Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 13/05/11. The contractual start date was in May 2015. The draft report began editorial review in May 2017 and was accepted for publication in September 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Beresford et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Context
In a recent James Lind Alliance (JLA) Childhood Disability Research Priority Setting Partnership for children with neurodisability,1 ‘therapy interventions’ featured strongly in its top 10 priority areas, or research questions (Box 1). Indeed, as we have highlighted in bold, this topic constituted 4 of those 10 areas.
-
Does the timing and intensity of therapies (e.g. physical, occupational and speech and language therapy, ‘early intervention’, providing information) alter the effectiveness of therapies for infants and young children with neurodisability, including those without specific diagnosis? What is the appropriate age of onset/strategies/dosage/direction of therapy interventions?
-
To improve communication for children and young people with neurodisability, (a) what is the best way to select the most appropriate communication strategies? And (b) how to encourage staff/carers to use these strategies to enable communication?
-
Are child-centred strategies to improve children’s (i.e. peers’) attitudes towards disability (e.g. buddy or circle of friends) effective in improving inclusion and participation within educational, social and community settings?
-
Does the appropriate provision of wheelchairs to enable independent mobility for very young children improve their self-efficacy?
-
Are counselling/psychological strategies (e.g. talking therapies) effective in promoting the mental health of children and young people with neurodisability?
-
What is the (long-term) comparative safety and effectiveness of medical and surgical spasticity management techniques (botulinum neurotoxin A, selective dorsal rhizotomy, intrathecal baclofen, orally administered medicines) in children and young people with neurodisability?
-
Does a structured training programme, medicines and/or surgery speed up the achievement of continence (either/or faecal or urinary) for children and young people with neurodisability?
-
What strategies are effective to improve engagement in physical activity (to improve fitness, reduce obesity, etc.) for children and young people with neurodisability?
-
Which school characteristics (e.g. policies, attitudes of staff) are most effective to promote inclusion of children and young people with neurodisability in education and after-school clubs?
-
What is the long-term safety, effectiveness and sustainability of behavioural strategies and/or drugs (e.g. melatonin) to manage sleep disturbance in children and young people with neurodisability (outcomes include time to onset, duration, and reducing the impact on the family)?
From Morris et al. 1 This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
The following overarching research question was generated from this process: what therapy interventions are, could and should be offered to children with neurodisability to help improve participation outcomes?
This question captures the complexity of this topic including issues such as the different ‘schools’, or approaches, to therapy; ‘dosage’ or intensity; the timing and duration of a therapeutic intervention; and the skills and qualifications of staff delivering the therapy. Over and above this is the challenge of identifying and measuring the ‘active ingredients’ of therapeutic interventions.
The existing evidence on this topic is very limited. For example, recent National Institute for Health and Care Excellence (NICE) guidance2 on the management of spasticity in children was not able to provide guidance on the timing or intensity of any of the interventions it included. The Guidance Development Group also noted that interventions are themselves poorly defined. 2 Evidence reviews in this area note the lack of rigorous research and the very limited nature of the current evidence base. 2–8 There are, however, indications of a growing interest, and investment, in research in this area. Studies to date have engaged in exploring the impact of therapy interventions on motor/physical functioning9–11 and participation12–14 using a range of study designs. The National Institute for Health Research (NIHR) itself has funded research in this area. 3,15
To inform future commissioning of research on this topic, the NIHR Health Technology Assessment (HTA) programme’s Maternal Neonatal and Child Health Panel commissioned a qualitative scoping study into current practice and perceived research needs through one of NIHR’s Health Services and Delivery Research (HSDR) programme’s Evidence Synthesis Centres.
Study objectives
The objectives of this scoping study were to:
-
identify and describe the current techniques, practices and approaches to delivering therapy interventions for children with non-progressive neurodisability that seek to improve participation as defined by the World Health Organization’s (WHO) 2002 International Classification of Functioning, Disability and Health (ICF) framework16
-
describe therapeutic approaches that are identified by professionals as promising or innovative but are not currently (routinely) delivered by the NHS
-
identify how and why these interventions may vary according to the nature and severity of the impairment
-
describe the factors that influence decision-making regarding the ‘therapeutic prescription’, including the nature and severity of the impairment
-
understand the dimensions that constitute a therapeutic intervention from the perspectives of NHS health professionals, children and parents (e.g. the physical environment, location, use of/access to equipment, staff skills/qualification, parent involvement/delivery and self-management)
-
seek the views of NHS health professionals, parents and children regarding the ‘active ingredients’ of therapy, and how to capture or measure these
-
understand, and compare, the ways in which professionals and families currently conceive therapy outcomes, the meaningfulness of ‘participation’ as a therapy outcome and how these may vary according to the nature and severity of the impairment
-
map NHS health professionals’, parents’ and children’s views of the evidence gaps related to therapy interventions for children with non-progressive neurodisability, and identify views on the issues that need to be accounted for in the design of any future evaluations.
Defining the scope
The scope of the study was set according to the following criteria.
-
Intervention: therapy interventions that meet the ‘patient group’ and ‘setting’ criteria below and target outcomes within the participation component of the ICF framework. 16 The domains captured by this concept include participation in learning and applying knowledge; general tasks and demands; communication; mobility; self-care; domestic life; interpersonal interactions and relationships; major life areas; and community, social and civic life. This criterion includes interventions delivered directly by therapy staff, or by school staff, parents and/or children, in the home or in a school setting, under instruction from therapy staff.
-
Patient group: children and young people up to school-leaving age with non-progressive neurodisability predominated by physical/motor impairment, including those without a specific diagnosis. This includes children with: cerebral palsy (defined as physical, medical and developmental difficulties caused by injury to the immature brain), brain injury, some metabolic and neurogenetic disorders and developmental co-ordination disorder, as well as those without a specific diagnosis. Within and across these patient groups, the extent to which physical/motor abilities are affected varies considerably. For many of these children and young people, the presence of neurodisability results in a number of physical/motor and cognitive impairments.
-
Setting: outpatient, community, school and/or home.
An overview of the therapies under investigation
At the outset, it is useful to offer a brief overview of the therapies included in this scoping study. Thus, this opening section offers a brief definition of each therapy and the ways in which it works in order to achieve its objectives. We also provide a brief history of each discipline within the UK context, noting here that its development and emergence in other countries may not be similar. Finally, in understanding what these three therapies do, it is important at this stage to point out that therapists’ work may involve direct work with a child and/or training and supporting others (e.g. parents, school staff and therapy assistants) to implement and use techniques, procedures and/or equipment.
Occupational therapy
The objective of occupational therapy with children with neurodisability is to provide practical support to enable them to overcome any barriers that prevent them from doing the activities (occupations) that matter to them. ‘Occupation’ refers to practical and purposeful activities that allow people to live independently and have a sense of identity. This could be essential day-to-day tasks, such as self-care, learning or leisure. Occupational therapists use the following techniques:
-
advising on alternative techniques to achieve a desired occupation
-
making changes to the child’s home or school environment
-
providing equipment.
The early history of occupational therapy is located in a response to the need to rehabilitate people recovering from tuberculosis who had been subject to extended periods of bed rest. The idea of graded engagement in activities emerged with the view to support and enable patients to return to employment once they were fully recovered. In responding to the need to rehabilitate soldiers returning from the first world war, the discipline took further significant steps forward, with national training courses and professional colleges established in the 1930s across the UK. These colleges merged in the 1970s, forming the Royal College of Occupational Therapists (RCOT).
Physiotherapy
For children with neurodisability, the objective of physiotherapy is to promote, develop or restore physical movement and strength and the ability of the child to perform functional activities in their daily lives. A further objective is to reduce pain. Physiotherapists treat or manage movement and body structure/function impairments or disorders through:
-
tailored exercises/physical activity
-
manual therapy
-
education and advice.
Physiotherapy’s origins can be traced back to Sweden and the sport of gymnastics. The Royal Central Institute of Gymnastics was established in Stockholm in 1813. [The Swedish word for physiotherapist (physical therapist) is ‘sjukgymnast’ = ‘sick-gymnast’.] In 1887, physiotherapists were officially recognised and other countries soon followed suit. In 1894, four nurses in Great Britain formed the Chartered Society of Physiotherapy (CSP), and this remains the profession’s national body. The need to rehabilitate individuals with polio and soldiers returning from the first world war served to promote and develop the profession during the first half of the 20th century.
Speech and language therapy
For children with neurodisability, speech and language therapy addresses difficulties with communication or with eating, drinking and swallowing. To address these difficulties, speech and language therapists can work in a number of ways:
-
providing education and advice
-
developing and supporting the implementation of programmes to help to develop communication and/or the management of eating and drinking problems
-
providing feeding/drinking equipment
-
providing communication aids and devices.
Speech and language therapy began to emerge as a distinct discipline in the late 1800s and early 1900s. A national professional body (the College of Speech and Language Therapy) was formed in 1945; again, the recovery and rehabilitation needs of soldiers returning from a world war drove developments within the profession. The college became the Royal College of Speech and Language Therapists (RCSLT) in 1995.
The structure of the report
Chapter 2 reports the study design and methods. Chapters 3–10 present study participants’ views of and beliefs about topics and issues relevant to, and contributing to, the study objectives. We start by providing a high-level picture of the way therapy services to children with non-progressive neurodisability are organised and delivered in England (see Chapter 3). Next, in Chapter 4, we move on to a detailed exploration of participants’ accounts of the overall approaches and schools of thought which currently inform physiotherapy, occupational therapy and speech and language therapy. Then, placed under that framework, we offer an overview of how these therapies are being practised. In Chapter 5 we present parents’ accounts of the provision and delivery of therapy. After this, we turn to exploring study participants’ views and beliefs about the active ingredients of therapy interventions: this is reported in Chapter 6. Following this, in Chapter 7, we describe their views about therapy outcomes, including the notion of participation. The next two chapters consider issues relevant to future research. Chapter 8 reports on accounts of the current ‘research environment’ within the therapy professions, and Chapter 9 describes participants’ views on the challenges of evaluative research and reports the methodological research, which participants identified as being necessary to progress research into therapy interventions, including their evaluation. Our final findings chapter (see Chapter 10) reports the priorities for research identified, or nominated, by study participants. The study findings are discussed (see Chapter 11) and reflected on in the remaining chapters of this report (see Chapters 11 and 12).
We would note at the outset that this is a complex topic area and some of the issues investigated were explored from two perspectives (e.g. describing current practice, and the challenges of researching practice). We have strived to avoid unnecessary repetition but it is sometimes required, particularly given that this report may not be read in its entirety.
Chapter 2 Methods
Study design
A descriptive case study design, taking the delivery and practice of therapy interventions as the case, was adopted. 17 Qualitative research methods (interviews and focus groups) were used and a purposive approach to sampling18 was implemented.
The proposed design was to use group and individual interviews and/or a brief online survey to ascertain the views and experiences of different stakeholder groups, namely:
-
child/disability leads in national professional groups
-
therapy practitioners and assistant practitioners based in community paediatric teams/services, paediatric specialties and tertiary clinics/centres
-
training placement supervisors within therapy services used by therapy training institutions (both undergraduate and master’s qualification routes)
-
clinical academics/researchers currently active in the field
-
community paediatricians and paediatric neurologists
-
parents
-
children and young people.
Deviation from the proposed design
Three changes were implemented during the early stages of fieldwork as it became clear that planned methods of data collection and choice of stakeholder group were not appropriate. The changes implemented were as follows.
-
The method used to consult with community paediatricians and paediatric neurologists was changed from a survey to an interview. Early into fieldwork it became clear that the topics under investigation were complex and nuanced and it was important that representatives of this particular participant group had the opportunity to contribute in the same way as other participant groups. Thus, the decision was made to change the design to individual interview, and to reduce the proposed sample size.
-
Early in the project we discovered that undergraduate qualifications in physiotherapy, occupational therapy, and speech and language therapy are generic, that is, not specific to particular age groups or conditions. Therefore, we decided that it would not be fruitful to pursue training placement supervisors as a key participant group. We did, however, record participants’ involvement in training and supervision of new trainees, and explored their views on general training curricula when appropriate.
-
Finally, following careful discussion within the team, we added a further ‘miscellaneous’ stakeholder group to the sample. This was in response to emerging findings regarding the importance of the perspectives of managers of children’s community health services, educationalists and private practitioners.
Study participants and rationale for inclusion
A number of different stakeholder groups were identified to take part in the study. Each group was selected on the basis of the unique and valuable perspective that it could bring to the project. Table 1 details each participant group, the data collection method used and the rationale for the group’s inclusion. It should be noted that some study participants were members of more than one stakeholder group (e.g. a research-active therapist). These participants were categorised according to our primary reason for seeking to recruit them to the study. However, we were cognisant of these multiple roles, and the interview topic guides were adjusted according.
| Stakeholder group | Method | Rationale |
|---|---|---|
| Clinical academics and researchers (including therapists, other clinicians and academics) | Individual interview | To provide evidence on recent or ongoing research and the issues and challenges associated with evaluating a therapy intervention, and in the case of those in teaching or supervisory roles, the content of training curricula |
| Representatives of national professional groups representing physiotherapists, occupational therapists and speech and language therapists | Individual interview | To offer a ‘high-level’ view of different practices and approaches currently being implemented by physiotherapy, occupational therapy and speech and language therapy services |
| Therapy practitioners | Focus groups | To supply a collective detailed picture of the delivery of therapy and decision-making around the therapeutic prescriptions |
| Consultant paediatricians and paediatric neurologists | Individual interview | To allow the scoping study to place and understand therapy interventions within the wider context of the care and management of children with neurodisabilities |
| Parents | Focus groups | To ensure that families’ views and perspectives are represented |
| Children and young people | Focus groups | To ensure that patients’ views and perspectives are represented |
Ethics approval
The study was approved by a subcommittee of the University of York’s Ethics Committee (Department for Social Policy and Social Work) (reference BB06/2016).
Recruitment and consenting
In building the overall sample, within each stakeholder group the research team adopted a purposive sampling approach that aimed to ensure a balance of representatives of physiotherapists, occupational therapists and speech and language therapists, as well as representation from different parts of the country. The target sample sizes for each stakeholder group are shown in Table 2.
| Stakeholder group | Sample size, (n) |
|---|---|
| Clinical academics and researchers | ≈10 |
| Representatives of national professional groups | ≈6 |
| Therapy practitioners | 8 × ≈7 group participants (N = ≈55) |
| Consultant paediatricians and paediatric neurologists | ≈6 |
| Parents | 4 × ≈8 group participants (N = ≈32) |
| Children and young people | 4 × ≈6 group participants (N = ≈25) |
Recruitment took place in two overlapping stages: a first stage to recruit individual interview participants, and a second stage to recruit group interview participants. Recruitment materials, including study information sheets and consent forms, can be found in Appendices 1–3.
Stage 1: recruitment
The first stage of recruitment comprised desk-based research to identify individual interview participants. This involved searches of the NIHR funding database and high-impact therapy journals for academic clinicians and researchers currently (or recently) active in the field of therapy interventions. At the same time, the professional bodies for the different therapies were approached, via the leads of their respective paediatric and/or specialist neurodisability divisions, to each nominate representatives who could provide a ‘national’ overview of their profession at a research and a practice level. The research team then used a snowballing method, whereby existing recruits were asked for suggestions of other relevant people to include in the study from among their colleagues and professional networks. This iterative recruitment process continued until, from initial analyses and discussions within the research team, data saturation on key or critical themes had been achieved.
All individual interview participants were sent an e-mail invitation to take part in the study. This e-mail introduced the research, the nature of the interview and the topics for exploration. A study information sheet was attached. If no response was received, a member of the research team followed this up by telephone or a further e-mail. Arrangements were then made with those who responded positively for a suitable date and time to conduct the interview. Finally, a confirmation e-mail was sent, to which was attached an additional information sheet setting out the scope of the interview and giving final details about the interview. For those taking part in a telephone interview, also attached to the confirmation e-mail was a consent form outlining the protocols of the interview so that participants could familiarise themselves with these before giving their recorded verbal consent at the beginning of the interview. The three people who were interviewed in person gave written consent before the interview took place.
Stage 2: recruitment to focus groups
In the second stage of recruitment, we sought groups of frontline practitioners, parents, and children and young people to take part in focus group discussions. Recruitment methods varied according to the group in question.
Practitioner groups were recruited through direct representations to the lead practitioners and heads of therapy services we had recruited to individual interviews, or by securing a workshop slot at forthcoming professional conferences. In the case of the former, a member of the research team liaised with a ‘site co-ordinator’ to make arrangements for the meeting. This included sending the co-ordinator an information sheet with details about the study to forward to all those taking part. This sheet also explained that, at the start of the meeting, participants would be asked to give their written consent to take part in the study. In the case of the latter, when recruitment took place on the day of a conference, participants were given both a study information sheet and a consent form to sign at the beginning of the focus group ‘workshop’. All practitioner focus group participants were also asked to complete a brief pro forma regarding their professional backgrounds. Those attending focus groups were offered a personalised certificate of attendance to include in their career portfolios.
In the case of parents and children and young people, we aimed to recruit pre-existing groups in the belief both that this would be more time efficient and that pre-existing groups can move more quickly onto the particular task or discussion and, within the context of a single data collection event, are therefore more likely to yield high-quality data. For parents, we were able to use an established parent group co-ordinated by our own research unit. The study topic was introduced as an agenda item and discussed accordingly at a regular meeting. We then approached several condition-specific voluntary organisations for potential parent groups as well as local groups of the National Network of Parent Carer Forums (www.nnpcf.org.uk). For children and young people, we took a similar route and made representations to sports teams, youth and social clubs and school/university groups, a national voluntary umbrella organisation that represents disabled children and their families, and, via colleagues, existing young people’s research advisory groups. A flier was designed and distributed for this purpose. A ‘thank-you’ shopping voucher (worth £20 for parents and £10–15 for children and young people) was used.
When groups agreed to participate, a member of the research team liaised with the group co-ordinator to arrange a venue, date and time for the meeting and to request that they distribute study information sheets on behalf of the research team. Participants were asked to sign a consent form at the start of the meeting.
Sample
In all, 109 people took part in the study. Thirty-eight individual interviews (including one joint interview) and 10 focus groups were carried out.
Individual interviews: sample
Ninety-three per cent of those invited to participate in an interview accepted the invitation. Of those who did not, one was unable to take part because they were abroad when fieldwork was taking place; one (who had recently changed jobs) failed to respond to our invitation; and one declined to take part as they felt that others would be more suitable. Table 3 displays the role, or post, of the professionals who took part in individual interviews.
| Role | Number of individual interview participants |
|---|---|
| Academic researcher based at university | 9 |
| Cliniciana based in the NHS | 17 |
| Cliniciana based in a specialist centreb | 5 |
| Private practitioner operating nationally | 3 |
| Professional body employee operating nationally | 5 |
| Total | 39 |
Some of those recruited were at the forefront of research on childhood neurodisability. Areas of research interest were diverse, encompassing a range of specific interventions and approaches within physiotherapy, occupational therapy and speech and language therapy, participation outcomes and tools of outcome measurement. Similarly, clinical expertise covered a range of health conditions associated with childhood neurodisability and significant motor impairment, but primarily neuromuscular and skeletal movement disorders and oromotor and communication disorders.
Academic researchers and clinical academics were based in universities and specialist research institutes, in NHS hospital and community trusts and in specialist treatment and rehabilitation centres serving the NHS. As well as leading their own research and managing under- and postgraduate teaching programmes or large clinical caseloads, many had additional roles and responsibilities. Within their own organisations these included managing research strategy, building research capacity and capability, providing clinical and student supervision, and positions as heads of service and professional leads. Externally they included providing strategic leadership via active membership of networks such as the British Academy of Childhood Disability; the European Academy of Childhood Disability; NHS clinical governance networks and independent clinical advisory bodies; and organisations such as Disability Matters. A few had been members of guidance development groups for NICE.
Individual interview participants were drawn from across the disciplines of physiotherapy, occupational therapy and speech and language therapy, and from paediatric medicine (Table 4). Of those recruited who had a therapy background, all were members of their national professional body. Within these organisations, some were members of specialist sections providing professional direction and guidance to their members, such as the Specialist Section Children, Young People and Families of the RCOT and the Association of Paediatric Chartered Physiotherapists within the CSP. Of those who were members of the RCSLT, some were voluntary specialist advisors in their field of expertise and/or members of local Clinical Excellence Networks that meet regularly to share and develop common interests and expertise. In the same way, some of the paediatricians recruited held voluntary roles within the Royal College of Paediatrics and Child Health, such as on the Specialist Advisory Committee for Neurodisability.
| Type of training | Number of individual interview participants |
|---|---|
| Occupational therapist | 12 |
| Physiotherapist | 7 |
| Speech and language therapista | 10 |
| Paediatrician/paediatric neurologist | 9 |
| Otherb | 1 |
| Total | 39 |
As was our aim, there was also representation in the interview sample from across the country as defined by the four broad areas of NHS England’s regional teams (Table 5). The largest group, from the North of England, was made up of nine people from the north-east and three from the north-west. Representatives from RCOT, CSP and RCSLT worked countrywide, as did two of the private practitioners.
| Region (based on NHS regional teams) | Number of individual interview participants |
|---|---|
| North of England | 12 |
| Midlands and East of England | 3 |
| London | 7 |
| South of England | 7 |
| Countrywide | 8 |
| Othera | 2 |
| Total | 39 |
Practitioner focus groups: sample
Forty-four therapists took part in one of six focus groups. Over half of these were physiotherapists, the smallest therapy profession represented among those interviewed individually. Most worked for the NHS in the community, predominantly in the north of England. Overall, the therapies they represented, and the organisation, type of setting and locations in which they were based, are reported in Table 6.
| Participant characteristics | Practitioner group (n) | Total (N) | |||||
|---|---|---|---|---|---|---|---|
| A (N = 4) | B (N = 7) | C (N = 15) | D (N = 9) | E (N = 3) | F (N = 6) | ||
| Therapy | |||||||
| OT | 4 | 5 | 9 | ||||
| PT | 2 | 14 | 9 | 25 | |||
| SLT | 3 | 6 | 9 | ||||
| Other | 1a | 1 | |||||
| Organisation base | |||||||
| NHS | 7 | 11 | 9 | 5 | 32 | ||
| Charitable | 4 | 3 | 1 | 8 | |||
| Private | 3 | 3 | |||||
| Other | 1a | 1 | |||||
| Practice base | |||||||
| Hospital | 1 | 1 | |||||
| Community | 5 | 10 | 9 | 5 | 29 | ||
| Mix | 2 | 2 | 1 | 5 | |||
| Other | 4b | 1a | 3b | 9 | |||
| Missing | 1 | ||||||
| Regional base (based on NHS regional teams) | |||||||
| North | 7 | 4 | 9 | 6 | 26 | ||
| Midlands and East | 3 | 3 | |||||
| London | 2 | 2 | |||||
| South | 4 | 1 | 3 | 8 | |||
| Other | 2c | 2 | |||||
| Missing data | 3 | 3 | |||||
The practitioners had wide-ranging experience within physiotherapy, occupational therapy and speech and language therapy. The mean number of years that practitioners had been qualified was 14.2 years (median 11 years). Most were employed in band 6 or 7 posts. Over 60% reported some previous experience of research, although this varied: investigator, involvement in delivering a programme under evaluation, research within undergraduate/postgraduate studies, service audit and/or membership of research discussion forums. These characteristics of the sample are reported in Table 7.
| Practitioner group | Number of years qualified | Grade of post | Previous research experience | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 3 | 3–10 | 11–20 | > 20 | Other | Band 5 | Band 6 | Band 7 | Band 8 | Other | Yes | No | |
| A (n = 4) | – | 2 | 2 | – | – | – | 2 | 2 | – | – | 4 | – |
| B (n = 7) | 1 | 3 | 3 | – | – | 1 | 3 | 3 | – | – | 3 | 4 |
| C (n = 15) | 1 | 6 | 2 | 5 | 1a | 1 | 5 | 5 | 2 | 2a,b | 12 | 3 |
| D (n = 9) | 2 | 1 | 4 | 2 | - | 2 | 3 | 4 | – | – | 1 | 8 |
| E (n = 3) | – | 2 | 1 | – | – | – | – | 3 | – | – | 3 | – |
| F (n = 6) | – | 1 | 2 | 3 | – | – | 2 | 3 | 1 | – | 4 | 2 |
| Total | 4 | 15 | 14 | 10 | 1 | 4 | 15 | 20 | 3 | 2 | 27 | 17 |
The participants’ caseloads were also diverse in the type of neurological conditions covered, but often their patients had multiple impairments. Box 2 lists the main neurodisabilities represented in the sample’s caseloads.
-
Acquired brain injury.
-
Cerebral palsy.
-
Complex motor disorders.
-
Congenital and rare syndromes.
-
Developmental co-ordination disorder.
-
Dysphagia.
-
Genetic disorders/chromosomal abnormalities.
-
(Global) developmental delay.
-
Head injuries.
-
Learning disabilities.
-
Metabolic disorders.
-
Neuromuscular conditions.
-
Spina bifida.
-
Spinal injuries.
Parent focus groups: sample
In total, four focus groups were conducted with 26 parents. Of these parents, 20 were mothers, five were fathers and one was a grandfather (Table 8).
| Parent group | Mothers (n) | Fathers (n) | Grandfathers (n) | Total in group (N) |
|---|---|---|---|---|
| A | 3 | 1 | 0 | 4 |
| B | 5 | 2 | 0 | 7 |
| C | 6 | 0 | 0 | 6 |
| D | 6 | 3 | 1 | 9 |
| Total | 20 | 6 | 1 | 26 |
Parents were recruited locally from parent-carer forums and our unit’s parent consultation group, and at a weekend-long event held by a condition-specific children’s charity and attended by parents of preschool-aged children from across the country (Table 9).
| Parent group | Type of organisation (n) | Regional base of parents (based on NHS regional teams) (n) | |||||
|---|---|---|---|---|---|---|---|
| Local parent-carer forum | Condition-specific charity | In-house parent consultation group | North of England | Midlands and East of England | South of England | Missing data | |
| A (N = 4) | – | – | 1 | 1 | – | ||
| B (N = 7) | 1 | – | – | 1 | – | ||
| C (N = 6) | 1 | – | – | 1 | – | ||
| D (N = 9) | – | 1 | – | 1 | 3 | 2 | 2 |
| Total | 2 | 1 | 1 | 3 | 1 | 2 | 2 |
Within these four parent focus groups, 28 children and young people (15 boys, 13 girls) were represented. There was some variation in age (Table 10).
| Parent group | Gender of children represented (n) | Total number represented (n) | Age of children (years) | ||
|---|---|---|---|---|---|
| Male | Female | Mean | Median | ||
| A (N = 4) | 3 | 0 | 3 | 14.5 | 16 |
| B (N = 7) | 7 | 3 | 10 | 13 | 14.5 |
| C (N = 6) | 2 | 4 | 6 | 9 | 8 |
| D (N = 9) | 3 | 6 | 9 | 4 | 3 |
| Total | 15 | 13 | 28 | 9 | 7 |
The health conditions represented by these groups were various and, again, included children with multiple complex needs. The conditions reported by parents are listed in Box 3. It should be noted that, as would be expected for this population, many children had more than one diagnosis, including some degree of learning disability and/or autism and/or sensory impairment.
-
Asperger’s, autism and ADHD.
-
Ataxia and dystrophy.
-
Cerebral palsy (mild to severe).
-
Communication and sensory processing needs.
-
Complex epilepsy.
-
Down syndrome.
-
Dyspraxia.
-
Fine motor impairments.
-
Genetic syndromes.
-
Hemiplegia.
-
Hydrocephalus.
-
Learning disabilities (mild to severe).
-
Non-verbal AAC users.
-
Scoliosis.
-
Spina bifida.
AAC, alternative communication; ADHD, attention deficit hyperactivity disorder.
Children typically had more than one diagnosis.
Challenges of recruitment
Whereas recruitment of the individual interview participants was straightforward, recruitment of the focus group participants proved more difficult. These challenges of recruitment are reported separately for the focus groups with practitioners, parents, and children and young people.
Practitioner groups
We aimed to recruit practitioner groups through therapy service departments. The practitioner contacts made through the individual interviews proved invaluable as a ‘way in’ to these departments. Although services were always supportive of the research, resource issues meant that our approaches were not always successful because of limited staff capacity.
Parent groups
With parents, the difficulty was finding pre-existing groups of parents with children who met the study inclusion criteria. There are many more parent-led/voluntary organisations for other neurodisabilties (e.g. autism or progressive conditions) or that focus particularly on learning difficulties. We approached several condition-specific voluntary organisations with this in mind, but we were unable to find existing groups of parents we could access. In the end, a compromise was reached, whereby we accessed groups of parents through voluntary organisations that were brought together specifically for the purpose of the study.
Children and young people groups
Various avenues were pursued to recruit pre-existing groups of children and young people with neurodisability. Given the abstract nature of the subject matter to be discussed, we were wary of the difficulties of capturing thoughts on this, in a meaningful way and in the time scale available, from young people who had moderate or severe learning disabilities. We therefore sought pre-existing groups of children and young people who did not have significant cognitive impairment.
Approaches were made to special schools, disability/special needs sports teams, youth and social clubs, and school/university groups, through a national umbrella organisation for disabled children’s charities, and through professional research networks with established young people’s research advisory groups. When relevant, we also sought suggestions from some of the practitioner and parent focus groups for appropriate children’s and young people’s groups to contact. In the event, none of these avenues was fruitful. We would note that this was not entirely unexpected. Securing meaningful engagement of children and young people in studies such as this – which are constrained by time and resources – is often very challenging. 1 We would recommend that a specific piece of work exploring children’s and young people’s views be carried out, informed by the findings from this scoping study. It is useful to note here that Morris et al. 1 made a similar recommendation in response to their experiences of conducting the JLA research priority setting exercise for children with neurodisability.
Data collection
Individual and group interviews were used to ascertain the views and experiences of different stakeholder groups. Individual interviews aimed to collect in-depth data on the participant’s particular area of expertise, whether that was within or across different therapy services. Group interviews allowed a collective exploration of the topics presented for discussion.
The interview topic guides
The content and focus of the interviews and focus groups differed across the stakeholder groups in accordance with the rationale for recruiting them to the study.
Semistructured topic guides of key themes and subthemes to cover were developed for the individual and group interviews. Table 11 reports on the broad themes covered in the different stakeholder topic guides. (See Appendix 4 for exemplar topic guides.)
| Stakeholder group topic guide | Themes covered | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Current state of research evidence | Participation outcomes and outcome measurement | Active ingredients of therapy interventions | Challenges to evaluating interventions | Research priorities | Overview/experiences of current therapy practice | Role in building and promoting evidence-based practice | Role of practice therapies | Parental involvement in delivering therapies | |
| Clinical academics/researchers (n = 13) | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Professional bodies (n = 7) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Other practitioners (n = 12) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Paediatricians (n = 7) | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Practitioner groups (n = 6) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||
| Parent groups (n = 4) | ✓ | ✓ | ✓ | ✓ | |||||
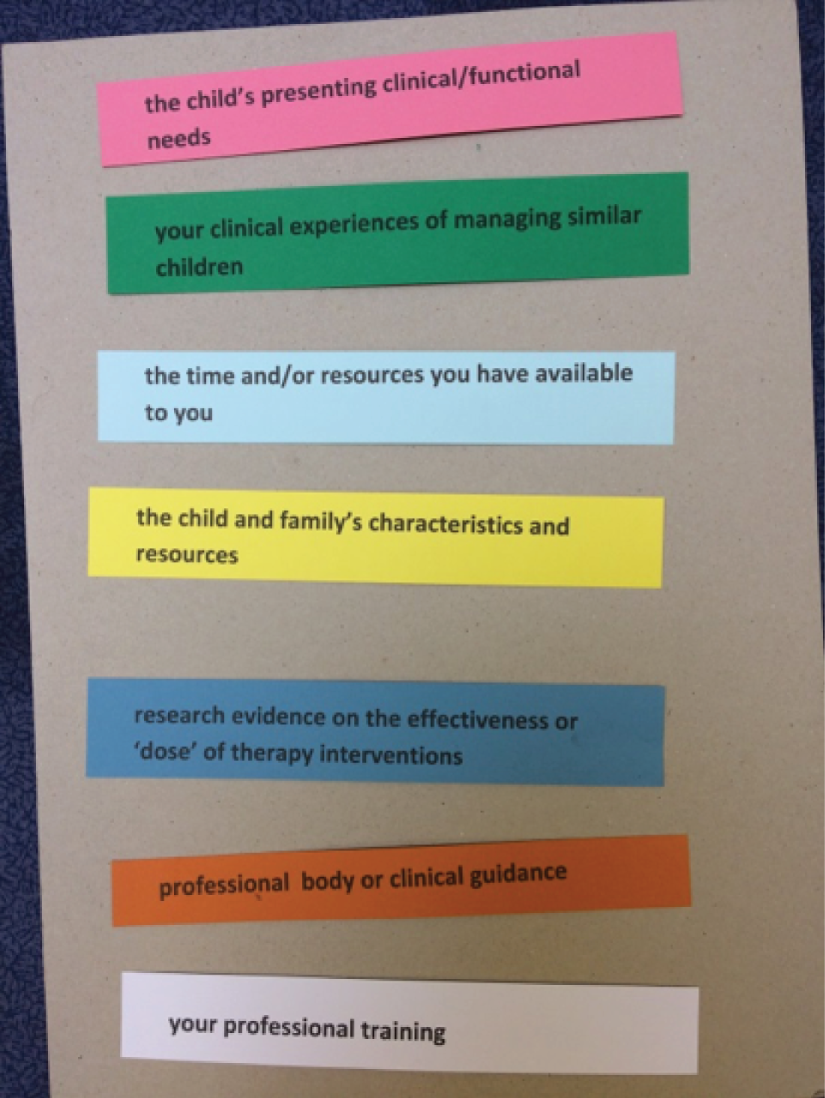
Two group exercises were used during the focus groups to facilitate discussion. In larger groups, subgroups were created to work on these tasks. The first was to rank, in order of priority, factors that influenced or informed decision-making about the management of a case. Participants were given a set of cards, each describing one factor. Once they had discussed and agreed a ranking order, they were asked to affix the cards to a mounting board in order of most to least important (Figure 1). The boards were then displayed and discussed among the whole group.
FIGURE 1.
Example of output from focus group ranking exercise.
The second exercise involved participants completing a worksheet about their priorities for research. The worksheet was divided into three sections for this purpose: research about specific interventions, research about particular groups of children (e.g. diagnosis, need, age) and research about the way therapy is organised and delivered. Participants were advised that they did not have to complete all of the sections. Again, the responses were shared and discussed among the group.
Fieldwork
Fieldwork took place between August and December 2016 and was shared by the three members of the research team. Most of the individual interviews were conducted over the telephone, but three were carried out face to face. Except for two instances when focus groups were convened via a national meeting with participants attending from across the country (one practitioner group and one parent group), the group interviews took place in the localities of the participants. The groups were facilitated by one or two researchers. Interviews lasted approximately 1 hour and, with permission, were digitally recorded.
Data analysis
Audio-recordings of the interviews and focus groups were used to create detailed summaries, using a template derived from the headings and subheadings of the relevant topic guide. These summaries included verbatim quotations. The position of verbatim quotations on the audio-recording (in terms of minutes and seconds) was noted.
The research team met regularly throughout the data collection period to reflect on a priori and emerging topics and issues. Once all interview/focus group summaries were complete, the team met again on three separate occasions to discuss and develop, through consensus, ‘mind maps’ of the themes and subthemes covered in the data relevant to the research questions.
These maps were then modified to create a structure into which analytical writings, summarising findings on each theme, could be organised. These formed the basis of the project report. Drafts of the findings sections of the project report were shared and reviewed by all members of the research team, and final versions were agreed.
Verbatim quotations are used extensively throughout the report to illustrate points made in the text and to ensure that the voices of study participants are directly presented. For professional study participants, each individual participant or focus group is identified by a unique code (A1–X2; C1–H1 focus group participant). The use of this coding system allows the reader to evaluate the use of quotations from across the breadth of the sample. To ensure anonymity, we do not provide details of the characteristics of individuals quoted. When appropriate, in the preceding text, we do specify individuals’ profession or other relevant information.
Chapter 3 An overview of the organisation and delivery of therapies
Introduction
This chapter reports the evidence gathered from professionals regarding the way in which therapy services for children with non-progressive neurodisability are currently organised and delivered, and non-statutory sources of physiotherapy, occupational therapy and speech and language therapy. It is important to note that this study did not systematically map service organisation and delivery issues. However, study participants included those with a ‘national-level’ view and those who had worked in a number of service settings and geographical locations, or reported themselves to be at the forefront of service development and service organisation. This chapter describes a variable and changing landscape, with those changes being driven by a number of different factors. Parents’ views and experiences of therapy provision are reported in Chapter 5.
The organisational settings of therapy services
Therapy services for children with non-progressive neurodisability are located in tertiary, secondary and community health-care settings. Tertiary provision includes single-centre and ‘hub-and-spoke’ models. Tertiary (and some secondary-level) services take the form of ‘standalone’ therapy-specific teams (e.g. complex communication needs, neurorehabilitation, respiratory physiotherapy) and therapists within specialist (sometimes residential) provision for particular populations (e.g. acquired brain injury, profound physical impairment, dysphagia) working within either multidisciplinary or single-therapy teams. Such services may also support the work of non-specialist children’s therapy teams.
Children with neurodisability may use one or more of these different levels of provision at some stage during their lives. For example, a child with acquired brain injury may be initially cared for in a specialist centre before being transferred to the care of the local community-based team. Therapists in secondary care settings tend to have a more time-limited involvement – addressing transitory, acute needs (e.g. respiratory interventions; rehabilitation following hip surgery) – or being the first point in a therapy intervention pathway before discharge to community teams (for example, early rehabilitation following a stroke). In terms of community-based therapy services, where therapy services sit, and how they are organised, is largely determined by the wider structure of community paediatric services in that locality. Within this provision, therapy teams or services may be organised in terms of population groups and/or the type of functional impairment. The usual care pathway appears to be referrals being made to therapy teams via a consultant paediatrician-led service. However, as described below, alternative models were reported.
Finally, in addition to occupational therapy services within the NHS, occupational therapists work in local authority housing and social care departments. Here they are involved in assessments and delivery related to the adaptation of children’s homes and the provision of associated equipment (e.g. hoists, bathing aids or toileting aids). They may also be directly employed by schools.
The locations in which therapists work
Therapists work in a number of settings: the hospital ward, outpatient clinic, nurseries, schools, homes and the community settings or services a child uses. However, this was reported to vary between therapies, the therapist’s remit and local practices or commissioning arrangements. Occupational therapists were most likely to report seeing children in their home or other community settings. Physiotherapists based in community health teams reported working out of clinics and through home visits, although the extent to which the latter was implemented appeared to be highly variable. A preference for this way of working appears to be connected to adopting participation-focused approaches and incorporating therapy exercises or procedures into everyday activities. However, local commissioning arrangements and a service lead’s opinion appeared to influence the extent to which this was routine practice. For children with long-term therapy needs, the move into school, particularly if to special school, typically meant that sessions or appointments with physiotherapists and speech and language therapists took place at school.
The organisation of therapy provision
The traditional model
Across all of these settings, the traditional model is that physiotherapy, speech and language therapy and occupational therapy services work as ‘unitherapy’ teams, with assessment and intervention delivery occurring separately, or in isolation, from other types of therapy interventions a child may be receiving. Physical barriers were reported as acting to prevent even informal modes of integrated working:
We are often still based in separate buildings by profession, or separate offices. Right down to what desk you sit at. A huge amount of clinician time and effort goes into trying to mitigate the negative impact of that.
L1
Although not necessarily regarded as a problematic model for children with a short-term need for a specific therapy, difficulties with this model with respect to children with complex long-term needs were identified across all study participant groups. It had the potential to lead to different or conflicting priorities in terms of the purpose or focus of therapy interventions and the perceived objectives.
Alternative models
In addition to the traditional model of service organisation and provision described above, study participants reported other models. These were typically presented as ‘atypical’ or ‘ground-breaking’ and were observed across all levels of care: tertiary, secondary and community services. They included the following.
Multitherapy teams
Perhaps the most frequently reported alternative to ‘unitherapy’ teams, multitherapy teams comprised two or all three therapies. When described, ‘joint/bitherapy’ teams were always a collaboration of physiotherapy and occupational therapy. This was explained by the two therapies being more likely to be interdependent in terms of achieving the desired outcomes for the child.
Integrated, multiprofessional approaches
This model comprises an integrated approach to the assessment and care of children with neurodisability involving therapists, relevant paediatric specialisms and, potentially, other professionals working together. This approach includes integrated working arrangements across teams as well as multiprofessional teams. There is also variability in the extent of integrated working. For example, the assessment and care planning process may be integrated but actual intervention delivery may still be located across ‘unitherapy’ rather than ‘multitherapy’ teams.
Transdisciplinary or ‘primary provider’ models
A couple of interviewees described a ‘transdisciplinary model of working’. For example, a joint physiotherapy and occupational therapy team had implemented a ‘generic therapist’ role. Here, a single therapist – physiotherapist or occupational therapist – works with the child, but draws on both occupational therapy and physiotherapy intervention approaches. A similar model was described within the context of a multitherapy occupational therapy/physiotherapy/speech and language therapy service, whereby each profession is recognised as having a ‘unique contribution’ but a single therapist acts as the main conduit by which all the therapies are delivered. These interviewees believed that families preferred this model, as it offered a co-ordinated approach.
Therapist-led services
Therapist-led services were also described. Regarded as innovative and recently implemented, this model appeared to be used to manage impairments of function that required brief, time-limited intervention, and when a diagnosis from a paediatrician, or another relevant specialist, was not required to proceed with therapy.
Factors driving changes in service organisation
Three main factors emerged from interviewees’ accounts as appearing to drive these changes.
-
A policy driver: the Children and Families Act (2014)19 – which demands joint working across health, education and social care, a single, overall assessment of need, and co-ordination and integration of services – was identified as prompting reviews of the way therapy services are organised.
-
Participation outcomes and goals-focused approaches: the shift to regarding participation as a key outcome for therapy interventions, and the accompanying move to goals-focused approaches to assessment and intervention, emerged as a key driver to changing the way therapy services were organised and delivered. (We report this in more detail in Chapter 4.) Interviewees described how the achievement of a goal will require the inputs and interventions from all, or two, of the therapies as well as from other professionals.
-
The need/desire for greater efficiency: reduced resources, coupled with high demand, were reported to have led to alternative approaches being sought. Reconfigurations of service models in order to reduce wait times, prevent duplication both within assessment processes and in the delivery of interventions, and make best use of therapists’ skills and expertise were all cited as reasons for seeking to change models of service organisation and delivery.
Interviewees who had been involved in restructuring or reorganising therapy provision typically described this as a difficult process. Creating multitherapy teams that were truly integrated was challenging and, often, ‘work in progress’.
Approaches to provision
Interviewees described two broad approaches to therapy provision, particularly within physiotherapy and speech and language therapy. First, and the more traditional approach, is open-ended involvement with a case until ‘recovery’ or broad therapy objectives have been achieved. For some children, this may mean a relatively short period of contact with a therapist. For others, with significant and enduring physical and motor impairment, their involvement with therapists is long term – often up to the point of transfer to adult services. Second, and presented as a relatively recent innovation, is an ‘episodes of care’ model, with re-referral into the service for further input.
The driver behind this shift in approach was primarily attributed to limited resources and managing demand. Managers and senior staff interviewed reported significant and sustained cuts in funding:
In the past children will have come on to our caseload and stayed on it. Now we discharge children after a block of intervention and then the child has to be re-referred after 12 weeks to get further support. A lot of services operate an episode of care model. It seems to be a capacity-based decision rather than a clinical need-based one.
V2
Within occupational therapy, given the focus of this particular therapy, it appears that involvement may have always been more episodic, although it is not clear from our data if the duration of those episodes is changing over time.
Across all approaches to provision, parents and school staff are often those delivering the actual intervention to the child. To some extent this model of delivery has been in place for a while, but interviewees’ accounts suggest that this is being further embedded in the way services are organised and therapy interventions are delivered. We return to this issue in Chapter 4.
Private providers
Among some groups of children with neurodisability, private providers are not an uncommon source of therapy provision. A number of factors seem to be at play here. Interviewees noted that a dominant belief among parents is that the amount and intensity of direct work on a child – delivered by a therapist (or themselves, under instruction from a therapist) – was the predominant reason for purchasing additional therapy:
Often parents come along with the idea that more therapy is always better . . .
W1
. . . [it] ends up with a battling mentality in which parents feel that NHS professionals aren’t doing their best for them. And that’s very, very counterproductive.
V1
This belief, coupled with concerns about the level, or amount, of therapy being received from statutory health care, led to parents seeking alternatives. It was frequently observed that private providers tended to use more traditional, high-dose/high-intensity intervention approaches. This aligned with parents’ desires to be ‘doing all they can’ for their child. For some parents, the appeal of private providers can be that it removes demands on them, as parents, to deliver therapy to their child. A further reason identified by study participants as to why parents seek private provision is that parents can learn (via word of mouth, or through internet searches) about an intervention, or intervention approach, that they believe would benefit their child but that is not available through the NHS, owing to a perceived evidence gap, resource constraints and/or commissioning decisions.
Professionals reported that the use of private providers could introduce another aspect of their management of a case. Sometimes this related to co-ordinating the two sources of therapy or managing conflicting advice. They were aware that parents did not always reveal the non-NHS interventions they were purchasing or using, which could, in itself, lead to difficulties.
Parent-identified and -delivered ‘therapies’
In addition, our work with parents revealed that some had sought out, and were using, additional therapy interventions without any therapy professional input or oversight. Again, seeking these alternative sources of therapy was driven by a perceived inadequacy of statutory provision. Some professionals expressed concerns that the roll-out of personal health budgets may mean increasing numbers of parents purchasing ‘unproven’ interventions:
I worry about the vested interests of companies trying to make money out of parents and their personal budgets. I would love a decent evidence base with which to advise families.
V1
There are companies selling things, yet what they do isn’t based on published evidence nor does it do what they claim. Yet parents will come to us and say ‘Why aren’t you doing this?’.
H1
As a parent, your natural instinct is to do anything you can for your child. But you are rubbing up against salesmen of equipment manufacturers, many of whom are very moral and decent people. [But] my fear is that sales sometimes drive the agenda.
O2
Chapter 4 Therapy interventions: approaches and techniques
Introduction
An objective of this study was to describe current approaches and practices in the delivery of therapy interventions to children with non-progressive neurodisabilities. In this chapter, we present findings regarding this that have emerged from our interviews with professionals. We offer a broad view of the current situation placing this, when necessary, in the historical context of the development of physiotherapy, occupational therapy, and speech and language therapy. Parents’ reports of their experiences of therapy – for example the approaches and specific techniques – are presented in Chapter 5.
Understanding therapy interventions
Physiotherapy, occupational therapy and speech and language therapy can be described and understood at three levels:
-
the overall approach a therapist brings to the assessment and management of a case
-
the schools of thought that inform views regarding the appropriate way to manage a case
-
the specific techniques, procedures, activities and equipment used.
There is some interaction, or interdependency, between these levels (Figure 2). Certainly, the two higher levels influence what a therapist actually ‘does’ with a child. Equally, the overall approach will determine, at least to some extent, what are regarded as legitimate or acceptable schools of thought.
FIGURE 2.
Therapy intervention constructs and their interconnections.

In this chapter, we report what our interviews with professionals reveal about these different ways of conceptualising or understanding therapy interventions. We also report how thinking on these matters is shifting and changing. We do not claim that this is the only way to understand and conceptualise therapy interventions, but is the clearest solution we found to presenting interviewees’ accounts.
The overall approach
Four different, but interconnecting, facets appear to contribute to this concept of the ‘overall approach’:
-
the objective of the intervention
-
the role of the therapist
-
the role of the child and family
-
the place of the therapy in the life of the child.
The World Health Organization’s International Classification of Functioning, Disability and Health
Before moving on to describe each aspect of ‘overall therapy approach’ in turn, it is useful to offer a brief overview of the WHO’s ICF, published in 2002. This conceptual model was widely referred to in our interviews. It was clear that it not only offers a language and framework by which therapy interventions can be understood, but has also been a catalyst for change in the overall approach of therapies. It is a conceptual model that has been endorsed by all three profession,20–22 with guidance issued to support its implementation (e.g. College of Occupational Therapists, 2004; Royal College of Speech and Language Therapists, 2005) as well as being integrated into the training of new therapists. 23
In 2002, WHO proposed a conceptual model of disability that sought to bring together elements of the pre-existing medical and social models of disability, and incorporate them into a biopsychosocial model of disability. 16 Figure 3 offers a representation of this model.
FIGURE 3.
The ICF model of disability and health.
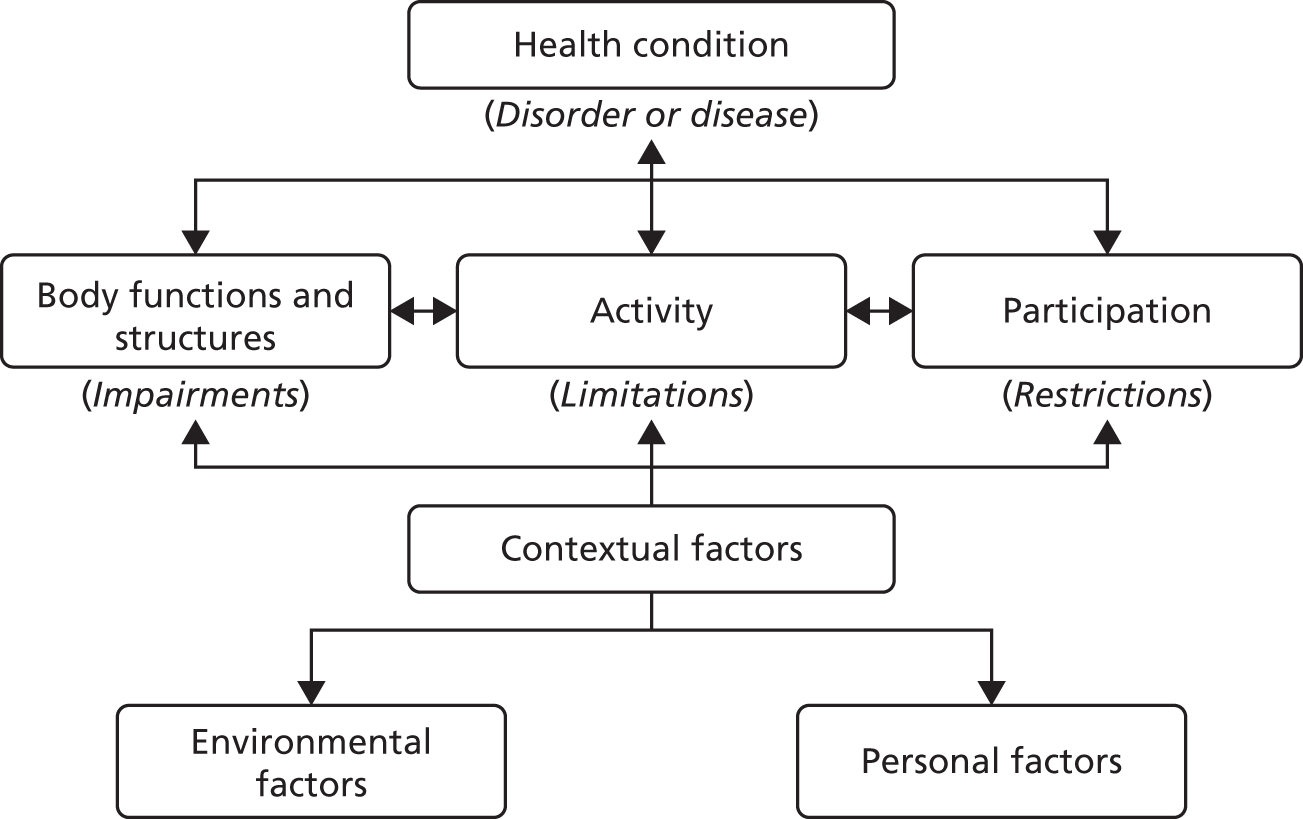
The meanings of the terms used in this model are as follows.
p. 10. 16 Reprinted from Towards a Common Languages for Functioning, Disability and Health: International Classification Framework. World Health Organization, © 2002. URL: www.who.int/classifications/icf/icfbeginnersguide.pdf (last accessed 21 December 2017)
Overall approach: the objective of the intervention
In describing the overall objectives of a therapy intervention, interviewees framed this in terms of the ICF model. Three possibilities were described.
-
First, the ‘deficit model’: here remedying physical/body dysfunction and distortion is seen as the end point, or objective, of therapy interventions or, as one interviewee described it, ‘fixing the child’ (OT-PB-01). This model can be regarded as the original starting point of all three professions.
-
The second approach focuses on the achievement of specific activities, or occupations, that the child’s physical impairments have limited or rendered difficult, for example walking or articulating verbal speech. When interviewees offered a chronology of the emergence of these different models, this approach was described as emerging in the 1990s.
-
The third approach is child/family focused, goals focused, in which the objectives of therapy are driven and guided by the child’s/family’s goals and desires. These goals should be expressed in terms of the child’s participation in everyday life, or life situations, that is relevant and meaningful for a child of that age (e.g. learning, self-care, communicating, moving about, friendships and being part of a family), rather than outcomes related to body structure/function or achievement of specific skills or activities. Within this approach, addressing dysfunction or impairment is no longer the key focus. This opens up alternative ways of intervening which may be as, or more, successful. One example is achieving independent mobility through the use of a wheelchair rather than through a lengthy and intensive physiotherapy programme. Another example is teaching a child to use augmentative and alternative communication systems and devices to communicate, or supplement verbal communication, rather than simply seeking to achieve verbal communication through speech and language therapy input:
The really complex ones, you can do as much therapy as you like, and it probably won’t make much difference – so let’s focus on the environment and the equipment and stuff . . .
A1
A slightly different, or concurrent, conceptualisation emerged from interviews with occupational therapists. It had a more dichotomous stance: a ‘deficit-focused’ model versus a focus on achieving occupation, or participation, through modifications to the environment and/or providing equipment to facilitate the child’s engagement or participation.
The operationalisation of these approaches
A number of issues emerged during our discussions with interviewees regarding these three possible approaches to understanding the objectives of a therapy intervention.
First, there was clear evidence that all the approaches are being used by therapists. Furthermore, not all interviewees believed that the different approaches were incompatible. Thus, some viewed them as being necessarily connected, with achievements of particular skills or reducing pain, for example enabling higher-level outcomes (expressed in the goals identified by children or parents) to be achieved, even if not explicitly identified at the outset of the intervention:
[Let me give you this example] . . . A 7-year-old boy, with quite a severe impairment, was delighted that his newly acquired ‘pick-up and release skills’ meant he could now take a tissue out of a box and wipe his nose himself. He is now independently participating in his own personal care, and this gave him better self-esteem in the classroom.
K1
Start with the child or impairment, working on the body structure and functions as a means to an end to achieving the desired occupation. Start with the occupation, looking both at the child and the environment to see what can be done to achieve the occupation. Both approaches are still occupational therapy. Yet the same situation can be looked at in different ways, involving different interventions, and with different people. That can be confusing and challenging . . . and it’s a sensitive topic within the profession. Some favour one, some the other, and others use a bit of both.
N1
Second, a goals-focused approach was widely endorsed and, reportedly, operationalised. However, the implementation of participation-oriented, goals-focused approaches within the therapies was viewed by some as ‘under development’ as opposed to already achieved:
. . . in my service you can see a three-generation approach. The first generation used to do ‘body function/structure stuff’ working on things like fine motor skills, co-ordination, range of movement and postural stability. Then, about 12 years ago, with the second generation, it became much more about targeting an activity and participation. However, in reality it was more about targeting activity and the child’s skills than true participation. Now a third-generation model is needed, where [we] really target participation. [So my question is] . . . ‘What’s our third-generation approach going to be so that it actually targets participation head-on through the right hypothesis-change mechanism?’.
L1
There’s been a bit of a shift in terms of whether body structure and function is meaningful in its own right, or whether it’s an intervention which enables children to participate in something. We’ve started on that shift, but we aren’t all the way.
F1
This was also evidenced in some of our interviews when interviewees described goals that ranged across all of the ICF concepts. Thus, a goals-focused approach was being operationalised, but not necessarily within a framework of participation.
Third, it was not clear whether the shift to goals-focused approaches was simply a matter of the influence of new ‘ways of thinking’ informed by both ICF and family-centred practice,24 or whether stringent cuts in funding had forced therapists and services into a position where intense work on body structure and function was no longer possible.
Fourth, there appeared to be a degree of confusion about the differences between the ICF concepts of ‘activities’ and ‘participation’, and the definitions offered for both varied considerably. Participation, as set out in the WHO report, was viewed by some as challenging in terms of its definition and measurement, in terms of both appropriate time points and the indicators of participation used. This is something we discuss in detail in Chapter 7.
Finally, new ways of working, intervention programmes and practices have emerged or been developed in response to this shift in approach from deficit to activities or goals-focused approaches. Examples of these referred to by study participants included, for physiotherapy, the MOVE programme (www.move-international.org/) and for occupational therapy, goals-directed training. 25
Overall approach: the role of therapist
There was a consistent view that, over recent years, the role of therapists in the delivery of interventions to children with neurodisability has shifted. A number of interviewees – and across all therapies – referred to a ‘consultative model’ whereby the therapist assesses the child, develops an intervention programme and then trains, or ‘upskills’, others (assistant practitioners, parents, child, classroom assistant and/or teacher) to deliver it, with supervision and ongoing monitoring. This approach was regarded as more prevalent within community, rather than secondary care or acute, settings.
Two drivers for this change were presented by interviewees. First, many interviewees noted the reduction in funding for therapies for children with neurodisability, which had forced changes in the way therapists worked. The way NHS trusts have chosen to address resource constraints has, however, differed. In some trusts, specialty posts have been maintained – albeit operating in a consultative role – whereas in others, posts have been lost and/or downgraded. A second driver – attributed to the number of ‘influential leaders’ in the field – was the acknowledgement that, to be effective, therapy interventions cannot be restricted to what are relatively occasional sessions with a qualified therapist in a clinic setting:
. . . it’s an intelligent way of capacity building. Also, in schools it’s the staff who know the children better than the therapist does. The therapist will come in one or two times a term so it would be ludicrous to expect a change with that amount of contact.
R2
There was a diversity of opinion as to whether or not this change is for the better. The dominant concern was that non-therapists may not be sufficiently skilled or competent to respond to changes in functioning or to evaluate the impact of the interventions and adjust the intervention accordingly:
There is something about the skill of the therapist in working with any one child with particularly complex needs, to be able to tune in to how the child is responding to what you are doing with them. . . . To make the kind of adjustment that you need to do to make the therapy work there and then, and to know whether you can push onto something more complex . . .
O2
. . . I think intervention effectiveness is actually being diluted . . . by having less skilled staff. I can understand why they are doing it, but I think it’s short-sighted.
Z1
A second concern was adherence to intervention programmes. This was typically spoken about in terms of the multiple demands on people’s time and/or a lack of understanding of the intervention programme and its objectives. Finally, this represented a very significant change in the day-to-day work of therapists that may be difficult to accept and assimilate:
Within practice there is a reluctance to change that [move to less hands-on and more activity-based therapy], particularly among those who have been trained in manual handling of patients and how to support and help them move.
F2
Furthermore, it was noted that parents may struggle to accept the consultative approach. Many interviewees believed that seeking the input of private practitioners was often due to a desire for more intense input from a qualified therapist.
Overall approach: the role of the child and family
The goals-focused approach described earlier was often spoken about alongside descriptions of a change in the way children, and their families, are regarded within the context of a therapy intervention. The shift in thinking described was from regarding the child/family as passive recipients to viewing them as active participants in the therapy intervention. Some interviewees referred to this is a move from the ‘expert practitioner’ model to the ‘expert parent’ model:
We are looking for children and families to be active in the rehabilitation process. So, instead of a child coming into hospital and having all this therapy done to them, they are a real active participant in what they are doing and they’re actively involved in their rehabilitation process.
L2
Occasionally, this shift was located, or attributed, within a wider change in the NHS to a focus on self-management. This was perceived to be driven by both an outcomes-focused approach and constrained resources.
Again, there was a sense that this study was being conducted at a time when thinking within each of the professions on such matters was in a state of change. Thus, we had interviewees who firmly advocated opposing approaches. Equally, there were interviewees who described the approach they were working towards, but had not yet attained:
I want us to get to the situation where we are working with families, giving them the right information – and doing that well and early enough – so that they can be empowered to . . . make decisions.
A1
Therapists have always worked very closely with parents, and older children too, in terms of goal-setting and goal preferences. The idea of offering people informed choice is not there . . . at the moment.
P2
With respect to the move to place children and families more centrally in decision-making and ‘condition management’ processes, a number of interviewees referred to ‘health-coaching’ models or programmes which were informing or influencing changes in their ways of working.
Overall approach: integrating therapy into everyday life
The final interconnecting strand within the concept of ‘therapy approaches’ is integrating therapy interventions into everyday life. Again, interviewees spoke of a shift in thinking: taking therapy out of clinic settings, and delivering in the settings and environments where the child spends his or her time. Linked to this were notions of integrating the therapy procedures into everyday activities and aiming to design the intervention to maximise engagement and motivation:
I say to families that it’s no good just doing things for a short time, so it’s better to incorporate activities into everyday life, or position their child so they can do something else as well. That way activities get embedded and done more often, and so more likely to make a difference.
F1
Once more, the extent to which this approach was dominant in an individual therapist’s practice was dependent on the extent to which their practice reflective goals-focused, participative approaches.
A number of constraints to adopting such an approach – particularly around the settings in which therapists practised – was noted, particularly when, in the past, therapy was delivered in outpatient clinic settings. Here, commissioners could be reluctant to resource therapists working in the child’s everyday settings.
Schools of thought
One of the topic areas NIHR wanted this study to investigate and report on was current ‘schools of thought’ within physiotherapy, occupational therapy, and speech and language therapy. This has proved difficult to elucidate.
However, it is possible to present three sets of ‘schools of thought’ revealed in our interviews with study participants:
-
‘traditional’ schools of thought
-
emerging schools of thought
-
early intervention.
We have conceived schools of thought as distinct from ‘overall approach’ that we reported in the previous section.
Traditional schools of thought
Different schools of thought advocate, or stipulate, different techniques or procedures to use with a child. Alternatively, they may posit different views on the mechanisms of change underlying technique or procedure. This notion of distinct schools of thought appears to be very similar to that observed in other specialisms. (For example, psychological interventions typically sit under different schools of thought, such as psychodynamic, gestalt and cognitive–behavioural.)
Although the notion of different specific schools of thought was referred to by interviewees across all three professions, it emerged most strongly in our interviews with physiotherapists. This was both in terms of the way they may act to firmly ground (or constrain) an individual therapist’s approach or, more typically, as an area of controversy or concern. In both respects, neurodevelopmental approaches (e.g. the Bobath approach), sensory integration theory and conductive education were the most frequently mentioned. Bobath and sensory integration theory also emerged as divisive schools of thought in our interviews with occupational therapists. A concern about, or active rejection of, these schools of thought was explained in terms of their basis being located within a ‘deficit model’ of intervention, and/or existing evidence on their impact/effectiveness.
As is a common theme through many of our data, there was a sense that these distinct, traditional schools of thought were, and would continue to become, less dominant. One of the key drivers for this appears to be the ongoing, higher-level reconstructions of what therapy is and what its objectives should be, which we described in the previous section.
Emerging schools of thought
The shifts in overall approach described earlier – from a deficit model to activity-based and now goals-focused/participation ways of working – appear, however, to have led to the emergence of new schools of thought within the professions. Of those described to us during the study, these typically drawing on principles or approaches developed within other specialisms. For example, cognitive–behavioural, problem-solving approaches, sometimes referred to as ‘coaching’, were reported as being used within occupational therapy. Global notions of ‘goals-focused approach’, family-centred practice and ‘evidence-based practice’ were referred to across all therapies as ‘schools of thought’ that the professions were adopting.
Early intervention
The final school of thought, applicable across all therapies, was the notion that early intervention is essential, and this should be the time when the intensity of the intervention is at its greatest. The rationale for early intervention is that it is likely to yield greater impact: supporting development and preventing permanent damage and/or deterioration. This argument is based on notions of neuroplasticity, physical and cognitive development.
Thus, it was also typically reported that the intensity of therapy interventions decreases as the child grows older (or in terms of time since brain injury). However, what was less clear was the rationale for tailing off therapy; indeed, it was a source of concern among some interviewees. Often this was expressed with respect to physical changes associated with puberty or to a child’s ongoing cognitive or communication development, and the implications this may have for the child’s needs for therapy input:
Younger children get more research and more therapy. Therapy is front-loaded so families get most at the preschool stage, some in primary school, rarely any in secondary school and none as adults.
N2
Techniques, procedures and equipment used by the different therapies
The purpose of this scoping study was not to provide an account of the enormous range of techniques, procedures and equipment currently being used by therapists in England. A different methodology would be required to generate such data. (We have, however, collated a list of all the techniques, procedures and equipment described to us by study participants. This can be found in Appendix 6.)
Rather, what this study has achieved is an overview of the practice of physiotherapy, occupational therapy and speech and language therapy. We describe this in terms of a number of concepts:
-
professional autonomy
-
responsive practice
-
managing prognostic uncertainty
-
the role of protocols and care pathways
-
working out of a tool box
-
mode of delivery.
Professional autonomy
A first overarching principle of practice within therapies is the concept of professional autonomy. In many interviews, therapists were presented as working in an autonomous, individualistic way within their scope of practice (or qualification):
Assessment and hands-on work is probably more individualised, but we all sign up from the same baseline.
F1
. . . certain institutions or individuals will have a favoured approach but ultimately it’s individual choice. Each physiotherapist is an autonomous practitioner . . .
M2
This autonomy operated both in the choice of interventions and in the intensity, or dose, of the interventions. Despite this notion of autonomy, some interviewees noted that, within the NHS, practice has become more standardised over the past decade, driven by emerging evidence and the shift in overall approach to providing these therapies. The publication of protocols and the implementation of care pathways – both described below – also contributed to a standardisation of practice.
Responsive practice
The ability to make an ongoing assessment, even within the context of specific session, of the way a child is responding to an intervention and/or their ability or motivation to engage with an activity or procedure (sometimes on a moment-by-moment basis) was regarded as a core therapy skill. Responding to the child, and their response to an intervention, meant that therapists may be continually tailoring either their work with a child or the overall management of the case:
At the beginning of a session I may not have a definitive goal in mind, but will have an idea of what I’m hoping to achieve and structure the session accordingly. Over time, I may adapt and change the goals in order to make progress. So it’s a very fluid process and we need to be responsive and adaptive to get the best out of the child.
M2
Managing prognostic uncertainty
With more complex cases, the issue of prognostic uncertainty and a lack of evidence of intervention effectiveness could lead therapists to trial a number of interventions, sometimes simultaneously, to establish a child’s potential capabilities and/or which technique suited the child best:
Parents with children with cerebral palsy always ask ‘[When] is my child going to talk, is spoken language going to be possible for them?’ And we can never answer that question because each child is so different. So it may be we set off on an eclectic approach, [thinking] . . . ‘let’s do some work on vocalisation or signing or symbols as well . . .
V2
The role of protocols and care pathways
Participants used the term ‘protocol’ in two distinct ways. First, it was used to refer to the way in which a team or service managed a referral to their service. Here, both the terms ‘protocol’ and ‘care pathway’ were used. Thus, some study participants described the development, and early implementation, of a number of care pathways within their service, each specific to a particular presenting need or diagnosis. Typically, these were multidisciplinary, or integrated, pathways specifying who and when different professional groups should become involved with a child, and for how long.
Second, and more specifically, some techniques or presenting clinical needs were identified as having clear protocols in terms of assessment and/or management. For example, frequent references were made to NICE guidance on the management of spasticity. Interviewees drew attention to the fact that for many children with neurodisability, especially those with complex needs, there will be individualistic practice happening alongside protocol-informed practice(s).
Issues were raised of adherence to protocols, particularly when others were delivering the treatment, and the potential difficulties of implementing a protocol in an appropriate way for a particular child:
Protocols are anyway problematic because children vary and delivery is not always under their control. Children are at different ages and different stages and living in different families. . . . [And] to have protocols – good, evaluated ones – is one thing, but to implement them in families’ everyday life is another.
M1
However, a much greater proportion of therapists’ work was reported as lacking any protocols. As a result, there could be great variation in the way in which a case was managed:
[There is] . . . huge variation in the interventions they receive. Not only in what they receive but in how often and from whom they receive it.
N2
It’s been quite easy to write a pathway [protocol] for children with, say, hemiplegia receiving CMIT [constraint-induced movement therapy], or for those having Botox [botulinum toxin] injections as there’s quite a lot of evidence or guidance to draw on. Whereas all the others just get based on your clinical experience of managing other children . . . and what you see in the child.
C1
Working out of a toolbox
Within the notion of professional autonomy described above, many interviewees described themselves as working out of a ‘toolbox’:
What you tend to find in practice is that most practitioners use an eclectic approach. It’s a little bit of this and a little bit of that. . . . it’s a little bit of what you’ve got in your toolbox.
K2
We have a great big menu of interventions to choose from.
P2
It’s about having that huge toolbox and choosing the right thing for the child, on the day almost.
W2
Thus, in each case, a therapist brings a range of techniques, procedures, activities or items of equipment. There follows, through assessment of the child and the wider context, a process of clinical decision-making as to what particular ‘tools’ to choose, something that we report on in the following section.
Our analysis suggests that a number of factors influence the content of an individual therapist’s toolbox:
-
the ‘overall therapy approach’ to which the individual therapist adheres
-
their position, or beliefs, regarding schools of thought
-
their training
-
practices they have learnt from colleagues
-
trends or ‘fads’
-
team/clinical lead views
-
the techniques, etc., that commissioners will fund
-
clinical guidance (e.g. from NICE) or guidance or recommendations from professional bodies
-
evidence.
There is a lot of individualistic work going on. We have very experienced therapists with strong beliefs based on their own clinical experience, which can be very powerful.
P1
The notion of ‘embedded’ or ‘inherited practice’ was frequently mentioned. This was much more likely to be grounded in clinical consensus rather than in any evidence base:
There is a good level of consensus of opinion in what’s best in treatments and approaches to treatment which is cascaded down to therapists. . . . the team generates practice which then perpetuates down.
I2
There is an awful lot of tacit knowledge that’s handed down through the profession . . . certain techniques, [and] ‘that is how you do it, [and] this is the right way to do it . . .’
F2
Embedded practice was also seen as a barrier to change in therapy approaches or to evidence suggesting that an intervention may not be effective:
. . . but a lot of therapists have done this [refers to a particular technique] for 30 years. [And] they can’t stop doing it if you don’t put anything in its place.
F2
Trends or ‘fads’ in terms of particular techniques, procedures, activities or equipment were frequently mentioned by interviewees. Some were enthusiastic in their descriptions of, for example, a new technique that they or their team had started to use. Others were greatly concerned about the lack of an evidence-based rationale for adopting new techniques, equipment or practices. Furthermore, the commercial interests of manufacturers, or organisations, in promoting new techniques or equipment worried some interviewees. A further concern was that the successful use of a technique with a small number of children, or with respect to children of a particular developmental stage or diagnosis, could lead to wide-scale roll-out within a locality (or more broadly), which may not be appropriate:
There’s a massive growth in [name of technology] at the moment . . . and that’s very liberating for lots of young people . . . but it’s often being rolled out to children who are not ready yet . . . families and teams are spending an awful lot of money on technology that’s not being used effectively, and ultimately gets abandoned.
O2
That said, there was an understanding of why therapists can be drawn to new (untested) practices and equipment. These are often presented, or marketed, with an anatomical or neuromuscular ‘rationale’ and some persuasive case studies. Furthermore, new techniques or practices may offer therapists a structure and process to their work. For example, a manual, an assessment pro forma and guidance on intervention intensity may be offered. Some interviewees believed that this could be very appealing to practitioners who were trained to be autonomous and work in a very individualistic way, but within a discipline where there is little sound evidence on which to base clinical decision-making:
You can book to go on your [name of course] or your [name of other course], and then you have your kit . . . [and then] . . . you know what you’re meant to be doing.
S1
You’re taught in a staged way. It’s a clear, almost manualised, road map of what to do. It’s a qualification ‘in something’. It fills a gap.
P1
Finally, the role of evidence in informing the content of a therapist’s ‘toolbox’ was typically regarded as very limited. However, included in our study sample were settings where sustained attempts were being made to use evidence, when possible, to specify intervention approaches. In these situations, evidence was (often) being drawn across from adult rehabilitation and/or other diagnostic groups.
Mode of delivery
A less common topic referred to in relation to therapy practice was mode of delivery. It appeared that, in the majority of interviews, study participants assumed that the research team already knew that they were referring to individually delivered interventions. However, a few interviewees reported using group-delivered interventions, and this typically appeared to be in relation to the management or treatment of non-complex issues.
Factors affecting decision-making in the management of a case
One of the objectives of this study was to describe the factors that therapists reported as influencing their decision-making regarding the ‘therapeutic prescription’. We explored this in our individual interviews and focus groups with physiotherapists, occupational therapists and speech and language therapists.
The focus groups provided a useful opportunity to explore frontline practitioners’ views of the relative importance of factors brought to play in clinical decision-making in the management of a case. This exercise was conducted during six focus groups, with a total of 14 groups or subgroups completing this exercise. Participants were asked to rank the following factors:
-
child’s and family’s characteristics and resources
-
child’s presenting clinical/functioning needs
-
clinical experiences managing similar children
-
professional training
-
research evidence on intervention effectiveness
-
time and/or resources available to the therapist.
Table 12 sets out the results of that ranking exercise.
| Factor | Number of times ranked | |||||
|---|---|---|---|---|---|---|
| First | Second | Third | Fourth | Fifth | Sixth | |
| The child’s presenting clinical/functioning needs | 11 | 3 | 0 | 0 | 0 | 0 |
| Your professional training | 3 | 0 | 3 | 4 | 1 | 3 |
| Your clinical experiences of managing similar children | 0 | 6 | 5 | 2 | 1 | 0 |
| The child’s and family’s characteristics and resources | 0 | 3 | 2 | 5 | 1 | 3 |
| The time and/or resources you have available to you | 0 | 1 | 2 | 2 | 6 | 3 |
| Research evidence on the effectiveness, or ‘dose’, of therapy interventions | 0 | 1 | 2 | 1 | 5 | 5 |
Not unexpectedly, the dominant factor in decision-making was the therapist’s assessment of the child’s presenting clinical/functional needs, and it is important to note here that some groups explicitly stated that they had assumed this to also refer to the child’s, or parents’, goals. Only 3 of the 11 groups identified a different factor as the most important in informing clinical decision-making. In all cases, this factor was their professional training. A number of groups noted that the nature of other health interventions a child is receiving (e.g. other therapies, or medical/surgical interventions) may influence clinical decision-making and, in some cases, play a dominant role.
Clinical experience typically featured as a strong, but not the most important, influence on clinical decision-making. Here, many groups reported that they drew on not only their own clinical experience, but also that of colleagues. Discussing cases was an inherent part of their practice, and thus turning to others for input and advice was important and, possibly, more valuable or relevant than research evidence.
Views regarding the strength of influence of family characteristics and resources varied between therapists working in different settings. Those based in community teams viewed this as having a greater influence on decision-making than did those based in residential or school settings. Furthermore, the extent to which this factor was relevant to decision-making varied between families. Here, the key issue was the family’s capacity to take on a programme of therapy:
We know that some families will be able to take on therapy programmes and carry out a significant amount, but for others we know that we can’t possibly ask them to take this on as it would put an unbearable load on them and create an additional stress.
G1
A further aspect of the role, or influence, of the family on clinical decision-making was revealed in our discussions with therapists. This concerned the pressure that therapists can feel parents place on them to ‘do something’ or try a particular approach.
A few interviewees developed this further, noting that a therapists’ implicit desire to help a child may influence their clinical decision-making:
. . . our own internal drivers to offer something positive into what can be quite catastrophic situations . . .
G2
Therapists typically stated that resource issues should not influence their clinical decision-making. However, it was acknowledged that local directives can restrict the options open to a therapist. This can be at the team level; for example, clinical leads may adhere to particular approaches and practices. It may also operate at a trust level, with clinical decision-making affected by directives about whether specific procedures will be funded, the intensity of input (e.g. the frequency, number and duration of sessions) and/or the settings in which a therapist is permitted to work (e.g. clinic vs. home- or community-based work).
Research evidence was typically identified as having the least, if any, influence on clinical decision-making. The most frequent explanation for this was that there was a lack of evidence or that the existing evidence was not applicable to a particular diagnostic group:
Dysathria research does not include participants with learning disabilities, so that rules out most of our kids.
G1
. . . it’s the same thing every time we try to do evidence-based guidelines: there is no evidence for use with children with ABI [acquired brain injury].
D1
Other explanations included scepticism about existing evidence, particularly if such evidence raised questions about a technique or approach that the therapist strongly believed, from their clinical experience, had positive impacts for children. In addition, therapists described coming to the decision that, for a particular child, existing evidence was not relevant or meaningful:
. . . research doesn’t necessarily work for everyone . . . it’s all about assessing it on a case-by-case basis.
G1
A number of therapists referred to the difficulty accessing or ‘keeping up with’ evidence:
. . . there are so many diverse presentations among people we see that it’s hard to know all of the evidence.
C1
Participants often reported looking to outputs from national professional bodies, or NICE, that summarised evidence and considered its implications. We also came across instances of services/teams or professional/clinical excellence networks seeking to collate and synthesise evidence in order to produce internal, or member, guidance:
It translates the evidence for you, and it’s really useful when it’s done like that.
C1
We further discuss views on the perceived state of evidence in Chapter 8.
Chapter 5 Meeting children’s therapy needs: parents’ views and experiences
Introduction
This chapter reports some of the findings from our focus groups with parents. Here we describe parents’ accounts of their experiences of therapy provision within the NHS, their use of private provision, their experiences of delivering therapy interventions at home and, finally, the practices and approaches they valued in the therapists they had worked with. This chapter is deliberately placed after the two chapters that have reported professionals’ views on issues of service organisation and delivery, and practice.
Experiences of NHS provision
A range of parents participated in this scoping study in terms of their children’s diagnosis, age, the NHS services they used, and the localities in which they lived. Some of the children represented had complex needs. Experiences of physiotherapy, occupational therapy, and speech and language therapy were represented. Occupational therapy was typically mentioned as a service with which they had periodic contact. Physiotherapy and speech and language therapy were more likely to be spoken about as therapies for which their child had an enduring need.
Clarity around the objectives of therapy interventions
Parents commonly expressed that they had no knowledge or understanding of the decision process and rationale behind the therapy that their child was being offered. Furthermore, many parents reported being unclear about the aims, or goals, of the therapy being provided, and how progress towards those goals would be monitored, reviewed and, if necessary, the goals revised or updated.
Satisfaction with the child’s therapy
Parents varied in terms of satisfaction with the amount of therapy that their child was receiving. Those more likely to be content were those with younger, preschool children. Some described therapy ‘dropping away’ once their child started school.
Two key factors emerged as associated with parents’ level of satisfaction: whether or not the level of contact with the therapist was perceived as adequate, and continuity of therapist:
They [speech and language therapists] don’t come often enough to get to know your child.
We’ve never had a good [occupational therapist] because we’ve never had one for more than one session.
There was general agreement among parents that their children did not get enough therapy. Although such statements were usually followed by a caveat expressing a belief that therapy services were significantly under-resourced, some parents noted that restricting access to therapy was short-sighted as it may lead to greater levels of dependency and/or more expensive treatments being required. The example provided was preventing contractures through physiotherapy, rather than managing them through surgery.
Parents reported experiences, or an awareness, of geographical differences in therapy access. The phrase ‘postcode lottery’ was used, with some parents aware that geographical differences were, to some extent, due to commissioning decisions. Some parents believed that therapy services were directed towards children with less severe needs who represented ‘quick wins’. Others noted that some of their child’s less prominent needs were not being addressed by therapy provision, and wondered if this was because they were not severe enough. Overall, there was confusion about how decisions were made about the acceptance of referrals and the resources allocated to a case.
Parents often described having to ‘push’ or ‘bang on’ to get the level of therapy that they felt their child needed. One parent described herself as a having to become a ‘warrior parent’ to secure therapies for her child at the level she felt they had to be, and a few parents reported unpleasant ‘confrontations’ when they protested about their child’s levels of therapy. Some had tried to argue for greater provision but had given up:
We’ve given up on speech and language: in the end we had to give in and accept our son as he is . . .
Concern was expressed for those children whose parents were not able to pursue issues of perceived deficiencies in care.
Models of provision: ongoing versus episodic care
Some parents reported experiences of repeated cycles of time-limited provision, discharge and re-referral. Parents consistently favoured arrangements that allowed ongoing access to therapy support, ideally from the same therapist. When parents felt that their child did not need continual input, open discharge arrangements (i.e. when re-referral was not necessary) were valued.
The key difficulty parents identified with episodic care was the lack of continuity of care. For example, one parent reported that her child had been seen by 12 occupational therapists. Another mentioned that seven physiotherapists had been involved with her child. This lack of continuity was viewed as problematic for two reasons. First, therapists were not in contact with the chid long enough to understand his or her needs and for the child to ‘get to know’ them. Second, some parents believed that it led to therapists having an incomplete understanding of conditions or diagnoses, in particular that the conditions are lifelong with changing needs.
Integrated care
A dominant theme in our conversations with parents was the integration of provision from the three therapies. The majority reported that they did not experience this. They were not aware of any joint or integrated assessment, outcomes/goals-setting, and therapy delivery between physiotherapy, occupational therapy and speech and language therapy. Parents reported that this left them, and school staff, confused about the correct approaches to supporting and working with the child. As one parent noted:
. . . they don’t work together, they look at the child just from their perspective so the teacher and parent get mixed messages . . .
This situation could also leave parents feeling overburdened about what they were expected to do with their child in terms of delivering the therapy programmes set out by the therapist. Parents with experience of specialist independent education provision (with places purchased by local authorities) noted that this seemed to be the only setting in which a true integration of therapies was achieved. This was because the therapists were core members of staff and always on site.
Parents also explored notions of integration in terms of the position of therapy provision with respect to the wider care and management of their children. They spoke positively about child development centres, believing that these supported integrated working owing to the co-location of professionals and joint working practices. Less positive were experiences of Education, Health and Care Plans, which are part of statutory assessment and planning processes for children with additional needs over and above those provided within usual special educational needs support,26 as these had not always led to co-ordinated approaches to therapy provision and interventions.
Parents’ roles
As noted in the previous section, there was general acceptance among parents that they needed to be actively involved in delivering their child’s therapy ‘prescription’ or intervention programme. We describe in a later section their experiences of assuming this role.
On a separate note, a common theme in parents’ accounts, albeit not expressed by all, was that therapists did not acknowledge or value parents’ unique and ‘expert’ knowledge of their child. The example given was that parents may be best placed to judge when to ‘push’ a child in terms of the challenges or expectations placed on them for a particular therapy intervention. More generally, parents spoke of how they knew their child best, including their strengths and weaknesses. Related to this was a desire for a greater sense of working in partnership. Some parents described a hierarchical model in which disapproval was expressed when parents failed to ‘adhere’ to a therapy programme. In contrast, parents believed that partnership working benefited the child.
Parents also regarded themselves as advocates for their child. This was represented in their desire to be actively involved in assessment and planning processes, seeking the best for their child and speaking on their behalf. In terms of the last of these, sometimes this was because the child had significant communication and learning impairments, and other times the child had requested this.
In addition, some parents reported assuming the role of training staff in settings where their child spent time, for example day-care nursery or school. Furthermore, they reported assuming a wider monitoring of therapy provision at school, particularly checking that the provision set out in their child’s Education, Health and Care Plan was being delivered.
Finally, some parents reported assuming a co-ordination role in which they held and appropriately disseminated the disparate (and sometimes contradictory) information and advice given to them by the professionals involved with the child. As one parent noted, ‘we are like a hub’.
Other issues
Wheelchair services
A number of parents reported difficulties with wheelchair services, a provision that interfaces closely with physiotherapy and occupational therapy, and is accessed via referrals from these services. Delays in provision, a lack of choice, restricted access to powered wheelchairs and policies stipulating the age at which equipment is provided, rather than making decisions on a case-by-case basis, were reported, along with wheelchair services staff disagreeing with the therapist’s assessment and providing a suboptimal solution.
Transferring to adult care
Looking forward, some parents expressed concerns about their child’s transfer to adult services. This was both in terms of being able to access therapy per se, and also because the dominant model in adult services is a fixed number of sessions. This was not felt to be appropriate for young people with severe physical impairments.
Children using tertiary services
Finally, a few of the parents who had a child under the care of a tertiary service reported poor co-ordination, or a ‘disconnect’, between this service and any local therapy provision. This appeared to be located in a lack of shared objectives and time scales, plus different approaches apparently being taken to the management of the child.
Parents’ reports of accessing private provision
Why look outside the NHS?
A number of parents reported paying for private therapy. This included buying the services of an individual therapist and purchasing an assessment (and possibly also therapy and ongoing review) from a private provider organisation. The predominate reason for doing this was concern about the level of therapy support that their child was receiving from NHS provision or that provision was not addressing all of their child’s perceived needs. Some parents also explained their decision to use private providers in terms of responding to their desire, as parents, to do or try anything that might help their child. It was noted that private providers were not constrained in what they could offer in terms of intensity and types of intervention. The latter sometimes referred to new procedures or programmes; as one parent remarked, ‘they can think outside the box’. Others had turned to private providers because their NHS service no longer offered an intervention that the parent felt benefited the child. One parent who had chosen this route explained that ‘sensory integration is something my child desperately needs’.
Parents’ experiences of the assessments conducted by private specialist centres (physiotherapy and speech and language therapy) were very positive and reported as taking goals-focused approaches. Parents also valued having a clear plan for ongoing review. However, a number of parents reported that, post assessment, achieving the intensity of delivery required by some of the ‘prescribed’ therapy programme could be very difficult as a result of the various demands on parents’ and children’s time, and children’s capacity to engage in therapy after a day at school. Indeed, understanding the demands that such provision may place on a family was the reason why one parent decided against pursuing this option, believing that it would put too much pressure on her with ‘everything else going on’. Other parents’ experiences were different and they had successfully integrated the programme recommended. Aside from private therapy provision, parents reported paying for other types of interventions such as complementary medicine.
We asked parents whether or not they reported to NHS services that they were using a private provider. Some reported deliberately choosing not to for fear of losing the NHS provision that their child currently received. Others reported taking recommendations from private assessments to their NHS therapists or paediatricians and, on occasion, this had resulted in changes in the provision or timing of interventions. Parents’ experiences of asking advice from NHS therapists about seeking privately delivered interventions were mixed: some had been encouraged, and others had not.
Parent-initiated and -delivered therapies
Parents also reported independently identifying and delivering interventions to address their child’s impairments. The reasons for this varied. Some felt that NHS services did not have sufficient aspirations for their child, or they did not believe the result of a NHS assessment. Others felt that the NHS interventions being offered were without structure and the end points or objectives were unclear. Others sought out alternative interventions as a means of supplementing what they viewed as insufficient levels of contact with NHS providers. Finally, and sometimes underlying some of the reasons already described, this option was pursued simply ‘in the hope it will help’. Some parents reported positive outcomes for the child as a result of their efforts. For example, one parent reported that, on the advice of a friend, she had attended training in a signs- and symbols-based communication system. She recounted how this had supported her child to use signing and develop some speech, even though she had initially been told by her speech and language therapist that ‘nothing could be done’.
Parent-sourced equipment
Parents also reported independently sourcing equipment for their child. The most common reason was believing that NHS therapists were not aware of the current range of equipment options and were unable to supply the best equipment for their child. Parents reported finding out about equipment from other parents (e.g. via web-based parent support networks) and attending demonstration days run by equipment suppliers. Other reasons for purchasing privately were unreliability of NHS equipment and long waiting times for repairs. Some parents reported carrying out fundraising activities to buy equipment. Parents’ stories of sourcing equipment often concerned mobility-related items such as walkers or different types of wheelchair. Sometimes it was a second version of equipment that the child had already but was not suited to all of the activities the child wanted or needed to engage in. One or two parents reported taking a suggestion for equipment to their NHS team and persuading them to order it for their child.
Parents’ experiences of delivering therapies at home
Changes over time
Parents typically described the preschool years as the most intense in terms of the time demands made on them to deliver therapy interventions. However, starting school could lead to its own difficulties as the opportunities to do therapy work reduced; children were tired after school, and the options and opportunities for other activities may have increased. A parent observed:
. . . having to do therapy after school means my child has much less of a life than she should have.
Conflicting feelings
Parents described a sense of conflict. They felt pressure to adhere to a therapy regime, fearing that their child would suffer if they did not. As one parent noted, ‘I’m scared she will deteriorate’. At the same time, however, parents felt guilty that their insistence on sticking to a regime meant their child was missing out. Parents could not identify a way to bring these competing priorities together, as one parent expressed:
There’s the real word and the therapy world . . . you can’t alter it, that’s how it is.
There was a sense that parents believed that therapists did not fully appreciate the demands and conflicts caused by introducing therapy interventions. For example, in replying to a question about how a therapist had reacted to finding out the parent had stopped implementing a particular therapy regime, this parent responded:
If they’re doing their job right they do listen to you and accept it. But you can understand their frustration that they want to improve the legs and so on . . . that’s their world.
Parents described having moments when they recognised that they had become overly zealous about maintaining therapy regimes. As one parent recounted:
You get ‘programmed’ as to why you’re doing it . . . but you want them to have a life as well. It’s a balancing act.
Impact on wider family life
Many parents described the struggle of fitting their child’s therapy programme into everyday family life. For those with more than one child with therapy or other additional needs, this issue was even more acute. All reported that, on occasion, and sometimes more frequently than that, ‘the exercises go out of the window!’.
Parents’ capacities
There was agreement that parents differ in their capacity to take on the delivery of a therapy intervention. Some remarked on the need to protect themselves from over-reaching. As one parent put it:
There’s a balance to be achieved between what you do for child and keeping yourself sane.
Supervision and support
Many parents reported concerns, and sometimes anger, about the level of supervision they received from therapists. These concerns related to whether they were still doing exercises, or other work with the child, in the way that they had been instructed. When the child started school and therapies were being delivered in that setting, parents often expressed confusion about what they should still be doing, if anything. Finally, parents agreed that guidance on what to prioritise would be extremely helpful.
Variation in advice and prescribing
Some parents reported that they had experienced receiving different advice regarding the implementation of a particular technique or exercise, or the way a piece of equipment should be used, or for how long. Parents reported feeling puzzled and confused. In one case, when the use of a standing frame over long periods had been causing a child considerable discomfort, an inconclusive discussion with the physiotherapist left the parent wondering whether even the therapist knew what the appropriate dose or intensity should be. Moreover, having adhered to the therapist’s previous guidance, the parent felt that they had been unknowingly complicit in delivering an intervention that may have caused unnecessary distress to their child.
Children’s responses
Almost all parents reported that their child resisted the implementation of therapy programmes, either routinely or occasionally. This included practising exercises related to motor or speech/communication, splinting and the use of sleep systems. The reasons why children resisted included the fact that the therapy restricted them doing other activities, that it was painful and that it disturbed their sleep. Various ways of managing this were reported, both between parents and on a situation-by-situation basis. Sometimes it led to a treatment being abandoned altogether. In a couple of instances, child mental health professionals had been brought in to support the child’s acceptance of an intervention.
Parents described strategies they developed to overcome these difficulties. For example, with younger children, physiotherapy exercises could be undertaken through play, and with older children this could be done by focusing on what one parent referred to as ‘recreational physio’, such as joining a sports club or team. Parents acknowledged these strategies as a ‘balance’, as using them could mean moving away from the specific exercises suggested by physiotherapists.
Valued therapy practices and approaches
Within the data gathered from parents are some clear themes about the therapy practices and approaches that parents valued. It is clear that parents valued enormously having a ‘good therapist’ and, in some instances, they had worked hard to ensure that their child remained under such a therapist’s care: ‘She (physiotherapist) tries to discharge us, but I don’t let her!’; ‘You fight “tooth and nail” to keep the good therapists!’.
Child-focused approaches
Parents particularly appreciated therapists who clearly appeared to value their child and want the best for them. Parents described a sense of isolation if this was not the case, whether experienced with respect to a particular aspect of their child’s care or to the wider situation:
I think in every area nobody thinks your child’s got potential. Why should our children not be pushed to reach their full potential? It’s like they’re written off and it’s up to you as a parent.
Goals-focused approaches
It was clear in discussions with parents that there was a preference for goals-focused approaches. As we reported in an earlier section, many parents did not report this experience. However, they were clear that they would value ways of working that offered a shared, transparent and structured plan for how their child’s therapy interventions were working towards agreed goals, including systems of review and subsequent adaptation as needed.
Furthermore, within a goals-focused approach, parents wanted the focus to be on higher-level outcomes. Some parents did not feel a longer-term view was in the minds of the therapists working with their child, or that it had certainly not been overtly expressed to parents in those terms. A parent expressed the sentiment in this way: ‘unlike parents, therapists just think about today, not what will benefit my child in the longer term’. This approach was regarded as leading to a focus on functional outcomes, rather than identifying alternative ways and means by which goals related to participation and well-being could be achieved.
Two parents described their situations thus:
We’ve had walkers shoved at us left, right and centre. But this has left my child feeling isolated at school because he couldn’t keep up with other children.
. . . my priority is that my daughter is mobile, regardless of how. I feel it would be better to work on her upper arm strength so she can use a wheelchair. She just needs to get [to places] because she’s got stuff to do.
Many parents stressed the need for greater clarity about the aims of therapy interventions. Some parents observed that they had experienced differences between therapists in terms of where the objectives of therapy were ‘pitched’ or presented to them. For example, one parent commented:
. . . it’s more the OT [occupational therapist] who looks at the overall picture [of participation and independence], the physio is more about specific movements . . .
Within this process, parents did not want resource constraints to limit their children’s aspirations. Some had experience of this. For example, one parent described a situation when their child had identified riding a bicycle as her goal, but instead she was offered a tricycle. The parent interpreted this response as being because ‘. . . that wouldn’t require their [i.e. the therapist’s] input’.
Follow-up and review
As noted in the previous section, but important to explicitly identify, parents consistently spoke of the need for therapy interventions to include systematic processes, of which they were aware, that monitored and responded to a child’s progress. Parents who had accessed private provision often identified this as one of the most valued aspects of using private providers.
Knowledgeable about the child’s condition and therapy options
Parents valued working with therapists who knew about and understood their child’s condition. Some parents of children with conditions other than cerebral palsy expressed concerns that therapists may be transferring practice from their better knowledge of cerebral palsy to their child’s condition without properly understanding the limitations, or consequences, of doing this.
In addition, parents valued feeling well informed about the therapy options available to their child. They found it helpful and reassuring if their child’s therapist had some awareness of alternatives.
Creativity
Some parents reported very positive experiences with therapists who had been willing to ‘think outside the box’ and pursue what might be quite unique approaches or solutions to their child’s therapy needs as an individual. Parents spoke very highly of such experiences.
A holistic, multidisciplinary approach
When parents had experienced therapy provision that was integrated across the therapies and integrated the collective aims of therapy into the school context and curriculum, this was highly valued. As this parent described:
My OT [occupational therapist] and physio communicate . . . they have a joint aim of working towards my child’s freedom and independence, and they are working closely with school on this.
Some parents were clearly frustrated that one element of their child’s needs remained unaddressed. They believed that, without the work and support to develop skills and abilities, or finding alternative ways to enable the child, interventions that focused on other aspects of the child’s impairments would be relatively meaningless and have little impact on overall outcomes. Often during these discussions reference was made to a perceived lack of attention and resources available for speech and communication support. As one parent observed, ‘if my child’s speech and language isn’t there, it means they don’t have the means to communicate with anyone, which then impacts on other areas of their life’.
Parents consistently valued therapists who took a wider interest in the child and family and who were able and prepared to offer, where appropriate, wider advice. Within this, parents welcomed therapists speaking with colleagues in other therapy teams or services to ensure co-ordinated and consistent approaches to the care and management of the child.
Finally, a few parents specifically mentioned the valuable role that therapists could play in supporting their child’s emotional well-being, particularly when the child is sensing their ‘differentness’ to peers.
Working in partnership with parents
Finally, we would note and reiterate material reported earlier in this chapter regarding the way therapists worked with parents, in particular whether or not there was a sense of partnership, respect and shared objectives.
Chapter 6 The active ingredients of therapy interventions: professionals’ views
Introduction
For pharmacologic interventions, the component of the intervention responsible for the therapeutic action is referred to as the ‘active ingredient’. There is increasing recognition of the importance of detailed and accurate reporting of the active ingredients of pharmacologic interventions in reports of evaluations and intervention manuals. 27–29
The concept of an ‘active ingredient’ is also used for non-pharmacologic interventions. However, as McCleary et al. 30 argue, adopting this term for such interventions is not necessarily straightforward. Referred to as complex interventions,31 they may well have one or more of the following features:
-
involve several interacting components
-
require many different behaviours from health-care professionals or participants for successful delivery
-
be aimed at different levels within an organisation
-
be tailored to different contexts or settings. 30
-
In addition, as Boutron et al. 32,33 note, the success of these interventions may well depend on the expertise of the providers.
A recent review comparing reporting of the active ingredients for pharmacologic interventions and non-pharmacologic interventions found it significantly poorer for the latter. The complexity of such interventions, and a lack of understanding or evidence regarding the mechanisms of change, are likely contributors to this. One of the key objectives of this scoping study was to explore stakeholders’ views on the ‘active ingredients’ of physiotherapy, occupational therapy and speech and language therapy for children with neurodisability. We report our findings in this chapter, including study participants’ views on the implications for research of an understanding of the active ingredients of therapy interventions. Before moving on to do so, we briefly discuss three overarching issues: levels of complexity, understandings of the active ingredients of therapies and therapist versus therapy.
Levels of complexity
All interviewees agreed that physiotherapy, occupational therapy and speech and language therapy are complex interventions. It was also argued that because the interventions are being delivered to children, and a diagnosis of neurodisability is present, the level of complexity increases. This was particularly the case when the neurodisabilty resulted in multiple and severe impairments. Four points were made.
-
Parents (and school staff) may also be involved in delivering the therapy.
-
The nature of the child’s impairments means that a single therapist may be delivering a number of interventions.
-
The child’s care and management plan may include other therapies and medical or surgical interventions.
-
The nature of the child’s impairments (e.g. the presence of learning difficulties, or frail health) may moderate or mediate the impact of the active ingredient(s).
Understandings of the active ingredient(s) of therapies
There was consensus among participants that there was limited or questionable understanding of the mechanisms by which therapy interventions effect change:
We need to start thinking clearly conceptually what the active ingredients might be, and making head-to-head comparisons and robustly evaluating them.
I1
We are dogged in therapy by multiple, sometimes not that plausible, hypothesised change mechanisms that are rarely explicitly articulated.
L1
The level of complexity, particularly the fact that a child may receive multiple interventions concurrently that may have shared objectives (especially higher-level outcomes such as participation or quality of life), led to a degree of scepticism among some interviewees about whether was possible to isolate and measure the active ingredient(s) of each intervention a child was receiving:
At some level we won’t ever be able to tease it out, because interventions are complex and lots of other things are happening around the child. The best way to work is multidisciplinary, but to show the contribution of SLT [speech and language therapy] there is very, very difficult. And, in reality, do we even want to do that? Or is it more about showing collectively what’s happening for the child? Those are real tough questions.
R2
It’s difficult to unpick how therapies impact on outcomes because there’s so much going on.
I2
This was the case even for longstanding techniques. The following quotation is on the use of standing frames in physiotherapy:
. . . is it stretching of the legs? Is it the weight bearing? Is it getting children to stand at the same height as their peers? By fixing them so their body’s nice and stable, does it enable them to move their hands better? People also report a benefit in breathing, and bladder and bowel function. There’s all these different ingredients you can measure. And so you may well [need] a series of different outcome measures for each individual child for one intervention.
I2
Therapist versus therapy?
There was widespread agreement that, for physiotherapy, occupational therapy and speech and language therapy, a key reason for an intervention’s complexity was that outcomes could be affected by the therapist, by their techniques, procedures and equipment, or by the wider therapeutic context:
. . . but was the benefit down to the therapy or the therapist? And I think that’s maybe what you’ve got to pull out: is the therapy or the person?
K2
So there’s definitely something about the therapist, and about the skills of the therapist and their passion and their engagement with that child.
T1
For each of these, participants identified a number of features regarded as active ingredients of a therapy intervention for a child with neurodisability. One way of presenting or understanding this is set out in Box 4.
-
The overall approach.
-
Schools of thought.
-
Techniques, procedures and/or equipment provided.
What a therapist brings:
-
knowledge
-
skills.
What a therapist does:
-
clinical decision-making
-
ongoing assessment and review
-
physical contact
-
creating a therapeutic team and therapeutic environment
-
the work with the family:
-
psychosocial support
-
‘activating’ the family to the intervention.
-
-
The capacity of the wider ‘therapeutic team’.
-
Setting.
-
Access to equipment.
-
Space to use equipment.
-
Access to clinical expertise.
Box 4 specifies three ‘sources’ of active ingredients identified by study participants: the therapy, the therapist and the wider therapeutic context. Although displayed as discrete entities, it is critical to note that the interviewees believed that, and described how, these components interacted and inter-related, an issue clearly and consistently identified in writings about the active ingredients of complex, non-pharmacological interventions. Finally, we would note that this will not be an exhaustive list: it is simply the one generated from our interviews with participants.
The following sections of this chapter offer further detail on each of these sources of active ingredient within therapy interventions for children with neurodisability. A final section reports study participants’ accounts of the impact of the active ingredients on ‘secondary outcomes’.
The therapy
As reported in Chapter 4, therapy interventions can be conceptualised as having three components:
-
the overall approach
-
schools of thought
-
techniques, procedures and/or equipment used or provided.
Overall approach and schools of thought
To a greater and lesser degree, these components intersect, with one informing, or influencing, the other. As described in Chapter 4, the views and practices regarding the overall approach to therapy interventions and schools of thought influence perceived objectives of therapy and decisions regarding the techniques, procedures and/or equipment used. The overall approach taken was viewed as being one of the ‘active ingredients’ of a therapy intervention. Indeed, some believed that this had a stronger impact on outcomes than the actual techniques used:
Child-centred goal setting is probably one of the many active ingredients of therapy, but there is as yet, little evidence to support this.
K1
The techniques, procedures and/or equipment used or provided
The intervention itself – and the duration and intensity of its delivery – was consistently identified as an active ingredient in the impact that physiotherapy, occupational therapy and speech and language therapy had on a child’s outcomes. It was noted, however, that this was a complex area because of the potentially eclectic nature of a therapist’s work with a child:
Therapists take elements of different interventions so it becomes such a mish-mash. And you don’t know what is what and what works . . . so you’re doing a bit of neurodevelopmental therapy and postural management and sensory integration and goal orientation. Research is needed to unpick this mix and identify the active ingredients of interventions.
Q1
Explanations were sometimes offered of the mechanism (anatomical, physiological or neurological) by which a technique or procedure had an impact on body structure or function.
In some instances, a theory and its associated evidence were described as informing the development of a particular technique, for example wider theories of how people learn motor or communication skills, physical development, exercise and fitness. For others, a ‘theory’ had been developed to offer a rationale for a particular technique or procedure. It is important to note, however, that the veracity of these theories had not necessarily been tested.
Intervention integrity
The degree to which an intervention is delivered in the way it should be delivered was also viewed as, potentially, having a role in the outcomes achieved from therapy. As we describe in a later section (see The therapeutic context), other individuals are usually involved in delivering an intervention. Furthermore, some interviewees noted that therapists may not be adequately trained in, or have complete understanding of, the techniques they use.
The therapist
Active ingredients were identified in both the roles a therapist assumed and the skills and knowledge they brought to those roles.
What the therapist brings to a therapy intervention
Knowledge
The therapist’s knowledge and understanding of the child’s condition and intervention options were regarded as two of the foundational aspects of the way a therapist had an impact on outcomes. The influence of this knowledge on clinical decision-making was regarded as a key mechanism by which knowledge affected outcomes.
Skills
A number of distinct skills were identified as active ingredients in therapy interventions. Some were viewed as able to be acquired through training and experience. Others spanned learned skills and personality characteristics. Together they influenced how a therapist worked. The following list, not necessarily comprehensive, demonstrates the broad range of skills that interviewees identified as active ingredients of a therapy intervention:
-
being sensitive; having the ability to empathise
-
able to communicate effectively with the child, family and others involved in intervention delivery
-
able to train others in techniques, procedures and/or use of equipment
-
able to motivate the child and/or wider ‘therapeutic team’ (e.g. parents and school staff) or negotiate ways in which intervention is delivered:Q1F2
Some therapists are better than others at getting the kids to respond to them.
. . . negotiation . . . particularly when children start to disengage and refuse to wear splints, etc.
-
able to judge when to intervene or adapt therapy and when to allow further time for child to achieve task or outcome
-
able to integrate intervention programme into everyday life and activities:Q2
You can set up switches to give a child with severe CP [cerebral palsy] the opportunity to experience environmental control, but unless you can find something they are interested in they’re not going to be motivated to do the switching and so won’t learn anything.
What the therapist does within an intervention
Box 4 also sets out a number of active ingredients located within the roles a therapist assumes in the context of an intervention. These include:
-
clinical decision-making
-
ongoing assessment and review
-
physical contact
-
the work with the family
-
creating a ‘therapeutic team’ and therapeutic environment.
We describe each of these in turn.
Clinical decision-making
Study participants believed that a therapist’s choice of procedures or techniques, and their decisions about the mode of delivery, had an impact on outcomes:
It’s having the right tools, for the right child, at the right time, with the right people surrounding them.
T2
A number of interviewees highlighted the skills involved when a therapist selected an intervention from their available ‘toolbox’ (see Chapter 4):
It is the clinical reasoning behind using that piece of equipment that makes the difference . . . it’s the thought processes and reasoning that goes into choosing to use a particular piece of equipment. It’s the knowing of the reasons why they are going to use it and how that is really impacting on outcomes.
K2
Many interviewees emphasised the contribution of clinical experience to this decision-making process, be that the therapist’s own, from the wider team or through supervision from a senior practitioner.
It is important to note here that many interviewees identified a number of factors, some of which were outside their influence and did not relate to the presenting clinical need, that affected their decisions about which intervention to use. These included parents’ and/or school staff’s capacity to partner in the delivery of the intervention, space or housing issues (particularly when equipment was involved), other presenting clinical or functional issues, and the equipment, interventions and resources the therapist had available to them, or was permitted to the deliver. Some of these factors also influenced a therapist’s decisions about when to intervene:
There is something about readiness for intervention. It’s not always the right time for a child if they’ve got other things going on, such as kidney dialysis which is about keeping the child alive. The hierarchy of need kicks in when you’ve got families with complex lives and they’re being evicted [from their home], or a parent’s in prison or something. So it’s about being sensitive to that and timing an intervention in the right way where it can be most effective.
V2
Ongoing assessment and review
Many interviewees drew attention to the way in which therapists continually observed and assessed a child, and how they tailored the intervention in response to that analysis. Within occupational therapy, for example, the term ‘dynamic performance analysis’ is used to describe this. There was a general belief that that this element of a therapist’s intervention with a child or family may be difficult to capture, or measure.
One interviewee described how, as part of this process, therapists were continually looking for the ‘nudge point’: the point at which it was necessary to push the child to the next stage in acquiring a particular skill or function. It was noted that this also needed to be taught to those who worked with, or supported, the child more frequently.
Physical contact
One interviewee was keen to draw attention to the potential, but poorly understood, role of touch as an active ingredient in a therapy intervention.
The work with the family
A dominant theme in many interviewees’ views on the ‘active ingredients’ of therapy interventions was the ‘work’ the therapists did with family. This was particularly highlighted when children with severe and complex needs were discussed, and when therapists were directly involved with families over a long time, and from the point of diagnosis onwards:
[The therapies are] absolutely crucial . . . and when we see sometimes for whatever reason families are referred late, I see the difference both in the way families are able to positively adjust their mind and move forward, as well as in the outcomes for the children: the two go hand in hand.
Z1
. . . there will be stuff in those interventions that will be exerting an effect, but . . . we underplay the importance of interactions of communication and relationship, and we’re more obsessed with the technical expertise.
L1
If you don’t have a relationship, and a trust and belief that what you are embarking upon is going to be effective, then you’re not going to get anywhere with the family or young person.
T2
This ‘work’ with families can be split into two main areas: psychosocial/emotional support and securing positive and effective engagement within the intervention (we discuss both in detail in the following sections). The success of the latter was seen, to a greater or lesser degree, as dependent on the former. Some interviews located this work within wider theory of behaviour change interventions, for example increasing a child’s motivation to practise an activity, or enabling a parent to feel confident to carry out a procedure. For example, one participant referred to the behaviour change technique taxonomy34 as a very useful framework through which to understand the components of occupational therapy.
Psychosocial/emotional support
The first area of work with families described by interviewees concerned the provision of psychosocial or emotional support. Sometimes this was presented as a consequence of prolonged contact and engagement with a family:
A key role of the therapist is to enable the parent to be an effective therapist, and parents can only do that if they’re feeling ‘buoyant’.
V1
A lot of therapists do an awful lot more than just therapy. The family do see them as a friend, a confider, that kind of thing.
W2
Others believed that providing psychosocial or emotional support was integral to their role and critical to the success of the therapy intervention and the work they did with families in terms of ‘activating’ the family to the intervention (see the following section). When this position was taken, reference was made particularly to work done with families on acceptance of and adjustment to the diagnosis, nurturing realistic but aspirational goals for the child, cultivating parents’ sense of confidence and efficacy as ‘co-therapists’, and mitigating a sense of social isolation.
‘Activating’ the family to the intervention
‘Activating families’ and ‘dynamic engagement’ were terms used to described an ongoing process of ‘actively engaging and collaborating with the child and the parent throughout’:
If families feel rail-roaded into an intervention, you’re not going to get the outcome you’re after.
J1
Work in this domain might also include helping families to identify goals for the child. When this role was described, reference was often made to the fact that the parents and/or the child may be adjusting to the news of a diagnosis or dealing with the aftermath of a traumatic injury:
. . . in which you are taking the family with you as an OT, helping them to elicit goals in face of adversity and grief, which sometimes you are, early on.
S1
This process was regarded not only in terms of facilitating and supporting the families’ ‘buy-in’ to the therapeutic prescription, but also as key to informing decisions about the prescription itself. For example, interventions that are regarded as ‘dose dependent’, with high-intensity input from a parent required, would not be selected for a family who had been assessed as not having the resources or capacity to deliver it:
For me, the ‘intervention’ is secondary, because if you haven’t really engaged, if you have put yourself there . . . It’s actually one of the most exhausting parts of being a therapist . . . active listening and taking in where the family is at, where the child is at. Is there a mismatch between the priorities of the young person and their parents? What’s going on there? You can’t prescribe an intervention until you’ve got that kind of thing. And the art of therapy is getting there as quickly as you can.
J1
Finally, it is important to note that different services’ approaches to staffing, and/or time allocated to families, were identified as affecting the effectiveness of therapists’ work with families (e.g. a lack of consistency of therapist and reduced duration and/or frequency of contact). In addition, some interviewees noted that therapists’ ability to engage in emotional work was threatened by work-related stress, which some participants believed to be an issue of increasing concern.
Creating a ‘therapeutic team’ and therapeutic environment
Many interviewees highlighted that their role as therapists could be conceived as ‘indirect’, and that interventions were principally delivered by others:
We actually don’t do a lot with children. We aren’t the ones who are going to make a difference. It is the people that are with that child every day at home and in an educational or nursery environment that are really going to be the ones that are implementing the techniques and delivering it.
U2
Thus, a key element of their role was the education and training of others, for example parents, Early Years workers, teachers and teaching assistants. These individuals needed to be ‘upskilled’ in a number of ways:
-
the understanding of the child’s impairment
-
the specifics of the therapy intervention and the rationale for its choice
-
how to embed the intervention across everyday activities
-
their role in helping the child
-
being able to identify when the child is ready to move on to the next stage of rehabilitation.
You can spot the families that have had some type of training from the way they talk about their children and how they describe their skills. And the parents say that after [a training course] they feel so much more skilled, they are much more informed and able to argue their children’s cases with professionals. [Then] they can enter into shared decision-making and shared therapy planning for them.
N2
[it’s also] the stuff going on between the therapist and, say, school staff. Because the therapist will often work through the classroom staff and train them so that the child is immersed in the milieu that is encouraging their development in a range of domains.
W1
A further element of supporting an effective ‘therapeutic team’ was getting ‘buy-in’ and commitment to the intervention from others and/or the organisations in which they were based. This was seen as essential for some children if optimal outcomes were to be achieved:
We know [of situations] where the child has got a communication aid [but] that it’s on the back of the wheelchair and not being used. And earlier today I came across [a situation where] a new teaching assistant was supporting a child with dysphagia and a risky swallow who was not using the child’s feeding mat or specialist cutlery because the message had not been passed on.
V2
Some expressed the opinion that there was minimal research and understanding of homes (and classrooms) as therapeutic environments, and the features of these environments – physical and social/relational – that mediate or moderate intervention effectiveness.
The therapeutic context
The capacity of the wider ‘therapeutic team’
The issue of capacity of both schools and families to fulfil their role in implementing a therapy prescription was raised many times. It was viewed as having the potential to play a significant role in the effectiveness of a therapy intervention. School staff undertaking this role (usually teaching assistants) may not be supported – in terms of the time allocated to the role, or the extent to which the school accommodates or integrates the child’s therapy requirements into the curriculum or usual practices. Participants reported that parents’ capacity to accept, understand and take on the role of supporting therapy programme delivery varied enormously (and, as noted earlier, itself influenced clinical decision-making):
Some families are more able than others, for different reasons, [to deliver interventions].
K1
Interviewees also described how a family’s capacity, including their levels of motivation, may change over time as a result of other events and situations. Thus, this was not necessarily a stable or predictable element of an intervention.
Setting
The setting of the intervention – whether a clinic or the home/community– was regarded as an active ingredient. Setting emerged as an important aspect of a therapy intervention in discussions about the shift towards participation-focused outcomes. This is because such outcomes are naturally focused on the everyday lives of children and the settings in which they find themselves, or want to participate.
The importance of the therapy setting was particularly voiced by physiotherapists. This may be because occupational therapists more typically work in home and community settings, and speech and language therapy is often introduced only during the nursery or early-school years. Traditionally, however, physiotherapy (especially in the preschool years) has been delivered in clinical settings. However, in seeking to adopt participation/goals-focused approaches, physiotherapists believed that, to be most effective, they needed to work with children and families in their everyday settings. Some reported that they were constrained in the extent to which they were permitted do this:
There’s quite a push from the manager’s point of view for us to do more stuff here where we work and less out in the community. To cut down on time and cost . . . [but] as a therapist I believe that therapy should take place where the child’s accessing or participating in a particular activity. I sometimes find it quite hard to argue that.
C1
Access to equipment
Study participants based in specialist services (residential schools or tertiary centres) often noted the value of that setting in terms of offering access to (specialist) equipment that supported positive outcomes. On a different note, it was reported that children might not have access to their equipment (or be able to transport it) in all of the different places and settings where they spent their time (e.g. home, school, nursery, respite/short breaks).
Space to use equipment
Some interviewees noted that a family’s housing situation, particularly in terms of space and levels of access, may influence the options available to them for equipment to be provided or installed.
Access to clinical expertise
It was acknowledged that some of a therapist’s skill set is acquired only through clinical experience. Many participants noted that senior posts had been or were being lost across therapy services owing to strategic decisions by NHS trusts. Thus, clinical experience and supervision was being removed from therapy teams, or had been made more difficult to access. This was an issue of grave concern among some interviewees:
I actually think they are diluting the effectiveness of the intervention by trying to save money by having less skilled staff . . . it’s understandable, but short-sighted. You need to have that level of expertise on a team in order to get the best outcomes.
X2
What they are drawing on there is lots of knowledge from other children they’ve seen, their knowledge about the theory, and their clinical experience and practice.
O2
Active ingredients having an impact on secondary outcomes
A final theme to report here was participants’ belief that there could be secondary outcomes of therapy interventions, in other words those outcomes not explicitly identified as the objective or focus of an intervention. Thus, either directly or indirectly, therapy interventions could further contribute to children’s, or parents’, outcomes.
Positive outcomes associated with mode of delivery
One interviewee observed that physical interventions delivered in hobby/skill acquisition groups (e.g. upper-limb therapy work delivered via magic or circus skills training camps) and/or involve participating in fun and enjoyable activities may result in secondary outcomes. Those outcomes identified included increased confidence, increased self-esteem and increased social networks:
The therapy programme is not supposed to be doing that, it’s supposed to be about hand function. [But], just by doing the activities and meeting other children, you’ve got the secondary impact of all the cognitive and social development things going on.
I2
Access to other services
It was also pointed out that, through signposting or referral to other services or resources, therapists may support wider outcomes being achieved, or have an impact on outcomes directly. This applied to both the child (e.g. through contributing to educational assessment processes; supporting referral to wheelchair services) and the parent (e.g. signposting to a local support group).
Chapter 7 Therapy outcomes
Introduction
One of the objectives of this scoping study commissioned by NIHR was to understand the ways that therapy outcomes are currently conceived and, specifically, whether or not participation is a meaningful outcome. In addition, it sought to identify the other outcomes that evaluations of therapy interventions may need to consider.
We report findings relevant to these study objectives in this chapter. We begin by briefly reminding the reader of the core constructs of the ICF outcomes framework. Next, we move on to reporting study participants’ understandings of the concept of participation. We follow this with an account of interviewees’ views and beliefs regarding participation as an appropriate outcome measure to use when evaluating physiotherapy, occupational therapy and speech and language therapy interventions for children with neurodisability. After this, we report on other outcomes that participants believed should be considered when evaluating therapy interventions. The final sections of this chapter explore issues of outcome measurement, including views about the adequacy of existing measures, goal attainment scaling and issues related to deciding follow-up time-points.
The International Classification of Functioning, Disability and Health outcomes framework
As reported in Chapter 4, in 2002 the WHO proposed a conceptual model of disability that identified three outcome domains: body structure and function, activity, and participation. 16 The WHO definitions of these concepts are:
-
body functions – physiological functions of body systems (including psychological functions)
-
body structures – anatomical parts of the body such as organs, limbs and their components
-
activity – the execution of a task or action by an individual
-
participation – the involvement in a life situation.
In the UK, this framework has been widely adopted and implemented within physiotherapy, occupational therapy and speech and language therapy, and this was evident through study participants’ consistent references to these concepts. However, as also reported in Chapter 4, the understandings of these concepts were not consistent, particularly with respect to ‘participation’ and the differences between ‘activity’ and ‘participation’.
Setting this issue aside for a moment, within this framework study participants identified three possible objectives of therapy interventions:
-
progress or improvement
-
maintenance or prevention of deterioration
-
recovery to previous levels of function, activities and participation.
Understandings of the concept of participation
A core feature of our interviews with study participants was an exploration of their views regarding participation as a legitimate, or appropriate, outcome by which to assess the impact of therapy interventions. In the majority of interviews, participation was spontaneously identified as an ultimate objective of therapy interventions. The move from an exclusive focus on functional, or clinical, outcomes was welcomed across all of the practitioner groups represented in this study:
One of the best things in the last ten to fifteen years has been the push towards the focus on what are the needs of the child in terms of outcomes, rather than specific clinical outcomes.
X1
It’s a bit of a shift in terms of whether [intervening on] ‘body structure and function’ is meaningful in its own right, or whether it’s actually an intervention which enables the child to participate in something.
F1
The ICF model of participation . . . gets across a holistic view of the child and their context. It’s a very useful model for thinking about that and moving away from the medical model.
O2
However, the way this concept of participation was defined, or interpreted, within the context of delivering physiotherapy, occupational therapy or speech and language therapy, varied between participants and across all three professions. Furthermore, some participants reported that it was also the case that other terms were being used to refer to what was, ostensibly, the same concept:
I think that participation would be a fairly strong shared outcome in occupational therapy. I think there would be variance about how much ownership people take of that outcome, and they might call it other things, but ultimately it’s what most of us are interested in . . . that’s what we’re about, children doing stuff in real life.
L1
Others described it as ‘vague’ or poorly defined, and that its interpretation, or points of emphasis, differed between theoretical and disciplinary positions:
From the medical and ICF perspective, it is about involvement in meaningful activity in daily life. From a social science perspective, it is much more around choice and having the opportunity to make a choice about what is meaningful to you. But children haven’t necessarily had enough life experience to know what choices are available. So it’s often the parents that know about things and give the child the opportunity to try it, and if they like it then to carry on with that activity.
F2
The notion of participation as a unidimensional concept, or something that can be captured using a single measure, was challenged by some interviewees, who argued that more work was needed to define, or specify, participation and participation outcomes. The absence of a conceptual framework was seen as contributing to confusion among practitioners about what constitutes participation. In addition, this was regarded as a key impediment to the use of participation as an outcome indicator:
Participation is a really complex issue.
O2
When we asked study participants to define participation, the concepts spontaneously elicited included:
-
engagement with their community
-
engagement with broader society
-
social experiences, relationships and social networks
-
employment
-
attendance at school and accessing the school curriculum
-
independence (in mobility, communication, self-care, etc.)
-
independence (from family)
-
having (and expressing) choice
-
full engagement in life situations
-
self-determination
-
some kind of engagement with someone else
-
self-expression
-
communication/taking part in communication interactions with others.
Within these concepts, some interviewees emphasised that the core feature of participation was having the opportunity to take part in activities, experiences and relationships, as opposed to taking part. The ease by which participation was achieved was also highlighted as an important, but perhaps under-recognised, facet:
. . . having the opportunity to explore or involve themselves in developmentally appropriate tasks and activities within their homes, communities and educational placements.
U1
Alternative understandings
Some interviewees used the ICF concepts of ‘activity’ and ‘participation’ interchangeably. Others queried whether these were distinct concepts:
There’s always a discussion about what’s an activity and what’s participation? . . . and how do you separate the two.
O2
Among some, the concept of participation appeared to be defined, to a greater or lesser extent, in terms of engagement with the mainstream world, and typical development. This understanding appeared to contribute to a belief that the concept of participation did not ‘work’ for children with severe or complex impairments, and had been inappropriately applied in these instances:
For me, with complex children, goals are often around being comfortable during the day and when they sleep so that they can participate in their education. Whereas, working with ‘mild to moderate’ children, it is about participation. For the child ‘to be part of normal society’, joining in activities, looking after themselves and having as much independence as possible.
F1
Concerns were expressed that (mistakenly) aligning the concept of participation with notions of ‘normality’ and ‘mainstream’ life could mean that therapy interventions had unhelpful objectives, and may incorrectly appear to be effective:
You might suggest that because they are attending a mainstream school they are participating as typically developing children. But actually sometimes you might find that a child finds it easier to interact in different educational provision [where] they aren’t as different.
I2
So sometimes participation goes along with inclusion, and everyone thinks they need to make sure little Jonny is going to a group where all the other children don’t have additional needs. But actually a lot of families like it when there are other children with similar difficulties. Families find it very supportive for themselves, and often their children [appear to] really enjoy it as well.
Z1
The need for individualistic, child-centred approaches to defining participation
The argument was made that it is critical not to make assumptions or be prescriptive about what participation is, or represents, for an individual child. The importance of finding out children’s own goals and aspirations was seen as a central and, indeed, fundamental requirement when defining participation outcomes. It was, however, acknowledged as highly challenging among some populations.
Does the concept work for all groups of children with neurodisability and for all therapy interventions?
Leading on from the previous point, some interviewees expressed the view that further work was required on what participation means, and what participation outcomes are, for certain populations. This included neonates and very young children, children with disordered states of consciousness, children with profound and multiple disabilities, and typically developing children with a recently sustained severe brain injury.
Participation as an outcome indicator for therapy interventions?
Although, broadly, there was a consensus that any therapy intervention should be grounded in the objective of participation, concerns were voiced about whether, or how, it could be operationalised as a measure of intervention effectiveness.
A common and consistent theme in many interviews was the notion that therapy is a ‘cog in the wheel’ and that its role in supporting participation may be indirect. One paediatrician asserted that ‘all our goals should be targeted towards participation . . . ’, and another described participation as ‘the overall aspirational outcome’. There is an implicit meaning in these words: that ‘participation’ is the point towards which all interventions with children with neurodisability should be navigating. It also suggests a view that participation is the end point of a collective effort, rather than something achieved by a single intervention. Among some study participants, this raised questions or concerns about the (universal) appropriateness of participation as an outcome indicator for therapy interventions. The following arguments were made to support this position.
-
A specific therapy intervention, or therapy discipline, may not be able to resolve issues of participation. The shift to multitherapy and integrated teams (see Chapter 3) working to the same goals is testament to the multifaceted approach required to support participation.
-
Therapies are just one of a number of health, educational, social care and housing interventions a child with neurodisability may be receiving:I1J1
We [as therapists] need to accept that we’re not going to come up with all-singing, all-dancing interventions for participation in all its aspects. For example, a child wants to take part in sport. Part of that is getting dressed in their kit. A physio will address posture and stability (and can measure that), but for the OT the focus is on the outcome of whether the child can take part in sport . . . and then it can be difficult to pin down the extent of the OT’s specific contribution.
Participation keeps the focus on the outcomes important for the child and family, regardless of who precisely did what to achieve them: the therapist, the doctor, the therapy assistant. While a therapist may not be able to say that they have enabled a child to achieve these things, they could pinpoint specific contributions – for example, the child bathing unaided, or able to get up and down stairs unaided. [And] these things mean something because they reduce carer burden and enable the child’s participation.
-
At the other end of the spectrum, questions were raised about the appropriateness of participation as an indicator of intervention effectiveness for a child referred to a therapist with a mild and specific physical impairment/functional difficulty.
-
A number of factors have an impact on participation, not all of which are under the control, or within the remit, of therapists. For example, special education settings, although having many benefits, can act as a significant barrier to participation in mainstream life and activities; other factors include parental beliefs and values, a family’s access to material resources, and opportunities and facilities available in the child’s local community.
Many of our ‘clinical academic’ interviewees expressed concern that requiring participation to be the main, or only, outcome of intervention studies would be incorrect. It would also be counterproductive, leading to the exclusion from future research of therapy interventions perceived as having a direct, or more significant, effect on other outcome domains:
We need to be more modest about the studies we are doing and actually, paradoxically, through that we will have more impact.
I1
However, it is also important to note that the concerns reported above arise from interviewees’ understandings, or definitions, of participation. When the concept was perceived as higher-level/global or longer-term outcome, its appropriateness as an outcome indicator was questioned. If, however, interviewees argued that it could (also) be conceptualised as relevant to particular times, setting or activities, then the notion of participation as an appropriate outcome measure was more meaningful and acceptable.
Operationalising participation as an outcome indicator
Concerns
A number of key concerns were raised about operationalising participation as an outcome measure in evaluations of therapy interventions. First, interviewees emphasised the importance of self-reported outcomes, which were regarded as highly challenging for some populations:
So measuring true participation can’t be kind of proxy. You’ve actually got to ask the children . . . and I don’t know how it’s best to do that.
I2
Second, the individualised nature of participation – replicated in goals-focused approaches to therapy interventions – was regarded as sitting uncomfortably with standardised measures. (We discuss the option of goal attainment scaling methods of outcome measurement later in this chapter.)
Third, capturing outcomes over the longer term was frequently regarded as an essential element of any programme of work evaluating therapy interventions, particularly, but not only, if participation was chosen as the primary outcome:
What would be amazing would be to have studies going over children’s lifetimes and to be able to say, for this generation: what does it look like? For example, if we do some work on participation when they’re 6, does it have benefits when they are teenagers?
S1
There were a number of reasons for this stance: the benefits of an intervention may take time to materialise, may be dependent on other changes happening in the child’s life or may require the child to reach a particular developmental stage or age:
The skills they learn in their early childhood should be equipping them for school, and be building blocks for the future. The children who have effective intervention early on should, theoretically, do better than those who don’t. But, to do that, you have to look several years down the line.
N2
It was noted that longer-term follow-up points may run counter to some models of research funding.
Finally, and with respect to particular populations (e.g. neonates and children in minimally conscious states), questions were raised about whether or not participation was an appropriate objective in the early stages of a treatment trajectory.
Perceived opportunities
On the other hand, some interviewees noted that using participation as the primary outcome usefully forces a particular type of research question. For example, which is more effective in achieving participation: a powered wheelchair or body structure and function interventions (which seek to develop child’s own mobility)? Thus, the focus is lifted away from questions about the type and/or dose of structure and function interventions that best support a child becoming independently mobile, and instead is given to comparing the very different means by which this might be achieved.
Methods
One consistently expressed view was that the measurement or assessment of participation outcomes required both quantitative and qualitative research methods:
You’ve got an element of quantitative and qualitative research. You’ve got to have something that you can genuinely hang information on. But the qualitative side of things is as important in many ways.
X1
In addition, many of the participants who had direct experience of leading or being involved in research noted the importance of having realistic outcome measures in terms of the time demands on families and professionals:
We don’t want death by questionnaire. They need to be fun and friendly and easy to do.
W1
Other outcomes relevant to investigating the impacts of interventions
When asked about therapy outcomes, the majority of study participants spontaneously mentioned outcomes other than participation. As reported above, although there was general ‘buy-in’ to participation being the core or ultimate objective of any intervention, interviewees were often keen to stress the importance of other outcomes when assessing the impact of interventions, or intervention effectiveness. These outcomes were often regarded as, potentially, less problematic in terms of their (quantitative) measurement. In addition, when to measure these outcomes was typically seen as less problematic, with short- and longer-term points being both appropriate and important. Importantly, all were regarded as intermediate outcomes to the overarching outcome of participation.
Body structure, functioning and activities
It was clear that the majority of study participants believed that outcomes related to the other ICF constructs of body structure and functioning, and activities, remained salient and should not be abandoned: ‘You have to think across the breadth of the ICF’:
Looking at the therapist who is working on stopping a joint contracture, this may not make any difference to the child’s life. [But] it may reduce pain around the joint, which is crucial . . . and [now] this same child isn’t in pain and has a few centimetres’ movement round the joint. [But] this doesn’t mean the child can then go to the playground and play a game. Whereas, if the therapist helps the same child use a trike, then the child can get over to the other side of the playground and have the opportunity to play.
U1
One interviewee referred to the stance that participation should be the only identified objective of any therapy interventions as a case of the ‘pendulum swinging too far’; it was believed to have led to a dangerous imbalance between what was understood as therapy and reference to body structure and function being seen as ‘taboo’. Indeed, there was agreement among many participants that when a therapy intervention was (appropriately) directed at a specific impairment of body structure/functioning (e.g. pain, cardiovascular fitness or muscle tone) or activity (e.g. handwriting), measuring outcomes in these terms could be more appropriate and legitimate, and certainly when evaluating outcomes in the shorter term.
Parent-level outcomes
All of our study participants talked about children in the context of a family, and the discussion was sometimes as much about the work therapists did with parents as about the work they did with the child. This was particularly the case when a child’s physical functioning was severely impaired and ‘recovery’ (or a return to previous levels of functioning) was not an appropriate outcome.
Parental well-being was the global outcome that interviewees typically identified as the most salient in terms of capturing the impacts of a therapist’s involvement with a family. This was usually explained as being the consequence of a number of intermediate outcomes, all of which therapists identified as objectives that they might work towards with a child and their family. These outcomes included:
-
adjustment to the child’s diagnosis or impairment
-
having appropriate, but aspirational, expectations for their child
-
knowledge and understanding of their child’s condition
-
perceived emotional and information support needs being met
-
understanding of the alternative ways to support their child achieving their goals, which may not follow the more traditional approach of intensive work on body structure and function
-
feeling comfortable and sufficiently skilled: these constructs, which capture notions of self-management, were discussed both in terms of a general sense of confidence as the mother or father of a child with neurodisability, and with respect to the work they did as parents to support their child’s development, functioning and participation in the context of physical (and sometimes learning) impairment:
A key role of the therapist is to enable the parent to be an effective therapist, and parents can only do that if they’re feeling ‘buoyant’. Therapists can help parents take pleasure in their child . . . to help parents see and celebrate the progress they can make.
V1
We often see children with CP [cerebral palsy], for example, who are GMS [gross motor skills] level 4 or 5, but the family are still working on goals around standing or walking and things like that. You often need an experienced positional therapist to say actually these [other goals] are the right things we should be working on, and guide the families in that sense. So they are very integral in setting the right outcome, the right goals, for families.
Y1
Importantly, interviewees often expressed their belief that parents’ outcomes moderated, or mediated, children’s outcomes:
Children’s physical mobility does impact on their participation and life choices, but as important is the family’s attitude to their child and what limitations they presume on that child.
V1
Child-level outcomes
In addition to body structure and function, activity and participation outcomes, constructs regarded as relevant domains for the evaluation of physiotherapy, occupational therapy and speech and language therapy in terms of children’s outcomes included emotional well-being, quality of life, acceptance of impairment and engagement with therapy. It should be noted that, during our discussions about outcomes, interviewees dwelt or expanded less on these other child outcomes. It is our view that this may reflect the confusion around what participation is, and is not, with the assumption being that, having discussed notions of children’s participation quite widely [see Chapter 6, Understandings of the active ingredient(s) of therapies], their focus shifted to parent-level outcomes.
Outcome measures
Work to identify/develop robust outcome measures was a common theme in interviewees’ discussions about research priorities. There was a belief that measures were needed for both short- and longer-term outcomes. The latter were regarded as particularly crucial when, if appropriate, a study was looking at more global outcomes, such as participation:
It’s relatively easy to measure just the child’s ‘deficit outcomes’ [e.g. a change in degree of body movement], but much more difficult to measure how a child is participating in play or life in general.
N1
That said, some interviewees referred to outcome tools or measures that they had used, for example the measure of participation developed by the SPARCLE (Study of Participation of Children with Cerebral Palsy Living in Europe) project,35 and, with respect to speech and language therapists, reference was frequently made to the Therapy Outcome Measure. 36 This was the measure chosen by the RCSLT in an ongoing project to standardise outcomes data collection across the profession.
The challenges, but imperativeness, of creating outcome measures that are robust and suitable for use with children and young people with complex needs were repeatedly raised:
We need outcome measures that are fit for purpose for the most complex disabling conditions, where the child is totally dependent on others for everything but can still enjoy a quality of life. So I think we need urgently to have tools that can celebrate enjoyment and sensory experiences, and those very small steps of achievement that families recognise.
W1
Some interviewees felt that this was a high priority in terms of future research. This was based on concerns that, if not available, evaluation of interventions within this population would not happen. This carried a risk of diverting services/resources away from this population owing to a lack of evidence on the impact of therapy interventions.
Many interviewees expressed concern that participation may come to be regarded as the only outcome to be measured. There was widespread belief that, aside from the conceptual or definitional issues associated with this term, participation alone is not adequate. Child, parent and family well-being, quality of life, indicators of social inclusion, parenting confidence, and mental and emotional well-being were all constructs with which study participants identified. In addition, as we noted in Chapter 6, there was some degree of consensus that outcomes related to body structure and function, pain, skills and abilities were also important and relevant. Depending on the intervention objectives, the follow-up points and the wider context of an intervention, these may sometimes be the primary outcomes, and at other times be more appropriately regarded as intermediate outcomes.
Many interviewees stressed the critical importance of holding children’s, young people’s and parents’ views central to any outcome measure development work:
We need better outcome measurement tools that are fitted to the outcomes that matter to children and young people, rather than what the therapist necessarily thinks is important.
W1
Goal attainment scaling
Goal attainment scaling methodologies were viewed as having considerable potential as a method for assessing and measuring therapy outcomes. The main strengths of this approach identified by study participants were twofold.
-
It addressed the need not to be prescriptive about, or assume, what participation is.
-
It was regarded as overcoming the enormous heterogeneity within the population of children with neurodisability, and the wide-ranging nature of therapy interventions in terms of their focus and duration.
A caveat was made, however, with regard to its use. If the setting of goals was led by the child or their family, this could risk over- or underestimating the expectations for a child. The importance of skilled work by the therapist in identifying appropriately aspirational goals was therefore stressed.
Taking a goals-focused approach to intervention research was identified as offering the opportunity for taking a different approach, in which study populations are defined not in terms of diagnosis or impairment, but by the goal they want to achieve. Finally, the approach was regarded as having a potentially useful role in enabling the establishment of routine outcome measurement practices across the therapies.
Follow-up points
Finally, in terms of measuring and evaluating outcomes, participants highlighted the importance of identifying appropriate follow-up points. Intervention objectives, and hypothesised mechanisms of change, were regarded as important steers in decisions regarding this.
Interviewees stressed that assumptions could not be made that, for an intervention, the same follow-up point(s) should be used across all studies. The nature of the population may influence when changes in outcomes are likely to be observed. For example, it was noted that for some children (and those with complex disabilities were highlighted here) change happens more slowly than for other groups. Finally, it was noted that the achievement of some outcomes (e.g. independent self-care, employment) may be dependent on the age, or developmental stage, of the child. The argument was made, therefore, that all of these factors need to be taken into account on a study-by-study basis when deciding follow-up points.
Chapter 8 The research environment
Introduction
In this chapter we report on data from professional participants’ interviews that provide insights into what we have termed ‘the research environment’ within the physiotherapy, occupational therapy and speech and language therapy professions. First, we present the professional participants’ opinions on the current state of the research evidence and its perceived uses. We then go on to report views about evidence-based practice and the place of evaluation research within the therapies. Finally we describe aspects of research infrastructure and research capacity: first by exploring participants’ accounts of engaging directly in research, and then by looking at the ways in which they access evidence, and the barriers encountered.
The current state of the research evidence and its perceived uses
It came as no surprise to the professionals taking part in the study that the JLA research priority-setting exercise for children with neurodisability identified evidence of the effectiveness of therapy interventions as its top priority. Most described an almost complete lack of high-quality evidence for or against specific therapeutic approaches, dosages of treatment or service-level issues. This concerned many interviewees.
Even in the limited areas where the evidence-base was regarded as reasonable – including evidence that refuted particular approaches or interventions –this was not believed to be routinely integrated into clinical decision-making. As a result, interventions were being delivered in a range of settings where, at best, the evidence for their effectiveness was weak and, at worst, existing evidence suggested that they could be damaging:
There is a lot of well-meaning work being done on a very limited evidence base.
O2
So even in the face of published evidence of what works, people still aren’t doing it.
W1
Study participants were also clear that this scarcity of evidence had led to wide variability in practice both across and within different parts of the country. In the absence of specific research evidence to guide their practice, there was concern among practitioners that they were not always ‘doing the right thing’:
You might not provide the best therapy for the child because you don’t know what it is so you go on either your clinical experience or your training or advice, or apply research from adults or apply research from paediatric development and try to make it fit, but you can’t be hundred per cent confident that that is the right thing to do and that is what’s going to give you the best outcome.
D1
There was also a sense among practitioners that, with increasing pressure on NHS resources, evidence of intervention effectiveness was needed to prove their own worth and guard against further cuts to their services. There was concern, too, that lack of evidence had made it more difficult to protect paediatric therapists and their teams from being ‘asset-stripped’ and from their expertise being ‘taken for granted’ (U1). Furthermore, the point was made that it does not necessarily follow that because there is no evidence of an intervention’s effectiveness, the intervention is not having a positive effect:
. . . we should be using an evidence base to be effective and prove what we are doing particularly to commissioners and again to make sure that we are doing the right thing . . .
C1
I’m concerned that this conversation [about evidence] is happening at the same time as major threats. I’ve been at meetings where managers hear that phrase ‘lack of evidence’ for an intervention and take it to mean that the intervention has no positive effect. That’s incredibly dangerous.
V1
Research evidence was also viewed by practitioners as a useful negotiating tool in decision-making with parents and families. Its absence meant that therapists could feel pressured to provide treatment regardless of any known difference this would make, in the face of parents’ expectations of regular, hands-on therapy or interventions that they had come across through their own investigations or word of mouth:
Parents would be more likely to listen if there was evidence to back up what the therapist is saying.
H1
Parents want to know what’s going to work best, and in the absence of any other offer of evidence they’re going to say more is better.
W1
A senior practitioner with a commissioning role also pointed out that a clear evidence base was invaluable when making decisions in relation to the commissioning of therapy services:
If you’ve got clarity of evidence then that makes the job easier to push for specific commissioning.
X1
Interventions regarded as having stronger evidence
Frequent reference was made to a recently published systematic review6 of interventions for children with cerebral palsy. This review used a ‘traffic light’ system to grade intervention effectiveness as follows: green represented ‘do it’, yellow represented ‘probably do it’ and red represented ‘do not do it’. However, views about this were mixed. Some believed that it offered a very helpful ‘line in the sand’, whereas others criticised it. Specifically, its reliability was questioned as some of the interventions included in the review were poorly described. The example of ‘home programme’ was mentioned by several interviewees:
While Novak [referring to systematic review6] is meaning a home programme [that is] based on a holistic, comprehensive and significant package of intervention in the child’s home that involves goal setting and demonstration [. . .] in general day-to-day NHS practice, a home programme means something quite different.
L1
Thus, overall, there was limited consensus as to which aspects of therapy practice were more evidence-based.
[For information, interventions relevant to this scoping study that received a ‘green light’ in the above systematic review were bimanual training, constraint-induced movement therapy, context-focused therapy and occupational therapy after botulinum toxin. A further few were graded green or yellow: fitness training, goal-directed training or functional training, and home programmes (for improving motor function or self-care). All other therapies reviewed were given ‘red light’ status.]
Views about research evidence and evaluation
Overall, there was a great desire for more robust evidence that could inform practice:
We all want to know whether we’re being effective.
C1
Nevertheless, concerns were expressed about the implications of moving towards evidence-based practice. First, there was suspicion among some that the motivation behind evidence-based practice was driven by the need to reduce spending, rather than a desire to improve patient outcomes:
You have to believe that people wouldn’t be looking at the research evidence so as to cut service. But in reality they would be, so that’s a massive barrier. People have to trust that research has the welfare of children at heart.
V1
Second, interviewees noted that there can be resistance, or a reluctance, to change long-standing practice, even in the face of robust evidence. Others referred to changing practice as causing anxiety and requiring therapists to move away from their own ‘sphere of knowledge’ and engage in doing something ‘different to their lived experience as a therapist’ (R1), and about which they may not be fully persuaded (R1):
And that is very difficult for all of us; to think: ‘Is what I’ve been doing for the last 20, 30 years actually helping?’
X1
Professional expectations regarding evidence-based practice
In order to practice, therapists must be registered with the Health and Care Professions Council, the UK regulatory body responsible for setting and maintaining standards of professional training, performance and conduct. In addition, most therapists are registered with their relevant professional body – RCOT, CSP or RCSLT – although this is not compulsory. Therapists’ engagement in evidence-based practice is an expectation of the Health and Care Professions Council and the three professional bodies: as one participant said, ‘it is in our job description to look at the evidence base’ (T2).
Direct engagement with research
Although there was general agreement that more research is needed on therapy interventions for children with neurodisability, direct engagement in research (e.g. supporting recruitment, and devising and implementing studies) was unusual for frontline staff, unless they were pursuing a postgraduate qualification. This situation was said to stem, in part, from insufficient training in basic research knowledge and skills to be ‘good consumers of research evidence’ (I1). Thus, unlike in the medical profession, there is no long-term tradition of research training in physiotherapy, occupational therapy and speech and language therapy. As one interviewee remarked, ‘It is not “ingrained in their thinking” in the same way as for medics’ (H2). For example, physiotherapy only gained degree status in the UK in 1994 and there is no obvious trajectory whereby therapists can engage in postgraduate studies. Typically, it appears that when therapists have engaged in research, it is more likely to have occurred some years after qualification. It was reported that very few therapists had doctorates:
It isn’t part of the culture with what we’ve grown up with really.
F2
Research training opportunities
Interviewees did note, however, that in recent years there has been a shift in thinking in both pre-registration training curricula and continuing professional development strategies. For example, research knowledge and skills have become part of pre-registration therapy programmes. Thus, therapists trained more recently are likely to be better equipped to engage in research activities and take research forward. However, as a number of interviewees noted, if these skills and knowledge are not built on and developed, confidence in research abilities is lost.
Some practitioners questioned how they were supposed to acquire research skills without ‘jumping two feet into a master’s’ (U2). Among some interviewees there was an anxiety about their lack of research skills, but no easy route was identified to begin developing those skills:
We do it as a team, we are constantly worried about it all the time, and feels like we could be doing more but don’t have those skills and don’t know where to get them from without signing up for a heavy commitment.
U2
For those able to make a commitment to pursue postgraduate training, the NIHR Fellowship Programme was praised for the opportunities it gives therapists who want to do this. However, other opportunities for therapists to study for master’s qualifications were, according to study participants, becoming few and far between owing to the financial pressures involved in releasing someone from clinical practice:
What worries me now is that with the funding squeeze in the NHS, we’re being squeezed and squeezed and squeezed and where we had the opportunity to send people on these [master’s] programmes, it may be more difficult in the future.
T2
Consequently, the only route open to those wanting to engage and develop their skills in research was to leave clinical practice for academia. This was regarded by some as reinforcing a gap between research and practice.
Time for research
Many interviewees noted the lack of protected time for research activities, whether this was to keep up to date with the research evidence, to take part in research-related activities or to write research proposals and submit bids for research funding. All agreed that clinical teams within NHS community and acute trusts were under a lot of pressure to meet their clinical demands and so there was little or no time left for research. These pressures, it was generally recognised, were increasing with recent austerity measures:
. . . we haven’t got enough posts to do the work and have free time to do the extra bits like research. So the pressure is very much you’ve got to do your caseload, you’ve got to do this, you’ve got to do that.
H2
Nobody’s going to want to do research if they’re going to have to add it on to what they are already doing. They don’t have time to even do what they need to do . . . they are in survival mode.
Q1
The constraints on therapists’ time were also referred to in the context of involving therapists in research, and it was felt that this situation would not change. Thus, clinical academics taking part in this study reported that, to engage with and support studies, therapists may have to squeeze appointments and/or do this work out of hours.
We have managed to do some research locally but it has been very much dependent on people’s goodwill; and unfortunately in the NHS at the moment, there’s less of that around.
Z1
Wider views about therapists’ engagement in research
Some interviewees (including therapists and paediatricians) believed that research may be actively discouraged among middle and senior management. It was neither valued nor perceived as a part of the therapist’s role:
[. . . They say] ’it’s not your job to do research’ kind of thing.
U1
One participant (a therapist) described the resistance to their research they had encountered from managers who argued that it did not fit into clinical practice. Others talked about having to ‘push’ to do research rather than it being the other way around, with managers reluctant to invest in research training or provide time for research opportunities.
However, in settings where there was a stronger culture of research, therapists described undertaking their own research projects. Experiences of support from local NHS research and development departments were variable.
Accessing research evidence
A number of issues associated with accessing evidence were described, including the challenges and difficulties, and the structures, systems and cultures that supported therapists to engage with research evidence.
The limitations of existing evidence
Some therapists commented that many children in their care had multiple disabling conditions and comorbidities and that this was not reflecting in existing evidence:
. . . So it’s finding evidence that actually reflects that complexity.
C1
The challenge of staying up to date
The wide variety of children on a caseload had implications in terms of the volume of research with which a therapist may want to keep up to date:
It’s about keeping up to date with the evidence and finding time in a busy clinical job to do that [. . .], timing can be critical when you’ve got a very broad and varied caseload . . . it can be more of a challenge to try to keep up and read across everything.
G1
The role of research culture and infrastructure
Participants reported several areas in which organisational culture and infrastructure facilitated accessing the evidence. Some, for example, talked about an ‘open flow of conversation’ between therapy practitioners that included an exchange of ideas and expertise about the research evidence. This could be discussion and learning through e-mail communication, individual or team meetings, continuing professional development activities or peer support initiatives.
When there was a stronger culture of research within an organisation, journal clubs were reported. These were described as providing an opportunity for groups of therapists to meet regularly to critically evaluate research articles relevant to their therapy practice. Teams not connected with a university or medical school reported that gaining access to journals could be problematic.
Professional and national clinical guidance
Many interviewees described using professional guidelines (developed by their national professional organisation) and NICE guidance. Occasionally, and usually in the larger and/or specialist teams/centres, evidence-based practice guidance was (being) produced for staff.
Professional networks
External professional networks were often mentioned as supporting the receipt and exchange of research knowledge. Many of the networks described to us were organised under the auspices of the three professional bodies (RCOT, CSP and RCSLT). Other networks reported by therapists as supporting them to stay informed about research and evidence relevant to therapy interventions were the British Academy of Childhood Disability and its European counterpart (the European Academy of Childhood Disability), and the British Association for Community Child Health. Some therapy-specific initiatives to support evidence-based practice were also reported, for example the CountMeIn! initiative within occupational therapy (www.thechildrenstrust.org.uk/count-me-in) and the What Works database within speech and language therapy (www.thecommunicationtrust.org.uk/whatworks).
Chapter 9 Perceived challenges for (evaluative) research
Introduction
A number of challenges for future research, particularly in terms of achieving robust evaluations, were identified by study participants. These challenges were located in the following areas:
-
the heterogeneous nature of the population
-
the nature of therapy interventions
-
research design issues
-
challenges associated with implementing evaluation studies
-
the requirements of funders.
In this chapter, we report and describe professional interviewees’ experiences of and beliefs about each of the above issues, and the implications of these challenges in terms of priorities for future research.
However, before moving on to this, we report a general challenge to future research in this area identified by study participants. Namely, honesty regarding the current state of evidence will be required. This may lead parents to question decisions about the care and management of their child, or their confidence in the child’s health-care team. It was noted that careful thought and planning may be required to pre-empt or address this issue:
I think families are interested in finding the best possible treatments and therapies and so are keen to participate in research. But I think we need to be more honest [to parents], and say . . . ‘we haven’t got a good evidence base for this but we believe it’s the right thing, but there might be other ways of doing this, or how we achieve that’.
I2
The heterogeneous nature of the population
The heterogeneous nature of the population of children with neurodisability, even within diagnostic groups, was frequently described as a research challenge. Heterogeneity was characterised as multifaceted, in terms of extent and severity of physical impairment, the presence of concurrent health conditions, and other impairments. (It was, however, noted that certain groups, such as children with hemiplegia, were more homogeneous.) A further challenge was where there was no confirmed diagnosis or an extremely rare condition:
I strongly feel that what works for a child with relatively straightforward cerebral palsy and no comorbidity won’t necessarily work for [a child with] four limb cerebral palsy, plus epilepsy, plus a gastrostomy. These two are not the same, and the way therapeutic input works may not be the same.
V1
. . . very often we’re looking at kids who don’t fall into neat groups. So they’re not homogeneous, and they’re also quite low incidence.
Q2
There was a perception that some, or much, existing research had not confronted the complexity of many children with neurodisability, with evaluative research focusing on ‘simple’ subgroups only:
Dysarthria research does not include participants with learning disabilities so that rules out most of our kids. They want to hone in on a very small section of our clients when, actually, it’s not very helpful because so many of our clients have these co-existing problems.
G1
Some participants believed that this lack of homogeneity meant that a randomised controlled trial (RCT) would be an inappropriate, or unachievable, research design:
Children are so individual in themselves, let alone in the family and school environment and everything else. So, to do an RCT isn’t really feasible as you wouldn’t be able to compare like with like.
C1
Others did not take that stance, although they believed that multisite, international studies may be needed if particular trial designs were used:
A key issue is the group of children we work with are heterogeneous which makes it more difficult to match groups, but it is not impossible. It’s been done. But it’s very different to doing a project on typically developing children where you can access a nursery and do hundreds.
O2
Some identified finding ways to overcome the issue of heterogeneity as a research priority. Typically, this referred to further testing of the validity and reliability of existing frameworks or systems for defining symptoms/impairments, and examining their application to other diagnostic groups within the neurodisablility population. Participants suggested the following frameworks: the Gross Motor Function Classification System (https://canchild.ca); the classification systems for cerebral palsy;37 the Pediatric Evaluation of Disability Inventory-Computer Aided Test (http://pedicat.com/category/home); the Functional Assessment Measure;38 and therapy outcome measures. 36
The nature of therapy interventions
A second area of research challenge was the nature of therapy interventions. Three particular issues were identified:
-
the individualised approach taken to the delivery of therapy interventions
-
the fact that interventions are not specified
-
the context of multiple, simultaneous interventions.
The individualised approach taken to the delivery of therapy interventions
A key theme in many interviews –with regard to both practice and research issues – was the belief that, to make an impact, a highly individualised approach was required when delivering therapy to a child with neurodisability. This was regarded as a barrier to conducting clinical trials and was a reason why, when opinions were expressed regarding study design, some believed that single subject/case study research was a more appropriate design because it could accommodate this individualised approach:
The problem is bridging these very strict research protocols within the context of the families and children who we actually deal with at a clinical level.
K1
Interventions are not specified
Closely connected to this notion of an individualised approach is the fact that most therapy interventions are not specified: there are no universal protocols or intervention manuals. This was regarded as a significant barrier to rigorous research. In response, some interviewees stressed the need for, or adoption of, systems or frameworks that allowed for a standardised approach to defining the content of an intervention. At the moment, it was argued, quite different interventions might carry the same label:
We need to get down to the content, because the labels mean absolutely nothing.
L1
A further concern was that this lack of specificity meant that intervention fidelity, or adherence, could not be assessed. In addition, within published intervention studies, the impact of poorly defined interventions was regarded as twofold: first, the synthesis of findings in evidence reviews may not be reliable, and, second, it prevents replication.
The context of multiple, simultaneous interventions
Many study participants described the multifaceted nature of the care of many children with neurodisability, especially those with more severe or complex impairments. In these instances, it is likely that a number of professions will be involved and the child may be receiving multiple interventions. It was noted that this may present challenges for evaluation studies, and would need to be controlled or accounted for:
. . . and there might be lots of other therapies that might be coinciding with the treatment. So there might be medical treatments ‘chinking’.
I2
Research design issues
There was a range of beliefs among participants about how therapy interventions could, or should, be evaluated. It should be noted that, quite understandably, sometimes these beliefs were based on a limited understanding of research. We have been circumspect, therefore, in how we report the issues and concerns about the design of evaluation research expressed by participants.
Some issues relevant to this topic have already been explored, or have been placed in Chapter 10 on research priorities, and we do not therefore cover them again here. This includes issues related to outcome, outcome measurement and follow-up points (see Chapter 7), and the measurement of active ingredients (see Chapter 10). Thus, here we focus on reporting participants’ views on the following issues:
-
the feasibility of trials
-
the potential of non-experimental study designs.
The feasibility of trials
Among interviewees who had some degree of experience of designing or conducting evaluations, trials were usually, although not always, regarded as an appropriate and/or feasible study design for some research questions or objectives. However, many stressed that realist evaluation principles needed to be incorporated into the design of trials so that questions about ‘what works, for whom, and in what circumstances’ could be answered:
I think we need to be changing our methods of analysis to hone down on which children are making the most progress, and what are the predictors of those that did not make progress. Rather than oversimplifying the [analysis] to: did the therapy make a difference, or not? So I think we could do more than just say ‘Here’s the money for an RCT’, we need to really plot what are the presenting features of the children, and what are the factors that cluster together to support a good outcome?
K1
Comparator groups
Across all three therapies and across a range of settings, participants said that it may not be possible, or ethical, to withhold treatment to create a no-treatment comparator. A rhetoric of equipoise was not presented within these reflections:
Within the population we see, it would not be feasible to have a control where we are doing nothing; there would have to be another sort of comparator.
R1
Some participants also noted that using ‘usual care’ comparator groups would be equally difficult, or unadvisable, given the enormous variation in individual practices and the approaches taken by, and organisation of, different services.
The potential of non-experimental study designs
Non-experimental study designs were viewed as having the potential to make a strong contribution to the evidence base on intervention effectiveness, and neurodisability per se. Particular reference was made to case studies and long-term cohort studies. Such designs were viewed as a potential solution to the heterogeneity of the population and small sample size, or when the intervention being evaluated was complex:
I think for some complex interventions and for heterogeneous populations, RCTs don’t tell you very much. Because what we’re interested in is not work what works, but what works for whom. So you’re almost at two ends of the scale. Either you need an enormous RCT with scope to look at subgroups with very complex cluster analysis, or you do some single case experimental designs which allow you to say what’s working for what type of child. [I think] we need to make more use of good, robust single case study experimental designs because we’re often looking at kids who don’t fall into neat groups: they’re heterogeneous and can be low incidence. A while ago I was trying to set up a study and was told by a medical statistician there needed to be a plague of cerebral palsy for me to do it. So we need to be more accepting of what are the appropriate methodologies.
N2
With respect to cohort studies, participants highlighted potential opportunities within the newly established Children and Young People Health Services Data Set (http://content.digital.nhs.uk/maternityandchildren/CYPHS). A number of interviewees also mooted the benefits of adopting of the hip surveillance strategy for children with cerebral palsy, which had been implemented recently in Scotland:
Epidemiological data is very important. So if you really want to understand the natural history of a condition like cerebral palsy, we need a large cohort disease registry so you can monitor the progress of children over time and perhaps then compare what interventions they’ve had as standard practice or compare how practice has changed over time . . . that means thinking very long term, rather than short term.
I2
There’s no point looking at short-term outcomes. For participation, you need to look at cohorts in the longer term, so 10-plus years.
X1
A number of interviewees noted the potential value of developing clear protocols for reporting case studies, which, if there was some sort of national repository, would allow the collation and synthesis of evidence. Research investment to support such initiatives, and ensure that they are robust and properly supported, was highlighted by many, from clinical academics through to frontline staff. It was also noted that case studies offered a means by which frontline therapists could actively engage in, and contribute to, research, thereby increasing the research capacity within the profession.
Reflection
Overall, therefore, there was strong support for a mixed research design strategy and approach to evaluating interventions:
All methodologies have pros and cons, but there’s room for them all if they are done well and are saying something important . . . and RCTs can’t always be used in isolation to answer the important questions: they need to be combined with other methodologies, for example, [in order to] find out the perceptions of families.
J1
The final sections of this chapter consider two further challenges: implementing evaluation studies in practice and securing research funding.
Challenges associated with implementing evaluation studies
Intervention adherence
There was strong consensus that research on therapies has to be practice based, rather than consisting of contrived clinic-based studies of efficacy. The latter, it was felt, do not reflect the true complexity of therapy interventions for children with neurodisability. That said, it was noted that this presented challenges, and ‘intervention adherence’ was one of them. This was described at two levels. First, as we have already noted, many therapy interventions are not manualised, or have no protocol. Second, many interventions are delivered by other people: parents, school staff and therapy assistants. This clearly introduces another source of deviation in terms of adhering to the intervention, or even doing it at all:
. . . so it might be the same principles of therapy, but the dosage might be different, so there’s a lack of consistency in that. [Many of these interventions] . . . are not like taking a pill, the intervention is an investment from people. To standardise that is difficult.
I2
You can give them some beautifully described exercises to do with their child . . . but they [parents] are not [necessarily] going to do them.
Q1
Sample selection and recruitment
Mixed views were presented on whether or not engaging families in research and recruiting them to studies would be a challenge:
Parents are bombarded with and sometimes worn down by paperwork. They have multiple appointments with professionals and so their diaries are full.
T2
Others noted that recruitment to research may be required at a time when families are highly traumatised, for example after they have learned a diagnosis, or after their child has had an accidental and severe head injury. The need for investment in feasibility studies was flagged up:
It’s crucial to acknowledge the reality of likely recruitment difficulties, and also the time you need to build into studies to get through the processes of agreement to take part, which can be lengthy.
P2
Concerns were also expressed that those families recruited to trials may not represent the entire patient group, an important issue given that there was consensus that family characteristics have an impact on an intervention’s effectiveness:
Research participants are often those families who are prepared to engage. But, in reality, we are working with a lot of families who are ‘difficult to reach’ and are not going to attend research appointments and follow-ups. So it is difficult to know what to base the decision-making for those families on.
G1
The requirements of funders
Finally, a common theme in discussions about future research was the importance of funders neither applying unfeasible standards to research designs that did not recognise the ‘real world’ of therapies for children with neurodisability, nor imposing inappropriate standards to the intervention under investigation. For example, it was regarded as more difficult to apply uniform study processes (e.g. referral and recruitment processes) in community settings than in acute settings:
It requires funders to think carefully about methodological standards, deciding where they can allow for leniency and risks to take account of complexity, and where they cannot. Therapy is complex and interventions, especially in the community, take place in the messy real world. What is needed is for designs which take that into account. And for funders to accept where methodological risks can be taken.
I1
It’s a medical approach to think that the only way to crack the nut is to do an RCT . . . if that’s the only method being considered then you’re not going to do a lot of research because it isn’t always appropriate.
J1
The studies may not be perfectly designed research and the confounders will be there. But as long as we try and identify what those confounders are, and at least accept them or account for them, we can still find useful information.
I2
Interviewees called for support for feasibility studies and the use of non-experimental designs, both to develop understanding of interventions and their impact (e.g. using case studies) and as an alternative to trials (e.g. observational cohort studies). Finally, some felt that funders should be open to accepting trials that had two active arms.
Chapter 10 Views on research priorities
Introduction
As reported in the previous chapter, there was agreement among study participants of the need for research into therapies for children with non-progressive neurodisability. The level of support for such research varied, with concerns most likely to be voiced with respect to evaluative research, specifically whether or not it was possible to measure, or demonstrate, impact.
Many, however, noted a ‘moral imperative’ to establish a deeper and more solid evidence base on therapy interventions for this group of children. This related to seeking both the best outcomes for the child and the best use of limited resources:
We need to think very carefully in these times of austerity about whether we are adding any value, whether we’re doing anything useful, or whether we are just pulling the child out of school and passing the time. We do need evidence of what works, and what doesn’t. And parents want to know what’s going to work best; and in the absence of any other offer evidence, they are going to say more is better.
W1
We need research to direct what to do as well as backing up what we do already.
C1
The previous chapter described a number of ‘research challenges’ identified by study participants. Some of these challenges generated methodological questions that could themselves be addressed by research. Research priorities of this nature were therefore described in that chapter. Here we turn to reporting the other topics and questions that study participants nominated as research priorities.
Topic areas
The research questions and issues suggested by interviewees can be organised into seven broad topic areas. We have further grouped them around two types of research:
-
foundational or underpinning research
-
understanding of neurodisability
-
understanding of the condition or condition trajectories
-
understanding of therapy interventions
-
defining participation
-
-
evaluation
-
evaluation of overall approaches to therapy
-
evaluation of service organisation and delivery
-
evaluation of techniques, procedures and equipment.
-
Thus, perceived research priorities did not just concern the evaluation of interventions; they also included topics that we have termed foundational to, or necessarily underpinning, evaluative research. We begin by reporting parents’ research priorities within this framework.
Parents’ research priorities
Parents’ views on research priorities were firmly grounded in and informed by their experiences of therapy provision for their child. Their priorities lay within evaluation research, with greater emphasis being placed on the evaluation of therapy approaches and service delivery than on, for example, evaluations of specific techniques.
Evaluations of approaches to therapy
Goals-focused approaches
We have already reported the way in which parents valued goals-focused approaches. They returned to this theme when research priorities were discussed, although they struggled to articulate specific research topics or questions.
Supporting and empowering parents
A second area prioritised for future research concerned studies to identify the best ways to enable and support parents in delivering therapies to the child. Parents often spoke about this notion broadly and in terms of working in partnership with therapists, rather than being regarded as a passive actor, unable to make decisions or be proactively involved in the assessment, planning, delivery and review of their child’s therapy.
Timing of interventions
Two different research priorities were identified relating to the timing of therapy interventions. First, parents called for research into the therapy needs of young people approaching and during puberty (and associated growth spurts and physical changes). Second, parents wanted research to be carried out that provided the evidence on when to start therapy interventions. One example given was parents’ experiences of current practices regarding speech and language therapy provision, believing that this was not started early enough: ‘. . . you’re lucky you get it at two-and-a-half years’.
Evaluations of service organisation and delivery
Integrated care
Parents called for research that would evidence and support integrated approaches to working and provision, both between therapies and in terms of the wider service context for children with neurodisability, including other elements of paediatric provision and schools. Included in this discussion were notions of services working towards shared and agreed goals. As one parent remarked, ‘It would be good to have evidence about the benefits of joint working, so if you can “buy” it all in one therapy, one activity and so on . . .’.
Models of provision
Parents who had experienced an ‘episodes of care’ service model expressed concerns about it. They felt that this approach should be investigated as they believed that the cycle of repeated discharge and lack of continuity of contact with the same therapist disadvantaged their child.
Evaluations of techniques, procedures and equipment
Dose
Parents also had questions about ‘dose’, that is, the frequency or duration of specific techniques or procedures (e.g. ‘how long should my child stay in a standing frame?’), or simply the length of contact time between the child and the therapist. These questions arose from a view both that their children did not have enough time with a therapist and that practices were inconsistent between therapists, even those working on the same team.
Within this discussion, parents gave the example of the greater intensity of contact they have with private providers compared with NHS provision. They felt that it was important to research the differences in children’s outcomes in terms of the ‘dose’ of therapy received.
Other research topics identified by parents
Equity of access: within and between localities
Parents believed that it was important to research, understand and describe what they regarded as ‘the massive inconsistencies’ in the therapies offered by different localities to families with a child with neurodisability. They asked if it would be possible to do research that would define what a ‘universal service’ should constitute, rather than the current ‘postcode lottery’ of provision or provision to families ‘who shout the loudest’.
Therapist training and practice
Finally, parents believed that research needed to be carried out to identify therapists’ training needs, and how best to meet these needs. Here they pinpointed topics that they had encountered in their contact with therapy services. First, they felt that therapists could improve their knowledge and understanding of conditions other than cerebral palsy, for example spina bifida. Second, parents called for research that identified how therapists could best be kept informed about new evidence, equipment and treatment options.
Foundational or underpinning research
Professionals identified three main streams of work that can be defined as foundational to, or underpinning, evaluation studies. These were:
-
understanding of neurodisability
-
understanding of therapy interventions
-
defining participation.
Understanding of neurodisability
Understanding of the conditions and condition trajectories
On numerous occasions, a desire for evidence on the long-term outcomes of children with neurodisability, including into adulthood, was voiced. The view was that very little is understood about this group, particularly those with complex needs and acquired brain injury (where understanding of the trajectory of, and potential for, recovery is poorly understood). Such evidence, it was argued, was needed so that therapy interventions could be designed or developed with longer-term outcomes in mind.
In addition to body function and structure issues, some interviewees highlighted the importance of research to develop understanding of symptoms such as pain and fatigue (this latter issue was noted particularly for children with acquired brain injury):
My first question would be, what is the prevalence of pain? What can we understand about their level of pain? Then, after looking at the prevalence of pain, then looking at strategies to reduce pain, and how pain impacts on participation and quality of life.
I2
A few interviewees specifically stressed the need for research on the social inclusion of disabled children in mainstream settings. The argument was made that higher-level outcomes (such as inclusion or participation) may not happen simply because wider issues have not been recognised or addressed:
. . . it’s all very well developing motor skills and communication skills. But if no one plays with you in the classroom it doesn’t do you much good.
Q2
Understanding the development of children with neurodisability
Addressing the lack of understanding of cognitive and motor development in children with neurodisability was also raised as key contextual, or background, evidence gap. Different topics or issues were identified. For example, a number of interviewees highlighted the lack of understanding about language and communication development in non-verbal children with learning difficulties. This meant that the design of communication systems (e.g. the way the vocabulary of a system is organised) had been based on various assumptions, leading to alternative approaches, or systems, being developed:
The trajectory of typical language development is another framework that’s used for this group of children. Whilst this makes complete sense, the slight concern is that we don’t know how this group of children learn language. There’s an assumption that they learn in the way that typically developing children do, but we’re learning that’s not quite the same. So, they learn vocabulary, but they don’t learn grammar.
O2
In addition, some interviewees reported a lack of agreement about whether or not working on some skills can result in improvements, or about what the maximum expected improvement might be. Systems and technologies to support the use of eye-gaze, and therefore to improve eye-gaze skills, for supporting communication was frequently mentioned in relation to this.
Understanding therapy interventions
Defining new and emerging approaches
A few interviewees pondered the implications of goals- and participation-focused approaches, and potential future shifts in their work or focus of activity. In terms of research, the implication was to ensure that these ‘newer’ aspects of a therapist’s role are understood:
One of my questions would be: if you’re a participation-oriented therapist, what does your intervention look like?
P1
Active ingredients and mechanisms of action
We have already reported (see Chapter 6) that many therapy interventions have not been specified in terms of a ‘theory of change’, that is, the mechanisms by which the ‘active ingredients’, or components, of an intervention achieve specified outcomes. Interviewees identified this as a significant barrier to research, and some participants prioritised future research to inform the development, and testing, of theories of change of therapy interventions:
We need to unpack the ‘black box’. Therapy interventions [sometimes] claim to target every outcome at every level of the ICF. We are targeting body function, body structure, activity limitation, participation, the social environment, or parents’ empowerment. I don’t blame therapists [for this rhetoric]: it’s the heritage they’ve got. But, sometimes you need to spend a bit of time working out what the heck is the intended outcome? And that, to medical leaders, can seem really weird. But it’s work that needs doing. That could be research in its own right.
L1
As well as preventing replication of studies, this lack of an existing evidence base was regarded as a barrier to the development of interventions that could then be taken forward to evaluation:
It’s an interesting dilemma from the point of view of developing an intervention. How strongly should it be based on a pragmatic ‘. . . this is what it would look like’? Or how far should it be [based on] a strong theoretical position?
P3
In addition, the need to identify and understand the active ingredients of an intervention – be it with respect to an overall approach, a care pathway, or specific techniques – was frequently raised by study participants as a key research area, and foundational to other research. As already reported, interviewees believed that the active ingredients were multifaceted:
In day-to-day practice we see the positive impacts on children, but we need the evidence to demonstrate and quantify this positive impact. What is it that therapists do that is effective?
M2
We need to understand more about contributing factors. Is it [the technique or approach], or is it motivation, or is it the family environment?
Q1
Related to this was the need for systems by which interventions can be specified, or defined, in order to allow the replication of studies. Thus, finding ways to systematically describe the complex and multifaceted nature of therapy interventions was identified by many as a research priority:
We have to have a way of describing the intervention in a succinct and manageable way.
N2
Some interviewees dwelt on the challenges this presented. It was felt that interventions that comprised the introduction of a piece of equipment, or a device, were easier to specify (and, to date, were more successful in securing funding to evaluate):
The difficulty with effectiveness research is that we’re not comparing like with like. And we’re not very specific about what we’re comparing. So I think that the state of our effectiveness research in therapies is at quite an early stage really. There are some very fundamental issues we need to address before we are able to meaningfully evaluate stuff.
L1
TIDieR (Template for Intervention Description and Replication) guidance29 on reporting interventions, and other guidance being specifically written for electronic device interventions,39 was identified as a useful resource and offering a way forward. A further, and significant, challenge identified by study participants was knowing which active ingredients ‘matter most’ and should be measured, or controlled for, in evaluative research. Interviewees appeared to think that this would vary between interventions and depending on factors such as intervention objectives and child and impairment characteristics.
Finally, the measurement of active ingredients was regarded as key element of future research on active ingredients. Many interviewees believed that some active ingredients would be particularly challenging to ‘measure’ or capture in a way that could be quantified and systematically replicated across studies:
It may be easier to capture the physical things around therapy, like the equipment pf the therapist’s communication style or knowledge base, than the ingredients around feelings and motivations.
R1
. . . with physios and other therapy services it’s very much about an ongoing relationship . . . and I don’t know how we capture this.
X2
Children’s and parents’ understanding and experiences of therapy
Many participants highlighted the lack of evidence on families’ understanding of therapy interventions and on the impact that interventions have on families’ lives:
We drop bits of equipment into the family situation. I’d be interested in the waves that causes.
X2
. . . we need to ask young people what they felt about therapy. Was it worth the effort? We need to ask these powerful questions.
J1
You’re asking them [parents] to do something that’s not a normal part of their role. So parents [can] become kind of medicalised. How do they feel about that?
I2
Two key reasons appeared to underlie the prioritising of research in this area. First, a lack of knowledge about families’ understanding of therapy stymied efforts to support family involvement in decision-making, goals-focused working and work to maintain engagement. Second, this meant that therapists had little idea of the impacts of therapy on the everyday lives of children and families. With respect to this, particular reference was made to situations in which parents may be quite intensively involved and/or multiple professionals are working with a family concurrently.
Therapists’ views of therapy
Related to the previous topic, a few interviewees suggested that an important area of research would be using qualitative methods to explore therapists’ views and beliefs about what they do: their practice, decision-making and perceived outcomes. One reason for prioritising this was its potential contribution to understanding interventions in terms of mechanisms of action and active ingredients. Another rationale was that it would help to inform ways to approach implementing evidence-based, or evidence-informed, change.
Defining participation
As reported earlier (see Chapter 7), the notion of participation, although widely accepted, was felt by many participants to be a nebulous, or poorly defined, construct. Conceptual work on its definition, and work to describe and understand the mechanisms and processes by which therapy interventions may influence it – directly or indirectly – was regarded as another aspect of ‘foundational research’ that should be prioritised and, once achieved, would support and enable work in other research areas.
One issue some participants highlighted was the need to further specify the different aspects of participation:
I think to treat participation as a single outcome is a bit crazy. We need to break participation outcomes into smaller parts, or it doesn’t really make sense.
O1
On a slightly different note, some interviewees believed that, for some groups of children (e.g. those in minimally conscious states, babies and very young children), there had been little thought or debate about the meaning of participation. These participants prioritised research in that area.
There was strong consensus that, in carrying out work on this topic, there needed to be extensive and close work and consultation with parents and children.
Evaluation
Three domains of evaluation research were identified: the evaluation of overall approaches to therapy; the evaluation of models or service organisation and delivery; and the evaluation of techniques, procedures and equipment.
Before we move on to describing participants’ views on research priorities within each of these domains, it is important to note that, in many of the suggestions made (by both parents and professionals), emphasis was placed on the fact that evaluation studies should include an economic evaluation, and that attention should also be paid to supporting the implementation of findings. We explore these two issues briefly here.
The need for evidence to support arguments for the investment of therapists’ time, skills or equipment was something that many interviewees raised. The need for research to be able to test and explore ‘value for money’ was, therefore, often articulated:
[Seating] is one of those things we’ve always overspent. There’s a lot of budget going into it and we need to be able to prove the outcomes of that really.
C1
Some interviewees, when discussing the importance of economic evaluation being nested within outcome evaluations, noted that a holistic approach would need to be taken, and one that could take a long-term view on outcomes (in terms of both child and parent) as well as on what an effective intervention prevents. In addition, some interviewees stressed that any economic evaluation needed to capture or incorporate notions of quality of life, including for those children with the most profound impairments:
. . . what people always want to see is that somehow you are showing cost effectiveness, but sometimes the cost effectiveness is in quality of life and productivity of individuals and the prevention of family breakdown and prevention of secondary issues, and sometimes that means you are having to invest early in to prevent all those other things which are actually covered by other people’s budgets.
Z1
Implementation science was identified by some as a core element of future evaluation research. This included developing an evidence base on effective ways to embed evidence-based, or evidence-informed, practice within therapy teams:
How do we train therapists in whatever the active ingredients are that make interventions work, and then how do we implement that within a clinical team in the community?
Q1
The problem is getting the research information to the jobbing physiotherapist and their managers. What is needed is to develop some pretty quick ways of telling the troops on the ground this way is better than that.
U1
There’s an ongoing perception that these children need treatment, treatment, treatment, but instead we should be giving families the freedom to participate, rather than bogging them down with therapy treatments. Somehow that message is hard to get through.
X2
A further issue concerned developing an evidence base on ways to maintain the implementation of proven interventions by others involved in delivering therapies to children with neurodisability, including parents and school staff.
We turn now to report the three domains of evaluation research identified by professionals taking part in our study. As noted earlier, these were:
-
evaluation of overall approaches to therapy interventions
-
evaluation of service organisation and delivery
-
evaluation of techniques, procedures and equipment.
Evaluation of overall approaches to therapy interventions
In Chapter 4 we described the shifts in thinking regarding therapy objectives and ways of working currently taking place across physiotherapy, occupational therapy and speech and language therapy. A number of research priorities were identified relating to the evaluation of these emerging approaches. Such research had two overall objectives: first, to establish whether or not they ‘worked’, and for whom and in what circumstances, and, second, to identify the best ways to implement and to deliver them. A number of diverse questions about the overall approach to therapy interventions were identified.
-
When should a child be accessing therapy interventions?
-
What supports families’ engagement in therapy interventions and notions of self-management?
-
What practices, or ways of working, best support children, young people and families to effectively engage in goal-setting?
-
What practices, or ways of working, best support a consultative model of delivering therapy interventions?
When should children and young people access therapy interventions?
Participants identified a number of research questions related to the age of the child and when to intervene. Sometimes these questions were grounded in a wider conversation about a lack of understanding of physical, communication and cognitive development of children with neurodisability.
As reported in Chapter 4, early intervention is the dominant model of therapy interventions for children with neurodisability. Research questions identified with respect to this practice were as follows.
-
Is early intervention the right approach, and are outcomes maintained?
-
Should therapy be maintained, and in what form, after the early intervention ‘window’ has passed?
-
Are there other time points in a child’s life when intervention intensity needs to be greater? A few physiotherapist interviewees, for example, raised questions about whether growth and structural changes associated with puberty should signal the reinvolvement, or greater involvement, of physiotherapy.
-
Should interventions start earlier than they currently do? This issue was predominantly raised by speech and language therapists, who typically become involved in the management of a child with neurodisability later than physiotherapists.
-
For children with complex and enduring needs, the issue of the consequences and impacts of the loss of access to therapy that typically happens at transition to adult services was, for some interviewees, regarded as a research priority.
Self-management and engagement in interventions
Given the changes and developments across all three therapies in terms of overall approach, it is not surprising that some research priorities concerned implementing family-centred and goals-focused approaches. In this context, notions of ‘engagement’, ‘coaching’, ‘enabling’, ‘educating/informing’ and ‘empowering’ were discussed. Although not necessarily labelled as such by interviewees, the notion of self-management skills and capacity emerged as a key concept, and the need for evidence on what works to facilitate and sustain this was referred to often. For some, research that answers questions about whether these approaches yield better outcomes, and the best ways of supporting these approaches, was a top priority:
My question would be, is it better to send parents back into the community with their child after intensive one-to-one therapy sessions where they are told what to do with their child, or after occupational therapy coaching sessions which give them the skills to problem-solve in relation to their child when back in community?
R1
Therapists know that parents delivering therapy interventions is the only practical way forward, given funding restrictions. But, for that to work, parents need to be not just an extra pair of hands, but to truly understand their child’s condition and for both parents and children to be able to manage changes ‘down the track’ to support well-being. We need to know what it takes to make that happen.
J1
Therapists are always reinventing the wheel by concocting little flyers and leaflets [for parents]. [Studies generating guidance on] informed parent decision-making and information to support them working with their child . . . would be really helpful.
P3
We need research which helps us to get to a situation where we’re working with families: giving them the right information, at the right time, and doing that well. So that families can be outcomes and goal-focused, and take a lead in decision-making – what do we want to prioritise for our child, how do we want to achieve this or that outcome?
A1
The notion of engagement was also discussed with respect to adherence to specific intervention programmes. Researching strategies to support engagement was regarded as a priority for some. To make their case, interviewees shared their experiences of adherence to intervention programmes lessening after a few weeks, even when the intervention used what were regarded as quite engaging, everyday life activities (e.g. virtual reality gaming):
Even if you have a brilliant form of therapy, if the child’s demotivated and has got bored, and the parents have had enough and let them go off and play, it’s not going to work.
H2
Finally, and more specifically, some interviewees highlighted the need for evidence on how therapists can best support a parent’s acceptance of their child’s condition, or impairments. This was regarded as an important prerequisite to engaging with interventions in a positive and helpful way, and having the confidence to self-manage appropriately.
Ways of working that support goal-setting
Supporting children, young people and parents to identify appropriate goals, and those relating to higher-level outcomes such as participation and well-being, was regarded as requiring a specific set of skills. The development of an evidence base to support this approach was prioritised by some interviewees. The fact that such approaches may run counter to families’ usual experiences of services, and to professionals’ original training, was felt to add to the argument for research into effective practices or ways of working.
The evaluation of service organisation and delivery
The second area of evaluation studies identified as research priorities concerned the organisation of therapy, and neurodisability services more widely. Studies in this area were frequently identified as a priority for evaluative research. The types of issues raised within this topic area include:
-
effective multidisciplinary team-working
-
multitherapy versus unitherapy teams
-
care pathways
-
the impact of skill/band level of therapists on intervention outcomes
-
the relative effectiveness of the consultative role versus the therapist having closer direct involvement in the delivery of therapy
-
the relative effectiveness of therapists versus others (e.g. parents and school staff) in the delivery of interventions
-
alternative approaches to assessment.
Interviewees involved in reformulating the organisation and delivery of therapy services in their locality typically identified the role of research in informing strategic decision-making and implementing change:
How do you identify family priorities and make sure that professionals bond to them in an integrated way?
L1
There’s plenty on the policy agenda about what we should do, but there’s not a lot of help, guidance or models for how we deliver it. So, how do we integrate effectively? Often the focus is on effectiveness research for clinical intervention but we also need effectiveness research around service delivery and implementation of interventions.
L1
The Trust get more money if we do face-to-face stuff with the child. But as soon as you take the child out of the equation, there is not as much funding . . . for going and sitting with the parent and discussing the logistics of getting to somewhere or whatever, which can be as useful to the child as spending time with them.
C1
Some topics related to service organisation, or ways of working, stemmed from changes to the way therapy interventions are being conceived and delivered. For example, in response to therapists increasingly assuming a consultative role, in which they ‘upskilled’ and supported others (parents, school staff, children and young people) to deliver interventions, some interviewees nominated research into techniques to improve the way therapists approach and deliver a consultative role. Here, comparative evaluations of consultative versus direct work approaches were mentioned, as were realist evaluations that provided evidence on ‘what works, for whom and in what circumstances’.
I think it would be great to have some research around what is the right intensity for doing things. Does therapy always have to be delivered by a therapist? Does is matter who’s delivered it, provided it has the child’s needs as its focus.
PHY-PB-02
Another area of interest for future research was the evaluation of a multidisciplinary care pathway, something that is beginning to be introduced in some localities:
There are lots of clinical pathways and packages of care now and it’s the way the NHS is going. It would be good to compare what different areas have in place for certain levels of need because everywhere is developing their own approach. This sort of approach comparison would help to support ‘what works’ well.
F1
Finally, research was called for that evaluated alternative methods of assessment. This was suggested as being useful in terms of supporting and informing the wider changes taking place across the professions. Specifically, interviewees identified a need for research in two areas: first, whether diagnosis per se was a useful construct around which to structure the care pathway, and, second, whether referral criteria and assessment should align more directly with functional impact and goals for different life domains or activities (e.g. mobility, social integration and self-care) as opposed to diagnostic or impairment criteria. Such an approach was regarded as having the potential to drive and support goals-focused working:
In some ways I think it’s more useful [for practice] to be looking at service criteria rather than diagnosis. So, focusing on finding out the functional impact for the child and whether the impact is sufficient for service support. Focusing on diagnosis means that waiting lists are long and we end up having a lot of services which are more or less assessment only, because by the point of diagnosis their resources are more or less used up. So [then] the child or family get a few activity ideas or suggestions, but therapists can’t work with them because they have no resource capacity left.
N1
The evaluation of specific techniques, procedures and equipment
In this section we report the research priorities related to the evaluation of specific techniques, procedures and equipment used by physiotherapists, occupational therapists and speech and language therapists. A wide range of specific interventions was nominated. Within this, there was a breadth in terms of the populations identified for whom evidence on intervention effectiveness was needed. Importantly, there was no clear indication of a body of support for research on, for example, a particular technique. Rather, research priorities in this area appeared to derive from personal or clinical interests and experiences. As a result, we do not specify any particular techniques, procedures or equipment here, and instead report on some key principles and overarching issues.
The range of interventions identified
Not unexpectedly, participants frequently mentioned evidence on intervention effectiveness. The techniques, procedures and equipment identified as priorities for research were wide-ranging and across all therapies. Furthermore, they concerned interventions related to prevention (e.g. pain, hip dislocation, deformity), recovery (e.g. traumatic brain injury in typically developing children) and children’s abilities to engage in tasks and activities and/or participate more fully in everyday life and the opportunities therein. Interviewees identified both interventions that had been used for many decades and more recent innovations. In addition, study participants identified a need for research on interventions delivered directly to the child (by therapists or others), parent-training interventions and interventions to support self-management. Finally, also suggested was an evaluation of the application of mainstream interventions, such as physical fitness and conditioning, to children with neurodisability:
I’d be interested in looking at whether we’ve looked at some of the other ways of improving outcomes by giving children with really significant difficulties the opportunity to be engaging in strengthening and cardiovascular activities. So, rather than concentrating on a particular area, look very much at the overall strength and cardiovascular and respiratory fitness of that child by some sort of mimicking of what normal levels of exercise would be for a child of that age.
Z1
Populations
Reference was made to children across the entire age range with respect to the evaluation of specific interventions.
The types of evaluation question
Questions about the effectiveness of specific techniques were expressed in various ways. Sometimes this was in terms of ‘should we still be doing this at all?’ or ‘what should we stop doing?’:
What really works? And what do we need to stop doing? What are we wasting our resources on? . . . but until we know it’s very difficult to take stuff away, especially from families that just want the reassurance that their child is actually receiving an intervention.
P1
Alternatively, the question was one of the relative effectiveness of two interventions, both designed to address the same presenting need or aspiration: ‘which should I choose?’.
Some interviewees extended their discussion of which interventions should be prioritised by future research to include questions of dose. When raised, questions of ‘dose’ were typically quite global; so, questions were about general levels of intensity in terms of frequency and duration of contact with a therapist, rather than concerned with, for example, the precise number of minutes for which a particular procedure or piece of equipment should be used. On this topic, it was suggested that families using private providers might be a useful comparator group, allowing a comparison of high-intensity, direct work (common among private providers) with the newer approaches being implemented within the NHS.
Others felt that, in some instances, it would be possible to be more specific about dose, referring to the notion of a ‘therapy prescription’ (in which the frequency, duration and intensity of an intervention was defined), and that this should be the objective of research:
The dose is what matters. Parents don’t complain about who is giving it . . . it’s the direct contact. So it’s the [evidence about] dose which we need.
A2
In addition, there were questions about mode of delivery. For example, some interviewees identified the relative benefits of individual versus group delivery of interventions as an important area for research. This included identifying factors that may reliably indicate to therapists and other health professionals whether they should offer group-delivered or individually delivered therapy to a child. It was felt that such indicators may be located in the intervention itself and/or in child or family characteristics.
The need for research on the setting of therapy was also expressed. Here questions related to investigating the relative effectiveness of clinic-based versus home-/community-based appointments. It was also discussed in relation to the rehabilitation of children with acquired brain injury in terms of whether residential or home-based care was more appropriate and effective.
Finally, research to identify the diagnostic features that indicate use of one intervention over another was commonly mentioned. This point was made in the context of participants describing instances when they did not know which of a range of options they should use to manage a particular need or goal, or having to try a number of different techniques/procedures with a child to identify the best approach.
Building an understanding and evidence base on an intervention
Discussions about research priorities regarding intervention effectiveness often included reflections on the need to build evidence slowly, and not to seek to carry out experimental studies from the outset. In this respect, single case series and cohort study designs were suggested as appropriate ways to start to build an evidence base. The notion of a programmatic approach to research was supported:
There may be a need to start back at single case series and cohort-type studies before we can get to [evaluating] interventions. But we also need a programmatic approach which goes beyond these studies, because, in the past, there have been single case series but the problem has always been that nobody follows it through.
P2
Transferring evidence on effectiveness from one group to another
Some study participants described having to recourse to evidence about an intervention derived from a different population, for example adults with brain injury, or a different neurodisability diagnosis. The extent to which this was an appropriate and legitimate practice was questioned. Research that identified when, and when not, to use such evidence was identified by some as a research priority. Occasionally, a similar question was applied to evidence derived from studies of typically developing children, particularly regarding the development of cardiovascular fitness and language interventions:
We try to apply ‘mainstream’ speech and language approaches but need to know when these are effective or what would make them effective for different groups.
G1
Future work on identifying research priorities
The involvement of children, young people and their parents
There was a strong and consistent view that it is essential, both in terms of setting research agendas and within specific projects or programmes of work, that children, young people and parents are directly and actively involved in meaningful ways:
We need to have parents and children from the outset of a research idea: a collegiate approach . . . And not just using the ‘usual group’ of parents who are consulted.
G2
They were involved in the JLA exercise but they need to be embedded and involved at every step.
W1
A number of interviewees noted the challenge of finding ways to involve children and young people who had severe impairments, including learning difficulties, in research:
It’s a huge struggle to involve in research in a meaningful and proper way people who have severe cerebral palsy.
Q2
Further devices to support research prioritisation
Some ideas or suggestions were offered as possible devices by which interventions could, or should, be used to prioritise research.
Current volumes of use or investment
One interviewee suggested prioritising for research those interventions that are widely used, but for which there is no evidence base. One reason for this is that these interventions may be ones that therapists are finding make some sort of difference, or have a positive impact. Here reference was made to Sackett et al. ’s40 discussion of evidence-based medicine. Such an approach, it was felt, would avoid individuals’ interests and agendas overly influencing the direction of future research. Another interviewee believed that priority should be given to evaluating interventions receiving the greatest investment, and/or when families typically expressed dissatisfaction with the level of therapy their child was receiving.
Feasible interventions
The notion that research should focus on interventions/approaches regarded as feasible and realistic within current health-care systems and resources, and also feasible and acceptable to families, was stressed by some interviewees. However, some interviewees noted that there may be value in evaluating interventions currently available only through private practitioners or third-sector providers, if these appeared ‘promising’.
Chapter 11 Discussion
Study overview
This scoping study was commissioned by NIHR’s HTA (Maternal and Child Health Panel) programme through one of the Health Services and Delivery Research programme’s Evidence Synthesis Centres. The agreed objectives of the study were to:
-
identify and describe the current techniques, practices and approaches to delivering therapy interventions for children with non-progressive neurodisability that seek to improve participation as defined by the ICF
-
describe the therapeutic approaches identified by professionals as promising or innovative but not currently (routinely) delivered by the NHS
-
identify how and why these interventions may vary according to the nature and severity of the impairment
-
describe the factors that influence decision-making regarding the ‘therapeutic prescription’, including the nature and severity of the impairment
-
understand the dimensions that constitute a therapeutic intervention from the perspectives of NHS health professionals, children and parents, for example the physical environment, location, use of/access to equipment, staff skills/qualification, parent involvement/delivery and self-management
-
seek the views of NHS health professionals, parents and children on the ‘active ingredients’ of therapy, and how to capture/measure them
-
understand, and compare, the ways in which professionals and families currently conceive therapy outcomes, the meaningfulness of ‘participation’ as a therapy outcome, and how these may vary according to the nature and severity of the impairment
-
map NHS health professionals’, parents’ and children’s views of the evidence gaps related to therapy interventions for children with non-progressive neurodisability, and identify views on the issues that need to be accounted for in the design of any future evaluations.
The research approach
Qualitative research methods were used to gather data to address these objectives. Professionals and parents participated in the study. Unfortunately, despite extensive efforts, the team was unable to secure the involvement of children and young people. We have already noted the importance of further work to allow children and young people’s voices to be heard.
Individual interviews and focus group discussions were held with therapists (frontline and service leads/managers) and included those working in private practice, those active in the research in this field, representatives of the therapies’ national professional bodies, professionals based in schools, and paediatricians. In recruiting to the study, we experienced extremely high levels of response and engagement with the study objectives.
Some overall impressions and comments
This scoping study has engaged with a highly complex and wide-ranging topic area, and one in which there are some sensitivities. The team who worked on the study are applied social scientists and none held any relevant professional qualifications. Although experienced in working on studies of this nature, and on the topic of childhood disability, they had not previously engaged closely with physiotherapy, occupational therapy and speech and language therapy. The ‘external’ nature of the team was referred to by many study participants, and this was consistently viewed positively as an indication of the team’s neutrality and independence.
As is clear in our report of the study findings, physiotherapy, occupational therapy and speech and language therapy are complex interventions. This study was concerned with their use with the highly heterogeneous population of children with non-progressive neurodisability. A further layer of complexity is the fact that there are multiple ways in which therapists may ‘work’ with a child with neurodisability. This made conducting a relatively brief piece of research – but with wide-ranging objectives – challenging, and decisions had to be made about the level of detail which could, or should, be usefully obtained. Furthermore, study participants sometimes held quite different and contradictory views.
Another finding was that physiotherapy, occupational therapy and speech and language therapy appear as professions in a state of change, even (r)evolution. As one would expect to find, there are mixed feelings, and sometimes strong views, about this: both for and against. We also observed both caution and impatience with regard to the changes under way. We believe that it is good and appropriate that this study has represented these different views and opinions. We also know that some of the changes reported were caused by externally imposed factors: principally, significant losses of NHS funding and resources. To a greater or lesser degree, therapy professionals felt beleaguered and under threat.
For these reasons, we have taken the approach of presenting the study findings in a very descriptive way, using verbatim quotations to illustrate the findings reported. This aligned with study objectives to offer a description of the current situation and understandings regarding therapies for children with neurodisability, and to elicit and report priorities for future research.
Study limitations
A key limitation is its failure to recruit children and young people to the study. We therefore cannot present data on their views on outcomes, perceptions regarding the active ingredients of an intervention, and research priorities. This is a significant omission and should be borne in mind when considering the implications of the study findings. Additional work will be required to secure the views and perspectives of this group; the findings from this study may well form a useful resource from which to build consultation tools and materials.
We would note that extensive efforts were made to recruit children and young people, and the research team has successfully recruited this population to many studies. Thus, this failure cannot necessarily be attributed to a lack of effort or insufficient experience. We have already drawn attention to the experiences of other researchers who have sought to include children and young people in research prioritisation exercises: it is possible that the rather intangible nature of projects of this study, compared with other health services research topics, makes participation in studies of this kind less compelling or meaningful.
A second limitation to the study is that the perspective of teaching/education professionals was limited to a single participant. Certainly, it is clear that schools are an environment in which much therapy is delivered, often by teaching assistants under the supervision or direction of a therapist or therapy assistant. Other studies have described a lack of knowledge and understanding of therapy interventions among teaching staff and negative or ambivalent feelings about therapy interventions and equipment. 41–46 These findings support the need for consultation with school staff, and therapists working in these settings, when refining research questions concerned with the models of service provision which may well include the provision of therapies in school settings. Linked to this, we would note a recently completed NIHR study within the Research for Patient Benefit programme, which evaluated training school staff (and parents) in postural care. 47
In the remainder of this chapter, we return to the study objectives, reporting for each the key findings and broad conclusions that can be drawn.
Objectives 1 and 2: the techniques, practices and approaches to delivering therapy
Objectives 1 and 2 were:
-
to identify and describe current techniques, practices and approaches to delivering therapy interventions for children with non-progressive neurodisability that seek to improve participation as defined by the ICF
-
to describe therapeutic approaches identified by professionals as promising or innovative but not currently (routinely) delivered by the NHS.
It is important to note that, from the outset, participation was consistently identified as a primary objective of any therapy intervention. Thus, our discussions with participants about techniques, practices and approaches were not restricted in any way. Chapters 3–5 reported the findings relevant to this objective.
The organisation of therapy services and service models
First, we described the ways in which therapy services are organised, and how they interface with, or are connected to, other services for children with neurodisability.
Predominantly, reference was made to other health services; however, the interface between health and education – particularly the delivery of therapy, or the implementation of therapy interventions, in schools – was regarded as a key issue. In addition, parents were identified as often playing a key role in implementing therapy programmes. To date, the role of ‘non-therapists’ in the delivery of therapy interventions, their experiences and its impact has been studied in a limited way. A number of barriers to implementing therapy regimes in school settings have been identified and reported, including issues of staff knowledge and confidence. 41,45 It has been suggested that parents may vary in their willingness and/or capacity to assume the role of ‘co-therapist’. 48–51 Notions of feeling overburdened by the requirements of a therapy regime, and a lack of ongoing training and support, have also been reported. 52 In terms of work within the existing NIHR portfolio, a study47 funded as part of the Research for Patient Benefit programme has been recently published, which evaluated a training intervention for parents and school staff on postural management.
Different models for organising therapy provision were reported, and alternatives to the traditional model of ‘unitherapy’ teams were presented. These included joint/multitherapy teams and integrated, multiprofessional teams. Transdisciplinary teams were also described, with therapists working across disciplines and/or one therapist acting as primary provider for all therapies to the child. Finally, therapist-led services, operating without referral from a paediatrician, were reported. Often, multiple factors were driving, or informing, the development of alternative service models. Certainly, resource constraints played a part, but the responses to these constraints were informed by new thinking about therapy interventions, particularly family-centred and goals-focused approaches. The influence of the ICF model of impairment and disability, which presents ‘participation’ as the key objective of any intervention, was explicitly referred to by study participants.
The use of private practice
Final key themes in Chapter 3 were the issues of private provision and parents identifying and delivering ‘therapy interventions’ themselves. Professionals taking part in the study reported that this was not uncommon, and this was certainly borne out in the experiences of parents recruited to the study. There was consensus that parents turning to alternative sources of provision was an indicator of their intense desire ‘to do the best’ for their child, and the frustrations that they may experience with NHS provision. Parents’ accounts supported these views, as reported in Chapter 5.
Overall approaches to therapy and schools of thought
In Chapter 4, we presented a model by which therapy interventions can be understood. It was argued that specific techniques, procedures, activities, practices and equipment need to be understood in the broader context. This broader context was occupied by two factors: first, the overall approach a therapist brought to the management of a case, and, second, whether the therapist adhered to, or was influenced by, particular schools of thought. We reported the strong, but partial, influence of WHO’s ICF model of disability and health, and family-centred practice, across the three professions.
Thus, there was a belief that the ‘deficit model’ and a focus on the achievement of specific activities were still routinely operationalised, and that goals-focused approaches to assessment and therapy provision were not yet fully ingrained in practice. Indeed, there was evidence of some confusion with concepts such as ‘goals-focused’ and ‘participation’, and differences in the way they were being defined and implemented. In addition, notions of parents and/or children and young people as active partners and decision-makers in the delivery of therapy intervention were viewed as aspirations or ‘work in progress’, as opposed to firmly bedded into practice.
Chapter 4 also described how, a few decades ago, certain schools of thought dominated the approaches taken by therapists. It was clear that some of these traditional schools of thought were no longer regarded, by some at least, as having any credibility. Other schools of thought – drawn from other disciplines or professions – were, however, reported to be influencing current therapy practice. These included cognitive–behavioural, problem-solving approaches; family-centred practice; and evidence-based practice. Importantly, the notion of early intervention continues to strongly guide the management of children with neurodisability.
The practice of therapies
The second half of Chapter 4 reported our findings on what we have termed ‘the practice of physiotherapy, occupational therapy or speech and language therapy’. Here we described and illustrated the key constructs that define these interventions, namely professional autonomy, responsive practice, managing prognostic uncertainty, protocols and pathways, working out of a tool box and mode of delivery. Throughout much of this account, the notion of therapies as, typically, highly individualised interventions has emerged strongly.
In Chapter 4 we referred readers to Appendix 6, which sets out the procedures, techniques and activities that interviewees reported using, or having come across, in NHS settings. This serves to portray the great diversity of practice, but we would stress that this list is, to no extent, comprehensive. The research team’s view is that to map all procedures, techniques and activities would, arguably, be an almost impossible task. Importantly, as Chapter 4 demonstrated, knowing the names of techniques or procedures is not the same as knowing how a therapist is using or implementing them.
In terms of new and emerging techniques, procedures or equipment that appear promising, this was not generally a topic interviewees regarded as important or relevant, as they believed that the priority should be research into existing practices and ways of organising and delivering therapy interventions. However, there was strong support for research that evaluated new and emerging approaches to service organisation and delivery (e.g. multi- and transdisciplinary working; upskilling/cascading skills) and ways of working (e.g. goals-focused approaches, family-centred practice and promoting self-management). We return to the topic of research priorities later in this chapter.
Parents’ experiences of services, reported in Chapter 5, generally aligned with professionals’ accounts of the way in which the majority of therapy services are organised. A predominant theme in parents’ accounts were dissatisfaction with the amount of therapy their child received and the lack of integration across therapies and other interventions. These are not newly identified issues; they have been reported by previous studies and, indeed, have stimulated policy responses. 19 However, we have not been able to identify any recent English research that has mapped this on a scale beyond specific localities. Parental dissatisfaction with the amount of therapy partly reflects the reality of significantly constrained resources for therapies within the NHS, but may also indicate a mismatch in understanding of appropriate levels of intensity in terms of contact with therapists. A strong thread throughout parents’ accounts was a desire to be doing all they could for their children, and this had led some to pay for the services of private providers and/or identify and deliver therapy interventions themselves.
We also explored the impact on parents of the expectation that, particularly in a child’s preschool years, they may assume a significant role in the delivery of therapy. Included in the stories they relayed were themes of guilt, conflict, exhaustion and a sense of working in isolation, all of which have been reported in previous studies. 48,52 In addition, they expressed concerns about the way therapies intruded into their child’s life and prevented the child from doing other activities. They also described their children’s responses to receiving therapy. Here parents focused on sharing experiences of negative reactions, which were attributed to pain, frustration and a desire to be doing something else. Sometimes these reactions were difficult to manage and this was a common reason why parents desisted from carrying out interventions and using equipment.
Objectives 3 and 4: factors influencing clinical decision-making
Objectives 3 and 4 were:
-
to identify how and why these interventions may vary according to the nature and severity of the impairment
-
to describe the factors that influence decision-making about the ‘therapeutic prescription’, including the nature and severity of the impairment.
Chapter 4 reported findings relevant to study objectives 3 and 4. References within these objectives to the potential influence of impairment-related characteristics on clinical decision-making could be perceived as sitting at odds with notions of goals-focused approaches to assessment and clinical decision-making. However, even within this approach, account may need to be taken of the child’s ability to learn new skills or manipulate equipment, so here issues of cognitive, rather than motor, impairment play a greater role.
In Chapter 4 we reported that, for the majority of therapy interventions, no protocols or manuals exist. It is possible to glean some explanations for this. First, children with neurodisability are highly diverse in both diagnosis and the way each diagnosis presents in terms of motor functioning and impairment. Second, the evidence base on therapy interventions is minimal. Taking these two factors into account, it is easy to see why manualised approaches and protocols are not common features of practice.
Furthermore, as we discuss in the following section, very little is understood about the active ingredients of interventions. There are, therefore, significant barriers to the development of protocols or manualised interventions for this population. One exception is interventions for the management of a specific presenting need and within a specific population. For these situations, interviewees did cite more routinised approaches, such as the management of hemiplegia by constraint induced movement therapy, and the management of spasticity in children with cerebral palsy.
As a result, clinical decision-making is typically highly individualised and becomes increasingly so the more complex and severe the presenting needs. The principle of professional autonomy, and the factors therapists reported as influencing clinical decision-making in the management of a particular case, are described in Chapter 4. Certainly the child’s presenting needs (or desired goals) were reported to be a key influence on decision-making. However, other factors were reported as significantly influencing the decision made.
A key issue, and one driven by the role parents often play in the implementation of therapy programmes, was family characteristics and resources. Therapists consistently reported that this influenced their decision-making about what interventions they selected and the intensity of their delivery. We also describe the emphasis placed by therapists on the role of clinical experience (sometimes gleaned from more experienced colleagues), in interaction with other factors such as family characteristics, in designing an intervention programme, including the ‘dose’ (i.e. the frequency and duration of each therapy session or episode).
Chapter 4 also described the wide range of factors influencing which interventions a therapist might bring to that decision-making process. Here we used the analogy of the ‘toolbox’, and reported how a number of diverse factors influenced what an individual therapist may have in his or her toolbox. These included their training, overall approaches to therapy interventions, practices learnt from colleagues, personal preferences, clinical guidance and what they were permitted to do by commissioners or service leads.
Thus, a picture is painted of highly individualistic practice, the outcome being that different therapists may choose to work with the same child in very different ways. This certainly aligned with professionals’ accounts and parents’ views and experiences (reported in Chapter 5).
Objectives 5 and 6: understanding therapy interventions and their active ingredients
Objectives 5 and 6 were:
-
to understand the dimensions that constitute a therapeutic intervention
-
to seek views regarding the ‘active ingredients’ of therapy, and how to capture and measure these.
In Chapter 6, we explored professionals’ views of what constitutes a therapy intervention, and what are its active ingredients. Chapter 5 included a description of parents’ views of valued practice, which is also relevant to this topic.
Therapies as complex interventions
Our opening sections of Chapter 6 presented the notion of physiotherapy, occupational therapy and speech and language therapy as complex interventions,31 and described the existing conceptualisations of the active ingredients of non-pharmacological interventions. We referred to work by McCleary et al. 30 and Bourton et al. 32,33 Both have highlighted the challenges of identifying, defining and measuring the active ingredients of complex, non-pharmacological interventions, and this offers an explanation of why, to date, the active ingredients have been poorly reported.
In essence, the argument is made that the following interconnecting features of complex, non-pharmacological interventions make it difficult and complicated to identify their active ingredients.
-
They may have several interacting components.
-
Different health-care professionals and other individuals may be involved in their delivery.
-
They may be tailored to specific situations or contexts.
-
Their success may be dependent on the expertise of the intervention provider.
Much of the remainder of Chapter 6 presented study participants’ views on what constitutes the active ingredients of an intervention, and these are summarised in Figure 4. First, there was clear consensus that a therapy intervention comprises the therapist, the work that therapist does and the work that others do under the training or supervision of the therapist. In terms of the therapist, as reported in Chapter 4, there are various levels of influence in terms of what they ‘bring’ to a case and the ‘work’ they decide to do. This includes the overall approach that they adopt (deficit vs. activity-focused vs. goals-focused) and the influence of particular schools of thought, as well as clinical decision-making processes and the factors that influence them. A further component of an intervention that emerged from participants’ accounts was the ‘therapeutic context’. We used this term to define elements such as the capacity of the wider therapeutic team (e.g. parents, school staff), the setting in which therapy may be delivered, and the access to, and space to use, equipment).
FIGURE 4.
The active ingredients of therapy interventions: study participants’ views.
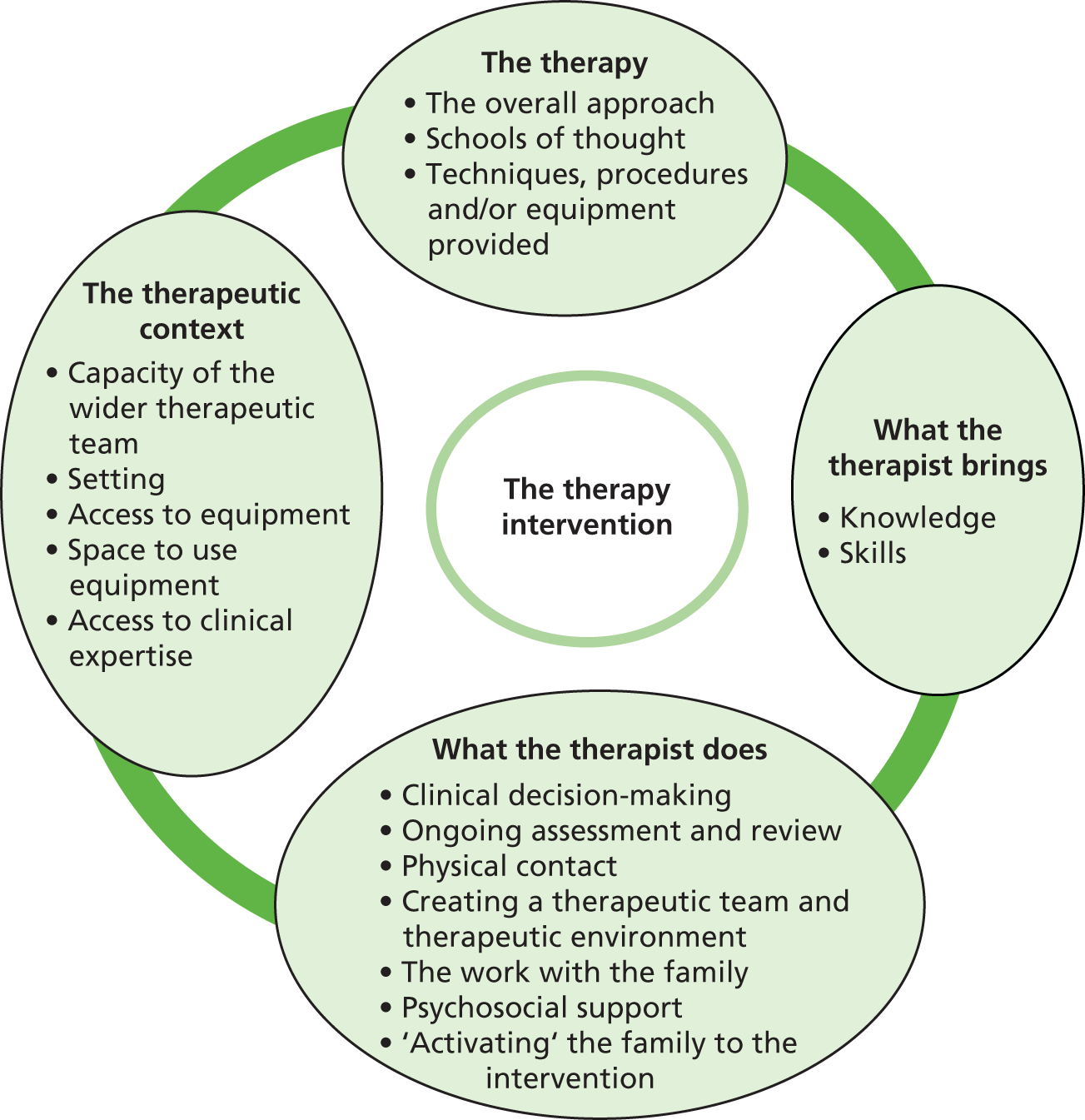
The final section of Chapter 6 reported professionals’ views on the measurement of these active ingredients. Certainly, both the lack of an understanding of active ingredients, which ones matter most, and systematic ways to describe, record and measure them were identified as significant barriers to future research, both in terms of the design of an evaluation (i.e. which factors, or ingredients, need to be controlled for, or manipulated), and in their execution. We return to this issue when reporting study participants’ research priorities.
Objective 7: therapy outcomes
Objective 7 was:
-
to understand, and compare, the ways that professionals and families currently conceive therapy outcomes, the meaningfulness of ‘participation’ as a therapy outcome, and how these may vary according to the nature and severity of the impairment.
Findings relating to this objective were presented in Chapter 7, with relevant material also appearing in Chapters 4 and 5.
Parents’ views
The outcomes identified by parents were consistently located within more global outcomes, such as participation, independence, quality of life and mental well-being. Although these outcomes were global, parents strongly believed in the potential of therapy interventions in supporting their achievement. Thus, improvements in physical functioning, acquiring new motor skills and having access to equipment were regarded as necessary, but intermediate, outcomes to the achievement of higher-level outcomes. These views align closely with other studies that have explored parents’ (and children’s) views on desired, or prioritised, outcomes of health and care provision. 53,54 However, as we reported in Chapter 5, some parents reported that therapists may not explicitly refer to these higher-level goals, and can appear to be focused on specific aspects of functioning, etc.
Professionals’ views
Our report on professionals’ views about outcomes was presented within the ICF framework, which distinguishes between outcomes related to body structure and function, outcomes related to the achievement of particular activities and outcomes that can be defined as being aligned with notions of participation. As reported in Chapter 4, the ICF framework16 and the concept of participation were adopted by the professions a number of years ago, although understanding of the meaning of the concept varied. Certainly, the term ‘participation’ was spontaneously offered as one of the main objectives of any therapy intervention, although we must be cautious about the consistency of definition applied to this term. The specifics of definition aside, participation was consistently regarded as a complex and multifaceted concept. Furthermore, it was clear that some study participants felt that further critical, conceptual work was required to clarify its definition, and the way in which it should be operationalised by the therapies.
Some helpful developments to the concept were, however, offered during our interviews. First, it was stressed that participation could sometimes simply be about opportunity (and choice), and, second, that it should include notions of ‘ease of participation’, and not just participation per se. There was also a clear view that participation had to be something defined by the child and/or their wider family, and that assumptions should not be made about what constitutes participation for an individual child.
Another thread in our discussions with professionals were concerns about the extent to which participation can be operationalised, or applied, to some groups of children with neurodisability, including neonates and very young children, children with disordered states of consciousness, children with multiple and profound disabilities, and typically developing children who have recently sustained a severe brain injury.
Participation as an outcome measure
A second, separate question explored in our interviews with study participants was to ask whether participation is an appropriate or meaningful concept to use with respect to the evaluation of interventions. A number of significant issues were raised and we will not rehearse them fully here. However, four key issues or concerns were raised. First, therapy interventions are often one aspect of a multifaceted, multidisciplinary programme of interventions that a child may be receiving. Second, any evaluation of intervention outcomes needs to take account of the impact of any age-/development-related changes in the child. Third, it was suggested that although participation should be the end point, or overall goal, a therapy intervention’s role in achieving this may come early on, in order to secure intermediate outcomes on which other interventions can build. Finally, questions about the appropriate time to ‘measure’ participation were raised, which in turn led interviewees to point to the myriad of other events and circumstances that may intervene in a child’s life before participation-related outcomes are investigated.
There was greater engagement with the notion of participation as an outcome indicator if the evaluation concerned the whole approach of services, or particular service models. However, questions about when, and what, to measure were still raised, and similar arguments rehearsed regarding the challenges and complexities of outcome measurement. A recently completed NIHR HSDR project55 on meaningful health outcomes for paediatric neurodisability – incorporating the collection and collation of the views of families and professionals, as well as a systematic review of existing outcome measures – makes an important contribution to moving forward on this issue. In addition, a similar project but specific to young children with autism has also been published recently. 56 Both of these studies identify measure development work as a research priority.
Goal attainment scaling
Given the move towards goals-focused approaches to therapy interventions, goal attainment scaling was suggested as an approach that had the potential to capture participation-type outcomes that may be more directly attributable to a specific intervention. It was also regarded as having the potential to be implemented routinely, and, if standardised and used routinely, could lead to the development of very useful data sets for cohort studies. To date, this approach has predominantly been confined to adult rehabilitation,57 although its use in paediatrics has been critically evaluated. 58 This latter piece of work called for more research into the reliability of goal attainment scaling within the paediatric context. A useful piece of work going forward would be to review evidence on this.
Finally, before this discussion is concluded, it is important to return to the issue of multiple definitions and understandings, which introduced this section. Readers need to be mindful that interviewees’ views on participation as an appropriate and meaningful outcome indicator will be based on their understanding of this concept.
Other child outcomes
Interviewees readily identified other outcomes that they believed to be appropriate and meaningful, and that should be considered when designing evaluations. These included measures of body structure and functioning, engagement in/achievement of activities, emotional well-being, quality of life, acceptance of impairment and engagement with interventions.
Parent outcomes
Outcomes for parents were also strongly emphasised. These were regarded as legitimate indicators of the impact of a therapy intervention. The parent-level outcomes suggested included quality of life, resilience, emotional well-being, perceived emotional and information support needs met, confidence in skills and abilities, and knowledge and acceptance of child’s impairment. Certainly some of these outcomes map well on to other research, referred to earlier in this discussion, which has explored parents’ experiences of delivering therapy interventions. 41,48,52
Objective 8: evidence gaps and issues of study design
Objective 8 was:
-
to map NHS health professionals’, parents’ and children’s views of the evidence gaps related to therapy interventions for children with non-progressive neurodisability, and identify views on the issues that need to be accounted for in the design of any future evaluations.
In Chapter 10 we reported study participants’ views on priorities for future research. This was preceded by a consideration of the nature of the ‘research environment’ within the therapy professions (see Chapter 8), in which we reported on the beliefs and cultural and infrastructural factors that relate to engagement with, and capacity to engage in, research. Following this, we reported on the perceived challenges of evaluative research (see Chapter 9), some of which generated research questions/priorities themselves. It is important to stress the significant limitation regarding this aspect of the study that we were unable to secure the involvement of children and young people and, thus, their views on research priorities are absent.
Views about the need for research
Chapter 8 began by reporting widespread acceptance and agreement that the current evidence base on therapy interventions for children with neurodisability is very limited. This very much concurs with the wider accepted view of the current situation1,6,59 and therapists’ views on the barriers to evidence-based practice. 60–68 These findings are not unique to the therapy professions investigated in this study, and have been reported across a wide range of health-care professions. 64–66 Furthermore, and as other studies report,61–63 the applicability of existing, higher-quality evidence (derived from studies not conducted in routine practice or clinical settings) was questioned.
This lack of evidence was generally viewed as causing variability in practice and models of service delivery, and inequity of provision. It was also seen as hindering professions’ abilities to argue their case for sufficient resources from commissioners. Some therapists also reported concerns about whether their practice, or that of others, was always ‘the right thing’ for the child.
Overall, therefore, there was strong support for research into therapies for children with neurodisability. However, this was sometimes tempered by concerns about whether or not it was possible to show that therapies make a difference. The notion of evidence-based practice was typically referred to as a ‘good thing’, and is enshrined within professional standards. However, sometimes there was a concurrent rhetoric about the importance of clinical experience and professional autonomy within the clinical decision-making process. Viewing clinical experience as being ‘at odds’ with a notion of evidence-based practice – an issue also identified by previous research61 – is perhaps a reflection of a common misunderstanding of this concept. 67 The true meaning, or application, of evidence-based practice is one in which existing research evidence is applied in the context of clinical experience and the patient’s values and preferences. 40 A range of views on the relative value of high-quality research evidence compared with clinical experience is something some other studies have also reported, with recency, level of training and characteristics of the workplace (e.g. university hospital vs. services unconnected with academic/research endeavours) being found to influence an individual’s viewpoint. 61–63
Research infrastructure within the therapy professions
There was a strong consensus that, currently, the majority of therapy services could not be described as research engaged or research active. Furthermore, time for research is not routinely incorporated into roles; indeed, engaging in research may not be supported by service leads or managers. Opportunities to review and discuss research evidence (e.g. holding journal clubs) were not widely reported. They appeared to be most likely to be located in services based in, or linked to, university hospitals. Instances of services actively seeking evidence to inform their practice and service development were, however, described to us. We also learned about a service (non-NHS) that had invested in research posts, which focused on both developing evidence-informed guidance and initiating primary research.
Interviewees noted that, in the past, research had not been part of the training curriculum but that this has changed over the past decade. However, although more recently qualified therapists might have had some exposure to research and research methods during their training, there had been little opportunity to pursue this. That said, it was reported that within continuing professional development provision, there had been a growing focus on research. Finally, there was a sense from participants’ accounts that there is a potential disconnect between current research activity and frontline therapy services, with much existing research being led from academic institutions.
This description of the research infrastructure within the therapy professions aligns closely with findings from other studies, carried out in England and other countries. 60–63
Perceived challenges of designing and conducting evaluative research
Study participants readily identified challenges with evaluating therapy interventions and a minority believed that these were insurmountable. Most regarded them as issues that may themselves need to be researched. The challenges identified included the heterogeneous nature of the population, the nature of therapy interventions, research design issues, the challenges associated with implementing evaluation studies and the requirements of funders. The main message arising from these debates was that evaluations of therapy interventions will require a range of study designs and methods, and a willingness on the part of funders to both invest in non-experimental designs and be cognisant, but accommodating, of the challenges of implementing experimental study designs when evaluating highly complex, non-pharmacological interventions.
Parents’ research priorities
The majority of research priorities identified by parents aligned with issues relating to the design and delivery of therapy provision and ways of working. Thus, parents called for research that supported and informed integrated care, goals-focused approaches and empowering parents. They also wanted research to be carried out that compared ongoing with episodic models of care, and studies that identified when children and young people should be receiving therapy interventions and/or have the intensity of these increased.
Some parents also identified specific intervention (e.g. should a technique or piece of equipment be used at all?) or had questions about dose or intervention intensity. However, no specific techniques were consistently mentioned by parents.
Professionals’ views on research priorities
Among our interviews with professionals, a wide range of research priorities were identified, not all of which were concerned with the evaluation of therapy interventions for children with neurodisability. We categorised their research priorities as follows: methodological research (reported in Chapter 9), and foundational, or underpinning, research and evaluation (both reported in Chapter 10).
Participants’ suggestions about methodological research included recommendations for feasibility studies, methodological work on trial design, investigating other study designs – particularly cohort studies and case studies – and the possibilities for establishing endeavours using these approaches, and, finally, outcome measures and outcome measurement.
In terms of foundational research, first, the case was made for the need to secure a better understanding of neurodisability per se and the trajectories of different conditions. This reflects the great range of children and conditions represented under this umbrella term, the fact that the impairment has a neurological origin, the relative infancy of the academic discipline of neurodisability, and, arguably, the lack of investment in research on this particular population. Second, some interviewees prioritised the need for research that would develop understanding of therapy interventions. The topic areas for this ranged from the mechanisms of change and active ingredients of interventions to families’ and practitioners’ beliefs and understandings. (This was also an area that was raised by participants of the JLA’s research prioritisation exercise for children with neurodisability1 but was not taken forward to the actual prioritisation because it was outside the scope of that particular piece of work.) The third area of ‘foundational research’ was work on further defining the concept of participation.
In terms of evaluation research, the research priorities identified can be split into two broad categories: the evaluation of overall approaches to therapy interventions and the evaluation of specific treatments, procedures or items of equipment.
In terms of overall approaches to therapy interventions, the following types of question were posed:
-
When should a child be accessing therapy interventions?
-
How should therapy services be organised in order to achieve the best outcomes for children (and parents) in both the short and the longer term?
-
Do goals- and participation-focused approaches improve children’s outcomes, and how can they best be implemented?
-
What practices, or ways of working, best support a consultative model of delivering therapy interventions?
-
What supports families’ engagement in therapy interventions and notions of self-management?
-
What practices, or ways of working, best support children, young people and families to effectively engage in goal-setting, and why?
Often questions of cost and cost-effectiveness were included in study participants’ discussions about these issues.
Regarding specific practices, techniques, procedures and equipment, a wide range was nominated as priorities for future research. None was mentioned consistently, reflecting the fact that these suggestions often appeared to be grounded in personal interest or experience. In addition to interventions specific to neurodisability, some interviewees stressed the need for research that evaluated the application of practices or approaches used with typically developing children and young people, particularly for cardiovascular fitness and language and communication development with children with neurodisabilities.
A number of different evaluation questions were posed. Some concerned evaluations of effectiveness per se, whereas others related to testing dose, mode of delivery and therapy setting. Another area of investigation was identification of diagnostic (or other) features that should be used to inform clinical decision-making. Some viewed research into specific practices and techniques as secondary to, or irrelevant compared with, research into models of care and ways of working.
The research priorities identified by professionals and parents generally aligned with those reported by Morris et al. ,1 which were generated from a wider research prioritisation exercise for children with neurodisabilities, although the emphasis is different. The research priorities pertaining to physiotherapy, occupational therapy and speech and language therapy identified by Morris et al. 1 were generally presented in terms of intervention approaches or strategies to improve function rather than research on approaches to practice (e.g. goals-focused working, family-centred practice) or the way in which services are organised and delivered. However, it is important to note that the two pieces of work had different parameters. First, Morris et al. ’s study was restricted to ‘interventions and process’: this was not specifically defined and might not have included the notion that service-/organisational-level issues and characteristics can be understood as interventions in themselves. 68 Second, this study would not have included the identification of methodological or more ‘foundational’ research within its scope. Third, the research prioritisation approach by Morris et al. 1 required the identification of research questions; however, they did report that many of the issues raised during the research prioritisation exercise could not be framed as such.
Chapter 12 Conclusions
Study overview
The overarching purpose of this scoping study was twofold. First, we aimed to provide contextual information to NIHR regarding current approaches, practices, service models and ways of working in the provision of physiotherapy, occupational therapy and speech and language therapy to children and young people with non-progressive neurodisability. Second, we wanted to consult with key stakeholders about research priorities, and to identify the challenges of carrying out research on therapy interventions, both in terms of methodological and study design issues and with respect to the current ‘research environment’ within therapies services.
Interviews and focus groups with a wider range of professionals – front line and managerial; research naive, research aware and research active; within the professions and based in services that interface with therapy provision; and across the country – were carried out. We also held focus groups with parents, and these parents represented children and young people across a wide range of ages, diagnoses, and types and severity of impairment.
Thus, we sought to capture a breadth of current knowledge, experiences and opinions. We would note that we experienced a high level of interest and willingness to participate in the project among both participant groups: therapies for children with neurodisability was an issue they wanted to discuss and debate.
Sadly, we found the identification and engagement of groups of children and young people to be a harder task and did not, within the fixed time frames of this project, manage to secure their involvement. In terms of further work to inform the direction and scope of research on therapies with children with neurodisability, we would stress the importance of working with children and young people, and indeed parents, a position fully endorsed by those who participated in this scoping study.
Key findings and conclusions
The key findings and conclusions are as follows.
-
Parents are clear in their belief about the necessity and importance of therapy interventions. In terms of provision, the predominant issue they report is insufficient therapy. It seems that it is not uncommon for parents to seek private providers, or to identify and self-deliver (untested) ‘therapy’ interventions.
-
The three professions are in a state of dynamic change and development. This appears to be taking place in response to three separate issues:
-
debates and conceptual understandings of disability and impairment
-
shifts taking place in other professions and disciplines, and related evidence, regarding goals-focused working, family-centred approaches and supporting self-management
-
significant resource constraints.
-
-
In terms of the practice of therapy, the key distinctive features are professional autonomy and highly individualised approaches to delivering therapy that are informed, or underpinned, by clinical experience, ‘philosophical positions’ regarding the purpose of therapy, and the specific procedures, techniques and/or equipment that the therapist has the skills, or resources, to deliver.
-
Manualised, or protocol-driven, interventions are unusual. There are early signs of a move to care pathways, and the application of protocols within this structure.
-
Much of the direct work of delivering therapy to a child is carried out by parents and school staff. Increasingly, therapists assume a consultative role. Their skills in this regard are therefore critical.
-
Therapy interventions are complex. Existing frameworks for understanding complex, non-pharmacological interventions offer a useful structure by which this complexity can be understood.
-
Children with non-progressive neurodisability are a highly heterogeneous population. Many have complex needs and require the support and care of a number of professionals and services. The neurological origins of their impairments mean that children with predominantly physical/motor impairments – specified as the population in question for this scoping study – may well have cognitive impairment. Additional or alternative approaches to defining populations – for example in terms of gross motor function or desired goals – may be more meaningful and appropriate.
-
Many potential ‘active ingredients’ were identified, some of which would appear to offer challenges in terms of their ‘measurement’. Related to this, understandings of mechanisms of change are limited.
-
Parents and professionals strongly identify participation as one of the overarching objectives of therapy interventions. However, study participants’ understanding of this term was extremely variable, and, furthermore, it may not be explicitly operationalised in practice.
-
The notion of participation as an appropriate and meaningful outcome indicator for therapy interventions was questioned, particularly evaluations of a specific procedure or technique. There was agreement that, when properly implemented into a study design, participation may be an appropriate indicator in studies evaluating the impact of wider models of care.
-
There was broad agreement that any evaluations should capture outcomes across the entire spectrum of the WHO’s ICF framework, including functioning/body structure, engagement in activities, and participation (as well as other, higher-level outcomes). Some of these outcomes may be better conceived as intermediate outcomes.
-
Quality of life, physical and emotional well-being, resilience and self-management were identified as potentially relevant higher-level outcomes.
-
Typically, there is not a strong culture of research within therapy services. However, within the professions there is growing engagement with and interest in research. There is recognition and acceptance of the need for research, although for some this is tempered by concerns about research’s ability to demonstrate the impact they believe therapies have on children’s lives.
-
A broad-ranging agenda of research priorities was identified. Some were regarded as ‘foundational’ or prerequisites of other types of studies.
-
A number of methodological and study design issues were identified as barriers to evaluation research.
-
Evaluations of ways of working (e.g. goals-focused approaches) and service models (e.g. integrated care, multi- or transtherapy teams) were frequently identified as research priorities. Overall, parents’ research priorities were located in these types of studies.
-
Research priorities concerning particular techniques, procedures or items of equipment generated a long list of potential studies. These appeared to be located in personal preferences and clinical experience, and none emerged as receiving strong and consistent support.
-
There was universal consensus that evaluative research needs to use mixed methods, and patient experience as well as outcomes should be captured.
-
Health economics and implementation science were consistently identified as needing to be core components of evaluation studies.
Study limitations
The main, and major, limitation of this study was its failure to recruit a sample of children and young people. This was despite extensive and creative efforts being made within the constraints of time and resources arising from the fact this was a commissioned study being delivered within a fixed 9-month timeline. Additional work is required to consult with children and young people, and we would suggest that the findings from this study would provide a useful and effective starting point for discussion and consultation. In addition, the study did not incorporate a patient and public involvement element, and nor did its design include sufficient representation from school/education staff.
Final comments
This study was commissioned by NIHR to inform strategic decision-making in terms of its response to the findings of a JLA research prioritisation exercise for children with neurodisability. Four of the top 10 priorities emerging from this exercise concerned therapy interventions. Within NIHR, it was the HTA programme that initiated this scoping study. The findings from this piece of work suggest that a much broader approach to tackling the significant evidence gaps related to therapy interventions for children with neurodisability would be appropriate, embracing, for example, the HSDR, Efficacy and Mechanism Evaluation and Programme Grants for Applied Research programmes, as well as the Medical Research Council-NIHR Methodology Research Programme.
Acknowledgements
We particularly acknowledge the contributions of the parents who participated in this study, many of whom made special arrangements to attend a focus group meeting. Our sincere thanks go to them for their interest and involvement.
We would also like to express our thanks to the individuals within parent-led support and advocacy organisations who brought together relevant parents on our behalf and co-ordinated arrangements for, and hosted, focus groups.
We would also like to acknowledge the efforts made by many of our professional interviewees to participate in this scoping study, protecting time and fully and thoughtfully engaging with the topics we wanted to explore. Some of these individuals also facilitated contacts with other research participants or organised focus groups with therapy practitioners. We are very grateful for this commitment and support to the project.
Finally, we would like to thank Teresa Frank, who ably provided administrative support to the project.
Contributions of authors
Bryony Beresford (Research Director) is an Applied Social Scientist working in health and care services research; was the chief investigator; contributed to data collection and data analysis; led writing of the final report.
Susan Clarke (Research Associate) is an Applied Social Scientist working in health and care services research; co-led on data collection and data analysis; contributed to writing of the final report.
Jane Maddison (Research Fellow) is an Applied Social Scientist working in health and care services research; co-led on data collection and data analysis; contributed to writing of the final report.
Data sharing statement
Requests for access to anonymised data should be made to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Morris C, Simkiss D, Busk M, Morris M, Allard A, Denness J, et al. Setting research priorities to improve the health of children and young people with neurodisability: a British Academy of Childhood Disability-James Lind Alliance Research Priority Setting Partnership. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006233.
- NICE . Spasticity in Under 19s: Management 2012. www.nice.org.uk/guidance/cg145 (accessed 26 July 2016).
- Pennington L, Goldbart J, Marshall J. Speech and language therapy to improve the communication skills of children with cerebral palsy. Cochrane Database Syst Rev 2004;2. https://doi.org/10.1002/14651858.CD003466.pub2.
- Tinderholt Myrhaug H, Ostensjo S, Larun L, Odgaard-Jensen J, Jahnsen R. Intensive training of motor function and functional skills among young children with cerebral palsy: a systematic review and meta-analysis. BMC Pediatr 2014;14. https://doi.org/10.1186/s12887-014-0292-5.
- Rameckers EA, Janssen-Potten YJ, Essers IM, Smeets RJ. Efficacy of upper limb strengthening in children with cerebral palsy: a critical review. Res Dev Disabil 2014;36C:87-101.
- Novak I, McIntyre S, Morgan C, Campbell L, Dark L, Morton N, et al. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol 2013;55:885-910. https://doi.org/10.1111/dmcn.12246.
- Franki I, Desloovere K, De Cat J, Feys H, Molenaers G, Calders P, et al. The evidence-base for basic physical therapy techniques targeting lower limb function in children with cerebral palsy: a systematic review using the International Classification of Functioning, Disability and Health as a conceptual framework. J Rehabil Med 2012;44:385-95. https://doi.org/10.2340/16501977-0983.
- Franki I, Desloovere K, De Cat J, Feys H, Molenaers G, Calders P, et al. The evidence-base for conceptual approaches and additional therapies targeting lower limb function in children with cerebral palsy: a systematic review using the ICF as a framework. J Rehabil Med 2012;44:396-405. https://doi.org/10.2340/16501977-0984.
- Yonetsu R, Iwata A, Surya J, Unase K, Shimizu J. Sit-to-stand movement changes in preschool-aged children with spastic diplegia following one neurodevelopmental treatment session – a pilot study. Disabil Rehabil 2014;37:1643-50. https://doi.org/10.3109/09638288.2014.972592.
- Schroeder A, Von Kries R, Riedel C, Homburg M, Auffermann H, Blaschek A, et al. Patient-specific determinants of responsiveness to robot-enhanced treadmill therapy in children and adolescents with cerebral palsy. Dev Med Child Neurol 2014;56:1172-9. https://doi.org/10.1111/dmcn.12564.
- Christy JB, Chapman CG, Murphy P. The effect of intense physical therapy for children with cerebral palsy. J Pediatr Rehabil Med 2012;5:159-70.
- Anaby D, Law M, Teplicky R, Turner L. Focusing on the environment to improve youth participation: experiences and perspectives of occupational therapists. Int J Environ Res Public Health 2015;12:13388-98. https://doi.org/10.3390/ijerph121013388.
- Piskur B, Meuser S, Jongmans J, Ketelaar M, Smeets R, Casparie B, et al. The lived experience of parents enabling participation of their child with a physical disability at home, at school and in the community. Disabil Rehabil 2015;38:803-12. https://doi.org/10.3109/09638288.2015.1061612.
- Van Wely L, Balemans A, Becher J, Dallemeijer A. The effectiveness of a physical activity stimulation programme for children with cerebral palsy on social participation, self-perception and quality of life: a randomized controlled trial. Clin Rehabil 2014;28:972-82. https://doi.org/10.1177/0269215513500971.
- Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ. Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial. Health Technol Assess 2007;11. https://doi.org/10.3310/hta11160.
- Towards a Common Language for Functioning, Disability and Health: International Classification Framework. Geneva: WHO; 2002.
- Simons H. Case Study Research in Practice. London: Sage; 2009.
- Emmel N. Sampling and Choosing Cases in Qualitative Research: A Realist Approach. London: Sage; 2013.
- Children and Families Act 2014. London: The Stationery Office; 2014.
- Sykes C. The International Classification of Functioning, Disability and Health: relevance and applicability to physiotherapy. Adv Physiother 2008;10. https://doi.org/10.1080.14038190802294617.
- Prodinger B, Darzins S, Magasi S, Baptise S. The International Classification of Functioning, Disability and Health (ICF): opportunities and challenges to the use of ICF for occupational therapy. World Federation Occup Ther Bull 2015;71. https://doi.org/10.1179/2056607715Y.000000000.
- Westby C. Application of the ICF in chidren with language impairments. Semin Speech Long 2007;28:265-72. https://doi.org/10.1055/s-2007-986523.
- Jelsma J, Scott D. Impact of using the ICF framework as an assessment tool for students in paediatric physiotherapy: a preliminary study. Physiotherapy 2011;97:47-54. https://doi.org/10.1016/j.physio.2010.09.004.
- Dunst CJ, Trivette CM, Hamby DW. Meta-analysis of family-centered helpgiving practices research. Ment Retard Dev Disabil Res Rev 2007;13:370-8. https://doi.org/10.1002/mrdd.20176.
- Mastos M. Goal-directed training: linking theories of treatment to clinical practice for improved functional activities in daily life. Clin Rehabil 2007;21:47-55. https://doi.org/10.1177/0269215506073494.
- Department for Education and Department of Health . Special Education Needs and Disability Code of Practice: 0 to 25 Years Statutory Guidance for Organisations Which Work With and Support Children and Young People Who Have Special Educational Needs or Disabilities n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/398815/SEND_Code_of_Practice_January_2015.pdf (accessed 14 December 2017).
- Hopewell S, Clarke M, Moher D, Wager E, Middleton P, Altzman D, et al. CONSORT for reporting randomized controlled trials in journal and conference abstracts: explanation and elaboration. PLOS Med 2008;5. https://doi.org/10.1371/journal.pmed.0050020.
- Davidson KW, Goldstein M, Kaplan RM, Kaufmann PG, Knatterud GL, Orleans CT, et al. Evidence-based behavioral medicine: what is it and how do we achieve it?. Ann Behav Med 2003;26:161-71. https://doi.org/10.1207/S15324796ABM2603_01.
- Hoffmann T, Glasziou P, Boutron I, Perera R, Moher D, Altman D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- McCleary N, Duncan E, Stewart F, Francis J. Active ingredients are reported more often for pharmacologic than non-pharmacologic interventions: an illustrative review of reporting practices in titles and abstracts. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-146.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. CONSORT Group . Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 2008;148:295-309. https://doi.org/10.7326/0003-4819-148-4-200802190-00008.
- Boutron I, Ravaud P, Boutron I, Ravaud P, Moher D. Randomized Clinical Trials of Nonpharmacological Treatments. Boca Raton, FL: Chapman & Hall/CRC Press; 2012.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behaviour change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behaviour change interventions. J Behav Med 2013;46:81-9. https://doi.org/10.1007/s12160-013-9486-6.
- Colver A, Thyen U, Arnaud C, Beckung E, Fauconnier J, Marcelli M, et al. Association between participation in life situations of children with cerebral palsy and their physical, social, and attitudinal environment: a cross-sectional multicenter European study. Arch Phys Med Rehabil 2012;93:2154-64. https://doi.org/10.1016/j.apmr.2012.07.011.
- Enderby P, John A, Petheram B. Therapy Outcome Measures for Rehabilitation Professionals. London: John Wiley & Sons; 2006.
- Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol 2007;109:8-14.
- Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil 2009;23:362-70. https://doi.org/10.1177/0269215508101742.
- Agarwal S, KeFevre A, Lee J, L’Engle K, Mehl G, Sinha C, et al. Guidelines for reporting health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist. BMJ 2016;352. https://doi.org/10.1136/bmj.i1174.
- Sackett D, Rosenberg W, Gray J, Haynes R, Richardson W. Evidence-based medicine: what it is and what it isn’t. BMJ 1996;312. https://doi.org/10.1136/bmj.312.7023.71.
- Hutton E, Coxon K. Involving parents as service users in an interprofessional research project. J Interprof Care 2008;22:661-3. https://doi.org/10.1080/13561820802038757.
- Hutton E, Coxon K. ‘Posture for Learning’: meeting the postural care needs of children with physical disabilities in mainstream primary schools in England – a research into practice exploratory study. Disabil Rehabil 2011;33:1912-24. https://doi.org/10.3109/09638288.2010.544837.
- Nash B, Norwich T. Preparing teachers to teach children with special educational needs and disabilities: the significance of a national PGCE development and evaluation project for inclusive teacher education. Jorsen 2011;11:2-11.
- Telfer S, Solomondis S, Spence W. An investigation of teaching staff members’ and parents’ views on the current state of adaptive seating technology and provision. Disabil Rehabil Assist Technol 2010;5:14-2. https://doi.org/10.3109/17483100903191334.
- Coster W, Law M, Bedell G, Liljenquist K, Kao YC, Khetani M, et al. School participation, supports and barriers of students with and without disabilities. Child Care Health Dev 2013;39:535-43. https://doi.org/10.1111/cch.12046.
- Brown J, Devecchi C. The impact of training on teaching assistants’ professional development: opportunities and future strategy. Professional Dev Educ 2013;39:369-86. https://doi.org/10.1080/19415257.2012.762720.
- Hotham S, Hamilton-West K, Hutton E, King A, Abbot N. A study into the effectiveness of a postural care training programme aimed at improving knowledge, understanding and confidence in parents and school staff. Child Care Health Dev 2017;43:743-51. https://doi.org/10.1111/cch.12444.
- Jansen LM, Ketelaar M, Vermeer A. Parental experience of participation in physical therapy for children with physical disabilities. Dev Med Child Neurol 2003;45:58-69. https://doi.org/10.1111/j.1469-8749.2003.tb00861.x.
- Marshall J, Goldbart J. ‘Communication is everything I think.’ Parenting a child who needs Augmentative and Alternative Communication (AAC). Int J Lang Commun Disord 2008;43:77-98. https://doi.org/10.1080/13682820701267444.
- Carroll C. ‘It’s not everyday that parents get a chance to talk like this’: exploring parents’ perceptions and expectations of speech-language pathology services for children with intellectual disability. Int J Speech Lang Pathol 2010;12:549-54. https://doi.org/10.3109/17549500903312107.
- Pappas N, McAllister L, McLeod S. Parental beliefs and experiences regarding involvement in intervention for their child with speech sound disorder. Child Lang Teach Ther 2015;32:1-17.
- Nicolson A, Moir L, Millsteed J. Impact of assistive technology on family caregivers of children with physical disabilities: a systematic review. Disabil Rehabil Assist Technol 2012;7:345-9. https://doi.org/10.3109/17483107.2012.667194.
- Rabiee P, Sloper P, Beresford B. Desired outcomes for children and young people with complex health care needs, and children who do not use speech for communication. Health Soc Care Community 2005;13:478-87. https://doi.org/10.1111/j.1365-2524.2005.00578.x.
- Allard A, Fellowes A, Shilling V, Janssens A, Beresford B, Morris C. Key health outcomes for children and young people with neurodisability: qualitative research with young people and parents. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2013-004611.
- Morris C, Janssens A, Allard A, Thompson Coon J, Shilling V, Tomlinson R, et al. Informing the NHS Outcomes Framework: what outcomes of NHS care should be measured for children with neurodisability. Health Serv Deliv Res 2014;2.
- McConachie H, Parr JR, Glod M, Hanratty J, Livingstone N, Oono IP, et al. Systematic review of tools to measure outcomes for young children with autism spectrum disorder. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19410.
- Hurn J, Kneebone I, Cropley M. Goal setting as an outcome measure: a systematic review. Clin Rehabil 2006;20:756-72. https://doi.org/10.1177/0269215506070793.
- Steenbeek D, Ketelaar M, Galama K, Willem Gorter J. Goal attainment scaling in paediatric rehabilitation: a critical review of the literature. Dev Med Child Neurol 2007;49:550-6. https://doi.org/10.1111/j.1469-8749.2007.00550.x.
- Baker E, McLeod S. Evidence-based practice for children with speech sound disorders: part 1 narrative review. Lang Speech Hear Serv Sch 2011;42:102-39. https://doi.org/10.1044/0161-1461(2010/09-0075).
- Stephens D, Upton D. Speech and language therapists’ understanding and adoption of evidence-based practice. Int J Ther Rehabil 2012;9:328-34. https://doi.org/10.12968/ijtr.2012.19.6.328.
- Scurlock-Evans L, Upton P, Upton D. Evidence-based practice in physiotherapy: a systematic review of barriers, enablers and interventions. Physiotherapy 2014;100:208-19. https://doi.org/10.1016/j.physio.2014.03.001.
- Upton D, Stephens D, Williams B, Scurlock-Evans L. Occupational therapists’ attitudes, knowledge, and implementation of evidence-based practice: a systematic review of published research. Br J Occup Ther 2014;77:24-38. https://doi.org/10.4276/030802214X13887685335544.
- da Silva TM, Costa Lda C, Garcia AN, Costa LO. What do physical therapists think about evidence-based practice? A systematic review. Man Ther 2015;20:388-401. https://doi.org/10.1016/j.math.2014.10.009.
- van Dijk N, Hooft L, Wieringa-de Waard M. What are the barriers to residents’ practicing evidence-based medicine? A systematic review. Acad Med 2010;85:1163-70. https://doi.org/10.1097/ACM.0b013e3181d4152f.
- Zwolsman S, te Pas E, Hooft L, Wieringa-de Waard M, van Dijk N. Barriers to GPs’ use of evidence-based medicine: a systematic review. Br J Gen Pract 2012;62:e511-21. https://doi.org/10.3399/bjgp12X652382.
- Ubbink DT, Guyatt GH, Vermeulen H. Framework of policy recommendations for implementation of evidence-based practice: a systematic scoping review. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-001881.
- Straus SE, McAlister FA. Evidence-based medicine: a commentary on common criticisms. CMAJ 2000;163:837-41.
- Cohen G, Schroeder J, Newson R, King L, Rychetnik L, Milat A, et al. Does health intervention research have real world policy and practice impacts: testing a new impact assessment tool. Health Res Policy Syst 2015;13. https://doi.org/10.1186/1478-4505-13-3.
Appendix 1 Recruitment materials: professionals
Appendix 2 Recruitment materials: parents
Appendix 3 Children and young people: recruitment flier
Appendix 4 Individual interview topic guides
Appendix 5 Focus group topic guides and materials
Appendix 6 Procedures, techniques and activities described by study participants
Procedures, techniques and activities described by study participants and used in NHS settings
| Physiotherapy | Occupational therapy | Speech and language therapy |
|---|---|---|
| Areas of intervention | ||
|
Gross motor skills: gait/walking/mobility; hand/arm function Pain/comfort Spasticity Body structure, core strength, bone density, muscle strength, posture and contractures |
Interventions to enable/support taking part in activities and occupations |
Communication, speech, language Eating, drinking, swallowing (including nutritional sufficiency, safety and enjoyment) |
| Procedures, techniques, activities and equipment described | ||
|
Strength training Resistance training Stretching (including positional stretching, splints) Endurance training Cardiovascular fitness training Specific techniques: Constraint-induced movement therapy Bimanual training Proprioceptive neuromuscular facilitation Hip and spine surveillance Acupuncture Standing frames Walking frames Postural management [sleep; 24-hour; different systems (e.g. micro-garments)] Stretches Splinting (traditional; Lycra®) Hydrotherapy Functional electrical stimulation Botulinum (botox) Sports (e.g. football or cycling) Wii-FitTM (Nintendo, Redmond, WA, USA) Move it to improve it [(Mitii https://mitii.com)] Rebound therapy (www.reboundtherapy.org) |
Teaching skills to enable child to engage in activitiesAdjusting/changing a task to support a child to manage it independently Providing equipment to enable child to engage in activitiesEquipment provision to supportChanging the environment to support engagement in activities or address care needsProviding settings/supporting access to settings |
Communication Oromotor skills Eye-gaze skills Language development Narrative/storytelling skills Reciprocal communication (e.g. baby-signing; intensive interaction) Aided Language Simulation Articulation therapy Breath support skills Facial oral tract therapy Dysphagia (swallowing, saliva control) and eating and drinking Modifying food, drinks Positioning Supporting non-oral feeding VitalStim Therapy Oral desensitisation Equipment Augmentive and alternative communication systems Feeding/drinking equipment |
| Across many of these | ||
|
Repetition Practice |
||
List of abbreviations
- CSP
- Chartered Society of Physiotherapy
- HSDR
- Heath Services and Delivery Research
- HTA
- Health Technology Assessment
- ICF
- International Classification of Functioning, Disability and Health
- JLA
- James Lind Alliance
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- RCOT
- Royal College of Occupational Therapists
- RCSLT
- Royal College of Speech and Language Therapists
- RCT
- randomised controlled trial
- WHO
- World Health Organization
