Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/141/02. The contractual start date was in October 2008. The draft report began editorial review in May 2016 and was accepted for publication in February 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Paul Salkovskis is Editor-in-Chief of Behavioural and Cognitive Psychotherapy, the official journal of the British Association for Behavioural and Cognitive Psychotherapy, but does not receive any money in connection with this work. Paul Salkovskis and Hilary Warwick developed cognitive–behaviour therapy for health anxiety but have no financial or other interests in its use. Helen Tyrer has written a book (Tyrer H. Tackling Health Anxiety: A CBT Handbook. London: RCPsych Press; 2013), and Peter Tyrer and Helen Tyrer have co-authored online teaching modules on the recognition and treatment of health anxiety for the Royal College of Psychiatrists. Peter Tyrer is Co-Editor of Personality and Mental Health, for which he receives an annual honorarium.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Tyrer et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction to health anxiety
Parts of this chapter have been reproduced from Tyrer et al. 1 This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Health anxiety – and its older synonym, hypochondriasis – is a relatively common problem in both primary and secondary medical care settings. 2–4 It also places a substantial burden on health services,5 as its central feature is sufficient fear of having a serious disease to lead to medical consultation, and, very commonly, this is followed by further investigations. This condition has only recently been recognised, despite its ubiquity and its ability to provoke considerable suffering. Even when the condition is recognised, concerns over litigation in hospital clinics may lead to expensive investigations being carried out unnecessarily. This may provoke further pathology when findings of marginal clinical significance are reported. The extra burden on services is particularly important in secondary medical care. Between 10% and 20% of all attenders at medical clinics have abnormal health anxiety6,7 and patients often rotate between different clinics depending on the focus of their symptoms. The symptoms of abnormal health anxiety show little tendency to spontaneous resolution and persist for months in the absence of treatment. 6
Potential benefits of psychological treatment and previous studies
The failure to detect this serious pathology is perhaps less surprising when there is, or at least has been until very recently, a general belief that there is no adequate treatment. Pharmacological management is generally unsatisfactory, but psychological treatment in the form of cognitive–behaviour therapy (CBT) has been shown to be effective both in primary care8,9 and, more recently, in secondary care. 10 Although these trials suggested efficacy of this intervention, it is less clear if it has a significant impact on costs. Although the total costs were somewhat reduced in those receiving CBT in the only trial in secondary care, these manifested only in the 6 months after treatment had been completed. 10 It is also not known to what extent health anxiety is found in patients with existing medical disease and whether or not this can be successfully treated, as almost all published trials exclude those with definite physical illness.
The precursors to the cognitive–behaviour therapy for health anxiety in medical patients (CHAMP) trial were a series of research studies, mainly carried out at King’s Mill Hospital in north Nottinghamshire. The first of these studies established, in a genitourinary medicine clinic setting, that health anxiety was relatively common, that it persisted in the absence of detection or intervention and that it led to more consultations with doctors. 6 The second suggested that the prevalence of health anxiety was somewhat higher (around 12%) in medical clinics such as cardiology and endocrinology clinics,7 and the third was a randomised controlled trial of a modified form of CBT for health anxiety (CBT-HA) developed earlier by Salkovskis and Warwick11 versus standard care in patients attending a genitourinary medicine clinic. 10 The last of these was the essential precursor to the CHAMP study. Since the trial began in 2008, there have been many more published trials but, as explained in full later in this report, these have all been concerned with somewhat different populations.
Chapter 2 Trial methods
Parts of this chapter have been reproduced from Tyrer et al. 1 This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Research objectives
The main objectives of the CHAMP trial were to examine the clinical value, cost and cost-effectiveness of the administration of CBT in health-anxious patients attending five medical clinics in secondary care. Specifically, we hypothesised that (1) between five and 10 sessions of health anxiety-directed CBT using the Salkovskis–Warwick model11,12 are more effective than standard care in reducing health-anxious symptoms measured by the Health Anxiety Inventory (HAI)13 1 year after randomisation to the trial; and (2) the costs of the CBT and the control are equivalent; the end point for this outcome is the cost of health service interventions at 2 years adjusted for baseline values.
The secondary hypotheses were that, compared with the control condition (single interview), CBT-HA would lead to significantly greater improvement in health anxiety at 3, 6, 24 and 60 months measured using the HAI,13 in self-rated generalised anxiety measured using the anxiety section of the Hospital Anxiety and Depression Scale (HADS),14 in quality of life using the EuroQol-5 Dimensions (EQ-5D) measure of health-related quality of life15 and in social functioning using the Social Functioning Questionnaire (SFQ),16 all at 6, 12, 24 and 60 months.
In addition, we tested a number of secondary hypotheses. The first of these was that health anxiety-focused CBT (CBT-HA) would be less effective in patients who had additional comorbid pathology in the form of obsessional symptomatology [measured using the Short Obsessive–Compulsive disorder Screener (SOCS)]. 17 We also hypothesised that personality status would have an impact on the effectiveness of treatment, and that those with dependent personalities [measured using the Dependent Personality Questionnaire (DPQ)]18 and other personality disorders19 [measured using the Quick Personality Assessment Schedule (PAS-Q)],20 which were subsequently converted into International Statistical Classification of Diseases, Eleventh Edition (ICD-11)21 personality disorder categories,22 would have a worse outcome with CBT-HA. We also expected that these comorbid disorders would be associated with increased costs.
The study also allowed prevalence estimates to be made for health anxiety in different age groups and in different medical clinics.
Patient and public involvement
We recognised at the outset of the study that one of the major problems in executing the trial was the relative lack of awareness of health anxiety in medical clinics. These clinics are busy places with clear tasks set for clinicians and, despite regular but fairly vague comments about the importance of mental pathology in patients who are attending, there is no requirement for mental health status to be assessed, with the possible exception of dementia.
With the help of a support group called Confederation of Health Anxiety Sufferers Supporting Increased Services (CHASSIS) we developed a strategy for identifying the patients who might have pathological health anxiety. In a previous study7 we found that many patients with existing, and often successfully treated, medical pathology had a high level of health anxiety, and so excluding such patients was felt to be a mistake.
This led to the two-way strategy of combining feedback from clinics about potentially unsuitable attendees (by consultation with clinical staff) with screening of attenders using the short form of the HAI. As broaching the subject of health anxiety with people who were attending the clinic ostensibly for medical follow-up and consultation only was potentially counterproductive, we asked our CHASSIS group of sufferers with health anxiety to advise on the best way of introducing the subject of health anxiety. We chose ‘worry about your health’ as the core component of this after this consultation.
The CHASSIS group has also been active in disseminating the results of the CHAMP trial, most recently (at the time of writing) by attending a meeting of the All Party Mental Health Group in the House of Commons in December 2014.
Trial summary
The study was a pragmatic randomised controlled trial with two parallel arms and approximately equal randomisation of eligible patients to an active treatment group of 5–10 sessions of CBT or to a control group. During the course of the baseline assessment an explanatory interview was given about the nature of health anxiety; this was the only specific health-anxiety intervention in the control group, but there is some evidence that a simple explanation is of benefit in its own right. 11
Settings
Patients attending cardiology, endocrinology, gastroenterology, neurology and respiratory medicine clinics in five general hospitals (King’s Mill Hospital, north Nottinghamshire; St Mary’s Hospital, London; Charing Cross Hospital, London; Chelsea and Westminster Hospital, London; and the Hillingdon Hospital, Middlesex) were considered for the study. A total of 107 consultants agreed to collaborate with the study and to allow their patients to be approached provided that they were not considered inappropriate for the study on account of the severity of their physical pathology.
Form of randomisation
After baseline assessment, randomisation was carried out by a computerised system [Open Clinical Data Management System (openCDMS), Centre for Health Informatics, University of Manchester, Manchester, UK] using block randomisation with no stratification in randomised blocks of four and six. The allocation was carried out by the UK Mental Health Research Network independently of CHAMP personnel.
Target population and procedure
Patients attending clinics of the collaborating consultants, apart from those who were specifically excluded, were approached while waiting for their outpatient appointments and, if they agreed, were given the short form of the HAI,13 a rating scale of 14 questions that takes 5–10 minutes to complete. Those that scored at least 20 points on the scale were offered the opportunity to take part in the trial and given an information sheet about the study. If the patients agreed immediately, they were given an information sheet about the study and baseline assessments were made, provided that they satisfied the inclusion criteria and the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV) diagnosis of hypochondriasis [derived from the Structured Clinical Interview for DSM-IV (SCID-IV) interview]. 23 Those who were uncertain were approached later.
When each patient had satisfied the criteria for entry to the study, formal consent was obtained and baseline assessments completed. At the baseline assessment all patients received a standard explanation of the nature and significance of health anxiety. After completion of the assessments, the research assistant entered and registered each patient to an online system (openCDMS) and this automatically led to the appropriate randomisation. The study co-ordinator was then informed of the details of the treatment arm allocation. Equal allocation was made to either (1) the active treatment group – between 5 and 10 1-hour sessions of CBT from a psychologist or research nurse at the clinic, backed up by a short take home manual; or (2) the standard care group, which received the normal care in the clinic.
The patients were recruited over a 21-month period beginning in October 2008 and ending in July 2010, and were followed up for 5 years. Because there were so many clinics running simultaneously, we required additional assessment help in recruitment. This was provided by Clinical Studies Officers of the North London and East Midlands hubs of the Mental Health Research Network, and proved to be invaluable.
Inclusion and exclusion criteria
Patients suitable for inclusion were those who satisfied the criteria for excessive health anxiety outlined above and who (1) were aged between 16 and 75 years, (2) were permanently resident in the area, (3) had a sufficient understanding of English to read and complete the questionnaires and (4) gave written consent for the interviews and audio-taping of 50% of treatment sessions, and for access to their medical records. The presence of existing medical pathology, provided that it was not new and required further investigation, was not a bar to treatment in the study, and as in preliminary work we had found that many patients with existing pathology have a high level of health anxiety.
Some patients who would otherwise satisfy the inclusion criteria above were excluded if (1) they were felt by their consultants to have a level of continuing major pathology that was too severe for them to take part in the study; (2) they were currently being actively investigated for significant pathology suspected by the clinician and for whom CBT might confuse or cause distress; (3) they had progressive cognitive impairment; or (4) they were currently under psychiatric care.
Assessments
The following assessments were carried out at baseline only:
-
personality assessment using the PAS-Q,20 followed by conversion to the ICD-11 personality levels22 but also including the questions from the hypochondriasis subsection of the full schedule19
-
the SOCS17 (a set of seven questions that identify the likely presence of obsessive–compulsive disorder); and
-
the DPQ,18 an assessment of dependent personality traits (this was included because both dependent personality and obsessional symptoms are associated conditions that may handicap or complicate treatment).
The remaining clinical assessments, in addition to the main health anxiety measure (HAI) were generalised anxiety and depression (measured with the HADS14), as these symptoms are common in patients with hypochondriasis, quality of life (EQ-5D)15 and social functioning (SFQ). 16 These assessments were given at baseline and at 6, 12, 24 and 60 months. To ensure the highest possible follow-up rate, patients were reminded of the next follow-up point at each assessment. The HAI was also given at 3 months by post or telephone with a research assistant.
Service use data for the economic evaluation were collected using the Adult Service Use Schedule (ADSUS).
Methods of overcoming bias
The independent central computerised system involved in randomisation (openCDMS) ensured no bias in allocation of treatments and also full baseline information, as it was only when all necessary data were entered that the patient was randomised. As this was a single-blind study, there was always the danger of disclosure of the form of treatment by the patient, therapist or other investigators in the study. This was minimised by (1) patients being asked by research assessors not to disclose their treatment to the research assessors, (2) the assessors and therapists working in different areas and (3) establishing a system whereby any assessor who was unwittingly informed about the nature of the treatment then ceased to assess that patient, and another research assessor was allotted for continued assessments.
Study interventions
Cognitive–behaviour therapy treatment arm
As the aim was to replicate the conditions of treatment that would be likely to prevail in the future if the trial found benefit from CBT, as much as possible it was aimed to give CBT within or close to the referring clinic, so that it was perceived by patients to be part of the clinic’s function in combining help for mental and physical problems, instead of being a potentially stigmatised external psychiatric service.
At each clinic we therefore trained a psychologist, research nurse or equivalent health professional (G-grade or equivalent) to administer the treatment. Each patient was invited to receive between 5 and 10 sessions of CBT with additional adaptations for health anxiety developed by HT and PS, reinforced by three booklets to be handed to patients at treatment sessions (Box 1). Each therapist attended two workshops at the beginning of the study and received up to 3 months’ training from the senior practitioners in the study, sometimes in vivo with two therapists being present in treatment sessions, before taking on the care of patients alone.
-
Recognition of fear of disease rather than actual disease.
-
Dangers of internet browsing.
-
Avoiding reassurance.
-
Negative consequences of body monitoring and hypervigilance.
-
Recognition that the awful possible explanations of symptoms are rare.
-
Reading of three booklets summarising health anxiety.
Because of the need for training, recruitment was planned to be slower in the first 3 months of the trial than in the later phases of the study. Following the initial period, therapists had fortnightly supervision from senior practitioners until the last patients had been recruited and treated. Therapists were also given a manual of CBT (written by PS and HT) developed for health anxiety. This was prepared in advance of training and used for refreshment during treatment.
Research assistants who had all been trained in the assessment procedures (by SC) carried out both baseline assessments and follow-up. The follow-up at 3 months concerned only the HAI, which was administered by post or telephone. Follow-ups from 6 months onwards were carried out by face-to-face interview with some patients but for those who preferred a telephone assessment this method was used. As the main clinical assessments were all self-ratings, this rarely presented a problem. The ADSUS is administered as a clinical interview, but the answers are all simple factual ones that readily allow the information to be gathered over the telephone.
Training and fidelity of intervention
Four of the applicants (PS, GS, DM and HS) were involved in the training of therapists in two all-day workshops, and also in the assessment of treatment fidelity, and HW, one of the originators of the treatment, also assessed the audio-taped interviews independently.
Approximately half of all treatment sessions were audio-recorded and tapes or discs of these sessions given to patients to help in their progress. Fidelity was tested using a health-anxiety modification of the Cognitive Therapy Rating Scale24 (Health Anxiety Version), in which all therapists were assessed before they were regarded as competent. Those who did not reach an accepted grade had further training until they achieved competence. Manuals for the training of therapists and to aid patients in their treatment were also prepared. This issue is important, as better treatment fidelity with CBT has been associated with better treatment effects. 25,26
Standard treatment arm
Patients allocated to the standard treatment arm continued their care in both primary and secondary care settings and were reminded that they would be followed up at regular intervals up to 5 years. No restrictions on treatment were given to this group as the study was a pragmatic trial and the follow-up period was long.
Sample size
We calculated sample sizes for both the primary outcome measure and the first secondary outcome measure, choosing the larger of the two for the study.
Based on the pilot study in a genitourinary medicine clinic,10 we assumed that the true difference in the change of HAI score between CBT and control at 2 years is 5.00 points and that the standard deviation (SD) for the change of HAI score at 2 years is 7.58 points. With these assumptions, the study needed 122 patients to detect the above difference with 95% power at a two-sided 5% significance level. Taking into account 20% dropout by 24 months, the sample size was estimated to be 152 patients. It is also fair to add that when the study was set up there was no knowledge on what was a minimally significant clinical difference in the HAI score, and even now there is little work on this subject, but an improvement of 2 points on the scale appears to be clinically important (see Chapter 5, Meaningful clinical difference in Health Anxiety Inventory scores).
There remains no agreed approach to calculate the sample size required for an economic evaluation, particularly in areas such as health anxiety, in which the willingness to pay for improvements in outcomes is unknown. Based on the pilot study, we considered that the CBT intervention would be cost-effective if it improved HAI score and that it was no more costly than the control treatment. The sample size calculation for the economic evaluation was therefore based on the total costs over 24 months being equivalent.
With a sample size of 186 per group, the study had 80% power to reject the null hypothesis that the costs of the CBT and control are not equivalent (when the difference in mean costs is ≈£150) in favour of the alternative hypothesis that the means of the two groups are equivalent, assuming that the expected difference in means is 0 and the common SD is 580 (from pilot study data).
The sample size was thus powered by the first secondary outcome of the CHAMP study, estimated as 466 patients, assuming a 20% dropout by 24 months, leading to a total of 372 completing treatment and equal randomisation between groups. The sample size calculation uses a one-sided (non-inferiority) test. Thus, with 466 patients, or fewer if the dropout rate was less, the study was adequately powered to both detect the assumed difference in the primary outcome and assess the equivalence in the secondary economic outcome between the CBT group and the control group.
Statistical analysis
All primary statistical analyses used the intention-to-treat principle using the statistical package SAS, version 9.3 (SAS Institute Inc., Cary, NC, USA). The numbers (with percentages) of losses to follow-up at 12, 24 and 60 months after randomisation will be reported and compared between the treatment arms with absolute risk differences [95% confidence intervals (CIs)]. Deaths were reported separately for each group. The Consolidated Standards of Reporting Trials (CONSORT) procedure was used for reporting flow through the trial.
The primary end point was analysed using a mixed model with time, treatment, and time × treatment interaction as fixed effects, baseline measurement as covariate and patient as random effect. The treatment differences at each time point together with the 95% CI were derived from the mixed model. Missing data were treated as missing at random in the mixed-model analysis. To assess the sensitivity of the result to missing values, the last observation carried forward strategy was used to compute the missing HAI score at the follow-up visits. Other assessments were analysed in a similar way. In addition, covariate-adjusted analysis was performed on the primary outcome analysis by mixed model, controlling for three pre-specified potential predictors for the primary end point (clinic type, site and age). In addition, the percentage of patients achieving normal levels of health anxiety (HAI score of ≤ 10 points) was compared using a generalised estimating equation model with visit, treatment, interaction between visits and treatment as fixed effect, baseline measurement of HAI score as covariate and patient as random effect (an exchangeable covariance structure).
Subgroup analyses were also carried out to determine if there was heterogeneity in any of the main groups identified for analysis.
Chapter 3 Results
Parts of this chapter have been reproduced with permission from Tyrer P, Wang D, Tyrer H, Crawford M, Cooper S. Dimensions of dependence and their influence on the outcome of cognitive behaviour therapy for health anxiety: randomized controlled trial. Pers Ment Health 2016;10:96–105. 27 Copyright © 2016 John Wiley & Sons, Ltd.
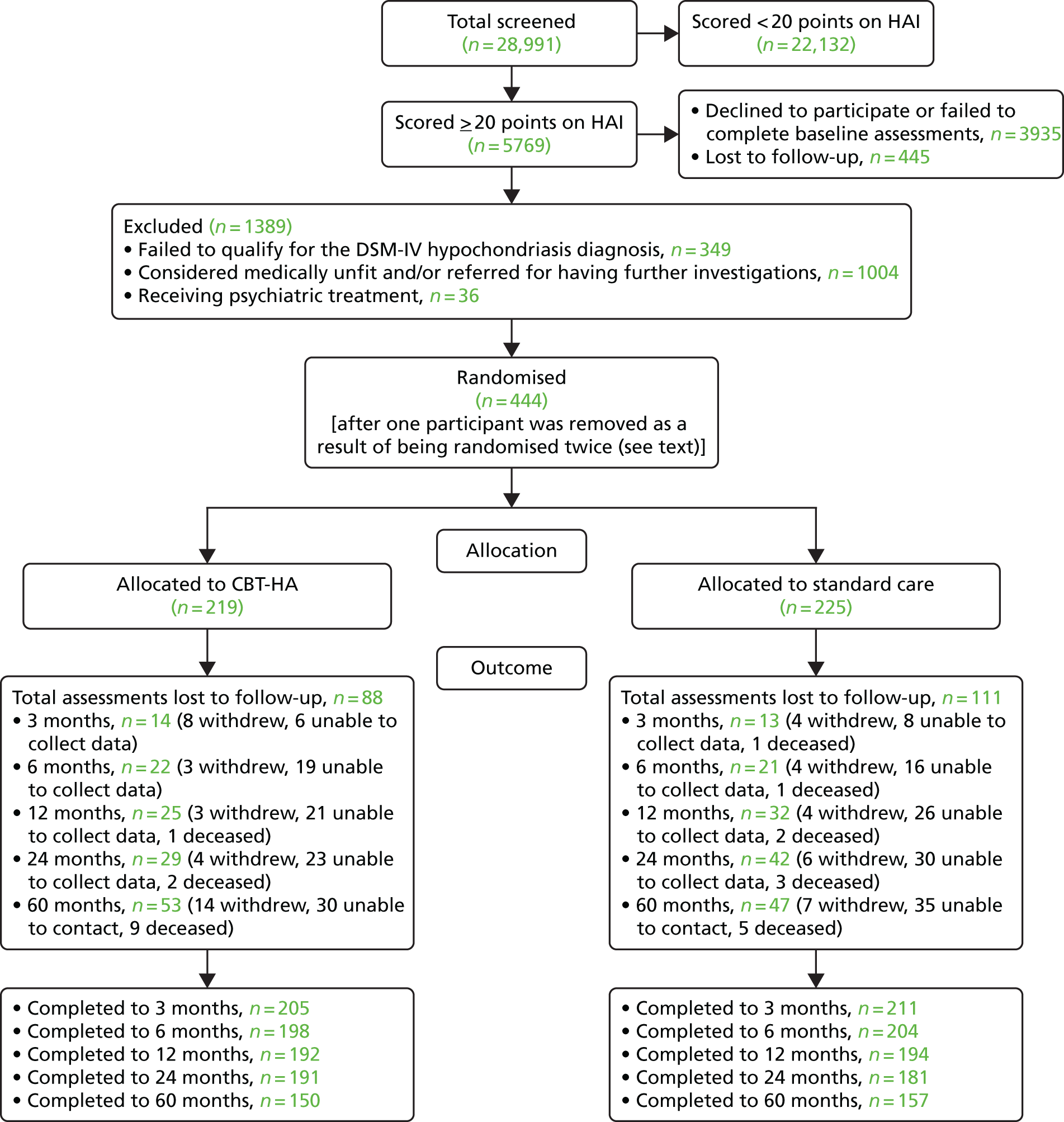
A total of 219 patients were allocated to CBT-HA and 225 to standard care. The CONSORT diagram for all phases in the trial is illustrated in Figure 1. Of the 444 patients (including those who had died), 416 (94%) were followed up at 3 months, 402 (91%) at 6 months, 386 (87%) at 12 months, 372 (84%) at 2 years and 308 (69%) at 5 years. The CONSORT details are notable in several respects. First, nearly 20% (2991) of all 5769 patients who completed the HAI scored ≥ 20 points and were therefore eligible to proceed to the next phase of the trial. After exclusions and refusals, only 444 were randomised. Possible explanations for this are given later in this report and, in particular, we suspect, but cannot confirm, that the sample that entered the trial was roughly a representative one. Second, although there were many reasons why high HAI scorers did not take part, only a minority (n = 349, 6%) were excluded because they did not have a DSM-IV diagnosis of hypochondriasis. The other finding worthy of note is that dropout rates were very similar in both groups, and at 5 years were greater in the CBT-HA group than in the standard care one. This is somewhat unusual in trials of psychological treatments, for which retention is usually greater in the psychological treatment arm.
FIGURE 1.
Consolidated Standards of Reporting Trials diagram (numbers assessed for some variables differ because of missing data). Reprinted from the Lancet, vol. 383, Tyrer P, Cooper S, Salkovskis P, Tyrer H, Crawford M, Byford S, et al. Clinical and cost-effectiveness of cognitive behaviour therapy for health anxiety in medical patients: a multicentre randomised controlled trial, pp. 219–25. Copyright (2014),28 with permission from Elsevier.
The main baseline characteristics of the two treatment groups are shown in Table 1; the table shows that the two groups were essentially similar in important respects.
| Variable | Treatment group | All (N = 444) | |
|---|---|---|---|
| CBT-HA (N = 219) | Standard care (N = 225) | ||
| Age (years) | |||
| Mean (SD) | 50.3 (13.6) | 47.0 (13.4) | 48.6 (13.6) |
| Gender, n (%) | |||
| Female | 113 (51.6) | 123 (54.7) | 236 (53.2) |
| Male | 106 (48.4) | 102 (45.3) | 208 (46.8) |
| Ethnicity, n (%) | |||
| White British | 145 (67.8) | 151 (68.0) | 296 (67.9) |
| White other | 26 (12.1) | 18 (8.1) | 44 (10.1) |
| Black/black British: African | 6 (2.8) | 9 (4.1) | 15 (3.4) |
| Black/black British: Caribbean | 5 (2.3) | 7 (3.2) | 12 (2.8) |
| Asian/Asian British | 15 (7.0) | 23 (10.4) | 38 (8.7) |
| Asian/Asian British: other | 8 (3.7) | 8 (3.6) | 16 (3.7) |
| Arab/Middle East | 7 (3.3) | 4 (1.8) | 11 (2.5) |
| Chinese/Far East | 2 (0.9) | 2 (0.9) | 4 (0.9) |
| Hospital, n (%) | |||
| Chelsea and Westminster Hospital | 26 (11.9) | 23 (10.2) | 49 (11.0) |
| Charing Cross Hospital | 31 (14.2) | 26 (11.6) | 57 (12.8) |
| Hillingdon Hospital | 56 (25.6) | 63 (28.0) | 119 (26.8) |
| King’s Mill Hospital | 70 (32.0) | 74 (32.9) | 144 (32.4) |
| St Mary’s Hospital | 36 (16.4) | 39 (17.3) | 75 (16.9) |
| Clinic type, n (%) | |||
| Cardiology | 53 (24.2) | 57 (25.3) | 110 (24.8) |
| Endocrinology | 41 (18.7) | 43 (19.1) | 84 (18.9) |
| Gastroenterology | 77 (35.2) | 72 (32.0) | 149 (33.6) |
| Neurology | 20 (9.1) | 22 (9.8) | 42 (9.5) |
| Respiratory medicine | 28 (12.8) | 31 (13.8) | 59 (13.3) |
| HAI score | |||
| Mean (SD) | 24.9 (4.2) | 25.1 (4.5) | 25.0 (4.4) |
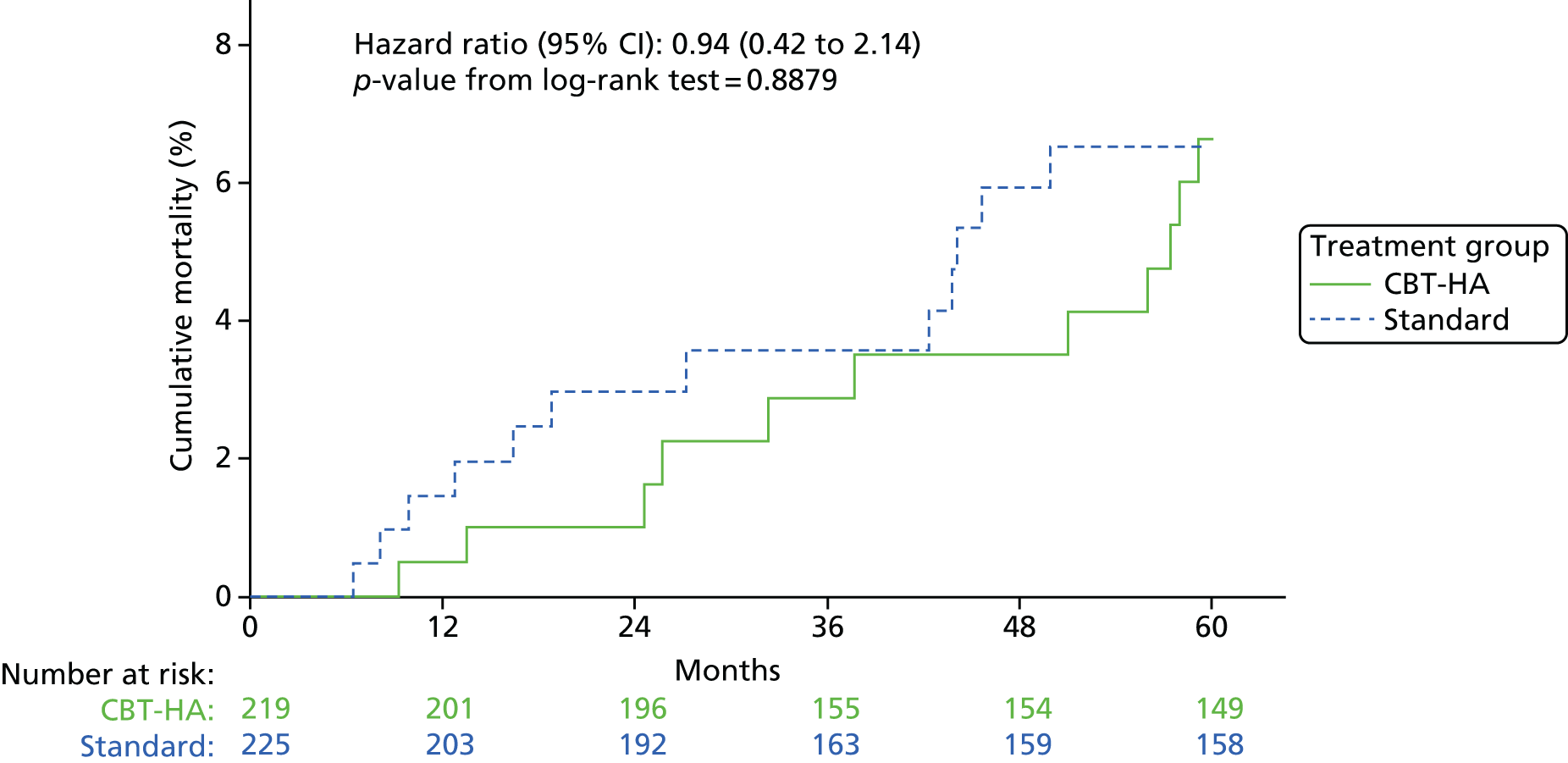
There were 24 deaths during the trial, 12 in each treatment group. All were from natural causes. The Kaplan–Meier plot of deaths showed a non-significant trend for lower mortality in the CBT-HA arm early in the trial (Figure 2). One patient in the standard care group had an episode of deliberate self-harm during follow-up. The 219 patients in the trial allocated to CBT-HA were seen by 11 therapists; assessment of the fidelity of therapists’ treatment showed that all except one scored at an adequate competence level or higher, and this was confirmed by the independent assessor (HW). The therapist who failed to achieve this level saw five patients in the trial.
FIGURE 2.
Kaplan–Meier plot of deaths over the 5-year period of the trial.
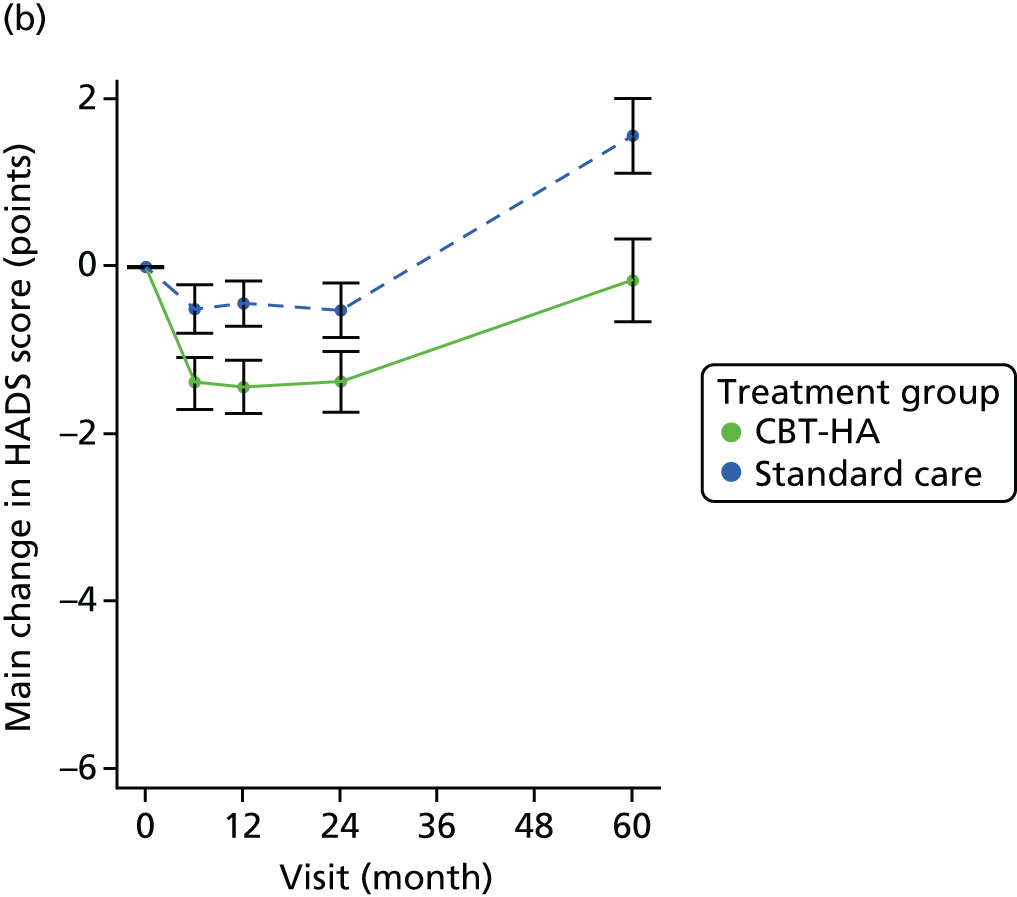
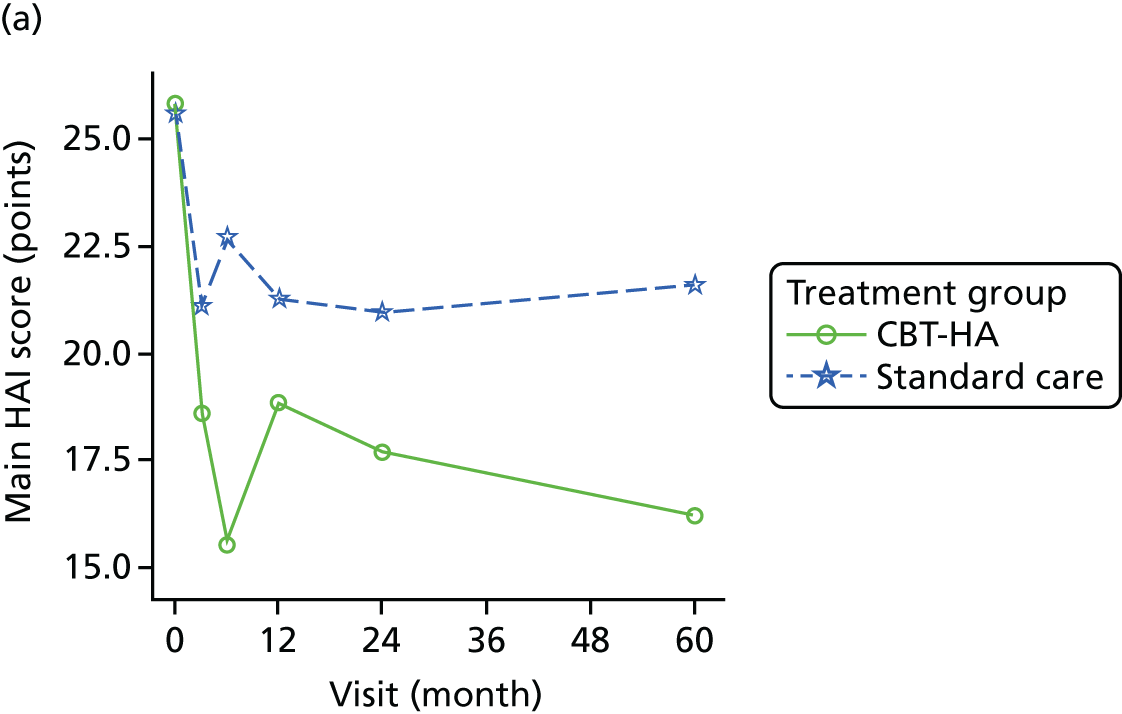
Primary outcome
The scores on the HAI showed greater improvement with CBT-HA than with standard care at all times of testing, with maximal differences at 6 months (Table 2 and Figure 3).
| Visit | Observed value | Mixed-model analysis | ||||
|---|---|---|---|---|---|---|
| CBT-HA | Standard care | Treatment difference (points) (95% CI) | p-value | |||
| n | Mean score (points) (SD) | n | Mean score (points) (SD) | |||
| Baseline | 219 | 24.88 (4.23) | 225 | 25.12 (4.52) | ||
| Improvement from baseline | ||||||
| 3 months | 205 | 4.41 (7.63) | 212 | 2.62 (6.17) | 1.74 (0.38 to 3.11) | 0.0123 |
| 6 months | 197 | 7.11 (7.83) | 204 | 2.33 (5.76) | 4.83 (3.45 to 6.21) | < 0.0001 |
| 12 months | 194 | 6.44 (7.47) | 193 | 3.20 (6.54) | 2.97 (1.57 to 4.37) | < 0.0001 |
| 24 months | 190 | 5.90 (7.54) | 183 | 3.66 (6.57) | 2.01 (0.60 to 3.42) | 0.0052 |
| 5 years | 149 | 6.45 (8.57) | 157 | 4.34 (7.75) | 2.20 (0.70 to 3.70) | 0.0040 |
| Overall | 2.75 (1.65 to 3.85) | < 0.0001 | ||||
FIGURE 3.
Change in HAI scores between CBT-HA and standard care (treatment as usual) over the 5-year period. Note: the change in HAI scores between the two treatments at 12 months is the primary outcome. Adapted from the Lancet, vol. 383, Tyrer P, Cooper S, Salkovskis P, Tyrer H, Crawford M, Byford S, et al. Clinical and cost-effectiveness of cognitive behaviour therapy for health anxiety in medical patients: a multicentre randomised controlled trial, pp. 219–25. Copyright (2014),28 with permission from Elsevier.

Last observation carried forward analyses
The analysis using the last observation carried forward method for the primary outcome (HAI) showed very similar results. Because similar agreement was found with other outcomes they are not included in the report.
| Comparison | Difference in score (points) (95% CI) | p-value |
|---|---|---|
| CBT-HA vs. standard care at 3 months | –1.72 (–3.03 to –0.41) | 0.0099 |
| CBT-HA vs. standard care at 6 months | –4.52 (–5.82 to –3.21) | < 0.0001 |
| CBT-HA vs. standard care at 12 months | –2.93 (–4.24 to –1.63) | < 0.0001 |
| CBT-HA vs. standard care at 24 months | –2.07 (–3.38 to –0.77) | 0.0019 |
| CBT-HA vs. standard care at 5 years | –2.06 (–3.36 to –0.75) | 0.0021 |
| CBT-HA vs. standard care at all times | –2.66 (–3.72 to –1.60) | < 0.0001 |
Secondary outcomes
Generalised anxiety and depression
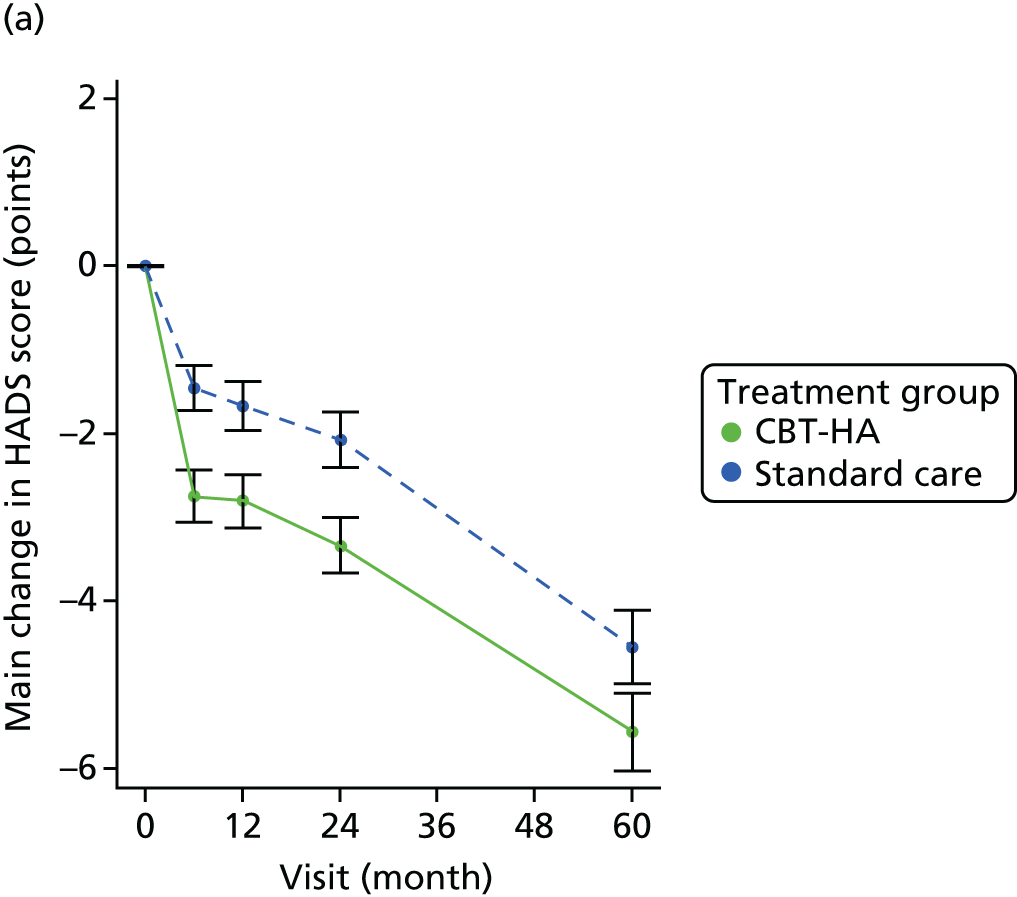
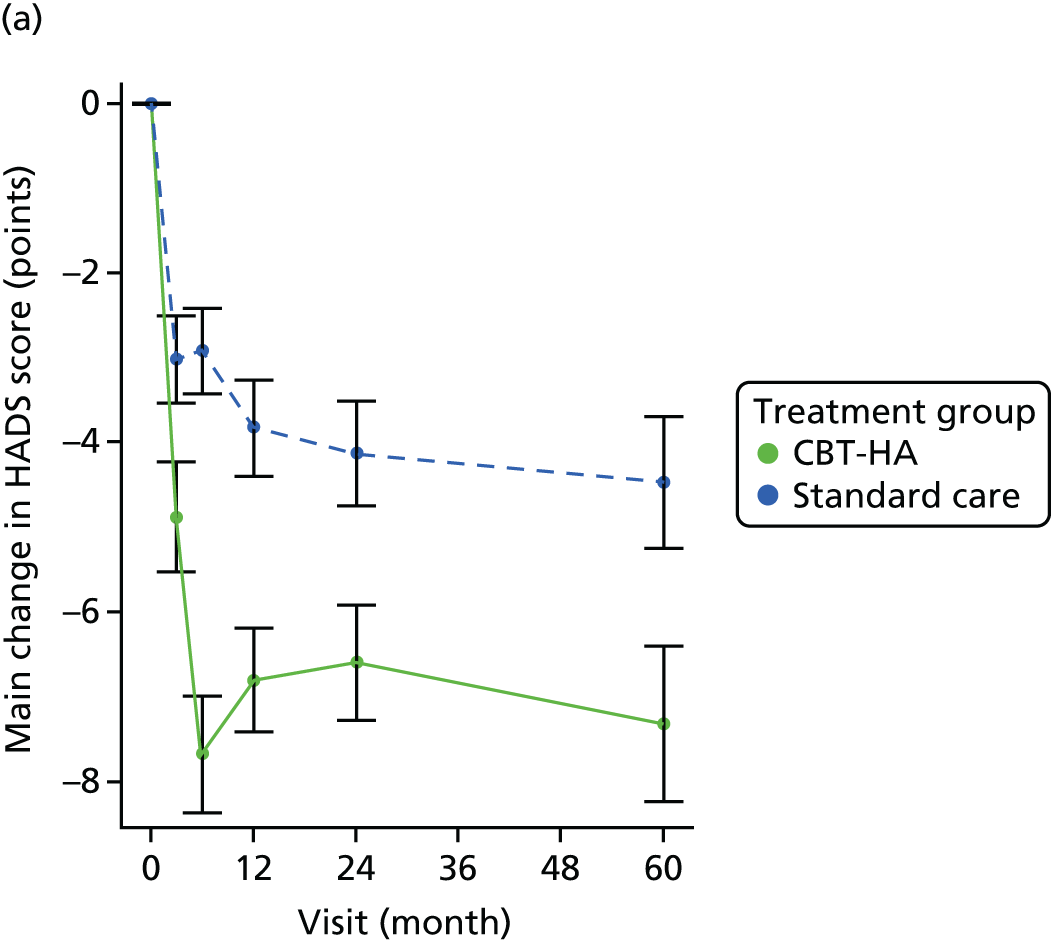
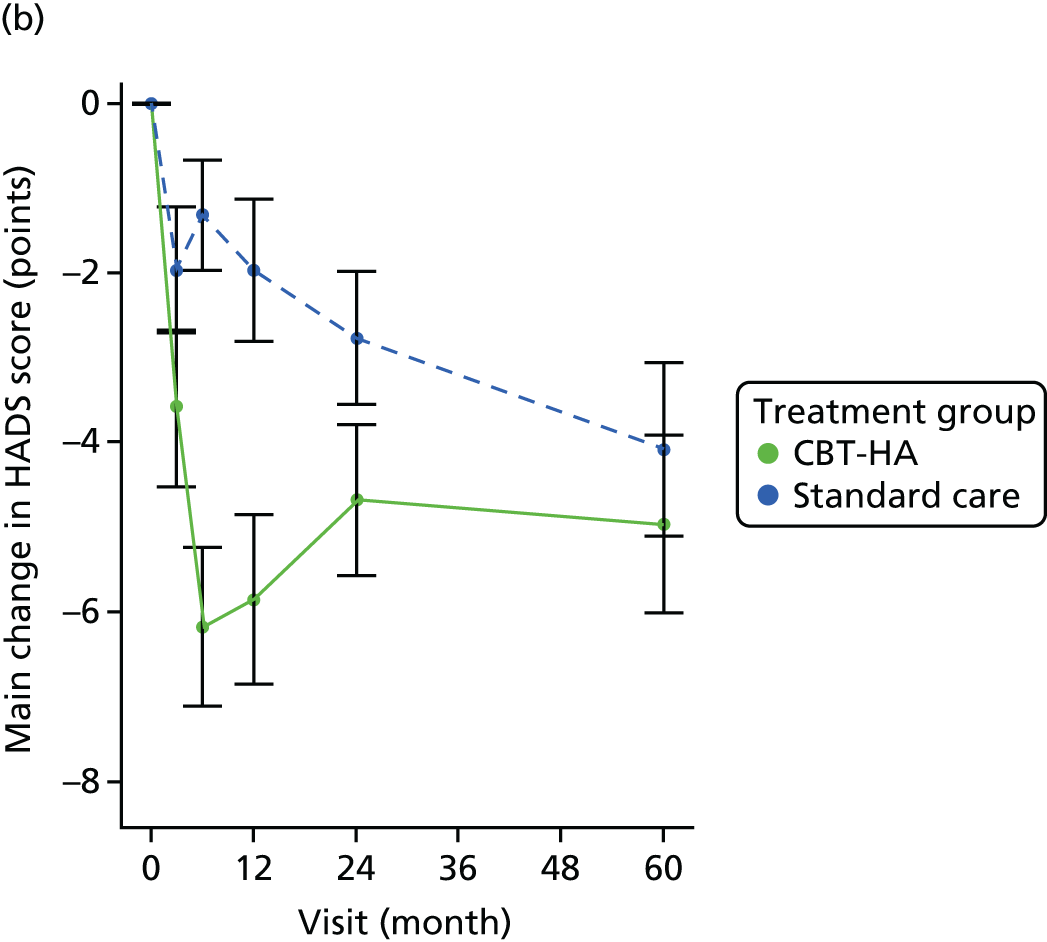
Generalised anxiety and depression as recorded using the HADS anxiety (HADS-A) and depression (HADS-D) sections also showed significant differences between the two treatments over the 5-year period, with those for generalised anxiety (HADS-A) being maximal at 6 months (Table 4 and Figure 4) and those for depression (HADS-D) being maximal at 5 years (Table 5 and Figure 4).
| Visit | Observed value | Mixed-model analysis | ||||
|---|---|---|---|---|---|---|
| CBT-HA | Standard care | Treatment difference (95% CI) | p-value | |||
| n | Mean score (points) (SD) | n | Mean score (points) (SD) | |||
| Baseline | 219 | 12.56 (3.74) | 225 | 12.25 (3.88) | ||
| Improvement from baseline | ||||||
| 6 months | 197 | 2.74 (4.41) | 204 | 1.46 (3.89) | 1.30 (0.48 to 2.11) | 0.0019 |
| 12 months | 194 | 2.80 (4.40) | 193 | 1.67 (4.04) | 1.02 (0.19 to 1.85) | 0.0165 |
| 24 months | 190 | 3.33 (4.57) | 183 | 2.07 (4.35) | 1.01 (0.17 to 1.86) | 0.0186 |
| 5 years | 150 | 5.56 (5.72) | 158 | 4.54 (5.48) | 0.71 (–0.20 to 1.61) | 0.1245 |
| Overall | 1.01 (0.38 to 1.64) | 0.0018 | ||||
| Visit | Observed value | Mixed-model analysis | ||||
|---|---|---|---|---|---|---|
| CBT-HA | Standard care | Treatment difference (95% CI) | p-value | |||
| n | Mean score (points) (SD) | n | Mean score (points) (SD) | |||
| Baseline | 219 | 9.12 (4.34) | 225 | 8.83 (4.58) | ||
| Improvement from baseline | ||||||
| 6 months | 197 | 2.74 (4.41) | 204 | 1.46 (3.89) | 0.75 (–0.09 to 1.58) | 0.0797 |
| 12 months | 194 | 2.80 (4.40) | 192 | 1.67 (4.04) | 0.75 (–0.10 to 1.60) | 0.0821 |
| 24 months | 189 | 3.33 (4.57) | 181 | 2.07 (4.35) | 0.63 (–0.23 to 1.49) | 0.1521 |
| 5 years | 150 | 5.56 (5.72) | 157 | 4.54 (5.48) | 1.41 (0.48 to 2.33) | 0.0029 |
| Overall | 0.88 (0.25 to 1.52) | 0.0065 | ||||
FIGURE 4.
Changes in the anxiety and depression sections of the HADS over 5 years. (a) HADS anxiety total score; and (b) HADS depression total score.
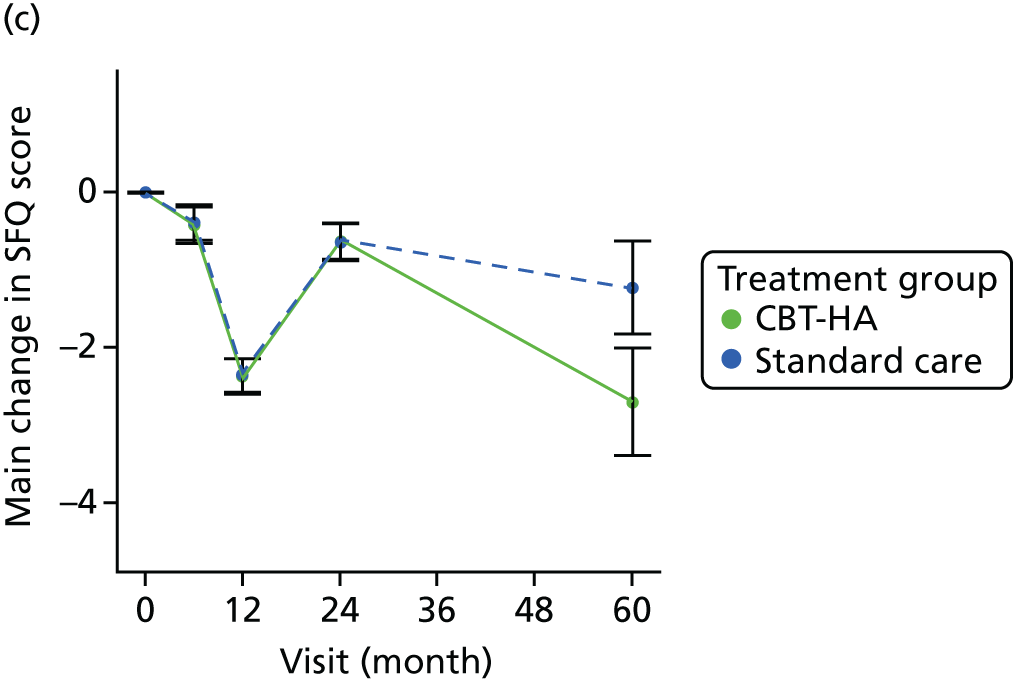
Social functioning
There was very little difference between the scores on the SFQ between the two groups over the 5-year period. The scores at baseline indicated a moderate degree of social dysfunction (the normal population average is 4.6 points and a mean score of 7.7 points is found with patients attending general practice with common mental disorders. 13 The higher than expected SFQ scores were partly explained by comorbid medical pathology but also by personality status (see Table 9). Over the course of the study there was a modest improvement in social functioning in both groups (Table 6).
| Visit | Observed value | Mixed-model analysis | ||||
|---|---|---|---|---|---|---|
| CBT-HA | Standard care | Treatment difference (points) (95% CI) | p-value | |||
| n | Mean score (points) (SD) | n | Mean score (points) (SD) | |||
| Baseline | 219 | 8.52 (2.07) | 225 | 8.59 (2.00) | ||
| Improvement from baseline | ||||||
| 6 months | 197 | 0.32 (1.71) | 204 | 0.33 (1.77) | 0.02 (–0.47 to 0.50) | 0.9508 |
| 12 months | 194 | 2.21 (1.75) | 192 | 2.30 (1.69) | –0.09 (–0.58 to 0.41) | 0.7335 |
| 24 months | 190 | 0.70 (1.93) | 182 | 0.58 (1.85) | 0.12 (–0.38 to 0.63) | 0.6355 |
| 5 years | 150 | 1.20 (4.88) | 157 | 1.27 (4.56) | –0.06 (–0.62 to 0.50) | 0.8367 |
| Overall | –0.00 (–0.32 to 0.32) | 0.9908 | ||||
Influence of obsessional symptoms on outcome
Scores on the SOCS scale were dichotomised at the level of 6 points, as recommended by the original and subsequent authors. 17,29 The results showed that patients with higher SOCS scores had somewhat lesser improvement in HAI scores with CBT-HA over the 5-year period (Figure 5) and that at 5 years the difference between CBT-HA and standard care was not significant (see Table 13).
FIGURE 5.
Mean change in HAI score by initial scores on the SOCS, with scores dichotomised at the recommended score of 6. (a) SOCS score of ≤ 6 points; and (b) SOCS score of ≥ 6 points.
Influence of personality status on outcome
Personality assessment was carried out using the PAS-Q,20 derived from its parent instrument,30 which records both the severity and the type of personality disorder with an algorithm to identify the International Statistical Classification of Diseases, Tenth Edition (ICD-10)31 personality disorders, including dependent personality disorder. SC trained all raters in advance on a standard course. During the progress of the study the Working Group for the Reclassification of Personality Disorder in ICD-11 completed its initial work on a classification based on severity criteria (April 2010). 22 The PAS-Q data were subsequently reclassified to the ICD-11 severity equivalents. Good reliability between assessors in this exercise was achieved. 32
Using the ICD-11 classification, only 63 (14.2%) had no personality dysfunction but 197 (44.3%) had personality difficulty (a subthreshold condition not qualifying for disorder). Only three people assessed had severe personality disorder and so they were included with the moderate group. No differences in patient characteristics at baseline were identified and there was an even spread of male/female and a similar age profile between the ICD-11 personality groups (Table 7). However, there were significant differences in symptoms of health anxiety and generalised anxiety, depression and social functioning at baseline; participants with moderate to severe personality disorder had significantly higher scores than those with no personality disturbance (see Table 7). There were no differences in total cost at baseline apart from somewhat greater costs for each increment of personality severity.
| Variable | Personality status | p-value | |||
|---|---|---|---|---|---|
| 0 (N = 63) | 1 (N = 197) | 2 (N = 142) | 3–4 (N = 42) | ||
| Sex, n (%) | |||||
| Female | 29 (46.0) | 109 (55.3) | 76 (53.5) | 22 (52.4) | 0.642 |
| Male | 34 (54.0) | 88 (44.7) | 66 (46.5) | 20 (47.6) | – |
| Age (years) | |||||
| Mean (SD) | 48.6 (14.8) | 49.5 (13.6) | 47.5 (13.6) | 47.9 (11.3) | 0.592 |
| Minimum to maximum (range) | 18.3 to 73.9 | 17.3 to 74.3 | 17.0 to 75.5 | 21.7 to 72.4 | – |
| HAI score | |||||
| Mean (SD) | 24.0 (3.2) | 24.8 (4.5) | 25.2 (4.3) | 26.9 (4.9) | 0.006 |
| HADS-A score | |||||
| Mean (SD) | 10.1 (3.6) | 12.1 (3.7) | 13.4 (3.6) | 14.0 (3.6) | < 0.001 |
| HADS-D score | |||||
| Mean (SD) | 6.7 (3.7) | 8.2 (4.1) | 10.0 (4.4) | 12.4 (4.7) | < 0.001 |
| SFQ score | |||||
| Mean (SD) | 5.9 (3.4) | 8.6 (4.0) | 11.3 (4.4) | 12.7 (3.8) | < 0.001 |
| Total cost (preceding 6 months) | |||||
| Mean (SD) | 2405.2 (2526.3) | 2601.8 (2837.2) | 2668.1 (2887.1) | 2692.5 (2708.3) | 0.954 |
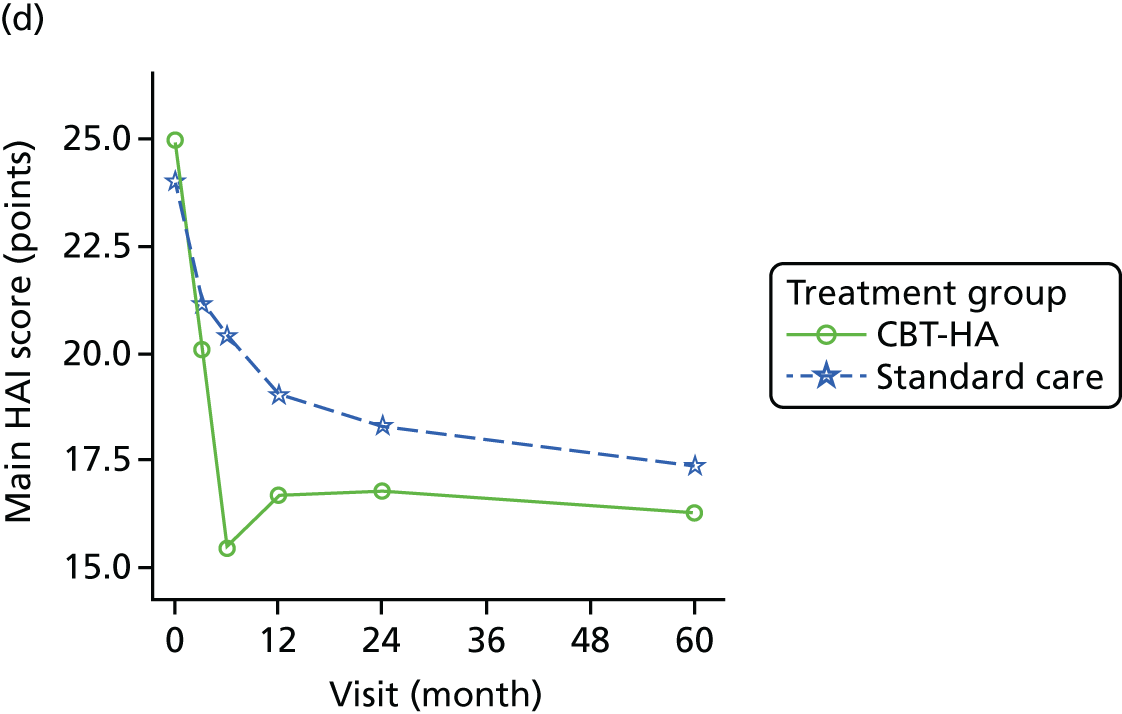
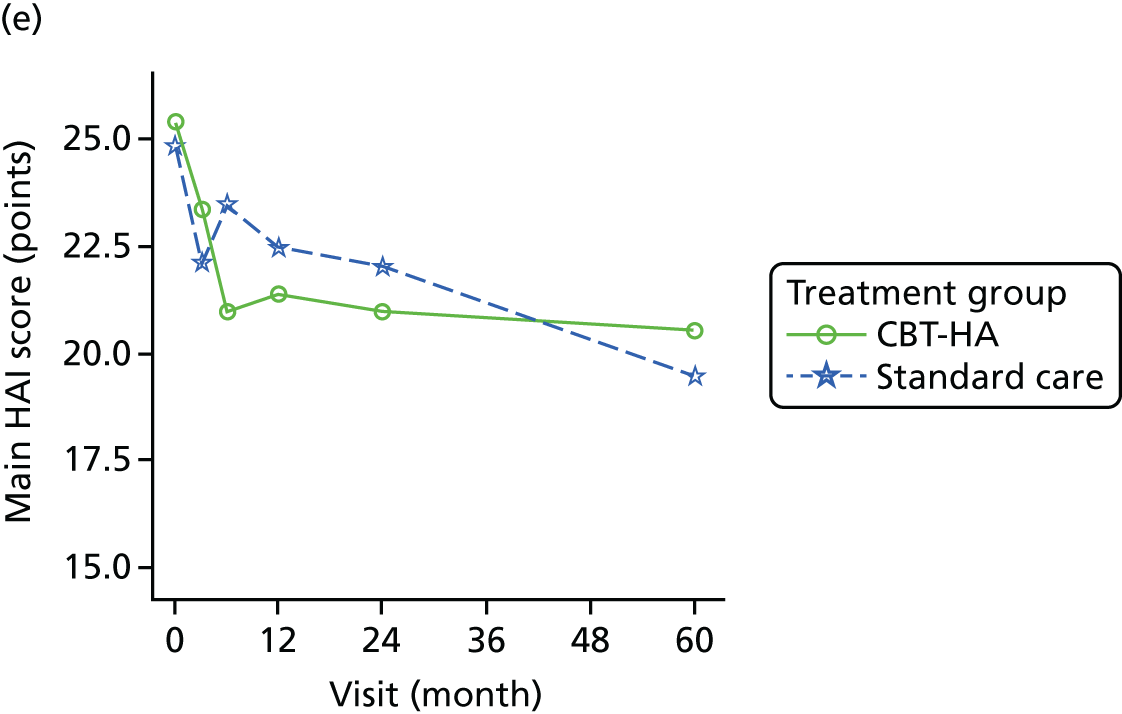
The outcome data over follow-up by ICD-11 classification are detailed in Table 8 and Figure 6. Contrary to our hypotheses, the results show that those with no personality dysfunction showed no benefit from CBT-HA at any time point in the study; overall standard care was superior (p < 0.05). For all other groups the picture was different. For participants with personality difficulty and mild personality disorder, there was evidence of strong gains from CBT-HA at all time points compared with standard care (p < 0.001), and these were maintained at 5 years, especially in those with mild personality disorder. For participants with moderate and severe personality disorder, the initial benefit was not retained at 2 years, resulting in a weaker relationship over follow-up (p < 0.05), and by 5 years benefit was lost. Improvement in social function was similar in all groups except in those with no personality dysfunction (p < 0.02 in favour of standard care) and in those of mild personality disorder at 5 years, whose SFQ scores were significantly lower in the CBT-HA group (Figure 7). Clinical symptomatology increased and social dysfunction was greater with each increment of personality pathology, and although the results were most marked in those with health anxiety they were also found with generalised anxiety and depressive symptoms (see Table 7).
| Variable | Difference between CBT-HA and standard care (95% CI) | |||
|---|---|---|---|---|
| ICD-11 personality level 0 (N = 63) | ICD-11 personality level 1 (N = 197) | ICD-11 personality level 2 (N = 142) | ICD-11 personality level 3–4 (N = 42) | |
| HAI score | ||||
| 3 months | 2.12 (–1.41 to 5.64) | –1.62 (–3.56 to 0.31) | –3.24** (–5.57 to –0.92) | –3.76 (–8.24 to 0.71) |
| 6 months | –1.29 (–4.9 to 2.31) | –4.80*** (–6.77 to –2.84) | –5.51*** (–7.85 to –3.16) | –8.13** (–12.59 to –3.66) |
| 12 months | 0.47 (–3.11 to 4.05) | –3.55** (–5.54 to –1.57) | –3.32** (–5.69 to –0.96) | –4.42 (–8.99 to 0.14) |
| 24 months | 1.45 (–2.12 to 5.03) | –2.98** (–4.98 to –0.97) | –2.96* (–5.35 to –0.56) | –0.31 (–4.93 to 4.31) |
| At all time points | 0.69 (–2.23 to 3.6) | –3.24*** (–4.84 to –1.64) | –3.76*** (–5.78 to –1.74) | –4.16* (–7.99 to –0.33) |
| HADS-A score | ||||
| 6 months | 1.45 (–0.5 to 3.39) | –1.47* (–2.64 to –0.29) | –1.71* (–3.05 to –0.36) | –2.03 (–4.7 to 0.65) |
| 12 months | 2.68 (0.75 to 4.62) | –1.70** (–2.89 to –0.51) | –1.42* (–2.78 to –0.06) | –1.32 (–4.05 to 1.41) |
| 24 months | 2.21* (0.25 to 4.16) | –1.81** (–3.01 to –0.60) | –1.00 (–2.38 to 0.38) | –1.00 (–3.77 to 1.77) |
| At all time points | 2.11** (0.51 to 3.71) | –1.66*** (–2.62 to –0.70) | –1.38* (–2.56 to –0.20) | –1.45 (–3.79 to 0.89) |
| HADS-D score | ||||
| 6 months | 2.17* (0.11 to 4.24) | –1.33* (–2.49 to –0.17) | –1.1 (–2.49 to 0.28) | –1.42 (–4.32 to 1.48) |
| 12 months | 1.79 (–0.27 to 3.85) | –1.27* (–2.45 to –0.09) | –0.69 (–2.10 to 0.71) | –2.64 (–5.62 to 0.33) |
| 24 months | 3.29** (1.22 to 5.36) | –0.69 (–1.88 to 0.49) | –1.84* (–3.27 to –0.41) | –2.06 (–5.08 to 0.96) |
| At all time points | 2.42** (0.62 to 4.21) | –1.10* (–2.06 to –0.13) | –1.21* (–2.41 to –0.02) | –2.04 (–4.55 to 0.47) |
| SFQ score | ||||
| 6 months | 2.32* (0.19 to 4.45) | –0.42 (–1.57 to 0.73) | –0.31 (–1.68 to 1.06) | –1.89 (–4.54 to 0.77) |
| 12 months | 1.52 (–0.61 to 3.64) | –0.08 (–1.25 to 1.09) | –0.66 (–2.05 to 0.73) | –1.91 (–4.64 to 0.82) |
| 24 months | 2.88** (0.75 to 5.01) | –0.19 (–1.37 to 0.98) | –1.49* (–2.9 to –0.08) | –0.88 (–3.65 to 1.89) |
| At all time points | 2.24* (0.41 to 4.07) | –0.23 (–1.19 to 0.73) | –0.82 (–1.97 to 0.33) | –1.56 (–3.83 to 0.71) |
FIGURE 6.
Differential outcome of patients over 5 years treated by CBT-HA and standard care groups separated by ICD-11 personality status at baseline (see Table 8 for significance of differences). (a) No personality dysfunction; (b) personality difficulty; (c) mild personality disorder; and (d) moderate/severe disorder.


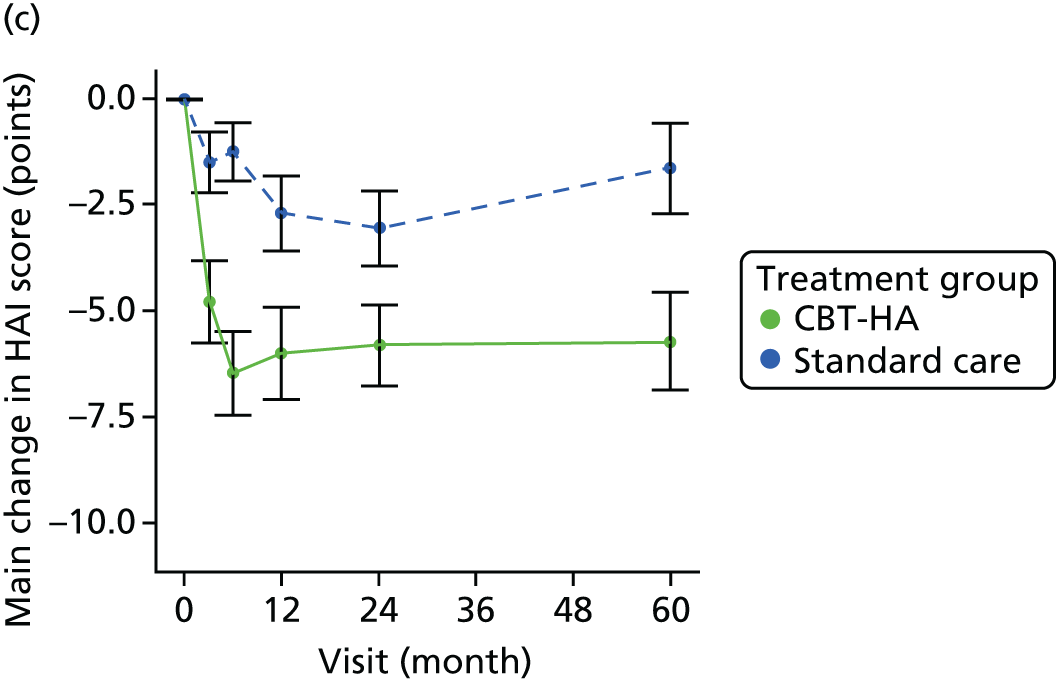
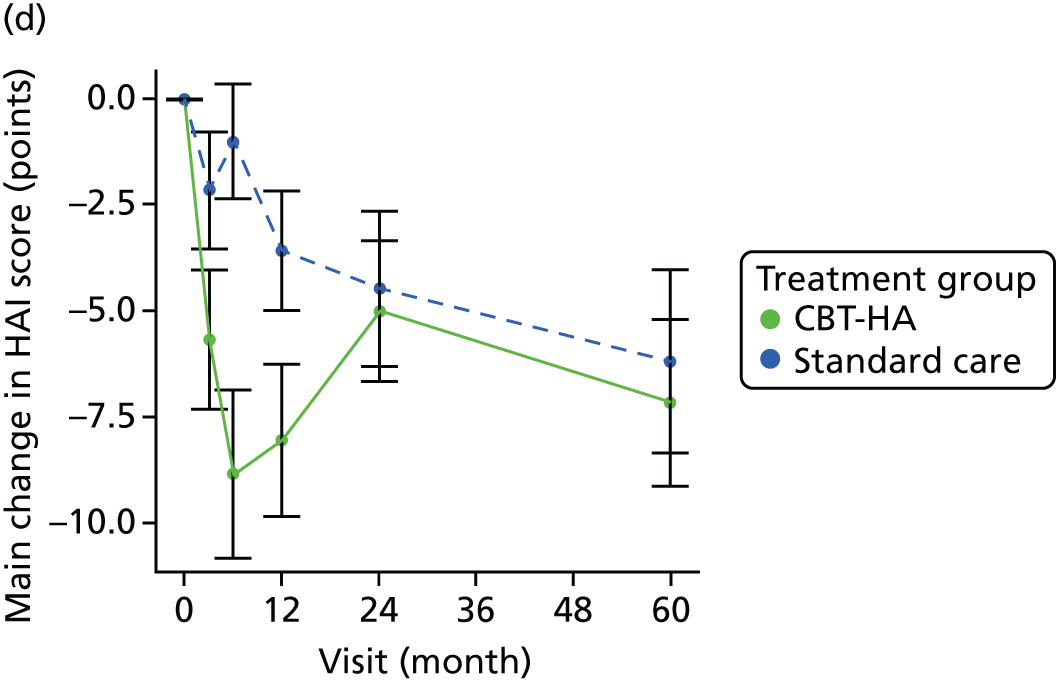
FIGURE 7.
Change in social functioning separated by ICD-11 personality status in CBT-HA and standard care groups over a 5-year period. (a) No personality dysfunction; (b) personality difficulty; (c) mild personality disorder; and (d) moderate/severe disorder.



Costs were lower in patients treated with CBT-HA for all levels of personality disturbance apart from moderate and severe personality disorder, when costs were greater (Table 9).
| ICD-11 personality status | Treatment group | Total | ||||
|---|---|---|---|---|---|---|
| Standard care | CBT-HA | |||||
| Mean | SD | Mean | SD | Mean | SD | |
| No personality disorder, 0 (n = 49) | 7565.45 | 9840.9 | 6204.83 | 5731.1 | 6926.79 | 8121.8 |
| Personality difficulty, 1 (n = 153) | 8436.81 | 8835.34 | 8166.55 | 9302.32 | 8297.26 | 9050.66 |
| Mild personality disorder, 2 (n = 106) | 7754.32 | 10021.78 | 6819.05 | 5558 | 7277.86 | 8037.21 |
| Moderate and severe personality disorder, 3 (n = 31) | 5363.28 | 3266.24 | 6529.42 | 3876.78 | 5927.54 | 3563.55 |
Effect of personality: dependent personality traits
Dependent personality status was also assessed dimensionally in the same way as the ICD-11 severity levels (range 0–24) using the DPQ. 18 A previous epidemiological study in general practice33 had identified the range of scores associated with disability with 0–6 (no personality dysfunction), 7–11 (personality difficulty), 12–16 (mild personality disorder) and ≥ 17 (moderate personality disorder) linking to ICD-11 severities. The DPQ does not allow severe dependent personality disorder to be identified because none of its questions address self-harm or aggression, even though these may sometimes be present in association with dependent personality. 34
As with the main study using ICD-11 diagnostic criteria for all personality disorders, most patients in the study had some degree of dependent personality disturbance at baseline, with women having more dependent traits than men (Table 10). The generalised anxiety and depression scores were higher in those who were more dependent, although this was not the case for the HAI scores, and there was significantly greater social dysfunction in higher scorers (see Table 10). The mean number of treatment sessions was higher in those with more dependent personality dysfunction (p < 0.005) (Table 11).
| Variable | Dependent personality dysfunction | ||||
|---|---|---|---|---|---|
| 0 (N = 76) | 1 (N = 186) | 2 (N = 141) | 3 (N = 41) | p-value | |
| Age (years), mean (SD) | 50.64 (13.03) | 49.88 (13.61) | 46.48 (12.89) | 46.56 (15.62) | 0.0507 |
| Female, n (%) | 29 (38.2) | 100 (53.8) | 85 (60.3) | 22 (53.7) | 0.0206 |
| HAI score, mean (SD) | 24.31 (4.18) | 24.85 (4.38) | 25.29 (4.50) | 25.95 (4.14) | 0.1957 |
| HADS-A score, mean (SD) | 10.46 (3.53) | 11.97 (3.81) | 13.45 (3.62) | 14.41 (2.86) | < 0.0001 |
| HADS-D score, mean (SD) | 7.70 (4.55) | 8.46 (4.44) | 9.42 (3.71) | 12.12 (5.22) | < 0.0001 |
| SFQ score, mean (SD) | 8.28 (4.41) | 8.70 (4.35) | 9.65 (4.09) | 12.88 (4.91) | < 0.0001 |
| Statistics | Dependent personality dysfunction group | p-value | |||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||
| n | 47 | 86 | 65 | 21 | 0.0046 |
| Mean | 5.40 | 5.28 | 6.49 | 8.62 | |
| SD | 4.174 | 3.794 | 3.857 | 5.390 | |
| Minimum | 0.00 | 0.00 | 0.00 | 0.00 | |
| Median | 5.00 | 5.00 | 8.00 | 7.00 | |
| Maximum | 21.00 | 15.00 | 14.00 | 22.00 | |
Of the 444 patients, 47 had an ICD-10 diagnosis of dependent personality disorder, seven with dependent disorder alone and 18 in conjunction with other personality disorders. Agreement between the DPQ and the PAS-Q groups was significant but relatively low (weighted kappa 0.16; p < 0.01).
Contrary to the initial hypotheses, patients treated with CBT-HA who had greater levels of dependence showed superior improvement in health-anxiety scores to those receiving standard care at all times of testing, and this was equally strong after 5 years (Table 12). The score differences were of greater magnitude in those with moderate dependent personality disorder, among whom, at 5 years, the mean score of 13.9 was fairly close to the normal level in the population (around 11)18 (see Table 12). Generalised anxiety and depression scores (HADS) were also significantly more improved in those who received CBT-HA than in those who received standard care. Social function showed no significant differences between the allocated treatments separated by dependence groups (see Table 12).
| Outcome (CBT-HA group vs. standard care group) | Dependent personality dysfunction | |||
|---|---|---|---|---|
| 0 (n = 76) | 1 (n = 186) | 2 (n = 141) | 3 (n = 41) | |
| HAI score | ||||
| 3 months | ||||
| Difference (95% CI) | –0.81 (–4.92 to 3.31) | –1.03 (–3.05 to 0.99) | –3.23 (–5.62 to –0.84) | –1.37 (–5.60 to 2.87) |
| p-value | 0.6998 | 0.3168 | 0.0082 | 0.5244 |
| 6 months | ||||
| Difference (95% CI) | –3.82 (–7.93 to 0.29) | –4.33 (–6.40 to –2.26) | –5.20 (–7.62 to –2.78) | –6.52 (–10.7 to –2.30) |
| p-value | 0.0683 | < 0.0001 | < 0.0001 | 0.0027 |
| 12 months | ||||
| Difference (95% CI) | –2.80 (–7.03 to 1.43) | –2.30 (–4.37 to –0.24) | –3.32 (–5.76 to –0.89) | –4.91 (–9.33 to –0.49) |
| p-value | 0.1938 | 0.0291 | 0.0076 | 0.0296 |
| 24 months | ||||
| Difference (95% CI) | 0.47 (–3.83 to 4.78) | –2.02 (–4.13 to 0.09) | –3.26 (–5.70 to –0.82) | –1.90 (–6.35 to 2.55) |
| p-value | 0.8292 | 0.0601 | 0.0090 | 0.3996 |
| 5 years | ||||
| Difference (95% CI) | –4.60 (–9.13 to –0.08) | –1.26 (–3.46 to 0.94) | –1.65 (–4.32 to 1.03) | –4.08 (–8.71 to 0.55) |
| p-value | 0.0463 | 0.2608 | 0.2273 | 0.0837 |
| Overall | ||||
| Difference (95% CI) | –2.31 (–5.66 to 1.03) | –2.19 (–3.80 to –0.58) | –3.33 (–5.28 to –1.38) | –3.76 (–7.29 to –0.23) |
| p-value | 0.1748 | 0.0078 | 0.0008 | 0.0372 |
| HADS-A score | ||||
| 6 months | ||||
| Difference (95% CI) | –1.75 (–3.83 to 0.34) | –1.22 (–2.53 to 0.08) | –1.08 (–2.49 to 0.33) | –2.41 (–5.00 to 0.18) |
| p-value | 0.0997 | 0.0658 | 0.1330 | 0.0676 |
| 12 months | ||||
| Difference (95% CI) | –0.80 (–3.00 to 1.40) | –0.57 (–1.87 to 0.73) | –1.21 (–2.63 to 0.21) | –2.87 (–5.65 to –0.09) |
| p-value | 0.4745 | 0.3907 | 0.0957 | 0.0433 |
| 24 months | ||||
| Difference (95% CI) | –0.79 (–3.02 to 1.43) | –0.90 (–2.25 to 0.44) | –1.09 (–2.51 to 0.34) | –1.89 (–4.69 to 0.92) |
| p-value | 0.4828 | 0.1884 | 0.1345 | 0.1843 |
| 5 years | ||||
| Difference (95% CI) | –0.80 (–3.18 to 1.58) | –0.72 (–2.12 to 0.69) | –0.98 (–2.57 to 0.60) | –1.53 (–4.49 to 1.43) |
| p-value | 0.5095 | 0.3147 | 0.2230 | 0.3064 |
| Overall | ||||
| Difference (95% CI) | –1.03 (–2.63 to 0.56) | –0.85 (–1.83 to 0.12) | –1.09 (–2.21 to 0.03) | –2.17 (–4.20 to –0.15) |
| p-value | 0.2031 | 0.0871 | 0.0572 | 0.0352 |
| HADS-D score | ||||
| 6 months | ||||
| Difference (95% CI) | –0.45 (–2.74 to 1.83) | –0.41 (–1.74 to 0.91) | –1.36 (–2.78 to 0.07) | –1.47 (–4.00 to 1.07) |
| p-value | 0.6950 | 0.5409 | 0.0626 | 0.2543 |
| 12 months | ||||
| Difference (95% CI) | –0.05 (–2.46 to 2.35) | –0.41 (–1.73 to 0.91) | –1.23 (–2.67 to 0.21) | –2.26 (–5.01 to 0.49) |
| p-value | 0.9644 | 0.5429 | 0.0929 | 0.1062 |
| 24 months | ||||
| Difference (95% CI) | 2.16 (–0.27 to 4.59) | –0.65 (–2.02 to 0.71) | –1.87 (–3.32 to –0.43) | –1.56 (–4.34 to 1.22) |
| p-value | 0.0808 | 0.3482 | 0.0111 | 0.2686 |
| 5 years | ||||
| Difference (95% CI) | –4.09 (–6.68 to –1.51) | –0.87 (–2.30 to 0.56) | –0.83 (–2.44 to 0.77) | –1.52 (–4.49 to 1.45) |
| p-value | 0.0021 | 0.2317 | 0.3083 | 0.3120 |
| Overall | ||||
| Difference (95% CI) | –0.61 (–2.42 to 1.20) | –0.59 (–1.57 to 0.40) | –1.32 (–2.46 to –0.18) | –1.70 (–3.42 to 0.01) |
| p-value | 0.5069 | 0.2414 | 0.0229 | 0.0519 |
| SFQ score | ||||
| 6 months | ||||
| Difference (95% CI) | –0.17 (–1.46 to 1.12) | 0.26 (–0.53 to 1.06) | –0.10 (–0.91 to 0.71) | –0.85 (–2.38 to 0.67) |
| p-value | 0.7946 | 0.5138 | 0.8094 | 0.2683 |
| 12 months | ||||
| Difference (95% CI) | –0.26 (–1.63 to 1.11) | 0.30 (–0.49 to 1.10) | 0.15 (–0.67 to 0.97) | –1.01 (–2.66 to 0.64) |
| p-value | 0.7090 | 0.4546 | 0.7231 | 0.2263 |
| 24 months | ||||
| Difference (95% CI) | –0.47 (–1.86 to 0.92) | –0.04 (–0.86 to 0.78) | 0.02 (–0.80 to 0.85) | –0.79 (–2.46 to 0.88) |
| p-value | 0.5067 | 0.9323 | 0.9556 | 0.3480 |
| 5 years | ||||
| Difference (95% CI) | 0.40 (–1.12 to 1.92) | –0.00 (–0.89 to 0.89) | –0.14 (–1.11 to 0.83) | –0.56 (–2.39 to 1.27) |
| p-value | 0.6041 | 0.9998 | 0.7772 | 0.5431 |
| Overall | ||||
| Difference (95% CI) | –0.12 (–1.05 to 0.80) | 0.13 (–0.37 to 0.64) | –0.02 (–0.56 to 0.53) | –0.81 (–1.87 to 0.26) |
| p-value | 0.7906 | 0.6052 | 0.9507 | 0.1357 |
Differences in outcome by site, clinic and age
These outcomes were considered relevant in the covariate-adjusted analyses and are summarised here, but it is important to emphasise that there were no particular hypotheses linked to these outcomes and randomisation did not take account of these. The five sites covered a mix of urban, suburban and rural areas, including two main teaching hospitals (St Mary’s Hospital and Charing Cross Hospital), two hospitals linked to teaching hospitals (Hillingdon and Chelsea and Westminster) and one district general hospital (King’s Mill Hospital). Four of the clinics concerned (cardiology, endocrinology, gastroenterology and respiratory medicine) had been identified previously as having at least 12% of attenders with a high level of health anxiety,7,35 and during the course of the study another clinic type, neurology, was added.
The differences between sites are shown in Figure 8. In general, the non-teaching hospitals showed the largest differences between the patients receiving CBT-HA and those receiving standard care. There is no obvious explanation for this difference except in terms of therapist type (see Subgroup analyses). There were also differences in HAI outcome by clinic. Patients seen in cardiology clinics showed the largest differences between those who received CBT-HA and those receiving standard care, maximal at 5 years (Figure 9), and respiratory medicine patients showed the least differences between groups (with no benefit after the first 6 months of treatment).
FIGURE 8.
Differences in outcome by HAI scores separated by site. (a) Chelsea and Westminster; (b) Charing Cross Hospital; (c) Hillingdon Hospital; (d) King’s Mill Hospital; and (e) St Mary’s Hospital.
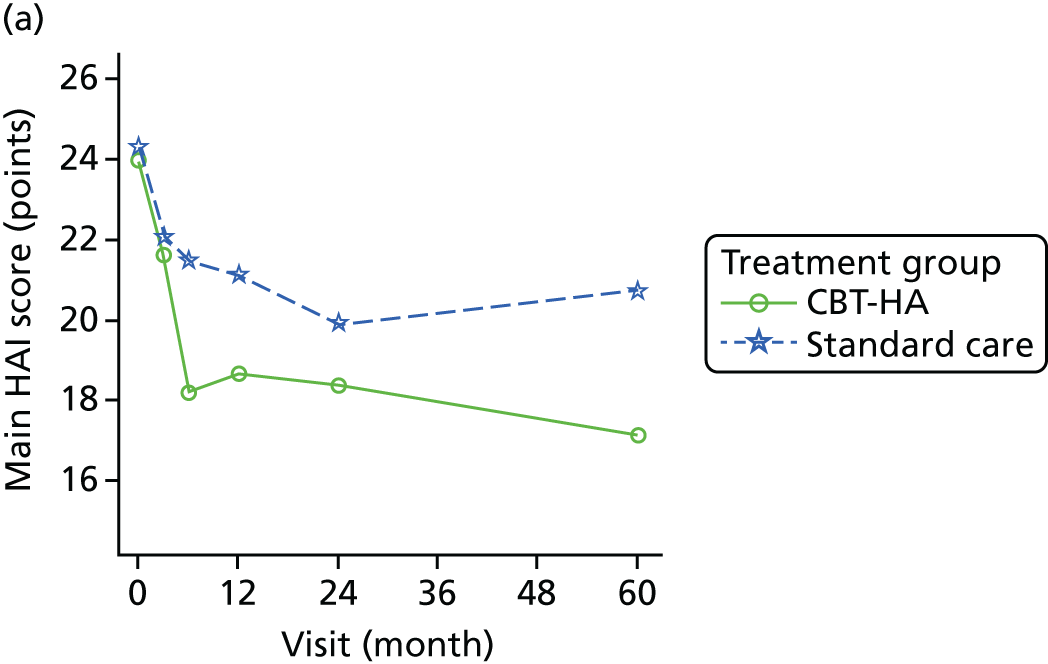

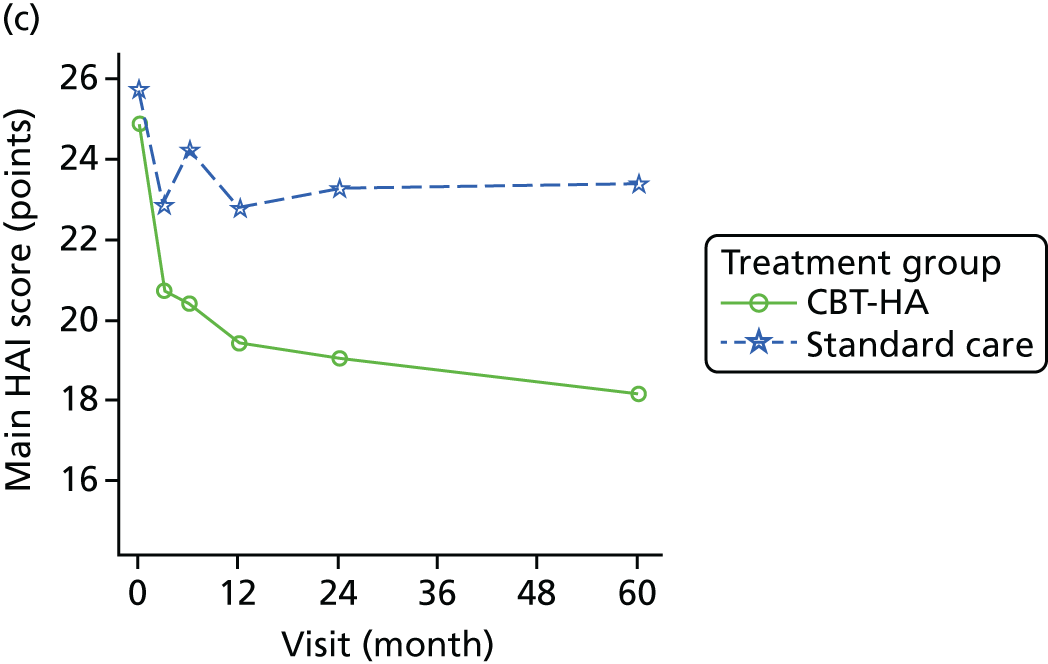
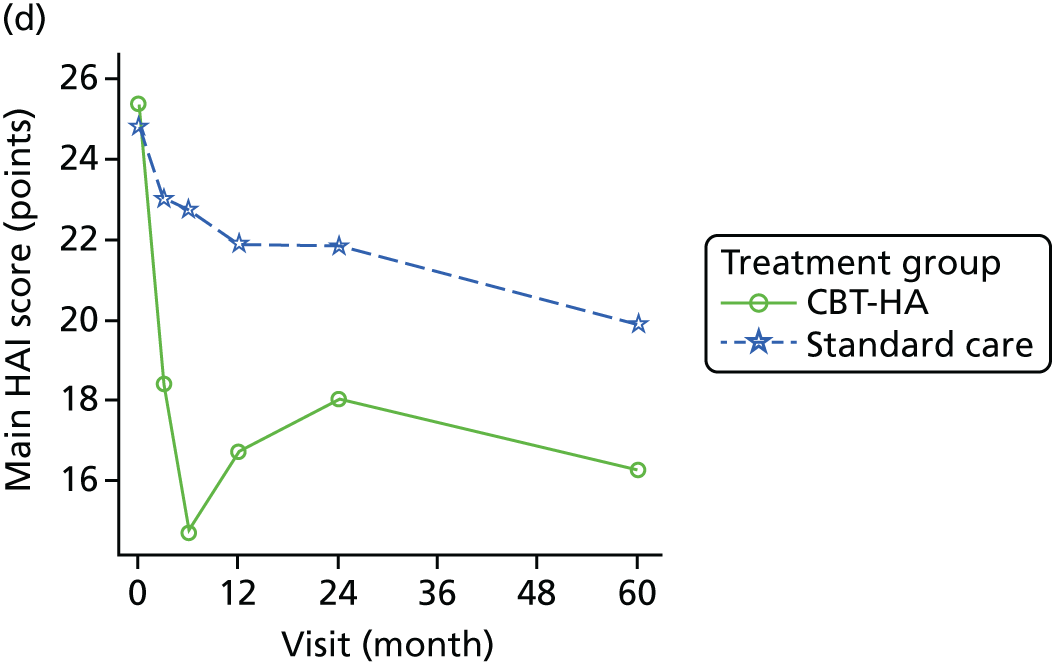

FIGURE 9.
Differences in outcome by HAI scores separated by clinic type. (a) Cardiology; (b) endocrinology; (c) gastroenterology; (d) neurology; and (e) respiratory medicine.


Older patients derived greater benefit from CBT-HA compared with standard care than younger patients. This was not an expected finding and possible reasons for it are discussed later in this report.
Subgroup analyses
There were several subgroup analyses that showed generally similar findings. The subgroup analysis to examine the heterogeneity of the variables of interest is shown for the primary outcome, the HAI, in Table 13. There were no significant interactions, suggesting that the data were consistent and robust. The only variable approaching heterogeneity was the study site. King’s Mill Hospital had a better outcome than the other sites over the period of the study; this was also the site where the nurses were the main therapists.
| Variable | Mixed-model result | ||||
|---|---|---|---|---|---|
| CBT-HA | Standard care | Difference (95% CI) | p-value | p-value from interaction test | |
| n, mean (SD) | n, mean (SD) | ||||
| Age group (years) | |||||
| ≤ 49 | 63, 6.68 (8.36) | 79, 5.69 (7.06) | 1.78 (–0.46 to 4.01) | 0.1197 | 0.2051 |
| > 49 | 86, 6.28 (8.76) | 79, 2.98 (8.21) | 2.78 (0.77 to 4.79) | 0.0067 | – |
| Hospital | |||||
| Charing Cross Hospital | 20, 5.10 (9.81) | 19, 6.58 (8.64) | –3.32 (–7.50 to 0.86) | 0.1186 | – |
| Chelsea and Westminster Hospital | 14, 6.93 (6.47) | 15, 3.12 (6.39) | 3.60 (–1.10 to 8.30) | 0.1321 | 0.0669 |
| Hillingdon Hospital | 43, 6.33 (8.47) | 46, 2.37 (7.09) | 3.56 (0.83 to 6.29) | 0.0107 | – |
| King’s Mill Hospital | 45, 8.89 (7.62) | 53, 4.85 (7.49) | 4.78 (2.15 to 7.42) | 0.0004 | – |
| St Mary’s Hospital | 27, 3.35 (9.50) | 25, 5.88 (9.06) | –1.66 (–5.32 to 2.00) | 0.3718 | – |
| Clinic | |||||
| Cardiology | 33, 8.73 (7.93) | 38, 3.56 (8.62) | 5.21 (2.08 to 8.34) | 0.0012 | 0.4715 |
| Endocrinology | 28, 4.89 (6.82) | 30, 3.70 (6.30) | 1.39 (–2.06 to 4.83) | 0.4286 | – |
| Gastroenterology | 57, 5.77 (9.02) | 55, 4.78 (7.73) | 1.45 (–1.07 to 3.98) | 0.2591 | – |
| Neurology | 13, 9.08 (9.05) | 17, 5.53 (8.19) | 1.15 (–3.52 to 5.82) | 0.6274 | – |
| Respiratory medicine | 18, 4.97 (9.87) | 18, 4.53 (8.27) | –0.13 (–4.39 to 4.12) | 0.9507 | – |
| SOCS score | |||||
| ≤ 6 points | 94, 7.32 (8.93) | 103, 4.47 (7.87) | 2.73 (0.87 to 4.58) | 0.0040 | 0.4376 |
| > 6 points | 55, 4.97 (7.76) | 55, 4.09 (7.59) | 1.31 (–1.23 to 3.84) | 0.3112 | – |
| DPQ score | |||||
| ≤ 15 points | 127, 6.51 (8.86) | 140, 4.57 (7.78) | 2.02 (0.41 to 3.64) | 0.0140 | 0.5229 |
| > 15 points | 22, 6.09 (6.75) | 18, 2.50 (7.52) | 3.30 (–0.62 to 7.22) | 0.0983 | – |
| PAS-Q | |||||
| 0 | 20, 5.02 (9.46) | 17, 4.59 (7.61) | 0.25 (–4.24 to 4.74) | 0.9118 | 0.2902 |
| 1 | 79, 6.27 (8.84) | 97, 4.05 (7.81) | 2.30 (0.35 to 4.25) | 0.0207 | – |
| 2 | 39, 8.10 (7.77) | 33, 4.03 (8.26) | 3.83 (0.62 to 7.03) | 0.0194 | – |
| 3 | 11, 4.55 (7.66) | 11, 7.36 (5.95) | –0.93 (–6.81 to 4.94) | 0.7537 | – |
Outcome by therapist type
When the CHAMP trial started it was hoped that sufficient excess treatment costs might be available to fund dedicated therapists at all sites in the study; this was not possible, but at one site (King’s Mill Hospital) a subvention grant allowed two general nurses (SM and YL-S) to be employed for approximately 80% of their time in giving CBT-HA. In other centres somewhat less funding was obtained for other therapists, mainly trainee psychologists, but also other health professionals, including a dietitian, to be employed on a mainly part-time basis.
Apart from the nurses and the dietitian, the other therapists had at least some knowledge of the principles of CBT before the trial began and some had practised, but none had been trained in, CBT-HA. All therapists were involved in the initial 2-day workshop and, once trained at this standard level, received supervision from established trainers at each site.
The results, also reported elsewhere,36 showed that although the patients treated by all three therapist groups (nurses, assistant psychologists and graduate workers) showed superior HAI outcomes after 6 months, the nurses group showed the largest benefit across the initial 2-year period (Figure 10 and Table 14). After 2 years, 23.5% of patients in standard care had improved to a score of 15 on the HAI (mild but not pathological health anxiety), whereas the proportions in the three therapist CBT-HA groups were 28.9% (assistant psychologists), 34% (graduate workers) and 44.3% (nurses) (Table 15).
FIGURE 10.
Mean differences in HAI scores between the outcomes of 219 patients with health anxiety treated by nurses (n = 66), graduate workers (n = 66) and assistant psychologists (n = 87) over 2 years. Reprinted from the International Journal of Nursing Studies, vol. 52, Tyrer H, Tyrer P, Lisseman-Stones Y, McAllister S, Cooper S, Salkovskis P, et al. Therapist differences in a randomised trial of the outcome of cognitive behaviour therapy for health anxiety in medical patients, pp. 686–94. Copyright (2015),36 with permission from Elsevier.

| Visit | HAI score (points), n of patients, mean score (SD) | Difference between nurses and other groups | ||||
|---|---|---|---|---|---|---|
| Standard care | CBT by assistant psychologists | CBT by graduates | CBT by nurses | All | Mean (95% CI); p-value | |
| Baseline | 225, 25.12 (4.52) | 87, 24.76 (3.91) | 66, 24.38 (4.15) | 66, 25.53 (4.67) | 225, 25.12 (4.52) | – |
| 3 months | 212, 22.37 (6.71) | 82, 21.65 (6.62) | 59, 21.33 (6.97) | 64, 18.15 (9.07) | 212, 22.37 (6.71) | 4.10 (6.1 to 3.1); p < 0.0001 |
| 6 months | 204, 22.62 (6.81) | 78, 20.13 (7.26) | 56, 17.77 (8.42) | 63, 14.67 (7.53) | 204, 22.62 (6.81) | 4.93 (7.0 to 2.9); p < 0.0001 |
| 12 months | 193, 21.54 (7.45) | 75, 19.80 (6.96) | 57, 18.53 (8.31) | 62, 16.81 (8.31) | 193, 21.54 (7.45) | 3.24 (5.3 to 1.2); p < 0.002 |
| 24 months | 183, 21.35 (7.67) | 76, 19.51 (7.22) | 53, 18.98 (8.14) | 61, 17.95 (8.63) | 183, 21.35 (7.67) | 2.49 (4.5 to 0.5); p < 0.02 |
| All periods | 3.7 (5.4 to 2.0); p < 0.0001 | |||||
| Therapist group | Number of patients (%) with HAI scores of ≤ 15 points | Odds ratio of improvement (CBT-HA vs. standard care): all times (significance) | 95% CI |
|---|---|---|---|
| Standard care | |||
| 3 months | 31 (14.6) | – | – |
| 6 months | 30 (14.7) | ||
| 12 months | 42 (21.8) | ||
| 24 months | 43 (23.5) | ||
| CBT-HA: assistant psychologists | |||
| 3 months | 16 (19.5) | 1.58 (p = 0.05) | 0.99 to 2.51 |
| 6 months | 24 (30.8) | ||
| 12 months | 19 (25.3) | ||
| 24 months | 22 (28.9) | ||
| CBT-HA: graduates | |||
| 3 months | 10 (16.9) | 2.05 (p = 0.005) | 1.25 to 3.36 |
| 6 months | 24 (42.9) | ||
| 12 months | 24 (42.1) | ||
| 24 months | 18 (34.0) | ||
| CBT-HA: nurses | |||
| 3 months | 28 (43.8) | 3.16 (p < 0.0001) | 1.97 to 5.06 |
| 6 months | 40 (63.5) | ||
| 12 months | 33 (53.2) | ||
| 24 months | 27 (44.3) | ||
Chapter 4 Economic evaluation
Perspective
The economic evaluation took a health and social care perspective, which included the costs of the CBT intervention, other health-care costs and other community health and social services. In addition, we completed the sensitivity analysis from a societal perspective, to include all resources in the health and social care perspective plus productivity losses.
Identification of resources
The calculation of costs was separated into three stages: identification, measurement and valuation of resources.
We identified relevant resources based on the results of our pilot study10 and in discussion with study clinicians and patient representatives. Resource use was collected in the following domains:
-
delivery of CBT-HA
-
use of NHS secondary care services
-
inpatient stays
-
day-case procedures
-
outpatient appointments
-
accident and emergency attendances
-
use of NHS primary care services
-
General practitioner [(GP) in practice, at home or by telephone]
-
community nurse (practice nurse, district nurse, health visitor, midwife)
-
community mental health services
-
community medical services (walk-in clinic)
-
community medical professional (physiotherapist, chiropodist)
-
use of all medication
-
use of social care and voluntary sector services
-
social worker
-
voluntary sector advice worker
-
housing services
-
service-provided accommodation
-
productivity losses measured as absenteeism.
Measurement of resources
The identified resources were measured using the following methods.
The CBT-HA therapists recorded information on attendance and non-attendance at treatment sessions together with the duration of each session. These data were extracted for analysis from trial records.
The computerised records of the host hospital trusts (Sherwood Forest Hospitals NHS Foundation Trust, Imperial College Healthcare NHS Trust, Chelsea and Westminster Hospital NHS Foundation Trust and The Hillingdon Hospitals NHS Foundation Trust) were examined and accident and emergency attendances, inpatient stays, day-patient procedures and outpatient appointments were extracted for analysis by hospital trust-based information specialists co-ordinated by AP.
Other service use data for the economic evaluation were collected using the ADSUS, based on previous economic evaluations in adult mental health populations37 and on the data collected in the pilot study. 10 The ADSUS was completed at baseline, at 6, 12 and 24 months and at the 5-year follow-up. At baseline, the ADSUS covered the previous 6 months and at each of the follow-up interviews, service use since the previous interview was recorded so that the entire period from baseline to final follow-up was covered. The ADSUS records the number and duration of contacts with a range of health and social service professionals and medications taken.
The number of days taken off work because of ill health was collected with the relevant questions from the World Health Organization Health and Work Performance Questionnaire. 38
Valuation of resources
The cost of the CBT-HA intervention was estimated using the bottom-up approach set out by the Personal Social Services Research Unit at the University of Kent. 39 The salary cost for the therapist was based on that of an experienced nurse or therapist (Agenda for Change Band 6),40 onto which employer costs (National Insurance and pension contribution) were added. Overhead costs were then added to include building costs, administrative and managerial costs and capital costs. An hourly cost was calculated on the working time assumptions set out in the Unit Costs of Health and Social Care,41 and then weighted to account for the therapist spending time on non-patient-facing activities. In addition, the final cost per hour included an allowance for the cost of time spent by the therapist in supervision and the cost of supervisor time.
For each type of other service use, an appropriate unit cost was identified. All unit costs were for the financial year 2009–10 and costs with their sources are listed in full in Table 16. When necessary, unit costs were inflated to 2009–10 costs using the Hospital and Community Health Services inflation index or the Retail Price Index as appropriate. 41 Costs in the second, third, fourth and fifth years were discounted at a rate of 3.5% per annum as recommended by the National Institute for Health and Care Excellence (NICE). 44
| Service | Unit | Cost (£) |
|---|---|---|
| Medication42 | Per daily dose | Various |
| Inpatient43 | Per night | 382–726 |
| Outpatient43 | Per appointment | 39–989 |
| Diagnostic procedure43 | Per procedure | 1–553 |
| Accident and emergency43 | Per attendance | 103 |
| Ambulance43 | Per trip | 222 |
| GP surgery41 | Per minute of patient contact | 2.40 |
| GP home41 | Per home visit minute | 4.00 |
| GP telephone41 | Per minute of patient contact | 2.40 |
| Community medical professionals41 | Per minute of contact | 0.37–1.13 |
| Community social care professionals41 | Per minute of contact | 0.42–2.63 |
The cost of productivity losses was calculated using the human capital approach, when each day off work is valued at the daily salary for that individual. 45
Calculation of quality-adjusted life-years
Quality-adjusted life-years (QALYs) were calculated on the basis of the EQ-5D health state classification instrument46 and the health states were assigned a utility score using responses from a representative sample of adults in the UK. 47 QALYs were then calculated as the area under the curve defined by the utility values at baseline and at the 6-, 12-, 24- and 60-month follow-ups. We assumed that changes in utility score over time followed a linear path. 48 QALYs in the second to fifth years were discounted at a rate of 3.5% as recommended by NICE44 and all analyses were adjusted for baseline utility scores to take into consideration the impact of baseline differences on the area under the curve. 49
Data analysis
For the economic evaluation the base case was a complete-case analysis.
We report the mean average resource use by randomised groups at 24 months’ and 5 years’ follow-up, as well as the percentage of people in each randomised group who have had at least one contact with each service. No between-group statistical comparisons are made in order to avoid the problems of multiple comparisons and because the focus of the economic evaluation is on cost and cost-effectiveness.
Our hypothesis was that the cost of the CBT intervention would be recouped through a reduction in the use of health and social care services. We tested this through a non-inferiority (equivalence) test, with a pre-specified equivalence test of £150. The equivalence was declared between active and control groups if the 95% CI fell between –£150 and £150. These analyses were adjusted for baseline differences in cost.
Cost-effectiveness was considered for two outcomes: QALYs and the HAI score. Cost-effectiveness was initially explored through the calculation of incremental cost-effectiveness ratios (ICERs), a ratio of differences in cost by differences in outcomes between the CBT-HA and standard care groups. ICERs are a useful decision-making tool when there is no uncertainty around the costs and outcomes used in the ratio. Here, the ICERs are based on four sample means; therefore, the uncertainty around the ICER was explored.
Cost-effectiveness planes were produced by the production of bootstrapped regressions (5000 replications) of study group on total costs and HAI score or QALYs, with covariates for baseline costs or outcomes as appropriate. The coefficients of group differences were then plotted on to a graph.
Replications in the north-east quadrant suggest that CBT-HA is more effective and more costly than standard care, replications in the south-east quadrant suggest that CBT-HA is more effective and less costly than standard care, replications in the south-west quadrant suggest that CBT-HA is less effective and less costly than standard care and replications in the north-west quadrant suggest that CBT-HA is more costly and less effective than standard care.
Knowledge of uncertainty around incremental cost-effectiveness is not sufficient for decision-making, which will depend on the how much society is willing to pay for improvements in outcomes. Cost-effectiveness acceptability curves (CEACs) were therefore constructed, and these show the likelihood that CBT is cost-effective for different values a decision-maker is willing to pay for improvements in outcome. 50 All analyses were adjusted for baseline costs and for baseline HAI and EQ-5D scores as appropriate.
We completed a number of sensitivity analyses. First, we used the Stata® (StataCorp LP, College Station, TX, USA) impute command (a regression-based single imputation) to impute missing costs at 24 months and 5 years. Second, we undertook an analysis of differences in costs, including the estimates of the cost of productivity losses.
Results
At 24 months, full ADSUS and hospital records data were available for 172 participants in the CBT-HA group and 170 in the standard care group (77% of those randomised). At 5 years, full ADSUS and hospital records data were available for 149 participants in the CBT-HA group and 157 in the standard care group (69% of those randomised). For total costs over 5 years we needed data from the 24-month and 5-year interviews and there were 141 participants in the CBT-HA group and 133 in the standard care group who met this criterion (62%). We were able to collect hospital service use for 442 randomised participants (99%).
We examined the cost data in order to examine the impact of highly influential observations, which, as defined by Weichle et al. ,51 were those that were above the 99th centile and when removed would have resulted in major changes to the results. Following this, two observations were identified and were removed from the main analysis as recommended.
Resource use
Service use over 24 months’ follow-up is detailed in Table 17. There were no between-group differences in service use and no evidence that CBT-HA reduced service use over this period, as the use of some hospital and community services remained high.
| Service | Treatment group | |||||
|---|---|---|---|---|---|---|
| CBT (n = 172) | Standard care (n = 170) | |||||
| Mean | SD | % | Mean | SD | % | |
| Service-provided accommodation | 0.13 | 0.87 | 2.33 | 0.27 | 1.49 | 3.53 |
| Inpatient number of nightsa,b | 2.57 | 7.09 | 32 | 2.18 | 8.07 | 29 |
| Outpatient number of appointmentsa,b | 13.08 | 13.64 | 99 | 12.88 | 16.84 | 99 |
| Accident and emergency number of attendancesa,b | 1.22 | 4.14 | 37 | 0.87 | 1.37 | 41 |
| GPa | 13.33 | 11.12 | 97.67 | 14.61 | 16.26 | 97.65 |
| Community medical professionalsa | 10.15 | 13.54 | 93.02 | 9.76 | 13.84 | 84.71 |
| Community social service professionalsa | 5.01 | 27.08 | 21.51 | 6.09 | 30.85 | 22.94 |
| Community mental health servicesa | 0.05 | 0.32 | 2.33 | 0.29 | 1.78 | 5.29 |
| Community other professionalsa | 0.43 | 1.52 | 11.05 | 1.39 | 6.65 | 11.76 |
Use of service-provided accommodation such as hotels, refuges and emergency accommodation (e.g. bed and breakfast) was low, being accessed by 2–4% of the sample over the 24 months.
Hospital outpatient appointments were attended by 99% of the study participants and the average number of appointments was 13. Around one-third of the study participants were admitted as inpatients and the average length of stay among the whole sample was between two and three nights. Attendance at accident and emergency departments was low.
The use of GPs and community medical services such as community nursing, physiotherapy, pharmacy and walk-in centres was common. Almost all participants (up to 98%) had at least one contact with a GP and the average number of appointments was between 13 and 16. Interestingly, the use of community mental health services was low; only 2–5% of participants had any contact with a community mental health professional.
In some areas, the use of services between 2 and 5 years continued the pattern set at 24 months, as detailed in Table 18. For example, around one-third of the sample in both groups had an inpatient stay. However, there was a 20% drop in the percentage of participants having at least one outpatient appointment and, as a yearly average, the number of appointments was lower. Similarly, over the 2–5-year period there were, on average, only five GP appointments, compared with 14 over the first 24 months.
| Resource use | Treatment group | |||||
|---|---|---|---|---|---|---|
| CBT-HA (n = 149) | Standard care (n = 157) | |||||
| Mean | SD | % | Mean | SD | % | |
| Inpatient number of nightsa | 3.05 | 9.52 | 29 | 3.85 | 17 | 30 |
| Outpatient number of appointmentsa | 11.5 | 14.97 | 78 | 12.01 | 15.27 | 78 |
| Accident and emergency number of attendancesa | 1.81 | 3.22 | 53 | 1.43 | 2.64 | 48 |
| GPb | 5.15 | 6.61 | 88 | 5.72 | 6.83 | 91 |
| Community medical professionalsb | 13.99 | 33.41 | 72 | 13.74 | 34.14 | 71 |
| Community social service professionalsb | 2.27 | 16.5 | 9 | 2.39 | 16.47 | 8 |
| Community mental health servicesb | 0.53 | 3.08 | 6 | 1.24 | 4.37 | 14 |
| Community other professionalsb | 0.43 | 2.65 | 7 | 0.39 | 2.63 | 4 |
Over the 5-year follow-up period, almost all inpatient stays were medical admissions and there were no admissions to mental health units. Similarly, almost all non-trial outpatient appointments were to medical specialties rather than to a mental health professional. In common with the numbers at 24 months, the use of community mental health services was very low.
Total cost
The mean cost of the CBT-HA intervention in the intervention group was £421.51 per patient (range 0–2383) for an average of six sessions.
Table 19 shows total costs per patient over 24 months’ follow-up. For all cost categories, total costs were lower for the CBT-HA group than for the control group. Overall, total health and social care costs, including the cost of the intervention, were lower in the CBT-HA group (mean £7314) than in the control group (mean £7727). In analyses adjusted for baseline cost, however, the adjusted mean difference between the two groups was £156 (95% CI –£1446 to £1758; p = 0.848). Although equivalence was not achieved, there was no evidence of a significant difference in cost between the CBT-HA and standard care groups.
| Individual cost item | Treatment group | Adjusted coefficient | 95% CI (adjusted, bootstrapped) | p-value | |||
|---|---|---|---|---|---|---|---|
| CBT (n = 172) | Standard care (n = 170) | ||||||
| Mean | SD | Mean | SD | ||||
| CBT-HA | 421.51 | 308.25 | 0.00 | 0.00 | – | – | – |
| Service-provided accommodation | 134.52 | 1025.45 | 235.83 | 1640.25 | – | – | – |
| Hospital services | 3946.81 | 5583.89 | 4223.31 | 6353.28 | – | – | – |
| Community services | 774.02 | 1153.36 | 891.53 | 1639.54 | – | – | – |
| Medication | 2037.33 | 2760.75 | 2376.74 | 4487.03 | – | – | – |
| Total | 7314.20 | 7429.58 | 7727.40 | 8970.80 | 155.86 | –1446.20 to 1757.93 | 0.848 |
The total cost for the 5-year follow-up is detailed in Table 20. The second row of the table reports costs in years 3, 4 and 5 as £5055 in the CBT-HA group and £4835 in the standard care group. The adjusted mean difference in cost is –£557, thus rejecting the null hypothesis that costs are equivalent at follow-up. Taking the costs between randomisation and 24 months and 2 and 5 years together gives the total costs over 5 years’ follow-up. These are also listed in Table 19. In total, costs were £12,591 in the CBT-HA group and £13,335 in the standard care group. The regression adjusted for baseline costs also showed that these costs were not equivalent [coefficient = 545, 95% CI (–2375 to 3466); p = 0.713]. The direction of the difference in costs changes when the adjustment is made for baseline costs.
| Cost | Treatment group | Adjusted mean difference | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|
| CBT | Standard care | ||||||
| Mean | SD | Mean | SD | ||||
| Years 1 and 2 (n = 342) | 7314.20 | 7429.58 | 7727.40 | 8970.80 | 155.86 | –1446.20 to 1757.93 | 0.848 |
| Years 3, 4 and 5 (n = 303) | 5054.56 | 6581.72 | 4834.74 | 6908.10 | 557 | –919.82 to 2034.65 | 0.458 |
| Total cost (n = 271) | 12,590.58 | 14,290.00 | 13,334.94 | 14,402.05 | 545 | –2374.78 to 3466.02 | 0.713 |
Outcomes
The EQ-5D tariff over the 5-year follow-up is detailed in Table 21 and shown graphically in Figure 11. Utility scores are very similar between groups over follow-up. When QALYs were calculated, these were 1.09 in both the CBT-HA group and the standard care group at 24 months, and 2.75 in the CBT-HA group and 2.64 in the standard care group at 5 years; this small difference at 5 years is not significant.
| EQ-5D variables and QALYs by visit | Treatment group | Adjusted mean difference | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|
| CBT | Standard care | ||||||
| Mean | SD | Mean | SD | ||||
| EQ-5D tariff | |||||||
| Baseline (n = 442) | 0.49 | 0.35 | 0.47 | 0.35 | – | – | – |
| 6 months (n = 401) | 0.52 | 0.4 | 0.52 | 0.36 | – | – | – |
| 12 months (n = 386) | 0.57 | 0.37 | 0.56 | 0.37 | – | – | – |
| 24 months (n = 371) | 0.57 | 0.38 | 0.55 | 0.37 | – | – | – |
| 5 years (n = 308) | 0.56 | 0.4 | 0.54 | 0.4 | – | – | – |
| QALYs | |||||||
| 24 months (n = 347) | 1.09 | 0.63 | 1.09 | 0.6 | –0.002 | –0.09 to 0.09 | 0.964 |
| 5 years (n = 303) | 2.75 | 1.55 | 2.64 | 1.58 | 0.09 | –0.16 to 0.33 | 0.482 |
| EQ-5D VAS | |||||||
| Baseline (n = 434) | 50.92 | 22.51 | 51.47 | 21.34 | – | – | – |
| 6 months (n = 389) | 56.91 | 25.78 | 52.71 | 23.75 | – | – | – |
| 12 months (n = 376) | 58.00 | 23.44 | 57.12 | 23.62 | – | – | – |
| 24 months (n = 363) | 59.94 | 25.43 | 55.67 | 23.63 | 4.27 | –0.80 to 9.34 | 0.098 |
| 5 years (n = 307) | 56.2 | 24.02 | 55.62 | 25.69 | –0.58 | –5.02 to 6.17 | 0.840 |
FIGURE 11.
Mean EQ-5D tariff by randomised group.
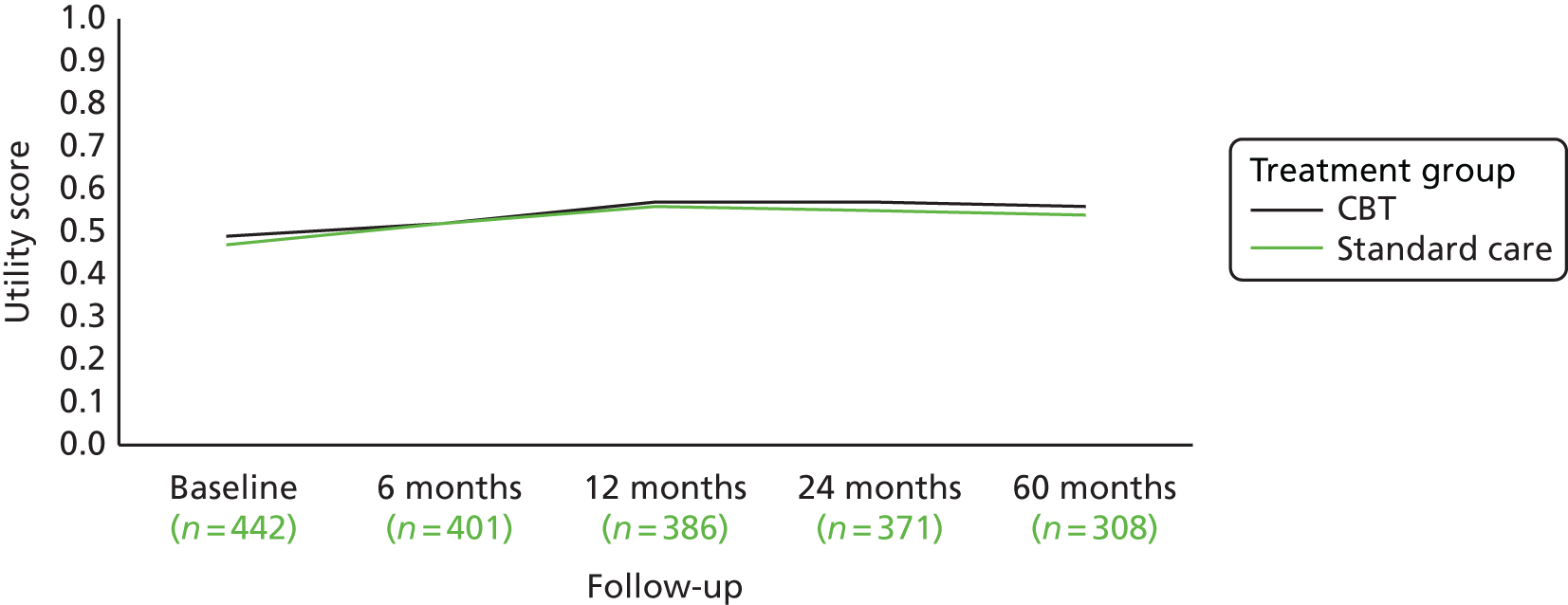
The EQ-5D visual analogue scale (VAS) scores are also presented in Table 21 and Figure 12. Again the results are generally similar between groups and, while there are some differences in VAS score at 24 months, the difference is not significant and not sustained at 5 years.
FIGURE 12.
Mean EQ-5D VAS by randomised group.

Cost-effectiveness analysis
In adjusted analyses, the ICER for QALYs was £14,169 (the difference in cost, £156, divided by the difference in QALYs, 0.011), which highlights that additional QALYs can be gained only with additional expenditure. The scatterplot and CEAC in Figures 13 and 14 demonstrate that there is substantial uncertainty around the mean values used in the ICER. In Figure 13, the bootstrapped replications of costs and outcomes fall almost equally across all four quadrants of the cost-effectiveness plane, suggesting that there is no clear evidence on the cost-effectiveness of either CBT-HA or standard care. The CEAC in Figure 14 suggests that CBT-HA is not cost-effective for the usually accepted values that a decision-maker would be willing to pay for improvements in outcomes.
FIGURE 13.
Cost-effectiveness plane showing bootstrapped cost and QALY pairs at the 24-month follow-up.
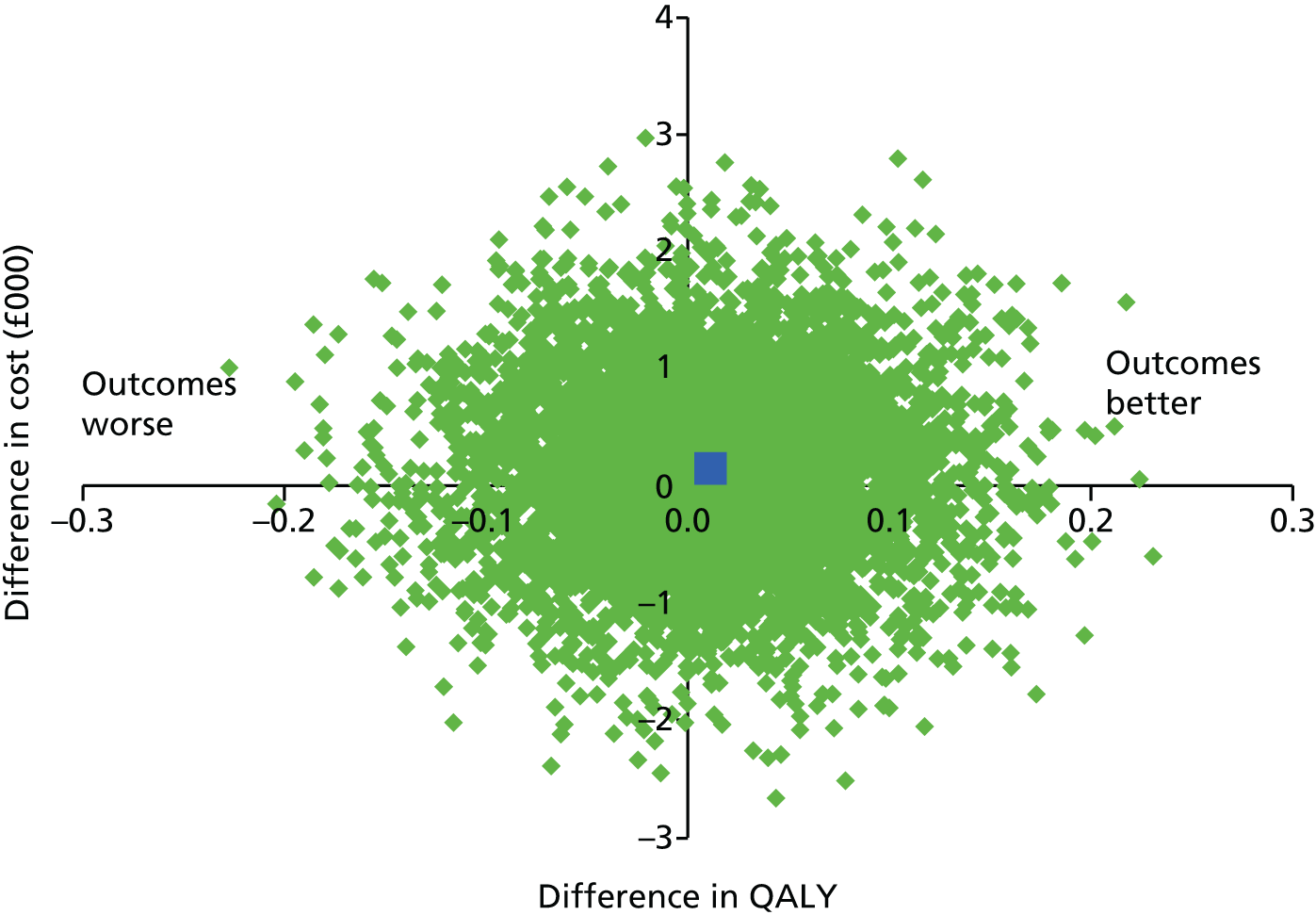
FIGURE 14.
Cost-effectiveness acceptability curve showing the probability that CBT-HA is more cost-effective than standard care in terms of QALYs at the 24-month follow-up.

The ICER for the HAI, adjusted for baseline costs, was £55.86 (the difference in cost, £156, divided by the difference in HAI score, 2.79 points). The adjusted scatterplot in Figure 15 shows replications in the north-west and south-west quadrants. Here, these quadrants represent better outcomes in the CBT-HA group because a higher score on the HAI denotes worse anxiety. There is clear evidence that CBT-HA improves outcomes, but the picture regarding costs is uncertain. The CEAC in Figure 16 reflects this uncertainty, demonstrating that, at a willingness to pay for an improvement in HAI score of zero points, there is only a 44% probability of CBT-HA being cost-effective. However, if willingness to pay per point change in HAI score increases to values over £53, there is a > 50% probability that CBT-HA is cost-effective.
FIGURE 15.
Cost-effectiveness plane showing bootstrapped cost and HAI score pairs at the 24-month follow-up.

FIGURE 16.
Cost-effectiveness acceptability curve showing the probability that CBT-HA is more cost-effective than standard care in terms of health anxiety at the 24-month follow-up.
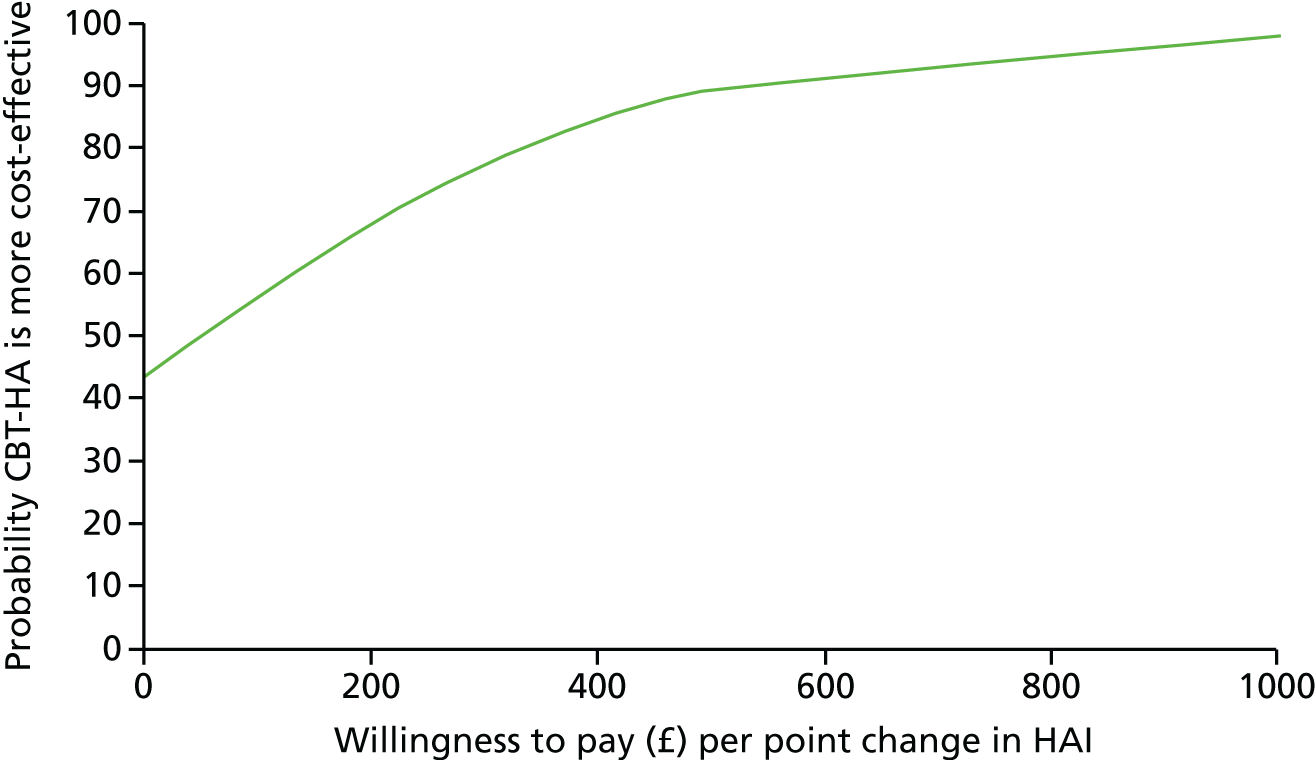
Over 5 years, costs are, on average, lower in the CBT-HA group than in the standard care group and outcomes in terms of QALYs and HAI scores are better. In these cases ICERs are not the most useful decision-making tool, as negative values can produce a positive ICER; we therefore leave them to one side in order to concentrate on the scatterplots and CEACs presented in Figures 17–20. The scatterplot in Figure 17 shows that the bootstrapped replications mainly fall to the right of the y-axis in the north-east and south-east quadrants, where outcomes are better but costs are either higher or lower. This finding is reflected in the CEAC for QALYs in Figure 18, which shows that there is little evidence that CBT-HA is cost-effective in terms of QALYs.
FIGURE 17.
Cost-effectiveness plane showing bootstrapped cost and QALY pairs at the 5-year follow-up.

FIGURE 18.
Cost-effectiveness acceptability curve showing the probability that CBT-HA is more cost-effective than standard care in terms of QALYs at the 5-year follow-up.
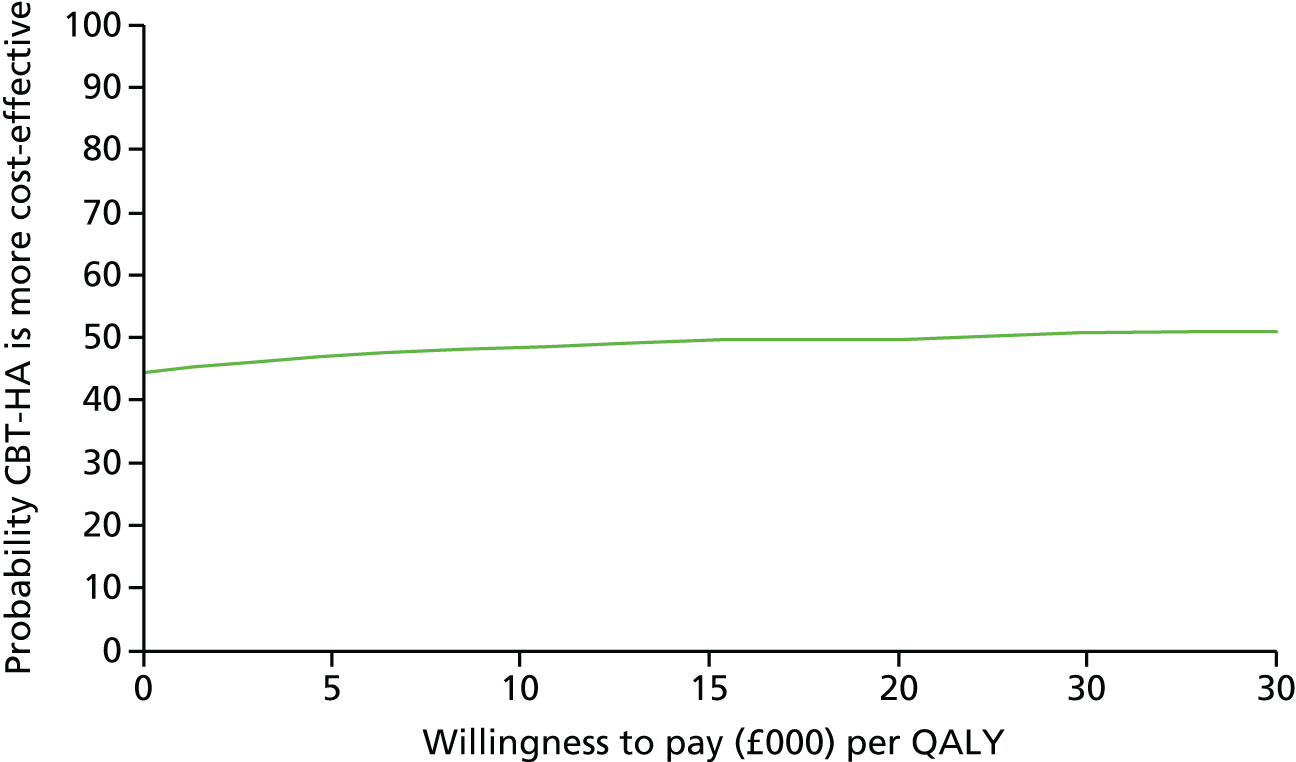
FIGURE 19.
Cost-effectiveness plane showing bootstrapped cost and HAI score pairs at the 5-year follow-up.
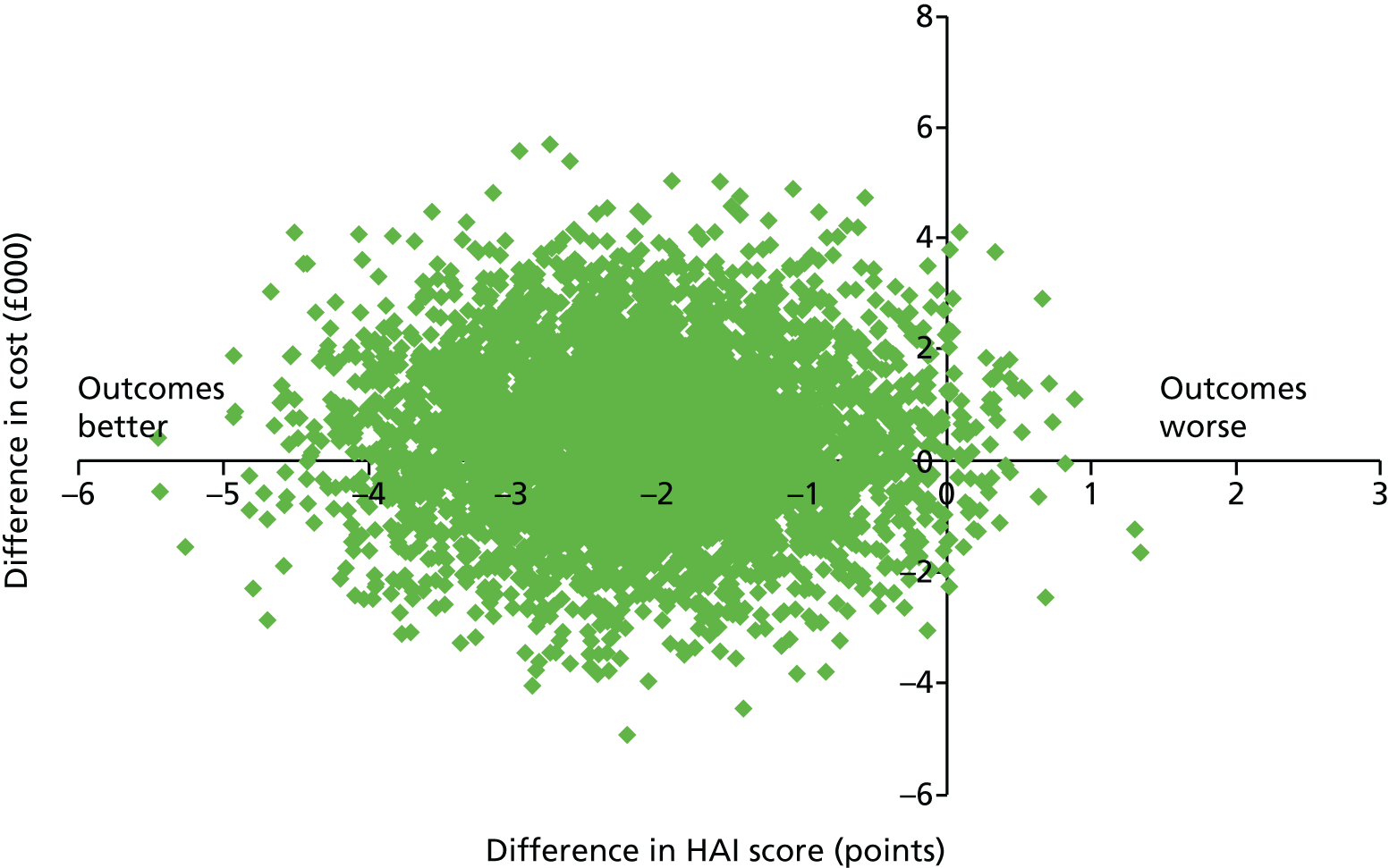
FIGURE 20.
Cost-effectiveness acceptability curve showing the probability that CBT-HA is more cost-effective than standard care in terms of health anxiety at the 5-year follow-up.
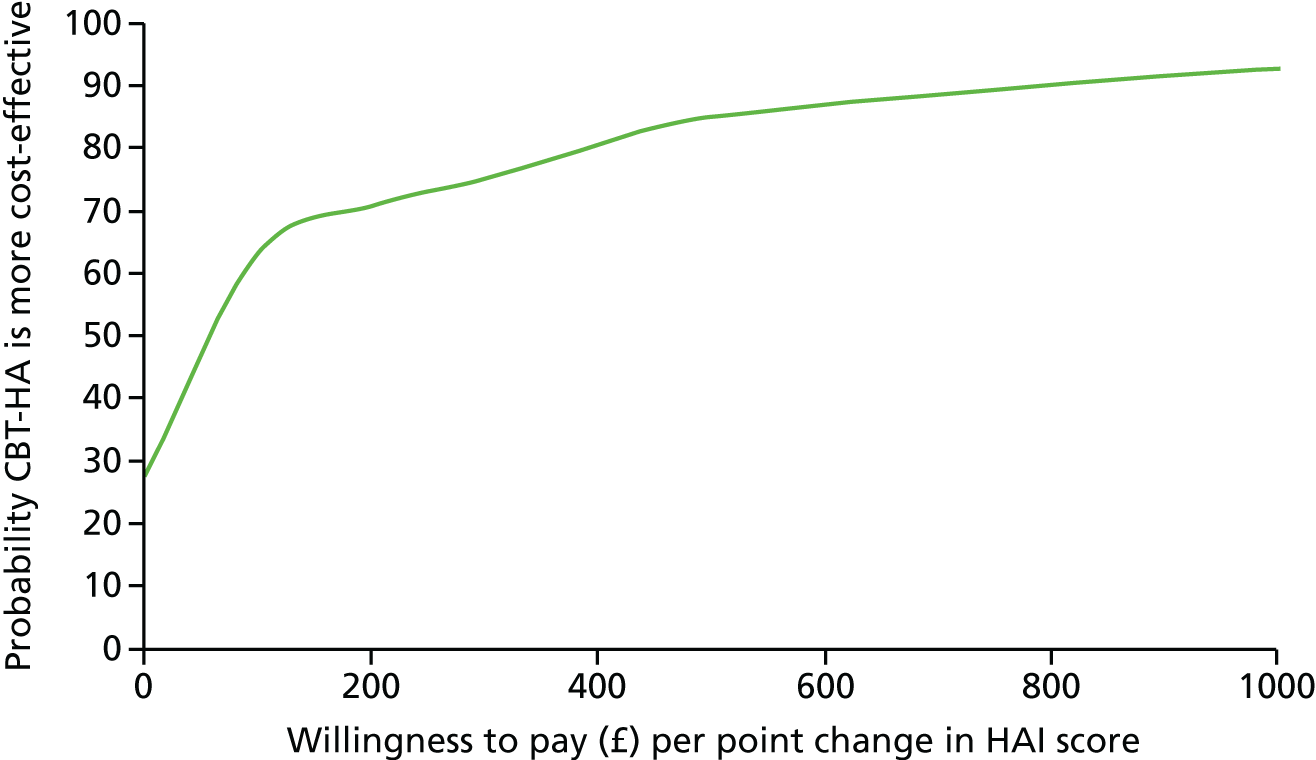
For the HAI score at 5 years, the bootstrapped replications in Figure 19 fall between the south-west and north-west quadrants (again these quadrants represent better outcomes in the CBT-HA group because a higher score on the HAI denotes worse anxiety). The related CEAC in Figure 20 generally supports the cost-effectiveness of CBT-HA, particularly for willingness-to-pay values for a unit change in HAI scores of > 100 points.
Sensitivity analysis
Imputation of missing data and the inclusion of productivity losses did not alter the finding that costs were not equivalent, as detailed in Table 22.
| Cost variable | Treatment group | Adjusted mean difference | 95% CI | p-value | |||
|---|---|---|---|---|---|---|---|
| CBT | Standard care | ||||||
| Mean | SD | Mean | SD | ||||
| Multiple imputation of total cost (n = 444) | 14,095.49 | 9780.85 | 14,748.15 | 10,648.14 | –368.80 | –1793.76 to 1056.17 | 0.611 |
| Total costs plus productivity losses (n = 258) | 14,437.41 | 16,379.47 | 14,455.54 | 15,488.24 | 1438.87 | –2050.26 to 4927.99 | 0.417 |
Chapter 5 Discussion
The CHAMP trial is the first large-scale trial of CBT-HA in secondary care. Although there has been increasing evidence of the clinical benefits of this treatment in primary care,52–56 particularly during the period of this trial, the added value of this treatment in secondary care in terms of cost-effectiveness is still uncertain, and explains the major argument for long-term follow-up. As our data showed that the benefit of CBT-HA extends far beyond the duration of treatment this has important implications.
Identification and classification of health anxiety
When the CHAMP trial started in 2008, health anxiety had uncertain status in international diagnostic systems. It was regarded as a synonym for hypochondriasis, although there was a suspicion among researchers that it was not exactly the same condition. Because of this uncertainty we also required patients to satisfy the diagnostic requirements of the DSM-IV for hypochondriasis, and so all who progressed to randomisation had this formal label, which placed patients in the somatoform disorder group.
Since then there have been new international classifications developed and a new diagnosis, illness anxiety (diagnostic code 300.7), was introduced to the fifth American classification Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition. This is very similar to health anxiety, as it incorporates excessive concern and monitoring of health, fear of developing or having a physical disease, bodily checking and high levels of anxiety, but an absence of marked somatic symptoms. 57 This last requirement serves to separate illness anxiety from what used to be called ‘medically unexplained symptoms’, but have been relabelled somatic symptom disorders. Because of the apparent close links between illness anxiety and these other conditions, illness anxiety is placed in the somatic symptom group, but paradoxically has introduced the requirement that ‘marked somatic symptoms’ must be absent. In the experience of therapists in the CHAMP trial, somatic symptoms of anxiety are very common.
The ICD-11 classification group has chosen differently; it has opted to place health anxiety in the obsessional group of disorders, as there is a degree of overlap between the excessive checking behaviour of the health-anxious patient and obsessional behaviour,58 and this is also noted in the CHAMP study. There is considerable dissatisfaction with the somatic group of psychiatric disorders, even after these revisions,59 and the CHAMP trial results suggest that health anxiety is primarily an anxiety disorder, not a somatic one. This suggestion is made as the results of the HADS-A scale paralleled those of the HAI throughout the 5 years of study, and when health anxiety reduced so did generalised anxiety. A similar recommendation that health anxiety is fundamentally an anxiety disorder has also been made on the basis of its links to other disorders. 60
Representativeness of sample
It could be argued that, as < 10% of those who were originally identified with a high level of health anxiety took part in the trial, those who did participate were unrepresentative. This cannot be answered definitively, as we had no data apart from the HAI scores on those who did not participate, but we were not surprised by the relatively low uptake of invitee participation in the trial. Patients were approached at ordinary outpatient clinics and were not seeking any form of intervention for health anxiety. As they were attending medical clinics, it is reasonable to suppose that patients were seeking medical advice and not expecting to be invited to take part in a psychological treatment.
If we had adopted other ways of recruiting, such as asking consultants to refer patients, we do not think that we would have recruited so many participants. Although the staff in some hospitals are conscious of the importance of health anxiety – several were noted in our study – they are currently in a minority, and most medical staff do not regard the psychological aspects of their patients as a priority when their main tasks are to treat and exclude organic disease. In this respect, the study population was very different from those in other recent trials of internet-delivered or group treatment of health anxiety,52–55 as clearly those populations recognised the problem of health anxiety and were seeking help for it.
Differences from recent studies
Since the CHAMP trial was started in 2008 there has been one meta-analysis and five other trials published of CBT and related psychological treatments in health anxiety,52–56,61 all of which showed positive results in favour of the CBT-linked psychological intervention. There were some important differences between the populations treated in these studies and those in the CHAMP trial that need to be highlighted. All of these other publications described populations that had consulted or responded to advertisements from professionals who were providing treatment for health anxiety (i.e. the patients understood fully that they had health anxiety and wanted treatment for it). Patients in the CHAMP study were not seeking treatment and > 90% of those who screened positively for health anxiety (HAI score of ≥ 20 points) did not proceed to randomisation, largely because of refusal rather than exclusion criteria. This is not really surprising, as the people approached in medical clinics had a predominantly medical consultation mindset, with the expectation that, whatever the nature of any worries that might beset them, these would be answered by doctors in the clinic, not external psychological sources.
The mean scores for the HAI (≈25 points at baseline) in CHAMP were also considerably lower than the equivalent scores in these other studies (≈40 points), and this explains why many of these other studies refer to ‘severe health anxiety’ in their titles. The population in CHAMP was not a highly handicapped one (except when there was associated significant medical pathology), and it is possible that the long-term benefits shown with CBT-HA in this group were achieved because of this lesser handicap. Put another way, once people had ‘seen the light’ and realised that health anxiety was an important part of their problem, it did not require a great deal of intervention to make this benefit semi-permanent. The additional evidence that this was achieved with benefits to generalised anxiety and depression over 5 years shows the degree of overlap between health anxiety and other common mental disorders.
This supposition is also supported by the improvement shown in the patients allocated to standard care. Over the course of 5 years the maximal improvement (60%) was shown in the first 3 months (see Figure 3), suggesting that even the relatively short and bland explanation of health anxiety during the baseline assessment was enough to give a degree of insight into the subject and yield some benefit.
Meaningful clinical difference in Health Anxiety Inventory scores
It is not known what constitutes a meaningful clinical difference (MCD) in scores on either the long or short form of the HAI. In very large trials it is possible to find statistically significant differences that are not clinically meaningful because the differences are so small. In our original sample size calculations we suggested that a difference of 5 points in treatment groups was meaningful, but this was based on limited evidence.
Previous studies of anxiety using the HADS have suggested that a reduction in the HADS-A score of 0.7 points or a reduction in the total scale score of 1.32 points is clinically meaningful62,63 and, if we take a conservative estimate of 1 point for a MCD for the HADS-A and 0.7 points for the HADS-D, this roughly equates to a MCD of 2 points on the HAI. On this basis, the differences between treatments at all assessment points after baseline suggest that CBT-HA is clinically effective as well as statistically superior to standard care.
Relevance of findings of personality status
The findings with regard to personality status were of particular interest in this study because they contradicted previous robust findings with regard to the outcome of depression and, to a lesser extent, anxiety. 62–65 The main studies, backed up by a substantial meta-analysis, showed that patients with comorbid depressive and personality disorder had an odds ratio of > 2 in having a worse symptomatic outcome than those who had depression alone. 64,65 It was expected that these findings would extend to health anxiety and a previous cohort study had found that those with hypochondriacal personality characteristics, possibly of sufficient severity to be called hypochondriacal personality disorder, had a much worse outcome than those without this disorder. 66
All studies in this subject carried out previously were with patients who had generalised anxiety or depression. The CHAMP study findings of greater improvement with CBT-HA than standard care, extending over 5 years, in those with personality difficulty and mild personality disorder, findings not shown with other personality groups, are striking. The additional evidence that this difference in improvement also extended to social functioning, and that standard care led to better social function in those with no personality dysfunction, adds to the impact of these findings.
However, there was an important difference between the assessment of personality in CHAMP and those of other studies. Currently personality disorder is diagnosed dichotomously in classification systems: patients either do or do not have personality disorder. The ICD-11 system of classification67 uses a single dimension of classification consistent with research evidence; of the two levels of personality disturbance that showed persistent preferential improvement with CBT-HA, one, personality difficulty, is classified as a ‘non-disorder’, and the other, mild personality disorder, is included among the personality disorders. Using the older dichotomous system of classification, the differences between outcomes would have been attenuated, but not to the extent that the previous findings of a poorer outcome in personality-disordered patients would be replicated.
The high proportion of patients with at least some level of personality disturbance (80%) may appear surprising but is also consistent with other data. 68–71 People with high levels of health anxiety and, to a lesser extent, generalised anxiety, often have personalities that are strong in avoidant, anxious and dependent characteristics, and this impairs both relationships and functioning, and adds to symptomatology (see Table 17). The evidence that this does not handicap patients’ responses to CBT-HA, in either the short or longer term, is encouraging. Whether or not the difference in response by personality level is sufficiently strong to suggest that personality assessment should be undertaken in ordinary practice is beyond the scope of this study, but there are cogent arguments in its favour. 70,71
It is not clear why those with no personality dysfunction did not respond to CBT-HA or why this treatment seemed to impair social functioning. One possible explanation is that this group had appropriate rather than pathological anxiety, and so the introduction of CBT-HA was regarded not only as unnecessary, but also as irritating or annoying.
Implications for health services
Our findings indicate that excessive health anxiety is common and, if untreated, tends to persist, which supports previous evidence from several sources. 6,72,73 Therefore, it appears that the natural course of health anxiety is quite different from that of generalised anxiety disorder, which tends to pursue a fluctuating path depending on circumstances. Possible reasons for health anxiety persisting without much improvement include the reinforcing aspects of reassurance and medical consultation, and these tend to continue in the absence of any appropriate management.
At the time of writing, in most parts of the UK this management can be accessed only through the Improving Access to Psychological Therapies (IAPT) programme but, although practitioners in the services were initially trained to have skills in CBT for depression and anxiety, the IAPT services have extended these to include health anxiety. However, the numbers potentially benefiting from therapy, possibly one in five of all medical outpatients, are far beyond the capacity of an external service to serve. It may appear too strong a claim, but the number of people with major health-anxiety concerns in general hospitals is both sufficiently large and undetected to be called a silent epidemic. 74 There is a growing realisation that better integration of medical and mental health services is necessary in general hospitals75 and that it would be a great advantage to develop skills within the general hospital to identify and treat patients with health anxiety, alongside the provision of normal care. The evidence from the CHAMP study that general nurses, when appropriately trained, were highly suitable practitioners of CBT-HA, suggests that an obvious way forward would be to train interested nurses in general hospitals in the principles of treatment and to raise awareness of the nature of health anxiety among their fellow professionals.
Comment was made after the first major CHAMP publication that the intervention could not be regarded as cost-effective because of the high degree of screening needed to recruit patients. 76 We argue that if health-anxiety literacy in medical clinics were greater, there would be no need for screening, and until this time comes it would be perfectly reasonable for the HAI or a similar scale to be given to patients when first registering at a medical outpatient clinic, at very low cost. In this way, patients who present recurrently with anxiety about problems that appear to have no physical cause would be identified in the clinic and an appropriate response made.
Long-term benefit of cognitive–behaviour therapy for health anxiety
The benefit of CBT-HA in reducing health anxiety appears to be long lasting. This finding was unexpected, not least as most interventions for anxiety and depression using CBT tend to diminish over time and are seldom present over 1 year after completing therapy. 77–81 There is no doubt that CBT is effective in treating both generalised anxiety and depression (these benefits often go together),80 but the evidence that these benefits extend beyond 1–2 years is very weak, partly because so many trials have waiting list controls that curtail comparison of groups over long periods. 79,80 There is one exception to this: the CoBalT study of CBT for depression showed continuing benefits of CBT 40 months after randomisation. 81 There is no equivalent for generalised anxiety.
The evidence that these benefits were maintained with gains at 2 years being just as strong at 5 years deserves discussion. There could be at least three reasons for this: first, the failure of those in standard care to improve beyond the initial gains at 3 months could have been a consequence of their continued concerns and consultations about their health, which only reinforced their symptoms. Second, in those who received CBT-HA in this particular population, the acquisition of insight into the presence of health anxiety, together with a relatively straightforward set of learnt procedures to overcome it, may have been a powerful restitutional force that kept people well (other general advice, including avoidance of internet browsing for health problems, may also have been of benefit). The third reason relates to psychological help-seeking – in most studies of psychological treatment for anxiety and depression the patients are seeking treatment, and if they do not receive it from one source they get it from another. In the words of a study of collaborative care, those in control populations ‘catch up’ on those who have more specific interventions over the course of time82 because they eventually receive the care that is needed.
The population with health anxiety in CHAMP was not help-seeking and so ‘catching up’ was not an issue for them. Before being involved in the CHAMP study, patients felt that it was quite in order for them to continue to express concerns about their health to their physicians and no further intervention was necessary. Therefore, there was no attempt from those in the control group to seek further assistance and, indeed, there was no evidence of crossover to CBT-HA or other related therapies in the standard care group over the 5-year period.
In view of the maintenance of benefit of CBT-HA after 5 years, the project group is now carrying out an 8-year follow-up. This will also examine costs again to see if the continued savings between 2 and 5 years are extended.
Interpretation of the economic evaluation
In terms of cost-effectiveness, our data suggest that the picture is more complex than our original hypothesis that successful CBT-HA would reduce health anxiety and, therefore, unnecessary service use would result in lower costs. The results of the cost-effectiveness analysis therefore require careful interpretation. Our original hypothesis was that savings would offset the additional costs of the CBT intervention elsewhere in the health system, resulting in equivalent costs between groups. We found evidence of offset but did not find hypothesised equivalence, nor did we find any noticeable or significant difference in cost between groups, except in personality status. As a consequence, it is right to state that the CHAMP trial did not find clear evidence of cost-effectiveness. These issues will be considered in the following section.
The inability to demonstrate equivalence and cost-effectiveness has its root in two key characteristics of the data and the patient group: that there is considerable variation in costs and that the costs are multifaceted. Variation in costs is not unusual in cost data; however, the variation in this group was substantial enough that it was necessary to remove two outliers from the main analysis as they met the criteria for influential outliers. The multifaceted nature of the costs needs to be unpacked a little. If we take costs back to service use, it allows us to try and explain what exactly this phenomenon might be. Table 17 shows that levels of hospital and GP use were considerable, and that use of these services continued in both randomised groups throughout follow-up. Given that we believe that the patient group is one with substantial medical pathology, it is perhaps unsurprising that use of these medical services remained high despite a noted and consistent reduction in health anxiety in the CBT-HA group. Thus, any reductions in service use as a result of changes in behaviour following successful CBT-HA are lost in the noise of all other medical service use.
A previous study of the cost-effectiveness of CBT-HA compared with control treatment was carried out in Sweden using internet-guided treatment. 83 This showed that the total costs were only a little higher (< 15%) than those of health care in this population, suggesting that future studies could rely on health-care costs alone.
There are a number of limitations of the economic evaluation, which resulted from both the duration of the analysis and the patient group. In terms of the duration of the analysis, collecting service use data over long periods generates a number of challenges. For the follow-up interviews up to 12 months, the ADSUS asked participants to recall their service use only for the previous 6 months. At the 24-month interview recall was for 12 months, and at the 5-year interview recall was for 3 years. We acknowledge that the accuracy of recall over long periods is limited and we sought to limit the impact of this in two ways. First, the list of services that we asked participants to recall was short and limited to services provided in the community. Second, we did not ask participants to recall use of hospital services and instead extracted these from hospital trust computer databases. In addition, we were able to extract hospital use data from the trial host hospital trust databases only, and it is likely that participants accessed services from other hospitals from which we were not permitted to access information. It is important to note that there is nothing to suggest that recall bias is not equally distributed across the whole cohort. If this were so, the randomised group differences are valid. However, recall bias may provide an explanation for the apparent reduction in community service use at 5 years.
Another important limitation was the choice of outcome measure for the economic evaluation. Our results suggest that it is likely that CBT-HA is cost-effective in terms of health anxiety and that the probability of it being cost-effective increases with positive values on the willingness to pay for an improvement in outcome. The difficulty with this is that the willingness-to-pay value for a change in HAI score is unknown, so it is therefore not possible to make clear statements in terms of policy-making. Regarding the economic outcomes, there were no noticeable improvements in quality of life as measured with the EQ-5D. One explanation for the inability of the EQ-5D to pick up the improvement in the CBT-HA group that was found with the HAI outcome links back to a key characteristic of the patient group; rather than being a group of individuals with health anxiety and medically unexplained symptoms, they are in many cases individuals with health anxiety and substantial medical pathology. These problems would inevitably have an impact on an individual’s quality of life. The EQ-5D contains only one domain on depression/anxiety and it is likely that study participants would continue to score highly in the other domains of the EQ-5D, making any differences in anxiety as a result of the intervention difficult to capture. It is also possible that the health-anxiety intervention did not have an impact on depression and, thus, there could be no impact on the EQ-5D scores in this way either. Future studies in health anxiety should consider a different measure of quality of life.
It does remain possible and important, however, to reach conclusions based on the evidence we have collected on the costs of health anxiety in medical patients. The first is that, in terms of the HAI score as an outcome, CBT-HA has a > 50% probability of being cost-effective for almost all willingness-to-pay values. The second is that, counter to this, there is no evidence that CBT-HA is cost-effective in terms of QALYs as measured using the EQ-5D.
Chapter 6 Recommendations for further research
We have identified pathological health anxiety as a highly prevalent problem in medical clinics and have developed a treatment that is clinically effective and possibly cost-effective. The work has posed many new areas for research.
-
Is the degree of health anxiety in patients attending all medical clinics clearly pathological? It is reasonable to argue that, when someone is medically ill, they should be more concerned about their health than at other times, and it could be argued that such anxiety is normal. The persistence of therapeutic value in the CHAMP study suggests that such anxiety is indeed pathological, as it would be likely to wax and wane in line with medical pathology. There is also evidence that worry over health leads to premature mortality84 and that cardiac anxiety is associated with later major cardiac pathology. 85 This may be of particular relevance to cardiology as, in the CHAMP study, the beneficial effects were maximal at 5 years.
-
What are the main reasons for poor recruitment of patients to receive psychological treatments, especially CBT, for the treatment of health anxiety? We have speculated about this in the report, but formal studies, probably qualitative in nature, are needed to explore this more fully.
-
Are general or specialised nurses in medical specialties better able to deliver CBT-HA in medical settings or is this work suitable for trained IAPT therapists, as current government strategy suggests?
-
Is there a good argument for a staged care strategy for health anxiety in medical settings? The improvement made by the standard care group in the first 3 months suggested that being made aware of health anxiety was of benefit. In such a staged strategy it would seem appropriate for the first stage to be carried out by nurses or other staff in the medical clinics concerned.
-
Why is it that older patients have a better outcome than younger ones? Is it likely to be related to comorbid pathology? It is reasonable to postulate that in the presence of any form of medical pathology health anxiety is likely to be activated, and the better response in older patients might be related to better understanding of heath-anxiety generation.
-
Is there a better way of measuring cost-effectiveness of psychological treatments in the presence of significant medical illness, when the costs of the latter far exceed those of the psychological intervention (taking into account its likely savings)? This, to some extent, may be determined by other studies in different populations, especially in primary care, when expensive medical costs are absent. One study followed the principles of CBT-HA and combined it with web-based video interaction with therapists instead of face-to-face contact86 and this is likely to report shortly.
-
Are the prevalence and incidence of health anxiety increasing as a consequence of cyberchondria (excessive use of the internet for health advice)?
The CHAMP study is continuing to a final follow-up after 8 years and it is hoped that some of these questions can at least be partially addressed in this last phase of the study.
Acknowledgements
We particularly thank the Mental Health Research Network, and especially Sandra O’Sullivan, for adopting and promoting the trial; we also thank Aaron Beck, who acted as trial adviser. We thank the editor and publishers of the Lancet, International Journal of Nursing Studies, British Journal of Psychiatry and Personality and Mental Health for permission to include material from previously published papers cited in this monograph.
Contributions of authors
The trial was initiated by Peter Tyrer and Helen Tyrer, who, with Paul Salkovskis, Michael J Crawford, Simon Dupont, John Green, David Murphy, Steven Reid, Sarah Byford and Barbara Barrett, designed the structure of the trial.
Duolao Wang and Barbara Barrett were involved primarily in developing the statistical analysis plan.
Sylvia Cooper was the trial co-ordinator and organiser of the recruitment strategy.
Georgina Smith, Rachel Evered, Yvonne Lisseman-Stones, Sharon McAllister and Jessica Nagar were the main therapists.
Rahil Sanatinia co-ordinated the acquisition of personality data for ICD-11 conversion.
Sharandeep Bhogal, Shaeda Nourmand, Valentina Lazarevic, Gemma Loebenberg, Stephanie Kings, Antoinette McNulty, Kofi Kramo, Katherine Whittamore and Gemma Walker were the main research assistants.
Aaron Philip assisted with the co-ordination and checking of hospital data, Hilary Warwick helped with assessment of treatment fidelity, and Sarah Byford and Barbara Barrett carried out the economic analysis.
All authors read and approved the final manuscript.
Publications
Tyrer P, Cooper S, Salkovskis P, Tyrer H, Crawford M, Byford S, et al. Clinical and cost-effectiveness of cognitive behaviour therapy for health anxiety in medical patients: a multicentre randomised controlled trial. Lancet 2014;383:219–25.
Tyrer H, Tyrer P, Lisseman-Stones Y, McAllister S, Cooper S, Salkovskis P, et al. Therapist differences in a randomised trial of the outcome of cognitive behaviour therapy for health anxiety in medical patients. Int J Nurs Stud 2015;52:686–94.
Sanatinia R, Wang D, Tyrer P, Tyrer H, Crawford M, Cooper S, et al. Impact of personality status on the outcomes and cost of cognitive-behavioural therapy for health anxiety. Br J Psychiatry 2016;209:244–50.
Tyrer P, Wang D, Tyrer H, Crawford M, Cooper S. Dimensions of dependence and their influence on the outcome of cognitive behaviour therapy for health anxiety: randomized controlled trial. Pers Ment Health 2016;10:96–105.
Data sharing statement
The full data set for this study can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Tyrer P, Cooper S, Tyrer H, Salkovskis P, Crawford M, Green J, et al. CHAMP: Cognitive behaviour therapy for health anxiety in medical patients, a randomised controlled trial. BMC Psychiatry 2011;11. https://doi.org/10.1186/1471-244X-11-99.
- Robbins JM, Kirmayer LJ. Transient and persistent hypochondriacal worry in primary care. Psychol Med 1996;26:575-89. https://doi.org/10.1017/S0033291700035650.
- Barsky AJ, Wyshak G, Klerman GL, Latham KS. The prevalence of hypochondriasis in medical outpatients. Soc Psychiatry Psychiatr Epidemiol 1990;25:89-94.
- Escobar JI, Gara M, Waitzkin H, Silver RC, Holman A, Compton W. DSM-IV hypochondriasis in primary care. Gen Hosp Psychiatry 1998;20:155-9. https://doi.org/10.1016/S0163-8343(98)00018-8.
- Barsky AJ, Orav EJ, Bates DW. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch Gen Psychiatry 2005;62:903-10. https://doi.org/10.1001/archpsyc.62.8.903.
- Seivewright H, Salkovskis P, Green J, Mullan N, Behr G, Carlin E, et al. Prevalence and service implications of health anxiety in genitourinary medicine clinics. Int J STD AIDS 2004;15:519-22. https://doi.org/10.1258/0956462041558122.
- Seivewright H, Mulder R, Tyrer P. Prevalence of health anxiety and medically unexplained symptoms in general practice and hospital clinics. Aust N Z J Psychiatry 2007;41.
- Clark DM, Salkovskis PM, Hackmann A, Wells A, Fennell M, Ludgate J, et al. Two psychological treatments for hypochondriasis. A randomised controlled trial. Br J Psychiatry 1998;173:218-25. https://doi.org/10.1192/bjp.173.3.218.
- Barsky AJ, Ahern DK. Cognitive behavior therapy for hypochondriasis: a randomized controlled trial. JAMA 2004;291:1464-70. https://doi.org/10.1001/jama.291.12.1464.
- Seivewright H, Green J, Salkovskis P, Barrett B, Nur U, Tyrer P. Randomised controlled trial of cognitive behaviour therapy in the treatment of health anxiety in a genitourinary medicine clinic. Br J Psychiatry 2008;192:332-7. https://doi.org/10.1192/bjp.bp.108.052936.
- Salkovskis PM, Warwick HM. Morbid preoccupations, health anxiety and reassurance: a cognitive-behavioural approach to hypochondriasis. Behav Res Ther 1986;24:597-602. https://doi.org/10.1016/0005-7967(86)90041-0.
- Warwick HM. A cognitive-behavioural approach to hypochondriasis and health anxiety. J Psychosom Res 1989;33:705-11. https://doi.org/10.1016/0022-3999(89)90086-X.
- Salkovskis PM, Rimes KA, Warwick HM, Clark DM. The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med 2002;32:843-53. https://doi.org/10.1017/S0033291702005822.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiat Scand 1983;57:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Tyrer P, Nur U, Crawford M, Karlsen S, McLean C, Rao B, et al. The social functioning questionnaire: a rapid and robust measure of perceived functioning. Int J Soc Psychiatry 2005;51:265-75. https://doi.org/10.1177/0020764005057391.
- Uher R, Heyman I, Mortimore C, Frampton I, Goodman R. Screening young people for obsessive compulsive disorder. Br J Psychiatry 2007;191:353-4. https://doi.org/10.1192/bjp.bp.106.034967.
- Tyrer P, Morgan J, Cicchetti D. The Dependent Personality Questionnaire (DPQ): a screening instrument for dependent personality. Int J Soc Psychiatry 2004;50:10-7. https://doi.org/10.1177/0020764004038754.
- Tyrer P, Alexander MS, Cicchetti D, Cohen MS, Remington M. Reliability of a schedule for rating personality disorders. Br J Psychiatry 1979;135:168-74. https://doi.org/10.1192/bjp.135.2.168.
- Tyrer P, Tyrer P. Personality Disorders: Diagnosis, Management and Course. London: Arnold; 2005.
- International Classification of Diseases. Geneva: World Health Organization; n.d.
- Tyrer P, Crawford M, Mulder R, Blashfield R, Farnam A, Fossati A, et al. The rationale for the reclassification of personality disorder in the 11th Revision of the International Classification of Diseases. Personal Ment Health 2011;5:246-59. https://doi.org/10.1002/pmh.190.
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for the DSM-IV Axis I Disorders. Washington, DC: American Psychiatric Press; 1996.
- Young J, Beck AT. Cognitive Therapy Scale Rating Manual. Philadelphia, PA: Psychotherapy Research Unit, University of Pennsylvania; 1980.
- Davidson K, Scott J, Schmidt U, Tata P, Thornton S, Tyrer P. Therapist competence and clinical outcome in the prevention of parasuicide by manual assisted cognitive behaviour therapy trial: the POPMACT study. Psychol Med 2004;34:855-63. https://doi.org/10.1017/S0033291703001855.
- Kingdon D, Tyrer P, Seivewright N, Ferguson B, Murphy S. The Nottingham Study of Neurotic Disorder: influence of cognitive therapists on outcome. Br J Psychiatry 1996;169:93-7. https://doi.org/10.1192/bjp.169.1.93.
- Tyrer P, Wang D, Tyrer H, Crawford M, Cooper S. Dimensions of dependence and their influence on the outcome of cognitive behaviour therapy for health anxiety: randomized controlled trial. Pers Ment Health 2016;10:96-105. https://doi.org/10.1002/pmh.1339.
- Tyrer P, Cooper S, Salkovskis P, Tyrer H, Crawford M, Byford S, et al. Clinical and cost-effectiveness of cognitive behaviour therapy for health anxiety in medical patients: a multicentre randomised controlled trial. Lancet 2014;383:219-25. https://doi.org/10.1016/S0140-6736(13)61905-4.
- Piqueras JA, Rodriguez-Jimenez T, Ortiz AG, Moreno E, Lazaro L, Godoy A. Validation of the Short Obsessive-Compulsive Disorder Screener (SOCS) in children and adolescents. BJPsych Open 2015;1:21-6. https://doi.org/10.1192/bjpo.bp.115.000695.
- Tyrer P, Alexander J. Classification of personality disorder. Br J Psychiatry 1979;135:163-7. https://doi.org/10.1192/bjp.135.2.163.
- International Classification of Diseases. Geneva: World Health Organization; 1992.
- Sanatinia R, Wang D, Tyrer P, Tyrer H, Crawford M, Cooper S, et al. Impact of personality status on the outcomes and cost of cognitive-behavioural therapy for health anxiety. Br J Psychiatry 2016;209:244-50. https://doi.org/10.1192/bjp.bp.115.173526.
- Chan A. Dependent Personality in General Practice: An Epidemiological Study 2003.
- Kane FA, Bornstein RF. Beyond passivity: dependency as a risk factor for intimate partner violence. Personal Ment Health 2016;10:12-21. https://doi.org/10.1002/pmh.1322.
- Tyrer H, Ali L, Cooper F, Seivewright P, Bassett P, Tyrer P. The Schedule for Evaluating Persistent Symptoms (SEPS): a new method of recording medically unexplained symptoms. Int J Soc Psychiatry 2013;59:281-7. https://doi.org/10.1177/0020764012438484.
- Tyrer H, Tyrer P, Lisseman-Stones Y, McAllister S, Cooper S, Salkovskis P, et al. Therapist differences in a randomised trial of the outcome of cognitive behaviour therapy for health anxiety in medical patients. Int J Nurs Stud 2015;52:686-94. https://doi.org/10.1016/j.ijnurstu.2014.11.013.
- Barrett B, Byford S, Crawford M, Patton R, Drummond C, Henry J, et al. Cost-effectiveness of referral to an alcohol health worker in patients attending an accident and emergency department: a decision-making approach. Drug Alcohol Depend 2006;81:47-54. https://doi.org/10.1016/j.drugalcdep.2005.05.015.
- Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Environ Med 2003;45:156-74. https://doi.org/10.1097/01.jom.0000052967.43131.51.
- Netten A, Knight J, Dennett J, Cooley R, Slight A. A Ready Reckoner for Staff Costs in the NHS. Canterbury: Personal Social Services Research Unit, The University of Kent; 1998.
- NHS Health Education England . Agenda for Change – Pay Rates 2017. www.healthcareers.nhs.uk/about/careers-nhs/nhs-pay-and-benefits/agenda-change-pay-rates (accessed 12 January 2017).
- Curtis L. Unit Costs of Health and Social Care 2010. Canterbury: Personal Social Services Research Unit, University of Kent; 2011.
- British National Formulary. London: Royal Pharmaceutical Society; 2010.
- NHS Reference Costs, 2010. London: Department of Health; 2011.
- Methods for Technology Appraisal. London: NICE; 2008.
- Koopmanschap MA, Rutten FF. A practical guide for calculating indirect costs of disease. PharmacoEconomics 1996;10:460-6. https://doi.org/10.2165/00019053-199610050-00003.
- Kind P, Spilker B. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia, PA: Lippincott-Raven; 1996.
- Dolan P, Gudex C, Kind P, Williams A. A Social Tariff for Euroqol: Results from a UK General Population Survey. York: University of York, Centre for Health Economics; 1995.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ 2004;13:1203-10. https://doi.org/10.1002/hec.901.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. https://doi.org/10.1002/hec.635.
- Weichle T, Hynes DM, Durazo-Arvizu R, Tarlov E, Zhang Q. Impact of alternative approaches to assess outlying and influential observations on health care costs. Springerplus 2013;2. https://doi.org/10.1186/2193-1801-2-614.
- Hedman E, Andersson G, Andersson E, Ljótsson B, Rück C, Asmundson GJ, et al. Internet-based cognitive-behavioural therapy for severe health anxiety: randomised controlled trial. Br J Psychiatry 2011;198:230-6. https://doi.org/10.1192/bjp.bp.110.086843.
- McManus F, Surawy C, Muse K, Vazquez-Montes M, Williams JM. A randomized trial of mindfulness-based cognitive therapy versus unrestricted services for health anxiety (hypochondriasis). J Consult Clin Psychol 2012;80:817-28. https://doi.org/10.1037/a0028782.
- Hedman E, Axelsson E, Görling A, Ritzman C, Ronnheden M, El Alaoui S, et al. Internet-delivered cognitive-behavioural therapy and behavioural stress management for severe health anxiety: randomised controlled trial. Br J Psychiatry 2014;205:307-14. https://doi.org/10.1192/bjp.bp.113.140913.
- Eilenberg T, Fink P, Jensen JS, Rief W, Frostholm L. Acceptance and commitment group therapy (ACT-G) for health anxiety: a randomized controlled trial. Psychol Med 2016;46:103-15. https://doi.org/10.1017/S0033291715001579.
- Olatunji BO, Kauffman BY, Meltzer S, Davis ML, Smits JA, Powers MB. Cognitive-behavioral therapy for hypochondriasis/health anxiety: a meta-analysis of treatment outcome and moderators. Behav Res Ther 2014;58:65-74. https://doi.org/10.1016/j.brat.2014.05.002.
- Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition. Washington, DC: American Psychiatric Association; 2013.
- Stein DJ, Kogan CS, Atmaca M, Fineberg NA, Fontenelle LF, Grant JE, et al. The classification of Obsessive-Compulsive and Related Disorders in the ICD-11. J Affect Disord 2016;190:663-74. https://doi.org/10.1016/j.jad.2015.10.061.
- Mayou R. Is the DSM-5 chapter on somatic symptom disorder any better than DSM-IV somatoform disorder?. Br J Psychiatry 2014;204:418-9. https://doi.org/10.1192/bjp.bp.113.134833.
- Scarella TM, Laferton JA, Ahern DK, Fallon BA, Barsky A. The Relationship of Hypochondriasis to Anxiety, Depressive, and Somatoform Disorders. Psychosomatics 2016;57:200-7. https://doi.org/10.1016/j.psym.2015.10.006.
- Sørensen P, Birket-Smith M, Wattar U, Buemann I, Salkovskis P. A randomized clinical trial of cognitive behavioural therapy versus short-term psychodynamic psychotherapy versus no intervention for patients with hypochondriasis. Psychol Med 2011;41:431-41. https://doi.org/10.1017/S0033291710000292.
- O’Neil A, Hawkes AL, Atherton JJ, Patrao TA, Sanderson K, Wolfe R, et al. Telephone-delivered health coaching improves outcomes after myocardial infarction: the ‘Pro-Active Heart’ trial. Eur J Prev Cardiol 2014;21:30-8. https://doi.org/10.1177/2047487312460515.
- Ihle-Hansen H, Thommessen B, Fagerland MW, Oksengård AR, Wyller TB, Engedal K, et al. Effect on anxiety and depression of a multifactorial risk factor intervention program after stroke and TIA: a randomized controlled trial. Aging Ment Health 2014;18:540-6. https://doi.org/10.1080/13607863.2013.824406.
- Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: a meta-analysis of published studies. Br J Psychiatry 2006;188:13-20. https://doi.org/10.1192/bjp.188.1.13.
- Newton-Howes G, Tyrer P, Johnson T, Mulder R, Kool S, Dekker J, et al. Influence of personality on the outcome of treatment in depression: systematic review and meta-analysis. J Pers Disord 2014;28:577-93. https://doi.org/10.1521/pedi_2013_27_070.
- Tyrer P, Seivewright N, Seivewright H. Long-term outcome of hypochondriacal personality disorder. J Psychosom Res 1999;46:177-85. https://doi.org/10.1016/S0022-3999(98)00072-5.
- Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet 2015;385:717-26. https://doi.org/10.1016/S0140-6736(14)61995-4.
- Tyrer P, Seivewright H, Johnson T. The Nottingham Study of Neurotic Disorder: predictors of 12-year outcome of dysthymic, panic and generalized anxiety disorder. Psychol Med 2004;34:1385-94. https://doi.org/10.1017/S0033291704002569.
- Skodol AE, Geier T, Grant BF, Hasin DS. Personality disorders and the persistence of anxiety disorders in a nationally representative sample. Depress Anxiety 2014;31:721-8. https://doi.org/10.1002/da.22287.
- Hengartner MP, De Fruyt F, Rodgers S, Müller M, Rössler W, Ajdacic-Gross V. An integrative examination of personality dysfunction in a large community sample. Personal Ment Health 2014;8:276-89. https://doi.org/10.1002/pmh.1263.
- Tyrer P, Yang M. The clinical implications of personality-generated mental illness. Personal Ment Health 2015;9:17-20. https://doi.org/10.1002/pmh.1286.
- Fink P, Ørnbøl E, Christensen KS. The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. PLOS ONE 2010;5. https://doi.org/10.1371/journal.pone.0009873.
- Eilenberg T, Frostholm L, Schroder A, Jensen JS, Fink P. Long-term consequences of severe health anxiety on sick leave in treated and untreated patients: analysis alongside a randomised controlled trial. J Anxiety Disord 2015;32:95-102. https://doi.org/10.1016/j.janxdis.2015.04.001.
- Tyrer P, Eilenberg T, Fink P, Hedman E, Tyrer H. Health anxiety: the silent, disabling epidemic. BMJ 2016;353. https://doi.org/10.1136/bmj.i2250.
- The Five Year Forward View for Mental Health: A Report from the Independent Mental Health Taskforce to the NHS in England. London: NHS; 2016.
- Williams C, House A. Cognitive behaviour therapy for health anxiety. Lancet 2014;383:190-1. https://doi.org/10.1016/S0140-6736(13)62107-8.
- Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al. Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland. Health Technol Assess 2005;9. https://doi.org/10.3310/hta9420.
- Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al. Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial. Health Technol Ass 2006;10:1-67. https://doi.org/10.3310/hta10190.
- Hunot V, Churchill R, Silva de Lima M, Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev 2007;1. https://doi.org/10.1002/14651858.CD001848.pub4.
- Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, Andersson G. Psychological treatment of generalized anxiety disorder: a meta-analysis. Clin Psychol Rev 2014;34:130-40. https://doi.org/10.1016/j.cpr.2014.01.002.
- Wiles NJ, Thomas L, Turner N, Garfield K, Kounali D, Campbell J, et al. Long-term effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary are: follow-up of the CoBalT randomised controlled trial. Lancet Psychiatry 2016;3:137-44. https://doi.org/10.1016/S2215-0366(15)00495-2.
- Richards DA, Bower P, Chew-Graham C, Gask L, Lovell K, Cape J, et al. Clinical effectiveness and cost-effectiveness of collaborative care for depression in UK primary care (CADET): a cluster-randomised controlled trial. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20140.
- Hedman E, Andersson E, Lindefors N, Andersson G, Rück C, Ljótsson B. Cost-effectiveness and long-term effectiveness of internet-based cognitive behaviour therapy for severe health anxiety. Psychol Med 2013;43:363-74. https://doi.org/10.1017/S0033291712001079.
- Berge LI, Skogen JC, Sulo G, Igland J, Wilhelmsen I, Vollset SE, et al. Health anxiety and risk of ischaemic heart disease: a prospective cohort study linking the Hordaland Health Study (HUSK) with the Cardiovascular Diseases in Norway (CVDNOR) project. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-012914.
- Van Beek MH, Zuidersma M, Lappenschaar M, Pop G, Roest AM, Van Balkom AJ, et al. Prognostic association of cardiac anxiety with new cardiac events and mortality following myocardial infarction. Br J Psychiatry 2016;209:400-6. https://doi.org/10.1192/bjp.bp.115.174870.
- Patel S, Malins S, Guo B, James M, Kai J, Kaylor-Hughes C, et al. Protocol investigating the clinical outcomes and cost-effectiveness of cognitive–behavioural therapy delivered remotely for unscheduled care users with health anxiety: randomised controlled trial. BJPsych Open 2016;2:81-7. https://doi.org/10.1192/bjpo.bp.115.002220.
List of abbreviations
- ADSUS
- Adult Service Use Schedule
- CBT
- cognitive–behaviour therapy
- CBT-HA
- cognitive–behaviour therapy for health anxiety
- CEAC
- cost-effectiveness acceptability curve
- CHAMP
- cognitive–behaviour therapy for health anxiety in medical patients
- CHASSIS
- Confederation of Health Anxiety Sufferers Supporting Increased Services
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DPQ
- Dependent Personality Questionnaire
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition
- EQ-5D
- EuroQol-5 Dimensions
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- HADS-A
- Hospital Anxiety and Depression Scale (anxiety section)
- HADS-D
- Hospital Anxiety and Depression Scale (depression section)
- HAI
- Health Anxiety Inventory
- IAPT
- Improving Access to Psychological Therapies
- ICD-10
- International Statistical Classification of Diseases, Tenth Edition
- ICD-11
- International Statistical Classification of Diseases, Eleventh Edition
- ICER
- incremental cost-effectiveness ratio
- MCD
- meaningful clinical difference
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- openCDMS
- Open Clinical Data Management System
- PAS-Q
- Quick Personality Assessment Schedule
- QALY
- quality-adjusted life-year
- SD
- standard deviation
- SFQ
- Social Functioning Questionnaire
- SOCS
- Short Obsessive–Compulsive disorder Screener
- VAS
- visual analogue scale