers from the different versions of the survey we sought to describe the organisation of services, including multidisciplinary working, working across acute and community settings in terms of discharge planning, liaison and signposting to supportive social groups and activities, and coverage of rehabilitation services. We also planned to be able to describe current clinical practice in terms of assessment and the content of routine rehabilitation.
Demographics
All versions of the questionnaire included questions on the location of the service and the hip fracture centres served, the respondent’s role in hip fracture rehabilitation and the profession of the respondent. In addition, the therapist versions asked for the respondent’s NHS clinical band and type of setting in which they worked (to direct them to the appropriate section of the questionnaire).
The study manager developed the questions in consultation with the chief investigator. The content of the questions and response options for the physiotherapy and occupational therapy questionnaires were developed by the study manager and the physiotherapist and occupational therapist members of the research team. Other members of the research team then commented on all of the questions to further refine them. All of the questionnaires were piloted on members of staff across one health board in Wales. This organisation has responsibility for both acute and community services and so all versions of the questionnaire could be piloted within this one organisation. The pilot was used to assess the content of the questionnaires and the functionality of the web-based survey. A few minor amendments were made following feedback from this pilot, for example adding ‘other’ as a response option for questions and correcting questions that referred to the wrong professions.
Organisation of services
The survey of managers focused on the organisation of services and included questions concerning:
-
the availability of different acute and community service provision models
-
the involvement of different professions in the multidisciplinary rehabilitation team both in acute centres and in the community
-
discharge planning and co-ordination with community services and signposting to social support or activities
-
the proportion of patients discharged from acute centres to their own homes who received rehabilitation after discharge.
A few service organisational questions were also included in the two therapist questionnaires. As for the managers, acute therapists were asked about the types of wards where patients were treated and how weekend care was organised. Community therapists were asked about their involvement in multidisciplinary team discharge planning meetings. Community hospital therapists were asked about discharge timing, that is, the length of time post-operatively before patients were usually transferred from an acute hospital.
All respondents were asked if they routinely signposted patients to formal/informal social support services or activities. They were also asked if they used a hip fracture integrated care pathway that included rehabilitation and, if so, to send it to the research team. Physiotherapists were also asked if they used patient information leaflets about exercises and, if so, to send examples to the research team.
Clinical practice
The physiotherapist and occupational therapist questionnaires addressed:
-
assessment, including its timing
-
the content of routine rehabilitation
-
the frequency and length of sessions
-
details of any home visits carried out before discharge from inpatient care and for which patients
-
whether or not they routinely assessed cognitive status, mood, self-efficacy or fear of falling, which tools were used and which profession conducted these assessments.
In addition, physiotherapists were asked on which post-operative day patients were mobilised.
Areas of good practice and those needing improvement
Open-ended questions were used to allow respondents to comment on good aspects of their service and anything that they thought could be improved. Open-ended questions were also used to give respondents the opportunity to add any further comments about aspects of rehabilitation not covered by the survey.
Data collection
The survey was open for 7 weeks from 6 August 2013 to 25 September 2013.
Strategies used to reach respondents
Survey of therapy managers
We purposively surveyed a sample of senior managers who had a strategic role in rehabilitation services for this group of patients. We aimed to achieve a 10% sample of all UK hip fracture centres. We identified centres in Wales, Northern Ireland and England from publicly available information on the National Hip Fracture Database. A list of acute centres in Scotland was obtained by contacting acute hospitals by telephone and e-mail. From the list of centres obtained, we purposively sampled for geographical spread and a range of centre sizes. An attempt was made to contact 62 of the 186 hospitals registered on the National Hip Fracture Database by telephone, as well as a further eight hospitals in Scotland not on the database. Of the 70 hospitals, three refused to take part in the survey, 11 did not reply, 26 provided a general enquiry e-mail addresses to contact managers and the remaining 30 gave direct contact details for therapy service managers. In total, we invited a sample of 56 therapy managers from 194 centres (29%), including five from Scotland. The sample came from a range of hospitals serving different geographical areas and with a range of hip fracture activity according to the number of hip fracture operations performed in the last year. High-activity hospitals performed > 700 operations, medium-activity hospitals performed 400–699 operations and low-activity hospitals performed < 400 operations. Twenty-four centres agreed to complete the survey from around the country (completion rate therefore 12%). Of these, 11 were high-activity hospitals, four were medium-activity hospitals and five were low-activity hospitals. The remaining four were located in Scotland. In addition to telephone contact, we advertised the survey on the National Hip Fracture Database website to obtain data from additional centres.
Survey of physiotherapists and occupational therapists
As there is no register or centrally held record of physiotherapists and occupational therapists working in hip fracture rehabilitation, we were not able to establish the population of such professionals in the UK or use such a register as a sampling frame. We decided to advertise the survey on the websites of the Chartered Society of Physiotherapists and the College of Occupational Therapists/British Association of Occupational Therapists to target special interest groups when possible, and on the National Hip Fracture Database website. We asked those who saw the advert to pass the survey web link on to any colleagues working in this field; we also asked therapy service managers completing the survey to pass the survey web link on to their therapy staff.
Analysis
Descriptive statistics were used to provide frequency (counts, percentages) data concerning current services and practice when the answer format provided predetermined response options. When the response format was open-ended, responses were coded and categorised into themes. The integrated care pathways and physiotherapy exercise sheets returned to the team were qualitatively reviewed to provide a description of commonalities and differences.
Results
Demographics
In total, 210 respondents completed the survey, consisting of 13 managers, 57 acute inpatient physiotherapists, 29 community inpatient physiotherapists, 43 community team physiotherapists, 37 acute inpatient occupational therapists, 18 community inpatient occupational therapists and 13 community team occupational therapists. Of the 70 hospitals contacted in relation to the survey of therapy service managers, 25 agreed to take part, with 13 actually completing the survey, as shown in Appendix 24. It was our aim to recruit therapy service managers from 10% of UK hip fracture centres to which we achieved 7%. Although 24 centres agreed to take part in the survey of managers, the survey links may have been passed on within the centre, resulting in respondents answering a more relevant version of the questionnaire. An example of this is that, although we were unable to recruit any managers from Northern Ireland, we did receive completed surveys from some therapists in Northern Ireland.
Geographical spread
Respondents were geographically spread across the UK, with respondents from community hospitals and teams generally being from the surrounding areas of respondents from acute hospital teams. Of the respondents to the survey of therapy managers, two were from Wrexham and two were from Portsmouth.
Respondents’ roles/job titles
The exact job roles and titles of the different groups varied, although managers were generally principals, leads or heads of departments. Eleven of the 13 manager respondents were physiotherapists and two were occupational therapists. In all three settings (acute hospitals, community hospitals and community teams) the majority of the physiotherapist and occupational therapist respondents reported spending most of their time delivering front-line clinical care, with some also having some management responsibility.
Table 4 denotes the workload structures for physiotherapists and occupational therapists in different settings.
| Role | Setting, n | |||||
|---|---|---|---|---|---|---|
| Acute hospitals | Community hospitals | Community teams | ||||
| Physiotherapists | Occupational therapists | Physiotherapists | Occupational therapists | Physiotherapists | Occupational therapists | |
| I spend most of my time delivering front-line clinical care and rehabilitation to proximal hip fracture patients | 14 | 10 | 7 | 4 | 8 | 5 |
| I spend a lot of my time delivering clinical care and rehabilitation with some management responsibility (e.g. line management for junior staff) | 29 | 24 | 15 | 10 | 22 | 5 |
| I spend most of my time managing the physiotherapy rehabilitation service for proximal hip fracture patients | 4 | 2 | 1 | 3 | 2 | 0 |
| I have a strategic managerial role in physiotherapy service provision including oversight of rehabilitation for proximal hip fracture patients | 5 | 0 | 1 | 0 | 1 | 0 |
| Other | 5a | 1b | 5a | 1b | 10a | 3b |
| Total | 57 | 37 | 29 | 18 | 43 | 13 |
Service organisation
Integrated care pathway
In the survey of managers, nine of the 13 centres said that they had a written integrated care pathway for patients with proximal hip fracture including rehabilitation; the remaining four did not. Four centres sent a copy of their integrated care pathway to the research team. The initial assessment of the patient varied between pathways but often included a specific falls assessment to identify patients at risk of further falls. This involved a review of medication and other physical factors, such as visual or auditory impairment, but may also have included an assessment of how the current fall happened, the circumstances that led to it and whether or not the patient had previously fallen. In addition to the falls assessment, the initial assessment often asked about the social history of the patient. This generally focused on the type of accommodation that the patient lived in, who he or she lived with, and where the bed and bathing facilities were located. There was also a pre-fracture mobility assessment that was relatively consistent across the pathways and that assessed the ability of patients to walk indoors and outdoors, and whether they needed a walking aid or assistance. It also addressed specific mobility areas such as transfers, stairs and some ADL. Although this information was consistently recorded across pathways, it may have been located in different sections of the pathways for completion by different staff members, for example in some cases it was included in the nursing assessment section and in others it was contained in a specific occupational therapist assessment section.
A number of the integrated care pathways had clearly defined criteria for the occupational therapy assessment. Those that had specific sections assessed personal and domestic ADL, transfers (chair, toilet and bed), general mobility, standing, walking and stairs. One also assessed home hazards and cognition, whereas, in another, specific assessments were carried out on each day post-operatively. Although there was some variation in how these assessments were carried out or presented in the pathways, the overall rehabilitation aims for the patients were very similar and tended to include a referral to the falls service or other outpatient referrals. These pathways were often written as checklists, with no specific details provided, although one integrated care pathway included a detailed list of inclusion/exclusion criteria for the different services.
Twenty-eight (49%) acute hospital physiotherapist respondents stated that there was an integrated care pathway for patients; however, only eight centres forwarded a copy of the integrated care pathway to the research team. Only three (10%) physiotherapist respondents from community hospitals stated that there was an integrated care pathway for their patients, with 18 (42%) community team physiotherapist respondents stating that there was no integrated care pathway. Seventeen (46%) occupational therapist respondents from acute inpatient hospitals stated that there was a written document describing the integrated care pathway. Only one occupational therapist respondent from a community hospital and three occupational therapist respondents from 10 community teams stated that there was a written document describing the integrated care pathway for patients. It was unclear whether the eight integrated care pathways submitted were sent by occupational therapists, physiotherapists or therapy managers.
Rehabilitation in acute hospitals
For all of the responding centres, the multidisciplinary rehabilitation team in acute hospitals included physiotherapists, occupational therapists and nurses. An orthogeriatrician was involved in 11 of the centres with general geriatricians involved in the others. A social worker and pharmacist were involved in 10 of the centres. A dietitian was routinely involved in five centres and a mental health professional in four. Some respondents also mentioned the pain team.
Type of hospital ward where post-operative rehabilitation was delivered
The wards used for post-operative rehabilitation by the 57 physiotherapist and 37 occupational therapist respondents from acute hospitals are described in Figure 4; the majority of respondents worked on orthopaedic trauma wards. Twenty (54%) occupational therapist respondents routinely saw proximal hip fracture patients pre-operatively.
FIGURE 4.
Acute hospital wards used for post-operative rehabilitation by physiotherapists and occupational therapists. GORU, geriatric orthopaedic rehabilitation unit; MARU, mixed assessment and rehabilitation unit.

Occupational therapist care delivered in acute hospitals
Occupational therapists working in acute inpatient routine rehabilitation responded that their care of these patients consisted of:
-
prescribing specific equipment (n = 37, 100%)
-
practising various ADL (n = 36, 97%)
-
providing education about hip precautions (n = 30, 81%)
-
providing information about falls services (n = 27, 73%)
-
other activities to encourage independence (n = 23, 62%)
-
providing information about falls prevention techniques (n = 19, 51%)
-
anxiety management (n = 16, 43%)
-
developing self-awareness (n = 9, 24%)
-
referring patients to a falls prevention service (n = 31, 84%)
-
referring patients to social services (n = 35, 95%)
-
referring patients to a discharge team (n = 34, 92%)
-
home visits with patients prior to discharge (n = 30, 81%)
-
home environment visits without the patient (n = 32, 86%).
Other duties included assessment and referral for minor adaptations in the home, such as grab rails, furniture height raisers and delivery of equipment, referral to community services for support, and liaising with families and carers to obtain information regarding home circumstances and the level of support available.
When patients were first seen by therapists in acute hospitals
Table 5 shows the responses given by physiotherapists and occupational therapists when asked when they first saw proximal hip fracture patients, whether or not they saw patients at weekends and when patients were first mobilised post-operatively.
| Patient variable | Physiotherapists, n (%) | Occupational therapists, n (%) |
|---|---|---|
| Patients seen Monday to Thursday | ||
| Pre-operatively | 19 (33) | – |
| Same day as the hip fracture surgery | 4 (7) | 4 (11) |
| Day after hip fracture surgery | 53 (93) | 17 (46) |
| By second day after hip fracture surgery | – | 7 (19) |
| By third day after hip fracture surgery | – | 2 (5) |
| By fourth day after hip fracture surgery | – | 1 (3) |
| Variable | – | 6 (16) |
| Patients seen Friday, Saturday or Sunday | ||
| Still seen on the regular nominated day | 42 (74) | – |
| Seen the following Monday | 10 (18) | 19 (51) |
| Same day, the day after or not depending on patient need | 5 (9) | |
| Have weekend therapy team | – | 16 (43) |
| Patients mobilised | ||
| On the same day as surgery | 4 (7) | – |
| The day after surgery | 51 (89) | – |
| The second day after surgery | 2 (3) | – |
| Who mobilised patient out of bed first | ||
| Physiotherapist | 39 (68) | – |
| Nurse | 2 (4) | – |
| Mixed | 16 (28) | – |
In one pathway the action planning also involved a pre-operative physiotherapy assessment but the rest of the pathways appeared to include physiotherapists and occupational therapists only after surgery, with multidisciplinary teams meeting from the first day post-operatively. There was considerable variation in the specific details of post-operative mobilisation and assessment, but the consensus was for early mobilisation on post-operative day 1 when possible, supported by physiotherapists. There was consensus across the pathways that the minimum expected mobilisation on day 1 was for the patient to transfer from bed to chair (with assistance as needed), with exercise discussions beginning. Increased mobilisation and practice of exercises was planned on subsequent days, with most pathways suggesting that the increase in mobilisation, that is, the number of steps taken, should be recorded and with one pathway specifying that this should include reduced supervision/assistance. Although the general aim of increasing mobilisation was seen across the different pathways, some included more detailed specific aims for daily rehabilitation and there was considerable variation in expectations, with one pathway encouraging bed exercises at day 3 and another expecting that an ADL assessment would be carried out by this point in recovery. There was also variation in who carried out the assessments, with one particular pathway allocating separate goals relating to rehabilitation and mobilisation to nursing staff and the therapy team.
Physiotherapy rehabilitation exercises
Forty-nine (86%) physiotherapist respondents on the acute ward used muscle-strengthening training, 27 of whom used progressive resistance training for at least some of their patients. However, 18 respondents stated that they did not use progressive resistance training. Other exercises used by all included walking, climbing stairs and transferring. Forty-five (79%) physiotherapist respondents used weight-bearing exercises, 37 (65%) gait training and 31 (54%) other exercises, as described in Box 4. Forty-two (74%) physiotherapist respondents from acute hospitals provided patients with exercise sheets.
-
Bed exercises (hip flexion and abduction, knee flexion, static contractions of the quadriceps and glutei, range of movement of ankle, circulatory).
-
Chair exercises (quadriceps strengthening).
-
Getting in and out of bed, toileting.
-
Repeated standing up and sitting down.
-
Standing exercises to increase strength and range of movement (hip abduction, flexion and extension, knee flexion, heel raises, double leg dips, weight transference in standing), sometimes using parallel bars.
-
Balance exercises including reaching and turning while standing, Otago balance exercises, functional balance activities (obstacle courses, stepping over sticks, etc.).
-
Step assessments.
-
Bed exercises including active range of movement with or without weights.
-
Balance exercises when standing and moving (walking forwards and backwards, sidestepping).
-
Exercise tolerance.
-
Referral to other exercise classes or groups in the community such as Nordic walking, falls prevention classes, Bone Boost programme for those identified as osteoporotic.
-
Otago exercises. a
-
Gym-based rehabilitation programme.
-
Outpatient clinic referrals for hydrotherapy, physiotherapy, day hospital balance classes.
-
Bed exercises.
-
Range of movement exercises in lying and standing, including the use of slide sheets.
-
Strengthening exercises for the quadriceps and glutei.
-
Balance and proprioception exercises, including postural stability, weight shift practice.
-
Outpatient clinic referrals for physiotherapy for gym-based exercise.
-
Referral to other exercise classes or groups in the community such as Nordic walking, falls prevention classes, Zumba Gold, bone health classes (specific bone-loading exercises, advice and education on osteoporosis, talk from dietitian and physiotherapist).
-
Backward chaining as part of exercise groups.
A series of progressive leg-strengthening and balance-retraining exercises and a walking plan.
Occupational therapist assessment
All occupational therapist respondents from acute inpatient hospitals performed an individual assessment of patients with regard to functional tasks, which included transfers and personal ADL. Thirty-four (92%) respondents stated that this included domestic ADL, 33 (89%) respondents stated that it included the environment and social support, and 16 (43%) respondents stated that they performed an individual assessment of posture and seating. Other comments concerning functional assessment included:
If needed we will complete access and home visits with patients’ consent.
Level of assessment varies for individual patients.
Mobility.
Equipment needs assessment including Telecare.
Due to time restraints within acute hospital, there is little time to assess patients carrying out domestic tasks. However, we always ask patients if they have support with such tasks at home and discuss with them any concerns that they may have.
Frequency and length of therapy sessions
Sixteen (28%) physiotherapy respondents gave physiotherapy twice a day, 12 (21%) once or twice a day, 27 (47%) once a day, one (2%) every other day and one (2%) only two to three times a week. The length of the sessions is shown in Figure 5.
FIGURE 5.
Length of physiotherapy and occupational therapy sessions in minutes.
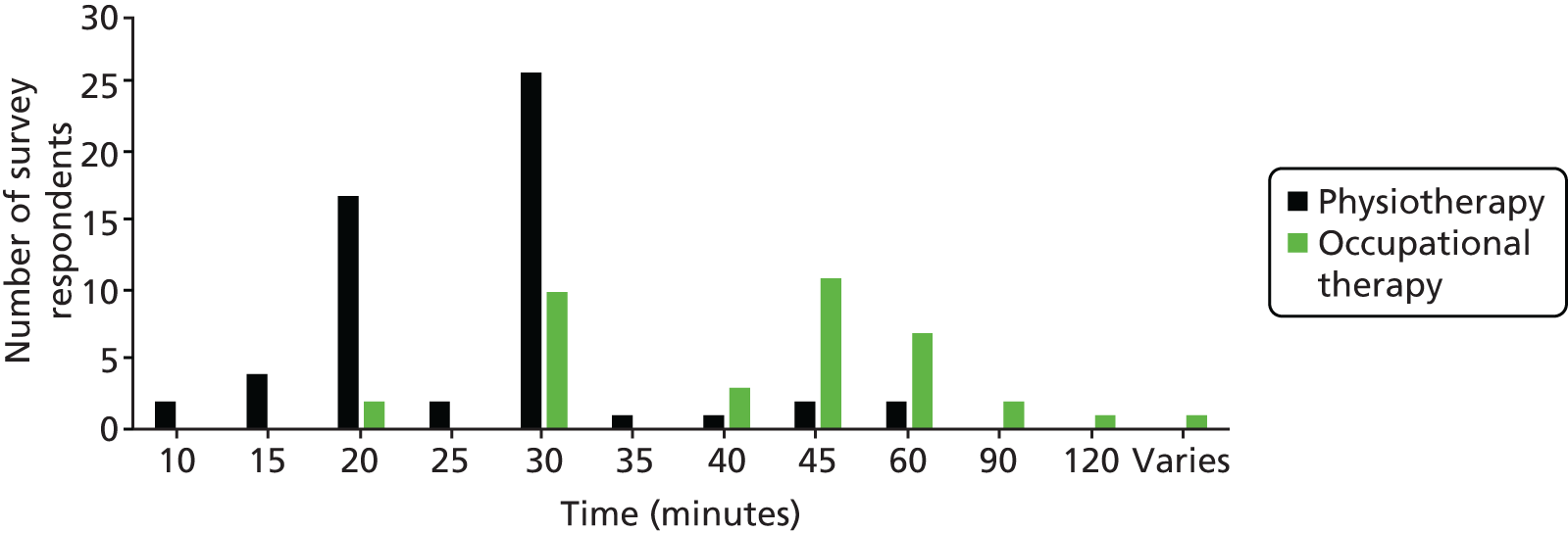
The number of times that occupational therapists in acute inpatient hospitals saw patients was variable. The minimum length of these sessions was 15 minutes and the maximum length was 2 hours (see Figure 5), with a mode of 30 minutes.
Assessment of mood and cognition
Routine assessments of cognitive status happened in 11 of the 13 centres responding to the therapy manager survey (one replied ‘no’ and one replied ‘don’t know’). The health-care professionals performing the assessment varied at different sites. Doctors, nurses and therapists all performed these assessments on admission and in pre- and post-operative assessments. Assessments were most often carried out using the Abbreviated Mental Test Score (AMTS)274 and the MMSE. 275 Routine assessments of mood occurred in five of the 13 centres (four replied ‘no’ and four replied ‘don’t know’), which were usually completed by the medical staff. The Geriatric Depression Scale (GDS)276,277 was used in one centre to assess mood, with a subjective assessment of mood carried out in four centres. Routine assessments of self-efficacy were carried out in four of the 13 centres (four replied ‘no’ and five replied ‘don’t know’). These assessments were performed by nursing staff, a psychologist or occupational therapists and could occur on admission, as required or prior to discharge.
Routine assessment of fear of falling was carried out in nine of the 13 centres by physiotherapists, occupational therapists, nursing staff or doctors. The tools used varied, from in-house tools to physiotherapy assessments, the Falls Efficacy Scale – International (FES-I),278,279 the Berg Balance Scale,280 the visual analogue scale for fear of falling (VAS-FOF)281 and the Timed Unsupported Steady Stand. 282
In terms of routine assessments, 47 (82%) acute hospital physiotherapist respondents reported that cognitive status was measured, 19 (33%) that mood was assessed, eight (14%) that self-efficacy was assessed and 23 (40%) that fear of falling was assessed. Doctors, nurses, physiotherapists and occupational therapists performed these assessments. The majority of physiotherapist respondents, 40 out of 57 (70%), did not use a standard assessment tool but relied on one developed in their locality. In terms of routine assessments, 32 (86%) occupational therapist respondents from acute inpatient hospitals reported that cognitive status was measured, 16 (43%) that mood was assessed, eight (22%) that self-efficacy was assessed and 18 (49%) that fear of falling was assessed. Instruments used to assess cognitive status included the Test Your Memory test283 and the Montreal Cognitive Assessment (MoCA). 284 Falls screening was carried out using the Falls Risk Assessment Tool (FRAT). 285
Good aspects of the service and areas for improvement
When asked to comment on what they felt were good aspects of the service, more than half of the inpatient acute physiotherapist respondents highlighted the benefits of having a multidisciplinary team available for patient treatment. This was followed by having good access to physiotherapists, in particular on weekends or soon after surgery, to allow for early mobilisation when appropriate. Other positive areas of the service referred to by a smaller number of respondents were the communication with patients/carers and access to specialist team members or ward staff. A similar number of respondents highlighted that they were able to provide a timely response to patient care, with a small number specifically mentioning early or pre-operative assessment within this. A number of respondents also commented on the seamless care provided, with referral to various groups and tailoring of treatment to the specific needs of patients and their families. A few respondents also added that they had access to specialist staff in their multidisciplinary team and that they provided patients with specific goals and educational tools.
When asked to identify where there was room for improvement in their service, more than half of the acute hospital physiotherapist respondents commented that there was a need for more resources for staff, beds in community hospitals and rehabilitation equipment. This was the most common theme emerging from the physiotherapists. A number of respondents also commented on the need for the development and use of existing follow-up programmes, such as referrals to falls groups and the use of workbooks and information sheets. Other aspects of care identified as having the potential for improvement included the treatment of dementia patients, communication with and the involvement of nursing staff, intermediate care and timing of input from physiotherapists. When occupational therapist respondents from acute hospitals were asked what aspects of their service could be improved, the responses were varied. Better communication within the multidisciplinary team, better external services (such as falls groups) and the provision of more staff to enable more time to be spent rehabilitating patients were all mentioned with similar frequency. A few respondents also commented that a more consistent service, the provision of office space and improved patient facilities for assessment would be beneficial.
Discharge planning
With regard to successful discharge planning, managers reported that multidisciplinary team meetings were important, although the frequency of these meetings differed between centres, ranging from daily to weekly. Managers commented that, when it was not already occurring, the input of community staff and social workers would improve outcomes for discharge planning. Managers felt that the close collaborative work of the multidisciplinary team was one of the positive aspects of their service, which contributed to improved discharge times and better patient care, and that having the same team throughout a patient’s care was beneficial. However, a small number of managers commented that liaison between primary services and secondary services could be improved. Other areas highlighted for improvement included better access to rehabilitation beds and therapy/nursing resources, and a ward with a dedicated multidisciplinary team.
Discharge and action planning could also be addressed on admission or within the pre-operative period. This could include an assessment of services that were currently used by patients and whether or not they had any home safety equipment already in place, such as alarm pull cords. Some pathways were quite general and contained only a space to indicate if patients had been given advice leaflets and told about follow-up services. In other pathways this information was more detailed and could include checklists that related to specific areas of recovery, for example patients’ understanding of plans for increasing their mobility post surgery or identifying patients’ needs for planned discharge. Some pathways also included an estimated date of discharge and an indication of which services would be involved in the different areas of discharge. In other pathways, discharge was not specifically mentioned until after surgery.
Routine multidisciplinary team meetings were held to discuss discharge planning in 12 of the 13 centres involved in the therapy manager survey. Comments on the survey about what worked well with regard to these meetings and what could be improved included ‘meeting nursing and occupational therapy staff daily’ and ‘weekly meeting with orthogeriatrician’ as well as ‘more social worker input would be helpful’. In the centre that did not hold multidisciplinary team meetings, the primary nurse was in charge of the discharge plans. Seven of the 13 centres held general multidisciplinary team meetings, whereas five held multidisciplinary team meetings at which only hip fracture patients were discussed. The professionals involved in the multidisciplinary team meetings are shown in Table 6. Community nurses attended multidisciplinary team meetings in only one of the 13 centres.
| Health professional | Number of centres |
|---|---|
| Physiotherapist | 12 |
| Occupational therapist | 12 |
| Orthopaedic ward nurse | 12 |
| Orthogeriatrician | 10 |
| Social worker | 7 |
| Clinical nurse specialist (hip fracture, orthogeriatric) | 5 |
| Other doctors (ward and junior) | 4 |
| Discharge planning team | 4 |
| Mental health professional | 2 |
| Community nurse | 1 |
| Total | 70 |
In two of the centres patients regularly attended discharge meetings and in three of the centres carers regularly attended discharge meetings. In six centres, specific responsibility for co-ordinating discharges was delegated to the following:
-
discharge link nurses on each ward whose role it was to expedite discharge
-
discharge facilitator
-
integrated discharge bureau to co-ordinate complex discharges or else nurses and the multidisciplinary team organised discharge back to a patient’s home when the social set-up was good, for example younger patients without dementia
-
hip fracture unit-based occupational therapist or physiotherapist co-ordinated most discharges, with some support from a hip fracture specialist nurse
-
hip fracture specialist nurse employed by secondary care with responsibility for co-ordinating care and discharge arrangements between professions
-
community liaison team employed by primary care with responsibility for co-ordinating follow-up in community care
-
ward nurse
-
unspecified.
In only two of the centres were there staff members with a specific responsibility for overall co-ordination between secondary care and community care services. These were specified as being rehabilitation nurses and ward nurses.
None of the 13 manager respondents from the community teams attended acute hospital-based multidisciplinary team discharge meetings. Other reasons for not attending meetings included ‘acute hip fracture centre too far away’, ‘not invited’ and ‘we have our own multidisciplinary team’.
Home visits
Forty-seven (83%) acute hospital physiotherapist respondents did not make home visits with patients prior to discharge. Only one respondent (2%) indicated that this happened in all cases, with the remaining nine respondents (16%) indicating that this happened for some patients.
Social support on discharge
We asked therapy service managers whether or not discharge plans included referral to or the provision of patients with information about social support and social activities. In five of the centres therapy service managers reported that patients were routinely referred or signposted to social support or activities on discharge. The following types of referral were mentioned:
-
home from hospital, Careline Services, befriending, luncheon clubs
-
referral by social worker for packages of care, which may involve third-sector activity clubs, etc.
-
an information leaflet given by ward nursing staff
-
to local exercise groups run by Age UK
-
routinely signposted to local exercise groups if appropriate after our 6 weeks of input; depending on the needs or wants of patients they may be referred to other groups.
Forty-seven (82%) acute hospital physiotherapist respondents referred or signposted at least some patients to social support or social activities on discharge. Other tasks that physiotherapists mentioned included confidence building, giving advice to patients and carers, referral to community rehabilitation and to falls groups, and attending multidisciplinary team meetings.
Rehabilitation in community hospitals
Occupational therapists from community hospitals reported that their routine rehabilitation consisted of prescribing specific equipment (such as long-handled aids) (n = 18, 100%), practising various ADL (n = 18, 100%), education about hip precautions (n = 15, 83%), providing information about falls services (n = 12, 67%), other activities to encourage independence (n = 12, 67%), falls prevention techniques (n = 15, 83%), anxiety management (n = 6, 33%) and developing self-awareness (n = 3, 17%). Eleven (61%) respondents referred some patients to a falls prevention service, 16 (89%) referred some patients to social services and 12 (67%) referred some patients to a discharge team. Seventeen (94%) respondents carried out home visits with patients prior to discharge and all made a home environment visit without the patient. Other duties included promoting patient empowerment and increased confidence in patients’ ability, teaching relaxation and pain management techniques, and providing advice to carers and patients about good moving and handling practices and joint protection.
When patients were transferred to community hospitals
Nineteen (66%) physiotherapist respondents from community hospitals reported that patients were transferred within the first week post-operatively, nine (31%) reported that patients were transferred in the second post-operative week and three (10%) reported that patients were transferred in the third post-operative week. The other seven respondents gave a variety of time periods, indicating that the timing of transfer varied according to patient and departmental factors. Factors influencing transfer to a community hospital included:
When the GP refers patients – they cannot be directly referred from the acute hospital following discharge.
As soon as medically stable and bed available.
After clinic review, often greater than 6 weeks post-operatively if they are still having difficulties.
When discharge is delayed.
Depends when the consultant or GP refers the patient.
Hard to clarify but some come to us straight from hospital at approximately three weeks post operation. Others go via intermediate care team services so would come to us at between 3–6 weeks post fracture.
Two (11%) occupational therapist respondents from community hospitals noted that their patients were usually transferred in the first post-operative week, eight (44%) that their patients were transferred in the second week and three (17%) that their patients were transferred in the third week, and five (28%) stated that it depended on the patient.
When patients were first seen by therapists in community hospitals
Therapy service managers reported that when the community team members saw their patients varied, with three respondents reporting that they were seen on the day of discharge, one the day after, two within 2 days, one within 7 days and one within 4–6 weeks; for five managers the timing varied according to circumstances. Therapy service managers responded that the services provided by community team physiotherapists were early supported discharge (n = 12), intermediate care (n = 5), neither early supported discharge nor intermediate care (n = 13) and other (n = 13). Most respondents who ticked ‘other type of service’ described it as a combination of early supported discharge and intermediate care.
Thirty-two (74%) physiotherapist respondents from community hospitals stated that the time after surgery at which they first saw patients varied, with most patients being seen within 1 week. Only three respondents saw patients on the day of discharge, with a further five respondents seeing them the day after discharge.
Frequency and length of therapy sessions
For 21 (49%) physiotherapy respondents from community teams the length of contact varied from patient to patient. For one (2%) respondent the contact time was 8 weeks, for 10 (23%) respondents it was 6 weeks, for two (5%) respondents it was 4 weeks and for one (2%) respondent it was only 1 week. Six respondents (21%) saw their patients twice a day, 13 (45%) saw them once a day, one saw them weekly, one saw them three to five times per week, one saw them daily, reducing as discharge planning took place, and one saw them four times a week and in cases of urgency. The minimum length of these sessions was 10 minutes, the maximum 60 minutes, with a mode of 30 minutes.
With regard to the frequency with which occupational therapists saw patients in community hospitals, three (17%) occupational therapists saw them daily, seven (39%) saw them on alternate days, one (6%) saw them every third day, two (11%) saw them twice a week and four (22%) stated that the frequency of sessions depended on the patient. The length of the therapy sessions was variable and depended on the patient; the minimum length of the sessions was 10 minutes and the maximum was 60 minutes, with a mode of 60 minutes.
Assessment of mood and cognition
Community hospital physiotherapists frequently commented on their ability to carry out thorough assessments and provide intensive input to patients, allowing them to tailor rehabilitation to an individual’s needs. A number of respondents also highlighted the good communication and working relationships within the multidisciplinary team, which allowed consistent and seamless care of patients. Some respondents felt that this contributed to safer or quicker discharge of patients. Ten (56%) occupational therapist respondents from community hospitals indicated that they employed a successful client-centred approach. Six (33%) respondents also highlighted the good multidisciplinary team working and six (33%) commented on good patient outcomes, engagement with family members/carers, the provision of intensive rehabilitation and that staff were experienced and of a high calibre.
Ten (34%) physiotherapist respondents from community hospitals used a standardised tool to assess progress: eight used the Elderly Mobility Scale,286 one used the EuroQol-5 Dimensions (EQ-5D)287 and one used the Timed Up and Go test. 288 How often progress was assessed varied from daily (n = 14, 48%) to weekly/fortnightly (n = 8, 28%). Sixteen (55%) physiotherapist respondents from community hospitals measured cognitive status, 11 (38%) assessed mood, seven (24%) assessed self-efficacy and 17 (59%) assessed fear of falling. Fourteen (78%) occupational therapist respondents from community hospitals measured cognitive status, 11 (61%) assessed mood, five (28%) assessed self-efficacy and nine (50%) assessed fear of falling.
Physiotherapist rehabilitation exercises
Twenty-five (86%) respondents from community hospitals gave out exercise sheets. In community hospitals, 27 (93%) respondents used strength exercises (quadriceps, hip abductors) in rehabilitation. Of these, four always used progressive resistance training, 10 used it for some patients, seven used it for a small minority of patients, one used it once patients were discharged and five did not use it at all. Twenty-seven (93%) respondents used weight-bearing exercise, 22 (76%) used gait training and one (3%) used treadmill gait training. Other exercises used are listed in Box 4.
In terms of ADL, 28 (97%) physiotherapist respondents from community hospitals encouraged walking and climbing stairs and 27 (93%) encouraged transferring. Other ADL addressed included:
-
indoor and outdoor mobility when possible
-
getting in and out of bed
-
managing clothing
-
getting on and off the toilet
-
getting in and out of a car
-
gait re-education
-
getting up from the floor
-
patient-specific goals
-
balance and falls prevention.
Other interventions that were used included acupuncture for pain relief, the provision of advice about, for example, seating at home, bed height and car seats, hydrotherapy, progression of walking aids and stretches.
Occupational therapist assessment
All occupational therapist respondents from community hospitals performed individual assessments of functional tasks, which included transfers, personal and domestic ADL and the environment, and car transfer practice and stair practice. Seventeen (94%) respondents stated that this also included an assessment of social support and 11 (61%) performed an individual assessment of posture and seating.
Discharge planning including referral to social support
Sixteen (89%) occupational therapist respondents from community hospitals stated that patients were routinely signposted to social support or social activities when discharged, such as day care, community resource teams, Age Concern, local charities, exercise classes and Crossroads.
Referral to social support or activities was reported by 14 (48%) community hospital physiotherapists; this included exercise groups, day centres, lunch clubs, care and repair agencies, falls groups, local charity support groups, Age UK, befriending, Bone Boost and Nordic walking.
Home visits
Sixteen (55%) physiotherapist respondents from community hospitals did not routinely make a home visit. One (3%) respondent always made a routine home visit, whereas 12 (41%) visited according to need.
Good aspects of the service and areas for improvement
Although the time spent with patients was identified as a good aspect of most services, when asked to comment on areas that could be improved, 10 (55%) occupational therapist respondents from community hospitals reported that increased staffing levels would be beneficial. Respondents felt that this would allow for an increased duration and frequency of visits. Five (28%) occupational therapist respondents commented that the provision of facilities and access to referral services could be improved, as well as there being better communication and consistency across the multidisciplinary team. One (6%) occupational therapist respondent also commented that links with the acute hospital could be improved.
Rehabilitation in the community
According to the occupational therapist respondents from community teams routine rehabilitation consisted of prescribing specific equipment (n = 13, 100%), practising various ADL (n = 13, 100%), education about hip precautions (n = 13, 100%), providing information about falls services (n = 12, 92%), other activities to encourage independence (n = 12, 92%), falls prevention techniques (n = 13, 100%), anxiety management (n = 6, 46%) and developing self-awareness (n = 6, 46%). Seven (54%) respondents referred some patients to a falls prevention service, 10 (77%) referred some patients to social services and one (8%) referred some patients to a discharge team. Other duties included checking medication, providing support and advice to family members, partners or carers and referring clients to intermediate care if they had complex needs.
Health professionals involved in community-based rehabilitation
The health professionals involved in community-based rehabilitation, according to the survey of therapy service managers, are shown in Table 7. Physiotherapists provided rehabilitation in all of the centres and occupational therapists provided rehabilitation in all but one centre.
| Health professional | Number of centres |
|---|---|
| Physiotherapist | 13 |
| Occupational therapist | 12 |
| District nurse | 10 |
| Falls prevention team | 8 |
| GP | 6 |
| Social worker | 4 |
| Dementia care team | 2 |
| Health care support worker | 1 |
| Mental health team | 1 |
| Total | 57 |
Types of community-based rehabilitation service
According to the survey of therapy service managers, the types of community-based rehabilitation service available to proximal hip fracture patients after discharge from the acute hospital were:
-
community hospital providing hip fracture rehabilitation or other community-run rehabilitation inpatient rehabilitation unit (n = 9)
-
early supported discharge service providing community-based multidisciplinary rehabilitation for about 4–6 weeks based in the patient’s own home (n = 10)
-
early supported discharge service providing community-based multidisciplinary rehabilitation for about 4–6 weeks based in the care home/nursing home where a patient has been discharged for the long term (n = 5)
-
traditional model of community care in which the patient is discharged home (to their own home or to a long-term care setting) under the care of a GP and with individual referral to community health and social care professionals as needed (n = 11).
Three respondents from community teams described their service as an early supported discharge scheme, two as intermediate care and two as neither of these. The remaining six respondents gave their own description of their service:
Intermediate care at home service.
All of the above, early supported discharge has no limit on the rehabilitation time and includes trying to prevent admission to hospital.
Intermediate care team who take rapid response patients for early discharge or prevention of admission.
We see clients for 4–6 weeks. They can be discharged directly from acute hospital or from intermediate care.
Intermediate care team providing community therapy. ‘I provide OT [occupational therapy] services to individuals who come from a variety of sources and who may have multiple conditions’. Work with some of those include individuals who may have been supported home with multidisciplinary team planning from acute or intermediate care beds or they may have suddenly been discharged due to a variety of reasons.
Our team also provides an in-reach therapy service to a 10 bedded rehabilitation unit in a care home. Our team also see people in their own home to deliver therapy interventions following proximal hip fracture.
When patients were discharged home
Community rehabilitation was available to over half of patients after discharge home in 11 centres and to > 75% of patients in five centres. One centre stated that < 10% of patients received community rehabilitation and one centre did not provide any information on this.
When patients were first seen and frequency and length of sessions
Occupational therapists in community teams saw patients in the community according to need. Five (38%) saw patients twice weekly and one (8%) saw patients once a week. The length of time that patients were seen for was variable and depended on the patient. The minimum length of the therapy sessions was 30 minutes and the maximum was 100 minutes, with a mode of 60 minutes.
Assessment of mood and cognition
Eighteen (42%) community team physiotherapist respondents measured cognitive status, 15 (35%) assessed mood, 11 (26%) assessed self-efficacy and 26 (60%) assessed fear of falling. The different assessment tools used by therapists are shown in Table 8. As well as using standardised measures, many respondents based their assessments on general observations and discussion with the patient or used local screening tools. Twelve (92%) occupational therapist respondents from community teams measured cognitive status, 12 (92%) assessed mood, seven (54%) assessed self-efficacy and 11 (85%) assessed fear of falling.
| Assessment | Acute hospitals | Community hospitals | Community teams |
|---|---|---|---|
| Cognitive status | AMTS, MMSE, 4AT, 6CIT, MoCA, ACE-R | 6CIT, MoCA, AMTS, MMSE, MEAMS | 6CIT, ACE-R, MMSE, MEAMS, MoCA, GPCOG test, RUDAS |
| Mood | HADS, GDS, unified assessment proforma, MoCA | GDS, HADS, SF-12, COPM | 6CIT, GDS, HADS, TOM |
| Self-efficacy | Unified assessment proforma, 10-m walk | FES, VAS, COPM | EQ-5D, TOM |
| Fear of falling | VAS, BBS, Elderly Mobility Scale, Oxford Hip Score, Tinetti Assessment Tool | FRAT, VAS, FES, FES-I, Tinetti Assessment Tool, COPM | FRAT, VAS |
| Health utility | EQ-5D | EQ-5D |
Physiotherapy rehabilitation exercises
All physiotherapist respondents from community teams indicated that they used strengthening exercises, with 39 (91%) respondents indicating that they used progressive resistance training with some of their patients. Forty-one (95%) respondents used weight-bearing exercises, whereas only 34 (79%) used gait training. None of the physiotherapists used treadmill gait training. Other exercises used are listed in Box 4. Thirty-nine (91%) physiotherapist respondents from community teams gave their patients exercise sheets. In terms of ADL, 42 (98%) physiotherapist respondents from community teams encouraged walking and climbing stairs and 39 (91%) encouraged transferring. Other ADL addressed included personal care and meal preparation, stair climbing, accessing the community, outdoor walking, car and bus transfers, feeding the cat, walking the dog and caring for a relative. The frequency of physiotherapy sessions varied from patient to patient but was either weekly or fortnightly. The minimum length of therapy sessions was 15 minutes and the maximum was 90 minutes, with a mode of 30 minutes (Figure 6).
FIGURE 6.
Length of community physiotherapy and occupational therapy sessions.
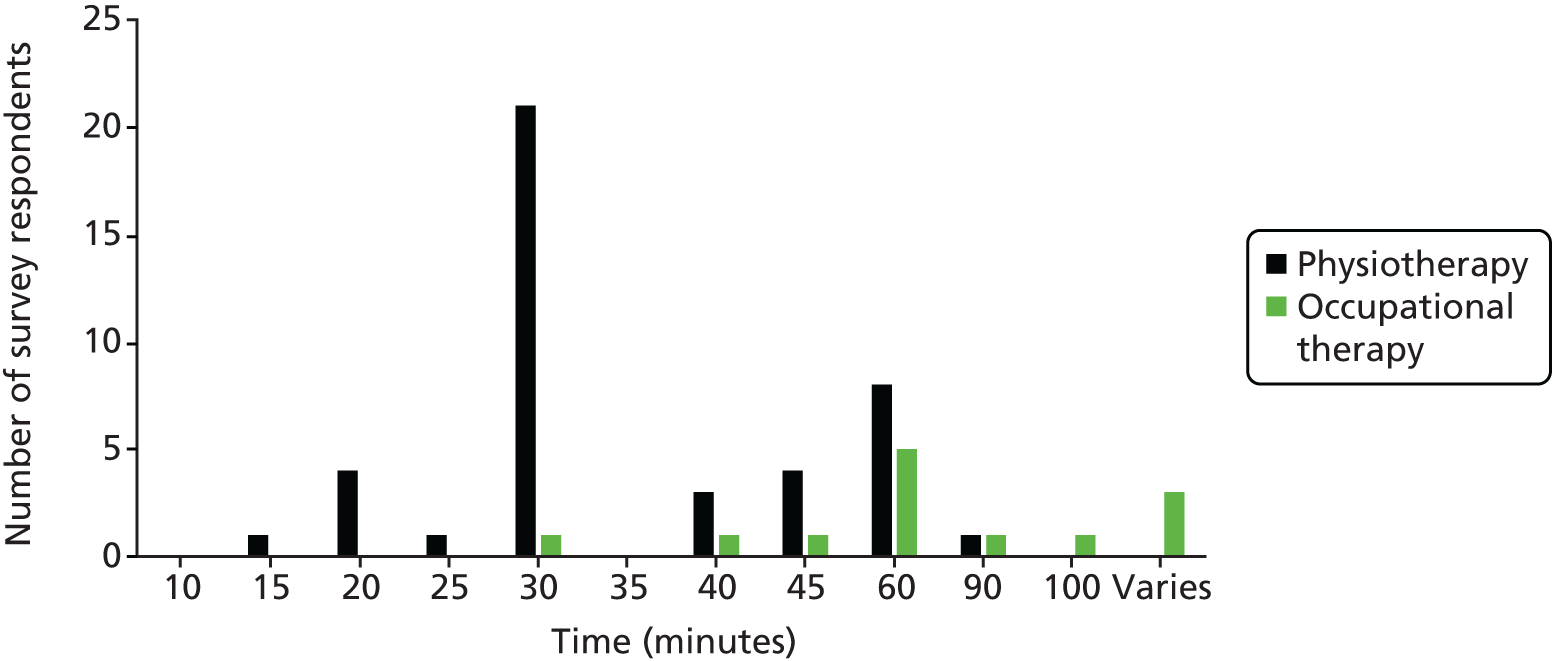
Occupational therapist assessment
All occupational therapy respondents from community teams carried out individual assessments of functional tasks, which included transfers, personal and domestic ADL, the environment and social support. Five (38%) respondents carried out an individual assessment of posture.
The frequency of occupational therapy sessions varied from patient to patient according to individual need. The minimum length of these sessions was 30 minutes and the maximum 90–100 minutes, with a mode of 1 hour (see Figure 6).
Referral to social support
Twenty-six (60%) of the community team physiotherapist respondents referred patients to social support or social activities when discharged. Other tasks performed by physiotherapists that have not already been mentioned included confidence building by performing balance and falls prevention exercises, the provision of home exercise programme/information, the provision of walking aids, orthotics assessment and contacting family members/carers.
Twelve occupational therapist respondents from community teams stated that patients were routinely signposted to social support or social activities when discharged, such as:
-
befriending services (Age UK/Red Cross)
-
day care or day centres (social services)
-
shopping services (Red Cross)
-
local charities and lunch clubs
-
Age UK and local voluntary good neighbouring and support services
-
Women’s Royal Voluntary Service to aid with transport and shopping
-
enablement services
-
long-term care services
-
sensory impairment services
-
art classes
-
exercise classes.
Good aspects of the service and areas for improvement
When commenting on good aspects of their service, the majority of community team physiotherapists mentioned the relationship with the patients and their ability to be responsive and flexible to tailor treatment to individual patients’ needs. Some respondents also highlighted strong links and communication within the multidisciplinary team as positive aspects of their service. More than half of the respondents from community teams felt that the amount of time that they were able to spend with patients, particularly in their own home, was a positive aspect of their service. A number of participants also commented on good multidisciplinary team working and a few individuals highlighted the inclusive nature of their service and how they were able to work to the goals of patients and their family.
When asked to comment on areas that needed improvement, a common response was that community teams would benefit from increased staffing levels and better links to hospitals. Smaller numbers of respondents also commented that improvements could be made by increasing the number of available rehabilitation beds, improving access to specific referral groups (e.g. falls, balance and exercise groups) and using standardised assessments for treatment. Only one community physiotherapist respondent routinely attended multidisciplinary team discharge meetings. The reasons for not attending included insufficient staffing levels and good links with inpatient staff, with the discharge of complex patients discussed on the telephone. A few respondents from community teams felt that communication with other services could be improved and that therapists had an overload of patients, which decreased the time that they were able to spend with each individual patient. One respondent felt that there should be less focus on outcome measurement sheets as they were a waste of time, whereas another respondent commented that the regular use of standardised outcome measures would be useful.
Discussion
Summary of survey findings
Survey respondents were geographically spread across the UK. Therapy service managers were principals, leads or heads of departments. Most therapy service managers had a written integrated care pathway for patients with proximal hip fracture that included their rehabilitation. In contrast, less than half of the physiotherapists and occupational therapists in all three settings stated that they had a written integrated care pathway. The initial assessment of patients varied between pathways but often included a specific falls assessment for identifying patients at risk of further falls.
Acute hospital rehabilitation consisted of strengthening exercises, the practice of ADL, education about hip precautions, the provision of information about falls services, other activities to encourage independence, the prescribing of specific equipment, falls prevention techniques, anxiety management and the development of self-awareness. Patients were mostly seen and mobilised by a physiotherapist the day after surgery and seen by an occupational therapist any time from the same day as surgery to up to 4 days later. How often a patient received physiotherapy and occupational therapy varied depending on patient need. In terms of routine assessment, acute hospitals measured cognitive status and assessed mood, self-efficacy and fear of falling. In most cases, patients were referred or signposted to social support or social activities on discharge. Patients were transferred into the community hospital variably according to patient and departmental factors.
Community hospital rehabilitation consisted of strengthening exercises, individual assessment of functional tasks, personal and domestic ADL and the environment, the prescribing of specific equipment and education about hip precautions and falls prevention. In most cases, progressive resistance training was not used. Most patients were given exercise sheets. As with the acute hospital, the frequency with which patients were seen by a therapist varied depending on patient need. Community hospitals measured patients’ cognitive status and assessed mood, self-efficacy and fear of falling. However, routine assessments using validated tools were not carried out in all centres and how often progress was assessed varied between centres.
Not all patients received community rehabilitation after acute hospital discharge. For those who did, community rehabilitation consisted of prescribing specific equipment, practising various ADL, education about hip precautions, providing information about falls services, other activities to encourage independence and falls prevention techniques. Most therapists said that they referred some patients to social services. As with community hospitals, routine assessments using validated tools were made of cognitive status, mood, self-efficacy, fear of falling, disability, mobility and balance.
Good points according to managers and therapists
The survey found that the range of rehabilitation programmes provided in all three settings had similar goals and highlighted the importance of multidisciplinary teams. Therapy service managers felt that the close collaborative work of the multidisciplinary team was one of the most positive aspects of their service, which contributed to improved discharge times and better patient care, and that having the same team throughout a patient’s hospital stay was beneficial. When asked to comment on good aspects of their service, more than half of the acute hospital physiotherapist respondents and most of the occupational therapists highlighted the benefits of having a multidisciplinary team for patient treatment. Similar numbers of respondents also highlighted that they were able to provide a timely response to patient care. Community hospital physiotherapists frequently commented on their ability to carry out thorough assessments and provide intensive input to patients, allowing them to tailor rehabilitation to individual patients’ needs. More than half of the community hospital occupational therapists indicated that they followed a successful client-centred approach. Some of the respondents also highlighted the good multidisciplinary team working. The majority of community team physiotherapists mentioned the relationship with the patients and their ability to be responsive and flexible to tailor treatment to individual patients’ needs. More than half of the community team occupational therapists felt that the amount of time that they were able to spend with patients, particularly in their own home, was a positive aspect of their service.
Areas for improvement according to managers and therapists
For therapy service managers, areas for improvement included better liaison between acute hospitals and community services, better access to rehabilitation beds and more therapy/nursing resources. More than half of the acute hospital physiotherapists wanted more resources for staff, more beds in community hospitals and more rehabilitation equipment; acute hospital occupational therapists wanted better communication within the multidisciplinary team, better external services (such as falls groups) and the provision of more staff to enable more time to be spent rehabilitating patients. The main area for improvement mentioned by more than half of the respondents from community hospitals and community teams was staffing levels. The community teams also wanted better links to hospitals.
Strengths and limitations of the survey
This is the first UK-wide survey aiming to describe rehabilitation for patients following hip fracture across acute and community settings since the introduction of NICE guidance in 20117 including recommendations for rehabilitation. A wide range of respondents was sampled in terms of profession, health-care sector and geographical spread of hip fracture centres. The link to the survey was easily circulated by e-mail to relevant potential respondents from the hip fracture centres. Because of data protection issues, the professional organisations could not provide us with their contact lists, but they did let their members know about the survey and provided the link to the survey itself. We were also able to place a notice about the survey on the National Hip Fracture Database website news section. We also encouraged people to pass on information about the survey to colleagues. As there is no register or centrally held record of physiotherapists and occupational therapists working in hip fracture rehabilitation, we were not able to establish the total number of these professionals in the UK or use such a register as a sampling frame.
We recruited therapy service managers by telephone, which enabled us to provide them with detailed information about the study as well as ask them to circulate the survey to their colleagues. Although this method did work well, with many asking to be informed of the results of the study and being happy to circulate the survey to their staff, it was time-consuming.
It is possible that our survey results may not have been entirely representative of the UK situation regarding rehabilitation for hip fracture patients because we were unable to sample settings and therapists and community service managers proportionately. However, we did sample acute hip fracture centre managers proportionately, aiming for a 10% sample of the hip fracture centres in the UK and obtaining a 7% sample. However, no acute hip fracture centre managers from Northern Ireland responded to the survey and so we were unable to obtain the perspectives of managers from Northern Ireland. We did, however, receive responses from therapists in England, Wales, Scotland and Northern Ireland. Our strategy for reaching respondents resulted in 210 respondents completing the survey, with a good geographical spread of respondents from different acute and community settings.
As with all surveys, the findings provide only a description of what was happening; causality for the variation found could not be demonstrated and may warrant further investigation.
Comparison with previous literature
Respondents in both acute and community hospital settings mostly reported that routine clinical practice followed the latest NICE7 and SIGN74 guidance. However, there was variability in the provision of services, especially in terms of what was available in the community. This variability in service provision has been reported elsewhere, for example in a report of physiotherapy services for rheumatoid arthritis. 289 Similar findings are reported for the focus groups involving hip fracture patients, described in Chapter 5.
Staffing levels were reported to be an issue that impacted on the level of service that could be provided in the community. This finding agrees with an earlier report of NHS physiotherapy waiting times and workload with regard to hip fracture and other conditions requiring rehabilitation. 290
Important psychological issues, such as fear of falling and self-efficacy, were not measured in many settings, although the realist review discussed in Chapter 2 found them to be important components of a successful rehabilitation programme. Previous qualitative research with Australian physiotherapists planning discharge home following hip fracture found that lack of confidence was seen as a barrier after hospital discharge but that this was not one of the discharge criteria. 185
Communication within teams in a particular setting was often seen as good; however, communication across boundaries between community services and acute services was more of a challenge. This has been noted previously. 176
The findings that therapy managers appreciated the role of integrated care pathways in streamlining the flow of patients rapidly through the health-care system, and that many of the health-care staff providing treatment felt that such a checklist approach devalued the human aspect of dealing with patients as individuals, agreed with the results of previous research. 176
Implications for rehabilitation programme
The variability in rehabilitation programmes could be reduced, particularly in the community, but not at the expense of tailoring programmes to individual need. There needs to be greater awareness of available resources for patients, carers and clinicians, with more standardised referral procedures and less reliance on the need for patients and their carers to push for access to services. Communication should be improved between acute hospitals and community services, and also with patients and their carers. There should be a more consistent assessment of important prognostic variables such as self-efficacy and fear of falling, perhaps by the adoption of a set of measures that could be used to evaluate the progress of patients during the course of their rehabilitation.
Chapter 5 Phase I focus groups
Introduction
The third component of Phase I (developing the multidisciplinary rehabilitation programme) consisted of two series of focus groups, one with health professionals who were part of the multidisciplinary rehabilitation teams treating patients following a fractured neck of femur and the other with patients who had experienced a hip fracture and their family carers.
Aim
To describe the experiences of multidisciplinary rehabilitation programmes in the North Wales area from the perspective of health-care professionals, patients and carers.
Objectives
To assess the views of patients and their carers on:
-
the rehabilitation that they received following surgical repair of a proximal hip fracture
-
how the programme could be improved
-
the intervention ideas emerging from the different strands of work in Phase I.
To assess the views of health professionals in the multidisciplinary rehabilitation teams on:
-
the rehabilitation programmes currently available to patients following surgical repair of a proximal hip fracture
-
how the programmes could be improved.
Ethics approval
The study received ethics approval from the UK NHS North Wales Research Ethics Committee – Gwynedd and Anglesey (reference number 12/WA/0355) and NHS research and development (R&D) approval from the BCUHB Internal Review Panel.
Methods
Focus groups with rehabilitation team members
Three focus groups were organised with members of multidisciplinary rehabilitation teams in the community around three North Wales hospital sites [north west (Ysbyty Gwynedd and surrounding areas), central (Ysbyty Glan Clwyd and surrounding areas) and north east (Ysbyty Maelor and surrounding areas)].
Sample and recruitment process
After gaining NHS ethics and R&D approval, the management team of the Therapies and Clinical Support Clinical Programme Group was contacted to inform it about the study and seek its co-operation in recruiting staff involved in managing and delivering rehabilitation care and services to hip fracture patients. The managers granted permission to contact hospital and community team leaders, who then assisted in the further identification of members of their teams who might wish to participate in the focus groups. These individuals were sent a letter or an e-mail inviting them to take part. This contained an information sheet and topic guide, a specimen consent form and a reply slip for either e-mail or postal return using a prepaid envelope for their use if they wished to take part. The sample was purposive, aiming to gain a wide variety of views of rehabilitation service delivery from a variety of grades of front-line staff and managers working in both the acute sector and community sectors.
Informed consent
On receipt of consent via the reply slip or e-mail, a member of the research team contacted potential participants by telephone or e-mail to provide a further opportunity to ask questions and to ensure that potential participants had read and understood the participant information sheet. Written informed consent was obtained just prior to starting the focus group from those who attended.
Focus groups with hip fracture patients and their carers
Three focus groups with patients and carers were originally planned, also based around the three main hospital sites within the BCUHB; however, as more than eight participants responded for one of the groups, two focus groups were run at this site.
Sample and recruitment process
The specific inclusion criteria for the focus groups were:
-
being aged ≥ 65 years
-
having recent proximal hip fracture, including intracapsular and extracapsular (pertrochanteric, intertrochanteric, reverse oblique or subtrochanteric) fracture
-
having undergone surgical repair by replacement arthroplasty or internal fixation
-
having completed some hip fracture rehabilitation
-
living independently prior to hip fracture
-
having capacity to give informed consent (in the case of patients lacking capacity, a carer was invited to represent their experiences).
Eligible participants were identified from local data returned to the National Hip Fracture Database,1 which includes data on age, length of hospital stay and discharge destination. Database information was accessed through medical and nursing staff responsible for maintaining the database at each site. Using these data, and electronic medical records at the three hospital sites, and with the assistance of the Health and Care Research Wales network, all those who had undergone surgery between 3 and 12 months previously were invited to take part. This time period was chosen to allow sufficient time for patients to have completed some post-operative rehabilitation while being recent enough that patients would have sufficient recall of their experiences. The carers of eligible patients with cognitive impairment were also invited to attend.
Potential patient/carer participants were sent an invitation letter containing an information sheet, a topic guide, a specimen consent form and a reply slip with a prepaid envelope.
We had hoped to purposively sample patients with different levels of disability, including those who were:
-
discharged home from the orthopaedic ward after recovering from proximal hip fracture surgery and who received a rehabilitation intervention in the community
-
transferred to an inpatient rehabilitation ward from the orthopaedic ward and then discharged home.
However, it was not possible to identify this differing rehabilitation pathway from the electronic medical records. We did, however, recruit patients with a range of ages and experiences of the two different pathways. The main subpopulations who were not represented were those who were living independently prior to hip fracture but who now lived in residential or nursing care and carers of those with cognitive impairment.
Informed consent
On receipt of the reply slip, a member of the research team contacted potential participants by telephone to give them a further opportunity to ask questions about the focus group and to ensure that they had read and understood the participant information sheet. Written informed consent was obtained just prior to starting the focus group from those who attended.
Data collection
The focus group discussions were semistructured and run by a moderator (the study manager) and co-moderator (study researcher) using a topic guide291,292 that contained open-ended questions regarding experiences of, and perceptions and beliefs about, rehabilitation following proximal hip fracture (see Appendix 25). In the later patient focus groups we were able to start exploring and gaining feedback on initial ideas for the intervention.
As the focus groups were held in an area where two languages are spoken (Welsh and English), we allowed participants to choose which language they wanted to participate in. As a result, one patient and carer focus group was run with the use of simultaneous translation, to enable all participants to discuss their personal experiences using the language that they were most comfortable with. In this focus group a third moderator (study researcher) was present who was fluent in both languages to ensure equality of access to both English- and Welsh-speaking participants. All of the study documentation was provided in both languages.
In the focus groups with professionals, in addition to the topic guide, we developed patient scenarios to stimulate discussion about the sorts of rehabilitation programmes patients would be likely to receive (see Appendix 26).
The focus group discussions were digitally recorded and fully transcribed. The transcriptions were made in the original language and any transcripts in Welsh were translated into English for analysis.
Analysis, credibility and plausibility
The focus groups were thematically analysed using the framework approach. 293 The initial framework used for this analysis was broadly developed from the theory areas identified as important in guiding the realist review (see Chapter 2). The framework (see Appendix 27) was used to index the transcripts and was populated with summaries of data by one researcher (the study manager). This was carried out separately for the patient and carer focus group data and the professionals’ focus group data. Once summarised, each subsection of the index was transferred onto a new sheet for coding. The coding was completed for both sets of data for a particular subsection of the framework in sequence, to begin identifying similarities and differences in the perspectives and to start the process of synthesising the analysis. The researcher was able to add reflective notes as the coding progressed. At the end of each section, emerging key ideas and issues were noted for development into categories and subcategories.
Once this process was completed for all sections of the framework, the researcher developed an initial interpretation using the categories, grouping them into themes. At this point a second researcher experienced in framework thematic analysis, and who had been a co-moderator in one focus group but who was otherwise independent of the study, reviewed the charts and agreed the plausibility of the emerging themes.
A third researcher involved in the study then reviewed the initial framework, the original transcripts and the draft of the initial analysis. This researcher then made the final decisions about theme structure and content. The initial and third researchers agreed on the final analysis. Involving three researchers in the analytical process strengthened the plausibility and credibility of the findings, as the identified themes were not generated from one person’s perspective. The indexing of the transcripts and the framework charts provided an audit trail connecting the themes back to the original data.
Patient and public involvement
A patient and public involvement representative commented on all aspects of the study protocol,294 including the content of the topic guides, and was actively involved in the design of the patient-facing materials, such as the information sheets and consent forms.
Results
Description of participants
Thirteen health-care professionals involved in delivering rehabilitation throughout the patient pathway consented to take part in the focus groups. These were:
-
one physiotherapist from an acute hospital orthopaedic trauma ward
-
one nurse manager of an acute hospital orthopaedic trauma ward
-
three occupational therapists from three different acute hospital orthopaedic trauma wards
-
one physiotherapist from a community hospital providing inpatient rehabilitation
-
one physiotherapist from a community rehabilitation unit who also saw patients at home
-
one physiotherapist from a community intermediate care team
-
one occupational therapist from a community intermediate care team
-
one occupational therapist from a local authority social services team
-
two local authority domiciliary support team managers (teams that provide reablement care as part of their remit)
-
one co-ordinator of a local authority leisure services centre providing the National Exercise Referral Scheme295 (a national scheme in Wales).
Thirteen hip fracture patients (11 women and two men) and four associated carers (two women and two men) consented to take part in the focus groups. Three of the carers were spouses and one was a friend. Patient and carer participant ages ranged from 60 to 90 years and participants were from both rural and urban areas of North Wales.
The numbers of participants in the patient and carer focus groups ranged from three to seven and in the health-care professional focus groups from two to six. Some participants in the health-care professional focus groups were unable to attend at short notice because of work commitments and two participants in the patient and carer focus groups were unable to attend because of illness.
Focus group themes
Four main themes emerged from the data analysis:
-
the variation in rehabilitation care provided
-
the need for information
-
facilitators of, and barriers to, rehabilitation
-
the psychosocial impact of hip fracture.
The variation in rehabilitation care provided
The prominent theme throughout all of the focus groups, and which defined the context in which rehabilitation was delivered, was the wide variability in care. In general, patient participants did receive some form of post-discharge rehabilitation. Provision in some areas was extensive, with patients receiving walking aids, home adaptations and varied physiotherapy sessions with one-to-one rehabilitation, gym classes and hydrotherapy. However, other patients reported receiving very little rehabilitation or having to overcome significant barriers to access services. This was particularly evident in the provision of community physiotherapy services, with some patients having only one or two sessions following discharge and others receiving many weeks of home visits and referral to ongoing physiotherapy programmes. Occupational therapy services, including the provision of walking aids and home adaptions, were more consistent across the North Wales area and patients typically viewed these services very positively:
The occupational therapy girls were brilliant, you know if you wanted anything, you just had to phone and they would get it for you, they were really really good.
Female carer, Flintshire and Wrexham
There were three main factors that this variability was attributed to:
-
geographical variation in resource availability
-
variation in referral procedures and service awareness
-
variation in the tailoring of rehabilitation to individual needs
Geographical variation in resource availability
Patients and health-care professionals attributed the variation in usual care, in part, to geographical variation in resource availability, leaving available staff and services overstretched, and unable to meet demands consistently across the whole North Wales area. This was reflected in comments from patients, such as the care received ‘depends where you live’ (male carer, Flintshire and Wrexham) and that optimal care may not be available ‘if you don’t live in the right postcode’ (female patient, Flintshire and Wrexham). Health-care professionals also acknowledged that the provision of NHS rehabilitation services, social care provision and access to charity services was a ‘postcode lottery’ (reablement team, Ysbyty Gwynedd) and that, even for services that are universally available, there may be variation in who is eligible to receive them:
We could provide a service under our eligibility criteria but other counties have got different eligibility criteria.
Reablement team, Ysbyty Glan Clwyd
The resultant variation in care was apparent in the acute setting and throughout patient rehabilitation. Although the patient and carer focus group participants particularly emphasised the impact of resource scarcity during the post-discharge rehabilitation period, they also raised it as an issue that they had experienced during their stay in the acute hospital. Patients observed that ward staff struggled to cope with the volume of highly dependent patients: ‘there is too much work, not enough nurses’ (female patient, Gwynedd and Conwy). As a result, some participants experienced delays in care and were incontinent or left in pain without medication:
I wet the bed a couple of times and I felt so embarrassed.
Female patient, Gwynedd and Conwy
I was initially in a room on my own because the place was so full, and I just could not get hold of anybody to give me the morphine when I needed it.
Female patient, Gwynedd and Conwy
Despite these challenges, findings from the focus groups with health-care professionals suggested that there was a good level of standardisation at the acute phase of rehabilitation, with early mobilisation being ‘quite routine’ (occupational therapist, Ysbyty Glan Clwyd) within 24 hours after surgery, which was in line with NICE guidance. 7 However, the impact of post-discharge resource availability on planning discharges from the acute setting, and consequently the therapy given in hospital, was apparent, with therapists often having to take a flexible approach:
We usually have plan A and plan B because if the bed [in community hospital] doesn’t come up they are going home.
Acute hospital occupational therapist, Ysbyty Gwynedd
The variation in post-discharge rehabilitation was not limited to patients who were discharged directly to their own home, but was also experienced by those discharged to community hospitals:
There was another ward with, they were all erm . . . different types of breakages and whether there wasn’t room the day I went there to go in that ward. I think if I had been in that ward I may have been, had more exercises to do you know.
Female patient, Flintshire and Wrexham
They taught us in detail how to climb stairs, with a stick, and with crutches, and they sent us to walk in the corridors and outside . . . I found that extra fortnight to be very valuable.
Female patient, Anglesey and Gwynedd
Although some patients had positive experiences or found that specific aspects of their rehabilitation were well implemented, there was a general sense of isolation and that they would have appreciated more consistent input from health-care professionals:
I don’t think the aftercare is what it should be. You are just left to look after yourself more of less.
Female patient, Conwy and Denbighshire
Health-care professionals in one area acknowledged that some patients may go home with no care, but postulated that it was ‘probably rare to have absolutely nothing’ (occupational therapist, Ysbyty Glan Clwyd) and that there would likely be some level of community service engagement, even if there was no occupational therapy or physiotherapy input from the hospital.
Referral procedures and service awareness
Variation in referral processes and in some cases the criteria for accessing a service meant that staff had to be aware of different referral pathways in different areas, which could cause delays in referral. In particular, a lack of uniformity in referral procedures for different community hospitals was identified as an issue by health-care professionals:
You have five referral forms, you can’t just have one, and there you are that’s done, so that takes time.
Nurse orthopaedic ward manager, Ysbyty Gwynedd
There was variation in the delay that patients experienced at the start of their rehabilitation and when progressing to more demanding activities. This was partly explained by different referral processes in health and social care. One physiotherapist commented:
Social workers have got their own timescale . . . they only have a panel once a week and that’s on a Monday, if you refer any day like Thursday afterwards they are going to miss that panel so you will have to wait an additional week.
Nurse orthopaedic ward manager, Ysbyty Gwynedd
A number of patients and their carers also commented that there had been a delay in their referral to physiotherapy. This was particularly noted to be a problem for patients who had received some physiotherapy after discharge but who had to be referred again by their GP when the initial sessions had come to an end:
If she goes to the doctor the doctor doesn’t really, he only refers you to the hospital, then you have got to wait an appointment, which there is no one you can actually say can you come next week and tell me if I am, if it’s . . . sort of all right.
Male carer, Gwynedd and Conwy
Patients experiencing delays because of problems with referral systems or variation in service provision in different areas felt that they would have benefited if they had access to these rehabilitation services immediately following discharge and that such delays in treatment were a barrier to them achieving their recovery potential:
There have been long gaps and that very slow start and I know, the physio[therapist] I saw, not immediately when I started but soon after, was very concerned about that delay it had made it a lot more difficult for me, and more difficult for her to get anything moving.
Male patient, Anglesey and Gwynedd
It took longer than perhaps it could’ve before I actually got to the stage where I did go to the gym. I think I could’ve done with that being happening a bit sooner.
Female patient, Anglesey and Gwynedd
Others were very pleased with the care that they received and felt that it had helped them progress quickly:
I was very grateful for the care I got . . . in the hospital and to resettle after being in hospital . . . within some 3 months I went back to driving a car.
Female patient, Anglesey and Gwynedd
Some therapists thought that it was challenging for the acute staff and GPs to know the full extent of services that were available in different areas and that this may have contributed to some patients not being referred to services that they were eligible to receive:
There is not always a great awareness of the acute team of exactly what services are in which place . . . I think we could definitely signpost them better to these . . . GPs need to know how to . . . what services there are and how to signpost.
Occupational therapist, Ysbyty Glan Clwyd
Physiotherapists based in community hospitals who ran the falls prevention classes also commented that, even when patients were referred, it was often at a later stage than they would expect:
You need to refer them the minute they are showing signs of impaired balance, or problems or at risk of falls. I think we are missing a lot, of the prevention stuff.
Community hospital physiotherapist, Ysbyty Gwynedd
It was also suggested that awareness in patients could be raised and that, if patients were able to self-refer, this might help to overcome the problems. However, therapists acknowledged that available resources would limit this and it also raised an issue of relying on the self-motivation of patients to seek out additional therapy:
Self-referral, you know making patients aware, posters up in GP surgery, have you lost your confidence, have you got a balance problem you can self-refer and then but it’s the resources to cope with that then, that are missing.
Community hospital physiotherapist, Ysbyty Gwynedd
Tailoring of rehabilitation to individual needs
Health-care professionals spoke extensively about tailoring patient care according to individual needs, which was determined by comprehensive assessment consisting of a background history, past medical history, social history, an assessment of the present condition, a physical assessment and an assessment of patient goals. The outcome of this assessment would determine where a patient might be referred. A recurring theme in the staff focus groups was that individual patient’s needs and situation varied greatly, so rehabilitation needs to be individualised.
It depends completely on the patient, you can’t just say well this is what is going to happen to every patient, they vary so much . . . there is different avenues depending on what they present.
Community hospital physiotherapist, Ysbyty Gwynedd
Health-care professionals’ knowledge of these factors was extensive and they were aware of several options for patient care that depended on a patient’s home situation and comorbidities. For initial rehabilitation, the type of surgery carried out was also a major factor:
It depends on what, what procedure she [the surgeon] has done to fix the fractured NOF [neck of femur] as to what level of interventions we do.
Occupational therapist, Wrexham Maelor
While discussing the patient scenarios, there was a consensus among the health-care professionals that the planned care for each patient would be tailored to his or her specific needs. This included signposting patients to certain services but the health-care professionals also highlighted the fact that they would not, for example, assess all patients as needing to attend falls prevention or balance classes, even if their fracture had occurred as the result of a fall; referral would depend on the cause of the fall:
You are dealing with very angry relatives who were under the presumption that because they are under our service, that they will automatically get care and they won’t, not unless there is a need.
Clinical specialist physiotherapist, Wrexham Maelor
Although the tailoring of post-fracture rehabilitation to individual patient needs is recommended in NICE guidelines,7 it may contribute to a significant degree of the variation reported within these broadly defined care pathways. Some participants held the perception that more comprehensive care was given only to patients who were assessed as being less able to cope alone, with others who may have been more independently mobile feeling that they would still have benefited from input from a health-care professional. One patient felt that, because she had shown self-motivation to exercise independently, it was difficult for her to receive physiotherapy input, commenting that ‘they just could see that I was motivated and doing things and they were needed somewhere else’ (female patient, Gwynedd and Conwy). Health-care professionals also commented that, although a patient might be referred to a service, they might not receive the maximum available input, for example 6 weeks with an intermediate care team; how much care was actually given would depend on an individual patient’s needs, which might be defined differently in different areas or by different therapists. ‘Usual care’, therefore, was hugely variable.
The need for information
As a consequence of the variability in usual care and available services in different areas, it was not possible to give patients definitive information on what would happen during their recovery period. This was compounded when communication links between different services providing care at different stages or providing different parts of a patient’s rehabilitation broke down. For example, an acute therapist could refer a patient for outpatient physiotherapy at a community hospital when he or she was discharged, but if the referral was delayed in the system the patient was left wondering if such a long wait was normal and what they should do about it. Patients and their carers often expressed uncertainty about the services that were available and which services they would be assessed as requiring. Patients and their carers perceived these issues as occurring because of a lack of communication from health-care staff and felt that they were not given adequate information about what to expect from their rehabilitation following hip fracture. The theme that emerged from the data was that there was a crucial need for better communication and dissemination of information to enable patients and carers to better cope with what had happened and to manage their expectations for recovery.
What to expect following hip fracture
Patients’ initial need for information related to the physical aspects of what had happened to them during their hip fracture and what they should expect during their recovery. In particular, there was a need for information about what activities they could do safely as they were uncertain whether they should exercise or ‘lie on your backside for 5 weeks’ (male carer, Flintshire and Wrexham). Another patient stated that:
I didn’t know what to do I didn’t know whether to sit, and rest or try to exercise or what nobody told me anything . . . people don’t explain . . . tell you so that you can understand. You just, left to ponder it over for yourself.
Female patient, Conwy and Denbighshire
There was confusion among patients regarding the hip fracture precautions given on discharge, with the wife of one patient reporting that, although they were told that her husband was not allowed to climb the stairs alone, they had no understanding of why this was as ‘nobody ever told us that’ (female carer, Flintshire and Wrexham). This lack of clarity left patients feeling isolated and unsure about what activities they should resume, a problem that was compounded by a feeling that the time post discharge was a ‘no man’s land’ (male carer, Gwynedd and Conwy), with patients and carers feeling unsure about who they could seek advice from.
Although some patients reported good experiences of ongoing rehabilitation after discharge from the hospital consultant, for others there was a perception that at this stage in recovery hospital consultants ‘didn’t want to see you’ (female patient, Gwynedd and Conwy) and that GPs felt that they were unable to help because of the responsibility lying with community therapy teams. This confusion surrounding where patients should ask for help meant that delays in receiving rehabilitation were not communicated to them, and patients did not know if they would receive any services at all. Although patient and carer focus group participants were dissatisfied with these delays, they also stated that they could have accepted them if it had been clearer at the beginning that rehabilitation would happen eventually:
The GP just seemed to be saying it’s the physio[therapist]’s responsibility. I didn’t know where the responsibility was at all. I think if there was someone to talk to or whatever, if I knew that it would lead into rehabilitation then that would have been better.
Male patient, Anglesey and Gwynedd
For patients who did receive rehabilitative input from health-care professionals, their need for information changed over time; although the initial input was especially helpful, they needed support throughout the entire recovery process:
There was a whole series of questions I had that had come up over the previous 3 weeks and I think the ability to go and talk to someone, with different experience and knowledge, was very important for me now.
Male patient, Anglesey and Gwynedd
There was also a common feeling among participants that the problems that they faced were related to accessing services, rather than the quality of the services that were provided, and once these services had been accessed patients were satisfied with the majority of the care that they received: ‘Care is good, communication is rubbish’ (male carer, Flintshire and Wrexham).
A draft of the intervention workbook had been developed by the time of the later focus groups. This contained information relating to the physical aspects of fracture and surgery and examples of people’s experiences of hip fracture. These focus group participants felt that such information would have been very useful for them in their recovery, as they were keen to achieve a greater understanding of their condition, and that such a workbook would still be useful in addressing some of their outstanding issues.
Information for carers
Carers of hip fracture patients also identified their own specific information needs. One participant who cared for his wife described how he was not given any information about when she would be discharged from the community hospital, or to where, leaving him feeling let down and overlooked:
No one said a word to me like, I was sort of invisible like, you know, it was a funny situation like you are nothing.
Male carer, Gwynedd and Conwy
Another carer was distressed and concerned about her husband’s well-being when she discovered that he was to be discharged home with insufficient warning for her to make adequate preparations:
They never discussed it with us the girls, I was panicking then . . . I was in such a state I was getting upset all the time.
Female carer, Flintshire and Wrexham
These responses related to communication with the acute hospital teams. In comparison, some of the community occupational therapists discussed the importance of involving family carers in patients’ rehabilitation and how this can be beneficial in encouraging patients to continue with their exercise practice, suggesting that there is variation in carer involvement between different services:
It’s important to engage with family or carers . . . you know making sure that they are aware of the exercise programme.
Acute and community occupational therapist, Ysbyty Glan Clwyd
We you know, invite the family to be there when we are discussing the precautions [post-discharge guidelines given to hip replacement patients] so that they can understand their importance and reinforce it to the patient as well.
Occupational therapist, Wrexham Maelor
Facilitators of, and barriers to, rehabilitation
The third theme that emerged concerned the perceived facilitators of, and barriers to, commencing and continuing a programme of physical activity. As well as system-level challenges, such as the variation in available resources, impacting on a patient’s access to rehabilitation, other factors also worked as facilitators of, and barriers to, rehabilitation. Whether or not patients were able to use the services made available to them effectively was often dependent on their ability, both physical and psychological (e.g. motivation), to negotiate challenges and make the most of what was offered to them.
Service reliance on patient self-motivation
Some patients or their families had to persistently ask to access rehabilitation services, which they did not feel was their responsibility. They felt that such services should be offered automatically or arranged by health-care professionals without instigation from patients and carers:
I phoned them and asked them would it be possible, I came on a, I think it was an 8-week course then.
Female patient, Conwy and Denbighshire
I had to do all the ringing up, which seemed a bit crazy.
Female patient, Gwynedd and Conwy
Some participants reported receiving basic therapy input initially but were told by therapists that ‘we are only at the end of a phone’ (female carer, Flintshire and Wrexham) or ‘we won’t come again unless you ask us’ (female patient, Gwynedd and Conwy), leaving the onus on patients to instigate further input from these services. Although this usually applied to patients who were progressing well and who were happy to be more independent, patients differed in the extent to which they were willing to ask for help; some ‘felt like we were just a total nuisance’ (female carer, Flintshire and Wrexham) if they pursued further care.
Although some patients ‘haven’t got the nerve or the nouse to ring up and badger them’ (female patient, Gwynedd and Conwy), it was evident that patients who were told to contact the therapist or encouraged by outside sources to seek additional help were more likely to do so, and this helped them overcome the feeling that they were a burden. This was also identified as a positive aspect of the proposed intervention workbook, a draft version of which was shown to participants in later focus groups, who commented that it would ‘prompt you to ask things’ (female carer, Flintshire and Wrexham).
Professionals also acknowledged that in some cases it was up to patients to request input from therapists or other services and that they would receive this only if they made contact with the services themselves.
Patients who had good levels of activity and mobility pre fracture and who were younger often received less input, as clinicians would expect them to resume their activities in a more independent manner. These patients might be assessed to check safety and progress with exercises but not necessarily referred for many organised sessions (e.g. group physiotherapy or more frequent appointments at a physiotherapy gym). If they were provided with exercises to do, these patients would be expected to continue with minimal input from therapists, relying on their own self-motivation:
They are expected to do them, of their own accord if they can.
Community hospital physiotherapist, Ysbyty Gwynedd
It’s a lot about their own mentality.
Nurse orthopaedic ward manager, Ysbyty Gwynedd
This reliance on patients and their family members to be the driving force in rehabilitation could cause problems for those who do not have a sufficient support network, who are less self-motivated or who lack confidence to ask for help.
One occupational therapist also commented that seemingly independent patients might not do as well as expected without input and may take longer in their recovery than originally anticipated:
Couple of women recently and have taken ages, whereas initially talking to them they are women you know sort of retired but really active, do loads, but then they have fallen and really I think it’s more, you know the shock of the falling over and not being able to do things it does take them quite a long time to get over it.
Acute hospital occupational therapist, Ysbyty Gwynedd
Even in patients who were self-motivated, there was an acknowledgement that it was difficult to maintain motivation over time and that it was not a limitless reserve:
Getting hold of numbers is quite difficult yes. You have to be motivated don’t you and I think a lot of people aren’t motivated. Well they have had it knocked out of them by that time.
Female patient, Gwynedd and Conwy
Patient engagement in rehabilitation
Another potential barrier was the lack of engagement of some patients in the available exercise programmes. Professionals described how, for these patients, they had to ‘sit down and reason why it is important for them to do exercises’ (health-care professional, Ysbyty Glan Clwyd) and that at this point it was often helpful to include family carers to help encourage the patients.
Some patients commented that it was important that the exercises that they were given were relevant to their everyday activities, rather than being focused entirely on more abstract strength training, with comments such as ‘doing normal things in the house was more beneficial to me’ (male patient, Flintshire and Wrexham). Professionals agreed that setting functional goals that related to ADL was helpful for engaging patients in their rehabilitation. This provided the basis for methods used in enablement units, which some patients were referred to, in which patients ‘can see themselves actually doing something that is worthwhile for them’ (community occupational therapist, Ysbyty Gwynedd).
Other patients valued continued therapist input to maintain momentum, commenting that being left with pre-printed exercise sheets without the input of a therapist ‘didn’t benefit anything’ (male patient, Flintshire and Wrexham), particularly when they were experiencing pain, as this was a common barrier to exercise:
Seeing the physio[therapist], it’s a mixture of more exercises and going through it but also it’s the ability just to have someone to talk through things like what to do with the pain.
Male patient, Anglesey and Gwnyedd
She didn’t do the exercise because she was in pain so much.
Male carer, Gwynedd and Conwy
Participants also referred to a need for their rehabilitation to evolve and progress as they started to regain function, as this gave them a sense of achievement that helped in motivating them to continue:
There’s a limit to what you can do at home, I got to the stage where I needed equipment . . . the first time I went to the gym and saw the physio[therapist] there, I thought yes . . . It hurt, it was painful, but at least I felt I’m sure I’m going to get somewhere, and it has it’s been brilliant.
Female patient, Anglesey and Gwynedd
When participants were able to see the progress that they have made, either independently or with the input of health-care professionals, this led to greater self-efficacy, strengthening their own beliefs that they could manage further challenges as they moved forward.
Although many participants were keen to exercise and resume activities quickly, they identified that what was useful for some might be ‘totally different for certain people’ (male carer, Flintshire and Wrexham). Many patients felt that a more individualised approach to their rehabilitation would have been beneficial.
One participant had very strong views that patients should be given more time in a community hospital to recuperate rather than being engaged in physical rehabilitation, stating that:
. . . there should be somewhere, where people can erm . . . are allowed to get more time to recover, a person my age or whatever, can’t recover in a few days, they should be given more help somewhere or another.
Female patient, Conwy and Denbighshire
Comorbidities and pre-fracture function
Patients’ pre-existing levels of fitness and comorbidities prior to their fracture had a significant impact on their ability to recover and influenced their perceptions of rehabilitation and how they might engage with it. Patients who were previously very active may have found it easier to engage in a new exercise programme after fracture, as they were already aware of the benefits that exercise could have and how exercise had previously helped them to maintain function. One participant had previously suffered organophosphorus poisoning and spoke of how, before her fracture, she would ‘go swimming first thing in the morning, because that is the way I have got myself to walk again. And I need to do it to keep being able to walk’ (female patient, Gwynedd and Conwy); this had motivated her to do the same after her fracture, to rebuild her strength a second time.
In contrast to this, therapists commented that patients who were ‘poorly, sort of, post-op, with various different sort of comorbidities’ (occupational therapist, Wrexham Maelor), could develop a perception that they should stay in bed to recuperate and that this could have a negative impact on rehabilitation.
Previous levels of activity also had an effect on patient expectations and could lead to a sense of frustration at what was often perceived as a slow recovery. One participant described how he had previously walked a lot and that he felt very unhappy that he had not been able to regain this previous level of activity:
Now I feel badly done by because I am nowhere near, and I’m never going to be fit enough for that.
Male patient, Anglesey and Gwynedd
Other participants commented on the length of time that it took them to return to pre-fracture function and how they found this especially difficult to cope with. One patient said that it had ‘ruined my life’ (female patient, Flintshire and Wrexham) because she felt that she was unable to return to her previous level of function. Another patients stated that ‘It’s a year now and I thought I would have been better by now, you know’ (female patient, Gwynedd and Conwy).
This unrealistic expectation of recovery is linked to the patient need for information and, as previously outlined, may be mediated in situations in which there is input from a health-care professional who is able to manage these expectations.
Transport
Professionals highlighted transport as a major barrier to patients being able to access available services and a factor that they had to consider when referring patients to ongoing rehabilitation services. This was identified as an aspect of services that could be improved, by increasing the provision of transport to rehabilitation programmes run within the community:
We refer a lot [to falls group], as long as they can get transport.
Health-care professional, Ysbyty Glan Clwyd
The problem we have is transport for a lot of the over-70s because they don’t drive.
Community hospital physiotherapist, Ysbyty Gwynedd
Physiotherapists identified lack of transport as one of the reasons that patients may have declined further therapy input, even if they had been progressing well. This could lead to their progress stalling if they were able to access classes only that were below their ability level:
The big stumbling block then is the transport. We will occasionally keep people on for another session another 12 weeks, if they really have no means of transport but then they are then being limited by the level of exercise that everybody else is doing. Erm . . . so that is our biggest concern is getting people to places.
Clinical specialist physiotherapist, Wrexham Maelor
Problems with patients having access to transport also contributed to the variation in geographical service provision, as patients in rural areas may not have been able to access all services.
Communication between service departments
One participant who had experienced gaps in her care stated that this had happened as a result of the hospital losing her notes, leaving her with a poor impression of the hospital referral system and its general co-ordination of post-discharge rehabilitation. On a wider scale, there was a consensus that communication between different areas of the health service was the main problem, rather than the people who were delivering the services.
One example of a breakdown in communication was that of a patient who required a corrective boot following surgery, which she was told by the district nurses and community therapists that she should wear at all times, including overnight, which caused a lot of pain. It was only on the insistence of the patient’s family that she received an earlier follow-up appointment with the orthopaedic consultant, who was then able to clarify how the boot should be used and rectify her treatment plan:
Communication is not very good, because although they said they had rung about what they needed to do about me boot, what they had been told, was that it wasn’t to be taken off at all . . . [the consultant] said well, no it shouldn’t have been left on, you should have been having physiotherapy.
Female patient, Conwy and Denbighshire
The lack of co-ordination between departments was a common theme that undoubtedly contributed to the variation in care that patients received. There was an expectation on the part of patients that health-care professionals were able to ensure that the correct information was passed on to where it was needed, but there were barriers within the system that often prevented this from happening:
Communication was absolutely shocking.
Female carer, Flintshire and Wrexham
Despite patient perceptions that communication between service departments was poor, health-care professionals reported examples of good communication between acute services and community therapy services, and liaison with carer support workers, social workers and other peripheral services.
One therapist who was part of a community-based intermediate care team commented that her domiciliary care staff ‘have weekly meetings . . . that will be sort of inviting certain individuals in to support them if they were having problems, it’s linking that with sort of other colleagues . . . Support workers are really good at liaising with us’ (physiotherapist, Conwy intermediate care, Ysbyty Glan Clwyd).
Other health-care professionals commented that working in teams within the acute sector or in different community regions had a positive impact on communication as they ‘know what is going on around them, you know who to contact and they have the networks there’ (reablement team, Ysbyty Glan Clwyd). Working in close proximity with other members of a wider multidisciplinary team was seen to make it easier to communicate about a patient’s care:
Things seem to happen an awful lot quicker because it’s sort of, a head pops over a computer and says oh.
Health-care professional, Ysbyty Glan Clwyd
Health-care professionals also acknowledged that there could be problems liaising with authorities in patients’ home area if they did not live locally, which was common in North Wales because of tourism. The therapists described this as ‘challenging’ (occupational therapist, Ysbyty Glan Clwyd) because of the different systems that were in place in different areas; sometimes it was not possible to follow the usual procedures for these patients as health-care professionals were unable to order equipment or arrange travel in different areas. This could delay hospital discharge, delay the start of community rehabilitation and lead to further burdens being placed on family members, who might have to take responsibility for arranging care in their local area:
It’s the practicalities of then how that patient is getting back to their local area and hospital transport and funding arrangements, then that delays discharge quite a bit.
Occupational therapist, Ysbyty Glan Clwyd
The psychosocial impact of hip fracture
A fourth theme was the psychosocial effects of fracturing a hip as a result of a fall. This was influenced by the commonly experienced variability in care and lack of information, as problems with accessing services left patients feeling unsupported and unsure of their recovery trajectory. This, coupled with anxiety about their ability to return to their previous level of function, contributed to their concerns about undertaking exercise, and this impacted on their engagement with the available rehabilitation services.
A prominent issue raised was an increased fear of falling, which often came as a shock to patients:
I am afraid of another fall, that is what worries me at the moment, so I do . . . I try to do things at my own pace, and I tend to grip onto everything. I am trying to avoid another fall but I don’t think I would survive another fall to be perfectly honest.
Female patient, Conwy and Denbighshire
That is something nobody tells you about I don’t think, is the fear of falling again.
Female patient, Conwy and Denbighshire
The anxiety around falling again often resulted in an over-reliance on walking aids, which, although helping with confidence, could hinder the progress of rehabilitation:
The stick gives you a bit of confidence I think.
Male carer, Gwynedd and Conwy
When I go out I still take a stick because I feel, I don’t know, it’s like a comfort blanket I suppose.
Female patient, Anglesey and Gwynedd
This over-reliance on walking aids was also commented on by therapists. The therapists recognised that this over-reliance occurred because patients were anxious about falling again and that it might not be possible to identify which patients would be at risk of developing these fears:
Fear. We don’t have any, any brilliant ideas of getting over people’s fear . . . You will have people who go home who you think will do very well, and you can’t get off the zimmer[frame], no thank you very much I am quite happy I feel safer, no I don’t want to go outside, and that is a big issue I think.
Occupational therapist acute hospital, Wrexham Maelor
Therapists at one site commented on the traumatic experience of a hip fracture, as opposed to a scheduled elective hip replacement, and how this might be responsible for some of the anxiety that patients experienced, and that regaining their confidence was an important part of rehabilitation:
Recently we have had some quite active people recently who take a long time because I think its more the psychological side the shock of the trauma isn’t it . . . They are scared and I think it’s their anxiety.
Acute hospital occupational therapist, Ysbyty Gwynedd
They are still anxious, they are bruised and battered as well from getting the injury so there is all that too.
Acute hospital physiotherapist, Ysbyty Gwynedd
Staff involved in rehabilitation acknowledged that, because of this anxiety, patients’ needs extended beyond physical rehabilitation to include the rebuilding of lost confidence, to allow them to engage fully in rehabilitation. Some patients who were assessed as being at risk of a further fall may have been referred to falls prevention or balance classes. These classes often focused on ‘backward training’, in which patients were taught how to get up safely if they did fall, which health-care professionals felt was an important part of addressing their fear of falling and improving patient confidence:
It’s to do with personal care as well, and to raise confidence as well, that’s a lot to do with it because people who have had the falls, it’s their confidence really that’s taken a big knock.
Reablement team, Ysbyty Glan Clwyd
It’s just really reinforcing good practice, encouragement . . . it’s reassurance, the mental barrier that you have to break through, sometimes you never do.
Nurse orthopaedic ward manager, Ysbyty Gwynedd
The anxiety surrounding the fear of falling could also delay hospital discharge:
Sometimes it’s also family or the patient that might influence that [discharge], they might say I am not . . . I don’t feel confident going straight home, or the family might feel that they shouldn’t be going straight home so soon.
Occupational therapist, Ysbyty Glan Clwyd
Patients who were able to access rehabilitation services identified this as an important factor in overcoming their fear of falling and discussed the impact that support and encouragement from therapists had on their recovery:
You think you are going to fall all the time, erm . . . so it is just practice I think, just keep doing it, keep doing little bits and erm . . . I had the reassurance from the physiotherapist who said ‘no, by next summer you will be doing exactly what you were doing last summer’.
Female patient, Gwynedd and Conwy
Another major psychological challenge was the potential loss of independence. The inability to perform usual activities independently, such as driving or going shopping, necessitated a reliance on social networks such as family and church groups, but many people found this difficult to accept, with one patient commenting ‘I want to do it myself though’ (female patient, Flintshire and Wrexham). Other patients reflected on how their inability to walk prevented them from attending social activities, causing them to feel isolated and less able to take part in activities that they had previously enjoyed:
Not being able to walk is a significant impact on all sorts of different layers.
Male patient, Anglesey and Gwynedd
I don’t feel I can go [on a walking trip] because I’m so slow, you know you feel that somebody will be waiting for you and ‘where is she sort of thing’ so I just don’t go. So I suppose in a way, well I am, I’m missing out on that socially.
Female patient, Anglesey and Gwynedd
Discussion
Summary of main findings
Four main themes emerged from the focus groups: (1) the variation in rehabilitation care provided, (2) the need for information, (3) the facilitators of, and barriers to, rehabilitation and (4) the psychosocial impact of hip fracture. The variation in care provided occurred partly because of the individual tailoring of treatment, but was also the result of geographical variation in the availability of resources, the complex variety of providers delivering different components of rehabilitation programme and the lack of awareness by referring clinicians of the full extent of available services. This complexity in programme provision meant that there was a strong need for more information to be provided to patients and their carers about what to expect following hip fracture and how to access all of the resources available for rehabilitation. Facilitators of, and barriers to, rehabilitation included the reliance on patients’ self-motivation for seeking out and accessing services, and also their confidence to do so, their engagement in the rehabilitation programme, which could depend on its relevance to their day-to-day activities, and their self-efficacy beliefs, as well as their pre-fracture level of functioning and comorbid conditions. As rehabilitation progressed, some flexibility in response to changing patient needs was required, such as requiring access to transport for community services when home visits were no longer required. Good co-ordination and communication between the different components of the programme were important; as different components were provided by different organisations or services, it was evident that failures in communication had the potential to cause problems at various stages along a patient’s rehabilitation journey. Finally, in addition to physical needs, falling and fracturing had an important psychosocial impact in terms of anxiety, fear of falling, loss of independence and loss of participation in previously enjoyed activities.
Strengths and limitations
Although the best efforts were made to ensure that participants in the health-care professional focus groups included representatives from across the whole multidisciplinary team involved in post-fracture care and rehabilitation, it was not possible for members from all disciplines to attend, for example pharmacists or orthogeriatricians. Therapy managers involved in the organisation of wider teams were also absent from the focus groups. Although the inclusion of such therapy managers may have provided further insights into the organisation of resources across areas, there is the potential for the presence of senior staff to limit the discussions generated from more junior members of teams. As the groups consisted generally of staff at similar levels of seniority, the inclusion of such therapy managers was avoided, and good levels of discussion were seen between focus group members. Representatives from social services from one council were able to attend one focus group, which was useful to obtain their perspectives; however, there are several other councils in this area so these perspectives may be limited, particularly in relation to the geographical variation that was apparent.
Similarly, the absence from focus groups of patients or the carers of patients who were living in residential care, or who had cognitive impairment, limits the breadth of information gathered from the patient and carer perspective. The patients who were able to attend had a broad range of functional abilities and comorbidities, allowing us to gain insight from patients with different experiences of rehabilitation. However, it is possible that those patients who declined to take part in the focus groups or who were unable to attend because of ill health may have been those who were struggling the most with their recovery.
Comparison with previous literature
There are significant similarities between the focus group findings and other published reports of qualitative research in comparable groups. Other studies have found a similar spectrum of patient participants with varying levels of post-fracture function and a range of levels of dependency on carers and available health services,296 but generally displaying strong self-motivation and ‘zest for life’. 88 A study exploring mobility levels pre and post fracture also reported a fear of falling, a lack of confidence (low self-efficacy) and reliance on others as having an impact on patients’ experiences of rehabilitation. 297 Patients and health-care professionals expressed a difficulty in predicting post-fracture self-efficacy and confidence, which has also been evidenced in a review of surgical outcomes in total hip and total knee replacements. 272 This review concluded that post-operative self-efficacy was a more consistent predictor of functional outcomes than pre-operative self-efficacy, highlighting the importance of feedback on post-operative achievements for continuing rehabilitation engagement. The patient need for information from health-care professionals and the importance of this in successful rehabilitation has also been previously identified. 298
A qualitative study of physiotherapist perceptions of rehabilitation also found that there is tailoring of care to patients’ individual needs, based on their own goals and level of support available. 185 A study into the challenges of team working in the rehabilitation of hip fracture patients also demonstrated that there are breakdowns in communication within multidisciplinary teams and issues relating to the organisation of resources and services that lead to variation in patient care. 299 In addition, this theme was prevalent in the survey findings (see Chapter 4).
The description of care across North Wales was also similar to the findings from across the UK, as presented in Chapter 4. There is an emphasis on early mobilisation after surgery and rehabilitation programmes vary according to the resources available and the individual needs of patients.
Implications for practice and future research
The goal of conducting focus groups was to gain insight into the perspectives of patients, carers and health-care professionals on the rehabilitation of patients following hip fracture and highlight areas that could be improved. This has been successfully achieved. The emergent themes encompassed a range of experiences and insights, which were used to inform the development of the study intervention (see Chapter 6) and further refine the theory areas of the realist review (see Chapter 2). In particular, they emphasised the need of patients for information following hip fracture, which led to the development of an information workbook to be used as part of the study intervention, the content of which was partially based on information requirements that were detailed in focus groups.
The variability in care provision was an important factor in both patient and professional perspectives of what constitutes a good package of rehabilitation, and the decision to provide six additional therapy sessions to intervention group participants aimed to address this issue.
On a wider scale, there are also implications in terms of informing health and social care services about areas that could be improved, particularly with regard to how to communicate information to patients and their families to support them during a time when they report feeling isolated and vulnerable. By including patients more explicitly in the decisions regarding their care, providing feedback on progress and being transparent around expectations, including the lack of service provision or potential treatment delays, it may be possible to improve patient engagement in rehabilitation and allow patients and families to regain control of their recovery.
Chapter 6 Development of the intervention
Summary of the main findings from Phase I
The three components of the first phase of the study aimed to systematically develop an enhanced rehabilitation intervention by collating the available evidence and developing theories on what current rehabilitation programmes consist of, how effective they are and how patients and health-care professionals view them.
From the realist review (see Chapter 2) an overarching theory was developed that, in our target population of patients who have varied pre-fracture functions and comorbidities, a tailored intervention incorporating increased quality and amount of practice of exercise and ADL could improve confidence, mood, self-efficacy, function and mobility, and reduce the fear of falling.
A survey of UK health-care professionals involved in the rehabilitation of hip fracture patients (see Chapter 4) identified the ability to tailor rehabilitation to individual needs and the role of multidisciplinary rehabilitation teams as important factors in patient recovery, but reported that communication between the different providers (e.g. acute and community services) required improvement in some areas. Survey respondents also reported variability in the provision of services, the availability of resources, the assessment of patient progress and the assessment of psychological mediators of recovery.
Focus groups with rehabilitation health-care professionals and hip fracture patients and their carers conducted across North Wales also identified variability as a pertinent theme that underpinned the delivery of rehabilitation programmes and how they were received by patients (see Chapter 5). This led to uncertainty for patients and carers in what to expect during recovery, and patients and carers identified a need for better communication and information from health-care professionals to help manage expectations and support patient recovery. Patient engagement in rehabilitation and confidence in seeking out and accessing services were also identified as potential barriers to recovery. The traumatic experience of falling and fracturing also had an important psychosocial impact in terms of anxiety, fear of falling and loss of independence.
Designing the enhanced rehabilitation intervention
Based on the findings described in the previous section, we identified four main criteria that our intervention should fulfil:
-
allow for tailoring to account for pre-fracture function and comorbidities
-
increase the amount and quality of exercise, and improve engagement and self-efficacy
-
address the psychological impact of hip fracture and patients’ need for information
-
improve the co-ordination of services.
With this in mind, we developed a programme comprising both physical and psychological components. The physical component consisted of the provision of six additional rehabilitation sessions made available to patients on discharge to their permanent place of residence. Physiotherapists and dual-trained technical instructors conducted these sessions and tailored the content of the sessions to individual needs. The psychological component consisted of a patient-held information workbook and goal-setting diary to be used in conjunction with the extra sessions and the support of the therapists. The physiotherapists used the initial extra session to assess each patient’s function and any existing comorbidities, and to discuss his or her individual aims for recovery. The physiotherapist then guided patients to set achievable goals, which were worked on with the technical instructors in the remaining five sessions.
A previously developed stroke rehabilitation workbook300 guided the topic areas of the workbook and the specific content was informed by the findings from the Phase I focus groups. The workbook contained information on:
-
the physiological aspects of hip fracture and surgery and how these could impact on recovery
-
what to expect during recovery from a hip fracture, including answers to common questions, details of other people’s experiences and the role of the health-care team
-
the variability in progress between individuals and the importance of physical exercise for progressing
-
fear of falling and fall prevention services
-
other services that may be useful, including charities.
The goal-setting diary included information on how to use the diary and emphasised the importance of making goals specific, measurable and achievable. The diary was designed to be introduced to patients prior to or during their first intervention session by a qualified physiotherapist, who could support them in the setting of their initial goals, making sure that they were appropriate for their individual capabilities. The format of the diary was set up to facilitate this and it encouraged patients and carers to review progress over a time period that they could set themselves and comment on (Figure 7). Both the goal-setting diary and the information workbook encouraged patients to ask their therapists and health-care professionals for guidance in their recovery, as well as providing signposting to other relevant services.
FIGURE 7.
Example page of the goal-setting diary.

The aim of the physical component of the intervention was to increase the intensity and/or frequency of physical exercise and ADL, with supervision from physiotherapists and occupational therapists. By providing additional therapy sessions and, thus, increasing the opportunity for practice and professional support, we aimed to improve overall mobility, independence and functional outcomes by:
-
improving muscle strength
-
improving mood and self-efficacy
-
increasing confidence and reducing fear of falling.
The psychological components aimed to improve patient engagement in the rehabilitation programme by giving patients a sense of ownership of their own recovery, with patient-led goals and patient-held documents. This was achieved by:
-
enhancing self-efficacy through goal-setting to increase motivation and promote participation in their rehabilitation
-
self-monitoring and feedback on goals
-
verbal encouragement and support from professionals
-
providing information on what to expect from recovery
-
increasing confidence through reassurance and encouraging patients to seek advice.
Although the psychological components were mediated through the workbook and goal-setting diary, the additional sessions were also an opportunity for patients to obtain reassurance and guidance from a qualified health-care professional. Similarly, the psychological components aimed to increase confidence and self-efficacy, which would affect patients’ ability and willingness to perform exercises, thus improving their physical outcomes. The complex nature of the intervention activities and their proposed outcomes were described in a logic model (Figure 8). This linked programme theory from the realist review with the relevant component of the intervention, the short- and long-term goals of the intervention and functional outcomes in terms of the International Classification of Functioning, Disability and Health. We also mapped the intervention components to the NICE recommendations for multidisciplinary rehabilitation of hip fracture7 (Figure 9).
FIGURE 8.
Logic model of intervention activities and proposed goals. ICF, International Classification of Functioning, Disability and Health.

Patient and public involvement
A patient and public involvement representative commented on all aspects of the intervention, including the content of the information workbook and the goal-setting diary.
Chapter 7 Randomised feasibility study
Introduction
The second phase of the study assessed the feasibility of conducting a future RCT.
Study objectives
-
To assess the acceptability of, and compliance with, the rehabilitation programme among patients, carers and clinicians, and identify any AEs.
-
To determine the feasibility of a future definitive RCT by assessing the number of eligible patients, monitoring recruitment and retention rates, and explore the willingness of patients to be randomised and the willingness of patients and carers to complete process and outcome measures.
-
To produce means and SDs for the quantitative measures so that effect sizes can be calculated for planning the future RCT.
Methods/design
Study design
Phase II encompassed the second stage of the MRC framework for assessing complex interventions,20 using a parallel-group randomised feasibility study to inform a definitive RCT comparing usual care with the enhanced rehabilitation package. It also consisted of a cohort study of all hip fracture patients (see Chapter 8). The acceptability of the new rehabilitation programme to multidisciplinary rehabilitation teams, hip fracture patients and their carers, as well as its feasibility, were assessed with further focus groups (see Chapter 9). An exploratory economic evaluation was conducted as part of the feasibility study (see Chapter 10). Patients recruited to the feasibility study were also recruited to a triangulation study that aimed to compare the quality of data on service use collected from patient-reported outcome measures with the quality of the same information extracted from patient electronic records (see Chapter 11).
Selection of subjects for the feasibility study
We anticipated that we would be able to identify and invite 150 patients admitted to all three hospital sites across the BCUHB to participate in the feasibility study comparing usual care with the enhanced rehabilitation package during the planned 6-month study period. We attempted to recruit 50 patients into the two groups using an allocation ratio of 1 : 1. The number of eligible patients, the recruitment and retention rates and the number who completed the outcome questionnaires were recorded. It was also important to determine whether or not random allocation to either group was acceptable to patients and carers and clinicians providing the service. The feasibility study was also an opportunity to test a package of outcome measures, including economic measures, for the main trial and to inform the effect size for a future sample size calculation.
Inclusion criteria
We aimed to recruit older adults recovering on an orthopaedic ward from proximal femoral fracture who were previously living independently and who had recently received surgical treatment. The specific inclusion criteria were:
-
being aged ≥ 65 years
-
having recent proximal hip fracture, including intra- and extracapsular (pertrochanteric, intertrochanteric, reverse oblique or subtrochanteric) fracture
-
having undergone surgical repair by replacement arthroplasty or internal fixation within the previous week
-
recovering as an inpatient on an orthopaedic ward, transferred to an inpatient rehabilitation ward or discharged home
-
living in their own home prior to hip fracture
-
having capacity to give informed consent, assessed by the clinical team in the acute hospital
-
living and receiving rehabilitation in the NHS in the area covered by the BCUHB.
Exclusion criteria
The exclusion criteria were:
-
living in a residential or nursing home prior to hip fracture
-
not able to understand Welsh or English.
Informed consent: patient participants
Clinical staff on the orthopaedic wards of the three main hospitals in the BCUHB screened patients for eligibility. If eligible, a clinician approached potential participants to see if they were interested in taking part and willing to be seen by a researcher. The study team researchers, supported by the Health and Care Research Wales research professionals, then recruited patients following the study’s informed consent process, which had been reviewed and approved by the NHS research ethics committee. Consent was obtained while patients were recovering on the acute ward, as soon after surgery as possible. Patients who had delirium were revisited if this had cleared prior to discharge. Patients who were not ready to consent but who expressed an interest in the study were revisited on the acute ward or in the community hospital or place of residence if they requested. Patients and carers who attended the Phase I focus groups provided input into the content of the information sheets and consent forms to improve clarity and suitability (see Appendix 28). Because of the challenges in engaging patients while still in the acute hospital, a patient information summary sheet was used to gauge initial interest in the study and this was followed up with a comprehensive information sheet for those who expressed an interest in participating.
It was possible that during the study the capacity of some participants may have changed. Consequently, at the follow-up visit, the researcher was asked to assess whether or not participants no longer had capacity to provide informed consent, using a research ethics committee-approved checklist. If a participant no longer had capacity, no follow-up data were collected, but the baseline and any other data collected to this point were used in the analysis. The study took place in an area where there are two official national languages, Welsh and English. Consequently, participants were given a choice of Welsh- or English-language patient information sheets and informed consent forms. When validated outcome measures existed in the Welsh language, participants had the option to complete them in that language. The researcher completed the outcome measures with participants before randomisation. The participants’ GP and treating consultants were informed of their participation and a record was made in their medical records.
Informed consent: carer participants
For the purpose of this study, a carer was defined as a friend or relative caring for a hip fracture patient recruited to the study by providing them with face-to-face support most days in the week, including help with ADL and/or physical care. The study team researchers, supported by the Health and Care Research Wales research professionals, identified and recruited carers following the study’s informed consent process (see Appendix 29). Carers were asked to complete a carer burden questionnaire [the Caregiver Strain Index (CSI)301] at baseline and at follow-up.
Randomisation
Patient participants who give their informed consent completed baseline process and outcome measures before being individually randomised. The randomisation was performed by dynamic allocation302 to ensure that good balance in the allocation ratio of 1 : 1 was maintained, both within each stratification variable and across the trial. Participants were stratified by (1) hospital and (2) gender.
Randomisation was requested by the researcher who had taken informed consent and was achieved by secure web access to the remote randomisation centre at the North Wales Organisation for Randomised Trials in Health (NWORTH) at Bangor University. This system was set up, maintained and monitored independently of the trial statistician and other trial staff. The randomisation procedures were aligned with NWORTH standard operating procedure 5.01 to ensure best practice. All of the team, except for the trial manager, were blinded within the study. The key to the randomisation code was held centrally by NWORTH.
Withdrawal of participants
Participant withdrawal from the study did not affect their medical care and this point was emphasised in the patient information sheet and during the informed consent process. Similarly, withdrawal of carer participants did not affect the medical or social care of the hip fracture patient who they were caring for.
Non-completion of the follow-up questionnaires or physical function tests did not constitute formal withdrawal from the trial and, unless a participant requested withdrawal of his or her data completely, they were used to impute values for the analysis. The imputation of missing values ensured that the data set was utilised to its full power.
Duration of the feasibility study
We recruited participants over a 9-month period and followed them up for 3 months. Baseline data were collected between June 2014 and March 2015 (January 2015 in Ysbyty Gwynedd), with collection stopping on schedule. The information was collected either on the ward following surgery or in the patients’ place of residence following discharge. Follow-up data were then collected from September 2014 to June 2015 in the patients’ place of residence.
Feasibility study interventions
We compared the enhanced rehabilitation intervention with usual rehabilitation care. Usual care was varied and consisted of a multidisciplinary rehabilitation delivered by the acute hospital, community hospital and community services depending on patients’ individual needs at different times during their recovery and on the availability and accessibility of services in different areas. The multidisciplinary teams delivering care and rehabilitation included orthopaedic surgeons, orthogeriatricians, nurses, physiotherapists, occupational therapists, dieticians, pharmacists, GPs and social workers. The settings for care included acute orthopaedic or orthogeriatric wards, rehabilitation units in community hospitals, rehabilitation beds in care homes, patients’ homes and care home settings.
The main aim of the intervention was to enhance usual rehabilitation by increasing the amount and quality of patients’ practice of physical exercise and ADL to improve their functional outcomes at 3-month follow-up. We also hypothesised that improving patients’ self-efficacy would increase their motivation to engage in the rehabilitation process and improve the quality and quantity of this practice.
Rehabilitation was enhanced by means of a patient-held information workbook and diary given to participants in the acute hospital and kept with them throughout the follow-up period of the study. Six additional therapist/technical instructor sessions were available to patients once they returned to their usual place of residence. These extra sessions were tailored to individuals’ needs at the discretion of the therapists allocated to deliver the extra sessions. The workbook also included information about what to expect from their recovery and information about NHS, council and voluntary sector services that they could use. This included a variety of community services such as falls preventions programmes.
The objectives of the workbook and diary and a logic model of the enhanced rehabilitation intervention are provided in Chapter 6.
Delivery of the intervention
The extra six sessions of rehabilitation were delivered by additional physiotherapists and therapy assistants in collaboration with the existing therapists delivering usual care. The intervention therapy teams were alerted to which group a patient was randomised to and arranged a time for an initial assessment and goal-setting session in the acute hospital or in a community setting. The remaining five sessions were structured according to the individual’s need and rehabilitation plan.
Feasibility study outcomes
The outcomes were collected in a variety of ways. Demographic data were collected from patients and from their medical records. Recruitment rates were collected by researchers from their screening and recruitment records. At baseline and at 3-month follow-up, patient-completed outcome measures were completed by participants, assisted by Health and Care Research Wales research professionals or a member of the research team, who were blind to treatment allocation. Participants were also given the choice to complete validated versions of outcome measures in Welsh when they existed. Fewer patient-completed outcome measures were used at baseline than at 3-month follow-up, as we wished to reduce the burden on patients so soon after surgery. Physical function was objectively assessed by the researcher at baseline using the grip strength test. At 3-month follow-up, a physiotherapist measured other objective tests of physical function, including the grip strength test. These were performed in the physiotherapy gym or, if the patient was unable to travel, in his or her own home. The timing of the outcome assessments is summarised in Table 9.
| Event | Baseline | 3-month follow-up |
|---|---|---|
| Patients | ||
| Eligibility screening | Full eligibility screening, including capacity assessment, by the clinical team | Checklist to confirm that capacity was maintained |
| Informed consent | Obtained | Confirmed |
| Outcome measures performed | BADL, NEADL, AMTS, EQ-5D, GSES, HADS, VAS, ICECAP-O, CSRI | BADL, NEADL, EQ-5D, GSES, HADS, VAS, ICECAP-O, FES-I, SEE, VAS-FOF, CSRI, DCE |
| Physical function tests | Hand grip strength | Hand grip strength, 8-foot up-and-go test, 50-foot walk test, 30-second sit-to-stand test |
| Randomisation | Performed following outcome measure completion | NA |
| Carers | ||
| Carer consent | Obtained | Confirmed |
| Outcome measures | CSI | CSI |
Routinely collected demographic, clinical and recruitment data
During recruitment to the feasibility study, we collected information on the number of patients approached, the number eligible, the numbers who did and did not consent and, when possible, the reasons for not consenting. The number of eligible patients who fulfilled the inclusion criteria and were willing to be randomised was expressed as a percentage of the number screened. In addition, we recorded the number who withdraw after the baseline assessment and randomisation and the number who completed the various outcome measures at baseline and at 3-month follow-up. The researchers who administered the outcome measures recorded the reasons for any non-completion.
The following demographic data and descriptors were collected:
-
date of birth (age)
-
gender
-
type of fracture
-
type of surgery
-
living arrangements
-
place of residence prior to admission
-
place of discharge from acute and/or community hospital.
Cognitive status
Abbreviated Mental Test Score
The AMTS274 is a validated test that is widely used in clinical and research settings in the UK for detecting and monitoring cognitive impairment. This was used to provide a baseline description of patients’ level of cognition. It is brief (10 items) and was recommended for cognitive screening in acute settings in the Alzheimer’s Society (2013) toolkit,303 Helping You to Assess Cognition: A Practical Toolkit for Clinicians. It is generally considered to be easily administered and well tolerated by raters and subjects. The score range is 0–10, with higher scores indicating worse cognitive function.
Patient-completed measures: primary outcome
Barthel Activities of Daily Living index
The Barthel Activities of Daily Living (BADL) index265 is a patient- or assessor-completed outcome measure of current functional status, which determines the individual’s ability to care for him- or herself. It is validated for use in patients with musculoskeletal or neuromuscular disorders and is considered easy to use, reliable and sensitive to change. It focuses on the person’s level of independence on the following items: feeding, bathing, grooming, dressing, bowel function, bladder function, toilet use, transfers and mobility on level surfaces and stairs. This measure was used at baseline and at the 3-month follow-up assessment. The score range is 0–20, with lower scores indicating increased disability.
Patient-completed measures: secondary outcomes
Nottingham Extended Activities of Daily Living scale
The Nottingham Extended Activities of Daily Living (NEADL) scale304 is a patient-completed outcome measure of ADL in the previous 4 weeks, which has been validated in stroke patients. The NEADL is a record of actual activity rather than capability, scoring patients in the areas of mobility and kitchen, domestic and leisure activities. A higher score indicates a greater level of independence. At baseline it was used to assess participants’ functional capacity prior to hip fracture; at the 3-month follow-up assessment it was used to assess the degree of functional recovery. The score range is 0–66, with higher scores indicating greater independence.
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS)305 is a patient-completed outcome measure of anxiety and depression, designed to measure anxiety and depression in patients with physical health problems. It has seven items related to common symptoms of anxiety and seven items for depression. Patients are asked whether they experience the symptom definitely, sometimes, not much or not at all. The HADS was designed for use in the hospital setting but has been used successfully with the general population. This measure was used at baseline and at the 3-month follow-up assessment. The two subscales have score ranges of 0 to 21, with higher scores indicating increased anxiety and depression.
Process measures (potential mediators of outcomes)
Visual analogue scale for hip pain intensity
This is a patient-completed measure of current hip pain intensity following surgery,306 which is an important factor affecting rehabilitation. This measure was used at baseline and at the 3-month follow-up assessment. We chose to use a visual analogue scale (VAS) as it has been reasonably well validated against the Oxford Hip Score307 and is much simpler and quicker to complete, thus reducing the burden on patients. The score range is 0–10 on a segmented line.
General Self-Efficacy Scale
The General Self-Efficacy Scale (GSES)308 is not behaviour specific and was chosen as a measure of general confidence when facing challenge. It has evidence of validity in populations of older people and surgical patients. It was used at the baseline assessment and at the 3-month follow-up to allow an assessment of change over time in such expectancy-based cognitions (as well as to test between-group differences at follow-up comparing the intervention with usual care). The more behaviour-specific FES-I and Self-Efficacy for Exercise (SEE) scale (see the following sections) were also completed at 3-month follow-up.
Falls Efficacy Scale – International (self-efficacy)
The FES-I309,310 measures how concerned a patient is about falling when performing ADL, both inside and outside the home. The scale includes 16 activities and patients rate each one activity with regard to how concerned they would be about falling if they performed that activity, from 1 (not at all concerned) to 4 (very concerned). The score range is 16–64, with higher scores indicating a greater fear of falling. The FES-I has been used successfully in older patients both with and without cognitive impairment.
Self-Efficacy for Exercise scale
The SEE scale311 is a revision of an unpublished self-efficacy barriers to exercise measure (McAuley W. Self-Efficacy Measures. Unpublished raw data; 1990). The scale consists of statements regarding participants’ confidence that they could exercise for 20 minutes, three times a week, depending on factors such as pain and mood. Participants were instructed to use numbers from 0 (not confident) to 10 (very confident) to rate their expectations. This measure assesses participants’ present expectations and so was used only at the 3-month follow-up point; pain from surgery would likely be the major factor in patients’ expectations at baseline and so normal levels of self-efficacy would not be measured at baseline. The score range is 0–90, with higher scores indicating greater confidence in capability.
Visual analogue scale for fear of falling
The VAS-FOF312 is a patient-completed VAS to measure fear of falling. A VAS is useful as it is easy to administer and brief. The VAS-FOF uses a numerical scale to measure perceived fear, with 1 representing no fear of falling and 10 representing an extreme fear of falling. It has previously been used in older adults with and without cognitive impairment with good results and was used to measure fear of falling in our study at 3-month follow-up.
Health economic measures
The following economic measures were used:
-
EuroQol-5 Dimensions, three-level version (EQ-5D-3L)287
-
ICEpop CAPability measure for Older people (ICECAP-O)313,314
-
Client Service Receipt Inventory (CSRI)315
-
discrete choice experiments (DCEs) (discussed in more detail in Chapter 10).
Objective measures of physical function
Grip strength
This is an objective measure of physical function316 that was administered by the researcher as part of the patient-completed questionnaires. Grip strength correlates well with general fitness and muscle strength relating to physical function. It is also a more appropriate measure for use at baseline, as performing other physical assessments at this time point may carry a risk to patients or would be likely to primarily reflect post-operative pain and not overall function. Grip strength was measured at baseline and at the 3-month follow-up assessment. Other objective measures, described in the following sections, were administered by a physiotherapist at the 3-month follow-up.
Thirty-second sit-to-stand test
The 30-second sit-to-stand test317,318 is used to measure lower body strength and is useful in older adults because it forms part of everyday activities, for example getting off the toilet and getting in and out of a car and in and out of a chair. It correlates reasonably well with other measures of lower body strength, such as knee extensor and knee flexor strength, and has been shown to have good test–retest reliability in older adults living in a community setting. From a seated position in a chair with no armrests, the participant rises to a full stand and returns to a fully seated position without using their arms to support him- or herself. An observer measures the number of stands completed in 30 seconds.
Eight-foot up-and-go test
The Timed Up and Go test (also known as the 8-foot up-and-go test)318 is used to assess mobility, agility and balance. An observer measures the time taken for a participant to stand up from a chair, walk 8 feet (2.5 m) with or without a walking aid, turn 180°, walk back to the chair and sit down. There is evidence of validity and reliability. 318
Fifty-foot walk test
The 50-foot (15.4-m) walk test319 is carried out on a level 50-foot walk test course (25 feet out and 25 feet back). On the command ‘go’ the participant walks as quickly as possible from the start line to the 25-foot mark and back. An observer records the time taken from the command ‘go’ until the start line is crossed on the way back. It has been shown that there are correlations between the recorded gait time and muscle strength, and also between the recorded gait time and the ability of older people living in the community to carry out ADL. 320
Carer-completed measure: secondary outcome
Caregiver Strain Index
Carers who were recruited onto the study were asked to complete the CSI. 301 The CSI is a 13-item tool that measures strain related to care provision. There is at least one item for each of the following major domains: employment, financial, physical, social and time. Positive responses to seven or more items indicates a greater level of strain. It can be used to assess individuals of any age who have assumed the role of caregiver for an older adult. This measure was completed at baseline and at the 3-month follow-up. The score range is 0–13, with higher scores indicating greater strain.
Therapist process outcomes and use of the intervention workbook
To describe the rehabilitation programme in both arms of the feasibility study, we accessed routinely collected data from the Therapy Manager System. The Therapy Manager System is an electronic system that allows therapy staff across different departments to log all direct and indirect activities relating to patient care in both hospital and community settings. This system is widely used only in the central region and so data were unavailable for the west and east regions.
An information technology (IT) manager at the BCUHB granted access for an unblinded researcher to extract the following data and return them anonymously to the research team [data were identifiable only by participants’ study identification (ID) number]:
-
patient study ID number and date of the extra session
-
whether the session was face to face or indirect
-
where the face-to-face session was held
-
who conducted the session.
Data were collected on the care received once patients had been discharged to their permanent residence until they reached the 3-month follow-up date for the study.
The intervention therapy teams completed a paper record of how they used the extra sessions, which also formed part of patients’ clinical records. We assessed whether or not the fidelity and dose of the enhanced rehabilitation programme delivered to participants were consistent with our programme theory. We evaluated how the programme was delivered along with patients’ views and their use of the workbook through the use of focus groups (see Chapter 9). The workbook contained a page of questions and Likert scale-type response options to encourage participants to provide feedback on their workbook. Researchers also collected the diary sections to assess how they were used. We evaluated engagement with the workbook by counting how many diaries were used, how regularly they were filled out and whether or not goals were set and quizzes completed.
Triangulation study of service use information
The health service use data obtained from the patient-completed CSRI questionnaires were compared with the same information obtained from routinely collected data recorded on computerised patient records. The routinely collected data were collected by NWORTH and BCUHB IT staff.
Assessment of safety
Recording adverse events
All AEs and serious adverse events (SAEs) were recorded in this study. AEs included the following:
-
non-injurious falls
-
an exacerbation of a pre-existing illness
-
an increase in the frequency or intensity of a pre-existing episodic condition
-
a condition detected after the start of the study (even though it may have been present prior to the start of the feasibility study)
-
continuous persistent disease or symptoms present at baseline that worsened during the study.
The following were not included as AEs:
-
medical or surgical procedures in which the condition that led to the procedure was the AE
-
pre-existing disease or conditions present before treatment that did not worsen
-
overdose of medication without signs or symptoms.
A SAE was any medical event that:
-
resulted in death
-
was life-threatening (refers to an event during which the participant was at risk of death at the time of the event; does not refer to an event that might have caused death had it been more severe in nature)
-
consisted of a fall and repeat fracture
-
required hospitalisation or prolongation of existing hospitalisation
-
resulted in persistent/significant disability or incapacity
-
based on appropriate medical judgement, may have jeopardised the participant and may have required medical or surgical intervention.
Process for recording adverse events
All AEs were recorded by researchers when they were made aware of the events by the patient, carer, treating clinician or therapist. AE reporting information was included in the training given to the therapy teams delivering the intervention and they were also given copies of the AE reporting forms (see Appendix 30) and details of how to return the forms to the research team. Details of the AE reporting procedure was also included in letters sent to the participants’ GP and consultants informing them of patients’ participation in the study. The AE form had two sections. The first section was completed by the health-care professional and then returned to the study manager. The study manager liaised with the chief investigator, who determined whether or not the AE was serious and whether or not it was related to the study. The chief investigator completed the second part of the form. All SAEs, along with the chief investigator’s assessments of whether or not events were related to the study, were sent to the Data Monitoring and Ethics Committee (DMEC) for a second opinion. The study manager recorded the information on the study master file and informed the clinical trials unit manager. Study-related SAEs were reported to the sponsor and to the academic school (School of Healthcare Sciences, Bangor University) within 24 hours of an event being determined as serious. They were also reported to the DMEC chairperson and the research ethics committee.
Referral of vulnerable adults to protection agencies (protection of vulnerable adults referral)
Staff and researchers recruiting patients were provided with statutory protection of vulnerable adults (POVA) training by the BCUHB within the vulnerable adult protection framework321 in accordance with Welsh Government guidance. 322,323 A mechanism of immediate risk assessment and onward referral to the appropriate local authorities, the police and the BCUHB POVA hub was developed within the framework of the Human Rights Act 1998324 and the Data Protection Act 1998325 if abuse or neglect was suspected, observed or disclosed by participants.
Statistics
Sample size
We estimated that we would recruit 25% of eligible patients with a proximal femoral fracture admitted to the three acute hospitals in the BCUHB and randomise them to either the enhanced rehabilitation programme or usual care. To estimate the SD of the primary outcome measure (BADL index) with a high level of confidence, for use in a power calculation for a future definitive RCT, a sample size of at least 50 participants completing the trial was advisable. 326 If the retention rate was 80% then 62 participants would need to be recruited.
Statistical analysis
The main outcomes of the feasibility study were the descriptive statistics for recruitment and retention, as follows:
-
The number of patients screened for eligibility.
-
The number of eligible patients and the number of eligible patients compared with the number of patients screened. A full trial would be considered feasible if 50% of the patients screened were eligible for inclusion in the trial.
-
The number of ineligible patients and the frequency of pre-determined reasons for ineligibility (lack of mental capacity to consent, not living independently, living outside the study area, age, did not have surgery for their hip fracture, living within the study area but outside the area where the intervention could be delivered, other).
-
The number of eligible patients recruited (and so, by implication, the number who were willing to be randomised) was expressed as a percentage of the number in the cohort data set and as a percentage of the number identified as eligible in the feasibility study. The full trial was considered feasible if the expected 25% of eligible patients were recruited to the trial.
-
The number of eligible patients not recruited and the reasons and frequencies for this (e.g. burden, did not want to take part in a research study).
-
The number who withdrew after the baseline assessment and randomisation, and the reasons for withdrawal.
-
The number who completed the various outcome measurements at baseline and at 3-month follow-up. The researchers who administered the outcome measures recorded the reasons for any non-completion of measures. The retention rate was set at 75% for the full trial to be feasible.
The following demographic descriptors were presented overall and per randomised group:
-
date of birth (age)
-
gender
-
type of fracture
-
marital status and living arrangements
-
place of residence prior to admission
-
place of discharge from acute or community hospital
-
AMTS.
All outcome measures were presented descriptively for all of the time points at which they had been collected.
An exploratory correlation analysis was performed. Correlations were calculated using Pearson’s product moment correlation coefficient for specific pairs of variables, as outlined in the following sections. All of the correlations were completed at both baseline and 3-month follow-up.
Barthel Activities of Daily Living index compared with the 8-foot up-and-go test
This explored the relationship between patients’ current functional status and the results of the physical function test used to assess their agility and dynamic balance.
Barthel Activities of Daily Living compared with the General Self-Efficacy Scale/Falls Efficacy Scale – International/Self-Efficacy for Exercise scale
Three different self-efficacy measures were used within the feasibility stage of this study. All three were correlated with the primary outcome measure to evaluate any differences between them and assist in the decision as to which measure to take forward to a full trial. The correlation aimed to compare patients’ self-efficacy with their current functional status to see whether or not a link was present.
Preliminary exploratory analysis of the primary outcome measure (BADL index) was performed to find estimates of the means, SDs and CIs for both of the treatment arms. These values also allowed the sample size calculation for a future RCT to be carried out. An exploration of any potential differences between the two groups in relation to the BADL index was completed using an analysis of covariance (ANCOVA). The effect sizes and CIs were calculated to evaluate any relationships present. It was envisaged that a more complex analysis would have been required to elicit an accurate description of the group differences; however, this would have been possible only with a larger sample size. The same procedure was followed for analysing the secondary outcome measures. The results and appropriateness of the outcomes were evaluated to determine if they would be suitable for use in a future RCT.
Trial management
Study Management Group
A Study Management Group (SMG) consisting of individuals responsible for the day-to-day running of the study was established and was responsible for overseeing the progress of the study throughout all of its phases. The SMG met regularly every 1–2 months. The SMG included the chief investigator (NHW), study manager (CH), study statistician (ZH), trial unit quality assurance manager and study co-applicants. The group ensured that the protocol294 was adhered to, took appropriate action to safeguard participants and ensured the overall quality of the study. The SMG reported to the Study Steering Committee (SSC) and the DMEC.
Study Steering Committee
A SSC meeting was held every 3–6 months to provide overall supervision of the study and ensured that the study was conducted to the rigorous standards set out in the principles of good clinical practice outlined by the International Conference on Harmonisation – Good Clinical Practice. 327 The SSC consisted of the following members: an independent chairperson (Dr Sharon Simpson), other independent members (Dr Fiona Wood, Dr John Belcher, Professor George Kernohan and Dr Tom Welsh), a patient representative (Ms Tricia Best), the chief investigator (NHW), the study manager (CH), a member observing from Bangor University as the sponsoring organisation (Bob Woods) and a representative from the National Institute for Social Care and Health Research Clinical Research Centre (NISCHR CRC) (Mrs Jayne Jones). The SSC considered study progress and adherence to the protocol,294 and provided advice to the study team. The SSC made recommendations to the SMG and reported to the sponsor and the funder.
Data Monitoring and Ethics Committee
Data monitoring and quality assurance was overseen by the DMEC. The DMEC was independent of the study organisers. It considered study progress, recruitment and retention, patient safety and any new information relevant to the study. The DMEC consisted of the following members: an independent chairperson and statistician (Professor Chris Robertson) and other independent members who were experts in the field of rehabilitation of older people (Professor Rowan Harwood, Dr Neil Artz and Dr Diane Dixon). The DMEC reported to the SSC.
Ethics and regulatory approvals
NHS research ethics (reference number 13/WA/0402) and NHS R&D approvals were obtained. All trial documentation, including participant information sheets, participant consent forms, template GP letters and questionnaires, were submitted for approval. To conform to the Data Protection Act 1998325 and Freedom of Information Act 2000,328 all data were anonymised and stored securely. No published material contained patient-identifying information.
Direct access to source data/documents
Source data were the hospital written and electronic medical records and routinely collected data, community electronic and written records, and audio-recordings and transcripts of the focus group interviews. Access to these data were through members of the NISCHR CRC, BCUHB IT staff and researchers on the team who had NHS research passports. Trial-related monitoring, audits, research ethics committee reviews and regulatory inspections were permitted, allowing access to data and documents when required.
Quality assurance and quality control
This study was conducted in line with the study protocol294 and followed the principles of good clinical practice outlined by the International Conference on Harmonisation – Good Clinical Practice327 and complied with European Union directive 2001/20/EC. 329
Regular monitoring activities were put in place based on a study risk assessment and were delegated to members of the study team to ensure that collected data adhered to the requirements of the protocol;294 only authorised persons completed case report forms; the potential for missing data was minimised; validation checks were performed on the data (e.g. range and consistency checks); and recruitment rates, withdrawals and losses to follow-up were reviewed overall and by hospital site. Only members of the research team who had completed good clinical practice training and who had received training in focus groups or who were supervised by an experienced team member conducted were co-moderators at these groups.
Patient and public involvement
A patient and public involvement representative was a member of the SSC and commented on all aspects of the study protocol,294 including outcome measurement, and was actively involved in the design of patient-facing materials such as information sheets and consent forms.
Data handling
Data-capturing method
Data were entered into the MACRO (version 4.2; InferMed, London, UK) data management programme, which is a web-based system that allows controlled access to data by all centres and that stores a full audit trail. Additional health service use data obtained from primary and secondary care records were recorded electronically on encrypted laptop computers or collected by NHS staff on secure computers and anonymised in an electronic data set that was ready for secure transfer to NWORTH.
Coding specifications
The design of the source documentation in MACRO was documented specifying the design, format, derivation and validations used for each type of question in the coding specification. The data captured were stored in a database running on servers maintained by Bangor University. Access to the complete database was limited to the core team members of the project involved in data management, data cleaning, analysis and study management. The physical storage of paper case report forms was documented within the data management plan. The coding was conducted in the design set-up phase of the source documentation for MACRO. The code book was shared along with the data in the data-sharing process to allow meaningful interpretation of the data set by other researchers in the project.
Data transfer process steps
Data on the MACRO data management programme were made available for analysis via IBM SPSS 20.0 (IBM Corporation, Armonk, NY, USA). Paper copies of case report forms (participant questionnaires) were stored securely on Bangor University premises during the trial. Photocopies, if needed, were made before returning any originals to NWORTH. The originals were returned to NWORTH by recorded delivery/courier for data entry, if necessary, and for archiving at the end of the study. The photocopies held at the site were destroyed at the end of the trial once the final data set was closed. Whenever possible, consent forms were stored securely at the NHS sites. Any consent forms (e.g. focus group consent forms) and paper-recorded data stored at Bangor University were kept in separate locked cabinets.
Review of the quantitative data
A periodic review of the quantitative data was performed to ensure the accuracy of data entered into the database. The researchers entering the data into the online system randomly checked each other’s entries against the paper case report forms to ensure consistency and accuracy; determined if all participant data had been entered; and checked for missing values and identified any obvious problems. A random check of ID numbers, number of entries and out-of-range values was also performed.
Data management
A data management plan was written that covered processes for auditing, cleaning and monitoring the quality of data.
Indemnity
Bangor University had appropriate clinical trials indemnity and professional indemnity insurance in place that covered members of the research team to conduct the research as per protocol. NISCHR CRC staff were on NHS contracts and their work was appropriately insured. NHS and social services staff who worked with patients involved in the intervention were not expected to do anything that was not covered by their contract and they remained covered by NHS or social services insurance arrangements.
Changes to the protocol
After the trial began some minor changes were made to the protocol. An additional patient information summary was provided alongside the patient information sheet to ensure that patients had a good understanding of the trial before recruitment. Reasons for declining participation that had not previously been collected were added to the screening information taken from participants. The DCE was also shortened to reduce patient burden and aid completion, and a Welsh version of the HADS was made available to Welsh speakers alongside the English version in an attempt to validate the Welsh version of the measure. As a result of recruitment being slow, the recruitment period was increased from 6 to 9 months in Ysbyty Glan Clwyd and Wrexham Maelor. Recruitment was not extended in Ybsyty Gwynedd as resources were not available to continue delivery of the intervention for an additional 3 months.
Results
Demographic characteristics
In total, 61 patients were randomised into the feasibility study and 49 patients subsequently completed the trial. Of the 61 participants, 32 were randomised into the control group and 29 were randomised into the intervention group, showing a good balance between the groups.
The characteristics of the recruited participants are shown in Table 10. Participants ranged in age from 66 to 99 years. The difference between the mean ages for the two groups was 2.9 years, which, within the 33-year age range, is a reasonably small difference.
| Characteristic | Overall, n (%) | Control, n (%) | Intervention, n (%) |
|---|---|---|---|
| Age (years), mean (SD); range | 79.4 (7.6); 66–99 | 78.0 (8.3); 66–99 | 80.9 (6.6); 69–94 |
| AMTS, mean (SD); range | 9.1 (1.3); 5–10 | 9.0 (1.2); 6–10 | 9.1 (1.3); 5–10 |
| Gender | |||
| Male | 15 (25) | 9 (28) | 6 (21) |
| Female | 46 (75) | 23 (72) | 23 (79) |
| Usually lives | |||
| Alone | 31 (51) | 16 (50) | 15 (52) |
| With others | 30 (49) | 16 (50) | 14 (48) |
| Accommodation | |||
| Owner-occupied property | 48 (79) | 24 (75) | 24 (83) |
| Privately rented property | 5 (8) | 2 (6) | 3 (10) |
| Housing association/local authority property | 6 (10) | 4 (13) | 2 (7) |
| Sheltered accommodation | 2 (3) | 2 (6) | 0 (0) |
| Type of fracture | |||
| Intracapsular | 27 (44) | 16 (50) | 11 (38) |
| Extracapsular | 20 (33) | 9 (28) | 11 (38) |
| Not recorded/available | 14 (23) | 7 (22) | 7 (24) |
| Type of surgery | |||
| Total hip arthroplasty | 5 (8) | 4 (13) | 1 (3) |
| Hemiarthroplasty | 29 (48) | 15 (47) | 14 (48) |
| Internal fixation | 17 (28) | 7 (22) | 10 (34) |
| Intramedullary nailing | 2 (3) | 2 (6) | 0 (0) |
| Not recorded/available | 8 (13) | 4 (13) | 4 (14) |
| Direct discharge | |||
| Yes | 27 (44) | 17 (53) | 10 (34) |
| No | 22 (36) | 7 (22) | 15 (52) |
| Missing | 12 (20) | 8 (25) | 4 (14) |
| Hospital | |||
| Ysbyty Gwynedd | 11 (18) | 6 (19) | 5 (17) |
| Ysbyty Glan Clwyd | 34 (56) | 17 (53) | 17 (59) |
| Wrexham Maelor | 16 (26) | 9 (28) | 7 (24) |
Most of the participants (75%) were female. The proportions of men and women were similar in both groups, which would be expected as gender was used as a stratification variable.
There was an even split in both groups between participants who lived alone and those who lived with others before being admitted to hospital. The majority (79%) lived in owner-occupied properties before they were admitted to hospital. After discharge there was a small difference between those who were discharged directly to their original accommodation (27 patients) and those who were not (22 patients). This was not consistent between the two groups, with 17 (53%) in the control group discharged directly home but only 10 (34%) in the intervention group discharged directly home.
The most common type of fracture was intracapsular (44%). There was a slight difference between the two treatment groups, with equal numbers in the intervention group having intra- and extracapsular fractures but more people in the control group having an intracapsular fracture than an extracapsular fracture.
Recruitment at each of the three centres was not equal, with 34 patients recruited at Ysbyty Glan Clwyd in Denbighshire, 16 patients recruited at Wrexham Maelor and 11 patients recruited at Ysbyty Gwynedd in Bangor. Hospital site was a stratification variable within the randomisation process to ensure that the proportions from each site were similar between the groups, which worked effectively.
Mean scores for most of the outcome measures and physical function tests at baseline were similar between the groups (see Table 17); however, there was an imbalance in NEADL scores, with a higher mean score in the control group.
Participant flow
Figure 10 shows the Consolidated Standards of Reporting Trials (CONSORT) diagram, detailing the flow of participants through the trial.
FIGURE 10.
Consolidated Standards of Reporting Trials (CONSORT) diagram.

A further breakdown by recruitment centre of the number of patients screened, the number of eligible patients and the numbers recruited and retained is provided in Tables 11 and 12 and Figure 11.
| Participants | Ysbyty Gwynedd, n | Ysbyty Glan Clwyd, n | Wrexham Maelor, n | Total, n |
|---|---|---|---|---|
| Screened | 147 | 235 | 211 | 593 |
| Eligible | 75 | 103 | 88 | 266 |
| Recruited | 11 | 35 | 16 | 62 |
| Retained | 4 | 29 | 16 | 49 |
| Variable | Target | Ysbyty Gwynedd (95% CI) | Ysbyty Glan Clwyd (95% CI) | Wrexham maelor (95% CI) | Total (95% CI) |
|---|---|---|---|---|---|
| Eligibility rate (%) | 50 | 51 (43 to 59) | 44 (38 to 50) | 42 (35 to 49) | 45 (41 to 49) |
| Recruitment rate (%) | 25 | 15 (7 to 23) | 34 (25 to 43) | 18 (10 to 26) | 23 (18 to 28) |
| Retention rate (%) | 75 | 36 (8 to 64) | 83 (71 to 95) | 100 | 79 (69 to 89) |
FIGURE 11.
Numbers of screened, eligible, recruited and retained patients within the trial by recruitment centre.
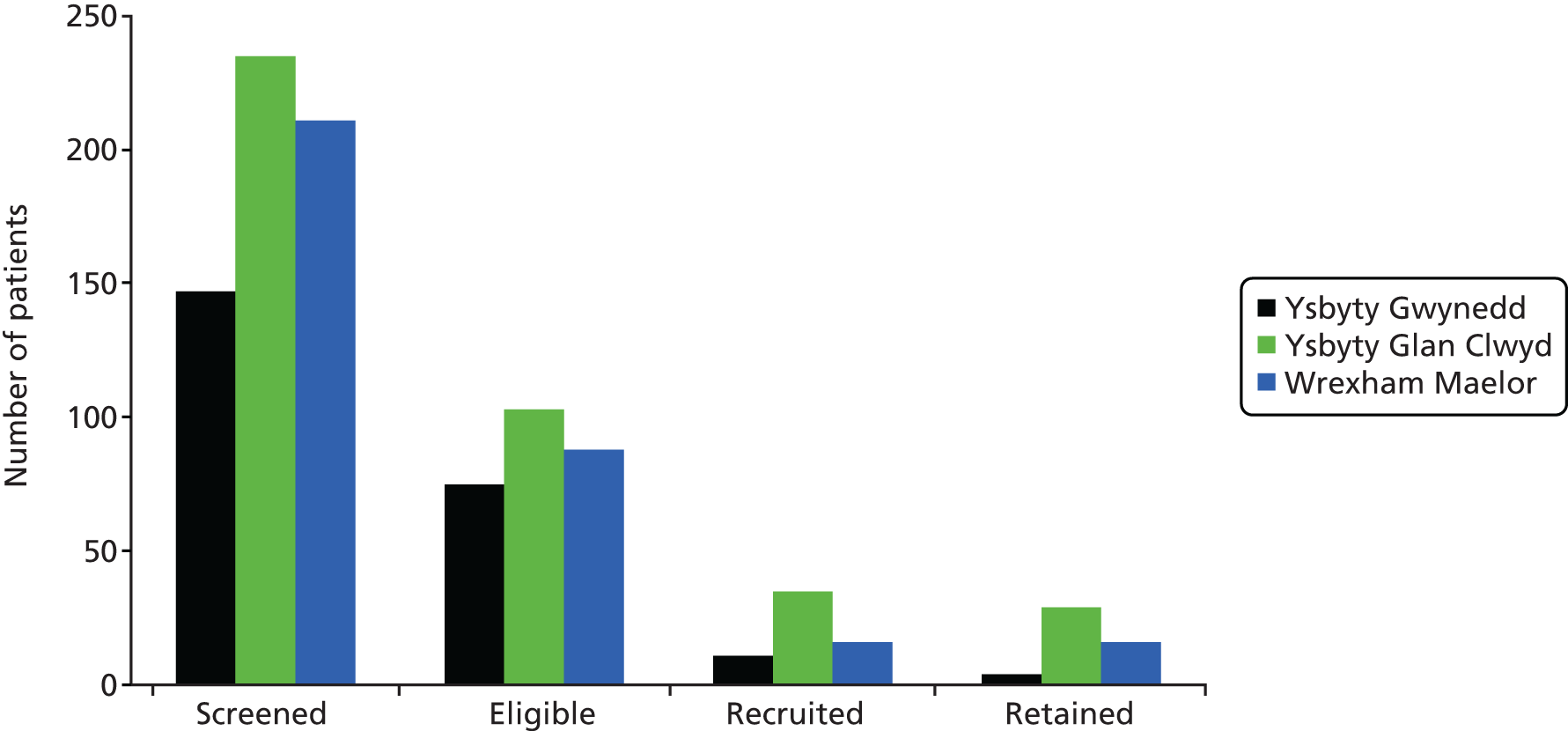
The overall eligibility rate was just short of the 50% target. There was some variation in eligibility rate between the centres, with Ysbyty Gwynedd reaching the target, and the other two centres being within approximately 10% of the target, which can be explained by natural variation. The main reason for ineligibility was a lack of mental capacity, which accounted for 49% of ineligible patients.
The recruitment rate was within the 95% CI of the 25% target. This rate differed between centres, with Ysbyty Glan Clwyd recruiting 34% of the eligible patients and the other two centres recruiting lower percentages of the eligible patients. Patients were recruited after 193 of 266 (73%) eligible patients were approached, with 176 (91%) of these agreeing to talk to the researcher. Those who were not approached lived in areas where it was not possible to deliver the intervention or were deemed by clinical staff to be too ill to take part in the study; in addition, in some cases there were safety concerns because of lone worker policies that would have prevented the intervention being delivered.
The CONSORT diagram in Figure 10 details the reasons for non-recruitment of eligible patients to the study, with the most common reason being the perceived study burden. Information concerning the number of visits it took to recruit participants was collected for 36 patients. The majority of patients had two visits and the researchers reported that, as recruitment occurred early in patients’ recovery from surgery, many requested a return visit to discuss the study after they had been discharged (Table 13). It may be worth considering the timing of when patients are approached in a future definitive RCT.
| Number of visits | n (%) |
|---|---|
| One | 11 (18) |
| Two | 17 (27) |
| Three | 8 (13) |
| Missing | 26 (42) |
The overall retention rate for the trial was satisfactory, but varied between centres. The retention rate in Wrexham Maelor was 100%, but in Ysbyty Gwynedd it was only 36%. This centre did encounter particular difficulties accessing staff for the trial, which might partly explain the poor retention rate observed. Nine of the patients who did not complete the study withdrew and the remaining four could not be contacted and so were lost to follow-up.
Alongside the recruitment of patient participants we also identified and recruited their carers. In total, 41 carers were identified and 31 (76%) of these agreed to participate. Six carers withdrew during the study and seven were lost to follow-up, leaving 18 (58%) carers who completed the follow-up questionnaire.
Defining usual therapy care
Data were collected from Therapy Manager manually by a researcher accessing individual patient entries, identified by name, address, date of birth and hospital ID number.
Of the 35 participants recruited at Ysbyty Glan Clwyd, all had entries on Therapy Manager relating to their post-fracture care in the acute hospital. Six of these participants withdrew from the study and no further data regarding usual care were collected. Following treatment at the acute hospital, patients were discharged to their place of residence or for further rehabilitation in a community hospital prior to going home (Figure 12).
FIGURE 12.
Rehabilitation pathways in usual care on discharge from Ysbyty Glan Clwyd following surgical repair of fracture.
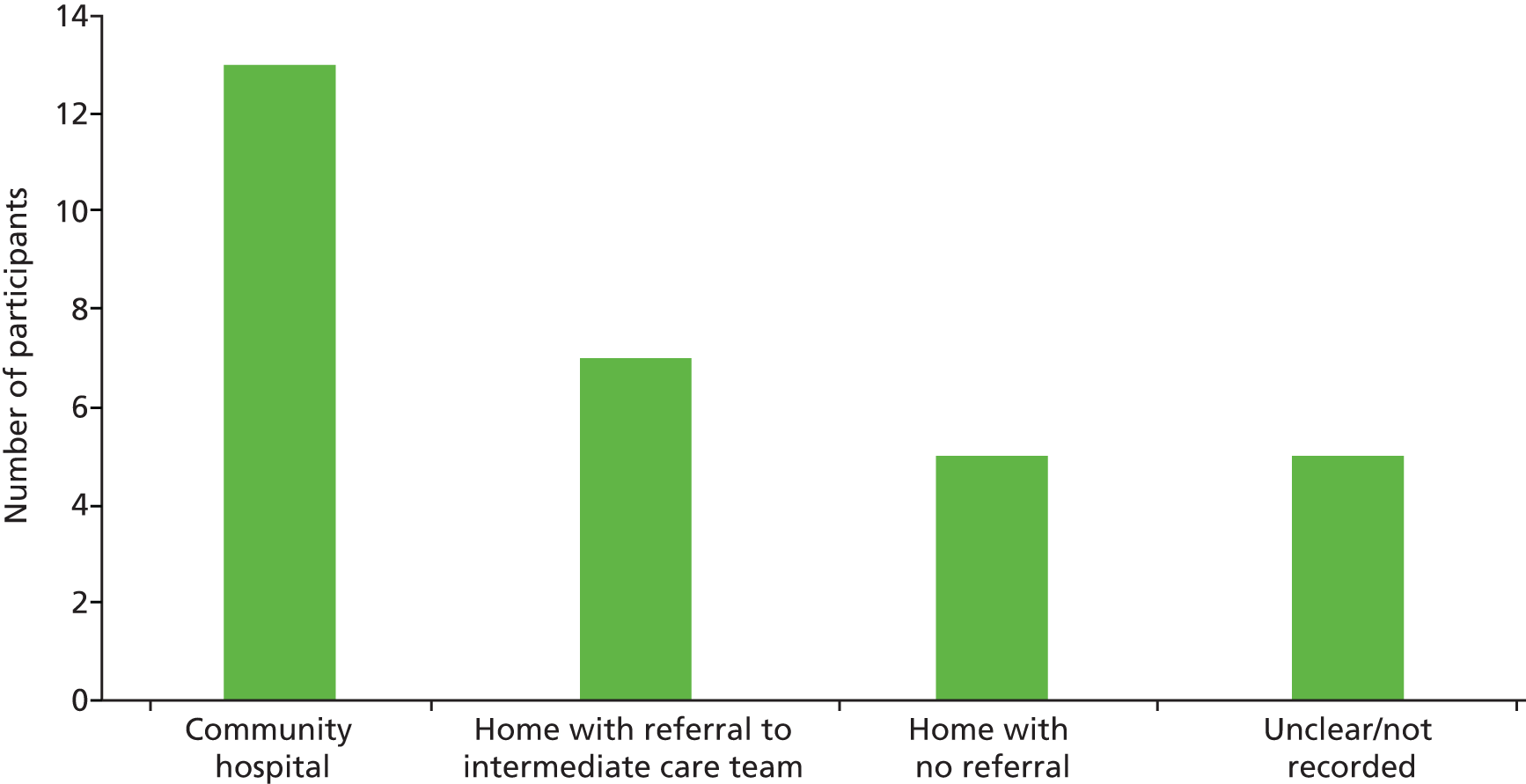
Ten patients had no details recorded relating to usual care following acute hospital discharge from Ysbyty Glan Clwyd. Of the 20 patients who did have entries on Therapy Manager, four did not receive any face-to-face appointments with a health-care professional; their entries related to telephone calls to patients who were either uncontactable or who declined further treatment. The 16 patients who did receive an appointment received a median of three appointments (n = 4). The maximum number of appointments for one patient was 21. In total, these 16 patients received a total of 81 appointments, with 73 of these appointments (90%) conducted as home visits. Home visits were completed by different members of the therapy team (Figure 13), whereas 90% of outpatient appointments were conducted by a physiotherapist (10% not recorded). In general, the time between outpatient follow-up appointments was longer than the time between home visits.
FIGURE 13.
Percentage of home visits for usual care conducted by different members of the rehabilitation team.
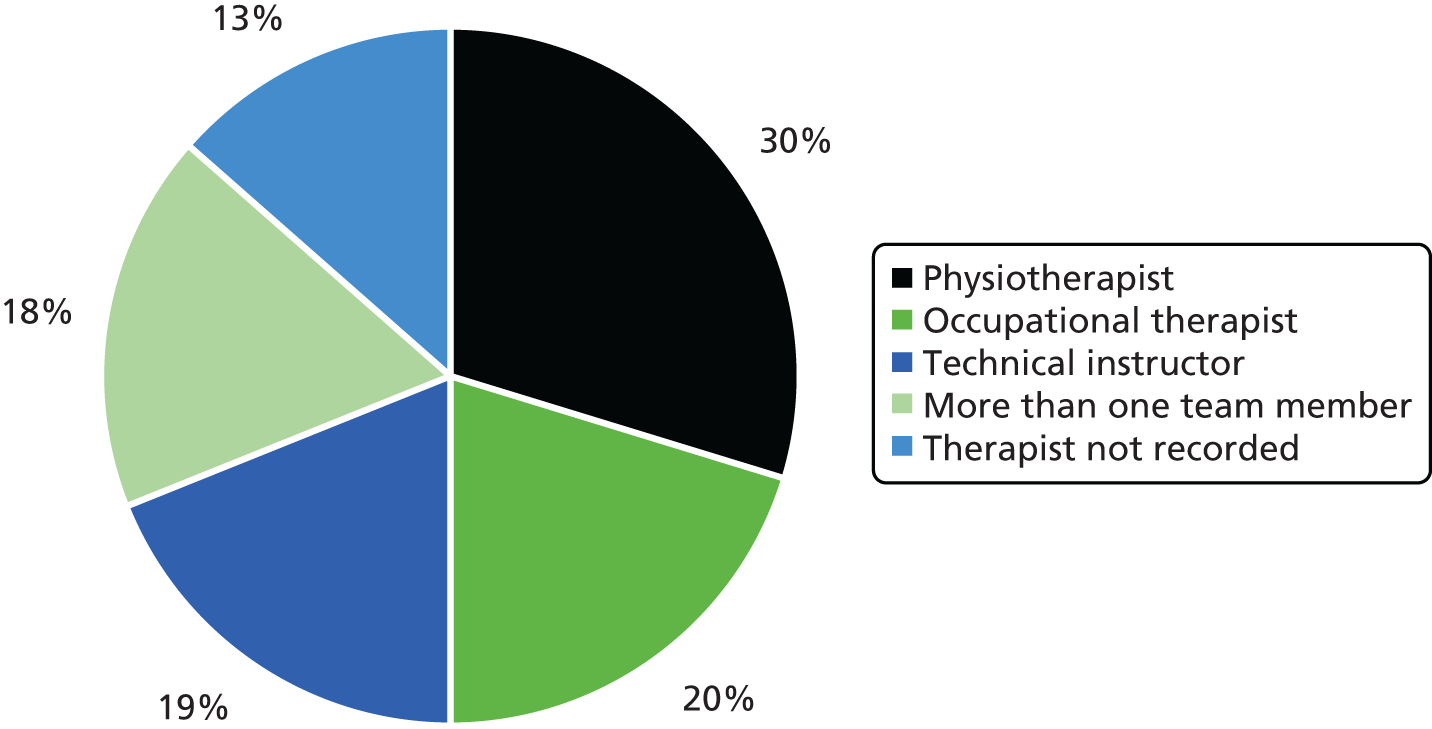
The role of the health-care professional carrying out a home visit appeared to be dependent on individual patient need. For example, if an assessment was required then a qualified physiotherapist or occupational therapist completed the visit, with subsequent visits, following an agreed care plan, conducted by a technical instructor. It was also common for more than one therapist to attend.
Although there was no universal format for recording how appointments were used, information was available about the activities that team members completed in relation to patients. These activities were categorised as direct or indirect. For usual care, the majority of direct activities involved the practice of ADL (25%) or physical exercise (23%). The remainder of the direct activities involved telephone calls with patients, discussion of progress and assessment of mood. Indirect activities were predominantly referrals to other services (33%) or contact with other members of the multidisciplinary team (30%).
Therapy Manager also allowed health-care professionals to record qualitative data relating to their interactions with patients. It was apparent from entries in the system that information given to patients about waiting times for usual care was inconsistent. In one case a patient was told that the standard wait for an appointment was a minimum of 4 weeks; however, this patient was seen within 1 week after she contacted the relevant department. The therapist who recorded this visit stated that the waiting list was based on patient need, as was the provision of sessions. This did not seem to be clear across the service and there was confusion for both patients and staff. A number of patients also reported to the therapy staff that they were reluctant to engage in physical activity until they had been seen by a physiotherapist, even though in many cases they were told that there would be a wait of at least 4 weeks.
Adherence to and fidelity of the intervention
Twenty-nine patients were randomised to the intervention group and details of intervention session use were available for 20 of these participants. Reasons for missing data are shown in Table 14.
| Reason | Number of participants | Area |
|---|---|---|
| Withdrawn | 4 | Gwynedd, Anglesey, Conwy and Denbighshire |
| Area not covered by therapist | 1 | Gwynedd and Anglesey |
| Declined intervention sessions | 1 | Conwy and Denbighshire |
| Could not be contacted to arrange sessions | 1 | Conwy and Denbighshire |
| Received intervention but therapist not returned paperwork | 1 | Gwynedd and Anglesey |
| Therapist delivering sessions moved to different area and could not complete the intervention | 1 | Gwynedd and Anglesey |
Of the 20 participants with information on intervention session use, the majority (n = 13) received all six sessions. Other participants did not feel that they needed all six sessions; this may have been a characteristic of the younger, healthier subpopulation recruited or may reflect the variability in usual care. The average number of sessions delivered to the intervention participants was five, four of which took place in their own home. One patient randomised to the intervention was discharged from the community hospital to a respite care home and so her intervention therapy sessions were delivered there.
A technical instructor alone conducted the majority (55%) of the intervention sessions, with 44% of sessions conducted by a physiotherapist and the remaining 1% conducted by more than one team member.
As with the usual care sessions, the content of the intervention sessions was determined according to individual patient need and was at the discretion of the therapist conducting each session. Therapists consistently completed the intervention paperwork detailing the types of activities that were carried out in sessions and the time taken for different activities in each session. Each session lasted for approximately 1 hour, with an additional hour spent travelling. Activities were categorised as direct or indirect, as with usual care. In the intervention sessions, a lower percentage of direct activities were categorised as the practice of exercises (15%) or ADL (14%) than in usual care; instead, there was a higher rate of activities such as answering questions raised by the intervention workbook, working with goal-setting diaries, giving feedback on progress and discussing the emotional needs of patients. For indirect activities, only 7% of the time was used for discussion with the wider team and 4% was used for referring to other services. This is likely to be a result of the intervention being used alongside usual care, with the referrals and multidisciplinary team discussions being covered by the usual care therapists. The remaining indirect activities for intervention therapists consisted of travel to appointments, writing notes, arranging further appointments and discussions with carers.
Ten participants returned their goal-setting diaries and workbooks to the study team following completion of their intervention sessions. All of the goal-setting diaries included input from a therapist detailing the goals that were set in the initial assessment session and five had also been updated by the patients and their carers. These participants used the diaries extensively, updating their progress on the initial goals agreed and entered by the therapist and adding new goals into the diary themselves. Three of these participants also completed the quizzes and hip fracture story sections of the workbook. One of the workbooks was also completed by a carer, who detailed the things that had been challenging in the patient’s recovery and what they were doing to overcome these problems.
Measure completion rate
There were good completion rates at baseline for all of the outcome measures (> 90%) (Table 15). Completion rates were reduced at follow-up, when there were particular problems with the GSES, SEE and grip strength test.
| Measure | Baseline (61 participants, 31 carers), n (%) | Follow-up (49 participants, 18 carers), n (%) |
|---|---|---|
| Outcome measure | ||
| AMTS | 55 (90) | Not collected |
| BADL index | 59 (97) | 44 (90) |
| CSI | 28 (90) | 18 (100) |
| CSRI | 59 (97)a | 37 (76) |
| EQ-5D | 61 (100) | 61 (100) |
| FES-I | Not collected | 37 (76) |
| GSES | 58 (95) | 42 (86) |
| HADS | 55 (90) | 45 (92) |
| ICECAP-O | 58 (95) | 46 (94) |
| NEADL scale | 56 (92) | 42 (86) |
| SEE scale | Not collected | 36 (73) |
| VAS-FOF | Not collected | 47 (96) |
| VAS for hip pain intensity | 60 (98) | 48 (98) |
| Physical function tests | ||
| 8-foot up-and-go test | Not collected | 37 (76) |
| 50-foot walk test | Not collected | 37 (76) |
| Grip strength test | 55 (90) | 31 (63) |
| 30-second sit-to-stand test | Not collected | 37 (76) |
Completion rates were based on the final score for a measure being present, with all individual scores having to be completed for the final score to be calculated. In some cases, one question might have been omitted and, as the final score could not be calculated, this measure would be classed as incomplete.
Exploratory correlation analysis
Correlations were calculated to assess the relationships between several variables as prespecified prior to the trial data becoming available. All correlations are shown in Table 16.
| Correlation measures | BADL index at baseline, correlationdf, p-value (95% CI) | BADL index at follow-up, correlationdf, p-value (95% CI) |
|---|---|---|
| 8-foot up-and-go test | Not collected | r31 = –0.151 (–0.716 to 0.349) |
| Self-efficacy measures | ||
| GSES | r55 = 0.427 (0.124 to 0.679) | r37 = 0.594 (0.231 to 0.821) |
| FES-I | Not collected | r34 = –0.680 (–0.831 to –0.447) |
| SEE scale | Not collected | r33 = 0.621 (0.263 to 0.819) |
Barthel Activities of Daily Living index compared with the 8-foot up-and-go test
The primary outcome, the BADL index, is a self-reported measure that assesses participants’ ADL and the 8-foot up-and-go test is a practical test used to assess participants’ agility and dynamic balance. As the 8-foot up-and-go test was not recorded at baseline, this comparison was carried out for the follow-up data only. The correlation between these two variables was not statistically significant for this population group (r31 = –0.151, p = 0.401).
Barthel Activities of Daily Living index compared with the self-efficacy measures
Within this feasibility study, three different self-efficacy measures were used to enable an evaluation of which would be the most appropriate to take forward to a full definitive RCT. These were the GSES, FES-I and SEE scale. The GSES was recorded at both baseline and follow-up and so the correlations were calculated at both time points. At both baseline (r55 = 0.427, p = 0.001) and follow-up (r37 = 0.594, p < 0.001) the relationship between the two variables was statistically significant, suggesting that, as participants’ ADL increased, so did their self-efficacy. The FES-I was completed only at follow-up and the correlation of this variable with the BADL index was statistically significant (r34 = –0.680, p < 0.001). With the FES-I, higher scores represent a greater fear of falling, and therefore the relationship showed that, as the fear of falling increased, ADL decreased. The SEE scale was also completed only at follow-up and the relationship with the BADL index was statistically significant (r33 = 0.621, p < 0.001), suggesting that as participants’ confidence in their capabilities within exercise increased, their ADL also increased.
These results were statistically significant, with correlation values ranging from 0.4 to 0.7, which suggests a moderate relationship. As expected, all correlations were in the same direction, suggesting that higher self-efficacy was associated with higher levels of activity. Of the three self-efficacy measures, the strongest correlation shown with the BADL index was from the FES-I.
Exploratory analysis of the primary outcome
Exploratory analysis was performed on the primary outcome measure, the BADL index. An ANCOVA was completed, which included the participants’ baseline score as a covariate, with the aim of achieving an effect size along with a 95% CI. 330 This resulted in an extremely low effect size of 0.29 (95% CI –0.31 to 0.89), which suggests that there was no discernible difference between the two treatments within this study. 331 All assumptions were tested and satisfied before completion of the analysis.
Exploratory analysis of the secondary outcomes
Further exploratory analysis was performed on the remaining outcome variables and physical function tests using the same methods. The baseline and follow-up scores, the differences between the groups and the effect sizes with CIs are shown in Tables 17 and 18. For the variables contained in Table 17, an ANCOVA controlling for baseline score was used to evaluate the effect sizes, and the mean differences shown in these tables have been adjusted for the baseline scores. When baseline scores were not collected, a t-test was completed on the follow-up data to obtain the effect sizes and 95% CIs (see Table 18). All analysis was completed on an intention-to-treat basis.
| Outcome measure | Baseline, mean (SD) | Follow-up, mean (SD) | Scale range | Adjusted mean difference between groups at follow-up (95% CI) | Cohen’s d effect size (95% CI) | ||
|---|---|---|---|---|---|---|---|
| Control group | Intervention group | Control group | Intervention group | ||||
| Primary outcome measure | |||||||
| BADL index | 17.8 (3.4), n = 32 | 17.8 (2.4), n = 27 | 17.7 (3.0), n = 22 | 18.2 (2.9), n = 21 | 0–20 | 0.5 (–0.5 to 1.6) | 0.29 (–0.31 to 0.89) |
| Secondary outcome measures | |||||||
| GSES | 31.6 (5.6), n = 31 | 33.6 (5.1), n = 27 | 30.5 (7.8), n = 19 | 33.7 (7.0), n = 22 | 10–40 | 1.3 (–2.5 to 5.0) | 0.20 (–0.42 to 0.81) |
| HADS | 12.8 (9.0), n = 31 | 11.0 (4.8), n = 24 | 11.0 (8.2), n = 22 | 8.7 (6.0), n = 20 | 0–42 | –1.2 (–4.8 to 2.6) | 0.20 (–0.41 to 0.81) |
| NEADL scale | 16.1 (5.5), n = 29 | 13.7 (7.4), n = 27 | 14.2 (5.7), n = 20 | 15.8 (6.0), n = 20 | 0–22 | 3.0 (–0.4 to 6.4) | 0.63 (–0.01 to 1.26) |
| VAS for hip pain intensity | 4.2 (2.4), n = 32 | 4.1 (2.3), n = 28 | 3.4 (3.1), n = 23 | 2.9 (2.9), n = 25 | 0–10 | –0.2 (–1.7 to 1.3) | 0.00 (–0.58 to 0.58) |
| Carer outcome measure | |||||||
| CSI | 2.6 (3.1), n = 12 | 3.5 (3.4), n = 16 | 3.3 (3.7), n = 8 | 2.7 (2.1), n = 7 | 0–13 | –1 (–5.1 to 3.0) | 0.35 (–0.68 to 1.37) |
| Physical function test | |||||||
| Grip strength | 21.0 (10.1), n = 30 | 20.0 (7.2), n = 26 | 23.4 (12.3), n = 17 | 19.5 (8.3), n = 12 | Unlimited | 1.2 (–1.7 to 4.2) | 0.35 (–0.40 to 1.09) |
| Outcome measure | Follow-up, mean (SD) | Mean difference between groups at follow-up (95% CI) | Scale range | Cohen’s d effect sizea (95% CI) | |
|---|---|---|---|---|---|
| Control group | Intervention group | ||||
| Secondary outcome measures | |||||
| FES-I | 36.2 (14.9), n = 17 | 32.0 (12.2), n = 20 | –4.2 (–13.2 to 4.8) | 16–64 | –0.31 (–0.96 to 0.35) |
| SEE scale | 49.9 (21.7), n = 18 | 58.2 (17.8), n = 18 | 8.3 (–5.2 to 21.7) | 0–80 | 0.42 (–0.25 to 1.08) |
| VAS-FOF | 4.8 (2.9), n = 24 | 5.0 (2.5), n = 23 | 0.2 (–1.4 to 1.8) | 0–10 | 0.07 (–0.50 to 0.64) |
| Physical function tests | |||||
| 8-foot up-and-go test | 13.6 (6.1), n = 15 | 12.9 (6.0), n = 12 | 0.6 (–5.4 to 4.2) | Unlimited | 0.12 (–0.64 to 0.88) |
| 50-foot walk test | 19.3 (6.7), n = 12 | 31.5 (42.3), n = 12 | 12.2 (–13.5 to 37.8) | Unlimited | 0.40 (–0.41 to 1.20) |
| 30-second sit-to-stand test | 11.0 (3.6), n = 11 | 10.1 (3.9), n = 10 | –0.9 (–4.3 to 2.5) | Unlimited | 0.24 (–0.62 to 1.10) |
Many of the effect sizes were extremely small; however, when considering the NEADL scale an effect size of 0.63 was found, which is considered a medium effect size. For this measure, the intervention group therefore achieved better results than the control group.
One further variable, the 50-foot walk test, had a Cohen’s d effect size of 0.40, which is a reasonable size. This variable represents the physical function of the patient and the results show that the control group completed the 50-foot walk in a shorter time than the intervention group, which suggests that the control group had better physical function than the intervention group. Those in the control group received their physical function appointment, on average, 22 days later than those in the intervention group because of the relocation of physiotherapy services in the central area where the majority of participants were recruited from, limiting access to the gym required for carrying out the tests. This may have affected the results as control group participants had longer to recover from surgery than intervention group participants. However, there was also one outlier in the control group who affected this result and so a sensitivity analysis was completed with this outlier removed. This resulted in an effect size of 0.02 (95% CI –0.80 to 0.84), which suggested that there was no longer a difference between the groups. In the analysis, only data for the physical function tests from patients who completed the tests unaided were used. When possible, participants completed the tests as intended; however, when problems occurred they were permitted to complete the test with the aid of a walking stick, using the arms of the chair, etc. These results were recorded but were not included in the analysis.
Discussion
Summary of findings
The trial methods were feasible in terms of recruitment, randomisation and follow-up, although recruitment was initially slow and the recruitment period was extended in two sites for an additional 3 months. In total, 45% of the potential participants screened were eligible, with the main reason for ineligibility being lack of mental capacity. Of the eligible population, 23% agreed to participate; the main reason for non-participation was the perceived study burden. The participation rate of identified carers was 76%. Although recruitment was challenging as patients were approached soon after a traumatic injury and subsequent surgery, the overall recruitment rate achieved was within the 95% CI of the target rate. The completion rate for the baseline questionnaires was > 90%.
The intervention and control groups were similar with respect to gender, living status, type of property, type of fracture, type of surgery and admitting hospital. After hospital admission there was a small discrepancy between the groups for those discharged directly home and those sent to a community hospital for rehabilitation. The baseline scores for the outcome measures and physical function tests were similar between the two groups. However, the NEADL score was higher in the control group.
At 3-month follow-up, the patient retention rate was 79% and the carer retention rate was 44%. The completion rate for the follow-up questionnaires varied from 64% to 100%. There were minimal differences between the two groups for most of the outcome measures, including the main outcome measure, the BADL index. In the intervention group there was a trend for a greater improvement in self-efficacy and mental health, but with small effect sizes. However, the intervention group showed a medium-sized improvement in the ability to perform ADL (as measured by the NEADL scale) relative to the control group. Paradoxically, one of the physical function tests, the 50-foot walk test, reported better function in the control group, with a medium effect size. However, this can be explained by one outlier, as without this participant the effect size was massively reduced. The improvement in the ability to perform ADL suggests that the community-based rehabilitation intervention could be beneficial in enabling participants to regain better levels of independence compared with usual care.
Strengths and limitations
This was a single-centre feasibility study conducted in one local health board at its three acute hospital sites in North Wales. It was able to assess the feasibility of the trial methods in terms of recruitment, randomisation and outcome measurement. It was not designed, or powered, to test the effectiveness or cost-effectiveness of the rehabilitation intervention.
As expected, usual care varied between patients. The provision of physiotherapy services in usual care was based on individual patient need, with variation in the number of sessions provided, how they were used and which health-care professional delivered them. There was less variation in the intervention sessions when considering which type of health-care professional conducted the sessions because of the limited number of staff involved in the delivery of the intervention. There were challenges in delivering the intervention in some areas, but there was good adherence to the planned intervention by those patients who did receive sessions, with a high level of detail provided in the completed intervention paperwork.
We were able to assess the different outcome measures to determine which would be the most suitable for a larger definitive RCT. The NEADL scale was more responsive than the BADL index for measuring the ability to perform ADL. The FES-I and SEE scale were more responsive than the GSES, but the researchers reported that many participants struggled to understand the SEE scale and so the FES-I seems the most appropriate measure of self-efficacy for the main definitive RCT. The most appropriate health economic outcome measure is discussed in Chapter 10.
The physical function test with a medium effect size, the 50-foot walk test, reported better function in the control group than in the intervention group. However, this can be explained by the outlier in the control group, as the effect size was greatly reduced by removing this outlier. This did, however, identify that those in the control group completed the 50-foot walk test later than those in the intervention group, which must be addressed within any future study.
A strength of the feasibility study was the high completion rates for the outcome measures. However, patients’ frailty, lack of manual dexterity and comorbid conditions, such as hearing or visual problems, sometimes meant that assistance was required from carers to complete the measures. This improved the completion rates but also might have introduced bias, as the carers might have influenced how the patients responded to some measures, especially the quality-of-life and mental health measures. 332
Examination of therapist notes using the Therapy Manager System highlighted the variability in usual care, which could impact on the ability to measure differences in patient outcomes between the two groups.
Originally, we had hoped to include participants who lacked mental capacity to assess if the rehabilitation intervention was feasible and acceptable for different levels of cognitive functioning. However, the NHS research ethics committee excluded participants who lacked capacity because the study was not investigating the condition causing this lack of capacity. Participants with cognitive impairment but with sufficient mental capacity were included, but the mean AMTS demonstrated a good level of cognitive functioning in the feasibility study participants. Hence, the findings might not be generalisable to patients with more severe cognitive impairment.
Comparison with previous literature
Previous studies of hip fracture rehabilitation interventions were reviewed in our realist review in Chapter 2. We identified previous studies of rehabilitation interventions that combined the promotion of physical exercise and practice of ADL with psychological interventions designed to tackle self-efficacy and fear of falling, for example the study by Resnick and Jenkins. 311 However, none of these studies was set in the UK and we are not aware of any other RCTs of similar interventions following hip fracture in the NHS.
As discussed, the overall recruitment rate of eligible patients was 23%, with the main reason for non-recruitment being the perceived study burden. Recruitment into trials, particularly those involving surgical treatments, is challenging and has been discussed previously. 333,334 Although the data show that a large number of patients would require screening in a full definitive trial, this was a relatively simple process as all patients admitted to the ward were assessed by the acute physiotherapist and the eligibility criteria for the trial would be included in such an assessment.
Phase II studies are primarily intended to test the feasibility and acceptability of the various trial methods prior to a larger definitive Phase III RCT. However, they also provide an opportunity to compare and contrast different methods, for example in this trial different patient-completed outcome measures for self-efficacy, functional ability and quality of life, and different objective measures of physical function were compared. Measuring outcomes comprehensively is important in health services research to inform improvements in clinical practice and improve patient outcomes. 335 However, reducing patient burden while completing such measures is also important for patient adherence and, hence, a core set of measurement instruments in hip fracture has been advocated. 336–338 Hip fracture populations pose particular challenges to researchers as a numerous outcomes have been reported in the literature (see Chapter 2) and deciding on a core set is difficult. 278 A recent UK consensus study has made recommendations on a core set of outcome measures338 and the current study complied with most of these recommendations, although it differed in the use of the NEADL scale to measure the ability to perform ADL. The NEADL scale is an instrument that measures patients’ actual ability to perform their day-to-day activities, rather than what they presume they can do, as is the case with the BADL index, which this study used as its primary outcome. As previously discussed, changing this will be considered for a future full RCT.
Implications for future research
This was a difficult population to recruit from, particularly because of the large number of patients with cognitive impairments and the perceived study burden. Recruitment was initially slow but the recruitment rate was acceptable and good completion rates for the different measures indicate that obtaining the required data was feasible. In future research it would be beneficial to capture the experiences of those patients who declined to take part to try and identify their needs. The intervention was generally delivered as planned and was well tolerated by participants.
Problems encountered with accessing the physiotherapy gym in some areas led to a delay in the physical function tests being conducted. Using an alternative test, the Short Physical Performance Battery (SPPB),279 could address this problem in future research as it does not require such a long distance to perform the walk test and could therefore be completed in a patient’s home. With sufficient training, this test could also potentially be conducted by researchers, further reducing problems with resource availability that are encountered when a therapist is required to complete the test.
Usual care data included notes from therapists and administration staff who had spoken to patients over the telephone. In some cases it was recorded that patients were reluctant to engage in physical activity without seeing a therapist for an initial ‘fact-finding’ session, to determine which activities were safe to perform. This theme is further explored in the focus groups presented in Chapter 9.
This feasibility study allowed us to refine the trial methods for a future definitive RCT. This is expanded on in Chapter 12.
Chapter 8 Cohort study of hip fracture patients within the Betsi Cadwaladr University Health Board
Introduction
The cohort study included an anonymised data set of all patients aged ≥ 65 years who were admitted with a hip fracture to one of the three acute hospitals in the BCUHB in North Wales (Ysbyty Gwynedd in Bangor, Ysbyty Glan Clwyd in Denbighshire and Wrexham Maelor) within the first 6 months of the feasibility study (from June to November 2014). Data were collected on serious complications and readmissions during the 3 months following surgical repair. All of the data were extracted from the BCUHB electronic system and from patients’ written records. The cohort study was carried out alongside the feasibility study to assess the representativeness of the recruited population in terms of its demographics and characteristics.
Methods
Selection of subjects for the cohort study
The BCUHB informatics department extracted data on all patients who were coded in the electronic system as having been admitted with a fractured neck of femur. Data were filtered to exclude patients aged < 65 years and were separated into three groups according to acute hospital using patients’ hospital numbers. Health and Care Research Wales researchers at each of the hospitals requested the notes for each patient after 3 months had passed from the initial admission. Data on demographic characteristics and events in the 3 months following fracture were then collected from the notes using a case report form and the anonymised forms were returned to NWORTH.
Cohort study outcomes
From the cohort anonymised data set we recorded the following:
-
The number of patients aged ≥ 65 years admitted with a proximal femoral fracture.
-
The number of patients who fulfilled the inclusion criteria for the randomised feasibility study.
-
The numbers of deaths, serious complications such as falls and repeat fractures, serious illnesses requiring hospital readmission and discharges to institutional care. This included details such as type of ward and type of residential care to enable the costs per night locally to be calculated. These costs were compared with Department of Health reference costs339 for proximal femoral fracture-related hospital stays.
Results
Demographic characteristics
The final data set for the cohort analysis consisted of 400 patients. The characteristics of patients in the cohort study and in the feasibility study are compared in Table 19. The cohort population was slightly older than the feasibility study population, with a mean age difference of 4.5 years. In both data sets there was a higher proportion of women (73–75%), with similar proportions of women in both data sets.
| Characteristic | Trial data, n (%) | Cohort data, n (%) | ||
|---|---|---|---|---|
| Age (years), mean (SD); range | 79.4 (7.6); 66–99 | 83.9 (7.7); 66–101 | ||
| Gender | ||||
| Male | 15 (25) | 108 (27) | ||
| Female | 46 (75) | 292 (73) | ||
| Type of fracture | ||||
| Intracapsular | 27 (44) | 195 (49) | ||
| Extracapsular | 20 (33) | 126 (32) | ||
| Missing | 14 (23) | 79 (20) | ||
| Extracapsular fracture | ||||
| Pertrochanteric | 1 (5) | 2 (2) | ||
| Intertrochanteric | 11 (55) | 103 (82) | ||
| Subtrochanteric | 2 (10) | 13 (10) | ||
| Missing | 6 (30) | 8 (6) | ||
| Type of surgery | ||||
| Total hip arthroplasty | 5 (8) | 27 (7) | ||
| Hemiarthroplasty | 29 (48) | 159 (40) | ||
| Internal fixation | 17 (28) | 151 (38) | ||
| Intramedullary nailing | 2 (3) | 16 (4) | ||
| No surgery | 0 (0) | 29 (7) | ||
| Missing | 8 (13) | 18 (5) | ||
| Hospital | ||||
| Ysbyty Gwynedd | 11 (18) | 146 (37) | ||
| Ysbyty Glan Clwyd | 34 (56) | 123 (31) | ||
| Wrexham maelor | 16 (26) | 131 (33) | ||
| Accommodation | Before admission | After discharge | Before admission | After discharge |
| Private property | 59 (97) | 44 (72) | 313 (78) | 104 (26) |
| Sheltered accommodation | 2 (3) | 3 (5) | 11 (3) | 1 (< 1) |
| Residential home | 0 (0) | 1 (2) | 34 (9) | 12 (3) |
| Nursing home | 0 (0) | 0 (0) | 36 (9) | 29 (7) |
| Community hospital | 0 (0) | 1 (2) | 3 (1) | 224 (56) |
| Other acute hospital | 0 (0) | 0 (0) | 1 (< 1) | 6 (2) |
| Missing | 0 (0) | 12 (19) | 2 (1) | 24 (6) |
Fracture details
Information relating to the type of fracture suffered by patients along with the type of surgery used to treat the fracture were recorded from patients’ medical records. Intracapsular fractures were more common than extracapsular fractures, with similar proportions in the two data sets. In the extracapsular group, intertrochanteric fractures were the most common type of fracture.
There was a higher percentage of unavailable information in the feasibility study than in the cohort study. This could be related to the timing of examination of the hospital records. For the cohort study the records were examined retrospectively by experienced researchers working for Health and Care Research Wales. Within the trial, the records were examined by study researchers while patients were being recruited. This occurred either while a patient was on the ward, when the hospital notes were also being used by the various clinical teams or after a patient was discharged home, when the hospital notes were not available.
Most of the cohort study population underwent hemiarthroplasty (40%) or internal fixation (38%). In the feasibility study population, a slightly higher proportion received hemiarthroplasty (47%) and a slightly lower proportion received internal fixation (28%). Within the trial, all of the patients underwent a surgical procedure, as this was one of the inclusion criterion; however, 7% of the cohort study population did not receive any surgery and would therefore have been excluded from the study during screening.
Living arrangements
The type of accommodation that patients lived in, both before and after their hospital admission, was recorded. The aim of this was to detect any change that had occurred in patients’ living conditions and related independence following their hip fracture and subsequent surgery.
Living independently prior to hip fracture surgery was an inclusion criterion for the feasibility study. Most of the cohort population (78%) lived in a private property before their admission to hospital and a further 3% lived independently in sheltered accommodation. The remaining 19% of patients admitted with hip fracture in the cohort study did not fulfil the living independently criterion for taking part in the feasibility study. In contrast, in the feasibility study, 10% of the assessed patients were ineligible because they were not living independently prior to hip fracture surgery. Some patients would have been ineligible for multiple reasons and, in particular, may not have been living independently because of a lack of capacity. As only the primary reason for ineligibility was recorded for the feasibility study, this may account for the discrepancy.
In the cohort study, the majority of patients (56%) were discharged from the acute hospital to a community hospital. Only 26% of patients were discharged directly back to their private property, with 11% discharged to other types of residential care. The same data were not available for the feasibility study population to allow a direct comparison to be made between the data sets. However, information was available at 3-month follow-up in the feasibility study on participants’ place of residence and whether or not this was the same place that they had been discharged to after their hospital stay. At 3-month follow-up, 27 patients were living in the same residence that they were discharged to and, in most cases (93%), this was a private property. The remaining 22 patients had an interim residence between discharge and their 3-month follow-up; however, details of where this was were not recorded.
Readmissions and deaths
In the cohort study, information was collected on the number of patients who had an unplanned readmission to hospital or who had died in the 3 months following their hip fracture. As shown in Table 20, 69 patients (17%) were readmitted to hospital and 68 patients (17%) died within 3 months of their hip fracture. As these numbers were very similar, additional information was collected to determine whether or not these two events occurred in the same patients. However, 117 patients either were readmitted or died during the 3 months post hip fracture, suggesting that the two events mostly occurred in separate populations.
| Hospital | Ysbyty Gwynedd, n (%) | Ysbyty Glan Clwyd, n (%) | Wrexham Maelor, n (%) |
|---|---|---|---|
| Patients admitted with a hip fracture | 146 | 123 | 131 |
| Patients with a readmission by 3-month follow-up | 17 (12) | 24 (20) | 28 (21) |
| Readmitted once | 12 | 24 | 22 |
| Readmitted twice | 4 | 0 | 5 |
| Readmitted three times | 1 | 0 | 1 |
| Patients deceased by 3-month follow-up | 17 (12) | 24 (20) | 27 (21) |
| Patients with either a readmission or death by 3 months’ follow-up | 32 (22) | 39 (32) | 46 (35) |
Table 20 also shows how many times patients were readmitted in the 3-month follow-up period for those patients who were readmitted. Most patients (n = 58) were readmitted only once; however, nine patients were readmitted twice and two were readmitted three times. In the feasibility study population, only one death (2%) and two readmissions to hospital (3%) were recorded. These proportions were much lower than those found in the cohort population, suggesting that the feasibility study recruited a younger and healthier subpopulation of patients.
Complications at initial admission
Information was collected in the cohort study on any serious complications that patients encountered during their initial admission for hip fracture. These serious complications included repeat falls, repeat fractures and adverse reactions to any drugs received.
In total, 160 (40%) patients experienced at least one complication during their initial admission. Some patients experienced numerous complications during their admission, which could be numerous instances of the same complication. Data on complications are provided in Table 21, which shows that, in total, 359 complications were experienced by patients in the cohort study. Examples of incidents that would come under the other medical complications category were myocardial infarctions, urinary tract infections or deep vein thromboses.
| Complication | Number (%) of patients who experienced complication | Total number of patients who experienced the complication | Total number of complication instances | ||
|---|---|---|---|---|---|
| Once | Twice | Three times | |||
| Repeat fall | 25 (78) | 7 (22) | 0 (0) | 32 | 39 |
| Repeat fracture | 5 (100) | 0 (0) | 0 (0) | 5 | 5 |
| Other accident or injury | 11 (100) | 0 (0) | 0 (0) | 11 | 11 |
| Adverse drug reaction | 2 (100) | 0 (0) | 0 (0) | 2 | 2 |
| Hospital-acquired infection | 39 (100) | 0 (0) | 0 (0) | 39 | 39 |
| Revision of surgery | 4 (100) | 0 (0) | 0 (0) | 4 | 4 |
| Unplanned transfer from general care to intensive care | 1 (100) | 0 (0) | 0 (0) | 1 | 1 |
| Cardiac arrest | 5 (100) | 0 (0) | 0 (0) | 5 | 5 |
| Other medical complicationsa | 98 (88) | 13 (12) | 1 (1) | 112 | 127 |
| Other complications | 90 (85) | 12 (11) | 4 (4) | 106 | 126 |
Screening logs
The numbers of patients identified for inclusion in the cohort study are shown by centre in Table 22. The cohort study identified 462 patients in total over a 6-month period. In this same period the feasibility study screened 372 patients for eligibility. Therefore, most of the potential feasibility study participants (81%) were identified by the researchers during screening. The majority of the patients’ hospital notes (87%) were pulled from the system. The reasons for patients’ hospital notes not being pulled are shown in Table 22, with the most common reason being that the notes were not available; some of the patients had been moved between hospitals and so would have been included within the cohort for the other hospital.
| Patient variable | Ysbyty Gwynedd, n (%) | Ysbyty Glan Clwyd, n (%) | Wrexham Maelor, n (%) | Total, n (%) |
|---|---|---|---|---|
| Patients identified | 177 | 133 | 152 | 462 |
| Patients’ hospital notes pulled | 146 (82) | 123 (92) | 131 (86) | 400 (87) |
| Reason patients’ hospital notes not pulled | 31 (18) | 10 (8) | 21 (14) | 62 (13) |
| Notes not available | 22 (71) | 10 (100) | 0 (0) | 32 (52) |
| Moved to another hospital | 8 (26) | 0 (0) | 16 (76) | 24 (39) |
| Duplicate patient | 0 (0) | 0 (0) | 5 (24) | 5 (8) |
| Unknown | 1 (3) | 0 (0) | 0 (0) | 1 (2) |
Discussion
Summary of findings
The anonymised cohort allowed us to assess the representativeness of the population recruited to the feasibility study in relation to the broader hip fracture population. Participants recruited to the cohort and feasibility studies were similar with respect to gender, type of hip fracture and type of surgery, but the feasibility study participants were younger and less likely to die or be readmitted to hospital. This suggests that the feasibility study recruited a healthier and younger subset of the total hip fracture population.
Strengths and limitations
One of the main strengths of the cohort study was that data were extracted and collated by experienced researchers working for Health and Care Research Wales, who have a great deal of expertise in and familiarity working with patients’ medical records. For reasons of patient confidentiality, this was an anonymised cohort and so it was not possible to match participants in the cohort with those in the feasibility study. In total, the feasibility study identified 81% of those in the cohort study. It is not known how the 19% who were not identified in the feasibility study differed, nor is it known why they were identified in the cohort study but not in the feasibility study.
A limitation that could have influenced the study was the search terms that were used to identify patients. It is possible that patients who had not been correctly coded on their admission with a hip fracture would not have been included in the cohort study. After identifying patients who fit the criteria for inclusion in the cohort study, their physical notes had to be located to capture any relevant information; this was often problematic and the research workforce was unable to locate 13% of the medical records. If hospital records were completely digitised this would avoid the problems associated with locating paper record folders.
Although not essential to the conclusions drawn, it may have been beneficial if the feasibility study had recorded the place of discharge in a more consistent manner, similar to that used in the cohort study. This would have allowed a closer comparison of the data. This could be considered in any future study.
Comparison with previous literature
The age and gender composition in the cohort study were similar to the age and gender composition in other studies from Sweden340 and the USA. 281 The mortality rate in the cohort study was higher than that reported in California, where 12.7% of patients died in the 3 months after hip fracture,341 in Sweden, where 13% of patients died in the 6 months after fracture,340 and in Northern Ireland, where 15.1% of patients died in the 12 months after fracture. 342 Readmission rates were not directly comparable but were similar: in the USA, 11.9%281 and 12.3%341 of patients were readmitted within 30 days; in Sweden, 32% of patients were readmitted within 6 months. 340
The proportion of patients identified as having non-surgical conservative management of their hip fracture appeared to be higher in our cohort (7%) than is reported elsewhere in the literature (between 2% and 5% in European studies342,343). The reason for non-surgical management was not collected in our cohort study.
There were fewer deaths and readmissions in the feasibility study population than in the cohort population. The recruitment of younger, healthier patients to a physical activity or exercise intervention study was not surprising and has been reported previously. 199
Implications for future research
Including an anonymised cohort has allowed us to consider the representativeness of the population recruited to the feasibility study. It is highly likely that a future definitive RCT of the rehabilitation intervention would recruit a younger, healthier, more motivated subgroup. One important group excluded from the feasibility study was those frail individuals who lack mental capacity. To ensure that a future RCT is more representative it will be necessary to include such groups. This is discussed further in Chapter 12.
Chapter 9 Phase II focus groups with patients, carers and health-care professionals
Introduction
Focus groups in Phase II of the study were conducted with patients and carers who took part in the feasibility study and health-care professionals who had been involved in recruiting patients, delivering the intervention sessions and conducting the physical function tests.
Methods
The acceptability and feasibility of the different components of the study, including the acceptability of the recruitment and randomisation processes and the delivery of the intervention, were explored in focus groups. Separate focus groups were conducted for health-care professionals involved in delivering the intervention and for patients and carers who were recruited into the study.
Patient focus group participants
All patient participants and their carers were asked when initially consenting to take part in the feasibility study whether or not they also agreed to be invited to a focus group later in their recovery. All those who agreed were invited to participate in a local focus group following completion of follow-up. Participants were contacted by telephone to gauge interest and those who expressed an interest in taking part were sent an information sheet, specimen consent form, topic guide and details of the venue. Separate focus groups were conducted for those in the control group and those in the intervention group. Written informed consent was obtained just prior to starting the focus group from those who attended. We aimed to recruit approximately eight participants to each focus group.
Health-care professional focus group participants
Staff who had been involved in the screening and recruitment of participants, delivery of the intervention and conducting physical function tests were approached by study researchers to ask if they would be willing to take part in a focus group. Focus groups were arranged at the hospital site where staff were based to minimise disruption to their working day and maximise the number of staff who could attend. When staff were unable to attend focus groups, one-to-one interviews were offered. Staff who expressed an interest in participating were sent an information sheet, specimen consent form and topic guide prior to the focus group. Written informed consent was obtained just prior to starting the focus group from those who attended. For telephone interviews, verbal consent was given and recorded, and written informed consent was posted back to the study team.
Focus group procedures
All participants gave written consent to participate and agreed that their comments could be recorded, transcribed and anonymised for analysis. The discussions in the focus groups were semistructured and run by a moderator (the study manager) and co-moderator (a study researcher) with the use of a topic guide (see Appendix 31). Topic guides were specific to patient and carer or health-care professional focus groups and contained open-ended questions regarding experiences, perceptions and beliefs about the rehabilitation that they had delivered or received, including the different aspects of the enhanced programme for those patients and carers in the intervention group. The topics covered were informed by the aims and objectives of the study and the intervention logic model. In focus groups with patients and carers randomised to the intervention, ranking exercises were also used to elicit discussion on the importance to patients of the different aspects of the intervention. Focus groups were run in English, although simultaneous translation into Welsh was offered to participants. Digital recordings of the focus group discussions were made and notes were taken during the focus groups by the moderator or co-moderator. At the end of the focus groups, the recordings were downloaded onto an encrypted NWORTH laptop and subsequently downloaded and stored on the university server. Access to the data was limited to core members of the study team. Transfer of the recordings to an approved transcriber and return of the transcripts involved encrypting the recordings and uploading them to/downloading them from a secure server.
Care was taken not to record personally identifiable data in written notes. Written notes were stored in a locked cabinet in a locked room in NWORTH and were accessible to authorised team members only.
Qualitative data analysis
Transcripts of the focus groups were analysed by the study manager, who had acted as group moderator, using the framework approach to thematic analysis. 293 Data from the focus group notes and transcriptions of the discussions were transferred to Microsoft Excel® version 2013 (Microsoft Corporation, Redmond, WA, USA) software for qualitative analysis. A framework was developed based on the programme theories, logic model and questions of feasibility and acceptability that the study was designed to answer. The transcripts were then coded and grouped together into categories. The study manager discussed, compared and named the categories that were used to populate and refine the framework with an objective researcher experienced in qualitative research who had not been present at the focus groups and not been directly involved in the study. A process of refinement of the overarching themes across the data set to more specific recurrent issues within these themes provided a more in-depth appreciation of the way in which the intervention was delivered and received. The simultaneous analysis of the transcripts and themes by two researchers prior to consultation with the chief investigator as a third reviewer ensured the plausibility and credibility of the findings.
Results
Four focus groups were conducted with patients and carers, and two focus groups were conducted with health-care professionals involved in delivering the intervention (Table 23). Because of the geographical spread of participants in the Gwynedd and Anglesey, it was not possible to conduct a focus group in this area, although one participant who was recruited from this area was able to attend a focus group in Conwy and Denbighshire. Health-care professionals involved in delivering the intervention in this area were also unable to attend focus groups but one acute physiotherapist and three technical instructors participated in a one-to-one telephone interview.
| Participant type | Location | Attendees |
|---|---|---|
| Patient and carers in control group | Flintshire and Wrexham | 2 female patients, 1 male patient, 2 male carers (n = 5) |
| Patient and carers in control group | Conwy and Denbighshire | 2 female patients, 1 male patient, 1 female carer (n = 4) |
| Patient and carers in intervention group | Flintshire and Wrexham | 3 female patients (n = 3) |
| Patient and carers in intervention group | Conwy and Denbighshire | 2 male patients, 2 female patients, 1 male carer, 2 female carers (n = 7) |
| Health-care professionals | Flintshire and Wrexham | Clinical specialist physiotherapist, 2 orthopaedic physiotherapists, physiotherapy technical instructor (n = 4) |
| Health-care professionals | Conwy and Denbighshire | Orthopaedic acute physiotherapist, rotational physiotherapist, physiotherapy technical instructor (n = 3) |
Patients’ and carers’ experiences of post-discharge rehabilitation following a fractured neck of femur
Five overarching themes emerged from the focus groups conducted with patients and their carers. These provided an overarching framework to delineate the key issues pertinent to patients regarding their post-hospital discharge rehabilitation.
Four themes related to general patient and carer experiences of the rehabilitation process following hip fracture:
-
the impact of variation within usual care on patient experiences and expectations
-
patient expectations of post-fracture recovery and their management by health-care professionals
-
patient preferences for individualised care and support
-
the relationship between the patient and the health-care professional and its role in patient engagement in rehabilitation.
The fifth theme related specifically to patient experiences of taking part in a research study and the acceptability of the intervention.
The impact of variation within usual care on patient experiences and expectations
The frequency and format of rehabilitation appointments in usual care varied across the region, depending on the availability of resources and the provision of support services such as reablement and falls prevention classes. Usual care was also tailored to an individual’s needs, leading to further variation within these services between different patients. This variation impacted on patients’ experiences of the care and information that they received, and was thought to be the result of what one carer termed a ‘postcode lottery’ (male carer, control group, Flintshire and Wrexham).
The issues raised by variation in care were compounded by a lack of communication with patients and their families. Following discharge from the acute hospital setting, patients were unaware when, or if, community rehabilitation would commence, leading to uncertainty for them and their families. One patient reported that this lack of clarity led to her feeling as though she was ‘just dumped, you know because everybody else I have spoken to or people say, oh somebody came to see me for a week or so afterwards, well I didn’t get anything whatsoever’ (female patient, intervention group, Flintshire and Wrexham).
Such uncertainty also resulted in expectations of post-discharge care that were not met, highlighted by a number of focus group participants and reflected in comments such as ‘when I came home, I thought I would most probably have a bit more sort of, well health-care person come round’ (female patient, intervention group, Flintshire and Wrexham).
In participants randomised to the control group, the provision of usual care that was ‘a bit fragmented and patchy’ (male patient, control group, Flintshire and Wrexham) highlighted two salient points that were less prominent in focus groups conducted with participants who had received the intervention. The first was the patients’ self-motivation to obtain rehabilitation support and the second was poor communication between the different multidisciplinary teams in the hospital and in the community, creating a barrier to this. Several patients recounted that they had to independently seek help and guidance, primarily from their GP, before they were able to access adequate rehabilitation services. One patient described how having ‘plenty of motivation’ (female patient, control group, Flintshire and Wrexham) facilitated this process, and patients were driven by the opinion that ‘physio[therapy] should be there as a right, it is part of the process’ (male patient, control group, Flintshire and Wrexham). Unfortunately, this patient felt that his rehabilitation was hindered by ‘the fragmented manner in which treatment is given’ (male patient, control group, Flintshire and Wrexham). There was a consensus among patients and carers in the control group that there was a lack of communication between the multidisciplinary teams in the hospital and the multidisciplinary teams in the community, with one carer commenting on the ‘lack of co-ordination . . . I found that very frustrating’ (female carer, control group, Conwy and Denbighshire) and a patient concluding that ‘it is only by virtue of my attitude and I suppose my limited medical knowledge that I have been able to chase [post-discharge care] myself’ (male patient, control group, Flintshire and Wrexham).
Although patients in the intervention group also identified themselves as self-motivated individuals, the provision of additional therapy sessions by the intervention team staff meant that it was not necessary for them to initiate contact with the health services to request rehabilitation support. Furthermore, patients in the intervention group did not comment on the disconnected nature of multidisciplinary teams, suggesting that this problem was being addressed to some level by providing sessions that were consistently delivered by the same therapist or group of therapists.
Patient expectations of post-fracture recovery and their management by health-care professionals
Patients recalled a general lack of communication from health-care professionals early in their fracture experience with regard to what to expect from their recovery, with one patient noting that in the acute hospital ‘they don’t really explain to you, because they have no time to explain to you the dos and the don’t sort of and what you would experience’ (female patient, intervention group, Flintshire and Wrexham). This lack of information can result in patients having unrealistic expectations of the speed of their recovery and, in some patients, led to an assumption that, after surmounting the initial hurdle of being discharged home, they would rapidly return to their pre-fracture function. However, most patients reported a post-discharge realisation of the challenges that they faced, acknowledging that ‘you think you can get back to normal . . . . It actually doesn’t happen does it’ (female patient, control group, Conwy and Denbighshire). One patient commented that ‘it’s a gradual thing I think accepting that you are now limited’ (female patient, control group, Conwy and Denbighshire). This problem was compounded in some instances because of patients lacking a post-discharge point of contact with rehabilitation services, as it is often only at this point that patients begin to identify their requirements for support in their recovery.
Managing expectations
The conflict between patient expectations and their physical ability to progress also resulted in significant frustration being expressed by the majority of the focus group participants. Patients reported feelings of anger and frustration directed at themselves and at their dependence on others, with one commenting that ‘being incapacitated infuriated me so much’ (female patient, intervention group, Conwy and Denbighshire). Similarly, the carer of another patient reflected on his wife’s frustration:
She is very erm . . . annoyed at her inability to immediately start running the marathon or something.
Male carer, intervention group, Conwy and Denbighshire
It was at this point, when recovery failed to follow patients’ expected trajectory, that the physiotherapist played a pivotal role in managing expectations and reassuring patients that they were progressing normally. In the absence of this support there was a risk of patients losing motivation with regard to their rehabilitation. In particular, there seemed to be a need for patients to gain this reassurance from a qualified and knowledgeable professional, to help them feel confident in their recovery:
You know when somebody says ‘yes that is fine’ . . . it is helpful when somebody explains to you.
Female patient, intervention group, Flintshire and Wrexham
This reassurance from a health-care professional was also important to patients in terms of giving them the confidence to perform their physical activities, as there was an underlying concern that they may otherwise carry out exercises that may be harmful to them:
I had the security to know they were the right exercises, somebody there who gave them to me and you know they are qualified and they are telling you the right thing to do.
Female patient, control group, Flintshire and Wrexham
For participants in the control group who did not have the intervention sessions for support, this lack of reassurance was a particular problem. Patients received a list of activities to avoid (hip precautions), but some were given no information about what exercises and activities were safe to perform. Once patients were discharged home and recommenced their usual activities, further questions were raised surrounding these precautions. Patients stated that they had felt confused about what they should or should not do, and many felt that it would have been helpful to have had access to ‘somebody I could have just picked up the phone and said, how about this, should this be happening’ (female patient, control group, Flintshire and Wrexham) during this time. Control group participants reiterated throughout the focus group sessions that the provision of a point of contact would have been particularly helpful, and this was highlighted by the intervention group participants as a particular benefit of their extra sessions. Both groups identified the initial contact with therapists as being pivotal in building their confidence and supporting their own self-motivation for recovery. One patient succinctly captured the views of the groups, stating that:
Once you have the information and the guidance on what to do, what not to do, I think we are intelligent enough to go away and do it, but it is just that initial guidance . . . we might be capable but you still need guidance.
Male patient, control group, Flintshire and Wrexham
Fear of falling
Within this theme of patient expectations and the psychological aspects of patient recovery, we also identified fear of falling following participants’ initial fracture. This was common in patients who had experienced a hip fracture resulting from a fall, in both the control group and the intervention group. Participants acknowledged that this fear of falling made them more cautious and more likely to rely on a mobility aid for both stability and reassurance:
That is why I like the stick still because you know I have had my two falls and you are scared stiff then.
Female patient, intervention group, Conwy and Denbighshire
I was back on [walking sticks] because I am so afraid of falling again and breaking the other hip.
Female patient, control group, Flintshire and Wrexham
Although some participants identified that their fear of falling held back their recovery because of the reliance on walking aids, which ‘affects your rehabilitation . . . your ability to exercise’ (male patient, control group, Flintshire and Wrexham), some individuals in the intervention group did not consider this fear to be an obstacle to recovery, but rather saw themselves behaving cautiously to avoid further falls:
I think it is a good thing, because you are more cautious.
Male patient, intervention group, Conwy and Denbighshire
It doesn’t make me frightened of falling but it makes me more aware of not falling.
Female patient, intervention group, Flintshire and Wrexham
Patient preferences for individualised care and support
This theme encompassed three subthemes, as detailed in the following sections.
Recognition of unique rehabilitation needs
Patients’ experiences of rehabilitation and their perceptions of its effectiveness and relevance were often associated with their own personal circumstances and how specifically the rehabilitation programme addressed their own personal needs. This was evidenced particularly by comments from intervention group participants relating to their home environment, the specific challenges that they faced there and how intervention therapists conducting sessions in their own home helped to address these individual needs:
It is nice when they come to the house, and show you how to get up your own stairs and what leg you should be using.
Female patient, intervention group, Conwy and Denbighshire
It gives you the more drive doing it at home, you know because you have got somebody coming there, specifically for me . . . you say what you want to do.
Female patient, intervention group, Conwy and Denbighshire
An individualised aspect of rehabilitation, a defining characteristic of the study intervention but also present in some usual care provision, allowed therapists to tailor rehabilitation exercises directly to specific activities that patients were keen to recommence. This enabled participants to identify the relevance of these exercises to their recovery and potentially improved their engagement with them. Many participants also spoke of how important it was to be able to adapt these exercises and aids to suit their needs, emphasising the fact that a ‘one size fits all’ approach is not optimal and that when rehabilitation is focused on function rather than an abstract concept of muscle strength, this may be more motivating.
Tailoring of care to suit the individual
Focus group participants from the intervention group consistently referred to their preference for this form of personalised one-to-one therapy, which specifically considered their own comorbidities and goals. There was an emphasis on being shown how to perform exercises and activities in their own home in the ‘correct’ way, which reassured them that they were carrying out the exercises and activities safely and in the optimal manner for their recovery, which linked to their need for reassurance and support.
Although some patients reflected that the provision of usual care was adequate, with ‘lots of people coming from the hospital’ (male carer, control group, Flintshire and Wrexham), criticisms from control group participants and their carers centred around the lack of personalisation of this care, stating that it consisted of ‘basic stuff’ (female patient, control group, Conwy and Denbighshire) and ‘very gentle, sort of exercises’ (male patient, control group, Conwy and Denbighshire), which often felt ‘a bit rushed’ (female carer, control group, Conwy and Denbighshire). One control group participant received extra physiotherapy that he sought out independently, which was comparable to that received in the study intervention sessions. He positively reflected on this rehabilitation programme, stating that it was ‘really quite challenging’ (male patient, control group, Conwy and Denbighshire) in comparison with usual care, and his wife also observed the beneficial impact that it had had on his progression, particularly in terms of supporting his own motivation, as previously ‘there was a fear of, of pushing yourself too far’ (female carer, control group, Conwy and Denbighshire).
Consistency within the rehabilitation programme was also important and some patients expressed a preference for seeing the same therapist each time, enabling them to build a relationship with the therapist. This personalised care also allowed many participants to overcome their concerns that they were a burden on therapists’ time in some situations and that there may be other patients who were waiting to be seen. One participant explained her preference as ‘One to one, not a queue waiting you know, “hurry up because I have got all these people to see”. The one to one is good’ (female patient, intervention group, Conwy and Denbighshire).
In contrast, with regard to outpatient appointments, when time was limited, there was a perceived pressure to be considerate of other patients who were waiting and in this context there was less of an established rapport with the therapists. These appointments were seen by some patients to be a ‘little bit of a waste of time’ (female patient, intervention group, Conwy and Denbighshire). Control group participants, in particular, commented that they felt that their usual care sessions were rushed, with one carer remarking that the therapist was just ‘dashing in and out’ (female carer, control group, Conwy and Denbighshire), which, again, emphasises patient and carer preferences for a more personal service. Patients appeared to lack enthusiasm with regard to the outcomes of these appointments and appeared less engaged in any ongoing exercise plans that may have been prescribed:
You haven’t got the drive when . . . you go into hospital, you need drive and you don’t get it there because it is so impersonal I think.
Female patient, intervention group, Conwy and Denbighshire
Personalised goal-setting as a motivational tool
Although goal-setting was used implicitly in usual care, it was not specifically identified as a factor in recovery by control group participants. These patients received limited written information and generally agreed that they would have ‘welcomed a bit more comprehensive stuff to read’ (female patient, control group, Flintshire and Wrexham). The inclusion of a patient-held goal-setting diary as part of the study intervention was well received by participants as it gave them a direct focus and accountability for their goals. This was reflected in comments such as ‘You feel as if you have got a goal to get to, because you have put it in that book and you have got a goal’ (female patient, intervention group, Conwy and Denbighshire).
Many of the focus group participants were self-motivated individuals, so it is not possible to attribute their engagement in rehabilitation entirely to the intervention materials such as the goal-setting diary. However, participants did acknowledge the impact that goal-setting activities had in terms of maintaining their enthusiasm for working towards long-term goals. In particular, the ability to choose their goals themselves and make them specific to them, linking to their desire for personalised one-to-one care, was seen to be beneficial and supported their innate determination to regain their pre-fracture function. There was a sense that generic exercise-based goals were less applicable to them and that the ability to choose something relevant to their lifestyle helped them maintain an enthusiasm for their rehabilitation activities. This may particularly be of relevance in terms of giving patients focus and a deadline to achieve their goals by. This can be evidenced in the following selected comments:
I felt encouraged to go on doing things, and not just let them slide. I felt determined, I must get it right before [the therapist] comes.
Female patient, intervention group, Flintshire and Wrexham
When you have written it down in a book it makes you feel well I have got, I know I want to do that but I have got to do it now.
Female patient, intervention group, Flintshire and Wrexham
That said, some participants felt that the goal-setting diaries were of minimal use in their recovery and conversely viewed such resources as burdensome. Rather than acting as an aide memoir for reviewing their own rehabilitative progress, they became burdened by and preoccupied with the completion of such documentation:
You sort of wonder how to, put this in, and how to put that in.
Male patient, intervention group, Conwy and Denbighshire
The relationship between the patient and the health-care professional and its role in patient engagement in rehabilitation
A number of therapists, with a range of qualifications and experience levels, were involved in delivering the extra sessions to participants as part of the intervention. All participants reported that this was an overwhelmingly positive experience and reflected on the importance of connecting with the therapists on a personal level, with comments such as, ‘Very helpful and very pleasant to deal with, which is important too isn’t it . . . Like a friend coming in which is good’ (female patient, intervention group, Conwy and Denbighshire). The recurrent theme was related to the support that the therapist(s) provided in terms of reassurance and encouragement, while also creating an environment that made patients feel involved in the decision-making process regarding their recovery. One aspect of this, which was emphasised by patients, was the importance of these sessions in giving them time to discuss their individual problems as well as an opportunity to ask questions, particularly in the early stages of their rehabilitation. This was facilitated by the relationships that they developed with the therapists or therapy team, which allowed them to feel comfortable enough to ask questions without the fear of being dismissed or considered a nuisance. This contrasted with how they felt, on occasion, in the acute hospital or in usual care, with patients feeling less well informed of the processes and less familiar with the staff. An established relationship with their therapist as a point of contact for their rehabilitation underpinned many of the important factors of successful rehabilitation for patients and, in particular, engaging with their therapist and their goals appeared important to the success of the intervention. The respect that participants had for their therapist enabled them to both engage in, and take responsibility for, their role within their recovery process. One respondent characterised the relationship between himself and his wife and the therapist as being part of a team:
I felt as though it was a sort of team effort, and she [the therapist] was sort of team leader, and knew what to do, and then it is sort of from part of the team if you like.
Male patient, intervention group, Conwy and Denbighshire
Acceptability of the study to patients and carers
A primary objective of the focus groups was to gain insight into participants’ reflections on taking part in this research. In particular, this study aimed to better understand participants’ experiences of recruitment and of completing study outcome measures as this relates to the primary aim of assessing the feasibility of a larger-scale definitive trial. Despite patients being approached to participate in this study while in the acute hospital-based phase of their recovery, and indeed soon after the occurrence of a traumatic injury and surgery, an evidently positive perception of having been approached to take part was detected. Patients commented that having the opportunity to take part in research that may direct the future organisation and delivery of post-operative care for femoral fracture was a source of altruistic satisfaction.
The participant information sheets were described as being understandable and clear, and provided the necessary information regarding participation in the study. Explanation of the study by team researchers was furthermore considered to be clear and was felt to provide an accurate overview of the study purpose and processes, including randomisation. Although control group participants expressed disappointment at having not received the intervention, they ‘didn’t mind’ (female patient, control group, Conwy and Denbighshire) and still provided positive accounts of taking part in the study. Participation in a focus group was in itself found to be a cathartic experience for patients and one that reduced social isolation:
It is nice to talk to other people about it too isn’t it, you are not on you own are you.
Female patient, intervention group, Conwy and Denbighshire
Patient feedback on the intervention workbook varied. Some patients expressed a particular interest in the information relating to the mechanics of their fracture and the surgeries used to fix this; they appreciated having this explained to them and being able to gain a better understanding of their condition:
I thought it was good because it did explain things, it did explain to you what happens with a fracture.
Female patient, intervention group, Flintshire and Wrexham
Explained the various things used in the fracture, like a bolt or whatever you know different bits of metal was used, that was very interesting to find.
Female patient, intervention group, Flintshire and Wrexham
Other patients reflected on the comfort that having this additional information gave them and spoke of the workbook as ‘having got a back-up . . . just an assurance really’ (female patient, intervention group, Flintshire and Wrexham). One participant who lived alone and had little support stated that she found this aspect very helpful:
I didn’t know what to expect but I found I read [the workbook] profusely every day, and I did, I found it very, very helpful. It made me feel that I wasn’t on my own.
Female patient, intervention group, Conwy and Denbighshire
Other participants were less engaged with the workbook and provided comments such as ‘I just didn’t bother with that’ (female patient, intervention group, Flintshire and Wrexham) and ‘I sort of read it once and thought well you know this isn’t very useful’ (male patient, intervention group, Conwy and Denbighshire).
Without exception, the most useful aspect of the intervention was seen to be the extra time that participants received with the therapy teams, with the goal-setting diary and information workbook seen as useful supporting documents to these extra sessions.
Therapist experiences of post-discharge rehabilitation of patients following a hip fracture and delivery of the study intervention
Four main themes emerged from the health-care professional focus groups in relation to general patient care and delivery of the study intervention:
-
the impact of variation within usual care on delivery of the intervention and overall therapist experiences
-
therapist perceptions of their role within the rehabilitation of hip fracture patients
-
patient-led goal-setting to facilitate engagement in rehabilitation
-
challenges of delivering the intervention.
The impact of variation within usual care on delivery of the intervention and overall therapist experiences
Focus groups with therapists who delivered the study intervention identified a very diverse range of services for people discharged home from hospital with a hip fracture, and discussion focused on the effect that this had. Therapists’ experiences of what was available to patients in each geographical area varied, with some patients receiving multiple same-day appointments for post-surgical rehabilitation in the home and other patients receiving no rehabilitation at all (with the exception of the study intervention). It is not surprising that this impacted widely on the delivery of the intervention. Therapists shared concerns about offering advice to patients or supporting them to set individualised goals in their recovery when these might inadvertently conflict with goals being supported by other rehabilitation providers. One therapist commented that ‘it was much harder when they had [another ongoing service], the reablement ones were much harder too actually, because somebody else was already setting what they were going to achieve’ (clinical specialist physiotherapist, Wrexham Maelor). It was also felt that some participants considered that they ‘don’t really need two of you because I am getting quite good now’ (physiotherapist, Wrexham Maelor), suggesting that in some cases the provision of additional physiotherapy sessions was regarded by patients as an unnecessary addition to usual care. This was also remarked on by another therapist, who concluded, however, that, even in situations in which usual care is of a high standard, the provision of additional intervention sessions may mean that the patient ‘probably did get on sooner than she would have normally’ (therapy assistant, Ysbyty Gwynedd telephone interview).
Although therapists acknowledged the complex nature of delivering intervention sessions in an environment of varied usual care, it was generally accepted that the extra sessions were of great benefit to patients. In those areas where only a modest amount of home-based rehabilitation was available, the additional therapy sessions provided as part of the intervention arm could potentially help to redress such an inequity. Therapists also accepted that the variation in usual care and the potential impact of this on patient recovery was rarely communicated to patients, leaving them unaware of the possibility that they may not receive any rehabilitation following discharge from hospital:
No, they don’t realise, that is why they are saying ‘well if you hadn’t have come what would we have had’ and the answer is nothing. But they don’t know that, before they leave.
Clinical specialist physiotherapist, Wrexham Maelor
Variation in usual care between regions also affected the timescale of delivery of intervention sessions. In particular, there was debate about when and how these sessions would be best utilised, given that individual patients might be receiving markedly different rehabilitation services, as determined by their region of residence. As a result of this, no prescribed optimum use for the intervention sessions could be asserted, although therapists were naturally anxious for more clarity and guidance from the study team during training sessions. Therapists were required to adapt session intervals to accommodate usual care sessions and to make best use of their clinical time. One lead therapist commented that when she delivered the intervention to patients living in areas with sparse usual care provision she would ‘spread out the sessions, and then just pushed [the patient] harder, in the 2 weeks’ (clinical specialist physiotherapist, Wrexham Maelor). This was in contrast to regions where a comprehensive rehabilitation programme was in place, where she could deliver intervention sessions weekly in the confidence that at the end of the intervention period this rehabilitation trajectory would be continued through such services as local groups for falls prevention or community-run exercise schemes.
Therapist perceptions of their role within the rehabilitation of hip fracture patients
The priority in rehabilitation sessions, from the perspective of therapists, was physical exercise. This was considered to underpin recovery, as ‘all the goals that [the patients] wanted to achieve would be dependent on them improving the balance, the muscle strength, whatever’ (clinical specialist physiotherapist, Wrexham Maelor).
Although this reflected the stance of the wider body of therapist participants, in regions where there was adequate provision of usual care to support physical exercise and strength rehabilitation, therapists tended towards using the additional interventional sessions as an opportunity to focus on ADL with patients, such as climbing stairs or getting into a car or on and off public transport. One therapist noted that although these sessions relied on prior strength training from physiotherapy sessions, the functional goals that were set by patients for the intervention ‘were more I suppose OT [occupational therapy] goal-setting rather than physiotherapy’ (therapy assistant, Ysbyty Gwynedd telephone interview).
The first appointment with a patient at home following his or her discharge from the acute hospital was a source of some contention in terms of ‘defining’ the therapist role. Some therapists held the opinion ‘that my first visit might be a waste of time’ (clinical specialist physiotherapist, Wrexham Maelor) because patients prioritised the opportunity to ask questions and gather information at this stage rather than receive physical rehabilitation. This was a common theme, with other therapists concurring that the first session involved a lot of ‘weird type of questions of what [the patient] can and can’t do’ (physiotherapist, Wrexham Maelor) and that it is often ‘a bit of a problem-solving visit’ (physiotherapy technical instructor, Wrexham Maelor).
However, not all therapists held the same view regarding their role and the prioritisation of exercise practice. For example, one technical instructor acknowledged that her role extended beyond teaching physical exercises alone and identified the importance of adopting a psychosocial function:
[The patient] just lacked a little bit of confidence which after one visit that soared . . . it is just, realising that even if they only have one visit and it gives them that confidence boost, because they are scared.
Physiotherapy technical instructor, Ysbyty Glan Clwyd
When considering the best utilisation of the additional therapy sessions, this therapist identified the apparent benefit to patients of practising ADL while recognising that her own focus would normally be on the promotion of physical exercises. She commented that having intervention sessions directed by patient-set goals allowed her to focus on providing psychological reassurance and enabling patients’ own self-motivation for recovery to be the platform from which they could overcome barriers (more often than not psychologically), which might normally be overlooked by the therapist:
A couple of them were wary of the stairs and things like that . . . and back doorsteps. You know they see these things as a huge problem, whereas they are not. So it was just overcoming that . . . in their head oh I can’t do the stairs . . . it is just that little bit of reassurance.
Physiotherapy technical instructor, Ysbyty Glan Clwyd
This perceived lack of role clarity influenced ideas about how the extra therapy sessions might be used: some therapists perceived early use of the intervention to be less useful in areas where there was limited follow-up care provided and instead favoured a later stage of input to focus on functional goals. The rationale for this was that functional goals set by patients might be dependent on them first achieving a certain level of basic mobility. However, this was potentially counterproductive as limited input in the early stages of recovery could result in inactivity and subsequent loss of muscle and function, thus preventing patients from reaching their full recovery potential. This was particularly relevant given the varied nature of usual care, as therapists delivering the intervention may have been unaware what local rehabilitation services, if any, were available to support the intervention sessions.
Patient-led goal-setting to facilitate engagement in rehabilitation
The act of ‘goal-setting’ was identified by therapists as playing an important function in engaging patients with their own recovery and in providing motivation to regain function and independence. As previously outlined, therapists tended to prioritise physical exercises for improving muscle strength above functional aspects of recovery, particularly in the early stages of rehabilitation. There was the potential for patients to see these exercises as somewhat abstract and removed from their personal goals. Therapists reflected on the ability of patient-led goal-setting exercises to facilitate patient understanding of the importance of muscle-strengthening exercises by emphasising their relevance to achieving the patient-set goals:
I think [patients] probably more motivated because they can see the steps, to getting to that point. And why you are doing it.
Clinical specialist physiotherapist, Wrexham Maelor
Therapists across regions had similar experiences and used goal-setting as ‘a tool’ to help manage the expectations of patients who were surprised by the pace of their own recovery. One therapy assistant recognised that the presence of goals had helped to ‘make her [patient] think of the little things she wasn’t doing . . . it definitely focused her to do more’ (therapy assistant, Ysbyty Gwynedd telephone interview).
With the use of the goal-setting workbook, therapists felt that patients were better enabled to be involved in their own rehabilitative journey; ‘we are meant to like involve them normally in goal-setting, aren’t we, but I would say we generally do the goal-setting’ (physiotherapist, Wrexham Maelor). Enabling patients to take a more proactive role in this process, with support from the therapist to ensure that feasible goals were set, had a positive impact on patient engagement:
I think they probably were more motivated to take part then, I think, because it was what they wanted.
Physiotherapy technical instructor, Wrexham Maelor
Therapists also commented that the workbook was particularly useful for helping patients track their own progress and highlighting their achievements, which helped to support patients’ own self-efficacy. One therapist also commented that the goal-setting diary enabled better inclusion of carers in the rehabilitation process, which was reflected in comments such as, ‘If they’ve got a diary to flick through they are like, oh yes, I have done that, I have done this and they can show it to their family’ (physiotherapy technical instructor, Ysbyty Glan Clwyd).
Of particular note was that patients, on occasion, did not have the goal-setting diary to hand when visited by the therapist for a follow-up session. One therapist reported that she ‘struggled because I didn’t have the guidance of the book’ (physiotherapy technical instructor, Ysbyty Glan Clwyd). It was felt that such situations should have been covered in training, or measures put in place to ensure that therapists visiting patients were also in possession of a copy of the original goals agreed. This was one significant disadvantage identified by therapists of an intervention supported by an entirely patient-held workbook, but, overall, the goal-setting diary and the intervention as a whole were well received by therapists, who reflected on the positive impact that it had had on their patients’ recovery:
Does the goal-setting diary, does that extra time and input make a difference. I am sure it probably does.
Clinical specialist physiotherapist, Wrexham Maelor
Therapists did, however, express concern about dedicating additional time to working on goal-setting with patients. Within the context of a time-pressured working environment and with relatively limited resources, this concern about workload implications was one that might be described as a potential barrier to the effective implementation of a goal-setting diary.
Finally, although this study excluded patients lacking mental capacity to consent to participation, therapists felt that the goal-setting diary would also be of benefit to those with mild to moderate cognitive impairment, particularly if used in co-operation with carers and family members, as it would give patients a reference to keep track of goals and progress.
Challenges of delivering the intervention
A number of problems were identified by therapists with regard to delivering the extra intervention sessions, and these often related to the variations seen in ‘usual’ care. This problem was compounded when, in some areas, the staff delivering the intervention sessions were also treating patients as part of the usual care programme. One therapist expressed the difficulties that she had at the beginning of the study, commenting that she was unclear how to use the extra intervention sessions in conjunction with the usual care that, in this case, she was also providing to the patient. She commented that this left her feeling that she ‘didn’t know what to deliver really’ (therapy assistant, Ysbyty Gwynedd telephone interview). This became confusing for both staff and patients, who were unable to distinguish between the care that they received as part of usual NHS rehabilitation services and what was, in fact, care received as part of the trial intervention. Having already been visited by the ‘study’ therapist, this led on a number of occasions to patients attempting to decline an appointment, assuming that ‘the system’ had duplicated a visit. There was a consensus across the therapy teams that it would have been advantageous if there had been a dedicated therapist appointed to deliver the extra (intervention) sessions and that it might be helpful if these therapists had been distinguishable from those delivering usual NHS care, for example by wearing a distinct uniform.
The provision of intervention sessions by members of usual care teams also presented difficulties with regard to resource allocation. In two of the three areas, therapists were delivering intervention sessions in addition to their usual clinical schedule, with no staff cover or backfill of time available. Subsequently, staff conducted intervention sessions as overtime or alternatively were left having to vacate a ward to undertake the required domiciliary visit.
Therapists felt that they would have benefited from more training prior to administering therapy sessions as part of the trial intervention. The retrospective desire for further training related mainly to the previously explored uncertainty around how best to use the additionally allocated therapy sessions and how to integrate their own usual care practice with patient-led goal-setting. This was particularly important when initially delivering the intervention, with one therapist describing feeling ‘left in the dark a little bit, I didn’t know what was, what was expected of me’ (therapy assistant, Ysbyty Gwynedd telephone interview). This highlights a clear need for the study team to maintain more contact with therapists once delivery of the intervention has commenced to ensure that the therapists feel adequately equipped, in practice, to deliver the intervention as intended.
Another recurrent and important trial recruitment consideration raised related to the time point at which patients were approached about the study. Therapists identified this as a potentially critical factor in determining whether or not patients were likely to be receptive to taking part in the trial. Requiring patients to read a participant information sheet soon after surgery and to make a decision about participation was strongly reflected on:
A lot of them don’t feel 100% do they after surgery, it takes them a few days to get back to sort of feeling bothered that they want to do things.
Acute orthopaedic physiotherapy, Ysbyty Glan Clwyd
They are asked too early and you know their head is elsewhere.
Technical instructor, Ysbyty Glan Clwyd
One therapist suggested that, while still in hospital, ‘the patients had other things to worry about’ (acute orthopaedic physiotherapist, Ysbyty Gwynedd, telephone interview) and that recruiting after discharge from the acute hospital would be preferable. This was the case in some hospitals but, as the initial session and goal-setting needed to be performed by a physiotherapist, this was not always possible, as in some areas the intervention physiotherapist was unable to carry out community visits and these had to be completed prior to discharge.
Therapists participating in focus groups provided both extensive and wide-ranging feedback about the content of the study documents, including the information sheets, goal-setting diaries and intervention workbooks. The content, layout and format of the participant information sheets were generally well received, although it was noted that some patients found them hard to read and, thus, the addition of a summary information sheet was considered particularly useful. It was also noted that a number of patients had disclosed to their therapist that they felt that participation in this research was ‘above their kind of level to be involved’, given its affiliation with a university, and that this ‘could be a barrier for some people’ (rotational physiotherapist, Ysbyty Glan Clwyd).
With reference to the patient workbook, therapists shared that, overall, this was a good reference point for patients and that the information contained within this resource was particularly useful during the early phase of recovery after leaving hospital.
It was felt that patients often have not fully processed what has happened to them physically and that explanation of this would be useful, with one physiotherapist commenting ‘that is just telling them about [their fracture] isn’t it? That is all right’ (physiotherapist, Wrexham Maelor).
One physiotherapist shared that she had previously attempted to develop such a workbook within her own team, identifying this as beneficial to patients in terms of providing evidence-based information about the rehabilitation journey. The management of patient expectations was emphasised during this early phase of recovery and the role that providing information to patients can play:
Just give [the patient] some erm . . . hope really . . . because some of them are quite disheartened you know falling and hurting themselves and it really affects their thinking about the future.
Acute orthopaedic physiotherapist, Gwynedd and Anglesey
However, some therapists expressed concern that when community hospitals or residential facilities were referred to in the book, with particular reference to aspects of longer-term recovery for some people, a sense of avoidable fear may be evoked:
Adding a fear that that patient may not have had and may never need.
Clinical specialist physiotherapist, Wrexham Maelor
Although perceived to be useful on many levels, one therapist did share anecdotally that features such as the quizzes could be considered condescending to patients. This was raised with her by a patient, who told her that it was ‘an insult to my intellect’ (clinical specialist physiotherapist, Wrexham Maelor) and that this prevented him from engaging with the resource.
The goal-setting diary was also considered to be a positive addition to the post-hospital recovery by therapists, and was perhaps more widely accepted, with most concurring that they were ‘very easy to fill in’ (physiotherapy technical instructor, Ysbyty Glan Clwyd). Minor alternations were recommended to increase the ease of use of the diary, such as ‘I think you could have a tick box . . . and then you could tick, you know, how often they had done it’ (physiotherapist, Wrexham Maelor).
Discussion
Summary of findings
Figure 14 provides a visual representation of the overarching themes relating to patients’ and health-care professionals’ experiences of post-discharge rehabilitation following hip fracture in this study. It shows, in the context of varied usual care, the pivotal role of the physiotherapist in managing patient needs and expectations through the use of personalised care and goal-setting. In the intervention group, these activities were well supported by the workbook and goal-setting diary.
FIGURE 14.
Overarching themes from the focus groups with patients and therapists with regard to post-hospital discharge rehabilitation following hip fracture.

The themes identified in the patient focus groups can be categorised according to three distinct levels. On a health services level we identified a concern over the large variation in usual care following discharge from hospital with a hip fracture. Patients described an ad hoc experience of home-based care and rehabilitation and, in some cases, no post-discharge physiotherapy at all. This variation in experience revealed an uncertainty and associated anxiety among patients about how they could safely promote their own recovery after they were discharged from hospital.
On a patient experience level, frustration at wanting to restore their former physical functioning coupled with a lack of clarity with regard to expectations of recovery (such as what could be considered achievable or not achievable on an individual basis) led to patients feeling demotivated and needing reassurance from a health professional. Patients stated a preference for individual therapeutic care at home on a one-to-one basis that was responsive to individual physical needs. In the absence of such support, patients felt a sense of frustration at the speed of their physical recovery, which was felt to have been poorly managed.
On an interventional level, the key recurring message with regard to community physiotherapy was the importance of regular home visits, particularly in the early phase of post-hospital recovery. These visits should provide tailored advice promoting confidence and enable patients to support their own recovery by providing reassurance about which physical activities can be safely performed, along with promoting self-efficacy by highlighting patient progress.
The themes identified in the therapist focus groups mapped onto the themes identified in the patient focus groups. For example, the successful delivery of the study intervention was affected by the highly varied nature of usual care. However, there was a disparity of views between the patient focus groups and the therapist focus groups regarding the initial contact with a therapist. For the therapists, this was merely information sharing prior to starting proper rehabilitation, including the practice of exercises and ADL. For the patients, however, this initial contact with their qualified community therapist was vital. Once at home, patients’ anxieties mainly related to the uncertainty about the trajectory of their physical recovery and which daily activities were safe to perform independently. Uncertainty about what was safe and the fear of causing further damage over-rode the impulse to begin exercising and resume normal ADL, thus becoming an obstacle in the early and critical phase of patients’ physical rehabilitation. Therapists provided reassurance about recovery and verbal guidance on strategies to support recovery in the context of patients’ homes. The provision of such evidence-based guidance on self-management and recovery optimisation was pivotal for a phased return to normal ADL, while ensuring that the return to pre-fracture activities was achieved safely. The therapists were not fully aware of the pertinence, for patients, of this early psychological support and reassurance in underpinning and directing a confident trajectory of recovery.
In summary, the therapists were providers of evidence-based guidance and provided reassurance and clarity on:
-
what was available to patients to support their rehabilitation, for example physical aids and psychosocial support
-
what could be realistically expected in terms of recovery, for example when to expect markedly increased mobility
-
what was safely achievable on an individual basis over a given time frame.
Strengths and limitations
Although we were able to conduct one-to-one interviews with staff at one of the hospital sites (Ysbyty Gwynedd, Bangor) where there had been problems with delivery of the intervention, these staff were unable to come together and discuss these issues in a focus group because of clinical commitments. As patient participants in this site were spread over a large geographical area, it was not possible to arrange a focus group that these participants could attend. Also, because of problems with intervention delivery in this area (see Chapter 9), only one participant actually received the extra sessions, and she was unable to attend the other groups that were arranged. Patient and professional participants from Gwynedd and Anglesey were therefore under-represented in this study.
The intervention was delivered only by physiotherapists and technical instructors; there was no involvement of occupational therapists as we had originally anticipated. This was because of resource availability. As such, the focus groups included only two types of professionals, although the physiotherapists were of differing grades and had different roles within the health board. Although we attempted to recruit nurses who had been involved in screening patients for eligibility, they were unable to attend the focus groups because of clinical commitments.
These factors also impacted on the number of participants in each group, which in some cases was as few as three. Although the participants represented a range of rehabilitation experiences, it would have been beneficial to reach our target of eight participants per focus group to encourage discussion from a variety of viewpoints.
Comparison with previous literature
Comments from health-care professionals and patients regarding the variable nature of usual care were comparable to those provided in the Phase I focus groups (see Chapter 5). Similar views have also been documented in the literature. 344–347
Goal-setting and supporting patients’ self-efficacy were seen to be important in helping patients to engage with their rehabilitation. Another study on patient empowerment347 also found that empowered patients were more likely to benefit from their rehabilitation and return to previous living.
The focus groups highlighted that, without involvement from a health-care professional, patients’ expectations of their recovery may be unrealistic. A previous study has also shown that patients need detailed counselling to create realistic expectations of their recovery and enable them to prepare for the outcomes. 348
Implications for practice and future research
The focus groups supported the findings from the wider feasibility study that usual care is variable and often unpredictable, and demonstrated that this had a negative impact on patient experience. Although this was expected, they highlighted the challenges that this can cause when delivering a rehabilitation intervention in this context and emphasised the need for more thorough training of intervention therapists, with continuing support for how the intervention can best be delivered. This should be considered in a definitive RCT and the training opportunities increased. Because of the challenges involved in delivering the intervention, which related to resource allocation, it would be beneficial to use a dedicated therapist to deliver the intervention sessions. This would also help to address the problems that were encountered when intervention therapists were left to provide usual care for the same patient, causing confusion for patients and therapists.
Therapists highlighted that in some cases patients felt that they did not need all six additional therapy sessions. This is supported by adherence data (see Chapter 7) and is likely to be influenced by the variability in usual care and also the specific population recruited to the feasibility study, who were shown to be a younger and healthier subpopulation of the whole cohort (see Chapter 8). This may be of relevance to future practice and to defining the minimum dose of therapy that is optimal for this population.
Patients’ perception of the therapist’s role in their rehabilitation appeared from the focus groups to be one of a guide during their recovery process. In these self-motivated and previously independent people, there was a requirement of the therapist to support a patient-led recovery process, allowing patients to take ownership of their recovery while being reassured by a professional that they were progressing safely. From the specific patient needs that were highlighted in the focus groups, and the disparities between the role perceptions of therapists, we have produced a mnemonic that could be used by therapy managers to assist their teams in rehabilitating these types of patients (Figure 15).
FIGURE 15.
The GUIDE (Guidance, Understanding, Individualised, Direction, Expertise) tool for therapists for rehabilitating hip fracture patients.

This aims to highlight the central role of the therapist in guiding patients to set realistic and achievable goals and providing feedback on progress to support patients’ own self-efficacy. It also reminds therapists of the information needs of patients and how addressing these psychological problems underpins their physical progress.
Although there were some significant challenges involved in delivering the study intervention, it was well tolerated by participants, who found taking part in the study a positive experience overall. Therapy staff involved in the delivery of the intervention also provided several suggestions that could be implemented in a future RCT of the intervention to overcome some of the problems that they encountered. One of the issues experienced by therapists was how best to utilise the intervention sessions in the context of variable usual care. They commented that they would have welcomed more training with regard to this; the use of the GUIDE tool (see Figure 15) in training may be helpful in this regard.
Chapter 10 Economics results
Introduction
In this chapter, we first provide an overview of the economic evidence relating to the rehabilitation of proximal femoral fracture in an elderly population. We then describe the measurement of outcomes and costs included in the economic evaluation of the feasibility study from a public sector, multiagency perspective. We report the study intervention costs and the type and frequency of contact with primary and secondary health-care, social care and charity and community-based services, and patterns of service use by the intervention and control groups, and the associated costs, over the 3-month follow-up period of the feasibility trial. We report health-related quality of life (EQ-5D-3L)287 and self-report capability (ICECAP-O)313 at baseline (prior to randomisation) and at 3 months post baseline. We report the results of a patient preference-based DCE349 that asked participants about the characteristics (attributes) of post-proximal femoral fracture rehabilitation services that they found to be the most important. Finally, we report whether or not a social return on investment (SROI) analysis would be possible as part of a full-scale RCT, acknowledging the lessons learned and based on the data obtained in the feasibility study.
Published economic evidence
The National Institute for Health and Care Excellence7 highlighted in its guidance on the management of hip fracture in adults the lack of cost-effectiveness evidence available. A Cochrane review conducted by Handoll et al. 8 concluded that there was no conclusive evidence on the effectiveness and cost-effectiveness of multidisciplinary inpatient rehabilitation following proximal femoral fracture surgery in older people. Our own systematic review of the economic evidence (see Chapter 3 for the full methods and results) identified seven published economic evaluations conducted alongside rehabilitation interventions for proximal femoral fracture in older people. 253,254,260–264 The year of publication in the included evaluations ranged from 1986 to 2009. The evaluations were conducted in Australia, New Zealand, the Netherlands, Sweden, the UK and the USA. The majority of the evaluations calculated costs from a hospital perspective, considering direct hospital costs only, such as the costs of treatment, medication and care. 254,260,261,264 Two of the three cost-effectiveness evaluations found that rehabilitation pathways were cost-effective. 253,260 Of the two cost–benefit analyses, only one found that the benefits of the intervention outweighed the costs. 262 Both cost-minimisation evaluations revealed that the interventions under study reduced costs without reducing outcomes compared with usual care, thus demonstrating that the interventions could provide lower-cost alternatives to regular practice. 263,264 The findings in Chapter 3 correspond with the findings of previous economic evaluations7,8 that there is a limited evidence base for multidisciplinary proximal femoral fracture rehabilitation, particularly from a UK perspective.
Objective of the feasibility study economic analysis
The objective of the feasibility study economic analysis was to explore the methodological issues around conducting an economic evaluation alongside a future RCT, including identifying the most efficient way of measuring patient-level costs and health benefits, and programme costs and identifying potential payer stakeholders.
The objective of the feasibility study economic analysis was divided across three work streams:
-
work stream 1 – assessing the feasibility of conducting an economic analysis from data collected in the feasibility study
-
work stream 2 – assessing the feasibility of measuring patients’ preferences for proximal femoral fracture rehabilitation services using a DCE
-
work stream 3 – scoping the potential to conduct SROI analysis in a future trial based on data gathered in the feasibility study.
These work streams are described in turn in the following sections.
Work stream 1: assessing the feasibility of conducting an economic analysis from data collected in the feasibility trial
Objective
The primary objective of the health economics analysis was to test whether or not it was feasible to conduct economic analysis using the data from the feasibility study. We also wished to explore the use of a generic health-related quality-of-life measure and a capability measure to explore the extent to which the two approaches could help guide commissioning decisions following a full trial and full economic evaluation.
Methods
Cost-effectiveness and cost–consequences analysis
National Institute for Health and Care Excellence guidelines7 recommended that further cost-effectiveness studies be conducted in the field of rehabilitation for proximal femoral fracture. However, as the small feasibility study was not powered to test an effect on the primary outcome measure (BADL index265), we report a cost–consequences analysis. Cost–consequences analysis is a variant of cost-effectiveness analysis in which an array of consequences/outcomes (e.g. health-related quality of life) and costs (e.g. health service use costs) are presented, comparing the two treatment arms of the trial (intervention group vs. control group) in a disaggregated form, without combining these into a cost-effectiveness ratio or a cost–utility ratio. This type of analysis lists the components of an intervention, without making judgements about their relative importance, which is left to the decision-maker. 350,351 Cost–consequences analysis is championed as being a method that is particularly relevant to economic evaluations carried out alongside public health interventions. 352 Kelly et al. 353 have argued that the QALY approach may be too narrow to capture the full range of benefits from public health interventions. Weatherly et al. 354 have argued for cost–consequences analysis to be carried out alongside cost-effectiveness or cost–utility analysis. This method requires the researcher to clearly set out a full range of disaggregated benefits alongside any cost per QALY results or cost-effectiveness ratios, allowing multiple outcomes to be assessed.
Perspective of the analysis
We adopted a public sector, multiagency perspective (including the NHS and primary care, social care and voluntary services) in accordance with our standard operating procedure for conducting an economic evaluation alongside RCTs. 355
Time horizon
Data were gathered at baseline (prior to randomisation) and at 3 months post baseline. As the time horizon was < 1 year, we did not discount costs or outcomes in the analysis.
Measurement of consequences
Measurement of generic health-related quality of life
Generic health-related quality of life was measured using the EQ-5D-3L. 287 This is a patient-completed index of health-related quality of life that gives a weight to different health states. It consists of five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has three possible responses (no problems, moderate problems and extreme problems); responses are converted into a single summary index by applying a formula that attaches weights to each of the levels in each dimension. This index score can be used to describe health states, including health states considered worse than death, and can be compared with population norms. The EQ-5D also includes a VAS, ranging from 0 to 100, with the participant drawing a line on the scale to rate his or her health state today. The EQ-5D-3L was administered at baseline and at the 3-month follow-up assessment.
Measurement of self-report capability
Self-report capability was measured using the ICECAP-O. 313 This is a patient-completed self-report measure of capability in older people, focusing on well-being rather than health. It has five attributes: attachment (love and friendship), security (thinking about the future without concern), role (doing things that make you feel valued), enjoyment (enjoyment and pleasure) and control (independence). Each attribute has four possible responses (all, a lot, a little and none) that record the extent of capability. It was administered at baseline and at the 3-month follow-up assessment, and the responses to each attribute were converted to a capability utility based on valuations derived from best/worst scaling. We calculated the difference in the mean capability index between the intervention group and the control group.
Measurement of type and frequency of health and social care service use
The type and frequency of health and social care service use was measured using the CSRI. 315 The CSRI is a questionnaire for collecting retrospective information about study participants’ use of health and social care services, including voluntary services (e.g. charity services). The questionnaire was administered as an interview, with the researcher asking the participants details about their contacts, for example who they saw, how long the appointments lasted and where the appointments took place (e.g. at the surgery/clinic or at home). An abbreviated version of the questionnaire was administered at baseline to reduce the participant burden, as patients completed the baseline measures while recovering from surgery for proximal femoral fracture. A more in-depth version was administered at the 3-month follow-up assessment. Services were grouped into categories [e.g. health services, consisting of inpatient admissions, outpatient procedures and attendances at accident and emergency (A&E) departments] in the questionnaire to make it easier to complete by the participants and to assist with reporting. We calculated the difference in mean service use between the intervention group and the control group.
Measurement of costs
Intervention costs
The enhanced rehabilitation programme was fully costed using unit costs from a NHS perspective. Unit costs were obtained from the local health board and applied to information received from the health professionals delivering the intervention, namely the salary band of therapists, the time spent with patients conducting rehabilitation, the costs of travel and the costs of any additional equipment.
Costs of services
The type and frequency of health and social care service use was measured using the CSRI. 315 The information obtained from the CSRI was combined with national sources of unit costs339,356,357 to calculate a mean cost per participant per arm for health and social care service use. A unit cost table is provided in Appendix 32, outlining the published unit costs used in this cost–consequences analysis and their sources. As already described, a reduced version of the CSRI was administered at baseline to reduce the participant burden, as patients completed the baseline measures soon after discharge from hospital. A more in-depth version was administered at the 3-month follow-up assessment. The 2013–14 cost year in UK pounds sterling was applied for all costs.
Analysis of consequences
For the analysis of the EQ-5D-3L data we calculated QALYs using the area-under-the-curve method, a standard approach in health economics. 358 QALYs measure health gain by aggregating the number of years gained from a drug or health-care intervention, weighted by the utility value associated with a given health state (utility). 359 We calculated mean QALYs for both the intervention group and the control group. We calculated the differences in mean QALYs between the groups and produced 95% CIs around these differences. For the ICECAP-O measure, responses to each attribute were converted to a capability index derived from UK norms. We calculated the change in the mean capability index for the intervention and the control groups. We also calculated the differences in mean capability index between the groups and produced 95% CIs around these differences.
Analysis of costs
We compared the frequency and cost of health and social care service use (including charity services) over 3 months between the intervention group and the control group. We calculated the mean total service use costs (including intervention costs) for the intervention group and the control group. We calculated the differences in mean total service use costs between the groups and produced 95% CIs around these differences. We also compared mean frequencies and costs using non-parametric Mann–Whitney U-tests, as the distributions were skewed.
Results
Health economics sample
In total, 61 participants were recruited in the feasibility study, of whom 12 withdrew during the course of the study, resulting in 49 sets of data available for analysis. We excluded six participants as they were missing data at either follow-up or both baseline and follow-up (one participant did not complete the EQ-5D-3L questionnaire at follow-up, one participant did not complete the CSRI at follow-up and four participants did not complete the ICECAP-O313 questionnaire at both baseline and follow-up). Therefore, the final sample for the economic complete case analysis included 43 sets of data (intervention, n = 21; control, n = 22). The six participants with missing data were excluded from the analysis because cost-effectiveness or cost–utility analysis requires complete data for both costs and outcomes. Although we were unable to perform cost-effectiveness or cost–utility analysis because of a lack of a significant effect for the primary outcome, we felt that it was important to use the feasibility data in this way to inform future economic evaluations. Therefore, we used only complete data across the three economic measures (EQ-5D, ICECAP-O and CSRI) in the final sample, as would be required by a full economic evaluation. Furthermore, as this was a feasibility study, we did not impute missing data, as stated in the statistical analysis plan.
The ICECAP-O questionnaire had a lower completion rate than the EQ-5D-3L. Three participants stated that they were unable to answer the questionnaire as they felt that the domains did not apply to them (e.g. they felt that they had no social life at the moment and so could not answer the questionnaire). One participant was not able to finish the questionnaire as one of the questions led her to think about something upsetting in her life and she became distressed. These participants were omitted from the analysis because, to calculate a capability index, all questions on the ICECAP-O questionnaire must be answered. 313
Table 24 summaries the characteristics of the economic sample at baseline; Table 25 shows the mean EQ-5D-3L utility scores, EQ-5D-3L VAS scores and ICECAP-O capability index scores at baseline and at 3-month follow-up; and Table 26 shows, for both the intervention and the control groups, the mean QALYs, change in the mean ICECAP-O capability index score and mean total service use costs (including the cost of the intervention for the intervention group) over the 3-month study period. The differences between groups in mean QALYs, capability indices and service use costs are also presented, with 95% CIs around these differences.
| Characteristic | Intervention (N = 21), n (%) | Control (N = 22), n (%) |
|---|---|---|
| Gender | ||
| Female | 17 (81) | 15 (68) |
| Male | 4 (19) | 7 (32) |
| Usually lives | ||
| Alone | 11 (52) | 11 (50) |
| With others | 10 (48) | 11 (50) |
| Accommodation type | ||
| Owner-occupied property | 17 (81) | 17 (77) |
| Privately rented property | 2 (10) | 2 (9) |
| Housing association/local authority property | 2 (10) | 2 (9) |
| Sheltered accommodation | 0 (0) | 1 (5) |
| Type of fracture | ||
| Intracapsular | 8 (38) | 12 (55) |
| Extracapsular | 9 (43) | 7 (32) |
| Not recorded in notes/notes unavailable | 4 (19) | 3 (14) |
| Type of surgery | ||
| Hemiarthroplasty | 9 (43) | 12 (55) |
| Internal fixation | 10 (48) | 4 (18) |
| Intramedullary nailing | 0 (0) | 1 (5) |
| Total hip arthroplasty | 1 (5) | 4 (18) |
| Not recorded in notes/notes unavailable | 1 (5) | 1 (5) |
| Direct discharge | ||
| Yes | 10 (48) | 16 (73) |
| No | 11 (52) | 6 (27) |
| Recruited from | ||
| Ysbyty Glan Clwyd | 12 (57) | 12 (55) |
| Wrexham Maelor | 7 (33) | 9 (41) |
| Ysbyty Gwynedd | 2 (10) | 1 (5) |
| Age at baseline (years), mean (SD); range | 80.95 (6.2); 69–89 | 76.82 (7.5); 66–89 |
| Outcome | Baseline, mean (SD), range | 3-month follow-up, mean (SD), range | ||
|---|---|---|---|---|
| Intervention group (n = 21) | Control group (n = 22) | Intervention group (n = 21) | Control group (n = 22) | |
| EQ-5D-3L utility score | 0.50 (0.26), 0.02–1.00 | 0.37 (0.43), –0.48 to 1.00 | 0.66 (0.27), 0.09–1.00 | 0.60 (0.27), 0.02–1.00 |
| EQ-5D-3L VAS score | 64.43 (16.37), 35.00–100.00 | 55.14 (25.72), 0.00–90.00 | 71.10 (17.89), 18.00–100.00 | 68.55 (18.44), 30.00–98.00 |
| ICECAP-O capability index score | 0.82 (0.11), 0.54–0.98 | 0.75 (0.21), 0.35–1.00 | 0.84 (0.13), 0.50–1.00 | 0.78 (0.19), 0.19–1.00 |
| Outcome | Intervention group (n = 21) (1000 bootstrapped 95% CI) | Control group (n = 22) (1000 bootstrapped 95% CI) | Difference between groups (1000 bootstrapped 95% CI) |
|---|---|---|---|
| Mean QALYs over 3 months | 0.15 (0.12 to 0.17) | 0.12 (0.09 to 0.15) | 0.02 (–0.02 to 0.06) |
| Mean change in ICECAP-O capability index scores over 3 months | –0.03 (–0.08 to –0.03) | –0.03 (–0.12 to 0.07) | 0.00 (–0.11 to 0.22) |
| Mean total service use costs at follow-up including cost of the intervention (£) | 149,243.02 (119,376.32 to 186,035.64) | 105,243.95 (78,934.94 to 132,971.08) | 43,999.07 (4026.98 to 88,818.07) |
The economic sample represented 72% of the main clinical sample. The characteristics of the two samples were the same (see Chapter 9 and Table 24), with more women recruited to the trial than men. The age of the participants was similar in both samples, with the intervention group slightly older (mean age 81.0 years in the economic sample and 80.9 years in the clinical sample) than the control group (mean age 76.8 years in the economic sample and 78.0 years in the clinical sample). The participants’ home circumstances were similar between the groups in the economic sample, with the same number of participants living alone or living with others (n = 11) in the control group and one more participant living alone (n = 11) than living with others (n = 10) in the intervention group. As in the clinical sample, the majority of participants in both groups in the economic sample owned their own home; experienced an intracapsular fracture and received hemiarthroplasty surgery, with internal fixation the second most common type of surgery; and were recruited from Ysbyty Glan Clwyd, with the lowest number of participants recruited from Ysbyty Gwynedd.
The control group had a lower EQ-5D-3L index score, EQ-5D-3L VAS score and ICECAP-O capability index score than the intervention group at baseline (see Table 25). However, both groups had improved scores at follow-up, with the maximum range being at the ceiling score of the measures (1.00 for the EQ-5D-3L and ICECAP-O indices, and 100 for the EQ-5D-3L VAS). Differences in EQ-5D-3L index scores, EQ-5D-3L VAS scores and ICECAP-O capability index scores between groups were assessed using Mann–Whitney U-tests, which found no statistically significant differences (p > 0.05).
Table 26 shows the mean QALY gains (if any) by each group over 3 months. For the control group we calculated a mean QALY gain of 0.12 (1000 bootstrapped 95% CI 0.09 to 0.15), equating to 45 days gained. The intervention group showed a slightly higher QALY gain of 0.15 (1000 bootstrapped 95% CI 0.12 to 0.17), equating to 53 days gained. The difference in QALYs between the two groups was 0.02 (1000 bootstrapped 95% CI –0.02 to 0.06), equating to 8 days gained.
The mean change in the ICECAP-O capability index scores over 3 months was –0.03 (1000 bootstrapped 95% CI –0.12 to 0.07) in the control group and –0.03 (1000 bootstrapped 95% CI –0.08 to –0.03) in the intervention group (see Table 26), indicating that both the intervention and the control groups reported lower levels of capability at follow-up than at baseline. This could be because of reduced mobility and independence while participants recovered from their fracture, resulting in lower perceived capability as measured by the ICECAP-O across the whole sample. The difference in capability index scores between the two groups was 0 (1000 bootstrapped 95% CI –0.11 to 0.22).
The intervention group reported mean total service use costs per participant at follow-up (including the cost of intervention) of £149,243.02 (1000 bootstrapped 95% CI £119,376.32 to £186,035.64), whereas the control group reported mean total service use costs at follow-up of £105,243.95 (1000 bootstrapped 95% CI £78,934.94 to £132,971.08). The difference in total service use costs at follow-up between the groups was £43,999.07 (1000 bootstrapped 95% CI £4026.98 to £88,818.07).
Mann–Whitney U-tests found no statistically significant differences between the groups in terms of QALYs gained (U = 184.00, p = 0.18) or ICECAP-O capability index scores (U = 249.00, p = 0.86). However, Mann–Whitney U-tests revealed a statistically significant difference in mean total service use costs per participant between the two groups (U = 136.00, p = 0.02).
Box 5 outlines how the service use categories – primary health-care and community services, secondary health-care services, social care services, proximal femoral fracture-specific services, voluntary/charity services and medication use – were derived from the contacts listed in the CSRI questionnaires. These service use categories are used throughout this chapter when describing participant service use and associated costs. Service use data were collected for the 3 months prior to baseline and the 3 months prior to follow-up.
GP.
Practice nurse.
District nurse.
Health visitor.
Physiotherapist.
Occupational therapist.
Technical instructors/rehabilitation assistants to physiotherapists or occupational therapists.
Community pharmacist.
Secondary (hospital) health-care servicesInpatient services.
Outpatient services.
A&E services.
Day hospital.
Any other hospital services not listed in the questionnaire.
Social care servicesSocial worker.
Community psychiatric nurse/community mental health nurse.
Psychologist.
Community psychiatrist.
Counsellor.
Home-care worker.
Care attendant.
Proximal femoral fracture-specific servicesEnablement centre for rehabilitation.
Nursing home for rehabilitation.
Falls prevention classes.
National Exercise Referral Scheme.
Voluntary/charity servicesBritish Red Cross.
Borrowing of equipment (e.g. wheelchairs).
Medication useAll medications used, including prescribed and over-the-counter medicines.
Figure 16 shows the mean total frequency of contacts and the mean frequency of contacts with primary and secondary health-care services in the intervention group (n = 21) and the control group (n = 22) during the 3 months prior to baseline.
FIGURE 16.
Mean frequencies of primary and secondary health-care service use by participants in the intervention group and the control group, as measured by the CSRI during the 3 months prior to baseline. Frequencies are presented to one decimal place.
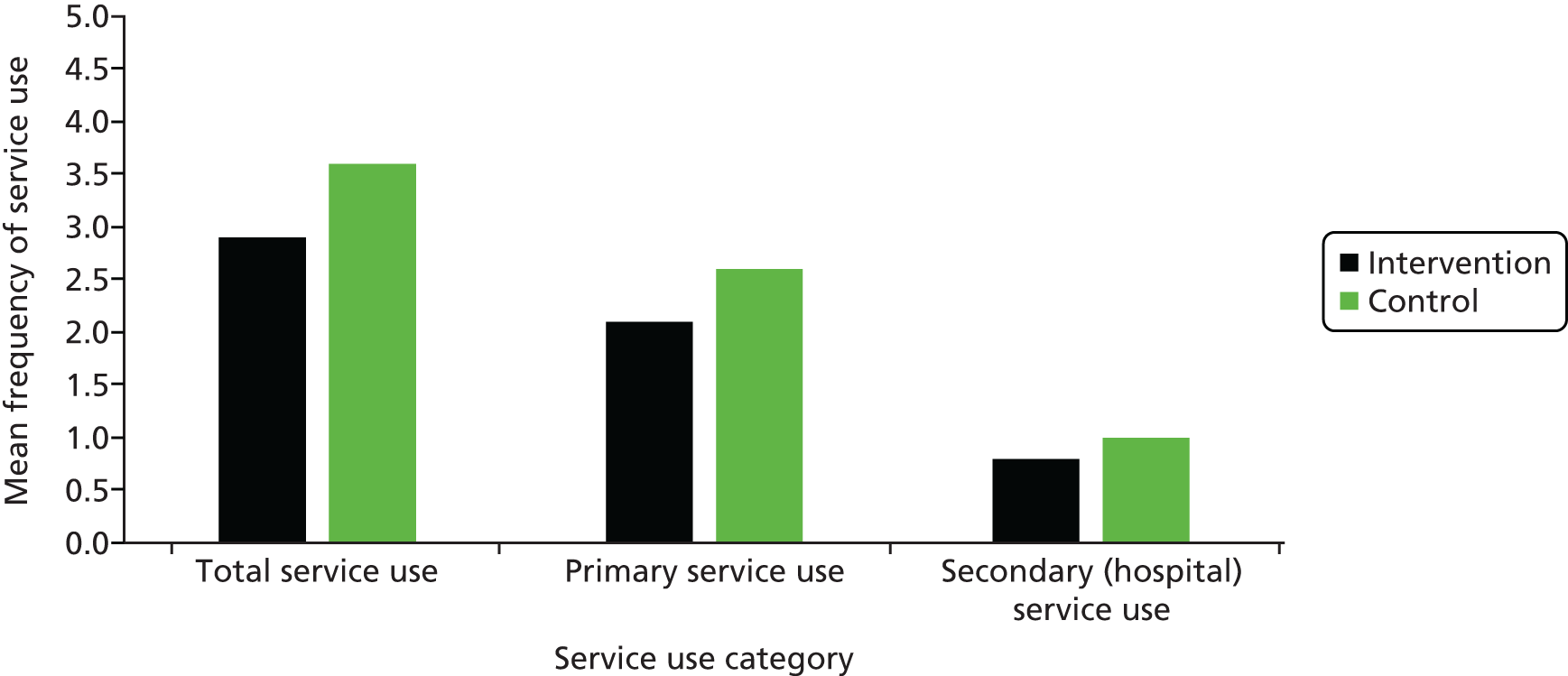
During the 3 months prior to baseline, participants in the control group accessed more services than participants in the intervention group. Participants accessed more primary care services than secondary care (hospital) services prior to their proximal femoral fracture. Participants were most likely to see a GP, with practice nurses the second-highest accessed health-care professionals. Participants underwent more outpatient procedures than inpatient procedures during this time period.
Figure 17 illustrates the mean costs of the service use associated with the intervention group and the control group during the 3 months prior to baseline. The mean costs of primary service use were minimal, with the costs of secondary (hospital) services accounting for the majority of the total service costs. Secondary (hospital) services accounted for 98% of the costs in the intervention group, with primary services accounting for the remaining 2%; the corresponding percentages for the control group were 99% and 1%. The majority of the hospital costs were related to multiple outpatient appointments attended by the sample.
FIGURE 17.
Mean costs of primary and secondary health-care service use by participants in the intervention group and the control group, as measured by the CSRI during the 3 months prior to baseline. Costs are rounded to the nearest pound and are presented for the cost year 2013–14.

Figure 18 shows the frequency of contacts with primary and secondary health-care services, social care services, proximal femoral fracture-specific services and voluntary/charity services, as well as medication use, in the intervention group (n = 21) and the control group (n = 22) during the 3 months prior to follow-up. Participants primarily accessed primary services and social services. There were high levels of polypharmacy within the sample, with the sample, on average, taking more than five medicines at the time of completing the CSRI. The most common medications prescribed were ramipril, omeprazole, alendronic acid, amlodipine, warfarin, calcium and vitamin D supplements. Differences in frequencies between the groups were assessed using Mann–Whitney U-tests. No statistically significant differences were found between the groups in the frequency of total health-care service use (U = 197.00, p = 0.41), primary health-care service use (U = 187.00, p = 0.28), secondary (hospital) health-care service use (U = 259.50, p = 0.48), social care service use (U = 215.00, p = 0.65), hip fracture-specific service use (U = 217.50, p = 0.61) or voluntary service use (U = 238.50, p = 0.74), or in the frequency of medication use (U = 189.50, p = 0.31).
FIGURE 18.
Mean frequencies of primary and secondary health-care, social care, proximal femoral fracture-specific and voluntary/charity service use and frequency of medication use by participants in the intervention group and control group, as measured by the CSRI during the 3 months prior to follow-up: (a) intervention group; and (b) control group. Frequencies are presented to one decimal place.
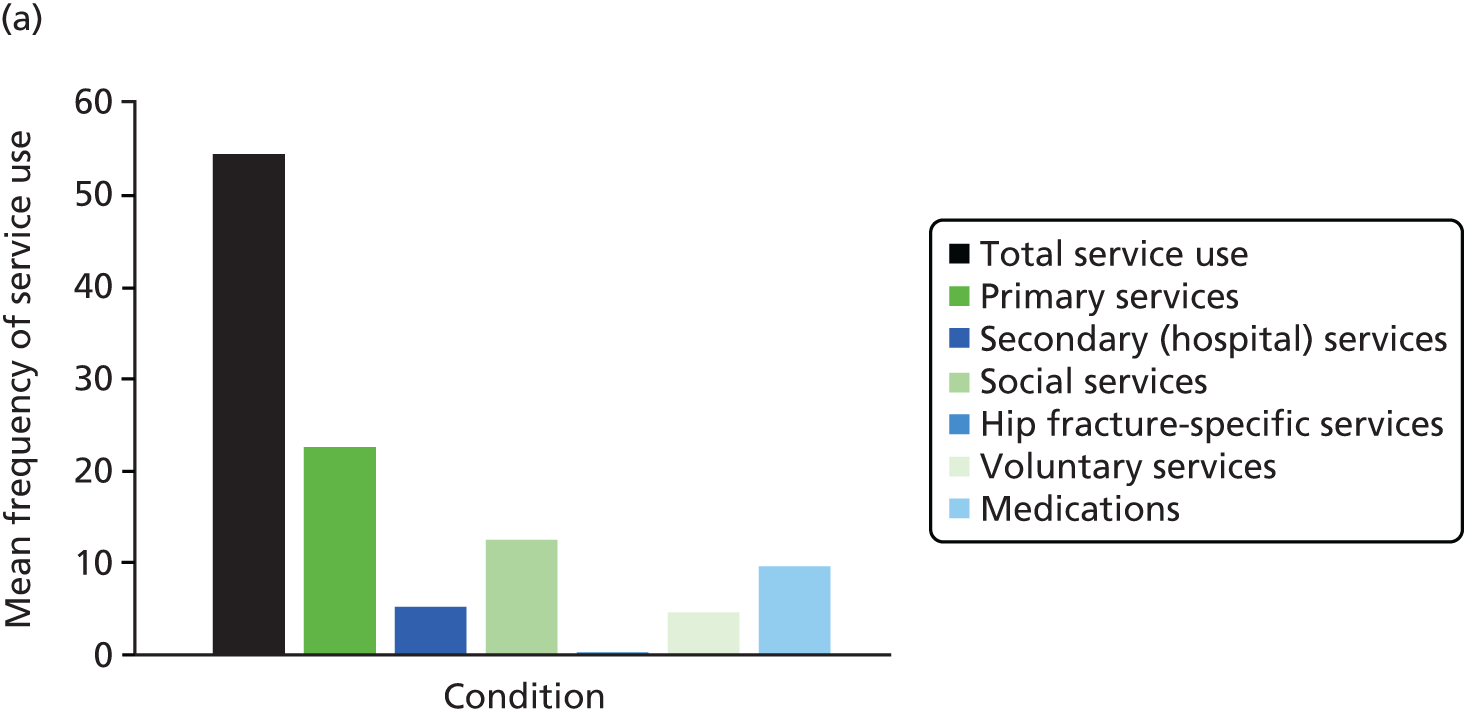
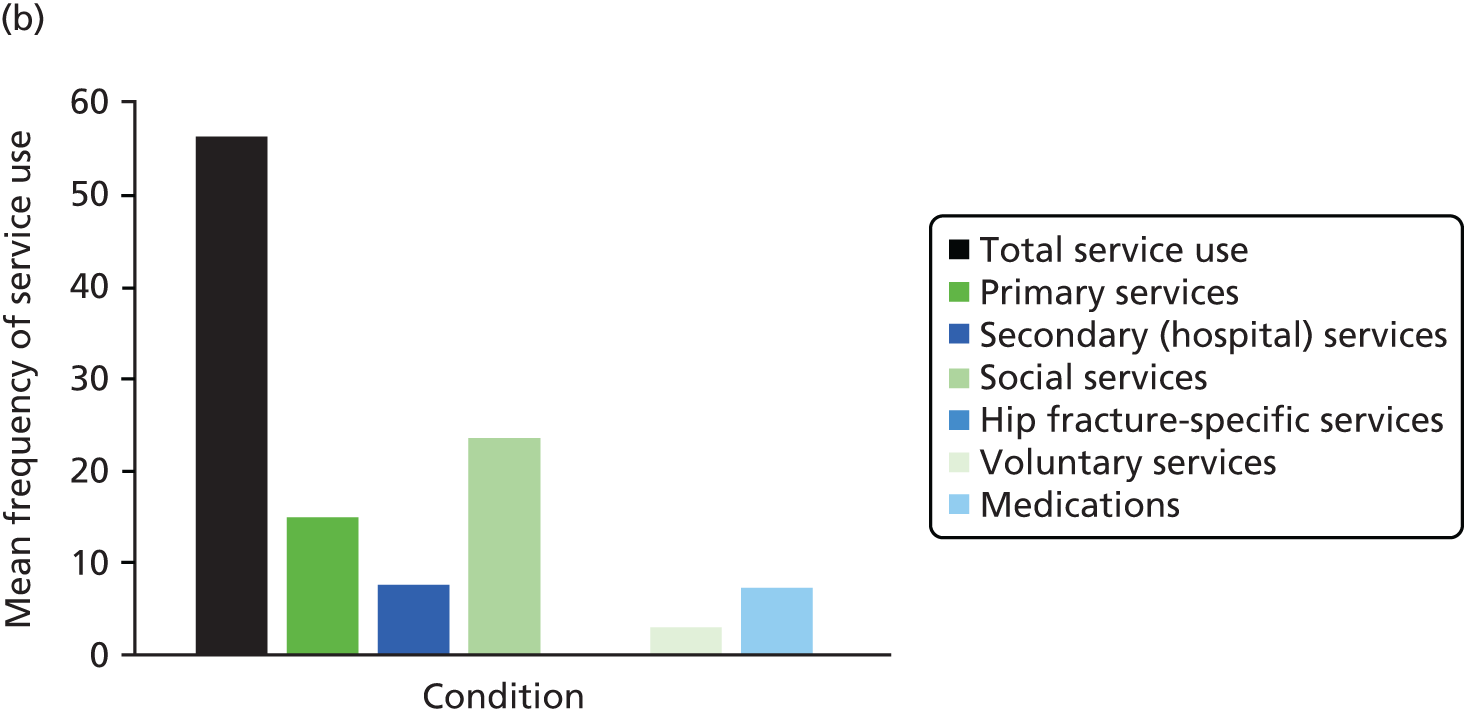
Figure 19 shows the costs of primary and secondary health-care service, social care service, proximal femoral fracture-specific service and voluntary/charity service use, as well as medication use, in the intervention group (n = 21) and the control group (n = 22) during the 3 months prior to follow-up. Service use costs were mainly accrued by secondary (hospital) health-care services, as patients underwent surgery and required time in hospital to recover. In total, 51% (n = 22) of the sample reported a longer than average inpatient stay post surgery. A longer inpatient stay was reported by 67% (n = 14) of the intervention group and 36% (n = 8) of the control group.
FIGURE 19.
Mean costs of primary and secondary health-care, social care, proximal femoral fracture-specific and voluntary/charity service use by participants in the intervention group and the control group, as measured by the CSRI during the 3 months prior to follow-up: (a) intervention group; and (b) control group. Costs are rounded to the nearest pound and are presented for the cost year 2013–14.

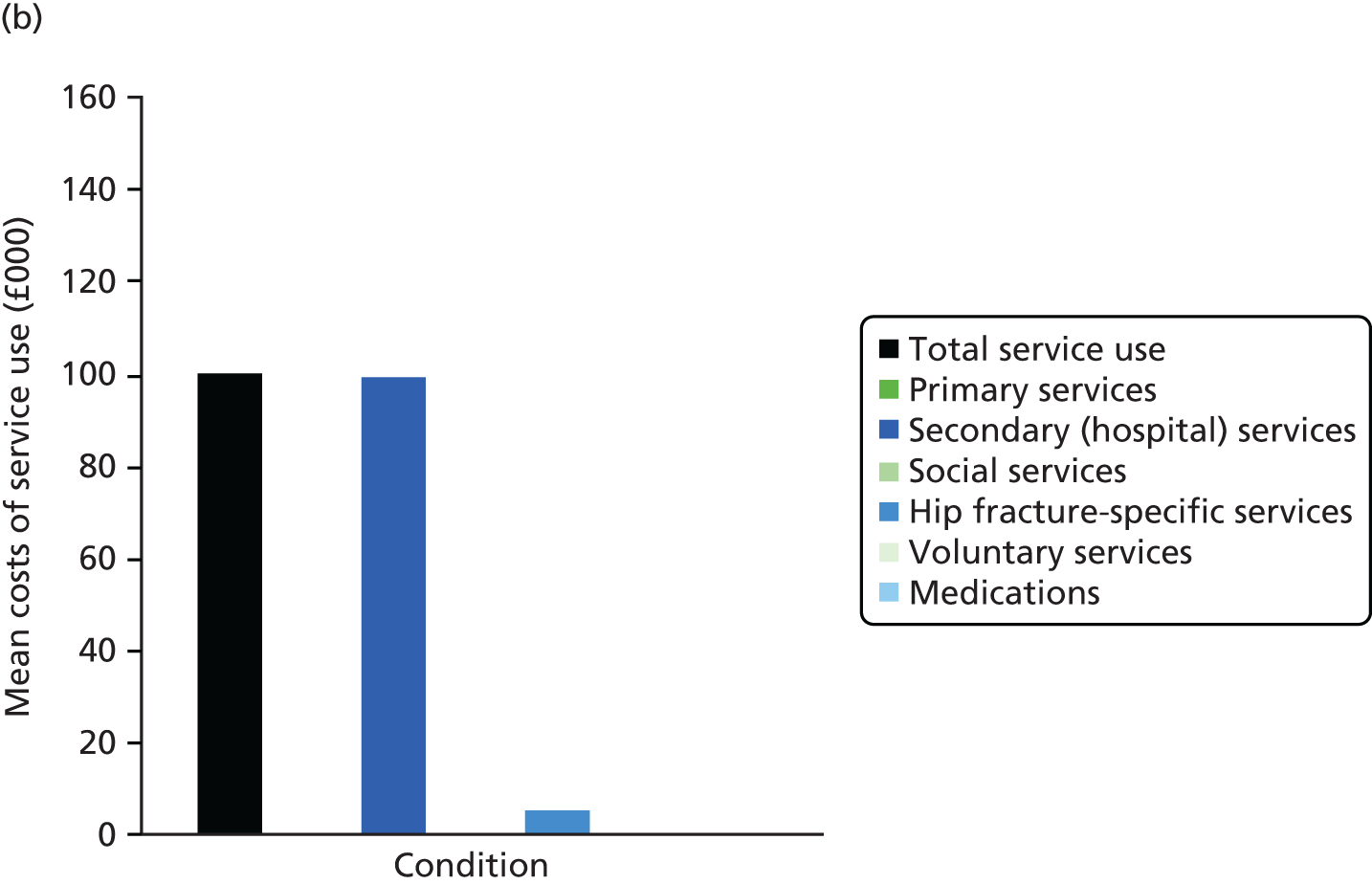
Secondary (hospital) health-care services accounted for 96% of the costs of service use at follow-up in the intervention group, with the remaining 4% accrued by hip fracture-specific services such as the National Exercise Referral Scheme and enablement centres. Similarly, in the control group, secondary (hospital) health-care services accounted for 95% of the costs of service use at follow-up, with the remaining 5% accrued by hip fracture-specific services.
Mann–Whitney U-tests revealed a statistically significant difference between the two groups in mean total hospital costs (U = 135.00, p = 0.02) and total service use costs per participant (U = 136.00, p = 0.02). This finding could be attributed to a larger proportion of the sample in one group than in the other experiencing a longer inpatient stay. No statistically significant differences were detected between the groups in the costs of primary health-care service use (U = 202.00, p = 0.48), social care service use (U = 208.00, p = 0.52), hip fracture-specific service use (U = 219.00, p = 0.65), voluntary service use (U = 240.50, p = 0.68) and medication use (U = 181.00, p = 0.22).
Table 27 shows that, when further exploring participant inpatient stays at baseline, the mean number of inpatient bed-days in both groups was less than the average length of stay specified by the Department of Health NHS reference costs 2013–14. 339
| Type of ward | Intervention group (n = 21) | Control group (n = 22) | Average number of bed-days according to the Department of Health339 | ||
|---|---|---|---|---|---|
| Inpatient bed-days, mean | Percentage of inpatient admissions that were readmissions | Inpatient bed-days, mean | Percentage of inpatient admissions that were readmissions | ||
| Orthopaedic trauma inpatient ward | 8.00 | 0 | 7.00 | 0 | 14.27 |
| Renal inpatient ward | 0.00 | 0 | 9.00 | 0 | 9.27 |
| Medical inpatient ward | 0.00 | 0 | 4.00 | 0 | 5.56 |
Table 28 shows similar data for inpatient stays during the 3 months prior to follow-up for both groups. More often than not, the mean number of inpatient bed-days in the two groups exceeded the average length of stay specified in the Department of Health NHS reference costs 2013–14. 339 This finding further explains the high cost of participant service use at follow-up, as higher-cost excess inpatient bed-day costs were applied in the majority of cases. Additionally, as shown in Table 28, 50% of surgical inpatient ward stays were stated by participants to be readmissions, demonstrating the complexity involved in treating this cohort of elderly patients.
| Type of ward | Intervention group (n = 21) | Control group (n = 22) | Average number of bed-days according to the Department of Health339 | ||
|---|---|---|---|---|---|
| Inpatient bed-days, mean | Percentage of inpatient admissions that were readmissions | Inpatient bed-days, mean | Percentage of inpatient admissions that were readmissions | ||
| Orthopaedic trauma inpatient ward immediately following hip fracture | 15.15 | 5 | 10.47 | 0 | 14.27 |
| Surgical inpatient ward immediately following hip fracture | 15.50 | 50 | 17.33 | 0 | 14.27 |
| Assessment inpatient ward | 7.50 | 0 | 7.00 | 0 | 14.27 |
| Rehabilitation inpatient ward | 12.11 | 0 | 18.80 | 0 | 11.57 |
| Continuing care inpatient ward | 21.00 | 0 | 70.00 | 0 | 11.57 |
| Respite inpatient ward | 10.00 | 0 | 0.00 | 0 | 7.83 |
| Medical inpatient ward | 13.00 | 0 | 0.00 | 0 | 8.92 |
Contacts with health and social care professionals for hip-related reasons
As part of the CSRI,315 we asked whether or not contacts with services were hip related. Table 29 shows the mean frequency of contact with services in the intervention and control groups for hip-related reasons and other reasons during the 3 months prior to baseline. Table 30 shows the mean frequency of contact with services in the intervention and control groups for hip-related reasons and other reasons during the 3 months prior to follow-up.
| Type of service | Intervention group (n = 21), mean frequency of contact | Control group (n = 22), mean frequency of contact | Mann–Whitney U-test | p-valueb |
|---|---|---|---|---|
| Primary services | ||||
| Hip-related reasons | 0.33 | 0.41 | 240.50 | 0.68 |
| Other reasons | 1.76 | 2.18 | 232.00 | 0.98 |
| Secondary (hospital) services | ||||
| Hip-related reasons | 0.10 | 0.50 | 282.50 | 0.51 |
| Other reasons | 0.62 | 0.50 | 198.50 | 0.33 |
| Type of service | Intervention group (n = 21), mean frequency of contact | Control group (n = 22), mean frequency of contact | Mann–Whitney U-test | p-valueb |
|---|---|---|---|---|
| Primary services | ||||
| Hip-related reasons | 18.19 | 12.41 | 196.00 | 0.39 |
| Other reasons | 4.10 | 2.32 | 145.00 | 0.02b |
| Secondary (hospital) services | ||||
| Hip-related reasons | 4.14 | 6.59 | 221.00 | 0.80 |
| Other reasons | 1.05 | 1.00 | 238.50 | 0.84 |
| Social services | ||||
| Hip-related reasons | 10.85 | 5.50 | 224.50 | 0.88 |
| Other reasons | 2.19 | 18.00 | 211.00 | 0.47 |
| Proximal femoral fracture-specific services | ||||
| Hip-related reasons | 0.19 | 0.09 | 208.00 | 0.35 |
| Other reasons | 0.10 | 0.09 | 230.00 | 0.96 |
| Medications | ||||
| Hip-related reasons | 1.33 | 1.05 | 199.00 | 0.41 |
| Other reasons | 5.57 | 4.82 | 183.50 | 0.25 |
As expected, a higher number of services was accessed for hip-related reasons in the 3 months prior to follow-up than in the 3 months prior to baseline. In total, 63% of the sample (n = 27) broke their hip after a fall and were admitted to hospital via A&E services. The only statistically significant difference between the groups was for contact with primary services for other reasons in the 3 months prior to follow-up (see Table 30). No other statistically significant differences were found between the groups using Mann–Whitney U-tests.
Costs of the intervention
Table 31 shows the unit costs of producing and implementing the intervention as part of the feasibility trial. The intervention consisted of a patient-held information workbook, a goal-setting diary and extra physiotherapy sessions. A mean of five additional therapist/technical instructor sessions were available to intervention participants once they returned home or were admitted permanently to a care home. These extra sessions were tailored to individuals’ needs at the discretion of the community occupational therapist or physiotherapist responsible for their care. The trial manager liaised with the local health board to purchase staff time to provide training in the intervention and intervention delivery; the study trial manager supplied these staff costs for the health economics analysis. The associated costs of printing the workbook and diary were also supplied by the study trial manager for the health economics analysis. Table 31 shows that it cost a total of £6711.46 to deliver the intervention to the 29 participants who were randomised to the intervention group, equating to £231.43 per person. However, only 21 participants received the intervention in the trial. It should be highlighted that the costs of developing the intervention and liaising with the local health board to operationalise the additional sessions are not included Table 31. We did not include these costs as we wished to focus on implementation costs rather than development costs.
| Type of cost | Units | Unit cost | Total cost (£) |
|---|---|---|---|
| Workbooks and goal-setting diaries | 135 workbooks and 135 diaries (90 workbooks and 90 diaries printed in English; 45 workbooks and 45 diaries printed in Welsh) | £3.78 per workbook and diary pair (£3.78 × 29 participants randomised to the intervention group) | 109.62 |
| Training | Six band 6 staff members and three band 4 staff members attended a 3-hour training session | Band 4 physiotherapy/occupational therapy assistant: £12.69 per hour (£12.69 × 3 × 3 = £114.21) | 447.03 |
| Band 6 physiotherapist/occupational therapist: £18.49 per hour (£18.49 × 3 × 6 = £332.82) | |||
| Travel to training | 240 miles total travelled | £0.67 per mile | 160.80 |
| Additional therapy sessions delivered to participants (physical exercise sessions, telephone calls to participants, referrals to other services, administrative tasks) | Five sessions delivered – on average, 1.08 hours (65 minutes) spent per session. On average, three sessions were conducted by a band 4 physiotherapy/occupational therapy assistant and two sessions were conducted by a band 6 physiotherapist/occupational therapist | Band 4 physiotherapy/occupational therapy assistant: (£16.03 per hour × 1.08) × 3 = £51.94; £51.94 × 29 participants randomised to the intervention group = £1506.26 | 2969.60 |
| Band 6 physiotherapist/occupational therapist: (£23.36 per hour × 1.08) × 2 = £50.46; £50.46 × 29 participants randomised to the intervention group = £1463.34 | |||
| Travel time to visit participants | On average, 1.1 hours (66 minutes) spent travelling to visit participants (round trip) | Band 4 physiotherapy/occupational therapy assistant: (£16.03 × 1.1) × 3 = £52.90; £52.90 × 29 participants randomised to the intervention group = £1534.10 | 3024.41 |
| Band 6 physiotherapist/occupational therapist: (£23.36 per hour × 1.1) × 2 = 51.39; £51.39 × 29 participants randomised to the intervention group = £1490.31 | |||
| Total cost of the rehabilitation intervention | 6711.46 | ||
| Cost per participant (based on 29 participants who were randomised to the intervention) | 231.43 |
Sensitivity analysis
As part of sensitivity analysis, we liaised with local health board staff to estimate the cost per participant of the intervention in a future full RCT using two separate costing models. Table 32 shows the cost of the intervention in the first model, in which a band 6 physiotherapist/occupational therapist conducted the first additional therapy session to assess the patient and conduct the initial goal-setting, with the subsequent four sessions conducted by a band 4 physiotherapy/occupational therapy assistant. Table 32 shows that it cost a total of £317.61 per participant to deliver the intervention using both band 6 and band 4 staff.
| Type of cost | Units | Unit cost | Total cost (£) |
|---|---|---|---|
| Workbooks and goal-setting diaries | 135 workbooks and 135 diaries (90 workbooks and 90 diaries printed in English; 45 workbooks and 45 diaries printed in Welsh) | £3.78 per workbook and diary pair | 3.78 |
| Training | One band 6 staff member and one band 4 staff member attended a 3-hour training session | Band 4 physiotherapy/occupational therapy assistant: £12.69 per hour (£12.69 × 3 × 1 = £38.07) | 93.54 |
| Band 6 physiotherapist/occupational therapist: £18.49 per hour (£18.49 × 3 × 1 = £55.47) | |||
| Travel to training | Average of 30 miles travelled per member of staff in the feasibility trial | £0.67 per mile (30 miles × 2 × £0.67) | 40.20 |
| Additional therapy sessions delivered to participants (physical exercise sessions, telephone calls to participants, referrals to other services, administrative tasks) | Five sessions delivered – on average, 1.08 hours (65 minutes) spent per session. One session was conducted by a band 6 physiotherapist/occupational therapist; four sessions were conducted by a band 4 physiotherapy/occupational therapy assistant | Band 4 physiotherapy/occupational therapy assistant: (£16.03 × 1.08) × 4 = £69.25 | 89.22 |
| Band 6 physiotherapist/occupational therapist: (£18.49 × 1.08) × 1 = £19.97 | |||
| Travel time to visit participants | On average, 1.1 hours (66 minutes) spent travelling to visit participants (round trip) | Band 4 physiotherapy/occupational therapy assistant: (£16.03 × 1.1) × 4 = £70.53 | 90.87 |
| Band 6 physiotherapist/occupational therapist: (£18.49 × 1.1) × 1 = 20.34 | |||
| Cost per participant | 317.61 |
In the second model, the health board advised that, if one member of staff was to conduct all five sessions, a band 5 physiotherapist/occupational therapist would be able to conduct the initial assessment and goal-setting session as well as the subsequent sessions. Table 33 shows that it would cost a total of £236.97 per participant to deliver the intervention if a band 5 physiotherapist/occupational therapist conducted all five additional therapy sessions.
| Type of cost | Units | Unit cost | Total cost (£) |
|---|---|---|---|
| Workbooks and goal-setting diaries | 135 workbooks and 135 diaries (90 workbooks and 90 diaries printed in English; 45 workbooks and 45 diaries printed in Welsh) | £3.78 per workbook and diary pair | 3.78 |
| Training | One band 5 physiotherapist/occupational therapist attended a 3-hour training session | Band 5 physiotherapist/occupational therapist: £15.33 per hour (£15.33 × 3 × 1 = £45.99) | 45.99 |
| Travel to training | Average of 30 miles travelled per member of staff in the feasibility trial | 0.67 per mile | 20.10 |
| Additional therapy sessions delivered to the participant (physical exercise sessions, telephone calls to participants, referrals to other services, administrative tasks) | Five sessions delivered – on average, 1.08 hours (65 minutes) spent per session. All sessions conducted by a band 5 physiotherapist/occupational therapist | Band 5 physiotherapist/occupational therapist: (£15.33 × 1.08) × 5 | 82.78 |
| Travel time to visit participants | On average, 1.1 hours (66 minutes) spent travelling to visit participants (round trip) | Band 5 physiotherapist/occupational therapist: (£15.33 × 1.1) × 5 | 84.32 |
| Cost per participant | 236.97 |
Tables 32 and 33 demonstrate two different costing models that could be employed to deliver the intervention in a full RCT. The cost per participant ranged from £236.97 to £317.61, with the least costly option being to use one member of staff to deliver all sessions. However, as the feasibility trial did not employ a band 5 physiotherapist/occupational therapist and this model is untested, future trials should ensure that staff are fully trained to deliver the intervention to ensure fidelity to the original programme.
Key findings
A sample of 43 participants was used for the cost–consequences analysis.
The ICECAP-O313 questionnaire had a lower completion rate than the EQ-5D questionnaire,287 which has implications for a full-scale future trial. The cost–consequences analysis demonstrated that it cost a total of £6711.46 to deliver the intervention (£231.43 per person, based on the 29 participants randomised to the intervention group).
Both the intervention and the control groups showed improvements in the EQ-5D health utility index, EQ-5D VAS score and the ICECAP O capability index at follow-up compared with baseline. There were no statistically significant differences between the groups in any of these three measures, but this small feasibility trial was not powered to test such a difference.
The intervention group had slightly higher mean QALY gains than the control group, although this difference was not statistically significant; however, this small feasibility trial was not powered to test such a difference.
There was a statistically significant difference between the two groups in mean total hospital costs and total costs of service use per participant. This could be attributed to a larger proportion of the sample in one group than in the other experiencing a longer inpatient stay. No other statistically significant differences were detected for the other service use categories.
Although in a disaggregated cost–consequences form our economic analysis shows that the multidisciplinary intervention, workbooks and diaries were no more effective than receiving usual care, this small feasibility trial was not powered to test such a difference.
Work stream 2: assessing the feasibility of measuring patients’ preferences for proximal femoral fracture rehabilitation services using a discrete choice experiment
Objective
The objective of this workstream was to assess the feasibility of using a DCE to measure participants’ preferences for proximal femoral fracture rehabilitation services.
Methods
A DCE is a method for eliciting individuals’ preferences about goods and services. 349 It is based on the theory that individuals make trade-offs between choices. 349 The DCE used in this trial explored participants’ preferences for rehabilitation services. Hypothetical rehabilitation services (A and B) were presented in the form of a questionnaire given to each participant according to a set number of characteristics, each of which had different levels. These characteristics and levels created a set of alternative scenarios. In each scenario, the participant was asked which service they preferred by ticking A or B. In the DCE, the characteristics and levels were chosen based on the outcomes of the literature review and focus groups conducted in Phase I of the study (see Chapters 2 and 5).
Table 34 describes the attributes (characteristics) and levels chosen to create the alternative scenarios used in the DCE questionnaire. The different attributes and levels yielded a total of 108 hypothetical scenarios. However, to create a manageable number of scenarios for participants, we used the appropriate mixed-level orthogonal arrays360 to derive a reduced number of 16 hypothetical scenarios. For each of the 16 scenarios, participants were presented with two hypothetical service scenarios and asked to choose the preferred service, A or B. A member of the research team was present during completion of the DCE questionnaire at the 3-month follow-up to answer queries and help participants understand the questions and how to complete the questionnaire.
| Attributes | Levels |
|---|---|
| 1. Time with health-care professional to conduct follow-up rehabilitation exercises or activities | 30 minutes |
| 60 minutes | |
| 90 minutes | |
| 2. Qualifications of health-care professional who provides my rehabilitation | Supervised, unqualified assistant |
| Fully qualified | |
| 3. How will my rehabilitation progress be monitored? | By health-care professionals in your medical records |
| By myself in a workbook/diary | |
| 4. Where will my rehabilitation take place? | In hospital with good gym equipment and health-care professionals experienced in rehabilitation |
| In the community (e.g. leisure centre) with good gym equipment and experienced exercise instructors | |
| At home with limited equipment (e.g. step) | |
| 5. Information about additional services to support rehabilitation | Hospital-based services only (e.g. hydrotherapy pool) |
| Community services only (e.g. National Exercise Referral Scheme) | |
| Both hospital and community services |
Analysis
Conditional logit regression techniques recommended by Ryan et al. 349 were used to assess which attributes were important to participants and the direction of participants’ preferences for rehabilitation services using Stata 10.1 (StataCorp LP, College Station, TX, USA). Non-parametric 5000 bootstrap replications using Stata 10.1 were also conducted as part of the analysis to gain stability around the coefficient estimates, to create a 95% CI.
Results
Of the 61 participants recruited to the trial, 12 withdrew. Of the remaining 49 participants, one participant completed the follow-up assessment over the telephone and therefore the DCE could not be completed as the measure cannot be administered over the telephone. One participant was given a previous version of the questionnaire that had more than 16 scenario choice sets. One participant was not available at follow-up to complete the measures. Eight participants did not receive any rehabilitation and therefore felt that the DCE questionnaire was not relevant to them and declined to complete it. Four participants struggled to understand the questionnaire and how to answer it, and therefore did not complete the measure. Two participants left questions blank; as the DCE questionnaire requires all questions to be answered for analysis to be conducted, these participants were removed from the final analysis. After removing the 12 withdrawn participants and the 17 non-completers, 32 participants remained in the DCE analysis. Ryan et al. 349 suggest that a sample size of at least 30 individuals is required to undertake DCE analysis; therefore, we analysed the results from the 32 sets of data received.
Table 35 describes the characteristics of the DCE sample. The DCE sample was similar to the main clinical and economic samples. There were more women than men in the sample and the mean age of the sample was 79.28 years. Slightly more participants in the DCE sample lived with others, whereas in the main clinical and economic samples there was an even split between those who lived alone and those who lived with others. As in the main clinical and economic samples, the majority of participants in the DCE sample owned their own home, with fewer participants living in privately rented properties, housing association/local authority properties or sheltered accommodation. Hemiarthroplasty surgery was the most common type of surgery received, followed by internal fixation. The majority of participants who completed the DCE questionnaire were recruited from Wrexham Maelor, with the fewest number recruited from Ysbyty Gwynedd.
| Characteristic | DCE sample, n (%) |
|---|---|
| Age at baseline (years), mean (SD); range | 79.28 (7.54); 67–91 |
| Gender | |
| Female | 22 (69) |
| Male | 10 (31) |
| Usually lives | |
| Alone | 15 (47) |
| With others | 17 (53) |
| Accommodation type | |
| Owner-occupied property | 25 (78) |
| Privately rented property | 4 (13) |
| Housing association/local authority property | 3 (9) |
| Sheltered accommodation | 0 (0) |
| Type of fracture | |
| Intracapsular | 14 (44) |
| Extracapsular | 14 (44) |
| Not recorded in notes/notes unavailable | 4 (13) |
| Type of surgery | |
| Hemiarthroplasty | 13 (41) |
| Internal fixation | 11 (34) |
| Intramedullary nailing | 1 (3) |
| Total hip arthroplasty | 5 (16) |
| Not recorded in notes/notes unavailable | 2 (6) |
| Direct discharge | |
| Yes | 22 (69) |
| No | 10 (31) |
| Recruited from | |
| Ysbyty Glan Clwyd | 14 (44) |
| Wrexham Maelor | 16 (50) |
| Ysbyty Gwynedd | 2 (6) |
During development of the DCE, we hypothesised that participants would prefer more time with the health-care professional and sessions to be delivered by a fully qualified physiotherapist or occupational therapist rather than a supervised unqualified assistant. We expected participants to prefer to monitor their own progress using a workbook/diary as opposed to progress monitoring being carried out by a health-care professional using medical records. We also hypothesised that participants would prefer to undertake any rehabilitation at home. Finally, we expected participants to prefer to receive information about both hospital and community additional services to support their rehabilitation. Table 36 provided the results of the conditional logit regression. The sign of the beta-coefficient indicates the direction of preference for each attribute; based on our hypotheses we expected positive beta-coefficients for all five attributes analysed.
| Attribute | β-coefficient | SE | p-valueb | 5000 bootstrapped 95% CI |
|---|---|---|---|---|
| Time with health-care professional delivering rehabilitation sessions | 0.005 | 0.002 | 0.043b | 0.000 to 0.010 |
| Qualifications of health-care professional delivering rehabilitation sessions | –0.596 | 0.094 | 0.000b | –0.862 to –0.445 |
| Rehabilitation progress monitoring | 0.088 | 0.094 | 0.344 | –0.112 to 0.299 |
| Venue of rehabilitation | 0.084 | 0.072 | 0.241 | –0.068 to 0.255 |
| Additional rehabilitation service information | –0.085 | 0.073 | 0.243 | –0.257 to 0.072 |
| Number of observations = 512 | ||||
| Number of individuals = 32 | ||||
| Log-likelihood function = –261.246 | ||||
Only two of the five coefficients (qualifications of health-care professional delivering the rehabilitation sessions and time with the health-care professional delivering the rehabilitation sessions) were statistically significant (p < 0.05), indicating that these attributes were important to the participants questioned. When these two significant results were ranked in order of importance, the qualifications of the health-care professional delivering the rehabilitation sessions was the most important. In accordance with our a priori hypotheses, the coefficients for time with the health-care professional delivering the rehabilitation sessions, rehabilitation progress monitoring and venue of rehabilitation were all positive. However, only time with the health-care professional delivering the rehabilitation sessions was statistically significant. In contrast to our a priori hypotheses, the coefficients for qualifications of the health-care professional delivering the rehabilitations sessions and additional rehabilitation service information were negative. This indicates that the participants preferred rehabilitation to be delivered by a supervised unqualified assistant rather than a fully qualified physiotherapist or occupational therapist and that participants also preferred the provision of additional information about hospital-based services only, rather than information about both hospital and community services. However, of these two attributes, only one was statistically significant: the qualifications of the health-care professional delivering the rehabilitations sessions. In the feasibility trial, physiotherapy/occupational therapy assistants delivered the majority of the five additional sessions received. Participants who had experienced the rehabilitation intervention may have had more contact with the assistants, thus building a relationship with them and preferring them to deliver rehabilitation. In addition, in usual care it is possible that physiotherapy/occupational therapy assistants conducted more of the rehabilitation sessions. There is further evidence from the Phase II focus groups (see Chapter 10) that physiotherapy/occupational therapy assistants focused more on ADL and confidence than physiotherapists/occupational therapists and that focus group attendees preferred these sorts of activities. With regard to the provision of additional information about services to support rehabilitation, following discharge from hospital, usual care in the trial was patchy and varied greatly across the region, and therefore participants were more likely to access community services such as the National Exercise Referral Scheme, leading them to prefer the provision of advice about additional hospital-based services.
Key findings
The results from this DCE analysis demonstrated that the methodology can be applied in an elderly population [mean age 79.28 years (SD 7.54 years)] following proximal femoral fracture.
Only four participants failed to complete the questionnaire because of a lack of understanding.
Two attributes were found to be important to participants: time with the health-care professional delivering the rehabilitation sessions and the qualifications of the health-care professional delivering the rehabilitation sessions.
The coefficients for three of the five attributes were positive (time with the health-care professional delivering the rehabilitation sessions, rehabilitation progress monitoring and venue of rehabilitation), as expected in our a priori hypotheses. However, in contrast to our a priori hypotheses, the coefficients for the qualifications of the health-care professional delivering the rehabilitation sessions and information about additional rehabilitation services were negative.
If DCE methods are to be used in a full-scale trial, further pilot work is required to ensure that the attributes and levels chosen for the feasibility trial are meaningful across the population of interest and to further test the questionnaire with regard to layout and wording.
Work stream 3: scoping the potential to conduct social return on investment analysis in a future trial based on data gathered in the feasibility trial
Objective
The objective of this workstream was to scope the potential of conducting a SROI analysis based on the data received from the feasibility trial to inform whether or not a full SROI analysis would be possible in a full-scale RCT of the multidisciplinary rehabilitation intervention.
Methods
Using the measures administered in this feasibility trial, we assessed the completeness of the responses and the level of detail provided by the respondents to scope the potential for using these as a source of data for a larger-scale SROI analysis. SROI analysis requires data to quantify the tangible and intangible outcomes from an intervention compared with those of a control condition, assign a monetary value to those outcomes, and assess attribution and the length of effect of an intervention.
Results
For the main outcomes of the feasibility trial (see Chapter 9) and in the health economics analysis (see Work stream 1), we received a high level of complete data from the sample. At baseline the measures were approximately 90% complete, although at follow-up this reduced to approximately 80%. The CSRI,315 in particular, was completed well by the participants, with good detail recorded of the services accessed. This made calculating the costs of service use by participants in the economic sample, using national sources of costs, very manageable. However, we recognise that the CSRI questionnaire administered at follow-up was lengthy and that other methods of data collection, such as using hospital records, may improve the efficiency of data collection, in particular for hospital service use, in the future.
The current measures collected in the feasibility trial would provide data to describe what changes have occurred for two potential payer stakeholders: patients and publicly funded services such as the NHS. Measures of health-related quality of life, self-reported capability, improvement following rehabilitation, ADL, anxiety and depression, pain, self-efficacy and fear of falling describe changes for patients, whereas the health, social care and voluntary service use data collected using the CSRI describe the changes that have occurred for these services.
The benefit of using SROI analysis is that it allows wider and intangible outcomes, for example happiness, leisure time and socialising, to be explored. The measures used in the feasibility trial assessed a wide range of outcomes including fear of falling and ADL. However, we did not further explore potential wider outcomes as we wanted the number of measures used in the trial to be appropriate for the sample in question. This consideration was particularly important at the baseline assessment, which occurred very soon after the participants had experienced a proximal femoral fracture. As we did not include these wider outcome measures in the feasibility trial, we cannot say whether or not their inclusion in a full-scale RCT would allow SROI analysis to be conducted. In addition, we would need to further explore the data available for this population of interest, with particular reference to data banks and valuation techniques such as well-being valuation, to place a value on non-market goods and services. 361,362
In SROI analysis, it is essential to calculate what would have happened without the intervention, to attribute how much change the intervention is responsible for. In RCTs, the control group can provide an estimate of what would have happened without a particular intervention. However, we note that in the feasibility trial, participants assigned to the control group requested additional help and support from NHS rehabilitation services. In the trial, usual care was patchy and varied greatly across the region. The majority of control participants who requested additional help and support did so because they knew they were part of a research trial and therefore expected to receive something. A large-scale full RCT would need to ensure that those in the control group do not receive an intervention or additional services. The issue of control group compared with intervention group is key, because if the groups in the trial are not distinct then SROI analysis will not be able to determine what changes are the direct result of the intervention. Furthermore, to assist attribution, questionnaires can be administered to participants assigned to the intervention group, asking them to what extent the outcomes that they have experienced are the result of the intervention. Figure 20 provides an example of an attribution question. The appropriateness of using an attribution questionnaire for the sample in question needs to be carefully considered. As mentioned previously, participant burden when completely questionnaires was a key consideration for the research team.
FIGURE 20.
Example attribution question.
Key findings
Based on the data collected in the feasibility trial we cannot currently answer the question of whether or not a SROI analysis would be possible in a full-scale trial.
We identified the patients and publicly funded health and social care services as potential payer stakeholders in our scoping exercise.
Measures administered in the feasibility trial were acceptable to participants; however, we recognise that the CSRI315 questionnaire administered at follow-up was lengthy. In a future trial, efficiency may be improved by gaining access to hospital records to collect data about hospital services used by participants (see Chapter 12).
Further work is required to test the completeness and acceptability of additional measures such as attribution questionnaires and questionnaires to assess wider outcomes, for example happiness.
Additionally, in further work, the added benefit of conducting a SROI analysis compared with cost-effectiveness or cost–utility analyses using a multiagency perspective needs to be determined.
Discussion
Summary of findings
We report a range of health economic analyses to address a number of objectives for this feasibility trial. A cost–consequences study explored the feasibility of conducting an economic evaluation in this trial, setting out disaggregated findings as the feasibility trial was not powered to test an effect in the primary outcome measure, the BADL index. Both the intervention group and the control group showed improvements in the EQ-5D health utility index, EQ-5D VAS score and ICECAP-O capability index at follow-up compared with baseline. There was no statistically significant difference between the groups for any of the measures, but this small feasibility trial was not powered to test such differences. The intervention group had slightly higher mean QALY gains than the control group, although this difference was not statistically significant. The only statistically significant differences between the groups were in mean total hospital costs and the total cost of service use per participant. However, this could be attributed to a larger proportion of the sample in one group than in the other experiencing longer inpatient stays. No other statistically significant differences were detected for the other service use categories. A DCE demonstrated that it is possible to use this method with an elderly population (mean age of 79.28 years). Only four participants failed to complete the questionnaire because of a lack of understanding. Two attributes were found to be important to participants: time with the health-care professional delivering the rehabilitation sessions, with participants preferring more time with the health professional, and the qualifications of the health-care professional delivering the rehabilitations sessions, with participants preferring supervised unqualified assistants to fully qualified physiotherapists/occupational therapists. A scoping study of the potential to conduct a SROI analysis as part of the feasibility trial identified that measures were well completed in the trial, with a small drop-off rate at follow-up (approximately 80% completion) compared with baseline (approximately 90% completion). Potential payer stakeholders included the patients and publicly funded health and social care services. Further work is needed in this area to assess the added value of conducting a SROI analysis compared with a cost-effectiveness or cost–utility analysis using a multiagency perspective.
Strengths and limitations
There is limited economic evidence relating to rehabilitation following proximal femoral fracture, particularly in a UK context. This feasibility trial and concurrent economic analysis, including a cost–consequences analysis, DCE and scoping study of SROI analysis, adds to the evidence base and addresses the particular need for more UK-based evidence, as highlighted by NICE. 7 We demonstrated that the intervention was relatively low cost, with a cost per participant of £231.43, and that measures such as the EQ-5D and ICECAP-O were acceptable to most participants. However, the ICECAP-O was subject to a lower completion rate than the EQ-5D (92% and 98%, respectively). Additionally, we demonstrated that a DCE questionnaire could be used with this elderly population. The lack of power to detect an effect in the main outcome measure (the BADL index) resulted in the use of cost–consequences analysis rather than cost–utility or cost-effectiveness analysis, which were specifically highlighted by NICE7 as being needed in the area of proximal femoral fracture. However, we used a range of methods to answer the specific objectives, including cost–consequences analysis, which is championed as a method that is particularly relevant to economic evaluations carried out alongside public health interventions. 352–354 The need to ensure that the battery of measures used in the feasibility trial was manageable for participants and reduce participant burden, particularly as the baseline assessment was conducted very shortly after participants had experienced their fracture, meant that the extent to which a SROI analysis could be conducted was limited. In the feasibility study, data were collected on outcomes such as health-related quality of life, self-reported capability, improvement following rehabilitation, ADL, anxiety and depression, pain, self-efficacy and fear of falling. However, wider and intangible outcomes, for example happiness, leisure time and socialising, were not assessed in the feasibility study. One of the main benefits of a SROI analysis is the ability to value intangible outcomes and further work is needed to assess the acceptability of such additional measures to the population included in this feasibility trial.
Comparison with previous literature
The systematic review reported in Chapter 3 did not identify any cost–consequences studies; therefore, we cannot make direct comparisons between our study and the previous literature. However, Olsson et al. 260 demonstrated using cost-effectiveness analysis in a Swedish hospital setting that an integrated care pathway, with a focus on motivation for rehabilitation and early first ambulation, was less costly and more effective than the usual care pathway for patients admitted with hip fracture. Additionally, Cameron et al. 253 found that, in an Australian general hospital setting, an accelerated rehabilitation intervention using early assessment, early mobilisation, physical independence and detailed discharge planning was more cost-effective than conventional rehabilitation in treating proximal femur fracture. These two analyses found that patient-centred approaches to rehabilitation were a good use of hospital resources. The intervention applied in this feasibility trial used personalised goal-setting and diaries to provide a record of progress during rehabilitation, utilising a similar ethos to that in the studies by Olsson et al. 260 and Cameron et al. 253 of patient-centred approaches to rehabilitation.
The mean EQ-5D health utility index scores for the intervention group [0.50 (SD 0.26)] and the control group [0.37 (SD 0.43)] were lower than the UK population mean score for men and women aged ≥ 75 years living in Wales [0.80 (SD 0.24)]. 363 At follow-up, the EQ-5D health utility index scores remained lower than the UK population mean score of 0.80 (SD 0.24), with the intervention reporting a mean score of 0.66 (SD 0.27) and the control group reporting a mean score of 0.60 (SD 0.27).
Additionally, the mean EQ-5D VAS scores for both groups were lower at baseline [intervention 64.43 (SD 16.37), control 55.14 (SD 25.72)] and follow-up [intervention 71.10 (SD 17.89), control 68.55 (SD 18.44)] than the UK population mean score for men and women aged ≥ 75 years living in Wales [82.91 (SD 12.33)].
Compared with the mean EQ-5D health utility index score reported by Davis et al. 364 for a female sample of older adults (mean age 79.3 years) with mobility impairments [0.701 (SD 0.291)], the mean EQ-5D health utility index scores in the feasibility study, which included a sample of predominantly women (women, n = 32, men, n = 11), were lower at both baseline and follow-up in both groups. The mean EQ-5D VAS scores in the feasibility study were also lower for both groups at both baseline and follow-up than the mean EQ-5D VAS score in the study by Davis et al. 364 [72.3 (SD 17.6)].
Davis et al. 364 administered the ICECAP-O to their female sample with mobility impairments, reporting a mean ICECAP-O capability index score of 0.815 (SD 0.177). In the feasibility study, the control group reported a lower mean score at both baseline and follow-up than the mean score reported by Davis et al. 364 Conversely, the intervention group in the feasibility study reported a slightly higher mean score at both baseline and follow-up than the mean score reported by Davis et al. 364
As in the feasibility study, previous DCE studies conducted by Milte et al. 365 and Laver et al. 366 demonstrated that this method can be used in a frail elderly population aged between 71 and 80 years who have experienced proximal femoral fracture, stroke and other neurological conditions. However, rather than focusing on the elements of rehabilitation as in this study, the line of inquiry in the study by Milte et al. 365 was to establish what frail older people in Australia are prepared to endure to achieve improved mobility following hip fracture. Attributes included the risk of falling and breaking another bone during rehabilitation, level of pain accepted to recover the ability to walk short distances, the level of effort needed during rehabilitation and ability to recover walking following participation in the programme. Laver et al. 366 conducted a DCE in southern Australia to explore the differences in preferences of patients, occupational therapists and other rehabilitation clinicians for the way in which rehabilitation services are provided.
Implications for practice and/or future research
The feasibility study demonstrated that measures such as the EQ-5D,287 ICECAP-O313 and CSRI315 are acceptable to participants, with an approximately 90% completion rate at baseline and an approximately 80% completion rate at follow-up. However, we note that the ICECAP-O was subject to a lower rate of completion in the economic sample. Although the measure was developed with a general population sample of older adults, we found that during the feasibility study three participants were unable to answer the questionnaire as they felt that the domains did not apply to them (e.g. they felt that they had no social life at the moment and so could not answer the questionnaire). Horwood et al. 367 conducted a think-aloud study of the face validity of the ICECAP-O with hip and knee arthroplasty patients. In the sample of 20 older individuals with hip or knee arthroplasty, a minority (n = 5) showed some confusion over, and had difficulty understanding, the questionnaire. Horwood et al. 367 commented that during the think-aloud exercise a minority of the sample interpreted the questions within their disease context, linking it directly with their joint replacement or other conditions such as arthritis. Horwood et al. 367 postulated that this context-specific answering was a result of the timing of the interview, which took place days before their joint replacement surgery. The acceptability of the ICECAP-O questionnaire in the feasibility study could also be linked with the timing of administration. This measure was administered shortly after fracture and then 3 months later. At 3 months post baseline, many participants still may not have gained mobility and, thus, may have felt dependent and frustrated that they could not currently do the things that they had previously enjoyed, such as gardening. The use of the ICECAP-O in a future RCT should be considered carefully. Although the measure explores a broader concept of well-being rather than being a purely health-related measure, the implication that participants may be answering it within a disease-specific context, and therefore find it distressing or difficult to answer, may mean that just administering the questionnaire is not sufficient. In a future RCT it may be useful to include an additional qualitative element as part of questionnaire administration to uncover how participants are interpreting the questionnaire.
Future research should also consider the value of conducting a SROI analysis compared with a cost-effectiveness or cost–utility analysis using a multiagency perspective. The feasibility study did not include the valuation of wider, intangible outcomes such as happiness, to keep the battery of measures manageable and to reduce the burden on participants. Further work is required to assess the acceptability and completeness of additional measures, such as attribution questionnaires and questionnaires, to assess wider outcomes.
Conclusion
The complete case cost–consequences analysis included a sample of 43 participants. The total cost of the intervention was £6711.46 (£231.43 per participant). There were improvements in both the intervention and the control groups in the EQ-5D health utility index, EQ-5D VAS score and ICECAP-O capability index at follow-up compared with baseline. However, these improvements were not statistically significant for any of the measures. The intervention group had slightly higher mean QALY gains than the control group, although this difference was not statistically significant. Statistically significant differences between the two groups in mean total hospital costs and total cost of service use per participant were found. In the DCE, participants indicated preferences for spending an increased amount of time with the health-care professional delivering the rehabilitation sessions and for a physiotherapy/occupational therapy assistant to deliver the rehabilitation sessions. The scoping SROI analysis showed high levels of completeness for the measures chosen for the feasibility study, although further work is needed to investigate more intangible outcomes and how these could be quantified.
In summary, although NICE7 has called for further cost-effectiveness evidence in this area, we have demonstrated that it is feasible to conduct a range of health economic analyses, including cost–consequences analysis, a DCE and a scoping SROI analysis. The intervention resulted in improvements in the economic measures used. These improvements were not statistically significant, but this small feasibility study was not powered to test such differences. The intervention adopted a patient-centred approach to rehabilitation following proximal femoral fracture, which has been highlighted by others in the field as being a cost-effective method. 253,260
Chapter 11 Triangulation study
Introduction
As part of the economic evaluation we collected heath service activity data using the patient-completed CSRI. 315 This asked for retrospective information about activities such as general practice appointments, outpatient referrals, inpatient admissions, prescribed medication and investigations. This process can be burdensome for participants and may be inaccurate, particularly if participants have problems with memory and recall. There is increasing interest in using routinely collected data for health service research as an adjunct to the patient-completed CSRI to reduce participant burden. Information on A&E attendances, hospital admissions and outpatient appointments is collected on the health board’s computerised Patient Administration System. Information on general practice consultations, prescribing, secondary care referrals and investigations is collected on each general practice’s computerised record database.
The aim of this triangulation study was to test new methodologies to obtain routinely collected data on service use and evaluate the quality of the data acquired, and compare these data with data collected using patient-reported outcome measures. If successful, replacing some or all of the patient-reported measures of service use with data collected by researchers and NHS IT staff would have the potential to reduce participant burden and increase the efficiency of trial methods.
Method
The health service use data obtained from the patient-completed CSRI were compared with the same information obtained from routinely collected data recorded on computerised patient records (see Chapter 7). Informed patient consent was obtained for carrying out this study.
Identifying patients
A patient identity check was undertaken through IDRIS (Identifying Data for Research in Information Systems), a bespoke software system designed by NWORTH and developed by the BCUHB informatics department. The identification number, surname, forename, date of birth, gender, postcode and NHS number of each of the trial participants were inputted into the IDRIS system, which resides on servers within the BCUHB network. Participant information was checked in real time against data held on the Master Patient Index at the Welsh Demographic Service to confirm (or fail to confirm) the identity of the participants. If the enquiry to the Welsh Demographic Service failed to confirm a participant’s identity, no data for that participant would be made available to the researchers. Data were extracted for the 49 participants in the study (which excluded those who had withdrawn from the main trial).
Extracting data
The following data were extracted from BCUHB systems: inpatient days and episodes, outpatient episodes and A&E department episodes. Each patient whose identity was confirmed by the IDRIS system was added to a register containing their details and participant identification number. Once all participants had been checked by IDRIS the register was closed and sent electronically to the BCUHB informatics department, remaining on BCUHB secure servers at all times. The previously agreed data records for each participant were then extracted and anonymised, and patient-identifiable information was removed, in accordance with BCUHB information governance instructions, leaving only the participant identification number to link the records to the other anonymised data held for each patient. The data were then transferred to the study researchers using a secure file transfer system.
Comparing data
Data extracted from BCUHB systems were compared with data obtained from the CSRI questionnaire for consistency using the intraclass correlation coefficient (ICC). A value on this measure of ≥ 0.7 shows good consistency between the two data sources.
Results
Accident and emergency department attendances
In total, 60 A&E department attendances were logged in medical records compared with 43 reported in the CSRI data, which equates to under-reporting by 28%. Records for 24 of the 49 participants were found in both sources. Of the 24 participants, 21 under-reported attendances compared with BCUHB records and three over-reported attendances compared with BCUHB records. Other possible causes of over-reporting were loss of NHS records or episodes in which the patient presented directly to the acute medical unit, which was mistaken for the A&E department. An ICC model found a medium degree of agreement between the CSRI data and the BCUHB data. The single-measure ICC was 0.45 (95% CI 0.20 to 0.64; F49,49 = 2.619; p < 0.001). This suggests that there was an approximately 45% agreement between the two data sets, but with a wide CI.
Outpatient episodes
For outpatient data, the under-reporting appeared to be less pronounced, with 204 reported episodes in the CSRI data compared with 215 reported episodes in the medical records. However, a review of the CSRI data for the two patients who were outliers (one participant reported 30 in the CSRI data, with five logged in the medical records; the other patient reported 42 in the CSRI data, with three logged in the medical records) suggested that the CSRI data represented the length in minutes of each episode, rather than the number of episodes. When these outliers were excluded, the CSRI data again suggested that patients were prone to under-reporting. Records from both sources matched for only seven participants, with 28 participants under-reporting compared with the medical records and 15 participants over-reporting compared with the medical records. The agreement between the CSRI data and the BCUHB data was low, with an ICC of 0.28 (95% CI 0.0 to 0.52; F49,49 = 1.774; p = 0.024). This suggests that there was little similarity between the two data collection methods.
Inpatient days
For inpatient days, the data from the CSRI forms were well matched with the data obtained from the medical records. In total, 1254 inpatient days were recorded on the CSRI forms and 1274 inpatient days were logged in BCUHB records. The single-measure ICC was 0.88, representing a strong agreement between the CSRI data and the BCUHB data (F49,49 = 15.311, p < 0.001), which suggests that the two methods reported similar results for the number of inpatient days. Only five of the individual patient records matched exactly between the two data sets, which may be because days is a more difficult unit to record accurately than episodes, as was used within the A&E attendances and outpatient episodes comparisons. After several weeks in hospital it may have been difficult for patients to recall the exact number of days that they had been admitted, or there may have been differences in the way that arrival and departure days were counted. If an error margin of 6 days was allowed to counter such small errors, 39 of the 49 patients correctly recorded their inpatient stay.
During the comparison of the two data sets three data input errors were identified, which occurred when inputting data from the hard-copy CSRI forms into the MACRO database. The errors seemed to have occurred at random and straddled both treatment groups and so the discrepancies did not generate bias. These errors were within the 2% error rate that would trigger a full data entry audit (as specified in the data management plan) and so no further action was required.
Discussion
Summary
The triangulation study embedded within the Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR) study tested the methodology devised by NWORTH and BCUHB to make routinely collected data in BCUHB secondary care systems available to researchers after informed consent has been given by study participants. The methodology to provide such data was successful and it was demonstrated that it was feasible to obtain research data in this manner. Although some areas showed high levels of comparability between data obtained from medical records and data obtained from the CSRI, the two methods did not universally produce the same results. Further investigation will be required to elucidate the reasons for the discrepancies and confirm which method of data collection provides a higher level of accuracy.
Strengths and limitations
Provision of routinely collected data using electronic methods for research purposes holds considerable potential for future studies. In this study a novel methodology was applied, which meant that the process of making the data from hospital records available was slow and laborious. The data required were confidential and of a potentially sensitive nature, and each stage of the process required careful planning and liaison with stakeholders to ensure that the correct procedures and security processes were followed. In particular, liaison with the data keepers and BCUHB information governance had to progress with care and there were understandable and valid delays. Despite these challenges, the data were successfully obtained and the software and methodology are now in place. Future uses of this process will thus be much more streamlined while still ensuring that security procedures and good practice are adhered to.
Although it was possible to account for some of the discrepancies in the data by identifying data input errors or accounting for errors in patient recall, it was not possible to check the accuracy of the data collected from BCUHB systems. This is a current limitation that should be addressed in future work as it is not currently possible to confidently conclude which of the data sets provides the most accurate representation of service use.
Comparison with previous literature
There have been many studies in which routinely collected administration data have been compared with data obtained from patient self-reporting. These studies have been carried out in different settings and in different countries, thus reflecting different methods of collecting routine data and different IT systems for storage. The results reported have been contradictory and inconclusive. For example, one study reported a high concordance between self-reported and claims-based hospital episodes, but concordance for physician visits was low. 368 Factors significantly associated with bidirectional (over- and under-reporting) and unidirectional (over- or under-reporting) error patterns were detected. Caution was advised when drawing conclusions based on just one physician visit data source. Consistent with our findings, another study found that patients tended to report a lower number of visits to physicians than was recorded in the computerised medical records. 369 Similarly, a study of external sources of secondary care data in older German adults showed that survey estimates based on self-report tended to underestimate true health-care use in the older population. 370 In a prospective cohort study in Germany, self-reports regarding psychiatric inpatient and day-care use collected by telephone interviews based on the Client Socio-Demographic and Service Receipt Inventory, as well as calculated costs, were compared with data from computerised hospital records. The different data sources resulted in similar estimates at the population level; however, there were pronounced differences for outpatient visits at an individual level. 371 The accuracy of the results was heavily dependent on context. For example, GP records provided more accurate data on primary care contacts than patient reports, but less reliable information on contacts with other health services. In a further study, reliance on GP records for data related to hospital services and other community health services based outside general practice surgeries was not recommended. 372 A recently published review of studies on the Database of Instruments for Resource Use Measurement (DIRUM)315 found evidence for a good correlation between medical records and patient or carer recall. 373
Finally, the conclusions of Williams et al. 374 are still valid today:
Routine data have the potential to support health technology assessment by RCTs. . . . further work is required to improve the validity of routine data . . . . Better knowledge of the capability of local systems and access to the data held on them is also essential.
Implications for future research
The use of routinely collected data has the potential to improve the efficiency of trials and other studies. Although the methodology to make the data available has been successfully demonstrated, further investigation is required to evaluate the quality and accuracy of the data obtained and to test the validity of different data sources in different contexts.
Chapter 12 Discussion
Summary of the main findings
There were three components to Phase I of the study (developing the rehabilitation intervention): a realist review, a survey and focus groups (see Chapter 1).
Three programme theories emerged from the realist review: improving patient engagement by tailoring the intervention according to individual needs and preferences; reducing the fear of falling and improving self-efficacy to exercise and perform ADL; and co-ordination of services and sectors delivering the rehabilitation (see Chapter 2).
The systematic review of the economic evidence relating to rehabilitation of proximal femoral fracture identified seven economic evaluations conducted in different countries (see Chapter 3). Two of the three cost-effectiveness studies found that rehabilitation pathways were cost-effective. One of the two cost–benefit analyses found that the benefits of the intervention outweighed the costs. The two cost-minimisation studies found that the intervention being studied reduced costs. Further economic evidence is needed, particularly in a UK context.
The survey found that routine clinical practice is broadly in line with current guidance (see Chapter 4). However, there was variability in the provision of services, especially in the community, and important psychological mediators such as self-efficacy and fear of falling were not routinely assessed using validated tools.
The focus groups also found variation in the care provided, which was partly because of the individual tailoring of treatment, but also because of geographical variation in the availability of resources, the complex variety of providers delivering different components of rehabilitation programme and the lack of awareness by referring clinicians of the full extent of available services (see Chapter 5). There was a need for more information to be provided to patients, carers and clinicians. Facilitators of, and barriers to, rehabilitation included reliance on self-motivation to seek out services and engage with the rehabilitation programme, the pre-fracture level of functioning, comorbid conditions, transport issues, and co-ordination and communication between different components of the programme. Falling and fracturing had an important psychosocial impact in terms of anxiety, fear of falling and loss of independence.
After considering these findings, we developed an intervention to enhance usual rehabilitation by improving patients’ self-efficacy, thereby increasing the amount and quality of patients’ practice of physical exercise and ADL, to improve functional outcomes (see Chapter 6). The intervention included a patient-held information workbook and goal-setting diary, with additional therapy sessions provided to patients once they had returned home.
In Phase II of the study the feasibility of the rehabilitation intervention was assessed in a randomised feasibility study. The trial methods were feasible in terms of recruitment, randomisation and follow-up rates; however, recruitment was challenging. Those in the intervention group showed a moderate improvement in their ability to perform ADL as well as small improvements in self-efficacy and mental health (see Chapter 7).
An anonymised cohort study of all patients admitted with hip fracture to one of the three acute hospitals in the BCUHB during the first 6 months of the feasibility study period was conducted, with demographic data and data on readmissions collected (see Chapter 8). Comparison of the anonymised cohort with the randomised feasibility study population demonstrated that participants recruited to the feasibility study were younger and less likely to die or be readmitted to hospital than the anonymised cohort.
The key finding from the focus groups to investigate the acceptability of the study and intervention to patients, carers and therapists was that, in the context of variable usual rehabilitation care, the role of the therapist was extremely important in managing patients’ needs and expectations (see Chapter 9). This was especially so at the beginning of rehabilitation, for giving guidance and reassurance about what physical activity was safe to do. Regular home visits allowed a relationship to build between the patient and the rehabilitation therapist, which was important for patient engagement. Patients valued the use of tailored care and personal goal-setting as a motivational tool. These activities were well supported by the workbook and the goal-setting diary.
The economic evaluation used a cost–consequences analysis (see Chapter 10). It found that the cost of delivering the intervention was £231 per patient. Both the intervention group and the control group showed improvements in the EQ-5D health utility index score and the ICECAP-O capability index score from baseline to the 3-month follow-up. The intervention group had slightly higher mean QALY gains than the control group. A difference was found in hospital costs between the groups because of longer inpatient stays in one group. The DCE found that two attributes were important to participants. Participants preferred more time with the health professional delivering the rehabilitation sessions and preferred unqualified therapy assistants to qualified therapists. The scoping SROI analysis identified that outcome measures were well completed in the trial. Potential payer stakeholders included the patient and publicly funded health and social care services.
Finally, an alternative method of obtaining health service activity data from routinely collected data was compared with patient-reported health service use as measured by the CSRI questionnaire (see Chapter 11). Agreement between these methods was poor, moderate or good, depending on the question asked.
Strengths and weaknesses
Multiple methods were used to develop the intervention during Phase I of the study, which complemented each other during different stages of the development process (see Chapter 1). The topic guide for the focus groups and the items in the survey were influenced by the findings of our initial scoping review. The initial focus groups and the preliminary survey findings contributed to theory development in the realist review. Finally, the materials developed for the intervention were discussed at the final focus groups by patients, carers and rehabilitation professionals.
The realist review of multidisciplinary rehabilitation following hip fracture was not a systematic review (see Chapter 2). As such, it did not attempt to summarise all of the evidence and judge whether or not rehabilitation programmes were effective, but rather to build an explanatory account of the mechanisms behind rehabilitation and establish which components were effective and in which circumstances.
We did, however, summarise the economic evidence using systematic review methods (see Chapter 3). This review found a lack of UK evidence, and no two papers compared the same intervention, making comparisons difficult. There was also a lack of recent economic evaluations; the latest evaluation included in the review was published in 2009. Another limitation was the lack of detail when describing how the costs of the interventions were calculated.
Our survey results may not have been entirely representative of the UK situation regarding rehabilitation for hip fracture patients because we were unable to sample settings, therapists and community service managers proportionately (see Chapter 4). Because of data protection issues the professional organisations could not give us their contact lists and, as there was no centrally held register of therapists working in hip fracture rehabilitation, we were not able to use such a register as a sampling frame. However, a good range of respondents was sampled in terms of profession, health-care sector and geographical spread. As with all surveys, the findings and results can be presented only as a description of what was happening; the cause of the variation in rehabilitation could not be demonstrated and may warrant further investigation.
Early focus group results contributed to theory development in the realist review; later focus groups were able to provide feedback on the preliminary findings of the review and our proposed rehabilitation intervention. However, some of the focus groups had fewer than five participants. Some participants in the professional groups were unable to attend at short notice because of work commitments, whereas two patient/carer participants were unable to attend because of illness. We had hoped to purposively sample patients with different levels of disability, including those who were discharged home from the orthopaedic ward and who received rehabilitation in the community and those who were transferred to an inpatient rehabilitation ward from the orthopaedic ward and then discharged home. However, it was not possible to identify from electronic medical records what type of rehabilitation programme patients had received. We did, however, include participants with a range of ages and experiences across the groups. The main groups not represented were those who were living independently prior to hip fracture but who now lived in residential or nursing care and those with a cognitive impairment (see Chapter 5).
A strength of the new rehabilitation intervention was that it was informed by the programme theories from the realist review, areas of good practice, and areas suggested in the survey and focus groups with patients and carers and the rehabilitation professionals delivering the intervention in which rehabilitation provision could be improved (see Chapter 6).
The feasibility study was conducted in only one local health board in North Wales and so the study may not be generalisable to the rest of the NHS throughout the UK. The study aimed to assess the feasibility of the trial methods in terms of recruitment, randomisation and outcome measurement. It was not designed, or powered, to test the effectiveness or cost-effectiveness of the rehabilitation intervention. As expected, usual care varied and there were challenges in delivering the intervention in some areas, but there was good adherence to the planned intervention in those patients who did receive the rehabilitation sessions, with a high level of detail provided in the completed intervention paperwork. We aimed to recruit 50 patients but, although 61 patients were randomised, only 49 completed the follow-up; however, this was within the 95% CI of our target. We were also able to assess different outcome measures to determine which would be the most suitable for a larger definitive RCT, particularly for measuring the ability to perform ADL and self-efficacy. This highlighted that our chosen primary measure (the BADL index) was not responsive enough in our recruited population. However, our use of a variety of measures allowed us to identify an alternative for use in a definitive RCT, the NEADL scale. A limitation of our data analysis was that some tests could not be measured at baseline and so no adjustment could be made for patients’ function at the beginning of the trial in some analyses. There were high completion rates for outcome measures, but carers’ assistance in completing the outcome measures may be a potential source of bias (see Chapter 7).
The anonymised cohort study allowed us to assess the representativeness of the population recruited to the feasibility study in relation to the broader hip fracture population in this area (see Chapter 8). Originally, we had hoped to include participants who lacked mental capacity to assess whether or not the rehabilitation intervention was feasible and acceptable for different levels of cognitive functioning; however, the NHS research ethics committee did not allow us to do so. We did not exclude patients based on their level of frailty, as long as they could give informed consent and there were no contraindications to physical activity. In comparison with the cohort population, the feasibility study population was less likely to die or be readmitted to hospital in the 3 months following fracture. Hence, the findings of the feasibility study might not be generalisable to all hip fracture populations. Because it was an anonymised cohort, it was not possible to match participants in the cohort with those in the feasibility study. The cohort identified 462 patients and the feasibility study identified 372 patients in the same time period, which is 81% of those in the cohort. Data were extracted from paper medical records but it was not possible to locate 13% of these records.
Focus groups were used to investigate the acceptability of the study and intervention to patients, carers and therapists (see Chapter 9). One focus group with rehabilitation professionals and one focus group with patients included only three participants each, which was not ideal. Participants in Gwynedd and Anglesey were spread over a large geographical area and it was not possible to arrange focus groups in this area. However, one patient from this area was able to attend a focus group in a neighbouring area and a physiotherapist and three technical instructors participated in one-to-one telephone interviews. The focus groups highlighted that the delivery of the intervention was challenging and that therapists would have benefited from more training on how the additional sessions could be used.
The small feasibility study was not powered to test for an effect on the main outcome measure; therefore, it was appropriate to perform a cost–consequences analysis. We demonstrated that a DCE could be used in this elderly frail population. We also conducted a scoping SROI analysis, identifying the patients and publicly funded health and social care services as stakeholders. However, to reduce participant burden when completing the measures, intangible outcomes, such as happiness, were not assessed in this feasibility study. Assessing these outcomes could prove beneficial in a future trial (see Chapter 10).
In the triangulation study it was possible to obtain routinely collected electronic records from the local health board (see Chapter 11). When these data were compared with patient-completed questionnaire data there were many discrepancies. Although some of the discrepancies in the data could be accounted for by data input errors, it was not possible to check the accuracy of the data collected from the electronic systems.
Comparison with previous literature
The most similar previously published intervention for rehabilitation following hip fracture is the Exercise Plus Program, which was one of the Baltimore hip studies. 73 The Exercise Plus Program combined an exercise programme with a motivational intervention. In the UK NHS there are too few clinicians available to enable a psychological intervention to be delivered for the rehabilitation of a physical illness. However, there are examples of workbooks designed to improve self-efficacy in coronary heart disease375 and following stroke. 376 In addition, a trial protocol has been published describing an intervention for patients with Huntington’s disease that consists of an activity workbook combined with six home visits to promote physical activity and exercise. 377
Implications for future research
Challenges in recruitment
Recruitment of elderly, frail individuals soon after surgery was challenging. The recruitment period needed to be extended and many individuals required at least two visits to gain consent. As different hospitals have different procedures for discharge, some patients were in the acute hospital for a short time only and, as such, it is important to have procedures in place to recruit interested participants after discharge to maximise recruitment.
Delivering the rehabilitation intervention
In the first phase of the study we developed an intervention to enhance usual rehabilitation by improving patients’ self-efficacy, to increase the amount and quality of patients’ practice of physical exercise and ADL to improve functional outcomes. The intervention consisted of a patient-held information workbook and goal-setting diary and additional therapy sessions available to patients once they had returned home. This phase of the study demonstrated the benefits of using realist synthesis in complex intervention development in conjunction with other traditional methods. The explicit reporting of how the different methods were used to collate information and inform theory to develop individual intervention components may be informative for the development of future complex interventions. The second phase of the study found that the intervention was acceptable to patients, carers and rehabilitation professionals; however, when considering the results from the process evaluation, the focus groups and the DCE, further improvements, as described in the following section, could be made.
Further improvements to the workbooks and goal-setting diaries
Ten participants returned their goal-setting diary and workbook to the study team. All of the goal-setting diaries contained input from the therapists and half of the diaries had been completed by the patients. In addition, three out of the 10 patients had completed some of the activities, including the quizzes about hip fracture preconceptions. However, in the focus groups some of the therapists who delivered the intervention reported that some patients disliked these aspects of the workbook and found them to be too simplistic. The content of these materials and how they are delivered may need to be revised, with further input from patient representatives and therapists, and also with the assistance of a graphic designer.
Delivering the extra therapy sessions
The majority of those in the intervention group who lived in areas that we were able to deliver the intervention to received all six of the extra therapy sessions. The average number of sessions received was five, four of which took place in the home. The focus groups with patients confirmed that they preferred these extra sessions to take place in their own home rather than in an outpatient physiotherapy department. The DCE results agreed with this preference for home-based therapy, but this preference was not statistically significant.
The DCE also found a statistically significant preference for longer rehabilitation sessions and a statistically significant preference for unqualified technical instructors to deliver the rehabilitation sessions under the supervision of qualified therapists, rather than the qualified therapists themselves. This latter finding seems counterintuitive at first. However, the technical instructors undertook a larger proportion of the additional therapy sessions and findings from the focus groups suggest that patients’ initial requirements on discharge from hospital were based on a need for information and guidance rather than commencement of physical exercise. These requirements appeared to be better understood and prioritised by technical instructors, who were seemingly more aware than higher-banded therapists of the important role of reassuring and supporting patients to boost their confidence and self-efficacy, to enable them to be more physically active.
There were issues with the delivery of the rehabilitation intervention in Anglesey and Gwynedd. This was partly because of the rural geography of these counties, but also because therapy managers could not find therapists to deliver the intervention because the existing therapists were working at full capacity. In Wrexham, one of the therapists was able to provide additional sessions to deliver the study intervention because it was possible to backfill her time. This will need to be taken into account when delivering the intervention in a full RCT. One way of addressing this might be for the research team to employ dedicated therapists to deliver the study intervention. However, this would have its own challenges when trying to integrate the intervention into the day-to-day practice of the health service. Consideration could also be given to integrating more with other existing NHS interventions such as falls services.
During the focus groups, the therapists also discussed the challenges involved in delivering the intervention in the context of variable usual care. Although the intervention was designed to augment rather than standardise usual care, this is an important point for future research that highlights the need for additional training of the intervention teams, with more support on how to use the additional sessions for individuals with varying needs. The GUIDE tool (see Chapter 9) could be used as the basis for this training, but specific training needs would also need to be addressed, with the input of the therapists who have experience of delivering the intervention. This is an important consideration for the continuation of our own research but should also be considered by others conducting research in this area and highlights the importance of comprehensive training for successful implementation on interventions.
A future definitive Phase III randomised controlled trial
The rehabilitation intervention was tested in a Phase II randomised feasibility study, which demonstrated that the trial methods for a full definitive RCT and economic evaluation were satisfactory. The criteria for judging the feasibility of a future RCT were as follows:
-
eligibility rate 50% of those screened – in the feasibility study the eligibility rate was 45% (95% CI 41% to 49%), which was just below the 50% criterion
-
recruitment rate 25% of those screened – in the feasibility study the recruitment rate was 23% (95% CI 18% to 28%) of those screened, which was just below the 25% criterion
-
retention rate at 3-month follow-up 75% of those screened – in the feasibility study the retention rate was 79% (95% CI 69% to 89%), which satisfied the 75% criterion.
The main reason for lack of eligibility was lack of mental capacity. Originally, we had hoped to include participants who lacked capacity to assess whether or not the rehabilitation intervention was feasible and acceptable for different levels of cognitive functioning. However, the NHS research ethics committee excluded participants who lacked capacity because the study was not investigating the condition causing this lack of capacity. Now that we have proof of concept in the population with capacity, we believe that we should now give future trial participants who lack capacity the opportunity to participate, with feasibility tested as an internal pilot study in a definitive RCT.
Although Phase II studies are primarily intended to test the feasibility of trial methods, they also provide an opportunity to compare and contrast different methods for use in a future definitive RCT. The following sections describe the different methods that were assessed.
Patient-completed outcome measures
We assessed the following different outcome measures to determine which would be the most suitable.
-
The NEADL scale was more responsive than the BADL index for measuring the ability to perform ADL. A ceiling effect was observed in the BADL index in our recruited population, who had a high level of function at baseline, and therefore the NEADL scale would be a more appropriate primary outcome measure for a definitive RCT. We tested the feasibility of using the NEADL scale only in participants who have mental capacity. Further testing will be needed in those who lack capacity, perhaps in an internal pilot study in a future RCT.
-
The self-efficacy scales for falls and exercise were more responsive than the GSES, but researchers reported that many participants struggled to understand the SEE scale and so the FES-I seems to be the most appropriate measure of self-efficacy.
-
For the health economic analysis the EQ-5D-3L was a more responsive outcome measure than the ICECAP-O questionnaire. The researchers also reported that some participants disliked answering the questions on the ICECAP-O questionnaire and so the EQ-5D-3L would be the most suitable health economic outcome measure. A five-level version of the EQ-5D is now available and could be used in a future RCT.
-
The other outcome measures assessed in the feasibility study (AMTS, HADS, VAS for hip pain intensity, VAS-FOF and CSRI) will be retained to provide a broad suite of outcome measures.
Objective measures of physical function
Of the four physical function tests used in the feasibility study, the most responsive was the 50-foot walk test, which showed a medium effect size in favour of the control group. This paradoxical result was caused by an outlier. However, it was also apparent that physical function tests were not consistently performed at the same point post fracture, with discrepancies between groups. This highlighted problems encountered with accessing physiotherapy facilities, which could be addressed by using alternative measures such as the SPPB,279 which can be performed in the home. Grip strength was the only physical function test that could be measured at baseline, as it was not possible for patients to perform the other physical tests so soon after their hip surgery. The most suitable physical function tests for a future RCT would therefore be the grip strength test and the 50-foot walk test or the SPPB, with other tests used to provide a broad picture of physical function. It would be beneficial to record patient weight in addition to grip strength as this would give additional insight into how muscle strength (as indicated by grip strength) related to performance in the other physical function tests at follow-up.
Collecting health and social care service activity data
Health-care, social care and voluntary (charity) service use data were obtained from patient-completed CSRI questionnaires and routinely collected health-care data from electronic records. Although the method for obtaining routinely collected health-care data from electronic records was successfully demonstrated for hospital-based services, there were many uncertainties regarding the quality, accuracy and validity of the data. Also, the records were limited to hospital data held by the local health board and primary care service data held by Secure Anonymised Information Linkage. Currently, data for social care or voluntary (charity) service use are not held in a central database; therefore, health and social care service activity data should be obtained from both sources in a future RCT.
Other methodological issues
Other methodological issues related to a definitive Phase III RCT were raised during a meeting held on 19 January 2016 at Bangor University, when the final study findings were presented to the wider research group.
Cluster or individual randomisation
The question of the unit of randomisation was raised after the final study results were presented. If the extra sessions were to be integrated into usual rehabilitation care then the future trial should be a cluster RCT. If the extra sessions were to be delivered as an additional intervention in the same manner as in the feasibility study, then the unit of randomisation should be the individual patient. For cluster randomisation there is an additional layer of complexity: the sample size would be larger and the ICC is not known and has not been estimated in the feasibility study. Also, the unit of randomisation (general medical practice, a locality, a community team delivering the intervention or the acute hospital) is uncertain. Individual randomisation is more feasible and would maintain continuity from the Phase II feasibility study. It would also be easier to employ a dedicated therapist to deliver the additional therapy sessions than to integrate the intervention into current rehabilitation provision. However, there would need to be a thorough implementation plan if the intervention was found to be effective and cost-effective in a definitive RCT.
Length of follow-up
It is possible that the intervention will have a longer-term effect on self-efficacy and psychological issues and resumption of ADL, and so the definitive trial should include an additional follow-up assessment at 12 months.
Timing of recruitment
Most patients received two visits from researchers before agreeing to participate. The researchers, and also the therapists in the focus groups, reported that, as recruitment occurred early in the patients’ recovery from surgery, many requested a return visit to discuss the study once they had been discharged. In a future RCT it may be worth delaying patient recruitment until after patients are discharged. Recruitment in Anglesey, Gwynedd, Conwy and Denbighshire was also affected by the availability of a physiotherapist to conduct the initial assessment and goal-setting session; the physiotherapist was available only at the acute hospital site and was not able to visit patients at home. In these circumstances, if patients did not give consent before they were discharged home, it would not be possible to recruit them. This could be addressed by the use of dedicated intervention therapists.
Sample size calculation
The adjusted mean difference in NEADL score between the groups in this feasibility study was 3, which is considered a clinically significant change. A study by Wu et al. 378 suggested that the minimum clinically significant difference in the total NEADL score is 2.4, so this has been used within the sample size calculation for a future study. Based on a t-test with an alpha value of 5% and 90% power to detect a difference of 2.4 (SD 5.86), 254 participants are required to complete the trial over both treatment groups. When considering the 79% retention rate, the trial would need to recruit 322 participants.
Economic evaluation
The feasibility study did not include the measurement of wider, intangible outcomes such as happiness. If economic methods such as SROI analysis are to be used in a future RCT, then further work is required to assess the acceptability of additional measures to gather information on intangible outcomes. It would also be necessary to assess the acceptability of measures such as attribution questionnaires, which would be used to ascertain if any changes occur and if any changes that do occur can be ascribed by participants to the intervention.
Although the eligibility and recruitment rates in the feasibility study were lower than expected and the recruitment period had to be extended, the feasibility criteria that we set out were met. As detailed, we have identified key areas of the study that were challenging and have proposed adaptations and additions to mitigate these challenges in a future study. Because of the social and clinical implications of this work, as discussed in Chapter 1, we believe that a larger definitive RCT should be undertaken, incorporating the valuable lessons learnt from this study to maximise its success in determining the effectiveness and cost-effectiveness of the enhanced rehabilitation programme.
Implications for practice
The focus groups with therapists and patients made some interesting findings, which have implications for usual rehabilitation practice by therapists. The patients found the initial consultation with a therapist to be particularly valuable, because it allowed them to ask questions about what activities were safe to perform and to seek guidance about returning to favoured activities and pastimes. Conversely, some physiotherapists considered that this initial session was not useful, as it merely involved information exchange, with subsequent sessions focusing on practising exercises and ADL. The therapy assistants were more aware of the importance of their role in reassuring patients and rebuilding their confidence, which is one possible explanation why patients indicated in the DCE that they would prefer the rehabilitation sessions to be delivered by therapy assistants rather than qualified therapists. Following the focus groups, we developed the GUIDE mnemonic as a tool for therapists when rehabilitating patients after hip fracture (see Chapter 9).
Acknowledgements
Particular thanks go to all of the FEMuR study participants who gave their time to take part in the study.
We would also like to thank the following:
Betsi Cadwaladr University Health Board – BCUHB IT department staff who provided assistance and expertise for the cohort study and the triangulation study, and provided the data from the Therapy Manager System in the feasibility study; BCUHB therapies senior managers and surgical nursing senior managers who provided support for the study as well as their staff who were involved; Glenys Mutter who maintains the National Hip Fracture Database in Conwy and Denbighshire and identified participants for Phase I of the study.
Betsi Cadwaladr University Health Board orthopaedic consultants – Glynne Andrew, Aeneas O’Kelly and Sara Gerrie for supporting the study and providing access for researchers to the orthopaedic wards and their patients.
Betsi Cadwaladr University Health Board therapy teams and orthopaedic ward staff for identifying and screening patients, recruiting participants and delivering the intervention – Anglesey and Gwynedd: Delyth Davies, Jackie Roberts, Nerys Jones, Marie Thorne, Hefin Jones, Janet Howarth, Llio Jones and Jane Boyd; Conwy and Denbighshire: Sarah Williams, Lorraine Baker-Foulds, Kate Lynch, Amy Hall and Alison Tardival; and Wrexham and Flintshire: Sylvia Tomassen, Laura Lane, Amy Charnock-Baron, Rachel Hawking, Joanne Barron, Jane Evans and Dawn Ross.
Health and Care Research Wales – Jayne Jones, Lucie Hobson, Jane Stockport, Eryl Roberts, Stella Wright, Pamela Martin-Forbes, Annette Bolger, Caroline Mulvaney-Jones and Karen Jones for their contributions to data collection and patient recruitment.
North Wales Organisation for Randomised Trials in Health – particularly David Hunnisett for setting up and maintaining the IT systems; Youngzhong Sun for statistical support; Lexi Bastable for constructing and maintaining the MACRO online databases; and Roumen Kountchev for maintaining the remote online randomisation system.
North Wales Centre for Primary Care Research – particularly Andrei Stanciu for help in data collection for the feasibility study; Dr Julia Hiscock for assistance with the focus groups and consultation on the qualitative analysis; Barbara France for running the electronic literature searches and for study document retrieval; and Annie Hendry for help in extracting the data from the included studies. We would also like to thank Dr Richa Sinha for help with reference screening and the conceptual categorisation of potentially relevant studies for the realist review, and John Spalding/Bangor University library staff for help with electronically inaccessible document retrieval through interlibrary loans.
Independent members of the SSC – Sharon Simpson (chairperson), Fiona Wood, John Belcher, Tricia Best, Jayne Jones, George Kernohan, Tom Welsh, Brendan McCormack and Antony Johansen.
Independent members of the DMEC – Chris Robertson (chairperson), Neil Artz, Rowan Harwood and Diane Dixon.
Contributions of authors
Nefyn H Williams (Clinical Senior Lecturer in General Practice) was the chief investigator and grant holder, was responsible for study design, conduct and analysis, led the writing of Chapters 1, 7 and 12, contributed to all other chapters, led the discussions of the implications of the study findings, and had overall responsibility for the study and final report.
Jessica L Roberts (Trial Development and Management Officer) was the study manager during data collection and intervention delivery, overseeing the day-to-day conduct of the study, provided methodological input, developed the intervention workbook, contributed to the qualitative analysis in Chapter 5, conducted the qualitative analysis in Chapter 9, led the writing of Chapters 5, 6 and 9, contributed to the other chapters in the report and contributed to the discussion of the implications of the study findings.
Nafees Ud Din (Research Officer) conducted the realist review, was involved in the acquisition of data and analysis, led the writing of Chapter 2, gave feedback on other chapters of the report and contributed to the discussion of the implications of the study findings.
Joanna M Charles (Research Fellow) conducted the economic review, economic analysis and realist review, contributed to the writing of Chapter 2, led the writing of Chapters 3 and 10, contributed to the triangulation study, gave feedback on other chapters of the report and contributed to the discussion of the implications of the study findings.
Nicola Totton (Trial Statistician) conducted the statistical analysis for the cohort, feasibility and triangulation studies, led the writing of Chapters 7 and 8 and provided feedback on the other chapters in the report.
Michelle Williams (Trial and Development Support Officer) was involved in the conduct of the study, including maintenance of the trial documentation and acquisition of the data, led the writing of Chapter 4, provided administrative support with regard to report production and provided feedback on other chapters of the report.
Kevin Mawdesley (IT Specialist) conducted the triangulation study and led the writing of Chapter 11.
Claire A Hawkes (Senior Research Fellow) was the study manager during study set-up, intervention implementation and initial data collection, made a significant contribution to drafting the main study protocol, provided methodological and clinical input, developed the survey for Chapter 4, conducted the initial qualitative analysis for Chapter 5, contributed to the writing of Chapters 5–9, provided feedback on the other chapters and contributed to the discussion of the implications of the study findings.
Val Morrison (Deputy Head of School for Impact) was a coinvestigator, was responsible for the study design, provided health psychology expertise and methodological oversight throughout the study, commented on all chapters of the final report and contributed to the discussion of the implications of the study findings.
Andrew Lemmey (Professor of Sport, Health and Exercise Science) was a coinvestigator, was responsible for the study design, provided methodological oversight throughout the study, commented on all chapters of the final report and contributed to the discussion of the implications of the study findings.
Rhiannon T Edwards (Professor of Health Economics) was a coinvestigator, contributed to the study design, was responsible for the economic evaluation design, and was involved in writing Chapters 3 and 10.
Zoe Hoare (Principal Trial Statistician) provided input to the study design, developed the survey, was responsible for the design of the statistical analysis, provided methodological oversight, provided support to the trial statistician and contributed to the discussion of the implications of the study findings.
Aaron W Pritchard (Trial Development and Management Officer) contributed to the qualitative analysis and the writing of Chapters 5 and 9.
Robert T Woods (Director of Dementia Services Development Centre) was a coinvestigator, contributed to the study design, provided clinical psychological expertise and contributed to the discussion of the implications of the study findings.
Swapna Alexander (Consultant Orthogeriatrician) was a coinvestigator and provided orthogeriatric expertise and input in relation to the design of the intervention.
Catherine Sackley (Professor of Rehabilitation) was a coinvestigator, contributed to the methodology and study design, provided physiotherapy and rehabilitation expertise, and provided input in relation to the design of the intervention.
Pip Logan (Professor of Rehabilitation Research) was a coinvestigator, contributed to the methodology and study design, provided occupational therapy and rehabilitation expertise, and provided input in relation to the design of the intervention.
Clare Wilkinson (Deputy Head of Research, School of Healthcare Sciences) was a coinvestigator, provided feedback on the study protocol and contributed to the discussion of the implications of the study findings.
Jo Rycroft-Malone (Professor in Health Services and Implementation Research) was a coinvestigator, provided methodological input into the conduct of the realist review and contributed to the writing of Chapter 2.
Publications
Williams NH, Hawkes C, Din NU, Roberts J, Charles JM, Morrison V, et al. Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR): study protocol for a Phase II randomised feasibility study of a multidisciplinary rehabilitation package following hip fracture [ISRCTN22464643]. Pilot Feasibility Stud 2015;1:13.
Williams NH, Roberts JL, Din NU, Totton N, Charles JM, Hawkes CA, et al. Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR): a phase II randomised feasibility study of a multidisciplinary rehabilitation package following hip fracture. BMJ Open 2016;6:e012422.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Currie C, Partridge M, Plant F, Roberts J, Wakeman R, Williams A. The National Hip Fracture Database National Report. London: British Orthopaedic Association; 2011.
- Osteoporosis: review of the evidence for prevention, diagnosis, and treatment and cost-effectiveness analysis . Osteoporos Int 1998;8:S1-88.
- Bertram M, Norman R, Kemp L, Vos T. Review of the long-term disability associated with hip fractures. Inj Prev 2011;17:365-70. http://dx.doi.org/10.1136/ip.2010.029579.
- Darowski A. The Care of Patients with Fragility Fracture. London: British Orthopaedic Association; 2007.
- Egan M, Jaglal S, Byrne K, Wells J, Stolee P. Factors associated with a second hip fracture: a systematic review. Clin Rehabil 2008;22:272-82. http://dx.doi.org/10.1177/0269215507081573.
- Healee DJ, McCallin A, Jones M. Older adults’ recovery from hip fracture: a literature review. Int J Orthop Trauma Nurs 2011;15:18-2.
- Hip Fracture: Management. Clinical Guideline CG124. London: Royal College of Physicians; 2011.
- Handoll HHG, Cameron ID, Mak JCS, Finnegan TP. Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev 2009;4. https://doi.org/10.1002/14651858.cd007125.pub2.
- Handoll HHG, Sherrington C, Mak Jenson CS. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev 2011;3. https://doi.org/10.1590/s1516-31802011000600012.
- Crotty M, Unroe K, Cameron I, Miller M, Ramirez G, Couzner L. Rehabilitation interventions for improving physical and psychosocial functioning after hip fracture in older people. Cochrane Database Syst Rev 2010;1. https://doi.org/10.1002/14651858.cd007624.pub3.
- Mossey JM, Mutran E, Knott K, Craik R. Determinants of recovery 12 months after hip fracture: the importance of psychosocial factors. Am J Public Health 1989;79:279-86. https://doi.org/10.2105/AJPH.79.3.279.
- Oude Voshaar RC, Banerjee S, Horan M, Baldwin R, Pendleton N, Proctor R, et al. Fear of falling more important than pain and depression for functional recovery after hip fracture surgery. Psychol Med 2006;36:1635-45.
- Proctor R, Wade R, Woodward Y, Pendleton N, Baldwin R, Tarrier N, et al. The impact of psychological factors in recovery following surgery for hip fracture. Disabil Rehabil 2008;30:716-22. http://dx.doi.org/10.1080/09638280701403536.
- Visschedijk J, Achterberg W, van Balen R, Hertogh C. Fear of falling after hip fracture: a systematic review of measurement instruments, prevalence, interventions and related factors. J Am Geriatr Soc 2010;58:1739-48. https://doi.org/10.1111/j.1532-5415.2010.03036.x.
- Peel NM, McClure RJ, Hendrikz JK. Psychosocial factors associated with fall-related hip fractures. Age Ageing 2007;36:145-51. http://dx.doi.org/10.1093/ageing/afl167.
- Poynter L, Kwan J, Sayer AA, Vassallo M. Do cognitively impaired patients benefit from rehabilitation?. Rev Clin Gerontol 2008;18:53-64.
- Allen J, Koziak A, Buddingh S, Liang J, Buckingham J, Beaupre LA. Rehabilitation in patients with dementia following hip fracture: a systematic review. Physiother Can 2012;64:190-201. http://dx.doi.org/10.3138/ptc.2011-06BH.
- Delirium: Diagnosis, Prevention and Management. Clinical Guideline 103. London: NICE; 2010.
- Clinical Practice Guideline for the Assessment and Prevention of Falls in Older People. London: Royal College of Nursing; 2004.
- Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2010.
- Auais MA, Eilayyan O, Mayo NE. Extended exercise rehabilitation after hip fracture improves patients’ physical function: a systematic review and meta-analysis. Phys Ther 2012;92:1437-51.
- Beaupre LA, Jones CA, Saunders LD, Johnston DW, Buckingham J, Majumdar SR. Best practices for elderly hip fracture patients. A systematic overview of the evidence. J Gen Intern Med 2005;20:1019-25. http://dx.doi.org/10.1111/j.1525-1497.2005.00219.x.
- Cameron ID. Coordinated multidisciplinary rehabilitation after hip fracture. Disabil Rehabil 2005;27:1081-90. https://doi.org/10.1080/09638280500061261.
- Chudyk AM, Jutai JW, Petrella RJ, Speechley M. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil 2009;90:246-62. http://dx.doi.org/10.1016/j.apmr.2008.06.036.
- Feehan LM, Beck CA, Harris SR, MacIntyre DL, Li LC. Exercise prescription after fragility fracture in older adults: a scoping review. Osteoporos Int 2011;22:1289-322.
- Halbert J, Crotty M, Whitehead C, Cameron I, Kurrle S, Graham S, et al. Multi-disciplinary rehabilitation after hip fracture is associated with improved outcome: a systematic review. J Rehabil Med 2007;39:507-12. https://doi.org/10.2340/16501977-0102.
- Handoll HH, Parker MJ, Sherrington C. Mobilisation strategies after hip fracture surgery in adults. Cochrane Database Syst Rev 2003;1. https://doi.org/10.1016/s0031-9406(05)61028-0.
- Lafferty G. Community-based alternatives to hospital rehabilitation services: a review of the evidence and suggestions for approaching future evaluations. Rev Clin Gerontol 1996;6:183-94.
- Leigheb F, Vanhaecht K, Sermeus W, Lodewijckx C, Deneckere S, Boonen S, et al. The effect of care pathways for hip fractures: a systematic review. Calcif Tissue Int 2012;91:1-14. http://dx.doi.org/10.1007/s00223-012-9589-2.
- Mehta SP, Roy JS. Systematic review of home physiotherapy after hip fracture surgery. J Rehabil Med 2011;43:477-80. http://dx.doi.org/10.2340/16501977-0808.
- Moffa-Trotter ME, Anemaet WK. Cost effectiveness of home rehabilitation: a literature review. Topics Geriatr Rehabil 1999;14:1-33.
- Nigwekar SU, Rajda J, Navaneethan SD. Hospitalist care and length of stay in patients with hip fracture: a systematic review. Arch Intern Med 2008;168:1010-1. http://dx.doi.org/10.1001/archinte.168.9.1010.
- Parker MJ, Handoll HH, Dynan Y. Mobilisation strategies after hip fracture surgery in adults. Cochrane Database Syst Rev 2000;3.
- Sherrington C. The Effects of Exercise on Physical Ability Following Fall-Related Hip Fracture. Sydney: University of New South Wales; 2001.
- Smith T, Hedges C, MacNair R, Schankat K. Early rehabilitation following less invasive surgical stabilisation plate fixation for distal femoral fractures. Physiotherapy 2009;95:61-75.
- Toussant EM, Kohia M. A critical review of literature regarding the effectiveness of physical therapy management of hip fracture in elderly persons. J Gerontol A Biol Sci Med Sci 2005;60:1285-91.
- Ward D, Drahota A, Gal D, Severs M, Dean Taraneh P. Care home versus hospital and own home environments for rehabilitation of older people. Cochrane Database Syst Rev 2008;4. https://doi.org/10.1002/14651858.cd003164.pub2.
- Yamamoto N. Rehabilitation and mobilization in hip fracture patients. Clin Calcium 2010;20:1402-6. http://dx.doi.org/CliCa14021406.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: Sage; 2006.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review: a new method of systematic review for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-21.
- Wong G, Greenhalgh T, Westhorp G, Pawson R. Development of methodological guidance, publication standards and training materials for realist and meta-narrative reviews: the RAMESES (Realist And Meta-narrative Evidence Syntheses – Evolving Standards) project. Health Serv Deliv Res 2014;2.
- Bowles S. Microeconomics: Behavior, Institutions, and Evolution. Princeton, NJ: Princeton University Press; 2006.
- Mongin P, Davis J, Hands W, Maki U. Handbook of Economic Methodology. London: Edward Elgar; 1997.
- Levitt S, Dubner S. Freakonomics: A Rogue Economist Explores the Hidden Side of Everything. New York: Harper Collins; 2005.
- Bachmann S, Finger C, Huss A, Egger M, Stuck AE, Clough-Gorr KM. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ 2010;340. https://doi.org/10.1136/bmj.c1718.
- Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al. Geriatric rehabilitation following fractures in older people: a systematic review. Health Technol Assess 2000;4.
- Cameron ID. Models of rehabilitation – commonalities of interventions that work and of those that do not. Disabil Rehabil 2010;32:1051-8. http://dx.doi.org/10.3109/09638281003672377.
- Cameron ID, Handoll HH, Finnegan TP, Madhok R, Langhorne P. Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures. Cochrane Database Syst Rev 2000;4.
- Chong CP, Savige J, Lim WK. Orthopaedic-geriatric models of care and their effectiveness. Australas J Ageing 2009;28:171-6. http://dx.doi.org/10.1111/j.1741-6612.2009.00368.x.
- Drenth JC, Hobbelen JSM. Assessment of physical fitness using upper extremity tests in elderly patients during the non-weight bearing stage after hip fracture: a systematic review. Ned Tijdschr Fysiother 2012;122:104-10.
- Egol KA, Koval KJ, Zuckerman JD. Functional recovery following hip fracture in the elderly. J Orthop Trauma 1997;11:594-9. https://doi.org/10.1097/00005131-199711000-00009.
- Green J, Hallett L, Zhao Y, Birt J, Foster T. Burden and medical needs in older patients with hip fractures and muscle atrophy or weakness. Osteoporos Int 2012;23:S93-94.
- Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury 2012;43:676-85. http://dx.doi.org/10.1016/j.injury.2011.05.017.
- Jelicic M, Kempen G, van Eijk L. Do psychosocial factors affect recovery from hip fracture in the elderly? A review of the literature. J Rehabil Sci 1996;9:77-81.
- Mauffrey C. The management of subcapital fractures in the elderly population. Eur J Orthop Surg Traumatol 2010;20:359-64.
- Muir SW, Yohannes AM. The impact of cognitive impairment on rehabilitation outcomes in elderly patients admitted with a femoral neck fracture: a systematic review. J Geriatr Phys Ther 2009;32:24-32. https://doi.org/10.1519/00139143-200932010-00006.
- Robinson KM. Efficacy of home care rehabilitation interventions. Ann Longterm Care 2000;8:68-71.
- Romeo R, Knapp M, Banerjee S, Morris J, Baldwin R, Tarrier N, et al. Treatment and prevention of depression after surgery for hip fracture in older people: cost-effectiveness analysis. J Affect Disord 2011;128:211-19. http://dx.doi.org/10.1016/j.jad.2010.07.026.
- Wang X, Emery L. Cognitive status after hip replacement. Phys Occup Ther Pediatr 2002;21:51-64.
- Pearson M, Hunt H, Cooper C, Shepperd S, Pawson R, Anderson R. Intermediate Care: A Realist Review and Conceptual Framework. Final Report 2013.
- Pearson M, Hunt H, Cooper C, Shepperd S, Pawson R, Anderson R. Providing effective and preferred care closer to home: a realist review of intermediate care. Health Soc Care Community 2015;23:577-93. http://dx.doi.org/10.1111/hsc.12183.
- Godfrey M, Keen J, Townsend J, Moore J, Ware P, Hardy B, et al. An Evaluation of Intermediate Care for Older People. Leeds: Institute of Health Sciences and Public Health Research, University of Leeds; 2005.
- Ritzer G. Meta-theorizing in Sociology. Lexington, MA: Lexington Books; 1991.
- Roen K, Arai L, Roberts H, Popay J. Extending systematic reviews to include evidence on implementation: methodological work on a review of community-based initiatives to prevent injuries. Soc Sci Med 2006;63:1060-71.
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions 2011. www.cochrane-handbook.org (accessed 27 March 2017).
- Pluye P, Robert E, Cargo M, Bartlett G, O’Cathain A, Griffiths F, et al. Proposal: A Mixed Methods Appraisal Tool for Systematic Mixed Studies Reviews 2011. www.webcitation.org/5tTRTc9yJ (accessed 10 December 2015).
- Resnick B, Orwig D, D’Adamo C, Yu-Yahiro J, Hawkes W, Shardell M, et al. Factors that influence exercise activity among women post hip fracture participating in the Exercise Plus Program. Clin Interv Aging 2007;2:413-27.
- Resnick B, Daly MP. The effect of cognitive status on outcomes following rehabilitation. Fam Med 1997;29:400-5.
- Resnick B, Magaziner J, Orwig D, Zimmerman S. Evaluating the components of the Exercise Plus Program: rationale, theory and implementation. Health Educ Res 2002;17:648-58. https://doi.org/10.1093/her/17.5.648.
- Resnick B, Orwig D, Wehren L, Zimmerman S, Simpson M, Magaziner J. The Exercise Plus Program for older women post hip fracture: participant perspectives. Gerontologist 2005;45:539-44. https://doi.org/10.1093/geront/45.4.539.
- Resnick B, Orwig D, Yu-Yahiro J, Hawkes W, Shardell M, Hebel JR, et al. Testing the effectiveness of the exercise plus program in older women post-hip fracture. Ann Behav Med 2007;34:67-76. https://doi.org/10.1007/BF02879922.
- Management of Hip Fracture in Older People: A National Clinical Guideline. Guideline No. 111. Edinburgh: SIGN; 2009.
- American Academy of Orthopaedic Surgeons . Management of Hip Fractures in the Elderly: Evidence-Based Clinical Practice Guideline 2014. www.aaos.org/cc_files/aaosorg/research/guidelines/hipfxguideline.pdf (accessed February 2014).
- The Bone and Joint Decade . National Hip Fracture Toolkit 2011. http://boneandjointcanada.com/wp-content/uploads/2014/05/National-hip-fracture-toolkit-June-2011.pdf (accessed February 2017).
- Australian and New Zealand Hip Fracture Registry . Australian and New Zealand Guideline for Hip Fracture Care: Improving Outcomes in Hip Fracture Management of Adults 2014. www.acem.org.au/getattachment/91169f29-890e-47c8-a4db-03e1ae0b716e/Australian-New-Zealand-Hip-Fracture-Registry-(ANZH.aspx (accessed February 2017).
- Bellelli G, Buccino G, Bernardini B, Padovani A, Trabucchi M. Action observation treatment improves recovery of postsurgical orthopedic patients: evidence for a top-down effect?. Arch Phys Med Rehabil 2010;91:1489-94. http://dx.doi.org/10.1016/j.apmr.2010.07.013.
- Buddenberg LA, Schkade JK. Special feature: a comparison of occupational therapy intervention approaches for older patients after hip fracture. Top Geriatr Rehabil 1998;13:52-68.
- Casado BL, Resnick B, Zimmerman S, Nahm ES, Orwig D, Macmillan K, et al. Social support for exercise by experts in older women post-hip fracture. J Women Aging 2009;21:48-62. http://dx.doi.org/10.1080/08952840802633719.
- Fortinsky RH, Bohannon RW, Litt MD, Tennen H, Maljanian R, Fifield J, et al. Rehabilitation therapy self-efficacy and functional recovery after hip fracture. Int J Rehabil Res 2002;25:241-6. https://doi.org/10.1097/00004356-200209000-00011.
- Huang TT, Acton GJ. Ways to maintain independence among Taiwanese elderly adults with hip fractures: a qualitative study. Geriatr Nurs 2009;30:28-35. http://dx.doi.org/10.1016/j.gerinurse.2008.03.006.
- Jackson J, Schkade J. Occupational adaptation model versus biomechanical-rehabilitation model in the treatment of patients with hip fractures. Am J Occup Ther 2001;55:531-7.
- Jellesmark A, Herling SF, Egerod I, Beyer N. Fear of falling and changed functional ability following hip fracture among community-dwelling elderly people: an explanatory sequential mixed method study. Disabil Rehabil 2012;34:2124-31. http://dx.doi.org/10.3109/09638288.2012.673685.
- McKee KJ, Orbell S, Austin CA, Bettridge R, Liddle BJ, Morgan K, et al. Fear of falling, falls efficacy, and health outcomes in older people following hip fracture. Disabil Rehabil 2002;24:327-33. http://dx.doi.org/10.1080/09638280110093686.
- McMillan L, Booth J, Currie K, Howe T. A grounded theory of taking control after fall-induced hip fracture. Disabil Rehabil 2012;34:2234-41. http://dx.doi.org/10.3109/09638288.2012.681006.
- Oldmeadow LB, Edwards ER, Kimmel LA, Kipen E, Robertson VJ, Bailey MJ. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg 2006;76:607-11. http://dx.doi.org/10.1111/j.1445-2197.2006.03786.x.
- Olsson LE, Nyström AE, Karlsson J, Ekman I. Admitted with a hip fracture: patient perceptions of rehabilitation. J Clin Nurs 2007;16:853-9. http://dx.doi.org/10.1111/j.1365-2702.2006.01635.x.
- Travis SS, McAuley WJ. Mentally restorative experiences supporting rehabilitation of high functioning elders recovering from hip surgery. J Adv Nurs 1998;27:977-85.
- Zidén L, Wenestam CG, Hansson-Scherman M. A life-breaking event: early experiences of the consequences of a hip fracture for elderly people. Clin Rehabil 2008;22:801-11. http://dx.doi.org/10.1177/0269215508090204.
- Allegrante JP, Peterson MG, Cornell CN, MacKenzie CR, Robbins L, Horton R. Methodological challenges of multiple-component intervention: lessons learned from a randomized controlled trial of functional recovery following hip fracture. HSS J 2007;3:63-70.
- Binder E, Brown M, Sinacore D, Steger-May K, Yarasheski K, Schechtman K. Effects of extended outpatient rehabilitation after hip fracture: a randomized controlled trial. JAMA 2004;292:837-46.
- Bischoff-Ferrari H, Dawson-Hughes B, Platz A, Orav E, Stahelin H, Willett W, et al. Effect of high-dosage cholecalciferol and extended physiotherapy on complications after hip fracture: a randomized controlled trial. Arch Intern Med 2010;170:813-20.
- Crotty M, Finucane P, Hayball N, Gray S, Krishnan J, Wells V. A trial of rehabilitation in the home (RITHOM) for patients with fractured neck of femur: an early report. Aus N Z J Med 2000;30.
- Crotty M, Whitehead C, Miller M, Gray S. Patient and caregiver outcomes 12 months after home-based therapy for hip fracture: a randomized controlled trial. Arch Phys Med Rehabil 2003;84:1237-9. https://doi.org/10.1016/S0003-9993(03)00141-2.
- Delmi M, Rapin CH, Bengoa JM, Delmas PD, Vasey H, Bonjour JP. Dietary supplementation in elderly patients with fractured neck of the femur. Lancet 1990;335:1013-16. https://doi.org/10.1016/0140-6736(90)91073-J.
- Deschodt M, Braes T, Broos P, Sermon A, Boonen S, Flamaing J, et al. Effect of an inpatient geriatric consultation team on functional outcome, mortality, institutionalization, and readmission rate in older adults with hip fracture: a controlled trial. J Am Geriatr Soc 2011;59:1299-308. http://dx.doi.org/10.1111/j.1532-5415.2011.03488.x.
- Elinge E, Lofgren B, Gagerman E, Nyberg L. A group learning programme for old people with hip fracture: a randomized study. Scand J Occup Ther 2003;10:27-33.
- Hagsten B, Svensson O, Gardulf A. Early individualized postoperative occupational therapy training in 100 patients improves ADL after hip fracture: a randomized trial. Acta Orthop Scand 2004;75:177-83. https://doi.org/10.1080/00016470412331294435.
- Huang T, Liang S. A randomized clinical trial of the effectiveness of a discharge planning intervention in hospitalized elders with hip fracture due to falling. J Clin Nurs 2005;14:1193-201.
- Huusko TM, Karppi P, Avikainen V, Kautiainen H, Sulkava R. Randomised, clinically controlled trial of intensive geriatric rehabilitation in patients with hip fracture: subgroup analysis of patients with dementia. BMJ 2000;321:1107-11. https://doi.org/10.1136/bmj.321.7269.1107.
- Kennie DC, Reid J, Richardson IR, Kiamari AA, Kelt C. Effectiveness of geriatric rehabilitative care after fractures of the proximal femur in elderly women: a randomised clinical trial. BMJ 1988;297:1083-6. https://doi.org/10.1136/bmj.297.6656.1083.
- Kuisma R. A randomized, controlled comparison of home versus institutional rehabilitation of patients with hip fracture. Clin Rehabil 2002;16:553-61. https://doi.org/10.1191/0269215502cr525oa.
- Lauridsen UB, de la Cour BB, Gottschalck L, Svensson BH. Intensive physical therapy after trochanteric femoral fracture. A randomized clinical trial. Ugeskr Laeg 2002;164:1040-4.
- Lin PC, Wang CH, Chen CS, Liao LP, Kao SF, Wu HF. To evaluate the effectiveness of a discharge-planning programme for hip fracture patients. J Clin Nurs 2009;18:1632-9. http://dx.doi.org/10.1111/j.1365-2702.2008.02695.x.
- Louie W-SS, Shuk-yiu Y, Wai-ling C, Kai-ming A, Kam-man W. Effectiveness of a patient/carer empowerment programme for people with hip fractures. Int J Ther Rehabil 2012;19:673-81.
- Mangione K, Craik R, Palombaro K, Tomlinson S, Hofmann M. Home-based leg-strengthening exercise improves function 1 year after hip fracture: a randomized controlled study. J Am Geriatr Soc 2010;58:1911-17. https://doi.org/10.1111/j.1532-5415.2010.03076.x.
- Mendelsohn ME, Overend TJ, Connelly DM, Petrella RJ. Improvement in aerobic fitness during rehabilitation after hip fracture. Arch Phys Med Rehabil 2008;89:609-17. http://dx.doi.org/10.1016/j.apmr.2007.09.036.
- Mitchell SL, Stott DJ, Martin BJ, Grant SJ. Randomized controlled trial of quadriceps training after proximal femoral fracture. Clin Rehabil 2001;15:282-90. https://doi.org/10.1191/026921501676849095.
- Moseley AM, Sherrington C, Lord SR, Barraclough E, St George RJ, Cameron ID. Mobility training after hip fracture: a randomised controlled trial. Age Ageing 2009;38:74-80. http://dx.doi.org/10.1093/ageing/afn217.
- Naglie G, Tansey C, Kirkland JL, Ogilvie-Harris DJ, Detsky AS, Etchells E, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ 2002;167:25-32.
- Peiris CL, Taylor NF, Shields N. Additional Saturday allied health services increase habitual physical activity among patients receiving inpatient rehabilitation for lower limb orthopedic conditions: a randomized controlled trial. Arch Phys Med Rehabil 2012;93:1365-70.
- Peterson MGE, Ganz SB, Allegrante JP, Cornell CN. High-intensity exercise training following hip fracture. Top Geriatr Rehabil 2004;20:273-84.
- Portegijs E, Kallinen M, Rantanen T, Heinonen A, Sihvonen S, Alen M, et al. Effects of resistance training on lower-extremity impairments in older people with hip fracture. Arch Phys Med Rehabil 2008;89:1667-74. http://dx.doi.org/10.1016/j.apmr.2008.01.026.
- Ryan T, Enderby P, Rigby AS. A randomized controlled trial to evaluate intensity of community-based rehabilitation provision following stroke or hip fracture in old age. Clin Rehabil 2006;20:123-31. https://doi.org/10.1191/0269215506cr933oa.
- Saltvedt I, Prestmo A, Einarsen E, Johnsen LG, Helbostad JL, Sletvold O. Development and delivery of patient treatment in the Trondheim Hip Fracture Trial. A new geriatric in-hospital pathway for elderly patients with hip fracture. BMC Res Notes 2012;5. http://dx.doi.org/10.1186/1756-0500-5-355.
- Sherrington C, Lord S. Home exercise to improve strength and walking velocity after hip fracture: a randomized controlled trial. Arch Phys Med Rehabil 1997;78:208-12. https://doi.org/10.1016/S0003-9993(97)90265-3.
- Sherrington C, Lord SR, Herbert RD. A randomized controlled trial of weight-bearing versus non-weight-bearing exercise for improving physical ability after usual care for hip fracture. Arch Phys Med Rehabil 2004;85:710-16. https://doi.org/10.1016/S0003-9993(03)00620-8.
- Shyu YI, Liang J, Wu CC, Su JY, Cheng HS, Chou SW, et al. Interdisciplinary intervention for hip fracture in older Taiwanese: benefits last for 1 year. J Gerontol A Biol Sci Med Sci 2008;63:92-7. https://doi.org/10.1093/gerona/63.1.92.
- Stenvall M, Olofsson B, Nyberg L, Lundstrom M, Gustafson Y. Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up. J Rehabil Med 2007;39:232-8.
- Tinetti ME, Baker DI, Gottschalk M, Williams CS, Pollack D, Garrett P, et al. Home-based multicomponent rehabilitation program for older persons after hip fracture: a randomized trial. Arch Phys Med Rehabil 1999;80:916-22. https://doi.org/10.1016/S0003-9993(99)90083-7.
- Tsauo JY, Leu WS, Chen YT, Yang RS. Effects on function and quality of life of postoperative home-based physical therapy for patients with hip fracture. Arch Phys Med Rehabil 2005;86:1953-7. http://dx.doi.org/10.1016/j.apmr.2005.04.020.
- Uy C, Kurrle SE, Cameron ID. Inpatient multidisciplinary rehabilitation after hip fracture for residents of nursing homes: a randomised trial. Australas J Ageing 2008;27:43-4.
- Vidán M, Serra J, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc 2005;53:1476-82.
- Vogler CM, Menant JC, Sherrington C, Ogle SJ, Lord SR. Evidence of detraining after 12-week home-based exercise programs designed to reduce fall-risk factors in older people recently discharged from hospital. Arch Phys Med Rehabil 2012;93:1685-91. http://dx.doi.org/10.1016/j.apmr.2012.03.033.
- Yu-Yahiro JA, Resnick B, Orwig D, Hicks G, Magaziner J. Design and implementation of a home-based exercise program post-hip fracture: the Baltimore hip studies experience. PMR 2009;1:308-18. http://dx.doi.org/10.1016/j.pmrj.2009.02.008.
- Zidén L, Frändin K, Kreuter M. Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities. Clin Rehabil 2008;22:1019-33. http://dx.doi.org/10.1177/0269215508096183.
- Richards SH, Coast J, Gunnell DJ, Peters TJ, Pounsford J, Darlow MA. Randomised controlled trial comparing effectiveness and acceptability of an early discharge, hospital at home scheme with acute hospital care. BMJ 1998;316:1796-801. https://doi.org/10.1136/bmj.316.7147.1796.
- Swanson CE, Day GA, Yelland CE, Broome JR, Massey L, Richardson HR, et al. The management of elderly patients with femoral fractures. A randomised controlled trial of early intervention versus standard care. Med J Aust 1998;169:515-18.
- Hauer K, Pfisterer M, Schuler M, Bärtsch P, Oster P. Two years later: a prospective long-term follow-up of a training intervention in geriatric patients with a history of severe falls. Arch Phys Med Rehabil 2003;84:1426-32. https://doi.org/10.1016/S0003-9993(03)00267-3.
- Carmeli E, Sheklow SL, Coleman R. A comparative study of organized class-based exercise programs versus individual home-based exercise programs for elderly patients following hip surgery. Disabil Rehabil 2006;28:997-1005. https://doi.org/10.1080/09638280500476154.
- Dai YT, Huang GS, Yang RS, Tsauo JY, Yang LH. Functional recovery after hip fracture: six months’ follow-up of patients in a multidisciplinary rehabilitation program. J Formos Med Assoc 2002;101:846-53.
- Di Monaco M, Vallero F, De Toma E, De Lauso L, Tappero R, Cavanna A. A single home visit by an occupational therapist reduces the risk of falling after hip fracture in elderly women: a quasi-randomized controlled trial. J Rehabil Med 2008;40:446-50.
- Giangregorio LM, Thabane L, Debeer J, Farrauto L, McCartney N, Adachi JD, et al. Body weight-supported treadmill training for patients with hip fracture: a feasibility study. Arch Phys Med Rehabil 2009;90:2125-30. http://dx.doi.org/10.1016/j.apmr.2009.06.022.
- Jones GR, Jakobi JM, Taylor AW, Petrella RJ, Vandervoort AA. Community exercise program for older adults recovering from hip fracture: a pilot study. J Aging Phys Act 2006;14:439-55. https://doi.org/10.1123/japa.14.4.439.
- Nicholson CM, Czernwicz S, Mandilas G, Rudolph I, Greyling MJ. The role of chair exercises for older adults following hip fracture. S Afr Med J 1997;87:1131-8.
- Ohsawa S, Miura A, Yagyu M, Oizumi A, Yamada E. Assertive rehabilitation for intracapsular fracture of the proximal femur. Clin Rehabil 2007;21:36-40. http://dx.doi.org/10.1177/0269215506069243.
- Adunsky A, Lusky A, Arad M, Heruti RJ. A comparative study of rehabilitation outcomes of elderly hip fracture patients: the advantage of a comprehensive orthogeriatric approach. J Gerontol A Biol Sci Med Sci 2003;58:542-7.
- Al-Ani AN, Flodin L, Söderqvist A, Ackermann P, Samnegård E, Dalén N, et al. Does rehabilitation matter in patients with femoral neck fracture and cognitive impairment? A prospective study of 246 patients. Arch Phys Med Rehabil 2010;91:51-7. http://dx.doi.org/10.1016/j.apmr.2009.09.005.
- Van Balen R, Steyerberg EW, Cools HJ, Polder JJ, Habbema JDF. Early discharge of hip fracture patients from hospital: transfer of costs from hospital to nursing home. Acta Orthop Scand 2002;73:491-5. https://doi.org/10.1080/000164702321022749.
- Bellelli G, Frisoni GB, Turco R, Trabucchi M. Depressive symptoms combined with dementia affect 12-months survival in elderly patients after rehabilitation post-hip fracture surgery. Int J Geriatr Psychiatr 2008;23:1073-7.
- Fredman L, Hawkes WG, Black S, Bertrand RM, Magaziner J. Elderly patients with hip fracture with positive affect have better functional recovery over 2 years. J Am Geriatr Soc 2006;54:1074-81. http://dx.doi.org/10.1111/j.1532-5415.2006.00786.x.
- Giusti A, Barone A, Oliveri M, Pizzonia M, Razzano M, Palummeri E, et al. An analysis of the feasibility of home rehabilitation among elderly people with proximal femoral fractures. Arch Phys Med Rehabil 2006;87:826-31. http://dx.doi.org/10.1016/j.apmr.2006.02.018.
- Hoekstra JC, Goosen JH, Wolf GS, Verheyen CC. Effectiveness of multidisciplinary nutritional care on nutritional intake, nutritional status and quality of life in patients with hip fractures: a controlled prospective cohort study. Clin Nutr 2011;30:455-61. http://dx.doi.org/10.1016/j.clnu.2011.01.011.
- Johansen I, Lindbaek M, Stanghelle JK, Brekke M. Structured community-based inpatient rehabilitation of older patients is better than standard primary health care rehabilitation: an open comparative study. Disabil Rehabil 2012;34:2039-46. http://dx.doi.org/10.3109/09638288.2012.667193.
- Koval K, Aharonoff G, Su E, Zuckerman J. Effect of acute inpatient rehabilitation on outcome after fracture of the femoral neck or intertrochanteric fracture. J Bone Joint Surg Am 1998;80:357-64.
- Levi SJ. Posthospital setting, resource utilization, and self-care outcome in older women with hip fracture. Arch Phys Med Rehabil 1997;78:973-9. https://doi.org/10.1016/S0003-9993(97)90060-5.
- Lieberman D, Lieberman D. Rehabilitation after proximal femur fracture surgery in the oldest old. Arch Phys Med Rehabil 2002;83:1360-3. https://doi.org/10.1053/apmr.2002.35113.
- Munin MC, Seligman K, Dew MA, Quear T, Skidmore ER, Gruen G, et al. Effect of rehabilitation site on functional recovery after hip fracture. Arch Phys Med Rehabil 2005;86:367-72. http://dx.doi.org/10.1016/j.apmr.2004.10.004.
- Pryor GA, Myles JW, Williams DR, Anand JK. Team management of the elderly patient with hip fracture. Lancet 1988;1:401-3. https://doi.org/10.1016/S0140-6736(88)91192-0.
- Röder F, Schwab M, Aleker T, Mörike K, Thon KP, Klotz U. Proximal femur fracture in older patients – rehabilitation and clinical outcome. Age Ageing 2003;32:74-80. https://doi.org/10.1093/ageing/32.1.74.
- Rösler A, von Renteln-Kruse W, Mühlhan C, Frilling B. Treatment of dementia patients with fracture of the proximal femur in a specialized geriatric care unit compared to conventional geriatric care. Z Gerontol Geriatr 2012;45:400-3. http://dx.doi.org/10.1007/s00391-012-0299-1.
- Host HH, Sinacore DR, Bohnert KL, Steger-May K, Brown M, Binder EF. Training-induced strength and functional adaptations after hip fracture. Phys Ther 2007;87:292-303. http://dx.doi.org/10.2522/ptj.20050396.
- Jensen JS, Tøndevold E, Sørensen PH. Social rehabilitation following hip fractures. Acta Orthop Scand 1979;50:777-85. https://doi.org/10.3109/17453677908991309.
- Roberts HC, Pickering RM, Onslow E, Clancy M, Powell J, Roberts A, et al. The effectiveness of implementing a care pathway for femoral neck fracture in older people: a prospective controlled before and after study. Age Ageing 2004;33:178-84. http://dx.doi.org/10.1093/ageing/afh063.
- Visser M, Harris TB, Fox KM, Hawkes W, Hebel JR, Yahiro JY, et al. Change in muscle mass and muscle strength after a hip fracture: relationship to mobility recovery. J Gerontol Ser A Biol Sci Med Sci 2000;55:M434-40. https://doi.org/10.1093/gerona/55.8.M434.
- Beaupre LA, Cinats JG, Senthilselvan A, Scharfenberger A, Johnston DW, Saunders LD. Does standardized rehabilitation and discharge planning improve functional recovery in elderly patients with hip fracture?. Arch Phys Med Rehabil 2005;86:2231-9. http://dx.doi.org/10.1016/j.apmr.2005.06.019.
- Boyd RV, Compton E, Hawthorne J, Kemm JR. Orthogeriatric rehabilitation ward in Nottingham: a preliminary report. Br Med J 1982;285:937-8. https://doi.org/10.1136/bmj.285.6346.937-a.
- Dy CJ, Dossous PM, Ton QV, Hollenberg JP, Lorich DG, Lane JM. Does a multidisciplinary team decrease complications in male patients with hip fractures?. Clin Orthop Relat Res 2011;469:1919-24. http://dx.doi.org/10.1007/s11999-011-1825-y.
- Holmberg S, Agger E, Ersmark H. Rehabilitation at home after hip fracture. Acta Orthop Scand 1989;60:73-6. https://doi.org/10.3109/17453678909150098.
- Whitehead C, Miller M, Crotty M. Falls in community-dwelling older persons following hip fracture: impact on self-efficacy, balance and handicap. Clin Rehabil 2003;17:899-906. https://doi.org/10.1191/0269215503cr695oa.
- Zabari A, Lubart E, Ganz FD, Leibovitz A. The effect of a pain management program on the rehabilitation of elderly patients following hip fracture surgery. Isr Med Assoc J 2012;14:104-6.
- Bäuerle D, Specht-Leible N, Voss E. Changes in needs for assistance and care after hip fractures in the elderly. Z Gerontol Geriatr 2004;37:351-3. https://doi.org/10.1007/s00391-004-0257-7.
- Takayama S, Iki M, Kusaka Y, Takagi H, Tamaki S. Factors that influence functional prognosis in elderly patients with hip fracture. Environ Health Prev Med 2001;6:47-53. https://doi.org/10.1007/BF02897309.
- Roberto KA. The role of social supports in older women’s recovery from hip fractures. J Appl Gerontol 1992;11:314-25. https://doi.org/10.1177/073346489201100305.
- Portegijs E, Edgren J, Salpakoski A, Kallinen M, Rantanen T, Alen M, et al. Balance confidence was associated with mobility and balance performance in older people with fall-related hip fracture: a cross-sectional study. Arch Phys Med Rehabil 2012;93:2340-6. http://dx.doi.org/10.1016/j.apmr.2012.05.022.
- Latham NK, Jette DU, Warren RL, Wirtalla C. Pattern of functional change during rehabilitation of patients with hip fracture. Arch Phys Med Rehabil 2006;87:111-16. http://dx.doi.org/10.1016/j.apmr.2005.08.121.
- Hoenig H, Rubenstein LV, Sloane R, Horner R, Kahn K. What is the role of timing in the surgical and rehabilitative care of community-dwelling older persons with acute hip fracture?. Arch Intern Med 1997;157:513-20. https://doi.org/10.1001/archinte.1997.00440260055009.
- Petrella RJ, Payne M, Myers A, Overend T, Chesworth B. Physical function and fear of falling after hip fracture rehabilitation in the elderly. Am J Phys Med Rehabil 2000;79:154-60. https://doi.org/10.1097/00002060-200003000-00008.
- Bellelli G, Guerini F, Trabucchi M. Body weight-supported treadmill in the physical rehabilitation of severely demented subjects after hip fracture: a case report. J Am Geriatr Soc 2006;54:717-18.
- De Jonge KE, Christmas C, Andersen R, Franckowiak SC, Mears SC, Levy P, et al. Hip Fracture Service – an interdisciplinary model of care. J Am Geriatr Soc 2001;49:1737-8. https://doi.org/10.1046/j.1532-5415.2001.49292.x.
- Edwards MM, Baptiste S. The HIPP consultation and rehabilitation team: developing a streamlined service and its implications for work processes. Work 2004;23:23-9.
- Kerr C, Gallop K, Nixon A, Naegeli A, Zhao Y, Burge R. Conceptual model of the impact of hip fracture on patients’ lives. Value Health 2011. https://doi.org/10.1016/j.jval.2011.08.452.
- Shawler C. The empowerment of older mothers and daughters: rehabilitation strategies following a hip fracture. Geriatr Nurs 2006;27:371-7. http://dx.doi.org/10.1016/j.gerinurse.2006.10.014.
- Cree M, Hayduk L, Soskolne CL, Suarez-Almazor M. Modeling changes in health perception following hip fracture. Qual Life Res 2001;10:651-9. https://doi.org/10.1023/A:1013880008217.
- Atwal A, Caldwell K. Do multidisciplinary integrated care pathways improve interprofessional collaboration?. Scand J Caring Sci 2002;16:360-7.
- Barone A, Giusti A, Pizzonia M, Razzano M, Oliveri M, Palummeri E, et al. Factors associated with an immediate weight-bearing and early ambulation program for older adults after hip fracture repair. Arch Phys Med Rehabil 2009;90:1495-8. http://dx.doi.org/10.1016/j.apmr.2009.03.013.
- Kammerlander C, Gosch M, Kammerlander-Knauer U, Luger TJ, Blauth M, Roth T. Long-term functional outcome in geriatric hip fracture patients. Arch Orthop Trauma Surg 2011;131:1435-44. http://dx.doi.org/10.1007/s00402-011-1313-6.
- Lieberman D, Friger M, Lieberman D. Inpatient rehabilitation outcome after hip fracture surgery in elderly patients: a prospective cohort study of 946 patients. Arch Phys Med Rehabil 2006;87:167-71. http://dx.doi.org/10.1016/j.apmr.2005.10.002.
- Lindelof N, Littbrand H, Lindstrom B, Nyberg L. Weighted belt exercise for frail older women following hip fracture – a single subject design. Adv Physiother 2002;4:54-6.
- Moore A. Functional outcomes of patients with hip fracture in the home health care setting. J Home Health Care Pract 1993;5:49-58.
- Morghen S, Gentile S, Ricci E, Guerini F, Bellelli G, Trabucchi M. Rehabilitation of older adults with hip fracture: cognitive function and walking abilities. J Am Geriatr Soc 2011;59:1497-502. http://dx.doi.org/10.1111/j.1532-5415.2011.03496.x.
- Robinson SB. Transitions in the lives of elderly women who have sustained hip fractures. J Adv Nurs 1999;30:1341-8. https://doi.org/10.1046/j.1365-2648.1999.01238.x.
- Rolland Y, Pillard F, Lauwers-Cances V, Busquère F, Vellas B, Lafont C. Rehabilitation outcome of elderly patients with hip fracture and cognitive impairment. Disabil Rehabil 2004;26:425-31. http://dx.doi.org/10.1080/09638280410001663148.
- Taylor NF, Harding KE, Dowling J, Harrison G. Discharge planning for patients receiving rehabilitation after hip fracture: a qualitative analysis of physiotherapists’ perceptions. Disabil Rehabil 2010;32:492-9.
- van der Sluijs JA, Walenkamp GH. How predictable is rehabilitation after hip fracture? A prospective study of 134 patients. Acta Orthop Scand 1991;62:567-72. https://doi.org/10.3109/17453679108994498.
- Walheim G, Barrios C, Stark A, Broström LA, Olsson E. Postoperative improvement of walking capacity in patients with trochanteric hip fracture: a prospective analysis 3 and 6 months after surgery. J Orthop Trauma 1990;4:137-43. https://doi.org/10.1097/00005131-199004020-00006.
- Borgquist L, Nordell E, Jarnlo GB, Strömqvist B, Wingstrand H, Thorngren KG. Hip fractures in primary health care. Evaluation of a rehabilitation programme. Scand J Prim Health Care 1990;8:139-44. https://doi.org/10.3109/02813439008994947.
- Li HJ, Shyu YI. Coping processes of Taiwanese families during the postdischarge period for an elderly family member with hip fracture. Nurs Sci Q 2007;20:273-9. http://dx.doi.org/10.1177/0894318407303128.
- Lin P, Chang S. Functional recovery among elderly people one year after hip fracture surgery. J Nurs Res 2004;12:72-8.
- Orwig D, Hochberg M, Yu-Yahiro J, Resnick B, Hawkes W, Shardeil M, et al. Delivery and outcomes of a yearlong home exercise program after hip fracture: a randomized controlled trial. Arch Intern Med 2011;171:323-31.
- Penrod JD, Boockvar KS, Litke A, Magaziner J, Hannan EL, Halm EA, et al. Physical therapy and mobility 2 and 6 months after hip fracture. J Am Geriatr Soc 2004;52:1114-20. http://dx.doi.org/10.1111/j.1532-5415.2004.52309.x.
- Sirkka M, Bränholm I. Consequences of a hip fracture in activity performance and life satisfaction in an elderly Swedish clientele. Scand J Occup Ther 2003;10:34-9. https://doi.org/10.1080/11038120310004501.
- Talkowski JB, Lenze EJ, Munin MC, Harrison C, Brach JS. Patient participation and physical activity during rehabilitation and future functional outcomes in patients after hip fracture. Arch Phys Med Rehabil 2009;90:618-22. http://dx.doi.org/10.1016/j.apmr.2008.10.024.
- Jones GR, Miller TA, Petrella RJ. Evaluation of rehabilitation outcomes in older patients with hip fractures. Am J Phys Med Rehabil 2002;81:489-97. https://doi.org/10.1097/00002060-200207000-00004.
- Shyu YI, Cheng HS, Teng HC, Chen MC, Wu CC, Tsai WC. Older people with hip fracture: depression in the postoperative first year. J Adv Nurs 2009;65:2514-22. http://dx.doi.org/10.1111/j.1365-2648.2009.05125.x.
- Burns A, Banerjee S, Morris J, Woodward Y, Baldwin R, Proctor R, et al. Treatment and prevention of depression after surgery for hip fracture in older people: randomized, controlled trials. J Am Geriatr Soc 2007;55:75-80.
- Long AF, Kneafsey R, Ryan J, Berry J. The role of the nurse within the multi-professional rehabilitation team. J Adv Nurs 2002;37:70-8. https://doi.org/10.1046/j.1365-2648.2002.02059.x.
- Sylliaas H, Brovold T, Wyller TB, Bergland A. Progressive strength training in older patients after hip fracture: a randomised controlled trial. Age Ageing 2011;40:221-7.
- Fox HJ, Hughes SJ, Pooler J, Prothero D, Bannister GC. Length of hospital stay and outcome after femoral neck fracture: a prospective study comparing the performance of two hospitals. Injury 1993;24:464-6. https://doi.org/10.1016/0020-1383(93)90151-U.
- Arinzon Z, Fidelman Z, Zuta A, Peisakh A, Berner YN. Functional recovery after hip fracture in old-old elderly patients. Arch Gerontol Geriatr 2005;40:327-36. http://dx.doi.org/10.1016/j.archger.2004.10.003.
- Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 2000;55:M498-507. https://doi.org/10.1093/gerona/55.9.M498.
- van Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ. Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res 2001;390:232-43. https://doi.org/10.1097/00003086-200109000-00027.
- Mutran EJ, Reitzes DC, Mossey J, Fernandez ME. Social support, depression, and recovery of walking ability following hip fracture surgery. J Gerontol B Psychol Sci Soc Sci 1995;50:S354-61.
- Lenze EJ, Munin MC, Skidmore ER, Dew MA, Rogers JC, Whyte EM, et al. Onset of depression in elderly persons after hip fracture: implications for prevention and early intervention of late-life depression. J Am Geriatr Soc 2007;55:81-6. http://dx.doi.org/10.1111/j.1532-5415.2006.01017.x.
- Bandura A. Self Efficacy: The Exercise of Control. New York, NY: WH Freeman; 1997.
- Young Y, Resnick B. Don’t worry, be positive: improving functional recovery 1 year after hip fracture. Rehabil Nurs 2009;34:110-17. https://doi.org/10.1002/j.2048-7940.2009.tb00265.x.
- Houwing RH, Rozendaal M, Wouters-Wesseling W, Beulens JW, Buskens E, Haalboom JR. A randomised, double-blind assessment of the effect of nutritional supplementation on the prevention of pressure ulcers in hip-fracture patients. Clin Nutr 2003;22:401-5. https://doi.org/10.1016/S0261-5614(03)00039-6.
- Ponzer S, Tidermark J, Brismar K, Söderqvist A, Cederholm T. Nutritional status, insulin-like growth factor-1 and quality of life in elderly women with hip fractures. Clin Nutr 1999;18:241-6. http://dx.doi.org/10.1054/clnu.1999.0029.
- Zidén L, Scherman MH, Wenestam CG. The break remains – elderly people’s experiences of a hip fracture 1 year after discharge. Disabil Rehabil 2010;32:103-13. http://dx.doi.org/10.3109/09638280903009263.
- Godfrey M, Townsend J. Older people in transition from illness to health: trajectories of recovery. Qual Health Res 2008;18:939-51. http://dx.doi.org/10.1177/1049732308318038.
- Manthorpe J, Cornes M. Intermediate care: older people’s involvement and experiences. J Integrated Care 2004;12:43-8.
- Thomas V, Lambert S. An ethnographic study of intermediate care services in Wales: the hidden work. J Nurs Manag 2008;16:181-7. http://dx.doi.org/10.1111/j.1365-2834.2008.00846.x.
- Trappes-Lomax T, Hawton A. The user voice: older people’s experiences of reablement and rehabilitation. J Integrated Care 2012;20:181-95.
- Joseph Rowntree Foundation . Older People Shaping Policy and Practice 2004. www.jrf.org.uk/report/older-people-shaping-policy-and-practice (accessed 27 January 2016).
- Swinkels A, Mitchell T. Delayed transfer from hospital to community settings: the older person’s perspective. Health Soc Care Community 2009;17:45-53. http://dx.doi.org/10.1111/j.1365-2524.2008.00796.x.
- Ryan-Woolley B, Wilson K, Caress A. The implementation and evaluation of a community rehabilitation team: a case study. Disabil Rehabil 2004;26:817-26. http://dx.doi.org/10.1080/09638280410001696737.
- Crotty M, Whitehead CH, Gray S, Finucane PM. Early discharge and home rehabilitation after hip fracture achieves functional improvements: a randomized controlled trial. Clin Rehabil 2002;16:406-13. https://doi.org/10.1191/0269215502cr518oa.
- Knowelden J, Westlake L, Wright KG, Clarke SJ. Peterborough Hospital at Home: an evaluation. J Public Health Med 1991;13:182-8. https://doi.org/10.1093/oxfordjournals.pubmed.a042616.
- Crotty M, Kittel A, Hayball N. Home rehabilitation for older adults with fractured hips: how many will take part?. J Qual Clin Pract 2000;20:65-8. https://doi.org/10.1046/j.1440-1762.2000.00367.x.
- Cicirelli V, Brubaker TH. Family Relationships in Later Life. Newbury Park, CA: Sage; 1990.
- Shyu Y-IL, Liang J, Wu C-C, Cheng H-S, Chen M-C. An interdisciplinary intervention for older Taiwanese patients after surgery for hip fracture improves health-related quality of life. BMC Musculoskelet Disord 2010;11. https://doi.org/10.1186/1471-2474-11-225.
- Collins R, Lee RE, Albright CL, King AC. Ready to be physically active? The effects of a course preparing low-income multiethnic women to be more physically active. Health Educ Behav 2004;31:47-64. http://dx.doi.org/10.1177/1090198103255529.
- Wilcox S, Bopp M, Oberrecht L, Kammermann SK, McElmurray CT. Psychosocial and perceived environmental correlates of physical activity in rural and older African American and white women. J Gerontol B Psychol Sci Soc Sci 2003;58:P329-37.
- Littbrand H, Rosendahl E, Lindelöf N, Lundin-Olsson L, Gustafson Y, Nyberg L. A high-intensity functional weight-bearing exercise program for older people dependent in activities of daily living and living in residential care facilities: evaluation of the applicability with focus on cognitive function. Phys Ther 2006;86:489-98.
- Resnick B, Vogel A, Luisi D. Motivating minority older adults to exercise. Cultur Divers Ethnic Minor Psychol 2006;12:17-29. http://dx.doi.org/10.1037/1099-9809.12.1.17.
- Resnick B, Hicks GE, Orwig D, Yu-Yahiro J, Magaziner J. Review of the impact of exercise interventions on function post hip fracture and recommendations for future interventions. Int J Disabil Community Rehabil 2010;9.
- Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res 1967;11:213-18. https://doi.org/10.1016/0022-3999(67)90010-4.
- Rotter J. Some problems and misconceptions related to the construct of internal versus external control of reinforcement. J Consult Clin Psychol 1975;43:55-67.
- Peterson C, Seligman ME. Explanatory style and illness. J Pers 1987;55:237-65. https://doi.org/10.1111/j.1467-6494.1987.tb00436.x.
- McAuley E, Konopack JF, Motl RW, Morris KS, Doerksen SE, Rosengren KR. Physical activity and quality of life in older adults: influence of health status and self-efficacy. Ann Behav Med 2006;31:99-103. https://doi.org/10.1207/s15324796abm3101_14.
- Lundström M, Olofsson B, Stenvall M, Karlsson S, Nyberg L, Englund U, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res 2007;19:178-86.
- Stenvall M, Berggren M, Lundström M, Gustafson Y, Olofsson B. A multidisciplinary intervention program improved the outcome after hip fracture for people with dementia – subgroup analyses of a randomized controlled trial. Arch Gerontol Geriatr 2012;54:e284-9. http://dx.doi.org/10.1016/j.archger.2011.08.013.
- Stenvall M, Olofsson B, Lundström M, Svensson O, Nyberg L, Gustafson Y. Inpatient falls and injuries in older patients treated for femoral neck fracture. Arch Gerontol Geriatr 2006;43:389-99. http://dx.doi.org/10.1016/j.archger.2006.01.004.
- Dai YT, Huang GS, Yang RS, Tsauo JY, Yang LH. Effectiveness of a multidisciplinary rehabilitation program in elderly patients with hip fractures. J Formos Med Assoc 2001;100:120-6.
- Zuckerman JD, Sakales SR, Fabian DR, Frankel VH. Hip fractures in geriatric patients. Results of an interdisciplinary hospital care program. Clin Orthop Relat Res 1992;274:213-25.
- Reid J, Kennie DC. Geriatric rehabilitative care after fractures of the proximal femur: one year follow up of a randomised clinical trial. BMJ 1989;299:25-6. https://doi.org/10.1136/bmj.299.6690.25-a.
- Galvard H, Samuelsson SM. Orthopedic or geriatric rehabilitation of hip fracture patients: a prospective, randomized, clinically controlled study in Malmö, Sweden. Aging 1995;7:11-6. https://doi.org/10.1007/bf03324284.
- Hempsall VJ, Robertson DR, Campbell MJ, Briggs RS. Orthopaedic geriatric care – is it effective? A prospective population-based comparison of outcome in fractured neck of femur. J R Coll Physicians Lond 1990;24:47-50.
- Cameron ID, Handoll HH, Finnegan TP, Madhok R, Langhorne P. Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures. Cochrane Database Syst Rev 2009;4. https://doi.org/10.1002/14651858.cd000106.pub2.
- Hutchings L, Fox R, Chesser T. Proximal femoral fractures in the elderly: how are we measuring outcome?. Injury 2011;42:1205-13. http://dx.doi.org/10.1016/j.injury.2010.12.016.
- Allegrante JP, MacKenzie CR, Robbins L, Cornell CN. Hip fracture in older persons. Does self-efficacy-based intervention have a role in rehabilitation?. Arthritis Care Res 1991;4:39-47. https://doi.org/10.1002/art.1790040108.
- Craik RL. Disability following hip fracture. Phys Ther 1994;74:387-98. https://doi.org/10.1093/ptj/74.5.387.
- Marks R. Physical activity and hip fracture disability: a review. J Aging Res 2011;2011. http://dx.doi.org/10.4061/2011/741918.
- Zijlstra GA, van Haastregt JC, van Rossum E, van Eijk JT, Yardley L, Kempen GI. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc 2007;55:603-15. http://dx.doi.org/10.1111/j.1532-5415.2007.01148.x.
- Krichbaum K. GAPN postacute care coordination improves hip fracture outcomes. West J Nurs Res 2007;29:523-44. http://dx.doi.org/10.1177/0193945906293817.
- Farnworth MG, Kenny P, Shiell A. The costs and effects of early discharge in the management of fractured hip. Age Ageing 1994;23:190-4. https://doi.org/10.1093/ageing/23.3.190.
- Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2009;2. https://doi.org/10.1002/14651858.cd007146.pub2.
- Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev 2009;3. http://dx.doi.org/10.1002/14651858.CD002759.pub2.
- Jung D, Lee J, Lee S-M. A meta-analysis of fear of falling treatment programs for the elderly. West J Nurs Res 2009;31:6-16. http://dx.doi.org/10.1177/0193945908320466.
- Di Monaco M, Vallero F, Tappero R, Cavanna A. Rehabilitation after total hip arthroplasty: a systematic review of controlled trials on physical exercise programs. Eur J Phys Rehabil Med 2009;45:303-17.
- Stewart LSP, McMillan IR. Rehabilitation schemes for elderly patients with a hip fracture. Br J Occup Ther 1998;61:367-71.
- Cameron ID, Lyle DM, Quine S. Cost effectiveness of accelerated rehabilitation after proximal femoral fracture. J Clin Epidemiol 1994;47:1307-13. https://doi.org/10.1016/0895-4356(94)90136-8.
- Fordham R, Thompson R, Holmes J, Hodkinson C. A Cost–Benefit Study of Geriatric Orthopaedic Management of Patients With Fractured Neck of Femur 1986. www.york.ac.uk/media/che/documents/papers/discussionpapers/CHE%20Discussion%20Paper%2014.pdf (accessed 16 February 2017).
- Huusko TM, Karppi P, Avikainen V, Kautiainen H, Sulkava R. Intensive geriatric rehabilitation of hip fracture patients: a randomized, controlled trial. Acta Orthop Scand 2002;73:425-31. http://dx.doi.org/10.1080/00016470216324.
- Coast J, Richards SH, Peters TJ, Gunnell DJ, Darlow MA, Pounsford J. Hospital at home or acute hospital care? A cost minimisation analysis. BMJ 1998;316:1802-6. https://doi.org/10.1136/bmj.316.7147.1802.
- Hollingworth W, Todd C, Parker M, Roberts JA, Williams R. Cost analysis of early discharge after hip fracture. BMJ 1993;307:903-6. https://doi.org/10.1136/bmj.307.6909.903.
- O’Cathain A. Evaluation of a Hospital at Home scheme for the early discharge of patients with fractured neck of femur. J Public Health Med 1994;16:205-10. https://doi.org/10.1093/oxfordjournals.pubmed.a042958.
- Parker MJ, Pryor GA, Myles JW. Early discharge after hip fracture. Prospective 3-year study of 645 patients. Acta Orthop Scand 1991;62:563-6. https://doi.org/10.3109/17453679108994497.
- Olsson LE, Hansson E, Ekman I, Karlsson J. A cost-effectiveness study of a patient-centred integrated care pathway. J Adv Nurs 2009;65:1626-35. http://dx.doi.org/10.1111/j.1365-2648.2009.05017.x.
- Kramer AM, Steiner JF, Schlenker RE, Eilertsen TB, Hrincevich CA, Tropea DA, et al. Outcomes and costs after hip fracture and stroke: a comparison of rehabilitation settings. JAMA 1997;277:396-404. https://doi.org/10.1001/jama.1997.03540290048031.
- Ruchlin HS, Elkin EB, Allegrante JP. The economic impact of a multifactorial intervention to improve postoperative rehabilitation of hip fracture patients. Arthritis Care Res 2001;45.
- Polder JJ, van Balen R, Steyerberg EW, Cools HJ, Habbema JD. A cost-minimisation study of alternative discharge policies after hip fracture repair. Health Econ 2003;12:87-100. http://dx.doi.org/10.1002/hec.690.
- Elliot JR, Wilkinson TJ, Hanger HC, Gilchrist NL, Sainsbury R, Shamy S, et al. The added effectiveness of early geriatrician involvement on acute orthopaedic wards to orthogeriatric rehabilitation. N Z Med J 1996;109:72-3.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J 1965;14:61-5.
- Ware JE, Snow KK, Kosinski MA, Gandek BG. SF-36 Health Survey: Manual and Interpretation Guide. Boston, MA: The Health Institute, New England Medical Center; 1993.
- Van Bennekom CA, Jelles F, Lankhorst GJ. Rehabilitation activities profile: the ICIDH as a framework for a problem-oriented assessment method in rehabilitation medicine. Disabil Rehabil 1995;17:169-75. https://doi.org/10.3109/09638289509166712.
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98. https://doi.org/10.1016/0022-3956(75)90026-6.
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963;185:914-19. https://doi.org/10.1001/jama.1963.03060120024016.
- Sikorski JM, Senior J. The Domiciliary Rehabilitation and Support Program. Rationale, organisation and outcome. Med J Aust 1993;159:23-5.
- Briggs AH, Gray AM. Power and sample size calculations for stochastic cost-effectiveness analysis. Med Decis Making 1998;18:81-92. https://doi.org/10.1177/0272989X98018002S10.
- Magklara E, Burton C, Morrison V. Does self-efficacy influence recovery and well-being in osteoarthritis patients undergoing joint replacement? A systematic review. Clin Rehabil 2014;28:835-46.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. https://doi.org/10.1037/0033-295X.84.2.191.
- Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972;1:233-8. https://doi.org/10.1093/ageing/1.4.233.
- Pangman VC, Sloan J, Guse L. An examination of psychometric properties of the Mini-Mental Status Examination and the Standardized Mini-Mental Status Examination: implications for clinical practice. Appl Nurs Res 2000;13:209-13. https://doi.org/10.1053/apnr.2000.9231.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37-49. https://doi.org/10.1016/0022-3956(82)90033-4.
- Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 1986;5:165-73. https://doi.org/10.1300/J018v05n01_09.
- Williamson PR, Altman DG, Blazeby JM, Clarke M, Devane D, Gargon E, et al. Developing core outcome sets for clinical trials: issues to consider. Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-132.
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85-94. https://doi.org/10.1093/geronj/49.2.M85.
- Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther 2008;88:559-6. https://doi.org/10.2522/ptj.20070205.
- Kates SL, Shields E, Behrend C, Noyes KK. Financial implications of hospital readmission after hip fracture. Geriatr Orthop Surg Rehabil 2015;6:140-6. http://dx.doi.org/10.1177/2151458515578265.
- Simpson J, Worsfold C. A simple test of balance for frail old people. Clin Rehabil 1996;10.
- Brown J, Pengas G, Dawson K, Brown LA, Clatworthy P. Self administered cognitive screening test (TYM) for detection of Alzheimer’s disease: cross sectional study. BMJ 2009;338. https://doi.org/10.1136/bmj.b2030.
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695-9. https://doi.org/10.1111/j.1532-5415.2005.53221.x.
- Nandy S, Parsons S, Cryer C, Underwood M, Rashbrook E, Carter Y, et al. Development and preliminary examination of the predictive validity of the Falls Risk Assessment Tool (FRAT) for use in primary care. J Public Health 2004;26:138-43. https://doi.org/10.1093/pubmed/fdh132.
- Smith R. Validation and reliability of the Elderly Mobility Scale. Physiotherapy 1994;80:744-7. https://doi.org/10.1016/S0031-9406(10)60612-8.
- EuroQol . EQ-5D User Guide Version 2 n.d. www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/EQ-5D-5L_UserGuide_2015.pdf (accessed 27 March 2017).
- Podsiadlo D, Richardson S. The timed ‘Up & Go’: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142-8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x.
- National Rheumatoid Arthritis Society and Chartered Society of Physiotherapy . RA and Physiotherapy: A National Survey 2011. www.csp.org.uk/publications/ra-physiotherapy (accessed 8 January 2016).
- Chartered Society of Physiotherapy . A Survey of NHS Physiotherapy Waiting Times, Workforce and Caseloads in the UK 2010–2011 2011. www.csp.org.uk/publications/survey-nhs-physiotherapy-waiting-times-workforce-caseloads-uk-2010-2011 (accessed 8 January 2016).
- Kitzinger J. The methodology of focus groups: the importance of interaction between research participants. Sociol Health Illness 1994;16:103-21. https://doi.org/10.1111/1467-9566.ep11347023.
- Kitzinger J. Qualitative research. Introducing focus groups. BMJ 1995;311:299-302. https://doi.org/10.1136/bmj.311.7000.299.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- Williams NH, Hawkes C, Din NU, Roberts J, Charles JM, Morrison V, et al. Fracture in the Elderly Multidisciplinary Rehabilitation (FEMuR): study protocol for a Phase II randomised feasibility study of a multidisciplinary rehabilitation package following hip fracture [ISRCTN22464643]. Pilot Feasibil Stud 2015;1. https://doi.org/10.1186/s40814-015-0008-0.
- Murphy S, Raisanen L, Moore G, Edwards RT, Linck P, Williams N, et al. A pragmatic randomised controlled trial of the Welsh National Exercise Referral Scheme: protocol for trial and integrated economic and process evaluation. BMC Public Health 2010;10:1-12.
- Griffiths F, Mason V, Boardman F, Dennick K, Haywood K, Achten J, et al. Evaluating recovery following hip fracture: a qualitative interview study of what is important to patients. BMJ Open 2015;5. http://dx.doi.org/10.1136/bmjopen-2014-005406.
- Taylor NF, Barelli C, Harding KE. Community ambulation before and after hip fracture: a qualitative analysis. Disabil Rehabil 2010;32:1281-90. http://dx.doi.org/10.3109/09638280903483869.
- McMillan L, Booth J, Currie K, Howe T. ‘Balancing risk’ after fall-induced hip fracture: the older person’s need for information. Int J Older People Nurs 2014;9:249-57. http://dx.doi.org/10.1111/opn.12028.
- Long AF, Kneafsey R, Ryan J. Rehabilitation practice: challenges to effective team working. Int J Nurs Stud 2003;40:663-73. https://doi.org/10.1016/S0020-7489(03)00015-4.
- Morrison VL, Johnston M, MacWalter RS, Pollard BS. Improving emotional outcomes following acute stroke: a preliminary evaluation of a work-book based intervention. Scott Med J 1998;43:52-3.
- Robinson BC. Validation of a Caregiver Strain Index. J Gerontol 1983;38:344-8. https://doi.org/10.1093/geronj/38.3.344.
- Russell D, Hoare ZS, Whitaker R, Whitaker CJ, Russell IT. Generalized method for adaptive randomization in clinical trials. Stat Med 2011;30:922-34. http://dx.doi.org/10.1002/sim.4175.
- Helping You to Assess Cognition: A Practical Toolkit for Clinicians. London: Alzheimer’s Society; 2013.
- Nouri F, Lincoln N. An extended activities of daily living scale for stroke patients. Clin Rehabil 1987;1:301-5.
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Brokelman RB, Haverkamp D, van Loon C, Hol A, van Kampen A, Veth R. The validation of the visual analogue scale for patient satisfaction after total hip arthroplasty. Eur Orthop Traumatol 2012;3:101-5.
- Martinelli N, Longo UG, Marinozzi A, Franceschetti E, Costa V, Denaro V. Cross-cultural adaptation and validation with reliability, validity, and responsiveness of the Italian version of the Oxford Hip Score in patients with hip osteoarthritis. Qual Life Res 2011;20:923-9. http://dx.doi.org/10.1007/s11136-010-9811-5.
- Schwarzer R, Jerusalem M, Weinman J, Wright S, Johnston M. Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs. Windsor: NFER-NELSON; 1995.
- Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005;34:614-19. http://dx.doi.org/10.1093/ageing/afi196.
- Hauer K, Yardley L, Beyer N, Kempen G, Dias N, Campbell M, et al. Validation of the Falls Efficacy Scale and Falls Efficacy Scale International in geriatric patients with and without cognitive impairment: results of self-report and interview-based questionnaires. Gerontology 2010;56:190-9.
- Resnick B, Jenkins LS. Testing the reliability and validity of the Self-Efficacy for Exercise scale. Nurs Res 2000;49:154-9.
- Scheffer AC, Schuurmans MJ, vanDijk N, van der Hooft T, de Rooij SE. Reliability and validity of the visual analogue scale for fear of falling in older persons. J Am Geriatr Soc 2010;58:2228-30. http://dx.doi.org/10.1111/j.1532-5415.2010.03105.x.
- Coast J, Peters TJ, Natarajan L, Sproston K, Flynn T. An assessment of the construct validity of the descriptive system for the ICECAP capability measure for older people. Qual Life Res 2008;17:967-76. http://dx.doi.org/10.1007/s11136-008-9372-z.
- Makai P, Brouwer WB, Koopmanschap MA, Nieboer AP. Capabilities and quality of life in Dutch psycho-geriatric nursing homes: an exploratory study using a proxy version of the ICECAP-O. Qual Life Res 2012;21:801-12. http://dx.doi.org/10.1007/s11136-011-9997-1.
- Database of Instruments for Resource Use Measurement . Client Service Receipt Inventory (CSRI) n.d. www.dirum.org/instruments/details/44 (accessed January 2015).
- Giampaoli S, Ferrucci L, Cecchi F, Lo Noce C, Poce A, Dima F, et al. Hand-grip strength predicts incident disability in non-disabled older men. Age Ageing 1999;28:283-8. https://doi.org/10.1093/ageing/28.3.283.
- Bohannon RW. Test–retest reliability of the five-repetition sit-to-stand test: a systematic review of the literature involving adults. J Strength Cond Res 2011;25:3205-7. http://dx.doi.org/10.1519/JSC.0b013e318234e59f.
- Rikli RE, Jones CJ. Senior Fitness Test Manual and Kit. Champaign, IL: Human Kinetics; 2001.
- Brown M, Sinacore DR, Binder EF, Kohrt WM. Physical and performance measures for the identification of mild to moderate frailty. J Gerontol Ser A Biol Sci Med Sci 2000;55:M350-5. https://doi.org/10.1093/gerona/55.6.M350.
- Brach JS, VanSwearingen JM. Physical impairment and disability: relationship to performance of activities of daily living in community-dwelling older men. Phys Ther 2002;82:752-61.
- Ramessur N. Policy and Procedures for the Protection of Vulnerable Adults (POVA). Safeguarding Vulnerable Adult Committee, BCUHB Safeguarding Children and Vulnerable Adult Board 2009. www.wales.nhs.uk/sitesplus/861/opendoc/144785 (accessed 2014).
- In Safe Hands: Implementing Adult Protection Procedures in Wales. Cardiff: Welsh Government; 2000.
- Wales Interim Policy and Procedures for the Protection of Vulnerable Adults from Abuse. Cardiff: Welsh Government; 2013.
- Human Rights Act 1998. London: The Stationery Office; 1998.
- Data Protection Act 1998. London: The Stationery Office; 1998.
- Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol 2012;65:301-8. http://dx.doi.org/10.1016/j.jclinepi.2011.07.011.
- ICH Harmonised Tripartite Guideline. Guideline for Good Clinical Practice. Geneva: International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use; 1996.
- Freedom of Information Act 2000. London: The Stationery Office; 2000.
- European Parliament and the Council of the European Union . Directive 2001 20 EC 2001 of the European Parliament and of the Council of 4 April 2001 n.d. http://eurlex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2001:121:0034:0044:en:PDF (accessed 16 February 2017).
- Kromrey JD, Bell BA. ES_ANOVA: A SAS® Macro for Computing Point and Interval Estimates of Effect Sizes Associated With Analysis of Variance Models n.d.
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. New York, NY: Academic Press; 1988.
- Sprange K, Mountain GA, Shortland K, Craig C, Blackburn D, Bowie P, et al. Journeying through dementia, a community-based self-management intervention for people aged 65 years and over: a feasibility study to inform a future trial. Pilot Feasibility Stud 2015;1:1-14.
- Thoma A, Farrokhyar F, McKnight L, Bhandari M. Practical tips for surgical research: how to optimize patient recruitment. Can J Surg 2010;53:205-10.
- Abraham NS, Young JM, Solomon MJ. A systematic review of reasons for nonentry of eligible patients into surgical randomized controlled trials. Surgery 2006;139:469-83. http://dx.doi.org/10.1016/j.surg.2005.08.014.
- Ward JA, Potter S, Blazeby JM. Outcome reporting for reconstructive breast surgery: the need for consensus, consistency and core outcome sets. Eur J Surg Oncol 2012;38:1020-1. http://dx.doi.org/10.1016/j.ejso.2012.07.108.
- Currie C, Partridge M, Plant F, Wakeman R, Williams A. National Hip Fracture Database National Report 2012. www.nhfd.co.uk/ (accessed 26 January 2015).
- Haywood KL, Brett J, Tutton L, Stanisewska S. Patient-reported outcome measures (PROMs) and fragility hip fracture: a systematic review of quality and acceptability. J Qual Life 2013;22.
- Haywood KL, Griffin XL, Achten J, Costa ML. Developing a core outcome set for hip fracture trials. Bone Joint J 2014;96-B:1016-23. http://dx.doi.org/10.1302/0301-620X.96B8.33766.
- Reference Costs 2013 to 2014. London: NHS England; 2014.
- Härstedt M, Rogmark C, Sutton R, Melander O, Fedorowski A. Impact of comorbidity on 6-month hospital readmission and mortality after hip fracture surgery. Injury 2015;46:713-18. http://dx.doi.org/10.1016/j.injury.2014.12.024.
- Lo JC, Srinivasan S, Chandra M, Patton M, Budayr A, Liu LH, et al. Trends in mortality following hip fracture in older women. Am J Manag Care 2015;21:e206-14.
- Heyes GJ, Tucker A, Marley D, Foster A. Predictors for 1-year mortality following hip fracture: a retrospective review of 465 consecutive patients. Eur J Trauma Emerg Surg 2017;43:113-19.
- Moulton LS, Green NL, Sudahar T, Makwana NK, Whittaker JP. Outcome after conservatively managed intracapsular fractures of the femoral neck. Ann R Coll Surg Engl 2015;97:279-82. http://dx.doi.org/10.1308/003588415X14181254788809.
- Drew S, Sheard S, Chana J, Cooper C, Javaid MK, Judge A. Describing variation in the delivery of secondary fracture prevention after hip fracture: an overview of 11 hospitals within one regional area in England. Osteoporos Int 2014;25:2427-33. https://doi.org/10.1007/s00198-014-2775-5.
- Neuburger J, Harding KA, Bradley RJD, Cromwell DA, Gregson CL. Variation in access to community rehabilitation services and length of stay in hospital following a hip fracture: a cross-sectional study. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005469.
- Millett R. Lack of community rehab consigns hip fracture patients to costly hospital stays, says CSP. Frontline 2013;19.
- Löfgren S, Hedström M, Ekström W, Lindberg L, Flodin L, Ryd L. Power to the patient: care tracks and empowerment a recipe for improving rehabilitation for hip fracture patients. Scand J Caring Sci 2015;29:462-9. http://dx.doi.org/10.1111/scs.12157.
- McBride TJ, Panrucker S, Clothier JC. Hip fractures: public perceptions. Ann R Coll Surg Engl 2011;93:67-70. http://dx.doi.org/10.1308/003588411X12851639107034.
- Ryan M, Gerard K, Amaya-Amaya M. Using Discrete Choice Experiments to Value Health Care Programmes. Dordrecht: Springer; 2008.
- Brazier J, Ratcliffe J, Saloman JA, Tsuchiya A. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford: Oxford University Press; 2007.
- Health Care Cost, Quality, and Outcomes. Lawrenceville, NJ: ISPOR Publications; 2003.
- Methods for the Development of NICE Public Health Guidance. London: NICE; 2012.
- Kelly MP, McDaid D, Ludbrook A, Powell J. Economic Appraisal of Public Health Interventions. London: Health Development Agency; 2005.
- Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy 2009;93:85-92. http://dx.doi.org/10.1016/j.healthpol.2009.07.012.
- Edwards RT, Hounsome B, Linck P, Russell IT. Economic evaluation alongside pragmatic randomised trials: developing a standard operating procedure for clinical trials units. Trials 2008;9. https://doi.org/10.1186/1745-6215-9-64.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2014.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: Personal Social Services Research Unit, University of Kent; 2012.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2007.
- Robinson R. Economic evaluation in health care. Cost–utility analysis. BMJ 1993;307:859-62. https://doi.org/10.1136/bmj.307.6908.859.
- Hahn GJ, Shapiro SS. A Catalog and Computer Program for the Design and Analysis of Orthogonal Symmetric and Asymmetric Fractional Factorial Experiments. Schenectady, NY: General Electric, Research and Development Center; 1966.
- Fujiwara D. A General Method for Valuing Non-Market Goods Using Wellbeing Data: Three-Stage Wellbeing Valuation 2013. http://cep.lse.ac.uk/pubs/download/dp1233.pdf (accessed 16 February 2017).
- Dolan P, Peasgood T. Measuring well-being for public policy: preferences or experiences?. J Legal Stud 2008;37:S5-31.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: University of York; 1999.
- Davis JC, Bryan S, McLeod R, Rogers J, Khan K, Liu-Ambrose T. Exploration of the association between quality of life, assessed by the EQ-5D and ICECAP-O, and falls risk, cognitive function and daily function, in older adults with mobility impairments. BMC Geriatr 2012;12. http://dx.doi.org/10.1186/1471-2318-12-65.
- Milte R, Ratcliffe J, Miller M, Whitehead C, Cameron ID, Crotty M. What are frail older people prepared to endure to achieve improved mobility following hip fracture? A discrete choice experiment. J Rehabil Med 2013;45:81-6.
- Laver K, Ratcliffe J, George S, Lester L, Crotty M. Preferences for rehabilitation service delivery: a comparison of the views of patients, occupational therapists and other rehabilitation clinicians using a discrete choice experiment. Aust Occup Ther J 2013;60:93-100.
- Horwood J, Sutton E, Coast J. Evaluating the face validity of the ICECAP-O capabilities measure: a think aloud study with hip and knee arthroplasty patients. Appl Res Qual Life 2014;9:667-82.
- Wolinsky FD, Miller TR, An H, Geweke JF, Wallace RB, Wright KB, et al. Hospital episodes and physician visits: the concordance between self-reports and Medicare claims. Med Care 2007;45:300-7. https://doi.org/10.1097/01.mlr.0000254576.26353.09.
- Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA, Lorig KR. Self-reports of health care utilization compared to provider records. J Clin Epidemiol 2001;54:136-41. https://doi.org/10.1016/S0895-4356(00)00261-4.
- Hunger M, Schwarzkopf L, Heier M, Peters A, Holle R. Official statistics and claims data records indicate non-response and recall bias within survey-based estimates of health care utilization in the older population. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-1.
- Heinrich S, Deister A, Birker T, Hierholzer C, Weigelt I, Zeichner D, et al. Accuracy of self-reports of mental health care utilization and calculated costs compared to hospital records. Psychiatry Res 2011;185:261-8. http://dx.doi.org/10.1016/j.psychres.2010.04.053.
- Byford S, Leese M, Knapp M, Seivewright H, Cameron S, Jones V, et al. Comparison of alternative methods of collection of service use data for the economic evaluation of health care interventions. Health Econ 2007;16:531-6. https://doi.org/10.1002/hec.1175.
- Ridyard CH, Hughes DA. Review of Resource-Use Measures in UK Economic Evaluations. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- Williams J, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT. Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment. Health Technol Assess 2003;7. https://doi.org/10.3310/hta7260.
- Peterson JC, Link AR, Jobe JB, Winston GJ, Marina Klimasiewfski E, Allegrante JP. Developing self-management education in coronary artery disease. Heart Lung 2014;43:133-9. http://dx.doi.org/10.1016/j.hrtlng.2013.11.006.
- Johnston M, Bonetti D, Joice S, Pollard B, Morrison V, Francis JJ, et al. Recovery from disability after stroke as a target for a behavioural intervention: results of a randomized controlled trial. Disabil Rehabil 2007;29:1117-27. http://dx.doi.org/10.1080/03323310600950411.
- Busse M, Quinn L, Dawes H, Jones C, Kelson M, Poile V, et al. Supporting physical activity engagement in people with Huntington’s disease (ENGAGE-HD): study protocol for a randomized controlled feasibility trial. Trials 2014;15:1-13.
- Wu C-Y, Chuang L-L, Lin K-C, Lee S-D, Hong W-H. Responsiveness, minimal detectable change, and minimal clinically important difference of the Nottingham Extended Activities of Daily Living scale in patients with improved performance after stroke rehabilitation. Arch Phys Med Rehabil 2011;92:1281-7.
- Dahlgren L-O, Fallsberg M. Phenomenography as a qualitative approach in social pharmacy research. J Soc Adm Pharm 1991;8:150-6.
- Bachrach-Lindstrom M, Unosson M, Ek AC, Arnqvist HJ. Assessment of nutritional status using biochemical and anthropometric variables in a nutritional intervention study of women with hip fracture. Clin Nutr 2001;20:217-23. https://doi.org/10.1054/clnu.2000.0383.
- Barrett-Connor E. The economic and human costs of osteoporotic fracture. Am J Med 1995;98:3S-8S. http://dx.doi.org/10.1016/S0002-9343%2805%2980037-3.
- Beaupre LA, Cinats JG, Jones CA, Scharfenberger AV, Johnston DWC, Senthilselvan A, et al. Does functional recovery in elderly hip fracture patients differ between patients admitted from long-term care and the community?. J Gerontol 2007;62A:1127-33. https://doi.org/10.1093/gerona/62.10.1127.
- Becker DJ, Kilgore ML, Morrisey MA. The societal burden of osteoporosis. Curr Rheumatol Rep 2010;12:186-91. https://doi.org/10.1007/s11926-010-0097-y.
- Beloosesky Y, Grinblat J, Epelboym B, Hendel D. Dementia does not significantly affect complications and functional gain in elderly patients operated on for intracapsular hip fracture. Arch Orthop Trauma Surg 2001;121:257-60. https://doi.org/10.1007/s004020000220.
- Bennett GC. After hip fracture repair. Lancet 1982;2:561-2. https://doi.org/10.1016/S0140-6736(82)90645-6.
- Berggren M, Stenvall M, Olofsson B, Gustafson Y. Evaluation of a fall-prevention program in older people after femoral neck fracture: a one-year follow-up. Osteoporos Int 2008;19:801-9. https://doi.org/10.1007/s00198-007-0507-9.
- Bitsch MS, Foss NB, Kristensen BB, Kehlet H. Acute cognitive dysfunction after hip fracture: frequency and risk factors in an optimized, multimodal, rehabilitation program. Acta Anaesthesiol Scand 2006;50:428-36. https://doi.org/10.1111/j.1399-6576.2005.00899.x.
- Borgquist L, Ceder L, Thorngren KG. Function and social status 10 years after hip fracture. Prospective follow-up of 103 patients. Acta Orthop Scand 1990;61:404-10. https://doi.org/10.3109/17453679008993550.
- Borgquist L, Nilsson LT, Lindelöw G, Wiklund I, Thorngren KG. Perceived health in hip-fracture patients: a prospective follow-up of 100 patients. Age Ageing 1992;21:109-16. https://doi.org/10.1093/ageing/21.2.109.
- Botella-Carretero JI, Iglesias B, Balsa JA, Arrieta F, Zamarron I, Vazquez C. Perioperative oral nutritional supplements in normally or mildly undernourished geriatric patients submitted to surgery for hip fracture: a randomized clinical trial. Clin Nutr 2010;29:574-9. http://dx.doi.org/10.1016/j.clnu.2010.01.012.
- Braid V, Barber M, Mitchell SL, Martin BJ, Granat M, Stott DJ. Randomised controlled trial of electrical stimulation of the quadriceps after proximal femoral fracture. Aging Clin Exp Res 2008;20:62-6. https://doi.org/10.1007/BF03324749.
- Bruce D, Laurance I, McGuiness M, Ridley M, Goldswain P. Nutritional supplements after hip fracture: poor compliance limits effectiveness. Clin Nutr 2003;22:497-500. http://dx.doi.org/10.1016/S0261-5614%2803%2900050-5.
- Cameron ID, Handoll HH, Finnegan TP, Madhok R, Langhorne P. Co-ordinated multidisciplinary approaches for inpatient rehabilitation of older patients with proximal femoral fractures. Cochrane Database Syst Rev 2000;4.
- Carinci F, Roti L, Francesconi P, Gini R, Tediosi F, Di Iorio T, et al. The impact of different rehabilitation strategies after major events in the elderly: the case of stroke and hip fracture in the Tuscany region. BMC Health Serv Res 2007;7. https://doi.org/10.1186/1472-6963-7-95.
- Carlsson P, Tidermark J, Ponzer S, Söderqvist A, Cederholm T. Food habits and appetite of elderly women at the time of a femoral neck fracture and after nutritional and anabolic support. J Hum Nutr Diet 2005;18:117-20. https://doi.org/10.1111/j.1365-277X.2005.00594.x.
- Ceder L, Lindberg L, Odberg E. Differentiated care of hip fracture in the elderly. Mean hospital days and results of rehabilitation. Acta Orthop Scand 1980;51:157-62. https://doi.org/10.3109/17453678008990780.
- Currie CT, Hoy D, Tierney AJ, Bryan-Jones J, Lapsley I. HipMod: development of a multi-agent audit-based computer simulation of hip fracture care. Health Inform J 2003;9:183-97. https://doi.org/10.1177/14604582030093005.
- Davis E, Biddison J, Cohen-Mansfield J. Hip fracture rehabilitation in persons with dementia: how much should we invest?. Ann Long Term Care 2007;15:19-21.
- Di Lorenzo L, Forte A, Formisano R, Gimigliano R, Gatto S. Low back pain after unstable extracapsular hip fractures: randomized control trial on a specific training. Eura Medicophys 2007;43:349-57.
- Dubljanin-Racpopoc E, Matanovic D, Bumbasirevic M. The impact of cognitive impairment at admission on short-term functional outcome of elderly hip fracture patients. Srpski Arhiv Za Celokupno Lekarstvo 2010;138:319-22. https://doi.org/10.2298/SARH1006319D.
- Duncan DG, Beck SJ, Hood K, Johansen A. Using dietetic assistants to improve the outcome of hip fracture: a randomised controlled trial of nutritional support in an acute trauma ward. Age Ageing 2006;35:148-53. http://dx.doi.org/10.1093/ageing/afj011.
- El Kadaoui Calvo N, Febres Panez D, Pareja Sierra T, Rodriguez Solis J, Hornillos Calvo M. Clinical features in the elderly patients admitted for hip fracture: benefits of geriatric intervention. Eur Geriatr Med 2011;2:S132-S3. http://dx.doi.org/10.1016/j.eurger.2011.06.002.
- Elliot JR, Wilkinson TJ, Hanger HC, Gilchrist NL, Sainsbury R, Shamy S, et al. The added effectiveness of early geriatrician involvement on acute orthopaedic wards to orthogeriatric rehabilitation. N Z Med J 1996;109:72-3.
- Espaulella J, Guyer H, Diaz-Escriu F, Mellado-Navas JA, Castells M, Pladevall M. Nutritional supplementation of elderly hip fracture patients. A randomized, double-blind, placebo-controlled trial. Age Ageing 2000;29:425-31. https://doi.org/10.1093/ageing/29.5.425.
- Folden S, Tappen R. Factors influencing function and recovery following hip repair surgery. Orthop Nurs 2007;26:234-41. https://doi.org/10.1097/01.NOR.0000284652.83462.7e.
- Fordham R, Thompson R, Holmes J, Hodkinson C. A cost–benefit Study of geriatric–orthopaedic Management of Patients With Fractured Neck of Femur 1986.
- Foss NB, Kristensen MT, Kehlet H. Anaemia impedes functional mobility after hip fracture surgery. Age Ageing 2008;37:173-8. https://doi.org/10.1093/ageing/afm161.
- French FH, Torgerson DJ, Porter RW. Cost analysis of fracture of the neck of femur. Age Ageing 1995;24:185-9. https://doi.org/10.1093/ageing/24.3.185.
- Galvard H, Samuelsson SM. Orthopedic or geriatric rehabilatation of hip fracture patients: a prospective, randomized, clinically controlled study in Malmo, Sweden. Aging Clin Exp Res 1995;7:11-6. https://doi.org/10.1007/BF03324284.
- Gerety MB, Soderholm-Difatte V, Winograd CH. Impact of prospective payment and discharge location on the outcome of hip fracture. J Gen Intern Med 1989;4:388-91. https://doi.org/10.1007/BF02599687.
- Gilchrist WJ, Newman RJ, Hamblen DL, Williams BO. Prospective randomised study of an orthopaedic geriatric inpatient service. BMJ 1988;297:1116-18. https://doi.org/10.1136/bmj.297.6656.1116.
- Strickland EM, Fares M, Krebs DE, Riley PO, Givens-Heiss DL, Hodge WA, et al. In vivo acetabular contact pressures during rehabilitation, Part I: Acute phase. Phys Ther 1992;72:691-9. https://doi.org/10.1093/ptj/72.10.691.
- Gorodetskyi IG, Gorodnichenko AI, Tursin PS, Reshetnyak VK, Uskov ON. Non-invasive interactive neurostimulation in the post-operative recovery of patients with a trochanteric fracture of the femur. A randomised, controlled trial. J Bone Joint Surg Br 2007;89:1488-94. https://doi.org/10.1302/0301-620X.89B11.19352.
- Granger CV, Reistetter TA, Graham JE, Deutsch A, Markello SJ, Niewczyk P, et al. The Uniform Data System for Medical Rehabilitation: report of patients with hip fracture discharged from comprehensive medical programs in 2000-2007. Am J Phys Med Rehabil 2011;90:177-89. https://doi.org/10.1097/PHM.0b013e31820b18d7.
- Guerini F, Morghen S, Lucchi E, Bellelli G, Trabucchi M. Depressive symptoms and one year mortality among elderly patients discharged from a rehabilitation ward after orthopaedic surgery of the lower limbs. Behavioural Neurology 2010;23:117-21. http://dx.doi.org/10.3233/BEN-2010-0274.
- Hagino T, Sato E, Tonotsuka H, Ochiai S, Tokai M, Hamada Y. Prediction of ambulation prognosis in the elderly after hip fracture. Int Orthop 2006;30:315-19. https://doi.org/10.1007/s00264-006-0086-y.
- Hall SE, Williams JA, Senior JA, Goldswain PR, Criddle RA. Hip fracture outcomes: quality of life and functional status in older adults living in the community. Aust NZ J Med 2000;30:327-32. https://doi.org/10.1111/j.1445-5994.2000.tb00833.x.
- Harwood RH, Sahota O, Gaynor K, Masud T, Hosking DJ. Nottingham Neck of Femur (NONOF) Study . A randomised, controlled comparison of different calcium and vitamin D supplementation regimens in elderly women after hip fracture: The Nottingham Neck of Femur (NONOF) Study. Age Ageing 2004;33:45-51. https://doi.org/10.1093/ageing/afh002.
- Hashmi MA, Tellisi N, Rigby AS, Wahab KHA. The value of a prognostic scoring system in the rehabilitation of elderly patients with proximal femoral fractures. Int J Clin Pract 2004;58:2-5. https://doi.org/10.1111/j.1368-5031.2004.0016.x.
- Hawkes WG, Wehren L, Orwig D, Hebel JR, Magaziner J. Gender differences in functioning after hip fracture. J Gerontol A Biol Sci Med Sci 2006;61A:495-9. https://doi.org/10.1093/gerona/61.5.495.
- Hedman AM, Grafström M. Conditions for rehabilitation of older patients with dementia and hip fracture – the perspective of their next of kin. Scand J Caring Sci 2001;15:151-8. https://doi.org/10.1046/j.1471-6712.2001.00013.x.
- Hedman AR, Heikkilä K, Grafström M, Strömberg L. Hip fractures and cognitive state: patient outcomes and proxies’ perceptions of the rehabilitation period. Int J Older People Nurs 2008;3:178-86. https://doi.org/10.1111/j.1748-3743.2008.00131.x.
- Hedman A, Stromberg L, Grafstrom M, Heikkila K. Hip fracture patients’ cognitive state affects family members’ experiences – a diary study of the hip fracture recovery. Scand J Caring Sci 2011;25:451-8. https://doi.org/10.1111/j.1471-6712.2010.00848.x.
- Henderson SA, Finlay OE, Murphy N, Boreham C, Mollan RA, Gilmore DH, et al. Benefits of an exercise class for elderly women following hip surgery. Ulster Med J 1992;61:144-50.
- Hershkovitz A, Kalandariov Z, Hermush V, Weiss R, Brill S. Factors affecting short-term rehabilitation outcomes of disabled elderly patients with proximal hip fracture. Arch Phys Med Rehabil 2007;88:916-21. https://doi.org/10.1016/j.apmr.2007.03.029.
- Heruti RJ, Lusky A, Barell V, Ohry A, Adunsky A. Cognitive status at admission: does it affect the rehabilitation outcome of elderly patients with hip fracture?. Arch Phys Med Rehabil 1999;80:432-6. https://doi.org/10.1016/S0003-9993(99)90281-2.
- Hoenig H, Rubenstein L, Kahn K. Rehabilitation after hip fracture – equal opportunity for all?. Arch Phys Med Rehabil 1996;77:58-63. https://doi.org/10.1016/S0003-9993(96)90221-X.
- Hollingworth W, Todd CJ, Parker MJ. The cost of treating hip fractures in the twenty-first century. J Public Health Med 1995;17:269-76.
- Holmberg S, Thorngren KG. Consumption of hospital resources for femoral neck fracture. Acta Orthop Scand 1988;59:377-81. https://doi.org/10.3109/17453678809149385.
- Horgan N, Cunningham C. Impact of cognitive impairment on hip fracture outcome in older people. Int J Ther Rehabil 2003;10:228-32. https://doi.org/10.12968/bjtr.2003.10.5.13547.
- Intrator O, Berg K. Benefits of home health care after inpatient rehabilitation for hip fracture: health service use by Medicare beneficiaries, 1987–1992. Arch Phys Med Rehabil 1998;79:1195-9. https://doi.org/10.1016/S0003-9993(98)90261-1.
- Jarnlo GB, Ceder L, Thorngren KG. Early rehabilitation at home of elderly patients with hip fractures and consumption of resources in primary care. Scand J Prim Health Care 1984;2:105-12. https://doi.org/10.3109/02813438409018083.
- Jones AW, Gummerson NW, Newman RJ. Predicting outcomes of proximal femoral fractures by analysis of ‘get well’ cards. Age Ageing 2001;30:267-8. https://doi.org/10.1093/ageing/30.3.267.
- Jongjit J, Komsopapong L, Songjakkaew P, Kongsakon R. Health-related quality of life after hip fracture in the elderly community-dwelling. Southeast Asian J Trop Med Public Health 2003;34:670-4.
- Keating JF, Robinson CM, Court-Brown CM, McQueen MM, Christie J. The effect of complications after hip fracture on rehabilitation. J Bone Joint Surg Br 1993;75.
- Kim SM, Moon YW, Lim SJ, Yoon BK, Min YK, Lee DY, et al. Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients. Bone 2012;50:1343-50. http://dx.doi.org/10.1016/j.bone.2012.02.633.
- Kirk-Sanchez NJ. Factors related to activity limitations in a group of Cuban Americans before and after hip fracture. Phys Ther 2004;84:408-18.
- Konnopka A, Jerusel N, Konig HH. The health and economic consequences of osteopenia- and osteoporosis-attributable hip fractures in Germany: estimation for 2002 and projection until 2050. Osteoporos Int 2009;20:1117-29. http://dx.doi.org/10.1007/s00198-008-0781-1.
- Kristensen MT, Foss NB, Kehlet H. Timed ‘up & go’ test as a predictor of falls within 6 months after hip fracture surgery. Phys Ther 2007;87:24-30. https://doi.org/10.2522/ptj.20050271.
- Kristensen MT, Foss NB, Kehlet H. Factors with independent influence on the ‘timed up and go’ test in patients with hip fracture. Physiother Res Int 2009;14:30-41. http://dx.doi.org/10.1002/pri.414.
- Kristensen MT, Jakobsen TL, Nielsen JW, Jorgensen LM, Nienhuis RJ, Jonsson LR. Cumulated Ambulation Score to evaluate mobility is feasible in geriatric patients and in patients with hip fracture. Dan Med J 2012;59.
- Laake K, Laake P, Ranhoff AH, Sveen U, Wyller TB, Bautz-Holter E. The Barthel ADL index: factor structure depends upon the category of patient. Age Ageing 1995;24:393-7. https://doi.org/10.1093/ageing/24.5.393.
- Lai H-YF, Wong M-CE, Poon M-Y, Louie W-SS, Wong K-MS. Validation on efficiency pattern analysis for geriatric hip fractures rehabilitation. J Orthop Trauma Rehabil 2010;14:14-20. http://dx.doi.org/10.1016/j.jotr.2010.08.003.
- Lamb SE, Oldham JA, Morse RE, Evans JG. Neuromuscular stimulation of the quadriceps muscle after hip fracture: a randomized controlled trial. Arch Phys Med Rehabil 2002;83:1087-92. https://doi.org/10.1053/apmr.2002.33645.
- Lau TW, Leung F, Siu D, Wong G, Luk KDK. Geriatric hip fracture clinical pathway: the Hong Kong experience. Osteoporos Int 2010;21:S627-S36. http://dx.doi.org/10.1007/s00198-010-1387-y.
- Leigheb F, Vanhaecht K, Sermeus W, Lodewijckx C, Deneckere S, Boonen S, et al. The effect of care pathways for hip fractures: a systematic review. Calcif Tissue Int 2012;91:1-14. https://doi.org/10.1007/s00223-012-9589-2.
- Lenze EJ, Munin MC, Dew MA, Rogers JC, Seligman K, Mulsant BH, et al. Adverse effects of depression and cognitive impairment on rehabilitation participation and recovery from hip fracture. Int J Geriatr Psychiatry 2004;19:472-8. http://dx.doi.org/10.1002/gps.1116.
- Licciardone JC, Stoll ST, Cardarelli KM, Gamber RG, Swift JN, Winn WB. A randomized controlled trial of osteopathic manipulative treatment following knee or hip arthroplasty. J Am Osteopath Assoc 2004;104:193-202.
- Lieberman D, Fried V, Castel H, Weitzmann S, Lowenthal MN, Galinsky D. Factors related to successful rehabilitation after hip fracture: a case-control study. Disabil Rehabil 1996;18:224-30. https://doi.org/10.3109/09638289609166305.
- Lieberman D, Galinsky D, Fried V, Grinshpun Y, Mytlis N, Tylis R. Geriatric Depression Screening Scale (GDS) in patients hospitalized for physical rehabilitation. Int J Geriatr Psychiatry 1999;14:549-55. https://doi.org/10.1002/(SICI)1099-1166(199907)14:7<549::AID-GPS960>3.0.CO;2-4.
- Lieberman D, Friger M. Visual and hearing impairment in elderly patients hospitalized for rehabilitation following hip fracture. J Rehabil Res Dev 2004;41:669-74. https://doi.org/10.1682/JRRD.2003.11.0168.
- Martin F. Improving functional status in rehabilitation. Eur Geriatr Med 2012;3. http://dx.doi.org/10.1016/j.eurger.2012.07.434.
- McGilton K, Wells J, Davis A, Rochon E, Calabrese S, Naglie G, et al. Rehabilitating Patients With Dementia Who Have Had a Hip Fracture: Part II: Cognitive Symptoms That Influence Care. Top Geriatr Rehabil 2007;23:174-82. https://doi.org/10.1097/01.TGR.0000270186.36521.85.
- McGilton K, Wells J, Teare G, Davis A, Rochon E, Calabrese S, et al. Rehabilitating patients with dementia who have had a hip fracture: part I: behavioral symptoms that influence care. Top Geriatr Rehabil 2007;23:161-73. https://doi.org/10.1097/01.TGR.0000270185.98402.a6.
- Miller RR, Ballew SH, Shardell MD, Hicks GE, Hawkes WG, Resnick B, et al. Repeat falls and the recovery of social participation in the year post-hip fracture. Age Ageing 2009;38:570-5. https://doi.org/10.1093/ageing/afp107.
- Munn Z. Mobilization strategies after hip fracture surgery in adults. J Adv Nurs 2008;63:343-4. http://dx.doi.org/10.1111/j.1365-2648.2008.04679.x.
- Myers JS, Grigsby J, Teel CS, Kramer AM. Nurses’ assessment of rehabilitation potential and prediction of functional status at discharge from inpatient rehabilitation. Int J Rehabil Res 2009;32:264-6. http://dx.doi.org/10.1097/MRR.0b013e32832a62c2.
- Neumann M, Friedmann J, Roy MA, Jensen GL. Provision of high-protein supplement for patients recovering from hip fracture. Nutrition 2004;20:415-19. https://doi.org/10.1016/j.nut.2004.01.004.
- Nevalainen TH, Hiltunen LA, Jalovaara P. Functional ability after hip fracture among patients home-dwelling at the time of fracture. Cent Eur J Public Health 2004;12:211-16.
- Nguyen-Oghalai TU, Kuo YF, Zhang DD, Graham JE, Goodwin JS, Ottenbacher KJ. Discharge setting for patients with hip fracture: trends from 2001 to 2005. J Am Geriatr Soc 2008;56:1063-8. https://doi.org/10.1111/j.1532-5415.2008.01688.x.
- Nguyen-Oghalai TU, Ottenbacher KJ, Kuo YF, Wu H, Grecula M, Eschbach K, et al. Disparities in utilization of outpatient rehabilitative care following hip fracture hospitalization with respect to race and ethnicity. Arch Phys Med Rehabil 2009;90:560-3. https://doi.org/10.1016/j.apmr.2008.10.021.
- Nightingale EJ, Sturnieks D, Sherrington C, Moseley AM, Cameron ID, Lord SR. Impaired weight transfer persists at least four months after hip fracture and rehabilitation. Clin Rehabil 2010;24:565-73. https://doi.org/10.1177/0269215509360753.
- Norton R, Butler M, Robinson E, Lee-Joe T, Campbell AJ. Declines in physical functioning attributable to hip fracture among older people: a follow-up study of case-control participants. Disabil Rehabil 2000;22:345-51. https://doi.org/10.1080/096382800296584.
- Nurmi I, Narinen A, Luthje P, Tanninen S. Functional outcome and survival after hip fracture in elderly: a prospective study of 106 consecutive patients. J Orthop Traumatol 2004;5:7-14. http://dx.doi.org/10.1007/s10195-004-0033-x.
- O’Malley NT, Blauth M, Suhm N, Kates SL. Hip fracture management, before and beyond surgery and medication: a synthesis of the evidence. Arch Orthop Trauma Surg 2011;131:1519-27. http://dx.doi.org/10.1007/s00402-011-1341-2.
- Parke B. Elderly women used interdisciplinary approaches to face obstacles and make a successful transition through recovery after hip fracture. commentary on Robinson SB. Transitions in the lives of elderly women who have sustained hip fractures. J Adv Nurs 1999;30:1341-8.
- Parker MJ, Palmer CR. Prediction of rehabilitation after hip fracture. Age Ageing 1995;24:96-8. https://doi.org/10.1093/ageing/24.2.96.
- Parker MJ. Evidence based case report: managing an elderly patient with a fractured femur. BMJ 2000;320:102-3. https://doi.org/10.1136/bmj.320.7227.102.
- Parker MJ. Current concepts in the treatment of hip fracture. Z Gerontol Geriatr 2001;34:74-7. https://doi.org/10.1007/s003910170096.
- Parker MJ, Lewis SJ, Mountain J, Christie J, Currie CT. Hip fracture rehabilitation – a comparison of two centres. Injury 2002;33:7-11. https://doi.org/10.1016/S0020-1383(01)00020-1.
- Penrod JD, Litke A, Hawkes WG, Magaziner J, Koval KJ, Doucette JT, et al. Heterogeneity in hip fracture patients: age, functional status, and comorbidity. J Am Geriatr Soc 2007;55:407-13. https://doi.org/10.1111/j.1532-5415.2007.01078.x.
- Penrod JD, Litke A, Hawkes WG, Magaziner J, Doucette JT, Koval KJ, et al. The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci 2008;63A:867-72. https://doi.org/10.1093/gerona/63.8.867.
- Press Y, Grinshpun Y, Berzak A, Friger M, Clarfield AM. The effect of co-morbidity on the rehabilitation process in elderly patients after hip fracture. Arch Gerontol Geriatr 2007;45:281-94. https://doi.org/10.1016/j.archger.2007.01.059.
- Pryor GA, Williams DR. Rehabilitation after hip fractures. Home and hospital management compared. J Bone Joint Surg Br 1989;71:471-4.
- Roberto KA. Coping strategies of older women with hip fractures: resources and outcomes. J Gerontol 1992;47:P21-6. https://doi.org/10.1093/geronj/47.1.P21.
- Rosler A, Krause T, Niehuus C, von Renteln-Kruse W. Dementia as a cofactor for geriatric rehabilitation-outcome in patients with osteosynthesis of the proximal femur: a retrospective, matched-pair analysis of 250 patients. Arch Gerontol Geriatr 2009;49:e36-9. http://dx.doi.org/10.1016/j.archger.2008.08.003.
- Salkeld G, Cameron ID, Cumming RG, Easter S, Seymour J, Kurrle SE, et al. Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ 2000;320:341-6. https://doi.org/10.1136/bmj.320.7231.341.
- Shabat S, Mann G, Nyska M, Maffulli N. Scoring systems to evaluate elderly patients with hip fractures. Disabil Rehabil 2005;27:1041-4. https://doi.org/10.1080/09638280500056642.
- Shardell M, Alley DE, Miller RR, Hicks GE, Magaziner J. Comparing reports from hip-fracture patients and their proxies: implications on evaluating sex differences in disability and depressive symptoms. J Aging Health 2012;24:367-83. http://dx.doi.org/10.1177/0898264311424208.
- Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison RS. Early ambulation after hip fracture: effects on function and mortality. Arch Intern Med 2006;166:766-71. https://doi.org/10.1001/archinte.166.7.766.
- Söderqvist A, Miedel R, Ponzer S, Tidermark J. The influence of cognitive function on outcome after a hip fracture. J Bone Joint Surg Am 2006;88:2115-23. https://doi.org/10.2106/00004623-200610000-00001.
- Stewart NA, Chantrey J, Blankley SJ, Boulton C, Moran CG. Predictors of 5 year survival following hip fracture. Injury 2011;42:1253-6. https://doi.org/10.1016/j.injury.2010.12.008.
- Strickland E, Fares M, Krens D, Riley P, Givens-Heiss D, Hodge W, et al. In vivo acetabular contact pressures during rehabilitation, part II: posacute phase. Phys Ther 1992;72:691-9. https://doi.org/10.1093/ptj/72.10.691.
- Sund R. Modeling the volume-effectiveness relationship in the case of hip fracture treatment in Finland. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-238.
- Tamulaitiene M, Alekna V. Incidence and direct hospitalisation costs of hip fractures in Vilnius, capital of Lithuania, in 2010. BMC Public Health 2012;12. https://doi.org/10.1186/1471-2458-12-495.
- Thomas S, Mackintosh S, Halbert J. Determining current physical therapist management of hip fracture in an acute care hospital and physical therapists’ rationale for this management. Phys Ther 2011;91:1490-502. http://dx.doi.org/10.2522/ptj.20100310.
- Thorngren KG. Cost comparison in hip fracture treatment. Acta Orthop Scand Suppl 1991;241:38-9. https://doi.org/10.3109/17453679109155104.
- Thorngren KG. Full treatment spectrum for hip fractures: operation and rehabilitation. Acta Orthop Scand 1997;68:1-2. https://doi.org/10.3109/17453679709003965.
- Tidermark J, Zethraeus N, Svensson O, Törnkvist H, Ponzer S. Femoral neck fractures in the elderly: functional outcome and quality of life according to EuroQol. Qual Life Res 2002;11:473-81. https://doi.org/10.1023/A:1015632114068.
- Tidermark J, Ponzer S, Carlsson P, Söderqvist A, Brismar K, Tengstrand B, et al. Effects of protein-rich supplementation and nandrolone in lean elderly women with femoral neck fractures. Clin Nutr 2004;23:587-96. https://doi.org/10.1016/j.clnu.2003.10.006.
- Toussant EM, Kohia M. A critical review of literature regarding the effectiveness of physical therapy management of hip fracture in elderly persons. J Gerontol A Biol Sci Med Sci 2005;60A:1285-91. https://doi.org/10.1093/gerona/60.10.1285.
- Tsushima E, Hada R, Iwata M, Tsushima H. Early prediction of gait ability in patients with hip fracture. Environ Health Prev Med 2009;14:188-95. https://doi.org/10.1007/s12199-009-0079-8.
- Weingarten S, Riedinger MS, Sandhu M, Bowers C, Ellrodt AG, Nunn C, et al. Can practice guidelines safely reduce hospital length of stay? Results from a multicenter interventional study. Am J Med 1998;105:33-40. https://doi.org/10.1016/S0002-9343(98)00129-6.
- Weinrich M, Good D, Reding M, Roth E, Cifu D, Silver K, et al. Timing, intensity, and duration of rehabilitation for hip fracture and stroke: report of a workshop at the National Center for Medical Rehabilitation Research. Neurorehabil Neural Repair 2004;18:12-28. https://doi.org/10.1177/0888439003262041.
- Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E. Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int 2001;12:271-8. https://doi.org/10.1007/s001980170116.
- Williams MA, Oberst MT, Bjorklund BC, Hughes SH. Family caregiving in cases of hip fracture. Rehabil Nurs 1996;21:124-31. https://doi.org/10.1002/j.2048-7940.1996.tb01690.x.
- Wykes C, Pryor J, Jeeawody B. The concerns of older women during inpatient rehabilitation after fractured neck of femur. Int J Ther Rehabil 2009;16:261-70. https://doi.org/10.12968/ijtr.2009.16.5.42103.
- Yau DTY, Chung RCK, Pang MYC. Knee muscle strength and visual acuity are the most important modifiable predictors of falls in patients after hip fracture surgery: a prospective study. Calcif Tissue Int 2013;92:287-95. http://dx.doi.org/10.1007/s00223-012-9681-7.
- Young Y, Fried LP, Kuo Y. Hip fractures among elderly women: longitudinal comparison of physiological function changes and health care utilization. J Am Med Dir Assoc 2010;11:100-5. http://dx.doi.org/10.1016/j.jamda.2009.09.005.
- Zerahn B, Olsen C, Stephensen S, Kanstrup IL, Schwarz Lausten G. Bone loss after hip fracture is correlated to the postoperative degree of mobilisation. Arch Orthop Trauma Surg 1998;117:453-6. https://doi.org/10.1007/s004020050291.
- Edwards RT, Linck P, Hounsome N, Raisanen L, Williams NH, Moore L, et al. Cost-effectiveness of a national exercise referral programme for primary care patients in Wales: results of a randomised controlled trial. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-1021.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2015.
Appendix 1 Nature of complex programmes
Complex programmes:
-
are active not passive (recipients have to choose to respond/participate)
-
have long implementation chains and multiple stakeholders
-
are embedded in complex social systems
-
are implemented against the background of other interventions/service changes
-
borrow and adapt from other programmes; they are rarely implemented exactly as originally envisaged
-
have typically evolved from previous interventions
-
change the conditions that made them work in the first place.
Appendix 2 Methodological differences between conventional systematic reviews and realist reviews
| Conventional systematic review | Realist review |
|---|---|
| 1. Identify the review question | 1. Clarify scope of the review: identify the review question, refine the purpose of the review, articulate key candidate theories to be explored |
| 2. Search for primary studies using clear pre-defined inclusion and exclusion criteria | 2. Search for relevant evidence, refining inclusion criteria in the light of emerging data |
| 3. Appraise the quality of studies using a pre-defined and validated critical appraisal checklist, considering relevance to the research question and methodological rigour | 3. Appraise the ‘quality’ of studies using judgement to consider relevance and rigour from a ‘fitness for purpose’ perspective |
| 4. Extract standard items of data from all primary studies using a template or matrix | 4. Extract different data from different studies using a range of tools (e.g. Microsoft Excel, NVivo) in an iterative fashion |
| 5. Synthesise data to obtain effect sizes and CIs and/or transferable themes from qualitative studies | 5. Synthesise data to achieve refinement of programme theory, that is, to determine what works for whom, how and under what circumstances |
| 6. Make recommendations, especially with reference to whether the findings are definitive or if further research is needed | 6. Make recommendations, especially with reference to contextual issues for particular policy-makers at particular times |
| 7. Disseminate the findings and evaluate the extent to which practitioners’ behaviour changes in a particular direction | 7. Disseminate the findings and evaluate the extent to which existing programmes are adjusted to take account of elements of programme theory revealed by the review |
Appendix 3 List of items to be included when reporting a realist synthesis
| Item | Description | Page number |
|---|---|---|
| Title | ||
| 1. Title | In the title, identify the document as a realist synthesis or review | 7 |
| Abstract | ||
| 2. Abstract | When acknowledging the publication requirements and house style, abstracts should ideally contain brief details of the study’s background, review question or objectives; the search strategy; the methods of selection, appraisal, analysis and synthesis of sources; the main results; and implications for practice | xxiv–xxxii |
| Introduction | ||
| 3. Rationale for the review | Explain why the review is needed and what it is likely to contribute to existing understanding of the topic area | 7 |
| 4. Objectives and focus of the review | State the objective(s) of the review and/or the review question(s). Define and provide a rationale for the focus of the review | 7, 8 |
| Methods | ||
| 5. Changes to the review process | Any changes made to the review process that was initially planned should be briefly described and justified | – |
| 6. Rationale for using realist synthesis | Explain why realist synthesis was considered the most appropriate method to use | 8 |
| 7. Scoping the literature | Describe and justify the initial process of exploratory scoping of the literature | 8, 9 |
| 8. Searching processes | When considering the specific requirements of the journal or other publication outlet, state and provide a rationale for how the iterative searching was carried out. Provide details on all of the sources accessed for information in the review. When searching of electronic databases has been carried out, the details provided should include the names of the databases, search terms, dates of coverage and date last searched. If individuals familiar with the relevant literature and/or topic area were contacted, indicate how they were identified and selected | 10, 11 |
| 9. Selection and appraisal of documents | Explain how judgements were made with regard to including and excluding data from documents and justify any decisions made | 11–13 |
| 10. Data extraction | Describe which data or information were extracted from the included documents and justify this selection | 12–15 |
| 11. Analysis and synthesis processes | Describe the analysis and synthesis processes in detail. This section should include information on the constructs analysed and a description of the analytical processes | 13–15 |
| Results | ||
| 12. Document flow diagram | Provide details about the number of documents assessed for eligibility and included in the review, with reasons for exclusion at each stage, as well as an indication of their source of origin (e.g. from searching databases, from reference lists). Consider using the example templates [(Appendix 7) which are likely to need modification to suit the data] that are provided | 16 |
| 13. Document characteristics | Provide information on the characteristics of the documents included in the review | 15–18 |
| 14. Main findings | Present the key findings with a specific focus on theory building and testing | 20–31 |
| Discussion | ||
| 15. Summary of findings | Summarise the main findings, taking into account the review’s objective(s), research question(s), focus and intended audience(s) | 31 |
| 16. Strengths, limitations and future research directions | Discuss both the strengths of the review and its limitations. This should include (but need not be restricted to) (a) a consideration of all of the steps in the review process and (b) comment on the overall strength of evidence supporting the explanatory insights that emerged. The limitations identified may point to areas where further work is needed | 31–33 |
| 17. Comparison with existing literature | When applicable, compare and contrast the review’s findings with the existing literature (e.g. other reviews) on the same topic | 32–33 |
| 18. Conclusion and recommendations | List the main implications of the findings and place these in the context of other relevant literature. If appropriate, offer recommendations for policy and practice | 33 |
| 19. Funding | Provide details of funding source (if any) for the review, the role played by the funder (if any) and any conflicts of interests of the reviewers | v |
Appendix 4 Intermediate programme theories
Theory level 1: individual patients
-
Comorbid conditions affecting the ability to participate in rehabilitation (physical health, mental health status, cognitive status).
-
How do other comorbid conditions, mental health status and cognitive status affect an individual’s rehabilitation?
-
-
Psychological models influencing rehabilitation (internal control, self-efficacy, outcome expectations, coping adjustment, stage of change).
-
What is the relationship between internal control, self-efficacy, outcome expectations, coping adjustment and stage of change?
-
-
Behavioural economic theories affecting patients’ choices concerning rehabilitation (rational/irrational choices; automatic/reflective thinking; sure short-term gains vs. uncertain long-term losses; expected utility gains; welfare judgements).
-
What choices are made when an individual decides on a particular form of rehabilitation? (‘rational’ and ‘irrational’; ‘automatic’ and ‘reflective’; sure short-term gains vs. uncertain long-term losses; expected utility gains; welfare judgements)
-
Theory level 2: team delivering the intervention
-
The level of skill and specialisation needed to deliver each component of the intervention.
-
How can the multidisciplinary team help patients to increase the time spent practising physical exercise and activities of daily living?
-
Which health professionals should provide the different components of multidisciplinary care?
-
-
Co-ordination of care between different disciplines in the hospital and the community.
-
How can the co-ordination of care between different disciplines in the hospital and the community be improved?
-
-
Reducing unnecessary variation in practice.
-
How can unnecessary variation in practice be reduced?
-
-
Configuration of the team delivering the intervention
-
What combinations of practitioners generate additional costs compared with usual practice?
-
Theory level 3: the rehabilitation intervention
-
The optimal type, intensity and frequency of physical exercise for rehabilitation.
-
What is the optimal type, intensity and frequency of physical exercise for rehabilitation?
-
-
Improving task-oriented activities of daily living to reduce disability.
-
Does improving task-oriented activities of daily living reduce disability?
-
-
Interventions to reduce fear of falling, improve self-efficacy or improve stage of change.
-
What interventions reduce fear of falling, improve self-efficacy or improve stage of change?
-
How do interventions that reduce fear of falling, improve self-efficacy or improve stage of change lead to improved functioning, reduce disability and promote independent living?
-
How does early resumption of self-care and domestic activities lead to improved self-efficacy?
-
-
Interventions to improve social inclusion.
-
Interaction between intervention components.
-
Individually tailored rehabilitation programme or group activities.
-
What is the effect of tailoring rehabilitation programmes according to patients’ individual health needs, disability status and living circumstances?
-
What is the effect of group learning programmes on rehabilitation activities?
-
-
Intervention costs.
-
Which elements of a rehabilitation programme generate additional costs compared with usual practice?
-
-
How does ease of implementability of an intervention affects its delivery?
-
How does the care pathway affect rehabilitation?
-
Nutritional aspects of rehabilitation.
Theory level 4: the setting for the intervention
-
Contextual factors.
-
What factors lead to increased time spent practising activities of daily living and physical exercise?
-
How can we implement ‘choice architecture’ to help individuals make better decisions about rehabilitation care packages?
-
-
Setting.
-
How does the setting influence participation in rehabilitation activities?
-
How do certain settings increase intervention costs?
-
-
Family and other sources of social support.
-
How can the family and other sources of social support encourage the practice of activities of daily living and physical exercise?
-
Interventions to improve social inclusion.
-
Why do peer groups influence health-care decision-making?
-
-
Cultural factors.
-
What cultural factors are important for the rehabilitation programme?
-
Why do peer groups influence health-care decision-making?
-
Appendix 5 Emerging programme theories
-
A multidisciplinary orthogeriatric assessment approach facilitates patients’ pre-fracture as well as post-surgery assessments, resulting in a rehabilitation programme that is resilient and tailored according to patients’ needs and capacities to facilitate participation and practice, which in turn increases muscle strength and improves confidence to continue practice into the community after discharge.
-
Continuity and smooth transition from hospital discharge to community support facilitates patients’ continuing practice and empowerment to gain independence.
-
Cognitively impaired patients need extensive supervision and prolonged rehabilitation to regain their pre-fracture function and mobility, and master self-care skills.
-
Rehabilitation programmes need to take into account pre-morbid/comorbid conditions and be adapted accordingly to ensure the safety of patients.
-
If the place of residence is made safe, patients will feel confident and improve their practice.
-
A home environment rehabilitation programme needs to be tailored according to the space/facilities available and patients’ abilities and capacities, with the aim of facilitating independence by reinforcing behaviour, increasing confidence, and reducing discomfort and the fear of falling.
-
Patients’ prolonged engagement with a specialist/supervised programme leads to participation persistence and increased confidence.
Appendix 6 Context–mechanism–outcome configurations of the theory areas
| Contexts | Mechanisms | Outcomes |
|---|---|---|
|
|
|
Appendix 7 Example data extraction forms for the realist review
| Study/participant details | Description of the intervention(s) | Comparator(s) | Explanation of the findings | Strengths and weaknesses | Conclusions |
|---|---|---|---|---|---|
| Resnick 200773 | Exercise Plus Program (exercise training component + motivational component: theory of self-efficacy) (n = 52) – home-based trainer administered aerobic, strengthening and stretching exercise intervention for all muscle groups and provided the Plus component (self-efficacy and outcome expectations, performance accomplishment, verbal encouragement, physiological feedback, cueing and self-modelling); a total of 42 supervised visits for face-to-face implementation of the motivational and exercise intervention; weekly telephone calls made in months 7–12 when visits were decreased to once per month; weekly aspects of the motivational intervention implemented by telephone contact. Plus-only intervention (motivational component: theory of self-efficacy) (n = 54) – participants in this group received sessions focused only on the Plus components (i.e. education about exercise, verbal encouragement, removal of unpleasant sensations and cueing); there were no exercise sesions with a trainer. Exercise-only intervention (exercise training component) (n = 51) – participants in the exercise-only group exercised with the trainer during the sessions but were not exposed to the Plus components of the intervention. In all treatment groups, visits from the trainer were initially twice per week for the first 2 months; this decreased to once per month in the final 4 months of the programme, with weekly telephone calls for those exposed to the Plus component of the intervention during the weeks when no visits were scheduled. All visits lasted for 1 hour. Participants were expected to exercise five times per week for 45 minutes | Inactive control – routine care (n = 51) – participants received physical and occupational therapy as prescribed by their orthopaedist and/or primary health-care provider | Lack of a statistically significant increase in the number of steps in the Exercise Plus group could be because these individuals spent more time carrying out resistive exercise activities, which were not captured by the Step Activity Monitor. Conversely, it is possible that combining exercise and the Plus components in the same hour-long session resulted in less intense exposure to one of the components, reducing the impact of the intervention. The study compared different components of the intervention and it is impossible to control exposure to sources of efficacy information in the real world. The Plus only participants had mastery experiences if and when they exercised, although this was not with the trainer. Likewise, the exercise-only participants, by virtue of the exercise programme provided, could establish goals for themselves and also received feedback (albeit not the same as the verbal persuasion provided through the Plus component) during the course of their exercise sessions. It is therefore impossible to conclude whether or not mastery alone is sufficient to motivate older women post hip fracture to exercise or if verbal persuasion, vicarious experience or altering unpleasant physiological and affective states is needed | Weaknesses – the older women in this study were relatively healthy, lived in the community prior to fracture and willingly participated in an exercise intervention study; there was variability in terms of when the intervention was initiated (because of participant unwillingness to allow the trainer to come out to the home setting) and some group differences in the number of visits to which participants were exposed; it was not possible to control the type and amount of efficacy information that participants were exposed to, limiting interpretation of the findings; multiple measures were based on recall; differences in time spent exercising could not be addressed because of the short follow-up. Strengths – it was possible to engage these women in a home-based exercise programme and all three intervention groups reported the desired outcome of increased time in exercise | Older adults should be helped to realistically assess their self-efficacy and outcome expectations related to exercise. Health-care providers and friends/peers should be encouraged to reinforce the positive benefits of exercise. Fear of falling should be addressed throughout the entire hip fracture recovery trajectory, well after the initial fracture. Interactions with peers, possibly peers who themselves exercise (and who may have experienced a hip fracture), have a positive influence on self-efficacy related to exercise post hip fracture. Practitioners should consider the use of peers to strengthen beliefs and thereby improve exercise behaviour in older adults post hip fracture. There was no evidence of a trainer effect during any of the testing time points; thus, the benefits of encouraging exercise are not trainer specific and the skills required to be an effective trainer may be easily learned. Self-efficacy and outcome expectations had no direct relationship with exercise; instead, they indirectly related to exercise through stage of change. Thus, the interventions might best be targeted at encouraging self-efficacy related to the readiness to adopt exercise behaviour, after which time the performance of exercise will increase. Future research is needed to replicate the findings of this study as demonstrating the beneficial impact of the Plus component alone has practical implications in clinical settings |
| Women with hip fracture who were otherwise medically fit and healthy and able to walk unassisted (n = 209) | |||||
| Cognitive impairment: no | |||||
| Setting: community | |||||
| Country: USA | |||||
| Study design: RCT | |||||
| Conceptual richness: rich |
| Study/participant details | Description of the intervention | Self-efficacy | Self-efficacy | Exercise behaviour | Exercise behaviour | Physical functioning | Depression |
|---|---|---|---|---|---|---|---|
| Self-Efficacy for Walking/Exercise Scale [nine items rated from 0 (no confidence) to 10 (high confidence); higher scores indicate stronger self-efficacy] | Outcome Expectations for Exercise Scale [nine items rated from 1 (strongly disagree) to 5 (strongly agree); higher scores indicate stronger outcome expectations] | Yale Physical Activity Survey | Step Activity Monitor – CHAMPS Physical Activity Questionnaire for Older Adults | SF-36 | Centre for Epidemiological Studies Depression Scale (0–5; higher scores indicate depressive symptoms) | ||
| Resnick 200773 | Exercise Plus (psychological component) (n = 52) vs. inactive control (n = 51) | 2 months == | 2 months == | 2 months ++ | 2 months ++ | 2 months ++ | 2 months <> |
| USA | 6 months == | 6 months == | 6 months ++ | 6 months ++ | 6 months ++ | 6 months <> | |
| RCT | 12 months == | 12 months == | 12 months ++ | 12 months ++ | 12 months ++ | 12 months <> |
| Study/participant/intervention details | Research methods | Theory/mechanisms/conclusions and comments |
|---|---|---|
|
Limitations:
|
|
| 1. Tailoring of the intervention: proximal hip fracture patients presenting with a range of pre-fracture physical and mental functioning and a variety of comorbidities affecting their ability to achieve rehabilitation goals (C) need a rehabilitation programme that is tailored to individual needs (M) to achieve appropriate outcomes such as improved physical functioning, greater mobility, reduced disability and independent living (O) | |
| Component | Detailed assessment of patients’ pre-fracture level of functioning, current cognitive status and other comorbid conditions |
| Mechanism | Substantial physical limitations, dependency in daily activities, social restrictions and depression are common after a hip fracture, especially during the first months after the injury. We think that it is essential for health professionals to learn more about patients’ situation after discharge from hospital, for example to be able to find ways to identify those who need extra rehabilitation interventions to improve the recovery process |
| 2. Practice of exercise and ADL: proximal hip fracture patients with poor physical functioning, who fear falling, who have low mood or who lack self-efficacy (C) require interventions that improve the quality and amount of practice of physical exercises, ADL and psychological tasks (M) to improve self-efficacy, reduce the fear of falling, improve confidence and increase mobility and physical functioning to promote independence (O) | |
| Component | Controlling anxiety symptoms |
| Mechanism | One of the categories showed that hip fracture was experienced as a distinct manifestation of being old and that this experience contained a variety of negative attributes. This may be seen as a reflection of society’s attitudes towards the elderly, who, in contrast to young people, are often given the attributes of worthlessness and a strain on society |
| 3. Fear of falling and lack of self-efficacy: hip fracture patients who fear falling, who have low mood or who lack self-efficacy (C) require interventions that improve psychological tasks and provide motivation and a sense of ownership to engage in exercises (M) to improve self-efficacy, reduce the fear of falling, improve confidence, provide a quicker progression through a programme of recovery, increase functional outcomes and increase mobility (O) | |
| Component | Signposting to other services and sources of help/support |
| Mechanism |
|
| 4. Co-ordination of services and sectors delivering the intervention: the diversity of services provided by different disciplines, across sectors from a variety of funders (C), requires the co-ordinated provision of a multidisciplinary rehabilitation programme (M) to deliver appropriate physical, functional and psychological interventions to patients in a timely manner (O) | |
| Component | Not reported |
| Mechanism | Not reported |
Appendix 8 Search strategies for the different databases searched in the realist review
MEDLINE (via Ovid)
-
exp Hip Fractures/
-
((femur$ or femoral$) adj3 (head or neck or proximal) adj4 fracture$).ti,ab.
-
((hip$ or femur$ or femoral$ or trochant$ or pertrochant$ or intertrochant$ or subtrochant$ or intracapsular$ or extracapsular$) adj4 fracture$).ti,ab.
-
1 or 2 or 3
-
exp rehabilitation/ or exp rehabilitation nursing/ or “Recovery of Function”/ or Subacute Care/
-
exp rehabilitation centers/ or Residential Facilities/ or Assisted Living Facilities/ or Halfway Houses/
-
Day Care/ or home care services/ or home care services, hospital-based/ or home nursing/ or hospital units/
-
exp Nursing Homes/ or exp Patient Care Team/ or exp Patient Care Management/ or exp Occupational Therapy/ or exp Physical Therapy Techniques/ or exp Physical Therapy Department, Hospital/
-
exp “Physical Therapy (Specialty)”/ or exp Critical Pathways/ or exp Therapy, Computer-Assisted/ or exp Exercise Therapy/ or exp Walking/
-
exp Social Work/ or exp Social Support/ or exp Pain Clinics/ or exp Patient Education/ or exp Health Education/ or Caregivers/
-
(rehab$ or habilitat$ or recover$).ti,ab.
-
(multidisciplinar$ or interdisciplinar$ or multiprofessional$ or multimodal$ or mdt or mdr).ti,ab.
-
(social adj1 (work$ or support or care)).ti,ab.
-
(pain clinic$ or pain service$ or pain relief unit$ or (pain center$ or pain centre$)).ti,ab.
-
((treatment$ or therap$ or training or education$ or healthcare) adj10 (program$ or intervention$ or approach$)).ti,ab.
-
(early adj1 (mobil$ or discharg$ or ambulat$)).ti,ab.
-
(occupational therap$ or physical therap$ or physiotherap$ or physio).ti,ab.
-
(exercis$ adj3 therap$).ti,ab.
-
((early or earli$ or immediat$ or initial$ or begin$ or first$ or first-line or first line or first choice or primar$ or preceed$ or original$) adj3 (interven$ or treat$ or therap$ or care or medicine$ or technique$ or strateg$ or activit$ or mobili$)).ti,ab.
-
(walk or walks or walking).ti,ab.
-
mobili?ation strateg$.ti,ab.
-
(ambulate$ or ambulation$ or ambulating$).ti,ab.
-
(exerci$ adj3 (rehab$ or habilitat$ or recover$ or therap$ or treat$ or medicine$ or intervention$ or technique$ or strateg$)).ti,ab.
-
((walk$ or mobil$ or mov$ or motor$ or physi$) adj3 (rehab$ or habilitat$ or recover$ or therap$ or treat$ or medicine$ or intervention$ or technique$ or strateg$)).ti,ab.
-
(extend$ adj2 care$ adj3 (facilit$ or service$ or unit$ or center$ or clinic$ or program$ or residen$ or home$ or hous$)).ti,ab.
-
((residen$ or intermediate$ or assist$ liv$) adj3 (facilit$ or care$ or service$ or unit$ or center$ or clinic$ or program$ or residen$ or home$ or hous$)).ti,ab.
-
((halfway or transition$) adj3 (home$ or hous$ or facilit$ or care$ or residen$ or service$ or unit$ or center$ or clinic$ or program$)).ti,ab.
-
(nurs$ adj2 home$).ti,ab.
-
(geriatr$-orthop$ or orthop?edic-geriatr$ or ortho$-geriatr$ or orthogeriatr$ or goru).ti,ab.
-
(orthop$ adj2 geriatr$).ti,ab.
-
rehabilitation unit$.ti,ab.
-
(mixed assessment or maru).ti,ab.
-
(geriatric hip fracture program$ or ghfp).ti,ab.
-
(day adj (hospital$ or care or unit$)).ti,ab.
-
((home-based or home based) adj care).ti,ab.
-
carer$ involve$.ti,ab.
-
(esd or early supported discharge).ti,ab.
-
sequential care.ti,ab.
-
or/5-38
-
4 and 39
-
limit 40 to humans
The Cochrane Library
-
MeSH descriptor Hip Fractures explode all trees
-
((hip* or pertrochant* or intertrochant* or trochant* or subtrochant* or intracapsular* or extracapsular* or ((femur* or femoral*) NEAR/3 (neck or proximal))) NEAR/4 fracture*):ti,ab,kw
-
#1 OR #2
-
MeSH descriptor Rehabilitation explode all trees
-
MeSH descriptor Rehabilitation Centers explode all trees
-
MeSH descriptor Rehabilitation Nursing explode all trees
-
MeSH descriptor Patient Care Team explode all trees
-
MeSH descriptor Patient Care Management explode all trees
-
MeSH descriptor Occupational Therapy explode all trees
-
MeSH descriptor Physical Therapy Modalities explode all trees
-
MeSH descriptor Physical Therapy Department, Hospital explode all trees
-
MeSH descriptor Physical Therapy (Specialty) explode all trees
-
MeSH descriptor Critical Pathways explode all trees
-
MeSH descriptor Therapy, Computer-Assisted explode all trees
-
MeSH descriptor Exercise Therapy explode all trees
-
MeSH descriptor Social Work explode all trees
-
MeSH descriptor Social Support explode all trees
-
MeSH descriptor Pain Clinics explode all trees
-
MeSH descriptor Patient Education as Topic explode all trees
-
MeSH descriptor Health Education explode all trees
-
MeSH descriptor Recovery of Function, this term only
-
MeSH descriptor Subacute Care, this term only
-
MeSH descriptor Residential Facilities explode all trees
-
MeSH descriptor Day Care, this term only
-
MeSH descriptor Home Care Services, this term only
-
MeSH descriptor Home Care Services, Hospital-Based, this term only
-
MeSH descriptor Home Nursing, this term only
-
MeSH descriptor Hospital Units, this term only
-
MeSH descriptor Nursing Homes explode all trees
-
MeSH descriptor Walking explode all trees
-
MeSH descriptor Caregivers, this term only
-
(rehab* or habilitat* or recover*):ti,ab,kw
-
(multidisciplinar* or interdisciplinar* or multiprofessional* or multimodal* or mdt or mdr):ti,ab,kw
-
(social NEAR (work* or support or care)):ti,ab,kw
-
(pain clinic* or pain service* or pain relief unit* or (pain center* or pain centre*)):ti,ab,kw
-
((treatment* or therap* or training or education* or healthcare) NEAR/10 (program* or intervention* or approach*)):ti,ab,kw
-
(early NEAR (mobil* or discharg* or ambulat*)):ti,ab,kw
-
(occupational therap* or physical therap* or physiotherap* or physio):ti,ab,kw
-
(exercis* NEAR/3 therap*):ti,ab,kw
-
((early or earli* or immediat* or initial* or begin* or first* or first-line or first line or first choice or primar* or preceed* or original*) NEAR/3 (interven* or treat* or therap* or care or medicine* or technique* or strateg* or activit* or mobili*)):ti,ab,kw
-
(walk or walks or walking):ti,ab,kw
-
mobili?ation strateg*:ti,ab,kw
-
(ambulate* or ambulation* or ambulating*):ti,ab,kw
-
(exerci* NEAR/3 (rehab* or habilitat* or recover* or therap* or treat* or medicine* or intervention* or technique* or strateg*)):ti,ab,kw
-
((walk* or mobil* or mov* or motor* or physi*) NEAR/3 (rehab* or habilitat* or recover* or therap* or treat* or medicine* or intervention* or technique* or strateg*)):ti,ab,kw
-
(extend* NEAR/2 care* NEAR/3 (facilit* or service* or unit* or center* or clinic* or program* or residen* or home* or hous*)):ti,ab,kw
-
((residen* or intermediate* or assist* liv*) NEAR/3 (facilit* or care* or service* or unit* or center* or clinic* or program* or residen* or home* or hous*)):ti,ab,kw
-
((halfway or transition*) NEAR/3 (home* or hous* or facilit* or care* or residen* or service* or unit* or center* or clinic* or program*)):ti,ab,kw
-
(nurs* NEAR/2 home*):ti,ab,kw
-
(geriatr*-orthop* or orthop?edic-geriatr* or ortho*-geriatr* or orthogeriatr* or goru):ti,ab,kw
-
(orthop* NEAR/2 geriatr*):ti,ab,kw
-
rehabilitation unit*:ti,ab,kw
-
(mixed assessment or maru):ti,ab,kw
-
(geriatric hip fracture program* or ghfp):ti,ab,kw
-
(day NEAR (hospital* or care or unit*)):ti,ab,kw
-
((home-based or home based) NEAR care):ti,ab,kw
-
carer* involve*:ti,ab,kw
-
(esd or early supported discharge):ti,ab,kw
-
sequential care:ti,ab,kw
-
#4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 or #56 or #57 or #58 or #59
-
#3 and #60
Cumulative Index to Nursing and Allied Health Literature (via EBSCOhost)
-
mh hip fractures+
-
femur* n3 proximal n4 fracture* or femur* n3 neck n4 fracture* or femoral* n3 proximal n4 fracture* or femoral* n3 neck n4 fracture* or pertrochant* n4 fracture* or intertrochant* n4 fracture* or trochanteric n4 fracture* or subtrochanteric n4 fracture* or extracapsular* n4 fracture* or hip* n4 fracture*
-
intracapsular* n4 fracture* or femur* n4 fracture* or femoral* n4 fracture*
-
S1 or S2 or S3
-
(MH “Rehabilitation+”)
-
(MH “Rehabilitation Nursing”)
-
(MH “Recovery”)
-
(MH “Subacute Care”)
-
(MH “Rehabilitation Centers+”)
-
mh residential facilities or mh Assisted Living Facilities or mh Halfway Houses
-
mh Day Care or mh home care services or mh home care services, hospital-based or mh home nursing or mh Hospital Units
-
mh Nursing Homes+ or mh Patient Care Team+ or mh Patient Care Management+ or mh Physical Therapy Techniques+ or mh Physical Therapy Department, Hospital+
-
mh Critical Pathways+ or mh Therapy, Computer-Assisted+ or mh Exercise Therapy+ or mh Walking+
-
mh Social Work+ or mh Social Support+ or mh Pain Clinics+ or mh Patient Education+ or mh Health Education+ or mh Caregivers
-
(MH “Multidisciplinary Care Team+”)
-
rehab* or habilitat* or recover*
-
multidisciplinar* or mdr or mdt or multimodal* or multiprofessional* or interdisciplinar*
-
social n1 work* or social n1 support or social n1 care
-
pain clinic* or pain service* or pain relief unit* or pain center* or pain centre*
-
treatment* n10 program* or treatment* n10 intervention* or treatment* n10 approach* or therap* n10 program* or therap* n10 intervention* or therap* n10 approach* or training n10 program* or training n10 intervention* or training n10 approach* or education* n10 program* or education* n10 intervention* or education* n10 approach*
-
healthcare n10 program* or healthcare n10 intervention* or healthcare n10 approach*
-
early n1 mobil* or early n1 discharg* or early n1 ambulat*
-
occupational therap* or physical therap* or physiotherap* or physio
-
exercis* n3 therap*
-
early n3 interven* or early n3 treat* or early n3 therap* or early n3 care or early n3 medicine* or early n3 technique* or early n3 strateg* or early n3 activit* or early n3 mobili*
-
earli* n3 interven* or earli* n3 treat* or earli* n3 therap* or earli* n3 care or earli* n3 medicine* or earli* n3 technique* or earli* n3 strateg* or earli* n3 activit* or earli* n3 mobili*
-
immediat* n3 interven* or immediat* n3 treat* or immediat* n3 therap* or immediat* n3 care or immediat* n3 medicine* or immediat* n3 technique* or immediat* n3 strateg* or immediat* n3 activit* or immediat* n3 mobili*
-
initial* n3 interven* or initial* n3 treat* or initial* n3 therap* or initial* n3 care or initial* n3 medicine* or initial* n3 activit* or initial* n3 technique* or initial* n3 strateg* or initial* n3 mobili*
-
begin* n3 interven* or begin* n3 treat* or begin* n3 therap* or begin* n3 care or begin* n3 medicine* or begin* n3 technique* or begin* n3 strateg* or begin* n3 activit* or begin* n3 mobili*
-
first* n3 interven* or first* n3 treat* or first* n3 therap* or first* n3 care or first* n3 medicine* or first* n3 technique* or first* n3 strateg* or first* n3 activit* or first* n3 mobili*
-
first-line n3 interven* or first-line n3 treat* or first-line n3 therap* or first-line n3 care or first-line n3 medicine* or first-line n3 technique* or first-line n3 strateg* or first-line n3 activit* or first-line n3 mobili*
-
primar* n3 interven* or primar* n3 treat* or primar* n3 therap* or primar* n3 care or primar* n3 medicine* or primar* n3 technique* or primar* n3 strateg* or primar* n3 activit* or primar* n3 mobili*
-
original* n3 interven* or original* n3 treat* or original* n3 therap* or original* n3 care or original* n3 medicine* or original* n3 technique* or original* n3 strateg* or original* n3 activit* or original* n3 mobili*
-
preceed* n3 interven* or preceed* n3 treat* or preceed* n3 therap* or preceed* n3 care or preceed* n3 medicine* or preceed* n3 technique* or preceed* n3 strateg* or preceed* n3 activit* or preceed* n3 mobili*
-
walk or walks or walking
-
mobili?ation strateg*
-
ambulate* or ambulation* or ambulating*
-
exerci* n3 rehab* or exerci* n3 habilitat* or exerci* n3 recover* or exerci* n3therap* or exerci* n3 treat* or exerci* n3 medicine* or exerci* n3 intervention* or exerci* n3 technique* or exerci* n3 strateg*
-
walk* n3 rehab* or walk* n3 habilitat* or walk* n3 recover* or walk* n3 therap* or walk* n3 treat* or walk* n3 medicine* or walk* n3 intervention* or walk* n3 technique* or walk* n3 strateg*
-
mov* n3 rehab* or mov* n3 habilitat* or mov* n3 recover* or mov* n3 therap* or mov* n3 treat* or mov* n3 medicine* or mov* n3 intervention* or mov* n3 technique* or mov* n3 strateg*
-
motor* n3 rehab* or motor* n3 habilitat* or motor* n3 recover* or motor* n3 therap* or motor* n3 treat* or motor* n3 medicine* or motor* n3 intervention* or motor* n3 technique* or motor* n3 strateg*
-
physi* n3 rehab* or physi* n3 habilitat* or physi* n3 recover* or physi* n3 therap* or physi* n3 treat* or physi* n3 medicine* or physi* n3 intervention* or physi* n3 technique* or physi* n3 strateg*
-
extend* n2 care* n3 facilit* or extend* n2 care* n3 service* or extend* n2 care* n3 unit* or extend* n2 care* n3 center* or extend* n2 care* n3 clinic* or extend* n2 care* n3 program* or extend* n2 care* n3 residen* or extend* n2 care* n3 home* or extend* n2 care* n3 hous*
-
residen* n3 facilit* or residen* n3 care* or residen* n3 service* or residen* n3 unit* or residen* n3 center* or residen* n3 clinic* or residen* n3 program* or residen* n3 residen* or residen* n3 home* or residen* n3 hous*
-
intermediate* n3 facilit* or intermediate* n3 care* or intermediate* n3 service* or intermediate* n3 unit* or intermediate* n3 center* or intermediate* n3 clinic* or intermediate* n3 program* or intermediate* n3 residen* or intermediate* n3 home* or intermediate* n3 hous*
-
assist* liv* n3 facilit* or assist* liv* n3 care* or assist* liv* n3 service* or assist* liv* n3 unit* or assist* liv* n3 center* or assist* liv* n3 clinic* or assist* liv* n3 program* or assist* liv* n3 residen* or assist* liv* n3 home* or assist* liv* n3 hous*
-
halfway n3 home* or halfway n3 hous* or halfway n3 facilit* or halfway n3 care* or halfway n3 residen* or halfway n3 service* or halfway n3 unit* or halfway n3 center* or halfway n3 clinic* or halfway n3 program*
-
transition* n3 home* or transition* n3 hous* or transition* n3 facilit* or transition* n3 care* or transition* n3 residen* or transition* n3 service* or transition* n3 unit* or transition* n3 center* or transition* n3 clinic* or transition* n3 program*
-
nurs* n2 home* or geriatr*-orthop* or orthop?edic-geriatr* or ortho*-geriatr* or orthogeriatr* or goru or orthop* n2 geriatr* or rehabilitation unit* or mixed assessment or maru
-
geriatric hip fracture program* or ghfp or day n1 hospital* or day n1 care or day n1 unit* or home-based n1 care or home based n1 care or carer* involve* or esd or early supported discharge or sequential care
-
S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 or S41 or S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 or S51
-
S4 and S51
EMBASE (via Ovid)
-
exp Hip Fracture/
-
((femur$ or femoral$) adj3 (head or neck or proximal) adj4 fracture$).ti,ab.
-
((hip$ or femur$ or femoral$ or trochant$ or pertrochant$ or intertrochant$ or subtrochant$ or intracapsular$ or extracapsular$) adj4 fracture$).ti,ab.
-
1 or 2 or 3
-
exp Rehabilitation/ or exp Rehabilitation Nursing/ or exp daily life activity/
-
assisted living facility/ or nursing home/ or pain clinic/ or rehabilitation center/ or residential home/ or halfway house/
-
day hospital/ or home care/ or home health agency/ or home physiotherapy/ or home rehabilitation/ or patient care/ or patient care planning/ or rehabilitation care/
-
exp mobilization/ or exp Occupational Therapy/ or exp Physiotherapy/ or exp kinesiotherapy/ or walking/
-
exp clinical pathway/ or social care/ or caregiver support/ or social support/ or caregiver/
-
(rehab$ or habilitat$ or recover$).ti,ab.
-
(multidisciplinar$ or interdisciplinar$ or multiprofessional$ or multimodal$ or mdt or mdr).ti,ab.
-
(social adj1 (work$ or support or care)).ti,ab.
-
(pain clinic$ or pain service$ or pain relief unit$ or (pain center$ or pain centre$)).ti,ab.
-
((treatment$ or therap$ or training or education$ or healthcare) adj10 (program$ or intervention$ or approach$)).ti,ab.
-
(early adj1 (mobil$ or discharg$ or ambulat$)).ti,ab.
-
(occupational therap$ or physical therap$ or physiotherap$ or physio).ti,ab.
-
(exercis$ adj3 therap$).ti,ab.
-
((early or earli$ or immediat$ or initial$ or begin$ or first$ or first-line or first line or first choice or primar$ or preceed$ or original$) adj3 (interven$ or treat$ or therap$ or care or medicine$ or technique$ or strateg$ or activit$ or mobili$)).ti,ab.
-
(walk or walks or walking).ti,ab.
-
mobili?ation strateg$.ti,ab.
-
(ambulate$ or ambulation$ or ambulating$).ti,ab.
-
(exerci$ adj3 (rehab$ or habilitat$ or recover$ or therap$ or treat$ or medicine$ or intervention$ or technique$ or strateg$)).ti,ab.
-
((walk$ or mobil$ or mov$ or motor$ or physi$) adj3 (rehab$ or habilitat$ or recover$ or therap$ or treat$ or medicine$ or intervention$ or technique$ or strateg$)).ti,ab.
-
(extend$ adj2 care$ adj3 (facilit$ or service$ or unit$ or center$ or clinic$ or program$ or residen$ or home$ or hous$)).ti,ab.
-
((residen$ or intermediate$ or assist$ liv$) adj3 (facilit$ or care$ or service$ or unit$ or center$ or clinic$ or program$ or residen$ or home$ or hous$)).ti,ab.
-
((halfway or transition$) adj3 (home$ or hous$ or facilit$ or care$ or residen$ or service$ or unit$ or center$ or clinic$ or program$)).ti,ab.
-
(nurs$ adj2 home$).ti,ab.
-
(geriatr$-orthop$ or orthop?edic-geriatr$ or ortho$-geriatr$ or orthogeriatr$ or goru).ti,ab.
-
(orthop$ adj2 geriatr$).ti,ab.
-
rehabilitation unit$.ti,ab.
-
(mixed assessment or maru).ti,ab.
-
(geriatric hip fracture program$ or ghfp).ti,ab.
-
(day adj (hospital$ or care or unit$)).ti,ab.
-
((home-based or home based) adj care).ti,ab.
-
carer$ involve$.ti,ab.
-
(esd or early supported discharge).ti,ab.
-
sequential care.ti,ab.
-
or/5-37
-
4 and 38
Allied and Complementary Medicine Database (via Ovid) (not National Institute for Health and Care Excellence) (using the MEDLINE search strategy as the basis)
-
exp Hip Fractures/
-
((femur$ or femoral$) adj3 (head or neck or proximal) adj4 fracture$).ti,ab.
-
((hip$ or femur$ or femoral$ or trochant$ or pertrochant$ or intertrochant$ or subtrochant$ or intracapsular$ or extracapsular$) adj4 fracture$).ti,ab.
-
1 or 2 or 3
-
exp rehabilitation/ or exp rehabilitation nursing/ or “Recovery of Function”/ or Subacute Care/
-
exp rehabilitation centers/ or Residential Facilities/ or Assisted Living Facilities/ or Halfway Houses/
-
Day Care/ or home care services/ or home care services, hospital-based/ or home nursing/ or hospital units/
-
exp Nursing Homes/ or exp Patient Care Team/ or exp Patient Care Management/
-
exp Therapy, Computer-Assisted/ or exp Exercise Therapy/ or exp Walking/
-
exp Social Work/ or exp Social Support/ or exp Pain Clinics/ or exp Patient Education/ or exp Health Education/ or Caregivers/
-
(rehab$ or habilitat$ or recover$).ti,ab.
-
(multidisciplinar$ or interdisciplinar$ or multiprofessional$ or multimodal$ or mdt or mdr).ti,ab.
-
(social adj1 (work$ or support or care)).ti,ab.
-
(pain clinic$ or pain service$ or pain relief unit$ or (pain center$ or pain centre$)).ti,ab.
-
((treatment$ or therap$ or training or education$ or healthcare) adj10 (program$ or intervention$ or approach$)).ti,ab.
-
(early adj1 (mobil$ or discharg$ or ambulat$)).ti,ab.
-
(occupational therap$ or physical therap$ or physiotherap$ or physio).ti,ab.
-
(exercis$ adj3 therap$).ti,ab.
-
((early or earli$ or immediat$ or initial$ or begin$ or first$ or first-line or first line or first choice or primar$ or preceed$ or original$) adj3 (interven$ or treat$ or therap$ or care or medicine$ or technique$ or strateg$ or activit$ or mobili$)).ti,ab.
-
(walk or walks or walking).ti,ab.
-
mobili?ation strateg$.ti,ab.
-
(ambulate$ or ambulation$ or ambulating$).ti,ab.
-
(exerci$ adj3 (rehab$ or habilitat$ or recover$ or therap$ or treat$ or medicine$ or intervention$ or technique$ or strateg$)).ti,ab.
-
((walk$ or mobil$ or mov$ or motor$ or physi$) adj3 (rehab$ or habilitat$ or recover$ or therap$ or treat$ or medicine$ or intervention$ or technique$ or strateg$)).ti,ab.
-
(extend$ adj2 care$ adj3 (facilit$ or service$ or unit$ or center$ or clinic$ or program$ or residen$ or home$ or hous$)).ti,ab.
-
((residen$ or intermediate$ or assist$ liv$) adj3 (facilit$ or care$ or service$ or unit$ or center$ or clinic$ or program$ or residen$ or home$ or hous$)).ti,ab.
-
((halfway or transition$) adj3 (home$ or hous$ or facilit$ or care$ or residen$ or service$ or unit$ or center$ or clinic$ or program$)).ti,ab.
-
(nurs$ adj2 home$).ti,ab.
-
(geriatr$-orthop$ or orthop?edic-geriatr$ or ortho$-geriatr$ or orthogeriatr$ or goru).ti,ab.
-
(orthop$ adj2 geriatr$).ti,ab.
-
rehabilitation unit$.ti,ab.
-
(mixed assessment or maru).ti,ab.
-
(geriatric hip fracture program$ or ghfp).ti,ab.
-
(day adj (hospital$ or care or unit$)).ti,ab.
-
((home-based or home based) adj care).ti,ab.
-
carer$ involve$.ti,ab.
-
(esd or early supported discharge).ti,ab.
-
sequential care.ti,ab.
-
or/5-38
-
4 and 39
PsycINFO (via Ovid)
-
hips/
-
((femur$ or femoral$) adj3 (head or neck or proximal) adj4 fracture$).ti,ab.
-
((hip$ or femur$ or femoral$ or trochant$ or pertrochant$ or intertrochant$ or subtrochant$ or intracapsular$ or extracapsular$) adj4 fracture$).ti,ab.
-
1 or 2 or 3
Appendix 9 Criteria used to conceptually categorise the documents for screening
Reproduced from Pearson M, Hunt H, Cooper C, Shepperd S, Pawson R, Anderson R. Intermediate Care: A Realist Review and Conceptual Framework. Final report. Southampton: NIHR Service Delivery and Organisation programme; 2013. 61 This report may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising.
Appendix 10 Key for outcome measures in the outcomes tables in Appendix 19
| Number | Outcome measurement instrument |
|---|---|
| 1 | Activities of Daily Living – Katz (kADL) index |
| 2 | Activities of Daily Living – NEADL – Instrumental (I-ADL) scale |
| 3 | Activities of Daily Living – Performance (P-ADL) index |
| 4 | Activities of Daily Living – Basic (BADL) index |
| 5 | Activities of Daily Living – Instrumental (I-ADL) index |
| 6 | Activities of Daily Living – Total (ADL) index |
| 7 | Activities-specific Balance Confidence (ABC) scale |
| 8 | Acute Physiology and Chronic Health Evaluation II scale (APACHE II) |
| 9 | Ambulation ability score |
| 10 | Barthel Index – Chinese (CBI) |
| 11 | Barthel Index – Modified (MBI) |
| 12 | Barthel Index |
| 13 | Barthel Index questionnaire – modified |
| 14 | Beck Depression Inventory (BDI) |
| 15 | Berg Balance Scale (BBS) |
| 16 | Centre for Epidemiologic Studies Depression Scale (CESD) |
| 17 | Chinese version of the ‘functional status subscale’ adapted from the OARS Multidimensional Functional Assessment Questionnaire (OMFAQ) |
| 18 | Clinical Outcome Variables (COVS) |
| 19 | Clinical Outcome Variables – Swedish (S-COVS) |
| 20 | Cumulative Illness Rating Scale (CIRS) |
| 21 | Discharge to care home |
| 22 | Discharge to previous place of residence |
| 23 | Elderly Mobility Scale (EMS) |
| 24 | EQ-5D |
| 25 | Established Populations for Epidemiologic Studies of the Elderly (EPESE) interview |
| 26 | Face pain scale |
| 27 | Falls Efficacy Scale – Chinese (CFES) |
| 28 | FES-I |
| 29 | Falls Efficacy Scale – Modified (MFES) |
| 30 | Falls Efficacy Scale – Swedish [FES(S)] |
| 31 | Falls Efficacy Scale (FES) |
| 32 | Frenchay Activity Index |
| 33 | Functional Ambulation Classification (FAC) |
| 34 | Functional efficiency – absolute (aFE) |
| 35 | Functional gain – absolute (aFG) |
| 36 | Functional gain – motor (mFG) |
| 37 | Functional gain – relative (rFG) |
| 38 | Functional Independence Measure (FIM) |
| 39 | Functional Independence Measure – motor (mFIM) |
| 40 | Functional Independence Measure – absolute total (tFIM) |
| 41 | Functional Independence Measure – cognitive (cFIM) |
| 42 | Functional Independence Measure – instrumental (iFIM) |
| 43 | Functional reach test |
| 44 | Functional Status Index |
| 45 | Functional Status Questionnaire (FSQ) |
| 46 | Gait speed test |
| 47 | Gait velocity |
| 48 | GDS |
| 49 | GDS – 15 items |
| 50 | Geriatric Depression Scale – Chinese version (cGDS) |
| 51 | Grip strength – Jamar® Hand Dynamometer (Takei Scientific Instruments Co., Ltd, Nigata, Japan) |
| 52 | Harris hip scores |
| 53 | Harris pain scores |
| 54 | Hip Fractures Knowledge Test |
| 55 | HADS |
| 56 | Hospital readmission rate |
| 57 | Health-related quality of life |
| 58 | Institutionalisation rate |
| 59 | Instrumental Activity Measure |
| 60 | Iowa Level of Assistance Scale (ILOA) |
| 61 | Iowa Level of Assistance Scale – modified (mILOA) |
| 62 | Isometric force of the hip, knee, and ankle extensors |
| 63 | Knee extension torque – asymmetric |
| 64 | Knee extension torque – isometric |
| 65 | Lawton and Brody Instrumental Activities of Daily Living (IADL) scale |
| 66 | Lawton Index |
| 67 | Leg extension power – asymmetric (aLEP) |
| 68 | Leg extension power – isometric (iLEP) |
| 69 | Length of hospital stay |
| 70 | London Handicap Scale (LHS) |
| 71 | Lower Extremity Gain Scale |
| 72 | Maximal gait speed test |
| 73 | Maximum step height test |
| 74 | Mental Component Summary (MCS) score |
| 75 | Merle d’Aubigné and Postel Hip Score |
| 76 | MMSE |
| 77 | Mobility function score |
| 78 | Mobility recovery score |
| 79 | Modified Physical Performance Test (mPPT) |
| 80 | Montebello Rehabilitation Factor Score (MRFS) |
| 81 | Morbidity rate |
| 82 | Mortality rate |
| 83 | Muscle strength – functional lower extremity |
| 84 | Muscle strength – knee extensor |
| 85 | Muscle strength – quadriceps |
| 86 | Nottingham Health Profile (NHP) questionnaire |
| 87 | Numerical rating scale (NRS) |
| 88 | OARS Multidimensional Functional Assessment Questionnaire (OMFAQ) |
| 89 | OARS Multidimensional Functional Assessment Questionnaire (OMFAQ) – Chinese |
| 90 | Older Americans Resources and Services Instrument |
| 91 | Outcome Expectations for Exercise Scale |
| 92 | Outpatient rehabilitation consumption |
| 93 | Pain – seven-item ordinal scale |
| 94 | Patient Satisfaction Questionnaire |
| 95 | Performance-Oriented Mobility Assessment (POMA) |
| 96 | Physical Performance and Mobility Examination (PPME) |
| 97 | Physical Performance Test (PPT) – nine items |
| 98 | Physical Performance Test (PPT) – modified |
| 99 | Positive affect (high/low) |
| 100 | Post-hospital institutional stay |
| 101 | Postural sway |
| 102 | Postural sway meter |
| 103 | Range of motion (ROM) |
| 104 | Rate of falls |
| 105 | Rate of repeat falls |
| 106 | RAP |
| 107 | Rehabilitation duration |
| 108 | Rehabilitation therapy self-efficacy |
| 109 | Rehabilitation therapy self-efficacy questionnaire |
| 110 | Satisfaction questionnaire |
| 111 | Self-care knowledge questionnaire |
| 112 | Self-Efficacy for Walking/Exercise Scale |
| 113 | Service utilisation |
| 114 | Short Form questionnaire-12 items (SF-12) |
| 115 | SF-36 |
| 116 | SPPB |
| 117 | Short Portable Mental Status Questionnaire (SPMSQ) |
| 118 | Sickness Impact Profile (SIP) |
| 119 | Sit-to-stand test |
| 120 | Social Activity Scale [adapted from the Established Populations for Epidemiologic Studies of the Elderly (EPESE) interview] |
| 121 | Social Support for Exercise Habits Scale (SSEH) |
| 122 | Spitzer Quality of Life Index |
| 123 | Step Activity Monitor (SAM) – CHAMPS Physical Activity Questionnaire for Older Adults |
| 124 | Therapy Outcome Measure (TOM) |
| 125 | Timed stair climb |
| 126 | Timed Up and Go scale |
| 127 | Tinetti scale score |
| 128 | VAS (1–10) |
| 129 | 10-minute walk test (10MWT) |
| 130 | 2-minute walk test (2MWT) |
| 131 | 6-minute walk test (6MWT) |
| 132 | Walking ability scale (0–15) |
| 133 | Walking ability scale (0–5) |
| 134 | Walking distance |
| 135 | Walking speed |
| 136 | Walking speed – fast |
| 137 | Walking speed – preferred |
| 138 | Wong–Baker pain scale |
| 139 | Yale Physical Activity Survey |
| 140 | Patient-reported outdoor mobility experience |
| 141 | Composite of knee strength and Timed Up and Go scale |
| 142 | VO2peak |
| 143 | Increase in body cell mass |
| 144 | Patient-reported risk of falling |
| 145 | New nursing home admission |
| 146 | Discharge destination |
| 147 | Cumulative sessions of physical and occupational therapy |
| 148 | Health-care utilisation |
| 149 | Patient-/carer-reported occurrence of falls |
| 150 | Malnourishment |
Appendix 11 Summary of outcome measure instruments used in the included studies
| Outcome category | Study | Outcome measure |
|---|---|---|
| ADL | Stenvall 2007120 | Activities of Daily Living – Katz (kADL) index |
| Giusti 2006143 | Activities of Daily Living – Katz (kADL) index/Barthel Index | |
| Saltvedt 2012;116 Sylliaas 2011199 | Activities of Daily Living – NEADL – Instrumental (I-ADL) scale | |
| Dai 2002;132 Koval 1998;146 Vidán 2005124 | Activities of Daily Living – Basic (BADL) index | |
| Al-Ani 2010139 | Activities of Daily Living – Katz (kADL) index | |
| Host 2007;153 Koval 1998;146 Louie 2012;106 Naglie 2002;111 Röder 2003151 | Activities of Daily Living index – Instrumental (I-ADL) index | |
| Binder 2004;92 Host 2007;153 Louie 2012;106 Naglie 2002;111 Röder 2003;151 Rösler 2012;152 Stenvall 2007;120 Tinetti 1999121 | Activities of Daily Living – Total (ADL) index | |
| Shyu 2008119 | Barthel Index – Chinese (CBI) | |
| Mitchell 2001;109 Whitehead 2003161 | Barthel Index – Modified (MBI) | |
| Di Monaco 2008;133 Huang 2005;100 Levi 1997;147 Ryan 2006;115 Uy 2008123 | Barthel Index | |
| Giusti 2006143 | Barthel Index/Lawton Index | |
| Zidén 200890 | Frenchay Activity Index | |
| Louie 2012;106 Zidén 200890 | Functional independence measure (FIM) – Motor (mFIM) | |
| Latham 2006;167 Zidén 200890 | Functional Independence Measure – instrumental (iFIM) | |
| Van Balen 2002140 | RAP | |
| ADL – instrumental | Orwig 2011191 | Older Americans Resources and Services Instrument |
| ADL – lower extremity | Orwig 2011191 | Functional Status Index |
| AEs | Hoekstra 2011144 | Malnourishment |
| Roberts 2004;155 Vidán 2005124 | Morbidity rate | |
| Huang 2005;100 Jensen 1979;154 Lieberman 2002;148 Naglie 2002;111 Roberts 2004155 | Mortality rate | |
| Bischoff-Ferrari 201093 | Rate of falls | |
| Huang 2005100 | Rate of repeat falls | |
| Balance | Whitehead 2003161 | Activities-specific Balance Confidence (ABC) scale |
| Binder 2004;92 Mendelsohn 2008;108 Moseley 2009;110 Sylliaas 2011;199 Tinetti 1999;121 Whitehead 2003161 | Berg Balance Scale (BBS) | |
| Sherrington 1997;117 Sherrington 2004118 | Postural sway metre | |
| Carer satisfaction | Crotty 200395 | SF-36 |
| Cognitive status | Van Balen 2002;140 Ohsawa 2007137 | MMSE |
| Giusti 2006143 | Short Portable Mental Status Questionnaire (SPMSQ) | |
| Depression | Nicholson 1997136 | Beck Depression Inventory (BDI) |
| Casado 2009;80 Fredman 2006;142 Resnick 2007;69 Fortinsky 200281 | Centre for Epidemiologic Studies Depression Scale (CESD) | |
| Shyu 2008;119 Shyu 2009196 | Geriatric Depression Scale – Chinese version (cGDS) | |
| Ryan 2006115 | HADS | |
| Depression/quality of life | Orwig 2011191 | GDS/SF-36 |
| Discharge destination | Kennie 1988;102 Roberts 2004155 | Discharge destination |
| Oldmeadow 200687 | Discharge home | |
| Fox 1993200 | Discharge to care home | |
| Jackson 2001;83 Fox 1993;200 Huusko 2000;101 Naglie 2002111 | Discharge to previous place of residence | |
| Disease burden | Giusti 2006143 | Cumulative Illness Rating Scale (CIRS) |
| Disease burden/severity of illness | Giusti 2006143 | Acute Physiology and Chronic Health Evaluation II scale (APACHE II) |
| Exercise behaviour | Resnick 200769 | Step Activity Monitor (SAM) – CHAMPS Physical Activity Questionnaire for Older Adults |
| Casado 2009;80 Resnick 200769 | Yale Physical Activity Survey | |
| Favourable clinical course | Delmi 199096 | Morbidity rate/mortality rate |
| Fear of falling | Louie 2012106 | Falls Efficacy Scale – Chinese (CFES) |
| Saltvedt 2012116 | FES-I | |
| Moseley 2009110 | Falls Efficacy Scale – Modified (MFES) | |
| Zidén 200890 | Falls Efficacy Scale – Swedish [FES(S)] | |
| Casado 2009;80 Nicholson 1997136 | Falls Efficacy Scale (FES) | |
| Sherrington 1997117 | Patient-reported fear of falling | |
| Sherrington 2004118 | Patient-reported risk of falling | |
| Function | Deschodt 201197 | Activities of Daily Living – Katz (kADL) index |
| Beaupre 2005157 | Barthel Index – Modified (MBI) | |
| Adunsky 2003138 | Functional efficiency – absolute (aFE) | |
| Adunsky 2003138 | Functional gain – absolute (aFG) | |
| Jackson 2001;83 Zabari 2012162 | Functional Independence Measure (FIM) | |
| Adunsky 2003138 | Functional Independence Measure – motor (mFIM) | |
| Adunsky 2003;138 Zabari 2012162 | Functional Independence Measure – absolute total (tFIM) | |
| Adunsky 2003138 | Functional Independence Measure – cognitive (cFIM) | |
| Oude Voshaar 200712 | Functional reach | |
| Oude Voshaar 200712 | Gait speed test (time) | |
| Oldmeadow 200687 | Iowa Level of Assistance Scale –modified (mILOA) | |
| Whitehead 2003161 | London Handicap Scale (LHS) | |
| Adunsky 2003138 | Montebello Rehabilitation Factor Score (MRFS) | |
| Sherrington 2004118 | Physical Performance and Mobility Examination (PPME) | |
| Moseley 2009110 | Physical Performance and Mobility Examination (PPME)/Barthel Index | |
| Mangione 2010107 | Physical Performance Test (PPT) – modified | |
| Mangione 2010107 | SF-36 | |
| Oude Voshaar 200712 | Timed Up and Go scale | |
| Functional recovery | Vidán 2005124 | Composite functional status score |
| Tsauo 2005122 | Harris hip scores | |
| Functioning – cognitive | Jones 2002195 | Functional Independence Measure – cognitive (cFIM) |
| Functioning – physical | Kennie 1988102 | Activities of Daily Living – Katz (kADL) index |
| Bischoff-Ferrari 201093 | Composite of knee strength and Timed Up and Go scale | |
| Arinzon 2005;201 Jones 2002;195 Lieberman 2002;148 Mendelsohn 2008;108 Ohsawa 2007;137 Penrod 2004;192 Rolland 2004184 | Functional Independence Measure (FIM) | |
| Bellelli 2010;78 Jones 2002;195 Munin 2005149 | Functional Independence Measure – motor (mFIM) | |
| Bellelli 201078 | Functional Independence Measure – absolute total (tFIM) | |
| Carmeli 2006131 | Functional reach test | |
| Binder 200492 | Functional Status Questionnaire (FSQ) | |
| Orwig 2011191 | Lower Extremity Gain Scale | |
| Ohsawa 2007137 | Merle d’Aubigné and Postel Hip Score | |
| Lin 2009105 | OARS Multidimensional Functional Assessment Questionnaire (OMFAQ) – Chinese | |
| Carmeli 2006131 | Physical Performance Test (PPT) | |
| Host 2007153 | Physical Performance Test (PPT) – nine items | |
| Binder 200492 | Physical Performance Test (PPT) – modified | |
| Allegrante 2007;91 Jensen 1979154 | SF-36 | |
| Bellelli 2010;78 Rösler 2012152 | Tinetti scale score | |
| Orwig 2011191 | 6-minute walk test (6MWT) | |
| Koval 1998146 | Walking ability | |
| Functioning – physical and emotional | Ryan 2006115 | Therapy Outcome Measure (TOM) |
| Functioning – social | Allegrante 200791 | SF-36 |
| Mobility | Crotty 2003;95 Kuisma 2002103 | Ambulation ability score |
| Naglie 2002111 | Barthel Index – Modified (MBI) | |
| Stenvall 2007120 | Clinical Outcome Variables – Swedish (S-COVS) | |
| Mitchell 2001109 | Elderly Mobility Scale (EMS) | |
| Ryan 2006115 | Frenchay Activity Index | |
| Vidán 2005124 | Functional Ambulation Classification (FAC) | |
| Fortinsky 200281 | Functional Independence Measure (FIM) | |
| Fortinsky 2002;81 Latham 2006167 | Functional Independence Measure – motor (mFIM) | |
| Sherrington 1997;117 Sherrington 2004;118 Binder 2004;92 Mangione 2010107 | Gait velocity | |
| Sylliaas 2011199 | Maximal gait speed test | |
| Sylliaas 2011199 | Maximum step height test | |
| Dai 2002;132 Roberts 2004;155 Tinetti 1999;121 Visser 2000156 | Mobility function score | |
| Portegijs 2008114 | Patient-reported outdoor mobility experience | |
| Tinetti 1999121 | Performance-Oriented Mobility Assessment (POMA) | |
| Nicholson 1997;136 Tsauo 2005122 | Range of motion (ROM) | |
| Naglie 2002111 | Rate of change in ambulation | |
| Saltvedt 2012116 | SPPB | |
| Oude Voshaar 200712 | Sickness Impact Profile (SIP) | |
| Sylliaas 2011199 | Sit-to-stand test | |
| Host 2007153 | Timed stair climb | |
| Mendelsohn 2008;108 Mitchell 2001;109 Saltvedt 2012;116 Sylliaas 2011;199 Zidén 200890 | Timed Up and Go scale | |
| Uy 2008123 | 10-minute walk test (10MWT) | |
| Mendelsohn 2008108 | 2-minute walk test (2MWT)/10-minute walk test (10MWT) | |
| Mangione 2010;107 Sylliaas 2011199 | 6-minute walk test (6MWT) | |
| Van Balen 2002;140 Al-Ani 2010;139 Shyu 2008119 | Walking ability scale (0–5) | |
| Walking ability scale (0–15) | ||
| Portegijs 2008114 | Walking distance | |
| Moseley 2009110 | Walking speed | |
| Host 2007153 | Walking speed – fast | |
| Host 2007153 | Walking speed – preferred | |
| Deschodt 2011;97 Huusko 2000101 | Mortality rate | |
| Muscle strength | Mitchell 2001;109 Nicholson 1997;136 Orwig 2011191 | Grip strength – Jamar Hand Dynamometer |
| Moseley 2009110 | Isometric force of the hip, knee and ankle extensors | |
| Portegijs 2008114 | Knee extension torque – asymmetric | |
| Mangione 2010;107 Portegijs 2008114 | Knee extension torque – isometric | |
| Portegijs 2008114 | Leg extension power – asymmetric (aLEP) | |
| Mitchell 2001;109 Portegijs 2008114 | Leg extension power – isometric (iLEP) | |
| Zidén 200890 | Muscle strength – functional lower extremity | |
| Sherrington 1997;117 Sherrington 2004118 | Muscle strength – quadriceps | |
| Pain | Ohsawa 2007137 | Face pain scale |
| Saltvedt 2012116 | Numerical rating scale (NRS) | |
| Moseley 2009110 | Pain – seven-item scale | |
| Zabari 2012162 | VAS (1–10) | |
| Patient-reported outcomes | Louie 2012106 | Hip Fractures Knowledge Test |
| Di Monaco 2008133 | Morbidity rate – occurrence of falls | |
| Lin 2009105 | Patient Satisfaction Questionnaire | |
| Shyu 2008119 | Patient-/carer-reported occurrence of falls | |
| Lin 2009105 | Self-care knowledge questionnaire | |
| Patient satisfaction | Jackson 200183 | Satisfaction questionnaire |
| Crotty 2003;95 Sylliaas 2011199 | SF-36 | |
| Physical activity levels | Orwig 2011191 | Yale Physical Activity Survey |
| Physical functioning | Casado 2009;80 Resnick 200769 | SF-36 |
| Physiological measurements | Orwig 2011191 | Bone mineral density |
| Hoekstra 2011144 | Increase in body cell mass | |
| Mendelsohn 2008108 | VO2peak | |
| Psychological morbidity | Röder 2003151 | MMSE |
| Quality of life | Hoekstra 2011;144 Moseley 2009;110 Ryan 2006;115 Saltvedt 2012116 | EQ-5D |
| Tsauo 2005122 | Health-related quality of life | |
| Van Balen 2002;140 Mitchell 2001109 | Nottingham Health Profile (NHP) questionnaire | |
| Binder 2004;92 Huang 2005;100 Lin 2009105 | SF-36 | |
| Shyu 2008119 | SF-36 (Taiwanese) | |
| Röder 2003151 | Spitzer Quality of Life index | |
| Self-efficacy | Whitehead 2003161 | Falls Efficacy Scale (FES) |
| Casado 2009;80 Resnick 200769 | Outcome Expectations for Exercise scale | |
| Fortinsky 200281 | Rehabilitation therapy self-efficacy questionnaire | |
| Casado 200980 | Self-Efficacy for Walking/Exercise Scale | |
| Resnick 200769 | ||
| Service resource use | Adunsky 2003138 | Length of hospital stay |
| Levi 1997147 | Cumulative sessions of physical and occupational therapy | |
| Moseley 2009110 | Falls and hospital readmissions | |
| Naglie 2002111 | Health-care utilisation | |
| Van Balen 2002;140 Bischoff-Ferrari 2010;93 Deschodt 2011;97 Huang 2005;100 Roberts 2004;155 Shyu 2008;119 Stenvall 2007120 | Hospital readmission rate | |
| Beaupre 2005;157 Arinzon 2005201 | Institutionalisation rate | |
| Arinzon 2005;201 Van Balen 2002;140 Beaupre 2005;157 Boyd 1982;158 Deschodt 2011;97 Fox 1993;200 Holmberg 1989;160 Huang 2005;100 Huusko 2000;101 Jensen 1979;154 Kennie 1988;102 Lin 2009;105 Oldmeadow 2006;87 Roberts 2004;155 Rösler 2012;152 Stenvall 2007;120 Vidán 2005;124 Zidén 200890 | Length of hospital stay | |
| Deschodt 201197 | New nursing home admission | |
| Stenvall 2007120 | Outpatient rehabilitation consumption | |
| Levi 1997147 | Post-hospital institutional stay | |
| Lieberman 2002148 | Rehabilitation duration | |
| Social support | Casado 200980 | Social Support for Exercise Habits Scale (SSEH) |
| Socialisation | Tinetti 1999121 | Established Populations for Epidemiologic Studies of the Elderly (EPESE) interview – modified |
Appendix 12 Results of the databases searches in the realist review
| Database | Dates covered | Date searched | Hits | Loaded to EndNote library | Database host |
|---|---|---|---|---|---|
| MEDLINE | 1946–present | 26 February 2013 | 6651 | 6651 | Ovid |
| EMBASE | 1947–present | 26 February 2013 | 8915 | 8915 | Ovid |
| CINAHL | 1981–2013 | 26 February 2013 | 2159 | 2159 | EBSCOhost |
| AMED | 1985–present | 5 March 2013 | 568 | 568 | Ovid |
| The Cochrane Library | To present | 27 February 2013 | 620 | 620 | Wiley |
| Other reviews | 11 | ||||
| CDSR | 33 | ||||
| Trials | 551 | ||||
| Methods studies | 4 | ||||
| NHS EED | 18 | ||||
| HTA database | 3 | ||||
| Total 18,913 | |||||
| After electronic deduplication (2098) 16,815 | |||||
| PEDro | 1929–8 April 2013 | 8 April 2013 | 113 | 96 |
Appendix 13 Reviewer final decisions about the conceptual categorisation of included studies
| Study | Conceptual categorisation |
|---|---|
| Adunsky 2003138 | Thick (motor and cognitive functional independence measure) |
| Al-Ani 2010139 | Thick (walking ability and ADL in demented patients) |
| Allegrante 200791 | Thick |
| Arinzon 2005201 | Thick (influence of age on rehabilitation outcomes) |
| Atwal 2002176 | Rich (model of integrated care and whether it leads to better outcomes) |
| Barone 2009177 | Thick (immediate weight bearing and early ambulation) |
| Bäuerle 2004163 (German) | Thick (formal/informal/financial support, ability to walk, cognition) |
| Beaupre 2005157 | Thick (RCT of discharge planning) |
| Bellelli 2006170 | Thick (case study, body weight-supported treadmill for functional recovery) |
| Bellelli 2008141 | Thick (depression and dementia) |
| Bellelli 201078 | Rich (action observation treatment plus conventional physiotherapy) |
| Binder 200492 | Thick (RCT of exercise rehabilitation) |
| Bischoff-Ferrari 201093 | Thick (standard physiotherapy vs. standard physiotherapy + home physiotherapy) |
| Borgquist 1990188 | Thick (rehabilitation in primary care + home walking + progressively no walking aid) |
| Boyd 1982158 | Thick (rehabilitation setting) |
| Buddenberg 199879 | Rich (occupational adaptation frame of reference approach combines biomechanical principles with focus on facilitation of the internal occupational adaptation process) |
| Burns 2007197 | Rich (model of fear of falling) |
| Carmeli 2006131 | Rich (supervised and non-supervised exercise programmes vs. outcomes) |
| Casado 200980 | Rich (model of self-efficacy, social support) |
| Cree 2001175 | Thick |
| Crotty 200094 | Thick (RCT of exercise rehabilitation) |
| Crotty 200395 | Thick (RCT of early discharge) |
| Dai 2002132 | Thick |
| De Jonge 2001171 | Thick (discharge planning) |
| Delmi 199096 | Thick (dietary planning and dietary supplementation of rehabilitation in hip fracture) |
| Deschodt 201197 | Thick |
| Di Monaco 2008133 | Thick (RCT of occupational therapy home visits and risk of falling) |
| Dy 2011159 | Thick |
| Edwards 2004172 | Thick |
| Elinge 200398 | Thick |
| Fortinsky 200281 | Thick (self-efficacy vs. locomotor recovery) |
| Fox 1993200 | Thick (outcomes, length of stay – comparison between two hospitals) |
| Fredman 2006142 | Thick |
| Giangregorio 2009134 | Thick |
| Giusti 2006143 | Thick (home/institutional rehabilitation vs. effect on function) |
| Hagsten 200499 | Thick |
| Hauer 2003130 | Thick |
| Hoekstra 2011144 | Thick (dietary planning and dietary supplementation of rehabilitation in hip fracture) |
| Hoenig 1997168 | Thick |
| Holmberg 1989160 | Thick (home rehabilitation, effect on use of hospital resources) |
| Host 2007153 | Thick (RCT of exercise rehabilitation) |
| Huang 2005100 | Thick (discharge planning is one of the theory areas) |
| Huang 200982 | Thick (qualitative) |
| Huusko 2000101 | Thick |
| Jackson 200183 | Rich (occupational adaptation model) |
| Jellesmark 201284 | Thick |
| Jensen 1979154 | Thick (social rehabilitation) |
| Johansen 2012145 | Thick |
| Jones 2002195 | Thick (functional evaluation for inpatient rehabilitation) |
| Jones 2006135 | Thick |
| Kammerlander 2011178 | Thick |
| Kennie 1988102 | Thick (RCT of the effectiveness of rehabilitation in elderly women) |
| Kerr 2011173 | Thick |
| Koval 1998146 | Thick (inpatient rehabilitation outcomes) |
| Kuisma 2002103 | Thick |
| Latham 2006167 | Thick |
| Lauridsen 2002104 | Thick |
| Levi 1997147 | Thick (post-hospital settings – influence on rehabilitation outcomes) |
| Li 2007189 | Thick |
| Lieberman 2002148 | Thick |
| Lieberman 2006179 | Thick |
| Lin 2004190 | Thick |
| Lin 2009105 | Thick (RCT of discharge planning) |
| Lindelof 2002180 | Thick |
| Long 2002198 | Thick |
| Louie 2012106 | Rich [RCT of empowerment intervention – ADL, Activities of Daily Living index – Instrumental (I-ADL) and falls] |
| Mangione 2010107 | Rich (interventions used by physiotherapists in home care for people after hip fracture; home-based leg-strengthening exercise rehabilitation following hip rehabilitation) |
| McKee 200285 | Thick |
| McMillan 201286 | Rich (grounded theory of taking control) |
| Mendelsohn 2008108 | Thick (improvement in aerobic fitness during rehabilitation following hip fracture) |
| Mitchell 2001109 | Thick (quadriceps training in rehabilitation following hip fracture) |
| Moore 1993181 | Thick (functional outcomes of patients with hip fracture in the home health-care setting) |
| Morghen 2011182 | Thick |
| Moseley 2009110 | Thick |
| Munin 2005149 | Thick (rehabilitation setting) |
| Naglie 2002111 | Thick (interdisciplinary inpatient care for elderly people following hip fracture) |
| Nicholson 1997136 | Thick (role of chair exercises following hip fracture) |
| Ohsawa 2007137 | Thick |
| Oldmeadow 200687 | Thick |
| Olsson 200788 | Thick |
| Orwig 2011191 | Thick |
| Oude Voshaar 200712 | Thick |
| Peiris 2012112 | Thick |
| Penrod 2004192 | Thick |
| Peterson 2004113 | Thick |
| Petrella 2000169 | Thick |
| Portegijs 2008114 | Thick (RCT of strength training intervention; effects of muscle strength and power training on mobility in older hip fracture patients) |
| Portegijs 2012166 | Thick |
| Proctor 200813 | Rich (theory of health locus of control) |
| Pryor 1988150 | Thick (home-based vs. institutional care rehabilitation) |
| Resnick 200572 | Rich (theory of self-efficacy; qualitative study of older women’s experiences of an exercise rehabilitation programme post hip fracture) |
| Resnick 200769 | Rich (attribution theory of achievement motivation; exercise programme for older women following hip fracture) |
| Richards 1998128 | Thick |
| Roberto 1992165 | Rich (coping strategies, internal locus of control) |
| Roberts 2004155 | Thick |
| Robinson 1999183 | Thick |
| Röder 2003151 | Thick (rehabilitation after hip fracture – effect on morbidity and mortality of older people) |
| Rolland 2004184 | Thick (effect of cognitive impairment on rehabilitation following hip fracture) |
| Rösler 2012152 | Thick (effect of cognitive impairment and dementia – cognitive geriatric unit vs. non-cognitive geriatric unit for dementia patients) |
| Ryan 2006115 | Thick (community-based rehabilitation, although mix of hip fracture and stroke patients) |
| Saltvedt 2012116 | Thick |
| Shawler 2006174 | Thick |
| Sherrington 1997117 | Thick |
| Sherrington 2004118 | Thick |
| Shyu 2008119 | Thick (predictors of depression in hip fracture patients; multidisciplinary intervention pilot following hip fracture; predictors of functional recovery following hip fracture) |
| Shyu 2009196 | Thick (RCT of inpatient and home rehabilitation physiotherapy intervention vs. hip flexion for ADL, walking, falls; interdisciplinary intervention for health-related quality of life following hip fracture; predictors of depression in hip fracture patients; interdisciplinary intervention following hip fracture) |
| Sirkka 2003193 | Rich (usual activities and life satisfaction following hip fracture) |
| Stenvall 2007120 | Thick (multidisciplinary rehabilitation) |
| Swanson 1998129 | Thick |
| Sylliaas 2011199 | Thick (exercise-based rehabilitation) |
| Takayama 2001164 | Thick (factors affecting recovery after hip fracture) |
| Talkowski 2009194 | Thick |
| Taylor 2010185 | Thick |
| Tinetti 1999121 | Thick (multicomponent home rehabilitation programme) |
| Travis 199889 | Rich (continuity theory of psychosocial ageing) |
| Tsauo 2005122 | Thick |
| Uy 2008123 | Thick |
| Van Balen 2002140 | Thick (cost analysis of early discharge from hospital to a nursing home) |
| van der Sluijs 1991186 | Thick |
| Vidán 2005124 | Rich (RCT of multidisciplinary geriatric intervention, functional outcomes) |
| Visser 2000156 | Thick (muscle mass and strength; balance and gait; patient-reported outcomes) |
| Vogler 2012125 | Thick |
| Walheim 1990187 | Thick |
| Whitehead 2003161 | Thick |
| Yu-Yahiro 2009126 | Thick |
| Zabari 2012162 | Thick |
| Zidén 2008127 | Thick |
| Zidén 200890 | Thick (home rehabilitation programme including efficacy and ADL; RCT of home rehabilitation and conventional care; qualitative description of patient experiences following hip fracture) |
Appendix 14 Reference list of thin studies that were not data extracted
| Study | Reviewer reason for conceptual thinness |
|---|---|
| Allegrante 2001 | Economic analysis only |
| Allegrante 200791 | Economic analysis only |
| Bachrach 2001380 | Nutritional status |
| Barrett Connor 1995381 | Economic analysis only |
| Beaupre 2007382 | Comparison of function between community dwelling and long term care |
| Becker 2010383 | Economic analysis only |
| Beloosesky 2001384 | No rehabilitation, subgroups of demented patients vs. ADL and functional outcomes |
| Bennett 1982385 | No rehabilitation, multidisciplinary team – orthopaedic + geriatrician + rehabilitation professional + environment |
| Berggren 2007386 | Rehabilitation programme description not provided |
| Bitsch 2006387 | Post-operative rehabilitation and cognitive dysfunction link |
| Borgquist 1990388 | Function and social function and predictors for living at home in the long term |
| Borgquist 1991389 | Cost analysis by type of fracture and functional status |
| Botella-Carretero 2008390 | RCT of nutrition – intermediate outcomes only |
| Braid 2008391 | RCT of electrical stimulation |
| Bruce 2003392 | RCT of nutrition – intermediate outcomes only, nutrition supplement vs. outcomes, namely mortality, body mass index, functional outcome |
| Cameron 1993253 | Accelerated rehabilitation, cost analysis |
| Cameron 1994253 | Economic analysis only |
| Cameron 2000393 | Review, therapy effectiveness not studied, although costs and some functional status included |
| Carinci 2007394 | Types of rehabilitation programmes and economic analyses but no intervention |
| Carlsson 2005395 | RCT of nutrition – intermediate outcomes only |
| Ceder 1980396 | Comparison between care and outcomes |
| Centre Medicare 2007 | Medicare funding discussion |
| Centre for Medicare 2007 | Cost analysis, compares inpatient rehabilitation facilities with skilled nursing facilities |
| Currie 2003397 | Statistical model of hip fracture care |
| Davis 2007398 | Case study, one patient, family experiences |
| Day 1988 | Vitamins – intermediate outcomes only |
| Day 2001 | Orthogeriatric liaison |
| Di Lorenzo 2007399 | Back pain only following fracture |
| Dubljanin-Racpopoc 2010400 | Undecided (foreign-language paper; introduction only) |
| Duncan 2006401 | RCT of nutritional status vs. muscle mass and handgrip strength |
| El Kadaoui 2011402 | Thin |
| Elliot 1996403 | Early geriatric care, cost analysis |
| Espaulella 2000404 | Nutritional supplement vs. function |
| Farnworth 1994247 | Early discharge, cost analysis |
| Folden 2007405 | Factors affecting recovery |
| Fordham 1986406 | Cost–benefit analysis |
| Foss 2008407 | Anaemia vs. functional recovery |
| French 1995408 | Costing study |
| Galvard 1995409 | RCT of orthopaedic vs. geriatric rehabilitation |
| Gerety 1989410 | Prospective payment system and rehabilitation |
| Gilchrist 1988411 | RCT of geriatric orthopaedic ward vs. standard orthopaedic ward |
| Givens 2008412 | Cognitive impairment + delirium + depression vs. functional recovery, no rehabilitation intervention mentioned |
| Gorodetskyi 2007413 | Neurostimulation for recovery in trochanteric fracture vs. pain and hip flexion, no functional outcome |
| Graham 1968 | Early weight bearing |
| Granger 2011414 | Functional status and length of stay |
| Guerini 2010415 | Depression vs. functional outcome and mortality |
| Hagino 2006416 | Prediction of ambulation prognosis |
| Hall 2000417 | Influence of functioning on quality of life, no rehabilitation intervention |
| Harwood 2004418 | Nutritional supplementation vs. falls |
| Hashmi 2004419 | Prognostic scoring system with ADL component, rehabilitation intervention not described |
| Hawkes 2006420 | Gender differences in functioning |
| Hedman 2001421 | Qualitative study, rehabilitation requirements from next of kin for demented patients |
| Hedman 2008422 | Patient outcomes and proxies’ perceptions about rehabilitation, rehabilitation intervention not discussed |
| Hedman 2011423 | Qualitative study of experiences of family members of patients with dementia who had hip fracture, no rehabilitation |
| Henderson 1992424 | Post-operative exercise classes |
| Herrmann 1999 | Undecided (paper in German) |
| Hershkovitz 2007425 | Factors affecting outcomes, rehabilitation intervention not studied |
| Heruti 1999426 | Cognitive status and rehabilitation |
| Hoening 1996427 | Factors influencing access to rehabilitation resources |
| Hollingworth 1993257 | Early discharge, cost analysis |
| Hollingworth 1995428 | Economic analysis only |
| Holtzman 2002 | Pain and baseline function vs. recovery after hip arthroplasty, no rehabilitation |
| Holmberg 1988429 | Thin |
| Horgan 2003430 | Cognitive impairment vs. outcome, physiotherapy intervention considered |
| Intrator 1998431 | Home rehabilitation, health service costs |
| Jarnlo 1984432 | Early rehabilitation and use of resources |
| Jones 2001433 | Outcomes (functional, pain, quality of life) after total knee and hip arthroplasty |
| Jongjit 2003434 | Function, quality of life, etc., no intervention |
| Keating 1993435 | Complications, further surgery, rehabilitation |
| Kennie 1989 | RCT follow-up, general recovery assessment |
| Kim 2012436 | No rehabilitation; prediction modelling of functional recovery and mortality after recurrent fracture |
| Kirk-Sanchez 2004437 | Thin |
| Konnopka 2009438 | Economic analysis only |
| Kramer 1997261 | Economic analysis only |
| Kristensen 2007439 | Fall prediction, physiotherapy intervention, although few details provided |
| Kristensen 2009440 | Factors affecting mobility |
| Kristensen 2012441 | Mobility related, physiotherapy intervention mentioned |
| Laake 1995442 | BADL index |
| Lai 2010443 | No description of reconditioning training and ADL training vs. functional outcome |
| Lamb 2002444 | RCT of neuromuscular stimulation |
| Lawson 2000 | Non-RCT of nutrition intervention, patient compliance |
| Lau 2010445 | Thin |
| Leigheb 2012446 | Review, primarily focused on hospital admission not rehabilitation |
| Lenze 2004447 | Depression, effects on rehabilitation |
| Licciardone 2004448 | RCT of osteopathic manipulation, limited discussion of hip fractures |
| Lieberman 1996449 | Factors associated with successful rehabilitation |
| Lieberman 1999450 | Depression and effects on functional state |
| Lieberman 2002 | Compared outcomes in younger and older elderly patients |
| Lieberman 2004451 | Compared rehabilitation in men and women, little conceptual content |
| Logters 2008 | Undecided (paper in German) |
| Maire 2003 | Upper-limb interval training following hip fracture |
| Maire 2004 | Arm-interval exercise rehabilitation programme following hip fracture |
| Martin 2012452 | Improving function following hip fracture |
| McGilton 2007453,454 | Effect of dementia on rehabilitation following hip fracture |
| Miller 2009455 | Depression as a factor in repeat falls post hip fracture |
| Muir 200957 | Review of effect of cognitive impairment on hip fracture rehabilitation |
| Munn 2008456 | Summary of Cochrane review of mobilisation strategies after hip fracture surgery |
| Myers 2009457 | Nurses’ assessment of rehabilitation potential and prediction function following inpatient rehabilitation |
| Neumann 2004458 | Provision of high-protein supplement for patients recovering from hip fracture |
| Nevalainen 2004459 | Functional ability following hip fracture in home-dwelling patients |
| Nguyen-Oghalai 2008460 | Trends in hospital discharge setting for hip fracture patients |
| Nguyen-Oghalai 2009461 | Effect of ethnicity on utilisation of outpatient rehabilitative care following hip fracture |
| Nightingale 2010462 | Weight transfer following hip fracture |
| Norton 2000463 | Physical function following hip fracture |
| Nurmi 2004464 | Functional outcome following hip fracture |
| O’Malley 2011465 | Review of hip fracture management, including multidisciplinary rehabilitation |
| Parke 2000466 | Experiences and recovery |
| Parker 1995467 | Predictors of rehabilitation success |
| Parker 2000468 | Case report, very limited discussion of rehabilitation |
| Parker 2001469 | Discussion of concepts, little mention of rehabilitation |
| Parker 2002470 | Comparison of two hospitals |
| Penrod 2007471 | Age, functional status and comorbidity |
| Penrod 2008472 | Race, gender and comorbidity – part of larger study |
| Pientka 1999 | Undecided (paper in German) |
| Press 2007473 | Comorbidity and rehabilitation outcomes, limited conceptual content |
| Pryor 1989474 | Limited conceptual content |
| Räsänen 2007 | Economic paper – health-related quality of life and cost–utility analysis |
| Roberto 1992475 | Coping strategies of older women following hip fracture |
| Rosler 2009476 | Effect of dementia on rehabilitation following hip fracture |
| Salkeld 2000477 | Quality of life in older women after hip fracture |
| Sashika 1996 | Physical therapy intervention following hip fracture |
| Shabat 2005478 | Commentary on hip fracture in the elderly |
| Shardell 2012479 | Sex differences in depressive and disability symptoms of hip fracture patients |
| Siu 2006480 | Immobilisation after hip fracture and outcomes |
| Soderqvist 2006481 | Cognitive function and outcomes after hip fracture |
| Stewart 1998 | Review of rehabilitation schemes for hip fracture |
| Stewart 2011482 | Predictors of 5-year survival following hip fracture |
| Strickland 1992412,483 | No rehabilitation description but a case study of acetabular contact pressures generated during selected rehabilitation activities |
| Sund 2010484 | No rehabilitation; policy implications of volume–effectiveness relationship in the case of hip fracture treatment |
| Talkowski 2009 | No intervention |
| Tamulaitiene 2012485 | Economic paper – cost comparison |
| Thomas 2011486 | Physiotherapy management including barriers |
| Thorngren 1991487 | Economic paper – cost comparison |
| Thorngren 1997488 | Treatment and rehabilitation of hip fracture |
| Tidermark 2002489 | Health-related quality of life and functional outcome |
| Tidermark 2004490 | Nutritional study |
| Toussant 2005491 | Review of physical therapy management |
| Tsushima 2009492 | Prediction of gait ability |
| Van Balen 2002 | Economic paper – cost–consequences analysis |
| Weingarten 1998493 | Hospital guidelines intervention, not all hip fractures |
| Weinrich 2004494 | Discussion of rehabilitation strategies |
| Wiktorowicz 2001495 | Economic analysis only |
| Williams 1996496 | Study of caregivers – part of larger study |
| Wykes 2009497 | Experiences and rehabilitation |
| Y-I Shyu 2006 | Emotional support and recovery |
| Y-I Shyu 2010 | Report on caregivers’ needs, part of larger study |
| Yau 2013498 | No rehabilitation |
| Young 2010499 | Longitudinal study using existing data |
| Zerahn 1998500 | Bone mineral density measurements only |
Appendix 15 Reference list of studies excluded from the review
| Study | Reason for exclusion |
|---|---|
| Akker-Scheek 2007 | Not hip fracture |
| Anakwe 2011 | Not hip fracture |
| Arinzon 2010 | No rehabilitation intervention |
| Avramidis 2003 | Not hip fracture |
| Bachrach 2001 | No rehabilitation intervention |
| Badura-Brzoza 2009 | Not hip fracture |
| Badura-Brzoza 2009 | Hip arthroplasty for osteoarthritis |
| Bastow 1983 | Nutritional intervention, not rehabilitation |
| Bateman 2012 | No rehabilitation, medical management |
| Beloosesky 2002 | No rehabilitation intervention |
| Bendall 1985 | No rehabilitation |
| Berend 2004 | Not hip fracture |
| Berman 1987 | Not hip fracture |
| Bernhardt 2005 | No rehabilitation |
| Bernhardt 2005 | No rehabilitation |
| Bjorkelund 2009 | No rehabilitation |
| Blake 2010 | Economic evaluation of geriatric fracture programme |
| Bonjour 1996 | No rehabilitation |
| Bottella Carretero 2008 | No rehabilitation |
| Brandis 1998 | No rehabilitation intervention |
| Brokelman 2008 | Not hip fracture |
| Buntin 2007 | No rehabilitation intervention |
| Burleigh 2011 | No rehabilitation intervention |
| Carlos 2009 | Economic analysis, no rehabilitation costs |
| Carlsson 2005 | No rehabilitation intervention or functional measurement |
| Chaudhry 2007 | Review, surgical management and economic considerations |
| Chen 2002 | Not a hip fracture-specific article |
| Chesser 2011 | Not a study but NICE guidance to improve hip fracture outcomes |
| Chesworth 2001 | Home-care utilisation, rehabilitation intervention not mentioned |
| Chin 2008 | No rehabilitation but predictors of outcome |
| Chrischilles 1994 | Costs of hip fracture but no rehabilitation costs |
| Cook 2011 | Protocol paper, no description of rehabilitation strategy, description of scales, good for methods |
| Cotter 2006 | Economic evaluation of falls |
| Cree 1999 | No rehabilitation intervention |
| Cree 2001 | No rehabilitation intervention |
| Cree 2001a | No rehabilitation intervention |
| Cree 2004 | No rehabilitation but perception of health pre and post hip fracture with respect to cognitive impairment |
| Day 1988 | No rehabilitation |
| Day 2001 | No rehabilitation |
| de Morton 2013 | Mobility instrument validation |
| Deakin 2008 | No rehabilitation but factors influencing discharge location |
| Denkinger 2001 | Questionnaire testing, no rehabilitation |
| Denkinger 2012 | Instrument validation |
| Dennett 2012 | No rehabilitation, methods |
| Di Lorenzo 2007 | Focus on low back pain rehabilitation after hip fracture |
| Di Monaco 2007 | No rehabilitation intervention, muscle mass vs. function |
| Doucette 2006 | No rehabilitation, discharge planning |
| Duclos 2010 | Burden on inpatient care |
| Duignan 2007 | Intervention for depression post hip fracture |
| Duncan 2006 | No rehabilitation intervention, methods |
| Edgren 2012 | No rehabilitation intervention |
| Egan 2008 | Factors for subsequent hip fracture |
| Ekstrom 2009 | Quality-of-life study |
| Eneroth 2006 | Nutrition, no rehabilitation |
| Eneroth 2006m | Nutrition, no rehabilitation |
| Esche 2005 | No rehabilitation |
| Farag 2012 | Validation article, methods |
| Farnworth 1994 | Duplicate |
| Farnworth 1995 | Duplicate |
| Farworth 1994 | Duplicate |
| Feng 2010 | No rehabilitation intervention |
| Friedman 2008 | Geriatric co-managed care with no rehabilitation |
| Gandhi 2008 | No rehabilitation, arthroplasty and not specific to hip fracture |
| Gandhi 2009 | No rehabilitation, arthroplasty and not specific to hip fracture |
| Gandhi 2010 | Total hip replacement outcomes, no rehabilitation |
| Granger 2003 | Letter |
| Gregersen 2012 | No rehabilitation intervention |
| Gutierrez 2012 | Costing study, not specifically hip fracture |
| Haentjens 2001 | Only costs |
| Haentjens 2005 | Economic analysis |
| Hartgrink 1998 | Pressure sores, no rehabilitation |
| Hauer 2003 | Falls in geriatric patients, not specifically hip fracture patients |
| Hayes 2000 | Length of stay vs. clinical outcomes and patients’ perceptions, no rehabilitation |
| Healy 1998 | Total hip replacements |
| Hedstrom 2002 | No rehabilitation, nutrition supplement vs. clinical outcomes, muscle mass |
| Heikkinen 2005 | Functional measurement, ADL, etc., no rehabilitation intervention |
| Heikkinen 2005a | No rehabilitation |
| Hershkovitz 2010 | Study of the relationship between the Clock Drawing Test (CDT) and psychological outcomes and not the effect of rehabilitation on outcomes |
| Holmes 2012 | No rehabilitation intervention, racial disparity in use of rehabilitation |
| Hommel 2007 | Nutritional status vs. pressure ulcers |
| Houwing 2003 | Nutrition intervention vs. pressure ulcers |
| Hutchings 2011 | Outcome measurement, no rehabilitation |
| Ingemarsson 2000 | Duplicate |
| Jellesmark 2012 | No rehabilitation intervention, prevalence of fear of falling and changed functional ability after hip fracture |
| Jones 2005 | Test–retest reliability of utility index |
| Keener 2003 | Efficacy of a surgical technique |
| Keisu 2001 | Hip surgery technique |
| Kempen 2003 | All fractures, not specific to hip fracture, and gender differences in functional recovery |
| Kondo 2005 | Reliability of an instrument |
| Kristensen 2008 | Reliability of mobility instrument |
| Kristensen 2009 | Reliability of mobility instrument |
| Kristensen 2010 | Reliability measure, applicable for methods |
| Kristensen 2011 | Inter-rater reliability |
| Laupacis 2002 | Total hip replacements |
| Liang 1987 | Total hip replacements |
| Licciardone 2004 | Hip and knee arthroplasty |
| Lieberman 2004 | No rehabilitation intervention, efficacy of standard rehabilitation programme in visual and hearing impaired hip fracture elderly |
| Mahomed 2002 | Post surgery, not hip fracture rehabilitation |
| Mahon 2002 | Health-related quality of life for patients awaiting hip arthroplasty, no rehabilitation |
| Maravic 2010 | Too broad, economic analysis of osteoporotic fracture |
| Marcantonio 2001 | Hospital management of hip fracture, not rehabilitation |
| Mauffrey 2010 | Surgical management of hip fracture, not rehabilitation |
| McCarthy 2011 | Post surgery, not hip fracture rehabilitation |
| McGilton 2009 | Post-surgery unit, not hip fracture rehabilitation |
| McGilton 2012 | Protocol |
| McMillan 2012 | No rehabilitation intervention, but what a rehabilitation intervention should aim for in terms of functional outcomes |
| Meyer 2000 | Factors associated with mortality after hip fracture |
| Miura 2009 | Post surgery, not hip fracture rehabilitation |
| Montalban Quesada 2012 | Post surgery, not hip fracture rehabilitation |
| Montero-Odasso 2009 | Mobility heterogeneity in the elderly, not hip fracture rehabilitation |
| Montin 2007 | Post surgery, not hip fracture rehabilitation |
| Moppett 2012 | Measure assessment, not hip fracture rehabilitation |
| Morghen 2010 | Excluded as duplicate of Morghen et al. |
| Mossey 1989 | Post surgery, not hip fracture rehabilitation |
| Munin 1998 | Hip and knee arthroplasty |
| Muraki 2006 | Post-surgery mortality, not hip fracture rehabilitation |
| Mutran 1995 | Post surgery, not hip fracture rehabilitation |
| Nurmi 2003 | Cost analysis of hip fracture treatment, not rehabilitation |
| O’Cathain 1994 | Hospital discharge scheme, not hip fracture rehabilitation |
| Oliver 2009 | Commentary of guidelines – risk of falls, not specific to hip fracture |
| Ostendorf 2004 | Total hip replacement |
| Penrod 2008 | No rehabilitation but predictors of outcome |
| Poynter 2008 | Not specific to hip fracture, effect of rehabilitation for cognitively impaired, review |
| Quintana 2009 | Health-related quality-of-life after surgery, not hip fracture rehabilitation |
| Ragab 1999 | Post surgery, not hip fracture rehabilitation |
| Rahme 2010 | Post surgery, not hip fracture rehabilitation |
| Reuling 2012 | Measure assessment, not hip fracture rehabilitation |
| Riediger 2010 | Post surgery, not hip fracture rehabilitation |
| Rolfson 2009 | Post surgery, not hip fracture rehabilitation |
| Romeo 2011 | Psychological rehabilitation for depression after hip fracture and cost-effectiveness study |
| Ruggiero 2005 | Critique of another study |
| Sahota 2012 | Cost analysis only |
| Salmon 2001 | Surgical treatment, not hip fracture rehabilitation |
| Sanders 2010 | No rehabilitation intervention |
| Scheerlinck 1998 | Surgical treatment, not hip fracture rehabilitation |
| Schlenker 1997 | Cost analysis only |
| Schurch 1996 | Incidence of hip fracture, not hip fracture rehabilitation |
| Sendi 2000 | Osteoporosis, not hip fracture rehabilitation |
| Shabat 2005 | Scoring systems for hip fracture, not hip fracture rehabilitation |
| Shakouri 2009 | No rehabilitation |
| Shaw 2003 | Recovery from surgery, not hip fracture rehabilitation |
| Sherrington 2005 | Reliability of portable tests of function, balance and strength, not hip fracture rehabilitation |
| Shiell 1993 | Nurse co-ordination of hospital care, not hip fracture rehabilitation |
| Shiell 1995 | Letter correcting a published version of study |
| Shiri-Sharvit 2005 | Medical intervention, not hip fracture rehabilitation |
| Shoemaker 2002 | Measure assessment, not hip fracture rehabilitation |
| Siggeirsdottir 2005 | Hospital stay, not hip fracture rehabilitation |
| Sipila 2011 | Protocol |
| Skelly 1992 | No hip fracture rehabilitation |
| Sletvold 2011 | Protocol |
| Smektala 1999 | Quality appraisal of report card system for hip fracture, not rehabilitation |
| Stromberg 1997 | No hip fracture rehabilitation |
| Sullivan 1998 | Nutrition post operation, not hip fracture rehabilitation |
| Sullivan 2004 | Nutrition post operation, not hip fracture rehabilitation |
| Svensson 1996 | Hospital stay, not hip fracture rehabilitation |
| Takahashi 2011 | Hospital stay, not hip fracture rehabilitation |
| Taylor 2010 | Physiotherapists’ perception of discharge criteria, barriers and difficulties |
| Theis 2003 | Not hip fracture rehabilitation |
| Thomas 2008 | Protocol |
| Thomas 2010 | Walking aids, not rehabilitation |
| Tidermark 2003 | Comparison of quality-of-life measures for hip fracture patients, not rehabilitation |
| Tidermark 2004b | Nutrition for osteoporosis, not rehabilitation |
| Tidermark 2004c | Comparison of quality of life measures for hip fracture patients, not rehabilitation |
| Trafton 2005 | Commentary of Binder et al. |
| Trudelle-Jackson 2004 | Total hip arthroplasty |
| Tudor 1998 | Orthopaedic discharge team, not hip fracture rehabilitation |
| Turner 1997 | No hip fracture rehabilitation |
| Van Balen 2003 | Measure assessment, not hip fracture rehabilitation |
| Vogler 2012 | Not hip fractures |
| Wang 2002 | Total hip replacements |
| Ward 1998 | No rehabilitation |
| Ward 2008 | Review, findings irrelevant |
| Weatherall 2001 | No rehabilitation intervention, economic analysis |
| Weaver 2003 | Total hip replacements |
| Werner 2004 | Total hip replacements |
| Willig 2002 | Questionnaire only |
| Wyers 2010 | Study design only, not rehabilitation |
| Yao 2009 | Questionnaire only |
| Zerahn 1998 | No hip fracture rehabilitation |
| Ziden 2008a | No rehabilitation intervention |
| Zimmerman 2006 | Measure assessment, not hip fracture rehabilitation |
Appendix 16 Characteristics of study participants
| Study details (author, year; country; study type; study design; setting; conceptual richness) | Participant characteristics | Exclusion criteria | Gender | Age (years) | n | Cognitive impairment | Intervention (n analysed) | Comparator (n analysed) | Intervention category |
|---|---|---|---|---|---|---|---|---|---|
| Adunsky 2003138 | Patients aged ≥ 65 years with pertrochanteric (extracapsular) or subcapital (intracapsular) hip fracture who were otherwise medically fit | Rehabilitation period of < 7 days; presence of other acute disabilities (such as multiple trauma); post-operative unstable (non-weight-bearing) hip fracture; medical conditions preventing active rehabilitation (e.g. cardiac failure with functional capacity stage III–IV of the New York Heart Association classification, severe chronic lung disease necessitating a constant use of oxygen); transfer to an acute care department as a result of complications; or death | Both | ≥ 65 | 320 | No | Orthogeriatric ward (n = 116) | Orthopaedic department (n = 204) | Place |
| Israel | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Al-Ani 2010139 | Patients with femoral neck fracture aged ≥ 65 years with cognitive impairment and able to walk before the fracture | NR | Both | ≥ 65 | 227 | Yes | Early discharge to a rehabilitation unit (n = 81) | Early discharge to previous residence (n = 146) | Discharge planning |
| Sweden | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Allegrante 200791 | Primary unilateral hip fracture patients aged ≥ 65 years who underwent successful surgical repair | Patients unable to consent or speak English or give coherent responses; pathological fracture; condition that contraindicated exercise (e.g. critical aortic stenosis, unstable angina, end-stage cardiomyopathy); no access to or accessibility by telephone; intention to relocate after discharge | Both | ≥ 65 | 176 | No | Hospital-based physical therapy plus motivational videos plus visits from recovered hip fracture patients (n = 90) | Usual care (n = 86) | Physical and psychological |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Arinzon 2005201 | Hip fracture patients aged ≥ 65 years operated for unilateral post-fall hip fracture and without clinical evidence of acute addicted disease | NR | Both | ≥ 65 | 102 | No | Old-old elderly (aged ≥ 85 years) geriatric rehabilitation in the community (n = 46) | Young elderly (aged 65–74 years) geriatric rehabilitation in the community (n = 56) | Psychological |
| Israel | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Atwal 2002176 | Health professionals providing rehabilitation services | NR | Both | NR | 48 health professionals | NA | NA (n = NA) | NA (n = NA) | NA |
| UK | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Barone 2009177 | Osteoporotic fracture of the proximal femur (a fracture that occurred in the absence of trauma or with minimal trauma and not related to secondary causes); aged ≥ 70 years; surgical stabilisation of the fracture; able to walk (with or without aid) in the 2 weeks before hospital admission | Secondary fractures (metastatic cancer, Paget’s disease of the bone), other fractures, fracture through a major trauma, another fracture on the same hip, patients who refused to give informed consent | Both | ≥ 70 | 469 | Partial | Immediate weight-bearing training (n = 469) | NA (n = NA) | Physical |
| Italy | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Bäuerle 2004163 (German) | Patients aged ≥ 65 years with a fall-related femur fracture | NR | Both | ≥ 65 | 332 | No | Service and health-care evaluation (n = 332) | NA (n = NA) | Process/system improvement |
| Germany | |||||||||
| Quantitative non-comparative | |||||||||
| Historical cohort study | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Beaupre 2005157 | Patients aged ≥ 65 years with a hip fracture who lived within local calling distance; patients with cognitive impairment and those residing in institutional settings before hip fracture were eligible for inclusion | Pathological fracture (i.e. primary/secondary tumour, Paget’s disease) or recurrent hip fracture; unable to communicate in English; no telephone access | Both | ≥ 65 | 919 | Yes | Clinical pathway consisting of standardised, current best evidence or clinical consensus (n = 451) | Pre-clinical pathway (n = 468) | Multidisciplinary co-ordination |
| Canada | |||||||||
| Quantitative comparative | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Bellelli 2006170 | Hip fracture patient | NA | Both | ≥ 80 | 1 | Yes | Body weight–supported treadmill technique (n = 1) | NA (n = NA) | Physical |
| Italy | |||||||||
| Quantitative non-comparative | |||||||||
| Case report | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Bellelli 2008141 | Hip frature patients aged ≥ 65 years admitted for rehabilitation (n = 211) | Advice not to ambulate; advanced malignancy; severe pneumonia or congestive heart failure; delirium | Both | ≥ 65 | 211 | Yes | Dementia (n = 40), depression (n = 54), both (n = 27) | No dementia or depression (n = 90) | Psychological |
| Italy | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Bellelli 201078 | Hip fracture patients aged 18–90 years undergoing first-time surgery and rehabilitation (n = 60) | Dementia or delirium; poor nutritional or somatic health status; severe reduction in vision acuity | Both | ≥ 18 | 60 | No | Conventional post-orthopaedic rehabilitation programme plus visual feedback (n = 30) | Conventional post-orthopaedic rehabilitation programme (n = 30) | Physical and psychological |
| Italy | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Binder 200492 | Age at least 65 years; community dwelling (not living in a nursing home) on discharge from physical therapy for hip fracture; screening evaluation within 16 weeks of hip fracture repair; modified Physical Performance Test score between 12 and 28; self-reported difficulty or requirement for assistance with one or more ADL | Pathological fracture, bilateral femur fractures or previous contralateral femur fracture; inability to provide informed consent because of dementia or cognitive impairment; inability to walk 50 feet (using an assistive device, if needed); visual or hearing impairments that interfered with following directions or that were judged to potentially interfere with performing exercises safely; cardiopulmonary disease or neuromuscular impairments that would contraindicate participation in a weight-training programme (unstable angina or congestive heart failure, spinal stenosis, symptomatic spondylosis, etc.); conditions that would not be expected to improve with exercise training (e.g. severe Parkinson’s disease, cerebrovascular disease with residual hemiparesis); initiation of medication for osteoporosis or hormone therapy within 12 months of screening; terminal illness with a life expectancy of < 1 year | Both | ≥ 65 | 90 | No | Tailored, supervised physical therapy and exercise training (n = 46) | Home exercise (n = 44) | Physical |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Bischoff-Ferrari 201093 | Hip fracture patients aged ≥ 65 years | MMSE score of < 15; conservative treatment; unable to communicate in German; severe hearing or visual impairment; death prior to inclusion; unwilling or unable to take study medication; early complications or transfer to intensive care; previous hip fracture of the same hip; plans to leave the city or country after surgery; chemotherapy in the last year or bone metastases; unable to walk prior to hip fracture; increased alcohol intake; creatinine clearance < 15 ml/minute; epilepsy | Both | ≥ 65 | 173 | No | Extended physiotherapy (n = 87) | Standard physiotherapy (n = 86) | Physical |
| Switzerland | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Borgquist 1990188 | Patients aged ≥ 50 years and surgically operated for hip fracture | NR | Both | ≥ 50 | 298 | No | Community rehabilitation (n = 298) | NA (n = NA) | Place |
| Sweden | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Boyd 1982158 | Female hip fracture patients with injury complicated by other disease or disability, trauma or any major rehabilitation problem | Fit patients who were expected to do well without special measures; gross physical or mental defects that would prevent mobilisation | Female | NR | 771 | No | Rehabilitation ward programme (n = 482) | No rehabilitation ward programme (n = 289) | Physical |
| UK | |||||||||
| Quantitative comparative | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Buddenberg 199879 | Caucasian women aged > 75 years with a surgically repaired hip fracture; fracture sustained secondary to a fall; living independently before fracture; independent in self-care before fracture | Male; non-Caucasian; aged ≤ 75 years; non-independent prior to fracture | Female | > 75 | 20 | Partial | Occupational therapy plus psychological therapy (n = 10) | Conventional occupational therapy (n = 10) | Physical and psychological |
| USA | |||||||||
| Quantitative comparative | |||||||||
| Non-randomised trial/quasi-experimental study | |||||||||
| Rehabilitation facility (no other details provided) | |||||||||
| Rich | |||||||||
| Burns 2007197 | Patients aged > 60 years who have undergone surgery for a fractured neck of femur | Significant cognitive impairment (score of < 15 on the MMSE), deafness significantly interfering with the assessments, severe physical illness, living > 30 miles from an assessment centre or unable to speak English | Both | > 60 | 293 | Partial | Psychological intervention (n = 121) | Usual care (n = 172) | Psychological |
| UK | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Carmeli 2006131 | Hip fracture patients aged ≥ 75 years undergoing rehabilitation after hip fracture surgery | Aged < 75 years; history of a diagnosed central or peripheral nervous system pathology such as Parkinson’s disease, cerebrovascular accident, Alzheimer’s disease, transient ischaemic attack, neuropathy or brain surgery; old/prior hip fractures; significant metabolic disorder (e.g. diabetes, hyperthyroidism); significant hearing or visual defects | Both | ≥ 75 | 63 | No | Class-based outpatient exercise programme (n = 34) | Home-based programme (n = 29) | Physical |
| Israel | |||||||||
| Quantitative comparative | |||||||||
| Quasi-randomised trial | |||||||||
| Hospital and community | |||||||||
| Rich | |||||||||
| Casado 200980 | Women aged ≥ 65 years who had had surgical repair of a non-pathological hip fracture; no medical problems with a risk for falls (e.g. neuromuscular conditions); ability to walk without human assistance pre fracture; mild cognitive impairment | NR | Female | ≥ 65 | 168 | Partial | Exercise Plus Program (exercise training component plus motivational component: theory of self-efficacy) (n = 126) | Routine care (n = 42) | Physical and psychological |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Cree 2001175 | Hip fracture patients aged ≥ 65 years | NR | Both | ≥ 65 | 222 | No | NA (n = NA) | NA (n = NA) | NA |
| Canada | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Crotty 200094 | Patients with hip fracture in need of rehabilitation; living in the community; gave consent | Living in residential care; needing more care than could be provided in the home | Both | ≥ 50 | 68 (59 analysed) | Partial | Early discharge for home-based rehabilitation (n = 29) | Normal discharge and hospital-based rehabilitation (n = 30) | Discharge planning |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Crotty 200395 | Patients aged ≥ 65 years admitted to hospital for surgical treatment for a fall-related hip fracture; medically stable; adequate physical and mental capacity to participate in a rehabilitation programme; expected to return home after discharge from hospital; home environment suitable for rehabilitation | Inadequate social support in the community, no telephone at home or did not live in the vicinity of the study hospitals | Both | ≥ 65 | 66 | No | Accelerated discharge and home rehabilitation (n = 34) | Usual or conventional care (n = 32) | Discharge planning |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Dai 2002132 | Patients aged ≥ 60 years; ability to walk independently with or without an assistive device; living in their own home pre fracture; no severe cognitive impairment | Pathological fracture; multiple fractures; unstable fracture; severe cognitive impairment | Both | ≥ 60 | 94 | No | Multidisciplinary rehabilitation programme (n = 50) | Conventional care (n = 44) | Multidisciplinary co-ordination |
| Taiwan | |||||||||
| Quantitative comparative | |||||||||
| Quasi-randomised trial | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| De Jonge 2001171 | NA | NA | NA | NA | NA | NA | Multidisciplinary evaluation (n = NA) | NA (n = NA) | Psychological |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Work process and service restructuring | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Delmi 199096 | Patients aged > 60 years with femoral neck fracture after an accidental fall | Fractures resulting from violent external trauma; pathological fractures as a result of tumours or non-osteoporotic osteopathy; overt dementia; renal, hepatic or endocrine disease; gastrectomy or malabsorption; treatment with phenytoin, steroids, barbiturates, fluoride or calcitonin | Both | > 60 | 59 | No | Dietary supplementation (n = 27) | Control (n = 32) | Physical |
| Switzerland | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Deschodt 201197 | Verbally competent individuals with traumatic hip fracture aged ≥ 65 years | Multiple trauma or metastatic cancer or other known comorbidity expected to reduce life expectancy to < 6 months | Both | ≥ 65 | 171 | Partial | Inpatient geriatric consultation (n = 94) | Usual care (n = 77) | Multidisciplinary co-ordination |
| Belgium | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Di Monaco 2008133 | Community-dwelling women who planned to return to the same dwelling at discharge (non-institutional); sustained their first hip fracture as a result of a fall; surgically operated on; referred for inpatient rehabilitation; no cognitive impairment, with a MMSE test score of > 23 | NR | Female | ≥ 60 | 95 | No | Hospital plus home rehabilitation (n = 45) | Hospital rehabilitation alone (n = 50) | Place |
| Italy | |||||||||
| Quantitative comparative | |||||||||
| Quasi-randomised trial | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Dy 2011159 | Medically stable male patients with hip fracture | NR | Male | ≥ 55 | 74 | No | Medical Orthopaedic Trauma Service programme (n = 74) | NA (n = NA) | Multidisciplinary co-ordination |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Edwards 2004172 | NA | NA | NA | NA | NA | NA | NA (n = NA) | NA (n = NA) | Process/system improvement |
| Canada | |||||||||
| Quantitative non-comparative | |||||||||
| Work process and service restructuring | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Elinge 200398 | Patients of any age from Umeå principality of any age who were admitted to the hospital with a diagnosis of hip fracture or vertebral fracture | Dementia or other severe cognitive impairment; psychiatric illness; other severe illness; inability to walk independently with or without assistive devices before fracture; fracture caused by high-energy trauma or pathological processes; previous fracture at the opposite hip | Both | ≥ 50 | 35 (30 analysed) | No | Supervised group learning (n = 18) | Usual care (n = 12) | Physical |
| Sweden | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Fortinsky 200281 | Hip fracture patients living in the community and ambulatory at the time of the index hip fracture; English speaking; fracture occurred as a result of reasons other than multitrauma accident (e.g. automobile accident) or metastatic cancer | NR | Both | ≥ 65 | 24 | No | Physical and occupational therapy (n = 24) | NA (n = NA) | Physical |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Fox 1993200 | Two hospitals managing patients with hip fracture | NR | NA | NA | 335 | No | In-hospital rehabilitation and discharge to own home policy (n = 142) | No in-hospital rehabilitation and discharge to own home policy (n = 193) | Place |
| UK | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Fredman 2006142 | Patients aged ≥ 65 years hospitalised for hip fracture | Pathological fractures; patients admitted from a nursing home, hospital or extended care facility | Both | ≥ 65 | 432 | NR | NA (n = NA) | NA (n = NA) | NA |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Giangregorio 2009134 | Patients treated for a hip fracture by an orthopaedic surgeon and admitted to the inpatient rehabilitation floor of a teaching hospital between September 2006 and November 2007. Patients were deemed suitable if they had a stable fracture, adequate fixation, were able to follow two-step commands; their rehabilitation restrictions were to be 50% weight bearing or weight bearing as tolerated; and they were able to take a few steps with an assistive device | Cultures positive for meticillin-resistant Staphylococcus aureus; able to walk without an assistive device; had hip, knee or ankle surgery before the hip fracture; unable to understand instructions or give informed consent; incontinent; uncontrolled cardiovascular disease, uncontrolled hypertension, uncontrolled diabetes, neuromuscular disease or other musculoskeletal disease such as rheumatoid arthritis or uncontrolled pain | Both | ≥ 70 | 21 (14 analysed) | No | Treadmill training (n = 10) | Standard physiotherapy (n = 4) | Physical |
| Canada | |||||||||
| Quantitative comparative | |||||||||
| Non-randomised trial/quasi-experimental study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Giusti 2006143 | Hip fracture patients aged ≥ 70 years living in the community | Fracture because of secondary causes (metastatic cancer, Paget’s disease of the bone); living in a nursing home at the time of fracture; refused to give informed consent (follow-up and in-hospital interviews) | Both | ≥ 70 | 199 (194 analysed) | No | Home-based rehabilitation (n = 95) | Institution-based rehabilitation (n = 99) | Place |
| Italy | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Hagsten 200499 | Hip fracture patients aged > 65 years; proficient in Swedish; lucid; living independently and not using walking aids (n = 100) | Aged ≤ 65 years; unable to speak Swedish; not lucid, living in residential care; using walking aids | Both | > 65 | 100 | No | Occupational therapy (n = 50) | Usual care (n = 50) | Physical |
| Sweden | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Hauer 2003130 | Hip fracture patients with a recent history of injurious falls; aged > 75 years; female; consent of their orthopaedic surgeon; willingness to participate in the study | Acute neurologic impairment, severe cardiovascular disease, unstable chronic or terminal illness, major depression, severe cognitive impairment or an inability to stand or walk | Female | > 75 | 57 | No | Strength training (n = 31) | Inactive control (n = 26) | Physical |
| Germany | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Hoekstra 2011144 | Hip fracture patients aged ≥ 65 years requiring surgical intervention | Additional fractures; severe dementia; diagnosed malignancy affecting nutritional status; suspicion of a pathological fracture; liver or kidney dysfunction; pacemaker or the impossibility to be weighed for bioelectrical impedance assessment; lack of a thorough command of the Dutch language; inability to communicate through family and update dietary records at home | Both | ≥ 65 | 127 | No | Multidisciplinary nutritional care (n = 61) | Standard nutritional care (n = 66) | Multidisciplinary co-ordination |
| The Netherlands | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Hoenig 1997168 | Hip fracture patients aged ≥ 65 years; hospitalised in one of 297 randomly selected hospitals from 30 areas in five states, with 20% of patients being drawn from each state. Hospitals were selected to provide a nationally representative sample in terms of size, percentage urban vs. rural, percentage of Medicare patients and teaching status. Hospitals caring for the poor were oversampled by a factor of 2. Patients were selected for inclusion in the study if the hospital had assigned them an International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code indicating acute hip fracture as the primary diagnosis (820.0X, except 820.01, 820.2X, 820.8X, in which X was any number or blank space) | Patients transferred from another acute care hospital whose fracture was not acute; acute myocardial infarction; comatose; suffered a cardiorespiratory arrest on admission; major competing conditions such as terminal cancer, acquired immune deficiency syndrome or end-stage renal disease; acute hip fracture not the primary reason for admission; hip fracture the result of multiple trauma; fracture occurred in a hip that had been previously fractured and had undergone surgical repair; fracture occurred in a hip that was a known site of cancer, metastasis or radiation therapy | Both | ≥ 65 | 2762 | NA | NA (n = NA) | NA (n = NA) | Physical |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Database analysis | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Holmberg 1989160 | Hip fracture patients aged ≥ 65 years | NR | Both | ≥ 65 | 170 | No | Discharge home (n = 84) | Discharge to a rehabilitation hospital (n = 86) | Place |
| Sweden | |||||||||
| Quantitative comparative | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Host 2007153 | Patients aged ≥ 65 years; community dwelling with a recent proximal femur fracture and having a screening evaluation within 16 weeks of hip fracture repair; modified Physical Performance Test score of 12–28; self-reported difficulty or requirement for assistance with one or more ADL | Pathological fracture, bilateral femur fractures or previous contralateral femur fracture; inability to provide informed consent because of dementia or cognitive impairment; inability to walk 15 m (50 feet); visual or hearing impairments that interfered with following directions or that were judged to potentially interfere with performing exercises safely; cardiopulmonary disease or neuromuscular impairments that would contraindicate participation in a weight-training programme; conditions that might not be expected to improve with exercise training (severe Parkinson’s disease or cerebrovascular disease with residual hemiparesis); initiation of medication for osteoporosis or hormone therapy within 12 months of screening; terminal illness with a life expectancy of < 1 year | Both | ≥ 65 | 31 | No | Supervised exercise training programme (n = 31) | NA (n = NA) | Physical |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Controlled before-and-after study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Huang 2005100 | Hip fracture patients aged ≥ 65 years, hospitalised as a result of falling; discharged from a medical centre to the catchment area of the study centre | Cognitively impaired or too ill to take part (e.g. with comorbidities, unable to communicate or needing to stay in the intensive care unit) | Both | ≥ 65 | 126 | No | Discharge planning (n = 63) | Routine care (n = 63) | Discharge planning |
| Taiwan | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Huang 200982 | Older people aged ≥ 65 years who had experienced a hip fracture because of a fall in the last 12 months; living in the community; capable of self-care; verbal communication ability in Mandarin, Minanese or Hakkanese | NR | Both | ≥ 65 | 15 | No | NA (n = NA) | NA (n = NA) | NA |
| Taiwan | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Huusko 2000101 | Patients aged ≥ 65 years with hip fracture; living independently; able to walk unaided before the fracture | Pathological/multiple fractures; serious early complications; receiving calcitonin treatment; terminally ill | Both | ≥ 65 | 243 | Yes | Geriatric rehabilitation (n = 120) | Standard care (n = 123) | Multidisciplinary co-ordination |
| Finland | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Jackson 200183 | Hip fracture patients aged 65–85 years willing to participate in the study and with the cognitive ability to participate in the therapy process | Major conditions that negatively affect participation in ADL (e.g. Parkinson’s disease, cerebrovascular accident, Alzheimer’s disease) | Both | 65–85 | 24 | No | Occupational adaptation model) (n = NR) | Biomedical rehabilitation model) (n = NR) | Physical |
| USA | |||||||||
| Quantitative comparative | |||||||||
| Quasi-randomised trial | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Jellesmark 201284 | Community-dwelling hip fracture patients aged ≥ 65 years who had the ability to walk independently at discharge. Criteria for participating in the in-depth interviews were high degree of fear of falling, varying levels of functional ability and ability to verbalise the situation in detail | Patients with readmission to hospital for ≥ 1 week; inability to read or understand Danish; living outside the Copenhagen area | Both | ≥ 65 | 33 surveys, 4 interviews | No | NA (n = NA) | NA (n = NA) | NA |
| Denmark | |||||||||
| Mixed methods | |||||||||
| Mixed methods | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Jensen 1979154 | Femoral neck or trochanteric fracture patients | NR | Both | Any | 518 | No | Physical rehabilitation (n = 518) | NA (n = NA) | Physical |
| Denmark | |||||||||
| Quantitative non-comparative | |||||||||
| Controlled before-and-after study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Johansen 2012145 | Men and women aged > 65 years considered to have rehabilitation potential with stroke, osteoarthritis, hip fracture, ageing disability, loss of function because of long periods of hospitalisation or other chronic, slowly progressing diseases | Patients not considered to have rehabilitation potential and those with highly progressive diseases and severe depression | Both | > 65 | 302 | Partial | District rehabilitation centre (n = 202) | Standard rehabilitation (n = 100) | Place |
| Norway | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Jones 2002195 | Hip fracture patients aged ≥ 60 years who had potential for improvement | Severe cognitive deficit (MMSE score of ≤ 14) or a consensus decision by the rehabilitative care team that the patient would not likely return to their pre-fracture residence | Both | ≥ 60 | 100 (44 analysed) | No | Inpatient rehabilitation (n = 44) | NA (n = NA) | Place |
| Canada | |||||||||
| Quantitative non-comparative | |||||||||
| Controlled before-and-after study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Jones 2006135 | Patients aged ≥ 65 years; good cognitive function (MMSE score of > 24); residing at and planning to return home after standard inpatient rehabilitation care for hip fracture | Serious medical conditions (i.e. cancer, cardiovascular disorders or stroke) or elective hip replacement surgery; poor cognitive function; residing in residential care | Both | ≥ 65 | 25 | No | Community exercise programme (n = 17) | Standard outpatient therapy (n = 8) | Place |
| Canada | |||||||||
| Quantitative comparative | |||||||||
| Non-randomised trial/quasi-experimental study | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Kammerlander 2011178 | Hip fracture patients aged ≥ 80 years | Pathological and multiple fractures; organ transplantation | Both | ≥ 80 | 246 | NR | NA (n = NA) | NA (n = NA) | NA |
| Austria | |||||||||
| Quantitative non-comparative | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Kennie 1988102 | Hip fracture female patients aged ≥ 65 years | Expected to die before being fit enough to enter the trial; pathological fracture; likely to be discharged within 7 days of entering the trial; unfit for transfer to a peripheral hospital | Female | ≥ 65 | 108 | No | Multidisciplinary rehabilitation in a community hospital (n = 54) | Routine care with early discharge home (n = 54) | Multidisciplinary co-ordination |
| UK | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Kerr 2011173 | Patients aged ≥ 50 years who experienced a hip fracture in the previous 2–18 months | NR | Both | ≥ 50 | 21 | No | NA (n = NA) | NA (n = NA) | NA |
| USA | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Koval 1998146 | Non-pathological fracture patients aged ≥ 65 years; able to walk before the fracture; cognitively intact; living in own home or apartment | NR | Both | ≥ 65 | 609 | No | Inpatient rehabilitation (n = 308) | Standard care available before implementation of inpatient rehabilitation programme (n = 301) | Place |
| USA | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Kuisma 2002103 | Patients aged > 50 years with a fractured proximal femur | Concomitant serious conditions; living alone or spends > 4 hours alone during the day | Both | > 50 | 81 | No | Home-based physiotherapy (n = 40) | Institution-based physiotherapy (n = 41) | Physical and place |
| Hong Kong | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Latham 2006167 | Hip fracture patients who received rehabilitation in skilled nursing facilities | Patients who died or who were admitted to an acute care facility from the skilled nursing facility | Both | Any | 351 | No | Rehabilitation in a skilled nursing facility (n = 351) | NA (n = NA) | Place |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Database analysis | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Lauridsen 2002104 | Women aged 60–89 years; fully mobile prior to fracture; full weight bearing; no concomitant disabling disorders; transferred for rehabilitation within 3 weeks of surgery | Patients who did not wish to participate; patients who fell ill during the trial with symptoms that prevented training; patients discharged before attaining planned functional capacity | Female | 60–89 | 88 | Partial | Intensified physical therapy (n = 44) | Usual care (n = 44) | Physical |
| Denmark | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Levi 1997147 | Community-living women aged ≥ 65 years with hip fracture treated surgically | Unable to mentally or physically participate in an interview | Female | ≥ 65 | 123 | No | Comparison of discharge practices of four hospitals and discharge destinations (n = 123) | NA (n = NA) | Discharge planning |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Li 2007189 | Care receivers: aged ≥ 65 years, hospitalised as a result of hip fracture and surgery for internal fixation or arthroplasty; living in northern Taiwan; no cognitive impairment. Caregivers had to be aged ≥ 18 years and taking primary responsibility for the care receiver | Care receivers: aged < 65 years; no hip fracture; cognitive impairment. Caregivers: aged < 18 years; not the primary caregiver | Both | ≥ 65 | 20 | No | NA (n = NA) | NA (n = NA) | NA |
| China | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital and Community | |||||||||
| Thick | |||||||||
| Lieberman 2002148 | Hip fracture patients aged ≥ 75 years hospitalised for rehabilitation after surgical repair | Patients with advanced dementia and/or those with a low pre-morbid functional status | Both | ≥ 75 | 424 | No | Older group (≥ 85 years) geriatric ward rehabilitation (n = 127) | Younger group (75–84 years) geriatric ward rehabilitation (n = 297) | Physical and psychological |
| Israel | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Lieberman 2006179 | Patients aged ≥ 65 years hospitalised for hip fracture and suitable for conventional rehabilitation | Advanced dementia and/or low pre-morbid functional status | Both | ≥ 65 | 946 | Partial | NA (n = NA) | NA (n = NA) | NA |
| Israel | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Lin 2004190 | Aged ≥ 65 years; men and women with either femoral neck fracture or intertrochanteric fracture | Pathological fractures | Both | ≥ 65 | 103 | No | NA (n = NA) | NA (n = NA) | NA |
| Taiwan | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Lin 2009105 | Hip fracture patients aged ≥ 65 years; able to walk; mentally alert and able to communicate; living in the vicinity of the study centre | Cognitive impairment; terminal disease | Both | ≥ 65 | 50 | No | Comprehensive discharge planning (n = 26) | Routine discharge nursing care (n = 24) | Discharge planning |
| Taiwan | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Lindelof 2002180 | Women aged 78–82 years and able to understand simple instructions and with perceived mobility problems following hip fracture at least 6 months previously | Severe pain affecting participants’ ability to participate and motor impairment from neurological disease | Female | 78–82 | 3 | No | Supervised functional training (n = 3) | NA (n = NA) | Physical and psychological |
| Sweden | |||||||||
| Quantitative comparative | |||||||||
| Controlled before-and-after study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Long 2002198 | Health professionals | NR | Both | NA | 49 health professionals | NA | NA (n = NA) | NA (n = NA) | NA |
| UK | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Louie 2012106 | Current diagnosis of avascular necrosis of the femoral head/osteoarthritis of the hip and traumatic hip fracture; fractures of the neck of the femur and trochanter of the femur; Cantonese version of the MMSE baseline score of ≥ 16; one main carer (able to provide > 8 hours’ care to the participant every day) willing to participate in the programme | Pathological fracture, bilateral femur fractures or fractures of other parts of the body in relation to the current admission; cardiovascular disease (cerebrovascular accident), Parkinsonism or psychiatric illness; visual or hearing impairments hinderinge participation in the programme | Both | ≥ 65 | 134 | No | Patient and Carer Empowerment Programme (n = 63) | Conventional care (n = 71) | Psychological |
| Hong Kong | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Mangione 2010107 | Successful fixation of a hip fracture within the previous 6 months; aged > 65 years; living at home before the fracture; physician referral; discharged from physical therapy | Unstable angina pectoris or uncompensated congestive heart failure; ongoing chemotherapy or renal dialysis; history of stroke with residual hemiplegia; Parkinson’s disease; absence of sensation in the lower extremities as a result of sensory neuropathy; life expectancy of < 6 months; cognitive impairment; fast or very slow walkers | Both | > 65 | 26 | No | Leg-strengthening exercises (n = 14) | Conventional transcutaneous electrical nerve stimulation (n = 12) | Physical |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Rich | |||||||||
| McKee 200285 | Hip fracture patients aged ≥ 65 years admitted to hospital as a result of a fall | NR | Both | ≥ 65 | 57 | No | NA (n = NA) | NA (n = NA) | NA |
| UK | |||||||||
| Mixed methods | |||||||||
| Controlled before-and-after study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| McMillan 201286 | Patients who sustained a fall-induced hip fracture and who were discharged home within 3 months | NR | Both | ≥ 65 | 27 | No | NA (n = NA) | NA (n = NA) | NA |
| UK | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital and community | |||||||||
| Rich | |||||||||
| Mendelsohn 2008108 | Unilateral hip fracture patients who had a weight-bearing capactiy of at least 25% | Limited cognitive function; unstable cardiovascular disease or unstable chronic obstructive lung disease; limited visual capacity; unstable metabolic disease; language, vision or hearing barriers that could limit participation; any medical problems other than the hip fracture that could interfere with rehabilitation and the required measurements of function | Both | ≥ 70 | 20 | No | Upper-body exercise plus standard rehabilitation care (n = 10) | Standard rehabilitation care (n = 10) | Physical |
| Canada | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Mitchell 2001109 | Age ≥ 65 years; fracture treated surgically | AMTS < 6; medically unstable; previously unable to walk | Both | ≥ 65 | 80 | No | Quadriceps training plus standard physiotherapy (n = 40) | Standard physiotherapy (n = 40) | Physical |
| UK | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Moore 1993181 | Hip fracture patients | NR | Both | NR | 32 | No | Physical therapy (n = 32) | NA (n = NA) | Physical |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Morghen 2011182 | Aged > 65 years and admitted to hospital for post-hip fracture surgery rehabilitation | Length of stay in the orthopaedic ward before admission > 1 week; written order not to ambulate after hip fracture surgery; pathological or multiple fractures and/or other illnesses reducing life expectancy to < 6 months; poor reliability of self-reported depressive symptoms with a score of < 15/30 on the MMSE; ability to walk independently or with minor assistance on admission to reduce interpatient variability at baseline | Both | > 65 | 230 | Yes | Intensive physical therapy (n = 230) | NA (n = NA) | Physical |
| Italy | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Moseley 2009110 | Hip fracture patients with surgical fixation admitted to the inpatient rehabilitation unit; approval to weight bear or partial weight bear; able to tolerate the exercise programmes; able to take four plus steps with a forearm support frame and the assistance of one person; no medical contraindications that would limit the ability to exercise; living at home or in a low-care residential facility prior to the hip fracture and planning to return to this accommodation at discharge. Subjects with cognitive impairment were included if a carer who was able to supervise the exercise programme was available | High-functioning patients who were discharged directly home and low-functioning patients who were discharged to a residential care facility from the acute orthopaedic ward; patients who had no carer available; patients with more than four adjusted errors on the Short Portable Mental Status Questionnaire; medical contraindications that would limit ability to exercise | Both | ≥ 70 | 160 | Yes (if carer available) | Higher-dose weight-bearing exercise (n = 80) | Lower-dose limited weight-bearing exercise (n = 80) | Physical |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Munin 2005149 | Hip fractures patients aged ≥ 60 years and who had surgical stabilisation of the fracture; living in the community pre fracture | Cognitive impairment hindering consent; metastatic cancer | Both | ≥ 60 | 76 | No | Inpatient rehabilitation facility (n = 42) | Skilled nursing facility rehabilitation (n = 34) | Place |
| USA | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Naglie 2002111 | Hip fracture patients from the community and from nursing homes who underwent surgical repair; aged ≥ 70 years | Fracture occurring in an acute care hospital; pathological fracture; multiple trauma; previous surgery on the fractured hip; expected survival < 6 months; residence in a nursing home and dependence on at least one person for ambulation before the fracture; residence outside metropolitan Toronto; failed surgery for technical reasons; requiring care in an intensive care unit; unavailability of beds on the interdisciplinary care ward | Both | ≥ 70 | 279 | No | Post-operative interdisciplinary care (n = 141) | Usual care (n = 138) | Multidisciplinary co-ordination |
| Canada | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Nicholson 1997136 | Patients unable to adequately perform essential ADL; lives alone or had other complications; in stable health | Impaired cognitive function; subsequent fall; premature discharge prior to the completion of the 6-week exercise programme; voluntary discontinuance | Both | ≥ 70 | 30 | No | Supervised exercise intervention (n = 20) | Routine care (n = 10) | Physical |
| South Africa | |||||||||
| Quantitative comparative | |||||||||
| Non-randomised trial/quasi-experimental study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Ohsawa 2007137 | Frail elderly patients with displaced intracapsular fracture of the proximal femur who had poor general condition and refused to have an operation | NR | Both | ≥ 80 | 20 | No | Assertive therapy (n = 13) | Conventional care (n = 7) | Psychological |
| Japan | |||||||||
| Quantitative comparative | |||||||||
| Non-randomised trial/quasi-experimental study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Oldmeadow 200687 | Patients with an acute neck of femur fracture | Pathological fracture; post-operative non-weight-bearing advice given for the operated hip; admitted from a nursing home; non-ambulant premorbidly | Both | ≥ 70 | 60 | No | Early ambulation (n = 29) | Delayed ambulation (n = 31) | Physical |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Olsson 200788 | Patients acutely operated on for a hip fracture; aged ≥ 70 years; non-institutional residence | Severe illness; cognitive impairment or dementia; pathological fracture | Both | ≥ 65 | 13 | No | NA (n = NA) | NA (n = NA) | NA |
| Sweden | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Orwig 2011191 | Community-dwelling women aged ≥ 65 years admitted within 72 hours of a non-pathological hip fracture receiving surgical repair | Pathological fracture; cardiovascular, neurological and respiratory diseases that could interfere with exercising independently at home; diseases of the bone (e.g. Paget’s disease, osteomalacia); metastatic cancer; cirrhosis; end-stage renal disease; hardware in the contralateral hip; conditions that increase the risk of falling while exercising independently; inability to walk without human assistance prior to the fracture; cognitively impaired | Female | ≥ 65 | 180 | No | In-home exercise intervention (n = 91) | Usual care (n = 89) | Physical and psychological |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Oude Voshaar 200712 | Patients aged > 60 years who had undergone surgery for a fractured neck of femur | Significant cognitive impairment (a score of < 15 on the MMSE); deafness significantly interfering with the assessments; severe physical illness; living > 30 miles from the assessment centre; unable to speak English | Both | > 60 | 291 | Partial | Psychological intervention (n = 291) | NA (n = NA) | Psychological |
| UK | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Peiris 2012112 | Patients aged ≥ 18 years admitted for rehabilitation in the orthopaedic ward with a lower-limb orthopaedic condition; able to walk independently or with assistance; cognitively alert | Age < 18 years; non-lower-limb orthopaedic condition; unable to walk; reduced cognitive function | Both | ≥ 18 | 105 | No | Additional physical therapy sessions at the weekend (n = 51) | Usual care (n = 54) | Physical |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Penrod 2004192 | Patients hospitalised for hip fracture | Patients aged < 50 years; sustained a fracture as an inpatient; transferred from another hospital post-operatively; sustained concurrent major internal injuries; pathological fractures; fractures limited to the pelvis or acetabulum; fractures ≥ 2 cm below the trochanter; bilateral hip fractures; fractures in which there was previous surgery on the same hip; previous ipsilateral hip fracture | Both | ≥ 50 | 443 | No | Physical therapy plus occupational therapy (n = 443) | NA (n = NA) | Physical |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Peterson 2004113 | Patients aged ≥ 65 years admitted to the fracture service; community dwelling within the tri-state area; ambulatory with or without assistive device prior to fracture; MMSE score of ≥ 24; able to understand English; fracture resulting from a mechanical fall | Aged < 65 years; living in care facility; living outside the tri-state area; non-ambulatory; MMSE score of < 24; unable to understand English; fracture non-fall related; comorbidity preventing the ability to exercise; patients who could not be medically cleared within 48 hours of surgery; patients without a telephone | Both | ≥ 65 | 70 | NA | Intensive strength training (n = 38) | Inactive control (n = 32) | Physical |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Petrella 2000169 | Hip fracture patients who were admitted to the rehabilitation facility | Not suitable to return home; significant comorbidities; non-weight-bearing at admission | Both | ≥ 65 | 56 | No | Intensive rehabilitation (n = 56) | NA (n = NA) | Physical |
| Canada | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Portegijs 2008114 | Community-living 60- to 85-year-old femoral neck or trochanteric fracture patients; fracture occurred from 6 months to 7 years before baseline | Patients not living independently in the vicinity of the study centre; neurological and progressive severe illnesses; unable to walk outdoors without assistance | Both | 60–85 | 46 | No | Tailored strength–power training (n = 24) | Usual care (n = 22) | Physical |
| Finland | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Portegijs 2012166 | Community-dwelling people aged > 65 years who had been previously operated on for femoral neck or trochanteric fracture | Inability to move outdoors without assistance; amputation of a lower limb; severe progressive or neurological diseases, alcoholism and severe memory problems | Both | ≥ 60 | 130 | Partial | NA (n = NA) | NA (n = NA) | NA |
| Finland | |||||||||
| Quantitative comparative | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Proctor 200813 | Three case studies | NR | Both | NR | 3 | No | NA (n = NA) | NA (n = NA) | Psychological |
| UK | |||||||||
| Case studies | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Pryor 1988150 | Hip fracture patients | NR | Both | Any | 208 | No | Early discharge plus inpatient rehabilitation (n = 154) | Standard care (n = 46) | Discharge planning |
| UK | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Resnick 200572 | Hip fracture patients who participated in the Exercise Plus Program and were living in the community prior to hip fracture; receiving some type of surgical repair of the fracture (e.g. open reduction internal fixation, hemiarthroplasty); able to walk at least 50 feet; MMSE score of 20; no medical problems that would put the individual at risk for exercising alone in the home setting, such as Parkinson’s disease or myocardial infarction within the past 6 months; long-term use of coumadin | NR | Both | ≥ 70 | 70 | No | NA (n = NA) | NA (n = NA) | Physical and psychological |
| USA | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Community | |||||||||
| Rich | |||||||||
| Resnick 200769 | Hip fracture females who were otherwise medically fit and healthy and able to walk unassisted | NR | Female | ≥ 70 | 208 | No | Exercise Plus Program: exercise plus motivation (n = 52); motivation only (n = 54); exercise only (n = 51) | Inactive control (n = 51) | Physical |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Rich | |||||||||
| Richards 1998128 | Adult patients (all but 16 were aged > 65 years) on an acute hospital ward and resident within catchment area of Frenchay NHS Trust; positive rehabilitative outcome expected; appropriate home circumstances (i.e. adequate heating, safety in relation to patient’s disability) and adequate support from carers available if necessary; would require further hospital care if team was not available; not awaiting a nursing home place or input of social care alone; expected to remain in hospital for between 1 and 28 days; GP accepts clinical responsibility | NR | Both | > 65 | 241 | No | Hospital at home (n = 160) | Usual care (n = 81) | Place |
| UK | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Roberto 1992165 | Caucasian hip fracture women aged 65–94 years | NR | Female | 65–94 | 101 | No | NA (n = NA) | NA (n = NA) | NA |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Historical cohort study | |||||||||
| Community | |||||||||
| Rich | |||||||||
| Roberts 2004155 | Patients aged ≥ 65 years with a femoral neck fracture | Multiple fractures, fractures resulting from malignancy or re-fracture; total hip replacement; previous entry into the study; operation performed elsewhere | Both | ≥ 65 | 764 | No | Integrated care pathway (n = 395) | Conventional care (n = 369) | Multidisciplinary co-ordination |
| UK | |||||||||
| Quantitative comparative | |||||||||
| Controlled before-and-after study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Robinson 1999183 | White female hip fracture patients aged > 70 years; living alone; able to read and speak English; discharged from the subacute unit within 9 months | NR | Female | > 70 | 15 | No | NA (n = NA) | NA (n = NA) | NA |
| USA | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Röder 2003151 | Patients aged ≥ 65 years who had a non-pathological hip fracture as a result of a fall; diagnosis confirmed by radiography; no dementia or higher cognitive deficits | NR | Both | ≥ 65 | 142 | No | Supervised inpatient rehabilitation in orthopaedic and geriatric hospitals (n = 108) | Usual care (n = 34) | Physical |
| Germany | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Rolland 2004184 | Hip fracture patients aged ≥ 70 years hospitalised for rehabilitation after hip fracture surgery; cognitive status and previous hip fracture were not exclusion criteria | Unable to walk a distance of 10 m without assistive devices; acute disease such as another orthopaedic injury (fracture, amputation); severe symptomatic arthritis; severe cardiac or pulmonary disease; depression; neurological conditions including Parkinson’s disease, polyneuropathy and stroke | Both | ≥ 70 | 61 | Yes | Multidisciplinary rehabilitation (n = 61) | NA (n = NA) | Multidisciplinary co-ordination |
| France | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Rösler 2012152 | Patients with fracture of the proximal femur and dementia | NR | Both | Any | 129 | Yes | Specialised ward (cognitive geriatric unit) (n = 53) | Geriatric ward (non-cognitive geriatric unit) of the same geriatric department (n = 76) | Multidisciplinary co-ordination |
| Germany | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Ryan 2006115 | Hip fracture patients aged ≥ 65 years | NR | Both | ≥ 65 | 58 | No | Intensive home-based rehabilitation (n = 30) | Less intensive home-based rehabilitation (n = 28) | Physical |
| UK | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Saltvedt 2012116 | Home-dwelling older people aged ≥ 70 years; previously able to walk 10 m and living in their own home or staying temporarily in an institution; intracapsular, trochanteric or subtrochanteric fracture; able to give an informed consent | Pathological fracture or multitrauma injuries; terminal illness and not expected to live > 3 months | Both | ≥ 70 | 401 | Yes | Comprehensive geriatric assessment (n = 15 beds) | Usual care (n = 24 beds) | Process/system improvement |
| Norway | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Shawler 2006174 | Mothers aged 76–85 years, post hip fracture and able to ambulate and living in a non-institutional setting. Adult daughters aged 49–67 years who provided some level of assistance to their mothers during the health crisis. All of the women were European American | NR | Female | Mothers 76–85; daughters 49–67 | 6 mother–adult daughter dyads | No | NA (n = NA) | NA (n = NA) | NA |
| USA | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Sherrington 1997117 | Aged > 60 years; living in the community at the time of fracture; fracture resulting from a fall; fracture occurring within the last 9 months; discharge within south-western Sydney | NR | Both | > 60 | 44 | No | Weight-bearing exercise (n = 22; 20 analysed) | No intervention control (n = 22; 20 analysed) | Physical |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Sherrington 2004118 | Aged ≥ 55 years; community or residential care dwelling; 80% women | Severe cognitive impairment; medical conditions; complications from the fracture resulting in delayed healing and associated weight-bearing restrictions | Both | ≥ 55 | 120 | No | Weight-bearing and non-weight-bearing home exercise (n = 80) | No intervention control (n = 40) | Physical |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Shyu 2008119 | Aged ≥ 60 years; admitted to hospital for an accidental single-side hip fracture; receiving hip arthroplasty or internal fixation; able to perform full range of motion against gravity and against some or full resistance; living in northern Taiwan | Severely cognitively impaired; terminally ill | Both | ≥ 60 | 162 | Yes, mild to moderate | Geriatric consultation services, a rehabilitation programme and discharge-planning services (n = 80) | Usual care (n = 82) | Multidisciplinary co-ordination |
| Taiwan | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Shyu 2009196 | Aged ≥ 60 years; no severe cognitive impairment; able to walk independently pre fracture | NR | Both | ≥ 60 | 147 | No | NA (n = NA) | NA (n = NA) | NA |
| Taiwan | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Sirkka 2003193 | Fall-related hip fracture patients living in their own home | NR | Both | ≥ 65 | 29 | No | NA (n = NA) | NA (n = NA) | NA |
| Sweden | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital and community | |||||||||
| Rich | |||||||||
| Stenvall 2007120 | Patients with femoral neck fracture aged ≥ 70 years | Patients with rheumatoid arthritis, severe hip osteoarthritis or pathological fracture, with severe renal failure and who were bedridden before the fracture | Both | ≥ 70 | 199 | Yes | Specialised geriatric ward (n = 102) | Specialist orthopaedic ward (n = 97) | Multidisciplinary co-ordination |
| Sweden | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Swanson 1998129 | Aged ≥ 55; both genders | Pathological fracture; not independently mobile; unable to give informed consent; inaccessible for follow-up; dementia; unable to understand English; nursing home resident | Both | ≥ 55 | 71 | No | Early intervention (n = 38) | Usual care (n = 33) | Multidisciplinary co-ordination |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Sylliaas 2011199 | Patients aged ≥ 65 years with a femoral neck or trochanteric fracture; living at home; able to undergo physical therapy for the hip fracture; no cognitive impairment | Permanently institutionalised before the hip fracture; metastatic cancer as presumed reason for the fracture; expected remaining lifetime < 6 months; hip fracture part of a multitrauma. Those who had been registered in the acute phase but who died, were moved or were institutionalised during the first 3 months or did not return for the 3-month follow-up were excluded | Both | ≥ 65 | 150 | No | Physiotherapist-supervised group and individual exercises (n = 100) | Routine care (n = 50) | Physical |
| Norway | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Takayama 2001164 | Hip fracture patients aged ≥ 60 years who had undergone surgery | Patients who died within 1 year; lack of walking data; pathological fractures; re-fracture during the course of the study | Both | ≥ 60 | 189 | Partial | Standard rehabilitation programme (n = 189) | NA (n = NA) | Physical |
| Japan | |||||||||
| Quantitative non-comparative | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Talkowski 2009194 | Community-dwelling adults aged ≥ 60 years admitted to skilled nursing facilities or inpatient rehabilitation facilities and who were ambulatory with or without assistance following a hip fracture. The majority of the participants were female | Non-weight bearing; bilateral or additional fractures other than the femur; cognitive deficits or haemodynamically unstable; active bleeding with hypotension, uncontrolled arrhythmias or uncontrolled hypertension | Both | ≥ 60 | 18 | No | NA (n = NA) | NA (n = NA) | Physical |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Taylor 2010185 | Female physiotherapists working in rehabilitation in both outpatient and inpatient settings | NR | Female | NR | 12 | NA | NA (n = NA) | NA (n = NA) | NA |
| Australia | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Tinetti 1999121 | Community-living individuals aged at least 65 years who have undergone surgical repair of a hip fracture | Known dementia or failed cognitive screen; known terminal illness defined as a life expectancy of < 1 year or who died in the hospital; lives > 25 miles from the two hospitals | Both | ≥ 65 | 304 | No | Home-based rehabilitation (n = 148) | Usual care (n = 156) | Physical |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Travis 199889 | Hip fracture patients aged ≥ 60 years having lower strength and muscle mass and lower levels of physical endurance | Unable to verbally communicate; blind; had a medical event during the subacute admission that interfered with recovery and rehabilitation; not receiving rehabilitation services; serious cognitive deficits; more than four dependencies in the ability to perform basic ADL | Both | ≥ 60 | 8 | No | NA (n = NA) | NA (n = NA) | NA |
| USA | |||||||||
| Mixed methods | |||||||||
| Mixed methods | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Tsauo 2005122 | Hip fracture patients admitted to hospital for surgery | Patient or family rejected further treatment and follow-up after discharge; patient unable to complete the entire follow-up because of transportation problems; mental or cognitive problems (e.g. psychiatric disorders, senile dementia); ongoing medical litigation | Both | ≥ 60 | 54 (25 analysed) | No | Physical therapy (n = 13) | Usual care (n = 12) | Physical |
| Taiwan | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Uy 2008123 | Cognitively impaired women with hip fracture; ambulant prior to fracture; able to follow commands at the time of seeking informed consent consent | NR | Female | ≥ 80 | 10 | Yes | Inpatient interdisciplinary rehabilitation (n = 3) | Discharge back to the nursing home (n = 7) | Multidisciplinary co-ordination |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick | |||||||||
| Van Balen 2002140 | Hip fracture patients aged ≥ 65 years | Patients with a hip fracture because of metastatic cancer or multitrauma | Both | ≥ 65 | 208 | No | Early discharge to a nursing home rehabilitation ward (n = 106) | Conventional discharge to a nursing home rehabilitation ward (n = 102) | Discharge planning |
| The Netherlands | |||||||||
| Quantitative comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| van der Sluijs 1991186 | Patients with a fresh hip fracture who were living independently in their own home or in an old people’s home | Patients from nursing homes and with a pathological fracture | Both | Any | 134 | NR | Weight-bearing training (n = 134) | NA (n = NA) | Physical |
| The Netherlands | |||||||||
| Quantitative non-comparative | |||||||||
| Controlled before-and-after study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Vidán 2005124 | Patients aged ≥ 65 years hospitalised for hip fracture surgery | Inability to walk before the fracture and dependency in all basic ADL (ADL50); pathological hip fracture; known terminal illnesses, defined as those associated with a life expectancy of < 12 months | Both | ≥ 65 | 319 | No | Comprehensive geriatric intervention (n = 155) | Usual care (n = 164) | Multidisciplinary co-ordination |
| Spain | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital | |||||||||
| Rich | |||||||||
| Visser 2000156 | Community-dwelling women aged ≥ 65 years with recent fracture of the proximal femur | NR | Female | ≥ 65 | 90 | NR | Physical therapy (n = 90) | NA (n = NA) | Physical |
| USA | |||||||||
| Quantitative non-comparative | |||||||||
| Controlled before-and-after study | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Vogler 2012125 | Patients hospitalised for hip fracture | Medical contraindications to exercise; cognitive impairment (MMSE score of ≤ 24); to be discharged to a high-care residential aged facility | Both | ≥ 65 | 180 | No | Home-based exercise programme (n = 120) | Social visits (n = 60) | Physical |
| Australia | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Walheim 1990187 | Patients aged > 50 years treated for trochanteric fracture | NR | Both | ≥ 50 | 92 | Partial | Physiotherapy (n = 92) | NA (n = NA) | Physical |
| Sweden | |||||||||
| Quantitative non-comparative | |||||||||
| Concurrent cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Whitehead 2003161 | Community-dwelling, cognitively intact older adults with a fall-related non-pathological hip fracture | NR | Both | ≥ 60 | 73 | No | Home rehabilitation (n = 73) | NA (n = NA) | Place |
| Australia | |||||||||
| Quantitative non-comparative | |||||||||
| Historical cohort study | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Yu-Yahiro 2009126 | Women aged ≥ 65 years recruited within 15 days of hip fracture; eligible patients were those with a non-pathological fracture who were admitted within 72 hours of injury, had surgical repair of the hip fracture and met medical inclusion criteria. Participants initially were randomised to exercise groups and then assigned to exercise trainers | Medical exclusions: presence of cardiovascular disease, neuromuscular conditions limiting exercise (e.g. Parkinson’s disease, amyotrophic lateral sclerosis, multiple sclerosis), respiratory conditions, diseases of the bone (e.g. Paget’s disease, osteomalacia), metastatic cancer, cirrhosis and end-stage renal disease. Other exclusions: increased risk of falling while exercising independently (e.g. history of seizures, alcohol abuse or narcotic or benzodiazepine use) or increased risk of injury if a fall occurred (e.g. recent gastrointestinal bleeding or the use of warfarin); inability to walk without human assistance (independent ambulation with or without an assistive device) before the fracture; and a score of < 20 on the Folstein MMSE | Female | ≥ 65 | 180 | No | Strengthening exercises (n = 91) | Usual care (n = 89) | Physical |
| USA | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Zabari 2012162 | Patients aged > 65 years with an operated hip fracture admitted to the geriatric rehabilitation department for treatment | Dementia; medical complications interrupting the rehabilitation process such as infections, acute coronary events and deep-vein thrombosis | Both | > 65 | 144 | NR | Pain management protocol (n = 67) | Usual care (n = 77) | Physical |
| Israel | |||||||||
| Quantitative non-comparative | |||||||||
| Historical cohort study | |||||||||
| Hospital | |||||||||
| Thick | |||||||||
| Zidén 2008127 | Aged 65–99 years; living in their own home; no cognitive impairment; able to understand and speak Swedish | NR | Both | ≥ 65 | 18 | No | NA (n = NA) | NA (n = NA) | NA |
| Sweden | |||||||||
| Qualitative | |||||||||
| Qualitative | |||||||||
| Community | |||||||||
| Thick | |||||||||
| Zidén 200890 | Community-dwelling hip fracture patients aged ≥ 65 years; medically approved by the responsible geriatric doctor as being in need of geriatric care and rehabilitation; able to speak and understand Swedish | Severe medical illness with expected survival of < 1 year; severe drug or alcohol abuse; mental illness or documented severe cognitive impairment | Both | ≥ 65 | 102 | No | Home-based rehabilitation (n = 54) | Conventional care (n = 48) | Multidisciplinary co-ordination |
| Sweden | |||||||||
| Quantitative comparative | |||||||||
| RCT | |||||||||
| Hospital and community | |||||||||
| Thick |
Appendix 17 Characteristics of the interventions in the included studies
| Study details (author, year; country; study type; study design; setting; conceptual richness) | Participants | Intervention (group) category (n allocated/n analysed) | Intervention description | Control (group) category (n allocated/n analysed) | Control description | Follow-up |
|---|---|---|---|---|---|---|
| Adunsky 2003138 | Patients with pertrochanteric (extracapsular) or subcapital (intracapsular) hip fracture who were otherwise medically fit (n = 320); age: ≥ 65 years; gender: both; cognitive impairment: no | Orthogeriatric ward (n = 116/116) | Patients were admitted directly from the emergency ward to the orthogeriatric ward and received all surgical, medical and rehabilitation therapy in a single setting. An interdisciplinary team approach was used in which medical personnel (two certified geriatricians, an orthopaedic consultant, nurses, physiotherapists, occupational and speech therapists, social workers, and psychologists) met twice a week to evaluate the status of each patient and formulate a treatment plan. On average, patients underwent 5 hours of physical therapy and 5 hours of occupational therapy per week (5 days per week). Additional rehabilitative services were provided whenever needed | Orthopaedic department (n = 204/204) | Patients admitted soon after surgery from the orthopaedic department to the orthogeriatric ward for further rehabilitation did not have any interdisciplinary team meetings or the same nurses or therapists before the transfer | Post discharge (6–8 weeks) |
| Israel | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Al-Ani 2010139 | Patients with femoral neck fracture with cognitive impairment and able to walk before the fracture (n = 227); age: ≥ 65 years; gender: both; cognitive impairment: yes | Early discharge to a rehabilitation unit (n = 81/81) | Patients received some physiotherapy directly after their operation and were assisted by physiotherapists to take a few steps using a walking table and with personal support when necessary untill discharge. Physiotherapists and occupational therapists were involved in daily rehabilitation activities of patients referred to these units | Early discharge to previous residence (n = 146/146) | Patients received some physiotherapy directly after their operation and were assisted by physiotherapists to take a few steps using a walking table and with personal support when necessary until discharge. No or minimal number of physiotherapists and occupational therapists were involved in daily rehabilitation activities of patients discharged back to their residential/care home | 12 months |
| Sweden | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Allegrante 200791 | Primary unilateral hip fracture patients who underwent successful surgical repair (n = 176); age: ≥ 65 years; gender: both; cognitive impairment: no | Hospital-based physical therapy plus motivational videos plus visits from recovered hip fracture patients (n = 90/90) | Intervention programme consisted of three components: (1) in-hospital, post-operative motivational patient videotape and a corresponding patient information booklet designed to address falls prevention and lack of self-efficacy; (2) in-hospital supportive visit by a recovered hip fracture patient of a similar age who had received brief training in peer counselling; and (3) hospital-based, 8-week outpatient programme of physical therapy consisting of tailored exercises including range of motion, flexibility and progressive muscle-strength training based on individual patient needs, ability and capacity. Patients were then scheduled for their supervised exercise programme as outpatients, consisting of individualised balance retraining and gait training. After discharge from hospital, all patients received weekly socially supportive telephone calls until they were seen by their surgeon for their first post-operative follow-up visit | Usual care (n = 86/86) | Patients received the usual post-operative care and rehabilitation services available to all patients seen in the fracture service at the participating hospitals. Usual care consisted of weight bearing on the leg of the fracture hip and routine range-of-motion and low-intensity strengthening exercises. Patients also received supportive telephone contact after discharge from the hospital almost identical to that of patients in the intervention arm | 6 months |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Arinzon 2005201 | Hip fracture patients operated for unilateral post-fall hip fracture and without clinical evidence of acute addicted disease (n = 102); age: ≥ 65 years; gender: both; cognitive impairment: no | Old-old elderly (aged ≥ 85 years) geriatric rehabilitation in the community (n = 46/46) | Geriatric rehabilitation at home or in the community | Young elderly (aged 65–74 years) geriatric rehabilitation in the community (n = 56/56) | Geriatric rehabilitation at home or in the community | At discharge |
| Israel | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Community | ||||||
| Thick | ||||||
| Atwal 2002176 | Health professionals providing rehabilitation services (n = 48 health professionals); age: NR; gender: both; cognitive impairment: NA | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| UK | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital | ||||||
| Rich | ||||||
| Barone 2009177 | Osteoporotic fracture of the proximal femur (a fracture that occurred in the absence of trauma or with minimal trauma and not related to secondary causes); surgical stabilisation of the fracture; able to walk (with or without aid) in the 2 weeks before hospital admission (n = 469); age: ≥ 70 years; gender: both; cognitive impairment: partial | Immediate weight-bearing training (n = 469/469) | Immediate weight-bearing and assisted ambulation training on the first post-operative day | NA (n = NA/NA) | NA | NA |
| Italy | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Bäuerle 2004163 (German) | Patients with a fall-related femur fracture (n = 332); age: ≥ 65 years; gender: both; cognitive impairment: no | Service and health-care evaluation (n = 332/332) | Service and health-care evaluation | NA (n = NA/NA) | NA | 12 months |
| Germany | ||||||
| Quantitative non-comparative | ||||||
| Historical cohort study | ||||||
| Community | ||||||
| Thick | ||||||
| Beaupre 2005157 | Patients with a hip fracture who lived within local calling distance; patients with cognitive impairment and those residing in institutional settings before hip fracture were eligible for inclusion (n = 919); age: ≥ 65 years; gender: both; cognitive impairment: yes | Clinical pathway (treatment) group (n = 451/451) | The clinical pathway consisted of a standardised rehabilitation regimen and discharge planning from the time of admission through to discharge from the surgical site. It also included medical care based on current best evidence or clinical consensus when no evidence was available. Consensus was reached using a multidisciplinary team that included orthopaedic surgeons, rehabilitation professionals and geriatric specialists. The multidisciplinary team defined goals of early mobilisation (with weight bearing as tolerated) when possible as important factors in assisting the progression of daily rehabilitation visits. The pathway also included standardised discharge planning to try to facilitate optimal subacute rehabilitation practice (i.e. rehabilitation offered 10–14 days post-operatively). To promote adoption of the new model of care, pre-printed orders accompanied the clinical pathway to minimise treatment delays associated with waiting for attending staff to write daily orders | Pre-clinical pathway (n = 468/468) | Control (pre-clinical pathway) group | 6 months |
| Canada | ||||||
| Quantitative comparative | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Bellelli 2006170 | Hip fracture patient (n = 1); age: ≥ 80 years; gender: both; cognitive impairment: yes | Body weight–supported treadmill technique (n = 1/1) | The training involved stepping on a motorised treadmill while unloading a percentage of a person’s body weight using a counterweight harness system. Manual assistance was provided as necessary to promote upright posture and lower-extremity trajectories associated with human normal gait, with the length of daily sessions progressively increasing. According to functional improvement, the body-weight suspension was progressively reduced to allow a task-specific repetitive approach and minimise the delay during which gait training can be initiated | NA (n = NA/NA) | NA | 6 weeks |
| Italy | ||||||
| Quantitative non-comparative | ||||||
| Case report | ||||||
| Hospital | ||||||
| Thick | ||||||
| Bellelli 2008141 | Hip frature patients admitted for rehabilitation (n = 211); age: ≥ 65 years; gender: both; cognitive impairment: yes | Dementia (n = 40), depression (n = 54), both (n = 27) | Dementia, depression or both | No dementia or depression (n = 90) | No dementia or depression | 12 months |
| Italy | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Bellelli 201078 | Hip fracture patients undergoing first-time surgery and rehabilitation (n = 60); age: ≥ 18 years; gender: both; cognitive impairment: no | Conventional post-orthopaedic rehabilitation programme plus visual feedback (n = 30/30) | Conventional post-orthopaedic rehabilitation programme for 1 hour per day, 6 days per week for 3 weeks. Each session consisted of a warm-up, strengthening and range-of-motion exercises, flexibility exercises, trunk and upper-extremity positioning, transfer, postural and gait training, functional and self-care retraining, adaptive equipment training (if needed) and a cool-down phase. Additionally, patients received an additional daily session during which they were asked to observe three short films showing an actor performing daily actions with the leg or trunk. After observation, patients were required to execute the observed actions to the best of their ability. Patients received written instructions to avoid being influenced by the unblinded treating physiotherapist. At the end of each session, patients were asked to recognise some of the observed video clips with motor content from a group of video clips, including some that were not presented | Conventional post-orthopaedic rehabilitation programme (n = 30/30) | Patients in the comparator group received the same programme except that they were asked to recognise some of the observed video clips with no motor content from a group of video clips, including some that were not presented | 12 months |
| Italy | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Rich | ||||||
| Binder 200492 | Community dwelling (not living in a nursing home) on discharge from physical therapy for hip fracture; screening evaluation within 16 weeks of hip fracture repair; modified Physical Performance Test score between 12 and 28; self-reported difficulty or requirement for assistance with one or more ADL (n = 90); age: ≥ 65 years; gender: both; cognitive impairment: no | Tailored, supervised physical therapy and exercise training (n = 46/46) | Two 3-month-long phases of exercise training. Phase 1: exercises were conducted by a physiotherapist using a group format (two to five subjects per group) designed to enhance flexibility, balance, co-ordination, movement speed and muscle stength. The programme consited of 22 types of exercise. Exercise sessions lasted for 45–90 minutes (with breaks). The exercises were made progressively more difficult by increasing the number of repetitions and by having the subjects perform the exercises in more challenging ways, tailored to each subject’s ability, tolerance and specific physical impairments. Participants also exercised on a stationary bicycle or treadmill if fit to do so. Phase 2: progressive resistance training was added to the programme with the aim of exercising for 60 minutes per session, with another 30 minutes spent on the phase 1 exercises (focusing on balance, flexibility and core abdominal exercises), at least three times per week | Home exercise (n = 44/4) | The home exercise protocol focused primarily on flexibility. Participants attended a 1-hour training session at an exercise facility and were then asked to perform the exercises at home three times per week but were not prohibited from performing them more often or from taking part in some other forms of exercise, such as walking or swimming. They were specifically prohibited from participating in a weight-training programme | 6 months |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Bischoff-Ferrari 201093 | Hip fracture patients (n = 173); age: ≥ 65 years; gender: both; cognitive impairment: no | Extended physiotherapy (n = 87/87) | The extended physiotherapy programme included 30 minutes of a home programme each day during acute care: standing on both legs and then standing on one leg while holding a handrail (simple balance component); pulling a rubber band while sitting for arm strength training; getting in and out of a chair and going up and down stairs (functional mobility). At discharge, the extended physiotherapy group also received a leaflet that illustrated the home programme, with a recommendation to follow the programme for 30 minutes each day | Standard physiotherpay (n = 86/86) | The standard physiotherapy group received 30 minutes per day of supervised therapy during acute care and no home programme | 12 months |
| Switzerland | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Borgquist 1990188 | Patients surgically operated for hip fracture (n = 298); age: ≥ 50 years; gender: both; cognitive impairment: no | Community rehabilitation (n = 298/298) | After internal fixation with immediate mobilisation and weight bearing, evaluation was performed of individual goals and planning for discharge was carried out, including consultation with a local community centre. After discharge, local health centre personnel received patients in their home, brought technical aids, checked their ability to manage minor houshold functions and determined their need for communal home help and physiotherapy. The treatment was carried out in the patients’ place of reidence by a physiotherapist or an occupational therapist and consisted mainly of walking instructions and a successive decrease in use of walking aids | NA (n = NA/NA) | NA | 4 months |
| Sweden | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Boyd 1982158 | Female hip fracture patients with injury complicated by other disease or disability, trauma or any major rehabilitation problem (n = 771); age: NR; gender: female; cognitive impairment: no | Rehabilitation ward programme (n = 482/482) | Fractured femur care in 1979 after introduction of a rehabilitation ward programme (the first complete year after the ward opened) | No rehabilitation ward programme (n = 289/289) | Fractured femur care in 1977 before introduction of a rehabilitation ward programme (the last complete year before the ward opened) | At discharge |
| UK | ||||||
| Quantitative comparative | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Buddenberg 199879 | Caucasian women with a surgically repaired hip fracture; fracture sustained secondary to a fall; living independently before fracture; independent in self-care before fracture (n = 20); age: ≥ 75 years; gender: female; cognitive impairment: partial | Occupational therapy plus psychological therapy (n = 10/10) | Patients received both standard occupational therapy using the biomechanical approach, which provides a therapist-driven programme focusing on strengthening exercises, activity tolerance and retraining in ADL, and occupational therapy using the occupational adaptation frame of reference. Patients were encouraged to take an active role in evaluation and treatment planning by asking each patient to identify three specific activities that they would like to be able to perform. These activities were incorporated into the goals of the treatment. The intervention emphasised improving patients’ performance in their chosen activities. Patients were encouraged to become active participants in the planning and problem-solving necessary to achieve their goals. The intervention was included to improve strength and activity tolerance when deficits in these areas resulted in a limitation in patients’ performance of their selected activities | Conventional occupational therapy (n = 10/10) | Customary occupational therapy using the biomechanical approach. A group format was often used for strength exercises and instructions for training in ADL were provided on an individual level | NA |
| USA | ||||||
| Quantitative comparative | ||||||
| Non-randomised trial/quasi-experimental study | ||||||
| Rehabilitation facility (no other details provided) | ||||||
| Rich | ||||||
| Burns 2007197 | Patients who have undergone surgery for a fractured neck of femur (n = 293); age: ≥ 60 years; gender: both; cognitive impairment: partial | Psychological intervention (n = 121/121) | Six weekly sessions consisting of meetings with a psychiatric nurse based on liaison principles (for referral or medication if needed), including a cognitive–behavioural approach to treat depression. The elements included compliance with antidepressant medication, assisting referral to other professionals (e.g. physiotherapy), advising on other services (e.g. social care), education about depression and problem-solving with support from a senior psychiatrist tailored to individual patient needs. A maximum of seven sessions was offered. After an initial assessment, the assistant psychologist worked with patients to introduce relevant psychoeducational material, identify and challenge negative thoughts and ideas about recovery, and introduce positive coping strategies | Usual care (n = 172/172) | Usual care | 6 months |
| UK | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Rich | ||||||
| Carmeli 2006131 | Hip fracture patients undergoing rehabilitation after hip fracture surgery (n = 63); age: ≥ 75 years; gender: both; cognitive impairment: no | Class-based outpatient exercise programme (n = 34/34) | Directed and administered in the outpatient clinic, the exercise programme aimed to improve balance, muscle strength and gait, and safety and included precautions relating to the timing and interval of exercising, with the overall aim of improving functional capacity. The exercise programme was administered over a period of 14 weeks with a total of 42 workout sessions at a frequency of three times per week, with sessions lasting 50 minutes each. Sessions consisted of warm-up, specific exercise and cool-down intervals (5 minutes). The class-based sessions were instructed alternately by two physiotherapists to ensure consistency | Home-based programme (n = 29/29) | The home-based programme group received the same exercise regimen and was monitored by the same two physiotherapists by a telephone call every other week and by a visit once per month. The telephone consultations lasted for 10–15 minutes and were designed to provide feedback as well as promote compliance. The group was instructed to keep a journal of their exercise performance | 14 weeks |
| Israel | ||||||
| Quantitative comparative | ||||||
| Quasi-randomised trial | ||||||
| Hospital and community | ||||||
| Rich | ||||||
| Casado 200980 | Women who had surgical repair of a non-pathological hip fracture; no medical problems with a risk for falls (e.g. neuromuscular conditions); ability to walk without human assistance pre fracture; mild cognitive impairment (n = 168); age: ≥ 65 years; gender: female; cognitive impairment: partial | Exercise Plus Program (exercise training component plus motivational component: theory of self-efficacy) (n = 126/126) | Exercise Plus Program (exercise training component plus motivational component: theory of self-efficacy): home-based trainer administered aerobic, strengthening and stretching exercise intervention for all muscle groups. The trainer exercised with the individual and provided the Plus component (self-efficacy and outcome expectations, performance accomplishment, verbal encouragement, physiological feedback, cueing and self-modelling). A total of 42 supervised visits were carried out for face-to-face implementation of the motivational and exercise intervention; weekly telephone calls were made in months 7–12 when visits were decreased to once per month; weekly aspects of the motivational intervention were implemented by telephone contact. Plus-only intervention (motivational component: theory of self-efficacy): the sessions focused only on the Plus components (i.e. education about exercise, verbal encouragement, removal of unpleasant sensations and cueing), with no exercise sessions with the trainers. Exercise-only intervention (exercise training component): participants in the exercise-only group exercised with the trainer during the session but were not exposed to the Plus components of the intervention. In all treatment groups, visits from the trainer were initially twice per week for the first 2 months, decreasing to once per month in the final 4 months of the programme, with weekly telephone calls for those exposed to the Plus component of the intervention during the weeks when no visits were scheduled. All visits were 1 hour in length. Subjects were expected to exercise five times per week for 45 minutes | Routine care (n = 42/42) | Participants received physical and occupational therapy as prescribed by their orthopaedist and/or primary health-care provider | 6 months |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Rich | ||||||
| Cree 2001175 | Hip fracture patients (n = 222); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 3 months |
| Canada | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital | ||||||
| Thick | ||||||
| Crotty 200094 | Patients with hip fracture in need of rehabilitation; living in the community; gave consent (n = 68); age: ≥ 50 years; gender: both; cognitive impairment: partial | Early discharge for home-based rehabilitation (n = 29/29) | Early discharge to home for hospital-at-home rehabilitation | Normal discharge and hospital-based rehabilitation (n = 29/29) | Normal discharge and rehabilitation at hospital | 10 months |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Crotty 200395 | Patients admitted to hospital for surgical treatment for a fall-related hip fracture; medically stable; adequate physical and mental capacity to participate in a rehabilitation programme; expected to return home after discharge from hospital; home environment suitable for rehabilitation (n = 66); age: ≥ 65 years; gender: both; cognitive impairment: no | Accelerated discharge and home rehabilitation (n = 34/34) | Paitients initially assessed by the study co-ordinator who also visited their home environment and organised any modifications, installation of equipment or assistive aids prior to discharge. Participants were discharged from acute care within 48 hours of randomisation and promptly visited by therapists from the home rehabilitation team, who negotiated realistic, short-term and measurable treatment goals with both participants and carers. The goals included outcomes relevant to participants’ day-to-day lives. Therapy frequency was tailored to the needs and rate of progress of individual participants and structured practice sessions were encouraged between visits. Standard therapy services such as podiatry, nursing care and assistance with light domestic tasks (shopping/cleaning) were provided as required | Usual or conventional care (n = 32/32) | Routine hospital care and rehabilitation consisting of inpatient services and involving the development of care pathways and discharge planning | 12 months |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Dai 2002132 | Ability to walk independently with or without an assistive device; living in their own home pre fracture; no severe cognitive impairment (n = 94); age: ≥ 60 years; gender: both; cognitive impairment: no | MRP (n = 50/50) | The MRP included the following four components: (1) pre-operative instruction and immediate post-operative commencement of in-bed mobilisation by nursing staff; (2) 20-minute bedside mobility training every weekday provided by a student physiotherapist under faculty supervision, including active range-of-motion exercise of the lower extremity, including hip and knee flexion, and functional training such as ankle pumping, gluteal and quadriceps setting, turning, transferring and ambulation; with the surgeon’s permission each patient practised weight bearing on the affected leg and ambulated as early as possible; (3) participation in a mobility training programme with instruction twice per day provided by a primary nurse until discharge; and (4) comprehensive discharge planning that included early assessment of needs for continuing care, adequate instruction for post-hospital care, care co-ordination and referral, and procurement of assistive devices | Conventional care (n = 44/44) | Patients received non-systematic instruction about range-of-motion and muscle-strengthening exercises from nurses after surgical treatment. Subjects were recruited in the last 6 months of a previous study | 6 months |
| Taiwan | ||||||
| Quantitative comparative | ||||||
| Quasi-randomised trial | ||||||
| Hospital | ||||||
| Thick | ||||||
| De Jonge 2001171 | NA (n = NA); age: NA; gender: NA; cognitive impairment: NA | Multidisciplinary evaluation (n = NA/NA) | Patients and their families received a brochure describing expectations of the hospital’s course of treatment, goals for the patient and contact numbers for various disciplines on admission. Education of clinical staff from all involved disciplines occured formally through a monthly case conference. All patients receive daily evaluation by geriatricians and orthopedists, who discussed active problems and reached a consensus on a treatment plan. Patients usually began physical therapy on the first post-operative day. For uncomplicated cases, the goal was to transfer patients to home or to a rehabilitation setting by post-operative day 3 | NA (n = NA/NA) | NA | NA |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Work process and service restructuring | ||||||
| Hospital | ||||||
| Thick | ||||||
| Delmi 199096 | Patients with femoral neck fracture after an accidental fall (n = 59); age: > 60 years; gender: both; cognitive impairment: no | Dietary supplementation (n = 27/27) | 250 ml of oral nutritional supplement provided (254 kcal, 20 g of protein, 29 g of carbohydrate, 5–8 g of lipid, 525 mg of calcium, 750 IU of vitamin A, 25 IU of vitamin D3, vitamins E, B1, B2, B6, B12, C, nicotinamide, folate, calcium pantothenate, biotin and minerals). Supplementation was started on admission to the orthopaedic unit and continued throughout the stay in the second (recovery) hospital | Control (n = 32/32) | Control group | 6 months |
| Switzerland | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Deschodt 201197 | Verbally competent individuals with traumatic hip fracture (n = 171); age: ≥ 65 years; gender: both; cognitive impairment: partial | Inpatient geriatric consultation (n = 94/94) | The intervention team consisted of a geriatrician, three nurses, a social worker, two occupational therapists and a physiotherapist. Other disciplines were available on call. The intervention by the team included four successive steps: (1) comprehensive geriatric assessment, (2) in-depth multidisciplinary evaluation, (3) formal clinical advice and recommendations, and (4) in-hospital follow-up on request. Within 72 hours of the initial comprehensive geriatric assessment or in-depth multidisciplinary evaluation, the inpatient geriatric consultation team made specific and individualised recommendations in addition to and different from the usual care delivered by the trauma care team. Recommendations were included in participants’ electronic file and discussed among the team, and additional recommendations were made when necessary and patients’ electronic records were updated accordingly | Usual care (n = 77/77) | Evaluation of living conditions before admission by social workers, early mobilisation and rehabilitation by the physiotherapist, treatment with anticoagulants and non-opioid pain medication, and post-operative radiography of the hip | 12 months |
| Belgium | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Di Monaco 2008133 | Community-dwelling women who planned to return to the same dwelling at discharge (non-institutional); sustained their first hip fracture as a result of a fall; surgically operated on; referred for inpatient rehabilitation; no cognitive impairment, with a MMSE test score of > 23 (n = 95); age: ≥ 60 years; gender: female; cognitive impairment: no | Hospital plus home rehabilitation (n = 45/45) | All patients received a multidisciplinary intervention to prevent falls, as part of the usual rehabilitation protocol, consisting of 1–3 hours per day for 5 days a week of physical exercise to improve strength and balance, advice and training on the use of assistive devices and training in ADL conducted by physiotherapists and occupational therapists. At least 3 hours were devoted to a skilled occupational therapist assessing home hazards of falling on the basis of a standard checklist that took into account both the home environment and behaviour during ADL. The occupational therapist suggested targeted modifications of the home environment and behavioural changes to prevent falls. In addition, the geriatrician checked the possibility of withdrawing all medications known to increase the risk of falling. All patients received daily oral supplementation with vitamin D plus calcium. Additionally, the intervention group received a home visit by an occupational therapist at a median of 20 days after discharge from hospital, to reiterate the advice on preventing falls | Hospital rehabilitation alone (n = 50/50) | All patients received a multidisciplinary intervention to prevent falls, as part of the usual rehabilitation protocol, consisting of 1–3 hours per day for 5 days a week of physical exercise to improve strength and balance, advice and training on the use of assistive devices and training in ADL conducted by physiotherapists and occupational therapists. At least 3 hours were devoted to a skilled occupational therapist assessing home hazards of falling on the basis of a standard checklist that took into account both the home environment and behaviour during ADL. The occupational therapist suggested targeted modifications of the home environment and behavioural changes to prevent falls. In addition, the geriatrician checked the possibility of withdrawing all medications known to increase the risk of falling. All patients received daily oral supplementation with vitamin D plus calcium | 6 months |
| Italy | ||||||
| Quantitative comparative | ||||||
| Quasi-randomised trial | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Dy 2011159 | Medically stable male patients with hip fracture (n = 74); age: ≥ 55 years; gender: male; cognitive impairment: no | MOTS programme (n = 74/74) | This service was co-managed by attending and resident physicians from the internal medicine and orthopaedic surgery departments. A dedicated physician extender (nurse practitioner or physician assistant) was assigned to care for all patients. The programme consisted of the following: daily inpatient walking rounds led by the medical attending and including the orthopaedic resident, MOTS physician extender, physiotherapists, social workers and nursing staff; a co-ordinated plan to facilitate inpatient care, rehabilitation progress and discharge planning, delivered to the patient each morning; plans for rehabilitation therapy and discharge, discussed by the orthopaedic resident, physiotherapists and social workers on a patient-by-patient basis throughout the day; pre- and post-operative plans of care, co-ordinated through the physician extender after communicating with the orthopaedic and internal medicine residents and attending physicians; discussion of medical and surgical plans and findings, as well as plans for rehabilitation progress and discharge; and an afternoon debriefing session involving the MOTS physician extender, medical attending and orthopaedic resident | NA (n = NA/NA) | NA | NA |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Edwards 2004172 | NA (n = NA); age: NA; gender: NA; cognitive impairment: NA | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| Canada | ||||||
| Quantitative non-comparative | ||||||
| Work process and service restructuring | ||||||
| Hospital | ||||||
| Thick | ||||||
| Elinge 200398 | Patients of any age from Umeå principality of any age who were admitted to the hospital with a diagnosis of hip fracture or vertebral fracture (n = 35); age: ≥ 50 years; gender: both; cognitive impairment: no | Supervised group learning (n = 21/18) | The intervention group participated in a group learning programme; the intervention was carried out in four consecutive groups of five to eight participants. A geriatric team consisting of a dietitian, an occupational therapist, a physician, a physiotherapist and a social worker lectured in the programme. The participants were taught about the effects of osteoporosis, the risk factors for osteoporosis, how to avoid further falls and how to perform ADL in a safe way. Each session involved 1 hour of education and 1 hour of physical training, with weight-bearing exercises focusing on muscle strength and balance. Each participant also received an individually tailored home training plan | Usual care (n = 14/12) | The control group received scheduled assessments | 1 year |
| Sweden | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Fortinsky 200281 | Hip fracture patients living in the community and ambulatory at the time of the index hip fracture; English speaking; fracture occurred as a result of reasons other than multitrauma accident (e.g. automobile accident) or metastatic cancer (n = 24); age: ≥ 65 years; gender: both; cognitive impairment: no | Physical and occupational therapy (n = 24/24) | Physical and occupational therapy both in the hospital post surgery and at home after discharge | NA (n = NA/NA) | NA | 6 months |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Fox 1993200 | Two hospitals managing patients with hip fracture (n = 335); age: NA; gender: NA; cognitive impairment: no | In-hospital rehabilitation and discharge to own home policy (n = 142/142) | Patients whose independence was threatened were able to transfer to an orthopaedic rehabilitation unit with intensive physiotherapy and occupational therapy input | No in-hospital rehabilitation and discharge to own home policy (n = 193/193) | Hospital did not have a rehabilitation ward, operated an early discharge policy and used community hospitals for rehabilitation and convalescence and had better access to nursing home accommodation. Patients were rehabilitated on the acute ward and discharged rapidly to community hospitals or nursing home accommodation | Discharge |
| UK | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Fredman 2006142 | Patients hospitalised for hip fracture (n = 432); age: ≥ 65 years; gender: both; cognitive impairment: NR | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 34 months |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Community | ||||||
| Thick | ||||||
| Giangregorio 2009134 | Patients treated for a hip fracture by an orthopaedic surgeon and admitted for inpatient rehabilitation. Patients were deemed suitable if they had a stable fracture, adequate fixation and were able to follow two-step commands; their rehabilitation restrictions were to be 50% weight bearing or weight bearing as tolerated; and they were able to take a few steps with an assistive device (n = 21); age: ≥ 70 years; gender: both; cognitive impairment: no | Treadmill training (n = 14/10) | A treadmill and a suspension system were used during the intervention. The Pneumex Pneuweight (Pneumex, Sandpoint, ID, USA) is a pneumetic unweighting system that allows for the provision of up to 136 kg of body weight support. Participants were fitted into a specialised harness secured to an overhead cable that supported their body weight but did not produce discomfort or alter their gait pattern. Participants self-selected their walking speed at the start of each session and this was progressively increased with their improvement. Participants completed 2–3 bouts of walking, with resting by either sitting or standing in between, according to preference. Participants were encouraged to increase the duration of exercise. Participants began with walking bouts of ≤ 2–5 minutes according to tolerance, up to a total maximum time of 20 minutes. The maximum of 20 minutes was chosen to resemble actual clinical conditions, such that the physiotherapist would not normally walk in the hallway with the participant for > 20 minutes in any one session | Standard physiotherapy (n = 7/4) | Standard physiotherapy sessions including walking and bed exercises | 3 months |
| Canada | ||||||
| Quantitative comparative | ||||||
| Non-randomised trial/quasi-experimental study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Giusti 2006143 | Hip fracture patients living in the community (n = 199); age: ≥ 70 years; gender: both; cognitive impairment: no | Home-based rehabilitation (n = 95/95) | A geriatric care nurse developed a discharge plan with each patient and his/her proxies, including the choice of rehabilitation setting. Patients and their proxies were given detailed information about home rehabilitation services and skilled rehabilitation facilities available in the area. The decision whether to discharge patients to a home-care programme or to rehabilitation facilities was made by the patients themselves and/or their families. The specific content and duration of the training programme therapy were left to the discretion of the individual therapists. Usually, physiotherapists provided strengthening and range-of-motion exercises and instructed patients in gait and transfer training | Institutional-based rehabilitation (n = 99/99) | The specific content and duration of the training programme therapy were left to the discretion of the individual therapists. Usually, physiotherapists provided strengthening and range-of-motion exercises, and instructed their patients in gait and transfer training | 12 months |
| Italy | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Hagsten 200499 | Hip fracture patients; proficient in Swedish; lucid; living independently and not using walking aids (n = 100); age: > 65 years; gender: both; cognitive impairment: no | Occupational therapy (n = 50/50) | All patients receieved the same care for the first 3–4 days following surgery. The occupational therapist then provided indiviualised training for 45–60 minutes every weekday morning. The therapist and patient planned the training activities that were important for self-care at home. With support and supervision, patients trained as independently as possible to get up from the bed, use the bathroom and dress. Patients received training when necessary regarding technical aids. The therapist and patient decided together how to prepare and adapt the home environment for maximum independence | Usual care (n = 50/50) | Conventional care from the nursing staff | 2 months |
| Sweden | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Hauer 2003130 | Hip fracture patients with a recent history of injurious falls; consent of their orthopaedic surgeon; willingness to participate in the study (n = 57); age: > 75 years; gender: female; cognitive impairment: no | Strength training (n = 31/31) | Patients in the intervention group underwent a regimen of high-intensity progressive resistance training of functionally relevant muscle groups and a progressive functional training programme for 3 days per week for 12 weeks. Intensity of strength training was adjusted to fall between 70% and 90% of each individual’s maximal workload. Basic training in functions such as walking, stepping or balancing was progressive, and training tasks with increasing complexity were introduced in the training regimen and protocol | Inactive control (n = 26/26) | Patients met three times per week for 1 hour of motor placebo activities such as stretching or playing ball games while in a predominantly sitting position | 2 years |
| Germany | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Hoekstra 2011144 | Hip fracture patients requiring surgical intervention (n = 127); age: ≥ 65 years; gender: both; cognitive impairment: no | Multidisciplinary nutritional care (n = 61/61) | The multidisciplinary intervention focused on nutritional care from nurses, doctors and dietitians, tailored to individual patients’ physiological and medical needs. Patients were provided with a ‘nutrition during admission’ leaflet containing advice about how to raise their nutritional intake. At discharge, all disciplines gave oral and/or written transfers to caretakers, GPs or nursing home doctors to guarantee nutritional care. If necessary, oral supplements were continued at home | Standard nutritional care (n = 66/66) | Standard nutritional care | 3 months |
| The Netherlands | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Hoenig 1997168 | Hip fracture patients hospitalised in one of 297 randomly selected hospitals from 30 areas in five states, with 20% of patients being drawn from each state. Hospitals were selected to provide a nationally representative sample in terms of size, percentage urban vs. rural, percentage of Medicare patients and teaching status. Hospitals caring for the poor were oversampled by a factor of 2 (n = 2762); age: ≥ 65 years; gender: both; cognitive impairment: NA | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Database analysis | ||||||
| Hospital | ||||||
| Thick | ||||||
| Holmberg 1989160 | Hip fracture patients (n = 170); age: ≥ 65 years; gender: both; cognitive impairment: NA | Discharge home (n = 84/84) | Physiotherapy was supervised by a district physiotherapist on an outpatient basis. A part-time occupational therapist performed the activitiy of daily living tests and acted as the co-ordinator between the hospital and the district level. No extra resources were allocated at this level. Patients were encouraged to undertake full weight-bearing exercises the day after operation if possible; after assessment on the 10th post-operative day they were discharged to their own home for rehabilitation | Discharge to a rehabilitation hospital (n = 86/86) | Discharge to a rehabilitation hospital after acute treatment | 4 months |
| Sweden | ||||||
| Quantitative comparative | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Host 2007153 | Community dwelling with a recent proximal femur fracture and having a screening evaluation within 16 weeks of hip fracture repair; modified Physical Performance Test score of 12–28; self-reported difficulty or requirement for assistance with one or more ADL (n = 31); age: ≥ 65 years; gender: both; cognitive impairment: no | Supervised exercise training programme (n = 31/31) | The programme included two 3-month-long phases of exercise training. Phase 1: exercises were conducted by a physiotherapist using a group format (two to five subjects per group) and were designed to enhance flexibility, balance, co-ordination, movement speed and the strength of all major muscle groups. Twenty-two exercises formed the basis of this programme. Exercise sessions lasted for 45–90 minutes (with breaks). The exercises were made progressively more difficult by increasing the number of repetitions and by having the participants perform the exercises in more challenging ways, with tailoring according to each subject’s ability, tolerance and specific physical impairments. Participants also exercised on a stationary bicycle or treadmill if the therapist thought the patients were fit enough. Phase 2: progressive resistance training was added to the programme with the aim of exercising for 60 minutes per session plus another 30 minutes for the phase 1 exercises (focusing on balance, flexibility and core abdominal exercises) at least three times per week | NA (n = NA/NA) | NA | 6 months |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Controlled before-and-after study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Huang 2005100 | Hip fracture patients, hospitalised as a result of falling; discharged from a medical centre to the catchment area of the study centre (n = 126); age: ≥ 65 years; gender: both; cognitive impairment: no | Discharge planning (n = 63/63) | This intervention was designed on the following principles: (1) structure – formalise the discharge plan by providing written information and structured interactions with health-care providers; (2) process – within 24–48 hours of patients’ admission, start to assess their health-care needs; visit regularly (every 48 hours at least) during hospitalisation to assess, counsel, educate, co-ordinate and evaluate the health-care needs of patients and caregivers; use a multidisciplinary approach; promote communication between health-care-providing organisations; establish a follow-up programme; and involve patient and family; and (3) outcome – an assumption of discharge planning programmes is that they will be cost-effective and enhance patients’ quality of life. The discharge planning intervention was provided by a full-time, master’s-prepared gerontological nurse with 7 years’ experience in hospital and home care of older adults from hospital admission to 3 months after discharge. The nurse visited patients regularly and was available by telephone 7 days per week. Patients received two brochures with coloured step-by-step pictures and information on self-care and falls prevention. The nurse provided direct care, education and confirmation of learning with regard to both medication and environmental safety, as well as the proper employment of assistance devices. The nurse executed the set-up of home-care services and the assessment of rehabilitation facility needs | Routine care (n = 63/63) | Patients received routine hospital discharge planning, provided by nurses who were primarily diploma- or bachelor’s-prepared generalists. No brochures or written discharge summaries were given to patients in this group, nor did they receive any home visits or telephone contact | 3 months |
| Taiwan | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Huang 200982 | Older people aged ≥ 65 years who had experienced a hip fracture because of a fall in the last 12 months; living in the community; capable of self-care; verbal communication ability in Mandarin, Minanese or Hakkanese (n = 15); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| Taiwan | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Community | ||||||
| Thick | ||||||
| Huusko 2000101 | Patients with hip fracture; living independently; able to walk unaided before the fracture (n = 243); age: ≥ 65 years; gender: both; cognitive impairment: yes | Geriatric rehabilitation (n = 120/120) | The geriatric team at the central hospital consisted of a geriatrician internist, a specially trained GP, nurses with training in the care of older patients, a social worker, a neuropsychologist, an occupational therapist and physiotherapists. A consultant specialist in physical medicine, a neurologist and a psychiatrist worked with the team for up to 4 days each week. The intervention consisted of assessment by the geriatric team. Patients received physiotherapy sessions twice a day and daily activities were practised throughout the day with the nurses. The nurses and the physiotherapists had weekly joint meetings to discuss methods of improving rehabilitation. The daily schedule for each patient was planned to support early ambulation, self-motivation and the best possible functional ability. The physiotherapist evaluated walking aids. An occupational therapist evaluated the need for daily living aids and occupational therapy was offered to those patients who were thought able to benefit from it. Individualised patient and family counselling was provided by physiotherapists and nurses on several occasions and this was reinforced with a brochure on hip fracture. The discharge plan was checked during weekly team meetings with patients and their family, and the physiotherapist made a home visit before patients were discharged if the team thought that it was necessary. All patients who were discharged to independent living had 10 home visits from the physiotherapist | Standard care (n = 123/123) | Standard post-operative rehabilitation in a local hospital | Post surgery |
| Finland | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Jackson 200183 | Hip fracture patients willing to participate in the study and with the cognitive ability to participate in the therapy process (n = 24); age: ≥ 65 years; gender: both; cognitive impairment: no | Occupational adaptation model (n = NR/NR) | The occupational adaptation intervention focused on occupational goals determined by the patient. Participants also had to evaluate themselves on their perceived progress. Participants were allowed to choose the activities that they would work on to address their goals. The therapist’s role was to facilitate restoration of a functional internal adaptation process. The therapist conducted the required evaluations. The intervention was planned around occupational readiness (e.g. increasing strength) and occupational activity (patient-selected activity that is personally meaningful). After the baseline assessments and with the patients’ agreement, the intervention was implemented in the following way: occupational roles or meaningful activities identified; required energy and assist levels for discharge discussed on the basis of patients’ desires and environment situation; training provided for occupational readiness tasks, such as education in hip precautions, ADL, functional mobility and environmental mobility, and for occupational activities based on patients’ identified roles, such as cooking, household tasks and car transfers, and patients were given the choice of tasks and activities and were able to control the therapy process by working on tasks important to them, with the therapist making suggestions and recommendations as needed | Biomedical rehabilitation model (n = NR/NR) | The biomedical rehabilitation intervention began with an evaluation of patients’ physical segments, including head, trunk and extremities, to determine the strengths and deficits that affect functional abilities for ADL. The environment was modified or assistive equipment was used to promote independence in ADL. After the baseline assessments and with the patients’ agreement, the intervention was implemented in the following way: identification of goals that the facility traditionally viewed as appropriate for this patient group; discussion of goals with patients; education in hip precautions provided as well as training in ADL, functional mobility, environmental mobility and upper-extremity strengthening; patients given formal weekly feedback on progress; and informal feedback given during the course of the intervention and when requested by patients | At discharge |
| USA | ||||||
| Quantitative comparative | ||||||
| Quasi-randomised trial | ||||||
| Hospital | ||||||
| Rich | ||||||
| Jellesmark 201284 | Community-dwelling hip fracture patients who had the ability to walk independently at discharge. Criteria for participating in the in-depth interviews were high degree of fear of falling, varying levels of functional ability and ability to verbalise the situation in detail (n = 33 surveys, n = 4 interviews); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 6 months post hospital discharge |
| Denmark | ||||||
| Mixed methods | ||||||
| Mixed methods | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Jensen 1979154 | Femoral neck or trochanteric fracture patients (n = 518); age: any; gender: both; cognitive impairment: no | Physical rehabilitation (n = 518/518) | The physical rehabilitation programme consisted of 6 weeks of partial weight-bearing mobilisation with emphasis on early weight bearing. If the rehabilitation programme did not progress satisfactorily within the first 2–3 weeks, patients were discharged to a convalescent home with facilities for physical therapy or to a rehabilitation clinic with a highly developed sociomedical care system. Patients were discharged from hospital or institutions as soon as they were able to walk and undertake ADL | NA (n = NA/NA) | NA | 6 months |
| Denmark | ||||||
| Quantitative non-comparative | ||||||
| Controlled before-and-after study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Johansen 2012145 | Men and women considered to have rehabilitation potential with stroke, osteoarthritis, hip fracture, ageing disability, loss of function because of long periods of hospitalisation or other chronic, slowly progressing diseases (n = 302); age: > 65 years; gender: both; cognitive impairment: partial | District rehabilitation centre (n = 202/202) | District rehabilitation centre (model 1) | Standard rehabilitation (n = 100/100) | Standard primary health-care rehabilitation (model 2) | 3 months after rehabilitation |
| Norway | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Community | ||||||
| Thick | ||||||
| Jones 2002195 | Hip fracture patients who had potential for improvement (n = 100); age: ≥ 60 years; gender: both; cognitive impairment: no | Inpatient rehabilitation (n = 100/44) | All patients with hip fracture were referred for intensive rehabilitation after surgical repair, which typically included both physical therapy (approximately 1.5 hours per day) and occupational therapy (approximately 1.0 hour per day), 5 days per week for a period of 3–6 weeks | NA (n = NA/NA) | NA | 6 weeks |
| Canada | ||||||
| Quantitative non-comparative | ||||||
| Controlled before-and-after study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Jones 2006135 | Good cognitive function (MMSE score of > 24); residing at and planning to return home after standard inpatient rehabilitation care for hip fracture (n = 25); age: ≥ 65 years; gender: both; cognitive impairment: no | Community exercise programme (n = 17/17) | The community exercise programme was led by an older adult-certified fitness instructor. The programme included a 5-minute warm-up period consisting of a range of exercises for the upper and lower body, 10–25 minutes of continuous stepping exercises, which involved participants ascending and descending a single-step platform, 10–15 minutes of lower-extremity strengthening exercises performed in a weight-bearing position and a 5- to 10-minute cool-down period that incorporated both range-of-motion and balance-training activities. The stepping exercises were performed using standard Reebok step platforms (Reebok, Canton, MA, USA) approximately 10.5-cm high. The height of the platforms was increased in 10.5-cm increments throughout the intervention. A wall-mounted safety bar was used for support, but as the participants progressed to the higher stepping levels they were encouraged to manage unassisted. Each stepping level was progressively more challenging, beginning with raising the step each time, to stepping without assistance to stepping over the platform entirely. Strengthening exercises were used to train muscle endurance. Particpants began with one set of five repetitions and progressed to two sets of 10–15 repetitions. All strengthening exercises were performed in a standing position so that muscle and joint positions were similar to those used for weight bearing. Ankle weights were used to provide resistance for hip-strengthening exercises. Participants started with 1.5 lb per ankle and progressed to a maximum of 3.5 lb per ankle. All exercises were performed slowly and with control | Standard outpatient therapy (n = 8/8) | Standard outpatient therapy | 16 weeks |
| Canada | ||||||
| Quantitative comparative | ||||||
| Non-randomised trial/quasi-experimental study | ||||||
| Community | ||||||
| Thick | ||||||
| Kammerlander 2011178 | Hip fracture patients (n = 246); age: ≥ 80 years; gender: both; cognitive impairment: NR | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 5 years |
| Austria | ||||||
| Quantitative non-comparative | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Kennie 1988102 | Hip fracture female patients (n = 108); age: ≥ 65 years; gender: female; cognitive impairment: no | Multidisciplinary rehabilitation in a community hospital (n = 54/54) | Patients were transferred to orthopaedic beds in a peripheral hospital. A GP provided day-to-day medical attention and a consultant physician in geriatric medicine attended two ward rounds and one conference of the multidisciplinary team each week. An orthopaedic specialist was not routinely present, but advice was available on demand. Patients received physiotherapy, occupational therapy and orthotic and other services | Routine care with early discharge home (n = 54/54) | Patients received regular attention on orthopaedic ward rounds and the demand for beds encouraged their early discharge. Patients received physiotherapy, occupational therapy and orthotic and other services | 1 year |
| UK | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Kerr 2011173 | Patients who experienced a hip fracture in the previous 2–18 months (n = 21); age: ≥ 50 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| USA | Non-pathological fracture patients; able to walk before the fracture; cognitively intact; living in own home or apartment (n = 609); age: ≥ 65 years; gender: both; cognitive impairment: no | Inpatient rehabilitation (n = 308/308) | In addition to standard care, patients received 2 hours of physical therapy 7 days per week for gait training, stair climbing, transfers, range-of-motion exercises and strengthening of the upper and lower extremities. They also received 1 hour of occupational therapy 7 days per week for instruction in ADL. There were weekly conferences with patients and family members, with an emphasis on establishing realistic short- and long-term goals and expectations. Family members were encouraged to participate in the therapy sessions and were taught how to perform range-of-motion and strengthening exercises. Decisions regarding the discharge of patients from the rehabilitation programme and the need for home-care services were made by consensus of a multidisciplinary group, with input from patients and family members, and were based on patients’ achievement of their short-term goals | Standard care available before implementation of the inpatient rehabilitation programme (n = 301/301) | Standard care involved early mobilisation on the first day post-operatively and walking with weight bearing as tolerated. During the acute care period, patients were seen by a physiotherapist for 30 minutes once or twice a day on weekdays and once a day at weekends and during holidays. The physical therapy sessions involved gait training, stair climbing, transfers, range-of-motion exercises and strengthening of the upper and lower extremities. Before discharge from hospital, patients were seen once by an occupational therapist for assessment and instruction in ADL | 12 months |
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital | ||||||
| Thick | ||||||
| Koval 1998146 | Non-pathological fracture patients; able to walk before the fracture; cognitively intact; living in own home or apartment (n = 609); age: ≥ 65 years; gender: both; cognitive impairment: no | Inpatient rehabilitation (n = 308/308) | In addition to standard care, patients received 2 hours of physical therapy 7 days per week for gait training, stair climbing, transfers, range-of-motion exercises and strengthening of the upper and lower extremities. They also received 1 hour of occupational therapy 7 days per week for instruction in ADL. There were weekly conferences with the patient and family, with an emphasis on establishing realistic short- and long-term goals and expectations. Family members were encouraged to participate in the therapy sessions and were taught how to perform range-of-motion and strengthening exercises. Decisions regarding the discharge of patients from the rehabilitation programme and the need for home-care services were made by consensus of a multidisciplinary group, with input from patients and their family, and were based on patients’ achievement of their short-term goals | Standard care available before implementation of inpatient rehabilitation programme (n = 301/301) | Early mobilisation and walking with weight bearing as tolerated was aimed for on the first day post-operatively. During the acute-care period, patients were seen by a physiotherapist for 30 minutes once or twice a day on weekdays and once a day at weekends and on holidays. The physiotherapy sessions involved gait training, stair climbing, transfers, range-of-motion exercises and strengthening of the upper and lower extremities. Before discharge from hospital, patients were seen once by an occupational therapist for assessment and instruction in ADL | 12 months |
| USA | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Kuisma 2002103 | Patients with a fractured proximal femur (n = 81); age: ≥ 50 years; gender: both; cognitive impairment: no | Home-based physiotherapy (n = 40/40) | Intervention (physiotherapy at home) group | Institution-based physiotherapy (n = 41/41) | Control (conventional institution-based rehabilitation) group | 12 months |
| Hong Kong | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Latham 2006167 | Hip fracture patients who received rehabilitation in skilled nursing facilities (n = 351); age: any; gender: both; cognitive impairment: no | Rehabilitation in a skilled nursing facility) (n = 351/351) | Rehabilitation in a skilled nursing facility | NA (n = NA/NA) | NA | At discharge |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Database analysis | ||||||
| Hospital | ||||||
| Thick | ||||||
| Lauridsen 2002104 | Fully mobile prior to fracture; full weight bearing; no concomitant disabling disorders; transferred for rehabilitation within 3 weeks of surgery (n = 88); age: 60–89 years; gender: female; cognitive impairment: partial | Intensified physical therapy (n = 44/44) | Training programme consisted of bench exercises (warming up, range of motion, strength, endurance, stretching, stabilising), gait training, balance and co-ordination training, stair climbing and, in some cases, hydrotherapy | Usual care (n = 44/44) | Usual care | NA |
| Denmark | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Levi 1997147 | Community-living with hip fracture treated surgically (n = 123); age: ≥ 65 years; gender: female; cognitive impairment: no | Comparison of discharge practices of four hospitals and discharge destinations (n = 123/123) | Comparison of discharge practices of four hospitals and discharge destinations | NA (n = NA/NA) | NA | 6 months |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Li 2007189 | Care receivers: age ≥ 65 years, hospitalised as a result of hip fracture and surgery for internal fixation or arthroplasty; living in northern Taiwan; no cognitive impairment. Caregivers had to be ≥ 18 years and taking primary responsibility for the care receiver (n = 20); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 3 months |
| China | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Lieberman 2002148 | Hip fracture patients hospitalised for rehabilitation after surgical repair (n = 424); age: ≥ 75 years; gender: both; cognitive impairment: no | Older group (≥ 85 years) geriatric ward rehabilitation (n = 127/127) | Patients eligible for rehabilitation were transferred to the geriatric ward, where they underwent a conventional rehabilitation programme | Younger group (75–84 years) geriatric ward rehabilitation (n = 297/297) | Patients eligible for rehabilitation were transferred to the geriatric ward, where they underwent a conventional rehabilitation programme | At discharge |
| Israel | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Lieberman 2006179 | Patients hospitalised for hip fracture and suitable for conventional rehabilitation (n = 946); age: ≥ 65 years; gender: both; cognitive impairment: partial | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| Israel | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Lin 2004190 | Patients with either femoral neck fracture or intertrochanteric fracture (n = 103); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 1 year |
| Taiwan | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Lin 2009105 | Hip fracture patients; able to walk; mentally alert and able to communicate; living in the vicinity of the study centre (n = 50); age: ≥ 65 years; gender: both; cognitive impairment: no | Comprehensive discharge planning (n = 26/26) | The programme consisted of a structured assessment of discharge planning needs, systematic individualised nursing instruction based on patients’ individual needs, monitoring of services and co-ordinated resources and arranging of referral placements for each patient. After discharge, two home visits were conducted to provide necessary support and consultation. Patients were provided with a health education booklet developed by the research team | Routine discharge nursing care (n = 24/24) | Nurses who cared for patients provided the discharge service and gave non-structured discharge instructions according to their own professional judgement, without following a standardised procedure | Post discharge |
| Taiwan | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Lindelof 2002180 | Able to understand simple instructions and with perceived mobility problems following hip fracture at least 6 months previously (n = 3); age: ≥ 78–82 years; gender: female; cognitive impairment: no | Supervised functional training (n = 3/3) | Combined functional training with a weighted belt, supervised by a physiotherapist. A detailed diary was also kept for each participant to record experiences of the intervention, feelings of well-being and any reported pain or discomfort | NA (n = NA/NA) | NA | 10 weeks |
| Sweden | ||||||
| Quantitative comparative | ||||||
| Controlled before-and-after study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Long 2002198 | Health professionals providing rehabilitation services (n = 49); age: NA; gender: both; cognitive impairment: NA | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| UK | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital | ||||||
| Thick | ||||||
| Louie 2012106 | Current diagnosis of avascular necrosis of the femoral head/osteoarthritis of the hip and traumatic hip fracture; fractures of the neck of the femur and trochanter of the femur; Cantonese version of the MMSE baseline score of ≥ 16; one main carer (able to provide > 8 hours’ care to the participant every day) willing to participate in the programme (n = 134); age: ≥ 65 years; gender: both; cognitive impairment: no | PCEP (n = 63/63) | The programme was designed as follows: (1) deliver disease-specific education and hands-on ADL skills training to both patients with hip fractures and their carers; (2) facilitate goal-setting and problem-solving skills of patients throughout the programme; and (3) improve the confidence of patients with hip fractures and reduce their fear of falling with regard to ADL. Five 1-hour sessions of PCEP for hip fractures were conducted once daily. Before the first session, the participants were asked to set their goals for the programme. The first session of the programme included a 1-hour educational group session on knowledge about hip fractures, adapted ADL skills and falls prevention strategies. An information booklet was provided for participants after the session. This was followed by four 1-hour sessions of ADL drills with a group size of six to eight patients and carers. Skills practised in these four sessions included bed-to-chair transfer, toileting, lower-garment dressing, and donning and doffing of socks and shoes. The techniques used throughout the sessions were teaching and learning methods, sharing, goal-setting for each session, peer support, hands-on demonstrations and practice. At least one session of carer training was provided to the main carers of the participants to strengthen their caregiving and proper handling techniques | Conventional care (n = 71/71) | Participants were provided with remedial activities and individual ADL training according to the conventional hip fracture rehabilitation protocol throughout the rehabilitation phase | 5 days post programme |
| Hong Kong | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Rich | ||||||
| Mangione 2010107 | Successful fixation of a hip fracture within the previous 6 months; living at home before the fracture; physician referral; discharged from physical therapy (n = 26); age: > 65 years; gender: both; cognitive impairment: no | Leg-strengthening exercises (n = 14/14) | Leg-strengthening exercises for the hip extensors and abductors, knee extensors and ankle plantar flexors bilaterally were provided by licensed physiotherapists twice a week for 10 weeks, with each session lasting approximately 30–40 minutes. A portable progressive resistive exercise machine was used for the hip and knee muscles; body weight was used for the ankle muscles. The physiotherapist determined the amount of resistance that the patient could push against to complete a maximum of eight repetitions. Intensity was re-evaluated every 2 weeks and the resistance was increased if the patient was able to complete eight repetitions at the higher load comfortably | Conventional transcutaneous electrical nerve stimulation (n = 12/12) | Bilateral gluteal muscles (hip extensors and abductors), knee extensors and ankle plantar flexors were stimulated for 7 minutes for a total of 21 minutes each session. The physiotherapist adjusted the intensity of the stimulation until the participant reported feeling a comfortable tingling in the muscle bellies. No visible muscle contraction was elicited. The initial intensity was not changed over the course of the study. During transcutaneous electrical nerve stimulation, guided imagery was used to encourage the participant to envisage the leg muscles being used in activities involving rising up on the toes, rising from a squatting position and climbing a steep incline | 6 months |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Rich | ||||||
| McKee 200285 | Hip fracture patients admitted to hospital as a result of a fall (n = 57); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 2 months |
| UK | ||||||
| Mixed methods | ||||||
| Controlled before-and-after study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| McMillan 201286 | Patients who sustained a fall-induced hip fracture and who were discharged home within 3 months (n = 27); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 3 months |
| UK | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital and community | ||||||
| Rich | ||||||
| Mendelsohn 2008108 | Unilateral hip fracture patients who had a weight-bearing capactiy of at least 25% (n = 20); age: ≥ 70 years; gender: both; cognitive impairment: no | Upper-body exercise plus standard rehabilitation care (n = 10/10) | The exercise-training programme included three sessions per week for 4 weeks. Each session included a warm-up period (5 minutes) at no resistance (0 W), an endurance phase (20 minutes) and a cool-down period (5 minutes) at 0 W. Intensive rehabilitation sessions (including physiotherapy and occupational therapy) were conducted 5 days per week for 45 minutes per session for a period of 4 weeks. Each session included range-of-motion, flexibility and strengthening exercises, balance, gait and stair retraining and training in ADL (e.g. assistive device use, co-ordination, dressing, grooming, eating and drinking, transferring in and out of bed, rising from a chair, going up and down stairs) | Standard rehabilitation care care (n = 10/10) | Intensive rehabilitation sessions (including physiotherapy and occupational therapy) were conducted 5 days per week for 45 minutes per session for a period of 4 weeks. Each session included range-of-motion, flexibility and strengthening exercises, balance, gait and stair retraining, and training in ADL (e.g. assistive device use, co-ordination, dressing, grooming, eating and drinking, transferring in and out of bed, rising from a chair, going up and down stairs) | At discharge |
| Canada | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Mitchell 2001109 | Fracture treated surgically (n = 80); age: ≥ 65 years; gender: both; cognitive impairment: no | Quadriceps training plus standard physiotherapy (n = 40/40) | Patients underwent twice-weekly progressive training of their quadriceps in both the recently fractured and the unaffected leg. Initially, the investigator determined the one-repetition maximum (1RM) of the quadriceps muscle group. This measure is the maximum load that an individual can lift through the full range of knee extension. The training was as follows. Weeks 1 and 2: training was carried out at 50% of the 1RM. The participants performed three sets of 12 repetitions of knee extension with each leg (6–9 seconds per repetition, with 2 minutes rest period between sets). These sets of exercises were carried out with a knee angle from 90° to 0° and then repeated with a knee angle from 10° to 0°. Weeks 3 and 4: patients’ 1RM was re-established and they then trained at 70% of their new 1RM, with sets and repetitions as above. Weeks 5 and 6: the 1RM was re-established and patients trained at 80% of the new 1RM, with sets and repetitions as for weeks 1 and 2 | Standard physiotherapy (n = 40/40) | Standard treatment consisted of physiotherapy (5 days per week) for approximately 20 minutes per day. Initially, the treatment included bed exercises with active assisted hip flexion and abduction of the fractured leg using a re-education board. This progressed to active exercises of both the affected and the unaffected limb. Once out of bed, the physiotherapist taught the patients bed and chair transfers and provided gait re-education and balance training. Practice of functional activities was carried out in the physiotherapy gym and involved sit-to-stand exercises and walking practice using an obstacle course. Walking aids were changed according to patients’ level of functional dependence. Activities in the parallel bars included sidestepping, backward walking and walking over obstacles. Balance exercises were also practised within the parallel bars | 4 months |
| UK | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Moore 1993181 | Hip fracture patients (n = 32); age: NR; gender: both; cognitive impairment: no | Physiotherapy (n = 32/32) | Physiotherapy (n = 32) and occupational therapy (n = 10) | NA (n = NA/NA) | NA | 6 weeks |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Morghen 2011182 | Admitted to hospital for post-hip fracture surgery rehabilitation (n = 230); age: > 65 years; gender: both; cognitive impairment: yes | Intensive physical therapy (n = 230) | All subjects received intensive physical therapy rehabilitation twice a day (6 days per week). Each session started with a 15-minute warm-up and ended with a 10-minute cool-down phase. The rehabilitation training included strengthening exercises, transfer, postural and gait training, and adaptive equipment training, according to physiotherapist evaluation of individual needs. At the beginning of each rehabilitation session the physiotherapist explained the nature and goal of the exercises. Strengthening exercises were initially used in all patients with gait disorders. Generally, each session consisted of a 40-minute phase including leg extension, leg curl, step-up, upright row, abductions, adductions and pelvic tilt. When patients required a rest, a brief interruption (no longer than 1 minute) was allowed | NA (n = NA/NA) | NA | 1 year |
| Italy | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Moseley 2009110 | Hip fracture patients with surgical fixation admitted to the inpatient rehabilitation unit; approval to weight bear or partial weight bear; able to tolerate the exercise programmes; able to take four plus steps with a forearm support frame and the assistance of one person; no medical contraindications that would limit the ability to exercise; living at home or in a low-care residential facility prior to the hip fracture and planning to return to this accommodation at discharge. Subjects with cognitive impairment were included if a carer who was able to supervise the exercise programme was available (n = 160); age: ≥ 70 years; gender: both; cognitive impairment: yes (if carer available) | Higher-dose weight-bearing exercise (n = 80/80) | Weight-bearing exercise was carried out twice daily for a total of 60 minutes per day for 16 weeks. Five weight-bearing exercises were prescribed in addition to walking on a treadmill with partial body weight support using a harness (for inpatients) or a walking programme (after hospital discharge at patients’ place of residence). The five weight-bearing exercises used for both legs were stepping in different directions, standing up and sitting down, tapping the foot and stepping on and off a block. The exercises were progressed by reducing support from the hands, increasing block height, decreasing chair height and increasing the number of repetitions. This commenced as an inpatient programme and was followed by home visits and a structured home exercise programme after inpatient discharge. All participants received usual post-operative mobilisation (e.g. walking practice in the ward) and the rehabilitation programme usually provided by other health professionals (e.g. occupational therapists) and any gait aids were progressed as per usual protocols. No other physiotherapy treatments were administered | Lower-dose limited weight-bearing exercise (n = 80/80) | Patients performed five exercises in a sitting or lying position plus a small amount of walking using parallel bars or walking aids for a total of 30 minutes each day for 4 weeks. The exercises were progressed by increasing the repetitions and resistance. This commenced as an inpatient programme and was followed by weekly home visits and a structured home exercise programme incorporating the same exercises. After 4 weeks, participants were provided with a tailored programme of limited weight-bearing exercises and were encouraged to continue exercising; no further physiotherapy home visits were undertaken. All participants received usual post-operative mobilisation (e.g. walking practice in the ward), and the rehabilitation programme usually provided by other health professionals (e.g. occupational therapists) and any gait aids were progressed as per usual protocols. No other physiotherapy treatments were administered | 16 weeks |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Munin 2005149 | Hip fractures patients who had surgical stabilisation of the fracture; living in the community pre fracture (n = 76); age: ≥ 60 years; gender: both; cognitive impairment: no | Inpatient rehabilitation facility (n = 42/42) | A minimum of 3 hours of combined physical therapy and occupational therapy was provided per day. Rehabilitation nurses and physicians also worked in a multidisciplinary fashion to provide daily care | Skilled nursing facilities rehabilitaiton (n = 34/34) | No specific intensity or type of therapy programme was provided. Weekend therapy services were not usually included, nursing staffing ratios were lower and patients had less contact with physicians | 6 months |
| USA | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Naglie 2002111 | Hip fracture patients from the community and from nursing homes who underwent surgical repair (n = 279); age: ≥ 70 years; gender: both; cognitive impairment: no | Post-operative interdisciplinary care (n = 141/141) | The programme included standardised measures to prevent common problems in patients with hip fracture (e.g. delirium, urinary problems, constipation, pressure sores, venous thrombosis, polypharmacy, malnutrition and depression), early mobilisation (full weight bearing and twice-daily physiotherapy sessions), early participation in self-care and individualised discharge planning (e.g. pre-discharge home visits, home care and additional rehabilitation in a rehabilitation facility). All nursing staff on the interdisciplinary care ward received specialised education about the care of elderly patients with hip fracture. A physiotherapist, occupational therapist, clinical nurse specialist and social worker assigned to the ward routinely assessed all study patients within 72 hours. Patients received routine post-operative surgical care, as well as daily medical care by a senior internal medicine resident supervised by an internist-geriatrician | Usual care (n = 138/138) | Patients had access to allied health-care professionals if a consultation was requested, but they had limited access to an occupational therapist or a clinical nurse specialist. Patients received routine post-operative surgical care only, which could include a geriatric consultation | 6 months |
| Canada | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Nicholson 1997136 | Patients unable to adequately perform essential ADL; lives alone or had other complications; in stable health (n = 30); age: ≥ 70 years; gender: both; cognitive impairment: no | Supervised exercise intervention (n = 20/20) | The programme consisted of supervised 50-minute chair exercise sessions. Participants sat facing inward on straight-backed chairs in a circle formation with adequate space to allow for unhindered lateral movements. The choreographed seated exercise routine was high paced and included relatively complex movement co-ordinations. The exercise was adapted to individual capacity and ability. Exercise sessions were conducted daily on a four exercise periods per subject basis. The same physiotherapist led all of the exercise classes. Classes began with a 10-minute warm-up and then the pace increased, with emphasis on both muscle endurance and range of movement | Routine care (n = 10/10) | Routine care (no detail provided) | 6 weeks |
| South Africa | ||||||
| Quantitative comparative | ||||||
| Non-randomised trial/quasi-experimental study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Ohsawa 2007137 | Frail elderly patients with displaced intracapsular fracture of the proximal femur who had poor general condition and refused to have an operation (n = 20); age: ≥ 80 years; gender: both; cognitive impairment: no | Assertive therapy (n = 13/13) | The programme consisted of standing on the fractured limb and walking in parallel bars as soon as possible after hospital admission for the fracture. Patients performed range-of-motion exercises for the affected hip joint within tolerable extent while sitting on one side of the bed. When patients could sit in a wheelchair for a while, they performed standing on the sound leg using a tilted table. This procedure started within 1 month of the start of rehabilitation. Gradual weight bearing was then imposed on the affected leg. When patients could tolerate weight bearing on the affected leg, they were encouraged to stand on both legs and to increase weight bearing on the affected leg | Conventional care (n = 7/7) | The injured limb was immobilised under skin traction and then patients gradually tried to use a wheelchair for pain reduction | 6 months |
| Japan | ||||||
| Quantitative comparative | ||||||
| Non-randomised trial/quasi-experimental study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Oldmeadow 200687 | Patients with an acute neck of femur fracture (n = 60); age: ≥ 70 years; gender: both; cognitive impairment: no | Early ambulation (n = 29/29) | Patients walked for the first time after their surgery with a physiotherapist(s) during standard work hours and as soon as possible on post-operative day 1 or 2. The physiotherapy ambulation re-education programme was implemented once per day over 7 days. This programme was the same for all and included walking re-education, bed exercises and chest physiotherapy as indicated. All patients received routine post-operative medical and nursing clinical care. All patients were transferred to sit out of bed as early as possible after surgery | Delayed ambulation (n = 31/31) | Patients did not commence walking until post-operative day 3 or 4. The physiotherapy ambulation re-education programme was implemented once per day over 7 days. This programme was the same for all and included walking re-education, bed exercises and chest physiotherapy as indicated. All patients received routine post-operative medical and nursing clinical care. All patients were transferred to sit out of bed as early as possible after surgery | 7 days |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Olsson 200788 | Patients acutely operated on for a hip fracture; non-institutional residence (n = 13); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | Post surgery |
| Sweden | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital | ||||||
| Thick | ||||||
| Orwig 2011191 | Community-dwelling women admitted within 72 hours of a non-pathological hip fracture receiving surgical repair (n = 180); age: ≥ 65 years; gender: female; cognitive impairment: no | In-home exercise intervention (n = 91/91) | The programme consisted of an exercise component and a self-efficacy-based motivational component, and was initiated at completion of skilled rehabilitation services by exercise trainers in participants’ post-acute discharge location. Participants received three trainer-supervised exercise sessions per week during the first 2 months and then two supervised sessions per week for the following 2 months. The frequency then dropped to once a week and then once every other week for a maximum of 56 supervised sessions by the end of the protocol. The trainer supplemented the decrease in supervised sessions with telephone calls to remind participants to exercise and address any questions or concerns. The exercise sessions combined aerobic exercise using a Stairstep, a comprehensive strengthening programme that covered the main muscle groups relevant to hip fracture recovery and stretching exercises (20- to 30-minute warm-up and cool-down periods). Strength training included a series of 11 exercises for the upper and lower extremities. The duration of each exercise was increased until participants could perform three sets of 10 repetitions on both sides. The intensity was then augmented by increasing the resistance of the exercises. The duration of aerobic stepping was increased with the goal of completing 30 minutes of continued stepping. Once participants could perform 20 minutes, light ankle weights were added to increase the exercise intensity | Usual care (n = 89/89) | Patients received the physician-prescribed post-fracture standard of care for patients with hip fracture, which included a relatively short hospital stay and approximately 2–4 weeks of rehabilitation | 1 year |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Oude Voshaar 200712 | Patients who had undergone surgery for a fractured neck of femur (n = 291); age: > 60 years; gender: both; cognitive impairment: partial | Psychological intervention (n = 291/291) | Six weekly sessions consisting of meetings with a psychiatric nurse based on liaison principles (for referral or medication if needed) and including a cognitive–behavioural approach to treat depression | NA (n = NA/NA) | NA | 6 months |
| UK | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Peiris 2012112 | Patients admitted for rehabilitation in the orthopaedic ward with a lower-limb orthopaedic condition; able to walk independently or with assistance; cognitively alert (n = 105); age: ≥ 18 years; gender: both; cognitive impairment: no | Additional physical therapy sessions at the weekend (n = 51/51) | Usual care physiotherapy and occupational therapy, 1–3 hours per day, from Monday to Friday plus an additional full occupational therapy and physiotherapy session on Saturday | Usual care (n = 54/54) | Usual care physiotherapy and occupational therapy, 1–3 hours per day, from Monday to Friday | 7 days |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Penrod 2004192 | Patients hospitalised for hip fracture (n = 443); age: ≥ 50 years; gender: both; cognitive impairment: no | Physiotherapy and occupational therapy (n = 443/443) | Patients were grouped into ‘early physiotherapy’ if they received physiotherapy from the day of surgery to post-operative day 3, and into ‘late physiotherapy’ if they received physiotherapy from post-operative day 4 to 8 weeks post admission. The number of physiotherapy and occupational therapy sessions the patients received and for how long were also taken into consideration | NA (n = NA/NA) | NA | 6 months |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Peterson 2004113 | Patients admitted to the fracture service; community dwelling within the tri-state area; ambulatory with or without assistive device prior to fracture; MMSE score of ≥ 24; able to understand English; fracture resulting from a mechanical fall (n = 70); age: ≥ 65 years; gender: both; cognitive impairment: NA | Intensive strength training (n = 38/38) | Following conventional rehabilitation, patients in the intervention group began a programe of high-intensity circuit training exercises based on the results of the physical therapy evaluation that took place in the first exercise session. Eight exercise stations were incorporated into the treatment sessions. At the first station exercises were performed with free weights, with the level of resistance set at 60% of the the one-repetition maximum (1RM) for hip flexors and knee extensors. Resistance was increased in accordance with participants’ tolerance. The second exercise station was the Kinetron (Cybex International, Inc., Medway, MA, USA), an isokinetic training device that provides resistance as the limb moves, at a constant speed of motion, to the hip flexors and knee extensors. The third station was an isotonic hip abduction machine, which provided constant resistance to the hip abductors. The fourth station was another isokinetic machine that provided resistance to the quadriceps and hamstrings. The fifth station was an upper-body ergometer that provided constant resistance and varied speed for cardiovascular endurance training. The sixth station was the total gym, which provided constant resistance and varied speed to the hip flexors and extensors and knee flexors and extensors. The seventh station was the therapy ball, used for balance activities. The eighth station was the stationary bicycle, used for cardiovascular training. Other components included a motivational video, a patient handbook and peer visiting | Inactive control (n = 32/32) | Conventional care | 1 year |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Petrella 2000169 | Hip fracture patients who were admitted to the rehabilitation facility (n = 56); age: ≥ 65 years; gender: both; cognitive impairment: no | Intensive rehabilitation (n = 56/56) | Intensive rehabilitation sessions (including occupational and physical therapy) on a daily basis (≈80 minutes per session) for an anticipated period of 3–6 weeks (average stay 31.8 ± 13.6 days) | NA (n = NA/NA) | NA | 12 months |
| Canada | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Portegijs 2008114 | Community-living femoral neck or trochanteric fracture patients; fracture occurred from 6 months to 7 years before baseline (n = 46); age: 60–85 years; gender: both; cognitive impairment: no | Tailored strength–power training (n = 24/24) | A 12-week individually tailored training programme carried out twice a week (1–1.5 hours) in a gym, supervised by an experienced physiotherapist. The weaker leg was trained first in every exercise, and more sets and repetitions and/or a higher resistance were used. Each training session included both strength and power exercises and started with a 10-minute warm-up sitting on a chair. The first two training sessions were used to familiarise participants with the facility, equipment and staff. A physician was consulted for all pain and other medical symptoms emerging during the training period. This was to ascertain which of the symptoms were likely to be related to the training and whether or not they affected the training | Usual care (n = 22/22) | The control group did not receive any intervention. Participants were encouraged to continue their lives as usual and maintain their pre-study level of physical activity during the 12-week trial | 3 months |
| Finland | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Portegijs 2012166 | Community-dwelling people who had been previously operated on for femoral neck or trochanteric fracture (n = 130); age: ≥ 60 years; gender: both; cognitive impairment: partial | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 7.5 years since fracture |
| Finland | ||||||
| Quantitative comparative | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Proctor 200813 | Case studies (n = 3); age: NR; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| UK | ||||||
| Case studies | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Rich | ||||||
| Pryor 1988150 | Hip fracture patients (n = 200); age: any; gender: both; cognitive impairment: no | Early discharge plus inpatient rehabilitation (n = 154/154) | Patients were suitable for early discharge and resided within the catchmnent of the hospital-at-home programme. After identification of patients suitable for early discharge, the process and the facilities available were explained to patients and relatives or friends. Occupational therapists visited the patients’ home before discharge to fit the necessary equipment. The hours of home nursing to be allocated to patients were determined initially by the liaison sister in consultation with patients, relatives and the community nursing service. Once patients were discharged, the team physiotherapist visited regularly (two to three times per week). Follow-up was by the surgeon at outpatient visits and by the occupational therapist and physiotherapist during home visits. Early discharge (n = 56); inpatient rehabilitation (n = 98) | Standard care (n = 46/46) | Patients were suitable for early discharge and did not reside within the catchmnent of the hospital-at-home programme. Patients in the control group received standard care | At discharge |
| UK | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Resnick 200572 | Hip fracture patients who participated in the Exercise Plus Program and were living in the community prior to hip fracture; receiving some type of surgical repair of the fracture (e.g. open reduction internal fixation, hemiarthroplasty) (n = 70); age: any; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 12 months |
| USA | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Community | ||||||
| Rich | ||||||
| Resnick 200769 | Hip fracture females who were otherwise medically fit and healthy and able to walk unassisted (n = 208); age: ≥ 70 years; gender: female; cognitive impairment: no | Exercise Plus Program: exercise plus motivation (n = 52); motivation only (n = 54); exercise only (n = 51) | Exercise Plus Program (exercise training component plus motivational component: theory of self-efficacy): a home-based trainer administered an aerobic, strengthening and stretching exercise intervention for all muscle groups. The trainer exercised with the individual and provided the Plus component (self-efficacy and outcome expectations, performance accomplishment, verbal encouragement, physiological feedback, cueing and self-modelling); there were a total of 42 supervised visits for face-to-face implementation of the motivational and exercise intervention; weekly telephone calls were made in months 7–12 when visits were decreased to once per month; weekly aspects of the motivational intervention were implemented by telephone contact. Plus-only intervention (motivational component: theory of self-efficacy): the sessions focused only on the Plus components (i.e. education about exercise, verbal encouragement, removal of unpleasant sensations and cueing) and participants did not exercise with the trainer. Exercise-only intervention (exercise training component): participants exercised with the trainer during the sessions but were not exposed to the Plus components of the intervention. In all treatment groups, visits from the trainer were initially twice a week for the first 2 months; this decreased to once per month in the final 4 months of the programme, with weekly telephone calls for those exposed to the Plus component of the intervention during the weeks when no visits were scheduled. All visits were 1 hour in length. Participants were expected to exercise five times per week for 45 minutes | Inactive control (n = 51/51) | Routine care: participants received physical and occupational therapy as prescribed by their orthopaedist and/or primary health-care provider | 12 months |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Rich | ||||||
| Richards 1998128 | Adult patients (all but 16 were aged > 65 years) on an acute hospital ward and resident within catchment area of Frenchay NHS Trust; positive rehabilitative outcome expected; appropriate home circumstances (i.e. adequate heating, safety in relation to patient’s disability) and adequate support from carers available if necessary; would require further hospital care if team was not available; not awaiting a nursing home place or input of social care alone; expected to remain in hospital for between 1 and 28 days; GP accepts clinical responsibility (n = 241); age: > 65 years; gender: both; cognitive impairment: no | Hospital at home (n = 160/160) | Hospital at home | Usual care (n = 81/81) | Routine hospital care | 3 months |
| UK | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Roberto 1992165 | Caucasian hip fracture patients (n = 101); age: 65–94 years; gender: female; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Historical cohort study | ||||||
| Community | ||||||
| Rich | ||||||
| Roberts 2004155 | Patients with a femoral neck fracture (n = 764); age: ≥ 65 years; gender: both; cognitive impairment: no | Integrated care pathway (n = 395/395) | The integrated care pathway was developed by a multidisciplinary team based on an extensive literature review and clinical consensus and covered patient care from admission through to discharge. Clinical care was provided by medical, nursing, physiotherapy and occupational therapy staff. A senior nurse specialist, experienced in orthogeriatric care, was responsible for staff training and implementation of the pathway | Conventional care (n = 369/369) | Conventional care | 1 month |
| UK | ||||||
| Quantitative comparative | ||||||
| Controlled before-and-after study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Robinson 1999183 | White female hip fracture patients; living alone; able to read and speak English; discharged from the subacute unit within 9 months (n = 15); age: > 70 years; gender: female; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | Post discharge |
| USA | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital | ||||||
| Thick | ||||||
| Röder 2003151 | Patients who had a non-pathological hip fracture as a result of a fall; diagnosis confirmed by radiography; no dementia or higher cognitive deficits (n = 142); age: ≥ 65 years; gender: both; cognitive impairment: partial | Supervised inpatient rehabilitation in orthopaedic and geriatric hospitals (n = 108/108) | Supervised inpatient rehabilitation in an orthopaedic hospital (n = 69) and a geriatric hospital (n = 39) | Usual care (n = 34/34) | No special rehabilitation and discharged home | 12 months |
| Germany | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Rolland 2004184 | Hip fracture patients hospitalised for rehabilitation after hip fracture surgery; cognitive status and previous hip fracture were not exclusion criteria (n = 61); age: ≥ 70 years; gender: both; cognitive impairment: yes | Multidisciplinary rehabilitation (n = 61/61) | The rehabilitation programme was carried out with a physiotherapist for 5 days per week in two daily sessions each lasting 1 hour. None of the groups received specific cognitive stimulation. Each week a team conference (including a geriatrician, physiotherapist, psychologist and geriatric nurse) was held to establish goals for each patient, organise the rehabilitation programme and assess the results | NA (n = NA/NA) | NA | 6 months |
| France | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Rösler 2012152 | Patients with fracture of the proximal femur and dementia (n = 129); age: any; gender: both; cognitive impairment: yes | Specialised ward (cognitive geriatric unit) (n = 53/53) | Some characteristics of cognitive geriatric units are extended geriatric assessment, special education of staff and particular equipment and architecture, which, in addition to conventional treatment including physiotherapy, occupational therapy and neuropsychological assessment, includes additional components such as hidden exit doors, increased light in hallways and patient rooms, night lights, a treatment room on the ward to decrease patient transferral, a living and eating room and a loop track for wandering patients. The number of beds on the cognitive geriatric unit was decreased and the number of nurses was increased. All team members in the cognitive geriatric unit volunteered to work on this specialised ward. Staff were provided with additional training if and when required | Geriatric ward (non-cognitive geriatric unit) of the same geriatric department (n = 76/76) | Conventional treatment including physiotherapy, occupational therapy and neuropsychological assessment (Consortium to Establish a Registry for Alzheimer’s Disease battery) | 12 months |
| Germany | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Ryan 2006115 | Hip fracture patients (n = 58); age: ≥ 65 years; gender: both; cognitive impairment: no | Intensive home-based rehabilitation (n = 30/30) | The service was provided by a local multidisciplinary team (physiotherapist, occupational therapist, speech and language therapist or therapy assistant) and included an augmented number of face-to-face contacts (six or more per week) | Less intensive home-based rehabilitation (n = 28/28) | The service was provided by a local multidisciplinary team (physiotherapist, occupational therapist, speech and language therapist or therapy assistant) and included a routine number of face-to-face contacts (three or fewer) | 3 months |
| UK | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Saltvedt 2012116 | Home-dwelling older people; previously able to walk 10 m and living in their own home or staying temporarily in an institution; intracapsular, trochanteric or subtrochanteric fracture; able to give an informed consent (n = 401); age: ≥ 70 years; gender: both; cognitive impairment: yes | Comprehensive geriatric assessment (n = 15 beds/15 beds) | The intervention programme was offered during the acute hospital stay in the dedicated department of geriatrics and included the following components. Comprehensive geriatric assessment, which is a systematic and multidimensional diagnostic process focusing on the evaluation of a frail elderly patient’s medical, psychosocial and functional capabilities and limitations in order to develop a co-ordinated and integrated plan for treatment and long-term follow-up by the primary health-care system, was performed by an interdisciplinary team consisting of geriatricians and residents, nurses, physiotherapists and occupational therapists with special competence in geriatrics. Emphasis was placed on adequate nutrition, early mobilisation and functioning in ADL, initial in-hospital rehabilitation and early discharge planning, which started as early as possible with a focus on the identification and treatment of comorbidities, pain relief, hydration, oxygenation, nutrition, elimination, prevention and management of delirium, assessment of falls and osteoporosis. A systematic approach was used, using checklists both for each professional category and for the interdisciplinary teamwork. These can be summarised as follows: (1) interdisciplinary teamwork – dedicated responsibilities; (2) interdisciplinary team meetings – first day post-operatively: plan for individual treatment, goal-setting, discharge planning; fourth day post-operatively: evaluation, discharge planning; (3) systematic approach – checklists, treatment protocols; (4) mobilisation/rehabilitation – mobilisation out of bed first day post-operatively, individualised plan for mobilisation and participation in ADL integrated in care plans and ward activities; and (5) discharge planning – collaboration with patients, caregivers and municipality, mapping of pre-fracture function, place of residence and social situation, discussion of discharge destination first day post-operatively, set realistic short- and long-term goals, organise institutional care, aids, assistance and physiotherapy when appropriate | Usual care (n = 24 beds/24 beds) | Patients received traditional treatment at the trauma unit and follow-up at the orthopaedic outpatient clinic. All patients were referred for in-hospital physiotherapy. Staff nurses were responsible for discharge planning. Patients were discharged from hospital as soon as they were medically stable after surgery and a suitable place of discharge was available | 12 months |
| Norway | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Shawler 2006174 | Mothers aged 76–85 years, post hip fracture and able to ambulate and living in a non-institutional setting. Adult daughters aged 49–67 years who provided some level of assistance to their mothers during the health crisis. All of the women were European American (n = 6 mother–adult daughter dyads); age: 76–85 years; gender: female; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| USA | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Community | ||||||
| Thick | ||||||
| Sherrington 1997117 | Patients living in the community at the time of fracture; fracture resulting from a fall; fracture occurring within the last 9 months; discharge within south-western Sydney (n = 44); age: > 60 years; gender: both; cognitive impairment: no | Weight-bearing exercise (n = 22/20) | Weight-bearing exercise (patient stood with both feet adjacent, placed one foot on a block and attempted to lift the contralateral leg off the ground by extending the hip and knee of the leg on a block) with telephone books (27 cm by 23 cm by 5 cm) as stepping blocks, corresponding to an appropriate thickness for the weight-bearing exercise (i.e. approximately one-third of the height of a standard house step). Participants were instructed to undertake the exercise at least once a day and were encouraged to slowly increase the number of repetitions. The number of daily repetitions initially prescribed ranged from 5 to 50. Subjects were given a photograph of themselves doing the exercise correctly and a written description of the exercise and a diary to record the number of repetitions performed each day. They were instructed to cease the exercise if they experienced chest pain or hip pain. The investigator visited once during the intervention phase to check whether or not the exercise was being carried out correctly and to increase the number of repetitions and the height of the block as necessary | No intervention control (n = 22/20) | Control group | 1 month |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Sherrington 2004118 | Community or residential care dwelling; 80% women (n = 120); age: ≥ 55 years; gender: both; cognitive impairment: no | Weight-bearing and non-weight-bearing home exercise (n = 80/80) | Weight-bearing exercise group (n = 40) performed exercises in weight-bearing positions. The exercises performed were sit-to-stand (repeated stands from a chair or adjustable-height exercise plinth), lateral step-up, forward step-up and over (stepping onto a block with both legs and down off it again), forward foot taps (tapping one foot up onto a block while supporting the weight on the other leg) and a stepping grid (stepping in different directions as guided by marks on the floor). These exercises were initially conducted with tables, chairs or walking aids as support. The exercises were progressed by increasing the number of repetitions, lessening the hand support, increasing the height of the blocks or decreasing the chair height. A physiotherapist prescribed the exercise programme based on pre-determined guidelines and the subjects’ performance of the exercises; this was modified at the follow-up visits as and when needed. Non-weight-bearing exercise group (n = 40) carried out all exercises in a non-weight-bearing (supine) position. The exercises were hip abduction (sliding the straight leg out to the side), hip flexion (lifting the straight leg), hip and knee flexion and extension (sliding the heel towards the buttock by bending the hip and knee), end-of-range knee extension (straightening the bent knee over a wedge) and ankle dorsiflexion and plantarflexion. The exercises were progressed by increasing the number of repetitions | No intervention control (n = 40/40) | Control group | 4 months |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Shyu 2008119 | Admitted to hospital for an accidental single-side hip fracture; receiving hip arthroplasty or internal fixation; able to perform full range of motion against gravity and against some or full resistance; living in northern Taiwan (n = 162); age: ≥ 60 years; gender: both; cognitive impairment: yes, mild to moderate | Geriatric consultation services, a rehabilitation programme and discharge-planning services (n = 80/80) | Participants received routine hospital care plus the intervention programme, which included three components: geriatric consultation services, a rehabilitation programme and discharge-planning services. The geriatric consultation was delivered by a geriatric nurse and a geriatrician. Before surgery, the geriatric nurse contacted the patient and completed the initial assessment to detect potential medical and functional problems and post-operative complications. Based on this assessment, the geriatric nurse revised suggestions in the post-operative care plan for the surgeon in charge with regard to time of surgery, use of infection and thromboembolic prophylaxis, post-operative nutrition management, urinary tract management and delirium prevention and management. The rehabilitation programme placed emphasis on providing early post-operative rehabilitation and in-home rehabilitation, delivered by the geriatric nurse, physiotherapist and rehabilitation physician, and contained a hip fracture-oriented intervention consisting of pain relief, range-of-motion, muscle strength and endurance, proprioceptive enhancement and balance challenges, as well as exercises to increase physical fitness, including aerobic capacity, anaerobic capacity, muscle strength and endurance and flexibility. Rehabilitation started on the first day post surgery, with exercises being customised to patients’ condition and ability, and was delivered once a day by a geriatric nurse, with input from a therapist and rehabilitation physician. After discharge, further flexibility-enhancing, knee extension and strengthening exercises were continued for up to 3 months, led the nurse and supplemented with therapist visits. The discharge service component was delivered by geriatric nurses to maintain continuity of care. Nurses assessed patients for caregivers’ competence, resources, family function, patient self-care ability, and patient and family caregiver needs for continuing health and social services and made necessary referrals during hospitalisation. Nurses also made home visits before discharge to assess the home environment and suggested environmental modifications. Nurses also made telephone calls to remind patients about follow-up visits to clinics | Usual care (n = 82/82) | Participants received only routine hospital care plus regular social contact provided by a research nurse. After a fall incident, patients were usually sent directly to the hospital emergency room and were cared for by orthopaedists. In the first 2–3 days after surgery, patients received antibiotics and pain medication and were taught to exercise with caution while still in bed. Physical therapy usually began on the second or third day. The usual hospital stay following surgery was around 7 days and no in-home programmes were provided. Patients were encouraged to ambulate with protected weight bearing for 3 months. Using a walker and touching the ground lightly were recommended | 2 years |
| Taiwan | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Shyu 2009196 | No severe cognitive impairment; able to walk independently pre fracture (n = 147); age: ≥ 60 years; gender: both; cognitive impairment: yes, mild to moderate | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 12 months |
| Taiwan | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Sirkka 2003193 | Fall-related hip fracture patients living in their own home pre fracture (n = 29); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 3 months |
| Sweden | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital and community | ||||||
| Rich | ||||||
| Stenvall 2007120 | Patients with femoral neck fracture (n = 199); age: ≥ 70 years; gender: both; cognitive impairment: yes | Specialised geriatric ward (n = 102/102) | The intervention unit was a geriatric unit specialising in geriatric orthopaedic patients. The staff worked in teams to apply comprehensive geriatric assessments and rehabilitation. Active prevention, detection and treatment of post-operative complications, such as falls, delirium, pain, decubital ulcers and malnutrition, were systematically implemented daily during the hospitalisation. Early mobilisation with daily training was provided by physiotherapists, occupational therapists and care staff during the hospital stay. A geriatric team, including a physician, assessed patients 4 months post-operatively to detect and treat any complicating disorders and to determine further rehabilitation needs | Specialist orthopaedic ward (n = 97/97) | The control unit was a specialist orthopaedic unit following conventional post-operative routines. A geriatric unit specialising in general geriatric patients was used for those who needed longer rehabilitation, but such patients were not admitted to the same ward as that used for the intervention | 12 months |
| Sweden | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Swanson 1998129 | Hip fracture patients (n = 71); age: ≥ 55 years; gender: both; cognitive impairment: no | Early intervention (n = 38/38) | Early surgery, minimal narcotic analgesia, intense daily therapy and close monitoring of patient needs using a multidisciplinary approach | Usual care (n = 33/33) | Standard care | NA |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Thick | ||||||
| Sylliaas 2011199 | Patients with a femoral neck or trochanteric fracture; living at home; able to undergo physical therapy for the hip fracture; no cognitive impairment (n = 150); age: ≥ 65 years; gender: both; cognitive impairment: no | Physiotherapist supervised group and individual exercises (n = 100/100) | Exercises were conducted by a physiotherapist using a combination of group and individual sessions. All patients exercised on a stationary bicycle or a treadmill for 10–15 minutes as a warm-up. The treadmill speed or bicycle resistance was set at the highest comfortable setting. Exercise sessions lasted for 45–60 minutes, depending on participants’ ability and tolerance. Patients completed four exercises: standing knee flexion, lunge (pass forward), sitting knee extension and leg extension. Each participant was required to attend exercise sessions twice per week and to complete a home-training programme once a week. The home exercise protocol included two exercises in the standing position: standing knee flexion and lunge (pass forward). If they were able to, patients were advised to walk for about 30 minutes every day | Routine care (n = 50/50) | Patients were asked to maintain their current lifestyle. No restrictions were placed on their exercise activities | 3 months |
| Norway | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Takayama 2001164 | Hip fracture patients who had undergone surgery (n = 189); age: ≥ 60 years; gender: both; cognitive impairment: partial | Standard rehabilitation programme (n = 189/189) | Patients were encouraged to walk with a cane at about 40 days after surgery and then a period of post-operative functional training commenced | NA (n = NA/NA) | NA | At discharge |
| Japan | ||||||
| Quantitative non-comparative | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Talkowski 2009194 | Community-dwelling adults admitted to a skilled nursing facility or an inpatient rehabilitation facility and who were ambulatory with or without assistance following a hip fracture (n = 18); age: ≥ 60 years; gender: both (majority female); cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 6 months |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Taylor 2010185 | Female physiotherapists working in rehabilitation in both outpatient and inpatient settings (n = 12); age: NR; gender: female; cognitive impairment: NA | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | NA |
| Australia | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Hospital | ||||||
| Thick | ||||||
| Tinetti 1999121 | Community-living individuals who have undergone surgical repair of a hip fracture (n = 304); age: ≥ 65 years; gender: both; cognitive impairment: no | Home-based rehabilitation (n = 148/148) | Physiotherapy component was designed to identify and ameliorate impairments in upper- and lower-extremity strength, balance, transfers, gait and stair climbing. Interventions for gait, transfers and bed mobility involved instruction in safer, more effective techniques, procurement of and training in the use of assistive devices and environmental modifications. Participants were instructed in the performance of progressive, competency-based exercises for balance (five levels), for upper- and lower-extremity conditioning (using four levels of colour-coded resistive bands) and, if indicated by the baseline assessment, for specific muscle and joint groups. Participants were then asked to complete their exercise programme by themselves once each day. To enhance and monitor adherence to the daily exercise programme, participants completed an exercise checklist each day. The functional therapy component of the intervention, based on the principles of occupational therapy, was designed to identify and improve inefficient and/or unsafe performance of tasks of daily life. A rehabilitation nurse, in consultation with an occupational therapist, administered the functional therapy programme. A rehabilitation nurse performed the assessment component, based on Occupational Therapy Functional Assessment Compilation, which involved observing the performance of medication management, oral care, eating, toileting, grooming, bathing, dressing, meal preparation, laundry, dishwashing, housekeeping and shopping. For tasks performed unsafely or ineffectively, the nurse determined which of 12 impediments [memory, problem-solving, decreased motivation, low confidence (fear), pain, decreased activity tolerance (endurance), vision, hearing, co-ordination (fine motor), strength, range of motion or balance] contributed to this unsafe or ineffective performance. Interventions targeted task performance based on the identified impediments and included (1) task modification; (2) use of adaptive equipment; (3) environmental modifications; (4) psychological interventions (to enhance confidence or motivation); (5) caregiver (usually family) education and involvement; and (6) referral to other health-care providers (e.g. to a physician for treatment of depression or pain). For both physiotherapy and functional therapy, the number of visits was tapered over time. Specific criteria and decision rules that linked assessment results with the appropriate interventions were developed for physiotherapy and functional therapy. Criteria for progression in each area were also articulated. The intervention continued for up to 6 months | Usual care (n = 156/156) | This consisted of traditional physiotherapy provided by physiotherapists. Only a few of the participants received occupational therapy. As is typical in home care, the specific content and duration of the therapy training programme for usual care patients was left to the discretion of the individual therapists. The usual care physiotherapists instructed their patients in gait and transfer training, and provided strengthening and range-of-motion exercises, usually without resistive bands or weights. No usual care patients received functional therapy | 12 months |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Travis 199889 | Hip fracture patients having lower strength and muscle mass and lower levels of physical endurance (n = 8); age: ≥ 60 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 10 post-operative days |
| USA | ||||||
| Mixed methods | ||||||
| Mixed methods | ||||||
| Hospital | ||||||
| Rich | ||||||
| Tsauo 2005122 | Hip fracture patients admitted for surgery (n = 54); age: ≥ 60 years; gender: both; cognitive impairment: no | Physical therapy (n = 28/13) | The home-based physiotherapy programme was an individualised training programme that encompassed (1) strengthening exercises, mainly for hip flexors, extensors, abductors and knee extensors; (2) range-of-motion exercises, mainly for the hip joint; (3) balance training; (4) functional training, such as sit-to-stand training, ambulation training and stair climbing, if needed in the home environment; (5) the practice of safe and efficient transfer techniques; (6) adjustment of walking aids; and (7) adaptation and modification of the home environment. The exercise items were given according to the individual capacity and general medical condition of each patient. In general, five exercise items were taught at each visit, initially in three sets of 10 repetitions per day for each item. The number of repetitions or sets increased if patients tolerated them well, based on the home visit evaluation by the physiotherapist. In most circumstances, a 1-kg sandbag was used as resistance. However, patients could discontinue the exercise whenever they experienced any discomfort. To improve the accuracy and compliance of the exercise prescription, the physiotherapist provided an exercise brochure and record sheet at each visit. The exercise brochure listed the possible problems and proper exercise protocols in the different stages after surgery. The amount of daily exercise was recorded every day by patients or familiy members and a telephone call reminder was given every week | Usual care (n = 26/12) | Patients were instructed to practise the exercise programme given at bedside before discharge | 6 months |
| Taiwan | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Uy 2008123 | Cognitively impaired women with hip fracture; ambulant prior to fracture; able to follow commands at the time of seeking informed consent consent (n = 10); age: ≥ 80 years; gender: female; cognitive impairment: no | Inpatient interdisciplinary rehabilitation (n = 3/3) | Inpatient interdisciplinary rehabilitation programme | Discharge back to the nursing home (n = 7/7) | Discharge back to the nursing home after surgery | 4 months |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick | ||||||
| Van Balen 2002140 | Hip fracture patients (n = 208); age: ≥ 65 years; gender: both; cognitive impairment: no | Early discharge to a nursing home rehabilitation ward (n = 106/106) | Early discharge | Conventional discharge to a nursing home rehabilitation ward | Conventional management | 4 months |
| The Netherlands | ||||||
| Quantitative comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| van der Sluijs 1991186 | Patients with a fresh hip fracture who were living independently in their own home or an old people’s home (n = 134); age: any; gender: both; cognitive impairment: NR | Weight-bearing training (n = 134/134) | Full weight bearing was allowed after 7 days, except in patients with cannulated screw fixation and in patients whose fracture stabilisation was considered inadequate for full weight bearing. All of the patients were mobilised with the help of a physiotherapist and the nursing team | NA (n = NA/NA) | NA | 12 months |
| The Netherlands | ||||||
| Quantitative non-comparative | ||||||
| Controlled before-and-after study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Vidán 2005124 | Patients hospitalised for hip fracture surgery (n = 319); age: ≥ 65 years; gender: both; cognitive impairment: no | Comprehensive geriatric intervention (n = 155/155) | A geriatric team that included a geriatrician, a rehabilitation specialist and a specific social worker treated patients in the intervention group. The intervention consisted of a complete geriatric evaluation to identify and quantify medical and psychosocial problems and functional capability to elaborate a comprehensive therapeutic plan. A geriatrician visited patients daily and was responsible for medical care. The rehabilitation specialist planned the schedule and the intensity and duration of physical therapy. The social worker assessed the social environment network and gave advice needed to improve social support when necessary. After the initial assessment, and within the first 72 hours of admission, an interdisciplinary meeting was held, including the orthopaedic and geriatric teams, to discuss patients’ medical, functional and social problems, and elaborate a comprehensive therapeutic plan. This meeting was repeated weekly to assess compliance | Usual care (n = 164/164) | All patients had an orthopaedic surgeon and a nurse assigned when they were admitted to hospital. The intervention and control groups shared the same orthopaedic wards and used the same hospital-wide support services, including physical therapy and social work. The orthopaedic surgeon made the decision of discharge moment in both groups. The surgeon and the orthopaedic nurses managed patients allocated to the usual care group, with counselling from different specialists as needed if medical problems occurred | 12 months |
| Spain | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital | ||||||
| Rich | ||||||
| Visser 2000156 | Community-dwelling women with a recent fracture of the proximal femur (n = 90); age: ≥ 65 years; gender: female; cognitive impairment: NR | Physical therapy (n = 90/90) | No details of the physical therapy given | NA (n = NA/NA) | NA | 12 months |
| USA | ||||||
| Quantitative non-comparative | ||||||
| Controlled before-and-after study | ||||||
| Community | ||||||
| Thick | ||||||
| Vogler 2012125 | Patients hospitalised for hip fracture (n = 180); age: ≥ 65 years; gender: both; cognitive impairment: no | Home-based exercise programme (n = 120/120) | Weight-bearing exercises (n = 60): lower-limb strength was targeted while standing, with a chair or bench for support if required. Exercises included heel raises, partial squats, sit-to-stand and stepping forward and sideways up onto blocks. Resistance was provided with weight-loaded waist belts aiming for a 10- to 12-repetition maximum load. Additional exercises aimed to enhance weight-bearing task performance and included reaching and leaning in standing, tapping one foot onto and off a block, controlled anterior–posterior weight shifts and controlled pelvic hitches, tandem standing and walking and getting up off the floor. If a participant was judged to be unable to complete all of the exercises, priority was given to the exercises that primarily targeted strength. Seated resistance exercises (n = 60): exercises targeted hip flexion, extension, abduction, knee flexion and extension and ankle plantar and dorsiflexion, and were undertaken while sitting on a standard dining room chair. Resistance from cuff weights and exercise bands was added to the exercises with the aim of a 10- to 12-repetition maximum load (i.e. the weight that could be lifted only 10–12 times). Weights began at 0.5 kg and were progressed according to participant capability in 0.5-kg increments | Social visits (n = 60/60) | Participants were visited by a research assistant, with visits at the same frequency as in the exercise group. The 1-hour visits consisted of playing board games and cards and general conversation. No exercises or walking were carried out during these visits. Participants were encouraged to exercise using their exercise booklets, as prescribed by the physiotherapist, at least three times per week. Participants completed an exercise diary that indicated how many exercise sessions were completed and which exercises were carried out in each session | 12 weeks |
| Australia | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Walheim 1990187 | Patients treated for trochanteric fracture (n = 92); age: > 50 years; gender: both; cognitive impairment: partial | Physiotherapy (n = 92/92) | Rehabilitation programme detail not provided | NA (n = NA/NA) | NA | 6 months |
| Sweden | ||||||
| Quantitative non-comparative | ||||||
| Concurrent cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Whitehead 2003161 | Community-dwelling, cognitively intact older adults with a fall-related non-pathological hip fracture (n = 73); age: ≥ 60 years; gender: both; cognitive impairment: no | Home rehabilitation (n = 73/73) | Home rehabilitation programme | NA (n = NA/NA) | NA | 4 months |
| Australia | ||||||
| Quantitative non-comparative | ||||||
| Historical cohort study | ||||||
| Community | ||||||
| Thick | ||||||
| Yu-Yahiro 2009126 | Women recruited within 15 days of hip fracture; eligible patients were those with a non-pathological fracture who were admitted within 72 hours of injury, had surgical repair of the hip fracture and met medical inclusion criteria. Participants initially were randomised to exercise groups and then assigned to exercise trainers (n = 180); age: ≥ 65 years; gender: female; cognitive impairment: no | Strengthening exercises (n = 91/91) | The exercise programme was started at the end of the physician-prescribed post-acute physical therapy period. Exercise sessions were carried out 5 days per week and participants received three trainer-supervised exercise sessions a week in the home during the first 2 months of the study. The frequency of supervised sessions then decreased, with participants receiving a maximum of 56 supervised sessions by 12 months after the fracture. Participants were expected to exercise five times per week for 45 minutes. Two sessions a week focused on strength training exercises performed with resistive bands and cuff weights, whereas three sessions a week (alternating days) involved aerobic activity using a specially designed stair step with handles. Exercise trainers documented the level, intensity and frequency of each exercise during supervised sessions. Participants received a calendar page each month on which they were asked to record all independent exercise. Individual exercises were modified in a standard way, for consistency, according to participant limitations, such as physical restriction, and were documented. All participants were advanced to a higher level of exercise in a standardised manner using the same equipment. In addition to the exercises, there was a self-efficacy-based motivational component. This component addressed patient education and encouragement, physiological feedback, and cuing and self-modelling | Usual care (n = 89/89) | Physician-prescribed usual care post fracture included a relatively short hospital stay and approximately 2–4 weeks of rehabilitation, with follow-up by the orthopaedist and primary care provider | Post discharge |
| USA | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Community | ||||||
| Thick | ||||||
| Zabari 2012162 | Patients with an operated hip fracture admitted to the geriatric rehabilitation department for treatment (n = 144); age: > 65 years; gender: both; cognitive impairment: NR | Pain management protocol (n = 67/67) | Daily pain evaluation followed by immediate titration of the pain using a flow chart of pain scores. Patients were asked about the presence and intensity of pain and were placed on a standard analgesic protocol that included one of the following drugs: acetaminophen, dipyrone, tramadol or oxycodone. Analgesic drugs were added according to patients’ self-reported pain levels. The medication was changed if the VAS pain score was ≥ 5 or whenever it was 2 points higher than on the previous day | Usual care (n = 77/77) | Usual care | Post discharge |
| Israel | ||||||
| Quantitative non-comparative | ||||||
| Historical cohort study | ||||||
| Hospital | ||||||
| Thick | ||||||
| Zidén 2008127 | Patients living in their own home; no cognitive impairment; able to understand and speak Swedish (n = 18); age: ≥ 65 years; gender: both; cognitive impairment: no | NA (n = NA/NA) | NA | NA (n = NA/NA) | NA | 1 year |
| Sweden | ||||||
| Qualitative | ||||||
| Qualitative | ||||||
| Community | ||||||
| Thick | ||||||
| Zidén 200890 | Community-dwelling hip fracture patients; medically approved by the responsible geriatric doctor as being in need of geriatric care and rehabilitation; able to speak and understand Swedish (n = 102); age: ≥ 65 years; gender: both; cognitive impairment: no | Home-based rehabilitation (n = 54/54) | Geriatric, multiprofessional home rehabilitation programme focused on supported discharge, independence in daily activities and enhancing physical activity and confidence in performing daily activities. All patients received early mobilisation, information leaflets and oral information about the surgical treatment and the prognosis as well as the importance of physical activity. All personnel were involved in the everyday rehabilitation, such as training bed transfer, dressing, grooming and walking to the toilet and dining room, after instruction from the physiotherapist and occupational therapist. When needed, the occupational therapist or physiotherapist made a home visit together with the patient to find out if the patient could manage at home and which technical aids would be needed. During the hospital stay, patients were offered an individually tailored rehabilitation programme with close co-operation between the occupational therapist, physiotherapist and the rest of the health-care staff. After this, patients underwent supported discharge for multiprofessional actions aimed at sensitising and mobilising patients’ motivation and individual self-efficacy, close contact with social home service and relatives to plan a smooth discharge and co-operation during the first weeks at home. Home rehabilitation consisted of a brief intervention period of a maximum of 3 weeks. The same occupational therapist and physiotherapist who had trained patients at the hospital performed the home visits to ensure continuity and advancement in the rehabilitation process. The focus of the physiotherapy intervention within the programme was to encourage and support self-efficacy, meaning confidence in locomotion and physical activity, with special attention paid to outdoor ambulation to attain as much pre-fracture mobility as possible. The mode of operation was inspired by the approach ‘learning by doing’. The focus of the occupational therapy intervention was to encourage safety and independence in fundamental activities of daily life, particularly basic transfers, dressing, grooming, bathing and cooking. All home rehabilitation interventions were individually designed based on individual goals and needs | Conventional care (n = 48/48) | Conventional care involved participation in the standard rehabilitation programme, including daily individual training in basic activities of daily life functions, transfer techniques, test of and training with technical aids and indoor and stair walking, as well as physiotherapy and occupational therapy group training sessions. No structured rehabilitation after discharge was included. Prior to discharge, the home service officer and patients’ next-of-kin were contacted to make plans for the future (e.g. to establish the appropriate level of social home service or home care as well as offer information about available outpatient rehabilitation facilities) | 1 month |
| Sweden | ||||||
| Quantitative comparative | ||||||
| RCT | ||||||
| Hospital and community | ||||||
| Thick |
Appendix 18 Strengths, limitations and author conclusions of the included studies
| Study details (author, year; country; study type; study design; setting; conceptual richness; participants) | Strengths and limitations | Author conclusions |
|---|---|---|
| Adunsky 2003138 | Limitations: (1) study design and the non-randomisation of patients; (2) multifactorial background of the patients and the non-inclusion in the analysis of some already well-known predictors of outcome, such as associated comorbidities, pre-fracture ambulating status and pre-fracture level of ADL; (3) the variable time interval from surgery to onset of the rehabilitation period was not analysed because a delay in a patient’s transfer (as well as the timing of surgical intervention) may depend on other medical and non-medical factors; (4) a specific adjustment for coexisting comorbidities was not performed, because patients with significant comorbidities that could affect rehabilitation outcome were excluded a priori; and (5) no cost and cost-effectiveness analysis was carried out because the purpose of the study was to look at functional rehabilitation outcomes rather than at associated expenses. Strengths: provides clinical evidence supporting the implementation of comprehensive orthogeriatric care, which can help manage the use of economic resources and the facilitation of effective treatment strategies | Rehabilitation functional outcomes of elderly hip fracture patients are better for those treated in an orthogeriatric setting than for those treated with the common two-phase model of surgery followed by transfer to a geriatric rehabilitation facility. This model of a comprehensive orthogeriatric ward is a practical and feasible service that covers the various needs of hip fracture patients, results in a shorter length of hospital stay and provides more efficient rehabilitation |
| Israel | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 320; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Al-Ani 2010139 | Limitations: (1) data were collected only from relatives/friends because the patients were selected because of their severe cognitive impairment; no reliability testing of this information was performed; (2) patients discharged to rehabilitation units may differ from those discharged directly to their previous living condition; and (3) although factors that might influence the outcome were adjusted for, data relevant for the decision of discharge to rehabilitation units were not collected. Strengths: (1) the choice of easily recognisable outcome variables: walking outside and inside, ability to walk and Activities of Daily Living – Katz (kADL) index; and (2) fairly low dropout rate | Discharge to the rehabilitation unit was associated with preserved walking ability and ADL in cognitively impaired patients with hip fracture |
| Sweden | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 246; age: ≥ 65 years; gender: both; cognitive impairment: yes | ||
| Allegrante 200791 | Limitations: (1) high attrition rate largely because of refusal to complete the entire outcome assessment protocol, mainly because of failure to return to hospital; (2) self-selection bias; and (3) inability to blind the surgeons leading to encouragement of control group patients to obtain more physical therapy, diluting the impact of the intervention | Role limitation as a result of physical health was reduced significantly but the results should be interpreted cautiously because of the large number of dropouts. Such results are likely to be expected in community settings when a multicomponent intervention is implemented in rehabilitation after hip fracture |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 176; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Arinzon 2005201 | NR | Geriatric rehabilitaion helped the younger age group more than the older age group achieve better results with regard to functional improvement; hence, older groups need more support to obtain better rehabilitation outcomes |
| Israel | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Community | ||
| Thick | ||
| Participants: n = 102; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Atwal 2002176 | NR | The key themes identified from the stakeholder interviews were (1) time constraints prevented professionals from completing and reading the multidisciplinary integrated care pathway; and (2) goal-setting was regarded as time consuming. The key findings from the analysis of the interprofessional integrated care pathways were interprofessional differences in the management of the patient caused discharge delays (discharges were not delayed by social services but by organisational aspects). If interprofessional working is to be encouraged, there must be a real commitment to this process. Health-care professionals must be able to state their opinions freely, be willing to share information, set goals with both the patient and other members of the team and be able to understand the value base of other professionals |
| UK | ||
| Qualitative | ||
| Qualitative | ||
| Hospital | ||
| Rich | ||
| Participants: n = 48 health professionals; age: NR; gender: both; cognitive impairment: NA | ||
| Barone 2009177 | NR | This study established that immediate weight-bearing and assisted ambulation is feasible in a high proportion of patients after surgical stabilisation of hip fracture. Neither cognitive impairment nor high comorbidity influenced significantly the adherence to the protocol, indicating that immediate weight-bearing and assisted ambulation may be offered to an unselected population of the elderly with hip fracture. The day of surgery (e.g. pre-holiday or not) was the only variable influencing adherence to the immediate weight-bearing and assisted ambulation protocol, suggesting the importance of maintaining the same standard of daytime care every day of the week |
| Italy | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 469; age: ≥ 70 years; gender: both; cognitive impairment: partial | ||
| Bäuerle 2004163 (German) | NR | The extent of help and care needed after a hip fracture depends on the subgroup categorisation of patients’ pre-fracture status, including cognitively sound, younger, frailer, very old, living alone or living with family |
| Germany | ||
| Quantitative non-comparative | ||
| Historical cohort study | ||
| Community | ||
| Thick | ||
| Participants: n = 332; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Beaupre 2005157 | NR | Standardised rehabilitation and discharge planning did not affect post-operative function or institutionalisation in elderly patients with hip fracture. In intervention patients with low levels of social support, function improved and institutionalisation was reduced |
| Canada | ||
| Quantitative comparative | ||
| Historical cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 919; age: ≥ 65 years; gender: both; cognitive impairment: yes | ||
| Bellelli 2006170 | NR | A body weight-supported treadmill technique was better at improving gait and balance than conventional training |
| Italy | ||
| Quantitative non-comparative | ||
| Case report | ||
| Hospital | ||
| Thick | ||
| Participants: n = 1; age: ≥ 80 years; gender: both; cognitive impairment: yes | ||
| Bellelli 2008141 | Limitations: (1) no formal clinical evaluation of depression; and (2) unclear whether depressive symptoms developed before or after surgery | The co-occurrence of depression and dementia significantly increases the 12-month risk of dying in elderly patients after rehabilitation post-hip fracture surgery |
| Italy | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 211; age: ≥ 65 years; gender: both; cognitive impairment: yes | ||
| Bellelli 201078 | NR | Action observation treatment is a useful approach in the rehabilitation of post-surgical orthopaedic patients and may be a complementary or an alternative approach to current well-assessed rehabilitation treatments |
| Italy | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Rich | ||
| Participants: n = 60; age: ≥ 18 years; gender: both; cognitive impairment: no | ||
| Binder 200492 | Limitations: (1) results can be generalised only to the subset of people with mild to moderate cognitive impairment or frailty after hip fracture; (2) transportation was provided to maximise study adherence, which may not be practical in many clinical settings, and the study sample may not reflect the eligible individuals who would be able to participate in this type of rehabilitation programme without such support; (3) individuals who dropped out of the control group between 3 and 6 months improved less on the FSQ at 3 months than individuals who continued, which may have biased the estimates of the magnitude of the group difference in FSQ score at 6 months; (4) the lack of a non-exercising control group limits the ability to determine the effect of different intensities of exercise on the functional outcomes and may have reduced the magnitude of the effect size of the physical therapy intervention; (5) physical therapy participants may have had greater social contact than control participants and it is possible that an increased level of socialisation enhanced their motivation more than in control participants and that this may account for some of the improvements observed, particularly in the SF-36 measures; however, the high compliance rate and lower dropout rate among control participants appear to reflect a high level of motivation and it is unlikely that differences in socialisation account for the changes observed in the modified PPT and strength measures, and this is supported by analyses of covariance that included the changes in SF-36 social functioning subscale scores; (6) the study was not designed to answer questions about the optimal timing of intensive physical therapy or weight training, and further study is needed to address this issue; and (7) most patients who had a hemiarthroplasty repair procedure were prescribed range-of-motion restrictions that prohibited them from performing some of the exercises, including lower-extremity weight training, until 10–12 weeks after their fracture | 6 months of extended outpatient rehabilitation that includes progressive resistance training can improve physical function and quality of life, and reduce disability compared with low-intensity home exercise in community-dwelling frail elderly patients with hip fracture |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 90; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Bischoff-Ferrari 201093 | Strength: with the high level of frailty after acute hip fracture, the trial was powered for the end points investigated despite its moderate size | Extended physiotherapy was successful in reducing falls but not hospital readmissions |
| Switzerland | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 173; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Borgquist 1990188 | NR | Routine follow-up of hip fracture patients in the orthopaedic department after discharge can be omitted. Follow-up in primary health care without radiography and orthopaedic expertise gives good functional results provided that patients with pain and walking problems from the hip are guaranteed rapid specialist treatment. Rapid specialist involvement should be possible because of the outpatient resources released at the hospital |
| Sweden | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 298; age: ≥ 50 years; gender: both; cognitive impairment: no | ||
| Boyd 1982158 | NR | The rehabilitation ward programme reduced the average length of hospital stay by 18 days (27%), saving 8676 patient bed-days. This also motivated patients to participate in the rehabilitation activities |
| UK | ||
| Quantitative comparative | ||
| Historical cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 771; age: NR; gender: female; cognitive impairment: no | ||
| Buddenberg 199879 | Limitations: (1) small sample size; (2) short follow-up period; and (3) lack of demographic variability in the study population | As participants were similar at baseline and on admission, and received the same number of hours of therapy, it appears that the improvements observed were due to the intervention received |
| USA | ||
| Quantitative comparative | ||
| Non-randomised trial/quasi-experimental study | ||
| Rehabilitation facility (no other details provided) | ||
| Rich | ||
| Participants: n = 20; age: ≥ 75 years; gender: female; cognitive impairment: partial | ||
| Burns 2007197 | NR | After hip fracture surgery, no statistically significant benefits can be achieved from a psychiatric intervention in people who are depressed or a psychological intervention to prevent the onset of depression |
| UK | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Rich | ||
| Participants: n = 293; age: ≥ 60 years; gender: both; cognitive impairment: partial | ||
| Carmeli 2006131 | Limitations: (1) small sample size; (2) high dropout rate; (3) patients from specific government-sponsored hospitals so might not be a representative population; and (4) concerns about the randomisation process | The supervised/class-based exercise group had better outcomes than the non-supervised/home-based exercise group with regard to quality of life and functional performance |
| Israel | ||
| Quantitative comparative | ||
| Quasi-randomised trial | ||
| Hospital and community | ||
| Rich | ||
| Participants: n = 63; age: ≥ 75 years; gender: both; cognitive impairment: no | ||
| Casado 200980 | Limitations: (1) limited generalisability because the participants were mostly Caucasian and willingly participated in the study; (2) only expert aspect of the social support tested in the model; and (3) there was a poor fit of the model to the data and the significant paths explained only a small per cent of the variance in exercise; the consideration of additional variables that explain exercise performance among these individuals is needed | The positive effect of social support for exercise by experts on the outcome expectations for exercise in older women recovering from a hip fracture provides an opportunity for health-care providers to improve physical activity in this population. Age and fear of falling were related to outcome expectations, with those who were younger and had less fear of falling having stronger outcome expectations. Mental health status was related to self-efficacy and depression, as the participants who reported better mental health reported higher self-efficacy and fewer depressive symptoms. Treatment group assignment was related to social support from the experts, such that those exposed to the trainer had stronger social support for exercise. Treatment group assignment (treatment was equivalent to being exposed to any of the treatment groups) also had direct impact on exercise behaviour, indicating that exposure to treatment increased participants’ exercise activities. Social support from experts showed a significant relationship with outcome expectations, such that those who had stronger social support to exercise from the expert reported stronger outcome expectations for exercise. Those who were not exposed to this type of encouragement and who exercised with the trainer only also had improvement in social support for exercise, showing that supervised exercise programmes produce more positive outcomes than unsupervised ones in older adults. There was no significant relationship between expert social support and self-efficacy expectations. Although the significant relationship between social support from experts and outcome expectations may not be influencing current exercise behaviour, it may be important for long-term adherence to exercise. Outcome expectations for exercise have repeatedly been identified as a significant predictor of exercise behaviour over time, pointing to a critical long-term impact of outcome expectations on exercise adherence. The influence of experts on strengthening outcome expectations may therefore have a lasting effect on the hip study participants |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Rich | ||
| Participants: n = 168; age: ≥ 65 years; gender: female; cognitive impairment: partial | ||
| Cree 2001175 | Limitation: retrospective nature of the questions | Interventions aimed at improving post-fracture social support could increase health perception following hip fracture |
| Canada | ||
| Qualitative | ||
| Qualitative | ||
| Hospital | ||
| Thick | ||
| Participants: n = 222; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Crotty 200094 | Limitations: (1) randomisation and research procedures may have discouraged some people; and (2) patients received conflicting information from practitioners about their ability to manage at home and so were confused about whether or not to consent | Given the choice, hip fracture patients and their carers are less likely to choose early discharge and home rehabilitation, preferring a longer hospital stay and hospital-based rehabilitation, particularly for those living alone. It is necessary to expand these home rehabilitation programmes to educate providers, patients and carers |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 68; age: ≥ 50 years; gender: both; cognitive impairment: partial | ||
| Crotty 200395 | Limitations: (1) insufficient power to detect differences in many outcome measures because of the small sample size; and (2) the consent process allowed patients with a pre-existing preference for hospital care to refuse the possibility of home rehabilitation and automatically transfer to hospital rehabilitation | The intervention group had greater physical independence and more confidence that they would avoid falling while undertaking ADL. Successful early discharge programmes depend on careful selection of patients (medically stable, assessed as needing, and having adequate physical and mental capacity to participate in, a formal rehabilitation programme, expecting to return home after discharge from hospital, having a home environment suitable for rehabilitation and having adequate social support in the community) and their caregivers, and consultation with families is important to explain the nature of the programme and to relieve their suspicions of the motives for early discharge. With this approach, generally good outcomes for both patients and caregivers can be achieved in 12 months |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 66; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Dai 2002132 | Limitations: (1) a younger and healthier population than most so not representative of the normal hip fracture population; (2) risk of confounding of data collection before and after the study because of changes in hospital practice or policy, although sensitivity analyses showed no significant effects; (3) lack of blinding of outcome assessors; and (4) instead of random assignment, consecutive sampling was used. Strength: follow-up data after hospital discharge were obtained by home visits and direct patient contact, which is more reliable than telephone interviews | A multidisciplinary rehabilitation programme had a continuous positive effect on hip fracture patients and successfully maintained the functional recovery in mobility in elderly patients with hip fracture 6 months after hospital discharge. Earlier discharge from hospital in the intervention group compared with the control group facilitated a better recovery in ADL and mobility 6 months after hospital discharge. Patients with independent mobility before fracture, those patients who did not receive the multidisciplinary rehabilitation programme and women were less likely than others to regain pre-fracture mobility within 6 months of discharge |
| Taiwan | ||
| Quantitative comparative | ||
| Quasi-randomised trial | ||
| Hospital | ||
| Thick | ||
| Participants: n = 94; age: ≥ 60 years; gender: both; cognitive impairment: no | ||
| De Jonge 2001171 | NR | A dedicated team with orthopaedic and geriatric leadership can lead to improved efficiency and quality of care for hip fracture patients |
| USA | ||
| Quantitative non-comparative | ||
| Work process and service restructuring | ||
| Hospital | ||
| Thick | ||
| Participants: n = NA; age: NA; gender: NA; cognitive impairment: NA | ||
| Delmi 199096 | NR | Clinical outcome of elderly patients with femoral neck fracture can be improved by once-daily dietary oral supplementation |
| Switzerland | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 59; age: > 60 years; gender: both; cognitive impairment: no | ||
| Deschodt 201197 | Limitation: no blinding of participants, health-care professionals or members of the inpatient geriatric consultation team | There were no functional benefits of a recommendation-based and patient-centred inpatient geriatric consultation team model for major outcome parameters such as functional status and length of stay in people with hip fracture |
| Belgium | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 171; age: ≥ 65 years; gender: both; cognitive impairment: partial | ||
| Di Monaco 2008133 | Limitations: (1) overall population not representative and so the results are not generalisable; (2) large number of dropouts; (3) no blinding of participants and hospital staff; (4) modest study follow-up period (about 6 months); and (5) no record of the time of the first fall and so no survival analysis performed | A single home visit by an occupational therapist after discharge from a rehabilitation hospital significantly reduced the risk of falling in a sample of elderly women following hip fracture. The results suggest that ameliorating adherence to falls prevention advice may result in a further decrease in falls risk. Home visits, mainly targeted at environmental hazards, significantly reduced the risk of falling in the elderly |
| Italy | ||
| Quantitative comparative | ||
| Quasi-randomised trial | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 95; age: ≥ 60 years; gender: female; cognitive impairment: no | ||
| Dy 2011159 | Limitations: (1) the study included only male patients; (2) the retrospective nature of the study had several inherent limitations – (a) the assessment of comorbidity and post-operative complications was dependent on the clinical evaluation and documentation provided by previous health-care providers, (b) the occurrence of some of the complications, including delirium and decubitus ulcers, was derived from clinical documentation; because of the retrospective nature of the study, it was not possible to use standardised measures to assess for delirium and to grade the severity of decubitus ulcers; however, these limitation are persistent across both study cohorts, which limits its likelihood of influencing the study results, (c) no follow-up of outcomes after discharge, such as return to pre-hospital function, cognition and residence, which are important after sustaining a hip fracture and (d) inability to evaluate the functional impact of the programme at further post-discharge time points; and (3) inclusion of in-hospital outcomes only | Multidisciplinary collaboration for patients with hip fractures can decrease the likelihood of experiencing inpatient complications in male patients. Focused multidisciplinary models of care may improve short-term outcomes for patients with hip fracture but may not yield longer-term benefits |
| USA | ||
| Quantitative non-comparative | ||
| Historical cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 74; age: ≥ 55 years; gender: male; cognitive impairment: no | ||
| Edwards 2004172 | Limitations: (1) issues related to system change; (2) resistance to change among staff – (a) staunch commitment to previous work patterns and relationships, (b) perceived lack of control by the care staff on the acute care units regarding the appropriate timing for referral to rehabilitation because of the consultation team automatically assessing all patients with hip fracture, and (c) patients were assessed within 2 days post-operatively and, in many instances, this may have been too soon to clearly identify rehabilitation potential. Strength: (1) advantages of the streamlined system – (a) potential to improve service coverage in times of staff shortage, (b) opportunity for new learning between two specialty teams, previously functioning separately, (c) this cross-fertilization shared office space and could become enhanced both formal and informal communication, (d) iterative discussions resulted in a more efficient, consolidated service with the potential for staff growth and expertise and (e) client-centred service means a shift in power to enable clients and families to have more control and be partners with service providers; there is greater flexibility in service delivery; thus, services fit the client rather than the reverse | The consolidated model of the HIPP consultation and rehabilitation team has the potential to improve service coverage. It was noted that this cross-fertilisation was facilitated when the staff shared office space and could become acquainted at a more personal level. Although the process of change required iterative discussions regarding both content and process of care, the effort expended resulted in a more efficient, consolidated service with potential for staff growth and expertise within the provision of a client-centred service |
| Canada | ||
| Quantitative non-comparative | ||
| Work process and service restructuring | ||
| Hospital | ||
| Thick | ||
| Participants: n = NA; age: NA; gender: NA; cognitive impairment: NA | ||
| Elinge 200398 | Limitations: (1) high refusal rate; (2) high dropout rate; (3) instruments not always sensitive enough to detect small changes and low levels of disability; and (4) small groups | A hip fracture may disrupt a person’s normal life in several ways and it is therefore important to give those elderly people who do not have the ability to participate in group activities, such as a learing programme, the rehabilitation that they are entitled to. In particular, this may be important for patients with low pre-fracture levels of physical and mental function, factors that strongly influence the rehabilitation outcome. This rehabilitation should be given in the home, so that patients do not have to decline a longer or more intense period of rehabilitation. Self-care and household activity training are important occupational therapy interventions for these patients but measures to support patients’ participation in society must not be disregarded, especially with regard to long-term rehabilitation |
| Sweden | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 35; age: ≥ 50 years; gender: both; cognitive impairment: no | ||
| Fortinsky 200281 | Limitation: small sample size, limiting the ability to evaluate the self-efficacy measure and preventing analyses that could shed light on important clinical variables that may independently affect reported rehabilitation therapy self-efficacy in the hospital setting, including medical comorbidities and physical symptoms such as pain and weakness | Patients with higher self-efficacy scores had a greater likelihood of locomotion recovery, controlling for pre-fracture locomotion function level and depressive symptoms |
| USA | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 24; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Fox 1993200 | NR | Resource savings made by early discharge and reduced length of stay will be borne elsewhere in the community and at the expense of significantly reduced numbers returned home and increased numbers placed in nursing homes |
| UK | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 335; age: NA; gender: NA; cognitive impairment: no | ||
| Fredman 2006142 | NR | High positive affect seems to have a beneficial influence on performance-based functioning after hip fracture |
| USA | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Community | ||
| Thick | ||
| Participants: n = 432; age: ≥ 65 years; gender: both; cognitive impairment: NR | ||
| Giangregorio 2009134 | Limitations: (1) it was not possible to blind outcome assessors; (2) patients were not randomised: (3) the control group had a longer length of stay on average and so may have received more therapy; and (4) therapists reported that it was easier to deliver hallway walking than body weight-supported treadmill training because of the time taken to put on the harness. Strength: body weight-supported treadmill training was particularly useful for obese patients and those with a great deal of pain on weight bearing | The current study provides preliminary evidence that it may be feasible to implement supported treadmill walking for patients with hip fracture in an inpatient rehabilitation setting. It also provides important feasibility information for future studies of interventions for patients with hip fracture in inpatient rehabilitation with respect to the screening-to-recruitment ratio, the recruitment challenges and the magnitude of loss to follow-up after discharge. Although evaluation of the efficacy of hip fracture rehabilitation interventions is needed, the challenges demonstrated here illustrate the difficulties of conducting rehabilitation research in this population. To optimise future research into hip fracture rehabilitation strategies, trials with sufficient sample sizes and rigorous methods for recruitment and retention are needed, as well as standardisation of outcomes to facilitate comparisons across studies |
| Canada | ||
| Quantitative comparative | ||
| Non-randomised trial/quasi-experimental study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 21; age: ≥ 70 years; gender: both; cognitive impairment: no | ||
| Giusti 2006143 | Limitation: lack of randomisation | Home-based rehabilitation seems to be a feasible alternative to institution-based rehabilitation for hip fracture in older adults previously living in the community with relatives |
| Italy | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 199; age: ≥ 70 years; gender: both; cognitive impairment: no | ||
| Hagsten 200499 | Limitation: it was not possible to hide the allocation of patients in each group from nursing staff | Individualised occupational therapy training can speed up a patient’s ability to perform ADL on discharge from hospital, which enhances the possibility of the patient returning to independent living at home. Follow-up visits are rational for these elderly patients to make sure that they are performing well and that they are not in need of further medical and/or nursing intervention or rehabilitation |
| Sweden | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 100; age: > 65 years; gender: both; cognitive impairment: no | ||
| Hauer 2003130 | NR | Improved functional performance in the training group did not lead to an increased level of physical activity after training, which might have preserved the functional improvements. In mobility-restricted, frail geriatric patients, training programmes should continue to keep patients active and prevent the decline in strength and functional performance that precedes loss of autonomy |
| Germany | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 57; age: > 75 years; gender: female; cognitive impairment: no | ||
| Hoekstra 2011144 | Limitations: (1) not a randomised study; (2) inability to determine the relative effectiveness of different components of the multidisciplinary nutritional care programme; (3) observer and patient bias; (4) intervention provided at different time points; and (5) the seasonal effects (autumn/winter for the control group and spring/summer for the intervention group) could have affected the findings | A multidisciplinary nutritional care strategy increased the intake of energy, protein, vitamin D, zinc and calcium in the immediate post-operative period compared with standard nutritional care. The intervention group experienced a significant beneficial effect on quality of life and nutritional status compared with the control group. The intervention could not prevent a decline in quality of life or nutritional status, but this decline was lower in the intervention group than in the control group |
| The Netherlands | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 127; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Hoenig 1997168 | NR | Surgical repair within the first 2 days of hospitalisation and more than five physiotherapy/occupational therapy sessions per week were associated with better health outcomes in a nationally representative sample of elderly patients with hip fracture |
| USA | ||
| Quantitative non-comparative | ||
| Database analysis | ||
| Hospital | ||
| Thick | ||
| Participants: n = 2762; age: ≥ 65 years; gender: both; cognitive impairment: NA | ||
| Holmberg 1989160 | Limitations: (1) historical cohort; and (2) selection bias | Discharging directly home for rehabilitation reduces the lenth of hospital stay significantly, with similar outcomes |
| Sweden | ||
| Quantitative comparative | ||
| Historical cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 170; age: ≥ 65 years; gender: both; cognitive impairment: NA | ||
| Host 2007153 | Limitations: (1) results can be generalised only to the subset of people with mild to moderate frailty after hip fracture; (2) a precise dose–response relationship could not be assessed for the phase 1 exercises because there was no quantitative measure of intensity, such as the one-repetition maximum (1RM), which was used in the progressive resistance training phase of the programme; and (3) during the progressive resistance training phase of the programme subjects performed bilateral exercises, but isokinetic strength assessments were performed unilaterally; the bilateral measures of exercise intensity (whether as the 1RM, as a percentage of the initial 1RM or as the training volume) were all highly correlated with the unilateral measurement of isokinetic peak torque | In frail elderly people after hip fracture and repair, a 6-month supervised exercise programme can induce gains in strength such that the fractured limb is essentially equivalent to the non-fractured limb. The concept of specificity of training does not apply to the fractured limb. There appears to be a strong relationship between exercise training intensity and functional performance adaptations |
| USA | ||
| Quantitative non-comparative | ||
| Controlled before-and-after study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 31; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Huang 2005100 | Limitations: (1) this study was limited to one hospital; (2) small size and included a 3-month follow-up period; and (3) potential for compromise of blinding of hospital staff and research assistant | Appropriate discharge planning by a nurse and designed by a multidisciplinary team can improve quality of life, survival and the ability to perform ADL, while reducing readmission rates and length of stay in hospital for older people with hip fracture |
| Taiwan | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 126; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Huang 200982 | NR | Clinicians need to determine how best to foster social support to help older people maintain high levels of a positive sense of self and engage them in conversations about ageing, including the positive and negative aspects of the ageing process, to promote independence |
| Taiwan | ||
| Qualitative | ||
| Qualitative | ||
| Community | ||
| Thick | ||
| Participants: n = 15; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Huusko 2000101 | Limitation: no physician or assessor blinding | Hip fracture patients with mild or moderate dementia undergoing active geriatric and intensive rehabilitation can return to the community, have a shorter length of hospital stay, succeed to return to independent living and need less institutional care than hip fracture patients in a standard care programme |
| Finland | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 243; age: ≥ 65 years; gender: both; cognitive impairment: yes | ||
| Jackson 200183 | Limitations: (1) substantial interpretational problems because of the quasi-experimental design; (2) therapist bias in reporting Functional Independence Measure (FIM) scores because of favour of the occupational adaptation approach; (3) researcher-constructed satisfaction questionnaire has not been subjected to rigorous reliability and validity studies | Occupational adaptation was associated with a more efficient outcome and greater patient satisfaction. The occupational adaptation approach provides one framework for offering an occupation-based intervention that is client-centred and can be efficient, effective and satisfying |
| USA | ||
| Quantitative comparative | ||
| Quasi-randomised trial | ||
| Hospital | ||
| Rich | ||
| Participants: n = 24; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Jellesmark 201284 | Limitations: (1) cross-sectional design, which meant that it was not possible to determine the causal association between fear of falling and functional ability; (2) underestimation of the prevalence of fear of falling in patients because of the exclusion of patients who were unable to walk independently at discharge; possibly, fear of stigma and institutionalisation may have prevented participants from admitting to fear of falling; and (3) in the qualitative subset saturation of the data may not have been reached, which is an inherent problem in the explanatory sequential mixed-method design, and this may reduce transferability. Strengths: (1) mixed-methods design that allowed us to investigate the prevalence of fear of falling and associations between fear of falling, avoidance of activities and functional ability and at the same time facilitate a deeper understanding of fear of falling through in-depth interviews with those who experienced a high degree of fear of falling; and (2) the use of validated instruments and conducting the survey face to face improved data collection | Fear of falling was common and significantly associated with activity avoidance and disability, and affected the lives of elderly people recovering from hip fracture. Some patients were physically incapacitated by fear of falling. Fear of falling screening at hospital discharge might be beneficial in tailoring rehabilitation efforts to individual patients. It is assumed that a reduction in fear of falling would enhance self-efficacy and improve physical ability related to balance and strength. Rehabilitation efforts should start early and combine hospital-based training and home training |
| Denmark | ||
| Mixed methods | ||
| Mixed methods | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 33 surveys, n = 4 interviews; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Jensen 1979154 | Limitation: the assessment system applied in this series does not consider walking ability or ADL | More patients discharged to their home maintained their social function than patients discharged to a convalescent home or rehabilitation clinic |
| Denmark | ||
| Quantitative non-comparative | ||
| Controlled before-and-after study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 518; age: any; gender: both; cognitive impairment: no | ||
| Johansen 2012145 | NR | Rehabilitation of older, multimorbid and disabled patients in a district inpatient rehabilitation centre improves independency to a higher degree and within a shorter time period than standard community rehabilitation in short-term beds in nursing homes. District rehabilitation centres seem to be an interesting model in societies challenged by increasing needs of primary health-care rehabilitation in an ageing population |
| Norway | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Community | ||
| Thick | ||
| Participants: n = 302; age: > 65; gender: both; cognitive impairment: partial | ||
| Jones 2002195 | Limitations: (1) no data available regarding the quantity and intensity of outpatient therapy; (2) observational study design with no comparable population; (3) large number of patients not analysed at the final outcome measurement point; and (4) no long-term follow-up measurements | Inpatient rehabilitation improved overall functional independence. Relative change indicated that the rehabilitation outcome for locomotion was not maximised, despite patients exhibiting large absolute gains during inpatient rehabilitation. The improvements demonstrated at discharge were maintained at follow-up Improved locomotion skills and maximising the ability to transfer independently are areas in which inpatient rehabilitation may be targeted to improve function |
| Canada | ||
| Quantitative non-comparative | ||
| Controlled before-and-after study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 100; age: ≥ 60 years; gender: both; cognitive impairment: no | ||
| Jones 2006135 | Limitations: (1) small sample size; and (2) lack of randomisation makes it difficult to generalise the results to a larger population | This study demonstrates the benefits of a functional (task-specific) group exercise programme administered to community-dwelling older adults post hip fracture. The next logical step for future investigations would be to determine, through a RCT, whether or not the exercise intervention will reduce overall mortality and morbidity and improve quality of life for hip fracture patients |
| Canada | ||
| Quantitative comparative | ||
| Non-randomised trial/quasi-experimental study | ||
| Community | ||
| Thick | ||
| Participants: n = 25; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Kammerlander 2011178 | NR | The duration of rehabilitation for an optimal outcome in geriatric hip fracture patients is very long, but the results also show that an early geriatric intervention may lead to better function |
| Austria | ||
| Quantitative non-comparative | ||
| Historical cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 246; age: ≥ 80 years; gender: both; cognitive impairment: NR | ||
| Kennie 1988102 | NR | This sudy confirms the effectiveness of geriatric rehabilitative aftercare for elderly women with hip fracture in terms of reducing the hospital stay and improving functional independence and the likelihood of patients returning to an independent life. Both hospital and patient benefited when post-operative rehabilitation was provided in a setting specialising in such care for elderly patients with trauma |
| UK | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 108; age: ≥ 65 years; gender: female; cognitive impairment: no | ||
| Kerr 2011173 | NR | The conceptual model summarised important experiences and related impacts of hip fracture from the patient’s perspective and demonstrates the wide-ranging effects on other areas of a patient’s life during the recovery process |
| USA | ||
| Qualitative | ||
| Qualitative | ||
| Hospital | ||
| Thick | ||
| Participants: n = 21; age: ≥ 50 years; gender: both; cognitive impairment: no | ||
| Koval 1998146 | Limitations: (1) results not generalisable to previously institutionalised or demented elderly patients; (2) follow-up data collected by telephone interview and so less accurate than data collected face to face; and (3) presence of selection bias because the request for a rehabilitation consultation and the ultimate discharge to the rehabilitation programme were at the physician’s discretion. Strengths: (1) patients were mobilised within 48 hours post-operatively, countering the potential confounding effect of differing weight-bearing protocols; and (2) prospective data collection and small number lost to follow-up | Use of the diagnosis-related-group-exempt rehabilitation programme increased the overall duration of hospitalisation, but decreased acute care hospitalisation. Patients discharged to the rehabilitation programme had no additional benefit with regard to recovering to their pre-fracture level of independence in basic ADL at the 3-month follow-up than patients who were not discharged to the programme |
| USA | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 609; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Kuisma 2002103 | Limitations: (1) treatment bias because of inability to blind health professionals; and (2) results of the study are not generalisable patients living alone or patients not having adequate support at home unless alternative community care is available | Five physiotherapy sessions in the patient’s home after discharge yielded equal or better results in ambulation ability than 1 month of conventional institution-based rehabilitation. All of the patients in the intervention group were able to walk independently in all circumstances at the completion of the study; hence, home-based physiotherapy for patients with hip fracture is an effective alternative to institutional care |
| Hong Kong | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 81; age: ≥ 50 years; gender: both; cognitive impairment: no | ||
| Latham 2006167 | Limitations: (1) use of secondary data generated for the purpose of clinical and utilisation management decision-making, so cautious interpretation required; and (2) external validity, because the study sample consisted only of patients covered under Medicare Advantage for their skilled nursing facilities stay | The pattern of functional change over time differed for ADL and mobility domains and for specific groups of patients. People with severe baseline mobility impairments experienced a slower rate of mobility improvement in the initial stage of rehabilitation, but the rate of change increased in the second phase. This pattern was reversed for patients with higher levels of mobility at baseline. For both domains, executive function and length of stay were associated with the overall rate of change. The results have implications for goal-setting and discharge planning |
| USA | ||
| Quantitative non-comparative | ||
| Database analysis | ||
| Hospital | ||
| Thick | ||
| Participants: n = 351; age: any; gender: both; cognitive impairment: no | ||
| Lauridsen 2002104 | Limitation: high withdrawal rate in the intervention group | Because of the high dropout rate in the intervention group intensive physical therapy may not be the way to reduce the duration of rehabilitation. Patients with hip fracture often have a multitude of problems requiring a multidisciplinary approach. A significant reduction in length of stay is likely to require a modified objective with more emphasis on outpatient rehabilitation |
| Denmark | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 88; age: 60–89 years; gender: female; cognitive impairment: partial | ||
| Levi 1997147 | Limitations: (1) sample not representative of the hip fracture population (women, community dwelling and mentally and physically fit); and (2) small numbers for multiple regression analyses | Type of post-hospital setting is associated with resource utilisation but not self-care outcome after hip fracture. Discharge to a skilled nursing setting rather than an inpatient rehabilitation setting is associated with more than double the number of days spent in post-hospital institutions, more sessions of physical therapy and more sessions of occupational therapy, and is not predictive of a decreased ability to perform ADL 2 and 6 months after hip fracture |
| USA | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 123; age: ≥ 65 years; gender: female; cognitive impairment: no | ||
| Li 2007189 | Limitation: the findings are limited because of the purposive sampling method used, chosen because of financial limitations, and the short follow-up period | The findings provide evidence to support and expand the application of the concept of interdependence in the Taiwanese context regarding the families of an elderly relative with hip fracture during the post-discharge period. The findings of this study may benefit health-care providers in other countries with an elderly Chinese population in terms of developing more culturally relevant discharge plans |
| China | ||
| Qualitative | ||
| Qualitative | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 20; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Lieberman 2002148 | Limitations: (1) selection bias; and (2) outcomes assessed at discharge only and no follow-up | Rehabilitation after proximal femur fracture surgery is much less successful in the ≥ 85 years age group than in the 75–84 years age group, but there were no differences in duration, the rates of most complications or mortality. A substantial percentage of patients in the older age group were rehabilitated successfully and they should not be denied the chance of successful surgery and rehabilitation, although the younger age group improved more than the older age group |
| Israel | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 424; age: ≥ 75 years; gender: both; cognitive impairment: no | ||
| Lieberman 2006179 | Limitations: (1) not all patients who underwent surgery were included, leading to an inevitable selection bias; and (2) rehabilitation outcome was assessed at the point of discharge from the hospital | The outome of rehabilitation of elderly patients after hip fracture surgery was associated with four correctable clinical and nutritional parameters. The other four associated significant variables cannot be corrected but may help in predicting outcomes and adjusting expectations of all individuals involved in the rehabilitation process |
| Israel | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 946; age: ≥ 65 years; gender: both; cognitive impairment: partial | ||
| Lin 2004190 | Limitations: (1) correlations between cognitive function and recovery were not studied and therefore the results must be interpreted with caution; and (2) many patients were lost to follow-up after discharge because of incorrect contact details provided or family refusal to answer the telephone or return items by post | Fracture leads to deterioration in physical function despite the high rate of surgical success. In addition, most elderly people suffer from chronic disease and therefore physical function cannot be recovered after 3–6 months of healing. Rehabilitation should be carried out to improve muscle strength and enhance the self-care ability of the elderly. Comprehensive discharge planning, including pre-discharge instruction, referral and home follow-up, is needed to ensure that patients are properly prepared for discharge |
| Taiwan | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 103; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Lin 2009105 | Limitation: small sample size | A comprehensive discharge planning service can improve hip fracture patients’ self-care knowledge, functional recovery and quality of life |
| Taiwan | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 50; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Lindelof 2002180 | Limitations: (1) greater variation between participants would have been desirable; and (2) the design used may have been unnecessarily cautious | The results of this treatment are promising and should offer encouragement to elderly patients with hip fracture to carry out these exercises. Functional training with a weighted belt seems to show broad effects with regard to mobility and could be suitable for frail elderly persons in general |
| Sweden | ||
| Quantitative comparative | ||
| Controlled before-and-after study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 3; age: ≥ 78–82 years; gender: female; cognitive impairment: no | ||
| Long 2002198 | Limitation: the fact that the study is based on fieldwork of contrasting case studies, clients and settings in one region of England may be seen to limit the generalisability, authenticity and credibility of the findings | Key elements of nurses’ contribution within rehabilitation should aim to maximise client choice to enhance independent living in the clients’ future environment. At a nursing educational policy level, nurses need to have a full understanding of the principles and models of rehabilitation. At a practice level, the nurse’s role must be valued and recognised, by nurses themselves and by other team members |
| UK | ||
| Qualitative | ||
| Qualitative | ||
| Hospital | ||
| Thick | ||
| Participants: n = 49 health professionals; age: NA; gender: both; cognitive impairment: NA | ||
| Louie 2012106 | Limitations: (1) small sample size; (2) no intention-to-treat analysis; (3) no outcome measures to investigate whether or not carers could carry out the necessary caregiving skills and the degree of change in carer stress after participating in the carer training sessions; and (4) no long-term follow-up | Participants who underwent the PCEP were more likely to build on the use of their newly adapted ADL skills. PCEP empowered patients to reinforce their skills and knowledge of hip fractures and ADL. The programme encouraged patients to take a more active role in their rehabilitation |
| Hong Kong | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Rich | ||
| Participants: n = 134; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Mangione 2010107 | Limitations: (1) small sample size; (2) single, unblinded interventionist; (3) high dropout rate; (4) baseline differences in modified PPT scores; and (5) lack of information regarding activities that participants performed from the end of the intervention period to the end of the trial. Strengths: (1) use of an attentional control for patients after hip fracture made it possible to control for attention and motivation, which physiotherapists are known to provide during treatment; (2) despite the small number in the trial, the strength of the design provides support for the leg-strengthening intervention being effective; (3) attempts were made to minimise bias with concealed randomisation and blinded outcome assessors; (4) outcomes measured several months after the intervention was completed; and (5) baseline differences were controlled for using ANCOVA | A 10-week programme of twice-weekly progressive resistance training for the leg muscles beginning 6 months after hip fracture was effective at improving force production, gait speed and endurance and physical performance 1 year after hip fracture |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Rich | ||
| Participants: n = 26; age: > 65 years; gender: both; cognitive impairment: no | ||
| McKee 200285 | Limitation: small, convenience sample prohibiting the exploration of interactions between a larger number of variables; thus, study findings not generalisable. Strengths: (1) sample representative of the target population; and (2) high recruitment rate and satisfactory response rate for the follow-up assessment | Assessing worry over further falls in hospital may help to identify older people with hip fracture at risk of poor health outcomes |
| UK | ||
| Mixed methods | ||
| Controlled before-and-after study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 57; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| McMillan 201286 | NR | Older people are vulnerable to losing a sense of control after a health trauma; hence, they and their families need tailored information and support to enable them to take control safely and appropriately. This is especially important for those who are able to return to their own home (and who might not have family and/or professional support) and engage in a precarious process of balancing as they strive to take control. Health-care professionals need to understand the perspective of older people and recognise that the efforts that people make to take control are a consequence of balancing. This understanding can enable health-care professionals to enhance their care of older people and will help them to facilitate successful balancing and progression through the recovery trajectory |
| UK | ||
| Qualitative | ||
| Qualitative | ||
| Hospital and community | ||
| Rich | ||
| Participants: n = 27; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Mendelsohn 2008108 | Limitations: (1) small sample size; (2) inclusion criteria of relatively high cognitive functioning and high physical functioning affect the generalisability of the results; (3) conflict between scheduled physiotherapy and occupational therapy sessions and the testing and training schedule in the study; and (4) no increase in intensity, duration or frequency of training during the training programme | The upper-body exercise programme had a significant effect on aerobic power and physical function, including mobility and balance; hence, aerobic endurance exercise should be integrated into standard rehabilitation to enhance patients’ aerobic fitness and mobility after hip fracture surgery |
| Canada | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 20; age: ≥ 70 years; gender: both; cognitive impairment: no | ||
| Mitchell 2001109 | Limitations: (1) low compliance rate (75%); (2) high rate of loss to follow-up; and (3) observer bias as researchers not blinded to treatment allocation. Strengths: (1) populations representative of the general population so the results are generalisable; and (2) study groups well matched in terms of baseline characteristics | A 6-week programme of twice-weekly progressive high-intensity quadriceps training in elderly proximal femoral fracture patients increased leg extensor power and reduced disability, accompanied by an increase in energy. Benefits persisted for at least 10 weeks after finishing the training programme. The programme was well tolerated by frail elderly subjects who are rehabilitating after proximal femoral fracture. The treatment requires only very basic, inexpensive equipment, such as weighted sandbags, which are placed over the ankle |
| UK | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 80; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Moore 1993181 | NR | Functional gains are made through both physiotherapy and occupational therapy during home care of patients with hip fracture |
| USA | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 32; age: NR; gender: both; cognitive impairment: no | ||
| Morghen 2011182 | Limitations: (1) the only measure used to assess depressive symptoms was the 15-item GDS, although previous studies have shown this to be reliable; (2) the study was conducted at only one site and it is not known whether patients lost to follow-up died or became institutionalised; and (3) variables with a possible influence on functional recovery, such as fracture site, type of anaesthesia, degree of pre-operative risk and vitamin D levels, were not assessed | Moderate to severe depressive symptoms in post-hip fracture surgery patients, as measured by the GDS, are associated with poor walking recovery after rehabilitation and an increased risk of institutionalisation or death at 1 year. In addition to those of previous studies, these results may provide valuable clues for designing trials of interventions and developing individualised rehabilitation pathways that consider moderate to severe affective disorders as a specific target of interest |
| Italy | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 230; age: > 65 years; gender: both; cognitive impairment: yes | ||
| Moseley 2009110 | Limitations: (1) insufficient differences between the high- and low-dose exercise programmes; and (2) relatively short duration of the exercise programmes (i.e. 16 weeks). Strengths: (1) trial carefully designed and implemented according to a strict experimental protocol; and (2) adequate sample size, with a very low dropout rate and good compliance with the exercise programmes | There was no benefit (or harm) of the higher-dose, weight-bearing exercise programme with respect to the primary outcome measures. However, patients with cognitive impairment gained greater benefit and there was a statistical and clinically relevant improvement in functioning, mobility, balance, ADL and quality of life from the higher-dose programme than from the lower-dose programme |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 160; age: ≥ 70 years; gender: both; cognitive impairment: yes (if carer available) | ||
| Munin 2005149 | Limitations: (1) no cost comparison; (2) subjects recruited from one facility, so limited generalisability; (3) incomplete follow-up data for some patients; (4) possible bias by the research occupational therapist, influencing FIM motor data; and (5) selection bias because group selection was based on clinical decision-making rather than on random group assignment. Strength: use of sensitive measures to evaluate cognition and behavioural domains | Hip fracture survivors treated in inpatient rehabilitation facilities had superior functional outcomes, as measured by the FIM motor score, than those treated in skilled nursing facilities. The improved outcomes with inpatient rehabilitation occurred during a significantly shorter rehabilitation length of stay |
| USA | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 76; age: ≥ 60 years; gender: both; cognitive impairment: no | ||
| Naglie 2002111 | Limitation: limited statistical power | Post-operative interdisciplinary geriatric care in an acute care hospital did not result in a significantly better 3- and 6-month combined outcome of the proportion of patients who were alive and had no change in ambulation, transfers or residence or in significantly better outcomes individually or in significantly better ADL in patients with hip fracture |
| Canada | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 279; age: ≥ 70 years; gender: both; cognitive impairment: no | ||
| Nicholson 1997136 | Limitations: (1) small sample size; (2) large dropout rate; (3) non-randomisation of study groups; (4) absence of a controlled intervention for the control group; and (5) short rehabilitation intervention of 6 weeks. Strengths: the exercise programme required no special equipment, was easily implemented, was safe and cost-effective and was applicable in a nursing home setting | The intervention contributed to the maintenance of the physical condition of older women temporarily disabled as a result of a fracture and subsequent hip surgery. Frail elderly participants were no worse off for their involvement in the 6-week chair exercise programme and showed some significant improvements in body composition |
| South Africa | ||
| Quantitative comparative | ||
| Non-randomised trial/quasi-experimental study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 30; age: ≥ 70 years; gender: both; cognitive impairment: no | ||
| Ohsawa 2007137 | Limitations: (1) small sample size; (2) non-randomised trial; (3) results not generalisable as the programme was indicated only for patients who accepted the programme and was suitable for more active and vigorous patients; (4) unblinded assessment of hip function; and (5) 6-month follow-up only | Assertive rehabilitation was more effective at restoring the ambulatory ability of frail elderly patients with intracapsular fracture of the hip than conventional care. Assertive rehabilitation is recommended as a conservative treatment for displaced intracapsular fractures of the proximal femur in frail elderly patients as it provides better improvements in ADL than conventional therapy and seems to be an alternative to surgery for patients with poor general condition |
| Japan | ||
| Quantitative comparative | ||
| Non-randomised trial/quasi-experimental study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 20; age: ≥ 80 years; gender: both; cognitive impairment: no | ||
| Oldmeadow 200687 | Limitations: (1) patients were not followed up beyond acute care and it is not possible to say if early ambulation, with its associated improved functional outcomes, resulted in shorter lengths of stay overall; given that early ambulation can be uncomfortable and challenging for patients, investigating their experiences would also have been informative; and (2) current clinical practice is to prescribe bed rest in the presence of cardiovascular challenge and so ambulation was not attempted for most of these patients | Early ambulation in the presence of medical stability accelerates functional recovery, contributes to shorter lengths of stay, is associated with more discharges directly home and less to high-level care and results in lower levels of dependency at discharge from acute care. These benefits justify the intense resources required. Cardiovascular stability is a major determinant of successful early ambulation after hip fracture surgery |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 60; age: ≥ 70 years; gender: both; cognitive impairment: no | ||
| Olsson 200788 | NR | Differences in patients’ perspectives on the rehabilitation process need to be taken into account to enhance outcomes. Inadequate knowledge and engagement on the part of patients with a hip fracture probably have an impact on their rehabilitation outcome, but the degree of this impact is uncertain |
| Sweden | ||
| Qualitative | ||
| Qualitative | ||
| Hospital | ||
| Thick | ||
| Participants: n = 13; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Orwig 2011191 | Limitation: study included a select group of female participants who were healthier than the average hip fracture patient and who showed greater physical functioning and a smaller relative decline in bone mineral density. Strength: the intervention was delivered in participants’ homes. Participants were visited by certified trainers early in the intervention period, leading to the high level of acceptance of the intervention and greater level of activity in the intervention group | Patients with hip fracture who participated in a year-long, in-home exercise programme increased their activity level than those receiving usual care; however, no significant changes in other targeted outcomes were detected |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 180; age: ≥ 65 years; gender: female; cognitive impairment: no | ||
| Oude Voshaar 200712 | Limitations: (1) patients with delirium and a severe cognitive impairment or other significant mental health conditions were excluded; and (2) short follow-up period of 6 months. Strengths: (1) large sample size; (2) the measurement of predictive variables at baseline and at 6 weeks and the assessment of different psychological variables within one study; and (3) use of highly validated and reliable outcome variables to measure performance-based functional outcome | Fear of falling and cognitive functioning may be more important than pain and depression in predicting functional recovery after hip fracture surgery. Cognitive impairment, depressive symptoms and a higher fear of falling are related to a less favourable functional recovery independent of age and pre-morbid level of functioning, whereas the effect of pain on functional recovery is less consistent. Depression increases the impact of a hip fracture on patients’ lives more than can be explained by the degree of objective functional impairment |
| UK | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 291; age: > 60 years; gender: both; cognitive impairment: partial | ||
| Peiris 2012112 | Limitation: the activity monitor recorded only steps with a cadence of ≥ 20 steps per minute and did not record activity in lying or sitting positions and so bed and sitting exercises were not recorded; monitors placed on the affected limb underestimated step counts at slower walking speeds but this was rectified by placing the monitor on the unaffected limb | Additional allied health rehabilitation services at the weekend increased activity levels of patients who received them, not only at the weekend but also on the following days. However, patients’ lower limbs may not be sufficiently active during inpatient rehabilitation as inpatients are most active during physical therapy and occupational therapy sessions and do little habitual physical activity when not under the supervision of therapists |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 105; age: > 18 years; gender: both; cognitive impairment: no | ||
| Penrod 2004192 | Limitations: (1) observational study design leading to differential provision of physiotherapy and/or occupational therapy to patients based on their likelihood of benefiting from these, as well as differences in timing and frequency; (2) limitation of the locomotion subscale of the FIM in terms of the amount of assistance that patients receive from a person or device to walk and climb stairs and not measuring gait speed or fear of falling that might have improved by early physiotherapy; (3) analysis performed of survivors only, who might have been healthier and hence may not represent the elderly/frail population; and (4) the number of therapy sessions is only one part of the rehabilitative and overall package of services received by patients with hip fracture; little is known about how the timing and intensity of therapy sessions might affect the outcomes and, moreover, the reimbursement policy, rather than clinical judgement or evidence of effectiveness, may largely dictate the prescription of the timing and intensity of therapy sessions | There was a mobility advantage at 2 months post hip fracture for patients who received more physiotherapy between the day of hip fracture surgery and the first 3 post-operative days. However, the association between early physiotherapy and mobility improvement was attenuated at 6 months post fracture. Hence, early mobilisation and physiotherapy sessions are prudent for patients undergoing surgical repair after fracture of a hip |
| USA | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 443; age: ≥ 50 years; gender: both; cognitive impairment: no | ||
| Peterson 2004113 | Limitations: (1) the peer visits were not well received and so that component was discontinued; (2) some patients were not discharged directly home but to acute and subacute care facilities, which delayed the start of the intervention; (3) some participants received care at home other than the intervention or standard care; and (4) participants were reluctant to return to the hospital for assessment | Although strength training and balance exercises may improve rehabilitation after hip fracture, it not possible to illustrate an effect from this study. Both intervention and control participants were involved in exercise programmes elsewhere and it was impossible to monitor the type of training received. This study attempted too much in a short time period when participants were showing rapid improvement anyway |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 70; age: ≥ 65 years; gender: both; cognitive impairment: NA | ||
| Petrella 2000169 | NR | There may be a discrepancy between the attention of the rehabilitation programme on functional outcomes and less emphasis being placed on confidence-building behaviours. Restrictions in function from a fear of falling may negate any gains made through rehabilitation and this could limit the long-term success of these programmes and patient outcomes after hip fracture |
| Canada | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 56; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Portegijs 2008114 | Limitations: (1) study was underpowered; and (2) the fractured leg was not always the weaker leg because of potential influences of other diseases and injuries affecting one leg since the hip fracture; the training, specifically aiming to reduce asymmetric deficit, may thus be more effective when targeted to a population with a clear and consistent deficit, such as in the rehabilitation phase after disease or injury affecting one leg only | Intensive resistance training is feasible for people with a hip fracture and helps improve muscle strength and power. The intervention group had better walking ability and outdoor mobility. Patients may be more responsive in the rehabilitation phase after major injury when the asymmetric deficit is likely to be large |
| Finland | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 46; age: 60–85 years; gender: both; cognitive impairment: no | ||
| Portegijs 2012166 | Limitations: (1) because of the exclusion criteria, participants had a relatively high level of functioning compared with hip fracture patients in general and so generalisation of the results should be carried out with caution; and (2) because of the cross-sectional study design, the chronological order of lack of balance confidence and limitations in mobility and balance performance and the relationship to the hip fracture event remain unclear | In older people with fall-related hip fracture, an independent relaptionship exists between balance confidence and a range of performance-based and self-reported mobility and balance performance measures. In this group of older people, a score of < 85 on the Activities-specific Balance Confidence scale identified those with mobility and balance limitation. Identification of those with a lack of balance confidence seems clinically relevant as it may compromise functional recovery. Potentially, rehabilitation may be more effective when lack of balance confidence is taken into account or targeted. However, further study is needed to develop existing strategies to improve balance confidence and reduce the functional decline associated with hip fracture |
| Finland | ||
| Quantitative comparative | ||
| Historical cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 130; age: ≥ 60 years; gender: both; cognitive impairment: partial | ||
| Proctor 200813 | NR | Psychological interventions should be formulation led and based on the specific individual needs of the person, a core prerequisite to any psychological approach. Therefore, it is essential that clinical psychologists facilitate and disseminate the use of psychological strategies by providing teaching, training and consultation to other professionals within health-care services |
| UK | ||
| Case studies | ||
| Historical cohort study | ||
| Hospital | ||
| Rich | ||
| Participants: n = 3 case studies; age: NR; gender: both; cognitive impairment: no | ||
| Pryor 1988150 | NR | A large proportion of patients need rehabilitation in hospital. The orthogeriatric system would seem most appropriate for such patients, and it can also significantly reduce the length of hospital stay |
| UK | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 200; age: any; gender: both; cognitive impairment: no | ||
| Resnick 200572 | Limitation: sample was selected based on specific inclusion criteria and hence the results may not be applicable to all hip fracture patients | The Exercise Plus Program had beneficial effects on hip fracture patients and lessons learned can be translated to the development of other motivational interventions to help engage older adults in exercise |
| USA | ||
| Qualitative | ||
| Qualitative | ||
| Community | ||
| Rich | ||
| Participants: n = 70; age: any; gender: both; cognitive impairment: no | ||
| Resnick 200769 | Limitations: (1) the older women in this study were relatively healthy, lived in the community prior to fracture and willingly participated in an exercise intervention study; (2) there was variability in terms of when the intervention was initiated (because of participant willingness to allow the trainer to come out to the home setting) and some group differences in the number of visits to which participants were exposed; (3) there was an inability to control the type and amount of efficacy information that participants were exposed to, limiting interpretation of the findings; (4) multiple measures were based on recall; and (5) differences in time spent exercising cannot be addressed because of the short follow-up. Strength: it was possible to engage these women in a home-based exercise programme and the Plus only, exercise only or combined Exercise Plus Program resulted in the desired outcome of increased time in exercise | Older adults should be helped to realistically assess their self-efficacy and outcome expectations related to exercise. Health-care providers and friends/peers should be encouraged to reinforce the positive benefits of exercise. Fear of falling should be addressed throughout the entire hip fracture recovery trajectory, well after the initial fracture. Interactions with peers, possibly peers who themselves exercise (and who may have experienced a hip fracture), has a positive influence on self-efficacy related to exercise post hip fracture. Practitioners should consider the use of peers to strengthen beliefs and thereby improve exercise behaviour in older adults post hip fracture. There was no evidence of a trainer effect during any of the testing time points. Thus, the benefits of encouraging exercise are not trainer specific and the skills to be an effective trainer may be easily learned. Self-efficacy and outcome expectations had no direct relationship with exercise. Instead, they indirectly related to exercise through stage of change. Thus, the interventions might best be targeted at encouraging self-efficacy related to readiness to adopt exercise behaviour, after which time exercising will increase. Future research is needed to replicate the findings of this study as demonstrating the beneficial impact of the Plus component alone has practical implications in clinical settings |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Rich | ||
| Participants: n = 208; age: ≥ 70 years; gender: female; cognitive impairment: no | ||
| Richards 1998128 | NR | The early discharge hospital-at-home scheme was similar to routine hospital discharge in terms of effectiveness and acceptability. Increased length of stay associated with the scheme must be interpreted with caution because of different organisational characteristics of the services |
| UK | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 241; age: > 65 years; gender: both; cognitive impairment: no | ||
| Roberto 1992165 | Limitations: (1) study design limitations: retrospective and cross-sectional and so has inherent biases; (2) the cross-sectional nature of this study limits the examination of coping to immediately after the hip fracture; it is not known if this strategy continued to be employed over the course of the recovery period; and (3) the women interviewed had survived an incident known for its high mortality rate; no information available about the resources or coping strategies of women who did not survive the trauma or who chose not to participate in the study | Coping with an enduring health condition is a daily challenge for many older adults. A better understanding of the types of strategies commonly used by older individuals to cope with health-related problems will provide greater insight into the reactions and behaviours of older adults |
| USA | ||
| Quantitative non-comparative | ||
| Historical cohort study | ||
| Community | ||
| Rich | ||
| Participants: n = 101; age: 65–94 years; gender: female; cognitive impairment: no | ||
| Roberts 2004155 | Limitation: study design was subject to contamination of the intervention effect, which was addressed by abstracting all data from the medical records prospectively and obtaining audit data from the nearby orthopaedic units for the same time frames to control for external influences during the study; this design represents a pragmatic solution to the difficulties of preventing contamination | The integrated care pathway was associated with improvements in the process and better outcomes of care, such as improved mobility on discharge, fewer infections and pressure sores, and a trend towards fewer admissions to institutional care for a group of patients with complex needs. Care pathways for hip fracture patients can be a useful tool for raising care standards but may require a longer hospital stay and additional resources such as greater occupational therapy use |
| UK | ||
| Quantitative comparative | ||
| Controlled before-and-after study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 764; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Robinson 1999183 | Limitation: it is possible that the researcher and moderator may have influenced the groups’ interactions; with focus group research, the researcher and moderator are actively involved in the production of data. Strength: both the moderator and the researcher attempted to be sensitive to this issue by ensuring that their interactions were open, authentic and sensitive to the participants | The participating women were confronted with an array of problems, which were labelled function-inhibiting factors. To overcome these problems, they mobilised their adaptive approaches to life. In addition, they identified various interdisciplinary interventions, labelled function-promoting factors, which helped to provide a successful transition. From these findings, a programme of interdisciplinary interventions was identified that could be implemented in subacute units and tested to establish its effectiveness in promoting a successful transition following hip fracture |
| USA | ||
| Qualitative | ||
| Qualitative | ||
| Hospital | ||
| Thick | ||
| Participants: n = 15; age: > 70 years; gender: female; cognitive impairment: no | ||
| Röder 2003151 | Limitations: (1) non-randomised study design; (2) small sample size; and (3) only patients with normal mental status were enrolled in the study, which might have meant that fitter individuals were recruited, and so the results might not be generalisable | After receiving institutional rehabilitation following surgical treatment of hip fracture there was improvement in patients’ activities of daily living and Instrumental Activities of Daily Living scale scores compared with pre-surgical evaluations; patients regained approximately 80–90% of their initial baseline scores (pre-fracture status) within 6 months of rehabilitation; and there was no significant impact on mortality and morbidity in patients of normal mental status |
| Germany | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 142; age: ≥ 65 years; gender: both; cognitive impairment: partial | ||
| Rolland 2004184 | Limitations: (1) assessments of comorbidity and medication use prone to reporting bias in cognitively impaired patients; (2) small sample size; and (3) underpowered study for analysis | Cognitively impaired elderly patients with hip fracture can benefit from participation in rehabilitation programmes and improve their functional status; this benefit can be small compared with the maximum theoretical functional gain but it is in accordance with their initial functional status |
| France | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 61; age: ≥ 70 years; gender: both; cognitive impairment: yes | ||
| Rösler 2012152 | NR | Treatment in a specialised cognitive geriatric unit resulted in better mobility of demented patients with proximal fracture of the femur but did not result in significant increases in ADL scores and number of patients discharged back home |
| Germany | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 129; age: any; gender: both; cognitive impairment: yes | ||
| Ryan 2006115 | Limitations: (1) low recruitment and uptake rate; (2) smaller sample size than calculated for power of the study; (3) large dropout rate (n = 13/58) and so the analysis was performed through simple imputation, which might increase the likelihood of detecting a significant difference; and (4) lack of information regarding the nature of the intervention | A more intensive community-based multidisciplinary therapy service after discharge from hospital following a hip fracture is unlikely to result in short-term benefit in relation to social participation and some aspects of health-related quality of life |
| UK | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 58; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Saltvedt 2012116 | Limitations: (1) study sample; (2) non-blinding of assessors; (3) choice of end points; and (4) content and performance of the experimental intervention programme | A new treatment program for old hip fracture patients was developed, introduced and run in the Department of Geriatrics, the potential benefits of which were compared in a RCT with those of traditional care of hip fracture patients in the Department of Orthopaedic Surgery; the results will be reported later |
| Norway | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 401; age: ≥ 70 years; gender: both; cognitive impairment: yes | ||
| Shawler 2006174 | Limitations: (1) despite attempts to include an ethnically diverse sample, all mothers and daughters in the study were European American; (2) even with prolonged engagement and multiple interviews, social desirability may have influenced the women’s reports; and (3) because mothers and daughters had to agree to participate together in this study, dyads with problematic relationships may not have been equally represented | Older women are at a much higher risk of disabling conditions as they age. Therefore, it is imperative that nurses recognise and acknowledge the courage needed and used by older mothers and their caregiving daughters during a health crisis. Nurses can reinforce the courage and inner strength of older women so that they may be empowered to manage and grow from the complicated times of the health crisis |
| USA | ||
| Qualitative | ||
| Qualitative | ||
| Community | ||
| Thick | ||
| Participants: n = 6 mother–adult daughter dyads); age: 76–85 years; gender: female; cognitive impairment: no | ||
| Sherrington 1997117 | Limitations: (1) no participant blinding so it is possible that part of the improvement found in the intervention group group may have been a result of the increased motivation and effort expended; (2) experimenter bias, as the investigator who assessed the subjects was not blind to treatment status; and (3) emphasis was placed on simple, portable tests for the measurements of strength, balance and gait; these assessment tools achieved this aim but may have lacked some of the precision of more sophisticated laboratory equipment | The exercise programme improved strength and mobility following hip fracture and significantly reduced fall risk factors, yet was relatively inexpensive as it was carried out in subjects’ home environment with basic equipment. Significant changes were noted in a short time frame and greater improvements may be possible with ongoing exercise of this nature |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 44; age: > 60 years; gender: both; cognitive impairment: no | ||
| Sherrington 2004118 | Limitations: (1) no assessor blinding; and (2) the exercise programme was conducted in the home with little supervision and so it was not possible to gather reliable information about the actual intensity of training; hence, practice recommendations cannot be made accurately and reliably. Strength: the external validity of the study is likely to be high; subjects were representative of those with fractured hips, people with a wide range of ages (57–95 years) were included and there were few exclusion criteria and, in addition, participants were recruited from several hospitals, both public and private care, and from several different settings (orthopaedic wards, rehabilitation wards, physical therapy departments); participants had received several different treatment approaches before entering the study and represented a range of socioeconomic and ethnic backgrounds | A weight-bearing home exercise programme with limited supervision can improve balance and functional ability to a greater extent than a non-weight-bearing programme or no intervention among older people with a fall-related hip fracture. All participants completed the usual post-fracture care, so it is evident that they had the potential for further improvements in physical functioning |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 120; age: ≥ 55 years; gender: both; cognitive impairment: no | ||
| Shyu 2008119 | Limitations: (1) older patients with severe cognitive impairment and weak muscle power were excluded and so the effect of the intervention can be generalised only to hip-fractured elders without severe cognitive impairment and with adequate muscle power in their extremities; (2) single-blind design in which the personnel delivering the intervention and assessing the outcomes were not blinded; (3) lack of baseline measures for health-related quality of life before implementing the intervention programme; (4) method of randomisation (coin flip) might have resulted in a dynamic bias; and (5) the effects of the intervention might not be observed if implemented in other countries because of different health systems, limiting the generalisability of the findings. Strength: intention-to-treat and on-protocol analyses had similar results | An interdisciplinary intervention for hip fracture with a geriatric hip fracture programme and a discharge support component benefited elderly patients without severe cognitive impairment by improving their self-care ability, walking ability and health-related quality of life, and decreasing depressive symptoms, number of subsequent falls and emergency department visits during the 2 years after hospital discharge. The results provide quantitative estimates for the trajectories of treatment effects and provide a reference for health-care providers in countries using similar programmes with Chinese/Taiwanese immigrant populations |
| Taiwan | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 162; age: ≥ 60 years; gender: both; cognitive impairment: yes, mild to moderate | ||
| Shyu 2009196 | Limitations: (1) convenience sample; (2) pre-fracture risk for depression was not assessed; (3) high rate of loss to follow-up; and (4) patients with severe mental impairment and physical disability prior to the fracture were excluded and so the results are not generalisable | Timely psychological interventions are suggested within the first 6 months after discharge. Health-care professionals need to pay attention to older patients with poorer pre-fracture functioning and particularly those with lower emotional–social support. The finding that the prevalence of risk for depression appeared to be high in this sample has several implications for nursing care – nurses should assess older patients for risk of depression during the first year following surgery for hip fracture |
| Taiwan | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 147; age: ≥ 60 years; gender: both; cognitive impairment: yes, mild to moderate | ||
| Sirkka 2003193 | Limitation: major domains of life satisfaction (e.g. satisfaction with ADL, leisure, financial situation and family life) were not investigated | The contribution of the occupational therapist should be to enable a person to live independently. Rehabilitation programmes should also be provided that focus on individuals’ needs and goals to allow participation in community life |
| Sweden | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital and community | ||
| Rich | ||
| Participants: n = 29; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Stenvall 2007120 | Limitations: (1) outpatient rehabilitation after discharge was not as standardised as during the in-hospital stay; in the intervention programme the aim was to have a well-planned discharge followed up with a telephone call and a home visit; (2) patients were offered further rehabilitation after discharge, but the intensity and quality of this outpatient rehabilitation is unknown; and (3) the assessors where not blinded concerning group allocation during the home visits. Strengths: the two groups had a small and similar dropout rate over time; only two people in each group refused the follow-up visits and one person in the control group moved to another part of the country | A multidisciplinary post-operative intervention programme enhances ADL performance and mobility (walking indoors without walking aids) after hip fracture, from both a short- and a long-term perspective |
| Sweden | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 199; age: ≥ 70 years; gender: both; cognitive impairment: yes | ||
| Swanson 1998129 | NR | Early intervention consisting of early surgery, minimal narcotic analgesia, intense daily therapy and close monitoring of patient needs through a multidisciplinary approach resulted in a shorter length of hospital stay |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Thick | ||
| Participants: n = 71; age: ≥ 55 years; gender: both; cognitive impairment: no | ||
| Sylliaas 2011199 | Limitations: (1) greater social contact in the intervention group; (2) healthier and more motivated people might have participated in this exercise intervention study; (3) exercises, other kinds of interventions or levels of physical activity for the control group were not registered; and (4) inclusion criteria restricted the findings to older people living on their own without cognitive impairment; the frailest patients were not included. Strengths: (1) trial designed and implemented according to a strict experimental protocol; (2) adequte sample size; (3) low dropout rate; (4) good compliance with the exercise programme; (5) use of standardised, validated instruments; and (6) blinded examiner | Home-dwelling hip fracture patients can benefit from an extended supervised strength-training programme in a rehabilitation setting. These patients are capable of high-intensity strength training, which should optimise gains in physical function, strength and balance. Resistance exercise training seems to influence functional performance adaptation |
| Norway | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 150; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Takayama 2001164 | Limitations: (1) retrospective study and so data obtained before fracture and at discharge depended on limited medical records and the memories of patients and their family members, introducing recall bias into the difference in duration between discharge from hospital and the time of investigation; and (2) proxy responses in a large number of patients (n = 121) | The findings of this study provide important information regarding current recommendations for shortening the duration of hospitalisation and the provision of appropriate post-operative rehabilitation programmes to patients with hip fracture, depending on their background factors |
| Japan | ||
| Quantitative non-comparative | ||
| Historical cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 189; age: ≥ 60 years; gender: both; cognitive impairment: partial | ||
| Talkowski 2009194 | Limitations: (1) no surgical or medical complications that may have affected activity were recorded; (2) data on body mass index or comorbidities were not collected; (3) three of the 18 patients did not complete their actigraph journal and therapists daily schedules had to be used to determine session times; (4) it was difficult to draw comparisons between inpatient rehabilitation facility and skilled nursing facility patients because of limted numbers of the latter; and (5) the study possibly suffered a type II error because of p-values being slightly higher than 0.5, but values appeared clinically meaningful. Strengths: (1) the longitudinal study allowed for the association between physical activity and future functional outcomes to be investigated; (2) the use of accelerometers was feasible and easily implemented and none of the accelerometers was lost or broken; and (3) the Pittsburgh Participation Rating Scale was simple to use in both settings and did not require excessive staff training or participant burden | Therapist-rated patient participation was associated with objective measures of patient activity, which added insight into future functional outcomes in patients after hip fracture |
| USA | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 18; age: ≥ 60 years; gender: both; cognitive impairment: no | ||
| Taylor 2010185 | Limitations: (1) interviews from a small number of physiotherapists; (2) one rehabilitation centre study so findings may not be generalisable; and (3) researchers’ backgrounds as physiotherapists and work colleagues might have influenced the interviews and the interpretation of the data. Strengths: the methods were rigorous as the participants were provided with transcribed interviews to check; transcripts were coded independently by two researchers and themes were developed by subsequent discussion with a third researcher; and the use of direct quotations in the results served to improve internal validity | In planning discharge after rehabilitation for hip fracture, clinicians place more emphasis on the individual needs and goals of the patient than on specifying objective performance criteria that must be met. The expectation that lack of confidence could be a problem after returning home suggests that this factor could be considered more in discharge planning |
| Australia | ||
| Qualitative | ||
| Qualitative | ||
| Hospital | ||
| Thick | ||
| Participants: n = 12; age: NR; gender: female; cognitive impairment: NA | ||
| Tinetti 1999121 | NR | The systematic multicomponent rehabilitation programme was no more effective in promoting recovery than usual home-based rehabilitation. No self-reported functional outcomes were better and only two physical performance outcomes were marginally better in the intervention group than in the usual care group. At 6 months, upper-extremity strength was significantly better in the intervention group than in the usual care group and the intervention group manifested marginally better qualitative gait performance than the usual care group |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 304; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Travis 199889 | Limitations: (1) no tape recording of the interviews, therefore missing the chance to capture the richness of the data; and (2) inability to gendralise the findings because the population was quite old | The actions that elderly people take to create opportunities for mentally restorative experiences are related to past patterns of restorative activities, opportunities made available by the facility, especially circumstances of their care, environmental limitations in the immediate care environment and the degree to which external factors (such as family visits) are readily available |
| USA | ||
| Mixed methods | ||
| Mixed methods | ||
| Hospital | ||
| Rich | ||
| Participants: n = 8; age: ≥ 60 years; gender: both; cognitive impairment: no | ||
| Tsauo 2005122 | Limitations: (1) small sample size; and (2) large number lost to follow-up | The home-based physiotherapy programme is associated with earlier functional recovery and better health-related quality of life than usual care |
| Taiwan | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 54; age: ≥ 60 years; gender: both; cognitive impairment: no | ||
| Uy 2008123 | NR | No definite conclusion can be drawn about the effectiveness of the intervention because of its premature termination. However, the study established that it is feasible to provide interdisciplinary rehabilitation to older people with hip fracture and severe disablement |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 10; age: ≥ 80 years; gender: female; cognitive impairment: no | ||
| Van Balen 2002140 | Limitations: (1) small sample size because of the time-consuming follow-up; and (2) study design non-randomised, so some variables (e.g. type of treatment and length of hospital stay) may have changed during the study | There was no clear advantage of discharging hip fracture patients 13 days earlier from the acute hospital. Patients who came from home in the early discharge group had better walking ability and improvements in ADL level at 1 month, but there was no difference at 4 months |
| The Netherlands | ||
| Quantitative comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 208; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| van der Sluijs 1991186 | NR | Rehabilitation after hip fracture is predominantly influenced by sociomedical factors, especially mental health status, whereas fracture type, treatment and ability for immediate weight bearing were not associated with success |
| The Netherlands | ||
| Quantitative non-comparative | ||
| Controlled before-and-after study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 134; age: any; gender: both; cognitive impairment: NR | ||
| Vidán 2005124 | Limitations: (1) sample size was estimated based on length of stay assumptions but not on clinical indices and so the study was not powered to detect differences in relevant low-incidence events; (2) this was an open trial and therefore subject to bias, such as changes in clinical management associated with observation; (3) these results may not be replicable in other clinical settings with a different health-care system organisation; (4) the functional evaluation was based on ADL and Functional Ambulation Classification scales. These are the most frequently used scales in clinical practice but probably lack sensitivity to detect subtle changes occurring during recovery from a hip fracture; and (5) this study lacked a cost-effectiveness analysis to help programme implementation | Early multidisciplinary daily geriatric care reduces in-hospital mortality and medical complications in elderly patients with hip fracture, but there is not a significant effect on length of hospital stay or long-term functional recovery |
| Spain | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital | ||
| Rich | ||
| Participants: n = 319; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Visser 2000156 | NR | Loss of muscle strength, but not loss of muscle mass, is an independent predictor of poorer mobility recovery 12 months after a hip fracture |
| USA | ||
| Quantitative non-comparative | ||
| Controlled before-and-after study | ||
| Community | ||
| Thick | ||
| Participants: n = 90; age: ≥ 65 years; gender: female; cognitive impairment: NR | ||
| Vogler 2012125 | Limitation: (1) the study population for this trial consisted of older people recently discharged from hospital, which may limit the generalisability of the findings to the broader community-dwelling population; and (2) given the short-term nature of the follow-up, it is not possible to draw any conclusions about health-care usage, costs or residential status | Balance improvements and fall-risk reductions associated with a 12-week home-based exercise programme in older adults were partially to totally lost 12 weeks after the cessation of the intervention. These significant detraining effects suggest that sustained adherence to falls prevention exercise programmes is required to reduce fall risk |
| Australia | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 180; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Walheim 1990187 | NR | Continued rehabilitation for > 3 months following surgery is absolutely worthwhile, especially in patients with an unstable trochanteric fracture |
| Sweden | ||
| Quantitative non-comparative | ||
| Concurrent cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 92; age: > 50 years; gender: both; cognitive impairment: partial | ||
| Whitehead 2003161 | Limitations: (1) inability to reliably measure pre-fracture disability; (2) London Handicap Scale component measuring economic self-sufficiency may be less relevant in this elderly group and overemphasise their degree of disability; (3) this scale has not previously been validated in an Australian sample; (4) results are not generalisable to the whole hip fracture population because of the exclusion of demented patients and those living in residential care; (5) small sample size; and (6) no assessment of the prevalence of mood disorders in the population, which could be a potential confounder | A clinical focus on the impairments that lead to slowed gait and falls following hip fracture could lead to lower levels of disability in this group. A focus only on self-care and simple ADL will not treat the key problems in this population, such as balance and strength. The range of outcome measures that are collected by rehabilitation wards should be expanded or revised in light of the findings of this study. Falls after hip fracture and slow gait speed lead to greater levels of disability and loss of self-efficacy. Measures of falls and gait speed following hip fracture should be considered as other outcomes in the rehabilitation of patients with hip fracture. Falls prevention following hip fracture should become an important target for the prevention of future disability |
| Australia | ||
| Quantitative non-comparative | ||
| Historical cohort study | ||
| Community | ||
| Thick | ||
| Participants: n = 73; age: ≥ 60 years; gender: both; cognitive impairment: no | ||
| Yu-Yahiro 2009126 | NR | It was possible to develop and implement, and engage a frail older population of post-hip fracture patients in, a home-based programme of aerobic and strength training exercise. The rate of participation in the programme was high |
| USA | ||
| Quantitative comparative | ||
| RCT | ||
| Community | ||
| Thick | ||
| Participants: n = 180; age: ≥ 65 years; gender: female; cognitive impairment: no | ||
| Zabari 2012162 | Limitations: (1) retrospective study; and (2) did not include data following discharge from the rehabilitation hospital | Proactive monitoring and management of pain in surgical hip fracture patients is associated with better outcomes and should be considered a standard in the rehabilitation of elderly patients following hip fracture surgery |
| Israel | ||
| Quantitative non-comparative | ||
| Historical cohort study | ||
| Hospital | ||
| Thick | ||
| Participants: n = 144; age: > 65 years; gender: both; cognitive impairment: NR | ||
| Zidén 2008127 | Limitations: (1) only two men included because of a lack of male candidates and because several men declined to participate; hence, the sample may not be representative of male gender views; (2) biases related to the inherent design of the interview study, making the validity questionable, as there is no way of ensuring that the subjects really shared their profound experiences or that the interpretation of what was said is correct; (3) the length of some of the interviews at 1 year of follow-up was relatively short; the interviews were performed at the end of the follow-up visit, after the completion of several self-report questionnaires and performance tests, which might have influenced their length, as the interviewees might have thought that they had already talked about various aspects of the fracture; (4) one interview was largely inaudible because of technical problems with the tape recorder; and (5) the participants knew the interviewer well as the visit was the last of at least four earlier encounters [one or two in hospital as well as follow-up visits (1 month, 6 months and 1 year after discharge) in the home], which may have led to the patients trying to please the interviewer; however, this familiarity may also mean that the interviewees were less afraid of sharing experiences. Strengths: (1) steps were taken to enhance the trustworthiness, reliability and validity of the results – (a) categories were illustrated with quotations from the interviews, (b) categories were double-checked by an independent assessor by first reading and analysing the interviews separately and then reflecting and discussing together until consensus about the category descriptions was reached and (c) the subjects, or the interviewer, were able to return to topics under discussion earlier if they wished because of the organic nature of the interview | The fracture caused social and existential cracks in sufferers’ thinking in the early phases after the injury, extending patients’ experiences beyond the actual injury. Hence, arranging health care and rehabilitation chains in order to link together different health-care organisations should be given priority. The findings indicate that the negative consequences of a hip fracture are substantial and long lasting. Hence, health professionals need to consider the patients’ own experiences and possible fear and not merely focus on the physical injury and disabilities |
| Sweden | ||
| Qualitative | ||
| Qualitative | ||
| Community | ||
| Thick | ||
| Participants: n = 18; age: ≥ 65 years; gender: both; cognitive impairment: no | ||
| Zidén 200890 | Limitations: (1) patients’ eligibility was not assessed before randomisation and so a considerable number of patients were excluded after randomisation; (2) baseline differences between the home rehabilitation group and the conventional care group; (3) ineffective use of the Falls Efficacy Scale to measure instrumental activities, resulting in weak measurements of confidence and efficacy; and (4) short follow-up duration. Strength: no dropouts and few missing values at the 1-month follow-up | A brief home rehabilitation programme focusing on enhancing self-efficacy improves patients’ balance confidence and makes them more independent and active in the early phase after hip fracture. Patients receiving home rehabilitation need less post-surgery time at health-care facilities. Home rehabilitation helped patients improve their outdoor activities, resume outdoor walking habits and improve balance confidence more quickly than conventional care |
| Sweden | ||
| Quantitative comparative | ||
| RCT | ||
| Hospital and community | ||
| Thick | ||
| Participants: n = 102; age: ≥ 65 years; gender: both; cognitive impairment: no |
Appendix 19 Outcomes reported in the included studies
All of the outcomes identified in the review were categorised into four major areas and effect sizes are presented for these subgroups of outcome measures in the following tables.
Key for effect sizes
++, intervention statistically significantly better than comparator.
==, no statistical difference between intervention and comparator.
–, comparator statistically significantly better than intervention.
<> statistical test(s) not reported.
Italic numerals relate to the outcome measure instruments reported in Appendix 10.
| Study details (author, year; country; study design) | Intervention and comparator | ADL | Composite scores: favourable clinical course/functional recovery | Exercise behaviour | Quality of life | Physical function/mobility/functional recovery/balance | Physiological measurements/muscle strength |
|---|---|---|---|---|---|---|---|
| Adunsky 2003138 Israel Concurrent cohort study |
Orthogeriatric ward (n = 116) vs. orthopaedic department (n = 204) | 39 – post discharge ++; 40 – post discharge ++ | 35 – post discharge ++; 34 – post discharge ++ | 80 – post discharge ++ | |||
| Al-Ani 2010139 Sweden Concurrent cohort study |
Early discharge to a rehabilitation unit (n = 81) vs. early discharge to previous residence (n = 146) | 6 – 4 months ++, 12 months ++ | 132 – 4 months ++, 12 months ++ | ||||
| Allegrante 200791 USA RCT |
Hospital-based physical therapy plus motivational videos plus visits from recovered hip fracture patients (n = 90) vs. usual care (n = 86) | 117 – 6 months ++ | |||||
| Arinzon 2005201 Israel Concurrent cohort study |
Old-old elderly (aged ≥ 85 years) geriatric rehabilitation in the community (n = 46) vs. young elderly (aged 65–74 years) geriatric rehabilitation in the community (n = 56) | 38 – at discharge -- | |||||
| Balen 2002140 Netherlands Concurrent cohort study |
Early discharge (n = 106) vs. conventional management (n = 102) | 108 – 4 months == | 86 – 4 months == | 135 – 4 months == | |||
| Beaupre 2005157 Canada Historical cohort study |
Clinical pathway consisting of standardised, current best evidence or clinical consensus (n = 451) vs. pre-clinical pathway (n = 468) | 11 – at discharge ++, 3 months ==, 6 months == | |||||
| Bellelli 201078 Italy RCT |
Conventional post-orthopaedic rehabilitation programme plus visual feedback (n = 30) vs. conventional post-orthopaedic rehabilitation programme (n = 30) | 40 – at discharge ++; 39 – at discharge ++; 129 – at discharge ++ | |||||
| Binder 200492 USA RCT |
Tailored, supervised physical therapy and exercise training (n = 46) vs. home exercise (n = 44) | 6 – 3 months <>, 6 months <> | 117 – 3 months ++, 6 months ++ | 15 – 3 months ++, 6 months ++; 45 – 3 months ++, 6 months ++; 100 – 3 months ++, 6 months ++; 47 – 3 months ++, 6 months ++ | |||
| Bischoff-Ferrari 201093 Switzerland RCT |
Physiotherapy (n = 87) vs. cholecalciferol therapy (n = 86) | 143 – 6 months ++, 12 months ++ | |||||
| Carmeli 2006131 Israel Quasi-randomised trial |
Class-based outpatient exercise programme (n = 34) vs. home-based programme (n = 29) | 99 – 3 months ++; 43 – 3 months ++ | |||||
| Casado 200980 USA RCT |
Exercise Plus Program: exercise plus motivation vs. exercise only vs. motivation only vs. routine care (n = 168) | 141 – 2 months ++, 6 months ++ | 117 – 2 months ++, 6 months ++ | ||||
| Crotty 200395 Australia RCT |
Accelerated discharge and home rehabilitation (n = 34) vs. usual or conventional care (n = 32) | 11 – 4 months ++, 12 months == | 128 – 4 months ==, 12 months ==; 9/15/70 – 4 months ==, 12 months == | ||||
| Dai 2002132 Taiwan Quasi-randomised trial |
Multidisciplinary rehabilitation programme (n = 47) vs. conventional care (n = 47) | 4 – 6 months == | 77 – 6 months ++ | ||||
| Deschodt 201197 Belgium RCT |
Inpatient geriatric consultation (n = 94) vs. usual care (n = 77) | 1 – 6 weeks ==, 4 months ==, 12 months == | |||||
| Di Monaco 2008133 Italy Quasi-randomised trial |
Hospital plus home rehabilitation (n = 47) vs. hospital rehabilitation alone (n = 48) | 12 – 6 months ++ | |||||
| Fortinsky 200281 USA Concurrent cohort study |
Physical and occupational therapy (n = 24) | 39 – 6 months ++; 38 – 6 months ++ | |||||
| Giusti 2006143 Italy Concurrent cohort study |
Home-based rehabilitation (n = 99) vs. institutional-based rehabilitation (n = 100) | 1/12 – 3 months ==, 6 months ++, 12 months ++; 12/66 – 3 months ++, 6 months ++, 12 months ++ | |||||
| Hoekstra 2011144 The Netherlands Concurrent cohort study |
Multidisciplinary nutritional care (n = 61) vs. standard nutritional care (n = 66) | 24 – 3 months ++ | 145 – 3 months == | ||||
| Host 2007153 USA Controlled before-and-after study |
Supervised exercise training programme (n = 31) | 5 – 6 months ++; 6 – 6 months ++ | 99 – 6 months ++; 139 – 6 months ++; 138 – 6 months ++; 127 – 6 months ++ | ||||
| Huang 2005100 Taiwan RCT |
Discharge planning (n = 63) vs. routine care (n = 63) | 12 – 3 months ++ | 117 – 3 months ++ | ||||
| Jackson 200183 USA Quasi-randomised trial |
Occupational adaptation model (n = NR) vs. biomedical rehabilitation model (n = NR) | 38 – at discharge == | |||||
| Jensen 1979154 Denmark Controlled before-and-after study |
Physical rehabilitation (n = 518) | 117 – 6 months ++ | |||||
| Jones 2002195 Canada Controlled before-and-after study |
Inpatient rehabilitation (n = 44) | 39 – 6 weeks ++; 38 – 6 weeks ++ | |||||
| Kennie 1988102 UK RCT |
Multidisciplinary rehabilitation in a community hospital (n = 54) vs. routine care with early discharge home (n = 54) | 1 – at discharge ++, 12 months ++ | |||||
| Koval 1998146 USA Concurrent cohort study |
Inpatient rehabilitation (n = 308) vs. standard care available before implentation of inpatient rehabilitation programme (n = 301) | 4 – 3 months ==, 6 months ==, 12 months ==; 5 – 3 months ==, 6 months ==, 12 months == | 135 – 3 months ==, 6 months ==, 12 months == | ||||
| Kuisma 2002103 Hong Kong RCT |
Home-based physiotherapy (n = 40) vs. institution-based physiotherapy (n = 41) | 8 – 4 months ++, 8 months ++, 12 months ++ | |||||
| Latham 2006167 USA Database analysis |
Rehabilitation in a skilled nursing facility (n = 351) | 42 – at discharge ++; 39 – at discharge ++ | |||||
| Levi 1997147 USA Concurrent cohort study |
Comparison of discharge practices of four hospitals and discharge destinations (n = 123) | 12 – 2 months ==, 4 months == | |||||
| Lieberman 2002148 Israel Concurrent cohort study |
Older group (≥ 85 years) geriatric ward rehabilitation (n = 127) vs. younger group (75–84 years) geriatric ward rehabilitation (n = 297) | 38 – at discharge ++ | |||||
| Lin 2009105 Taiwan RCT |
Comprehensive discharge planning (n = 26) vs. routine discharge nursing care (n = 24) | 117 – 3 months ++ | 90 – 3 months ++ | ||||
| Louie 2012106 Hong Kong RCT |
Patient and Carer Empowerment Programme (n = 63) vs. conventional care (n = 71) | 6 – 5 days post programme ++; 5 – 5 days post programme ==; 39 – 5 days post programme == | 54 – 5 days post programme == | ||||
| Mangione 2010107 USA RCT |
Leg-strengthening exercises (n = 14) vs. conventional transcutaneous electrical nerve stimulation (n = 12) | 117 – 3 months ==, 6 months == | 100 – 3 months ++, 6 months ++; 133 – 3 months ==, 6 months ++; 47 – 3 months ++, 6 months ++ | 64 – 3 months ==, 6 months ++ | |||
| Mendelsohn 2008108 Canada RCT |
Upper-body exercise plus standard rehabilitation care (n = 10) vs. standard rehabilitation care (n = 10) | 38 – at discharge == | 15 – at discharge ++; 128 – at discharge ++; 132/131 – at discharge ++ | 144 – at discharge ++ | |||
| Mitchell 2001109 UK RCT |
Quadriceps training plus standard physiotherapy (n = 40) vs. standard physiotherapy (n = 40) | 11 – 6 weeks ++, 4 months ++ | 87 – 6 weeks ++, 4 months ++; 128 – 6 weeks ++, 4 months ++; 23 – 6 weeks ++, 4 months ++ | 68 – 6 weeks ++, 4 months ++; 51 – 6 weeks ++, 4 months ++ | |||
| Moseley 2009110 Australia RCT |
Higher-dose weight-bearing exercise (n = 80) vs. lower-dose limited weight-bearing exercise (n = 80) | 97/12 – 4 weeks ==, 4 months == | 24 – 4 weeks ==, 4 months == | 15 – 4 weeks ==, 4 months == | 62 – 4 weeks ==, 4 months ==; 137 – 4 weeks ==, 4 months == | ||
| Munin 2005149 USA Concurrent cohort study |
Inpatient rehabilitation facility (n = 42) vs. skilled nursing facility rehabilitation (n = 34) | 39 – 3 months ++, 6 months ++ | |||||
| Naglie 2002111 Canada RCT |
Post-operative interdisciplinary care (n = 141) vs. usual care (n = 138) | 5 – 3 months ==, 6 months ==; 6 – 3 months ==, 6 months ==; 11 – 3 months ==, 6 months == | 8 – 3 months ==, 6 months == | ||||
| Nicholson 1997136 South Africa Non-randomised trial/quasi-experimental study |
Supervised exercise intervention (n = 20) vs. routine care (n = 10) | 105 – 6 weeks == | 51 – 6 weeks == | ||||
| Ohsawa 2007137 Japan Non-randomised trial/quasi-experimental study |
Assertive therapy (n = 10) vs. conventional care (n = 10) | 38 – 6 months ++; 75 – 6 months ++ | |||||
| Oldmeadow 200687 Australia RCT |
Early ambulation (n = 30) vs. delayed ambulation (n = 30) | 61 – 7 days post discharge ++ | |||||
| Oude Voshaar 200712 UK RCT |
Psychological intervention (n = 145) vs. usual care (n = 146) | 120 – 6 months ++ | 120 – 6 months ++ | 128 – 6 months ++; 46 – 6 months ++; 43 – 6 months ++ | |||
| Penrod 2004192 USA Concurrent cohort study |
Physical therapy plus occupational therapy (n = 443) | 38 – 2 months ++, 6 months == | |||||
| Portegijs 2008114 Finland RCT |
Tailored strength–power training (n = 24) vs. usual care (n = 22) | 136 – 3 months ==; 142 – 3 months ++ | 64 – 3 months ++; 63 – 3 months ==; 68 – 3 months ==; 67 – 3 months == | ||||
| Resnick 200769 USA RCT |
Exercise plus programme (n analysed): Exercise plus motivation (n = 52) Motivation only (n = 54) Exercise only (n = 51) vs. inactive control (n = 51) |
141 – 2 months ++, 6 months ++, 12 months ++; 125 – 2 months ++, 6 months ++, 12 months ++ | 117 – 2 months ++, 6 months ++, 12 months ++ | ||||
| Roberts 2004155 UK Controlled before-and-after study |
Integrated care pathway (n = 395) vs. conventional care (n = 369) | 77 – 1 month ++ | |||||
| Röder 2003151 Germany Concurrent cohort study |
Supervised inpatient rehabilitation in orthopaedic and geriatric hospitals (n = 69 and n = 39, respectively) vs. control (n = 34) | 6 – 6 months ++, 12 months ++; 5 – 6 months ++, 12 months ++ | 124 – 6 months ++, 12 months ++ | ||||
| Rolland 2004184 France Concurrent cohort study |
Multidisciplinary rehabilitation in a geriatric unit (n = 61) | 38 | |||||
| Rösler 2012152 Germany Concurrent cohort study |
Specialised ward (cognitive geriatric unit) (n = 53) vs. geriatric ward (non-cognitive geriatric unit) of the same geriatric department (n = 76) | 6 – 12 months ==; 129 – 12 months ++ | |||||
| Ryan 2006115 UK RCT |
Intensive home-based rehabilitation (n = 30) vs. less intensive home-based rehabilitation (n = 28) | 12 – 3 months == | 24 – 3 months == | 32 – 3 months ==; 126 – 3 months == | |||
| Sherrington 1997117 Australia RCT |
Weight-bearing exercise (n = 21) vs. usual care (n = 21) | 47 – 1 month ++; 103 – 1 month == | 85 – 1 month ++ | ||||
| Sherrington 2004118 Australia RCT |
Weight-bearing exercise (n = 60) vs. usual care (n = 60) | 98 – 1 month ==, 4 months ++; 47 – 1 month ==, 4 months ==; 103 – 1 month ++, 4 months ++ | 85 – 1 month ==, 4 months ++ | ||||
| Shyu 2008119 Taiwan RCT |
Geriatric consultation services, a rehabilitation programme and discharge-planning services (n = 81) vs. usual care (n = 81) | 10 – 1 month ++, 3 months ++, 6 months ++, 12 months ++, 24 months ++ | 117 – 1 month ++, 3 months ++, 6 months ++, 12 months ++, 24 months ++ | 134 – 1 month ++, 3 months ++, 6 months ++, 12 months ++, 24 months ++ | |||
| Stenvall 2007120 Sweden RCT |
Specialised geriatric ward (n = 102) vs. specialist orthopaedic ward (n = 97) | 6 – at discharge ==, 4 months ==, 12 months ++; 1 – at discharge ++, 4 months ==, 12 months ++ | 19 – at discharge ==, 4 months ==, 12 months == | ||||
| Sylliaas 2011199 Norway RCT |
Physiotherapist-supervised group and individual exercises (n = 100) vs. routine care (n = 50) | 2 – 3 months ++ | 117 – 3 months ++ | 15 – 3 months ++; 128 – 3 months ++; 121 – 3 months ++; 72 – 3 months ++; 73 – 3 months ++; 133 – 3 months ++ | |||
| Tinetti 1999121 USA RCT |
Home-based rehabilitation (n = 148) vs. usual care (n = 156) | 6 – 6 months ==, 12 months == | 77 – 6 months ==, 12 months ==; 15 – 6 months ==, 12 months ==; 96 – 6 months == 12 months == | ||||
| Tsauo 2005122 Taiwan RCT |
Physical therapy (n = 13) vs. usual care (n = 12) | 57 – at discharge ==, 1 month ++, 3 months ++, 6 months == | 105 – 1 month ==, 3 months ==, 6 months ==; 53 – at discharge ==, 1 month ++, 3 months ++, 6 months ++ | ||||
| Uy 2008123 Australia RCT |
Inpatient interdisciplinary rehabilitation (n = 3) vs. discharge back to the nursing home (n = 7) | 12 – 1 month ++, 4 months ++ | 131 – 1 month ++, 4 months ++ | ||||
| Van Balen 2002140 The Netherlands Concurrent cohort study |
Early discharge to a nursing home rehabilitation ward (n = 106) vs. conventional discharge to a nursing home rehabilitation ward (n = 102) | 106 – 4 months == | 86 – 4 months == | 133 – 4 months == | |||
| Vidán 2005124 Spain RCT |
Comprehensive geriatric intervention (n = 155) vs. usual care (n = 164) | 4 – at discharge ==, 3 months ++, 6 months ==, 12 months == | 44 – at discharge ==, 3 months ++, 6 months ==, 12 months == | 33 – at discharge ==, 3 months ++, 6 months ==, 12 months == | |||
| Visser 2000156 USA Controlled before-and-after study |
Physical therapy (n = 90) vs. NA | 77 – 12 months ++; 78 – 12 months ++ | |||||
| Whitehead 2003161 Australia Historical cohort study |
Home rehabilitation (n = 73) vs. NA | 11 – 4 months == | 70 – 4 months ++; 15 – 4 months ++; 9 – 4 months ++ | ||||
| Zabari 2012162 Israel Historical cohort study |
Pain management protocol (n = 67) vs. usual care (n = 77) | 40 – post discharge ++ | |||||
| Zidén 200890 Sweden RCT |
Home-based rehabilitation (n = 54) vs. conventional care (n = 48) | 39 – 1 month ++; 42 – 1 month ++; 32 – 1 month ++ | 128 – 1 month ++ | 83 – 1 month ++ |
| Study | Intervention and comparator | Patient satisfaction | Carer satisfaction | Cognitive function/dementia | Depression | Fear of falling | Psychological morbidity | Self-efficacy/falls efficacy | Socialisation | Social support |
|---|---|---|---|---|---|---|---|---|---|---|
| Adunsky 2003138 Israel Concurrent cohort study |
Orthogeriatric ward (n = 116) vs. orthopaedic department (n = 204) | 41 – post discharge ++ | ||||||||
| Casado 200980 USA RCT |
Exercise Plus Program (exercise training component plus motivational component: theory of self-efficacy) (n = 126) vs. routine care (n = 42) | 16 – 2 months ++, 6 months ++ | 31 – 2 months --, 6 months -- | 92 – 2 months ++, 6 months ++; 114 – 2 months ==, 6 months == | 123 – 2 months ++, 6 months ++ | |||||
| Crotty 200395 Australia RCT |
Accelerated discharge and home rehabilitation (n = 34) vs. usual or conventional care (n = 32) | 117 – 4 months ==, 12 months == | 117 – 4 months ++, 12 months ++ | 31 – 4 months ++, 12 months ++ | ||||||
| Fortinsky 200281 USA Concurrent cohort study |
Physical and occupational therapy both in the hospital post surgery and at home after discharge (n = 24) | 16 – 6 months ++ | 110 questionnaire – 6 months ++ | |||||||
| Giusti 2006143 Italy Concurrent cohort study |
Home-based rehabilitation (n = 99) vs. institutional-based rehabilitation (n = 100) | 119 – 3 months ++, 6 months ++, 12 months ++ | ||||||||
| Jackson 200183 USA Quasi-randomised trial |
Occupational adaptation model (n = 20) vs. biomedical rehabilitation model (n = 20) | 112 – at discharge ++ | ||||||||
| Jones 2002195 Canada Controlled before-and-after study |
Inpatient rehabilitation (n = 44) | 41 – 6 weeks == | ||||||||
| Lin 2009105 Taiwan RCT |
Comprehensive discharge planning (n = 26) vs. routine discharge nursing care (n = 24) | 95 – 3 months ==; 113 – 3 months ++ | ||||||||
| Louie 2012106 Hong Kong RCT |
Patient and Carer Empowerment Programme (n = 67) vs. conventional care (n = 67) | 27 – 5 days post programme == | ||||||||
| Moseley 2009110 Australia RCT |
Higher-dose weight-bearing exercise (n = 80) vs. lower-dose limited weight-bearing exercise (n = 80) | 29 – 4 weeks ==, 4 months == | ||||||||
| Nicholson 1997136 South Africa Non-randomised trial/quasi-experimental study |
Supervised exercise intervention (n = 20) vs. routine care (n = 10) | 14 – 6 weeks == | 31 – 6 weeks == | |||||||
| Ohsawa 2007137 Japan Non-randomised trial/quasi-experimental study |
Assertive therapy (n = 10) vs. conventional care (n = 10) | 76 – 6 months ++ | ||||||||
| Resnick 200769 USA RCT |
Exercise plus programme (n analysed): Exercise plus motivation (n = 52) Motivation only (n = 54) Exercise only (n = 51) vs. inactive control (n = 51) |
16 – 2 months <>, 6 months <>, 12 months <> | 114 – 2 months ==, 6 months ==, 12 months ==; 92 – 2 months ==, 6 months ==, 12 months == | |||||||
| Röder 2003151 Germany Concurrent cohort study |
Supervised inpatient rehabilitation in orthopaedic and geriatric hospitals (n = 69 and n = 39, respectively) vs. control (n = 34) | 76 – 6 months ==, 12 months == | ||||||||
| Ryan 2006115 UK RCT |
Intensive home-based rehabilitation (n = 30) vs. less intensive home-based rehabilitation (n = 28) | 55 – 3 months == | ||||||||
| Sherrington 1997117 Australia RCT |
Weight-bearing exercise (n = 21) vs. usual care (n = 21) | 146 – 1 month ++ | ||||||||
| Sherrington 2004118 Australia RCT |
Weight-bearing exercise (n = 60) vs. no intervention usual care (n = 60) | 146 – 1 month ==, 4 months == | ||||||||
| Shyu 2008119 Taiwan RCT |
Geriatric consultation services, a rehabilitation programme and discharge-planning services (n = 81) vs. usual care (n = 81) | 50 – 1 month ++, 3 months ++, 6 months ++, 12 months ++, 24 months ++ | ||||||||
| Shyu 2009196 Taiwan Concurrent cohort study |
Risk of depression in the first year after discharge (n = 147) | 50 – 1 month ++, 3 months ++, 6 months ++, 12 months ++ | ||||||||
| Tinetti 1999121 USA RCT |
Home-based rehabilitation (n = 148) vs. usual care (n = 156) | 25 – 6 months ==, 12 months == | ||||||||
| Whitehead 2003161 Australia Historical cohort study |
Home rehabilitation (n = 73) | 31 – 4 months ++ | ||||||||
| Zidén 200890 Sweden RCT |
Home-based rehabilitation (n = 54) vs. conventional care (n = 48) | 30 – 1 month ++ |
| Study | Intervention and comparator | Physical and occupational therapy sessions | Discharge destination/new nursing home admissions | Falls and hospital readmissions | Health-care utilisation | Length of hospital stay | Severity of illness/disease burden |
|---|---|---|---|---|---|---|---|
| Adunsky 2003138 Israel Concurrent cohort study |
Orthogeriatric ward (n = 116) vs. orthopaedic department (n = 204) | 69 – post discharge ++ | |||||
| Arinzon 2005201 Israel Concurrent cohort study |
Old-old elderly (aged ≥ 85 years) geriatric rehabilitation in the community (n = 46) vs. young elderly (aged 65–74 years) geriatric rehabilitation in the community (n = 56) | 58 – at discharge -- | 69 – at discharge -- | ||||
| Beaupre 2005157 Canada Historical cohort study |
Clinical pathway consisting of standardised, current best evidence or clinical consensus (n = 451) vs. pre-clinical pathway (n = 468) | 58 – 3 months ==, 6 months == | 69 – at discharge == | ||||
| Bischoff-Ferrari 201093 Switzerland RCT |
Physiotherapy (n = 87) vs. cholecalciferol therapy (n = 86) | 56 – 6 months ++, 12 months ++ | |||||
| Boyd 1982158 UK Historical cohort study |
Rehabilitation ward programme (n = 482) vs. no rehabilitation ward programme (n = 289) | 69 – at discharge ++ | |||||
| Deschodt 201197 Belgium RCT |
Inpatient geriatric consultation (n = 94) vs. usual care (n = 77) | 147 – 6 weeks ==, 4 months ==, 12 months == | 56 – 6 weeks ==, 4 months ==, 12 months == | 69 – 6 weeks ==, 4 months ==, 12 months == | |||
| Fox 1993200 UK Concurrent cohort study |
In-hospital rehabilitation and discharge to own home policy (n = 142) vs. no in-hospital rehabilitation and discharge to own home policy (n = 193) | 22 – at discharge ++; 21 – at discharge ++ | 69 – at discharge ++ | ||||
| Giusti 2006143 Italy Concurrent cohort study |
Home-based rehabilitation (n = 99) vs. institutional-based rehabilitation (n = 100) | 7 – 3 months ==, 6 months ==, 12 months ==; 20 – 3 months ==, 6 months ==, 12 months == | |||||
| Holmberg 1989160 Sweden Historical cohort study |
Discharge home (n = 84) vs. discharge to a rehabilitation hospital (n = 86) | 69 – at discharge ++ | |||||
| Huang 2005100 Taiwan RCT |
Discharge planning (n = 63) vs. routine care (n = 63) | 56 – 3 months ++ | 69 – at discharge ++ | ||||
| Huusko 2000101 Finland RCT |
Geriatric rehabilitation (n = 120) vs. standard care (n = 123) | 22 – 3 months ++, 12 months ++ | 69 – at discharge ++ | ||||
| Jackson 200183 USA Quasi-randomised trial |
Occupational adaptation model (n = 20) vs. biomedical rehabilitation model (n = 20) | 22 – at discharge ++ | |||||
| Jensen 1979154 Denmark Controlled before-and-after study |
Physical rehabilitation (n = 518) | 69 – at discharge ++ | |||||
| Kennie 1988102 UK RCT |
Multidisciplinary rehabilitation in a community hospital (n = 54) vs. routine care with early discharge home (n = 54) | 148 – at discharge ++, 12 months ++ | 69 – at discharge ++ | ||||
| Levi 1997147 USA Concurrent cohort study |
Comparison of discharge practices of four hospitals and discharge destinations (n = 123) | 149 – 2 months ++, 6 months ++ | 102 – 2 months ++, 6 months ++ | ||||
| Lieberman 2002148 Israel Concurrent cohort study |
Older group (≥ 85 years) geriatric ward rehabilitation (n = 127) vs. younger group (75–84 years) geriatric ward rehabilitation (n = 297) | 109 – at discharge == | |||||
| Lin 2009105 Taiwan RCT |
Comprehensive discharge planning (n = 26) vs. routine discharge nursing care (n = 24) | 69 – at discharge ++ | |||||
| Naglie 2002111 Canada RCT |
Post-operative interdisciplinary care (n = 141) vs. usual care (n = 138) | 22 – 3 months ==, 6 months == | 150 – 3 months ==, 6 months == | ||||
| Oldmeadow 200687 Australia RCT |
Early ambulation (n = 30) vs. delayed ambulation (n = 30) | 22 – 7 days post discharge == | 69 – 7 days post discharge == | ||||
| Roberts 2004155 UK Controlled before-and-after study |
Integrated care pathway (n = 395) vs. conventional care (n = 369) | 148 – 1 month == | 56 – 1 month ++ | 69 – 1 month ++ | |||
| Rösler 2012152 Germany Concurrent cohort study |
Specialised ward (cognitive geriatric unit) (n = 53) vs. geriatric ward (non-cognitive geriatric unit) of the same geriatric department (n = 76) | 69 – at discharge ++ | |||||
| Shyu 2008119 Taiwan RCT |
Geriatric consultation services, a rehabilitation programme and discharge-planning services (n = 81) vs. usual care (n = 81) | 56 – 1 month ==, 3 months ==, 6 months ==, 12 months ++, 24 months == | |||||
| Stenvall 2007120 Sweden RCT |
Specialised geriatric ward (n = 102) vs. specialist orthopaedic ward (n = 97) | 22 – at discharge ==, 4 months ==, 12 months == | 56 – at discharge ==, 12 months == | 93 – at discharge == | 69 – at discharge ++ | ||
| Van Balen 2002140 Netherlands Concurrent cohort study |
Early discharge (n = 106) vs. conventional discharge (n = 102) | 56 – 4 months == | 69 – 1 week ++, 1 month ++, 4 months == | ||||
| Vidán 2005124 Spain RCT |
Comprehensive geriatric intervention (n = 155) vs. usual care (n = 164) | 69 – at discharge == | |||||
| Zidén 200890 Sweden RCT |
Home-based rehabilitation (n = 54) vs. conventional care (n = 48) | 69 – at discharge == |
| Study | Intervention and comparator | Malnourishment | Morbidity rate | Mortality rate | Pain | Rate of (repeat) falls |
|---|---|---|---|---|---|---|
| Bischoff-Ferrari 201093 Switzerland RCT |
Extended physiotherapy (n = 87) vs. standard physiotherapy (n = 86) | 104 – 6 months ++, 12 months ++ | ||||
| Delmi 199096 Switzerland RCT |
Dietary supplementation (n = 27) vs. control (n = 32) | 81 – 6 months ++ | 82 – 6 months ++ | |||
| Deschodt 201197 Belgium RCT |
Inpatient geriatric consultation (n = 94) vs. usual care (n = 77) | 82 – 6 weeks ==, 4 months ==, 12 months == | ||||
| Di Monaco 2008133 Italy Quasi-randomised trial |
Hospital plus home rehabilitation (n = 47) vs. hospital rehabilitation alone (n = 48) | 151 – 6 months ++ | ||||
| Hoekstra 2011144 The Netherlands Concurrent cohort study |
Multidisciplinary nutritional care (n = 61) vs. standard nutritional care (n = 66) | 152 – 3 months -- | ||||
| Huang 2005100 Taiwan RCT |
Discharge planning (n = 63) vs. routine care (n = 63) | 82 – 3 months ++ | 107 – 3 months ++ | |||
| Huusko 2000101 Finland RCT |
Geriatric rehabilitation (n = 120) vs. standard care (n = 123) | 82 – 3 months ==, 12 months == | ||||
| Jensen 1979154 Denmark Controlled before-and-after study |
Physical rehabilitation (n = 518) | 82 – 6 months ++ | ||||
| Lieberman 2002148 Israel Concurrent cohort study |
Older group (≥ 85 years) geriatric ward rehabilitation (n = 127) vs. younger group (75–84 years) geriatric ward rehabilitation (n = 297) | 82 – at discharge == | ||||
| Moseley 2009110 Australia RCT |
Higher-dose weight-bearing exercise (n = 80) vs. lower-dose limited weight-bearing exercise (n = 80) | 94 – 4 weeks ==, 4 months == | ||||
| Naglie 2002111 Canada RCT |
Post-operative interdisciplinary care (n = 141) vs. usual care (n = 138) | 82 – 3 months ++, 6 months ++ | ||||
| Ohsawa 2007137 Japan Non-randomised trial/quasi-experimental study |
Assertive therapy (n = 10) vs. conventional care (n = 10) | 26 – 6 months == | ||||
| Roberts 2004155 UK Controlled before-and-after study |
Integrated care pathway (n = 395) vs. conventional care (n = 369) | 81 – 1 month ++ | 82 – 1 month ++ | |||
| Shyu 2008119 Taiwan RCT |
Geriatric consultation services, a rehabilitation programme and discharge-planning services (n = 81) vs. usual care (n = 81) | 151 – 1 month ==, 3 months ==, 6 months ==, 12 months ==, 24 months ++ | ||||
| Vidán 2005124 Spain RCT |
Comprehensive geriatric intervention (n = 155) vs. usual care (n = 164) | 81 – at discharge ++ | ||||
| Zabari 2012162 Israel Historical cohort study |
Pain management protocol (n = 67) vs. usual care (n = 77) | 130 – post discharge == |
Appendix 20 Quality assessment
Appendix 20.1: qualitative studies
Item 1: are the sources of qualitative data (archives, documents, informants, observations) relevant to the research question (objective)?
Item 2: is the process for analysing qualitative data relevant to the research question (objective)?
Item 3: is appropriate consideration given to how findings relate to the context, for example the setting in which the data were collected?
Item 4: is appropriate consideration given to how findings relate to researchers’ influence, for example through their interactions with participants?
| Study | Country | Item 1 | Item 2 | Item 3 | Item 4 | Rating |
|---|---|---|---|---|---|---|
| Huang 200982 | Taiwan | Yes | Yes | Yes | Yes | **** |
| Kerr 2011173 | USA | Yes | Yes | Cannot tell | Cannot tell | ** |
| Li 2007189 | China | Yes | Yes | Yes | Yes | **** |
| Long 2002198 | UK | Yes | Yes | Yes | Yes | **** |
| McMillan 201286 | UK | Yes | Yes | Yes | Cannot tell | *** |
| Olsson 200788 | Sweden | Yes | Yes | Yes | Yes | **** |
| Resnick 200572 | USA | Yes | Yes | Yes | Yes | **** |
| Resnick 200773 | USA | Yes | Yes | Yes | Yes | **** |
| Robinson 1999183 | USA | Yes | Yes | Yes | Yes | **** |
| Shawler 2006174 | USA | Yes | Yes | Yes | Yes | **** |
| Taylor 2010185 | Australia | Yes | Yes | Yes | Yes | **** |
Appendix 20.2: quantitative studies: randomised controlled trials
Item 1: is there a clear description of the randomisation (or an appropriate sequence generation)?
Item 2: is there a clear description of the allocation concealment (or blinding when applicable)?
Item 3: are complete outcome data provided (≥ 80%)?
Item 4: is there a low withdrawal/dropout rate (< 20%)?
| Study | Country | Item 1 | Item 2 | Item 3 | Item 4 | Rating |
|---|---|---|---|---|---|---|
| Allegrante 200791 | USA | Yes | No | No | No | * |
| Bellelli 201078 | Italy | No | No | Yes | Yes | ** |
| Binder 200492 | USA | Yes | Yes | Yes | Yes | **** |
| Bischoff-Ferrari 201093 | Switzerland | Yes | Yes | Yes | Yes | **** |
| Casado 200980 | USA | Yes | Yes | Yes | Yes | **** |
| Crotty 200094 | Australia | Yes | Yes | Yes | Yes | **** |
| Crotty 200395 | Australia | Yes | Yes | Yes | Yes | **** |
| Delmi 199096 | Switzerland | No | No | Yes | Yes | ** |
| Deschodt 201197 | Belgium | Cannot tell | Yes | No | No | ** |
| Elinge 200398 | Sweden | No | No | No | No | * |
| Hagsten 200499 | Sweden | Yes | Yes | Yes | Yes | **** |
| Hauer 2003130 | Germany | Yes | Cannot tell | No | No | ** |
| Host 2007153 | USA | Yes | Yes | Yes | Yes | **** |
| Huang 2005100 | Taiwan | No | No | Yes | Yes | ** |
| Huusko 2000101 | Finland | Yes | Yes | Yes | Yes | **** |
| Kennie 1988102 | UK | Cannot tell | No | Yes | Yes | ** |
| Kuisma 2002103 | Hong Kong | No | No | No | No | * |
| Lauridsen 2002104 | Denmark | Cannot tell | No | No | No | * |
| Lin 2009105 | Taiwan | No | No | Yes | Yes | ** |
| Louie 2012106 | Hong Kong | Yes | No | Yes | Yes | *** |
| Mangione 2010107 | USA | Yes | Yes | Yes | Yes | **** |
| Mendelsohn 2008108 | Canada | Yes | No | Yes | Yes | *** |
| Mitchell 2001109 | UK | Yes | Yes | No | No | ** |
| Moseley 2009110 | Australia | Yes | Yes | Yes | Yes | **** |
| Naglie 2002111 | Canada | Yes | Yes | Yes | Yes | **** |
| Oldmeadow 200687 | Australia | Yes | Cannot tell | Yes | Yes | *** |
| Orwig 2011191 | USA | Yes | Yes | No | No | ** |
| Oude Voshaar 200712 | UK | No | No | No | No | * |
| Peiris 2012112 | Australia | Yes | Yes | Yes | Yes | **** |
| Peterson 2004113 | USA | No | No | No | No | * |
| Portegijs 2008114 | Finland | Cannot tell | Cannot tell | Yes | Yes | ** |
| Resnick 200773 | USA | Yes | Yes | Yes | Yes | **** |
| Ryan 2006115 | UK | Yes | Yes | Yes | Yes | **** |
| Saltvedt 2012116 | Norway | Yes | Yes | Yes | Yes | **** |
| Sherrington 1997117 | Australia | Cannot tell | No | Yes | Yes | ** |
| Sherrington 2004118 | Australia | No | No | Yes | Yes | ** |
| Shyu 2008119 | Taiwan | Cannot tell | No | Yes | Yes | ** |
| Stenvall 2007120 | Sweden | Yes | Yes | Yes | Yes | **** |
| Swanson 1998129 | Australia | No | No | Yes | Yes | ** |
| Sylliaas 2011199 | Norway | Yes | No | Yes | Yes | *** |
| Tinetti 1999121 | USA | No | Yes | Yes | Yes | *** |
| Tsauo 2005122 | Taiwan | No | No | No | No | * |
| Uy 2008123 | Australia | Yes | Yes | No | No | ** |
| Vidán 2005124 | Spain | Cannot tell | No | Yes | Yes | ** |
| Vogler 2012125 | Australia | Yes | Yes | Yes | Yes | **** |
| Yu-Yahiro 2009126 | USA | Yes | Cannot tell | Yes | Yes | *** |
| Zidén 200890 | Sweden | Cannot tell | No | No | No | * |
Appendix 20.3: quantitative studies: non-randomised controlled trials (non-randomised/quasi-randomised trials, cohort studies, case–control studies, cross-sectional studies)
Item 1: are participants (organisations) recruited in a way that minimises selection bias?
Item 2: are measurements appropriate (clear origin, or validity known, or standard instrument; absence of contamination between groups when appropriate) regarding the exposure/intervention and outcomes?
Item 3: in the groups being compared (exposed vs. non-exposed; with intervention vs. without; cases vs. controls), are the participants comparable or do researchers take into account (control for) the differences between these groups?
Item 4: are complete outcome data provided (≥ 80%) and, when applicable, is there an acceptable response rate (≥ 60%) or an acceptable follow-up rate for cohort studies (depending on the duration of follow-up)?
| Study | Country | Study design | Item 1 | Item 2 | Item 3 | Item 4 | Rating |
|---|---|---|---|---|---|---|---|
| Adunsky 2003138 | Israel | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Al-Ani 2010139 | Sweden | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Arinzon 2005201 | Israel | Concurrent cohort study | Yes | Yes | No | Yes | *** |
| Beaupre 2005157 | Canada | Historical cohort study | Yes | Yes | Yes | Yes | **** |
| Bellelli 2008141 | Italy | Concurrent cohort study | Yes | Yes | No | Yes | *** |
| Boyd 1982158 | UK | Historical cohort study | No | Yes | Yes | Yes | *** |
| Buddenberg 199879 | USA | Non-RCT/quasi-experimental study | Yes | Yes | Yes | Yes | **** |
| Carmeli 2006131 | Israel | Quasi-randomised trial | Cannot tell | Yes | Cannot tell | Yes | ** |
| Dai 2002132 | Taiwan | Quasi-randomised trial | Yes | Yes | Yes | Yes | **** |
| Di Monaco 2008133 | Italy | Quasi-randomised trial | Cannot tell | Yes | Yes | No | ** |
| Dy 2011159 | USA | Historical cohort study | Cannot tell | Yes | Yes | Yes | *** |
| Fox 1993200 | UK | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Giangregorio 2009134 | Canada | Non-RCT/quasi-experimental study | Yes | Yes | Cannot tell | No | ** |
| Giusti 2006143 | Italy | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Hoekstra 2011144 | Netherlands | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Holmberg 1989160 | Sweden | Historical cohort study | Yes | Yes | Yes | Yes | **** |
| Jackson 200183 | USA | Non-RCT/quasi-experimental study | Cannot tell | Yes | Cannot tell | Yes | ** |
| Jensen 1979154 | Denmark | Controlled before-and-after study | Cannot tell | Yes | Yes | Yes | *** |
| Johansen 2012145 | Norway | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Jones 2006135 | Canada | Non-RCT/quasi-experimental study | Yes | Yes | Yes | Yes | **** |
| Levi 1997147 | USA | Concurrent cohort study | Yes | Yes | Cannot tell | Yes | *** |
| Lieberman 2002148 | Israel | Concurrent cohort study | Yes | Yes | No | Yes | *** |
| Munin 2005149 | USA | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Nicholson 1997136 | South Africa | Non-RCT/quasi-experimental study | No | Yes | No | Yes | ** |
| Ohsawa 2007137 | Japan | Non-RCT/quasi-experimental study | Cannot tell | Yes | No | Yes | ** |
| Pryor 1988150 | UK | Concurrent cohort study | Cannot tell | Yes | Cannot tell | Yes | ** |
| Roberts 2004155 | UK | Controlled before-and-after study | Yes | Yes | Yes | Yes | **** |
| Röder 2003151 | Germany | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Rösler 2012152 | Germany | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Van Balen 2002140 | Netherlands | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Zabari 2012162 | Israel | Historical cohort study | Cannot tell | Yes | Cannot tell | Yes | ** |
Appendix 20.4: quantitative studies: non-comparative/non-interventional descriptive studies (case series, cohort studies, case–control studies, service evaluations, service restructuring, database analyses etc.)
Item 1: is the sampling strategy relevant to address the quantitative research question (quantitative aspect of the mixed-methods question)?
Item 2: is the sample representative of the population under study?
Item 3: are measurements appropriate (clear origin, or validity known, or standard instrument)?
Item 4: is there an acceptable response rate (≥ 60%)?
| Study | Country | Study design | Item 1 | Item 2 | Item 3 | Item 4 | Rating |
|---|---|---|---|---|---|---|---|
| Barone 2009177 | Italy | Case series | Yes | Yes | Yes | Yes | **** |
| Bäuerle 2004163 | Germany | Health-care service evaluation | Yes | Yes | Yes | Yes | **** |
| Bellelli 2006170 | Italy | Case report | NA | NA | Yes | NA | * |
| Borgquist 1990188 | Sweden | Case series | Yes | Yes | Yes | Yes | **** |
| Cree 2001175 | Canada | Case series | Yes | Yes | Yes | Yes | **** |
| De Jonge 2001171 | USA | Service restructuring | NA | NA | NA | NA | * |
| Fortinsky 200281 | USA | Case series | Yes | Yes | Yes | Yes | **** |
| Fredman 2006142 | USA | Concurrent cohort study | Yes | Yes | Yes | Yes | **** |
| Jones 2002195 | Canada | Case series | Cannot tell | Yes | Yes | Yes | ** |
| Kammerlander 2011178 | Austria | Case series | Yes | Yes | Yes | No | *** |
| Koval 1998146 | USA | Concurrent cohort study | Cannot tell | Yes | Yes | Yes | *** |
| Latham 2006167 | USA | Database analysis | Cannot tell | Cannot tell | Yes | NA | ** |
| Lieberman 2006179 | Israel | Case series | Yes | Yes | Yes | Yes | **** |
| Lin 2004190 | Taiwan | Case series | Yes | No | Yes | Yes | *** |
| Lindelof 2002180 | Sweden | Case series | Cannot tell | No | Yes | Yes | ** |
| McKee 200285 | UK | Case series | Cannot tell | Yes | Yes | Yes | *** |
| Moore 1993181 | USA | Case series | Yes | Cannot tell | No | Yes | ** |
| Morghen 2011182 | Italy | Case series | Yes | Yes | Yes | Yes | **** |
| Penrod 2004192 | USA | Case series | Yes | Cannot tell | Yes | Yes | *** |
| Petrella 2000169 | Canada | Case series | Cannot tell | Yes | Yes | Yes | *** |
| Portegijs 2012166 | Finland | Analyses of pre-trial data | Cannot tell | Yes | Yes | Yes | *** |
| Proctor 200813 | UK | Case studies | Cannot tell | No | Yes | Yes | ** |
| Roberto 1992165 | USA | Case series | Yes | Yes | Yes | Yes | **** |
| Rolland 2004184 | France | Case series | Cannot tell | Yes | Yes | Yes | *** |
| Shyu 2009196 | Taiwan | Case series | Cannot tell | Cannot tell | Yes | Yes | ** |
| Sirkka 2003193 | Sweden | Case series | Yes | Yes | Yes | Yes | **** |
| Takayama 2001164 | Japan | Case series | Cannot tell | Yes | Yes | Yes | *** |
| Talkowski 2009194 | USA | Case series | Cannot tell | Cannot tell | Yes | Yes | ** |
| van der Sluijs 1991186 | Netherlands | Case series | Yes | Yes | Cannot tell | Yes | *** |
| Visser 2000156 | USA | Controlled before-and-after study | Cannot tell | No | Yes | No | * |
| Walheim 1990187 | Sweden | Case series | Cannot tell | Yes | Yes | No | ** |
| Whitehead 2003161 | Australia | Historical cohort study | Yes | Yes | Yes | Yes | **** |
Appendix 20.5: mixed-methods studies (involving both quantitative and qualitative data and integrating the findings from both)
Item 1: is the mixed-methods research design relevant to the qualitative and quantitative research questions (or objectives), or the qualitative and quantitative aspects of the mixed-methods question (or objective)?
Item 2: is the integration of qualitative and quantitative data (or results*) relevant to address the research question (objective)?
Item 3: is appropriate consideration given to the limitations associated with this integration, for example the divergence of qualitative and quantitative data (or results*) in a triangulation design?
Criteria (i.e. the items in Appendices 20.1–20.4) for the qualitative component (1.1–1.4) and appropriate criteria for the quantitative component (2.1–2.4 or 3.1–3.4 or 4.1–4.4) must be also applied.
*These two items are not considered to be double-barreled items as, in mixed-methods research, (1) there may be research questions (quantitative research) or research objectives (qualitative research) and (2) data may be integrated, and/or qualitative findings and quantitative results can be integrated.
| Study | Country | Quantitative | Qualitative | Mixed | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item 1 | Item 2 | Item 3 | Item 4 | Rating | Item 1 | Item 2 | Item 3 | Item 4 | Rating | Item 1 | Item 2 | Item 3 | Rating | ||
| Jellesmark 201284 | Denmark | Yes | Yes | Yes | Yes | **** | Yes | Yes | Yes | Yes | **** | Yes | Yes | Yes | *** |
| Travis 199889 | USA | Yes | Yes | Yes | Yes | **** | Yes | Yes | Yes | Yes | **** | Yes | Yes | Yes | ** |
Appendix 21 Physiotherapist survey questions
Section 1: demographics
-
What is the name of the hip fracture centre where patients you treat have their hip fracture surgery (e.g. name of acute hospital)?
-
What is your role in hip fracture rehabilitation?
-
What Agenda for Change band are you?
-
– 5.
-
– 6.
-
– 7.
-
– 8a.
-
– 8b.
-
– Other, please specify.
-
-
Where do you work? (Ask them to decide whether they are an inpatient or outpatient/community-based physiotherapist and choose which set of questions to answer)
-
– Acute hospital: route to inpatient physiotherapist questions.
-
– Community hospital: route to community rehabilitation questions.
-
– Primary care: route to community rehabilitation questions.
-
– Other, please specify.
-
Section 2: inpatient physiotherapist questions (routed from Q4a)
-
What sort of ward do the hip fracture patients you treat usually go to after surgery for their rehabilitation? Tick all that apply.
-
– Orthopaedic trauma ward.
-
– GORU – geriatric orthopaedic rehabilitation unit.
-
– MARU – mixed geriatric assessment and rehabilitation unit.
-
– Outliers/sleepers on any type of ward.
-
– Other.
-
– If ticked more than one please, write provide approximate proportions of patients going to each type of unit.
-
-
Do you follow a multidisciplinary team integrated care pathway for hip fracture patients? If yes, please attach a copy of the pathway when you return this questionnaire.
-
Do physiotherapists (or physiotherapy assistants) routinely see patients needing hip fracture surgery pre-operatively?
-
How are patients assessed and when (e.g. pre-operatively, post-operative day 0, 1, 2 etc.) and is a particular hip fracture assessment tool used? If so, please describe this assessment tool.
-
When do physiotherapists (or physiotherapy assistants) usually first see patients following hip fracture surgery?
-
– Post-operative day 0.
-
– Post-operative day 1.
-
– Post-operative day 2.
-
– Post-operative day 3.
-
– Post-operative day 4.
-
– Other.
-
-
When are patients usually mobilised following hip fracture surgery?
-
– Post-operative day 0.
-
– Post-operative day 1.
-
– Post-operative day 2.
-
– Post-operative day 3.
-
– Post-operative day 4.
-
-
Which health-care professional usually mobilises the patient out of bed first?
-
– Nurse.
-
– Physiotherapist.
-
– Either nurse or physiotherapist.
-
– Other, please state.
-
-
What exercises do physiotherapists routinely use with patients following hip fracture surgery?
-
– Strength training – if yes, does this involve progressive resistance training and, if yes, is progressive resistance training part of routine strength training or used only sometimes.
-
– Treadmill gait training.
-
– Weight-bearing exercises other, please specify.
-
– ADL exercises – yes/no, occupational therapists do them.
-
– Other, please specify.
-
-
How often do patients receive physiotherapy following hip fracture surgery?
-
– Once a day.
-
– Twice a day.
-
– Three times a day.
-
– Four times a day.
-
– Other, please specify how many times.
-
-
How long are the physiotherapy sessions on average (in minutes)?
-
Do physiotherapists routinely make a home visit for patients following hip fracture prior to discharge?
-
– Yes, for the majority of patients. If yes, is the home visit usually carried out with the patient or carer or patient and carer?
-
– Yes, for some patients. If yes, is the home visit usually carried out with the patient or carer or patient and carer? Please also describe which patients receive a home visit and how this is decided
-
– No routine home visits are carried out. If ticked, is any assessment of the home made? Please describe.
-
-
Do your proximal hip fracture patients have a routine assessment of any of the following? Please tick all that apply.
-
– Cognitive status.
-
– Mood.
-
– Self-efficacy.
-
– Fear of falling.
-
-
12b. For each answer ticked above, which professional makes this assessment and which tool, if any, do they use (e.g. Mini Mental State Examination)?
-
Please describe anything else that physiotherapists routinely do as part of rehabilitation for patients after hip fracture surgery.
Section 3: community rehabilitation questions (routed from Q4c)
-
How would you best describe the community service you are part of? Please tick one option.
-
– Early supported discharge service in which patients are discharged home and receive a package of rehabilitation care for a short period (e.g. 4–6 weeks).
-
– Intermediate care in which patients are transferred form the acute hospital to a community rehabilitation unit or nursing home where they receive their rehabilitation before being discharged home or to long-term care.
-
– Community physiotherapy team that is not part of the early supported discharge or intermediate care team.
-
– Other, please describe.
-
-
Do community physiotherapists/you routinely make a home visit for patients who have had hip fracture surgery prior to discharge? Please tick one option.
-
Do physiotherapists from the community team attend multidisciplinary team discharge meetings at the acute hip fracture centre that most of your patients are treated in?
-
– Yes, routinely.
-
– Yes, for some patients.
-
– No.
-
Comments:
-
How soon after discharge do community physiotherapists usually see patients who have had hip fracture surgery?
-
– Day of discharge.
-
– 1 day after discharge.
-
– 2 days after discharge.
-
– Other, please specify.
-
-
What exercises do physiotherapists routinely use with patients following hip fracture surgery?
-
– Strength training. If yes, does this routinely involve progressive resistance training?
-
– Treadmill gait training.
-
– Weight-bearing exercises other, please specify.
-
– ADL exercises – yes/no, occupational therapists do them.
-
– Other please specify.
-
-
How often do patients on average receive physiotherapy following hip fracture surgery?
-
– Once a day.
-
– Every other day.
-
– Every third day.
-
– Other, please specify how often.
-
-
How long are the physiotherapy sessions on average (in minutes)?
-
Do your proximal hip fracture patients have a routine assessment of any of the following? Please tick all that apply.
-
– Cognitive status.
-
– Mood.
-
– Self efficacy.
-
– Fear of falling.
-
-
8b. For each answer ticked above, which professional makes this assessment and which tool, if any, do they use (e.g. Mini Mental State Examination)?
-
Please describe anything else that physiotherapists routinely do as part of rehabilitation for patients after hip fracture surgery.
Appendix 22 Occupational therapist survey questions
Section 1: demographics
-
What is the name of the hip fracture centre where patients you treat have their hip fracture surgery (e.g. name of acute hospital)?
-
What is your role in hip fracture rehabilitation?
-
What Agenda for Change band are you?
-
– 5.
-
– 6.
-
– 7.
-
– 8a.
-
– 8b.
-
– Other, please specify.
-
-
Where do you work? (Ask them to decide whether they are an inpatient or outpatient/community-based occupational therapist and choose which set of questions to answer.)
-
– Acute hospital: route to inpatient occupational therapist questions.
-
– Community hospital: route to community-run hospital/rehabilitation unit occupational therapist questions.
-
– Community care: route to community occupational therapist questions.
-
– Other, please specify.
-
Section 2: inpatient occupational therapist questions (routed from Q4a)
-
What sort of ward do the hip fracture patients you treat usually go to after surgery for their rehabilitation? Tick all that apply.
-
– Orthopaedic trauma ward.
-
– GORU – geriatric orthopaedic rehabilitation unit.
-
– MARU – mixed assessment and rehabilitation unit.
-
– Outliers/sleepers on any type of ward.
-
– Other.
-
– If ticked more than one please, write provide approximate proportions of patients going to each type of unit.
-
-
Do you follow a multidisciplinary team integrated care pathway for hip fracture patients? If yes, please attach a copy of the pathway when you return this questionnaire.
-
Are patients with hip fracture routinely seen by an occupational therapist (or an occupational therapy assistant) pre-operatively?
-
When are patients with hip fracture usually seen by an occupational therapist (or an occupational therapy assistant)?
-
– Post-operative day 0.
-
– Post-operative day 1.
-
– Post-operative day 2.
-
– Post-operative day 3.
-
– Post-operative day 4.
-
– Post-operative day 5.
-
– Other.
-
-
What do occupational therapists assess for? ADL, anything specific for hip fracture patients?
-
What intervention do you give?
-
– Assessment of home for modifications and aids.
-
– ADL practice. Please specify, e.g. kitchen practice.
-
-
How often do occupational therapists usually see patients following hip fracture surgery during their inpatient rehabilitation? Please write in how many times over how many days.
-
7b. How long are these sessions?
-
Do occupational therapists routinely make a home visit for patients following hip fracture prior to discharge?
-
– Yes, for the majority of patients. If yes, is the home visit usually carried out with the patient or carer or patient and carer?
-
– Yes, for some patients. If yes, is the home visit usually carried out with the patient or carer or patient and carer? Please also describe which patients receive a home visit and how this is decided.
-
– No routine home visits are carried out. If ticked, is any assessment of the home made? Please describe.
-
-
Do your proximal hip fracture patients have a routine assessment of any of the following? Please tick all that apply.
-
– Cognitive status.
-
– Mood.
-
– Self-efficacy.
-
– Fear of falling.
-
-
9b. For each answer ticked above, which professional makes this assessment and which tool, if any, do they use (e.g. Mini Mental State Examination)?
-
Are patients routinely referred to or signposted to social support or activities when discharged? If yes, what sort of activities and who provides them (e.g. Age Concern, local charity running a voluntary befriending service)?
-
Please describe anything else that occupational therapists routinely do as part of rehabilitation for patients after hip fracture surgery.
Section 3: community-run hospital/rehabilitation unit occupational therapist questions (routed from Q4b)
-
On which post-operative day are patients usually transferred to your hospital/unit?
-
– Mostly within the first week post-operatively.
-
– Mostly in the second week post-operatively.
-
– Mostly in the third week post-operatively.
-
– Other, please specify.
-
-
What assessments do occupational therapists use as part of routine rehabilitation for patients aged > 65 years who have had surgery for proximal hip fracture at your centre?
-
– An individual assessment of functional tasks? Does this include any of the following?
-
– Transfers.
-
– Personal ADL.
-
– Domestic ADL.
-
– Environment.
-
– Social support.
-
– Other, please specify.
-
-
– An individual assessment of posture and seating?
-
– A routine assessment of any of the following?
-
– Cognitive status.
-
– Mood.
-
– Self-efficacy.
-
– Fear of falling.
-
– None of the above.
-
-
-
For cognitive status, mood, self-efficacy, fear of falling: who (which profession) makes this assessment, when and which, tool do they use if any (e.g. mini mental state)?
-
What does occupational therapist rehabilitation routinely consist of at your centre? Please tick all that apply.
-
– Practising various ADL.
-
– Other activities to encourage independence.
-
– Education about hip precautions.
-
– Anxiety management.
-
– Developing self-awareness.
-
– Falls prevention techniques.
-
– Providing information about falls prevention services.
-
– Referral to falls prevention services.
-
– Referral to social services.
-
– Referral to the discharge team.
-
– Prescribing specific equipment (e.g. raised toilet seat, banister rails).
-
– Other, please describe.
-
-
How frequently do occupational therapists usually see patients following hip fracture surgery during their community rehabilitation?
-
– Every day.
-
– Every other day.
-
– Every third day.
-
– Twice a week.
-
– Once a week.
-
– Once a fortnight.
-
– Other, please specify.
-
-
How long are these sessions?
-
Do occupational therapists make a home visit for patients following hip fracture prior to discharge?
-
– Yes, always.
-
– Yes, for some patients according to need.
-
– No.
-
-
Are patients routinely referred to or signposted to social support or activities when discharged? If yes:
-
– What sort of activities and who provides them (e.g. Age Concern, local charity running a voluntary befriending service)? Please describe.
-
-
Please describe anything else occupational therapists routinely do as part of rehabilitation for patients after hip fracture surgery.
-
Please describe what you think are the good aspects of your service.
-
Please describe anything about your service that could be improved and how.
Section 4: community occupational therapist questions (routed from Q4c)
-
How would you best describe the community rehabilitation service that you are part of? Please tick one option.
-
– Early supported discharge service in which patients are discharged home and receive a package of rehabilitation care for a short period (e.g. 4–6 weeks).
-
– Intermediate care in which patients are transferred form the acute hospital to a community rehabilitation unit or nursing home where they receive their rehabilitation before being discharged home or to long-term care.
-
– Community occupational therapy team that is not part of the early supported discharge or intermediate care team.
-
– Other please describe.
-
-
Do community occupational therapists routinely make a home visit for patients who have had hip fracture surgery prior to discharge?
-
– Yes, for the majority of patients. If yes, is the home visit usually carried out with the patient or carer or patient and carer?
-
– Yes, for some patients. If yes, is the home visit usually carried out with the patient or carer or patient and carer? Please also describe which patients receive a home visit and how this is decided.
-
– No routine home visits are carried out. If no, is any assessment of the home made? Please describe.
-
-
Do occupational therapists from the community team attend multidisciplinary team discharge meetings at the acute hip fracture centre that most of your patients are treated in?
-
– Yes, routinely.
-
– Yes, for some patients.
-
– No.
-
Comments:
-
How soon after discharge do community occupational therapists usually see patients who have had hip fracture surgery?
-
– Day of discharge.
-
– 1 day after discharge.
-
– 2 days after discharge.
-
– Other, please specify.
-
-
What do you assess for? ADL, anything specific for hip fracture patients?
-
What intervention do you give?
-
– Assessment of home for modifications and aids.
-
– ADL practice. Please specify, e.g. kitchen practice.
-
-
How often do occupational therapists usually see patients following hip fracture surgery during their community rehabilitation? Please write in how many times over how many days.
-
7b. How long are these sessions?
-
Do your proximal hip fracture patients have a routine assessment of any of the following? Please tick all that apply.
-
– Cognitive status.
-
– Mood.
-
– Self efficacy.
-
– Fear of falling.
-
-
8b. For each answer ticked above, which professional makes this assessment and which tool, if any, do they use (e.g. Mini Mental State Examination)?
-
Are patients routinely referred to or signposted to social support or activities when discharged? If yes, what sort of activities and who provides them (e.g. Age Concern, local charity running a voluntary befriending service)?
-
Please describe anything else that occupational therapists routinely do as part of rehabilitation for patients after hip fracture surgery.
Appendix 23 Therapy service manager survey questions
Section 1: demographics
-
What is the name of your hip fracture centre where surgery is performed (e.g. name of acute hospital, hospital trust)?
-
Which part of the UK is your centre in?
-
– Wales.
-
– Northern Ireland.
-
– Scotland.
-
– England.
-
-
How many proximal hip fracture patients had surgery at this centre in the last 12 months? Enter number:
-
What is your profession?
-
– Physiotherapist.
-
– Occupational therapist.
-
– Other, please specify.
-
-
What is your job title?
-
Please describe briefly what your responsibility is in care and service provision for the rehabilitation of patients who have had surgery for proximal hip fracture?
Please note the following questions are about patients aged > 65 years who have surgery following proximal hip fracture.
Section 2: service delivery organisation
-
On which type of ward do your patients aged > 65 years who have had surgery for proximal hip fracture have their post-operative rehabilitation in your centre? Tick all that apply.
-
– Orthopaedic trauma ward.
-
– GORU – geriatric orthopaedic rehabilitation unit.
-
– MARU – mixed assessment and rehabilitation unit accepting patients with a variety of medical, surgical and orthopaedic conditions.
-
– Other, please specify.
-
-
What community-based service(s) are available to your proximal hip fracture patients who live in the local area served by your centre when they are discharged? Tick all that apply.
-
– Community hospital providing hip fracture rehabilitation or other community-run inpatient rehabilitation unit.
-
– Short-term nursing home rehabilitation and assessment places specifically for hip fracture rehabilitation.
-
– Early supported discharge service providing community-based multidisciplinary rehabilitation for about 4–6 weeks based in the patient’s own home.
-
– Early supported discharge service providing community-based multidisciplinary rehabilitation for about 4–6 weeks based in a care home/nursing home where a patient has been discharged for the long term.
-
– A traditional model of community care in which the patient is discharged home (own home or long-term care setting) under the care of the GP and with individual referral to community health and social care professionals as needed.
-
-
Do you have an integrated multidisciplinary approach to the rehabilitation of hip fracture patients? If yes, which of the following does it include? Tick all that apply.
-
– Orthogeriatric assessment and rapid optimisation of fitness for surgery.
-
– Early identification of individual goals for multidisciplinary rehabilitation to recover mobility and independence and to facilitate return to pre-fracture residence and long-term well-being.
-
– Continued, co-ordinated orthogeriatric and multidisciplinary review liaison or integration with related services. If yes, which services are included:
-
– mental health.
-
– falls prevention.
-
– bone health.
-
– primary care.
-
– social services.
-
-
– Clinical and service governance responsibility for all stages of the pathway of care and rehabilitation, including those delivered in the community.
-
– Other, please specify.
-
Section 3: inpatient care
-
Who takes the medical lead for your patients having rehabilitation following surgery for proximal hip fracture?
-
– It is a collaborative role shared between the orthopaedic surgeon and the geriatrician/orthogeriatrician?
-
– Orthopaedic surgeon only.
-
– Other, please specify and describe their role in rehabilitation.
-
-
Patients having rehabilitation following surgery for proximal hip fracture are also usually seen by a variety of other health professionals. Which of these professions are routinely involved in the inpatient rehabilitation of proximal hip fracture patients at your centre? Tick all that apply.
-
– Physiotherapy.
-
– Occupational therapy.
-
– Nursing:
-
– orthopaedic ward nurse.
-
– specialist orthopaedic senior nurse (e.g. advanced nurse practitioner).
-
– specialist senior nurse for older people (e.g. advanced nurse practitioner) (if ticked route to questions on role in rehabilitation/describe role in rehabilitation).
-
– other, please specify and briefly describe their role in rehabilitation.
-
-
– Social work.
-
– Dietetics.
-
– Clinical psychology.
-
– Pharmacy.
-
– Other, please specify and briefly describe their role(s) specifically related to rehabilitation.
-
-
Do your proximal hip fracture patients have a routine assessment of any of the following? Please tick all that apply.
-
– Cognitive status.
-
– Mood.
-
– Self-efficacy.
-
– Fear of falling.
-
-
3b. For each answer ticked above, which professional makes this assessment and which tool, if any, do they use (e.g. Mini Mental State Examination)?
Section 4: discharge planning and co-ordination from acute services to the community
-
Do you have routine multidisciplinary team meetings to discuss discharge plans for patients following hip fracture surgery?
-
If yes, which professions from the hospital team are routinely involved in the multidisciplinary team discharge meeting? Tick all that apply.
-
– Orthopaedic surgeons.
-
– Orthogeriatricians.
-
– Other doctors (please specify).
-
– Orthopaedic ward nurses.
-
– Other specialist nurses (e.g. advance nurse practitioner in orthopaedics) (please state specialist role).
-
– Occupational therapists.
-
– Physiotherapists.
-
– Social workers.
-
– Pharmacists.
-
– Mental health professionals (please state which).
-
-
Do your community health-care professionals routinely attend multidisciplinary discharge meetings in your acute centre? If yes, does this routinely include community rehabilitation service (intermediate care services or early supported discharge service) professionals? Yes/no/service not available.
-
– If yes, please specify which professionals routinely attend, e.g. physiotherapists, occupational therapists.
-
– If no or service not available, do you include any community professionals on an ad hoc basis? If yes, please specify which professionals, e.g. occupational therapists.
-
-
Do patients routinely attend your discharge meetings?
-
Do carers routinely attend your discharge meetings?
-
Do carers of patients with cognitive impairment routinely attend your discharge meetings?
Comments:
If no, please describe how discharge plans are made and by whom.
Ask all:
-
Does anyone have specific responsibility for co-ordinating discharges? If yes, who? Please describe their role.
-
Does anyone have a specific responsibility for overall co-ordination between secondary and primary care services? If yes, please describe their professional role and what they do.
-
Are patients routinely referred to or signposted to social support or activities when discharged?
-
If yes, what sort of activities and who provides them (e.g. Age Concern, local charity running a voluntary befriending service)?
Appendix 24 Recruitment of therapy service managers flow chart
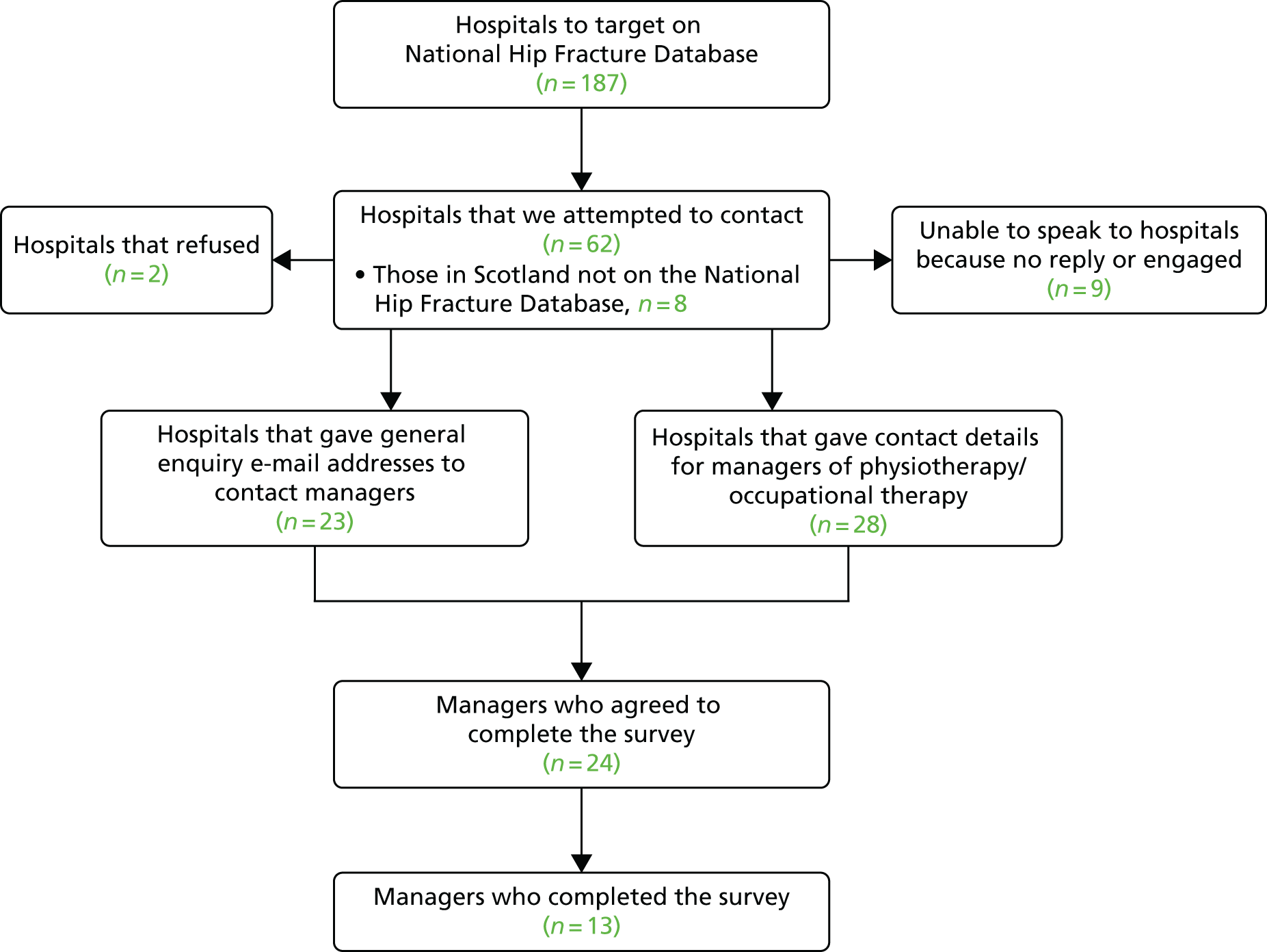
Appendix 25 Topic guides (Phase I)
Topic guide for focus groups with hip fracture patients and their carers (version 1, 30 October 2012)
-
Introduction:
-
background to project
-
explanation of process
-
consent forms.
-
-
Pre-injury beliefs about hip fracture.
-
Experience of the pre- and perioperative period.
-
Aftercare:
-
experience of aftercare following hip fracture surgery
-
what went well
-
what did not go well
-
factors that aid recovery
-
barriers to recovery.
-
-
Rehabilitation programme:
-
what does rehabilitation mean?
-
what are the important goals for recovery and rehabilitation?
-
experience of rehabilitation programme
-
rehabilitation in hospital:
-
what did it consist of?
-
what went well?
-
what went badly?
-
-
rehabilitation at home/in the community:
-
what did it consist of?
-
what went well?
-
what went badly?
-
-
what should a rehabilitation programme consist of?
-
self care and domestic activities
-
exercises
-
strength training
-
balance training
-
improving self-confidence
-
improving mood
-
social engagement
-
other
-
-
features that aid rehabilitation
-
barriers to rehabilitation:
-
fear
-
lack of confidence.
-
-
Topic guide for focus groups with health and social care professionals (v1, 30 October 2012)
-
Introduction:
-
background to project
-
explanation of process
-
consent forms.
-
-
Aftercare:
-
pathway for patients following hip fracture surgery
-
factors that aid recovery
-
barriers to recovery.
-
-
Rehabilitation programme:
-
what does rehabilitation mean?
-
what are the important goals for recovery and rehabilitation?
-
what does the rehabilitation programme consist of?
-
rehabilitation in hospital:
-
what does it consist of?
-
what works well?
-
what it does not consist of?
-
-
rehabilitation at home/in the community:
-
what does it consist of?
-
what works well?
-
what it does not consist of?
-
-
what should a rehabilitation programme consist of?
-
self care and domestic activities
-
exercises
-
strength training
-
balance training
-
improving self-confidence
-
improving mood
-
social engagement
-
other
-
-
features that aid rehabilitation
-
barriers to rehabilitation:
-
fear
-
self-confidence.
-
-
Appendix 26 Patient scenarios for the focus group with health and social care professionals
A
Mr Meirion Huws is a 70-year-old man who has led an active life and still enjoys hill walking and volunteers with outdoor activities for young people. He tripped and fell while supervising a group of young people and fractured his hip. He has no other comorbidities. He is really keen to get back to his previous level of fitness or at least to continue some sort of hill walking. Mr Huws lives with his wife in a modern house. Their bedroom is upstairs, as is the bathroom. There is a cloakroom with a toilet and handbasin downstairs.
B
Mrs Gwynedd Jones is 85 years old and was living independently at home in a large village with a reasonable range of facilities (small supermarket, good bus service to local town, post office, pubs, chapel). She is widowed and lives with a 19-year-old grandson, who is able to help a bit at home but does not have the same standards of housekeeping as Mrs Jones. He is working full time and has a busy social life.
Mrs Jones has osteoarthritis and fell over when stepping out of her back door. There is a steep step out of the back door and the ground slopes away from the house. There is a flagstone path to step on to, but some stones are uneven. The front door has a smaller step straight onto a path through the front garden. Her bedroom and bathroom are up steep, narrow stairs in her 19th-century end-of-terrace house. There is a kitchen downstairs but no toilet facilities.
Mrs Jones also has diabetes, which prior to her fall she managed well with insulin. Her GP has recently referred her for an appointment to assess whether or not she needs a knee replacement caused by her arthritis. Her mobility has been affected by the pain and stiffness in her knee, but she could still get about well enough (e.g. catching the bus to visit friends in the next village) as long as she did not have to walk too far.
C
Mrs Evelyn Wilson is a 79-year-old woman who is married. She is a carer for her husband who has Parkinson’s disease. He has nursing care from the district nursing team, who monitor his condition and ensure that he has the correct medication. Carers also come in in the morning and evening to help him get up and go to bed. Apart from that, Mrs Wilson cares for him. She slipped and broke her hip when she fainted while shopping in the local supermarket. There is a family history of syncope and hypotension, although Mrs Wilson has never been diagnosed with either. The supermarket staff, who know her from her regular shopping visits, mentioned to the paramedics that she has seemed increasingly forgetful over the past 6 months. This is confirmed by a friend who came in with her when she was admitted.
Appendix 27 Initial framework for coding transcripts
| Theory area 1: individual patient | Theory area 2: team delivering the intervention | Theory area 3: the rehabilitation intervention | Theory area 4: setting for the intervention |
|---|---|---|---|
|
|
|
|
Appendix 28 Patient participant information sheets and consent form
Appendix 29 Carer participant information sheet and consent form
Appendix 30 Adverse event reporting
Appendix 31 Focus group topic guides (Phase II)
Patient and carer topic guide: control group
-
What was your experience of the rehabilitation you received after your hip fracture, specifically regarding physiotherapy and exercise?
-
What went well, what could be improved? Having experienced fracture and the rehabilitation involved, what would you recommend to improve care?
-
If there are any attending the focus group, what were the experiences of participants who were discharged to nursing/residential care or those who were more dependent on carers?
-
-
Did your therapists give you exercises to do?
-
How confident did you feel about practising them?
-
Did your confidence change over time? What changed this?
-
-
Were you given any written information to keep with you?
-
How helpful was this? Was there any other information you would have found useful?
-
-
How involved did you feel in planning your recovery and rehabilitation?
-
Often people say they were afraid of falling again after having a hip fracture. Did you experience this?
-
Was there anything in your rehabilitation that helped reduce the fear of falling?
-
Did you attend a falls prevention class? How did you find out about this and was it useful?
-
-
How did you feel about being approached to take part in the study?
-
Did you understand the information you were given?
-
What made you decide to take part?
-
How did you feel about the questions you were asked in the hospital and at the follow-up, especially about how long they took and how well you were able to understand the questions and their relevance?
-
-
How did you feel about not knowing which study group you would be in when you agreed to take part?
-
How would you have felt if you had been in the other group?
-
-
Did you do some exercise tests with your community physiotherapists at the end of the study?
-
How did you feel about being asked to do these?
-
-
Has anything changed for you as a consequence of being in the study?
-
If you were asked to take part now, would you make the same decision?
-
Patient and carer topic guide: intervention group
-
What was your experience of the rehabilitation you received after your hip fracture?
-
What went well and what could be improved?
-
If there are any attending the focus group, what were the experiences of participants who were discharged to nursing/residential care or those who were more dependent on carers?
-
Task
Rank the following aspects of the intervention according to how useful they were:
-
extra time with a therapist
-
information in the workbook
-
being involved in setting your own goals
-
keeping a diary to look at progress.
Discussion of ranking:
-
Did you feel confident to suggest goals to your therapists and how did that help you?
-
What did you like best about the workbook? Was there anything you felt the workbook was missing?
-
Were you aware of the extra sessions which you received because you were in the study?
-
Were these sessions used differently to the care as usual sessions?
-
Did you notice any improvements in your recovery as a result of this extra time?
-
Did your therapists give you exercises to do?
-
How confident did you feel about practising them?
-
Did your confidence change over time? What changed this?
-
-
Often people say they were afraid of falling again after having a hip fracture. Did you experience this?
-
Was there anything in your rehabilitation that helped reduce the fear of falling?
-
Did you attend a falls prevention class? How did you find out about this and was it useful?
-
-
How did you feel about being approached to take part in the study?
-
Did you understand the information you were given?
-
What made you decide to take part?
-
How did you feel about the questions you were asked in the hospital and at the follow-up, especially about how long they took and how well you were able to understand the questions and their relevance?
-
-
Did you do some exercise tests with your community physiotherapists at the end of the study?
-
How did you feel about being asked to do these?
-
-
How did you feel about not knowing which study group you would be in when you agreed to take part?
-
How would you have felt if you had been in the other group?
-
-
Has anything changed for you as a consequence of being in the study?
-
If you were asked to take part now, would you make the same decision?
-
Health-care professional topic guide
-
Experiences of the enhanced rehabilitation intervention:
-
What went well?
-
What could be improved?
-
-
Experiences of extra therapist time:
-
Awareness of extra time available to patients in the study:
-
How did it work, what went well, what needs to be improved?
-
How did you use the extra time with patients? Do you think it made a difference?
-
-
Views of the workbook:
-
Did you use it?
-
If so, how? What was useful, what could be improved, was anything missing that you think would have been helpful?
-
-
-
Do you feel that the intervention made any difference to the way patients engaged with you and participated in their rehabilitation?
-
If so, how/if not, why?
-
What was your experience of the goal setting and feedback in the work book?
-
Similar to/different from usual way you work.
-
Good points.
-
Areas for improvement.
-
-
What was your experience of the information sections?
-
Useful to you/useful to patients/anything you weren’t aware of before/anything that was missing.
-
-
Experiences of working with patients with cognitive impairments and their carers:
-
How did the intervention go?
-
-
Experiences of working with patients who were discharged to long-term residential/nursing care:
-
How did the intervention go?
-
-
-
Feasibility of physiotherapists conducting the physical measures at 3-month follow-up.
-
Acceptability of the outcome measures for patients:
-
timing
-
number
-
content.
-
-
Anything else we haven’t talked about that you think has been important in working with this intervention.
Appendix 32 Unit costs of service use for the cost year 2013–14
| Health-care resource | Unit | Unit cost (£)a | Details and source |
|---|---|---|---|
| Primary health care and community services | |||
| GP (clinic) | Visit | 234 | Per hour of patient contact (including qualifications)b |
| Nurse (GP clinic) | Visit | 53 | Per hour of face-to-face patient contactb |
| District nurse | Visit | 66 | Per hour of patient-related workb |
| Physiotherapist (community) | Home visit | 36 | Per hourb |
| Occupational therapist (community) | Home visit | 37 | Per hourb |
| Technical instructors/assistants of physiotherapists or occupational therapists | Home visit | 23 | Per hourb |
| Community pharmacist | Consultation | 71 | Per hour of patient-related activitiesb |
| Social care services | |||
| Social worker | Visit | 79 | Per hour of client-related workb |
| Psychologist | Consultation | 138 | Per hour of client contactb |
| Home-care worker | Home visit | 24 | Per hour weekdayb |
| Care attendant | Home visit | 8 | Per hourc |
| Voluntary/charity services | |||
| British Red Cross | Home visit | 6.19 | Per hourb |
| Macmillan nurse | Home visit | 74 | Per hour of patient-related workb |
| Loan of equipment | Wheelchair | 30 | Per 6 weeks of loan (donation costs)d |
| Secondary care | |||
| Inpatient services | Bed-day | Various | Costed by proceduree |
| Outpatient services | Consultation | Various | Costed by proceduree |
| A&E services | Attendance | Various | Costed by proceduree |
| Day hospital | Procedure | Various | Costed by proceduree |
| Proximal femoral fracture-specific services | |||
| Falls prevention classes | Class | 3 | Per classf |
| National Exercise Referral Scheme | Session | 385 | Per person for 16 weeks, two sessions per weekg |
| Medications | Various | Various | Costed by specific medicationh |
List of abbreviations
- A&E
- accident and emergency
- ADL
- activities of daily living
- AE
- adverse event
- AMTS
- Abbreviated Mental Test Score
- ANCOVA
- analysis of covariance
- BADL
- Barthel Activities of Daily Living
- BCUHB
- Betsi Cadwaladr University Health Board
- CI
- confidence interval
- CMO
- context, mechanism and outcome
- CONSORT
- Consolidated Standards of Reporting Trials
- CSI
- Caregiver Strain Index
- CSRI
- Client Service Receipt Inventory
- DCE
- discrete choice experiment
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- FEMuR
- Fracture in the Elderly Multidisciplinary Rehabilitation
- FES-I
- Falls Efficacy Scale – International
- FRAT
- Falls Risk Assessment Tool
- GDS
- Geriatric Depression Scale
- GP
- general practitioner
- GSES
- General Self-Efficacy Scale
- GUIDE
- Guidance, Understanding, Individualised, Direction, Expertise
- HADS
- Hospital Anxiety and Depression Scale
- ICC
- intraclass correlation coefficient
- ICECAP-O
- ICEpop CAPability measure for Older people
- ICER
- incremental cost-effectiveness ratio
- ID
- identification
- IDRIS
- Identifying Data for Research in Information Systems
- IT
- information technology
- MMSE
- Mini Mental State Examination
- MoCA
- Montreal Cognitive Assessment
- NEADL
- Nottingham Extended Activities of Daily Living
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NISCHR CRC
- National Institute for Social Care and Health Research Clinical Research Centre
- NWORTH
- North Wales Organisation for Randomised Trials in Health
- OR
- odds ratio
- POVA
- protection of vulnerable adults
- QALY
- quality-adjusted life-year
- R&D
- research and development
- RAP
- Rehabilitation Activities Profile
- RCT
- randomised controlled trial
- SAE
- serious adverse event
- SD
- standard deviation
- SEE
- Self-Efficacy for Exercise
- SF-36
- Short Form questionnaire-36 items
- SIGN
- Scottish Intercollegiate Guidelines Network
- SMG
- Study Management Group
- SPPB
- Short Physical Performance Battery
- SROI
- social return on investment
- SSC
- Study Steering Committee
- VAS
- visual analogue scale
- VAS-FOF
- visual analogue scale for fear of falling
