Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 13/144/01. The contractual start date was in October 2015. The draft report began editorial review in November 2017 and was accepted for publication in March 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Understanding Frames is independent research funded by the National Institute for Health Research (NIHR) under its Health Technology Assessment programme (13/144/01). Anna Basu and Niina Kolehmainen report grants from NIHR outside the submitted work. Anna Basu reports employment as consultant paediatric neurologist in the Newcastle upon Tyne Hospitals NHS Foundation Trust and an educational grant from Ipsen outside the submitted work. Sarah Crombie is employed by Sussex Community NHS Foundation Trust and works at Chailey Clinical Services, which supply standing frames. From 2013 to 2016, Elaine McColl was an editor for the NIHR Programme Grants for Applied Research programme and her employer received a fee for her work. Andrew Roberts and Keith Miller are employed by the Robert Jones and Agnes Hunt Orthopaedic Hospital, which designs, builds and supplies standing frames within the NHS. Jill Cadwgan reports honoraria from Ipsen for delivery of a lecture and support for the development of training materials for botulinum toxin treatment outside the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2018. This work was produced by Goodwin et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2018 Queen’s Printer and Controller of HMSO
Chapter 1 Background and aims
Context
Cerebral palsy (CP) affects 1 in 400 children and young people. CP is associated with spasticity and secondary musculoskeletal complications. Twenty-five per cent of young people with CP are non-ambulant [Gross Motor Function Classification System (GMFCS) levels IV or V]. 1,2 These young people frequently experience joint contractures, loss of bone mineral density (BMD), fractures and hip dislocation, leading to pain and progressive disability. 3 Postural management, including standing frame use, is recommended4 and widely used in clinical practice for young people with CP. A standing frame has a rigid frame with a wide base. A child is positioned in the standing frame with variable support that may enable movement of the head, upper body and upper limbs, thus potentially improving their function and participation. For the lower limbs, standing is usually passive (i.e. continuous and stationary loading) but can be dynamic (i.e. simulating the forces applied during natural walking). Standing frames are predominantly used in non-ambulant young people (GMFCS III–V), but in the younger age range it may also be used in those with some independent mobility (GMFCS III).
Research objectives
The overall purpose was to answer the question: what is the likely acceptability of a trial to determine the clinical effectiveness of standing frames? To do this, we undertook two surveys as well as focus groups and in-depth interviews to assess the feasibility and potential design of a trial (or trials) of standing frame use for young people with CP.
Aims and objectives
Aim 1. To determine current standing frame use in UK practice for the postural management of young people with CP aged 1–18 years with severe movement impairment (GMFCS IV and V).
This aim was addressed by:
-
Objective 1: conduct a survey (survey 1) of parents, health-care providers and education staff to determine current standing frame use for young people with CP. The questions comprised treatment indications, treatment goals, types of frame, duration of intended and actual use, and perceptions and practicalities of standing frame use.
Aim 2. To assess the willingness of parents to have their child randomised in a potential trial, including the acceptability of different treatment regimens, and to assess the preparedness of health-care providers to recruit to a potential randomised controlled trial (RCT).
This aim was addressed by:
-
Objective 2: undertake qualitative research to explore attitudes to standing frame use and acceptability of evaluating their benefit through a trial or trials. This comprised (1) focus groups with parents, health-care providers and education staff and (2) in-depth interviews with young people.
-
Objective 3: propose a small number of potential trial designs, structured around a population, intervention, comparison, outcome, timing, setting (PICOTS) framework and informed by the results of survey 1 and the qualitative research.
-
Objective 4: conduct a second survey (survey 2) of parents, health-care providers and education staff regarding the acceptability and feasibility of these potential trial designs.
Aim 3. To propose a substantive trial design (or designs) that is informed by, and acceptable to, parents and health-care providers.
This aim was addressed by:
-
Objective 5: combine the results from survey 1, focus groups, interviews and survey 2 to develop a substantive trial design or designs.
Literature review
A consensus statement4 recommended the use of standing frames as part of a postural management programme for young people with CP (GMFCS IV and V) from the age of 12 months, but acknowledged the lack of an evidence base for this intervention; the evidence that there was came from small case series, which were not blinded or randomised.
Reviews of standing frames5–7 and this Health Technology Assessment (HTA) programme-commissioned call concurred that the evidence base was limited. The most recent review7 claimed a positive effect on BMD, hip stability and joint range of movement at the hip, knee and ankle with variable duration of standing frame use, but Fehlings et al. 6 found the evidence unconvincing. Frames may also be disadvantageous. Young people have reported pain and discomfort, and families have reported increased demands on their time. 5 Furthermore, standing frames are expensive (they cost around £800–2500 each), require adaptation with the young person’s growth and use therapist time to prescribe and monitor their use. We are aware of a UK group currently conducting a systematic review of supported standing in CP, although we were advised that it will not be published until 2018 (Rachel Rapson, Bidwell Brook School, 2017, personal communication).
Gibson et al. 8 conducted a small case series that examined the effect of standing frame use for 1 hour every day for 6 weeks in five non-ambulant young people with CP, aged 6–9 years. Two 6-week intervals of standing frame use were alternated with two 6-week periods of no standing frame use. There was a suggestion of an improvement regarding hamstring stretches with standing frame use.
Caulton et al. 9 reported a RCT of a standing frame programme on BMD in 26 prepubertal young people (aged 4–11 years) with CP. This was a heterogeneous group, paired according to vertebral and tibial BMD scores and then randomised to either their usual standing duration or 50% increased duration of standing. There was, on average, an increase of 6% in vertebral BMD in the intervention group but no significant change in proximal tibial BMD in either group. The authors concluded that by increasing vertebral BMD through increased duration of standing there might be a potential to reduce risk of vertebral fractures. However, National Institute for Health and Care Excellence (NICE) guidance10 recommends that standing frames should not be used for the sole purpose of preventing low BMD.
There is variability in the amount of weight bearing in different standing frames, which may affect BMD outcomes. 11 Dynamic standing interventions may have more potential to improve bone health than passive standing frames. 12
How did the literature inform this study?
Synthesis of the literature revealed evidential equipoise (i.e. conflicting results from a weak evidence base). This justifies the need for further study, particularly to better understand the impact of standing frames at different stages in the lives of individuals with CP, with respect to their participation and subjective well-being rather than simply changes in their body structure and body function.
Current practice in the use of standing frames
Little is known about current UK practice with respect to the prescribing or actual use of standing frames, at home or in the community. Clinical experience from co-applicants suggests that most young people with CP have a physiotherapy programme that includes standing frame use, but prescription, timing, and dosage of intervention may be varied. To our knowledge, there is no previously published description of current UK practice.
Why this research is needed
There is a large population for whom obtaining clarity on the benefits of standing frame use is important. The birth prevalence of CP is about 2.5 per 1000 live births, so approximately 1740 CP births annually in England and Wales. 13 Approximately 25% of young people with CP are GMFCS level IV or V, and are therefore likely to have standing frames considered as part of their postural management.
The potential impact of standing frame use extends beyond childhood. Life expectancy in those with GMFCS level IV or V cannot be precisely estimated because published studies use different classifications of severity; however, 89% of those with only motor impairment and who need a self-propelled wheelchair lived to age 30 years, and 42% of those who could not self-propel lived to age 30 years. 14
For a young person, a standing frame may reduce risks of joint contractures, hip dysplasia and scoliosis. It may improve BMD and increase the likelihood, as a non-ambulant adult, that they will be able to assist a caregiver in a standing or weight-bearing transfer. It may reduce pain and make daily care easier. By enabling the young person to be vertical, a standing frame may improve head and trunk control; fine motor skills; gastrointestinal, bladder and respiratory function; self-esteem; and social, communicative and exploratory participation. 7
However, these are only potential benefits. The NHS needs to know if these benefits are real, given that there are significant cost implications of use and also reported negative effects: some young people experience discomfort in standing frames, and families and education staff describe practical difficulties in their use. 15
If there is clinical benefit in the use of standing frames, then the costs need to be balanced against the cost of long-term health-care needs (including quality of life), and secondary musculoskeletal complications of spasticity in CP, such as management of hip migration and dislocation, neuromuscular scoliosis, pathological fractures, pain and respiratory compromise that might have been prevented.
The NICE guideline16 for spasticity highlighted the limited evidence base for all interventions for young people with spasticity and specifically for postural management programmes. NICE proposed a trial of standing frame use for young people aged 1–3 years with GMFCS level IV or V. Our study was designed in the light of the 2013 National Institute for Health Research (NIHR) HTA commissioning brief, which widened the question to include young people < 18 years. We agreed that this was appropriate because of clinical indications for frames and changing neurodevelopmental profiles of young people at different ages.
A future trial of standing frame use would also fit with the CMO’s 2012 annual report17 which highlighted the need for research into effective intervention for long-term conditions in childhood, particularly in neurodevelopmental disorders where the health needs may be great but for which the evidence base for interventions is weak. A standing frames trial also aligns with the top research question identified for young people with neurodisability:18 does the timing and intensity of therapies alter the clinical effectiveness of therapies for infants and young children with a neurodisability? This includes strategies, dosage and direction of therapeutic interventions.
Co-applicant clinical experience shows that some parents and professionals have strong preformed views about standing frame use. Some professionals may have opinions that have been informed by their training or subsequent clinical experience, and this may lead them to making persuasive arguments to parents despite the weak evidence base. Parents in turn may have invested time, effort and faith in standing frames. Thus, although the current paucity of evidence demonstrates a clear need for evaluative research, a substantive trial will be difficult to design. The challenges for trial design arise from the heterogeneity of current practice regarding the purpose and delivery of standing frame intervention, and the many variables in each of the PICOTS frameworks that need to be considered. Depending on the young person’s neurodevelopmental profile and the goal of standing frame use, a variety of different comparators in a trial may be appropriate.
Furthermore, parents, professionals and young people report benefits of standing frames with respect to activity and participation that is not included in the current literature and has not been explored. Research needs to consider further aspects of the International Classification of Functioning, Disability and Health: Children and Youth version (ICF-CY),19 such as participation factors, along with body structure. The ICF-CY is a useful framework for examining the impact of the surrounding environment (including therapeutic interventions such as standing frames) and individual characteristics on a young person’s health-related functioning; it encompasses functions and structures of the body, activity, participation, personal factors and environmental factors.
This study was designed to address these issues and consider how a trial could be designed by determining current UK practice in the use of standing frames for young people with CP and by consultation with young people, parents and professionals who use standing frames.
Chapter 2 Methodology
During the conduct of this study we adopted a view of health as conceptualised by the ICF-CY. 19
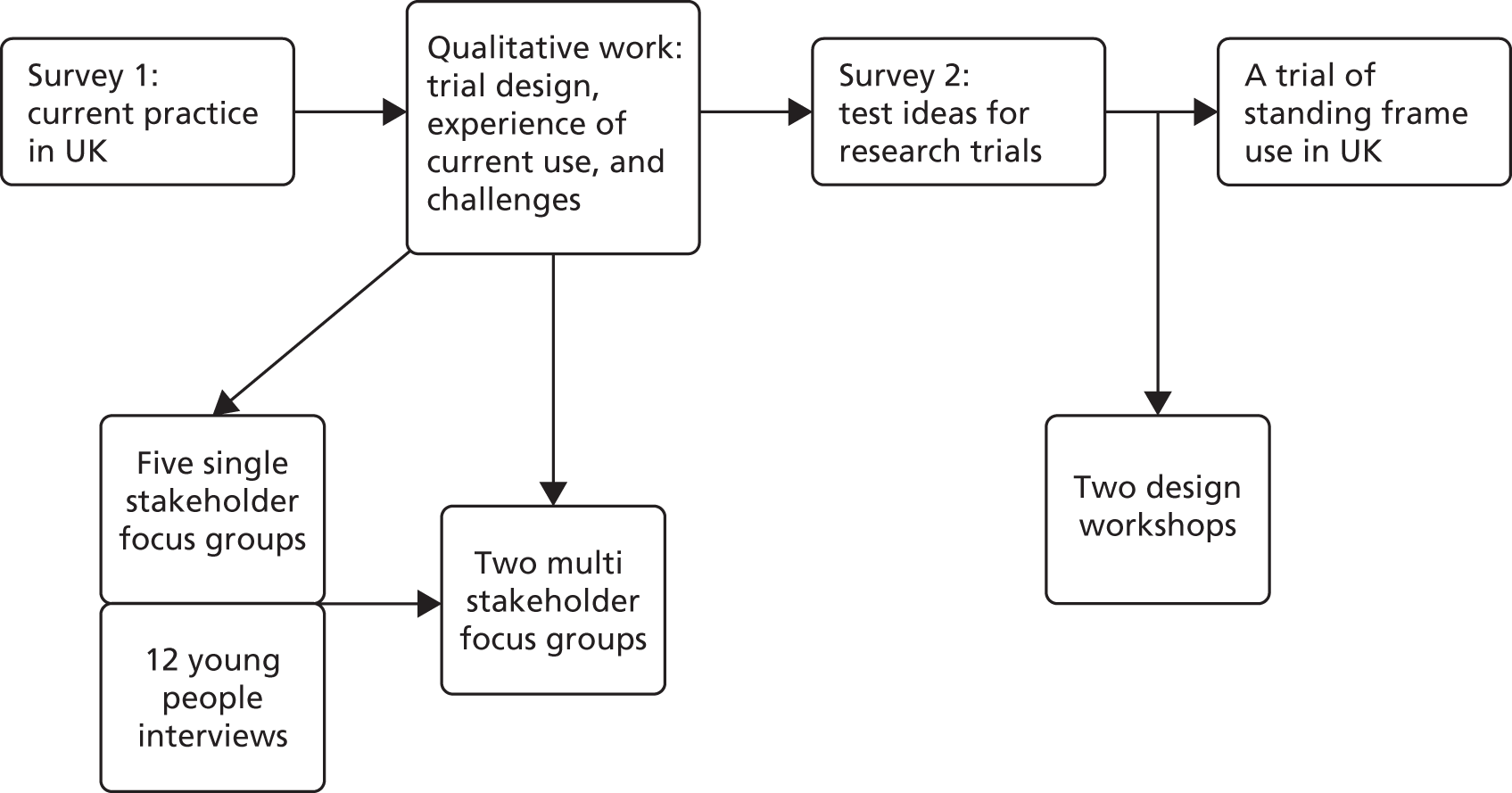
We used a sequential mixed-methods design, as outlined in Figure 1, whereby the findings from each stage informed the subsequent stage. The quantitative and qualitative findings are synthesised in Chapters 9 and 10. This process involved accounting for convergence (i.e. providing research recommendations) and divergence (i.e. highlighting potential challenges) between the data sources. People could take part in all stages if eligible, with the exception of the multistakeholder focus groups. Single stakeholder focus group participants could not participate in the multistakeholder focus groups.
FIGURE 1.
Flow of sequential mixed-methods design.
There were multiple study populations: prescribing professionals, professionals who work with standing frame users, parents of young people who currently use or have previously used a standing frame and young people who currently use or have previously used a standing frame.
Analysis
Quantitative data analysis was descriptive, largely reporting percentages of respondents in each category for each question. For survey 2, if there was a large spread of responses for particular items, the related open-ended responses were examined and then grouped into themes to explore the reasons behind participants’ closed-answer choices.
The qualitative analysis was informed by the framework method,20 which is not aligned with a particular epistemological or philosophical approach. 21 The framework method was chosen because it allowed for systematic data analysis that was accessible for our multidisciplinary research team. Table 1 outlines the stages of analysis. We used a deductive–inductive approach; although certain themes and codes were preselected based on the ICF-CY or the PICOTS, any new themes that were elicited were added to the framework and codes were then created. NVivo qualitative data analysis software version 11 (QSR International, Warrington, UK) was used to manage the data.
| Stage | Description |
|---|---|
| 1 | Verbatim transcription |
| 2 | Familiarisation with the interview (e.g. reading and rereading transcripts, relistening to the audio-recording) |
| 3 | Coding as per the ICF-CY. Although deductive coding was used, some open coding took place at this stage to ensure that important aspects of the data were not missed |
| 4 | Developing a working analytical framework through discussion and definition of labels after coding the first three interviews |
| 5 | Applying the analytical framework by indexing subsequent transcripts using existing codes |
| 6 | Charting data into the framework matrix (i.e. data were summarised by category for each transcript, with illustrative quotations) |
| 7 | Interpreting the data through discussion, reflection and writing up |
Reflexivity
All of the research team were active in disability research. Anna Basu, Jill Cadwgan, Sarah Crombie, Andrew Roberts, Jeremy R Parr, Keith Miller and Niina Kolehmainen work clinically with young people with CP who use standing frames. Johanna Smith is a parent of a young person with CP who uses a standing frame.
Mixed-methods design
A mixed-methods (qualitative and quantitative) design was chosen to provide a comprehensive means of researching this topic. Mixed-methods research has many benefits such as the ability to have an exploratory approach (rather than needing clear hypotheses), richer data from a variety of stakeholders and greater confidence in research findings through a holistic examination. Using only quantitative methods can produce results that may not reflect stakeholders’ experiences accurately because the researchers’ own agendas are driving the study. Using only qualitative methods can produce findings that are not generalisable to the understanding or prediction of issues affecting the wider population. Using both allows for weight to be given to the meanings, experiences and views of a variety of stakeholders. 22 Another advantage is that paradoxes between the data sources can open up new ways of thinking about a particular topic and enable further theory conceptualisation and the creation of recommendations for future research. 23
Trustworthiness in qualitative research
Each focus group was facilitated by Jane Goodwin and Jan Lecouturier, with the exception of the physiotherapist focus group (JG and SC) and the medical professional focus group (JG and JC). Sarah Crombie (Physiotherapist) and Jill Cadwgan (Consultant Paediatrician In Neurodisability) were chosen as secondary facilitators in the focus groups related to their discipline because it was anticipated that their specialist knowledge would be necessary to facilitate an in-depth discussion, including answering any clinical questions. Jane Goodwin conducted all of the interviews.
We approached clinicians who completed survey 1, personal contacts and professional networks (including via social media); however, it was difficult gathering a group of clinicians at the same time in the same place for a research focus group owing to their clinical commitments and other responsibilities. Two members of the research team (KM and AR) participated in the clinician single stakeholder focus group as we experienced trouble with recruitment (including having two clinicians recruited to the focus group who did not show up on the day due to urgent clinical commitments), and because they met eligibility criteria for the target population.
All qualitative data were analysed by Jan Lecouturier and Jane Goodwin. Although they had experience in disability research, they were naive about standing frames in research and clinical practice. This meant that they were fully in equipoise at the point of data collection. They had a greater awareness of stakeholders’ views about standing frames at the end of the focus groups and interviews, but, as these views were mixed, it is unlikely that they would have had any influence on the interpretation of the data at the analysis stage. They also independently coded all transcripts. A robust discussion followed to resolve any discrepancies, of which there were few. The coding was discussed and clarified with the co-applicants as a means of quality control and rigour check. Clinical members of the co-applicant team (e.g. JC, SC and AB) and the parent co-applicant (JS) were available to sense check the meaning of the transcripts and advise on the interpretation. Each researcher remained conscious of their biases to avoid them negatively influencing the analysis and write up. However, it is important to note that the researchers’ relevant knowledge and experience was also a strength because it allowed for in-depth engagement with the data, including unexpected themes. The transcripts and recordings were referred to continuously to ensure that the analysis and interpretation were staying true to the data. Quotations from participants are provided as supporting evidence for the themes. The transparent audit trail in NVivo 11 accounted for the systematic examination at each level of analysis.
Patient and public involvement
Patient and public involvement (PPI) was vital to this study from the outset; we outline PPI contributions at each stage. PPI was important for piloting surveys, creating topic guides and providing advice on interviewing young people with CP. A nominated Research Advisory Group (RAG) with six parents of young people with CP was convened. The parents were approached through the parent co-applicant’s (JS’s) contacts. A flexible approach to PPI was taken; as a result of the nature of parents’ caring roles and the complexity of CP, it was difficult at times for our nominated RAG to engage as outlined in the study timelines. Therefore, informal discussions with families known to the co-applicant team were held throughout, as well as two design workshops after all the data had been collected. In addition, the North East Young Persons Advisory Group was approached, with co-applicant Johanna Smith presenting and receiving feedback on study content at two of its meetings. This group comprises teenagers in the local area who are interested in medical research. Although at the time of our contact there were no members with CP, some had siblings or friends affected by disability. The young people provided invaluable input on how to engage young people in research and PPI. They also contributed extensively to a booklet of interview findings, which was then sent to the young people who participated in the interviews.
We learnt valuable lessons about the involvement of parents in PPI. We found that an online RAG allowed parents to engage in the study on their own terms [six parents joined a private Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) group for this purpose]. For example, they could provide feedback on documents in their own home after their children had gone to bed. Furthermore, the parent co-applicant (JS) ensured that the study was grounded in what was accessible (e.g. language used in documents), acceptable and reasonable (e.g. appropriate times to approach for consent), and feasible (e.g. which trial designs would be possible pragmatically) for families at all times. For example, from a research design perspective, a trial could (in theory) have recruited families to a ‘delayed start’ research study at the time of standing frame prescription because many families have a lengthy waiting period before receiving the prescribed standing frame anyway. Although acceptable to other participant groups, parent participants had commented that this would be unacceptable because it would be around the same time as the child’s CP diagnosis. Given the amount of complex information being processed by families during this time it would be difficult to ascertain informed consent to participate in a research trial. The appropriate weight may not have been given to the parents’ voices if Johanna Smith had not continued to speak on their behalf in research team meetings.
Research Ethics Committee approval and study governance
The study sponsor was Newcastle upon Tyne Hospitals NHS Foundation Trust. The research was approved by the Health Research Authority East Midlands – Nottingham 1 Research Ethics Committee (15/EM/0495, 9 December 2015).
Changes to the protocol
Originally, the protocol stated that four of the focus groups would be single stakeholder, one each for parents, therapists, medical staff (orthopaedic surgeons and paediatricians) and educational professionals. However, the parent co-applicant (JS), PPI advisors and other parents highlighted that it would be difficult for parents to travel long distances to attend a focus group, and that there may be important differences in opinion that are associated with where the parents live. After discussion, we decided to convene two parent focus groups, one in the north of England and one in the south. This was a substantial amendment and, therefore, required review and approval from the Research Ethics Committee. These were the only changes to the protocol (version 4, May 2016).
Initially, participants in the multistakeholder focus groups were going to be selected from those who had previously taken part in the single stakeholder focus groups. After co-applicant discussion, we decided to recruit new participants for the multistakeholder groups. This was because our knowledge about the acceptability and feasibility of a research trial had evolved, and we did not want to replicate the discussion in the single stakeholder focus groups.
Chapter 3 Survey 1: UK standing frame practice
Objectives
A survey was conducted from March to May 2016 to determine current UK standing frame practice, as well as the perceived benefits and challenges of standing frame use.
Methods
Population
Three populations in the UK were sampled:
-
professionals, such as physiotherapists, who prescribe standing frames for young people with CP
-
professionals, such as paediatricians, orthopaedic surgeons, physiotherapists, and education staff, who do not prescribe standing frames but work with young people with CP who use them
-
parents of young people (aged < 18 years) with CP who currently use or have used a standing frame.
Questionnaire development: UK standing frame practice
A questionnaire was developed to explore current standing frame practice. Following a literature review, parents and paediatric health professionals were consulted regarding ideas for appropriate questionnaire content. Based on this information, the co-applicant study group devised the content of the questionnaires, drawing on their clinical expertise and background experience of survey design for similar studies. Multiple drafts were circulated via e-mail and discussed prior to production of the three final drafts, that is, separate versions for the three populations sampled for this study (prescribers, professionals and parents). These drafts were then piloted with a small number of people known to the researchers (i.e. three prescribers, six professionals and five parents. Prescribers and professionals who worked across both private practice and the public sector were asked to respond in relation to their public sector work). Based on PPI advice, piloting using cognitive interviews was considered but rejected. The individuals provided feedback regarding the comprehensibility and acceptability of the questions and associated instructions, as well as the usability and technical functionality of the electronic questionnaire. Minor changes, such as wording and question logic, were made at this time. The authors then reviewed the questionnaires again in a co-applicant meeting prior to dissemination.
The final survey questions comprised: (1) demographic characteristics of respondents, (2) experience and use of standing frames as part of a postural management programme for young people with CP, (3) factors influencing standing frame choice and prescribing practice, (4) challenges of standing frame use, (5) indications for prescribing standing frames and (6) perceived benefits of standing frame use. The survey also identified any differences between recommended or prescribed use versus actual use. Most questions offered fixed-choice responses, though there were some brief free-text responses. Participants could use a ‘back’ button to review or change their answers as required (see Appendices 1–3).
Procedure
A convenience sample of prescribing clinicians and non-prescribing professionals were approached through relevant national royal colleges, professional bodies and their national newsletters, and child development teams via the British Academy of Childhood Disability. Parents were approached via clinical services located in the North, South, and West Midlands of England, and through the following national organisations: the National Network of Parent Carer Forums, Contact a Family and the Peninsula Cerebra Research Unit for Childhood Disability Research. In addition, we approached parents directly through school newsletters and peer-to-peer support groups. Facebook pages (e.g. Cerebra) and the study’s Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com) feed (@UnderstandFrame) were used to allow those interested to link to the study website (https://research.ncl.ac.uk/understandingframes/) and access the questionnaire. A £10 voucher was offered to all who completed the questionnaire.
Recruitment was UK-wide and took place between March and May 2016. The survey questionnaires were hosted on SurveyMonkey® (Palo Alto, CA, USA), with paper versions available on request. E-mail and web-based flyers were sent to potential participants with a link to the appropriate version of the questionnaire.
Results
Participants
Numbers included in the final analysis are presented here. Figure 2 indicates participant flow through the study from responses received to responses included in the final analysis.
-
Prescribing clinicians: professionals, such as physiotherapists, who prescribe standing frames for young people with CP, n = 305.
-
Non-prescribing professionals: professionals, such as paediatricians, orthopaedic surgeons, physiotherapists and education staff, who do not prescribe standing frames but work with young people with CP who use them, n = 155.
-
Parents: parents of young people with CP who currently use or have used a standing frame, n = 91.
FIGURE 2.
Survey 1: participant flow through the study from responses received to responses included in the final analysis.

Tables 2 and 3 outline the respondent characteristics. Most prescribing clinicians and a large number of non-prescribing professionals were physiotherapists working in community settings. The majority had > 10 years’ experience and used a variety of standing frame types.
| Characteristics | Prescribing clinicians, n (%) | Non-prescribing professionals, n (%) |
|---|---|---|
| Occupation | ||
| Physiotherapist | 302 (99) | 49 (31.6) |
| Occupational therapist | 1 (0.3) | 39 (25.2) |
| Paediatrician | 0 | 29 (18.7) |
| Classroom teacher or support teacher | 0 | 15 (9.6) |
| Therapy assistant or technical instructor | 1 (0.3) | 11 (7.1) |
| Other health professional | 0 | 7 (4.5) |
| Technician – engineering background | 0 | 3 (1.9) |
| Orthopaedic surgeon | 0 | 2 (1.3) |
| Missing | 1 (0.3) | 0 |
| Current working environmenta | ||
| Inpatients | 34 (11.1) | 32 (20.6) |
| Outpatients | 153 (50.2) | 77 (49.7) |
| Community – home | 263 (86.2) | 79 (51) |
| Community – education centre (school/preschool) | 279 (91.5) | 107 (69) |
| Other | 1 (0.3) | 6 (3.9) |
| Missing | 4 (1.3) | 2 (1.3) |
| Number of children on current case load who are prescribed standing frames | ||
| < 10 children | 126 (41.3) | 66 (42.6) |
| 11–20 children | 123 (40.3) | 35 (22.6) |
| 21–30 children | 23 (7.5) | 12 (7.7) |
| > 30 children | 21 (6.9) | 20 (12.9) |
| Missing | 12 (3.9) | 8 (5.2) |
| Did not know | – | 14 (9) |
| Years working with children who use standing frames | ||
| < 2 | 25 (8.2) | 14 (9) |
| 2–5 | 44 (14.4) | 24 (15.5) |
| 6–10 | 59 (19.3) | 32 (20.6) |
| > 10 | 173 (56.7) | 83 (53.5) |
| Missing | 4 (1.3) | 2 (1.3) |
| Groups of children with whom the clinicians worka | ||
| GMFCS I | 15 (4.9) | 9 (5.8) |
| GMFCS II | 79 (25.9) | 33 (21.3) |
| GMFCS III | 244 (80) | 74 (47.7) |
| GMFCS IV | 289 (94.8) | 105 (67.7) |
| GMFCS V | 277 (90.8) | 95 (61.3) |
| Would rely on prescriber | – | 25 (16.1) |
| Reported not familiar with GMFCS | 5 (1.6) | 12 (7.7) |
| Missing | 12 (3.9) | 9 (5.8) |
| Experience with types of standing framea | ||
| Fixed prone standing frame | 282 (92.5) | 116 (74.8) |
| Upright standing frame | 282 (92.5) | 136 (87.7) |
| Supine standing frame | 281 (92.1) | 111 (71.6) |
| Dynamic frame | 162 (53.1) | 53 (34.2) |
| Sit-to-stand frame | 116 (34.8) | 33 (21.3) |
| Missing | 13 (4.3) | 12 (7.7) |
| Children whose parents responded | n (%) |
|---|---|
| Child’s distribution of CP | |
| Whole body | 72 (79.1) |
| Both sides of the body but legs more than arms | 14 (15.4) |
| One side of the body only | 5 (5.5) |
| Missing | 0 |
| Child’s school typea | |
| Specialist school | 68 (74.7) |
| Mainstream | 29 (31.9) |
| College (post 16 years of age, with additional or special provision) | 5 (5.5) |
| Other | 11 (12.1) |
| Missing | 4 (4.4) |
| Child’s age (years) | |
| > 10 | 46 (50.5) |
| 6–10 | 25 (27.5) |
| 2–5 | 14 (15.4) |
| < 2 | 1 (1.1) |
| Missing | 5 (5.5) |
| Child’s estimated GMFCS level | |
| GMFCS I or II | 8 (8.8) |
| GMFCS III | 20 (22) |
| GMFCS III or IV | 10 (11) |
| GMFCS IV | 36 (39.6) |
| GMFCS V | 17 (18.7) |
| Missing | 0 |
| Experience with types of standing framea | |
| Fixed prone standing frame | 34 (37.4) |
| Upright standing frame | 43 (47.3) |
| Supine standing frame | 32 (35.2) |
| Dynamic frame | 10 (11) |
| Sit-to-stand frame | 6 (6.6) |
| Missing | 0 |
| Funding source for standing framea | |
| Statutory services (health, social care or education) | 76 (83.5) |
| Charity funding | 7 (7.7) |
| Private or self-funding | 7 (7.7) |
| Did not know | 3 (3.3) |
| Missing | 8 (8.8) |
| Professional who assessed and fitted the standing framea | |
| Physiotherapist | 78 (85.7) |
| Occupational therapist | 23 (25.3) |
| Frame manufacturer or representative | 21 (23.1) |
| Paediatrician | 2 (2.2) |
| Therapy assistant or technical instructor | 5 (5.5) |
| Did not know | 3 (3.3) |
| Missing | 8 (8.8) |
| Professional who monitors the use of the standing framea | |
| Physiotherapist | 74 (81.3) |
| Occupational therapist | 25 (27.5) |
| Frame manufacturer or representative | 6 (6.6) |
| Therapy assistant or technical instructor | 8 (8.8) |
| Paediatrician | 1 (1.1) |
| Did not know | 2 (2.2) |
| Missing | 14 (15.4) |
Sixty-five per cent of parents had children who used or had used only one type of standing frame that was assessed, fitted and monitored by a physiotherapist. The standing frames were generally funded by statutory services (see Table 3).
Children of the parent respondents were aged 1–18 years (median 10 years and 6 months). They began standing frame use at 1–11 years (median 3 years) and stopped use at 3–16 years (median 9 years and 7 months). Waiting times to receive a standing frame after it had been recommended ranged between the response options ‘less than 4 weeks’ and ‘more than 26 weeks’ (see Table 8).
Patient and public involvement work had indicated that asking parents to categorise their child based on their GMFCS level was inappropriate. Therefore, we estimated the GMFCS level from reported information about independent walking, use of mobility aids, weight bearing and maintenance of head position. However, for ten young people, it was not possible to determine whether they were GMFCS III or GMFCS IV based on the information provided. We therefore categorised them as ‘GMFCS III or IV’ (see Table 3).
Prescribing practice and actual use of standing frames
Standing frame recommendations and prescriptions for use were primarily based on clinical experience rather than national or local guidance, as reported by both non-prescribing professionals and prescribing clinicians (81% and 89%, respectively).
Of prescribing clinicians, 82% suggested that standing frames should be used daily; however, only 21% of parents reported that this was achieved. Furthermore, 76% of prescribers recommended that the duration of standing should be 30–60 minutes, yet only 39% of parents reported this duration of use (Tables 4–6). In terms of frequency of standing frame use, 59% of parents reported at least as much use as prescribed, and 91% reported a duration at least as much as described (see Tables 5 and 6).
| Frequency and duration of use | Prescription of prescribing clinicians, n (%) | Views of non-prescribing professionals, n (%) |
|---|---|---|
| Frequency of use | ||
| Every day | 251 (82.3) | 93 (60) |
| More than three times each week | 38 (12.5) | 15 (9.7) |
| More than once each week | 0 | 0 |
| Once each week | 0 | 0 |
| Less than once each week | 0 | 0 |
| Did not know | – | 27 (17.4) |
| Missing | 16 (5.2) | 20 (12.9) |
| Duration of standing | ||
| < 30 minutes | 9 (3) | 4 (2.6) |
| 30–60 minutes | 233 (76.4) | 66 (42.6) |
| 1–2 hours | 46 (15.1) | 18 (11.6) |
| > 2 hours | 1 (0.3) | 1 (0.6) |
| Did not know | – | 46 (29.7) |
| Missing | 16 (5.2) | 20 (12.9) |
| Prescribed usea | Actual usea | |||||
|---|---|---|---|---|---|---|
| Every day | More than three times each week | More than once each week | Once each week | Less than once each week | Did not know | |
| Every day | 13 | 5 | 6 | 0 | 1 | 0 |
| More than three times each week | 1 | 7 | 1 | 1 | 0 | 1 |
| More than once each week | 0 | 0 | 1 | 1 | 1 | 0 |
| Once each week | 0 | 0 | 0 | 1 | 0 | 0 |
| Less than once each week | – | – | – | – | – | – |
| I do not know | 0 | 0 | 0 | 0 | 0 | 5 |
| Prescribed usea | Actual usea | |||||
|---|---|---|---|---|---|---|
| > 2 hours | 1–2 hours | 30–60 minutes | Less than 30 minutes | Not recommended in this location (home or school) | Did not know | |
| > 2 hours | 0 | 0 | 0 | 0 | 0 | 0 |
| 1–2 hours | 0 | 3 | 2 | 1 | 0 | 0 |
| 30–60 minutes | 0 | 1 | 23 | 0 | 0 | 0 |
| < 30 minutes | 0 | 0 | 0 | 5 | 0 | 1 |
| Not recommended in this locationb (home or school) | 0 | 0 | 0 | 0 | 3 | 0 |
| Did not know | 0 | 0 | 1 | 0 | 0 | 7 |
Professionals considered a variety of factors, including physical space and cost, when choosing standing frames. They generally considered starting standing frame use by 18 months of age (Table 7).
| Factors | Prescribing clinicians, n (%) | Non-prescribing professionals, n (%) |
|---|---|---|
| External factors influencing choice of standing frame | ||
| Physical space | 225 (73.8) | 88 (56.8) |
| Cost of standing frames or funding pathways | 214 (70.2) | 96 (61.9) |
| Availability of standing frames | 206 (67.5) | 87 (56.1) |
| Parent or young person choice of standing frame | 163 (53.4) | 63 (40.6) |
| Other | 45 (14.7) | 22 (14.2) |
| Missing | 19 (6.2) | 20 (12.9) |
| Age at which they would first consider starting standing frame use | ||
| < 6 months | 1 (0.3) | 4 (2.6) |
| 7–12 months | 75 (24.6) | 29 (18.7) |
| 13–18 months | 171 (56.1) | 57 (36.8) |
| 19–24 months | 34 (11.1) | 29 (18.7) |
| 25–30 months | 4 (1.3) | 9 (5.8) |
| > 30 months | 5 (1.6) | 10 (6.5) |
| Missing | 15 (4.9) | 17 (11) |
Most professionals and parents reported waiting times for standing frames to be up to 13 weeks from identification of need to commencing a standing frame programme (Table 8).
| Average waiting time | Prescribing clinicians, n (%) | Non-prescribing professionals, n (%) | Parents, n (%) |
|---|---|---|---|
| < 4 weeks | 23 (7.5) | 3 (1.9) | 16 (17.6) |
| 4–8 weeks | 106 (34.8) | 25 (16.1) | 25 (27.5) |
| 9–13 weeks | 86 (28.2) | 18 (11.6) | 12 (13.2) |
| 14–20 weeks | 29 (9.5) | 10 (6.5) | 5 (5.5) |
| 21–25 weeks | 5 (1.6) | 1 (0.6) | 2 (2.2) |
| > 26 weeks | 2 (0.7) | 0 | 5 (5.5) |
| Did not know | 38 (12.5) | 82 (52.9) | 15 (16.5) |
| Missing | 16 (5.2) | 16 (10.3) | 11 (12.1) |
Tables 9 and 10 show that most prescribing clinicians suggested that standing frame use should be monitored (for suitability of the standing frame) and reviewed (for the suitability of the standing frame programme) every 3 months or more often.
| Monitoring: ideal | Monitoring: in practice | ||||||
|---|---|---|---|---|---|---|---|
| More than once per week | Weekly | Fortnightly | Monthly | Every 3 months (or termly) | Less than termly | When requested | |
| More than once per week | 3 | 1 | 0 | 0 | 0 | 0 | 0 |
| Weekly | 1 | 7 | 2 | 13 | 8 | 0 | 1 |
| Fortnightly | 0 | 0 | 1 | 5 | 9 | 0 | 0 |
| Monthly | 0 | 0 | 0 | 19 | 68 | 3 | 9 |
| Every 3 months (or termly) | 0 | 0 | 0 | 1 | 65 | 30 | 20 |
| Less than termly | 0 | 0 | 0 | 0 | 1 | 6 | 0 |
| When requested | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Reviewing: ideal | Reviewing: in practice | ||||||
|---|---|---|---|---|---|---|---|
| More than once per week | Weekly | Fortnightly | Monthly | Every 3 months (or termly) | Less than termly | When requested | |
| More than once per week | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| Weekly | 1 | 5 | 0 | 5 | 2 | 0 | 1 |
| Fortnightly | 0 | 0 | 2 | 8 | 3 | 0 | 1 |
| Monthly | 0 | 0 | 0 | 14 | 62 | 6 | 5 |
| Every 3 months (or termly) | 0 | 0 | 0 | 3 | 86 | 31 | 19 |
| Less than termly | 0 | 0 | 0 | 0 | 0 | 8 | 2 |
| When requested | 0 | 0 | 0 | 1 | 0 | 1 | 8 |
Reasons for use, and perceived benefits and difficulties associated with standing frames
Parents reported all the benefits they observed for their child, including opportunities for a change of position, participation and enjoyment in activities, and interaction with peers (Table 11). Eighty-nine per cent of parents reported more than one benefit. When parents were asked to indicate the three most important benefits of standing frames, the most frequently selected choice was the opportunity for a change of position, second was a reduced risk of hip dislocation or damage, and equal third were improvement of bladder and bowel function and a reduced risk of joint contractures (see Table 15).
| Benefits of standing frame use | Parent-reported benefits for their child, n (%) |
|---|---|
| Enjoy activities | 39 (42.9) |
| Help child communicate | 12 (13.2) |
| Help child stand independently in future | 29 (31.9) |
| Help child use their vision | 21 (23.1) |
| Help child walk in future | 17 (18.7) |
| Improve bladder and bowel functions | 52 (57.1) |
| Improve bone density/strength | 56 (61.5) |
| Improve breathing | 25 (27.5) |
| Improve motor abilities (head control) | 34 (37.4) |
| Improve motor abilities (trunk control) | 45 (49.5) |
| Improve motor abilities (upper limbs) | 40 (44) |
| Interact with peers | 42 (46.2) |
| Opportunity for a change of position | 72 (79.1) |
| Participate in activities | 52 (57.1) |
| Reduce risk of fractures | 23 (25.3) |
| Reduce risk of hip dislocation or damage | 47 (51.6) |
| Reduce risk of joint contractures | 52 (57.1) |
Prescribing clinicians and non-prescribing professionals consistently reported that they used the frames to offer the young person a change of position; improve BMD, breathing, bladder and bowel functions; reduce the risk of fractures and joint contractures; reduce the risk of hip dislocation or damage; and improve motor abilities, communication, vision, activity enjoyment, participation in activities and peer interaction (Table 12).
| Benefits | Patient age (years), n (%) | |||||
|---|---|---|---|---|---|---|
| < 5 | 5–11 | 12–18 | ||||
| Prescribing cliniciansa | Non-prescribing professionals | Prescribing cliniciansa | Non-prescribing professionals | Prescribing cliniciansa | Non-prescribing professionals | |
| Enjoy activities | 231 (75.7) | 77 (49.7) | 230 (75.4) | 79 (51) | 222 (72.8) | 77 (49.7) |
| Help child communicate | 217 (71.1) | 68 (43.9) | 217 (71.1) | 67 (43.2) | 212 (69.5) | 67 (43.2) |
| Help child stand independently in future | 59 (19.3) | 46 (29.7) | 96 (31.5) | 36 (23.2) | 55 (18) | 23 (14.8) |
| Help child to use their vision | 173 (56.7) | 58 (37.4) | 170 (55.7) | 56 (36.1) | 169 (55.4) | 54 (34.8) |
| Help child walk in future | 120 (39.3) | 29 (18.7) | 77 (25.2) | 22 (14.2) | 38 (12.5) | 15 (9.7) |
| Improve bladder and bowel function | 225 (73.8) | 66 (42.6) | 231 (75.7) | 69 (44.59) | 229 (75.1) | 65 (41.9) |
| Improve bone density/strength | 217 (71.1) | 70 (45.2) | 224 (73.4) | 71 (45.8) | 208 (68.2) | 64 (41.3) |
| Improve breathing | 205 (67.2) | 59 (38.1) | 207 (67.9) | 61 (39.4) | 208 (68.2) | 60 (38.7) |
| Improve motor abilities (head control) | 243 (79.7) | 74 (47.7) | 234 (76.7) | 75 (48.4) | 196 (64.3) | 64 (41.3) |
| Improve motor abilities (trunk control) | 221 (72.5) | 60 (38.7) | 217 (71.1) | 62 (40) | 176 (57.7) | 54 (34.8) |
| Improve motor abilities (upper limbs) | 226 (74.1) | 70 (45.2) | 222 (72.8) | 72 (46.5) | 201 (65.9) | 62 (40) |
| Interact with peers | 238 (78) | 75 (48.4) | 239 (78.4) | 76 (49) | 233 (76.4) | 73 (47.1) |
| Opportunity for a change of position | 245 (80.3) | 81 (52.3) | 246 (80.7) | 82 (51.6) | 244 (80) | 81 (52.3) |
| Participate in activities | 243 (79.7) | 79 (51) | 242 (79.3) | 81 (52.3) | 238 (78) | 79 (51) |
| Reduce risk of fractures | 175 (57.4) | 47 (30.3) | 175 (57.4) | 51 (32.9) | 172 (56.4) | 52 (33.5) |
| Reduce risk of hip dislocation or damage | 225 (73.8) | 60 (38.7) | 219 (71.8) | 63 (40.6) | 195 (63.9) | 56 (36.1) |
| Reduce risk of joint contractures | 234 (76.7) | 67 (43.2) | 237 (77.7) | 72 (46.5) | 232 (76.1) | 69 (44.5) |
Both prescribing clinicians and non-prescribing professionals reported that as well as child-specific factors, environmental and personal factors, such as cost, space for use and storage, availability of frames and parent/young person’s choice of frame also determined the most appropriate standing frame to use.
Tables 13 and 14 outline the difficulties that prescribing clinicians, non-prescribing professionals and parents experienced with the prescription and use of standing frames. Resourcing and environmental factors included funding for frames (87% of non-prescribing professionals), physical space in the home (78% of prescribing clinicians) and a child having a standing frame at nursery/school but not at home (55% of parents). Child-specific factors as identified by the respondents included needing a rest from using a frame (25.3%), dislike of using a standing frame (19.8%) and experiencing pain (14.3%). These were more frequently reported by parents of children who no longer used frames (31.6% of parents of previous users reported pain compared with 10.4% of parents of current users).
| Difficulties identified by professionals | Prescribing clinicians, n (%) | Non-prescribing professionals, n (%) |
|---|---|---|
| Resources | ||
| Allocation of resources or funding for frame | 183 (60) | 89 (87.4) |
| Allocation of resources for staff to prescribe/monitor use | 64 (21) | 42 (27.1) |
| Availability of parents/carers at home to help position the child | 166 (54.4) | 74 (47.7) |
| Availability of staff/carers in school to help position the child | 176 (57.7) | 72 (46.5) |
| Environment | ||
| Physical space at home | 238 (78) | 96 (61.9) |
| Physical space at school | 124 (40.7) | 53 (34.2) |
| Transportation of equipment | 106 (34.8) | 55 (35.5) |
| Other | 62 (20.3) | 26 (16.8) |
| Difficulties identified by parents | Parents (previous users and current users at home only),a n (%) | Parents (current users but not at home),b n (%) |
|---|---|---|
| Resources | ||
| Time | 25 (48.1) | 4 (12.1) |
| Do not have a standing frame at home | – | 18 (54.6) |
| Using a standing frame at home was not recommended | – | 2 (6.1) |
| Availability of parents/carers to help position the child | 14 (26.9) | 9 (27.3) |
| Environment | ||
| Physical space | 19 (36.5) | 16 (48.5) |
| Sometimes moving and handling difficulties at home for child | 14 (26.9) | 6 (18.2) |
| Difficulty with access to other equipment used to position child in the frame | 10 (19.2) | 3 (9.1) |
| Child factors | ||
| Child dislikes standing in their frame | 14 (26.9) | 4 (12.1) |
| Child sometimes wants a rest from using the frame | 19 (36.5) | 4 (12.1) |
| Child experiences pain when standing in their frame | 12 (23.1) | 1 (3) |
| Other | 7 (13.5) | 6 (18.2) |
What did survey 1 add?
Survey 1 provided insight into current standing frame use. Standing frames were widely used as part of postural management for young people with CP, despite limited evidence of clinical effectiveness. Prescribing practice was generally consistent across the UK, but achieving the prescribed use was not always possible because of resources or environment/child factors. Professionals and parents of young people with CP were invested in using standing frames. They reported a variety of benefits, although they also recognised many challenges associated with standing frame use.
How did survey 1 inform the next step?
Survey 1 was primarily used to inform the content in the next stages of the Understanding Frames study; that is, single stakeholder focus groups, interviews and multistakeholder focus groups. For example, survey 1 gave the research team insight into the perceived benefits of standing frames. However, it was unclear which benefits were research priorities for different stakeholder groups. There were also specific topics and/or issues raised in survey 1 that were necessary to explore with particular stakeholder groups, and these are outlined here.
The large number of physiotherapist respondents in survey 1 demonstrated that they are a key stakeholder group with an interest and investment in standing frames. This led to the following topics for exploration: whether or not physiotherapists are prepared to recruit to a trial, their anticipated barriers to trial recruitment and what kind of outcomes that they believe would be appropriate to use to examine the clinical effectiveness of standing frames. In terms of education professionals, we wanted to explore which of the challenges identified in survey 1 were specific to the classroom. We also asked for their opinions on adherence to a standing frame prescription, and how they would feel if they could not meet such requirements for the purposes of a trial. For parents, survey 1 revealed that many older young people were not using a standing frame, particularly during the school holidays. We needed to explore whether or not suspending standing frame use for this amount of time for the purposes of a trial (or switching standing frame use for an appropriate comparator) would be acceptable to parents. We explored all of these issues in the qualitative stages of the study.
Finally, participants in survey 1 provided contact details if they wished to participate in further stages of the Understanding Frames study (e.g. focus groups). Parents also provided contact details if their child was interested in being interviewed. Therefore, survey 1 was vital for participant recruitment for the later stages of the study.
Chapter 4 First stage focus groups: single stakeholder
Objectives
Five single stakeholder focus groups were held to explore views on the design and challenges of a trial to determine the clinical effectiveness of standing frame use in young people with CP.
Methods
Population
Single stakeholder focus groups were conducted with the same populations as survey 1; that is, clinicians, physiotherapists, education staff and parents. Respondents to survey 1 provided their contact details if they were willing to take part in other stages of the research. From this, a shortlist of potential participants was created for each group to ensure a representative sample. Potential participants were contacted via telephone or e-mail (depending on the contact details they provided in survey 1); the study was explained, and if the person was interested an information sheet and invitation to attend the appropriate focus group were posted or e-mailed to them, depending on preference.
Topic guide development and conduct of focus groups
A meeting was held with co-applicants Jill Cadwgan, Jan Lecouturier, Johanna Smith and research associate Jane Goodwin to discuss how the survey 1 results should inform the topic guide, and which topics should be explored. It was agreed that information on the context (e.g. purpose of study, findings from our study so far) would be helpful. Rather than rely on attendees reading materials sent beforehand, it was decided to give a presentation [Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) Presentation Manager 2013] about the study, the current evidence base and the results from our study so far. In addition, it was deemed important to explain levels of evidence and elements of trial design (i.e. PICOTS framework). Furthermore, it was suggested that we give participants time to introduce themselves, especially parents, so that there would be an informal, friendly start to the conversation with everyone given equal status. We chose a few topics to explore in detail with the aim of stimulating rich, thoughtful discussion. The topics were chosen to clarify the findings from survey 1 (e.g. why was an opportunity for change of position a benefit of standing frames?) and increase our understanding of research feasibility (e.g. would school or home be a better setting for a research trial?).
Following the meeting, there was an e-mail conversation with the wider team, and informal discussions with PPI members, as well as parents and health professionals known to the co-applicant team, were conducted. Minor adjustments were made as a result of these conversations, such as reducing the amount of information on the PowerPoint slides. We were also mindful that participants may have invested in standing frames and may not be aware that there is limited evidence for their use, and sought to handle this sensitively. The facilitators for each focus group were also decided at this stage. Each focus group had a lead facilitator and co-facilitator, at least one of whom was a qualitative researcher (JL or JG). The second facilitator was selected depending on background and logistics.
The final topic guide included (1) opinions on survey 1 results, (2) perceived benefits of standing frames, (3) challenges associated with standing frame use and (4) feasibility aspect of a future trial (see Appendix 4). Minor amendments were made to the topic guide for each group, which evolved iteratively. For example, we asked education staff about their experiences of how young people ‘perform’ in a standing frame at school, and we asked parents how they felt on learning that there is limited evidence for standing frame use. The brief PowerPoint presentation given at the beginning of the focus group, which informed the participants and framed the discussion around pertinent issues, is provided in Appendix 5.
Procedure
Five single stakeholder focus groups were conducted, with one each for physiotherapists, medical professionals and education professionals, and two for parents. One group was held for parents residing in the north and one in the south of England to ensure that we captured any geographical variation while minimising travel burden for parents.
The process of contacting and recruiting participants was identical for each of the focus groups. Potential participants were contacted via telephone or e-mail to explain the study, then an information sheet was e-mailed or posted out to them if they expressed an interest. Written consent was obtained on the day of the focus groups, before discussion commenced. Focus groups were digitally recorded with the permission of the participants. Sound files were transcribed verbatim and anonymised.
Findings
Participants
Five focus groups were convened in June and July 2016: two with parents of young people with CP (one in the North and one in the South), one with physiotherapists from around the UK (including London, Newcastle, Leeds, Leicester and Liverpool) who worked in a variety of services, one with clinicians (in the West Midlands) and one with education staff from a specialist school (in the North East). The numbers attending the groups ranged from three to nine. The numbers in one of the parent groups and the clinician group were lower than anticipated, three and five respectively, but the data were rich and all attendees participated fully in the discussion. It is important to note that because of difficulty in recruiting non-prescribing clinicians, two members of the research team (AR and KM) participated in the clinician focus group. Therefore, caution must be taken when interpreting the results, and we have indicated which quotes were from members of the research team.
Focus group format
Focus groups were scheduled for two hours including breaks. Refreshments were provided at each group. As a gesture of goodwill, attendees were offered a £10 Amazon voucher (Amazon.com, Inc., Bellevue, WA, USA). At the beginning, the study information sheet was provided to each attendee and they were given time to read through it. Written consent was obtained and ground rules agreed. Before the discussion, and to set the scene, a member of the research team gave a 10-minute PowerPoint® presentation. This presentation covered background information around the levels of evidence on which clinical decisions are made and the evidence base for standing frame use, results from the Understanding Frames survey 124 (see Chapter 3), the purpose of the focus groups and the topic questions.
Perceived benefits of standing frame use and potential outcomes for a trial
Participants in survey 1 had been asked to identify the three most important benefits of standing frame use. We then ranked these based on frequency (Table 15) and presented them on the screen, and a member of the research team summarised these verbally. The aims were to generate discussion, elicit attendees’ views on these perceived benefits and ascertain what would be useful and meaningful to measure to determine the outcome of standing frame use.
| Rank | Benefit |
|---|---|
| 1 | Opportunity for a change of position |
| 2 | Reduce risk of hip dislocation or damage |
| = 3 | Reduce risk of joint contractures |
| = 3 | Improve bladder and bowel function |
| 5 | Improve bone density/strength |
| 6 | Enjoy activities |
| 7 | Interact with peers |
| 8 | Participate in activities |
| 9 | Help child stand independently in future |
| 10 | Improve motor abilities (trunk control) |
| 11 | Improve motor abilities (upper limbs) |
| 12 | Help child walk in future |
| 13 | Improve motor abilities (head control) |
| 14 | Improve breathing |
| 15 | Help child use their vision |
| 16 | Help child communicate |
| 17 | Reduce risk of fractures |
Opportunity for a change of position
As illustrated in Chapter 3, ‘change of position’ was one of the most commonly mentioned benefits of standing frame use cited in survey 1. As there was no opportunity in the survey to elicit why a change of position was a benefit, this was explored in the groups. Two main reasons were given by parents, physiotherapists and education staff. The first was that it supports social interactions and enables the child to be able to see what is happening at a different level:
It was a social thing . . . he had a lot of young friends in the community who used to come in and I think being able to stand when they were standing as well, it was good for him to be at a similar height.
Parent group
From the educational point of view what is often forgotten about is if you find a different position your perspective on the world and how you feel about the world and what you see . . . is totally different . . . as soon as you put them in a standing frame you’ve changed that so they are going to get a totally different feedback . . . about their environment, about everything.
Education staff group
In the clinician group there was recognition of the importance of standing frames in facilitating social interaction but also that, depending on the situation, this could be isolating for children:
Because the point about social interaction, I think it’s all very well if you’re in a standing frame but if you’re static in the classroom with all the other kids running around, you’re not socially interacting.
Clinician group
This was also raised in the physiotherapist group, and one attendee said they had overcome this problem by having a number of children using standing frames at the same time to form a group. However, the education staff group, which was from one specialist school, commented that in their school there were too few standing frames to have one per child, limiting the number who could be standing at the same time.
The physiotherapist group recognised the importance of participation and commented that there sometimes had to be a trade-off between participation and maintaining body structure and body function. They commented that standing can improve participation in the classroom for some children, particularly those who use assistive technology such as switches. An example was given of one child who communicated to the physiotherapist that she felt more alert in the classroom when standing. Education staff were of the same opinion, and talked of children who were more involved in group discussions when standing, and could participate in classroom activities such as arts and crafts. The physiotherapist group thought that some children had better head control when standing, which could facilitate participation in certain classroom tasks or subjects.
On a less positive note, education staff were also aware of children whose participation was restricted when standing. For example, when using a communication aid, such as a voice output communication aid (VOCA), there were problems situating the device at the child’s eye level. They also believed that some children are not comfortable when standing, either because it is painful or unfamiliar to them:
If you put them in a stander you know they’re not going to perform because they are so concerned over how they feel because they are not used to being in those positions . . . it overrides everything and they can’t actually focus on anything else.
Education staff group
The second reason for the importance in a change of position was to give the young person the opportunity to stretch out after being in a sitting position for sometimes up to 10 hours a day; standing was thought to combat stiffness. Parents considered how they themselves would feel being restricted to a sitting position for hours on end and that ‘most people wouldn’t be able to tolerate it at all’. For one parent, the standing frame achieved both perceived benefits of a change of position:
We usually have the choice of either his wheelchair or his bed. So to keep him in the living room and keep him with everybody else where everything is going on, transfer him to a standing frame and allow him to have a bit of a stretch out and still be with everybody.
Parent group
For those in the education staff group, standing fulfilled the need for the children to stretch their muscles, particularly the hamstrings, and reduce the risk of contractures. They commented that, with some children, they could see a deterioration in skills (e.g. posture, joint range of movement) and an increase in stiffness when they had not been using a standing frame.
Parents said a change of position led to something tangible where they could ‘see the relief in a change of position’ whereas other ‘clinical’ effects were not easy for them to recognise. For this and the other reasons mentioned, a change of position was considered very important for the majority of parents.
Improve bladder and bowel function
Most parents also supported the survey result of standing frames being beneficial to digestion and bowel function, and reported that not using a frame had an impact on bowel movement. This was evidenced by parents who noticed a difference in the school breaks or following surgery when their child did not use a standing frame:
I know for a fact if he doesn’t stand his bowels do block up.
Parent group
The use of a standing frame to encourage bowel movements was also mentioned in the physiotherapist and education staff focus groups. The latter said some children stand during or following lunch to aid digestion. The physiotherapist group commented that, for the older children in particular, this was the main purpose of using a standing frame:
We have children who remain medication free and better managed by their families because of that reason. And they say if the child doesn’t stand then they have to use medication and that makes it very difficult to manage the bowels and makes it harder for them to go out.
Physiotherapist group
Improve bone mineral density and reduce risk of contractures
In the clinician group there was a discussion about the potential of standing frames in improving bone strength and reducing the risk of contractures. BMD was considered to be a surrogate measure of benefit but if the child ‘does not have an increased rate of fractures, what does it matter?’. One parent attributed improved bone density to using a standing frame but another parent commented that a trial where this was the main measure of effect may not be appealing to parents:
When my son had his hip operation, they said that his bone density was really good therefore the operation was a lot . . . there was a good fix with the pins and stuff. I think had he not used the standing frame, they wouldn’t have been as strong.
Parent group
I think you’d need a list . . . rather than just one specific thing. Because I think if it was just bone density . . . I don’t know how eager I would have been to put him in it and go through that every day when he was younger I think you need to have all the potential benefits to weigh up.
Parent group
Physiotherapists commented that measuring bone density would not be appropriate in children who use supine boards rather than standing frames, as they are not weight bearing. Another raised the issue of which bone to measure, and referred to a study where time in a standing frame was doubled but the team did not measure bone density in the femur: ‘I’m sure if they’d have got different results if they’d measured the femur instead’. In the clinician group it was thought that a longitudinal study would be needed to measure the impact of standing on BMD; to date only short-term studies have been conducted using this as an outcome.
In terms of reducing the risk of contractures, there were mixed feelings in the clinician group about whether or not this was important in determining the impact of standing frames. One person thought that if a child uses a wheelchair all of the time, then reducing the risk of contractures was not as important. There was an alternative view from another in the group which said that pain from contractures was an important issue; interestingly, pain reduction was not included as a benefit of standing frames in the responses to survey 1. As well as stressing the importance of reducing pain, the group also concurred with what was said by physiotherapists, namely that there should be a consideration of what happens to children in later life:
Standing is a physiological need of the body, it’s not a luxury – long-term pain and contractures do have . . . a knock-on effect on the rest of the joint . . . long term they may have the effect in their adulthood as an result of not doing the physiotherapy and the stretching early on.
Clinician group
This person went on to say that if a child is compliant with standing frame use ‘the outcomes that we see are completely different in terms of contractures and pain’. It was felt in the clinician group that it could be possible to measure a change in contractures in a 12-month period.
Improve motor abilities – trunk, head and upper limbs
The physiotherapist group raised the issue of maintaining movement and mobility of the joints because of the ‘unknowns’ for these children as they grow. They commented on pain, which was also mentioned as an important factor by the clinician group:
I think it’s a pain factor and I wonder whether it’s important to maintain a range of movement and some sort of mobility for all the joints because as they transition into adulthood . . . the debilitating factor is the pain.
Physiotherapist group
Physiotherapists also believed that maintaining alignment of the trunk and pelvis was important for respiratory function and preventing scoliosis. Parents and education staff mentioned the benefits of standing frames in relation to posture:
His core stability is really bad so he leans all the time which I think is making his scoliosis worse as well. Whereas he hasn’t got as much pressure through his back if he’s in a stander.
Parent group
Education staff gave an example of the difference a standing frame was making for one child by enabling her to achieve and maintain a straight position while in her wheelchair:
We have one [child] who only recently started going in [standing frame] every morning . . . we’re at 45 minutes of standing, to keep the head up and straighten up and you can’t half see the difference. . . . It’s working for her.
Education staff group
Prevention or delay of surgical intervention
The potential for standing frames to prevent or delay surgical intervention was a perceived benefit mentioned by physiotherapists and parents that had not been reported as a finding from survey 1. For physiotherapists, using a standing frame to prevent surgery would depend on the child’s gross motor function:
We use standing frames a lot with GMFCS V to maintain and prevent surgery and try and give them that prolonged stretch that we can’t necessarily do in other positions, whereas then we have GMFCS II who we would use to try and increase lower limb strength or try to build up the function.
Physiotherapist group
Another commented that they use standing frames primarily to provide a change of position but perhaps in the back of their mind to prevent surgery:
And I kind of think, well I’m not sure but I’d use it to kind of help prevent hip surgery but I don’t know whether it does long term or not because I’ve had a few kids who have refused to use standing frames and use their walkers instead and they’re still doing okay without needing surgery.
Physiotherapist group
A number of parents said their child had undergone surgery despite using a standing frame. There was a discussion and a belief that their children would have needed surgery regardless, but that use of the standing frame had delayed it. Despite the fact that the standing frame did not prevent surgery, one parent said there had been other benefits. Another parent, whose child used a walker and needed hip surgery, said, ‘I do not know if that’s down to me not having a standing frame at home’. A suggestion was made by the parent group for a study to determine the impact of surgery:
So if you can get X-rays [radiographs] from young babies who are likely to have cerebral palsy or mobility issues, then you’ll be able to watch the hip X-rays [radiographs] and see whether that’s making any difference and whether it changes the outcome of them having to have major hip surgery or not.
Parent group
This reflects the point made by the clinician group that hip dislocation would be difficult as an outcome measure because of the length of time in which children would have to be followed up. Clinicians also added that the pathology was little understood and there were a number of confounding variables.
Reduce risk of pressure sores
One parent commented that as children with CP tend to be very thin there is an increased risk of pressure sores from sitting, and standing reduces that risk. The education staff focus group also mentioned that a long time spent in a wheelchair can become uncomfortable for children and the opportunity to stand is a relief for them and ‘takes the pressure off their bottoms’.
Other benefits
Other benefits of standing frames mentioned were improved respiratory function (particularly an improvement in breathing), helping the child to relax (as they have more support in a standing frame than in a wheelchair), and reduced spasms. Parent participants also felt emotional seeing their non-ambulant child in a standing position. These feelings were still very strong, even years later, with participants becoming teary while discussing it.
What should the trial intervention and comparator be?
In the presentation to the groups the following examples were given of interventions and comparators: delayed or suspended use of a standing frame, a comparison of other devices, or therapies.
Current standing frame versus no standing frame use
Delayed start
The question was posed, would parents have taken part in a trial in which the introduction of a standing frame was delayed by 6 months? Clinicians had reservations about the ability to recruit to such a study and commented that most parents would feel that their child was missing out on a potentially beneficial therapy. One of the physiotherapists thought that a waiting list control of delayed standing frame introduction would be an acceptable study design, but then added that they were unsure whether or not this was ethical. When broached with parents, this option was not popular, despite accounts of delays of months in obtaining a standing frame when their child was first prescribed one, and the lack of evidence for their clinical effectiveness:
I can see why it would be useful in a study, but I wouldn’t want to be in the group that didn’t [get it].
Parent group
You’d go out of your way to get it if you thought it was going to make any difference at all and I don’t think I’d want to be a parent in the ‘wait and see group’ if I thought there was something there that could help.
Parent group
The reason for this parental stance was that, even in the face of a lack of evidence of clinical effectiveness, parents want to ensure that they have tried everything that may benefit their child; they would feel that they were missing out in a ‘delayed use’ trial design. Parents mentioned they would feel guilty if they delayed the introduction of anything that may help:
. . . it would always be in the back of your head that if they had been in it sooner would it have made any difference.
Parent group
Some commented that it would be unlikely that parents would be happy to participate if they had to delay the intervention onset, particularly as it would be around the same time as receiving their child’s diagnosis of CP. Only one parent disagreed:
You see I would have done. My daughter, she was 9 months old before she was diagnosed and . . . I saw the standing frames in a line and they looked like pieces of torture equipment . . . so if they’d given me a choice I’d have said no.
Parent group
This parent said she had not been aware of the lack of evidence of the benefits of standing frames at that time. One parent in the other group felt that an awareness of the rationale for, and the benefits of, standing frame use would ‘give the parent more of an understanding of whether they would want to take part in something like that or not’.
Even when an alternative therapy was suggested for the delayed standing frame group, opposition to the idea remained in the parent group. However, one parent said that it would depend on the alternative therapy and mentioned their experience of having physiotherapy ‘with a lot of standing’ when her child was younger. In the other parent group, hydrotherapy was mentioned as an alternative and this appeared to have the approval of the other parents.
Suspended standing frame use
Withdrawal of the standing frame was not a popular option and the majority were uncomfortable with this as a trial design. It was not something clinicians or physiotherapists would feel happy to approach parents about and recruit children to. Education staff would be unhappy to deliver this type of intervention based on the belief that standing frames are beneficial:
If you said, ‘don’t stand this student and stand that student to see if it’s any different’, because their overall health is obviously what’s going to come first and we couldn’t do that because of the implications of not standing . . . and it would be too risky.
Education staff group
A suggested option was to provide an alternative therapy rather than having nothing at all. In addition, to withdraw standing frame use would require the staff who prescribe them to communicate to parents and children the uncertainty around the benefits:
It’s difficult to do a comparison with no equipment whatsoever because lots of the equipment that we use has been used for years and years so how can we say ‘we’ve suddenly decided it might not be useful anymore so we’re just going to remove it’ . . . so I think you’d definitively have to compare one equipment versus another.
Physiotherapist group
One other option identified would be to take advantage of the ‘natural’ breaks in the use of a standing frame. Parents suggested that, for example, bowel function and opportunity for change in position could be measured when children have surgical intervention. Another disruption in standing frame use for most children is the school summer break (discussed below) and parents commented that when the children returned to school the physiotherapists knew whether or not they had been standing during the holiday:
The first thing he’d say is . . . hasn’t done any stretches. His legs would be crossed and they’d be bent.
Parent group
Fifteen other potential interventions were suggested (Table 16) across the five focus groups, with the current standing frame as a comparator. Some involved increased time in the current standing frame or additional therapies and others suggested different means of postural management. These are discussed in the following sections.
| Participant group | Comparator | Intervention |
|---|---|---|
|
Parents Education staff Physiotherapists Clinicians |
Increased/reduced time in standing frame per day | Standing frame use according to prescription |
|
Parents Physiotherapists Clinicians |
Use standing frame in summer holiday period/school breaks | |
|
Parents Education staff Clinicians |
No standing framea | |
|
Parents Physiotherapists Clinicians |
Delayed start and other therapy | |
|
Parents Education staff |
New/different model of standing frame | |
|
Parents Education staff |
Other therapies (e.g. physiotherapy, botulinum toxin injections, stretching, massage rebound therapy) | |
|
Parents Physiotherapists |
Powered/mobile standing frame | |
| Parents |
Standing frame plus physiotherapy Hydrotherapy Other equipment (e.g. seating systems, sleep systems, power chair) |
|
| Physiotherapists |
Supine board Night-time positioning Sleep system Abducted standing frame Suspended standing – sling or hoist |
|
| Clinicians | Contracture correction device |
Increased time in standing frame per day
The option of an intervention to compare two specified periods of time spent in a standing frame was raised spontaneously (i.e. without prompting from the facilitators) by the clinician focus group. This option was preferable to an intervention where one group of children would delay or stop using a standing frame for a certain period:
There certainly will be an intervention where two identical children, one had an hour, one has half an hour and see what the difference is. So rather than none at all just reduce the amount of therapy. Would that provide an answer? I don’t know.
Clinician group – co-applicant KM
Increased time spent in a standing frame compared with the standard prescribed time was a more popular option with the parent focus group, who thought that this would assuage any guilt parents may feel about delaying standing frame use. However, the issue of whether or not the child would be able to tolerate the recommended time was raised. Rather than a specified time, some in the parent focus group thought that a trial of frequency of standing frame use for a time that the child could tolerate may be more acceptable to parents:
So you could say to a parent . . . ‘You do once a day of your maximum toleration’ and another parent, ‘do twice a day at the maximum toleration’. I think that’s the only way you could get the benefit of . . . a standing frame.
Parent group
Although not raised as an intervention by the education staff group, they did comment that standing for 40 minutes ‘must be uncomfortable’. They said that while some children do enjoy standing, particularly the pressure from being strapped in and held securely (also raised by the parent group), others do not. Some children are visibly tired at the end of the specified period. One also thought that certain children say it is painful as an excuse for being taken out of the standing frame:
He just wants out. He doesn’t like being in it so everything will hurt because he knows that that’s a way of getting down.
Education staff group
Other issues were raised about the feasibility of adhering to a prescribed frequency of standing. For example, parents mentioned that periods when the child is in hospital for surgery and is not able to stand as a result of this would interfere with such an intervention. In addition, one parent felt that not having the freedom to get their child into a standing frame when they thought that they had been sitting for too long would be a struggle for parents. Moreover, as another parent pointed out, when the standing frame is used to facilitate other functions a specified frequency of standing could be a problem:
If [child] needed to open her bowels I’m not going to say, ‘Oh she’s been in this morning, I’m not going to put her in.’ How would you control it? I’d have to put her in then say, ‘She’s been in twice today’.
Parent group
Parents’ focus was primarily on the practical implications of the proposed trial intervention occurring in the home setting. They commented that time (to lift and position the young person in the standing frame) was an issue, particularly when juggling other demands and with the need for ‘several hands’ to do it effectively. Another area of concern was lifting and handling with only one parent or carer present because of the risk of injury to the child and difficulty in attaining the correct positioning. Space was also an issue as many parents are unable to have a standing frame in the home because of its size. Some parents thought that this could have an impact on quality of life, particularly on the time they have available should they want to take their child out. It was also considered too burdensome and impractical for families:
Prescribing to parents that [children] have to go in it this many times, actually that could be really hard. If someone’s ill or something else has happened, I just think there are enough pressures on parents.
Parent group
There was mention in the parent group that the trial could be conducted in a home setting with younger children (2–7 years of age), but recruiting parents to it could be problematic and they would have to fully understand the rationale for the study.
The parent group introduced the idea of conducting the intervention in a school setting because of these difficulties. However, the education staff group raised a number of problems with standing frame use in schools. Apart from the shortage of equipment, there was the extra time and manpower required to get the child into the frame, which could interfere with class activity. In addition, there was the fact that the frame may have been adjusted to meet the needs of the last child who used it and would then need to be readjusted for the next user. Although not averse to the idea of running a trial in the school setting, education staff stressed there would have to be adequate support and resources in place to do so. Clinicians thought that teachers and teaching assistants may struggle to find the time to put a child in their standing frame, and that adherence to study protocol may be difficult.
Standing frame use outside the school term
Most parents said their child was not able to use a standing frame in the school summer break as they did not have the equipment at home. This period of non-use of standing frames was considered to cause problems with chest infections, bowel functions and returning to standing frame use when back to school. This view was shared by the physiotherapist group, who mentioned the difficulties of getting children back to using a frame. However, they thought that increased standing would only make a difference to a certain proportion of children with CP:
For some children who are on a fine line of maintaining function – and we’ve all probably got them – that you just know that they’re going to go one way and then you’ll never get then back on [standing]. Those types of children I feel are the ones that 6 weeks without a standing frame . . . have secondary complications that cause a big effect.
Physiotherapist group
One physiotherapist had experience of providing a standing frame for a child over the summer period and it was not used. The education staff group mentioned using the half term and/or six week summer break as an opportunity for children to continue to use a standing frame ‘if there was somewhere they could go to use a stander’ and ‘see the difference before and after summer’.
Current standing frame versus other equipment/therapies
Non-static standing
Parents asked if the future trial could explore the impact or benefits of different types of standing frames rather than concentrate solely on the current standard in a delayed or increased frequency intervention. There was discussion around a non-static or motorised standing frame and the idea that this would make standing a more pleasurable experience and potentially improve compliance in standing:
My son hated standing for a long time and we realised it was because we took him from his wheelchair that he could self-propel, put him in a standing frame where he couldn’t move so we were taking away his independence . . . So when we found a standing frame with big wheels he loves it. His default is now standing and he sits for his change of position. Sometimes I think that the whole culture needs to be changed. Who picked sitting as the standard?
Parent group
Parents wondered if factors, such as boredom, rather than solely pain, may explain why children do not enjoy their time in a standing frame. One parent used videos to distract their child from the fact he was in a standing frame. Being able to control movement while in the standing frame was said to make them forget that ‘they are trussed up in a standing frame’. It was considered that this would make a difference to their children in terms of emotions, including their levels of happiness:
You can actually get wheels for the EasyStand as well, or you can get the motorised ones. You can get different additions to it, which would obviously help with greater independence if they’re able to move around the home in a standing position because they can choose their own position.
Parent group
Non-static standing frames or ‘walkers’ were also mentioned by physiotherapists when asked what other therapies could be compared with current standing frames in a future trial. One had experience of reviewing one of these with children in her care:
I think walking frames would be a good comparison because then you’re still getting the upright posture, you can still get quite a lot of support but then it’s more of an active intervention rather than a passive stretch.
Physiotherapist group
A lot of the improvements were parents felt [the child had] looser bladder and bowels but the fun they had out of it was fantastic . . . it was wonderful seeing the child moving and the child loved it as well. So on that participation and function, on normality it was fantastic.
Physiotherapist group
Non-static standing frames were also mentioned in the physiotherapist focus group when discussing the children’s enjoyment of being in a standing frame. The group believed that mobile standing frames could enhance participation in a number of ways:
It gives them more participation and it gives them more function and a bit of freedom and they can go around the playground with the others.
Physiotherapist group
Clinicians also commented that, in contrast to a static standing frame where a child may feel isolated in the classroom, participation may be improved if children are in ‘that sort of rabbit walker thing, yes, maybe you can engage more’. However, the cost of mobile standing frames was mentioned by both parents and physiotherapists as being prohibitive. Physiotherapists added that training in how to secure the child in the mobile standing frame would be required to ensure that they were safe.
Supine positioning
Physiotherapists also discussed supine positioning as a comparator to static standing, but the choice of this within a trial context would depend on what outcome was being measured. They considered supine boards, which can be tilted from flat to upright, which would be suitable if the outcome of interest was trunk and pelvis alignment. This was felt to be important in maintaining the ‘range of movements at the pelvis and the trunk in order to sit and function’. It was said also to help with respiratory function and as a way of stretching without standing. Supine positioning is suitable for children with poor head control whereas standing frames often are not:
If you brought them from supine all the way up they wouldn’t be able to lift their heads up. So they are children who are from say between 9 and 12, 13. They still get that benefit of stretching out and a couple of them really struggle to tolerate sitting for longer periods, they become really uncomfortable, so they like to come out.
Physiotherapist group
Continuing with the discussion of maintaining alignment, hip integrity was thought by other physiotherapists in the group to be important, but with the end point being the prevention of surgical intervention. Night-time positioning and sleep systems were thought to help with hip integrity and were raised as other potential comparators to standing frames:
There’s an Acheeva® [Ledbury, UK] bed which is like a sleep system but you use it during the daytime and you can put an incline on it. You can use it prone or supine . . . though for some kids it doesn’t hold their posture quite as firmly as a standing frame does.
Physiotherapist group
The physiotherapists said they would be happy to recruit to this type of intervention and there was a discussion around whether or not this could be introduced in term time and then continued throughout the 6-week summer break. There was some anxiety around the withdrawal of standing frames for the group who would be randomised to supine positioning and it was stressed that it would have to be for a ‘limited period’.
Other standing frames and therapies
Abducted standing frames and suspended standing were also mentioned by physiotherapists. The former were said to have been around for years but do not appear to have been popular or commonly available among school equipment.
Target population in a trial of standing frame use
Apart from clinicians, the general view across the stakeholder groups was that the target sample should be younger children, ideally aged around 2–7 years. Education staff commented that the use of standing frames is easier with younger children because they can be distracted by play activities, and moving and handling take less time. Parents mentioned that, with younger people, the prevention of hip contractures and the delay of surgery is something that it would be feasible to measure. Clinicians considered age to be unimportant, unless the intervention was to delay the introduction of a standing frame, yet recognised that it would be an impacting variable.
For the physiotherapists the exceptions were if the intervention was ‘all year’ standing frame use (i.e. including the summer break) versus treatment as usual, in which case a suitable group would be children aged 14 or 15 years, where maintaining function is critical.
Time and again the issue of the variability of how children are affected by CP was raised. Parents commented on the heterogeneity of children with CP and how this could be problematic in a trial as there are ‘no two children the same’:
Cerebral palsy affects them in so many different ways. My son’s a GMFCS V so he’s the most severe but then he doesn’t have dystonia, he’s got the other type where he gets stiff.
Parent group
The physiotherapy group demonstrated that standing frames were prescribed for different reasons and this was very much dependent on the child:
What am I using this piece of equipment for? Am I trying to . . . Is it the only way they’re going to get any weight bearing? So even if I don’t think it’s the best way to strengthen their bones it might be the only way available. Or do I want them to be able to stand with their family in the kitchen and cook? Then it’s your goals around participation.
Physiotherapist group
Education staff believed that further inclusion criteria would have to be children who (1) could tolerate the standing position, (2) did not have problems with their vision and (3) were able to communicate. Parents concurred and commented that to compare increased standing ‘may skew results’ if children who could and could not tolerate increased standing were included. Although they did not suggest this in the context of which children to include in a trial, education staff contrasted children who have used a standing frame from a very young age with those, where it has been introduced later, who ‘struggle a bit more’:
Kids who have come in from being 3 years old and they’ve been put in the little standing frames . . . they’ll accept it as part of the day because that’s what you do, like washing your hands . . . whereas the other kids they haven’t got their head around it as much.
Education staff group
Other challenges
The challenges identified were around the ‘noise’ from other therapies and interventions and the ‘fidelity’ of an intervention. That is, most groups talked about the fact that children would be having other interventions, not solely a standing frame, and how can you determine what results were caused by the standing frame?:
Because of all the input that children have I think it’d [be] very difficult to define what is exclusively because of the stander.
Parent group
It was considered unreasonable to stop these other interventions. It was also said that some parents do more at home with their children than others do and it would be difficult to expect them to stop. Parent participants noted that they were not particularly concerned with the lack of research evidence for standing frames. They would always choose the option that may benefit their child, and if they could see a positive outcome, they would continue to do what they think is best:
I think we do a lot of things for our children where there’s very limited evidence, because they are so complex. As parents, we’re used to a stab in the dark. If a therapist says ‘We think this will help, anecdotally this kind of helps’ then we’ll try it. It’d be lovely if there was clear evidence, because it would help with funding, getting consistent provision.
Parent group
Similarly, physiotherapists focused on the needs of the individual young person, and suggested that standing and/or walking was not always the best way to promote positive outcomes for them:
I think there is an emphasis in paediatric physiotherapy very much on the walking and the standing of the child and it’s this goal that we have to achieve walking – even [though] we know now that many children GMFCS IV and V will not achieve independent functional walking, and yet we strive for that in maintaining, in particular, hip extension at the cost of everything else . . . I think we sometimes really need to re-focus . . . We need to look at each child individually and what they’re actually doing and how it functions.
Physiotherapist group
There was some discussion in the clinician group around dependency on the ‘operator’ during a trial and the need to ensure that the child is correctly positioned and secured in the standing frame or whatever is used. Education staff also mentioned a lack of confidence in knowing they had done this correctly with the current standing frames they use in schools. There was the view that the physiotherapists were the most skilled at this. Comments were also made about the design of fastenings when hook and loop fasteners could creep out, or that the child’s family might loosen them if they felt they were too tight.
What did the single stakeholder focus groups add?
The single stakeholder focus groups added greater understanding to the survey 1 results, including highlighting some issues not identified through the survey responses. They provided vital information about potential designs of and the feasibility of a standing frames trial. The main findings are outlined in Chapter 5.
Emotional equipoise was an issue across all groups apart from the clinician group. Orthopaedic surgeons and physiotherapists had a strong belief that without standing frames there may be progressive deterioration in young people with CP. The views of parents in particular were entrenched in the idea that standing frames are good, which was not surprising as most had invested time and effort over the years in using them with their children. This would have to be managed in a future trial when recruiting participants. Parents themselves raised the issue of educating other parents to help them make an informed decision in the context of a trial.
Parents across both the Northern and Southern groups suggested more potential benefits of standing frame use compared with other stakeholders. It was a surprise to parents that there was no robust evidence for standing frame use. Health professionals had a greater awareness of what can/cannot be altered or improved in the condition and mentioned fewer potential benefits of standing frames. A number of the proposed outcomes would require a longitudinal study in order to answer the question about the impact of standing frames. Some would be feasible to measure in some children but not in others, depending on their GMFCS level.
The type of intervention was in some ways determined by the outcome of interest. Physiotherapists stressed that if the goal is to maintain hip integrity the child should be able to move; if the goal is to stretch then the child should not be able to move. The most popular intervention by far, and the one considered to have an impact on participation and probably compliance in standing, was the non-static standing frame, but there would be significant cost implications for this to be a comparator in a trial.
There was no consensus about how long the intervention should last and this would be dependent on the choice of intervention and the outcome of interest.
How did the single stakeholder focus groups inform the next step?
The single stakeholder focus groups provided essential information about potential benefits and challenges of standing frame use. This informed the topic guides for the subsequent interviews and multistakeholder focus groups.
Chapter 5 Interviews
Objectives
The objective of the interviews was to explore the attitudes of young people with CP to standing frame use.
Methods
Population
Young people were identified as potential participants by their parents, who had completed the survey 1 questionnaire, or through the clinical services of members of the co-applicant group. Young people were eligible to take part if they were aged 8–18 years and currently used or had used a standing frame.
Topic guide development and conduct of interviews
The young person was given the option to have a communication support person of their choice. At times, the choice of the young person’s communication support was crucial to the success of the interview, as it enhanced the young person’s understanding of the questions and as well as the interviewer’s understanding of their response. A number of steps were taken to ensure the trustworthiness of the interview data. The interviewer (JG) was experienced and confident in communicating with young people. This was enhanced through regular visits to a local specialist school to spend time with young people with CP and learn about their communication methods and equipment use. The interviewer built up a rapport with the young people to enable her to feel confident that they understood the questions and were giving their honest answers, rather than the answers that they felt the researcher would like to hear. Building a rapport took a variety of forms, including playing games, singing, sitting in on classroom activities, chatting about the young person’s toys, playing with family pets and generally trying to make the situation informal and fun. Importantly, the interviewer emphasised that she did not know much about standing frames, and as such, it was helpful for the young person to explain both what they liked and disliked about them; they would not get in trouble for anything they said. Furthermore, the interviewer was creative about how they talked to the young people. Answering direct questions was not always possible; alternatives were used such as showing pictures of standing frames, and asking the young person to show the interviewer their own standing frame. Following each interview, the researchers were debriefed to determine whether or not the topic guide should be amended. Only minor changes were deemed necessary to capture aspects of the experience not initially considered; for example, whether or not the young peoples’ opinions on standing frames had changed over time and how they would feel if they were not allowed to use a standing frame any more. See Appendix 6 for the topic guide.
Based on the developmental and cognitive level of the young people we interviewed, discussion about participating in a hypothetical trial was an idea that was too complex and abstract. However, we explored the idea of randomisation by asking the young people about choice in standing (e.g. ‘if this group of young people used a standing frame and that group didn’t, which group would you rather be in? Should young people be able to choose which group they are in?’).
Procedure
Parents of potential participants were contacted via telephone or e-mail to explain the study. Following this, an information sheet for both parent and young person were sent out. There were two versions of the young people’s information sheet to accommodate different methods of communication and cognitive ability. The parents then received a follow-up phone call and if the young person was interested, an interview was arranged. Each young person was offered an opportunity to meet the interviewer for familiarity and topic planning prior to the interview. Recruitment continued until data saturation, defined as three consecutive interviews not returning new themes,25 by agreement among the research team. The young people were purposively selected to ensure that there was representation from a range of ages, GMFCS levels, gender, educational settings and regions of the UK.
Assent to participate from the young person and consent from the young person’s parent was obtained. The two participants aged 18 years consented for themselves, although this decision was made in collaboration with their parents. All interviews were audio-recorded for transcription and transcribed verbatim. Pseudonyms have been used to preserve anonymity.
Findings
Participants
Participants were 12 young people with CP who were currently using or had used standing frames at some point in the past. Their characteristics and experience with standing frames are outlined in Table 17. For the participant given the pseudonym Tiffany we have included her mother’s quotes as she spoke for her and Tiffany indicated agreement by enthusiastically nodding. Tiffany’s mother made comments about Tiffany’s experience, then checked whether or not Tiffany agreed. The interviewer then re-confirmed with Tiffany. Although Tiffany had the opportunity to disagree with her mother’s statements, it is important to note that she may have felt unable to do this because of her rapport with the interviewer or her relationship with her mother. However, the interviewer was confident that Tiffany could express her opinion comfortably because of conversations unrelated to the interview content; for example, when the interviewer commented that Tiffany must be excited to return to school after holidays, she strongly disagreed.
| Name | Sex | Age (years) | GMFCS | Predominant motor pattern | Age of first standing frame use (years) | Currently using a standing frame? | Standing frame setting | Standing programme | Support person in interview | Communication method in interview |
|---|---|---|---|---|---|---|---|---|---|---|
| Connor | Male | 8 | IV | Spasticity | 2 | Yes | School | More than three times per week for 30–60 minutes | Class teacher | Speech, some comments/probing from support person |
| Olivia | Female | 9 | IV | Spasticity | 1 | Yes | Home | Every day for 30–60 minutes | Mother and sister | Speech, some comments from support people |
| Kyle | Male | 11 | V | Dystonia | 1 | No, stopped aged 9 years | N/A | N/A | Mother and teaching assistant | Limited speech, comments and probing from support people |
| Brooke | Female | 12 | IV | Mixed | 2 | Yes | Home | More than three times per week for 30–60 minutes | Mother | Speech, a little input from support person |
| Will | Male | 13 | IV | Spasticity | 6 | No, stopped aged 11 years | N/A | N/A | N/A | Speech |
| Tiffany | Female | 13 | V | Dystonia | 1 | Yes | Home | More than three times per week for 30–60 minutes | Mother and respite carer | Voice output communication aid. Comments from support person, Tiffany indicated agreement or disagreement |
| Fred | Male | 14 | IV | Spasticity | 3 | Yes | Home | More than three times per week for 30–60 minutes | Mother | Limited speech, some comments and probing from support person |
| Sophia | Female | 14 | IV | Spasticity | 6 or 7 | Yes | Home | Not known | Friend | Speech, a little input from support person |
| Gemma | Female | 15 | IV | Mixed | 5 | Yes | School | One per week, < 30 mins | N/A | Speech |
| Robert | Male | 17 | IV | Spasticity | 3 | Yes | School | More than three times per week for 30–60 minutes | Mother | Speech, some comments/probing from support person |
| Maddie | Female | 18 | IV | Spasticity | 6 | Yes | School | More than three times per week for 30–60 minutes | School physiotherapist | Speech, a little input from support person |
| Bart | Male | 18 | IV | Mixed | 4 | Yes | School | Once per week for 30–60 minutes | N/A | Speech |
Interview format
Interviews were conducted between June and November 2016 at a location of the young person’s or carer’s choosing. All elected to be interviewed at school or home. These settings were primarily chosen for the participants’ comfort and ease of access. At the beginning of the interview, the young people’s study information sheet was provided to each participant (and their support people) and the researcher talked them through it, particularly emphasising that they did not have to answer any questions they did not want to, and could stop the interview at any time. Written consent and assent was obtained. Interviews ranged between 10 minutes and 38 seconds and 35 minutes and 11 seconds in length. As a gesture of goodwill, participants were offered a £10 Amazon voucher.
Attitudes to standing frames
Understanding standing frame use
Participants were asked why they used their standing frames. The young people thought that standing frames were primarily used for improving aspects of body structure and body function. In particular, they suggested that standing frames were beneficial for bone strength, leg strength, growth, posture and general physical health:
[Standing frames help you] to stand up tall and make your legs get straight and not bendy. Make your body stronger, not weaker.
Fred
Another reported physical benefit was an extended stretch of their muscles. Some participants said they really enjoyed this sensation, especially after sitting for long periods. They believed it helped with their overall comfort, particularly in relation to their range of movement (or ‘flexibility’) and contracture prevention. The standing frame was perceived to be the only way to properly stretch their muscles:
I’m getting a stretch at every part, your hip flexors, your knees, your hamstrings and because there’s no other way . . . where you can get a better stretch.
Will
Standing frames gave the participants an opportunity for a change of position, which could be enjoyable for a variety of reasons, including having a ‘different view of surroundings’, ‘being in the upright position’ and ‘the feeling of being tall’. The importance of a position change was also related to pain management. Although participants enjoyed the mobility and independence of their wheelchairs, sitting for long periods was reported to be ‘uncomfortable’ and could make the young people ‘achy and hurty’:
I know that if I sat in here 24 hours a day, 7 days a week I would get quite tight and I would get probably a lot more pain than I do if I wasn’t in the standing frame.
Bart
Despite these benefits pain was an issue for many of the participants. General pain, knee pain and foot pain were all reported, especially after standing for ‘a while’ or ‘too long’:
I can’t, like, wait there for too long because otherwise it hurts my foot.
Gemma
Pain did not necessarily dissuade the young people from using (or asking to use) their standing frame. Rather, they were pragmatic about their pain and believed it was something to be endured in order to obtain positive outcomes for their physical health. Participants tolerated the discomfort of standing frames and focused instead on the advantages they believed that standing might give them in the long term:
I had an operation on my hip and they said, ‘Not many people get to 17 without needing the hip done.’ . . . For me to get to this age with only needing one [hip operated on] is all to do with standing, so there are benefits to go with the pain.
Bart
Bart also commented that he did not always feel this way. When he was younger, he never wanted to be put in his standing frame. His understanding of the (perceived) importance of standing frame use had developed with age:
. . . When I was much younger I never wanted to be going in it. I always used to complain . . . Then I would have to go in. Now that I’m older, I feel the benefit of it.
Bart
Experience of standing frame use
Being in a standing frame could allow the young people to participate in activities that would otherwise be impossible. Compared with a wheelchair, the standing frame gives the young person a different perspective on the world, and thus they have the freedom to independently engage in different tasks:
I had a bit more independence as well because I could actually wash the dishes or stand up . . . That is incredible how a stand can change how independent a person is.
Will
On the other hand, standing frames could also be quite restrictive and inhibited independence. As Olivia commented: ‘I cannot get around in the stander like everyone else can. [The powered wheelchair] is ‘sort of my legs’’. A static standing frame limits the young people’s mobility and forces them to rely on others for help:
There’s not many things you can do in the stander that involves you by yourself . . . I do a lot of independent things inside my wheelchair that I can’t do in the standing frame.
Bart
One participant mentioned that using the standing frame was an activity in itself and thus did not facilitate her ability to engage in other tasks. Standing required a lot of effort and concentration, much like going to the gym. Brooke did not see the need to do additional activities while in her standing frame:
I don’t like to do something. I just feel like it’s already doing something and I’d rather be in my wheelchair or on the floor when I’m doing anything else.
Brooke
In addition, standing frame use could be associated with discomfort and pain for a variety of reasons beyond standing for too long (as mentioned previously). Sometimes this was perceived to be caused by the general way the young person’s CP presents:
He tends to pull at everything. That is why in those frames he would extend and pull and twist. That is probably why it ended up being uncomfortable.
Kyle’s mother
Other times, it was related to a specific body part or injury which the standing frame could aggravate. For example, Gemma had particular trouble with her foot, and as such found it difficult to bear weight:
I don’t want to really force myself to use the stander at the moment, because my foot – it doesn’t know how it’s going to react to it. Because obviously it is getting really, really painful for me to do anything.
Gemma
Several participants also mentioned how frightening being in a standing frame could be. Because they spent the majority of their life in a wheelchair, standing was an unusual position for them. Sophia commented that standing frames were too high, and she was ‘scared of heights’. The fears could persist despite the fact that they knew logically they did not need to be scared while in the standing frame:
I must seem like a big baby or scaredy-cat to some people, but I am actually genuinely frightened and nervous. No matter how much people say I’m safe, that doesn’t help me because I know I’m safe, but a part of my brain just tells me I’m not safe.
Brooke
Although standing could feel quite strange and scary, some young people suggested that it is possible to become accustomed to the sensation. For young people using a standing frame for the first time they emphasised the importance of self-pacing:
It is very weird standing at first. But I would say, ‘if you’re uncomfortable just take your time.’ It does take time to get used to one, so I’d say, ‘just take your time and build up the confidence.’
Robert
Impact on peer interaction
Participants often used their standing frames for specific (sometimes solitary) tasks, such as school work. However, their positioning also had an impact on their social interactions, both positively and negatively. Connor found standing frames problematic particularly for peer interaction, describing time in his standing frame as ‘boring’ and ‘stinky’. Using his standing frame at school meant he was much higher/taller than his peers, who sat at desks. This meant it was difficult to engage socially:
I think that you like your chair better than your stander because . . . when you’re in your stander you’re a bit higher than everyone else . . . You don’t like standing up, separate.
It’s really boring, isn’t it?
However, another participant felt that being in a standing frame improved her peer interaction, particularly when she had attended a mainstream school. Standing allowed her to ‘fit in’:
The able-bodied children would relate to her differently and she was more like them because she was upright. It’s strange just changing position meant that.
Tiffany’s mother
Play
Olivia used her standing frame routinely for many tasks, such as toileting, eating and drinking. However, it also featured regularly in her play, especially with her sister, Olga:
I do painting and colouring and marking, like playing schools.
Olivia
Olivia stood in her frame to give herself a more dominant role in games, such as pretending to be a school teacher in front of her ‘class’. Her sister sometimes ‘wants to be disabled’ during play, so puts herself into the standing frame. Their mother noted that play between the sisters naturally incorporated the standing frame which, as a by-product, then teaches Olga about Olivia’s care needs. For example, as part of their role-playing games, Olga would strap Olivia in her hoist or position her in the standing frame.
Choice in standing
The young person’s choice about if and when they use their standing frame was a particularly salient issue. One young person was very keen to use a standing frame but did not have access to one. Others were frustrated about having to stand even though they did not want to. Some young people were happy not to have a choice about their standing:
I don’t mind what they say. I just go in the stander.
Fred
Although some participants technically had a choice about when they used their standing frame (e.g. they were asked whether or not they want to stand rather than being told they have to), they experienced negative reactions when they chose not to stand:
It is just the fact that we have to stand it for quite a long time . . . I can say no, but I always get moaned at for saying no because it is what is best for me.
Sophia
Many young people preferred the comfort and independence of their wheelchair over being stationary in a standing frame. Several participants commented on how society has dictated ‘normal’ postural positioning, which did not suit them as individuals:
I’m not a big fan of standing and I call it ‘the fault of life’ because I’m like, ‘Why do we have to?’ It’s like, ‘Why was this even invented and why did the world turn out this way?’.
Brooke
Interestingly, when asked if young people should have a choice about using a standing frame, one participant suggested that they should not:
Even though it’s pretty horrible to say, it’s probably the best thing for them, because when I was much younger I never wanted to be going in it . . . [but] now that I’m older, I feel the benefit of it.
Bart
Bart emphasised the need to explain the potential benefits of using a standing frame, even to very young children. This type of pragmatism was again evident when young people thought about long-term goals, rather than the discomfort of standing. They could weigh up the positive and negative aspects and make their choice about whether or not to stand:
I ask to go in it because I know it will help me with standing, but I’m reluctant to actually. I don’t really feel like the whole of me wants to go.
Brooke
Although the young people discussed many obstacles, one factor that actually helped them to use their standing frame was emotional support. It was important to have an opportunity to complain every so often, even if the young person was generally willing to use their standing frame:
My mum is very good. She listens to me. Even though she might be tired about it and heard it five million times, she still goes, ‘OK,’ and still tries to talk me through it because she’s my mum and she’s very supportive. All my family are really supportive.
Brooke
Challenges of standing frames
A major challenge for standing frame use was the manual lifting and handling it requires. Generally, two people were needed to make it possible for the young person to be positioned properly in their standing frame:
It’s a right job to get you transferred from the chair into the standing frame, and then out the standing frame into the chair.
Robert
The person or people positioning the young person not having the requisite skills could also be problematic, affecting the young person’s ability to use their standing frame. The carers required comprehensive training to ensure that the young person is comfortable and has their needs met:
It hurts because some people ping it so hard and I feel like saying, ‘Do you want to hurt me? Do you want to . . .?’ But I don’t . . .
Olivia
This issue was exacerbated for Tiffany, who had to have her VOCA adjusted with the change of position. If it was not set up correctly, she could not communicate the way she needed to while standing:
I think the challenge is with the people helping her need to know the equipment well and need to know how to position the communication equipment for her.
Tiffany’s mother
Another challenge when using the standing frame was interference from siblings. Parts of the standing frame (e.g. the angle adjustments) were at an accessible height for siblings, which could leave the young person in the standing frame vulnerable:
You used to happily be standing in it and then [your brother] used to adjust it and you used to be at a funny angle. Or he would take all your toys away.
Kyle’s mother
Standing frame design
The young people were particularly concerned with the type of standing frame they were using. It was important for them to feel safe and comfortable. As it was also desirable to be able to distract themselves from the pain, the young people tried to engage themselves in activities to keep themselves occupied. Some types of standing frame enhanced their ability to do this because of the size or attachments. For example, standing frames with tray attachments enabled them to enjoy particular activities independently:
The older ones have a tray or bowl in the middle so you could put cake mixture in it. There was a plastic tray that goes on top of the bowl . . . it’s the world’s best invention.
Will
Participants suggested that having a TV or music player connected to the frame would be beneficial. Aesthetics were thought to be important too and it was felt that young people would be more enthusiastic about using their standing frames if they could choose the colours and patterns. It would make standing less ‘boring’:
[I’d] change the colour of the standing frame because it’s boring . . . It would look colourful and look nice.
Maddie
Flexibility of the standing frame was also valued. Tiffany’s sit-to-stand frame was favoured because the level of stretch she received could be adjusted depending on her tolerance each day. An added benefit of this type of standing frame was that Tiffany had the independence to control her own standing (and comfort) using the levers:
She can say when it’s a comfortable stretch. Different days can be different, so she could have a bigger stretch one day and a smaller stretch another day . . . when she’s had enough she can let herself back down for the sitting position.
Tiffany’s mother
Size: lack of space
Another challenge of standing frames is their physical size. Standing frames take up a lot of space, and this causes difficulty in the home. It also means that the standing frame cannot always be used as intended. For example, Kyle was not able to move around in his dynamic stander:
The stand was at the back and the back legs came out so far that we couldn’t actually move me in it that well.
Kyle
Some young people overcame this issue by storing and using their standing frame at a place that is big enough, for example, school:
I tend to use it at school because we really haven’t got the space at home to accommodate it, have we?
Robert
What did the interviews add?
The interviews provided essential information regarding young people’s perceptions and experiences of using standing frames. Based on PPI advice and the experience of the co-applicant team, this was the most appropriate way to gain young people’s views (as opposed to the surveys and focus groups that were used for other stakeholders). Therefore, these interviews were a proxy for the stages of the Understanding Frames study that were inaccessible for young people with CP. The interviews have shown that young people have clear opinions but do not often get the chance to express them. Feelings about standing frames are unique to the individual; however, we now know that participation and activity engagement are particularly important to young people.
How did the interviews inform the next step?
The interviews informed the co-applicant team’s understanding of how a research trial might feasibly be designed, keeping in mind the issues that are most important to the users themselves (e.g. participation). This was particularly useful in the final stages of the study, when different trial designs were being considered.
Chapter 6 Multistakeholder focus groups
Objectives
The objective of the multistakeholder focus groups was to explore views on the acceptability and feasibility of potential trial designs to examine the clinical effectiveness of standing frame use in young people with CP. Mixed groups were chosen to allow for rich and meaningful discussions between different stakeholders.
Methods
Population
Eligibility was the same as for the single stakeholder focus groups, for parents and professionals. None of the single stakeholder focus group participants were approached as we did not want the group to be influenced by previous discussions. Again, potential participants were sought from survey 1 who were willing to take part in further stages of the research (with priority given to those approached for the single stakeholder focus groups who had expressed keen interest but were unable to attend) and personal contacts.
A shortlist of potential participants was created by Jill Cadwgan, Sarah Crombie, Jan Lecouturier and Jane Goodwin to ensure a sample with representation from a variety of stakeholders, including, but not limited to, physiotherapists, parents, paediatricians, orthopaedic surgeons and education professionals.
Topic guide development and conduct of focus groups
A topic guide was developed based on the previous stages to examine the stakeholders’ perceptions of standing frames research. Topics included (1) perceptions of research priorities, (2) acceptable periods of non-use and (3) support needs to ensure that a standing frame is used as prescribed. A brief PowerPoint presentation of the study results thus far was made at the start of the focus groups to inform the participants and frame the discussion of pertinent issues. See Appendix 7 for the PowerPoint presentation and topic guide.
Procedure
Two multistakeholder focus groups were conducted. One focus group was held in the north and the other was held in the south of England to allow for a representative sample without requiring too much travel for participants. Multistakeholder focus groups were convened to allow for discussion between different stakeholder groups.
The process of contacting and recruiting participants was identical for each of the focus groups. Potential participants were contacted via telephone or e-mail to explain the study, then an information sheet was e-mailed or posted to them if they expressed an interest. Written consent was obtained on the day of the focus groups before discussion commenced. Focus groups were digitally recorded with the permission of the participants. Sound files were transcribed verbatim and anonymised.
Findings
Participants
Two focus groups were convened in December 2016, one in the north and one in the south of England. In the Northern group, participants were two education professionals (mainstream – classroom support assistants), one parent, one orthopaedic surgeon, one neurodisability paediatrician, one paediatric neurologist, one research occupational therapist and one physiotherapist. In the Southern group, participants were five physiotherapists, one community occupational therapist, one paediatrician and one education professional (early years key worker). Although we invited three–five parents to each of these focus groups and had confirmed attendance, many cancelled at the last minute because of their child’s health. Therefore, we only had one parent participant across both groups.
Focus group format
Focus groups were scheduled for 2 hours and refreshments were provided. Participants were offered a £10 Amazon voucher as a gesture of goodwill. At the beginning, the study information sheet was provided to each participant and they were given time to read it through. Written consent was obtained and the ground rules were agreed. Before the discussion, and to set the scene, a member of the research team gave a 10 minute presentation. This presentation covered results to date from survey 1, the single stakeholder focus groups and interviews, potential PICOTS for a standing frames trial, the purpose of the focus groups and the topic questions.
The findings are outlined here in the PICOTS framework, to provide a clear outline of how the data from these multistakeholder focus groups could be incorporated into a standing frames trial. A section about the participants’ reservations for a trial has also been added to highlight the potential challenges, particularly regarding ethics issues of research in this population.
Population
Throughout the focus group discussions and the exploration of the most appropriate group to participate in a future trial, it was clear that the age, GMFCS level and cognitive ability would determine the choice of intervention and/or the outcome. Participants also noted that age, school setting and cognitive ability may have an impact on standing frame perceptions.
Age
It was thought that an intervention to introduce standing frame use in the 6-week summer break would be problematic in the preschool-age young people who tend to have a standing frame in the home. This would require those randomised to the control group to stop using their standing frame at home, which was considered ‘tricky’ and unlikely to be acceptable to parents. However, older young people usually do not have a standing frame at home because of the lack of space and could be a suitable group for such a design. In addition, it was recognised that preschool children generally enjoy being in their standing frames; it is the older children who often are reluctant and this could have implications for compliance in a future study. Nevertheless, participants in the South felt that a range of ages should be included and divided into preschool, primary and secondary school children, but the issue of conducting a trial in mainstream schools was acknowledged as something that would have to be thought through. Issues highlighted in the single stakeholder groups about the potential for children or young people in mainstream schools to feel isolated if they are the only people standing in the classroom were also raised.
Gross Motor Function Classification System level
Gross Motor Function Classification System level was an important consideration for all focus group participants. The groups reported that some young people were put in standing frames unnecessarily, for example, with GMFCS II, because the activities they could do, such as walking, were likely to have more impact on bone density and hip migration than passive standing. This means that GMFCS I and II would be considered groups to exclude from a standing frame study. Owing to the variation in how children are affected by CP across and within the GMFCS levels, selection of the most appropriate level for any research study was felt to be crucial. Alternatively, if a range of levels was included then they could potentially be separated at the analysis stage:
I think even within one level you can get so much variation that you’re going to find it really difficult to show significant differences unless that group is really, really narrow.
Southern group – physiotherapist
The intervention of the use of standing frames in the summer break was also thought to be more appropriate for GMFCS IV and V. This group of children ‘would be the ones who would probably deteriorate’ if they were not using a standing frame and a difference could be detected in those who continue standing throughout the break. Participants commented that the selection of GMFCS level would also determine the type of equipment used in a trial:
So like for the GMFCS level IV and maybe some of the Vs you could look at, for example, a kid walker versus a standing frame.
Southern group – physiotherapist
If the outcome of interest is participation, this could look very different, as the activities would vary considerably depending on GMFCS level. If hip dislocation is the selected outcome then participants were not convinced that the standing frame would help young people with more severe CP, such as GMFCS V:
I think a lot of parents have a lot of guilt and . . . the last thing we want to do as therapists is add to that guilt. So if they think, ‘if my child isn’t in their standing frame twice a day for 30 minutes then now they’ve got contractures or their hip is dislocated, this is all my fault.’ Well, the evidence quite strongly shows us that’s not the case and that that was going to happen regardless of whether they were in the standing frame or not.
Southern group – physiotherapist
Cognitive ability
The fact that some children do not enjoy being in a standing frame, and find standing painful, was raised. One suggestion for future research was to explore whether or not the standing frame is useful for the individual and whether or not they choose to use it. In the Southern group, cognitive ability was raised as a potential barrier to measuring participation if it were chosen as an outcome, particularly if the means of measurement was feedback from the child or young person or an interview. This was picked up in the Northern group, where there was some frustration about young people with severe learning disabilities generally being excluded from research; differences in intellectual functioning may be related to standing frame experiences, and a research trial must capture this:
I do struggle sometimes, because there’s so much research for children who can show an ability, or do motor skills, or this, that and the other. It’s like, ‘oh, OK. Could you just try and find a way to help those who can’t? Who haven’t got the motor skills, who can’t do a clear yes/no?’ But I absolutely appreciate that it’s incredibly difficult to find a way to do it.
Northern group – parent
Both groups were particularly keen to make the study as inclusive as possible and a possible solution was proposed that parents could act as a proxy to read the young person’s ‘signs’. For example, a smile can mean they enjoy standing.
Intervention
The interventions discussed in the focus groups were: no standing versus standing, increased standing time and comparison of different types of standing frames.
No standing versus standing
With a treatment versus no treatment trial, participants noted the difficulty of measuring outcomes such as body structure and body function outcomes because treatment would need to be withdrawn for too long to see any difference:
You’d have to remove it for long enough to actually believe there could be a difference. If you were going to be thinking about ‘does using the standing frame help constipation?’ ‘Does using the standing frame make a child less stiff or reduce their tone?’ . . . You’d have to remove it for quite a long period.
Southern group – physiotherapist
Withdrawing standing frames when they are already used in routine practice was considered problematic (and potentially unethical), and other 24-hour postural management may have an effect on a study’s outcome measures. It was thought that families would be uncomfortable with withdrawing standing frames as an intervention, as some believe ‘that it’s really making a difference to their child’. Even if parents did accept withdrawal, what would parents consider an acceptable period? What they think is acceptable may not be sufficient time to measure any changes.
Increased standing time versus current standing time
Based on the experience of a number of participants in the Southern group who have cared for young people with CP who disliked standing, there was a slightly more negative view of standing frames. They felt compliance with increased standing could be a major problem. There were certain young people for whom standing improved things like function, integration and communication, and compliance would not be a problem; it would be possible to select such young people, but this would have implications for trial design. On the other hand, in the Northern group standing duration was considered to be a viable option, but the most appropriate outcome would be difficult to determine, practical issues were identified and it may not be feasible in practice:
In terms of looking at an outcome like bone density – frames are already widely used, you’re not looking at a study that would be no use of the standing frame over 6 years. So it’s going to be a difference in time. So we have to say, ‘how much more would they have to do to be different from what is used now, and closer to where they need to be?’ It’s then very difficult to power the difference, and it may not be practical. Although it may be something that we all want to know the answer to . . . it’s just too difficult to detect the difference, because we can’t go back to zero, we can’t go back in time and not use standing frames.
Northern group – orthopaedic surgeon
The practicalities of implementing an increased standing time intervention in schools were also raised.
Another option, rather than increased time standing per day, would be to continue standing for a group of young people over the 6-week summer break. A number of participants in the Northern group expressed views on the impact of the 6-week break in standing:
A lot of physios will tell you that children who haven’t stood over the 6-week holiday do come back to school more contracted, less head control . . . it may be that you could look at that side of things for some children.
Northern group – physiotherapist
However, one person in the group asked whether or not this deterioration over the holiday period was ‘retrievable’:
Hey, we can get back there, and actually they’ve had some mental space during their holiday.
Northern group – paediatric neurologist
It was generally agreed that this intervention would be more suitable with older children who are unlikely to have and use a standing frame in the home. Then there would be no need to ask certain families to stop using the standing frame if they were randomised into the control group. The logistics were discussed, in particular where young people would go to use a standing frame in the summer break; several suggestions were made, including specialist schools’ facilities, although this could result in a long distance to travel for some families.
Delayed standing
Delaying the introduction of a standing frame at the time when the young person was diagnosed with CP was discussed in the groups. Some participants thought that delaying standing frame use would be acceptable from a clinical perspective but not to parents. The parent perspective was that the point when parents receive the diagnosis is too stressful a time to make such a decision:
At an early stage you’re just bombarded. You’re in this new world and you just don’t know what to do, where to turn and to be faced with a decision like ‘Are you happy for your child to be delayed starting?’ It’s a massive, massive decision to take.
Northern group – parent
This led to a discussion about equipoise and that ‘many therapists and many clinicians will perceive (standing frames) as best practice’. Furthermore, standing frames are already used and being prescribed. Both of these factors make it difficult for parents to believe that they may not be of benefit.
In the Southern group, delayed standing was not discussed in any depth. However, during the discussion of the results of survey 1, one participant expressed reservations about the early introduction of standing frames:
The ages that we are recommending, so we are going down sometimes even young than a year to start standing up and I’m not always sure parents are ready for that equipment to be in their lives because they have not really had time to come to terms with their child’s diagnosis.
Southern group – physiotherapist
Similarly, in the Southern group a discussion about equipoise ensued. This was in relation to therapists and the need for honesty when explaining to parents the reasons a standing frame is being prescribed and the lack of evidence for their use.
Comparison of different standing frames
There was also discussion about the type of standing frame a research trial could and should use. Rather than withdraw standing, one preference was to introduce something different. The Southern group thought that it would be worthwhile comparing static standing versus a supportive walker (or equipment such as trikes). The intervention might be more enjoyable if it was more active, because the young person and their family might be more motivated to use it. There might need to be different comparators for each GMFCS level, and it would be challenging to do such a study:
It means it would be easier to do a comparison, I think, with supported walkers instead. It depends. I still think that the outcome should be about child activity and participation. It’s not going to be easy.
Southern group – physiotherapist
Participants in the Northern group concluded that the type of frame probably does not matter as long as the young person is as perpendicular as possible:
I do not know whether it makes such a huge difference once the child’s standing. If they are in the most appropriate frame for them, then I would not think that would make a huge difference.
Northern group – physiotherapist
However, participants in the Southern group noted challenges with this approach; different needs were met for young people with CP in terms of standing frame type, positioning and alignment. This was seen as creating difficulties for standardising standing frame practice for the purposes of a research trial, and impacting on outcome variables related to activity and participation:
There does not seem to be consensus as to the best, the right way – not only the best standing frame, but the best way of positioning and placing a child and that may, again, impact on the activity and participation that’s possible, the comfort that’s possible, you know, how are they going to deal with that, that there is some children who are more difficult to position than others? What’s your best possible alignment? What do we mean by that?
Southern group – physiotherapist
Participants in the Southern group suggested choosing a specific standing frame for a trial because ‘otherwise you’re not comparing like with like’.
Although driven primarily by the outcome of participation, a comparison of standing versus sitting was suggested. This would involve the young person carrying out an activity they enjoy (tailored for each person) in their standing frame and in their wheelchair. It may require qualitative methods, observing whether or not the young person seems happier if they are not able to express this themselves, and quantitative, for example, measuring whether or not they can engage in the activity for longer. Outcomes could be determined for each individual, rather than having an overall outcome measure across participants. That is, using an individualised, goal-oriented outcome.
Comparator
A number of the controls or comparators have been described in relation to the intervention: standing frame as currently prescribed (treatment as usual). The Southern group also suggested identifying a place where standing frames are not prescribed to compare with groups who do use standing frames. Certain variables related to activity and participation may be compared in this way:
I think it’s a really interesting idea is finding a natural group where people do not stand, so using countries where people perhaps cannot access . . . You could measure the same, from a participation point of view.
Southern group – physiotherapist
However, the other participants pointed out that the trial would then need to consider confounders such as culture, diet and medication differences.
Outcome
Participants believed that it is important to have information about the body structure and functional benefits of standing frames as primary evidence for their use. The parent participant commented that the standing frame helped with digestion and bowel movements, and if these are not managed correctly, there is an effect on the rest of the young person’s functioning (and the family’s happiness). The young person’s quality of life is also extremely important. Although these are potential outcome variables, it is difficult for parents to isolate each benefit of standing frame use, as they all overlap:
If I picked one, I cannot single them, but two. The first one that has an impact on lots of other things [is] his digestion and bowel movement. If he gets constipated, that has a real knock-on effect on everything he can do. So helping his bowel and digestion actually facilitates him doing lots of other things. Then the second one is just his enjoyment. He just absolutely loves standing up.
Northern group – parent
What came across quite strongly in the groups was the importance participants placed on measuring activity and participation in activities as outcomes of standing frame use. When considering the benefits of standing frames, the views of equipment users are most important. Participants believed that what is measured should be guided by what young people want. It was suggested that we need to investigate whether or not standing is a positive experience for the young person, and if so, in what way. The young person’s motivation for standing must be considered, especially if they did an activity they particularly liked or disliked in a standing frame:
I think we need to focus on the users of that equipment . . . regardless of what it provides for everyone else. Because an added benefit . . . would be improved alignment or reduced bone density or reduced joint contractures. But their actual ability to participate with their friends does much more for their confidence and their self-esteem.
Southern group – physiotherapist
Professionals monitor . . . the body structure and function, and then there is more what I call a subjective benefit, related to the participation and the activity, and then there’s the question of the environment. I call that subjective, because I believe what the family feeds back to me, or the physio feeds back to me.
Northern group – orthopaedic surgeon
Throughout the discussion, participants commented that outcome variables for a trial would also depend on the young person’s age, GMFCS level and school setting. They felt that it would be difficult to design a trial because therapies were tailored to the individual, and there would be challenges investigating each potential benefit. Each benefit might require a different approach to investigation and different resource depending on the intervention and outcome. For example, the ‘change of position’ identified by parents as important was considered likely to be part of pain management. Other comparator positions might be painful (e.g. lying on their stomach), so this would need to be considered when designing a trial:
Yes, but they do not like that [lying on their stomach], and also most young children, especially the ones that have got poor head control, hate going on their tummy.
Northern group – physiotherapist
Participants suggested that a mixed-methods approach would be appropriate to explore the clinical effectiveness of standing frames because, although functional assessments are important, qualitative research can provide rich insights on life:
You can do both quantitative and qualitative. So you can use your health-related quality-of-life measures. You can use your CP child, you can use elements of functional assessment, functional outcome. But I think it would be a strongly important thing to have a reflection running alongside . . .
Southern group – paediatrician
Timing
Owing to the in-depth discussion and focus on the most appropriate intervention and outcome, the duration of a potential trial and data collection time points were not discussed in great depth. Where this was discussed was in relation to withdrawal of standing frame. Apart from the fact this may not be popular with parents, one participant commented that a 6-week to 3-month withdrawal period would be required for a difference in body structure to become noticeable. Another person felt that up to 3 months’ withdrawal was too short and indicative of the problem with previous research:
All the bad evidence that is out there is because it’s done for too short a period of time with too little follow-up. Imagine if you, fundamentally, really want to look at something, it’s got to be a long trial and it’s got to have a long-term follow-up. A lot of decisions are being made . . . on poor quality data short period and it’s not appropriate.
Southern group – paediatrician
In the Southern group, the importance of study duration and follow-up was emphasised. It was expressed that 2 years might not be long enough to determine the impact of using/not using a standing frame. In terms of securing a research grant, it was thought that funding for a 2-year intervention study was feasible but ideally, there should be scope to follow participants up over a further 2 years. This led the group to suggest a cohort study rather than a trial:
This is not some sort of thing that you can get a big difference quickly by doing something. This is almost a cohort trial rather than anything that is more specifically interventional. So you are probably going to be having to look at relatively high numbers.
Southern group – paediatrician
Also, if it was a cohort you could follow the same children through that age range as well instead of having different children, which would be a helpful thing to do.
Southern group – physiotherapist
Setting
Participants perceived that few young people use standing frames in mainstream schools, especially secondary school, as a result of logistics, such as changing classrooms, stairs and young people wanting to sit like their peers. Therefore, a standing frames trial should focus on young people at specialist schools.
The intervention to extend standing frame use in the summer break could be challenging because there may not be enough caregivers or physical space for the young person to use their standing frame. Furthermore, a lot of other things change during this period (e.g. therapy), and it would be difficult to determine what impact was caused by the standing frame:
We see a lot of the children who come up for surgery, who have interventions. They always want to come in the holidays to kind of deal with it, that’s another confounding – how do you exclude people from the study. So do you exclude people who are having botulinum toxin injections or surgery . . .
Southern group – physiotherapist
Reservations about a trial
Participants acknowledged that a trial would be difficult because of the variation in CP presentation and the individual benefits the standing frame has. Furthermore, some benefits are unlikely to be anticipated during prescription, such as ‘feeling tall’. The young person’s well-being is important, and careful consideration must be given to the priorities in their life at the time. Standing frames should not be used at the cost of all other activities:
When there is a split placement, it’s more important that they are doing the things that they are coming to a mainstream school for. Well, I think it is, than actually being in a standing frame at that time. There are other opportunities to be in a standing frame.
Northern group – physiotherapist
There were a number of issues highlighted that should be explored. First, withdrawing treatment may not be acceptable to parents, young people or health professionals. It is important to know what it means for the young person to not be able to access their standing frame. Furthermore, if not standing results in loss of function, can it be regained?
Secondly, parents may question delaying standing frame use when it is considered best (or at least routine) practice. Along with this, when considering a trial with younger children (e.g. delayed start), participants emphasised that it would be essential to be mindful of the parents’ journey with CP. Parents are bombarded with information at the time of diagnosis and rely on people to help them navigate. They may not be able to consent and fully understand the implications of participation. Seeing their child standing can be very emotional for parents. It remains a salient memory even years later. Therapists in the Southern group spoke of their responsibility to be honest in the way they introduce standing frames. They wanted to work towards honest goals with families to avoid adding guilt and burden. Open communication is required so families understand that therapies can be adapted and adjusted. Potential benefit needs to be balanced with what is possible and comfortable:
I think that’s one of the challenges isn’t it, working long term, is to be open and honest and to say, ‘we are working together on this. And if it’s not working for you or your child, you must tell us, so that we can adapt it or adjust it.’ As you said, be honest and say, ‘these are the reasons we are using it.’
Southern group – physiotherapist
Similarly, despite the perceived need for evidence, focus group participants from the South particularly warned of creating unnecessary emotional distress for families through a trial. Tension may arise between parents and young people if the young person was forced to use the standing frame even if it was uncomfortable. Parents can also feel guilty for not using the standing frame if they believed that they were effective:
They also have that guilt of not knowing [who] to listen to when their children is complaining in pain. And they still feel obliged to put their child in a standing frame, because they believe all of these things will go wrong, if they do not. And I think we do not help parent and child relationships in that instance, because we have got a child who’s saying they do not want to do it and we are causing a level of conflict between the parent and the child, which in any other situation, where the child did not have a disability we would not necessarily accept. So I think we open ourselves up to affecting that sort of family relationship.
Southern group – physiotherapist
Finally, in order to take part in a standing frame trial, the people positioning the young person would need to have adequate training to achieve the optimum effect. This could be feasible using technology:
You could make little videos on iPads [Apple Inc. Cupertino, CA, USA] that the school have.
Northern group – occupational therapist
What did the multistakeholder focus groups add?
The multistakeholder focus groups added more in-depth clinical insight into potential trial designs for different stakeholder groups and reinforced some of the findings from the single stakeholder groups. The variety of participants allowed for rich discussion of the different priorities for each stakeholder group. Participants delineated appropriate parameters for each section of the PICOTS. There would be interaction between each aspect; for example, the chosen outcome would affect the type of participants (in terms of age, GMFCS level and cognitive ability) and vice versa. A mixed-methods design was repeatedly suggested in order to adequately capture the outcomes and experiences of young people with CP.
Generally, both focus groups from the North and South were in agreement, with a few exceptions. The Northern group believed that the type of standing frame used would not affect the study (as long as it was prescribed appropriately for the individual), whereas the Southern group felt that the type of standing frame would need to be the same to properly compare the young people. However, this would reduce the potential participant pool, as only some young people would be suitable for a specified standing frame.
For a trial, there would be barriers to overcome for all stakeholders as each person brings their unique experiences and biases to their perceptions of the value of standing frames. Professionals, parents, and young people are not in emotional equipoise despite understanding the evidential equipoise. Standing frames are currently regularly used as part of postural management, and some participants believed that this indicates they are clinically effective.
How did the multistakeholder focus groups inform the next step?
Overall, there was a strong theme throughout the multistakeholder focus groups of participation and/or the young person’s well-being. All stakeholders emphasised how important it is to consider the individual, because young people with CP are different in many ways. This is a major challenge to a standing frames trial. Studies related to long-term body structure outcomes are unlikely to be feasible or funded. This is because of difficulties with timelines (e.g. length of time required to show differences in body structure), populations (e.g. variation in young people with CP), and confounders (e.g. other therapies). Therefore, innovative thinking is required to design a research study that is feasible. It is important to give insight into the clinical benefit of standing frames beyond body structure and body function, including participation and quality of life. A mixed-methods design, with a qualitative process evaluation, alongside a RCT and economic evaluation, is likely to be most appropriate to capture the broader experiences of the young people, their families and professionals (health care and education), as well as the clinical effectiveness and cost-effectiveness end points. The information provided by the multistakeholder focus groups informed the questions for survey 2, which explored the acceptability and feasibility of a research trial.
Chapter 7 Survey 2: research trial acceptability and feasibility
Objectives
A survey was conducted from April to May 2017 to explore the perceived value of standing frames research. Opinions were gathered on a specific research design as well as the practicalities of conducting the research more generally, including feasibility and acceptability. Owing to the anonymous nature of the questionnaires, it was impossible to determine how many participants took part in both survey 1 and survey 2 or to link responses across the two surveys.
Methods
Population
Three populations in the UK were sampled for this study:
-
Health professionals: physiotherapists and paediatricians who work or have worked with young people with CP who use standing frames.
-
Education professionals: teachers who work or have worked with young people with CP who use standing frames.
-
Parents: parents of young people with CP who currently use or have used a standing frame.
Young people with CP who currently use or have used a standing frame were not participants in this stage of the study because completing a survey was not an appropriate way to collect their data. This is because young people with CP GMFCS III–V have a variety of communication methods, and reading and writing are less likely to be an accessible communication style for this particular group. However, we included young people’s voices in the interview stage, and used parents as a proxies (surveys, focus groups and PPI).
Questionnaire development: research trial acceptability and feasibility
Survey 2 was developed using the same procedure as survey 1. The questionnaire was devised based on the information gathered in the previous stages of the study. Separate versions of the questionnaire were designed for the three participant populations to ensure that the questions were relevant and used appropriate language, although all versions explored similar concepts.
The questions related to the perceived value of standing frames research and opinions about how a research study could be conducted (e.g. Which age group of young people with CP do you think would be most suitable for a standing frames research study?). Furthermore, an example research study was presented, and participants were asked to provide their views about its feasibility and factors that would prevent them from recruiting to, or participating in, such a study. Most questions had fixed-choice responses with a free-text box to explain the response (see Appendices 8–10).
Procedure
Survey 2 followed the same procedure as survey 1 (see Chapter 3) and was conducted from April to May 2017. As per protocol, ethics approval was sought and approved for the final version of survey 2, as it was dependent on the results from all previous stages of the study.
Results
Participants
Numbers included in the final analysis are presented here. Figure 3 indicates participant flow through the study from responses received to responses included in the final analysis. In survey 2, we did not distinguish between prescribers and non-prescribers as per survey 1 (current UK standing frame practice; see Chapter 3):
-
Health professionals – physiotherapists and paediatricians who work with young people with CP who use standing frames, n = 467.
-
Education professionals – teachers who work with young people with CP who use standing frames, n = 44.
-
Parents – parents of young people with CP who currently use or have used a standing frame, n = 74.
FIGURE 3.
Survey 2: participant flow through the study from responses received to responses included in the final analysis.
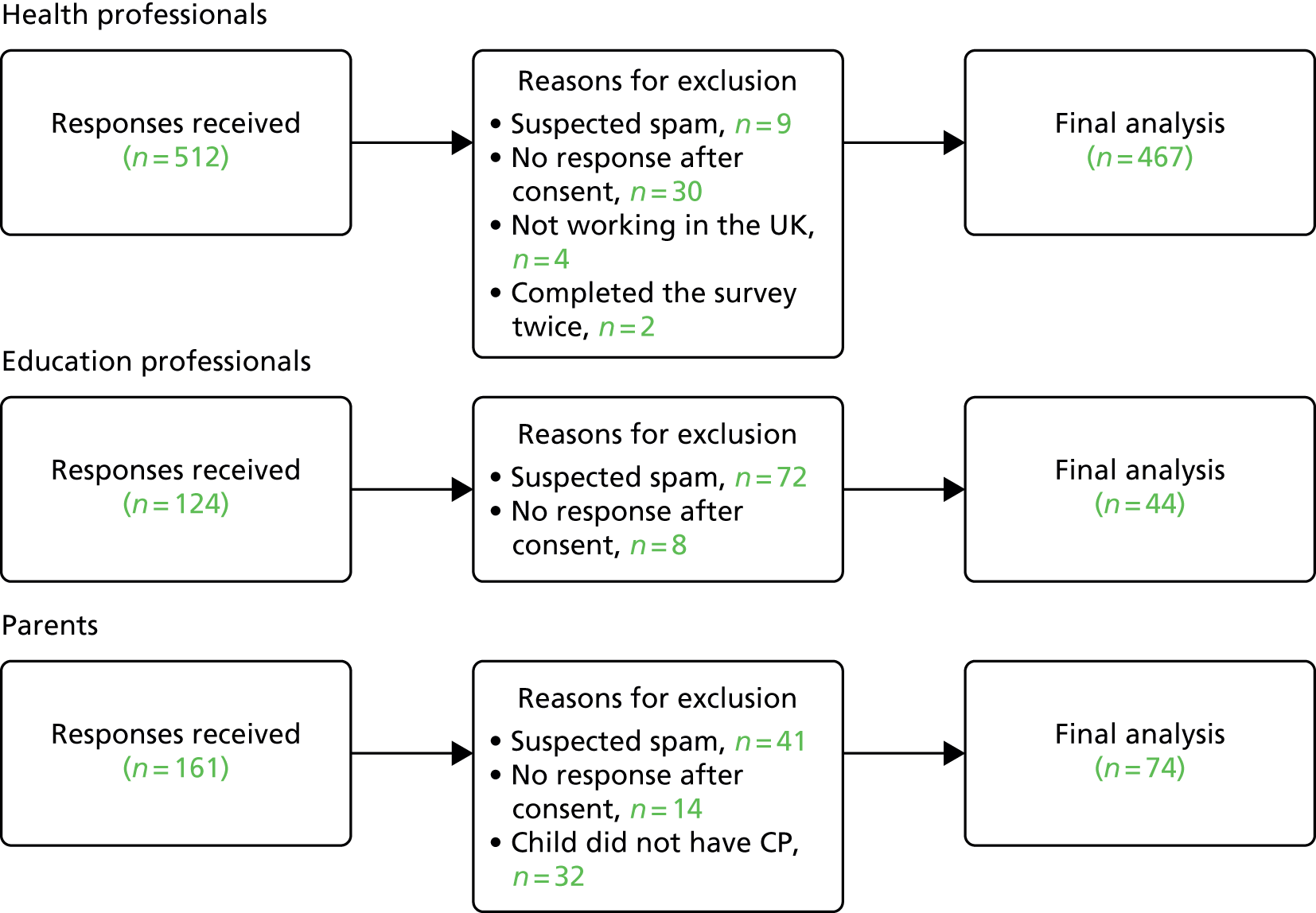
Unfortunately, during recruitment, we identified that there was a sudden significant increase in responses over a 12-hour period. The responses did not seem genuine; for example, false postcodes and unusual e-mail addresses were provided, there were odd responding patterns (e.g. participants identifying as physiotherapists and parents and paediatricians and speech pathologists), and answers were in Chinese script. Following urgent co-applicant discussion, the surveys were closed. On the next working day, Jill Cadwgan sought advice from the HTA and the chair of the steering committee. It was decided that further recruitment should be discontinued for the following reasons:
-
Genuine responses were reviewed. Participants provided the first two letters of their postcode, and we could see that there was already a spread across the UK.
-
A detailed examination of the responses, including the open-ended answers, revealed a consistent message. It seemed unlikely that new participants would add new information.
-
We analysed the data using descriptive statistics only. Therefore, we did not need a certain amount of participant numbers to meet the assumptions of any statistical tests.
-
It would have required a significant amount of resources, may have delayed study progress and may have only resulted in an extra few responses.
-
We felt that our resources in the closing months of the study would be better spent engaging with key stakeholders to inform our recommendations.
Table 18 outlines the respondent characteristics. Most health-care respondents were physiotherapists (83.5%) and most education respondents were classroom teachers or support assistants (77.3%). The majority of health professionals worked in community settings: at home (n = 300), in specialist education (n = 299), and/or in mainstream education (n = 272) (multiple responses were allowed). Education professionals tended to work in specialist schools (79.9%). Seventy-four per cent of parent respondents had a child who currently used a standing frame and most had a child who attended a specialist school (64.8%).
| Characteristic | Health professionals, n (%) | Education professionals, n (%) | Parents, n (%) |
|---|---|---|---|
| Rolea | |||
| Physiotherapist | 390 (83.5) | – | – |
| Paediatrician | 24 (5.1) | – | – |
| Therapy assistant or technical instructor | 21 (4.5) | – | – |
| Occupational therapist | 15 (3.2) | – | – |
| Other | 10 (2.1) | 4 (9.2) | – |
| Orthopaedic surgeon | 4 (0.9) | – | – |
| Classroom teacher or support teacher | 2 (0.4) | 34 (77.3) | – |
| Parent | 1 (0.2) | – | 74 (100) |
| Health professional | – | 7 (15.9) | – |
| Missing | 0 | 0 | 0 |
| Education setting | |||
| Specialist school (private/other e.g. charity funding) | – | 28 (63.6) | 26 (35.1) |
| Specialist school (state funded) | – | 7 (16.3) | 22 (29.7) |
| Mainstream (state funded) | – | 4 (9.1) | 13 (17.6) |
| Other | – | 3 (6.8) | 8 (10.8) |
| Mainstream school with additional resource for SEND | – | 1 (2.3) | 2 (2.7) |
| Mainstream (private) | – | 0 | 2 (2.7) |
| Missing | – | 1 (2.3) | 1 (1.4) |
| Current working environmenta | |||
| Community – home | 300 (64.2) | – | – |
| Community – special education centre | 299 (64) | – | – |
| Community – mainstream education centre | 272 (58.2) | – | – |
| Child development or family centre clinic | 237 (50.7) | – | – |
| Outpatients | 138 (29.6) | – | – |
| Inpatients | 79 (16.9) | – | – |
| Other | 36 (7.7) | – | – |
| Missing | 70 (14.9) | – | – |
Importance of a research study
The majority of respondents in all participant groups suggested that further research into standing frames was needed but one-quarter of education professionals were not sure, and their open-ended responses indicated that this was because they were not aware of the findings from existing standing frames research. Most respondents in each participant group thought that standing frames should be used for non-ambulant young people with CP, and 78.2% of health professionals believed that they are clinically effective.
There were mixed responses as to whether or not health and education professionals would agree to young people with CP ceasing standing frame use if there was good-quality evidence showing that standing frames were not beneficial. The open-ended responses indicated that health professionals do not believe that there is any point in continuing with ineffective interventions, but research demonstrating that that was the case would need to be supported by professional bodies. Other health professionals did not routinely use standing frames in their practice anyway and as such felt that the state of the research would not change their practice. Those who disagreed with, or were unsure about, stopping standing frame use, even if there was good-quality evidence to do so, cited reasons such as the importance of giving young people an opportunity for a change of position, not being confident enough to make the decision themselves, perceptions of benefits regardless of evidence, and difficulty persuading parents to stop anyway. Many health professionals also commented that there would need to be evidence that standing frames caused harm, not simply that there were no benefits; the research would need to be extremely robust and conclusive. Education professionals also noted that there was no need to continue an intervention, such as a standing frame, if it proved not to be beneficial, but they would primarily follow advice from their health professional colleagues (e.g. physiotherapists). Others did not agree or were unsure because they felt that the young person’s preference and individual needs, rather than research evidence, should dictate standing frame use. Professional experience was in support of the positive effects of a change of position through standing frame use.
Most respondents indicated that young people ≤ 11 years of age were most suitable to be recruited to standing frame research. Approximately half of each professional group said they would be willing to change their standing frame practice for a research trial compared with 63.6% of parents. It was considered acceptable by most participants to suspend or delay standing frame use for up to 12 weeks (Table 19).
| Perception | Health professionals, n (%) | Education professionals, n (%) | Parents, n (%) |
|---|---|---|---|
| Standing frames should be used for children with CP GMFCS III–V | |||
| Yes | 415 (88.9) | 34 (77.3) | 62 (83.8) |
| No | 2 (0.4) | 0 (0) | 1 (1.4) |
| Did not know | 12 (2.6) | 2 (4.5) | 6 (8.1) |
| Missing | 38 (8.1) | 8 (18.2) | 5 (6.8) |
| I personally believe that standing frames are clinically effective | |||
| Yes | 365 (78.2) | – | – |
| No | 8 (1.7) | – | – |
| Did not know | 56 (12) | – | – |
| Missing | 38 (8.1) | – | – |
| Further research into standing frames is necessary | |||
| Yes | 400 (85.7) | 26 (59.1) | 62 (83.8) |
| No | 3 (0.6) | 0 | 1 (1.4) |
| Did not know | 29 (6.2) | 11 (25) | 6 (8.1) |
| Missing | 35 (7.5) | 7 (15.9) | 5 (6.8) |
| I would agree to change my practice for a research study | |||
| Yes | 237 (50.7) | 23 (52.3) | 35 (63.6) |
| No | 26 (5.6) | 6 (13.6) | 1 (1.8) |
| Did not know | 154 (33) | 5 (11.4) | 18 (32.7) |
| Missing | 50 (10.7) | 10 (23.7) | 1 (1.8) |
| If there was good-quality evidence that standing frames were not beneficial, I would agree for children with CP to stop using them | |||
| Yes | 159 (34) | 21 (47.7) | – |
| No | 35 (7.5) | 4 (9.1) | – |
| Did not know | 221 (47.3) | 10 (22.7) | – |
| Missing | 52 (11.1) | 9 (20.5) | – |
| Suitable age groups (years) for a standing frames research studya | |||
| 0–5 | 341 (73) | 18 (40.9) | 42 (56.8) |
| 6–10 | 363 (77.7) | 26 (59.1) | 49 (66.2) |
| 11–15 | 248 (53.1) | 18 (40.9) | 37 (50) |
| 16–18 | 151 (32.3) | 12 (27.3) | 28 (37.8) |
| No age groups are suitable | 4 (0.9) | 3 (6.8) | 0 |
| Missing | 51 (10.9) | 9 (20.5) | 11 (14.9) |
| Longest possible time to delay/suspend standing frame use (weeks) | |||
| < 2 | 21 (4.5) | – | 10 (18.2) |
| 2–6 | 117 (25.1) | – | 13 (23.6) |
| 7–12 | 76 (16.3) | – | 7 (12.7) |
| 13–18 | 20 (4.3) | – | 1 (1.8) |
| 19–24 | 12 (2.6) | – | 0 |
| > 24 | 10 (2.1) | – | 0 |
| It is not appropriate to delay or suspend use of a standing frame for a research study | 27 (5.8) | – | 7 (12.7) |
| Did not know | 49 (10.5) | – | 14 (25.5) |
| Other | 68 (14.6) | – | 0 |
| Missing | 67 (14.3) | – | 3 (5.5) |
Feasibility of a research study
Over 55% of health professionals suggested that they would be willing to recruit participants to a standing frames trial, although only 22% thought that they would have time to do this in their current role and only 19% currently have good clinical practice training (Table 20). Open-ended responses indicated that health professionals who were willing to recruit participants in principle believed in the importance of research, were happy to be of help and were interested and/or invested in the topic. Those who were not willing or were unsure cited reasons such as time limitations; case loads (including heavy case loads and case load mix) and/or professional roles (e.g. believing young people on their case load would be too young or old to take part in a research study); the need for team support and/or decisions; perceived reluctance from parents and other staff; and the need for more information about the study.
| Perception | Health professionals, n (%) |
|---|---|
| Appropriate person to recruit participantsa | |
| Physiotherapist | 383 (82) |
| Occupational therapist | 65 (13.9) |
| Therapy assistant or technical instructor | 106 (22.7) |
| Paediatrician | 95 (20.3) |
| Orthopaedic surgeon | 81 (17.3) |
| I do not know | 5 (1.1) |
| Other (please specify) | 22 (4.7) |
| Missing | 72 (15.4) |
| In principle, I would be willing to recruit participants | |
| Yes | 261 (55.9) |
| No | 43 (9.2) |
| I do not know | 89 (19.1) |
| Missing | 74 (15.8) |
| In reality, I could recruit participants | |
| Yes | 195 (41.8) |
| No | 63 (13.5) |
| I do not know | 135 (28.9) |
| Missing | 74 (15.8) |
| I would have time to recruit participants to a research study in my current role | |
| Yes | 102 (21.8) |
| No | 112 (24) |
| I do not know | 177 (37.9) |
| Missing | 76 (16.3) |
| I have relevant clinical training which allows me to consent participants to a research study | |
| Yes | 89 (19.1) |
| No | 246 (52.7) |
| I do not know | 62 (13.3) |
| Missing | 70 (15) |
| I would be prepared to do relevant training which allows me to consent participants to a research studyb | |
| Yes | 188 (61) |
| No | 37 (12) |
| I do not know | 83 (26.9) |
| Missing | 0 |
| I would be prepared for a research physiotherapist to be involved in the child’s care for the duration of the study | |
| Yes | 322 (69) |
| No | 19 (4.1) |
| I do not know | 47 (10.1) |
| Missing | 79 (16.9) |
Health professionals who indicated that they could recruit participants thought that they had appropriate case loads and could persuade parents to participate, had previously been involved in research, and believed in the importance of research. Those who thought that they could not recruit participants did not have appropriate case loads, lacked time, or did not think that they could convince parents to take part. Health professionals who were unsure whether or not they could actually recruit participants for a trial gave reasons such as the decision would not be made by them (e.g. management would have to choose whether or not to take part), it would depend on the time commitment, limited resources, inappropriate work setting, changing professional roles, and perceptions that the families they work with would not be willing to take part.
More than half of the education professionals would be happy for young people at their school to take part (regardless of their allocation to an intervention or control group), would agree to a research physiotherapist visiting the school, and would find it easy to keep a diary of standing frame use, bowel functions, medications and pain.
Table 21 shows that although only 43% of parents expressed a willingness in principle for their child to take part in a research study regardless of their allocation, 25.7% were unsure. Open-ended responses indicated that parents who were willing believed that there was no negative difference between intervention and control groups, the study findings would benefit their child anyway by contributing to knowledge about young people with CP, and their child prefers not to use a standing frame over summer anyway. Those who would not be willing to have their child randomised (13.5%) or were unsure (25.7%) cited the following reasons: needing more information about the study, their child’s tolerance and/or pain, fear of putting their child at risk, going against advice they have received, belief in the benefits of standing frames, uncertainty about what interventions the control group would receive and their child did not currently use a standing frame anyway. Similar to education professionals, parents reported that they would find it relatively easy to keep research diaries.
| Perception | Education professionals, n (%) | Parents, n (%) |
|---|---|---|
| I would be happy for children at my school/my child to take part regardless of whether or not they were in the experimental or control group | ||
| Yes | 25 (56.8) | 32 (43.2) |
| No | 2 (4.5) | 10 (13.5) |
| I do not know | 4 (9.1) | 19 (25.7) |
| Missing | 13 (29.5) | 13 (17.6) |
| I would agree to a research physiotherapist visiting children at school for assessments | ||
| Yes | 27 (61.4) | – |
| No | 0 | – |
| I do not know | 3 (6.8) | – |
| Missing | 14 (32.6) | – |
| Keeping a daily diary of standing frame use would be | ||
| 1 (impossible) | 2 (4.5) | 7 (9.5) |
| 2 | 1 (2.3) | 7 (9.5) |
| 3 | 2 (4.5) | 7 (9.5) |
| 4 | 8 (18.2) | 12 (16.2) |
| 5 (easy) | 17 (38.6) | 26 (35.1) |
| Missing | 14 (31.8) | 15 (20.3) |
| Keeping a detailed diary of bowel functions, medication and pain would be | ||
| 1 (impossible) | 3 (6.8) | 4 (5.4) |
| 2 | 2 (4.5) | 7 (9.5) |
| 3 | 5 (11.4) | 13 (17.6) |
| 4 | 11 (25) | 13 (17.6) |
| 5 (easy) | 9 (20.5) | 22 (29.7) |
| Missing | 14 (31.8) | 15 (20.3) |
| Preferred method to keep a diarya | ||
| Electronic (e.g. iPad, phone, computer) | 1 (2.3) | 13 (17.6) |
| Hard copy (e.g. a book) | 14 (31.8) | 20 (27) |
| Either hard copy or electronic | 10 (22.7) | 20 (27) |
| I would not keep a diary | 0 | 3 (4.1) |
| Other | 5 (11.4) | 3 (4.1) |
| Missing | 14 (31.8) | 15 (20.3) |
| I would agree to work with a research physiotherapist | ||
| Yes | 22 (20) | – |
| No | 2 (4.5) | – |
| I do not know | 6 (13.6) | – |
| Missing | 14 (31.8) | – |
| It would matter if children in the same class were in different groups for the research study | ||
| Yes | 2 (4.5) | – |
| No | 21 (47.7) | – |
| I do not know | 7 (15.9) | – |
| Missing | 14 (31.8) | – |
Parents were also willing to be approached by health professionals about a standing frame research study (64.9%), as well as to provide medical information (71.6%), to complete questionnaires (66.2%) and to have detailed physiotherapy assessments (66.2%) of their child (Table 22).
| Perception | Parents, n (%) |
|---|---|
| I would be prepared to/for my child to be asked by a health worker if we would be interested in taking part in a research study | |
| Yes | 48 (64.9) |
| No | 7 (9.5) |
| I do not know | 6 (8.1) |
| Missing | 13 (17.6) |
| I would be prepared for me/my child toa | |
| Provide medical information for the purpose of research | 53 (71.6) |
| Complete questionnaires about their participation and activities | 49 (66.2) |
| Allow them to have a detailed assessment by the research physiotherapist | 49 (66.2) |
| I would not agree to any of these | 4 (5.4) |
| Missing | 14 (18.9) |
| The best location for assessments during a research study would bea | |
| School | 40 (54.1) |
| Home | 38 (51.4) |
| A clinic or centre where my child receives care usually | 29 (39.2) |
| A different clinic or hospital to where my child usually visits | 13 (17.6) |
| Missing | 18 (24.3) |
Barriers to a research study
The most common ethical reason identified by each participant group for not recruiting or participating in a standing frames research study was fear that stopping standing frame use could cause irreversible harm to the young person. Health professionals also reported that a research study would be too labour-intensive to be feasible (56.2%), whereas 29.5% of education professionals and 35.1% of parents did not believe any of the practical issues were applicable (Table 23).
| Difficulties | Health professionals, n (%) | Education professionals, n (%) | Parents, n (%) |
|---|---|---|---|
| Practicala | |||
| A research study would be too resource intensive to be feasible | 129 (27.6) | – | – |
| A research study would be too labour intensive to be feasible | 150 (56.2) | – | – |
| Children with CP are individual. It is impossible to research the impact of standing frames | 44 (9.4) | 4 (9.1) | 1 (1.4) |
| Some benefits of standing frames cannot be measured (e.g. ‘feeling tall’) | 107 (22.9) | 8 (18.2) | 6 (8.1) |
| It would be too difficult to get children and parents to participate in a research study | 79 (16.9) | 0 | – |
| It would be too difficult to get professionals to participate in a research study | 41 (8.8) | – | – |
| I would not have the support in my workplace to take part in a research study | 64 (13.7) | – | – |
| There would not be enough space for children’s standing frames | – | 0 | 7 (9.5) |
| Other | 76 (16.3) | 7 (15.9) | 21 (28.4) |
| None of these apply | 0 | 13 (29.5) | 26 (35.1) |
| Missing | 141 (30.2) | 18 (40.9) | 20 (27) |
| Ethical or personal choicea | |||
| It is not right to withdraw standing frame treatment for a research study | 51 (10.9) | 3 (6.8) | 6 (8.1) |
| Stopping standing frame use for a research study could cause harm that could not be reversed | 186 (39.8) | 13 (29.5) | 16 (21.6) |
| Participating in a research study about standing frames may affect the child’s quality of life negatively | 102 (21.8) | 6 (13.6) | 4 (5.4) |
| The child’s choice, rather than a research study, should dictate their standing frame use | 107 (22.9) | 7 (29.5) | 7 (9.5) |
| I would feel guilty if I could not do everything I needed to do for the study | – | – | 14 (18.9) |
| It is an emotionally significant moment to see my child stand; it is more important to me than a research study | – | – | 2 (2.7) |
| Other | 55 (11.8) | 2 (4.5) | 10 (13.5) |
| None of these apply | 0 | 9 (20.5) | 19 (25.7) |
| Missing | 164 (35.1) | 18 (40.9) | 22 (29.7) |
What does survey 2 add?
Survey 2 demonstrated that the majority of participants believe that more standing frames research is necessary. Most respondents suggested that they were willing in principle to engage in a trial. For example, most parents were willing to be approached by health professionals about participating in a research study, have their child randomly allocated to experimental or control groups and change how their child uses a standing frame for the purposes of a research study. Furthermore, approximately 50% of health and education professionals would agree to change their standing frame practice for a research study.
In addition, the results of survey 2 provided vital information about ‘deal breakers’ in a standing frames research study. The maximum amount of time most health professionals and parents would agree to suspend/delay standing frame use is 12 weeks. There are factors that would stop a relatively small proportion of professionals and parents participating in a standing frames study, such as fear, that suspending use would cause irreversible damage. Although these may not appear to be major issues at this stage, they are important factors for consideration when calculating the number of potential participants that would need to be approached.
Survey 2 has also showed that stakeholders have different perceptions regarding challenges to a research study. Feasibility is a major issue. For example, a higher proportion of health professionals than parents indicated that there were issues that would stop them recruiting for, or participating in, a study. Health professionals are clearly invested in standing frames, and education and resource may be required to enhance engagement in a research study.
How has survey 2 informed the next step?
Survey 2 allowed us to see if the discussions in our qualitative work were generalisable to a wider population. It also enabled us to explore ‘deal breakers’ in a trial for potential participants.
Large numbers of data were collected throughout the study. It was essential to record, analyse and share this information in order to understand it. Therefore, the next phase of the study was engaging stakeholders in sense checking and interpreting the findings. A secondary outcome of this was engagement of potential future participants and dissemination of findings.
Analysis of the results led the co-applicants to consider and ask stakeholders the following questions in two design workshops (see Chapter 8):
-
What are the research priorities as related to standing frames?
-
What are the pros and cons of different research study designs?
-
Should a standing frames research trial be explanatory or pragmatic?
Chapter 8 Robustness of results: stakeholder involvement and patient and public involvement
Objectives
The collated study results (survey 1, single stakeholder focus groups, interviews, multistakeholder focus groups, survey 2) were taken to two multistakeholder design workshops in June 2017. The aims of these design workshops were to discuss (1) the study’s findings, (2) priorities for research studies, (3) potential trial designs and (4) produce conclusions and recommendations. Potential research designs that were discussed were (1) standing frame use versus no standing frame use and (2) treatment as usual standing frame use (i.e. participants would continue to use their standing frame as they usually would) versus ‘super standing’ [i.e. extra support provided to use the standing frame as generally prescribed (five times per week for 30–60 minutes)]. The design workshops were also to ensure that the results were robust and the co-applicants’ ideas were staying true to the data.
Attendees at the design workshops included co-applicants, steering group members and various stakeholders, such as physiotherapists, orthopaedic surgeons, paediatricians, parents and a young person with CP. Stakeholders were identified through the PPI group, clinical connections or participants who had expressed interest and consented to further contact either via the survey or after the focus group. Three of the physiotherapists had been focus group attendees but none of the other stakeholders had taken part in a focus group. A medical professional who was naive to the study took notes on the discussion. Jill Cadwgan and Jane Goodwin were particularly mindful not to lead the conversation based on their own biases because they had been immersed in the data from the outset and throughout. The discussions are summarised here.
Design workshop: various stakeholders
Co-applicants Jill Cadwgan, Allan Colver, Anna Basu, Denise Howell, Sarah Crombie, Jan Lecouturier and Johanna Smith were in attendance, along with a member of the steering group (paediatrician), five physiotherapists and an orthopaedic surgeon.
Research priorities
A detailed discussion of research priorities revealed that participation should be a primary outcome with body function as a secondary outcome. That is:
-
Primary outcome: quality of participation (including, but not necessarily limited to, interaction, communication, vision, using upper limbs/motor abilities). Related to this, it is important to examine what elements of participation are associated with being upright.
-
Secondary outcome: body function (including, but not limited to, bowel function, speech, breath control, feeding).
Throughout this, it would be important to ensure that everyone involved understands the concepts of evidential and emotional equipoise. It would also be important to shift from the value of body structure to the importance of participation. Both of these would require significant education for professional and parent stakeholders.
Trial design
In principle, it was agreed that a trial would need to be pragmatic rather than explanatory. Intervention versus no intervention was preferable to standing versus an increased dose of standing because of the perception that it would be impractical and prohibitively expensive to introduce ‘super standing’. Furthermore, it would be more difficult to show a significant difference between two slightly different doses. Useful comparators include walkers, standing slings, supported lying positioning and powered chairs. A qualitative component would be required to adequately capture experiences. However, any type of research study in this population would require significant resources, even to facilitate adherence to the prescribed standing frame use. Therefore, trial settings (e.g. specific specialist schools) and stakeholder engagement would need to be established as early as possible.
Reservations about a trial
Design workshop attendees had several reservations about a standing frames research study. Some major concerns centred on the ethics of conducting research that may demonstrate standing frames do not achieve certain outcomes. This has implications for commissioners, and there were fears that standing frames may not be funded in future, even though many families and young people with CP enjoy using their standing frames (regardless of any body structure, body function, participation or activity benefits). Some people have such strong beliefs about the benefit of standing frames on the body that they are likely to continue to use them, despite any evidence that is produced. Commercial companies are likely to continue to market their products as helpful for body structure, and this may have more of an influence on professionals and families than the results of a scientifically robust research study. Furthermore, the intrinsic perception regarding the body structure benefits of standing is difficult to overcome because it is virtually impossible to design research that isolates the impact of standing frames alone.
The design workshop highlighted a number of topics for discussion. The importance of clinically relevant outcomes was raised. For example, is bone density worthwhile exploring if it does not affect the risk of fractures? Exploring the idea of reducing sedentary time and increasing metabolic rate may also be worthwhile. The physiotherapists were particularly concerned that a research study (and potential findings) could increase parental guilt and create additional practical difficulties. If participation outcomes are being measured, the standing frame should be used to access existing activities, not new activities, because otherwise we will be enhancing participation by default.
Design workshop: parents
A second design workshop was held with five parents and one young person who uses a standing frame because we were unable to get representation from these groups at the first workshop. It was facilitated by co-applicant Johanna Smith and research associate Jane Goodwin. The aims were the same as the first workshop, and the discussions from the day are summarised here. It is important to note that parents were reacting to the information given to them on the day from a lay perspective; therefore, some of their ideas had previously been explored. The summary reports the parents’ views only, and we have not further justified and analysed them in this section. However, these ideas have contributed to the final recommendations in Chapter 9 in combination with the synthesis of all the results of the study.
Research priorities
Parents suggested that the research priority should be the change of position that comes with standing frames, because they believe that it gives their child access to, for example, eye contact, general participation and life in a different position:
-
Primary outcome: change of position (including, but not necessarily limited to, access, stretch, comfort, functional ability, interaction, being like other young people and enjoyment).
-
Secondary outcomes:
-
Physiological measures (including, but not limited to, bowel function and breathing). Parents believed that it was important to have a medical reason for using standing frames so that they could continue to use the standing frame for participation. They suggested that body structure/function and participation cannot be separated, and, as such, neither should be neglected. Parents also perceived that it would be easier to persuade schools to use standing frames if there was physiological science behind it, rather than simply parents’ beliefs about what is best for their child.
-
Young person’s quality of life (including, but not necessarily limited to, how the standing frame affects how they feel about themselves and being disabled, and their self-awareness). Parents commented that young people often realise in their teen years that their disabilities are permanent, and that this realisation can cause major psychological distress.
-
Parents also believed that standing frames research did not necessarily have to be about progress (e.g. improving function). It could be about maintaining existing skills or preventing any deterioration and this would be enough to justify the use of standing frames.
Trial design
Attendees at this workshop had alternative suggestions for standing frame research designs. For a study regarding change of position, they recommended monitoring young people to see how much they get to move. Parents believed that there was an evidence base for the health benefits of changing positions. They also suggested a retrospective study could be conducted with older young people, investigating body structure outcomes (e.g. bone density) then examining their medical records to see how much they had used their standing frame. Finally, parents proposed conducting a study with a group of young people who do not already use a standing frame and have them use one for 12 weeks to see the results. This way, nobody ‘loses out’ on using a standing frame. Some of these ideas are not likely to be feasible (discussed in Chapter 9) or scientifically robust, and as such highlight the need to educate families at recruitment about the trial’s research priorities and methods.
They suggested sit-to-stand wheelchairs (which allow the young person to keep up with friends and siblings without manual lifting) as a potential comparator.
Pros and cons of trial designs
Parents generally agreed that 12 weeks was acceptable for delaying or suspending standing frame use, especially if the study was built into the school holidays. However, one parent commented on the struggle between wanting research and her child’s individual needs. She is desperate for research that might help her child but she would not feel comfortable withdrawing her child’s standing frame for the purposes of a study because her child enjoys standing so much.
Parents were also worried about one of the potential trial designs presented to them. That is, standing treatment as usual versus ‘super standing’. They did not think that it was right to introduce an intervention (such as an enhanced standing programme) then take it away, especially if the young person really enjoyed it. They would want a guarantee that the intervention would still be available after the research study. This would not be feasible in current UK practice according to our survey 1 results. Likewise, the parents expressed concern that if a young person is not used to standing five times per week, it may be a shock. However, the young person who attended the workshop indicated that it would be acceptable to stand that often. Another concern was the variability in function of young people with CP. Energy levels and muscle tone can vary on an hourly or daily basis and parents felt that as a result it would be difficult to determine what changes were caused by the standing frame use.
Parents had some recommendations for a research study with standing frames. First, it may be more feasible to do with younger children because it is physically easier and they can engage in activities like painting. Older young people find the use of a standing frame more difficult (especially at mainstream schools) because of room changes, space and wanting to fit in with peers. It would be better to have young people participating in a research study standing at the same time in a classroom so that they can be the same as their peers. Lots of activities can be done in a group if everyone is in a standing frame.
Reservations about a trial
Parents were ‘disappointed with science’. They have learnt that health professionals use their best guess, and that parents receive anecdotal evidence (which is useful) from other families. It had been surprising and disappointing to learn about the lack of evidence for the many treatments their children undergo (e.g. postural management), even if they do make logical sense. Therefore, they do believe that there is a need for research, yet they worry that studies may demonstrate that standing frames have no clinical effect, which could mean they are no longer funded. This would be very distressing because many families believe that the standing frame is worthwhile, especially if their child enjoys using it. They wondered whether or not their child’s enjoyment would count for anything with commissioners.
In terms of practicalities of a study, parents suggested that the best way to achieve compliance would be if it was carried out at school. It is asking a lot of parents to meet study requirements, such as standing five times per week. However, it is difficult for parents to know what is being done at school. They noted that the child receives a prescription for standing frame use which may be different from what is actually happening at school, and parents may not be included in any part of this process.
Chapter 9 Discussion
Introduction
The overall purpose of this study was to answer the question: what is the likely acceptability of a trial to determine the clinical effectiveness of standing frames? To do this, we undertook two surveys, focus groups and in-depth interviews.
Summary of findings
The range of clinical indications and benefits described by all participants throughout the study included body structure and body function, such as bladder or bowel functions, activity, such as improved motor abilities, and participation, such as interaction with peers. They also reported other benefits, such as improvement in BMD and prevention of hip dislocation. They noted challenges related to environmental and personal factors such as physical space and the child’s pain. With respect to body structure and body function, participants perceived benefits despite the lack of evidence in the literature. For example, 73.8% of prescribing clinicians in survey 1 (current UK standing frame practice) (see Table 12) reported a belief that frames improve bladder and bowel functions, yet we found only one single-case study in a child with CP and chronic constipation. 26 Furthermore, although using a standing frame to support hip joint development has some scant evidence, participants identified this as a benefit of standing frames. More research is needed for guidance on positioning, as well as the duration and frequency of standing. 5
Participants also perceived standing frames to help with participation, enjoyment and communication. Physical assistance and environmental adaptations improve participation in children with CP,27 but to our knowledge, there is no research relating specifically to standing frames. Being at standing height may be advantageous for social interaction and independence, but this is dependent on the position and activities of other individuals. When a person is using a wheelchair, a standing companion receives more eye contact from third parties, giving the impression that the wheelchair user depends on their standing companion. 28 In terms of activity, upper limb function can be affected by positioning. Self-feeding may be enhanced by standing, but picking up small objects is easier if sitting. 29 The young people with CP who were interviewed (Chapter 5) also commented on the importance of independence. Young people have previously reported that independence is essential for self-sufficiency and making choices. 30 Some young people in the current study thought that the standing frame limited their mobility and independence because they had to rely on others for help while in the standing frame. Static standing frames take away the young person’s ability to move freely and can isolate them from their peers. Therefore, they preferred their powered wheelchairs. This is similar to previous research that highlighted the positive effect of powered wheelchairs in terms of social activities and being able to engage in the environment without constant supervision and assistance from others. 31 However, others thought that their standing frame allowed them to participate more in activities such as cooking.
There are significant challenges with regards to standing frame use. Participants in survey 1 (current UK standing practice) and the qualitative studies identified physical space as a particular difficulty. Huang et al. 32,33 also found space to be a major factor restricting assistive device use (including standing frames) by parents and teachers in their study in Taiwan. Other barriers in their study included inadequate teacher training and personal factors such as feeling pressured to use equipment at school but not at home. 32 Huang et al. 32,33 did not report on carer availability for moving and handling, which was a reported difficulty in our study.
What have we found?
The results from survey 1 (UK standing frame practice) and the focus groups, along with discussions at design workshops and PPI events, showed that standing frames are largely prescribed to ameliorate difficulties or potential difficulties of body structure and body function. Other benefits (e.g. participation and activity) are considered to be useful by-products rather than primary aims. Despite the lack of supporting evidence, the majority of stakeholders have strong beliefs about the benefits for body structure and body function. Prescription is based on clinical experience and pragmatism.
Thus, there is not universal emotional equipoise about whether or not standing frames work.
What would not be feasible in a trial?
Despite the emphasis on body structure and body function in the prescription and use of standing frames, we found that body structure outcomes would be challenging as the focus of a trial. We outline the reasons for this view:
-
Timelines: responses from parents and professionals suggest that 12 weeks is the maximum amount of time they would delay starting or withdrawing standing frame use. An intervention would need to be longer than this to have an effect on body structure.
-
Carry over effects: although a crossover study was used as a potential study design for survey 2, it was decided (based on co-applicant discussions and the design workshops) that this was impractical because of carry over effects.
-
Co-interventions: standing frames are just one aspect of young people’s postural management. Other health and therapeutic interventions, such as walkers, are likely to impact on the same outcomes that standing frames might influence. Co-interventions would also be problematic in a trial with a short intervention period and long-term follow-up.
-
Type of standing frame/position: as a result of the different types of standing frames and positioning within them, there are too many variables which may impact on the outcome being measured, such as bone density. For example, prone standing may provide a different level of weight bearing compared with being upright.
What might be feasible in a trial?
If young people are not being prescribed standing frames, or are not using their standing frames solely to improve body structure, we should examine the other indications for use that have been identified in our study. That is, body functions (e.g. bowel function) and other benefits (e.g. choice, change of position, participation, enjoyment and communication).
These ‘other benefits’ are broad, including aspects of quality of life, participation and subjective well-being, and could be explored in a trial as patient-reported outcomes. The World Health Organization defines ‘quality of life’ as an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. 34 It is a broad-ranging concept, affected in a complex way by the person’s physical health, psychological state, personal beliefs, social relationships and their relationship to salient features of their environment. Participation is involvement in a life situation19 and subjective well-being is self-reported well-being, including happiness, pleasure and fulfilment.
To the authors’ knowledge, there is no published research into the clinical effectiveness of standing frames with respect to patient-reported outcomes. A potential study design is proposed in Chapter 10.
Limitations of our study
It is likely that the study attracted participants who were interested, engaged and had strong opinions, whether positive or negative, about standing frames. Therefore, they may not be representative of the general population of people who work with standing frames, have a child who uses or has used a standing frame, or of young people who use standing frames. A limitation of the parent groups was that their children had all used a standing frame for a number of years. We were not able to explore views on delayed start with parents who were within a year or two of diagnosis when that could be an option.
Furthermore, because of the nature of recruitment and the anonymity of surveys 1 and 2, we could not calculate response rates or determine non-response bias. There were also challenges in engaging education staff and parents. It is likely that education staff were difficult to recruit for face-to-face events (e.g. focus groups) because there are no other people to cover their duties during the day and after school hours they have further work and personal commitments. This reflects what we would anticipate in trial. Therefore, a trial would need to specifically target schools for recruitment and arrange the study in a way that was acceptable to and convenient for education staff. Parents were also hard to recruit for face-to-face events, with many cancelling just prior to the focus group. This is not surprising because they have significant caregiving responsibilities. Therefore, the education staff and parents who were able to participate in the Understanding Frames study may not be representative of the underlying populations.
Professionals’ experiences of standing frames may be coloured by a variety of factors including their training, the region of the UK they work in, and the population of young people they work with. As the study progressed, we realised that education professionals would be major stakeholders in a trial. Therefore, it would have been helpful to have a separate survey 1 for this participant group to give more information on use of standing frames within the school context, which would have been useful considering the proposed trial within the school context. Parents’ experiences are likely to be influenced by demographic factors (e.g. socioeconomic factors), their emotional journey with having a child with CP, the support they receive, and the way their child reacted (and continues to react) to their standing frame use.
In terms of participation in research, different factors may influence parents and young people. This has been highlighted in our current study and is relevant in future trials. For example, depending on their level of education a visit to a university may be intimidating, or, as a result of previous experiences, hospital visits may be upsetting. Lack of interest in research, time to participate and the priority of the research question in relation to the family’s own interests and priorities are also important factors to consider. The young people’s experiences may be affected by their cognitive and communicative abilities. Although we aimed to include participants with a variety of experiences and abilities, the sample is more representative of young people with CP who have the capacity to provide assent, and understand relatively complex questions about their standing frame use. Five out of the 12 participants attended mainstream school (including one mixed placement), and only one participant used a VOCA. Although the qualitative findings may not be representative of all standing frame stakeholders, they contribute to the body of knowledge surrounding young people, CP and standing frames, by highlighting both positive and negative impacts on these participants.
Strengths of our study
We received rich data from a variety of stakeholders. Mixed methods has given us confidence in our research findings because of the holistic examination. Data from survey 1 (current UK standing frame practice) informed us of the wide range of perceived benefits and challenges to standing frame use, but in-depth understanding of these could only be extracted during the focus groups and interviews. Young people in particular added understanding of the complexities of how using frames may affect participation, activity, interaction and emotional well-being. Survey 1 also contributed to our understanding of study designs (e.g. delayed or suspended use) that could be explored in the qualitative phase of the study. Ideas produced in the qualitative stage gave us priorities for research and potential trial designs. The qualitative aspect allowed for in-depth examination of what was acceptable for various stakeholders and the reasoning for their comments. Final feasibility of these trial designs was then tested in a wide population through survey 2 (research trial acceptability and feasibility). The benefits of mixed-methods design have been outlined in Chapter 2.
There were a large number of survey participants from all over the UK. We had representation from professionals who work in a variety of settings. We also had strong PPI from the outset and throughout. PPI advisory group members (as well as informal PPI) provided feedback on the initial application, study documents (e.g. information sheets), surveys (1 and 2), potential trial designs, the co-applicants’ interpretation of the data and dissemination. Furthermore, having a parent of a young person with CP on the co-applicant team was a great strength of this study. The PPI allowed the research to be grounded in the practicalities of conducting research with families affected by CP (e.g. holding focus groups in the middle of the day because of commitments before and after school hours, allowing time for introductions to make parents more comfortable), as well as remaining accessible (e.g. avoiding overloading participants with information) and respectful (e.g. type of language used).
Chapter 10 Conclusions
Recommendations for research
Current research priorities
We found that patient-reported outcomes (e.g. quality of life, participation and subjective well-being) are important to young people, parents and professionals (both health and education professionals) and feasible for a trial with a short intervention. This was recognised in each stage of the study, particularly the design workshops held after the study data had been collated. Body structure and body function characteristics are also important and would be of interest to a variety of stakeholders, but we found they would be difficult to use as primary outcomes. We have proposed body structure as a secondary outcome. Despite the clinical impression that long-term effects on body structure (e.g. bone density and preventing the need for surgery) may take several years to evaluate, our study showed that parents and professionals are worried that harm may occur from not using a standing frame relatively quickly (e.g. loss of joint range of movement over a summer holiday). Using body structure as a secondary outcome would allow any harms to be identified.
We recommend trials that focus on the following outcomes:
-
Primary outcome:
-
selected from patient-reported outcomes (e.g. participation).
-
-
Secondary outcomes:
-
patient-reported outcomes not included as a primary outcome (e.g. quality of life, subjective well-being)
-
body function (e.g. bowel function, speech, breath control and feeding)
-
body structure (e.g. loss of range of movement).
-
Recommendation of, and rationale for, particular trial designs
We recommend a mixed-methods design. A qualitative process evaluation alongside the quantitative data collection could help understand the complexity of the intervention and social contexts, and the clinical effectiveness of the intervention. 35 Qualitative data could also capture the experience of young people when they are (or are not) using standing frames, as well as all stakeholders involved in standing frame use.
As we found that ‘prescribed’ standing frame use was generally not achieved because of a variety of factors, a trial should be pragmatic (i.e. able to work in everyday practice) rather than explanatory (i.e. work in ideal circumstances). Survey 1 (current UK standing frame practice) and focus group results showed that physiotherapists were not monitoring as often as they would have liked to because of lack of resources. Therefore, a trial should also include a health economic evaluation.
We present our recommendations for a research trial using the PICOTS framework.
Population: young people with cerebral palsy (Gross Motor Function Classification System III–V)
A study in those children of infant and primary school age (4–11 years) is likely to be the most practical with respect to ease of facilitation of standing frame use in school, size of standing frames and the typical age at which most young people with CP start using standing frames. A study with preschool children was considered, but we decided against it because of such factors as the developmental age of the child and preparedness of families to be recruited to a trial when their child had been recently diagnosed with CP (as advised by parent participants and co-applicant Johanna Smith reflecting on their past experiences). Using standing frames at secondary school age, particularly in school, is a challenge because of environmental considerations, and young people and professionals may be less able to adhere to a trial protocol.
The commissioned call suggested research into young people with CP GMFCS IV and V; however, our survey shows that standing frame use in younger people with GMFCS III is widespread, in keeping with our clinical experience, and we therefore recommend that inclusion criteria should include young people with CP GMFCS III. Classification of young people on the basis of their pattern of motor impairment (e.g. dystonia vs. spasticity vs. mixed) would be difficult because it is clinically difficult for clinicians and parents to distinguish. Both boys and girls should be included. Data capture for the current study was predominantly in England, but there is no reason why study sites in Scotland, Wales and Northern Ireland should not be included.
Intervention: standing frame use (3 days per week)
We found that recommended standing frame use was 30–60 minutes daily for 5 days or more each week, but that this was not usually achieved. Pragmatically, a standing frame intervention for a duration tolerated (for longer or shorter periods) by the young person for 3 days per week would be an appropriate dosage based on the results from survey 1 (UK standing frame practice).
Adherence to a trial regime greater than this would be likely to require significant resource to ensure implementation and may be susceptible to reduced compliance and fidelity. Some young people use standing frames at home, and there would need to be consideration of a standardisation of standing frame use at home.
Many types of standing frames are used and prescription should be appropriate to the individual young person. Because the primary outcome will be selected from patient-reported outcomes (e.g. participation), the specific type of standing frame is less important. It would be unfeasible to recommend exactly which standing frame the young person should use. More important is consideration of the suitability and availability of the standing frame to the individual child. Angle and position may need to be considered and could be examined in the qualitative component of the trial. For example, if a young person is looking up in the air or down at the floor, participation and activity may be more limited.
Comparator: no standing frame use
Standing frame use versus no use, or versus alternative therapy or equipment (e.g. hydrotherapy or disability exercise bike) has been discussed in detail throughout the study. Consensus suggests that standing frame use versus no use would be most likely to detect change and be feasible. All young people would be likely to have other therapy, orthotics and activities regardless of whether they were in the intervention or non-intervention group (‘treatment as usual’) but randomisation should lead to a balance with respect to these factors across trial groups. Careful consideration of trial design will be necessary in order to control for these, or to define and standardise ‘treatment as usual’ for the duration of the trial. This may be a consideration for the final population or setting; for example, control of ‘treatment as usual’ may be easier in one particular location or setting.
Outcomes: selected patient-reported outcomes (e.g. quality of life, participation, subjective well-being), body function and structure
-
Primary outcome:
-
selected patient-reported outcome (e.g. participation).
-
-
Secondary outcomes:
-
patient-reported outcomes not included as a primary outcome (e.g. quality of life, subjective well-being)
-
body function (e.g. bowel function, speech, breath control and feeding)
-
body structure (e.g. loss of range of movement).
-
Measures should address the primary and secondary outcomes of the study. Selected patient-reported outcome measures could assess quality of life, participation, and subjective well-being. All measures should ideally be adaptable to the young person’s communication level and cognitive ability. There may be a need for parent- and/or education staff-proxy reports of the child’s patient-reported outcomes (e.g. quality of life, participation and subjective well-being), although the ideal would be young people’s self-report. It will also be important to assess impact on parents and family life. Secondary outcome measures of body function may include respiratory function, bowel function and pain, and of body structure may include clinical measures of joint range of movement and growth.
Adherence to trial protocol would need to be carefully monitored as our survey highlights that ‘treatment as prescribed’ is not always achieved. Both quantitative and qualitative methods should be included. This is particularly important when considering young people’s voices and the individuality of standing frame prescription (i.e. what works for one child may not work for another, and quantitative research may not capture this variation).
Timing: 6–12 weeks
We found through survey 1 and the qualitative work that young people often have a break from standing frame use during school holidays. Survey 2 demonstrated that suspending or delaying standing frame use would be acceptable and ethical for a period of 6–12 weeks. However, qualitative data from parents reflecting on their experiences revealed that delayed use (i.e. a waiting list control design) would not be an acceptable trial design. It must be noted, however, that we did not have any parent participants who had a child who had recently been diagnosed with CP to confirm whether or not a delayed start would be acceptable. Therefore, we recommend suspended use for 6–12 weeks. Furthermore, there may be other variables (e.g. other therapies and activities) that need to be taken into account in the school holidays compared with school term time.
Anxieties highlighted by stakeholders regarding deterioration in body structure for longer durations of ‘non-use’, could be alleviated by including clinical assessments at the time of the outcome assessments.
Setting: specialist school environment
We recommend that standing frame use should be explored in the specialist school environment, because this is where most young people with GMFCS III–V are educated; furthermore, specialist schools would be better equipped to support standing frame use for the purposes of a trial, as they tend to be used in this environment anyway. There may be challenges with education, training and support of educational professionals in conducting a trial in that setting. Although our survey 2 data suggested that education staff would be willing, and find it acceptable, to recruit to a trial, our focus group data from a single specialist education school highlighted issues with staff confidence and achieving prescribed standing in a classroom because of conflicting interests between therapy and education. Furthermore, we experienced difficulties with education staff recruitment to both focus groups and the surveys, likely because they do not have other people to cover their duties and they have other work and personal commitments. This may have implications for trial buy-in from education staff, and adherence to treatment as prescribed in the school setting.
For adequate statistical power, a trial would need multicentre recruitment. Describing, and potentially balancing or adjusting for ‘treatment as usual’ would need to be considered. For example, young people are more likely to receive a similar therapy or orthotic programme in one school, but these interventions are likely to vary between schools.
Potential challenges
Our study identified significant challenges for a research trial but we believe that they are surmountable with careful planning. PPI (including young people with CP) would be required from the development of a funding application for a future trial through to the dissemination of the results. This level of PPI could be achieved by allowing members to take part flexibly (e.g. via online forums) and having representatives on the co-applicant team (parent and/or young person with CP) as well as on the Trial Steering Committee and/or a separate PPI RAG.
Recruitment and attrition
Allied health professionals, particularly physiotherapists, were the main professional stakeholders (in terms of prescribing, monitoring, and supporting standing frame use) for standing frames. Physiotherapists would therefore be the most appropriate professionals to recruit participants.
We had problems finding education staff willing and able to participate in our study, which might mean there will be difficulties engaging schools in a full trial, although it is the preferable setting. However, for the purposes of our study, we were asking education staff to leave the school setting and participate in research that was beyond their role. If the setting for a trial was in a specialist school, education staff would be asked to position their students in a standing frame, which is something they often do anyway.
Consent and assent
We found that young people with CP may have different opinions to their parents about their standing frame. This has implications for the young people’s assent to a trial. Furthermore, if young people have strong feelings (positive or negative) about using a standing frame, their allocation to intervention or control could have a significant confounding effect on the outcome measures, including quality of life and subjective well-being. It would be important to note reasons for non-recruitment of screened population including lack of assent from the young person for trial. Legal and ethics frameworks around consent and assent would also need consideration.
Engagement in a trial
We found that engagement of stakeholders in a trial may be challenging because of the emphasis currently placed on body structure. Professionals may be unaware of how their conversations with families may lead to families sharing the same views about frames. Shifting the framework to patient-reported outcomes (e.g. quality of life, participation and subjective well-being) and body function outcomes will require education to engage professionals and families in a trial and to inform thinking in clinical practice.
Moreover, young people with CP may have multiple comorbidities and/or general health issues which may prevent them from participating in a trial.
Need for equipoise
In one sense standing frames work because they do make the young person stand. What we need to ask is ‘what is the standing for?’. Professionals, parents and young people entering the trial should think that the trial is worthwhile because it is an open question whether or not standing frames have benefit. If they are certain of benefits, they may not consent to the trial. Personal preferences for standing frame use may thus affect recruitment.
Implications for health care and the need for a pilot phase
Although there is no strong evidence that standing frames are beneficial, they still might be. We found that it will be difficult to develop a robust evidence base. We also found that many stakeholders (including physiotherapists, parents and young people) are invested in standing frames despite the paucity of evidence for their use. Therefore, standing frames may continue to be prescribed and used even if a future trial demonstrates that they are not effective with respect to selected patient-reported outcomes (e.g. quality of life, participation and subjective well-being) and body function. Participants suggested that there would need to be evidence that standing frames cause harm for people to stop using them.
For all of the above challenges identified, it is not feasible or cost-effective to progress to a full multicentre RCT. This leaves a question regarding the logical next step. There are two possibilities:
-
A randomised feasibility study – an external stand-alone pilot.
-
A randomised feasibility study – an internal pilot with clear progression criteria to a full trial.
We would recommend a randomised feasibility study (an internal pilot phase with clear progression criteria to a full trial), and summarise the reasons:
-
To determine that physiotherapists have the capacity to recruit, especially for a trial in the specialist school setting.
-
To explore the extent to which parents and professionals are agreeable to the primary outcome of a selected patient-reported outcome (i.e. participation). What people say they will do may be quite different from what they do when confronted with a real-life decision.
-
To establish whether or not education staff in specialist schools are prepared to ‘buy in’ to the study, and to facilitate the prescribed standing programme.
-
To establish that sufficient staff and families are in equipoise.
-
To establish that the proposed outcomes can be collected.
The researchers considered a randomised feasibility study (an external stand-alone pilot), that is, data would be collected on the feasibility of a future trial (e.g. recruitment, retention and choice of outcomes), but would not be used in the definitive trial. However, they decided against it for the reasons summarised:
-
It would be at least 8–10 years before any definitive conclusion about standing frames could be obtained. The current study has highlighted that families would value evidence about the benefits of standing frames as soon as possible, and may object to waiting for this amount of time.
-
With recruitment and power concerns, data captured in a pilot would be valuable.
-
A pilot would require much effort and commitment from staff, young people and parents. It might be considered unethical to then omit them from the main study if the design was feasible.
Therefore, there is a strong argument for an internal pilot (i.e. data collected at this stage would be included in a main trial). Although the internal pilot reduces waste, there would need to be consideration of how to manage the data collected if the trial design was adjusted to improve feasibility of the main trial. 36
Concluding statement
Our findings suggest that a trial could examine standing frame use in young people with CP GMFCS III–V. The primary outcome of the trial should be a selected patient-reported outcome (e.g. participation), with other selected patient-reported outcomes (e.g. quality of life, subjective well-being body function and body structure) as secondary outcomes. There would be multiple factors to consider in the trial design including the heterogeneity of the population, significant challenges to recruitment and retention and adherence to protocol. These challenges can be overcome by clinical understanding of the population and careful trial design to include a randomised feasibility trial (i.e. an internal pilot). Consideration of issues including knowledge of treatment as usual, other postural management approaches and outcome measures will be required. A mixed-methods approach, which captures quantitative and qualitative data about users’ experience, is necessary.
Standing frames are one part of postural management for young people with CP GMFCS III–IV. Many of our findings are relevant to potential trials of many interventions for young people with neurodisability. We have shown that it is possible to obtain young people’s views, which are highly valuable with respect to their engagement in clinical intervention and research.
Parents and professionals engaged in the qualitative aspect of this research, and stakeholders who took part in the design workshops understood the concept of evidential equipoise and appreciated the lack of clinical evidence. However, our surveys and qualitative information (and PPI) demonstrated that most people are not in a position of individual emotional equipoise and have strong beliefs regarding the clinical effectiveness of standing frames.
Despite the publication of the International Classification of Functioning, Disability, and Health in 2001 (and the ICF-CY in 2007),37 research and clinical focus still tends to be based only on body structure and body function. To engage stakeholders in a trial, there needs to be explanation of why patient-reported outcomes (e.g. quality of life, participation, and subjective well-being) are important clinical outcomes.
Acknowledgements
Contributions of authors
Dr Jane Goodwin (Research Associate, Psychology) developed the survey materials, ran the survey and analysed the data; conducted and analysed the interview data; cofacilitated the focus groups and analysed the data; prepared the results from survey 1 and the interviews for publication; and contributed to writing the report and approved the final version.
Ms Jan Lecouturier (Senior Research Associate and Deputy Director, NIHR, Research Design Service North East and study co-applicant) was involved in the design of the study; led the qualitative research, cofacilitated the focus groups and supported the research associate with the conduct of the qualitative research and analysis of the data; and was involved in preparing the report and approved the final version.
Dr Anna Basu (NIHR Career Development Fellow and Honorary Consultant Paediatric Neurologist and study co-applicant) was involved in the design of the study. She commented on results from all stages of the research as they emerged. She was an author on papers published from the research. She contributed to the final report and approved the final version.
Professor Allan Colver (Professor of Community Child Health and study co-applicant) was involved in the design of the study. He commented on results of all stages of the research as they emerged. He was an author on papers published from the research. He contributed to the final report and approved the final version.
Dr Sarah Crombie (Clinical Specialist Physiotherapist and study co-applicant) was involved in the design of the study. She was involved in participant recruitment. She commented on results of all stages of the research as they emerged. She was an author on papers published from the research. She contributed to the final report and approved the final version.
Mrs Johanna Smith (Parent and study co-applicant) was involved in the design of the study. She was PPI lead during the project, recruiting parents to the RAG, facilitating and comoderating the RAG Facebook group and disseminating information to wider parent groups. She cofacilitated the parent focus group (Northern England). She commented on results of all stages of the research as they emerged. She was an author on papers published from the research. She drafted the Plain English summary, contributed to the final report and approved the final version.
Ms Denise Howel (Senior Lecturer in Epidemiological Statistics and study co-applicant) was involved in the design of the study. She led the quantitative research and supported the research associate with the conduct of the quantitative data analysis. She commented on results of all stages of the research as they emerged. She was an author on papers published from the research. She contributed to the final report and approved the final version.
Professor Elaine McColl (Professor of Health Service Research and study co-applicant) was involved in the design of the study and provided particular expertise in respect to survey methods and trial design. She commented on results of all stages of the research as they emerged. She was an author on papers published from the research. She contributed to the final report and approved the final version.
Dr Jeremy R Parr (Clinical Senior Lecturer/Honorary Consultant and study co-applicant) was involved in the design of the study and the analysis of results. He commented on results of all stages of the research as they emerged. He was an author on papers published from the research and approved the final version of the report.
Dr Niina Kolehmainen (Senior Clinical Lecturer and Honorary Consultant Allied Health Professional and study co-applicant) supported the design of the study and the analysis of results. She was an author on papers published from the research and approved the final version of the report.
Mr Andrew Roberts (Consultant Orthopaedic Surgeon and study co-applicant) supported the design of the study and the analysis of results. He was involved in participant recruitment. He was an author on papers published from the research and approved the final version of the report.
Mr Keith Miller (Rehabilitation Engineer) supported the study design and the analysis of results. He was an author on papers published from the research and approved the final version of the report.
Dr Jill Cadwgan (previously Kisler; Consultant Paediatrician and Associate Clinical Researcher) was lead applicant and was ultimately responsible for the conduct of the study, including design, ethics approval, analysis, and dissemination. She was the corresponding author on papers published from the research. She contributed to the final report and approved the final version.
Dissemination
Publications
Goodwin J, Lecouturier J, Crombie S, Smith J, Basu A, Colver A, et al. Understanding frames: a qualitative study of young people’s experiences of using standing frames as part of postural management for cerebral palsy. Child Care Health Dev 2018;44:203–11.
Goodwin J, Colver A, Basu A, Crombie S, Howel D, Parr JR, et al. Understanding frames: a UK survey of parents and professionals regarding the use of standing frames for children with cerebral palsy. Child Care Health Dev 2018;44:195–202.
Conferences
Crombie S, Goodwin J, Cadwgan J. Understanding Frames: A UK Survey of Parents and Professionals Regarding the Use of Standing Frames for Children with Cerebral Palsy. The Association of Paediatric Chartered Physiotherapists Conference, Cardiff, 3–4 November 2017.
Cadwgan J, Goodwin J. Understanding Frames: Evaluating ‘Inherited’ Clinical Practice in Children and Young People with Cerebral Palsy. Royal College of Paediatrics and Child Health Annual Conference, Birmingham, 24–6 May 2017.
Goodwin J, Lecouturier J, Crombie S, Smith J, Cadwgan J. Understanding Frames: Young People’s Experiences of Using Standing Frames as Postural Management in Cerebral Palsy. European Academy of Childhood Disability Annual Meeting, Amsterdam, 17–20 May 2017.
Goodwin J, Lecouturier J, Crombie S, Smith J, Cadwgan J. Understanding Frames: Implementation of Standing Frames as Part of Postural Management for Children with Cerebral Palsy in the Classroom. European Academy of Childhood Disability Annual Meeting, Amsterdam, 17–20 May 2017.
Goodwin J, Colver A, Basu A, Crombie S, Howel D, Parr J, et al. Understanding Frames: A UK Survey of Parents and Professionals Regarding the Use of Standing Frames for Children with Cerebral Palsy. European Academy of Childhood Disability Annual Meeting, Amsterdam, 17–20 May 2017.
Goodwin J, Lecouturier J, Crombie S, Smith J, Cadwgan J. Understanding Frames: Young People’s Experiences of Using Standing Frames as Postural Management in Cerebral Palsy. Great North Children’s Research Community Conference, Newcastle upon Tyne, 10 March 2017.
Goodwin J, Lecouturier J, Crombie S, Smith J, Cadwgan J. Young People’s Experiences of Using Standing Frames as Postural Management in Cerebral Palsy. Young Person’s Advisory Group – North England. Young People’s Voices: Shaping the Future of Research and Healthcare, Newcastle upon Tyne, 1 December 2016.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Gross motor function classification system (GMFCS). Dev Med Child Neurol 1997;39:214-23. https://doi.org/10.1111/j.1469-8749.1997.tb07414.x.
- Westbom L, Hagglund G, Nordmark E. Cerebral palsy in a total population of 4–11 year olds in southern Sweden. Prevalence and distribution according to different CP classification systems. BMC Pediatr 2007;7. https://doi.org/10.1186/1471-2431-7-41.
- Shevell MI, Dagenais L, Hall N. REPACQ CONSORTIUM* . The relationship of cerebral palsy subtype and functional motor impairment: a population-based study. Dev Med Child Neurol 2009;51:872-7. https://doi.org/10.1111/j.1469-8749.2009.03269.x.
- Gericke T. Postural management for children with cerebral palsy: consensus statement. Dev Med Child Neurol 2006;48. https://doi.org/10.1017/S0012162206000685.
- Bush S, Daniels N, Caulton J, Davis A, Jex J, Stern G, et al. Guidance on assisted standing for children with cerebral palsy. APCP Journal 2010;2:3-10.
- Fehlings D, Switzer L, Agarwal P, Wong C, Sochett E, Stevenson R, et al. Informing evidence-based clinical practice guidelines for children with cerebral palsy at risk of osteoporosis: a systematic review. Dev Med Child Neurol 2012;54:106-16. https://doi.org/10.1111/j.1469-8749.2011.04091.x.
- Paleg GS, Smith BA, Glickman LB. Systematic review and evidence-based clinical recommendations for dosing of pediatric supported standing programs. Pediatr Phys Ther 2013;25:232-47. https://doi.org/10.1097/PEP.0b013e318299d5e7.
- Gibson SK, Sprod JA, Maher CA. The use of standing frames for contracture management for nonmobile children with cerebral palsy. Int J Rehabil Res 2009;32:316-23. https://doi.org/10.1097/MRR.0b013e32831e4501.
- Caulton JM, Ward KA, Alsop CW, Dunn G, Adams JE, Mughal MZ. A randomised controlled trial of standing programme on bone mineral density in non-ambulant children with cerebral palsy. Arch Dis Child 2004;89:131-5. https://doi.org/10.1136/adc.2002.009316.
- Cerebral Palsy in Under 25s: Assessment and Management. London: NICE; 2017.
- Herman D, May R, Vogel L, Johnson J, Henderson RC. Quantifying weight-bearing by children with cerebral palsy while in passive standers. Pediatr Phys Ther 2007;19:283-7. https://doi.org/10.1097/PEP.0b013e318156cc4d.
- Damcott M, Blochlinger S, Foulds R. Effects of passive versus dynamic loading interventions on bone health in children who are nonambulatory. Pediatr Phys Ther 2013;25:248-55. https://doi.org/10.1097/PEP.0b013e318299127d.
- Births in England and Wales: 2016. Newport: ONS; 2017.
- Hutton JL, Pharoah PO. Effects of cognitive, motor, and sensory disabilities on survival in cerebral palsy. Arch Dis Child 2002;86:84-9. https://doi.org/10.1136/adc.86.2.84.
- Hutton E, Coxon K. ‘Posture for Learning’: meeting the postural care needs of children with physical disabilities in mainstream primary schools in England – a research into practice exploratory study. Disabil Rehabil 2011;33:1912-24. https://doi.org/10.3109/09638288.2010.544837.
- Spasticity in Under 19s: Management. London: NICE; 2012.
- Davies SC, Lemer C, Hargreaves D, Cheung R, Strelitz J, Weil L, et al. Annual Report of the Chief Medical Officer. Our Children Deserve Better: Prevention 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/255237/2901304_CMO_complete_low_res_accessible.pdf (accessed 1 November 2017).
- Morris C, Simkiss D, Busk M, Morris M, Allard A, Denness J, et al. Setting research priorities to improve the health of children and young people with neurodisability: a British Academy of Childhood Disability – James Lind Alliance Research Priority Setting Partnership. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006233.
- International Classification of Functioning, Disability, and Health: Children and Youth Version: ICF-CY. Geneva: World Health Organization; 2007.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. New York, NY: Routledge; 1994.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 1995;311:42-5. https://doi.org/10.1136/bmj.311.6996.42.
- Rossman GB, Wilson BL. Numbers and words: combining quantitative and qualitative methods in a single large-scale evaluation study. Eval Rev 1985;9:627-43. https://doi.org/10.1177/0193841X8500900505.
- Goodwin J, Colver A, Basu A, Crombie S, Howel D, Parr JR, et al. Understanding frames: a UK survey of parents and professionals regarding the use of standing frames for children with cerebral palsy. Child Care Health Dev 2017;44:1-8.
- Francis JJ, Johnston M, Robertson C, Glidewell L, Entwistle V, Eccles MP, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health 2010;25:1229-45. https://doi.org/10.1080/08870440903194015.
- Rivi E, Filippi M, Fornasari E, Mascia MT, Ferrari A, Costi S. Effectiveness of standing frame on constipation in children with cerebral palsy: a single-subject study. Occup Ther Int 2014;21:115-23. https://doi.org/10.1002/oti.1370.
- Schenker R, Coster W, Parush S. Personal assistance, adaptations and participation in students with cerebral palsy mainstreamed in elementary schools. Disabil Rehabil 2006;28:1061-9. https://doi.org/10.1080/09638280500526461.
- Edelmann RJ, Done B, Easterbrook J, Evans J, Foster T, Green M. Disablement and eye contact. Percept Mot Skills 1984;58:849-50. https://doi.org/10.2466/pms.1984.58.3.849.
- Noronha J, Bundy A, Groll J. The effect of positioning on the hand function of boys with cerebral palsy. Am J Occup Ther 1989;43:507-12. https://doi.org/10.5014/ajot.43.8.507.
- Palisano RJ, Shimmell LJ, Stewart D, Lawless JJ, Rosenbaum PL, Russell DJ. Mobility experiences of adolescents with cerebral palsy. Phys Occup Ther Pediatr 2009;29:133-53. https://doi.org/10.1080/01942630902784746.
- Evans S, Neophytou C, de Souza L, Frank AO. Young people’s experiences using electric powered indoor – outdoor wheelchairs (EPIOCs): potential for enhancing users’ development?. Disabil Rehabil 2007;29:1281-94. https://doi.org/10.1080/09638280600964406.
- Huang IC, Sugden D, Beveridge S. Assistive devices and cerebral palsy: the use of assistive devices at school by children with cerebral palsy. Child Care Health Dev 2009;35:698-70. https://doi.org/10.1111/j.1365-2214.2009.00968.x.
- Huang IC, Sugden D, Beveridge S. Assistive devices and cerebral palsy: factors influencing the use of assistive devices at home by children with cerebral palsy. Child Care Health Dev 2009;35:130-9. https://doi.org/10.1111/j.1365-2214.2008.00898.x.
- Development of the World Health Organization WHOQOL-BREF quality of life assessment . Psychol Med 1998;28:551-8. https://doi.org/10.1017/S0033291798006667.
- O’Cathain A, Thomas KJ, Drabble SJ, Rudolph A, Hewison J. What can qualitative research do for randomised controlled trials? A systematic mapping review. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-002889.
- Wittes J, Brittain E. The role of internal pilot studies in increasing the efficiency of clinical trials. Stat Med 1990;9:65-71. https://doi.org/10.1002/sim.4780090113.
- International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY. Geneva: WHO; 2007.
Appendix 1 Survey 1: parents
Appendix 2 Survey 1: prescribing clinicians
Appendix 3 Survey 1: non-prescribing professionals
Appendix 4 Single stakeholder focus groups: topic guide
Appendix 5 Single stakeholder focus groups: PowerPoint presentation
Appendix 6 Interviews: topic guide
Appendix 7 Multistakeholder focus groups: PowerPoint presentation with topic guide included
Appendix 8 Survey 2: parents
Appendix 9 Survey 2: health professionals
Appendix 10 Survey 2: education professionals
Glossary
- Activity
- The execution of a task or action by an individual.
- Body function
- The physiological functions of body systems (including psychological functions).
- Body structure
- Anatomical parts of the body such as organs, limbs and their components.
- Children and young people
- Children and young people aged 0–19 years with cerebral palsy. Throughout the report, children and young people are referred to as young people unless referring to the young people in relation to their parents; for example, ‘children of the parent respondents’.
- Classroom support assistant
- An individual who supports a teacher in the classroom setting by helping disabled young people with their learning through one-on-one support or in small groups.
- Emotional equipoise
- A state of genuine uncertainty regarding the clinical effectiveness of standing frames based on an individual’s personal beliefs and feelings (e.g. parents’ experience of their child standing).
- Environmental factors
- External influences on functioning and disability. That is, the physical, social and attitudinal environment in which people live and conduct their lives.
- Evidential equipoise
- A state of genuine uncertainty about the clinical effectiveness of standing frames based on an individual’s knowledge of the research literature (e.g. conflicting results, weak evidence base).
- International Classification of Functioning, Disability and Health: Children and Youth version
- A framework that encompasses functions and structures of the body, activity, participation, personal factors and environmental factors. We have used it to examine the impact of standing frames on a young person’s health-related functioning.
- Participation
- Involvement in a life situation (as per the International Classification of Functioning, Disability and Health: Children and Youth version).
- Patient-reported outcomes
- For the purposes of our report, patient-reported outcomes refers to quality of life, participation and subjective well-being.
- Personal factors
- Internal influences on functioning and disability, that is, individual attributes of the person.
List of abbreviations
- BMD
- bone mineral density
- CP
- cerebral palsy
- GMFCS
- Gross Motor Function Classification System
- HTA
- Health Technology Assessment
- ICF-CY
- International Classification of Functioning, Disability and Health: Children and Youth Version
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PICOTS
- population, intervention, comparison, outcome, timing, setting
- PPI
- patient and public involvement
- RAG
- Research Advisory Group
- RCT
- randomised controlled trial
- VOCA
- voice output communication aid
- WHO
- World Health Organization
