Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 10/104/13. The contractual start date was in November 2012. The draft report began editorial review in May 2017 and was accepted for publication in October 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Rumana Omar reports membership of the Health Technology Assessment General Board. Michael King is a member of the PRIMENT Clinical Trials Unit, which is funded by the National Institute for Health Research.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Hassiotis et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Several passages in this chapter are adapted from Hassiotis et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Introduction
Intellectual disability (ID) is characterised by significant impairments in cognitive, social and practical skills including activities of daily living and work tasks. 2 Prevalence estimates suggest that as many as 2 in 100 adults have ID worldwide, although prevalence rates may vary according to country, age and socioeconomic status. 3 Individuals with ID have complex and unique care needs, given their pronounced vulnerability to biological, psychological and environmental stressors compared with the general population. 4 A reduced ability to cope with these stressors makes individuals with ID more likely to experience challenging behaviours. 5 Between 10% and 15% of adults with ID present with challenging behaviour, most commonly aggression, which may result in long-term hospitalisation, often in out-of-area facilities, restrictive care practices and neglect as well as an increase in receipt of antipsychotic medication and service use. 6–9 Therefore, effective treatment approaches for challenging behaviour are vital. However, the wide range of factors that could trigger challenging behaviour, as well as the many psychiatric conditions associated with ID, make a clear understanding of challenging behaviour in ID difficult. Although there have been a number of interventional approaches over the years, the literature on pharmacological and psychosocial interventions is limited to observational studies and single-site randomised controlled trials (RCTs) with short follow-up periods, which therefore are subject to significant bias. 10–13 Furthermore, these studies did not include a health economic evaluation, which is important in guiding policy-makers and service commissioners.
Cost of challenging behaviour to society
The presence of challenging behaviour increases the cost of care for people with ID, mostly due to increases in support and long-term inpatient care, often in expensive out-of-area placement;14–17 and also increases family-carer burden. 18 Hunter19 argues that the limited economic data currently available make use of information based on services that are many years old and superseded by advances in community health and social care.
The psychosocial intervention with the greatest evidence base for efficacy is Positive Behaviour Support (PBS). It is described in detail in the following section.
Positive Behaviour Support
Positive Behaviour Support has arisen out of the tenet that challenging behaviour is shaped by personal and psychological experiences and helps the person to exert some control over their environment. It is considered a cornerstone of good-quality care that is also supported by policy objectives to maintain individuals in their local communities and encourage commissioning that rewards skilled care provision. 20,21 The challenging behaviour may be a response to environmental cues or ‘schedule induced’, that is, may be the result of interactions between the individual and the environment. 22 These concepts have influenced the definition of challenging behaviour as ‘behaviour of such intensity, frequency or duration that the physical safety of the person or others is placed in serious jeopardy or behaviour which is likely to seriously limit or deny access to the use of ordinary community facilities’. 23 PBS is ‘the application of the science of applied behaviour analysis (ABA) in the support of people with challenging behaviour’ and is an essentially complex intervention in terms of its components and range of outcomes. 24 PBS is a flexible, multicomponent approach that takes a lifespan perspective and emphasises prevention, and so far is the only treatment with evidence of efficacy. It focuses on reducing challenging behaviour and improving quality of life in individuals with intellectual disabilities25 and other population groups across the lifespan, for example in education or in individuals with brain injury. 26–29 It aims to help professionals and family or paid carers understand the behaviour that an individual displays by focusing on the individual’s interaction with his/her environment and identifying the context in which the behaviour takes place by means of a functional assessment that should lead to personalised, non-restrictive approaches to challenging behaviour designed to foster prosocial actions.
Staff training in Positive Behaviour Support
Positive Behaviour Support can be implemented in a number of ways, including by a single practitioner co-ordinating all elements of the framework and leading each stage of the process,30–32 by professional teams in which different members contribute to different elements of the PBS framework or process,13,33 and systemwide, whereby the PBS framework is implemented at varying levels of intensity via a tiered model of prevention that covers an entire organisation or geographical area. 33–35 Specific staff competencies have an impact on the effectiveness of PBS in improving challenging behaviour. However, as a result of the resources required to deliver PBS, this type of support is not always available. Despite PBS being a well-known intervention framework, only about half of adults with ID and challenging behaviour may receive it. 36 Even in areas with specialist support teams providing applied behaviour analysis or PBS, patients often have to wait several months to receive help. Therefore, training paid carers and professional staff in PBS is thought to increase awareness of good care for this population group and extend the expertise in managing challenging behaviour in the community. McClean et al. 36 and Grey and McClean37 have reported on training 132 paid carers in a non-randomised clinical study (n = 60). The authors found significant reductions in challenging behaviour in groups supported by trained carers compared with controls. However, the instrument used to measure the primary outcome does not have established psychometric properties and the study was uncontrolled and included training paid carers (rather than professionals) who are likely to require a different set of skills and knowledge from the outset. The authors estimated that paid carer training in PBS may lead to savings of €2000 per person treated.
A pilot RCT of PBS incorporating applied behaviour analysis delivered by a specialist behaviour team in one area in England showed significant reductions in irritability, lethargy and hyperactivity. 11 A naturalistic 2-year follow-up of the same cohort showed a continued positive effect of the intervention on reducing challenging behaviour compared with TAU. 13
The National Institute for Health and Care Excellence (NICE) in the UK has produced a guideline38 that recommends the implementation of PBS in routine care and highlights the importance of working with the individual and their carers, understanding the function of the behaviour and ensuring that interventions are provided in the least restrictive manner. However, it has been acknowledged that staff in community ID services are not sufficiently skilled to deliver PBS. Training programmes for front-line staff have been developed and delivered nationally, showing an increase in knowledge and perceived confidence in understanding and managing challenging behaviour. 39
In the light of the widespread implementation of PBS, a rigorous evaluation of the clinical effectiveness of staff training in PBS was required. Furthermore, the economic evaluation would test whether or not any reductions in challenging behaviour resulted in reduced service-use costs and improved health-related quality of life. Therefore, we conducted a real-world multicentre evaluation of the clinical effectiveness and cost-effectiveness of staff training in PBS for treating challenging behaviour in adults with ID compared with TAU in ID services in England.
Trial objectives
Primary objective
Examine the clinical effectiveness of staff training in PBS on carer-reported ratings of challenging behaviour over 12 months as measured by the Aberrant Behaviour Checklist – Community total score (ABC-CT)40 in community-dwelling adults with ID.
Secondary objectives
-
Examine the cost-effectiveness of staff training in PBS.
-
Examine the impact of the intervention on the prescription of psychotropic medication, paid-carer and family-carer burden, and service user mental status as well as participation in community-based activities over 12 months when compared with treatment as usual (TAU) alone.
-
Measure the influence on the primary outcome of the level of ID, adaptive behaviour scores, mental health status and autism spectrum disorder (ASD) status.
-
Carry out an exploratory analysis of the impact of the intervention on all measures in a subsample of participants with an ASD over 12 months.
-
Understand factors that promote and hinder the successful training of staff and the delivery of PBS within community ID services.
Rationale for the long-term follow-up
It has been suggested that some treatments may have delayed beneficial or harmful effects, which may not be known until well after the trial has been completed, showing that the true value of a therapy may change in the light of long-term data. 41,42 There is some evidence from cancer research, cardiovascular medicine and mental health research for long-term treatment effects. A recent RCT of prevention of depression in primary care43 showed little difference in the incidence of major depression after 6 months, but a substantial reduction after 18 months. The collection and analysis of longitudinal data can provide further insight into not only clinical, but also economic, outcomes.
The PBS study is the first large-scale RCT of a complex behavioural intervention for adults with ID and challenging behaviour. Conducting an additional final follow-up assessment would provide further information about the clinical and economic long-term outcomes as well as any potential treatment effect of PBS compared with TAU over time, and would therefore contribute to the existing knowledge of evidence-based care for people with ID who have challenging behaviour.
Chapter 2 Methods
Several passages in this chapter are adapted from Hassiotis et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Trial design
This was a multicentre, single-blind, parallel two-arm cluster RCT evaluating clinical outcomes of manual-based face-to-face staff training in PBS for managing challenging behaviour in adults with ID. A cluster randomised designed was deemed appropriate for this type of complex educational intervention in order to avoid transfer of the intervention skills between the two different arms. 44
Sample size
The primary outcome is the ABC-CT measured repeatedly at 6 and 12 months following recruitment. The pilot study11 generated a mean baseline Aberrant Behaviour Checklist – Community (ABC-C) score of 45.4 [standard deviation (SD) 26.4]. A SD reduction of 0.45 on the ABC-C score in the PBS arm compared with the control arm is considered to be clinically important. Using an analysis of covariance approach, based on a correlation of 0.48 between the baseline and post-intervention ABC-C measurements (estimated from the pilot study), 80 participants per arm were required to detect a SD difference of 0.45 with 90% power and 5% significance level. Inflating for clustering within the community ID services, using the formula proposed by Eldridge et al. ,45 which accounts for variable cluster sizes and an intracluster correlation of 0.062 (estimated from the pilot study), an average cluster size of 12 (we expected it to be 13, however, allowing for 10% attrition and rounding it up to the nearest integer we have used a cluster size of 12 in our calculations) and a SD for the cluster size of 3, a total of 276 participants were required. However, this sample size can be reduced as each participant provided two measurements of ABC-C score. Using a correlation of 0.6 between the 6 and 12 months’ post-intervention ABC-C measurements (estimated from the pilot study) and a cluster size of 2, a total of 442 ABC-C measurements; thus, 221 participants, were required. In performing this calculation, we have assumed that there would be no treatment by time period interaction over 12 months, which was supported by the pilot studies. 11,13 To allow for 10% attrition over the 12-month period, a total of 246 participants had to be recruited in to the trial thus requiring 19 clusters. The sample size calculation was based on the program and formulae in Stata® version 12 (StataCorp LP, College Station, TX, USA).
Service and participant recruitment
Twenty-three community ID services in England were recruited to the study. All participating services treat adults with ID and challenging behaviour, which tends to be remitting and relapsing so that patients may experience periods of exacerbation of behaviours but also periods of relative stability. The services were recruited through the Clinical Research Networks across several regions in England (London, Leicestershire, Kent, Surrey, Bradford, and Coventry and Warwickshire), which cover urban, semi-rural and rural areas. The number of registered adults with ID ranged from 100 to 1000 and ID services employed a median of 23 full-time equivalent health and/or social care staff (range 4–70). A maximum of 16 participants (range 5–16) with ID were recruited from each cluster.
Two volunteer health staff in each service (henceforth called therapists) from a variety of professions (i.e. psychiatrists, psychologists, nurses, occupational therapists and speech and language therapists) received PBS training. We considered it beneficial to have two therapists per team, as this would enable peer support and cover in the event that one of the therapists subsequently became unavailable, thus ensuring continuity of the intervention and implementation. Interested staff required the agreement of their line managers to take part.
Each therapist had a maximum caseload of eight individuals at any time during the trial, which meant a maximum of 16 service users having treatment per team. Therapists may have continued to provide generic input for other service users, such as taking part in dysphagia assessments, assessment of capacity or day activities/home environment if practicable. However, as therapists who received PBS training were delivering an intensive intervention (suggested time of 12.5 hours per participant excluding travel and writing up), we asked their clinical managers to reduce their routine caseloads to allow them sufficient time to deliver the intervention. We anticipated that, once the training was completed, 12–14 service users per month would be taken on for treatment across the intervention sites.
Randomisation and masking
Once the clusters were recruited and potential participants had been screened for eligibility by their participating ID services and had provided verbal consent to be approached about the study, they were randomised using an independent web-based randomisation system (Sealed Envelope Ltd, London, UK) and random permuted blocks on a 1 : 1 basis. The following data were taken into account in our randomisation planning: team size (number of full-time equivalent staff), clusters located in or out of London and number of service users registered per team (cluster). We calculated the ratio of staff to service users in in-London and out-of-London teams and no difference was found. We stratified the randomisation by calculating the staff-to-patient ratio for each cluster, thus creating a binary factor that indicated whether a cluster was below or above the median ratio. A second wave of randomisation was prepared because of delays in the recruitment of some of the participating teams. The sites were informed of their treatment allocation by the trial manager.
Although clusters, participants and carers were aware of arm allocation, the research assistants (RAs) and clinical studies officers (CSOs) from the National Institute for Health Research (NIHR) Clinical Research Network conducting the study assessments were blind to treatment arm allocation. They were asked to guess treatment allocation for each participant at each follow-up assessment and to report any incident of unblinding. In the analysis, we compared treatment allocation guesses to identify potential bias attributable to unblinding.
Possible sources of bias
One possible source of bias we took into account was the transfer of PBS-trained therapists between the intervention and control teams during the trial. We examined the health staff turnover rates in a number of services that had expressed interest in participating and this was well below 13%, which is considered very low based on agreed service performance data such as balanced scorecards. Therefore, the chance of such leaks of the intervention were considered to be very small. Any therapist changes were recorded throughout the study duration and none found a new post within teams in the control arm. We judged that contamination between study arms was unlikely given the more intensive nature of the intervention. However, PBS principles are being taught widely and, therefore, some knowledge of PBS in teams in the control arm was unavoidable. Selection bias resulting from recruiting participants after cluster allocation is revealed was avoided by completing recruitment and screening assessment prior to randomisation. A degree of variation in participant characteristics between the study arms can be accounted for by the cluster RCT design. 46
Inclusion criteria
Participants
The inclusion criteria for participants were as follows:
-
eligible to receive care from ID services
-
age ≥ 18 years
-
mild to severe ID
-
an ABC-CT of ≥ 15 at initial screening (indicating a degree of challenging behaviour taking place at least weekly, including verbal or physical aggression, hyperactivity, refusal to attend activities and non-responsiveness that requires professional input).
Community intellectual disability services
The inclusion criteria for community ID services were as follows:
-
willingness to participate in the study
-
availability of at least two staff members willing to train
-
written agreement by the service manager to participate.
Exclusion criteria
Participants
Participants could not be included in the study if:
-
they had a primary clinical diagnosis of personality disorder or substance misuse, as PBS is not considered first-line treatment for those disorders
-
there was a relapse in pre-existing mental disorder
-
there was a decision by the clinical team that a referral to the study would be inappropriate.
Community intellectual disability services
Community ID services could not be included in the study if:
-
there were not two team members who were willing to train
-
the service has already received PBS training and was implementing PBS for their service users.
Interventions
Positive Behaviour Support-based staff training (in addition to treatment as usual)
The therapists from clusters randomised to the intervention arm received face-to-face PBS training supported by a training manual,47 which consisted of the following topics:
-
functional behavioural assessment and formulation skills using the Brief Behavioural Assessment Tool (BBAT) for brief functional analyses
-
primary prevention
-
secondary prevention and reactive strategies
-
periodic service review and problem solving –
-
developing individualised periodic service reviews
-
troubleshooting.
-
The training was delivered by expert trainers who deliver training in PBS in a variety of health and social care settings, run accreditation and academic courses in PBS and also carry out research on this topic. It was conducted over a total of 6 days and delivered in three 2-day workshops that were 6–8 weeks apart, over a course of 15 weeks. Between the first and second workshop, the therapists were expected to begin undertaking work with participants who had completed a baseline assessment. The final 2-day workshop focused on effective implementation of behavioural plans and providing problem-solving strategies. The training outline is shown in Appendix 1.
The therapists were offered post-training mentoring for the time they were treating participants and they were responsible for utilising this facility. The mentoring was intended to maintain motivation and enhance practice skills. The mentoring arrangements were as follows:
-
Months 1–6 post training – therapists were offered up to 2 hours of support per month (1 hour for the mentor to read the submitted materials and 1 hour for feedback). Therapists were asked to submit the following material for two further cases: BBAT/summary statement, intervention plan table, PBS plan, training plan and fidelity checklist. Subsequently, they received feedback on all submitted material from their designated mentor (mentoring responsibility was shared equally among the four tutors).
-
Months 7–12 post training – therapists were offered up to 1 hour of support per month, during which they could raise specific technical or theoretical issues about their remaining sample cases.
-
In all, therapists were offered detailed mentoring on three cases (one during training and two post training).
-
This model reflected a tapering mentoring model that fits ‘real-world’ conditions.
-
Although mentors took all practical steps to ensure that appropriate contacts were put in place, responsibility for making the best use of supervision rested with the therapists.
In addition, the trial manager, the chief investigator and trainers held monthly teleconferences with therapists in order to discuss issues in relation to the treatment delivery, aiming to maintain and enhance practice skills and motivation.
Clinical responsibility of the cases remained with the local clinical teams, which also managed any emergencies as they arose.
Treatment as usual
Staff in the clusters that were randomised to TAU continued with their existing treatment approaches and were able to use any resource they had available to them. Most community ID services in England employ a variety of health and social care professionals, and patients have access to standard behavioural, psychosocial and pharmacological interventions, for example strategies to improve communication, physical health checks, simple behavioural modification and prescribing and monitoring of psychotropic medication. In some cases, the participants lived in accommodation where paid carers were PBS aware, that is, the accommodation provider had offered PBS-awareness seminars or employed an external consultant to advise care staff on PBS. We did not influence the approaches that those teams used. All clinical and social care aspects of TAU were also available to the participants in the intervention arm.
Initially, we had committed to offer a 1-day seminar in PBS for the services in the control arm. However, because of the long-term follow-up, this has not been carried out, in order to minimise systematic bias. Policy changes post 2014 meant that teams in the control arm were subsequently able to access such training through an NHS England initiative. 48
Frequency and duration of follow-up
All participants received a baseline assessment and were followed up at 6 and 12 months after baseline. We allowed for a window of ± 4 weeks around the due date for each follow-up assessment with every individual participant.
Ethics issues, research governance and consent
The study received ethics approval from the National Research Ethics Service Committee London – Harrow (reference 12/LO/1378). Research and development approvals were obtained from all NHS trusts involved in the study. Details can be found in Appendix 2. The study was sponsored by University College London (UCL). It was conducted in compliance with Good Clinical Practice,49 the Research Governance Framework50 and according to the standard operating procedures of the PRIMENT Clinical Trials Unit at UCL. All data were stored securely and anonymised in accordance with the Data Protection Act. 51
The study’s Trial Steering Committee (TSC) consisted of two independent and two non-independent members and met twice per year. The study’s Data Monitoring and Ethics Committee (DMEC) consisted of three independent members and convened twice a year.
Easy-to-read information sheets and consent forms for the study were prepared with the assistance of the study service users reference group Camden SURGE (Speaking Up Rights Group Experts), The Advocacy Project. RAs and CSOs were trained in obtaining informed consent (including assessing capacity to consent), good clinical practice and data collection. Initially, they contacted those who had given verbal consent to be approached about the study by telephone to discuss the study. Subsequently, they sent written information about the study procedures to family or paid carers and participants with ID, and followed this up with a telephone call ≥ 7 days later to discuss whether or not they were interested in taking part in the study. The RAs or CSOs then visited the participants and carers in their home (or place of work for paid carers) and obtained their written informed consent to take part in the study. If the participants with ID lacked capacity as per the Mental Capacity Act 2005,52 a person was identified or nominated to act as consultee on their behalf.
We notified the participant’s general practitioner (GP) of his/her participation in the trial. All of the research team members followed the required risk assessment procedures including the guidelines for risk management and safeguarding processes.
Serious adverse events
Reports of serious adverse events (SAEs) were collected for the duration of the trial. They were defined as events that:
-
resulted in death
-
were life-threatening
-
required hospitalisation or prolonged existing hospitalisation
-
resulted in persistent or significant disability or incapacity
-
were otherwise considered medically significant by the investigator.
Any events that were related to the trial (i.e. resulted from the administration of any of the research procedures) and were unexpected (i.e. the type of event was not listed in the protocol as an expected occurrence) were reported to the Research Ethics Committee in line with their reporting timelines. The SAE form is shown in Appendix 3.
In addition, we collected information on the following events for participants for the duration of the study: medications taken including psychotropic medication, out-of-area placements and police contacts.
Outcome measures and instruments
Quantitative assessments
The Case Report File collected participant demographic information (sex, age and ethnicity), level of ID as measured by the Wechsler Abbreviated Scale of Intelligence (WASI)53 and carer-reported adaptive behaviour as measured by the Adaptive Behaviour Scale (ABS)54 at baseline (Tables 1 and 2). Information on the cause of ID was recorded if known. The postcode of the participant’s residence was recorded for linkage with the Index of Multiple Deprivation,55 obtained via the UK Data Service website. 56
| Measures | Assessment time point | ||
|---|---|---|---|
| Baseline (T1) | 6 months (T2) | 12 months (T3) | |
| WASI | ✓ | ||
| Short-form ABS | ✓ | ||
| ABC-C | ✓ | ✓ | ✓ |
| Mini PAS-ADD | ✓ | ✓ | ✓ |
| ASD scale | ✓ | ||
| EQ-5D-Y | ✓ | ✓ | ✓ |
| GCPLA | ✓ | ✓ | ✓ |
| Uplift/Burden Scale | ✓ | ✓ | ✓ |
| CDS-ID | ✓ | ✓ | ✓ |
| GHQ-12 | ✓ | ✓ | ✓ |
| CSRI-LD | ✓ | ✓ | ✓ |
| Medication use including psychotropic medication | ✓ | ✓ | ✓ |
| Measures | Respondent | ||
|---|---|---|---|
| Service user | Paid carer or family carer/keyworker | Family carer | |
| WASI | ✓ | ||
| Short-form ABS | Either family or paid carer | ||
| ABC-C | Either family or paid carer | ||
| Mini PAS-ADD (including ASD scale) | ✓ (if able) | Either family or paid carer | |
| GCPLA | Either family or paid carer | ||
| Uplift/Burden Scale | ✓ | ||
| CDS-ID | Paid carer only | ||
| CSRI-LD | ✓ | ✓ | |
| GHQ-12 | ✓ | ||
| EQ-5D-Y | ✓ (if able) | Either family or paid carer | |
Primary outcome measure
The primary outcome was challenging behaviour as measured by the ABC-CT at 6 and 12 months. 40 The ABC-C has been widely used for monitoring changes in behaviour in people with ID following treatment and has demonstrated acceptable reliability and validity. The ABC-C scores can be separated into five different domains: (1) irritability, agitation and crying (15 items), (2) lethargy and social withdrawal (16 items), (3) stereotypic behaviour (seven items), (4) hyperactivity and non-compliance (16 items) and (5) inappropriate speech (four items). Each domain is rated on a 4-point scale (0–3). A total score can be obtained by adding up all domain scores. A higher score indicates more severe challenging behaviour. The ABC-CT was administered by a paid carer or family carer at all three assessment time points.
Secondary outcome measures
Participants were screened for mental health and ASDs using the Mini Psychiatric Assessment Schedules for Adults with Developmental Disabilities (Mini PAS-ADD). 57 The instrument comprises 86 psychiatric symptoms with threshold scores for the following psychiatric disorders: depressive disorder, anxiety disorder, hypomania/mania or expansive mood, obsessive–compulsive disorder, psychosis, dementia or an unspecified disorder, and a screen for pervasive developmental disorder.
The EuroQol-5 Dimensions Youth (EQ-5D-Y) was used to calculate quality-adjusted life-years (QALYs) in line with accepted guidance. 58 The EQ-5D-Y is a five-domain (usual activity, self-care, mobility, pain and anxiety/depression), three-level (no problems, some problems and extreme problems) questionnaire. It was administered at all time points. The youth version was used in our study, as it was assumed that individuals with ID would find this version easier to complete.
Community participation was measured by the Guernsey Community Participation and Leisure Activities Scale (GCPLA). 59 It was developed to monitor the impact of interventions on the service user’s daily living. It contains six categories of activity that refer to 49 operationally defined contacts. The frequency of participation in any of the activities over the course of the previous 6-month period is rated on a five-point scale.
Family-carer burden was assessed by the Uplift/Burden Scale,60 which is a 23-item scale that has six uplift and 17 burden items. The scale has been used previously with individuals with ID. 61
Family carer psychiatric morbidity was assessed using the General Health Questionnaire – 12 items (GHQ-12). 62
Paid-carer burden was measured by the Caregiving Difficulty Scale – Intellectual Disability (CDS-ID). 63 It is adapted from an existing scale and measures subjective burden.
Costs of care were collected using a modified version of Client Services Receipt Inventory (CSRI) for people with ID. 64 It was administered at all time points, asking about health care, social care, housing, carer input and criminal justice contacts for the preceding 6 months.
All secondary outcome measures were administered by a family carer or paid carer at all three assessment time points.
The instruments were piloted prior to commencing assessments in order to establish any problems in their administration and completion. A RA guidance document was developed and all RAs and CSOs had an induction and monthly supervision.
Data entry
Data were entered into a study-specific web-based database developed by Sealed Envelope Ltd. Data entry was undertaken by the study researchers. As agreed with the trial statisticians, the trial manager conducted source data verification (SDV) checks on 100% of the primary outcome measure (ABC-C) at all three assessment time points; for secondary outcome measures, 100% SDV checks were conducted for 20% of all study participants at all three assessment time points. The trial manager prepared a SDV check report that was discussed with the trial statisticians. No further SDV checks were required.
Statistical analysis
Baseline characteristics
The baseline characteristics of the PBS and control arms have been summarised using means, SDs and proportions as appropriate. These summaries are based on observed ratings only.
Primary outcome
A three-level regression model, adjusting for baseline ABC-C measurements, time period and effects of clustering by services, and accounting for repeated measures within subjects, was used for the primary analysis. We adjusted for the staff-to-service user ratio (low/high) stratification variable. In a supportive analysis we adjusted for the participant characteristics that are not balanced across arms and are potentially related to the primary outcome (ethnicity and the accommodation that the service user lived in). For the primary analysis, we used an all-available-case analysis. As we have two follow-up time points for the ABC-CT, the missing post-randomisation data should be dealt within our model.
The primary analysis was performed by two statisticians (VV and RO) separately to ensure its accuracy.
Bias attributable to missing data was initially investigated by comparing the characteristics of the trial participants with complete follow-up measurements and the characteristics of those with incomplete follow-up or no outcome data, descriptively. No predictors were found that were associated with both the missing data and the outcomes.
Subgroup analyses
In order to explore the heterogeneity (or otherwise) of the intervention effect, we examined the treatment effect across the following characteristics: sex, age, ethnicity, ASD and mental disorder (if the participant is positive on Mini PAS-ADD). The estimates of intervention effect in each subgroup is shown in a forest plot. The results from these analyses should be treated as exploratory.
Sensitivity analyses
The following sensitivity analyses were carried out: (1) adjusting for area deprivation as measured using the Index of Multiple Deprivation;55 (2) the primary outcome score can be completed either by a family carer or by a paid carer – we fitted the primary analysis model adjusting for this variable; (3) exploring a model that includes two random effects at the service level, one for each of the intervention and control arms;65 (4) adjusting for the percentage of participants per cluster who had a completed PBS plan; and (5) a ‘Baseline Observation Carried Forward’ approach was also used to include participants with missing values for the ABC-CT.
Exploratory multivariate analysis
An exploratory analysis was carried out to examine the effect of the staff training in PBS on the different domains of the ABC-CT using a three-level multivariate outcome linear regression model with outcomes nested within time periods, which are nested within patients. 66 This model allows an estimation of the intervention effects for multiple outcomes (all five subscales of the ABC-C) simultaneously. We adjusted for each baseline subscale score and time period.
Secondary outcomes
Similar analyses were conducted for the secondary outcomes using appropriate regression models depending on the type of outcome. The results from all secondary analyses have been presented as estimates with confidence intervals (CIs) and should be treated as exploratory.
Blinding and unmasking
The researchers’ treatment arm allocation guesses were evaluated using a chi-squared test.
All statistical tests and CIs are two-sided. Statistical analysis was performed using Stata® version 14 (StataCorp LP, College Station, TX, USA). We conducted all analyses by treatment allocation. A detailed statistical analysis plan was developed and discussed with the Trial Management Group and further agreed with the DMEC and the TSC prior to the analysis of unblinded data.
Health economic evaluation
The primary aim of the economic evaluation was to calculate the mean incremental cost per QALY gained by the intervention arm compared with the control arm from a health and social care perspective. Utility scores calculated from proxy responses to the EQ-5D-Y were used to calculate QALYs over 12 months.
A secondary aim of the economic evaluation was to calculate the mean incremental cost per QALY gained of staff training in PBS compared with TAU from a societal cost perspective. In addition to health and social care costs, the societal perspective includes the cost of housing, criminal justice costs and out-of-pocket costs for health and social care.
The mean incremental cost per change in ABC-C from a health and social care cost perspective and societal cost perspective will also be reported in Chapter 3.
Quality-adjusted life-years
Utility scores were calculated from proxy responses to the EQ-5D-Y at baseline, 6 and 12 months and the EuroQol-5 Dimensions, three-level version (EQ-5D-3L) tariff formula. 67 The EQ-5D-Y was used instead of the EQ-5D-3L as patients with ID find it easier to complete than the EQ-5D-3L and so the same version was completed by proxies and participants to allow for comparability. QALYs were calculated from the baseline, 6-month and 12-month utility scores as the area under the curve adjusting for the baseline responses.
Mean utility scores at baseline, 6 months and 12 months, and for the intervention arm and the control arm, were calculated using bootstrapped 95% CIs based on 5000 draws. Baseline-adjusted total QALYs for the treatment and control arms, including clustering by site, were calculated along with 95% CIs. 68 For the primary economic analysis, the complete case for QALYs is reported assuming that data are missing at random and that there is a low level of missing data (< 15%).
Cost of training in Positive Behaviour Support
To calculate the cost of the intervention, data were collected on the resources associated with training the therapists. This included the cost of staff time to attend the training sessions, the cost of specialist and academic staff time to run the training sessions, training materials and travel costs. The total cost of training per patient is calculated as the total cost of training divided by the number of participants in the intervention arm as a conservative estimate. This is because a clinical staff member’s caseload (and hence the number of participants that PBS training for a staff member may have an impact on) will be greater than the number of patients who consent to be involved in the trial.
Information was also collected on the amount of time that community team staff spent on delivering the intervention. This included the time spent on conducting assessments, direct contact time with patients delivering PBS and time spent assessing and working with other staff, patients and carers, and having an impact on the wider environment. Trial-related activities were not included in the calculation of the resources required to deliver PBS. The mean total hours spent per participant was calculated and multiplied by the cost per hour of a band 6 community-health professional to deliver the intervention. 69
Health-care, social care, criminal justice and out-of-pocket costs
We calculated the percentage of participants that used the service and the mean number of contacts greater than zero for each resource category at each assessment point; the 95% CIs are based on bootstrapping with 5000 draws.
Resource use was multiplied by the unit costs reported in Appendix 4, Table 21, to calculate the mean total cost per participant of each resource use type at baseline, 6 months and 12 months. The total cost of each contact has been calculated as the hourly cost of face-to-face contact [based on Personal Social Services Research Unit (PSSRU) costs] multiplied by the average duration of an appointment for that service. Medication has been costed using the British National Formulary 2016 costs. 70 All costs are in 2014/15 Great British pounds (GBP).
The mean incremental total cost of the intervention compared with control and 95% CIs were calculated using regression analysis adjusting for baseline, and includes clustering by site and bootstrapping with 5000 draws. The unit costs are shown in Appendix 4.
Incremental cost-effectiveness ratio
The mean costs and QALYs calculated above were used to calculate the mean incremental cost per QALY gained with PBS compared with TAU.
Cost-effectiveness plane and cost-effectiveness acceptability curve
The results of the bootstrap are presented on a cost-effectiveness plane (CEP). A cost-effectiveness acceptability curve (CEAC) is also reported using the bootstrap data for a range of values of willingness to pay per QALY gained. 68 The probability that the intervention is cost-effective compared with TAU at a threshold for willingness to pay per QALY gained of £20,000 is reported.
Discounting
As costs and QALYs are for 12 months only, no discounting was included.
Missing data
For the primary analysis, participants lost to follow-up were not included in the calculation of resource use and costs for the CSRI. Participants who reported that they used a resource but did not report the number of times they used the resource were not included in the calculation of means and SDs, but were included in the proportion of those who used a service. For their total health and social care and societal cost, that service is missing from their total cost and hence is effectively included as zero.
Reported total costs and QALYs used in calculating the incremental cost-effectiveness ratio (ICER), CEP and CEAC were based on complete case analysis given that no baseline predictors of missing outcomes were identified and missingness occurred at a low level (< 15%).
Societal costs
Unpaid carers (family and close others) often provide essential support and care to patients with ID. Their contribution to care needs to be recognised and valued. If it is not, this can represent an undervaluing of the total cost of care if an unpaid carer provides a significant amount of care for a patient. As a result, an analysis will include health and social care costs in addition to the cost of care if the unpaid carer was paid at the same rate as a paid carer. This has been costed based on the cost of an hour of face-to-face time with a home care worker at £24 per hour. 69 We asked about the typical number of hours spent per week providing informal care over the past 6 months and what categories these included.
Societal costs also include private service use or out-of-pocket costs. These were costed at the same level as health-care costs.
Housing costing methodology
Data on participant employment and benefits, carer employment and benefits, and criminal justice contacts were also collected. Descriptive statistics, costs per unit change and mean total participant costs for the intervention and control arms are reported with 95% CIs.
Accommodation was divided into residential, supported living and independent living with floating support. Costs for residential accommodation were based on the number of bedrooms in the property. 70,71 The cost of supported living was divided into (1) with 24-hour care and (2) without 24-hour care.
Cost-per-point change on the Aberrant Behaviour Checklist – Community
As there were concerns about the performance of the EQ-5D-Y in this trial, a secondary analysis was conducted in which the cost-per-point change in ABC-C was calculated for health and social care costs as well as societal costs.
Incremental cost-effectiveness ratios, CEACs and CEPs are reported for the secondary analyses.
Sensitivity analyses
Participant-completed responses to the EQ-5D-Y are available for those who had the capacity to complete the questionnaire. The mean incremental cost per QALY gained for the intervention compared with TAU for these participants only is reported in Health economic evaluation.
We have reported the total cost of training in PBS for staff on different pay bands, assuming a range of caseloads, to estimate the cost per participant of training. If a staff member has a higher caseload, the cost of training will be lower because the total cost of training is divided by a larger number of potential participants.
Participants with autism
All participants were screened for the presence of an ASD using the autism subscale of the Mini PAS-ADD. However, as this is unreliable in ascertaining all those who are likely to have an ASD, we examined the clinical record documented by the researchers in the Case Report File. These records stated if participants had a diagnosis or suspected diagnosis of ‘autism spectrum disorder’, ‘ASD’ or ‘Asperger syndrome’ and the clinical records had a higher yield of cases than screening alone (37 vs. 113). We therefore concluded that an autism spectrum group should be defined using clinical data, and used a two-stage process to validate our assumptions: first, two raters (AH and AS) independently grouped the clinical diagnoses and relevant terms into those that could help to define an autism and non-autism group, reaching consensus by discussing any cases that were unclear (see Appendix 5); second, we tested the Mini PAS-ADD ASD scores between the two categories. The autism group had higher overall scores than the non-autism group (mean of 8.14 vs. 5.76; Figure 1). A total of 113 participants were thus identified as having broadly defined autism (46%).
FIGURE 1.
Comparison of Mini PAS-ADD scores between participants with and without autism. Kernel density plot of Mini PAS-ADD score. N, threshold of 4; P, threshold of 1; R, threshold of 3.

Changes to study protocol
The following changes were made to the original study protocol:
-
Five community ID teams dropped out prior to randomisation.
-
In the Trial Management Group meeting on 10 May 2013, it was agreed that the screening assessment would be completed before randomisation and this was subsequently amended in the study protocol.
-
In addition to interviewing staff, service managers and carers, we also intended to interview service users with severe ID as part of the process evaluation. This has been amended in the protocol.
-
A protocol addendum describes the rationale and procedure for using video recordings for qualitative interviews with service users with severe ID in order to capture visual responses by service users during the interview.
-
A no-cost long-term follow-up of the participants was conducted at a mean of 36 months post randomisation. The rationale for this is described in Chapter 1. The procedures of the long-term follow-up are further described in the following section.
Long-term follow-up
Once the National Research Ethics Service and Health Research Authority approval had been obtained for the long-term follow-up, we contacted all available participants and carers who had taken part in the PBS study to discuss the additional final follow-up assessment with them. We obtained either verbal or written consent for the long-term follow-up assessment prior to conducting it. Verbal consent was obtained from carers and consultees of participants lacking capacity. We obtained written consent from participants who had capacity to consent. For written consent, we followed the same consent procedures as per the original protocol. Prior to obtaining verbal consent, we sent the relevant information sheet in advance and subsequently contacted the person by telephone in order to gain their consent to participate. The verbal consent process was audio-recorded and the recordings were securely stored.
Follow-up assessments were conducted either face to face or over the telephone. The follow-up data are limited to the primary outcome (ABC-C40) as well as service use (CSRI64), health-related quality of life (EQ-5D-Y58) and medication use including psychotropic medication (Table 3).
| Measures | 19–44 months (T4) |
|---|---|
| ABC-C | ✓ |
| EQ-5D-Y | ✓ |
| CSRI-LD | ✓ |
| Medication use including psychotropic medication | ✓ |
Furthermore, we collected information on SAEs including hospital admissions. A total of 184 participants (75%) were seen at a mean of 36 months after entry to the study (range 19–44 months). Fifty-nine participants dropped out (reasons include refused consent, died, were uncontactable and did not returned consent forms). The PRIMENT Clinical Trials Unit continued to provide statistical and health economical support for the analyses. The DMEC and TSC agreed to, and remained involved in, the study overview during the long-term follow-up.
Sample size estimates and analysis plan
The outcome of interest was the ABC-CT measurements using the total score at three time points (6 months, 12 months and a mean final follow-up time point of 36 months).
The analysis estimated the difference in the ABC-CT between participants randomised to intervention or TAU on an intention-to-treat basis over time. A three-level regression model (adjusting for baseline ABC-CT measurements and time period, and accounting for clustering within services and the repeated measures of the ABC-CT at 6 months, 12 months and the final follow-up time point) was used to examine the intervention effect over time. This model also investigated whether or not the intervention effect varied over time by including an intervention by time period interaction term in the model. We carried out an all-available-case analysis but were aware of the fact that some data would be missing and the proportion was likely to increase sequentially at each follow-up point. We dealt with this by adopting the assumption that the missing data were missing at random. We also investigated whether there were any outliers or observations with high leverage. We had already recruited 246 participants, and this number was required in the original study to detect a difference of 0.45 SD with 90% power at a 5% significance level, accounting for the repeated measures at 6 months and 12 months, the effect of clustering and 10% attrition over the 12-month period. The design of the extended follow-up remained the same. Attrition was 4% at 12 months, but we predicted that this figure was likely to be larger for the additional final follow-up, leading to a smaller sample size, and our analysis could therefore be underpowered. As a result, we regarded the results from the extended follow-up analysis as exploratory.
The study statisticians were unblinded following the original study and, therefore, were not blinded for the analyses of the long-term follow-up data. However, we did not unblind the RAs who carried out the long-term follow-up assessments.
Health economic evaluation
The primary cost-effectiveness analysis for the long-term follow-up remained the same and was conducted from a health and social care perspective as well as a societal cost perspective. The cost-effectiveness measure was the incremental cost per QALY gained from the intervention compared with TAU. This was calculated as the mean cost difference between the intervention and TAU divided by the mean QALY difference to derive at the ICER. QALYs were calculated using the EQ-5D-Y, as recommended by NICE. 72 Missing data were imputed using multiple imputation by chained equations given the high percentage of missing data at 36 months. Current living situation, accommodation and level of disability were found to be predictors of missing EQ-5D-Y and CSRI at 36 months.
Process evaluation
The aim of process evaluations was to facilitate the understanding of complex observed phenomena needed to guide policy-makers in allocating resources and contributing to improvements in delivery and implementation of evidence-based clinical practice. 73
Interventions usually aim to alter the regular functioning of a system with unpredictable consequences and non-linear outcomes. 74 The Medical Research Council framework73 established a series of dimensions to assess the complexity of the intervention:
-
the number of skills required to deliver the intervention
-
the number of groups affected by the intervention
-
the variability and number of outcomes (i.e. unattended outcomes)
-
how flexible the intervention is to be adapted to different circumstances.
Process evaluations can further facilitate the understanding of how the intervention may be implemented elsewhere75 by examining the context, implementation and mechanisms of impact. The process evaluation covered the domains of (1) context, (2) implementation and (3) mechanisms of impact.
Context
Context responds to the questions ‘what is facilitating the delivery?’ and ‘what is challenging the delivery?’.
The context represents anything external to the intervention that may act either as a barrier to or as a facilitator of its delivery. 76 Many pre-existing factors (i.e. factors intrinsic to the population receiving the intervention) also play a role in determining the effect of the intervention and this explains the high variability of an intervention when implemented in different contexts. 77
Implementation
Implementation responds to the questions ‘how is delivery carried out?’ and ‘what is delivered?’.
The implementation further describes the process of delivery of the intervention through the assessment of key dimensions:
-
implementation process: comprising the resources and mechanisms essential for the intervention to be delivered
-
fidelity: representing the consistency of what is delivered
-
adaptations: representing the changes made to the intervention to reach a better fit with the context
-
dose: describing how much of the intervention has been implemented
-
reach: reporting how many participants received the intervention.
Mechanisms of impact
Mechanisms of impact responds to the question ‘how is change attained through intervention?’.
The understanding of the participants’ experience of the intervention can be achieved through the employment of qualitative interviews.
Logic model
Although all interventions assume that change is gained on delivery, the theory behind the functioning of interventions is far more complex and it requires a logic model, that is, a description of the mechanisms of the intervention to allow the consideration of all of the interplaying factors and expected outcomes. 73
The logic model is based on Kirkpatrick’s Four-Level Training Evaluation Model. 78 This logic model is further used as a reference framework against which we compare the views of our participants to assess the effectiveness of the training in PBS (Figure 2), comprising the following.
-
Level 1: inputs. This level measures what has been put in place to enable the carrying out of the training and intervention. This includes the quality and number of professionals acting as therapists, the trainers employed and the type of training delivered, the quality and quantity of support provided by the PBS research team (teleconference meetings, telephone calls and site visit), the quality and type of support provided for clinical supervision for therapists training in PBS, the quality and type of mentoring scheme offered by the trainers throughout the engagement of therapists with participants for the duration of the trial.
-
Level 2: processes. This level measures how the training was delivered and what has been delivered.
-
Level 3: actions. This level measures what elements of the interventions have been implemented by therapists and the quality of the plans implemented.
-
Level 4: results. This level measures what outcomes have been achieved as a consequence of the delivery of PBS. This last level of investigation takes into account the qualitative interviews of stakeholders in the intervention arm.
FIGURE 2.
Logic model for PBS-based staff training intervention.

Each level measures key dimensions of delivery of the intervention: the initial inputs provided in order for the intervention to be delivered, the training received by therapists, the intervention including the specific components implemented and the resulting outcomes.
Objectives
The process evaluation aimed to identify the different mechanisms of the staff training in PBS, to explore the factors that had an impact on the outcome of the intervention and to present stakeholders’ (participants with ID, paid and family carers, therapists, managers and trainers) experiences of taking part in the trial.
Participants
For the process evaluation, we interviewed the following stakeholder groups:
-
participants with ID in the intervention arm
-
family and paid carers for their views and experience of the intervention
-
service managers to explore their viewpoint regarding the impact of the training on the service
-
therapists who received PBS training, to explore their views on the training and challenges that they experienced because of participation in the study
-
the PBS trainers who delivered the training and provided mentoring to therapists during and after the training.
Procedure
Interview guides were developed by a group of co-applicants with extensive experience in qualitative research (further described in Qualitative data analysis) and were based on research literature. Further advice on the wording of interview questions for service users was provided by the study service users reference group Camden SURGE, The Advocacy Project. Individual semistructured qualitative interviews were conducted with all participants. Interview questions varied according to the group of participants and questions were revised iteratively to further explore any issues that arose from the interviews. The interviews were conducted by the qualitative research assistant and audio-recorded. In accord with existing literature on good practice in qualitative interviewing,79 general questions about participants’ experience of PBS were discussed in the first part of the interview and more specific questions about the study were asked further on.
Qualitative data analysis
The audio-recordings of the interview sessions were transcribed verbatim and data were extracted by means of NVivo version 10 (QSR International, Warrington, UK). For the analysis of the transcripts, we used the inductive approach of thematic analysis by Braun and Clark,80 according to whom themes and subthemes emerge from the text and are not predefined by the researcher. Topics were given the status of ‘theme’ when they emerged more than twice from the transcript. However, when a topic did not appear at least twice in the text, but was still deemed relevant to the present work, the researcher would consider whether or not to include it in the analysis. Subthemes were further developed for each of the themes.
Once themes and subthemes had been generated, the RA created a codebook to be utilised by co-raters to test inter-rater reliability by independently rating the interviews. Co-raters were co-applicants: one lead clinical psychologist, three consultant ID psychiatrists and one representing the family carers’ group for people with ID. Inter-rater reliability was measured using the Kappa coefficient (Cohen’s Kappa). 81 The parameters were based on the ranges proposed by Landis and Koch,82 as follows:
-
< 0.00 = poor
-
0.00–0.20 = slight
-
0.21–0.40 = fair
-
0.41–0.60 = moderate
-
0.61–0.80 = substantial
-
0.81–1.00 = almost perfect.
Co-raters met frequently during the qualitative analysis to discuss the accuracy and quality of the codebook. A total of three rounds of codebook revisions were necessary to define themes and subthemes.
The frequency of themes was further calculated through an aggregate mean, weighted according to the number of stakeholders interviewed in the study. This strategy helped to factor the number of participants for each stakeholder group into the calculation.
Fidelity assessment
The quality assessment of behavioural plans was conducted by an independent reviewer (a consultant clinical psychologist with extensive PBS experience) by means of the Behaviour Intervention Plan Quality Evaluation Scoring Guide II (BIP-QE II). 83
The BIP-QE II is designed to measure the extent to which key domains of a behaviour plan are present in the plan assessed. This scale comprises 12 domains for behavioural plan evaluation: problem behaviour, predictors of behaviour, analysis of what is supporting the problem behaviour, environmental changes, predictors related to function, function related to replacement behaviours, teaching strategies, reinforcement, reactive strategies, goals and objectives, team co-ordination and communication.
Good reliability and validity were found to be associated with the BIP-QE II. Scores from the scale are interpreted according to the following ranges: a score of ≤ 12 points indicates a weak plan, a score of 13–16 points indicates an underdeveloped plan, a score of 17–21 points indicates a good plan and a score of 22–24 indicates a superior plan (Box 1). A higher score on the scale indicates an increased likelihood that a behaviour intervention plan will be implemented with fidelity.
-
Problem behaviour.
-
Predictors of behaviour.
-
Analysing what is supporting problem behaviour.
-
Environmental changes.
-
Predictors related to function.
-
Function related to replacement behaviours.
-
Teaching strategies.
-
Reinforcement.
-
Reactive strategies.
-
Goals and objectives.
-
Team co-ordination.
-
Communication.
-
≤ 12 points (weak plan): this plan may affect some change in behaviour but the written plan is weak.
-
13–16 points (underdeveloped plan): this plan may affect some change in problem behaviour but would require a number of alterations.
-
17–21 points (good plan): this plan is likely to affect a change in behaviour.
-
22–24 points (superior plan): this plan is likely to affect a change in problem behaviour and embodies best practice.
Patient and public involvement
A local group of service users with ID from the Camden SURGE, The Advocacy Project, provided advice for the entire duration of the trial. One of the study’s RAs and the chief investigator met with the group on a regular basis. The group provided support for the development of accessible information materials for the study instruments, participant information sheets and consent forms, the study website, topic guides for qualitative interviews, recruitment and the dissemination of findings. Reports from the meetings between the RA and the group were provided to the TSC.
Mrs Vivien Cooper, OBE, the founder and Chief Executive of the Challenging Behaviour Foundation, is one of the study’s co-applicants. Mrs Cooper was involved in the development of the study, advised on recruitment, reviewed study-related documentation such as information sheets, consent forms and qualitative interview topic guides and was involved in the dissemination of the findings.
The study team produced a newsletter twice a year that was disseminated to the participants, their family or paid carers and the local investigators.
Chapter 3 Results
Participants
A total of 23 clusters took part in the study, of which 11 were allocated to the intervention plus TAU arm and the remaining 12 to TAU-only arm. In the 11 intervention clusters, one therapist provided training in four clusters, two therapists provided training in another four clusters and three therapists provided training in the remaining three clusters. A total of 382 potential participants were screened, of whom 246 (64%) consented to take part in the trial. One participant was erroneously consented as they did not meet the inclusion threshold on the ABC-CT and, therefore, was excluded from the analysis.
The median number of participants who were recruited per cluster was 13 [interquartile range (IQR) 6–14]. The details are shown in the trial Consolidated Standards of Reporting Trials (CONSORT) flow diagram (Figure 3). Recruitment took place from 2 June 2013 to 24 November 2014. The 6-month follow-up assessments were conducted between 10 December 2013 and 21 May 2015, and 12-month follow-up assessments were conducted between 3 June 2014 and 30 November 2015.
FIGURE 3.
Trial flow chart. nfc, number of family carers; npc, number of paid carers; nsu, number of service users; nt, number of teams. From Hassiotis A, Poppe M, Strydom A, Vickerstaff V, Hall IS, Crabtree J, et al. Clinical outcomes of staff training in positive behaviour support to reduce challenging behaviour in adults with intellectual disability: cluster randomised controlled trial. Br J Psychiatry, vol. 212, iss. 3, pp. 161–8, 2018,84 reproduced with permission.

A total of 215 participants (87%) completed the 6-month follow-up and 225 (92%) completed the 12-month follow-up assessments. There was no difference in attrition between the arms (7% in the intervention arm and 9% in the control arm). Table 4 shows the baseline demographic and clinical characteristics of the participants.
| Characteristics | Total (N = 245) | Trial arm | |
|---|---|---|---|
| TAU (N = 137) | PBS (N = 108) | ||
| Demographic | |||
| Age (years), median (IQR) | 37 (25–51) | 33 (24–51) | 42 (27–50) |
| Sex: male, n (%) | 157 (64) | 90 (66) | 67 (62) |
| Ethnic origin: white, n (%) | 176 (72) | 95 (69) | 81 (75) |
| Service-reported level of ID, n (%) | |||
| Mild | 41 (17) | 17 (12) | 24 (22) |
| Moderate | 77 (31) | 46 (34) | 30 (28) |
| Severe | 127 (52) | 73 (53) | 54 (50) |
| Short-form ABS score, median (IQR) | 48 (29–68) | 42 (25–64) | 55 (35–73) |
| WASI score (full scale IQ 4) (N = 95) | 44 (40–52) | 43 (40–50) | 46 (41–53) |
| Current accommodation, n (%) | |||
| Residential | 105 (43) | 52 (38) | 53 (49) |
| Supported living | 69 (28) | 36 (27) | 33 (30) |
| Family home | 64 (26) | 47 (34) | 17 (16) |
| Own flat/house | 7 (2) | 2 (1) | 5 (5) |
| Clinical | |||
| ABC-C score, median (IQR) | |||
| Total score | 64 (44–86) | 68.5 (47–87.5) | 60 (43–80) |
| Irritability | 20 (13–29) | 21.5 (15–29) | 18 (11–26) |
| Lethargy | 12 (7–21) | 13 (6.5–21) | 12 (7–21) |
| Stereotypy | 5 (2–10) | 5.5 (2–10) | 4 (2–9) |
| Hyperactivity | 20 (12–26) | 21 (13–28) | 18 (11–24) |
| Inappropriate speech | 4 (1–8) | 4 (1–8) | 5 (1–8) |
| Medications, n (%) | |||
| Any | 217 (89) | 122 (89) | 95 (88) |
| Antipsychotic | 162 (66) | 89 (65) | 73 (68) |
| Other psychotropic | 177 (72) | 100 (73) | 77 (71) |
| Mini PAS-ADD, n (%) | |||
| Common mental disorder | 117 (49) | 61 (46) | 56 (52) |
| Severe mental illness | 47 (20) | 27 (20) | 20 (19) |
| ASD | 50 (21) | 31 (23) | 19 (18) |
| ASD broad definition | 113 (46) | 66 (58.4) | 47 (41.6) |
| Physical health problems, n (%) | 180 (74) | 107 (80) | 73 (68) |
| Mobilitya (N = 180) | 64 (36) | 38 (36) | 26 (36) |
| Sensory | 43 (24) | 29 (27) | 14 (19) |
| Epilepsy | 67 (37) | 42 (39) | 25 (34) |
| Incontinence | 78 (43) | 46 (43) | 32 (44) |
| Other | 103 (57) | 63 (59) | 40 (55) |
Primary outcome
At baseline, the median ABC-CT was 60 (IQR 43–80) in the intervention arm, compared with 68.5 (IQR 47–87.5) in the control arm. In the intervention arm, the median ABC-CT reduced to 50.5 (IQR 30–75) at 6 months and to 49.0 (IQR 32–73) at 12 months. In the control arm, the median ABC-CT was 54 (IQR 37–81) at 6 months and 55 (IQR 42–75) at 12 months. The primary model used 439 ABC-CT measurements from 233 participants over the two follow-up time points. There was no statistically significant difference between arms in ABC-CT over 12 months (mean ABC-CT difference –2.41, 95% CI –8.79 to 4.51; p = 0.528) (Table 5 and Figure 4).
| Time point | Trial arm | n | Mean | SD | Median | IQR |
|---|---|---|---|---|---|---|
| Baseline | TAU | 136 | 68.5 | 29.0 | 68.5 | 47–87.5 |
| PBS | 107 | 61.8 | 27.7 | 60 | 43–80 | |
| 6 months | TAU | 116 | 60.6 | 32.6 | 54 | 37–81 |
| PBS | 98 | 55.0 | 32.5 | 50.5 | 30–75 | |
| 12 months | TAU | 125 | 59.2 | 28.8 | 55 | 42–75 |
| PBS | 100 | 54.0 | 32.1 | 49 | 32–73 |
FIGURE 4.
Aberrant Behaviour Checklist – Community total score over 12 months. From Hassiotis A, Poppe M, Strydom A, Vickerstaff V, Hall IS, Crabtree J, et al. Clinical outcomes of staff training in positive behaviour support to reduce challenging behaviour in adults with intellectual disability: cluster randomised controlled trial. Br J Psychiatry, vol. 212, iss. 3, pp. 161–8, 2018,84 reproduced with permission.
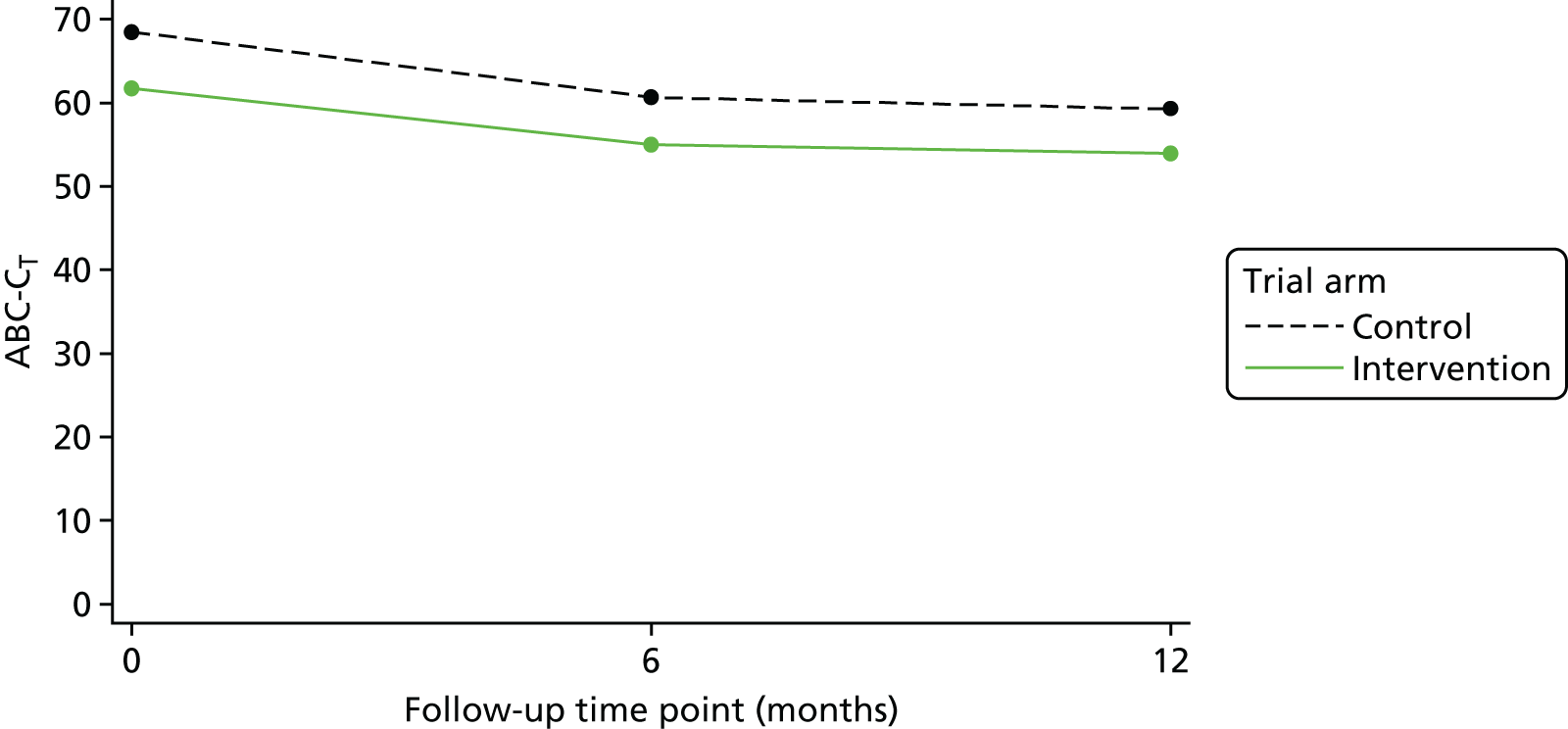
The intracluster correlation coefficient (ICC) for the ABC-CT at the service level was 0.021 (95% CI 0.001 to 0.286). The ICC for the repeated measures within participants was 0.625 (95% CI 0.542 to 0.702).
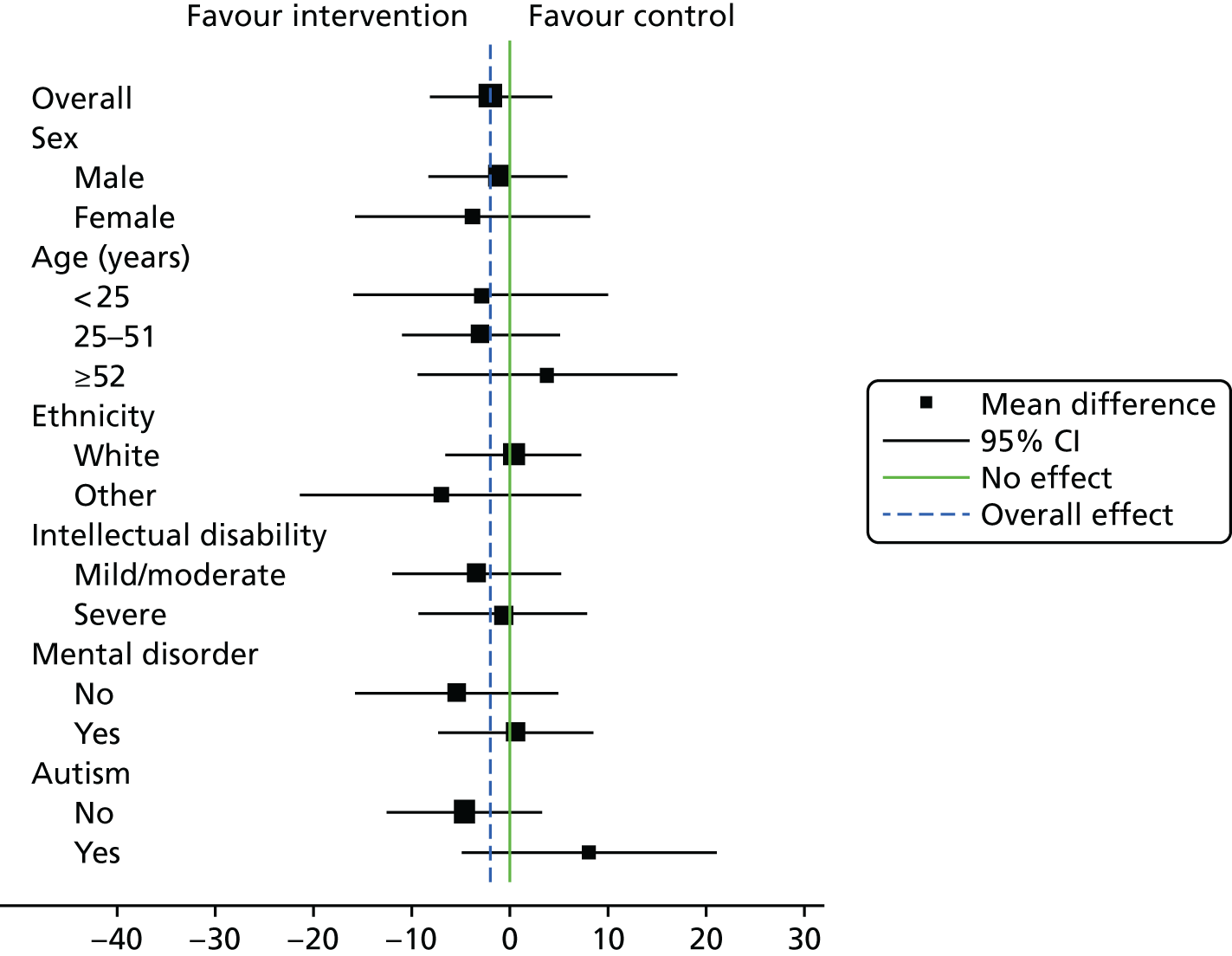
Subgroup analysis
The estimates of the intervention effect on participant sociodemographic and clinical characteristics are shown in a forest plot (Figure 5).
FIGURE 5.
Subgroup analysis. From Hassiotis A, Poppe M, Strydom A, Vickerstaff V, Hall IS, Crabtree J, et al. Clinical outcomes of staff training in positive behaviour support to reduce challenging behaviour in adults with intellectual disability: cluster randomised controlled trial. Br J Psychiatry, vol. 212, iss. 3, pp. 161–8, 2018,84 reproduced with permission.
Sensitivity analysis
A series of analyses were conducted as follows: (1) adjusting for area deprivation, (2) adjusting for the nature of the respondent (participant or carer), (3) adjusting for the unbalanced baseline characteristics (ethnicity and participant’s cohabitant), (4) adjusting for the percentage of PBS plans written, (5) a model including two random effects and (6) imputing missing values with ‘Baseline Observation Carried Forward’. All of these analyses gave similar results, with differences in ABC-CT between the arms ranging from –3.45 to –0.81. None of the service user baseline demographics nor the presence of a mental disorder predicted missing data and, therefore, no further analyses were conducted.
Exploratory multivariate analyses
Multivariate analysis examined the effect of training staff in PBS on the individual domains of the ABC-C. The inappropriate speech domain was not included in the multivariate model as it had low correlations (0.300, 0.094, 0.175 and 0.360) with the (1) irritability, agitation and crying, (2) lethargy and social withdrawal, (3) stereotypic behaviour and (4) hyperactivity and non-compliance domains, respectively. The intervention had a similar effect on all four domains; it varied from a standardised difference of –0.016 (95% CI –0.22 to 0.19) for the lethargy and social withdrawal domain to –0.050 (95% CI –0.25 to 0.14) for the stereotypic behaviour domain between the two arms. These analyses are shown in Table 6.
| Model | Difference | 95% CI | p-value |
|---|---|---|---|
| Sensitivity analyses | |||
| Primary model | –2.14 | –8.79 to 4.51 | 0.528 |
| Area deprivation | –2.39 | –9.19 to 4.41 | 0.491 |
| Completed by family/paid carer | –1.21 | –8.20 to 5.79 | 0.735 |
| Missing data (BOCF) | –1.83 | –8.42 to 4.76 | 0.586 |
| Heteroscedastic model | –2.35 | –9.24 to 4.55 | 0.505 |
| Imbalance in baseline characteristics | –0.81 | –7.95 to 6.32 | 0.824 |
| % of participants who had at least one intervention component (e.g. plan, observations, goodness to fit) | 1.41 | –15.5 to 18.3 | 0.870 |
| Multivariate analysis (ABC-C subdomains) | |||
| Irritability, agitation and crying | –0.041 | –0.22 to 0.14 | |
| Lethargy and social withdrawal | –0.016 | –0.22 to 0.19 | |
| Stereotypic behaviour | –0.050 | –0.25 to 0.14 | |
| Hyperactivity and non-compliance | –0.049 | –0.23 to 0.13 | |
Secondary outcomes
There was no difference in the prevalence of mental disorders (measured using the Mini PAS-ADD) or frequency of activities (measured using the GCPLA) over 12 months. In total, 69 family carers were included in the study, 19 in the intervention arm and 50 were in the control arm. The majority (n = 59, 86%) were female with a median age of 54 years (IQR 48–59 years). As a result of the small numbers in the intervention arm, only descriptive analyses of these secondary outcomes were performed. There was no difference in the Uplift/Burden Scale and GHQ-12 scores over the 12 months. A total of 175 paid carers took part in the study, 89 in the intervention arm and 86 in the control arm. Two-thirds of the paid carer participants (n = 108, 67%) were female and the median age was 41 years (IQR 32–53 years). Over the 12 months, 86 paid carers (49%) left their posts (control arm, n = 49; intervention arm, n = 37) and, therefore, no further analyses were carried out. Details of the treatment effect on the secondary outcomes are given in Table 7.
| Outcomes | Descriptive | Analysis over 12 months | ||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | Number of service users | Odds ratio/difference | 95% CI | |
| Service users | ||||||
| Mini PAS-ADD, n (%) | ||||||
| Common mental disorder | ||||||
| Control | 61 (46) | 43 (37) | 54 (44) | 230 | 1.07 | 0.61 to 1.87 |
| Intervention | 56 (52) | 45 (46) | 42 (42) | |||
| Severe mental illness | ||||||
| Control | 27 (20) | 13 (11) | 21 (17) | 229 | 1.24 | 0.32 to 4.81 |
| Intervention | 20 (19) | 17 (18) | 15 (15) | |||
| Autistic spectrum | ||||||
| Control | 31 (23) | 31 (27) | 40 (33) | 230 | 0.70 | 0.26 to 1.88 |
| Intervention | 19 (18) | 24 (24) | 22 (22) | |||
| GCPLA, median (IQR) | ||||||
| Range | ||||||
| Control | 17 (12–22) | 16.5 (13–21) | 17 (13–21) | 232 | 0.587 | –0.57 to 1.74 |
| Intervention | 19 (13–23.5) | 19 (14–23) | 17 (13.5–22) | |||
| Busy | ||||||
| Control | 10 (7–13) | 11 (7–13) | 11 (8–13) | 232 | 0.377 | –0.59 to 1.34 |
| Intervention | 11 (8–15) | 11 (8–14) | 12 (8–14) | |||
| Family carers, median (IQR) | ||||||
| Uplift | ||||||
| Control | 15 (13–17) | 15 (12–17) | 15 (13–17) | |||
| Intervention | 14 (13–16) | 15 (14–17) | 15 (13–16) | |||
| Burden | ||||||
| Control | 33 (28–39) | 31 (25–36) | 30 (25–39) | |||
| Intervention | 28 (26–31) | 29 (25.5–32.5) | 30 (28–32.5) | |||
| GHQ-12 score | ||||||
| Control | 4 (1–8) | 4 (2–7) | 3 (1–6) | |||
| Intervention | 3 (0–4) | 2.5 (1–6.5) | 2 (0–3) | |||
| Paid carers, median (IQR) | ||||||
| CDS-IDa | ||||||
| Control | 24 (15–37) | |||||
| Intervention | 21 (13–31) | |||||
Subsample with autism spectrum disorders
A total of 113 participants (46.1%) constituted the ASD+ group (control arm, n = 66; intervention arm, n = 47) and 132 participants constituted the ASD– group (control arm, n = 71; intervention arm, n = 61). The baseline demographic and clinical characteristics of a subgroup of participants with broadly defined ASD compared with those without can be found in Table 8.
| Characteristics | Total (N = 245) | Participant group | |
|---|---|---|---|
| ASD– (N = 132) | ASD+ (N = 113) | ||
| Demographic | |||
| Age (years), median (IQR) | 37 (25–51) | 43 (30–53) | 31 (22–48) |
| Sex: male, n (%) | 157 (64) | 74 (56) | 83 (73) |
| Ethnic origin: white, n (%) | 176 (72) | 101 (77) | 75 (66) |
| Service-reported level of ID, n (%) | |||
| Mild | 41 (17) | 31 (24) | 10 (9) |
| Moderate | 77 (31) | 39 (30) | 37 (33) |
| Severe | 127 (52) | 61 (47) | 66 (58) |
| Short-form ABS score, median (IQR) | 48 (29–68) | 53 (29–73) | 45 (28–62) |
| Current accommodation, n (%) | |||
| Residential | 105 (43) | 64 (48) | 41 (36) |
| Supported living | 69 (28) | 32 (24) | 37 (33) |
| Family home/own home | 71 (29) | 36 (27) | 35 (31) |
| Clinical | |||
| ABC-CT score, median (IQR) | 64 (44–86) | 60 (41–80) | 73 (47–89) |
| Medications, n (%) | |||
| Any | 220 (90) | 118 (89) | 102 (90) |
| Antipsychotic | 165 (67) | 91 (69) | 74 (65) |
| Other psychotropic | 180 (73) | 100 (76) | 80 (71) |
| Both antipsychotic and other psychotropic | 139 (57) | 78 (59) | 61 (54) |
| Physical health problems, n (%) | |||
| Mobilitya (N = 180) | 64 (36) | 47 (46) | 17 (22) |
| Sensory | 43 (24) | 28 (27) | 15 (19) |
| Epilepsy | 67 (37) | 40 (39) | 27 (35) |
| Incontinence | 78 (43) | 49 (48) | 29 (37) |
| Other | 103 (57) | 54 (53) | 49 (63) |
At baseline, the median ASD+ ABC-CT in the intervention arm was 66 (IQR 45–85) compared with 75 (IQR 51–93) in the control arm. In the intervention arm, the median ABC-CT reduced to 55 (37–78) at 6 months and to 53 (35–72) at 12 months. In the control arm, the median ABC-CT was 62 (IQR 43–90) at 6 months and 60 (IQR 43–66) at 12 months. The difference in the reduction in challenging behaviour over 12 months between the intervention arm and the control arm was not statistically significant (mean difference –2.10, 95% CI –11.3 to 7.13; p = 0.655) (Figure 6).
FIGURE 6.
Aberrant Behaviour Checklist – Community total score over 12 months: ASD.

A total of 102 participants with an ASD received any type of medication, 74 (65%) received antipsychotic medication and 80 (71%) also received other psychotropic medication.
With regard to the subgroup comparisons between the ASD+ and ASD– groups for common mental disorder (CMD) and severe mental illness (SMI), differences at baseline were not statistically significant (CMD, p = 0.625; SMI, p = 0.615). The analysis over 12 months revealed that the CMD and SMI symptoms were stable in both the ASD+ and ASD– group (Table 9).
| Mini PAS-ADD result | Time point, n (%) | ||
|---|---|---|---|
| Baseline | 6 months | 12 months | |
| CMD | |||
| All | 117 (49) | 88 (41) | 96 (43) |
| ASD– | 65 (50) | 45 (39) | 54 (45) |
| ASD+ | 52 (47) | 43 (43) | 42 (40) |
| SMI | |||
| All | 47 (20) | 30 (14) | 36 (16) |
| ASD– | 27 (21) | 17 (15) | 23 (19) |
| ASD+ | 20 (18) | 13 (13) | 13 (13) |
Patterns of prescribing did not differ between the ASD+ and ASD– groups, irrespective of the presence of mental health comorbidity.
Eighty-five per cent of individuals with CMD in both the ASD+ and ASD– groups were prescribed medication. Sixty-five per cent of individuals in the ASD+ group received antipsychotic medication, compared with 60% of individuals in the ASD– group, whereas 63% in the ASD+ group received other psychotropic medication (i.e. anxiolytic medication), compared with 66% in the ASD– group.
A similar number of participants with SMIs in the ASD+ and ASD– groups received medication (90% in the ASD+ group vs. 89% in the ASD– group), with 75% of the ASD+ group and 70% of the ASD– group receiving antipsychotic medication, and 75% of the ASD+ group and 78% of the ASD– group receiving other psychotropic medication.
In the group with neither CMD nor SMI (i.e. without any evidence of mental illness diagnosis), 91% of participants from both the ASD+ and ASD– groups were prescribed medication; 70% of the ASD+ group and 65% of the ASD– group were prescribed antipsychotic medication, and 73% of the ASD+ group and 80% of the ASD– group received other psychotropic medication.
Serious adverse events
Twenty-nine participants experienced a total of 45 SAEs, including the death of one participant in the intervention arm. Twenty-six of the SAEs were in the intervention arm and 19 were in the control arm. Two participants were admitted to hospital because of mental illness and challenging behaviour and the remaining SAEs were hospitalisations attributable to physical ill-health including falls, or acute exacerbation of chronic conditions, for example respiratory disease and epilepsy. Thirteen participants (intervention arm, n = 3; control arm, n = 10) moved from their original addresses to a new home because of either closures of previous accommodation or a change in the participant’s needs.
Blinding and unmasking
There were six cases of unmasking researchers to the participant’s trial arm allocation; another researcher collected data from those sites. Researchers accurately predicted the arm allocation of 123 participants (59%) at 6 months and 126 participants (56%) at 12 months; thus, the predictions were considered to be no better than chance.
Health economic evaluation
Cost of the intervention
Details of the cost components of training staff in PBS are reported in Table 10. The cost of training per participant was £397.
| Activity | Total cost (£) |
|---|---|
| Preparation and printing of training manual and material | 873 |
| Workshops | |
|
6669 |
| Preparation for workshops (6 days × 7 hours × £50) | 2100 |
| Reading and commenting on participant assessments and PBS plans between workshops 1, 2 and 3 (4 hours × 2 workshops × 20 participants × £50) | 8000 |
| Mentoring post workshops (2 hours per month × 12 months × 20 participants × £50) | 24,000 |
| Travel and expenses | 1200 |
| Total | 42,842 |
Details of the activities and the time and cost of delivering PBS were available for 65 participants (60%) in the intervention arm, reported in Table 11. Assuming that a band 6 NHS Agenda for Change nurse is the typical therapist trained in the intervention, the total average cost per participant (of training plus delivery) is estimated to be £1598.
| Elements of PBS intervention | Average number of hours | Cost (£) of a band 6 nurse |
|---|---|---|
| Assessment: direct observation of client | 3.6 | 157 |
| Assessment: contact with staff team, parents/carers, wider system | 5.2 | 227 |
| Assessment: indirect work | 3.8 | 169 |
| Intervention: direct contact with client | 2.4 | 104 |
| Intervention: contact with staff team, parents/carers, wider system | 3.2 | 143 |
| Report writing and other administration not accounted for in other categories | 6.9 | 302 |
| Other work not accounted for in other categories | 2.7 | 118 |
| Total spent on case | 27.3 | 1201 |
Resource use and costs
Descriptive statistics for resource use are reported in Appendix 5. Total costs for each resource type are reported in Table 12. GPs and primary care were used by more than 80% of participants, with psychiatrists being the second most frequently consulted professionals (see Appendix 5). The cost per participant of the intervention including training and delivery is £1251.
| Resource use costs | Time point | Difference | Baseline-adjusted difference | 95% CI | |||
|---|---|---|---|---|---|---|---|
| Baseline | 12 months | ||||||
| Intervention arm | Control arm | Intervention arm | Control arm | ||||
| Community | 1175 | 988 | 1470 | 1648 | –178 | –293 | –817 to 231 |
| Mental health – secondary care | 48 | 94 | 74 | 544 | –469 | –457 | –1237 to 322 |
| Physical health – secondary care | 369 | 610 | 1281 | 996 | 284 | 425 | –220 to 1070 |
| Medication | 160 | 156 | 285 | 294 | –9 | –10 | –94 to 74 |
| Total health and social care costs excluding medication | 1592 | 1692 | 2827 | 3189 | –362 | –346 | –1518 to 825 |
| Total health and social care costs including medication | 1752 | 1848 | 3112 | 3483 | –371 | –361 | –1532 to 810 |
| Voluntary | 43 | 21 | 16 | 9 | 11 | 11 | –23 to 47 |
| Private and out of pocket | 345 | 539 | 757 | 440 | 362 | 353 | –128 to 834 |
| Accommodation | 24,469 | 19,217 | 51,291 | 41,557 | 9734 | 954 | –2206 to 4114 |
| Criminal justice | 170 | 88 | 46 | 166 | –120 | –148 | –379 to 81 |
| Unpaid/family carers | 13,815 | 22,821 | 19,691 | 31,194 | –11,503 | –4472 | –14,418 to 5475 |
| Total societal costs | 41,398 | 43,856 | 74,951 | 77,021 | –2069 | –719 | –9902 to 8464 |
The total cost of health and social care at 12 months (excluding the cost of medication and training in PBS) per participant is estimated at £2827 in the intervention arm and £3189 in the control arm. Adjusting for baseline costs, the mean incremental health and social care cost of the intervention compared with TAU is –£346 (95% CI –£1518 to £825).
When medication costs are added, the average adjusted incremental total health and social care cost per participant is –£361 (95% CI –£1532 to £810) for a total cost of £1237 including training and delivery.
Societal costs
Societal costs, including out-of-pocket costs, accommodation, criminal justice and unpaid carers, are reported in Table 12. Accommodation costs make up between 44% and 68% of the total societal cost. Contributions of unpaid carers make up the second largest contribution to costs, making up between 26% and 52% of costs.
At baseline, the number of hours per week spent by unpaid carers on care or support averaged 22 hours (95% CI 12 to 32 hours) in the intervention arm and 36 hours (95% CI 26 to 46 hours) in the control arm. At 12 months, carers in the intervention arm provided 15 hours a week of care and support (95% CI 7 to 22 hours) and those in control arm 27 hours a week (95% CI 18 to 36 hours): a baseline-adjusted difference of –6 hours a week of care and support for the intervention arm compared with the control arm at 12 months (95% CI –4 to 15 hours).
Cost utility and quality-adjusted life-years
Descriptive statistics for EQ-5D-Y proxy-completed utility scores and QALYs are reported in Table 13. Complete data to calculate QALYs were available for 96 participants (88%) in the intervention arm and 108 participants (78%) in the control arm. We found an adjusted difference in QALYs between the two arms of 0.076 in favour of the intervention (95% CI 0.011 to 0.140 QALYs).
| Time point | QALYs | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | ||||||
| Intervention arm | Control arm | Intervention arm | Control arm | Intervention arm | Control arm | Intervention arm | Control arm | |
| n | 103 | 127 | 102 | 120 | 103 | 125 | 96 | 108 |
| Mean | 0.565 | 0.478 | 0.638 | 0.497 | 0.617 | 0.483 | 0.612 | 0.492 |
| SD | 0.38 | 0.37 | 0.33 | 0.36 | 0.32 | 0.33 | 0.292 | 0.230 |
Cost-effectiveness: incremental cost-effectiveness ratio, cost-effectiveness acceptability curves and cost-effectiveness plane
As reported in Primary outcome, the average decrease in the primary outcome of ABC-CT was 2.14 (95% CI –8.79 to 4.51). This translates to a mean incremental cost per 1-point reduction in ABC-C over 12 months of £578 from a health and social care perspective and £411 from a societal cost perspective. At a threshold for willingness to pay for a point change in ABC-CT of £5000, there is an 87% probability that the intervention is cost-effective from a health and social care perspective and an 88% probability that it is cost-effective from a societal cost perspective (Figure 7).
FIGURE 7.
Cost-effectiveness acceptability curve of willingness to pay for a 1-point change in the primary outcome (ABC-CT).

Over 12 months, the incremental cost per QALY gained of training in PBS compared with TAU is £17,871 excluding medication costs and £16,276 including medication costs from a health and social care perspective. The probability that PBS is cost-effective for a range of values of willingness to pay for a QALY is presented in Figure 8. Figure 9 shows the results of the bootstrap analysis on a CEP. At a threshold for willingness to pay for a QALY of £20,000 per QALY gained, there is a 60% chance that the intervention is cost-effective from a health and social care perspective. When out-of-pocket costs, costs for voluntary services, the criminal justice sector, accommodation and unpaid carer time are included, the incremental cost per QALY gained is £11,566. From a societal cost perspective, there is a 54% probability that training staff in PBS is cost-effective at a cost-effectiveness threshold of £20,000. The lower probability of training staff in PBS being cost-effective from a societal perspective (even although it has a lower ICER) is attributable to the wider variation in costs.
FIGURE 8.
Cost-effectiveness acceptability curve for a range of values of willingness to pay per QALY gained.

FIGURE 9.
Cost-effectiveness plane of bootstrapped values for training in the intervention arm compared with the control arm: health and social care costs only.

Sensitivity analysis
The EQ-5D-Y was self-completed by 26 participants with ID (intervention arm, n = 14; control arm, n = 12) at baseline, 6 months and 12 months. Therefore, we were able to generate QALYs. The adjusted average QALYs over 12 months were 0.782 (95% CI 0.749 to 0.815 QALYs) for the intervention arm and 0.735 (95% CI 0.639 to 0.830 QALYs) for the control arm, with a mean baseline-adjusted difference of 0.043 QALYs (95% CI –0.075 to 0.170 QALYs). This equates to a mean incremental cost per QALY gained of £30,925 from the health-care perspective and £21,975 from a societal cost perspective.
To provide an estimate of the cost-effectiveness of training in PBS compared with TAU, the average cost per participant of both aspects needs to be estimated. We made the conservative assumption that the average cost of training per participant was the total cost of training divided by the number of therapists in the intervention arm. In reality, this may be larger, as other participants in the therapist caseload may benefit from the training, particularly those allocated after the trial or those who did not consent to provide data. The cost may also be lower as a result of staff turnover, for example. If a therapist’s caseload is, on average, 25% larger than it was in the trial, the total cost of the intervention per participant would be £317. If it is 25% smaller, then it would be £529 per participant.
Clinical staff delivering the intervention may also have been graded at bands other than band 6. Some may be more junior, for example at band 5, at £36 per hour and a total cost of delivering the intervention per participant of £982. If they were more senior (band 7, at a cost of £52 per hour), the average cost per participant would be £1419.
Combining the upper and lower estimates for training and delivery, the total health and social care service use cost, and dividing by proxy-reported QALYs, the ICER may be as low as £13,257 per QALY gained or as high as £22,538 per QALY gained.
If accommodation costs are removed from the societal analysis, given that they take up the largest proportion of costs and that the data are potentially unreliable, the additional total mean cost per participant of training in PBS compared with TAU is £452 (95% CI –£12,233 to £13,138), with an ICER of £5947 per QALY gained.
Long-term follow-up
Participants and outcomes
The final assessments took place between July 2016 and March 2017. On average, the third follow-up took place 36 months (SD 4.7 months) after the baseline assessment. A total of 184 individuals were seen (intervention arm, n = 79; control arm, n = 105). A total of 50 participants dropped out and a further 11 were uncontactable. Table 14 shows the baseline characteristics of the participants who were seen at 36 months and those who dropped out.
| Characteristics | Total (N = 245) | Completed 36 months (N = 184) | Missing at 36 months (N = 61) |
|---|---|---|---|
| Demographic | |||
| Age (years), median (IQR) | 37 (25–51) | 38 (25–51) | 34 (24–50) |
| Sex: male, n (%) | 157 (64) | 118 (64) | 39 (64) |
| Ethnic origin: white, n (%) | 176 (72) | 131 (71) | 45 (74) |
| Service-reported level of ID, n (%) | |||
| Mild | 41 (17) | 24 (13) | 17 (28) |
| Moderate | 77 (31) | 64 (35) | 13 (21) |
| Severe | 127 (52) | 96 (52) | 31 (52) |
| Living situation, n (%) | |||
| Living alone | 39 (16) | 29 (16) | 10 (16) |
| Living with parents/others | 206 (84) | 155 (84) | 51 (84) |
| Current accommodation, n (%) | |||
| Residential | 105 (43) | 87 (47) | 18 (30) |
| Supported living | 69 (28) | 51 (28) | 18 (30) |
| Family home | 64 (26) | 44 (24) | 20 (33) |
| Own flat/house | 7 (2) | 2 (1) | 5 (8) |
| Clinical | |||
| Mini PAS-ADD, n (%) | |||
| CMD | 117 (49) | 83 (46) | 34 (57) |
| SMI | 47 (20) | 33 (18) | 14 (23) |
| Autistic spectrum | 50 (21) | 37 (20) | 13 (22) |
| ABS (median, IQR) | 48 (29–68) | 48 (28–68) | 44 (32–71) |
| WASI score (full scale IQ 4) (N = 95), median (IQR) | 44 (40–52) | 43 (40–49) | 53 (42–65) |
| Physical health problems, n (%) | 180 (74) | 132 (72) | 48 (81) |
| Mobilitya (N = 180) | 64 (36) | 41 (31) | 23 (48) |
| Sensory | 43 (24) | 33 (25) | 10 (21) |
| Epilepsy | 67 (37) | 48 (36) | 19 (40) |
| Incontinence | 78 (43) | 53 (40) | 25 (52) |
| Other | 103 (57) | 78 (59) | 25 (52) |
| ABC-CT score, median (IQR) | |||
| Total score | 64 (44–86) | 63 (45–86) | 65 (43–82) |
| Irritability (15 questions) | 20 (13–29) | 21 (13–29) | 20 (14–25) |
| Lethargy (16 questions) | 12 (7–21) | 12 (7–20) | 14 (7–21) |
| Stereotypy (7 questions) | 5 (2–10) | 5 (2–10) | 6 (2–9) |
| Hyperactivity (16 questions) | 20 (12–26) | 19 (12–26) | 21 (12–27) |
| Inappropriate speech (4 questions) | 4 (1–8) | 5 (1–8) | 3 (1–7) |
Further reductions in challenging behaviour were noted in both arms of the study but, as previously stated, the mean difference in ABC-CT between arms was non-significant. The median ABC-CT was 49 (IQR 32–78) and 38 (IQR 25–56) in the control and intervention arms, respectively. The mean difference was –3.70 (95% CI –9.25 to 1.85; p = 0.191). Figure 10 shows the change in ABC-CT at all four assessment points. The ABC-C subscale scores at long-term follow-up are shown in Appendix 6.
FIGURE 10.
Aberrant Behaviour Checklist – Community total scores over 36 months.

All other sensitivity and subgroup analyses followed the same pattern as in the main study, revealing no significant differences between the study arms.
Regarding the longer-term impact of the intervention on medication, the proportion of participants in the intervention arm being on any medication, antipsychotic medication and other psychotropic medication remained unchanged over time, as shown in Table 15.
| Medications | Time point, n (%) | |||
|---|---|---|---|---|
| Baseline | 6 months | 12 months | 36 months | |
| Any | ||||
| All | 217 (89) | 195 (91) | 205 (91) | 165 (90) |
| Control | 122 (89) | 108 (92) | 115 (92) | 96 (91) |
| Intervention | 95 (88) | 87 (89) | 90 (90) | 69 (87) |
| Antipsychotic | ||||
| All | 162 (66) | 139 (65) | 145 (64) | 123 (67) |
| Control | 89 (65) | 77 (66) | 79 (63) | 69 (66) |
| Intervention | 73 (68) | 62 (63) | 66 (66) | 54 (68) |
| Other psychotropic | ||||
| All | 177 (72) | 163 (76) | 172 (76) | 142 (77) |
| Control | 100 (73) | 92 (79) | 97 (78) | 84 (80) |
| Intervention | 77 (71) | 71 (72) | 75 (75) | 58 (73) |
| Antipsychotic and at least one other psychotropic | ||||
| All | 136 (56) | 121 (56) | 125 (56) | 110 (60) |
| Control | 75 (55) | 68 (58) | 67 (54) | 61 (58) |
| Intervention | 61 (56) | 53 (54) | 58 (58) | 49 (62) |
| Antipsychotic with no other psychotropic | ||||
| All | 26 (11) | 18 (8) | 20 (9) | 13 (7) |
| Control | 14 (10) | 9 (8) | 12 (10) | 8 (8) |
| Intervention | 12 (11) | 9 (9) | 8 (8) | 5 (6) |
Resource use and quality-adjusted life-years
The total cost of health and social care at 36 months for the previous 6 months (excluding the cost of medication and training in PBS) was £1540 in the intervention arm and £1100 in the control arm. The adjusted mean incremental health and social care cost of the intervention compared with TAU is £501 (95% CI –£270 to £1274). From a health and social care perspective, adding 6-month and 12-month costs and PBS training and delivery costs, the mean incremental cost per participant in the intervention arm compared with the control arm is £1931 undiscounted (95% CI £260 to £3402) and £1898 discounted (95% CI £480 to £3318).
From a societal perspective, the adjusted mean incremental total societal cost of the intervention compared with TAU is –£4874 (95% CI –£14,485 to £4736). When 6-month and 12-month costs and PBS training and delivery costs are added, the mean incremental cost per participant is –£1235 undiscounted (95% CI –£19,347 to £16,874) and –£879 discounted (95% CI –£18,405 to £16,648). Details are given in Appendix 7.
At 36 months, complete data were available to calculate QALYs for 73 participants (68%) in the intervention arm and 90 participants (66%) in the control arm. The discounted adjusted difference in utility scores between the two arms was 0.160 (95% CI –0.034 to 0.355). Over the duration of the trial, 12 participants died (intervention arm, n = 5; control arm, n = 7). Including those participants in the calculation of QALYs (assuming a straight line from the participant’s last utility score to 0, representing death), there was a difference in adjusted discounted QALYs of 0.150 (95% CI –0.064 to 0.364 QALYs).
The discounted incremental cost per QALY gained of training in the PBS arm compared with the control arm over 36 months from a health and social care perspective, excluding medication costs, is £12,653. The probability that PBS is cost-effective for a range of values of willingness to pay for a QALY is presented in Figure 11, which shows discounted costs and QALYs. At a threshold for willingness to pay for a QALY of £20,000 per QALY gained, there is a 67% chance that the intervention is cost-effective from a health and social care perspective.
FIGURE 11.
Cost-effectiveness acceptability curve per QALY gained at 36 months (discounted).
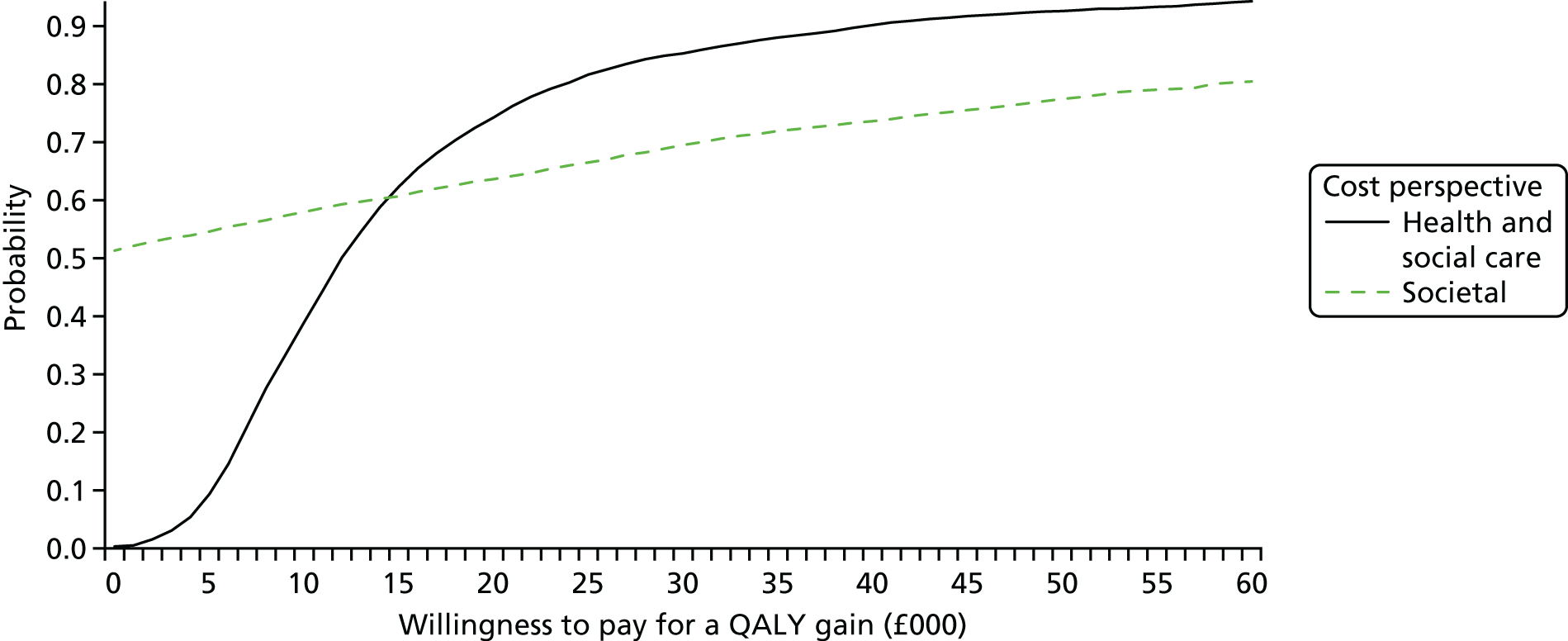
Multiple imputation of missing data
Given the high percentage of missing data at 36 months (> 30%), multiple imputation was used to generate 35 complete data sets for discounted QALYs and discounted total health-care costs. Current living situation, accommodation at baseline and level of disability were all found to be predictors of missing data at 36 months and hence were used to generate the multiple imputation data sets.
Regression analysis of the multiple imputation data sets found no significant difference in adjusted, discounted QALYs for the intervention arm compared with the control arm (0.166 additional QALYs in the intervention arm, 95% CI –0.083 to 0.416 QALYs) and no significant difference in discounted adjusted health and social care costs excluding intervention costs (the intervention arm cost an additional £405, 95% CI –£1271 to £2080). The mean incremental cost per QALY gained using the imputed data sets and including intervention costs is £12,060.
Relationship between EuroQol-5 Dimensions Youth proxy and Aberrant Behaviour Checklist – Community
We evaluated if there was a significant relationship between the EQ-5D-Y proxy utility scores and the primary outcome of ABC-CT using a multilevel model accounting for individual-level variability over time and variability within and between sites.
For every 1-point increase on the ABC-C, there is a significant decrease on the EQ-5D-Y, as reported by proxies of –0.002 (95% CI –0.003 to –0.002), with a constant of 0.69 (95% CI 0.63 to 0.75). Given the significant relationship between the two measures, there is no need to calculate any further CEACs or ICERs for the primary outcome. This is because changes in the ABC-C should be captured by changes in EQ-5D-Y utility scores. These have the additional benefit of being converted into QALYs and a standardised and comparable cost-per-QALY threshold is calculated.
Process evaluation
Implementation of Positive Behaviour Support training
Resource and training
Thirteen therapists attended each of the two training courses. Of these 26 therapists, 21 completed the full training. Five dropped out early because of long-term illness, maternity leave or work pressures that were deemed incompatible with taking on study-related tasks. Another seven therapists left at some point during the study (because of a job change, sabbatical or long-term illness). Some of those plans were not communicated to the research team until the last moment and changes were then difficult to implement, for example training new staff.
All therapists received a PBS workbook including assessment forms (hard copies and electronic versions) and they were expected to reduce their general caseload in order to treat eight participants each, which would include completing paperwork such as treatment logs, carrying out observations and writing and implementing PBS plans. Therapists received support from the research administrator (two weekly calls, e-mail communication and collection of treatment data).
Fidelity, dose and reach
The elements of the PBS intervention that were expected to be delivered by therapists comprised the BBAT, observations, PBS plan, goodness of fit, fidelity checklist and log of engagement. Of the 108 data sets returned, 33 were complete (i.e. they included all elements), 47 were incomplete and in 28 cases we did not receive any data because the participant was not seen, refused to work with the therapist or did not present with challenging behaviour at the time of contact. For 12 participants, it became apparent that the they resided in accommodation in which the providers had enlisted external training in PBS. The study therapists faced a dilemma regarding whether or not they should carry on with the study tasks, thus over-riding the support plans put in place by the care providers. This was discussed with the trainers (Professor David Allen, consultant to the study) and a decision was made not to carry on. The therapists reported spending a median of 11.5 hours (IQR 8–32.7 hours) for each participant. An external assessment of the quality of the delivery and the therapist competence was carried out throughout the study (for further details please refer to Appendix 8). Table 16 lists a summary of the reasons that therapists reported as underlying the incomplete or missing PBS data sets.
| Reason for missing data | n |
|---|---|
| Workload too large | 23 |
| Challenging behaviour (none or mild at point of contact) | 16 |
| Staff leaving | 12 |
| Organisational issues affecting the study (external PBS providers, guidelines already in place, participant under the care of another team/professional, managers unwilling to assist with workload management) | 14 |
| Participant/family carer dropped out of the study | 7 |
| Referral to other teams (inpatient, other professionals) | 2 |
| Unavailable information | 10 |
| Total | 84 |
Fidelity assessment
Thirty-three data sets contained a PBS plan. Twenty-one plans (63.7%) were produced by community nurses, three (9.1%) by occupational therapists, three (9.1%) by consultant psychiatrists, three (9.1%) by a combination of mental health professionals, two (6.0%) by speech and language therapists and one (3.0%) by a clinical psychologist. Additionally, 17 of the participants (51.5%) with a plan had mental health diagnoses such as depression (12.1%), schizophrenia (9.1%) and anxiety (6.1%). Physical and verbal aggression was the most prevalent challenging behaviour, exhibited by 20 participants (60.6%), followed by verbal aggression (60.6%), property destruction (39.4%) and other challenging behaviours (42.4%). Fifteen out of 33 participants (45.5%) had pervasive challenging behaviours, which were evident in different settings.
Applying the fidelity checklist contained within the manual,47 the mean score was 17.7 (SD 6, range 2–24) with the highest score indicating that most elements of the intervention were present. Two hand-written plans contained only a few sentences describing the primary intervention in an understandable manner and thus scored two points on the fidelity checklist. Nearly all of the plans (97%) had a section to provide a service user’s name, age and address (anonymised) and most (93.9%) had a section entitled ‘understanding their behaviours’. Twenty-three plans (69.7%) had logical summaries of the formulation explaining the challenging behaviour, whereas 10 plans (30.3%) did not provide possible explanations for challenging behaviour but described it in an ambiguous and vague manner, for example ‘the person can be challenging in more than one way’.
In the primary prevention section, 87.9% of the plans addressed slow triggers and 84.9% of the plans targeted fast triggers. The most frequently-targeted slow and fast triggers were levels of activity and interaction style (51.5% and 75.8%, respectively). By contrast, broad ecological strategies, skills teaching and differential reinforcement were the least frequently implemented strategies (24.2%, 21.2% and 15.2%, respectively) as the primary prevention.
In the secondary prevention, most of the plans (81.8%) had a description of early warning signs and 78.8% of the plans mentioned how to interact with a person at this stage. However, the majority of the plans (54.6%) did not mention any strategies regarding how to understand why a person is exhibiting challenging behaviour. The most frequently mentioned reactive strategies in the plans were self-protection/breakaways and how to interact verbally (both mentioned in 63.6% of the plans). Only 13 of the plans (39.4%) reported steps on how to help an individual get back to a normal emotional state after an incident.
A total of 61 data sets (complete and incomplete) from 18 therapists were sent to an independent reviewer to assess procedural integrity. All 33 PBS plans were given a score of ≤ 12 point;, therefore, they were deemed to be weak plans. The remaining 28 data sets did not contain sufficient documentation to assess procedural integrity (see Appendix 8).
Mechanisms of impact: stakeholder interviews
A total of 13 service users, 11 family carers, 10 paid carers, 12 service managers, 12 therapists and four PBS trainers were interviewed to explore their experience of taking part in the study.
Three rounds of revisions of the codebook were necessary to reach agreement among co-raters for the coding of the interviews. A subsequent inter-rater reliability exercise revealed a range of 0.8–1 for the different subgroups of stakeholders.
The views of the service user advisory group from Camden SURGE, The Advocacy Project, were recorded at regular meetings convened to discuss the interpretation of emerging themes and subthemes from the qualitative interviews. The SURGE members also took the opportunity to reflect on their own past experience of having been in hospital or having received treatment for challenging behaviour and how it matched or differed from the experiences of the study participants.
Participants’ experience of Positive Behaviour Support: thematic analysis
A total of seven themes and a number of subthemes emerged from the transcripts of the interviews with stakeholders participating in the study. Details on the frequency of the themes per stakeholder group are reported in Table 17.
| Themes | Stakeholder | ||||
|---|---|---|---|---|---|
| Family carer | Manager | Paid carer | Therapist | Service user | |
| Impact on organisation | ++++ | ++++ | |||
| Engagement with the study | ++++ | +++ | ++++ | ++++ | |
| Implementation | ++ | ++ | ++++ | ||
| Managing difficult situations | ++++ | + | ++++ | ||
| Research impact | +++ | ++++ | ++++ | ++ | |
| Understanding of the concepts of PBS | + | + | ++++ | + | |
| Understanding of the behaviour | ++ | ++ | +++ | ||
The three themes most frequently reported by the stakeholders were (1) impact on organisation, (2) engagement with the intervention and the study and (3) implementation, with a weighted mean of 84%, 78%, and 70%, respectively.
Impact on organisation
Motivation to change
There was a strong motivation to utilise the PBS intervention for challenging behaviour. This was already a priority for some services:
We have got a new psychiatrist that has just started this week for example, and we are getting more energy into the service and PBS is something that our psychology team is very keen on using so we are using it eh, so . . . you know, we need to focus on the more complex population and this has been a key process to it to do that so yeah.
Community ID team manager
. . . I already have with a couple of cases of people presenting with quite severe challenging behaviour and other lighter, less-time-intensive interventions hadn’t proved helpful. And absolutely, it was helpful . . . I’ve encouraged trainees, trainee psychologists who are in placement with us, to use this approach and they found it helpful.
Therapist
Embedding PBS as an intervention in the service provided by the community ID team was seen as a positive outcome:
We feel we should incorporate it into our initial assessment documents and use it as an initial assessment. It’s our only initial assessment tool.
Therapist
Therapists saw PBS as an approach that was inclusive of other professions and almost in place of care co-ordination:
It is an intervention that to my mind aims to co-ordinate other interventions; so, for example, we might have speech and language therapy in the course and that speech and language therapy can be integrated into the PBS approach, for what the PBS approach does is that hopefully all the people involved in that person’s care are aware of the goals they’re trying to achieve.
Therapist
Another therapist added:
It fits quite nicely with communication. Being a speech language therapist it is something we think about it anyway, we are looking at triggers, we are looking at how we can manage that . . . so it fits quite nicely with what I do.
Therapist
However, some therapists felt that PBS was very similar to the approach they already used in the service:
The PBS and what we do are so the same that the only real difference was the tool we used and then how we wrote it up in the first person.
Therapist
Engagement with the intervention and the study
Stakeholders experienced their engagement during participation in the study as positive, negative or absent. The theme ‘relationship’ includes the degree of support and communication that took place during PBS.
The role of therapists was central to the delivery of the intervention and in supporting the carers in difficult moments:
I have got a very good help from E [community nurse] because F [service user] had a hernia, F [service user] has been to the hospital, and every call he has been by my side.
Family carer
Oh excellent. Yes, yes I have been very pleased; just thank you!
Family carer
Family and paid carers found the intervention to have had a positive impact on both their life and the participant’s life:
The quality of the help I would say, it was excellent. V is a professional . . . and as I see her intervention has helped in the sense that, yeah has improved A’s [service user] life for sure and ours.
Paid carer
Support from the study team, including mentoring, was welcome:
The support from the PBS team I think helped, so the training and the mentoring and it was also useful to have site visits from the PBS team.
Therapist
Equally, therapists rated the support from the service as high, which was associated with the allocation of time to dedicate to research cases:
My manager was quite diligent, saying you can work once a week so we did not need to take work home.
Therapist
Participants with ID reported contact with their carers as desirable outcomes and strategies that help them relax and settle:
Gives me a cuddle.
Service user
Yeah I am getting that help; what he has been doing . . . he’s on the computer watching TV with me.
Service user
Family carers perceived the research assessments as useful and as a sign of engagement with the study team:
Yeah, [RA] was in contact quite regularly and you know, she called back and forth to arrange the visits and explain what she needed to do, what she wanted from us and that she was there if we had any questions.
Family carer
Communication with the researchers was important for several stakeholders, including team managers and service users, as it was also part of the treatment plans:
It was a positive experience overall. The guidance was available and the support was there, especially from the research team in the organisation, and the monitoring was also well organised and with regular feedback.
Manager
. . . if I do not understand things then my mum explains it to me carefully and then I can understand it because sometimes I get . . . if I am not too sure about it then my mum helps.
Service user
Some carers were disappointed by not receiving the PBS intervention:
I do not know why we did not receive the intervention. Maybe they felt we were managing his behaviour, but how to manage his behaviour, then that is the crucial question.
Family carer
A perceived lack of support, including therapist absence, had a negative impact on the carers, who thought that they may adopt inappropriate or unsuitable management strategies:
How do we stop major incidents happening? I am going to tell you how, that we do not take Y [service user] out in public at all.
Paid carer
I felt that sometimes things did not get like I was said because she was off sick and she did not come back or she did not contact probably as much as she should have done.
Family carer
Buying-in from the managers of services was a constant difficulty throughout the study, and this lack of buying-in was seen as a lack of commitment:
Yeah. I think we’re doing it right. Yeah. Which was nice, but frustrating for the research because for me it is the right thing, but I’m not sure whether our involvement is actually supported enough . . . In this case all fell on me to implement everything, really.
Therapist
Staff who were put forward to volunteer in the study were undertaking more tasks without having been briefed adequately:
It would be interesting to look at the figures actually with an estimate of how many hours we would be . . . working with each client and I think it was roughly under-represented because . . . somebody has to do the work for us, there were three people in my little cohort and we were all shocked about the amount of work that we were asked to undertake.
Therapist
I was asked at the last moment because one of my colleagues was not able to complete, so I was not really 100%. I knew what PBS was, but I was not, I suppose, I had not been briefed in regards to what is involved.
Therapist
Implementation
The PBS training was experienced positively by most therapists, although some thought that the format might not have been optimal:
I think the training we have been having was excellent . . . really clear, great examples. People took us through the things step by step . . . it was really practical in terms of what we have done.
Therapist
The training dates were quite close together and I think it would have made the training more cohesive if we’d had time to complete the components before the next step, so I found myself having the next stage of training before I’d finished implementing the first part.
Therapist
Specific elements of the intervention were thought to have been effective in improving the participant’s behaviour:
We have this time plan to follow and it has improved the evening routine and the morning routine . . . it just made life slightly easier for me because he is now following a routine rather than me just keep nagging him all the time, you know, come on it is bed time, or come on it is time to get up but rather say, this is what we are going to do today . . . we are going to follow this.
Family carer
We went over questions, she asked me about C’s [service user] temperament, she explained things I needed to know, good and bad things, you know, and why C [service user] was anxious and why she was not . . . she got to the bottom of few things with us, so worthwhile.
Family carer
What helped me? I suppose knowledge of the person, working as part of a team and writing a robust plan that everybody could work with.
Therapist
. . . I think what actually was really helpful was the kind of rigorous approach in terms of really thinking about the kind of functions of behaviour and checking that out and trying relating your initial ideas . . . but also that is going to work within that setting and have a kind of fit for the people involved.
Therapist
In addition, a paid carer reported that the learning of new activities increased a participant’s skills and choices:
For example . . . before now, he could not, maybe . . . let’s say make a cup of tea, but with the PBS we have broken it down into steps . . . and now when you talk to him and say ‘bring milk’ he knows to go to the fridge, open the fridge and he knows how to recognise milk.
Paid carer
Several challenges derived from involvement in the PBS study.
Time management was consistently reported as a challenge by managers. This complaint related to the resource needed to complete the study tasks by the therapists:
I think people have not quite realised the impact of doing that work how much time it will take.
Manager
I think the issue was competing priorities, so when you have got day-to-day operational work and research work where the priority goes, I mean people quite often go to the operational end and I think start trying to do the research work around that and that time has been difficult.
Manager
A common challenge for therapists was staff leaving, which affected the delivery of the intervention:
We were reduced to less than half of the staff and that meant that our caseload increased and there was definitely not time for reflection and for doing PBS paperwork and that was my biggest challenge.
Therapist
Home visits, although much appreciated most of the time, may also be seen as a hindrance:
I found it, probably for my son it was positive but overwhelming . . . having different people in, having him assessed. It was quite difficult, I found it quite difficult myself and . . . yeah . . . I think I was judged in lots of ways so it made me think twice about doing it.
Family carer
Alternatively, they can be insufficiently frequent and, therefore, not effective in producing change:
It was not frequent, it was once every 6 months so by the time the person meets after 6 months the person can forget you or something like that.
Paid carer
Because of the relapsing–remitting nature of challenging behaviour, in a few cases the participant did not present with difficulties at the time of initial contact:
We found that some [service users] when we came to visit them, actually there wasn’t any current challenging behaviour. So, possibly there had been some issues in the past, but at the current time they were very settled, so then it was hard to find a clinical rationale to prioritise them above somebody else who was presenting a new or some kind of really challenging.
Therapist
Finally, paid carer opinions and beliefs about the participant’s behaviour were often difficult to challenge or even change:
If they [paid carers] have worked with the client for a long period of time and their employers have told they were doing a good job and then we come in and say you could do differently you know, all of a sudden.
Therapist
Additional topics brought up by stakeholders
The least frequently reported themes were (1) managing difficult situations, (2) research impact, (3) understanding of the concepts of PBS and (4) understanding of the behaviour, with weighted means of 65.0%, 63.0%, 45.4%, and 40.0%, respectively.
Carers reported their own strategies when dealing with challenging behaviour, which may have been helpful:
He is not able to tell you when he is thirsty . . . So we have to know oh, could M [service user] be thirsty? If he is getting hot or cold, could M [service user] be too hot? Does he need to take his coat off? Does he need to take extra, has he got too many layers.
Family carer
I think with P [service user] you just have to be motivational with him, and very consistent with him and this is what we have got at the moment we are very consistent with P [service user] and if you are not consistent he breaks down so joint consistency is what really matters.
Paid carer
This was also the case for participants with ID, who described techniques they had learnt over time to help manage frustration or anger:
No because if I do not like shouting I go somewhere else where it is quieter for me and it is easier. If I am in a crowd, if I cannot handle the crowd sometimes, if I cannot handle it I say my mum, ‘mum I cannot handle this, it is too much for me, I want to go somewhere else’.
Service user
Managing the challenging behaviour of participants was associated with carer burden:
You know, it gets just a bit you feel worn out when he gets a bit fed up. So if you have got somebody coming in to encourage you, it cheers you up again.
Family carer
Managing carer burnout was also of concern to family carers:
Being positive with yourself and also being a carer is looking also after yourself so that you can look after.
Family carer
The implementation of PBS was associated with positive outcomes for many of the stakeholders who were interviewed:
I have seen a lot of differences in the cases that I have actually completed and implemented and on post treatment; I have been able to actually reduce some of the medications and depot medications, so the frequency and severity of those behaviours have been significantly reduced.
Therapist
Yeah, because my mum knows how to make me calm.
Service user
That has helped in terms of finding out really what she likes and what does not like.
Paid carer
Having seen some of the work that E [therapist] has done and L [therapist] has done with some of the service users, they have seen some measureable improvements. It has been definitely worthwhile.
Home manager
In addition, a benefit was reported with respect to the research study. According to a manager:
I think it is important that research is done on the ground, actually in real services to actually get the impact of intervention with real people in real times. Our staff being trained . . . we were lucky. We were in the intervention, it is part of the study.
Manager
Stakeholders reported differing views around their participation in the study, ranging from positive to negative:
There has been regular input to our meetings and from the staff who are participating in it from E [NHS site], so we get feedback from them on the nature of the research and we have the opportunity to look at the issues that are coming up.
Manager
My experience of that was slightly frustrating for the clinician, because of the amount of time the work around the research took. So my experience was to try to negotiate with people within the service and to try to have free time for the individual.
Manager
There appeared to be a consensus that the newly acquired skills were useful for the professional development of staff:
On the positive perspective, by having a member of staff who is very knowledgeable or becoming more knowledgeable about PBS and now she is implementing her role as an OT [occupational therapist] into something that is, could be more of a generic way of approaching working.
Manager
It makes a difference to the staff in the way think about things . . . so people who have done the training they do, they approach things slightly differently, and think things through quite differently.
Manager
Similar thoughts were shared by paid carers, who commented on the change in perspective they had gained through PBS:
I think it has helped us a lot immensely as I see it. We are now much more focused on meeting others’ needs in a positive way and trying to put ourselves in her shoes and see the world through her eyes, rather than us trying to fit her into our world.
Paid carer
Therapists reported that the involvement in the study enabled them to refine their existing knowledge about behavioural interventions and challenging behaviour:
Definitely being on the training, I was struck by the fact that it is, it’s a lot to kind of learn. I’ve had three trainings, part of which was on understanding behavioural approaches and behavioural theory and of all of these things . . . and for me it was kind of revising what I knew and then placing it maybe within a kind of slightly more elaborated and refined approach.
Therapist
The skills obtained by the training, for example how to make an effective behavioural assessment, seem to be a fundamental starting point to appreciate the understanding of the behaviour:
It is a capacious and open approach and it’s just that kind of beginning part, making sure that you’ve done a really good assessment and you have a good understanding, a kind of starting point for why and what the function of the behaviour is.
Therapist
Stakeholders saw PBS as a system supportive of a variety of methodological approaches but also as a person-centred intervention:
If you have done a good assessment and you understand what the issues are, then there are other pieces of work like sensory assessment and also communication assessment in order to understand people’s needs and develop the skills of the people around them.
Therapist
The intervention . . . it kind of invites all the patient’s support network to be involved, puts the patient at the centre of the intervention and it is kind of a holistic kind of intervention, so it is very comprehensive and includes all the aspects of the service user’s life.
Therapist
It has seemed to me that if you are looking at patterns of behaviour and within those patterns of behaviour you might be able to see certain trend . . . so see if certain times of day affect different behaviours.
Paid carer
It is a series of behaviour observations, ruling out any other sort of reasons that somebody might present with some sort of challenges so there is some similarities between SCIP [Strategies for Crisis Intervention and Prevention] and PBS in what I have read.
Manager
The PBS plan appears to have the most currency when discussing PBS:
We did a lot of talking about S’s [service user] everyday life and everything he did he likes to do and what he likes and what he dislikes which obviously S [community learning disability nurse] was putting together to do the PBS plan.
Family carer
Various explanations were provided for the presence of challenging behaviour:
She wants attention and all of the time to herself from staff so, yeah, those who were improved you know the destructive behaviour that has actually almost disappeared . . . because we know how to kind of praise her for the work she does.
Paid carer
S [service user] is receiving a benefit from meeting people when going to the A&E [accident and emergency]. Why should he stop?
Paid carer
The function of the behaviour is, however, essential, as the same behaviour may have different triggers:
Although she has the same behaviour, it is actually as if the function is different, so it is usually when she cannot do something and thinks she finds it hard or she finds it hard being asked to do something that she does not want to do.
Therapist
The analysis found three major themes describing the trainers’ experience of the impact of the pragmatic conditions on the delivery of PBS by the therapists in the study, each with a number of subthemes (Table 18).
| Themes | Subthemes |
|---|---|
| Positive outcomes of training in PBS | Increased performance with moderate challenging behaviour |
| Generating knowledge through training | |
| Challenges in delivering PBS | Issues with service management |
| Staff-related issues | |
| Diversity of professional roles | |
| No challenging behaviour to treat | |
| Potential improvements | Role of champion |
| Service support for therapists | |
| Three-way approach to training |
Trainers reported that the implementation of the intervention was mediated by the level of severity of challenging behaviour in the service user. A moderate level of challenging behaviour was associated with the therapist achieving better outcomes:
When someone had a case that was within . . . the moderate range of challenge, where the training sort of fitted the levels of the BBAT, the person was motivated and had fair chances to give it a go, then it flows pretty well.
According to the trainers, one of the major benefits associated with the therapists’ participation in the study was the PBS-based training they received. One trainer commented:
I think actually people got a good deal, a substantial manual you know, which would have cost them a lot of money trying to do it elsewhere, they got, you know, 6 days’ input from people who have been doing that for a long time.
They further reported that another major benefit of the training was the constant support that therapists received during the workshops and follow-ups:
They got the offer of follow-up support for that training, they had the opportunity to practise their skills and they learned and got feedback on that.
The degree of support from the respective services was strongly felt to be a challenge in the delivery of the intervention by most trainers. Trainers noticed that, even in the presence of good training and the participation of therapists in the workshops, a lack of support in the workplace had a negative impact on the delivery of PBS:
If you were the participant who is being trained by us but you are working in a service context that isn’t supportive of what we are trying to do then . . . your power to affect change is hugely reduced.
A trainer added that poorly managed staff caseloads had implications for the number of PBS plans implemented by the therapists:
There is practice leadership issue. She [therapist] was trying to get things implemented in a staff team and there was no manager or the manager was not ever there . . . we provided a lot of training . . . but ultimately is the management with all staff that will implement PBS plan without our support.
The trainers reported that the constant change of professionals in the service may have had an impact on the delivery of the behavioural assessments:
There was a very high staff turnover in one site in particular so she [therapist] talked to one [therapist] staff one day who the week later no longer worked and she did some training with some staff, you know, never seen again really, and these concerns were serious that escalated locally.
Trainers agreed on the fact that the difficulty of managing PBS cases on top of their work cases represented a common challenge for therapists, especially for ID community nurses, who already had a substantial number of cases allocated to them:
I did not realise this was on top of someone’s existing cases and if you are a community nurse you have kind of ridiculous amount of caseloads, like 60 or 70.
The trainers felt that the selection of therapists with different professional roles had a negative effect on the quality of the assessments delivered:
One of the issues we all thought was that people with very different roles attended the training . . . not many had some prior knowledge of PBS and struggled to see the role of using the BBAT to achieve functional analysis and struggled to fit the PBS plan within their role.
The trainers found that the absence of challenging behaviour in some participants was one of the major issues related to the small number of cases receiving the PBS intervention:
She [therapist] was with people who had no challenging behaviour, no current challenging behaviour. [The therapist reported] ‘I looked at them and I really cannot do much, what if there are no challenging behaviours’.
According to the trainers, the inclusion of an on-site champion to motivate the therapists to deliver the intervention may have helped to increase the number of participants receiving PBS:
What it is all about is a strong senior nurse on the study telling them what to do and what not to do and watching them.
One trainer also commented on the overall level of support that services should have had towards participating therapists to enable them to dedicate time to deliver PBS to their cases:
A major factor was, you can’t have one individual, two individuals in a service implementing it.
Chapter 4 Discussion
Summary of main findings
In this cluster RCT, we evaluated the clinical outcomes of a training programme in PBS that was delivered to qualified health professionals, who are specialists in working with adults with ID, supported by a training manual and mentoring to reduce challenging behaviour in adults with ID. To our knowledge, this is the first large-scale, pragmatic RCT of this intervention. The results revealed that training in PBS was not clinically and statistically significant in reducing challenging behaviour, measured by the ABC-CT over 12 months. Thus, we conclude that the training in PBS of qualified health professionals in this study was no more effective than TAU in reducing challenging behaviour. Secondary outcomes were also similar between the two arms. Crucially, compliance and treatment fidelity to the PBS model, as well as the reach of PBS, appeared to be low and may go some way to account for the lack of effect of the intervention. The 36-month follow-up showed that the differences in the primary and secondary outcomes between the study arms remained non-significant and the initial gains in health-related quality of life also dissipated.
A subsample of participants with broadly defined ASD presented with higher challenging behaviour scores than participants without an ASD. However, the intervention did not significantly reduce challenging behaviour in participants with an ASD.
Resource use was similar across both arms but costs were lower, particularly from a societal cost perspective, although not significantly so, than resource use costs in the control arm. The mean incremental cost per QALY gained for training in PBS compared with TAU was £16,276 from a health and social care cost perspective and £11,566 from a societal cost perspective, with both estimates falling below the cost-effectiveness threshold of £20,000 per QALY. Although this finding is mostly driven by a greater number of QALYs over 12 months for participants in the intervention arm, it should be considered with caution because of the proxies being unblinded to arm allocation and the study not being powered to detect significant differences in costs. The relatively low probability of cost-effectiveness at a threshold of £20,000 per QALY gained is primarily attributable to the large variability in costs between participants, as reflected in the wide 95% CIs for the difference in costs between the intervention and control arms. As a result, there is great uncertainty regarding the cost-effectiveness of the intervention compared with TAU. The relatively high cost per participant of the training and delivery of PBS of £1597 also has an impact on the cost-effectiveness of the intervention.
Process evaluation
Despite the lack of clinical effectiveness, a number of findings from this investigation are quite promising. The training in PBS was very well received by therapists, and the majority of therapists completed the training workshops. With respect to the experience of those who were interviewed, several positive outcomes relating to the training and interventions within the PBS framework were found. Despite their different roles, therapists reported an increased knowledge of the nature of the challenging behaviour experienced by participants and of the intervention itself. The training programme was also reported to be an important asset for the service, as it enhanced the skills of health staff and improved the quality of the care delivered. The PBS framework was perceived as helpful in co-ordinating different approaches delivered by a multidisciplinary team.
Challenges were instead found in practice post training, despite great efforts to improve buy-in and implementation. The setting in which the intervention was delivered was highly complex and the intervention was superseded by, or competed with, other service requirements. This suggests that, although the training was carried out successfully, its delivery by therapists at the level of participants with challenging behaviour and their family or paid carers was inadequate. This may have also been compounded in the few cases in which the person did not show challenging behaviour at the time of contact with the therapists as well as by the need for extra resources to manage the workload.
However, although all of the reviewed PBS plans were rated as unlikely to affect behaviour, some limitations of the BIP-QE II may have had an impact on the ratings. The effectiveness of the BIP-QE II has been mainly evidenced in educational settings and with a young population, whereas the participants taking part in this trial were adults with ID living in a variety of community settings (i.e. supported living and residential care). 85 It is possible that training in PBS may need to be more tailored to the setting and other factors across the lifespan and this, in turn, may improve the quality of the support plans.
Although there is an indication of poor-quality PBS plans, it should be noted that there is a lack of research suggestive of a positive correlation between the (better) quality of PBS plans and better outcomes in the person’s challenging behaviour. Thus, we cannot be certain that this was a definitive reason for the lack of effectiveness.
Paid and family carers and participants with ID reported certain techniques they have learnt to help the participant with ID manage their anger or other behaviours. Such strategies were usually along behavioural lines, for example ‘time out’. However, other aspects of PBS, such as functional analysis and its association with improving the understanding of challenging behaviour, were reported by service managers and therapists. It is possible that lay people and participants with ID are not able to differentiate the varying domains of PBS or even identify them from a list of generic behavioural approaches. For example, the use of a time plan for activities for the participant was seen as helpful in creating structure in their daily routine and, in turn, facilitating the caring process. PBS plans were also valued as a helpful tool that enabled the understanding of the participants’ needs. Other elements that were valued were the relationships with the therapists, which, through non-specific treatment effect, may help to engage individuals and their families and promote a therapeutic alliance.
The preliminary analysis of the impact of the intervention in adults with ID and autism (ASD+) also shows that it was not clinically effective or cost-effective for this group either, although they appeared to have a higher ABC-CT than the ASD– group. Surprisingly, the ASD+ group reported a lower level of access to any services than the ASD– group, except for art therapy (ASD+ 8% vs. ASD– 6%) and contact with social workers (ASD+ 50% vs. ASD– 49%) and psychologists (ASD+ 18% vs. ASD– 17%).
Finally, medication use did not change overall over time, with the same proportions of participants being prescribed psychotropic medication over 12 and 36 months’ follow-up. This pattern was the same in the ASD+ and ASD– groups.
Results in context
MacDonald and McGill86 conducted the only systematic review to date on outcomes of training staff in PBS. The authors argue that the training in PBS of community services staff increases their competence in managing challenging behaviour and reduces the use of restrictive practices and the reliance on other professional support. However, the research is undertaken within fairly controlled environments with little evidence of how to translate practice into real-world conditions. The therapist professions, study settings and training courses in the present study mirror those reported in the review. 86 Despite the review finding that the training led to reductions in challenging behaviour, when this was measured and reported, none of the included studies used a randomised or quasi-randomised design and the follow-up was limited to 6 months, if included at all. Therefore, previously reported significant effects of the intervention on challenging behaviour are likely to be attributable to study bias. 37
There was a risk that some form of PBS-based care would be gradually adopted in some of the clusters in the control arm during the trial and that this may have reduced any differences between the trial arms. However, we explicitly excluded teams that had implemented PBS provided by practitioners, either embedded in services or through tertiary specialist teams. This was further confirmed by the responses to a survey of the participating ID teams prior to the study commencing, which explored the pre-existing behavioural approaches, training and resources in each cluster. The local and principal investigators at each site reported that they had no specific service pathways relating to challenging behaviour; PBS-trained staff had left the services and specialist teams for challenging behaviour, when previously available, had been decommissioned.
It is possible, nevertheless, that the results of the present study have been affected by improvements in the quality of care in the TAU-only clusters, which may have attenuated the impact of more specialist interventions such as staff training in PBS. Our study began just after the Winterbourne View scandal,21 which exposed the poor care and abuse perpetrated on adults with ID and challenging behaviour in an inpatient facility in England. By the time that the report21 was completed 4 years later, NHS England and the Department of Health and Social Care had made serious efforts to counteract complacency and improve the standards of practice for people with ID. 87 However, such policy changes are slow to be implemented and to reach a sustained local impact; therefore, we argue that such changes are unlikely to account for the findings. Furthermore, we did not measure staff skills or knowledge per se, so those aspects that may have been improved by the training in PBS were not captured. 88,89 It is often repeated that functional analysis is an important element of behavioural approaches and this may not have been carried out consistently in this study. However, a recent multilevel analysis of one experimental study showed that functional analysis does not moderate the relationship between an intervention and its impact on challenging behaviour, so it is unlikely that omission of a functional analysis would have had a significant impact on participant outcomes. This is further supported by McClean and Grey,90 who carried out a 26-month follow-up of paid carers as part of a 5-year rolling PBS training programme. They found that no specific PBS components accounted for reductions in challenging behaviour.
This is the first RCT that we are aware of to conduct an extensive cost-effectiveness analysis of a PBS-related intervention, with most studies in this area predominantly using a before-and-after design. 19 Whereas before-and-after studies have hypothesised a decrease in accommodation costs for participants who are provided with PBS, this study has echoed the findings of other economic evaluations of person-centred interventions for participants with challenging behaviour in that there is no reduction in costs. 16 This is likely to be because of changes in community care for people with challenging behaviour and ID, which require significant changes in the commissioning of appropriate services, therefore taking time to implement fully. Other research in which resource use has been investigated91 suggests that the type of challenging behaviour, for example externalising, and whether or not mental illness/other mental disorder is present, is linked to higher costs. Although we did not look specifically at types of behaviour in this study, some costs may potentially have been driven by the severity of behaviour and/or comorbid conditions. Given the paucity of economic studies in the field of ID in general, and in the context of psychosocial intervention effectiveness in particular,92 our findings provide the first indications of resource use and cost-effectiveness of a widely rolled-out intervention.
Strengths and limitations
Our study had several strengths, including the recruitment of the required number of participants and clusters, testing a single primary outcome, achievement of a low attrition rate at an individual level and an a priori analysis plan, all of which reduce the risk of bias. Furthermore, the ICC for the primary outcome is smaller than originally assumed for the sample size calculation and the sensitivity analyses support the main findings of the study, suggesting that the findings are robust.
Our design aimed to maximise the external validity and generalisability of the study. The trial was conducted within the NHS in 23 community ID services in different parts of England, covering urban, semi-rural and rural areas, from which we recruited 246 service users. Despite the geographical spread of the services, we found that services were not very different. Although there were some minor differences in baseline participant characteristics, adjusting for these variables in the main analysis had no bearing on the study outcomes. Our inclusion and exclusion criteria closely resembled the cases that were likely to be referred for assessment and treatment to those services. The overall median level of challenging behaviour of the participants was higher than that reported in a trial of antipsychotic medication by Tyrer et al. 61
In order to guard against the tendency for the impact of training to dissipate over time, we set up mentoring and peer support during the study period. 1,28,93 Our process evaluation indicated that training in PBS was well received by the therapists and the delivery of PBS was welcome and highly valued by the service managers of participating services, carers and participants with ID.
The study also has limitations, including low fidelity and a less than optimal engagement of the therapists with the intervention. We found that 30% of participants received all elements of PBS as specified in the training and 43.5% received only partial input, mainly observations. In addition, there was a low uptake of the mentoring support that was offered by the PBS trainers. A reason for poor implementation was the difficulty experienced by some of the participating NHS organisations to assist their staff in undertaking the additional responsibilities of the study procedures by failing to reduce therapist caseloads. Therefore, the therapists either undertook the delivery of PBS in addition to their normal workload or were unable to implement it. Furthermore, therapists were embedded in the ordinary community ID team and, therefore, clinical procedures including managing emergencies and interprofessional referrals may have also hindered the delivery of the intervention as intended. This may be a reflection of the realities of implementing PBS in community ID services without the provision of additional resources, such as specific posts for accredited behavioural therapists.
Regarding the lack of impact on the subgroup with broadly defined ASD, it may be that interventions that are not specific to ASD are less likely to help improve behaviour. However, the findings in this respect are preliminary but worth considering in the context of investigating treatment approaches for this population.
There was a considerable turnover of paid carers in the study. This may also have affected some of the delivery of PBS, as the therapists were meant to work closely with family and paid carers, and any change in paid carers would have required the therapists to continue this work with a new carer, possibly having an impact on the continuity of their work. Also, because of the considerable turnover in paid carers and the small number of family carers in the intervention arm, we were unable to further explore the secondary outcomes in paid and family carers.
As a result of the nature of the intervention, it was not possible to blind carers and participants to treatment arm allocations. There were six cases in which researchers were unblinded to a cluster’s treatment arm allocation, which indicates a small possible risk of bias. In such cases, another researcher subsequently collected data from those sites. Moreover, our analysis showed that researchers’ predictions of treatment arm allocation were considered to be no better than chance.
Costing for accommodation was based on very broad assumptions because of poor data on accommodation costs. There was no evidence of changes in participants’ accommodation throughout the study. We were unable to provide any estimates of the impact on employment or state benefits as a result of the intervention due to poor reporting and a large number of missing or inconsistent data. This points to the need for better methods of collecting data on accommodation, employment and state benefits for people with ID. The self-reported questionnaire for unpaid carer time was limited to four questions and it is potentially unreliable as it has not been extensively validated. 94 It was reported that 14 participants did not have challenging behaviour at the time of first contact with the therapist. This may have been attributable to a number of factors such as (1) challenging behaviour being a relapsing–remitting disorder and, therefore, not being acutely present at the time; (2) other interventions may have been delivered by other team members with positive outcomes; and (3) the behaviour being mild enough not to cause any harm or severely reduce quality of life and so treatment was not seen as priority by the carers. Paid carer turnover was significant and limited the undertaking of some of the PBS-related tasks such as goodness of fit, which requires discussion of the plans and their implementation in the patient’s home or activity setting. Finally, because of the design and logistics of the study, we were unable to train new staff to undertake PBS in place of the therapists who left. Therefore, the therapist cohorts were fairly static and any changes meant that participants allocated to the intervention arm did not receive it as we were unable to replace therapists. The study began at a time of increasing awareness of PBS as a preferred psychosocial approach to manage challenging behaviour and ended at a time when training in PBS at scale was implemented. 95 These changes in health and social care service approaches may have closed the gap between the intervention and TAU. There is currently a debate on whether PBS is delivered as it should be or if cursory attention is paid to its delivery across multiple services. Although we had considered this issue at the inception of the trial, we believe that we had offered significant incentives and support to motivate and entice services to participate. However, we were unprepared for the wide variation in delivery that we encountered and the opposition at times from services allocated to the intervention to make adjustments to accommodate research activity. Although our results may be disappointing to many in the PBS community, they nevertheless present a fair account of how PBS as an intervention may be corrupted96 and the extent to which it requires further modification in both content and delivery in order to provide the benefits that its proponents advocate. At 12 months, the intervention appeared to increase QALYs and, in this context, society may be willing to pay a higher price given the intractable problem of challenging behaviour. However, it is also important to take into account the fact that the measures used for cost-effectiveness (i.e. EQ-5D-Y) may have uncertain validity in this population with long-term disability.
Implications for practice
Our study is important because it was randomised and had a longer follow-up time than most studies in ID literature. It raises important issues in relation to the expectations that providing training in PBS to health professionals in community ID services may be sufficient to confer significant reductions in challenging behaviour beyond what is currently achieved by TAU. The UK is relatively unique in the provision of multidisciplinary teams that are specialised in working with individuals with ID.
Our findings are relevant to many professional groups, ranging from service planners for adults with ID to policy-makers who are responsible for setting nationwide directives about the care of adults with ID and challenging behaviour, including that of universal PBS training. For example, the PBS and Autism Training Fund, part of the Positive and Safe initiative that was launched in 2014,48 has supported training events for 2900 health and social care staff and family carers at a cost of > £500,000. 93 During the 36-month follow-up, we found that all but one of the clusters in the control arm had received such training since the end of recruitment in 2014. In the light of the main study findings, however, there is doubt as to the added benefit of such training.
It is also striking that, over the time of the study, the proportion of participants on psychotropic medications has remained stable. This may be attributable to medication reduction not being a specific target of the treatment or that issues around medication review/reduction may require another approach to address systemic beliefs about their benefits or otherwise. The identification of patient-reported outcome measures is another important consideration, as there may be discrepancies between what professionals and patients and their families think of as recovery-focused achievements.
Recommendations for future research
We believe that we have carried out a carefully conducted clinical trial, which has moved from small uncontrolled or feasibility studies to a fully powered pragmatic multicentre RCT in NHS community ID services. The behavioural aspects of the PBS framework have sufficient evidence of efficacy behind them and, potentially, an explanatory trial rather than a pragmatic one might have been a useful alternative design. A further concern is whether an implementation plan should have been considered at the outset to explore any issues that may arise in the intervention delivery. 97 Such blended designs may consider both the conduct of the clinical trial and issues in its implementation or may test both domains at the same time. We did collect implementation data but, because of the limitations, we were unable to react to the challenges in a flexible way, as reported in Chapter 2, Positive Behaviour Support-based staff training (in addition to treatment as usual). The trial raises important questions about (1) the content of staff training in PBS, (2) the optimisation of implementation in ordinary care and (3) the elements of a person’s life that it is most likely to have an impact on. It is crucial to understand the mechanisms by which PBS has an impact on behaviour as this would lead to targeted implementation and would clarify training objectives. As this is the first cost-effectiveness study of training in PBS, further studies about its delivery in different settings should include a health economic component to ensure that resources are prioritised and allocated in the most effective way.
Positive Behaviour Support is the only intervention with efficacy evidence, but not evidence of clinical effectiveness, in adults with ID and challenging behaviour. The 2015 NICE guideline38 on behaviour that challenges failed to find other candidate psychosocial interventions to ameliorate this long-term condition. Evidence-based care must be a top priority in the care of people with ID as it is for the care of other population groups. It is therefore imperative to develop new, or optimise existing, interventions for this population in order to improve care and quality of life in addition to making the best use of resources.
Acknowledgements
We would like to thank all of the study participants and carers who kindly donated their time to complete the study assessments, local and principal investigators and therapists for their continued support during the study, members of the study’s DMEC and TSC, the CSOs who conducted the study baseline assessments and the service user study group from Camden SURGE, The Advocacy Project, for providing valuable advice and feedback throughout the study.
Trial collaborators
Participating services
-
Camden Learning Disability Service.
-
Islington Learning Disability Partnership.
-
Tower Hamlets Community Learning Disability Service.
-
Hackney Learning Disabilities Service.
-
Barnet Learning Disabilities Service.
-
Enfield Integrated Learning Disabilities Service.
-
Barking and Dagenham Learning Disability Service.
-
Havering Learning Disability Service.
-
Waltham Forest Learning Disability Team.
-
Bexley and Greenwich Learning Disability Services.
-
Wandsworth Community Learning Disability Team.
-
Leicester City (East) Community Learning Disability Team.
-
Leicester City (West) Community Learning Disability Team.
-
Charnwood Community Learning Disability Team.
-
Coalville and Hinckley Community Learning Disability Team.
-
Market Harborough, Oadby and Wigston Community Learning Disability Team.
-
Dartford, Gravesend and Swanley Mental Health of Learning Disability Service.
-
Medway Mental Health of Learning Disability Service.
-
East Surrey Community Team for People Learning Disabilities.
-
South West Surrey, North East Hants and North West Surrey Community Team for People Learning Disabilities.
-
Mid Surrey Community Team for People Learning Disabilities.
-
Coventry, South Warwickshire and Rugby Community Learning Disabilities Team.
-
Bradford Learning Disabilities Service.
Recruitment and follow-up: clinical studies officers from the NIHR Clinical Research Networks
-
Kirsty Collins.
-
Megan Lawrence.
-
Tara Harvey.
-
Naomi Bateman.
-
Karishma Jivraj.
-
Lisa Russell.
-
William Morgan.
-
Sheetal Dandgey.
-
Angeliki Kassari.
-
Hannah Kelly.
-
Michael Kelly.
-
Augustine Musa.
-
Anna Weller.
-
Andra Cosma.
-
Neisha Rhule.
-
Sophie Oram.
-
Precina Pankhania.
-
Imogen Sargent.
-
Sarah Dickens.
-
Tessa Saunders.
-
Eliza Jane Corson.
-
Emily Williams.
-
Ruth Charig.
-
Claire Price.
-
Emily Benson.
-
Elizabeth Nyamadzawo.
-
Former PBS study RAs: Natalie Cook and Lisa Dockery.
Contributions of authors
Angela Hassiotis (Professor in Learning Disability and Consultant Psychiatrist) was the chief investigator for the study, designed the study with input from the other authors, was involved in all aspects of management and implementation of the study and drafted and edited the final report.
Michaela Poppe (Trial Manager) co-ordinated the study as the trial manager and drafted the final report.
Andre Strydom (Consultant Psychiatrist and Reader in Intellectual Disabilities) was a principal investigator for the study, was involved in study design and management and provided key revisions and detailed feedback for the final report.
Victoria Vickerstaff (Medical Statistician) was a statistician for the study and conducted the statistical analysis, contributed to the funding application and protocol and drafted sections of the final report.
Ian Hall (Lead Clinician) was a principal investigator for the study and was involved in study design and management, advised on the methodology and analysis of qualitative interviews and provided key revisions and detailed feedback for the final report.
Jason Crabtree (Lead Consultant Psychologist) was a principal investigator for the study and was involved in study design and management, advised on the methodology and analysis of qualitative interviews and provided key revisions and detailed feedback for the final report.
Rumana Omar (Professor of Medical Statistics) was the senior statistician for the study and conducted the statistical analysis, contributed to the funding application and protocol and provided key revisions and detailed feedback for the final report.
Michael King (Professor of Primary Care Psychiatry and Joint Director of PRIMENT Clinical Trials Unit) was the triallist for the study and was involved in study design, management and analysis, and provided key revisions and detailed feedback for the final report.
Rachael Hunter (Senior Research Associate, Health Economics) was the health economist for the study and was involved in study design and management, conducted the health economic analysis and drafted sections of the final report.
Alessandro Bosco (Research Assistant) was a qualitative research assistant for the study and carried out the process evaluation (including conducting and analysing all qualitative interviews) and drafted sections of the final report.
Asit Biswas (Consultant Psychiatrist) was a principal investigator for the study and was involved in study design and management and provided key revisions and detailed feedback for the final report.
Victoria Ratti (Research Assistant) was a research assistant for the study and was responsible for participant recruitment, collected the study data and contributed to the protocol paper submission.
Jessica Blickwedel (Research Assistant) was a research assistant for the study and was responsible for participant recruitment, collected the study data and contributed to the protocol paper submission.
Vivien Cooper (Chief Executive of the Challenging Behaviour Foundation) is a family carer of a person with ID and a co-investigator for the study. She was involved in study design and management, advised on the methodology and analysis of qualitative interviews and provided key revisions and detailed feedback for the final report.
William Howie (Consultant Psychiatrist in Learning Disability) was a principal investigator for the study and was involved in study design and management and provided key revisions and detailed feedback for the final report.
Mike Crawford (Professor of Mental Health Research) was a principal investigator for the study and was involved in study design and management and provided key revisions and detailed feedback for the final report.
Publications
Ali A, Blickwedel J, Hassiotis A. Interventions for challenging behaviour in intellectual disability. Adv Psychiatr Treat 2014;20:184–92.
Ratti V, Hassiotis A, Crabtree J, Deb S, Gallagher P, Unwin G. The effectiveness of person-centred planning for people with intellectual disabilities: a systematic review. Res Dev Disabil 2016;57:63–84.
Ratti V, Vickerstaff V, Crabtree J, Hassiotis A. An exploratory factor analysis and construct validity of the Resident Choice Assessment Scale with paid carers of adults with intellectual disabilities and challenging behavior in community settings. J Ment Health Res Intellect Disabil 2017;10:198–216.
Hassiotis A, Poppe M, Strydom A, Vickerstaff V, Hall IS, Crabtree J, et al. Clinical outcomes of staff training in positive behaviour support to reduce challenging behaviour in adults with intellectual disability: cluster randomised controlled trial. Br J Psychiatry 2018;212:161–8.
Data sharing statement
Appropriately anonymised copies of the research databases will be made available in UCL Discovery (http://discovery.ucl.ac.uk) (https://doi.org/10.14324/000.ds.10041531). Please contact the corresponding author with queries.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Hassiotis A, Strydom A, Crawford M, Hall I, Omar R, Vickerstaff V, et al. Clinical and cost effectiveness of staff training in Positive Behaviour Support (PBS) for treating challenging behaviour in adults with intellectual disability: a cluster randomised controlled trial. BMC Psychiatry 2014;14. https://doi.org/10.1186/s12888-014-0219-6.
- American Psychiatric Association . Diagnostic and Statistical Manual Version 5 (DSM V). Intellectual Disability 2013. www.psychiatry.org/psychiatrists/practice/dsm (accessed 12 March 2018).
- Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Res Dev Disabil 2011;32:419-36. https://doi.org/10.1016/j.ridd.2010.12.018.
- Allen D. Positive behavioural support as a service system for people with challenging behaviour. Psychiatry 2009;8:408-12. https://doi.org/10.1016/j.mppsy.2009.07.001.
- Grey IM, Hastings RP. Evidence-based practices in intellectual disability and behaviour disorders. Curr Opin Psychiatry 2005;18:469-75. https://doi.org/10.1097/01.yco.0000179482.54767.cf.
- Allen D, Lowe K, Brophy S, Moore K. Predictors of restrictive reactive strategy use in people with challenging behaviour. J Appl Res Intellect Disabil 2009;22:159-68. https://doi.org/10.1111/j.1468-3148.2008.00484.x.
- Webber R, Bowers B, Bigby C. Hospital experiences of older people with intellectual disability: responses of group home staff and family members. J Intellect Dev Disabil 2010;35:155-64. https://doi.org/10.3109/13668250.2010.491071.
- The Australian Psychological Society . Evidence-Based Guidelines to Reduce the Need for Restrictive Practices in the Disability Sector 2011. www.psychology.org.au/Assets/Files/Restrictive-Practices-Guidelines-for-Psychologists.pdf (accessed December 2016).
- Neidert PL, Dozier CL, Iwata BA, Hafen M. Behavior analysis in intellectual and developmental disabilities. Psychol Service 2010;7:103-13. https://doi.org/10.1037/a0018791.
- Didden R, Korzilius H, van Oorsouw W, Sturmey P. Behavioral treatment of challenging behaviors in individuals with mild mental retardation: meta-analysis of single-subject research. Am J Ment Retard 2006;111:290-8. https://doi.org/10.1352/0895-8017(2006)111[290:BTOCBI]2.0.CO;2.
- Hassiotis A, Robotham D, Canagasabey A, Romeo R, Langridge D, Blizard R, et al. Randomized, single-blind, controlled trial of a specialist behavior therapy team for challenging behavior in adults with intellectual disabilities. Am J Psychiatry 2009;166:1278-85. https://doi.org/10.1176/appi.ajp.2009.08111747.
- Heyvaert M, Maes B, Onghena P. A meta-analysis of intervention effects on challenging behaviour among persons with intellectual disabilities. J Intellect Disabil Res 2010;54:634-49. https://doi.org/10.1111/j.1365-2788.2010.01291.x.
- Hassiotis A, Canagasabey A, Robotham D, Marston L, Romeo R, King M. Applied behaviour analysis and standard treatment in intellectual disability: 2-year outcomes. Br J Psychiatry 2011;198:490-1. https://doi.org/10.1192/bjp.bp.109.076646.
- Knapp M, Comas-Herrera A, Astin J, Beecham J, Pendaries C. Intellectual disability, challenging behaviour and cost in care accommodation: what are the links?. Health Soc Care Community 2005;13:297-306. https://doi.org/10.1111/j.1365-2524.2005.00539.x.
- Mansell J, Knapp M, Beadle-Brown J, Beecham J. Deinstitutionalisation and Community Living – Outcomes and Costs: Report of a European Study. Volume 2: Main Report. Canterbury: University of Kent; 2007.
- Robertson J, Emerson E, Hatton C, Elliott J, McIntosh B, Swift P, et al. Longitudinal analysis of the impact and cost of person-centered planning for people with intellectual disabilities in England. Am J Ment Retard 2006;111:400-16. https://doi.org/10.1352/0895-8017(2006)111[400:LAOTIA]2.0.CO;2.
- Hassiotis A, Parkes C, Jones L, Fitzgerald B, Romeo R. Individual characteristics and service expenditure on challenging behaviour for adults with intellectual disabilities. J Appl Res Intellect Disabil 2008;21:438-45. https://doi.org/10.1111/j.1468-3148.2007.00413.x.
- Barron DA, Molosankwe I, Romeo R, Hassiotis A. Health Soc Care Community 2013;21:283-92. https://doi.org/10.1111/hsc.12015.
- Hunter R. Evaluating the costs and cost-effectiveness of interventions for people with learning disabilities and behaviour that challenges: the need to improve the evidence base. Tizard Learning Disability Review 2016;21:181-5. https://doi.org/10.1108/TLDR-06-2016-0016.
- Department of Health and Social Care . Services for People With Intellectual Disability and Challenging Behaviour and Or Mental Health Needs (Revised Edition) 2007. www.kent.ac.uk/tizard/staff/documents/dh2007mansellreport%20_revised.pdf (accessed May 2016).
- Department of Health and Social Care . Transforming Care: A National Response to Winterbourne View Hospital: Department of Health Review Final Report 2012. www.gov.uk/government/uploads/system/uploads/attachment_data/file/213215/final-report.pdf (accessed April 2017).
- Chowdhury M, Benson BA. Use of differential reinforcement to reduce behavior problems in adults with intellectual disabilities: a methodological review. Res Dev Disabil 2011;32:383-94. https://doi.org/10.1016/j.ridd.2010.11.015.
- Emerson E. Challenging Behaviour: Analysis and Intervention in People with Intellectual Difficulties. Cambridge: Cambridge University Press; 1995.
- LaVigna GW, Willis TJ. The efficacy of positive behavioural support with the most challenging behaviour: the evidence and its implications. J Intellect Dev Disabil 2012;37:185-95. https://doi.org/10.3109/13668250.2012.696597.
- Gore NJ, McGill P, Toogood S, Allen D, Hughes JC, Baker P, et al. Definition and scope for positive behavioural support. International Journal of Positive Behavioural Support 2013;3:14-23.
- Goh AE, Bambara LM. Individualized positive behavior support in school settings: a meta-analysis. Remedial Spec Educ 2013;33:271-86. https://doi.org/10.1177/0741932510383990.
- Rothwell NA, LaVigna GW, Willis TJ. A non-aversive rehabilitation approach for people with severe behavioural problems resulting from brain injury. Brain Inj 1999;13:521-33. https://doi.org/10.1080/026990599121421.
- Bradshaw CP, Waasdorp TE, Leaf PJ. Effects of school-wide positive behavioral interventions and supports on child behavior problems. Pediatrics 2012;130:e1136-45. https://doi.org/10.1542/peds.2012-0243.
- Waasdorp TE, Bradshaw CP, Leaf PJ. The impact of schoolwide positive behavioral interventions and supports on bullying and peer rejection: a randomized controlled effectiveness trial. Arch Pediatr Adolesc Med 2012;166:149-56. https://doi.org/10.1001/archpediatrics.2011.755.
- Emerson E, Toogood A, Mansell J, Barrett S, Bell C, Cummings R, et al. Challenging behaviour and community services: I. introduction and overview. Mental Handicap 1987;15:166-9. https://doi.org/10.1111/j.1468-3156.1987.tb00430.x.
- Toogood S, Bell A, Jaques H, Lewis S, Sinclair C, Wright L. Meeting the challenge in Clwyd: the intensive support team. Br J Learn Disabil 1994;22:18-24. https://doi.org/10.1111/j.1468-3156.1994.tb00107.x.
- Blunden R, Allen D. Facing the Challenge: An Ordinary Life for People with a Learning Disability and Challenging Behaviour. London: The King’s Fund; 1987.
- Allen D, James W, Evans J, Hawkins S, Jenkins R. Positive behavioural support: definition, current status and future directions. Tizard Learning Disability Review 2005;10:4-11. https://doi.org/10.1108/13595474200500014.
- Sugai G, Horner RH, Sailor W, Dunlap G, Sugai G, Horner R. Handbook of Positive Behaviour Support. New York, NY: Springer; 2009.
- Allen D, Kaye N, Horwood S, Gray D, Mines S. The impact of a whole organisation approach to positive behavioural support on the use of physical interventions. International Journal of Positive Behavioural Support 2012;2:26-30.
- McClean B, Dench C, Grey I, Shanahan S, Fitzsimons E, Hendler J. Person focused training: a model for delivering Positive Behaviour Supports to people with challenging behaviours. J Intellect Disabil Res 2005;49:340-52. https://doi.org/10.1111/j.1365-2788.2005.00669.x.
- Grey IM, McClean B. Service user outcomes of staff training in Positive Behaviour Support using person-focused training: a control group study. J Applied Res Intellect Disabil 2007;20:6-15. https://doi.org/10.1111/j.1468-3148.2006.00335.x.
- National Institute for Health and Care Excellence (NICE) . Challenging Behaviour and Learning Disabilities: Prevention and Interventions for People With Learning Disabilities Whose Behaviour Challenges 2015. www.nice.org.uk/guidance/ng11/resources/challenging-behaviourand-learning-disabilities-prevention-and-interventions-for-people-withlearning-disabilities-whose-behaviour-challenges-1837266392005 (accessed August 2016).
- Lowe K, Jones E, Allen D, Davies D, James W, Doyle T, et al. Staff training in Positive Behaviour Support: impact on attitudes and knowledge. JARID 2007;20:30-4. https://doi.org/10.1111/j.1468-3148.2006.00337.x.
- Aman MG, Singh NN, Stewart AW, Field CJ. The aberrant behavior checklist: a behavior rating scale for the assessment of treatment effects. Am J Ment Defic 1985;89:485-91.
- Wellens HJ. Randomized clinical trials: how long should they last?. Circulation 2004;110:107-8. https://doi.org/10.1161/01.CIR.0000134919.98104.22.
- Knight BP. The long-term benefits of long-term follow-up in clinical trials. EP Lab Digest 2013;13:1-2.
- Bellón JÁ, Conejo-Cerón S, Moreno-Peral P, King M, Nazareth I, Martín-Pérez C, et al. Intervention to prevent major depression in primary care: a cluster randomized trial. Ann Intern Med 2016;164:656-65. https://doi.org/10.7326/M14-2653.
- Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al. Contamination in trials of educational interventions. Health Technol Assess 2007;11. https://doi.org/10.3310/hta11430.
- Eldridge SM, Ashby D, Kerry S. Sample size for cluster randomized trials: effect of coefficient of variation of cluster size and analysis method. Int J Epidemiol 2006;35:1292-300. https://doi.org/10.1093/ije/dyl129.
- Hahn S, Puffer S, Torgerson DJ, Watson J. Methodological bias in cluster randomised trials. BMC Med Res Methodol 2005;5. https://doi.org/10.1186/1471-2288-5-10.
- Smith MP, Nethell G, Allen D, Jones E. Positive Behavioural Support – Assessment and Intervention for Challenging Behaviour – Manual. NHS Wales: Abertawe Bromorgannwg University Health Board; 2013.
- Department of Health and Social Care, The Rt Hon Norman Lamb . Positive and Safe: Reducing the Need for Restrictive Interventions n.d. www.gov.uk/government/speeches/positive-and-safe-reducing-the-need-for-restrictive-interventions (accessed 19 January 2018).
- ICH Harmonised Tripartite Guideline . Guideline for Good Clinical Practice E6(R1) 1996. www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R1_Guideline.pdf (accessed January 2018).
- Department of Health and Social Care . Research Governance Framework for Health and Social Care. Second Edition 2005. www.gov.uk/government/uploads/system/uploads/attachment_data/file/139565/dh_4122427.pdf (accessed March 2017).
- Data Protection Act 1998. London: The Stationery Office; 1998.
- Great Britain . Mental Capacity Act 2005 2005. www.legislation.gov.uk/ukpga/2005/9/pdfs/ukpga_20050009_en.pdf (accessed May 2013).
- Wechsler D. Wechsler Abbreviated Scale of Intelligence – Second Edition (WASI-II). San Antonio, TX: Psychological Corporation; 2011.
- Hatton C, Emerson E, Robertson J, Gregory N, Kessissoglou S, Perry J, et al. The adaptive behavior scale-residential and community (part I): towards the development of a short form. Res Dev Disabil 2001;22:273-88. https://doi.org/10.1016/S0891-4222(01)00072-5.
- Department for Communities and Local Government . English Indices of Deprivation 2015 2005. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed January 2016).
- Department for Communities and Local Government . English Indices of Deprivation 2015 n.d. http://imd-by-postcode.opendatacommunities.org/ (accessed March 2018).
- Prosser H, Moss S, Costello H, Simpson N, Patel P, Rowe S. Reliability and validity of the Mini PAS-ADD for assessing psychiatric disorders in adults with intellectual disability. J Intellect Disabil Res 1998;42:264-72. https://doi.org/10.1046/j.1365-2788.1998.00146.x.
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. https://doi.org/10.1007/s11136-010-9648-y.
- Baker PA. Measurement of community participation and use of leisure by service users with intellectual disability: the Guernsey community participation and leisure assessment. J Applied Res Intellect Disabil 2000;13:169-85. https://doi.org/10.1046/j.1468-3148.2000.00015.x.
- Pruchno RA. The effects of help patterns on the mental health of spouse caregivers. Res Aging 1990;12:57-71. https://doi.org/10.1177/0164027590121003.
- Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al. Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID). Health Technol Assess 2009;13. https://doi.org/10.3310/hta13210.
- Goldberg D, Williams P. A User’s Guide to the General Health Questionnaire. Windsor: NFER-Nelson; 1988.
- McCallion P, McCarron M, Force LT. A measure of subjective burden for dementia care: the Caregiving Difficulty Scale – Intellectual Disability. J Intellect Disabil Res 2005;49:365-71. https://doi.org/10.1111/j.1365-2788.2005.00670.x.
- Strydom A, Romeo R, Perez-Achiaga N, Livingston G, King M, Knapp M, et al. Service use and cost of mental disorder in older adults with intellectual disability. Br J Psychiatry 2010;196:133-8. https://doi.org/10.1192/bjp.bp.108.060939.
- Omar RZ, Thompson SG. Analysis of a cluster randomized trial with binary outcome data using a multi-level model. Stat Med 2000;19:2675-88. https://doi.org/10.1002/1097-0258(20001015)19:19<2675::AID-SIM556>3.0.CO;2-A.
- Goldstein H. Multilevel Statistical Models. London: Arnold; 2003.
- Dolan P. Modelling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ 1997;6:327-40. https://doi.org/10.1002/(SICI)1099-1050(199707)6:4<327::AID-HEC282>3.0.CO;2-W.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- British National Formulary. London: British Medical Association and Royal Pharmaceutical Society; 2016.
- Illustrative Cost Models in Learning Disabilities Social Care Provision. London: Department of Health; 2011.
- Guide to the Methods of Technology Appraisal 2013. London: National Institute for Health and Care Excellence; 2013.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Keshavarz N, Nutbeam D, Rowling L, Khavarpour F. Schools as social complex adaptive systems: a new way to understand the challenges of introducing the health promoting schools concept. Soc Sci Med 2010;70:1467-74. https://doi.org/10.1016/j.socscimed.2010.01.034.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Jansen YJ, Foets MM, de Bont AA. The contribution of qualitative research to the development of tailor-made community-based interventions in primary care: a review. Eur J Public Health 2010;20:220-6. https://doi.org/10.1093/eurpub/ckp085.
- Bonell C, Oakley A, Hargreaves J, Strange V, Rees R. Research methodology: assessment of generalisability in trials of health interventions, suggested framework and systematic review. BMJ 2006;333:346-9. https://doi.org/10.1136/bmj.333.7563.346.
- Kirkpatrick DL. Techniques for evaluating training programs. Journal of the American Society of Training Directors 1959;13:21-6.
- Stewart DW, Shamdasani PN. Focus Groups: Theory and Practice. Newbury Park, CA: Sage Publications; 1990.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960;20:37-46. https://doi.org/10.1177/001316446002000104.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. https://doi.org/10.2307/2529310.
- Browning-Wright D, Mayer GR, Saren D. The Behavior Support Plan – Quality Evaluation Guide II 2013. www.pent.ca.gov (accessed July 2014).
- Hassiotis A, Poppe M, Strydom A, Vickerstaff V, Hall IS, Crabtree J, et al. Clinical outcomes of staff training in positive behaviour support to reduce challenging behaviour in adults with intellectual disability: cluster randomised controlled trial. Br J Psychiatry 2018;212:161-8. https://doi.org/10.1192/bjp.2017.34.
- Browning-Wright D, Mayer GR, Cook CR, Crews D, Kraemer BR, Gale B. A preliminary study on the effects of training using behavior support plan quality evaluation guide (BSP-QE) to improve positive behavioural support plans. Educ Treat Children 2007;30:89-106. https://doi.org/10.1353/etc.2007.0017.
- MacDonald A, McGill P. Outcomes of staff training in Positive Behaviour Support: a systematic review. J Dev Phys Disabil 2013;25:17-33. https://doi.org/10.1007/s10882-012-9327-8.
- NHS England . Transforming Care for People With Learning Disabilities – Next Steps 2015. www.england.nhs.uk/wp-content/uploads/2015/01/transform-care-nxt-stps.pdf (accessed December 2016).
- Deveau R, McGill P. Leadership at the front line: impact of practice leadership management style on staff experience in services for people with intellectual disability and challenging behaviour. J Intellect Dev Disabil 2014;39:65-72. https://doi.org/10.3109/13668250.2013.865718.
- Hutchinson LM, Hastings RP, Hunt PH, Bowler CL, Banks ME, Totsika V. Who’s challenging who? Changing attitudes towards those whose behaviour challenges. J Intellect Disabil Res 2014;58:99-109. https://doi.org/10.1111/j.1365-2788.2012.01630.x.
- McClean B, Grey I. A component analysis of Positive Behaviour Support plans. J Intellect Dev Disabil 2012;37:221-31. https://doi.org/10.3109/13668250.2012.704981.
- Adams D, Handley L, Simkiss D, Walls E, Jones A, Knapp M, et al. Service use and access in young children with an intellectual disability or global developmental delay: associations with challenging behaviour. J Intellect Dev Disabil 2016;10:1-10. https://doi.org/10.3109/13668250.2016.1238448.
- Romeo R, Molosankwe I. Economic evidence in intellectual disabilities: a review. Curr Opin Psychiatry 2010;23:427-31. https://doi.org/10.1097/YCO.0b013e32833ad946.
- Personal Communication . Angela Hassiotis n.d.
- McCrone P. Capturing the costs of end-of-life care: comparisons of multiple sclerosis, Parkinson’s disease, and dementia. J Pain Symptom Manage 2009;38:62-7. https://doi.org/10.1016/j.jpainsymman.2009.04.006.
- Positive Behavioural Support Academy . PBS Academy n.d. http://pbsacademy.org.uk/ (accessed February 2018).
- Department of Health and Social Care, PbR Finance and Costing Team . National Schedule of Reference Costs 2013–14 2014. www.gov.uk/government/uploads/system/uploads/attachment_data/file/380322/01_Final_2013-14_Reference_Costs_publication_v2.pdf (accessed January 2018).
- Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012;50:217-26. https://doi.org/10.1097/MLR.0b013e3182408812.
- Ball J, Philippou J, Pike G, Sethi G. Survey of District and Community Nurses in 2013. Report to the Royal College of Nursing National Nursing Research Unit. London: King’s College London; 2014.
- Cruz M, Roter DL, Cruz RF, Wieland M, Larson S, Cooper LA, et al. Appointment length, psychiatrists’ communication behaviors, and medication management appointment adherence. Psychiatr Serv 2013;64:886-92. https://doi.org/10.1176/appi.ps.201200416.
- Pomerantz AS, Corson JA, Detzer MJ. The challenge of integrated care for mental health: leaving the 50 minute hour and other sacred things. J Clin Psychol Med Settings 2009;16:40-6. https://doi.org/10.1007/s10880-009-9147-x.
- Renforth P, Yapa RS, Forster DP. Occupational therapy predischarge home visits: a study from a community hospital. Br J Occup Ther 2004;67:488-94. https://doi.org/10.1177/030802260406701104.
- Heslin M, Callaghan L, Barrett B, Lea S, Eick S, Morgan J, et al. Costs of the police service and mental healthcare pathways experienced by individuals with enduring mental health needs. Br J Psychiatry 2017;210:157-64. https://doi.org/10.1192/bjp.bp.114.159129.
- Hayhurst KP, Leitner M, Davies L, Flentje R, Millar T, Jones A, et al. The effectiveness and cost-effectiveness of diversion and aftercare programmes for offenders using class A drugs: a systematic review and economic evaluation. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19060.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
Appendix 1 Positive Behaviour Support training outline
-
The overall model includes three separate workshops over a total of 6 days. The workshops will aim to train participants in a complete pathway from assessment to intervention implementation of PBS. Training will focus around participants developing competencies around one specific service user with the assumption that they are then able to roll out these competencies to a further cohort of nine or 10 service users post training.
-
The target competencies are:
-
completion and interpretation of a brief functional behavioural assessment
-
ability to construct a functionally relevant individualised PBS plan on the basis of this assessment
-
ability to assess mediator competency to implement the plan and provide supportive preinterventions as appropriate
-
support mediators to implement the plan in practice
-
conducting an initial assessment of plan effectiveness
-
identifying and overcoming problems in implementation.
-
-
The mentoring will provide participants with further technical guidance on the tools and concepts taught during the course – it will not provide participants with individual clinical supervision on their full cohort of service users. In order to meet clinical governance requirements, this supervision needs to be provided for participants at a local level. Any emergency scenarios will similarly be managed at the local level.
| Training phase | Content |
|---|---|
| Workshop 1 |
Behavioural theory – revision and update Principles of functional assessment Using the BBAT |
| 6-week interval | Participants complete a BBAT on their identified service user and submit this for feedback at least 7 working days before workshop 2 |
| Workshop 2 |
Feedback on completed BBAT Designing individualised PBS interventions based on functional assessment Competency-based training model Mediator interventions |
| 8-week interval |
Participants draft intervention (3 weeks) Implement intervention (3 weeks) Submit intervention plan and initial feedback at least 7 working days before workshop 3 |
| Workshop 3 |
Feedback on intervention plan design and implementation Troubleshooting and solutions Individualised periodic service reviews Aims of and procedures for mentoring support |
Appendix 2 Research and development departments and corresponding sites in the participating NHS trusts
| Research and development departments that gave approval | Team |
|---|---|
| Camden and Islington NHS Foundation Trust (NoCLoR) | Camden Learning Disability Service |
| Islington Learning Disabilities Partnership | |
| Barts Health NHS Trust and East London NHS Foundation Trust | Tower Hamlets Community Learning Disability Service |
| Homerton University Hospital NHS Foundation Trust | Hackney Learning Disabilities Service |
| Barnet, Enfield and Haringey Mental Health NHS Trust (NoCLoR) | Barnet Learning Disabilities Service |
| Central and North West London NHS Foundation Trust (NoCLoR) | Enfield Integrated Learning Disabilities Service |
| North East London NHS Foundation Trust | Barking and Dagenham Community Learning Disability Service |
| Havering Community Learning Disability Service | |
| Waltham Forest Community Learning Disability Team | |
| Oxleas NHS Foundation Trust | Bexley Learning Disability Team and Greenwich Community Learning Disability Team |
| South West London and St George’s Mental Health NHS Trust | Wandsworth Community Learning Disability Team |
| Leicestershire Partnership NHS Trust | Leicester City (East) Community Learning Disability Team |
| Leicester City (West) Community Learning Disability Team | |
| Charnwood Community Learning Disability Team | |
| Coalville and Hinckley Community Learning Disability Team | |
| Market Harborough, Oadby and Wigston Community Learning Disability Team | |
| Kent and Medway NHS and Social Care Partnership Trust via RM&G Consortium for Kent and Medway | Dartford, Gravesend and Swanley Mental Health of Learning Disability Service |
| Medway Mental Health of Learning Disability Service | |
| Surrey and Borders Partnership NHS Foundation Trust | East Surrey Community Team for People with Learning Disabilities |
| South West Surrey, North East Hants and North West Surrey Community Team for People with Learning Disabilities | |
| Mid Surrey Community Team for People with Learning Disabilities | |
| Coventry and Warwickshire Partnership NHS Trust | Coventry, South Warwickshire and Rugby Community Learning Disabilities Teams |
| Bradford District NHS Care Trust | Bradford Learning Disabilities Service |
Appendix 3 National Research Ethics Service serious adverse event form
Appendix 4 Unit costs for health, social care and criminal justice
| Type of service | Unit cost per contact (£) | Source |
|---|---|---|
| Community care | ||
| GP (surgery) | 33 | PSSRU69 |
| GP (home) | 68 | PSSRU69 |
| GP (telephone) | 20 | PSSRU69 |
| District nurse | 39 | PSSRU,69 Ball et al.98 |
| Mental health nurse | 17.50 | PSSRU,69 Ball et al.98 |
| Learning disabilities nurse | 17.50 | PSSRU69 |
| Psychiatrist | 39 | PSSRU,69 Cruz et al.99 |
| Psychologist | 52 | PSSRU,69 Pomerantz et al.100 |
| Social worker | 55 | PSSRU69 |
| Occupational therapist | 33 | PSSRU,69 Renforth et al.101 |
| Art/drama/music therapy | 68 | Reference costs96 |
| Alternative therapy | 85 | Reference costs96 |
| Counsellor | 44 | PSSRU69 |
| Physiotherapist | 52 | Reference costs96 |
| Dentist | 85 | Reference costs96 |
| Speech and language therapist | 84 | Reference costs96 |
| Community support worker | 51 | PSSRU69 |
| Chiropodist/podiatrist | 44 | Reference costs96 |
| Optician | 97 | Reference costs96 |
| Behavioural therapist | 85 | Reference costs96 |
| Acute and specialist care | ||
| Mental health (per bed-day) | 223 | PSSRU69 |
| Short non-elective stay | 608 | PSSRU69 |
| Long non-elective stay | 2863 | PSSRU69 |
| Planned (elective) acute care | 3405 | PSSRU69 |
| Critical care stay | 1207 | Reference costs96 |
| Mental health (outpatient) | 107 | PSSRU69 |
| General medical outpatient | 112 | PSSRU69 |
| Day case | 704 | PSSRU69 |
| A&E attendance (admitted) | 167 | Reference costs96 |
| A&E attendance (not admitted) | 108 | Reference costs96 |
| Criminal justice | ||
| Police contact (arrested) | 267 | Heslin et al.102 |
| Police contact (not arrested) | 841 | Heslin et al.102 |
| Learning disabilities assessment | 284 | PSSRU68 |
| Probation | 2690 | Hayhurst et al.103 |
Appendix 5 Resource use: main study
| Resource | Time point | |||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | ||||
| PBS arm (N = 108) | Control arm (N = 136) | PBS arm (N = 103) | Control arm (N = 130) | PBS arm (N = 103) | Control arm (N = 132) | |
| GP (surgery) | ||||||
| Yes (n) | 88 | 103 | 85 | 105 | 83 | 103 |
| Yes (%) | 82 | 76 | 83 | 81 | 81 | 78 |
| For those who used the service | ||||||
| Mean | 5.1 | 4 | 4.3 | 4.2 | 5 | 3.5 |
| SD | 6.6 | 4 | 8.4 | 6.6 | 11 | 3.3 |
| GP (home) | ||||||
| Yes (n) | 14 | 30 | 12 | 23 | 13 | 21 |
| Yes (%) | 13 | 22 | 12 | 18 | 13 | 16 |
| For those who used the service | ||||||
| Mean | 2 | 3.3 | 2.6 | 3.4 | 1.5 | 2.1 |
| SD | 1.7 | 4.8 | 2.8 | 5.6 | 0.9 | 2.5 |
| GP (telephone) | ||||||
| Yes (n) | 29 | 50 | 24 | 46 | 20 | 28 |
| Yes (%) | 27 | 37 | 24 | 36 | 20 | 29 |
| For those who used the service | ||||||
| Mean | 2.4 | 4.1 | 3.6 | 6.4 | 2.6 | 2.7 |
| SD | 2.1 | 7.4 | 4.8 | 15.4 | 1.7 | 2.5 |
| Community/district nurse | ||||||
| Yes (n) | 24 | 46 | 23 | 31 | 33 | 31 |
| Yes (%) | 22 | 34 | 23 | 24 | 32 | 23 |
| For those who used the service | ||||||
| Mean | 4 | 11.6 | 5.7 | 10.2 | 6 | 5 |
| SD | 5.5 | 33.0 | 6.3 | 34.1 | 13.1 | 8.6 |
| Community psychiatric nurse | ||||||
| Yes (n) | 26 | 12 | 17 | 14 | 17 | 15 |
| Yes (%) | 24 | 9 | 17 | 11 | 17 | 11 |
| For those who used the service | ||||||
| Mean | 5.2 | 3.1 | 5.4 | 2.9 | 3.5 | 4.3 |
| SD | 7.6 | 3.1 | 6.1 | 3.2 | 4.1 | 5.6 |
| Learning disabilities nurse | ||||||
| Yes (n) | 38 | 40 | 26 | 22 | 24 | 27 |
| Yes (%) | 35 | 29 | 26 | 17 | 23 | 20 |
| For those who used the service | ||||||
| Mean | 4.3 | 12.5 | 4.4 | 20.2 | 4.4 | 2.9 |
| SD | 4.7 | 35.9 | 5.9 | 54.2 | 4.7 | 4.7 |
| Psychiatrist | ||||||
| Yes (n) | 79 | 88 | 66 | 81 | 60 | 78 |
| Yes (%) | 73 | 65 | 65 | 63 | 58 | 59 |
| For those who used the service | ||||||
| Mean | 2 | 1.8 | 1.7 | 2 | 1.4 | 2.1 |
| SD | 2.9 | 1.5 | 1.3 | 1.8 | 0.9 | 1.8 |
| Psychologist | ||||||
| Yes (n) | 16 | 26 | 8 | 23 | 13 | 29 |
| Yes (%) | 15 | 19 | 8 | 18 | 13 | 22 |
| For those who used the service | ||||||
| Mean | 3.7 | 4.1 | 4.4 | 2.3 | 2.2 | 3.1 |
| SD | 6.3 | 6.4 | 5.6 | 2.4 | 2.2 | 4.6 |
| Social worker/care manager | ||||||
| Yes (n) | 64 | 57 | 48 | 63 | 55 | 60 |
| Yes (%) | 59 | 42 | 47 | 48 | 53 | 46 |
| For those who used the service | ||||||
| Mean | 5.2 | 2.5 | 2 | 2.3 | 2.6 | 2.4 |
| SD | 23.2 | 2.5 | 2.0 | 3.5 | 7.7 | 2.5 |
| Occupational therapist | ||||||
| Yes (n) | 20 | 17 | 17 | 22 | 12 | 22 |
| Yes (%) | 19 | 13 | 17 | 17 | 12 | 17 |
| For those whoused the service | ||||||
| Mean | 2.2 | 3.2 | 3.9 | 2.5 | 2.5 | 1.9 |
| SD | 2.3 | 2.7 | 6.0 | 1.9 | 2.2 | 1.5 |
| Art/drama/music therapy | ||||||
| Yes (n) | 7 | 5 | 9 | 6 | 8 | 7 |
| Yes (%) | 6 | 4 | 9 | 5 | 8 | 5 |
| For those who used the service | ||||||
| Mean | 20.6 | 16.2 | 18.7 | 21.9 | 12.25 | 11.1 |
| SD | 17.1 | 11.8 | 9.7 | 17.2 | 18.7 | 6.6 |
| Alternative therapist | ||||||
| Yes (n) | 6 | 5 | 1 | 8 | 1 | 2 |
| Yes (%) | 6 | 4 | 1 | 6 | 1 | 2 |
| For those who used the service | ||||||
| Mean | 14.8 | 18.8 | 13 | 16 | 48 | 19 |
| SD | 12.1 | 10.0 | 9.3 | 9.9 | ||
| Counsellor | ||||||
| Yes (n) | 2 | 2 | 0 | 2 | 0 | 0 |
| Yes (%) | 2 | 1 | 0 | 2 | 0 | 0 |
| For those who used the service | ||||||
| Mean | 4.7 | 6 | 13.5 | |||
| SD | 6.4 | 17.7 | ||||
| Physiotherapy | ||||||
| Yes (n) | 6 | 21 | 6 | 16 | 7 | 8 |
| Yes (%) | 6 | 15 | 6 | 12 | 7 | 6 |
| For those who used the service | ||||||
| Mean | 2.7 | 4.8 | 7.7 | 6.1 | 6.3 | 3 |
| SD | 7.1 | 8.8 | 9.6 | 8.4 | 7.9 | 3.8 |
| Dentist | ||||||
| Yes (n) | 81 | 77 | 72 | 81 | 69 | 79 |
| Yes (%) | 75 | 57 | 71 | 63 | 67 | 60 |
| For those who used the service | ||||||
| Mean | 1.7 | 1.5 | 1.5 | 1.7 | 1.5 | 1.5 |
| SD | 1.5 | 0.9 | 1.5 | 1.8 | 1.0 | 1.0 |
| Speech and language therapy | ||||||
| Yes (n) | 14 | 14 | 14 | 26 | 17 | 26 |
| Yes (%) | 13 | 10 | 14 | 20 | 17 | 20 |
| For those who used the service | ||||||
| Mean | 2.2 | 2.1 | 5.6 | 6 | 3.5 | 2.1 |
| SD | 2.0 | 2.0 | 6.7 | 7.9 | 2.9 | 1.3 |
| Community support worker | ||||||
| Yes (n) | 6 | 9 | 6 | 9 | 4 | 15 |
| Yes (%) | 6 | 7 | 6 | 7 | 4 | 12 |
| For those who used the service | ||||||
| Mean | 89.7 | 59.4 | 99.7 | 54.7 | 98.3 | 79.7 |
| SD | 79.7 | 122.0 | 76.7 | 58.7 | 97.8 | 106.2 |
| Acute care and specialist services | ||||||
| Mental health inpatient | ||||||
| Yes (n) | 0 | 2 | 0 | 1 | 0 | 2 |
| Yes (%) | 0 | 1 | 0 | 1 | 0 | 2 |
| For those with an admission | ||||||
| Number of admissions, mean (SD) | 1 (0.0) | 1 | 1 | |||
| Number of bed-days, mean (SD) | 12 (12.7) | 30 | 110 (110.3) | |||
| General medical planned admission | ||||||
| Yes (n) | 0 | 3 | 1 | 0 | 2 | 1 |
| Yes (%) | 0 | 2 | 1 | 0 | 2 | 1 |
| For those with an admission | ||||||
| Number of admissions, mean (SD) | 1 (0.0) | 2 | 1 (1.0) | 1 | ||
| Number of bed-days, mean (SD) | 1 (0.0) | 8 | 7.7 (11.6) | 0 | ||
| General medical unplanned admission | ||||||
| Yes (n) | 5 | 11 | 4 | 5 | 4 | 5 |
| Yes (%) | 5 | 8 | 4 | 4 | 4 | 4 |
| For those with an admission | ||||||
| Number of admissions, mean (SD) | 2.5 (1.9) | 1.3 (0.7) | 2.25 (1.5) | 1.9 (0.6) | 1.25 (0.5) | 1 (0.0) |
| Number of bed-days, mean (SD) | 5.3 (4.8) | 4.2 (5.8) | 6.25 (3.9) | 6.4 (6.2) | 6 (7.4) | 4 (5.6) |
| Medical ICU/HDU | ||||||
| Yes (n) | 2 | 1 | 0 | 1 | 0 | 0 |
| Yes (%) | 2 | 1 | 0 | 1 | 0 | 0 |
| For those with an admission | ||||||
| Number of admissions, mean (SD) | 1 (0.0) | 2 | 1 | |||
| Number of bed-days, mean (SD) | 4.5 (2.1) | 4 | 17 | |||
| Physical-health-related A&E attendance | ||||||
| Yes (n) | 20 | 31 | 12 | 32 | 15 | 18 |
| Yes (%) | 19 | 23 | 12 | 25 | 15 | 14 |
| For those who used the service | ||||||
| Mean | 1.6 | 1.8 | 2.2 | 1.6 | 3.4 | 1.4 |
| SD | 1.0 | 1.5 | 22 | 1.7 | 7.5 | 1.0 |
| Mental-health-related A&E attendance | ||||||
| Yes (n) | 3 | 1 | 1 | 3 | 2 | 2 |
| Yes (%) | 3 | 1 | 1 | 2 | 2 | 2 |
| For those who used the service | ||||||
| Mean | 7 | 26 | 7.5 | 1 | 1.5 | |
| SD | 1.4 | 9.2 | 0.0 | 0.7 | ||
| Psychiatric outpatient appointment | ||||||
| Yes (n) | 28 | 43 | 31 | 49 | 21 | 40 |
| Yes (%) | 26 | 32 | 31 | 38 | 21 | 30 |
| For those who used the service | ||||||
| Mean | 1.7 | 1.7 | 1.4 | 1.6 | 1.6 | 1.4 |
| SD | 1.0 | 1.0 | 1.1 | 1.3 | 1.2 | 0.7 |
| Day patient procedure | ||||||
| Yes (n) | 13 | 40 | 24 | 32 | 32 | 39 |
| Yes (%) | 12 | 29 | 24 | 25 | 31 | 30 |
| For those who used the service | ||||||
| Mean | 2.1 | 1.6 | 1.9 | 1.5 | 2.2 | 1.8 |
| SD | 1.3 | 0.8 | 1.6 | 1.0 | 2.2 | 1.3 |
| Medical outpatient appointment | ||||||
| Yes (n) | 25 | 36 | 21 | 27 | 24 | 24 |
| Yes (%) | 23 | 27 | 21 | 21 | 23 | 18 |
| For those who used the service | ||||||
| Mean | 2.4 | 2.2 | 3 | 2.2 | 2.6 | 3.3 |
| SD | 2.7 | 3.0 | 2.4 | 3.7 | 2.0 | 5.0 |
Appendix 6 Aberrant Behaviour Checklist – Community subscales at 36 months
FIGURE 12.
Aberrant Behaviour Checklist – Community subscales at 36 months. Subscales for (a) irritability and agitation; (b) lethargy and social withdrawal; (c) stereotypic behaviour; (d) hyperactivity and non-compliance; and (e) inappropriate speech.
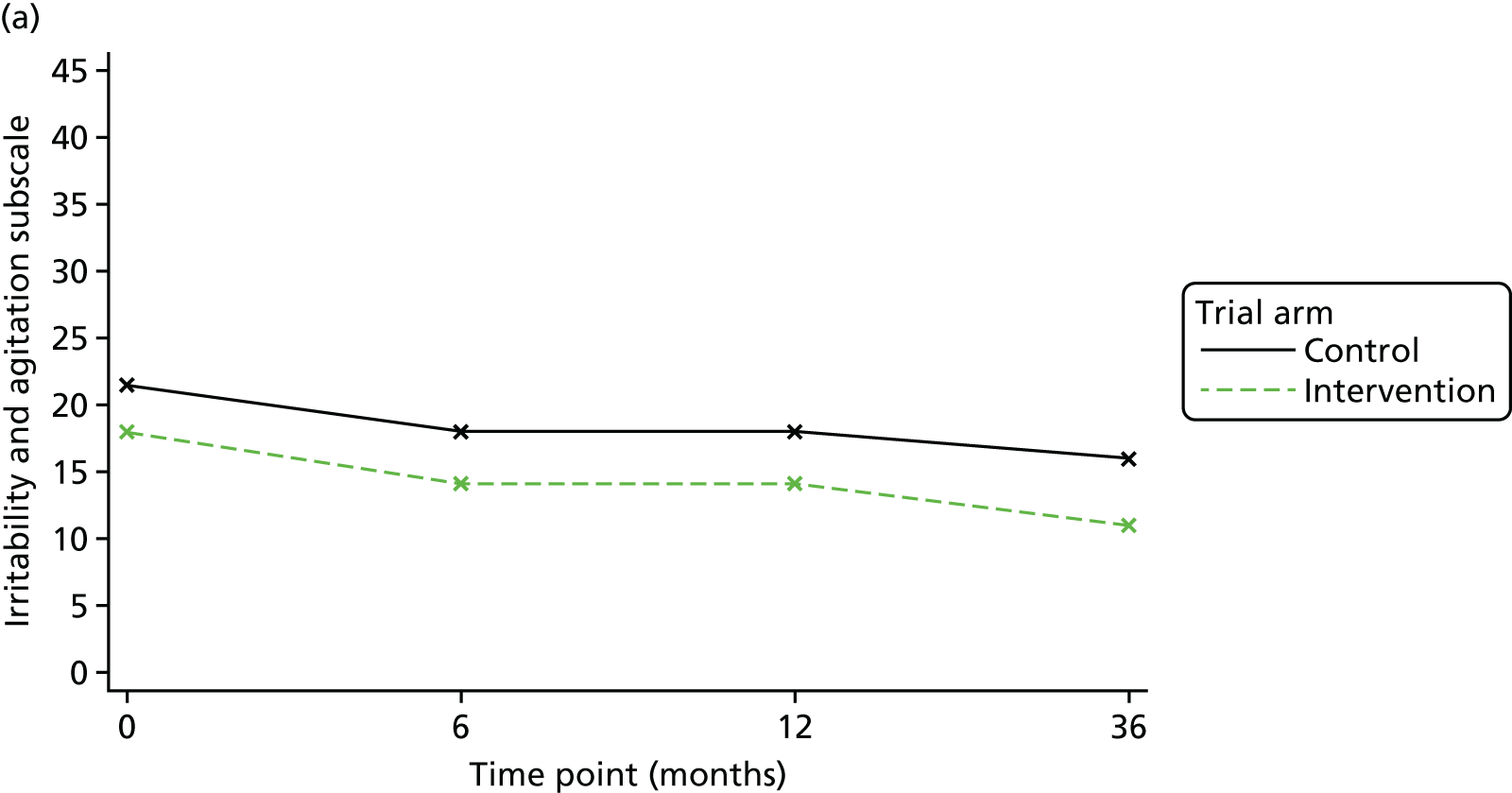
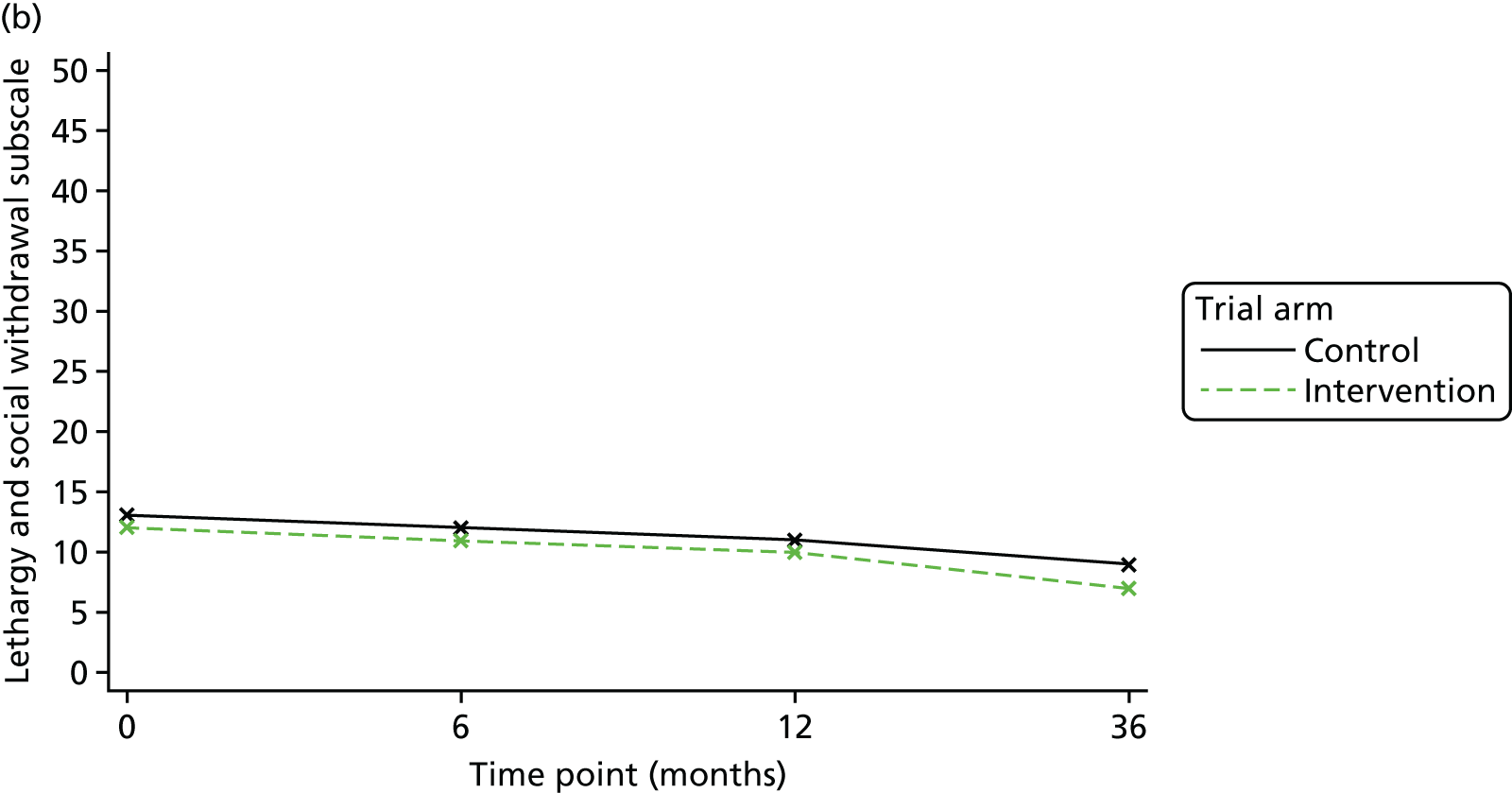

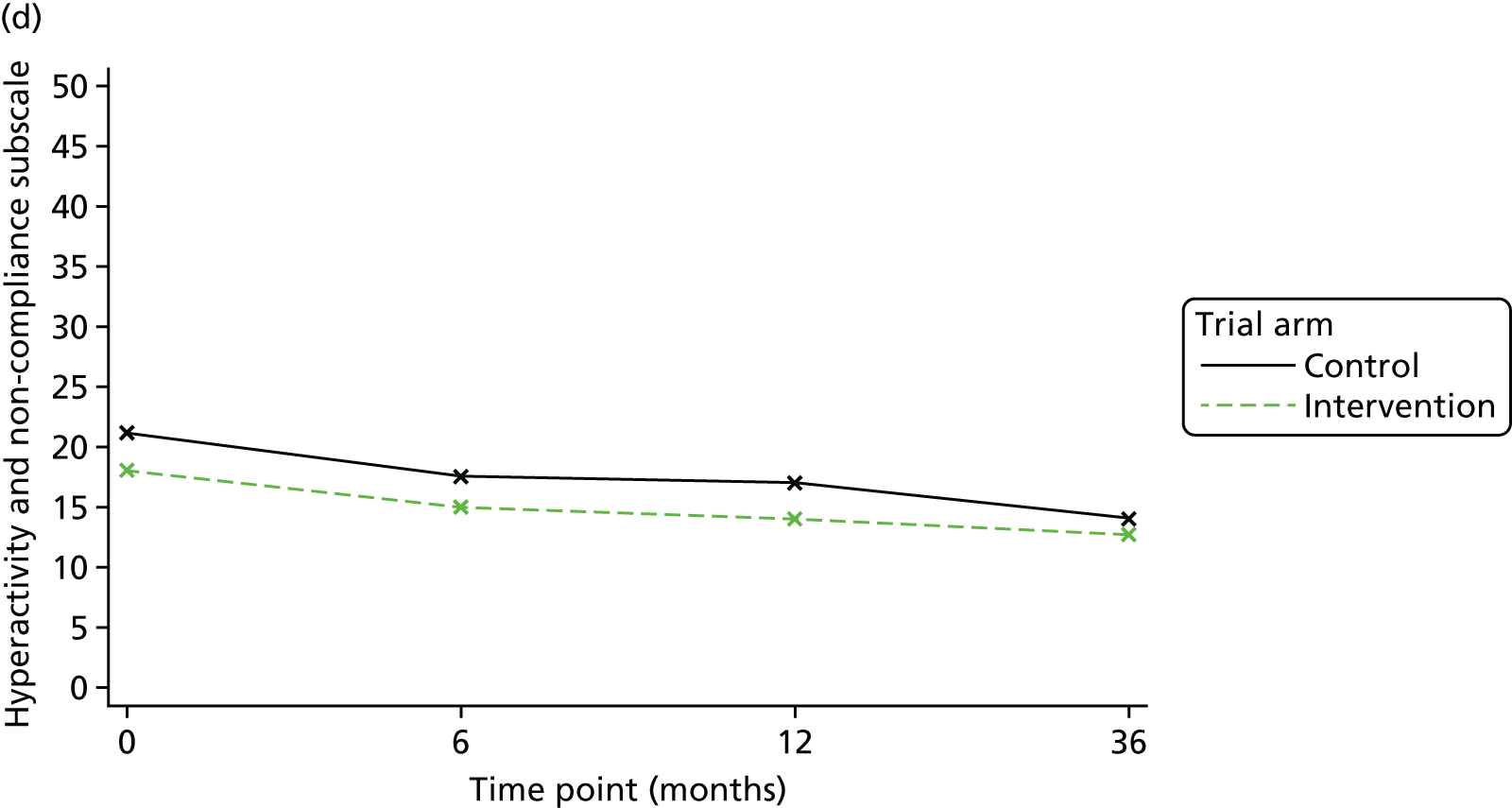
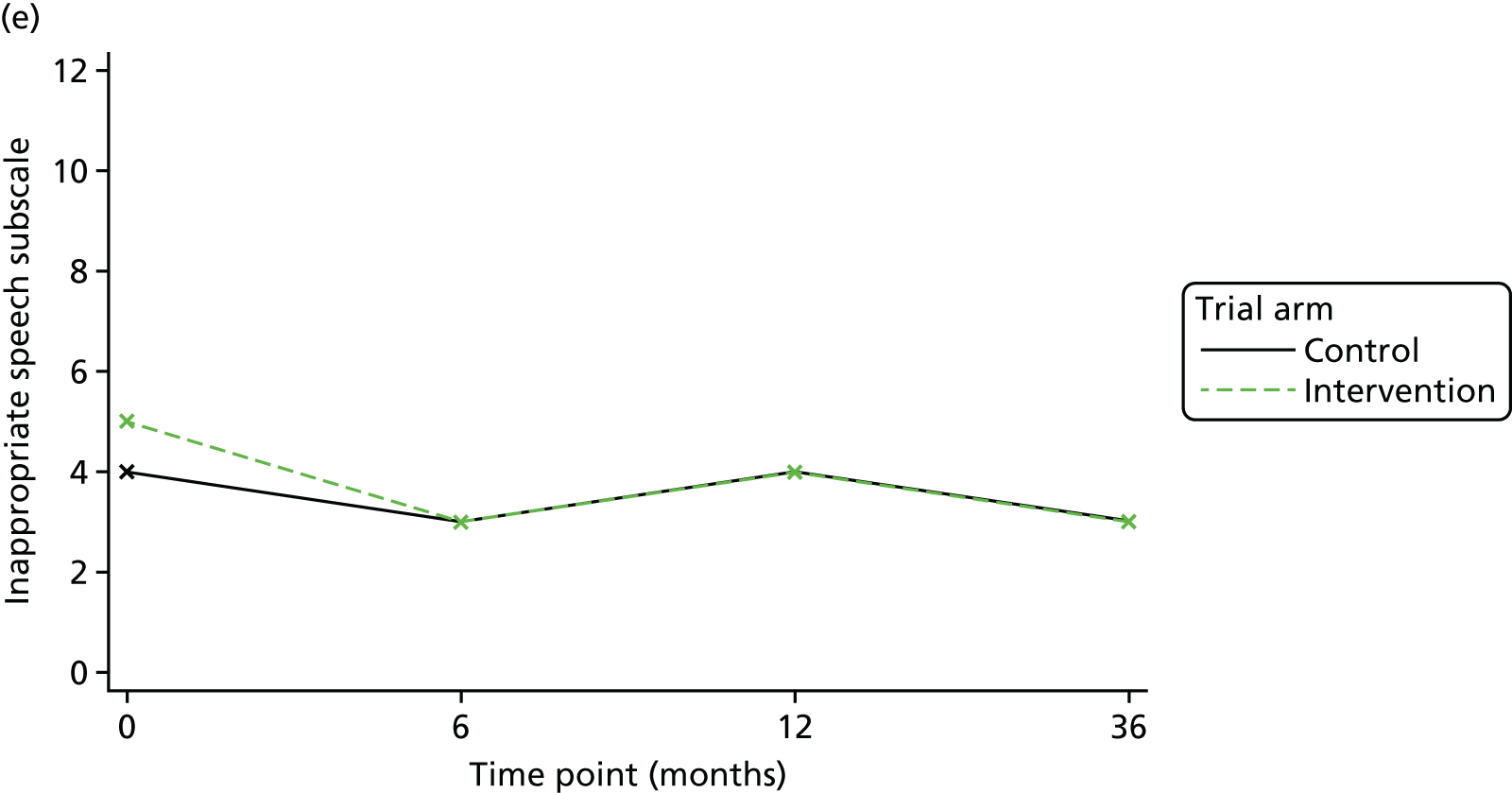
Appendix 7 Resource use and societal costs: long-term follow-up
| Resource | Time point | |||
|---|---|---|---|---|
| Baseline | 36 months | |||
| PBS arm (N = 108) | Control arm (N = 136) | PBS arm (N = 79) | Control arm (N = 105) | |
| GP (surgery) | ||||
| Yes (n) | 88 | 103 | 63 | 78 |
| Yes (%) | 82 | 76 | 80 | 74 |
| For those who used the service | ||||
| Mean | 5.1 | 4 | 3.9 | 3.1 |
| SD | 6.6 | 4.0 | 6.6 | 3.9 |
| GP (home) | ||||
| Yes (n) | 14 | 30 | 7 | 13 |
| Yes (%) | 13 | 22 | 9 | 12 |
| For those who used the service | ||||
| Mean | 2 | 3.3 | 1.4 | 2.3 |
| SD | 1.7 | 4.8 | 0.5 | 2.2 |
| GP (telephone) | ||||
| Yes (n) | 29 | 50 | 11 | 16 |
| Yes (%) | 27 | 37 | 14 | 15 |
| For those who used the service | ||||
| Mean | 2.4 | 4.1 | 1.9 | 5.9 |
| SD | 2.1 | 7.4 | 0.9 | 7.7 |
| Community/district nurse | ||||
| Yes (n) | 24 | 46 | 18 | 29 |
| Yes (%) | 22 | 34 | 23 | 28 |
| For those who used the service | ||||
| Mean | 4 | 11.6 | 15.4 | 7.9 |
| SD | 5.5 | 33.0 | 41.9 | 33.5 |
| Community psychiatric nurse | ||||
| Yes (n) | 26 | 12 | 2 | 4 |
| Yes (%) | 24 | 9 | 3 | 4 |
| For those who used the service | ||||
| Mean | 5.2 | 3.1 | 6 | 4.5 |
| SD | 7.6 | 3.1 | 1.4 | 3.5 |
| Learning disabilities nurse | ||||
| Yes (n) | 38 | 40 | 10 | 18 |
| Yes (%) | 35 | 29 | 12 | 17 |
| For those who used the service | ||||
| Mean | 4.3 | 12.5 | 1.9 | 7.7 |
| SD | 4.7 | 35.9 | 1.5 | 12.9 |
| Psychiatrist | ||||
| Yes (n) | 79 | 88 | 35 | 62 |
| Yes (%) | 73 | 65 | 44 | 59 |
| For those who used the service | ||||
| Mean | 2 | 1.8 | 1.6 | 1.9 |
| SD | 2.9 | 1.5 | 1.2 | 1.8 |
| Psychologist | ||||
| Yes (n) | 16 | 26 | 11 | 12 |
| Yes (%) | 15 | 19 | 14 | 11 |
| For those who used the service | ||||
| Mean | 3.7 | 4.1 | 2.2 | 2.7 |
| SD | 6.3 | 6.4 | 1.7 | 1.9 |
| Social worker/care manager | ||||
| Yes (n) | 64 | 57 | 29 | 45 |
| Yes (%) | 59 | 42 | 37 | 43 |
| For those who used the service | ||||
| Mean | 5.2 | 2.5 | 1.5 | 3 |
| SD | 23.2 | 2.5 | 1.2 | 5.4 |
| Occupational therapist | ||||
| Yes (n) | 20 | 17 | 11 | 14 |
| Yes (%) | 19 | 13 | 14 | 13 |
| For those who used the service | ||||
| Mean | 2.2 | 3.2 | 4.3 | 2.9 |
| SD | 2.3 | 2.7 | 7.9 | 2.1 |
| Art/drama/music therapy | ||||
| Yes (n) | 7 | 5 | 11 | 17 |
| Yes (%) | 6 | 4 | 14 | 16 |
| For those who used the service | ||||
| Mean | 20.6 | 16.2 | 12.3 | 16.2 |
| SD | 17.1 | 11.8 | 11.4 | 9.5 |
| Alternative therapist | ||||
| Yes (n) | 6 | 5 | 8 | 8 |
| Yes (%) | 6 | 4 | 10 | 8 |
| For those who used the service | ||||
| Mean | 14.8 | 18.8 | 17.8 | 20.1 |
| SD | 12.1 | 10.0 | 9.0 | 15.9 |
| Counsellor | ||||
| Yes (n) | 2 | 2 | 0 | 0 |
| Yes (%) | 2 | 1 | 0 | 0 |
| For those who used the service | ||||
| Mean | 4.7 | 6 | ||
| SD | 6.4 | |||
| Physiotherapy | ||||
| Yes (n) | 6 | 21 | 5 | 12 |
| Yes (%) | 6 | 15 | 6 | 11 |
| For those who used the service | ||||
| Mean | 2.7 | 4.8 | 3.8 | 2.2 |
| SD | 7.1 | 8.8 | 5.2 | 1.4 |
| Dentist | ||||
| Yes (n) | 81 | 77 | 48 | 63 |
| Yes (%) | 75 | 57 | 60 | 60 |
| For those who used the service | ||||
| Mean | 1.7 | 1.5 | 1.2 | 1.2 |
| SD | 1.5 | 0.9 | 0.6 | 0.6 |
| Speech and language therapy | ||||
| Yes (n) | 14 | 14 | 3 | 16 |
| Yes (%) | 13 | 10 | 4 | 15 |
| For those who used the service | ||||
| Mean | 2.2 | 2.1 | 4.7 | 3.7 |
| SD | 2.0 | 2.0 | 2.3 | 6.4 |
| Community support worker | ||||
| Yes (n) | 6 | 9 | 8 | 10 |
| Yes (%) | 6 | 7 | 10 | 10 |
| For those who used the service | ||||
| Mean | 89.7 | 59.4 | 65.3 | 176.9 |
| SD | 79.7 | 122.0 | 49.7 | 156.0 |
| Acute care and specialist services | ||||
| Mental health inpatient | ||||
| Yes (n) | 0 | 2 | 1 | 0 |
| Yes (%) | 0 | 1 | 1 | 0 |
| For those with an admission | ||||
| Number of admissions, mean (SD) | 1 (0.0) | 1 | ||
| Number of bed-days, mean (SD) | 12 (12.7) | 120 | ||
| Mental health rehabilitation | ||||
| Yes (n) | 0 | 0 | 0 | 1 |
| Yes (%) | 0 | 0 | 0 | 1 |
| For those with an admission | ||||
| Number of admissions, mean (SD) | 1 | |||
| Number of bed-days, mean (SD) | 42 | |||
| General medical planned admission | ||||
| Yes (n) | 0 | 3 | 0 | 0 |
| Yes (%) | 0 | 2 | 0 | 0 |
| For those with an admission | ||||
| Number of admissions, mean (SD) | 1 (0) | |||
| Number of bed-days, mean (SD) | 1 (0) | |||
| General medical unplanned admission | ||||
| Yes (n) | 5 | 11 | 4 | 9 |
| Yes (%) | 5 | 8 | 5 | 9 |
| For those with an admission | ||||
| Number of admissions, mean (SD) | 2.5 (1.9) | 1.3 (0.7) | 1.25 (0.5) | 1 (0.0) |
| Number of bed-days, mean (SD) | 5.3 (4.8) | 4.2 (5.8) | 20.8 (33.0) | 6.1 (5.1) |
| Medical ICU/HDU | ||||
| Yes (n) | 2 | 1 | 0 | 0 |
| Yes (%) | 2 | 1 | 0 | 0 |
| For those with an admission | ||||
| Number of admissions, mean (SD) | 1 (0.0) | 2 | ||
| Number of bed-days, mean (SD) | 4.5 (2.1) | 4 | ||
| Physical-health-related A&E attendance | ||||
| Yes (n) | 20 | 31 | 9 | 22 |
| Yes (%) | 19 | 23 | 11 | 21 |
| For those who used the service | ||||
| Mean | 1.6 | 1.8 | 1.3 | 1.6 |
| SD | 1.0 | 1.5 | 0.7 | 2.0 |
| Mental-health-related A&E attendance | ||||
| Yes (n) | 3 | 1 | 2 | 1 |
| Yes (%) | 3 | 1 | 3 | 1 |
| For those who used the service | ||||
| Mean | 7 | 75.5 | 1 | |
| SD | 1.4 | 105.4 | ||
| Psychiatric outpatient appointment | ||||
| Yes (n) | 28 | 43 | 3 | 8 |
| Yes (%) | 26 | 32 | 4 | 7 |
| For those who used the service | ||||
| Mean | 1.7 | 1.7 | 1 | 1.25 |
| SD | 1.0 | 1.0 | 0.0 | 0.5 |
| Day patient procedure | ||||
| Yes (n) | 13 | 40 | 16 | 27 |
| Yes (%) | 12 | 29 | 20 | 26 |
| For those who used the service | ||||
| Mean | 2.1 | 1.6 | 1.8 | 1.3 |
| SD | 1.3 | 0.8 | 1.6 | 0.8 |
| Medical outpatient appointment | ||||
| Yes (n) | 25 | 36 | 13 | 16 |
| Yes (%) | 23 | 27 | 16 | 15 |
| For those who used the service | ||||
| Mean | 2.4 | 2.2 | 1.5 | 1.4 |
| SD | 2.7 | 3.0 | 0.9 | 0.8 |
| Costs (£) | Time point | Difference | Baseline-adjusted difference | 95% CI | |||
|---|---|---|---|---|---|---|---|
| Baseline | 36 months | ||||||
| Intervention arm | Control arm | Intervention arm | Control arm | ||||
| Community costs | 1175 | 988 | 559 | 635 | –76 | –80 | –276 to 115 |
| Mental health: secondary care | 48 | 94 | 343 | 47 | 296 | 309 | –256 to 874 |
| Physical health: secondary care | 369 | 610 | 638 | 418 | 220 | 275 | –204 to 756 |
| Total health and social care costs excluding medication | 1592 | 1692 | 1540 | 1100 | 440 | 501 | –270 to 1274 |
| Voluntary | 43 | 21 | 0 | 0 | 0 | 0 | 0 to 0 |
| Private and out of pocket | 345 | 539 | 672 | 1377 | –705 | –682 | –1669 to 304 |
| Accommodation | 24,469 | 19,217 | 25,714 | 21,705 | 4009 | 0 | –2002 to 2002 |
| Criminal justice | 170 | 88 | 27 | 31 | –4 | –17 | –59 to 25 |
| Unpaid/family carers | 13,815 | 22,821 | 10,180 | 28,796 | –18,616 | –6294 | –16,217 to 3628 |
| Total societal costs | 41,398 | 43,856 | 38,133 | 45,280 | –7147 | –4874 | –14,485 to 4736 |
Appendix 8 External assessment of plan quality
| Therapist | Component | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | K | L | ||
| 1 | 1 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 8 |
| 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 5 | |
| 1 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 9 | |
| 0 | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 7 | |
| 1 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 9 | |
| 2 | 0 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 9 |
| 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | |
| 3 | 1 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 10 |
| 4 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 3 |
| 2 | 2 | 2 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 9 | |
| 5 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 |
| 6 | 2 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 11 |
| 1 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 10 | |
| 1 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | |
| 7 | 1 | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 8 |
| 8 | 1 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 6 |
| 9 | 1 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 11 |
| 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 4 | |
| 1 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 9 | |
| 10 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 12 |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 11 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 6 |
| 1 | 2 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 6 | |
| 1 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 11 | |
| 0 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 10 | |
| 12 | 1 | 1 | 1 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 7 |
| 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 12 | |
| 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 12 | |
| 13 | 1 | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 8 |
| 14 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 11 |
| 15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 |
| 17 | 2 | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 8 |
Appendix 9 Topic guides for qualitative interviews
Images in this appendix made with Photosymbols, with permission from Photosymbols Ltd.
Appendix 10 Client Service Receipt Inventory104 modified for the Positive Behaviour Support study
List of abbreviations
- ABC-C
- Aberrant Behaviour Checklist – Community
- ABC-CT
- Aberrant Behaviour Checklist – Community total score
- ABS
- Adaptive Behaviour Scale
- ASD
- autism spectrum disorder
- BBAT
- Brief Behavioural Assessment Tool
- BIP-QE II
- Behaviour Intervention Plan Quality Evaluation Scoring Guide II
- CDS-ID
- Caregiving Difficulty Scale – Intellectual Disability
- CEAC
- cost-effectiveness acceptability curve
- CEP
- cost-effectiveness plane
- CI
- confidence interval
- CMD
- common mental disorder
- CSO
- clinical studies officer
- CSRI
- Client Service Receipt Inventory
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-Y
- EuroQol-5 Dimensions Youth
- GBP
- Great British pounds
- GCPLA
- Guernsey Community Participation and Leisure Activities Scale
- GHQ-12
- General Health Questionnaire – 12 items
- GP
- general practitioner
- ICC
- intracluster correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- ID
- intellectual disability
- IQR
- interquartile range
- Mini PAS-ADD
- Mini Psychiatric Assessment Schedules for Adults with Developmental Disabilities
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PBS
- Positive Behaviour Support
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- RA
- research assistant
- RCT
- randomised controlled trial
- SAE
- serious adverse event
- SD
- standard deviation
- SDV
- source data verification
- SMI
- severe mental illness
- SURGE
- Speaking Up Rights Group Experts
- TAU
- treatment as usual
- TSC
- Trial Steering Committee
- UCL
- University College London
- WASI
- Wechsler Abbreviated Scale of Intelligence
