Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/62/02. The contractual start date was in May 2013. The draft report began editorial review in March 2016 and was accepted for publication in January 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Ulph et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Newborn (neonatal) bloodspot screening (NBS) is seen as one of the most significant public health achievements in the developed world. 1 In England, NBS began in 1969 with screening for phenylketonuria (PKU)2 and over the following 40 years four additional disorders were added: congenital hypothyroidism (CHT), cystic fibrosis (CF), sickle cell disorders (SCDs) and medium-chain acyl-CoA dehydrogenase deficiency (MCADD). Three of these disorders were added since 2007, in keeping with NBS worldwide, where panel expansion has been most noticeable in the last decade. 3 Most recently, in January 2015, four further conditions were added: maple syrup urine disease (MSUD), homocystinuria (HCU) (pyridoxine unresponsive), glutaric aciduria type 1 (GA1) and isovaleric acidaemia (IVA).
In England, NBS involves collecting a blood sample between 5 and 8 days after birth. The premise behind screening is that there is a clinical benefit to affected infants of being identified and treated in the neonatal phase. 4 In 2014–15, > 666,000 babies were screened in the UK, of whom 590 had a positive screening result, leading to an urgent referral for diagnostic tests and treatment when necessary. 5 The annual report for the UK National Blood Screening Programme (NBSP) stated that the cost of screening for that year was £1,911,677. 5 Existing economic evaluations of NBS (e.g. Bunnik et al. 6), as well as studies such as retrospective cohort studies,7 have concluded that NBS is a cost-effective use of resources. However, the costs of the associated communication are not currently known.
The prescreening newborn bloodspot screening communication model in England
Newborn bloodspot screening is introduced to parents as a recommended routine screen with the proviso that screening occurs only after parents have given informed consent. 8 The latest version of the Health Professional Handbook9 states that:
When obtaining consent for newborn blood spot screening, you must ensure that parents understand they are consenting to the following:
The sample being taken
The sample being booked in and analysed in the NBS laboratory and used for quality assurance
The laboratory sending the results to the child health records department
The results being stored on the child health information system
The potential identification of their baby as a ‘carrier’ of SCD or CF
A referral to specialist services if a result is positive
The blood spot card being stored for a minimum period by the laboratory, as detailed in the Code of Practice for the Retention and Storage of Residual Spots (see 4.3; please note that this document is currently under review)
Their baby’s anonymised data being used for research studies that help to improve the health of babies and their families in the UK, for example population studies (see 4.3)
In rare circumstances, receipt of invitations from researchers who would like to use their baby’s blood spot card for research (this is optional – see 4.3)
The use of identifiable data on babies, or children under age 5, with SCD or thalassaemia by the NHS Sickle Cell and Thalassaemia Screening Programme (see 4.4)
Contains public sector information licensed under the Open Government Licence 3.09
The handbook guides health professionals to discuss and provide an information booklet, Screening Tests For You and Your Baby,10 at booking (the first appointment) and again after birth. It is recognised in the handbook that not all parents receive the booklet at booking and so health professionals are advised to provide the Screening Tests for Your Baby booklet later in pregnancy. (We refer to these texts as booklets as they are over 30 pages long; however, later in the report the interviewees may refer to them as leaflets.)
The booklets supporting communication changed during the project. As described, at the start of the project there were two booklets: Screening Tests For You and Your Baby was 72 pages long and was given early in pregnancy; Screening Tests For Your Baby was a shorter booklet designed to be given to parents in the last trimester or after birth. In October 2014 Screening Tests For You and Your Baby was revised10 and midwives were told to remove old copies from circulation. Although the Health Professional Handbook refers to both booklets, the provision of Screening Tests For Your Baby was also stopped in October 2014. Screening Tests For You and Your Baby is now 49 pages long, with NBS being covered on pages 44–9. If parents require further information they are signposted back to the booklet, which is available in 12 languages. 11 Thus, the dominant communication model is of midwives communicating with parents using generic screening booklets for support.
Acceptability, parental understanding and the broader impact of current consent and communication models
Provision of information is seen as central to ensuring that the potential harms of NBS (distress following an unexpected diagnosis, concerns about carrier status) are minimised12,13 and the benefits (ensuring quick follow-up of children with abnormal results) are maximised. 12,14–26 Clear screening information and effective communication between health professionals and parents is also seen as a way of balancing the conflicting needs of a public health screening programme with respect for parents’ autonomy. 14 Despite NBS being in place for almost 50 years in some countries, there is still a need to establish an evidenced-based and effective communication model. Although globally both the number and the type of conditions included in the panel vary considerably, as does opinion regarding the appropriate level of consent, there is universal concern regarding the efficacy of communication. 15,16
Consent models for NBS vary along a continuum, from the decision being made by the state (mandatory screening) through to ‘opt-out models’, in which the state advises screening but with parents able to object, and models in which parents are the decision-makers (informed consent). Consent for NBS involves a number of special considerations. First, parents are asked to make screening decisions on behalf of their newborn child – proxy consent. Second, the information provided is complex; screening covers a range of rare diseases that many people will not have heard of previously;17 the blood sample will be used for diagnostic testing, but also potentially anonymised research; across the different conditions there is a range of outcomes from diagnosis to inconclusive diagnosis, carrier, suspected carrier, false positive and normal; and the results of screening can have important implications for people other than the newborn child. Third, consent is often taken just a few days after birth when parents are tired and are being provided with large amounts of information regarding looking after a newborn. Thus, consent in this context is potentially quite different from consent in a range of other settings.
Concerns have been raised about the efficacy of informed consent as there is almost universal uptake of screening across countries. 4,6,15,18–20 Rather than this being because of positive regard, the concern is that parents are not truly making an informed decision because of limitations in the communication or consent process. 21 It has been argued that by making screening a routine part of postnatal care, and aiming for high uptake, NBS is incompatible with the concept of informed consent usually required for testing for serious diseases and disorders. 22
Additional concerns surround repeat findings that parents whose children have been screened have limited knowledge about screening. 19,23–30 Indeed, some parents were unaware that their child had been screened. 25,28,31–33 Within the UK a health technology assessment (HTA) study reported concerns over whether or not parents were adequately informed prior to screening,34 linking this to subsequent distress and resource use when adapting to carrier results. That such anxiety has been linked to impaired relationships with the baby35–37 and stress-related problems enduring into childhood38 demonstrates that lessons from PKU screening, which has triggered the vulnerable child syndrome for some parents,39,40 have not been learned. Unfortunately, such distress commonly has an impact on the wider family. 34 In these scenarios multiple and/or specialist health professional consultations are often needed to allay such anxiety. 34,41 However, the resources related to this further service need are not included in NBS cost estimates. 42 Thus, providing parents with NBS information appears to be complex, with no evidence-based, effective and standardised model in existence, and, critically, the provision of NBS information can have an impact on families and resource use.
Crucially, research suggests that such distress may be avoidable as not only can parents understand NBS information and assimilate the results into their lives with minimal distress but they also positively value the results. 34 The key difference between parents who reported distress and those who received carrier results with minimal service need is that parents who adapted well had a prior awareness of the disease and could understand the relevance of the NBS information provided antenatally. 34 Thus, there are calls for antenatal communication to be optimised to minimise the distress from false-positive37 or carrier13 results. Parents who reported distress did not feel prepared for screening, felt overloaded by information provided antenatally26,34 and felt that the NBS information provided did not meet their needs or was not relevant. 27,34 This fits with an argument made by Climb (an organisation that provides information on metabolic diseases for parents, children and health professionals) that the NBS booklets require users to have pre-existing knowledge to appreciate their relevance. 16
Expanded newborn bloodspot screening
The advent of tandem mass spectrometry (MS/MS) provided the means to screen for numerous disorders with few extra costs. 43 As NBS panels include increasingly rare diseases with less clear treatment benefits, communication will become ever-more critical and yet challenging. 16 Specifically, there is a recognised need to inform parents prior to screening,34,43,44 preferably antenatally,34,45 and that current models may not be meeting parents, needs for clear and timely information. 34 A potential expansion to the NBS panel in England (which was enacted in January 2015) necessitated revisiting the efficacy of providing relevant information antenatally and how to prepare parents for the possibility that their child may have a positive result. 16
The introduction of the expanded NBS panel, within England specifically, needed also to be viewed in the context of providing a national health service from a finite budget, with a requirement to consider the opportunity cost. The additional cost of expanding the NBS panel, potentially requiring extra input from midwives and removing them from other duties, needed to be worth the potential benefits for parents and babies. These may come in the form of both health and non-health benefits, such as the value of the additional information per se that comes from a NBS result and the minimising of distress if parents are adequately prepared. 34
Summary
There is a need to review communication and consent models currently used in NBS in England because of concerns about the efficacy of the current models, which have been further exaggerated by the expansion of the panel. Although there is a paucity of guidelines for developing communication and consent models for NBS, it has been suggested that the National Institute for Health and Care Excellence (NICE) report on guideline development8 can be used as a model. 46 This study used the definition in Stewart et al. 46 of evidence-based medicine as the template for the methods:
the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. It requires a bottom-up approach that integrates the best external evidence with individual clinical expertise and patient-choice.
Thus, published research on the efficacy, impact and parent understanding of NBS communication and consent was evaluated. Parents and both front-line and clinical specialists were then engaged in qualitative research to develop alternative communication models for use with expanded NBS. These models were then evaluated using quantitative and qualitative methods in the remainder of the study.
Aim
The overall study aimed to determine service providers’ and users’ views about the feasibility, cost, efficiency, impact on understanding and consent process of current practice and preferences for alternative methods of conveying NBS information antenatally. There were nine objectives, which were addressed in two phases:
Phase 1: generation of alternative models, establishing costs and implications of current best practice for parent understanding:
-
collate the characteristics of alternative communication and consent models for NBSPs through a realist review of current NBSP communication models within the UK and countries operating extended NBSPs
-
explore how providers and users envisage that information given antenatally can best meet the challenge of effectively and efficiently providing parents with sufficient understanding of an extended NBSP, including their reflections on the alternatives identified through the review
-
examine parents’ understanding and experiences of NBSP communication to draw inferences regarding best practice within an extended NBSP
-
establish the resource use and costs associated with the current practice(s) of providing NBSP information antenatally.
Phase 2: acceptability, preferences, cost and broader impact of alternative models:
-
examine the preferences of midwives, parents and prospective parents for different models of conveying NBSP information antenatally
-
establish the key parameters affecting the cost-effectiveness of new modes of information provision compared with the current practice(s) of providing NBSP information antenatally
-
outline the key uncertainties in the current evidence base and the value of future research to evaluate the effectiveness and cost-effectiveness of providing NBSP information antenatally
-
explore providers’ and users’ views on the study suggestions, focusing on acceptability, broader impact, effectiveness, efficiency and parent understanding
-
establish how generalisable the study findings are across conditions screened for in the UK NBSP.
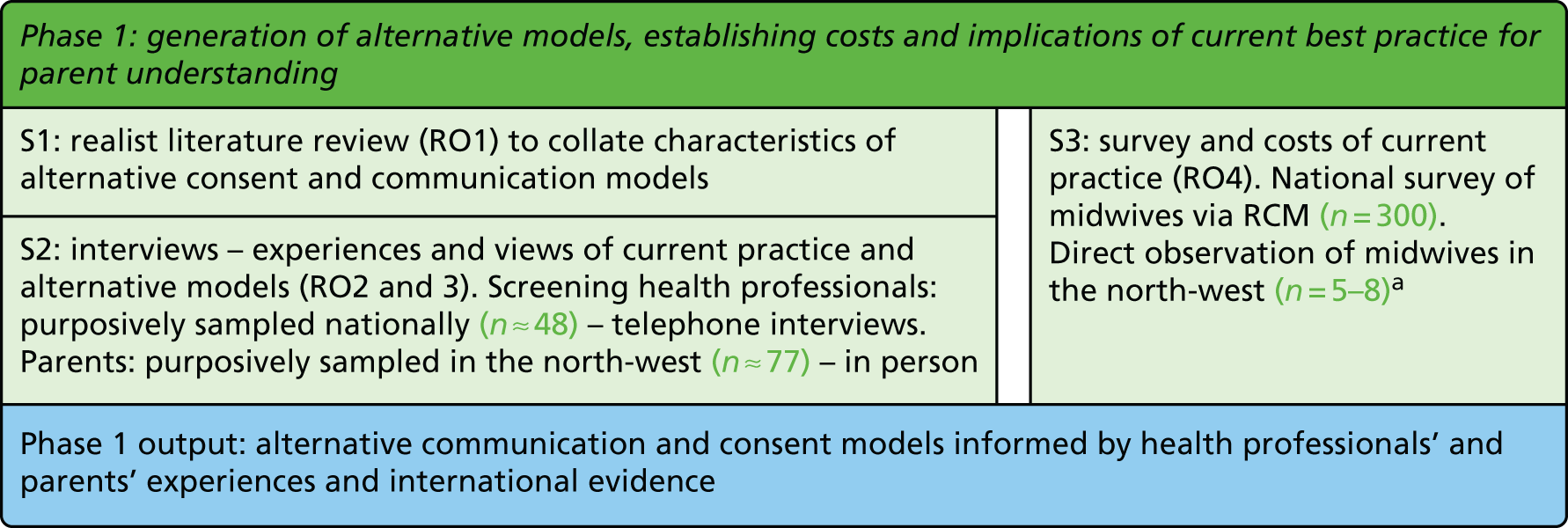
These objectives were met though six studies (Figure 1).
FIGURE 1.
Phases of the study. DCE, discrete choice experiment; RCM, Royal College of Midwives; RO, research objective; S, study. a, Number is planned sample size a priori.

Structure of this report
The next six chapters report each of the studies outlined in Figure 1. The findings of these studies are discussed in Chapter 8. The input of patient and public involvement (PPI) is discussed within each study chapter and is summarised in the following section.
Patient and public involvement
Given that the central aim of this project focused on a communication event between midwives and parents, with the desire to create alternative models that were acceptable to both groups, the involvement of parents and midwives in the research process was crucial. Three groups of advisors worked with the project team.
Parent reference group
Parents were invited to become members of the parent reference group. Four parents joined with differing experiences of NBS results and numbers of children, and differences in how recent their NBS experience was. They advised the team on the interview schedule and study materials for the study reported in Chapter 3. Their opinions were sought about how to introduce the observation study to parents (see Chapter 4). They also advised on the design of the discrete choice experiment (DCE) survey for parents, which led to a complete reformatting of the layout of the information and how questions were phrased (further explanation of the DCE is provided in Chapter 5). They were given the first overview of the project findings and helped design the summaries for parents and advised on the timing of focus groups and strategies to facilitate engagement in the groups. They were invited to the stakeholder consultation. Their involvement was encouraged through a range of face-to-face meetings, e-mail correspondence and telephone calls. Parents had the option to attend meetings on their own, with childcare provided, or with their children. Travel expenses were also provided.
The duration of meetings was kept to a minimum given the competing roles that the parents had. The principal investigator met with group members and asked if they wanted a reminder of the study aims before an overview was provided on the findings to date. The relevant researcher for the task then introduced the problem that the team was considering before handing over to the parent reference group to hear the views of its members. Study materials or measure ‘mock-ups’ were given to the parent reference group to handle and interact with, with notes taken regarding their advice. In subsequent meetings the team reported back to the parent reference group about how their advice had altered the study design. Study updates were sent to parent reference group members when appropriate between meetings, with an open invitation to contact the team should they have any views that they wished to share. When parents were unable to attend, telephone conversations were held to maintain two-way communication between parents and the team. At the final meeting members were asked whether or not they wanted to receive any outputs from the study.
Newborn screening advisory group
The newborn screening advisory group consisted of a NBS laboratory director, a senior quality advisory manager and a research midwife. Meetings with these advisors were held to discuss the project aims and they were invited to participate in the stakeholder consultation at the end of the project. Although advice was sought from group members in terms of measures, for example the interview schedule for the health professional interviews and the DCE for midwives (available on request), the majority of their advice surrounded recruitment issues. This was central to the project’s success. Group members provided guidance on structures within NBS and from that developed the idea of snowball sampling in study 2 (see Chapter 3). They also provided guidance on the observation study practicalities and advised on which trusts to approach (see Chapter 5). They were central to the recruitment of parents in study 2, in which the team approached laboratory directors and midwives to ask them to recruit for the study.
Given that it was less important to seek consensus in the advice arising from this group, the challenges of ensuring that three health professionals were available to meet and the focus of some questions on certain professional groups, engagement more commonly occurred in a way that was directed by the availability of the members. Thus, engagement ranged from semi-formal office-based meetings to informal coffee shop brainstorming sessions, e-mails and telephone calls.
Scientific advisory board
The scientific advisory board included a laboratory scientist, representatives from Genetic Alliance and Climb, and a senior midwife. Formal meetings were held at which overviews of study progress were reported. The board advised on future fieldwork and current policy and practice issues that might impact on the studies. Board members were provided with summaries of the project findings and were invited to comment. They advised on interview schedules for parents and recruitment strategies, specifically for parents whose children had been diagnosed through NBS or who had received a false-positive result.
Key outputs arising from patient and public involvement
Key outputs from PPI were:
-
the interview schedules for study 2 (see Chapter 3)
-
the DCE (see Chapter 5)
-
the stakeholder consultation summary (see Chapter 7)
-
methods for recruiting parents to the interview study, focusing on fathers and specific subgroups of parents
-
methods for recruiting health professionals for interviews and the DCE
-
the observation study protocol.
This project benefited enormously from the combined expertise of the parent reference group, the NBS advisors, the scientific advisory board and the research team. Without this collaborative way of working key questions would have been missed, measures would have been less valid or would have been less likely to engage people in completing them, responses could have been misinterpreted and the quality of the research would have suffered as a result. Each group had a unique insight that, when combined, ensured the quality of the research.
One of the markers of quality engagement is low levels of withdrawal. Despite each parent juggling competing priorities and a young family, and health professionals often doing the same, all members engaged throughout the course of the research, for which we are extremely grateful.
Phase 1 Generation of alternative models, establishing costs and implications of current best practice for parent understanding
This phase consisted of three studies (Figure 2). A realist review (see Chapter 2) was carried out to collate existing research and practice regarding communication and consent in NBS. From this the range of alternative models in communication and consent practice were mapped out and explored in interviews with health professionals and parents (see Chapter 3). Simultaneously, a costing study was carried out to establish the current cost of the communication and consent model practised in England (see Chapter 4).
FIGURE 2.
Phase 1 of the study. RCM, Royal College of Midwives; RO, research objective; S, study. a, Number is planned sample size a priori.
Chapter 2 Study 1: realist review
Study objectives
-
Collate the characteristics of alternative communication and consent models for NBSPs.
-
Review research examining procedures for consent in NBSPs.
-
Establish what works, for who and under what circumstances to assimilate suggestions for alternatives to the current UK NBSP communication model.
Introduction
As stated in Chapter 1, there is variation across NBSPs in the conditions included, the communication methods and the consent models. Despite universal acknowledgement of the importance of communication, there is not yet an effective, evidence-based approach to providing NBS prescreening information. Thus, a realist review was conducted to examine underlying theories of informed consent, review the empirical literature and populate our theoretical framework. From this we assimilated suggestions for alternative communication and consent models.
Methods
The methodology of realist review focuses first on developing a conceptual or theoretical framework to understand the phenomenon or intervention being studied and then on undertaking a review of the empirical literature to populate that framework. 47 The intention is that the underlying programme theory is used to organise and structure the presentation of the available empirical evidence, while the synthesis of the empirical evidence is used to test out and refine the programme theory. The aim is to bring together our theoretical and empirical understanding.
Publications in English were searched for from the inception of the databases to 2015 using the search terms ‘informed consent’, ‘theor*’, ‘concept*’, ‘defin*’, ‘framework’ and ‘model’. This yielded 214 papers and all titles and abstracts were reviewed for relevance independently by KW and FU. The following papers were excluded: those that were primarily empirical studies of informed consent, with little or no theoretical or conceptual content, those that focused on informed consent primarily in relation to a particular clinical domain and those that were primarily aimed at training or professional development in relation to informed consent. In total, the full texts of 37 papers were retrieved, which were read and summarised to identify key concepts, theories and methodological developments in relation to informed consent.
Theories of informed consent: developing an analytical framework
The dominant theoretical perspective of informed consent was first framed by Faden and Beauchamp48 and is rooted in both legal thinking and ethical theory. It is centred on the concept of autonomous authorisation – the idea that consent requires an act of authorisation undertaken autonomously and that this requires evidence of intentionality, understanding and control.
-
Intentionality means that the person wants or wills what is being consented to and has gone through some cognitive process to reach this position. Of course, capacity to do this may be constrained by the circumstances in which consent is being given or by personal characteristics of the person.
-
Understanding means that the person understands what he or she is consenting to, which involves him or her in both having or receiving relevant information about it and being capable of retaining and grasping that information and using it to reach the decision to consent. Achieving what is sometimes called full and true understanding may be constrained by the complexity of the information and by the personal characteristics of the person.
-
Control means that the person is free of external influences and makes the decision to consent independently. Distinguishing between legitimate advice and forms of persuasion, manipulation and coercion is not straightforward. Control over a decision may be exercised through social norms or expectations and by legal obligations on the person or others.
This approach to defining and operationalising arrangements for informed consent has been widely used in both clinical practice and research and in many areas where consent is often a contested and difficult matter to negotiate, for example neuroscience,49 child psychiatry,50 dementia51 and end-of-life care. 52
It has been observed that the concept of autonomous authorisation leads to ‘theoretical confidence, and practical disquiet’,53 providing a theoretical framework for informed consent that is, in practice, difficult to realise and can be problematic ethically when operationalised. Many authors have argued that it is rare in practice to achieve intentionality, understanding and control,54–56 leaving health-care providers and researchers in a vulnerable position. As a consequence, lower standards of consent are often adopted – ideas such as presumed consent, broad consent and open consent may represent necessary compromises if the ideal of informed consent cannot be realised, but may also dilute and devalue the concept of informed consent. 57
More fundamentally, some have suggested that the theory of autonomous authorisation puts personal sovereignty and autonomy above well-being and can run counter to the established ethical principle of beneficence. 52 In addition, it is noted that wider ideas of the common good, public interest or the collective needs of society are not represented. 58,59 Some have suggested that autonomous authorisation represents a particular set of Western social and cultural values and is not simply transferable to other societies and cultural settings. 60
An alternative and more recent approach to informed consent, termed the ‘fair transaction model’, sets the idea of informed consent in the wider context of consent to other social transactions (e.g. in commerce, employment or personal relationships). 53 It argues that consent is a morally transformative act in that it makes morally permissible something that would otherwise not be morally permissible and asserts that, to be valid, consent must achieve this moral transformation. In this context, it is suggested that we should consider both autonomy and well-being, for the consenter, the health-care provider and in some cases for wider society as well. This means that the balance of risks and benefits in the thing being consented to becomes part of our consideration, as do the effects on those other than the person giving consent.
The prevailing model of autonomous authorisation was widely used and cited in the NBS literature and so it was selected to be the theoretical framework for this chapter. For the review of the empirical literature on informed consent and communication in NBS, the three main concepts of autonomous authorisation (intentionality, understanding and control) formed the analytical framework. However, understanding was subdivided into four subcomponents: the provision of relevant information, information retention, understanding that information and the capacity to use that information while consenting. This was done partly because initial scoping suggested that the literature was largely focused on understanding, rather than on intentionality and control, and because some literature reported on research in jurisdictions where mandatory screening is practised and issues of intentionality and control are not addressed, although there is still a belief that understanding is important. Also, subdividing the model more closely aligned it with the applied legal test of informed consent to medical treatment, testing or research, which involves enabling individuals to make as authentic a decision as possible. For this decision to be deemed valid, a number of conditions need to apply. Individuals must have the intellectual capacity to make this decision, they must have relevant information to make this decision, they must be able to understand and retain this information and they must not be coerced in their decision. The resultant framework was as follows:
-
Relevant information. Had papers examined whether or not relevant information was provided? (content). How was information given, for example in person, through leaflets, through media or via the internet? (mode). Did the information provided meet parents’ needs (i.e. what information did parents want)? Was there a difference between parents’ information needs and those inferred by the authors?
-
Understanding. Had papers examined parents’ understanding of the information (through surveys, interviews or direct tests of knowledge)? Is there any evidence that parents’ knowledge/understanding was checked (by a health professional)? Were there any language barriers that prevent understanding? Was information on readability tests of the written information provided or is there any evidence that the necessary understanding to make this decision was lacking?
-
Retention. Had it been assessed whether or not parents retained the information that they were given about NBS? Could parents recall the information at the time of the decision? Were any attempts made to check whether parents retained this information? How long was the gap between the provision of information and the decision being made?
-
Intellectual capacity. Had papers considered the capacity of parents at the time of the screening decision (e.g. in high-stress/emotive circumstances, such as with premature or special care babies)? Had papers examined any key groups who might have compromised capacity (e.g. people with learning difficulties, mental illness or brain injury, or teenagers), and is there any evidence that capacity was lacking or that the issue of capacity was ignored?
-
Control. Had papers examined the level of control/coercion/influence/persuasion that was at play during the decision? Is there any information on the level of choice that parents had over whether or not their baby was screened? How much of the screening decision was part of parents’ free will? Is there any evidence that screening was carried at as routine practice/proceduralised or that the parents’ decision was coerced in any way?
-
Intentionality. Had papers examined whether a cognitive process took place (e.g. weighing up of the risks and benefits of screening) or whether the decision was based on individuals’ pre-existing beliefs/values? Did parents intend to have their baby screened? Is there any evidence on how valued (important to parents) the decision was? Did parents know that their child was being screened?
Regardless of the consent model, it is hoped that prescreening communication provides relevant information that is understood and retained to maximise benefits (follow-on care) and limit harms (such as the psychological impact of a false-positive result). All other concepts become important once the goal of the communication model is to achieve informed consent.
Search strategy for empirical newborn bloodspot screening research
Publications in English were searched for from the inception of the databases to 2015. Search terms, databases and inclusion and exclusion criteria are detailed in Figure 3.
FIGURE 3.
Search strategy for empirical literature. CHD, congenital heart disease; HMIC, Health Management Information Consortium.
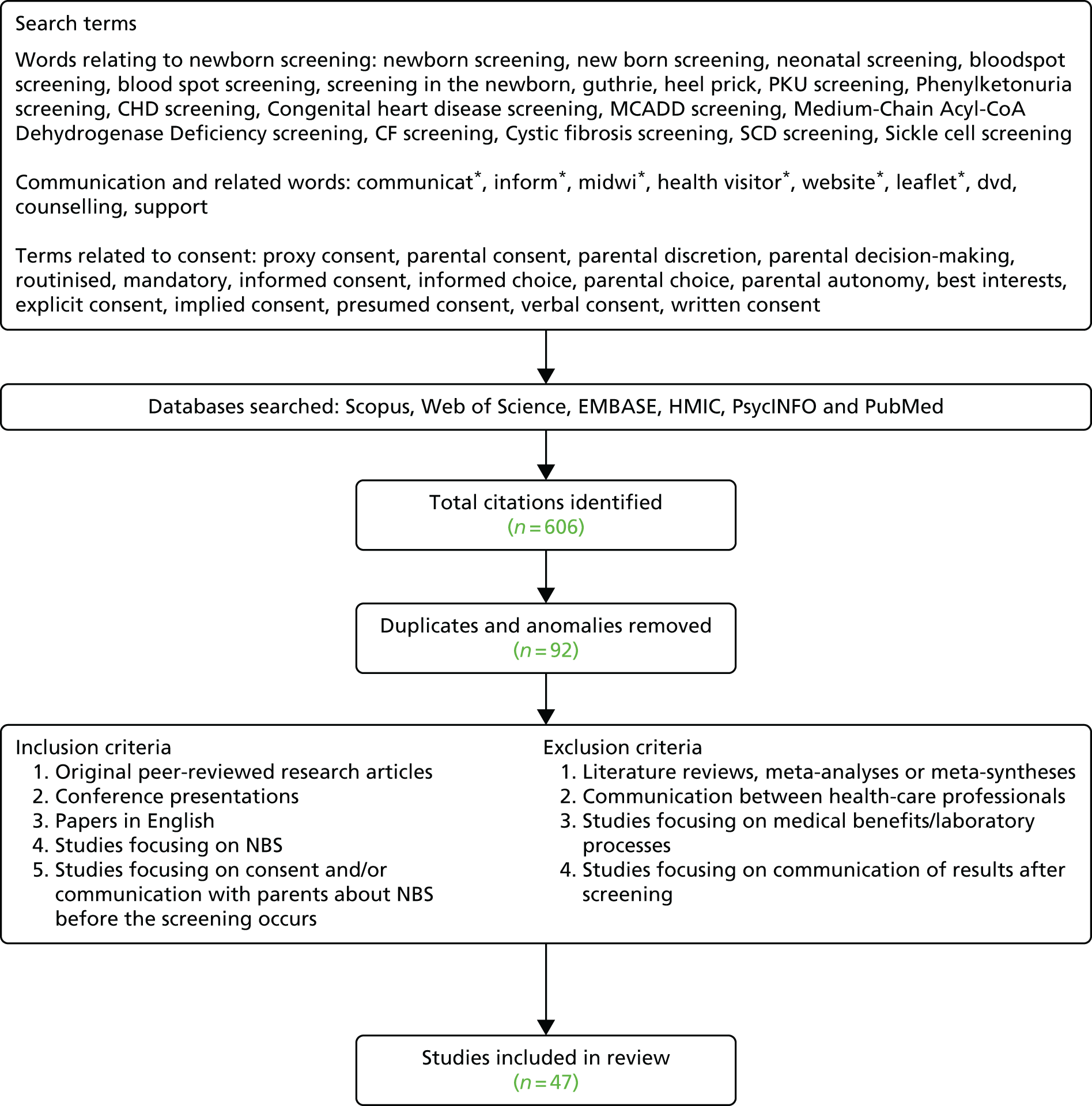
Searches were iterative and the final searches were completed in August 2015. The consent and communication searches were conducted separately and then combined. The database searches yielded 606 articles. These were entered into EndNote (version 5; Thomson Reuters, CA, USA). Next, all titles and abstracts were scanned by ND and FU for relevance according to the following inclusion/exclusion criteria. Papers were included if they reported empirical peer-reviewed research and focused on research on consent and/or communication in NBS, research on the knowledge of consent and/or communication and attitudes towards consent and/or communication of parents who had experienced NBS or the views of health professionals involved in the consent and communication process. Papers were excluded if they were commentaries or review papers, reported screening policy or different screening technologies, described communication between health professionals or focused on post-result communication, the impact of false-positive results or the medical benefits of screening. Papers without abstracts were retained for examination of the full text. When the full text of a paper was not available, authors were contacted for further information on whether or not a manuscript was available. In total, this strategy resulted in 47 papers being included in the review,8,12,14,15,17,19,20,25,26,28–30,33,61–94 covering NBS in a number of different countries: England (n = 118,14,25,62,66,70,72,78–80,83), Wales (n = 285,86), France (n = 189), Germany (n = 115), the Netherlands (n = 129), USA (n = 2017,19,26,30,33,61,63,64,71,74–76,81,82,84,87,88,90,91,93), Canada (n = 412,65,73,77), Australia (n = 320,28,68), New Zealand (n = 269,94), Taiwan (n = 192) and Hong Kong (n = 167). Within this there were variations in the conditions screened for and the consent models used, which are noted in the literature overview table in Appendix 1.
Synthesis
The following information was extracted from papers: country, tests included in screening, consent practice, aim of the study, relevant participant characteristics (e.g. sex, ethnicity, socioeconomic status, language), study design, sample size, any outcome measures and findings (see Appendix 1). The included papers were then imported into NVivo (version 10; QSR International, Warrington, UK) and coded according the programme theory concepts.
Results
The results are split into two sections: concepts that are central to all communication models irrespective of consent model and concepts that become important once parents are asked to make a decision.
Universal goals of all communication models
This section discusses the literature related to relevant information, understanding and retention. In doing so it looks at what is considered to be relevant information in NBS and how this might be provided. It also examines when information should be provided so that it can be retained for use by parents. In the setting where decisions are not necessary parents would need to recall the information to prepare for, and adapt to, NBS results.
Relevant information
Providing relevant information was valued across consent models. 12,19,61 Indeed, one paper suggested that information was valued more than choice. 45 Although effective information provision was seen as central to choice12 and the quality of the choices made,62 it was also valued for minimising distress if further testing was required or a diagnosis given. 63 In countries that rely on parents actively seeking further care this was improved if parents were given relevant information. 64 Others argued that information enabled parents to feel respected65 or that parents had a need to know what was happening to their child. 19 Of concern, then, is the finding that numerous papers reported that parents believed that they had never received any information. 29,66,67 For example, parents in the Netherlands reported that they had received no or little official NBS information, including about what the screening programme was for. 29 Parents cited their information sources as being the television and pregnancy books. More recently, 19.8% of parents in England reported that they had received no information on NBS66 and 83% of 177 parents in Hong Kong were not aware of NBS (although their child would have recently had it), with 99.4% of the sample wanting more information. 67 This was a repeated claim in the papers. 29,33,63,66–68
There may be numerous reasons for this pattern. First, it could be that the information really is not given for some reason. Interestingly, even health professionals have reported that parents do not receive any information. 69 Although their study took place in a research setting, Hargreaves et al. 70 showed that midwives would sometimes select not to give women leaflets if they felt that they would not be able to understand them or appeared uninterested. Also, if parents were having their second or subsequent child, either party may have assumed that they already had knowledge and so NBS information was not given. 18 Indeed, parents reported that they probably say that they have enough information without actually having a full awareness of the current screening information. 18 Another factor could be the lack of a clear protocol stating which health professional is responsible for providing information. This has been shown to result in health professionals assuming that it is someone else’s responsibility. 69,71 These issues appear to feed into another narrative in the data about who is responsible for ensuring that parents have the relevant information. Hayeems et al. 61 found that health professionals recognised their responsibility to provide parents with information by signposting, but felt that it was the responsibility of parents to educate themselves. In a public engagement exercise by the same team, participants thought that parents were able to, and would, take such a responsibility. 12
Second, it could be that information is given but parents cannot assimilate it for some reason. Indeed, it has been argued that it is difficult to establish if information is not given or if it is given but not recognised/read by parents. 66 For example, it is a repeat finding that parents do not read leaflets,12,29,66,68,72 sometimes because of time constraints. It is questionable whether or not ensuring that parents read leaflets would solve this issue as a paper that examined information resource use found that very few parents used leaflets to make their NBS decision. 72
One of the dominant narratives about relevant information surrounded the level of detail needed. However, although a common finding was that parents want more information,29,63,67,68 it was rarely stated what this would look like. Focusing specifically on expanded screening, two characteristics appeared to trigger parents to want more information: the inclusion of diseases for which treatment benefits were less clear and asking parents to be more involved in the decision. 29 However, the issue of providing more NBS information to parents is complicated by the repeat finding that parents feel overwhelmed by information in pregnancy (e.g. Tluczek et al. 63). Indeed, papers talked about the need for brief information29,66 or needing not to overload parents. 61 In one study, participants in a focus group evaluating the current screening booklet for use in England talked about the balance needing to be in favour of not enough information rather than too much. 66 One suggestion was to convey a sense of what is being screened for (i.e. metabolic conditions) without naming all of the conditions. 73 However, work with the public has stated that ‘parents need to be informed about every single part of the screening’ (citizen focus group)12 or that parents could make a decision only if ‘all the implications were clear’. 29 One possible solution to this is that health-care professionals should ask parents how much they want to know. 73 This may address the issue of parents varying in the amount of information sought, implied by differences not only between papers but also within them. For example, in one study, 45% of parents reported that they wanted more information whereas 51% reported that they wanted the same amount of information. 66 Some parents felt that they had the right level of information, others wanted more and some suggested that they had already received too much and that it had triggered anxiety. Thus, taking a population-wide approach to balance overwhelming parents and creating anxiety with underpreparing parents and triggering profound distress may not be effective. One suggestion is that people receive ‘basic’ facts but can access more detailed information on an individually driven level. However, what the basic level of information would be is rarely specified.
Content of relevant information
Establishing what information is deemed relevant is the first step in establishing whether the standard of providing relevant information has been met. Some guidance comes from the American Academy of Pediatrics (AAP) Newborn Screening Task Force95 and some have used this as a yardstick to see whether or not materials are suitable. 74 It suggests that the following should be included: the purpose of NBS, benefits of NBS, how testing is carried out, how results will be received, the need for repeat testing/follow-up, the purpose of the repeat testing/follow-up, the importance of responding quickly to results, how to make contact with the NBS programme, the risk of a false-positive result, the risk of pain/infection, a list of the conditions screened and information regarding storage and the use of bloodspot samples. Additional information found in documents included whether or not consent was needed and whether or not parents had the option to refuse. 75
Another way to address this issue is to examine what information parents want. Nicholls and Southern72 highlighted that, if the information provided does not match what parents think is important, it is likely to be dismissed. Although numerous papers focused on parents’ information needs, these were sometimes inferred from guidelines or from health professionals’ views rather than by asking parents directly. Studies using parent samples found that the following topics were valued:
-
the need for further samples/how to respond if in the USA26,78
-
where to get further information70
-
reassurance70
-
results – range and meaning77
-
what happens if a test is positive70
-
test accuracy70
-
information about the fact that screening uses deoxyribonucleic acid (DNA)70
-
heritability76
-
screening alternatives (e.g. testing later in life)76
Although placed in order of frequency, little can be inferred from this as often papers would use the generic term ‘more information’ and cite examples of information that were particularly salient or currently missing from the information that parents received. A clear message from the literature was the value of tailored information, with parents choosing the level of information received. This was either explicitly found or implied by findings that parents reported wanting very different levels of information. 12,66
How can relevant information be provided?
Parents most frequently received verbal information from health professionals,68,69 leaflets66,69 or leaflets plus verbal information from health professionals. 66,69 Some concerns in an evolving screening programme were reports that the second most likely information source was a previous pregnancy. 68
The use of leaflets seems ubiquitous in NBS. However, concerns have been raised about inherent barriers as a result of literacy levels or cultural competency74 (this will be addressed further in Understanding). In addition, information coverage in leaflets has been reported as being incomplete or presenting a biased picture. 14 As stated previously, it was repeatedly found that parents do not read leaflets12,29,66,68,72 and their efficacy in providing useful information has been argued to be limited in this setting. 30 These issues may explain the finding that only half of the parents sampled in one study had read the leaflets. 72 A related finding is that, in research carried out to evaluate leaflets, they were not given to women who appeared uninterested or for whom English was not their first language. 70 Thus, in this study leaflet design was informed by interested women who may not have had access issues. A further issue is that when leaflets are provided alongside non-health service materials they are not seen as being important. 72 As the authors of this study argue, one of the key issues with the effectiveness of written information is its visibility.
Parents indicated that leaflets should not be relied on and that health professionals should discuss NBS with them directly. 63 However, health professionals appeared to value leaflets, with 80% of them finding leaflets extremely or very useful. 69 Even when leaflets were used, parents wanted information confirmed by verbal communication with a health professional,70 known as a ‘layered approach’. 65 Parents who had questions after reading a brief leaflet wanted to be able to have a discussion with a health professional and written information to back this up. 66
The accessibility of information in leaflets may have contributed to the repeat finding that parents in England wished to receive information from a health professional. 66,72,79 Asian participants or participants for whom English was not their first language were especially likely to prefer information provision by a health professional. 66 This option has some merit as it has been found to be the most effective way to convey complex information96 and parents had a higher recall after verbal conversations45 with midwives. 72 In addition, in a study that reported some of the highest levels of awareness across the literature, the majority of mothers in the sample (34%) had received their information from midwives. 68 Likewise, post-partum nurses were the most frequent informers in a study in Texas. 30 Importantly, although this study uncovered important omissions in the mothers’ knowledge, those who had been informed by a health professional were significantly more likely to know about key issues. Of interest, a range of health professionals were included in this study.
Another way that health professionals were viewed was as ‘gatekeepers’ to information for parents. 72 It has been argued that they can be central in ensuring that parents are sufficiently informed about NBS. 66 Another benefit is the universal acceptance of health professional communication; passive information processers gained information only from midwives, whereas active information processors valued communication with a midwife even though they sought information from other sources. 72 Some reasons offered for this were that parents had already allocated time for this communication (i.e. they did not need to find time to seek information) and that it was easy. 72 Health professionals were valued also in terms of being able to clarify existing understanding, provide sufficient information or signpost to further information.
In some samples parents of affected children suggested that website addresses should be provided to signpost to support groups. 78 This sample also endorsed the internet as a way of providing NBS information antenatally. However, the internet appeared to be used by some parents to gain supplemental information, rather than being a central information source. 72 Such usage may be appropriate currently as mothers who received information via the internet were less likely to have key information, such as how to seek further testing. 30 This was a crucial omission in a sample from the USA, where parents need to actively seek further testing from their provider. However, screening programme websites were used as a key way to engage the public in 13 states in the USA. 17 One benefit is that it may engage parents with low levels of trust in their health-care professionals, as those who reported gaining information primarily from the internet had the lowest levels of trust in midwives. 18 In a study in England, parents indicated that they were less inclined to use the internet because they could not judge whether or not the information was trustworthy and there was a lack of guidance to navigate them to appropriate sites. 62
The use of videos antenatally has generated mixed findings. Yang et al. 64 reported that a brief 10-minute video resulted in parents being more likely to retain information postnatally and engage in appropriate post-result behaviours. However, others have reported that mothers did not find videos to be an effective communication model30 or that few parents value videos and posters beyond their use during antenatal classes. 78 Indeed, in one study a majority of health professionals (70%) believed that parents received information about NBS through antenatal classes. 69 It should be noted, however, that one of these samples78 was supportive of providing audio information and it could be that the use of the term ‘video’ has changed. Once it was a static format but now it is commonly embedded in websites. Indeed, the comments from the participants in this study suggest that this is the case. Therefore, views of video usage may change.
Understanding
Parents who felt that they understood NBS information were more likely to say that they believed that they had made an informed choice. 80 Likewise, although the data are very sparse, they do suggest that the main reason that parents refuse screening is a lack of understanding. 19 Thus, understanding is central to parents’ views on their choice, but also the choices that they make. A recent report on the expansion of NBS in England argued that midwifery support is needed to ensure that parents’ understanding is checked. 73 However, few studies reported whether or not health professionals checked parents’ understanding. 18
One study suggested that health professionals believe that parents can understand NBS information – it is ‘not rocket science’. 73 However, a common finding in the literature was that parents have knowledge gaps that raise concerns about their preparedness to make an informed decision. 26,28–30,33,68,93 Some parents were aware of this and admitted that they had made a decision about NBS without knowing information about symptoms, treatment, severity and hereditability. 76 Other studies, however, suggested that parents were not aware of their limited knowledge. For example, in one of the studies reporting the highest levels of awareness of the purpose of NBS (82%; n = 712), only one-third of parents knew that it was possible to receive a false-positive result,77 an important part of preparing parents for the outcomes of NBS. A further survey of 154 parents from one laboratory in England found that parents had a greater understanding of the process of and rationale for screening than of condition-related information. 80 In addition, although parents in the Netherlands recognised the term ‘heel prick’ and knew that it had been performed, this had usually been without their knowledge of what the screening was for. 29 This pattern has subsequently been reported in a sample of English parents. 66 Interestingly, within this study, parents were asked directly whether or not they understood the NBS information, with 62% indicating that they did. However, within this sample there was poor knowledge and understanding of the conditions screened for or the implications of screening. Furthermore, in a sample of 750 mothers in Ontario, the variation in understanding across topics was as follows: purpose of NBS, 88% understood; how screening is conducted, 85%; the importance of screening, 72%; and how the results would be stored or what happens to the sample after testing, < 15%. 77 This pattern was repeated in a study of 548 post-partum mothers in Texas: 59.1% of women did not know what newborn bloodspots were30 and 68.2% and 71.4%, respectively, did not realise that a positive result indicated that there could be alterations in either their own or the father’s DNA. Knowledge about where they would go to get a second sample or how they would receive the results of screening was also very low, which is of importance in the USA as there is a reliance on parents to proactively seek further testing. The authors of this study highlighted that this raises questions about whether or not parents were aware of the retention of bloodspots. Concerns about the level of understanding that parents have about the retention of bloodspots were also raised by Tarini et al. ,81 who suggested that parents might not understand the utility of the stored bloodspots as those who refused storage were more likely to have lower education levels or children with good health, potentially suggesting a conflation with umbilical storage.
Some of the studies that assessed the readability of NBS materials repeatedly found that materials were written at too high a level. 74,82 One study that examined parent educational materials82 found that the mean Flesch Reading Ease score of the materials was at 10th grade level (the recommendation is grade 6 or below), with one-quarter of leaflets written at college level. Grade 10 was also used for consent forms in a different study. 19 Indeed, only 8% of the materials about NBS designed for parents were written at an accessible level. There were also issues with the images used, which were felt to be misleading, such as ones depicting a toddler, which may lead parents to infer that this is information needed at a later stage. A survey of 106 materials from the USA, the UK and Australia found that 36 used unexplained technical terms and 14 would need expert levels of knowledge to understand. 14 These results are similar to those of an earlier study that reported that 60% of materials provided by USA NBS programmes were at grade 10–11 level. 74 However, importantly, this study found that materials that covered more of the recommended messages did not necessarily have a higher reading age. Thus, there is nothing inherent in the information that causes materials to be complex. Indeed, although a pilot study of earlier versions of the UK NBS materials found few issues, a repeat criticism was that they were too technical and that parents did not need a ‘biology lesson’. 70,78 This was also raised in the piloting of the expanded NBS materials. 66 Collectively, then, there are repeat recommendations that information should be provided in as simple a form as possible,66,78 with a specific finding that the current information booklet in England may benefit from further simplification. 66
There were some more basic, yet hugely important, barriers identified, for example information and consent forms not being provided in the appropriate language,70 despite this repeatedly being highlighted as important17,69,70,78,83 and being policy in many countries. Reasons for this may be gleaned from the study by Stewart et al. ,78 in which health professionals queried who was going to fund these alternative versions. Not having the leaflet available in the language needed was a rationale given by health professionals in New Zealand for not using leaflets at all. 69
Thus, there are issues over information being provided in such a way that it creates barriers to understanding, in terms of level, language or timing. It has recently been highlighted that there is still insufficient evidence regarding the optimal communication model for NBS to achieve understanding. 77 One interesting finding that may suggest a solution to this is that women’s understanding of, and ability to recall information about, NBS increased remarkably if they were asked to sign a consent form. It appears that this process triggered parents to attend to and assimilate information. 19,84 Indeed, this appeared to account for more of the variance in knowledge scores than demographic variables. 84
Some of the issues with research in this area include the difference between understanding per se and knowledge. For example, although 62.2% parents reported that they understood the information that they were given, they also thought that they had low levels of knowledge about the conditions screened for. 66 The link between understanding and choice should also be carefully handled as parents have reported being happy with the decision that they have made, despite illustrating low levels of knowledge of screening, the conditions screened for and the impact of screening. 66
Retention
Although few papers addressed this concept directly, some of the findings discussed in Relevant information are relevant here. One of the standard ways to measure retention is to ask whether or not parents can recall receiving information about NBS or what information they can recall about NBS (it is accepted that the two are not entirely synonymous). For example, the finding that parents reported that they received no information may be linked to retention, as in many studies there was a significant time lag between NBS and parents’ participation in the research. Thus, it is hard to establish whether or not it was the study design or the communication model that was causing the recall problems. In studies in which there was a delay in measuring retention, retention levels varied from 69% of parents recalling having received NBS information77 to the majority of parents of healthy and affected children not being able to recall being given any explicit information about NBS. 29 This lower level of awareness was repeated across several studies,19,33,66,67 with parents also reporting being unaware of what conditions their children had been screened for. 14,28,33 There were also issues over study design in terms of how retention should be measured. For example, although parents might have NBS knowledge that they could recall, this might have been derived from other sources such as the television;29 thus, measuring knowledge is not a direct measure of the success of a NBS communication model as that material may not have been retained.
Although it is arguably very important that parents can recall information if one wants to moderate the levels of anxiety that parents feel when receiving further testing, from the perspective of consent a potentially more important question was whether or not parents could recall the information at the point of making the decision. Newcomb et al. 30 surveyed mothers within 24–72 hours of their child being screened and found incomplete knowledge about NBS and bloodspot storage. Important gaps in their knowledge were that just under half did not know whether or not further tests would be performed, the majority did not know when they would receive the test results or what the implications of positive results were for family members and 63% did not realise that their child’s blood would be stored. Whether or not this is truly an issue of retention and subsequent recall, however, is a moot point as there were significant differences between the mothers based on how they had received their information. Furthermore, Nicholls and Southern62 put forward a very valid argument that measuring recall alone is insufficient as it does not indicate that those recalled facts actually contributed to decision-making. However, the above indicates that, if parents wanted to incorporate information provided by their health service, there is a barrier to them doing so and that parents appear to have low levels of knowledge to draw from.
When should information be given so that it can be retained at the time of decision-making?
One school of thought is that the most likely factor affecting retention is the delay in the time between receiving information and utilising it in a decision. However, it is also possible in this setting that, if information is provided at a time when it can not be assimilated, this would also lower retention levels. Indeed, a main conclusion from a survey of 600 mothers post birth is that information needs to be provided at a time that enables assimilation. 68 This study found that, although 51% of mothers were satisfied with the information that they had been given, they felt that the time at which it was provided determined whether or not they could use it. Another study reported that parents felt that they had received information at the wrong time. 29 Although this is not necessarily easily solved, as parents have different views on when information should be provided, there appears to be a clear message that information should not be provided post birth. 63 Some argue that providing information after birth does not give parents sufficient time to absorb the information. 96 Thus, there appears to be no doubt that there may be barriers to interacting with information,18,66 with communication policies seeming to recognise this. For example, the AAP Newborn Screening Task Force suggests that information on NBS be provided in the third trimester. 74 However, providing information just before the test or at the time of the test (i.e. after birth) is a common finding. 30,33,69,77
There is strong support for information provision in pregnancy. 17,29,33,66,78 An interesting study that explored the impact of providing information about SCD prenatally found that parents were more likely to retain the information given postnatally if they had also received some information prenatally,64 suggesting that priming parents, or providing information repeatedly, may aid retention. Some reported that information should be provided in early pregnancy,29,78 with it being refreshed after birth. 66 However, Moody and Choudhry66 suggested that information is often forgotten if given in early pregnancy. Indeed, this is cited as a reason why some health professionals do not give information in early pregnancy70 and across the literature there seem to be relatively low levels of people giving information at that time. 69
Another common message was that parents wanted information to be given at 36 weeks or during the last trimester. 66,70 They believed that this would provide them with the time to assimilate the information70 and was a time when thoughts of the child were more central. 29 Health professionals also reported that this is the most common time at which they provide information. 69 However, interestingly, midwives have also been reported as stating that parents would not appreciate the provision of NBS information at 28 weeks,78 believing that it is best to give NBS information early in pregnancy and in a written format only. Furthermore, another study based on an English sample reported that some midwives thought that it was not feasible to provide information leaflets at 28 weeks. 70 This partly seemed to be because of workload, but was also driven by a belief among health professionals that providing information postnatally is preferable to prevent it being lost or forgotten. 70 Although this belief was held by a minority of participants, and in this study there was also a discourse about information not being given ‘too late’,70 it does show that there can be resistance to providing information antenatally and that there are differing views between and within parent and health professional samples. What this highlights is that people may want information at different times. 29 For example, it has been reported that first-time mothers especially wanted time to read and digest the information. 66 This was also echoed in data from a CF nurse in the study by Hargreaves et al. 70 To fit this need a flexible approach could be taken, with information provided any time after the anomaly scan. 78
Concepts that are important when parents are decision-makers
The following concepts became more important to factor into communication models when the aim was to enable informed consent. In this section the literature related to intellectual capacity, control and intentionality is reviewed. Suggestions for alternative models of consent based on the literature are also outlined.
Intellectual capacity
There is a reported belief among parents that teenage parents may struggle with NBS information,33 yet there were no data in the papers examining this. There were also no data that examined directly whether or not certain groups of parents would lack intellectual capacity to understand NBS information.
Another consideration is whether or not NBS occurs at a time when parents may temporarily lack capacity. Currently in England, although policy states that parents should be informed about NBS before birth, they are asked to consent to NBS after birth. Parent data suggest that this is a time when there are competing demands on parents’ attention. 66,69,70,78 Mothers are recovering from the birth69 and will be tired78 and some parents admitted that this meant that they probably did not pay attention to what was being said to them. 14 A lot of information is provided at this time70 and new parents are having to make many decisions. 69 However, direct data examining parents’ intellectual capacity at this time seem sparse. 73 Hargreaves et al. 70 appear to suggest that parents’ ability to assimilate information may be hampered and Nichols79 reports data from mothers suggesting that this is the case. It should be noted that not all data fitted with this pattern, as Nicholls and Southern62 found that only 10.6% of 154 parents felt that they were too tired and 9.7% felt that they were too emotional to make a decision.
Control
The requirement to gain informed consent from individuals before they undergo medical treatment or procedures is founded on the idea that individuals should have control over what happens to them in a health-care setting. Thus, even if individuals make what others see as an unwise decision, as long as we feel that those making the decision are sufficiently informed, have the mental capacity to make this decision and are not coerced, we feel that this decision should be accepted. To do otherwise would be to move backwards to the days of medical paternalism. Thus, one of the main foundations of valid consent is that people have control and are not coerced into giving consent against their wishes. Therefore, for consent to be judged as valid, parents must be clearly aware that there is a choice to be made, that is, it must be made clear to parents that they can decline NBS screening. Indeed, if parents recalled that screening was presented as optional, this was a significant predictor of whether or not they felt that they had made an informed choice. 80 The literature discussed previously suggests that there are many cases in which is it not clear that the ability to refuse was made clear to parents and thus whether or not the voluntariness of the consent given could be said to be confidently met.
Another related question is whether or not parents feel that they really do have a choice to decline, even when the option of declining testing is made clear. One study suggested that only 7% of health professionals would accept a parent’s choice to refuse NBS without taking further steps. 69 Although most commonly this would be providing more information (64%), it could also include actively persuading (13%). 69 Liebl et al. 15 report that if screening has not been performed parents are contacted and counselled on the importance of NBS. Thus, although declining screening may well be theoretically possible, the reality is often that parents are not aware of this option or a great deal of pressure is put on parents to agree.
Nicholls and Southern62 argue that there is a need to look at context to understand parents’ decision-making. What follows is an overview of a range of contextual factors that may contribute to parents’ feeling of choice. Kemper et al. 17 report that 15 out of 51 states in the USA have no requirement to inform parents that they have a right to refuse the screening. In an evaluation of 106 leaflets from the UK, the US and Australia, only 38 mentioned whether or not screening was mandatory. 14 Of the 25 leaflets that discussed choice, 10 presented this along with a recommendation for screening and four highlighted the negative consequences of declining screening. Furthermore, there was an overwhelming bias towards presenting the benefits of NBS compared with the limitations. Nicholls18 used this to argue that subtle pressures operate in NBS rather than overt coercion. This was also echoed by Newson,83 who stated that, although legal intervention is unjustified in PKU screening refusal, the state still has an influence (not overt coercion) through health professionals. It is important to note, however, that some parents do welcome direction. 79 Some studies examined whether or not parents felt that they had a choice and found that parents were not aware that they could opt out of or decline screening,19,20,29,66,77 as it was not presented as optional14,18,66,80 or midwives just assumed that screening would take place. 14,66,70 Some parents also feel that choosing screening is expected of them. 80 In a recent study in England, 41% of parents felt that they could not decline NBS and believed it to be compulsory. 66 Nicholls18 argues that the lack of perceived choice or the perception that NBS is mandatory may suppress parents’ information seeking or knowledge, possibly as parents perceive little need for it. However, parents who perceive greater choice have higher perceived knowledge of NBS and hold more positive attitudes towards screening. 18
Another form of coercion is to allow insufficient time for parents to make their decision, resulting in them being more likely to follow the guidance of the person offering the intervention. Indeed, Nicholls and Southern80 found that, if parents felt that they had had sufficient time to make a decision, it significantly predicted a feeling that they had made an informed choice. When asked how long they needed to make a decision regarding expanded NBS, 58% of parents reported that they wanted between 1 day and 1 week to decide. 66 However, parents also reported not being given any time to decide; they were just told that screening would be carried out or were given information just before the bloodspot was taken. 18
The timing of information provision can also be detrimental to informed decision-making, for example being asked to make an informed decision postnatally,18 which some may argue is a form of coercion. Indeed, Moody and Choudhry66 argue that parental control is lacking in NBS for a number of reasons, including because of anxiety, dependence on and trust in health-care professionals, the challenge of new parenthood and the ability to read and retain information in the postnatal period. 66 In one of the largest interview studies of parents’ experiences of being informed about NBS, the issue of the timing of information provision was more prominent than how parents were informed or who informed them. 63 However, in one study most parents (68%) felt that they had had enough time to make some form of a decision and > 70% felt that they had made an informed choice. 80 The problem with this may be that people do not know what they do not know, as highlighted earlier.
In the study by Nicholls,18 participants stated that they believed that raised hormone levels had altered their ability to make decisions. This led some participants to talk about how, even if they would have questioned the screening information antenatally, they would fail to do so postnatally. This is a vitally important insight that illustrates how, although parents may not lack the intellectual capacity to make a decision per se, actively engaged people can become passive if information is provided postnatally. Nicholls18 concluded that this highlights that the postnatal period is not the right time for information to be provided. Arguably, this could be extended to include that the decision should not be made at this time either if the goal is to ensure that parents make an autonomous decision.
Another practice that is recognised as being detrimental to a person’s ability to make a choice is to make a process routine. It can be argued that making the screening process routine sends a message to parents that screening is important and recommended, which may make it increasingly difficult for them to voice alternative views. This was indicated across multiple studies, with parents reporting routinisation of NBS and that they had not explicitly consented but health-care professionals had assumed consent. 14,18,29,65,79,85,86 Even when explicit consent was sought, parents were encouraged to comply with a highly routinised procedure. 73 Nicholls79 argues that the inclusion of NBS with the other postnatal checks that are readily accepted makes NBS more automatic.
Intentionality
Although a minimal number of data related to the concept of intentionality directly, tangential evidence raises concerns whether or not a cognitive process took place whereby parents made a choice. Stewart et al. 78 outlined that an informed decision is one where all the available information about the health alternatives is weighed up and used to inform the final decision: the resulting choice should be consistent with the individual’s values.
However, Nicholls18 raised the concern that the view that parents consider the information provided by the health professional and then make a decision based on this is not only simplistic, but also wrong in some cases. In addition, as discussed earlier, many parents were unaware that screening had taken place,28,97 indicating that no cognitive appraisal of beliefs and choice could have been made. This raises the question of how to change the current process to ensure that a cognitive appraisal is made and that parents feel that they have a choice. One suggestion from parents was that asking them to sign a form would make intentions clearer. 14 This process was seen as being even more important if the bloodspot sample was going to be stored. 70 There was also a belief that this would trigger cognitive appraisal, but it was also noted that for parents to engage with the screening properly they must be provided with all of the necessary information. There was recognition, however, that parents may need different information depending on their values to support them in their decision-making. 65
Part of intentionality is how much a person wants or wills what has happened. This was echoed in the literature as several authors felt that NBS decisions should reflect parents’ social and cultural values,18,69,78,83 as in many other decisions that parents make for their children. 83 Although there is a recognised lack of data regarding this issue,80 it is known that uptake rates are high for NBS69 and therefore if choices are being made in line with attitudes then parents’ attitudes should be similarly positive. When asked directly, parents do indicate that, had they been aware of the choice, they would have chosen to have their child screened14 or that they are supportive of screening for serious disorders, whether or not treatment is available,12,87,93 and expanded screening. 67 It has also been reported that 42% of parents would agree to screening immediately (i.e. without needing further time to think about it) if offered expanded NBS,66 suggesting that this is seen as something that is essentially so positive that it does not require consideration. One study reported that 95% of parents agreed that NBS was valuable. 68 This is possibly because of inherent recruitment biases, whereby those who value screening are more likely to participate in research. Indeed, one comment in the data – ‘if it’s a screening thing then that can only be good can’t it’14 (author italics) – may indicate a concern about how informed these views are if people think that screening is without harm. Across studies, parents who refuse NBS are rarely included in samples. One repeat finding suggests that parents whose children screened positive are most pro-screening. 14 Although this is understandable, what is not clear is whether or not it is because these parents are also the most educated about screening or because they have derived a benefit from screening. Another possibility is that studies recruited information seekers, as inherent in some data were perceptions that all knowledge that you receive about your child is good. 87
How much do parents value choice?
The consent model and how this is enacted can also link to coercion, as shown in the finding that both health professionals and parents of affected children preferred a model of verbal consent and written dissent as it made it easier to ‘give rather than withhold’ consent,14 although others in this study did not support this as they felt that it would seem coercive. On a policy level, the most common view appears to be that NBS should be strongly recommended to parents, despite there being a right to decline. 65,83 However, Newson83 argues that the state should not interfere even if parents act recklessly or wrongly as long as there is no serious threat to the child’s life or welfare, with others suggesting that the state should get involved only in ‘extreme circumstances’69 (e.g. when there is danger to life). Linked to this was a concern that if parents feel pressurised to participate in NBS it could jeopardise future attitudes towards health care. 83 However, it was also argued that parents have an obligation to make choices that do not foreclose choices that children may want themselves when older. 83 This is most commonly linked to outcomes for children who screen positive who may not get treatment quickly enough otherwise. Indeed, some parents and health professionals use this to argue for mandatory screening. 14 One study suggested that health professionals believe that NBS is part of the moral imperative to save life and therefore one should not worry about ‘delicate issues about consent’. 73 That the benefit to the child was more important than the parental rights to decision-making was also argued elsewhere. 88
Mandatory screening has some support from data from parents of children identified with conditions through NBS,14 with support also coming from health professionals. 12,14 However, some of this support comes from studies examining PKU and CHT, for which there appears to be more consensus among clinicians and more support from parents for mandatory screening than for other conditions. 33 Likewise, in the Netherlands, when asked to reflect on screening for PKU, CHT and adrenogenital syndrome, as many parents were in favour of mandatory screening as were in favour of informed choice. 29 A very important caveat is that respondents did not feel that mandatory screening was important for them, rather that other parents may need it. For example, some parents raised concerns that others may refuse screening out of ignorance,33 focusing especially on teenage or less educated parents. Of interest, these same parents discovered through participating in the research that they had limited understanding themselves. However, it has been shown repeatedly that implementing informed consent models does not affect uptake20 and has actually lowered refusal rates. 89 Grob90 also argues that the above is a weak argument when one examines the outcome of informed choice models on uptake compared with the impact of positive results with low awareness. Another argument for seeking mandatory testing is provided by data which suggest that health professionals believe that informed consent is not possible because of the amount of information that would need to be covered. 73 Although providing information to enable informed choice in NBS will always be a challenge, it is not clear that this is a challenge that cannot be met; levels of support for mandatory screening can be low (23%), with up to 61% of health professionals actively disagreeing with this model. 69
In assumed consent models, parents can opt out of screening if desired, although the onus is on parents to make this clear to the health professional. A small proportion (11%) of health professionals suggested that this was being practised in New Zealand as they reported that, although parents were aware of the need for screening, they were not asked for consent. 69 Interestingly, 77–88% of participants in focus groups supported the idea of screening without explicit consent when treatments were available. 12 This changed if treatments were not available. Another form of informed consent is an opt-out model and this was endorsed by most parents if screening could prevent harm to their child. 29 This model had the highest levels of support from parents in the most recent study regarding expanded screening in England. 66
Data suggested that, when conditions are included in NBS panels for which the arguments regarding the need for screening may be weaker, it was important that parents were able to make a choice. 12,70 Interestingly, this was more commonly argued by health professionals than parents. 14 However, a preference for informed consent is a repeat finding in samples of health professionals69 and parents. 67,98 Parents have also been reported as wanting choice in expanded screening in England,66 yet, interestingly, in this sample only 27% supported an opt-in model of consent.
Choice appears to be valued, especially regarding the retention of bloodspots. 14,68 Indeed, a sense of a lack of control has been cited as a reason for parents opting out of storage. 30 A repeat finding is that storage of bloodspots triggers people to want a choice, with 49% indicating that it was not permissible for the state to store bloodspots without permission from parents. 30 A benefit of informed consent was found to be that practices such as storage could be accomplished with public support,20 rather than with concerns of a backlash/drop in engagement. This fits with findings from the USA where, although parents were positive about the idea of bloodspots being used for research, this was only with parental consent. 68
Interestingly, although 65% of health professionals reported that parents were asked for verbal consent, only 39% endorsed this model of consent. 69 Verbal consent was seen as sufficient by parents, though, even when considering expanded NBS. 66
Hargreaves et al. 14 reported that many health professionals and parents in their English sample valued written consent. However, this is not practised in England. In the USA only five states require parents to consent and each of these require parents to sign a consent form. 17 In a study from New Zealand, although only 20% of health professionals asked for written consent, 55% felt that there should be written consent. 69 Importantly, most of these respondents felt that consent for screening and consent for storage should be split. 69 There is some merit in this given that it is a reason cited for parents opting out of screening. 69 Split consent models are also used in three states in the USA, where the core panel is mandatory but parents are able to decide about additional tests. 17 Again, there seem to be benefits of this flexibility, with the authors stating that it enables pilot studies to scale up more quickly. Some concerns have been raised about written consent models, with parents reporting that it would cause them to be suspicious as other screening programmes do not require it and that it could lead to mistrust, worry or a perception that the decision must be difficult. 66
What is important to note is that countrywide research appears to show that health professionals can be practising up to three different forms of consent simultaneously69 and may be practising consent models that they do not believe in. 69 There is also a consistent finding that parents within one study can have very different views about the level of consent needed. 19
Discussion
This study created an analytical framework from the autonomous authorisation model and populated it with empirical data. Overall, many of the concepts of the framework were neglected. Although most studies studied some aspect of the consent model, none did so holistically. There seemed to be a predominant focus on ‘relevant information’ and ‘not coerced’ and yet intentionality and intellectual capacity are neglected and information about understanding and retention is sparse.
Thus, although the above suggests that there is a fairly good consensus on what constitutes core topics of relevant information, there are a lack of data regarding whether or not this information is understood or retained at a time when parents need to use it. Focusing on just one of these factors can render the information useless, for example if relevant information is provided but it cannot be understood or retained. This highlights one of the most important messages regarding communication and consent models in NBS implicit in the literature: when evaluating a communication model it is important to look at information receipt rather than the far more common focus of information provision. In some of the above studies it was very difficult to state categorically what the information provision had been and whether or not parents had been provided with information or a choice at all. However, in terms of assessing whether or not someone has made an informed choice or is trying to reduce the potential psychological harms of NBS, what is important is whether or not parents had sufficient information to be prepared or to make a sufficiently informed decision. 13 This is of concern as, although variation existed in terms of preferences for consent models, knowledge was universally valued. 12,19,61 The finding repeated throughout this review, however, is that data suggest that parents did not have full knowledge of what was happening. 26,28–30,33,68,93 The finding that parents are not adequately informed fits with what is known from research conducted with parents after they have received their child’s result, which shows that their awareness is linked to how well they adapt to the results. 99
There was also variation in the literature in how and when29 parents should be informed about NBS and the level of detail sought. It may be that these factors make it impossible to design a uniform communication model that works optimally across all populations. It could be that some flexibility is needed whereby there are standard goals of information provision, with these met by enabling varied delivery methods and timings. 65
The review also suggested that there could be differences in parents’ and health professionals’ views regarding the timing of information provision and consent models. 91 As this may explain one of the barriers to effective NBS, it is important that future research examines this. However, one of the issues that this review highlights is the difficulty of comparing midwives’ (or health professionals’) views with those of parents if the research is conducted at different time points, as changes in screening could account for differences in opinion. Therefore, to truly understand NBS communication issues, research needs to sample health professionals and parents simultaneously.
Another concern from the literature is that there appears to be evidence that, when choice is given, the level of choice falls below what would normally be expected to meet the current legal test of informed consent. Additionally, there appears to be evidence of coercion18,83 in the way that NBS is presented to parents. That current practice may not fit with existing standards of informed consent may support critics of the autonomous authorisation model, who argue that, although it may be a useful theoretical model, the challenges of achieving such consent in practice mean that alternative practice occurs. This may also explain the variation in consent models that health professionals are practising within one region. 69 It could be, therefore, that the fair transaction model may be quite relevant to NBS, in which issues arise such as the complexity of information provision; giving communication and understanding; the pervasiveness of indirect and direct coercion; the limited cognitive space and time for decision-making; the complex risks and benefits of screening; the giving of surrogate consent by parents; the potential effects on others of screening; and the wider societal attitudes to and values placed on such screening.
However, the autonomous authorisation model of consent is more in line with current English law on this issue and with parents’ clearly expressed views that they would like to be given clear information12,19,61 and have the ability to make decisions for themselves and their families. It is not yet clear whether or not alterative models of communication in NBS could be designed to enable parents to make decisions that would meet the criteria for informed consent. Rather, the central dialogue implicit in the data appears to be that special consideration needs to be taken of the complexity of NBS when designing communication and consent models for this screening programme. It may not be sufficient to ‘just follow the standard template’ of other screening programmes, as this screening programme is unique in (1) asking for proxy consent, (2) at a time when it is challenging to make decisions and assimilate information and (3) for a number of different conditions simultaneously.
The range of alternatives in communication and consent was used to generate a pre-interview tool to give participants a chance to consider alternatives to current practice. The subsequent interviews are reported in the following chapter.
Chapter 3 Study 2: interview study
Study objectives
-
Explore how providers and users envisage that information given antenatally can best meet the challenge of effectively and efficiently providing parents with sufficient understanding of an extended NBSP, including their reflections on the alternatives identified in the review.
-
Examine parents’ understanding and experiences of NBSP communication to draw inferences regarding best practice within an extended NBSP.
Introduction
There were recognised gaps in the research regarding the effectiveness of NBS information provision, including information provision antenatally;100 the effectiveness of alternative communication models;101,102 and parents’ views. 21,34,101 Thus, this project focused on a need to develop the evidence base to produce acceptable, efficient and effective models of NBS communication in the antenatal phase.
Methods
Design
A qualitative design was employed whereby semistructured face-to-face and telephone interviews were conducted. We began with the interviews with health professionals, with parent interviews starting once approximately one-third of the health professional interviews had been completed. This overlap in data collection allowed the emergent data from the health professional and parent interviews to be incorporated into the remaining interviews for both groups, enabling the team to explore emerging ideas in subsequent interviews.
Health professional sample
All senior quality assurance managers (SQAMs) in England were invited to participate as previous work103 has shown evidence of variation in NBS communication practice and discussions with screening co-ordinators about the design of this project suggested that variation in practice persists. Current communication practice will affect views of alternative models and thus we sought to capture maximum variation in practice. Midwives in the community and hospital setting were sampled nationally, proportional to those involved in NBS, and purposively to capture variation in experience. Preliminary discussions with screening co-ordinators and research midwives suggested that the following numbers of health professionals would provide a sample that proportionally represents front-line professionals involved in the communication of NBSP information: 18 hospital screening co-ordinators, 14 community midwives and four hospital-based midwives.
Using publicly available details, initial contact was made with SQAMs. Subsequent participants were identified and recruited through snowball sampling in which SQAMs forwarded the study information to trust screening co-ordinators who forwarded the information to community midwives. Although all participants were qualified midwives, those involved in quality assurance did not practise clinically.
Parent sample
Within the parent interviews, views were sought representing parents across the screening pathway and with experience of different outcomes. Parents were purposively sampled from different stages of the NBS pathway to include parents-to-be, parents of children with a normal NBS result, parents of children with a metabolic condition, parents whose child had had a false-positive result/avoidable repeat sample and parents awaiting their child’s NBS result. Sample frameworks were based on discussions with local NBSP advisors, data from previous annual reports for the Manchester Newborn Screening Laboratory and experience of conducting interview studies with parents with regard to NBSP communication. Participants were recruited through screening co-ordinators and midwives, NBS laboratories across England, and Sure Start and family centres to reach more diverse parents. Throughout recruitment the team interrogated participant demographics and emerging narratives to direct further theoretically driven sampling. 104
Measures and procedure
Prior to the interviews, participants in the parent sample were presented with a summary of alternative consent and communication models for expanded NBS (see Appendix 2). A semistructured interview schedule was designed by members of the team with expertise in qualitative methods and NBS communication. This was developed from the findings of the realist review, guided by the scientific advisory board, parent reference group and advisors, and was piloted with two parents. Participants were asked about their views on alternative consent and communication models, with prompts directing them to discuss factors that might affect acceptability or understanding within each model. Parents were also asked how they were informed about NBS antenatally and to reflect on their level of understanding and if/how this was affected by content or mode of information provision. Interviews were audio recorded and transcribed by a professional company.
Interviews were conducted in parents’ homes for the parent samples and by telephone for health professionals.
Analysis
The majority of the data was analysed using thematic analysis, which seeks and reports the patterns that are inherent within the data collected. 105 Thematic analysis is a commonly used method that results in a rich and complex yet accessible account of the data. 105 It has been widely used in evaluative and health-care studies similar to this one. 13,106 Thematic analysis was chosen as it allowed for an understanding of the data to be developed and patterns within the thoughts and views of participants to be examined. 105 It was also chosen as it would ultimately allow for the views and opinions of all participant groups to be expressed and heard, in their own way. 107 One major advantage of thematic analysis is its flexibility, whereby the researcher can take either an inductive or a deductive approach, or even a combination of both approaches. 108 Analysis of the data was conducted using a realist method, by which the participants’ reality, experiences and meanings were reported. 105 A hybrid process of both inductive and deductive thematic analysis was used to code the data. 108 Aspects of grounded theory that enhance rigour were used, such as iterative data generation and analysis, constant comparative analysis,109 and detailed line-by-line coding.
For the health professional sample two researchers independently coded six transcripts each in NVivo. The first researcher (ND) followed an inductive approach whereby themes were generated by examining the data alone. The second researcher (FU) followed a more deductive approach by coding data using preselected categories outlined in the protocol. Comparison of the thematic frameworks revealed that almost identical categories and themes were developed by both researchers. The parent data were coded by ND and the emerging coding framework was developed with guidance from FU.
For both analyses, to develop recommendations on alternative NBS communication models, most themes were coded at the manifest level;110 however, when appropriate, a latent analysis was conducted to enhance the depth of the analysis, utilising the flexibility inherent in thematic analysis. 111 Coding was conducted systematically and iteratively. Deviant cases were sought to test the emerging framework. Coding continued until the analysis team was satisfied that the framework adequately described and captured the data and saturation had been achieved. ‘Member checking’ is a form of validation in qualitative research112 whereby initial findings are reported to participants to elicit feedback, as detailed above. This process is inherent in the final study (see Chapter 7).
A subset of data from the health professional interviews pertaining to information content was analysed using content analysis. 113 Interview transcripts were scanned for content terms, which were then collated into NVivo nodes and grouped for similarity of topics. The frequency of topics was then calculated.
Ethics approval
Ethics approval for the health professional interview study was obtained from the University of Manchester Research Ethics Committee (reference number 13198). Ethical approval for the parent interview study was obtained from the NHS West Midlands Edgbaston Research Ethics Committee (reference number 13/WM/0438). Research and development (R&D) approval was gained from trusts for the health professional and parent interviews.
Health professional participants provided verbal consent for the telephone interviews whereas written consent was obtained from all parents. Interview transcripts were fully anonymised with all identifiable information removed.
Results
Participants
Health professionals across the NBS pathway participated in interviews (n = 37). The sample consisted of SQAMs (n = 6), a regional quality assurance manager (n = 1), hospital screening co-ordinators (n = 13), community midwives (n = 14) and hospital midwives (n = 3). Participants employed by the NHS were based across 16 trusts in rural and urban areas of England. All regions of England were represented in the sample. At the time of interview, 19 participants were working in a trust implementing the expanded NBSP pilot.
Semistructured interviews were conducted with 45 adults (37 women and eight men). Participants were recruited from different stages of the NBS pathway, with the sample consisting of parents-to-be (n = 14), parents awaiting their child’s screening result (n = 6), parents of children with a normal NBS result (n = 15), parents of children with a metabolic condition [n = 8 (PKU, n = 4; MCADD, n = 2; GA1, n = 2)] and parents whose child required a repeat bloodspot sample (n = 2). The mean age of parents was 38.82 years (standard deviation 5.10 years). The majority of parents had one or more children at the time of interview. Table 1 provided the sociodemographic characteristics of the parent sample.
| Characteristic | n (%) |
|---|---|
| Age (years) | |
| 18–25 | 5 (11.1) |
| 26–30 | 8 (17.8) |
| 31–35 | 15 (33.3) |
| 36–40 | 17 (37.8) |
| Ethnicity | |
| White British | 26 (57.8) |
| White European | 6 (13.3) |
| Black African | 3 (6.7) |
| Pakistani | 3 (6.7) |
| White Irish | 2 (4.4) |
| Black Caribbean | 1 (2.2) |
| North African | 1 (2.2) |
| British Chinese | 1 (2.2) |
| Mixed | 1 (2.2) |
| White other | 1 (2.2) |
| Primary language | |
| English | 35 (77.8) |
| Urdu | 3 (6.7) |
| French | 2 (4.4) |
| Polish | 2 (4.4) |
| German | 1 (2.2) |
| Romanian | 1 (2.2) |
| Ukrainian | 1 (2.2) |
| Employment status | |
| Employed full-time | 25 (55.6) |
| Employed part-time | 7 (15.6) |
| Full-time parent | 3 (6.7) |
| Full-time student | 2 (4.4) |
| Self-employed | 5 (11.1) |
| Maternity leave | 3 (6.7) |
| Highest educational attainment | |
| Degree or higher degree | 30 (66.7) |
| NVQ, Diploma, A level, HND or equivalent | 13 (28.9) |
| GCSE or equivalent | 2 (4.4) |
| Number of children | |
| Pregnant with first child | 12 (26.7) |
| Parent of one child | 11 (24.4) |
| Parent of two or more children | 22 (48.9) |
Results overview
Although the focus of this chapter is on communication strategies to ensure parent understanding, as outlined in Chapter 2 the design of communication models can depend on the NBS consent model. Therefore, data on health professionals’ and parents’ views about consent are presented first. Next, data relating to what health professionals and parents felt constituted ‘sufficient understanding’ are presented before considering the findings on parent experience and understanding. These data are contrasted with the ‘sufficient understanding’ data to foreground the findings relating to alternative models. The third section outlines the challenges of providing NBS information and how best they can be met to ensure sufficient understanding. In addition to data from the interviews, data from the stakeholder consultation are included, in which participants reflected further on their experiences.
Although the aim of the last qualitative study was to ask parents and health professionals to reflect on the project’s findings, it was found that many participants provided further depth on their original data in line with repeat interview methodology. Owing to the ability for these data to inform the research objectives of this study, relevant information from the final study was incorporated into the data set for this chapter. To provide clarity regarding the source of data, however, any data from the final study that are reported here are marked up with ‘i’ or ‘fg’ to indicate that it came from an interview or a focus group, respectively, in the final study.
Views on consent models
As consent is not an everyday topic that people discuss, parents were provided with consent options in a pre-interview tool so that they could consider their views before the interview, rather than being asked on the spot for their views. As health professionals should have received training on consent issues it was deemed reasonable to ask them directly for their views. The parent consent preferences in the pre-interview tool are provided in Table 2.
| Preference | Number of parents |
|---|---|
| Parents can choose if their baby will be screened or not | 9 |
| Parents can choose if their baby will be screened or not and, if they say yes, they can choose which conditions they would like their baby to be screened for | 7 |
| Health-care professionals will assume that parents want their baby to be screened. If parents do not want their baby to be screened, they will have to explain the reason why to a health-care professional | 19 |
| Parents do not have any choice about screening as screening is compulsory for all babies | 10 |
Because of the sampling strategies adopted in this study, the numbers in Table 2 should not be used to indicate preferences for consent models in a population; rather, they simply outline the range of views of parents within our sample. Although there was variation in the level of choice that parents wanted for NBS, there was a unanimous consensus that it was important that parents were fully informed about NBS and its implications:
I suppose it’s about being involved and being made aware as to what is happening, what the options are, what are the advantages, disadvantages, effects, that kind of thing. And just about, yeah, sort of being fully informed as to what’s happening to my child. And for my husband as well, not just for me.
#6, mother-to-be
Informed consent
The majority of health professionals stressed the importance of informed parental consent:
I think it’s important in everything we do. At the end of the day it’s the woman, it’s their baby and they’ve got a right to say what tests they want for themselves and their children. I certainly wouldn’t have appreciated it if somebody had have said to me when I had my children that this is what we do and that’s it, they just get on with it.
#22, trust screening co-ordinator
Parents, however, varied considerably in terms of their preferred model of consent. For parents who valued having a choice with regard to screening, their perceived responsibility to act in their child’s best interest appeared to underlie their views on choice:
Because even though obviously they’re their own person, you are responsible for them and until they’re of legal age, they are your responsibility. So it’s a bit like a freedom, isn’t it, and it’s the right to choices and things like that.
#42, mother, second child, both negative results
For one parent, the opportunity to make a choice about NBS appeared to foster empowerment and confidence as a mother, compared with her experience with her previous children when screening was not perceived to be a choice:
[. . .] because I had a choice and that made me feel good because it made me feel like a parent, whereas with the other two children I felt like I had no choice and she just came and did it.
#41, mother, third child, all negative results
There was also widespread acknowledgement that true informed consent was often difficult to obtain in practice as many parents had not read the information leaflet or fully grasped the implications of screening:
I think it is quite tricky to get informed consent on some occasions because some parents they just consent and they don’t really know what it’s for but at the end of the day they don’t really want to know. They don’t want to read the leaflets, they don’t want to be told about it, but they’re happy to have any tests done on their baby for the health of their baby.
#30, community midwife
Thus, the reason why parents are ill-informed was placed onto parents’ lack of engagement. In contrast, although parents also queried whether or not informed consent really occurred, they had a different view on the reasons for non-engagement:
I think maybe option B is a better option of parents actually saying yes, I would like this screening. But for it to be offered, so this is what we offer; would you like to have that? And then maybe that should be documented as you . . . so not just having the leaflet and that’s you giving your consent because you’ve been given a leaflet.
#1, mother, English, second child, negative result
Indeed, the overarching message from parents was that they would have wanted and accepted more involvement in learning about NBS and felt that the distribution of leaflets was not enabling this. However, some parents did feel that they had been informed and one parent felt that she had made the choice to have their child screened. This participant was a doctor and may therefore have had prior awareness of the relevance of this information.
Assumed consent/opt-out
Health professionals were generally not in favour of assumed consent/opt-out because of concerns that such a model may not place sufficient onus on the health professional to ensure that parents are informed. Front-line professionals could see how this might lead time-pressured health professionals to prioritise other tasks. For health professionals involved in training and quality assurance the link between professionalism and rigorous informing practice was key:
You’ve got to maintain your professionalism and in something like screening if you just have an opt-out policy, you are, kind of, doing your own profession an injustice by not giving all the information that you should be giving to the parent.
#3, SQAM
However, several front-line professionals acknowledged that there was often an assumption of parental consent in current practice as NBS was offered as part of routine care:
I think there’s an element of that, to be honest with you, that we already do assume [. . .] Yeah, we do actually, because we diary it in, that’s a routine sort of midwifery . . . see them on the day they come out of hospital, you then see them on day 5 for bloodspot and weight, and then you see them on day 10.
#12, trust screening co-ordinator
This highlights how practices that are not directly linked to information provision can convey the extent of choice to parents. This aligned with the experience reported by most of the parent interviewees:
Because you just kind of almost go along with it, I felt you’re just going along with what they’re telling you, and they’re not telling you that much.
#2, mother, English, two children, normal result, focus group
Of interest, parental views that this model would be an improvement were based on the belief that it should trigger communication between health professionals and parents, as their experience had been of minimal or no communication about NBS. That all health professionals reported that communication was occurring highlights the discrepancies in views between health professionals and parents:
Like even though I had said that I’d be perfectly happy with the health-care professional handling everything but, you know, with the caveat that they can actually explain the rationale rather than just go ahead and do it without explaining anything.
#27, father-to-be
At least you would know whether they’d been informed or not, because the health-care professional could be like, well, you know what might happen if you don’t have it. So then they are being informed actually because they’re talking to the health-care professional on why they don’t want it.
#17, mother, child has PKU
Generic consent
As with assumed consent, midwives emphasised the need for parents to be fully informed prior to screening. However, midwives did admit that further expansion of screening may require changing the consent model, depending on the number of conditions:
Again, if it was to be a case of in 10 years’ time we’re now testing for 20 conditions I think it would have to be a case of looking at a different way of consenting and perhaps examining more closely something like a generic consent.
#19, trust screening co-ordinator
These sentiments were echoed by parents, who reflected on the amount of information that may need to be conveyed in the future if further conditions were included and whether or not this was necessary or desirable.
Mandatory screening
Mandatory screening was not supported by any of the health professionals. Of particular concern to health professionals was the added vulnerability that they faced as professionals by collecting a sample without parents’ consent, something they felt was incongruent to the ethos of providing choice in midwifery practice:
I’m thinking of all of the screening programmes that we offer and yet have different means of consenting for different tests within the antenatal and newborn screening programme. So while most things its informed consent such as the Down’s syndrome screening and then to have a mandatory consent for another part of the screening programme it seems to be that the principles are seen to be a little bit conflicting.
#19, trust screening co-ordinator
Several participants were also concerned that making screening mandatory for all babies could result in a backlash, with parents rejecting screening as well as other health services for their newborn child:
I think when we absolutely mandate that you have to have these things is when you risk women registering their babies in the first place and slipping under the radar.
#1, SQAM
Interestingly, the vast majority of parents reported that they were unaware that they had a choice over NBS, with many believing that it was a mandatory procedure, although, on the whole, parents were happy that their child had been screened:
I didn’t realise I had a choice to opt out but I think it’s a bit crazy if you opt out really, especially if you can find out and do something about it.
#7, mother, second child, both negative
No, no, it wasn’t, do you want your child to have this test, it was she is having it.
#13, mother, pregnant, second child
Many parents contrasted their experience of choice with regard to NBS with their experience of antenatal screening and noted the differences between these:
When you have the testing done in your pregnancy, the scans, that felt like an option. It was like would you like to have this? That was never presented to me with the newborn screening. It was like we’re coming to your house to do this. So it was never an option of not having it really. And I never questioned that.
#1, mother, second child, normal result
I think it should be down to the parents, just like the Down’s syndrome test is completely optional and up to yourself.
#21, mother-to-be
Summary
There appeared to be variation in the parent sample regarding the level of choice that they wished to have with regard to screening. However, health professionals felt strongly that an informed choice model should be followed and, regardless of their views on consent, parents felt that it was necessary that they were fully informed about NBS. The next section examines what information would need to be provided to achieve this.
Sufficient understanding and parents’ actual experiences and understanding of newborn screening
The goal of NBS communication globally is to ensure that parents receive ‘sufficient information’, yet this is poorly defined. This study sought to establish what ‘sufficient information’ is within England. The second objective of this study was to examine parents’ understanding and experiences of NBSP communication to draw inferences regarding best practice within an extended NBSP.
Sufficient understanding
All participants emphasised the importance of parental understanding of NBS information prior to screening. Participants were asked what information they thought parents would need to enable them to have sufficient understanding of NBS (Table 3). Again, little inference can be taken from the frequencies of responses, other than that they indicate the variation within one sample. Examining the data in more detail showed that midwives placed importance on parents being aware not only of the conditions being screened but also of the potential implications of the conditions and the importance of early detection through screening:
I think that all of the midwives that I know, [. . .] would agree that it’s our responsibility to make sure that any intervention that we’re carrying out, that women need to know why we’re doing it and how we’re going to do it and what the repercussions would be.
#32, trust screening co-ordinator
| Information required | Number of midwives/parents |
|---|---|
| Midwives | |
| Conditions being screened, with some detail on implications of the conditions | 34 |
| When and how results will be received | 19 |
| Possible outcomes of screening | 16 |
| How screening takes place | 15 |
| Importance and objectives of screening, including the benefits of having their child screened | 9 |
| Timing of screening | 4 |
| Rarity of conditions | 4 |
| Possibility of repeat samples | 3 |
| Storage of bloodspot cards | 2 |
| Screening is not diagnostic | 2 |
| Screening is optional | 1 |
| Parents | |
| What the implications are if your child screens positive – treatments available | 10 |
| Brief information on conditions – treatable | 8 |
| How screening takes place | 5 |
| When and how results will be received | 4 |
| What has changed since previous pregnancy | 4 |
| Where to get further information | 3 |
| Benefits of screening | 2 |
| Timing of screening | 2 |
| How to calm your child | 1 |
| Implications of not screening | 1 |
| Probability of child having condition | 1 |
| Symptoms | 1 |
| Recommended | 1 |
| Family may not be aware of illness | 1 |
Data from the interviews showed that parents who asked for brief information on the conditions being screened for did so because they had received no information previously, rather than wanting a reduction in the amount of information provided:
So, yeah, this heel prick, like maybe a little, brief introduction about what’s the heel prick and what we are testing or screening would be better, just without . . . it’s better than not saying anything about it, I think so.
#44, mother, second child, first child negative result, waiting for second child’s result
However, when asked to indicate on the pre-interview tool their preferred level of information, the majority of parents selected the option in which only the names of the conditions being screened for were provided (Table 4). They also wanted to be given procedural information about screening, the time frame for the results and where to access further information if desired.
| Preference | Number of parents |
|---|---|
| Parents receive information about how the heel prick test will be carried out, when they will receive the results of the test and information about each of the conditions their baby is being screened for | 12 |
| Parents receive information about how the heel prick test will be carried out, when they will receive the results of the test and the names of the conditions being screened for. Parents will be told where they can obtain further information about each condition their baby is being screened for should they want it | 32 |
| Parents are told only that screening will take place and when they will get the results | 33 |
The parental responses in Table 4 suggest that different parents have different information needs. For example, parents who were experiencing NBS for the first time wanted step-by-step information about significant events occurring in the postnatal period, such as screening, whereas parents whose previous children had been screened preferred more concise information about any changes to screening since their previous child had been screened. Also, although the majority of parents just wanted to know the names of the conditions being screened for, some also wanted to be given more thorough information about each of the conditions being screened for.
Instead of just listing off the names, when you don’t really know what they are anyway. You don’t want to be saying, well, could you explain what that is and that, because I don’t know what that is either?
#39, mother, first child negative result
Only one parent (father) did not want any information prior to screening as he tended not to desire detailed health information in general. However, the partner of this parent did want information about the process of screening, the receipt of results, the names of the conditions being screened for and where to obtain further information, further highlighting that even within parenting couples there can be different information needs.
Health professionals’ focus on informing parents was driven by their duty to obtain parents’ consent prior to screening. Indeed, one midwife defined midwifery practice as:
It’s giving the information; it’s giving the information at the right pitch to the right women so that they’ve got a full understanding or a good understanding of what the screening is about and that they can make their choices.
#35, trust screening co-ordinator
However, only one health professional mentioned that it was important that parents knew that screening was optional. On the other hand, only one parent also thought that it was important to know that screening was recommended, as mentioned in the information leaflet.
Parental understanding
Although many parents knew that the heel prick test was carried out, the majority of parents, with the exception of those in the medical profession, lacked knowledge about the conditions included in NBS, both prior to screening occurring and after screening had occurred. Furthermore, many parents did not fully understand why their children had been screened:
Well, I knew there was a heel prick test, so yeah, I knew that, but . . . and I knew that they take a few other samples, but not really. [. . .] I don’t know what the actual . . . why he had it done.
#8, mother, third child, all negative results
Some parents appeared to be fully informed only when they had their second or third child, as midwives took the opportunity to actively engage parents by providing detailed information, as illustrated by the following parent:
Well I’ve had two other children before so obviously they were doing it back then and I wasn’t really aware of why they had to do it [. . .] During my third pregnancy my midwife told me during the pregnancy why. She gave me a leaflet as well about it and told me why the babies have to have it done and what the screening’s for and the conditions that they can have.
#34, mother, third child, normal result
Regardless of their child’s screening result, many parents were concerned that they did not realise the seriousness and importance of NBS earlier and linked this to the lack of information provided:
I just don’t remember being really on the ball with that and really understanding how serious it can be.
#13, mother, expecting second child, first child negative result
I don’t feel that we were told why it was happening and what the results would be, and what the consequences would be. I think we would have taken it a bit more seriously than we did.
#18, father, first child, PKU result
Moreover, parents whose child had a condition detected through screening reflected on the impact of their lack of awareness about the conditions being screened for and the possible outcomes of screening. Some parents expressed their initial shock and surprise at their child’s result, whereas for others the consequences of a positive result appeared to extend for far longer:
I think in hindsight, once we got the result then we certainly didn’t . . . we didn’t even know really what they fully tested for [. . .] when they said the word ‘GA1’, we didn’t have a clue and we’re like, well, did you even test for that?
#14, mother, second child; first child negative result, second child GA1
Our world had come crashing down. In fact, the next 3, 4 weeks, even the next few months really . . . because then you have to come to terms with it, you have to learn how to deal with it, it was really hard.
#11, mother, second child; first child negative result, second child PKU
Challenges and strategies for effective communication with parents
The next section defines what the challenges are to effective communication and what solutions the participants offered. When appropriate, example quotations from health professionals and parents are provided to contrast the similarities and differences in views.
Problem: incorrect timing of information
Both health professionals and parents felt that the timing of information delivery was a pivotal factor in determining whether or not information was engaged with, understood and retained by parents.
Booking: irrelevant
Both participant groups felt that giving information at booking was difficult for both the health professional and the parent because of the amount of information exchanged and the competing demands on parents’ time:
They’re so busy doing other things that I just don’t think they have time to pick up the leaflet and read it.
#29, community midwife
I was given a leaflet but I wasn’t very far gone, I think I’d just had my first scan, and it just went to the back of a cupboard.
#11, mother, second child; first child negative result, second child PKU
Many parents did not remember discussing or receiving any information prior to birth. However, of those who did, the majority of parents admitted not getting around to reading the information leaflet and there appeared to be many reasons for this. Some parents were not focused on the baby as they were preoccupied with other aspects of the pregnancy, such as antenatal screening. Others echoed the sentiments of the health professional above, explaining that the information was deemed irrelevant as the baby was not perceived as a tangible entity prior to the 20-week scan:
I think you’re more focused on [. . .] being pregnant and what kind of complication can happen than you are of what’s going to happen after [. . .] when the baby comes it’s going to have to have this test and stuff.
#43, mother, third child, negative result last child, previous two not screened
Birth: too tired
Participants also recognised that communicating with parents post birth was also not optimal as ‘you can see that glazed look coming over’ (#25, community midwife). There was also awareness of the implications that such information giving had on consent, with a concern that this was ‘possibly the worst way to consent somebody’ (#15, community midwife). The majority of parents whose children had been screened reported being informed about screening following the birth of their child. Although some parents were informed when they were being discharged from hospital that screening would take place, a significant proportion of parents reported being informed only when a midwife visited them at home for the first time after the birth:
From what I can remember, it was when the midwives came round to my house to visit. They told me that the next time they were coming, they’d be doing the heel prick test. And they explained a little bit about it . . . That was the first time I heard of it.
#39, mother, negative result
Of greatest concern was the finding that some parents were informed only on the day that screening was due to take place. Parents who received NBS information postnatally discussed the difficulties that they faced in processing and retaining information at such a busy and tiring time:
When you do have the time [post birth] you’re just too tired to take anything in; you can’t read anything, you can’t . . . I personally couldn’t retain any information [. . .] The first few weeks are so hard.
#9, mother, second child, both negative results
This was a uniform statement from parents, even for those, as in the case of the mother above, who had had a previous child and received a negative result.
Solution: focus discussion and consent in the third trimester
The most appropriate time to discuss NBS and signpost parents to information resources was perceived to be the third trimester, when information would be more relevant to parents as they began preparing for the arrival of their newborn child:
I think 36 weeks is a good time [. . .] I do think that’s probably the best time when women are most sort of receptive to taking that information in because they’re not rushing out to work, they’re starting to have that sort of nesting instinct and they’re kind of happy to absorb information that is going to affect their baby.
#25, community midwife
Given the dominance of the narrative that the postnatal period was a difficult time for parents to process information, this led the research team to start testing out whether or not it would be better to move information provision and decision-making into the antenatal phase. Interestingly, the majority of participants felt that moving consent into the antenatal period would enable parents to make informed decisions about screening, providing that the decision could be revisited after birth:
[. . .] if the baby’s only 24 hours old, and actually the last thing on their mind is, do they want to make a decision about these tests for their baby? [. . .] I think the discussion about gaining consent would be better done in the antenatal period, and obviously reviewed when we’re about to actually perform the tests in the postnatal period.
#33, community midwife
Parents were also asked about their views on the timing of consent and most agreed that it would be better to indicate consent in pregnancy, as they would have more time to engage with the information and would have the mental capacity to make an informed decision:
I think it will be good to ask during pregnancy as well because sometimes during pregnancy you can have all sorts of thoughts running through your mind, so I think talking about it during pregnancy, it’s really important. So if the midwife asks the question, would you like to have it done, and if the mum or dad says, no we don’t want to have it done, then I think that should be respected and then as well after the baby’s born, just to make sure that they don’t change their mind or anything.
#23, mother, first child, normal result
One parent raised concerned about this practice, but her views seemed to be linked to the idea that parents might initially decline screening:
I think women change and women’s emotions change so they might be on a hormone high during pregnancy and think, oh, everything will be fine and then the baby will be born and suddenly they are more anxious and might change their mind to do want to know now so depending on the hormone state of every woman, I think you should give them time until the baby is born.
#30, mother, pregnant with first child
Although this was a common concern and was also evident in the health professionals’ narratives, there was no indication from any of the parents at any stage that any would consider declining NBS.
Problem: information not prioritised
Several parents also commented on the lack of emphasis on NBS and little awareness of the possibly that their child could potentially have a health problem after birth, and rather appeared to remember the multiple reassurances that their child was healthy:
In fact, all the way through your pregnancy, you kind of . . . there’s a lot of emphasis on things like Down’s syndrome test and things like that, and it seems that you tick all these boxes and then you get through to the stage they’ve been born, somebody’s laid out and measured, that’s all ticked away. So you think, in theory, you’ve passed, you know, you’ve got a healthy baby.
#18, father, first child, PKU result
Parents also commented on the emphasis placed on antenatal screening compared with NBS screening.
Because usually people think they have their babies and that’s it, there’s nothing really offered after that. Because during pregnancy you have all sorts of screening done, like the Down’s syndrome, the glucose tolerance test and other pregnancy-related screenings. But after the baby’s born usually people think that’s it, they don’t do anything.
#41, mother, third child due, previous two children negative result
I think more needs to be said about it, not just there is a leaflet in your folder, please go away and read it, and no one mentions it again. Or certainly, no one did to me. It was never checked up on, have you read that information. There wasn’t . . . there was a lot about breastfeeding in the information but not about that.
#2, mother, two children, pregnant sample, fg
This mother, from the stakeholder consultation, reflected that she was able to remember some complex health information provided during pregnancy – the four chambers of the heart, from a waiting room poster – and attributed her lack of knowledge about the NBS conditions screened for to the lack of attention drawn to NBS. Later, this mother highlighted that it was not only NHS services that appeared to not raise awareness, but also other frequently used services:
Even on the . . . I mean, I was quite . . . you know, I’ve been on baby centre twice through both pregnancies and I don’t even remember it being quite a topic of conversation on there.
#2 mother, two children, pregnant sample, fg
Parents also commented on the general lack of awareness about NBS by others, further emphasising the idea that NBS is conspicuously absent in discussions around pregnancy:
Because everybody that I speak to about it, I say [child’s] got PKU and they’re like, oh, how did you find out? And blah, blah, blah, what is it? Nobody’s ever heard of it.
#12, mother, second child; first child negative result, second child PKU
In terms of awareness about NBS, some parents who were days away from giving birth at the time of their interview reported that they became aware only through being invited to take part in the present study:
Yes, the first I’d heard about it was reading the information that you’d given to us when you introduced yourself.
#31, father-to-be
One suggestion throughout the data was that most of the NBS information was directed at mothers, despite an awareness that fathers needed to be equally aware of NBS. If information provision for mothers was poor, it appeared to be completely absent for fathers, with very little chance of a father being informed directly about NBS prior to the screening occurring. However, as noted above, some mothers in our sample also reported that they became aware of NBS only through the research team. Of note, the mother in the following quotation was pregnant with her second child, further highlighting the lack of knowledge of NBS in the population:
So when you told me, 1 day before her birth, then I got told.
#38, mother, pregnant with second child, first child not screened, Urdu, does not need interpreter
Problem: leaflets not read
Interestingly, both health professionals and parents discussed how information materials were not engaged with. Health professionals reported that, although much of the necessary information was featured in the Screening Tests For You and Your Baby booklet, parents often lacked understanding and awareness of screening:
I mean I can give them a leaflet but I can’t guarantee they’ve actually read it because most people don’t, even on . . . you know, even at booking when we give the screening leaflet or currently you’ll say, you were given, you know, the screening leaflet on discharge from hospital. On the first home visit you’d remind them that the information’s there. You’d talk about the conditions that we’re screening for, the nine conditions, how we take the sample. Then we can go back in on day 5 when we’re actually doing the sample but they haven’t actually read the information, and you can see sometimes with their face that they haven’t.
#1, senior community midwife, stakeholder interview
Although the view that parents did not engage with the information materials was a strong discourse running through the health professional and, indeed, the parent data, there were differing views as to why this occurred. Midwives attributed this to parents not reading the booklet, whereas parents attributed this to not being made aware of the importance of engaging with the information. The way in which parents were given information about NBS also appeared to closely reflect how they engaged with the information. The majority of parents who recalled being given information antenatally tended to report receiving a leaflet, with little verbal discussion:
I’m nearly 27 weeks now and it hasn’t been spoken about.
#13, mother, pregnant with second child
I haven’t been told. We’ve been given information in the form of leaflets and all I know is it’s done quite soon after the baby’s born.
#21, mother-to-be
With regard to the information booklet, many parents reported that they did not realise that the information required their attention as they were not explicitly told to read it by their midwife:
I think I saw a leaflet on it, but it wasn’t really pointed out to me by the midwives [. . .] It’s more like they just gave a whole bunch of stuff and then, you know, read it if you want to and don’t read it if you’re not too interested.
#19, mother-to-be
This parent’s data highlights the problematic nature of designing information interventions within pregnancy, which was echoed across the parent data and acknowledged by health professionals – booklets can be effectively designed but, if they are evaluated using a design in which parents are given only that material, they have not been robustly evaluated in the environment in which they need to perform, namely in competition with a deluge of other information sources and topics.
In terms of parental engagement with the information, both of the samples raised the issue that existing parents had a different antenatal experience from first-time parents. Health professionals believed that existing parents were less engaged in screening and did not see the relevance of the information, whereas some parents were concerned that they were offered a different service. This was such a concern to these parents that this issue was raised again by parents in the stakeholder consultation study:
And the other thing I felt left out, like, when you are an experienced parent, some of the information they give you when you are a first parent, it is completely different. I had a bit gap between my kids, so actually I felt as I wasn’t able to burp my child. They assume that you can know everything, how to put the nappy on, how to burp the baby, when you have the reflux, what you need to do. Meanwhile I was blank like a jacket potato, I didn’t know what to do. Even though I had a kid, just the gap, assuming in medical ways just gross negligence.
#3, mother, second child, focus group
Problem: parents not aware of the need to engage as unaware of the choice
Many parents also cited their trust in midwives and their lack of awareness that they had a choice as possible reasons for their lack of engagement and why they did not seek further information:
I guess it’s just, I just accept it as a routine thing, I didn’t even realise that you had the option to opt out of it. I just saw it as if it was just routine screening. I just thought it was just a thing that was done.
#7, mother, second child, both negative results
I don’t know, kind of, put my trust in the midwives and the NHS and, you know, just let them get on with it, do what you need to do.
#9, mother, second child, both negative results
Reading across the parent data there was a strong sense of this being a huge period of change for parents in terms of roles and identities, but also a time when they were being overburdened with information. This was not only because they needed to learn a lot about the pregnancy, tests, screening, the birth and parenthood, but also because they appeared to be targeted continuously by marketing companies, given the multitude of products available to sell to parents. These factors combined to create a situation in which, unless information was clearly marked as needing their attention and directed them to take action (i.e. you need to make a decision), their limited attentional resources were directed to other information. Thus, their accounts provided a rationale as to why they did not engage with the information, especially if this was coupled with a view of inevitability that the screening would occur or an inherent trust that a NHS service would be without risk. Thus, the parents’ accounts illustrated that, without knowing that they needed to make a decision, or that there may be other factors to consider, they were more likely to store the information away, with some making the analogy with the terms and conditions of a purchase, for a time when it was needed, rather than engaging with it a priori.
Problem: rare event so not relevant
The focus on the rarity of the diseases also drove some parents to disengage with the information, leading them to fail to see the relevance of knowing about screening before the event:
I know these things are all rare and it’s just come to it when you cross the bridge type of thing. Like really to me, like one in 200,000 or whatever, as long as I read that that’d be like, oh OK, you know, I’ll forget about it until if I get a positive result then I’ll read up about it.
#19, mother-to-be doctor
Thus, factually correct information, such as the incidence of the individual diseases, can act as a barrier to engagement with the information. Indeed, a review of the website available to parents at the time of this study revealed that parents would have needed to scroll down through a number of pages of information about the rarity of diseases to discover that they had a choice as parents about whether or not to have their child screened. It also shows how the importance of the information is judged based on the likelihood of a disease state being found, rather than recognising the other potential outcomes that parents may need to be prepared for, such as carrier status or a false-positive result. Although there was some discourse in the health professional and parent data about the need for parental choice, the role of the information in enabling parents to make this choice was absent from most participants’ accounts. For some, the link between the likelihood of a diagnosis and the need for information actually acted as a way to shut down, probably unintentionally, parental requests for information:
The midwife said, we’re going to come and do a heel prick test for some rare conditions, and you’ll probably hear nothing back from them. [. . .] But it’s just a blood test and it’s over in seconds and it goes off and you usually never hear anything back.
#12, mother, second child; first child negative result, second child PKU
Solution: separate health information from other materials/mark up appropriately
Several parents also described difficulties with identifying which pieces of information were relevant to read among the volume of information leaflets that they had been given at the beginning of pregnancy. Parents particularly referred to being overloaded with information leaflets as well as promotional material for baby products:
Because a lot of it actually is probably rubbish and some marketing material, so I think it’s fairly difficult to actually figure out what’s worth reading and what’s not from what you get given.
#2, father, first child, normal result
We shouldn’t be using things like the Bounty programme to promote information, but actually they do promote it fairly well in their little booklets and what have you. I think we need to make sure that anything that is produced doesn’t look like some sort of marketing because those leaflets just go in the recycling for a lot of people.
#1, SQAM
However, many parents reported that they would have engaged with the leaflet had it been more explicitly pointed out to them. Thus, a simple and cost-effective way of making leaflets more effective would be to place greater emphasis on their importance:
But if I was told, listen this is, you need to read this, this is serious, you’ve got to read it, then yeah I would take it and read it, obviously.
#11, mother, second child; first child negative result, second child PKU
Solution: drip feed
Drip feeding information at multiple time points and a verbal discussion of screening antenatally were approaches that were appreciated by parents and which appeared to facilitate engagement with information:
So I think if it’s going to be discussed antenatally then perhaps it could be brought up somewhere around the 6-month pregnancy mark, 6 or 7 months and then it could be re-discussed at the following antenatal appointment, sort of, 4 weeks later or whatever. I think that would be an adequate length of time for most parents to make an informed decision.
#20, mother, first child, negative result
Health professionals also felt that information should ideally be given incrementally at different time points during pregnancy to both ensure that parents had sufficient time to understand the information prior to birth and facilitate absorption. It was thought that mentioning NBS multiple times would prompt parents to access and engage with relevant information resources:
But they need time to digest that, and maybe you need to revisit these things more than once to be honest, I think. I think giving it them once is perhaps not enough. Because they get bombarded with stuff, don’t they, in pregnancy?
#36, antenatal clinic midwife
But there could be little tick boxes at various gestations, to say, has this been discussed again? Have you ensured that they’ve got the information? And just as a little aide memoire to midwives really, to keep on bringing it up, because I think the more it’s referred to, the more likely it is that people are going to go and have a look at it.
#15, community midwife
Both of these accounts acknowledge the contextual factors relevant to information engagement in pregnancy discussed previously, such as the overwhelming amount of competing information and the need for midwives to drive engagement with information. Across the data sets, no parent or health professional provided an account that would counter the idea of drip feeding as an improvement in NBS communication. Rather, it was a concept that emerged from the accounts of the interviewees as being a necessary approach to information provision.
Solution: raise general awareness of newborn screening
Related to the drip-feed approach was raising awareness of NBS more generally. Thus, it would become part of the known pregnancy pathway. One suggestion was to ensure more comprehensive dissemination such as through family centres, antenatal clinics and general practice waiting areas:
I think we need to make sure there’s good information in family centres where they still exist, because those are often targeted at people who have issues already and they’re the ones that probably need the information most.
#1, SQAM
Another benefit was that people would receive repeated ‘nudges’ to engage with the information:
I think posters you could have, antenatal clinic, you could have on the postnatal ward, you could even have in the GP [general practice] surgery. You’re not really going to miss people out there.
#17, regional quality assurance manager
Another suggestion to enhance parents’ engagement with and acceptance of expanded NBS was to raise awareness nationally using the media to promote screening:
So you can increase awareness by putting adverts in those sorts of things; TV, radio, free newspapers and local newspapers as well [. . .] Yeah, just to make it nationally known, national because the more aware the parents are, know about it, that it’s going to happen, the more they’re likely to respond to it. So advertising and awareness really, where people will read about it.
#23, trust screening co-ordinator
Alongside engaging both parents in the NBS communication process, one midwife gave an example from her own trust of holistic communication focusing on awareness across the wider family, which appeared to have had a positive impact on parent engagement:
There’s been a massive, massive re-launch of our information-giving processes and how we access women to give that information, parent education being a massive, massive way forward. We have dads’ nights, we have grandparents’ nights, we have all sorts.
#12, trust screening co-ordinator
Inherent in this account is the multitude of people who may be making decisions on behalf of a newborn child, rather than focusing purely on mothers as the decision-makers for children. Such multifaceted attempts to ensure that parents were informed appeared to be working, according to parents’ accounts.
I believe I remember reading about it in literature that was given to me by the hospital and also literature that was given to me in the Bounty pack. And then it was verbally discussed with me with my midwife at my birth plan meeting. So I was, sort of, you know, a four-pronged attack as it were with regards to actual information about it.
#22, mother, first child, negative result
Problem: effective newborn screening communication takes time and training
Problem: midwives’ need for comprehensive training
Participants who practised clinically emphasised the importance of ensuring that their own knowledge of the additional conditions in expanded NBS was sufficient to effectively relay this to parents and answer their questions:
I think obviously it’s important that we understand what the other four conditions are so we can make sure people understand before we consent them for it and also we have to have a certain level of understanding.
#20, community midwife
Participants also acknowledged the importance of having well-trained and knowledgeable staff to facilitate the effective implementation of expanded NBS and obtain parental consent:
And that the requirement to have knowledgeable, well trained staff prior to implementation, is clear that that needs to be in place.
#2, SQAM
One participant who had experience of the expansion highlighted that some of the challenges may be at quite a basic level, yet they represent a real communication barrier:
I think it’s the same way as for the other newborn bloodspot screening. However, when we did introduce this [expansion] the challenges were first of all the names of all the tests, they’re unpronounceable and so that was a real barrier for getting the information over.
#11, trust screening co-ordinator, taking part in pilot
Additionally, participants discussed needing sufficient knowledge so that they could provide information to parents according to the amount and type of information that they desired:
There might be parents who want more in-depth information about the conditions before they test for it and then there will be the people who want, sort of, more of a basic understanding of what they’re testing for. So we need to have different levels of knowledge really.
#20, community midwife
Furthermore, participants who organised and delivered training sessions for midwives reported concerns regarding the amount of content to fit into already time-constrained training sessions, how to reach all midwives in a timely manner and how to provide information in a standardised manner:
And I do training every month. Unfortunately I’ve been cut back. I used to get an hour, I now only get half an hour. But in that half an hour I have to roll out training for the whole seven screening programmes that I co-ordinate.
#12, trust screening co-ordinator
I mean, you know, from my point of view I prefer to have a session where somebody comes along where I don’t have to think about anything else, anybody coming in interrupting me. It’s protected time where I can go and learn about whatever it is that’s going to be new [. . .] If it just drops into my inbox we’re all so busy and, again, you know, interruptions, you go to look at it and working in a clinical area it doesn’t work like that.
#31, trust screening co-ordinator
In addition, participants who were responsible for informing parents and collecting bloodspot samples raised concerns about the lack of time to access training materials outside of protected mandatory training. Taken together, these data show how there are challenges in terms of the content of the information and the amount of information. The data regarding the need to tailor information sufficiently to diverse parent needs highlight how midwives need to have a deep knowledge of NBS. Placing these data alongside the acknowledgement from those involved in training of the constraints on training time and the reports from midwives that they are rarely given permission to attend training because of staff shortages highlights how challenging it is to rely on midwives to convey information.
Problem: effective newborn screening takes time
Several participants raised concerns about the impact of the expansion on their time and how this would then impact on their ability to effectively obtain parental consent for screening:
I think it probably impacts on our time because there’s more to explain obviously and to go through with the parents and the more anxious parents, they need more time to go through each of the conditions [. . .] It would mean you wouldn’t be able to see as many women that day because the appointments are taking longer.
#30, community midwife
There will be the odd case where it’s not going to be able to be done in 10 minutes if you want informed consent done appropriately. If you want it done badly, sure, you can do it in 10 minutes.
#24, community midwife
Many participants also expressed concerns regarding the ongoing expansion and how this would affect effective communication:
Once it gets to then [past 9–10 conditions], then people are going to have to sit down and think, how are we going to deliver this information? It’s massive. Are we going to deliver it all in one fell swoop? Are you going to have to break it up into three different sections? You’d have to think, it depends how many. Because, eventually, it will become unmanageable, won’t it?
#36, hospital antenatal clinic midwife
Solution: reconsider information content
Throughout the interviews with both samples there was a concern that an overwhelming amount of information was provided during pregnancy and that the NBS information itself had reached a point of being too voluminous to still have utility. Participants sought to consolidate information in different ways. Health professionals focused on how to group the diseases into meaningful groups based on their holistic knowledge of NBS:
I can’t pronounce the name so there’s no way parents are going to remember all the names of all those conditions, so I think grouping them together so potentially we still have maybe four or five different conditions to tell them about. But definitely we need good-quality succinct information that they’ll read.
#4, SQAM
I think sometimes grouping them together simplifies it so we want to make sure is yes it’s an informed decision but they’ve got to understand it in the first place haven’t they and I think we can’t be expected to go into a great deal of information for every test, it’s not practical, we’d be there for ages.
#22, trust screening co-ordinator
In contrast, parents appeared to focus on grouping information across the pregnancy, making it meaningful to stages and easy to find:
Think if they took all the information on everything and redefined it all and sectioned it off like the book, I found the book really useful, I’ve still got it on my shelf in there in the other room. It takes you from pre-pregnancy right through to 5 years old like development as well and the health conditions I think, something like that would be beneficial.
#7, mother, first child, negative result
Thus, whereas health professionals sought to solve the challenge of how to convey NBS information in one session, parents were grappling with the wider issue of keeping track of a multitude of new information across the pregnancy.
Solution: parents’ active role
Both midwives and parents valued the midwife discussion as a way of ensuring that parents were informed and midwives had fulfilled their role. Given the complexity of expanded NBS and the additional challenges involved, discussed by participants in the previous section, several health professionals thought that communication could be enhanced if parents took on some of the responsibility to engage with the information that they were given:
We have to be aware that the responsibility partly is on the woman. We’re giving them literature and advising them to read further, and they have to be responsible for taking some of that on board so that they are informed of what will be offered after their baby is born.
#34, trust screening co-ordinator
Some of this stuff has to sit with the woman, or the couple. You can take a horse to water, but you can’t make it drink, can you?
#36, hospital antenatal clinic midwife
An additional benefit of parents being more active in the NBS communication process prior to screening was the potential impact on midwives’ time, allowing them to spend more time with parents who required further informational support:
If you’re going out to do four bloodspots and two of them have already read the information, it’s still going to, you know, make your time more effective, and potentially give you more time to spend with the people that haven’t.
#9, SQAM
I would rather that we retained the consent element and that the information element became more generic, if you like, in that women were signposted away from midwives to get the informed information if you like.
#32, trust screening co-ordinator
Some participants felt that utilising technology could change the emphasis from midwives being the main informant to midwives focusing on checking parents’ knowledge and understanding gained from the information resources:
Getting the women to utilise their time to look at [the information], and then when they see the midwife, it would be just reflecting on what they’ve looked at and what their perception and understanding of that is, so it’s not like going to . . . going through it all from scratch. They would have had a look at it hopefully and then you’d just be ensuring that they understand everything.
#6, community midwife
As articulated by the midwife above, participants perceived their role as being more effective in terms of signposting parents to appropriate information resources and checking understanding prior to obtaining consent:
I think being able to encourage women to do some of the information finding themselves, with the right signposting, to the right technology, is helpful these days.
#9, SQAM
Another suggested way of maximising communication further was to ensure that information was conveyed to both parents:
I think that it’s also important that both the partner and the mother understand what the process is and what it entails, and what the screening is for.
#7, community midwife
Certainly fathers can be very influential to mothers, can’t they, even if they’re not with the mother of the baby, they can be very influential and making sure that everybody understands how important these things are and why they do need to have them done.
#32, trust screening co-ordinator
Another potential reason for not engaging with information may be inferred from a latent analysis of the following quotation:
It’s just kind of a no-brainer to me. If it’s a test and it looks for nasty things, then, you know, I’m all for it, kind of thing. There was no way I’d ever dispute it or even question why it was being done.
#12, mother, second child; first child negative result, second child PKU
The pro-screening sentiments in this parent’s comment were echoed throughout the parent sample. This implies that, when a service is seen as such a positive step, it can lead people to ‘not question it’ and passively receive the service. There may be a need, therefore, to highlight to parents that they are expected to make a decision about screening.
Solution: information tool kit
The availability of additional information resources was also seen to alleviate midwives’ concerns regarding the impact of expanded screening on their time, as discussed earlier, as well as save resources:
I think just having the resources that we do already have, but just making more use of them, so that the parents can have them to go to rather than getting all the information from the midwives.
#30, community midwife
Related to the theme of involving both parents was the need for more holistic and flexible communication strategies to engage parents. Participants advocated the use of multiple communication strategies to facilitate parents’ engagement with NBS information, which would also enable parents to take on responsibility for being informed:
Communication with parents does not mean just give them a leaflet. That’s it I think. There’s more ways of communicating than just that. You have to explore them all to make sure the message gets across.
#3, SQAM
Recognising individual differences in information needs and preferences, there was an overarching consensus among midwives that parents should have the flexibility to choose the information format that was best suited to them:
I think to have as large a variety of options as possible, that then people could pick and choose the way in which they accessed the information [. . .] I think people access and interpret information in different ways.
#15, community midwife
I mean that discussion and a range of materials to be able to say to them, this is available, this is available how would you prefer to access this info?
#35, trust screening co-ordinator
Midwives also emphasised the importance of making information more accessible by removing some of the key obstacles to parents’ engagement, such as language and literacy barriers. A repeated concern expressed throughout the interviews was the need for more readily available translated information to enable an equitable service to be provided to an increasingly diverse population:
Again, a lot of my women who I look after just don’t speak English so we give them a leaflet and I know they can’t read it, but we have to give them a leaflet because we’ve got to tick the box to say that they’ve had the leaflet.
#29, community midwife
Recognising the increasing diversity of parents that they were seeing, midwives acknowledged that a single communication approach was not likely to be appropriate for all parents:
I think they need to be tailored to different groups, different languages; other groups as well, vulnerable groups. So I don’t think you could just have one general leaflet, I think you’d have to put it into different formats and different languages for people.
#17, regional quality assurance manager
Format of information included in the tool kit
Group discussion
For some parents, receiving information verbally from a midwife would be the only effective method for them as they were too busy juggling other priorities to self-educate about NBS:
I wouldn’t have had time to read it, because I’m very busy with children. My own health problem, the baby and the children. Maybe giving advices [sic] by talking would be better.
#10, mother, primary language French, fourth child, all children negative results
One parent recounted her unique experience of receiving detailed verbal information prior to being discharged from hospital:
Before I was discharged I had one of the midwives sit with me for a good half an hour, 40 minutes [. . .] she sat there and explained in detail this is what it’s going to be. It’s going to be on such and such a date. This is how the process goes.
#24, mother, second child, screened awaiting result
Although the detailed verbal explanation was helpful in preparing this mother for screening, she did acknowledge that face-to-face communication may not be effective at ensuring parents’ understanding if screening were to be further expanded in the future:
If they expanded to more conditions I think they’re going to make things more complicated. So, if someone sat there and explained to me the intricate details of every single condition I probably wouldn’t be able to take it all in.
#24, mother, second child, screened awaiting result
One way that parents could receive information from a health professional was through group discussions. The majority of midwives supported incorporating NBS into antenatal parent education classes, with perceived benefits of the group setting including having the opportunity to engage partners, who often attended antenatal classes, and being able to encourage parents to ask questions:
We try and encourage the women in the team of midwives I work for to come to antenatal classes, because we’ll talk about it there and that allows the partners if they’re present to talk about it with us and the women to ask us questions. So hopefully we’re capturing those women who wouldn’t be inclined to read a pamphlet, and it maybe if they want more information then they know where to get it and to look it up and to think about it.
#24, community midwife
Many parents were in favour of receiving NBS information as part of group discussions on the proviso that the sessions took place antenatally, to ensure that they were able to understand and retain the information as well as have the opportunity to ask questions:
I’ve got a class on Friday and I’m hoping that they are going to mention what’s going to happen afterwards just because I’m so close now. I’ve only got 4 weeks, so yes, it would be really useful and then if you don’t understand you’ve got somebody there to ask questions.
#21, mother-to-be
Again, this seems to suggest that women become psychologically ready towards the end of pregnancy to hear information about their child.
However, both samples raised the issue that not all parents attended antenatal classes and that those who did might attend only for their first child. Therefore, there was a need to ensure that information was available from other resources to ensure that all parents were informed. Some midwives worked in hospitals where there was a group discharge policy and suggested that this would be another opportunity to remind parents postnatally about NBS. As reflected in Problem: incorrect timing of information above, postnatal information sessions were generally not perceived as desirable by parents because of the practical barrier of agreeing on a convenient time for all, as well as parents’ exhaustion in the early postnatal period:
Trying to find a time where a whole group of women can go and sit down and listen and concentrate on some information giving when they have probably had no sleep for a couple of days. They’ve got a newborn baby, I think that’s probably unrealistic to be honest.
#20, mother, first child, negative result
One suggestion from multiple parents was to incorporate the information session within existing antenatal appointments as a way of engaging all parents and saving NHS time and resources:
You see you know when you go and kind of get your bloods done and whatnot throughout pregnancy is there any way of amalgamating people that way? So they’re doing it in an hour and going through it as a kind of process.
#7, mother, second child, both negative results
Dedicated newborn screening helpline
When asked about their thoughts on a dedicated NBS helpline the majority of midwives were supportive of the initiative, as long as it was promoted well and monitored closely to ensure equitable access by parents. Another aspect favoured by midwives was the potential support that a helpline could offer in terms of providing tailored information to parents who preferred to access information via an application (app) or website and who could use the helpline to answer any questions that they might have. This would enable midwives to spend more time with parents requiring more direct informational support:
So if women feel that they want information they can phone and speak to somebody, access the information online and then phone to fill in the gaps if they felt there were some.
#34, trust screening co-ordinator
The majority of parents thought that such a resource would be helpful and easy to access rather than taking up the time of midwives during antenatal appointments. However, parents emphasised the need for clear signposting to ensure that there would be sufficient awareness of the helpline among parents:
I think that’d probably be a good idea, you know, especially if you’ve maybe taken some information home [. . .] if you know somebody’s going to be at the end of the line, then it’s a lot easier. Obviously, you can’t always make contact with your midwife straightaway.
#22, mother, first child, negative result
Leaflets
Virtually all participants who we interviewed advocated the use of technology as fundamental to improving the efficiency and effectiveness of expanded NBS communication with parents, with health professionals recognising that leaflets may not be how people currently access information:
I think in this day and age leaflets might be a little bit old fashioned, if I’m being honest. I think they need to look at a more modern form of information giving.
#3, SQAM
I think the population is changing and I think that the old way of sending out letters and, you know, giving the books, and things, I’m not entirely sure this is the most efficient way for information to be given, because in my experience, the young people around me seem to live on their phones.
#32, trust screening co-ordinator
For others, the content of the current booklets created barriers. A repeated pattern in the data from both parents and health professionals was how the current system of leaflets does not work for women whose first language is not English. Indeed, even parents whose first language was English struggled with some of the terms.
I think that at the back they should include like a glossary or something to explain the terms better for parents to understand, because you know, sometimes you don’t always know and you don’t always have a dictionary handy to find the word, and what does that mean.
#41, mother, third child due, previous two children negative results
There were also examples of leaflets being given that were not actually about NBS or trusts placing limits on whether or not midwives could print translated leaflets. Although these comments were directed at the existing system of booklet provision, they do highlight further how the static nature of leaflets can place restrictions on how services can meet recipients’ needs for information. Of interest, across the samples there was a preference to keep leaflets as one format that could be provided, yet the reliance on them should be reduced:
I think simple information, probably I think the initial information in almost an easy read format, then that’s sort of accessible to everybody.
#13, SQAM
I think having clear, concise explanations of what they are, as opposed to sort of long-winded, quite difficult to read and understand. It’s going to be really important because certainly, a lot of my clientele would have a screening pamphlet and really not quite understand what they’re reading.
#15, community midwife
Participants appeared to recognise that leaflets were useful as a means of enabling a concrete act of ‘giving’, in terms of literally handing over, information. It was reassuring to health professionals that they had performed an act of information provision, which could be a useful way of starting the conversation about NBS. However, it is likely that other approaches would need to be used to fully provide information about NBS.
Applications
An app was endorsed by all midwives as an effective communication strategy given that many parents were existing users of pregnancy apps. However, midwives felt that, as well as being free to download, a NBS information app needed to be NHS endorsed to be a trusted and regulated source of information for parents:
[. . .] it’s Royal College of Obstetrics approved and Royal College of Midwives approved, so it isn’t just a company that have set up, you know, with an idea, it’s all legitimate information.
#32, trust screening co-ordinator
Additionally, participants felt that an app encompassing all of the relevant information about pregnancy and the newborn period would be more useful for parents, would have a higher uptake if it contained more holistic information and would possibly help overcome resource issues regarding translated information:
If you download this app and it’s on your phone and you can read about different screening that’s going on maybe they would use that, especially if it was in their own language.
#29, community midwife
The facility to send push notifications via apps and text messages was seen as a further benefit as these could serve as prompts and reminders to parents to read information at the appropriate times. Overall, midwives were happy to support the introduction of an app including NBS information providing that there was an opportunity for them to check that parents had accessed and understood the information prior to obtaining their consent for screening. However, although midwives recognised that an app would be a useful and acceptable information resource, they were also aware that not all parents had access to a smartphone and so multiple resources would still be required:
A lot of them use their phones all the time so I think if there’s an app there I suppose obviously if it’s a free app which obviously we can signpost the ladies to then yeah, I’m sure they probably would do. Obviously not all of them but again some of them will.
#21, trust screening co-ordinator
As well as improving the efficiency of communication, a further perceived benefit of using technology was improving access to information for parents living in rural areas:
We’re quite unique sort of geographically, and with how sometimes it is difficult to access things, and I think our ladies tend to like technology, for that reason . . . They don’t have a lot of the social stuff that maybe people, in bigger cities, would have. Sort of drop in and have a chat and the information sharing, sort of face-to-face with a group of friends or family, or things like that, doesn’t tend to happen very easily here.
#5, community midwife
Many parents were supportive of an app, providing that it was linked to the wider aspects of pregnancy and early neonatal period. Further benefits of an app noted by parents included the ability to keep track of key milestones for their child as well as notifications to remind parents about upcoming events such as NBS:
If you were going to have an app, I think it would have to be maybe not just be about this screening, but if it was a whole pregnancy type app, you know, akin to the BabyCenter so women could use it throughout the pregnancy.
#20, mother, first child, negative result
I have used apps for the pregnancy, so because of the apps you have these reminders, you have these kinds of notifications, it can remind you.
#44, mother, pregnant with second child
Importantly, the fathers who did talk about apps suggested that these were a form of information that they felt they could access. The timeline nature of the app content appeared to enable fathers to feel that they were able to track the progress of the pregnancy. Moreover, apps were perceived to be a consolidated, more accessible and convenient information resource for parents, many of whom were usual smartphone users:
I think if it was all in one place, it was easy to access, people could find it straightaway, I think it would really work.
#7, mother, second child, both negative results
One of the benefits of having information accessible by phone would be that people constantly have the means to access such information on their person:
My phone’s constantly in my hand anyway, so that’s easy to, sort of, pick up and read.
#22, mother, first child, negative result
So what my midwife tells me is different from what her midwife told her, so I think this can be easier on an app or a website or whatever, a better understanding of what they’re really going to be doing.
#14, mother, second child, GA1 result
Furthermore, many parents also felt that presenting NBS information via an app could potentially mitigate barriers to information engagement, such as information overload, described earlier, as they could access the appropriate level of detail that they desired:
And then you know you’ve got then you can shorten any links then to go into more detail if they want to do that. Because I think sometimes you’re given too much, you just go oh there’s too much to read.
#6, mother, pregnant with second child
Like, when you first find out you’re pregnant or whatever, they give you loads of leaflets, like about 10–12 leaflets. That’s information overload [. . .] But if it was, like, an app, you could just take your time to read through your app.
#14, mother-to-be
Although the majority of parents endorsed an app as a useful information resource, not all parents interviewed possessed a smartphone and so there would be a need to ensure that a range of information resources were available.
Websites
Midwives were generally supportive of directing parents to a website as an alternative information resource. The perceived benefits of using a website included easier access for parents following clear signposting by midwives to a trusted and credible source as well as the capacity to include varying levels of detail to suit parents’ information needs without the space constraints of a printed leaflet. Moreover, midwives thought that the use of graphics and multimedia, for example podcasts and video clips, could potentially enhance the user-friendliness of the information by catering for the needs of a range of parents. However, as with apps, there was an acknowledgement that a website would be an accessible source of information only for some parents:
But I think it’s important that they know which websites, you know, the recommended websites, and obviously we’ve got no control over which website people might choose to access beyond that. And then, obviously, not everybody has got access to the internet, but a lot more people have now. You know, a lot of people have smartphones from all backgrounds.
#13, SQAM
Virtually all parents supported the idea of a dedicated website as a useful and accessible resource for NBS information. Notable benefits of a website cited by parents included easy retrieval of information, knowing that the information was up-to-date and the capacity to include different levels of detail that parents could access according to their needs:
I think I would find that more useful than as a leaflet because you have it in your e-mails and you can always go back because you know it’s there.
#37, mother, first child, negative result
Then, you know, rather than having all these leaflets revised, it’s all there, it’s up to date if it’s changed you can see when it’s been revised as well.
#7, mother, second child, both negative results
A recurrent message by all parents was the need to ensure that a NBS website was NHS based so that it could be trusted to provide accurate and balanced information. Furthermore, parents thought that it was important that they were clearly signposted to the website rather than having to search for it themselves and suggested sending e-mail reminder alerts to ensure that parents were accessing the correct website:
My first port of call would be an NHS website just because you know what you’re getting is fact whereas sometimes some websites you come across they’re a bit scaremongering.
#40, mother, twin children, negative results
I think it would need to be written down rather than just been told to Google it or, you know, told what the website was, because I’m not sure that many people would remember.
#47, mother, second child; first child negative result, second child repeat testing returned negative result
Although there was widespread acceptance of a website as a valuable information resource, there were parents who did not have internet access at home or who lived in areas with weak internet connectivity and thus would not be able to access such a website.
Digital versatile discs
On the whole, midwives felt that a digital versatile disc (DVD) containing NBS information may not be a cost-effective communication strategy given the costs associated with producing and disseminating it. However, many midwives touched on the success of a similar information resource for breastfeeding and thought that some form of visual information may be appropriate for parents who struggled to read written information. As an alternative, midwives suggested that a video clip incorporated on a NBS information website would be a better use of resources, coupled with showings on clinic and bedside televisions as well as during antenatal classes:
Well, it’s going to be very expensive as well, isn’t it, to mass produce, for every pregnant woman in the country. I’m not sure that it would work. Unless you played it at the parent education sessions, but I don’t think all trusts are doing that now anyway.
#17, regional quality assurance manager
For many parents, a DVD containing NBS information was not their preferred method of information provision as they felt that they would not have time to watch it. Quite a few parents also reported not having access to a DVD player but indicated that they would welcome being shown a NBS information DVD during their antenatal classes or as an embedded clip on a website. As well as being more resource efficient and convenient, an online video was desirable for parents whose first language was not English as well as for parents who related better to visual information:
Because to be honest, in England it is a lot of people from different countries, so all the mums . . . some of the mums, they can’t understand at all English, so reading, watching . . . maybe watching like the movies or something would be easy.
#34, mother, first child, screened awaiting result, Polish, no interpreter required
Another suggestion from parents was to use hospital/clinic waiting room television screens to visually remind parents about NBS, to help raise awareness among the constant flow of advertising material currently displayed on clinic television screens:
Different ads are given on them, like pram and baby seat. Why not, this information should be displayed on that.
#45, mother, second child, screened awaiting result
Discussion
This study combined data from parents and health professionals to further understand the communication that occurs between them. In so doing it elucidated how and why communication can sometimes be less than efficient, despite the common goal of both parties. Regardless of their views on consent, with the exception of one father all parents and health professionals unanimously valued the idea that parents should be fully informed about NBS. 45 As shown in previous research, however, the amount of information needed to achieve this differed between parents,12,66 even within couples, with parents also differing depending on whether or not they had had previous children. Thus, although there is a uniform ideal goal of being informed, the information needed to achieve this is unlikely to be uniform.
There was also variation in the parent sample regarding the level of choice that parents wished to have about screening. However, health professionals felt strongly that an informed choice model should be followed and were strongly against mandatory screening, as found in other studies. 69 Of interest, however, in line with other research,22,27,30–32,41,44,75,82 few parents were aware that screening was optional, highlighting a disconnect between how midwives wish to practise and how screening is perceived by many parents.
Of concern, despite attempts to optimise information provision in England, our data suggest that the problem of very low levels of parental knowledge about NBS persists. There were also data to suggest that this caused distress for parents whose children were diagnosed. 63 In addition to the suggestion that key items of information could have reduced such distress, parents also valued this information as it caused them to feel respected65 and fulfilled their need to know what was happening to their child. 19 Of more concern are the data indicating that it was only by participating in the study that parents found out about NBS, suggesting that the findings that parents are not receiving any information29,66,67 and are unaware about screening8,67,78,86,93 are not purely historical. These data also highlight that the practice of assuming that existing parents are informed about NBS through previous pregnancies, which has also been documented in other studies,18 needs to be questioned.
Rather than suggesting that information is simply not provided, the data appear to show that key factors may be reducing how effective communication about NBS is, with the central issue being the timing of information provision. This study adds to the findings that information provision post birth is not effective, nor is the provision of information too early in the pregnancy when the focus is on the pregnancy rather than the eventual child. Within this study we developed the idea that once parents have seen their child on the anomaly scan they are more able to concretely identify him or her as a person for whom they need to make decisions, with many parents endorsing information provision in the third trimester. Although midwives recognise that post-birth communication is not effective, many parents report that they were given information about NBS at this time. Further research should explore whether or not this is indeed the case and, if so, what is driving midwives to provide information at this stage, given the strong evidence base suggesting that communication at this time is ineffective.
As in the literature reviewed in Chapter 2, the data suggest that participants had clear ideas of what should be covered in the information provided, but that differences exist between health professionals and parents. Thus, information provision that follows the priorities of health professionals or information provided in the NBS leaflet may be at too great a level or in the wrong order for parents, causing it to be dismissed. 72 As argued in previous work, it may be more beneficial to first describe why this information could be of relevance to the recipient (i.e. you have a decision to make) before providing the information, especially if the diseases screened for are seen as rare and lack personal relevance. 114 Indeed, not knowing that screening was optional appeared to be a barrier to engagement with information in the current study, with parents citing the fact that they thought that screening was routine as a reason not to scrutinise leaflets or engage with health professionals. Thus, rather than highlighting that not knowing about their ability to choose constitutes purely a lack of knowledge, this study illustrates how this knowledge deficit can become a barrier to engagement itself.
Although the current model of communication may be based on effective modes of communication, such as health professional communication and a booklet that contains relevant information, this study highlights that there are concerns over whether or not parents are adequately informed. The booklets provided appeared to be underused, with few being read. Although this finding is in line with previous research, which suggests that time constraints have a part to play here,12,29,66,68,72 this study suggests that there are also more nuanced barriers that combine, such as providing NBS materials along with other information, failing to mention NBS during standard pregnancy interactions and a generalised lack of promotion, which is out of line with other screening programmes such as that for Down syndrome. The data suggest that altering the time at which parents are given information and separating important information from other materials and highlighting it as such could provide great benefits. It appears that, although health professional interaction is valued by parents and is very much felt by health professionals to be part of a midwife’s role, the size of the NBS panel may already have reached a point at which it is not realistic to expect every midwife to be trained to a sufficient level and to have the time to individually inform all parents. However, both parents and midwives were optimistic that good information provision could occur if additional strategies were employed. There did not appear to be a view that NBS communication was overly complex and certainly that informed consent was not possible, as per some arguments reported in the literature review. 73
One suggestion in the data is that NBS may have reached a point at which communication needs to occur in a group setting. There also appears to be a recognition in the data that, to communicate with parents effectively and to be able to answer questions in a diverse population, the information provider needs to undergo in-depth training, with there being doubts about whether or not this is possible given the existing shortage of midwives and the effect that this shortage has on midwives’ ability to access training. Thus, it may be preferable to ensure that a smaller number of midwives are trained to provide information to groups of patients, with other mechanisms used to provide additional information, such as information tool kits and national helplines.
Midwives emphasised the importance of multiple communication strategies to ensure that all parents can access an information resource appropriate to their language, literacy and learning needs. With regard to each of the alternative information resources discussed in this chapter, clear signposting by midwives was seen to be integral to the successful uptake of the resources. Despite the focus on technology, midwives felt that the NBS information leaflet was still an important resource for parents who did not have a smartphone or internet access, as well as for parents who prefer to have a hand-held written information resource. In terms of combining strategies and information timing, midwives thought that an effective way to communicate with parents would be to begin with a verbal introduction to NBS, followed by signposting to an app or a website or providing a leaflet that parents could access in their own time in the third trimester. Multiple reminders in pregnancy using e-mail-, text- or app-based notifications were also seen to be effective prompts for parents, as well as postnatal reminders at discharge and on the day 1 midwife visit.
Chapter 4 Study 3: costing studies
Study objective
The objective of this study was to establish the resource use and costs associated with the current practice(s) of providing NBSP information antenatally.
Introduction
The process of providing information in the context of the UK NBSP has resource implications for the recipients of the information (parents) and those providing the information (midwives). As outlined in Chapter 1, the latest version of the Health Professional Handbook9 suggests that midwives provide parents with a copy of the Screening Tests For You and Your Baby booklet and verbally provide information about NBS. They should seek consent after checking that parents understand 10 different points. It is not known, however, what practice is actually followed and what resources and how much time are required when delivering the current model of UK NBSP information provision. Evidence on the required resources and associated unit costs is necessary to inform future evaluation studies of new models of information provision to identify their incremental benefits and costs.
Methods
This study identified the key items of resource use and potential cost drivers in current practice using the perspective of NHS England. The time frame for the analysis was from the time of initial information provision to the time at which informed consent is obtained. Two types of direct health-care costs were identified and quantified: (1) semi-fixed costs, such as staff time, and (2) variable costs, such as the number of leaflets provided. Two modes of data collection were used: (1) a survey of midwives and (2) direct observation of midwife practice. NHS ethics approval was obtained.
Survey of midwives
The survey aimed to identify current practice, any regional variations in current practice and the key cost drivers of current practice, using the views of a national sample of midwives. Initially, a postal survey was planned but a lack of response meant that the survey was redesigned to be conducted as a telephone interview.
Observation study
The direct observation of midwives aimed to provide information on actual practice by making ‘real-time’ recordings of staff grade and the time taken to perform duties associated with the provision of NBSP information. This study sent a researcher alongside practising midwives on their visits. R&D approval for the observation study was sought for a range of NHS trusts in the north-west region of England.
Study samples
The relevant study population for this study was midwives working in NHS England and currently providing antenatal care for parents in the hospital and community setting. Different approaches to sampling were used for the survey and observation study.
A target sample size of 30 respondents was set for the telephone survey. This sample size was deemed to be sufficiently large to identify the full range of resources used across the information pathway, along with heterogeneity in practice across NHS England. Only midwives in England were approached as the number of conditions screened for in the different countries of the UK varies and therefore the resource use and cost implications in these different regions will vary. The sampling framework for the survey was informed using advice from the project scientific advisory board and local NBSP advisors (n = 5). A list of senior midwives (n = 80) was generated along with their e-mail contact details. The list ensured a geographical representation of NHS England. An initial e-mail containing details of the study was sent to these 80 senior midwives, who were asked to pass the information on to midwives in their trusts. Potential participants then contacted the researcher (SW), who arranged a telephone interview at a time that was convenient for each midwife. Survey respondents were entered into a draw for the chance to win a £50 Marks & Spencer voucher as a thank you for their time.
For the observation of midwife practice, the target sample was midwives working in up to eight different NHS hospital trusts. The NHS hospital trusts were based in the north-west of England but were selected to allow some variation in the demographic and geographical make-up of populations served to try to capture heterogeneity in practice. The sampling frame was heads of midwifery at the trusts that had given approval for contact to be made. A researcher (SW) first contacted the heads of midwifery to explain what the process of observation would involve and for support in recruiting midwives to the observation study. The heads of midwifery were asked to circulate an e-mail request to their midwives. Midwives who expressed an interest by return of e-mail were provided with an information sheet and a date was then arranged for the observation. In the information sheet midwives were informed that the researcher wanted to observe routine practice in NBS. On the first day of the observation the researcher again explained the study and gained written consent from the midwife for the observation of practice to take place.
The telephone survey: design
The telephone survey used a structured interview schedule that consisted of closed and open questions (see Appendix 3). Two sources (Tina Lavender, University of Manchester, 5 November 2013, personal communication, and UK Newborn Screening Programme Centre115) were used to develop an understanding of the current model of information provision in the UK NBSP and hence inform the key questions to include in the survey to be able to identify the resources required to provide NBSP information. The survey was prepiloted by a sample of senior midwives, including the north-west region SQAM, a newborn bloodspot project manager, a research midwife co-ordinator and practising midwife, and a senior academic midwife.
The interview schedule was tailored to the roles of hospital and community midwives respectively. The main focus of the questions was to understand when and how midwives give information to parents about the NBSP. Additionally, questions were included to account for the resources used to provide this information, including asking midwives how long they spent discussing NBS and what materials they used to help them. Midwives were asked how they obtained consent from parents and how many parents a week they gained consent from. The free-text questions focused on exploring whether or not there were any barriers to the provision of information.
The observation data collection tool
A data collection tool was designed to facilitate the timely and accurate recording of the resources used while observing a midwife providing information in practice (see Appendix 4). The data collection tool also recorded the time spent travelling to visits as well as the total length of the visits. This information would allow the proportion of the resources required for the visit to be allocated specifically to NBS information provision. The types of information provided were recorded to identify how resource use may change if additional information were to be provided in future models of information provision. The types of information that may be important were identified as part of a systematic review of DCEs (see Chapter 5) of screening, and diagnostic and genetic technologies, as well as maternity care (see Appendix 5). Box 1 shows the types of information included in the initial spreadsheet. Additional types of information that were provided by midwives were added when encountered in an observation.
-
The names of the conditions included in the screening.
-
How you can prepare your baby for the sample.
-
How the sample is taken.
-
Whether your baby would suffer any pain or side effects when the sample is taken.
-
The time it takes to receive the results.
-
How I will receive the results.
-
Whether you could receive a result which suggests that your baby does not have a condition when in reality he or she does.
-
Whether you could receive a result which suggests that your baby has a condition when in reality he or she does not.
-
The effect that having one of the conditions would have on your baby’s health.
-
How common or rare the conditions are.
-
What can be done to treat your baby if he or she has one of the conditions.
Data collection
The data from the structured telephone interviews were directly entered into a bespoke Microsoft Excel® (2010; Microsoft Corporation, Redmond, WA, USA) spreadsheet. Drop-down menus with categories of response were created, although the interviewers were encouraged to allow respondents to give a free answer before providing them with these responses. All responses were anonymised.
For the direct observation process, the researcher (SW) assumed the role of a (hypothetical) student midwife, with midwives knowing that they were being shadowed. The researcher shadowed the workday of each midwife. Shadowing midwives involved travelling with them in their car to visits if they were community based. The midwives conducted routine checks and procedures with the parents first while the researcher waited outside the room/in the car. Midwives then explained that a researcher was observing them provide information about NBS and asked parents to give verbal consent for this observation. The researcher then entered the room and observed the provision of information, recording resource use and the types of information provided on an Apple iPad (Apple Inc., Cupertino, CA, USA) using the observation data collection tool (see Appendix 4). The time spent discussing NBS was recorded subtly using a wristwatch, as many visits took place in the home and the use of a stopwatch was deemed to be obtrusive. It may have also added a sense of pressure to the midwives providing the information. No information about the parents or baby was recorded. When information about NBS had been provided, the researcher left the room.
Data analysis
Data collected from the survey and direct observation were first analysed separately. Responses to the closed-ended questions in the telephone survey were analysed using descriptive statistics. If respondents gave a range for an answer (e.g. the duration of information provision), the mid-point value was taken for calculation of medians and means. The data from the open-ended questions were transcribed into a Microsoft Word® (Microsoft Corporation, Redmond, WA, USA) document and analysed using content analysis to identify common arguments. The observational data were analysed using descriptive statistics to summarise the types and quantities of resources used, together with the types of information provided.
The data from the survey and direct observations were then combined to produce a list of the types and range of resources required to provide information about NBS. In addition, a narrative approach was taken to draw similarities and make comparisons between the data collected from the survey (stated use of resources) and the data collected in the observation study (observed actual resource use).
Unit costs to attach to the items of resource use were identified using published sources combined with personal communication (Tina Lavender, University of Manchester, 25 September 2014). It was not possible to use the Personal Social Services Research Unit’s Unit Costs of Health and Social Care 2015116 to provide the cost of a midwife. Therefore, after consultation with a senior academic midwife, it was decided to use the cost information for community nurses as a proxy for community midwives, given the similar salary level and working patterns involved in the roles.
Results
The findings from the survey and direct observation are first presented separately and then combined to provide an overview of the types and quantities of resources used and the information provided by midwives in the current practice of NBSP information provision in the NHS.
Telephone survey
A total of 22 midwives completed the telephone survey. Twenty of the midwives worked in the NHS but two were subsequently identified as midwives working in the private sector. The NHS midwives represented 20 distinct NHS trusts across England, with the two private midwives working in a variety of areas in the north-west of England. Nearly half of the midwives (n = 10) were community midwives, 27% (n = 6) were screening co-ordinators and 14% (n = 3) were community midwife team leaders. The remaining three midwives were caseload midwives (n = 2) and a research midwife (n = 1). Most midwives were either at band 6 (n = 12) or at band 7 (n = 7) on the NHS central pay scale. One midwife had a mixed role that was part band 6 and part 7, one of the private midwives was at band 8 and one midwife did not provide a pay band.
Information provision and resource use
Tables 5 and 6 summarise the findings from the telephone survey. Multiple answers were available for some questions, resulting in percentages that sum to > 100%. An extended table displaying the full combinations of answers that midwives gave is provided in Appendix 6. The resources used to provide information about the NBSP depended on the time during pregnancy or after birth at which information was provided. Information about NBS is potentially given by midwives at five different time points: at booking (8–12 weeks of pregnancy), late in pregnancy (after 30 weeks’ gestation), on discharge from hospital, on day 3 (after the baby is born) and on day 5. The majority of midwives provided information at booking (n = 19; 95%) and on day 3 (n = 17; 85%) (excluding information from private midwives).
| Topic | Number of midwivesa,b (%) |
|---|---|
| Antenatal information | |
| Do you give information before birth? | |
| Yes | 19 (95) |
| No | 1 (5) |
| If you give information before birth, how do you do this? | |
| Individual discussion | 7 (35) |
| Give the general screening leaflet | 19 (95) |
| Give a specific NBS leaflet | 1 (5) |
| If you discuss NBS before birth, when would this be? | |
| At booking (< 12 weeks) | 2 (10) |
| At 32–36 weeks | 5 (25) |
| If you discuss NBS before birth, where would you do this? | |
| In an antenatal clinic | 3 (15) |
| In a hospital | 0 (0) |
| In the parents’ home | 2 (10) |
| Other, including Sure Start centres, GP surgery and antenatal clinic | 4 (20) |
| If you provide a screening leaflet before birth, when would you do this? | |
| At booking | 17 (85) |
| At > 30 weeks | 2 (10) |
| If you provide a screening leaflet before birth, where would you do this? | |
| In an antenatal clinic | 9 (45) |
| In the parents’ home | 5 (25) |
| Other (Including GP surgery, children’s centres and by post) | 9 (45) |
| Postnatal information | |
| Do you give information after birth? | |
| Yes | 20 (100) |
| No | 0 (0) |
| If you give information after birth, how do you do this? | |
| Individual discussion | 19 (95) |
| Give the general screening leaflet (if parents do not have one) | 12 (60) |
| Give a specific NBS leaflet (if parents do not have one) | 2 (10) |
| If you discuss NBS after birth, when would this be? | |
| Immediately before the test | 8 (40) |
| 24 hours before the test | 4 (20) |
| > 24 hours before the test | 17 (85) |
| At hospital discharge | 1 (5) |
| If you discuss NBS after birth, where would you do this? | |
| In hospital | 6 (30) |
| In the parents’ home | 19 (95) |
| Other (community clinic or specific NBS clinic) | 2 (10) |
| Consent for screening | |
| Do you personally take informed consent for screening? | |
| Yes | 19 (95) |
| No | 1 (5) |
| How do you take informed consent for screening? | |
| Verbal | 17 (85) |
| Written | 3 (15) |
| Question | Mean | 95% confidence interval | Median |
|---|---|---|---|
| If you discuss NBS before birth, how long would you spend doing this? | 5.07 minutes | 0.87 to 9.23 minutes | 2.50 |
| If you discuss NBS after birth, how long would you spend doing this? | 5.18 minutes | 3.73 to 6.64 minutes | 5.00 |
| If you personally take consent for screening, how many times a week would you do this? | 8.00 occasions | 3.65 to 12.35 occasions | 4.50 |
| If you personally explain why a repeat screening test may be necessary, how long do you spend explaining this? | 4.94 minutes | 2.65 to 7.24 minutes | 2.50 |
| On average, how many second bloodspot samples do you take in a week? | 0.69 samples | 0.31 to 1.06 samples | 0.50 |
In the antenatal period information was generally given in an antenatal clinic (n = 9; 45%) or in the parents’ home (n = 5; 25%), but other settings such as general practice surgeries and children’s centres were also mentioned by nine (45%) of the midwives as potential locations at which parents may receive information. In contrast, virtually the entire sample reported that all information provided after the birth was given in the parents’ home (n = 19; 95%), although one midwife said that some information may be given on hospital wards at discharge.
Only two key physical information resources were used to convey the information: a general leaflet about all types of screening that are offered during and after pregnancy and a leaflet containing only information about NBS. The general leaflet was given to parents by all midwives who provided information in the antenatal period and most midwives (n = 12; 60%) stated that they also checked that parents still had this leaflet after their baby was born, replacing it if it had been lost. The NBS-specific leaflet was used by only two midwives and in both instances this was provided after birth.
Alongside providing parents with physical information in the form of a leaflet, midwives also discussed the information, to different extents. In the antenatal period, NBS was discussed by seven (35%) of the NHS midwives surveyed. At this time, information provision was brief, taking a median of 2.5 minutes (mean 5.07 minutes). However, 19 (95%) of the NHS midwives discussed NBS with parents after their baby was born and this discussion lasted for a median of 5.0 minutes (mean 5.18 minutes). The two private midwives both stated that they spoke about NBS for 20–30 minutes and, as this duration of time far exceeded the times suggested by the NHS midwives, the responses of the private midwives were excluded from the analysis. When midwives were required to obtain a repeat sample for screening, the reasons for this were also explained in an individual discussion, with this lasting for a median of 2.5 minutes (mean 4.94 minutes).
Consent for screening was nearly always obtained verbally (n = 17; 85%), although in some trusts the midwife obtained written consent so that a health visitor or maternity support worker could take a screening sample at a later date. In this sample, midwives took consent for screening, and therefore conducted screening, a median of 4.5 times per week (mean 8 times).
Content analysis of free-text comments
Just over half (52%) of the midwives said that they believed that their other duties limited the amount of time that they could spend explaining NBS to parents. This meant that many midwives felt the need to rush the provision of information. When additional time was needed to explain the information, this was often simply added to the midwife’s day, which resulted in a late finish with no extra pay.
The potential addition of four new conditions was reported as a cause for worry by some midwives, who could not see how they would be able to provide all of the information required in their consultation time. Other time demands such as the need to vaccinate against flu and whooping cough in autumn and winter might result in less information being provided at these times. One midwife stated that if policy-makers wanted true informed consent to be taken then they would need a lot more than 30 minutes for the first postnatal visit, suggesting that an hour might be more appropriate.
Sometimes the time spent giving information was seen to be constrained by the lack of desire or ability of parents to take on the information. For example, some midwives (9%) perceived that NBS was not seen as a priority by first-time mothers and in other cases midwives felt that they had to rush when women were already very stressed or tired (14%). Other midwives (9%) felt that they were limited in the amount of detail that they could give to parents while at the same time ensuring that they understood it.
Some of the midwives (14%) mentioned that the amount of information given to parents who had had previous children was generally less detailed as it was assumed that they would remember the information from previous births. One midwife mentioned that parents sometimes insist that they know the information and so do not need to hear it again.
The midwives who were interviewed gave mixed messages about when information should be provided. One midwife believed that, after the birth, parents would be more concerned about receiving information and help on how to breastfeed and change nappies and, because of this, information about NBS should ideally be given in the less stressful antenatal period.
The perceived lack of confidence of the midwives to provide information and answer questions was a recurring theme. One midwife stated that she struggles with the names of the conditions and many others (23%) suggested that updated training would be useful as midwives often need to move between different roles. The need for evidence-based guidance on information provision was seen as important by one midwife.
Some of the midwives (18%) suggested a need for simpler, less scientific information in ‘plain English’ to improve the current NBS leaflet. One midwife mentioned that an app for tablets or smartphones might be useful as parents often use these devices.
Direct observation
In total, eight midwives were observed providing NBS information in five NHS hospital trusts, which yielded 14 observed instances of information provision. On three occasions it was not possible to directly observe information provision: on one occasion, consent was not given for observation by a parent; on another, the parent had another medical problem; and, on the third, the parent was not at home at the time of the appointment.
Information provision and resource use
Of the observed 14 instances of information provision, eight took place on day 5 after the birth, four took place on day 3 after the birth, one took place at week 20 of pregnancy and one took place at hospital discharge. The majority of the observed information provision, therefore, took place post birth, with most occurring in the parents’ home (n = 11; 79%). On one occasion information was provided on discharge from hospital and on another occasion it was provided in hospital on day 5 for medical reasons relating to the parent.
Midwives checked that parents had received the general screening leaflet in 4 of the 14 observations. One of these observations took place at week 20 during pregnancy, one was on day 3 post birth and two were on day 5 post birth. However, midwives were observed providing the NBS-specific leaflet on eight occasions, one at week 20, one at hospital discharge, four at day 3 post birth and two at day 5 post birth.
On average, neonatal home visits lasted for 40.27 minutes. The direct observation allowed the duration of the discussion about NBS to be recorded. In the one observation of information being provided before birth, the midwife spent 1.5 minutes discussing NBS. When information was given after birth (13 observations), the median time spent discussing NBS was 4.00 minutes (mean 3.67 minutes).
Midwives who visited parents’ homes used their own car. Midwives were observed on 13 occasions to spend a median of 12 minutes (mean 12 minutes) travelling to and from visits in parents’ homes.
Table 7 summarises the types and quantity of information offered during the direct observation of 14 episodes of information provision. These findings identified that, on average, 6.57 pieces of information were offered: five pieces of information at 20 weeks, five pieces of information at hospital discharge, eight pieces of information at day 3 post birth and 6.25 pieces of information at day 5 post birth.
| Type of information | Number of times information presented at different time points (n = 14 observations) | ||||
|---|---|---|---|---|---|
| 20 weeks | Hospital discharge | Day 3 | Day 5 | Total (%) | |
| The names of the conditions | 1 | 1 | 3 | 7 | 12 (86) |
| The health effects for the child of having one of the conditions | 1 | 1 | 3 | 7 | 12 (86) |
| Screening is voluntary | 0 | 0 | 4 | 7 | 11 (79) |
| The time until results are received | 0 | 0 | 4 | 7 | 11 (79) |
| The treatability of the conditions | 1 | 1 | 3 | 6 | 11 (79) |
| How the sample is taken | 1 | 0 | 4 | 6 | 11 (79) |
| The rarity of the conditions | 1 | 1 | 4 | 3 | 9 (64) |
| The storing of bloodspots is voluntary | 0 | 0 | 4 | 0 | 4 (29) |
| The possibility of false positives, false negatives or repeat tests | 0 | 0 | 1 | 3 | 4 (29) |
| How parents can prepare their baby for screening | 0 | 1 | 2 | 1 | 4 (29) |
| Whether the child will feel any pain from screening | 0 | 0 | 0 | 3 | 3 (21) |
| Who will take the sample | 0 | 0 | 0 | 0 | 0 (0) |
Resources and unit costs
Table 8 summarises the unit costs for each type of resource use, identified from the telephone survey and direct observation study, together with the sources of the costs. These costs are provided in 2015 UK pounds.
| Resource use | Level of resource use (range) | Unit cost (£) | Total cost (range) (£) | Assumption | Source |
|---|---|---|---|---|---|
| Cost of a midwife’s time to discuss the information | 3.31 minutes (1.5–6 minutes) | 50.00 per houra (0.83 per minute) | 2.75 (1.25–4.98) | Community nurse (grade 6) as a proxy for community midwife | Curtis116 |
| Printed leaflet | 1.00 | 0.11 | Not applicable | Mean cost per leaflet from all 2015 orders | Personal communicationb |
| Cost of a midwife’s time to discuss the leaflet | 0.55 minutes (0.30–1.00 minutes) | 0.83 | 0.46 (0.17–0.83) | Assumed that the same amount of time is taken to explain the leaflet as to provide one type of information verbally | Curtis116 |
| Cost of a midwife’s time to travel between visits on days 3 and 5 | 12 minutes (2.00–19.00 minutes) | 0.83 per minute travelled | 10.00 (1.66–15.77) | Mean of 12.00 minutes spent travelling to and from visits | Curtis,116 observation study |
| Mileage for midwife travel between visits on days 3 and 5 | 6.00 miles (0.90–9.25 miles) | 0.56 per mile | 3.36 (0.50–5.18) | Assumed 6 miles travelled per visit and an average speed of 30 miles per hour | NHS Employers117 |
The cost of providing newborn screening information in current practice
Combining the data collected from the telephone survey and the data collected in the observation study suggested that the median time spent presenting information about NBS was 2.25 minutes (mean 4.63 minutes, range 1.5–17.5 minutes) in the antenatal period and 4.00 minutes (mean 4.82 minutes, range 1.25–12.5 minutes) in the postnatal period.
The survey and direct observations indicated that there is some variation in practice between midwives. To produce an ‘average cost’ for the current model of information provision in NBS, a simple information provision pathway was modelled to represent the potential use of resources by midwives in NHS England. Figure 4 represents the potential pathways and associated use of resources, from the initial discussion about NBS to the provision of informed consent.
FIGURE 4.
Model representing potential information provision pathways.
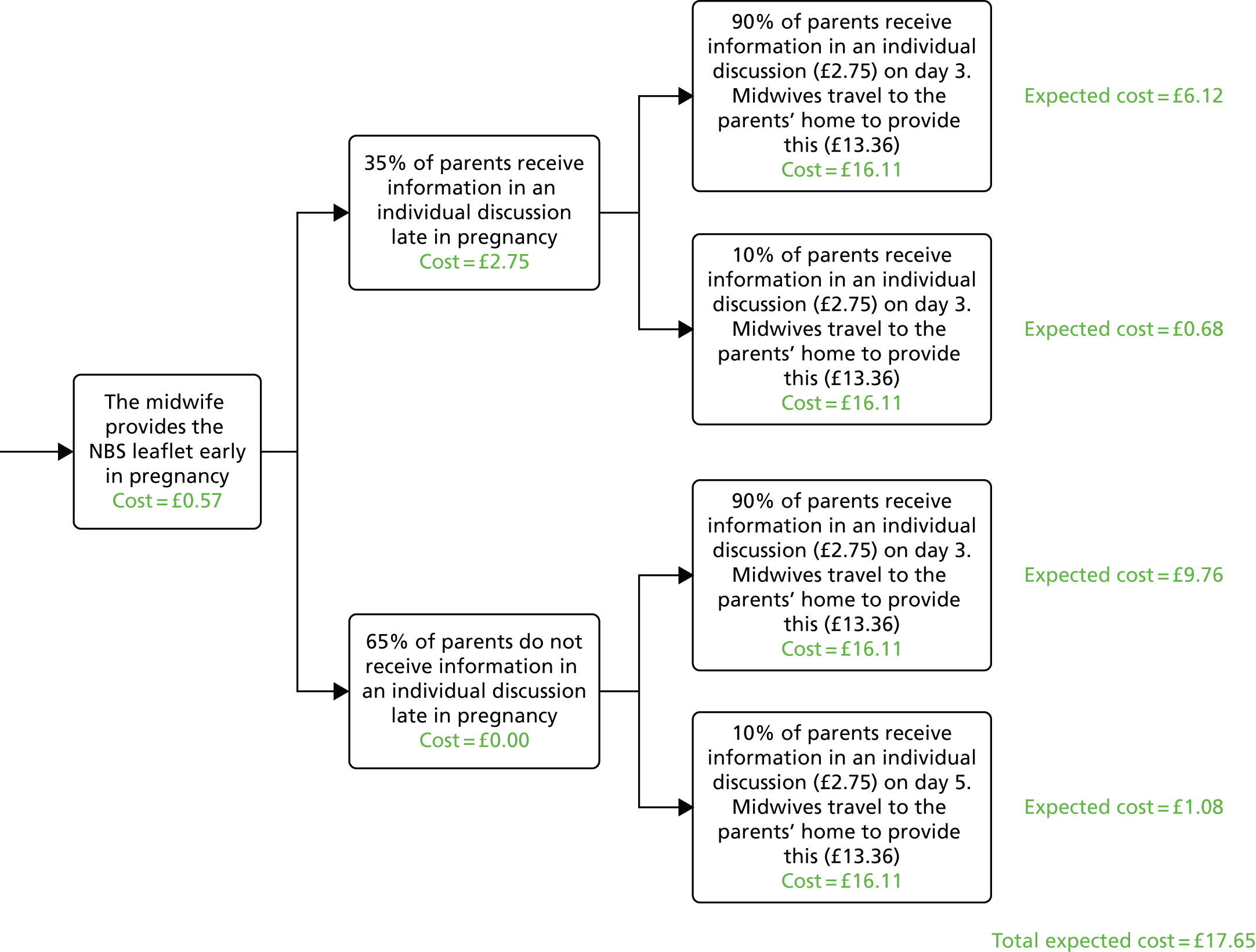
Table 9 shows the values of the input parameters used to generate an estimate of the total expected cost per parent receiving information over the duration of the pregnancy and birth until the provision of informed consent. The estimated total expected cost per parent was £17.65. Assuming that there are 661,496 live births annually, using 2014 data from England,118 the total cost of the current information provision model in England is £11,675,404 per annum. This estimate assumes that all children survive until NBS is conducted.
| Parameter | Value | Source/assumption |
|---|---|---|
| Proportion of parents participating in a discussion late in pregnancy | 0.35 | Telephone survey: mean proportion of midwives stating that they did provide a discussion late in pregnancy (n = 7/20) |
| Proportion of parents receiving information on day 3b | 0.90 | Telephone survey: mean proportion of midwives stating that they provided information on day 3 or day 3 and day 5 (n = 18/20) |
| Proportion of parents receiving information on day 5 | 0.10 | Telephone survey: mean proportion of midwives stating that they provided information on day 5 only (n = 10/20) |
| Cost of receiving information in a discussiona | £2.76 | Observation: mean time taken to provide a piece of information (0.55 minutes) multiplied by the mean number of types of information provided (n = 6) multiplied by the cost per minute for a midwife’s time (£0.83) |
| Cost of receiving information in a leafleta | £0.57 | Observation: average time taken to provide one piece of information (0.55 minutes) multiplied by the cost per minute of a midwife’s time (£0.83) added to the cost of printing a single leaflet (£0.11) |
| Cost of midwife travel to provide information on day 3 or day 5 | £13.36 | Observation: mean time taken to travel to the visit (12 minutes) multiplied by the cost per minute of a midwife’s time (£0.83) added to the cost of travelling for that amount of time at 30 miles per hour [£0.56 × 12 × (30/60) = £3.36] |
Summary
This study identified the key items of resource use and the quantities of resources used when providing NBS information using the current model of information provision. There was some variation between the reported and the observed duration of individual discussions. The times associated with information provision stated in the telephone survey were generally longer than those observed in real practice. Although it is possible that midwives deliberately overstated the duration of information provision, there may also have been a tendency for individuals to report round number values, for example 5 minutes, or take the midpoint value when a range was given. It is possible that the results of the observation study were influenced by the Hawthorne effect, whereby the observed party behaves differently because he or she is being observed. A trade-off was required between observing the midwives for a whole week each, involving the observation of a large amount of irrelevant activities, and observing them only providing NBS information. The latter was chosen despite the fact that it meant that midwives might not become used to being observed, heightening the risk of the Hawthorne effect. The former strategy of observing all of a midwife’s activities was deemed to be too intrusive to the midwife’s other patients who were not receiving NBS information. Using a combination of the data from the telephone survey and the data from the observation study, the estimated expected cost per parent was £17.65, which can be extrapolated to a total cost of £11,675,404 per annum to NHS England using the estimate of the number of babies born in 2014. To our knowledge this is the first estimate made of the cost of information provision for NBS in NHS England.
A systematic review of published economic evaluations of NBS (reported in Chapter 6) identified five studies that included a cost associated with information provision related to NBS. 119–123 In the two identified studies relevant to the UK setting,119,120 an incremental cost of providing information, based on the additional time that it would take a midwife to explain the additional tests being evaluated, was used (£0.30119 and £0.40120). Pandor et al. 119 provided little information on how the cost they used was derived, but did refer to being informed by a consultation with a midwife. Simpson et al. 120 based their cost on the salary cost for a midwife providing 2.1 minutes of information. In a study carried out in Australia, Geelhoed et al. 121 used a similar method, multiplying the salary cost for a midwife by the amount of time spent providing information. Wildhagen et al. 122 estimated the cost of providing information about neonatal CF carrier screening by taking a value from a previous study124 and scaling it by a factor of 60%. This study used a top-down approach that provided little information about how individual items of resource use were valued. No reason was provided for using the adjustment value of 60%. Autti-Rämö et al. 123 used a cost of €5.41 for information provision, which included the costs of a nurse providing verbal information, a leaflet and visits to a physician for additional information (10% of parents).
With the exception of the study by Autti-Rämö et al. ,123 these published estimates of the cost of information provision in NBS did not account for aspects of resource use that would be involved in providing information other than midwives’ time. The observation of midwives as part of this study suggested that travel costs were the most significant contributor to the total cost and so it is crucial that such costs are included in estimates. The total cost calculated in this study suggests that previous estimates of the cost of providing information about NBS may be significantly lower than the costs actually incurred by the health-care system. To provide an accurate estimate of the cost-effectiveness of an expansion in NBS, the full cost of providing information about the service to parents must be incorporated.
There is likely to be significant uncertainty in our estimated cost of information provision in NBS using the current approach (midwives and leaflets). However, the cost estimate of £11,675,404 per annum provides a starting point for a subsequent evaluation of the incremental costs associated with alternative modes of information provision in the context of a national NBSP in NHS England.
Phase 2 Acceptability, preference, cost and broader impact of alternative models
This phase of the study sought to test out and narrow down some of the alternative models of communication and consent (Figure 5). Two DCEs were carried out, one with the public and one with midwives (see Chapter 5). Economic modelling was used to determine the cost of the most likely alternative model (see Chapter 6) and findings from all of the studies in this project were fed back to participants in study 2 (qualitative interviews; see Chapter 3) to explore their views about the acceptability of, their preferences for and the broader impact of the study recommendations (see Chapter 7).
FIGURE 5.
Phase 2 of the study. RCM, Royal College of Midwives; RO, research objective; S, study.
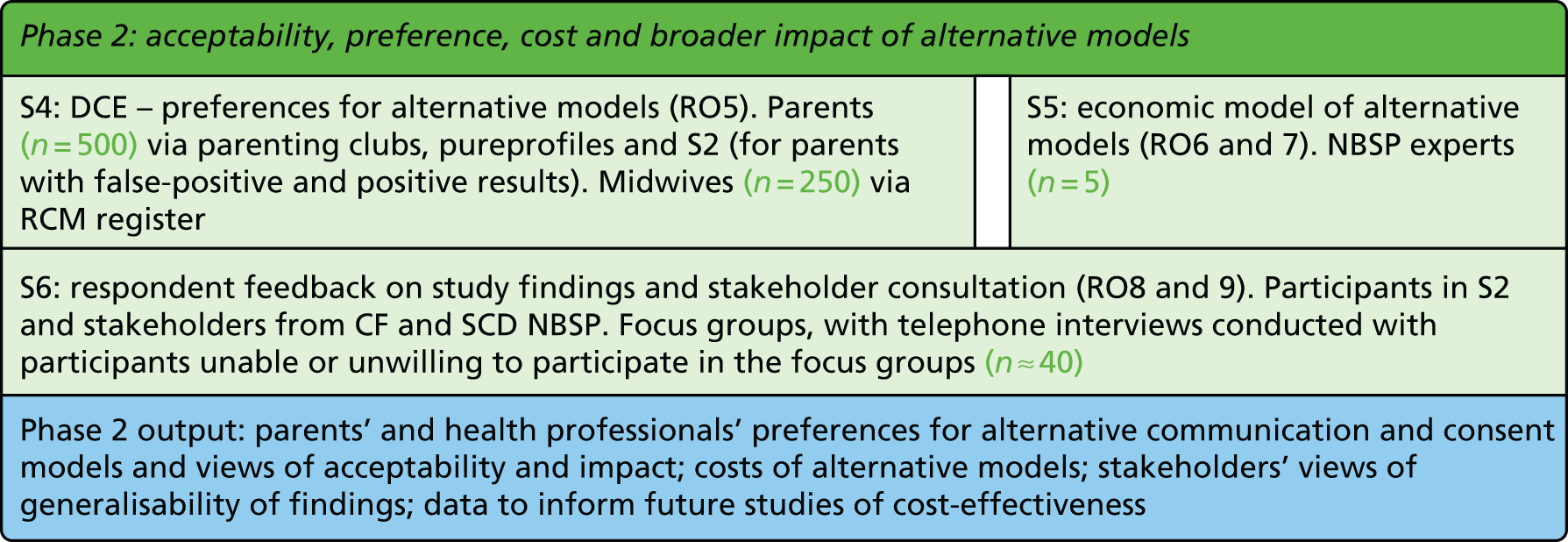
Chapter 5 Study 4: preferences for information provision
Study objective
The objective of this study was to examine the preferences of midwives, parents and prospective parents for different models of conveying NBSP information antenatally.
Introduction
As stated in the introduction (see Chapter 1), information received as part of the NBSP has some unique characteristics in terms of volume and timing. 62 The challenge, therefore, is to ensure that health-care professionals, using information materials, are able to adequately inform parents of the different diseases and screening process when each disease is rare and there are increasing numbers of diseases included in NBSPs. This involves the provision of an adequate type and volume of information while also considering how, and when in relation to the birth, this information is provided.
In the absence of testable existing models of information provision, one option is to identify the preferences of parents and health-care professionals (midwives) for different types of information and different modes of information provision. A DCE is a survey-based method that is commonly used to value different models of health-care programmes and allows the measurement of preferences, underpinned by robust economic theories. 125 A DCE is a form of survey that identifies and measures what outcomes or aspects of service delivery service users or providers prefer and value the most and which can be used to incorporate patient-stated preferences into resource allocation decisions. Importantly, a DCE enables the identification of the trade-offs that people make between different attributes of a service, such as being prepared to wait longer to achieve better-quality information. An understanding of parents’ and midwives’ preferences for the process and outcomes of information provision has the potential to improve the allocation of resources when designing new programmes or expanding existing NBSPs to include more conditions.
Research questions
This study was designed to answer four research questions:
-
What types of information are perceived to improve parents’ ability to make a decision about screening?
-
How and when should information be provided?
-
What is the relative value placed by parents on the process of information provision compared with the quality of information provided in terms of its impact on parents’ ability to make a decision?
-
How do the preferences of parents compare with those of midwives?
Methods
This study used a hybrid survey design consisting of a rating-based conjoint analysis and separate, but linked, binary DCE with opt-out. The rationale for using this hybrid approach was driven by the complexity of the choice question being addressed in that parents may value both the way in which information is provided and the impact of that information on their ability to make a decision about screening: (1) what are the types of information that should be provided about the NBSP so that parents feel able to make an informed decision and (2) how should information be provided and traded against the outcome of the information provision process (ability to make an informed decision)? The study was designed in accordance with published guidelines for the design of studies using conjoint analysis. 126
Attributes and levels
The same attributes and levels were used in the different versions of the survey for parents and midwives. Mixed methods were used to identify and frame the attributes and levels for the conjoint analysis and DCE: a systematic review of published DCEs relevant to screening programmes; a rapid review of NHS NBSP policy and practice documents and training materials; consultation with NHS NBSP experts; and semistructured interviews with parents, midwives and regional quality assurance co-ordinators.
The systematic review identified 58 published DCEs relevant to screening programmes (see Appendices 5 and 7 for a full list). All attributes were tabulated from each identified DCE and grouped by intervention. Duplicate attributes were combined and unique attributes were collated to give 20 distinct starting themes. Themes that were deemed not to be relevant to the policy context were removed, leaving 13 attributes. Eleven of these attributes represented the type of information and were used in the conjoint analysis. Two of these attributes were related to the process of information provision and were used in the DCE. The out-of-pocket cost for parents of receiving information and the impact of information on parents’ ability to make a decision about screening were also added as attributes in the DCE.
Three NHS NBSP policy documents were identified: the current Screening Tests For You and Your Baby leaflet,10 a set of postnatal notes that are given to parents and which contain some information on NBS127 and a handbook designed for health professionals who take the bloodspot sample. 115 These documents were used to validate the attributes to be included in the conjoint analysis (reflecting the types of information required), with the current screening leaflet representing current practice.
Semistructured interviews with parents (n = 20), midwives (n = 29) and NBSP regional quality assurance managers (n = 7) were also used to inform the selection and framing of the attributes and levels. The semistructured interviews did not identify any new potential attributes but suggested that it was necessary to try to elicit how preferences for information may change given the number of conditions included in the NBSP. These interviews also informed how we could modify the framing of the survey to make the same attributes and levels clear and relevant for parents and midwives.
The findings from each of these studies were triangulated128 to identify areas of dissonance, agreement or silence and create a ‘shortlist’ of potential attributes and levels. Consultation with NHS NBSP experts (n = 3) and the parent reference group confirmed the relevance of the attributes and levels. A set of attributes and levels for the conjoint analysis and DCE were then piloted using think-aloud methods in a sample of five members of the public and university researchers and three midwives and analysed using content analysis before the final list of attributes and levels was selected and framed. This pilot phase indicated that the types of conditions being screened should not be included as an attribute as this would correlate directly with the attribute in the conjoint analysis that asked respondents if they wanted to know what conditions were included. Subsequent piloting confirmed that a feasible approach in the parent sample to determine the impact of the number of conditions in the NBSP and effect on preferences for information provision would be to create two survey versions: (1) one for a NBSP that screened the baby for nine conditions, as has recently become current practice in the UK, and (2) one for a NBSP that screened the baby for 20 conditions, representing a further expanded NBSP. However, for midwives, it was not feasible to include a survey related to 20 conditions as they knew that the current programme included only nine conditions. For this reason, one version of the survey was created for midwives, relating to nine conditions. Box 2 and Table 10 show the final list of attributes and levels for the conjoint analysis and DCE respectively.
-
The names of the conditions included in the screening.
-
How you can prepare your baby for the sample.
-
How the sample is taken.
-
Whether your child would suffer any pain or side effects when the sample is taken.
-
The time it takes to receive the results.
-
How I will receive the results.
-
Whether you could receive a result which suggests that your child does not have a condition when in reality they do.
-
Whether you could receive a result which suggests that your child has a condition when in reality they do not.
-
The effect that having one of the conditions would have on your child’s health.
-
How common or rare the conditions are.
-
What can be done to treat your child if they have one of the conditions.
Each attribute had two levels (present or absent).
| Attributes | Levels |
|---|---|
| How information is provideda | Discussion |
| Leaflet | |
| Internet | |
| Mobile/tablet app | |
| Group session | |
| When information is provideda | Early pregnancy |
| Late pregnancy | |
| When the baby arrives | |
| Post birth (day 3) | |
| When the sample is taken (day 5) | |
| Parent(s)’ ability to make a decisionb | It would be very hard to make a decision |
| It would be hard to make a decision | |
| It would be easy to make a decision | |
| It would be very easy to make a decision | |
| Cost to the parent(s)b | £5 |
| £25 | |
| £50 | |
| £75 | |
| £100 |
Experimental design
Separate approaches to experimental design were used for the conjoint analysis and DCE. The conjoint analysis used an orthogonal main-effects design with fold-over to allow the unbiased estimation of main effects and two-way interactions among types of information. 129 This design created a total of 24 conjoint analysis questions, which were randomly separated into four blocks so that each respondent answered six conjoint analysis questions. For the DCE, a D-efficient design was initially created for the pilot study using NGene version 1.1.2 (ChoiceMetrics, Sydney, NSW, Australia). The design included constraints such that unrealistic combinations of attributes and levels could not occur. This design created 40 DCE questions that were randomly divided into four blocks, with each respondent answering 10 DCE questions.
Following a quantitative pilot of the initial survey design in a sample of 66 members of the public between the ages of 18 and 45 years representing future and current parents, priors were assigned to the coefficients of the attributes and levels of the DCE and a new Bayesian D-efficient design was created for the parent arm of the study. Because of the smaller sample of midwives available, a quantitative pilot was not feasible and so the original D-efficient design with zero priors was used for this DCE.
The survey
An online survey was created using SSI Web version 8.3.10 (Sawtooth Software, Orem, UT, USA) and housed on a secure university web server. Two versions of the survey were created for parents, relating to a NBSP for nine conditions and a NBSP for 20 conditions (available on request). One survey for midwives was created, relating to a NBSP for nine conditions. All versions of the survey were presented in five sections. Training materials were included at the start of the survey. Respondents were asked to watch a video embedded into the online survey that explained the role of a NBSP and why information provision may be important. They also received detailed information about how to complete each type of question in each section.
Section 1: the effect of information provision on the ability to make decisions about newborn screening
Respondents were asked to complete six conjoint analysis questions each that asked them to consider scenarios in which some types of information were provided and other types of information were not provided. Figure 6 provides an example of a conjoint analysis question. Respondents then had to rate how easy or hard they thought it would be to make a decision about NBS given the type of information provided. Answers were provided on a five-point scale ranging from ‘It would be very hard to decide whether to take part’ to ‘It would be very easy to decide whether to take part’. The framing of the conjoint analysis questions allowed the effect of each type of information on the ability to make a decision to be identified.
FIGURE 6.
Example of a conjoint analysis question.

Section 2: choosing a preferred way of receiving information about newborn screening
In this task respondents completed 10 DCE questions that asked them to choose their preferred way for parents to receive information about NBS out of two possible scenarios (Figure 7). An opt-out was included to allow participants to choose for parents to receive no information about NBS if neither of the presented alternatives was attractive to them. The framing of the DCE questions allowed the identification of the relative value placed by respondents on the process (how information is provided) and outcomes (the ability to make a decision) of information provision. The DCE was linked with the conjoint analysis through the attribute ‘ability to make an informed decision’, which was the rating scale used in the conjoint analysis questions.
FIGURE 7.
Example of a DCE question.

Section 3: making a decision about newborn screening
All respondents, both parents and midwives, were asked to state on a standardised scale, the Patient Preference for Control (PPC) measure,130 how much involvement they would want in the decision about whether or not to have their child screened. There were seven possible responses divided into three categories: passive, active and collaborative. These three categories were defined by Bradley et al. 130 The seven possible responses ranged from ‘I prefer that my midwife tells me what to do’ (labelled as passive) to ‘I prefer that I make the decision without any information or recommendation from the midwife’ (labelled as active) and ‘I prefer that my midwife and I make the decision together’ (labelled as collaborative).
Section 4: attitudes to health information
All respondents, both parents and midwives, were asked a series of questions about how they use information to make decisions about their own health. These questions were taken from the Health Information Orientation Scale (HIOS)131 and aimed to measure the degree to which an individual engages with health information and/or experiences apprehension when dealing with health information. 132
Section 5: background
The fifth section of the survey asked respondents to answer up to nine questions about themselves, with the number of questions answered being dependent on previous answers. In the surveys for parents, the background questions covered aspects such as sex, age, marital status, level of education, ethnicity and whether or not they had previous children. In the survey for midwives, the background questions asked about their sex, age, primary place of work, pay grade, ethnicity and whether or not they had any children. Questions were also asked to determine how easy or hard respondents found the conjoint analysis and DCE tasks and whether or not they had based their choices on a subset of attributes in the DCE.
Study population
Two study populations were relevant to this study: (1) current and future parents and (2) practising midwives. The population of current and future parents (aged between 18 and 45 years) was represented using a sampling frame consisting of members of the UK public. A market research company (Research Now, London, UK) was used to recruit 700 survey respondents. This sample size allowed a reasonable number of responses (≈350) to be obtained for each survey (nine and 20 conditions). Given that the survey aimed to elicit the preferences of current or future parents, respondents who stated that they were in a relationship (in the characteristics held by Research Now) were oversampled. The population of practising midwives was identified by contact with the heads of midwifery at NHS hospital trusts across England through the Royal College of Midwives (RCM). A practical sample size of 250 midwives was set as the target number of respondents. The heads of midwifery were asked to forward to midwives an e-mail containing details of the DCE, a link to the survey and a participant information sheet. As an incentive to complete the survey, the first 100 midwives to complete the survey were e-mailed a £10 Amazon voucher. Screening co-ordinators were also targeted through a Public Health England mailing list for NBS. To verify that midwives were practising midwives, they were asked to supply their RCM registration number.
Data collection
The survey for parents was conducted in April 2015. Respondents were randomised to receive one of two survey versions that asked them to consider either a NBSP that screened their baby for nine conditions or a NBSP that screened their baby for 20 conditions. After completing both the conjoint analysis and the DCE questions, respondents to each survey were asked to state whether or not they thought that their answers would have changed if the screening had been for the alternative number of conditions (nine not 20 and vice versa). The survey for midwives was conducted in November 2015. Midwives were sent one version of the survey relating to a NBSP that screened the baby for nine conditions.
Data analysis
The responses to questions in sections 3, 4 and 5 of the survey were analysed using summary statistics. Five distinct steps were used for data analysis of the responses to the conjoint analysis questions and the DCE questions. The responses to both versions of the survey for parents (nine conditions and 20 conditions) and the responses to the survey for midwives (nine conditions) were analysed separately. In the first step, responses to the conjoint analysis questions and responses to the DCE questions were analysed separately. Marginal rates of substitution were then calculated to generate estimates of willingness to pay (WTP) for a unit change in attribute levels in the DCE. The findings from the conjoint analysis and DCE were then linked before using bootstrapping to calculate confidence intervals (CIs) around the estimated WTP values. Finally, the estimated coefficients for the three surveys (parents: nine or 20 conditions; midwives: nine conditions) were compared to identify similarities and differences in the results. All data analyses were conducted in Stata® version 14 (StataCorp LP, College Station, TX, USA).
Analysis of the conjoint analysis data
An ordered logit regression model was used to analyse the influence of preferences for different types of information on the ability to make an informed decision, measured on a five-point rating scale. The dependent variable was defined as taking one of five values (ranging from –2 to 2), which reflected the five-point rating scale. The independent variables were each of the 11 attributes, with the binary levels (reflecting present/absent) represented using effects coding.
Analysis of the discrete choice experiment data
A conditional logit regression model was used to analyse the DCE data. The data were collected in long form with the dependent variable being whether or not a profile was chosen (coded as ‘1’) or not chosen (coded as ‘0’). The independent variables were the five attributes. These attributes were the two continuous attributes (ability to make a decision and cost) and the effects-coded categorical variables for the levels of the attributes relating to how and when information is provided. Effects coding results in coefficients that are relative to a mean effect for any information provision as opposed to dummy coding where coefficients are relative to an omitted base case of information provision. 133 No attributes or levels were specified for the opt-out choice meaning that the probability of choosing this option was represented in the analysis by a fixed alternative specific constant.
Calculating marginal rates of substitution
The use of cost as a value attribute allowed estimation of marginal rates of substitution and calculation of the WTP for changes between the continuous attribute in the DCE (the ability to make a decision about screening) and the categorical levels of two DCE attributes (when information is given and how it is given). The beta coefficients for the estimated cost attribute were first checked to be linear by plotting the cost levels as effects-coded variables. To calculate the WTP, the estimated beta coefficient for a given attribute or level from the conditional logit model was divided by –1 multiplied by the estimated beta coefficient for the cost attribute.
Linking the conjoint analysis and discrete choice experiment data
To link the conjoint analysis and DCE data, the first step involved concatenation of the beta coefficients estimated from the ordered logit model (conjoint analysis data) and conditional logit model (DCE data). First, the effect of each information attribute on parents’ ability to make a decision was calculated by turning this attribute ‘on’ while leaving all other attributes ‘off’. This produced a value on the scale from –2 to 2, which represented the extremes of ‘it would be very hard to make a decision’ and ‘it would be very easy to make a decision’ respectively. This value was then multiplied by the value of the beta coefficient for the ability to make a decision in the DCE to obtain a beta coefficient for participant preferences for each specific type of information attribute. This value was then divided by the negative value of the estimated beta coefficient for the cost attribute to obtain a WTP value for the conjoint analysis attribute. This process was repeated for each of the 11 conjoint analysis attributes.
Bootstrapping was used to generate 95% CIs for the WTP values. 134 A sample of 700 participants was drawn from the data with replacement, and ordinal logistic regression was conducted on their conjoint analysis data followed by conditional logistic regression on their DCE data. This process was repeated 800 times so that a distribution of WTP values for attributes in the conjoint analysis and DCE could be obtained.
Results
In total, 702 respondents representing current and future parents completed one of the versions of the online parent survey (366 respondents completed the survey relating to screening for nine conditions and 336 respondents completed the survey relating to screening for 20 conditions). Table 11 summarises the characteristics of the parent samples completing each version of the survey. In both parent samples there were more female respondents [nine conditions, n = 211 (58%); 20 conditions, n = 193 (57%)] and the majority of people defined themselves as being white British/Irish [nine conditions, n = 315 (86%); 20 conditions, n = 285 (85%)]. In line with predefined sampling requirements, most respondents were aged between 25 and 44 years and most were currently in a relationship.
| Characteristic | Number (%) of respondents completing the nine-condition survey (N = 366) | Number (%) of respondents completing the 20-condition survey (N = 336) |
|---|---|---|
| Sex | ||
| Male | 152 (42) | 141 (42) |
| Female | 211 (58) | 193 (57) |
| Missing | 3 (1) | 2 (1) |
| Age band (years) | ||
| 16–19 | 7 (2) | 5 (1) |
| 20–24 | 12 (3) | 11 (3) |
| 25–34 | 176 (48) | 165 (49) |
| 35–44 | 168 (46) | 153 (46) |
| 45–54 | 3 (1) | 2 (1) |
| Marital status | ||
| Single | 117 (32) | 116 (35) |
| Separated/divorced | 17 (5) | 8 (2) |
| Living with partner | 79 (22) | 68 (20) |
| Married | 149 (41) | 143 (43) |
| Widowed | 3 (1) | 1 (0.3) |
| Missing | 1 (0.3) | 0 (0) |
| Education | ||
| No formal qualifications | 8 (2) | 5 (1) |
| One to four O levels/GCSEs | 19 (5) | 17 (5) |
| Five or more O levels/GCSEs | 32 (9) | 23 (7) |
| NVQs | 44 (12) | 44 (13) |
| A levels/AS levels | 86 (23) | 71 (21) |
| Undergraduate degree | 112 (31) | 114 (34) |
| Master’s degree | 45 (12) | 48 (14) |
| PhD | 11 (3) | 6 (2) |
| Other formal qualifications | 8 (2) | 8 (2) |
| Missing | 1 (0.3) | 0 (0) |
| Ethnicity | ||
| White British/Irish | 315 (86) | 285 (85) |
| White other | 17 (5) | 24 (7) |
| Mixed | 9 (2) | 3 (1) |
| Black/black British | 3 (1) | 3 (1) |
| Asian/Asian British | 18 (5) | 21 (6) |
| Other | 4 (1) | 0 (0) |
| Children | ||
| Has children | 187 (51) | 151 (45) |
| Does not have children | 178 (49) | 184 (55) |
| Missing response | 1 (0.3) | 1 (0.3) |
| Aware that child has taken part in NBSPa | ||
| Yes | 111 (59) | 83 (55) |
| No | 76 (41) | 67 (44) |
| Missing | 0 (0) | 1 (1) |
| Desired involvement in decision-making | ||
| I prefer that my midwife tells me what to do | 29 (8) | 26 (8) |
| I prefer that my midwife tells me what to do and explains the choice briefly | 26 (7) | 32 (10) |
| I prefer that my midwife tells me what to do and explains the choice, including other choices and consequences | 60 (16) | 57 (17) |
| I prefer that my midwife and I make the decision together | 77 (21) | 62 (18) |
| I prefer that I make the decision with the midwife giving me both information and a recommendation | 137 (37) | 125 (37) |
| I prefer that I make the decision with the midwife giving me information but no recommendation | 27 (7) | 29 (9) |
| I prefer that I make the decision without any information or recommendation from the midwife | 10 (3) | 5 (1) |
A total of 134 midwives completed the survey. Table 12 summarises the characteristics of the midwife sample. All but one of the respondents were female and 98% (n = 131) were aged between 25 and 64 years, with over one-third aged between 45 and 54 years. Half of the sample (n = 69) was currently working in a community setting, with one-third (n = 46) based in a hospital and 12% working in a midwife-led unit. The majority of midwives were on a pay grade of either 6 (65%) or 7 (24%).
| Characteristic | Number (%) of midwives (N = 134) |
|---|---|
| Sex | |
| Male | 1 (0.8) |
| Female | 133 (99.2) |
| Age band (years) | |
| 16–19 | 0 (0) |
| 20–24 | 2 (1) |
| 25–34 | 29 (22) |
| 35–44 | 31 (23) |
| 45–54 | 50 (37) |
| 55–64 | 21 (16) |
| ≥ 65 | 1 (0.8) |
| Current work location | |
| Hospital | 46 (34) |
| Midwife-led unit | 16 (12) |
| Community | 69 (51) |
| Other | 3 (2) |
| Pay grade | |
| 2 | 0 (0) |
| 3 | 1 (0.8) |
| 4 | 2 (1) |
| 5 | 8 (6) |
| 6 | 87 (65) |
| 7 | 32 (24) |
| 8A–C | 3 (2) |
| Student | 1 (0.8) |
| Ethnicity | |
| White British/Irish | 124 (93) |
| White other | 4 (3) |
| Mixed | 0 (0) |
| Black/black British | 3 (2) |
| Asian/Asian British | 2 (1) |
| Other | 1 (0.8) |
| Children | |
| Has children | 103 (77) |
| Does not have children | 30 (22) |
| Unknown | 1 (0.8) |
| Aware that child has taken part in NBSP | |
| Yes | 94 (70) |
| No | 2 (1) |
| Don’t know | 8 (6) |
| Desired involvement in decision-making | |
| I prefer that my midwife tells the parent what to do | 0 (0) |
| I prefer that my midwife tells the parent what to do and explains the choice briefly | 2 (1) |
| I prefer that my midwife tells the parent what to do and explains the choice, including other choices and consequences | 18 (13) |
| I prefer that my midwife and the parent make the decision together | 8 (6) |
| I prefer that the parent make the decision with the midwife giving me both information and a recommendation | 36 (27) |
| I prefer that the parent make the decision with the midwife giving me information but no recommendation | 69 (51) |
| I prefer that the parent make the decision without any information or recommendation from the midwife | 1 (0.8) |
Table 11 summarises the views in the parent sample on the preferred level of decision-making in relation to participation in a NBSP. Parents responding to the online surveys relating to nine conditions and 20 conditions gave similar answers. The most common (modal) category was ‘I prefer that I make the decision with the midwife giving me both information and a recommendation’ [nine conditions, n = 137 (37%); 20 conditions, n = 125 (37%)], indicating a desire for an ‘active’ role in decision-making. The modal category for desired role in decision-making, as defined by parent responses to the PPC measure, was an ‘active’ role [nine conditions, n = 174 (48%); 20 conditions, n = 159 (47%)]. A substantial number of respondents stated a desire for a ‘collaborative’ role (‘my midwife and I make the decision together’) [nine conditions, n = 77 (21%); 20 conditions, n = 62 (18%)] or a ‘passive’ role (‘my midwife tells me what to do and explains the choice, including other choices and consequences’) [nine conditions, n = 60 (16%); 20 conditions, n = 57 (17%)]. Very few parents stated a desire for complete control, with no midwife input in the decision-making process [nine conditions, n = 10 (3%); 20 conditions, n = 5 (1%)].
The scores on the HIOS questionnaire were used to summarise the degree to which parents were information engaging or suffered information apprehension. In line with published recommendations, the answers on the HIOS questionnaire were given scores ranging from 0 (not at all true) to 4 (very much true). 132 The scores for questions 1, 4, 6 and the inverse of 5 were averaged to give a score for information engagement, with the scores for the other questions forming the score for information apprehension. Parents were found to be moderately information engaging (nine conditions: HIOS score 2.56; 20 conditions: HIOS score 2.61) and had a relatively low level of information apprehension (nine conditions: HIOS score 1.41; 20 conditions: HIOS score 1.31). The differences in HIOS scores between parents who answered the nine-condition survey and those who answered the 20-condition survey were not statistically significant when tested using a t-test (information engaging, p = 0.840; information apprehension, p = 0.0708).
Table 12 summarises the views in the midwife sample on the preferred mode of decision-making. Midwives preferred parents to make the decision about screening, with information provided by the midwife but no recommendation given (n = 69, 51%). Only 15% (n = 20) of midwives advocated that parents should have a ‘passive’ role in decision-making, with 6% favouring a ‘collaborative’ role and 79% (n = 106) believing that parents should be ‘active’ in the decision-making process. The midwife sample had a similar mean information engaging score (2.653) to that of the parent sample when completing the HIOS. However, with a mean score of 0.905 they appeared to be less information apprehensive, as might be expected from professionals who deliver such information regularly.
Preference data
All respondents were asked whether they found the conjoint analysis and DCE easy or difficult. The modal answer given by all three samples was ‘quite easy’. The preference data elicited from the hybrid conjoint analysis–DCE survey are presented in three sections. The first section presents the results of the conjoint analysis along with the generated WTP values. The second section presents the results of the DCE and generated WTP values. The final section presents the generated WTP estimates for the conjoint analysis attributes calculated using the concatenation of the ordered logistic regression.
Conjoint analysis data
Table 13 presents the results of the ordered logit regression analysis of the conjoint analysis data from the two parent samples, who completed surveys relating to screening of nine conditions and screening of 20 conditions. In both surveys, all types of information were identified as statistically significantly improving parents’ ability to make a decision about taking part in a NBSP. The most preferred piece of information was whether or not the child would suffer any pain or side effects from screening. A heteroscedastic ordered logistic regression model was run separately to determine whether or not scale effects would affect the direct comparison of the coefficients from the nine-condition and 20-condition surveys. The scale parameter was not statistically significant (p = 0.6210), indicating that a comparison could be made.
| Attribute | Parent sample: nine-condition survey | Parent sample: 20-condition survey | ||||
|---|---|---|---|---|---|---|
| Coefficient (SE) | Mean WTP (£) | WTP 95% CI (£) | Coefficient (SE) | Mean WTP (£) | WTP 95% CI (£) | |
| The names of the conditions included in the screening | 0.439*** (0.078) | 1.89 | 0.85 to 2.96 | 0.564*** (0.082) | 2.86 | 1.61 to 4.42 |
| How you can prepare your baby for the sample | 0.249*** (0.077) | 0.64 | –0.18 to 1.49 | 0.428*** (0.081) | 1.90 | 0.90 to 3.04 |
| How the sample is taken | 0.489*** (0.078) | 2.31 | 1.25 to 3.56 | 0.502*** (0.081) | 2.72 | 1.43 to 4.32 |
| Whether your child would suffer any pain or side effects when the sample is taken | 0.580*** (0.078) | 2.76 | 1.89 to 3.90 | 0.560*** (0.081) | 2.96 | 1.86 to 4.29 |
| The time it takes to receive the results | 0.373*** (0.078) | 1.35 | 0.51 to 2.16 | 0.489*** (0.081) | 2.41 | 1.40 to 3.56 |
| How I will receive the results | 0.491*** (0.078) | 2.21 | 1.37 to 3.19 | 0.332*** (0.081) | 1.52 | 0.69 to 2.57 |
| Whether you could receive a result which suggests that your child does not have a condition when in reality they do | 0.430*** (0.078) | 1.77 | 0.91 to 2.79 | 0.374*** (0.081) | 1.64 | 0.58 to 2.94 |
| Whether you could receive a result which suggests that your child has a condition when in reality they do not | 0.232*** (0.077) | 0.59 | –0.40 to 1.62 | 0.467*** (0.081) | 2.34 | 1.17 to 3.71 |
| The effect that having one of the conditions would have on your child’s health | 0.315*** (0.078) | 1.10 | 0.50 to 1.91 | 0.353*** (0.081) | 1.47 | 0.68 to 2.42 |
| How common or rare the conditions are | 0.330*** (0.078) | 1.25 | 0.43 to 2.20 | 0.313*** (0.081) | 1.34 | 0.40 to 2.35 |
| What can be done to treat your child if they have one of the conditions | 0.487*** (0.078) | 2.18 | 1.23 to 3.28 | 0.494*** (0.081) | 2.44 | 1.08 to 4.01 |
| Cut 1 constant | –0.241 (0.161) | –0.207 (0.165) | ||||
| Cut 2 constant | 1.714 (0.160) | 1.796 (0.165) | ||||
| Cut 3 constant | 2.960 (0.165) | 2.988 (0.169) | ||||
| Cut 4 constant | 4.766 (0.187) | 4.754 (0.189) | ||||
| Observations | 2208 | 2022 | ||||
| Pseudo-R2 | 0.035 | 0.042 | ||||
Table 14 presents the results of the ordered logit regression analysis of the conjoint analysis data from the midwife sample. All attributes apart from the possibility of false-positive results were statistically significant. However, the possibility of receiving false-negative results was statistically significant only at the 0.05 level, whereas all of the other significant attributes were significant at the 0.001 level. For midwives, the types of information that were perceived to be the most important for parents were the names of the conditions being screened for and the way in which the sample is taken. Whether or not the baby would feel any pain, the attribute most favoured by parents, was only the sixth most important attribute for midwives (Table 15).
| Attribute | Midwife sample: nine-condition survey | ||
|---|---|---|---|
| Coefficient | Mean WTP (£) | WTP 95% CI (£) | |
| The names of the conditions included in the screening | 1.111*** | 10.23 | 6.54 to 15.36 |
| How you can prepare your baby for the sample | 0.582*** | 3.17 | 0.98 to 5.96 |
| How the sample is taken | 1.010*** | 10.41 | 6.43 to 16.22 |
| Whether your child would suffer any pain or side effects when the sample is taken | 0.658*** | 5.23 | 2.78 to 8.45 |
| The time it takes to receive the results | 0.599*** | 3.52 | 1.21 to 6.52 |
| How I will receive the results | 0.659*** | 1.71 | –0.57 to 4.16 |
| Whether you could receive a result that suggests that your child does not have a condition when in reality they do | 0.334* | 0.09 | –2.63 to 3.10 |
| Whether you could receive a result that suggests that your child has a condition when in reality they do not | 0.066 | –0.63 | –3.40 to 1.96 |
| The effect that having one of the conditions would have on your child’s health | 0.871*** | 5.88 | 3.50 to 9.30 |
| How common or rare the conditions are | 0.916*** | 6.47 | 3.90 to 10.25 |
| What can be done to treat your child if they have one of the conditions | 0.594*** | 5.46 | 2.25 to 10.01 |
| Cut 1 constant | 1.666 | ||
| Cut 2 constant | 4.098 | ||
| Cut 3 constant | 5.144 | ||
| Cut 4 constant | 6.971 | ||
| Observations | 804 | ||
| Pseudo-R2 | 0.102 | ||
| Ranking | Order of importance of information attributes | ||
|---|---|---|---|
| Parent sample: nine-condition survey | Parent sample: 20-condition survey | Midwife sample: nine-condition survey | |
| 1 | Whether your child would suffer any pain or side effects when the sample is taken | Whether your child would suffer any pain or side effects when the sample is taken | How the sample is taken |
| 2 | How the sample is taken | The names of the conditions included in the screening | The names of the conditions included in the screening |
| 3 | How I will receive the results | How the sample is taken | How common or rare the conditions are |
| 4 | What can be done to treat your child if they have one of the conditions | What can be done to treat your child if they have one of the conditions | The effect that having one of the conditions would have on your child’s health |
| 5 | The names of the conditions included in the screening | The time it takes to receive the results | What can be done to treat your child if they have one of the conditions |
| 6 | Whether you could receive a result that suggests that your child does not have a condition when in reality they do | Whether you could receive a result that suggests that your child has a condition when in reality they do not | Whether your child would suffer any pain or side effects when the sample is taken |
| 7 | The time it takes to receive the results | How you can prepare your baby for the sample | The time it takes to receive the results |
| 8 | How common or rare the conditions are | Whether you could receive a result that suggests that your child does not have a condition when in reality they do | How you can prepare your baby for the sample |
| 9 | The effect that having one of the conditions would have on your child’s health | How I will receive the results | How I will receive the results |
| 10 | How you can prepare your baby for the sample | The effect that having one of the conditions would have on your child’s health | Whether you could receive a result that suggests that your child does not have a condition when in reality they do |
| 11 | Whether you could receive a result that suggests that your child has a condition when in reality they do not | How common or rare the conditions are | Whether you could receive a result that suggests that your child has a condition when in reality they do not |
Discrete choice experiment data
Table 16 reports the results of the conditional logit regression analysis of the DCE data from the parent samples together with the generated mean WTP values and 95% CIs. The estimated coefficients for the two continuous attributes (ability to make an informed decision and cost) were found to have the expected sign (positive and negative respectively). When these continuous variables were estimated using effects coding, the resulting coefficients were identified to be linear on visual inspection when plotted.
| Attribute | Parent sample | |||||
|---|---|---|---|---|---|---|
| Nine-condition survey | 20-condition survey | |||||
| Coefficient (SE) | Mean WTP (£) | WTP 95% CI (£) | Coefficient (SE) | Mean WTP (£) | WTP 95% CI (£) | |
| When information is given | ||||||
| Early in pregnancy | 0.220*** (0.050) | 11.88 | 5.56 to 19.53 | 0.211*** (0.051) | 11.73 | 4.69 to 19.59 |
| Late in pregnancy | 0.128*** (0.048) | 6.40 | 1.86 to 11.52 | 0.283*** (0.050) | 15.91 | 10.64 to 21.63 |
| At hospital discharge | –0.054 (0.050) | –2.80 | –7.84 to 2.39 | –0.088 (0.052) | –4.79 | –10.61 to 1.27 |
| Day 3 post pregnancy | –0.194*** (0.050) | –10.31 | –15.90 to –4.87 | –0.206*** (0.051) | –11.65 | –17.96 to –5.16 |
| Day 5 post pregnancy | –0.100 | –5.15 | –11.61 to 0.49 | –0.200 | –11.20 | –18.40 to –5.72 |
| How information is given | ||||||
| Individual discussion | 0.307*** (0.050) | 15.92 | 10.54 to 21.39 | 0.211*** (0.053) | 11.81 | 5.34 to 17.44 |
| Leaflet | 0.082 (0.056) | 4.61 | –0.90 to 11.10 | 0.076 (0.059) | 4.56 | –1.67 to 11.03 |
| Internet | –0.081 (0.057) | –4.50 | –10.26 to 1.42 | –0.089 (0.059) | –5.28 | –10.76 to 4.66 |
| Tablet or smartphone app | –0.068 (0.058) | –4.04 | –9.67 to 1.59 | –0.031 (0.061) | –2.21 | –8.26 to 4.66 |
| Group discussion | –0.240 | –11.99 | –18.79 to –5.14 | –0.168 | –8.87 | –16.83 to –1.52 |
| Ability to make a decision | 0.192*** (0.017) | 9.97 | 7.84 to 12.37 | 0.198*** (0.017) | 11.19 | 8.62 to 14.41 |
| Cost | –0.020*** (0.001) | NA | NA | –0.018*** (0.001) | NA | NA |
| Opt-out constant | –0.688*** (0.058) | NA | NA | –0.864*** (0.062) | NA | NA |
| Observations | 10,980 | 10,080 | ||||
| Pseudo-R2 | 0.110 | 0.125 | ||||
The predicted probability that participants would opt out was similar between the nine-condition survey (33% of respondents) and the 20-condition survey (30% of respondents). A heteroscedastic logit model suggested that there was not a statistically significant scale effect between the two samples (p = 0.1510) and so the estimated coefficients from the nine- and 20-conditions surveys could be directly compared.
In both surveys in the parent sample, respondents’ choices indicated that receiving NBS information before the baby was born was important. Parents completing the survey relating to screening for nine conditions preferred to receive information before 20 weeks of pregnancy (WTP £11.88, 95% CI £5.56 to £19.53). In contrast, for parents completing the survey relating to screening for 20 conditions, the highest WTP was obtained for receiving information after 20 weeks (£15.91, 95% CI £10.64 to £21.63). None of the parents in either survey wanted to receive information 3 days after the baby was born. For parents completing the survey relating to screening for 20 conditions, this was indicated by the negative WTP for receiving information immediately before the test (WTP –£11.20, 95% CI –£18.40 to –£5.72). Discussing NBS individually with parents was the only mode of information provision with a statistically significant positive coefficient. The WTP for group discussions was negative and significant in both surveys (nine conditions: WTP £11.99, 95% CI –£18.79 to –£5.14; 20 conditions: –£8.87, 95% CI –£16.83 to –£1.52).
For the sample of midwives, the best times to receive NBS information were perceived to be late in pregnancy (WTP £13.57, 95% CI £2.44 to £26.16) and on day 3 (WTP £11.77, 95% CI £1.23 to £22.61) (Table 17). Unlike the parent sample, the sample of midwives stated that information should not be provided early in pregnancy (WTP –£23.29, 95% CI –£36.43 to –£11.66). Similarly to the parents, the midwives preferred information to be provided by discussing it with parents on an individual basis (WTP £12.52, 95% CI £2.79 to £22.60), but they differed from parents in disliking the provision of information on the internet (WTP –£10.67, 95% CI –£22.41 to –£0.78). The generation of WTP values should be treated with caution in the midwife sample. The two attributes assumed to be continuous and linear, the ability to make a decision about screening and cost attributes, were found to be non-linear when effects coded. With regard to parents’ ability to make a decision, midwives were very averse to scenarios in which it would be very hard for parents to make a decision. On the other hand, there was no statistically significant difference in the coefficients for ‘it would be easy to make a decision’ and ‘it would be very easy to make a decision’. With regard to cost, midwives appeared to be disproportionately likely to choose profiles that cost £5.
| Attribute | Midwife sample: nine-condition survey | ||
|---|---|---|---|
| Coefficient (SE) | Mean WTP (£) | WTP 95% CI (£) | |
| When information is given | |||
| Early in pregnancy | –0.387*** (0.088) | –23.29 | –36.43 to –11.66 |
| Late in pregnancy | 0.323*** (0.088) | 13.57 | 2.44 to 26.16 |
| At hospital discharge | –0.040 (0.083) | 7.41 | –2.06 to 18.52 |
| Day 3 post pregnancy | 0.260*** (0.0844) | 11.77 | 1.23 to 22.61 |
| Day 5 post pregnancy | –0.156 | –9.26 | 1.96 to –22.78 |
| How information is given | |||
| Individual discussion | 0.493*** (0.086) | 12.52 | 2.79 to 22.60 |
| Leaflet | –0.162 (0.098) | 3.70 | –6.34 to 16.30 |
| Internet | –0.307*** (0.094) | –10.67 | –22.41 to –0.78 |
| Tablet or smartphone app | –0.168 (0.104) | –1.63 | –12.70 to 9.30 |
| Group discussion | 0.144 | –4.15 | –16.36 to 7.30 |
| Ability to make a decision | 0.370*** (0.030) | 18.98 | 13.90 to 27.16 |
| Cost | –0.025*** (0.002) | NA | NA |
| Opt-out constant | –0.930*** (0.062) | NA | NA |
| Observations | 4020 | ||
| Pseudo-R2 | 0.213 | ||
Linking the conjoint analysis and discrete choice experiment: generating willingness-to-pay values
Tables 13 and 14 report the generated WTP values for the attributes in the conjoint analysis that were estimated by linking the responses from the DCE with the conjoint analysis data for the parent samples and midwife samples respectively. There were clear differences observed between the parents who completed the survey relating to screening for nine conditions and the parents who completed the survey relating to screening for 20 conditions. For the parents completing the nine-condition survey, the WTP values for ‘How you can prepare your baby for the sample’ and ‘Whether you could receive a result which suggests that your child has a condition when in reality they do not’ were not statistically significant. In contrast, all of the WTP values for the information attributes were statistically significant for the parents who completed the 20-condition survey. In general, all of the estimated WTP values tended to be higher, but not statistically significantly higher, for the 20-condition survey than for the nine-condition survey. The two exceptions to this general trend were for the attributes ‘How I will receive the results’ and ‘Whether you could receive a result which suggests that your child does not have a condition when in reality they do’. The estimated WTP values for the midwife sample were statistically significant except for the possibility of false positives and false negatives. The WTP values estimated for the midwife sample were generally larger than those estimated for the parent samples.
Summary
The results of this study confirmed that a representative sample of current and potential future parents do want information when deciding whether or not to consent for their newborn child to take part in a UK-based NBSP. Two standardised measures, the PPC and the HIOS, were completed by the sample and the results indicated a desire for an ‘active’ role in decision-making and that more respondents were information engaging than were afraid of information in the context of a NBSP. Similarly, the sample of midwives believed that parents should be involved in decision-making, although this sample surveyed seemed more reluctant to offer a recommendation about whether or not parents should have their child screened.
The results from the hybrid conjoint analysis–DCE stated preference survey supported a desire for information provision. The responses to the DCE questions had face validity as the estimated coefficients were in line with a priori expectations, with a desire for an increased ability to make an informed decision with lower out-of-pockets costs attached to gaining information for the parent making the decision. To maximise the ability to make an informed decision, respondents wanted comprehensive types of information covering a range of topics. All of the attributes reflecting the types of information required when participating in a NBSP were found to have a statistically significant influence on preferences in the parent sample. In the midwife sample, only one type of information, the possibility of false-positive results, was viewed to not improve the perceived ability to make a decision about screening.
There were some important differences between the types of information preferred when comparing the responses of the parents with those of the midwives. For parents, the key concern was whether or not their child would feel any pain as a result of screening and this has been identified in the literature as one of the most memorable aspects of screening for parents. 74 The process of screening, the names of the conditions that are being screened for and the treatability of the conditions were also identified as key drivers of preferences. However, although the midwives also believed that how the sample is taken and the names of the conditions were important pieces of information, they also placed an emphasis on conveying the rarity and health impact of the conditions.
The results of this survey also indicated some clear preferences for when, and how, information is provided. It was evident that receiving information before the baby was born was important and parents wanted to be able to have an individual discussion with the midwife when information was provided. Although the midwives surveyed agreed that information provision late in pregnancy would be beneficial, they stated a strong dislike for providing information early in pregnancy. This finding contradicts current practice, in which information is given in the form of a leaflet early in pregnancy. Currently, midwives also have an individual discussion about NBS with parents on day 3 or day 5 after the baby is born. 115 Neither the parents nor the midwives surveyed supported giving information on day 5 and the results of the DCE provide evidence which suggests that, although parents valued an individual discussion, giving information on day 3 after the baby is born should also be avoided. A mutually approved solution may be for midwives to provide information during an individual discussion after the 20-week scan.
The sample representing the views of current and future parents was split to allow an exploration of the impact of the number of conditions included in the NBSP (nine or 20 conditions). The results suggested that there was a minimal effect on the overall stated need for information provision when respondents considered a NBSP for 20 conditions rather than nine conditions. However, the estimated rank order of the coefficients, and implied order of importance of the attributes in the conjoint analysis, did differ between the two parent samples. For parents completing the 20-condition survey, the names of the conditions being screened as well as the possibility of false-positive results appeared significantly higher in the ranking of types of information. Therefore, if midwives are constrained in the amount of time that they have available to provide information, it may be important to tailor the information provided depending on the number of conditions included in the NBSP. Importantly, it was found that parents completing the 20-condition survey felt that not receiving any information was more detrimental than receiving information in terms of their ability to make an informed decision. There was an overwhelming preference for information to be provided before the baby was born in both groups. However, although the sample completing the nine-condition survey placed the highest value on information provision early in pregnancy, the respondents to the 20-condition survey preferred to receive the information after the 20-week scan. The respondents to the 20-condition survey were also more averse to receiving information immediately before the test, potentially because of the need for more time to digest a greater amount of information. It has previously been identified that, in the time period following the birth of a child, parents may not be able to take in and process information because of stress and tiredness. 38
A key finding was that, as the number of conditions screened for increased from nine to 20, the possibility of receiving false-positive results became a more important piece of information for parents. Effectively communicating about the possibility of false-positive results and repeat samples may help to reduce the anxiety that parents feel about these results13,135 and any additional health-care resource use as a result. 34,136 A number of previous studies have identified the potential impact of the receipt of false-positive results on anxiety and subsequently health status42,137–139 and also the impact on health-care resource use. 140 Combined with the results of this study, this evidence base provides support for the need for parents to be made aware, before screening is completed, of the possibility of false-positive results.
This study has identified that, in a UK NBSP, the preferences for information provision of a sample of the general public, representing the views of current and potential future parents, and a sample of midwives, obtained using a linked conjoint analysis–DCE, did differ from how information is provided in current UK practice in the NBSP. Therefore, some realignment of information provision to match these preferences could help to improve parents’ ability to make a decision about participation and help midwives to focus what information is provided. The results of this preference study suggest that one potential model of information provision for a NBSP may be for midwives to provide information during an individual discussion after the 20-week scan. Future work is needed to understand the financial and economic impact of new models of information provision in the context of a UK-based NBSP, particularly when there is a continued call for expansion of screening programmes to include more conditions.
Chapter 6 Study 5: economic impact of models of information provision
Study objectives
-
Establish the key parameters affecting the cost-effectiveness of new modes of information provision compared with the current practice(s) of providing NBSP information antenatally.
-
Outline the key uncertainties in the current evidence base and what is the value of future research to evaluate the effectiveness and cost-effectiveness of providing NBSP information antenatally.
Introduction
In England, the NBSP screened 666,671 babies from 2014 to 2015. 141 The potential scale of population-level screening programmes means that even small incremental increases in the unit cost can add up to substantial total costs for health-care providers. The impact on limited health-care resources and the associated need to understand the opportunity cost of changing or expanding NBSPs has stimulated the production of a growing literature in which methods of economic evaluation are applied to help policy-makers decide whether or not a NBSP is an effective use of health-care budgets and which specific conditions should be included in a NBSP. The ultimate aim of these economic evaluations is to guide whether or not the proposed NBSP is a cost-effective use of finite health-care resources.
The unit cost of adding new conditions into existing screening programmes is apparently low; however, there are additional costs associated with the methods of information provision and communication that should, ideally, also be taken into account. Evidence suggests that there is an appreciation of the centrality of communication in ensuring that benefits from NBSPs are realised and the probability of potential harms is reduced. 42,63,142–149 Specifically, there is a recognised need to inform parents prior to screening,34,44,52 preferably antenatally. 34,72
Without effective communication the validity of consent is questioned, as, although parents consent to screening, many are not aware that screening has occurred28,31–33 or have limited knowledge about it. 19,23,24,62,63,150 Poor communication of key pieces of information can cause anxiety and distress when unexpected results are received,148,151 which in turn has been shown to impact on relationships, the ability to work and engagement in society. 13 In turn, there may be consequences in terms of the use of health-care services, as parents may seek additional consultations to reduce anxiety. 13,140
As NBSPs include increasingly rare diseases with fewer clear treatment benefits, communication will become ever more critical. 152 In summary, it is apparent that the process of information provision as part of a NBSP may have implications in terms of health-care resource use and also subsequent health-related and non-health-related outcomes, such as the capability to make an informed decision about whether or not to participate in the NBSP and/or the need to use subsequent health-care services.
Aim
The aim of this study was to identify and quantify the key drivers of the relative cost-effectiveness of alternative modes of providing information as part of a NBSP.
Research questions
This study was designed to address three research questions:
-
Have existing published economic evaluations of NBSP taken into account the role of information provision and its consequences?
-
What are the key parameters affecting the cost-effectiveness of new modes of information provision compared with the current practice(s) of providing NBSP information?
-
What is the value of future research needed to evaluate the cost-effectiveness of providing NBSP information?
Existing economic evidence
A systematic review, in accordance with published guidelines,153,154 was used to identify economic evaluations of screening technologies or NBSP screening published up to the search date of November 2014.
Three electronic databases [MEDLINE, EMBASE and the Cumulative Index to Nursing and Allied Health Literature (CINAHL)] were searched using a structured electronic search strategy (see Appendix 8 for an example used for MEDLINE). The electronic search strategies, specific for each database, combined relevant index and free-text terms for NBS with the Centre for Reviews and Dissemination (CRD)’s economic evaluation search filter. 155 The electronic searches were supplemented by examining the reference lists of each identified study and by carrying out a keyword search of the NHS Economic Evaluation Database (NHS EED).
Three independent reviewers screened the identified titles and abstracts for inclusion in the review according to the following criteria: the intervention should be a NBSP or relevant screening technology offered to a population of neonates, infants or children; the study should be a full economic evaluation (cost-effectiveness analysis; cost–utility or cost–benefit analysis); and the study should be published in English and available as a full text. Two reviewers extracted the data from each included study using a structured data collection form based on the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) checklist. 156 Specifically, data on the valuation of the cost of information provision and the valuation of benefits were extracted. The results were tabulated and summarised as part of a narrative synthesis.
Existing economic evaluations
In total, 22 economic evaluations were included in the review, of which 10 evaluated screening technologies used in NBSPs43,57,119,137,138,157–162 and 12 evaluated NBSPs. 42,121,122,139,163–170 Figure 8 summarises the study selection process. Nineteen were model-based economic evaluations (NBSPs, n = 10; screening technologies, n = 9).
FIGURE 8.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of search results.
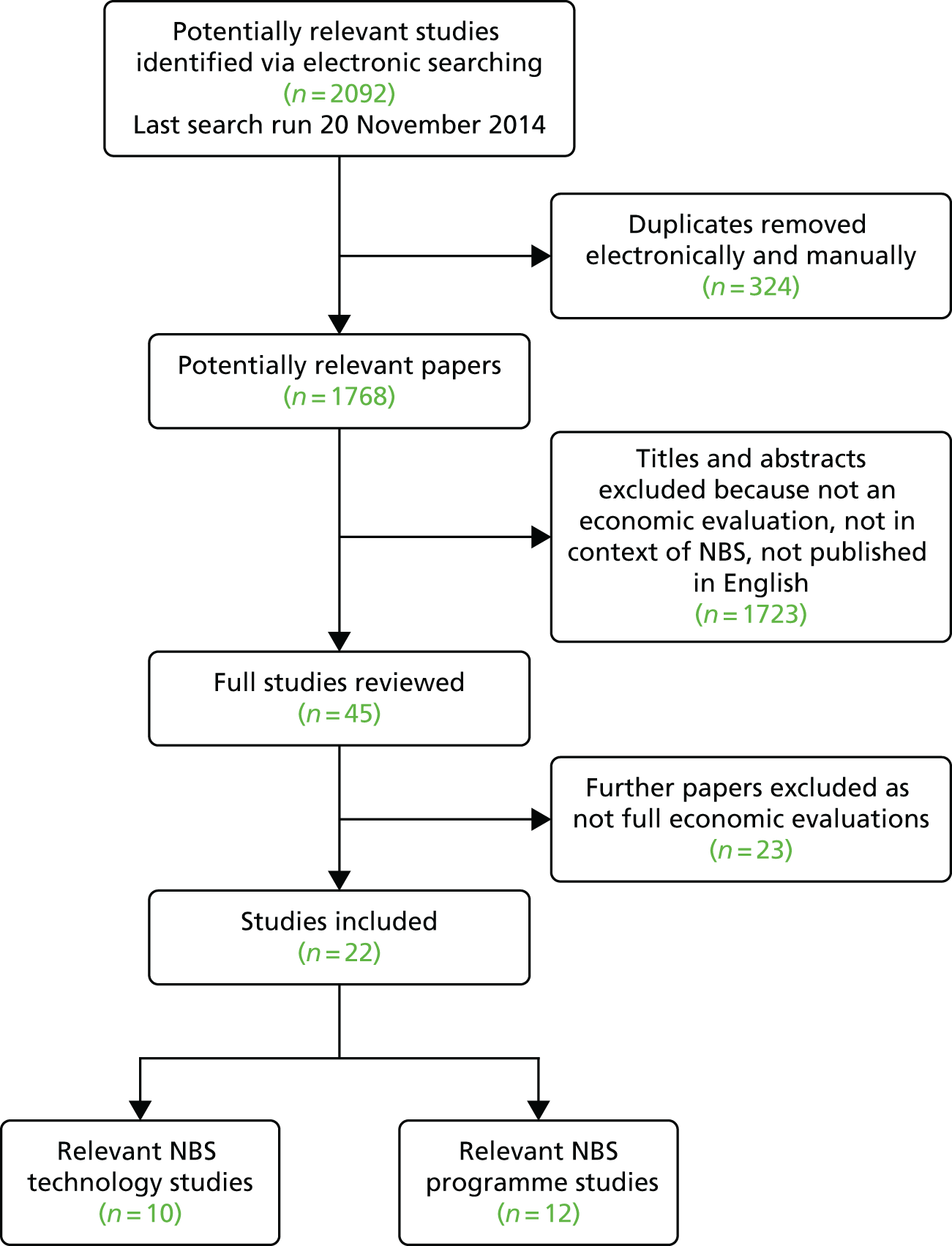
Two types of technology were evaluated in the 10 economic evaluations of screening technologies (see Appendix 5): the Guthrie method157 and MS/MS. 43,57,119,137,138,158–162 Shamshiri et al. 157 compared the Guthrie method with no screening from the Iranian health service perspective. Iran has a voluntary NBSP with the exception of screening for CHT. Nine studies evaluated MS/MS and three of these studies used no screening as the relevant comparator137,158,159 but did not justify the choice of comparator. Four studies compared new MS/MS with existing technologies. 43,52,138,160 Tran et al. 162 compared MS/MS screening with clinical diagnosis. The study by Schoen et al. 161 did not clearly specify a comparator but it can be inferred that no screening was used.
The review identified a relatively low number of published economic evaluations of NBSP (n = 12), given the extent of national screening programmes on a global basis (see Appendix 7). Five of the studies compared the NBSP with no screening. 122,163–166 The remaining seven studies compared screening with existing strategies. 42,121,139,167–170
Seven studies discussed the implications of using screening strategies such as universal or targeted strategies. 121,163–165,168–170 Three studies focused on expanded screening programmes, including additional screening for MCADD,42,139,167 and two studies reported screening strategies specifically for CF122 and MCADD. 166
Around half of the identified studies focused on understanding the economic impact of newborn screening as a national programme. Of these studies, half were based in countries that all require parental consent prior to performing a NBS test (Australia, France and the Netherlands). Table 18 shows the content of existing national NBSPs.
| Country | Region/state/territory | Current conditions screened (2015) | Source |
|---|---|---|---|
| Australia | New South Wales | PKU, CHT, CF, galactosaemia and a range of aminoacidopathies, organic acidaemias and fatty acid oxidation defects | Norman et al.160 |
| Western Australia | PKU, CHT, CF, galactosaemia and a range of aminoacidopathies, organic acidaemias and fatty acid oxidation defects | Geelhoed et al.121 | |
| Canada | Nova Scotia | PKU, CHT, CF, MCADD, MSUD, SCD, GA1, IVA, LCHAD, very long-chain acyl-CoA dehydrogenase deficiency and four other conditions | Tran et al.162 |
| Ontario | PKU, CHT, CF, galactosaemia, MCADD, MSUD, SCD, GA1, HCU, IVA and 16 other conditions | Cipriano et al.138 | |
| Iran | Whole country | CHT | Shamshiri et al.157 |
| France | Whole country | PKU, CHT, CF, SCD, CAH and MCADD | Hamers and Rumeau-Pichon167 |
| Netherlands | Whole country | PKU, CHT, CF, galactomsaemia, SCD, CAH, GA1, MCADD, HCU, IVA and six other conditions | Lanting et al.,168 van den Akker-van Marle et al.,169 van der Hilst et al.,166 Wildhagen et al.122 |
| UK | Whole country | PKU, CHT, CF, SCD, MCADD, MSUD, GA1, IVA and HCU | Pollitt et al.,43 Pandor et al.119 |
| USA | Alaska | PKU, CHT, CF, CAH, SCD, MSUD, MCADD, GAI, IVA, LCHAD and 36 other conditions | Gessner et al.164 |
| California | PKU, CHT, CF, CAH, SCD, MSUD, MCADD, GAI, IVA, HCU and 47 other conditions | Feuchtbaum and Cunningham,158 Schoen et al.161 | |
| Indiana | PKU, CHT, CF, CAH, SCD, MSUD, MCADD, GA1, IVA, LCHAD and 40 other conditions | Carroll and Downs163 | |
| Kentucky | PKU, CHT, CF, CAH, SCD, MSUD, MCADD, GA1, IVA, LCHAD and 42 other conditions | Wells et al.170 | |
| Pennsylvania | PKU, CHT, CF, CAH, SCD, MSUD, MCADD, GA1, IVA, LCHAD and 23 other conditions | Venditti et al.137 | |
| Texas | PKU, CHT, CF, CAH, SCD, MSUD, MCADD, GA1, IVA, LCHAD and 20 other conditions | Tiwana et al.139 | |
| Wisconsin | PKU, CHT, CF, CAH, SCD, MSUD, HCU, galactosaemia, severe combined immune deficiency, argininosuccinic aciduria and 34 other conditions | Insinga et al.159 |
Existing evidence on the costs of information provision
The need for parental consent infers a requirement for a clear mechanism of information provision to be built into a national NBSP. This need for information provision will have associated resource use implications.
Two studies explicitly mentioned the omission of the cost of information provision in their evaluation of a NBSP. Hamers and Rumeau-Pichon’s167 economic evaluation of universal screening for MCADD in France included the start-up costs of the programme but excluded the costs of ‘producing information and education materials’. No justification for this omission was given. Van den Akker-van Marle et al. 169 explained that they did not include information provision in their model of the cost-effectiveness of differing methods of screening for CF because the assumed cost of updating the information leaflet would be insignificant.
Three studies (two on NBSPs,121,122 one on screening technologies118) included an estimate of the cost of information provision in their analyses. Two of these studies were model-based evaluations118,122 whereas the other was based on a retrospective cohort of newborn children. 121 Costs were developed from a range of sources including cost data from existing programmes, the cost of information provision in similar health-care programmes (e.g. information provision for prenatal or antenatal screening) and the estimated time for a consultation with a midwife.
All three studies used different assumptions and methods to estimate the cost of information provision. In the UK-based analysis, Pandor et al. 119 included a unit cost of £0.30 (2001 prices) per baby screened to account for the extra (incremental) time taken by a midwife to explain the test, although the actual length of additional time was not specified. This cost was identified through a consultation with a midwife. The evaluation conducted by Geelhoed et al. ,121 based in Western Australia, included a cost for the 15 minutes per child that a nurse would spend providing information about the test. An individual figure for the cost of providing information was not given but it can be calculated by dividing the total cost of nursing input in the sample (AU$326,875) by the number of babies seen (25,000) and multiplying this by the proportion of nurse time spent giving information (0.5), resulting in a value of AU$6.54 (2001 prices) per child screened. Wildhagen et al. ,122 based in the Netherlands, evaluated a CF NBSP but calculated the cost of information provision by using the mass media costs of information provision for a breast cancer screening programme. 124 The analysis assumed that the relative cost of providing a NBSP compared with a breast cancer screening programme would be reduced by 40% to account for the greater ease of introducing NBS into clinical practice. The final value included in the analysis was £136,956.60 (1996 prices), which was then combined with the cost of providing information at the individual level (assumed to be £1.19). This resulted in a cost of information of £2.13 (1996 prices) per child screened.
Existing evidence on the harms of information provision
Two of the studies in this review43,161 made a link between the level of information that a parent had received about NBS and the magnitude of the anxiety that they would experience on receipt of a false-positive result. These studies argued that the more information a parent was given about screening, the lower the level of anxiety they would experience on receipt of a false-positive result. However, these studies did not quantify the impact of information provision on anxiety levels following a false-positive result.
Four studies included valuations of the impact of parental anxiety. Prosser et al. 135 used the time trade-off approach and showed that, on average, parents were willing to give up 1 week of their life to not receive a false-positive result, which yielded a utility estimate of 0.003 for a health-related quality of life loss. Prosser et al. 42 then used this estimate in a model-based analysis of MCADD in a NBSP but found that the resulting 0.0005 quality-adjusted life-years (QALYs) lost from false-positive results had no significant impact on the relative cost-effectiveness. In absolute terms, including the anxiety costs raised the incremental cost-effectiveness ratio (ICER) by £50 per QALY. In a cost-effectiveness analysis of NBS for MCADD by Venditti et al. ,137 in the absence of finding a relevant disutility value for anxiety from a false-positive result, they used a value (0.03) based on the anxiety that oncology patients experience when receiving a false-positive result. This value was varied between 0.01 and 0.03 in sensitivity analysis, which resulted in a QALY loss of between 0.0025 and 0.0075, which again did not significantly affect the results. Two subsequent studies also used the disutility value of 0.03 used by Venditti et al. 137 In an economic analysis of an expanded NBSP, the authors allowed the effect of parental anxiety to vary from a disutility of 0.01 to a value of 0.05 (a QALY loss of 0.0125). 138 This study did not report the impact of including this disutility on the relative cost-effectiveness of the expanded NBSP. In a study by Cipriano et al. ,138 based in Canada, including a disutility for parental anxiety appeared to have a significant impact on the relative cost-effectiveness of expanding a NBSP. 138 Including the disutility value caused the intervention to not be cost-effectiveness when 15 conditions were included in the NBSP.
Pandor et al. 119,171 did not include an explicit value to quantify the impact of this ‘harm’ in their model even though the study described the need to provide information to reduce the anxiety that parents feel on the receipt of a false-positive result. The authors justified this omission by stating that any psychological disbenefits caused by screening would be far outweighed by the improvement in quality of life for children that a screening programme would bring. Two studies assumed that the disutility associated with parental anxiety would be negligible and so omitted this parameter from their model. Geelhoed et al. 121 suggested that only five children had received a false-positive result in Western Australia in 2001 and this meant that the total ‘negative benefit’ of the screening programme would be small. Hamers and Rumeau-Pichon167 also excluded anxiety because of its negligible potential impact and cited papers from the USA which suggested that parents had a high tolerance for false-positive results and that including them in a model made no significant difference to the outcome.
Existing evidence on the costs of imperfect information
One study161 mentioned costs related to the impact of imperfect information, specifically in reference to false-positive results and when part of the resulting anxiety could possibly be attributed to a lack of understanding. Schoen et al. 161 identified that, although false-positive results could cause increased parental anxiety, such results could also lead to ‘a cascade of costly clinical events, including emergency department visits, hospital admissions, additional definitive laboratory studies, and use of on-call medical personnel’. It was not possible to identify the actual increase in the resources used caused by this assumption.
Summary
This review has systematically identified if, and how, published economic evaluations took account of information provision within NBSP and related screening technologies. There is limited evidence in the literature as to the impact of information provision on the health-care costs and on the users of NBSP, the parents of newborn children.
Decision problem
The objective of this study was to begin to quantify the potential impact of different modes of information provision as part of a national NBSP and understand the key drivers of relative cost-effectiveness. Table 19 describes the decision problem addressed by this study and the key design criteria for the economic evaluation.
| Key design criteria | Description |
|---|---|
| Decision problem | What are the key drivers of the incremental costs and benefits of example modes of information provision used in a national NBSP including nine conditions? |
| Interventions | The personalised information provision approach involves offering mothers a choice of how they receive information |
| The universal information provision approach involves offering information to all mothers in the same way | |
| Mothers receiving information in both of the new modes of information provision are assumed to receive all 11 types of information recommended as part of the NBSP | |
| Comparators | The current ‘recommended’ information provision approach was assumed to follow published guidelines and mothers were assumed to receive all 11 types of information about NBS |
| The current ‘actual’ information provision approach was informed by the findings from the observation study (see Chapter 4) | |
| Model type | Decision tree |
| Population | Mothers of newborn babies in England |
| Setting | Health-care services |
| Time horizon | From conception of the baby to the point at which the result from the NBSP is provided |
| Costs | National currency (£) at 2015 prices |
| Benefits | QALYs in 1 year |
| Discounting | Not appropriate given the time horizon of the analysis |
| Cost-effectiveness threshold | NICE UK-recommended threshold of £20,000 per QALY gained |
Methods
This study used decision-analytic modelling methods to conduct an early economic evaluation comparing alternative modes of information provision in a national NBSP.
Model conceptualisation
The first stage in structuring the decision-analytic model that formed the basis for the economic evaluation was to conceptualise how the proposed modes of information provision and comparator with subsequent events should be represented. The challenge when conceptualising a decision-analytic model is to make it sufficiently complex to capture the relevant screening and treatment pathways but also to maintain a level of simplicity to allow the model to be populated with data. This process is called model conceptualisation and was completed in line with published recommendations. 172 Several important decisions and assumptions were made during the model conceptualisation process. The decisions were made with input from the scientific advisory board and members of the research team. The key decisions and assumptions made are described in the following sections.
Study perspective
The model-based economic evaluation assumed the perspective of NHS England, which provides the current mode of information provision as part of the NBSP in England. NHS Wales and NHS Scotland have their own approach to information provision in the NBSP.
Time horizon
A number of alternative time horizons were possible. This study chose to focus on the time from when the baby is conceived up to and including the point at which the final result from the NBSP is returned. The focus on events occurring within this time horizon was used as the objective of this study was to understand the key drivers of the relative cost-effectiveness of information provision rather than the impact of the NBSP. A definitive study that wanted to understand if, and how, information provision affected the relative cost-effectiveness of a NBSP would ideally assume a lifetime horizon of the baby.
Study population
Three types of individuals are potentially affected by a NBSP: the baby, the mother and the ‘family’ unit. This study assumed that the relevant study population was made up of mothers expecting a baby in England. The ‘family’ unit would have included the view of the birth father or a person acting in the position of ‘father’ and in some cases may extend to the wider family. There is substantial evidence from published studies and the findings of this study that it is the mother who is the primary decision-maker when deciding whether or not the baby should participate in the NBSP, which was why this focus was taken. The majority of published economic evaluations of NBSP all use the baby as the relevant study population. However, the baby is clearly not a decision-maker receiving information about the NBSP and so was not the relevant study population for this study. The size of the relevant population of mothers was informed by the number of live births in England.
Mode of information provision
Two new modes of information provision were proposed: personalised information provision and universal information provision. These potential new modes of information provision were informed by the findings from Chapters 3 and Chapter 5. Both modes would involve providing information on 11 elements of the NBSP, as described in Chapter 5.
The personalised information provision approach involves offering mothers a choice of how they receive information. Information can be provided by face-to-face discussions with a midwife (discussion based) or by providing written information in the form of leaflets, websites and smartphone apps (written materials). If discussion-based information is chosen, the mother would have a face-to-face discussion with a midwife and be provided with a leaflet late in pregnancy. The mother could also receive information face-to-face in a group appointment late in pregnancy. If written materials were selected the mother would receive a leaflet, which would also signpost the mother to information available on the internet and on smartphone apps. The mother would also be given the opportunity to request a face-to-face discussion with a midwife about the NBSP at a later point in the pregnancy. Mothers receiving information through both approaches would also receive a brief reminder about the NBSP after the baby was born.
The universal information provision approach involves offering information to all mothers in the same way. Information is provided through an individual face-to-face discussion with a midwife late in pregnancy, with the midwife also providing a leaflet about screening. In this approach, some information can also be received in group appointments and all mothers also receive a brief reminder about the NBSP after the baby is born.
Comparator
Two approaches to current practice were used as comparators to reflect current ‘recommended’ approaches to information provision115 and the current ‘actual’ approach to information provision used in the NBSP (see Chapter 4).
The current recommended approach to information provision was assumed to involve a mother being offered a leaflet early in pregnancy followed by an individual face-to-face discussion with a midwife late in pregnancy. The mother would then receive information in another discussion with the midwife on day 3 after the baby is born. Mothers who received the current ‘recommended’ information approach were assumed to receive all 11 types of information about NBSP, as described in Chapter 5.
The current actual approach to information provision was informed by the findings from the observation study (see Chapter 4). This approach was assumed to involve a mother being offered a leaflet early in pregnancy. It was then assumed that a proportion of mothers receive information in an individual face-to-face discussion with a midwife late in pregnancy. Regardless of whether the mother had received information late in pregnancy, a proportion of mothers would then be offered information in a face-to-face discussion with the midwife on day 3 after the birth of the baby and the remainder of mothers would receive the information in a face-to-face discussion with the midwife on day 5 after the birth of the baby.
Taking account of conditions included in the newborn screening programme
The current national NBSP includes nine conditions: PKU, CHT, CF, SCD, MCADD, MSUD, GA1, IVA and HCU (see Table 18). This study assumed that the same information provision model would be used for all of these nine conditions up until the point at which the first result from the NBSP is known. If a positive result is identified for four selected conditions (MCADD, MSUD, GA1 or IVA) then it becomes a matter of urgency to conduct a confirmatory screening test and the situation is labelled ‘urgent’ and an associated process of events is put in place by the health-care system. At this point a significant effort is made to contact the mother/parents of the newborn baby as it is imperative that the diagnosis is confirmed and treatment started. In this study, we represented this urgent situation by including a pathway representing the need for an urgent response following the first analysis of the bloodspot in the NBSP.
This model does not explicitly account for the anxiety caused by the receipt of a carrier result for CF or SCD. This is because parents experiencing these results were excluded from study 2 and so parents’ views about receiving carrier status information are omitted. However, it is likely that the anxiety caused by receiving a CF or SCD carrier result is captured in the sensitivity analysis.
Taking account of events following a screening result
This study focused on identifying the impact of alternative modes of information provision up until the point at which the result from the screening programme is confirmed. The next event that will occur is dependent on whether or not a positive or a negative screening result is reported. If a negative result is returned, this effectively signals the end of the use of health-care resources. However, if a positive result is returned then the baby will be referred to the relevant service for a formal diagnosis of the identified inherited condition. Although not within the scope of this study, it is necessary to consider this when conceptualising the model because, in theory, this model could be ‘bolted-on’ to a subsequent model that aimed to quantify the incremental costs and benefits of a screening programme for that specific named condition within the screening panel.
Modelling methods
A decision tree was chosen to create the mathematical representation of the decision-analytic model structure. In accordance with the recommendations of Brennan et al. ,173 a decision tree was the most suitable type of model as this was an early economic analysis that aimed to capture a linear pathway of information provision in a large population of mothers. The model structure was developed using an iterative process with input from the research team and members of the scientific advisory board.
Populating the model
‘Populating the model’ refers to the process of selecting values for all of the parameters defined in the decision-analytic model. Parameter values were drawn from a range of sources including the midwife survey (see Chapter 4), the midwife observation study (see Chapter 4), a systematic review of the NBS literature and consultation with experts. Appendix 9 provides a summary of all of the model input parameters and values. The process of populating the model is described for each parameter in turn in the following sections.
Probabilities
The values for the probability input parameters for the current actual information provision approach were derived from the midwife survey reported in Chapter 4. There were no probabilistic events associated with the current recommended information provision pathway.
For both the proposed universal information provision approach and the personalised information provision approach a probabilistic event was included to capture whether or not the mother opted to receive information in a group appointment. As there were no data to populate this parameter, in the base-case analysis it was assumed that the mother would not have access to such classes and so the probability was set at zero. Including this probability in the model structure meant that the impact of this assumption could be explored in the one-way sensitivity analysis.
The personalised information provision approach included a probability event to capture whether or not the information was provided using a discussion-based or a materials-based approach. In the base-case analysis it was assumed that the population would be evenly split in terms of choosing one of these options and the probability input parameter was set to 0.50; this was changed in the one-way sensitivity analysis. In the base-case analysis the probability that a mother who accessed the materials-based approach would then later request a discussion-based approach was set to zero.
The values for the probabilities included in the post-screening tree were taken from relevant NBSP literature. The probability of a repeat sample being required was set at 0.044, representing an unweighted mean of the reported annual repeat rates for each geographical region in England. 174 The probability of receiving a true-positive result was established from the incidence estimates reported in the study by Pandor et al. 119 The probability of receiving a false-negative result was set at zero. The probability of parents receiving a positive result for an ‘urgent’ condition was estimated by calculating the proportion of children diagnosed with MCADD, MSUD, GA1 or IVA compared with the total number of children diagnosed post screening.
The model also captured whether or not a mother’s capability of making an informed decision would be affected by the mode of information provision by including an event to represent either decision-making that was unaffected or decision-making that was affected. In the base-case analysis this chance event was assumed to be relevant only for the two current modes of information provision. In the base-case analysis, the value for the probability of affected decision-making was set to zero for each of the proposed new modes of information provision.
Resource use and costs
All estimates for resource use and costs were informed by the costing study reported in Chapter 4. The approach taken to calculate the resource use and costs for the current actual information provision pathway is described in Chapter 4. The results of the costing study were also used to inform resource use for new approaches to information provision and the current recommended approach. For these approaches it was assumed that a mother would receive 11 pieces of information, as described in Chapter 5, at a unit cost of £0.46 (see Chapter 4). This equated to a cost of £5.05. The cost of signposting the mother to use the internet and app-based information was estimated to equate to the cost of providing one piece of information. The cost of a group appointment was calculated by assuming that there would be six mothers in each group and dividing the time that it would take to provide an individual discussion (6.05 minutes) by six. If a midwife provided a brief reminder about screening this was assumed to take 1 minute, which was taken from the observation study (see Chapter 4).
Additional use of resources was required if a midwife had to obtain a second bloodspot sample for analysis. This resource use was informed by the observation study (see Chapter 4) and was estimated from the cost of travelling back to the parents’ home (£13.36) and the cost of providing all 11 pieces of NBSP information (£5.05).
It was also assumed that additional health-care resource use in the form of visits to a general practitioner (GP) would be incurred if the mother received a false-positive result and her decision-making was affected because she had received one of the current approaches to information provision. For the pathway in which a false-positive result was returned for a condition that required urgent attention, an additional visit to the GP was assumed as the timescale for conducting a repeat sample would not allow time for more visits. Two visits to a GP were assumed to be incurred in the pathway for non-urgent conditions and confirmed negative results. The cost of a GP visit was obtained from Curtis. 116
Consequences
The consequence of receiving each information provision model was captured using QALYs over 1 year. This required the identification of a utility value for each pathway in the model. Published preference weights for the health status of a woman aged between 18 and 44 years were used for the utility value (0.91) attached to all of the pathways. 175
The systematic review of published economic evaluations of NBSP (see earlier in this chapter) was used to inform the disutility value associated with receiving a false-positive result in the pathway representing current practice. Four studies were identified in the systematic review that included a utility decrement for parents whose child had received a false-positive result. 42,137–139 These disutility values ranged between 0.01 and 0.05. In this model, the mean of the reported published values (0.018) was used for the utility decrement in the base-case analysis. This utility decrement was assumed to last for 3 months in accordance with the assumptions made in the published studies. The utility decrement, and the duration of the harm, were changed in the one-way sensitivity analysis.
Data analysis
A base-case analysis was used to calculate the total expected costs and QALYs for each mode of information provision received by a mother. All costs and QALYs were discounted at a rate of 0% as the time from birth to the return of screening results is < 1 year.
A full incremental analysis was planned that would involve, first, calculating the total costs and QALYs for each intervention and then putting the interventions in order of expected QALYs. Each intervention would then be compared with the next best alternative in terms of the order inferred by the expected QALYs. In practice, however, the expected QALYs for each intervention, other than current actual practice approach, were estimated to be the same. This meant that a full incremental analysis was not appropriate and each intervention was compared with current actual practice using the formula shown in Equation 1.
where QALY2 is the total expected QALYs for the new intervention and QALY1 is the total expected QALYs for current actual practice and C2 and C1 are the respective total expected costs.
One-way sensitivity analysis
One-way sensitivity analyses, in which a single parameter is systematically varied over a predefined range of values, were used to explore the key drivers of relative cost-effectiveness. The parameters selected for inclusion in the one-way sensitivity analyses were:
-
the proportion of parents receiving information in the personalised, universal or current recommended strategies whose decision-making was affected as a consequence of the information provision
-
the utility decrement for parents receiving a false-positive result in the current actual practice arm
-
the duration of the quality of life decrement for parents receiving a false-positive result
-
the proportion of parents choosing to receive information in a discussion-based format rather than materials-based information in the personalised information provision approach
-
the proportion of parents receiving information in group appointments in the personalised and universal information provision pathways
-
the proportion of parents in the materials-based information arm of the personalised practice pathway who then requested additional information in a discussion-based format.
Probabilistic sensitivity analysis
To account for uncertainty in the values of multiple parameters simultaneously, a probabilistic sensitivity analysis (PSA) was conducted. In the PSA, ranges and distributions were assigned to selected model input parameters (see Appendix 9). Monte Carlo simulation was then used to rerun the analysis over 10,000 times using the values drawn from the predefined ranges and the distributions of the model input parameters. The ranges and distributions for resource use parameter values were obtained from the survey and observation study (see Chapter 4). A hypothetical distribution of disutility values was generated using nine example utility values and by creating a gamma distribution. Distributions were also added to the proportion of mothers attending group appointments, using a wide range of values, as it was assumed that this parameter would vary substantially and might have an impact on the model results.
Value of future research
To quantify the potential value of future research, the expected value of perfect information (EVPI) was calculated using the results of the PSA. 176 Calculating the EVPI provides an estimate of the value of research that would eliminate all uncertainty associated with selected inputs for parameter values in the model. The EVPI analysis involves calculating the difference in the net benefit achieved by choosing the ‘optimal’ intervention, as defined by the expected net benefit, compared with selecting another intervention for each run of the PSA. The EVPI is dependent on the assumed duration of the effective lifetime of the intervention. This study estimated the EVPI for five example lifetimes for the information provision approach (between 1 year and 5 years). The population EVPI was estimated by assuming a eligible population of mothers, based on 2014 data on the number of live births in England. 118
Results
This section presents the results of the base-case analysis, the one-way sensitivity analysis for each predefined parameter included in the decision-analytic model, the PSA and the EVPI analysis.
Base-case analysis
Table 20 shows the results of the base-case analysis for a population of 661,496 mothers, which is consistent with the number of lives births in England in 2014. 118 The mode of information provision with the lowest total expected cost (£12,269,487) was personalised information. Universal information provided in the recommended way was slightly more expensive (£13,635,077) because of the increase in the quantity of information provided in individual discussions. Information provided as per current guidelines was the most expensive because of the repetition of all information late in pregnancy as well as after the baby is born. The expected QALYs accrued for each of the new modes of information provision and current recommended practice were assumed to be the same as the same proportion of mothers would have their decision-making affected by the different approaches. Personalised information and universal information dominated current actual practice as they were less expensive and provided more QALYs. This finding would hold only if these modes of information provision completely prevented mothers from having their decision-making affected by raised anxiety levels. Current recommended practice was more expensive than current actual practice and resulted in a gain in QALYs and, with an ICER of £3272 per QALY gained, would be deemed a cost-effective use of resources, given the NICE WTP threshold of £20,000 per QALY.
| Pathway | Expected QALYs | Expected cost (£) | Incremental QALYsa | Incremental cost (£)a | ICER (£)a |
|---|---|---|---|---|---|
| Current actual practice | 604,254 | 15,987,415 | Not appropriate | ||
| Current recommended practice | 604,387 | 16,421,935 | 133 | 434,519 | 3272 |
| Universal practice | 604,387 | 13,635,077 | 133 | –2,352,340 | Dominates current practice |
| Personalised practice | 604,387 | 12,269,487 | 133 | –3,717,930 | Dominates current practice |
One-way sensitivity analysis
Table 21 shows the results of the one-way sensitivity analysis. The only model input parameter that affected the relative cost-effectiveness of the different modes of information provision was the assumption about how many mothers would have their decision-making affected because of raised anxiety levels. If > 46% of mothers receiving information in the current recommended practice arm had their decision-making affected then this mode of information provision was no longer cost-effective. Increases in the proportion of mothers having their decision-making affected decreased the relative cost-effectiveness of the universal and personalised information provision strategies but they continued to have ICERs below the WTP threshold of £20,000 per QALY up until the point at which all mothers had their decision-making affected.
| Scenario | Values | ICER (£) vs. current practicea | ||
|---|---|---|---|---|
| Current recommended practice | Universal practice | Personalised practice | ||
| Proportion of parents with affected decision-making | 1.00 | Infinity | Infinity | Infinity |
| 0.75 | 98,413 | 14,620 | –26,512 | |
| 0.50 | 35,035 | –6936 | –27,502 | |
| 0.25 | 13,860 | –14,121 | –27,832 | |
| Impact of anxiety on quality of life | 0.01 | 5972 | –32,328 | –51,095 |
| 0.05 | 1194 | –6466 | –10,219 | |
| Duration of utility decrement for anxiety | 2 weeks | 21,269 | –115,141 | –181,984 |
| 1 year | 818 | –4429 | –6999 | |
| Proportion of parents receiving information in group appointments in the personalised and universal practice arms | 1.00 | 3272 | –13,524 | –25,903 |
| 0.75 | 3272 | –14,572 | –26,426 | |
| 0.50 | 3272 | –15,619 | –26,950 | |
| 0.25 | 3272 | –16,667 | –27,474 | |
| Proportion of parents choosing individual discussion in the personalised practice arm | 1.00 | 3272 | –17,713 | –17,714 |
| 0.75 | 3272 | –17,713 | –22,856 | |
| 0.25 | 3272 | –17,713 | –33,139 | |
| 0.00 | 3272 | –17,713 | –38,281 | |
| Proportion of parents choosing written materials and also discussion-based information in the personalised practice arm | 1.00 | 3272 | –17,713 | –15,429 |
| 0.75 | 3272 | –17,713 | –18,571 | |
| 0.50 | 3272 | –17,713 | –21,713 | |
| 0.25 | 3272 | –17,713 | –24,855 | |
Changes in the proportion of parents receiving information in group appointments in the personalised and universal strategy arms had virtually no impact on the relative cost-effectiveness of these approaches. Similarly, the proportion of patients choosing discussion-based information to begin with, or after receiving written materials, in the personalised strategy arm had very little impact on relative cost-effectiveness. This lack of impact was because the cost element of these strategies, as well as that of current recommended practice, was dominated by the cost of GP appointments. These additional anxiety-related health-care costs meant that changes in the QALY impact of false-positives had little impact on the results, suggesting that the true value of improved decision-making may lie in reducing unnecessary health-care resource use.
Probabilistic sensitivity analysis
The strategy of providing personalised information to parents had the highest probability of being cost-effective across all potential threshold values of additional cost per QALY gained. However, the probability of cost-effectiveness peaked at < 45%, indicating that there was a significant amount of uncertainty in the results. Universal information provision had the second highest probability of being cost-effective at WTP thresholds between £20,000 and £30,000 per QALY, followed by current actual practice and current recommended practice (Figure 9).
FIGURE 9.
Cost-effectiveness acceptability curve.

Value of future research
Table 22 shows the value of additional research that would remove all uncertainty using the stated assumptions for the model input parameters. Given the rapidly changing make-up of the UK NBSP, the EVPI results are shown for different assumptions about the duration for which the information provision mode remains relevant. The high EVPI estimates, assuming a threshold of either £20,000 or £30,000 per QALY, suggest a high level of uncertainty in the choice of optimal information provision strategy in NBS and a need for further research.
| Value of information parameter | Cost per QALY threshold | |
|---|---|---|
| £20,000 | £30,000 | |
| Individual EVPI (£) | ||
| EVPI per parent | 2.67 | 3.52 |
| Population EVPI (£)a | ||
| Time horizon of information mode (years) | ||
| 1 | 1,764,616 | 2,330,326 |
| 2 | 3,469,559 | 4,581,849 |
| 3 | 5,116,847 | 6,757,233 |
| 4 | 6,708,430 | 8,859,053 |
| 5 | 8,246,191 | 10,889,798 |
Discussion
This study aimed to identify the key drivers of the relative cost-effectiveness of different modes of information provision compared with current actual practice for a national NBSP. The proposed new modes of information provision were informed by the findings from qualitative semistructured face-to-face interviews (see Chapter 3) and a stated preference survey (see Chapter 5). Current ‘actual’ practice was defined as involving the resource use identified in an observation study (see Chapter 4). It is important to note that the absolute values for and relative ordering of the intervention and comparator strategies should be interpreted with caution as the population of the model-based cost-effectiveness analysis was challenging owing to a paucity of robust data for many of the input parameters. With the data available and assumptions made, in the base-case analysis, using a personalised or universal approach to information provision dominated current ‘actual’ practice. Current ‘recommended’ practice was estimated to have an ICER well below the threshold of £20,000 per QALY. The relative cost-effectiveness of these three approaches was driven by the assumed effect of removing unnecessary GP visits following a positive first test result and subsequently avoiding anxiety that would cause decision-making to be negatively affected. The analysis suggested that a personalised approach to information provision would be the least expensive option. The lower cost of this approach was driven by the significantly lower number of resources required to provide information (the use of leaflets, the internet or smartphone apps rather than all parents having an individual face-to-face discussion with a midwife). Even factoring in an assumption that, on some occasions, a proportion of mothers may later ask for a discussion with the midwife, this personalised approach proved to be a potentially cost-effective option. However, introducing this option into practice would require a mechanism for identifying which mothers would prefer a discussion-based approach to information provision and which would prefer the provision of written material.
The lack of data to populate this model-based cost-effectiveness analysis resulted in substantial uncertainty surrounding the decision about which strategy would be the most cost-effective if introduced into practice. The EVPI analysis confirmed this uncertainty by suggesting that future research is required to improve the parameter estimates. Taking account of the one-way sensitivity analysis, it is likely that a key area of uncertainty is in quantifying the extent of decision-making affected by an initial positive test result. There are three elements to this uncertainty: how many mothers would have their decision-making affected in a negative manner; what is the value of the assumed utility decrement associated with the resulting anxiety levels and for how long should it be applied; and what additional level of resource use should be assumed before a final confirmatory test result is received.
This analysis assumed that the impact of information provision would primarily be on the mother. A key consideration for future research is how the approach taken in this model-based cost-effectiveness analysis, which assumed the mother’s perspective, can be combined with existing economic analyses that have quantified the impact of NBS on the health of the baby. In theory, the model structure proposed in this study could be put in front of a subsequent model that captures the impact of screening for any of the nine conditions currently in the NBSP (or more if the programme is expanded). However, this would mean that a future analysis would have to consider how to combine the impact of the NBSP on two populations, mothers and their babies.
Conclusion
This model-based cost-effectiveness analysis developed potential pathways for four modes of information provision in a national NBSP. The key driver of the relative cost-effectiveness of the different modes of information provision was how effective each approach would be in allaying anxiety potentially caused by mothers being poorly informed and hence making inappropriate decisions. Using an effective information provision strategy could avoid the unnecessary use of health-care resources and/or reduce the negative impact on the anxiety levels of the individual caring for a newborn. There was insufficient evidence to inform the values assumed in this model-based cost-effectiveness analysis. Future research is required to improve the robustness of key model inputs and considerable investment in future research would be valuable to inform which mode of information provision for NBSP is the best use of NHS resources.
Chapter 7 Study 6: stakeholder consultation
Study objectives
-
To explore providers’ and users’ views on the study suggestions, focusing on acceptability, broader impact, effectiveness, efficiency and parent understanding.
-
To establish how generalisable the study findings are across conditions screened for in NBS in England.
Introduction
There are recognised gaps in the research regarding the effectiveness of NBS information provision, including the provision of information antenatally;100 optimal communication during follow-up testing33 and for conveying carrier results;34,101 the effectiveness of alternative communication models;101,102 and parents’ views. 34,101 Thus, this study focused on a need to develop the evidence base to produce acceptable, efficient and effective models of NBS communication. Existing research appears to show that the main additional communication resources required during the NBS pathway are for parents receiving carrier results or false-positive results. 34,43 This is because routine information provision is conducted alongside other activities and so resources are shared across interventions. However, when carrier or false-positive results are received, an additional visit is required with the sole purpose of providing additional information. Both were highlighted as important areas requiring further research with regard to NBS communication. 100 There are, however, large enough differences between the implications and experiences of receiving a carrier result and the implications and experiences of receiving a false-positive metabolic result to warrant detailed examination of these situations independently. Research conducted for the NIHR HTA programme has focused on the communication needs and experiences of parents receiving carrier test results from CF and SCD screening and has provided many findings relevant to this project. 34 Thus, this project focused initially on screening for metabolic diseases and then tested how transferable the findings were for screening of CF and SCD by inviting relevant stakeholders to participate in the consultation alongside participants from study 2 (see Chapter 3).
Methods
Design
A qualitative design was employed using focus groups and telephone interviews to validate the team’s interpretation of the qualitative data and the participants’ views regarding the project’s conclusions and examine how generalisable suggestions for practice were to wider NBS. This approach has been used previously177 and follows recommendations of how to test NBS materials. 33 This model of modifying research-based policy recommendations through focus groups with providers and users has been used previously by the principal investigator when making recommendations about NBSP communication issues. 34 Furthermore, focus groups enabled observation of how the recommendations were discussed and concerns were negotiated, providing insight into the implicit processes and potential barriers that may affect the success of alternative models of communication. 178 Those who were not available or who did not want to participate in focus groups were offered the option of taking part in a telephone interview, thus enabling involvement through group discussion and ‘private’ interviews, in keeping with best practice in developing guidance. 179 Separate focus groups were held for health professionals and parents as the data gathered earlier in the project suggested that this may allow participants to speak more freely about their concerns and views.
Sample
All participants from the interview study (see Chapter 3) were sent an invitation to participate in a focus group or a telephone interview. Additionally, key stakeholders in the NBSP for CF and SCD and from the RCM, as well as NBS laboratory directors, were invited to participate to discuss the project findings in relation to screening for these diseases to determine how transferable the project findings based on metabolic disorders are to wider NBS.
Procedure
The focus groups were hosted at the University of Manchester, with refreshments provided and travel expenses covered. Given the volume of findings, the research team split the findings into four key areas linked to communication and consent: how, when, what and why. Taking each topic in turn, first, participants were asked to discuss their views and experiences this and then the team provided an overview of the findings. The content was identical for both the health professional and the parent focus groups, but it was delivered to parents using a quasi-informal discussion, with the findings presented on sticky notes, and to health professionals by way of a presentation. A presentation was used for the health professionals as they are used to receiving information in this way prior to discussion (see Appendix 10). For parents, the verbal discussion and sticky note approach was adopted to break down the formality of the process and hopefully reduce the potential perception that the researchers are experts providing information to parents. It also made abstract concepts concrete by enabling parents to ‘handle’ the suggestions and move them around. The participants read the sticky notes out to each other rather than the researchers reading them, after which they were asked to discuss them. This was to try to ensure that participants felt empowered. In the health professional group a similar pattern was followed whereby health professionals’ views were sought afresh on topics. This was partly because this group contained new participants, but it also provided a sense of the participants driving the data. The research team then provided brief presentations around the topics. Within the presentations any uncertainties or contradictions in the results or any aspects for which clarification of meaning was sought were highlighted. This focus group ran after the parent focus group and so there was a further layer to the health professional presentations in which they were shown the written notes from the parent focus group (see Appendix 11). This is because our existing data set suggested a disconnect somewhere between health professionals’ and parents’ experiences and it was deemed important to bring these ‘voices’ into the health professionals’ discussions. There was also an awareness that the service users may have suggestions that logically sound viable but that health professionals may have service knowledge which explains why this is not so. Thus, this process sought a way of bringing the data together.
Additionally, participants who were willing to be interviewed by telephone were sent a summary of the project findings by e-mail (see Appendix 12). A convenient time for a telephone interview was arranged within 1 week of receiving the project summary. Interviews lasted between 20 and 40 minutes. Participants provided verbal consent and interviews were audio recorded and transcribed in the same manner as for the interviews reported in Chapter 3.
Ethics approval
Ethics approval for this study was gained at the same time as approval for the interview study (see Chapter 3) as the interview participants were invited to participate in this study. Thus, approval for participation of the health professionals was obtained from the University of Manchester Research Ethics Committee (reference number 13198) and approval for participation of the parents was obtained from the NHS West Midlands Edgbaston Research Ethics Committee (reference number 13/WM/0438). R&D approval was gained from trusts under the same approval as for study 2 (see Chapter 3).
Analysis
Data were analysed using thematic analysis. 105 As participants discussed their own experiences again while reflecting on the project summary, the data were first divided into ‘actual experience’ and ‘experience wanted’ to make it clear when people were talking about their previous experiences and when they were talking about how they felt the service should be provided. Actual experience data were added to the data set for study 2 (see Chapter 3) as the focus of the stakeholder consultation was to examine future models. Following a deductive approach, data were further divided into ‘communication’ and ‘choice’ as these were the central areas of a future service of interest. 110 Within these areas codes were created using a deductive framework of how, when and what. Coding was conducted by FU at the manifest level110 to maintain a direct link between participants’ expressed views and the findings. An overview of this was presented to the wider team, with requests for feedback. Analysis ceased once saturation had been achieved. Negative case analysis180 was conducted rigorously to seek out examples that did not fit the pattern of results so that the limits of the suggestions could be identified.
Results
In total, 12 health professionals and five parents participated in this study. The health professional sample consisted of midwives (n = 4), SQAMs (n = 2), a senior representative of the RCM, a NBS laboratory director, a trust screening co-ordinator, a screening link health visitor and a representative of NBS screening for CF. The health professionals were located in the north-west, the East Midlands and London, although some could provide a national perspective given their role. The parent sample included mothers aged 29–35 years. Two did not speak English as their first language and all were educated to college or university level. Contextual data are provided in the data identifiers, with ‘i’ denoting interview and ‘fg’ indicating that the participant took part in a focus group. Throughout the presentation of the results, data excerpts from health professionals and parents are contrasted to highlight areas of convergence and divergence in views.
Views on the research summary
Although the data relating to actual experiences are not reported in detail here (see Chapter 3), it is important to note that comments made about the summary of results presented to the parents indicated that the summary matched their experience or desired experience and views. There was one exception, a mother who at first could not engage with the idea that screening would be anything other than mandatory given her experience. In contrast, the comments from the health professionals varied. Many front-line staff suggested that they did provide the service as per the project recommendations. However, this did not fit with parent reports or the views of some health professionals involved in working with parents later in the screening pathway. This anomaly was brought up spontaneously in the health professional focus group:
What you’re saying [midwife describing her practice] sounds really good, it sounds perfect, really. Yet, what we’re experiencing at the other end is completely different. And every single parent, and this is not just one or two parents, the vast majority of them will say, never heard about [name of condition], didn’t even know it was, didn’t even know you were screening for it. [. . .] a remarkable number get to a result, and are traumatised by it and say, well nobody ever told me this was gonna happen. So there’s a disconnect somewhere.
CF screening representative, fg
This triggered the midwives to reflect that, although those participating may provide a very good service, they were aware of some very poor examples, which were almost exclusively driven by the time pressures and staff shortages that midwives were working under, driving them to prioritise clinical care over communication. Another central concern was that of lack of resources, in terms of both trust-level barriers to accessing translated materials and the lack of interpreters. All of the parents stated that what was represented in the summary is what they would have liked but did not receive. That some of the practices are currently part of policy recommendations (i.e. informing parents what conditions are screened for) suggests that there are still issues with ensuring that all midwives are able to follow standardised guidelines. This may also be the result of another system-related barrier that health professionals raised, which was the need to convey ever-increasing amounts of information without increasing the length of appointments.
Communication model
In line with how the summary was presented to participants, the following analysis is presented within the areas of what information, how and when.
What
In the summary it was reported that the interview data suggested that the following messages were important:
-
the purpose of screening and why it is important
-
the names of the conditions being screened
-
how the sample will be taken
-
whether or not the baby will feel any pain or side effects
-
when and how the results will be received
-
what has changed (for parents who have been through the screening process with previous children)
-
where to get further information
-
what will happen to the baby’s bloodspot sample card after screening.
There appeared to be broad agreement from our respondents on the usefulness of these messages. With regard to differences between health professionals and parents, health professionals discussed the balance of information and the utility of the different messages – rarity of conditions, condition names, etc. – whereas parents were more interested in a general raising of awareness and simple messages about what the implications were if they refused screening and what symptoms to look out for in their child.
The following quotation illustrates what many parents would have liked:
I would have just loved to have known what the heel prick was testing for. Even if it was just a really brief one-line thing, it would have been really helpful.
Mother, English, second child, PKU result, i
In general, front-line health professionals reported that this was closely aligned with what they covered now and was in the booklet. However, others, involved in more managerial and training roles, held a view that practice did not need to be changed, suggesting that they were aware of instances where current practice did not fit with the recommendations coming from the data:
They’ve just said just the names of conditions being screened for, and that’s probably fair, because I think at the moment it’s just too much information.
SQAM, i
However, the health professionals’ discussion very much focused on the variation in information needs of parents, with some questioning the utility of knowing a condition name given the low levels of knowledge in the population of these conditions. Although there was a recognition that different parents may seek differing types and levels of information, there did not seem to be much variation in the views of health professionals dependent on their role, with the exception of the need to prepare parents for carrier status. This was a central information omission raised by the CF screening representative and supported by the health visitor (i.e. professionals working with parents after they receive the results of screening) and was not initially seen as being very important by those providing prescreening information. Although factually correct, there were also concerns about how useful the message about the rarity of the diseases screened for is for parents.
One health professional raised concerns about ethical practice if communication focused only on the names of conditions. Of note, she did so while reflecting on her current practice:
I know that they’re incredibly rare, but I don’t feel like I’m getting an informed consent for those four because all I’m getting consent for is the name not the actual condition.
Community midwife, London, i
The problem driving such behaviour was seen as information overload, which encompassed both the limits of training and the ability of midwives to retain information and parents’ ability to receive information. Both front-line and policy-orientated health professionals felt that, in practice, they had already reached the point at which the goal of providing complete information was actually so overwhelming those involved in NBS communication (both the midwife and the parent) that it was rendering information ineffective even on basic levels:
Historically in this country we were giving information about every condition weren’t we and what that means whereas that becomes more and more impossible I think as the number of metabolic conditions that are screened for increases and I think we’ve probably reached that point now with the expanded programme.
NBS laboratory director, i
However, there was a recognition that parents may need more than the names of the conditions being screened for and the health professionals went on to suggest a solution:
Perhaps you should say, well, and we screen for a range of metabolic conditions which are serious and treatable and I think that’s the important thing, isn’t it, that they understand that the criteria that are used for screening one of them is that that condition is treatable and that their baby is going to benefit really.
NBS laboratory director, i
Of interest, the treatability of the conditions being screened for was one of the key pieces of information that was missing according to the mother of a child who had experienced receiving a positive NBS result. In her experience it was not until she met the specialist paediatrician that she heard that the condition was treatable, which significantly reduced her anxiety levels
. . . she came round in the morning and said, oh, he’s had an abnormal heel prick, after telling us that it was fine, nothing would come of it, and that we had to go to the hospital on the Tuesday, and that it was fine because there was a dietary treatment. But then there was no one to talk to. No, she did give us a mobile number actually of the woman, didn’t she, if we had any questions. But obviously, the first thing that you do is go on the internet. So we just got ourselves in absolute . . . really upset. And then went to hospital on the Tuesday first thing in the morning. And then they had another . . . they did his blood test again and then it was confirmed. And then he was on the diet straightaway. But then when we spoke to the consultant and everyone was really like, you know, if he starts on the diet now, he’ll be absolutely fine.
#17, mother, child has PKU
But, I do think, at the moment, in the screening tests You and Your Baby booklet, there’s way too much information on the conditions, I think that could be just condensed to a couple of lines. Because, for most families, it’s not going to be relevant, and then, with those sorts of, if the baby has a problem, then that’s the point for more information.
SQAM, i
Thus, again, the need to clarify the goals of the communication, the why in the communication model, is implicit in these data, as are the issues around using one piece of information for the wide range of parental information needs. Thus, the focus of fully informing – providing all information on a topic – may have reached a point where it is no longer meaningful for some parents, nor effective. Rather, it runs the risk of being ineffective in terms of achieving other communication goals, such as preparing parents for the outcomes of screening. The responses from the health professionals included consideration of which messages were most important for all parents to appreciate. One of these was the need to be clear about storage of bloodspots:
It’s important to understand that we do store the bloodspots and why we store them because that might obviate people getting concerned after the event really. Yes, I think all of those are . . . I mean, I would hope all of those things are covered currently. They should be.
NBS laboratory director, i
Unfortunately, across the study parents appeared to have little awareness that samples may be stored:
What happens to bloods – yes I don’t know that what happens to the bloodspot sample card after screening – yes that needs to be elaborated on as well because I have no idea.
Mother, English, pregnant, i
Of note, although this mother was recruited into the ‘pregnant’ sample at the time of the interview, she had recently become a parent at the time of the stakeholder consultation. She therefore represented parents with a recent experience of NBS communication. Even though the parent focus group attendees reflected on the fact that they felt that they had more awareness and understanding of NBS given their participation in two parts of this research project, they still were shocked when the researcher asked them their views about storage, stating that they had no idea that this happened. This highlights again how challenging it appears to be to convey key simple messages about NBS, even though this information is provided in the leaflet:
For me, I’m angry that they are using my kid’s blood without me even knowing. Even though I know that I will never say no, but doing it almost in a hiding way, it’s not really right. Then you are regretting that you have given the consent form, or you have the right to say no. Yeah, honesty is just enormous. It’s like I take something from you without you knowing.
Mother, English, two children, negative result, fg
This mother verbally reported that she was shocked and was visibly upset in the focus group. Her response highlights how detrimental it could be to the public image of a screening programme and trust if key pieces of information are not made clear to parents. Furthermore, it highlights the differences in parental reactions to screening and storage. Although a lot of parents said that they had not felt that they had a choice about screening and had limited knowledge of the conditions screened for, few parents were angry that screening per se had been performed (rather, they may have preferred a different communication experience), whereas, when they became aware that storage of bloodspots may occur following NBS, they were upset. This highlights how the prioritising of NBS information messages should not necessarily align with what are medically seen as the most important pieces of information. For example, the storage of bloodspot samples is not seen as a primary goal of NBS, but it may be one of the most important pieces of information that parents want to receive in relation to NBS and their role in making decisions about it.
One of the items on the list that was definitely novel was the idea of a screening update tool whereby the date of birth of previous children could be put into a computer and a document could be generated to highlight to parents what the changes in screening had been in the interim to ensure that they did not consent based on information provided for a previous, smaller screening panel. This was in part to address the issue of health professionals and/or parents assuming that parents were already informed if they had had a previous pregnancy. This idea was supported by all parents in the focus group and was highlighted as the most important finding by front-line midwives, who felt that this would also be useful for them.
Early in the focus group the health professionals brought up the need to make it clear to parents that screening was optional. This was also raised spontaneously in the parent focus group in reaction to an introduction about NBS provided by the research team that mentioned that screening is optional:
I mean, if, right now, there is a choice, I think it should be . . . parents should be aware of that, and I don’t think they are.
Mother, English, two children, negative result, fg
Of interest, although the focus group members had differing views on whether or not parents should have a choice about screening, they agreed on the view that, if NBS policy is that NBS is the parents’ choice, this must be made explicit. During this discussion parents demonstrated their passion about this and, indeed, not ensuring that parents were aware of this was seen as breaking their trust in the NHS, showing the detrimental effect that receiving information about NBS after experiencing the event could have on parents.
How
The summary stated that:
-
rather than everyone receiving the same leaflet, a range of information resources should be available, for example leaflets, websites, apps and video clips, with parents choosing the format that is best for them
-
NBS information provision should be more parent led
-
information provision should be modernised using technology, for example apps and websites
-
a brief discussion with a midwife is still required to introduce and signpost parents to information resources
-
information overload should be minimised by separating NBS information
-
parents’ understanding of information should be checked.
During the interviews participants were asked what was the most important point that they felt had come from the study; because of time limitations this was inferred from the focus group discussions. Of interest, all of the data related to the issue of how to provide information, from aligning the mode of information provision with how people currently obtain information (i.e. on their phones) to drip-feeding, updating, empowering parents to be active and providing a range of formats to match the diverse needs of the population. Optimising information provision was a vital part of the study findings for most participants:
I think it’s [the most important point] the information sharing and how we’re going to move forward to make sure that we do get the information across at the most up to date and in the right format for the right person.
Senior community midwife, i
Within this response one can unpick the need to improve, the evolving nature of NBS and individual preferences. Thus, unless one has the ‘how’ sorted, the needs of a NBS communication model cannot be met. The ability of these approaches to also address the issue discussed earlier about the surfeit of information was also part of the attraction and this was recognised among parents through to policy-level participants who did not have a front-line role:
The key thing is that parents want it to be given in a way that’s more digestible and that we need to try and get on and do it I suppose.
NBS laboratory director, i
I think there was something – I think probably the new technology thing having that available would have been good [. . .] Then having the information drip fed at multiple points at the beginning, in the middle and then like you say right at the end would have been better as well.
Mother, English, pregnant sample, i
Although participants supported the need to vary the approaches used to convey NBS information, there was a desire to ensure that the leaflet format was still available:
I think the information being available in different formats for different people; I think that’s a really key thing. Because, you know, people do like information in different forms, apps and websites, and . . . But, I do think that the initial leaflet should almost be given in a very easy read format, so it’s acceptable to everybody.
SQAM, i
The discourse about enabling parents to be ‘active’ in gaining NBS information was dominant across both sample groups in terms of providing an efficient service. Giving some of the responsibility to parents was also seen as having additional benefits:
I think like we can’t underestimate how much parents would like to be involved. We tend to take a paternalistic model of care to health care in general but I think it needs to be a bit more putting the power back in the parents’ hands because, I mean, they’re going to be the parents of this child for the rest of its life and they’re going to be making all these decisions so I don’t see why we can’t not get them involved as early as possible in that decision-making process.
Community midwife, i
Although a repeated message in the data was that parents are not encouraged to engage with NBS, the following comment by a mother also queried how adequately midwives are trained for this role:
The main thing is just to get the information out there and also for the midwives to be up to date with the information as well. You know, I’m sure some of them are but I also think some of them aren’t, and it’s just a bit of a cop-out to kind of say, oh yeah, it tests for all sorts of things, rare things, you don’t need to really worry about it.
Mother, second child, PKU result, i
Indeed, when compared with the dialogue from parents during the focus group, it is clear that this concept of the damage done when parents feel that they are not made aware of what happens during NBS is still dominant. In a lengthy response one mother summed up the discussion of the group, covering several points:
Just make sure that information’s available. It’s so, so important. As a new parent, you should know, when you do get the baby, the baby’s here, that there could potentially be something wrong. And you’re not fully aware of that. [. . .] And I just think that people need to be informed properly of what they’re testing for, in a user-friendly way and be fair about it. Instead of it being an elephant in the room, you know. Because people don’t want to talk about what could happen. [. . .] And for me, I feel that I wasn’t aware. I feel very lucky; both my children seem to be okay. But yeah, I would like to have known.
Mother, English, two children, negative result, fg
Changing roles in expanded newborn screening: change in the role of the midwife
Part of the rationale for this suggestion was the recognised time constraints of midwives. Across health professionals, changing the role of the midwife was supported for this reason. Midwives also viewed this as a form of positive engagement with parents:
Yeah, I mean me personally I’d be happy to ask the mums and the dads the questions to make sure they’ve read the information or gone on the website, used the app. I’d be quite happy to sort of, you know, use resources to be able to ensure they’ve understood what’s actually happening and what’s being screened for.
Senior community midwife, i
Of interest, when comparing the spontaneous reactions from health professionals and parents it is possible to see how this approach is actually bringing practice into line with both actors’ views of a service that they would want to be involved with:
I think something like that would be a very good compromise by putting the power, empowering parents to find out but also it would give the midwife some time back to actually not just do the check on mother and baby and like have to rush through all the information they have to get through for that appointment. It would actually maybe give them 5 minutes to actually answer questions or concerns that parents might have in the antenatal period. I think it’s a good compromise.
Community midwife, London, i
And I think they should have the opportunity to call back to the midwife or have another meeting even with another midwife, to be able to just ask things that they didn’t think about at the beginning. Because I know that I didn’t have that opportunity. I didn’t need it, but some people might need it.
Mother, Spanish, one child, negative result, fg
The negative case analysis found one participant with concerns about this approach:
It’s easier to tell somebody something, rather than to try and work out whether you feel that they understand something. And I think that’s a real skill. And I’m sure that midwives could do it, but it’s actually a very different philosophy to what you’ve done year on year.
CF screening representative, fg
Within the focus group discussion the researchers made it clear that they envisaged that key questions would need to be developed to appropriately assess parents’ understanding and that guidance would be given. However, those in the group who carry out this role felt that this approach was feasible and was something that midwives were used to engaging with:
But in the woman’s hand-held notes, there’s set information that you have to give anyway, on safe sleeping, if a woman is smoking in pregnancy, you have to ask the questions at certain stages in the pregnancy. [. . .] so it’s there. So it can be done, you can put it into the process.
SQAM, fg
What may be contributing to these differing views between representative and midwives is midwives’ experiences of educating parents about novel information throughout their pregnancy compared with their experiences of having to support parents post results when they are experiencing anxiety because of misconceptions and a lack of information. Interestingly, concerns about their experience and current practice where a light-touch approach was taken to checking parents’ understanding was spontaneously brought up by the parents in their focus group:
You’ve been given this, da-da-da. So actually, at some point for this information, have you read that leaflet? Yes, and it’s signed off. Do you understand? And maybe you sign it.
And maybe not do it, the midwife, but you do it. Yeah.
[. . .]
Because they’re very keen for you to sign the breastfeeding things, they’re very keen for you to do that.
Although parents’ views appeared to be broadly in line with those of health professionals, overall they had much less to say about a change in the midwife role and instead focused their discussions on the idea of the tool kit. This may be because their predominant concern was ensuring that they were given the relevant information. No concerns were expressed by parents about changing the role of midwives other than by one parent who stressed that the change would need to include ensuring that midwives had the time to check on a deeper level whether information had been understood:
I think that would be OK, so long as the role did include them checking that the parents understood and it wasn’t just the midwife saying, oh, you know, these are the things you can look at to look into newborn screening, and leave them to it. Because some people may take them up on that and some people may just completely dismiss it and think oh well, you know, it’s fine.
Mother, English, second child, PKU result, i
This mother’s concerns are understandable given that she experienced the shock of receiving a positive result when insufficiently prepared (the harm that communication is seeking to minimise).
Changing roles in expanded newborn screening: parental responsibility
The other part of the proposed change in the communication interaction would be that parents themselves would have a more active role to play in learning about NBS. Of note, this proposal was supported by both groups of participants:
I think, as midwives, we have a responsibility to give information at certain times. But then, also, it’s the parents as well, isn’t it. Accessing, and being proactive, if you like.
Antenatal clinic midwife, fg
Interestingly, although in the research team this idea dovetailed with the idea that the role of the midwife would also change (i.e. the role of the midwife could not change to one of understanding checker without parents becoming more independent learners), there appeared to be more concerns about this approach from some participants. Concerns were raised by some health professionals either that this would be seen as a way of devolving responsibility away from midwives completely, although this was refuted by midwives in the group including the screening co-ordinator, who said that midwives would see it as their role to give some information, or that there was a need for a basic uniform level of information to be provided by health professionals. Of note, these concerns were not raised in relation to a change in roles; rather, they represented a need for clarity in defining and communicating the new roles. The team’s recommendation included the idea that parents are made aware of NBS and the importance of engaging with the information before they go and access further information themselves. However, within one of the interviews a concern was raised that, although this approach may reduce costs, it could also lead to scenarios in which parents are not informed:
I think that is a bit risky just signposting them and not following it up with a bit of a detailed conversation. I understand the implications are yes it saves time, obviously it saves resources, it saves midwife resource, but I think there’s still a risk there.
RCM representative, i
The reason for this concern may be elucidated in another comment from this interview:
I know you can come back and check it out but the women may just say yes, yes, I’ve read it, but haven’t read it and doesn’t really understand it.
RCM representative, i
It seems that this interviewee believed that the midwife would simply check whether or not parents had interacted with the material rather than whether or not they understood it. This appears to be similar to the trigger question that is provided to midwives in the latest available training materials. 9 For clarification, the new model would include the midwife asking more involved questions to truly check understanding, rather than simply receipt of the information material. As stated previously, one parent was also concerned that parents may not see the importance of engaging with the information once signposted. Again, inherent in her response was that this change in the role of parents would be made without also changing some of the key messages to alert parents to the relevance of NBS information:
It wasn’t just the midwife saying, oh you know, these are the things you can look at to look into newborn screening, and leave them to it.
Mother, English, second child, PKU result, i
Crucially, both groups valued the recommendation of a change in the role of parents, not only in terms of saving time for the NHS, but also in terms of moving away from the paternalistic model of health inherent in this parent’s phrase, ‘letting us be independent’:
It’s almost like letting us be independent with the information, as long as we know how to get it. We don’t need to rely on the midwife person, who don’t have enough time for each person. Like, almost we are taking a certain burden from them, even though they are there when we need them.
Mother, French, one identified as a sickle cell carrier, three children, fg
Crucially, both groups raised the point that this approach could also ensure that midwives were able to focus on the consent aspect of NBS:
Yeah. And on the midwife visit, you know, did you read the information, are you sure about . . . do you want to have it done. You know, I don’t remember being asked if I wanted to have it done.
Mother, English, two children, both negative results, focus group
I think like you said like most research does show that parents do want to be involved and they do want to be actively taking a role in how these processes work so I think we actually need to start listening to that research and working with them not like talking at them or taking that sort of approach because they’re intelligent people and just because they don’t have a midwifery or a medical degree it doesn’t mean that they’re not intelligent people in their own right.
Community midwife, London, works with young parents, i
Another health professional recounted a development in another field in which health professionals had given patients more access to records and how this had driven up patient involvement and that this could be seen as an analogous situation:
I know it’s not . . . they haven’t got a disorder but they’re obviously, they’re nurturing their baby and you would think they would want to be actively involved in understanding what’s happening in their care antenatally and what’s happening to their investigations to their baby postnatally so it just seems to . . . you just seem to feel that if it’s done in the right way it has to work better, don’t you?
NBS laboratory director, i
Although it was not a dominant view held in this study or in the interview study (see Chapter 3), one mother did highlight a limitation of relying on health professionals to verbally provide information:
In my case, I think it’s not enough. I tend to receive the information, and then after think about and process it later. So it doesn’t help me that much. I prefer maybe to sit down and be able to really think about that in that moment, more than receive the information. Sometimes I cannot process all the information I’m given verbally, so I prefer to read it.
Mother, Spanish, one child, negative result, fg
This further highlights the need to have a non-rigid, responsive model of information provision that enables communication to take place in a variety of ways to best fit with the recipients’ needs. This idea is expanded on further in the following section.
Tailoring information provision
There was a view that, with expansion of NBS, health professionals would be reliant on using other information sources to provide details of the screening programme as it would become impossible to do this verbally. Both parents and health professionals recognised that different people need different levels of information and prefer different modes of receiving information:
. . . because even though everyone has babies but our needs are different.
Mother, French, three children, one identified as a sickle cell carrier, fg
Because we all digest information differently and some people will take on board the information that I’m giving but a different midwife might give it in a different way. Then they can always go back to the written information and, you know, fill in the gaps or maybe come up with more questions, assuming, like I said, they’re able to read.
Senior community midwife, i
Indeed, one midwife outlined the limitation of not having a variety of materials available and for her this was one of the key findings from the research that she felt was most important:
If we’re just giving information because we think that’s how they want to receive it and they’re not taking it in or it’s not the sort of way that they want to be informed, well, then there’s just no point because then you’re still not going to get informed consent at the end of the day.
Community midwife, London, i
Overall, therefore, implicit in the data was the fact that a range of information tools would need to be accessible to parents to meet their needs. However, this was also said more explicitly at times:
I think face-to-face is important, but I think there needs to be like a portfolio of available information that . . . [. . .] . . . people are different.
I think that’s a very sensible approach, because we’re all human beings, aren’t we. We all need things in different ways, and it’s up to the health professional, who sees the parents at that time, to help guide them. And there needs to be many different solutions to fit everybody.
One size doesn’t fit all.
[. . .]
And it’s a new way of thinking, and a change really. But it sounds good!
Information tool kit
As discussed in Chapter 3, there was a recognition of the limitations of different formats of information provision. In summary, the issues that were raised again here were that leaflets were not read, not every parent attends classes, not all midwives are sufficiently trained to answer parents’ questions and not every parent has access to a smartphone. It was felt there were merits of the tool kit containing information provision in the following formats.
Leaflets
Novel insights in this study included that parents did still value the idea of receiving leaflets.
Previous data presented in this chapter also indicate that parents do not want to move away from being given some sort of leaflet about NBS. This was seen as a way of providing standard, basic information across populations. However, it was suggested that there could be scope to modify the leaflets, with this aligned to the idea of providing specific, relevant information at key times:
Yeah, like I said before, I think a leaflet is a great idea because if you’re kind of told a website or an app, you could go away and forget about them. But so long as that leaflet perhaps is given.
Mother, English, second child, PKU result, i
I don’t know but yeah, it would be more beneficial to give information that they need at that point rather than the whole screening information because the leaflet covers everything from booking, bloods, all the way through, doesn’t it, to scans, which they don’t need that information. So it’s a . . . it would be a postnatal leaflet rather than . . . yeah.
Senior community midwife, i
Again, there was also an idea that the leaflet may serve to benefit the health service more as midwives are pushed for time and have a sense that they need an auditable trail to document that they have provided parents with information:
Because it’s so difficult to document everything, a transaction, a conversation between a midwife and a family about blood spot screening, so the information leaflet is given as a proxy to summarise up the discussions taking place.
SQAM, i
However, very much in line with the discourses outlined in the interview study (see Chapter 3), there was a recognition that, although providing leaflets was a concrete way of showing that information had been ‘given’, even current materials were not suitable for some parents:
At the moment it does require quite a high level of reading skills, and I know it said it’s been informed by user input, but I still think it’s way too complicated.
SQAM, i
Group appointments
Another mechanism for providing standard, universal information to all was the idea of presenting information during a routine appointment in the third trimester that women already took time to attend, such as a measurement appointment. Rather than providing individual appointment times, a group appointment time would be given (similar to some hospital clinics) with six women attending simultaneously. This would create a situation in which, rather than having < 5 minutes to provide identical information to each woman separately, the midwife would have 30 minutes to provide the information to the whole group. There were concerns raised by some midwives about how the logistics of this would fit within current staff shift designs, but other midwives felt that this could work as it had been achieved for other key messages such as breastfeeding:
That sounds reasonable, that makes sense, if you can get the women to that assessment that sounds totally fine. As you say if it ties in with the normal antenatal, you know, health screening part of the pathway yes absolutely. I think we need normal in the more you can make it, you know, as natural and normal as possible then the better the uptake that would be absolutely fine.
RCM representative, i
Parents unanimously supported this suggestion. Importantly, given the concerns around engagement, parents reported that this was a format that they would access:
I would have definitely attended that, absolutely, yes. For me that would have been a really good thing and I would have definitely, definitely have made use of that resource, yes.
Mother, English, pregnant, i
Parents also valued the social aspect of meeting other women locally, with babies due at similar times. Parents also appeared more confident about receiving information in this format, with some suggesting that other parents might ask questions and they might benefit from hearing the answers; for others, the other parents in the group could themselves become sources of information. For example, one mother who did not need an interpreter but whose first language was not English talked of how she would look out for other parents who seemed to understand the information and then chat with them to be able to understand further herself. Thus, the group appointment appeared to make maximal use of the midwives’ time, but also enable parents to start discourses with others and gain from their understanding, rather than NBS being the ‘silent’ screening programme.
Parent-led approaches
The following were seen as forming part of the information tool kit that midwives should offer to parents. Parents could select to use these sources of information at a time and level that suited them.
Applications
There was a general view from health professionals that applications were used extensively by parents throughout pregnancy to obtain information:
Some of them download lots of apps, and they get information from that. I’ve never listened to one of these apps, but this woman told me the other day, she had five pregnancy apps on her mobile phone.
Wow.
And they’re information apps?
Yes, they are.
They’re really good, actually, very, very good.
It was recognised that this form of technology enabled parents to obtain tailored information relevant to their stage of pregnancy. It was also felt that this could be one of the mechanisms by which parents could obtain details about the screening programme that it was not possible to provide verbally. Parents also reported they valued apps because information could be found easily again and did not get lost in the way that leaflets might be lost. One mother highlighted that the potential use of apps was one of the most important parts of the discussion for her, as:
Good for me anyway because I use my phone all the time but I suppose a lot of people don’t.
Mother, English, pregnant
There was also a view that NBS ran the risk of being out of sync with how people naturally seek information today:
I mean, you would think in this electronic age that there would be a lot of younger parents who would prefer not to have a big war and peace book to lug around and read. Inherently it feels right and so I think it’s inevitably the road that it really needs to go down for sure otherwise we’re a bit stuck in the dark ages really, aren’t we, and it does work for everything else.
NBS laboratory director, i
It was commented on that parents would use social media anyway [e.g. Mumsnet (www.mumsnet.com)] and there were concerns that such formats may demonstrate a preference for experiences over fact. Therefore, there was a view that the lack of NHS information in this format may be driving people to seek information from such sites and that the NHS needed to provide the counter voice to such outlets:
But I mean, we should be ahead of the game on social media, we should actually be not scared of it. We should be embracing it and making sure it works for our parents. But maybe we are, I don’t know what these apps do.
CF screening representative, fg
We need to be modern and on the ball and update it more quickly and economically as we can do.
Senior community midwife, i
Through the health professionals’ discussion of apps it became apparent that a range of apps is currently available and that, although some are very good, parents are currently left to decide without guidance which apps to use and that this could lead to misinformation spreading. Again, similar to previous discussions, there was a recognition that not providing a NHS-developed app may in itself not just be an absence of information, but may be driving parents towards poorer sources of information and contributing to misunderstandings about NBS.
National telephone line
Another approach that sought to enable parents to engage with NBS information at a time that suited them was a 24-hour national telephone line. Although there were concerns about who would staff it, the idea of a national telephone line was seen to have its merits as it would be available at times that parents were more likely to be concerned (i.e. outside clinic hours). It was also seen to align with a vision of the NHS in the future:
I think it’s a tremendous idea, and it’s the way the NHS is going. Increasingly, there will be . . . it would be expensive, but the NHS would like it ‘cos it’s a national resource. So, would families use it, parents . . . I don’t know whether apps and things will then become more useful, or some sort of more formal version.
CF screening representative, fg
The parents in the focus group unanimously supported this idea and became quite animated in their discussions:
[. . .] you can call this line.
Yeah.
Yeah, I like that.
Uh-huh.
Everyone seems to be nodding at that.
It’s a really good idea.
Yeah. As I said before, in my case, I process the information later, so I can have all my questions later and I have to wait 2 weeks to see again the midwife or . . . and maybe that anxiety . . . I mean, you can have anxiety during all 2 weeks or just take the phone, make a call, everything resolved.
One development suggested in this study was that this resource did not have to be limited to telephone calls and that it would be good if parents could also send e-mails to a national centre:
You can write an e-mail, it doesn’t really need to be a phone line, but you know that you can . . . sometimes just you have a question and you’re getting anxiety on that, just let it go and say it. Even if you know it’s going to take maybe 1, 2 days to have the answer, you know you’re going to have the answer on the phone or e-mail would work as well.
Mother, Spanish, one child, negative result, fg
This mother had previously said that she preferred to receive written information.
Another resource that was suggested as feeding into this approach was using other specialised health professionals:
I don’t even see why within the laboratory we shouldn’t have more interaction with the parents themselves in terms of . . . because often the midwives they may need to go either to ourselves or to see specialist nurses or their colleagues because they can only have a certain level of understanding about every one of those conditions so there almost needs to be a network of support where patients can go and midwives can also go to gather answers.
NBS laboratory director, i
Again, these data appear to be aligned with the idea of having a wider range of options open to optimise communication and help parents understand NBS.
Websites
This was one of the parent-led strategies that was already in use to a certain extent, as reported by both health professionals and parents:
You see with the website it’s a touch of a button, it can be updated really quickly compared to written information, but I agree we need to be modern and on the ball and update it more quickly and economically as we can do.
Senior community midwife, i
Websites were valued for their ability to provide detailed information:
I would have thought that it was better to give a smaller amount of information with the option that there is information available on websites, podcasts, apps or whatever, that people can look at in more detail if they want more detail but every mother’s understanding is different, isn’t it.
NBS laboratory director, i
As mentioned previously, there was a thought that a frequently asked questions section could be made for the NHS Choices website. This could be responsive to parents’ needs and could be updated economically.
Strategies to raise awareness
Classes
Although there was recognition from both health professionals and parents that not all parents attend antenatal classes, both samples believed that providing information about NBS in these classes would be an effective way of informing parents:
That class is split over 6 weeks. Not everyone can get on those classes because they’re often full, so you’ve got to book early to get on. But there should be some part . . . I remember there was some part of them bathing a baby, and that was very vague, you know. There was bathing a baby but there wasn’t actually these other conditions that your baby could potentially have, and they won’t be picked up on a scan or they might not be picked up on a scan.
Mother, English, two children, negative results, fg
Parents went further by commenting on how it appeared strange that NBS was not mentioned in these classes as being part of postnatal care. This echoes parents’ concerns reported in the interview study in Chapter 3, in which they commented on the contrast between the focus on tests and screening in pregnancy and the absence of information provision on NBS, which created a false reassurance in some that their baby would be born healthy. Thus, incorporating NBS information into such classes was not only effective but could also minimise some of the shock that parents felt when they learned about NBS after the birth of their baby.
One of the ways to mitigate some of the access issues with regard to antenatal classes would be to turn a routine measurement appointment into a group appointment. This was unanimously supported by parents, who felt that it would also add to the practice of drip-feeding information:
If you give too much information on different things it obviously, it’s like you say information overload, but if you just stick to half an hour on the screening, half an hour on something else I think that would be better separating it than just doing it all in one go. No that would be really good, a good idea.
Mother, English, pregnant, i
E-mails
E-mails were seen as a valuable way to nudge parents and indeed there seemed to be some indication that e-mail addresses were already being collected by midwives at booking for other purposes. Another insight was given when talking about how brands target parents at key stages in their pregnancy. As discussed earlier, this led to parents feeling overwhelmed with information. The following quotation not only highlights this but also illustrates that, during a phase when parents are already overwhelmed with information, marketing is being delivered more skilfully than health-care messages:
Like Bounty and Boots, they’re always sending us information 8 months, 9 months, child development, it’s really useful. This is one way of penetrating parents with the information that they need and it would cost less. And once they have it in their system, just kind of like e-mail.
Mother, French, three children, one identified as a sickle cell carrier, fg
Thus, marketing companies have found ways to permeate the voluminous amounts of information that are given to parents, whereas, as the designers of health information models do not use these strategies, health messages are at a disadvantage.
Posters
The idea of continuously nudging parents to remind them about NBS was also brought up in terms of using posters in the community. Participants also came up with their own ideas for driving up awareness and felt that lessons could be learned from other areas of antenatal care:
Would it be appropriate to have it in places where parents go, like Tesco, or Asda, or Mothercare, or anywhere like that. You could have little subtle reminders, as you say. That would be a new way of thinking. They have it for breastfeeding now, don’t they?
SQAM, fg
There’s often big posters about meningitis and what to look for in babies, they’re often at the midwife appointments.
When you’re waiting, you always have to wait, so yeah.
So that would be at GP clinics, at . . .?
Yeah, the midwife . . .
Yeah, where the midwives, because a lot of them, mine was in like a sports hall place.
Oh, okay. So wherever the midwives are?
Yeah. And even I would say in the hospital when you’re doing the – I can’t remember the name . . .
When you’re having your scan?
Yeah, when you have . . .
Thus, even though posters are a static and uniform information source, similar to leaflets, they were valued by both groups of participants as being a beneficial way of raising awareness. Thus, it appears that the short, simplistic, static forms of information are best used to drive awareness, whereas the multilayered, tailorable, timeline framework of apps, e-mails and websites is more beneficial to convey the content of NBS information.
Clinic televisions
Parents reported that they spent a significant amount of time in NHS waiting rooms and this was also observed by the research team. Almost without exception waiting rooms had televisions for parents to watch, which screened a mixture of adverts and health-related messages. Parents would spontaneously talk about the products or messages that they had seen on the television and could clearly recall almost verbatim what the messages had been. There was a belief among health professionals that clinic televisions could be used to convey information about NBS:
What about, most places are like . . . I think in [name of trust], there’s a television in front of the antenatal clinic. Could you not have a rolling TV . . .?
Screening link health visitor, fg
Interestingly, this was also commented on by parents and was seen as being part of the much-needed strategy for ensuring that NBS becomes part of a process that parents recognise as being to check on the health of their baby. Linked to this was also the concern that the absence of information about NBS on such channels further instils the idea that NBS is the screening programme/health-care initiative that is not talked about.
Blended
There was also an idea that by blending learning each individual component could become more effective. For example:
Put the information in about the website, definitely, and that could shorten the written leaflet quite a lot, so parents would be more likely to read it.
SQAM, i
Participants in both samples appeared to identify a blended learning environment whereby communication would be dovetailed from midwives and apps:
You might go and see your midwife but the information is on an app you can upload and read it again on your phone at any point, I think that would be really helpful.
Mother, English, pregnant, i
Of interest, the idea of a ‘blended approach’ to communication, a common idea throughout this study, arose from the idea that communication around checking understanding and answering questions did not necessarily need to be the role only of midwives. The solution below blends an in-person and online learning approach:
There are going to be questions that crop up frequently and so there could be obviously a frequently asked questions section on the website that might answer some of those things but there’d need to be perhaps a network of support for more complicated or difficult questions that might be asked.
NBS laboratory director, i
When
When information should be given:
-
parents and midwives thought that information about NBS should be given for the first time in pregnancy and not after birth
-
information should be ‘drip fed’ at multiple time points, with added reminders provided towards the end of pregnancy
-
the third trimester/36 weeks is the ideal time to discuss NBS
-
parents should be asked to consent for screening when discussing their birth plan.
Drip feed
Health professionals responsible for communicating with parents about NBS reported that they used a ‘drip feed’ approach and commented on how this approach fits with the guidelines. However, other health professionals involved in the delivery of the screening programme and working with parents subsequently asked if this approach was actually used:
Because what you describe sounds to me, eminently logical, it shouldn’t be seen as a one-off, you know, opportunity. But it should be a staged approach of taking every opportunity of seeing them, and the father, and educating them. But then, we get the other end of the scale, where it doesn’t seem that that is . . .
CF screening representative, fg
The feedback from parents suggested that they had not experienced receiving information at multiple time points and indeed one parent selected this as the most important part of the summary for her:
I think the key thing is for me that it should be drip fed at multiple points. [. . .] Then having the information drip fed at multiple points at the beginning, in the middle and then like you say right at the end would have been better as well.
Mother, English, pregnant, i
The importance of ensuring that information is provided at multiple and varied times (i.e. not always when the mother is visiting the midwife, but also during classes) becomes more apparent when one considers data from both health professionals and parents showing not only that fathers are missing out on the information but also the impact that this can have when fathers act as interpreters for mothers. Indeed, the effect that the current time-limited practice has on English-speaking, experienced parents is illustrated by one mother:
Because I’ll be totally honest – I mean, I don’t know how you feel about this – but I actually probably can’t name you three things that my child was tested for. I actually don’t even know. I couldn’t recall it. I’ll have known at the time but I can’t recall it to you. [comment by interviewer] Whereas I can recall what injections my children have had because I knew prior to that what was coming up. But I don’t actually know what they’ve been tested for.
Mother, English, two children, fg
Thus, current communication practices may lead to transient knowledge, which leaves parents with a sense that they are not aware of what has happened to their child. Indeed, although the drip-feed approach should represent what is happening as it is contained in policy documents, some health professionals also appeared to think that this was a novel approach:
I quite like those points, I like the drip fed at multiple time points, with added reminders, I thought that’s really good.
SQAM, i
Third trimester
All participants in this study emphatically supported the idea of information being provided during the third trimester. One of the reasons for this is that it fits better with the focus of parents at this time:
It becomes more about baby and what’s going to happen when baby is here whereas prior to that it’s like just, you know, oh, is everything okay with baby? How is baby growing and things like that?
Community midwife, i
At the beginning of your pregnancy, you’ve kind of got enough things to worry about. And like I say, it’s not going to come into effect until the baby’s born anyway, until you have that heel prick test done. [. . .] It would have made me really think, I think, right, oh, you know, this is becoming real now, my baby is soon going to be here, and the next things to think about are things like immunisations and heel prick test, and screening and that kind of thing.
Mother, English, second child, PKU result, i
This parent went on to report that she felt that there was a temporary lull in information provision at this time, further highlighting the benefits of communication at this time:
And then it seemed to peter off a little bit towards the end, so the scans kind of stop and that kind of thing. So maybe it would just be a nice timely little point to say, you know, when your baby is here, they will have the heel prick test and these are the kind of things that they will be looking for. Yeah.
Mother, English, second child, PKU result, i
Discussion of the provision of information during the third trimester identified a need to review the use of appointment times:
If we’re going to potentially give information at 36 weeks you’re probably going to be looking at probably half an hour because of everything else you need to discuss as well, because the things we discuss currently, we run out of time anyway.
Senior community midwife, i
Thus, although issues were raised about finding time during appointments to discuss required information, this did not appear to be a new problem as the pathway appears to be already overcrowded at this time.
Not at the same time as advertising
As in the interview study (see Chapter 3), parents and health professionals discussed the scenario of mothers being laden with information during routine appointments. Health professionals reflected on their own experiences:
When we asked women about information there were quite a lot of women that said, well I didn’t really read the information, all I looked for in the Bounty bag were the freebies. That, kind of, worries me about that, you know, about the timings – so whether you are chucking everything in the one bag whether it’s antenatal, postnatal et cetera, et cetera. I think we have to be really careful what information we put in the bag and what advertising goes in and the message is about, you know, screening information, it’s not about advertising and getting freebies.
RCM representative, i
I can remember having a giant bag of quite a lot of rubbish as a mother and thinking, oh, you know what . . . trying to sift through it all and you’re absolutely right, yes.
NBS laboratory director, i
This last quotation further highlights that even medically trained mothers who are perhaps more aware of the salience of key materials can feel overwhelmed. Within the study we tested out the idea of separating the materials provided to parents, which was supported by all:
[. . .] we should maybe perhaps separate the screening information from other information. So for example, the information you get about prams and what have you, right at the beginning.
Yeah. No, I agree with that. And I think it perhaps would be better if it came later on. Because at the beginning of your pregnancy, you’ve kind of got enough things to worry about. And like I say, it’s not going to come into effect until the baby’s born anyway, until you have that heel prick test done. So I think it would be actually . . . I think it says at the top, at some point in the third trimester towards the end of the pregnancy, that you’re given that information. Because I can’t really remember what information I was given but I know at the start, I got quite a lot.
Consent
The summary stated that:
-
parents want to be informed and be more active in information exchange
-
the majority of parents supported compulsory and assumed screening providing that they had received adequate information in advance.
Compulsory screening
Although the idea of compulsory screening surprised some respondents in both samples, those in policy-level positions could see the merits of such a system. However, all front-line midwives in the focus group were very uncomfortable with such a model and felt that it went against the wider ethos of their practice. One supporter was a parent of a child who had been identified as having a condition through NBS and a laboratory director felt that as long as this was truly what parents wanted this could be a beneficial step, given the strict controls in the UK about the conditions on the panel. Interestingly, parents in the focus group began by offering their views that screening should be compulsory given the way that they perceived the risk:
You’re not pumping anything into the child at that point, you’re taking blood, you’re taking a sample. So you’re not injecting anything in, it’s not the decisions when you come into immunisation, which, whatever your stance is on that. If your child is found to have something, there is a massive cost on the NHS to treat your child. So for me, it should be done as standard because there shouldn’t be a choice for that, personally.
Mother, English, two children, negative results, fg
Indeed, in the group discussion after this one mother stated that there were ‘no risks for the baby’ (mother, Spanish, one child, negative result). These views may be a result of the way that the mothers categorised risk, as most screening experts would not have the view that a screening programme is without risks. One mother did have a different view, based on her different culture:
Meanwhile . . . someone from my culture, taking my baby’s blood is really, really important, it’s the life of my baby. You are taking it while doing exams. So by giving at least the information and the consent form, at least you are putting me at ease.
Mother, French, three children, one identified as a sickle cell carrier, fg
Of interest, when parents were asked about the issue of storage, their views changed dramatically. This highlights the problem of polling parents’ views on consent when they have incomplete knowledge of what they have/are consented/ing to:
They can be used for research purposes.
Oh.
In that case, I think that part should be . . .
Honest.
. . . that should be told to the parents, and that part should be a choice.
[. . .]
Yeah, I didn’t know that. I don’t mind but . . .
I need to know that. I’m quite happy, I mean . . .
No, I’m happy for that, I don’t have a problem.
But I don’t think everybody . . .
A tad naughty to do that and not tell you. But yeah, I don’t mind that, yeah.
It’s really shocking.
Importantly, this triggered some views about trust:
It just makes you question what else they keep doesn’t it. They keep so much that they never ever tell you.
For me, I’m angry that they are using my kid’s blood without me even knowing. Even though I know that I will never say no, but doing it almost in a hiding way, it’s not really right. Then you are regretting that you have given the consent from, or you have the right to say no. Yeah, honesty is just enormous. It’s like I take something from you without you knowing.
Importantly, even when these parents were in the phase of believing that screening should be mandatory, they felt that it was important that they were given the full spectrum of information and had a belief that ‘it doesn’t cost them anything to tell you verbally and to give you one set of information’ (mother, English, two children, focus group). This participant later balanced this against their opinion that, ‘ultimately, it’s your right to know that as a parent’. Of concern, this parent also raised the belief that some information was purposively withheld:
Risk of not communicating
I think they also choose not to tell you certain things. I don’t think anybody likes to have to sit down with somebody and say these are the nine things that potentially could be wrong with your child. They don’t want to do that. So on the day they come and take the test, they say, oh, we’re going to test for some things, but it will be okay. And I remember her saying that with a, oh, you know, he’ll be fine, it’s very rare that anything comes back on the test. But she didn’t . . .
Mother, English, two children, negative results, fg
Others had quite strong beliefs that screening should not be compulsory, citing other screening programmes such as that for Down syndrome. There was also a concern that by making screening compulsory it may be more likely that parents’ support would be lost:
In all my time in 12/14 years of being a midwife I’ve never had one person saying no but potentially I think you could do if it was compulsory.
Senior community midwife, i
Inherent in this response is the lack of need to make screening compulsory given that people do not tend to refuse. Indeed, parents repeatedly stated in this study that they would not decline screening:
It’s quite important – even though I would have chosen to have had it done, I think that having the choice there is quite important.
Mother, English, pregnant, i
It’s just I cannot understand why that parent would say no.
Mother, English, two children, fg
Assumed consent
Respondents seemed in favour of a model of assumed consent, with some midwives feeling that it reflected current practice and fits with developments in other areas of health care. This support appeared to be with the caveat that the health professional needed to be assured that the woman knew what decision she was making:
You have to have a well-educated population – they all have to be on board with what population health and public health is about and they have to be really clear what screening tests are about in terms of their child – so assuming all that’s done then yes it’s fine. [. . .] However, not doing any education and just assuming that women know what the screening tests are, no you can’t do that – that would be a risk, that’s a no.
RCM representative, i
Interestingly, the opposite view came from a parent, who appeared to be more concerned that someone could opt-out of screening without having full knowledge of what it entailed:
Like, maybe if they had to opt out, then there’d be more information given on why . . . more advice given to them on why perhaps they shouldn’t opt out, just to make sure that they’re fully aware. Because they could be taking a bit of a gamble.
Mother, English, second child, PKU result, i
Some interesting data came from a mother who, throughout both her interviews, was supportive of screening being mandatory. Indeed, even when first asked about choice she could not consider the question as she was so concerned about the implications for the child’s health should a parent say no. However, when asked about making a choice in pregnancy she said:
I think if it became the parents’ decision, like an active decision for them to make, then it would at least make people consider . . . [. . .] if I was asked to make the decision, it would make me want to make sure that I knew what exactly they were being screened for. So it might kind of get that awareness out there.
Mother, English, second child, PKU result, i
The need for this to be a real choice was also voiced by a midwife:
think obviously consent needs to be obtained as well for obvious reasons but I think it needs to be done properly not just like, oh, are you happy to have this? We offer all babies this in the United Kingdom.
Community midwife, London, i
Consent in pregnancy
Respondents were asked what they thought of the idea of parents being asked to consent during pregnancy. This would not be binding and the choice could be revisited, but it would enable parents to make a decision at a time when they were more likely to be able to make an informed decision. Within the focus group with health professionals this idea was developed by tying it in with when women made their birth plan. This was tested out in the telephone interviews:
I like the parents should be asked for consent for screening when discussing birth plans, because then it, sort of, helps to keep all the information in one place. [. . .] Because, that’s the sort of appointment where you’re checking through, is everything all right, have you got any concerns, so it seems like a nice one to do that, and to get the consent at that point.
SQAM, i
This approach was also valued as saving the midwives time on the day of the screening visit, reiterating again the pressures that midwives are under in the current system.
However, a couple of health professionals were uncertain about the validity of consent if it was taken prior to birth or if parents would feel able to make a decision at this point. When this was raised in the health professional focus group, these concerns were dismissed with examples of other times when parents are asked to, and do, make decisions on behalf of their child before birth. Parents generally supported the idea of providing consent in pregnancy with the caveat that they would be able to change their decision post birth:
I think definitely towards the end to, kind of, remind people that it’s going to happen fairly soon after you’ve had the baby and to make plans, and yes I would have put it into my birthing plan if I had one.
Mother, English, pregnant, i
One of the health professionals who raised concerns about parents’ views changing later reflected that one benefit was that it enabled parents some time before the event to fully engage with the information and suggested a middle ground of still keeping formal consent after birth:
I suppose you could provide the information when discussing the birth plans and then explain that you were going to take consent at the point of taking the sample and then they would definitely have had a clear window of time to consider the information before the actual point when the blood was . . . the baby’s blood was taken.
NBS laboratory director, i
In contrast, parents were all in agreement with the idea of providing consent during pregnancy and could see the merits of not being asked to consent after the birth of their baby:
Yes, I think that kind of discussing that and saying yes you would like that done before the birth would be better. People, they’d have more information and make more of an informed decision rather than just like, oh God I’m knackered yes, whatever, whatever you need to do.
Mother, English, pregnant, i
As with all suggestions, however, there was a recognition that not all women make a birth plan, with respondents having the view that such women usually accept whatever happens during the birth. This is not the same as not being prepared to make a decision on behalf of the baby prior to birth and so it would be worth testing whether or not such parents would be prepared to provide consult during pregnancy.
Summary
This study examined health professional and parent views on study recommendations that they were involved in generating. Of note, responses in the parent and health professional samples were largely in agreement. Both groups were highly supportive of an information tool kit and ensuring that NBS conversations happen in the last trimester. This was seen as being more effective in terms of ensuring parent understanding and more efficient in terms of using midwives’ time. The importance of utilising a range of information formats was reinforced in the data from this study in terms of recognising both that different parents have different modes of optimal learning and that all information formats have limitations. Thus, the best way to optimise learning was suggested to be to provide a range of information formats that parents can self-select and blend. Inherent in many of the health professionals’ and parents’ responses was that there are already a number of information provision strategies in the NHS that are working to drive awareness of key NHS strategies and parents and health professionals felt that these could be utilised for NBS.
Central challenges in NBS communication have been balancing information provision about a diverse screening programme against not overwhelming parents to the extent that they do not engage, and ensuring that a large workforce of midwives is trained in an evolving screening programme for rare diseases that they may seldom encounter. It would appear that some of the technologically based solutions suggested in the data, such as apps, websites and series of e-mails, could be helpful as they have the ability to contain vast amounts of information yet present it in layers so that the reader never sees the full amount of information and thus is not overwhelmed. Another solution, which is novel in the literature, of midwives providing NBS information in group settings was also supported and may help meet the second challenge of ensuring that all midwives are adequately trained in-depth in NBS. It was also suggested that health professionals other than midwives could be involved in answering parents’ questions. Previous work suggests that, with regard to NBS results, parents value interactions with health professionals who can answer their questions rather than being concerned about who the health professionals are. 34 There is no reason to believe that their views would be different regarding questions pre screening.
Although the majority supported consent in pregnancy, some were concerned about foreclosing post-birth decisions. Perhaps, rather than taking ‘legally binding’ consent in pregnancy, parents should be asked to state their intentions, with these being checked on the day of the screen. However, there were some concerns that an overly stretched workforce may see this as repeating work already carried out, with the most likely part to be dropped being the discussion during pregnancy. Therefore, a potentially more effective middle ground is that parents consent for screening and retention in pregnancy, but consent for the actual blood sample at the time of the event. This would fit with English law, whereby parents can consent for their child once the child is born. Thus, parents could still decline NBS after birth if desired, but hopefully awareness of NBS and engagement with information would be driven up, which would reduce distress and the associated costs and maintain trust.
Moving communication to the third trimester seemed to be of central importance to these participants. This fits with current research which suggests that people must understand the relevance of information to engage72 and understand why they should invest time in absorbing it. 114 Research is now needed to establish if ensuring that the first message regarding NBS is that ‘NBS is a parents’ choice’ is more effective in conveying the relevance of information than information about rare diseases, which may be more likely to lead parents to assume there is a lack of personal relevance.
The concerns about information overload in pregnancy, which were documented in the literature review (see Chapter 2) and in the interviews with parents (see Chapter 3), were also brought up in this study, further emphasising the need to ensure that any attempts to provide information to parents in pregnancy are timed correctly and do not just add to the burden of unattended-to information. It is of great concern that a leaflet designed to be used during the third trimester has recently been removed from use, as parents appear most receptive to information provision at this time and this is therefore a key time when midwives and parents could have a discussion about NBS.
Of interest, although there was variation in parents’ support for different consent models in the interview study (see Chapter 3), parents in the focus group demonstrated that they supported mandatory screening because they were unaware of sample storage. Once aware of this facet of the current screening programme, their consent preferences became uniform and they stressed the need for parent choice in line with previous research,14,68 which has shown that parents consistently value parent choice with regard to storage. The data tracking this change in response illustrated how learning key bits of NBS information after screening has occurred is detrimental to trust and the public view of NBS.
Conclusion
Previous work in this project had highlighted the discrepancies in accounts and views between information providers (health professionals) and information recipients (parents), with both groups highlighting concerns about whether or not current information provision met the goals of informed choice. Successful communication requires moving from a position where the information provider and the information recipient have differing views of the interaction and thoughts on efficacy to a place where they have convergent views on how best to achieve the communication outcome. Data from this study suggest that a range of solutions are possible, which are seen by both information providers and recipients as feasible, able to meet the needs of a diverse group of parents and able to achieve the goal of enabling parents to make an informed choice. By exploring in detail the content, timing, mode and goals of communication, adaptations can be made to enable resources to be used most effectively. For example, it was accepted by all that midwives should introduce NBS and that leaflets were beneficial in terms of auditing communication and providing simplistic introductions to topics. However, neither midwives nor leaflets were likely to be able to provide detailed explanations of NBS. This was partly because of the range of issues and conditions covered in NBS. This was further compounded by the huge diversity in parents’ needs, in terms of both information amount and tailoring. However, technology-assisted communication (television, websites, apps, e-mails) was seen as a way to individually tailor information for parents and also match their current information sources. Importantly, ensuring that key messages were conveyed was more likely to engage parents, as was structuring time within pregnancy appointments to convey information and make decisions on NBS.
Chapter 8 Discussion
This project provides evidence about the experiences and preferences of health professionals and parents regarding communication and consent models in NBS and the impact of these on understanding, costs and effectiveness. The project included a realist review to both inform the studies and foreground the results. Evidence comes from five further studies employing a range of methods to determine the views of parents from the first stages of pregnancy through to a range of screening outcomes and the views of health professionals, including midwives, quality assurance managers, laboratory directors, health visitors and screening representatives. In particular, this project appears unique in linking the views on communication and consent simultaneously in samples of service providers and samples of recipients, with some of the largest sample sizes in the respective studies. The accumulated evidence can be used to move the field forward. This project suggests that the use of information materials to support communication and consent models could be enhanced to improve parent understanding, engagement, efficacy and cost. Specifically, the research highlighted that:
-
Most parents held positive views about a national NBSP and would want their child screened, but they also require relevant information and want to be actively involved in making a decision about screening. Health professionals also want to practise an informed consent model.
-
Parents have low levels of awareness that participation in screening requires them to make a choice, rather than screening being routine. Parents also had poor levels of knowledge about what they had agreed to once their child had been screened. This lack of knowledge included understanding which conditions are screened for, that blood samples are stored and how the results of screening are received.
-
Key messages regarding the possibility of false-positive results and of being a carrier are not effectively being conveyed.
-
There is a clear need for information to be provided at a relevant time to parents to make the best use of midwives’ time. The third trimester was identified as being the most appropriate time to provide information, but minimal information was conveyed at this time in current practice.
-
There is evidence to suggest that the most common time point at which information is provided is post birth, even though this does not fit with current policy. This approach to information provision may be driven by time pressures, resulting in communication occurring only at a time when midwives are seeking consent.
-
Although in-person communication is most highly valued, the timing and goal of this face-to-face interaction could be changed to optimise the outcomes of the communication process and use of resources such as midwives’ time.
-
It is clear that new information cannot be assimilated by parents post birth. Although they are able to understand information at that moment, the ability to retain this information may be transient in nature, which may lead to parents feeling underinformed and underprepared when they receive the results of screening up to 6 weeks later. However, it is potentially useful for parents to be reminded of NBS information after birth.
-
All parents and most health professionals agreed that the decision whether or not to participate in NBS should be made in the third trimester rather than postnatally.
-
Parents wanted guidance from midwives that NBS was important and that they should engage with the information as they have a choice to make, and they preferred having someone to talk to if they had any questions.
-
There is an opportunity to utilise the information sources that parents are already using to seek more general information about their pregnancy (apps, websites, posters, clinic television) and adapt content to include key information about NBS and raise awareness.
-
Both parents and health professionals believe that there is a benefit in making knowledge acquisition parent led rather than it being directed by the midwife.
-
Telling parents about the storage of bloodspots could be seen as an opportunity to engage parents in learning about NBS, rather than potentially causing concern, resulting in a lower uptake of screening. The importance of being honest and not treating this issue like ‘an elephant in the room’ was highlighted by the shock and anger that parents feel when they find out about storage at a later date.
-
There was a recognition that the number of conditions in NBS panels has already reached a size where a single information source (health professional or leaflet) is unlikely to be effective or feasible. Rather, it was suggested that blended learning models could be potentially useful, particularly using online technology rather than leaflets.
-
Both health professionals and parents reported a need for easily accessible resources to help with communication with parents who do not read or whose first language is not English. This need suggests that, although existing resources are available, there are barriers to their usage.
-
Some realignment of the goal of communication is required so that all parents have a basic knowledge of core topics, which is subsequently checked by midwives. This would replace the current goal that midwives should check that parents have received a universal information booklet.
-
All formats of information provision have some limits with regard to accessibility and parents were identified to have different learning needs. Therefore, providing a personalised approach to information provision using a range of formats and levels of detail, which parents can self-select, is likely to be more effective than a uniform model of provision when engaging a diverse population of parents.
-
The relative cost-effectiveness of alternative modes of information provision could not be robustly quantified using the existing levels of evidence. The key drivers of cost-effectiveness were related to the events that would occur if poor levels of information provision result in raised anxiety levels that impact on the health status of the mother and also in subsequent inappropriate consultations to allay the fears of anxious parents.
-
More research is needed before a new mode of information provision can be recommended for use in a national NBSP.
Strengths
This project used mixed methods underpinned by qualitative and quantitative paradigms. A diverse set of skills and views were captured in the individual study designs and overall project. The research team was multidisciplinary, representing midwifery, bioethics, research synthesis, health economics, health psychology, communication research, statistics and qualitative methods. Importantly, this project benefited throughout from guidance provided by three advisory groups containing members who represented parents and health professionals, covering the full range of NBS issues. This project collated the experiences, views, understanding and preferences of a range of parental and stakeholder perspectives.
A particular strength of this project is that the parent sampling framework enabled the communication experience to be tracked in ‘real time’ as parents were sampled in pregnancy, when NBS communication is meant to occur, but also immediately after screening but before they received the results. This reduced the impact of recall bias that some may argue contributed to the low levels of information recall found in the literature reviewed in Chapter 2. These data were also combined with data from parents whose children had received a range of results from NBS to address the concern that some parents do not know what information they need pre screening until they have received the results. Of interest, the key issues that were raised by parents were similar across the sample, suggesting that a sense of knowing what is happening to your child is a universal need and that it is not just the parents of children with a positive result who want more information. Also, the parent sample in this study was one of the largest for an in-depth qualitative study in this field and one of the most diverse in terms of age range, ethnicity and languages spoken.
Combining these viewpoints with those of health professionals experiencing the same NBS programme furthered our understanding of the communication challenges; it could be seen that both parties in the communication event valued information provision and it was not as simplistic as health professionals not providing information or parents not engaging with the information. Of particular use was comparing the views of parents and health professionals on information needs within the different studies. The initial interviews enabled participants to convey their concerns about how the other actors may be hampering information provision (e.g. enabling midwives to raise their concerns that parents were not engaging and parents to reflect on how midwives had not highlighted the need for them to engage). Bringing participants together in focus groups then allowed additional important data to be collected. The experiences of some health professionals who worked with parents post results suggested that there must be a disconnect between policy and parents’ experiences and this enabled midwives to reflect that good practice may not be uniform and discuss ways in which improvements could be made. In the parent focus group the discussion enabled parents to hear others’ very different experiences, learning needs and cultural needs with regard to information provision and choice. The focus groups also enabled the team to track changes in opinions as new knowledge was gleaned about NBS.
Samples of parents and midwives were combined in both the interview and the DCE studies, which enabled differing information priorities and levels of detail between the groups to be illustrated. This work highlighted how, by starting with information prioritised by health-care professionals, parents may be triggered to ‘tune out’ of the discussion. The data from parents suggested that, if the order and level of information could be matched more closely to their needs, information receipt may be enhanced.
The national NBS panel was expanded to include nine conditions at the start of 2015 whereas this project began in May 2013. This overlap of events provided an opportunity to explore the potential impact of expanding the NBS panel. The interviews with health professionals (see Chapter 3) were conducted before the four additional conditions were added to the national panel, but some interviewees were sampled from the pilot sites and so their views reflected what happens when additional conditions are added to the NBS panel. The interviews with parents (see Chapter 3) were conducted both before and after the inclusion of the additional conditions, which allowed a mix of views to be collated. The stated preference study was run after the expansion of the NBS panel and therefore captured the views of parents who had experienced both panels. The findings from the realist review and the stated preference study implied that information provision would be more highly valued as the number of conditions included on a NBS panel increased.
Limitations
The main limitations in this project centred on key challenges around the recruitment of study participants. Despite exhaustive recruitment efforts the number of parents identified who had received a false-positive result was low. However, previous experience suggests that recruiting such samples is always highly challenging. The final sample size of those who received a false-positive result in this study was still commensurate with that of previous studies that included only parents who had received a false-positive result. The team worked with both the NBS advisors and the parent reference group to specifically target younger parents and those will a lower educational background. Although the overall numbers in the sample coming from these groups were low, relative to other studies this sample is diverse and a testament to the hard work of the research team. Further work with these groups would be beneficial, although given that our findings suggested that even well-educated and engaged service users did not feel suitably informed, it is likely that our findings are highlighting barriers that could have an even more profound impact on parents without these characteristics. One group not represented is parents whose child is born preterm. It is important to recognise that these parents would potentially not benefit from information provision in the third trimester; however, it does further highlight the need to engage parents throughout pregnancy. Likewise, these parents are likely to be further disadvantaged by the current practice of focusing information provision in the post-birth period.
The aim of the resource use study was to obtain a representative sample to understand how information is currently provided by midwives in NBS. The types of resources used in the current information provision pathway were established, but the small sample sizes in the survey and observation study mean that there may be significant uncertainty in the point estimates of the levels of resource use. For pragmatic reasons, the observation study involved only midwives working in the north-west of England. It is possible that the results from the observation study may not be generalisable beyond this region. For example, all of the observed information provision after birth occurred in urban locations. It is likely that travel costs for midwives based in rural locations will be significantly higher because of the lower population density in such regions. As travel costs were the most significant costs in the provision of NBS information, the total cost of providing such information at a national level may be significantly higher than that estimated. The impact of these uncertainties was investigated in the model-based economic evaluation reported in Chapter 6.
The stated preference study used a pragmatic and purposive approach to sampling but this may affect the generalisability of the findings. The sampling frame of current and future parents, consisting of members of the public between the ages of 18 and 45 years, was chosen to try to best represent the people who receive information about NBS. However, as only 48% of the participants were actually current parents, the sample may not provide a true representation of the preferences of parents who are receiving information about screening.
The resource use identified in this study was collected up until the point at which consent for screening was given. In practice, additional information resources may sometimes be required on receipt of positive screening results, before confirmatory diagnostic tests are conducted. There are also likely to be significant costs involved in educating parents about their child’s condition on receipt of a confirmed diagnosis but these costs form part of the diagnosis and treatment care pathway as opposed to being related to screening-based information. However, because of the rarity of the conditions screened for, the limited geographical range of the observation study and the ethical issues related to the observation of information provision at a time of high potential anxiety for parents, information provision at this time point was not observed.
What does this study add?
This project, with its collective studies, confirmed the existing evidence base supporting the idea that the importance of effective communication with parents should not be underestimated in a national NBSP. Some literature suggests that communication is valued more than choice itself. 33 The findings from the qualitative interviews showed how much parents and midwives valued parents being informed and a key theme from the focus groups with stakeholders was the negative feelings of parents when they became aware that their agreement was not as informed as they believed.
Some participants in this project had the view that mandatory screening could, in theory, replace informed consent. This view was largely driven by a wish to ensure that children could benefit from being identified as having a condition and receive timely treatment, which is in line with previous arguments in the literature. 14,33 However, there is no indication either in the data in this report or in the international literature that informed choice would result in parents declining testing. 20,89 Also, as in previous research, the advocates of mandatory screening focused on the identification of children with conditions14 and showed no awareness of carrier identification or storage issues. That parents’ views changed dramatically to preferring informed choice once they were aware of the storage of bloodspots after discussion in the focus groups highlights the danger of basing consent policy on incomplete parent knowledge profiles. The data may also suggest that, were NBS in England to move to a mandatory screening model, the storage of bloodspots would need to be considered in a separate consent model.
Furthermore, the findings from the stated preference study suggested that making screening mandatory may result in more parents trying to opt out of NBS. In the interviews, some parents explicitly said that they would not like mandatory screening, and midwives also did not feel comfortable with this model as it did not fit with their wider remit of being women’s advocates. Midwives also felt they would need more training and would need to be more knowledgeable about a screening programme that is somehow imposed on parents to ensure that they were confident about delivering the relevant information. A well-functioning informed consent and choice model was both acceptable and desirable, which fits with existing health professional guidance. 9 However, this project suggests that, in practice, an informed choice was not made by many parents and as a result they did not view NBS positively as trust in the health-care system was lost. This places the onus on midwives to ensure that the first message that is imparted to all parents is that they are expected to make an informed decision.
Of interest, although there seems to be a surface-level acceptance that information is provided to enable parents to make informed decisions, there appears to be an implicit view, driven by fear, that if we make certain messages clear (choice, storage) then parents are more likely to decline screening or that there is a need to really emphasise some messages (impact of condition) to ensure that parents do not decline. However, there does not appear to be any evidence in any of our studies, including the literature review, that parents contemplate refusing NBS. Indeed, many parents appear to be hugely supportive of NBS and see it as a ‘no brainer’. However, there is ample evidence that when parents are not adequately informed or prepared then the negative impact on their well-being is increased and their trust in the NHS is shaken. Interestingly, they do not appear to suggest that they would now refuse NBS, but rather that they would have wanted the information and choice to be provided honestly. Thus, NBS communication may well be more about maintaining trust with parents and encouraging them to be active decision-makers in the best interests of their child than it is about a true choice being made (if all parents are going to say yes anyway).
In line with previous research, the qualitative data suggested that parents did not feel that they had been made fully aware of NBS and its consequences. The storage of bloodspots was one of the least frequently discussed topics and when it was discussed this occurred after the birth. Poor communication can lead to negative effects for parents and their wider family, an increased need for support and resources and long-term breakdown of relationships between parents and health professionals,34 but it also represents a missed opportunity for NBSPs to have a positive impact. 181 Parents taking part in NBS who feel adequately informed and empowered have reported feeling a duty to inform other family members of the potential risks, correct misperceptions and challenge stigma and misunderstanding more widely in their communities. 181 Within both antenatal screening and NBS there is an increasing recognition of the important role that families and social networks can play in informing parents45,181 and shaping their choices about and adaptation to screening. 181 Thus, optimising communication is likely to have a much broader impact than the impact on the original target set of parents.
This project has suggested why there may be apparently conflicting situations in which health professionals report that they do provide NBS information but parents report that they were not sufficiently aware of this information. Although there was evidence that not all messages were conveyed to parents, it did appear that most parents were given some form of information, albeit it may not have been effectively given. This project has illustrated that this contradiction in perspectives may be a result of the timing of the communication event, which, currently, occurs immediately after the birth. Anecdotal evidence, observed during the observation study, provided examples of parents being provided with information by a midwife but the next day appearing to be completely unaware of this information. The data from the parents in this sample and from the literature review raise concerns about whether or not such information can be meaningfully stored by parents. Current guidance for midwives advises that parents in England should not be told about NBS for the first time post birth, but the interviews and the observation study provided examples of parents recalling information provision or receiving information for the first time post birth. Both the survey and the observation study results suggested that the longer conversations with parents were occurring after the birth, with midwives spending a minimal amount of time providing information antenatally. Some central messages were observed to be conveyed only after birth, such as messages about the chance of false-positive results, whereas the possibility of being a carrier was never mentioned in the observation study. One of the most important messages to arise is therefore the need to move information provision from after the birth to the third trimester, which is consistent with the published literature. 11,75 Parents can, at least temporarily, become passive during this time (i.e. become willing to let health professionals do whatever they see fit), presumably because of exhaustion from caring for a newborn. 18 The current approach to information provision, and the design of materials for communication in NBS, have not been informed by a recognised evidence base from the discipline of cognitive psychology, which suggests that women perform more poorly on memory tests in pregnancy and shortly after birth. 182–187 It is important to recognise that parents whose children are born preterm may not benefit from information provision in the third trimester; however, they should still benefit from more effective awareness strategies and drip-feeding of information across pregnancy, resulting in an enhanced likelihood that they are able to make a decision about NBS compared with current practice.
This project was not able to establish why health professionals were providing information after birth, in contradiction to current guidance. One possibility is that midwives have multiple competing priorities and so have insufficient time to provide information during pregnancy. This could result in midwives needing to prioritise other information in appointments during the pregnancy and only being able to prioritise NBS information at a time when they are required to seek consent. One possible solution would be to move the consent process into pregnancy, as is the case in New Zealand, to ensure that the communication and decision-making process take place at a time when parents are most receptive to the information29,66,70 and are able to make decisions.
The one mode of information provision that was consistently valued was having a discussion with a health professional. 66,72,79 A discussion is potentially the most beneficial way of providing NBS information, but also the most expensive, and therefore it is vital that it is employed effectively. Our data suggest that parents want the health professional both to be trained and to have the time to perform this role. An example of the need for up-to-date training not being currently met was identified when the Health Professional Handbook was accessed in March 2016 and was found to refer to only five conditions in the NBS panel, despite the panel having been expanded in January 2015. It is a concern that health professionals are not being adequately informed of the conditions being screened for as this has been shown to feed into parents’ reactions when they first hear that their child may be affected. 34,99 The data suggest that one solution may be for midwives to provide information in group sessions and for parents to be able to access a national telephone line to receive further information, while simultaneously moving the time for informing parents to the third trimester. To adequately train the entire midwifery workforce and allow them the 30 minutes that they feel they would need with each parent using the current approach to communication is not likely to be feasible within current health-care budgets. Midwives’ time is likely to be much better spent having more lengthy conversations in the third trimester, when parents are more receptive to information. Another message that was explicit in the data, but also implicit given the lack of knowledge of key messages that are included in the current screening booklet,188 is that the current practice of using leaflets needs optimising. Although the realist review reported in Chapter 2 raised some concerns about the use of leaflets, they may still be an effective mode of information provision if they are provided at a time when parents are more receptive to information, such as in the third trimester of the pregnancy, and ensuring that midwives’ time is used instead in helping parents check their understanding or make decisions in line with their personal preferences.
A key central message from this project was the potential value of making the learning experience parent led, rather than perceiving parents as being passive recipients of information given to them by midwives and through leaflets. Both parents and health professionals in the interview and stakeholder studies valued this development. This also fits with emerging dialogues in the literature61 and the lack of an optimally effective communication mode evidenced by multiple Cochrane reviews. 189,190 The supplementary questions included in the stated preference study identified some differences in attitudes to receiving information, which introduces the concept of personalising information provision. For personalised information provision to occur there is a need for multiple formats to be available, giving rise to the idea of an ‘information tool kit’. The information tool kit could use alternative information routes such as embedded videos on trusted websites and waiting room televisions. Pooling existing resources by providing information in a group setting antenatally, rather than on an individual parent basis, could also be offered within a personalised information provision model.
Within such a model, midwives could change their remit and act as ‘trusted guides’, who could direct parents to important information and then use their constrained time to answer specific questions. Robust training, however, would be required for midwives to meet this new role, which may not be feasible for the entire midwifery workforce. A solution would be to offer a national telephone line for parents to seek further information that would reduce the number of midwives who would need to be NBS experts. Indeed, there was some suggestion from other health professionals that midwives may not need to fulfil this role and there is evidence from another NBS publication that it is more important to parents that the health professional can answer their questions effectively. 34
It is also necessary to be clear about what information is best provided within a personalised information provision model. This project, using data from the interviews, focus groups and stated preference study, suggested that the type of information provided should also be personalised to parents. There were differences identified between what parents perceived to be important and what health professionals perceived to be important, with parents prioritising information about pain and side effects and midwives prioritising the names of the conditions and the way that the sample is taken. However, it was also clear from the stakeholder study that it was possible to generate a list of core types of information required by all parents.
Carrier results are the most frequent results conveyed across a NBSP because of the number of sickle cell carriers identified. 34 Previous work suggests not only that carrier results can trigger psychological distress and impact on child bonding, parental relationships and the ability to engage with daily life,13 but also that this distress is a key driver for parents seeking further support from the NHS, usually in the form of specialists. 34 It has been shown that when parents are adequately informed of the likelihood of a carrier result being returned, or that further testing may be needed, this impact and service need can be minimised or removed altogether. 34 This project did not focus on recruiting carriers as previous work had already focused on this need to adequately inform parents about carrier results. 13,34 Yet it is of concern that few parents and no health professionals, with the exception of one in the focus group, raised the need for NBS prescreening information to contain information about carriers. Furthermore, the observation study suggested that parents were generally not told that a range of potential results were possible outcomes of the screen and, when parents were told, this occurred after birth when they were unlikely to absorb this information.
In addition to contributing to distress further on in the screening pathway for some parents, the omission of this message may be a missed opportunity to engage parents. It has been shown previously that young adults who dismissed the relevance of NBS information did start engaging with the information once they realised that they could potentially be carriers of one or other of the conditions. 114
Ultimately, the question of why communication and information provision in NBS is necessary should be revisited. If the view is that communication is occurring to enable informed consent, then the data within this project suggest that the markers of informed consent are currently not being met. However, there are suggestions that, with modifications, this could be achievable and would be desirable. Likewise, if the view is that communication is happening so that parents have an understanding of the screening programme for disease, then it is understandable that midwives will focus their communication on providing information about the types of diseases in the panel and the likelihood of a ‘rare’ positive result. In contrast, if the remit of information provision is reframed as being to make parents aware of the implications of their child being screened and preparing them for the most likely outcomes of the screening, then the importance of conveying the possibility of false-positive and carrier results increases. It is a dominant view within the medical profession that carrier results do not have a medical impact on the child, but it has repeatedly been shown that these results, as well as false-positive results, often have a psychological and financial impact. 13,35–38,43 Therefore, the need to make parents aware that they have a choice whether or not to take part, that samples will be stored and that carrier status might be revealed are key messages within an antenatal communication programme that is meant to prepare parents for the outcomes of NBS.
Further research
This project has identified a number of key areas for future research. Importantly, the value of information analysis suggested that there are key areas of uncertainty that merit investment in future research.
-
The development and robust evaluation of an information tool kit to provide a personalised approach to information provision in NBS through a trial of the personalisation mechanism and information tool kit offered to parents in the third trimester of pregnancy compared with current actual practice.
-
The development of a mechanism with which to target the components of the information tool kit to subgroups of parents such that the mode of communication matches parents’ attitude (active or passive) to information provision.
-
Use of this trial of the information tool kit to examine the effect of changing the role of midwives from providing a list of information to becoming a signposter and checker of parental understanding.
-
Use of the current practice arm of the trial to understand why health professionals currently provide information at the time that do and in the way that they do.
-
Identify the appropriate primary outcome measure to capture the effectiveness of the information tool kit for parents taking part in a NBSP.
-
Quantify the impact of different approaches to information provision on anxiety levels in parents.
-
Quantify the impact of different approaches to information provision on the use of health-care resources and specifically understand the level of uptake of visits to health-care professionals and the NHS when a positive result has been received and a confirmatory test is awaited.
-
Within this study explore how to trigger understanding in parents rather than focusing on information provision to parents.
Acknowledgements
This report presents independent research commissioned by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the NIHR Evaluation, Trials and Studies Coordinating Centre (NETSCC), the Health Technology Assessment programme or the Department of Health. The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, the NHS, the NIHR, the Medical Research Council, the CCF, NETSCC, the Health Technology Assessment programme or the Department of Health.
We would like to acknowledge the contribution of Denise Kasperkiewicz for her assistance with producing the report, retrieving publications for the review, compiling study summaries, compiling tables, figures and abstracts and managing the project administration.
We would like to thank all of the health professionals who assisted with recruiting participants and all of the participants who gave up their time. We are indebted for your time.
We would like to thank the members of our newborn screening advisory group and our scientific advisory board for their support and advice. A huge thank you also to our parent reference group: Natalie Cano Sclare, Tom Millard, Sarah Woolner and Suzanne Hayes.
Contributions of authors
Fiona Ulph (Senior Lecturer in Qualitative Methods, Newborn Screening Communication, Health Psychology; principal investigator and grant holder) designed and supervised the qualitative work, led the literature review and the stakeholder consultation and completed development and writing of all sections of the report.
Stuart Wright (Research Associate, Health Economics) contributed to obtaining ethical approval and managed the R&D approval for the health economic work, collected and analysed the costing data and DCE data and carried out the economic modelling, contributed to formulation of the review framework and assisted with synthesis of the literature and drafted the costing, DCE and economic modelling chapters.
Nimarta Dharni (Research Associate, Qualitative Methods) managed the ethical and R&D approval for the qualitative studies, collected and analysed interview data, contributed to formulation of the review framework and the pre-interview tool, maintained communication with the parent advisory group, ran the literature searches and assisted with synthesis of literature and drafted the interview study chapter.
Katherine Payne (Professor of Health Economics; grant co-applicant) designed and supervised the health economic work and completed development and writing of all sections of the report.
Rebecca Bennett (Professor in Bioethics; grant co-applicant) advised on bioethical aspects of study, contributed to formulation of the review framework and the pre-interview tool and advised on drafts of the literature review and developments of the alternative consent model.
Stephen Roberts (Statistician; grant co-applicant) advised on statistical aspects of the study and general study design and data interpretation and assisted with drafting all sections of the report.
Kieran Walshe (Professor of Health Policy and Management; grant co-applicant) advised on the review methodology, contributed to formulation of the review framework, synthesised the consent theory literature and oversaw the synthesis of the empirical NBS communication and consent literature and contributed to realist review chapter.
Tina Lavender (Professor of Midwifery; grant co-applicant) advised on all aspects of the study design, assisted with recruitment of both the parent and the midwifery samples, advised on midwifery practice in relation to NBS and wider policy issues regarding midwifery and assisted with drafting all sections of the report.
Data sharing statement
The data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Bombard Y, Miller FA, Hayeems RZ, Carroll JC, Avard D, Wilson BJ, et al. Citizens’ values regarding research with stored samples from newborn screening in Canada. Pediatrics 2012;129:239-47. http://dx.doi.org/10.1542/peds.2011-2572.
- Simpson N, Randall R, Lenton S, Walker S. Audit of neonatal screening programme for phenylketonuria and congenital hypothyroidism. Arch Dis Child Fetal Neonatal Ed 1997;77:F228-34. https://doi.org/10.1136/fn.77.3.F228.
- Ahmed S, Bryant L, Hewison J. ‘Balance’ is in the eye of the beholder: providing information to support informed choices in antenatal screening via Antenatal Screening Web Resource. Health Expect 2007;10:309-20. https://doi.org/10.1111/j.1369-7625.2007.00455.x.
- Pollitt RJ. Compliance with science: consent or coercion in newborn screening. Eur J Pediatr 2004;163:757-8. http://dx.doi.org/10.1007/s00431-004-1557-z.
- Mackie A, Fenton K. NHS Screening Programmes in England 2014–2015. London: Public Health England; 2015.
- Bunnik EM, de Jong A, Nijsingh N, de Wert GM. The new genetics and informed consent: differentiating choice to preserve autonomy. Bioethics 2013;27:348-55. http://dx.doi.org/10.1111/bioe.12030.
- Sheehy A, Davis D, Homer CS. Assisting women to make informed choices about screening for group B streptococcus in pregnancy: a critical review of the evidence. Women Birth 2013;26:152-7. http://dx.doi.org/10.1016/j.wombi.2012.10.004.
- Nicholls SG. Knowledge or understanding? Informed choice in the context of newborn bloodspot screening. Public Health Ethics 2010;3:128-36. https://doi.org/10.1093/phe/phq016.
- Health Professional Handbook: A Guide to Newborn Bloodspot Screening for Health Professionals. London: UK Newborn Screening Programme Centre; 2012.
- Screening Tests for You and Your Baby. London: Public Health England; 2014.
- Screening Tests for You and Your Baby: Translations. London: Public Health England; n.d.
- Hayeems RZ, Miller FA, Bombard Y, Avard D, Carroll J, Wilson B, et al. Expectations and values about expanded newborn screening: a public engagement study. Health Expect 2015;18:419-29. https://doi.org/10.1111/hex.12047.
- Ulph F, Cullinan T, Qureshi N, Kai J. Parents’ responses to receiving sickle cell or cystic fibrosis carrier results for their child following newborn screening. Eur J Hum Genet 2015;23:459-65. https://doi.org/10.1038/ejhg.2014.126.
- Hargreaves KM, Stewart RJ, Oliver SR. Informed choice and public health screening for children: the case of blood spot screening. Health Expect 2005;8:161-71. https://doi.org/10.1111/j.1369-7625.2005.00324.x.
- Liebl B, Nennstiel-Ratzel U, von Kries R, Fingerhut R, Olgemöller B, Zapf A, et al. Very high compliance in an expanded MS-MS-based newborn screening program despite written parental consent. Prev Med 2002;34:127-31. http://dx.doi.org/10.1006/pmed.2001.0952.
- Ross LF. Mandatory versus voluntary consent for newborn screening?. Kennedy Inst Ethics J 2010;20:299-328.
- Kemper AR, Fant KE, Clark SJ. Informing parents about newborn screening. Public Health Nurs 2005;22:332-8. https://doi.org/10.1111/j.0737-1209.2005.220408.x.
- Nicholls SG. Considering Consent: An Analysis of Factors Infuencing Parental Perceptions of Decisional Quality in the Context of Newborn Screening 2010.
- Faden R, Chwalow AJ, Holtzman NA, Horn SD. A survey to evaluate parental consent as public policy for neonatal screening. Am J Public Health 1982;72:1347-52. https://doi.org/10.2105/AJPH.72.12.1347.
- Charles T, Pitt J, Halliday J, Amor DJ. Implementation of written consent for newborn screening in Victoria, Australia. J Paediatr Child Health 2014;50:399-404. http://dx.doi.org/10.1111/jpc.12484.
- Hewlett J, Waisbren S. A review of the psychosocial effects of false-positive results on parents and current communication practices in newborn screening. J Inherit Metab Dis 2006;29:677-82. https://doi.org/10.1007/s10545-006-0381-1.
- Bennett R. Routine antenatal HIV testing and informed consent: an unworkable marriage?. J Med Ethics 2007;33:446-8. https://doi.org/10.1136/jme.2006.018861.
- Dankert-Roelse JE, Knol K, ten Kate LP. Effects of neonatal screening for cystic fibrosis on reproduction, attitudes toward reproductive behaviour and genetic knowledge. Acta Univ Carol Med (Praha) 1990;36:99-101.
- Statham H, Green J, Snowdon C. Mothers’ consent to screening newborn babies for disease. BMJ 1993;306:858-9. https://doi.org/10.1136/bmj.306.6881.858-c.
- Campbell ED, Ross LF. Incorporating newborn screening into prenatal care. Am J Obstet Gynecol 2004;190:876-77. https://doi.org/10.1016/j.ajog.2003.12.026.
- Davis TC, Humiston SG, Arnold CL, Bocchini JA, Bass PF, Kennen EM, et al. Recommendations for effective newborn screening communication: results of focus groups with parents, providers, and experts. Pediatrics 2006;117:S326-240. https://doi.org/10.1542/peds.2005-2633M.
- Locock L, Kai J. Parents’ experiences of universal screening for haemoglobin disorders: implications for practice in a new genetics era. Br J Gen Pract 2008;58:161-8. https://doi.org/10.3399/bjgp08X277276.
- Suriadi C, Jovanovska M, Quinlivan JA. Factors affecting mothers’ knowledge of genetic screening. Aust N Z J Obstet Gynaecol 2004;44:30-4. http://dx.doi.org/10.1111/j.1479-828X.2004.00171.x.
- Detmar S, Hosli E, Dijkstra N, Nijsingh N, Rijnders M, Verweij M. Information and informed consent for neonatal screening: opinions and preferences of parents. Birth 2007;34:238-44. https://doi.org/10.1111/j.1523-536X.2007.00176.x.
- Newcomb P, True B, Walsh J, Dyson M, Lockwood S, Douglas B. Maternal attitudes and knowledge about newborn screening. MCN Am J Matern Child Nurs 2013;38:289-94. http://dx.doi.org/10.1097/NMC.0b013e31829a55e2.
- Smith RA, Williams DK, Sibert JR, Harper PS. Attitudes of mothers to neonatal screening for Duchenne muscular dystrophy. BMJ 1990;300. https://doi.org/10.1136/bmj.300.6732.1112.
- Tluczek A, Mischler EH, Farrell PM, Fost N, Peterson NM, Carey P, et al. Parents’ knowledge of neonatal screening and response to false-positive cystic fibrosis testing. J Dev Behav Pediatr 1992;13:181-6. https://doi.org/10.1097/00004703-199206000-00005.
- Campbell E, Ross LF. Parental attitudes regarding newborn screening of PKU and DMD. Am J Med Genet A 2003;120A:209-14. http://dx.doi.org/10.1002/ajmg.a.20031.
- Kai J, Ulph F, Cullinan T, Qureshi N. Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice. Health Technol Assess 2009;13. https://doi.org/10.3310/hta13570.
- Merelle ME, Nagelkerke AF, Lees CM, Dezateux C. Newborn screening for cystic fibrosis. Cochrane Database Syst Res 2001;3.
- Tluczek A, Mischler EH, Bowers B, Peterson NM, Morris ME, Farrell PM, et al. Psychological impact of false-positive results when screening for cystic fibrosis. Pediatr Pulmonol Suppl 1991;7:29-37. https://doi.org/10.1002/ppul.1950110707.
- Gurian EA, Kinnamon DD, Henry JJ, Waisbren SE. Expanded newborn screening for biochemical disorders: the effect of a false-positive result. Pediatrics 2006;117:1915-21. https://doi.org/10.1542/peds.2005-2294.
- Fyrö K, Bodegård G. Four-year follow-up of psychological reactions to false positive screening tests for congenital hypothyroidism. Acta Paediatr Scand 1987;76:107-14. https://doi.org/10.1111/j.1651-2227.1987.tb10424.x.
- Green M. Vulnerable child syndrome and its variants. Pediatr Rev 1986;8:75-80. https://doi.org/10.1542/pir.8-3-75.
- Rothenberg MB, Sills EM. Iatrogenesis: the PKU anxiety syndrome. J Am Acad Child Psychiatry 1968;7:689-92. https://doi.org/10.1016/S0002-7138(09)62188-9.
- Waisbren SE, Albers S, Amato S, Ampola M, Brewster TG, Demmer L, et al. Effect of expanded newborn screening for biochemical genetic disorders on child outcomes and parental stress. JAMA 2003;290:2564-72. http://dx.doi.org/10.1001/jama.290.19.2564.
- Prosser LA, Kong CY, Rusinak D, Waisbren SL. Projected costs, risks, and benefits of expanded newborn screening for MCADD. Pediatrics 2010;125:e286-94. http://dx.doi.org/10.1542/peds.2009-0605.
- Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al. Neonatal screening for inborn errors of metabolism: cost, yield and outcome. Health Technol Assess 1997;1.
- Morrison DR, Clayton EW. False positive newborn screening results are not always benign. Public Health Genomics 2011;14:173-7. http://dx.doi.org/10.1159/000322527.
- Potter BK, Avard D, Entwistle V, Kennedy C, Chakraborty P, McGuire M, et al. Ethical, legal, and social issues in health technology assessment for prenatal/preconceptional and newborn screening: a workshop report. Public Health Genomics 2009;12:4-10. https://doi.org/10.1159/000153430.
- Stewart R, Hargreaves K, Oliver S. Evidence informed policy making for health communication. Health Educ J 2005;64:120-8. https://doi.org/10.1177/001789690506400204.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications; 1997.
- Faden RR, Beauchamp TL. A History and Theory of Informed Consent. New York, NY: Oxford University Press; 1986.
- Schmitz D, Reinacher PC. Informed consent in neurosurgery – translating ethical theory into action. J Med Ethics 2006;32:497-8. https://doi.org/10.1136/jme.2005.013144.
- Hattab JY, Kohn Y. Informed consent in child psychiatry – a theoretical review. J Ethics Mental Health 2007;2:1-6.
- Meulenbroek O, Vernooij-Dassen M, Kessels RPC, Graff MJL, Sjogren MJC, Schalk BWM, et al. Informed consent in dementia research. Legislation, theoretical concepts and how to assess capacity to consent. Eur Geriatr Med 2010;1:58-63. https://doi.org/10.1016/j.eurger.2010.01.009.
- Freeman JM. Rights, respect for dignity and end-of-life care: time for a change in the concept of informed consent. J Med Ethics 2010;36:61-2. http://dx.doi.org/10.1136/jme.2009.031773.
- Miller FG, Wertheimer A. The fair transaction model of informed consent: an alternative to autonomous authorization. Kennedy Inst Ethics J 2011;21:201-18. https://doi.org/10.1353/ken.2011.0013.
- Freedman B. A moral theory of informed consent. Hastings Cent Rep 1975;5:32-9. https://doi.org/10.2307/3561421.
- Kluge EH. Competence, capacity, and informed consent: beyond the cognitive-competence model. Can J Aging 2005;24:295-304. https://doi.org/10.1353/cja.2005.0077.
- Dolan T. Autonomy as a negotiated concept: the case of informed consent. AJOB Neurosci 2013;4:69-70. https://doi.org/10.1080/21507740.2013.828111.
- Karlsen JR, Solbakk JH, Holm S. Ethical endgames: broad consent for narrow interests; open consent for closed minds. Camb Q Healthc Ethics 2011;20:572-83. http://dx.doi.org/10.1017/S0963180111000314.
- Simm K. The concepts of common good and public interest: from Plato to biobanking. Camb Q Healthc Ethics 2011;20:554-62. http://dx.doi.org/10.1017/S0963180111000296.
- Sutrop M. Changing ethical frameworks: from individual rights to the common good?. Camb Q Healthc Ethics 2011;20:533-45. http://dx.doi.org/10.1017/S0963180111000272.
- Levine RJ. Informed consent: some challenges to the universal validity of the Western model. Law Med Health Care 1991;19:207-13. https://doi.org/10.1111/j.1748-720X.1991.tb01816.x.
- Hayeems RZ, Miller FA, Little J, Carroll JC, Allanson J, Chakraborty P, et al. Informing parents about expanded newborn screening: influences on provider involvement. Pediatrics 2009;124:950-8. https://doi.org/10.1542/peds.2008-3148.
- Nicholls SG, Southern KW. Parental decision-making and acceptance of newborn bloodspot screening: an exploratory study. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0079441.
- Tluczek A, Orland KM, Nick SW, Brown RL. Newborn screening: an appeal for improved parent education. J Perinat Neonatal Nurs 2009;23:326-34. http://dx.doi.org/10.1097/JPN.0b013e3181a1bc1f.
- Yang YM, Andrews S, Peterson R, Shah A, Cepeda M. Prenatal sickle cell screening education effect on the follow-up rates of infants with sickle cell trait. Patient Educ Couns 2000;39:185-9. https://doi.org/10.1016/S0738-3991(99)00022-1.
- Potter BK, Etchegary H, Nicholls SG, Wilson BJ, Craigie SM, Araia MH. Education and parental involvement in decision-making about newborn screening: understanding goals to clarify content. J Genet Couns 2015;24:400-8. https://doi.org/10.1007/s10897-014-9780-x.
- Moody L, Choudhry K. Parental views on informed consent for expanded newborn screening. Health Expect 2013;16:239-50. http://dx.doi.org/10.1111/j.1369-7625.2011.00710.x.
- Mak CM, Lam CW, Law CY, Siu WK, Kwong LL, Chan KL, et al. Parental attitudes on expanded newborn screening in Hong Kong. Public Health 2012;126:954-9. http://dx.doi.org/10.1016/j.puhe.2012.08.002.
- Davey A, French D, Dawkins H, O’Leary P. New mothers’ awareness of newborn screening, and their attitudes to the retention and use of screening samples for research purposes. Genomics Soc Policy 2005;1. https://doi.org/10.1186/1746-5354-1-3-41.
- Kerruish NJ, Webster D, Dickson N. Information and consent for newborn screening: practices and attitudes of service providers. J Med Ethics 2008;34:648-52. http://dx.doi.org/10.1136/jme.2007.023374.
- Hargreaves K, Stewart R, Oliver S. Pilot Study of Pre-screening Parent Leaflet on Newborn Blood Spot Screening and Health Professional Communication Guidelines. London: UK Newborn Screening Programme Centre; 2004.
- Faulkner LA, Feuchtbaum LB, Graham S, Bolstad JP, Cunningham GC. The newborn screening educational gap: what prenatal care providers do compared with what is expected. Am J Obstet Gynecol 2006;194:131-7. https://doi.org/10.1016/j.ajog.2005.05.075.
- Nicholls SG, Southern KW. Parental information use in the context of newborn bloodspot screening. An exploratory mixed methods study. J Community Genet 2012;3:251-7. http://dx.doi.org/10.1007/s12687-012-0082-4.
- Miller FA, Hayeems RZ, Carroll JC, Wilson B, Little J, Allanson J, et al. Consent for newborn screening: the attitudes of health care providers. Public Health Genomics 2010;13:181-90. http://dx.doi.org/10.1159/000240966.
- Fant KE, Clark SJ, Kemper AR. Completeness and complexity of information available to parents from newborn-screening programs. Pediatrics 2005;115:1268-72. https://doi.org/10.1542/peds.2004-0834.
- Araia MH, Potter BK. Newborn screening education on the internet: a content analysis of North American newborn screening program websites. J Community Genet 2011;2:127-34. http://dx.doi.org/10.1007/s12687-011-0046-0.
- Lipstein EA, Nabi E, Perrin JM, Luff D, Browning MF, Kuhlthau KA. Parents’ decision-making in newborn screening: opinions, choices, and information needs. Pediatrics 2010;126:696-704. http://dx.doi.org/10.1542/peds.2010-0217.
- Araia MH, Wilson BJ, Chakraborty P, Gall K, Honeywell C, Milburn J, et al. Factors associated with knowledge of and satisfaction with newborn screening education: a survey of mothers. Genet Med 2012;14:963-70. http://dx.doi.org/10.1038/gim.2012.87.
- Stewart R, Hargreaves K, Oliver S. Telling Parents about the Heelprick Test: Consultation Results and Resource Development. London: UK Newborn Screening Programme Centre; 2004.
- Nicholls SG. Proceduralisation, choice and parental reflections on decisions to accept newborn bloodspot screening. J Med Ethics 2012;38:299-303. http://dx.doi.org/10.1136/medethics-2011-100040.
- Nicholls SG, Southern KW. Informed choice for newborn blood spot screening in the United Kingdom: a survey of parental perceptions. Pediatrics 2012;130:e1527-33. http://dx.doi.org/10.1542/peds.2012-1479.
- Tarini BA, Goldenberg A, Singer D, Clark SJ, Butchart A, Davis MM. Not without my permission: parents’ willingness to permit use of newborn screening samples for research. Public Health Genomics 2010;13:125-30. http://dx.doi.org/10.1159/000228724.
- Arnold CL, Davis TC, Frempong JO, Humiston SG, Bocchini A, Kennen EM, et al. Assessment of newborn screening parent education materials. Pediatrics 2006;117:S320-5. https://doi.org/10.1542/peds.2005-2633L.
- Newson A. Should parental refusals of newborn screening be respected?. Camb Q Healthc Ethics 2006;15:135-46. https://doi.org/10.1017/S0963180106060166.
- Holtzman NA, Faden R, Chwalow AJ, Horn SD. Effect of informed parental consent on mothers’ knowledge of newborn screening. Pediatrics 1983;72:807-12.
- Parsons EP, King JT, Israel JA, Bradley DM. Mothers’ accounts of screening newborn babies in Wales (UK). Midwifery 2007;23:59-65. https://doi.org/10.1016/j.midw.2006.05.008.
- Parsons E, Moore C, Israel J, Hood K, Clarke AJ, Bradley DM. Emphasizing parental choice on newborn screening. Br J Midwifery 2005;13:165-8. https://doi.org/10.12968/bjom.2005.13.3.17637.
- Etchegary H, Dicks E, Hodgkinson K, Pullman D, Green J, Parfey P. Public attitudes about genetic testing in the newborn period. J Obstet Gynecol Neonatal Nurs 2012;41:191-200. http://dx.doi.org/10.1111/j.1552-6909.2012.01341.x.
- Feuchtbaum L, Cunningham G, Sciortino S. Questioning the need for informed consent: a case study of California’s experience with a pilot newborn screening research project. J Empir Res Hum Res Ethics 2007;2:3-14. http://dx.doi.org/10.1525/jer.2007.2.3.3.
- Dhondt JL. Implementation of informed consent for a cystic fibrosis newborn screening program in France: low refusal rates for optional testing. J Pediatr 2005;147:106-8. https://doi.org/10.1016/j.jpeds.2005.08.008.
- Grob R. Parenting in the genomic age: the ‘cursed blessing’ of newborn screening. New Genet Soc 2006;25:159-70. https://doi.org/10.1080/14636770600855218.
- Hasegawa LE, Fergus KA, Ojeda N, Au SM. Parental attitudes toward ethical and social issues surrounding the expansion of newborn screening using new technologies. Public Health Genomics 2011;14:298-306. https://doi.org/10.1159/000314644.
- Huang MC, Lee CK, Lin SJ, Lu IC. Parental consent for newborn screening in southern Taiwan. J Med Ethics 2005;31:621-4. https://doi.org/10.1136/jme.2004.010074.
- Lang CW, Stark AP, Acharya K, Ross LF. Maternal knowledge and attitudes about newborn screening for sickle cell disease and cystic fibrosis. Am J Med Genet A 2009;149A:2424-9. http://dx.doi.org/10.1002/ajmg.a.33074.
- Forman J, Coyle F, Levy-Fisch J, Roberts P, Terry S, Legge M. Screening criteria: the need to deal with new developments and ethical issues in newborn metabolic screening. J Community Genet 2013;4:59-67. http://dx.doi.org/10.1007/s12687-012-0118-9.
- Serving the family from birth to the medical home . Newborn screening: a blueprint for the future – a call for a national agenda on state newborn screening programs. Pediatrics 2000;106:389-422.
- Bailey DB, Bann C, Bishop E, Guarda S, Barnum L, Roche M. Can a decision aid enable informed decisions in neonatal nursery recruitment for a fragile X newborn screening study?. Genet Med 2013;15:299-306. http://dx.doi.org/10.1038/gim.2012.135.
- Campbell E, Ross LF. Professional and personal attitudes about access and confidentiality in the genetic testing of children: a pilot study. Genet Test 2003;7:123-30. http://dx.doi.org/10.1089/109065703322146803.
- Etchegary H, Perrier C. Information processing in the context of genetic risk: implications for genetic-risk communication. J Genet Couns 2007;16:419-32. http://dx.doi.org/10.1007/s10897-006-9082-z.
- DeLuca JM, Kearney MH, Norton SA, Arnold GL. Parents’ experiences of expanded newborn screening evaluations. Pediatrics 2011;128:53-61. http://dx.doi.org/10.1542/peds.2010-3413.
- Stewart R, Oliver S. What is Known about Communication with Parents about Newborn Bloodspot Screening?. London: UK Newborn Screening Programme Centre; 2003.
- Oliver S, Dezateux C, Kavanagh J, Lempert T, Stewart R. Disclosing to parents newborn carrier status identified by routine blood spot screening. Cochrane Database Syst Rev 2004;4. http://dx.doi.org/10.1002/14651858.CD003859.pub2.
- Kladny B, Gettig EA, Krishnamurti L. Systematic follow-up and case management of the abnormal newborn screen can improve acceptance of genetic counseling for sickle cell or other hemoglobinopathy trait. Genet Med 2005;7:139-42. https://doi.org/10.1097/01.GIM.0000153662.88425.68.
- Parker H, Qureshi N, Ulph F, Kai J. Imparting carrier status results detected by universal newborn screening for sickle cell and cystic fibrosis in England: a qualitative study of current practice and policy. BMC Health Serv Res 2007;7:203-11. https://doi.org/10.1186/1472-6963-7-203.
- Draucker CB, Martsolf DS, Ross R, Rusk TB. Theoretical sampling and category development in grounded theory. Qual Health Res 2007;17:1137-48. https://doi.org/10.1177/1049732307308450.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Shaw A, Hurst JA. ‘What is this genetics, anyway?’ Understandings of genetics, illness causality and inheritance among British Pakistani users of genetic services. J Genet Counsel 2008;17:373-83. https://doi.org/10.1007/s10897-008-9156-1.
- Patton MQ. Qualitative Evaluation and Research Methods. Newbury Park, CA: Sage; 1990.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:1-11. https://doi.org/10.1177/160940690600500107.
- Rolfe G. Validity, trustworthiness and rigour: quality and the idea of qualitative research. J Adv Nurs 2006;53:304-10. https://doi.org/10.1111/j.1365-2648.2006.03727.x.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage Publications; 1998.
- Hargreaves K, Stewart R, Sinclair J, Oliver S, Thorogood J, Coppinger C. Health visitors’ role in newborn blood spot screening. Community Pract 2006;79:221-4.
- Lincoln YS, Guba GE. Naturalistic Inquiry. Thousand Oaks, CA: Sage Publications; 1985.
- Krippendorff K. Content Analysis: an Introduction to its Methodology. London: Sage Publications; 1980.
- Noke M, Ulph F. Young adults’ pre-existing knowledge of cystic fibrosis and sickle cell diseases: implications for newborn screening. J Genet Couns 2014;23:121-30. http://dx.doi.org/10.1007/s10897-013-9622-2.
- NHS Screening Programmes . Health Professional Handbook 2012.
- Curtis L. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- NHS Employers . Section 17 – Reimbursement of Travel Costs n.d. www.nhsemployers.org/tchandbook/part-3-terms-and-conditions-of-service/section-17-reimbursement-of-travel-costs-1 (accessed 8 June 2017).
- Birth Summary Tables in England and Wales: 2014. Newport: Office for National Statistics; 2014.
- Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S. Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review. Health Technol Assess 2004;8. https://doi.org/10.3310/hta8120.
- Simpson N, Anderson R, Sassi F, Pitman A, Lewis P, Tu K, et al. The cost-effectiveness of neonatal screening for cystic fibrosis: an analysis of alternative scenarios using a decision model. Cost Eff Resour Alloc 2005;3. https://doi.org/10.1186/1478-7547-3-8.
- Geelhoed EA, Lewis B, Hounsome D, O’Leary P. Economic evaluation of neonatal screening for phenylketonuria and congenital hypothyroidism. J Paediatr Child Health 2005;41:575-9. https://doi.org/10.1111/j.1440-1754.2005.00725.x.
- Wildhagen MF, Hilderink HB, Verzijl JG, Verheij JB, Kooij L, Tijmstra T, et al. Costs, effects, and savings of screening for cystic fibrosis gene carriers. J Epidemiol Community Health 1998;52:459-67. https://doi.org/10.1136/jech.52.7.459.
- Autti-Rämö I, Mäkelä M, Sintonen H, Koskinen H, Laajalahti L, Halila R, et al. Expanding screening for rare metabolic disease in the newborn: an analysis of costs, effect and ethical consequences for decision-making in Finland. Acta Paediatr 2005;94:1126-36. https://doi.org/10.1080/08035250510029497.
- Van der Mass P, van Ineveld B, van Oortmarssen G. The Costs and Effects of Mass Screening for Breast Cancer. Rotterdam: Department of Public Health and Social Medicine; 1988.
- de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ 2012;21:145-72. http://dx.doi.org/10.1002/hec.1697.
- Bridges J, Hauber A, Marshall D, Lloyd A, Prosser L, Regier D, et al. Conjoint analysis applications in health – a checklist: a report of the ISPOR good research practices for conjoint analysis task force. Value Health 2011;14:403-13. https://doi.org/10.1016/j.jval.2010.11.013.
- Postnatal Notes for Baby. Birmingham: Perinatal Institute; 2013.
- Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res 2006;16:377-94. https://doi.org/10.1177/1049732305285708.
- Sloane N. A Library of Orthogonal Arrays 2016. http://neilsloane.com/oadir/.
- Bradley JG, Zia MJ, Hamilton N. Patient preferences for control in medical decision making: a scenario-based approach. Fam Med 1996;28:496-501.
- Bernard LL. Needs of Famililar Caregivers of Cancer Patients Across the Advanced Cancer Disease Trajectory 2004.
- DuBenske LL, Burke Beckjord E, Hawkins RP, Gustafson DH. Psychometric evaluation of the Health Information Orientation Scale: a brief measure for assessing health information engagement and apprehension. J Health Psychol 2009;14:721-30. https://doi.org/10.1177/1359105309338892.
- Bech M, Gyrd-Hansen D. Effects coding in discrete choice experiments. Health Econ 2005;14:1079-83. http://dx.doi.org/10.1002/hec.984.
- Gray E, Eden M, Vass C, McAllister M, Louviere J, Payne K. Valuing preferences for the process and outcomes of Clinical Genetics Services: a pilot study. Patient 2016;9:135-47. https://doi.org/10.1007/s40271-015-0133-0.
- Prosser LA, Ladapo JA, Rusinak D, Waisbren SE. Parental tolerance of false-positive newborn screening results. Arch Pediatr Adolesc Med 2008;162:870-6. http://dx.doi.org/10.1001/archpediatrics.2008.1.
- Tarini BA, Clark SJ, Pilli S, Dombkowski KJ, Korzeniewski SJ, Gebremariam A, et al. False-positive newborn screening result and future health care use in a state Medicaid cohort. Pediatrics 2011;128:715-22. http://dx.doi.org/10.1542/peds.2010-2448.
- Venditti LN, Venditti CP, Berry GT, Kaplan PB, Kaye EM, Glick H, et al. Newborn screening by tandem mass spectrometry for medium-chain Acyl-CoA dehydrogenase deficiency: a cost-effectiveness analysis. Pediatrics 2003;112:1005-15. https://doi.org/10.1542/peds.112.5.1005.
- Cipriano LE, Rupar CA, Zaric GS. The cost-effectiveness of expanding newborn screening for up to 21 inherited metabolic disorders using tandem mass spectrometry: results from a decision-analytic model. Value Health 2007;10:83-97. https://doi.org/10.1111/j.1524-4733.2006.00156.x.
- Tiwana SK, Rascati KL, Park H. Cost-effectiveness of expanded newborn screening in Texas. Value Health 2012;15:613-21. http://dx.doi.org/10.1016/j.jval.2012.02.007.
- Karaceper MD, Chakraborty P, Coyle D, Wilson K, Kronick JB, Hawken S, et al. The health system impact of false positive newborn screening results for medium-chain acyl-CoA dehydrogenase deficiency: a cohort study. Orphanet J Rare Dis 2016;11. https://doi.org/10.1186/s13023-016-0391-5.
- NHS Screening Programmes in England 2014 to 2015. London: Public Health England; 2015.
- La Pean A, Farrell MH. Initially misleading communication of carrier results after newborn genetic screening. Pediatrics 2005;116:1499-505. https://doi.org/10.1542/peds.2005-0449.
- Farrell M, Certain L, Farrell P. Genetic counseling and risk communication services of newborn screening programs. Arch Pediatr Adolesc Med 2001;155:120-6. https://doi.org/10.1001/archpedi.155.2.120.
- Farrell MH, Farrell PM. Newborn screening for cystic fibrosis: ensuring more good than harm. J Pediatr 2003;143:707-12. http://dx.doi.org/10.1016/j.jpeds.2003.09.022.
- Southern KW. Newborn screening for cystic fibrosis: the practical implications. J R Soc Med 2004;97:57-9.
- Dillard JP, Tluczek A. Information flow after a positive newborn screening for cystic fibrosis. J Pediatr 2005;147:94-7. https://doi.org/10.1016/j.jpeds.2005.08.021.
- Burgard P, Cornel M, Di Filippo F, Haege G, Hoffmann GF, Lindner M, et al. Report on the Practices of Newborn Screening for Rare Disorders Implemented in Member States of the European Union, Candidate, Potential Candidate and EFTA Countries 2012.
- Waisbren SE. Newborn screening for metabolic disorders. JAMA 2006;296:993-5. https://doi.org/10.1001/jama.296.8.993.
- Wilcken B. Expanded newborn screening: reducing harm, assessing benefit. J Inherit Met Dis 2010;33:S205-10. https://doi.org/10.1007/s10545-010-9106-6.
- Davis T, Humiston S, Arnold C, Bocchini J, Bass P, Kennen E, et al. Recommendations for effective newborn screening communication: results of focus groups with parents, providers, and experts. Pediatrics 2006;117:S326-40. https://doi.org/10.1542/peds.2005-2633M.
- Schmidt JL, Castellanos-Brown K, Childress S, Bonhomme N, Oktay JS, Terry SF, et al. The impact of false-positive newborn screening results on families: a qualitative study. Genet Med 2012;14:76-80. http://dx.doi.org/10.1038/gim.2011.5.
- Burton H, Moorthie S. Expanded Newborn Screening: a Review of the Evidence. Cambridge: PHG Foundation; 2010.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Healthcare. York: Centre for Reviews and Dissemination, University of York; 2009.
- Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4. https://doi.org/10.1186/2046-4053-4-1.
- NHS Economic Evaluation Database Handbook, 2007. York: Centre for Reviews and Dissemination, University of York; 2007.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f1049.
- Shamshiri AR, Yarahmadi S, Forouzanfar MH, Haghdoost AA, Hamzehloo G, Holakouie Naieni K. Evaluation of current guthrie TSH cut-off point in Iran congenital hypothyroidism screening program: a cost-effectiveness analysis. Arch Iran Med 2012;15:136-41. http://dx.doi.org/012153/AIM.006.
- Feuchtbaum L, Cunningham G. Economic evaluation of tandem mass spectrometry screening in California. Pediatrics 2006;117:S280-6. https://doi.org/10.1542/peds.2005-2633G.
- Insinga RP, Laessig RH, Hoffman GL. Newborn screening with tandem mass spectrometry: examining its cost-effectiveness in the Wisconsin Newborn Screening Panel. J Pediatr 2002;141:524-31. https://doi.org/10.1067/mpd.2002.128116.
- Norman R, Haas M, Chaplin M, Joy P, Wilcken B. Economic evaluation of tandem mass spectrometry newborn screening in Australia. Pediatrics 2009;123:451-7. http://dx.doi.org/10.1542/peds.2008-0911.
- Schoen EJ, Baker JC, Colby CJ, To TT. Cost–benefit analysis of universal tandem mass spectrometry for newborn screening. Pediatrics 2002;110:781-6. https://doi.org/10.1542/peds.110.4.781.
- Tran K, Banerjee S, Li H, Noorani HZ, Mensinkai S, Dooley K. Clinical efficacy and cost-effectiveness of newborn screening for medium chain acyl-CoA dehydrogenase deficiency using tandem mass spectrometry. Clin Biochem 2007;40:235-41. https://doi.org/10.1016/j.clinbiochem.2006.10.022.
- Carroll AE, Downs SM. Comprehensive cost–utility analysis of newborn screening strategies. Pediatrics 2006;117:S287-95. https://doi.org/10.1542/peds.2005-2633H.
- Gessner BD, Teutsch SM, Shaffer PA. A cost-effectiveness evaluation of newborn hemoglobinopathy screening from the perspective of state health care systems. Early Hum Dev 1996;45:257-75. https://doi.org/10.1016/0378-3782(96)01761-6.
- Panepinto JA, Magid D, Rewers MJ, Lane PA. Universal versus targeted screening of infants for sickle cell disease: a cost-effectiveness analysis. J Pediatr 2000;136:201-8. https://doi.org/10.1016/S0022-3476(00)70102-8.
- van der Hilst CS, Derks TG, Reijngoud DJ, Smit GP, TenVergert EM. Cost-effectiveness of neonatal screening for medium chain acyl-CoA dehydrogenase deficiency: the homogeneous population of the Netherlands. J Pediatr 2007;151:115-20.
- Hamers FF, Rumeau-Pichon C. Cost-effectiveness analysis of universal newborn screening for medium chain acyl-CoA dehydrogenase deficiency in France. BMC Pediatr 2012;12. http://dx.doi.org/10.1186/1471-2431-12-60.
- Lanting CI, van Tijn Da, Loeber JG, Vulsma T, de Vijlder JJM, Verkerk PH. Clinical effectiveness and cost-effectiveness of the use of the thyroxine/thyroxine-binding globulin ratio to detect congenital hypothyroidism of thyroidal and central origin in a neonatal screening program. Pediatrics 2005;116:168-73. https://doi.org/10.1542/peds.2004-2162.
- van den Akker-van Marle ME, Dankert HM, Verkerk PH, Dankert-Roelse JE. Cost-effectiveness of 4 neonatal screening strategies for cystic fibrosis. Pediatrics 2006;118:896-905. https://doi.org/10.1542/peds.2005-2782.
- Wells J, Rosenberg M, Hoffman G, Anstead M, Farrell PM. A decision-tree approach to cost comparison of newborn screening strategies for cystic fibrosis. Pediatrics 2012;129:e339-47. http://dx.doi.org/10.1542/peds.2011-0096.
- Pandor A, Eastham J, Chilcott J, Paisley S, Beverley C. Economics of tandem mass spectrometry screening of neonatal inherited disorders. Int J Technol Assess Health Care 2006;22:321-6. https://doi.org/10.1017/S026646230605121X.
- Weinstein MC, O’Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, et al. Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on Good Research Practices – Modeling Studies. Value Health 2003;6:9-17. https://doi.org/10.1046/j.1524-4733.2003.00234.x.
- Brennan A, Chick SE, Davies R. A taxonomy of model structures for economic evaluation of health technologies. Health Econ 2006;15:1295-310. http://dx.doi.org/10.1002/hec.1148.
- Screening KPI Data: Q1 (April to June) 2015 to 2016. London: Public Health England; 2015.
- Janssen B, Szende A, Szende A, Janssen B, Cabases J. Self-Reported Population Health: an International Perspective Based on EQ-5D. Heidelberg: Springer Netherlands; 2014.
- Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S. A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme. Health Technol Assess 2004;8. https://doi.org/10.3310/hta8310.
- Lewis MH, Scheurer ME, Green RC, McGuire AL. Research results: preserving newborn blood samples. Sci Transl Med 2012;4. http://dx.doi.org/10.1126/scitranslmed.3004474.
- Heary CM, Hennessy E. The use of focus group interviews in pediatric health care research. J Pediatr Psychol 2002;27:47-5. https://doi.org/10.1093/jpepsy/27.1.47.
- Richer J, Ghebremichael MS, Chudley AE, Robinson WM, Wilfond BS, Solomon MZ. Research use of leftover newborn bloodspots: attitudes of Canadian geneticists regarding storage and informed consent requirements. Genet Med 2011;13:305-13. https://doi.org/10.1097/GIM.0b013e3181f69da0.
- Denzin NK, Lincoln YS. Handbook of Qualitative Research. London: Sage Publications; 2011.
- Vansenne F, de Borgie CA, Legdeur M, Spauwen MO, Peters M. Providing genetic risk information to parents of newborns with sickle cell trait: role of the general practitioner in neonatal screening. Genet Test Mol Biomarkers 2011;15:671-5. http://dx.doi.org/10.1089/gtmb.2010.0232.
- Rendell PG, Henry JD. Prospective-memory functioning is affected during pregnancy and postpartum. J Clin Exp Neuropsychol 2008;30:913-19. http://dx.doi.org/10.1080/13803390701874379.
- de Groot RH, Vuurman EF, Hornstra G, Jolles J. Differences in cognitive performance during pregnancy and early motherhood. Psychol Med 2006;36:1023-32. https://doi.org/10.1017/S0033291706007380.
- Silber M, Almkvist O, Larsson B, Uvnäs-Moberg K. Temporary peripartal impairment in memory and attention and its possible relation to oxytocin concentration. Life Sci 1990;47:57-65. https://doi.org/10.1016/0024-3205(90)90566-A.
- Crawley RA, Dennison K, Carter C. Cognition in pregnancy and the first year post-partum. Psychol Psychother 2003;76:69-84. https://doi.org/10.1348/14760830260569265.
- de Groot RH, Hornstra G, Roozendaal N, Jolles J. Memory performance, but not information processing speed, may be reduced during early pregnancy. J Clin Exp Neuropsychol 2003;25:482-8. http://dx.doi.org/10.1076/jcen.25.4.482.13871.
- Henry JD, Rendell PG. A review of the impact of pregnancy on memory function. J Clin Exp Neuropsychol 2007;29:793-80. https://doi.org/10.1080/13803390701612209.
- NHS Screening Programmes . Screening Tests for You and Your Baby 2016.
- Saeterdal I, Lewin S, Austvoll-Dahlgren A, Glenton C, Munabi-Babigumira S. Interventions aimed at communities to inform and/or educate about early childhood vaccination. Cochrane Database Syst Rev 2014;11. https://doi.org/10.1002/14651858.CD010232.pub2.
- Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for communicating results of medical investigations. Cochrane Database Syst Rev 2012;6. https://doi.org/10.1002/14651858.CD007456.pub2.
- Adewuyi JO. Knowledge of and attitudes to sickle cell disease and sickle carrier screening among new graduates of Nigerian tertiary educational institutions. Niger Postgrad Med J 2000;7:120-3.
- Centers for Disease Control and Prevention (CDC) . Sickle Cell Quiz n.d. www.cdc.gov/ncbddd/sicklecell/quiz/.
Appendix 1 Realist review summary table
| Author | Country | Tests included in screening | Consent practice | Aim of study | Relevant participant characteristics | Study design | Sample size | Any outcome measures | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Faden et al. 198219 | USA (Maryland) | 56 conditions | Consent required for testing. Second screening strongly recommended for all newborns at 1–2 weeks | Maryland adopted a regulation designed to respect parents’ rights to refuse neonatal screening by imposing a parental consent requirement. This is reviewed and evaluated in this study | The study was conducted in two phases. In phase 1, health-care providers who were involved in implementing the parental consent regulation were interviewed. In phase 2, women from whom consent had been solicited under the regulation were interviewed | Qualitative | Phase 1, n = 39 obstetrical units; phase 2, n = 418 | Health-care providers were oblivious to laws requiring parental consent. Hospitals were generally in agreement with any technical requirements with regard to the regulations. Little evidence that these requirements resulted in any extra costs generally. Mothers supported the view that they wanted to be informed about NBS screening and learned a lot of new information through the consent process. Mothers were split evenly with regard to whether or not they favoured actual parental consent | |
| Holtzmann et al. 198384 | USA (Maryland) | 56 conditions | Consent required for testing. Second screening strongly recommended for all newborns at 1–2 weeks | To determine whether or not knowledge is improved through parental consent for NBS screening for PKU and other disorders | New mothers in seven Maryland hospitals | Quantitative | Mothers were interviewed either before receiving a standard disclosure (n = 210) or after giving consent (n = 418) | An increase in knowledge may be expected from informed consent. The authors believed that their findings indicated that information provision could lower anxiety and better prepare parents for outcomes of screening | |
| Yang et al. 200064 | USA | Up to 58 conditions in different states | Mandatory | Looked at the effects of prenatal instructions regarding sickle cell screening on parental compliance with follow-up for infants with sickle cell trait | Expectant mothers whose prenatal education included information about newborn sickle cell screening made up the study group and those whose prenatal education did not include such information made up the control group | Quantitative – case–control study | Control group, n = 606; study group, n = 41 | State Trait Anxiety Inventory (STAI) prior to the notification and counselling/education session | The use of prenatal instruction regarding sickle cell screening considerably increased the follow-up rate for those infants with sickle cell trait and also helped with the recall of information |
| Liebl et al. 200215 | Germany | 14 conditions in 2014 | Optional | To evaluate the influence of implementing informed consent on compliance by systematic demographic tracking | NA | Quantitative | Babies born from 1 August 1999 to 31 July 2000 (n = 123,284) | Implementing written consent does not hinder a high rate of compliance with NBS if applicable information is used and tracked | |
| Campbell and Ross 200333 | USA (Chicago) | 58 conditions | Mandatory | To retrieve information on the attitudes, beliefs and concerns of parents about NBS conditions that are treatable and untreatable in childhood | 84 women and 18 men ranging in age from 18–69 years, with an average age of 39.36 years; African American and Caucasian. On average, respondents had 2.47 children, ranging from one to seven children, aged between 3 weeks and 50 years, with the youngest child averaging 8.52 years and the oldest averaging 14.74 years. One-quarter (24/102) reported living with a child with a chronic illness. On the advice of the advisory board to this project, extensive demographic information, including education and income data, were not collected | Qualitative | 102 participants spread over 12 focus groups | All participants believed that PKU screening was beneficial given the need for timely treatments. Concerns raised were linked to insurance, research on retained bloodspots and whether or not breastfeeding was permissible if diagnosed. Mandatory screening was supported by many because of concern that less educated or very young parents would decline. Many participants were surprised by their own ignorance. More education was sought. Information was valued over choice. Many wanted information to be provided antenatally, not post birth. DMD screening was valued for different reasons – emotional and financial preparation. Levels of support for screening varied across groups. In this scenario it was thought that screening should be offered but parents should be able to choose | |
| Hargreaves et al. 200470 | UK | Three to five conditions | Voluntary – informed consent | Pilot study reviewing the look of and detail included in the leaflets used for NBS for both parents and midwives so that changes could be made if necessary | Parents and midwives through 13 pilot sites | Quantitative and qualitative – questionnaire with closed and open questions | 228 parents (21%) and 25 midwives (22%) completed and returned questionnaires | Changes made to the leaflet in 2004 included (1) more detailed information about conditions and treatments; (2) more information about carrier status with regard to CF and SCD, including how gene testing is carried out; (3) results section reworded and organised differently to make it easier to understand; (4) added information on the storage and retention of bloodspots, including with contact details for further information; (5) new photographs added that were more ethnically diverse and more appropriate to NBS; (6) communication guidelines restructured into a brief summary. Further detail is provided in the training handbook | |
| Stewart et al. 200478 | UK | Three to five conditions | Voluntary – informed consent | To outline the details of national communication and information resources about NBS. Also, to present the results of the consultation on the prescreening information leaflet and guidelines for communication and outline the decisions and revisions made as a result of this | Parents whose children have been screened, n = 21; health professionals who take part in NBS screening, n = 23; nurse specialist, NBS screening manager, developmental psychologist, NBS administrator, a researcher and two others (n = 8) | Consultation document | 52 respondents | CF and carrier testing: findings included evidence suggesting that parents do not receive much information about the heel prick test and that this affects the screening process. The use of communication materials such as videos and paper leaflets does aid understanding. Findings also suggested a need for health professional training in the language of risk | |
| Suriadi et al. 200428 | Australia | Victoria – 25 conditions, New South Wales – 30 conditions, Western Australia – 22 conditions | Voluntary | To evaluate the knowledge of women with regard to Down syndrome counselling and NBS screening and to look at any demographic factors involved in the knowledge process. Additionally, to find out if the women could identify that they had had a diagnostic test for Down syndrome and NBS | A total of 232 consecutive women delivering a live-born baby | Quantitative – cross-sectional survey | A total of 200 women consented to participate in the study (86.2%) | Findings suggested that practices for NBS need to be looked at, especially in those hospitals with larger non-English-speaking populations or those speaking English as a second language, to ensure that information about screening is understood correctly | |
| Davey et al. 200568 | Australia (Western Australia) | 22 conditions | Voluntary | To find out mothers’ knowledge about the NBS process and how they felt about the retention of samples and future need for samples to be used for research purposes | Women who gave birth during the month of January 2005 | Quantitative | A total of 600 women completed the survey | Access to the Midwives Notification Database | Mothers need to be given appropriate information at a time when they are able to retain it. Ethically, the retention of samples needs to be seen to be being dealt with appropriately, before the long-term storage of the samples |
| Dhondt 200589 | France | Five conditions | Voluntary – informed written consent | To determine the effects of the educational efforts used to obtain informed consent for NBS for CF | NA | Quantitative | NA | There was a significant decrease in the refusal rate of testing for CF if an effort was made to inform parents and health professionals appropriately about NHS | |
| Fant et al. 200574 | USA | Up to 58 conditions in different states | Mandatory | To look at the educational materials in NBS programmes to check for any difficulties in terms of reading ability required or if they were easy to understand | NA | Telephone survey and then content analysis | NBSP screening co-ordinators (n = 51) | Parent educational materials for NBS do not meet AAP standards. There are significant variations between state programmes. Further research is needed to establish how close practice is to achieving the goals of good communication set out in the American Academy of Pediatrics blueprint and how practice changes have an impact on the care patients receive | |
| Hargreaves et al. 200514 | UK | Three to five conditions | Voluntary – informed consent | Examined views of parents and health professionals about informed choice in NBS and assessed information and communication needs | Parents: 42 mothers and 5 fathers – 19 parents of unaffected babies, 6 parents of PKU babies, 10 parents of CHT babies, 6 parents of SCD babies, 6 parents of CF babies. Health professionals: 6 midwives, 4 health visitors, 4 CF nurses, 8 sickle cell counsellors/specialist nurses, 6 paediatricians, 7 GPs (one parent was a GP who was interviewed as a health-care professional and then separately as a parent) | Qualitative | 47 parents of children who screened positive and negative and 35 NBS health-care professionals | Parents and health professionals recognise that there is a conflict between informed choice and screening of children. NBS information for parents needs to be brief and accurate and communication between health professionals and parents needs to be effective and address individual parental needs | |
| Hargreaves et al. 200514 | UK | Nine conditions | Voluntary – informed consent | To assess NBS leaflets from different countries for both parents and health professionals | NA | Quantitative | 106 leaflets: UK, n = 68; USA, n = 34; Australia, n = 4 | Appraisal tool based on DISCERN criteria plus UK National Screening Committee screening criteria | Health information in the leaflets is shown in a positive light and difficulties are not communicated. The study recommended using specific measures of standard patient information in addition to specific advice on certain conditions to develop further information for both parents and health professionals |
| Huang et al. 200592 | Taiwan | Information not available for 2005 | Voluntary | To look at current practice in Taiwan with regard to the parental consent process in NBS | Five obstetricians, 22 nurses, two administrative staff members and one medical technician were included, all with at least 2 years of work experience | Qualitative | 30 staff members from the 23 obstetric clinics/hospitals were interviewed | Staff treat NBS as routine practice and fail to appreciate new versions of NBS may be different. Decisions about consent have historically been driven by financial incentives. The authors urge a new framework where consent is based on a parents’ right to know and an awareness that preparing parents reduces psychological impact | |
| Kemper et al. 200517 | USA (Michigan) | 56 conditions | Mandatory | To assess the current procedure for communicating with parents and educating them about NBS | Officials from all 51 NBSPs participated in the telephone survey | Quantitative – standardised semistructured interview | NBSP co-ordinators in all 50 states and the District of Columbia | The complexity of NBSPs and the likely future expansion in the number of conditions being screened for presents a unique opportunity for the creation of effective measures of communication and integration of care | |
| Parsons et al. 200586 | Wales, UK | Four conditions included in the Welsh NBS programme (CF, PKU, CHT and DMD) | Parents have to opt in for DMD by giving signed consent. No signature required for other conditions | To assess the implications of changing the protocol for NBS for DMD to make the choice more clear and open to parents | All participants were mothers. No other demographics reported | Mixed-methods intervention study. An extra spot of blood was put on a separate screening card in the intervention group. In the control group, practice remained unchanged (only one screening card used). Both groups gave signed informed consent | n = 1347 (response rate 37%) – intervention, n = 788; control: n = 559 | Protocol and procedures for testing of DMD are not always informed or consented. This raises other questions with regard to other treatable diseases such as PKU and the ability to obtain true informed consent from parents | |
| Arnold et al. 200682 | USA | Up to 58 conditions in different states | Mandatory | To assess the readability, ease of use and understanding of parents’ education materials about NBS | NA | Quantitative | Brochures from 48 states and Puerto Rico | Flesch reading ease formula used – measure to determine readability of text | Revision of parent education materials needed to increase understanding and ease of use – should be at 8th grade level or lower and should focus on layout, pictures, the message and cultural diversity. In developing these materials parents need to be involved in the initial process to determine key messages and how to get these messages across appropriately |
| Davis et al. 200626 | USA | Up to 58 conditions in different states | Mandatory | To find out parent and health providers’ knowledge of NBS and interview parents and health professionals to gather opinions about the content of education materials and the timing of the use of those materials to develop recommendations for future use | Purposeful sampling of English- and Spanish-speaking parents of infants aged < 1 year who had experience of initial testing, retesting or false-positive screenings; health professionals who provide prenatal care or health care for newborns; and state NBSP health professionals | Qualitative – focus groups and individual interviews | The focus groups and individual interviews involved 51 parents, 78 health-care providers and nine state NBSP health professionals; 22 focus groups and three individual interviews were carried out | Focus group moderator’s guide with scripted questions | Improvements such as the need for prenatal education materials that are easy to use and understandable were recommended by parents, providers and state NBSP professionals. Education materials need to be understood by all (patients and providers). Provided some examples of recommendations and layouts in the study |
| Faulkner et al. 200671 | USA (California) | 57 conditions | Mandatory | To assess care providers’ knowledge of attitudes towards and possible barriers to information provision in NBS and MS/MS screening | Prenatal care providers in California: obstetrician/family practitioner, midwives, nurse practitioner/physician assistant and others | Quantitative – survey mail-out | Prenatal care providers (n = 6197) | Returned and completed surveys were scanned and reviewed using TeleForm Verifier | Pregnant women and state professionals rely on prenatal care providers to educate pregnant women about NBS; however, many providers do not appear to view it as part of their responsibility. Therefore, the state needs to improve communication with both providers and the public about NBS |
| Grob 200690 | USA | Up to 58 conditions in different states | Mandatory | To explore the dominant narratives structuring public understanding about the need for mandatory screening and about screening programmes’ unprecedented practice of testing for non-infectious diseases without parental consent | None provided | Commentary using data from a primary qualitative study | 25 parents of a child affected by CF, detected through NBS | The author argued that the state’s interest in preventing the birth of children with expensive genetic disorders can certainly be seen as one underlying motivation for the recent expansion of NBS programmes to cover conditions for which the benefits to the identified newborn are minimal, but the potential savings in terms of care for future children ‘prevented’ from being born can be significant. The state’s delivery of unsolicited genetic risk information to women of childbearing age is a real threat to reproductive autonomy, yet a sustained dialogue about this consequence of universal screening is sorely lacking amid the rush to expand state programmes. In relation to the mandatory nature of NBS, the author argued that the underlying rationale of this can be summarised as follows:
|
|
| Newson 200683 | UK | Three to five conditions | Voluntary – informed consent | NA | NA | NA | NA | Pressures between parents, health professionals and the state are to increase with the developments in genetics and new methods of analysis. Future advances such as whole-genome sequencing are already being reflected on by policy-makers. Reflection on ethics, legalities and any possible barriers or conflicts are therefore necessary over time | |
| Detmar et al. 200729 | The Netherlands | 17 conditions (expanded to 35 in 2015) | Optional | To gauge the opinions of parents and future parents with regard to information about and consent for NBS and the possible future expansion of the programme | Included 10 parents-to-be, nine parents of healthy children and 12 parents of children with disorders (29 woman and seven men). Education: low, n = 2; intermediate, n = 14; high, n = 20. Age: 20–29 years, n = 9; 30–39 years: n = 20; > 40 years, n = 7 | Qualitative | 36 participants across seven focus groups | Parents would prefer to receive information about NBS during their pregnancy if the programme is to be expanded. Parents’ preference is for an opt-out approach, providing that screening is for the sole use of preventing permanent harm. If NBS were to be expanded parents were further divided on this issue | |
| Feuchtbaum et al. 200788 | USA (California) | 57 conditions | Mandatory | The idea of informed consent was assessed using interviews and was further examined in the context of parents, the newborn and society | No demographic information provided | Pregnant women | 198 interviews with parents | The authors argue that parents’ autonomy should not over-ride the interests of children and as such studies that are investigating new screening technologies should not require parental consent | |
| Parsons et al. 200785 | Wales, UK | Four conditions included in the Welsh NBS programme (CF, PKU, CHT and DMD) | Parents have to opt in for DMD by giving signed consent. No signature required for other conditions | To look at mothers’ experiences of the screening process, examining how they define screening and the process of consent | 100% female sample including mothers who had recently given birth and who had been offered screening for their newborn baby. All of the mothers had accepted screening for PKU, CHT and CF and the 10 mothers with a baby boy had chosen the DMD test. Sixteen respondents were first-time mothers; the remaining two mothers had one other child. All of the mothers reported that they had been in work before the birth of their baby, with eight in professional/semi-professional occupations and the rest classified as being in skilled, semi-skilled or other occupational groups | Qualitative | n = 18 | A semistructured framework was devised with four main topics | Mothers liked the information about screening to be given out during pregnancy, in line with recent recommendations from the UK Newborn Screening Programme Centre (2007). This needs to be implemented into everyday practice. The consent process needs to be made clear so that midwives are not compromised and mothers are fully aware of the different diseases being screened for and that they have a choice about which tests to undertake |
| Kerruish et al. 200869 | New Zealand | > 20 conditions | Voluntary | To evaluate the information gathered from health professionals regarding informed consent for NBS | 85% of the sample were female, 82% were midwives, 13% were GPs and 5% were obstetricians; 69% of the participants were aged 40–59 years and 25% were aged 20–39 years | Quantitative – questionnaire survey | 769 completed surveys were returned (74% response rate) | Information about NBS should be of a good quality and should be given before the baby is born as a matter of course. Consent is a complex issue and consensus is lower among health professionals regarding the degree of parental involvement. A policy of strong endorsement for NBS but allowing for parental choice appears to be the most reliable method to use with regard to NBS | |
| Hayeems et al. 200961 | USA | Up to 58 conditions in different states | Mandatory | Aimed to look at parents being informed appropriately before NBS sample collection | NBS care providers – obstetricians, midwives, family physicians and obstetric/post-partum nurses. Also genetics professionals and haematologists | Quantitative | 2410 eligible surveys were returned | This research shows a need to raise the confidence and capacity of those who provide NBS information to parents prior to screening. Included in this is a need to raise the perceived importance of this activity | |
| Tluczek et al. 200963 | USA (Wisconsin) | 44 conditions | Mandatory | To determine how parents are informed about NBS and to ask for ideas on how to improve this education process | Convenience sampling used. Parents were recruited on the basis of their infant’s NBS results and subsequent diagnostic testing. Families qualified for inclusion if their infant was aged < 6 months and had an abnormal NBS result in the state of Wisconsin and subsequent testing showed the infant to have (a) CF, (b) CHT, (c) one CF mutation, considered to be a CF carrier or (d) a normal NBS result | Qualitative | 193 parents of 100 infants | On the basis of criteria described by Hsieh and Shannon (2005),63 a directed content analysis was chosen to extend an emergent conceptual framework describing parents’ experiences of the NBS process | A trend towards preventative health care has led to an increasingly complex NBS process. This study found a lack of uniformity in NBS parent education materials. Parents requested information about NBS to be given before the birth of the baby. The findings highlight the need to develop more effective evidence-based approaches to parent education about NBS |
| Lang et al. 200993 | USA (Chicago) | 58 conditions | Mandatory | Study looked at mothers’ understanding of the NBS process for SCD and CF in addition to their understanding of genetics, symptoms and possible treatments involved | Women in the post-partum unit of the University of Chicago Hospitals whose infant was admitted to the general care nursery. Predominantly African American post-partum women | Qualitative | 388 participants | The questions about SCD were adopted from Adewuyi191 and a website sponsored by the Centers for Disease Control and Prevention192 | Women were more informed about SCD than CF but had substantial gaps in knowledge for both conditions. Women stated that information provided about NBS was insufficient but that they were in favour of NBS. Further educational materials are needed to inform women of all educational backgrounds appropriately |
| Lipstein et al. 201076 | USA | Up to 58 conditions in different states | Mandatory | To look at how parents view disease and how they make decisions about NBS | The majority of participants were mothers with at least a college education; 69% of participants self-reported their ethnicity as white | Qualitative | Six primary care focus groups with a total of 40 participants, and four interviews (three individual interviews and one group interview with two participants) with parents from the genetics clinic | There was strong support for NBS alongside well-defined and effective treatments, even if the disorders were associated with increased morbidity. Opinions were less constant for disorders with a late onset or with less definitive treatments. Optional screening was increasingly preferred for these types of conditions. Parents often requested further information about testing and the features of diseases when taking part in the study. Some parents stated that they had made decisions about screening without receiving the appropriate detailed information | |
| Miller et al. 201073 | Canada | 29 conditions | Voluntary | To look into current parental consent and whether or not this needs to be defined further with the current expansion of NBS | Obstetrician/gynaecologists (n = 498), midwives (n = 339), obstetrical/post-partum nurses in hospitals (n = 725), family physicians (n = 729), paediatricians (n = 569), genetics professionals (clinical and biochemical geneticists, genetic counsellors) (n = 105), haematologists (n = 148) | Mixed methods analysis of health-care provider attitudes towards consent for NBS | Survey (n = 1615) and semistructured interviews (n = 36) | Providers did not like the idea of a detailed consent process for NBS and wanted to continue with it as a simple process, reflecting the past service and not a future expanded version. Concerns were raised that the way in which health professionals communicated with NBS was in line with an older model of NBS. Suggestions were that either screening panels needed to be changed to ensure that they fitted with such communication or professionals needed training and resources to ensure a more nuanced conversation could occur | |
| Nicholls 20108 | UK | Nine conditions | Voluntary – informed consent | For informed consent to work it must be understood fully. This study looked at whether or not parents were able to fully recall their experiences of NBS | Parents of children who have undergone NBS | Qualitative | 18 interviews were conducted with both primaparous (n = 12) and multiparous (n = 6) parents | In line with existing evidence, parents had poor recall of their experiences with NBS | |
| Tarini et al. 201081 | USA | Up to 58 conditions in different states | Mandatory | To look at the storage of NBS dried bloodspots for research and determine parental attitudes to this | Mean age: 38.1 years; sex: 57% female; race/ethnicity: white 67.3%, black 11.0%, Hispanic 14.8%, other, non-Hispanic 6.9%; education: high school or less 39.6%, more than high school 60.4%; median number of children: 2 | Quantitative | 1508 respondents (49.5% response rate) | If their permission is sought, three-quarters of parents would allow their child’s NBS sample to be used for research purposes. Those not in favour generally did not agree with samples being used for research purposes | |
| Araia and Potter 201175 | USA | Up to 58 conditions in different states | Mandatory | Study looked at websites that provided information on NBS and whether or not they were consistent with current guidelines for parents | NA | Quantitative – content analysis | 85 documents containing educational materials (76 documents from US websites and nine documents from Canadian websites) | A standardised data collection instrument for content evaluation was developed and pilot tested by both authors | Further evaluation of NBS educational internet resources is needed, especially in terms of the messages that parents receive and the impact that they may have on their attitudes and behaviours |
| Hasegawa et al. 201191 | USA (Alaska, California, Hawaii and Washington) | Alaska – 46 conditions, California – 57 conditions, Hawaii – 47 conditions, Washington – 29 conditions | All mandatory | To assess parents’ knowledge of NBS and their attitudes towards NBS for untreatable conditions and late-onset disorders and towards informed consent in NBS | Mothers of healthy children with normal NBS results aged ≤ 10 years. A total of 114 women ranging in age from 18–49 years participated in the focus groups. The majority were college educated (60.5%), Japanese American or African American (23.7% and 21.1% respectively) and between the ages of 31 and 40 years (51.8%) and had a child aged between 1 and 5 years (62.3%) | Qualitative – focus groups | 114 women | Parents need to be included in the development of NBS policy now that NBS is expanding. There was general agreement in the focus groups about the issues that cause conflict among public health and health-care professionals. Parents are generally in opposition to professionals in terms of the timing of NBS education, informed consent, NBS for disorders with ineffective treatments and NBS for late-onset disorders | |
| Araia et al. 201277 | Canada | 29 conditions | Voluntary | To determine whether or not mothers’ knowledge about NBS is in line with the current NBS education materials provided | 1712 mothers residing in Ontario, Canada, and whose infants had recently undergone NBS | Quantitative | 750 completed questionnaires were returned (response rate 47%) | More effective engagement is needed with prenatal providers to increase mothers’ understanding and expectations of NBS. More effective engagement is also needed when communicating with mothers about the retention and handling of samples and the results that come back to them | |
| Mak et al. 201267 | Hong Kong | Three conditions | Voluntary | This is the first study looking at parental knowledge and attitudes towards NBS in Hong Kong | All participants were Chinese. No other details were provided | Cross-sectional survey in one of the major obstetric units in Hong Kong. Parents with babies born from 1 July to 31 October 2010 were randomly recruited to participate | 172 parents | The survey questions were set in accordance with the recommendations from the conjoint analysis survey of parental attitudes towards NBS | Parents are in favour of expanded NBS in Hong Kong. Parental tolerance was high. Parents liked the independence and choice gained from informed consent and the provision of counselling before the test the most |
| Nicholls 201279 | UK | Five conditions | Voluntary – informed consent | To determine how parental decisions are affected by the current NBS routine procedural process in terms of the timing and presentation of information | Parents (both mothers and fathers) were recruited between December 2008 and May 2009 and were eligible for inclusion if their child was born up to 2 years before being interviewed | Qualitative | 18 interviews were conducted | Participants reported proceduralisation of NBS. This impacted on their perception of autonomy. The way in which information was provided was also important. Participants highlighted the importance of antenatal information provision in enabling consideration of the information and informed consent | |
| Nicholls and Southern 201272 | UK | Five conditions | Voluntary – informed consent | To look into the selection process used by parents when they are gaining information about NBS | Parents were eligible for inclusion if their child’s bloodspot had been analysed by the Merseyside and Cheshire Regional Screening laboratory and their child had been born in 2008 | Mixed methods | Random sample of 500 parents – survey. Interviews – 18 parents who had accepted NBS; 12 interviewees were first-time parents | The midwife was the main information source for parents; only half of parents used the official leaflets provided. Barriers to gaining information included the provision of information postnatally. Demographics such as age, education level and income level did not affect the number of information sources used, which was limited. The use of written materials requires effective communication initially with a health professional for parents to fully understand the information | |
| Nicholls and Southern 201280 | UK | Five conditions | Voluntary – informed consent | To look at parental understanding of NBS and consent processes | The population selected was that served by the Clinical Biochemistry Department at the Royal Liverpool Children’s Hospital in in its role as part of the UK NBS Laboratories Network, an association of NHS laboratories that provide screening services for newborn babies | Qualitative | 154 questionnaires were returned, giving a response rate of 32% (154/488) | The majority of parents understood why NBS was carried out but only one-third understood what would happen if conditions were found that had to be treated. One-third of parents felt that they had no choice to decline screening but 70% felt that they had received an informed choice. A feeling of having made an informed choice was linked to whether parents had previous children, understanding why screening was necessary, having sufficient time to make a decision and sense that they had a choice | |
| Bailey et al. 201396 | USA | Up to 58 conditions in different states | Mandatory | To determine whether or not the provision of a brochure on informed decision-making improved attention to educational materials and led to a change of decision by parents in a fragile X syndrome NBS study | Mothers who had given birth in a university-based hospital | Quantitative | 1323 families | The brochure helped focus parents’ attention and with their perceptions of how helpful the study was but the majority of the families did not read it all. It was suggested that even if the study materials are well designed someone is still required to explain the study to gain fully informed consent | |
| Forman et al. 201394 | New Zealand | > 20 conditions | Voluntary | This study considered the international criteria for newborn metabolic screening | NA | NA | The proposed criteria will be beneficial in terms of balancing interests and modernising historic criteria to fit the contemporary culture and factors of the newborn situation | ||
| Moody and Choudhry 201366 | UK | Nine conditions | Voluntary – informed consent | To determine what parents and future parents think about NBS and expanded NBS in the UK and what information with regard to consent needs to be provided for this expansion | Parents and future parents. Survey participants: 124 females, 16 males; parents of a healthy child: 108, parents-to-be: 6, parents of a child with a disorder: 13, none of the above: 15. Focus group participants: 27 female, 2 males; ethnicity: South Asian, white British and mixed; parents of a healthy child: 24, parents-to-be: 5, parents of child with a disorder: 0 | Mixed methods | Focus groups (n = 29) and a web survey (n = 142) were undertaken with parents and future parents | Parents want guaranteed information provision with clear decision-making powers and an awareness of the choices available to them. The difference between existing screening provision and expanded screening was not considered to be significant enough by participants to warrant formal written, informed consent for expanded screening. It is argued that the ethical review processes need to be more flexible towards the provision of information and consent processes for service developments in NBS | |
| Newcomb et al. 201330 | USA (Texas) | 53 conditions and a further 24 secondary conditions | Mandatory unless parent refuses for religious reasons | To determine whether or not mothers of newborns understand basic facts about NBS and how they feel about state retention of dried bloodspots for research use | 55.7% were aged 25–35 years; ethnicity: 45.4% Caucasian, 19.2% African American, 25% Hispanic, 6.1% Asian, 4.3% other; education: less than high school 11.2%, high school diploma 23.8%, some college 29.7%, degree 25.1%, advanced degree 10.3%; 45.3% had health insurance; 56.9% had more than one child | Quantitative – cross-sectional survey | 548 mothers | Maternal Attitudes and Knowledge about Newborn Screening Survey | Mothers had insufficient knowledge about NBS and the retention of dried bloodspots. The most used source of information about NBS was the post-partum nurse. Most agreed that using the bloodspots was a good thing but minority groups and Medicaid participants were more hesitant than others about the use of dried bloodspots for research |
| Nicholls and Southern 201362 | UK | Five conditions | Voluntary – informed consent | To determine the factors affecting parents’ decisions about the acceptance of NBS | Parents whose children were screened in 2008 and who resided in Merseyside and Cheshire. Respondents to the survey were relatively representative in terms of ethnic mix but were generally older and more educated than the population from which they were drawn. In total, 67.5% of parents were aged > 30 years. The majority had multiple children (64.3%), 95% were white and 57.2% had an undergraduate degree or higher | Quantitative – cross-sectional survey | n = 154 | The main outcome measure was the quality of the decision made, assessed using the uncertainty and effective decision subscales of the Ottawa Decisional Conflict Scale | How NBS is presented to parents impacts on decision quality. This includes the information content in terms of benefits and risks, but also how consent processes are managed. Research should consider the context around NBS provision to further understand parents’ decision-making. Focusing on information content or parental recall is limiting |
| Charles et al. 201420 | Australia (Victoria) | 25 conditions | Voluntary | To be able to introduce a written consent process across Victoria to strengthen transparency, quality and parental choice in NBS | NA | Quality improvement project | Four pilot hospital sites and subsequently implemented state wide | Parents can take part more fully in NBS without reducing uptake. Retention of dried bloodspots can be maintained with the support of parents. In the future the quality of the consent process needs to be investigated, as well as why some parents choose to decline this process | |
| Hayeems et al. 201512 | Canada | 29 conditions | Voluntary | To investigate Canadian expectations and values with regard to the conditions that should be included in NBS and whether or not parents should provide consent | 60% of participants were female, 60% were single/separated/divorced or widowed; 87% were educated to at least college or university level; 27% were aged 18–29 years, 43% were aged 30–49 years and 30% were aged > 50 years; 43% had children | Mixed methods – focus group and pre/post questionnaires | Eight focus groups (n = 60). Six groups were conducted in English and two groups were conducted in French | Parental choice using five-point Likert scales | Anticipated benefits of expanded infant screening were prioritised over harms, with information provision perceived as a mechanism for mitigating harms and enabling choice. However, the study argued for caution around the potential for public enthusiasm to foster unlimited uptake of infant screening technologies |
| Potter et al. 201565 | Canada | 29 conditions | Voluntary | To outline existing implementation models for NBS, map the potential goals of parental education onto these models and consider the content that may be needed to support the goals | NA | Conceptual framework | NA | Comprehensive information for parents about NBS is important given the value of meeting parental expectations and preferences for communication. This infers respect and enhanced parental trust of NBS. A flexible approach enabling core messages to be relayed to all with tailored additional information provided is most likely to be effective |
Appendix 2 Pre-interview tool: alternative consent and communication models
Appendix 3 Telephone survey (version 3)
Appendix 4 Observation data collection Excel spreadsheet
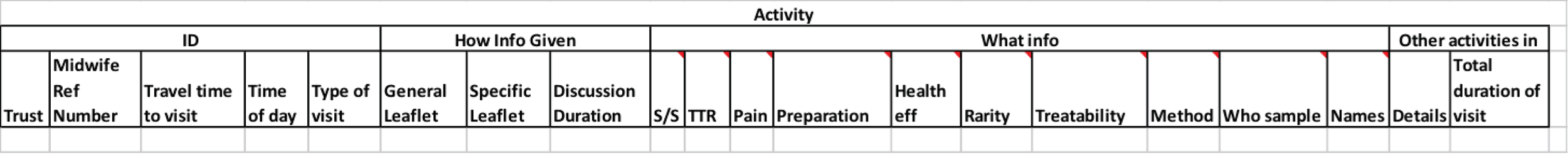
Appendix 5 Summary of identified economic evaluations of technologies used in newborn screening programmes
| Author and country | Intervention and comparator | Study viewpoint and population | Evaluation vehicle (type) and time horizon (discount rate) | Resource use and price year (currency) | Costs and harms related to information provision | Valuation of benefits | Key results |
|---|---|---|---|---|---|---|---|
| Cipriano et al. 2007,138 Canada (Ontario) | Intervention: MS/MS for 21 conditions; comparator: Guthrie test for PKU and hypothyroidism | Viewpoint: Canadian health service; study population: neonates born in Ontario in 1 year (n = 130,000) | Model based (decision tree); time horizon: lifetime (3%) | Resources: start-up costs, confirmatory testing, treatment, hospitalisation, social services and education; cost sources: primary data (trial), literature review; price year: 2004 (C$) | Costs: no; harms: yes. Quality of life decrement of between 0.01 and 0.03 for parents during the uncertain diagnosis period. The authors accounted for this decrement by decreasing each life-year saved by the quality of life loss | Life-years gained | Incremental analysis: yes. ICER: C$5,492,114 per life-year gained screening for PKU only, C$68,346 per life-year gained screening for PKU plus the 14 most cost-effective conditions. When parents experienced a quality of life decrement of 0.01, the ICER was C$73,500 per life-year gained for PKU plus the 14 most cost-effective conditions; when parents experienced a quality of life decrement of 0.03, the ICER was C$104,000 per life-year gained for PKU plus the 14 most cost-effective conditions |
| Feuchtbaum and Cunningham 2006,158 USA (California) | Intervention: MS/MS for screening for PKU; comparator: no screening for PKU | Viewpoint: Californian payers; study population: neonates born in California in 1 year (n = 540,000) | Model based (unspecified); time horizon: lifetime (3%) | Resources: personnel and administration, equipment, supplies, laboratory contracts, follow-up centres; cost sources: primary data (pilot study), literature review; price year: 2004 (US$) | Costs: no; harms: no | Life-years saved, cases detected, monetary benefits (for life-years saved), QALYs | Incremental analysis: yes. ICER: US$708,000 per life-year saved, US$132,000 per case detected, between US$11,000 and US$19,000 per QALY. Incremental net benefits: US$47.1M for the best-case scenario, US$14.1M for the worst-case scenario; benefit to cost ratio: US$9.32 for the best-case scenario, US$8.65 for the worst-case scenario |
| Insinga et al. 2002,159 USA (Wisconsin) | Intervention: MS/MS screening for 14 fatty acid disorders and organic acidaemias; comparator: no screening | Viewpoint: societal; study population: infants in the Wisconsin Newborn Screening Programme (n = 100,000) | Model based (decision tree); time horizon: lifetime (3%) | Resources: MS/MS screening test, MS/MS test confirmation (positive for MCADD), MS/MS test confirmation (negative for MCADD), lifetime carnitine supplementation, lifetime follow-up testing, routine hospital admission, neurological impairment; cost sources: literature review; price year: 2001 (US$) | Costs: no; harms: no | Life expectancy, QALYs | Incremental analysis: yes. ICER: US$41,862 per QALY |
| Norman et al. 2009,160 Australia | Intervention: MS/MS for five categories of disorders: aminoacidurias, urea cycle disorders, organic acidurias, MCADD and other fatty acid oxidation defects; comparator: individual screening for five categories of conditions | Viewpoint: health service; study population: neonates | Retrospective cohort based (before and after cohort study); time horizon: 4 years (6%) | Resources: screening (including follow-up testing for true-positive and false-positive cases), treatment of conditions, general health care; cost sources: primary data (trial), literature review; price year: 2002 (AU$) | Costs: no; harms: no | Life-years saved, death-years averted | Incremental analysis: yes. ICER: AU$472,913 per death averted, AU$10,779 per life-year saved |
| Pandor et al. 2004,119 UK | Intervention: MS/MS screening for PKU and MCADD; comparator: traditional screening for PKU only | Viewpoint: health and other public sector providers; study population: neonates (n = 100,000) | Model based (not specified); time horizon: lifetime (6%) | Resources: screening, treatment of condition, treatment of symptomatic presentation, social care and education; cost sources: literature review; price year: 2001 (UK£) | Costs: yes (£0.30 per specimen collected); harms: no | Life-years gained | Incremental analysis: yes. ICER: –£395 per life-year saved (intervention dominates) |
| Pollitt et al. 1997,43 UK | Intervention: MS/MS screening for a large range of conditions; comparator: standard screening for PKU | Viewpoint: health service; study population: neonates (n = 100,000) | Model based (decision tree); time horizon: lifetime (6%) | Resources: specimen collection costs, laboratory analysis, follow-up, treatment, misclassification; cost sources: primary data (surveys), literature review; price year: not reported | Costs: no; harms: no | Life-years saved | Incremental analysis: yes. ICER: £31 per life-year saved |
| Schoen et al. 2002,161 USA (California) | Intervention: MS/MS screening for PKU, galactosaemia, CHT and haemoglobinopathies; comparator: usual screening for the above conditions | Viewpoint: payer (HMO); study population: neonates (n = 100,000) | Model based (not reported); time horizon: lifetime (3%) | Resources: diagnosis, false-positive results, lifetime treatment; cost sources: literature review; price year: not reported (US$) | Costs: no; harms: no | QALYs | Incremental analysis: yes. ICER: US$5827 per QALY |
| Shamshiri et al. 2012,157 Iran | Interventions: various screening thresholds for CHT; comparator: the current cut-off point for Guthrie testing for CHT | Viewpoint: Iranian health service; study population: neonates (n = 10,000) | Model based (decision tree); time horizon: lifetime – up to 82 years (3%) | Resources: Guthrie test, confirmatory tests, diagnosis, laboratory tests, visits by physicians, drugs, education, care; cost sources: literature review; price year: not reported (US$) | Costs: no; harms: no | Disability-adjusted life-years (DALYs) | Incremental analysis: yes. ICER: –US$4580 per DALY (intervention dominates) for best-case scenario with a cut-off point of 5 mU/l |
| Tran et al. 2007,162 Canada (Nova Scotia) | Intervention: MS/MS screening for MCADD; comparator: clinical diagnosis of MCADD | Viewpoint: Canadian health-care system; study population: not reported explicitly | Model based (decision tree); time horizon: lifetime (not reported) | Resources: screening, acute episode, management, severe neurological impairment; cost sources: primary data (Nova Scotia Screening Programme), systematic review; price year: not reported (C$) | Costs: no; harms: no | QALYs | Incremental analysis: yes. ICER: C$2676 per QALY |
| Venditti et al. 2003,137 USA (Pennsylvania) | Intervention: MS/MS screening for MCADD; comparator: no screening | Viewpoint: societal; study population: infants up to age 19 years | Model based (decision tree and Markov model); time horizon: 20 and 70 years (3%) | Resources: screening and follow-up, confirmatory evaluation for positive screen, carnitine measurement in those screened for MCADD, care for those severely affected; cost sources: primary data (patient/family interviews), literature review, expert opinion; price year: 2001 (US$) | Costs: no; harms: yes (false-positive result: disutility between 0.01 and 0.03 for 3 months) | Life-years gained, QALYs | Incremental analysis: yes. ICER: US$11,000 per life-year gained (20 years), US$300 per life-year gained (70 years), US$5600 per QALY (20 years), US$100 per QALY (70 years) |
Appendix 6 Telephone data entry Excel spreadsheet
| Number | Question | Possible answers |
|---|---|---|
| Midwife initials | Midwife reference no. | |
| Before birth | ||
| 1 | Do you give information about NBS before birth? | Yes/no |
| 2 | Which of the following do you use to give information about screening? | Discussion |
| Screening For You and Your Baby | ||
| Bloodspot Screening For You and Your Baby | ||
| Other | ||
| 3 | When would you discuss NBS? | Date given |
| Category | ||
| 4 | Where would you discuss NBS? | Antenatal clinic |
| In hospital | ||
| At the parent’s home | ||
| Midwife-led delivery unit | ||
| 5 | How long do you spend discussing NBS? | Number given |
| Category | ||
| 6 | If you provide a leaflet, when would you do this? | Date given |
| Category | ||
| 7 | Where would you provide the leaflet? | Antenatal clinic |
| In hospital | ||
| At the parent’s home | ||
| Midwife-led delivery unit | ||
| After birth but before the test | ||
| 8 | Do you give information after the baby is born but before the test? | Yes/no |
| 9 | How long before the test would you give information? | Immediately before the test |
| 24 hours before the test | ||
| > 24 hours before the test | ||
| 10 | Where would you give this information? | In hospital |
| At the parent’s home | ||
| Midwife-led delivery unit | ||
| 11 | How would you give this information? | Discussion |
| Screening For You and Your Baby | ||
| Bloodspot Screening For You and Your Baby | ||
| Other | ||
| 12 | If you discuss screening with parents, how long would you spend doing this? | Number given |
| Category | ||
| Informed consent for NBS | ||
| 13 | Do you take informed consent for NBS? | Yes/no |
| 14 | How many parents would you see a week to take consent for NBS? | Number given |
| Category | ||
| 15 | Who do you prefer to take informed consent from? | Category |
| Other | ||
| 16 | If you prefer to gain informed consent from a certain person why is this? | Text answer |
| 17 | How do parents give consent? | Open answer but probably verbal or written |
| 18 | Do you use interpreters to help give information about NBS? | Yes/no |
| 19 | How frequently do you need to use interpreters? | Open answer but examples would be once a week/month, etc. |
| Providing information about repeat tests | ||
| 20 | If a repeat sample is needed, who explains the reasons for this to the parents? | Category |
| Other | ||
| 21 | If you explain why a repeat test is needed, how long would you spend on this? | Number given |
| Category | ||
| 22 | On average, how many second bloodspot samples do you take in a week? | Number given |
| Category | ||
| General questions about NBS | ||
| 23 | How important is presenting information relative to your other duties? | Category |
| 24 | Please explain your answer | Text answer |
| 25 | Do your other duties limit your ability to give information to parents? | Yes/no |
| 26 | Please explain your answer | Text answer |
| Some questions about you | ||
| 27 | What is your role in the NHS? | Free answer, ideally specific job title |
| 28 | What is your pay grade? | Category |
| 29 | What is the name of the NHS trust you work in? | Free answer |
| 30 | Is your trust involved in the pilot for expanded newborn screening? | Yes/no/don’t know |
| 31 | Do you have any other comments about providing information? | Text answer |
| 32 | Do you have any further comments about this survey? | Text answer |
| 33 | Would you be willing to receive information about further studies? | Yes/no |
Appendix 7 Summary of identified economic evaluations of newborn screening programmes
| Study and country | Intervention and comparator | Study viewpoint and population | Evaluation vehicle (type) and time horizon (discount rate) | Resource use and price year (currency) | Costs and harms related to information provision | Valuation of benefits | Key results |
|---|---|---|---|---|---|---|---|
| Carroll and Downs 2006,163 USA (Indiana) | Intervention: cost-effectiveness of each component part of a MS/MS screening panel; comparator: no screening | Viewpoint: societal; study population: not reported | Model based (decision tree); time horizon: lifetime (3%) | Resources: screening tests, caring for those with disease, sequelae from disease; cost sources: literature review, expert opinion; price year: 2004 (US$) | Costs: no; harms: no | QALYs | Incremental analysis: yes. ICER: US$4838.71 per QALY |
| Geelhoed et al. 2005,121 Australia | Intervention: PKU and CHT screening; comparator: symptomatic diagnosis (late detection) | Viewpoint: public sector; study population: newborns (n = 25,000) | Retrospective cohort based; time horizon: lifetime (5%) | Resources: programme (specimen collection, equipment, staff, reagents, paper and printing), treatment, intellectual disability, maternal PKU, productivity losses; cost sources: primary data (Western Australia screening programme), literature review; price year: 2001 (AU$) | Costs: yes (AU$6.54 per child screened); harms: no | Monetary benefit of a child becoming healthy rather than having intellectual disability (avoided costs from gain in life-years) | Incremental analysis: yes. ICER: cost per case of PKU or CHT detected AU$59,340; AU$4,375,442 total averted cost of PKU, AU$12,236,160 total averted cost of CHT, AU$2,879,776 net annual cost savings |
| Gessner et al. 1996,164 USA (Alaska) | Intervention: universal screening for SCD; comparator: targeted screening of African Americans for SCD | Viewpoint: payers; study population: not reported | Model based (decision tree); time horizon: 1.75 years (no discounting) | Resources: screening, physician visits, programme, medical and home care; cost sources: primary data (Oregon Public Health Laboratory), literature review; price year: 1993 (US$) | Costs: no; harms: no | Death-years averted, cases of mental retardation averted | Incremental analysis: yes. ICER: US$2,040,000 per death averted, US$53M per case of mental retardation averted |
| Hamers and Rumeau-Pichon 2012,167 France | Intervention: screening for five conditions plus MCADD and switching PKU screening to MS/MS; comparator: screening for current five conditions only | Viewpoint: societal; study population: birth cohort (n = 821,000) | Model based (decision tree); time horizon: lifetime (4%) | Resources: screening test, confirmatory test, treatment of MCADD sequelae; cost sources: literature review; price year: not reported (€) | Costs: no; harms: no | QALYs, life-years gained | Incremental analysis: yes. ICER: €19,478 per life-year gained (MCADD), €18,033 per QALY (MCADD), €8189 per life-year gained (MCADD with PKU), €7851 per QALY (MCADD with PKU) |
| Lanting et al. 2005,168 the Netherlands | Intervention: cost-effectiveness of various laboratory methods for the identification of children with CHT | Viewpoint: health service; study population: newborns (n = 1,181,079) | Retrospective cohort study based (cohort study); time horizon: 5 years (not reported) | Resources: laboratory, initial diagnostic tests; cost sources: primary data (Dutch Neonatal Screening Programme), literature review; price year: not reported | Costs: no; harms: no | Number of cases of CHT detected | Incremental analysis: no. Average cost per case detected by strategy: (T4) + TSH US$6353, T4 + TSH US$6209, T4 + TSH + TBG US$6851 |
| Panepinto et al. 2000,165 USA (not limited to one state) | Intervention: universal screening and targeted screening of African Americans for SCD; comparator: no screening | Viewpoint: health service; study population: newborns (n = 1,000,000) | Model based (Markov model); time horizon: birth to 3 years (3%) | Resources: screening test, confirmatory tests, follow-up, treatment of condition, treatment of serious sequelae; cost sources: literature review; price year: 1994 (US$) | Costs: no; harms: no | Life-years saved | Incremental analysis: yes. ICER: US$6709 per additional year of life saved (targeted screening vs. no screening), US$30,760 per additional year of life saved (universal screening vs. targeted screening) |
| Prosser et al. 2010,42 USA (not limited to one state) | Intervention: MS/MS screening for MCADD; comparator: clinical diagnosis of MCADD | Viewpoint: payers; study population: newborns (n = 100,000) | Model based (patient-level simulation); time horizon: lifetime (3%) | Resources: treatment, hospitalisation, caring for a child with developmental delay, screening test, clinical workup, treating a presumed diagnosis; cost sources: primary data (New England Newborn Screening Programme), literature review; price year: 2006 (US$) | Costs: no; harms: yes (TTO values: loss from false-positive results = 0.0005) | QALYs | Incremental analysis: yes. ICER: US$21,273 per QALY |
| Tiwana et al. 2012,139 USA (Texas) | Intervention: expanded screening programme (27 disorders); comparator: current screening programme (seven disorders) | Viewpoint: payers; study population: Texas birth cohort | Model based (Markov model); time horizon: lifetime (3%) | Resources: screening, confirmatory testing, false-positive results, disease management, disease sequelae; cost sources: literature review; price year: 2007 (US$) | Costs: no; harms: yes (Venditti et al.136 published disutility for false-positive result = 0.03) | QALYs | Incremental analysis: yes. ICER: US$11,560 per QALY |
| van den Akker-van Marle et al. 2006,169 the Netherlands | Intervention: different laboratory tests to identify children with CF: IRT-IRT, IRT-DNA, IRT-DNA-IRT, IRT-DNA-DGGE; comparators: comparison depended on strategy but comparators included no screening, IRT-DNA-DGGE and IRT-IRT | Viewpoint: health service; study population: neonates (n = 200,000) | Model based (not reported); time horizon: lifetime (3%) | Resources: organisation, screening and diagnosis, genetic counselling for carriers, clinical diagnosis of CF carriers, diagnosis of non-CF patients, treatment of patients identified by screening, treatment for clinically diagnosed patients; cost sources: literature review, expert opinions; price year: not reported (€) | Costs: no; harms: no | Life-years gained | Incremental analysis: yes. ICER: €24,800 per life-year gained IRT-IRT vs. no screening, €2,154,300 per life-year gained IRT-DNA vs. IRT-DNA-DGCE, €133,700 per life-year gained IRT-DNA-DGGE vs. IRT-IRT |
| van der Hilst et al. 2007,166 the Netherlands | Intervention: MS/MS screening for MCADD; comparator: no screening for MCADD | Viewpoint: societal; study population: newborns (n = 66,216) | Model based (decision tree); time horizon: lifetime (4%) | Resources: inpatient and outpatient visits, travel expenses, ambulance services, laboratory tests, consultations, diagnostic imaging, medication and food supplements, special education, institutionalisation, parents’ productivity losses; cost sources: primary data (five Dutch screening centres), literature review; price year: 2004 (US$) | Costs: no; harms: no | Life-years gained | Incremental analysis: yes. ICER: US$1653 per life-year gained |
| Wells et al. 2012,170 USA (Kentucky) | Cost and consequences comparison of two strategies of laboratory testing for CF: IRT-DNA and IRT-IRT | Viewpoint: societal; study population: newborns (n = 100,000) | Model based (decision tree); time horizon: from birth to confirmed diagnosis (not reported) | Resources: screening, laboratory equipment and personnel, insurance for parents and parents productivity (missed work, travel, etc.); cost sources: literature review; price year: 2010 (US$) | Costs: no; harms: no | Number of newborns diagnosed with CF | Incremental analysis: no. Cost $45,400 per diagnosis for IRT-IRT, $39,700 per diagnosis for IRT-DNA |
| Wildhagen et al. 1998,122 the Netherlands | Four strategies: prenatal screening [single-entry two-step couple screening (SETS) and double-entry two-step couple screening (DETS)], preconceptional screening (SETS and DETS), school screening and neonatal carrier screening; comparator: no CF gene carrier screening | Viewpoint: societal; study population: depended on the intervention – couples; schoolchildren in last year of compulsory education, neonates | Model based (simulation model); time horizon: 2 years (5%) | Resources: information provision before screening, testing, further diagnosis and treatment; cost sources: primary data (Dutch screening programme), literature review; price year: 1996 (UK£) | Costs: yes (£5.36 per child); harms: no | Number of detected carrier couples, number of avoided patients | Incremental analysis: no. Cost £58,000 per detected carrier couple (prenatal SETS), £70,000 per detected carrier couple (prenatal DETS), £69,000 per detected carrier couple (preconception SETS), £80,000 per detected carrier couple (preconception DETS), £85,000 per detected carrier couple (school screening), £21,000 per detected carrier couple (neonatal screening), £177,000 per avoided patient (prenatal SETS), £213,000 per avoided patient (prenatal DETS), £223,000 per avoided patient (preconception SETS), £258,000 per avoided patient (preconception DETS), £367,000 per avoided patient (school screening), £178,000 per avoided patient (neonatal screening) |
Appendix 8 Economic modelling electronic search strategy: example for MEDLINE
-
exp Infant, Newborn/
-
(neonat* or newborn or baby or babies or perinat*).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
-
1 or 2
-
exp Neonatal Screening/
-
(screen* or test* or program* or procedure).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
-
4 or 5
-
guthrie.ab,ti.
-
(blood spot* or bloodspot*).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
-
(heel-prick* or heelprick*).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
-
7 or 8 or 9
-
Economics/
-
exp ‘costs and cost analysis’/
-
Economics, Dental/
-
exp economics, hospital/
-
Economics, Medical/
-
Economics, Nursing/
-
Economics, Pharmaceutical/
-
(economic$or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab.
-
(expenditure$not energy).ti,ab.
-
value for money.ti,ab.
-
budget$.ti,ab.
-
or/1–11
-
((energy or oxygen) adj cost).ti,ab.
-
(metabolic adj cost).ti,ab.
-
((energy or oxygen) adj expenditure).ti,ab.
-
23 or 24 or 25
-
22 not 26
-
letter.pt.
-
editorial.pt.
-
historical article.pt.
-
28 or 29 or 30
-
27 not 31
-
exp animals/not humans/
-
32 not 33
-
bmj.jn.
-
‘cochrane database of systematic reviews’.jn.
-
health technology assessment winchester england.jn.
-
journal of medical economics.jn.
-
35 or 36 or 37 or 38
-
34 not 39
-
3 and 6 and 10 and 22 and 27 and 32 and 34 and 40
Appendix 9 Model parameters and structure
| Variable | Base-case value | Values used in one-way sensitivity analysis | Distribution used in PSA |
|---|---|---|---|
| Probabilities | |||
| Receiving an individual discussion late in pregnancy in current actual practice | 0.35 | Not appropriate | X ≈ Beta(7,13) |
| Receiving information on day 5 as opposed to day 3 in current actual practice | 0.90 | Not appropriate | X ≈ Beta(18,2) |
| Receiving information in an antenatal class in personalised or universal practice | 0 | 0.25, 0.50, 0.75, 1.00 | X ≈ Beta(1,1) |
| Requesting information based on individual discussion in personalised practice | 0.5 | 0, 0.25, 0.75, 1.00 | X ≈ Beta(1,1) |
| Requesting individual discussion after initially requesting written materials in personalised practice | 0 | 0.25, 0.50, 0.75, 1.00 | X ≈ Beta(1,1) |
| Requiring a repeat sample | 0.044 | ||
| Receiving a first sample true-positive result | 0.01 | ||
| Receiving a false-negative result | 0 | ||
| Receiving an ‘urgent’ positive result | 0.066 | ||
| Receiving a ‘non urgent’ positive result | 0.934 | ||
| Decision-making is affected in current actual practice | 0 | X ≈ Triangular(0,1,1) | |
| Decision-making is affected in personalised, universal and current recommended practice | 0 | 0.25, 0.5, 0.75, 1 | X ≈ Triangular(0,1,0) |
| Outcomes | |||
| Quality of life of a healthy individual | 0.91366 | ||
| Quality of life decrement caused by repeat samples | 0.01825 | 0.01, 0.05 | X ≈ Gamma(0.50,0.02) (QALY loss) |
| Duration of quality of life decrement | 3 months | 2 weeks, 1 year | X ≈ Gamma(0.50,0.02) (QALY loss) |
| Costs (£) | |||
| Parents in the personalised practice group choose discussion-based information and receive information in a group appointment | 21.45 | X ≈ Gamma(82.43,0.26) | |
| Parents in the personalised practice group choose discussion-based information but do not receive information in a group appointment | 20.61 | X ≈ Gamma(101.12,0.20) | |
| Parents in the personalised practice group choose leaflet-, internet- and app-based information but then ask for a discussion later | 21.53 | X ≈ Gamma(81.05,0.27) | |
| Parents in the personalised practice group choose leaflet-, internet- and app-based information and do not ask for a discussion later | 16.48 | X ≈ Gamma(1034.64,0.02) | |
| Parents in the universal practice group receive information in a group appointment | 21.45 | X ≈ Gamma(82.43,0.26) | |
| Parents in the universal practice group do not receive information in a group appointment | 20.61 | X ≈ Gamma(101.12,0.20) | |
| Current recommended practice | 24.83 | X ≈ Gamma(44.23,0.57) | |
| Parents in the current actual practice group receive a discussion late in pregnancy | 20.24 | X ≈ Gamma(91.44,0.22) | |
| Parents in the current actual practice group do not receive a discussion late in pregnancy | 17.49 | X ≈ Gamma(234.14,0.08) | |
| Repeat sample information | 18.41 | X ≈ Gamma(95.96,0.19) | |
| GP visits for parents of children receiving false-positive or repeat results that are later confirmed to be urgent positive results | 65 | ||
| GP visits for parents of children receiving false-positive or repeat results that are later confirmed to be non-urgent positive results | 130 | ||
| GP visits for parents of children receiving false-positive or repeat results that are later confirmed to be negative results | 130 | ||
Appendix 10 Presentation shown to health professionals during the focus groups






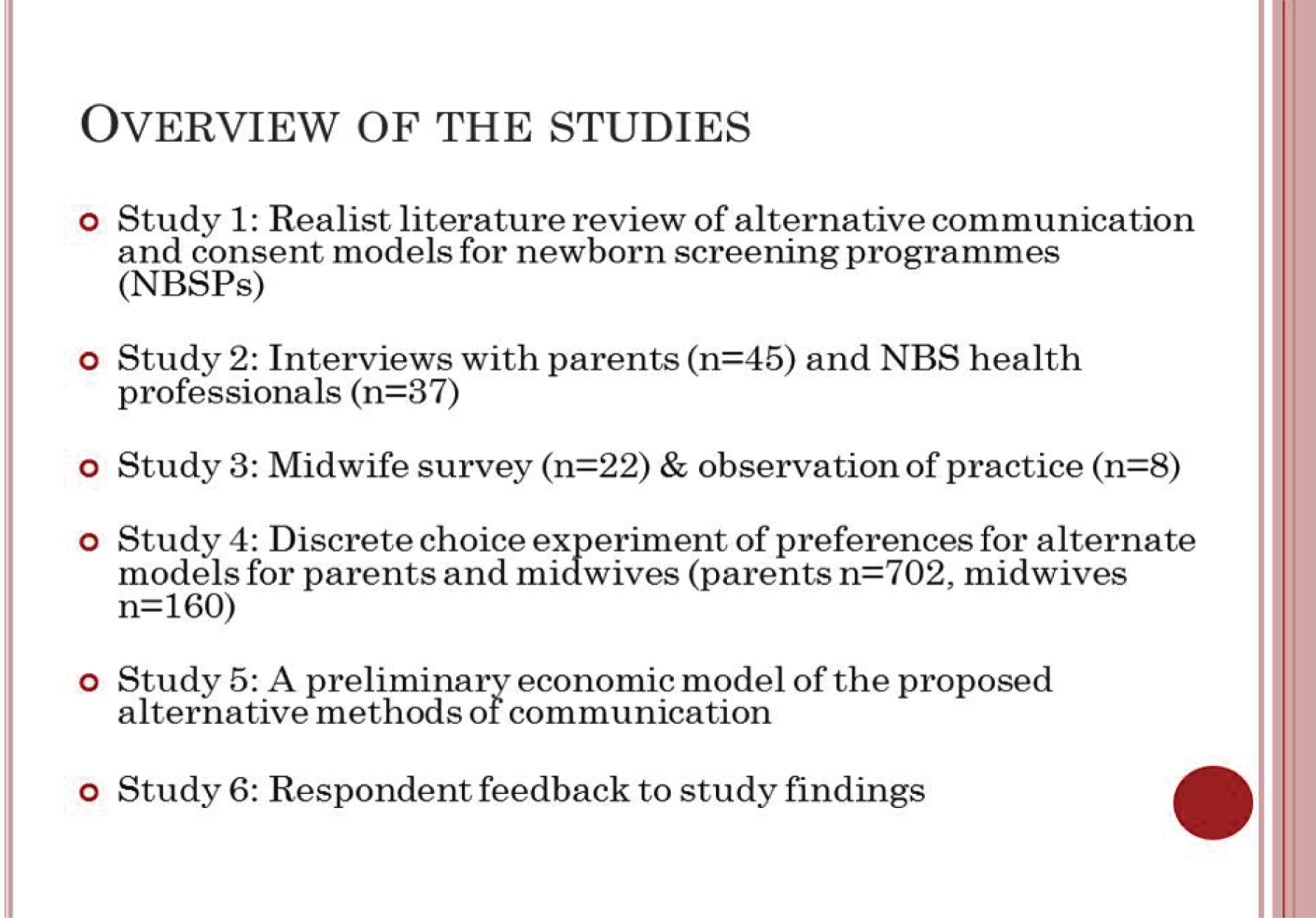



Appendix 11 Focus group written notes
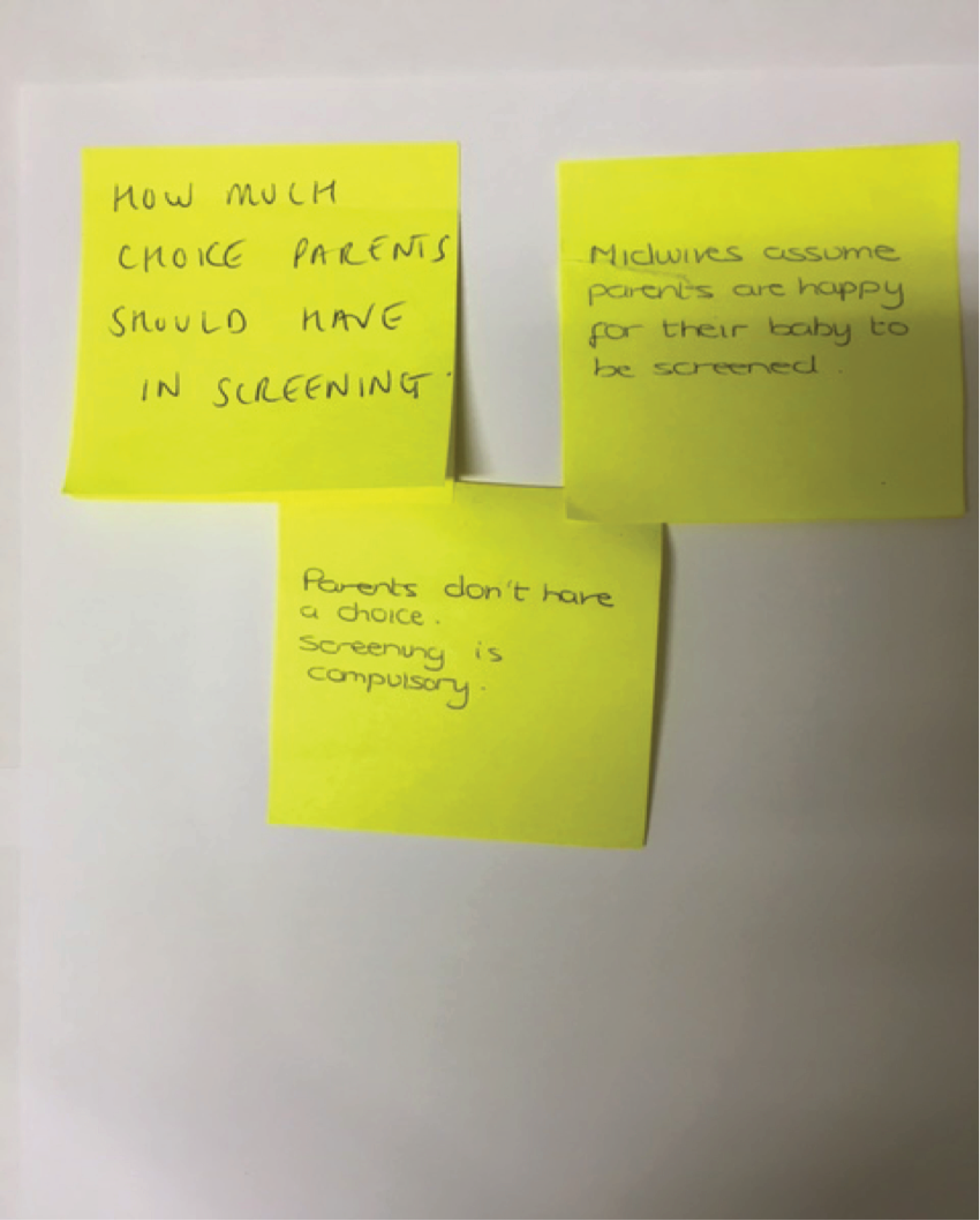


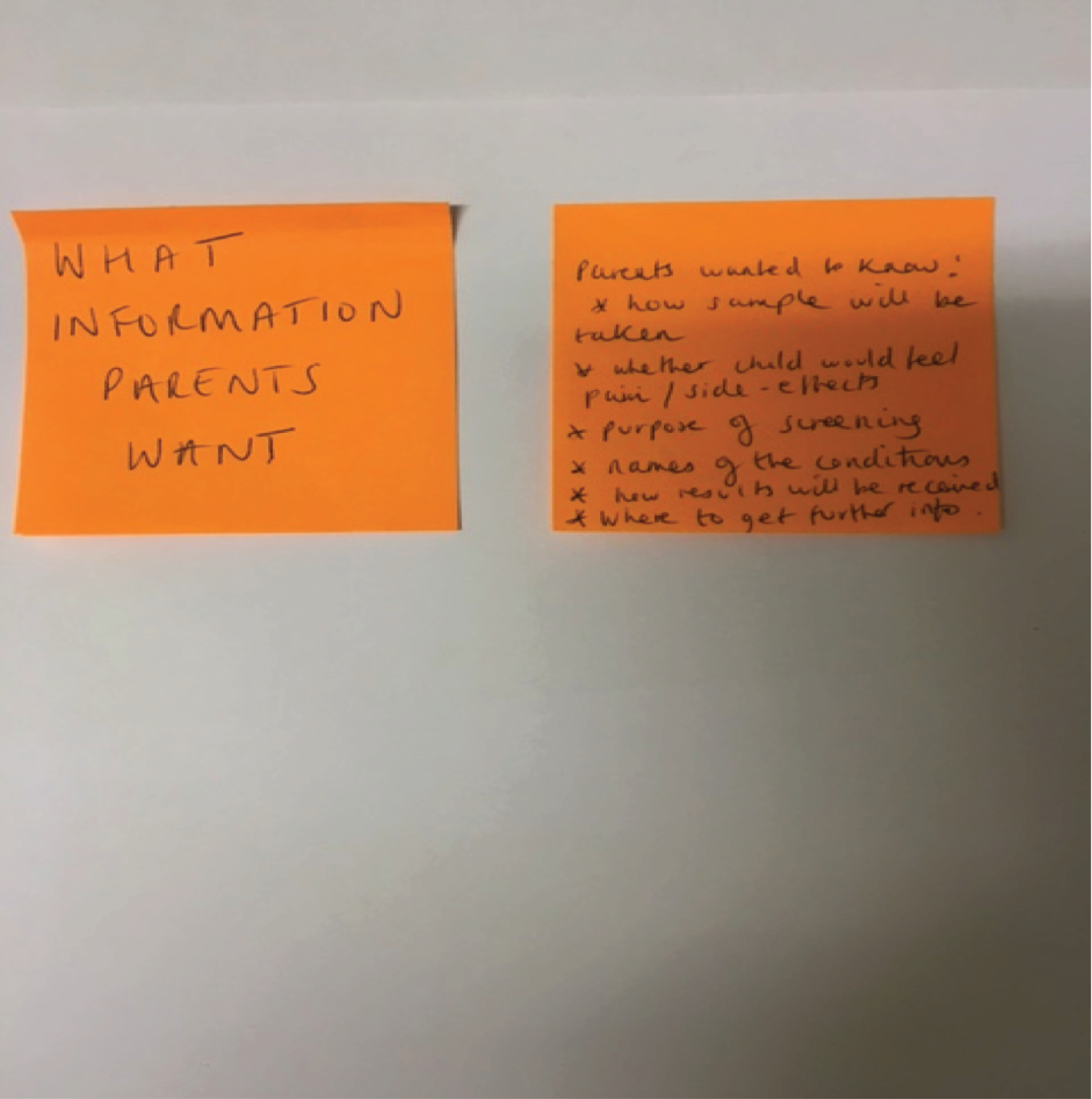
Appendix 12 Summary of the study findings sent to telephone interviewees
Providing Information about Newborn Screening (PINSA)
Summary of the study findings
Thank you once again for taking part in our interview study. The views you shared with us in the interviews were very important and helpful. We would now like to hear your thoughts on our findings.
Main findings
Across the different studies, the messages from parents and midwives focused on four main areas:
-
when information should be given to parents
-
what information should be given to parents
-
how information is given
-
parent choice in newborn screening.
When information should be given to parents
-
Parents and midwives thought that information about newborn screening should be given for the first time in pregnancy and not after birth.
-
Information should be ‘drip fed’ at multiple time points, with added reminders towards the end of pregnancy.
-
The third trimester/36 weeks is the ideal time to discuss newborn screening.
-
Parents should be asked to consent for screening when discussing their birth plan.
What information should be given to parents
-
Purpose of screening and why it is important.
-
Names of the conditions being screened.
-
How the sample will be taken.
-
Whether the baby will feel any pain or side effects.
-
When and how the results will be received.
-
What has changed (for parents who have been through the screening process with previous children).
-
Where to get further information.
-
What will happen to the baby’s bloodspot sample card after screening.
How information is given
-
Rather than everyone receiving the same leaflet, a range of information resources are available, for example leaflet, website, app and video clip, and parents can choose the format best for them.
-
Make the provision of newborn screening information more parent led.
-
Modernise information through technology, for example apps and websites.
-
Brief discussion with a midwife is still required to introduce and signpost parents to information resources.
-
Minimise information overload by separating NBS information.
-
Check parents’ understanding of information.
Parent choice in newborn screening
-
Parents want to be informed and be more active in the information exchange.
-
The majority of parents supported compulsory and assumed screening providing that they had received adequate information in advance.
We also want to know what strategies you think would be effective when providing information about newborn screening to parents and we will ask you more about that when we speak with you, for example what you think about our message about when and how information is given.
Many thanks once again. Please do get in touch if you have questions or would like to know more before giving your feedback. To keep up to date with study news, please visit our website (www.psych-sci.manchester.ac.uk/PINSA) or our Twitter page (@PINSAstudy).
If you are interested in where our findings have come from:
-
We interviewed a total of 45 parents and 37 health professionals from around the country about their views and experiences.
-
To find out more about current information-giving practice, we surveyed 22 midwives and observed eight midwives in practice.
-
We also conducted an online survey with 702 parents and 160 midwives to find out more about what information strategies parents and midwives preferred.
-
We conducted focus groups and telephone interviews with parents and health professionals to gather feedback on our study findings and recommendations for the future.
Appendix 13 Realist review search strategies
Newborn screening and consent search strategy
-
newborn screening or new born screening or neonatal screening or blood spot screening or bloodspot screening or screening in the newborn or Guthrie test or heel prick test or PKU screening or phenylketonuria screening or CHD screening or congenital heart disease screening or MCADD screening or medium-chain-acyl-CoA dehydrogenase deficiency screening or CF screening or cystic fibrosis screening or SCD screening or sickle cell screening
-
proxy consent or paren* consent or parent* discretion or parent* decision making or routinised or mandatory or informed consent or informed choice or parent* choice or parent* autonomy or best interests or explicit consent or implied consent or presumed consent or verbal consent or written consent or intellectual capacity or intentionality or coerc* or retention or understanding or relevant information
-
1 AND 2
All results limited to title and abstract in all databases.
Informed consent theory search
Six databases [EMBASE, Scopus, PubMed, PsycINFO, Web of Science, HMIC (Health Management Information Consortium)]
Terms
-
informed consent
-
theor* OR concept* OR defin* OR framework OR model
-
1 AND 2
Appendix 14 Parent demographic form
Appendix 15 Discrete choice experiment cognitive interview schedule
Appendix 16 Information provision strategies before the bloodspot sample is taken
FIGURE 10.
Information provision strategies before bloodspot sample is taken.
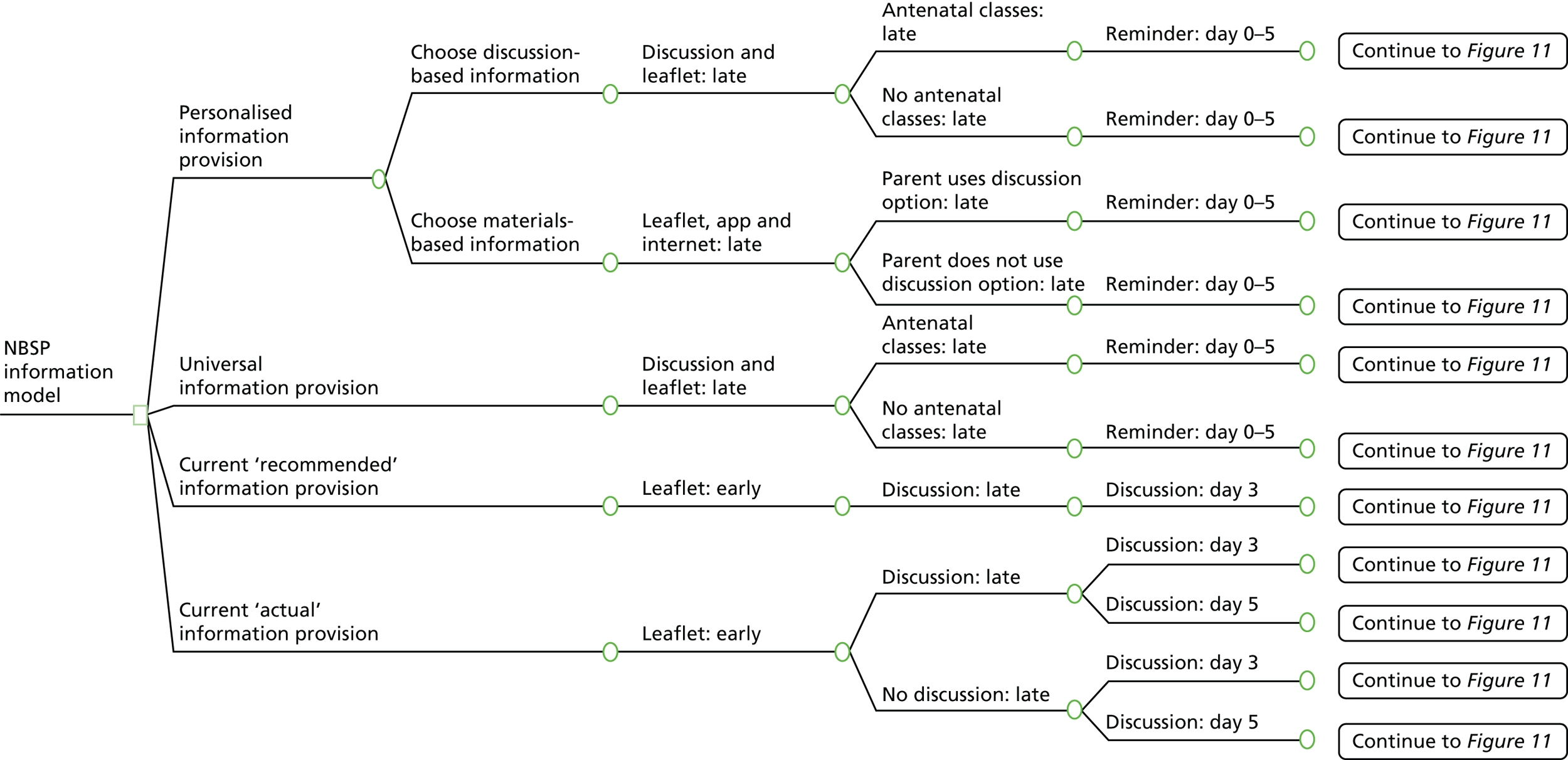
Appendix 17 Post-sample events
FIGURE 11.
Post-sample events.
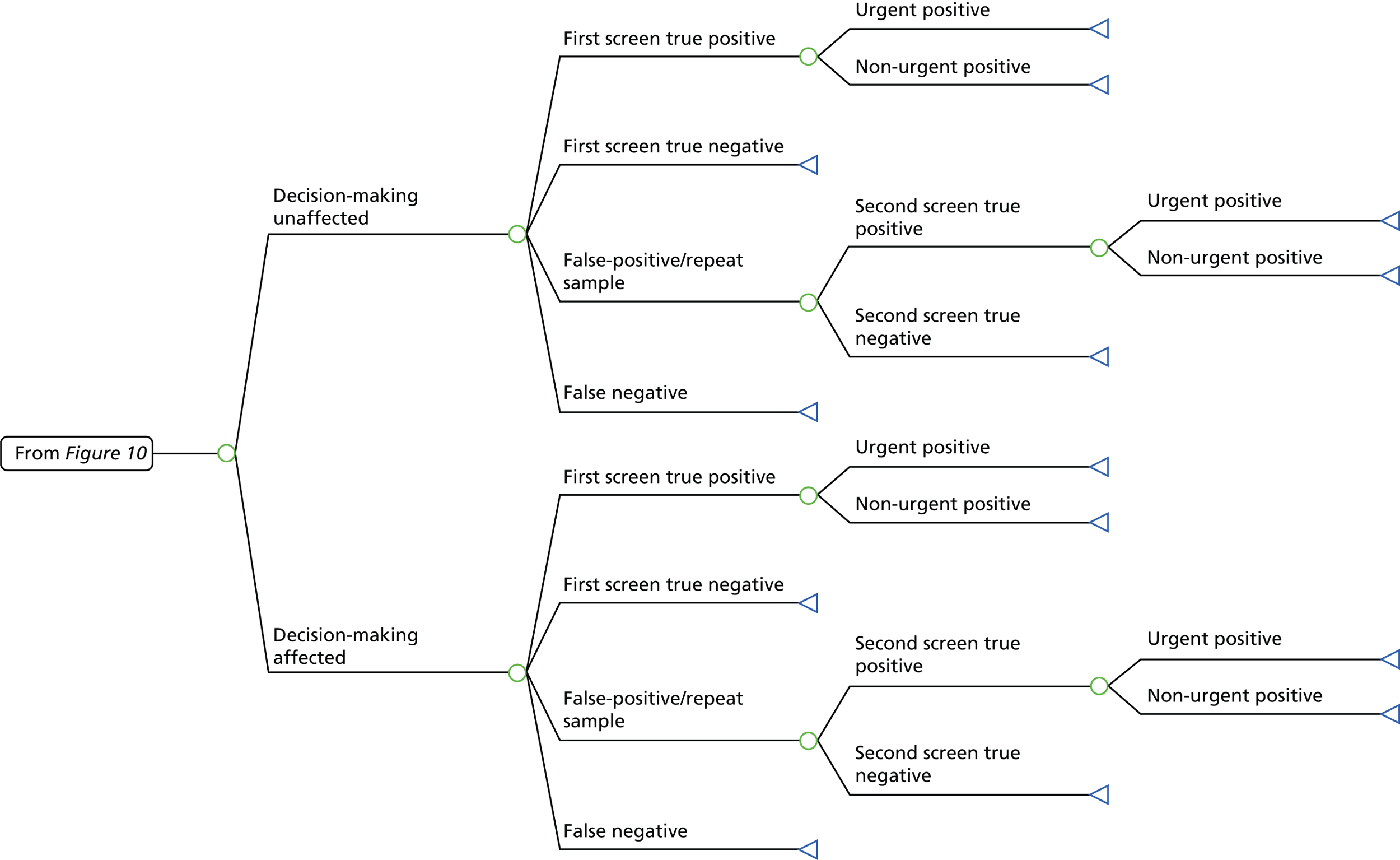
Appendix 18 Description of decision tree branches
| Tree label | Definition |
|---|---|
| Personalised information provision | |
| Choose discussion-based information | The mother chooses to receive information based on an individual discussion rather than in written materials |
| Choose materials-based information | The mother chooses to receive information based on written materials: a leaflet, website-based information and a smartphone app |
| Discussion and leaflet: late | Parents receive 11 types of information in an individual discussion, supported by a leaflet. Information is provided late in pregnancy |
| Leaflet, app and internet: late | Parents receive information by way of a leaflet, website and smartphone app. Information is provided late in pregnancy |
| Antenatal classes: late | Parents receive information in antenatal classes late in pregnancy |
| No antenatal classes: late | Parents do not receive information in antenatal classes late in pregnancy |
| Parent uses discussion option: late | Parents who choose to receive information by way of written materials later choose to additionally receive information in a discussion. This information is provided late in pregnancy |
| Parent does not use discussion option: late | Parents who choose to receive information by way of written materials do not later choose to additionally receive information in a discussion |
| Brief reminder: days 0–5 | Parents receive a short reminder about NBS between birth and the sample being taken |
| Universal information provision | |
| Discussion and leaflet: late | Parents receive 11 types of information in an individual discussion, supported by a leaflet. Information is provided late in pregnancy |
| Antenatal classes: late | Parents receive information in antenatal classes late in pregnancy |
| No antenatal classes: late | Parents do not receive information in antenatal classes late in pregnancy |
| Brief reminder: days 0–5 | Parents receive a short reminder about NBS between birth and the sample being taken |
| Current recommended information provision | |
| Leaflet: early | Parents receive a leaflet early in pregnancy |
| Discussion: late | Parents receive 11 types of information in an individual discussion late in pregnancy |
| Discussion: day 3 | Parents receive 11 types of information on day 3 post birth in an individual discussion |
| Current actual information provision | |
| Leaflet: early | Parents receive a leaflet early in pregnancy |
| Discussion: late | Parents receive six types of information in an individual discussion late in pregnancy |
| Discussion: day 3 | Parents receive six types of information on day 3 post birth in an individual discussion |
| Discussion: day 5 | Parents receive six types of information on day 5 post birth in an individual discussion |
| Post-sample tree | |
| Decision-making unaffected | Parents’ ability to make decisions about their child’s health is not affected as a result of the information that they are given. They do not experience additional anxiety if their child requires a repeat sample and will not visit their GP unnecessarily because of any anxiety |
| Decision-making affected | Parents’ ability to make decisions about their child’s health is affected as a result of the information that they are given. They may experience additional anxiety if their child requires a repeat sample and may also visit their GP unnecessarily because of this anxiety |
| First screen true positive | A positive result is returned from screening |
| First screen true negative | A negative result is returned from screening and the child does not later develop an illness. This is an end point for the model |
| False-positive/repeat sample | The initial results of the first screening sample are equivocal or the initial sample was inadequate for avoidable reasons and another sample is required for confirmation |
| False negative | The screening returns a negative result. However, the result is false and the child later develops one of the conditions. This is an end point for the model. Because of the difficulty in identifying false-negative cases, it is assumed that no children receive a false-negative result |
| Second screen true negative | The second sample is returned with a negative result. This is an end point for the model |
| Second screen true positive | The second sample is returned with a true-positive result |
| Urgent positive | Children receiving positive results for MCADD, MSUD, IVA or GA1 are immediately asked to attend their local hospital so that diagnostic tests can be completed and treatment started. This is an end point for the model |
| Non-urgent positive | Children receiving positive results for PKU, CHT, CF, SCD or HCU are referred to the relevant health-care professional within a week of the results being received from the laboratory |
Glossary
- False positive
- Some women are told that tests have shown that their baby may have a problem. If further tests then show that this is not the case, that result is called a false positive.
- National Screening Committee
- The UK National Screening Committee is a national advisory body that makes recommendations about screening for the Department of Health.
- Newborn Bloodspot Screening Programme
- The Newborn Bloodspot Screening Programme’s overall objective is the assurance of high-quality screening services for babies and their parents.
- Newborn (neonatal) screening
- A public health screening programme to screen newborn children for the presence of certain metabolic or genetic conditions. Screening is carried out within days of birth to identify infants at increased risk of specific genetic or endocrine disorders so that treatment can begin as soon as possible. When a newborn screening result is ‘out of the expected range’, further diagnostic testing is usually required to confirm or specify the results.
- Positive result
- A positive result is a result which shows that the child does have (or is likely to have) the condition that is tested for. Sometimes people will say that the child is affected.
- Royal College of Midwives
- The Royal College of Midwives is the only professional organisation and trade union dedicated to serving midwifery and the whole midwifery team, providing workplace advice and support, professional and clinical guidance and information, and learning opportunities, including a broad range of events, conferences and online resources.
List of abbreviations
- AAP
- American Academy of Pediatrics
- app
- application
- CF
- cystic fibrosis
- CHT
- congenital hypothyroidism
- CI
- confidence interval
- DCE
- discrete choice experiment
- DNA
- deoxyribonucleic acid
- DVD
- digital versatile disc
- EVPI
- expected value of perfect information
- GA1
- glutaric aciduria type 1
- GP
- general practitioner
- HCU
- homocystinuria
- HIOS
- Health Information Orientation Scale
- HTA
- health technology assessment
- ICER
- incremental cost-effectiveness ratio
- IVA
- isovaleric acidaemia
- MCADD
- medium-chain acyl-CoA dehydrogenase deficiency
- MS/MS
- tandem mass spectrometry
- MSUD
- maple syrup urine disease
- NBS
- newborn (neonatal) bloodspot screening
- NBSP
- Newborn Bloodspot Screening Programme
- NETSCC
- NIHR Evaluation, Trials and Studies Coordinating Centre
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PKU
- phenylketonuria
- PPC
- Patient Preference for Control
- PPI
- patient and public involvement
- PSA
- probabilistic sensitivity analysis
- QALY
- quality-adjusted life-year
- R&D
- research and development
- RCM
- Royal College of Midwives
- SCD
- sickle cell disorder
- SQAM
- senior quality assurance manager
- WTP
- willingness to pay