Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/175/02. The contractual start date was in February 2017. The draft report began editorial review in October 2017 and was accepted for publication in March 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
William McGuire is a member of the Health Technology Assessment Commissioning Board and the Health Technology Assessment and Efficacy and Mechanism Evaluation Editorial Boards.
Disclaimer
The views expressed in this report are those of the authors and not necessarily those of the NIHR Health Technology Assessment programme. Any errors are the responsibility of the authors.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Corbett et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Intravenous (i.v.) access for the provision of medication and nutrition is a common, and in many cases essential, procedure used for children and infants in hospitals. Although adverse outcomes resulting from i.v. access are rare, the procedure is not without risk. Extravasation injuries are caused by unintended leakages from i.v. lines in which a fluid deviates from its planned pathway (the vein) into surrounding tissue. Extravasation of fluid can cause pain, inflammation, tendon or nerve damage and predispose to local and invasive infection. Initial treatments aim to reduce pain and prevent or minimise local tissue necrosis and associated functional and cosmetic impairment. Longer term treatment of severe extravasation episodes may require skin grafts and prolonged hospitalisation. The severity of injury and likelihood of long-term damage depends on a number of factors, including the type and amount of fluid extravasated, the injury site, how quickly treatment is administered and the treatment itself. 1
The terms ‘extravasation’ and ‘infiltration’ are often used interchangeably in the literature but are sometimes defined separately, based on the type of fluid being administered. 2 A vesicant is any medication or fluid with the potential for causing blisters, severe tissue injury, or necrosis primarily due to biochemical reactions. Vesicants can vary in type but include many cytotoxic agents (such as chemotherapies). Non-vesicants include fluids such as parenteral nutrition and antibiotics that can cause damage primarily due to the mechanical forces exerted. The distinction between ‘extravasation’ (i.e. leakage of a vesicant) and ‘infiltration’ (i.e. leakage of a non-vesicant) can sometimes cause undue confusion as these two types of event are often indistinguishable externally. 3
Prevalence of extravasation injuries and risk factors
There is some uncertainty about the incidence of extravasation injuries in children in the NHS because of the absence of a centralised register, a paucity of data available from prospective studies and heterogeneity in definitions used to describe injury occurrence. 1 Estimates of between 0.01% and 7% have been reported, although there is some evidence to suggest that this has reduced considerably since 2002. 1 Age is an important risk factor and injuries that result in tissue necrosis seem to be more prevalent in neonates and younger infants. This is likely to be owing to their immature skin, fragile veins, lack of subcutaneous tissue, likelihood of needing longer periods of i.v. treatment and their limited ability to report pain. 4,5 A UK-based survey of regional neonatal intensive care units5 (NICUs), published in 2004, estimated the incidence of extravasation injuries resulting in skin necrosis to be 38 per 1000 babies. Most (70%) of these occurred in preterm infants born before 27 weeks’ gestation. 5 More recently, a Greek study4 of 1409 neonates reported a severe injury rate of 2.4%, and a Canadian children’s hospital-based study6 reported an overall rate of 0.04% per patient-day, in a population with a median age of 10 months. Nearly all of the injuries were at peripheral i.v. sites. 6
The Great Ormond Street Hospital guidelines for the recognition, management and prevention of infiltration and extravasation injuries2 categorise risk factors as being device related, drug related, patient related and clinician related. Device-related factors refer to how the drug was administered and include the infusion site (distal limb vs. centrally placed), the type of cannula used and how the cannula was secured. Drug-related factors refer to what was administered and include the vesicant potential of the solution, the volume of fluid that is extravasated and the concentration of the drug. Patient-related factors refer to characteristics such as age and communication impairment. Finally, clinician-related factors refer to those administering the i.v. treatment and include: lack of knowledge of extravasation events, lack of i.v cannula or catheter placement skills and interruptions or distractions during i.v. treatment.
Managing these risk factors to prevent extravasation occurring is preferable to treating an injury. Immediate removal of the catheter and prompt treatment is thought to be important in such cases. This is often hampered by the unreliability of alarms on i.v. pumps in detecting elevated perfusion pressures that may indicate extravasations. These alarms are not intended to detect extravasations but are often the only warning sign the clinicians have to indicate flow faults during infusions. 7 These devices have been shown to detect extravasation in only 19% of cases because of the variability in resistance to flow due to the rate and site of infusion. 8
Litigation in extravasation injuries
About 65% of clinical negligence claims in paediatric surgery in the UK result in payment to the claimant. 9 Of these, between 2% and 4% are due to extravasation events. 10,11 However, a severe extravasation injury does not constitute negligence in itself. Any claims would be assessed with careful consideration of the risk factors outlined above. 12,13 Specifically, it is the failure to take special precautions to minimise the potential for extravasation injury that determines fault. Demonstration of the following would be important: effective securement of the i.v. device, appropriate monitoring of the site, timely recognition of the extravasation, immediacy of intervention and the completeness of documentation.
Severity of injury
Extravasation injuries have been classified into four stages of increasing severity, which are thought to be useful in predicting injury prognosis and in determining the best treatment results. 14 The four stages are:
-
Stage 1: a painful i.v. site, no erythema and swelling, flushes with difficulty.
-
Stage 2: a painful i.v. site, slight swelling, redness, no blanching, brisk capillary refill below infiltration site, good pulse volume below infiltration site.
-
Stage 3: a painful i.v. site, marked swelling, blanching, cool to touch, brisk capillary refill below infiltration site, good pulse volume below infiltration site.
-
Stage 4: a painful i.v. site, very marked swelling, blanching, cool to touch, capillary refill of > 4 seconds, decreased or absent pulse, skin breakdown or necrosis.
Objectively assessing injuries according to these criteria has been recommended both in treatment and in research so that accurate outcome data can be collected. Researchers have suggested that these can be used to guide assessments and interventions. Clifton-Koeppel8 goes further, stating that using a protocol based on these criteria would improve consistency in assessment, increase compliance, decrease the incidence of extravasation and allow for prompt treatment. The author also suggests that stage 4 injuries should be further categorised to include a stage 5 injury that is distinguishable from a stage 4 injury by also including extensive or very deep wounding. However, this extra criterion has not been widely adopted.
There have been attempts to adapt, rather than subdivide, the stages of injury. 3 The Infusion Nurses Society adapted the scale by including guidelines3 for the size of the injury and by suggesting that infiltrations involving vesicant solutions should automatically be considered as stage 4 injuries. Other researchers have argued that the Millam guidelines are not appropriate for paediatric populations. 3,15 The smaller size of children means that similarly sized injuries (to those seen in adults) are actually much more severe. To counter this, researchers have proposed alternative guidelines. 3,15 Amjad et al. 3 accomplished this by referring to the number of joints involved, rather than overall size of the injury, to determine scale of injury. Similarly, Simona15 used percentage of the limb affected, rather than measurements, to determine the injury’s grading.
Treatment options
The main objective for treating extravasation injuries is to prevent pain and progression to tissue necrosis, ulceration, and scarring. 16 However, there is no consensus on the best approach to management. 17–19 The intervention strategies used are normally driven by the type and extent of the injury and by the time interval between injury and intervention. Treatment options are many and varied, but broadly fall under the following categories.
Conservative management strategies
This typically involves elevating the affected limb to reduce oedema by decreasing the hydrostatic pressure in the capillaries. Carers may administer hot or cold dressings. Heat promotes the absorption of extravasated fluids and oedema, whereas cold dressings may limit inflammation. The standard dressing of wounds and administration of analgesics would come under this category of treatment.
Topical treatments
Topical treatments are most often used when an open wound is present. These include nitroglycerin or silver sulfadiazine ointment and dimethyl sulfoxide (DMSO). These attempt to promote a moist wound environment, which, it is argued, reduces healing time, reduces likelihood of infection and prevents scarring. 8
Antidotes
Some vesicant solutions may have a particular antidote which can be infused or injected into an affected area. This approach appears to be most often used for treating chemotherapy extravasations. Among the antidotes recommended for use are sodium thiosulfate for mechlorethamine, hyaluronidase for plant alkaloids and dexrazoxane for anthracyclines. 20 However, guidelines published by the European Society for Medical Oncology1 indicate that specific antidotes are not commonly used and their effectiveness has been questioned. It should also be noted that the specific antidotes have limited access for use in European countries. 1
Hyaluronidase injections
Subcutaneous hyaluronidase injections can be used in an attempt to break down connective tissue and facilitate absorption of the extravasated fluid into the vascular and lymphatic systems. It has been recommended that the administration of these injections should take place within one hour of the extravasation. 18
Saline flush-out and liposuction
Both saline flush-out and liposuction are administered with the aim of removing the extravasated fluid before it can cause damage. As such, there is an implicit requirement that these treatments are undertaken as soon as possible. Gault21 has described both techniques, which can be administered alone or together, although various modifications to these techniques have also been reported.
Flush-out techniques typically involve skin incisions being made in the extravasation injury and saline injected into each incision, the aim being that this process will flush out the infusate via the remaining puncture points. The process is sometimes preceded by injection of hyaluronidase to break down the hyaluronic acid in connective tissues, thus aiding infusate dispersal. The procedure is often performed under a local anaesthetic, although a general anaesthetic may sometimes be necessary, especially if liposuction is also to be performed. Liposuction is a minimally invasive surgical technique in which a cannula with side holes is inserted into the wound, and fluid and subcutaneous fat is aspirated out.
Surgery
If less invasive treatments are unsuccessful and necrotic tissue is unresolved after an extended period of time, the next option on the treatment pathway is surgical debridement, or plastic surgery, or both. The purpose of debridement is the removal of necrotic tissue (eschar), which impairs wound healing. It typically involves either a surgical technique (the use of sharp instruments to excise the eschar under general anaesthesia) or an enzymatic approach (which promotes softening of eschar tissue). Once the wound is clean, application of a skin graft or artificial skin may be necessary.
Current guidelines on treatment
Few treatment guidelines have been published, and recommendations are often conflicting. 1,8,16,18,19 For example, the saline flush-out treatment, as originally proposed by Gault21 has been described as very effective and to be recommended,8 as having achieved good results,2 as potentially effective but lacking in evidence18 and as not to be recommended as routine management. 1 This finding is unsurprising given the inconsistency of the approach to treatment and given that many of the published, peer-reviewed guidelines and reviews that exist are based on limited research evidence. 17,19,22,23 Reviews of the area highlight a paucity of good-quality comparative research between treatments for extravasations of cytotoxic drugs. The literature appears even sparser for the management of paediatric populations and for treating extravasation injuries resulting from non-cytotoxic drugs. 16,24
Despite published guidelines,2 evidence from surveys suggests there is a lack of consensus on the best course of treatment for extravasation injuries. The lack of consensus is also illustrated by the existence of the many local hospital guidelines on management as indicated by UK survey findings. 5 The pattern appears to be replicated internationally, as reported in surveys conducted in the USA25 and Australia and New Zealand. 26 A British survey conducted by Wilkins et al. 5 found that exposing the wound to the air alone was used for 29% of cases, 43% of cases were treated with saline wash-out (85% of which also included the use of hyaluronidase), 20% were treated with hydrocolloids and 5.5% with hydrogels. A similar survey was conducted in Australia and New Zealand by Restieux et al. 26 This study found that limb elevation was used in 63% of cases, saline wash-out in 67%, hyaluronidase in 38% and 27% used a specific antidote. There is a very different distribution of treatments between the two regions, with only the proportion of hyaluronidase use being equivalent. Pettit et al. 25 used a sample in the USA to look specifically at hyaluronidase and phentolamine use. They found that only 57% had a procedure for hyaluronidase use and only 29% had a procedure for phentolamine.
Aside from the specifics of the management techniques reported in these surveys, two of the surveys revealed that there appeared to be a significant proportion of centres which did not have a written policy for the treatment of extravasation injuries. Restieaux et al. ’s26 survey of 27 NICUs in Australia and New Zealand reported this rate as 35%, whereas Pettit and Hughes’25 survey of nine geographical areas in the USA reported a rate of 27%.
The lack of consensus in sites, and within and between these surveys, is concerning, particularly with regard to the finding in the UK study5 that a substantial minority of cases were being treated solely by exposure to air. However, it should be noted that this study is somewhat outdated, with current NHS practice likely to be different. An up-to-date survey is therefore warranted. Despite this, it is still apparent that policies are largely based on historical practice within hospitals, on prior experience and on expert opinion, rather than on published guidelines. 22
Overall aims and objectives of the study
This study aims to begin the process of resolving the uncertainty surrounding which treatments are the best for treating extravasation injuries in babies and young children. Results from a scoping review will determine which treatments are likely to be the most promising, and results from a NHS survey will inform on which treatment approaches are currently used across the NHS and provide opinions about which interventions are most worthy of future research.
Chapter 2 Scoping review of treatments for extravasation injuries
Methods
Our scoping review was undertaken based on the methodological framework proposed in papers by Arksey and O’Malley,27 Levac et al. 28 and Daudt et al. 29 Briefly, the framework involves six core stages: identifying the research question; identifying relevant studies; study selection; charting the data (data extraction); collating, summarising, and reporting results; and consultation (consumer and stakeholder involvement). This is an area of review methodology which continues to evolve. 30 A key difference between a scoping review and a systematic review is that scoping reviews do not usually encompass a formal quality assessment of all included studies. It seems likely that, for many scoping reviews, some form of quality assessment – whether formal or informal – of at least some of the included studies may be necessary to allow informed recommendations for research.
Literature searching
The aim of the literature search was to identify studies of interventions for treating extravasation injuries in infants, children or adolescents. An information specialist developed the search strategy in MEDLINE (via Ovid). The strategy included a set of terms covering extravasation injuries, combined using the Boolean operator ‘AND’, with a set of terms for infants, children and adolescents. No date, language, geographical or study design limits were applied to the strategy. The MEDLINE strategy was adapted for use in all resources searched.
The searches were carried out during February 2017. The following databases were searched without date restrictions: MEDLINE (including: Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE), British Nursing Index, Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews (CDSR), Cumulative Index to Nursing & Allied Health (CINAHL Plus), Database of Abstracts of Reviews of Effects (DARE), Excerpta Medica dataBASE (EMBASE), Ovid Emcare, Health Technology Assessment (HTA) Database, Maternity and Infant Care, PubMed and Science Citation Index.
The following resources were searched for ongoing, unpublished or grey literature: ClinicalTrials.gov, Conference Proceedings Citation Index: Science, EU Clinical Trials Register, Proquest Dissertations & Theses: UK & Ireland, PROSPERO and the WHO (World Health Organization) International Clinical Trials Registry Platform portal.
A search for relevant guidelines was carried out via the following websites: National Institute for Health and Care Excellence (NICE), National Guideline Clearinghouse and the Turning Research into Practice database. Reference lists of key studies were scanned for any further relevant studies. The search results were imported into EndNote X8® (Clarivate Analytics, PA, USA) and deduplicated. The full search strategies for all sources searched can be found in Appendix 1. The reference lists of reviews were also checked for any further relevant studies.
Study selection
The following criteria were used to select studies for inclusion:
-
Population: children (aged < 18 years) with an extravasation or infiltration injury associated with central or peripheral i.v. access. Animal studies were excluded. For the purposes of this review we were interested in extravasation injuries which involved leakage into the skin or subcutaneous tissue, or into muscle tissue. Studies of injuries termed as ‘extravasation’ but which related to leakages into cavities or viscera were excluded (these references are documented in Appendix 2). Our definition of extravasation covers ‘infiltrations’ (i.e. it includes leakages of vesicants and non-vesicants).
-
Interventions: any intervention for treating an extravasation injury.
-
Comparators: any comparator (or no comparator).
-
Outcomes: any of the following – wound healing time, scarring, infection, pain, contractures, functional impairment, disfigurement, requirement for surgery, mortality, anaphylactic reactions to extravasation treatments.
-
Study design: any study design was eligible including comparative studies, case series, case reports, reviews and guidelines.
Two reviewers independently assessed titles and abstracts for these eligibility criteria. The full text of potentially relevant titles and abstracts were sought and assessed independently by two reviewers. Any reviewer disagreements were resolved through discussion and, when necessary, through consultation with a third member of the study team. Titles, abstracts and full papers were screened using EPPI-Reviewer 4 software (Evidence for Policy and Practice Information and Co-ordinating Centre, University of London, London, UK). For the titles and abstracts the ‘key term highlighting’ function was used to help make decisions more quickly. Terms which indicated an abstract that may have been an ‘exclude’ appeared as red text, and terms suggesting that an abstract might have been relevant to the review appeared in green. Full papers published in French and German were single-screened by native speakers (and data were extracted, when appropriate, with the help of one of the review team). Full papers published in Spanish were screened (and data were extracted) by one of the review team who spoke Spanish as a second language.
In addition to the studies in children identified, we also used any reviews which had a focus on treatments, and guidelines identified, to provide the basis for an overview of the evidence for extravasation treatments more broadly (i.e. studies which included adults because it was possible that some of this evidence might have been more methodologically robust than the studies in children).
Data extraction
Data extraction forms were developed for three different study designs: comparative studies, non-comparative studies and case reports. These forms were piloted on a selection of studies and amended when necessary; few iterations were needed. The extracted data included details of basic study methods, population characteristics (such as age, type of vesicant, injury severity), intervention (type, number and frequency of treatments), comparators, outcome measures and results. Any recommendations for future research that were relevant to this review were also extracted. Data were extracted by one researcher and checked by another, with discrepancies resolved by discussion or consultation with a third member of the study team where necessary.
Collating, summarising and reporting results
Study details were presented in structured tables based first on study design and then on intervention type. For each type of study design, the extent, range and nature of the identified research was described. Study parameters and results were then described and summarised narratively.
Results
Quantity and quality of research available
Following the removal of duplicates retrieved from the database searches, a total of 3830 records were identified for title and abstract screening, from which 289 records were selected as potentially being of interest. Of those records excluded at the title and abstract phase, 63 were excluded for relating to events which were termed ‘extravasation’ but which did not involve skin or muscle tissue, for example events such as cardiac tamponade or pleural effusion (these studies are listed in Appendix 2). Copies of the full texts of 271 papers were assessed for inclusion in the review. Six papers were identified from other sources: checking references or citation searching of key papers. Figure 1 illustrates the flow of studies through the review process and the number of included studies, by study design. Translators were not available for the nine foreign-language papers published in languages other than French, German or Spanish. Of the 26 group studies included in the scoping review,4,21,31–54 only two were comparative. 16,55
FIGURE 1.
Flow chart showing the number of studies identified and eligible for inclusion.

Primary studies of clinical effectiveness and safety
Comparative studies
Only two comparative studies were identified and included in the review, and both were set in the USA. 16,55 Full details of the studies are presented in Table 1. In 1979, Brown et al. 55 published results for a quasi-randomised study which compared three types of treatment: silver sulfadiazine cream with sterile saline cleansing, povidone-iodine with sterile saline cleansing and sterile saline cleansing alone. The 34 study participants had extravasation injuries resulting in skin loss, and were mostly aged < 1 year. Each of the three treatments was given according to one of two possible protocols, depending on the type of skin loss, classified as either full-thickness loss (24 participants) or partial-thickness loss (10 participants). Participants were allocated treatment according to calendar month. The types of infusate causing injury varied, but they mostly comprised parenteral nutrition, with or without antibiotics. The main outcome reported was the time required for wound healing. The authors reported that there were no significant differences between the three treatment protocols in the rate of healing. Four of the children in the full thickness group died and a further two participants died before receiving treatment.
| Study details | Population characteristics | Injury details | Intervention | Results |
|---|---|---|---|---|
|
Authors Brown et al. 197955 |
Age Range: 5 days–12 years. 22 were aged < 1 year |
Method of delivery Varied, but mostly infusions |
All patients had their i.v. therapy stopped, the apparatus removed and the affected area elevated. Patients were then allocated one of the following treatments – |
Time for wound healing Silver sulfadiazine: ranged between 3 and 10 weeks in the 11 children with full-thickness loss, and 1–5 weeks in the four children with partial-thickness loss |
For patients with partial-thickness skin loss:
|
||||
|
Design Quasi-randomised study. Treatment allocation changed with the calendar month. The study ran for 6 months. Each of the three treatments was therefore used for 2 full months |
Comorbidities Varied range, with respiratory distress syndrome, leukaemia, septicaemia, necrotising enterocolitis and Wilm’s tumour among the most frequent |
Types of eligible injury Only children with skin loss: partial (e.g. blistering or discolouration) or full thickness |
For patients with full-thickness skin loss:
|
Povidone-iodine: ranged between 2 and 6 weeks in the six children with full-thickness loss and 3 weeks in the one child with partial-thickness loss |
|
Setting Children’s hospital in PA, USA |
Duration of i.v. NR |
Sites Mostly dorsum of foot or the hand. Some injuries on shin, ankle, wrist, scalp, arm and abdomen |
Saline: ranged between 4 and 8 weeks in the four children with full-thickness loss and 2 and 3 weeks in the three children with partial-thickness loss | |
|
Sample size 34 |
Mean time to treatment NR |
Infusates Varied, but mostly parenteral nutrition (0.5% to 2% amino acids in 10% to 12.5% glucose solution) sometimes with antibiotics |
No significant difference in the rate of healing among the three treatment protocols is readily apparent. Nevertheless, primary healing occurred in all patients without the need for skin grafting and without loss of function of the affected part | |
| Four of the full thickness group died. A further two patients died before receiving treatment | ||||
|
Authors Hanrahan 201316 |
Age NR (‘paediatric population’) |
Injury details NR | Hyaluronidase (n = 37) or no hyaluronidase (n = 76) | AHRQ Common Format harm scores were used as an outcome measure |
|
Design Before-and-after study of the implementation of a guideline for using hyaluronidase. 56 Other outcomes included costs, knowledge, extravasation incident reports, hyaluronidase usage reports |
Comorbidities NR |
To determine if treatment resulted in less harm, subjects were collapsed into two groups: those receiving hyaluronidase (n = 37) and those who did not (n = 76). Mean harm scores were similar: 5.29 and 5.27, respectively | ||
|
Setting Children’s hospital in Iowa, USA |
Duration of i.v. NR |
Most of the no hyaluronidase group were treated before the guideline was implemented and most of the hyaluronidase group were treated post implementation. An increase in the frequency of treatment with hyaluronidase was reported from baseline (9%) to implementation (63%) | No events resulted in permanent harm, severe permanent harm, or deaths (harm score > 6) | |
|
Sample size 113 |
Mean time to treatment Pre implementation: 125 minutes (SD = 75) |
|||
| Post implementation: 76 minutes (SD = 38) |
The second study was a pre–post study on the implementation and evaluation of a guideline for using hyaluronidase. 16 Although very few population details were reported, the study cohorts appeared quite different from the Brown trial,55 as patients were treated quite quickly (within a few hours of injury). Most of the no-hyaluronidase group were treated before the guideline was implemented and most of the hyaluronidase group were treated post implementation. The mean time to receiving treatment was 125 minutes before guideline implementation and 76 minutes post implementation. Most of the outcomes studied did not relate to the effectiveness or safety of hyaluronidase treatment. The exception was the reporting of Agency for Healthcare Research and Quality (AHRQ) Common Format harm scores. To determine if hyaluronidase treatment resulted in less harm, subjects were collapsed into two groups: those receiving hyaluronidase (n = 37) and those not (n = 76). The mean harm scores were very similar, that is, 5.29 and 5.27, respectively. No events resulted in permanent harm, severe permanent harm or deaths (i.e. a harm score of > 6).
Summary
The comparative study evidence identified was scarce and had important limitations in relation to the aims of this scoping review. The Brown et al. 55 study is an old trial of treatments which are little used in the NHS. It was performed in a population of patients with quite severe wounds, where the extravasation injuries may not have been identified for quite some time. The quasi-randomised design meant that the study results may have been influenced by selection bias. The study was also small and, therefore, underpowered to detect treatment differences. The Hanrahan hyaluronidase guideline study16 was not really designed to evaluate treatment effectiveness. Although it did endeavour to determine if hyaluronidase treatment resulted in less harm than no hyaluronidase treatment, the before-and-after design, lack of population details and lack of details on interventions given to the no hyaluronidase group mean that the study’s ‘harm score’ result should not be regarded as a reliable estimate of hyaluronidase effectiveness.
Non-comparative group studies
Details of the identified non-comparative studies are presented in Tables 2–6. Studies were published over the time period 1975–2016. Most were set in Europe or North America and four studies were set in the UK. 21,31,32,57 Most studies were published as full papers, but the exceptions were two studies that were published as letters. 32,33 The included studies covered conservative management interventions (n = 7),34–40 flush-out methods with or without hyaluronidase (n = 7),4,21,31,32,41,42,57 hyaluronidase injections without flush out (n = 2),45,46 artificial skin treatments (n = 2),33,41 and debridement and/or plastic surgery (n = 7). 21,48–53
Conservative management
Seven case series studies described using a conservative management approach to treatment. 34–40 A minority of patients also went on to receive surgery in one study. 34 Study details are reported in Table 2. Only one study was performed prospectively. 39 Sample sizes ranged from 6 to 19 participants. The studies covered the following interventions: hot compress with topical ointment;37 antibiotic/anti-inflammatory ointment mixture followed by dressing;36 wet dressing and localised massage;35 alcohol based dressing;34 cold compresses and elevation;38 a wound care protocol comprising aqueous gel; a hydrofibre sheet; and a hydrocolloid dressing. 39 The final study used a mixed-management approach utilising puncture points (similar to those made in the Gault21 technique) followed by hydrocolloid dressing before scalpel debridement only of dead tissue (so anaesthesia was not needed). 40 The approach used in this study was decided on the basis of the uncertainty encountered when selecting adequate treatments at an early stage because of difficulties in determining the depth and extent of injuries. The treatment goals were to remove infusates and promote wound healing by inducing autolytic debridement and providing a moist environment.
| Study details | Population characteristics | Injury details | Intervention | Results |
|---|---|---|---|---|
|
Authors An and Ning 201537 |
Age Mean 4 months (range 1–9 months) |
Method of delivery NR |
Wet-hot compresses by small sterile gauze 3 or 4 times per day, with temperature at 40–45 °C and duration of 20–30 minutes per session. Next, MPS cream was applied topically, followed by tender massage for 3–5 minutes | After a median duration of 3 days’ treatment, all patients had complete fluid absorption and were discharged without adverse outcomes at 3 months |
|
Design Retrospective case series |
Comorbidities Respiratory tract infection |
Types of injury Swelling, masses |
||
|
Setting Children’s hospital emergency department, China |
Duration of i.v. therapy 2–3 days |
Sites All scalp |
||
|
Sample size Six |
Mean time to treatment NR |
Infusates Mezlocillin and sulbactam sodium |
||
|
Authors Moon et al. 201236 |
Age Mean 20 days (31 weeks’ gestation) [range 14–50 days (28–35 weeks’ gestation)] |
Method of delivery NR |
Local conservative management was given with healing by secondary intention. An antibiotic and anti-inflammatory ointment mixture was topically applied to the whole region of the wound site, followed by a dressing. This was performed twice a day during the acute phase and once a day during the convalescent phase. Systemic prophylactic antibiotics were also given. The necrotic tissue was removed when it was clearly demarcated. After wound closure, topical oil moisturisation and mild compression were applied | The defects had completely closed 14 to 55 days after injury, the vast majority by wound contraction. Parents were shown photos of the initial defects and the final scar. The degree of the parents’ satisfaction was excellent in nine cases of pinpoint scars and linear scars, good in three cases of depressed or mild contracted linear scars and fair in two cases of round hypertrophic scars |
|
Design Retrospective case series |
Comorbidities Prematurity |
Types of injury Full-thickness defects |
||
|
Setting Plastic surgery department, South Korea |
Duration of i.v. therapy NR |
Sites Hand/wrist (n = 5), ankle/foot (n = 8) and elbow (n = 1) |
||
|
Sample size 13 (14 injuries) |
Mean time to treatment NR |
Infusates Total parenteral nutrition |
||
|
Authors Mu et al. 199935 |
Age NR (neonates) |
Method of delivery NR |
Wet dressing and localised massage, followed by rehabilitation programme | It took 18 to 50 days for functional recovery. Five lesions still had cosmetic residuals but none required a skin graft |
|
Design Case series (unclear whether retrospective or prospective) |
Comorbidities All had neonatal hypocalcaemia. Premature (n = 4) and perinatal asphyxia (n = 2) |
Types of injury Calcinosis cutis |
||
|
Setting Paediatric department, Taiwan |
Duration of i.v. therapy Range 5–11 days |
Sites Wrist (n = 4), forearm (n = 4), elbow (n = 3), ankle (n = 3) |
||
|
Sample size Nine |
Mean time to treatment NR |
Infusates Calcium gluconate |
||
|
Authors Nandiolo-Anelone et al. 201434 |
Age Mean 3.6 days. (range 1–9 days) |
Method of delivery NR |
Alcohol-based dressing 48 hours to 72 hours (n = 6), pre-surgical pro-inflammatory dressing up to 15 days (n = 6), graft excision (n = 4 primary; n = 4 secondary), including 1 with fasciotomy |
Total scores VSS: 53% with scores 0 or 1, 26% with scores 2–4, 13% with score 9, 6% lost to follow-up Two deaths: linked to prematurity (n = 1) and oesophageal atresia (n = 1) |
|
Design Retrospective case series |
Comorbidities Maternal and fetal infections (n = 6), fetal distress (n = 4), respiratory distress (n = 4), premature birth (n = 2), denutrition (n = 1) and oesophageal atresia (n = 1) |
Types of injury Stage III (n = 6) and IV (n = 9) extravasation injuries |
||
|
Setting Children’s Hospital, Ivory Coast |
Duration of i.v. therapy NR |
Sites Upper (n = 9) and lower limbs (n = 6) |
||
|
Sample size 15 |
Time to injury treatment Mean 3.93 days, (range 1–9 days) |
Infusates Serum 10% glucose and calcium chloride |
||
|
Authors Sawatzky-Dickson and Bodnaryk 200639 |
Age 1–40 days (24 to 40 weeks’ gestation) |
Method of delivery NR |
Wound care protocol developed by the authors. Aqueous gel was applied to coat the area of tissue damage but not the surrounding skin. A hydrofibre sheet was placed over the gel. A thin hydrocolloid dressing covered the area for 7 days (or changed sooner if necessary). Antibiotics were given for wound infections | Wound healing times ranged from 1 to 6 weeks. No wounds showed any signs of infection. One patient died before wound healed. Notes on research design:
|
|
Design Prospective case series |
Comorbidities NR |
Types of injury Sloughing or necrosis. Stage III or IV injuries |
||
|
Setting Neonatal intensive care unit, Canada |
Duration of i.v. therapy NR |
Sites Foot (n = 5), hand (n = 3) and forearm (n = 1) |
||
|
Sample size Nine |
Mean time to treatment NR |
Infusates Blood transfusion, sodium bicarbonate, parenteral nutrition and dextrose |
||
|
Authors Sung and Lee 201640 |
Age 30–39 weeks’ gestation |
Method of delivery NR |
Multiple wound punctures (using scalpel blade tip) were made and a hydrocolloid dressing applied. This was changed every 6 hours on the first day and with decreasing frequency thereafter. Debridement performed gradually when devitalised tissue began to be demarcated and autolysed – done with a scalpel and without anaesthesia. Mean duration of treatment was 25 days. After healing, silicone gel was recommended for 3 months to prevent hypertrophic scars |
|
|
Design Retrospective case series |
Comorbidities Nine were preterm |
Types of injury Skin discolouration (n = 7), bleb (n = 2), necrosis (n = 2) and swelling (n = 1). Nine eventually progressed to full-thickness open wounds |
||
|
Setting Plastic surgery department, South Korea |
Duration of i.v. therapy NR |
Sites Wrist (n = 5), ankle (n = 5), hand (n = 1) and antecubital (n = 1) |
||
|
Sample size 12 |
Mean time to treatment Between 1 and 10 hours for all but one patient (52 hours) |
Infusates Parenteral nutrition |
||
|
Authors Wang 200738 |
Age NR |
Method of delivery Injections |
Cold compresses and elevation | All wounds healed without necrosis |
|
Design Retrospective case series |
Comorbidities NR |
Types of injury Swelling (n = 13) and pain (n = 4) |
||
|
Setting NR, USA |
Duration of i.v. therapy NR |
Sites Arm (n = 10), hand (n = 3), shoulder (n = 1), ankle (n = 1), foot (n = 1) and groin (n = 1) |
||
|
Sample size 17 |
Mean time to treatment NR |
Infusates Contrast agent |
Five of the studies were of neonates,34–36,39,40 one was of infants (mean age 4 months)37 and one did not report on age. 38 Only two studies reported details relating to the delay between the extravasation event and treatment for the extravasation. 34,40 Both the types of infusate extravasated and the extravasation sites varied widely.
Two studies of milder injuries reported that all injuries healed well and without complications. 37,38 The four studies which covered more severe injuries such as full-thickness defects,36 stage III and IV injuries34,39 and calcinosis cutis35 reported long recovery times (typically between 1 and 8 weeks) and scarring in some patients. The mixed-management approach study reported on different severities of injury caused by parenteral nutrition extravasations in preterm neonates. 40 Wound healing times ranged from 8 to 41 days, with one contracture, no secondary infections and minor scarring. 40 It was also reported that parents were ‘satisfied with the final results’. Although 2 out of the 12 patients presented with necrotic lesions, nine patients eventually progressed to full-thickness open wounds.
Across studies, the outcomes used and result details reported were generally limited, although one study did report total scores on the Vancouver Scar Scale (VSS). 34
Flush-out methods
Seven studies reported using a flush-out technique,4,21,31,32,41,42,57 with sample sizes ranging from 14 to 96 patients. All but one of the studies21 was published after the year 2000. Study details are presented in Table 3. Two studies were prospective case series,32,57 with the remainder being retrospective case series (or having unclear methods). 4,21,31,41–43 Four studies used hyaluronidase before saline flush-out21,31,42,57 and three used saline flush-out alone in all patients,4,32 or nearly all patients. 41 Two studies additionally used liposuction in nearly all patients42 or only in a few patients. 21 Two studies reported on both an early referral group (seen within 24 hours) which received flush-out, and a late referral group which received surgical interventions. 21,41
| Study details | Population characteristics | Injury details | Intervention | Results |
|---|---|---|---|---|
|
Authors Andres et al. 200641 (published in Spanish) |
Age Mean 3 years |
Method of delivery NR |
For cases of < 24 hours, the Gault method with saline (500 cc) was used. In two patients hyaluronidase was used before saline flush-out. Includes eight patients who received artificial skin, see Table 5 | Seven of the 10 patients treated by the Gault method avoided necrosis and recovered fully |
|
Design Retrospective case series |
Comorbidities One with necrotising enterocolitis, one with hyaline membrane disease, five oncology patients, one severe head trauma and one liver transplant patient |
Types of injury Not reported for whole cohort though five patients had established necrosis |
||
|
Setting Paediatric hospital, Spain |
Duration of i.v. therapy NR |
Sites Dorsum of hand or foot (n = 14) and forehead (n = 1) |
||
|
Sample size 15 (includes eight patients who received artificial skin, see Table 5) |
Mean time to treatment < 24 hours |
Infusates Parenteral nutrition (n = 7), calcium gluconate (n = 4) and doxorubicin (n = 4) |
||
|
Authors Casanova et al. 200142 |
Age 20 days (1 day to 6 months) (mean weight 2.5 kg) |
Method of delivery NR |
Gault procedure with hyaluronidase under general anaesthesia in 11 cases. Mild aspiration with a 2-mm microcannula, following a liposuction technique, was then performed through the micro incisions. Aspiration with a 20-mm syringe or by mild mural aspiration. Procedure repeated several times, rinsing the area with saline after each infiltration of hyaluronidase. Extravasation site protected with an oily dressing. In two cases saline was used instead of hyaluronidase. In one case, only the hyaluronidase flush-out was performed | Eleven patients improved, with no skin involvement in ten cases. In one case a pre-existing blister subsided and healed. Three patients developed skin necrosis, which was treated and healed spontaneously |
|
Design Retrospective case series |
Comorbidities Six babies were premature |
Types of injury Swelling, discolouration, skin damage, blisters, induration |
||
|
Setting Plastic surgery department, France |
Duration of i.v. therapy NR |
Sites Foot/ankle (n = 9), hand/wrist (n = 3), elbow (n = 1) and forehead (n = 1) |
||
|
Sample size 14 |
Mean time to treatment 3–12 hours |
Infusates Dopamine (n = 9), caffeine (n = 2), beta-blocker (n = 1), calcium (n = 1), calcium and amikacine (n = 1) |
||
|
Authors |
Age Mean 36 months (1 day to 17 years) |
Method of delivery NR |
A total of 62% of patients received an early saline wash-out using the Gault technique. The technique involved creating multiple skin punctures around the periphery of the injury area with an atraumatic cannula and flushing each puncture with 0.9% sodium chloride. All the wash outs also used hyaluronidase | None of the patients who received the Gault technique developed complications. Of the remainder, there were three cases of associated infection, one case of ischaemic toe with subsequent digit amputation and one case of calcinosis cutis (involving prolonged hospitalisation and readmission for secondary infection) |
|
Design Retrospective case series |
Comorbidities Prematurity (40%), gastrointestinal (21%), cardiorespiratory (16%), sepsis (16%) and other (7%) |
Types of injury NR |
||
|
Setting Plastic surgery department, UK |
Duration of i.v. therapy NR |
Sites Upper limb (65%; 40% on the dorsum of hand), lower limb (25%) and other (10%) |
||
|
Sample size 69 |
Mean time to treatment 4 hours (range 0.2–24 hours) |
Infusates 32% maintenance fluids (glucose, or sodium or potassium chloride), 23% TPN and 45% others |
||
|
Authors Gault 199321 |
Age Mean 10 years (range 0–70 years). The study includes some adults but the mean age (and range) suggests most of the population were children |
Method of delivery NR |
‘Early referral’ group: of the 44 patients seen within 24 hours, 37 were treated with saline flush-out (500 ml) following prior infiltration with hyaluronidase. One with liposuction alone, and six with both. Prophylactic antibiotics were also used for immunosuppression. Following flush-out, a layer of Jelonet™ (Smith & Nephew, Canada) and betadine-soaked gauze was applied, and limb was elevated for 1 day. ‘Late referral’ group needed extensive reconstructive surgery (see Table 6) | Flush-out group (early referral): no tissue damage (n = 39), minor skin necrosis or delayed healing (n = 5) |
|
Design Retrospective case series |
Comorbidities NR |
Types of injury NR |
||
|
Setting Plastic surgery unit, UK |
Duration of i.v. therapy NR |
Sites Varied greatly but mostly hand/forearm or foot/ankle |
||
|
Sample size 96 (includes patients needing surgery see Table 6) |
Mean time to treatment 44 patients within 24 hours |
Infusates Varied greatly but mostly calcium, parenteral nutrition, dextrose, vincristine, daunorubicin or doxorubicin |
||
|
Authors Ghanem et al. 201557 |
Age Mean 3.2 years, median 0.2 years (range 1 day–16.7 years) |
Method of delivery 89% peripheral lines, 9% central lines and 2% other |
Evaluation of a hospital guideline of early referral to plastic surgeons and wash out of high-risk cases. Extravasation injuries were diagnosed in 48 out of 82 cases (i.e. vesicant involved). The rest were classed as infiltration injuries. Twenty-two out of the 48 extravasation injuries required wash-out with hyaluronidase, the remainder were treated conservatively with elevation and analgesia. None of the infiltration injuries required wash-out | Limited outcome data reported. Three patients had tissue necrosis. There was satisfactory healing with no requirement for surgical intervention. Two of these three cases were referred later than 24 hours after the injury |
|
Design Prospective case series (audit) |
Comorbidities NR |
Types of injury NR |
||
|
Setting Children’s hospital, UK |
Duration of i.v. therapy NR |
Sites Varied, but most were the upper limbs (60%) or lower limbs (30%) |
||
|
Sample size 78 (82 injuries) |
Time to injury treatment Mean 8.3 hours |
Infusates Varied, though TPN for 46% of the extravasation injury group (n = 48). Antibiotics and sodium chloride caused over half the injuries classed as infiltration. No chemotherapeutic extravasation injuries |
||
|
Authors |
Age NR (neonates) |
Method of delivery NR |
Modification of Gault’s saline flush-out technique: 500 ml of saline, to exit via puncture wounds | No episodes of skin or soft tissue loss were recorded and no reconstructive surgery was required |
|
Design Prospective case series (reported in a letter) |
Comorbidities NR |
Types of injury NR |
||
|
Setting Neonatal unit, UK |
Duration of i.v. therapy NR |
Sites NR |
||
|
Sample size 56 confirmed injuries from 82 referrals |
Time to injury treatment Unclear ‘immediately assessed’ |
Infusates Parenteral nutrition, inotropes, dextrose, calcium, potassium, and bicarbonate |
||
|
Authors Kostogloudis et al. 20154 |
Age Mean age 11.6 days. Four neonates were extremely preterm, nine were very preterm, 14 were late preterm and seven were full term. Gestational age range: 24–42 weeks |
Method of delivery Peripheral i.v. infusion |
Normal saline flush-out (mean 60 ml, range 10–160 ml), two to six full-thickness incisions made. Dressing (paraffin- and povidone-iodine-soaked gauze) and elevation for 24 hours. Dressing changed daily until healing complete | Wound healing in 1–25 days. All infants responded well to wash-out – clinical findings subsided significantly within 24 hours. Twenty-one neonates showed no signs of soft tissue damage 24 hours after treatment and only minor findings, such as blistering and epidermolysis were still present in seven neonates in the next few days |
|
Design Case series (unclear whether or not prospective) |
Comorbidities NR |
Types of injury Neonates with stage III and IV extravasation injuries were included in the study |
||
|
Setting Neonatal intensive care unit, Greece |
Duration of i.v. therapy NR |
Sites Ankle (n = 22 patients), dorsum of hand (n = 6), dorsum of foot (n = 3) and thigh (n = 3) |
||
|
Sample size 34 |
Time to injury treatment Range 10–30 minutes |
Infusates Parenteral nutrition (n = 28), dextrose 10% (n = 4) and cephalosporin (n = 2) |
||
| Ischaemic signs recorded in six neonates by day 2, but gradually subsided within 25 days. Incisions healed uneventfully within 7–13 days and with minimal scar formation | ||||
| Hypoplasia of the toenails noted in one case at 26 months. One neonate had compartment syndrome – emergency fasciotomies, followed by saline irrigation were performed. All incisions healed uneventfully by secondary intention, resulting in fully functional upper extremities with aesthetically acceptable scar formation |
Three studies were in neonates,4,32,42 three studies had populations with mean ages of around 3 years,31,41,57 and in one study the mean age was around 10 years. 21 Where such data were reported, patients were treated within 24 hours of the extravasation event, with the quickest treatment (within 10–30 minutes) seen in a study of preterm neonates with stage III and IV extravasation injuries (Millam criteria were used for staging). 4 Infusate types and the extravasation injury sites varied both within and across studies.
For the three studies of neonates, two reported generally positive results but provided little in terms of result details. 32,42 The study of 34 (mostly) preterm neonates presented more result details, reporting good responses with clinical findings subsiding significantly within 24 hours and wound healing in 1 to 25 days. Twenty-one neonates showed no signs of soft tissue damage 24 hours after treatment and only minor findings, such as blistering and epidermolysis, were still present in seven neonates in the next few days. One child had hypoplasia of the toenails at 26 months. One neonate had compartment syndrome; therefore, emergency fasciotomies, followed by saline irrigation were performed. All incisions healed uneventfully by secondary intention with aesthetically acceptable scar formation. 4 This study also reported that gestational age was not significantly related to the incidence of extravasation injuries (p = 0.87), although it did affect the incidence of skin necrosis after severe extravasation injury (p = 0.009); this was more common in extremely low-birthweight neonates. Similar to most of the neonatal studies, there was a lack of detailed results data for the four studies of older children,21,31,41,43,57 with outcome reporting largely focusing on presence/absence of necrosis.
Other studies of hyaluronidase
Two retrospective studies evaluated hyaluronidase injections without flush out. 45,46 One was a study of extravasations from iodinated contrast material and included both adults and children. 45 For the eight included children, the only treatment-related details presented were that two were treated with hyaluronidase, and brief details were reported for one child whose extravasation had a prolonged course. The other study was of 13 neonates and infants, treated within a median time since injury of around 6 hours. Treatment comprised hyaluronidase injections followed by massage with Hirudoid Cream™ (Mobilat Produktions GmbH, Pfaffenhofen, Germany) around the affected area. 46 Brief results were presented with the authors reporting that symptoms improved and no complications were noted at the 48-hour and 3-month follow-ups.
Another study had a much broader scope: to summarise adverse drug event reporting. 47 In this retrospective hospital database study, extravasation injuries accounted for 10% of the 863 events. The paper reported that infants were ‘treated with hyaluronidase’ for 31 out of the 38 parenteral nutrition extravasations, but no details were reported about whether or not flush-out was also used. Details of the population studied and details on outcome data were also very limited. Study details are presented in Table 4.
| Study details | Population characteristics | Injury details | Intervention | Results |
|---|---|---|---|---|
|
Authors Cochran et al. 200245 |
Age 3 months to 9 years |
Method of delivery Four were manual injection |
Two were treated with hyaluronidase | No results data relating to all eight children were presented other than ‘one extravasation had a prolonged course’; brief details were reported for this child |
|
Design Retrospective database study |
Comorbidities NR |
Types of injury NR |
||
|
Setting Radiology department, USA |
Duration of i.v. therapy NR |
Sites NR |
||
|
Sample size Eight children (study also reported data for adults) |
Mean time to treatment NR |
Infusates All contrast material |
||
|
Authors Yan et al. 201446 |
Age Mean 26 days (range 5–150 days) |
Method of delivery NR |
Hyaluronidase injections and Hirudoid Cream. A 25-gauge needle was used and a total of 1-ml solution (150 U/ml) of hyaluronidase was divided into five 0.2-ml injections: one in the centre and four along the edge of the extravasation sites. Some cases needed another injection several hours after the first injection (contained five 0.2-ml injections). Hirudoid cream was massaged around the affected area | After the treatment, the symptoms improved, and no complications were noted at the follow-up within 48 hours and 3 months. Negligible loss of functional movements of the fingers, hands, arms, feet, or legs was noticed |
|
Design Retrospective case series |
Comorbidities Prematurity (n = 5), pneumonia (n = 4), gastrointestinal disorders (n = 2), malnutrition (n = 1) and neonatal jaundice (n = 1) |
Types of injury Swelling in all 13, with erythema (n = 5), blister (n = 3) and necrosis (n = 1) |
||
|
Setting Neonatal department, China |
Duration of i.v. therapy NR |
Sites Hand (n = 4), leg (n = 3), forearm (n = 3) wrist, armpit and scalp (all n = 1) |
For the calcium chloride-treated patient, a scar developed 2 days after treatment, and calcinosis developed 3 weeks after hospital discharge | |
|
Sample size 13 |
Mean time to treatment Median 6.4 hours for 12 cases. For the calcium chloride-treated patient, the hyaluronidase was given after 14 hours |
Infusates Total parenteral nutrition (n = 9), calcium chloride, 10% dextrose, immunoglobin and para-aminomethylbenzoic acid + etamsylate (all n = 1) |
||
|
Authors Crowther et al. 201147 |
Age Mean 28 days (range 2–93 days) for the 38 patients with extravasation of parenteral nutrition |
Method of delivery Mostly peripheral i.v. lines |
‘Treated with hyaluronidase’ for 31 of the 38 parenteral nutrition extravasations. No further details were reported about how hyaluronidase was used | A total of 46% full recovery, remainder were referred to wound care (10%) or did not have a documented outcome (44%) |
|
Design Retrospective hospital database study |
Comorbidities NR |
Infusates A total of 42% parenteral nutrition, other agents such as dopamine, dextrose, potassium chloride, contrast media, ciprofloxacin and fentanyl each made up ≤ 5% of total |
||
|
Setting Children’s hospital, USA |
Duration of i.v. therapy NR |
Types of injury NR |
||
|
Sample size 90 |
Time to injury treatment NR |
Sites NR |
Other treatments included elevation, hot or cold compresses, and analgesic use but these were not consistently documented |
Artificial skin treatments
Two studies reported the use of artificial skin. 33,41 One was of 26 preterm neonates with partial- and full-thickness wounds arising from hypertonic solutions. 33 The treatment was Hyalomatrix PA (Anika Therapeutics, Bedford, MA, USA), a tissue reconstruction matrix composed of two layers. Eighteen patients had restoration of dermal quote and a rapid re-epithelialisation process after 21 days. Patients were followed up for up to 14 months; four patients had pathological scars and four had debilitating scar contractures needing secondary surgery. The other study reported on the use of artificial skin with two membranes (silicone and bovine tendon collagen mesh) and debridement and skin grafts in children with necrotic extravasation injuries. 41 All eight patients recovered full functionality with only minor scars; no secondary surgery or amputation was necessary. Study details are presented in Table 5.
| Study details | Population characteristics | Injury details | Intervention | Results |
|---|---|---|---|---|
|
Authors Andres et al. 200641 (published in Spanish) |
Age Mean 3 years |
Method of delivery NR |
For cases of < 24 hours, the Gault method with saline (500 cc) was used. In five patients, where necrosis was already established (and in three in which it started after the flush-out), the area was covered with artificial skin consisting of two membranes: one comprised a three-dimensional porous fibrillar mesh of bovine tendon collagen next to chondroitin-6-sulfate. The other was a thin sheet of silicone. Necrotic tissue was debrided and after 2 or 3 weeks a partial skin graft was performed | In total, eight patients needed the artificial skin and skin grafts. All recovered full functionality with only minor scars; no secondary surgery or amputation was necessary |
|
Design Retrospective case series |
Comorbidities One with necrotising enterocolitis, one with hyaline membrane disease, five oncology patients, one severe head trauma and one liver transplant patient |
Types of injury Not reported for whole cohort although five patients had established necrosis |
||
|
Setting Paediatric hospital, Spain |
Duration of i.v. therapy NR |
Sites Dorsum of hand or foot (n = 14) and forehead (n = 1) |
||
|
Sample size 15 (includes 10 flush-out patients, see Table 3) |
Mean time to treatment < 24 hours |
Infusates Parenteral nutrition (n = 7), calcium gluconate (n = 4) and doxorubicin (n = 4) |
||
|
Authors Onesti et al. 201233 |
Age Mean gestational age 32 weeks (range 28–36 weeks) |
Method of delivery NR |
Hyalomatrix PA (a dermal substitute composed of two layers): first, topical collagenase was applied, then 72 hours later debridement, followed by application of Hyalomatrix PA. After 1 week the area was cleaned and Hyalomatrix PA applied and kept in place for 7 to 11 days. This procedure was continued for a total of 21 days | Eighteen patients had restoration of dermal quote and a rapid re-epithelialisation process after 21 days. Patients were followed up for up to 14 months. Four had pathological scars, four had debilitating scar contractures needing secondary surgery. There were no wound infections |
|
Design Case series (reported in a letter). Unclear whether or not prospective |
Comorbidities Preterm neonates |
Types of injury Patients with partial- and full-thickness wounds. Cutaneous eschar (n = 8), ulcers, blisters and erythematous wound margins (n = 18) |
||
|
Setting Plastic surgery department, Italy |
Duration of i.v. therapy Mean 3 days (range 2 days–1 week) |
Sites Dorsum of hand (n = 11), dorsum of foot (n = 6), forearm (n = 3), ankle (n = 1), leg (n = 3) and scalp (n = 2) |
||
|
Sample size 26 |
Time to injury treatment NR |
Infusates Hypertonic solution |
Debridement and plastic surgery
Seven studies, which were all retrospective, reported on patients who needed debridement and/or plastic surgery. 21,48–53 Most studies were small (sample sizes ranged from 4 to 51 patients) and all except one50 were published before the year 2000. Study details are presented in Table 6. Three studies reported on outcomes following debridement,48,50,53 three reported on debridement and skin grafts,49,51,52 and one reported different types of reconstructive surgery. 21
| Study details | Population characteristics | Injury details | Intervention | Results |
|---|---|---|---|---|
|
Authors Falcone et al. 198948 |
Age Mean gestational age 28.5 weeks (range 26–33 weeks) |
Method of delivery NR |
Enzymatic debridement | All wounds healed completely with no infections and no functional scar contractions at up to 16 months’ follow-up. No skin grafts were needed |
|
Design Retrospective case series |
Comorbidities Preterm, hyaline membrane disease, rule out sepsis, patent ductus arteriosus, necrotising enterocolitis, seizures and bronchopulmonary dysplasia |
Types of injury Full-thickness injury |
||
|
Setting Plastic surgery department, USA |
Duration of i.v. therapy NR |
Sites Foot (n = 13), hand (n = 2) and scalp (n = 1) |
||
|
Sample size 15 (16 injuries) |
Mean time to treatment NR |
Infusates Parenteral nutrition (n = 9), electrolyte solution (n = 3) and unknown (n = 3) |
Debridement and topical fibrinolysin/deoxyribonuclease ointment (Elase, Parke-Davis, Morris Plains, NJ, USA) every 8 hours. After 5–7 days, process is repeated until the wound begins to re-epithelialise (3–4 weeks) | |
|
Authors Gault 199321 |
Age Mean 10 years (range 0–70 years). The study includes some adults but the mean age (and range) suggests that most of the population were children |
Method of delivery NR |
‘Early referral’ group: 44 patients, see Table 3 | Late referral: no tissue damage (n = 8 patients), minor skin necrosis or delayed healing (n = 17), scar revision (n = 5), skin graft (n = 6), contractures (n = 6), flap coverage required (n = 6), amputation (n = 3 neonates) and infection (n = 1) |
|
Design Retrospective case series |
Comorbidities NR |
Types of injury NR |
||
|
Setting Plastic surgery unit, UK |
Duration of i.v. therapy NR |
Sites Varied greatly but mostly hand/forearm or foot/ankle |
||
|
Sample size 96 (includes patients receiving flush-out, see Table 3) |
Mean time to treatment 44 patients within 24 hours |
Infusates Varied greatly but mostly calcium, parenteral nutrition, dextrose, vincristine, daunorubicin or doxorubicin |
‘Late referral’ group: 15 of the 51 patients needed extensive reconstructive surgery | |
|
Authors |
Age From 6 months to 14 years |
Method of delivery Some i.v. drip, some push |
Surgery – debridement and wound closure: mostly split-thickness skin grafts or delayed primary closure | The mean time for wound closure was 49 days (range 10–85 days). Three patients died before wound closure. At least one patient needed a split thickness skin graft but could be more as results not given separately for children and adults. One child developed sympathetic dystrophy syndrome. Some children developed permanent joint stiffness. Other negative outcomes are mentioned but unclear if they were experienced by the child sample |
|
Design Retrospective case series |
Comorbidities Mostly acute myelogenous leukaemia or lymphoma |
Types of injury Only patients with extensive injuries, defined as 300 cm2 of tissue loss |
||
|
Setting Plastic surgery department, USA |
Duration of i.v. therapy NR |
Sites Upper arm, forearm or hand, foot and leg |
||
|
Sample size 18 (study also included 22 adults) |
Mean time to treatment Range 6–62 days |
Infusates Doxorubicin hydrochloride |
Sodium hypochlorite dressings | |
| All patients had at least two operations | ||||
|
Authors Sivrioglu 201450 |
Age 26 days (range 1 day–3 months) |
Method of delivery NR |
Injuries were initially flushed with saline and a cold compress applied. Oily dressings were applied and skin necrosis developed within a week. Debridement with the VersajetTM Hydrosurgerical system (Smith & Nephew, London, UK) (a waterjet debriding tool) under general anaesthesia. Oily dressings used after debridement | Wounds healed spontaneously by re-epithelialisation. The mean time of full epithelialisation was 14 days. At 1 year, minimal scar formation was noted with no hypertrophic scars |
|
Design Retrospective case series |
Comorbidities NR |
Types of injury Skin necrosis |
||
|
Setting Plastic surgery department, Turkey |
Duration of i.v. therapy NR |
Sites Hand/wrist (n = 5), foot (n = 3) and scalp (n = 1) |
||
|
Sample size Nine |
Mean time to treatment All within 12 hours |
Infusates Calcium gluconate |
||
|
Authors Upton et al. 197951 |
Age 5.6 years (range 1 week–11 years) |
Method of delivery Varied |
Debridement and skin grafts. All patients needed two or more operations | Below elbow amputation (n = 1), contractures (n = 2), extensor loss (n = 2), hair loss (n = 1), loss of motion (n = 1) and reconstruction needed (n = 1) |
|
Design Retrospective case series |
Comorbidities Varied, including acute leukaemia, head trauma and gastroenteritis |
Types of injury Major injuries with full-thickness tissue loss |
||
|
Setting Various departments in five US hospitals |
Duration of i.v. therapy NR |
Sites Hand, scalp, forearm, wrist, foot or ankle |
||
|
Sample size Seven (study also reported on 24 adults) |
Mean time to treatment Range 1–42 days |
Infusates Varied including dextrose, potassium chloride, doxorubicin hydrochloride, tetracycline |
||
|
Authors von Heimburg and Pallua 199852 (published in German) |
Age Five infants (no further details other than minimum age 2 weeks) |
Method of delivery NR |
Debridement, temporary wound coverage by allogeneic donor tissue grafts, and autologous split-skin graft | After 15 days there was full healing (defined as time at which no further wound coverage changes were required) in all five infants |
|
Design Actual design is retrospective comparative study. But extractable data for five infants |
Comorbidities NR |
Types of injury Late phase, requiring surgical intervention |
||
|
Setting Germany, specialised clinic for plastic, hand and burns surgery |
Duration of i.v. therapy NR |
Sites Bridge of foot |
||
|
Sample size Extractable: five infants (one case report) |
Mean time to treatment 19 days (range 2–10 weeks), but these figures include 19 adult cases |
Infusates NR |
||
|
Authors Weiss 197553 |
Age NR (but premature neonates) |
Method of delivery NR |
Wet dressings and repeated economical debridement | Wounds healed well in 15 to 40 days. Scars were visible but without discolouration |
|
Design Retrospective case series |
Comorbidities Neonatal hypocalcaemia |
Types of injury Localised skin necrosis |
||
|
Setting Department of premature infants, Israel |
Duration of i.v. therapy Up to 15 days |
Sites All scalp |
||
|
Sample size Four |
Mean time to treatment NR, but lesions developed after needle removal |
Infusates Calcium gluconate |
Three studies were in neonates and all evaluated debridement techniques. 48,50,53 Two were of skin necrosis wounds caused by calcium gluconate,50,53 one of them being in preterm neonates. 53 The other was in preterm neonates with full-thickness injuries, mostly caused by parenteral nutrition. 48
Two studies were in older children: one in children (mean age 5.6 years) with full-thickness tissue loss arising from different types of infusate,51 and one in children with cancer diagnoses such as acute myelogenous leukaemia or lymphoma who had extensive injuries caused by doxorubicin hydrochloride. 49 In two studies, only limited population details for surgery patients were available. 21,52
As would be expected in studies of more severe injuries, the delay between the extravasation event and (surgical) treatment was longer than in the studies of the interventions previously discussed. However, in one neonatal study of debridement, patients were treated within 12 hours of injury. 50 This was because this study actually used a combination of intervention approaches, rather than just debridement. It used conservative management methods and flush-out before debridement using a waterjet debriding tool. 50
Only basic result details were reported for the debridement studies in neonates. The two calcium gluconate studies reported wound healing in 15 to 40 days,53 and a mean of 14 days for full epithelialisation,50 with minimal scar formation at 1 year. 50 The parenteral nutrition study, which was of enzymatic debridement, reported that all 16 wounds healed completely, with no infections and no functional scar contractions at up to 16 months. 48 A study of five infants receiving debridement and skin grafts reported full healing at 15 days. 52 The study in seven older children (mean age 5.6 years) reported an amputation, two contractures, hair loss and loss of motion. 51 The doxorubicin hydrochloride study of children with extensive injuries reported a mean time for wound closure of 49 days. 49 Other outcomes were reported, but this study also reported on adults and separate results for children were not always available.
Summary
Although many types of extravasation injury treatments have been studied in non-comparative studies, the limitations inherent in these studies makes it very difficult to compare results across treatments. Some results have probably been subject to chance effects or biases because most studies were very small and were retrospective in design: 17 out of the 24 studies had sample sizes of < 20 and only three studies were reported as having a prospective design. Furthermore, there was considerable clinical heterogeneity across study populations in factors such as age, types of infusate, injury severity, location of injury and the time gaps between injury and treatment. Differences in results might be a reflection of variation in one or more of these parameters, rather than differences in treatment effect. Volume of infusate may have been another important factor, though this was very rarely reported. Although data on injury severity grading could have helped with interpreting the importance of these issues, few studies reported such data. Finally, the results sections for most studies were very brief and reported limited data for outcomes which were often related to short-term time points. No studies reported pain as an outcome and few studies quantified outcomes, for example, by using measures of scarring, such as scar scores. Only one study reported on whether or not interventions resulted in adverse effects. 46
Uncertainty exists regarding which treatments may be the most promising, particularly with respect to how to treat earlier stage injuries (i.e. injuries which have not become necrotic). Some of the better evidence (in terms of study size and a prospective design) relates to studies of saline flush-out techniques. Notwithstanding the reporting limitations of the results sections of many studies, these techniques appear to be quite promising treatments. The effect of prior infiltration with hyaluronidase before wash out is unclear though.
Neonates were the most frequently studied population, being evaluated in around half of the non-comparative studies. Neonates have more fragile skin and veins and are less able to communicate the presence of injuries compared with older infants; Sung and Lee40 suggested that the use of flush-out methods in neonates may be too invasive to perform and, therefore, proposed a middle ground between conservative management and flush-out: puncture points and hydrocolloid dressing. However, although 2 out of the 12 (mostly) preterm neonates in this South Korean study presented with necrotic lesions, nine eventually progressed to full-thickness open wounds. Additionally, two group studies have performed flush-out treatments in neonates. 4,32 One of them was prospectively performed in a UK neonatal unit, but it was only published as a letter and so only reported the population as ‘neonates’ along with very basic results. 32 The other was conducted in a Greek neonatal intensive care unit in mostly very preterm or late preterm neonates with quite severe (stage III or IV) extravasation injuries. 4 This study reported impressive results with 21 out of the 34 neonates showing no signs of soft tissue damage 24 hours after treatment, and only minor findings (blistering and epidermolysis) still present in seven neonates in the following few days. These results might therefore suggest that flush-out treatments may be more worthy of further study than the middle ground of puncture (without flush-out) and dressing. However, this is merely a suggestion, as although both the studies were of parenteral nutrition extravasations, they differed in an important way: in the Greek study the neonates were treated within 10–30 minutes of injury compared with between 1 and 10 hours in the South Korean study.
Case report studies
There were 106 case report studies identified,58–163 23 of which detailed more than one participant. 62,64,70,75,79,87,102,104,108–111,121,123,129,147,148,153,157,159–162 In total, 163 individual participants were studied. Study characteristics are summarised in Table 7 with full treatment, intervention and outcome details presented in Appendix 3. The age range of the participants was from newborn to 17 years old, with a mean age of 2.1 years. The majority of the case reports were on neonates or young infants with 93 case reports detailing those < 1 month old and 122 examining those < 1 years old.
| Study authors and date | Design | Age | Infusate | Intervention |
|---|---|---|---|---|
| Abraham et al. 201258 | Case report | 9 years | Chloramphenicol and ampicillin | Fasciotomy |
| Altan et al. 201359 | Case report | 23 days | Packed red blood cells | Conservative, nitroglycerin |
| Altmann et al. 201460 | Extractable: case report | 2 years | Doxorubicin | Conservative, debridement |
| Amano et al. 200861 | Case report | 3 years | Parenteral nutrition | Conservative, antibiotics, silver sulfadiazine, debridement |
| Amaya 201662 | Multiple case reports (four patients) | 4–32 weeks old (three preterm) | Parenteral nutrition | Saline wash, fasciotomy, debridement, skin graft |
| Amhaz et al. 201663 | Case report | 10 days | Adrenalin | Conservative, antibiotics |
| Aribit et al. 200064 | Multiple case reports (two patients) | 6 and 11 months | Parenteral nutrition and intralipid | Antibiotics, drainage |
| Baker et al. 199165 | Case report | 7 years | Nafcillin sodium | Antibiotics (n = 1), silver sulfadiazine (n = 2), debridement (n = 1), skin graft (n = 1) |
| Bassi et al. 200766 | Case report | 10 months | Contrast agent | Conservative, fasciotomy |
| Berger et al. 1974162 | Multiple case reports (three patients) | 2 days to 1 month (two preterm) | Unspecified antibiotic | Debridement, skin graft |
| Beytut et al. 2014163 | Case report | 7 years | NR | Honey, debridement, skin graft |
| Bhosale et al. 201267 | Case report | 16 years | Blood | Conservative, saline wash |
| Borman et al. 199868 | Case report | 4 years | Glucose 10% (n = 1), NR (n = 1) | Saline wash |
| Boyar et al. 201469 | Case report | 3 weeks (preterm) | Calcium gluconate | Debridement (n = 2), antibiotics (n = 2) |
| Broom et al. 201670 | Multiple case reports (two patients) | 6 months to 1 year | NR | Conservative, topical, oxygenotherapy |
| Chait et al. 197571 | Case report | 2 years | Dopamine | Antibiotics, debridement, skin graft |
| Chen et al. 201072 | Case report | 4 days (preterm) | NR | Fasciotomy |
| Chiang et al. 200473 | Case report | 11 days (preterm) | Calcium gluconate (10%) | Conservative, antibiotics, fasciotomy (n = 2) |
| Ching et al. 201474 | Case report | 4 days | Calcium gluconate (10%) | Conservative, antibiotics |
| Cho et al. 200775 | Multiple case reports (five patients) | 17 to 50 days | Calcium gluconate | Conservative |
| Cohan et al. 199076 | Case report | 12 months | Iopamidol | Conservative |
| D’Acunto et al. 201577 | Case report | 2 months (preterm) | Balanced electrolyte solution | Conservative, debridement, skin graft |
| Davé 199378 | Case report | 3 years | Undefined fluids (no drugs) | Conservative, debridement, skin graft |
| Davies et al. 199479 | Multiple case reports (two patients) | 26 and 11 days (both preterm) | Dopamine | Conservative, nitroglycerin |
| Denkler et al. 198980 | Case report | 1 day (preterm – two sites: hand/foot) | Dextrose and 25% normal saline | Conservative |
| Domizio et al. 200681 | Case report | 2 days (two sites) | Doxorubicin | Debridement, skin graft |
| Dunn et al. 198482 | Case report | 5 months | Dextrose saline | Conservative |
| Duray et al. 198683 | Case report | 5 years | Calcium gluconate | Conservative |
| Eckersall et al. 199684 | Case report | 3 years | i.v. fluids | Antibiotics, debridement, skin graft |
| Eroglu et al. 200485 | Case report | 17 years | Parenteral nutrition (lipid infusate) | Drainage |
| Garcia-Alverez et al. 199986 | Case report | 2 weeks (administered over first 3 days of life) | Sodium bicarbonate | Conservative |
| Gibboney et al. 198687 | Multiple case reports (two patients) | 17 days and 4 weeks (both preterm) | Dextrose solution (5%), 25% saline and potassium chloride | Conservative, fasciotomy, skin graft |
| Govind et al. 201488 | Case report | 27 days (preterm) | Erythromycin | Conservative, saline wash, debridement, skin graft |
| Grabois et al. 200889 | Case report | 19 days (preterm) | Phenytoin | Fasciotomy |
| Handler 199090 | Case report | 4 years | Calcium gluconate (10%) | Conservative, debridement |
| Hankin et al. 198491 | Case report | 17 years | Vincristine | Hyaluronidase |
| Harb et al. 201092 | Case report | 1 year (preterm) | Parenteral nutrition | Antibiotics, hyaluronidase |
| Hasija et al. 201493 | Case report | 3 years | Dextrose solution | Conservative, hyaluronidase |
| Hey et al. 200594 | Case report | 12 months | Sodium bicarbonate | Conservative, hyaluronidase |
| Hironaja et al. 198295 | Case report | 6 days | Parenteral nutrition (lipids) plus antibiotics | Conservative, hydrogel |
| Hirsch et al. 201696 | Case report | 4 days (preterm) | Anthracycline (idarubicin) | DMSO |
| Hooke 200597 | Case report | Adolescent | Antibiotics, NR | Silver sulfadiazine, honey, hydrogel, hyaluronidase |
| Kameo et al. 201598 | Case report | 2 years | NR | Conservative |
| Khan et al. 201499 | Case report | 29 days (preterm) | Calcium gluconate | Conservative, antibiotics, oxygenotherapy, debridement |
| Kishi et al. 2014100 | Case report | 17 years | Intralipid and parenteral nutrition | Conservative |
| Kuensting 2010101 | Case report | 6 days | Calcium gluconate | Conservative |
| Kumar et al. 2001102 | Multiple case reports (six patients) | Neonate (preterm) to 2 years | Propofol and lidocaine | Saline wash, debridement, skin graft |
| Lee et al. 2013103 | Case report | 1 month (preterm) | Sodium bicarbonate (NaHCO3) | ACTICOAT™ (Smith & Nephew, London, UK) |
| Lehr et al. 2004104 | Multiple case reports (three patients) | 4 to 24 days (two preterm) | Arginine | Conservative, debridement, skin graft |
| Leung et al. 1980105 | Case report | 6.5 years | Phenobarbital | Antibiotics, debridement, skin graft |
| Llinares et al. 2005106 | Case report | 4 years | NR | Ultrasound, hydrogel, debridement |
| Martin et al. 1994107 | Case report | 4 months | Phenytoin | NR |
| Meszes et al. 2017108 | Multiple case reports (six patients) | Neonates (range 1–23 days) | NR | Antibiotics, debridement |
| Mohr et al. 2014109 | Multiple case reports (two patients) | 3 weeks (preterm), 19 days (preterm) | Parenteral nutrition (dextrose, calcium, potassium, etc) | Saline wash, hyaluronidase |
| Morrison et al. 1999110 | Multiple case reports (four patients) | Neonates (preterm) | Dopamine | Phentolamine |
| Mukherjee et al. 1977111 | Multiple case reports (four patients) | 5 years and NR | Phenytoin (diazepam before) | Conservative, hydrocortisone |
| Nissim et al. 2008112 | Case report | 1 day | Calcium gluconate | None |
| Onesti et al. 2012113 | Case report | 2 days (preterm) | Calcium gluconate | Antibiotics |
| O’Reilly et al. 1988114 | Case report | Neonate | Ceftriaxone sodium | Conservative, fasciotomy |
| Ozcan et al. 2015115 | Case report | 14 years | Mannitol | Fasciotomy |
| Pantelides et al. 2013116 | Case report | 1 day (preterm) | Dextrose | Conservative, drainage, antibiotics |
| Park et al. 2015117 | Case report | 7 months | Two NR, one hydration | Conservative (n = 1) and fasciotomy (n = 2) |
| Phillips et al. 2009118 | Case report | 3 months | Calcium gluconate | Antibiotics, debridement |
| Raffaella et al. 2009119 | Case report (two extravasations) | 5 years | Calcium solution | Other surgery |
| Ravenel 1983120 | Case report | 6 days | Dextrose | Conservative, hyaluronidase |
| Reilly et al. 1977121 | Multiple case reports (three patients) | 13, 15 and 17 years | Calcium solution | Conservative, antibiotics |
| Reynolds 2007122 | Case report | 2 days (preterm) | Dopamine | Conservative (n = 1) and nitroglycerin (n = 1) |
| Roberts 1977123 | Multiple case reports (five patients) | Neonates (range 1 day–1 year) | Calcium gluconate | Conservative |
| Rosales et al. 2004124 | Case report | 75 days (preterm) | Dopamine and tromethamine | Debridement, skin graft and other surgery (n = 1) |
| Roth et al. 2006125 | Case report | 31 days | Nafcillin sodium | Conservative (n = 1), hyaluronidase (n = 2) and skin graft (n = 1) |
| Rustogi et al. 2005126 | Case report | 4 days (preterm) | Flucloxacillin, calcium gluconate, human immunoglobulin, sodium bicarbonate, dextrose solution and 20% lipid nutrition | Conservative, debridement (n = 3), skin graft |
| Salameh et al. 2004127 | Case report | 3.5 years | Fatty acid, lipid and amino acid infusion (n = 4), glucose (n = 1) and dobutamine (n = 1) | Conservative (n = 3), hydrogel (n = 2), debridement (n = 1) and none (n = 1) |
| Samiee-Zafarghandy et al. 2014128 | Case report | 1 day (preterm) | Adriamycin | Conservative (n = 1), antibiotics (n = 1) and hydrocortisone (n = 1) |
| Sanpera et al. 1994129 | Multiple case reports (two patients) | 3 days and neonate (preterm) | Dextrose (10%) or calcium solutions | Debridement, skin graft (n = 4) |
| Santoshi et al. 2008130 | Case report | Neonate (preterm) (seen at 5 years) | Fluids or electrolyte solution (n = 5; 1 plus erythromycin) and phenytoin (n = 1) | Saline wash, debridement, skin graft (n = 2) |
| Schäfer et al. 2005131 | Case report | 2 weeks | Parenteral nutrition (sixth case blood transfusion) | Antibiotics, debridement (n = 2) |
| Schie et al. 2013132 | Case report | 33 weeks (preterm) | Calcium gluconate | Antibiotic corticosteroid |
| Schumacher et al. 1987133 | Case report | 7 years | Azithomycin | Conservative, antibiotics |
| Sharief et al. 1994134 | Case report (two extravasations) | 1 day (and 3 days) | 8.4% bicarbonate 20 ml, 10% calcium gluconate 10 ml, 50% glucose 5 ml, 1 : 1000 adrenaline 3 ml and 4.5% human albumin solution 50 ml | Saline wash, liposuction, hyaluronidase |
| Shenaq et al. 1996135 | Case report | 10 years | Parenteral nutrition | Topical |
| Sindal et al. 2015136 | Case report | Neonate (preterm) | Dextrose solution (12.5%) | Conservative |
| Siu et al. 2007137 | Case report | 2 days (preterm) | Calcium gluconate | Antibiotics |
| Siwy et al. 1987138 | Case report | 2 days | Dopamine | Phentolamine |
| Sokol et al. 1998139 | Case report | 14 months (preterm) | Arginine and 10% glucose | Conservative |
| Sonohata et al. 2006141 | Case report | 14 years | Arginine monohydrochloride (10% in sodium chloride) | Conservative, silver sulfadiazine |
| Sonohata et al. 2008140 | Case report | 3 days | 6 cc arginine monohydrochloride, 50% diluted in 12 cc of sodium chloride 0.9% | Conservative, topical, Debridement |
| Soon et al. 2001142 | Case report | 38 weeks | NR | Honey |
| Spenny et al. 2004144 | Case report | 3 years | Oncovin dauno rubicin | Conservative |
| Stahl et al. 2000143 | Case report | 10 years | Parenteral nutrition | Saline wash, hyaluronidase |
| Subedi et al. 2011145 | Case report | 16 years | Mannitol (20%) | Fasciotomy |
| Subhani et al. 2001146 | Case report | 1 day | Doxorubicin | Conservative, DMSO, debridement, skin graft |
| Talbot et al. 2011147 | Multiple case reports (three patients) | 7 to 10 months | Hydroxyzine | Conservative, silver sulfadiazine |
| Tilden et al. 1980148 | Multiple case reports (four patients) | 15 days to 4 months | Contrast medium (sodium iothalamate 54%) | Antibiotics, debridement, skin graft |
| Tiras et al. 2005149 | Case report | 2 days | Calcium gluconate | Skin graft |
| Tobin 2007150 | Case report | 1 day (preterm) | Blood, fluids and antibiotics | Other surgery |
| Tuncer et al. 2006151 | Case report | 6 years | Phenytoin | Hyaluronidase |
| Vanwijck and Lengele 1994152 | Case Report | 9 years | Parenteral nutrition | Conservative, antibiotics |
| von Muhlendahl 2012153 | Multiple case reports (six patients) | 14 days (preterm) to 14 months | Arginine monohydrochloride (10%) | Conservative, silver sulfadiazine, debridement, skin graft |
| Wada et al. 2003154 | Case report | Neonate | Dextrose solution; NR (rehydration) | Debridement, skin graft |
| Wiegand et al. 2010155 | Case report | 17 years | Parenteral nutrition | Conservative, silver sulfadiazine, debridement, artificial skin |
| Wolfe et al. 1983156 | Case report | 2 days | Dopamine | Conservative, topical, antibiotics, debridement |
| Wong et al. 1992157 | Multiple case reports (two patients) | 4 and 15 days (both preterm) | Calcium solution and NR | Debridement |
| Wong et al. 2015158 | Case report | 4 days | Calcium disodium edetate (EDTA) | Conservative |
| Yamamoto et al. 1994159 | Multiple case reports (two patients) | 1 and 4 years | Adriamycin (doxorubicin) | Debridement, skin graft |
| Yosowitz et al. 1975160 | Multiple case reports (seven patients) | 2 days to 10 years (two preterm) | Meglumine ioxitalamate | Conservative, antibiotics, saline wash, drainage |
| Zenk et al. 1981161 | Multiple case reports (three patients) | 3 days to 4 months | Calcium solution | Conservative, debridement, skin graft |
The range of extravasated fluids examined was varied. The majority of individual case reports examined calcium gluconate, amounting to 19% (n = 31) of the total. Parenteral nutrition and dextrose solutions made up the next highest frequency at 12% (n = 19) and 9% (n = 15), respectively. Other extravasated fluids examined were dopamine at 5% (n = 8), nafcillin sodium at 4% (n = 7), phenytoin at 4% (n = 6), arginine at 2% (n = 4), sodium bicarbonate at 2% (n = 4) and doxorubicin at 2% (n = 3). The extravasated material was not reported in 8% of case reports (n = 13).
The extent and quality of reporting of extravasation treatments varied across the studies. The majority of the studies (n = 56) reported the use of conservative management at least initially. 58,59,61,63,65,66,71–74,76–78,80,82,84,86,89–92,94–97,100–104,108,112,113,115,116,118,119,121–123,127,128,133,141,144,145,147,150,152,154–158,161,163 Only 17 of these studies, however, reported using conservative management in isolation for any case report. 58,71,74,76,82,84,86,89,112,116,121–123,133,147,157,158 Topical treatments were reported in 14 studies,61,62,65,69,96,97,100,104,106,108,109,113,132,148 including seven examining silver sulfadiazine,61,65,96,100,109,113,148 two using DMSO,97,106 three using medical honey62,69,109 and four reporting on hydrogel. 104,108,109,132 Hyaluronidase was used in 11 studies79,98,99,101,103,107,109,137,139,155,161 and saline wash out in 10 studies. 63,64,79,92,109,117,125,137,152,153
Surgical techniques were required in at least one participant in 49 of the studies,59,60,62,65–68,70,72,75,77,78,83,85,87,90–93,95–97,102,105,108,110,111,113,117–119,125,127,129,131,132,135,136,143,144,147–149,153,154,159–162 a significant proportion at 46%. Of these, 11 studies included fasciotomies,59,68,70,72,85,90,93,117,143,144,147 37 included case reports where debridement was necessary60,62,65–67,75,77,78,83,87,91,92,95–97,102,105,108,111,113,117–119,125,127,129,131,132,135,136,148,149,153,154,159,160,162 and 26 studies had case reports that required skin grafts. 60,62,65,67,77,78,83,87,90,92,97,102,105,110,111,117,125,127,131,135,148,153,154,159–161 Only one study reported a skin graft that had not also undergone debridement or a fasciotomy. 110
Outcomes were generally poorly reported and lacking in detail. The majority of studies (n = 90) reported a functional or full recovery for all their participants. 58–67,69–90,92–95,97–110,112,114,116,119–123,125–127,130–132,134,136–147,149–151,153,155–163 However, few of these (n = 25) reported on whether or not adverse outcomes such as scarring occurred. 58,61,65,66,69,71,75,79,81,85,94,97,100,102,105,107,110,114,116,120,130,139,146,150,153 Of these 25 studies, 17 indicated some scarring but how this was reported was inconsistent across studies and was usually vague. 58,61,65,66,69,71,79,85,97,100,102,105,110,130,139,150,153 In addition, the time points at which scars were assessed varied widely across the studies, ranging from within 24 hours to three years.
Summary
Overall, the case reports point to a lack of methodological consistency in the area. Little, if any, information is given about the extent of injury before treatment, and outcomes were measured and reported inconsistently. In a similar vein to the non-comparative studies, inconsistency of treatment variables such as dosage and delay until treatment make any comparisons of the findings of these reports of limited use.
Reviews and guidelines
Reviews
Three reviews, one narrative8 and two systematic,17,164 were identified that synthesised the evidence on treatment for extravasation events and injuries. Clifton-Koeppel8 conducted a broad narrative review of extravasation injuries across a range of patient populations which included a review of initial treatments and subsequent wound care options. The author recommended the use of clinical staging criteria of the severity of wounds to help determine the appropriate treatment. The author also indicated that, although there was agreement that immediate treatment is needed for the best outcomes, there is no consensus regarding which treatments are best. Saline wash-out and hyaluronidase treatments appeared to be frequently studied. The review also reported that reduced wound healing time and scarring can be achieved from the promotion of a moist environment using topical ointments/gels and dressings, while also noting the toxicity problems that may result from using topical treatments in newborns. The local application of heat or cold were not well studied treatments, with no studies found in newborns. Although this review was not systematic (so some relevant studies may have been missed), the author’s conclusions, in which they lament the very limited evidence available and call for further research, nevertheless, seem appropriate.
The second review was a Cochrane systematic review which examined the evidence for a specific type of technique, saline irrigation with or without prior hyaluronidase, on wound care in neonates with extravasation injuries. 17 The authors conducted an extensive search of the literature with clear search criteria to identify randomised controlled trials (RCTs) and quasi-RCTs comparing the intervention with no intervention or normal wound care. Despite the rigorous methodology, the authors found no eligible studies. They repeated the searches without an age restriction but still identified no studies that matched the inclusion criteria. They therefore performed a descriptive review of some case reports, case series and cohort studies. These indicated that several different methods were in current practice for the management of extravasation injuries; therefore, the review authors expressed the opinion of an impression that mild injuries (stages 1 and 2) may heal well under conservative management, whereas more severe injuries (stages 3 and 4) may need more invasive treatment. However, these recommendations are based on a very limited evidence base.
In 2015, Harrold et al. 164 published a systematic review of the management of cytotoxic chemotherapy extravasations. The review focused on strategies aimed at preventing the need for surgical debridement. Six databases were searched and eligibility criteria were specified for including studies in the review. Study quality was evaluated using a levels of evidence approach. The 31 included studies were mostly case series which evaluated dextrazoxane, DMSO, saline wash-out, hyaluronidase or steroids with or without sodium thiosulphate. However, no conclusive evidence was found to favour one strategy over another. The authors noted that, despite this, some ‘expert opinion’ guidelines favour the use of specific antidotes over saline wash-out. The authors also noted that no studies evaluated outcomes relating to patient experience or patient perspective on extravasation management.
Guidelines
The searches identified seven references relating to guidelines on the management of extravasation injuries. 1,2,18,19,165–167 Two of the references165,166 reported on the same set of guidelines but both were available only as conference abstracts, limiting the information that could be extracted from them. Of the remaining five references, one was a general document which included guidelines for all types of extravasation injuries,2 one focused on a paediatric population,19 and the remaining three limited their scope according to the type of fluid extravasated. 1,18,167
Great Ormond Street Hospital published a set of guidelines online, which cover the prevention, recognition and management of extravasation injuries. 2 The guidelines emphasised the need for immediate management of extravasation injuries by immediately stopping the infusion and aspirating the area of the wound, but the device should not be flushed. Plastic surgeons should determine treatment which includes analgesia, as required; elevation of the affected limb; conservative management, which may involve the use of hot or cold compresses, or antidotes; and saline wash-out. Extravasation kits should be available to the plastic surgeon. This guideline made reference to only a few studies that its recommendations were based on. It did not clarify the basis by which studies were selected, and the quality (i.e. strengths/weaknesses) of the studies was not assessed or discussed. The guideline did not state the circumstances where they are best applied and did not report on the potential harms or side effects that may occur from the listed treatments.
Flemmer and Chan19 limited their guidelines to the management of extravasation injuries in paediatric populations. Their article described a hospital treatment protocol developed to identify and treat extravasation injuries. Consistent with other guidelines, they reported on the inconsistency of approaches but discounted the practice of injecting treatments around the infiltrated site, as they argued this made infection and skin breakdown more likely. Rather, they proposed aspirating the wound to remove the extravasated fluid, then infiltrating it with the chosen treatment. They emphasised that appropriate treatment is dependent on the degree of severity of the wound, indicating that a stage 1 or 2 infiltrate can normally be managed conservatively through elevation. They stated that warm or cold packs have not been shown to significantly alter the clinical course. They recommended a more aggressive approach to treating stage 3 and 4 infiltrates, emphasising immediate and intrusive intervention. They recommended hyaluronidase treatment within 2 hours of the injury, together with glyceryl trinitrate (a vasodilator). Phentolamine was considered effective for treating vasoconstrictor extravasations.
Flemmer and Chan’s guideline19 is narrower in scope than Great Ormond Street’s guidelines and is, therefore, somewhat clearer in defining the health question. They stated that they conducted a review of the literature before creating the guideline but it is unclear if the recommendations are made on the basis of the literature search or on the clinical experience of their team. Despite conducting a review, the criteria on which they included studies, the nature of these studies and an assessment of their quality were not reported in the article. Some potential adverse treatment effects were mentioned. The article was published in 1993 and is, therefore, very likely to be out of date.
The guideline published by Bellin et al. 18 was specifically targeted towards contrast medium extravasations. They highlighted infants, young children, unconscious and debilitated patients as being particularly at risk for these types of injuries. Those receiving chemotherapy were also considered at risk because of the fragility of their vein walls. The guidelines stated that there is no consensus regarding treatment but that most extravasations involve small amounts of fluid inducing minimal swelling or redness. However, they emphasised that necrosis and ulceration do occur more commonly with high-volume extravasations than with low-volume extravasations. Despite the acknowledgement of these risk factors, the guidelines argued that it is not possible to predict whether these types of injuries will resolve or worsen at initial examination, but skin blistering, altered tissue perfusion, paraesthesia and persistent pain after 4 hours suggest severe injuries. They suggested that most contrast medium extravasations are not serious and only require conservative management. Silver sulfadiazine ointment was recommended for blistering to prevent secondary infections. Hyaluronidase injections (administered within 1 hour) have been used for large extravasations of contrast medium and chemotherapeutic agents, although conflicting efficacy results have been published. 45–47 DMSO, corticosteroids and vasodilators were mentioned as potential treatments but studies have either failed to demonstrate benefits or treatments have not been tested for extravasations of this type.
Bellin et al. ’s18 guidelines have a clear focus, acknowledge the limitations of the evidence and back up statements by reference to relevant studies. However, similar to the previous guidelines, they do not assess the quality of the studies they base their assertions on nor give the criteria with which they included these studies. This guideline is also somewhat dated, having been published in 2002.
The guideline published by Pérez Fidalgo et al. ,1 which focused primarily on chemotherapy extravasations, emphasised the importance of classifying extravasated fluids by their potential to cause damage (vesicant, irritant and non-vesicant categories were used). The authors noted a number of difficulties in recommending appropriate treatment, including the lack of any RCTs, likely due to ethics complications and potential difficulties in recruiting patients. The authors stated that an extravasation kit containing instructions, materials and medication to handle any incidence should be always available. The guideline covered many treatment options. Hydrocortisone injections have been shown to have some potential in preventing tissue necrosis but intralesion corticoids seem to do more harm than good. Subcutaneous corticoids were, therefore, not recommended. They reported that topical DMSO is an option for treating extravasation of anthracyclines, mitomycin C or platin salts, but the concentration of the drug should be kept low (50%). Dexrazoxane was also recommended for anthracycline extravasations. Hyaluronidase (injected through the existing i.v. line) was recommended to prevent skin necrosis following vinca alkaloid extravasation. Subcutaneous wash-out procedures were also reported to have shown encouraging results. The authors reported that around one-third of cytotoxic extravasations lead to ulceration and, hence, surgical procedures should be limited to those patients where conservative therapy has failed. They recommended surgical debridement of wounds for unresolved necrosis lasting > 10 days, followed by a skin graft where necessary.
These guidelines1 have a precise focus which, although making for a clear definition of the health question, restricts the generalisability to a paediatric population. The authors made no mention of the criteria with which they included the studies on which they based their recommendations. They did, however, provide details of the included studies and made explicit links to the recommendations and the supporting evidence. Levels of evidence gradings were also provided. The guidelines are also relatively current, having been published in 2012.
In 2015, Boulanger et al. 167 published a guideline on the management of antineoplastic agent extravasations to inform clinical practice in Quebec. Studies were identified using a search of PubMed, although few eligibility criteria were stated. Levels of evidence were used to grade recommendations. Separate guidance was made for peripheral line and central line extravasations of specific chemotherapies. Recommendations were similar to those published by Pérez Fidalgo et al. 1 and included dry warm compress, dry cold compress, DMSO, dexrazoxane and hyaluronidase. However, most recommendations were based on studies supported by little or no empirical evidence.
Only abstracts were available for the remaining two guideline articles. 165,166 An algorithm was developed guiding wound care for three potential wound types but little detail was provided. 165
Summary
Of the three reviews identified, none found any substantial comparative studies examining treatment effectiveness. 8,17,164 All reviews agreed that, although immediate treatment is needed for the best outcome, there is no consensus regarding which treatments are the best practice. They all mention saline wash-out with or without hyaluronidase as a frequently studied treatment, but no review could make conclusive statements on its effectiveness compared with other treatments, because of the limited quality of evidence.
Seven published guidelines were discovered which detailed the management of extravasation injuries. 1,2,18,19,165–167 All were limited in their applications to different patient groups and few reported on the potential harms or side effects that may occur from a particular course of treatment. In addition, the criteria on which studies were included and an assessment of the quality of these studies were not reported in any of the published guidelines. Their recommendations were often conflicting on treatments, such as for saline wash-out,1,2 specific antidotes1,19 and conservative management. They did report some similar findings on hyaluronidase as being an effective treatment and on corticosteroids as being an ineffective treatment. They also agreed that treatment should be started as soon as possible after injury.
Overall, the results from the reviews and guidelines that included evidence from studies in adults add little to the evidence seen in the primary studies in babies and children for identifying the most promising treatments for extravasation injuries.
Chapter 3 Survey of NHS practice
The primary aims of the survey were to determine how extravasation injuries in babies and young children are treated across the NHS, and to elicit opinions regarding future research studies.
Methods
A survey questionnaire was designed and distributed using Qualtrics software (version May 2017; Qualtrics, Provo, UT, USA). A systematic approach was used to develop the survey content which was informed by initial findings from the scoping review, peer-to-peer consultation and patient and public involvement feedback. The questionnaire was piloted among peers at neonatal and paediatric units in York, Bradford and Leeds. Our aim was to distribute the survey via the e-mail lists of the National Neonatal Audit Programme, the British Association of Perinatal Medicine (BAPM), the Neonatal Nurses Association, the Paediatric Intensive Care Audit Network and the Children’s Cancer and Leukaemia Group (CCLG). However, access could only be obtained to the BAPM and CCLG lists (for BAPM, the survey weblink was sent as part of an e-mailed newsletter).
Therefore, we had to utilise our extensive personal contact e-mail lists to achieve adequate distribution of the survey. This list was comprised primarily of consultant neonatologists, consultant paediatricians and consultant paediatric oncologists. A snowballing approach was adopted, with the e-mail recipients asked to either complete the questionnaire or to forward the link to another appropriate member of staff. Responses were made anonymously, although responders had the option of providing an e-mail address should they wish to be notified about the publication of this report. As such, and bearing in mind the survey link was also sent out in a BAPM newsletter, it was not possible to calculate an overall response rate. The survey was distributed between May and August 2017.
The survey asked questions about the use of guidelines for treating extravasation injuries, types of injury, frequency of use of specific treatments, litigation cases and thoughts on future research priorities/preferences. The full content of the questionnaire can be found in Appendix 4. No imputations were used for missing data in partially completed questionnaires. Data were assumed to be missing at random, with the most likely reasons for missing data assumed to be lack of time (the questionnaire was begun but the respondent did not have time to complete it) and a lack of information or knowledge (to hand) to complete the survey.
Results were analysed and presented narratively, with accompanying figures where appropriate. The unit of analysis was at the individual level for all questions, except for questions relating to unit-level protocols and lists; for these unit-level analyses, if any responses from within the same unit were found to be contradictory the response from the most senior individual was used.
Results
A total of 63 questionnaires were received from 56 different hospitals. Fifty-five questionnaires (87%) were fully completed and eight (13%) were partially completed. Key summary results relating to each question are presented below. Additional results data for some questions are reported in Appendix 5.
Respondent characteristics
Forty-eight (76%) questionnaires were received from units in England, six (10%) from Scotland, five (8%) from Northern Ireland and two (3%) from Wales. Although the survey was intended to be only of NHS units, the snowballing approach used resulted in two responses from outside the NHS: one from the USA and one from Canada. Given that the responses on these two questionnaires were broadly in line with those from other questionnaires, these data were included in our analyses.
Forty-five (71%) responses were from neonatal units, 13 (21%) were from principal oncology/haematology units and five (8%) were from paediatric intensive care units (PICU). Most responders were either consultant neonatologists (31 responders, 48%), nursing staff (10 responders, 16%) or consultant paediatricians (eight responders, 13%). Details of all responder positions are presented in Table 8.
| Position | Number (%) of responders |
|---|---|
| Consultant neonatologist | 31 (48) |
| Nursing staff | 10 (16) |
| Consultant paediatrician | 8 (13) |
| PICU consultant | 4 (6) |
| Consultant paediatric oncologist | 2 (3) |
| Clinical nurse educator | 2 (3) |
| Specialist registrar | 2 (3) |
| Associate specialist | 1 (2) |
| Paediatric registrar | 1 (2) |
| Ward manager | 1 (2) |
| Neonatal midwife | 1 (2) |
Hospital unit documentation
Does your unit have a written protocol or guideline for treating extravasation injuries?
This answer was analysed at the hospital-unit level (rather than by individual respondents). Overall, of the 57 unit responses to this question, 47 (82%) said they had a written protocol or guideline, nine (18%) said they did not and one (2%) did not know. In neonatal units, 29 (73%) had a written protocol or guideline, 10 (25%) did not and one unit (3%) did not know. All 13 principal oncology/haematology units and all four PICUs had a written protocol or guideline. Units answering ‘yes’ to this question were then asked about the inclusion of an injury severity staging system.
Does the protocol or guideline contain a staging system for grading severity of extravasation injury?
Of the 30 responses from neonatal units, 11 (37%) were ‘yes’, 16 (53%) were ‘no’ and three (10%) were ‘do not know’. Of the 13 principal oncology/haematology unit responses, 5 (38%) were ‘yes’ and 8 (62%) were ‘no’. Of the four PICU responses, one was ‘yes’ and three were ‘no’.
Does your unit have a list which identifies infusates which may cause serious problems when extravasated?
Overall, of the 55 units responding, 39 (71%) did have a list and 16 (29%) did not have a list. For neonatal units, 23 had a list and 16 did not. All 13 principal oncology/haematology unit responses and all three PICU responses were ‘yes’.
Injury parameters
Please select the type of access site most associated with extravasation injuries in your unit’s patients.
Of the 42 responses from individuals in neonatal units, 40 (95%) chose peripheral line and two (5%) chose peripheral central line. Of the 13 principal oncology/haematology unit responses, eight (62%) chose peripheral line, three (23%) indicated that extravasation injuries were too rare to choose an access site option, one (8%) chose central line and one (8%) did not know. All five PICU responses were peripheral line.
Please select the type of infusate which causes the largest proportion of all the extravasation injuries in your unit’s patients.
For this question, more than one answer could be selected if the proportions were equal. For neonatal units, 29 out of the 59 answers (49%) identified parenteral nutrition as the infusate causing the largest proportion of injuries. Other infusates were calcium (nine answers, 15%), blood (8 answers, 14%), do not know (5 answers, 8%), antibiotics (3 answers, 5%), inotropes or pressors (2 answers, 3%), 10% dextrose (2 answers, 3%) and caffeine (1 answer, 2%).
Vesicant chemotherapies caused the largest proportion of injuries in principal oncology/haematology units (9 out of 17 answers, 53%), followed by non-vesicant chemotherapies (three answers, 18%) and blood, saline and sodium bicarbonate (one answer each). One respondent opted for ‘do not know’ and one noted that there were ‘too few incidents to comment’. The seven PICU answers varied, without any infusate dominating; they included parenteral nutrition, calcium, antibiotics, 10% dextrose, ‘sodium benzoate, phenytoin, acyclovir’ and ‘i.v. fluids’.
The following question was asked of those responders selecting parenteral nutrition/calcium/blood or vesicant chemotherapies for the previous question:
What proportion of the extravasation injuries in your unit would you estimate is caused by extravasation of infused parenteral nutrition/calcium/blood/vesicant chemotherapies?
Of the 29 responders from neonatal units who said that parenteral nutrition caused the largest proportion of injuries, most indicated that these injuries constituted a large or very large majority of all the extravasation injuries encountered (Figure 2).
FIGURE 2.
Percentage of neonatal unit extravasation injuries caused by parenteral nutrition in units indicating parenteral nutrition as the main cause of injuries.

For the neonatal unit calcium extravasation responses, 5 out of 9 chose the 75–100% option. For the eight blood extravasation responses, the proportions were more varied (see Appendix 5). Of the principal oncology/haematology unit responses which indicated that vesicant chemotherapies caused the largest proportion of extravasation injuries, 6 out of 9 indicated that the proportions were large (see Appendix 5).
Interventions used to treat extravasation injuries
Please consider the list below of possible treatments for extravasation injuries. How frequently is each of them used in your unit?
The results of neonatal unit responders are reported in Table 9. The most frequently used intervention approaches were elevation of the affected area and administration of analgesics. In most units, warm or cold compresses were rarely or never used. There was notable variation across the responses regarding the use of occlusive dressings, ranging from always being used (8% of responses) to never being used (31% of responses). Variation in the use of saline irrigation, either with or without hyaluronidase, was also evident; these interventions seem to be either usually used or sometimes used in around half of neonatal units, although they are never used in around one-third of units. Results for principal oncology/haematology units (Table 10) and PICUs (Table 11) were broadly similar to the neonatal units results. However, there were some key differences in the principal oncology/haematology unit responses, including a more widespread use of cold and warm compresses and the use of antidotes to specific infusates.
| Treatment | Number of responses (% of total) | Total number of responders | ||||
|---|---|---|---|---|---|---|
| Always | Usually | Sometimes | Rarely | Never | ||
| Elevation of affected area | 12 (29) | 12 (29) | 13 (31) | 4 (10) | 1 (2) | 42 |
| Warm compress | 1(3) | 2 (6) | 3 (8) | 13 (36) | 17 (47) | 36 |
| Cold compress | 1(3) | 0 | 3 (9) | 11 (33) | 18 (55) | 33 |
| Analgesia | 9 (21) | 19 (45) | 10 (24) | 4 (10) | 0 | 42 |
| A specific topical cream or ointment | 0 | 3 (8) | 7 (19) | 6 (17) | 20 (56) | 36 |
| Occlusive dressing | 3 (8) | 6 (15) | 8 (2) | 10 (26) | 12 (31) | 39 |
| Saline irrigation without hyaluronidase | 0 | 6 (15) | 15 (38) | 5 (13) | 13 (33) | 39 |
| Saline irrigation with hyaluronidase | 2 (5) | 9 (23) | 11 (28) | 7 (18) | 11 (28) | 40 |
| Antidotes to specific infusates | 0 | 2 (6) | 2 (6) | 7 (20) | 24 (69) | 35 |
| Treatment | Number of responses (% of total) | Total number of responders | ||||
|---|---|---|---|---|---|---|
| Always | Usually | Sometimes | Rarely | Never | ||
| Elevation of affected area | 4 (40) | 3 (30) | 2 (20) | 1 (10) | 0 | 10 |
| Warm compress | 2 (22) | 1 (11) | 5 (56) | 0 | 1 (11) | 9 |
| Cold compress | 3 (33) | 0 | 5 (56) | 0 | 1 (11) | 9 |
| Analgesia | 6 (67) | 1 (11) | 2 (22) | 0 | 0 | 9 |
| A specific topical cream or ointment | 3 (33) | 1 (11) | 3 (33) | 0 | 2 (22) | 9 |
| Occlusive dressing | 0 | 0 | 3 (38) | 1 (13) | 4 (50) | 8 |
| Saline irrigation without hyaluronidase | 1 (11) | 0 | 2 (22) | 2 (22) | 4 (44) | 9 |
| Saline irrigation with hyaluronidase | 2 (22) | 1 (11) | 3 (33) | 1 (11) | 2 (22) | 9 |
| Antidotes to specific infusates | 3 (50) | 0 | 1 (17) | 0 | 2 (33) | 6 |
| Treatment | Number of responses (% of total) | Total Number of responders | ||||
|---|---|---|---|---|---|---|
| Always | Usually | Sometimes | Rarely | Never | ||
| Elevation of affected area | 4 (80) | 1 (20) | 0 | 0 | 0 | 5 |
| Warm compress | 0 | 0 | 0 | 1 (25) | 3 (75) | 4 |
| Cold compress | 0 | 0 | 0 | 2 (50) | 2 (50) | 4 |
| Analgesia | 3 (60) | 1 (20) | 1 (20) | 0 | 0 | 5 |
| A specific topical cream or ointment | 1 (25) | 0 | 0 | 2 (50) | 1 (25) | 4 |
| Occlusive dressing | 0 | 0 | 0 | 2 (40) | 3 (60) | 5 |
| Saline irrigation without hyaluronidase | 1 (20) | 0 | 3 (60) | 0 | 1 (20) | 5 |
| Saline irrigation with hyaluronidase | 2 (40) | 0 | 2 (40) | 1 (20) | 0 | 5 |
| Antidotes to specific infusates | 0 | 0 | 1 (33) | 0 | 2 (67) | 3 |
Approximately what proportion of extravasations injuries that you have actively treated have resulted in a need for plastic surgery at any stage?
Forty-four of the 59 responders (75%) answered ‘< 5%’. Nine responders (15%) did not know. Four responders answered ‘5–24%’ (three were from neonatal units) and two responders answered ‘> 50%’ (one each from a PICU and a principal oncology/haematology unit).
Litigation
In the last 10 years did any of the extravasation injuries which occurred in your unit result in litigation?
Of the 59 responses to this question, 30 (51%) answered ‘no’, 23 (39%) answered ‘do not know’ and six (10%) answered ‘yes’. The litigation cases related to injuries in three neonatal units, two PICUs and one principal oncology/haematology unit.
For those units which indicated there had been litigation, the following question was asked:
How many litigation cases were there in the last 10 years?
Four units reported one case, one unit did not know the number of cases and one PICU reported six cases.
Research
Regarding a future research study in this area, do you think a randomised trial design can be successfully undertaken to compare different treatments for extravasation injuries in babies and young children?
Of the 57 responses, 37 (65%) thought a future RCT might be viable, 12 (21%) did not think a RCT was viable and eight (14%) did not know. However, the results varied by setting; the proportion answering ‘yes’ to this question was 83% of the 40 neonatal unit responses, 33% of the 12 principal oncology/haematology unit responses (33% also responded ‘no’ and 33% responded ‘do not know’) and 0% of PICUs (of the five responses, three thought ‘no’ and two ‘do not know’).
For those who thought a future RCT was viable, the following question was asked:
Please tell us which treatment(s) you would most like to see studied in a randomised trial.
This was answered using a free text field. Almost all of the 28 responders mentioned one or more treatments: saline irrigation/wash-out, hyaluronidase and conservative management. Few details were given about conservative management approaches, although dressings, analgesia and hydrocolloid were mentioned. Two responders suggested trialling glyceryl trinitrate (GTN): comparing its use with no GTN, or compared with wash-out. The results are best summarised as a word cloud (Figure 3).
FIGURE 3.
Word cloud representing treatment suggestions for a randomised trial.

For those respondents who thought a future RCT was not viable, the following question was asked:
It would be helpful if you could say why a randomised trial design might not be viable. If you have any thoughts on alternative study designs, which you think might be more appropriate, please also state them here.
Of the five responders from neonatal units who did not think a RCT was viable, four provided further details. Two responders referred to there being too many variables, in terms of types of injury and other clinical factors (beyond infusate and volume) which could affect outcomes. One responder noted that, for total parenteral nutrition, the infusates may ‘be very different day by day, or between units’. Issues around timeliness of treatment when using randomisation, low numbers of patients and unwillingness to deviate from current practice were also stated as potential problems.
All the responders from principal oncology/haematology units (n = 4) and PICUs (n = 3) who did not think a RCT was viable provided further details. In principal oncology/haematology units, the rarity of extravasation events was mentioned as a potential problem by two responders. Reluctance to deviate from current practice (‘procedures which are currently working well’) was mentioned by the other two responders; the exception was blood transfusion extravasations where there were no guidelines on appropriate management (mentioned by one responder). In PICUs, the low incidence of injuries was raised as an issue. One responder thought that, although there was no equipoise for a placebo controlled trial, a comparison between two therapeutic options might be viable.
Are you aware of any summary data on the effectiveness or safety of treatments for extravasation injury which we are unlikely to have been identified in our searches of literature databases (e.g. unpublished data)?
None of the 55 responders were aware of any unpublished summary data (46 responded ‘no’ and nine responded ‘do not know’).
Any other comments or suggestions about this study?
Three principal oncology/haematology unit responders mentioned how rare extravasation injuries were, with two stating that they were so rare they struggled to provide answers for some questions (other than ‘do not know’). Three neonatal responders also mentioned the rarity of extravasation events, especially significant injuries (in other words, most of the injuries seen in practice are mild).
One principal oncology/haematology unit responder wanted to stress that their treatment protocol describes very specific management based on the infusate. A responder from a neonatal unit thought that the use of BadgerNet© (Clevermed Ltd, Edinburgh, UK) data would be good in order to study variation in the incidence of extravasation injuries (and the possible reasons for variation).
Chapter 4 Discussion
Principal findings
The evidence identified in the scoping review mostly comprised small, retrospective, uncontrolled group studies (such as case series) or case report studies. Although the published studies covered a wide range of treatments for extravasation injuries, few studies formally graded injury severity at baseline and the results sections of most studies were brief and lacking important information. Furthermore, there was considerable clinical heterogeneity across study populations in age, types of infusate, injury severity, location of injury and the time gaps between injury identification and subsequent treatment. Differences in results across studies might be a reflection of variation in one or more of these parameters, rather than differences in treatment effect. Consequently, uncertainty exists regarding which treatments may be the most promising, particularly with respect to how to treat earlier stage injuries (i.e. injuries which have not become necrotic). Notwithstanding the study limitations, some of the better evidence, in terms of study size and a prospective design, related to studies of flush-out techniques, which appear to be quite promising treatments. However, the effect of prior infiltration with hyaluronidase before flush-out is unclear.
The use of a scoping review, rather than a full systematic review, to assess the literature was justified on the expectation that any review was very unlikely to produce evidence robust enough to allow treatment recommendations to be made with sufficient confidence. Scoping reviews are broader and more exploratory in nature than full systematic reviews. They are often undertaken when an evidence base is expected to be either very large or have important limitations; the latter being the case for this review.
The NHS survey results showed that, although most units (82%) had a written protocol or guideline for treating extravasation injuries, a staging system for grading severity of extravasation injury was included in just over one-third of protocols or guidelines. Almost all responders indicated that peripheral lines were the access site most associated with extravasation injuries. In neonatal units, parenteral nutrition caused the largest proportion of extravasation injuries, whereas in principal oncology/haematology units, the largest proportion of injuries was due to the extravasation of vesicant chemotherapies.
The survey showed that the most frequently used intervention approaches were elevation of the affected area and analgesics. The results also revealed that, in most units, warm or cold compresses were rarely or never used. In neonatal units, there was notable variation regarding the use of occlusive dressings, ranging from always being used (8% of responses) to never being used (31% of responses). Variation in the use of saline irrigation (or wash-out), either with or without hyaluronidase, was also evident; these interventions seem to be usually or sometimes used in around half of the neonatal units, although they are never used in around one-third of units. Results for principal oncology/haematology units and PICUs were broadly similar to the neonatal unit results.
When asked about a future research study, most responders (65%) thought a RCT would be viable, although these results varied by setting: 83% of neonatal unit responses, 33% of principal oncology/haematology unit responses and 0% of PICUs. Almost all the responders who thought a RCT was viable mentioned one or more of the following treatments when asked which treatments they would most like to see studied: saline irrigation/wash-out, hyaluronidase and conservative management. Of those who thought a RCT was not viable, the reasons included too many variables which could affect outcomes, timeliness of treatment when using randomisation, low numbers of patients and unwillingness to deviate from current practice.
Strengths and limitations
The scoping review was performed using systematic, reproducible, transparent and robust methods. Our bibliographic database searches were comprehensive to allow identification of all relevant published studies and searches were also made to identify any unpublished studies. These methods minimised the possibility of publication or language biases affecting the review. The possibility of reviewer errors and biases affecting this review were minimised by performing review processes in duplicate. The sample for our NHS survey was large and diverse enough to be representative of NHS staff who treat extravasation injuries. The main limitation of the scoping review related to the evidence identified. Most studies were limited in helping to evaluate which treatments might be best and also in presenting ideas regarding which direction future research studies should take.
Patient (parent) and public involvement
Extravasation injuries are quite rare events and patient groups specifically in this area do not exist. However, one of our clinical team discussed this study with the parents of an infant who had suffered a severe extravasation injury. This proved to be useful in informing the survey content. For example, in the section of the survey where we asked questions about how frequently specific interventions were used, there was initially no question about use of analgesics. The importance of pain relief was emphasised by this parental input and, consequently, a question on analgesic use was added to the survey.
Future research on treatments for extravasation injuries
The survey results indicated that, across NHS neonatal units generally, there was optimism about randomised trial feasibility, although this was not the case for other types of units. The scoping review studies yielded little information about future research. Only three of the comparative or non-comparative studies mentioned issues relating to research study design. 31,39,40 In two studies, this was very brief: mention was made of the need for a prospective controlled study for confirmation of findings,40 and that a randomised trial was not possible because of the low incidence of injuries. 39 The authors of the third study commented, somewhat vaguely, that optimal management is uncertain because of ethics considerations limiting controlled research, although they added that a centralised register of extravasation events would be a useful means to monitor, assess and review outcomes. 31 One of the systematic reviews (of chemotherapy extravasations) also discussed the challenges of undertaking further research, noting key issues which may preclude the use of a randomised design. 164 These included the sporadic occurrence and low incidence of extravasations, and the complexity involved in controlling the many extraneous variables associated with extravasations: age, sex, comorbidities, type of infusate, site and volume of extravasation and time to intervention. The authors commented that the sample size required to properly control for these factors will probably be prohibitively large. Notwithstanding the discussion in this systematic review,164 the very limited insight on future research provided by the scoping review studies means that further exploration is needed. This is in relation to decisions regarding the study design, treatments to be studied, population to be studied and the outcome measures needed. Such decisions should not be made independently of each other. For example, a randomised trial would probably involve fewer, and more defined, interventions and a narrower population than an observational database study. As these two study designs, randomised trial and a database study, appear to be important options for any future study, the key issues relating to each will be discussed to help inform a decision on future research.
Randomised trials
Exploration of feasibility issues
Treatment delays and selection bias
Extravasation injuries require urgent treatment. The time gap between identifying and treating an injury is a key factor which determines important clinical outcomes. However, the process of recruiting and randomising patients into a clinical trial often results in treatment delays. Initial delays may arise when ascertaining whether or not a patient is eligible to participate. For those who are eligible, further delays may arise from the randomisation process. This is most likely to occur where the procedure of allocating treatment is performed in real time. For example, some delay would be inevitable when contacting a central randomisation service provider, either via the internet or by telephone. The scoping review identified that the time delay between injury identification and treatment varied widely across studies. Important questions when considering trial procedures are ‘what is the typical time gap between identification and treatment of an injury in the NHS?’, and, ‘is this short enough to accommodate a delay due to randomisation?’ (i.e. would the randomisation delay be acceptable or difficult to justify clinically?). Arguably, the most impressive results identified in the scoping review were from a study in which neonates with stage III and IV injuries were treated within just 10–30 minutes of injury. 4
A frequently used method of randomisation is the use of sequentially numbered, opaque, sealed envelopes containing randomly generated treatment allocations. Adoption of this method might minimise such delays, but this approach has been demonstrated to be prone to investigator selection bias. Reports of surgeons opening envelopes in order to subvert randomisation, and of trials using sequentially numbered, opaque, sealed envelopes being more likely to show statistically significant treatment effects than trials using more secure allocation methods, suggest that envelope-based methods should be used cautiously. 168 The risk of bias might only be reduced when the personnel with access to the envelopes are different from those actually recruiting participants. Of course, having an added layer of trial personnel involved in the recruitment process might itself add to treatment delays (and also to the administrative cost and burden of the trial). However, these concerns may have more limited relevance to trials performed in emergency or urgent care settings, where there is some evidence to suggest that the risks of selection bias may be low. 169
In trials where interventions exist in discrete packs and look indistinguishable from each another, or can be made to look so, a different type of time-saving method may overcome concerns about using envelopes. In this approach, randomisation identification labels which are pre-coded would be attached to ‘extravasation kits’ which would then be placed in order and allocated to patients sequentially. The pre-coded labels would be meaningless to the investigator, who would have only very restricted access to the randomisation coding system (e.g. where a serious adverse event was suspected). Heat-sealed bags could be used to reduce the risk of tampering and subverting the randomisation sequence. This type of method should obviate concerns about both selection bias and delays in receiving treatment as a result of randomisation because the randomisation process would simply involve the next kit being taken, used and recorded.
Nevertheless, many interventions cannot be code labelled as identical-looking, discrete packages, for example, different types of debridement or surgery. In these situations, a real-time randomisation process may be needed, which could lead to treatment delays. A possible alternative here might be the use of quasi-randomisation methods. This typically involves the use of a pre-defined participant or setting characteristic, such as date of birth or day of the month, to determine treatment allocation (e.g. odd days indicate treatment A and even days treatment B). The scoping review identified an old quasi-randomised trial reported by Brown et al. 55 which allocated treatment according to calendar month. Quasi-randomised studies often allocate treatments based on day of the month, but, given the scarcity of extravasation events, this idea of using alternate months seems a pragmatic approach to recruitment and treatment allocation. Quasi-randomisation would solve the time delay issue, but the selection bias issue would remain; however, as already noted, the risks of selection bias appear to be low in urgent care trials.
The requirement for urgent treatment also raises the issue of consent to participate, as this might also lead to treatment delays. However, in urgent care settings, a case can be made for using deferred consent, rather than prior consent. Deferred consent enables children to be included in trials without prior informed parental/carer consent, but requires such consent to be acquired as soon as possible for continued trial participation.
Recruitment
Perhaps the most important barriers to successfully executing a randomised trial are those which hinder the accrual of enough participants to yield meaningful and reliable results. Extravasation injuries are quite rare events which are also subject to variation, particularly in terms of patients (ages, comorbidities), causes (infusates), injury sites and severities and the speed at which injuries are detected and treated. Consequently, careful consideration would be needed when devising trial eligibility criteria to enable the recruitment of both a sufficiently homogeneous sample of participants and a sample which would be large enough to minimise the impact of chance differences across treatment groups in any of these factors. Failure to do so would increase the risk of false-positive trial results; small trials are more prone to yielding chance results than larger trials.
It is likely that a large number of participating hospital sites would be needed to allow adequate recruitment. Although the scoping review focused on children, it also involved an informal assessment of a broader range of papers on extravasation treatments in adults; however, only one randomised trial was identified. 170 The trial, reported as a conference abstract, compared different cooling treatments for doxorubicin extravasation; after 7 years, only 37 patients had been randomised (the study began in 1987 and ended in 1994). 171 This example serves to highlight the recruitment difficulties which might be encountered in any future RCT in children.
The discontinuation of randomised trials wastes research resources and also raises ethical concerns. A study of 1017 RCTs172 found that 25% were discontinued, the most frequent reason being poor recruitment (occurring in 10% of the 1017 trials). Trials discontinued because poor recruitment achieved a median percentage of target sample size of 41%. Trials with investigator sponsorship (compared with industry sponsorship) and trials with smaller planned sample sizes were at higher risk of discontinuation because of poor recruitment. A UK HTA study of 114 multicentre RCTs,173 which were funded by the Medical Research Council or the NHS (HTA), found that less than one-third of trials recruited their original target within the time originally specified and around one-third had extensions. The following factors were observed more frequently in trials that recruited successfully: having a dedicated trial manager, being a cancer or drug trial and use of treatments only available within the trial setting. Results from a survey of 181 principal investigators in a large US paediatric hospital174 found that the method of recruitment appeared to be the only significant and independent factor associated with achieving 80% or more of target enrolment; protocols that used recruitment in person were 4.6 times (95% confidence interval 1.3 to 15.9; p = 0.02) more likely to achieve 80% or more of their target enrolment when compared with those that used other recruitment methods. Utilisation of electronic data recorded in clinical practice databases or registries could reduce recruitment problems; therefore, randomised registry trials, sometimes referred to as pragmatic randomised electronic point of care trials, may be a useful approach and will be discussed in Database studies.
Small sample sizes are a common problem in paediatric trials, which, consequently, are often insufficiently powered to detect true treatment effects. Innovative approaches may, therefore, be considered to overcome this issue. 175 Sample size estimation can be a particular challenge when designing paediatric trials; this would be an issue for any trial of extravasation treatments because the effectiveness data available to inform such calculations will be minimal. However, in trials using a ‘sequential’ design, the sample size at the end of the trial is not known at the beginning; trial stopping rules are defined based on the accumulated data and, therefore, trials can end on the basis of efficacy or futility. This design may be suitable in trials where outcome results are available quickly in relation to the patient recruitment rate. Analyses from a systematic review of paediatric sequential trials176 (24 were published between 1963 and 2005) indicated a median reduction in sample size of 52 subjects (range −22 to 229 subjects) or 35% (range −42% to 90%) for sequential trials when comparing with a classical fixed sample size approach. Only nine trials reported sufficient information about assumptions to allow calculation of a corresponding fixed sample size. Thirteen of the 24 trials were performed in a NICU setting. Although for any given sequential trial it remains a possibility that the eventual sample size may turn out to be larger than the fixed sample size, it is evident that fewer patients are generally necessary to reach a conclusion, compared with a fixed sample size design, thus providing some ethical advantages. The unknown sample size at the start of sequential trials may be problematic for funders, although some trials pre specify a maximum number of participants. 176
Another strategy to address likely sample size problems is responsive–adaptive randomisation: a ‘play the winner’ approach that maximises allocation to the most effective treatment. Outcomes for previous participants affect subsequent treatment allocation probabilities. This design is, therefore, also limited to studies which assess outcomes quite quickly. However, the Food and Drug Administration177 has expressed concerns regarding the magnitude of the risk of bias and the size of the potential bias, and how to eliminate these effects, as they are not yet well understood for adaptive trial designs.
Blinding
A lack of blinding (also known as treatment masking) could be a source of bias in a trial of treatments for extravasation injuries. Although blinding would certainly be possible for some treatments, for example, hyaluronidase injections, where placebos could be used, it would not be viable for others, for example, when comparing saline flush-out with a conservative management intervention. In an extravasation trial of infants, there would be two mechanisms by which a trial might be biased by lack of blinding. First, via systematic differences between the care provided (e.g. cointerventions) to the different treatment groups (i.e. performance biases), and second, where outcomes assessors are aware of intervention assignments (i.e. detection biases). For example, detection bias may occur where it would be possible to distinguish between an injury treated with saline flush-out, which may still have puncture marks, and one treated with conservative management, which will not. With this in mind, it is not helpful that most outcomes in an extravasation trial would be subjective in nature (e.g. scarring, wound healing time). However, the risk of detection bias can be considered to be low if the outcome assessor used is an independent researcher, rather than a trial investigator; the latter may have treatment preferences, the former probably would not. Blinded assessment of photographs may also be a useful way of evaluating wounds over time. The use of parental assessment of outcomes could also be considered. An evaluation of performance bias can be made by recording, and later assessing, any deviations in the care provided which are beyond what would be expected in usual practice.
Treatments, populations and outcomes
The low rates and sporadic incidence of extravasation injuries are important issues to consider in any future research; this was evident from the survey where low incidence of injuries was noted several times as a barrier to a RCT, particularly any trial involving principal oncology/haematology units. As outlined in Chapter 1 Prevalence of extravasation injuries and risk factors, the incidence of extravasation injuries seems to be higher in preterm neonates (particularly those receiving an i.v. intervention at a peripheral site) than in other infants, making this, perhaps, the most viable population for a randomised trial. Restriction to parenteral nutrition infusions should further reduce population heterogeneity, although one survey respondent noted that, even here, there may be significant heterogeneity to overcome. Our survey results indicate that parenteral nutrition infusions at peripheral sites are the most frequent cause of extravasations in neonates. It is unclear, however, whether the preterm neonate population would be large enough for a randomised trial. The severities of injury to include in a trial would depend on the treatments being studied and on which paediatric injury grading scale is adopted. 3,15
For a preterm neonate population, the likely treatments to compare could be a specific form of conservative management compared with a saline flush-out technique. This is based on both the scoping review and survey results. The parameters used for saline flush-out can vary, such as the number of puncture points and the volume of saline; fewer puncture points and lower volumes (than is used for older infants) would seem appropriate in preterm neonates.
Although it is medically plausible to expect that prior hyaluronidase injection plus saline flush-out may be more effective than saline flush-out alone, there is little robust clinical research evidence to support this. The magnitude of any differences in outcome between these treatments could be small; therefore, a sizeable trial would be needed to allow such a difference to be demonstrated. Also, the appropriateness of using hyaluronidase in pre-term neonates is unclear. One study included in the scoping review noted that infiltration with hyaluronidase is an invasive procedure and the British National Formulary46 has advised caution in the use of hyaluronidase in infants and to control the speed and total volume of injection.
The degree of scarring following extravasation injury treatment will be an important outcome in any future study. In the scoping review, very few studies quantified scarring outcomes. Several measures exist for assessing scarring, but there is little consensus as to which is the optimal scale or tool to use. 178 A gold standard scar scale does not currently exist, although, ideally, such a scale should address cosmetic, functional and psychological sequelae. 179 Outcomes which involve parental evaluation, in addition to clinician evaluation, should also be considered for certain assessments, including scarring. The reliability and validity of outcome measures would need to be established for use in neonatal populations.
Database studies
Exploration of feasibility issues
A prospective database or registry study may be appropriate where a randomised trial is not considered to be viable for practical reasons. A database study would likely result in a larger sample than would be obtained in a RCT because of simpler recruitment processes and a broader population from which to recruit. The downside, or trade-off, with adopting such a non-randomised approach to comparing interventions is that the results would inherently be less reliable than those of a RCT; although, as previously discussed, RCTs which do not recruit enough participants may also produce unreliable results. The most important methodological difference between randomised and non-randomised studies arises as a result of confounding, caused by selection bias, which will often be encountered in non-randomised studies. Methods exist to adjust for confounding, such as regression analysis, propensity scoring, instrumental variables, stratification and matching, but it is unclear which methods are most appropriate in any given circumstance. 180 When aiming to generate believable estimates from non-randomised studies, it is necessary to identify the important confounding factors which need to be measured validly and precisely. 181 The risk of confounding arising from some factors might also be reduced by narrowing eligibility criteria. This would, however, limit the generalisability of the study results to wider patient groups.
However, we have already noted the extent of variation in important baseline characteristics in the studies identified in the scoping review: consideration would be needed regarding adjustments for variation in comorbidities, injury sites, methods of delivery, duration of i.v. therapy, the amount of fluid extravasated (very difficult to estimate) and the speed at which injuries are detected and treated. It could, perhaps, be argued that the latter four factors might be covered by use of a staging system for grading the severity of injuries. However, our survey results indicate that most units do not use a staging system to grade injury severity. Furthermore, variation is likely across units which do use such a system, since different approaches to grading injury severity have been published (see Chapter 1). An observational database study would also inevitably result in variation in the treatments given, even where they might be considered to be the same. For example, for flush-out techniques, variation exists in the number of puncture points made and the volume of saline used.
Nevertheless, a database study would be considerably cheaper to undertake than a randomised trial, especially if it were to utilise existing relevant database facilities such as the UK National Neonatal Research Database (NNRD). This database holds data entered by UK neonatal professionals. However, it does not currently routinely record data on extravasation injuries.
Randomised registry trials
If such data were recorded in a database in the future, the possibility of a randomised registry trial (also known as pragmatic randomised electronic point of care trials) could be explored, as the results of a UK survey of neonatal health professionals suggest this approach would be both feasible and acceptable in neonates. 182 Randomised registry trials are pragmatic randomised trials performed in usual clinical care conditions, which utilise routinely collected data. Trial interventions fall within accepted professional standards but, as yet, have uncertain comparative effectiveness. Ideally, the recruitment and follow-up procedures would be naturalistic and mimic actual clinical decisions and practices, except for the randomisation process. 183
These trials use the registry as a platform for recruitment and trial administration. Theoretically, this approach is appealing because it keeps the best aspects of both RCTs (i.e. robust, unbiased estimates of effectiveness) and registry studies (i.e. larger sample sizes) and, consequently, dispenses with some of the worst aspects (e.g. small samples with limited generalisability and estimates which are inherently unreliable). Importantly, registry RCTs should also be cheaper and quicker to undertake than conventional RCTs. A more detailed discussion of this trial design, including example trials, was published in 2016. 184
Some of the challenges to consider when planning a registry RCT include ensuring that the data are of high enough quality, consideration of blinding and the standardisation and adjudication needed for certain outcomes. 185 For any extravasation trial some key issues could include achieving a consistent use of a single staging system to grade injury severity when recruiting patients, the degree of standardisation/consistency needed when administering the studied treatments and the choice of outcome measures, which would need to be clinically practicable yet also demonstrate adequate reliability and validity.
Treatments, populations and outcomes
The treatments, populations and outcomes most viable for a randomised registry trial would be the same as those discussed in the previous section on randomised trials. But consideration should also be made regarding which treatments and populations might be studied in a prospective observational (i.e. non-randomised) database or registry study.
Usually, a key advantage of a prospective database study over a randomised trial is that a larger number of treatment approaches and a broader population could be studied. However, in this area of research, such benefits might, in reality, be quite small. Consider, for example, a population such as children receiving i.v. chemotherapy. The scarcity of chemotherapy extravasations, evident from the survey, coupled with the wide variation in infusates, subpopulations and injury treatment approaches, evident from reviews and guidelines, mean that accruing a cohort sufficiently large enough to produce meaningful comparative results may be very difficult. It is somewhat unclear to what extent this might be said for extravasations of other infusates such as calcium, contrast agents and blood. In mitigation, database studies by their very nature are able to accrue data over very many years. A database study might be useful for evaluations where there is less variation in the treatment options available. For example, for injuries which have become necrotic, comparison might be made of outcomes following different methods of debridement: mechanical, enzymatic and surgical.
Although beyond the scope of this review, research is also needed on interventions to prevent extravasation injuries. Ideally this would begin with a systematic review.
Summary
Careful thought is needed when considering any future comparative study of extravasation injury treatments. Decisions regarding the study design, treatments, population and outcome measures should not be made independently of each other. Some of the practicalities involved in undertaking a conventional RCT, such as recruiting adequate numbers, avoiding treatment delays and selection bias, could be difficult to overcome. Although a prospective observational database study would maximise the number of patients recruited, and eliminate concerns about treatment delays, its results would inherently be subject to uncertainty as a result of the likelihood of selection bias.
Several alternatives exist to a conventional RCT design, which still include a randomisation element. Perhaps the most promising is the randomised registry trial, which incorporates many of the best aspects of both conventional RCTs and observational database studies. Although this design is relatively new, and few trials have been performed, its relevance to a trial of treatments for extravasation injuries is worthy of exploration. However, a key relevant database, the UK NNRD, does not currently record data on extravasation injuries. Further issues to be considered in any randomised registry trial of neonates include the lack of a protocol or guideline for treating extravasation injuries in 25% of units, and the absence of the use of a staging system for grading injury severity in over half of the units which do have access to a protocol or guideline.
The low rates and sporadic incidence of extravasation injuries and population heterogeneity are key issues when considering the population to be studied. As such, preterm neonates receiving i.v. parenteral nutrition at a peripheral site may perhaps be the most viable population for any randomised trial. The main treatment candidates receive are a standardised conservative management intervention, saline flush-out without hyaluronidase and saline flush-out with hyaluronidase; the choice of treatment would depend on the injury severity grades chosen to be eligible for inclusion. A number of different methods exist for grading injury severity, with variation likely across the NHS; for example, some units do not formally grade injury severity. A paucity of standardised outcome measures used in previous studies in neonates is also a concern. Outcome measures used in a future study would need to be clinically practicable yet also demonstrate adequate reliability and validity.
Chapter 5 Conclusions
Although studies exist that, together, cover a wide range of treatments for extravasation injuries, most studies are small and lack comparator groups. The studies are also very varied in terms of patient, intervention and outcome characteristics. The quality of evidence overall is, therefore, very low. Consequently, there is uncertainty about which treatments are most promising, particularly with respect to treating earlier-stage injuries. Notwithstanding the evidence limitations, the results of studies of flush-out techniques suggest that these treatments may be worthy of further research. This finding was echoed in the NHS survey results, with flush-out techniques, hyaluronidase and conservative management frequently suggested as being the treatments where further study would be most worthwhile.
In planning a future comparative study of extravasation injury treatments, population heterogeneity and low rates and sporadic incidence of injuries are key issues. The most viable population for any randomised trial may, therefore, be preterm neonates receiving i.v. parenteral nutrition at a peripheral site. However, a paucity of standardised relevant outcome measures used in previous studies in neonates is a concern. Outcome measures used in a future study would need to be clinically practicable, yet also demonstrate adequate reliability and validity. Some of the practicalities involved in undertaking a conventional RCT, such as recruiting adequate numbers, avoiding treatment delays and selection bias, could be difficult to overcome. Although a prospective observational database study would maximise the number of patients recruited, and eliminate concerns about treatment delays, its results would inherently be subject to uncertainty because of the likelihood of selection bias. An alternative to a conventional RCT design is the randomised registry trial, which incorporates many of the best aspects of both conventional RCTs and observational database studies. However, a key relevant database – the UK NNRD– does not currently record data on extravasation injuries. Further issues to be considered in any randomised registry trial of neonates include the lack of a protocol or guideline for treating extravasation injuries in 25% of units, and the absence of the use of a staging system for grading injury severity in over half of the units which do have access to a protocol or guideline.
Acknowledgements
We thank both Georgina Mackenzie and Claire Khouja from Centre for Reviews and Dissemination for obtaining papers from The British Library, and Claire Khouja for checking the data extracted for case reports. We thank Nigel Davies from the British Association of Perinatal Medicine for distributing the survey link in an e-mailed newsletter. We thank Alexis Llewellyn and Kristina Dietz from Centre for Reviews and Dissemination for translating papers published in French and German.
Contributions of authors
Mark Corbett (Research Fellow) wrote the first draft of the protocol, led on designing and undertaking the scoping review and survey, and contributed to writing all sections of the report.
David Marshall (Research Fellow) screened studies and extracted data for the scoping review and contributed to the writing of the report.
Melissa Harden (Information Specialist) contributed to the protocol, developed the search strategies, conducted a range of searches to locate studies and wrote the sections of the report relating to the literature searches.
Sam Oddie (Consultant Neonatologist) contributed to the protocol, the survey design and distribution, and the writing of the report.
Robert Phillips (Senior Clinical Academic) contributed to the protocol, the survey design and distribution, and the writing of the report.
William McGuire (Professor of Child Health) contributed to the protocol, the survey design and distribution, and the writing of the report.
Data-sharing statement
All of the available scoping review data are included in this report. Most of the survey questionnaire results data are also included either in the main report or in the appendices. All requests for other data should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Pérez Fidalgo JA, García Fabregat L, Cervantes A, Margulies A, Vidall C, Roila F. ESMO Guidelines Working Group . Management of chemotherapy extravasation: ESMO-EONS Clinical Practice Guidelines. Ann Oncol 2012;23:vii167-73. https://doi.org/10.1093/annonc/mds294.
- Extravasation and Infiltration. London: Great Ormond Street Hospital for Children; n.d.
- Amjad I, Murphy T, Nylander-Housholder L, Ranft A. A new approach to management of intravenous infiltration in pediatric patients: pathophysiology, classification, and treatment. J Infus Nurs 2011;34:242-9. https://doi.org/10.1097/NAN.0b013e31821da1b3.
- Kostogloudis N, Demiri E, Tsimponis A, Dionyssiou D, Ioannidis S, Chatziioannidis I, et al. Severe extravasation injuries in neonates: a report of 34 cases. Pediatr Dermatol 2015;32:830-5. https://doi.org/10.1111/pde.12664.
- Wilkins CE, Emmerson AJ. Extravasation injuries on regional neonatal units. Arch Dis Child Fetal Neonatal Ed 2004;89:F274-5. https://doi.org/10.1136/adc.2003.028241.
- Paquette V, McGloin R, Northway T, Dezorzi P, Singh A, Carr R. Describing Intravenous Extravasation in children (DIVE study). Can J Hosp Pharm 2011;64:340-5. https://doi.org/10.4212/cjhp.v64i5.1069.
- Hee HI, Lim SL, Tan SS. Infusion technology: a cause for alarm. Paediatr Anaesth 2002;12:780-5. https://doi.org/10.1046/j.1460-9592.2002.00993.x.
- Clifton-Koeppel R. Wound care after peripheral intravenous extravasation: what is the evidence?. Newborn Infant Nurs Rev 2006;6:202-11. https://doi.org/10.1053/j.nainr.2006.10.001.
- Thyoka M. Clinical negligence claims in pediatric surgery in England: pattern and trends. Eur J Pediatr Surg 2015;25:66-70. https://doi.org/10.1055/s-0034-1395485.
- Raine JE, Williams K, Bonser J. An analysis of successful litigation claims in children. Arch Dis Child 2011;96. https://doi.org/10.1136/adc.2011.212563.138.
- Bhananker SM, Liau DW, Kooner PK, Posner KL, Caplan RA, Domino KB. Liability related to peripheral venous and arterial catheterization: a closed claims analysis. Anesth Analg 2009;109:124-9. https://doi.org/10.1213/ane.0b013e31818f87c8.
- Roth D. Legally speaking. Pediatric infiltration and extravasation. J Assoc Vasc Access 2006;11. https://doi.org/10.2309/java.11-1-5.
- Roth D. Extravasation injuries of peripheral veins: a basis for litigation?. J Vasc Access Devices 2003;8:13-9. https://doi.org/10.2309/108300803775307729.
- Millam DA. Managing complications of i.v. therapy (continuing education credit). Nursing 1988;18:34-43. https://doi.org/10.1097/00152193-198803000-00020.
- Simona R. A pediatric peripheral intravenous infiltration assessment tool. J Infus Nurs 2012;35:243-8. https://doi.org/10.1097/NAN.0b013e31825af323.
- Hanrahan K. Hyaluronidase for treatment of intravenous extravasations: implementation of an evidence-based guideline in a pediatric population. J Spec Pediatr Nurs 2013;18:253-62. https://doi.org/10.1111/jspn.12035.
- Gopalakrishnan PN, Goel N, Banerjee S. Saline irrigation for the management of skin extravasation injury in neonates. Cochrane Database Syst Rev 2012;2. https://doi.org/10.1002/14651858.CD008404.pub2.
- Bellin MF, Jakobsen JA, Tomassin I, Thomsen HS, Morcos SK, Thomsen HS, et al. Contrast medium extravasation injury: guidelines for prevention and management. Eur Radiol 2002;12:2807-12. https://doi.org/10.1007/s00330-002-1630-9.
- Flemmer L, Chan JS. A pediatric protocol for management of extravasation injuries. Pediatr Nurs 1993;19:355-8.
- Schulmeister L. Extravasation management: clinical update. Semin Oncol Nurs 2011;27:82-90. https://doi.org/10.1016/j.soncn.2010.11.010.
- Gault DT. Extravasation injuries. Br J Plast Surg 1993;46:91-6. https://doi.org/10.1016/0007-1226(93)90137-Z.
- Harrold K, Gould D, Drey N. The efficacy of saline washout technique in the management of exfoliant and vesicant chemotherapy extravasation: a historical case series report. Eur J Cancer Care 2013;22:169-78. https://doi.org/10.1111/ecc.12023.
- Pare JR, Moore CL. Intravenous infiltration resulting in compartment syndrome: a systematic review [published online ahead of print July 31 2015]. J Patient Saf 2015. https://doi.org/10.1097/PTS.0000000000000233.
- Beall V, Hall B, Mulholland JT, Gephart SM. Neonatal extravasation: an overview and algorithm for evidence-based treatment. Newborn Infant Nurs Rev 2013;13:189-95. https://doi.org/10.1053/j.nainr.2013.09.001.
- Pettit J, Hughes K. Neonatal intravenous therapy practices. J Vasc Access Devices 1999;4:7-16. https://doi.org/10.2309/108300899775703689.
- Restieaux M, Maw A, Broadbent R, Jackson P, Barker D, Wheeler B. Neonatal extravasation injury: prevention and management in Australia and New Zealand – a survey of current practice. BMC Pediatr 2013;13. https://doi.org/10.1186/1471-2431-13-34.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-69.
- Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksy and O’Malley’s framework. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-48.
- Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D. An evidence-based approach to scoping reviews. Worldviews Evid Based Nurs 2016;13:118-23. https://doi.org/10.1111/wvn.12144.
- Ching DL, Wong KY, Milroy C. Paediatric extravasation injuries: a review of 69 consecutive patients. Int J Surg 2014;12:1036-7. https://doi.org/10.1016/j.ijsu.2014.08.355.
- Harris PA, Bradley S, Moss AL. Limiting the damage of iatrogenic extravasation injury in neonates. Plast Reconstr Surg 2001;107:893-4. https://doi.org/10.1097/00006534-200103000-00053.
- Onesti MG, Carella S, Maruccia M, Ciotti M, Scuderi N. The use of hyalomatrix PA in the treatment of extravasation affecting premature neonates. Plast Reconstr Surg 2012;129:219e-221e. https://doi.org/10.1097/PRS.0b013e3182365e16.
- Nandiolo-Anelone KR, Allah KC, Cissé L, Bankolé SR, Oulaï M, Aké AY. Extravasation injuries in newborns: our experience about 15 cases. Chir Main 2014;33:44-50. https://doi.org/10.1016/j.main.2013.11.007.
- Mu SC, Lin CH, Sung TC. Calcinosis cutis following extravasation of calcium gluconate in neonates. Acta Paediatr Taiwan 1999;40:34-5.
- Moon HS, Burm JS, Yang WY, Kang SY. Prognosis of full-thickness skin defects in premature infants. Arch Plast Surg 2012;39:463-8. https://doi.org/10.5999/aps.2012.39.5.463.
- An B, Ning H. Accidental infusion leakage at subgalea in infants: report of 6 cases. Int J Clin Exp Med 2015;8:11943-6.
- Wang CL, Cohan RH, Ellis JH, Adusumilli S, Dunnick NR. Frequency, management, and outcome of extravasation of nonionic iodinated contrast medium in 69,657 intravenous injections. Radiology 2007;243:80-7. https://doi.org/10.1148/radiol.2431060554.
- Sawatzky-Dickson D, Bodnaryk K. Neonatal intravenous extravasation injuries: evaluation of a wound care protocol. Neonatal Netw 2006;25:13-9. https://doi.org/10.1891/0730-0832.25.1.13.
- Sung KY, Lee SY. Nonoperative management of extravasation injuries associated with neonatal parenteral nutrition using multiple punctures and a hydrocolloid dressing. Wounds 2016;28:145-51.
- Andrés AM, Burgos L, López Gutiérrez JC, Encinas JL, Díaz M, Rivas S, et al. Treatment protocol for extravasation lesions. Cir Pediatr 2006;19:136-9.
- Casanova D, Bardot J, Magalon G. Emergency treatment of accidental infusion leakage in the newborn: report of 14 cases. Br J Plast Surg 2001;54:396-9. https://doi.org/10.1054/bjps.2001.3593.
- Wong KY, Ching D, Milroy C. Paediatric Extravasation Injuries: A Review of 69 Consecutive Patients n.d.
- Harris PA, Moss AL. Management of extravasation injuries. ANZ J Surg 2002;72. https://doi.org/10.1046/j.1445-2197.2002.02496.x.
- Cochran ST, Bomyea K, Kahn M. Treatment of iodinated contrast material extravasation with hyaluronidase. Acad Radiol 2002;9:544-6. https://doi.org/10.1016/S1076-6332(03)80288-X.
- Yan YM, Fan QL, Li AQ, Chen JL, Dong FF, Gong M. Treatment of cutaneous injuries of neonates induced by drug extravasation with hyaluronidase and hirudoid. Iran J Pediatr 2014;24:352-8.
- Crowther DM, Buck ML, McCarthy MW, Barton VW. Improving pediatric adverse drug event reporting through clinical pharmacy services. J Pediatr Pharmacol Ther 2011;16:285-90. https://doi.org/10.5863/1551-6776-16.4.285.
- Falcone PA, Barrall DT, Jeyarajah DR, Grossman JA. Nonoperative management of full-thickness intravenous extravasation injuries in premature neonates using enzymatic debridement. Ann Plast Surg 1989;22:146-9. https://doi.org/10.1097/00000637-198902000-00010.
- Linder RM, Upton J, Osteen R. Management of extensive doxorubicin hydrochloride extravasation injuries. J Hand Surg Am 1983;8:32-8. https://doi.org/10.1016/S0363-5023(83)80048-3.
- Sivrioğlu N, Irkören S. Versajet hydrosurgery system in the debridement of skin necrosis after Ca gluconate extravasation: report of 9 infantile cases. Acta Orthop Traumatol Turc 2014;48:6-9. https://doi.org/10.3944/AOTT.2014.2941.
- Upton J, Mulliken JB, Murray JE. Major intravenous extravasation injuries. Am J Surg 1979;137:497-506. https://doi.org/10.1016/0002-9610(79)90121-1.
- von Heimburg D, Pallua N. Early and late treatment of iatrogenic injection damage. Chirurg 1998;69:1378-82. https://doi.org/10.1007/s001040050588.
- Weiss Y, Ackerman C, Shmilovitz L. Localized necrosis of scalp in neonates due to calcium gluconate infusions: a cautionary note. Pediatrics 1975;56:1084-6.
- Linder RM, Upton J. Prevention of extravasation injuries secondary to doxorubicin. Postgrad Med 1985;77:105-9. https://doi.org/10.1080/00325481.1985.11698920.
- Brown AS, Hoelzer DJ, Piercy SA. Skin necrosis from extravasation of intravenous fluids in children. Plast Reconstr Surg 1979;64:145-50. https://doi.org/10.1097/00006534-197908000-00002.
- Hanrahan K. Evidence-Based Practice Guideline: Hyaluronidase for Treatment of Intravenous Extravasations. Iowa City, IA: University of Iowa College of Nursing; 2012.
- Ghanem AM, Mansour A, Exton R, Powell J, Mashhadi S, Bulstrode N, et al. Childhood extravasation injuries: improved outcome following the introduction of hospital-wide guidelines. J Plast Reconstr Aesthet Surg 2015;68:505-18. https://doi.org/10.1016/j.bjps.2014.12.029.
- Abraham MB, van der Westhuyzen J, Khanna V. Arginine extravasation leading to skin necrosis. J Paediatr Child Health 2012;48:E96-7. https://doi.org/10.1111/j.1440-1754.2011.02074.x.
- Altan E, Tutar O, Senaran H, Aydın K, Acar MA, Yalçın L. Forearm compartment syndrome of a newborn associated with extravasation of contrast agent. Case Rep Orthop 2013;2013. https://doi.org/10.1155/2013/638159.
- Altmann S, Damert HG, Schneider W. Clinical manifestation of extravasation caused by infusion and its therapeutic management. Zentralbl Chir 2014;139:83-8. https://doi.org/10.1055/s-0031-1271432.
- Amano H, Nagai Y, Kowase T, Ishikawa O. Cutaneous necrosis induced by extravasation of arginine monohydrochloride. Acta Derm Venereol 2008;88:310-11. https://doi.org/10.2340/00015555-0420.
- Amaya R. Use of active Leptospermum honey (ALH) and dehydrated amniotic membrane allograft (DAMA) to manage extravasation wounds in neonates. J Wound Ostomy Continence Nurs 2016;43.
- Amhaz HH, Buretta K, Jooste EH, Machovec K, Marcus JR, Ames WA. Upper extremity peripheral intravenous line infiltration with concomitant loss of pulses treated with lipoaspiration: a case report. A A Case Rep 2016;7:185-7. https://doi.org/10.1213/XAA.0000000000000381.
- Aribit F, Laville J, Baron J. Extravasation injuries and subcutaneous aspiration in children. Rev Chir Orthop Reparatrice Appar Mot 2000;86:87-8.
- Baker GL, Franklin JD. Management of arginine monohydrochloride extravasation in the forearm. South Med J 1991;84:381-4. https://doi.org/10.1097/00007611-199103000-00018.
- Bassi E, Lonati D, Pandolfi R, Gatti M, Jolliffe VM, Del Forno C. Case of skin necrosis due to arginine monohydrochloride extravasation. J Dermatol 2007;34:198-200. https://doi.org/10.1111/j.1346-8138.2007.00249.x.
- Bhosale GP, Shah VR. Extravasation injury due to dopamine infusion leading to dermal necrosis and gangrene. J Anaesthesiol Clin Pharmacol 2012;28:534-5. https://doi.org/10.4103/0970-9185.101954.
- Borman H, Tuncali D, Apak A, Kostakoğlu N. Progressive gangrene of the hand following extravasation of antibiotics associated with hereditary resistance to activated protein C. Ann Plast Surg 1998;41:194-6. https://doi.org/10.1097/00000637-199808000-00014.
- Boyar V, Handa D, Clemens K, Shimborske D. Clinical experience with Leptospermum honey use for treatment of hard to heal neonatal wounds: case series. J Perinatol 2014;34:161-3. https://doi.org/10.1038/jp.2013.158.
- Broom A, Schur MD, Arkader A, Flynn J, Gornitzky A, Choi PD. Compartment syndrome in infants and toddlers. J Child Orthop 2016;10:453-60. https://doi.org/10.1007/s11832-016-0766-0.
- Chait LA, Dinner MI. Ulceration caused by cytotoxic drugs. S Afr Med J 1975;49:1935-6.
- Chen TK, Yang CY, Chen SJ. Calcinosis cutis complicated by compartment syndrome following extravasation of calcium gluconate in a neonate: a case report. Pediatr Neonatol 2010;51:238-41. https://doi.org/10.1016/S1875-9572(10)60045-9.
- Chiang MC, Chou YH, Wang CR, Huang CC. Extravasation of calcium gluconate concomitant with osteomyelitis in a neonate. Acta Paediatr Taiwan 2004;45:35-7.
- Ching DL, Wong KY, Milroy C. Latrogenic calcinosis cutis following a neonatal extravasation injury. Br J Hosp Med 2014;75. https://doi.org/10.12968/hmed.2014.75.5.295.
- Cho KY, Lee SJ, Burm JS, Park EA. Successful combined treatment with total parenteral nutrition fluid extravasation injuries in preterm infants. J Korean Med Sci 2007;22:588-94. https://doi.org/10.3346/jkms.2007.22.3.588.
- Cohan RH, Dunnick NR, Leder RA, Baker ME. Extravasation of nonionic radiologic contrast media: efficacy of conservative treatment. Radiology 1990;176:65-7. https://doi.org/10.1148/radiology.176.1.2353113.
- D’Acunto C, Neri I, Purpura V, Orlandi C, Melandri D. Extravasation injury of balanced electrolyte solution simulates the clinical condition of necrotizing fasciitis: a case report. J Pediatr Surg Case Rep 2015;3:466-8. https://doi.org/10.1016/j.epsc.2015.09.006.
- Davé AL. Third-degree burn following use of microwave-heated cryogel pack. Clin Pediatr 1993;32:191-2. https://doi.org/10.1177/000992289303200318.
- Davies J, Gault D, Buchdahl R. Preventing the scars of neonatal intensive care. Arch Dis Child Fetal Neonatal Ed 1994;70:F50-1. https://doi.org/10.1136/fn.70.1.F50.
- Denkler KA, Cohen BE. Reversal of dopamine extravasation injury with topical nitroglycerin ointment. Plast Reconstr Surg 1989;84:811-13. https://doi.org/10.1097/00006534-198911000-00017.
- Domizio S, Puglielli C, Barbante E, Sabatino G, Amerio P, Artese O, et al. Calcinosis cutis in a newborn caused by minimal calcium gluconate extravasation. Int J Dermatol 2006;45:1439-40. https://doi.org/10.1111/j.1365-4632.2006.02693.x.
- Dunn D, Wilensky M. Median and ulnar nerve palsies after infiltration of intravenous fluid. South Med J 1984;77. https://doi.org/10.1097/00007611-198410000-00044.
- Duray PH, Cuono CB, Madri JA. Demonstration of cutaneous doxorubicin extravasation by rhodamine-filtered fluorescence microscopy. J Surg Oncol 1986;31:21-5. https://doi.org/10.1002/jso.2930310104.
- Eckersall SJ, Spreadbury PL. Severe forearm oedema after intravenous infusion with a IMED 960 infusion pump. Eur J Anaesthesiol 1996;13:39-41. https://doi.org/10.1097/00003643-199601000-00008.
- Eroglu A, Uzunlar H. Forearm compartment syndrome after intravenous mannitol extravasation in a carbosulfan poisoning patient. J Toxicol Clin Toxicol 2004;42:649-52. https://doi.org/10.1081/CLT-200026975.
- Garcia-Alvarez F, Bello ML, Albareda J, Seral F. Neonatal tumoration in the secondary to calcium extravasation. Rev Esp Pediatr 1999;55:279-80.
- Gibboney W, Lemons JA. Necrotizing fasciitis of the scalp in neonates. Am J Perinatol 1986;3:58-60. https://doi.org/10.1055/s-2007-999829.
- Govind B, Tete PI, Thomas N. Percutaneous central line extravasation masquerading as an abscess. Indian Pediatr 2014;51:309-10. https://doi.org/10.1007/s13312-014-0384-1.
- Grabois FS, Voievdca T, Aqcuavita A, Kizlansky V, Saint Genez D, Vidaurreta S. Use of sterile petrolatum for extravasation injury in a premature infant. Arch Argent Pediatr 2008;106:533-5. https://doi.org/10.1590/S0325-00752008000600011.
- Handler EG. Superficial compartment syndrome of the foot after infiltration of intravenous fluid. Arch Phys Med Rehabil 1990;71:58-9.
- Hankin FM, Louis DS. Surgical management of doxorubicin (Adriamycin) extravasation. J Pediatr Orthop 1984;4:96-9. https://doi.org/10.1097/01241398-198401000-00018.
- Harb A, Sawyer A, Pandya A. Erythromycin extravasation mimicking necrotising fasciitis in the infant. Eur J Plast Surg 2010;33:159-61. https://doi.org/10.1007/s00238-010-0401-0.
- Hasija N, Hazarika AJ, Sokhal N, Kumar S. Tissue necrosis of hand caused by phenytoin extravasation: An unusual occurrence. Saudi J Anaesth 2014;8:309-10. https://doi.org/10.4103/1658-354X.130766.
- Hey DM, Koontz SE. Azithromycin extravasation in a pediatric patient. J Pharm Technol 2005;21:83-6. https://doi.org/10.1177/875512250502100206.
- Hironaga M, Fujigaki T, Tanaka S. Cutaneous calcinosis in a neonate following extravasation of calcium gluconate. J Am Acad Dermatol 1982;6:392-5. https://doi.org/10.1016/S0190-9622(82)70035-0.
- Hirsch SD, Powers JM, Rhodes JL. Neonatal soft tissue reconstruction using a bioengineered skin substitute. J Craniofac Surg 2017;28:489-91. https://doi.org/10.1097/SCS.0000000000003346.
- Hooke MC. Clinical nurse specialist and evidence-based practice: managing anthracycline extravasation. J Pediatr Oncol Nurs 2005;22:261-4. https://doi.org/10.1177/1043454205279289.
- Kameo SY, Silva GM, Sawada NO, Hardman GL. Hyaluronidase post extravasation of intravenous vincristine: use in children with cancer. J Nurs UFPE 2015;9:9239-45.
- Khan I, Rizvi SSA, Malik I, Weinberger B, Puvabanditsin S, Hegyi T. Extravasation of intravenous fluid in a preterm neonate. Consultant 2014;54:188-90.
- Kishi C, Amano H, Shimizu A, Nagai Y, Ishikawa O. Cutaneous necrosis induced by extravasation of hydroxyzine. Eur J Dermatol 2014;24:131-2. https://doi.org/10.1684/ejd.2013.2251.
- Kuensting LL. Treatment of intravenous infiltration in a neonate. J Pediatr Health Care 2010;24:184-8. https://doi.org/10.1016/j.pedhc.2010.02.001.
- Kumar RJ, Pegg SP, Kimble RM. Management of extravasation injuries. ANZ J Surg 2001;71:285-9.
- Lee HJ, Kwon SH, Choi JW, Park KC, Youn SW, Huh CH, et al. The management of infantile extravasation injury using maternal platelet-rich plasma. Pediatr Dermatol 2013;30:e114-7. https://doi.org/10.1111/j.1525-1470.2012.01815.x.
- Lehr VT, Lulic-Botica M, Lindblad WJ, Kazzi NJ, Aranda JV. Management of infiltration injury in neonates using duoderm hydroactive gel. Am J Perinatol 2004;21:409-14. https://doi.org/10.1055/s-2004-835309.
- Leung PC, Cheng CY. Extensive local necrosis following the intravenous use of X-ray contrast medium in the upper extremity. Br J Radiol 1980;53:361-4. https://doi.org/10.1259/0007-1285-53-628-361.
- Llinares ME, Bermúdez M, Fuster JL, Diaz MS, Gonzalez CM. Toxicity to topical dimethyl sulfoxide in a pediatric patient with anthracycline extravasation. Pediatr Hematol Oncol 2005;22:49-52.
- Martin PH, Carver N, Petros AJ. Use of liposuction and saline washout for the treatment of extensive subcutaneous extravasation of corrosive drugs. Br J Anaesth 1994;72:702-4.
- Meszes A, Tálosi G, Máder K, Orvos H, Kemény L, Csoma ZR. Lesions requiring wound management in a central tertiary neonatal intensive care unit. World J Pediatr 2017;13:165-72. https://doi.org/10.1007/s12519-016-0070-6.
- Mohr LD, Reyna R, Amaya R. Neonatal case studies using active Leptospermum honey. J Wound Ostomy Continence Nurs 2014;41:213-18. https://doi.org/10.1097/WON.0000000000000028.
- Morrison WA, Hurley JV, Ahmad TS, Webster HR. Scar formation after skin injury to the human foetus in utero or the premature neonate. Br J Plast Surg 1999;52:6-11.
- Mukherjee GD, Guharay BN. Digital gangrene and skin necrosis following extravasation of infusion fluid. J Indian Med Assoc 1977;68:77-9.
- Nissim L, Gilbertson-Dahdal D. An unusual complication of an infiltrated intravenous catheter: heterotopic ossification in a newborn. J Radiol Case Rep 2008;2:13-5. https://doi.org/10.3941/jrcr.v2i2.30.
- Onesti MG, Carella S, Maruccia M, Marchese C, Fino P, Scuderi N. A successful combined treatment with dermal substitutes and products of regenerative medicine in a patient affected by extravasation injury from hypertonic solution. In Vivo 2012;26:139-42.
- O’Reilly C, McKay FM, Duffty P, Lloyd DJ. Glyceryl trinitrate in skin necrosis caused by extravasation of parenteral nutrition. Lancet 1988;2:565-6.
- Ozcan A, Baratalı E, Meral O, Ergul AB, Aslaner H, Coskun R, et al. Bullous dermatitis and skin necrosis developing after adrenalin extravasation. Eurasian J Med 2015;47:226-8. https://doi.org/10.5152/eurasianjmed.2015.58.
- Pantelides NM, Shah AK. Extravasation injury: a simple technique to maintain limb elevation within a Neonatal Intensive Care Unit. J Neonatal Nurs 2013;19:243-5.
- Park HJ, Kim KH, Lee HJ, Jeong EC, Kim KW, Suh DI. Compartment syndrome due to extravasation of peripheral parenteral nutrition: extravasation injury of parenteral nutrition. Korean J Pediatr 2015;58:454-8. https://doi.org/10.3345/kjp.2015.58.11.454.
- Phillips RA, Andrades P, Grant JH, Ray PD. Deep dopamine extravasation injury: a case report. J Plast Reconstr Aesthet Surg 2009;62:e222-4. https://doi.org/10.1016/j.bjps.2008.11.064.
- Raffaella C, Annapaola C, Tullio I, Angelo R, Giuseppe L, Simone C. Successful treatment of severe iatrogenic calcinosis cutis with intravenous sodium thiosulfate in a child affected by T-acute lymphoblastic leukemia. Pediatr Dermatol 2009;26:311-15. https://doi.org/10.1111/j.1525-1470.2008.00776.x.
- Ravenel SD. Cellulitis from extravasation of calcium gluconate simulating osteomyelitis. Am J Dis Child 1983;137:402-3.
- Reilly JJ, Neifeld JP, Rosenberg SA. Clinical course and management of accidental adriamycin extravasation. Cancer 1977;40:2053-6.
- Reynolds BC. Neonatal extravasation injury: case report. Infant 2007;3:230-2.
- Roberts JR. Cutaneous and subcutaneous complications of calcium infusions. JACEP 1977;6:16-20.
- Rosales CM, Jackson MA, Zwick D. Malassezia furfur meningitis associated with total parenteral nutrition subdural effusion. Pediatr Dev Pathol 2004;7:86-90. https://doi.org/10.1007/s10024-003-4030-5.
- Roth W, Eschertzhuber S, Gardetto A, Keller C. Extravasation of propofol is associated with tissue necrosis in small children. Paediatr Anaesth 2006;16:887-9.
- Rustogi R, Mill J, Fraser JF, Kimble RM. The use of Acticoat in neonatal burns. Burns 2005;31:878-82.
- Salameh Y, Shoufani A. Full-thickness skin necrosis after arginine extravasation – a case report and review of literature. J Pediatr Surg 2004;39:e9-11.
- Samiee-Zafarghandy S, van den Anker JN, Ben Fadel N. Topical nitroglycerin in neonates with tissue injury: a case report and review of the literature. Paediatr Child Health 2014;19:9-12.
- Sanpera I, Fixsen JA, Hill RA. Injuries to the physis by extravasation. A rare cause of growth plate arrest. J Bone Joint Surg Br 1994;76:278-80.
- Santoshi JA, Pallapati SC, Thomas BP. Hand contracture: an unusual sequel of intravenous fluid extravasation in the neonatal period. J Postgrad Med 2008;54:244-5.
- Schäfer T, Kukies S, Stokes TH, Levin LS, Donatucci CF, Erdmann D. The prepuce as a donor site for reconstruction of an extravasation injury to the foot in a newborn. Ann Plast Surg 2005;54:664-6.
- Schie JC, Goodman KL. Treatment of neonatal extravasation injuries using non-contact, low-frequency ultrasound: development of a new treatment protocol. Newborn Infant Nurs Rev 2013;13:42-7.
- Schumacher HR, Osterman AL, Choi SJ, Weisz PB. Calcinosis at the site of leakage from extravasation of calcium disodium edetate intravenous chelator therapy in a child with lead poisoning. Clin Orthop Relat Res 1987;219:221-5.
- Sharief N, Goonasekera C. Soft tissue injury associated with intravenous phenytoin in a neonate. Acta Paediatr 1994;83:1218-19.
- Shenaq SM, Abbase EH, Friedman JD. Soft-tissue reconstruction following extravasation of chemotherapeutic agents. Surg Oncol Clin N Am 1996;5:825-45.
- Sindal MD, Nakhwa CP. Metastatic Serratia endophthalmitis associated with extravasation injury in a preterm neonate. Oman J Ophthalmol 2015;8:114-16. https://doi.org/10.4103/0974-620X.159261.
- Siu SLY, Kwong KL, Poon SST, So KT. The use of hyaluronidase for treatment of extravasations in a premature infant. HK J Paediatr 2007;12:130-2.
- Siwy BK, Sadove AM. Acute management of dopamine infiltration injury with Regitine. Plast Reconstr Surg 1987;80:610-12.
- Sokol DK, Dahlmann A, Dunn DW. Hyaluronidase treatment for intravenous phenytoin extravasation. J Child Neurol 1998;13:246-7. https://doi.org/10.1177/088307389801300512.
- Sonohata M, Akiyama T, Fujita I, Asami A, Mawatari M, Hotokebuchi T. Neonate with calcinosis cutis following extravasation of calcium gluconate. J Orthop Sci 2008;13:269-72. https://doi.org/10.1007/s00776-007-1217-z.
- Sonohata M, Asami A, Tsunoda K, Hotokebuchi T. Purple glove syndrome associated with intravenous phenytoin administration in a patient with severe mental and motor retardation. J Orthop Sci 2006;11:409-11. https://doi.org/10.1007/s00776-006-1024-y.
- Soon SL, Chen S, Warshaw E, Caughman SW. Calcinosis cutis as a complication of parenteral calcium gluconate therapy. J Pediatr 2001;138.
- Stahl S, Lerner A. Compartment syndrome of the forearm following extravasation of mannitol in an unconscious patient. Acta Neurochir 2000;142:945-6.
- Spenny ML, Moen KY, Dinulos JG. Acute bullous eruption with compartment syndrome due to intravenous infiltration. Arch Dermatol 2004;140:798-800. https://doi.org/10.1001/archderm.140.7.798.
- Subedi A, Bhattarai B, Biswas BK, Khatiwada S. Complex Regional Pain Syndrome (CRPS type-1) in an adolescent following extravasation of dextrose containing fluid – an underdiagnosed case. Korean J Pain 2011;24:112-14. https://doi.org/10.3344/kjp.2011.24.2.112.
- Subhani M, Sridhar S, DeCristofaro JD. Phentolamine use in a neonate for the prevention of dermal necrosis caused by dopamine: a case report. J Perinatol 2001;21:324-6. https://doi.org/10.1038/sj.jp.7200493.
- Talbot SG, Rogers GF. Pediatric compartment syndrome caused by intravenous infiltration. Ann Plast Surg 2011;67:531-3. https://doi.org/10.1097/SAP.0b013e3182085915.
- Tilden SJ, Craft JC, Cano R, Daum RS. Cutaneous necrosis associated with intravenous nafcillin therapy. Am J Dis Child 1980;134:1046-8.
- Tiras U, Erdeve O, Karabulut AA, Dallar Y, Eksioglu HM. Debridement via collagenase application in two neonates. Pediatr Dermatol 2005;22:472-5.
- Tobin C. Managing an extravasation wound in a premature infant. Wounds UK 2007;3:90-1.
- Tuncer S, Aydin A, Erer M. Extravasation of calcium solution leading to calcinosis cutis surrounding the dorsal cutaneous branch of the ulnar nerve. J Hand Surg Br 2006;31:288-9. https://doi.org/10.1016/J.JHSB.2005.12.001.
- Vanwijck R, Lengele B. Liposuction as a help for radiologists. Ann Chir Plast Esthet 1994;39:744-9.
- von Muhlendahl KE. Complications due to infusions in infants and young children. Lessons from six cases of litigation of the Norddeutsche Schlichtungsstelle fur Arzthaftpflichtfragen. Monatsschr Kinderheilkd 2012;160:988-91.
- Wada A, Fujii T, Takamura K, Yanagida H, Matsuura A, Katayama A. Physeal arrest of the ankle secondary to extravasation in a neonate and its treatment by the Gruca operation: a modern application of an old technique. J Pediatr Orthop B 2003;12:129-32. https://doi.org/10.1097/01.bpb.0000049576.53117.ae.
- Wiegand R, Brown J. Hyaluronidase for the management of dextrose extravasation. Am J Emerg Med 2010;28:257.e1-2. https://doi.org/10.1016/j.ajem.2009.06.010.
- Wolfe MS, North ER. Extravasation of injected calcium solution leading to calcifications in the upper extremity of the neonate. Report of a case. J Bone Joint Surg Am 1983;65:558-9. https://doi.org/10.2106/00004623-198365040-00022.
- Wong AF, McCulloch LM, Sola A. Treatment of peripheral tissue ischemia with topical nitroglycerin ointment in neonates. J Pediatr 1992;121:980-3. https://doi.org/10.1016/S0022-3476(05)80356-7.
- Wong KY, Ching D, Milroy C. Iatrogenic Calcinosis Cutis Following a Neonatal Extravasation Injury n.d.
- Yamamoto Y, Igawa H, Minakawa H, Sugihara T, Yoshida T, Minamimoto T, et al. Reconstruction of iatrogenic dorsal skin defects of hands with reverse forearm flaps. Eur J Plast Surg 1994;17:104-5. https://doi.org/10.1007/BF00176927.
- Yosowitz P, Ekland DA, Shaw RC, Parsons RW. Peripheral intravenous infiltration necrosis. Ann Surg 1975;182:553-6. https://doi.org/10.1097/00000658-197511000-00003.
- Zenk KE, Dungy CI, Greene GR. Nafcillin extravasation injury. Use of hyaluronidase as an antidote. Am J Dis Child 1981;135:1113-14. https://doi.org/10.1001/archpedi.1981.02130360021008.
- Berger PE, Heidelberger KP, Poznanski AK. Extravasation of calcium gluconate as a cause of soft tissue calcification in infancy. Am J Roentgenol Radium Ther Nucl Med 1974;121:109-17. https://doi.org/10.2214/ajr.121.1.109.
- Beytut D, Ozdamar N, Isler N, Turgut N. Extravasation injury: lokal oxigene therapy application within pediatric intensive care unit. Pediatr Crit Care Med 2014;1:134-5. https://doi.org/10.1097/01.pcc.0000449320.67961.46.
- Harrold K, Gould D, Drey N. The management of cytotoxic chemotherapy extravasation: a systematic review of the literature to evaluate the evidence underpinning contemporary practice. Eur J Cancer Care 2015;24:771-800. https://doi.org/10.1111/ecc.12363.
- Phillips A. Peripheral intravenous (PIV) catheter extravasation wound care guidelines. J Pediatr Nurs 2011;26. https://doi.org/10.1016/j.pedn.2011.01.264.
- Timmons J. Peripheral intravenous catheter extravasation wound care guidelines. J Pediatr Nurs 2011;26. https://doi.org/10.1016/j.pedn.2010.12.033.
- Boulanger J, Ducharme A, Dufour A, Fortier S, Almanric K. Comité de l’évolution de la pratique des soins pharmaceutiques (CEPSP) . Management of the extravasation of anti-neoplastic agents. Support Care Cancer 2015;23:1459-71. https://doi.org/10.1007/s00520-015-2635-7.
- Clark L, Fairhurst C, Torgerson DJ. Allocation concealment in randomised controlled trials: are we getting better?. BMJ 2016;355. https://doi.org/10.1136/bmj.i5663.
- Corbett MS, Moe-Byrne T, Oddie S, McGuire W. Randomization methods in emergency setting trials: a descriptive review. Res Synth Methods 2016;7:46-54. https://doi.org/10.1002/jrsm.1163.
- Langer SW, Sehested M, Jensen PB. Anthracycline extravasation: a comprehensive review of experimental and clinical treatments. Tumori 2009;95:273-82. https://doi.org/10.1177/030089160909500301.
- Harwood K, Gonin R. Short term vs long term cooling after doxorubicin (DOX) extravasation: an Eastern Cooperative Oncology Group (ECOG) study. Proceed Am Soc Clin Oncol 1994;13.
- Kasenda B, von Elm E, You J, Blümle A, Tomonaga Y, Saccilotto R, et al. Prevalence, characteristics, and publication of discontinued randomized trials. JAMA 2014;311:1045-51. https://doi.org/10.1001/jama.2014.1361.
- Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al. Recruitment to randomised trials: strategies for trial enrollment and participation study. The STEPS study. Health Technol Assess 2007;11. https://doi.org/10.3310/hta11480.
- Denhoff ER, Milliren CE, de Ferranti SD, Steltz SK, Osganian SK. Factors associated with clinical research recruitment in a pediatric academic medical center – a web-based survey. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0140768.
- Baiardi P, Giaquinto C, Girotto S, Manfredi C, Ceci A. TEDDY Network of Excellence . Innovative study design for paediatric clinical trials. Eur J Clin Pharmacol 2011;67:109-15. https://doi.org/10.1007/s00228-011-0990-y.
- van der Lee JH, Wesseling J, Tanck MW, Offringa M. Sequential design with boundaries approach in pediatric intervention research reduces sample size. J Clin Epidemiol 2010;63:19-27. https://doi.org/10.1016/j.jclinepi.2009.07.005.
- Adaptive Design Clinical Trials for Drugs and Biologics. Draft Guidance. Silver Spring, MD: US Food and Drug Administration; 2010.
- Brusselaers N, Pirayesh A, Hoeksema H, Verbelen J, Blot S, Monstrey S. Burn scar assessment: a systematic review of different scar scales. J Surg Res 2010;164:e115-23. https://doi.org/10.1016/j.jss.2010.05.056.
- Nguyen TA, Feldstein SI, Shumaker PR, Krakowski AC. A review of scar assessment scales. Semin Cutan Med Surg 2015;34:28-36. https://doi.org/10.12788/j.sder.2015.0125.
- Woolacott N, Corbett M, Jones-Diette J, Hodgson R. Methodological challenges for the evaluation of clinical effectiveness in the context of accelerated regulatory approval: an overview. J Clin Epidemiol 2017;90:108-18. https://doi.org/10.1016/j.jclinepi.2017.07.002.
- Valentine JC, Thompson SG. Issues relating to confounding and meta-analysis when including non-randomized studies in systematic reviews on the effects of interventions. Res Synth Methods 2013;4:26-35. https://doi.org/10.1002/jrsm.1064.
- Gale C, Modi N. WHEAT trial development group . Neonatal randomised point-of-care trials are feasible and acceptable in the UK: results from two national surveys. Arch Dis Child Fetal Neonatal Ed 2016;101:F86-7. https://doi.org/10.1136/archdischild-2015-308882.
- van Staa TP, Dyson L, McCann G, Padmanabhan S, Belatri R, Goldacre B, et al. The opportunities and challenges of pragmatic point-of-care randomised trials using routinely collected electronic records: evaluations of two exemplar trials. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18430.
- Li G, Sajobi TT, Menon BK, Korngut L, Lowerison M, James M, et al. Registry-based randomized controlled trials - what are the advantages, challenges, and areas for future research?. J Clin Epidemiol 2016;80:16-24. https://doi.org/10.1016/j.jclinepi.2016.08.003.
- Lauer MS, D’Agostino RB. The randomized registry trial – the next disruptive technology in clinical research?. N Engl J Med 2013;369:1579-81. https://doi.org/10.1056/NEJMp1310102.
Appendix 1 Database search strategies
MEDLINE [Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)]
Via Ovid; http://ovidsp.ovid.com/.
1946 to present.
Searched on: 1 February 2017.
Records retrieved: 1969.
Search strategy
-
“Extravasation of Diagnostic and Therapeutic Materials”/ (3147)
-
extravasat$.ti,ab. (15,523)
-
(infiltrat$ adj2 (intravenous$ or IV or infus$ or catheter$ or cannula$)).ti,ab. (239)
-
infiltrat$ adj2 (injur$ or wound$)).ti,ab. (874)
-
((intravenous$ or IV or infus$) adj2 leak$).ti,ab. (152)
-
(infus$ adj2 (injur$ or wound$)).ti,ab. (289)
-
(PIV adj2 (injur$ or wound$)).ti,ab. (2)
-
(PIV adj2 infiltrat$).ti,ab. (3)
-
(catheter$ adj2 (injur$ or wound$)).ti,ab. (708)
-
or/1-9 (19,211)
-
exp Child/ (1,703,797)
-
exp Infant/ (1,029,438)
-
Adolescent/ (1,782,430)
-
(child$ or infant$ or infancy or pediat$ or paediat$ or preschool$ or pre school$ or schoolchild$ or school age$ or schoolage$ or schoolboy$ or schoolgirl$).ti,ab. (1,552,190)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (201,718)
-
(adoles$ or young people or young person$ or teen$ or youth$ or preteen$ or juvenil$).ti,ab. (345,875)
-
(neonat$ or neo nat$).ti,ab. (225,315)
-
(newborn$ or new born$ or newly born$).ti,ab. (146,891)
-
(preterm or preterms or pre term or pre terms).ti,ab. (58,825)
-
(preemie$ or premie or premies).ti,ab. (140)
-
(prematur$ adj3 (birth$ or born or deliver$)).ti,ab. (13,561)
-
(low adj3 (birthweight$ or birth weight$)).ti,ab. (29,760)
-
(lbw or vlbw or elbw).ti,ab. (6880)
-
(baby or babies).ti,ab. (60,639)
-
or/11-24 (3,777,516)
-
10 and 25 (2131)
-
exp animals/ not humans/ (4,311,358)
-
26 not 27 (1969)
Key
/ = indexing term [medical subject heading (MeSH) heading]
exp = exploded indexing term (MeSH heading)
$ = truncation
ti,ab = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
British Nursing Index
Via ProQuest; www.proquest.com/.
1994 to present.
Searched on: 1 February 2017.
Records retrieved: 30.
Search strategy
(TI,AB(extravasat*) OR TI,AB(infiltrat* NEAR/2 (intravenous* OR IV OR infus* OR catheter* OR cannula*)) OR TI,AB(infiltrat* NEAR/2 (injur* OR wound*)) OR TI,AB((intravenous* OR IV OR infus*) NEAR/2 leak*) OR TI,AB(infus* NEAR/2 (injur* OR wound*)) OR TI,AB(PIV NEAR/2 (injur* OR wound*)) OR TI,AB(PIV N2 infiltrat*) OR (catheter* NEAR/2 (injur* OR wound*))) AND ((SU.EXACT.EXPLODE(“Infants”) OR SU.EXACT.EXPLODE(“Neonates”) OR SU.EXACT.EXPLODE(“Children”) OR SU.EXACT(“Adolescents”) OR SU.EXACT(“Neonates: Birthweight”) OR TI,AB(child* OR infant* OR infancy OR pediat* OR paediat* OR preschool* OR pre-school* OR schoolchild* OR school-age* OR schoolage* OR schoolboy* OR schoolgirl*) OR TI,AB(girl OR girls OR boy OR boys OR kid OR kids) OR TI,AB(adoles* OR “young people” OR “young person” OR “young persons” OR teen* OR youth* OR preteen* OR juvenil*) OR TI,AB(neonat* OR neo-nat*) OR TI,AB(newborn* OR new-born* OR “newly born”) OR TI,AB(preterm OR preterms OR pre-term OR pre-terms) OR TI,AB(preemie* OR premie OR premies) OR TI,AB(prematur* NEAR/3 (birth* OR born OR deliver*))) OR TI,AB(low NEAR/3 (birthweight* OR “birth weight” OR “birth weights”)) OR TI,AB(lbw OR vlbw OR elbw) OR TI,AB(baby OR babies))
Key
SU.EXACT = subject heading
SU.EXACT.EXPLODE = exploded subject heading
TI,AB = terms in the title or abstract fields
NEAR/2 = terms within two words of each other (any order)
* = truncation
” “ = phrase search
Cochrane Central Register of Controlled Trials
Via Wiley Online Library; http://onlinelibrary.wiley.com/.
Issue 1 of 12, January 2017.
Searched on: 1 February 2017.
Records retrieved: 200.
Search strategy
The strategy below was used to search CENTRAL and CDSR.
-
MeSH descriptor: [Extravasation of Diagnostic and Therapeutic Materials] this term only (54)
-
extravasat*:ti,ab,kw (312)
-
(infiltrat* near/2 (intravenous* or IV or infus* or catheter* or cannula*)):ti,ab,kw (41)
-
(infiltrat* near/2 (injur* or wound*)):ti,ab,kw (349)
-
((intravenous* or IV or infus*) near/2 leak*):ti,ab,kw (7)
-
(infus* near/2 (injur* or wound*)):ti,ab,kw (154)
-
(PIV near/2 (injur* or wound*)):ti,ab,kw (0)
-
(PIV near/2 infiltrat*):ti,ab,kw (0)
-
(catheter* near/2 (injur* or wound*)):ti,ab,kw (106)
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 (934)
-
MeSH descriptor: [Child] explode all trees (212)
-
MeSH descriptor: [Infant] explode all trees (14,891)
-
MeSH descriptor: [Adolescent] this term only (89,013)
-
(child* or infant* or infancy or pediat* or paediat* or preschool* or pre next school* or schoolchild* or school next age* or schoolage* or schoolboy* or schoolgirl*):ti,ab,kw (120,389)
-
(girl or girls or boy or boys or kid or kids):ti,ab,kw (6504)
-
(adoles* or young next people or young next person* or teen* or youth* or preteen* or juvenil*):ti,ab,kw (113,415)
-
(neonat* or neo next nat*):ti,ab,kw (13,221)
-
(newborn* or new next born* or newly next born*):ti,ab,kw (20,677)
-
(preterm or preterms or pre next term or pre next terms):ti,ab,kw (7960)
-
(preemie* or premie or premies):ti,ab,kw (20)
-
(prematur* near/3 (birth* or born or deliver*)):ti,ab,kw (1473)
-
(low near/3 (birthweight* or birth next weight*)):ti,ab,kw (3916)
-
(lbw or vlbw or elbw):ti,ab,kw (1157)
-
(baby or babies):ti,ab,kw (4157)
-
{or 11-24} (201,937)
-
10 and 25 (209)
-
10 and 25 in Cochrane Reviews (Reviews and Protocols) (7)
-
10 and 25 in Trials (200)
Key
MeSH descriptor = indexing term (MeSH heading)
* = truncation
ti,ab,kw = terms in either title or abstract or keyword fields
near/2 = terms within two words of each other (any order)
next = terms are next to each other
Cochrane Database of Systematic Reviews
Via Wiley Online Library; http://onlinelibrary.wiley.com/.
Issue 1 of 12, January 2017.
Searched on: 1 February 2017.
Records retrieved: 7.
See above under CENTRAL for search strategy used.
Cumulative Index to Nursing and Allied Health
Via EBSCOhost; www.ebscohost.com/.
Inception to 31 January 2017.
Searched on: 1 February 2017.
Records retrieved: 382.
| Number | Search term | Hits |
|---|---|---|
| S1 | (MH “Extravasation of Diagnostic and Therapeutic Materials”) | 930 |
| S2 | TI extravasat* OR AB extravasat* | 1224 |
| S3 | TI ( infiltrat* N2 (intravenous* or IV or infus* or catheter* or cannula*) ) OR AB ( infiltrat* N2 (intravenous* or IV or infus* or catheter* or cannula*) ) | 94 |
| S4 | TI ( infiltrat* N2 (injur* or wound*) ) OR AB ( infiltrat* N2 (injur* or wound*) ) | 214 |
| S5 | TI ( (intravenous* or IV or infus*) N2 leak*) ) OR AB ( (intravenous* or IV or infus*) N2 leak*) ) | 23 |
| S6 | TI ( infus* N2 (injur* or wound*) ) OR AB ( infus* N2 (injur* or wound*) ) | 73 |
| S7 | TI ( PIV N2 (injur* or wound*) ) OR AB ( PIV N2 (injur* or wound*) ) | 2 |
| S8 | TI PIV N2 infiltrat* OR AB PIV N2 infiltrat* | 3 |
| S9 | TI ( catheter* N2 (injur* or wound*) ) OR AB ( catheter* N2 (injur* or wound*) ) | 144 |
| S10 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 | 2265 |
| S11 | (MH “Infant+”) | 185,131 |
| S12 | (MH “Child+”) | 475,232 |
| S13 | (MH “Adolescence+”) | 370,678 |
| S14 | TI ( (child* or infant* or infancy or pediat* or paediat* or preschool* or pre N1 school* or schoolchild* or school N1 age* or schoolage* or schoolboy* or schoolgirl*) ) OR AB ( (child* or infant* or infancy or pediat* or paediat* or preschool* or pre N1 school* or schoolchild* or school N1 age* or schoolage* or schoolboy* or schoolgirl*) ) | 393,895 |
| S15 | TI ( girl or girls or boy or boys or kid or kids ) OR AB ( girl or girls or boy or boys or kid or kids ) | 37,933 |
| S16 | TI ( adoles* or young N1 people or young N1 person* or teen* or youth* or preteen* or juvenil* ) OR AB ( adoles* or young N1 people or young N1 person* or teen* or youth* or preteen* or juvenil* ) | 122,298 |
| S17 | TI (neonat* or neo N1 nat*) OR AB (neonat* or neo N1 nat*) | 38,395 |
| S18 | TI ( newborn* or new N1 born* or newly N1 born* ) OR AB ( newborn* or new N1 born* or newly N1 born* ) | 18,282 |
| S19 | TI ( preterm or preterms or pre N1 term or pre N1 terms ) OR AB ( preterm or preterms or pre N1 term or pre N1 terms ) | 18,728 |
| S20 | TI ( preemie* or premie or premies ) OR AB ( preemie* or premie or premies ) | 220 |
| S21 | TI ( prematur* N3 (birth* or born or deliver*) ) OR AB ( prematur* N3 (birth* or born or deliver*) ) | 2597 |
| S22 | TI ( low N3 (birthweight* or birth N1 weight*) ) OR AB ( low N3 (birthweight* or birth N1 weight*) ) | 7601 |
| S23 | TI ( lbw or vlbw or elbw ) OR AB ( lbw or vlbw or elbw ) | 1922 |
| S24 | TI ( baby or babies ) OR AB ( baby or babies ) | 19,968 |
| S25 | S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 | 847,079 |
| S26 | S10 AND S25 | 382 |
Database of Abstracts of Reviews of Effects
Via www.crd.york.ac.uk/CRDWeb/.
Inception to 31 March 2015.
Searched on: 1 February 2017.
Records retrieved: 9.
Search strategy
The strategy below was used to search DARE and the HTA database.
-
MeSH DESCRIPTOR Extravasation of Diagnostic and Therapeutic Materials IN DARE,HTA (5)
-
(extravasat*) IN DARE, HTA (12)
-
((infiltrat* NEAR2 (intravenous* or IV or infus* or catheter* or cannula*))) IN DARE, HTA (3)
-
(((intravenous* or IV or infus* or catheter* or cannula*) NEAR2 infiltrat*)) IN DARE, HTA (0)
-
(((intravenous* or IV or infus*) NEAR2 leak*)) IN DARE, HTA (0)
-
((leak* NEAR2 (intravenous* or IV or infus*))) IN DARE, HTA (1)
-
((infiltrat* NEAR2 (injur* or wound*))) IN DARE, HTA (3)
-
(((injur* or wound*) NEAR2 infiltrat*)) IN DARE, HTA (13)
-
((infus* NEAR2 (injur* or wound*))) IN DARE, HTA (5)
-
(((injur* or wound*) NEAR2 infus*)) IN DARE, HTA (5)
-
((PIV NEAR2 (injur* or wound* or infiltrat*))) IN DARE, HTA (0)
-
(((injur* or wound* or infiltrat*) NEAR2 PIV)) IN DARE, HTA (0)
-
((catheter* NEAR2 (injur* or wound*))) IN DARE, HTA (3)
-
(((injur* or wound*) NEAR2 catheter*)) IN DARE, HTA (12)
-
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 (47)
-
MeSH DESCRIPTOR child EXPLODE ALL TREES IN DARE,HTA (3236)
-
MeSH DESCRIPTOR infant EXPLODE ALL TREES IN DARE,HTA (1704)
-
MeSH DESCRIPTOR adolescent IN DARE,HTA (2377)
-
((child* or infant* or infancy or pediat* or paediat* or preschool* or pre-school* or schoolchild* or school-age* or schoolage* or schoolboy* or schoolgirl*)) IN DARE, HTA (8684)
-
((girl or girls or boy or boys or kid or kids)) IN DARE, HTA (196)
-
((adoles* or “young people” or “young person” or “young persons” or teen* or youth* or preteen* or juvenil*)) IN DARE, HTA (3352)
-
(neonat* or neo-nat*) IN DARE, HTA (1345)
-
((newborn* or “new born” or “new borns” or “newly born”)) IN DARE, HTA (1324)
-
((preterm or preterms or “pre term” or “pre terms”)) IN DARE, HTA (826)
-
((preemie* or premie or premies)) IN DARE, HTA (0)
-
((prematur* NEAR3 (birth* or born or deliver*))) IN DARE, HTA (182)
-
(((birth* or born or deliver*) NEAR3 prematur*)) IN DARE, HTA (31)
-
((low NEAR3 (birthweight* or “birth weight” or “birth weights”))) IN DARE, HTA (317)
-
(lbw or vlbw or elbw) IN DARE, HTA (43)
-
(baby or babies) IN DARE, HTA (425)
-
16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 (10,207)
-
15 AND 31 (10)
Key
MeSH DESCRIPTOR = indexing term (MeSH heading)
* = truncation
NEAR2 = terms within two words of each other (order specified)
” “ = phrase search
Excerpta Medica dataBASE
Via Ovid; http://ovidsp.ovid.com/.
1974 to 2017 January 31.
Searched on: 1 February 2017.
Records retrieved: 2413.
Search strategy
-
extravasation/ (12,184)
-
drug extravasation/ (717)
-
injection site extravasation/ (177)
-
contrast medium extravasation/ (3027)
-
extravasat$.ti,ab. (20,642)
-
(infiltrat$ adj2 (intravenous$ or IV or infus$ or catheter$ or cannula$)).ti,ab. (328)
-
(infiltrat$ adj2 (injur$ or wound$)).ti,ab. (1228)
-
((intravenous$ or IV or infus$) adj2 leak$).ti,ab. (196)
-
(infus$ adj2 (injur$ or wound$)).ti,ab. (447)
-
(PIV adj2 (injur$ or wound$)).ti,ab. (3)
-
(PIV adj2 infiltrat$).ti,ab. (5)
-
(catheter$ adj2 (injur$ or wound$)).ti,ab. (951)
-
or/1-12 (27,430)
-
exp infant/ (1,003,813)
-
prematurity/ (97,200)
-
exp low birth weight/ (53,279)
-
exp child/ (2,555,921)
-
exp adolescent/ (1,418,617)
-
juvenile/ (62,534)
-
(child$ or infant$ or infancy or pediat$ or paediat$ or preschool$ or pre school$ or schoolchild$ or school age$ or schoolage$ or schoolboy$ or schoolgirl$).ti,ab. (1,915,425)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (261,278)
-
(adoles$ or young people or young person$ or teen$ or youth$ or preteen$ or juvenil$).ti,ab. (431,418)
-
(neonat$ or neo nat$).ti,ab. (287,782)
-
(newborn$ or new born$ or newly born$).ti,ab. (176,924)
-
(preterm or preterms or pre term or pre terms).ti,ab. (80,398)
-
(preemie$ or premie or premies).ti,ab. (200)
-
(prematur$ adj3 (birth$ or born or deliver$)).ti,ab. (17,938)
-
(low adj3 (birthweight$ or birth weight$)).ti,ab. (36,605)
-
(lbw or vlbw or elbw).ti,ab. (9134)
-
(baby or babies).ti,ab. (80,717)
-
or/14-30 (3,867,788)
-
13 and 31 (2670)
-
(animal/ or nonhuman/) not exp human/ (5,056,272)
-
32 not 33 (2413)
Key
/ = indexing term (Emtree heading)
exp = exploded indexing term (Emtree heading)
$ = truncation
ti,ab = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
Ovid Emcare
Via Ovid; http://ovidsp.ovid.com/.
1995 to 2016 week 49.
Searched on: 6 February 2017.
Records retrieved: 572.
Search strategy
-
extravasation/ (2254)
-
drug extravasation/ (151)
-
injection site extravasation/ (63)
-
contrast medium extravasation/ (927)
-
extravasat$.ti,ab. (2870)
-
(infiltrat$ adj2 (intravenous$ or IV or infus$ or catheter$ or cannula$)).ti,ab. (94)
-
(infiltrat$ adj2 (injur$ or wound$)).ti,ab. (290)
-
((intravenous$ or IV or infus$) adj2 leak$).ti,ab. (42)
-
(infus$ adj2 (injur$ or wound$)).ti,ab. (102)
-
(PIV adj2 (injur$ or wound$)).ti,ab. (1)
-
(PIV adj2 infiltrat$).ti,ab. (2)
-
(catheter$ adj2 (injur$ or wound$)).ti,ab. (171)
-
or/1-12 (4719)
-
exp infant/ (150,126)
-
prematurity/ (30,020)
-
exp low birth weight/ (17,249)
-
exp child/ (492,360)
-
exp adolescent/ (264,126)
-
juvenile/ (30,797)
-
(child$ or infant$ or infancy or pediat$ or paediat$ or preschool$ or pre school$ or schoolchild$ or school age$ or schoolage$ or schoolboy$ or schoolgirl$).ti,ab. (484,484)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (63,264)
-
(adoles$ or young people or young person$ or teen$ or youth$ or preteen$ or juvenil$).ti,ab. (151,694)
-
(neonat$ or neo nat$).ti,ab. (56,554)
-
(newborn$ or new born$ or newly born$).ti,ab. (27,827)
-
(preterm or preterms or pre term or pre terms).ti,ab. (25,003)
-
(preemie$ or premie or premies).ti,ab. (66)
-
(prematur$ adj3 (birth$ or born or deliver$)).ti,ab. (3898)
-
(low adj3 (birthweight$ or birth weight$)).ti,ab. (10,789)
-
(lbw or vlbw or elbw).ti,ab. (3242)
-
(baby or babies).ti,ab. (19,426)
-
or/14-30 (790,276)
-
13 and 31 (600)
-
(animal/ or nonhuman/) not exp human/ (292,084)
-
32 not 33 (572)
Key
/ = indexing term (Emtree heading)
exp = exploded indexing term (Emtree heading)
$ = truncation
ti,ab = terms in either title or abstract fields
adj2 = terms within two words of each other (any order)
Health Technology Assessment database
Via www.crd.york.ac.uk/CRDWeb/.
Inception to 31 January 2017.
Searched on: 1 February 2017.
Records retrieved: 1.
See above under DARE for search strategy used.
Maternity and Infant Care
Via Ovid; http://ovidsp.ovid.com/.
1971 to December 2016.
Searched on: 1 February 2017.
Records retrieved: 65.
Search strategy
-
extravasat$.ti,ab,de. (45)
-
(infiltrat$ adj2 (intravenous$ or IV or infus$ or catheter$ or cannula$)).ti,ab,de. (5)
-
(infiltrat$ adj2 (injur$ or wound$)).ti,ab,de. (10)
-
((intravenous$ or IV or infus$) adj2 leak$).ti,ab,de. (3)
-
(infus$ adj2 (injur$ or wound$)).ti,ab,de. (4)
-
(PIV adj2 (injur$ or wound$)).ti,ab,de. (0)
-
(PIV adj2 infiltrat$).ti,ab,de. (0)
-
(catheter$ adj2 (injur$ or wound$)).ti,ab,de. (4)
-
or/1-8 (65)
Key
ti,ab,de = terms in either title or abstract or descriptor fields
$ = truncation
adj2 = terms within two words of each other (any order)
PubMed
Via www.ncbi.nlm.nih.gov/pubmed/.
Searched on: 1 February 2017.
Records retrieved: 327.
Search strategy
Search (((((((((((((((“Extravasation of Diagnostic and Therapeutic Materials”[Mesh:noexp])) OR extravasat*[Title/Abstract]) OR ((infiltrat*[Title/Abstract]) AND (intravenous*[Title/Abstract] OR IV[Title/Abstract] OR infus*[Title/Abstract] OR catheter*[Title/Abstract] OR cannula*[Title/Abstract]))) OR ((infiltrat*[Title/Abstract]) AND (injur*[Title/Abstract] OR wound*[Title/Abstract]))) OR (((intravenous*[Title/Abstract] OR IV[Title/Abstract] OR infus*[Title/Abstract])) AND leak*[Title/Abstract])) OR ((infus*[Title/Abstract]) AND (injur*[Title/Abstract] OR wound*[Title/Abstract]))) OR ((PIV[Title/Abstract]) AND (injur*[Title/Abstract] OR wound*[Title/Abstract]))) OR ((PIV[Title/Abstract]) AND infiltrat*[Title/Abstract])) OR ((catheter*[Title/Abstract]) AND (injur*[Title/Abstract] OR wound*[Title/Abstract])))) AND ((((((((((((((“Child”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh:noexp]) OR ((child*[Title/Abstract] OR infant*[Title/Abstract] OR infancy[Title/Abstract] OR pediat*[Title/Abstract] OR paediat*[Title/Abstract] OR preschool*[Title/Abstract] OR pre-school*[Title/Abstract] OR schoolchild*[Title/Abstract] OR school-age*[Title/Abstract] OR schoolage*[Title/Abstract] OR schoolboy*[Title/Abstract] OR schoolgirl*[Title/Abstract]))) OR ((girl[Title/Abstract] OR girls[Title/Abstract] OR boy[Title/Abstract] OR boys[Title/Abstract] OR kid[Title/Abstract] OR kids[Title/Abstract]))) OR ((adoles*[Title/Abstract] OR young people[Title/Abstract] OR “young person”[Title/Abstract] OR “young persons”[Title/Abstract] OR teen*[Title/Abstract] OR youth*[Title/Abstract] OR preteen*[Title/Abstract] OR juvenil*[Title/Abstract]))) OR ((neonat*[Title/Abstract] OR neo-nat*[Title/Abstract]))) OR ((newborn*[Title/Abstract] OR “new born”[Title/Abstract] OR “new borns”[Title/Abstract] OR “newly born”[Title/Abstract]))) OR ((preterm[Title/Abstract] OR preterms[Title/Abstract] OR “pre term”[Title/Abstract] OR “pre terms”[Title/Abstract]))) OR ((preemie*[Title/Abstract] OR premie[Title/Abstract] OR premies[Title/Abstract]))) OR ((prematur*[Title/Abstract]) AND (birth*[Title/Abstract] OR born[Title/Abstract] OR deliver*[Title/Abstract]))) OR ((low[Title/Abstract]) AND (birthweight*[Title/Abstract] OR “birth weight”[Title/Abstract] OR “birth weights”[Title/Abstract]))) OR ((lbw[Title/Abstract] OR vlbw[Title/Abstract] OR elbw[Title/Abstract]))) OR ((baby[Title/Abstract] OR babies[Title/Abstract]))))) NOT ((animals[mh] NOT humans[mh])))) AND ((pubstatusaheadofprint OR publisher[sb] OR pubmednotmedline[sb]))
The above search strategy incorporates the following search line to limit to studies found in PubMed but not available in Ovid MEDLINE: (pubstatusaheadofprint OR publisher[sb] OR pubmednotmedline[sb]).
Key
[Mesh] = exploded indexing term (MeSH heading)
[Mesh:noexp] = indexing term (MeSH heading) not exploded
* = truncation
” “ = phrase search
[Title/Abstract]) = terms in either title or abstract fields
Science Citation Index
Via Web of Science, Thomson Reuters
URL: http://thomsonreuters.com/thomson-reuters-web-of-science/.
1900 to 31 January 2017.
Searched on: 1 February 2017.
Records retrieved: 1018.
Search strategy
22 21 AND 9 (1018)
21 20 OR 19 OR 18 OR 17 OR 16 OR 15 OR 14 OR 13 OR 12 OR 11 OR 10 (1,920,782)
20 TS=(baby or babies) (43,069)
19 TS=(lbw or vlbw or elbw) (6578)
18 TS=(low NEAR/3 (birthweight* or “birth weight” or “birth weights”)) (33,946)
17 TS=(prematur* NEAR/3 (birth* or born or deliver*)) (10,333)
16 TS=(preemie* or premie or premies) (127)
15 TS=(preterm or preterms or “pre term” or “pre terms”) (71,557)
14 TS=(newborn* or “new born” or “new borns” or “newly born”) (128,013)
13 TS=(neonat* or neo-nat*) (217,907)
12 TS=(adoles* or “young people” or “young person” or “young persons” or teen* or youth* or preteen* or juvenil*) (384,736)
11 TS=(girl or girls or boy or boys or kid or kids) (142,187)
10 TS=(child* or infant* or infancy or pediat* or paediat* or preschool* or pre-school* or schoolchild* or school-age* or schoolage* or schoolboy* or schoolgirl*) (1,407,704)
9 8 OR 7 OR 6 OR 5 OR 4 OR 3 OR 2 OR 1 (16,789)
8 TS=(catheter* NEAR/2 (injur* or wound*)) (969)
7 TS=(PIV NEAR/2 infiltrat*) (3)
6 TS=(PIV NEAR/2 (injur* or wound*)) (4)
5 TS=(infus* NEAR/2 (injur* or wound*)) (468)
4 TS=((intravenous* or IV or infus*) NEAR/2 leak*) (170)
3 TS=(infiltrat* NEAR/2 (injur* or wound*)) (1492)
2 TS=(infiltrat* NEAR/2 (intravenous* or IV or infus* or catheter* or cannula*)) (306)
1 TS=extravasat* (13,541)
Key
TS = topic tag; searches terms in title, abstract, author keywords and keywords plus fields
* = truncation
” “ = phrase search
NEAR/2 = terms within two words of each other (any order)
On-going, unpublished or grey literature search strategies
ClinicalTrials.gov
URL: https://clinicaltrials.gov/.
Searched on: 3 February 2017.
Records retrieved: 42.
1. 25 studies found for: extravasation | Child
2. 20 studies found for: infiltration AND (intravenous OR IV OR PIV OR infusion OR catheter OR cannula OR injury OR wound OR leak) | Child
3. 2 studies found for: (intravenous OR IV OR infusion) AND leak | Child
Conference Proceedings Citation Index: Science
Via Web of Science, Thomson Reuters.
http://thomsonreuters.com/thomson-reuters-web-of-science/.
1990 to 31st January 2017.
Searched on: 1 February 2017.
Records retrieved: 61.
Search strategy
22 21 AND 9 (61)
21 20 OR 19 OR 18 OR 17 OR 16 OR 15 OR 14 OR 13 OR 12 OR 11 OR 10 (191,435)
20 TS=(baby or babies) (3359)
19 TS=(lbw or vlbw or elbw) (649)
18 TS=(low NEAR/3 (birthweight* or “birth weight” or “birth weights”)) (2670)
17 TS=(prematur* NEAR/3 (birth* or born or deliver*)) (904)
16 TS=(preemie* or premie or premies) (9)
15 TS=(preterm or preterms or “pre term” or “pre terms”) (7407)
14 TS=(newborn* or “new born” or “new borns” or “newly born”) (8707)
13 TS=(neonat* or neo-nat*) (17,826)
12 TS=(adoles* or “young people” or “young person” or “young persons” or teen* or youth* or preteen* or juvenil*) (34,295)
11 TS=(girl or girls or boy or boys or kid or kids) (8171)
10 TS=(child* or infant* or infancy or pediat* or paediat* or preschool* or pre-school* or schoolchild* or school-age* or schoolage* or schoolboy* or schoolgirl*) (141,665)
9 8 OR 7 OR 6 OR 5 OR 4 OR 3 OR 2 OR 1 (1222)
8 TS=(catheter* NEAR/2 (injur* or wound*)) (104)
7 TS=(PIV NEAR/2 infiltrat*) (0)
6 TS=(PIV NEAR/2 (injur* or wound*)) (0)
5 TS=(infus* NEAR/2 (injur* or wound*)) (45)
4 TS=((intravenous* or IV or infus*) NEAR/2 leak*) (22)
3 TS=(infiltrat* NEAR/2 (injur* or wound*)) (117)
2 TS=(infiltrat* NEAR/2 (intravenous* or IV or infus* or catheter* or cannula*)) (27)
1 TS=extravasat* (925)
Key
TS = topic tag; searches terms in title, abstract, author keywords and keywords plus fields
* = truncation
“ ” = phrase search
NEAR/2 = terms within two words of each other (any order)
EU Clinical Trials Register
www.clinicaltrialsregister.eu/ctr-search/search.
Searched on: 3 February 2017.
Records retrieved: 30.
-
2 result(s) found for: extravasat* limited to adolescent, children, infant and toddler, newborn, preterm new born infants, under 18
-
22 result(s) found for: infiltration AND (intravenous* OR IV OR PIV OR infus* OR catheter* OR cannula* OR injur* OR wound* OR leak*) limited to adolescent, children, infant and toddler, newborn, preterm new born infants, under 18
-
6 result(s) found for: (intravenous* OR IV OR infus*) AND leak* limited to adolescent, children, infant and toddler, newborn, preterm new born infants, under 18
ProQuest Dissertations & Theses: UK & Ireland
Via ProQuest www.proquest.com/.
Inception to present.
Searched on: 1 February 2017.
Records retrieved: 4.
Search strategy
(TI,AB,SU(extravasat*) OR TI,AB,SU(infiltrat* NEAR/2 (intravenous* OR IV OR infus* OR catheter* OR cannula*)) OR TI,AB,SU(infiltrat* NEAR/2 (injur* OR wound*)) OR TI,AB,SU((intravenous* OR IV OR infus*) NEAR/2 leak*) OR TI,AB,SU(infus* NEAR/2 (injur* OR wound*)) OR TI,AB,SU(PIV NEAR/2 (injur* OR wound*)) OR TI,AB,SU(PIV NEAR/2 infiltrat*) OR TI,AB,SU(catheter* NEAR/2 (injur* OR wound*))) AND (TI,AB,SU(child* OR infant* OR infancy OR pediat* OR paediat* OR preschool* OR pre-school* OR schoolchild* OR school-age* OR schoolage* OR schoolboy* OR schoolgirl*) OR TI,AB,SU(girl OR girls OR boy OR boys OR kid OR kids) OR TI,AB,SU(adoles* OR “young people” OR “young person” OR “young persons” OR teen* OR youth* OR preteen* OR juvenil*) OR TI,AB,SU(neonat* OR neo-nat*) OR TI,AB,SU(newborn* OR “new born” OR “new borns” OR “newly born”) OR TI,AB,SU(preterm OR preterms OR “pre term” OR “pre terms”) OR TI,AB,SU(preemie* OR premie OR premies) OR TI,AB,SU(prematur* NEAR/3 (birth* OR born OR deliver*)) OR TI,AB,SU(low NEAR/3 (birthweight* OR “birth weight” OR “birth weights”)) OR TI,AB,SU(lbw OR vlbw OR elbw) OR TI,AB,SU(baby OR babies))
Key
TI,AB,SU = terms in the title or abstract or subject heading fields
NEAR/2 = terms within two words of each other (any order)
* = truncation
” “ = phrase search
PROSPERO
Via www.crd.york.ac.uk/PROSPERO/.
Searched on: 1 February 2017.
Records retrieved: 13.
Search strategy
-
MeSH DESCRIPTOR Extravasation of Diagnostic and Therapeutic Materials (1)
-
extravasat* (16)
-
infiltrat* ADJ2 (intravenous* OR IV OR infus* OR catheter* OR cannula*) (2)
-
infiltrat* ADJ2 (injur* OR wound*) (1)
-
(intravenous* OR IV OR infus*) ADJ2 leak* (1)
-
leak* ADJ2 (intravenous* OR IV OR infus*) (0)
-
(intravenous* OR IV OR infus* OR catheter* OR cannula*) ADJ2 infiltrat* (1)
-
(injur* OR wound*) ADJ2 infiltrat* (11)
-
infus* ADJ2 (injur* OR wound*) (2)
-
(injur* OR wound*) ADJ2 infus* (4)
-
PIV ADJ2 (injur* OR wound* OR infiltrat*) (0)
-
(injur* OR wound* OR infiltrat*) ADJ2 PIV (0)
-
catheter* ADJ2 (injur* OR wound*) (1)
-
(injur* OR wound*) ADJ2 catheter* (7)
-
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 (33)
-
MeSH DESCRIPTOR child EXPLODE ALL TREES (1522)
-
MeSH DESCRIPTOR infant EXPLODE ALL TREES (491)
-
MeSH DESCRIPTOR adolescent (609)
-
(child* OR infant* OR infancy OR pediat* OR paediat* OR preschool* OR pre-school* OR schoolchild* OR school-age* OR schoolage* OR schoolboy* OR schoolgirl*) (6160)
-
girl OR girls OR boy OR boys OR kid OR kids (240)
-
adoles* OR “young people” OR “young person” OR “young persons” OR teen* OR youth* OR preteen* OR juvenil* (2259)
-
neonat* OR neo-nat* (884)
-
newborn* OR “new born” OR “new borns” OR “newly born” (350)
-
preterm OR preterms OR pre-term or pre-terms (559)
-
preemie* OR premie OR premies (1)
-
prematur* ADJ3 (birth* OR born OR deliver*) (88)
-
(birth* OR born OR deliver*) ADJ3 prematur* (66)
-
low ADJ3 (birthweight* OR “birth weight” OR “birth weights”) (252)
-
(birthweight* OR “birth weight” OR “birth weights”) ADJ3 low (57)
-
lbw OR vlbw OR elbw (50)
-
baby OR babies (330)
-
16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 (7139)
-
32 AND 15 (13)
Key
MeSH DESCRIPTOR = indexing term (MeSH heading)
* = truncation
ADJ2 = terms within two words of each other (order specified)
“ ” = phrase search
World Health Organization’s International Clinical Trials Registry Platform
Via www.who.int/ictrp/search/en/.
Searched on: 1 February 2017.
Records retrieved: 62.
Search strategy
All searches below were limited to clinical trials in children.
-
6 records for 6 trials found for: extravasat*
-
11 records for 11 trials found for: infiltrat* AND intravenous*
-
13 records for 13 trials found for: infiltrat* AND IV
-
No results were found for: infiltrat* AND PIV
-
9 records for 5 trials found for: infiltrat* AND infus*
-
2 records for 2 trials found for: infiltrat* AND catheter*
-
1 trial found for: infiltrat* AND cannula*
-
2 records for 2 trials found for: infiltrat* AND injur*
-
13 records for 13 trials found for: infiltrat* AND wound*
-
1 trial found for: infiltrat* AND leak*
-
1 trial found for: intravenous AND leak*
-
2 records for 2 trials found for: IV AND leak*
-
1 trial found for: infus* AND leak*
Guideline searches
The following websites were searched on 3 February 2017.
National Institute for Health and Care Excellence
Via www.nice.org.uk/.
-
Searched the guidance and advice section of the website with terms extravasation or infiltration – 0 results.
-
Searched the website with the terms extravasation (6 results) or infiltration (27 results) – all results browsed for relevance – no relevant guidelines found.
-
Browsed guidance by topics - infants and neonates, children and young people – no relevant guidelines found.
National Guidelines Clearinghouse
Via www.guideline.gov/.
-
extravasat* - 24 results found, browsed for relevance – no relevant guidelines found.
-
infiltrate* AND (intravenous* OR IV OR PIV OR infus* OR catheter* OR cannula* OR injur* OR wound* OR leak*) – 5 results found, browsed for relevance – no relevant guidelines found.
-
(intravenous* OR IV OR infus*) AND leak* - 40 results found, browsed for relevance – 1 relevant guideline found.
Trip
-
extravasation OR extravastions OR extravasted OR extravasate OR extravasates, filtered to guidelines – 49 results.
-
(infiltration AND (intravenous* OR IV OR PIV OR infus* OR catheter* OR cannula* OR injur* OR wound* OR leak*) AND (child* OR infant* or adolescen*)), filtered to guidelines – 139 results.
Results from the above searches were browsed for relevance – three relevant guidelines found.
Appendix 2 Studies excluded as being about other extravasations
Seventy studies (63 titles and abstracts and seven full papers) were excluded from the scoping review for being about other types of extravasation. The references of these studies are listed below in alphabetical order.
-
Adesanya O, Naqvi M. Term neonate with liver laceration, obstructive uropathy, and ascites-secondary to extravasation of total parenteral nutrition: a complication of malpositioned umbilical venous catheter. Glob Pediatr Health 2016;3:2333794X16670494. https://doi.org/10.1177/2333794X16670494
-
Akar S, Topcuoglu S, Dincer E, Sancak S, Karatekin G, Ovali F. A rare umbilical venous catheter complication miscible with necrotizing enterocolitis: intraperitoneal extravasation of total parenteral nutrition. Guncel Pediatri 2015;13:77–80.
-
Akkan K, Cindil E, Kilic K, Ilgit E, Onal B, Erbas G. Misplaced central venous catheter in the vertebral artery: endovascular treatment of foreseen hemorrhage during catheter withdrawal. J Vasc Access 2014;15:418–23. https://doi.org/10.5301/jva.5000267
-
Alia R, Ali H. 2 years follow up of intra-abdominal extravasation of TPN causing liver necrosis in a preterm infant. Arch Dis Child Fetal Neonatal Ed 2014;99(Suppl 1):A65–6.
-
Altunhan H, Annagur A, Ertugrul S, Yuksekkaya HA, Örs R. Coexistence of congenital chylous ascites and congenital hypothyroidism: case report. Turkiye Klinikleri Journal of Medical Sciences 2012;32:1486–9.
-
Ancora G, Soffritti S, Faldella G. Diffuse and severe ischemic injury of the extremities: a complication of umbilical vein catheterization. Am J Perinatol 2006;23:341–4. https://doi.org/10.1055/s-2006-946721
-
Au SH, Sun DC, Lue HC. Cardiac tamponade from percutaneous central venous catheterization: report of one case. Acta Paediatr Taiwan 2003;44:235–7.
-
Ayalon A, Anner H, Berlatzky Y, Schiller M. A life-threatening complication of the infusion pump. Lancet 1978;1:853–4.
-
Baker J, Imong S. A rare complication of neonatal central venous access. Arch Dis Child Fetal Neonatal Ed 2002;86:F61–2.
-
Bala I, Pratap M, Nakra D, Jain K. Retroperitoneal extravasation of i.v. fluid following femoral venepuncture. Paediatr Anaesth 2006;16:803–4.
-
Been JV, Degraeuwe PL. Pleural effusion due to intra-abdominal extravasation of parenteral nutrition. Pediatr Pulmonol 2008;43:1033–5. https://doi.org/10.1002/ppul.20891
-
Bergman KA, Doedens R, vd Akker E, Wüst AF. Displacement and extravascular position of a saphenous vein catheter: a serious complication. Eur J Pediatr 1999;158:868–9.
-
Blackwood BP, Farrow KN, Kim S, Hunter CJ. Peripherally inserted central catheters complicated by vascular erosion in neonates. JPEN J Parenter Enteral Nutr 2016;40:890–5. https://doi.org/10.1177/0148607115574000
-
Bolton DT. Extravasation associated with a multilumen central catheter. Anaesthesia 1997;52:1119.
-
Bothur-Nowacka J, Czech-Kowalska J, Gruszfeld D, Nowakowska-Rysz M, Kościesza A, Polnik D, Dobrzańska A. Complications of umbilical vein catherisation. Case Report. Pol J Radiol 2011;76:70–3.
-
Čače IB, Krajina R, Čače N. Umbilical vein catheterization – when complications occur a case report. Signa Vitae 2014;9:73–5.
-
Campistol J, Krauel J, Baraibar R. Hydrothorax: a rare complication of parenteral feeding in a new born. Z Kinderchir 1980;29:251–3.
-
Coley BD, Seguin J, Cordero L, Hogan MJ, Rosenberg E, Reber K. Neonatal total parenteral nutrition ascites from liver erosion by umbilical vein catheters. Pediatr Radiol 1998;28:923–7. https://doi.org/10.1007/s002470050500
-
Currarino G. Migration of jugular or subclavian venous catheters into inferior tributaries of the brachiocephalic veins or into the azygos vein, with possible complications. Pediatr Radiol 1996;26:439–49.
-
Das D, Datta M, Dey S, Parida J, Kumar R, Pande A. An unusual cause of cardiac tamponade during cardiac catheterization study. Case Rep Cardiol 2014;2014:652592. https://doi.org/10.1155/2014/652592
-
D’Elia C, Correia MS, de Oliveira SD, Barbosa NM. Bronchovascular fistula – complication of percutaneous central venous catheter in a neonate. J Pediatr 2002;78:347–50.
-
Department of Health and Social Care. Review of Four Neonatal Deaths due to Cardiac Tamponade Associated with the Presence of a Central Venous Catheter: Recommendations and Department of Health and Social Care Response. London: Department of Health and Social Care; 2001.
-
Edmonds LK, Craw S. Extravasation & UVC’s: a cautionary case series. J Paediatr Child Health 2015;51(Suppl 1):92.
-
Gomes ACR, da Silva CAG, Gamarra CJ, Faria JCdO, Avelar AFM, Rodrigues EdC. Assessment of phlebitis, infiltration and extravasation events in neonates submitted to intravenous therapy. Anna Nery School Journal of Nursing 2011;15:472–9.
-
Gonzalez-Tarancon R, Lasierra Monclus AB, Murillo Peruga O, Garcia-Rodriguez B, Puzo Foncillas J. Hydrothorax in an infant induced by central venous catheter malposition after cardiac surgery. A case report. Revista del Laboratorio Clinico 2015;8:127–30.
-
Grizelj R, Vukovic J, Bojanic K, Loncarevic D, Stern-Padovan R, Filipovic-Grcic B, et al. Severe liver injury while using umbilical venous catheter: case series and literature review. Am J Perinatol 2014;31:965–74. https://doi.org/10.1055/s-0034-1370346
-
Guzoglu N, Erdeve O, Yilmaz Y, Dilmen U. Intraperitoneal extravasation from umbilical venous catheter in differential diagnosis of neonatal chylous ascites. Acta Paediatr 2010;99:1284. https://doi.org/10.1111/j.1651-2227.2010.01893.x
-
Haass C, Sorrentino E, Tempera A, Consigli C, De Paola D, Calcagni G, et al. Cardiac tamponade and bilateral pleural effusion in a very low birth weight infant. J Matern Fetal Neonatal Med 2009;22:137–9. https://doi.org/10.1080/14767050802509561
-
Hager J, Menardi G. Retroperitoneal extravasation – rare complication with parenteral nutrition (author’s transl). Padiatr Padol 1981;16:227–31.
-
Hagerott HE, Kulkarni S, Restrepo R, Reeves-Garcia J. Clinical-radiologic features and treatment of hepatic lesions caused by inadvertent infusion of parenteral nutrition in liver parenchyma due to malposition of umbilical vein catheters. Pediatr Radiol 2014;44:810–15. https://doi.org/10.1007/s00247-014-2895-2
-
Hanta D, Gulcan H, Torer B, Ozdemir Z, Temiz A. Neonatal total parenteral nutrition ascites following umbilical venous catheterization in a preterm newborn. Early Hum Dev 2010;86:S82–3.
-
Jardine LA, Inglis GD, Davies MW. Aspiration of parenteral nutrition – a previously unreported complication of central venous access in an infant: a case report. J Med Case Rep 2008;2:63. https://doi.org/10.1186/1752-1947-2-63
-
Keeney SE, Richardson CJ. Extravascular extravasation of fluid as a complication of central venous lines in the neonate. J Perinatol 1995;15:284–8.
-
Kingsley DP, Kendall BE, Greitz T, Hoare RD. Extravasation of contrast-enhanced blood into the subarachnoid space during computed tomography. Neuroradiology 1979;18:259–62.
-
Knobel RB, Meetze W, Cummings J. Case report: total parenteral nutrition extravasation associated with spinal cord compression and necrosis. J Perinatol 2001;21:68–71.
-
Korver AM, Walther FJ, van der Molen AJ, de Beaufort AJ. [Serious complications of umbilical venous catheterisation.] Ned Tijdschr Geneeskd 2007;151:2219–23.
-
Krasna IH, Krause T. Life-threatening fluid extravasation of central venous catheters. J Pediatr Surg 1991;26:1346–8.
-
Kreusser KL, Volpe JJ. Peroneal palsy produced by intravenous fluid infiltration in a newborn. Dev Med Child Neurol 1984;26:522–4.
-
Krüse-Ruijter MF, Robben SG, Degraeuwe PL. Hydrocoele and periorchitis after extravasation of parenteral nutrition solution. Arch Dis Child Fetal Neonatal Ed 2011;96:F359. https://doi.org/10.1136/adc.2011.210914
-
Kundra P, Chandran BV, Subbarao KS. Unanticipated complication of a malpositioned central venous catheter. J Anesth 2009;23:275–7. https://doi.org/10.1007/s00540-008-0724-1
-
Kurepa D, Sankararaman S, Patra K, Kakkilaya V, Thomas G. Pleural effusion caused by ‘correctly’ placed umbilical venous catheter. J Investig Med 2011;59:454.
-
Lee SD, Kao TH, Cheng WY, Wang YC. Malposition of central venous catheter eliciting fluid leakage in the lumbar wound: a case report. Formosan J Surg 2001;34:153–7.
-
Lin C, Elsey N, Corridore M, Grischkan J, Shiels WE, Tobias JD. Dye extravasation during radiography for branchial cleft sinus compromising airway in an infant. Anaesth Pain Intensive Care 2015;19:192–5.
-
Mahajan V, Rahman A, Tarawneh A, Sant’anna GM. Liver fluid collection in neonates and its association with the use of a specific umbilical vein catheter: report of five cases. Paediatr Child Health 2011;16:13–15.
-
Meeks SL, Ciambotti JM, Rodgers BM, Gordon PV. Extravasation of hyperalimentation into the liver parenchyma from a peripherally inserted central catheter. J Pediatr Surg 2003;38:E8. https://doi.org/10.1053/jpsu.2003.50146
-
Nadroo AM, al-Sowailem AM. Extravasation of parenteral alimentation fluid into the renal pelvis – a complication of central venous catheter in a neonate. J Perinatol 2001;21:465–6.
-
Namachivayam P, Tibballs J. Methylene blue for diagnosis of displaced atrial lines. Anaesth Intensive Care 2006;34:280–1.
-
Nath MP, Gupta S, Chakrabarty A. Extravasation of catheter tip following central venous catheterisation: a near fatal complication. Indian J Anaesth 2010;54:572–3. https://doi.org/10.4103/0019-5049.72651
-
Nour S, Puntis JW, Stringer MD. Intra-abdominal extravasation complicating parenteral nutrition in infants. Arch Dis Child Fetal Neonatal Ed 1995;72:F207–8.
-
Onal EE, Saygili A, Koc E, Turkyilmaz C, Okumus N, Atalay Y. Cardiac tamponade in a newborn because of umbilical venous catheterization: is correct position safe? Paediatr Anaesth 2004;14:953–6.
-
Ozdemir R, Oğuz S, Uras N, Erdeve O, Yilmaz Y, Ulu H, Dilmen U. Phrenic nerve injury due to thoracentesis for TPN effusion in a preterm newborn: consecutive two unusual complications. Tuberk Toraks 2011;59:384–7.
-
Oztan MO, Ilhan O, Abay E, Koyluoglu G. An umbilical venous catheter complication presented as acute abdomen: case report. Arch Argent Pediatr 2016;114:e429. https://doi.org/10.5546/aap.2016.eng.e429
-
Perry MS, Billars L. Extravasation of hyperalimentation into the spinal epidural space from a central venous line. Neurology 2006;67:715.
-
Pignotti MS, Messeri A, Donzelli G. Thoracentesis in pericardial and pleural effusion caused by central venous catheterization: a less invasive neonatal approach. Paediatr Anaesth 2004;14:349–51. https://doi.org/10.1046/j.1460-9592.2003.01225.x
-
Rizzo AJ, Haller JO, Mulvihill DM, Cohen HL, Da Silva MG. Calcification of the ductus venosus: a cause of right upper quadrant calcification in the newborn. Radiology 1989;173:89–90. https://doi.org/10.1148/radiology.173.1.2675191
-
Sankararaman S, Kurepa D, Kakkilaya V, Patra K, Gates T. Pleural effusion: an extremely uncommon complication of correctly placed umbilical venous catheter. J Neonatal Perinatal Med 2012;5:269–73.
-
Schiavetti A, Ventriglia F. Contrast echocardiography test for intrapleural extravasation by central venous catheter. Imaging Med 2014;6:21–4.
-
Scott JJ, Ireland S, Kandasamy Y. Conservative management of TPN extravasation into the liver from UVC: a case series. J Paediatr Child Health 2015;51(Suppl 1):92.
-
Servetar EM. A case report of Twiddler’s syndrome in a pediatric patient. J Pediatr Oncol Nurs 1992;9:25–8. https://doi.org/10.1177/104345429200900105
-
Shareena I, Khu YS, Cheah FC. Intraperitoneal extravasation of total parental nutrition infusate from an umbilical venous catheter. Singapore Med J 2008;49:e35–6.
-
Spicer KM, Gordon L. Extravasation from venous catheter: a serious complication potentially missed by lung imaging. J Nucl Med 1983;24:1023–6.
-
Spriggs DW, Brantley RE. Thoracic and abdominal extravasation: a complication of hyperalimentation in infants. AJR Am J Roentgenol 1977;128:419–22. https://doi.org/10.2214/ajr.128.3.419
-
Sztajnbok J, Troster EJ. Acute abdomen due to late retroperitoneal extravasation from a femoral venous catheter in a newborn. São Paulo Med J 2002;120:59–61.
-
Tosello B, Michel F, Merrot T, Chaumoître K, Hassid S, Lagier P, Martin C. Hemidiaphragmatic paralysis in preterm neonates: a rare complication of peripherally inserted central catheter extravasation. J Pediatr Surg 2011;46:E17–21. https://doi.org/10.1016/j.jpedsurg.2011.03.065
-
van der Putten ME, Been JV, Robben SGF, Zimmermann LJI. An unusual cause of hydronephrosis in a preterm infant. Neth J Crit Care 2011;15:149–51.
-
Vidwans A, Neumann DP, Hussain N, Rosenkrantz T, Sanders MR. Diagnosis and management of spinal epidural space extravasation complicating percutaneous central venous line placement in a premature infant: case report and review of literature. Conn Med 2000;64:79–82.
-
Watterson J, Heisel M, Cich JA, Priest JR. Intrathoracic extravasation of sclerosing agents associated with central venous catheters. Am J Pediatr Hematol Oncol 1988;10:249–51.
-
Williams JH, Hunter JE, Kanto WP, Bhatia J. Hemidiaphragmatic paralysis as a complication of central venous catheterization in a neonate. J Perinatol 1995;15:386–8.
-
Yeh J, Vargas JH, Wozniak LJ, Smith JB, Ines Boechat M, Touma M. Massive liver mass and parenteral nutrition extravasation secondary to umbilical venous catheter complications. J Clin Neonatol 2014;3:158–60.
-
Yeoh HA, Chou YH, Wong HF. Migration of a central venous catheter into pulmonary vein complicated with lung edema in a premature infant. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 1997;38:303–5.
Appendix 3 Case report study details
Further details of the included case reports are presented in Table 12.
| Authors | Design | Age | Infusate | Intervention | Outcome |
|---|---|---|---|---|---|
| Abraham et al. 201258 | Case report | 9 years | Arginine and 10% glucose | Cool compresses and dressings | Residual scar but no other complications |
| Altan et al. 201359 | Case report | 23 days | Contrast agent | Elevation and cold compresses. Volar fasciotomy for compartmental syndrome | No functional complications |
| Altmann et al. 201460 | Extractable: only one case (rest mixed with adult population) | 2 years | Unspecified antibiotic |
Radical debridement Wound conditioning either by vacuum assisted closure or temporary wound coverage by allogeneic donor-tissue grafts (unclear which) Full-thickness skin graft |
Full restoration of right hand function |
| Amano et al. 200861 | Case report | 3 years | Arginine monohydrochloride (10% in sodium chloride) | Conservative therapy with 1% silver sulphadiazine | One month after the accident the ulcer healed, leaving a slight hypertrophic scar |
| Amaya 201662 | Multiple case reports (four patients) | 4–32 weeks old (three preterm) | NR | ALH, debridement and dehydrated amniotic membrane allograft | Needed skin graft but no untoward effects seen (healed 21 to 41 days). |
| Amhaz et al. 201663 | Case report | 10 days | Blood | Lipoaspiration cannula to evacuate the hematoma, elevation and compress | Healed over 2 weeks |
| Aribit et al. 200064 | Multiple case reports (two patients) | 6 and 11 months | Glucose 10% (n = 1), NR (n = 1) | Lipoaspiration, followed by local care until healed | Full recovery at 4 months other than postepidermolysis dyschromia, no other trophic or neurological adverse event |
| Baker et al. 199165 | Case report | 7 years | Arginine monohydrochloride (10%) | Elevate, cold compress. Topical silver sulphadiazine after twice daily hydrodebridement. Surgical debridement and skin graft | Nerve and tendons destroyed. Skin graft necessary and was 98% viable fully functional after 5 days. Full function at 4 weeks |
| Bassi et al. 200766 | Case report | 10 months | 6 cc arginine monohydrochloride, 50% diluted in 12 cc of sodium chloride 0.9% | Managed conservatively. Enzymatic debridement by collagenase ointment (clostridiopeptidase A) together with local antiseptics | Complete resolution within 2 months with hypertrophic scar (see Figure 2). There was no need for skin grafting |
| Berger et al. 1974162 | Multiple case reports (three patients) | 2 days to 1 month (two preterm) | All calcium gluconate | Soaks and mechanical debridement in two. Antibiotics in two | Took between 3 weeks and 6 months to heal depending on severity |
| Beytut et al. 2014163 | Case report | 7 years | NR | Oxygenotherapy, heat treatment and dressings with dextrose | 12 days to full recovery |
| Bhosale et al. 201267 | Case report | 16 years | Dopamine | 4 days of antibiotics, and noradrenaline with dopamine. Followed by skin debridement and grafting | Needed skin graft |
| Borman et al. 199868 | Case report | 4 years | Chloramphenicol and ampicillin | Dermatofasciotomy, heparin infusion | Day 20 gangrene and amputation of hand |
| Boyar et al. 201469 | Case report | 3 weeks (preterm) | NR | MEDIHONEY® (Derma Sciences, Plainsboro, NJ, USA) gel and dressing | Healed over 3 weeks with some scarring |
| Broom et al. 201670 | Multiple case reports (two patients) | 6 months to 1 year | NR | All underwent fasciotomy for compartment syndrome | Both had excellent outcome |
| Chait et al. 197571 | Case report | 2 years | Oncovin dauno rubicin | Moist dressings and elevation | Healed within 3 months with some scarring |
| Chen et al. 201072 | Case report | 4 days (preterm) | Calcium gluconate (10%) | Elevation, cold packs. Oxacillin, ampicillin and gentamicin, fasciotomy ( × 2) for compartment syndrome, vancomycin and ceftazidime. Wet dressings | Improved after 3 months |
| Chiang et al. 200473 | Case report | 11 days (preterm) | Calcium gluconate (10%) | Elevation, cold packs, oxacillin and gentamicin, vancomycin (4 weeks) | Improved after 45 days |
| Ching et al. 201474 | Case report | 4 days | Calcium gluconate | Managed conservatively | Improved after 20 weeks |
| Cho et al. 200775 | Multiple case reports (five patients) | 17 to 50 days |
Parenteral nutrition (6th case blood transfusion) |
Antibacterial (antibiotic) ointment, sesame oil, anti-inflammatory herbal mixture, dressings (one debridement, one escharectomy and oral antibiotic), Vitamin C | 1 month–2 years: no scar and no functional abnormalities |
| Cohan et al. 199076 | Case report | 12 months | Iopamidol | Elevation and warm compresses | 2 days to full recovery |
| D’Acunto et al. 201577 | Case report | 2 months (preterm) | Balanced electrolyte solution | Elevation, proteolytic cream, escharectomy as well as autograft skin | Total recovery after 1 year |
| Davé 199378 | Case report | 3 years | Undefined fluids (no drugs) | Wet gauze, hot packs, debridement and skin graft | No long-term functional complications |
| Davies et al. 199479 | Multiple case reports (two patients) | 26 and 11 days (both preterm) | Parenteral nutrition | Subcutaneous hyaluronidase and saline flushing | Healed with minimal scarring/no sign of injury |
| Denkler et al. 198980 | Case report | 1 day (preterm – two sites: hand/foot) | Dopamine | 2% nitroglycerin ointment and elevation | Full recovery same day |
| Domizio et al. 200681 | Case report | 2 days (two sites) | Ampicillin (50 mg/kg/day) and cefotaxime (100 mg/kg/day) added with 10% calcium gluconate | 7 days later treated topically with an antibiotic–corticosteroid cream | 20 days later, only whitish subcutaneous nodules from which tiny white pieces of calcific masses were eliminated spontaneously without signs of inflammation |
| Dunn et al. 198482 | Case report | 5 months | Dextrose and 25% normal saline | Elevation | 2 months later, no movement or feeling in parts of hand. 9 months after injury, improvement |
| Duray et al. 198683 | Case report | 5 years | Doxorubicin | Excision of surrounding skin | Skin graft needed but healed |
| Eckersall et al. 199684 | Case report | 3 years | Dextrose saline | Elevation (24 hours) | 3 days to full recovery |
| Eroglu et al. 200485 | Case report | 17 years | Mannitol (20%) | Fasciotomy for compartment syndrome | Fully functional, with a scar |
| Garcia-Alverez et al. 199986 | Case report | 2 weeks (administered over first 3 days of life) | Calcium gluconate | Managed conservatively | Full recovery 10 weeks later |
| Gibboney et al. 198687 | Multiple case reports (two patients) | 17 days and 4 weeks (both preterm) | i.v. fluids | Surgical debridement and antibiotics, one received several skin grafts | 5.5 to 9 months, healed |
| Govind et al. 201488 | Case report | 27 days (preterm) | Parenteral nutrition (lipid infusate) | Incision and drainage, flushing of central line | 18 months, healed naturally |
| Grabois et al. 200889 | Case report | 19 days (preterm) | Sodium bicarbonate | Clean wound and covered with Vaseline (Unilever, Surrey, UK; sterile petrolatum) for 20 days | Recovered after 20 days |
| Handler 199090 | Case report | 4 years | Dextrose solution (5%), 25% saline, and potassium chloride | Elevated and warm dressing. Fasciotomy for compartment syndrome, skin graft | Needed skin graft |
| Hankin et al. 198491 | Case report | 17 years | Doxorubicin | Cold packs. Wet to dry dressings. Conservative management. Debridement after 7 months | Healed with contracture of arm |
| Harb et al. 201092 | Case report | 1 year (preterm) | Erythromycin | Area was irrigated with saline through small punctures in the skin around the injury site. Managed initially conservatively, with regular dressing changes and delayed surgical intervention. At 3 weeks – debridement and skin graft | 1 week later – healing well |
| Hasija et al. 201493 | Case report | 3 years | Phenytoin | Fasciotomy for compartment syndrome | After a few days, normal tissue texture and the injury was managed |
| Hey et al. 200594 | Case report | 12 months | Azithomycin | Warm compresses, adaptic dressing, splint, elevation, topical antibiotics | Small area of unusual pigmentation, but otherwise healthy |
| Hironaja et al. 198295 | Case report | 6 days | Calcium gluconate (10%) | Warm soaks, debridement, soaks of (2%) ethylenediaminetetraacetic acid | At 4 months, full recovery but does not mention scarring, etc. |
| Hirsch et al. 201696 | Case report | 4 days (preterm) | Parenteral nutrition | Elevated, antibiotic ointment, slightly compressive gauze, 13 days debridement, collagenase, silicone dressing, splint, silver nitrite, Apligraf® (Organogenesis, Canton, MA, USA) | Day 16 wound closure, at 2 years, wrist contracture |
| Hooke 200597 | Case report | Adolescent | Doxorubicin | Aspirated, cold packs DMSO solutions topically, three debridements, skin graft | Large scar, but full use of area |
| Kameo et al. 201598 | Case report | 2 years | Vincristine | Hyaluronidase for 3 days, warm compresses | Full recovery |
| Khan et al. 201499 | Case report | 29 days (preterm) | Parenteral nutrition | Hyaluronidase and bacitracin | After 9 days, full recovery |
| Kishi et al. 2014100 | Case report | 17 years | Hydroxyzine | Conservative therapy and 1% silver sulphadiazine | After 2.5 months, slight scarring |
| Kuensting 2010101 | Case report | 6 days | 10% dextrose and 0.25% normal saline solution administered at 10ml per hour with the addition of ampicillin (135 mg every 8 hours) and cefotaxime (135 mg every 8 hours) | Elevation and warm packs, hyaluronidase and general wound care | Recovered within 24 hours, discharged at 8 days |
| Kumar et al. 2001102 | Multiple case reports (six patients) | Neonate (preterm) to 2 years | Flucloxacillin, calcium gluconate, human immunoglobulin, sodium bicarbonate, dextrose solution, 20% lipid nutrition | Dressings for three. Split skin graft and debridement for three, elevation and warm packs | Two excellent (one with scar), one fair and three moderate scarring (one contractures treated) |
| Lee et al. 2013103 | Case report | 1 month (preterm) | Sodium bicarbonate | Hyaluronidase, epithelial growth factor dressings and platelet-rich plasma dressings | 4 days after PRP, completely healed with no limitation of movement |
| Lehr et al. 2004104 | Multiple case reports (three patients) | 4 to 24 days (two preterm) | Parenteral nutrition (lipids) plus antibiotics | Compression, elevation and hydroactive gel | Healed no complications |
| Leung et al. 1980105 | Case report | 6.5 years | Contrast medium (sodium iothalamate 54%) | Repeated incisions, antibiotics, excision of necrotic skin and skin grafts | At 6 months, scarring, no limits on movement |
| Llinares et al. 2005106 | Case report | 4 years | Anthracycline (idarubicin) | Topical DMSO and cooling, antiseptic and moisturiser | Pain from application but recovered. At 4 weeks, loss pigmentation and focal induration |
| Martin et al. 1994107 | Case report | 4 months | 8.4% bicarbonate 20 ml, 10% calcium gluconate 10 ml, 50% glucose 5 ml, 1 : 1000 adrenaline 3 ml and 4.5% human albumin solution 50 ml | Hyaluronidase, liposuction and saline wash-out | 2 weeks later, no signs of soft tissue damage |
| Meszes et al. 2017108 | Multiple case reports (six patients) | Neonates (1 to 23 days) | Fatty acid, lipid and amino acid infusion (n = 4), glucose (n = 1) and dobutamine (n = 1) | Epithelising ointment (n = 3), hydrogels (n = 2), surgical necrectomy (n = 1) and observation (n = 1) | Transfer to NICU (n = 4), home (n = 1), surgery (n = 1) |
| Mohr et al. 2014109 | Multiple case reports (two patients) | 3 weeks (preterm), 19 days (preterm) | Antibiotics, NR | Hyaluronidase, ALH hydrogel, ALH calcium alginate, silver/collagen dressings | No negative side effects |
| Morrison et al. 1999110 | Multiple case reports (four patients) | Neonates (preterm) | Calcium gluconate | Skin grafts | 3 years later, visible scarring |
| Mukherjee et al. 1977111 | Multiple case reports (two patients) | 5 years, and NR | Dextrose solution; NR (rehydration) | Skin grafts; debridement | Gangrene, disfigured, and incapacitated |
| Nissim et al. 2008112 | Case report | 1 day | NR | Conservative treatment | Interval shrinkage and dissolution of the mass |
| Onesti et al. 2012113 | Case report | 2 days (preterm) | Parenteral nutrition | Elevation, topical silver sulphadiazine, some debridement, acellular dermal substitute, autologous keratinocytes | 9 months, scars and deformed foot (surgical correction); 14 months, fully healed |
| O’Reilly et al. 1988114 | Case report | Neonate | Parenteral nutrition | Glyceryl trinitrate patch | Healed without scarring (small area not covered, skin lost) |
| Ozcan et al. 2015115 | Case report | 14 years | Adrenalin | Elevation, local antibiotic ointment and pentoxyphilline | Patient died due to septic shock |
| Pantelides et al. 2013116 | Case report | 1 day (preterm) | Dextrose solution (12.5%) | Elevation | No scarring or functional deficit |
| Park et al. 2015117 | Case report | 7 months | Parenteral nutrition | Fasciotomy for compartment syndrome. Irrigation with saline solution. Debridement, after 4 months skin graft | Needed rehabilitation for contracture, healed with scar |
| Phillips et al. 2009118 | Case report | 3 months | Dopamine | Conservative treatment, topical antibiotics, debridement, physical therapy | Needed 12 months of physical therapy. May need secondary surgery |
| Raffaella et al. 2009119 | Case report (two extravasations) | 5 years | Calcium gluconate | Treated conservatively (limb elevation, daily wound care, and warm compresses), antibiotics, disinfection, and physiotherapy, daily hyperbaric oxygen therapy, weekly surgical debridement and escharectomy, sodium thiosulphate for calcification | 8 months to fully healed |
| Ravenel 1983120 | Case report | 6 days | Calcium gluconate | Antibiotics, nafcillin sodium | 6 weeks, swelling subsided |
| Reilly et al. 1977121 | Multiple case reports (three patients) | 13, 15 and 17 years | Adriamycin | Cold compress (n = 1), antibiotics (n = 1) and hydrocortisone (n = 1) | Two lost functional use; less serious, one healed |
| Reynolds 2007122 | Case report | 2 days (preterm) | Intralipid and parenteral nutrition | Elevation | 12 hours to heal completely |
| Roberts 1977123 | Multiple case reports (five patients) | Neonates (range 1 day–1 year) | Calcium gluconate | Conservative treatment (none or warm soaks) | Resolved spontaneously |
| Rosales et al. 2004124 | Case report | 75 days (preterm) | Parenteral nutrition and intralipid | Antibiotics, drained | Died of sepsis |
| Roth et al. 2006125 | Case report | 31 days | Propofol and lidocaine | Saline, debridement, skin graft | Satisfactory functional healing |
| Rustogi et al. 2005126 | Case report | 4 days (preterm) | Sodium bicarbonate | ACTICOAT™ dressing | 57 days to heal |
| Salameh et al. 2004127 | Case report | 3.5 years | Arginine | Compressive dressing, debridement, skin grafts | Functional result |
| Samiee-Zafarghandy et al. 2014128 | Case report | 1 day (preterm) | Packed red blood cells | Conservative management, topical nitroglycerin | Loss of two toes |
| Sanpera et al. 1994129 | Multiple case reports (two patients) | 3 days and neonate (preterm) | Calcium solution and NR | Eusol and debridements, dressings | Limb shortening and deformity |
| Santoshi et al. 2008130 | Case report | Neonate (preterm) (seen at 5 years) | Blood, fluids and antibiotics | NR – claw deformity at 5 years – fibrous sheet was excised, the extensor tendons were tenolysed and full correction was obtained | Some scarring but functional |
| Schäfer et al. 2005131 | Case report | 2 weeks | Phenobarbital | Topical antibiotics, debridement and skin graft | Fully recovered |
| Schie et al. 2013132 | Case report | 33 weeks (preterm) | NR | Non-contact low-frequency ultrasound (19 sessions), debridement, amorphous hydrogel and covered with a thin film or hydrocolloid, silicone sheet | 32 days, healed without complication |
| Schumacher et al. 1987133 | Case report | 7 years | Calcium disodium edetate (EDTA) | Warm soaks and splints | Calcification needed surgery (1.75 years later) |
| Sharief et al. 1994134 | Case report (two extravasations) | 1 day (and 3 days) | Phenytoin | NR | 1 week, complete resolution |
| Shenaq et al. 1996135 | Case report | 10 years | Adriamycin (doxorubicin) | Left for 4 months, debridement, physical therapy, dressings, skin graft, capsulotomies | Not fully functional |
| Sindal et al. 2015136 | Case report | Neonate (preterm) | NR | Debridement and topical antibiotic ointment | 2 weeks, healed completely |
| Siu et al. 2007137 | Case report | 2 days (preterm) | Parenteral nutrition (dextrose, calcium, potassium, etc) | Hyaluronidase and saline flushes, dressings | Healed within 5 days |
| Siwy et al. 1987138 | Case report | 2 days | Dopamine | Infusion of phentolamine (Regitine®,Novartis Pharmaceuticals Corporation, NJ, USA) in saline solution, kept at heart level | Healed after 9 days |
| Sokol et al. 1998139 | Case report | 14 months (preterm) | Phenytoin | Hyaluronidase | Barely visible scar |
| Sonohata et al. 2006141 | Case report | 14 years | Phenytoin (diazepam before) | Hydrocortisone injections, elevation, warm packs | 5 weeks to fully recovered |
| Sonohata et al. 2008140 | Case report | 3 days | Calcium gluconate | No treatment | 5 months, fully recovered |
| Soon et al. 2001142 | Case report | 38 weeks | Calcium gluconate | Local skin care and topical antibiotic | 3 months, recovered |
| Spenny et al. 2004144 | Case report | 3 years | Ceftriaxone sodium | Cold pack, diphenhydramine hydrochloride and adrenaline, clindamycin and morphine, fasciotomies | 3 months, healed with complete function |
| Stahl et al. 2000143 | Case report | 10 years | Mannitol | Fasciotomies | 1 year, no neurological or vascular damage |
| Subedi et al. 2011145 | Case report | 16 years | Dextrose | Analgesics and antibiotics followed by local incision and drainage. Managed conservatively for almost 5 months. Oral medications (gabapentin, amitriptyline, tramadol), a series of stellate ganglion blocks with bupivacaine, and limb physiotherapy | 6 months, pain and swelling subsided drastically with marked functional recovery |
| Subhani et al. 2001146 | Case report | 1 day | Dopamine | Phentolamine | Within the next few hours, there was complete resolution of the discoloration |
| Talbot et al. 2011147 | Multiple case reports (three patients) | 7 to 10 months | Two NR, one hydration | Fasciotomies for compartment syndrome, vacuum-assisted closure (n = 2) or moist dressings (n = 1) | Full functional recovery |
| Tilden et al. 1980148 | Multiple case reports (four patients) | 15 days to 4 months | Nafcillin sodium | Saline dressing and sulphadiazine silver (n = 2), debridement and skin graft (n = 1), bacitracin ointment (n = 1) | Healing well (n = 3), bacitacin not improved, died |
| Tiras et al. 2005149 | Case report | 2 days | Calcium gluconate | Debridement using collagenase clostridipeptidase A and bacitracin ointment mixture in gauze after wetting the wound with sterile saline | Healed without surgery |
| Tobin 2007150 | Case report | 1 day (preterm) | Parenteral nutrition | Oral antibiotics, ActiFormCool® (Activa Healthcare, Burton upon Trent, UK) dressings | 6 weeks, the wound had healed, with scarring |
| Tuncer et al. 2006151 | Case report | 6 years | Calcium solution | Surgery for calcinosis (4 years later) | Full recovery |
| Vanwijck and Lengele 1994152 | Case Report | 9 years | Meglumine ioxitalamate | Lipoaspiration with saline wash, followed by liposuction, under LA (n = 8) or GA (n = 1). Redon’s drain kept under aspiration for 24 hours. Perioperative and postoperative i.v. antibiotics, NSAIDS, elevated arm with light compress for 48 hours. Lymphatic drainage for persistent oedema at 1 week follow-up | Absent pulse in one child reappeared immediately after liposuction. Moderate reduction in extension (20 °) of two fingers extension in one patient. No other adverse events. |
| von Muhlendahl 2012153 | Multiple case reports (six patients) | 14 days (preterm) to 14 months | Fluids or electrolyte solution (n = 5; one plus erythromycin), phenytoin (n = 1) |
Immediate/early stage: within 24 hours of extravasation injury, complete removal of the aggravating substance via pressure-relieving incisions and flushing with Ringer’s solution or removal by aspiration (whichever is more appropriate); or Later than 24 hours: debridement and defect coverage (e.g., grafts) Standard care (n = 6), skin grafts (n = 2) |
Scars (n = 3), loss of fingers due to sepsis (n = 1), successful grafts (n = 2) |
| Wada et al. 2003154 | Case report | Neonate | Calcium solution | Conservative treatment, debridement, skin graft | 6 years, surgery for physeal arrest and short leg; further surgeries up until 12 years; 16 years, deformity remained |
| Wiegand et al. 2010155 | Case report | 17 years | Dextrose | Elevation, cold compresses, hyaluronidase | Full recovery |
| Wolfe et al. 1983156 | Case report | 2 days | Calcium solution | Antibiotics, immobilisation, and dressings | 6 months, full recovery |
| Wong et al. 1992157 | Multiple case reports (two patients) | 4 and 15 days (both preterm) | Dopamine | Nitroglycerin ointment, phentolamine (n = 1), elevation (n = 1) | 24 hours, full recovery |
| Wong et al. 2015158 | Case report | 4 days | Calcium gluconate | Managed conservatively | 20 weeks, healed |
| Yamamoto et al. 1994159 | Multiple case reports (two patients) | 1 and 4 years | Dopamine and tromethamine | Debridement and skin grafts (n = 2), scar surgery (n = 1) | Functional recovery |
| Yosowitz et al. 1975160 | Multiple case reports (seven patients) | 2 days to 10 years (two preterm) | Dextrose (10%) or calcium solutions | Debridement (n = 7) and skin grafts (n = 4) | Functional (n = 3), NR (n = 1), healed (n = 2), leg amputated (n = 1) |
| Zenk et al. 1981161 | Multiple case reports (three patients) | 3 days to 4 months | Nafcillin sodium | Hyaluronidase (n = 2); warm compresses and elevation, and 2 months skin graft (n = 1) | Healed (n = 3; two given hyaluronidase healed within a day) |
Appendix 4 Survey questionnaire content
The full questionnaire is detailed in Table 13.
| Question | Answers and format |
|---|---|
| What is your position? (e.g. consultant paediatrician): | Free text |
| What is the name and location of your unit? | Free text |
| Which of the following best describes your clinical setting: | Neonatal unit |
| Paediatric intensive care unit | |
| Principal oncology/haematology unit | |
| Shared care oncology/haematology unit | |
| Other (please state) | |
|
Does your unit have a written protocol or guideline for treating extravasation injuries? If yes, ask: |
Yes |
| No | |
| Does the protocol or guideline contain a staging system for grading severity of extravasation injury? | Yes |
| No | |
| Does your unit have a list of treatments/interventions which may cause serious problems when extravasated? | Yes |
| No | |
|
Please consider the list below of possible treatments for extravasation injuries. How frequently is each of them used in your unit? Elevation of affected area Warm compress Cold compress Analgesia Specific topical cream or ointment (please state) Occlusive dressing Saline irrigation without hyaluronidase Saline irrigation with hyaluronidase Antidotes to specific infusates |
For each, choose one of: Always Usually Sometimes Rarely Never Do not know |
|
Apart from plastic surgery, are there any other interventions you would use for extravasation injuries which were not listed in the previous question? If yes please list the other intervention(s) and indicate frequency of use. Please note that our study does not cover preventative interventions |
Yes No Free text along with one of: Always Usually Sometimes Rarely |
| Please select the type of access site most associated with extravastion injuries in your unit’s patients: |
Peripheral line (hands, feet) Peripheral central line Central line Other (please state) Do not know |
| Please select the type of infusate which causes the largest proportion of all the extravastion injuries in your unit’s patients |
More than one option may be selected if the proportion of injuries is around the same for two or more types of infusate: Parenteral nutrition Contrast agents Calcium Blood Vesicant chemotherapies Non-vesicant chemotherapies Inotropes or pressors Other (please state) Do not know |
| What proportion of the extravasation injuries in your unit would you estimate is caused by extravasation of infused (insert above response) |
75–100% 50–74% 25–49% 11–24% 1–10% Not sure, but > 50% Not sure, but < 50% |
| Approximately what proportion of extravasations injuries that you have actively treated have resulted in a need for plastic surgery at any stage? |
More than 50% 25–50% 5–24% < 5% Do not know |
|
In the last 10 years did any of the extravasation injuries which occured in your unit result in litigation? If yes, please state how many cases resulted in litigation: |
Yes No 1 2 3 4 5 ≥ 6 Do not know |
|
Regarding a future research study in this area, do you think a randomised trial design can be successfully undertaken to compare different treatments for extravasation injuries in babies and young children? If yes: Please tell us which treatment(s) you would most like to see studied in a randomised trial (state one or two treatments): If no: It would be helpful if you could say why a randomised trial design might not be viable. If you have any thoughts on alternative study designs, which you think might be more appropriate, please also state them here. |
Yes No Free text Free text |
|
Are you aware of any summary data on the effectiveness or safety of treatments for extravasation injury which we are unlikely to have identified in our searches of literature databases (e.g. unpublished data)? If yes display: ‘We would be very grateful if you could e-mail details on the summary data to mark.corbett@york.ac.uk within the next three weeks.’ |
Yes No |
| If you have any comments or suggestions about our study which have not been covered in this survey please add them here | Free text |
| Would you like to receive an e-mail notification when our final report is published online (it will be open-access)? |
Yes No thanks |
| If yes display: ‘Please tell us the e-mail address you would like the link sending to:’ | Free text |
| End message: Thank you very much for completing the survey |
Appendix 5 Further questionnaire results
Graphs summarising responses to the question ‘What proportion of the extravasation injuries in your unit would you estimate is caused by extravasation of infused calcium/blood/vesicant chemotherapies?’ (asked of those responders selecting calcium/blood or vesicant chemotherapies for the previous question) are summarised in Figures 4–6.
FIGURE 4.
Percentage of neonatal unit extravasation injuries caused by calcium in units, indicating calcium as the main cause of injuries.

FIGURE 5.
Percentage of neonatal unit extravasation injuries caused by blood in units, indicating blood as the main cause of injuries.
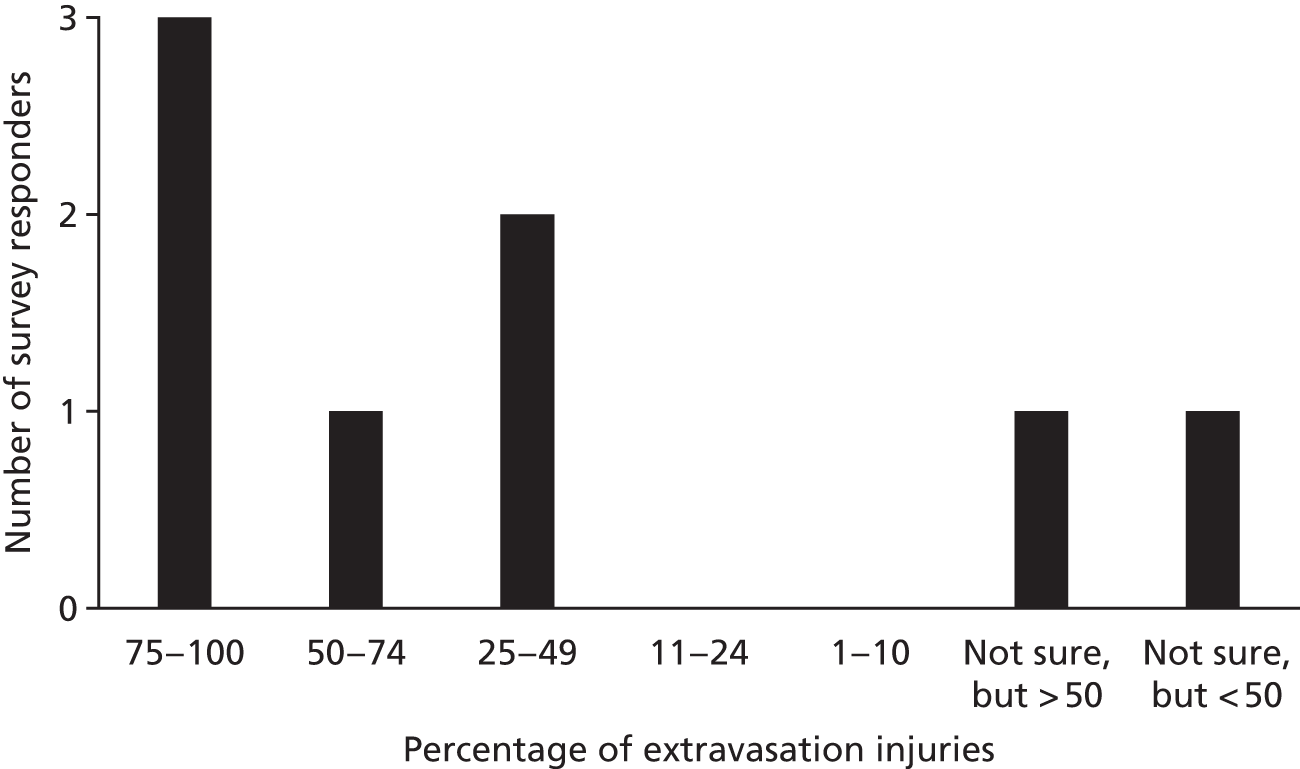
FIGURE 6.
Percentage of principal oncology/haematology unit extravasation injuries caused by vesicant chemotherapies in units, indicating vesicant chemotherapies as the main cause of injuries.

List of abbreviations
- AHRQ
- Agency for Healthcare Research and Quality
- BAPM
- British Association of Perinatal Medicine
- BNI
- British Nursing Index
- CCLG
- Children’s Cancer and Leukaemia Group
- CDSR
- Cochrane Database of Systematic Reviews
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CINAHL Plus
- Cumulative Index to Nursing and Allied Health Literature
- DARE
- Database of Abstracts of Reviews of Effects
- DMSO
- dimethyl sulfoxide
- EMBASE
- Excerpta Medica dataBASE
- GTN
- glyceryl trinitrate
- HTA
- Health Technology Assessment
- i.v.
- intravenous
- MeSH
- medical subject heading
- NICE
- National Institute for Health and Care Excellence
- NICU
- neonate intensive care unit
- NNRD
- National Neonatal Research Database
- PICU
- paediatric intensive care unit
- RCT
- randomised controlled trial
- VSS
- Vancouver Scar Scale
- WHO
- World Health Organization
