Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 13/18/05. The contractual start date was in September 2014. The draft report began editorial review in February 2017 and was accepted for publication in August 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Billie Hunter’s professorship is partly funded by the Royal College of Midwives.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Paranjothy et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2017 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Breastfeeding rates in the UK
The benefits of breastfeeding for the short- and longer-term health and well-being of babies and mothers in low- and high-income countries are well established. 1 If 45% of women in the UK exclusively breastfed for 4 months, it is estimated that at least £17M could be saved in treatment costs annually for acute illness in infants, in addition to incremental benefits over the lifetime of each annual cohort of first-time mothers. 2
The UK has exceptionally low breastfeeding rates. 1 The 2010 Infant Feeding Survey3 indicated that the majority of mothers in the UK (81%) initiate breastfeeding but that around two-thirds of these women stop breastfeeding before 6 weeks. For most women this is earlier than planned. 1 Only 1% of mothers in the UK currently exclusively breastfeed for 6 months,3 which is the World Health Organization (WHO)-recommended duration. 4 In 2010, eight in 10 mothers who stopped breastfeeding in the first 6 weeks did so before they had planned to, whereas, over the first 9 months, around three-quarters of mothers who stopped had intended to continue for longer. 3 Women’s experience of breastfeeding is not always straightforward, with around one-third reporting problems. In the first weeks, the most commonly given reasons for stopping breastfeeding are a perception of ‘insufficient milk’, a perception that the baby is rejecting the breast, ‘painful breasts/nipples’ and finding that breastfeeding takes too long or is tiring. 1
There are marked inequalities in breastfeeding rates. Geographically, low breastfeeding rates correlate with higher indices of social deprivation. 5 Younger mothers (aged < 20 years) of white British ethnicity and of lower socioeconomic status are less likely to start or continue breastfeeding beyond 6 weeks. 1 Midwives and health visitors provide professional support for breastfeeding and the majority of maternity units and health-visiting services are now working towards the United Nations International Children’s Emergency Fund (UNICEF)’s UK Baby Friendly Initiative (BFI) standards for support with infant feeding. 6 Nonetheless, mothers who give birth in the UK frequently feel underprepared for breastfeeding and many mothers who might benefit from breastfeeding support do not access professional help. 7
Medical conditions that prevent women from breastfeeding are rare;8 infant feeding decisions involve a complex interplay of psychological, social and cultural factors. 9 At the level of the individual mother, motivation to breastfeed and breastfeeding self-efficacy are associated with continuation of breastfeeding. 10–13 However, a broader set of social and societal drivers are at play, many of which can interact with individual mothers’ confidence, self-efficacy and determination to breastfeed. Extensive marketing of formula milk can denormalise breastfeeding;14 social attitudes and norms, including attitudes and norms of experiencing breastfeeding vicariously, can affect mothers’ confidence; and women’s work and employment conditions can make decisions to continue breastfeeding more difficult. 9,15
Women who are supported and encouraged to breastfeed by key members of their social network are more likely to start and continue breastfeeding for longer. 16 A review of the literature on differences between mothers who continue to breastfeed until 6 months and those who stop indicated that feeding intention and self-efficacy are inter-related with factors relating to social support. 17 Several UK studies have confirmed that attitudes, perceptions and experiences of immediate family members and friends have a strong influence on breastfeeding. 18–22 Mothers benefit from being part of a supportive community of other mothers who breastfeed,23 and women who have friends who have breastfed are more likely to breastfeed their own baby. 1 On the other hand, negative or mixed messages from partners, family, friends and health-care professionals can be confusing and can undermine decisions to breastfeed. 14,22,24 New approaches to support women who are at the highest risk of not continuing breastfeeding are urgently needed. There is a need for interventions that make appropriate use of theory and take into account the circumstances of women who are least likely to continue breastfeeding.
Breastfeeding peer-support interventions
In her concept analysis of ‘peer-support’ interventions, as applied to a wide range of health topics, Dennis25 notes that peer-support interventions seek to extend ‘natural embedded social networks and complement professional health services’. Dennis25 defines peer support as ‘the provision of emotional, appraisal and motivational assistance by a created social network member who possesses experiential knowledge of a specific behaviour or stressor, and has similar characteristics to the target population’. The importance of ‘similar characteristics’ relates to the principle of homophily,26 a key underpinning idea for peer-support interventions. This is the principle that (health education) messages will be more credible and support offered more acceptable because the peer delivering the message and offering the support is perceived by the recipient as being in some way similar to him- or herself – someone who is experiencing or who has experienced the problem being addressed and who shares the same frame of reference in terms of wider social and cultural norms and values.
Breastfeeding peer-support (BFPS) interventions that have been subject to experimental study have paid varying levels of weight to the principle of homophily. Peer supporters tended to be women who had experience of breastfeeding, in some cases from a similar sociodemographic and cultural background to the women whom they were supporting. This principle is itself linked to social learning theory,26 the idea that individuals compare themselves with others who occupy a social role to which they aspire and posits that people learn from one another through mechanisms of observation, imitation and modelling. Compared with health-care professionals, peer supporters may be more approachable, provide role models that mothers can relate to and have direct experience of the challenges of breastfeeding within a social context where it may not be the norm.
A second key underpinning principle for BFPS is the theory of social support, used to explain the ways in which social networks help individuals to manage stressful events. Four types of social support have been distinguished:27 emotional support, instrumental support, informational support and appraisal support. Informational support involves advice and suggestions that can be used to solve problems. Emotional support comes from sharing life experiences and providing empathy, love and caring built on relationships of trust. Instrumental support consists of providing tangible aid and services. Appraisal support facilitates self-evaluation through constructive feedback, for example through motivational interviewing (MI). 28 Intervention theorists distinguish between perceived support (i.e. the mother knows the help is there if she needs it and that in itself helps her to get through a stressful experience) and received support (direct interaction with the peer). The perception that help will be available when needed may be an attribute of BFPS interventions. 29
Breastfeeding peer-support interventions exhibit considerable design heterogeneity. 30 In some cases, BFPS is integrated within an existing health-care system, with peer supporters working alongside/reporting to health-care professionals. In other cases, the support is developed by a third-sector agency and delivered in community settings. Help is sometimes provided on a one-to-one basis (mother to peer) and is sometimes delivered in group settings. Modes of delivery include face to face, over the telephone, by text and online (e-mail, social media, forums). Some interventions are proactive (the peer contacts the mother directly), whereas others are reactive (the mother asks for help). Proactive interventions vary in intensity (the number of contacts) and in the timing of delivery (antenatal or postnatal; starting within 24 hours of the birth or several days afterwards).
Experimental evidence for the effectiveness of BFPS provides an unclear picture. A Cochrane review of ‘additional support’ from lay and professional supporters found that additional help can have an impact on breastfeeding rates. 31 The reviewers concluded that help is more likely to be effective in areas with high initiation rates, that face-to-face interventions are more likely to succeed and that reactive support is unlikely to be effective. The authors also recommended that support should be delivered in a predictable manner and be tailored to the needs of the population group targeted. A systematic review of 11 randomised controlled trials (RCTs) of antenatal BFPS found that targeted antenatal BFPS may lead to increases in breastfeeding initiation rates, whereas universal BFPS interventions tended not to be effective. 32
Another systematic review of RCTs looked at the impact of BFPS interventions on exclusive breastfeeding and breastfeeding continuation rates. 33 This review found these interventions to be effective in increasing breastfeeding maintenance in low- or middle-income countries, reducing the risk of not exclusively breastfeeding by up to 28%. However, the UK-based RCTs of BFPS interventions included in this review did not find increases in breastfeeding continuation rates,34–37 with no increase in breastfeeding maintenance at 8–10 weeks35,37 and 4 months. 36
Two quasi-experimental UK-based studies of BFPS have been published. The first, a community-based controlled trial of peer support delivered in a low-income area with very low breastfeeding rates (around 10%) resulted in no overall change in continuation rates at 6 weeks. 38 More recently, a time series analysis of a UK-based BFPS intervention delivered to a geographically defined population of adolescents found that, after adjusting for underlying trends, by the end of the study period, an additional 6.6 women in every 100 were initiating breastfeeding. 39
The UK-based interventions that have been studied were delivered as low-intensity interventions34,37,38 and several did not include an intended first contact with the mother in the days after the birth;34–36 in one UK-based study mothers were not contacted until their babies were around 3 months old. 36 In a UK context, this lack of early contact means that the intervention misses an important window, as breastfeeding discontinuation in the UK is highest during the early days and weeks after birth. 1 Four UK-based RCTs reported difficulty in achieving the intended number of contacts. 34,37–39
Motivational interviewing
Motivational interviewing is a counselling approach that is designed to build a client’s confidence and motivation for change, with a focus on eliciting the client’s reasons for behaviour change. MI is a well-defined approach that could be used within the context of BFPS to help provide a clear model for BFPS provision. Miller and Rollnick28 developed MI to be less confrontational, authoritarian and directing than other counselling styles that were available in the 1980s. MI addresses the therapist’s ‘righting reflex’ wherein therapists have the desire to ‘fix’ what seems to be wrong and tell the client how to change. MI has been called a person-centred collaborative conversation,40 as it is designed to ‘strengthen personal motivation for and commitment to a specific goal by eliciting and exploring the person’s own reasons for change within an atmosphere of acceptance and compassion’ (p. 29). 28 It was initially developed to help people with addictions, but has since been used in many areas such as medication adherence, weight loss and dental health care. 41,42
Motivational interviewing has been demonstrated to be effective across many areas of health. There have been at least 12 systematic reviews that have found statistically significant effects of MI in relation to health outcomes41–52 and three RCTs53–55 examining MI and breastfeeding support. A health educator,53 a research nurse54 and a practice nurse55 delivered the MI in the RCTs. Two of these RCTs53,54 found no significant effect of MI. The other RCT55 found statistically significant effects of MI on breastfeeding status at 2 and 4 months but not at 6 months post birth. In all three RCTs, it was difficult to disentangle the effects of MI from the other aspects of the intervention. Two of the interventions were MI-based interventions, in which only elements of MI were delivered. 53,55 None of the RCTs was based in the UK. It is possible that MI has a role in helping women to continue breastfeeding by increasing their intrinsic motivation to breastfeed, but there is limited evidence available on the effectiveness of MI in this context. The feasibility and acceptability of using a MI-based approach within a BFPS intervention has not been investigated.
The behaviour change wheel
Developing a complex intervention that utilises both peer support and MI-based techniques to support breastfeeding continuation requires integration of the MI and peer-support approaches, identification of potential mechanisms and consideration of how the intervention could be implemented. The behaviour change wheel (BCW) provides a unified and systematic framework for developing and characterising complex behaviour change interventions. 56 The BCW outlines a process for working out what needs to change (sources of behaviour), how to change it (intervention functions and behaviour change techniques) and how the intervention can be implemented (mode of delivery). 56 Within the BCW framework, the capability opportunity motivation – behaviour (COM-B) model helps to explain how interactions between people’s physical and psychological capability (C), social and physical opportunity (O) and automatic and reflective motivation (M) can influence behaviour (B). 57 The BCW uses the Behaviour Change Technique Taxonomy v1 (BCTTv1)58 to identify and classify the content of behaviour change interventions. The affordability, practicability, effectiveness and cost-effectiveness, acceptability, side effects and safety and equity (APEASE) criteria are used within the BCW process as a control point to consider the feasibility of an intervention. 56 The BCW process would therefore provide a unified framework for developing and characterising a MI-based BFPS intervention that could both guide its design and categorise the behaviour change techniques included in the intervention. This would provide a much greater understanding of the potential mechanisms of the intervention, which would facilitate future evaluation, refinement and replication of the intervention.
Mam-Kind: a UK feasibility study
The National Institute for Health Research Health Technology Assessment programme called for primary research in the form of a feasibility study to answer the following research question: ‘Can peer support for breastfeeding in the UK contribute to the maintenance of breastfeeding, particularly in groups of the population who are less likely to breastfeed?’.
This study aimed to develop and test the feasibility and acceptability of delivering a BFPS programme using a MI approach. The target population was women living in areas with lower than average breastfeeding initiation rates and high levels of social deprivation, who have expressed an interest in breastfeeding. We identified the key feasibility questions to be addressed prior to a full trial (outlined below) and designed our study to address these.
Although BFPS is recommended as part of the strategy for increasing breastfeeding rates in the UK, current National Institute for Health and Care Excellence (NICE) guidance does not specify how this should be provided, resulting in a variety of models being used across the UK. We therefore planned a rapid evidence review to understand how BFPS is currently provided in the UK and identify any underpinning theoretical models, elements of best practice and facilitators of, and barriers to, implementation of the service within a NHS or community setting. These data would also allow us to contextualise usual care across the UK and inform the care pathway in the control group of a full trial.
We planned to carry out qualitative research in the form of focus groups and interviews with pregnant women, mothers, fathers, peer supporters and health-care professionals to inform the intervention content and design and develop a training module that was specific to the intervention being developed.
Four UK RCTs,34–37 both individual and cluster randomised trials, had already demonstrated that it was feasible and acceptable to randomise pregnant women in the antenatal period to receive either BFPS or usual care. Two RCTs that randomised individuals recruited 70%35 and 82%34 of their intended sample size and cited difficulties in recruitment resulting from resource constraints. We therefore planned to use the qualitative work in the developmental phase of our study to explore the challenges to recruitment, investigate specific barriers to participation and develop strategies for recruitment and consent. Our approach was based on the work by the Bristol Medical Research Council (MRC) ConDuCT (Collaboration and innovation in Difficult and Complex randomised controlled Trials In Invasive procedures) methods hub,59 which demonstrated the utility of qualitative work for developing and testing optimal strategies for recruitment during the feasibility stage of trials to improve recruitment.
The previous UK RCTs of BFPS34–37 also highlighted the uptake of, and adherence to, the intervention as possible reasons for non-effectiveness. We therefore included a process evaluation in the design of this feasibility study, to include an assessment of the extent to which the MI-based BFPS intervention that we developed can be delivered as intended to the target population. We planned to test the feasibility of the MI-based BFPS intervention in three community maternity sites that had high levels of social deprivation [most deprived quintile of the Welsh Index of Multiple Deprivation (WIMD)60 and below UK average rate of breastfeeding initiation (< 70%)]. We were specifically interested in establishing the feasibility and acceptability of:
-
recruiting and retaining peer supporters from the community of women to whom MI-based BFPS is to be delivered
-
delivering MI-based BFPS as specified, including an assessment of the extent to which peer supporters utilised MI techniques in their interactions with the mothers they were supporting
-
the recruitment, data collection and follow-up strategies (for clinical outcome measures and resource usage and costs) and study materials.
A summary of the study aims and objectives are provided in Box 1. We intended to use the results from objectives 1–5 to inform the optimal strategy for recruitment, consent timing and approach and data collection in a full trial. Figure 1 provides a schematic representation of the different components of this study.
-
Develop a novel BFPS intervention for breastfeeding maintenance based on MI.
-
Test the feasibility of delivering MI-based BFPS to mothers living in areas with high levels of social deprivation.
-
Establish the necessary parameters to inform a possible full trial to test the effectiveness of MI-based BFPS for breastfeeding maintenance.
-
Identify, categorise and describe the range of BFPS interventions in the UK.
-
Develop MI-based BFPS programme content and identify the requirements for implementation using a user-informed approach, guided by the BCW framework.
-
Finalise the specification of MI-based BFPS (using the BCTTv1 to categorise behaviour change techniques) and the corresponding logic model with stakeholders.
-
Assess the feasibility and acceptability of providing MI-based BFPS to women living in areas with high levels of social deprivation.
-
Assess the feasibility of collecting resource usage and costs associated with the implementation of the Mam-Kind intervention.
-
Use the findings from objectives 1–5 to make recommendations about the need for and design of a full RCT to test the effectiveness of MI-based BFPS for breastfeeding maintenance compared with usual care.
FIGURE 1.
Schematic representation of the Mam-Kind study.

Chapter 2 Availability and range of breastfeeding peer-support interventions in the UK: a cross-sectional survey of infant feeding co-ordinators
In this chapter we address the first study objective, which was to identify, categorise and describe the range of BFPS interventions used in the UK.
Introduction
Peer support was recommended by NICE61 as part of the strategy to increase breastfeeding in the UK. Current NICE guidance on the commissioning of BFPS in England does not specify the theoretical basis, critical components or optimal delivery mode of BFPS. 62 This has resulted in a wide variety of models being used in current practice. 63,64 We wanted to explore the range of BFPS interventions that were currently available to identify lessons from current practice that could be used to inform intervention development. We carried out a survey of infant feeding co-ordinators (IFCs) in the four UK nations to map the current provision of BFPS and obtain an understanding of what peer-support services consist of and how these are provided. In addition to informing intervention development, these data would provide an understanding of ‘usual care’ to inform the planning of a future effectiveness trial, if warranted.
Method
Survey development and piloting
We adapted a previous survey of IFCs carried out in the seven health boards in Wales. 63 We invited three IFCs who worked outside Wales to pilot the adapted questionnaire and provide feedback to us on the acceptability and clarity of the questions. All three agreed to take part; they were sent the link to the questionnaire and provided verbal feedback to a member of the study team. This pilot work identified the need to update the list of potential employers in England to take account of recent changes affecting service commissioners and providers following public health’s move from the NHS to local government in April 2013. We amended the participant information, first, to highlight the ways in which the data collected would be used and, second, to inform respondents of the need to access reports and statistics relating to their service to fully complete the survey. As all questions remained the same, we included the data obtained in the pilot phase in the main analysis.
Sample
Infant feeding co-ordinators from the UK were invited to take part in the online survey or to pass the details on how to access the survey to a colleague if they did not feel that they had the appropriate knowledge to complete the survey themselves. We raised awareness of the survey at the annual UNICEF BFI conference (Newcastle upon Tyne, 27 November 2014), which is the annual professional meeting for UK IFCs. An e-mail invitation to complete the survey was circulated to those listed on four national e-mail distribution lists in December 2014: (1) the National Infant Feeding Network (serving England), (2) the Scottish Infant Feeding Advisors Network, (3) the All Wales IFC Forum and (4) the Northern Ireland Breastfeeding Coordinators Forum (total n = 696 individuals within 177 NHS trusts). We believe that these distribution lists included all individuals who undertook an IFC role in the UK, and also included some other health-care professionals and academics with an interest in infant feeding. Follow-up e-mails were sent to members of all four networks 1 week later, and a final reminder was circulated 12 days after the initial invitation.
Questionnaire and data collection
Participants completed a questionnaire consisting of a combination of closed- and open-text questions. The questions examined the way in which BFPS was organised in the geographical area for which participants had responsibility, with a focus on breastfeeding groups and other activities that breastfeeding peer supporters were engaged in (Table 1). For the majority of questions, participants were asked to describe their service using closed responses or to rate how well they perceived their service to be doing on a six-point Likert scale. Participants were then asked to provide more detail regarding why they answered in that way using open-text boxes. All data collection took place using a purpose-built web-based survey hosted on a secure server at the Centre for Trials Research, Cardiff University.
| Theme | Subquestion topics |
|---|---|
| Demographics | Nation; NHS trust; annual number of births in area; staff roles in relation to breastfeeding; IFC role descriptiona |
| Breastfeeding support groups | Number of groups; who organises groups; presence of records on attendance, support provided, problems with feeding, referrals, other records;a other thoughts on support groups;a funding for non-NHS breastfeeding groupsa |
| Training peer supporters | Number of trained peer supporters; what training is provided; who delivers training;a additional training for peer supportersa |
| Peer support | Recruitment of new peer supporters; supervision; activities that peer supporters are engaged in; integration of peer support with NHS services;a accessibility of peer support for mothers from poorer backgrounds;a other thoughts on peer supporta |
| Other non-NHS support for breastfeeding | Details of support available; provider of support; third-sector activities; presence of active breastfeeding counsellors |
We searched the internet for breastfeeding services in all NHS trusts and health boards (n = 177) to obtain data for the 75 sites for which we did not receive a survey response. We validated the information from sites that responded to the survey and found that the two sources of information were consistent, making it feasible to combine these data. In this report, we present a map of the provision of BFPS and breastfeeding support groups in the UK using data from both of these sources (see Figure 2). There were no material differences in the maps produced using the two sources of data.
Data analysis
We adopted a mixed-methods analysis strategy. Descriptive statistics summarising responses were generated from closed questions using IBM SPSS Statistics version 20 (IBM Corporation, Armonk, NY, USA). Open-text responses were thematically coded by one researcher facilitated by NVivo version 10 (QSR International, Warrington, UK). Individual case studies that illustrated barriers to, and facilitators of, successful delivery were extracted and discussed, but these are not reported here, to maintain anonymity. Themes were developed from responses within each question domain (such as barriers to, and facilitators of, training peer supporters) and across domains throughout the data set (e.g. financial issues, staffing levels). We used inductive thematic analysis to understand responses. 65 Open-text responses were interpreted alongside Likert scale scores when appropriate.
Ethics issues
We received confirmation from the chair of the NHS Wales Research Ethics Committee (REC) 3 that this survey constituted an audit of current service provision of BFPS and did not require ethics approval. Participants were provided with an information sheet and consented to take part in the survey via the web-based platform prior to completing the survey. All responses were anonymised.
Results
The following sections provide an overview of respondents’ characteristics, followed by the survey results in relation to six key themes: (1) recruitment, training and support for breastfeeding peer supporters, (2) peer-supporter roles, (3) descriptions of the management and implementation of breastfeeding groups, (4) the interaction between BFPS and health-care professionals, (5) the accessibility of BFPS and (6) resource and financial considerations.
Respondents
A total of 136 individual responses with usable data were received (response rate 19.5%), representing 58% of NHS trust/health board areas (Table 2). Within the 136 responses, there were multiple responses (total n = 34) from 21 NHS trust/health board areas. Seven of these were instances in which provision in England was split between the NHS trust and another provider, such as the local authority. We retained all individual responses in the analysis because the multiple responses from NHS trust/health board areas provided different information in response to open-text questions.
| Response | Location, n (%) | Total | |||
|---|---|---|---|---|---|
| England | Scotland | Wales | Northern Ireland | ||
| Individual responses | |||||
| Individual invitations | 617 | 40 | 19 | 20 | 696 |
| Individual responses | 113 | 11 | 8 | 4 | 136 |
| NHS trust/health board coverage | |||||
| NHS trusts/health boards | 151 | 14 | 7 | 5 | 177 |
| Total response within NHS trust/health board areas | 84 (56)a | 9 (64) | 7 (100) | 2 (40) | 102 (58) |
Breastfeeding peer support was available in 80 (78%) NHS trust/health board areas and breastfeeding support groups were available in 92 (90%) NHS trust/health board areas of the UK for which we had survey data. These data should be interpreted with caution, as we attributed individual responses to NHS trusts and, for larger trusts, these responses may not be representative of the whole catchment area. Neither BFPS nor breastfeeding support groups were available in 10% (n = 10) of the areas for which we had survey data. About half of the survey respondents reported that there were breastfeeding groups in their NHS/health board area that were funded by local authority or non-NHS organisations (n = 62, 54%) and that there were breastfeeding counsellors working in the area who regularly received referrals from health-care professionals (n = 31, 46%).
In total, 62% of the survey respondents (n = 66) reported that there had been a review, evaluation or report of the breastfeeding support service in their NHS trust/health board area. We requested copies of evaluations and received six reports from two respondents and written descriptions of evaluations from two further respondents. These reports were aimed at evaluating service development, such as breast pump loans and attempting to standardise delivery of breastfeeding support within an area, as opposed to evaluating the effectiveness of BFPS.
We searched the internet for information on the availability of BFPS services in the 81 (46%) NHS trusts that did not provide data on breastfeeding support (either because there was no response to the survey or no data were provided in response to the question). In total, 58% (n = 47) of these non-responder trusts provided breastfeeding support groups, 15% (n = 12) provided a one-to-one peer-supporter service, 24% (n = 20) provided both groups and a one-to-one peer-supporter service and 3% (n = 2) provided neither.
Combining the results from the survey and online search, 40% (n = 71) of NHS trusts provided breastfeeding support groups, 7% (n = 13) provided a peer-supporter service, 49% (n = 86) provided both groups and a peer-supporter service and 3% (n = 5) provided neither. Data were unobtainable for two NHS trusts (1%).
Figure 2 illustrates the areas in which breastfeeding support (groups, peer support, both groups and peer support or neither groups nor peer support) was provided throughout the UK, with Figure 3 providing a detailed map of London. It should be noted that these data indicate which services were available in any given region, but do not provide information on service coverage within the region, accessibility or uptake.
FIGURE 2.
The provision of BFPS and breastfeeding support groups in the UK.
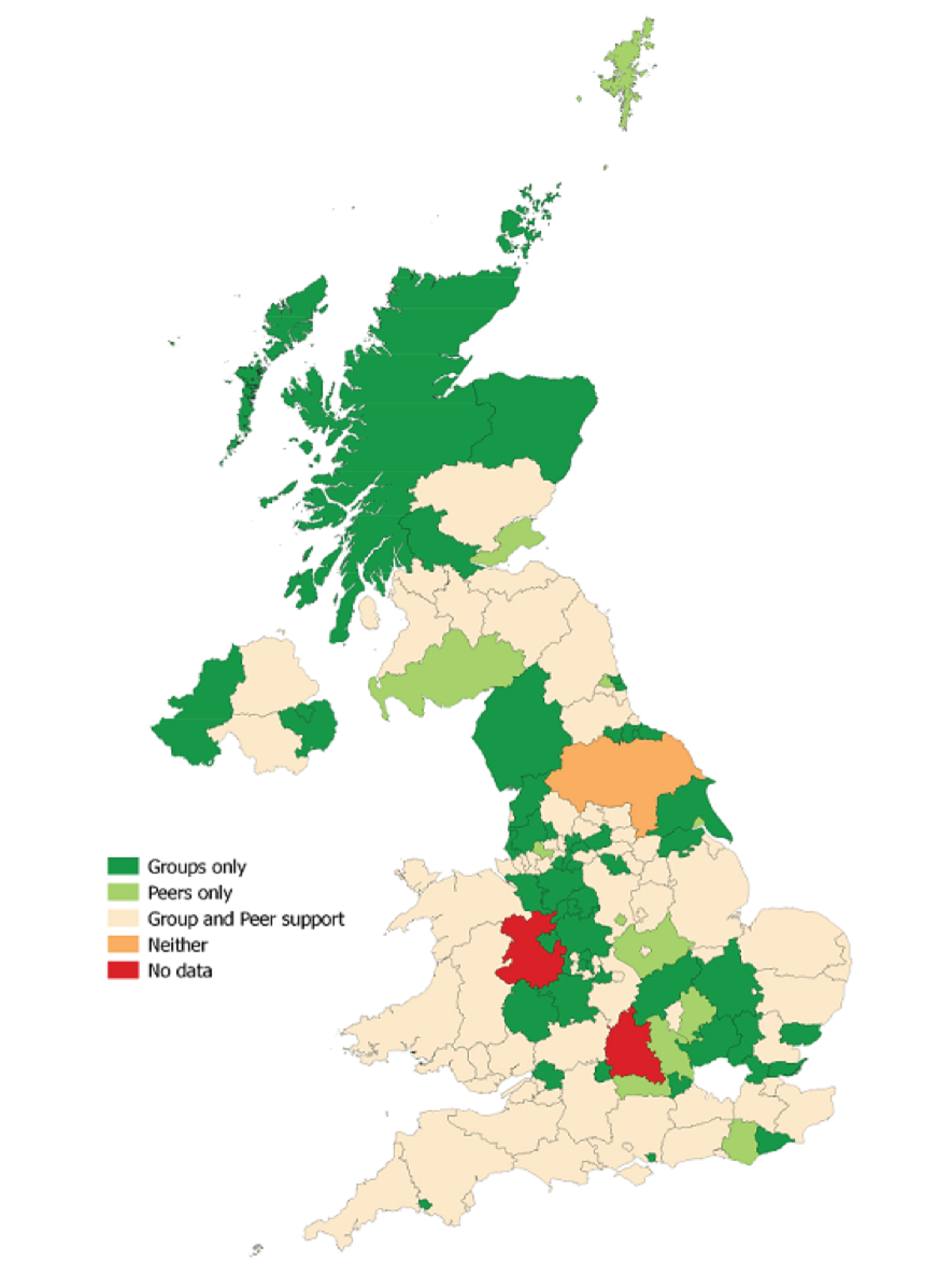
FIGURE 3.
The provision of BFPS and breastfeeding support groups in the London region.
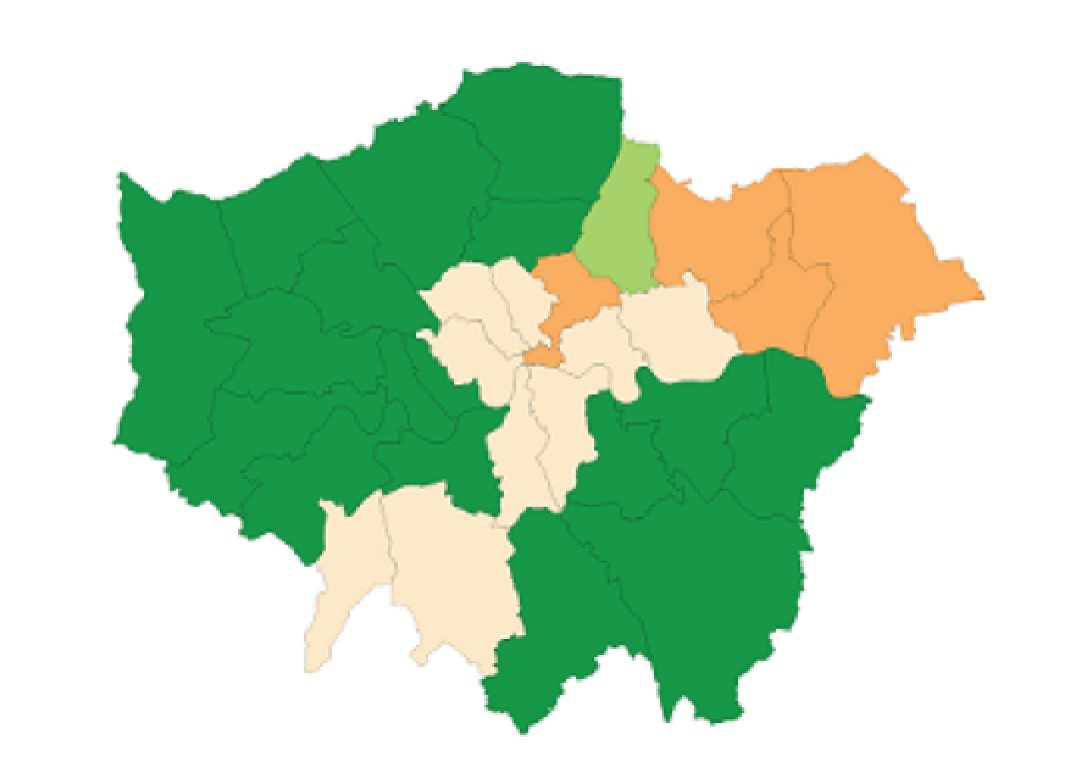
The visual representation uses current health board boundaries in Scotland, Wales and Northern Ireland. We were unable to produce a map for England using current health board boundaries and, therefore, we used primary care trust boundaries as a proxy, as these were most closely matched. However, some NHS trusts in England covered multiple geographical areas and, in these cases, all areas of the map have been coloured. Service coverage may vary within these boundaries, as some participants reported variation within the areas they managed in open-text responses and it was not possible to tease out the exact coverage from the available data.
Recruitment, training and support for breastfeeding peer supporters
The survey responses indicated that IFCs, who were employed by the NHS, were most often involved in managing peer supporters, although, in some cases, this was reported to be a shared responsibility between staff from the NHS, local authority staff and third-sector staff.
There was a multipronged approach to the recruitment of peer supporters (using multiple sources such as breastfeeding groups, midwives, health visitors, children’s centre staff and peer supporters), with 26 out of 103 (25%) respondents selecting all five responses available and only 11 out of 103 (11%) respondents selecting a single recruitment approach. Other methods used to recruit participants included external advertisements, which were disseminated via social media, traditional media and volunteering forums.
The median number of peer supporters who had been provided with initial training over the previous 12-month period in each area was 15 (range of 0–64). Participants were asked to describe in an open-text box who provided the training. The third sector was the most common provider for the initial training of peer supporters [including the Breastfeeding Network (BfN) and the National Childbirth Trust (NCT)], with IFCs and NHS and community centre staff also playing a key role. Initial training varied in duration and some included the potential for participants to gain qualifications. Some respondents (n = 45) provided further details about the initial training that was provided to peer supporters. This included examples of highly structured and comprehensive training in some areas, to less structured examples or no training provided in other areas. Based on the information in the survey responses, we developed a framework to illustrate the range of training approaches that were in use (Table 3).
| Framework | Content | |
|---|---|---|
| Highly structured and comprehensive | Less structured or comprehensive | |
| Availability | Available to all peer supporters | Available to selected peer supporters (e.g. regular group attendees) |
| Integration with health-care professionals | Joint training with health-care professionals | Available only to peer supporters |
| Content | Infant feeding plus additional professional training (e.g. confidentiality, child protection, setting boundaries, public health) | Infant feeding only |
| Formal qualifications from peer-support training | Available | Not available |
| Duration | Training plus ongoing support | Training with no ongoing support |
Training and/or ongoing support in addition to the initial training was provided in 70 of the 107 (65%) areas for which we had data and, in two-thirds of these areas (63%, n = 44), more than one type of support was provided. This was commonly in the form of regular local training (n = 69, 64%). In 13 of the areas, peer supporters were able to access BFI training. Other types of training included safeguarding (n = 15), joint training with NHS staff (n = 13), mandatory NHS staff training and local service updates. The extent to which training was mandated or optional varied between areas.
Peer supporters’ roles
Attending breastfeeding groups was the main activity that peer supporters were involved in, followed by working on the postnatal ward (Figure 4). In general, delivery seemed to be more focused on group support, with one-to-one forms of delivery being less common. Most peer supporters saw mothers in both the antenatal and postnatal periods (50% of survey responses, n = 68), but some saw mothers only in the postnatal period (29%, n = 39). The comprehensiveness of services was described through open-text responses, with some areas viewed as having a complete model of service delivery:
The Peer-support Service is a 7 days service 356 days of the year. Team of 10 members, total 7.5 whole time equivalent from 9–5 man a 24 telephone support line. The Service is integrated into [child health care], works alongside Health Visitors, School Nurses, and support staff. The service delivers Health Promotion sessions within Primary schools, they provide bedside support within the three feeder hospitals, provide support groups with Children’s Centre Groups. It is an excellent service provided by a dedicated team.
FIGURE 4.
What activities are peer supporters in your area engaged in?

In contrast, other areas indicated that they were not currently resourced to provide a comprehensive service:
I have one breastfeeding support worker who is employed by [the NHS], this isn’t enough for a birth rate of 2500. We are currently writing a business case for 10 × paid peer-support workers.
Breastfeeding support groups
It was most commonly reported that > 10 groups were running within individual areas (Figure 5). Respondents stated that NHS staff, children’s centre staff and trained peer supporters most commonly organised breastfeeding support groups. Alongside this, it was noted in open-text responses that coverage of breastfeeding support groups was not uniform throughout NHS trust areas and that this was not necessarily related to the numbers of births. Respondents also noted within the open-text boxes that group sessions took place in a broad range of settings, including community venues (café, garden centre café) and children’s centres, and alongside health visitor (weighing) clinics. Some groups ran as ‘baby cafes’, ‘first friends’ or generic ‘parenting support groups’ with a focus on breastfeeding, rather than explicitly as breastfeeding support groups. In response to questions about record-keeping in the groups, less than one-third of survey respondents reported that notes were kept on individual mothers who received support (n = 31, 26%), mothers who have problems (n = 34, 29%) and referrals for additional support (n = 32, 27%).
FIGURE 5.
If you have peer-support groups, how many groups are currently running?

Interaction between breastfeeding peer support and health-care professionals
The majority of participants (63%, n = 67) felt that peer support was well integrated with other NHS services (Figure 6). Alongside the closed question, which asked participants to describe how well they thought peer support was integrated with other health services, respondents were asked to explain their answer. The majority of open-text comments were consistent with respondents’ answers on the six-point Likert scale. Participants described a range of factors that were responsible for integration, including:
-
guidance on peer-supporters’ roles, with clear responsibilities (n = 15)
-
visibility to health-care professionals, such as working on postnatal wards or other shared working practices (n = 14)
-
peer support being trusted and valued by local health-care professionals (n = 9), including as a result of an evaluation or feedback from parents (n = 3)
-
a health-care professional acting as a ‘champion’ and communicating the value of peer supporters to other health-care professionals (n = 5).
FIGURE 6.
Do you think that BFPS provided in your area is well integrated with the breastfeeding support work that health-care professionals do?
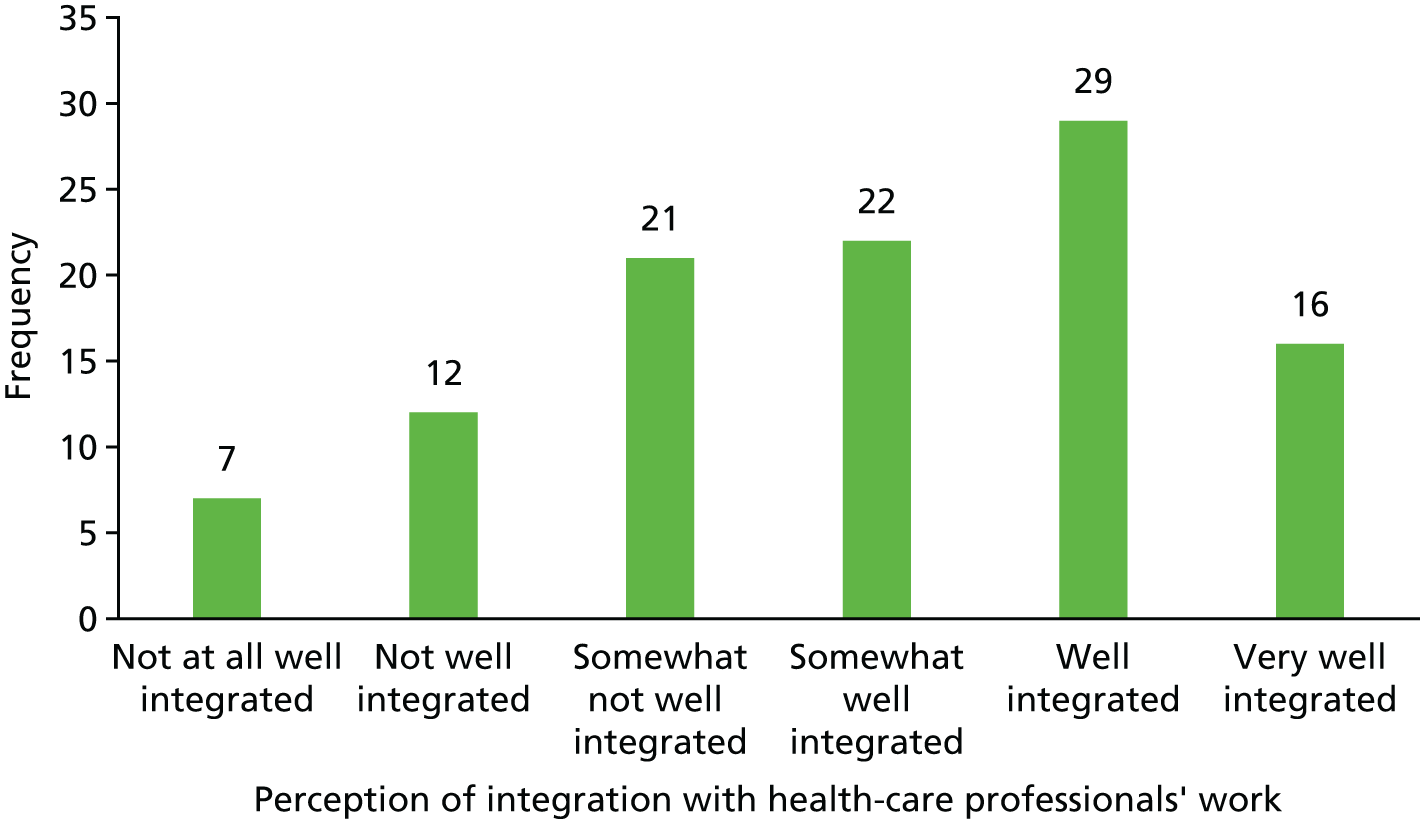
In areas with less integration, the converse occurred: staff did not understand the peer-supporter role and did not feel that peer supporters were suitably qualified and, as such, there was a lack of trust, resulting in a lack of referrals from health-care professionals to peer supporters.
Accessibility of breastfeeding peer support
In response to the question about how accessible peer support was to mothers from poorer social backgrounds, 24% (n = 25) of respondents used the three negative options (not/moderately, not/somewhat, not accessible) (Figure 7). However, some responses did not corroborate with the additional open text provided, suggesting that some respondents may have unintentionally ticked the wrong box. An example of this was a response that indicated an accessible service on the Likert scale, but conversely stated that ‘the most vulnerable and poorer mothers may be “put off” from attending groups as the groups are seen to have women in a slightly higher social class than themselves’.
FIGURE 7.
Is the BFPS provided in your area accessible to breastfeeding mothers from poorer social backgrounds?
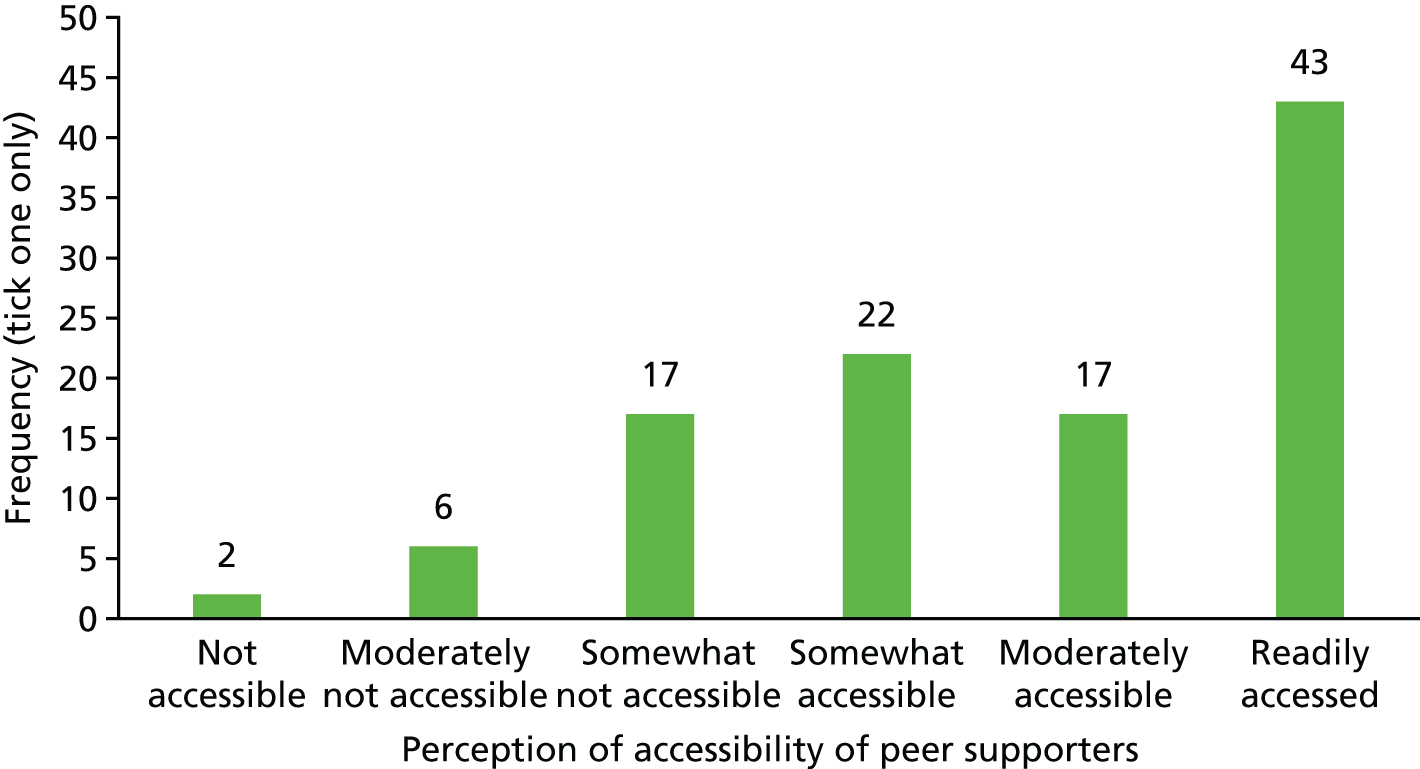
However, this could also mean that, although access is good overall, there are certain aspects of the service that could be improved. When asked to explain the rationale for their responses to the above question, participants suggested that services were working well when they:
-
were held in areas of high deprivation, and worked with providers who aimed to support women in areas of high deprivation and used informal conversations in areas with low levels of breastfeeding (school gates, social media)
-
were well accessed by mothers living in deprived areas (some responders had data to show this and, when there were no data, this was supported by the breastfeeding co-ordinators’ impressions)
-
recruited peers from areas of deprivation and provided proactive contact.
Barriers to accessibility included:
-
attracting women from deprived areas to breastfeeding support groups
-
inadequate numbers of peer supporters
-
being reactive as opposed to proactive
-
not being able to provide home visits.
Resource and financial issues
One of the main themes interwoven throughout the open-text responses was financial support for community breastfeeding services. This was often referred to as a problematic issue throughout the data, with some services continuing to face a reduction in available funding. Some respondents from England noted that their services had previously been funded through NHS community budgets and that NHS hospital budgets were not continuing to fund peer-support services following the move of public health from the NHS to local government in England. The reported shortfall affected finances to train peer supporters and pay travel expenses and health-care professional time for the supervision of peer supporters. In a small number of cases it was reported that BFPS services had been decommissioned. In a minority of areas, respondents reported that peer supporters were paid for their time, but, in most services, funds were not available for this. Several respondents noted that they were attempting to secure funding from charitable trusts or their own employers by writing business cases, and this was often to provide a basic service (supervisor time, travel expenses for peer supporters) rather than to pay for peer-supporters’ time. In contrast, in some areas, investment was being made in peer-supporter co-ordinator roles.
Discussion
Peer support for breastfeeding is recommended as part of a strategy to address low breastfeeding rates in the UK. 62 Within this context, our UK-wide survey of 136 UK-based IFCs found wide variation in service provision. As in previous studies,63,66,67 we found that there was wide availability of peer supporters across the country, both within and between NHS trust/health board areas. A key finding from our survey was that there was no standardised provision of BFPS in the UK. Services were regularly adapted in response to unstable financial circumstances, with services being reduced or increased in line with the funding available. None of the models that were implemented at the time of this survey had been robustly evaluated for effectiveness.
This survey has provided information about how peer support for breastfeeding is provided in the UK and identified some of the facilitators of, and barriers to, the delivery of peer-support services, which were further explored in our qualitative research and through discussions with the Stakeholder Advisory Group (see Chapter 3). A clear tension was reported in some areas between BFPS and health-care professionals, and this may be related to a lack of clear guidance regarding roles and responsibilities and a lack of visibility of BFPS to health-care professionals. We explored this further in our discussions with the Stakeholder Advisory Group and in qualitative work with health-care providers to ensure that the local health service context was considered in planning for intervention delivery in the feasibility sites (see Chapter 3). Accessibility to parents from poorer backgrounds was noted as a challenge. Services that considered themselves to be accessible to poorer mothers noted elements of good practice, including being held in areas of deprivation, working in partnership with organisations who support women from deprived areas and the use of informal conversations with peers.
A further issue was that, in many sites, the current level of support provided was not regularly documented or evaluated. Two-thirds of participants reported that registers of attendees were kept in their area, but details of any support provided or signposting to additional services were rarely kept. Documentation and record-keeping are important to enable evaluation in the context of a research study. This highlights the importance of engaging with peer supporters during the development phase of the study to explore the options for data collection to capture reliable information.
The most common theme found in the open-text responses was the challenge of running services with limited financial support, although this was not experienced equally by all services, with a minority of services reporting recent investment. Linked to this financial shortfall, some services reported the challenges of recruiting, training and providing ongoing supervision for peer supporters, with one-third of participants reporting no ongoing training and support in their area. Understanding this variation will enable the selection of sites in which a future RCT could be undertaken and may influence the extent to which sites are able to fully roll out an intervention.
The majority of survey respondents indicated that there had been a review or evaluation of BFPS in their NHS trust/health board area over the last 5 years; however, to our knowledge, these were service evaluations to inform service provision rather than formal assessments of efficacy or effectiveness.
This study is the first attempt to map and describe the provision of peer support for breastfeeding throughout all four nations of the UK. We received responses from around the UK and achieved a response rate that covered 58% of NHS trusts/health board areas. We searched the internet to obtain information about the availability of BFPS in the NHS trust/health board areas for which there were no survey data available to describe the current provision. We checked the consistency of the data provided in survey responses and those obtained from the internet and were satisfied that these two sources of information were compatible. The survey was open for a period of 3 weeks in December 2014, and it may be that we would have received further responses if the survey had been kept open for a longer period. We were also made aware that two participants were unable to access our online survey from their NHS computers. Although we provided support that enabled those participants to take part, it may be that other potential participants did not contact us and were thus unable to access the survey. The response rate to the survey was low. We did not receive a response from 42% of the NHS trust/health board areas, and, although we were able to obtain internet information on the types of BFPS available, we were unable to understand how these services were run and any potential facilitators or barriers in these areas. We mapped the data on BFPS availability to NHS trust and health board areas and, in doing so, we have had to assume that the responses for each health-care area were applicable across the board. This may not be the case for larger NHS trusts, in which the availability of services may vary greatly; however, our survey was not sensitive enough to capture availability at smaller geographical levels. Further information on the availability and accessibility of BFPS could potentially have been obtained through direct contact with NHS trust/local authorities and third-sector organisations, but we did not have the resources to do this within the scope of this study.
Chapter 3 Development of a novel motivational interviewing-based breastfeeding peer-support intervention to support breastfeeding maintenance
This chapter addresses study objective 2, to develop MI-based BFPS programme content and identify the requirements for implementation, and study objective 3, to finalise the specification of MI-based BFPS and the corresponding logic model with stakeholders.
Introduction
The theoretical basis of BFPS and its active behaviour change components have not been well described or characterised, so there is currently limited understanding of what components are required for an effective BFPS intervention. Motivation, self-efficacy, affective attitudes, social norms and strong beliefs that breastfeeding is the normal and healthiest way to feed an infant are associated with continuation of breastfeeding. 10,11,18,68 Applying the theory of constraints thinking to breastfeeding problems, Trickey and Newburn7 found that support should be proactive and mother centred, consistent with the data from our survey of IFCs. It is therefore important to address the ‘why’ (motivation) and ‘how’ (confidence, skills, resources) of breastfeeding maintenance in this context.
Framework for intervention development
The BCW57 provided a framework for identifying the behaviours to be addressed, the required functions of the MI-based BFPS intervention and the relevant service requirements. 56 We utilised the COM-B theoretical model, which hypothesises that interactions between people’s physical and psychological capability (C), social and physical opportunity (O) and automatic and reflective motivation (M) can be used to understand what needs to change to achieve the desired behaviour change (B). 57
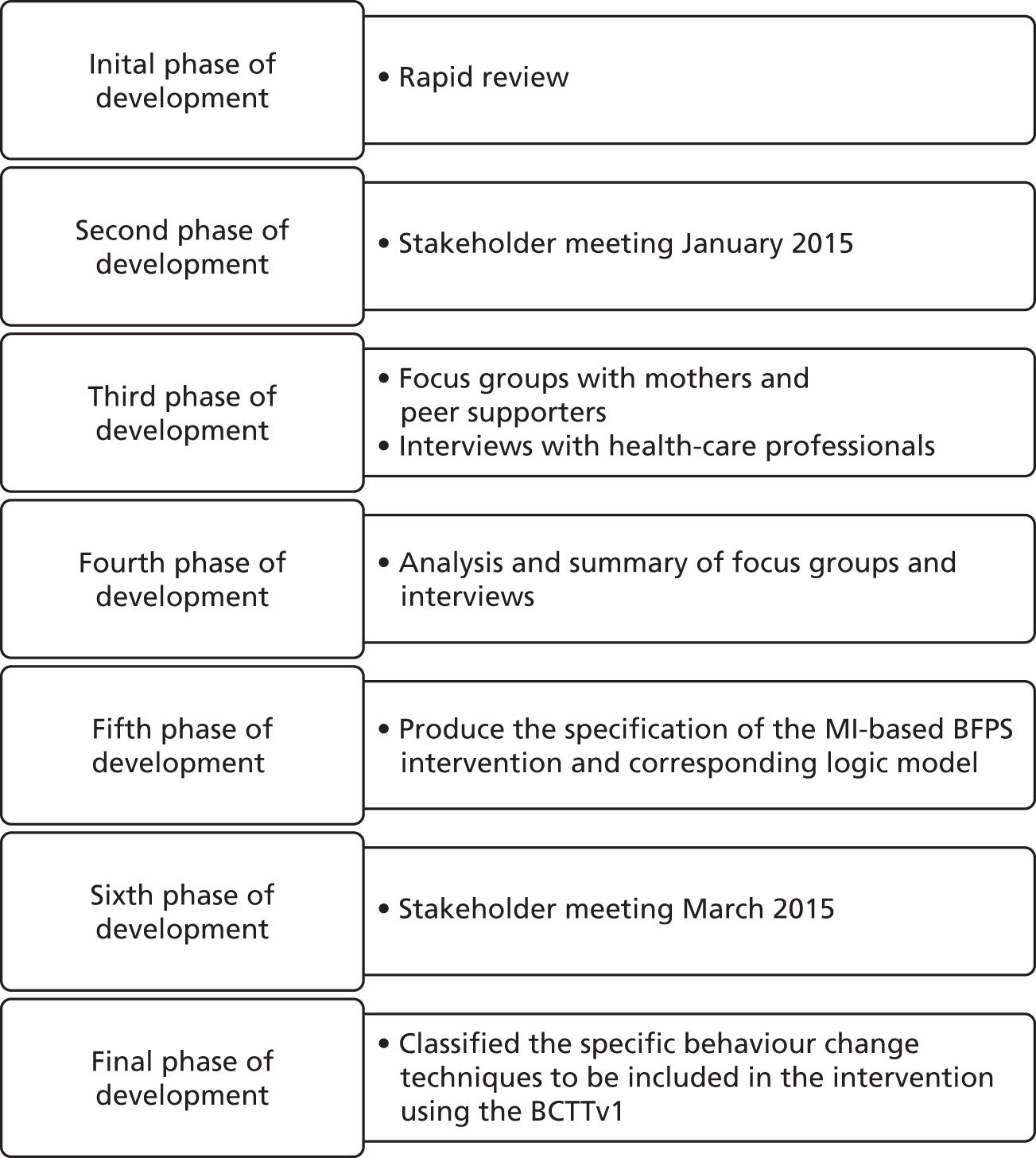
We used a flexible iterative process to develop this intervention, which is summarised in Figure 8. We used the survey findings reported in Chapter 2, a rapid literature review and qualitative research to identify the behaviours associated with breastfeeding to be addressed by the intervention and the underpinning theoretical models and design factors that influenced the delivery of the BFPS intervention. We aimed to explore parental, health-care professionals’ and peer-supporters’ views of what the features of a feasible, acceptable and effective BFPS intervention would be. We examined their perceived barriers to, and facilitators of, breastfeeding that a BFPS intervention would be able to address, what current peer support is like and what it should be like. We clarified the sources of behaviour to be addressed by the intervention through discussion with the Stakeholder Advisory Group, informed by the findings from the rapid evidence review and qualitative research, and categorised these according to the COM-B model. This enabled us to follow up on issues identified in the survey and literature review in more depth and explore issues directly relevant to the design of a MI-based BFPS intervention and define its function, content and mode of delivery.
FIGURE 8.
Development process.
Integrating the motivational interviewing approach with breastfeeding peer support
We proposed to develop a BFPS intervention that uses a MI approach. Self-determination theory (SDT) has been proposed as an explanatory theory for MI. 69,70 SDT is a theory about a person’s self-motivation to change behaviour. It shares a common principle with MI that ‘people have an innate organisational tendency toward growth, integration of the self and the resolution of psychological inconsistency’. 69 SDT seeks to explain what drives human behaviour and places motivation on a continuum of autonomy ranging from external regulation (no autonomy) to intrinsic regulation (full autonomy). By examining people’s different motivations for achieving goals, for example pleasure compared with obligation,71 SDT identifies three elements that are critical to support the process of changing motivation from external to intrinsic: competence support, autonomy support and relatedness. MI provides support for each of the psychological needs that are identified by SDT. 72
Motivational interviewing involves four key processes: engaging [establishing a ‘mutually trusting and respectful helping relationship to collaborate toward agreed-upon goals’ (p. 3)73], evoking (eliciting the client’s own motivation for a particular change), focusing (clarifying a particular goal or direction for change)73 and planning (developing a specific change plan that the client is willing to implement). 28 These processes are sequential and recursive and are used throughout the MI session. 28 A MI practitioner aims to clarify and resolve a client’s ambivalence about choosing a particular behaviour and does so in conversation with the client in a spirit of acceptance and collaboration. The process aims to help make complex behaviour changes feel clear and more achievable by allowing the client to decide on the changes in their life that they feel that they can make. Skilful MI practitioners use a range of skills and techniques to guide clients through this process. Central to these is a technical skill of attending differentially to client language that is indicative of change (change talk), while consciously not reinforcing client sustain talk, which is language in favour of the status quo. As MI is a conversation style, these techniques are not specific to a type of behaviour change; rather, they are used in response to where the client is in the MI process. In the case of breastfeeding, these techniques can be used to support initiation and continuation (Box 2).
An example of an interaction in which the client is expressing change talk:
I think I want to give breastfeeding a try. I know it is really good for my baby’s health.
Your baby is so important to you and you want to provide him with a healthy start.
An example of an interaction in which the client is expressing sustain talk:
I’m not sure breastfeeding is right for me as I really want my partner to be involved in feeding baby as well.
Whether you choose to breastfeed is your choice. Are there any ways you can think of in which your partner could be involved in feeding if you decide to breastfeed?
Self-determination theory is one of the theories that was considered during the development of the BCW framework56,74 and, therefore, it is likely that the BCW framework will be applicable in the context of MI-based BFPS. However, it has been suggested that the BCW may not capture some of the therapist skills that form a key element of the MI approach. 75 Therefore, in addition to using the BCW as a guide in developing and characterising the MI-based BFPS intervention, we assessed its applicability in the context of a MI-based approach and investigated whether or not there were any important potential mechanisms for change included in the intervention that were not incorporated in the current BCW framework and BCTTv1 taxonomy.
Methods
Rapid literature review
We searched 14 electronic databases on Ovid for BFPS studies to identify the features of one-to-one peer support that contributed to the successful delivery (or otherwise) of the interventions. The search was carried out in December 2014, with an update search carried out in March 2016. We used both keywords and medical subject heading (MeSH) terms, as detailed in the search strategy in Appendix 1. The literature review was designed to examine how BFPS interventions were provided: who provided peer support, where, when and how. The search was limited to English-language-only publications between the years 2000 and 2014, and was restricted to studies undertaken in Organisation for Economic Co-operation and Development (OECD) countries. We included RCTs and controlled studies that evaluated BFPS interventions that included one-to-one support. We extracted data from these studies to describe the study population, intervention (including any cited or explicitly described underpinning theories), delivery context and usual care, characteristics of peer supporters, factors associated with the uptake of the intervention, outcomes and lessons for study design and intervention delivery. We used this information to develop a narrative summary of the key features of BFPS interventions and the facilitators of, and barriers to, delivery of the interventions. These findings were presented at the first Stakeholder Advisory Group meeting in January 2015. Prior to writing this report, we updated the search to include publications up to 2016 and contacted study authors to obtain supplementary information, for example the results of process evaluations, when there was insufficient information in the primary publication of a study.
Qualitative interviews and focus groups
We conducted focus groups with mothers, fathers and peer supporters to understand their expectations and the required functions of MI-based BFPS, explore factors relevant to the delivery of the intervention and identify different experiences and perspectives within and across the groups. 76,77 Focus groups were chosen to facilitate reflections on the social realities of infant feeding. Participants all had experience of either being a new mother/father or being a peer supporter. By discussing this in a group, it is likely that new insights were extracted beyond those that we would have uncovered if we had discussed these issues with each participant alone during an interview. 78 One-to-one in-depth telephone interviews were conducted with health-care professionals to enable them to discuss their views on, and experiences of, BFPS within their local service and perceived facilitators of, and barriers to, implementation. We interviewed health-care professionals separately for two reasons. First, we may reasonably expect that, when investigating a relatively homogeneous group of health-care professionals, their experiences may vary. This may be problematic when health-care professionals do not know each other well, are at different levels of the professional hierarchy (e.g. some band 3 unqualified maternity care assistants and some band 7 infant feeding leads) and may be aware of practices that are not officially sanctioned. Accordingly, we believed that it was ethically appropriate to undertake individual interviews. 79 In addition, from a practical perspective, using individual interviews rather than focus groups allowed us to complete the data collection more easily, without having to co-ordinate the busy diaries of health-care professionals.
Setting
The qualitative work to inform intervention development was conducted in the three sites that would later be used to test the feasibility of the intervention. The study sites, two in South Wales and one in England, were selected because they included communities with high levels of socioeconomic deprivation and low breastfeeding rates. In two study sites, the existing peer-support services were voluntary and group based, whereas, in the other site, there was a one-to-one BFPS service that employed peer supporters. Prestudy discussions in the third site indicated that the model of peer support provided was proactive and peer-supporter led in the early postnatal period, and it was felt that it would be possible to adapt this and test the feasibility of delivering the new MI-based BFPS intervention that was being developed. Interviews with health-care professionals and focus groups with peer supporters were conducted in all study sites; focus groups with pregnant women, mothers and fathers were held in two of the three study sites for logistical reasons.
Participants and sampling
We conducted one focus group with fathers (n = 3), three focus groups with mothers and pregnant women (n = 14) and three focus groups with peer supporters (n = 15). Mothers and fathers were recruited through existing community-based antenatal and parenting groups, who invited parents to participate in a local focus group. They were the intended target population for the intervention and therefore did not necessarily have experience of peer support or breastfeeding. Peer supporters working in the study areas were identified through local service managers/IFCs or through databases of qualified peer supporters and were invited by e-mail, telephone and social media to participate in focus groups held in their local community. No incentives were offered for participation.
We conducted 14 telephone interviews with health-care professionals whose role included breastfeeding support: health visitors (n = 2), service managers (n = 2), community midwives (n = 4), postnatal/hospital-based midwives (n = 3), an early years practitioner (n = 1) and midwifery support workers (n = 2). We worked with the service managers in these areas to develop a sampling frame of health-care professionals who had managerial and/or service delivery roles to support breastfeeding. The service managers sent out invitations to those in the selected health-care professional roles. Fifteen of the 18 invited health-care professionals responded and consented to take part.
Ethical considerations
Ethics approval for the qualitative work that informed the intervention development was granted by the NHS Health Research Authority, Wales REC 3 Panel, in November 2014 (reference 14/WA/1123). All focus group participants provided written informed consent. Health-care professionals provided audio-recorded verbal consent for their interviews following a standardised script.
Procedure
Flexible topic guides were developed for each participant group (see Appendices 2–5). These were based on emergent themes from the rapid evidence review that required further development or clarification and the proposed research design (e.g. challenges for recruitment, retention and data collection, and study materials, such as information leaflets and consent forms). Intervention topics included past experience of breastfeeding support, BFPS, the appropriate timing and method of contact between mothers and peer supporters, training and support needs of peer supporters, partners’ involvement in peer support, factors that would encourage/discourage engagement with the intervention and intervention integration with local services. The MI concept was briefly described and participants were asked for their views on using this approach when providing breastfeeding support. All participants were given a study information sheet and completed a consent form or gave verbal consent. All interviews and focus groups were digitally audio-recorded.
Qualitative analysis
Qualitative data were fully transcribed, anonymised and analysed thematically using an approach that was both deductive and inductive. 65 An initial coding framework was developed using the BCW as a guide. This enabled us to map themes identified in the data against the different levels of the BCW (i.e. sources of behaviour, intervention functions, service/policy categories and mode of delivery). Analysis was facilitated by the use of NVivo 10 qualitative software. The qualitative researchers (LC and HT) met regularly during the analysis process to discuss coding and the interpretation of the findings. A sample of transcripts (one focus group and three interviews) was independently dual coded by a third researcher (HS) to assess the validity of the coding framework and showed a high level of agreement between coders. When NVivo identified discrepancies of > 10% during dual coding, this was the result of differences in how coded sections were highlighted or a lack of description within the coding framework. These discrepancies were discussed and resolved, leading to some themes in the initial coding framework being more explicitly defined, collapsed and relabelled, to simplify the coding structure and ensure that it fitted with the BCW definitions. Pseudonyms were allocated to participants to protect anonymity in reporting findings.
Production of the intervention specification
The results of the rapid review and qualitative work were mapped onto the COM-B model and the BCW to identify the relevant sources of behaviour to be addressed and the relevant behaviour change techniques and implementation requirements using the BCTTv1. 58 We then produced the specification of the MI-based BFPS intervention and corresponding logic model for discussion and endorsement by the Stakeholder Advisory Group.
Consultation with the Stakeholder Advisory Group
A Stakeholder Advisory Group (n = 23) was convened to advise on all aspects of study design, including intervention development. This group consisted of service users (n = 2), peer supporters (n = 1), peer-support co-ordinators (n = 3), IFCs (n = 1), service managers (n = 4), midwives (n = 1), health visitors (n = 2), MI trainers (n = 2) and voluntary sector representatives (n = 7). Two half-day creative workshops were held. In January 2015, the stakeholder group met to discuss the preliminary findings from the rapid evidence review and qualitative research and the initial generation of the intervention plan by the research team. Between January and March 2015 the analysis of the qualitative work was completed and used to inform the development of a more detailed specification of the intervention; this was presented to the stakeholder meeting in March 2015. The multidisciplinary research team led the sessions and moderated group work. Group discussions were audio-recorded and key points extracted. Drafts of the intervention description and logic model were circulated to this group for comment between meetings.
We consulted with mothers who were waiting to be trained by the NHS as peer supporters and those going through the training using a closed Facebook group (Facebook, Inc., Menlo Park, CA, USA). This group was also consulted on the name of the intervention and the participant materials.
Results
Rapid evidence review
The rapid literature review aimed to (1) describe heterogeneity in intervention theory and design among one-to-one BFPS interventions delivered in developed country settings that have been subject to experimental study and (2) identify opportunities and modifiable weak points associated with the design of BFPS interventions delivered across different contexts that could be addressed in the design and implementation of the MI-based BFPS intervention that we were developing.
The rapid review identified 15 BFPS interventions that were subject to experimental study, which were reported in 16 papers published between the start of January 2000 and the end of January 2016. 29,34,35,37–39,80–89 Nine interventions were delivered in the USA, all associated with the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). 80–87,89 Five papers related to UK-based interventions34,35,37–39,88 and one intervention was delivered in Canada. 29
Studies were included if they pertained to a model of BFPS that included planned one-to-one contact between a mother and a peer supporter, reported breastfeeding rates (initiation, continuation or exclusivity) as an outcome measure and if they had been delivered in a developed country setting. Studies were excluded if the support was primarily intended to be group based. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram90 describing the different stages of study identification is presented in Figure 9.
FIGURE 9.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram. BF, breastfeeding. Adapted from Moher et al. 90 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

Study quality
Eleven studies were RCTs,29,34,35,37,80,81,84,86–89 three were area-based controlled studies38,82,83 and two were natural experiments. 39,85 Applying Cochrane risk of bias criteria,91 we found that only three studies had a low risk of bias. 34,81,86 Six of the evaluations were at a risk of selection bias,29,38,39,82,83,85 attrition may have affected six evaluations35,37,80,83,87,88 and one evaluation89 was at a risk of detection bias. Implementation issues affected 11 of the 15 evaluations. 34,35,37–39,80,84,86–89 Among the five UK studies, there were difficulties in achieving the intended number of contacts34,38,39,88 and in ensuring intervention fidelity. 35,37,88. Of the nine studies of US-based cases, four reported significant implementation problems. 80,86,87,89
Heterogeneity between studies
Within the relatively narrow inclusion criteria, the rapid review found considerable heterogeneity in the type and scale of the breastfeeding rate ‘problems’ that were addressed, the background social norms and the wider health-care delivery context, as well as the underpinning intervention theory and specific intervention components.
With regard to the breastfeeding rate problem being addressed in the studies, nine interventions aimed to increase initiation rates33,35,38,39,80,83,85,87,88 and 12 sought to improve continuation rates,29,34,35,37–39,80,81,84,85,87,89 measured at varying time points. Two interventions were intended to improve the rates of exclusive breastfeeding. 86,89 The scale of the problem of low rates of breastfeeding varied. One intervention was implemented against a backdrop of a breastfeeding continuation rate of around 10% at 6 weeks,38 whereas two interventions were delivered in the context of background initiation rates of 90% in a low-income population of Latina – predominantly Puerto Rican – women. 86,87 The majority of included studies focused on populations that were socially deprived. 38,39,80–87,89 Many interventions were interlinked with a wider agenda to reduce health inequalities. Only three studies were not specifically located/targeted to address the needs of mothers experiencing social disadvantage. 29,34,35
Overwhelmingly, study papers did not include a description of the theoretical models underpinning the interventions that they described. The theory of social support27 seemed to be implied across many studies; however, different configurations of intervention components suggested differences of emphasis on informational, emotional, instrumental or appraisal support among the included interventions. Two studies explicitly referred to social influence or role modelling as a concept underpinning intervention design. 29,89
The emphasis on a similarity between the mother and the peer (adherence to the principle of homophily) varied. Most used peers selected on a locality basis, suggesting an intention to recruit from a similar social background. Six interventions attempted to individually match mothers to peers by ethnicity or language. 80,82,84,86,87,89 Two interventions targeted to adolescents used adolescent peers. 39,84 One intervention, targeted to recent Spanish-speaking immigrants, did match peers by first language. 87
Interventions differed considerably in accordance with indicators of peer professionalisation,25 and were not equally well embedded in existing health services. At one extreme, peers were trained to university diploma level34 whereas, at the other, peers received only 2 hours of orientation. 29 In some cases, peers were employed or were managed by health-care professionals. 37,39,80,83,85–88 Several settings had previous experience of BFPS. 81,85–87 In most settings, the intervention was funded for the lifetime of the evaluation only.
Comparison across interventions indicated considerable heterogeneity in the timing, frequency and intensity of contacts and the setting for contacts. Two interventions did not include an antenatal contact29,84 whereas one was entirely reactive in the postnatal period. 34 Six interventions intended more than five contacts with each mother. 35,80,81,84–86 Three interventions involved contact in hospital prior to discharge. 80,81,86
Design opportunities and modifiable weak points
Within these included studies, peer supporters were described as role models, affirming and normalising experiences and empowering mothers to identify solutions that work for them. The BFPS interventions across these studies aimed to address issues related to the mothers’ own capacity and resources (lack of knowledge, unhelpful beliefs, attitudes, low breastfeeding self-efficacy) and issues related to health-care professional support or capacity. All studies applied the principle of homophily (the tendency for people to identify with others who are similar to themselves)92 such that peer supporters were mothers who had breastfed, but there was variation between studies in the extent to which peers had similar social or cultural backgrounds to the mothers who they supported. The content of the interventions included in these studies is summarised in Appendix 6 (see Table 22).
Thematic cross-case analysis of extracted data resulted in the identification of five areas for consideration in intervention development. These were:
-
achieving cultural acceptance
-
successfully integrating with existing health-care services
-
ensuring that peer qualities enhance uptake and acceptance
-
ensuring that the peer is practically and emotionally accessible to the mother
-
ensuring that the peer–mother relationship promotes change in line with intervention goals.
We summarised the facilitators of, and barriers to, the delivery of BFPS within the context of each theme and identified delivery implications for the MI-based BFPS intervention. These lessons for design were endorsed by the Stakeholder Advisory Group in January 2015 (Table 4).
| Characteristic of BFPS | Facilitators | Barriers | Implications for the Mam-Kind BFPS intervention design |
|---|---|---|---|
| Sociocultural norms |
|
|
|
| Qualities of the peer |
|
|
|
| Accessibility of the peer |
|
|
|
| Peer–mother relationship |
|
|
|
| Successfully integrating with existing health-care services |
|
|
|
Intervention functions
We mapped the sources of behaviour identified in the literature review and our findings from the qualitative work to the COM-B model and the corresponding intervention functions (Table 5). The relevance and acceptability of these intervention functions were explored in the qualitative interviews and focus groups. These results are presented in the following sections.
| Sources of behaviour: barriers (–) and facilitators (+) to breastfeeding continuation | COM-B domain | Potential BCW intervention functions |
|---|---|---|
| Social norms: formula feeding (–) or breastfeeding (+) – includes wider cultural/social norms and beliefs and attitudes of significant others (e.g. partner, mother, sister) that formula feeding (–) or breastfeeding (+) is easier/convenient/healthier/more natural |
|
|
| Feel comfortable (+) or uncomfortable (–) about breastfeeding in front of others |
|
|
| Social support: social isolation (–) or feeling emotionally supported (+) |
|
|
| Beliefs that formula feeding (–) or breastfeeding (+) is easier/convenient/healthier/more natural; beliefs/expectations about what is ‘normal’ breastfeeding (e.g. frequency of feeding or how milk let-down feels) |
|
|
| Planning for formula feeding (–) or breastfeeding (+), e.g. buying equipment, formula, clothing |
|
|
| Intention to breastfeed: determination to overcome challenges encountered (+) vs. intention to formula feed if there are difficulties (–) |
|
|
| Confidence (+) and autonomy (+), for example feeling able to try out and find their own techniques for feeding rather than having to stick to ‘textbook’ methods |
|
|
| Positive (+) or negative (–) prior experience of breastfeeding and/or breastfeeding support |
|
|
| Quality of information and advice – consistent (+) or inconsistent (–) and accurate (+) or inaccurate (–) advice and information from social and professional sources of support |
|
|
| Being able (+) or unable (–) to access support services at the right time (e.g. to plan/prepare prior to birth, soon after birth, at crisis points) |
|
|
| Physical barriers and facilitators, e.g. difficult birth (–), hospital environment (–), positioning (+/–), pain (–), latching (+/–), milk supply (+/–), frequent feeding (–), return to work or other separation from baby (–), managing siblings and other demands on time/resources (–), lack of sleep (–), change in routine (–), skin-to-skin contact (+) |
|
|
Environmental restructuring
Feeling supported was perceived to be important by all participant groups, particularly in the narratives of mothers and peer supporters. One mother reflected that women can feel ‘that little bit on your own breastfeeding’ when support from midwives and health visitors tailed off. Peer supporters perceived the provision of social support to be one of the most important functions of their role:
I think the social aspect is really important, I think it’s the main key, because as a breastfeeder you feel quite isolated, whether it’s within your family, within your friends, so belonging to a breastfeeding community, gives you the encouragement to keep breastfeeding and to keep following what you want to do. I think without this community most of us probably wouldn’t have got anywhere as far on our own.
Sally, peer supporter, focus group 1
Fathers wanted to be acknowledged and respected by those providing support rather than being told that they are ‘just a dad’. Mothers and peer supporters discussed the variability in the quality and availability of breastfeeding support from health-care professionals. Some felt that peer supporters had more time to spend with individual mothers and build up a relationship, and were able to empathise with mothers to a greater extent and also provide practical support, for example linking mothers with other services, including health-care professionals and local groups, and accompanying mothers when appropriate (e.g. to breastfeeding groups).
Peer support was seen as being particularly valuable in areas where breastfeeding is not the norm. This was seen as being important in counteracting negative attitudes towards breastfeeding:
And quite often you’ll have mothers being told by relatives and friends, ‘Are you feeding again, he’s hungry again, you only just fed him’, you know, this type of thing, and of course the mothers get very demoralised then, and they start questioning the breastfeeding, they start thinking that you know, they’re not producing enough milk and all this sort of stuff. It takes quite a strong-willed woman, and if she’s a young girl . . .
Wendy, health-care professional
Education, training and modelling
All participant groups considered improving knowledge (education), skills and confidence (training) to be important functions of BFPS. There was also consensus across the participant groups about the importance of modelling. Training was a prominent theme among peer supporters and health-care professionals, and some mothers and fathers also recognised the importance of this as part of a peer-supporter’s role. Peer supporters viewed counteracting negative attitudes and misinformation as an important part of their role. The importance of consistency of information and advice was a recurrent theme for all participant groups:
But I think in the early days, before I joined this [parenting] group, I had like eight different people telling me how to feed. And they were all different. Whereas when you come to this group, you might get a different midwife, you might get a different health visitor, but they are saying the same sort of thing.
Maya, mother, focus group 2
There was also a desire among the fathers to be informed so that they could support their partners:
Then both parents are getting told the same information so they both know what to do.
Dave, father, focus group
Enablement
For mothers, normalising the breastfeeding experience, that is, that all mothers go through ups and downs with feeding their baby, was an important aspect of peer support:
It’s nice to have a reminder of what’s normal, as well, isn’t it, because by the time you’ve had the baby and like you say, you are sleep deprived, and everything else has gone out of your head.
Jade, mother, focus group 3
Mothers valued the experiences of other mothers who had breastfed, as this was perceived to be a more ‘realistic’ view of what to expect and what constitutes ‘normal’ breastfeeding, in addition to ‘textbook’ advice. Peer supporters felt that sharing their own experience was important in supporting mothers. They felt that they had an opportunity to give mothers ‘honest’ information and provide a ‘realistic view’ so that they were prepared for the ‘bumps in the road’:
We’re all realistically saying you know what, we’ve had nights like this, and it’s not uncommon.
Kate, peer supporter, focus group 1
Preparing mothers for the ‘bumps in the road’ can provide them with confidence and motivation to develop coping strategies to deal with difficulties.
Persuasion, incentivisation and coercion
The BCW includes intervention functions that involve overt attempts to persuade, incentivise or coerce individuals or populations into changing behaviour. However, a strong theme emerged from all participant groups, suggesting that mothers should not be pressurised into breastfeeding:
What are you going to do when your baby is born, are you breastfeeding or are you bottle feeding? That’s the first question they ask. So, you know. Like I say, you can’t go too persuasive. Because you might actually put them off in the end.
Jess, mother, focus group 2
Mothers and fathers felt that building a personal relationship with the people supporting them was important. Parents preferred a gentle and co-operative approach to an authoritarian one. They wanted peer supporters to be ‘supportive’ and ‘not judgemental’. Some of the health-care professionals also acknowledged the importance of mothers being able to talk to someone they could relate to:
If you actually speak to somebody else that’s done it, that you realise that it’s not forever, that things will improve, things will get better. So I think from an, er, like emotional point of view, often I think the peer supporters are really good because they’ve got credibility, because they’ve actually got a baby.
Jan, community midwife
Although the experience of other mothers was valued, the style of communication was considered important when providing support. Mothers and fathers expressed a preference for a supportive, collaborative relationship and valued positivity and encouragement. This was in agreement with our rapid literature review, which concurred that the peer supporter should have experience of breastfeeding and credibility, an effective listening style, the appropriate social skills to be able to develop personal relationships and should be sensitive to the mother’s agenda in relation to breastfeeding.
Policy categories: service delivery
Integrating with existing breastfeeding support
Health-care professionals were generally positive about the role of breastfeeding peer supporters, but, consistent with the rapid literature review, a key theme that emerged was the need for peer support to be integrated with local health services. Peer support was viewed as something that would be used in addition to existing services. It was seen as an opportunity to provide additional focused support from an approachable and relatable source, not as a means of patching up deficits in existing services. Good communication between peer supporters and health-care professionals, clear roles and responsibilities, good training and support and familiarity with the local service context were viewed as being important to facilitate integration.
Behaviour change techniques
We categorised the behaviour change techniques using the BCTTv1 categories to ensure that the specific behaviour change techniques that we proposed matched the intervention functions (identified from the literature and qualitative work) in the intervention description (see Table 6). The BCTTv1 enabled us to categorise the technical aspects of peer support and MI, although some adaptation of the categories was required to reflect the MI ethos of working in partnership with clients, drawing on their own strengths and assets, rather than doing things to them. With some minor adaptation of the way in which the BCTTv1 categories were described, it was possible to classify most of the technical aspects of the MI-based BFPS intervention. For example, using the MI approach, a peer supporter would seek to guide a mother in reflecting on her breastfeeding goals and outcomes, using open questions and simple and complex reflections to explore her own beliefs, motivations and ambivalence, which broadly fits within the ‘review behavioural goals’ and ‘review behavioural outcomes’ BCTT v1 categories. However, there were categories of the BCTTv1 relating to providing information, but not to eliciting information from people. ‘Commitment’ is described by Michie et al. 56 as asking a person to affirm or reaffirm their commitment to behaviour change, but, in the context of a MI-based intervention, this is likely to come from the mother herself, with the peer supporter using reflection and affirmation to reinforce this when appropriate. We categorised affirmation as ‘social reward’, that is, providing positive reinforcement of the mother’s efforts. We categorised conveying empathy and emphasising autonomy, which are key features of the MI approach, as ‘social support (emotional)’, although these were not explicitly described in the BCTTv1 definition.
In MI, there is an emphasis on working collaboratively with clients, engagement, valuing people and respecting and building autonomy. These aspects were presented as overarching ‘guiding principles’ for working with mothers in the context of the intervention.
Mode of delivery
There was no consensus on the exact timing and frequency of contact between mothers and peer supporters, but being flexible enough to meet individual mothers’ needs was consistently considered to be important. For mothers, not wanting to feel pressurised to breastfeed was a prominent factor in determining the frequency of contact with the peer supporter, and providing proactive support had to be balanced against frequency of contact. The review found that contact should be proactive, but that there should be an incorporation of a mother-led schedule of contacts into intervention guidelines. All participant groups felt that initial contact between peer supporters and mothers during the antenatal period, to facilitate building up a rapport, would be beneficial:
You’d have to do it before the baby arrives because you don’t want just some stranger, once the baby’s born, going, this is what you do . . . You want somebody you know, don’t you.
Mille, mother, focus group 3
Some of the mothers, and the fathers, felt that they did not want to be given a lot of advice and information before the baby was born, as this could be overwhelming. It was generally agreed that support with breastfeeding should be provided early on in the postnatal period. Many participants felt that support would ideally start while mothers were in hospital, as they felt that midwives were busy and under pressure:
I think sooner rather than later. When the baby is actually born, you could be in there [in hospital] a few days before you get home. So if you don’t latch on or anything in that time, it could put you off doing it at all, whether you’ve got help at home or anything then. I think it needs to be there when the baby is actually born, they can go through it with everyone, show them how it’s done properly.
John, father, focus group
Health-care professionals had mixed views about providing BFPS in the hospital environment. Although some supported the idea, others felt that the hospital environment was already too busy and that ‘another body’ would not be helpful in this ‘delicate place’. This was consistent with what was reported in the published literature, which suggested that early intervention by the peer supporter was important for breastfeeding continuation. We concluded that some of the perceived tension between BFPS and health-care professionals, as identified in the survey (see Chapter 2), was possibly related to a lack of clear guidance regarding roles, responsibilities and minimum standards.
There were no strong views about when BFPS should end. Mothers, fathers and peer supporters generally felt that peer support should be able to continue in a flexible way until mothers had stopped breastfeeding. Fathers felt that support was most critical in the period up until feeding was established. Peer supporters felt that ending the intervention should be handled sensitively so that mothers did not ‘just feel dumped’. For example, there should be provision for women to contact their peer supporter should they need further advice or referral to other support groups.
Acceptability of motivational interviewing as a component of the breastfeeding peer-support intervention
Health-care professionals reported that they were mostly familiar with the basic principles of MI and most felt that it would be useful to provide peer supporters with MI training to develop communication and listening skills:
I think you need to know how to phrase things, you need to know how to listen as well. I think that sometimes, that’s what a woman needs. Is somebody to just listen to her and actually hear what she’s saying. And then I think if the peer supporters are trained in that way, then the conversation is more going to be woman centred rather than the peer supporter just giving her views, it’s going to be more, sort of, directed in the woman in front of her . . . I think the motivational interviewing will allow them to open up a little bit more.
Jan, community midwife
Health-care professionals commented that mothers sometimes felt guilty about telling them that they had stopped and that a MI approach could help counteract this:
They’ve [peer supporters] got to be well trained not to put that feeling of guilt over if they [mothers] do fail or if they are having difficulties.
Helen, health visitor
Overall, MI was viewed as a positive communication style that could help the peer supporters communicate with mothers in a mother-led, non-judgemental, empathic style.
Recruitment of peer supporters
Health-care professionals viewed peer supporters as being highly motivated and passionate about helping mothers. They felt that it was an appealing role for mothers living in these areas, particularly when they themselves had young children and recent experience of breastfeeding. However, they felt that there was a shortage of peer supporters relative to demand. Consistent with the findings of our survey of IFCs (see Chapter 2), changes in midwifery and health visiting service staffing and funding arrangements were seen as potential barriers to recruiting, training and supporting peer supporters.
Paying peer supporters was generally seen as a positive thing, although there were some concerns about having both paid and volunteer peer supporters working in the same areas. Payment could facilitate a more professional relationship and enable a clearer specification of what the peer supporter’s role would be. From the peer supporters’ perspective, the advantages of a paid service included making the job more viable for many women whose families relied on a second income and the ability to commit to providing support as required by the job specification.
Health-care professionals noted that there was likely to be a relatively high turnover of peer supporters as mothers returned to their usual work routine, and, therefore, a network of peer supporters covering an area was important in ensuring the sustainability of the intervention.
Peer supporters considered establishing boundaries to be important in relation to working hours and their expected availability, acknowledging the potential tension between the need for flexible and responsive support and a practical and manageable role.
Training
All participant groups in our qualitative work agreed that peer supporters needed to have adequate training (including in local health service policies and procedures), good links with the local health-care team and complete the relevant checks, for example the Disclosure and Barring Service (DBS) check, to ensure that they could work safely and competently with mothers and babies. These themes were consistent with the findings from the literature review and were key for integrating the peer supporter with the local health-care service. Good relationships and communication with other peer supporters and health-care professionals and regular supervision were considered to be important in providing one-to-one support. The ability to access good training and support was viewed as important in the personal and professional development of peer supporters. Health-care professionals highlighted the importance of training in practical issues relating to breastfeeding, safeguarding, lone-worker policies, data protection and confidentiality. From the health-care professionals’ perspective, training of peer supporters and ensuring channels for communication with health-care professionals were seen as being key in providing consistent advice across the multiple sources of breastfeeding support for women. Health-care professionals felt that robust training for peer supporters was needed for them to have confidence in recommending the service to mothers. Peer supporters needed to have an awareness of how to work with mothers during a vulnerable time in their lives, when they may be emotional, tired or suffering from postnatal depression. Developing interpersonal relational skills was therefore important, including listening skills, communication and how to read body language. Responsibility for training needed to be clear and appropriately resourced. It was felt that training was currently community based and typically fell within the remit of health visitors.
Stakeholder Advisory Group view on the mode of delivery
Through discussion with the Stakeholder Advisory Group, we concluded that there should be at least one antenatal contact between the peer supporter and mother to enable information exchange and build a rapport and some contact in the first few days after birth (to include the time around the 72-hour weighing of the baby) and that ongoing support during the postnatal period should be flexible enough to meet individual mothers’ needs. There was consensus that the ending of the intervention should provide affirmation of the mother’s efforts and enable her to access other sources of support in the longer term (e.g. breastfeeding groups, online communities) should she require these. Boundaries around the peer-supporters’ role should be clearly set from the outset, be generated by an external party to provide consistency, ensure safety and acknowledge the limits of peer supporters’ knowledge and skills and be discussed and reflected on during supervision sessions. The intervention should focus on enabling mothers to cope outside of the peer supporters’ working hours by activating their social networks and signposting them to other services. This was supported by the rapid literature review, which signalled that peer supporters have an important role in acting as advocates for breastfeeding mothers within their own social groups and helping to change the culture. It was agreed that, following on from initial training, peer supporters would need support from midwives and health visitors to help with their practice and to deal with any issues or questions that they were uncertain about. The Stakeholder Advisory Group developed ‘principles of good practice’ for the delivery of MI-based BFPS, stating that peer supporters should be supportive, positive, non-judgemental, approachable, honest, down to earth and good listeners. Peer supporters should also be facilitated to make links with each other, for example by having a meeting once per month in which they could share their experiences and good practice.
The intervention name ‘Mam-Kind’ was developed in conjunction with the Stakeholder Advisory Group and peer supporters, who were part of a closed online social media group, hosted on Facebook. The Stakeholder Advisory Group generated a list of possible names. These were shortlisted by the study team and the final choice of three was presented to the closed online group of peer supporters. This group then voted for their preferred name. Box 3 summarises the defining characteristics of the Mam-Kind intervention.
-
There should be at least one antenatal contact to enable information exchange and build rapport, some contact in the first few days after birth (to include the time around the 72-hour weighing of the baby) and flexible ongoing support in the postnatal period to meet individual mothers’ needs, and ending of the intervention should provide affirmation of the mother’s efforts and enable her to access other sources of support in the longer term (e.g. breastfeeding groups, online communities).
-
Boundaries around the peer-supporters’ role should be clearly set from the outset, be generated by an external party to provide consistency and ensure safety, acknowledge the limits of peer-supporters’ knowledge and skills and be discussed and reflected on during supervision sessions.
-
The intervention should focus on enabling mothers to cope outside of the peer-supporters’ working hours by activating their social networks and signposting to other services.
-
Following initial training, peer supporters need support from midwives and health visitors to help with their practice and to deal with any issues or questions that they are uncertain about.
-
Peer supporters should be linked up with each other, for example by having a meeting once a month where they can share their experiences and good practice.
Content of the programme
Table 6 summarises the objectives and content of the sessions mapped onto the BCW within each time frame for the Mam-Kind intervention. In line with the intervention’s guiding principles, there was flexibility in the method of delivery, content and resources used to ensure a mother-centred approach. The emphasis was on achieving a high-quality contact, regardless of method. Appendix 7 (see Figure 11) shows the logic model that describes the theory of change underpinning the Mam-Kind intervention. An adaptation of this model, which includes the requirements for implementation, is provided in Appendix 7.
| Time period | Mode of delivery | Scope of session content | Intervention functions | Behaviour change techniques (BCTT v1) |
|---|---|---|---|---|
| Antenatal | Face-to-face visit (or telephone call if this is a mother’s preferred option) | Engagement and building a rapport with the mother and significant others (if present) | Restructuring the social environment | Social support (unspecified) |
| Information about accessing the intervention: what it’s about, how it works, letting the peer supporter know when the baby has arrived | Education, training | Instruction on how to perform a behaviour | ||
| Discuss an agenda with mothers: what can they expect and what they would like to get from the programme | Enablement | Action planning | ||
| Affirmation of the mother’s strengths and capability, emphasising her autonomy | Enablement, restructuring the social environment | Social support (emotional), social reward | ||
| Explore mothers’ current knowledge and information needs and provide information as appropriate. Use open questions, reflective listening and elicit–provide–elicit approaches to exchanging information with mothers | Education, training | Instruction on how to perform a behaviour, information about health, social and environmental and emotional consequences | ||
| Guide mothers in understanding their beliefs, motivations and intentions with regard to breastfeeding. Strengthen ‘change talk’ about breastfeeding and soften ‘sustain talk’ about not breastfeeding | Education, enablement | Identity associated with changed behaviour, framing/reframing, incompatible beliefs, pros and cons (including decision balance tool), goal-setting (behaviour), goal-setting (outcome), self-talk | ||
| Planning for breastfeeding (e.g. resources needed, how to overcome difficulties, how to get support) | Training, enablement | Instruction on how to perform a behaviour, problem-solving, action planning | ||
| Postnatal | A face-to-face visit (or a telephone call/text if not feasible) within 48 hours of birth, either in hospital or at home; contact every other day (face to face, by telephone or by text) from days 3–14, including a visit close to the 72-hour weighing of the baby; provide a graded exit from the intensive one-to-one service from 2 weeks onwards. Note: additional contact by telephone/text/in person can be provided if required | Engagement and building a rapport – introductions, congratulations on the new arrival (first visit), seek collaboration; convey empathy, affirm mothers’ strengths and capability and emphasise her autonomy | Enablement, restructuring the social environment | Social support (unspecified), social support (emotional),social comparison, social reward, demonstration of behaviour |
| Use open questions and reflective listening to elicit from the mother how she is doing, how the feeding is going and what support (if any) she would like; explore ambivalence and concerns and identify potential barriers to, and facilitators of, continued breastfeeding; provide information and skills training based on individual needs on breastfeeding relevant to the first few days and weeks | Education, training, enablement | Review behaviour goals, review outcome goals, instruction on how to perform a behaviour, information about health, social and environmental and emotional consequences. Identity associated with changed behaviour, pros and cons (including decision balance tool), framing/reframing, incompatible beliefs, social support (practical) | ||
| Provide a role model for continued breastfeeding | Modelling | Demonstration of the behaviour | ||
| Normalising experiences | Restructuring the social environment | Social comparison | ||
| Strengthen ‘change talk’ about continuing to breastfeed and soften ‘sustain talk’ about discontinuing breastfeeding earlier than the mother would like to | Enablement |
Commitment Self-talk |
||
| Planning for overcoming barriers to breastfeeding | Enablement | Problem-solving, action-planning | ||
| Graded exit from the intervention | Use open questions and reflection to elicit from mothers what other sources of breastfeeding support they might need now and in the longer term; signpost/refer to relevant services and act as an advocate when required; offer practical support to overcome barriers to accessing support, such as accompanying mothers to a breastfeeding group or to a public place (e.g. local café) if they have concerns about feeding in public | Enablement, training | Action-planning, instruction on how to perform a behaviour, social support (practical) |
Mam-Kind buddies
The peer supporters who delivered the Mam-Kind intervention were called Mam-Kind buddies and will be referred to as such from here on. Mam-Kind buddies should be women from the same locality as the women they support, who have breastfed and (1) have already completed BFPS training accredited at level 1 (e.g. Agored Cymru); (2) have the necessary personal attributes (warm, likeable, discreet, good communication skills and the ability to listen) and (3) are able to work within guidelines.
Support provided for Mam-Kind buddies
The Mam-Kind buddies were provided with additional breastfeeding and MI training. The training was based around the intervention description, ensuring that learning objectives were identified relating to breastfeeding, MI and professional practice (e.g. safeguarding). Specialists in each of these areas (NG, ST, JS) contributed to the development of the training programme. Further details of the training programme can be found in the training manual in Appendix 7 (see Report Supplementary Material 1). Mam-Kind buddies were provided with an intervention handbook, training materials and intervention-specific resources, as detailed in Appendix 8 and Report Supplementary Material 1. They were also provided with monthly one-to-one coaching sessions in using a MI-based approach and initial weekly supervision from a midwife, which was tailored to meet their needs.
Supervision from a midwife
The supervising midwives provided breastfeeding support to the Mam-Kind buddies. The supervising midwives were all provided with study and MI training. The Mam-Kind buddies met face to face with their supervising midwife, initially once a week, and this was reduced over time as the peer supporters and midwives saw fit. The midwives also provided support over the telephone with any queries the Mam-Kind buddies might have. Finally, the midwives were there to provide a link between the Mam-Kind buddies and health-care professionals, such as community midwives and health visitors.
Motivational interviewing supervision
Motivational interviewing supervision was provided to the Mam-Kind buddies over the course of the intervention. This consisted of one-to-one support by telephone once a month. The MI trainer listened to an audio recording of a face-to-face intervention session between the peer supporter and the mother prior to the telephone call and then provided feedback on the peer supporter’s MI skills.
Discussion
We used a systematic, user-informed approach, guided by the BCW, to develop a novel MI-based peer-support intervention to support breastfeeding maintenance. We pooled data from a range of sources (published and unpublished literature, qualitative research findings and discussions with experts in our Stakeholder Advisory Group) to understand the behaviours associated with breastfeeding that can be targeted by this intervention. We found that psychological capability, social opportunity and reflective motivation were the key sources of behaviour that the intervention should address to support women to continue breastfeeding. We used the BCW framework to link these behaviours with the relevant functions of the intervention and service requirements for implementation. To our knowledge, the BCW has not previously been used in this context.
The BCW is an extensive but not exhaustive model. 56 The BCW was developed in the context of professional-led interventions, primarily in the areas of diet and smoking. 57 Components of the BCW have since been used in a variety of behaviour change contexts, including improving the uptake of health checks for children,93 medication management for multimorbidity94 and understanding prescribing errors by junior doctors. 95 Using the BCW as a guide in this study enabled us to characterise the sources of behaviour targeted by the intervention and its functions, service implications and mode of delivery.
Motivational interviewing is currently included in the BCTTv1 under ‘emotional social support’. 58 However, this does not reflect the complexity of MI, which has both technical and interpersonal/relational dimensions. 96 There were several techniques used within MI that could be mapped on to behaviour change techniques included in other taxonomies. 75 One of the challenges that we encountered was that the terminology used in the BCTTv1 was not always consistent with the MI approach. The types of intervention that the BCW and BCTTv1 have been built on are in the main part directive and are often focused on doing things to a person to elicit behaviour change. The underlying ethos of MI is quite different, in that it values autonomy and draws on a person’s own strengths and assets. One of the guiding principles of MI is to resist the ‘righting reflex’, wherein health-care workers have a powerful desire to ‘set things right’, which can have paradoxical effects of increasing resistance to a given behaviour. 28
In working through the process of characterising the intervention, it became apparent that the BCTTv1 was not well suited to describing how the intervention content would be delivered in terms of style of communication, the quality of the interpersonal relationship between peer supporters and mothers and the underlying ethos of the intervention approach. Much of MI focuses on relational and interpersonal techniques, known as ‘the MI spirit’, which can strongly influence its effectiveness. 28 Building a collaborative relationship is a key feature of MI. 28 MI interventions that had a strong emphasis on improving fidelity to intervention content (i.e. using manuals) were less effective,97 whereas those focusing on adherence to relational–interpersonal style techniques had larger effects. 98 We addressed this by developing a set of ‘guiding principles’ to clarify the underlying ethos and interpersonal style that guides the way in which the technical behaviour change content of the intervention is delivered. These ‘non-specific’ factors apply to many types of intervention and can be challenging to measure and assess, but they are important and need to be given sufficient attention in future iterations of the BCTTv1 and other behaviour change technique taxonomies.
Chapter 4 Feasibility study
This chapter addresses study objective 4: to assess the feasibility and acceptability of providing MI-based BFPS to women living in areas with high levels of social deprivation.
Introduction
We aimed to assess (1) whether or not the intervention could be delivered as intended, with proactive Mam-Kind buddy-led support during the early postnatal period; and (2) whether or not the intervention and research processes were acceptable to pregnant women who lived in areas with high levels of social deprivation, Mam-Kind buddies and health-care professionals. We used quantitative data to assess adherence to the Mam-Kind intervention by examining the number, timing and duration of one-to-one contacts with Mam-Kind buddies. We used qualitative data from interviews with participants, Mam-Kind buddies and health-care professionals involved with the delivery of the Mam-Kind intervention in the study sites to assess the feasibility and acceptability of the method of recruiting pregnant women, and the study materials to understand what worked well and any areas for improvement. We also explored fidelity to the intervention by examining the extent to which Mam-Kind buddies met the objectives of the intervention as intended and the range of MI techniques used in their interactions with the mothers who they supported.
We considered the possible inclusion of a control group and randomisation process, but concluded that this would be premature at this stage. Previous studies had already demonstrated that it was feasible to conduct RCTs of BFPS, but highlighted problems with poor uptake and adherence to the intervention. We therefore considered that it was most important to establish the feasibility of providing a MI-based BFPS intervention as intended to the target population and designed the study to address this.
Ethics considerations
Ethics approval for the feasibility study was granted by the NHS Health Research Authority, Wales REC 3 Panel, in June 2015 (reference 15/WA/0149). All participants provided written informed consent. Health-care professionals provided audio-recorded verbal consent for their interviews following a standardised script.
Study design
This was a non-randomised multisite before-and-after study with a process evaluation.
Setting
The study was carried out within community maternity services in three areas with high levels of social deprivation and low breastfeeding initiation rates. Each site was in the 20% of most deprived communities based on the English Indices of Deprivation99/WIMD60 and had lower rates of breastfeeding than the UK average (< 70%) and a higher-than-average proportion of teenage pregnancies (> 41.9 conceptions per 1000 women aged < 18 years). One of the sites (site 3) had an existing paid peer-support service. This allowed us to test the feasibility of implementing the intervention within an existing service, which required a shift in the way of working to deliver Mam-Kind as specified in the context of a research study. The other two sites had a voluntary peer-support service that provided group support in community settings. In sites 1 and 2, we estimated that there would be approximately 528 women with an expected date of delivery during the recruitment period. Based on experience in other studies, we assumed that approximately half of these women (n = 264) would be considering breastfeeding and that 55% of these women (n = 145, based on breastfeeding initiation rates) would be interested in the study, with at least half (n = 73) consenting into the study. In site 3, we estimated that there would be approximately 264 women with an expected date of delivery during the recruitment period. By applying the same assumptions that were used in the other two sites, we estimated that approximately 34 women would consent to take part in the study.
Inclusion and exclusion criteria
All English-speaking pregnant women (at least 28 weeks’ gestation) who were considering breastfeeding were eligible for inclusion in this study. We chose to recruit and consent women who were considering breastfeeding in the antenatal period because the primary outcome that we wanted to affect was maintenance of breastfeeding. This was consistent with the finding from the rapid literature review, which suggested that a change in outcome was more likely if the intervention was targeted to a subpopulation that was inclined to value the offer of help. We anticipated that recruitment from 28 weeks onwards would provide sufficient time for women to have an antenatal contact with their Mam-Kind buddy in accordance with the intervention specification. Women with multiple pregnancies (twins, triplets, etc.) were eligible for inclusion in the study as long as they met the other inclusion criteria. This would have allowed us to explore the feasibility of providing MI-based BFPS to this group of women. We excluded women who were unable to provide written informed consent, who were unable to use conversational English, who did not plan to breastfeed, who had a clinical reason that precluded breastfeeding (e.g. baby with a major congenital anomaly) or who had a planned admission to a neonatal unit following birth.
Recruitment of Mam-Kind buddies
We recruited seven Mam-Kind buddies to work in the two sites that did not have a pre-existing service. In the site with an existing paid peer-support service, two peer supporters took on the Mam-Kind buddy role. An additional Mam-Kind buddy was recruited and trained to provide cover in sites 1 and 2 if needed; however, we retained all Mam-Kind buddies throughout the study and no cover was required. The post of breastfeeding peer supporter was advertised through the Cardiff University job vacancies web page. Local breastfeeding groups and peer supporters were approached via social media to reach potential applicants. All candidates (n = 15) who applied for the post were invited to attend the first 3 days of training, which included information about the study and an introduction to MI. When possible, video conferencing was used to deliver training for those who were unable to attend. The 3 days of training were unpaid with the exception of travel expenses and childcare costs. Following this training event, candidates were shortlisted and asked to attend for an interview to complete the selection process. Following recruitment, Mam-Kind buddies were given further study-specific training over 4 consecutive days to integrate breastfeeding and MI skills. One further training day was provided in final preparation for the role. Training was provided by Cardiff University and, although childcare costs and travel expenses were covered for the Mam-Kind buddies, attending further training was not feasible for the Mam-Kind buddies in site 3 because of the geographical distance and family commitments. All nine Mam-Kind buddies were provided with an intervention handbook containing information about the intervention and training materials and a resource pack with information about MI (see Report Supplementary Material 1). All eight Mam-Kind buddies who delivered the intervention were asked to take part in a process evaluation interview to understand their experiences of the study.
Recruitment of supervising midwives
We recruited one practising midwife in each site to provide supervision to the Mam-Kind buddies delivering the intervention at their site. We requested expressions of interest for the role, in collaboration with heads of midwifery. All three midwives attended the 1-day study-specific training, which included an introduction to MI.
Site set-up
Study promotion
Following study training, the study managers visited labour and postnatal wards at sites 1 and 2 to liaise with midwives, maternity care assistants, managers and IFCs to promote the study. Study posters were placed in prominent areas to provide further information and remind midwives to notify peer supporters of a birth so that they could contact the mother. Study information was cascaded via the daily safety briefing for staff at each shift change for approximately 1 week, when it was anticipated that the majority of staff would have been notified of the study. In site 3, the study midwife, who was the local site principal investigator (PI), took on the role of promoting the study and setting up the site for recruitment, with support from the study managers.
Recruitment of feasibility study participants
Midwives introduced the study to pregnant women at around 28 weeks’ gestation and obtained agreement to forward potential participants’ contact details to the research team. Midwives were asked to introduce the study by giving a study leaflet to women who met the eligibility criteria. We tested the feasibility of two models of obtaining consent. These were developed in response to discussion with local site PIs. In sites 1 and 2, potential participants’ contact details were passed to the study manager, who then organised and completed the recruitment visit. The study manager confirmed eligibility and provided a participant information sheet before obtaining consent to participate and collecting baseline data. In site 3, this process was carried out by a research midwife and a health visitor. Research midwives, who took over from the study manger part-way through the recruitment process, later provided recruitment support in site 2. They obtained consent and completed the baseline questionnaire with participants. Participants were assigned a Mam-Kind buddy and provided with details of the other Mam-Kind buddies in their area, whom they could contact in the event that their assigned buddy was not available. We did not match participants to their peer supporter based on need or preference. Participants were also asked if they would be willing to (1) have their sessions with the Mam-Kind buddy audio-recorded and (2) participate in a telephone interview (process evaluation interview) to evaluate their experiences of the study.
Sampling and recruitment of participants for the process evaluation interviews
The study manager contacted the participants who indicated that they would be willing to take part in the process evaluation interviews at approximately 8 weeks post birth to confirm their agreement to participate and arrange a time for the process evaluation interview. Mothers who took part in these interviews were provided with a £20 high street voucher to thank them for their time.
In addition to the study participants, we interviewed all of the Mam-Kind buddies and supervising midwives from the three feasibility study sites. We also purposively sampled two midwives (one midwife who was a high recruiter into the study and one midwife who was a low recruiter, selected based on the advice of the supervising midwife), one health visitor and one service manager from each feasibility study site (n = 12). All of those who were invited agreed to take part.
Outcome measures
We used a range of measures to assess the feasibility of delivering the Mam-Kind intervention, as shown in Box 4.
-
Feasibility of (1) recruiting and retaining peer supporters from the community of women to whom MI-based BFPS is to be delivered and (2) delivering MI-based BFPS as specified in objective 3, including an assessment of whether or not the intervention objectives were met and the extent to which Mam-Kind buddies utilise MI techniques in their interactions with the participants who they support (intervention fidelity).
-
Uptake of, acceptability of and adherence to MI-based BFPS by participants according to age and parity.
-
Number and duration of one-to-one contacts with Mam-Kind buddies and transition to use of breastfeeding groups.
-
Feasibility and acceptability of the method of recruiting pregnant women (including the timing of approach) to inform a possible full trial.
-
Acceptability of the study materials (study information leaflets, consent forms, toolkit for Mam-Kind buddies).
-
Suite of primary and secondary outcome measures for a possible full trial.
-
Optimal follow-up options of (1) using telephone interviews with participants, (2) obtaining data routinely collected by health visitors at the source and (3) using routine NHS databases (e.g. child health systems) to collect the recommended suite of outcome measures in a possible full trial.
Data collection
Baseline data items (see Report Supplementary Material 1) were collected at the time of obtaining consent, including sociodemographic variables, infant feeding intentions and maternal health and well-being. The study manager conducted a brief follow-up telephone interview at 10 days (see Report Supplementary Material 1) that asked about skin-to-skin contact post delivery, breastfeeding initiation, breastfeeding self-efficacy, support received, sources of influence and feeding method. A further, more detailed follow-up interview was conducted at 8–10 weeks after birth (see Report Supplementary Materials 1and 2) to ascertain the duration of exclusive or partial breastfeeding, breastfeeding attitudes, use of health-care professionals or groups for breastfeeding support and maternal and child health and well-being. A 10-day minimum data set questionnaire was completed at 8–10 weeks for participants who could not be contacted at 10 days. Well-being was measured using the Edinburgh Postnatal Depression Scale. 100 Breastfeeding status has been linked to mental health status and so we wanted to capture this as a potential confounder. Although we were not testing confounders in the feasibility study, we were testing the acceptability of collecting these types of data. Mam-Kind buddies completed a diary to provide data about their contacts with the women they were supporting. Mam-Kind buddies were also asked to audio-record all of their face-to-face sessions with participants who had consented to this. Midwives completed screening logs to record the number of women who did not want to participate in the study. Supervising midwives completed contact logs of their contacts with the Mam-Kind buddies. A summary of data items collected is provided in Table 7.
| Time point | Measure |
|---|---|
| Baseline | Educational status |
| Employment status | |
| NS-SEC – employment code | |
| Marital status | |
| Ethnicity | |
| Pregnancy status | |
| Number of babies expected | |
| Parity | |
| Feeding status of previous children | |
| How participant was fed as a child | |
| Knowledge of other mothers’ feeding methods | |
| Feeding intentions | |
| Social support | |
| Relationship questionnaire | |
| Edinburgh Postnatal Depression Scale | |
| GAD-2101 | |
| EQ-5D-5L102 | |
| Smoking status | |
| 10-day follow-up | Skin-to-skin contact |
| Breastfeeding initiation | |
| Feeding status at hospital discharge | |
| Feeding status at 10 days | |
| Reason for giving formula | |
| Breastfeeding Self-Efficacy Scale Short Form103 | |
| Breastfeeding experience | |
| Breastfeeding influence | |
| Breastfeeding support | |
| 8–10 weeks’ follow-up | Feeding status at 8 weeks |
| Feeding status in past 7 days | |
| Reason for giving formula | |
| Breastfeeding experience | |
| Breastfeeding influence | |
| Breastfeeding support | |
| Social support | |
| Breastfeeding Self-Efficacy Scale Short Form | |
| EQ-5D-5L102 | |
| Edinburgh Postnatal Depression Scale | |
| GAD-2101 | |
| Health resources utilisation | |
| MI fidelity | MITI 4.1 tool104 |
The process evaluation interviews were conducted by experienced qualitative researchers, facilitated by a topic guide (Box 5). The interviews were conducted by telephone, audio-recorded and transcribed verbatim by a professional transcription company. The duration of the interviews ranged from 16 to 41 minutes for health-care professionals, from 15 to 70 minutes for mothers who received the intervention, from 36 to 75 minutes for Mam-Kind buddies and from 29 to 35 minutes for supervising midwives.
Feeding experience.
Introduction to the study by the midwives.
Experience of the Mam-Kind buddies.
Experience of the intervention at the specified time points.
Birth notification.
Relationship with Mam-Kind buddies.
Help with breastfeeding.
Social support.
Consent and baseline.
10-day and 8-week follow-ups.
Topics covered in health-care professional interviewsIntroduction and training on the study.
Participant introduction to the study by the community midwives.
Study materials.
Research paperwork.
Experience of the Mam-Kind buddies.
Views of the study and intervention acceptability.
Birth notification.
How the Mam-Kind buddies worked with existing services.
Topics covered in peer-supporter interviewsRecruitment to Mam-Kind buddy role.
Training, including breastfeeding and MI.
Contact with participants, partners and families.
Birth notification.
Work–life boundaries.
Supervision.
Contact with health-care professionals.
Completion of research paperwork (Mam-Kind buddy diary) and audio-recording.
Topics covered in supervising midwife interviewsViews on the support given by peer supporters to the participants.
Training.
Supervision experience.
Use of supervision by the Mam-Kind buddies.
Completion of research paperwork (supervising midwife diary).
For the telephone interviews with mothers across the three sites, we used a purposive sampling process based on four factors: study site, Mam-Kind buddy delivering the intervention, success at breastfeeding at 10 days and level of engagement with the intervention. We approached a total of 43 mothers and 29 (67%) agreed to take part in the interviews. We originally aimed for the sample to consist of at least 50% of young mothers (aged ≤ 21 years). However, as the feasibility study had recruited only four mothers who were aged ≤ 21 years, we interviewed all eight mothers who were aged ≤ 25 years. We further interviewed mothers aged 26–30 years (n = 12), 31–35 years (n = 8) and ≥ 36 years (n = 1).
Fidelity to the content of the intervention sessions and MI was assessed using audio-recordings of face-to-face sessions between Mam-Kind buddies and mothers. Sessions were recorded on a Dictaphone (Olympus digital voice recorder VN-731PC, Olympus, Southend-on-Sea, UK) with the participants’ permission and transcribed verbatim for analysis. We initially selected two sessions per Mam-Kind buddy to be coded: the first antenatal session that the Mam-Kind buddy had audio-recorded and a postnatal session that occurred 2 months after the first session. An additional five audio-recordings were also included in the sample to ensure full representation of all key time points in the intervention (antenatally, 48 hours, 2–13 days and 2–6 weeks), resulting in an overall sample size of 21.
We used a validated measure of MI, the Motivational Interviewing Treatment Integrity (MITI 4.1) tool,104 to measure the extent to which the peer supporters used MI. Twenty-minute segments are usually randomly selected for MITI 4.1 assessment; however, we adapted this method of measurement for pragmatic reasons, as follows. In our sessions, Mam-Kind buddies shifted focus across a number of different topic areas, which meant that there was not necessarily a continuous 20-minute section in which they talked about ‘feeding baby’. Therefore, we first conducted a content analysis of the audio-recordings, which helped us to identify conversations focused on ‘feeding baby’, and then applied the MITI 4.1 tool to a 20-minute collection of these segments per audio-recording.
Quantitative data analysis
Summary measures [frequencies/percentages and means/standard deviations (SDs)] were tabulated for all quantitative data at each time point (baseline, 10 days and 8 weeks), including missing data for each measure.
Process evaluation data analysis
An initial coding framework for the interview data was developed, based on the analysis of three interviews with participants. The themes were further updated and refined in an iterative manner throughout the analysis.
The content of the audio-recordings was assessed using deductive content thematic analysis. The coding framework was based on the content guide of the intervention (see Table 6), to outline the content of the conversation against the specified intervention objectives at each stage of the intervention (antenatally – six objectives; 48 hours – five objectives; postnatally – five objectives). The coding framework was then applied to all of the participant interview and session data by two researchers (LC and LM). The team discussed any new analytical themes that emerged; these were added to the framework and previous transcripts were recoded accordingly until all of the data had been coded. The transcripts and the coding framework were uploaded to NVivo 10, where both researchers coded a subset of the data to test reliability.
We mapped session content against the objectives in the intervention content guide to assess whether or not (1) objectives had been met and (2) the content of the sessions was appropriate to the stage of the intervention.
Motivational interviewing fidelity was assessed using the MITI 4.1 tool. The MITI rating tool consists of a number of count and score variables. ‘Global’ ratings are divided into technical (cultivating change talk and softening sustain talk) and relational (partnership and empathy). These are scored on a scale from 1 to 5. Behaviour count scores are provided for giving information, persuade, persuade with permission, questions, simple reflections and complex reflections, affirm, seek collaboration, emphasising autonomy and confront.
A number of composite scores are calculable from these variables, including the technical rating (which encompasses scores on cultivating change talk and softening sustain talk), relational rating (which encompasses scores on partnership and empathy), percentage complex reflection, reflection-to-question ratio, total MI adherent and total MI non-adherent. There is no overall score to indicate ‘basic competence’ or ‘proficiency’ incorporating all of the measures. MITI guidance indicates that, to reach basic competence in each of the measures, a practitioner must achieve an average global technical score of 3, an average global relational score of 4 and a reflection-to-question ratio of 1 : 1 and that at least 40% of all reflections should be complex reflections. To reach proficiency, a practitioner must achieve 4, 5, 2 : 1 and 50% for these items, respectively. The Mam-Kind buddies were not expected to reach these thresholds, but we used this assessment to obtain an understanding of the extent to which peer supporters were able to use MI techniques in their interactions with mothers.
Intercoder reliability
Intercoder reliability was used to assess the reliability of the coded interview and peer-supporter session data. A random selection of 10% of the interviews and 30% of the content sessions was independently coded by a second researcher. A number of themes had > 5% disagreement, as calculated using NVivo 10. The majority of these were the result of differences in the amount of text included by the coders when coding themes. Discussion between both researchers led to the refinement of some definitions, but no substantial changes were made to the coding framework.
Sixteen MI sessions were rated by one member of the research team (LC) using the MITI 4.1 tool. A random selection of 30% of the peer-supporter sessions were double-coded by another member of the research team (SC).
The agreement level was summarised for each of the global rating scales using Fleiss’ multirater kappa. The behaviour counts were examined using an intracluster correlation coefficient (ICC), as is appropriate for continuous data. These methods produced an acceptable level of agreement and reliability (global score κ = 0.49 and ICC = 0.93). The detail of this assessment is provided in Appendix 9 (see Tables 23 and 24).
Feasibility study results
Feasibility of recruiting and retaining Mam-Kind Buddies
Recruitment and retention of Mam-Kind buddies
No difficulties were encountered in recruiting peer supporters at the two study sites where there was no pre-existing service, with 15 applications received for eight posts. We aimed to recruit women who had experience of breastfeeding and who had previously successfully completed accredited BFPS training. We had intended to recruit women who lived in the same locality (community maternity service catchment area) as the women who they would be supporting, but this was found to be incompatible with university recruitment regulations. Five of the eight Mam-Kind buddies lived in the same area in which they were supporting participants, two lived within a 10-mile radius and one lived approximately 20 miles away. All Mam-Kind buddies who passed the initial job checks continued in their role for the full 6 months’ duration of the study, demonstrating that it was feasible to retain peer supporters for the 9 months during which the intervention was delivered.
Mam-Kind buddies’ views on training
Feedback on the training provided to Mam-Kind buddies was obtained at the end of the training, by completion of a questionnaire and from the qualitative interviews carried out as part of the process evaluation. We did not collect feedback from potential Mam-Kind buddies who undertook initial training but who were not subsequently appointed.
The qualitative interviews provided mixed feedback about the recruitment process. Some Mam-Kind buddies felt that the initial mandatory 3 days of preselection training was a good networking opportunity and useful for their personal development, and felt that it would have been beneficial even if the post had not been subsequently offered to them. Others reflected that they felt overwhelmed by the training because of the numbers who attended and the study staff observing. Mam-Kind buddies felt that the initial 2-day basic MI training that they received was interesting and that there was a good balance between theory and practical application. Some participants felt that they were able to see how it could fit into their peer-support/Mam-Kind buddy role and also outside of this remit, whereas others felt that they lacked clarity on how to deliver the MI intervention in the context of the study:
With breastfeeding, [were we to] say that breastfeeding was the goal, or? Or . . . because then we also were supposed to be supporting people if they’re bottle feeding, so . . . and also just empowering mums. And if we’re empowering mums, the change talk might be that they do decide to bottle-feed, and that they become happier or . . . That wasn’t . . . So in terms of the training and clarity of what was . . . what are we listening for?
Mam-Kind buddy 4
The Mam-Kind buddies reported that the 5 days of integrated MI and breastfeeding training provided time to think about, and practise, their MI skills in the context of the study.
Some Mam-Kind buddies were unable to attend the whole programme of training and expressed that they found it more challenging to communicate with the Mam-Kind buddy group and study team, explaining that travelling and childcare was difficult to arrange because of the distance needed to travel. The Mam-Kind buddies felt that the continuity and support of the breastfeeding trainer throughout the training period was beneficial.
Mam-Kind buddies’ views on supervision
To support them with any clinical issues related to breastfeeding and to provide a link with other health-care professionals, Mam-Kind buddies received weekly supervision from a local community midwife. The Mam-Kind buddies valued the supervising midwife and found the format of supervision to be acceptable. The supervising midwives were able to schedule a weekly hour-long meeting and were also available to respond to telephone calls from the Mam-Kind buddies within the 3 hours per week of allocated time assigned to the study in their job plan (Table 8). The Mam-Kind buddies most frequently contacted the supervising midwife by telephone outside of their weekly meetings, to discuss breastfeeding issues and/or obtain reassurance about the appropriateness of the information that they were providing to mothers. Mam-Kind buddy attendance at the weekly supervision meetings was good. Although the Mam-Kind buddies valued the contact that they had with the supervising midwives, not all of them felt that the weekly hour-long face-to-face meeting was necessary, and they recommended a reduction in the frequency of these sessions. The supervising midwives agreed with this view.
| Site | Type of contact | Number of contacts |
|---|---|---|
| 1 | Face to face | 8 |
| 1 | Telephone | 20 |
| 2 | Face to face | 4 |
| 2 | Telephone | 10 |
| 3 | Telephone | 0 |
| 3 | Face to face | 14 |
Mam-Kind buddies received MI supervision from a qualified MI trainer. Each Mam-Kind buddy received at least two one-to-one sessions and three group sessions over the 6-month period. There was poor uptake of the final one-to-one session. This final session included a new task in which the Mam-Kind buddies had to listen to one of their own sessions and complete a self-evaluation form, reflecting on their use of MI techniques. Only three Mam-Kind buddies sent through an audio-recording and subsequently completed the self-evaluation and associated one-to-one feedback and supervision session. During the qualitative interviews, Mam-Kind buddies reported that the MI supervision sessions provided constructive feedback, furthered their understanding of how to use MI techniques, identified areas for improvement and provided reassurance that they were using MI techniques to a certain degree. Although some Mam-Kind buddies felt uncomfortable with one-to-one supervision, as they did not enjoy reflecting on their own audio-recorded sessions, they all enjoyed the group supervision sessions. This provided the Mam-Kind buddies with a supportive environment in which to reflect on their MI practice as a group and discuss any techniques that they were struggling with. Overall, the Mam-Kind buddies found the supervision to be beneficial for improving their skills, but found reflecting on their practice and listening to their sessions challenging.
Acceptability of the Mam-Kind buddy role requirements
One of the key aspects of acceptability that was explored with the Mam-Kind buddies through the qualitative interviews was the need for flexibility in when and how Mam-Kind buddies were contacted by mothers. Some of the Mam-Kind buddies reported that they chose to be available almost 24 hours a day at times for the participants. All reported that women did not text or ring at inappropriate times:
Yeah weekends I did yeah . . . and trying to think now . . . yeah sometimes it was in the early morning, but nothing ridiculous, nothing that I would think oh that’s a bit you know.
Mam-Kind buddy 1
The Mam-Kind buddies defined the appropriate time of contact individually. The flexible working pattern was welcomed by some of the Mam-Kind buddies, as it allowed them to work around other jobs or commitments. Others said that they found the unstructured nature of the job difficult, especially when trying to arrange childcare. The buddies that were recruited specifically for this study reported that the 15 hours pay per week either reflected the number of hours that they actually worked or provided some spare capacity to complete study paperwork. The buddies that were providing the Mam-Kind intervention in addition to an existing peer-support service in their area found it difficult to balance both roles within the 15 hours that they were paid for. In this site, it was intended that the Mam-Kind intervention would be provided instead of the usual service model; however, this could not be practically implemented, leading to the peer supporters providing both the Mam-Kind intervention and the usual service model for the duration of the study.
We were obviously doing our job role that we’re paid for and then with the additional work on for the [site name] study, we were having to do that out of our spare time really . . . It was quite hard work.
Mam-Kind buddy 8
Feasibility and acceptability of the method of recruiting pregnant women
Feasibility of recruitment
Feasibility of participant recruitment was demonstrated by the numbers recruited in each site, as shown in Figure 10 (for recruitment by site see Appendices 10–12). Of the 292 women who were assessed and met the eligibility criteria for the study, 39% (n = 115) expressed an interest in taking part. Of these 115 women, 61% (n = 70) completed the consent process and were recruited into the study. The majority of women (94%, n = 108) who expressed an interest in taking part in the study were contacted by the study team to carry out the recruitment process; however, of those contacted, 35% (n = 38) declined to participate. The percentage who declined to participate varied between sites (site 1: 34%, 11/32; site 2: 46%, 27/59; site 3: 0%, 0/17). The reasons given for declining were that it was a very busy time for them and they did not have time to take part in a study or they felt that it was not right for them. In site 3, the high rate of non-participation in the study may be explained by the availability of an existing one-to-one peer-support service that women could access without having to consent to a research study. There were four withdrawals across the three sites because of participants feeling that they had sufficient breastfeeding support systems in place.
FIGURE 10.
Recruitment flow diagram (all sites). EDD, estimated due date.

Demographic characteristics of participants
The mean age of participants was 29 years (Table 9). Three participants (4%) had no qualifications, nine participants (13%) had General Certificate of Secondary Education (GCSE) qualifications as their highest qualifications and 23 participants (33%) had a degree or higher qualification (Table 10). The majority of participants were employed in full-time (n = 46, 66%) or part-time (n = 7, 10%) work, with 14 participants (20%) unemployed. The majority of participants (43%) were in either managerial or professional occupations or intermediate occupations (23%).
| Site | Age (years) | |
|---|---|---|
| Mean (SD) | Min., max. | |
| 1 (n = 21) | 28.3 (5.09) | 19.2, 41.1 |
| 2 (n = 32) | 29.6 (4.14) | 20.5, 36.6 |
| 3 (n = 17) | 27.9 (4.13) | 20.9, 35.6 |
| Total (n = 70) | 28.8 (4.44) | 19.2, 41.1 |
| Characteristic | Participants (N = 70), n (%) |
|---|---|
| Marital status | |
| Married/civil partnership | 27 (38.6) |
| Living together | 27 (38.6) |
| Have partner but not living together | 6 (8.6) |
| Single | 9 (12.9) |
| Widowed/divorced/separated | 0 (0.0) |
| Missing | 1 (1.4) |
| Highest educational achievement | |
| GCSE grades A–C | 9 (12.9) |
| A or AS or S levels | 7 (10.0) |
| Certificate or diploma in higher education | 14 (20.0) |
| First degree (e.g. BA or BSc) | 20 (28.6) |
| Higher degree | 3 (4.3) |
| Other | 13 (18.6) |
| None of these qualifications | 3 (4.3) |
| Missing | 1 (1.4) |
| Employment status | |
| Full-time work | 46 (65.7) |
| Part-time work | 7 (10.0) |
| Unemployed/seeking work | 3 (4.3) |
| Unemployed/not seeking work | 11 (15.7) |
| Full-time education/training | 2 (2.9) |
| Part-time education/training | 0 (0.0) |
| Rather not say | 0 (0.0) |
| Missing | 1 (1.4) |
| NS-SEC – socioeconomic code | |
| Managerial and professional occupations | 30 (42.9) |
| Intermediate occupations | 16 (22.9) |
| Small employers and own-account workers | 3 (4.3) |
| Lower supervisory and technical occupations | 8 (11.4) |
| Semiroutine and routine occupations | 8 (11.4) |
| Not applicable (never worked) | 2 (2.9) |
| Missing | 3 (4.3) |
| Ethnicity | |
| White British | 66 (94.3) |
| Any other white background (Romanian) | 1 (1.4) |
| White and black Caribbean | 1 (1.4) |
| White and Asian | 1 (1.4) |
| Missing | 1 (1.4) |
| First baby? | |
| Yes | 43 (61.4) |
| No | 26 (37.1) |
| Missing | 1 (1.4) |
The majority of participants were married (n = 27, 39%) or living with a partner (n = 27, 39%). In total, 9% (n = 6) of participants reported that they had a partner that they were not living with and 13% (n = 9) were single. The majority of participants (n = 66, 94%) were white British. All participants were expecting one baby and for 61% (n = 43) it was their first baby. Among the 26 participants who had other children, about one-third had previously breastfed. Nearly all participants (n = 65, 93%) planned to exclusively breastfeed their child or to combine breast and formula milk (n = 2, 3%). The majority of women (n = 26, 37%) reported that the mothers they knew had mostly formula fed, with only 6% (n = 4) reporting that they knew mothers who had breastfed (Table 11). Half of participants reported that, as babies, they had been entirely formula fed (n = 35).
| Breastfeeding experiences | Participants (N = 70), n (%) |
|---|---|
| How participants were fed as a baby | |
| Breastfed entirely | 19 (27.1) |
| Formula entirely | 35 (50.0) |
| Mixed feeding | 8 (11.4) |
| Do not know | 0 (0.0) |
| Missing | 8 (11.4) |
| Know any mothers with young babies? | |
| Yes | 55 (78.6) |
| No | 14 (20) |
| Missing | 1 (1.4) |
| How other mothers you know have fed | |
| Mostly formula only | 26 (37.1) |
| Mostly breastfed | 4 (5.7) |
| Mostly mixed | 8 (11.4) |
| Mixture of above | 16 (22.9) |
| Do not know | 1 (1.4) |
| Not applicable | 14 (20.0) |
| Missing | 1 (1.4) |
| Plan to feed baby | |
| Formula (not eligible) | 0 (0.0) |
| Breastfeed | 65 (92.9) |
| Mixed | 2 (2.9) |
| Undecided | 1 (1.4) |
| Missing | 2 (2.9) |
Acceptability of recruitment methods to participants and health-care professionals (data from qualitative interviews)
The study training provided to midwives and maternity care assistants about introducing the study to potential participants was received positively, although fewer than expected attended because it took place during the summer holiday period. Midwives expressed that the training was clear and that they had a good understanding of their role within the study. The following insights were obtained through the qualitative interviews that were carried out during the process evaluation.
Community midwives felt that it was appropriate and acceptable to introduce the study to potential participants at 28 weeks’ gestation, as it coincided with the stage in their pregnancy when participants were starting to consider how they would feed their baby. However, midwives reported that they occasionally found that they had little time to explain the study to women. Participants felt reassured that they would get extra support with breastfeeding, and this was expressed as the primary reason for participating in the study:
And she said oh she said there’s people that are going to, you know are doing a study and they’re going to be able to support you through breastfeeding and I read all about it and I was like oh yes, you know it made me feel more at ease knowing that I’m going to get support.
Participant 103
Participants and midwives expressed that meeting with Mam-Kind buddies would be beneficial for study promotion and recruitment in a future trial. Midwives were requested to complete a screening log for all women who were approached about the study, but acknowledged that sometimes they forgot because of other time pressures:
And we have so many things to, to discuss and talk about and obviously we’ve only got 20-minute appointment, we’d obviously ask all the information but then sometimes it may just be that, because we’re so busy, we’ve forgotten to put it on the screen, the log at that point.
Midwife 2001
The process for referring potential participants who expressed an interest in the study for a consent visit needed refinement, and additional support was provided from the research and development office at the largest site (site 2). Written consent was obtained by a member of the research team, usually in the participant’s home, and this was acceptable to participants. The research team monitored recruitment and, when there was a noticeable plateau, a site visit was initiated or the local study team was contacted to remind midwives about the study and find out if there were any issues that needed to be resolved.
Overall, midwives expressed satisfaction with the training that they received. They felt that their role was clearly explained and expressed that they had the opportunity to discuss the study further. Midwives liked the study resource pack that they were given, consisting of BFI information leaflets for participants, screening logs, copies of the study invitation letter and procedures for introducing the study to women. There was only a short interval between the health-care professionals’ training and the commencement of study recruitment and some health-care professionals stated that they would have liked a few weeks to consider the study information before introducing the study to women.
Follow-up options
This section reports on data collection and considers the options for follow-up to collect the recommended suite of outcome measures in a possible full trial: (1) using telephone interviews with participants, (2) obtaining data routinely collected by health visitors at the source (directly from the mothers’ medical records) and (3) using routine NHS databases (e.g. child health systems).
Follow-up data collection
The recruitment chart (see Figure 10) presents the number of women who completed the baseline, 10-day and 8-week postnatal assessments. The study team attempted a maximum of three contacts (by telephone, text, e-mail or a combination) with participants before categorising them as ‘lost to follow-up’. Some participants stated that they would have preferred to complete the questionnaires electronically or by a messenger application (such as Facebook).
Baseline data were collected for 99% of participants (n = 69). Overall, data collection at 10 days postnatally was acceptable to participants, although some who had a longer stay in hospital or a difficult birth expressed that 10 days was early to be contacted. Data collection at 10 days’ follow-up by telephone was successful for 63% (n = 44) of participants. For participants who we were unable to contact at 10 days, a further attempt was made to collect these data using a minimum data set at 8 weeks. These data included skin-to-skin contact at birth and infant feeding at 10 days. This resulted in 10-day postnatal follow-up data being collected for an additional 11 participants (16%). This method of data collection was reported to be acceptable to participants in the qualitative interviews. We considered that the risk of inaccurate measurement associated with collecting 10-day data at 8 weeks because of the long period of recall was low, given the nature of the data items being collected. This approach enabled us to increase the completeness of follow-up data at 10 days for a minimum set of variables from 63% to 78%.
In total, 64% (n = 45) of participants completed the 8- to 10-week telephone follow-up. Data collection took, on average, 30–40 minutes (n = 28 questions). At 8 weeks’ follow-up, 51.1% of participants followed up were breastfeeding, with 42.2% exclusively breastfeeding (Table 12).
| Feeding at 8 weeks | All data (N = 45), n (%) |
|---|---|
| Only breast milk | 19 (42.2) |
| Only formula | 22 (48.9) |
| Mixed | 4 (8.9) |
| Missing | 0 (0.0) |
We tested the feasibility of collecting data on a suite of primary and secondary outcomes that would be relevant in a future trial of effectiveness. Data completeness was > 80% for all variables with the exception of questions within the breastfeeding self-efficacy scale at 10 days (66.5%) and the reasons for giving formula milk at 10 days (79%) and 8 weeks (51.1%).
Overall, the participants found the follow-up questions to be acceptable, although some participants reported that the mental health questions were quite personal and difficult to answer:
I found them OK a bit personal . . . so if I was you know a self-harmer or something like that . . . I think for somebody that does or has done it in the past . . . I think they’d find it a bit daunting to talk about it.
Participant 115
We explored the feasibility of collecting feeding status at 8 weeks from routine data collected by the health service that are usually collated within NHS databases. Of the 21 participants who could not be contacted for their 8-week follow-up, we obtained data for 10 participants on their breastfeeding status from their health-care provider. For three of these participants, breastfeeding data were collected at 4–8 weeks and, therefore, did not meet the definition of our primary outcome measure. In site 1, we were able to access data on breastfeeding at 6 weeks from the externally available child health system for four of the 10 participants. In site 2, we were unable to access these routinely available data from the child health system because the wording on the consent form was deemed insufficient to allow the research team to access these data.
Uptake of the Mam-Kind intervention
All participants were offered an antenatal contact with their Mam-Kind buddy and the majority of participants had an antenatal contact (face to face or by telephone) (primiparous women: 66%, n = 35; multiparous women: 72%, n = 18). There was no difference in the mean age of women according to whether or not they received an antenatal contact (mean age: 28 years); 74% of participants (n = 52) engaged with the intervention. Engagement was defined as accepting at least one antenatal and one postnatal contact, and this was not influenced by maternal age. The majority of women who received an antenatal and postnatal contact from the Mam-Kind buddy reciprocated this contact by texting the Mam-Kind buddy back, answering the call or meeting the Mam-Kind buddy face to face (primiparous women: 67%, n = 35; multiparous women: 68%, n = 17).
Fidelity to the Mam-Kind intervention
Number, timing and duration of one-to-one contacts with Mam-Kind buddies
We used the quantitative data from the Mam-Kind buddy diaries to determine the timing, location and type of contact (call, text or face to face) with Mam-Kind buddies, including who initiated the contact across the three sites. The intervention specification required Mam-Kind buddies to contact participants within 48 hours of the birth of their baby. In total, 73% of participants (n = 51) received a contact within 48 hours of birth, but this was not associated with whether or not antenatal contact with the Mam-Kind buddy had occurred (no 48-hour contact, n = 19; 10 had antenatal contact and nine did not). The Mam-Kind buddies reported that the main reason for not achieving contact within 48 hours of birth was a lack of notification of the baby’s birth by either the mother or the midwife.
In total, there were 1137 contacts between the Mam-Kind buddies and the participants. The mean number of contacts that each participant received from their Mam-Kind buddy was 16 (range 0–44).
The contact time was similar across all types of contact, with a mean contact time of 16 minutes (Table 13). The travel time for Mam-Kind buddies was similar for sites 1 and 2, but less for site 3. This was expected, because the buddies lived further away in site 1, site 2 covered a large geographical area and site 3 covered a smaller geographical area.
| Variable | Site, mean (SD) | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Contact time (minutes) | 15.8 (24.4), n = 399 | 15.9 (20.4), n = 469 | 16.2 (20.7), n = 163 |
| Travel time (minutes) | 58.1 (23.3), n = 50 | 56.7 (19.7), n = 32 | 5.4 (1.9), n = 16 |
When recorded, the majority of contacts occurred between 0900 and 1700 across all three sites, particularly in site 3, where 99% of contacts were made within this period (Table 14). Across all three sites, 74% of the face-to-face contacts took place at the participant’s home. There was limited contact at hospital sites, mainly because it was not possible for peer supporters to negotiate research governance procedures in line with the requirements of the study timelines. A ‘research passport’ was required by the respective health board in sites 1 and 2 to enable the Mam-Kind buddies to visit participants on the postnatal ward. To be issued with a research passport, the Mam-Kind buddies required an employment contract, a health check from occupational health and a DBS check. Delays across human resources and the health board research and development departments led to the relevant permissions taking up to 6 months to be issued. All peer supporters had a DBS and occupational health check before seeing mothers. The impact on the study was that, in two sites (sites 1 and 2), peer supporters were unable to have face-to-face contact with new mothers in the hospital setting until the last month of recruitment (January 2016).
| Variable | Site, n (%) | ||
|---|---|---|---|
| 1 (N = 414) | 2 (N = 511) | 3 (N = 212) | |
| Time of day | |||
| 0000–0859 | 25 (6.6) | 18 (3.7) | 0 |
| 0900–1659 | 219 (57.9) | 373 (76.4) | 93 (98.9) |
| 1700–2359 | 134 (35.4) | 97 (19.9) | 1 (1.1) |
| Missing | 36 | 23 | 118a |
| Type of contact | |||
| 0 | 2 (0.4) | 1 (0.5) | |
| Breastfeeding group | 1 (0.2) | 0 | 0 |
| Face to face | 61 (14.7) | 55 (10.8) | 33 (15.6) |
| 65 (15.7) | 0 | 0 | |
| No contact | 4 (1.0) | 0 | 0 |
| Telephone | 61 (14.7) | 69 (13.5) | 144 (67.9) |
| Text | 216 (52.2) | 373 (73.0) | 33 (15.6) |
| Missing | 6 | 12 | 1 |
| Location of all face-to-face contacts | |||
| Breastfeeding group | 4 (1.0) | 2 (0.4) | 2 (0.9) |
| Coffee shop | 2 (0.4) | 4 (0.8) | 1 (0.5) |
| Hospital | 3 (0.7) | 0 | 0 |
| Home | 40 (9.7) | 42 (8.2) | 27 (12.7) |
| NA (i.e. all contact made by telephone or social media) | 362 (87.4) | 458 (89.6) | 181 (85.4) |
| Missing | 3 | 5 | 1 |
| Who initiated contact | |||
| Family/friend | 1 (0.2) | 0 | 0 |
| Health-care professional | 5 (1.2) | 26 (5.1) | 3 (1.4) |
| Mam-Kind buddy | 294 (71.0) | 332 (65.0) | 181 (85.4) |
| Mother | 107 (25.8) | 131 (25.6) | 18 (8.5) |
| Missing | 7 | 22 | 10 |
| Prompts used | |||
| Agenda map | 2 (0.5) | 0 | 0 |
| Making a decision | 3 (0.7) | 0 | 0 |
| Mam-Kind toolkit | 4 (1.0) | 1 (0.2) | 0 |
| None | 397 (95.9) | 426 (83.4) | 212 (100) |
| Missing | 8 | 84 | 0 |
Some births were not reported to peer supporters during the period of the hospital stay. The research team had provided training on birth notification to midwives during the set-up of the study sites and also asked mothers to notify their peer supporter of their baby’s birth. A sticker was placed on participants’ hand-held maternity records to communicate to maternity staff that they were part of the study; however, this process had varied success across the sites. The failure of peer supporters to be notified of births contributed to the low frequency of hospital visits in sites 1 and 2. Any delay in birth notification and initiating contact with the peer supporter could potentially have a detrimental effect on subsequent engagement with the peer supporter and motivation to continue with breastfeeding:
I had the sticker on the front of the folder, but nobody [from the hospital] had actually rung [the Mam-Kind buddy]. And then it was, I think it was 2, 2 or 3 days after he’d been born, because I just completely forget really to be honest. Yeah, so then she didn’t really get a chance to come up, but then we’d switched over in the hospital.
Participant 201
The qualitative interviews with health-care professionals suggested that birth notifications could be improved by making the study stand out from the many other studies that are being run in hospitals:
There’s so many blinking trials going on . . . you just get mind, mind boggled with it all.
Health-care professional 0001
Mam-Kind buddies suggested that they could have visited the wards to introduce themselves to the staff, engage them and increase awareness of the intervention:
I don’t know if that would have been useful maybe before we sort of met mums to have gone up to the ward and just say, here we are, so they didn’t think we’re just . . .
Mam-Kind buddy 4
In site 3, mothers received peer support on the ward from a different peer-support service, according to the usual care available in that site, and were transferred to the care of a Mam-Kind peer supporter when they returned home.
As demonstrated by data from the Mam-Kind buddy diaries, the majority of contacts in sites 1 (52%) and 2 (73%) were made by text message, whereas in site 3 the majority of contacts (68%) were made by telephone (see Table 14). The interviews with mothers suggested that they found the variety of types of contact acceptable. Mothers reported that they found text-message contacts especially helpful, as they could text their Mam-Kind buddy at any time. This allowed the mothers to express their feelings at a particular point in time in the knowledge that a Mam-Kind buddy would reply to them as soon as they were able:
I was able to do that, and even writing it down saying ‘This is what I’m struggling with’. Makes a big difference with how you’re coping with it.
And at least get it down, did she ever get back to you at like 2 o’clock in the morning, did she?
More normal times, yeah.
The majority of contacts across all sites (74%) were initiated by the Mam-Kind buddies, which was consistent with the requirement in the Mam-Kind specification for proactive contact. In total, 20% of contacts were initiated by participants, suggesting that some participants also felt comfortable contacting their peer supporter. The reason for the higher rate of Mam-Kind buddy-initiated contact at site 3 is unknown, but may reflect established practices. In the interviews, the health-care professionals reported that they received positive feedback from participants about the amount of contact, although some of the participants stated that the proactive contact was too much for them:
One of the other mums had said it was too much . . . whereas another mum loved it, and just lapped it up, she could have been visited 100 times and would have enjoyed it.
Health-care professional 001
During the interviews, participants reported that the antenatal contact helped them to feel comfortable with their Mam-Kind buddy in terms of discussing personal and sensitive information, and that it facilitated the Mam-Kind buddy–mother relationship. During the postnatal period, participants reported that the Mam-Kind buddies provided guidance and signposting to appropriate forms of support on problems such as thrush (Candida albicans), mastitis or colic. Participants also stated that the Mam-Kind buddies pre-empted any problems that they thought the participants might develop based on what the participants were telling them. Participants reported that the Mam-Kind buddies helped to build their confidence and provided reassurance and emotional support.
Completeness of diary data
We used diaries completed by the Mam-Kind buddies to collect data on the number of contacts between the Mam-Kind buddies and the participants. Mam-Kind buddies reported in the qualitative interviews that the layout of the diary was acceptable and that it was straightforward to complete. However, some Mam-Kind buddies were uncertain about whether or not their documentation would have sufficient information about a contact if a participant experienced a health or social issue:
I didn’t think it covered enough . . . for safety reasons for staff and for parents . . . because that’s one of our things, we have to document everything that’s there, just in case.
Mam-Kind buddy 7
These diaries were developed primarily as a tool for data collection to support the process evaluation in the study. Further discussion is needed with health service managers to clarify the necessary documentation from the service perspective for the implementation of the Mam-Kind intervention.
Transition to breastfeeding support groups
Two weeks after birth, the Mam-Kind buddies were required to facilitate the transition of support to other community breastfeeding support services, such as breastfeeding groups. The interviews with participants and Mam-Kind buddies provided an insight into this process. Some mothers felt that they did not receive a graded exit from the study (i.e. being signposted onto other services, such as breastfeeding groups, with gradually reduced contact) and would have preferred a more gradual transition:
Well I don’t know, maybe it could be phased out a bit more. Erm, maybe you know not full-on support, but just you know have a conversation a couple of weeks after the follow-up and then maybe a month after or something so that there’s not an end until, you know the end becomes further away each time . . . so it feels like it’s not really an end by the time you get to that point.
Participant 109
Some Mam-Kind buddies accompanied mothers to breastfeeding groups and this was seen as a gentle way to encourage mothers to seek support from other sources following the intervention:
I wouldn’t have done it on my own . . . So she [peer supporter] took me to the first one and then I went on my own afterwards, so I welcomed it.
Participant 113
Some mothers felt supported by their Mam-Kind buddy in attending groups and felt that this experience helped them to normalise breastfeeding and also provided some structure to their day:
And I think it was a good place to start feeding in public there because everybody else was feeding as well . . . So it was nice to see other mums feeding and then you wasn’t as anxious to do it yourself.
Participant 315
In some cases the Mam-Kind buddies supported mothers for > 6 weeks, with some mothers reporting that they received contact from their Mam-Kind buddy at 8 weeks and 15 weeks. This was also reflected in the Mam-Kind diary data. This suggested that the Mam-Kind buddies may not have been signposting participants to breastfeeding groups to facilitate a graded exit from the service and preferred to continue to support women.
Fidelity to the Mam-Kind intervention content and use of motivational interviewing
Assessing fidelity was important to understand whether or not the intervention was being delivered as specified. We assessed fidelity using recorded sessions between Mam-Kind buddies and mothers. Audio-recordings were completed in 78 (52%) of the 149 face-to-face sessions that the Mam-Kind buddies delivered. In this section, we present data to show the level of MI skill demonstrated by the peer supporters and the extent to which the content of the intervention delivered by the Mam-Kind buddies matched the intervention specification.
Fidelity to the intervention content
Content analysis was conducted for 21 peer-support sessions, as described in Process evaluation data analysis. The Mam-Kind buddies had objectives to fulfil at each time point (six objectives at the antenatal contact and five at each postnatal contact) (see Appendix 13, Table 25). The extent to which these objectives were covered is presented in Table 15.
| Mam-Kind buddy–participant dyad | All time points | Topic | All postnatal time points | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antenatal | Postnatal | |||||||||||||
| 48 hours | 3–14 days | 15 days–6 weeks | ||||||||||||
| Emotional support | Social support | Engage with women and start to develop rapport | Information about the programme/what to expect | Information about breastfeeding (getting started) | Agree how peer supporter will be informed about birth | Engage with women and develop a rapport | Information about breastfeeding (relevant to first few days) | Maintain relationship with mothers (and their supporters) | Information about breastfeeding (relevant to first few weeks) | Provide graded exit from intensive one-to-one service | Information about breastfeeding (relevant to ongoing feeding) | Address queries or concerns | ||
| Antenatal session | ||||||||||||||
| Mam-Kind buddy 4, PID 230 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | |
| Mam-Kind buddy 7, PID 311 | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | – | – | – | – | – | – | – | |
| Mam-Kind buddy 8, PID 302 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | ✓ | – | |
| Mam-Kind buddy 2, PID 109 | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | – | – | – | – | – | ✓ | – | |
| Mam-Kind buddy 5, PID 226 | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | – | – | – | – | – | – | – | |
| Mam-Kind buddy 5, PID 207 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | |
| Mam-Kind buddy 3, PID 121 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | ✓ | – | |
| Mam-Kind buddy 6, PID 217 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | ✓ | – | |
| Mam-Kind buddy 1, PID 103 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | |
| Mam-Kind buddy 3, PID 101 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | |
| Mam-Kind buddy 6, PID 202 | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | – | – | – | – | – | ✓ | – | |
| Mam-Kind buddy 4, PID 210 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | |
| Postnatal session (48 hours) | ||||||||||||||
| Mam-Kind buddy 3, PID 121 | ✓ | ✓ | – | – | – | – | ✓ | ✓ | – | – | – | – | ✓ | |
| Mam-Kind buddy 7, PID 308 | ✓ | ✗ | – | – | – | – | ✓ | ✓ | – | – | – | – | ✓ | |
| Mam-Kind buddy 6, PID 205 | ✓ | ✓ | – | – | – | – | ✓ | ✓ | – | – | – | – | ✓ | |
| Postnatal session (3–14 days) | ||||||||||||||
| Mam-Kind buddy 2, PID 108 | ✓ | ✓ | – | – | – | – | – | – | ✓ | ✓ | – | – | ✓ | |
| Mam-Kind buddy 6, PID 217 | ✓ | ✓ | – | – | – | – | – | – | ✓ | ✓ | – | – | ✓ | |
| Mam-Kind buddy 3, PID 113 | ✓ | ✓ | – | – | – | – | – | – | ✓ | ✓ | – | – | ✓ | |
| Postnatal session (15 days–6 weeks) | ||||||||||||||
| Mam-Kind buddy 2, PID 112 | ✓ | ✓ | – | – | – | – | – | – | – | – | ✗ | ✓ | ✓ | |
| Mam-Kind buddy 1, PID 119 | ✓ | ✓ | – | – | – | – | – | – | – | – | ✗ | ✓ | ✓ | |
| Mam-Kind buddy 8, PID 315 | ✓ | ✓ | – | – | – | – | – | – | – | – | ✗ | ✓ | ✓ | |
Overall, Mam-Kind buddies met the majority of the content objectives in each session, with 93% of the objectives met (109 of the 117 total number of objectives for each of the analysed sessions). A maximum of one objective was not met in any one session. Mam-Kind buddies engaged with participants, provided emotional support and information about breastfeeding, discussed social support and addressed participants’ queries and concerns. Ten of the 21 sessions met all of the objectives of the content guide and included breastfeeding support that was relevant to the stage of the intervention. Eight sessions did not cover one of the objectives and five included breastfeeding information that was time inappropriate, that is, information that was beyond the scope of the session and was not asked for by the mother.
Key objectives related to discussion of how the Mam-Kind buddies would be informed about the birth and information about the programme were not met in four out of 12 antenatal sessions. However, it is possible that these objectives were covered before the antenatal session, as all of the Mam-Kind buddies who did not discuss these objectives in the antenatal session had previous contact with participants by telephone or text that lasted longer than 10 minutes.
The key objectives, providing a graded exit and providing social support, were not met in four of the nine postnatal sessions. However, all of the participants in the postnatal sessions between 15 days and 6 weeks who were included in the content analysis had subsequent contact with Mam-Kind buddies over 2 weeks by a combination of text, telephone calls, Facebook and face-to-face meetings. During these contacts, peer-supporter diaries indicated that participants were given links to further information such as information on expressing and bottle feeding and leaflets for support groups, potentially indicating that a graded exit was provided later on.
Five out of 12 antenatal sessions included information that was not relevant to the stage of the intervention. For example, the discussion extended beyond how to get started with breastfeeding to discussion of ongoing feeding, formula feeding and weaning. In two of these sessions, participants prompted discussion of long-term feeding plans. In the remaining three sessions, the Mam-Kind buddy provided information about long-term feeding without being prompted by the participant. One of the participants reported feeling overwhelmed by this discussion:
So if you decide that breastfeeding is going well, this is great, it’s something I want to carry on with, if you can do the first month just exclusively breastfeeding and then is a good time to start introducing bottles . . . It sounds like a lot doesn’t it.
Yeah, overwhelming.
Have you had any thoughts on um sort of how long?
I don’t know, because some people have said you know breastfeed up until about 6 months and then go to formula and then some people are like a year plus . . . by then obviously they’ll be starting to feed with solid food . . .
So you start to introduce solids at 6 months and yes, what they say is food before 1 is just for fun . . . even after 1 it’s very, very rare that a baby under 18 months would stop having milk.
Although some participants felt overwhelmed when given information that was not relevant to their stage of infant feeding, they felt reassured when Mam-Kind buddies addressed specific queries or concerns:
I’ve never fed a baby before . . . I just want to know I’m doing the right thing.
All you can do is try…you’ve asked us for our information . . . I’ve talked through everything with you. I’m on the phone whenever you want.
You’ve reassured me . . . that I’m doing OK . . .
It sounds like you’re doing great.
The content analysis demonstrated that prespecified objectives were met in most antenatal and postnatal sessions. However, greater emphasis is needed during the training to ensure that Mam-Kind buddies discuss birth notification during the antenatal session, provide information that is relevant to the stage of the intervention, discuss social support needs and provide a graded exit from the one-to-one service.
Fidelity to motivational interviewing
Sixteen recordings were assessed for fidelity to MI (Table 16). The global scores and behaviour counts must reach the thresholds specified in the MITI tool for the Mam-Kind buddies to have achieved basic competence or proficiency. We found that some Mam-Kind buddies developed certain MI skills to a competency level. Mam-Kind buddies avoided reinforcing talk about formula feeding (sustain talk), and there were some attempts to reinforce the participants’ talk about breastfeeding (change talk). Although the scores suggest weak efforts at collaboration and partnership working, there was evidence of empathy being communicated during intervention delivery. Mam-Kind buddies were able to learn reflective listening skills and five of the eight Mam-Kind buddies demonstrated at least a fair level of complex reflections compared with simple reflections. There was some indication of MI-consistent practice, evidenced through affirming, seeking collaboration or emphasising autonomy, and no evidence of MI-inconsistent practice involving confronting or explicitly disagreeing with participants. There was, however, clear evidence of efforts to persuade participants to breastfeed by offering opinions, suggestions or advice without explicitly reinforcing the participants’ autonomy in accepting these. Although Mam-Kind buddies did not directly confront or disagree with participants’ choices, they did attempt to persuade them to take specific actions rather than offer suggestions in a MI-consistent, autonomy-supporting manner.
| Mam-Kind buddy | Session | Global scores | Behaviour counts | ||||
|---|---|---|---|---|---|---|---|
| Technical | Relational | Percentage complex reflections | Total reflection-to-question ratio | Total MI adherent | Total MI non-adherent | ||
| 7 | PID 311 | 2.5 | 2.5 | 0 | 0.33 | 2 | 10 |
| 7 | PID 308 | 3 | 1.5 | 20 | 0.5 | 3 | 12 |
| 8 | 302 Oct S1 | 2 | 1.5 | 0 | 0 | 0 | 6 |
| 8 | 31530.12.15 | 2 | 1 | 33 | 0.6 | 3 | 10 |
| 1 | 10330.09.15S1 | 3.5 | 3.5 | 36 | 1.83 | 5 | 2 |
| 1 | 119.09.02.16 | 4 | 4 | 44 | 1.2 | 6 | 5 |
| 4 | 210.22.10.15S1 | 2.5 | 3.5 | 55 | 2.25 | 2 | 2 |
| 4 | 230.26.01.16 | 3.5 | 3.5 | 75 | 0.5 | 2 | 0 |
| 3 | 10118.11.15S1 | 4 | 3 | 38 | 0.89 | 2 | 18 |
| 3 | 12128.01.16S3 | 2.5 | 1.5 | 17 | 1.2 | 0 | 7 |
| 2 | 1009.10.15S1 | 2.5 | 3.5 | 67 | 3 | 2 | 2 |
| 2 | 11207.01.16S3 | 2.5 | 1.5 | 38 | 0.89 | 2 | 5 |
| 6 | 20213.10.15S1 | 3.5 | 3.5 | 17 | 1.5 | 3 | 1 |
| 6 | 20505.11.15S2 | 2.5 | 3.5 | 43 | 3.5 | 2 | 4 |
| 5 | 131015S1207 | 3 | 2.5 | 18 | 2.2 | 5 | 17 |
| 5 | 22608.12.15S1 | 2.5 | 2.5 | 60 | 1.25 | 1 | 4 |
Reflecting the MITI results, the Mam-Kind buddies reported that they found it challenging to use MI in the context of breastfeeding. They found it challenging to practice MI in the antenatal session, as it was the first conversation that they had had with the participants in which they were getting to know each other, which they found easier to do while having a sociable conversation. Mam-Kind buddies reported that they sometimes struggled to use their MI skills to engage with participants. Some of the Mam-Kind buddies felt pressured to use MI during all of the sessions, leading to them having difficulties with really listening to the participants. There was a perception that MI may have been easier to use if they had had more practice, which may have led to increased levels of proficiency.
Acceptability of the study materials (study information leaflets, consent forms and toolkit for Mam-Kind buddies)
The participants were given various study materials, including two leaflets explaining the study (an introduction leaflet and a participant information sheet) and contact cards for the Mam-Kind buddies. The interviews demonstrated that, overall, the mothers and health-care professionals liked the study materials and the health-care professionals felt that they were acceptable in terms of BFI standards:
No, absolutely, I thought it was appropriate, I thought it was enough, it wasn’t complicated.
Participant 213
Participants found that the study materials were clear and easy to read. The participants liked being able to show members of their family the materials to help them explain the study. Some participants stated that the format of the materials could be made electronic:
You get given a lot of information through health visitors and midwives and things and I think it could’ve really got mixed up in the mix of all the other things that . . . so I think maybe an e-mail.
Participant 303
Mam-Kind buddies infrequently documented in their diaries when they used the study materials (see Table 14). However, the interview data and audio-recordings of sessions suggested that the Mam-Kind buddies did use the Mam-Kind toolkit in many of their antenatal sessions:
Um and then you know, they’ve given a chance to talk about that, and then I would say ‘So um do you understand what the study’s all about, obviously, you know, you’ve enrolled on the study, do you understand what it’s all about?’, and they would say ‘Oh I think so yes’, and so then we would go through the timeline. That was really helpful.
Mam-Kind buddy 3
Amendments to the intervention based on the feasibility study findings
The findings from the feasibility study led us to make improvements to the Mam-Kind intervention. The findings from the MI fidelity work suggested that the Mam-Kind buddies struggled to implement their MI skills in the sessions and tended to default to an information-giving style of conversation. To address this, we simplified the objectives for each session of the intervention (Table 17). We adapted the intervention to clarify the structure of each session. For the antenatal session, this included an opportunity for the Mam-Kind buddies to have a purposeful and focused conversation about the mothers’ aspirations for breastfeeding. In postnatal sessions, this included an opportunity to simply understand the mothers’ experiences before stepping in to offer practical advice. In this way, we hope to have changed the emphasis of the sessions to reflect the collaborative and supportive nature of the conversations before Mam-Kind buddies step in and provide the participants with information and advice. This structure should help the Mam-Kind buddies in a future RCT to know how to use their MI skills throughout the sessions.
| Contact | Objectives | Method of delivery | Scope of the sessions |
|---|---|---|---|
| Antenatal |
|
Face-to-face visit with women during the antenatal period. Note: a telephone contact may be used as an alternative to provide flexibility for women who do not want a face-to-face visit at this stage (e.g. successfully breastfed before, not enough time before due date to arrange a visit) |
|
| First 48 hours after birth |
|
A face-to-face visit within 48 hours of birth, either in hospital or at home. Note: there will be some flexibility to allow contact by telephone or text, as a face-to-face visit may not always be possible. The participant knows that this is a standard visit as part of the intervention and so a face-to-face visit is preferable |
|
| 3–14 days after birth |
|
Every other day contact face to face, by telephone or by text, depending on the needs and preferences of individual mothers. Within this period there must be three face-to-face contacts with the mother. Note: this should include contact soon after the 72-hour weighing of the baby, recognising that this is a critical time when mothers may need additional support. Proactive support is gradually withdrawn (based on mothers’ individual needs), but mothers are still able to contact peer supporters if they would like support (by text, by telephone or face to face) |
|
| 15 days to 5 weeks after birth |
|
||
| 6 weeks after birth |
|
Last contact with mothers, which takes the form of a face-to-face or telephone session (i.e. contact should not be by text) |
|
The feasibility study results also demonstrated that the contact between Mam-Kind buddies and the participants mostly took place by telephone call or text. We had anticipated more face-to-face contact within the first 2 weeks after birth. We felt that face-to-face contact was an important part of the intervention, as it allowed the Mam-Kind buddies to assess any potential feeding problems. Therefore, we have changed the intervention specification to include two further face-to-face contacts between birth and 2 weeks (see Table 17). In addition, we have also included a face-to-face ending session with the participant. It was reported by participants that there was variation in how and when the Mam-Kind buddies ended support. Building in a structured face-to-face ending session would standardise the provision of support at the end of the intervention (see Table 17).
Stakeholder review of refinement to the intervention event
We held a third stakeholder event in November 2016 to present the findings of the feasibility study and the proposed changes to the intervention based on our findings. At this meeting, we sought feedback on our proposed changes. Our proposal for a more structured intervention with clear definitions of the scope of each session and increasing levels of face-to-face contact was positively received by all stakeholders, including the Mam-Kind buddies who delivered the intervention during the feasibility study. It was generally felt that increasing the face-to-face contact time would be acceptable, although it was noted that there may be issues with the availability of Mam-Kind buddies at short notice, for example with regard to arranging childcare. A further requirement for a future RCT is the need to recruit and pay Mam-Kind buddies through the NHS. Stakeholders thought that it was important that Mam-Kind buddies were integrated within the existing NHS team. Finally, we explored with stakeholders the possibility of improving data collection by collecting feeding status data from routinely collected data. However, the stakeholders’ feedback was that routinely collected data varied across regions in terms of completeness, who collects these data, where they are collected and where they are stored. Therefore, it was recommended that bespoke data collection would be required as part of a future RCT.
Discussion
In this section we summarise the key findings from the feasibility study and discuss the implications for a future trial.
Recruiting peer supporters (Mam-Kind buddies)
We have established that it is feasible to recruit Mam-Kind buddies and retain them, albeit within the context of the short duration of this feasibility study. We have tested a method for recruiting that included the provision of information about the study and MI as part of a preselection process and found that this worked well. We recruited Mam-Kind buddies through Cardiff University, and the buddies experienced delays in obtaining their research passports from the respective health boards, which impacted on their ability to visit the mothers who they were supporting on postnatal wards. We therefore recommend that, in a future trial, Mam-Kind buddies should be employed through the NHS health board/trusts where they will be working. This will also serve to ensure that they will be integrated with the local community maternity service that they will be working with, facilitating closer links with midwives. It will be important to ensure that sites participating in a future RCT are able to recruit Mam-Kind buddies and have the capacity to deploy midwifery time to provide supervision to the Mam-Kind buddies. Discussions with our Stakeholder Advisory Group, which included representation from community maternity services in England and Wales, suggested that this would be possible, but we would wish to formally establish this with sites considering taking part in a future full trial.
We tested the feasibility of delivering the Mam-Kind intervention in a site that has an existing peer-support service providing intensive, proactive support, similar to that required in the Mam-Kind intervention. We found that this could not be easily implemented in practice. There were barriers to study recruitment, as eligible women could access the existing peer-support service that was available through usual care without having to participate in the data collection and follow-up sessions required through participation in the research study. Interviews with health-care professionals from the two sites that did not have a paid pre-existing peer-support service were satisfied that the Mam-Kind intervention could be easily integrated with existing services. Therefore, we conclude that the effectiveness of the Mam-Kind intervention for breastfeeding maintenance should be tested in sites without an existing paid NHS trust-/health board-based one-to-one peer-support service. The results from our mapping of BFPS service provision (see Chapter 2) show that at least half of the current NHS trusts/health boards in England and Wales have community maternity services that would meet these criteria.
Intervention delivery
We have established that it is feasible to deliver the Mam-Kind intervention as per the specification described in Chapter 3. Previous RCTs described low uptake34,37–39,88 and adherence35,37,88 to the breastfeeding intervention. Our results demonstrate that uptake of, and engagement with, the Mam-Kind intervention was high, with about 75% of participants having received and reciprocated antenatal and postnatal contacts. The majority of participants were contacted by their Mam-Kind buddy within 48 hours of the birth of their baby, and this could be increased by improving the process for birth notifications and enabling Mam-Kind buddies to access postnatal wards. The average number of contacts that mothers received was 16, the majority of which occurred by text, with a range of other methods also being used, including the telephone, Facebook and face to face contacts. The qualitative interviews showed that the flexibility in terms of the method of contact was appreciated by mothers and was feasible for Mam-Kind buddies to provide. The majority of contacts were initiated by the Mam-Kind buddies, consistent with the requirement for proactive contact in the Mam-Kind specification. We found, however, that provision of a graded exit from the intervention to help participants transition to using breastfeeding groups could be improved. The qualitative interviews provided useful insights into the process, and we have used these data to refine the intervention session content and specification, to provide a structured approach for the final intervention session.
We found that Mam-Kind buddies delivered the intervention with high fidelity to the content and that some buddies developed certain MI skills to a competency level. However, some of the Mam-Kind buddies reported difficulties in providing MI, particularly with changing from an expert role to taking a collaborative approach. This is consistent with previous research,105 which has suggested that it is difficult to suppress prior counselling habits (i.e. prior peer-supporter experience), including practices that are inconsistent with MI. Although the MITI 4.1 tool scores suggest weak efforts at collaboration and partnership working, there was evidence of empathy being communicated during intervention delivery. However, there was also evidence of efforts to persuade mothers to breastfeed by offering opinions, suggestions or advice, without explicitly reinforcing the mothers’ autonomy in accepting these. These observations led us to refine the structure and scope of the sessions to clarify and place stronger emphasis on providing collaborative and mother-centred support.
As the Mam-Kind intervention uses a MI approach in its delivery of support, we did not expect or require Mam-Kind buddies to achieve a level of competence required by MI practitioners, but we used the MITI 4.1 tool to allow us to examine the extent to which they were using MI techniques in their practice. The MITI thresholds were determined by expert opinion and are not empirically derived, and so it is difficult to define thresholds that are relevant for this intervention. The data from the feasibility study appear to be similar to data from other studies that have used the MITI tool rating,106,107 although direct comparisons are limited because of the use of an earlier version of the tool (MITI 3.1,108 which uses different global and behavioural ratings) in the other studies. We discussed our findings with Professor Teri Moyers, an expert in the field, who confirmed that our data concur with experience in the field, that one-third of trainees will naturally take to MI, one-third will acquire skilfulness with added support and training and one-third might never develop the skills. 109
The training was provided by Ms Sally Tedstone, breastfeeding co-ordinator and study co-applicant, Professor Steve Rollnick, MI trainer and study co-applicant, and Dr Nina Gobat, MI trainer and MI supervisor for the Mam-Kind buddies. The training module evolved in response to the needs of the Mam-Kind buddies, utilising a holistic and integrated approach that included MI and an update on breastfeeding knowledge. The training aimed to provide the Mam-Kind buddies with an understanding of the expectations of the role, an understanding of MI in a generic form and the opportunity to spend some time exploring and practising MI skills in the context of the Mam-Kind buddy role. The trainers found that allowing participants to practise MI skills was pivotal and supported the development of key skills such as skilful engagement, focused respectful information exchange using the elicit–provide–elicit structure and developing a mindset that affirmed the mothers in the study as wise, skilful and able to problem solve. The trainers reflected that this was more important than trying to ensure that the peer supporters were able to problem solve all of the possible breastfeeding challenges that might arise.
Informed by the results of the feasibility study, we identified areas for refinement in the MI training in a full trial. Given our finding that a proportion of Mam-Kind buddies could improve their relational score based on the MITI analysis, an empathy prescreen could be used in a full trial to aid candidate selection. Although this may raise the threshold for recruiting eligible buddies, it would allow us to determine whether or not it would make any improvements to MI adherence practice and (possibly) outcome.
The role description of the Mam-Kind buddy should be reframed to allow measurement of their success based on collaboration rather than information-giving. The tension between this role and system drivers for information provision would need to be addressed during training and supervision. Revised training materials could be developed to support a more collaborative approach or to focus on change talk and step away from information provision. We consider face-to face group supervision to be the best forum for skills development, possibly including reflection on audio-recordings with a standardised client. There is also the potential to assess Mam-Kind buddy audio-recordings using the MITI 4.1 tool to monitor the use of MI techniques throughout the period of intervention delivery in a full trial. This monitoring during the intervention could allow for any suboptimal MI practice to be flagged and addressed in real time, reflecting what might happen in an implemented service. However, such an approach would require time investment from individual buddies and may not be feasible in practice. On balance, we anticipate that the changes that we have made to the training and intervention specification will facilitate improvements in how the Mam-Kind intervention is delivered. Although it is possible that there may be suboptimal levels of MI practice in some cases, we anticipate that, overall, practice will be acceptable and sufficient to provide a pragmatic BFPS intervention that uses a MI approach.
Study design parameters
We have developed methods for recruitment that are acceptable to health-care professionals and mothers and which appear to be feasible to implement in a full trial. We based this feasibility study on the assumption (informed by our experience from other studies) that 55% of eligible women would express an interest in the study and that 50% of these would consent to take part. Our recruitment data were broadly consistent with these assumptions: 39% of eligible women expressed an interest in taking part and 60% of these women consented to the study. We had intended to recruit 90 women to the feasibility study, but recruitment was slower than expected. We discussed the recruitment trajectory with our Study Steering Committee, who agreed with our decision not to extend the recruitment period, as sufficient data had been collected to address the feasibility questions that were the primary aim of the study. The process evaluation data confirmed that the process for recruitment and the timing of the approach worked well and were acceptable, although, in a full trial, we anticipate that more support for recruitment would be needed in larger sites; research midwives based at the recruiting sites could provide this. The importance of site monitoring by face-to-face contact and video link to promote the study has been highlighted.
Although this feasibility study was carried out in sites (community maternity services) in areas with high levels of social deprivation, high teenage pregnancy rates and low breastfeeding initiation rates, the sociodemographic profile of recruited participants did not fully reflect the target population. This could be because feasibility testing took place over a short period of time. Review of the recruitment data showed that the majority of women with an expected date of delivery during the study period were not approached or assessed for eligibility, and this could have had an impact on the participant profile that was achieved. However, the women who were recruited came from backgrounds and social circles in which breastfeeding was not the norm. The majority had been formula fed as babies themselves. We discussed this participant profile with our Stakeholder Advisory Group and, with their input, have established a range of strategies that can be used in a full trial to maximise reach of the intervention to younger mothers (aged < 20 years). Public engagement activities with the targeted communities will also have a critical role to play in encouraging women to participate in a full trial, as well as other research studies.
The process evaluation provided evidence that the suite of study materials that we have developed were useful and acceptable, and that these can easily be adapted for use in a full trial.
We identified a core set of primary and secondary outcome measures and tested the feasibility of collecting these data using telephone interviews. Our proposed primary outcome measure for a full trial is the receipt of any breast milk at 8 weeks. Using telephone interviews, we achieved a follow-up rate of 64% at 8 weeks. Less than optimal follow-up rates in research with new mothers is a known weakness in the field, and strategies are needed to address this. The study managers carried out the telephone interviews in our study during working hours, making a maximum of three attempts to contact each participant (as this was what was possible within the constraints of the study). We propose that data collection in a full trial should utilise a dedicated team with flexible working hours to carry out the telephone follow-up interviews, as this is likely to achieve a higher response rate (based on our experience in other studies such as Building Blocks110). In addition to telephone follow-up with participants, research midwives based in participating sites could collect breastfeeding status data at 8 weeks. We did not collect any data on birth characteristics that could influence breastfeeding (such as birthweight, gestation at birth, mode of delivery) and propose that research midwives could extract these data from the routine maternity data systems that are in use locally. These strategies for enhancing data collection were discussed and endorsed by our Stakeholder Advisory Group.
The main strength of this feasibility study is that fidelity to the content of the intervention and MI was specified and measured. This provided insight into whether or not the intervention was delivered as intended and identified areas for improvement. This led to clarifications over, and changes to, the intervention objectives to potentially improve the delivery of the intervention in a full RCT. A limitation of the process evaluation is that we did not manage to follow up many women at interview who disengaged from the Mam-Kind intervention and, therefore, we may not have gained the views of those who possibly did not like the intervention. The results of the acceptability assessment may therefore be positively biased.
In conclusion, we consider that the Mam-Kind intervention can be delivered as intended by the specification and is acceptable to mothers and stakeholders, and that the study procedures appear feasible to deliver. Our process evaluation provided some insights into how intervention fidelity can be further improved and we have made refinements and changes to the intervention specification to reflect this. The effectiveness of the refined Mam-Kind intervention for increasing the duration of breastfeeding can now be tested in a full RCT.
Chapter 5 Feasibility of the economic evaluation
This chapter addresses objective 5, which was to assess the feasibility of collecting resource usage and costs associated with the implementation of the Mam-Kind intervention.
Introduction
Given the importance of health economics in informing decision-making, the incorporation of a health economics work package would be fundamental to the success of a future RCT evaluating clinical effectiveness and cost-effectiveness. Within the context of public health interventions and programmes, attention should be paid to ensure that the aims and methods are congruent with UK decision-making bodies such as NICE, which published a generic manual for guideline development, including in public health, in 2014,111 with specific reference to consideration of incorporating economic evidence within the context of public health interventions. Key questions, such as which perspective should be adopted in the analysis and which measures of health and non-health benefits should be considered, are essential questions to address in the early stages of planning.
This part of the study (study objective 5) evaluated the feasibility of undertaking an economic evaluation of the effectiveness of the Mam-Kind intervention. Specifically, it was designed to assess whether or not accurate and comprehensive data could be collected on health and relevant resource use in this population and consider the key cost drivers associated with the Mam-Kind intervention and which relevant perspectives should be incorporated into a future trial. Early-stage identification of the resources needed to deliver the Mam-Kind intervention and the associated costs was undertaken as part of the feasibility testing. Alongside the data provided in Chapter 4, we considered the most appropriate measures to inform the collection of salient health and non-health benefits.
Objectives
The objectives of the economic evaluation were to:
-
assess the feasibility of collecting resource usage and costs associated with the implementation of the Mam-Kind intervention
-
provide an early-stage assessment of the costs associated with implementing the Mam-Kind intervention
-
identify the relevant perspectives to adopt in a future trial and related resource use categories for health economic analysis and consider outcome measures (and challenges associated), taking into account current thinking and practice in the design of economic evaluations of public health interventions
-
provide commentary on a suitable economic evaluation framework for a future RCT.
Methods
The evaluation was divided into the following consecutive stages, following the overall study process. We reviewed the health economic literature derived from the literature search and, when data allowed, aimed to provide a narrative synthesis of the current evidence base on the use of MI-based BFPS. Based on the results of the review (when applicable) and discussion with the research team on the findings from the qualitative component, we identified the initial perspective and key resource categories to adopt in the adaption or, if required, construction of a bespoke or adapted resource use measure, drawing on a search of the DIRUM (Database of Instruments for Resource Use Measurement) website112 for candidate measures.
Review of the health economic literature
The review methods were described in Chapter 3 and the search strategy is provided in Appendix 1. For the health economic component, a generic filter was applied to the search strategies to provide as sensitive a strategy as possible to identify potentially relevant papers. This strategy was similar to the approach taken in recent NICE guidelines113 to identify relevant health economic analyses alongside the main clinical searches.
From the initial searches, 1070 articles were retrieved. Deduplication and the removal of obviously irrelevant articles resulted in 435 articles being retained, which were subjected to review against the selection criteria in Table 18. For papers that fitted the PICO (participants, interventions, comparisons, outcomes) framework, a narrative synthesis was intended to be undertaken, with key features of papers described and appraised using the GRADE (Grading of Recommendations Assessment, Development and Evaluation) format utilised by NICE. 111 This review was undertaken in December 2013.
| Criterion | Descriptor |
|---|---|
| Population | Women who are considering breastfeeding |
| Intervention | Peer-support interventions |
| Comparator | Any |
| Outcomes | Reporting a full economic analysis:a cost-effectiveness study; cost–utility study; cost–consequences study; cost –benefit study |
| Setting | All settings, but country specifically identified and commented on in terms of applicability to a UK setting |
| Perspective | All relevant perspectives, e.g. health-care provider/insurer, public sector, societal |
We did not identify any suitable papers, because none of the 435 abstracts reviewed met the selection criteria.
Feasibility of capturing resource usage in the study population
Although considerable interest is paid to the methods (and particularly outcome measures) used to capture the most relevant health and non-health benefits in a trial, in comparison, little attention is usually paid to the methods and design of suitable measures used to capture and evaluate all relevant costs associated with the intervention (in this case the Mam-Kind intervention). 114
The costs associated with the Mam-Kind intervention were divided into the following categories:
-
the costs of the new intervention (i.e. the costs associated with the implementation of the Mam-Kind intervention)
-
the resources used during the Mam-Kind intervention and follow-up, to identify salient drivers of costs to include when assessing any resulting change in resource use and associated costs as a result of the Mam-Kind intervention in a future trial.
Costs associated with the Mam-Kind intervention
The resources associated with the Mam-Kind intervention were identified through discussion with the Mam-Kind team, while considering the description of the intervention within the study protocol. The focus was on establishing key drivers of costs involved in delivering the Mam-Kind intervention.
These costs were divided into the following:
-
the costs of training the Mam-Kind peer supporters – data were collected on staff time and grade, venue hire, training materials, catering and travel across the course of the Mam-Kind intervention
-
the costs of midwifery supervision to support the Mam-Kind peer supporters – data were collected on staff time and mode of contact
-
the costs of employing the Mam-Kind peer supporters for the duration of the study.
Perspective costs associated with resource use as a result of the Mam-Kind intervention
To undertake the development of a suitable resource use measure, the choice of perspective needed to be captured. Based on discussion with the research team during the early study phases and in consultation with the wider literature and guidelines (e.g. NICE111), a wider societal perspective was used to assess the feasibility of capturing relevant and important costs associated with the Mam-Kind intervention (Table 19).
| Perspective | Rationale |
|---|---|
| UK NHS | The Mam-Kind intervention could impact on health-care utilisation (primary, secondary and community services), for example a reduction in the number of visits to the general practitioner for feeding problems |
| Individual and family | The Mam-Kind intervention could impact on individual and family resources, for example purchase of over-the-counter medication and equipment, carer time (paid and unpaid) |
| Third sectora | The Mam-Kind intervention could influence breastfeeding uptake and access to other services, such as NCT or other volunteer-based groups |
| Lost productivitya | The Mam-Kind intervention could influence lost productivity, for example as a result of extended maternity leave to continue breastfeeding |
To assess resource use across these perspectives, a bespoke resource use questionnaire (RUQ) was adapted, drawing on the Client Service Receipt Inventory115 and consulting the DIRUM website for relevant measures used in other studies. 112 The RUQ was peer-reviewed for comprehensiveness of coverage and utility (i.e. whether or not it would be easy to understand by research staff and participants) by the Mam-Kind Study Management Group and health economists not associated with the Mam-Kind study. After two rounds of review, the RUQ was included as part of the suite of measures administered during the feasibility testing. It was administered by structured telephone interview with the participants as part of the data collection schedule (8–10 weeks after birth). This allowed a recall period that was within 3 months, which is often seen as a suitable recall period to use in RUQs. 112
Although the design of the feasibility study precluded any formal assessment of resulting changes in resource utilisation, capturing the costs at this early stage may help to identify potential cost drivers to inform the design of a future study. Thus, the health-care costs were identified and described as part of the preliminary assessment of the costs of the Mam-Kind intervention.
Valuation of costs
Costs were monetised into Great British pounds using the price year of 2016. The costs associated with the Mam-Kind intervention were based on the recorded costs supplied by the Mam-Kind research team. These included the costs of the external training and delivery, salary costs of the Mam-Kind peer supporters employed for the duration of the study (6 months) and the costs of midwifery supervision time. Staff costs were based on the NHS Agenda for Change 2016 (Cardiff and Vale University Health Board). 116 For prescribed medicines and primary, secondary and community care, appropriate unit costs were applied. 117–120
Feasibility of measuring and collecting health outcomes to inform a health economic analysis
The provisional focus in this feasibility study was to assess the potential to collect a wide range of health and non-health outcomes to inform a suitable economic analysis, for example cost–consequences and/or cost–utility analysis, in accordance with NICE recommendations. 121
The study outcomes collected are reported in Chapter 4.
Although the resources available precluded an assessment of the EuroQoL-5 Dimensions, five-level version (EQ-5D-5L)102 in detail, a basic assessment of coverage suggests that further examination of potential ceiling effects and the extent of missing data should be considered further in choosing suitable outcome measures for the calculation of utilities, for example whether or not the Short Form questionnaire-6 Dimensions (SF-6D)122 is a possible candidate measure. Further exploration of the literature and discussion will be needed to determine the relevant outcomes to be included in an economic analysis in a future trial.
Feasibility of measuring and collecting resource use information from the resource use questionnaire
The primary focus was to assess the feasibility of collecting resource use information from the RUQ developed for the study.
For illustrative purposes only, the health-care resource use and captured associated costs were valued in Great British pounds (using published costs) and costed using the British National Formulary,117 British National Formulary for Children,118 NHS Reference Costs 2014–2015,119 British Medical Association data123 and Unit Costs of Health and Social Care 2015120 (further information is available from the authors). Feedback from the Mam-Kind research team suggests that the RUQ was comprehensive in terms of coverage, although further refinement will be required to ensure that it focuses on salient cost drivers to minimise the burden of completion. A formal exploration of the range of resources consumed by the participants, for example over-the-counter medication, was beyond the scope of this study. Preliminary investigation suggests that this approach captures salient information for the wider costs associated with the Mam-Kind intervention. The limitation, however, is that the resource use data were collected for 45 out of the 70 participants (response rate 64%). Further investigation is needed to ensure that the data collection instrument (and approach) for collecting resource use data can support a good response rate, particularly during follow-up. These issues were discussed in Chapter 4 (see Study design parameters).
As noted in Chapter 4, data collection using the RUQ was acceptable to participants and it was feasible to collect data over the telephone. However, the practicalities (and costs) of implementing this model of data collection in a full trial may mean that alternative approaches should be considered, for example the use of participant diaries to support the telephone-administered RUQ at assessment points.
This study did not extract any routine data on health service utilisation and so no commentary can be provided on the use of routine data to inform resource use and costing. There is a potential for such approaches to be considered, although this is likely to be restricted to NHS resource use. Thus, a RUQ is likely to have value in a future trial, but further consideration is needed as part of the work-up for a future trial of the best sources of data to inform the identification and measurement of resource use and costs.
Intervention costs
A summary of the intervention costs associated with the Mam-Kind intervention is reported in Table 20. The overall cost of delivering the Mam-Kind intervention, based on the current feasibility study, was £33,595.
| Resource | Summary | Cost (£) | Unit cost (£/hour) | Reference |
|---|---|---|---|---|
| Training of peer supporters in the Mam-Kind intervention | Includes staff time, venue hire, refreshments and training materials | 2400 | Mam-Kind study records | |
| Two one-to-one sessions for peer supporters | 1280 | Mam-Kind study records | ||
| Three 2-hour group supervision sessions | Includes preparation, materials, facilitations | 1350 | Mam-Kind study records | |
| Total training costs | 5030 | |||
| Midwifery supervision: site 1 | 21 individual telephone contacts, median length 3 minutes (range 3–10 minutes); eight face-to-face contacts with three peer supporters (group supervision), median length 90 minutes (range 90–90 minutes); total 10.5 hours of supervision | 158 | 15a | NHS Agenda For Change 2015 (Cardiff and Vale University Health Board); Curtis and Burns120 |
| Midwifery supervision: site 2 | 16 individual telephone contacts, median length 11 minutes (range 2–65 minutes); four face-to-face contacts (three sessions with three peer supporters, one with two peer supporters), median length 90 minutes (range 60–120 minutes); total 12 hours of supervision | 180 | 15a | NHS Agenda For Change 2015 (Cardiff and Vale University Health Board); Curtis and Burns120 |
| Midwifery supervision: site 3 | No individual telephone contacts; 14 face-to-face contacts, seven with one peer supporter, seven with two peer supporters; median length 30 minutes (range 30–75 minutes), total 9.75 hours | 147 | 15a | NHS Agenda For Change 2015 (Cardiff and Vale University Health Board); Curtis and Burns120 |
| Total costs of midwifery supervision | 485 | 15a | NHS Agenda For Change 2015 (Cardiff and Vale University Health Board); Curtis and Burns120 | |
| Salary costs | Eight peer supporters recruited for 26 weeks for 15 hours per week | 28,080 | 9a | NHS Agenda For Change 2015 (Cardiff and Vale University Health Board) |
| Total cost of the Mam-Kind intervention | 33,595 | |||
| Total cost per participant (n = 70) | 480 | |||
| Total cost per participant (n = 96) | 350 |
The Mam-Kind intervention costs were based on delivery as in the feasibility study, and important factors should be considered in determining the reliability and validity of these costs, particularly with regard to how the Mam-Kind intervention would be delivered in the context of a RCT or in usual practice. The training costs were based on senior experts providing the MI-based training, with follow-up from members of the research team. An important consideration in developing this intervention for use in any future trial is to ensure that the skill mix of the training team is carefully considered, for example intervention costs could be reduced by ‘training’ others to deliver this important component of the Mam-Kind intervention.
With respect to the midwifery supervision, there was variation in practice across the three sites, with different modes of supervision provided (e.g. telephone vs. face to face; individual vs. group supervision). Although the cost of the supervision time is largely determined by the time spent, efficiencies could be achieved by optimising the model of supervision. Travel costs were not recorded and, thus, training and the provision of information to ensure accurate data collection for this component of the intervention should be undertaken for any future trial. Acknowledgement is also made that we used local financial records rather than published unit costs120 to calculate salaries and may have underestimated the on-costs associated with these salaries.
The opportunity cost of employing the peer supporters warrants further consideration, as it represents the most costly driver in delivering the Mam-Kind intervention. One important factor to consider is the workload of the peer supporters, with variation seen across the peer supporters, ranging from a workload of six participants to a workload of 11 participants. The base-case analysis showed that, for the 70 participants recruited to the study, the intervention cost per participant was £480. This did not take into account participants who withdrew from the Mam-Kind intervention. Although further in-depth examination was not carried out, the costs were re-examined based on a scenario in which the peer supporters recruited in accordance with the maximum number of participants allowed in the study protocol (12 per peer supporter; total of 96 participants). In this case, the costs would be reduced to £350, reflecting the need for any future trial or roll-out of the Mam-Kind intervention to fully consider the capacity of peer supporters to ensure the most effective and efficient delivery of the intervention. However, these costs associated with the Mam-Kind intervention must be considered early-stage estimations. Further consideration of how the feasibility study reflects the broader clinical sites that would be included in a future trial will also play a part in assessing the validity of these costs.
Health-care utilisation costs
The costs associated with NHS health-care resource usage are available from the authors, and a summary of the costs is shown in Table 21.
| Resource | Estimated cost (£) |
|---|---|
| Primary care | 835 |
| Hospital outpatient and day-case attendances | 4849 |
| Hospital admissions | 13,093 |
| Prescribed medications | 641.42 |
| Total costs | 19,418 |
| Total cost per participant | 431.51 |
Important caveats need to be placed around the estimations provided in Table 20. In total, 45 out of 70 questionnaires were available for analysis and, thus, these costs may not be reflective of all participants within the feasibility study. Even if a full response had been achieved, given the small sample size and the spread across the three sites, it is doubtful that these costs would be representative.
As expected, resource utilisation was skewed, with six hospital admissions (all related to the baby) being the biggest cost driver. This was weighted by one admission resulting from a urinary tract infection, resulting in a hospital stay of 10 days (NHS reference cost £9137). In addition, with the reliance on self-reported data, these costs could not be verified against routine records. Self-report also required participants to make a judgement on whether or not this was the result of a problem with feeding. In a subsequent trial, attention should be paid to the wording of questions, with a focus on whether this should be ‘specific to feeding issues’ (as used in this feasibility study) or should capture all health-care costs within the post-partum and longer period in a future economic analysis.
Nonetheless, this illustration of costs associated with the intervention indicates that a number of important cost drivers should be captured in a future study. Although not formally costed, the costs to the individual and the family (costs of over-the-counter medication, equipment, travel, carer time and paid help) will also be important determinants in establishing the wider costs associated with the Mam-Kind intervention.
Discussion
There is little health economic evidence to date on the use of peer-support interventions in breastfeeding. We identified the resources and associated costs involved in delivering the Mam-Kind intervention and considered the most appropriate measures to inform the collection of selected health and non-health benefits. We found that the questionnaire that was used captured salient information about the wider costs associated with the Mam-Kind intervention. With the focus on the impact of the Mam-Kind intervention on NHS maternity services, a NHS/Personal Social Services perspective should be adopted in a future trial. However, the feasibility study confirmed that capturing the wider costs to the family should also be considered. Feedback from the Mam-Kind research team suggested that it is feasible to use a telephone-administered RUQ. Based on the conduct of the feasibility study and recruitment of 70 participants, an intervention cost of £480 per participant was estimated. The number of participants recruited is an important factor in determining the intervention cost; if recruitment had been at the optimum capacity level for each peer supporter (12 participants), the intervention would have an estimated cost of £350 per participant. Appropriate consideration should be paid to the method of training peer supporters in the use of the Mam-Kind intervention. The cost estimation for the peer supporters included all of the development work that was conducted. If this intervention was to be rolled out, then a different training model could be used. This warrants further consideration, as efficiencies in delivery of the training and economies resulting from a longer duration of intervention delivery will have an impact on the cost of the intervention. An initial examination of health-care costs and costs to the individual and the family indicates that the costs of hospital admissions and outpatient/day-case and primary care costs make up the majority of the costs; prescribed medication for the baby and the purchase of equipment to support feeding are other important costs to consider, including potential cost offsets, such as reduced purchase of formula milk, over-the-counter medications and feeding equipment.
Although not formally explored, the impact of participants lost to follow-up is an important determinant in establishing intervention costs in a future trial; similarly, the importance of ensuring optimal capacity of peer supporters and variance in workload should also be considered in a future trial of clinical effectiveness and cost-effectiveness. Although brief consideration of the use of the EQ-5D-5L within the feasibility study suggests that it is feasible to collect data from mothers, careful consideration is needed to establish the most appropriate choice of outcomes to be included (and measure) to provide as comprehensive a picture as possible of the economic impact of the Mam-Kind intervention in a future trial. We propose that consideration should be given to generating a cost per quality-adjusted life-year (QALY)124 as a secondary objective in both any planned within-trial analysis and any subsequent model-based analysis to estimate the longer-term cost-effectiveness of the Mam-Kind intervention. A future framework for health economics analysis should consider the short- and longer-term outcomes of the Mam-Kind intervention, drawing on similar work that goes beyond trial modelling to examine the cost-effectiveness of breast feeding over the longer term. We suggest that the use of the NICE reference case,125 with specific consideration of the economic evidence to inform public health interventions, provides a useful framework for setting out the key requirements for such an analysis.
Chapter 6 Discussion
In this section we summarise the key findings from the study, discuss the strengths and limitations of the study, describe public involvement in the research and set out our recommendations for a future RCT to test the effectiveness of the Mam-Kind intervention for breastfeeding maintenance.
Summary of key findings
Our first objective was to carry out a rapid evidence review to describe the range of BFPS interventions in use in the UK. Our survey of UK IFCs showed that the provision of BFPS across the UK was not standardised. Services were regularly adapted in response to changing financial contexts, and none of the models in use were reported to have an underpinning theoretical model or to include results from robust evaluations of clinical effectiveness or cost-effectiveness. Although there was wide availability of peer supporters across the country, the majority were engaged in providing group support, with little provision of one-to-one support in the early postnatal period. The findings from this survey and our rapid literature review highlighted a number of potential facilitators of, and barriers to, implementing BFPS. Specifically, these included the need for clarity about the peer-supporter role and responsibilities and professional boundaries, the need for integration with existing local health-care services and close working with health-care professionals and a strategy for ensuring that peer supporters are informed of births and have access to postnatal wards.
We further clarified the content of the intervention and the requirements for implementation (our second objective) using focus groups with pregnant women, mothers, fathers and peer supporters and qualitative interviews with health-care professionals. The focus groups highlighted that peer supporters had an important role to play in normalising breastfeeding and supporting mothers, particularly in areas where breastfeeding was not the norm. In training for the peer-supporter role, the need to provide consistent advice (and the need for integration into local health services) was a prominent theme for both peer supporters and health-care professionals. A Stakeholder Advisory Group (n = 23) was also convened to advise on all aspects of study design, including intervention development. The qualitative work was finalised and used to inform the development of a more detailed specification of the intervention, which was presented to and endorsed by the Stakeholder Advisory Group.
We used the BCW framework to understand the behaviours associated with breastfeeding that can be targeted by this intervention. We determined that the intervention should address psychological capability, social opportunity and reflective motivation to enable women to continue breastfeeding. We used the BCW framework to link these behaviours with the relevant functions of the intervention and service requirements for implementation. To our knowledge, the BCW has not previously been used in this context. By the end of the process we produced the specification and corresponding logic model for the Mam-Kind intervention, fulfilling our third objective.
Our fourth objective was to assess the feasibility of delivering the Mam-Kind intervention to women living in areas with high levels of social deprivation. We were specifically interested in the recruitment and retention of peer supporters (Mam-Kind buddies), the recruitment of women to the study, the uptake of the intervention and intervention fidelity. We had no difficulties in recruiting Mam-Kind buddies who met our specification and all of the Mam-Kind buddies who successfully completed the initial job check continued in their role for the full duration of the study. In total, 39% of eligible women (n = 115) approached expressed an interest in taking part in the study, of whom 61% (n = 70) completed the consent process and were recruited. Although broadly consistent with our assumptions, the proportion of eligible women expressing an interest in the study was lower than we expected, which is possibly explained by a number of factors. In one site, only a proportion of midwives working in the area received training about the study. In another site with a pre-existing peer-support service, women were reluctant to take part in the Mam-Kind study when they could access peer support without having to consent to the research process. The recruitment rate, although reasonable, could be improved by a number of strategies discussed later in this section. Further to the recruitment and retention of participants, we were also interested in the recruitment and retention of supervising midwives. We managed to recruit and retain all three supervising midwives, who reported that they found the role to be acceptable and that it was feasible to deliver the supervision required by the Mam-Kind buddies. It was noted that the midwife supervision role should be kept distinct from other roles associated with the study, such as being a local champion, and recruitment in a full RCT.
Uptake of the intervention was good and the majority of participants had an antenatal contact with their Mam-Kind buddy, demonstrating that it was feasible to deliver this aspect of the intervention. In total, 73% of participants received a contact within 48 hours and this did not vary according to whether or not there was antenatal contact with the Mam-Kind buddy. The qualitative interviews carried out during the process evaluation provided some useful insights to inform future strategies to improve the birth notification process. Fidelity testing showed that the Mam-Kind buddies delivered the intervention content with high fidelity and, encouragingly, some Mam-Kind buddies developed MI skills to basic competency level. We did not make reaching competency on the MITI 4.1 scale a requirement for delivering the intervention, as this is the level expected by a trained and experienced MI counsellor. Instead, we used the MITI 4.1 tool to assess the extent to which the Mam-Kind buddies were using MI techniques in their contacts with the women who they were supporting. The process evaluation highlighted that there was a tension between information-giving and providing support in a MI-consistent manner. We have used these insights to refine the scope and objectives of the Mam-Kind sessions and refined the training module to increase the emphasis on providing support.
Strengths and limitations
The main strength of this study was the use of a systematic approach, consistent with MRC guidance for the development of complex interventions,126 to intervention development. We were able to validate the key findings from the rapid evidence review in the qualitative work that was carried out to support intervention development, and through discussion with the Stakeholder Advisory Group. In doing so, we have developed a detailed specification and logic model for the Mam-Kind intervention.
We engaged a stakeholder expert advisory group during the early stages of the study, which enabled us to adopt an interactive and iterative process for intervention development. This allowed us to develop an intervention that was informed by the views and perspectives of intended service users, peer supporters and health-care service providers and to ensure that the design of the intervention included practical strategies for recruitment, consent and data collection. We identified the key feasibility questions to be addressed prior to a full trial, and designed our study to address these.
However, there were some limitations. The response rate to our web-based survey was low. To mitigate this, we used publicly available data from organisational websites to supplement our survey findings. Although this provided data about the availability of peer support, it did not provide detail about how services were run or how training and supervision for peer supporters were provided. We mapped the data on BFPS availability to NHS trust and health board areas and, in doing so, we have had to assume that the responses for each health-care area were applicable across the board. This may not be the case for larger NHS trusts in which the availability of services may vary greatly within the trust; however, our survey was not sensitive enough to capture availability at smaller geographical levels. We did not have the resources within the scope of the project to directly contact local authority or voluntary groups to obtain further information about available services.
We included fathers in our intervention development work and used a pre-existing fathers’ parenting group to ensure that they felt comfortable talking to us about this emotive topic. Although this had the advantage of securing open talk about infant feeding, it attracted a smaller number of fathers than we had hoped to engage with.
Delivery of the Mam-Kind intervention was hindered in some cases by significant delays in the process of obtaining research passports for Mam-Kind buddies, which resulted in their inability to access postnatal wards and provide support within 48 hours, as specified by the intervention. A further limitation was that, although we managed to recruit in areas with high levels of social deprivation and low breastfeeding initiation rates, our participants had, on average, high levels of education and were mostly employed. The small number of mothers recruited who were aged < 20 years limited our ability to assess the acceptability of the Mam-Kind intervention to this group. The sample that we recruited may not be representative of the whole population in the study sites. A further limitation was the increase in loss to follow-up at 8 weeks, which has implications for the RCT; these are described in Strategies for the recruitment and retention of peer supporters and participants. These areas need further consideration before undertaking a future RCT. We have discussed these issues with our Stakeholder Advisory Group and used their input to develop strategies for addressing them in a full trial.
This study has demonstrated the levels of study uptake, levels of intervention usage, follow-up rates and levels of data completion. It has also provided an indication of how some of these processes may either be streamlined or improved (e.g. by providing additional training and redesigning some of the participant materials).
The incorporation of an early-stage assessment of the requirements and parameters for an economic analysis in a future trial has allowed a provisional assessment of this, with evidence from the feasibility study providing a useful basis for the development of a suitable framework. Because of resource constraints, in-depth examination was not intended and the provisional assessments (e.g. early assessment of the intervention costs associated with the Mam-Kind intervention) must be interpreted with appropriate caution. A key learning point was the need for health economics to be embedded into the feasibility study to ensure that important insights and lessons can be used to develop the framework for an economic analysis within a future trial. The considerations given to economic evaluation in this feasibility study provide a good basis for further development of the design of an economic analysis in a full trial.
Patient and public involvement in the study
In this section we describe how we involved the public in the design and conduct of the research. The aim of patient and public involvement (PPI) in this study was to improve the design, conduct and dissemination of the research. We achieved this using a range of methods to fulfil the following objectives:
-
inform the design of the study so that it addresses relevant questions and is acceptable and feasible from the perspective of service users and members of the public
-
contribute to oversight of the conduct of the research
-
provide a lay perspective on the analysis and interpretation of the data
-
facilitate public engagement and dissemination activities
We included a PPI representative as a co-applicant on the project and as a member of the Study Management Group for the duration of the project, to advise on study conduct and the materials to be used with service users and the public (Box 6). Our representative was a member of the Involving People (Wales) Network who had completed the network formal training days and was provided with ongoing support from the Involving People Network. We ensured that she was briefed about the project and was given opportunities to debrief with a member of the research team. She also attended the stakeholder events (see Box 6) and assisted with communication with other mothers and peer supporters through her own contacts with peer-support groups and online communities for breastfeeding mothers/peer supporters.
My baby was 8 weeks old when a friend sent me the advert from the Involving People Network for a PPI representative for the Mam-Kind study. Looking back at the sleep-deprived haze I was in then, I’m not sure how I got it together to write the application, let alone how I thought I would be able to contribute to the development of the research study, something I had no experience of. However, I’m glad that I did.
Initially I was involved with the project application process, providing comments on the application form from my experience as a breastfeeding mum. It felt good when the project was shortlisted and then approved. My role then focused more on communicating around different aspects of the study with other mums and breastfeeding peer supporters, as by this time I had trained to be a peer supporter myself, partly inspired by my involvement with the study. For example, I gathered comments on participant information sheets through Facebook and my breastfeeding support group. It was really interesting to be able to connect with others passionate about supporting breastfeeding mums. This, to me, was one of the highlights of being involved in the study. Being able to take part in the motivational interviewing training that was given to the peer supporters recruited for the study, as well as other Involving People Network training, was also a great chance to connect with people as well as being great learning opportunities. In terms of learning, just being part of the study group, a world that I didn’t have any experience of, gave me a great insight into the research process and the commitment and dedication needed to follow through a piece of work until the end.
I will admit that I found the experience a challenging one at times. It was a world of acronyms to get to grips with, and I didn’t always find it easy to understand who all the stakeholders were and what role they played. When I first got involved in the study I don’t think I appreciated how long the research process could take (that 8-week-old baby is now at school nursery!) and I found the time commitment more of a challenge once my maternity leave had ended and I was back at work. However, the study team were great when I needed help understanding something and were flexible in terms of the time I could give.
I feel that patient and public involvement is really important in the research process. Much like BFPS itself, it can really help to engage with someone with lived experience, not only theoretical knowledge. Being part of the study was really beneficial to me on a personal level, but I am also sure that the work will contribute to what we know about how to best support mothers in their breastfeeding goals.
We collaborated with the NCT, the UK’s largest charity for new and expectant parents, to secure additional PPI input. The Research Operations Manager, a collaborator on this study, was our link with the NCT. The NCT assisted with publicising the study and disseminating findings via web-based information, its information for volunteers and Maternity Services Liaison Committee representatives and through articles in NCT’s range of publications for parents, practitioners and commissioners.
We formed an online closed Facebook group to gather additional feedback from mothers and peer supporters. There were 30 members of this closed group. We asked them to provide feedback on the name of the study and to review patient-facing materials, such as the patient information sheet and the leaflets. The group also assisted with disseminating information about the peer-support job opportunities associated with the feasibility study.
Our Stakeholder Advisory Group included representation from two service users, three peer supporters and breastfeeding groups. The group worked across all of the study objectives, advising on the development of the intervention, the study materials and the management of any potential issues that arose during the course of the study and the interpretation of the findings, plans for dissemination and future plans for the research (including the design of a full trial). The group met on four occasions over the course of the project.
Our PPI representatives on the Study Management Group and the Stakeholder Advisory Group were mothers who had had a child (or children) in the last 5 years and who had experience of breastfeeding. Mothers were welcome to bring young babies along to meetings or childcare costs could be provided for older children if required. We provided payment at the Involving People Network-recommended rate (equivalent to £150 per day) to our PPI representatives for attending meetings and stakeholder events.
The PPI input on this project was invaluable in developing study procedures that were feasible and acceptable, given the sensitive nature of the topic at hand and that we were working with women during a busy and potentially vulnerable period in their lives. This meant that all study procedures and service user-facing materials were designed with the needs of mothers in mind. This mother-centred ethos was carried through all aspects of the study, ensuring that the information was relevant and easy to read, the burden of the study assessments was kept to a minimum and women were engaged at all stages of the research. It has also been invaluable in planning and designing the next steps in this research, particularly in terms of ensuring that planned future work is relevant and acceptable and that barriers to participation are addressed at the early design stage.
Patient and public involvement outputs
Rhiannon Phillips participated in an interview about PPI involvement in this research and how the research had benefited from this, which was published in the Involving People Network newsletter. 127
Sian Regan, the study’s PPI representative, took part in a short film for the Royal Society for Public Health to showcase the breadth of public health activity in the UK.
Lauren Copeland and Shantini Paranjothy published an article in the NCT’s Perspective journal in 2015128 examining the role of MI in the transition to parenthood, including breastfeeding.
Implications for a future randomised trial
Overall, we consider that the intervention can be delivered with fidelity and is acceptable to women, and that the core study procedures appear to be feasible to deliver. Further, we still consider that there is a pressing clinical need to better support women to breastfeed, as only 1% of mothers in the UK currently exclusively breastfeed for 6 months, which is the WHO-recommended duration. 129 Currently, there remains no good UK-based evidence of effective interventions to support breastfeeding, as indicated by the findings of our rapid review. In this section, we describe the implications for a future RCT to test the clinical effectiveness and cost-effectiveness of the Mam-Kind intervention for breastfeeding. We have focused on recommendations for the design of a future trial, strategies for the recruitment and retention of participants, measurement of primary and secondary outcomes and a framework for economic evaluation.
Study design
We considered that an individual RCT would be the most appropriate study design for testing the effectiveness of the Mam-Kind intervention. The advantage of randomising individuals over clusters is the smaller sample size required. A potential disadvantage is the risk of contamination, either Mam-Kind buddies or mothers in the intervention group coming into contact with mothers in the control arm; however, we considered this risk to be low. There is, however, the possibility of compensatory practice, whereby mothers in the control arm have ‘additional’ support provided or flagged up to them. Any changes to usual care will be captured within the process evaluation by maintaining regular contact with site principal investigators, recorded in a research diary and interviews with health-care professionals and participants, and focus groups with peer supporters. These changes to usual care can be mapped alongside quantitative outcome data.
The RCT will have two arms, with the intervention arm receiving the Mam-Kind intervention and the control arm receiving usual care. Our survey of IFCs has provided the context and map of the care pathway for the control group. The control group will be provided with usual NHS care; although this is likely to include some variability, it would probably involve support for breastfeeding provided by health-care professionals within standard midwifery and health visiting services that have achieved or are working towards UNICEF UK BFI accreditation, supported by a network of peer-support and breastfeeding groups, with contact between peer supporters and women usually occurring only at breastfeeding groups when their babies are several weeks old.
The RCT will include an in-built pilot phase to enable the early testing of recruitment and retention in one or two areas. Included in the RCT will be a PPI work package based on the work that we conducted during the feasibility study. We also plan to build in a process evaluation to map usual care services and intervention implementation, to assess whether intervention logic model assumptions hold true across different service contexts. Thematic analysis of interviews with participants, Mam-Kind buddies and health-care professionals will explore barriers and facilitators, broader acceptability and intervention, reach. Fidelity will be assessed using audio-recorded peer-support sessions and structured diary data from peer supporters. We anticipate that running the RCT in a relatively small number of representative sites over a longer duration (e.g. 1 year) will allow us to learn about the viability and sustainability of the intervention, while allowing the Mam-Kind buddies to develop their MI skills in delivering the intervention. The study training that was provided in the feasibility study has been adjusted for the RCT to allow it to be replicated. The feasibility study has provided insight into the required training for the peer supporters and has allowed the study team to focus and refine the training so that it can be delivered within a 3-day period.
Population
We will aim to recruit all English-speaking pregnant women from 28 weeks’ gestation onwards who are considering breastfeeding. Women who are unable to provide written informed consent, who do not plan to breastfeed or who have a clinical reason that precludes breastfeeding (e.g. major congenital anomaly) or a planned admission to a neonatal unit following birth will not be eligible for the study. We believe that the target population for the RCT should be all women, as the drop-off in breastfeeding rates from initiation to 6 weeks is 20% in the least deprived quintile to 30% in the most deprived quintile, indicating that women struggle to maintain breastfeeding across the range of social deprivation levels. 3 This approach is consistent with the principles of proportionate universalism130 to avoid stigmatising women at highest risk.
We had planned to include women with multiple pregnancies (twins, triplets, etc.) in the feasibility study but did not recruit any participants who met this criterion during the short period of recruitment. On reflection, we consider that women with multiple pregnancies should be excluded, as women in this group have a different profile of breastfeeding rates from women with singleton pregnancies.
Setting
Sites included in the trial will be community maternity services in England and Wales that include areas with high levels of social deprivation within their catchment. Sites participating in the RCT will need to be able to recruit Mam-Kind buddies and have the capacity to provide midwifery supervision for the duration of the study. The sites should not be providing any individual BFPS, which minimises the risk of contamination and facilitates intervention implementation, as we will not be cutting across or duplicating existing services.
Measurement of primary and secondary outcomes
We tested the acceptability of collecting a suite of primary and secondary outcome measures in the feasibility study and found high levels of data completeness. We recommend that receipt of any breast milk at 8 weeks should be the primary outcome measure to test the effectiveness of the Mam-Kind intervention. We did not collect any data relating to birth outcomes (such as gestation at birth, birthweight or mode of delivery), but recommend collecting these data in a future trial, as they are important influencers of breastfeeding duration.
Strategies for the recruitment and retention of peer supporters and participants
We plan to employ the peer supporters within the NHS at all sites participating in a RCT, which will allow the peer supporters access to the postnatal wards at any time. We will also introduce the midwives on the hospital wards to the peer supporters, which should encourage the staff to notify the peer supporters when a mother has given birth. Peer supporters will be encouraged to make a plan with mothers and birth partners about how they will be notified of the birth (e.g. by adding them to the list of people who they notify of the birth). These strategies should lead to an improvement in the level of face-to-face contacts at the 48-hour time point.
We recruited 39% of eligible women in our feasibility study and the process evaluation provided useful information to inform a strategy to increase the rate of recruitment. Specifically, this includes the importance of maintaining regular contact with clinical areas. This can be achieved either by having a member of the research team co-located with a recruitment site or by identifying a local champion to provide ongoing oversight and support for recruitment activities. The Mam-Kind buddies could also attend breastfeeding antenatal sessions to introduce themselves and the intervention to potential mothers. Participants in the feasibility study expressed a preference for being able to meet the Mam-Kind buddies prior to signing up to the study. We have developed a number of strategies to address the issue of recruiting a more representative sample of participants from our potential sites. This includes introducing the study through local community groups, such as Flying Start in Wales/Sure Start in England, or children’s centres that run pregnancy groups or groups for young mothers. These groups have established relationships within the community that are known and trusted. The recruiting research team could also attend these groups to allow the mothers to meet the researchers on the study who will be obtaining consent and collecting data. This could help to improve familiarity with research processes and negate any misunderstandings about research. 131 A further strategy would be to introduce the study through pregnancy-related Facebook sites and closed groups, providing a link to the study website, with people able to provide their contact details if they are interested in participating in the study. This would increase the reach of the study within a forum that people are comfortable using. 132
In our feasibility study, we achieved 78% follow-up at 10 days and 64% follow-up at 8 weeks. The two study managers carried out all of the follow-up telephone interviews within the time that they had available. Our experience from other studies (e.g. Building Blocks110) has demonstrated that using a participant resource centre for conducting follow-up telephone interviews is successful in achieving high follow-up rates with similar study populations, and we would recommend utilising this approach to maximise follow-up rates in a future trial. There is also the potential to utilise text messages to collect primary outcome data. In a full RCT we could open two or three sites early in a pilot phase to test these strategies for recruitment and retention.
Framework for economic evaluation
We consider that an in-trial economic evaluation alongside the RCT proposed in the previous sections would be the most appropriate method to use. We propose carrying out an incremental cost-effectiveness analysis based on the primary outcome, with a cost–utility (incremental cost per QALY) analysis based on the mother also undertaken. Further exploration is needed of potential suitable measures (e.g. EQ-5D-5L102 vs. SF-6D,122 using the Short Form questionnaire-12 items133 as a secondary outcome) to inform the economic analysis. Other outcomes would be presented in a cost–consequences analysis. The cost–consequences approach presents all relevant outcome measures alongside the costs (without combining them into an incremental cost-effectiveness ratio), allowing decision-makers to form their own opinion of their relative importance.
We suggest, in line with the NICE reference case,125 that a NHS/Personal Social Services perspective is taken, with an additional examination of the wider societal costs (to the family) included. The proposed follow-up period of 6 months would allow examination of the cost-effectiveness of the Mam-Kind intervention for the range of outcomes within the study. As this follow-up period is < 12 months, discounting would not be applied.
However, this approach will achieve only a short-term understanding of cost-effectiveness based on the success of breastfeeding at 8 weeks (primary end point) and a cost per QALY at 6 months. Further exploration is needed of whether or not health outcomes and/or model-based analysis could be conducted to examine the longer-term effects of the Mam-Kind intervention. We plan to do so by utilising the logic model to link to the economic model developed, with further consideration of what the important costs and health outcomes would be (for the mother and/or child) over a longer timeline, for example drawing on those outcomes that are considered to be part of policy initiatives such as Healthy Start, with utilisation of an appropriate time horizon, such as 5 years. As part of this, the collection of appropriate evidence to inform and populate a model would need to be built into the health economic methods, for example data inputs from the literature and/or expert opinions gathered in a systematic and rigorous but practical way. Further consideration is needed of the subgroups/scenarios to be examined in the economic analysis. To provide a comprehensive picture to decision-makers and service commissioners, a budget impact model (UK NHS) would be included as part of the economic evaluation, based on good practice guidelines.
The health economic analysis plan will take into account appropriate methods to adjust costs and outcomes, commensurate with the statistical analysis plan, including suitable imputation methods to handle missing data. Appropriate deterministic sensitivity analyses will also be required. Scenario analyses will enable consideration of different contexts for the Mam-Kind intervention, to reflect the appropriate settings within which the Mam-Kind intervention could be delivered. Subgroup analyses will be included if appropriate. Probabilistic sensitivity analysis will assess joint uncertainty, with cost-effectiveness acceptability curves and net benefit values presented to assess the willingness to pay of the Mam-Kind threshold for both cost-effectiveness (based on the primary clinical outcome) and cost per QALY.
Conclusion
We have established that there is no standardised provision of BFPS in the UK and that the models that are currently in use are not explicitly linked to theory nor have they been robustly evaluated for effectiveness. We have systematically developed a BFPS intervention that uses a MI approach, using the BCW and informed by service users, peer supporters and health-care professionals. Previous UK RCTs have not shown that BFPS interventions are effective at increasing breastfeeding maintenance, possibly because of their use of low-intensity interventions that relied on mothers to seek support. The Mam-Kind intervention, by contrast, is characterised by proactive Mam-Kind buddy (peer-supporter)-led support in the first 2 weeks post-partum. We have tested and established the feasibility of delivering the Mam-Kind intervention, with high uptake of the intervention and fidelity to intervention content. We have addressed the findings from the feasibility study by applying modifications and refinements to the intervention specification and have developed study materials that can be adapted for use in a full trial. We have established data collection methods for outcome data, including the feasibility of collecting salient information about the wider costs of the Mam-Kind intervention. This feasibility study was focused on developing and testing the delivery of the Mam-Kind intervention and the feasibility of research processes, such as data collection. A full RCT is now required to test the effectiveness of the Mam-Kind intervention at increasing the duration of breastfeeding, with a built-in pilot phase to ensure the recruitment and retention of participants.
Acknowledgements
We would like to acknowledge Professor Stephen Rollnick for his contribution to the development of the intervention, the delivery of MI training and the integration of MI in the intervention.
We would like to acknowledge Mala Mann for her contribution to the literature search, and are grateful to Cheryl McQuire for her contribution to the content analysis section.
We would like to acknowledge Kirsten McEwan for her statistical analysis of the survey data and Giles Greene for creating the maps in the survey.
We would also like to thank Joanna Lourenco, Avril Jones and Nicki Symes, members of the Stakeholder Advisory Group, for providing their thoughts and feedback to the study team. We would also like to acknowledge Mary Whitmore for her contribution to the Study Management Group and site set-up.
We would like to thank Sam Clarkson for designing the database.
We would like to thank Sue Channon and Helen Stanton for independently coding data.
We would also like to thank all of the administrative staff within the South East Wales Trials Unit who worked on the study for their hard work and support.
Finally, we would like to thank the participants and their families, the peer supporters and the health-care professionals who kindly took the time to participate in the study.
Contributions of authors
Shantini Paranjothy (Mansel Talbot Professor of Preventive Medicine, Population Health) was the Chief Investigator. She led the design of the study, interpretation of the data and drafting and approval of the final study report and provided oversight for all aspects of the study.
Lauren Copeland (Research Associate, Behaviour Change and MI) co-managed the study, providing a significant contribution to the final report, and led on several chapters. She also contributed to the design of the intervention and to the evaluation of MI fidelity and was involved in the recruitment of participants and data collection.
Laura Merrett (Research Associate, Midwifery) co-managed the study and contributed to the recruitment of participants and data collection. She also conducted, analysed and wrote up the qualitative research as part of the process evaluation and provided input into the final report.
Aimee Grant (Research Associate, Qualitative Research) oversaw the qualitative research. She conducted data collection for the peer-supporter interviews, provided an analysis of the survey data and wrote up the relevant part of the report.
Rhiannon Phillips (Research Fellow, Health Psychology) applied the BCW to the qualitative data analysis to develop the intervention. She contributed to the intervention development chapter of the report.
Nina Gobat (Research Fellow, MI and Behaviour/Motivation) developed and delivered the MI training and supervision to peer supporters, including integration of MI in the intervention. She also contributed to the process evaluation of MI fidelity and commented on the final report.
Julia Sanders (Consultant Midwife and Reader in Midwifery) was a study co-investigator providing senior clinical input to the study and was involved in the design of the study, intervention development and delivery and report writing.
Deborah Fitzsimmons (Professor of Health Outcomes Research and Academic Director, Health Economics) supervised the health economics aspects of the study, wrote the health economics plan and drafted the health economics chapter.
Billie Hunter (Royal College of Midwives Professor of Midwifery, Qualitative Research and Midwifery Practice) contributed to the conception and design of the study and the interpretation of the data and commented on and revised the final study report.
Sian Regan (PPI Representative, Involving People Network) contributed to the Stakeholder Advisory Group, provided feedback on the study documents and provided reflections in the PPI section of the report.
Rebecca Playle (Senior Lecturer, Medical Statistics) was responsible for the statistical design and analysis of the study.
Amy Brown (Associate Professor in Child Public Health, Infant Feeding Research) contributed to the design of the study and commented on the final report.
Sally Tedstone (Infant Feeding Specialist) contributed as a midwifery advisor to the development of the intervention, site set-up and breastfeeding peer-supporter training.
Heather Trickey (Research Associate, Social Science/Public Health, Infant Feeding Policy and Intervention) contributed to the rapid evidence review and to the qualitative research for the intervention development.
Mike Robling (Director of Population Health Trials, Psychology) was a co-investigator and funding co-applicant. He contributed to the design of the study, interpretation of the data and drafting and approval of the final study report.
Publications
Grant A, McEwan K, Tedstone S, Greene G, Copeland L, Hunter B, et al. Availability of breastfeeding peer support in the UK: a cross-sectional study. Matern Child Nutr 2017;e12476.
Trickey H, Thomson G, Grant A, Sanders J, Mann M, Murphy M, Paranjothy S. A realist review of one-to-one breastfeeding peer support experiments conducted in developed country settings. Matern Child Nutr 2017; in press.
Data sharing statement
We will make data available to the scientific community with as few restrictions as feasible, while retaining exclusive use until the publication of major outputs.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet 2016;387:475-90. https://doi.org/10.1016/S0140-6736(15)01024-7.
- Renfrew MJ, Pokhrel S, Quigley M, McCormick F, Fox-Rushby J, Dodds R, et al. Preventing Disease and Saving Resources: The Potential Contribution of Increasing Breastfeeding Rates in the UK. London: UNICEF; 2012.
- McAndrew F, Thompson J, Fellows L, Large A, Speed M, Renfrew MJ. Infant Feeding Survey 2010. Leeds: NHS Digital; 2012.
- WHO and UNICEF . Global Nutrition Targets 2025: Breastfeeding Policy Brief 2014. http://apps.who.int/iris/bitstream/10665/149022/1/WHO_NMH_NHD_14.7_eng.pdf?ua=1 (accessed 10 December 2015).
- Brown AE, Raynor P, Benton D, Lee MD. Indices of Multiple Deprivation predict breastfeeding duration in England and Wales. Eur J Public Health 2010;20:231-5. https://doi.org/10.1093/eurpub/ckp114.
- UNICEF . UNICEF UK Baby Friendly Initiative Standards 2014. https://353ld710iigr2n4po7k4kgvv-wpengine.netdna-ssl.com/babyfriendly/wp-content/uploads/sites/2/2014/02/Baby_Friendly_guidance_2012.pdf (accessed 21 February 2016).
- Trickey H, Newburn M. Goals, dilemmas and assumptions in infant feeding education and support. Applying theory of constraints thinking tools to develop new priorities for action. Matern Child Nutr 2014;10:72-91. https://doi.org/10.1111/j.1740-8709.2012.00417.x.
- WHO . Acceptable Medical Reasons for Use of Breast-Milk Substitutes 2009. http://apps.who.int/iris/bitstream/10665/69938/1/WHO_FCH_CAH_09.01_eng.pdf (accessed 5 November 2015).
- Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, et al. Why invest, and what it will take to improve breastfeeding practices?. Lancet 2016;387:491-504. https://doi.org/10.1016/S0140-6736(15)01044-2.
- Dyson L, Green JM, Renfrew MJ, McMillan B, Woolridge M. Factors influencing the infant feeding decision for socioeconomically deprived pregnant teenagers: the moral dimension. Birth 2010;37:141-9. https://doi.org/10.1111/j.1523-536X.2010.00394.x.
- Lawton R, Ashley L, Dawson S, Waiblinger D, Conner M. Employing an extended theory of planned behaviour to predict breastfeeding intention, initiation, and maintenance in white British and South-Asian mothers living in Bradford. Br J Health Psychol 2012;17:854-71. https://doi.org/10.1111/j.2044-8287.2012.02083.x.
- Forster DA, McLachlan HL, Lumley J. Factors associated with breastfeeding at six months postpartum in a group of Australian women. Int Breastfeed J 2006;1:1-12. https://doi.org/10.1186/1746-4358-1-18.
- Racine EF, Frick KD, Strobino D, Carpenter LM, Milligan R, Pugh LC. How motivation influences breastfeeding duration among low-income women. J Hum Lact 2009;25:173-81. https://doi.org/10.1177/0890334408328129.
- Parry K, Taylor E, Hall-Dardess P, Walker M, Labbok M. Understanding women’s interpretations of infant formula advertising. Birth 2013;40:115-24. https://doi.org/10.1111/birt.12044.
- Dyson LM. Interventions for promoting the initiation of breastfeeding. São Paulo Med J 2014;132:1-40. https://doi.org/10.1590/1516-3180.20141321T1.
- Avery A, Zimmermann K, Underwood PW, Magnus JH. Confident commitment is a key factor for sustained breastfeeding. Birth 2009;36:141-8. https://doi.org/10.1111/j.1523-536X.2009.00312.x.
- Meedya S, Fahy K, Kable A. Factors that positively influence breastfeeding duration to 6 months: a literature review. Women Birth 2010;23:135-45. https://doi.org/10.1016/j.wombi.2010.02.002.
- Brown A, Lee M. An exploration of the attitudes and experiences of mothers in the United Kingdom who chose to breastfeed exclusively for 6 months postpartum. Breastfeed Med 2011;6:197-204. https://doi.org/10.1089/bfm.2010.0097.
- Hoddinott P, Pill R. Qualitative study of decisions about infant feeding among women in East End of London. BMJ 1999;318:30-4. https://doi.org/10.1136/bmj.318.7175.30.
- Scott JA, Mostyn T. Greater Glasgow Breastfeeding Initiative Management Team . Women’s experiences of breastfeeding in a bottle-feeding culture. J Hum Lact 2003;19:270-7. https://doi.org/10.1177/0890334403255225.
- Hoddinott P, Britten J, Prescott GJ, Tappin D, Ludbrook A, Godden DJ. Effectiveness of policy to provide breastfeeding groups (BIG) for pregnant and breastfeeding mothers in primary care: cluster randomised controlled trial. BMJ 2009;338. https://doi.org/10.1136/bmj.a3026.
- McInnes RJ, Hoddinott P, Britten J, Darwent K, Craig LC. Significant others, situations and infant feeding behaviour change processes: a serial qualitative interview study. BMC Pregnancy Childbirth 2013;13:114-27. https://doi.org/10.1186/1471-2393-13-114.
- Brown A, Raynor P, Lee M. Young mothers who choose to breast feed: the importance of being part of a supportive breast-feeding community. Midwifery 2011;27:53-9. https://doi.org/10.1016/j.midw.2009.09.004.
- Larsen JS, Hall EO, Aagaard H. Shattered expectations: when mothers’ confidence in breastfeeding is undermined – a metasynthesis. Scand J Caring Sci 2008;22:653-61. https://doi.org/10.1111/j.1471–6712.2007.00572.x.
- Dennis CL. Peer support within a health care context: a concept analysis. Int J Nurs Stud 2003;40:321-32. https://doi.org/10.1016/S0020-7489(02)00092-5.
- McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: homophily in social networks. Annu Rev Sociol 2001;27:415-44. https://doi.org/10.1146/annurev.soc.27.1.415.
- House JS. Work Stress and Social Support. Boston, MA: Addison-Wesley Longman; 1981.
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. New York, NY: Guilford Press; 2012.
- Dennis CL. Breastfeeding peer support: maternal and volunteer perceptions from a randomized controlled trial. Birth 2002;29:169-76. https://doi.org/10.1046/j.1523-536X.2002.00184.x.
- Trickey H. Peer support for breastfeeding continuation: an overview of research. Perspective 2013;21:15-20.
- Renfrew MJ, McCormick FM, Wade A, Quinn B, Dowswell T. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev 2012;5. https://doi.org/10.1002/14651858.CD001141.pub4.
- Ingram L, MacArthur C, Khan K, Deeks JJ, Jolly K. Effect of antenatal peer support on breastfeeding initiation: a systematic review. CMAJ 2010;182:1739-46. https://doi.org/10.1503/cmaj.091729.
- Jolly K, Ingram L, Khan KS, Deeks JJ, Freemantle N, MacArthur C. Systematic review of peer support for breastfeeding continuation: metaregression analysis of the effect of setting, intensity, and timing. BMJ 2012;344. https://doi.org/10.1136/bmj.d8287.
- Graffy J, Taylor J, Williams A, Eldridge S. Randomised controlled trial of support from volunteer counsellors for mothers considering breast feeding. BMJ 2004;328:26-9. https://doi.org/10.1136/bmj.328.7430.26.
- Muirhead PE, Butcher G, Rankin J, Munley A. The effect of a programme of organised and supervised peer support on the initiation and duration of breastfeeding: a randomised trial. Br J Gen Pract 2006;56:191-7.
- Watt R, Tull K, Hardy R, Wiggins M, Kelly Y, Molloy B, et al. Effectiveness of a social support intervention on infant feeding practices: randomised controlled trial. J Epidemiol Community Health 2009;63:156-62. https://doi.org/10.1136/jech.2008.077115.
- Jolly K, Ingram L, Freemantle N, Khan K, Chambers J, Hamburger R, et al. Effect of a peer support service on breast-feeding continuation in the UK: a randomised controlled trial. Midwifery 2012;28:740-5. https://doi.org/10.1016/j.midw.2011.08.005.
- McInnes RJ, Love JG, Stone DH. Evaluation of a community-based intervention to increase breastfeeding prevalence. J Public Health Med 2000;22:138-45. https://doi.org/10.1093/pubmed/22.2.138.
- Scott S, Pritchard C, Szatkowski L. The impact of breastfeeding peer support for mothers aged under 25: a time series analysis. Matern Child Nutr 2017;13. https://doi.org/10.1111/mcn.12241.
- Sim MG, Wain T, Khong E. Influencing behaviour change in general practice: part 2 – motivational interviewing approaches. Aust Fam Physician 2009;38:986-9.
- Lundahl B, Moleni T, Burke BL, Butters R, Tollefson D, Butler C, et al. Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns 2013;93:157-68. https://doi.org/10.1016/j.pec.2013.07.012.
- Martins RK, McNeil DW. Review of motivational interviewing in promoting health behaviors. Clin Psychol Rev 2009;29:283-93. https://doi.org/10.1016/j.cpr.2009.02.001.
- Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev 2011;12:709-23. https://doi.org/10.1111/j.1467–789X.2011.00892.x.
- Knight K, McGowan L, Dickens C, Bundy C. A systematic review of motivational interviewing in physical health care settings. Br J Health Psychol 2006;11:319-32. https://doi.org/10.1348/135910705X52516.
- Britt E, Hudson SM, Blampied NM. Motivational interviewing in health settings: a review. Patient Educ Couns 2004;53:147-55. https://doi.org/10.1016/S0738-3991(03)00141-1.
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction 2001;96:1725-42. https://doi.org/10.1046/j.1360-0443.2001.961217253.x.
- Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract 2005;55:305-12.
- Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: conceptual issues and evidence review. J Am Diet Assoc 2006;106:2024-33. https://doi.org/10.1016/j.jada.2006.09.015.
- Erickson SJ, Gerstle M, Feldstein SW. Brief interventions and motivational interviewing with children, adolescents, and their parents in pediatric health care settings: a review. Arch Pediatr Adolesc Med 2005;159:1173-80. https://doi.org/10.1001/archpedi.159.12.1173.
- Resnicow K, DiIorio C, Soet JE, Ernst D, Borrelli B, Hecht J. Motivational interviewing in health promotion: it sounds like something is changing. Health Psychol 2002;21:444-51. https://doi.org/10.1037/0278-6133.21.5.444.
- VanWormer JJ, Boucher JL. Motivational interviewing and diet modification: a review of the evidence. Diabetes Educ 2004;30:404-6. https://doi.org/10.1177/014572170403000309.
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of motivational interviewing: twenty-five years of empirical studies. Res Soc Work Pract 2010;20:137-60. https://doi.org/10.1177/1049731509347850.
- Taveras EM, Blackburn K, Gillman MW, Haines J, McDonald J, Price S, et al. First steps for mommy and me: a pilot intervention to improve nutrition and physical activity behaviors of postpartum mothers and their infants. Matern Child Health J 2011;15:1217-27. https://doi.org/10.1007/s10995-010-0696-2.
- Wilhelm SL, Flanders Stepans MB, Hertzog M, Callahan Rodehorst TK, Gardner P. Motivational interviewing to promote sustained breastfeeding. J Obstet Gynecol Neonatal Nurs 2006;35:340-8. https://doi.org/10.1111/j.1552-6909.2006.00046.x.
- Elliott-Rudder M, Pilotto L, McIntyre E, Ramanathan S. Motivational interviewing improves exclusive breastfeeding in an Australian randomised controlled trial. Acta Paediatr 2014;103. https://doi.org/10.1111/apa.12434.
- Michie S, Atkins L, West R. The Behaviour Change Wheel Guide to Designing Interventions. London: Silverback Publishing; 2014.
- Michie S, van Stralen M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42-53. https://doi.org/10.1186/1748-5908-6-42.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The Behavior Change Technique Taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Research Councils UK . The MRC ConDuCT-II Hub. COllaboration and INnovation in DifficUlt and Complex Randomised Controlled Trials In Invasive Procedures 2014. http://gtr.rcuk.ac.uk/projects?ref= MR%2FK025643%2F1 (accessed 29 September 2017).
- Noble M, Smith GAN, Wright G, Dibben C, Lloyd M, Penhale B. Welsh Index of Multiple Deprivation. London: National Statistics; 2000.
- Maternal and Child Nutrition. London: NICE; 2008.
- A Peer-Support Programme for Women Who Breastfeed: Commissioning Guide. London: NICE; 2008.
- Tedstone S. Audit of Breastfeeding Support Groups and Peer Support Network in Wales 2013. www.wales.nhs.uk/publications/bfeedingstrategy-e.pdf (accessed 7 January 2015).
- Grant A, Sims L, Tedstone S, Ashton K. A Qualitative Evaluation of Breastfeeding Support Groups and Peer Supporters in Wales. Cardiff: Public Health Wales; 2013.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Britten J, Hoddinott P, McInnes R. Breastfeeding peer support: health service programmes in Scotland. Br J Midwifery 2006;14:12-9. https://doi.org/10.12968/bjom.2006.14.1.20255.
- Dykes F. Government funded breastfeeding peer support projects: implications for practice. Matern Child Nutr 2005;1:21-3. https://doi.org/10.1111/j.1740-8709.2004.00006.x.
- Bai Y, Middlestadt SE, Peng CY, Fly AD. Predictors of continuation of exclusive breastfeeding for the first six months of life. J Hum Lact 2010;26:26-34. https://doi.org/10.1177/0890334409350168.
- Markland D, Ryan RM, Tobin VJ, Rollnick S. Motivational interviewing and self-determination theory. J Soc Clin Psychol 2000;24:811-31. https://doi.org/10.1521/jscp.2005.24.6.811.
- Vansteenkiste M, Sheldon KM. There’s nothing more practical than a good theory: integrating motivational interviewing and self-determination theory. Br J Clin Psychol 2006;45:63-82. https://doi.org/10.1348/014466505X34192.
- Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act 2012;9. https://doi.org/10.1186/1479-5868-9-78.
- Ryan RM. Psychological needs and the facilitation of integrative processes. J Pers 1995;63:397-42. https://doi.org/10.1111/j.1467-6494.1995.tb00501.x.
- Miller WR, Rollnick S. Glossary of Motivational Interviewing Terms: Updated July 2012 2012. http://drug-films.com/docs/Glossary_MI_Terms.pdf (accessed 12 August 2017).
- Michie S, West R, Campbell R, Brown J, Gainforth H. ABC of Behaviour Change Theories. London: Silverback Publishing; 2014.
- Hardcastle S. Identification of the motivational techniques within motivational interviewing and relations with behaviour change techniques from the BCTTv1. Eur Health Psychol 2015;17:115-21.
- Fern E. Advanced Focus Group Research. London: Sage; 2001.
- Kitzinger J. The methodology of focus groups: the importance of interaction between research participants. Sociol Health Illn 1994;16:103-21. https://doi.org/10.1111/1467-9566.ep11347023.
- Morgan DL, Krueger RA, King J. The Focus Group Kit. Thousand Oaks, CA: Sage; 1998.
- Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. Singapore: Sage; 2014.
- Chapman DJ, Damio G, Perez-Escamilla R. Differential response to breastfeeding peer counseling within a low-income, predominantly Latina population. J Hum Lact 2004;20:389-96. https://doi.org/10.1177/0890334404269845.
- Anderson AK, Damio G, Young S, Chapman DJ, Pérez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Arch Pediatr Adolesc Med 2005;159:836-41. https://doi.org/10.1001/archpedi.159.9.836.
- Gross SM, Resnik AK, Cross-Barnet C, Nanda JP, Augustyn M, Paige DM. The differential impact of WIC peer counseling programs on breastfeeding initiation across the state of Maryland. J Hum Lact 2009;25:435-43. https://doi.org/10.1177/0890334409342070.
- Yun S, Liu Q, Mertzlufft K, Kruse C, White M, Fuller P, et al. Evaluation of the Missouri WIC (Special Supplemental Nutrition Program for Women, Infants, and Children) breast-feeding peer counselling programme. Public Health Nutr 2010;13:229-37. https://doi.org/10.1017/S1368980009990668.
- Di Meglio G, McDermott MP, Klein JD. A randomized controlled trial of telephone peer support’s influence on breastfeeding duration in adolescent mothers. Breastfeed Med 2010;5:41-7. https://doi.org/10.1089/bfm.2009.0016.
- Olson BH, Haider SJ, Vangjel L, Bolton TA, Gold JG. A quasi-experimental evaluation of a breastfeeding support program for low income women in Michigan. Matern Child Health J 2010;14:86-93. https://doi.org/10.1007/s10995-008-0430-5.
- Chapman DJ, Morel K, Bermúdez-Millán A, Young S, Damio G, Pérez-Escamilla R. Breastfeeding education and support trial for overweight and obese women: a randomized trial. Pediatrics 2013;131:e162-70. https://doi.org/10.1542/peds.2012-0688.
- Reeder JA, Joyce T, Sibley K, Arnold D, Altindag O. Telephone peer counseling of breastfeeding among WIC participants: a randomized controlled trial. Pediatrics 2014;134:e700-9. https://doi.org/10.1542/peds.2013-4146.
- MacArthur C, Jolly K, Ingram L, Freemantle N, Dennis CL, Hamburger R, et al. Antenatal peer support workers and initiation of breast feeding: cluster randomised controlled trial. BMJ 2009;338. https://doi.org/10.1136/bmj.b131.
- Srinivas GL, Benson M, Worley S, Schulte E. A clinic-based breastfeeding peer counselor intervention in an urban, low-income population interaction with breastfeeding attitude. J Hum Lact 2015;31:120-8. https://doi.org/10.1177/0890334414548860.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Harris J, Springett J, Booth A, Campbell F, Thompson J, Goyder E, et al. Can community-based peer support promote health literacy and reduce inequalities? A realist review. J Public Health Res 2015;3.
- Alexander KE, Brijnath B, Mazza D. Barriers and enablers to delivery of the Healthy Kids Check: an analysis informed by the theoretical domains framework and COM-B model. Implement Sci 2014;9. https://doi.org/10.1186/1748-5908-9-60.
- Sinnott C, Mercer SW, Payne RA, Duerden M, Bradley CP, Byrne M. Improving medication management in multimorbidity: development of the MultimorbiditY COllaborative Medication Review And DEcision Making (MY COMRADE) intervention using the behaviour change wheel. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0322-1.
- Duncan EM, Francis JJ, Johnston M, Davey P, Maxwell S, McLay J, et al. Learning curves, taking instructions, and patient safety: using a theoretical domains framework in an interview study to investigate prescribing errors among trainee doctors. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-86.
- Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol 2009;64:527-37. https://doi.org/10.1037/a0016830.
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol 2005;1:91-111. https://doi.org/10.1146/annurev.clinpsy.1.102803.143833.
- O’Halloran PD, Blackstock F, Shields N, Holland A, Iles R, Kingsley M, et al. Motivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysis. Clin Rehabil 2014;28:1159-71. https://doi.org/10.1177/0269215514536210.
- Departments for Communities and Local Government . English Indices of Deprivation 2015 2015. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 17 January 2015).
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. https://doi.org/10.1192/bjp.150.6.782.
- Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 2007;146:317-25. https://doi.org/10.7326/0003-4819-146-5-200703060-00004.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20. https://doi.org/10.1007/s11136-011-9903-x.
- Dennis CL. The breastfeeding self-efficacy scale: psychometric assessment of the short form. J Obstet Gynecol Neonatal Nurs 2003;32:734-44. https://doi.org/10.1177/0884217503258459.
- Moyers TB, Rowell LN, Manuel JK, Ernst D, Houck JM. The motivational interviewing treatment integrity code (MITI 4): rationale, preliminary reliability and validity. J Subst Abuse Treat 2016;65:36-42. https://doi.org/10.1016/j.jsat.2016.01.001.
- Söderlund LL, Madson MB, Rubak S, Nilsen P. A systematic review of motivational interviewing training for general health care practitioners. Patient Educ Couns 2011;84:16-2. https://doi.org/10.1016/j.pec.2010.06.025.
- Mounsey AL, Bovbjerg V, White L, Gazewood J. Do students develop better motivational interviewing skills through role-play with standardised patients or with student colleagues?. Med Educ 2006;40:775-80. https://doi.org/10.1111/j.1365-2929.2006.02533.x.
- Bennett GA, Roberts HA, Vaughan TE, Gibbins JA, Rouse L. Evaluating a method of assessing competence in motivational interviewing: a study using simulated patients in the United Kingdom. Addict Behav 2007;32:69-7. https://doi.org/10.1016/j.addbeh.2006.03.022.
- Moyers T, Martin T, Manuel J, Miller W, Ernst D. Revised Global Scales: Motivational Interviewing Treatment Integrity 3.1. 1 (MITI 3.1. 1). Albuquerque, NM: University of New Mexico; 2010.
- Berg-Smith SM. The Art of Teaching Motivational Interviewing: A Resource for MINT Trainers 1994. www.stephenrollnick.com/resources/The%20Art%20of%20Teaching%20MI%201.1.pdf (accessed 17 January 2017).
- Robling M, Bekkers M-J, Bell K, Butler CC, Cannings-John R, Channon S, et al. Effectiveness of a nurse-led intensive home-visitation programme for first-time teenage mothers (Building Blocks): a pragmatic randomised controlled trial. Lancet 2016;387:146-55. https://doi.org/10.1016/S0140-6736(15)00392-X.
- National Institute for Health and Care Excellence . Developing NICE Guidelines: The Manual 2014. www.nice.org.uk/process/pmg20/chapter/introduction-and-overview (accessed 21 March 2016).
- DIRUM . DIRUM: Database of Instruments for Resource Use Measurement 2013. www.dirum.org/ (accessed 19 April 2016).
- National Institute for Health and Care Excellence . The Social Care Guidance Manual 2016. www.nice.org.uk/process/pmg10/chapter/incorporating-economic-evaluation (accessed 19 April 2016).
- Edwards RT, Charles JM, Lloyd-Williams H. Public health economics: a systematic review of guidance for the economic evaluation of public health interventions and discussion of key methodological issues. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-1001.
- DIRUM . Client Service Receipt Inventory 1997. www.dirum.org/assets/downloads/634462388066137028-CSRI.pdf (accessed 5 February 2015).
- NHS Employers . Agenda for Change Pay Scales – Annual 2016. www.nhsemployers.org/your-workforce/pay-and-reward/agenda-for-change/pay-scales/annual (accessed 21 August 2016).
- British National Formulary. London: BMJ Group and Pharmaceutical Press; n.d.
- British National Formulary for Children. London: BMJ Group, Pharmaceutical Press, and RCPCH Publications; n.d.
- Department of Health . NHS Reference Costs 2014 to 2015 2015. www.gov.uk/government/publications/nhs-reference-costs-2014-to-2015 (accessed 15 October 2016).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- Claxton K, Sculpher M, Drummond M. A rational framework for decision making by the National Institute for Clinical Excellence (NICE). Lancet 2002;360:711-15. https://doi.org/10.1016/S0140-6736(02)09832-X.
- Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ 2004;13:873-84. https://doi.org/10.1002/hec.866.
- British Medical Association . NHS Direct Telephone Contact 2008. www.bma.org.uk/ (accessed 3 December 2016).
- Sassi F. Calculating QALYs, comparing QALY and DALY calculations. Health Policy Plan 2006;21:402-8. https://doi.org/10.1093/heapol/czl018.
- Langley PC. The NICE reference case requirement. PharmacoEconomics 2004;22:267-71. https://doi.org/10.2165/00019053-200422040-00005.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Health and Care Research Wales. Researcher interview: Rhiannon Phillips. Your Involvement Matters 2016:13-6. www.healthandcareresearch.gov.wales/uploads/Public/Noticeboard/Newsletter/Your_Involvement_Matters_February_2016.pdf (accessed 11 October 2017).
- Copeland L, Paranjothy S. Motivational interviewing: a key approach for supporting the transition to parenthood including breastfeeding?. Perspective 2015;27:17-20.
- The Optimal Duration of Exclusive Breastfeeding. Report of an Expert Consultation. Geneva: WHO; 2001.
- Marmot MG, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, et al. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post-2010 2010. www.parliament.uk/documents/fair-society-healthy-lives-full-report.pdf (accessed 17 September 2016).
- Bonevski B, Randell M, Paul C, Chapman K, Twyman L, Bryant J, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol 2014;14:42-54. https://doi.org/10.1186/1471-2288-14-42.
- Balfe M, Doyle F, Conroy R. Using Facebook to recruit young adults for qualitative research projects: how difficult is it?. Comput Inform Nurs 2012;30:511-15. https://doi.org/10.1097/NXN.0b013e31826e4fca.
- Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. https://doi.org/10.1097/00005650-199603000-00003.
- Moyers TB, Miller WR, Hendrickson SML. How does motivational interviewing work? Therapist interpersonal skill predicts client involvement within motivational interviewing sessions. J Consult Clin Psychol 2005;73:590-8. https://doi.org/10.1037/0022-006X.73.4.590.
- Carels RA, Darby L, Cacciapaglia HM, Konrad K, Coit C, Harper J, et al. Using motivational interviewing as a supplement to obesity treatment: a stepped-care approach. Health Psychol 2007;26:369-74. https://doi.org/10.1037/0278-6133.26.3.369.
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Dismantling motivational interviewing and feedback for college drinkers: a randomized clinical trial. J Consult Clin Psychol 2009;77:64-73. https://doi.org/10.1037/a0014472.
- Moyers TB, Manuel JK, Wilson PG, Hendrickson SML, Talcott W, Durand P. A randomized trial investigating training in motivational interviewing for behavioral health providers. Behav Cogn Psychother 2008;36:149-62. https://doi.org/10.1017/S1352465807004055.
Appendix 1 Rapid review search strategy
Search methods: breastfeeding peer support
Research question
-
What is the role of peer support for breastfeeding maintenance?
Methods
The protocol was registered with PROSPERO and the review was conducted and reported in compliance with PRISMA guidelines. 90
Search methods for the identification of studies
A search strategy was developed for electronic databases on Ovid using both keywords and MeSH terms. The search strategy was modified to search other bibliographic databases (Box 7).
Applied Social Sciences Index and Abstracts (ASSIA).
CENTRAL.
Cumulative Index to Nursing and Allied Health Literature (CINAHL).
EMBASE.
Education Resources Information Center (ERIC).
Health Management Information Consortium (HMIC).
MEDLINE.
MEDLINE In-Process & Other Non-Indexed Citations.
Scopus.
Social Services Abstracts.
Sociological Abstracts.
Web of Knowledge: Science Citation Index Expanded, Social Sciences Citation Index, Conference Proceedings Citation Index – Science.
Supplementary searchesBFI.
Breastfeeding Medicine.
Journal of Human Lactation.
Maternal & Child Nutrition.
metaRegister of Controlled Trials (mRCT).
Midwifery.
In addition, to maximise recall and minimise the potential for publication bias, a range of supplementary (‘snowballing’) techniques were used to increase the sensitivity of the search and to ensure coverage of grey literature and unpublished studies. These include reference list follow-up, searching websites and scanning content tables for the journals that appear most frequently in the list of relevant studies (see Box 7). Finally, all systematic reviews on relevant topics were unpicked for primary studies meeting the inclusion/exclusion criteria.
The search was limited to English-language studies and publication years 2000–16. In addition, the search was restricted to studies undertaken in OECD countries. These countries are likely to have similar economies and therefore the studies will be of equal relevance.
Ovid MEDLINE(R) (1946 to January week 4 2016)
Search strategy
-
exp Breast Feeding/
-
Milk, Human/
-
(infant feed* or breast feed* or breastfeed* or breast-feed* or breast fed or infant fed).mp.
-
or/1-3
-
Peer Group/
-
(lay adj5 (expert* orworker* or person* or advisor* or consultant* or leader* or educator* or tutor* or instructor* or facilitator*)).tw.
-
(volunteer* adj5 (trained or aide*)).tw.
-
(peer adj5 (expert* or worker* or advisor* or consultant* or leader* or educator* or tutor* or instructor* or facilitator*orcounsellor or counselor or coach)).tw.
-
(peer-support* or peer group or peer*).mp.
-
((support* or befriend* or advice* or advis* or counsel* or help* or assist* or encourag* or meeting* or visit* or program*) adj3 (peer-support or lay worker* or voluntary worker*)).tw.
-
mother to mother.tw.
-
lactation consultants.tw.
-
(support adj (volunteer or lay or social)).tw.
-
(or/5-13) and 4
-
((activist or advocate) adj3 (breastfeeding or breast feed* or breast-feed*)).tw.
-
((breastfeeding or breast feeding or breast feed* or breast-feed*) adj (counsellor* or counselor or group or groups or volunteer*1)).tw.
-
(volunteer support adj5 (breastfeeding or breast feeding or breast feed* or breast-feed*)).tw.
-
or/15-17
-
14 or 18
-
19 not (“Africa South of the Sahara”/ or Algeria$ or Egypt$ or Liby$ or Morocc$ or Tunisia$ or Western Sahara$ or Angola$ or Benin or Botswana$ or Burkina Faso or Burundi or Cameroon or Cape Verde or Central African Republic or Chad or Comoros or Congo or Djibouti or Eritrea or Ethiopia$ or Gabon or Gambia$ or Ghana or Guinea or Keny$ or Lesotho or Liberia or Madagasca$ or Malawi or Mali or Mauritania or Mauritius or Mayotte or Mozambiq$ or Namibia$ or Niger or Nigeria$ or Reunion or Rwand$ or Saint Helena or Senegal or Seychelles or Sierra Leone or Somalia or South Africa$ or Sudan or Swaziland or Tanzania or Togo or Ugand$ or Zambia$ or Zimbabw$ or China or Chinese or Hong Kong or Macao or Mongolia$ or Taiwan$ or Belarus or Moldov$ or Russia$ or Ukraine or Afghanistan or Armenia$ or Azerbaijan or Bahrain or Cyprus or Cypriot or Georgia$ or Iran$ or Iraq$ or Jordan$ or Kazakhstan or Kuwait or Kyrgyzstan or Leban$ or Oman or Pakistan$ or Palestin$ or Qatar or Saudi Arabia or Syria$ or Tajikistan or Turkmenistan or United Arab Emirates or Uzbekistan or Yemen or Bangladesh$ or Bhutan or British Indian Ocean Territory or Brunei Darussalam or Cambodia$ or India$ or Indonesia$ or Lao or People's Democratic Republic or Malaysia$ or Maldives or Myanmar or Nepal or Philippin$ or Singapore or Sri Lanka or Thai$ or Timor Leste or Vietnam or Albania$ or Andorra or Bosnia$ or Herzegovina$ or Bulgaria$ or Croatia$ or Faroe Islands or Greenland or Liechtenstein or Lithuani$ or Macedonia or Malta or maltese or Romania or Serbia$ or Montenegro or Svalbard or Argentina$ or Belize or Bolivia$ or Brazil$ or Colombia$ or Costa Rica$ or Cuba or Ecuador or El Salvador or French Guiana or Guatemala$ or Guyana or Haiti or Honduras or Jamaica$ or Nicaragua$ or Panama or Paraguay or Peru or Puerto Rico or Suriname or Uruguay or Venezuela or developing countr$ or south America$).ti,sh.
-
limit 20 to (english language and humans and yr=“2000 – 2016”)
Health economic review search strategy
Research questions
-
What is the cost-effectiveness of different interventions for breast feeding maintenance?
-
What resource usage and costs are associated with these interventions?
Methods
The protocol was registered with PROSPERO and the review was conducted and reported in compliance with PRISMA guidelines. 90
Search methods for the identification of studies
A search strategy was developed for electronic databases on Ovid using both keywords and MeSH terms. The search strategy was modified to search other bibliographic databases (Box 8).
Applied Social Sciences Index and Abstracts (ASSIA).
CENTRAL.
Cumulative Index to Nursing and Allied Health Literature (CINAHL).
EconLit.
EMBASE.
Education Resources Information Center (ERIC).
Health Management Information Consortium (HMIC).
MEDLINE.
MEDLINE In-Process & Other Non-Indexed Citations.
NHS Economic Evaluation Database (NHS EED).
Scopus.
Social Services Abstracts.
Sociological Abstracts.
Web of Knowledge: Science Citation Index Expanded, Social Sciences Citation Index, Conference Proceedings Citation Index – Science.
In addition, to maximise recall and minimise the potential for publication bias, a range of supplementary (‘snowballing’) techniques were used to increase the sensitivity of the search and to ensure coverage of grey literature and unpublished studies. These included reference list follow-up, searching websites and table of contents scanning for the journals that appear most frequently in the list of relevant studies (see Box 8). Finally, all systematic reviews on relevant topics were unpicked for primary studies meeting the inclusion/exclusion criteria.
The search was limited to English-language studies and the publication years 2000–14. In addition, the search was restricted to studies undertaken in OECD countries. These countries are likely to have similar economies and, therefore, the studies are likely to be of equal relevance.
Ovid MEDLINE(R) (1946 to November week 1 2014)
Search strategy
-
exp Breast Feeding/ (27,270)
-
Milk, Human/ (16,033)
-
(infant feed* or breast feed* or breastfeed* or breast-feed* or breast fed or infant fed).mp. (37,802)
-
or/1-3 (48,065)
-
Intervention studies/ (7515)
-
evaluation studies/ (206,080)
-
program evaluation/ (48,168)
-
Comparative study.pt. (1,730,486)
-
quasi-experiment$.tw. (5648)
-
(pre test or pretest or (posttest or post test)).tw. (15,502)
-
trial.ti. (128,505)
-
(time adj series).tw. (14,872)
-
(pre test or pretest or (posttest or post test)).tw. (15,502)
-
((evaluat$ or intervention or interventional) adj8 (control or controlled or study or program$ or comparison or “before and after” or comparative)).tw. (469,133)
-
((intervention or interventional) adj8 (effect$ or evaluat$ or outcome$)).tw. (62,603)
-
((process or program$) adj3 (effect$ or evaluat$)).tw. (43,146)
-
follow up assessment.tw. (2400)
-
controlled before.tw. (697)
-
“before and after stud$”.tw. (1491)
-
Cohort stud*.tw. (89,976)
-
or/5-20 (2,508,997)
-
animals/ not (humans/ and animals/) (3,998,169)
-
21 not 22 (2,026,432)
-
4 and 23 (8352)
-
Health Care Costs/ or Cost-Benefit Analysis/ (85,502)
-
economic evaluation.tw. (4985)
-
Economics/ or “costs and cost analysis”/ (69,986)
-
Cost control/ or Cost savings/ or Cost allocation/ or “Cost of Illness”/ (50,114)
-
Direct service costs/ (1058)
-
(low adj cost).tw. (21,904)
-
(high adj cost).tw. (6644)
-
(cost adj estimate*).tw. (1431)
-
Cost Analysis.tw. (3907)
-
(cost-effectiveness or cost consequence or cost-utility or cost-benefit or cost-minimisation).tw. (41,379)
-
cost burden.tw. (429)
-
or/25-35 (232,382)
-
24 and 36 (181)
-
Breast Feeding/ec [Economics] (39)
-
((infant feed* or breast feed* or breastfeed* or breast-feed* or breast fed or infant fed) adj6 cost).mp. (130)
-
38 or 39 (156)
-
37 or 40 (304)
-
“Africa South of the Sahara”/ (8256)
-
(Algeria$ or Egypt$ or Liby$ or Morocc$ or Tunisia$ or Western Sahara$ or Angola$ or Benin or Botswana$ or Burkina Faso or Burundi or Cameroon or Cape Verde or Central African Republic or Chad or Comoros or Congo or Djibouti or Eritrea or Ethiopia$ or Gabon or Gambia$ or Ghana or Guinea or Keny$ or Lesotho or Liberia or Madagasca$ or Malawi or Mali or Mauritania or Mauritius or Mayotte or Mozambiq$ or Namibia$ or Niger or Nigeria$ or Reunion or Rwand$ or Saint Helena or Senegal or Seychelles or Sierra Leone or Somalia or South Africa$ or Sudan or Swaziland or Tanzania or Togo or Ugand$ or Zambia$ or Zimbabw$ or China or Chinese or Hong Kong or Macao or Mongolia$ or Taiwan$ or Belarus or Moldov$ or Russia$ or Ukraine or Afghanistan or Armenia$ or Azerbaijan or Bahrain or Cyprus or Cypriot or Georgia$ or Iran$ or Iraq$ or Jordan$ or Kazakhstan or Kuwait or Kyrgyzstan or Leban$ or Oman or Pakistan$ or Palestin$ or Qatar or Saudi Arabia or Syria$ or Tajikistan or Turkmenistan or United Arab Emirates or Uzbekistan or Yemen or Bangladesh$ or Bhutan or British Indian Ocean Territory or Brunei Darussalam or Cambodia$ or India$ or Indonesia$ or Lao or People's Democratic Republic or Malaysia$ or Maldives or Myanmar or Nepal or Philippin$ or Singapore or Sri Lanka or Thai$ or Timor Leste or Vietnam or Albania$ or Andorra or Bosnia$ or Herzegovina$ or Bulgaria$ or Croatia$ or Faroe Islands or Greenland or Liechtenstein or Lithuani$ or Macedonia or Malta or maltese or Romania or Serbia$ or Montenegro or Svalbard or Argentina$ or Belize or Bolivia$ or Brazil$ or Colombia$ or Costa Rica$ or Cuba or Ecuador or El Salvador or French Guiana or Guatemala$ or Guyana or Haiti or Honduras or Jamaica$ or Nicaragua$ or Panama or Paraguay or Peru or Puerto Rico or Suriname or Uruguay or Venezuela or developing countr$ or south America$).ti,sh. (890,609)
-
42 or 43 (894,209)
-
41 not 44 (170)
-
limit 45 to (english language and humans and yr=“2000 – 2014”) (122)
Appendix 2 Topic guide for focus groups: fathers
Appendix 3 Topic guide for focus groups: mothers
Appendix 4 Topic guide for focus groups: peer supporters
Appendix 5 Topic guide for interviews: health-care professionals
Appendix 6 Type of peer support provided
| Study | Antenatal contact | Face-to-face contact outside of the health-care setting | Effective listening style: training in listening and communication skills | Providing expert knowledge | Peer supporter as paraprofessional |
|---|---|---|---|---|---|
| Anderson 200581 | ✗ | ✗ | ✗ | ✗ | |
| Chapman 200480 | ✗ | ✗ | ✗ | ✗ | |
| Chapman 201386 | ✗ | ✗ | ✗ | ✗ | ✗ |
| Dennis 200229 | ✗ | ✗ | |||
| Di Meglio 201084 | ✗ | ✗ | ✗ | ||
| Graffy 200434 | ✗ | ✗ | ✗ | ||
| Gross 200982 | ✗ | ✗ | ✗ | ||
| MacArthur 200988 | ✗ | ✗ | ✗ | ✗ | ✗ |
| McInnes 200038 | ✗ | ✗ | ✗ | ✗ | |
| Muirhead 200635 | ✗ | ✗ | ✗ | ||
| Olson 201085 | ✗ | ✗ | ✗ | ✗ | |
| Reeder 201487 | ✗ | ✗ | ✗ | ||
| Scott 201739 | ✗ | ✗ | ✗ | ✗ | |
| Srinivas 201589 | ✗ | ✗ | ✗ | ||
| Yun 201083 | ✗ | ✗ | ✗ |
Appendix 7 Logic model with requirements for implementation
FIGURE 11.
Logic model.
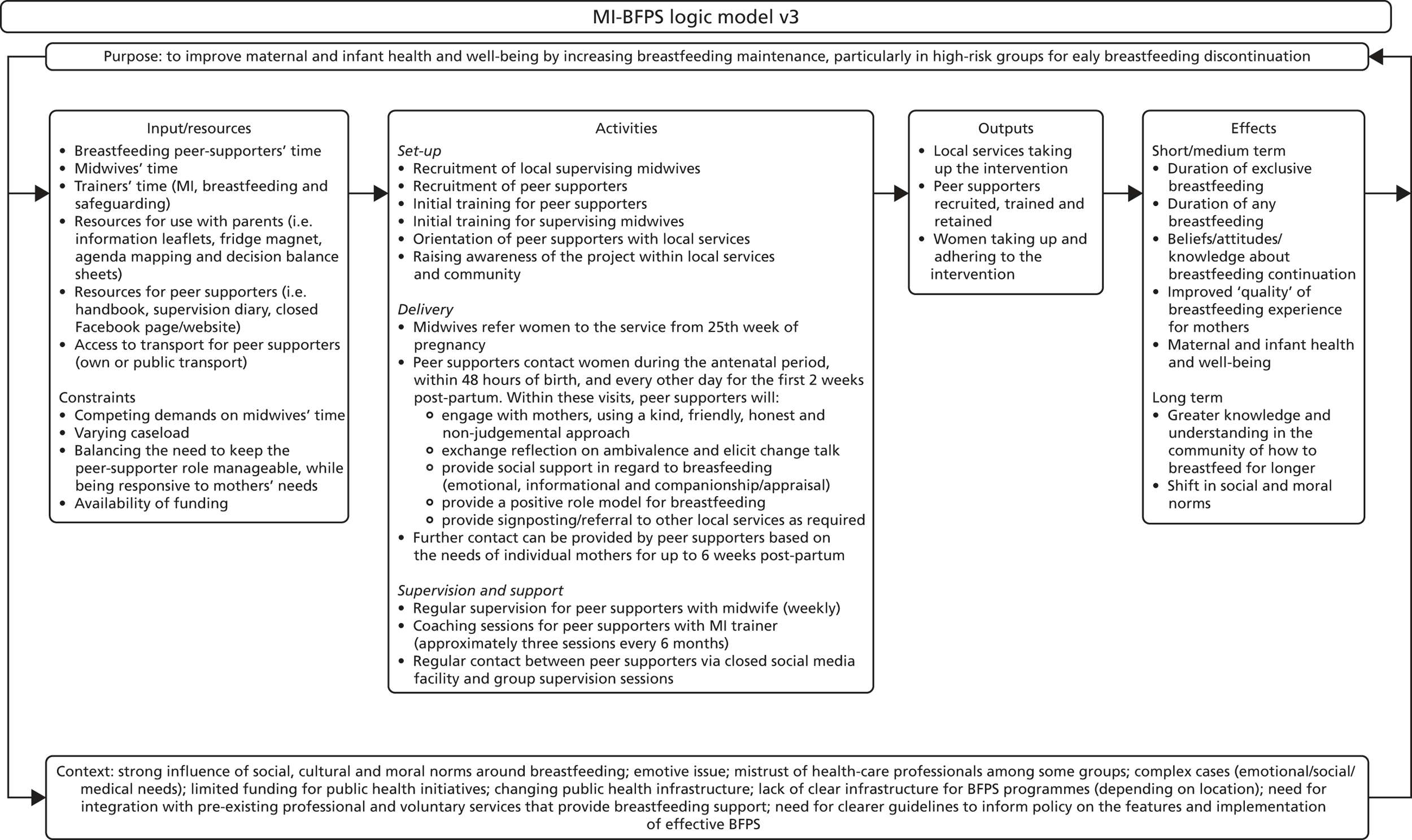
Appendix 8 Peer-supporter resources
Peer supporters were provided with an intervention handbook, training materials and intervention-specific resources, including:
-
an information leaflet about the intervention, including a graphical representation of a mother’s journey through breastfeeding (given to all participants)
-
an information leaflet for partners, family and friends (given to all participants)
-
a postcard and business card with the intervention name, web address and contact details for the participants’ primary peer supporter, other local peer supporters (Back-up Buddies) and support services (given to all participants)
-
links to closed Facebook groups in each area (that only participating mothers from development work focus groups, peer supporters currently working in the different site areas and the research team could access)
-
information leaflets from external providers to be given to participants on request, including those produced by the NHS, UNICEF UK BFI, BfN and NCT. These included Baby Tom’s First Week (BfN), Off to the Best Start (Start for Life, BFI), Building a Happy Baby (BFI), Caring for your Baby at Night (BFI), What’s in a Nappy (NCT), Expressing and Storing Breastmilk (BfN), Mastitis (BfN), Breastfeeding at Work or Study (Start for Life, BFI), A Guide to Infant Formula for Parents who are Bottle Feeding (BFI) and Bump, Baby and Beyond, 2nd edn (Public Health Wales).
Appendix 9 Motivational interviewing fidelity intercoder reliability results
Sixteen MI sessions were rated using the MITI 4.1 tool by one member of the research team (LC) and 30% of these (n = 5) were double-coded by another member of the research team (SC) to explore agreement prior to assessing fidelity (Table 23). Further details can be found in Chapter 4 (see Intercoder reliability). Increasing the number of sessions that were double-coded would have led to an increase in the values of the kappa statistic. The global score kappa statistic of 0.49 sits within the range of 0.41–0.60, which is considered to represent moderate agreement. We hypothesise that the raters and the MITI tool used could have had a role to play in the low global score kappa statistic. With regard to the raters, the global scores within the MITI tool are more subjective than the behaviour counts. This is in line with other studies,134–137 which have found lower global scores than behaviour counts. With regard to the method used, the MITI tool is designed to rate MI sessions, and it may not be the most appropriate tool for measuring MI-based approaches; however, this is the measure that is recommended and commonly used to measure the skilfulness of therapists.
| Measure | Kappa statistic | Number of sessions double-coded | Proportion in agreement |
|---|---|---|---|
| Change talk | 0.667 | 5 | 4/5 |
| Empathy | 1.000 | 5 | 5/5 |
| Partnership | 0 | 5 | 1/5 |
| Sustain talka | –0.250 | 5 | 3/5 |
| Overall | 0.493 | 5 | 11/20 |
The behaviour count analyses indicated high reliability overall, as demonstrated by the ICC of 0.93 (Table 24).
| Behaviour | ICC (95% confidence Interval)a | n |
|---|---|---|
| Affirmation | 0.72 (0.09 to 0.97) | 5 |
| Confront | No counts | 5 |
| Complex reflection | 0.78 (–0.07 to 0.98) | 5 |
| Emphasise | 0.91 (0.46 to 0.99) | 5 |
| Giving information | 0.84 (0.17 to 0.98) | 5 |
| Persuade | 0.95 (0.59 to 0.99) | 5 |
| Persuade with | 0.89 (0.36 to 0.99) | 5 |
| Questions | 0.88 (0.37 to 0.99) | 5 |
| Seek | 0 (–0.81 to 0.81) | 5 |
| Simple reflections | 0.89 (0.24 to 0.99) | 5 |
| Overall | 0.93 (0.89 to 0.96) | 50 |
| Overall (excluding ’confront’) | 0.93 (0.87 to 0.96) | 45 |
Appendix 10 Site 1 recruitment flow chart
FIGURE 12.
Site 1 recruitment flow chart.

Appendix 11 Site 2 recruitment flow chart
FIGURE 13.
Site 2 recruitment flow chart. EDD, estimated due date.
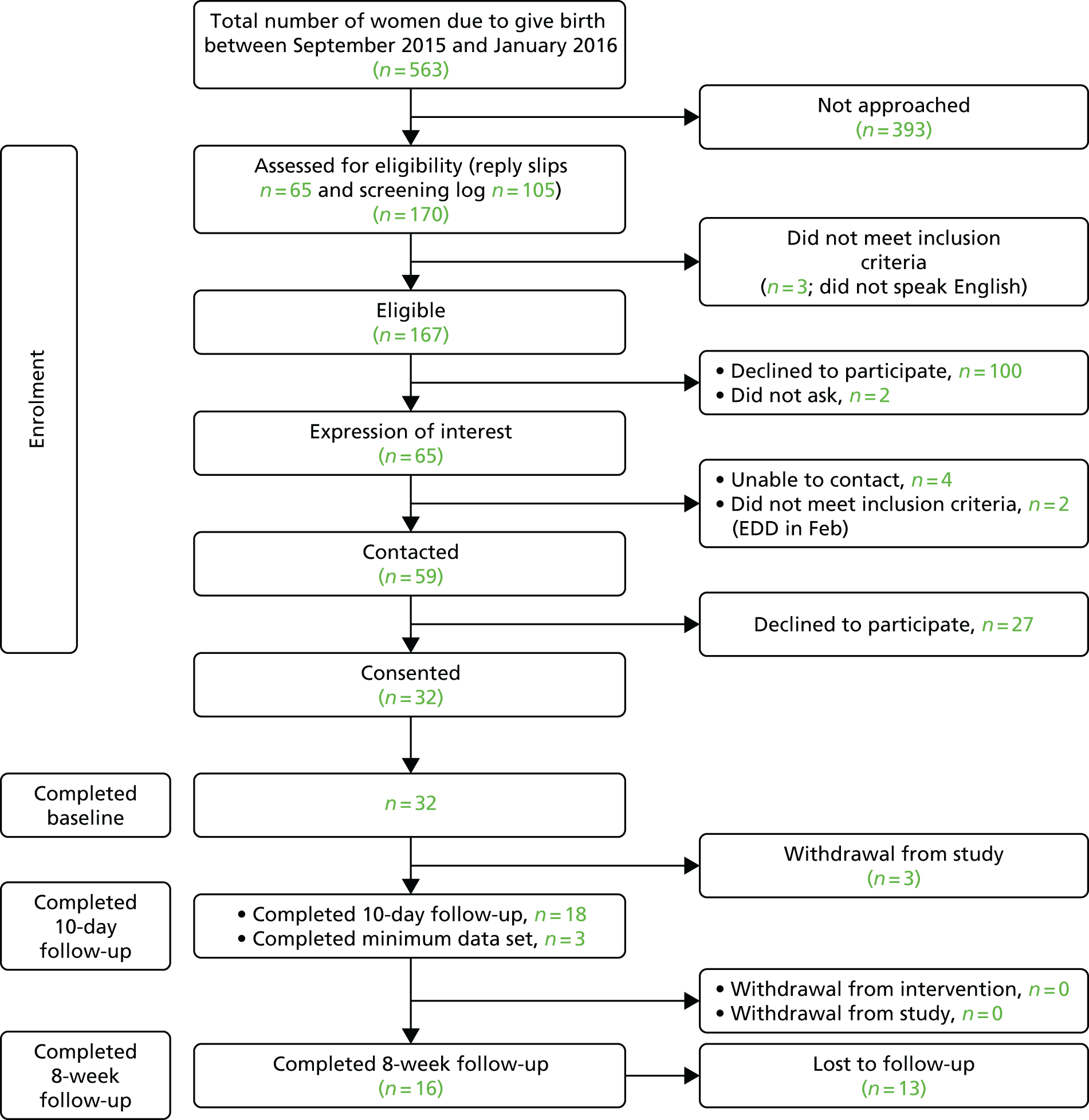
Appendix 12 Site 3 recruitment flow chart
FIGURE 14.
Site 3 recruitment flow chart.

Appendix 13 Content guide for the motivational interviewing-based breastfeeding peer-support intervention
| Contact | Objectives | Method of delivery | Scope of sessions |
|---|---|---|---|
| Antenatal |
|
Face-to-face visit with women during the antenatal period. Note: a telephone contact may be used as an alternative to provide flexibility for women who do not want a face-to-face visit at this stage (e.g. successfully breastfed before, not enough time before due date to arrange a visit) |
|
| First 48 hours after birth |
|
A face-to-face visit within 48 hours of birth, either in hospital or at home. Note: there will be flexibility to allow contact by telephone or text, as a face-to-face visit may not always be possible. Additional contact by telephone/text/in person can be provided if required |
|
| 3–14 days after birth. Note: This should include contact soon after the 72-hour weighing of the baby, recognising that this is a critical time when mothers may need additional support |
|
Daily contact – face to face, by telephone or by text depending on the needs and preferences of individual mothers |
|
| 15 days to 6 weeks after birth |
|
Proactive support is gradually withdrawn (based on mothers’ individual needs), but mothers are still able to contact peer supporters if they would like support (by text, telephone or face to face) |
|
Glossary
- Birth notification
- To notify the Mam-Kind buddy of the birth of the baby.
- Mam-Kind buddy
- Peer supporter who delivered the Mam-Kind intervention.
- Mam-Kind supervisor
- A local community midwife from the study site who supported the peer supporters with clinical queries and in liaising with other health-care professionals.
List of abbreviations
- BCTTv1
- Behaviour Change Technique Taxonomy v1
- BCW
- behaviour change wheel
- BFI
- Baby Friendly Initiative
- BfN
- Breastfeeding Network
- BFPS
- breastfeeding peer support
- COM-B
- capability opportunity motivation – behaviour
- DBS
- Disclosure and Barring Service
- DIRUM
- Database of Instruments for Resource Use Measurement
- EQ-5D-5L
- EuroQoL-5 Dimensions, five-level version
- GCSE
- General Certificate of Secondary Education
- ICC
- intracluster correlation coefficient
- IFC
- infant feeding co-ordinator
- MeSH
- medical subjects heading
- MI
- motivational interviewing
- MITI
- Motivational Interviewing Treatment Integrity
- MRC
- Medical Research Council
- NCT
- National Childbirth Trust
- NICE
- National Institute for Health and Care Excellence
- OECD
- Organisation for Economic Co-operation and Development
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RUQ
- resource use questionnaire
- SD
- standard deviation
- SDT
- self-determination theory
- UNICEF
- United Nations International Children’s Emergency Fund
- WHO
- World Health Organization
- WIMD
- Welsh Index of Multiple Deprivation