Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 12/138/02. The contractual start date was in June 2014. The draft report began editorial review in October 2016 and was accepted for publication in June 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Fiona Burns reports grants from the National Institute for Health Research (NIHR) for other projects during the conduct of the study, and personal fees and other from Gilead Sciences Ltd (London, UK), outside the submitted work. Rachael Hunter reports grants from the NIHR Health Technology Assessment (HTA) programme for other projects, during the conduct of the study. Ibidun Fakoya reports a grant from NIHR for another project, during the conduct of the study. Eleni Nastouli reports personal fees from Roche (Burgess Hill, UK), grants from Viiv Healthcare (London, UK), grants from the European Union (H2020) and personal fees from NIHR, outside the submitted work. Lisa McDaid reports grants from the NIHR HTA programme for other projects, during the conduct of the study. Jane Anderson reports grants and personal fees from Gilead Sciences Ltd, and personal fees from ViiV Healthcare, Merck Sharp & Dohme Limited (Hoddesdon, UK), Bristol-Myers Squibb (Uxbridge, UK), Jansen-Cilag Limited (High Wycombe, UK) and AbbVie (Maidenhead, UK), outside the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Seguin et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
HIV in the UK
Since 2003, more people have been living with heterosexually acquired human immunodeficiency virus (HIV) in the UK than those with HIV acquired via sex between men. Black Africans account for 55% of people with heterosexually acquired HIV and 2% of new HIV diagnoses in men who have sex with men (MSM); thus, people of black African ethnicity account for almost one-third of the 103,000 (95% credible interval 97,500 to 112,700) adults estimated to have HIV in the UK. 1 This equates to nearly four out of every 100 black African people being HIV positive. 2
Effective antiviral therapy means that HIV incidence is likely to be driven by the fraction of undiagnosed people living with HIV, and most HIV-related morbidity and mortality is increasingly associated with diagnosis at a late stage of infection [as defined by a cluster of differentiation 4 (CD4) white cell count of < 350 cells/mm3]. 2–4 Black African people in the UK are more likely to present to HIV services with an advanced infection than people in other ethnic groups. 5,6
Late diagnosis is associated with a 10-fold increased risk of death in the first year post diagnosis, when compared with people who are diagnosed with less advanced infection. 2 Late diagnosis also implies that a person has been living with undiagnosed HIV for a substantial period of time, which increases the risk of HIV transmission to other people. Reducing the incidence of late presentation to HIV services is the single most useful way of decreasing the ill health and death associated with HIV, and reducing late diagnosis is the only HIV-specific indicator within the 2013–16 Department of Health Public Health Outcomes Framework. 7 HIV prevention efforts have increasingly focused on increasing opportunities for people to have a HIV test, which reduces both the incidence of late presentation and undiagnosed HIV infection. The Joint United Nations Programme on HIV and AIDS (UNAIDS) has set a global target of 90% of people living with HIV to be aware of their diagnosis by 2020; increasing the uptake of HIV testing is the only means by which this can be achieved. 8
HIV testing among black African communities in the UK
HIV testing in the UK is predominantly offered at sexual health clinics. Black African people are less likely to use these services than other higher-risk communities. 1 General practice (GP) is accessed by this population, but opportunities for earlier HIV diagnosis are often missed. 9 Black African men in particular have high rates of undiagnosed infection and late presentation,10 in part because they have less contact with health services than women. In addition, concerns regarding confidentiality,11,12 stigma and discrimination11–13 and fear of a HIV-positive status14 present barriers to effective testing initiatives. These obstacles are compounded by structural issues that discourage access to HIV prevention, diagnostic and treatment services, such as poverty, unemployment and lack of child care,11 the reticence of non-specialist health staff to offer HIV testing,15 a lack of political will to recognise the pervasive health inequalities faced by many migrants16 and a lack of African representatives in decision-making processes. 14 Despite these obstacles, there is evidence to suggest that many black African people will test for HIV if provided the opportunity. 10,17
At a population level, no single intervention is likely to control HIV. However, HIV testing is the starting point from which to build effective strategies. A negative test result can support individual vigilance to remain uninfected. For those who test positive for HIV, the test result opens treatment and prevention options. Timely diagnosis and treatment means that those affected can expect near-normal life expectancy. 18
Owing to the challenges associated with traditional HIV testing options for black African people, innovative methods to increase the uptake and opportunities for testing among this population are required. Interventions should extend testing opportunities and directly address the barriers that foster late and undiagnosed infection. Such interventions could incorporate developments in testing technology that reduce the need to attend specialist services [e.g. use of self-sampling or self-testing kits (STKs)] or target testing interventions to specific populations (e.g. considering the psychosocial and sociocultural contexts of target populations, such as black African communities, rather than the general population). These interventions must also address the barriers that exist at a service provider level. Interventions need to be time and cost efficient, easy to use and deliver, and supported by robust clinical pathways.
Self-sampling kits
The range of HIV testing options continues to expand, with community-based point-of-care testing (POCT) and blood and oral self-sampling kits (SSKs) increasingly available. 19 In addition, HIV STKs are now licensed for use in the UK. Self-sampling negates the need for dedicated staff or special infrastructure for specimen collection, and can be used at a time and in a setting of the user’s choice. SSKs, accessed via clinical settings and online, have been shown to be an acceptable and feasible alternative to clinic attendance for HIV testing, and may increase the uptake of testing among hard-to-reach MSM. 20–22 Testers have shown an overall preference for oral-based sampling rather than blood-based sampling, especially among first-time testers. 23 Research among young men in the UK has also demonstrated the acceptability of SSKs for HIV testing, with health-care settings being the preferred venue for accessing kits. 24
Despite the burgeoning research base focused on SSKs, there is little evidence to support the acceptability or feasibility of using SSKs to increase the uptake of HIV testing among black African people in the UK. A pilot study, initiated by the Terrence Higgins Trust/HIV Prevention England and Dean Street at Home, has documented success in reaching black African people through internet-based SSK distribution. 25 Though the study had greater success in uptake among MSM than black African people of all sexualities, it found that 9.8% of the 7761 kits were requested by black African people and 7.3% of those were returned, with a positivity rate of 2.6%.
Embedding SSKs within existing health services (including health promotion initiatives and NHS screening) may facilitate the uptake of HIV testing. A cross-sectional study undertaken among black African people in England revealed that nearly one-third of participants without diagnosed HIV said that they would prefer to have a future HIV test at their GP surgery. 26 This may indicate the acceptability of offering SSKs via existing primary care venues. However, a lack of evidence persists regarding testing preferences by ethnicity, gender and age.
In 2012, the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme released a commissioned call (12/138) driven by the following research question: ‘what is the feasibility and acceptability of interventions to overcome individual and health-care professional barriers to the provision and uptake of HIV testing in black African adults in the UK?’.
The hypothesis behind the following research was that embedding SSKs for HIV testing in existing services is an acceptable and feasible means to increase the provision and uptake of HIV testing among black African people residing in the UK.
Aims
The overall aims of our research were to:
-
develop a SSK-based intervention to increase the provision and uptake of HIV testing among black African people using existing community and health-care provision (stage 1 of the project)
-
conduct an evaluation of selected SSK distribution models to assess feasibility and optimal trial design for a future Phase III evaluation (stage 2 of the project).
To answer the research question, the following objectives and outcomes were established.
Objectives
Stage 1
-
Examine/evaluate barriers to, and facilitators of, provision, access and use of HIV SSKs by black African people, in primary care, pharmacies and community outreach settings.
-
Determine appropriate SSK-based intervention models for different settings.
-
Determine robust HIV result management pathways.
-
Develop an intervention manual to enable intervention delivery.
Stage 2
-
Determine the feasibility and acceptability of a provider-initiated, HIV SSK distribution intervention targeted at black African people in two settings:
-
GP surgeries
-
community-based organisations (CBOs).
-
Secondary objectives
-
Establish the acceptability of interventions for service providers and service users.
-
Evaluate the clinical effectiveness of self-sampling for HIV in increasing the uptake of HIV testing by black African people.
-
Determine the cost-effectiveness of distributing SSKs among black African people compared with other screening methods.
-
Monitor the ability to trace participants with reactive results, confirmatory testing and linkage into specialist care.
-
Determine the cost per kit distributed and cost per HIV diagnosis per setting.
-
Assess the feasibility of collecting data for a lifetime cost-effectiveness model.
-
Assess the feasibility and, if appropriate, the optimal trial design (including sample size parameters) for a future Phase III evaluation.
Outcomes
Primary outcome
HIV SSK return rate.
Secondary outcomes
Point-of-delivery outcomes:
-
acceptability of the targeted HIV SSK distribution
-
acceptability and feasibility of the targeted SSK distribution among specified service providers.
Data collection outcomes:
-
ability to record the number of people offered SSKs, accepting SSKs and returning SSKs
-
feasibility of collecting correct contact details enabling follow-up, reminders and communication of results.
Pathway-to-care outcomes:
-
proportion of those whose samples are reactive, who –
-
are informed of the results in person
-
attend for confirmatory testing at a NHS setting of their choice.
-
Overarching outcomes:
-
cost per kit distributed and cost per HIV diagnosis per setting
-
attrition rates
-
confirmatory testing, proportion of those receiving a HIV-positive diagnosis and clinical stage at diagnosis
-
feasibility and sensitivity of outcome measures (testing, behavioural and economic) for a definitive trial.
Structure of the report
The report is structured in accordance with the aims and objectives of stages 1 and 2 of the study. Chapters 2–5 address the objectives of stage 1, and Chapters 6–10 address the objectives for stage 2, with the discussion and conclusions in Chapter 11.
Chapter 2 Study design and methodology of stage 1
To develop a SSK-based intervention to increase the provision and uptake of HIV testing among black African people, using existing community and health-care provisions, we first needed to address the following objectives:
-
examine/evaluate barriers to, and facilitators of, provision, access and use of HIV SSKs by black African people in primary care, pharmacies and community outreach
-
determine appropriate SSK-based intervention models for different settings
-
determine robust HIV result management pathways
-
develop an intervention manual to enable intervention delivery.
The objectives were met via the following three main research activities:
-
Conducting a systematic literature and policy review exploring the feasibility and acceptability of self-sampling for HIV testing, and the clinical effectiveness of self-sampling for HIV in increasing the uptake of HIV testing (see Chapter 3).
-
Conducting focus group discussions (FGDs) with non-specialists and service providers, and one-to-one interviews with the latter to gain stakeholder input into the development of an acceptable SSK distribution pathway and protocol via community-based health and HIV prevention services already accessed by black African people (see Chapter 4).
-
Developing an intervention manual for the feasibility trial in stage 2, drawing on theoretical frameworks and findings from the first two research activities (see Chapter 5).
The remainder of this chapter focuses on the methodological and analytical approaches to the literature review; qualitative data collected through FGDs and one-to-one interviews; and the intervention manual development.
Methodology of the systematic literature review
Search strategy and identification of studies
Ten electronic databases were searched using detailed search strategies:
-
OvidSP MEDLINE
-
OvidSP EMBASE Classic and EMBASE
-
OvidSP Global Health
-
OvidSP Social Policy and Practice
-
OvidSP PsycINFO
-
OvidSP Health Management Information Consortium
-
EBSCOhost Cumulative Index to Nursing and Allied Health Literature Plus with Full Text
-
The Cochrane Library
-
Web of Science Core Collection
-
Scopus.
The search strategy used for OvidSP MEDLINE is provided in Appendix 1.
Only studies written in English were included. The results were downloaded into a deduplicated database in EndNote 7 [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA]. The initial search was undertaken on 26 September 2014. Two further searches to update the database were undertaken on 17 April 2015 and 3 May 2016. Additional grey literature was retrieved from websites operated by the following organisations:
-
Avert (www.avert.org)
-
Terrence Higgins Trust (www.tht.org.uk)
-
National AIDS Trust (www.nat.org.uk)
-
Lambeth Council (www.lambeth.gov.uk/consultations/lambeth-southwark-lewisham-sexual-health-strategy-consultation)
-
Naz Project London (http://naz.org.uk)
-
Sexual Health Sheffield (www.sexualhealthsheffield.nhs.uk).
Inclusion and exclusion criteria
Only studies published since 1 January 2000 were included, as studies published earlier would be unlikely to reflect current technology or attitudes to HIV testing. Only studies conducted in the European Union/European Free Trade Agreement countries, North America, New Zealand or Australia were included, as studies conducted in other locations (particularly resource-poor settings) would probably have markedly different contexts and, thus, their results would not be applicable to the UK. Study populations that included lay groups, as well as health professionals, were included. Only studies that examined home/self-sampling tests for HIV were included as intervention studies. Studies without comparators were also included, as well as studies that compared home/self-sampling tests for HIV with routine service provision or other HIV testing interventions. Studies were included if they reported on any of the following outcomes:
-
increase/decrease in the number of HIV tests
-
proportion/number of confirmatory tests
-
proportion/number of participants linked into care
-
adverse events associated with HIV self-sampling
-
proportion/number of false positives or failed tests
-
increase/decrease in the reported history and frequency of taking HIV tests
-
increase/decrease in the number and types of venue where HIV testing is offered.
Qualitative studies were included only if they reported one or both of the following:
-
barriers to, or facilitators of, self-sampling reported by the general population
-
barriers to, or facilitators of, self-sampling reported by service providers.
The following study designs were considered for inclusion:
-
randomised or non-randomised controlled trials
-
prospective or retrospective cohorts
-
cross-sectional studies/prevalence studies
-
pilot or feasibility studies
-
qualitative studies (using in-depth interviews, FGDs and document analysis).
Studies that examined the use of, or views about, self-sampling for HIV in health-care workers were excluded, because the review focus was on uptake among testers, not service providers, as were all conference communications, because of insufficient detail and lack of peer review. Studies that focused solely on, or the outcomes of which were predominantly about, self-testing for HIV were also excluded at the study selection stage.
Study selection
Studies were selected using a two-stage screening approach. Reviewers Ibidun Fakoya and Esther Mugweni devised a checklist to independently screen titles and abstracts (see Appendix 1). When a consensus could not be reached about study inclusion, a third reviewer (FB) was consulted. Full-paper copies of the selected studies were screened and assessed independently by Ibidun Fakoya and Esther Mugweni, using a screening tool (see Appendix 1). Updated searches were screened using the same approach by Caroline Park, Thomas Hartney and Lisa McDaid. Inter-reviewer reliability scores of the different stages of the review were calculated using kappa in Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA). The full-paper screening achieved a kappa score of 1.0, which indicates a high level of agreement between reviewers.
Data extraction, analysis and synthesis
Structured data extraction tools were developed to capture the required information from the included papers on study types, populations, SSK interventions and acceptability, feasibility and efficacy outcomes. Data were extracted by Caroline Park and checked by Thomas Hartney.
A meta-analysis was not conducted, as a result of the heterogeneity of the designs, methods, samples and outcomes of the included studies. There are a number of narrative approaches to data synthesis, including integrative synthesis, to primarily combine and summarise data, and interpretative synthesis that aims to generate new concepts and theory. 27 An integrative approach to summarising and presenting the data was appropriate to this review. The narrative synthesis is supported by tables in Results of the systematic literature review, which outline the key characteristics and findings of each included study, as relevant to the research questions. To reduce the risk of bias, the extracted data were first summarised by Lisa McDaid and then reviewed by Thomas Hartney. Disagreements in interpretation were resolved through discussion between the two authors.
Quality appraisal
The quality of the eligible papers was appraised by Thomas Hartney using the National Institute for Health and Care Excellence (NICE) quality appraisal checklist for quantitative papers. 28 Each quantitative paper was assigned a score for internal and external validity, from ++ (high quality) to – (poor quality). Each qualitative paper was assigned a single overall score. The appraisal process was validated by a second researcher (Lisa McDaid) assessing a sample of papers with a high level of agreement reached. Any papers that did not present self-sampling data separately from other forms of testing were excluded, but papers were not excluded on the basis of quality.
Methodology of focus group discussions and one-to-one interviews
Qualitative research methods were used to collect data using FGDs and one-to-one interviews in late 2014. Ethics approval was obtained from the University College London (UCL) Research Ethics Committee [REC; project identification (ID) number 3321/001].
The study team conducted 12 FGDs, a method which was selected to maximise the extent of interaction between research participants in order to establish group similarities, as well as differences, by encouraging discussion, exchange and justification of divergent viewpoints. 29 Six of these groups were conducted with non-specialist members of the public who identified as black African and six were conducted with professionally, culturally and ethnically diverse people who provide HIV and other social services to black African people. From the latter group, nine participants also participated in one-to-one interviews, a choice that was made primarily to enable interviewers to tailor the topic guide in ways that would help to best capture the specific world view of these expert interviewees. 30
Topic guides for the non-specialist and service provider FGDs (see Appendices 1 and 2, respectively) were developed in consultation with members of the steering group and study team. The topic guide for the one-to-one interviews was adapted from that for service provider FGDs. These guides structured flexible discussions about participant views towards SSKs, community trust of SSKs, the practicalities and rationales for selecting potential community settings outside sexual health clinics, mechanisms for returning the sample, and communicating and confirming results to users, and the content of SSK packs. Group facilitators and interviewers sought to create a balance between the a priori issues outlined above, while also harnessing participant-led articulation of perspectives, social norms and discourses.
During the FGDs, participants were shown a video made by the producers of the TINY vial SSK (www.tdlpathology.com/test-information/test-service-updates/tdl-tinies). In a number of groups, participants were also shown an instructional video developed by a community organisation (www.youtube.com/watch?v=FSm0zP1TGUo) on self-use of dried blood spot sampling kits. TINY vial SSKs were displayed, distributed and discussed in all groups. As it was known that the use of an oral fluid kit was not possible within the context of the HAUS study, no oral-based kit was demonstrated during the groups. However, these kits were discussed by participants.
Participatory methods, such as ranking activities, were used to enhance data collection and participant engagement during FGDs. 29 The study team members who collected qualitative data in this stage were Catherine Dodds, Esther Mugweni, Sonali Wayal, Caroline Park, Gemma Philips and Ingrid Young. Catherine Dodds, Sonali Wayal and Ingrid Young already possessed extensive training and experience in this format of data collection in the HIV field among specialist service providers and non-specialists alike, and Catherine Dodds and Ingrid Young in particular were responsible for training and overseeing the research development of Esther Mugweni, Gemma Philips and Caroline Park. All FGDs were initially led by those with the greatest experience and ‘seconded’ by Esther Mugweni, Gemma Philips and Caroline Park, and, over time, these roles started to switch as the last group gained familiarity and experience with the method and the research tools being used. Two researchers attended every group to better enable data capture (including observation). All those involved in data collection had considerable opportunity to discuss challenges, successes and possible improvements to data collection during fortnightly core team meetings, designed to assist such exchange. Esther Mugweni and Gemma Philips undertook all one-to-one interviews, and each had considerable experience and training in this method.
Non-specialist black African focus group discussions
Participants in the non-specialist FGD included members of the public who self-identified as being black African (n = 48). Three of the FGDs occurred in Greater Glasgow, and three occurred in Greater London. The participants were recruited via social media (n = 1) and African embassies in London (n = 6), as well as university student groups (n = 16), and CBOs (n = 24) in both Glasgow and London (missing data, n = 1). Participants were eligible if they self-identified as being black African and were aged ≥ 18 years. The sample was purposively selected sequentially during recruitment (with some interested individuals being set aside into a ‘pool’ of recruited participants in case they were needed at a latter stage) to ensure diversity of age, region of birth and HIV testing experience. Men were slightly over-represented in the sample, with 28 out of 48 male participants (58%), compared with 20 female participants (42%). The age ranged from 18 to 60 years. Participants were born in various regions of Africa, including East Africa (n = 17), Southern Africa (n = 10), West Africa (n = 10) and Central and North Africa (n = 3), and some were born in the UK, Europe or the USA (n = 7; missing data, n = 1). In order to ensure a balance of voices, one of the FGDs consisted only of people aged < 30 years (in London), another group consisted of men only (in London) and a further group consisted of people living with diagnosed HIV (in Glasgow). The other three FGDs were mixed in terms of participant gender, age and HIV testing experience (London and Glasgow). Nineteen participants had never tested for HIV. The black African non-specialist FGD participants were compensated £25 for participating in the discussion. Each FGD lasted between 1.5 and 2 hours, with an average of nine participants in each group (range of 7–11 participants). The FGDs were audio-recorded and transcribed verbatim.
Service provider focus group discussions and interviews
Six FGDs were conducted with service providers: three in Glasgow and three in London. Sequential purposive sampling (undertaken with the support of simple screening questions asked during the recruitment process) ensured the diversity of service providers from a range of professional backgrounds, all of whom provided HIV-related or other social services to black African people. Black African ethnicity was not a criterion for involvement in these FGDs. GPs were recruited via Clinical Research Networks (CRNs) in London and through established working relationships with members of the research team in both Glasgow and London. Community workers in both cities were recruited from organisations with extensive experience of delivering HIV prevention and care, as well as a range of other non-HIV-specific services to black African people. The research team approached pharmacies in areas with high numbers of African residents in Glasgow and London, with support from local pharmacy associations. Almost all specialist FGDs comprised those from diverse working backgrounds, in order to elicit contrasts within working and experiential contexts.
In total, 53 service providers participated in either a FGD or a supplementary interview. Those taking part in FGDs included HIV CBO staff (n = 15), pharmacists and pharmacy assistants (n = 9), general practitioners (n = 7), those who provided services to black African people (non-HIV focused) (n = 5), GP and specialist nurses (n = 3), African faith leaders (n = 3) and a health-care assistant (HCA; n = 1). The service provider FGD participants were offered reimbursement for their travel and their time given to the study. The level of reimbursement varied according to profession. The service provider FGDs lasted between 1.5 and 2 hours, with an average of seven participants in each group (range of 4–10 participants). These sizes fell within the ideal range to prompt discussion, while ensuring the participation of everyone in the group. 30
Following the FGDs, interviews with 10 highly specialised HIV service providers (including HIV clinicians, HIV service managers and service commissioners) in London (n = 3) and Glasgow (n = 7) were conducted to help check the acceptability of the intervention and procedures. This approach was undertaken to include diversity of voice in FGDs, accompanied by highly specialised expertise gained through interviews. Each interview lasted between 30 and 45 minutes. The FGDs and interviews were audio-recorded and transcribed verbatim.
Analysis of focus group discussions and interviews
An analysis of the qualitative data was undertaken using a ‘blended’ thematic approach drawing heavily on framework analysis. 31 NVivo version 10 (QSR International, Warrington, UK) was used to synthesise and code data within a thematic matrix to enable elucidation of conceptual associations. Both a priori concepts used in the development of the FGD topic guide, as well as emergent concepts arising from the data, informed the process of identifying the key thematic categories used in data coding. Two researchers devised an agreed coding frame, which was then used to index and chart the findings. The integrated model of behavioural prediction and change was used as the theoretical framework to assess attitudes, willingness and perceived behavioural control to use HIV SSKs. 32
Broad descriptive themes included the feasibility and accessibility of HIV testing, and existing knowledge and uptake of SSKs, and the practicalities of distribution emerged. Cross-cutting themes also surfaced, which influenced our analysis, particularly those concerned with trust and HIV-related stigma. The themes were then refined to devise a more detailed participant-led, inductive, thematic framework. Researcher team discussions and iterative analysis focused on the internal coherence and face validity of the resulting analytic structure.
Methodology and analytic approach of intervention development
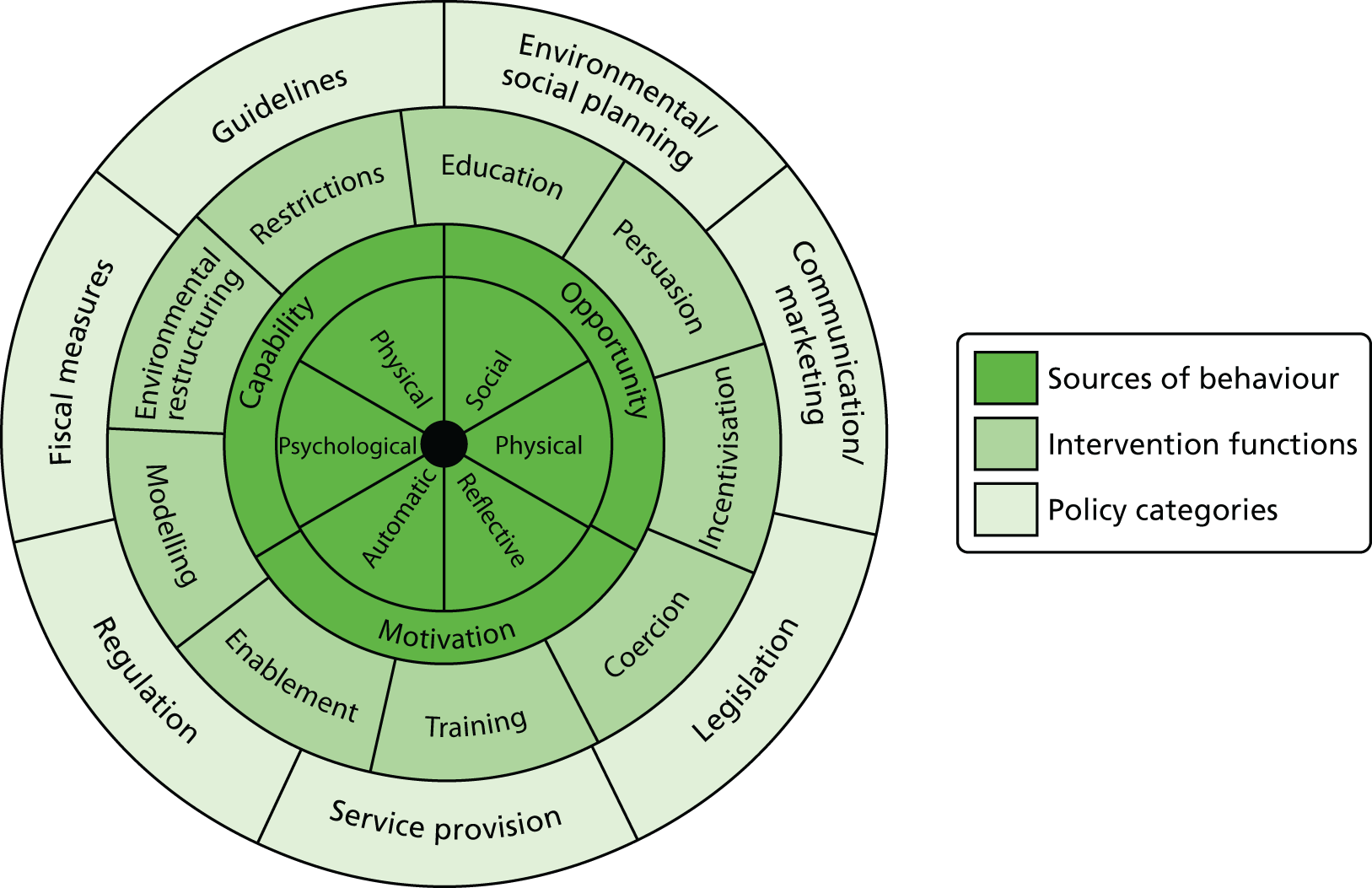
At the outset, it was recognised by the study team that successful interventions to increase the uptake of HIV testing are particularly challenging, as a result of the sexual transmission aspect and stigma associated with HIV, the latter being particularly prevalent among African communities in the UK. To mitigate the complexity inherent in developing and implementing a HIV SSK intervention, a systematic four-step approach to intervention development was adopted, drawing on the behaviour change wheel33 (Figure 1).
FIGURE 1.
The behaviour change wheel. Reproduced from Michie et al. 33 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Step 1: delineate key intervention components
The intervention development process began with identifying and conceptualising the diverse intervention components arising from a combination of existing SSK distribution practice and process-oriented data emerging from stage 1. The research team considered the sequential flow across social contexts, health professionals, SSK recipients and clinical governance procedures. In this way, the study team systematically considered the segmentation and flow of the intervention chain. This conceptual work also assisted in informing the topic guides for follow-up interviews with participants who agreed to take a SSK (regardless of whether or not they ultimately used it; see Appendix 4) and the choice of analytical approach for the intervention development work that followed.
Step 2: intervention barriers and facilitators, and relation to theoretical domains
Step 2 involved further consideration of the key intervention components identified in step 1 by utilising stage 1 data on barriers to, and facilitators of, the intervention. Appendix 5 provides an example of how the study team analysed the relevant data regarding the component ‘appearance and packaging of the HIV SSK’. Key barriers and facilitators were then mapped onto the theoretical domains framework (TDF). 34
The TDF is a metatheoretical framework that integrates key theoretical domains known to be important in understanding behaviour change across a range of populations. It provides a coherent way of organising explanations of why things do or do not happen in relation to either behaviour change or the implementation of particular intervention components. It enables insights into potential mechanisms of action for developing or optimising interventions. Table 1 illustrates the key domains of the TDF and provides a brief explanation of the content to which the particular domain refers.
| Domains | Explanatory statement of the domain |
|---|---|
| Knowledge | An awareness of the existence of something |
| Skills | Ability or proficiency acquired through practice |
| Professional roles/identity | Coherent set of behaviours and personal qualities of an individual in a work setting |
| Beliefs about capabilities | Acceptance of the truth or validity of an ability that a person can put to constructive use |
| Optimism | Confidence that things will happen for the best or that desired goals will be obtained |
| Beliefs about consequences | Acceptance of the truth or validity about the outcomes of a behaviour |
| Reinforcement | Increasing the probability of a response by arranging a dependent relationship between the response and a contingency |
| Intentions | Conscious decisions to perform a behaviour or act in a certain way |
| Motivation and goals | Representation of the outcome that an individual wants to achieve |
| Memory and decision processes | Ability to retain information, focus selectively and choose between two or more alternatives |
| Environmental context and resources | Any circumstances of a situation or environment that discourage/encourage development of skills, abilities and competencies |
| Social influences (norms) | Interpersonal processes that can cause individuals to change their thoughts, feelings or behaviours |
| Emotions | Complex reaction pattern, involving experiential, behavioural and physiological elements |
| Behavioural regulation | Anything aimed at managing or changing objectively observed or measured actions |
Analysis and the mapping of barriers to, and facilitators of, the TDF domains were discussed within a single all-day event attended by the research team. Differences of opinion were resolved through consensus.
Step 3: identifying intervention components that could overcome barriers and enhance facilitators
In step 3, an ideal hypothetical intervention that minimised key barriers and amplified key facilitators was constructed. The behaviour change wheel33 was then used to structure the intended intervention, guided by the ideal intervention.
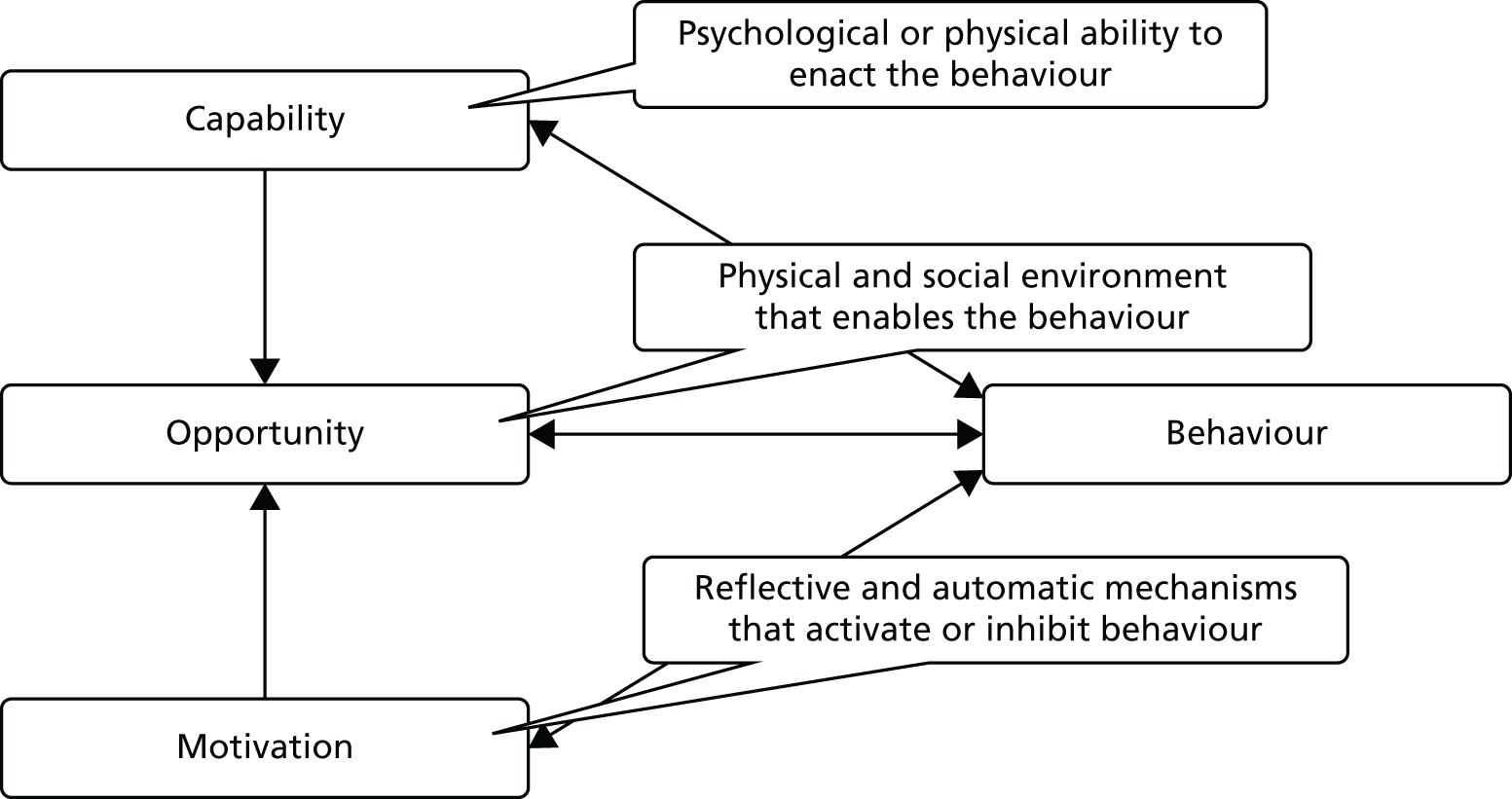
The behaviour change wheel33 links the domains of the TDF to the COM-B (capability, opportunity, motivation and behaviour) model of behaviour change36 (Figure 2). The COM-B model suggests that behaviour change is related to three key factors: (1) capability, (2) opportunity and (3) motivation. These three factors can be broken down into fine-tuned categories and, eventually, the TDF domains. Table 2 shows how the TDF domains relate to each COM-B component.
FIGURE 2.
The COM-B model. Adapted from Michie et al. 33 This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
| COM-B component | TDF domain |
|---|---|
| Capability | |
| Psychological | Knowledge |
| Cognitive and interpersonal skills | |
| Memory, attention and decision processes | |
| Behaviour regulation | |
| Physical | Skills |
| Opportunity | |
| Social | Social influences (norms) |
| Physical | Environmental context and resources |
| Motivation | |
| Reflective | Professional roles/identity |
| Beliefs about capabilities | |
| Optimism | |
| Beliefs about consequences | |
| Motivation and goals | |
| Intentions | |
| Automatic | Reinforcement |
| Emotions | |
Step 4: viability of the intervention
The outcome of step 3 provided a range of potential ways in which the intervention could be structured that would reflect key mechanisms of action and reduce barriers to effective implementation. However, it was important to ensure that the resulting intervention was viable within busy service delivery contexts. Thus, the study team evaluated the intervention content with the APEASE (affordability, practicability, effectiveness and cost-effectiveness, acceptability, site-effects/safety and equity) criteria,32 assessing the viability of intervention function and behaviour change techniques for a real-world intervention implementable within the UK.
Summary of stage 1 methods
This chapter has described and provided a rationale for each of the activities undertaken to meet the key objectives for this stage of the project, namely to:
-
review the available literature on SSKs with regard to the feasibility, acceptability and clinical effectiveness of this technology at increasing the uptake of HIV testing
-
gain insight from experts and non-experts into the best means of targeted distribution of SSKs for the benefit of black African people in the UK, as well as their perspective on kit use and functionality; and
-
convert these insights using a systematic four-step approach to intervention development, drawing on the behaviour change wheel. 33
Strengths and limitations
Although limited in scope and scale, the range of methods used in stage 1 enabled the team to select a mix of data sources and analytical approaches in its systematic, theoretically driven approach to intervention development.
Findings of the formative stage 1 FGDs and interviews with specialist service providers and non-specialist members of the public, and the ensuing intervention development process, are presented in Chapters 4 and 5, respectively. The next chapter presents the methodology and results from the policy and systematic literature review.
Chapter 3 Systematic policy and literature review
A systematic literature and policy review exploring the feasibility and acceptability of self-sampling for HIV testing, and the clinical effectiveness of HIV self-sampling in increasing the uptake of HIV testing, was conducted. The overall purpose of this exercise was to address the first three objectives of stage 1: (1) to clarify barriers to, and facilitators of, provision, access and use of HIV SSKs by black African people, in primary care, pharmacies and community outreach; (2) to determine appropriate SSK-based intervention models for different settings; and (3) to determine robust HIV result management pathways. This review also informs the fourth objective, to develop an intervention manual to enable intervention delivery. This chapter contains the methodology and results of the policy and systematic literature review.
The systematic review was registered as PROSPERO CRD42014010698.
Policy review
A policy review was conducted with the aim of summarising current approaches to, and policies/protocols around, the use of SSKs for the detection of HIV in the UK to add context to, and inform the development of, the HAUS SSK intervention manual. Eleven policy statements, clinical guidelines, reports and strategies that contained programmatic or clinical guidance on HIV self-sampling or on HIV testing in the UK or specific guidance on HIV testing for black African people in the UK, published between January 2008 and July 2016, were included (see Appendix 6). In the section below, we provide an overview of the policy approaches and recommendations relevant to SSKs.
Policy approaches and recommendations relevant to self-sampling kits
Most of the policy guidance documents yielded by this search were not specific to SSKs. The UK National HIV testing guidelines were produced by the British HIV Association (BHIVA), the British Association of Sexual Health and HIV (BASHH) and the British Infection Society in 2008, against the background of late HIV diagnosis and undiagnosed HIV status in the UK. 37 The guidelines advocated for the expansion of HIV testing services, including routine offering of HIV testing in GPs, in areas where the prevalence is higher than two per 1000 among 16- to 59-year-olds, to patients attending specified services, such as sexual health clinics or pregnancy termination services, and to patients who report practising high-risk behaviour and patients with indicator conditions. 37 Implementation of these guidelines was assessed using eight pilot projects in acute medical settings, emergency departments, primary care and community settings. 38 Findings from the pilot projects showed that the implementation of guidelines to expand HIV testing in the medical and community settings was both feasible and acceptable; HIV SSKs were successfully used in one of the pilot projects. A later review by Public Health England (PHE) on the evidence of the clinical effectiveness of HIV testing in medical and community settings noted that self-sampling could broaden the available testing options. 39 Other strategies have advocated for self-testing as an alternative option. 40 Indeed, the national response to HIV continues to evolve and, in April 2014, HIV STKs became legal in the UK. 41,42
With regard to policy specific to the black African community, NICE published specific guidance on increasing the uptake of HIV testing among black African people in 2011. 43 In 2014, NICE provided detailed recommendations for commissioners, including local authorities, Clinical Commissioning Groups and NHS England, on delivering HIV testing services. 44 NICE recommended that commissioners assess the local need for HIV testing for black African people and then develop a local HIV testing strategy with clear referral pathways, particularly for outreach point-of-care services. To address undiagnosed HIV and late diagnosis of HIV, NICE recommended that commissioners promote HIV testing, including through the use of modern HIV tests, and reduce barriers to HIV testing among black African people. In line with the 2008 guidelines mentioned above,37 NICE recommended that HIV testing should be offered by health professionals in primary and secondary care. Although SSKs were not specifically mentioned in these guidelines, SSKs have been commissioned by some local authorities as part of their HIV testing services. The NICE guidelines were updated in December 2016 and SSKs were considered a potentially innovative way of increasing the uptake of HIV testing among black African people, given that these kits may address known barriers to HIV testing in this risk group. 45 In the draft guidelines issued for consultation earlier this year, SSKs and STKs were endorsed as innovative ways of increasing uptake of HIV testing among black African people, given that they may potentially address the known barriers to HIV testing in this group. 45 Despite support within the policy documents for HIV SSKs as a means of increasing uptake of testing, evidence on the impact of SSKs on uptake compared with clinic-based testing was limited to one study.
Results of the systematic literature review
A total of 4052 documents were retrieved, of which 1994 were duplicates. Reviewers identified 85 papers eligible for full-paper screening, with 1973 excluded as they did not meet the inclusion criteria. Seventy-two papers were excluded after full-paper screening as a result of not including SSKs for HIV testing or presenting only combined results with other types of testing (n = 38), inappropriate publication type (n = 26), inappropriate study type (n = 6) or irrelevant country setting (n = 2). Figure 3 contains a flow chart of the study search and selection process. Thirteen studies were selected for inclusion in the literature review.
FIGURE 3.
Flow chart of the study search and selection process.

Description of included studies
Table 3 presents the description of the 13 studies included in the review. 21,46–57 Of the included studies, nine were conducted in the USA21,46,47,50–55 and four were conducted in the UK. 48,49,56,57 Eight were cross-sectional surveys,47,49–55 three were prospective cohort studies,21,48,57 one was a qualitative study56 and one was a randomised controlled trial (RCT). 46 The total sample size across the papers was 15,816, with an average response rate of 78% (range 38–100%; information was not provided in two studies47,57). The majority of the studies included communities at high risk of HIV infection. Ten studies included MSM,21,47–53,56,57 three included people who inject drugs (PWID)46,47,50 and three included non-specified individuals or clinic populations who practised high-risk activities. 21,54,55 Only two studies focused on heterosexual populations who practised high-risk activities (both studies were based in the USA);47,50 all of the UK studies included only MSM. The only RCT in the included studies was conducted with PWID. 46 Most studies reported a predominantly white sample, although the sample in the RCT was 48% African American. 46 Among the studies that provided this information, the average age of participants ranged from 18 to 47 years.
| Study number | First author (year of publication) and reference number | Study design | Study aims | Setting | Population (i.e. clinic, MSM, etc.) | Sample size, n | Response rate, % | Sample characteristics (i.e. age, gender, ethnicity) | Type of HIV testing sample | Method of SSK distribution | Method of return | Quality appraisal score (internal/external)a |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Bartholow (2005)46 | RCT | To compare the likelihood of HIV testing and obtaining test results between participants randomised to:
|
USA | PWID | 489 | 92 | Mean age of 40 years; 71% male; and 48% African American | Dried blood spot | Provided in drug clinic | Post | ++/++ |
| 2 | Colfax et al. (2002)47 | Multiple cross-sectional surveys | An examination of intent to use a SSK, actual use and barriers to use among persons at high risk of HIV | USA | MSM, PWID, heterosexuals at high risk of HIV | 3471 | Not reported | 74% male; and 44% white | Dried blood spot | Purchased (presumably from a pharmacy) | Not specified | +/+ |
| 3 | Fisher et al. (2015)48 | Prospective observational cohort | To determine the uptake of SSKs for HIV and STIs compared with conventional clinic-based testing, and to determine whether or not the availability of SSKs would increase the uptake of STI testing among HIV-infected MSM and those attending a community-based HIV testing service compared with historical controls | UK | MSM | 433 (80 for HIV testing) | 75 | Median age of 33 years; and 84% white British | Oral fluid | By post | Post | +/+ |
| 4 | Formby et al. (2010)49 | Cross-sectional survey | To evaluate the ‘Time 2 Test’ pilot study, which was based on the use of SSKs | UK | MSM | 126 | 100 | Median age of 24 years; and 89% white British | Oral fluid | Postal and public sex environments | Post | –/– |
| 5 | Greensides et al. (2003)50 | Cross-sectional survey | To determine the levels of awareness and use of alternative HIV tests (SSKs and rapid tests among people at high risk of HIV) | USA | MSM, PWID, heterosexuals at high risk of HIV | 2836 | 66 | Mode age of 25–34 years; 73% male; and 39% white | Dried blood spot | Not specified | Not specified | +/+ |
| 6 | Osmond et al. (2000)51 | Cross-sectional survey | To test the feasibility of obtaining HIV test results by SSKs from a probability telephone sample of MSM | USA | MSM | 490 | 78 | Urban areas; 67% white; and 71% aged 18–29 years | Oral fluid | Mailed | Post | ++/+ |
| 7 | Sharma (2011)52 | Cross-sectional survey with randomisation | To describe the factors associated with the willingness of internet-using MSM to take a free anonymous home HIV test as part of online prevention activities | USA | MSM | 6163 | 68 | Median age of 18–24 years; 43% white; and 31% Hispanic | Not specified | Not specified | Post | +/+ |
| 8 | Sharma et al. (2014)53 | Cross-sectional survey | To investigate attitudes towards six different HIV testing modalities presented collectively to internet-using MSM and identify which options rank higher than others in terms of intended usage preferences | USA | MSM | 973 | 38 | Median age of 26 years; and 77% white | Dried blood spot | Not specified | Not specified | +/+ |
| 9 | Skolnik et al. (2001)54 | Cross-sectional survey | To examine preferences for specific types of HIV tests (public clinic test, doctor test, SSKs, home self-test), as well as for test attributes, such as cost, counselling and privacy | USA | Public clinics | 354 | 96 | Mean age of 34 years; 77% male; and 63% white | Dried blood spot | Mailed or pharmacy | Post | +/+ |
| 10 | Spielberg et al. (2000)21 | Prospective cohort | To assess the feasibility and acceptability of bimonthly home oral fluid and dried blood spot collection for HIV testing among individuals at high risk of HIV | USA | At-risk individuals enrolled in vaccine study | 241 | 84 | Mainly white males; 58% MSM; and mean age of 36 years | Dried blood spot or oral fluid | Choice of having the test mailed or collecting it from the study site | Post | ++/+ |
| 11 | Spielberg et al. (2001)55 | Cross-sectional survey | To evaluate attitudes about SSKs and telephone counselling among participants, HIV counsellors, community advisory board members and cohort participants | USA | Clinic staff and at-risk individuals | 126 | ≈80 | Mean age of 35 years; 71% male; and 54% white | Dried blood spot or oral fluid | Not specified | Post | –/– |
| 12 | Wayal et al. (2011)56 | Qualitative interviews | To explore the preferred mechanism for offering home sampling kits, perceptions about using SSKs to screen for STIs and HIV and views about STI clinic use and SSKs | UK | MSM | 24 | 80 | Median age of 39 years; and mainly white | Not specified | Range of options assessed | Several options | + (overall) |
| 13 | Wood et al. (2015)57 | Prospective cohort | To compare the results of a pilot outreach STI service using nurse-delivered screening and SSKs at a sex-on-premises venue with screening within a sexual health clinic | UK | MSM | 90 | NA | Median age of 47 years | Dried blood spot | Collected in a sauna | Post | –/+ |
The majority of the studies evaluated a dried blood spot SSK (n = 8),21,46,47,50,53–55,57 whereas five studies assessed an oral fluid test21,48,49,51,55 (two studies assessed both types of sampling21,55 and another two did not specify the type of test52,56).
The methods by which SSKs were distributed varied across the studies, with five studies including the option of kits being mailed out to participants21,48,49,51,54 and six studies requiring participants to pick up a SSK from a study site21 (including a pharmacy,47,54 a drug clinic,46 a public sex environment49 and a sauna;57 the remainder did not specify the method of SSK distribution50,52,53,55). Three studies offered participants a choice of both options21,49,54 and four studies did not specify how kits were distributed. 50,52,53,55 Nine studies required participants to return kits by post (the remainder did not specify the method of return or it was not applicable to the study type). 21,46,48,49,51,52,54,55,57 The qualitative study assessed a range of options with participants. 56
Quality appraisal
In accordance with the criteria used for both qualitative and quantitative studies, only a few high-quality papers were identified that related to the study outcomes. The majority of studies took the form of cross-sectional surveys47,49–55 (eight out of 13 papers), with only one RCT identified. 46
Only the RCT scored ‘++’ for both internal and external validity. 46 Two21,48 of the three prospective cohort studies21,48,57 scored ‘+’ or higher for both categories, as did six47,50–54 of the eight cross-sectional studies. 47,49–55 The qualitative study scored ‘+’ overall. 56 Two of the cross-sectional studies assessed the acceptability of a hypothetical offer of self-sampling and, overall, few of the studies directly compared the efficacy of different forms of testing. Those studies that scored poorly on both categories commonly featured a small sample size and/or deficient level of analysis.
Acceptability, feasibility and clinical effectiveness of self-sampling
All but one of the included studies50 reported on some measure of the acceptability of self-sampling (Table 4). In total, only five studies21,46,48,49,51 (three studies21,46,51 from the USA and two studies48,49 from the UK) reported on the distribution and return of SSKs. Within these, 1652 SSKs were distributed (range 80–716 SSKs) and 1373 participants returned a specimen (range 60–665 participants who returned a specimen). This suggests a median return rate of 77.5% (range 47.6–92.9%). The two UK studies48,49 distributed 80 and 126 HIV SSKs, with 62 (77.5%) and 60 (47.6%) returned, respectively. Both of these studies used oral fluid sampling, and no inadequate samples were reported. Twelve of the included studies did include (self-reported) data on the acceptability of SSKs to participants,21,46–49,51–57 but the measures used were inconsistent. Self-reported acceptability was generally high, with self-sampling reported to be broadly acceptable to participants (see Table 4). For example, Spielberg et al. 21 reported that 98% of participants agreed to take part in either oral fluid or dried blood spot bimonthly sampling in the future. Similarly, Fisher et al. 48 reported that 81% of MSM found (oral fluid) SSKs to be acceptable. However, Colfax et al. ,47 Wood et al. ,57 Skolnik et al. 54 and Sharma et al. 53 reported that few participants took up the offer of testing and/or it was the least preferred option among participants – it is notable that all of these studies used blood sampling. In terms of comparing the different types of tests, Spielberg et al. 21 found no difference in testing rates between dried blood spot and oral fluid testing, but this was the only study to compare the two methods. 21 Acceptability did not vary significantly by distribution method.
| Study number | First author (year of publication) and reference number | Number of SSKs returned/number of SSKs distributed | Completion rate, % | HIV positivity rate, % | Self-reported acceptability | Feasibility | Efficacy (i.e. increases in uptake of HIV testing) |
|---|---|---|---|---|---|---|---|
| 1 | Bartholow (2005)46 | 174/240 (self-reported; not clear if all were self-sampled tests) | 72.5 | 3.4 (6/174) | Those in the SSK arm rated their satisfaction as being higher than those in the clinic testing arm | 37 (22%) of those who reported being tested did not report receiving their test results | Those in the SSK arm were twice as likely to have tested in the past month. However, they were not more likely to obtain their results |
| 2 | Colfax et al. (2002)47 | NA | NA | NA | 19% of participants chose SSKs for their next test in the first survey (pre-marketing), but in the second survey only 1% had used them | NA | Availability of SSKs did not increase testing rates among those not tested previously |
| 3 | Fisher et al. (2015)48 | 62/80 | 77.5 | 0 (0/62) | Acceptable to 81% of MSM in a sexual health clinic setting | Two out of 62 participants required a reminder to return the sample | Greater acceptance level than that for clinic-based testing (62.5% vs. 37.5%) |
| 4 | Formby et al. (2010)49 | 60/126 | 47.6 | 0 (0/60) | Pre-study survey showed that 52% of MSM chose SSKs as their preferred method of testing. Anecdotal evidence suggested that there was demand for the pilot to continue | Some samples were delayed in getting to the laboratory, meaning that participants had to be contacted to resend their samples. Seven samples had equivocal results and were retested (all negative). Capacity issues within virology for processing oral samples | Pilot successfully reached those not regularly engaging with HIV testing, including higher than expected numbers of bisexual men, men not otherwise tested in the last year and those not accessing GUM |
| 5 | Greensides et al. (2003)50 | NA | NA | NA | – | NA | High levels of awareness, but low reported usage of SSK use in the past year (4%) |
| 6 | Osmond et al. (2000)51 | 412/490 | 84 | 1.5 (6/412) | Many participants commented on how easy it was to provide oral fluid samples | Two indeterminate test results. Ten insufficient samples. Six new diagnoses made. Only half of participants tested telephoned for their results | SSKs found to be an effective method for estimating population seroprevalence among MSM |
| 7 | Sharma et al. (2011)52 | NA | NA | NA | 62% likely and 20% somewhat likely to take an offered SSK | NA | SSKs are acceptable, and future research and interventions should focus on addressing self-identified barriers faced by MSM to testing using SSKs |
| 8 | Sharma et al. (2014)53 | NA | NA | NA | SSKs were the least likely option among those available: appealed to less than half the participants | NA | Novel approaches are needed to increase HIV testing frequency, including combination packages |
| 9 | Skolnik et al. (2001)54 | NA | NA | NA | 1% preferred the SSK option of clinic or self-testing | NA | Most preferred self-testing and clinic testing to the SSK |
| 10 | Spielberg et al. (2000)21 | 665/716 | 92.9 | 0 (0/665) | 98% agreed to participate in bimonthly testing in the future. 99% said the test was easy to use | Staff concerns raised about the efficacy of telephone counselling. Anxiety reported among 28% of male PWID. 99% test adequacy: no positive diagnoses were made | No detectable difference in testing rates between dried blood spot and oral fluid samples |
| 11 | Spielberg et al. (2001)55 | NA | NA | NA | 92% of participants were willing to enrol in a monthly SSK study | NA | Despite staff concerns, the majority of participants expressed willingness to submit regular SSKs |
| 12 | Wayal et al. (2011)56 | NA | NA | NA | Acceptability of oral specimens examined with different parameters; broadly acceptable to MSM | NA | SSKs could be a viable alternative to meet the increasing demand for sexual health services, but, to improve uptake, the method of service provision must be culturally sensitive and acceptable |
| 13 | Wood et al. (2015)57 | NA | NA | NA | Lower rates of acceptance for SSKs than nurse-delivered testing (33 SSK users compared with 80 nurse-delivered tests) | Three out of 30 tests not processed. Four out of 30 test results not communicated | A combination outreach screening approach, including SSKs, is effective in targeting MSM using sex on premises venues |
In terms of feasibility, only six studies included any documentation of how tests were completed, errors in testing, communication of results or linkage to care. Three of these studies used oral samples, two studies used blood samples and one study used both. There were few reports of errors in testing. Spielberg et al. 21 reported that 99% of both oral fluid and dried blood spot samples were adequate for testing, whereas Osmond et al. 51 reported two indeterminate results and 10 insufficient samples (out of 412 returned oral fluid samples) and Formby et al. 49 reported that seven (out of 126) equivocal oral fluid samples had to be retested (all tests gave negative results). Wood et al. 57 reported that three out of 30 tests of dried blood spot samples were not processed. Spielberg et al. 21 reported that staff members were concerned about the efficacy of telephone counselling and Osmond et al. 51 found that only half of participants tested telephoned for their results. Similarly, Bartholow46 reported that 22% of those tested did not report receiving their test results and Wood et al. 57 reported that 4 out of 30 test results were not communicated to participants. Fisher et al. 48 reported that 2 out of 62 required a reminder to return their sample. Formby et al. 49 also reported that oral fluid samples were delayed in getting to the laboratory, which required participants to be contacted and asked to resend their samples to ensure accuracy of results. Linkage to care was not assessed, because most studies (n = 9) had no reactive results. The studies that did have reactive results were unable to check on outcomes for linkage to care because of the features of their methodology.
Only six studies provided data on the clinical effectiveness of SSKs for HIV in increasing the uptake of HIV testing. In the one RCT included in the review, Bartholow46 reported that those in the self-sampling arm were twice as likely to have tested for HIV in the past month, but were not more likely to obtain their results than those in the clinic-based testing arm. In the USA, Colfax et al. 47 reported that the availability of SSKs had not increased testing rates among those not tested previously, nor had it significantly changed testing behaviour among those who do get tested. In the UK studies, Formby et al. 49 reported that SSKs offered an alternative means of testing, with 35% of participants having never tested for HIV before, while Fisher et al. 48 reported greater uptake of SSKs (62.5%) than clinic-based testing (37.5%). Formby et al. 49 concluded that the pilot successfully reached those not regularly engaging in HIV testing, including higher than expected numbers of bisexual men, men not otherwise tested in the last year and those not accessing existing sexual health services. Other studies provided data in support of this stance as well. For example, the only qualitative study included in the review noted that the use of SSKs could be a viable alternative to meet increasing demand for sexual health services, but to improve uptake, the method of service provision must be culturally sensitive and acceptable. 56 Wood et al. 57 concluded that including self-sampling in outreach settings could be effective in targeting MSM using sex on premises venues. Finally, five studies21,46,48,49,51 reported the HIV positivity rate, which was an average of 0.9% (12/1311). Two studies48,49 (both including MSM in the UK) reported a positivity rate of 0%.
Barriers and motivators to, and facilitators of, self-sampling for HIV
The final section of the review assessed the barriers and motivators to, and facilitators of, HIV self-sampling (Table 5). Key barriers included anxiety, concerns over the accuracy of testing, concerns about confidentiality, privacy and the lack of face-to-face counselling and fears about the difficulty or pain involved in collecting samples. On the other hand, one of the UK studies reported that there was no difference in uptake related to the importance of accuracy of results or willingness to wait for results. 48 Test reliability was reported to be a barrier in the other UK study. 49 In addition, Wayal et al. 56 reported potential barriers to uptake among British MSM, including preference for medical venues (which were perceived as discrete and appropriate, especially if symptomatic), fear that distribution in gay social venues could trivialise testing or promote stigma, concerns about the unreliability of the postal service for delivering samples and anxiety over waiting for the results.
| Study number | First author (year of publication) and reference number | Barriers | Facilitators | Motivators (i.e. factors contributing to the acceptability of SSKs) |
|---|---|---|---|---|
| 1 | Bartholow (2005)46 | Difficulty of collecting blood sample. Negative reactions from others if diagnosed | Attendance at syringe exchange | Perceptions of personal risk of HIV. Perceived benefits of regular testing |
| 2 | Colfax et al. (2002)47 | Most common concern was accuracy (56%) | – | – |
| 3 | Fisher et al. (2015)48 | No difference in uptake related to the importance of accuracy of the results or willingness to wait for the results | – | – |
| 4 | Formby et al. (2010)49 | Reliability of test result. Speed of obtaining test results | Ease of use of kit. Ease of following instructions. Lack of embarrassment | Number of partners in previous year |
| 5 | Greensides et al. (2003)50 | Concerns raised about accuracy, privacy and cost by those who had not used self-sampling | Convenience and privacy cited as main advantages. Ease of use also mentioned | Awareness of alternative testing methods |
| 6 | Osmond et al. (2000)51 | 42% of study subjects (241/568) expressed concerns:
|
– | Cash incentive used to recruit to study (resulting in high uptake among those with previous HIV diagnosis) |
| 7 | Sharma et al. (2011)52 | Barriers cited:
|
– | Hypothetical cash incentive was offered for testing |
| 8 | Sharma et al. (2014)53 | – | – | Motivations for HIV test (across all methods):
|
| 9 | Skolnik et al. (2001)54 | 99% of participants selected other test methods; the most important attributes were:
|
Reasons for selecting self-sampling as their first choice (n = 2):
|
– |
| 10 | Spielberg et al. (2000)21 | Reasons for refusal to participate in the study:
|
|
Agreement that early treatment for HIV results in prolonged health |
| 11 | Spielberg et al. (2001)55 | Anxiety over receiving regular test results. Fear of pain of collecting a sample. Concerns over inaccuracy of results. Waiting time for blood spots to dry | Key themes: convenience (51%), ease of use (32%) and time efficiency (29%) | Help with reducing high-risk behaviour |
| 12 | Wayal et al. (2011)56 |
|
|
|
| 13 | Wood et al. (2015)57 | – | Clear supporting information and the opportunity to access health promotion advice | – |
Conversely, reported facilitators of SSKs were the availability of telephone (as opposed to face-to-face) counselling, and perceived anonymity, accuracy, convenience and ease of use. Finally, additional motivating factors that were reported to contribute to the acceptability of self-sampling were awareness of the seriousness of HIV56 and the benefits of regular/early testing,21,46 and agreement or awareness of being at risk of HIV. 21,46,53,56 Two studies also noted that a cash incentive could be a motivating factor to test. 51,52
Summary
Few studies have examined the acceptability or feasibility of self-sampling for HIV testing, and only 13 studies met the inclusion criteria to be included in this review. The majority of the evidence came from cross-sectional surveys or cohort studies, and there was only one qualitative study and one RCT. Most studies were conducted in the USA, with just four conducted in the UK. The majority of the studies, and all of those conducted in the UK, focused on MSM. The overall quality of the studies was mixed and relatively poor.
Few studies assessed acceptability and feasibility in terms of actual uptake and return of tests, with only five studies assessing distribution and return of SSKs. Acceptability varied by sample type. The majority of the studies evaluated a dried blood spot SSK and these appeared somewhat less acceptable to participants than oral fluid sampling. 47,53,54,57 However, the one study that directly compared the two types of test found no difference in testing rates between dried blood spot and oral fluid sampling. 21 Only one UK study (with MSM) included dried blood spot SSKs, and this method proved less acceptable than nurse-led testing. 57 The methods by which SSKs were distributed varied across the studies, but acceptability did not differ substantially by distribution method. It was not possible to assess acceptability by method of return, because all of the studies that specified a return method reported that SSKs were returned by post. Overall, feasibility was mixed and problems were reported with the return of tests and communicating results to participants. Again, there did not appear to be any significant difference by sample type; three of the studies reported on feasibility having used oral samples, two studies having used blood samples and one study having used both. Evidence on linkage to care was particularly lacking and not assessed, because most studies had no reactive results.
Evidence on the clinical effectiveness of self-sampling for HIV in increasing the uptake of HIV testing was also limited. In the one RCT included in the review, Bartholow46 reported that those in the self-sampling arm were twice as likely to have tested for HIV in the past month, but were not more likely to obtain their results. Two of the UK studies reported increased testing among groups never tested before, including higher than expected numbers of bisexual men, men not otherwise tested in the last year and those not accessing existing genitourinary medicine (GUM) services, but neither study included African communities. 48,49 Although other studies reported that using SSKs could be a viable means of reducing pressure on existing sexual health services,56,57 the HIV positivity rate (where reported) was low for the high-risk populations included (two studies48,49 with MSM in the UK reported a positivity rate of 0%), suggesting that those most at risk of contracting HIV were not using this method of testing.
Despite the limitations in assessing acceptability, feasibility and efficacy, all 13 studies in the review included some data to inform understanding of how SSKs could work in practice, with concerns about anxiety over the testing process, the accuracy of testing, confidentiality and privacy being key barriers. The qualitative study also noted that there was a preference among the MSM interviewed for testing to remain in clinical settings. Conversely, key facilitators were the availability of telephone (as opposed to face-to-face) counselling, perceived anonymity, accuracy (although this was also identified as a barrier), convenience and ease of use (again, somewhat in contrast to opposing fears about difficulties in collecting samples). A number of studies also noted that awareness and the perceived personal risk of contracting HIV were motivating factors for testing. 21,46,53,55,56
Strengths and limitations
The studies included in this review were of relatively poor quality, with most data derived from cross-sectional studies and only one RCT included in the review. Most studies were conducted in the USA, which raises questions about the transferability of the findings to a UK context. Most of the studies, and all of the UK studies, were conducted with MSM, which again raises questions about the transferability of the findings to black African people not identifying as MSM in the UK. Furthermore, data on actual uptake and return of tests, the clinical effectiveness of self-sampling to increase the uptake of HIV testing and the clinical effectiveness of processes for linkage to care were largely absent, and this represents key knowledge gaps. The lack of standardised reporting of outcomes also made it difficult to compare findings across studies. Only one qualitative study was yielded by the search, despite the potential for such studies to inform the design and implementation of self-sampling for HIV interventions.
Conclusion
Self-sampling for HIV testing has been suggested as an approach to broaden the available testing options,39 and was successfully used in one pilot project set up to assess implementation of the UK national HIV testing guidelines. 37 In the 2016 NICE guidelines, SSKs were endorsed as a potentially innovative way of increasing the uptake of HIV testing among black African people, given that these kits may address known barriers to HIV testing in this risk group. 45 In the draft guidelines issued for consultation, SSK sand STKs are endorsed as innovative ways of increasing uptake of HIV testing among black African people. However, our review suggests that evidence to support the acceptability, feasibility and clinical effectiveness of this as an approach to increase the uptake of HIV testing is limited, and absent for black African people of all sexualities in the UK. There is a need for well-conducted trials of self-sampling interventions to assess acceptability, feasibility and whether or not the approach can increase the uptake of HIV testing among all high-risk populations, and black African people in particular. It is important that these studies include detailed description of processes for, and the acceptability, feasibility and clinical effectiveness of, the processes for linkage to care, including uptake of confirmatory testing and methods for linking those who test positive for HIV to care and treatment services. This will be particularly important for self-sampling (and self-testing) interventions to be implemented in practice.
The next chapter presents the findings yielded via FGDs with non-specialists and service providers, and one-to-one interviews with the latter regarding the development of an acceptable SSK distribution pathway and protocol via community-based health and HIV prevention services already accessed by black African people.
Chapter 4 Findings from focus group discussions and one-to-one interviews
As stated in Chapter 1, the aim of stage 1 of the HAUS study was to develop a SSK-based intervention that could increase the provision and uptake of HIV testing among black African people using existing community and health-care provisions. In doing so, it was important to understand the barriers to, and facilitators of, HIV testing in general, to consider how participants responded to the SSK itself and to gain their insights into the most feasible distribution, collection and communication of results procedures. This chapter presents qualitative findings drawing on FGDs and interviews, as described in Chapter 2, Methodology of focus group discussions and one-to-one interviews.
Perceptions of HIV testing interventions
Non-specialist black African participants demonstrated awareness of the range of settings in which most HIV testing currently takes place. It was clear among all participants, however, that specialist sexual health and HIV services were regarded as playing a crucial role in recommending and facilitating HIV testing, as well as providing ongoing social support for those who are diagnosed with or affected by HIV. Experience of, and opinions about, community and non-HIV/sexual health clinic offers of HIV testing were varied, with most mentioning HIV testing during antenatal care, new GP registrations in high prevalence areas and POCT in community-based HIV charities. The vast majority of participants regarded HIV testing as an acceptable and effective intervention because of the universal availability of antiretroviral treatment in the UK.
Some service providers highlighted that undocumented African migrants were often isolated from the UK medical system and unaware of free access to HIV treatment, presenting barriers to HIV testing. One non-specialist participant commented that:
I think on a social level, from what I have experienced while working, is that a lot of people who are undocumented in this country don’t understand the fact that the test is free, and the treatment is free.
London non-specialist group 3
Furthermore, there was some concern that a profusion of HIV testing interventions could lead to a disjointed and confusing service landscape. Some felt that unfamiliarity with the NHS could mean that a proportion of black African people may be unaware of the confidentiality provisions, particularly those pertaining to HIV and sexual health.
There was considerable agreement that the stigmatising association of HIV with ‘sexual immorality’ and promiscuity (an association that many FGD participants and interviewees described as being heightened within black African communities) provides an ongoing disincentive to test.
Aligned with findings from previous research,9,58 some service provider and non-specialist participants alike pointed out that testing uptake may continue to be low, because a HIV diagnosis was regarded as having profound health, social, financial, insurance and immigration implications. These views were often based on assumptions or considerably outdated information, even among service providers. One service provider had the following query regarding HIV testing:
I don’t know if I’m right about this, but does that not affect your credit rating?
Glasgow service provider group 1
Furthermore, a strong association between HIV and mortality among black African people was repeated across service providers and non-specialists.
Some participants also believed that HIV exceptionalism had structurally prevented the integration of HIV testing into mainstream health services, such as primary care. They described the historic requirements for pre- and post-test counselling and the requirements of careful results management as barriers to both offers and uptake of tests.
Recognition of risk as a precursor to HIV testing
In many cases, a crucial factor that determines whether or not an individual undertakes a HIV test is the recognition that they have faced an elevated risk of exposure to HIV (i.e. a motivation to test), along with having the capacity and opportunity (time and skills) to act on that concern. With the exception of interviews undertaken among HIV clinicians and some service providers in London, improved recognition of personal HIV risk and the need for awareness of the disproportionate impact of HIV among black African people in the UK were rarely linked with the need for improved HIV testing uptake in this population. The findings summarised in this chapter draw attention to the ways that HIV-related stigma and fear are inevitably linked to inaccurate risk perception, which in turn influences the motivation and capacity to test for HIV.
Perhaps unsurprisingly, the findings reveal a dissonance in perceptions of HIV risk between the epidemiological data on black African communities and the way that the risk is perceived by individuals within such communities. What we are referring to here specifically is the lack of awareness (and acceptance) of surveillance estimates that reveal that people of black African ethnicity account for almost one-third of adults with HIV in the UK. 1 Some participants felt that when potential targets were unaware of the scientific rationale for segmenting the population in relation to epidemiological categories, such approaches would be met with resistance:
I just see there being a bit of a disconnect, unless people are made to understand that this is, these are the clear [epidemiological] results that have been found, and this is why we’re, you know, suggesting to you. Until that gap is bridged, I just don’t. I just believe you’re going to be almost, you know, you’re just going to be met with, you know . . . ’Uh’?
London non-specialist group 3
At least some service provider participants felt that the dissonance that emerged between individual risk perception and community risk profiling was a challenge that may often be beyond the capacity of the service provider to bridge in ‘one-off’ encounters. These findings demonstrate that the diverse range of participants had pervasive concerns about the interpersonal and wider social implications of targeting HIV testing interventions for black African people in the UK.
Competing imperatives
The relatively low priority of HIV screening among people who had many more pressing needs to be met was frequently raised, as was a lack of time or funds to reach a testing site. In addition, some participants highlighted that there are those who lack the freedom or control in their lives to undertake a test while maintaining adequate levels of privacy to avoid HIV-related stigma. Qualms were also expressed about the extent to which confidentiality within health services could be trusted, which meant that the prospect of disclosure presented too much risk for vulnerable individuals.
Targeting HIV testing on the basis of actual or perceived ethnicity
A range of issues emerged among participants about the underlying inequalities that can impede the success of HIV testing interventions designed to target black African people. There were intense concerns about such offers being perceived to be driven by racism and discrimination among both service providers and non-specialist participants, awareness of the particular sensitivities that targeting could fuel antimigrant discourse and the threat that targeting would be perceived as divisive. Similarly, a concern was expressed that targeting all people considered by a service provider to be black African implied complicity with the homogenisation of highly diverse cultures and communities. Finally, there was discomfort with the assumption that targeting would probably rely on appearance and colour of skin (being ‘black enough’, as one specialised HIV health-care provider mentioned). Therefore, imbalances of power pervade accounts of black African people’s engagement with HIV testing to a considerable extent. Participants reflected on the way that such imbalances affected offers and uptake of HIV screening, and this is amplified rather than minimised when it comes to interventions that are designed to disproportionately benefit black African people.
This concern was further evidenced by a few non-specialist participants who raised concerns about HIV testing interventions in acute services that they perceived to be based on skin colour, rather than an individual’s actual risk of contracting HIV. It was argued that black African people had valid reasons to distrust health services as a result of previous experiences of racism, being patronised, not having the opportunity to give fully informed consent or being exposed to racial microaggressions in these settings:59
By the way, if you find yourself in an A&E [accident and emergency (department)], and if you’re black African, you will get a test anyway. So . . . [others laugh].
He is right.
They will just . . . They will just, you know, shove it into you, and when you ask a question, why didn’t you tell me, they go, oh, oh we are very sorry. But it’s always like that. It’s just not new, particularly if you’re in South London.
London non-specialist group 2
Concerns were also expressed about the difficulty of ensuring fully informed consent in the busy and emotionally heightened environment of acute care services. Other participants mused that they assumed that most blood samples drawn for routine purposes were already being screened for HIV, and that HIV screening was happening ‘behind closed doors’. In both types of discussions, non-specialists demonstrated little confidence in mainstream NHS providers’ judgement and communication strategies when it came to HIV.
Not all discussion about targeted approaches focused on their negative impact or repercussions. Some service providers noted that rationing limited resources made sense within a current climate of reduced public spending. As such, although targeting HIV testing to black African people was seen as problematic for a number of reasons, it was often counterbalanced by the epidemiological and practical need for such targeting:
I have trouble just targeting just black communities with that kit, for me it has to be universal for everyone I wouldn’t like to just target a specific population group.
This is screening! If the epidemiological studies that there’re high prevalence and new incidence rate in that race, in that particular community, that is really . . . really where resources should be.
London service provider group 2
Epidemiological evidence was presented as a neutral counterpoint to the barriers to targeting:
I think you can target in a way that’s honest . . . Because, for example, I think it’s very clear and honest to say, if you are from a high-prevalence area – if you’ve had unprotected sex in a high-prevalence area of HIV and then name where the high-prevalence areas are – you are at more risk of acquiring it.
London service provider interview 1
Furthermore, some service providers argued that the offer of a HIV test may be catalytic for individual testing decisions. From a provider perspective, acknowledging the consequences of not offering a HIV test to a black African service user or patient was considered as being one way to support providers in deciding to offer the test, even when they acknowledged that a challenging discussion could follow.
Finally, participants focused on reducing barriers to targeting through participant-led and culturally sensitive ‘approaches to enhancing targeting’. These included embedding the offer of a HIV test within a wider ‘bundle’ of targeted interventions to diffuse the specific stigma of HIV (e.g. within offers of targeted approaches to address sickle cell or bone marrow transplant donations or hypertension). A culturally sensitive approach to targeting that ensured the coproduction of targeting approaches with representatives of black African communities was also suggested, as was the introduction of such interventions by black African providers. These approaches were seen to reduce barriers to targeting by being particularly sensitive to the ethnic mix of those involved within the targeting interaction. Participants further noted that attention needs to be paid to the potential for health promotion or research materials to link HIV to black African people in the minds of the general public, and the harmful social outcomes that could result if such interventions were misconstrued by a wider audience.
Perspectives on the use of HIV self-sampling kits
There was considerable (although not universal) enthusiasm around the abstract notion of distributing SSKs to black African people.
Device practicability
Prior to taking part in this research, awareness of SSKs was not widespread among the non-specialist participants, and only a handful disclosed having used one in the past. A considerable proportion of participants initially assumed that results would be instant (i.e. self-testing), as there were national media reports about that technology being licensed just before the period of research. In addition, participants were invariably surprised by the volume of blood (400 µl) required for a sufficient TINY vial sample, and service providers in particular stressed routinely that they did not think that most members of the public would be able to produce a sufficient sample:
I mean, we do health checks and we take blood from the finger and our machines just been changed to take a much smaller sample, we have to take 40 microns [sic] of the blood, not a big amount which is why I kind of, I was a bit shocked at this. And just getting that amount of blood is actually sometimes quite traumatic for a person.
London service provider group 1
While fear of needles and blood was also discussed, a few pharmacists, nurses and general practitioners held the view that, physiologically, their black patients often struggled to produce finger-prick samples because of thickened skin on the fingertips.
Many of the service providers and non-specialist participants felt that the TINY vial kits would prove to be too complex for most people to use correctly. As one participant in a service provider group in Glasgow expressed:
I think that will be quite tricky. Certainly, I don’t think it’s one that you can tell them it’s that easy to do [. . .] maybe if the test was simpler.
Glasgow service provider group 3
Furthermore, a number of participants expressed concern that SSKs could be easily contaminated by users. Participants questioned the robustness of the technology and procedures on offer to the public, and also whether or not samples would be mismatched between two users. There was also an underlying worry that unskilled members of the public who used SSKs might introduce a risk to others (through contamination or spills) or increase the chance of invalid/inconclusive results in some way:
Can I be very honest? I don’t like this, and the reasons why I don’t like it is because it isn’t simple . . . It isn’t easy and, of course, this will not be popular. [. . .] By the time people put a jab and then put their hands and blood starts dripping, one, two, three, four, five, six, seven, eight, up to 20, I find it a bit . . . very, very cumbersome. It makes it very, very . . . It’s liable to a lot of mistakes. And so what do you then do?
London non-specialist group 2
In many of the discussions with service providers, they raised comparisons between these HIV SSKs and a range of kits for other conditions that are now designed for self-sampling. These comparisons highlighted that many such kits had not had great success (chlamydia and bowel screening kits in particular were perceived as underused and not cost-effective). In contrast, HIV service providers with experience in using dried blood spot kits for HIV self-sampling among MSM were encouraged by the benefits that self-sampling could bring to black African users.
HIV stigma and the need for privacy and discretion
HIV-related stigma was among the most pervasive concern emerging within these data, which supports extensive theoretical and empirical work in the field more broadly. 13,60,61 All participants were clear about the profound challenges that HIV-related stigma presents for prevention and testing interventions. The role of stigma was particularly evident in the concerns about potential isolation and resulting harm that could be experienced by SSK users. Indeed, it is this pervasive stigma that continues to make the promotion of HIV testing within this population so challenging. Stigma predicates against self-perception of risk and promotes profound fear about being seen to be accessing a HIV testing service, as a result of the social implications that may follow. It also makes providers uncomfortable in offering the test, because they too are aware of these social implications. Although SSKs were considered by many participants as having some scope in reducing these social risks of discovery, they were simultaneously understood to be a means of ‘keeping HIV underground’, providing cover to those who desire increasingly secretive means of confirming whether or not they are infected with HIV.
Closely connected to the matter of HIV-related stigma, and directly related to the feasibility and acceptability of the distribution of SSKs within the community, were the many facets of privacy that participants discussed. Although service providers may consider health providers and pharmacists to be trusted professionals who understand and adhere to data protection requirements, non-specialists were far less likely to share this view. Not only did they worry that presenting in such environments and requesting a HIV test might result in judgement and bias, it was also clear that a considerable proportion of these participants held deep-seated fears about who else may acquire access to their most personal health information as a result of such an interaction. In conjunction with this concern, other non-specialist participants pointed out that some potential users may lack power vis-à-vis their partner in order to independently use a SSK. One participant offered a scenario of a husband and wife, in which the former possessed control over the latter and prevented her from using the SSK, or in which the intention to use the SSK would lead to conflict in the household.
Among the many beneficial elements identified, privacy, discretion and the capacity to determine one’s own status in an environment of relative anonymity were regarded as considerable strengths, particularly among potential lay users of the kit. Participants felt that the ability to use a kit privately was an essential benefit for those who were frightened about attending a sexual health clinic, raising the issue in a clinical setting or seeking out a community organisation that provides HIV testing. To this extent, taking a sample in private was regarded as a means of avoiding the stigma that is heavily associated with those who seek out a HIV test:
[It’s] quite hard for some people to go and approach GPs or doctors to explain their situation. Like myself, I’ve been thinking about it. It’s been in my mind for a long time to do a test, because I’ve been hearing people, I’ve been watching this, I’ve been . . . you know what I mean, media’s talking about it, so I don’t even know my status, but when something like this came up, if it’s, like you said, I think it’s an opportunity for people like me to take the chance to do it.
Glasgow non-specialist group 3
But you’ve got to understand, most people, especially with location, where people live, they don’t have that time to go to the hospital and go through the whole process of getting a HIV test. And it’s not even a matter of going to the hospital. It’s a matter of I could just come home, I could do this and I could keep going with what I do in a normal day and then get my results, like they did [with] chlamydia tests.
London non-specialist group 1
Thus, for some, SSK distribution was regarded as a way to access HIV testing that was non-stigmatised, highly accessible and convenient, potentially increasing its appeal to those who had not considered testing in the past.
Choice and autonomy as both opportunity and risk
The findings described above should not be interpreted to mean that SSKs were perceived by research participants as a means of replacing traditional HIV testing and POCT. Instead, SSKs were described as a means to bolster the array of options on offer:
I like the idea of home sampling because it gives more choice, flexibility and opportunity for people to have an HIV test. So for example, if people are worried about confidentiality, they can do the test in the privacy of their own home. And even though they still have to send the result in to a lab, at least it’s not done through a third person, having to disclose their history and why they’re worried about HIV.
London service provider interview 1
Service providers and non-specialists alike were interested in the extent to which the SSK increased an individual’s autonomy over their health, their HIV testing options, and their decision-making around how, when and where to have a test. There was also an extent to which this autonomy introduced a sense of liberation around HIV, and a few participants (mainly service providers) mentioned that making SSKs available in public spaces for private use might help to tackle HIV-related stigma at a structural level. Not everyone agreed with this last point, however, as it was also mentioned that increasing the extent of privacy through the use of SSKs may serve to hide the issue of HIV even further away.
Chief among the concerns expressed about SSK distribution was that the kits appeared to circumvent the provision of sustained interpersonal engagement and support. In almost all groups and several interviews, participants voiced their concern that users would be alone while waiting to hear their results and, most crucially, when discovering the results. In a considerable proportion of groups and interviews, participants felt that the risk of suicide and self-harm was elevated among SSK users learning of a reactive result, because they would not be in the physical presence of a professional for this discussion. When self-testing for HIV was discussed, this concern was even greater, and the SSK was at least regarded as a means of better ensuring linkage to care than self-testing technologies. There was an assumption embedded within these exchanges that linkage to support and care services was far more assured with face-to-face testing services, and there was considerable doubt that this could always be achieved with SSKs.
To some extent, such comments reveal a fundamental concern about the loss of systems control that SSKs represent. This is ultimately a direct consequence of increased user autonomy. It is not surprising that this was a key tension that emerged among participants with regard to this technology, and it is of note that potential isolation being a key drawback of SSKs was raised by service providers and non-specialist participants in equal share.
Self-sampling kits and point-of-care testing
There was also considerable discussion about ensuring that HIV testing is accompanied by a talking intervention given by a skilled professional, enabling risk assessment and pre-test counselling (and, potentially, advice on the use of a SSK). To this extent, guidance suggesting that pre- and post-test discussions are not entirely necessary is not universally accepted by service providers or non-specialists. 37 In all focus groups, and several interviews, there were those who made it clear that their preferred testing pathway involved direct contact and a risk assessment discussion with a skilled service provider, followed up by immediate on-site POCT. Such individuals considered SSKs to be a ‘poor relation’ to POCT. One participant had the following query:
If you’re going to start offering it as an anonymous kind of thing that’s not connected to services, well, what’s the reason for doing that? What problem are you trying to solve by offering that?
Glasgow service provider interview 1
Those who thought testing should be delivered with interpersonal engagement said that it seemed peculiar to distribute SSKs when POCT afforded immediate sample and results collection, with full support and advice on offer.
Essentially, these findings highlight participants’ ambivalence to SSKs. On the one hand, participants expressed enthusiasm about the freedom and autonomy that this technology offers. However, they were also concerned that this comes at the sacrifice of immediate results, professional contact, support and clinically robust procedures. It was widely held by most participants that SSKs needed to be embedded in larger support interventions that involved discussions with skilled professionals.
Self-sampling kit distribution options
The privacy afforded to individuals in each potential SSK distribution setting was ultimately the over-riding factor in participants’ assessments of their suitability. However, for every setting, there were disagreements on whether or not privacy and confidentiality could be guaranteed. Therefore, although some participants saw GP surgeries as providing an ideal combination of privacy and medical expertise, others worried that Home Office officials could be notified of an outcome via the medical facility, and there were concerns that even the discussion of a HIV test could persist on a medical file with negative consequences.
Furthermore, although some participants argued that ordering such a kit to be delivered through the post at home might be ideal, this suggestion was almost always vetoed by others who felt that most black African people did not live alone, and the arrival of such a kit in the post (or even the carrying of a package that is distributed in the community) would always elicit questions about what was inside:
I worry that we’re not understanding the home environment in which this will land in enough. That needs to be understood. There are so many other issues going on with our communities that the context in which this lands, it needs to be understood.
London service provider group 3
Many participants favoured voluntary pick-up of SSKs in key community sites (similar to what has been done with chlamydia SSKs), rather than service provider-initiated distribution, as this affords greater privacy while simultaneously reducing the potential for black African people to feel targeted and potentially stigmatised. At the same time, it was recognised that promotion of the kit to reluctant or unfamiliar users would be required. Indeed, there was considerable support for the proposition that first-time users should be shown how to use the kit, in order to ensure efficiency in SSK use and uptake.
Some participants delineated the need for a user-led approach within a fuller HIV prevention paradigm, starting with a discussion about HIV awareness, elevated prevalence among black African people in the UK, individual risk perception and the importance of prompt access to antiretroviral treatment for people infected with HIV, prior to a potential offer to take away a SSK. To this extent, it was agreed that assumptions of universal willingness (or, indeed, need) to use SSKs among all black African people were problematic, and that, on balance, participants recommended that a user-led and needs-led approach involving some dynamic interaction with a skilled distributor would often be required. To this end, service providers suggested that such distribution would be best placed within existing service specifications, with additional resourcing to ensure adequate staffing and promotion.
In terms of the best sites for accessing SSKs in the community, there was near-uniform support for distribution of the kits to black African people through GP surgeries. The confidentiality and privacy afforded in a GP setting was seen by many as a gold standard option for SSK distribution. However, there was concern about the capacity of surgery staff to appropriately target black African people while avoiding racist and stigmatising approaches:
Do you think it’s possible to target these [SSKs] mainly, or exclusively at black Africans?
I think in general practice that would be quite difficult.
Yes, it’s difficult from the point of view that you shouldn’t discriminate.
Glasgow service provider group 3
Some participants were confident that developing cultural competence training for GP staff could help to overcome this risk. Furthermore, it was thought that, on balance, the strong accessibility of the setting could outweigh the perceived shortcomings of distributors.
Other concerns, voiced particularly by service providers, included the length of time that such an intervention would take during the brief 10-minute appointments typically allocated in primary care, given that raising the topic of HIV requires some sensitivity, and the complex TINY vial kits (in particular) needed to be explained and demonstrated. There was considerable variation of opinion on the role that various GP surgery staff could play in active/passive distribution of SSKs, with a consensus on the fact that a specific appointment should not be required to acquire a kit. Some favourable comparisons were made with the way in which chlamydia SSKs were made discreetly available in such locations. However, the majority of service providers took the view that nurses and general practitioners should actively target and initiate distribution in order to increase cost-effectiveness by sharing information and assessing the likelihood of need, and increasing motivation.
There was also nearly universal approval of HIV specialist community organisations distributing SSKs alongside current outreach work. This workforce was deemed to have the expertise required to target this population sensitively, with less risk of causing offence or generating responses that might exacerbate HIV-related stigma:
You can say: You know what? We’ve got these kits and you can test in your home. The results won’t come back to me. I don’t really need to know until maybe you are confident enough maybe to discuss it with me. So I think it’s a good opportunity.
Glasgow service provider group 2
For the most part, SSK distribution by African-focused HIV specialist community service providers was regarded as having the potential to work seamlessly with community HIV promoters’ existing skills and approaches, as well as benefiting from existing relationships and infrastructures for setting access and referrals.
Further discussions were prompted about the appropriateness of pharmacies, faith-based organisations, higher education institutions, dental surgeries, hairdressers and salons with high numbers of African users, as well as targeted online ordering systems for home delivery of kits. While the ‘normalisation of HIV’ was regarded as a potential strength of all of these distribution sites, the over-riding response from service providers and non-specialist participants alike was that clinical governance concerns ruled out these options:
It’s because in a pharmacy it’s not like a GP. There’ll be someone else picking up different drugs or waiting behind you or whatever. So that’s where you feel, ‘God, there’s someone right here . . .’. There’s no, like, privacy in the pharmacy. You’re not going into the little room; you’re going to a counter.
Glasgow non-specialist group 1
I would say nobody would be courageous enough, especially if they are married or even if they want to get married in the next year or so to go to your pastor and ask for an HIV test kit, that’s almost impossible.
London service providers group 3
Lack of privacy (including the arrival of a kit through the post), and lack of appropriate HIV expertise, impartiality, or guarantees of confidentiality among other distributors, were at the forefront of participants’ rejection of using such settings for targeted distribution of SSKs to black African people.
Summary
The data from this stage of research fed directly into the process of intervention development, described in Chapter 2, Service provider focus group discussions and interviews. In particular, these findings are perhaps best summarised in relation to the COM-B model of behaviour change,36 which was ultimately applied to determine the best way forward for the intervention development for stage 2, as described in Chapter 5.
With regard to the capability of service users and providers to distribute and use SSKs, concerns were highlighted about the amount of time that service providers had (particularly general practitioners) to initiate discussion and encourage use, and, furthermore, there was also a fundamental concern raised in all groups about the volume of blood required to provide a TINY vial sample.
On the other hand, targeted distribution of SSKs was seen as a broadly positive means of expanding the range of opportunities for black African people to test for HIV. There was widespread enthusiasm about SSKs as one of many new technologies that comprise an improved array of HIV testing options for black African people. There was specific support for the fact that SSKs could provide an opportunity for the initiation and follow-through of a HIV testing discussion in a setting that black African people were already accessing, so convenience was regarded as a significant gain.
Finally, these findings offer us considerable insight into the potential motivation issues arising with targeted offers of SSKs. Participants advised that targeted offers (particularly those made in health-care settings and/or made by non-black African people to black African service users) needed to be couched in clear terms, using epidemiological evidence to help people consider their likely risk, and to work to avoid the perception that offers were being made because of racist or xenophobic sentiment. Instead, it was deemed of utmost importance that distributors were regarded as trustworthy, knowledgeable and non-judgemental, and that they could encourage a realistic degree of reflection about HIV risk among those for whom they encouraged SSK use. There was a universal view that SSK distribution needed to actively resist HIV-related stigma, rather than potentially reinforce it.
Ultimately, these data demonstrate that we cannot underestimate the extent to which considerations of privacy (and its limits) are at the centre of considerations for SSK feasibility and acceptability among black African people in the UK. Central to this concern is the pervasive presence of HIV-related stigma, which has an impact on service providers and black African people alike. Finding the correct mechanisms for highlighting epidemiological realities among members of ethnic minority communities, without engendering feelings of imposed stigma and blame, is not easy.
Strengths and limitations
Although limited in scope and scale, the range of recruitment methods used for our FGDs helped to ensure that we had a diverse mix of non-specialist participants, most of whom were unlikely to have taken part in similar research previously. We started to approach data saturation by the time of the last focus groups and interviews, demonstrating that our use of purposive sampling for both specialist and non-specialist participants had helped to achieve a balanced range of perspectives and experiences. The decision to make some of the non-specialist groups more homogeneous (all male, younger, HIV-positive participants) was a benefit overall, as it helped to ensure careful consideration of distinct subject positions during both data collection and analysis. Although the decision to hold one-to-one interviews with HIV clinicians and other decision-makers ultimately resulted in divergent and multiple data sources for this phase, the option of mixing them in groups with other specialist providers was not only less feasible in terms of availability to attend, but it was also clear that, given the strongly divergent insights expressed by those in this sample (influenced by clinical experience and policy involvement), it was ultimately best to collect their data separately.
Ultimately, the use of these qualitative methods to collect data in two geographically distinct locations enabled the study team to (1) triangulate findings across study populations and geographic areas; (2) compare and contrast specialist/non-specialist perspectives on SSKs and their targeted distribution, and their rationales for these viewpoints; and (3) directly address these perspectives in the design of the intervention to be assessed in stage 2 of the study.
Conclusion
As the introduction of this new technology is meant to assist in circumventing the problems of low uptake of HIV testing among black African people, these findings remind implementers to be cautious about not introducing new problems while trying to address existing ones. The next chapter builds on the findings presented in this chapter to develop the intervention that was implemented in stage 2 of this study.
Chapter 5 Intervention development
This chapter addresses the first aim of stage 1, to develop a SSK-based intervention to increase the provision and uptake of HIV testing among black African people using existing community and health-care provision.
The methods for intervention development comprising the four-step process, informed by the behaviour change wheel, are described fully in Chapter 2, Non-specialist black African focus group discussions. The four-step process is as follows:
-
step 1: delineate key intervention components
-
step 2: map barriers to, and enablers of, the implementation of intervention components in relation to theoretical domains
-
step 3: identify potential intervention components that can overcome modifiable barriers and enhance the enablers within a future intervention
-
step 4: ensure viability of the intervention using the APEASE criteria.
The sections below discuss the results at each point of this process.
Step 1: delineate key intervention components
The research team identified eight key intervention components:
-
setting and location
-
the targeted offer of a HIV SSK to black African people
-
participant personal information collection
-
the SSK itself
-
the appearance and packaging of the HIV SSK
-
information leaflet and instructions for the correct use of the SSK
-
kit return
-
result communication.
In order to facilitate focused consideration of the key intervention components, each component and its implications for the research team, participants and service providers are presented in Table 6. Each component is then explored in detail within step 2.
| Intervention components | Requirements | Notes regarding the component and associated behavioural domains |
|---|---|---|
| Setting and location | Research team needs to engage with professionals and black African, non-specialist members of the public to assess relative opportunities presented by a range of potential testing settings and their acceptability and assess the pragmatic aspects of intervention delivery within these diverse settings | Not a behavioural domain per se
|
| The targeted offer of a HIV SSK | Two distinct behavioural domains suggested for the health provider:
|
|
| Participant personal information collection | The participant must provide accurate information to enable processing of the sample and provision of results |
|
| The SSK itself |
|
|
| The appearance and packaging of the HIV SSK | Participant and outreach distributor must transport the SSK without damaging it, and may wish its contents to remain unknown to others |
|
| Information leaflet and instructions for correct use of the SSK | Participant must comply with kit instructions and understand result process and meaning |
|
| Kit return | The participant must return the kit to get it processed within the laboratory and to enable results to be communicated |
|
| Result communication | Researchers and providers to give results in acceptable ways and specify patient pathways when relevant |
|
Step 2: map barriers to, and enablers of, the implementation of intervention components in relation to theoretical domains
Key theoretical domains (see Table 1) were important for most, if not all, intervention components. Skills, beliefs about consequences, social influence and environmental context and resources were particularly important theoretical domains across many of the intervention components and their target populations. Below, we map the key barriers and enablers that we identified for each intervention component; these could relate to the service provider, the service user or both.
Setting and location
This is not a behavioural domain, but it is important to secure locations that maximise opportunities to reach African communities and settings that could facilitate trust in the intervention process. Furthermore, the limited amount of time with a potential user in some settings may prohibit intervention delivery on top of meeting the individual’s presenting needs.
The targeted offer of a HIV self-sampling kit
A central dimension of the intervention outline contained within the NIHR’s commissioned call was the specificity to black African people. It was imperative to reflect on which person or persons would be most appropriate to make a targeted approach. It was also important to consider which point in the path of the patient/client journey through routine services was the most appropriate time to make an offer of a SSK. It was equally vital to address risks about the potential implementation of the targeted offer to minimise harm and maximise uptake.
Key barriers in relation to the relevant TDF domain were:
-
knowledge – lack of knowledge as to why they would target HIV testing at black African people (service provider)
-
skills – lack of skills in initiating conversations about targeted self-sampling (service provider)
-
social/professional identity – service providers may or may not see routine or universal testing as part of their day-to-day role (service provider)
-
beliefs about capabilities – sense of low self-efficacy and capability concerning the targeted offer of a kit (service provider)
-
beliefs about consequences – perceptions that a targeted offer will be perceived as racist and that this may compromise their relationship with a person they have targeted and other community members, and could lead to a damaged reputation (service provider)
-
intentions – potential service users and providers may have prior intentions of testing through other routes (not self-sampling; both user and service provider)
-
the environmental context and resources – population-level exposure to targeting of black African populations may lead to heightened stigma and disincentivise testing (both user and service provider)
-
social influences – strong social norms concerning the avoidance of conduct that can be perceived as racist and discriminatory within a cultural context of xenophobia, racism, intergroup conflict, identity and social identity (service provider)
-
emotions – service providers’ distress and negative affect will be a barrier to the targeted offer of a test (service provider).
Participant personal information collection
Recipients of SSKs must provide accurate personal information to enable their sample to be processed and the results returned to them. This is central to facilitate the later communication of a negative, unsuitable sample or reactive test results, and to secure an entry into HIV care for anyone who obtained a reactive result. Although providing this information is within the behavioural domain of the participant, the service provider who makes the targeted offer of the SSK may be instrumental in explaining or reassuring the participant of the need and safety of disclosing personal information within the context of the HIV test.
Key barriers in relation to the relevant TDF domain were:
-
beliefs about consequences – personal details may not be confidential and could be seen by others or shared across agencies, with a negative impact on future health and social care (user).
Key facilitators in relation to the relevant TDF domain were:
-
beliefs about consequences – clear information detailing exactly how personal information would be used and why it was required would reduce perceptions of negative future consequences (user)
-
the environmental context and resources – using minimal information to enable the laboratory to contact the participant (user)
-
the environmental context and resources – using online systems for completing study procedures and data collection (user).
The testing kit itself
Although not a behavioural domain, the choice of SSK represents a central component of the intervention. Regulatory and clinical standards would limit options and create challenges if we wanted to use a non-Conformité Européenne (CE)-approved kit or enhance current kit options (see Challenges to the development of an optimal self-sampling kit intervention).
The appearance and packaging of the HIV self-sampling kit
There were three particularly important dimensions to consider: (1) how to ensure that the kit was packaged in a way to lessen the risk of damage during transport from the setting in which it was offered to the setting in which it was used; (2) how to address and minimise the effects of the social stigma associated with being seen to be in possession of a HIV test; and (3) how the intervention packaging could support the recipient in their testing behaviour.
Key barriers in relation to the relevant TDF domain were:
-
beliefs about consequences – the packaging may be recognised as a HIV SSK, and the users ‘reputation’ within their communities may be damaged (user)
-
the environmental context and resources – use of any external label/packaging that mentions HIV or the test kit (both user and service provider)
-
the environmental context and resources – concerns relating to the safety of the kit and potential damage to it (both user and service provider)
-
social influences – perceived HIV-related stigma shaping interpretations of carrying a kit if it is recognisable to others (user).
Key facilitators in relation to the relevant TDF domain were:
-
the environmental context and resources – use brown paper bags (or other generic material) to distribute/carry the kit (both user and service provider)
-
the environmental context and resources – use non-transparent materials to distribute/carry the kit (both user and service provider)
-
the environmental context and resources – the kit has to be convenient to carry (both user and service provider)
-
the environmental context and resources – tight, secure packaging that will not break/open/tear prior to use of the kits (both user and service provider)
Information leaflet and instructions for correct use of the self-sampling kit
Given that SSK recipients were likely to use the kit without the support of the service provider who distributed it, potentially days after this interaction and predominantly in a domestic setting, it was important to optimise the information on the participant information sheet (PIS) and kit instructions for acceptability and usability. Irrespective of the complexity of the intervention components, the correct use of the kit represents a complex multidimensional behavioural domain, as it involves 13 distinct steps (see Appendix 7).
Key barriers in relation to the relevant TDF domain were:
-
skills – lack of English-language skills could hamper use of the kit (user)
-
skills – lack of perceived skill in compliance with complex instructions (user)
-
beliefs about capabilities – concerns that test instructions may be too complex and difficult to follow (user)
-
beliefs about capabilities – concerns that language used will not be understood (user)
-
memory and decision processes – perception that instructions are too difficult and complex to follow (user)
-
memory and decision processes – the medical language concerning test results may be confusing and have a negative impact on testing decisions (perceptions of test efficacy; user)
-
the environmental context and resources – the perception that readability and font size of instructions are too small to read (user)
-
the environmental context and resources – medical language and terminology could be alienating to participants (e.g. ‘lancet’, ‘non-dominant hand’; user)
-
emotion – words/graphics on the printed instructions or instructional video could increase anxiety and fear and may lead to avoiding the kit (user)
-
emotion – anxiety levels and fear of test results may influence compliance with instructions (user).
Key facilitators in relation to the relevant TDF domain were:
-
skills – video/voice provision of test instructions to facilitate compliance with test instructions (user)
-
beliefs about capabilities – use of clear simple messages and pictures (user)
-
beliefs about capabilities – translate into other languages (user)
-
the environmental context and resources – having an additional online video of someone using the kit (user)
-
social influences – the perceived need for the service provider to have used the test themselves (user)
-
social influences – the perceived need for the service provider to explain the test process in person (user)
-
social influences – 24-hour access to a pre- and post-test counselling service may facilitate uptake (user)
-
social influences – signal clearly sources of, and provide easy access to, social support regarding testing within instructions to facilitate testing (user).
Kit return
A further core component was the process of the participant returning the collected sample with sufficient information to enable processing and result communication. This element, again, represented a relatively complex self-managed behavioural domain. Having used the kit, the participant must properly enclose the sample along with an ID label and sample return form within the protective packaging and ensure that it is posted via the supplied postage-paid addressed envelope.
Key barriers in relation to the relevant TDF domain were:
-
beliefs about consequences – perception that participants will not return the kit if they believe it will get lost or spoiled within the postal system (user)
-
the environmental context and resources – Royal Mail (Royal Mail Group, London, UK) system would disincentivise kit return through widespread perception of distrust with the system (user)
-
social influences – returning the kit to a community setting, for example, through faith leaders (as potential distributors), was linked to privacy concerns and disincentivising kit return (user)
-
emotion – concerns about the affective impact of information if the testing process was not confidential (user).
Key facilitators in relation to the relevant TDF domain were:
-
skills – previous competence with online tracking systems may facilitate kit return (user)
-
beliefs about consequences – participants should be given a choice of how to return the kit to accommodate beliefs about consequences (user)
-
intentions – intentions to test in situ at a distributor venue may enable uptake (user)
-
memory and decision processes – having choices of ways of returning the kit was seen as facilitating test kit return (user)
-
the environmental context and resources – postboxes are ubiquitous and can enable kit return with minimal effort (user)
-
the environmental context and resources – medical facilities, such as GP surgeries, were trustworthy with management of samples (user).
Result communication
The final component of the intervention related to the processing and communication of test results. These processes are subject to clinical governance regulations, and identifying mechanisms by which best practice would be delivered was crucial (see Aligning the study protocol with quality care and research governance framework).
Step 3: identify potential intervention components that can overcome modifiable barriers and enhance the enablers within a future intervention
Table 7 illustrates the mapping of the key barriers to, and facilitators of, potential intervention implementation against COM-B elements and the concomitant specific behaviour change theory that could enhance implementation. The intervention components each present different foci in relation to the COM-B elements; for example, some components highlight the need for focus on capability (the targeted offer of a SSK and compliance with kit instructions) and some focus on opportunity (the appearance and packaging of the SSK). The table also highlights how different components demand the use of different intervention functions (i.e. the way that the intervention content should be delivered). For example, the table shows that much of the proposed intervention content relating to the targeted offer of a test should be delivered within training and education of providers. In contrast, much of the active intervention content regarding the appearance and packaging relates to the redesign of the pack and persuading people to use the kit.
| Requirement | COM-B analysis | Broad function for training and intervention | Potential behaviour change techniques (numbers refer to behaviour change techniques taxonomy) |
|---|---|---|---|
| The targeted offer of a HIV SSK |
Capability Major psychological Some physical |
C – education, training, persuasion and modelling, enablement Environmental restructuring |
Within training sessions:
|
|
Opportunity Some physical Some social |
O – training, restructure environment | ||
|
Motivation Major reflective Some automatic |
M – training, incentivisation, coercion, environmental restructuring | ||
| Participant personal information disclosure |
Capability Minor physical Minor psychological |
In provider script:
|
|
|
Opportunity Major physical Minor social |
O – training, restructure environment (design a process to minimise perceived barriers) | ||
|
Motivation Major reflective No automatic |
M – education, persuasion and modelling (to improve disclosure) | ||
| Appearance and packaging |
Capability Minor physical Minor psychological |
|
|
|
Opportunity Major physical Minor social |
O – training, restructure environment (design pack) | ||
|
Motivation Major reflective No automatic |
M – education, persuasion and modelling (to take the kit and carry it) | ||
| Participant must comply with kit instructions |
Capability Major physical Major psychological |
C – training, education, environmental restructuring, enablement, modelling (redesign kit instructions) | Design of kit:
|
|
Opportunity Minor physical Minor social |
O – training, restructure environment | ||
|
Motivation Major reflective Minor automatic |
M – education, persuasion, modelling and enablement | ||
| Participant kit return |
Capability Minor physical Minor psychological |
O – restructure environment |
|
|
Opportunity Major physical Minor social |
M – education, persuasion, modelling and enablement | ||
|
Motivation Major reflective Minor automatic |
Finally, Table 7 addresses the particular behaviour change techniques that could be used within an intervention (adding much more specificity in relation to the broad and more generalised COM-B elements). The numbers provided relate to the behaviour change technique taxonomy. 62 For example, the motivational elements of training providers to deliver a targeted offer of the test can be achieved through the specific use of techniques that increase motivation to offer the test, that is, the technique ‘provide information about health consequences (5.1)’, wherein, within training sessions, providers are given details about the consequences of late diagnosis for potential test users in order to motivate them to overcome their perceived barriers for the targeted offer of a test. Equally, motivating the providers to overcome their perceived barriers could be achieved by using the technique ‘salience of consequences (5.2)’. In this way, motivation to overcome perceived barriers for the targeted offer of a test is achieved by highlighting the consequences of effectively performing targeting (e.g. reduction of the number of new HIV infections or details regarding the future health of patients, rather than their future disability). Using the behaviour change wheel, thus, enables a range of highly specific potential intervention elements that can be used in relation to each of the intervention components.
Step 4: ensure viability of the intervention using the APEASE criteria
Challenges to the development of an optimal self-sampling kit intervention
One of the key components of the HAUS intervention is the SSK itself. The type of specimen (saliva or blood) can have implications for its acceptability and for the accuracy of test results. The following section presents an overview of the UK regulations for medical devices for HIV testing and the resulting implications for development and viability of an optimal SSK intervention for HIV testing.
Current UK regulations for HIV testing and diagnostics
Self-sampling kits are required to meet the legal criteria, which aim to ensure the quality and performance of these kits. They have to be approved by the Medicines and Healthcare Agency (MHRA) and the European Medicines Agency. They cannot be sold without the CE mark, which indicates that the manufacturer has met the required standards in relation to test performance, directions for use and labelling.
HIV SSKs can take many forms, employing dried blood spot, saliva and blood collection devices. This is because the diagnosis of HIV is usually made on the basis of a serological test; the detection of HIV-1/2 antibodies (Abs) or simultaneous detection of HIV-1/2 Abs and the HIV-1 p24 antigen (Ag). In the UK, HIV testing using ‘fourth-generation’ assays (i.e. combined Ab and HIV p24 Ag detection) is recommended over ‘third-generation’ assays that detect only Abs against HIV. 37 The ability to detect the HIV-1 p24 Ag has enabled the reduction of the window period between exposure to HIV and detection of infection from 3 months to 1 month, thereby enabling detection of recent infections. Currently, all saliva-based testing options and a lot of POCTs using whole blood are third-generation only.
Although we did not formally assess the acceptability of various HIV self-sampling methods in FGDs (as we did not believe we would have a choice), strong concerns about the proposed TINY vial collection device arose (see Chapter 4).
Discordance between acceptable self-sampling methods among study participants and UK regulations for HIV testing and diagnostics
The discordance between preferences of black African communities, service providers and UK regulations for HIV testing had several implications on development of an optimal intervention.
Preference for oral specimen collection compared with a blood collection device among users and service providers
Stage 1 of the project elicited significant concerns about the only CE-marked SSK currently available in the UK. This SSK relies on the collection of 400 µl of blood into a vial. A finger is pricked with a lancet and droplets of blood are collected. Collecting a blood sample was viewed as a significant barrier to HIV testing for this population in community settings. As set out in Chapter 4, Perspectives on the use of HIV self-sampling kits, concerns about the volume of blood required, the fear of needles, presumed difficulty in using the kit, fear of contamination of the vial and fears about contaminating others were expressed. Among those familiar with SSKs, collection of an oral specimen using a swab was identified as an easier alternative to the TINY vial, in terms of use, acceptance and the amount of support required to promote its use. For these reasons, the study team perceived that usage of the TINY vial device constituted a barrier to the successful delivery of the intervention.
Lack of availability of Conformité Européenne-marked assay for saliva HIV testing and implications for development of the HAUS intervention
Owing to the concerns over the TINY vial, the study team proposed to use an oral self-sampling device, such as Orasure® (Orasure Technologies, Inc., Bethlehem, PA, USA), which is commercially available and CE marked in order to optimise testing in the study population. However, there is currently no CE-marked saliva-based HIV assay available in the UK. In the original grant application, we proposed to use the GENSCREEN™ ULTRA Ag–Ab assay (Bio-Rad Laboratories, Paris, France) for HIV testing. This test is CE marked for use on human blood serum and plasma, but not saliva. When used with plasma and serum, it is considered a fourth-generation assay, and has a sensitivity of 100% (93.2% in the seroconversion scenario), according to the manufacturer. 63 The test is a reliable indicator when a result is negative, which is important to consider, as incident infection in the black African population in the UK is likely to be low. 1 However, when used with saliva it is regarded as a third-generation assay, as it is unable to reliably detect the HIV-1 p24 Ag. This means that it is less sensitive to very recently acquired infection and can detect HIV that was caught > 14 weeks ago. The performance of the GENSCREEN ULTRA Ag–Ab assay with saliva has been evaluated and is considered appropriate for use. 64 All people with indeterminate and reactive results are strongly advised to attend confirmatory testing using serum or plasma (according to the standard practice of the NHS centre that they attend), so any false positives would be identified.
Given that the GENSCREEN ULTRA Ag–Ab assay for testing saliva for HIV is not CE marked, we obtained MHRA guidance on whether or not we would be able to use the assay on saliva within our research study. The MHRA responded positively on the proviso that a NHS trust would accept liability for using a product ‘off label’ for research purposes. Indeed, owing to user and provider demand for kits that use saliva, there are commercial and NHS services throughout the UK that are willing to take on this liability and use saliva-based HIV SSKs. 65 Exploring these options took up a considerable amount of time at a key point in our intervention development.
The University College London Hospital (UCLH) NHS Foundation Trust agreed to be our clinical partner organisation and assume the liability for using the GENSCREEN ULTRA assay off label, conditional on the study team obtaining permission from NIHR to use the assay. However, The Doctors Laboratory (TDL; The Doctors Laboratory, London, UK) – the processing laboratory for this study – declined to assume liability to test saliva specimens in the context of a research study, even though they provide saliva testing for some NHS services and SSKs could not be seen as NHS service provision (as UCLH do not offer a saliva-based self-sampling service).
University College London Hospital also stipulated that the only way they could accept the clinical responsibility for proceeding with a saliva option was if a formal evaluation of the kit was included in the study design, as this was not a test that the service was providing and, therefore, not evaluated previously. This would entail participants being provided both sampling options (blood and saliva) and both needing to be returned to TDL for processing. This was not a viable option, as it would represent a significant shift in the original research question and design. Furthermore, the requirement for both samples raised ethics issues about what to do should only a saliva kit be returned. Following consultation with the study steering committee, the research team decided that such a radical alteration in our proposed study design was not an appropriate option for the HAUS study.
The steering committee advised that stage 2 of the study should proceed, despite not being able to proceed with the optimal kit in terms of user and provider preference. Thus, it was agreed to continue with the TINY vials as part of the HAUS intervention. This decision was also supported by NIHR, because it was felt that the usage of the TINY vial method would not comprise a shift in the research design of the study. The stage 2 evaluation was also considered worthwhile, because a national HIV prevention initiative in the UK is based on HIV SSKs using TINY vials, with currently little evidence to support its clinical effectiveness or cost-effectiveness, in particular for black African communities. The stage 2 study would demonstrate whether or not the approach and distribution methods were feasible and acceptable, along with the return rate. In addition, the evaluation plan (which included qualitative interviews both with people returning kits and those not returning kits) would assess kit acceptability.
Aligning the study protocol with quality care and research governance framework
The best practices for provision of sexual health care in England are outlined in Standards for the Management of Sexually Transmitted Infections (STIs),66 developed by BASHH. These clinical recommendations also apply to Wales and Northern Ireland. Sexual health service standards for Scotland were published by NHS Quality Improvement Scotland in 2008. 67 Both of these standards provide guidance for achieving safe, high-quality services for management of sexually transmitted infections (STIs). According to these guidelines, development of clear care pathways to be utilised by all STI service providers both statutory and non-statutory is a vital component of STI management. Specialist GUM providers are advised to have an explicit leadership role for clinical expertise and clinical governance in the management of STIs. Provision of results as quickly as possible to service users, whether positive or negative, is emphasised for effective clinical management of infections and for user satisfaction. The recommended time period between consultation and receipt of results is ideally no more than 14 working days, taking account of the laboratory turnaround times. The guidelines emphasise that people accessing non-specialist or outreach services should receive the same standard of care as those accessing any other service for the testing and treatment of STIs. The Research Governance Framework for Health and Social Care68 outlines the responsibilities of researchers and care providers that apply to all research within the remit of Secretary of State. Ensuring confidentiality and quality of care provided to research participants is at the core of this framework.
In the context of SSKs for HIV testing, clear and robust pathways of care are needed for participants to send specimens for testing; delivery of test results; offering retests to those with indeterminate results and confirmatory tests to those with reactive results; and linking those who test positive for HIV to care. In order to align with the principles of the governance framework and given the sensitivities around HIV, the research team felt that it was important that an organisation with previous experience of managing HIV results, and ideally SSKs, was involved – this organisation would also need to be willing to assume the liability for the quality of care provided. Establishing collaboration with an organisation willing to accept the duty of care for all study participants, and not just those with reactive (positive) results, took considerable time and led to substantial delay. The reasons for the delay are described below.
The study team collaborated with TDL for the provision and processing of SSKs. A NHS trust initially agreed to take responsibility for the duty of care for all study participants. However, this arrangement was complicated by the fact that the team intended to use an ‘off-label’ assay to test for HIV. Although this trust had previously provided the same saliva-based SSKs using the GENSCREEN ULTRA Ag–Ab assay as part of outreach work to increase HIV testing in the gay community, they were unwilling to assume liability in the context of a research study. Eventually, the trust withdrew their support to fully partner the study and, in particular, to take responsibility of care for those participants who did not require direct personal contact. Cost pressures within the trust, leading to a reduction of staff as a result of the restructuring of commissioning of sexual health services, also made involvement problematic. Besides, for a NHS trust to assume liability for the assay, the assay would need to be supported by a performance evaluation. This was not feasible, as the trust did not house the required laboratory.
Similarly, other NHS trusts with SSK experience approached by the study team were unwilling to provide a duty of care to participants testing negative for HIV, because they would effectively have no contact at all with the individual (as the kits would be distributed in the community, processed by TDL and the patients informed of the results via text message sent by TDL). Eventually, UCLH agreed to be the ‘organisation providing care’ for all study participants; with laboratory services provided via a subcontract with TDL and a subcontract with the Central and North West London NHS Foundation Trust (CNWL) to deliver all results requiring direct contact with participants, given that UCLH did not have the prior experience or services in place to provide this. The process of establishing the clinical care pathways and necessary contracts took over 10 months, which adversely affected the ability to deliver the study on time and to scale.
Collaborating with general practices/community-based organisations
One of our study aims was to assess the feasibility of using existing services for a SSK intervention for a future Phase III evaluation. Based on results from stage 1, the study team decided to distribute HIV SSKs targeted at black African people in (GP) surgeries and CBOs working in HIV prevention in both London and Glasgow. Unfortunately, implementation of the HAUS study in Glasgow and collaborations with CBOs in London did not occur as intended.
Recruitment of general practice sites in Glasgow
Recruitment of GP surgeries for research purposes in Scotland is carried out by the Scottish Primary Care Research Network (SPCRN). Owing to the SPCRN’s previous experience of delays in gaining ethics approval and its impact on the willingness and interest of surgeries in participating in research, the SPCRN now declines to make contact with GP surgeries without ethics and NHS research and development (R&D) approvals being in place. In fact, no information on research projects can even be sent to GP surgeries prior to these approvals being in place, making it difficult to gauge interest and the likelihood of support for a project. The NHS R&D approvals in Scotland were also dependent on an agreement between GPs in Glasgow and UCL – something not required in London as no financial reimbursement would occur between London GP sites and UCL. Because CRN support differs between England and Scotland, there was a need for some reimbursement to Glasgow practices from UCL to ensure that these received the same support as their London counterparts. Despite beginning the contracting process in November 2015, it took until the end of April 2016 before the necessary contracts to enable payment were in place.
The SPCRN was provided with an introduction letter to the project, which was distributed to 17 GP surgeries across three regions within the Greater Glasgow and Clyde health board, namely Glasgow City, Clydebank and Paisley. Unfortunately, none of the surgeries responded to either accept or decline the request to participate. Owing to the lack of response, another letter was distributed, which did not yield any responses from surgeries. It is not possible to know the reasons behind this lack of willingness to participate. Anecdotally, staff at the SPCRN believed that recruitment would be low because of the low numbers of black African people attending GP nurse appointments within the Greater Glasgow and Clyde region. Owing to a lack of research sites in Scotland, the HAUS intervention could not be implemented through GP surgeries in Glasgow.
Recruitment of community-based organisations
A total of 10 CBOs were intended CBO partners in London; however, several declined to participate, because at the time of setting up this study, these organisations had to cease their services that had previously delivered HIV prevention that targeted black African people as a result of funding cuts. This meant that the burden of recruiting the required sample size for the study had to be shared by fewer CBOs than originally planned.
Waverly Care in Glasgow was involved in the project from its inception. One of the first exploratory focus group sessions (see Chapter 2, Methodology of focus group discussions and one-to-one interviews) was held on its premises, and many of its staff attended, as they had a great interest in the development of, and participation in, the intervention. Unfortunately, as a result of the delays in getting REC approval, it withdrew as distributors in order to work on developing its own HIV testing intervention, which was to be implemented for World Aids Day in 2015. As such, the HAUS intervention could not be implemented through CBOs in Glasgow.
Final intervention content
Table 8 illustrates the intervention functions and behaviour change techniques that were agreed across the team to become part of the HAUS intervention. These are the core components to be used within the intervention manual and within intervention training. As described in Step 4: viability of the intervention, these were derived after systematically having applied the APEASE criteria. 32 These criteria assess the viability of intervention function and behaviour change techniques for a real-world intervention implementable within the UK. In this way, the content of the HAUS intervention was finally agreed and drafted.
| Intervention component | Following application of APEASE criteria, intervention function and behaviour change theories to be used within the HAUS intervention in both training and the manual |
|---|---|
| The targeted offer of a HIV SSK |
|
|
|
| Participant personal information disclosure |
|
|
|
| The appearance and packaging |
|
|
|
| Compliance with kit instructions |
|
|
|
| Kit return |
|
|
Conclusion of the development of the HAUS intervention phase 2
A theoretically informed and implementable intervention was developed, specifying the active ingredients of the intervention content. It focused upon the targeted offer of a HIV SSK distributed by both practice nurses (PNs) in GP clinics and by community workers from community organisations. The study recruiters were trained using the training manual to offer black African people a SSK, using a scripted discussion that provides a rationale for HIV testing and explains how the kit is to be used. Use of the script would ensure consistency of approach across distributors. Intervention recipients were given a brief explanation of how to take the sample. They were asked to return their sample within 2 weeks using a stamped, addressed envelope provided with the kit. Using a structured approach to intervention development enabled a high degree of specificity regarding the content of the intervention training and intervention manual, and enabled clarity of focus for both process and outcome measures within the trial evaluation. The intervention manual and training materials are available on request.
Chapter 6 Study design and methodology for stage 2
The aim of stage 2 was to assess the feasibility, appropriateness of settings and optimal intervention design for a future Phase III evaluation. The objectives of stage 2 were addressed through three main research activities:
-
a feasibility study
-
a process evaluation
-
an economic analysis.
This chapter focuses on the study design and methodology for the feasibility study (see Methodology and design of the feasibility study) and the process evaluation (see Methodology and design of the process evaluation). The methodology and findings of the economic analysis are presented separately in Chapter 11.
Ethics approval was obtained from the East of England Cambridge South REC [reference number 15/EE/0412; Integrated Research Assessment System (IRAS) project ID 184223].
Methodology and design of the feasibility study
Study settings
The intervention was intended to be offered in GP surgeries and CBOs in both London and Greater Glasgow. Unfortunately, for the reasons described in Chapter 5, Collaborating with general practices/community-based organisations, implementation of stage 2 of the HAUS study in Glasgow did not occur.
London general practice surgeries
Recruitment was to be focused on areas with relatively large black African communities. South London, particularly Lambeth, Lewisham and Southwark, and Croydon and Bexley were identified via 2011 census data. Many GP surgeries within East London had recently participated in a HIV POCT intervention,69 so this area was initially excluded from recruitment, despite having a large black African population.
In mid-November 2015, staff at the South London CRN introduced the HAUS study via e-mail to practice managers whose surgeries were members of the ‘Research Sites Initiatives’ scheme. This was followed by e-mail communication to contacts at practices not part of the scheme in late November. In December 2015, the chief investigator of the HAUS study delivered a presentation on the study at a research event at Guy’s Hospital, London, to an audience of GP practice managers located in South London. This event introduced the study to a wide variety of practices, and resulted in interest in participation in the HAUS study from GP surgeries outside the initial target boroughs. As the practice recruitment rate was slower than expected, the geographical recruitment area was expanded to include all areas in South London (excluding Richmond, Kingston, Sutton and Bromley) and, eventually, North London. The study team were careful to ensure that the HAUS intervention would not interfere with recent interventions aiming to increase the level of POCT. 69
Twelve GP surgeries agreed to deliver the intervention. These sites were trained over a period spanning from mid-March to mid-June 2016 (training materials are available on request). All attendees evaluated the training received. All training sites received a trial site file, which contained the study protocol and study instruments.
London community-based organisations
Community-based organisations involved with HIV prevention in London were also recruited as distribution settings. Only organisations with experience of targeting black African people, and of which the existing scale and scope of work with this population were strong, were approached for involvement in the study.
A longlist of 10 London-based HIV CBOs that serve African people was drafted based on the extensive contacts held by members of the study. Of these, those CBOs with a predominant focus on HIV prevention were shortlisted (n = 8) and approached to attend phase 1 FGDs. This enabled the study team to identify four well-placed CBOs to be potential distributors, and one further CBO was identified at that stage to make a total of five. Ultimately, because two of these CBOs lost funding to undertake HIV prevention activity prior to the start of fieldwork (following a pattern that unfolded across the HIV sector during our study), we ultimately had three CBOs recruited as study distributors: Positive East (www.positiveeast.org.uk), NAZ Project London (http://naz.org.uk) and KwaAfrica (http://kwaafrica.org). Initial training sessions occurred in February 2016 before appropriate contracts outlining the CBO staff’s involvement and obligations to the study were finalised. There was a delay of several months between the training session and the signing of the contracts (see Chapter 5, Aligning the study protocol with quality care and research governance framework). As such, the CBO sites required retraining, as a result of the delay and staff turnover. These training sessions were delivered in April and May 2016 and focused more on data processing.
Each attendee was invited to evaluate the training sessions (the results of which are reported in Chapter 9, Acceptability and utility of training). Each CBO received a trial site file that contained the study protocol and study instruments.
Inclusion and exclusion criteria
To be eligible, potential participants needed to consider themselves to be ethnically black African, aged ≥ 18 years and able to provide informed consent. Potential participants were excluded if they were unable to read and understand English and/or could not provide a means of contact for result notification.
Statistical methods and sample size calculation
The sample size is based on the precision of the estimate of the return rate [e.g. the width of the confidence interval (CIs)]. The numbers were estimated using the well-known Wald approximation. As the primary measure is based on attrition (the return rate), no further allowance has been made for precision.
The HIV SSK projects, in the UK, (which primarily target MSM online) achieved return rates in the region of 60%. 20 Given that, in the UK, HIV testing rates tend to be lower in black African communities, the study team assumed a return rate of 50%. Distribution of a total of 600 kits per setting would enable a precision rate of at least ± 4.0% and distribution of a total of 380 kits per setting would enable a precision rate of at least ± 5.0%. Should the return rate be lower or higher with a fixed sample size, the size of the standard error would be smaller and the resulting CIs narrower.
More SSKs were to be distributed in London than in Glasgow, because the former has a larger population of black African people, and recruitment was limited in Glasgow to GP surgeries. We planned to distribute 600 SSKs in each site (GP surgeries and CBOs) in London and 380 in GP surgeries in Glasgow. Prior to the commencement of SSK distribution, it became clear that no SSKs would be distributed from Glasgow sites (for reasons outlined in Chapter 5, Collaborating with general practices/community-based organisations). Accordingly, the recruitment target was reduced from 1580 to 1200 participants.
Proportions were described using the number and percentage, and continuous data are described using the median and interquartile range. The relationship between baseline characteristics and enrolment is described using simple univariate logistic regression models. All analyses were conducted in SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Self-sampling kit
The TINY collection device in conjunction with the ROCHE HIV Combi assay (Roche Diagnostics GmbH, Mannheim, Germany) was used to test for the presence of HIV Ab in participants who consented to take part in this study. The ROCHE HIV Combi is a fourth-generation assay, used for the detection of the HIV p24 Ag and Abs to HIV-1 (groups M and O) and HIV-2. It can detect HIV that was acquired > 4 weeks ago, and is CE marked. The ROCHE HIV Combi assay has a sensitivity of 100% (95% lower confidence limit 99.8%) and a specificity of 99.63% (95% lower confidence limit 99.42%). 70 This test requires collection of 400 µl of blood (obtained by pricking a finger with the supplied lancet) in a small collection tube. The test enables the specimen to be transported to a laboratory, by post, in a vial that contains preservatives that stabilise the sample for up to 21 days if temperatures are between 4 °C and 37 °C.
The package distributed to participants included (1) the TINY kit sample collection device (including self-retracting lancets); (2) a sample data form, which required three unique sample identifiers from the participants in order for the laboratory to be able to process the sample and to enable result notification; (3) the acceptability questionnaire (see Appendix 9); (4) a paid return envelope for sample and questionnaire return to the laboratory; and (5) the sample collection instruction sheet. The instruction sheet provided information on how to collect the sample; a link to a video demonstration (www.haus.org.uk); information on labelling the sample and postage; information on how the result would be communicated and why participants may be contacted; and a reminder about completion of the acceptability questionnaire. Both the instruction sheet and the video demonstration used black African imagery.
The Doctors Laboratory, a Clinical Pathology Accreditation provider, which takes part in NEQAS (National External Quality Assurance Scheme), supplied the kits, with each featuring a unique identifier. Sites were instructed to store the kits in a locked cupboard until distribution to avoid tampering and theft. Kit distribution to all sites was tracked by the project manager.
Screening procedures
General practice surgeries
The plan was for PNs at GP surgeries to go through their patient list each morning and identify potentially eligible patients. Ethnicity information is often routinely gathered for new patients at GP surgeries in London and available on the electronic patient record, thus, enabling ID of eligible patients; this information was recorded on an enrolment log. Where ethnicity information was not available, or patients attended unexpectedly, recruiters were also encouraged to offer the intervention to others who were potentially eligible, and to record this retrospectively.
Community-based organisations
Details of all potential participants were also to be listed by CBO workers on the enrolment log, regardless of whether or not the potential participant ultimately enrolled in the study. CBOs did not always have the information required for the enrolment log (such as age) for all potential participants (especially for those who did not enrol in the study). The study team asked community workers to insert approximate age ranges when exact ages could not be ascertained.
Participant recruitment
An intervention script was provided to distributors in both GP surgeries and CBOs to introduce and initiate discussion about the study. This was supplemented by an aide-memoire in the form of key bullet points derived from the longer script. It was anticipated that this scripted interaction with potential participants would occur during routine consultations at GP surgeries or regular outreach activities undertaken by CBOs. Interested eligible potential participants were given the PIS, asked to read it, and given the opportunity to ask any questions. At this point potential participants were invited to enrol in the study and, if accepted, their eligibility was established.
If the participant declined, distributors were instructed to state, ‘That’s absolutely fine. We would really like to understand why people do not want to participate in the study. On this card are some of the common reasons why people say no’. They then showed the participant a card with nine reasons why people may not want to participate. The listed reasons were:
-
I have recently tested for HIV.
-
I do not believe I am at risk of HIV.
-
I would prefer to test elsewhere.
-
I would prefer not to use a SSK.
-
I would prefer not to know my HIV status.
-
I do not like being offered a HIV test just because I am black African.
-
I already know that I am HIV-positive.
-
I would prefer not to say.
-
Another reason.
If asked what was meant by the term ‘black African,’ distributors were instructed to clarify that this category included anyone who identified themselves as black African, whether they were migrants from Africa, African descendants or African nationals. A ‘frequently asked questions’ section was provided in the intervention manual to support distributors in fielding any questions that they may receive about HIV or the study process. If the potential participant was ineligible, the distributor thanked them for their interest, explaining that they did not meet the eligibility criteria, and suggested an alternative method of HIV testing.
Consent process
Informed consent was obtained from all participants. Though the study team intended for the majority of consent to be obtained via tablets, most sites used paper forms. In the case of GP surgeries, there was overwhelming preference for paper forms. Reasons for this preference usually centred on the lack of dependable Wi-Fi at GP surgeries and concern that the tablets would be stolen. As such, only the CBO sites were provided with study tablets, though the CBOs also relied on paper forms when the tablets were not feasible. Responses entered via tablets were automatically recorded and stored in the study database. Completed paper consent forms were sent to the trial manager via secure fax or e-mail.
The consent forms contained both mandatory and optional components. For those participants recruited from GP surgeries, notifying the general practitioner of the HIV test result was an optional consent item. If consent to this item was granted, the general practitioner was notified via letter from the chief investigator. The general practitioner was not informed if consent was not obtained for this item, and was also not informed if a participant decided not to return the kit to the laboratory for analysis. Participants recruited at both sites were given the option of consenting to be contacted for follow-up telephone interviews.
Baseline data
Participants were asked to complete a short baseline questionnaire (see Appendix 10) in situ either on paper or via a tablet. The baseline questionnaire collected demographic data and provided a brief assessment, which asked about country of birth, duration of UK residence, HIV testing history and sexual activity within the last 12 months. The baseline data were for research and governance purposes, and were not intended to be used or seen as a risk assessment screening tool.
Distribution of the kit
The distributors then gave the participant a SSK and briefly explained the processes involved with kit use. Distributors also explained how results would be communicated. Additional information on how to use the SSK, how to access the online video of someone using the kit, the importance of posting the sample to the laboratory for processing and the use of reminder text messages to participants should the sample not be received at the laboratory were highlighted in the PIS and instruction sheet.
Sample collection and analysis
Participants who self-collected a sample were also required to complete the sample form with three unique identifiers (initials, date of birth and a unique ID number) to enable the sample to be processed at the laboratory. The ID number was prepopulated on both the sample form and the acceptability questionnaire.
Follow-up of participants
Acceptability questionnaire
Every kit included an optional brief acceptability questionnaire (see Appendix 9), which was completed and returned with the sample. The questionnaire explored the acceptability of being offered a SSK in the setting, acceptability of targeting and the process of using the kit. The unique ID number enabled linkage with test results and baseline data.
Telephone interviews
At enrolment, participants were asked if they would be willing to take part in optional follow-up telephone interviews. The study team initially aimed to complete 30 interviews, purposively sampled to include participants across age ranges and genders, and to ensure a balance between participants who did and those who did not return a sample, in each of the intended study cities, as well as those recruited through each distribution setting (CBO or GP surgery). Because the overall recruitment target was not met, and this stage did not ultimately take place in Glasgow, the number of participants targeted for interviews was revised to 20. We sought to maintain a balance between those who did and those who did not use the kit. Furthermore, as this stage of the study progressed, a substantial proportion of kits were returned with insufficient samples, so we expanded our purposive sample to ensure that we interviewed a balanced sample between three groups: (1) those who accepted a kit but did not return a sample, (2) those who used a kit and received a negative result and (3) those whose sample was unable to be processed as a result of underfilling of the blood vial. Interviewing participants with reactive results was never part of our purposive sampling strategy, as we felt that this would probably cause distress; as it was, no reactive results emerged from within the study sample. This revision of the purposive sampling strategy enabled us to be responsive to the conditions and realities faced by our study population as they emerged in real time.
A topic guide (see Appendix 4) exploring kit distribution, kit use and return and the implications of the intervention was used for the interviews. Participants provided verbal consent to proceed with the interviews at a mutually convenient time. Interviews lasted approximately 30 minutes, and interviewees were sent a £10 voucher for their time. Interviews were recorded and transcribed. Detailed notes were taken during non-recorded interviews in lieu of transcription.
Anonymised transcribed interviews, along with notes from non-recorded interviews, were imported into an NVivo 10 file for coding and analysis. The interviews were analysed using a thematic approach.
Results communication and management
Anonymised results were communicated from TDL to the project manager at UCL on the same day that sample analysis occurred, via secure encrypted e-mail. There were three possible test results: (1) HIV not detected, (2) reactive sample or (3) insufficient sample (as a result of either underfilling of the TINY vial or gross haemolysis). UCLH provided a duty of care to all participants who returned a SSK, regardless of whether they were recruited at a GP surgery or a CBO. However, the duty of care was passed to CNWL for reactive results, insufficient samples and those without a mobile phone number. This arrangement arose because UCLH does not currently provide a self-sampling or HIV result notification service for patients. CNWL does, and its staff members have clinical expertise in the provision of HIV results. If a participant were to require confirmatory testing, the duty of care would pass to the health-care institution attended.
Non-reactive results
In line with standard practice in most NHS sexual health clinics, non-reactive results were delivered via text message. TDL, under contract to UCLH, was responsible for the delivery of these messages. If a participant provided only alternative contact means (e.g. a landline telephone number), then the study team tasked a health advisor (HA) at CNWL to notify the participant as per normal clinic practice.
Reactive results and insufficient samples
Participants with reactive results or insufficient samples were notified by telephone by CNWL HAs. HAs attempted to make contact directly with participants, rather than leaving a message for the participant to call back.
The Doctors Laboratory notified the project manager at UCL of any reactive or insufficient results on the day of the sample analysis via secure encrypted e-mail. At this stage, the names of participants with reactive samples were unknown to all parties, as only initials were required with the return of the SSK. The study manager would link the study ID number to the associated consent form and baseline questionnaire, thus obtaining the participant’s name. This information was passed to the HA in person, enabling them to contact the participant. Should any reactive results have been obtained, the HA would also have made follow-up telephone contact with the participant to ensure linkage to care had occurred. It was anticipated that this would also provide an opportunity to identify any unexpected consequences of the testing process.
For those with reactive results, the study team planned to offer follow-up for confirmatory testing within 1 working day of the test result. As postal code information was gathered, HAs were enabled to contact the sexual health clinic nearest any participant with a reactive result, to arrange for confirmatory testing. Thus, there was a process in place to ensure that any participant with a reactive result would be linked to specialist care.
For those with insufficient samples, a process identical to that in the case of reactive results was followed. The participant with the insufficient sample was offered three options via telephone communication: to have a second SSK posted, to be advised on where to access alternative HIV testing or to discuss alternative testing options with their general practitioner.
For both reactive results and insufficient samples, the HA was responsible for documenting the pathways into care and recording follow-up attempts and next steps, including linkage to care.
A schematic of the HAUS fieldwork process is provided in Appendix 8.
Methodology and design of the process evaluation
Purpose and scope of the evaluation
An understanding of what was implemented and how it was implemented is integral to explaining how an intervention works, in order to address questions of feasibility, or whether or not it was possible to deliver the intervention as planned in the chosen settings.
The principal concern of early process evaluation frameworks was capturing what was delivered in practice in order to avoid dismissal of sound intervention theories as a result of a failure to implement them effectively. 71 Most frameworks focus on the precise ‘form’ of delivery in terms of whether or not this represents fidelity to what was intended to be delivered, as well as measuring the reach of delivery (the dose). There is debate about whether or not adaptations in programme delivery, decided locally, enhance intervention clinical effectiveness or lead to poorer outcomes. 71,72
Advocates of strict fidelity73 argue that fidelity is essential if effective interventions are to be replicated, especially when an intervention’s ‘active ingredient’ may not be known. Advocates of local adaptation argue that interventions need to be tailored to local circumstances. 72 Durlak and DuPre74 propose a compromise, whereby the ‘core components’ of an intervention should be delivered in standard form, but less central intervention components or features can be modified to fit local needs. They present research that suggests that a balance between fidelity and adaptation is likely to be most effective, with the precise balance being dependent on the specific intervention.
The process evaluation was informed by Medical Research Council guidance75,76 and the wider implementation science literature. 77–79 It investigated not just implementation of the intervention (that is, fidelity, reach and acceptability), but also considered mechanisms of action (the impact in context) and potential future normalisation of the intervention. These three areas of exploration are described in fuller detail below.
-
Implementation:
-
Were standardised intervention components implemented with fidelity of form?
-
Where deviations from fidelity of form occur, do these reflect intentional adaptation (and, if so, with what motivation), unintentional drift or simple omission?
-
What was the reach of the intervention?
-
How did reach and acceptability vary across key subgroups of African people, and what contextual factors appear to affect this?
-
-
Mechanisms of action:
-
Does the intervention increase access to HIV testing (opportunity)?
-
Does the intervention provide an acceptable and viable option to establish HIV status (capability)?
-
Does the intervention increase motivation to test for HIV?
-
Are any potential harms suggested by qualitative data?
-
-
Normalisation:
-
Is the intervention likely to be supported by key stakeholders in future funding and delivery of SSKs? Do they –
-
view the intervention as coherent?
-
commit to future participation?
-
commit to collectively take on the work arising from the intervention?
-
review progress in implementing the intervention?
-
-
To address these areas, the process evaluation collated information from the inception of stage 2. Figure 4 contains a flow chart of the data collection points relevant for the process evaluation. The following data were intended to be collected:
-
study diaries – the study team routinely recorded challenges and issues encountered in all aspects of the implementation of the feasibility study
-
training evaluation – distributors were asked to complete a before/during/after survey assessing the value of the training, the extent to which the training met its stated aims and their comfort and confidence in delivering the HAUS intervention
-
screening and recruitment logs – these data assisted in monitoring progress during recruitment and facilitated early intervention if support in recruitment was required
-
distributor weekly log – distributors were asked to complete a weekly log to monitor their recruitment progress and report any problems with recruitment (see Appendix 11); they were asked to rate how they felt about recruiting people to the HAUS study, their confidence level in targeting black African people and answering questions about the study, and whether or not they used techniques provided in the training session or study manual
-
site visits – up to two site visits were planned with each distributor, to support implementation of the intervention; detailed notes were taken during the visits to aid with understanding of the environments and circumstances in which the intervention was being delivered
-
data flow – the speed and success of data flow through all elements of stage 2 were monitored to assess intervention feasibility
-
support queries and responses – any contact with the study team by distributors or study participants was logged
-
site summaries – throughout the distribution period, data from distributors were collated and synthesised into a one-page intervention summary for each site, describing their key successes, challenges and experiences along the way; each summary was cross-checked by the project manager, and then e-mailed to each distributor in turn, for their consideration and comments
-
site close-down interviews – the site summaries were used as the basis for undertaking final face-to-face interviews with distributors at each site; focus groups were originally planned; however, as few individuals at each site undertook distribution (in many cases, only one individual took up distribution), one-to-one or small group interviews were a more feasible format; interviews lasted for approximately 30 minutes (range: 5–60 minutes); a semistructured topic guide (see Appendix 12) was used to structure these discussions; the focus of the interviews was to gauge acceptability of the intervention, and distributors’ experience of undertaking targeting, recruitment and consenting procedures, and fielding questions; the interviews were recorded when possible, and notes were taken throughout; annotations formed the basis of analysis, with recordings providing back-up when needed
-
qualitative interviews with study participants – the process evaluation also drew from the qualitative follow-up interviews with participants (see Follow-up of participants above).
FIGURE 4.
The HAUS study process evaluation plan. LA, local authority.

The raw and synthesised data were then coded and analysed, with a focus on eliciting themes relevant to the organising principles of feasibility (fidelity) and acceptability.
Chapter 7 Results
The recruitment period for London-based CBOs and GP surgeries was reduced from 6 to 4 months (April to July 2016), as a result of delays caused by the kit selection and governance issues (see Chapter 2, Step 4: viability of the intervention). As such, the study team anticipated that recruitment would fall short of the revised target of 1200 participants.
Overall results
The recruitment rate from all sites (even when accounting for the truncated recruitment period) was substantially slower than expected, with only 349 eligible persons approached in total; 229 from GP settings and 120 in CBO settings. Of those 349 people approached, 125 (35.8%) agreed to participate. However, six participants who all returned their SSKs, subsequently had to be excluded because of errors with the consent process, providing a final total of 119 participants. Figure 5 illustrates the participant flow from screening to enrolment for GP and CBO settings.
FIGURE 5.
Participant flow from screening to enrolment per recruitment setting.
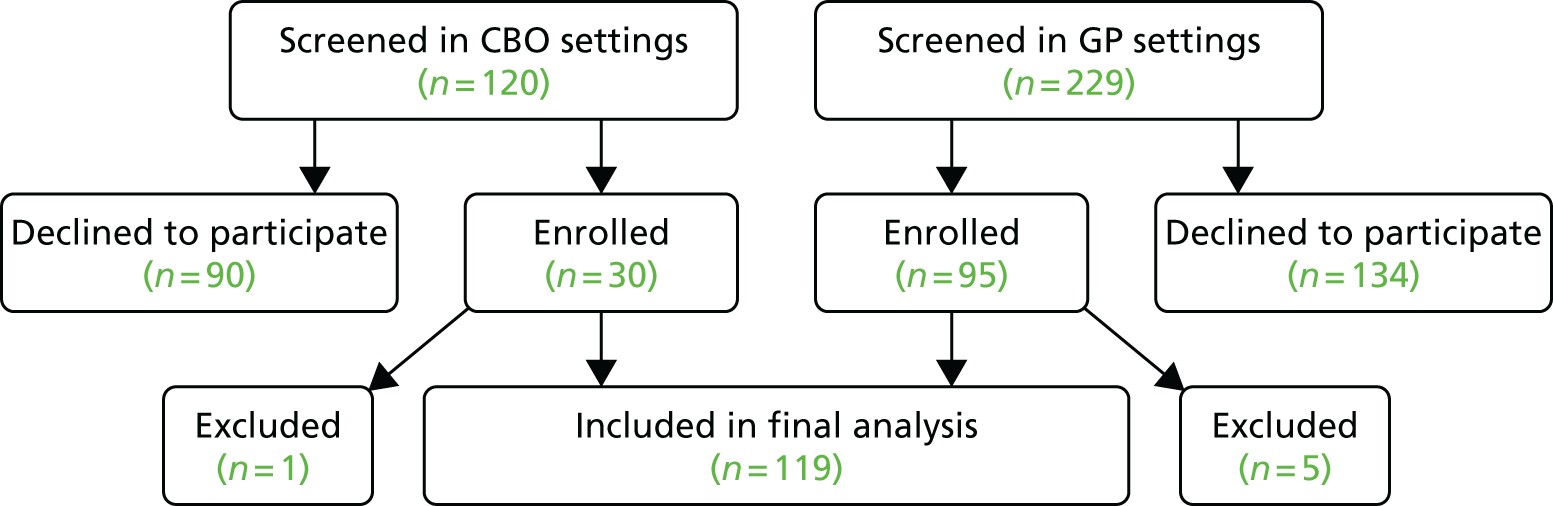
The most common reason for declining to participate was that the person had recently tested for HIV (25%), followed by lack of perceived risk (18.7%; Table 9). Six (2.7%) people stated that they did not like being offered a HIV test just because they were black African and a further 17.4% declined as they wanted to either test elsewhere or not use a SSK. We were unable to assess if the reasons for declining varied according to whether recruitment was in a GP surgery or via a CBO, as a result of the number of reasons presented and insufficient degrees of freedom.
| Reason for declining to participate | Frequency, n (%) |
|---|---|
| I have recently tested for HIV | 56 (25.0) |
| I do not believe I am at risk of HIV | 42 (18.7) |
| I would prefer to test elsewhere | 19 (8.5) |
| I would prefer not to use a SSK | 20 (8.9) |
| I would prefer not to know my HIV status | 15 (6.7) |
| I do not like being offered a HIV test just because I am black African | 6 (2.7) |
| I already know that I am HIV positive | 4 (1.8) |
| I prefer not to say | 19 (8.5) |
| Another reason (unspecified) | 43 (19.2) |
| Total | 224 (100) |
Eligible people visiting their GP were significantly more likely to be recruited than those approached via a CBO [odds ratio (OR) 1.96, 95% CI 1.21 to 3.19]. There was no observed relationship between gender or age and enrolment status (OR for greater recruitment among women 1.12, 95% CI 0.72 to 1.75; and OR for greater recruitment with increased age 1.02, 95% CI 0.997 to 1.034).
In total, 119 participants were correctly enrolled: there was a median age of 42.6 years (range 18–79 years); 58 participants (48.7%) were men; and the majority of participants (90; 75.6%) were recruited from GPs (Table 10). The SSK return rate was 55.5% (66/119, 95% CI 46.1% to 64.6%).
| Characteristic | Overall (N = 119), n (%) | SSK returned, n (%) | |
|---|---|---|---|
| Yes (N = 66) | No (N = 53) | ||
| Age (years), median (interquartile range) | 42.6 (32.7–51.7) | 41.6 (32.7–51.6) | 44.6 (36.7–53.7) |
| Male | 58 (48.7) | 33 (50.8) | 25 (46.3) |
| Recruitment site (n = 119) | |||
| GP | 90 (75.6) | 45 (50.0) | 45 (50.0) |
| CBO | 29 (24.4) | 21 (72.4) | 8 (27.6) |
| Country of birth (n = 109) | |||
| Africa | 89 (74.8) | 45 (50.6) | 44 (49.4) |
| Elsewhere, including the UK | 20 (16.8) | 12 (60.0) | 8 (40.0) |
| Time in the UK (n = 113) | |||
| < 1 year | 6 (5.0) | 3 (50.0) | 3 (50.0) |
| 1–2 years | 1 (0.8) | 0 (0) | 1 (100) |
| 2–5 years | 7 (5.9) | 4 (57.1) | 3 (42.9) |
| 5–10 years | 16 (13.4) | 8 (50.0) | 8 (50.0) |
| > 10 years | 6 (5.0) | 36 (52.9) | 32 (47.1) |
| Born in the UK | 15 (12.6) | 9 (60.0) | 6 (40.0) |
| Time since last HIV test (n = 113) | |||
| Never previously tested | 30 (26.5) | 12 (40.0) | 18 (60.0) |
| < 1 year ago | 19 (16.8) | 10 (52.6) | 9 (47.4) |
| 1–2 years | 17 (15.0) | 12 (70.6) | 5 (29.4) |
| 2–5 years | 17 (15.0) | 11 (64.7) | 6 (35.3) |
| > 5 years | 22 (19.5) | 12 (54.5) | 10 (45.5) |
| Prefer not to say | 8 (7.1) | 3 (37.5) | 5 (62.5) |
| Sex in the past 12 months (n = 113) | |||
| I have not had sex | 21 (18.6) | 15 (71.4) | 6 (28.6) |
| With both men and women | 1 (0.9) | 1 (100) | 0 (0) |
| Only with the opposite sex | 86 (76.1) | 41 (47.7) | 45 (52.3) |
| Unsure or prefer not to say | 5 (4.4) | 3 (60.0) | 2 (40.0) |
There was a reduced odds of SSK return with increasing age, although this was not statistically significant (OR 0.98, 95% CI 0.96 to 1.01; p = 0.212). Similarly, there was a non-significant reduction in the odds of returning a kit among women than with men (OR 0.84, 95% CI 0.41 to 1.72; p = 0.627). Kit return may vary according to whether recruitment occurred in a GP site or a CBO (OR 2.63, 95% CI 1.05 to 6.54). Twelve people who returned a kit had never previously tested for HIV and a further 12 had not tested for over 5 years.
The majority (83.1%) of tests returned HIV-negative results. However, 11 samples (16.9%) were unable to be processed, as a result of the vial being underfilled or the sample being grossly haemolysed. There were no reactive results. Of the 11 participants who returned insufficient or grossly haemolysed samples, only one requested a further SSK be mailed to them (unfortunately, this was also returned as an insufficient sample). Three were unable to be directly contacted and, after three attempts, a text message informing them of the outcome was sent. Most participants (n = 5) opted to discuss alternative testing options with their general practitioner when they next attended.
Acceptability data
Of the 65 participants who returned a SSK, 62 (95.4%) also returned the acceptability questionnaire (see Appendix 9). The offer of the test directly helped 79.0% of respondents to decide to test for HIV. The overwhelming majority (59/62; 93.7%) also reported that the person who offered the kit helped them to feel more confident about knowing their HIV status. Just under one-third (19/62; 32.2%) reported watching the video online; of these, 19 people found the video to be helpful, and 14 (83.3%) stated that it made them feel more confident. The majority of kit returners (73.2%) reported that they would be willing to use one of these kits again.
Participants were asked to rank how they found aspects of the intervention (Table 11), using a visual scale (Figure 6).
| Item | Level of acceptability, n (%) | ||||
|---|---|---|---|---|---|
| Very unacceptable (–2) | Unacceptable (–1) | Neutral | Acceptable (+1) | Very acceptable (+2) | |
| Acceptable to be offered a HIV test in this manner | 0 (0) | 3 (4.8) | 7 (11.3) | 9 (14.2) | 43 (69.4) |
| Acceptable to be offered a HIV test because you are African (n = 61) | 18 (29.6) | 3 (4.9) | 13 (21.3) | 3 (4.9) | 24 (39.3) |
| Location where the participant was offered the kit (n = 60) | 0 (0) | 0 (0) | 4 (6.7) | 10 (16.7) | 46 (76.7) |
| Item | Level of difficulty, n (%) | ||||
| Very difficult (–2) | Difficult (–1) | Neutral | Easy (+1) | Very easy (+2) | |
| Instructions in the kit were easy to understand (n = 61) | 4 (6.6) | 2 (3.3) | 5 (8.2) | 17 (27.9) | 33 (54.1) |
| Item | Level of comfort, n (%) | ||||
| Very uncomfortable (–2) | Uncomfortable (–1) | Neutral | Comfortable (+1) | Very comfortable (+2) | |
| How the participant felt about taking the sample themselves (n = 61) | 10 (16.4) | 4 (6.6) | 10 (16.4) | 14 (23.0) | 23 (37.7) |
FIGURE 6.
Visual scale used with the acceptability questionnaire.

The least acceptable aspect of the intervention was the targeting of black African people, with just over one-third of participants (34.5%) reporting that it was unacceptable. No one felt that the location in which they were offered the kit was unacceptable. The majority of participants (82%) found the SSK instructions easy to understand, and most (67.7%) felt comfortable with taking the sample themselves.
Limitations
The small sample size limits our ability to make associations and draw conclusions as to who did and who did not participate and/or return their sample. However, the baseline demographic and behavioural data of participants suggest that the intervention was reaching a black African population at risk of living with undiagnosed HIV, and four people approached to participate disclosed that they were already known to be HIV positive.
Acceptability data in this format are provided only on those who returned their sample, and, by definition, this is the group most likely to have found the intervention acceptable. Further qualitative data exploring acceptability with participants who did and those who did not return their sample are provided in Chapter 9. Finally, the failure of intervention implementation in Glasgow means that we were unable to assess whether or not acceptability or feasibility may vary across the UK. We had specifically wanted to test the intervention in two distinct health-care systems, which differed in the proportion of African people within their population, and in the provision of HIV and community services, in case this impacted on the acceptability and cost-effectiveness of the intervention.
Summary
Our findings demonstrate that users of the SSK liked being able to access HIV testing in this manner, and in the locations provided. The proactive opportunistic offer of the kit was directly responsible for the majority of kit users deciding to have a HIV test. Although numbers were small, there was a suggestion that distribution of HIV SSKs in these settings could help to increase the uptake of HIV testing in black African communities as 12 kit returners (18.5%) had never previously tested for HIV, and a further 12 (18.5%) had tested over 5 years ago. However, recruitment was low, with only 128 people (35.8%) approached consenting to participate. Although it is reassuring that 56 (25%) people declined participation in the study because they had recently tested for HIV, 42 (18.7%) did not perceive themselves to be at risk, and a further 15 (6.7%) did not want to know their HIV status – both potentially reflecting the impact of HIV-related stigma. A further 39 (17.4%) may have tested if an alternative method or location were available.
Although acceptability of the intervention was probably higher in those returning a kit, over one-third of participants still reported that it was not acceptable to be offered a HIV test because of their ethnicity. It is unclear whether or not these participants were aware that they had been explicitly targeted as black African people, as the findings from the follow-up interviews (see Chapter 9, Acceptability of targeting to African people in London) suggest that not all participants had realised this. Only six (2.7%) of those declining to participate indicated that targeting was responsible for their decision.
The kit return rate of 55.5% is in keeping with similar projects65 and, somewhat concerningly, so is the proportion of samples received that were unable to be processed as a result of underfilling or gross haemolysis. Our finding that 16.9% of samples (11/65) were unable to be processed is similar with the 15.4% reported by the national HIV self-sampling service among their 1125 black African users to date (Tim Alston, Preventx Ltd, 2016, personal communication). This suggests that an alternative to the TINY vial is required if HIV SSKs are to be an effective means of increasing the uptake of HIV testing in black African communities. There is also the potential that a negative experience with a SSK may put people off alternative or future HIV tests; therefore, the choice of SSK and its acceptability to participants should not be compromised in future research.
Chapter 8 Process evaluation: intervention fidelity and reach
The HAUS study aimed to establish whether or not it was feasible and acceptable to distribute and monitor the distribution of HIV SSKs to black African people using GP surgeries and community outreach services. This chapter describes findings from key elements of the process evaluation, which linked to the feasibility trial to allow for a fuller interpretation of the findings for potential further application.
There were three broad areas of interest within the purview of the process evaluation related to the implementation of the HAUS intervention: (1) fidelity, (2) reach and (3) acceptability. This chapter addresses fidelity and reach; the acceptability of the intervention for kit users and service providers is explored in Chapter 9.
Purpose and scope of the process evaluation
Fidelity
The HAUS intervention was designed to be implemented with highly standardised inputs and processes, with little or no site-specific tailoring. However, in practice, substantial local tailoring was observed. Therefore, our approach to evaluating implementation focuses both on fidelity of form and fidelity of function. Fidelity of form refers to the extent to which the intervention followed the standardised structures and processes developed for stage 2 of the HAUS study, as described in Chapter 6. This process evaluation examines the extent to which these standardised intervention components were implemented with fidelity of form. When we observed deviations from fidelity of form we assessed whether or not these were intentional adaptations (and, if so, what motivated them), unintentional drift or simple omission, and whether or not the adaptations ran with or against the logic of our theory of change (that behaviour is an outcome of three necessary conditions: capability, opportunity and motivation). This was a substantial issue in the HAUS study, as the intervention was delivered across 12 GPs and three African CBOs throughout London. We also examine fidelity of function, that is, the extent to which locally decided adaptations to the intervention processes were consistent with the overall theory of change.
Reach
Reach is the extent to which the target audience come into contact with the intervention. Moore et al. 75 recommend that process evaluations should include quantitative assessments of reach, in terms of, for example, proportions of the target audience who are aware of, and come into contact with, the intervention.
Assessing the reach of awareness of the HAUS intervention across the whole population of black African people in England and Scotland was not appropriate or feasible within the context of this study. Unfortunately, we were also unable to accurately determine what proportion of eligible persons in contact with the recruiters were actually exposed to the intervention. It was intended that the enrolment log would capture this information, but, in reality, these were often poorly completed. The data we have show that 349 people were offered the intervention, with 125 people agreeing to participate. In excess of 37,000 black African people are resident in the borough of Lambeth alone.
Normalisation
A further component of this process evaluation is to better understand the process by which interventions might best become embedded in distributors’ routine policies and systems of service delivery. This is often described in terms of ‘normalisation’ or ‘sustainability.’
There is a variety of frameworks that help evaluators assess intervention normalisation (e.g. the RE-AIM framework). 80,81 However, the study team chose to use the normalisation process theory. 77 The focus of this theory is to consider how implementers can enable the embedding of interventions within institutions and social contexts so that they are ultimately integrated. 77 The theory suggests that whether or not this happens depends on the following four ‘generative mechanisms’ that those working on implementation engage in individually and collectively:
-
coherence (how people make sense of a new practice)
-
cognitive participation (the willingness of people to sign up and commit to the new practice)
-
collective action (people’s ability to take on the work required of the practice)
-
reflexive monitoring (activity undertaken to monitor and review the practice).
The HAUS study: fidelity and feasibility
We start by examination of those areas where fidelity to the intended ‘form’ (by this we mean the structural and procedural issues) of the intervention either proved difficult or required adaptations to the agreed protocol. The second part of this section relates to aspects in which fidelity to key aspects of the intervention ‘function’ proved difficult for some distributors and/or participants. Intervention function relates to the central mechanisms that underpin the intended study and intervention design. Quotations are taken from the weekly distributors’ experience survey, e-mails to the project manager and the final distributor interviews.
Distributors
Within CBO settings, it was intended that community outreach workers would be the distributors of the SSKs, and this was what was reported from these distributors. Although the distributors within GP settings were intended to be PNs, during the training it became clear that this was not always going to be feasible. A range of GP locations told the project manager from the outset that other staff members in the surgery would be undertaking study recruitment and distribution, including: general practitioners, HCAs and practice managers. In all, 8 of the 12 practices used one or more of these alternate members of staff as recruiters and distributors for the study.
Discussions during site visits established that each practice took a different approach to managing staff workloads. This sometimes meant that HCAs were regarded by their senior colleagues as having more time to devote to research tasks than others, even if that was not actually the experience of HCAs. Alternatively, in a number of cases, general practitioners with a particular interest in sexual health took on responsibility for recruitment and distribution themselves. Though they were working under time pressures to stay within the typical 10-minute appointment schedule, they distributed the SSKs because they had a particular commitment to the issue. The following quotation is from a GP surgery where two general practitioners participated as distributors:
Why was it you two who did this?
Because we volunteered for it! We were the ones who were interested.
You got the e-mail, didn’t you?
Yeah, and I knew you would be keen.
Because we are doing a lot of gynae, and sexual health generally. So, it’s an area of interest.
In the main, we can conclude that in the majority of GP surgeries, it was not PNs (or not PNs alone) who recruited participants into the study and distributed kits. This action, while deviating from study intention, facilitated recruitment by increasing the opportunities in which it could be delivered, and, as such, should be considered a logical adaptation.
The intervention was designed to work alongside distributors’ existing commitments. However, it was reported to us by one general practitioner that staff members’ days off were used to attend HAUS training, and, in another instance, a general practitioner came into the surgery on her days off to undertake recruitment. Other distributors explained that it took a lot of additional time in the day (including overtime and loss of breaks) to fit in study recruitment, kit distribution and the associated research tasks.
Targeting
Within CBO outreach settings, it was intended that community workers would identify black African people whom they encountered in their routine outreach activities and locations to approach for study participation, and this is what was (in the main) reported by these distributors. In some cases, community workers also undertook special outreach events at settings, such as barbershops, in order to specifically recruit to the study.
Within GPs, it was intended that eligible individuals would primarily be identified from patient lists (using recorded ethnicity and/or country of birth data) at the start of the day, prior to the initiation of appointments. That way, a prepared enrolment log could be in front of each distributor, ready for when the patient came to them, and they could log the patient’s reason for refusal, or their agreement to take part on the enrolment log. This method was also intended to eliminate the need for practice staff to try to identify a patient’s ethnicity visually or to ask them their ethnicity prior to offering them the intervention.
Five GP surgeries informed us that there were usually or always insufficient data available to them to identify potential participants’ ethnicity in this way. As a result, practices resorted to a variety of alternative means of targeting black African people. Staff in at least four practices described using visual cues (both in the waiting room and in the consultation room) to identify potential participants. One practice, in particular, reported that this meant that many of those approached were ultimately found to be ineligible, as the majority were black Caribbean, rather than black African. Other tactics were also used to identify potential participants, in particular, knowledge of patient backgrounds, especially for those recruited in primary care. Having a range of practices to assess potential eligibility could cause confusion, as indicated by this comment:
Dr X asked the patient, who was happy to participate. I’m not sure if this particular patient fitted into the category though so was a little confused. The patient was born in the UK, so I could not remember whether this mattered or not.
Some practices did effectively use ethnicity data contained within their databases to identify some or all those eligible for participation. One practice designed a prompt to remind the distributor to introduce the study to come up on the practitioner’s screen when that patient was being seen. Another practice wanted to initiate such a system, but was ultimately unable to do so.
One GP used the ethnicity data that they held on patient lists to screen for eligibility and then contacted patients to invite them to make an appointment, so that the HAUS study could be introduced and discussed. This represents a considerable departure from the intention that the intervention was to take place alongside existing routine service delivery in GP settings when patients presented for other reasons.
Script to introduce the study
It was intended that distributors in CBO and GP settings would use the agreed script to present the study to eligible participants. The script and its importance were underlined at all training events, and laminated cards with the script wording were made available in each site manual.
When asked at follow-up about the extent to which they had adhered to the script, the staff at eight study sites said that they had not used the script consistently. Most said that they had used either the script or the PIS to become familiar with what information was to be communicated, and then they summarised it in their own words. One distributor remarked:
I used my own words, because it’s something I do on a daily basis. I just use my words, and the statistics are very important, they don’t lie. As well, I try to find out what part of Africa they are from.
Another distributor clarified that they did not follow the script word for word, preferring to memorise the key facts and state them in their own way.
It was felt that reading from a card could undermine confidence in the distributor, and one distributor said he was ‘not a robot’ and, therefore, needed to put things into his own words.
It was clear that, in most cases, the number of approaches made by each distributor in a single day or even a single week was too low to expect them to have committed the script to memory. Furthermore, at many GPs, study paperwork (including the site file) may not have been in the same room as the distributor, so they needed to raise the issue opportunistically and then find the relevant PIS and consent form afterwards. None of the CBO distributors reported adherence to the intervention script, as, once again, they had found it more comfortable to summarise and put things into their own words. Again, this can be regarded as a purposeful deviation from the intended intervention design, based on the practicalities of delivering it in busy settings and the professional expertise of health-care staff to put things in the most-appropriate language for a particular patient or situation.
When asked to confirm that they had all introduced the study in a way that made it clear that black African people were being targeted for distribution because of a higher prevalence of HIV in this population, all distributors agreed that they had made this clear in their tailored introductions to the study.
Recruitment process
In the intervention protocol, it was intended that one single distributor would take the participant through the entire recruitment process themselves, and that this would all happen within one 10-minute time period. Research paperwork (the consent form and the baseline questionnaire) was to be completed within this period, along with kit distribution and answering of any questions.
In the main, all CBO distributors attempted to adhere to this process, and all struggled to keep the required components to a 10-minute time frame. On at least one occasion during distribution at a barbershop, the barber first introduced the study to potential participants, and then sent interested participants to community workers at the back of the shop.
This practice of ‘funnelling’ potential study participants to other distributors who would then take them through the eligibility criteria and the study documentation was also evident in a few GPs. In these cases, a PN or a general practitioner would introduce the study, and then send interested individuals on to a designated colleague to complete the process. This was regarded as a means of extending reach, while utilising time and expertise efficiently. One distributor explained: ‘It was easy to do in surgery as another member of staff does the consent’.
Another variation, applied in a few practices, was for staff to break the recruiting process down into distinct stages, in order to avoid appointments backing up. For example, general practitioners at one surgery introduced the study during the appointment, and then asked interested individuals to go out into the waiting room to review and complete the study documentation on their own. These patients were then called in between appointments until all questions were answered and all documents completed. Again, this represents an opportunistic departure from intervention fidelity, as an attempt to undertake at least some recruitment in this setting.
At another practice, a HCA approached patients who looked to be black African and introduced the study to them in the waiting room (rather than in private as had been intended). Individuals were left with a copy of the PIS and invited to approach the HCA in her consultation room if they wanted to take part, and the rest of the process was carried out there. Finally, a HCA at a third practice said that he tended to introduce the study at the start of the consultation, and then, based on the patient’s response, gauged the remaining consultation time. If the patient seemed interested, the distributor tried to make sure he had time to go through all the stages of study recruitment by the end of the appointment. He felt that this tactic helped to prioritise the patients’ presenting health needs over the needs of the research study, while also ensuring that they did not leave the consultation without his having mentioned it.
Although in CBO settings it was suggested that the instruction video could be shown to potential participants as a part of the recruitment process, this option was not often utilised, because of time pressures or internet connectivity problems, or because it was felt that it could be ‘off-putting’ by at least one distributor.
Study procedures
It was intended that the introduction and recruitment components of the study, including sharing of the PIS and completion of the consent and baseline questionnaires, would take no more than 10 minutes. Feedback from almost all distributors indicated that it took considerably longer to get through the entire process, which, in the particular case of oversubscribed GP surgeries, caused major feasibility issues:
The only problem is the time, as no extra time has been allocated for this study while some minutes are needed to provide the information to patients as well as when patients asked questions to understand more about the study.
Difficult time wise to fit/ add into a 10 min[utes]. GP consultation when all the time has already been used up with the patient’s agenda/ symptoms.
There was a considerable burden of data management and data tracking expected of each distributor. A few sites (particularly CBOs) found it difficult at first to keep a log of those who they had approached who had refused, partly because of the perception that the study team needed an age and other data for each person who had refused, as well as a reason for their refusal. Once the study team intervened to suggest that estimates and null values were acceptable entries in the enrolment logs, tracking of refusals improved.
Furthermore, it was essential that in all cases an identical kit ID number was attached to the paperwork an individual had completed, which matched with the kit ID number on their SSK. In at least one case, the SSK kit ID did not match that on the paperwork received by the study team.
There was a range of data flow that was essential to the smooth running of the research study, including electronic or faxed copies of consent and baseline forms and enrolment logs being sent to the project manager, and completion of weekly distributor logs to identify and respond to emergent challenges. Both sets of data were generally very slow to be returned to the study team. This introduced a number of unintended challenges, as the project manager was frequently not in possession of the consent form or contact details of a participant who had, for instance, sent back an insufficient sample, and who therefore needed to be called by telephone to be advised of their options (see Chapter 6, Results communication and management). In this way, the participants, Royal Mail and TDL were able to jointly act with far greater efficiency than the distributors and the study team in terms of relaying required information through to one another. These logjams occasionally meant that results could not be clearly communicated to individuals until the paperwork had caught up. Occasionally, these logjams took a number of weeks to resolve and, in a small number of cases, the paperwork never materialised, so the individuals had to be excluded from the study. All individuals who returned a sample were informed of their results regardless of whether or not they were subsequently included in study.
Connection to other HIV testing interventions
The HAUS study was not intended to be delivered (either as a follow-on or a precursor) with any other HIV testing interventions being undertaken by the distributing agencies. However, it was reported by one CBO that, following an event where the SSKs had been introduced, a group of interested people accompanied the individual back to the CBO office to undertake a POCT HIV test, because they regarded this testing option as more acceptable than the SSK on offer in the HAUS study.
Distributor support to take blood sample
The study was designed to assess the acceptability and feasibility of the targeting and use of HIV SSKs among black African people. However, two distributors (one CBO and one GP surgery) described assisting participants with the blood sample collection. In the case of the GP surgery, the practice manager decided that, as she found the kit so difficult to use, she would support every single participant she recruited, and reported that the entire time spent with each participant was between 30 and 40 minutes. The following excerpt is from an enrolment log:
I helped another patient today, and again the whole process took ages to complete. This was because the patient’s blood wouldn’t flow from her fingers, we used all the lancets in the box plus another 4, in the end the nurse came in to help but the patient’s blood seemed to be clotting the minute it started to flow. I’m not sure whether there is enough blood in the bottle to test. We really persevered and the patient said that if she was at home she would have discarded the whole thing. For me it’s becoming a very time consuming exercise.
Two further general practitioners reported that they had requests from participants to support them with the use of the kit, because of its complexity, but each of these distributors refused, because of a desire to maintain fidelity with the research protocol.
There were further data emanating from one CBO (and the participants whom it recruited) that during one distribution event in a barbershop, at least some participants took their blood samples together at the same time, with support from the distributor.
Location for sample return
There was one reported instance in which a sample was returned to a GP surgery rather than being posted by the participant to TDL via Royal Mail. Because the distributor in this practice was not working on the day the sample arrived, it was stored in the practice refrigerator until a few days later, when that staff member returned to work and was informed about the sample. The distributor then posted it.
Further data collected from distributors and participants at the CBO also led us to infer that, after this event at the barbershop, it is likely that the distributor posted the samples via Royal Mail, rather than the participants doing this themselves.
Communication with participants after sample return
There were a number of occasions when participants and distributors reported that a 2-week text reminder to return a sample was sent to people who had already returned their sample. This created some concern among participants about the potential for lost samples, and made some doubt the veracity of their results.
Although it was intended that a HA at CNWL would have access to the secure database to enable them to directly obtain contact information for those participants with reactive or insufficient results, this did not occur, as sites predominantly used paper forms, so there was delay in getting this information onto the database. Instead, the project manager notified the HAs directly when an insufficient sample had been received at TDL. Occasionally, because of missing or delayed consent and baseline data forms, there was a delay in access to sufficient information to contact the participant immediately. Furthermore, as a result of the HAs’ working context, there were occasionally further delays between notifying the HA team and communication of the result to a participant. The protocol does not state a time limit for these activities, but, in the training, distributors were told to inform participants that it could take up to 5 days for them to receive a result.
It was also reported that, in at least a few cases, a negative result was received by participants via text from TDL within 24–48 hours of a sample being posted, which appears to have caused concern among some participants that the result may not be trustworthy, as it had arrived more quickly than anticipated.
Summary
The planned SSK intervention was not feasible in GP surgeries or during outreach from CBOs, and progression to a future Phase III evaluation is not supported. Although some form of the intervention was delivered by almost all distributors, most distributors found it difficult to recruit to and almost all found it too time-consuming to deliver in the context of a busy GP surgery or during community outreach. The research process attached to the intervention was the principal driver of this barrier.
Total fidelity in relation to the proposed intervention structures was not the norm, as local adaptations were common in most of the GP surgeries and all of the CBOs. Although these adaptions were not always agreed in advance, almost all might be considered to be reasonable tailoring of the intervention to the specific local context in which it was being delivered.
Most local adaptions maintained the fidelity of form for the intervention, in that they followed the standardised structures and processes developed for stage 2 of the HAUS study. Examples include broadening the range of staff recruiting to the intervention within a GP surgery or breaking up the offer and sign-up of patients into smaller blocks of time, to better suit the workflow of GP staff. The exception to this was the routine distributor support offered at two sites. This fundamentally changed the structure of the intervention from one of routine offer and self-completion of a SSK to a fully assisted intervention. Almost all the deviations from the proscribed fidelity of form for the intervention were intentional, and were motivated by a desire to speed up the process of recruitment or offer the intervention to a larger proportion of patients.
Chapter 9 Acceptability of the HAUS intervention
This chapter seeks to address the objective for stage 2 of establishing the acceptability of the intervention to black African people and service providers. The chapter is divided into two sets of findings: (1) acceptability of the intervention to participants, followed by (2) acceptability of the entire study process and the intervention among distributors. For each of these, we discuss findings related to those aspects of the intervention that compromised acceptability, followed by aspects that promoted acceptability. In quotations from study participants, their age, sex and HIV test outcome are stated. A range of data sources were used in this analysis, including interviews with a sample of study participants and staff from all distributing organisations, study team diaries and site visit notes, e-mails exchanged with distributors and weekly distributor experience surveys.
Acceptability to the black African community
Descriptive results
The total number of study participants interviewed was 21, the median age was 40 years (range 18–67 years) and 12 participants were women. Of the 21 participants interviewed, nine received negative results, four sent samples that were unable to be processed (as a result of the samples being underfilled) and eight did not return their sample. Seventeen interviewees were recruited at GP surgeries and four interviewees were recruited at CBOs. Approximately half of the interviewees (n = 9) had previously had a HIV test. However, the majority were unaware that SSKs existed prior to participation in the study. Some interviewees had a notion that a kit could be ordered online, but did not have a more specific knowledge of either SSKs or STKs before enrolment.
Barriers to the acceptability of self-sampling kits
There were five inter-related themes that emerged as barriers to the acceptability of the SSKs. The first three all pertained specifically to the kit used (fear of needles, insufficient blood flow and issues with the vial). The last two meant that several interviewees submitted an underfilled sample, resulting in their being contacted by HAs, who explained that the interviewee’s sample could not be processed and described future testing options (see Results communication and management above). Those who experienced this problem reported several concerns that had an impact on the acceptability of the intervention. Finally, interviewees identified the stigma, fear and taboo surrounding HIV and HIV testing as a barrier, not only to SSKs, but to all methods of HIV testing. Each of these themes are discussed in greater detail below.
Fear of needles
Of the interviewees who had not returned their sample, fear of needles and pricking one’s own finger were commonly mentioned obstacles to using the SSK. One interviewee recounted that she opened her SSK when she returned from her GP appointment and could not bring herself to prick her own finger. She explained:
I opened it, but I can’t do it by myself. I can’t use the needle to pinch myself. I can’t do it.
45-year-old female, non-returner
She subsequently returned to her GP surgery for a health check and requested assistance from two nurses in drawing blood for the SSK. The nurses apparently stated that they could not help, so the interviewee brought the SSK back home and did not try to use it. Another interviewee shared:
The reason why I didn’t [use the SSK] is because even though the doctor explained that it was really simple, I’m scared of needles, so I was actually waiting for someone to be with me to do it, in case, like, I started freaking out. [. . .] I’d prefer, like, a friend to do it, rather than me, ‘cause if I see a needle I’ll, like, freak out. Even though it was explained that it’s really easy. But I don’t know what’s easy in [general practitioner’s] terms. Like, for me, it’s not easy at all to, like, prick myself.
23-year-old female, non-returner
When asked whether or not they would consider using a SSK in the future, a number of participants replied that they would not consider future use, as a result of a lack of comfort in pricking one’s own finger and seeing one’s own blood. However, not all interviewees were squeamish about the lancets, and many found the lancets acceptable.
Insufficient blood flow
The interviews were replete in accounts describing the difficulties faced in maintaining sufficient blood flow to fill the vial. One woman who had consecutively submitted two insufficient samples expressed dissatisfaction and frustration with the process of drawing blood. She recounted:
The first time when I used it I thought the blood was enough and then [. . .] I posted it and they called that the blood wasn’t enough and then I got another [SSK] and then they said still the blood wasn’t enough, so I just couldn’t be bothered.
26-year-old woman, insufficient sample
This interviewee recalled that it had taken approximately half an hour each time she took the sample. She described being offered alternative HIV testing via a sexual health clinic near her home during a telephone call from a HA, but felt discouraged as a result of her negative experiences of using the SSKs. She shared:
They explained I can go and get a HIV test in [an area in London] or in where I live but I said, I say I can’t be bothered. They wanted to give me another home test but I say no, ‘cause two times, [loud sigh].
26-year-old woman, insufficient sample
One interviewee, a 52-year-old female, attributed issues in getting blood to flow to a pre-existing nerve problem. Her sample was underfilled, even though she used all of the lancets and ‘tried everything’ to get the blood to flow, including milking her finger.
Issues with the TINY vial
Frustration was also expressed regarding difficulty in getting blood to drop into the vial provided in the SSK. Lack of clarity over the best angle to hold the finger to facilitate the flow of blood into the vial was voiced, along with feedback that the vial was too narrow to allow the blood droplets to collect at the bottom. A few interviewees reported that the process was quite messy as a result of these issues:
This is where the flaws come into it. You know like you use the lancet, and then you try to get the droplets of blood to go in at a certain angle [. . .] it’s very hard to get the blood to drop freely as well, and it doesn’t collect enough.
39-year-old woman, insufficient sample
Another interviewee recounted:
It took me a while to get the rhythm of it. I mean basically the first finger was a dud. I completely mucked it up. Blood was everywhere and I think it was partly the nerves. [. . .] I couldn’t get it into [the vial]. [. . .] So I basically abandoned that finger and moved onto the second one and that one was much better. Yes.
Why do you think it went better?
I don’t know. Because I had a second go at it and probably made mistakes the first time around I would have been more aware the second time round. Like I didn’t handle my finger right in terms of how it was sort of placed above the little one tube. So when I changed the angle the blood was more prone to coming out in droplets that way than the other way. The other way was sort of messy [. . .] With the little bottle thing, the blood had a tendency not to go all the way down. It would sort of float at the top.
The issues of inadequate blood flow and difficulty in collecting blood droplets into a narrow vial were echoed in the following account:
The most difficult part was trying to get the blood out of my finger and I managed to put blood all over the table, and my mom came in and she thought that I was not doing it properly, so she helped me to do it, and I think that was just the most difficult part getting the blood to come out my finger and put it into that little tube.
18-year-old woman, negative
When asked whether or not they would be willing to consider using a SSK in the future, the vial was frequently cited as a factor that discouraged participants from future use. It was viewed as ‘tricky’ to use, and a few interviewees specifically recommended providing a wider vial to improve the ease of blood droplet collection.
Despite such comments, not all interviewees reported problems in filling the vial. For instance, a 67-year-old man reported that his blood flowed very easily. In fact, he reported that taking his sample had been a very positive experience: ‘It was so easy. It’s stress free. I really enjoyed it.’ Similarly, an 18-year-old female reported that she had trouble stopping her finger from bleeding, even after she had filled the vial. A 49-year-old female whose first sample was indeterminate, and second was negative, recounted that the second time drawing blood had been much easier than the first.
Many interviewees, especially those who did not return their sample or returned an insufficient sample, felt that issues regarding needle squeamishness, blood flow and collection in the vial could be overcome by having general practitioners and other health staff assist participants in taking their blood samples. One young female interviewee stated:
If they had been offered to me in the doctor’s and then he, sort of, helped me do it, I think it would’ve been a lot easier. But I think sometimes, when you take things away it’s, sort of, kind of, like, it’s a lot harder to get round to doing it, if that makes sense, and then there’s the whole hassle of having to send it off. That, sort of, factors in and it’s just . . . it might not be the best way to get, like, someone like me to do something.
23-year-old woman, non-returner
Another participant who did not return her kit felt uncomfortable about drawing her own blood and, similarly, would have preferred a health-care professional to take the blood for her. She shared:
It would be good if you invite the person in the hospital or somewhere and then do it for them, because if you give it to me like this I can’t use the needle to pinch my finger. It’s very hard for me to do it. [. . .] If someone is doing it for me I would do it, but doing it for myself I can’t. [. . .] It would be better if they can do it in the surgery or hospital. They invite you. You know, when you go and they can take your blood and then do it. That would be better if it was possible for that.
45-year-old woman, non-returner
This was echoed in a suggestion offered by a 52-year-old female who returned an insufficient sample. She thought that the aspect of the patient posting the kit could be retained, but that the sample collection could be assisted by a health-care professional, for those who had difficulty maintaining blood flow. Another interviewee, whose sample was indeterminate, suggested that providing a walk-in option where people could go to receive assistance in using the SSK would be beneficial. She stated:
Perhaps have a place within each locality where one could just walk in and do the test and have someone to assist them with the test as well. That could be another alternative as well.
39-year-old woman, insufficient sample
Issues with follow-up for insufficient samples
Several of the interviewees whose samples were unable to be processed as a result of being underfilled were critical of the way in which they received their result, and the options offered for further testing. One such interviewee was distributed two kits consecutively. The first one was never received by the laboratory. After receiving a reminder text from the study team to send in her sample, she returned to her GP surgery to obtain a second kit and presumed that the first one had been lost in the post. The second sample was insufficient, as it was underfilled. The interviewee recalled being contacted by a HA:
Someone called me from the study. Said there wasn’t a sufficient sample, and then I did a sample, I did the test twice. One, the study never received it, then the second one they didn’t get in time or something like that, and then they didn’t send me another kit or anything like that again. And I just thought okay, well, can I come in to do a face to face or, if need be, can I not just come in face to face and get it done as well, and that wasn’t offered. [. . .] I think going forward what would be useful would be to have the option of coming into a centre, not necessarily . . . like any of the hospitals, whichever was in that locality, or even up to the GP to obtain a sample.
39-year-old woman, insufficient sample
As the HAs were instructed to offer another SSK to anyone producing an insufficient sample, this would appear to conflict with the interviewee’s statement that an offer to send another kit was not made. Notably, she attributes the problem with the second kit to the study team not receiving the kit in time, which was not the case – the problem was that the vial was underfilled. She also stated that she was not offered a face-to-face test, although, according to the records kept by the study team, she was advised by the HA to discuss alternative testing options with her general practitioner upon her next visit. These anomalies demonstrate the gap between the process outlined in the study protocol for handling indeterminate samples and the process as perceived by the study participant.
This interviewee also referenced the delay she experienced between sending in the sample and hearing the result:
[Results notification] takes 5 days and no one knows what’s happening in between that 5 days before they call you, and then they’ll call you to say . . . I mean, I had two calls where I was told that they hadn’t received and I sent a text back and nobody actually replied back to that actual text, but you phoned back and said actually I did send it. [. . .] So I think maybe a better communication will be better as well. Also 5 days, depending on some people [. . .], they would feel more anxious. I wasn’t, but some people might have been. So, to alleviate that kind of anxiety, [. . .] if there’s another number for people to call. Because I got a call from somebody and they left a mobile number and, again, it wasn’t clear enough. Sometimes, it’s very hard to say what you want to say in a more succinct way. So, maybe better communication in terms of who calls and when they call, etc., and if there’s a standalone number that someone can leave a message and say call me back. Sorry, not a standalone number, but an actual mobile that’s actually manned as opposed to just you leave a message and then whoever will come back to you at a time that’s even more inconvenient because it’s convenient for them.
39-year-old woman, insufficient sample
Contained in this passage are several learning points for future interventions featuring SSKs and/or text messaging to participants. The respondent pointed out that no one responded to her text, which is accurate; the study protocol did not plan for study staff to respond to text messages received from participants who were sent reminder text messages by the study team. As this participant may have been comforted by receiving a text message back from the study team, future interventions may be improved by adding this capability into the process. Moreover, she suggested that an improved communication pathway with the HA is needed, as there was a lot of back and forth communication and leaving of messages by herself and the HA in this particular scenario.
Despite these experiences, other interviewees with insufficient samples found the follow-up process unproblematic. No participants had a reactive sample, so pathways for linkage to confirmatory testing remained untested.
Stigma, taboo and fear regarding HIV and HIV testing
Many interviewees cited stigma, taboo and/or fear around HIV testing, in general, as a barrier to the acceptability of SSKs. Several felt that others – as a result of HIV-related stigma – would rather remain ignorant of their HIV status than be tested (via a SSK or otherwise), even when they recognised that their behaviours may have put them at risk. One interviewee stated that some African people would never willingly be tested, based on a belief that HIV only becomes problematic once it is diagnosed.
Facilitators of the acceptability of self-sampling kits
The convenience of the SSK emerged as a very salient theme in the data. The comprehensive kit was thought to have many positive features, including the lancets (perceived by many interviewees as non-threatening) and clear instructions – features that were frequently cited as making the SSK acceptable to use. In addition, participant trust in the SSK distributor facilitated SSK acceptance. Each of these facilitators is discussed in the sections below.
Convenience
Comments on the convenience of the SSK were widespread, and centred on related themes regarding ease of use, speed and the delivery mechanism of results, flexibility on when and where to use the kit, and the privacy afforded by the kit. An 18-year-old female participant whose test was negative remarked on the convenience of not having to provide a blood sample at a medical facility, supervised by staff: ‘I would not need to come back another time to come and redo the test, and I could do it in the comfort of my own home, without anyone pestering me, or having to watch me do the test.’ The privacy afforded by the test was recognised even by an interviewee who did not return her test, who stated that:
It’s not like you going to a centre, standing there they take your blood, other people are watching; so you do it yourself. And then you post it.
41-year-old female, non-returner
Though some potential participants voiced a preference for POCT because of the immediacy of results, those who used the SSKs recognised that the SSK process delivered results quicker than some sexual health clinics:
Sometime before, 2 years ago, when I did it they just told me that they wanted to try using a pack to do a HIV test and I said I’m interested and they asked me to go to King’s College for the blood and they send the result to them and the nurse phoned me and said that I was negative. It took almost a week to get the result. This one it does not take, it’s almost within 24 hours I got my result.
And you didn’t have to travel to the hospital or anything like that?
Exactly. I would have to take a bus to the hospital.
Several interviewees appreciated that using a SSK negated the need to schedule time specifically for a HIV test at a clinic. Coupled with the speed of the result, the lack of need to travel to give the blood sample was cited as an attractive feature of the SSK. Related to this was the convenience of posting the sample once complete, though a minority of interviewees voiced concerns over the sample going missing in the post or felt that posting a sample was a ‘hassle.’ One shared:
I worried, because I did not know if it was going to get delivered to the right place.
18-year-old female, negative
In at least one case, a participant erroneously received a text message prompting her to return her kit when she had already returned it, causing the participant to wonder whether or not the kit had arrived at its intended destination. She later received a telephone call from a HA, as her sample was insufficient, which relieved her anxiety over whether or not the SSK had gone missing. She received and used another SSK, and was more confident about it not going missing in the post the second time, as it had arrived the first time.
The convenience of receiving the test result via text message was frequently linked to the speediness of this result notification method. The majority of those who received negative results via text message were comfortable with this method. In fact, some specifically stated that they were more comfortable with a text message than with a telephone call, as the latter method would have made them feel more nervous. When prompted to elaborate why he felt this way, one interviewee explained:
I probably would have felt more awkward if it was like a phone call. I probably would’ve gotten more nervous with a phone call. [. . .] Because you try to read into it. You try and read into the person’s tone and how they sound over the phone. And you try to like guess what it is before they say it.
25-year-old male, negative
Some interviewees specifically commented that the content of the text message was clear and, because of its format as a text message, it could easily be sent to others if desired. For instance, one interviewee recounted:
I did not expect [the test result] so soon. [. . .] I was happy because it was negative. So I was very happy. It was very straightforward and I sent it to my girlfriend [. . .] so that she would know that I am free.
64-year-old male, negative
However, one respondent felt that the message reporting the negative result could be misconstrued or misunderstood by some, as ‘negative’ may be interpreted as meaning ‘bad news’ rather than the absence of HIV Abs.
Interviewees received a text message reminder if more than 2 weeks passed between obtaining a SSK and reception of the SSK at TDL. This appeared to be an effective method to remind participants to use and post their SSKs. One interviewee recounted how the texted reminder prompted him to use the SSK:
I was reminded because you know I got the kit – I put it somewhere where I can usually see it. But I received a text message to remind me of it. [. . .] So that was when – it is like oh, I have been reminded now I think I have to do it.
50-year-old male, negative
The majority of interviewees, including those who submitted insufficient samples, stated that they were willing to use a SSK in the future, based on the convenient nature of the kits:
I’d be willing to use something similar to this, yeah. Definitely. [. . .] Because I just think the privacy is definitely like a win-win situation. I would prefer to not have to go somewhere I think. Yeah, I’d rather just do it in my own environment. If you do it where you’re comfortable as well, if you need the support of someone else close to you, you can do it with them. It’s just, yeah, I think it’s a really good idea.
18-year-old female, negative
One interviewee felt that the SSKs could be made even more convenient by storing them behind the counter at GP surgeries and having them available on request to anyone who wanted one, without having to book an appointment with health staff.
Non-threatening lancet
Though some interviewees (especially those who did not return their samples) were fearful of pricking their own fingers to draw the blood sample, many other interviewees found the supplied lancets acceptable and less ‘scary’ than other types of needles used to draw blood. One 25-year-old male liked the lancets because the sharp needle was not visible (it only emerged when the device was pressed against the finger, and then it retracted). Another man favourably compared the SSK lancets with needles used at hospitals to draw blood, and reported that having blood drawn by the latter method was ‘very painful’ and ‘caused anxiety’ for him. He viewed the lancets, by contrast, as being ‘very easy and simple’ to use. He recounts:
I pressed [the lancet against the finger] and there was blood coming out. It was very easy and very simple. Simple, easy, anxiety free, painless. I’m okay. I did enjoy it. If I had to do it every week I would do it.
66-year-old male, negative
Similarly, a male 26-year-old explained that he was motivated to use the SSK because it seemed to be a ‘less inconvenient and less painful’ HIV testing option than other testing methods. The lancets were also deemed acceptable by a 39-year-old woman, who recounted her first impression of the lancets in the following statement: ‘Then I looked at the lancet, and it wasn’t something that I was like oh it’s going to hurt me or anything like that, and I just did it’.
Clear instructions
Several interviewees opined that the instructions, both the paper version included with the SSK and the online version, assisted them in using the SSK. One young woman felt that the process seemed very complicated initially, until she referred to the instructions. She recounted her impression when she first opened her SSK at home:
Well, it looked very complicated because there was so many things inside the kit. But once I laid it out into where it is meant to go and read the instructions, it was actually a lot less than I expected, because most of it was just packaging and some of it I did not even have to use. It was just extras.
18-year-old female, negative
General comments about the video were positive, with one interviewee speculating that it would particularly appeal to young SSK users. One interviewee shared the following positive opinion:
I liked the video – you had the video which helped to go through the instructions a lot easier.
18-year-old female, negative
A minority felt that the written instructions were too complicated, and could have been simplified or made less ‘wordy.’ The small text size of the instructions was also referenced as a potential area for improvement.
Trust in distributor
A small number of interviewees mentioned that a high level of trust and regard for the distributor who offered the test motivated them to accept a SSK. Examples of this were evident in recruitment from both CBOs and primary care. One interviewee was offered the SSK via a CBO at a barbershop and was encouraged by his trusted barber to take the test. Similarly, a GP surgery-recruited participant referenced his high level of comfort and rapport with the HCA as motivating him to enrol in the study. One interviewee, a 50-year-old male, suggested that having black African distributors who had personally used a SSK may increase trust in distributors and thereby increase the acceptability of the kits and HIV testing more generally.
Awareness-raising of HIV testing and treatment
Increasing awareness of HIV testing and treatment options arose as a major theme when interviewees were prompted to suggest other or better ways to encourage black African people to be tested for HIV more regularly. One woman provided several suggestions on how to increase awareness:
Well, there’s like family planning clinics, church groups, invite people from various communities, from the black community, talk a bit more, put it into music, into sports, into drama, just get it out there and just try and . . . just try and talk to people in the community where you can do. You can do it with like a part of a general health thing, like if they’re doing a health focus on diabetes and other blood-borne viruses and other things, pneumonia, keeping well, health awareness sort of programme. Why not attach this along with it?
39-year-old female, insufficient sample
A 36-year-old male suggested that the SSKs and/or POCT could be offered out of health vans, or at events run by African organisations.
Another interviewee argued that increasing awareness could ‘normalise’ discussions about HIV, to decrease fear and stigma and, thereby, facilitate HIV testing efforts, including SSKs.
Acceptability of targeting to African people in London
Over half of the participants interviewed indicated that they did not mind that the intervention targeted black African people specifically. One interviewee commented that the way she was offered the kit was non-discriminatory, even though it was made clear that the intervention was targeting only black African people. Another interviewee mentioned that he liked the way his doctor approached him about the SSK, mentioning that his doctor ‘invited’ him to take part and that he felt privileged to be given a kit. Several interviewees thought that the intervention was a good idea, and that it should be expanded to be offered to other ethnic groups, even if they were not offended that it was limited to black African people. One participant pointed out that sexual relationships are not necessarily formed within ethnic boundaries, so the intervention should similarly not be limited in accordance with ethnicity. She stated that:
It becomes an African thing, like you know this test, there is intermarriages of different nationalities. [. . .] What about those who are married with the Africans, or those Africans who are married with the whites?
45-year-old female, insufficient sample
Only one interviewee, a 26-year-old male whose sample was negative, felt offended that he had been offered the test because of his ethnicity. He stated that the targeting of black African people was ‘quite racist,’ and that surely the SSK could have been beneficial for other groups as well.
Though the majority of the interviewees were not personally offended by the targeted aspect of the intervention, some participants speculated that the targeting of black African people may offend other African people. For instance, a 50-year-old male speculated that some would react to the offer of a SSK by thinking:
Oh, why Africans, why not other people? [. . .] They may get the message wrongly thinking oh it is just for Africans, why not for Americans, why not for other people from other races. [. . .] Some people might feel offended. Oh, why Africans, oh, they have come again, why Africans. No. You see such people might need some maybe literature to read.
50-year-old man, negative
The interviewee suggested that informing black African people of the reasoning behind the targeting would help in the acceptance of the SSKs. He recommended that ‘such people need to be informed, need to be lectured so that they understand why it is being carried out, otherwise they will get the message wrong’.
A minority of interviewees stated that they were unaware that the intervention was targeted at all. This may reflect the nervousness expressed by some sites to make it clear that the intervention was targeted exclusively at black African people, or simply misunderstandings among the interviewees about the targeted nature of the intervention. One interviewee described the interaction with a PN when he was offered the kit, which appears to support the former consideration:
How did you feel about being offered the HIV test because you were African?
I didn’t think about that. Because it was on the sign-up form so it was generic and for everybody. It never crossed my mind that it was because I was African or anything. You know?
Right. So no one specifically said that this was a programme that had been set up for the African community?
No.
In cases when interviewees were apparently unaware about the targeted nature of the intervention, the project manager contacted the sites from which the interviewees were recruited to inquire as to whether or not the distributors were fully informing potential participants of the targeting aspect of the study. In all of these instances, the distributor reported that they were indeed informing all potential participants that the SSKs were being offered only to black African people.
Acceptability to service providers
Thirteen GP surgeries and three CBOs in London judged the HAUS SSK intervention as likely to be acceptable to their staff and clients when they volunteered for the study, and all but one GP surgery maintained this judgement throughout the process of training prior to implementation; that London surgery withdrew from the study during training when substantial opposition was voiced by a range of staff members, both on the grounds of insufficient time and as a consequence of concerns about targeting black African people.
Acceptability and utility of training
All distributing organisations undertook mandatory training prior to the initiation of fieldwork. In total, 18 training sessions were delivered across London. These were delivered in the premises of 12 GP practices and three CBOs that participated, with the CBOs receiving two training sessions each. Some distributors asked for, and received, follow-up sessions, either to review key elements or to allow staff members who were unable to attend the first training session to catch up.
In total, 70 people attended the training sessions, following which 47 people (67%) voluntarily completed and returned an evaluation form anonymously. The participants identified their job roles as follows: professional health worker, including general practitioners, GP nurses, pharmacists, HCAs (n = 33); peer support worker (n = 4); CBO service manager (n = 8); and other (n = 2).
Training sessions typically lasted around 2 hours, and participants were asked to complete an evaluation form at the outset and following the training. These brief evaluations were primarily intended to be used iteratively to improve subsequent training sessions, but they also helped to assess the overall value that the training gave to intervention delivery.
Participants were asked to rate components of the training on a scale of 1 to 5, where 1 was ‘no benefit’ and 5 was ‘great benefit’ (Table 12). Each of these components received an average score of between 4 and 5, with the two highest-rated items being the overview of SSKs and study paperwork, as well as the clarification of study inclusion criteria. Some feedback demonstrated that a few participants were less confident about the benefit of the training to help them describe and model the use of the kit, and to explain to patients how their sample results would be delivered, but these views were very much in the minority.
| Component of training | Average score |
|---|---|
| Clarification of inclusion criteria | 4.60 |
| Overview of SSKs and study paperwork | 4.50 |
| Overview of the intervention | 4.45 |
| Explaining how results will be delivered | 4.44 |
| Alleviating concern and motivating potential participants | 4.42 |
| How to target individuals and gain consent | 4.36 |
| How to describe and model use of the kit | 4.29 |
| Building confidence in potential participants | 4.10 |
The vast majority of participants (96%) agreed that the range of topics covered within the training was good. When asked ‘Did you get what you were looking for from the training event?’, one-third of respondents (n = 16) said that they had ‘completely’ got what they wanted, with half of respondents (n = 23) saying that they had ‘mostly’ got what they wanted. Four participants were ambivalent, with their responses to this question being ‘somewhat’. All those who responded to ‘The training has increased my understanding of the HAUS study and what is expected of me as a distributor’ agreed with this statement (n = 45; two responses were missing). Similarly, the majority of respondents (87%) reported that any questions or concerns they had at the start had been answered, with the remaining six people neither agreeing nor disagreeing.
Each individual was asked to summarise what they understood the HAUS study to be about and their role within it, both at the start and at the completion of training. Following the training, all participants gained a stronger understanding of the study aims and objectives, and clarity about their roles and responsibilities also became more pronounced. A range of other responses further reflected on the excitement participants felt at having a new way to encourage HIV testing, and there was a comment that this could be a helpful route to ensuring ongoing support for African people with diagnosed HIV.
The clear shift in participants’ responses indicates that participation helped to increase their knowledge about the study and their roles as recruiters. Indeed, several GP distributors at the subsequent exit interviews (see Acceptability of the HAUS intervention to primary care staff) indicated that, prior to the training, they were unaware of the epidemiology relating to HIV in the UK in general, and to HIV in black African communities in particular.
Acceptability of the HAUS intervention to primary care staff
Broadly speaking, the level of acceptability of the intervention to staff at GP surgeries remained relatively high, even after, in many cases, a relatively unsuccessful period of intervention implementation.
The only universal impediment to the acceptability of this intervention in primary care was the time it took to recruit to the study. In the context of 10-minute consultations, the research requirements of the study were the major impediment. Moreover, some felt that there was insufficient time to describe and execute the SSK intervention without causing a backlog of other patients. All the GP surgeries struggled to find sufficient time to implement the intervention routinely and most offered the intervention to far fewer patients than they had hoped, because of the pressure of time. Problems with the time it took to deliver the research requirements were exacerbated by concerns about the kit itself among some distributors, especially among those surgeries that allowed the patient to take the sample on-site. However, there did remain a degree of enthusiasm about the potential use of SSKs in GP settings as ‘add-ons’ for patients, especially where phlebotomy was based off-site or POCT was not perceived as feasible. In our closing interviews, a number of GP-based distributors talked about the way in which a SSK could benefit some of the people they see, and, in the main, it tended to be the research process that prevented timely distribution. There was even more support for SSKs that used an oral sample or a blood-based sample, provided that these would be simpler to use than the TINY vial (for African people and for all potential users).
The other key issue in the perceived acceptability of the intervention was targeting. The majority of recruiting staff found the concept of targeting black African people acceptable, at least during training, and relatively few reported adverse reactions from patients once the intervention was implemented, though some patients required an explanation as to why they were being targeted. One distributor noted that ‘the black community are more receptive and recognise [HIV] is an issue. Don’t take it personally, not a slight’.
Some surgery staff found the process of targeting difficult, usually because it was not feasible to establish the ethnicity of patients from patient databases, as these were often incomplete or contained erroneous data, or because staff did not have the time to check through patient notes. In the absence of pre-existing data, clinics adopted a range of strategies to identify potentially eligible patients that often varied between staff, even in the same clinic. In some settings, there was discomfort with the concept of targeting based on visible race, because this often led to a discussion about the intervention with patients who were not ultimately eligible. This was especially pertinent in areas where the majority of black patients were of Caribbean, rather than African, origin.
In up to half of the clinics, some (but often not all) distributors felt some unease with targeting black African patients. The concept of targeting black African people raised concerns about exacerbating both HIV-related stigma and xenophobia. In three clinics, the proposed targeting based on ethnicity was accepted during HAUS study training, but rejected once the distribution period began, resulting in little or no recruitment occurring at these sites. In all these sites, most recruiters seemed uncomfortable with the concept of targeting black African people largely for fear of causing offence.
In one clinic, after training, staff decided that discussing the study openly with patients or even asking patients whether or not they were black African could be considered offensive and give rise to accusations of racism. In other surgeries, there was some mild concern that targeting migrants and visible ethnic minorities might exacerbate racism and xenophobia. One distributor noted: ‘I am always a bit cautious about offering based on ethnicity because of what has been happening, in our country, and people feeling a bit uneasy about the colour of their skin and where they are from’.
Acceptability of the HAUS intervention to the staff of community-based organisations
The level of acceptability of the intervention to staff at CBOs remained high throughout the study, in spite of substantial recruitment difficulties. CBOs maintained that SSKs were a useful additional intervention for their choice of services when targeting black African people; they also felt that the SSKs were considered convenient by their clients, though HIV-related stigma clearly presented a barrier to some enrolment. Broadly speaking, SSKs remained acceptable to CBO staff in spite of evidence that SSKs were not necessarily a feasible add-on intervention to the outreach activities that formed a large part of their existing funded work. For all CBOs, pre-existing commitments to funded interventions meant that they had limited capacity to recruit to the HAUS intervention. CBO staff had varied perceptions as to the likelihood of acceptability among black African people as a result of HIV stigma, the time required to complete research processes and the process of using the kit itself.
Although the staff and volunteers at one of the CBOs struggled to implement the intervention, they reported that it ‘felt good’ to be able to offer SSKs as an option for their clients. Furthermore, they reported that participation in the HAUS intervention increased morale among staff, partly because ‘they had something concrete to give out to people’, but also because it allowed them to have a dialogue with clients about HIV testing. Staff at this CBO had hoped to integrate the SSK offer into the standard outreach work that they are funded to provide to black African people, but this proved difficult because the HAUS process was too time-consuming. The staff members reported trialling the intervention at three ‘events’ at barbershops in Lambeth, but they also reported that there was some resistance to their activities in these settings, with a high number of refusals, which they assumed was a consequence of a lack of privacy in these settings.
Staff from another CBO had a little more success with recruitment, but still found it difficult to implement the intervention. In spite of difficulties, the intervention remained acceptable to the organisation and its staff, and they reported fewer acceptability concerns for their clients than staff from the first CBO described above. They were comfortable with targeting African people (as they too were black African) and with the element of providing information required alongside the intervention, even though this could be time-consuming. Staff at both CBOs felt that participating in the HAUS intervention was a good experience, as it filled gaps in their existing range of services. For instance, even though they had a mobile testing unit, the HAUS intervention allowed them to distribute kits where the mobile unit could not go.
Staff at the third CBO expressed considerable enthusiasm about the HAUS study during initial contact and training. Like staff at the other participating CBOs, they felt that the HAUS SSKs would give them an important new tool to engage with service users, and would help to supplement their office-based point-of-care HIV testing service. Distributors felt that their service users had benefited from the intervention; although not many kits were distributed, they felt that awareness of testing had increased as a result of the discussions prompted by the offer of the SSK.
All CBOs reported that they approached many eligible people who refused to participate. CBOs reported two key barriers to participation that might be considered evidence that the intervention was not acceptable to the intended target audience. The primary acceptability problems identified by the CBOs were very similar to those identified by the GP surgeries, with the added complication that the CBOs’ recruitment tended to focus their recruitment efforts on outreach interventions, rather than selecting among their existing clients.
Although the staff at CBOs had no initial qualms about targeting only black African people, they subsequently reported that some people approached were hostile about being targeted and even aggressive. African men were reported as especially challenging to engage. Even though staff at all three CBOs had experience of recruiting African people to other HIV prevention interventions, they all expressed surprise that there was still so much stigma associated with HIV among the wider community of African people in London. They felt disappointment that the intervention was limited to black African people, as it disqualified other black groups from participation. This issue was a bit off-putting to some black people approached, as they would indicate interest in the SSK, only to be turned away as a result of their black Caribbean status. This issue became especially problematic when the SSK was offered to a group of people, some of whom were eligible for participation and some of whom were not. One CBO also reflected that the usual users of their office-based HIV testing service were highly self-selecting, in that they were already primed to consider HIV testing, which was not the case in the wider community. The extent of disengagement from HIV, framed in hostile or suspicious responses, was described as being difficult to bear during kit distribution. Some staff felt that ignorance of HIV (including beliefs that HIV was a conspiracy or could be cured with prayer) was a barrier to using a SSK, but this is likely to be a disincentive to all types of HIV testing.
The second major barrier to recruitment was the amount of time it took to explain the study, fill out the paperwork and go over the kit contents. All CBOs intended to distribute SSKs in outreach sessions already scheduled for other funded projects, but this was not always feasible, as it took much more time than they expected to explain the study to potential participants, especially if they showed the video to potential testers.
As in the GP surgeries, CBO distributors reported problems with the actual intervention, including the amount of blood needed to fill the vial, the requirement to provide personal details to receive the result and the preference of some people to know the outcome of the test immediately. Some distributors reported that potential participants felt that they should be paid to participate in the research study.
Summary
The interviewees widely reported that the targeting of black African people specifically was acceptable. This was in contrast to the experience of distributors at GP surgeries, who, despite the training and provision of a script to initiate this discussion, often felt unease at targeting black African patients only. Concerns about exacerbating HIV-related stigma and xenophobia were expressed. Lack of willingness to target black African people ultimately led to little or no recruitment at three GP surgeries. Despite these misgivings, many primary care staff felt that the intervention was worthwhile, and expressed disappointment when the distribution period finished. Distributors at GP surgeries also reported having been unaware of the HIV epidemiology in relation to black African communities in the UK prior to participation in the study. Provision of this information did facilitate the targeting process for many.
Some distributors at GP surgeries noted that targeting was complicated, as information on ethnicity in patient databases is sparse and, moreover, there was limited time to check these data prior to appointments. These issues manifested in a large variety of methods employed at GP surgeries to select patients to whom to offer the intervention.
The level of acceptability of the intervention to staff at CBOs remained high throughout the study, with the SSKs generally viewed as a valuable add-on to service options. However, significant barriers to recruitment were noted, including stigma around HIV testing and limited time and capacity to conduct the intervention.
The acceptability of the HAUS intervention was also compromised by the specific SSK used, as well as issues with follow-up for insufficient samples, and the stigma, fear and taboo around HIV and HIV testing. Conversely, acceptability was supported by the convenience and privacy afforded by the use of SSKs, clear instructions and trust in the distributor. In a broad sense, users felt that acceptability, not only for SSKS, but for all HIV testing, could be increased through awareness-raising activities.
Based on these findings, suggestions to improve the acceptability of the SSK specifically included the development of a more user-friendly SSK and, ideally, the option of either a saliva-based kit or a blood-based kit.
Chapter 10 Cost-effectiveness
The aim of the economic model was to determine if offering a HIV SSK is a cost-effective means to increasing the provision and uptake of HIV testing among black African people in the UK compared with current practice, from a health-care perspective. The model assessed the lifetime cost per quality-adjusted life-year (QALY) gained of SSKs compared with current practice among black African people in the UK.
Methodology
We developed a hypothetical cohort of 8000 individuals of black African descent to populate the model. The hypothetical cohort was representative of the current black African population in the UK in regard to age, gender and HIV status. The cohort size was chosen so that sufficient infections of HIV were present in the model to test the hypothesis, but not so great that the model could not run as a result of computational load. All patients were aged 18–80 years and proportioned according to their current sex and age band distributions, as defined in Table 13.
| Characteristic | Sex | Reference | ||
|---|---|---|---|---|
| Male | Female | Male and female | ||
| Age (years) distribution (black African population in the UK), n | ||||
| 0–15 | 137,565 | 140,073 | ONS (2015)82 | |
| 15–24 | 80,175 | 80,468 | May and Finch (2009)77 | |
| 25–49 | 205,934 | 230,281 | May and Finch (2009)77 | |
| 50–64 | 39,182 | 40,322 | May and Finch (2009)77 | |
| ≥ 65 | 10,500 | 13,241 | May and Finch (2009)77 | |
| Total | 335,791 | 364,312 | May and Finch (2009)77 | |
| HIV-positive people in the black African population, n | ||||
| Diagnosed | 8312 | 17,730 | Skingsley et al. (2015)1 | |
| Undiagnosed | 1530 | 2380 | Skingsley et al. (2015)1 | |
| Percentage at each CD4 count (cells/mm3) | ||||
| < 350 | 20 | Skingsley et al. (2015)1 | ||
| 350–499 | 25 | Skingsley et al. (2015)1 | ||
| ≥ 500 | 55 | Skingsley et al. (2015)1 | ||
| Proportion receiving ART (all), % | 85 | Skingsley et al. (2015)1 | ||
| Proportion receiving ART and with a CD4 count of < 350 cells/mm3, % | 89 | Skingsley et al. (2015)1 | ||
| Average viral load for people infected with HIV (HIV RNA log10) | 4 | Nakagawa et al. (2015)83 | ||
Population
Sex-specific prevalence rates of HIV, including diagnosed HIV and estimated undiagnosed HIV, were used to determine the baseline number of HIV infections in our model population. 1 Data from PHE also provided information on the proportion of individuals with early- and late-stage HIV, and the proportion receiving antiretroviral therapy (ART)1 (see Table 13).
Model structure
A patient-level simulation was developed to assess the cost-effectiveness of SSKs among black African people in the UK compared with current practice. The model was developed using published data and results from the HAUS trial to predict individual participants’ transitions, costs and health outcomes. The model was created in Microsoft Excel 2010 in accordance with methodological recommendations for evaluations of new health-care technologies and interventions. 84,85
The same hypothetical cohort of 8000 patients was tested under two different HIV screening arms, similar to the trial: (1) intervention (SSK) or (2) comparator (current practice) (Figure 7).
FIGURE 7.
Decision tree of patient movements through the model.
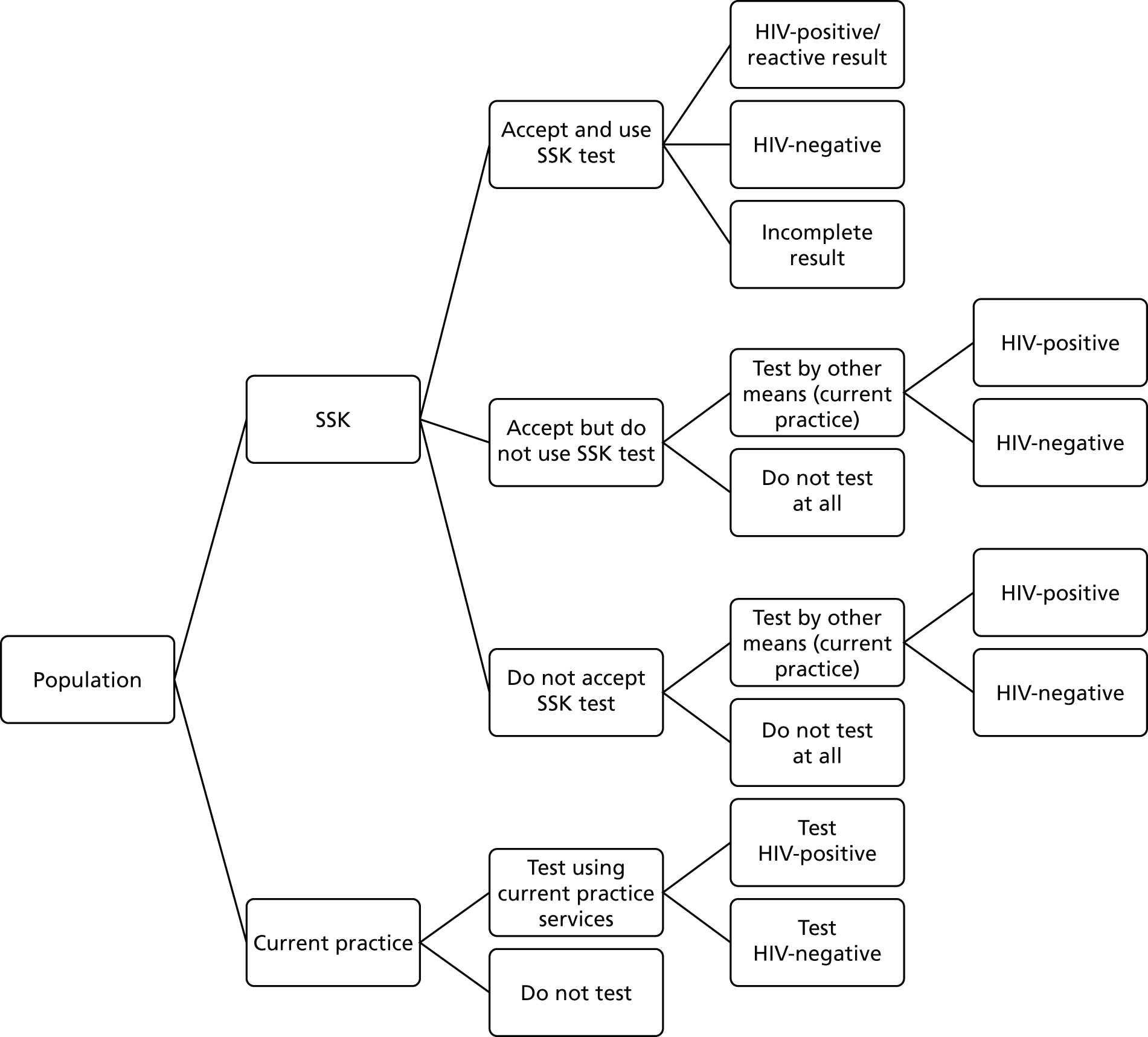
The patient-level model is a lifetime patient-level simulation with the following three components:
-
the simulation of HIV disease progression
-
the probability of HIV transmission from HIV-positive to HIV-negative patients
-
the clinical effectiveness of SSKs in increasing the uptake of HIV testing and reducing the number of undiagnosed and untreated infections of HIV in black African people in the UK.
The model consists of cycles of 3 months’ duration. In each cycle, patients are in one of six health states or two death states (Figure 8). All patients enter the model alive and in one of the six health states. There is a 10-cycle run-in period to stabilise the model, during which no outcomes are measured. After the 10th cycle, patients who are not dead and not in the state ‘diagnosed HIV’ are offered a SSK when they are in the SSK screening arm.
FIGURE 8.
Model structure for health states.

During each cycle, patients can remain in their current health state or move to a new one, based on the following rules.
-
Only sexually active patients can move from being HIV-negative to being newly HIV positive.
-
Newly HIV-positive patients move directly into ‘HIV undiagnosed’ in the next cycle; patients can only move from ‘HIV undiagnosed’ to ‘HIV diagnosed’ if:
-
they are in the SSK arm, and accept and return a SSK test
-
it is done through current screening practices in both arms.
-
-
Once a patient is ‘HIV diagnosed’, they have a probability of either receiving ART or not receiving ART; in both regimes, patients who are diagnosed as being HIV-positive receive ART, in line with HIV best-practice guidelines, whereby all patients start ART following diagnosis, regardless of CD4 count. 86
-
Diagnosed and undiagnosed HIV patients have a 3-month probability per cycle of either HIV-related causes or death from other causes; HIV-negative patients have a risk of death from other causes only. This was taken from Office for National Statistics’ (ONS) life tables. 82
-
All patients continue to cycle through the model until they reach an absorbing state of ‘dead’.
In the primary analysis, the SSK screening tool was only offered at one time point (baseline). A secondary analysis evaluated offering SSK screening tools at multiple time points (annually).
Clinical effectiveness of screening tools
Our model assessed two HIV screening tools: (1) SSKs and current practice, and (2) current practice only.
The clinical effectiveness of screening tools is dependent on the percentage of:
-
HIV-negative and undiagnosed HIV patients who are given a HIV SSK (acceptance rate)
-
patients given a SSK who return the SSK (return rate)
-
returned tests that provide a complete result
-
patients with undiagnosed HIV who are diagnosed as being HIV-positive after using the screening tool (dependent on the sensitivity of the screening tool used).
The SSK screening tool employed in this study, was a blood test sampling kit, with a sensitivity and specificity of 0.999 (95% CI 0.999 to 1.000) and 0.992 (95% CI 0.982 to 0.998), respectively. The percentage of patients who are given a SSK and who return the SSK was based on data from the HAUS trial. A range of values of acceptance and return rates were tested within sensitivity tests of the model.
HIV screening tools in current practice settings, such as sexual health clinics, GP clinics and antenatal services, are typically blood tests. The sensitivity and specificity of current practice screening tools were assumed to be the same as those for SSKs. The probability of testing was taken from the National Survey of Sexual Attitudes and Lifestyles (Natsal)-3, according to which the 5-year rate of HIV testing in black African men and women was 43.9% (95% CI 30.3% to 58.6%) and 46.1% (95% CI 35.6% to 57.0%), respectively. The probability of having a test in the past 5 years was based on HAUS trial data in a sensitivity test.
All individuals in the model who are diagnosed using a SSK receive confirmatory testing in current practice settings. In addition, all those who are not diagnosed as being HIV positive, and who are sexually active, could have additional testing in current practice settings, as per current practice testing rates.
Transition probabilities
In our model, events were assumed to have occurred when the patient-specific probability of an event was greater than a random number generated in Microsoft Excel. For example, if an individual who was HIV negative had a probability of HIV in a cycle of 0.4%, and the random number generated was 0.001 (0.1%), the individual would move to the ‘new HIV’ state. If, however, the random number generated was 0.553 (55.3%), the patient would stay in the HIV-negative health state. Events for patients were carried over cycles and, hence, the model has memory of past health states for each patient.
The probability of being infected with HIV was determined by four factors:
-
the transmission rate of HIV to HIV-negative patients for HIV-positive patients receiving ART87
-
the transmission rate of HIV to HIV-negative patients for HIV-positive patients not receiving ART87
-
the prevalence of HIV in the model population during that cycle
-
the probability that HIV-negative patients are sexually active; this was taken from the African Health & Sex Survey 2013–14: Headline Findings,26 which reported that 84.2% of men and 73% of women had a sexual partner in the previous year. A sensitivity analysis was conducted using the percentage of sexually active patients reported in the HAUS study.
A weighted average risk of HIV infection was applied to all patients who were HIV negative and sexually active in the model.
Patients who were HIV positive progressed through the stages of HIV (stage I, stage II, stage III and stage IV: death from HIV). At baseline, individuals infected with HIV were proportioned to the stage of disease. The proportions of individuals in the early and late stages of the disease were equal to the proportions of patients in each group reported by PHE in 201588 (see Table 14). Individuals who were free of HIV at baseline, and subsequently infected with HIV during the model, entered stage I of the disease. Progression through the stages of having HIV was determined by changes in CD4 count, whereby stages I, II and III were designated by a CD4 count of > 499, 350–499 and < 350 cells/mm3, respectively. Baseline CD4 count for newly infected patients and change in CD4 count were calculated using the algorithms reported in an economic model of lifetime outcomes and costs of HIV in MSM in the UK. 83 Patients who were HIV positive, receiving ART and adherent with medication, changed viral load and CD4 count in line with the algorithm set out in Nakagawa et al. ,83 based on treatment strategy and adherence.
The probability of dying from HIV was applied to all HIV-positive patients. Risk was stratified by sex and CD4 count, whereby risk increased 10-fold for those in the late stages of HIV (i.e. a CD4 count of < 350 cells/mm3). One-year probabilities were converted to 3-month rates, and then probabilities. 89
The probability of dying from non-HIV related causes was calculated from the ONS 2015 data,82 according to which death from non-HIV-related causes was equal to total mortality minus HIV-related mortality (International Classification of Diseases, Tenth Edition codes B20 to B24, as per the ONS guidelines). As mortality is higher in those with HIV, the probability of death from non-HIV-related causes was increased by 50%. 83 The risk of death from non-HIV-related causes was age and sex specific. We conducted a sensitivity analysis that increased the probability of death by 100% for non-HIV-related causes.
Clinical effectiveness of antiretroviral therapy
The clinical effectiveness of ART was applied to the transmission probability of HIV, whereby patients receiving ART were at a lower risk of transmitting HIV than those who were not. All patients who were newly diagnosed with HIV were assumed to be prescribed ART in line with current guidelines. Adherence with ART was based on the rate of adherence from PHE HIV statistics88 (see Table 14).
Costs
The costs included in our model were the cost of the HIV screening tool and the cost of HIV (Table 14). The cost of the HIV screening tool included the cost of SSKs and/or current practice screening tools, the cost of confirmatory testing, any additional testing and pre- and post-test counselling.
| Variable | Value | Reference |
|---|---|---|
| SSK related | ||
| Specificity | 99.24% | WHO (2013)90 |
| Sensitivity | 100% | WHO (2013)90 |
| HIV related | ||
| Rate of HIV testing in the previous 5 years | ||
| Male | 44% | Sonnenberg et al. (2013)91 |
| Female | 46% | Sonnenberg et al. (2013)91 |
| Specificity | 99.24% | WHO (2013)90 |
| Sensitivity | 100% | WHO (2013)90 |
| 1-year probability of death from HIV-related causes | ||
| Early-stage HIV (CD4 count of > 350 cells/mm3) | ||
| Male | 0.005 | ONS (2015)82 |
| Female | 0.003 | ONS (2015)82 |
| Late-stage HIV (CD4 count of < 350 cells/mm3) | ||
| Male | 0.05 | ONS (2015)82 |
| Female | 0.03 | ONS (2015)82 |
| Death from non-HIV related causes | ||
| Receiving ART | 0.03 | Cohen et al. (2011)87 |
| Not receiving ART | 0.022 | Cohen et al. (2011)87 |
| Compliance with ART | 0.85 | Skingsley et al. (2015)88 |
| Proportion of population sexually active | ||
| Male | 0.842 | Bourne et al. (2014)26 |
| Female | 0.73 | Bourne et al. (2014)26 |
| Viral loadb for people newly infected with HIV | 4 | Nakagawa et al. (2015)83 |
| Viral loadb change for all those people with HIV and not receiving ART | ||
| 0 to < 3 | 0.11 | Nakagawa et al. (2015)83 |
| 3 to < 3.5 | 0.13 | Nakagawa et al. (2015)83 |
| 3.5 to < 4 | 0.14 | Nakagawa et al. (2015)83 |
| 4 to < 4.5 | 0.15 | Nakagawa et al. (2015)83 |
| 4.5 to < 5 | 0.17 | Nakagawa et al. (2015)83 |
| 5 to < 5.5 | 0.18 | Nakagawa et al. (2015)83 |
| 5.5 to < 6 | 0.20 | Nakagawa et al. (2015)83 |
| 6 to < 6.5 (max.) | 0.21 | Nakagawa et al. (2015)83 |
| CD4 counta change for all those people with HIV and not receiving ART | ||
| 0 to < 3 | –0 | Nakagawa et al. (2015)83 |
| 3 to < 3.5 | –0.016 | Nakagawa et al. (2015)83 |
| 3.5 to < 4 | –0.04 | Nakagawa et al. (2015)83 |
| 4 to < 4.5 | –0.12 | Nakagawa et al. (2015)83 |
| 4.5 to < 5 | –0.04 | Nakagawa et al. (2015)83 |
| 5 to < 5.5 | –0.08 | Nakagawa et al. (2015)83 |
| 5.5 to < 6 | –1.6 | Nakagawa et al. (2015)83 |
| 6 to < 6.5 (max.) | –2 | Nakagawa et al. (2015)83 |
| Costs | ||
| Current practice/confirmatory testing | ||
| Of those tested, percentage tested in each setting | Health Protection Agency (2011)38 | |
| GP clinic | 10% | |
| Sexual health clinic | 61% | Health Protection Agency (2011)38 |
| Antenatal clinic | 29% | |
| Cost per test for each setting | ||
| GP clinic | £8.67 | |
| Sexual health clinic | £9.12 | |
| Antenatal clinic | £8.90 | |
| Cost of behaviour counselling per hour | £41.06 | |
| HIV events while receiving ART | ||
| CD4 count of > 200 cells/mm3 | £11,960 | Beck et al. (2011)92 |
| CD4 count of ≤ 200 cells/mm3 | £7307 | Beck et al. (2011)92 |
| HIV events while not receiving ART | ||
| CD4 count of > 200 cells/mm3 | £3145 | Beck et al. (2011)92 |
| CD4 count of ≤ 200 cells/mm3 | £7307 | Beck et al. (2011)92 |
| Undiagnosed HIV | £3145 | Beck et al. (2011)92 |
| Utility scores for QALYs | ||
| Healthy | 0.82 | |
| HIV-positive utility decrements | ||
| Receiving ART, VL ≤ 50 copies/ml, CD4 count of ≤ 200 cells/mm3 | –0.13 | Miners et al. (2014)93 |
| Receiving ART, VL ≤ 50 copies/ml, CD4 count of ≤ 200 cells/mm3 | –0.11 | Miners et al. (2014)93 |
| Receiving ART, VL > 50 copies/ml, CD4 count of ≤ 200 cells/mm3 | –0.15 | Miners et al. (2014)93 |
| Receiving ART, VL > 50 copies/ml, CD4 count of ≤ 200 cells/mm3 | –0.11 | Miners et al. (2014)93 |
| Stopped ART, CD4 count of ≤ 200 cells/mm3 | –0.18 | Miners et al. (2014)93 |
| Stopped ART, CD4 count of ≤ 200 cells/mm3 | –0.13 | Miners et al. (2014)93 |
| Never started ART, CD4 count of ≤ 200 cells/mm3 | –0.17 | Miners et al. (2014)93 |
| Never started ART, CD4 count of ≤ 200 cells/mm3 | –0.04 | Miners et al. (2014)93 |
The cost of the SSK was calculated from the HAUS study and includes the cost of the test kit itself, as well as the time taken to deliver the kit. The cost of the current practice screening tool was calculated as £9.33. 38 In addition, pre- and post-test counselling was valued at £46.45 per test.
The cost of HIV was extracted from an economic analysis of early access to HIV services. 92 The cost of HIV included the cost of hospital inpatient, outpatient and day ward services, determined by the mean number of days spent in each service. The cost of HIV was stratified by CD4 count and the presence of ART. For undiagnosed HIV, the cost was estimated to be equivalent to individuals with early-stage HIV (CD4 count of > 200 cells/mm3) and who were not receiving ART, as these individuals are likely to have more illnesses/visits to the doctor than HIV-negative individuals.
All costs were inflated to 2015 values, using relevant national price index conversion rates. 94
Outcomes
The outcomes assessed in this analysis included societal and individual-level outcomes. Societal outcomes included the number of HIV prevented, while individual-level outcomes included the impact of HIV on mortality and morbidity.
The impact on mortality and morbidity was evaluated using QALYs, as recommended by NICE in the UK. 95 QALYs are calculated by multiplying a preference-based value of a health state (a utility score) by the amount of time spent in that health state, whereby 1 represents perfect health and 0 represents death. All individuals who were HIV negative were assumed to be in a ‘healthy’ state with a utility score of 0.824. If an individual was infected with HIV, a utility decrement was applied. 93 This was applied at the time of infection, as well as every cycle thereafter until the individual died. The utility values were taken from a cross-sectional study of health-related quality of life of people infected with HIV compared with the general population. Utility decrements were dependent on viral load, CD4 count and the use of, and adherence to, ART. As individuals progressed through disease stages, and/or the use of ART changed, the utility decrement applied was updated accordingly.
Cost-effectiveness was evaluated as the mean incremental cost per QALY gained of 8000 patients over a lifetime horizon. 96 The incremental cost-effectiveness ratio (ICER) for the HAUS study is defined as the total discounted cost of the intervention (SSKs) minus the total discounted cost of current practice, divided by the total discounted QALYs of the intervention minus the total discounted QALYs of current practice. An ICER of £30,000 per QALY is generally reported as the maximum value at which NICE is likely to approve the implementation of a new technology. However, Claxton et al. 97 have calculated that it currently costs £12,936 to generate an additional QALY in the English NHS. 97 As a result, it has been argued that this value may represent a more appropriate cost-effectiveness threshold to use.
The random numbers in the model meant that each run of the model would give a different result. As such, we took the average of each parameter in the ICER from 10 runs of the model. A Monte Carlo Error from the 10 runs of the model is reported to provide an estimation of the precision of 10 runs of the model.
All future benefits (QALYs) and costs were discounted at 3.5% per annum, converted to a 3-month rate. 95
Sensitivity analyses
We conducted a number of sensitivity analyses. The analyses were conducted in line with the Decision Support Unit guidance. 98
Results
The average age of the hypothetical population in the model was 37 years, and 53% of the population were female. This compares with the population from the HAUS trial, with a median age of 42.6 years, and 51.3% of the population being female. In the baseline population, the prevalence of HIV was 4.2%, or a total of 335 HIV infections per 8000 people. Of the 335 HIV-positive people, 48 (14%) were undiagnosed.
As reported in Chapter 7, Overall results, 125 out of 349 patients (35.8%) approached agreed to take part in the HAUS trial. Of those who agreed, six patients were excluded from the trial as a result of problems with the consent process. For the purposes of this analysis, the participants excluded for consent reasons were considered to have ‘agreed to use a SSK’, as the consent process was separate to agreeing to take a SSK. Removing the six participants left 119 eligible participants remaining in the trial, 65 (54%) of whom returned the SSK. Of those SSKs returned, 11 (16.7%) were incomplete and the participants were contacted for a retest. In the model, we assumed that 100% of the patients who had incomplete tests were contacted to retake the test.
Qualitative investigation of the research process suggested that, of the 15- to 20-minute appointments that the nurses, community workers or HCAs had with patients to conduct the study, the majority of the time was spent on the research process (explaining the study, taking consent and administering baseline questionnaires), with only a few minutes dedicated to explaining the SSK and how to use it. As a result, a conservative estimate of 5 minutes with the patient per kit was used. The cost for the highest-paid professional, a PN, to give the test to the patient and explain how to use it was estimated as £4 for the 35.8% of patients who agreed to use a SSK. The test itself cost £3.24 if not used, and a returned kit cost £13.24 or £15, if including the cost of retest for incomplete tests.
In addition to the conservative estimate of time, and staff with a lower cost per minute dispensing the kit, there was discussion as well of the possibility of patients being able to collect the kit from reception or pharmacies, further reducing the cost of dispensing the SSKs. This was tested as part of a sensitivity analysis.
The results of 10 runs of the model for SSKs versus current practice are reported in Table 15. There were eight new cases of infection detected using SSKs, with a cost per infection detected of £6431. SSKs dominated current practice, resulting in an additional 24 QALYs and a cost-saving of £17,208 over 8000 patients and a maximum of 75 years, or until they died. The Monte Carlo error for the difference in QALYs was 735. As a result, the 95% CI for the difference in QALYs between SSKs and current practice is –432 to 480 QALYs. The Monte Carlo error for costs was 515,078, with a 95% CI for a difference in costs of –£336,451 to £302.035.
| Outcomes | Intervention | Difference | |
|---|---|---|---|
| SSK | Current practice | ||
| Total number of people tested for HIV using a SSK | 1502 | 0 | 1502 |
| Total number of HIV diagnoses made using a SSK | 8 | 0 | 8 |
| Total number of HIV diagnoses via other services | 57 | 60 | 3 |
| Total number of new HIV infections | 37 | 39 | 2 |
| Cost of SSK test (£) | 48,883 | 0 | 48,883 |
| Cost of other screening (£) | 1,530,123 | 1,528,834 | 1289 |
| Cost of HIV treatment (£) | 39,425,225 | 39,648,006 | –222,781 |
| Total cost (undiscounted) (£) | 41,004,231 | 41,179,840 | –172,609 |
| Total cost (discounted) (£) | 21,319,574 | 21,336,782 | –17,208 |
| Total QALYs (undiscounted) | 1,108,243 | 1,107,969 | 274 |
| Total QALYs (discounted) | 509,704 | 509,680 | 24 |
| ICER (discounted) | Dominant | ||
To test the robustness of some of the values used in the model, values from completion of the questionnaires completed as part of the HAUS study were used in the model instead. In the HAUS study, 50% of patients reported having been tested for HIV in the past 5 years. This is similar to the value reported in Natsal-3, in which 45% of black African people reported having been tested for HIV in the past year. In the HAUS study, 81% of patients reported being sexually active. This is compared with 79%, as reported in the African Health Survey & Sex 2013–14. 26 Changing the values in the model to those reported in the HAUS study does not give significant changes to the results.
The results of the sensitivity tests are reported in Table 16. None of the changes made to the model had an impact on the results.
| Results | Updated for results of the trial | 65% who accepted a SSK test | 75% who returned the test | 5% of tests returned incomplete | Assume death for HIV-related causes is twice as high for a CD4 count of < 200 cells/mm3 | SSKs dispensed by | |
|---|---|---|---|---|---|---|---|
| Reception | GP at £50 per patient | ||||||
| SSK | |||||||
| Total number of HIV-positive patients diagnosed using a SSK | 8 | 12.4 | 10 | 8 | 8 | 8 | 8 |
| Cost of SSK test (£) | 49,375 | 87,304 | 60,041 | 46,739 | 49,133 | 42,875 | 246,217 |
| Total number of new infections | 35 | 34 | 36 | 34 | 33 | 35 | 36 |
| Total cost, including HIV treatment (discounted) (£) | 21,824,075 | 20,706,392 | 22,082,340 | 21,736,367 | 19,991,397 | 21,313,567 | 21,809,262 |
| QALYs discounted | 509,956 | 509,853 | 509,899 | 509,877 | 509,633 | 509,956 | 509,816 |
| Current practice | |||||||
| Total number of new infections | 38 | 39 | 39 | 39 | 35 | 39 | 39 |
| Total cost, including HIV treatment (discounted) (£) | 21,360,691 | 21,336,782 | 21,336,782 | 21,336,782 | 20,562,684 | 21,336,782 | 21,336,782 |
| QALYs discounted | 509,645 | 509,680 | 509,680 | 509,680 | 509,531 | 509,680 | 509,680 |
| ICER (£) | 1489 | Dominant | 3407 | Dominant | Dominant | Dominant | 3468 |
Summary
This preliminary model of a SSK test dispensed to black African people in the GP or in community settings suggests that SSKs are a cost-effective way to identify new infections of HIV, with SSKs dominating current practice, resulting in more QALYs for less cost. Using the Monte Carlo error to test uncertainty, there does not appear to be significant differences in QALYs or costs. The results would benefit from additional runs of the model. This was not possible within the limited timelines of the project and computational power to run the model.
Chapter 11 Discussion
The overarching principles in the selection of our intervention were that it had to expand on current HIV testing opportunities for black African people, it had be acceptable to intervention users and providers and it had to be sustainable in the current economic climate. It also had to address the known barriers to HIV testing for these communities. This chapter comprises a discussion focused on how the aims and objectives of this study were addressed.
Discussion of stage 1
Barriers to, and facilitators of, the use of self-sampling kits
The first objective of stage 1 was to clarify barriers to, and facilitators of, provision, access and use of HIV SSKs by black African people in community settings. The policy review revealed a facilitative environment for STKs and SSKs for HIV, with the use of these kits being viewed as an innovative method of increasing uptake. Guidelines have shown that HIV testing in medical and community settings is both feasible and acceptable, with SSKs suggested as a route to broaden testing options. Evidence on the use and clinical effectiveness of SSKs, however, was scant – especially for black African groups.
The data yielded through interviews and FGDs echoed many of these reported barriers to, and facilitators of, SSK use. The privacy and convenience afforded by SSKs were viewed as major strengths, as they negated the need to attend a sexual health clinic and potential stigma. Service providers and non-specialists alike felt that SSKs increased individual autonomy and testing opportunities. However, both the FGD participants and the interviewees voiced concern over the volume of blood required to provide a TINY vial sample. Service providers in particular voiced doubts over the ability of members of the public to produce a sufficient sample. Participants also pointed out that fear of needles and blood, and the complexity of using the kit, could discourage some people from using the SSKs. Another concern was the potential isolation that could be experienced by users of the SSKs.
Many participants mentioned the stigmatising association of HIV with ‘sexual immorality’ and promiscuity (an association that many FGD participants and interviewees described as being heightened within black African communities) as a barrier to testing among black African people. SSKs, however, helped to mitigate the risk of others discovering that one was testing for HIV, as a result of the privacy afforded; however, as described above, what was regarded as the ‘benefit’ of privacy by some was regarded by others as carrying a risk of increased isolation for those receiving news of a reactive result.
The difference between individual- and community-level risk perception was also viewed as a barrier, with participants stating that those targeted may not appreciate the epidemiological data used as a justification to target black African people exclusively for the intervention. Participants recognised that, because of pervading HIV-related stigma and perceptions of being at a low risk of acquiring HIV, an opportunistic provider-led offer of a SSK was more likely to increase HIV testing than a user-led model. The participants warned that offers of SSKs exclusively to black African people may be perceived as racist and as fuelling anti-immigrant rhetoric.
Determining appropriate self-sampling kit-based intervention models for different settings
As participants in FGDs and interviewees recognised that black African people were already accessing primary care and CBOs, the addition of SSKs into their service options was viewed as a convenient extension that would immediately increase testing opportunities. There was almost universal approval of CBOs working with African communities and HIV prevention to be involved in distribution, as their staff members were considered to possess the expertise required to target black African people in a sensitive manner. CBOs, however, would not be extending their outreach activities, and HIV testing was already widely integrated into their services; therefore, there was some concern from the research team that this would not significantly increase HIV testing opportunities for the wider African community.
Participants advised that targeted offers needed to be couched in clear terms, using epidemiological evidence, and in a way that would avoid the perception that offers were being made because of racist or xenophobic sentiment. It was deemed of utmost importance that distributors were regarded as trustworthy, knowledgeable and non-judgemental in order to foster a realistic degree of reflection about HIV risk among those to whom they encouraged SSK use; it was felt that staff in GP settings and outreach teams in CBOs possessed all of these qualities. Ultimately, there was a universal view among participants that SSK distributors needed to actively resist HIV-related stigma, rather than potentially reinforce it.
The formative work revealed concerns about the limited amount of time available to providers to initiate discussions and gain informed consent, especially in GP surgeries. Embedding the intervention into routine practice was considered to be a critical component by the research team if the intervention was to be sustainable. Therefore, specific appointments for intervention delivery should not be part of the model.
Prior to intervention development, it was apparent that, ideally, a saliva-based test or a more user-friendly SSK would be preferable to the TINY vial. Unfortunately, despite this knowledge, and as described in Step 4: viability of the intervention, we were unable to proceed with an alternative option, as we could not identify a service provider that was willing to assume the liability for using an off-licence product in the context of a research project. At the time of writing, the TINY vial was the only CE-approved HIV SSK available in the UK. An alternative option would have been to formally test a saliva-based SSK against the TINY vial; however, this would have represented a significant shift in the original research question and design, which was not considered an appropriate option for the HAUS study.
The final intervention model for both settings utilised a theoretically informed scripted conversation in conjunction with distribution of a SSK during a routine encounter. The script was designed to assist providers in overcoming their anxieties about targeting black African communities (addressing the issue of capability), while also motivating users and increasing opportunities for HIV testing; it also ensured that the message was consistent, in order to enable intervention fidelity. The information supplied with the kit (including a web link to a video demonstration) and via the provider was designed to further increase the capability and motivation of service users. The study team were not able to deliver the intervention with what they believed would be the optimum SSK, owing to governance and regulation restrictions. A copy of the intervention and training manuals are available on request.
Determining robust HIV result management pathways
The formative work highlighted a disconnect between the accepted current practice of delivery of results by text message or telephone call, and the relatively widespread concern that SSK users may be isolated and at risk of self-harm when receiving test results. The use of SSKs was perceived to reduce opportunities for HIV prevention, with a lack of recognition that there is no strong evidence that routine pre- or post-test counselling subsequently affects the behaviour of those who receive a negative test result. Participants also warned that a profusion of HIV testing interventions could lead to a disjointed and confusing service landscape.
The clinical pathways within the HAUS study were all subject to clinical governance regulations and designed to ensure that best practice would be delivered. The research team felt that it was important that an organisation with experience and expertise in managing HIV results, and ideally SSKs, were involved to ensure appropriate and sensitive delivery of the test results, including the offering of retests to those with indeterminate results and confirmatory tests to those with reactive results, and linking those who tested positive for HIV to care.
The process of establishing these clinical pathways highlighted the uncertainty and confusion over where the duty of care and liability should lie for a SSK intervention delivered in community settings by non-NHS trust employees.
The provision of results as quickly as possible to service users, whether positive or negative, is emphasised throughout clinical standards, and the recommended time period for receipt of results is ideally within 48 hours, and no more than 14 working days. The process evaluation demonstrated that, although this was achieved for everyone testing negative, for those with insufficient samples, there was an occasional delay while information from recruiting sites was awaited. The FGDs highlighted significant concerns regarding confidentiality and privacy among potential users; this led us to request only initials (rather than a full name) with the returning sample, which, in hindsight, was an error, as it meant that we could not make contact with participants until the additional information was received from the recruitment site. All negative results were delivered by short message service (SMS) via an automated system, and this worked well. No reactive results were received, so the processes for confirmatory testing and linkage to care were not tested. There was also concern that people may not test if their general practitioner was automatically informed of the result. As a consequence, we obtained specific consent to notify general practitioners of the test results; 98.9% of participants recruited through primary care consented to this, suggesting that this concern was unfounded.
Discussion of stage 2
In November 2015, PHE launched a national HIV self-sampling service. This initiative enabled people at a higher risk of contracting HIV across the country to order a HIV SSK online. Self-sampling is further promoted by the London HIV Prevention Programme, which is aimed at black African communities and MSM; through its ‘Do it London’ website [https://doitlondon.org/ (accessed 28 January 2018)], users can click on a link to directly order a SSK. Similarly, sexual health services are increasingly trying to reduce costs by encouraging asymptomatic individuals to utilise self-sampling technologies, usually through web portals. To comply with BHIVA guidance (to use only approved SSKs and that testing should be fourth generation), most of these initiatives use the TINY vial SSK. 86 Despite this relatively rapid expansion of sexual health and HIV testing through self-sampling, there remains little evidence to support its clinical effectiveness or cost-effectiveness for communities beyond MSM.
The aim of stage 2 was to conduct an evaluation of selected SSK distribution models to assess the feasibility of a future Phase III evaluation. The specific objectives are discussed in the sections below.
Establishing the feasibility and acceptability of interventions for providers and service users
The primary objective of stage 2 was to determine the feasibility and acceptability of a provider-initiated, HIV SSK intervention targeted at black African people in two settings: GP surgeries and CBOs. Our findings indicate that, although many aspects of the intervention were acceptable, scale-up of the intervention to a Phase III evaluation is not feasible. All sites reported that the time it took to offer the kit and complete the research-relevant forms (consent, baseline questionnaire and enrolment log) was a major impediment to the feasibility and acceptability of the trial. With hindsight, a pilot of stage 2 in a GP surgery and a CBO might have identified some of these issues; however, project timelines and resources did not enable this. Consent at an individual level was sought to enable the collection of baseline data, tracking of data and follow-up interviews. Consent at a group (GP or CBO) level, and limiting data collection to service evaluation, may have proved more feasible and better reflected how the intervention would be implemented in practice.
Although interviewed participants reported that the targeting of black African people was acceptable, this is in contrast to the large proportion of respondents who indicated on the acceptability questionnaire that it was not acceptable to offer a HIV test based on a patient’s ethnicity. Many distributors, especially at GP surgeries, also continued to express unease at targeting black African patients only, despite the provision of training and a script designed to specifically overcome these barriers. This unease arose from concerns about exacerbating HIV-related stigma and xenophobia.
Our findings highlighted that community providers, as well as many black African people, would prefer to use SSKs that involve the collection of an oral specimen as opposed to a blood specimen. However, at the time of writing, in the UK, there are no CE-marked HIV testing assays that can be used on saliva. Not being able to proceed with a saliva-based option had a direct impact on the study feasibility. It meant that the SSK took longer to distribute, as there was more to explain and greater motivation required for a blood-based SSK; it was no longer possible to demonstrate kit use in the field, and the more complicated procedure to collect the sample was likely to have influenced the return rate and to be responsible for the extremely high rate (16.9%) of insufficient samples. This figure is remarkably similar to that reported by the national HIV self-sampling service among their black African users to date (Tim Alston, personal communication). This suggests that an alternative to the TINY vial is required if HIV SSKs are to be an effective means to increasing the uptake of HIV testing in black African communities.
Evaluating the clinical effectiveness of self-sampling for HIV in increasing the uptake of HIV testing by black African people
As a result of the failure of the study to recruit adequate numbers to the study, we were unable to evaluate the clinical effectiveness of SSKs in increasing the uptake of HIV testing in black African people.
The fact that 12 of the 65 participants who returned a kit reported having never previously tested, and that most kit returners tested because of the opportunistic offer of the test, suggests that if distribution of HIV SSKs in these settings were rolled out at scale as part of the range of available HIV testing options, there would be the potential for increasing the uptake of HIV testing. However, at a structural level, these services do not have time to ‘bolt on’ a SSK intervention (or indeed anything else), unless there is a strong benefit or incentive to do so.
Determining the cost-effectiveness of distributing the self-sampling kits among black African people over other screening methods
The model of a SSK dispensed to black African people in GP surgeries or in CBOs presented in Chapter 10 suggests that SSKs may be a cost-effective way to identify new infections of HIV, as SSKs resulted in more QALYs for less cost.
We showed that it was feasible to collect data as part of the HAUS trial in order to update values in the model. However, there were challenges in collecting data on the time taken to explain SSKs to participants. Although there were limited data available on the time taken, this proved to be inconsequential to the model, given that SSKs could cost as much as £50 per test and still be cost-effective.
The estimation of the uptake rates of SSKs taken from the HAUS study and used in the model may not reflect real life. The uptake rate for SSKs might be higher, as patients may have been put off by the research process. It is also possible that the use of an alternative SSK, which is easier to use, may increase return rates and reduce the number of incomplete results. It is likely that these improvements would improve the cost-effectiveness of the SSK.
Further work required includes running the model and the probabilistic sensitivity analysis more times, whereby values in the model are varied within given CIs and distributions to provide an estimate of the probability that SSKs are cost-effective compared with current practice. The extra value of perfect information would provide a monetary estimate of the value of additional research to provide more certainty of the result. However, the computational load required to run this analysis is significant, potentially taking days to run, and was not possible as part of this study.
Monitoring the ability to trace participants with reactive results, confirmatory testing and linkage into specialist care
No reactive results were obtained, so we were unable to assess the ability to trace participants with reactive results through the process of confirmatory testing and linkage to care.
Determining the cost per person of distributed kits and the cost per HIV diagnosis per setting
Data on the cost per kit distributed were collected as part of the trial. This was dependent, however, on who distributed the SSK. If a conservative upper estimate was made of a PN taking 5 minutes to explain the kit, the cost of staff time was £4. The economic model did not determine cost per setting as originally planned. It is unlikely that community workers would be paid more than a PN; thus, the cost-effectiveness could be expected to be greater in CBO settings, unless the time taken to explain the kit differed by setting. A limitation of the model is that the time to specifically target the individual and explain the kit could not be determined, as, within the study, the research components were so enmeshed with this process.
The cost of the SSK itself was £3.24 if not used, and a returned kit cost £15 (as this included the cost of a retest for incomplete tests). In a lifetime patient-level model of 8000 black African people in the UK, the cost per detected infection of HIV using a SSK was £6000. However, SSKs resulted in more QALYs for a total lower cost once the cost of treating HIV was included, dominating current practice. The Monte Carlo CI of 10 runs of the model suggested a significant increase in QALYs, but not cost.
Assessing the feasibility of collecting data for a lifetime cost-effectiveness model alongside the potential Phase III evaluation
Limited data were able to be collected to inform the cost-effectiveness model, because of a need to reduce the time taken for patients to complete questionnaires as part of the baseline assessment. The values that were collected as part of the questionnaire that could inform the model (the percentage of sexually active patients and the proportion of people tested in the past 5 years) tallied with the best-available data in the literature, suggesting that data from the literature are likely to be adequate and a better source of information. We were able to obtain better estimates of the proportion of people who agreed to use a SSK and returned the SSK to inform the model, although real-life scenarios, rather than trials, are likely to provide more realistic data.
Assessing the feasibility and, if appropriate, the optimal trial design for a future Phase III evaluation
Based on the findings of the HAUS study, in particular the challenges with recruitment in both GP and via CBOs, a future Phase III evaluation was not considered feasible by the study team.
Patient and public involvement
The HAUS project has been about listening to black African people and community-based service providers, with the aim of adapting HIV testing practice to better meet their needs. We found the additional perspectives of community representation to be invaluable in the design and implementation of our research. The project has also benefited from the inclusion of participants who were recruited via community contacts, as we believe that this improved our focus group diversity.
Our findings were fed back to participating sites, and a summary of the findings will be published on www.haus.org.uk, our study website.
Conclusions
Our findings indicate that, although many aspects of the intervention were acceptable, scale-up of the intervention to a Phase III trial is not feasible. Alternative, user-friendly SSKs that meet user and provider preferences and UK regulatory requirements are needed. In particular, blood-based kits not requiring users to ‘milk’ blood, and diagnostic assays that meet the CE criteria for testing saliva are required. The preliminary economic model suggests that, for the rates of acceptance and return of the tests seen in the trial, SSKs are a cost-effective way to identify new infections of HIV, but further work is needed to validate this result. Importantly, the study also found that busy services do not have time to ‘bolt on’ a SSK intervention or research generally, unless there is a strong incentive to do so.
To maximise the individual and public health benefits of HIV testing interventions, we must consider the technological, psychosocial and sociocultural contexts of HIV testing. The increasing diversification of the tests available demands systematic consideration of the right test for particular circumstances and particular subpopulations, and recognition that, over time, the same person may well require different testing methods and settings.
There is a danger that, by not grasping the complexity of HIV testing, we only reach the low-hanging fruit, designing, evaluating and implementing testing interventions that work for limited groups of people, but do not have an impact on the actual drivers of HIV transmission, such as HIV-related stigma. This is particularly important when considering how to implement NICE HIV testing guidance, which recommends the expansion of targeted testing in community settings for at-risk populations, including black African communities. 43,99 Ethnic targeting remained problematic; despite the fact that service providers couched the scripted intervention in epidemiological terms, this was not always perceived as neutral, and was the least acceptable aspect of the intervention for service users.
Research studies comparing the acceptability and return rates of different types of self-sampling methods can help people to better understand their impact on recruitment.
The challenges in setting up reliable pathways of care for research participants who accepted a SSK were reflected in the understandable lack of willingness of the NHS trusts to accept a duty of care for participants accessing SSKs at sites distinct from their own service provision sites. However, this arrangement is necessary if research participants, or users of SSKs outside research, are to have the benefit of having their results managed by people with experience in providing HIV-related services. Given that existing national initiatives in the UK and non-NHS service providers are offering SSKs for HIV testing, standardised protocols for setting up pathways of care should be developed and made accessible to service providers, as well as researchers conducting SSK research.
Changes in the commissioning of sexual health services, as well as funding for HIV prevention initiatives in the UK, are already affecting research capacity. Our experience also demonstrates how variation in the funding models of the CRN and SPCRN has implications for research studies that work across national borders. Researchers doing studies in different regions of the UK need to be aware of these differences and budget accordingly. Despite efforts to reduce the time taken to obtain REC and R&D approvals, continually changing systems breed confusion and affect study timelines and the feasibility of assessing research questions substantially.
Although our intervention was not suitable for scale-up to a Phase III evaluation because of process-related factors, this does not mean that the intervention is not feasible in practice, and we hope that our findings will prove useful for future service provision through evidence synthesis.
Future work
Sexual and public health services are increasingly utilising self-sampling technologies; however, alternative, user-friendly SSKs that meet user and provider preferences and UK regulatory requirements are needed, and additional research is required to understand the clinical effectiveness and cost-effectiveness for black African communities and the population as a whole.
Acknowledgements
We are immensely grateful to all the patients, the community participants and the key informants who contributed to the study. We are also very grateful to the services that supported our study (see Appendix 13), with particular thanks to all the distributors at participating sites, Dr Danielle Mercey and the Health Advisor team at CNWL, and Mr Abraham Roodt and Ms Annette Wilkinson at TDL. Special thanks to the BHA for Equality in Health and Social Care and NHS Greater Glasgow and Clyde that agreed to financially support the intervention.
We would like to thank the UK Community Advisory Board, the BHA for Equality in Health and Social Care and the members of our Advisory Group and Study Steering Committee (see Appendix 13) for their invaluable contribution to our work.
We are very grateful to Dr Gemma Philips for her work on the focus groups in Glasgow, and to Caroline Park for her contribution to the qualitative analysis in stage 1 and the intervention development, and for leading on the writing of the training manual. We are also grateful to Gary Hammond, S Benedict Dossen and Lee Marshall, who contributed their expertise and time in making the instructional video, and to the staff at Yorkshire MESMAC, for sharing their information and expertise on self-sampling interventions.
Contributions of authors
All authors contributed to the design of the study and approved the final report.
Dr Maureen Seguin (Research Associate) was responsible for project management and the data collection for stage 2 of the study. She led on the authorship of the report.
Dr Catherine Dodds (Assistant Professor of HIV and Sexual Health) was the lead investigator of stage 1 of the project. She also contributed to all qualitative components throughout the study, including the process evaluation. She led on engagement with the CBOs and the development of the study website and video.
Dr Esther Mugweni (Senior Research Associate) was responsible for project management and the data collection for stage 1 of the study. She led on developing the intervention manual.
Professor Lisa McDaid (Programme Leader – Social Relationships and Health Improvement) led on the systematic review and project oversight in Glasgow. She contributed to the analysis of the FGDs and intervention development.
Dr Paul Flowers (Professor of Sexual Health Psychology) led on the intervention development and contributed expert knowledge on the theory of behaviour change in relation to health, and its application to intervention development.
Dr Sonali Wayal (Research Associate) advised on the content of questionnaires, topic guides and the systematic review process, and assisted with the FGDs and analysis of qualitative work. She led on the sections in the report relating to challenges to implementation.
Dr Ella Zomer (Health Economist) contributed to the development of the cost-effectiveness model and led on this section of the report.
Mr Peter Weatherburn (Director of Sigma Research) led on the process evaluation and contributed to the analysis of the qualitative data from stage 1. He also helped develop the study website.
Ms Ibidun Fakoya (Research Associate) contributed to the systematic review protocol and the screening of abstracts. She also advised on the content of questionnaires, topic guides and the intervention development, and provided expertise on engaging black African communities.
Mr Thomas Hartney (PhD student) helped with data extraction and quality appraisal for the systematic review. He led the writing up of this section of the report.
Dr Lorraine McDonagh (Research Associate) undertook participant interviews and assisted with the coding, analysis and writing up of this section.
Dr Rachael Hunter (Health Economist) was the lead investigator on the cost-effectiveness and economic components of the study.
Dr Ingrid Young (Chancellor Fellow) provided project oversight in Glasgow for stage 1. She also undertook FGDs, and contributed to the analysis and writing up of these discussions.
Ms Shabana Khan (Senior Data Manager) helped to create the study database and study instruments. She contributed expert knowledge on trial processes.
Professor Nick Freemantle (Senior Statistician) contributed expert statistical knowledge and advice. He conducted the analysis of the quantitative data in stage 2.
Mr Jabulani Chwaula (Associate Director of Programmes, BHA for Equality in Health and Social Care) provided patient and public involvement throughout the project. He advised on the content of questionnaires, topic guides, the intervention script and the plain English summary. He also provided expertise on working and engaging with CBOs.
Ms Memory Sachikonye (Co-ordinator, UK Community Advisory Board) was the lead for patient and public involvement. She advised on the content of questionnaires, topic guides, the intervention script and the plain English summary, and contributed to the production of the intervention video.
Professor Jane Anderson (Consultant Physician) provided expertise in engaging with service providers and black African communities with regard to HIV. She also contributed expert knowledge on the epidemiology of HIV and public health interventions.
Dr Surinder Singh (Senior Lecturer in General Practice) advised on the content of questionnaires, topic guides and the intervention script. He also provided expertise on working and engaging with GP.
Dr Eleni Nastouli (Consultant Virologist) provided a duty of care for all participants in stage 2, oversaw all clinical governance aspects and provided expert advice on HIV testing and diagnosis.
Dr Greta Rait (Reader in Primary Care/GP and Triallist) contributed expertise on the design, implementation and evaluation of complex interventions. She advised on the content of questionnaires, topic guides and the intervention manual. She also provided expertise on working and engaging with GP.
Dr Fiona Burns (Reader and Honorary Consultant Physician, HIV) was the principal investigator, with overall responsibility for the study, and was the lead investigator for stage 2. She advised on all elements of data collection and analysis, and is the corresponding author for the report.
Data sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Skingsley A, Yin Z, Kirwan P, Croxford S, Chau C, Conti S, et al. HIV in the UK: Situation Report 2015. London: Public Health England; 2015.
- Yin Z, Brown A, Hughes G, Nardone A, Gill O, Delpech V, et al. HIV in the United Kingdom: 2014 Report. London: Public Health England; 2014.
- Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS 2006;20:1447-50. https://doi.org/10.1097/01.aids.0000233579.79714.8d.
- Skarbinski J, Rosenberg E, Paz-Bailey G, Hall HI, Rose CE, Viall AH, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med 2015;175:588-96. https://doi.org/10.1001/jamainternmed.2014.8180.
- Iwuji C, Churchill D, Gilleece Y, Weiss H, Fisher M. Older HIV-infected individuals present late and have a higher mortality: Brighton, UK cohort study. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-397.
- Burns FM, Fakoya AO, Copas AJ, French PD. Africans in London continue to present with advanced HIV disease in the era of highly active antiretroviral therapy. AIDS 2001;15:2453-5. https://doi.org/10.1097/00002030-200112070-00015.
- Public Health Outcomes Framework 2013 to 2016. London: Department of Health and Social Care; 2013.
- 90–90–90: An Ambitious Treatment Target to Help End the AIDS Epidemic. Geneva: UNAIDS; 2014.
- Burns FM, Johnson AM, Nazroo J, Ainsworth J, Anderson J, Fakoya A, et al. Missed opportunities for earlier HIV diagnosis within primary and secondary healthcare settings in the UK. AIDS 2008;22:115-22. https://doi.org/10.1097/QAD.0b013e3282f1d4b6.
- HIV in the United Kingdom: 2012 Report. London: Health Protection Agency; 2012.
- Burns FM, Imrie JY, Nazroo J, Johnson AM, Fenton KA. Why the(y) wait? Key informant understandings of factors contributing to late presentation and poor utilization of HIV health and social care services by African migrants in Britain. AIDS Care 2007;19:102-8. https://doi.org/10.1080/09540120600908440.
- Prost A, Elford J, Imrie J, Petticrew M, Hart G. Social, behavioural, and intervention research among people of Sub-Saharan African origin living with HIV in the UK and Europe: literature review and recommendations for intervention. AIDS Behav 2008;12:170-94. https://doi.org/10.1007/s10461-007-9237-4.
- Dodds C. HIV-related stigma in England: experiences of gay men and heterosexual African migrants living with HIV. J Community Appl Soc Psychol 2006;16:472-80. https://doi.org/10.1002/casp.895.
- Fakoya I, Reynolds R, Caswell G, Shiripinda I. Barriers to HIV testing for migrant black Africans in Western Europe. HIV Med 2008;9:23-5. https://doi.org/10.1111/j.1468-1293.2008.00587.x.
- Deblonde J, De Koker P, Hamers FF, Fontaine J, Luchters S, Temmerman M. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health 2010;20:422-32. https://doi.org/10.1093/eurpub/ckp231.
- Deblonde J, Sasse A, Del Amo J, Burns F, Delpech V, Cowan S, et al. Restricted access to antiretroviral treatment for undocumented migrants: a bottle neck to control the HIV epidemic in the EU/EEA. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2571-y.
- Prost A, Griffiths CJ, Anderson J, Wight D, Hart GJ. Feasibility and acceptability of offering rapid HIV tests to patients registering with primary care in London (UK): a pilot study. Sex Transm Infect 2009;85:326-9. https://doi.org/10.1136/sti.2008.033233.
- May M, Gompels M, Delpech V, Porter K, Post F, Johnson M, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ 2011;343. https://doi.org/10.1136/bmj.d6016.
- Westrop S, James C, Edwardes D, Brady M, Gillespie R, Gill O, et al. Testing History and Risk Behaviour of Individuals Requesting an HIV Test Through an Online Self-Sampling Service n.d.
- Elliot E, McCowan A, McCormak S, Rossi M, van Every T. Home sampling through social network websites: can we reduce undiagnosed HIV?. Sex Transm Infect 2012;88. https://doi.org/10.1136/sextrans-2012-050601a.20.
- Spielberg F, Critchlow C, Vittinghoff E, Coletti AS, Sheppard H, Mayer KH, et al. Home collection for frequent HIV testing: acceptability of oral fluids, dried blood spots and telephone results. HIV Early Detection Study Group. AIDS 2000;14:1819-28. https://doi.org/10.1097/00002030-200008180-00018.
- Dodds JP, Johnson AM, Parry JV, Mercey DE. A tale of three cities: persisting high HIV prevalence, risk behaviour and undiagnosed infection in community samples of men who have sex with men. Sex Transm Infect 2007;83:392-6. https://doi.org/10.1136/sti.2006.021782.
- Pant Pai N, Joshi R, Dogra S, Taksande B, Kalantri SP, Pai M, et al. Evaluation of diagnostic accuracy, feasibility and client preference for rapid oral fluid-based diagnosis of HIV infection in rural India. PLOS ONE 2007;2. https://doi.org/10.1371/journal.pone.0000367.
- Saunders JM, Mercer CH, Sutcliffe LJ, Hart GJ, Cassell J, Estcourt CS. Where do young men want to access STI screening? A stratified random probability sample survey of young men in Great Britain. Sex Transm Infect 2012;88:427-32. https://doi.org/10.1136/sextrans-2011-050406.
- Elliot E, Rossi M, McCormak S, McOwan A. Identifying undiagnosed HIV in men who have sex with men (MSM) by offering HIV home sampling via online gay social media: a service evaluation. Sexually Transm Infect 2016;92:470-3. https://doi.org/10.1136/sextrans-2015-052090.
- Bourne A, Reid D, Weatherburn P. African Health & Sex Survey 2013–14: Headline Findings. London: Sigma Research, London School of Hygiene and Tropical Medicine; 2014.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy 2005;10:45-53. https://doi.org/10.1177/135581960501000110.
- Methods for the Development of NICE Public Health Guidance. London: NICE; 2012.
- Kitzinger J. The methodology of focus groups: the importance of interaction between research participants. Sociol Health Illn 1994;16:103-21. https://doi.org/10.1111/1467-9566.ep11347023.
- Bryman A. Interviewing in Qualitative Research. Social Research Methods. Oxford: Oxford University Press; 2012.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage Publications; 2003.
- Atkins L, Michie S, Wood C. Applying Evidence-Based Theory To Behavioural Interventions 2014.
- Michie S, van Stralen M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26-33. https://doi.org/10.1136/qshc.2004.011155.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-37.
- Webster R, Estcourt C, Gerressu M, Bailey J. Increasing condom use in heterosexual men: development of a theory-based interactive digital intervention. Transl Behav Med 2016;6:418-27. https://doi.org/10.1007/s13142-015-0338-8.
- UK National Guidelines for HIV Testing 2008. London: BHIVA, BASHH, British Infection Society; 2008.
- Time to Test for HIV: Expanding HIV Testing Services in Healthcare and Community Settings in England. London: HPA; 2011.
- Addressing Late HIV Diagnosis through Screening and Testing: An Evidence Summary. London: PHE; 2014.
- HIV Testing Action Plan to Reduce Late HIV diagnosis in the UK. London: NAT; 2012.
- HIV Instant Result Self-Testing in Scotland: Addressing Key Questions and Recommending Good Practice. Edinburgh: HIV Scotland; 2014.
- Instant Result HIV Self-Test Kits: Information for the Public in England and Wales. London: NAT; 2015.
- Increasing the Uptake of HIV Testing Among Black Africans in England. Manchester and London: NICE; 2011.
- HIV Testing. Manchester and London: NICE; 2014.
- HIV Testing: Increasing Uptake Among People Who May Have Undiagnosed HIV. London: NICE; 2016.
- Bartholow B. A Comparison of Consumer-Controlled and Traditional HIV Counseling and Testing: Implications for Screening and Outreach Among Injection Drug Users 2005.
- Colfax GN, Lehman JS, Bindman AB, Vittinghoff E, Vranizan K, Fleming PL, et al. What happened to home HIV test collection kits? Intent to use kits, actual use, and barriers to use among persons at risk for HIV infection. AIDS Care 2002;14:675-82. https://doi.org/10.1080/0954012021000005533a.
- Fisher M, Wayal S, Smith H, Llewellyn C, Alexander S, Ison C, et al. Home sampling for sexually transmitted infections and HIV in men who have sex with men: a prospective observational study. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0120810.
- Formby E, Hirst J, Cripps C. Evaluation of Time 2 Test Pilot: Final Report. Sheffield: Sheffield Hallam University, Sheffield Teaching Hospitals, Centre for HIV & Sexual Health; 2010.
- Greensides DR, Berkelman R, Lansky A, Sullivan PS. Alternative HIV testing methods among populations at high risk for HIV infection. Public Health Rep 2003;118:531-9. https://doi.org/10.1016/S0033-3549(04)50289-3.
- Osmond DH, Catania J, Pollack L, Canchola J, Jaffe D, MacKellar D, et al. Obtaining HIV test results with a home collection test kit in a community telephone sample. J Acquir Immune Defic Syndr 2000;24:363-8. https://doi.org/10.1097/00126334-200008010-00011.
- Sharma A, Sullivan PS, Khosropour CM. Willingness to take a free home HIV test and associated factors among internet-using men who have sex with men. J Int Assoc Physicians AIDS Care 2011;10:357-64. https://doi.org/10.1177/1545109711404946.
- Sharma A, Stephenson RB, White D, Sullivan PS. Acceptability and intended usage preferences for six HIV testing options among internet-using men who have sex with men. SpringerPlus 2014;3. https://doi.org/10.1186/2193-1801-3-109.
- Skolnik HS, Phillips KA, Binson D, Dilley JW. Deciding where and how to be tested for HIV: what matters most?. J Acquir Immune Defic Syndr 2001;27:292-300. https://doi.org/10.1097/00042560-200107010-00013.
- Spielberg F, Critchlow C, Vittinghoff E, Gross M, Doherty-Iddings P, Scotti R, et al. Slow diffusion of home HIV-specimen collection: provider concerns at odds with client preferences. Sex Transm Dis 2001;28:51-7. https://doi.org/10.1097/00007435-200101000-00012.
- Wayal S, Llewellyn C, Smith H, Fisher M. Home sampling kits for sexually transmitted infections: preferences and concerns of men who have sex with men. Cult Health Sex 2011;13:343-53. https://doi.org/10.1080/13691058.2010.535018.
- Wood M, Ellks R, Grobicki M. Outreach sexual infection screening and postal tests in men who have sex with men: are they comparable to clinic screening?. Int J STD AIDS 2015;26:428-31. https://doi.org/10.1177/0956462414539668.
- Smith M. Africans in Scotland: Heterogeneity and Sensitivities to HIV. Glasgow: University of Glasgow; 2016.
- Sue DW, Capodilupo CM, Torino GC, Bucceri JM, Holder AM, Nadal KL, et al. Racial microaggressions in everyday life: implications for clinical practice. Am Psychol 2007;62:271-86. https://doi.org/10.1037/0003-066X.62.4.271.
- Auerbach JD, Parkhurst JO, Cáceres CF. Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations. Glob Public Health 2011;6:S293-309. https://doi.org/10.1080/17441692.2011.594451.
- Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med 2003;57:13-24. https://doi.org/10.1016/S0277-9536(02)00304-0.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Genscreen™ ULTRA HIV Ag-Ab: Screening Kit for the Detection of Hiv P24 Antigen and Antibodies to HIV-1 And HIV-2 in Human Serum/Plasma by Enzyme Immunoassay. Paris: Bio-Rad Laboratories; 2010.
- Rayment M, Rae C, Ghooloo F, Doku E, Hardie J, Finlay S, et al. Routine HIV testing in the emergency department: tough lessons in sustainability. HIV Med 2013;14:6-9. https://doi.org/10.1111/hiv.12069.
- Dean Street at Home . Postal HIV Testing for Gay Men Living in Greater London n.d. www.deanstreetathome.com (accessed 29 September 2016).
- Standards for the Management of Sexually Transmitted Infections (STIs). Macclesfield and London: BASHH and the Medical Foundation for HIV & Sexual Health; 2014.
- Standards – March 2008: Sexual Health Services. Edinburgh: NHS Health Scotland; 2008.
- Research Governance Framework for Health and Social Care. London: Department of Health and Social Care; 2005.
- Leber W, McMullen H, Anderson J, Marlin N, Santos AC, Bremner S, et al. Promotion of rapid testing for HIV in primary care (RHIVA2): a cluster-randomised controlled trial. Lancet HIV 2015;2:e229-35. https://doi.org/10.1016/S2352-3018(15)00059-4.
- HIV Combi. HIV-1 Antigen and Total Antibodies to HIV-1 and HIV-2 v5. Elecsys and Cobase Analyzers. Burgess Hill: Roche Diagnostics; 2010.
- Linnan L, Steckler A, Steckler A, Linnan L. Process Evaluation for Public Health Interventions and Research. San Francisco, CA: Jossey-Bass; 2002.
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control?. Clin Psychol Rev 1998;18:23-45. https://doi.org/10.1016/S0272-7358(97)00043-3.
- Mihalic S. The importance of implementation fidelity. Emotion Behav Disord Youth 2004;4:83-105.
- Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol 2008;41:327-50. https://doi.org/10.1007/s10464-008-9165-0.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- Bumbarger B, Perkins D. After randomised trials: issues related to dissemination of evidence-based interventions. J Child Serv 2008;3:55-64. https://doi.org/10.1108/17466660200800012.
- Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Community Psychol 2009;43:267-76. https://doi.org/10.1007/s10464-009-9229-9.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7. https://doi.org/10.2105/AJPH.89.9.1322.
- Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management?. Patient Educ Couns 2001;44:119-27. https://doi.org/10.1016/S0738-3991(00)00186-5.
- Mortality Statistics: Metadata July 2015. Newport: ONS; 2015.
- Nakagawa F, Miners A, Smith CJ, Simmons R, Lodwick RK, Cambiano V, et al. Projected lifetime healthcare costs associated with HIV infection. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0125018.
- Petrou S, Gray A. Economic evaluation using decision analytical modelling: design, conduct, analysis, and reporting. BMJ 2011;342. https://doi.org/10.1136/bmj.d1766.
- Husereau D, Drummond M, Petrou S. on behalf of the CHEERS Task Force . Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013;346. https://doi.org/10.1136/bmj.f1049.
- British HIV Association Guidelines for the Treatment of HIV-1-Positive Adults with Antiretroviral Therapy 2015. London: BHIVA; 2015.
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011;365:493-505. https://doi.org/10.1056/NEJMoa1105243.
- Skingsley A, Kirwan P, Yin Z, Nardone A, Gill O, Hughes G, et al. HIV New Diagnoses, Treatment and Care in the UK 2015 Report: Data to End 2014. London: Public Health England; 2015.
- Fleurence RL, Hollenbeak CS. Rates and probabilities in economic modelling: transformation, translation and appropriate application. PharmacoEconomics 2007;25:3-6. https://doi.org/10.2165/00019053-200725010-00002.
- WHO Prequalification of Diagnostics Programme Public Report. Produce: Genscreen Ultra HIV Ag-Ab. Geneva: WHO; 2013.
- Sonnenberg P, Clifton S, Beddows S, Field N, Soldan K, Tanton C, et al. Prevalence, risk factors, and uptake of interventions for sexually transmitted infections in Britain: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet 2013;382:1795-806. https://doi.org/10.1016/S0140-6736(13)61947-9.
- Beck EJ, Mandalia S, Sangha R, Sharott P, Youle M, Baily G, et al. The cost-effectiveness of early access to HIV services and starting cART in the UK 1996–2008. PLOS ONE 2011;6. https://doi.org/10.1371/journal.pone.0027830.
- Miners A, Phillips A, Kreif N, Rodger A, Speakman A, Fisher M, et al. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: a cross-sectional comparison with the general population. Lancet HIV 2014;1:e32-40. https://doi.org/10.1016/S2352-3018(14)70018-9.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Briggs A, Claxton K, Sculpher M. Decision Modelling for Health Economic Evaluation. Oxford: University of Oxford; 2006.
- Claxton K, Martin S, Soares M, Rice N, Spackman E, Hinde S, et al. Methods for the estimations of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technol Access 2015;19.
- Davis S, Stevenson M, Tappenden P, Wailoo A. Cost-effectiveness Modelling Using Patient-level Simulation: Report by the Decision Support Unit. Sheffield: Decision Support Unit, School of Health and Related Research, University of Sheffield; 2014.
- Ogaz D, Furegato M, Connor N, Gill O. HIV Testing in England: 2016 Report. London: Public Health England; 2016.
- National AIDS Trust . NAT Calls for Annual Testing Recommendation for African Men and Women 2012. www.nat.org.uk/press-release/nat-calls-annual-testing-recommendation-african-men-and-women.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
Appendix 1 Systematic review screening criteria and search strategy
Systematic review of self-sampling kit acceptability
Inclusion criteria: quantitative studies
-
Population: any lay population in any country.
-
Intervention: SSKs for the detection of HIV.
-
Comparison: any other HIV testing method.
-
Outcomes: completion of a SSK for HIV; participant-reported acceptability; adverse events; first-time testers; test/strategy; linkage; accuracy; and cost-effectiveness.
-
Study design: any randomised or non-randomised evaluation or observational design.
-
Publication date: 2000 to present.
-
Language: English.
Inclusion criteria: qualitative studies
Studies in any population group in any country describing, summarising or analysing the experiences and perceptions of any population group about SSKs for the detection of HIV. This will include studies of experiences of, and responses to, personal completion of SSKs for HIV detection and also perceptions and opinions of potential use. Any text-based qualitative research methodology will be included: interviews, focus groups and ethnography. Studies published from 2000 until the time of searching will be included.
Screening
Titles and abstracts of studies retrieved using the search strategy and those from additional sources will be screened by two researchers to identify studies that potentially meet the inclusion criteria outlined in Inclusion criteria: qualitative studies. Studies excluded at this stage will be excluded as ‘not relevant to SSKs for HIV’ and will be counted to allow completion of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram. At this stage, both quantitative and qualitative studies of SSKs for HIV will be retained together. When an abstract is not available and the title cannot be used to assess relevance, the article will be retained for full-text screening.
The full text of these potentially eligible studies will be retrieved and assessed for eligibility. All the PDF files will be incorporated into the bibliographic database, which will be delivered to the rest of the team. A more detailed coding scheme for exclusion reasons will be developed and recorded for completion of the PRISMA flow diagram. Eligible quantitative and qualitative studies will be separated at this stage and treated separately in the PRISMA flow diagram.
At each stage, the two researchers (EM and Gemma Philips) will:
-
complete a 5% sample of records in parallel to check the consistency and feasibility of inclusion/exclusion criteria application
-
split the remaining records and screen individually, with a 10% sample being double-screened.
Any disagreement between the two researchers (EM and GP) over the eligibility of particular studies will be resolved through discussion and, when needed, a third researcher will be consulted (FB and/or CD?). For all the excluded references, the exclusion reason will be recorded in an EndNote/Microsoft Excel spreadsheet.
The researchers will contact the investigators for clarification when eligibility cannot be determined from the published study, and for any new studies or references that may not be published yet, and to check that the search has captured important articles in the field. We will review backward and forward citation of Web of Knowledge for the publications finally identified as relevant after the screening process.
Full-paper screening
Was the study carried out in any of the following countries?
|
Yes/unclear – go to Q2 | No – exclude |
| Was the study published in 2000 or later? | Yes/unclear – go to Q3 | No – exclude |
| Does the paper include information about self-sampling for HIV? | Yes/unclear – go to Q4 | No – exclude |
Is the paper/study about interventions that include any of the following outcomes:
|
Yes/unclear – go to Q5 | No – exclude |
| Does this paper describe a primary study or is it a review (of primary studies) (e.g. randomised or non-randomised controlled trials, prospective observational analyses, retrospective observational analyses, cost–benefit analyses, cost-consequence analyses, cost-effective analyses and cost–utility analyses | Yes/unclear – go to Q6 | No – go to Q6 |
| Is the study exclusively measuring the validity or diagnostic clinical effectiveness of different types of HIV test; are the interventions examining testing following exposure to HIV in the workplace? | Yes – exclude | No/unclear – include for full-paper review |
MEDLINE (via OvidSP)
Date range searched: 2000 to week 3 September 2014.
Search strategy
-
exp HIV Infections/ (238,345)
-
exp HIV/ (86,013)
-
hiv.ti,ab. (225,871)
-
‘hiv1’.ti,ab. (710)
-
‘hiv2’.ti,ab. (149)
-
‘hiv type 1’.ti,ab. (3784)
-
‘hiv type 2’.ti,ab. (186)
-
human immunodeficiency virus.ti,ab. (69,068)
-
human immunedeficiency virus.ti,ab. (4)
-
human immuno-deficiency virus.ti,ab. (186)
-
human immune-deficiency virus.ti,ab. (245)
-
(human immun* adj3 deficiency virus).ti,ab. (435)
-
acquired immunodeficiency syndrome.ti,ab. (14,483)
-
acquired immunedeficiency syndrome.ti,ab. (10)
-
acquired immuno-deficiency syndrome.ti,ab. (94)
-
acquired immune-deficiency syndrome.ti,ab. (4904)
-
(acquired immun* adj3 deficiency syndrome).ti,ab. (5037)
-
Sexually Transmitted Diseases, Viral/ (1207)
-
or/1-18 (313,426)
-
(sample adj1 collect*).ti,ab. (5944)
-
home dried blood spot.ti,ab. (0)
-
(alternative adj3 test*).ti,ab. (3862)
-
(option* adj1 test*).ti,ab. (270)
-
((Home* or self* or mail*) adj3 (collection* or sampl* or specimen* or test* or kit)).ti,ab. (10,969)
-
or/20-24 (20,907)
-
19 and 25 (1003)
-
limit 26 to (english language and yr=‘2000 -Current’) (673)
Appendix 2 Topic guide for phase 1 non-specialist focus group discussion
Appendix 3 Topic guide for phase 1 service provider focus group discussions and interviews
Appendix 4 HAUS study semistructured interview topic guide
Appendix 5 Barriers and facilitators relevant to the intervention component ‘the appearance and packaging of the HIV self-sampling kit’
| Thinking about improving the acceptability of your component | ||
|---|---|---|
|
Key barriers to implement (Indicate score out of 10 to indicate relative strength) |
Key facilitators to implement (Indicate score out of 10 to indicate relative strength) |
Conceptual coherence (What is the specific focus of the barrier/facilitator) |
| Clear plastic bag containing the kit (9) will not be acceptable as it will be difficult to carry them around | Non-transparent material bags for packaging the kits (9) | Confidential packaging material |
| Avoid using packaging that is unique/can be identified as the one used only for HIV testing kits (9) as it will lead to involuntary disclosure of HIV test seeking/breach of confidentiality | Use generic/commonly used materials for packaging the kits, like brown paper bags or coloured bags (9) | Confidential packaging material/design |
| Concerns about the kit being tampered with/opened/torn prior to being used (7), leading to contamination and subsequent impact on reliability of the test results | Tight, secure packaging that will not break/open/tear prior to use of the kits (6) | Contamination-secure packaging |
| Concerns about contamination of the specimens when posting back to the laboratory (9) | Good packaging to send the specimens back to the laboratory and assurance that it does not get contaminated (9) | Contamination-secure packing for specimens |
| Not very big or long kit (5) | Small, compact packaging that can be easy to carry (4) | Convenient size of packaging |
| No mention of HIV on the package (10) because of concerns regarding privacy and confidentiality | Plain packaging with no reference to the kit containing a test for HIV | Confidential packaging design |
Appendix 6 Overview of policies and guidelines relating to HIV testing and self-sampling in the UK between 2008 and 2016
| Author/source | Year | Title | Policy content | Policy change over time/policy in practice |
|---|---|---|---|---|
| BHIVA/BASHH | 2008 | UK National Guidelines for HIV Testing 2008 37 |
|
|
| Health Protection Agency (now PHE) | 2011 | Time to Test for HIV: Expanding HIV Testing Services in Healthcare and Community Settings in England 38 | This report describes eight pilot projects that were commissioned by the Department of Health and Social Care after publication of the BHIVA HIV testing guidelines. The pilot projects assessed how the guidelines might be implemented in acute admissions units, emergency departments and primary care settings, as well as in community and outreach settings. HIV SSKs were successfully used in one of the pilot projects | Findings from the pilot projects indicated that HIV testing in various medical and community settings was feasible and acceptable, further supporting the implementation of the BHIVA HIV testing guidelines |
| NICE | 2011 | Increasing the Uptake of HIV Testing Among Black Africans in England 43 | National guidance providing specific recommendations on methods of increasing the uptake of HIV testing among black African people in the UK. Suggested recommendations include:
|
Guidance has been influential in the expansion of HIV testing services for black African people; NICE guidelines were updated in December 2016, and SSKs were considered a potentially innovative way of increasing the uptake of HIV testing among black African people, given that they may address known barriers to HIV testing in this risk group45 |
| National AIDS Trust | 2012 | NAT Calls for Annual Testing Recommendation for African Men And Women 100 | Policy briefing suggesting that NICE could introduce annual HIV testing for black African people in order to reduce undiagnosed HIV. The policy briefing does not discuss self-sampling specifically, but reiterates the need for wide-scale testing in primary, secondary and community settings, as indicated in the BHIVA 2008 HIV testing guidelines37 | NICE recommends regular testing for individuals with new or casual sexual partners; however, NICE has not specified the frequency of testing for black African people |
| National AIDS Trust | 2012 | HIV Testing Action Plan to Reduce Late HIV Diagnosis in the UK 40 | This strategy provides rationale and evidence to support increasing the uptake of HIV testing and screening to address late HIV diagnosis in the UK. In line with the 2008 BHIVA guidelines,37 the paper advocates priority actions to reduce undiagnosed HIV, including:
|
This paper is based on the 2008 BHIVA guidelines37 and the national response to HIV has changed (e.g. the legislation of self-tests in 2014) |
| Department of Health and Social Care | First published in 2012; revised in 2015 | Public Health Outcomes Framework 2013 to 2016 7 | The framework details the national public health vision, the national public health outcomes to be achieved and measurable indicators that can be used to evaluate and monitor the progress towards achieving the given outcomes. The proportion of people presenting at a late stage of HIV infection, that is, with a CD4 count of < 350 cells/mm3 has been identified as an indicator of essential actions to be taken to protect the public’s health | Addressing late diagnosis of HIV is a high public health priority for addressing the epidemic in the UK, and this indicator provides measurable progress towards addressing late diagnosis |
| NICE | 2014 | HIV Testing 44 | Guidance and recommendations for local authorities and other clinical commissioning groups on delivering HIV testing services. NICE recommends that commissioners conduct an assessment of local need for HIV testing for black African people and then develop a local HIV testing strategy with clear referral pathways, particularly for outreach point-of-care services. To address undiagnosed HIV and late diagnosis of HIV among black African people, NICE recommends that commissioners promote HIV testing, including the use of modern HIV tests, and reduce barriers to HIV testing among black African people. In line with the BHIVA 2008 guidelines,37 NICE recommends that HIV testing is offered by health professionals in primary and secondary care | Although this guidance does not discuss commissioning of HIV self-sampling initiatives by local authorities, under the Health and Social Care Act 2012,101 local authorities are responsible for commissioning comprehensive sexual health services, including HIV testing. HIV self-sampling has been offered in community settings and medical settings40 |
| HIV Scotland | 2014 | HIV Instant Result Self-Testing in Scotland: Addressing Key Questions and Recommending Good Practice 41 | This document provides guidance on HIV self-testing in Scotland. It provides a rationale for self-testing; discusses legislation of HIV self-testing in the UK and elaborates on how STKs may address known barriers to HIV testing and possible ways of supporting patients through the process | STKs are now in use in the UK. Their impact on late diagnosis has not yet been evaluated |
| PHE | 2014 | Addressing Late HIV Diagnosis through Screening and Testing: An Evidence Summary 39 |
|
Self-testing became legal in 2014 and is viewed as another innovative testing strategy in addition to HIV self-sampling |
| National AIDS Trust | 2015 | Instant Result HIV Self-Test Kits: Information for the Public in England and Wales 42 | Patient information sheet on the use of SSKs, including the meaning of results and linkage into care and support | Although STKs became legal in 2014, there are no publications evaluating this type of test in the UK |
| NICE | 2015 | HIV Testing: Increasing Uptake Among People Who May Have Undiagnosed HIV 45 | Consultation for this guidance at the time of writing was ongoing; however, the final guidance has now been published.45 It gives an update to the 2011 guidance on increasing the uptake of HIV testing among black African people and MSM in the UK. NICE provides guidance on interventions to raise public awareness and interventions to increase the type of and opportunities for HIV testing. The guidance specifically identifies self-sampling and self-testing as possible ways to increase HIV testing | To be published in 2016 |
Appendix 8 Fieldwork schematic diagram
FIGURE 9.
Fieldwork schematic diagram. CRF, case report form; CSV, comma separated value; CW, community worker.
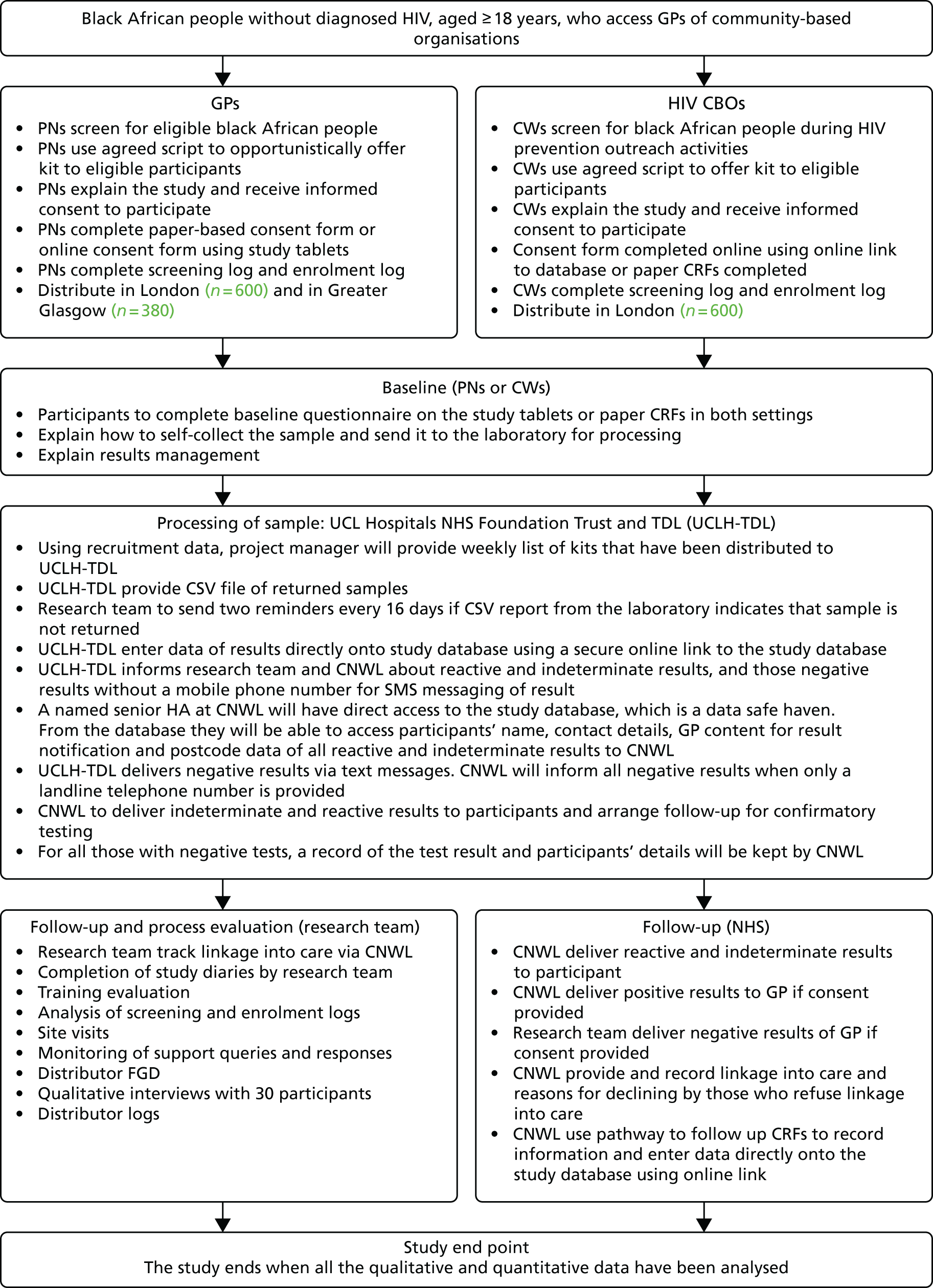
Appendix 9 Acceptability questionnaire
Appendix 10 Baseline questionnaire
Appendix 11 Distributor weekly log
Appendix 12 Study close-down interviews/group interviews with distributors
Appendix 13 Further acknowledgements
Distribution sites
Community-based organisations
KwaAfrica
Amanda Amito, Daniel Baliikya, Martha Bisirikirwa and Esther Namutoosi.
Naz
Parminder Sekhon Priyanka Goel.
Positive East
Amanda Amito, Daniel Baliikya, Martha Bisirikirwa and Esther Namutoosi.
General practice
Brigstock Medical Practice
Dr Dipti Gandhi, Nilgun Ahmed and Pat Southam.
Crawley Road Medical
Dr Rameet Singh Uberoi and Shiraaz Ibrahim.
Eagle House Surgery
Dr Claire Murphy and Dr Margaret Barnes.
Manor Place Surgery
Ahmed Faheem and Mohammad Halim.
Minet Green Health Practice
Dr Louise Medforth and Sue Chard.
Morden Hall Medical Centre
Dr Fiona White, Dr Ravi Patel and Emma Scerri.
Open Door Surgery
Dr Punam Mittal and Paula Batson.
Paxton Green
Dr Stephen Miller and Alison Peat.
Royal Arsenal Medical Centre
Dr Yann LeFeuvre.
Sir John Kirk Close Surgery
Dr Richard Proctor and Mohammad Halim.
Streatham Common Practice
Dr Ruth Danson and Tracy Hayward-Allingham.
The Corner Surgery
Dr David Wickstead, Filipa Pereira and Michelle Panton.
Advisory group membership
PHE
Dr Anthony Nardone.
Terrence Higgins Trust and King’s College Hospital NHS Foundation Trust
Dr Michael Brady.
Pharmacist
Mr Alistair Murray.
Positively UK
Ms Rebecca Mbewe.
Study Steering Committee
Dr Philippa James (chairperson): general practitioner, Cornbrook Medical Practice, Manchester.
Dr Suzanne Audrey: University of Bristol.
Dr Claudia Estcourt: Queen Mary University of London.
Collaborators
Dr Alan McOwan: Chelsea and Westminster Hospital NHS Foundation Trust.
Professor Graham Hart: UCL.
Glossary
- Non-specialist
- A person who does not work in the field of sexual health or HIV.
- Service provider
- A medical doctor, nurse, health-care assistant or provider of community-based sexual health and health promotion services.
- Service user
- An attendee of sexual health services and general practice surgeries, and of community-based health promotion and HIV prevention services.
List of abbreviations
- Ab
- antibody
- Ag
- antigen
- APEASE
- affordability, practicability, effectiveness and cost-effectiveness, acceptability, site-effects/safety and equity
- ART
- antiretroviral therapy
- BASHH
- British Association of Sexual Health and HIV
- BHIVA
- British HIV Association
- CBO
- community-based organisation
- CD4
- cluster of differentiation 4
- CE
- Conformité Européenne
- CI
- confidence interval
- CNWL
- Central and North West London NHS Foundation Trust
- COM-B
- capability, opportunity, motivation and behaviour (model of behaviour change)
- CRN
- Clinical Research Network
- FGD
- focus group discussion
- GP
- general practice
- GUM
- genitourinary medicine
- HA
- health advisor
- HCA
- health-care assistant
- HIV
- human immunodeficiency virus
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- ID
- identification
- IRAS
- Integrated Research Assessment System
- MHRA
- Medicines and Healthcare Agency
- MSM
- men who have sex with men
- Natsal
- National Survey of Sexual Attitudes and Lifestyles
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- ONS
- Office for National Statistics
- OR
- odds ratio
- PHE
- Public Health England
- PIS
- participant information sheet
- PN
- practice nurse
- POCT
- point-of-care testing
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PWID
- people who inject drugs
- QALY
- quality-adjusted life-year
- R&D
- research and development
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SMS
- short message service
- SPCRN
- Scottish Primary Care Research Network
- SSK
- self-sampling kit
- STI
- sexually transmitted infection
- STK
- self-testing kit
- TDF
- theoretical domains framework
- TDL
- The Doctors Laboratory
- UCL
- University College London
- UCLH
- University College London Hospital
