Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 14/168/02. The contractual start date was in May 2016. The draft report began editorial review in June 2018 and was accepted for publication in February 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Lewis et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background and overview ofthe research
In this chapter we set the scene for the research study, by providing background information regarding the function of perinatal and paediatric autopsy examination and how it is conducted, including new developments, contribution to clinical care, factors influencing its value, the consent process and current barriers. We also present an overview of the research study.
Introduction
In England and Wales, there are around 3000 terminations of pregnancy for fetal abnormality per annum and there are estimated to be at least 3000 miscarriages at 12–24 weeks’ gestation. 1 From approximately 700,000 births per annum, around 3000 result in stillbirth (SB), 2000 in neonatal death and 800 in infant death (of which 250 are unexplained). There are also around 50 unexpected child deaths (children aged 1–14 years) annually. 2–4 In those cases in which a coronial autopsy examination (otherwise known as a post-mortem) is not required, parents may be offered an autopsy examination to try to establish the cause of death and, when appropriate, to estimate the risk of problems recurring in future pregnancies. Standard autopsy examination results in clinically significant findings in 22–76% of cases, depending on the type of loss. 5,6 Without an autopsy, many parents are left with no understanding of the disease process related to their child’s death, and regret for some parents who decline autopsy has been identified. 7 Despite this, consent rates for prenatal, perinatal and paediatric autopsy have dropped significantly in the UK,7–9 Western Europe10,11 and the USA12,13 in the past 30 years. In the UK, less than half of parents of stillborn babies and only one-quarter of parents of neonates who die provide consent for standard autopsy examination. 9
Autopsy examination as a component of investigation of prenatal and paediatric death
The perinatal autopsy represents part of a specialist obstetric, fetal medicine or paediatric service and current guidelines recommend that the option of an autopsy, performed by specialist paediatric/perinatal pathologists, should be offered for all perinatal deaths, including miscarriages, SBs, termination of pregnancy for fetal abnormality (ToP) and neonatal deaths. 14 A sudden unexpected death in infancy (SUDI) or a sudden unexpected death in childhood (SUDC) require referral to the Her Majesty’s (HM) Coroner and, in most cases, a coronial autopsy is indicated.
Functions of perinatal and paediatric autopsy
The aim of investigation after death is to provide information for a number of functions, ranging from information relevant to the parents that may influence further management, through to providing data for clinical governance and service development.
Determination of cause of death or major diagnosis
In the majority of paediatric settings, the primary role of the autopsy, usually performed on behalf of HM Coroner, is to determine the likely underlying cause of death. In fetal cases, the aim is to confirm findings and determine undiscovered pathology in cases in which pregnancy was terminated for abnormality, and to determine the cause of death in SBs. However, it should be recognised that in the majority of clinically unexpected SBs, the precise cause of death may remain unexplained even after autopsy examination, highlighting the need for further research in this area. 15 Confirmatory findings following prenatal diagnosis of abnormalities or disease diagnosed during life may also be of benefit, providing reassurance and governance to clinicians and parents, and may assist some parents in their grieving process.
Management of future pregnancies and siblings
In around 10–20% of cases, additional information from autopsy may have a direct effect on the recurrence risk and counselling of future pregnancies, or may have implications for other family members. For example, detection of additional malformations may lead to a specific underlying syndromic diagnosis or the identification of a hereditary disorder, which may modify genetic counselling and/or management of future pregnancies. The detection of such underlying genetic or metabolic disorders may also have implications for other family members. Likewise, although uncommon, placental histological examination may reveal potentially recurrent disorders, including massive perivillous fibrin deposition and chronic histiocytic intervillositis, both of which are associated with adverse pregnancy outcome and a high risk of recurrence.
Research
In some cases, autopsy findings may provide little immediate clinical benefits for the parents, but information derived from pooled data from such studies may lead to improved understanding of a variety of pathological processes, with subsequent modification of clinical care and benefit for future patients. Autopsy data are also important when evaluating the possible effects of new treatment modalities and therapeutic interventions, including complications and side effects, new diagnostic procedures and the pathological features of diseases, providing data for improved health policies.
Audit, quality control and teaching
Comparisons between autopsy findings and antenatal or antemortem diagnoses represent an important audit function, which may serve to improve diagnostic accuracy. Similarly, regular discussion at multidisciplinary team meetings, regarding findings and discrepancies between clinical and autopsy findings, should be encouraged to improve patient care and service provision. The autopsy examination may also play an important role in teaching medical staff, including surgeons, trainee pathologists and undergraduate medical students. 16
Medicolegal issues/malpractice litigation
This function has been a relatively minor one until recently. Increasingly, perinatal and paediatric pathologists may be requested to perform an autopsy investigation on behalf of HM Coroner in cases in which there is risk of litigation relating to an intrapartum, neonatal or childhood death. In these circumstances, there may be issues relating to the timing of events, such as hypoxic–ischaemic injury, meconium passage or iatrogenic injury. If possible litigation or negligence is suspected, the case should be referred to HM Coroner and less invasive approaches may not be suitable in this clinical setting.
Contribution of the perinatal and paediatric autopsy to clinical care
In both perinatal and paediatric practice, with reduced exposure of doctors in training to autopsy, there is a perception that with improvements in medical care the relevance of investigation after death is declining; however, published data suggest otherwise. A systematic review17 reported substantial discrepancies between clinical diagnoses and autopsy findings in many cases. ‘Major errors’ (previously unrecognised diagnosis of the cause of death) were reported in around one-quarter of cases, with 10% ‘class I errors’, defined as previously unknown conditions that may have affected patient outcome had they been diagnosed in life. 17 A further meta-analysis demonstrated a 15–40% discrepancy for major diagnoses and a 30–60% discrepancy for cause of death in adults, with 45–75% of autopsies demonstrating at least one additional finding. 18 Similar data are available for perinatal autopsies specifically, with a review of 27 studies reporting that perinatal autopsy resulted in a change in diagnosis or additional findings that might have influenced management or counselling in 22–76% of cases. 5 In this study, 35% of antenatal ultrasound diagnoses were modified by additional autopsy findings. If only studies reported in the last decade are included, significant additional information required to change the underlying diagnosis or counselling is reduced to around 10%; however, this still represents a significant proportion, with a detection rate far above the majority of investigations performed in routine critical practice.
The process of autopsy involves several procedures and the data presented in most studies do not allow information to be obtained regarding which component of the investigation provided the most useful additional information. A change in perspective from considering autopsy examination as one investigation, to a more targeted investigation after death, using an algorithmic approach, would allow optimal resource use to target those in whom the various components of the autopsy are likely to be most contributory. Furthermore, in some clinical circumstances, although an autopsy investigation may provide information which may be useful for the purposes listed above, such as governance and quality assurance, in these settings the underlying diagnosis and counselling of parents is unchanged.
Factors influencing the value of the perinatal and paediatric autopsy
Several factors influence the usefulness of autopsy, including the type of antenatal or antemortem care; the accuracy and availability of previous investigations; and the level of clinical expertise, which may all affect the likelihood of identifying additional findings. Autopsies performed by specialist perinatal or paediatric pathologists in tertiary centres are significantly more likely to provide useful additional information than those performed by general pathologists in this clinical setting. In addition, in highly complex cases, pathologists with specific expertise in, for example, complex congenital cardiac disease or neuropathology, may be required for optimal interpretation.
Various technical variables may limit the pathologist’s ability to identify abnormalities. The most important of these are the effects of secondary changes following fetal death, either in utero (maceration) or during the delivery to post-mortem interval. For example, 10–20% of antenatally detected brain abnormalities cannot be confirmed at autopsy due to the degree of maceration and/or post-mortem autolysis. 19 It is therefore important that if an autopsy is to be performed, the body be refrigerated and the procedure performed as soon as possible after death. The number and type of ancillary investigations performed (e.g. example microbiological investigations or genetic testing) will also affect yield.
From a practical perspective, rapid turnaround times and high-quality autopsy reports that include a comprehensive, inclusive and directed clinicopathological correlation, improve the usefulness of perinatal autopsy for contributing to patient management.
Indications of particular value and of limited value
Based on available data and empirical practice, the potential value of autopsy examination to contribute to future patient management is dependent on the clinical circumstances. For example, in termination of pregnancy for prenatally diagnosed chromosomal abnormalities, although autopsy may provide confirmation and allow detection of subtle features, which may contribute to detailed understanding, the underlying diagnosis and, hence, patient management, is unlikely to be altered. In contrast, in the case of a patient undergoing termination for a prenatally diagnosed abnormality which may have a wide range of underlying aetiologies, such as central nervous system malformations and cystic renal disease, autopsy investigation is highly likely to provide a specific diagnosis which cannot be achieved by other means. Other examples include prenatally diagnosed skeletal dysplasias, in whom the specific type of dysplasia, relevant for management of future pregnancies and prenatal testing, is often not determined until after death.
It is impossible to provide a definitive list of indications representing ‘high’ or ‘low’ autopsy yields, as the individual circumstances, clinical questions, and availability of specialist antenatal investigations and pathologists, will vary between centres. Nevertheless, it is suggested that this process is performed locally in order to maximise use of resources and to ensure that expectations of both parents and clinicians are realistic and evidence based.
Classification systems of perinatal and paediatric deaths and their issues
For the purposes of epidemiological studies and research, a range of classification systems have been used in order to categorise the type of perinatal and paediatric death and/or the underlying pathophysiological mechanism involved. No universally accepted classification system exists. Those in use range from simple systems with only a few generic categories (e.g. Wigglesworth and Singer20), to more recent and complex systems which attempt to take account of not only autopsy findings, but also any potentially relevant conditions from the clinical history or other investigations [e.g. Relevant Condition at Death (ReCoDe21)]. By using different classification systems it is possible to use the same underlying data sets but significantly alter the proportion of cases in a specific category, such as ‘unexplained’. However, the clinical and epidemiological usefulness of each system largely depend on the purpose for which the data will be used. It is therefore important to be aware of which system was used so that erroneous conclusions are not drawn when comparing data classified in different ways.
Consent process
Types of autopsy: consented versus coronial
The vast majority of perinatal autopsy examinations require consent by one or both parents, as the immediate cause of death will be known and appropriate certification can be completed. In contrast, SUDI and SUDC cases represent unexpected deaths for whom a death certificate cannot be issued and therefore require referral to HM Coroner. Occasionally, intrapartum and neonatal deaths may also be referred to HM Coroner, who may decide to instruct a pathologist to perform an autopsy examination on their behalf; in these circumstances, parental consent is not required and the Coroner’s decision over-rides that of the parents. In general, SBs do not fall under the Coroner’s jurisdiction, as no death certificate is issued; however, HM Coroner may decide to investigate in some circumstances and this is becoming more common following precedents. In any case, once the Coroner has completed the investigation, tissue samples then fall under the jurisdiction of the Human Tissue Act,22 as for consented cases, and should be handled according to parents’ wishes. If there is a potential issue of litigation due to neglect or malpractice by hospital staff, the case should always be discussed with HM Coroner, as a Coronial autopsy may be performed and an inquest held, which results in the detailed circumstances of the case being reviewed but without assigning blame.
Consent requirements for autopsy
Following issues associated with organ retention in UK, the Human Tissue Act came into force in 2006, overseen by the Human Tissue Authority (HTA), which has published Codes of Practice and licensed organisations. 22 The Human Tissue Act covers almost any activity related to human tissue, including autopsy examination, and requires consent for the removal, storage and use of human tissue. The Human Tissue Act applies to all SBs, neonatal, infant and child deaths, but it is recommended that consent be obtained for the examination of all fetal tissue and for its use for scheduled purposes, regardless of gestational age.
Giving consent must be a positive action following the provision of appropriate information and with adequate understanding. The absence of refusal is not adequate consent. Consent must be given voluntarily by an appropriately informed person who has the capacity to agree, which in the setting of perinatal autopsy examinations will usually be one or both parents. For SBs and neonatal deaths, it is recommended that, if possible, consent is obtained from the mother and, when appropriate, both parents are involved. Under the Human Tissue Act, consent from one parent is sufficient. However, if there is disagreement between the parents, it is recommended that this be sensitively discussed before proceeding. It is important that the consent process is not viewed as the single act of signing the consent form, but rather as a process in which parents can discuss the issues, ask questions and make an informed decision.
The responsibility to seek consent is usually the treating clinician’s who should be sufficiently senior and well informed, with an adequate knowledge of the post-mortem procedure. It is recommended that consenting clinicians are trained in the management of bereavement and should have witnessed an autopsy examination. As valid consent can only be given if appropriate communication has taken place, information leaflets and consent forms should be available in the main local community languages for patients whose first language is not English, and interpreters should be used.
Practical aspects of the standard autopsy examination
External and macroscopic examination
The request for investigation after death should be seen as a request for a clinical consultation by a specialist colleague, which therefore requires the provision of both appropriate clinical information and documentation of the particular question to be addressed. Once clinical details have been reviewed and the case has been discussed, the consent status is verified, the body identified and an external examination is performed. According to the particulars of the consent, local policy and specific indications, autopsy imaging may also be performed at this stage.
The fetus, infant or child is weighed and measured, and external features are assessed. Significant tissue changes begin to occur following death and delivery, and the likelihood of an adequate detailed autopsy examination reduces with increasing time for which the body is not refrigerated. Furthermore, this process of autolysis appears to occur even more quickly in cases following feticide using potassium chloride, and in such cases, particularly for those with cardiac or brain abnormalities, the body should be refrigerated as soon as possible, with the minimum delay between delivery and autopsy examination.
Particular emphasis is placed on identifying external anomalies or dysmorphic features. Routine photographs are usually taken as part of the medical record, with more detailed photographs to document specific abnormalities. In standard autopsy, external examination is followed by a detailed macroscopic investigation of the body, usually via a mid-line incision through the anterior thorax and abdomen. Inspection of the internal organs is performed, which are then removed, weighed, dissected and sampled for histological examination. Organs are then returned to the body, which is reconstructed prior to release. If the head is to be examined, the scalp is incised, and the skull and the brain removed for formalin fixation, which may take several weeks for complex brain anomalies.
Histological examination
Small tissue samples of major organs are examined under the microscope for identification of specific histological changes, for cases in which the consent status allows this. Tissue samples are processed into small paraffin wax blocks and tissue sections on glass slides, 3–5 microns in thickness, are stained for detailed characterisation of the underlying disease process as required.
Ancillary investigations
Radiology
Although in some circumstances it had been standard practice to perform whole-body X-ray examinations, the diagnostic yield from this approach in the era of routine antenatal ultrasound screening is very low. However, if there are structural abnormalities, in particular skeletal abnormalities, detailed whole-body radiography is mandatory and often provides the specific underlying diagnosis. Other imaging modalities specific to minimally invasive autopsy (MIA) and non-invasive autopsy (NIA) are discussed in the section New developments in autopsy investigation: less invasive autopsy approaches.
Other
A wide range of other ancillary investigations may be performed according to clinical indications, including microbiological and virological analyses, metabolic studies (blood and bile spots for acylcarnitine profiling by tandem mass spectrometry, or enzyme assays using cultured fibroblasts), and cytogenetic and deoxyribonucleic acid (DNA) analysis for genetic disease.
Retention of organs
Occasionally, it may be necessary to retain an organ temporarily for further examination. In the vast majority of cases this will be known before the autopsy is conducted, based on the clinical circumstances. Retention involves removal of the organ from the body and fixing in formalin, which hardens the tissues by cross-linking proteins, enabling more detailed macroscopic examination and high-quality histological sections. Such temporary retention is usually required only for the brain, which is very friable and soft, and prone to disintegrate on handling, thus limiting the extent of the examination. Formalin fixation is also recommended for detailed examination of the heart in cases with suspected complex structural cardiac malformations. It is important that parents are informed that in such cases, particularly terminations of pregnancy or deaths with suspected brain abnormality, fixation of the brain is likely to be required for adequate examination.
Disposal of retained tissue samples, including blocks and slides
The blocks and slides taken as part of the autopsy examination are usually kept as part of the permanent medical record. Parents have the option to consent to the use of tissue for research which may help other families in the future, and surveys of bereaved parents have shown that the majority of parents are keen to participate in research.
Alternatively, parents can request that all samples are disposed of, either by the hospital or by the parents making their own arrangements, usually via their designated undertaker. If parents choose either of these options, it is important that they understand that subsequent review and further diagnosis will not be possible. Note that any tissue samples taken during a Coronial autopsy are under the authority of the HM Coroner and remain so until their investigation has ceased.
Limitations of autopsy examination
Despite the potential benefits, as outlined above, it is important that parents do not have unrealistic expectations. The examination may not answer their questions and in a significant number of cases may not establish a cause of death, especially for clinically unexpected third trimester SBs. Conversely, as outlined in Functions of perinatal and paediatric autopsy, although the autopsy examination may find ‘nothing new’, this too may be clinically helpful, providing reassurance to both clinicians and parents that nothing important had been overlooked during life.
The autopsy report
It is recommended that a final autopsy report, incorporating histological findings and results of further investigations, is provided 6 weeks after the autopsy examination. 23 The report should document the major findings and results of ancillary investigations, and also include an appropriate clinicopathological correlation and a summary. Parents are entitled to a copy of the report, but it is recommended that the contents be discussed with them by their clinician prior to receipt, preferably in person, as some parents may find the technical language used in such reports insensitive or distressing.
Prevalence of perinatal autopsy and reasons for consent refusal
Despite the potential benefits noted above, perinatal autopsy rates have decreased over recent years. The perinatal autopsy rate (including late fetal losses, SBs, and neonatal and postneonatal deaths) decreased from 48% of potential cases in 2000, to 39% in 2003, continuing to fall in recent years, with marked regional variation across the UK. Recent data have revealed a plateau for the proportion of neonatal deaths referred for consented autopsy examination, with 22% in 2003 and 21% in 2007. 15
In most cases, autopsy is offered by the clinical team but consent is not given by the parents. Although parents’ opinions regarding autopsy have been influenced by the organ retention issues in some hospitals in the UK,24 the main reason for refusal of standard autopsy is fear that the child will be mutilated or disfigured by the procedure. 25 It is of note that in a study of women’s reactions, 30% who refused autopsy subsequently regretted the decision, possibly as their questions remained unanswered. 26
Cultural and religious considerations also play a role, although most major religions do not explicitly prohibit an autopsy, especially if there is a perceived benefit to public health. The exception to this is in Islam and Judaism, in which cutting and disfigurement of the deceased, and removing internal organs, tissue and fluids, is forbidden. In addition, there is a religious requirement to bury the body as soon as possible. 27–30 Empirical evidence has highlighted uptake rates of fetal or neonatal autopsy among Muslim parents of 23%31 and 42%,32 compared with 77%31 and 75%32 among non-Muslim parents, respectively.
Clinicians find discussing the option of autopsy examination with bereaved parents difficult and distressing. This is further influenced by the complex and often lengthy consent forms now required. In conjunction with reduced exposure to autopsy, younger clinicians regard the autopsy as less useful, compared with senior colleagues. 33 Finally, perceptions may be influenced by the attitudes of pathologists, delays in issuing final autopsy reports, lack of clinicopathological correlation, and paucity of appropriate multidisciplinary team meetings contributing to the notion that the autopsy is of limited value in the immediate and subsequent management of the patient and/or parents.
New developments in autopsy investigation: less invasive autopsy approaches
To the best of our knowledge, traditional standard autopsy, based on prosection and dissection, has remained largely unchanged for hundreds of years. However, increasingly, parents are declining, such that at present the majority of parents do not agree to standard autopsy. In order to address these concerns and to improve uptake rates, the feasibility of less invasive autopsy (LIA) techniques has been developed and evaluated in recent years. 34 One promising approach is the use of cross-sectional imaging techniques, in particular magnetic resonance imaging (MRI). MRI provides excellent soft tissue imaging resolution in this patient population and MRI scanners are readily available in most hospitals.
A large Department of Health and Social Care-funded prospective, blinded trial comparing NIA, based on post-mortem MRI along with other ancillary investigations such as placental examination, genetic and metabolic tests, with standard autopsy, reported that there was around 95% concordance for major diagnoses for fetuses. Accuracy was less for infants and children (85% and 54%, respectively), as imaging alone is unable to detect cases of systemic disease with no anatomical features, such as sepsis. 35
In order to address this shortcoming, the combination of MRI plus targeted laparoscopic examination and biopsy of visceral organs (MIA) has been proposed as a possible alternative, as it combines the advantages of both imaging and tissue sampling; it is estimated that > 90% of significant histology findings from standard perinatal autopsies could be detected using a minimally invasive approach, although further evaluation in large numbers of cases would be required to provide accurate data for all pathologies. 36
This LIA approach was recommended as a realistic alternative to current invasive post-mortems in adults by the Department of Health and Social Care Post Mortem Forensic and Disaster Imaging Group in 2012, with the acknowledgement that there are important religious, cultural and humanitarian benefits offered by non-invasive post-mortems. 37
Less invasive autopsy has the potential to address sensitivities around organ retention, as well as accommodate the need to respect religious and cultural diversity. However, currently, very little is known about the acceptability of these alternative methods. A small study of 70 parents conducted in Belgium found a hypothetical increase in uptake of fetal and neonatal autopsy from 60% to almost 80% if MIA was offered. 32 Moreover, around 60% [95% confidence interval (CI) 35% to 82%] of Muslim participants in that study would hypothetically consent for MIA, although the sample size was small (n = 13). In a questionnaire study conducted in the UK, the authors found that parents preferred a full autopsy over a less invasive procedure if they were told it might provide more information. 38 However, owing to the small size of these studies, it is not possible to make generalisations about the acceptability of LIA and therefore further research is required, particularly to explore whether or not these alternative methods would be acceptable to those religious groups that traditionally decline autopsy. Among health professionals, MIA has been shown to be highly acceptable and its availability is considered beneficial for discussing autopsy with parents. 39
However, several important questions remain to be addressed, including likely acceptability in the wider population, how it might be implemented into existing care pathways, training requirements for staff offering LIA and which patient populations it is most appropriate for.
Importance of research on less invasive autopsy
Developing more acceptable alternatives could allow more parents to benefit from gaining information regarding prenatal and paediatric deaths, inform recurrence risk and have secondary benefits for researchers, policy-planners and society, by providing improved information regarding causes of fetal, infant and child deaths as a result of increased uptake. There are currently very few data regarding the acceptability of MIA and NIA compared with standard autopsy. If LIA represents an acceptable alternative to standard autopsy, this could radically change the future approach to investigating such deaths. Reducing perinatal mortality is a World Health Organization priority, ‘health of children and young people’ is a stated key priority for the European Commission and reducing premature mortality is one of the current NHS priority areas. 40,41 Improving the range of investigative strategies available for post-death investigation also aligns with NHS England’s goal of significantly improving patient choice by 2020. 42
Research aims
This research programme was submitted in response to the National Institute for Health Research commissioned call for its Health Technology Assessment programme.
The aims of this programme of research were as follows:
-
Provide empirical data on the acceptability and likely uptake rates for different types of autopsy among various patient groups and other key stakeholders (health professionals, coroners, religious leaders), using a mixed-methods approach. In particular the study set out to address –
-
if MIA and/or NIA were more acceptable to parents than standard autopsy methods
-
how alternate methods of investigating death should fit into existing care pathways
-
which patient populations these methods are most appropriate for
-
how best to offer such a service to groups for whom standard autopsy is never acceptable, including specific ethnic and religious populations.
-
-
Analyse existing autopsy data sources, including national data, retrospective autopsy series and existing LIA and MIA series, to provide estimates of the potential efficacy of MIA (incorporating a range of either no value or as good as standard autopsy) and its projected utility in clinical practice.
Components of the research programme
There were three components of the research programme: (1) a systematic review of factors having an impact on consent for autopsy; (2) empirical research with key stakeholders to determine the acceptability and likely uptake of LIA; and (3) a retrospective analysis of existing autopsy data.
A systematic review of factors having an impact on consent for autopsy
A systematic review was conducted in order to synthesise the current knowledge on bereaved parents’ motivations for accepting or declining autopsy and to identify any knowledge gaps that called for more research. The evidence generated was used to inform the empirical research with key stakeholders.
Empirical research with key stakeholders
This is the main component of the research programme and it involved three substudies.
Substudy 1: mixed-methods study with bereaved parents to determine acceptability and likely uptake of less invasive autopsy
A cross-sectional survey study was conducted with bereaved parents to examine acceptability and likely uptake of LIA. Recruitment occurred in two ways: (1) prospectively through hospitals [antenatal clinics, fetal medicine departments, intensive care units (ICUs)]; and (2) retrospectively through the support groups [Antenatal Results and Choices (ARC), Stillbirth and Neonatal Death Society (Sands), Child Bereavement UK and The Lullaby Trust]. Qualitative interviews were conducted with a subset of survey responders to explore issues around acceptability and likely uptake of LIA in more depth.
Substudy 2: interview study with health professionals and HM Coroners
Qualitative interviews were conducted with health professionals and HM Coroners to explore views towards LIA, perceived benefits, and concerns and issues regarding implementation into clinical practice. A focus group with patient advocates was also conducted.
Substudy 3: interview and focus group study with religious leaders and community members
Qualitative research was conducted with religious and community leaders, as well as community members. This comprised (1) interviews with religious and community leaders from the Muslim and Jewish faith, as well as interviews with religious leaders from other faith groups (Christian, Roman Catholic and Hindu) as comparators; and (2) focus groups with members of the community from the Muslim and Jewish faith.
Retrospective analysis of existing autopsy data
For this component of the research we examined national data in addition to detailed information from an existing in-house autopsy database of > 5000 cases. 43 From these data sets we determined the proportion of cases by clinical indication group for which tissue sampling of specific internal organs significantly contributed to the diagnosis and the maximum potential performance for MIA was estimated. This cannot theoretically be better than the gold standard of using samples obtained during full autopsy.
The proportions were compared between different diagnostic subgroups, in order to identify those subgroups for whom MIA was likely to be useful and whether or not these groups could be identified before any autopsy or investigation. The data were used to inform a proposed targeted approach to sampling by clinical indication and, combined with the data from the empirical research with key stakeholders, to estimate the potential impacts of a less invasive approach to national perinatal and paediatric autopsy services.
Chapter 2 Evidence synthesis: a systematic review of factors affecting uptake of autopsy examination
In this chapter we present the findings from a systematic review conducted to examine the key factors that motivate or prevent bereaved parents from consenting to autopsy examination. The findings from this work were used to inform the empirical research with key stakeholders, in particular the survey questions and topic guides used in the interviews and focus groups. The review was initially performed in year 1 of the study and published, and updated in April 2018 for the final report. This chapter is partly reproduced from Lewis et al. ,44 published in BJOG in 2017. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC 4.0) license, which permits others to copy, remix, transform, build upon and redistribute the material in any medium or format, for non-commercial use, provided the original work is properly cited and changes made are indicated. See: https://creativecommons.org/licenses/by-nc/4.0/.
Methods
We followed the method described by the Centre for Reviews and Dissemination45 and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist46 to conduct this systematic review. We undertook a quality assessment of the studies before conducting a narrative synthesis47 of the results. The initial search was undertaken in December 2015, repeated in August 2016 and again in April 2018.
Eligibility criteria
Criteria for included studies were:
-
bereaved parents [with experience of ToP, SB, neonatal or childhood death (aged < 16 years)], health professionals or general public
-
those for whom a diagnosis was known (e.g. childhood cancer), as well as when there was no confirmed diagnosis, in order to explore whether motivations and barriers were similar or significantly different
-
factors affecting uptake or decline of perinatal/paediatric autopsy examination
-
qualitative, quantitative or mixed-method studies that are in English and had been peer reviewed.
Criteria for excluded studies were:
-
study included adult autopsy examination, uptake rates (unless they subdivide participant characteristics influencing autopsy rates), a focus on verbal, social or psychological autopsy and studies of bereavement
-
non-English-language papers, owing to resource constraints
-
editorials, letters, abstracts or commentaries, non-research articles or case reports.
Search methods
In order to avoid publication bias, the search (conducted by CL) incorporated a variety of sources and methods:
-
an electronic database search using Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycARTICLES, PsycINFO, PubMed and Web of Science, The Cochrane Library, Google Scholar and websites of relevant patient organisations
-
a hand-search of the first and last authors of the initial set of papers and reference lists of those papers
-
a hand-search of the 5 previous years of publication of eight relevant journals
-
no time limit was set
-
data related to autopsy and post-mortem examination as defined by the studies; data were not available on specific components of the autopsy examination (such as placental examination, imaging, etc.) for the purposes of this study.
Search strategy
Search question
The SPIDER (sample, phenomenon of interest, design, evaluation, research type) acronym is an established model for aiding systematic searches that include qualitative and mixed-methods research. 48 SPIDER was used to delineate the elements of the research question and search strategy.
Sample
Bereaved parents with experience of termination of pregnancy, fetal death, SB, neonatal death or childhood death.
Phenomenon of interest
Post-mortem examination.
Design
Interview, survey or focus group.
Evaluation
Motivation or barrier.
Research type
Qualitative, quantitative or mixed methods.
Search strategy
‘Autops*’ OR ‘post mortem*’ OR ‘investigation* after death’ OR ‘minimally invasive autops*’ OR ‘less invasive autops*’ OR ‘non-invasive autops*’ OR ‘perinatal autops*’ OR ‘perinatal patholog*’ AND
‘Termination of pregnanc*’ OR ‘stillbirth*’ OR ‘stillborn’ OR ‘neonatal death*’ OR ‘childhood death*’ OR ‘infant death*’ OR ‘paediatric death*’ OR ‘pediatric death*’ OR ‘fetal death*’ OR ‘fetal loss*’ OR ‘foetal death*’ OR ‘foetal loss*’ OR ‘bereaved parent*’ OR ‘pregnancy loss*’ OR ‘child death*’ OR ‘perinatal death*’ AND
‘Consent*’ OR ‘attitude*’ OR ‘view*’ OR ‘opinion*’ OR ‘experience*’ OR ‘motivation*’ OR ‘barrier*’ OR ‘decision mak*’ OR ‘discussion*’ OR ‘accept*’ OR ‘factor*’ OR ‘reaction*’ AND
‘Qualitative’ OR ‘interview*’ OR ‘focus group*’ OR ‘quantitative’ OR ‘survey*’ OR ‘questionnaire*’
Study selection
Initial searches identified 1484 potential articles. Independent assessment by two researchers reduced these to 35 papers included for the quality assessment (Figure 1). A further five relevant papers were identified in April 2018 which were then included in the review.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 flow diagram.

Quality assessment
The Centre for Reviews and Dissemination underscores the importance of assessing the quality of the research included in systematic reviews. 45 We used the quality assessment tool described by Kmet et al. ,49 which provides two sets of questions, one for qualitative studies and one for quantitative studies, the responses to which are converted into a percentage. A cut-off point of 55%, described by Kmet et al. 49 as liberal, was used. One paper was excluded after using this methodology.
Data extraction
Key features of each study were extracted and tabulated (see Appendix 1).
Synthesis
As both quantitative and qualitative studies with diverse approaches were included, a narrative synthesis was considered most appropriate. Using NVivo 10 software (QSR International, Warrington, UK), study findings were coded using the framework of barriers to or facilitators of post-mortem uptake. For quantitative studies, statistical results and descriptions were tabulated and coded in terms of types of barriers or facilitators. For qualitative studies, direct quotations and descriptions were coded for all knowledge, beliefs, attitudes and practices in relation to the barriers to and facilitators of post-mortem. Findings were then compared across studies to examine interrelations (i.e. whether or not the same findings, concepts and theories existed across different studies), based on Noblit and Hare’s method of meta-ethnography. 50 During this process it became apparent that a number of studies highlighted examples of what might be considered best practice, irrespective of whether or not people consented to post-mortem. Therefore, a third overarching theme of ‘best practice’ was included to document these findings.
Results
Study and participant characteristics
An overview of the studies is presented in Appendix 1. Thirty-nine studies published between 1982 and 2018 were included in the final review. The majority (n = 31) had been published since 2000. Twenty-one studies were quantitative, 12 studies were surveys7,31,32,38,39,51–57 and nine studies were retrospective audits. 8,13,58–64 Ten studies were qualitative, consisting of semistructured interviews,65–71 qualitative analysis of free text in surveys 6,72 and focus groups. 71,73 Seven studies were mixed methods74–80 and one study was a systematic review. 81
Impact of parent or patient characteristics and experience on autopsy uptake
Thirteen studies13,31,32,58,62–64,66–68,75,77,79 addressed the impact of parent or patient characteristics on autopsy uptake. Three58,62,63 of the four31,58,62,63 prenatal studies concerning gestation showed that later gestation was significantly associated with increased autopsy uptake (p < 0.001, p = 0.006 and p = 0.016), with the fourth study31 indicating a significant association with earlier gestation (p < 0.001). However, as the authors of this last study31 point out, one explanation for this finding may be the significant number of Muslim women (23%) in the study for whom autopsy is permitted up to 120 days’ gestation. In postnatal studies, consent was significantly more likely to be given for autopsy when babies or children were older in two US studies13,63 (p < 0.001 and p = 0.007), but less likely in studies conducted in Zambia66 and Scotland. 67 Known cause of death was also identified as a factor affecting autopsy uptake in three studies. 63,67,75 Parents’ characteristics, ethnicity or educational level were not significant factors in four studies,13,31,62,77 but they were in one study79 on SB, in which single mothers and women who had left full-time education before the age of 16 years were significantly less likely to consent to a full autopsy (p < 0.01 and p < 0.05, respectively). Uptake was positively related to the mother being non-Muslim in two studies31,32 (p = 0.019 and p = 0.007).
Impact of health professional characteristics and experience on post-mortem uptake
Six studies8,31,39,52,56,77 addressed the impact of health professionals’ characteristics and experiences on post-mortem uptake. Health professional role and experience were significantly associated with seeking consent,52 perceived importance of post-mortem,77 parental satisfaction with the consent discussion56 or autopsy uptake. 8,31 Neonatologists and obstetricians were more likely to seek consent for autopsy than neonatal nurses or midwives (p < 0.001) and neonatal nurses with > 10 years’ experience were more inclined to suggest autopsy than those with less experience (p < 0.01) in an Australian postal survey study. 52 Seniority was also a positive factor in a retrospective Malaysian cohort study conducted in Scotland, in which specialists were judged to have provided a ‘good’ explanation compared with house or medical officers. 56 In the USA, advancement in staff position was associated with positive attitude regarding the importance of neonatal autopsy. 77 Conflictingly, in a UK study, Ben-Sasi et al. 39 did not find any significant association between job type (physician vs. nursing vs. other) and autopsy acceptability. 39 However, they did report that there were significant effects of demographic variables on the importance of factors which may prevent parental agreement for autopsy, including concerns regarding possible disfigurement among non-white groups and concerns regarding delays to the funeral, particularly for those of Indian, Asian or Arab ethnicity compared with white participants.
Barriers to uptake of autopsy
We identified seven major themes for barriers to autopsy uptake: (1) dislike of invasiveness, (2) practicalities of the procedure, (3) organ retention issues, (4) protective parenting, (5) communication and understanding, (6) religion and culture and (7) professional or organisational barriers.
Dislike of invasiveness
A recurring theme related to parents’ concerns about the invasiveness of the procedure51,54,68,79,81 and the baby’s appearance following autopsy,39,54,67,69,73 as illustrated by one mother who declined autopsy because she would rather not know the cause of her baby’s death than have her ‘all cut up’. 68 Comparable results were found in quantitative studies, with concern about the examination of the baby being a frequently cited reason for declining autopsy. 51,67 Concerns around disfigurement, particularly among non-white responders, also existed in health professionals. 39 Specifically, discussion around the removal of the brain was found to be distressing for parents67 and professionals. 70
Practicalities of the procedure
Other barriers included the need to transfer babies to another hospital for autopsy,7,81 which was considered to be a strong barrier in one study7 by 33% of parents but not by health professionals; turnaround time for results;6,7 and the prohibitive cost or lack of insurance cover in the only international study, in which most respondents were from the USA. 57
Organ retention issues
Organ retention issues were described as a barrier to autopsy in six studies,6–8,39,59,69 with autopsy rates falling significantly for SBs and neonatal deaths since organ retention controversies (between 1996 and 2001) both in Australia59 and in the UK8 following disclosures of unlawful organ retention. These findings are supported by a qualitative study in which a midwife commented that ‘after the Alder Hey82 episode many parents had been put off [autopsy] as they imagine parts of their baby sitting in specimen jars’. 6 Negative press coverage was felt by 41–62% of health professionals to be a significant barrier to uptake in a study conducted in 2012,7 although the majority (76%) of parents indicated that this factor had little influence on their decision.
Protective parenting
One of the main psychological barriers to uptake of autopsy was parents wanting to ‘protect’ their baby or child from unnecessary harm. 66,68,69,73,75 Parents commented that their children had ‘suffered enough’,66 were ‘fragile like dolls’69 and should be ‘left in peace’,75 with ‘I already felt my baby had suffered enough’ being the most frequently chosen response (44%) for respondents declining autopsy in a quantitative UK study. 54 Adopting this protective role has been suggested as one way parents could retain some degree of control over their situation. 68 Emotional distress during the autopsy discussion was also identified as a barrier. 7,56,68,73,81 One parent described being an ‘emotional wreck’ and that being asked about autopsy was ‘just too much all at once’,73 highlighting that the timing of the autopsy discussion is important. Shock and grief hindering decision-making was also found to be an important factor in parents’ decision about post-mortem in a systematic review on parental experience of SB. 81 In a qualitative study on SB, several women spoke of their fear that an autopsy would show that they were somehow to blame for their baby’s death, although this theme did not occur elsewhere in the literature. 73
Communication and understanding
One of the most commonly cited barriers for both parents and health professionals was ambivalence about the value of the procedure. 7,51,52,54,57,66,67,69,75,79,81 Twenty-six per cent of autopsy decliners in a UK study54 and 43% of decliners in a Zambian study66 cited this as their reason for declining autopsy. Declining an autopsy because parents felt that the cause of death was already known was cited in five studies,51,52,68,69,75 including those focused on SB51,68,79 as well as childhood cancer. 75 Thirty-eight per cent of women who declined post-mortem indicated that they already knew why their baby had died and 26% thought that it would not provide an answer in a survey of parents’ experience following SB. 79 Many midwives (35%) and obstetricians (32%) underestimated the value of autopsy in a UK study, which reported a likelihood of < 20% that useful information would be obtained. 7 A finding that some parents thought that staff discouraged them from having an autopsy was identified in a qualitative study on SB. 71 In a systematic review to understand and improve care after SB, the authors found that some parents had not been counselled about the advantages of autopsy, even through many had additional counselling. 81
Embarrassment or feeling uncomfortable asking were also identified as barriers,6,7,65,70 with ‘professional discomfort and lack of knowledge about the role and value of post-mortems’ quoted in a qualitative study exploring attitudes of neonatologists and pathologists. 70 Lack of knowledge about the procedure, staff workload and lack of rapport with patients, particularly among midwives, were also all identified as professional barriers to consenting parents in an internet-based survey about SB. 7 Similarly, only 58% of parents thought information about autopsy was explained clearly and 26% of parents said that the information was not given by knowledgeable professionals in a survey on SB conducted in Ireland. 80 Poor communication about the procedure was cited by both parents56,79 and health professionals. 60 Henderson et al. 79 identified that there was, in some instances, a lack of sensitivity on the part of clinical staff when discussing post-mortem and a sense of needing to get the task done. The quality and length of the consent form was cited as a barrier to consent by health professionals in two studies,6,70 as the NHS consent form was felt to be too long and drawn out. 6 Timing of the information provision about autopsy was also found to be a barrier to uptake. 72,78–80 In two qualitative studies, one on termination of pregnancy72 and one on SB,79 participants felt that the topic had been raised too soon and felt that they were rushed to make a decision. In a quantitative study on SB, just 67% of parents felt that the topic was addressed at an appropriate time. 80 Lack of trust in health professionals, either as a consequence of the organ retention scandal80 or because parents thought that a diagnosis should have been made prior to the child’s death, was also identified. 6,66
Religion and culture
Religious and cultural issues, including concerns about funeral delays and the cutting of the body being prohibited in Islamic law, were frequently discussed. 6,7,38,51,54,56,66,68,69 A number of quantitative studies conducted in the UK, Ireland, Sweden and Zambia found that religion was not a frequently chosen reason for declining post-mortem. 38,51,54,66,68 However, in a study conducted in Malaysia,56 28% cited this reason, possibly owing to the large Muslim population. In the study conducted in Zambia, nearly 10% of participants declined post-mortem because of concerns that the mutilation of dead bodies would result in ancestral spirits making all women in their family infertile. 66
Professional or organisational barriers
A key barrier to autopsy concerned the lack of specialist training among health professionals to consent patients (raised in five studies6,7,39,65,70). Varying levels of training reported among clinicians in two quantitative UK studies (21–82%)7,39 was supported by qualitative research conducted in the UK and the USA. 6,65,70 Similarly, Epstein65 commented that residents and fellows desired more guidance on the post-mortem consent procedure.
Facilitators of autopsy consent
We identified six major themes related to factors that facilitated parental consent to autopsy: (1) desire for information; (2) contributing to research; (3) coping and well-being; (4) respectful care; (5) minimally invasive options; and (6) policy and practice.
Desire for information
Desire for information was a commonly noted factor as to why parents consented to autopsy, with this being the most frequently cited reason in a number of quantitative studies. 7,51,54,76 Parents wanted an explanation for what had happened7,38,51,52,54,67–69,73,76 and to understand the impact on future pregnancies,38,51,52,54,67,68,73,81 the latter being rated the most important in the study conducted by Breeze et al. 38 on perinatal post-mortems. This was also a prominent theme in qualitative research, as highlighted by Meaney et al. 68 who commented that ‘all parents searched for meaning and aimed to uncover a reason why such an event had happened.’
Contributing to research
Advancement of medical knowledge7,38,51,54,74,76 and other altruistic motivations7,38,67,69,74–76,81 were frequently cited, as illustrated by a parent who commented that ‘our heartbreak could be somebody else’s gain’. 67 The desire to contribute to research was the dominant motivating factor for those parents who consented to autopsy when a diagnosis was already known. 74–76 In one US study74 of parental attitudes to autopsies in children with lethal brain tumours, parents most frequently mentioned their wish to advance medical knowledge when asked why they agreed to autopsy. Similarly, in a study76 on childhood cancer, most parents wanted to know how autopsy could help other children (90%) and how autopsy could help the medical team learn more about their child’s cancer (90%).
Coping and well-being
Consenting to autopsy was identified as a coping strategy in two studies. 51,69 Parents talked about ‘getting a positive from a negative’ in a qualitative study on parental attitudes,69 and 23 of the 54 participants in a Swedish study of mothers’ attitudes towards perinatal autopsy after SB cited ‘to better cope with the loss’ as their reason for agreeing to autopsy. 51 Information to help provide ‘closure’ was cited by 10%54 and 15%74 of participants. A further benefit identified in two studies54,68 related to ruling out self-blame. Meaney et al. 68 identified that fathers wanted to rule out the potential that it was their genetic material that was a contributing factor to the death, whereas mothers with an antepartum SB wanted to rule out the possibility that they had been negligent in some way during pregnancy.
Respectful care
Motivating procedural factors to consenting to autopsy were familiarity with the autopsy procedure,73,78 reassurance that the procedure would be carried out with care and dignity67 and knowing that their child’s body would be respected. 76 Parents found the ‘drip-feeding’ of information by the health professionals and the trusting relationships they formed useful, especially with the midwives, in a qualitative study conducted in the UK to understand challenges in care after SB. 71
Minimally invasive options
In four studies, the availability of a less invasive method of autopsy was found to be a motivating factor. 32,38,39,70 One study reported that 46% of parents who refused conventional post-mortem hypothetically consented to a minimally invasive option. 32 Notably, less than half (42%) of Muslim participants consented to conventional autopsy compared with 65% for a minimally invasive procedure, suggesting that less invasive methods would be more acceptable to that religious group. A study of health professional views found that 40% of health professionals thought that MIA was more acceptable than traditional autopsy (p < 0.001). 39
Policy and practice
Two studies identified departmental policies as facilitating parental consent. 6,8 One study8 noted that improvement of autopsy rates coincided with relocation of perinatal pathology services to the same site as the obstetric unit, thereby improving local availability of specialist perinatal pathologists to perform more timely autopsies. In addition, perinatal pathology involvement in multidisciplinary meetings, case discussions and teaching was also found to improve staff perception of the value of autopsy. Finally, unit guidelines were changed to stipulate that only senior staff should offer autopsy, and an increase in the uptake of autopsy rates had been evident since that particular policy change.
Models of best practice
There were a number of themes in the literature that reflected what was considered best practice, regardless of whether or not people consented to autopsy. These are highlighted in Box 1.
-
Having education materials available with words and phrases chosen that provide maximum comfort to the family. 39,74,78
-
National, standard information sheets and consent forms. 6
-
Ample time given for discussion and questions about the autopsy procedure. 23,81
-
Having a trusted health professional who is understanding and empathetic to the parents’ situation. 6,73,74
-
Training and support for staff to improve their knowledge and ability to guide and support parents. 6,71,81
-
Explicitly building support amid the core labour group to release staff to spend time with bereaved women. 6
-
Home visits to discuss autopsy and flexible timelines for decision-making. 6,73,74,76,78
-
If considered appropriate, the option of discussing autopsy prior to termination of pregnancy, SB or neonatal death, or on multiple occasions before decision-making. 71,73
Discussion
Conducting research into parental experience and attitudes towards autopsy examination has been recognised as being particularly challenging due to the sensitivity of the subject matter. 83,84 Despite these difficulties, these data indicate that researchers are attempting to meet these challenges, as a relatively large number of studies exploring the reasons parents accept and decline autopsy were identified. This systematic review highlights that current low autopsy uptake rates are a consequence of numerous factors encompassing not only procedural, psychological and cultural barriers from the parental perspective, but also a number of professional barriers, many of which were common across countries. This is not surprising, as parents are likely to have the same concerns around the invasiveness of the procedure and appearance of the body irrespective of where they live, their culture or their religious beliefs. This review also identified examples of best practice that may provide valuable evidence to health professionals and policy-makers around how these sensitive services should be delivered.
The concept of a less invasive approach to autopsy is relatively new85 and has thus far been considered in only four studies, all of which found it to be more acceptable than traditional autopsy for most participants, particularly those of Muslim faith who have low rates of acceptance of traditional autopsy. 32,39 This supports the view that less invasive methods may be more acceptable to those parents who currently decline autopsy. Professional concerns around the limitations of the technology were raised,6,38 highlighting that both advantages and limitations need to be made clear when discussing the various options for autopsy with bereaved families, which will require evidence-based data related to particular clinical circumstances. Although non-invasive imaging-only approaches may provide useful additional information in some circumstances, such as underlying structural malformations, they are unlikely in isolation to be useful for identification of many pathologies, such as metabolic diseases or infections. 86 However, when augmented with minimally invasive ancillary investigations (needle biopsy, placental examination, etc.), overall accuracy rates similar to that of conventional autopsy (> 90%) can be achieved in many circumstances. 35 Further work with key stakeholders, particularly parents and community leaders from those religious groups who traditionally decline autopsy, would be valuable to determine whether or not less invasive methods as part of routine clinical care would be religiously and culturally permissible and acceptable. In addition, as less invasive methods of autopsy become increasingly available, research to explore whether or not the psychological barriers identified in this review remain prominent factors would be useful. Finally, future studies reporting on autopsy yield should provide data regarding which specific aspects of the procedure contributed to the diagnosis or main findings, in order to allow appropriate counselling for parents considering more limited approaches.
Health professionals’ reluctance to raise the topic of autopsy was identified as a major barrier to uptake. Unless the death is being referred to the coroner, it is recommended that all parents should be offered the opportunity to discuss having an autopsy examination so that they can make an informed choice. 87 For this reason, creating environments that support health professionals to do this is critical. A number of studies identified examples of good practice when consenting parents for autopsy underscoring the importance of national guidelines. In the UK, the HTA have recently addressed this issue with the introduction of codes of practice for autopsy examination. 88 Many of the examples of best practice identified in this review are echoed in this document. The quality and appropriateness of the consent form and the need for national, standard information sheets and consent forms were also raised by health professionals. 6,70 In 2013, Sands launched the Sands perinatal post-mortem consent package, which was developed to provide information and guidance about post-mortems for health professionals seeking consent. 89 Research to determine the impact of this new consent package, as well as the HTA guidance, would be valuable to identify whether or not it has a significant impact on autopsy consent rates.
A notable facilitator of autopsy uptake was parental desire to contribute to research, as this created an opportunity for their child’s life to have meaning and value. Health professionals may be reluctant to ask bereaved parents about research as they are a potentially vulnerable group with high levels of distress, but it is clear that an opportunity for involvement in research is in fact valued by many families. Some research has specifically focused on including bereaved parents in research studies,83,90,91 with one study83 reporting that 73% of parents stated that taking part in research about autopsy decision-making had helped them to feel better about the decision, and they regarded such studies as valuable and important. These findings support the findings from this review and underscore the importance of health professionals explaining the potential for autopsy to contribute to medical knowledge when discussing the value of the procedure with parents.
The strengths of this review are the comprehensive search strategy used to identify papers and the use of a quality appraisal tool. Regarding limitations, older papers are not always well indexed, particularly if they are qualitative studies, and this is likely to be the reason why a significant number were identified through hand-searching of authors and reference lists. The quality appraisal identified variability in the methodological rigour of the included studies, including low response rates, lack of detail regarding data analysis (particularly in qualitative studies), omission of statistical significance testing or analysis of the influence of variables such as age, education, ethnicity, etc. Qualitative studies were predominantly limited to simple thematic analysis with very little interpretive content. Some papers included professional perceptions of parental views; these may not be consistent with the views of parents themselves as indicated by the diversity in patient and professional views, as reported in one study7 describing the impact of the organ retention publicity.
Conclusion
In summary, this review provides an insight into the parental and professional barriers around consent to autopsy that have resulted in suboptimal uptake rates. We have identified a number of important barriers, including system-level barriers within the NHS, as well as practical, psychological and religious parental barriers that impact consent uptake. We have also identified a number of facilitators that highlight the need for better health professional education and the fact that some of these concerns may be mitigated if less invasive methods of autopsy were routinely available to bereaved parents. Furthermore, new consent packages and HTA guidance may have a positive impact on the perception of examination after death in the UK. The landscape is changing; further research is necessary to assess its impact on autopsy uptake rates.
Chapter 3 Empirical research with key stakeholders: design and methods
In this chapter we present the study design used to conduct the empirical research with key stakeholders, including recruitment and methods for data analysis.
The research team and advisory group
The multidisciplinary research team included academics from the following disciplinary backgrounds: paediatric pathology (NS and CH), clinical radiology (OA), genetics and fetal medicine (LC), clinical psychology (MR), genetic counsellor (MH) and health psychology (CL). An advisory group was established at the start of the study in order to monitor the progress of the research and to include the perspectives of those with a stake in the research. The group included an academic clinical psychologist with expertise in bereavement research; a senior clinical lecturer in obstetrics with a special interest in SB research; and representatives from the patient groups Sands, The Lullaby Trust and Genetic Alliance UK. The advisory group had a bi-annual conference call and a written update was circulated every 3 months.
Ethics approval
NHS Research Ethics Committee approval for this empirical research was obtained in April 2016 (16/LO/0248 from London – Bloomsbury Ethics Committee).
Overall study design
This was a mixed-methods study comprising standard data collection approaches, namely a cross-sectional survey, semistructured interviews and focus groups. Mixed-methods research has been defined as ‘research in which the investigator collects and analyses data, integrates the findings, and draws inferences using both qualitative and quantitative approaches or methods in a single study or program of inquiry’. 92 By using a mixed-methods approach we aimed to ensure the validity of the research by cross-checking the findings from the different methods of data collection, increase the level of knowledge and capture different dimensions of the same phenomenon. 93 Data were collected by one of two researchers: a social scientist with experience in conducting qualitative studies on sensitive topics (CL) and a postdoctoral clinical psychologist experienced in conducting qualitative interviews (MR).
Substudy 1: mixed-methods study with bereaved parents to determine acceptability and likely uptake of less invasive autopsy
Study design and data collection
This substudy comprised (1) a cross-sectional survey, including quantitative-type questions (multiple choice, Likert scale) and free-text comments with bereaved parents; and (2) semistructured qualitative telephone interviews with a subset of the survey responders.
Cross-sectional survey with bereaved parents
The main aim of the survey was to elicit participants’ attitudes and likely uptake and preferences for NIA, MIA and conventional autopsy. A secondary aim was to understand the importance of a set of factors associated with decision-making for autopsy.
The survey was developed specifically for this study, with support from the research team and patient advocates from the support groups ARC, Sands, The Lullaby Trust and Genetic Alliance UK. Drafts of the survey were sent to three bereaved parents from these groups to ensure the descriptions of autopsy were sensitively worded and to test layout and readability. We also drew on a survey developed by Breeze et al. ,38 exploring parental views towards autopsy and a systematic review of factors associated with uptake of autopsy. 44
The survey presented a brief description of NIA, MIA and conventional autopsy. Following each description, responders were asked to indicate if they would consent to that particular method of investigation (yes/no/not sure), record acceptability on a 5-point Likert scale and indicate their preference. Following each set of questions, participants were invited to provide free-text comments. We assessed the importance of a number of factors associated with decision-making for autopsy using a 5-point Likert scale. Finally, responders were asked to complete a set of demographic questions and questions to assess their loss and autopsy experience. At the end of the survey, participants could either remain anonymous or choose to provide contact details if they wished to take part in an interview. The survey was made available through the online survey website SurveyMonkey® (Survey Monkey Inc., Palo Alto, CA, USA), as well as in paper format. In the online survey, there were no compulsory questions and skip logic was used so that participants were directed through different paths depending on their responses. Returning a completed survey was considered as implied consent to take part.
Recruitment
Recruitment into the survey was conducted both retrospectively and prospectively.
Retrospective recruitment
Bereaved parents were recruited retrospectively through the support groups ARC, Sands, The Lullaby Trust and Child Bereavement UK between June and September 2016. Anyone who had experienced the loss of a pregnancy (through miscarriage, ToP or SB) or had experienced a neonatal or infant death, was eligible to take part irrespective of whether they had been offered an autopsy or an autopsy had been requested by HM Coroner’s office.
Prospective recruitment
Bereaved parents were prospectively recruited through the fetal medicine unit, delivery unit or neonatal intensive care unit (ICU) of seven hospitals across England between September 2016 and December 2017. Women and their partners who were ≥ 18 years of age and had experienced loss of pregnancy (see Retrospective recruitment) or neonatal or infant death were eligible to participate in the study. Participants were recruited into the study by a member of the health-care team (such as an obstetrician, bereavement midwife or ICU consultant) following the autopsy examination discussion, irrespective of whether they consented or declined. Potential participants were briefly informed about this study and, if they were interested in taking part or finding out more, they were given a study pack containing a participant information sheet, the survey and a freepost envelope. The participant information sheet also included an online link to the survey. We included a question at the end of the survey to assess the burden of asking parents to take part in the survey at a time that we acknowledged was extremely sensitive. 83 We closely monitored the responses to this question to ensure that we were not creating any additional distress. No time frame was set with regards to returning the survey and no reminder was sent. In February 2017, the protocol was amended to include bereaved parents who had not been offered the option of an autopsy examination. This was because at one of the participating neonatal ICUs autopsies are rarely offered, but we felt that it was important to incorporate these parents’ views.
Semistructured telephone interviews with survey responders
Study design
Semistructured telephone interviews were conducted with a subset of survey responders. The topic guide explored participants’ experience of being approached about standard autopsy (for those for whom a coronial autopsy was not required), including reasons for accepting or declining; their views towards NIA and MIA, including perceived advantages and potential concerns or limitations; and their preference for standard autopsy, MIA, NIA or no autopsy, including the reasoning behind their preference.
Data collection and recruitment
A subset of survey responders who had indicated their willingness to take part in an interview by leaving their contact details at the end of the survey were purposively sampled to ensure a range of data in terms of preferences towards different types of autopsy and demographics. No time limit was set in terms of how many months prior to the interview the loss occurred. Potential participants were contacted either by e-mail or by telephone and were invited to take part in a telephone interview on a date suitable for them. Interviews were conducted by either Megan Riddington or Celine Lewis between November 2016 and May 2017. Participants were offered a gift voucher as a token of appreciation for their time. Interviews were digitally recorded and transcribed verbatim.
Substudy 2: interview study with health professionals and HM Coroners
Study design and data collection
This was a qualitative study using semistructured interviews conducted either face to face or by telephone. The semistructured discussion guide was developed with input from the advisory team and was informed through previous work. 44 It included three topic areas: (1) views regarding full autopsy, factors affecting uptake and experience of consenting parents; (2) views towards NIA and MIA, including perceived benefits and potential limitations or concerns; and (3) views regarding implementation of NIA and MIA into clinical or coronial practice. At the start of the interview, participants were provided with a standardised overview of NIA and MIA.
Recruitment
Health professionals in the UK from a range of clinical backgrounds, who would be involved in discussions with parents about autopsy examination or who would conduct or interpret autopsy results, were purposively sampled. HM Coroners, who are responsible for requesting autopsies in cases of unnatural or sudden deaths, including those in infancy and childhood, were also included. Potential participants were initially identified by Neil J Sebire, Lyn S Chitty, John C Hutchinson and Celine Lewis with the aim of recruiting participants from a range of specialties from various locations across England. We aimed to include anatomical pathology technologists (APTs), perinatal and paediatric pathologists, obstetric and fetal medicine consultants, bereavement midwives, paediatric radiologists, neonatologists, intensive care consultants and intensive care nurses. During the initial set of interviews, we asked interviewees if they could suggest any other health professionals or coroners that might be interested in taking part in the study. Using this ‘snowballing’ approach we identified further participants to interview. Potential participants were contacted by e-mail, sent a participant information sheet and asked to respond to Celine Lewis if they were interested in taking part. Interviews were conducted by Celine Lewis between April 2016 and July 2017.
Substudy 3: interview and focus group study with religious leaders and community members
Study design
This was a qualitative study incorporating (1) interviews with religious and community leaders; (2) focus groups with members of the Muslim and Jewish community; and (3) interviews with Muslim or Jewish participants from substudy 1. Separate but related topic guides were developed for interviews and focus groups. The following topic areas were included: participants’ personal views regarding acceptability of traditional autopsy examination and when, if at all, it would be acceptable; acceptability of traditional autopsy from a Muslim and a Jewish perspective; personal views regarding NIA and MIA; permissibility of NIA and MIA from a Muslim and a Jewish perspective (both religious belief and practice); likely uptake of NIA and MIA both personally and within the community more generally; and developing awareness of NIA and MIA within the community. At the start of the interview, participants were provided with a standardised overview of NIA and MIA. Focus group participants were also shown an image of a MRI machine and laparoscopic equipment to enhance understanding of NIA and MIA.
Recruitment
This study took place between April 2016 and May 2017. The methodological approach taken to recruit participants followed recognised approaches for working with minority ethnic communities in the UK. 94,95 This includes involving key community representatives as study personnel, as well as developing positive relationships between research staff and minority ethnic communities. 96
Interviews with religious and community leaders
A Muslim chaplain and an Orthodox rabbi based in London with links to a participating hospital were identified as key informants. They were initially contacted via e-mail with further face-to-face follow-up, including taking part in an interview for the study and discussion about recruiting additional participants. Those key informants then identified other religious (rabbi or imam) and community leaders (e.g. hospital chaplain, religious scholar, spokesperson for the Muslim burial society) to invite into the study. Purposive sampling was used to include participants with diverse backgrounds (e.g. health advocate, spokesperson for the Jewish Medical Association), beliefs and practices who spoke English. For example, to explore potentially diverse viewpoints among the Jewish key informants we included rabbis from within the Haredi, Orthodox, Masorti and Liberal movements who have differing beliefs and practices. We also used a ‘snowballing’ approach, whereby interviewees suggest other religious or community leaders. Interviews with religious leaders from other faiths (Christian, Catholic and Hindu) were also included, in order to explore how the Muslim and the Jewish viewpoint differed from that of other dominant faiths in the UK.
Community focus groups
Focus groups with members of two Muslim communities were arranged through representatives from the East Midlands Centre for Black and Minority Ethnic Health in Leicester and a Muslim community centre in Tower Hamlets, East London. At both sites, the recruiter was a member of the Muslim community. Leicester is one of the most ethnically and culturally diverse cities in the UK, with 37% of residents classifying their ethnicity as Asian or Asian British (28% as Indian, 2% Pakistani and 1% Bangladeshi) and 19% classifying their religion as Muslim. 97 In the London borough of Tower Hamlets, 41% of the population classify themselves as Asian or Asian British (32% as Bangladeshi, 3% as Indian and 1% as Pakistani),98 and 38% classify their religion as Muslim. 99 For the Muslim focus groups, we ensured that the two main South Asian ethnic groups in the UK (Pakistani and Bangladeshi) were represented. 100 Participants who spoke English, Urdu or Bengali were included.
For the Jewish community, focus groups were arranged through a rabbi from the Orthodox community and a community leader with close links to the Haredi community, both in London, which has the UK’s largest Jewish community. 101 Around 50% of the 300,000 or so Jewish people that live in the UK are affiliated with Orthodox Judaism and 13% with Strictly Orthodox (Haredi). 102
Purposive sampling was used to recruit parents (male and female) who were of child-bearing age (18–50 years).
Recruitment occurred in a number of ways: direct contact with participants attending community centres to discuss the study and invite them to take part (Bangladeshi and Pakistani community in Leicester); approaching community members by telephone (Haredi community in London and members of the Muslim community in East London); approaches at coffee mornings (Muslim community in East London); asking female participants to invite their husbands to take part (Bangladeshi and Pakistani Muslim community in Leicester); and circulating an e-mail to members of a synagogue (Orthodox Jewish community in London). Interested participants from the Muslim groups were asked to reply to the community representative, interested participants from the Jewish Orthodox groups were asked to reply to Celine Lewis directly and interested participants from the Jewish Haredi group were asked to reply to the community leader.
Interviews with bereaved parents
For this substudy, we included Muslim or Jewish parents who had experienced bereavement and had completed the questionnaire for substudy 1. Survey responders who had indicated their willingness to be interviewed were contacted to arrange an interview at a mutually convenient time.
Data collection
Interviews were conducted either face to face or by telephone. Celine Lewis conducted interviews with religious leaders and either Celine Lewis or Megan Riddington conducted interviews with bereaved parents. Focus groups were facilitated by Celine Lewis and a translator from within the community who was present at groups when the lack of English language was a potential barrier. When non-English-speaking participants were present, the translator began by translating the participant information sheet and the consent form into Urdu or Bengali. During the focus groups, there was two-way translation between the facilitator and participants who did not speak English. Audio-recordings were translated into English. Focus groups with Muslim participants were conducted at Muslim community centres in Tower Hamlets and Leicester, and focus groups with Jewish participants were conducted at the home of a rabbi and a community leader. Focus groups consisted of between 6 and 10 participants and lasted 1.5–2 hours. When advised, focus groups were divided by gender to take account of religious or cultural requirements. Written consent was sought to record the discussion and use anonymised quotations in papers or reports. Focus group participants received a gift voucher as appreciation for their time and contribution.
Data analysis
Quantitative data
For the quantitative survey data, frequencies were used to summarise the findings around autopsy acceptability, likely uptake and preferences, as well as decision-making factors. A chi-squared test and an independent samples t-test were used to determine significant associations between variables. McNemar’s tests were used to identify any statistically significant changes in proportions when comparing likely uptake of standard autopsy, MIA and NIA. Likert scales were dichotomised before analysis (e.g. for the analysis on questions around acceptability, the responses ‘totally acceptable’ or ‘acceptable’ were collapsed together; similarly, ‘totally unacceptable’ and ‘unacceptable’ were collapsed together due to small numbers in the extreme categories). Estimates of percentages and differences between subgroups and modes of examination are presented with 95% CIs. Questionnaires were excluded if data were missing for the questions on acceptability, likely uptake and preferences. Quantitative data were analysed using IBM SPSS Statistics version 22 (IBM Corporation, Armonk, NY, USA) and p < 0.05 was used as the cut-off point to define statistical significance.
Qualitative data
For the qualitative data, free-text comments, interviews and focus groups were analysed as one data set, using thematic analysis. 47 Data were collected and analysed concurrently, with data collection ceasing once saturation had been reached. Four researchers were involved in the coding process (CL, MH, MR, ZL). A subset of transcripts was coded by at least two researchers to agree on a coding framework that was related to the semistructured topic guides, with code names derived inductively from the data. The remaining transcripts were independently coded according to the framework. For substudy 3, in the final stages of analysis, findings relating to the religious viewpoints were discussed with key informants from both the Muslim and Jewish faiths (member checking), to check the validity of the interpretation of the data. 103 Analysis was facilitated using NVivo software.
Patient and public involvement
Patients were involved in the design of the Health Technology Assessment application. Two patient and public involvement meetings were held prior to writing the grant application – one involving the parent support groups (Sands, ARC and The Lullaby Trust) and one involving representatives from specific religious groups (Muslim, Jewish, Christian and Hindu). One of the patient representatives (Jane Fisher from ARC) is a co-applicant on this grant and was involved in writing the grant and the design of the study.
Patient representatives were involved in the management of the research on both the Study Steering Committee, in which we had representatives from The Lullaby Trust, Sands and Genetic Alliance UK, and on the advisory team (Jane Fisher from ARC). There were bi-annual meetings (as well as written updates every 3 months) with the Study Steering Committee, who oversaw the research.
Patients and patient representatives were involved in developing participant information resources, the interview topic guide and the bereaved parent survey. The survey was initially designed by Celine Lewis and revised by members of the advisory team. It was then circulated to three bereaved parents (from The Lullaby Trust and Sands) who reviewed the survey, including the descriptions of standard autopsy, NIA and MIA. The three bereaved parents also checked the survey for comprehension and their comments were incorporated into the final version. Participants for the survey and for the parent interviews were recruited by the patient groups Sands, The Lullaby Trust, ARC and Child Bereavement UK.
Key findings from the research were presented to the advisory team and the Study Steering Committee, who helped to translate the findings into implications for practice. The findings from this body of research were also presented to the advisory team, Study Steering Committee, as well as health professionals and religious/community leaders, at a dissemination meeting which took place at the University College London Great Osmond Street Hospital Institute of Child Health on 3 May 2018. Key findings from the empirical research will be summarised and disseminated through the support groups who were recruited into the study, following publication in academic journals (either through a newsletter or on the website), to ensure that those parents who took part have access to the results.
Chapter 4 Results: mixed-methods study with bereaved parents to determine acceptability and likely uptake of less invasive autopsy
In this chapter we present the results from the mixed-methods study looking at the acceptability and the likely uptake of LIA among bereaved parents. We present both quantitative and qualitative data. This chapter is partly reproduced from Lewis et al.,104 published in BJOG in 2018. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY-NC 4.0) licence, which permits others to copy, remix, transform, build upon and redistribute the material in any medium or format, for non-commercial use, provided the original work is properly cited and changes made are indicated. See: https://creativecommons.org/licenses/by-nc/4.0/.
Survey participants
In total, 938 questionnaires were returned: 870 through retrospective recruitment (655 via Sands, 108 via ARC, 81 via The Lullaby Trust and 26 via Child Bereavement UK) and 68 through prospective recruitment. Seventy-nine questionnaires were excluded because of missing data [whereby questions on likely uptake, acceptability and preferences for the different methods were omitted (questions 1–7)], leaving 859 questionnaires for inclusion in the analysis (79 from the retrospective recruitment and 0 from the prospective recruitment). Owing to the nature of the retrospective recruitment, it is not possible to calculate a recruitment rate. For the prospectively recruited participants, 23 participants actively declined to take part at the time of discussing the study and 160 participants passively declined (study packs were taken home and not returned) (30% response rate). Over 99% of respondents had experienced a perinatal or child loss (0.7% did not answer this question) and 48.6% of parents consented to a standard autopsy. Survey responder characteristics are presented in Table 1.
| Participant characteristic | Total sample (N = 859) | Prospective recruitment (N = 68) | Retrospective recruitment (N = 791) |
|---|---|---|---|
| Age (years), mean (SD), range | 35.9 (8.1), 18–73 | 32.6 (5.5), 20–50 | 36.2 (8.3), 18–73 |
| Sex, % (n) | |||
| Female | 94.9 (615) | 94.1 (64) | 97.5 (751) |
| Male | 2.7 (23) | 5.9 (4) | 2.5 (19) |
| Country of birth, % (n) | |||
| UK | 94.5 (774) | 76.1 (51) | 96.1 (723)*** |
| Other | 5.5 (45) | 23.9 (16) | 29 (3.7) |
| Education, % (n) | |||
| No formal qualification | 1.7 (14) | 1.5 (1) | 1.7 (13) |
| GCSE or equivalent | 21.5 (177) | 23.9 (16) | 21.2 (161) |
| A level or equivalent | 24.4 (201) | 20.9 (14) | 24.7 (187) |
| Degree or equivalent | 32.8 (271) | 26.9 (18) | 33.4 (253) |
| Postgraduate qualification | 19.5 (161) | 25.4 (17) | 19.0 (144) |
| Ethnicity, % (n)a | |||
| White or white British | 95.0 (783) | 64.2 (43) | 97.8 (740)*** |
| Black or black British | 2.5 (21) | 23.9 (16) | 0.7 (5) |
| Asian or Asian British | 1.3 (11) | 10.4 (7) | 0.5 (4) |
| Mixed | 0.6 (5) | 1.5 (1) | 0.5 (4) |
| Other | 0.5 (4) | 0 (0) | 0.5 (4) |
| Do you have a religious faith?, % (n) | |||
| Yes | 48.2 (393) | 68.9 (42) | 46.5 (351)** |
| No | 51.8 (423) | 31.1 (19) | 53.5 (404) |
| If ‘yes’, which faith?, % (n)b | |||
| Christian | 44.8 (358) | 72.7 (32) | 93.2 (326)*** |
| Muslim | 0.8 (6) | 4.5 (2) | 0.5 (4) |
| Jewish | 0.8 (6) | 4.5 (2) | 0.5 (4) |
| Sikh | 0.5 (4) | 6.8 (3) | 0.1 (1) |
| Hindu | 0.4 (3) | 4.5 (2) | 0.1 (1) |
| Jehovah’s Witness | 0.4 (3) | 2.3 (1) | 0.3 (2) |
| Buddhist | 0.1 (1) | 0 (0) | 0.1 (1) |
| Other | 1.5 (12) | 0 (0) | 1.6 (12) |
| Experience of loss (tick all that apply), % (n) | |||
| Miscarriage (loss up to 12 weeks’ gestation) | 34.3 (295) | 30.9 (21) | 34.6 (274) |
| Late miscarriage/fetal loss (12–24 weeks’ gestation) | 18.7 (161) | 38.2 (26) | 17.1 (135) |
| SB | 47.4 (407) | 26.5 (18) | 49.2 (389) |
| Termination for fetal anomaly | 18.3 (157) | 26.5 (18) | 17.6 (139) |
| Neonatal/infant death (aged 0–12 months) | 22.0 (189) | 17.6 (12) | 22.4 (177) |
| Child death (aged 1–16 years) | 2.3 (20) | 7.4 (5) | 1.9 (15) |
| None | 0 (0) | 0 (0) | 0 (0) |
| If ‘yes’, were you approached about autopsy in any of those cases?, % (n) | |||
| Yes | 83.2 (711) | 89.2 (58) | 82.7 (653) |
| No | 7.4 (63) | 7.7 (5) | 7.3 (58) |
| Not sure | 2.1 (18) | 1.5 (1) | 2.2 (17) |
| Coroner’s office issued a compulsory autopsy | 7.4 (63) | 1.5 (1) | 7.8 (62) |
| If ‘yes’, which type of autopsy were you offered? (Tick all that apply), % (n) | |||
| Standard autopsy examination | 67.1 (477) | 84.4 (49) | 65.5 (428) |
| Limited autopsy, only certain organs you consent to are examined | 21.8 (155) | 36.2 (21) | 20.5 (134) |
| MIA with tissue sampling and MRI | 6.3 (45) | 19.0 (11) | 5.2 (34) |
| NIA with MRI | 3.5 (25) | 15.5 (9) | 2.5 (16) |
| NIA with X-ray | 4.5 (32) | 17.2 (10) | 3.4 (22) |
| Not sure | 31.6 (225) | 10.3 (6) | 33.5 (219) |
| Which type of autopsy did you accept?, % (n) | |||
| Standard autopsy examination | 48.6 (346) | 58.6 (34) | 47.8 (312) |
| Limited autopsy, only certain organs you consent to are examined | 6.5 (46) | 1.7 (1) | 6.9 (45) |
| MIA with tissue sampling and MRI | 1.5 (11) | 0.0 (0) | 1.7 (11) |
| NIA with MRI | 0.6 (4) | 1.7 (1) | 0.5 (3) |
| NIA with X-ray | 1.8 (13) | 3.4 (2) | 1.7 (11) |
| Not sure | 9.1 (65) | 1.7 (1) | 9.8 (64) |
| None, I declined an autopsy | 33.5 (238) | 34.5 (20) | 33.4 (218) |
Quantitative results
Likely uptake of standard autopsy, minimally invasive autopsy and non-invasive autopsy
Overall, 90.5% (n = 777, 95% CI 88.3% to 92.2%) of participants indicated that they were likely to consent to some form of LIA (MIA, NIA or both). In total, 53.8% (n = 462, 95% CI 50.4% to 57.1%) indicated that they were likely to consent to a standard autopsy; 74.3% (n = 638, 95% CI 71.2% to 77.1%) were likely to consent to MIA; and 77.3% (n = 664, 95% CI 74.4% to 79.9%) were likely to consent to NIA (Table 2). A significant difference was found for likely uptake of MIA and acceptability of MIA when comparing participants who had experienced fetal loss (miscarriage, ToP and/or SB) with participants who had experienced neonatal and/or paediatric death (71.6% vs. 82.0%, p = 0.003 and 84.6% vs. 91.2%, p = 0.016, respectively) (Table 3).
| Likely uptake of . . . | Yes, % (n) | No, % (n) | Not sure, % (n) |
|---|---|---|---|
| Standard autopsy | 53.8 (462) | 26.0 (223) | 20.3 (174) |
| MIA | 74.3 (638) | 8.3 (71) | 17.5 (150) |
| NIA | 77.3 (664) | 5.2 (45) | 17.5 (150) |
| Acceptability of . . . | Acceptable, % (n) | Unacceptable, % (n) | No strong opinion, % (n) |
| Standard autopsy | 77.3 (664) | 9.4 (81) | 13.3 (144) |
| MIA | 86.3 (741) | 3.0 (26) | 10.7 (92) |
| NIA | 87.3 (750) | 3.1 (27) | 3.0 (26) |
| Likely uptake of . . . | Miscarriage/ToP/SB, % (n) | Neonatal/paediatric, % (n) |
|---|---|---|
| Standard autopsy | 53.7 (348) | 53.7 (110) |
| MIA | 71.6 (464) | 82.0 (168)** |
| NIA | 76.5 (496) | 79.5 (163) |
| Acceptability of . . . | Acceptable, % (n) | Acceptable, % (n) |
| Standard autopsy | 76.1 (493) | 81.5 (167) |
| MIA | 84.6 (548) | 91.2 (187)* |
| NIA | 87.5 (567) | 86.8 (178) |
Participants who indicated that they would decline standard autopsy but would consent to a less invasive option (excluding those who were not sure for either) were more likely to have a lower educational level [35.7% General Certificate of Secondary Education (GCSE) or lower, 37.7% Advanced level (A level) or equivalent, 25.5% degree or equivalent, 15.7% postgraduate qualification or equivalent; p < 0.0001]. There was no significant difference in age, gender, country of birth, ethnicity, religious faith, recruitment method or experience of loss (p > 0.05 for all). A McNemar’s test indicated that people were more likely to consent to a LIA than to standard autopsy (90.5% vs. 53.8%, respectively; p < 0.0001). Similarly, people were more likely to consent to MIA than to standard autopsy (74.3% vs. 53.8%, respectively; p < 0.0001) and to NIA than to standard autopsy (77.3% vs. 53.8%, respectively; p < 0.0001).
Acceptability of standard autopsy, minimally invasive autopsy and non-invasive autopsy
Regarding acceptability of the three options, 77.3% (n = 664, 95% CI 74.4% to 79.9%) thought that standard autopsy was acceptable, 86.3% (n = 741, 95% CI 83.8% to 88.4%) thought that MIA was acceptable and 87.3% (n = 750, 95% CI 84.9% to 89.4%) thought that NIA was acceptable (see Table 2). A McNemar’s test with continuity correction indicated that people found MIA more acceptable than standard autopsy (86.3% vs. 77.3%, respectively; p < 0.0001) and NIA more acceptable than standard autopsy (87.3% vs. 77.3%, respectively; p < 0.0001). No significant difference was found regarding the acceptability of standard autopsy, MIA and NIA when comparing participants who had experienced fetal loss with participants who had experienced neonatal and/or paediatric death (p > 0.01 for all) (see Table 3).
Preferences for different options
When asked to choose between the different options, 45.5% (n = 391, 95% CI 42.2% to 48.9%) of participants preferred MIA, 30.8% (n = 265, 95% CI 27.9% to 34.0%) of participants preferred NIA, 14.3% (n = 123, 95% CI 12.1% to 16.8%) of participants preferred standard autopsy, 7.7% (n = 66, 95% CI 6.0% to 9.7%) of participants had no strong preference and 1.6% (n = 14, 95% CI 1.0% to 2.7%) of participants would not choose any of the options. No significant associations were found between participant characteristics, recruitment method or type of loss with preference for the different options (p > 0.01 for all).
Factors associated with decision-making
Items rated extremely important by around 85% of study participants were ‘to understand why it happened’ (85.7%) and ‘to understand if it might happen again’ (85.3%). An item rated extremely important by around 60% of study participants was ‘to prevent this from happening to others’ (63.1%). Items rated extremely important by around 50% of study participants were ‘to reassure me it was not my fault’ (50.7%), ‘feeling that my baby/child had suffered enough’ (49.3%) and ‘not wanting my baby/child to be cut’ (49.1%). Items most frequently rated as not at all important by study participants were ‘my religion’s views about autopsy’ (84.7%) followed by ‘concern it would delay funeral arrangements’ (46.3%) (Table 4).
| Not at all important (%) | Not very important (%) | Neither important nor unimportant (%) | Quite important (%) | Extremely important (%) | |
|---|---|---|---|---|---|
| To understand why it happened | 1.7 | 1.6 | 4.2 | 6.8 | 85.7 |
| To understand if it might happen again | 2.4 | 1.2 | 3.8 | 6.7 | 85.3 |
| To prevent this from happening to others | 1.8 | 3.1 | 10.5 | 21.4 | 63.1 |
| To reassure me that it was not my fault | 10.2 | 6.6 | 17.6 | 14.8 | 50.7 |
| Feeling that my baby/child had ‘suffered enough’ | 8.5 | 6.6 | 22.0 | 13.4 | 49.3 |
| Not wanting my baby/child to be cut | 7.3 | 9.6 | 19.8 | 14.1 | 49.1 |
| To improve medical knowledge | 6.4 | 6.6 | 16.9 | 21.2 | 48.7 |
| Concern about the baby/child’s appearance afterwards | 8.6 | 9.0 | 19.4 | 20.0 | 42.9 |
| Concern about what would happen to the tissue/organs afterwards | 8.4 | 12.0 | 19.3 | 17.6 | 42.6 |
| To help with the grieving process | 13.1 | 7.5 | 20.1 | 18.3 | 40.9 |
| The description of autopsy given by the health professional | 17.7 | 10.2 | 21.8 | 16.1 | 34.1 |
| Concern that my baby/child might be moved to another hospital | 19.8 | 12.1 | 20.2 | 13.9 | 33.9 |
| Concern about the length of time it may take to get the results | 24.2 | 12.0 | 20.6 | 19.7 | 23.3 |
| Feeling that I already knew what caused the loss of my baby/child | 28.4 | 12.5 | 29.2 | 10.3 | 19.5 |
| Feeling that it would add to my grief | 30.7 | 13.6 | 25.3 | 16.7 | 13.5 |
| The complexity and length of the consent form | 43.3 | 12.9 | 20.8 | 9.9 | 12.9 |
| Concern that it would delay funeral arrangements | 46.3 | 13.3 | 18.6 | 10.3 | 11.4 |
| My religion’s views about autopsy | 84.7 | 4.8 | 5.3 | 1.9 | 3.2 |
Interview participants
For the interviews, 36 participants were contacted following their initial voluntary expression of interest and 20 consented and took part (56% response rate). Interview participant characteristics are presented in Table 5.
| Participant characteristic | Total sample (N = 20) |
|---|---|
| Age (years): mean (SD), range | 39.6 (9.5), 25–64 |
| Sex, % (n) | |
| Female | 90 (18) |
| Male | 10 (2) |
| Country of birth, % (n) | |
| UK | 85 (17) |
| Other | 15 (3) |
| Education, % (n) | |
| A level or lower | 20 (4) |
| Degree or higher | 80 (16) |
| Ethnicity, % (n) | |
| White or white British | 85 (17) |
| Other | 15 (3) |
| Do you have a religious faith?, % (n) | |
| Yes | 55 (11) |
| No | 45 (9) |
| If ‘yes’, which faith?, % (n) | |
| Christian | 73 (8) |
| Jewish | 27 (3) |
| Experience of loss (tick all that apply), % (n) | |
| Miscarriage (loss up to 12 weeks’ gestation) | 25 (5) |
| Late miscarriage/fetal loss (12–24 weeks’ gestation) | 15 (3) |
| SB | 45 (9) |
| ToP | 20 (4) |
| Neonatal/infant death (aged 0–12 months) | 35 (7) |
| Child death (aged 1–16 years) | 5 (1) |
| None | 0 (0) |
| Approached about autopsy, % (n) | |
| Yes | 75 (15) |
| No | 5 (1) |
| Coroner requested an autopsy, % (n) | 20 (4) |
| Consented to autopsy | |
| Yes (standard) | 60 (9) |
| Yes (limited) | 13 (2) |
| No | 27 (4) |
| Preference for type of autopsy, % (n) | |
| Standard | 25 (5) |
| MIA | 50 (10) |
| NIA | 25 (5) |
Qualitative findings
The findings below summarise the overall themes that emerged from the qualitative analysis around acceptability and likely uptake of standard autopsy, MIA and NIA.
Standard autopsy
Acceptability of standard autopsy was linked to comments around the thoroughness of the procedure:
I wanted to ensure there was every possible avenue, comprehensive procedure completed and explored that would, if possible, provide the answers to why my baby died.
The Lullaby Trust 73
Consenting to a standard autopsy was associated with ‘taking all steps possible’, and one which ‘gives the best chance of determining the cause of death’ or identifying information that would be relevant for future pregnancies:
I had an absolute need to know if there were any clues to why my daughter had died.
Sands 88
I understood that the procedure was invasive on my daughter’s body; however, it was extremely important for us to understand why she died after a seemingly healthy pregnancy. It was difficult to think of what would happen to her body; however it was worth this distress to get an answer.
Sands 110
Better information is the basis for better decision about future pregnancies.
Hospital P1
However, for many parents, the invasiveness was perceived to be too traumatic to consent to the procedure:
I couldn’t bear the idea of cutting my new baby I’d taken care of for 39 weeks.
Sands 510
There was a strong parental drive to protect the baby from ‘harm’ and to let the child ‘rest in peace’. Post-mortem was seen as furthering physical and psychological harm to the parent and baby/child without any prospect of ‘bringing the child back’:
I see the importance of an autopsy but my view is the child and parents have suffered enough through the loss. Nothing will ever bring the child back. Let sleeping babies sleep in peace.
Sands 602
I fear the complete autopsy will leave the child looking like a rag doll afterwards.
Hospital P9
Moreover, some parents had concerns about standard autopsy disrupting rituals around death:
Some people would like to bath their baby and get them dressed in their last outfit. And it’s just – with the amount of invasiveness that’s involved in the standard autopsy, it’s – that’s – not nice.
The Lullaby Trust 41
Babies and children were often positioned as special cases. The acceptability of standard autopsy for this ‘tiny’, ‘fragile’ group was called into question, and alternative options sought that would minimise parental burden and safeguard the dignity and respect of the infant or child:
It’s your baby they take away and cut into. It made me feel sick knowing that some unknown unfeeling professional was weighing my child’s organs like weighing fruit at the supermarket. There must be a more respectful manner in which to investigate an unexpected death.
The Lullaby Trust 6
Non-invasive autopsy
Non-invasive autopsy was acceptable for the majority of parents, primarily because the lack of any incision enabled the child to ‘rest in peace’ and put parents ‘more at ease’ consenting to the procedure:
Our child would have been kept as she was when she was born and wouldn’t have any further trauma.
Sands 274
Non-invasive autopsy was viewed as a more ‘comforting’ choice for parents, one that would not contribute further to the distressing ‘thoughts’ and ‘guilt’ that many were already experiencing:
It was upsetting to think of your beloved child/grandchild being cut open, so if this could be avoided and a cause of death could be ascertained I think this preferable.
The Lullaby Trust 64
Moreover, because there were no incisions to the body, parents felt that it would enable them to participate in rituals around death, such as washing, holding and dressing their babies before the funeral, found to be important in moving forward:
I didn’t feel able to see my baby before burial after having an autopsy but if there had been no cuts to her body I would’ve spent more time with her before her funeral.
Sands 345
Nevertheless, some participants raised concerns about the completeness of the information that NIA could gather and acknowledged that it might be unsuitable in certain circumstances:
A less invasive procedure would have appealed to me at the time. However, I felt the need to know everything I possibly could about what was wrong with my baby so would struggle with the idea that something might be missed that could have been picked up from a different method.
ARC 14
This would be my ideal but I appreciate that the tissue sampling may be necessary to give a fuller picture.
The Lullaby Trust 65
Other parents stated that they were prepared to accept a reduced chance of finding an answer if it meant that their child would not be cut:
[NIA] might not give all the answers, but personally I would prefer to have less chance of knowing a cause for death than I would consenting to an invasive autopsy.
Sands 396
Personally, I don’t think it’s a method that would pick up as much as you need to pick up. Obviously if a child has some kind of infection an MRI is not going to pick that up.
Hospital P40
Minimally invasive autopsy
Minimally invasive autopsy was considered to be a ‘good compromise’, as it overcame some of the limitations of NIA but enabled tissue samples to be taken without requiring large incisions to the body. Thus, it allowed parents to balance their need for thoroughness and answers, while easing the parental burden by protecting the baby or child from further ‘harm’:
This seems like the best of both worlds – you can physically see organs, and take samples, whilst at the same time being minimally invasive and less distressing for parents to agree to.
ARC 18
This would enable a more comprehensive examination which would be able to gain the maximum possible amount of information with only minimal desecration of a very precious little body.
Sands 418
Nonetheless, for some parents, MIA was still perceived as invasive and any level of invasiveness remained intolerable:
Personally, anything that involves cutting the baby or removing anything is not acceptable.
Sands 523
In addition, some parents raised concerns about whether or not there was a risk that conditions might not be detected and whether or not it could reach the same level of diagnostic yield as standard autopsy. The importance of research to compare both approaches was discussed:
As it’s new would it find the answers parents need from an autopsy? If results came back inconclusive would parents then be left wondering if the answer was in a full autopsy?
Sands 553
I think this would be my preferred option, as long as research shows it is as reliable as a full post-mortem.
Sands 153
Many parents thought that MIA and NIA were likely to result in an increased uptake of autopsy and would benefit those parents for whom standard autopsy is unacceptable, including those parents whose religion prohibits it. A number commented that there was the potential for parents who would have previously consented for standard autopsy to opt for NIA or MIA because it was emotionally easier:
This option would be ideal for those parents who find the invasiveness of post-mortem difficult and would potentially give them the opportunity to find out cause of death when they would possibly have refused a complete post-mortem. However, I think it may also reduce the number of complete post-mortems as parents may choose this option rather than the complete post-mortem, opting for a compromise/less invasive method.
Sands 650
Concerns were raised that parents might later regret not opting for standard autopsy if NIA or MIA did not result in a cause of death. Many parents supported a step-by-step approach to consenting for autopsy, whereby parents would agree to the most invasive approach they would accept, but if significant findings or a cause of death was found, no further procedure would be conducted:
I think [NIA] should be offered first with perhaps the option being there for a full autopsy if a cause isn’t found, should the parents agree to it.
ARC 3
Parental views about research participation
The vast majority (87.9%; n = 58) of prospectively recruited parents were glad to have been asked to take part in this study, 12.1% (n = 8) were unsure and none regretted it. Some parents commented that being asked to take part in research enabled something good to come out of a terrible experience, as exemplified by the following quotation:
Thank you for taking to time to find out our opinions. It feels very empowering to think that our experience, no matter how dreadful at the time, can be used to support others and make a difference.
The Lullaby Trust, P65
Discussion
This is the largest UK study examining the views and preferences of bereaved parents towards standard and less invasive forms of autopsy. The findings suggest a likely large overall increase in uptake, which could be as high as 90% if less invasive methods were available, although in practice this will depend on availability and effectiveness of different methods of autopsy in specific circumstances. Both MIA and NIA were clearly the more acceptable approaches (86% and 87%, respectively, compared with 77% for standard autopsy), a finding supported by the qualitative work, in which less invasive approaches were preferable, as they were considered ‘kinder’ to both parent and child. If asked to choose between the different approaches, nearly half of participants (46%) would choose MIA, as it enables tissue sampling without requiring large incisions to the body and is therefore perceived as a ‘good compromise’.
Although 74–77% of participants reported that they would consent to MIA or NIA, around 20% of responders remained undecided (‘not sure’). This uncertainty might indicate that further information about the procedure is required, including details of under which circumstances it is likely to result in a diagnosis. If the full range of approaches for examination after death were available, around 15% of responders indicated that they would still chose standard autopsy, highlighting the need for provision of choice. This finding suggests that some parents will continue to opt for the method which can theoretically provide the most information.
Notably, there was a marked difference (24%) in the proportion of responders in our study who thought that standard autopsy was acceptable (77%), compared with the number who would consent to it themselves (54%). This indicates that there is a difference between a procedure that is considered theoretically acceptable for ‘others to have’ and what parents would choose for themselves in practice.
Small, early studies with bereaved parents suggest that less invasive approaches are preferable to standard autopsy for some parents;31 however, other studies have found that the method likely to provide the most information is preferred. 38 Consistent with our study, Henderson et al. 79 found that fewer well-educated women were significantly less likely to consent to a standard autopsy. Our finding that survey responders who were less well-educated and would decline standard autopsy were likely to consent to LIA highlights that this would open up opportunities for this group that would otherwise be unavailable.
Although our findings support those of Cannie et al. 31 in that, overall, there was a preference for less invasive methods, 15% of participants still indicated a preference for standard autopsy as it was the most complete test available. Around half of parents (54%) stated that they would consent to a standard autopsy, findings which align with recent UK national data9 and an international survey of parents following SB,105 although a recent study in the UK found that around 80% of parents who experienced SB consented to a standard autopsy. 79 The primary reasons why bereaved parents consented to autopsy in this study, namely to understand why it happened and if it would happen again, have also been identified as the main motivators in other studies,7,38,54,68 supporting the importance of information to inform recurrence risk for many parents.
In the current survey, religion was not found to be an important factor in decision-making around autopsy. However, this is likely to be because of the small number of Muslim and Jewish responders (12 in total) and therefore should not be considered generalisable. Our qualitative research with parents and religious leaders from these two religious groups has shown that the invasiveness of standard autopsy is a key reason why Muslim and Jewish families decline, along with the requirement to bury the body as soon as possible, and that less invasive methods, in particular non-invasive approaches, would be considered religiously permissible and much preferred.
A major strength of the present study is the large number of participants and the use of a mixed-methods approach, which enabled corroboration of findings and a deeper understanding of the topic. Moreover, responses from prospectively recruited parents suggest that the majority of survey responders did not experience any adverse effect from taking part in the study. Although there was a significantly larger number of participants recruited retrospectively than prospectively, there was no overall difference in preferences for autopsy between the two cohorts. Moreover, we did not identify any differences in autopsy preferences across participant characteristics or loss experience (late miscarriage, SB, etc.), despite the majority of survey responders self-selecting their ethnicity as white and their education level as well educated. There was a greater proportion of responders who had experienced SB than other forms of perinatal loss, but this mirrors the proportions from recent national data on childhood, infant and perinatal mortality106 and, similarly, 49% of parents in our sample had previously consented to a standard autopsy, which is comparable to the national average of around 45%. 9 Not unexpectedly given the sensitive subject matter, there was a low response rate from parents recruited prospectively, which may have biased findings (30%). Women with poorer emotional health may have been less likely to respond. However, this figure is comparable with a recent survey of parental experience of autopsy following SB, in which the response rate was also 30%. 79 In addition, there was a low response rate for the interview study (56%). Thus, the qualitative findings may not be representative of the broader sample. Online recruitment enabled us to recruit a much larger sample than was likely to have been possible prospectively, yet it is subject to non-response bias, as participants may have been more interested in or enthusiastic about the topic. Finally, the hypothetically high uptake of MIA and NIA seen in our findings may not concur with actual uptake in a real-life scenario.
Conclusion
Further clinical work is required to assess concordance between MIA, NIA and standard autopsy so that appropriate counselling can be provided across a range of specific clinical scenarios (e.g. SB vs. infant death). Furthermore, economic and implementation evaluations are required to assess cost implications, as well as how LIA could be offered routinely as a clinical service within the NHS.
Chapter 5 Interview study with health professionals and HM Coroners
In this chapter we present the findings from qualitative semistructured interviews with health professionals and coroners. This chapter is partly reproduced from Lewis et al. ,107 published in the Archive of Disease in Childhood in 2018. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Sample characteristics
Forty health professionals were contacted and 25 from 11 hospitals consented and took part in the study (63% recruitment rate). Ten coroners were approached: one actively declined, five did not respond and four participated (40% recruitment rate). At the time of the interview, nine health professionals were already offering NIA to parents as a clinical service and all four coroners explained that it was available in their jurisdictions at a cost, although none recalled using it for infant or childhood deaths. Six health professionals were offering MIA either as part of a study or as a clinical service. None of the coroners were offering MIA (Table 6).
| Characteristic | Total (n) |
|---|---|
| Total participants | 29 |
| Profession | |
| Bereavement midwife | 6 |
| APT | 4 |
| HM Coroner | 4 |
| Intensive care consultant | 4 |
| Obstetrics/fetal medicine consultant | 4 |
| Perinatal/paediatric pathologist | 3 |
| ICU family liaison nurse | 2 |
| Consultant neonatologist | 1 |
| Paediatric radiologist | 1 |
| Gender | |
| Female | 17 |
| Male | 12 |
| Location | |
| London | 16 |
| Regional England | 13 |
| Offering/conducting NIA or MIA | |
| NIA | 13 |
| MIA | 6 |
Four overarching themes were established during the coding process: (1) benefits, (2) concerns, (3) implementation issues and (4) predicted uptake.
Benefits of minimally invasive autopsy and non-invasive autopsy
Health professionals and coroners acknowledged that availability of less invasive methods of autopsy was a positive development which would be of benefit to bereaved parents and potentially increase uptake:
Who in their right mind wants interference with a body of a loved one, if you didn’t have to? No one would. So I think I would encourage research into ways of replacing, augmenting and providing an alternative to traditional autopsy.
Coroner 1
They both sound really good, and I think you’d get a lot more uptake of post-mortem by having them available.
Obstetrician 1
Procedural benefits
Participants acknowledged that there were certain circumstances when autopsy imaging would be particularly useful, including congenital anatomical abnormalities such as ‘brain malformations’, ‘cardiac conditions’ and ‘skeletal dysplasias’. Several participants highlighted instances when NIA could provide greater diagnostic accuracy than a full autopsy, such as when looking at ‘very, very young babies where you’re not necessarily going to get as much information as you want with the naked eye’ or that ‘it might show up things you weren’t expecting’, such as a variety of abnormalities suggesting a syndrome. Additionally, NIA could be useful in confirming abnormal prenatal ultrasound findings. The main procedural benefit of MIA was the opportunity for tissue sampling without the need for large incisions, which was likely to be preferable to parents.
In terms of feeding back autopsy results to parents, five participants noted the potential benefits of MRI or computerised tomography (CT) images:
I would never show a family a photograph of say the liver, that would be inappropriate, but I would be comfortable showing them an MRI scan of the brain or the spinal cord . . . that would allow you to put a picture on something that you probably couldn’t do now.
Consultant neonatologist 1
Seven interviewees speculated whether or not NIA would be quicker than a full autopsy. Others noted that although the procedure might be quicker, it may be the ancillary investigations (histology, genetics, etc.) that delay reporting. Some participants speculated whether or not NIA and MIA would be more cost-effective as ‘you wouldn’t have to do the lengthy evisceration and evaluation’. Moreover, there was a potential cost saving to the mortuary in terms of length of time storing the body and costs associated with ‘reconstruction and body washing’. However, this cost saving may be offset if there was increased uptake. One participant pointed out that a ‘hard economic analysis’ in this area was required.
Psychological benefits
Psychological benefits included health professionals ‘feeling more comfortable having that conversation’, as well as parents feeling more comfortable consenting:
We’re very clear about what they do in a post-mortem and you can see them physically recoil sometimes. It’s often too much for them to take and I really do think a laparoscopic method would be much easier for them to cope with.
Bereavement midwife 3
It was also noted that parents were likely to be familiar with the concepts of MRI and CT, as well as keyhole surgery. Regarding MIA, health professionals commented that, psychologically, a small incision would be easier for parents to consent to than the large one and, similarly, parents were likely to find removal of small tissue samples preferable to whole organs:
I never found that talking about removing tissue samples and putting stuff in wax blocks was an issue. It was just the cutting the head and opening the chest cavity.
Bereavement midwife 2
Benefit to faith groups
Health professionals acknowledge that less invasive methods of autopsy, particularly NIA, would be preferable to members of the Muslim and Jewish communities who traditionally decline autopsy, as cutting of the body after death is prohibited:
There were certainly several Muslim families that haven’t been able to agree to a full post-mortem, but happily agreed to just MRI.
Bereavement midwife 1
There was, however, awareness that with NIA a key factor would be returning the body for burial as quickly as possible. Two coroners commented that the availability of NIA was particularly welcomed by members of the Muslim and Jewish communities who increasingly requested it. One coroner discussed how the availability of NIA had improved relations between the coroners’ office and the faith community, which had been ‘a game changer, it has a hugely positive effect’.
Neither coroner had requests for NIA from families outside the Muslim and Jewish faiths, although it was acknowledged that this was probably because it was not widely known about.
Concerns
Limitations of the technology
One of the main concerns raised related to whether or not one could reach the same level of certainty with NIA and MIA as with a traditional autopsy, and the potential for missing or misdiagnosis:
In sepsis or infection actually sometimes the most important thing is the sort of microbiology and sometimes it’s the combination of things which really sort of helps you . . . you might miss that with a minimally invasive approach.
Paediatric pathologist 1
Two participants worried about parents consenting to NIA or MIA ‘inappropriately and not getting the information out of it they thought they were going to get’ and one pathologist raised concerns about if he would be able to say to parents ‘look, we’ve done everything we possibly could’. A great deal of importance was therefore placed on ensuring further validation, as well as developing official guidance regarding in which circumstances NIA and MIA would be appropriate.
More specifically, there were various circumstances when participants noted that NIA was unlikely to be suitable. These included ‘infections’, ‘complex cases where tissue from multiple sites is required’, ‘aneurysms’, ‘stillbirth where the baby dies abruptly’ and coronial cases in which there was ‘negligent surgery’ or a ‘suspicious death’. Intensive care consultants discussed whether or not there would be added value of doing NIA on a child that had already been scanned:
Is there much mileage in doing a post-death imaging when we’ve already done pre-death imaging? That needs researching, is it something useful? I don’t know, possibly.
Consultant ICU 1
However, one ICU consultant did comment that NIA might be useful for a neonate ‘with a constellation of congenital abnormalities’. Two participants commented on the importance of tissue for DNA analysis as ‘that’s the sort of information on which future pregnancies are advised’.
Regarding MIA, it was acknowledged that this method had the added benefit over NIA of having tissue for analysis. However, the main concern related to whether or not there was the potential for ‘false negatives’. One participant commented that for complex cases tissue may be required from multiple organs, thus requiring a ‘maximum minimally invasive approach’. Finally, an APT commented that we still need a ‘way of sampling the brain’ in a minimally invasive way.
De-skilling the workforce
Concerns around ‘de-skilling’ pathologists to conduct traditional autopsies was raised by one health professional, particularly in relation to NIA:
My concern is that . . . if we go down that [NIA] route do we deskill our pathologists from doing the full post-mortem? We don’t want to end up being lazy, abandoning the methods that are the best we currently have.
Paediatric pathologist 3
Similarly, two APTs raised concerns around loss of skills in conducting reconstructions and how their role would fit in with these new technologies, asking ‘will we even be needed any more?’. One APT commented that perhaps their role would change and they would take on some of the laparoscopic work or be trained in using scanning equipment.
Implementation
Skills and training
Some of the most frequently cited issues around NIA and MIA related to the training that would be required for radiologists and pathologists to enable them to set up the service and to conduct procedures. For radiologists, it was acknowledged that, as well as having an interest in NIA, there would be a ‘learning curve because it’s a completely different set of reporting’. A paediatric pathologist commented that some pathologists might be ‘put off by trying to use a tiny telescope and just having very minimal access as pathologists [are] used to doing large incisions and dissecting organs’. Moreover, the current lack of pathologists working in clinical practice was identified as a potential barrier.
Health professionals commented that there would need to be training for staff both to have sufficient understanding of the techniques to be able to consent parents, and ‘to make sure the right type of post-mortem is offered to the right type of patient’. One of the pathologists queried whether or not health professionals might be discouraged from consenting parents for a traditional autopsy because of the availability of NIA and MIA.
Logistics
Most participants acknowledged that successful implementation of NIA and MIA would require a multidisciplinary approach, with pathologists and radiologists working together to decide when each method was most suitable and to ‘review the images and put the whole story together’. Other key logistical challenges concerned having sufficient access to MRI and CT machines, particularly given that ‘everyone’s priority in radiology is for the live patients’, as well as having the ‘electronics and wide bandwidth to transmit digital images because you might have to send the images to experts’. One paediatric pathologist acknowledged that access to MRI scanners had already ‘been the limiting factor for us in terms of imaging’. Regarding coronial cases, one of the coroners discussed how, for cases from the Muslim and Jewish community, they ‘made use of hospital scanners out of hours’ so that the body could be returned to the family as soon as possible. A few health professionals raised concerns around whether or not you would ‘swamp the pathology department’ if there was a significant increase in the number of autopsies being conducted.
Cost implications and equity of access
A range of costs associated with implementing NIA and MIA were identified. These included costs associated with training pathologists and radiologists, including covering their time in the clinic; the cost of the laparoscopic equipment; the potential costs if the pathology department required their own MRI or CT machine, if there was increased uptake; and the costs associated with using scanning equipment out of hours.
Concerns around equity of access and NIA and MIA becoming a ‘postcode lottery’ were raised. Three health professionals commented that a pragmatic solution would be to offer MIA and NIA through specialist centres ‘so it might be something that only happens in five or six centres around the UK’, although a midwife acknowledged that some parents may have concerns about their baby being moved to another hospital. In coronial cases, it was acknowledged that NIA is generally requested only by members of the Muslim and Jewish communities, with one coroner noting that he would ‘be far, far happier . . . if it was advertised to everyone, to take away from this being only for faith groups’.
Acceptance and governance
Acceptance from health professionals that NIA and MIA were reliable alternatives and the will to change current practice on the part of the paediatric pathology and radiology community were identified as key requirements for successful implementation:
We need to generate that evidence that MRI [Magnetic Resonance Imaging] autopsy is as good and then it would need to gain acceptance within the pathology community and I think we would need to do a lot of education of obstetricians and midwives to show that this was an effective alternative.
Obstetrician 3
One paediatric pathologist acknowledged that there might be some resistance from pathologists because ‘there is always a certain amount of “oh, we’ve always done it this way and it works for us”’. However, another paediatric pathologist addressed this concern by noting that in all specialties ‘practice changes’ and that minimally invasive techniques have become the standard for many operations that formerly required invasive procedures. A radiologist reflected that ‘simply the fact that it’s novel and I would need some experience or training to do it . . . is not a reason not to do it’.
The need for buy-in from hospital management to fund training and resources, including an out-of-hours service to use scanning equipment, was also discussed:
Reconfiguring a service would require a lot of resources and my reflection is it would be a bit of a difficult sell to a management, which I think understandably is very preoccupied about things like the numbers of people coming through the door of [accident and emergency] and whether we could get them a bed that night.
Paediatric pathologist 2
For coronial cases, two coroners identified the need for guidance from the Royal College of Pathologists (RCPath) as to when MIA and NIA would be acceptable alternatives to a standard autopsy, with one commenting that current guidance requires ‘a thorough examination’. Two coroners highlighted the ‘political will’ that would be required for authorities to fund ‘a comprehensive out-of-hours service’, although one noted that this might be more likely if an economic evaluation showed NIA to be cost-effective.
Predicted uptake of minimally invasive autopsy and non-invasive autopsy
All participants felt that the availability of NIA and MIA would increase uptake, although this varied from a ‘much, much bigger uptake’ (bereavement midwife) to ‘you might adjust the margins somewhat’ (consultant ICU). For health professionals who were already offering NIA or MIA, there had already been an increase in uptake:
I can certainly think of quite a number of people that it was like ‘no, no, no’ to the full post-mortem and then you would say ‘well, actually there is this that we can offer’ and that they would agree to that.
Bereavement midwife 1
It was acknowledged that some parents may prefer a traditional autopsy if it was likely to yield the most information.
Regarding how NIA and MIA should be offered, the vast majority advocated an approach whereby parents’ consent to the most invasive option they would consider acceptable, but if a diagnosis could be made less invasively, nothing further would be done.
Discussion
This study provides a unique insight into the views of health professionals and coroners working in perinatal and paediatric settings towards LIA. Examining the views of health professionals who discuss and consent bereaved parents is important, as paediatric and perinatal autopsy examination represent the largest group of consented autopsies. 108 Overall, participants viewed NIA and MIA as positive developments, likely to increase uptake of post-mortem, as they anticipated that parents would find it more acceptable, particularly those for whom current options are morally or religiously objectionable. These findings are consistent with a questionnaire study,39 in which LIA was found to be an acceptable alternative to traditional autopsy for most health professionals.
Participants in this study acknowledged a number of practical challenges that require attention before widespread implementation of less invasive perinatal and paediatric autopsy into clinical practice, many of which were identified when considering the use of autopsy imaging in adults. 109,110 Recommendations from that work included standards of practice and training programmes for pathologists, radiologists and APTs to be developed to deliver a trained workforce (e.g. APTs trained to operate scanners and undertake some minimally invasive procedures); imaging to be performed in any hospital equipped with scanning equipment, which could be used out of hours, with images then sent to a centre of expertise for reporting; and LIA to be conducted within already established centres of pathology based regionally across England, addressing concerns around equity of access. 109 Such strategies require investment and support from clinicians, as well as hospital decision-makers, royal colleges and local authorities. A detailed cost–benefit economic analysis to determine the true cost of implementing the service is therefore required.
Health professionals identified numerous situations in which imaging could be as reliable as, or even superior to, a full autopsy; comments that are supported by the current evidence. 111–113 Nevertheless, there were some circumstances in which it was unclear if imaging would be useful; for example, imaging of a child who had already had scans prior to death. This highlights the importance of ongoing research to understand which circumstances are most suitable for which method of autopsy, and development of formal guidance is required, both to ensure application in appropriate settings and also to inform clinicians’ consultations with bereaved parents regarding the likely yield of imaging or other investigations.
Further work is also required to determine the effects on reporting times for NIA and MIA. Despite NHS England recommending that 60% of autopsy reports should be issued within 42 days of examination,114 lengthy reporting times with current autopsy practice have been identified as a critical issue for parents, many of whom feel that they cannot move on until they receive a result. 79 The need for approaches that reduce the time required for laboratory processing and sample analysis may help to create a viable clinical service. 115 To the best of our knowledge, there is no published evidence to date demonstrating that MIA reduces the time from examination to final autopsy report, although NIA should result in much shorter turnaround times as there is no requirement for histological examination of internal organs.
The main strengths are that a range of health professionals were included with diverse views and experiences, and recruitment continued until saturation was reached. Participants were self-selecting, hence there may be responder bias towards people who have strong views. We tried to minimise this by purposely inviting people with varied views towards the technology. Snowball sampling is associated with problems of representativeness. There was a low response rate from coroners (40%). Finally, this research was conducted with health professionals and coroners in the UK only; opinions may differ outside the UK.
Conclusion
This work provides useful insights into the acceptability and the potential challenges of implementing LIA in clinical practice. Further research with bereaved parents, as well as research with religious groups, is required and forms aspects of the larger study of which this is part.
Chapter 6 Results: interview and focus group study with religious leaders and community members
In this chapter we present the findings from the interviews with religious and community leaders and the focus groups with members of the Muslim and Jewish communities. This chapter is partly reproduced from Lewis et al. ,116 published in PLOS ONE in 2018. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Study participants
Sixteen of 19 (84%) religious or community leaders participated (Table 7). Eight focus groups comprising 60 Muslim participants and two with 16 Jewish participants were conducted (Table 8).
| Religious or community leader | Total (N = 16), n |
|---|---|
| Muslim | 6 |
| Muslim chaplain | 3 |
| Imam | 1 |
| Spokesperson for Muslim Cemetery Trust | 1 |
| Scholar in Islamic Bioethics | 1 |
| Jewish | 6 |
| Rabbi | 3 |
| Spokesperson for Jewish Medical Association | 1 |
| Spokesperson for Jewish Burial Society | 1 |
| Orthodox Jewish health advocate | 1 |
| Christian | 3 |
| Church of England chaplain | 1 |
| Anglo-Catholic chaplain | 1 |
| Roman Catholic chaplain | 1 |
| Hindu | 1 |
| Hindu chaplain | 1 |
| Participant characteristics | Total (N = 76) | Muslim (N = 60) | Jewish (N = 16) |
|---|---|---|---|
| Age (years): median (range) | 39 (19–49) | 40 (19–49) | 37 (29–49) |
| Gender, n | |||
| Male | 25 | 20 | 5 |
| Female | 51 | 40 | 11 |
| Religion, n | |||
| Muslim | 60 | – | – |
| Jewish | 17 | – | – |
| Religiosity, n | |||
| Very religious | 23 | 12 | 11 |
| Quite religious | 45 | 43 | 2 |
| Not very religious | 5 | 3 | 2 |
| Country of birth, n | |||
| UK | 24 | 11 | 13 |
| Bangladesh | 24 | 24 | 0 |
| Pakistan | 16 | 16 | 0 |
| Somalia | 5 | 1 | 0 |
| Philippines | 1 | 5 | 0 |
| Thailand | 1 | 1 | 0 |
| Morocco | 1 | 1 | 0 |
| Indonesia | 1 | 1 | 0 |
| Belgium | 1 | 0 | 1 |
| South Africa | 1 | 0 | 1 |
| USA | 1 | 0 | 1 |
| Education, n | |||
| No formal qualification | 11 | 9 | 2 |
| GCSE or equivalent | 19 | 14 | 5 |
| A level or equivalent | 14 | 14 | 0 |
| Degree or equivalent | 17 | 16 | 1 |
| Postgraduate degree | 14 | 6 | 8 |
| Experience of loss, n | |||
| Miscarriage (< 12 weeks’ gestation) | 26 | 21 | 5 |
| Miscarriage (12–24 weeks’ gestation) | 8 | 7 | 1 |
| SB | 4 | 2 | 2 |
| ToP | 2 | 1 | 1 |
| Neonatal/infant death (aged 0–12 months) | 2 | 1 | 1 |
| Child death (aged 1–16 years) | 3 | 1 | 2 |
| If ‘yes’, were you approached about autopsy in any of those cases?, n | |||
| Yes | 13 | 9 | 4 |
| No | 15 | 12 | 3 |
| Not sure | 3 | 3 | 0 |
| If ‘yes’, did you consent?, n | |||
| Yes | 5 | 4 | 1 |
| No | 8 | 5 | 3 |
Three Jewish questionnaire responders were contacted and agreed to take part in an interview (age range 50–64 years; all educated to A Level or above; two were ‘quite’ religious, one was ‘not very’ religious). One responder had experienced a neonatal/infant death and had a coronial autopsy, one responder had a SB and one responder a ToP; the latter two responders had consented to a full autopsy. None of the questionnaire responders from the Muslim community (n = 6) agreed to be contacted further.
Key themes
Participants acknowledged that religious devotion involved a negotiation between religious observance and the complexities of daily life. For some participants, it was not always possible to ‘live our lives as strictly as we would like’ (FG9, Pakistani Muslim, women), or that sometimes, for example when a tragedy occurs, one’s emotions over-rode one’s observance of religious beliefs and practices:
Everyone’s faith goes up and down, so when the tragedy does happen to you, it depends what emotional state you’re at, a lot of things comes into it, sometimes instead of religion coming into it, it’s more your personal feelings.
FG7, mixed ethnicity, Muslim, women
Others discussed how their religion gave them comfort in times of tragedy and that the rituals around death ‘were just incredibly supportive’ (FG8 Jewish Orthodox, mixed gender). Moreover, there was an understanding that everyone interprets and practices their religion differently and that religion is not always ‘black and white, cast in stone’ (FG5 Bangladeshi Muslim, women). These factors influenced discussions around the different types of autopsy and accounted for the variation in viewpoints that were observed.
Religious teaching on traditional autopsy
It was widely recognised in both the key informant interviews as well as among lay participants in the focus groups that, according to the teachings of both Islam and Judaism, traditional autopsy was not religiously permitted because ‘our custom, together with our Muslim cousins, is to bury as soon as possible’ (Spokesperson for Jewish Burial Society), ‘that after the death the body should be left intact and it should not be disturbed unnecessarily’ (Imam) and the body ‘has to be returned in the manner in which it arrived’ (P39, Jewish bereaved parent):
The ruling in Islam on post-mortem, why we are so against it, is because the prophet Muhammed said that the one who cuts a dead body commits a sin, it’s like breaking the bones of a body which is alive. So, for us, a dead body will feel that pain, so it’s a sin to cut them up’.
FG7, mixed ethnicity, Muslim, women
The one example of when this view was not supported was in Liberal Judaism in which ‘there isn’t the same reluctance for post-mortems amongst the Reform communities generally . . . It’s completely acceptable.’ (Liberal rabbi). However, it was also recognised that, although Islam and Judaism may have very specific teachings on this topic, not everyone followed their religion to the same extent on this matter:
There are Jews who are very religiously observant, there are Jews who don’t care at all. Families vary enormously.
Masorti rabbi
Overall, the religious viewpoints from Muslim and Jewish participants differed significantly from those within the Christian faith in which there’s no ‘real set religious prohibition’ against autopsy (Anglo-Catholic chaplain) and the consensus is that ‘when a person dies their soul is with God and therefore their body, whilst it has encapsulated that soul, is no longer needed’ (Church of England chaplain). Similarly, in Hinduism, autopsy is not forbidden as ‘the body has no spiritual significance at all, it’s just an instrument’, although traditionally the ‘body needs to be cremated before the sunset’ (Hindu chaplain). Despite religious attitudes differing across the faith groups, it was acknowledged that regardless of religion, no parent would want their child to be cut or disfigured if it could be avoided:
It’d be very difficult to see your dead child with, you know, a huge cut along the head, and it would be painful . . . There’s something about body intactness that is almost sacred I think, whatever your faith.
Roman Catholic chaplain
Circumstances in which traditional autopsy is acceptable
The majority of parents stated that a traditional autopsy was not acceptable to them and that if a choice was offered they would be likely to decline. Nevertheless, for both Muslim and Jew people, the ‘religion does recognise the fact that if you’re staying in a country, one has to abide by the laws of the country.’ (spokesperson for Muslim Cemetery Trust) and hence it was accepted that in many cases, when an infant or child dies ‘you need to have a cause of death so you have to have a post-mortem’ (Jewish Burial Society). Participants from both faiths also acknowledged that, according to their religions, saving a life was one of the most important acts one could do: ‘the Koran says if you have saved one human being you have saved the whole humanity’ (Muslim chaplain 2). Thus, there was a strong case for allowing an autopsy ‘if say for instance, somebody’s had repeated SBs or problems in pregnancy and it might help save a future baby’ (Orthodox Jewish Health Advocate).
Similarly, if:
. . . parents whose young child or baby has died and . . . if there is a necessity to look into that in more detail then generally, you know, I can’t imagine there would be many scholars who would disagree that that is a legitimate reason.
Islamic scholar
Non-invasive autopsy and religious permissibility
All the religious and community leaders who took part in this study agreed that, from a religious perspective, NIA was permissible because it did not require any incisions or interference with the body:
The Jewish Law has a very specific definition of what’s considered violating the body, and imaging doesn’t violate that.
Orthodox rabbi
This viewpoint was also shared by many of the focus group participants who commented that ‘even if [someone is] very religious, they shouldn’t have a problem with going through this machine . . . You’re not harming the body. No cutting, no chemicals’ (FG10, Pakistani Muslim, men).
Most of the religious leaders and community leaders that were interviewed were aware that NIA had been used for coronial cases in adults in some areas and were very much in favour of that approach:
We have been working very closely with the Jewish community ourselves with the various institutions, to ensure that where there is a possibility, a non-invasive post-mortem method should be utilised. So we’re very much in favour of CT scans.
Muslim Burial Society
Uptake
Muslim and Jewish community members were positive towards the concept of NIA, with the majority indicating that they would potentially consent to the procedure:
My initial thought would be, absolutely 100% I would go for a non-invasive, without any hesitation . . . you’re keeping the body intact.
P43, Jewish bereaved participant
I personally would say probably yes, because it’s non-invasive, it’s not going to take as long, you know, and the body’s not going to be cut.
FG5, Bangladeshi Muslim, women
Religious leaders and community leaders also acknowledged the potential for an increase in uptake of autopsy if a non-invasive option was available, noting that ‘we might get a lot more families who will agree’ (Muslim chaplain 1) and that ‘there would be a much higher uptake, and not just amongst the Jewish community’ (Jewish Burial Society). Not only does NIA not violate any religious laws, but it was also considered to be psychologically easier for parents to accept because it was ‘kinder to the baby’ (P44, Jewish bereaved parent), ‘in terms of your mind, you’re put at rest. You don’t have that image of oh, gosh someone’s been cut up and then everything’s been taken out’ (FG6, Somali Muslim, women). Familiarity with the MRI machine was also cited as a reason why some participants would be more likely to consent to NIA. There were, however, certain caveats raised, namely turnaround time, circumstances of the loss and accepting God’s will.
Turnaround time
Members from both faith groups discussed the importance of burying the body as soon as possible and that ‘the actual soul of the person who’s passed away can’t come to eternal rest until their bodies have been buried’ (Orthodox Jewish Health Advocate), that prior to the burial ‘you’re in this horrific limbo’ (FG8, Jewish Orthodox, mixed gender) and that the grieving process cannot begin until after the funeral. Most participants would be prepared to wait 24 hours, although others cited 2 or 3 days, acknowledging that the particular circumstances would be a key factor:
I would wait 1 or 2 days. I think where there were lots of miscarriages people would wait 2 to 3 days.
FG9, Pakistani Muslim, women
When the turnaround time was likely to be longer than 24 hours, some participants would seek advice from a religious leader. Although a swift burial was an important aspect of Jewish religious life, one Jewish leader commented that for coronial cases, ‘the community would prefer to wait longer and have a non-invasive autopsy than a full autopsy and a quick burial’ (Jewish Burial Society).
Circumstances of the loss and likelihood of a diagnosis
Community members indicated that they were more likely to consent to NIA (or seek consent from a religious leader) if there had been multiple miscarriages or neonatal deaths, or when the information might ‘help us concretely in the future’ (FG11, Jewish Haredi, mixed gender), such as if ‘you might have more children’ (FG9, Pakistani Muslim, women). Similarly, participants indicated that they would be more likely to consent ‘if the doctor said we have no idea [why this child died] then I would probably say yes’ (FG7, mixed ethnicity, Muslim, women). Acceptability also depended on the chance that useful information would be found:
If the doctor said, ‘Well, you know, it’s a 50/50 chance we might not get anything, then I don’t know if I would.
FG5, Bangladeshi Muslim, women
Accepting God or Allah’s will
Despite NIA being religiously permissible, some participants still commented that they would decline on the basis that it was unnecessary because it was the will of God:
. . . it was destined, his time was up . . . I don’t need any more answers.
FG5, Bangladeshi Muslim, women
This view was particularly prominent in the Jewish Haredi focus group:
As part of our religion, we’re not so interested in why did this happen, because we look at things that happen maybe with a higher purpose . . . the reason and the causes doesn’t really make a difference to us because, for us, if it was meant to happen.
FG 11, Jewish Haredi, mixed gender
Placental examination
Most participants did not have any concerns with placental examination in cases of SB and were unaware of any religious observances associated with handling the placenta. A few participants commented that in cases of SB, ‘if the placenta is connected it gets buried.’ (FG11, Jewish Haredi, mixed gender).
Minimally invasive autopsy and religious permissibility
It was acknowledged by both Muslim and Jewish focus group participants that, strictly speaking, MIA was not religiously acceptable: ‘you’re still making an incision . . . you’re still taking samples’ (FG8, Jewish Orthodox, mixed gender). ‘In the Islamic perspective, it’s still forbidden because of the cutting, whether it’s a big cut or a small cut’ (FG7, mixed ethnicity, Muslim, women). This viewpoint was supported by religious leaders and community leaders who cited that ‘it still constitutes violation of the body’ (Orthodox rabbi) and ‘from a Muslim perspective it’s not acceptable’ (Muslim Burial Society). Nevertheless, the majority acknowledged that MIA was more acceptable than a full post-mortem, ‘while it’s still forbidden it’s less forbidden’, and ‘if there was no alternative one would definitely choose the latter [MIA over full autopsy]’ (Orthodox rabbi). Some community leaders also commented that it could be religiously justified ‘if parents have had more than one SB or neonatal death and they are very concerned’ (Muslim Burial Society) or ‘if it’s important for us to discover what happened, this might help us save future lives or it may be relevant to your other children’ (Masorti rabbi), highlighting that like a traditional autopsy there are times when it could be argued that MIA is religiously permissible.
Uptake
Despite acknowledgement that from a religious perspective MIA was questionable, around half of focus group participants thought that this approach was acceptable, recognising that ‘it’s only a small cut’ (FG4, mixed ethnicity, Muslim, mixed gender) and ‘it would be a much more palatable offer than full autopsy’ (FG8, Jewish Orthodox, mixed gender). As with NIA, participants’ comments suggested that they would be more likely to consent to MIA if there had been multiple unexplained losses. Some stated that they would first opt for NIA but ‘If there is still confusion, then go for minimally invasive autopsy’ (FG10, Pakistani Muslim, men). Certain comments alluded to the fact that psychologically, MIA was preferable to a full autopsy because it was more ‘respectful’ to the body (Muslim chaplain 1), ‘it sounds nicer, the child would look the same afterwards’ (FG8, Jewish Orthodox, mixed gender) and ‘psychologically it makes you think it’s OK, it’s just a tiny cut’ (FG7, mixed ethnicity, Muslim, women). One Muslim woman was reassured that parents would potentially be able to ‘direct it [the laparoscopic equipment] to where you want . . . they’re not going to fiddle around and take other things’ (FG6, Somali Muslim, women). Some would first want to discuss the procedure with a religious leader before consenting. Others cited that although it was preferable to a full autopsy, they would still decline because ‘the principle of cutting up, it still remains the same for me’ (FG10, Pakistani Muslim, men). This viewpoint was particularly pronounced for members of the Jewish Haredi community, all of whom said that they would not consent to MIA unless it was required by law:
Unless it’s requested by a coroner then the answer would be no.
FG11, Jewish Haredi, mixed gender
Preference for the ‘gold standard’
A small minority of focus group participants commented that they would still choose a full autopsy over NIA or MIA, as it was about ‘finding answers’ (FG9, Pakistani Muslim, women) and they would ‘want to go with what has the highest success rate’ (FG8, Jewish Orthodox, mixed gender).
Recommendations for improving uptake of less invasive autopsy
Suggestions for raising awareness and improving uptake of LIA related to four themes: (1) knowledge and awareness within the community; (2) advice and support; (3) challenging the status quo; and (4) terminology (Box 2).
-
Improving awareness of the value of autopsy among community members.
-
Educating religious leaders about LIA.
-
Educating the community through educational sermons at mosques/synagogues.
-
Hosting a conference on LIA for religious leaders and community leaders.
-
Raising awareness of LIA through social media platforms.
-
Citing the views of religious authorities in any written or online information about LIA.
-
Having hospital chaplains from the Muslim and Jewish communities with knowledge of LIA who can advise and support families.
-
Training of midwives, doulas and general practitioners who work within the Muslim and Jewish communities about LIA.
-
Training and awareness for health professionals who might speak with parents following a loss to understand Muslim/Jewish laws and customs relating to autopsy.
-
Moving away from the idea that all autopsy is forbidden.
-
Reducing stigma associated with autopsy among the Muslim and the Jewish community.
-
Using words such as ‘imaging’, ‘scanning’, ‘MRI’, etc., when describing NIA.
-
Using words such as ‘keyhole surgery’ when describing MIA.
-
Acknowledging that the word ‘autopsy’ or ‘post-mortem’ is likely to have a negative impact and being mindful of when and how it is used.
Discussion
There are 2.7 million Muslims and 263,000 Jewish people currently living in England and Wales, and both populations are growing. 100 Moreover, in the UK, two-thirds of Muslims are of Asian origin (primarily Pakistan and Bangladesh) and they have the second highest risk for SB (6.3/1000 births vs. 4.16/1000 births for UK population), neonatal death (2.3,1000 births vs. 1.77/1000 for UK population) and extended perinatal death (8.7/1000 births vs. 5.92/1000 for UK population). 9 To our knowledge, this is the first study to explore in depth the acceptability of LIA among members of the Muslim and Jewish communities. Even though the study was conducted in the UK, the findings may be of relevance to other countries with significant Muslim and/or Jewish populations.
In this unique exploration of the acceptability of LIA, we have shown that there are no religious objections to NIA and that it is far more acceptable to Muslim and Jewish parents than a traditional autopsy, which, as other studies have also demonstrated,31,32,39,117,118 most would decline. Although MIA is still viewed as invasive and is therefore not strictly religiously permissible, it is less objectionable than a traditional autopsy, particularly in circumstances when investigation is required (such as a coronial procedure), and it would be acceptable to a significant number of Muslim and Jewish parents if the information could help prevent losses in future pregnancies.
In most focus groups and parent interviews, a diverse range of views and attitudes were expressed relating to the acceptability of the three methods of autopsy, irrespective of ethnic group (for the Muslim participants), gender or previous experience of loss. The one group in which this differed was the Jewish Haredi focus group, in which all the participants identified themselves as being ‘very religious’ and attitudes towards the different types of autopsy were homogeneous. Only NIA was seen as acceptable in specific circumstances and with consent from a rabbi, with all other types of autopsy considered unacceptable when not required by HM Coroner. This is likely to reflect the strict observance to Jewish law within this community and the common viewpoint that the loss of a baby or a child is the will of God and, as such, does not require further explanation (a view also expressed by a number of Muslim participants). Seeking advice from a rabbi when faced with important life decisions is common among this religious group and it is rooted in the principle of da’as Torah (Torah knowledge), which mandates that one must seek Torah-based guidance from a rabbinic authority on all matters of life. 119
Most religious leaders and community leaders who took part in this study were aware of the use of NIA for adult coronial cases and valued this option in those circumstances in which an autopsy was legally required. The use of NIA for adult coronial cases was established at the request of the Jewish community in Manchester in 1997120 and has gained increasing awareness among the Muslim and Jewish communities in recent years. 121–123 In most of the adult cases, however, the cost of the service is covered by the community themselves124 at a cost of around £500–900. 125 The new Coroners and Justice Act 2009 recognised the importance of religious requirements relating to autopsy examination and permitted expeditions release of bodies where appropriate, as well as permitting less invasive post-mortem examinations. 126 Moreover, in 2015 a high court judge backed the religious right of Muslim and Jewish people to ask for NIA and that it must be considered by the coroner if there was a ‘reasonable possibility’ that it could establish the cause of death. 123 Given that NIA has been allowed within both communities for coronial cases, it is unsurprising that extending its use for non-coronial cases in childhood was perceived to be acceptable.
The findings from this study suggest that the availability of LIA may result in an increase in uptake from members of the Muslim and Jewish communities, although this is likely to require a quick turnaround to enable burial, preferably within 24 hours. Implementing such a service raises a number of practical and ethical challenges. Providing a 24 hours a day, 7 days a week service would require capital investment, training and support of health-care management to provide dedicated autopsy imaging facilities and personnel, including pathologists, radiographers and APTs. These implementation challenges have been identified in previous research with health professionals and HM Coroner. 107 Moreover, important questions around prioritising access for Muslim and Jewish parents at the expense of other parents having to wait longer, who may also prefer a less invasive approach, need addressing. Further thought will need to be given as to how LIA might be implemented into clinical practice in a way that is sensitive to the preferences and needs of all parents. In addition, as part of any possible future implementation study, the impact of timing of release and burial in relation to examination type should be assessed.
Participants identified a number of practical recommendations for the successful implementation of LIA among the Muslim and Jewish communities, largely related to raising awareness among the community as well as religious leaders and health professionals. Pathologists, radiologists and other professionals with experience of LIA will need to play a key role in terms of training and community outreach. One recommendation related to the importance of training health professionals about Muslim and Jewish laws and customs concerning autopsy, particularly as many health professionals lack confidence in communicating across cultural groups different from their own. 127 However, as participants had varying attitudes towards the acceptability of different types of autopsy, health professionals must avoid cultural assumptions or stereotyping and focus on facilitating individualised care.
Less invasive autopsy was preferable to full autopsy, not just for religious reasons but also because it was perceived to be ‘kinder’ and less traumatic to both parent and child. These viewpoints align with those that have been observed among the general parent population, for whom dislike of the invasiveness of the procedure and the desire to protect one’s baby or child from harm have been identified as key barriers to autopsy. 44 As such, it is highly likely that many non-Muslim and non-Jewish parents will find LIA preferable to a traditional autopsy. Further research with bereaved parents across a wider range of cultural, ethnic and religious groups is therefore required.
Key strengths of the study lie in the high response rate from the religious leaders and community leaders (thus reducing the risk of non-response bias), the range of religious leaders and community leaders that were included, the inclusion of community members from different religious and ethnic backgrounds and locations, and the range of experiences of loss, thus ensuring a wide range of viewpoints. Furthermore, we validated the findings through member checking with key informants to increase rigour. Although focus groups offer advantages associated with insights into attitudes and opinions that group interactions can enable, a challenge is the possibility of group dynamics promoting uniformity of views. We tried to address this by emphasising our interest in different perspectives at the start of each focus group. A further limitation is that in some cases community facilitators and key informants supporting recruitment into focus groups approached community members drawn from an established group of contacts, and in some cases focus group participants knew each other. This may have had an impact on the diversity of opinions expressed in the group. However, given the range of opinions expressed in most group discussions, this is unlikely to have influenced our conclusions. We provided a generalised description of MIA to study participants, involving a small incision to the stomach. It is possible that additional or alternative approaches may be developed that involve more puncture sites (e.g. up the nasal cavity or at the base of the brain), which will require comparative evaluation with parents to assess acceptability. Finally, the discussion around acceptability and likely uptake of NIA and MIA with the parents was hypothetical and may not reflect decisions people make in real life. Further research to assess actual uptake is required if LIA becomes routinely offered in clinical practice.
Conclusion
Less invasive autopsy is more acceptable to the Muslim and Jewish communities in the UK and has the potential to increase uptake in these religious groups, particularly if turnaround times can be minimised and awareness raised among community members. Our findings are likely to be useful for health professionals and decision-makers who direct future clinical practice in this area and may be of relevance to other countries with significant Muslim and/or Jewish populations. Further work with bereaved parents from other cultural, religious and ethnic groups, as well as quantitative data to provide more accurate estimates of potential uptake, is required.
Chapter 7 Retrospective analysis of existing autopsy data
In this chapter we present an evaluation of histological yield in a large series of previously performed standard autopsies at Great Ormond Street Hospital, based on indication group and tissue. We estimate the likely impact of a policy of widespread availability of LIA on national perinatal and paediatric autopsy activity, incorporating the acceptability findings from previous sections and the numbers of cases using national data.
Methods
Great Ormond Street Hospital is a tertiary referral centre for perinatal and paediatric autopsies, with several hundred cases performed per annum by specialist pathologists. Detailed data from all such autopsies since 1995 are recorded in a dedicated autopsy database, including > 400 variables/fields, with associated objective criteria described in a database handbook. The database allows identification of cases for research use, has Research Ethics Committee approval and has been used for several previous research studies. 128,129
Specifically, for the purposes of this study, each case was classified as SB/intrauterine fetal death (IUFD), ToP, SUDI or SUDC, according to clinical presentation. For each case, all organs examined were recorded as being normal, abnormal but not relevant to cause of death or main diagnosis, abnormal and possibly relevant to cause of death or main diagnosis, or abnormal and definitely relevant to cause of death or main diagnosis, based on both macroscopic appearance and histological (microscopic) examination.
As part of data entry, judgements made by the reporting pathologist regarding the abnormalities present at internal examination and on histological examination were recorded according to predefined categories (Figure 2). These categories were independent of each other, so they could be used in any combination for macroscopic and microscopic examination, and could be explored further within free-text boxes within the database. These categories were also applied to placental examination and placental histology, when appropriate.
FIGURE 2.
Categories of abnormalities.
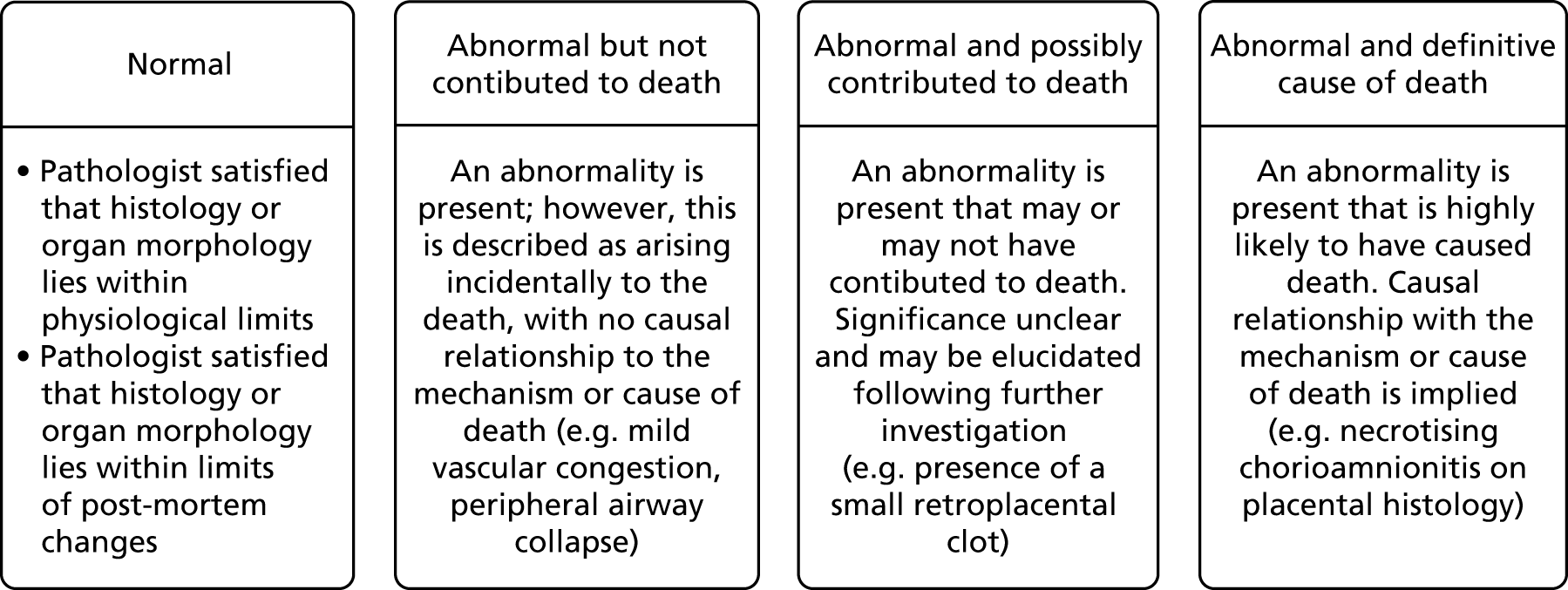
Following completion of data entry, data were extracted for all completed cases between 2005 and 2016, according to referral category (SUDI, SUDC, IUFD or ToP) and were analysed using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and StatsDirect (StatsDirect, Altrincham, UK), using descriptive statistics, chi-squared and comparison of proportions tests when appropriate.
Results
The relative yield (displayed as a percentage of the total number of cases in the relevant referral category in which data on that specific organ were available) of macroscopic examination and histological examination of organs by referral category are presented in Table 9 and Figure 3.
| Organ | Number of SUDC cases with adequate macroscopic and histological comment | Percentage of SUDC cases with adequate macroscopic and histological comment |
|---|---|---|
| Heart | 739 | 90 |
| Lungs | 786 | 95 |
| Brain | 661 | 80 |
| Adrenals | 654 | 79 |
| Thyroid | 466 | 57 |
| Liver | 735 | 89 |
| Kidney | 715 | 87 |
| Pancreas | 539 | 65 |
FIGURE 3.
Percentage of cases of SUDC for which cause of death was determined by macroscopic examination of organs.
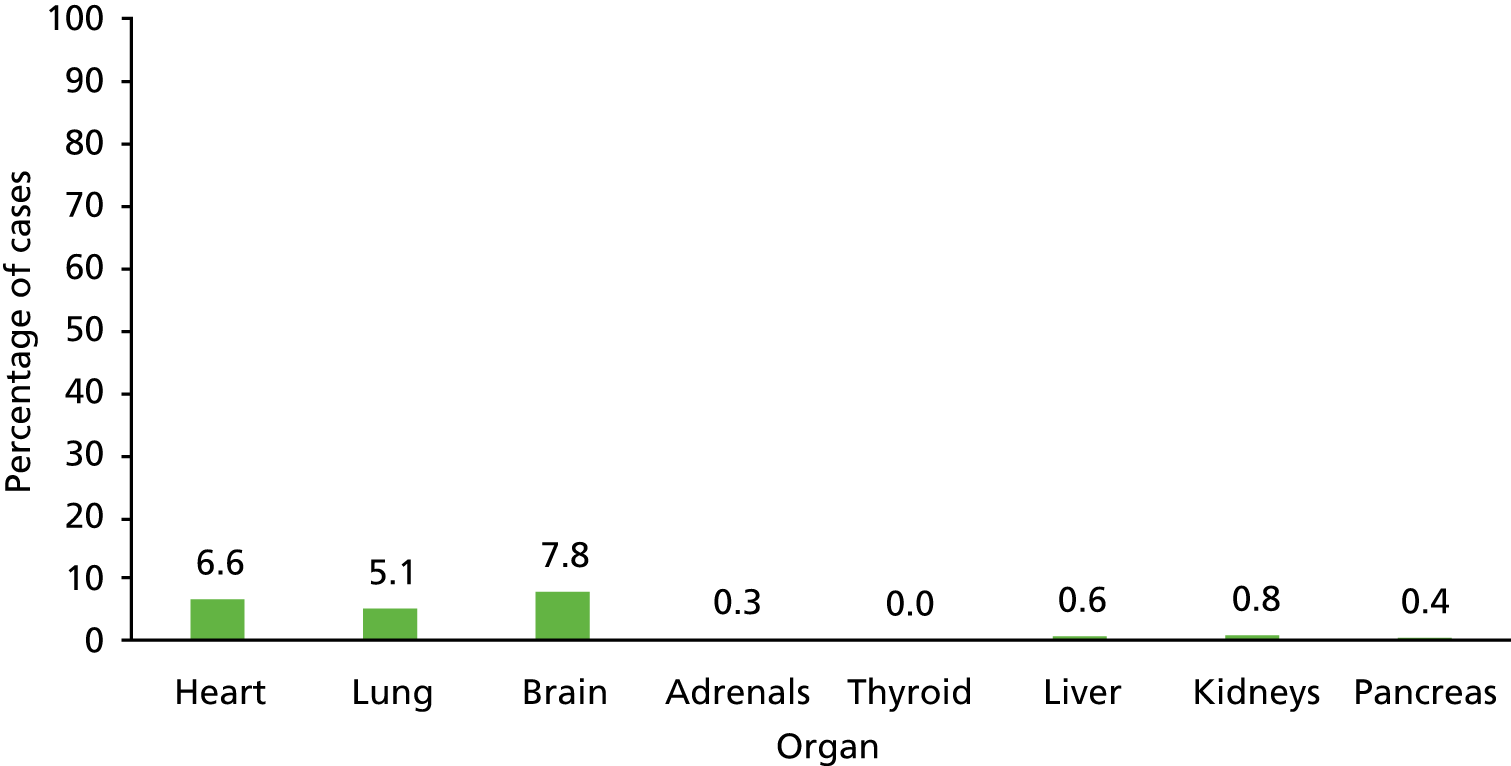
Sudden unexpected death in childhood
There were 824 cases of SUDC recorded in the database. Analysis of the cases revealed enough information to code the organs appropriately for both macroscopic and histological examination in most cases (range 65–95%); reasons that data for an organ may have been unavailable for analysis include lack of sampling, autolysis, or failure of the target tissue to survive histological processing.
Figure 4 demonstrates the percentage of SUDC cases in which a microscopic abnormality was discovered on histological investigation of an organ when the macroscopic evaluation of that organ was described as normal.
FIGURE 4.
Yield of histological examination in cases of SUDC (% of cases with a microscopic abnormality representing the cause of death when macroscopy was normal).
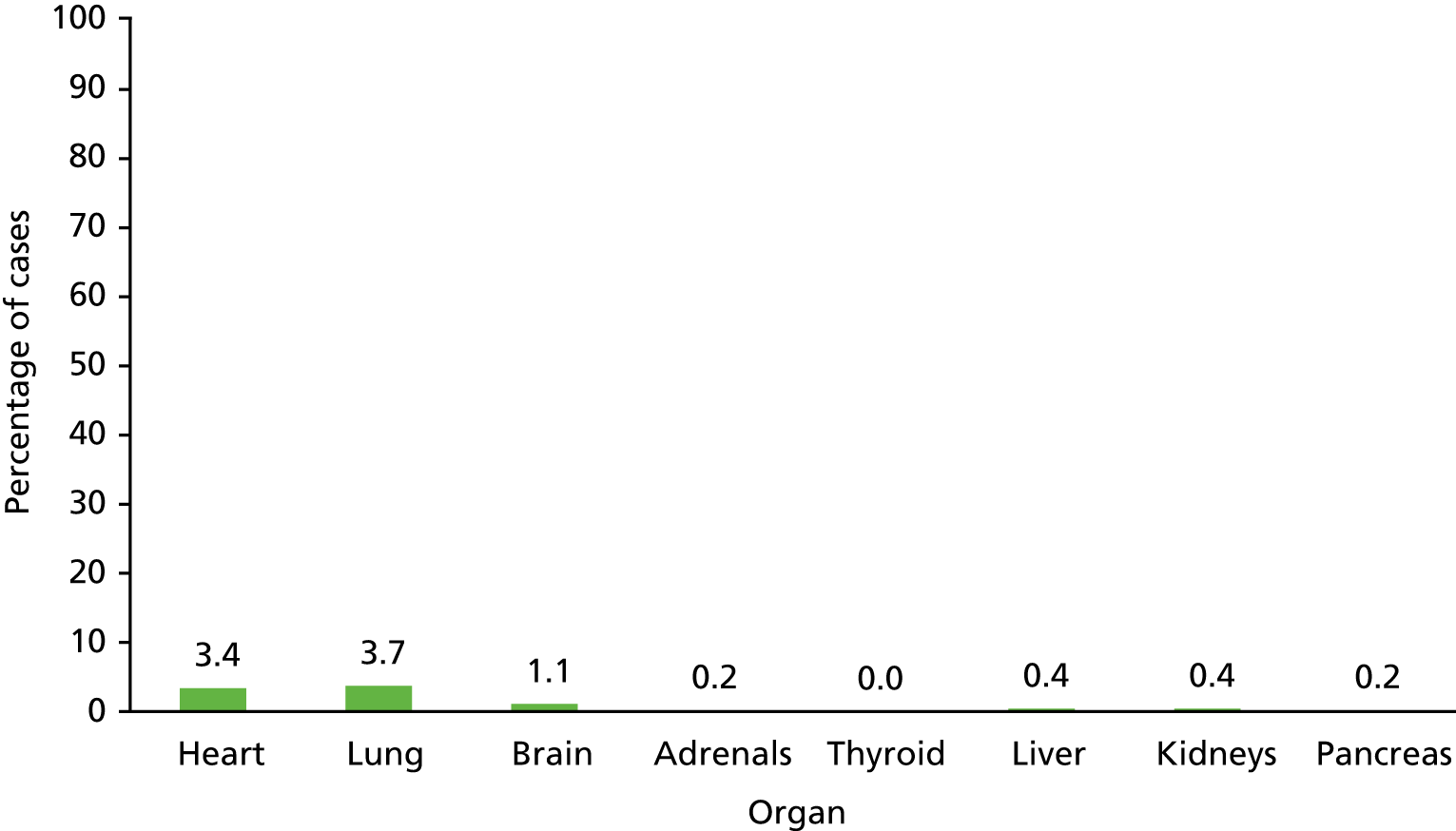
Sudden unexpected death in infancy
There were 1739 SUDI cases within the database. Analysis of the cases revealed enough information to code both the macroscopic and microscopic (Table 10 and Figures 5–10).
| Organ | Number of SUDI cases with adequate macroscopic and histological comment | Percentage of SUDI cases with adequate macroscopic and histological comment |
|---|---|---|
| Heart | 1638 | 94 |
| Lungs | 1680 | 97 |
| Brain | 1503 | 86 |
| Adrenals | 1586 | 91 |
| Thyroid | 1210 | 70 |
| Liver | 1647 | 95 |
| Kidney | 1631 | 94 |
| Pancreas | 1447 | 83 |
FIGURE 5.
Percentage of cases in SUDI for which cause of death was determined by macroscopic examination of organs.

FIGURE 6.
Yield (% of cases) of histological examination in SUDI (microscopic abnormality representing cause of death when macroscopy is normal).
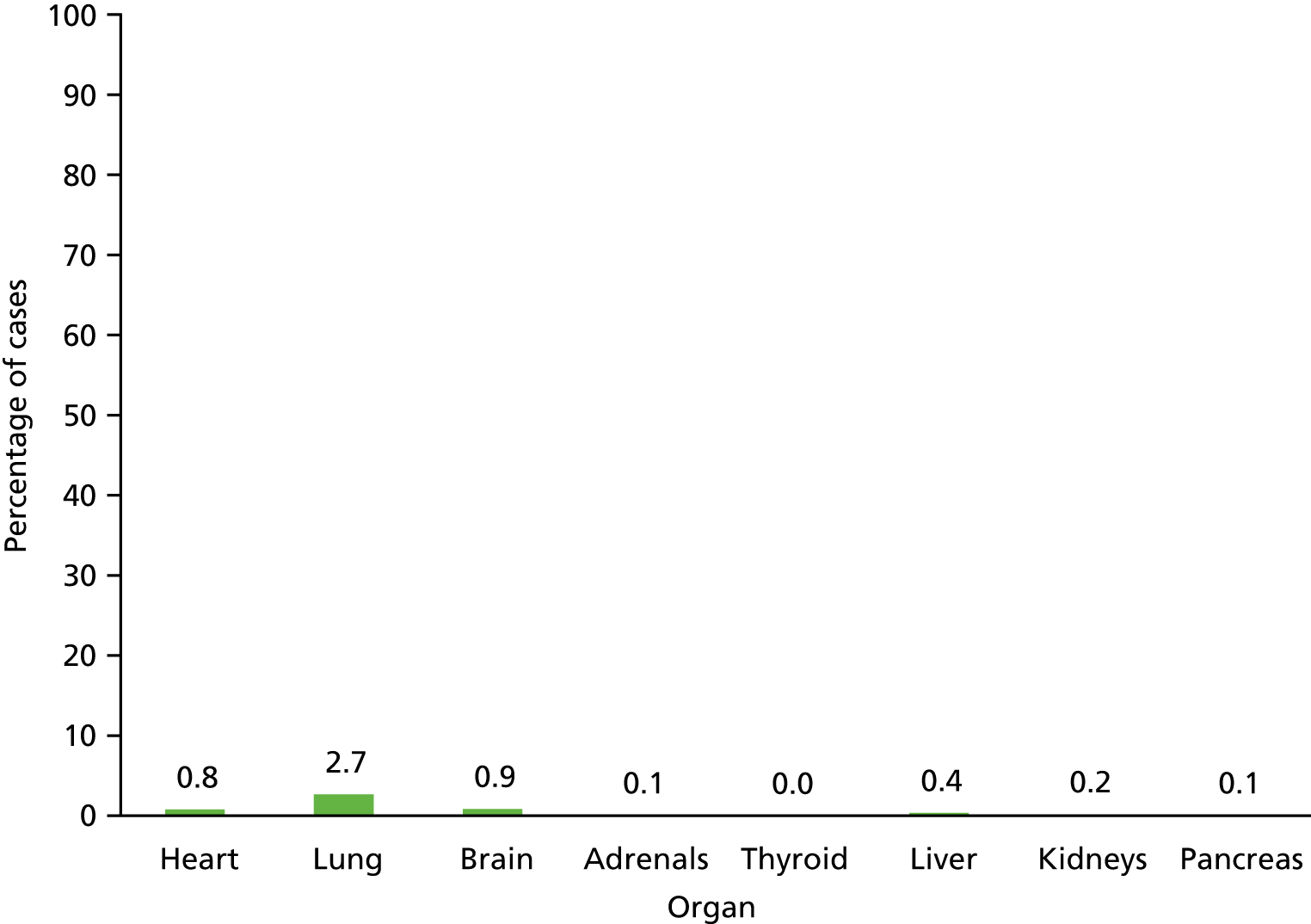
FIGURE 7.
Percentage of cases in SB/IUFD for which cause of death was determined by macroscopic examination of organs.

FIGURE 8.
Yield (% of cases) of histological examination in SB/IUFD (microscopic abnormality representing cause of death when macroscopy is normal).
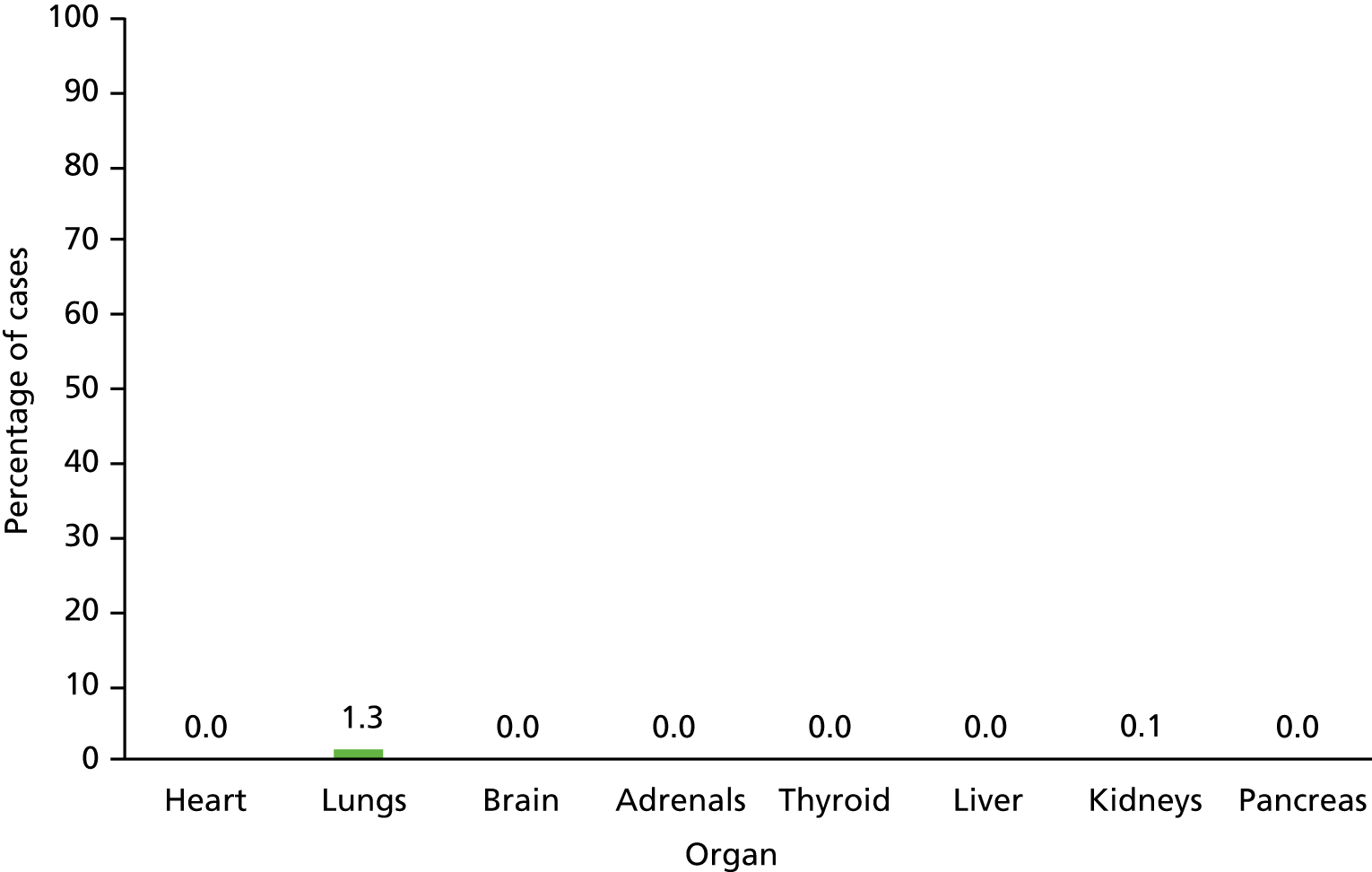
FIGURE 9.
Percentage of cases in ToP for which cause of death was determined by macroscopic examination of organs.
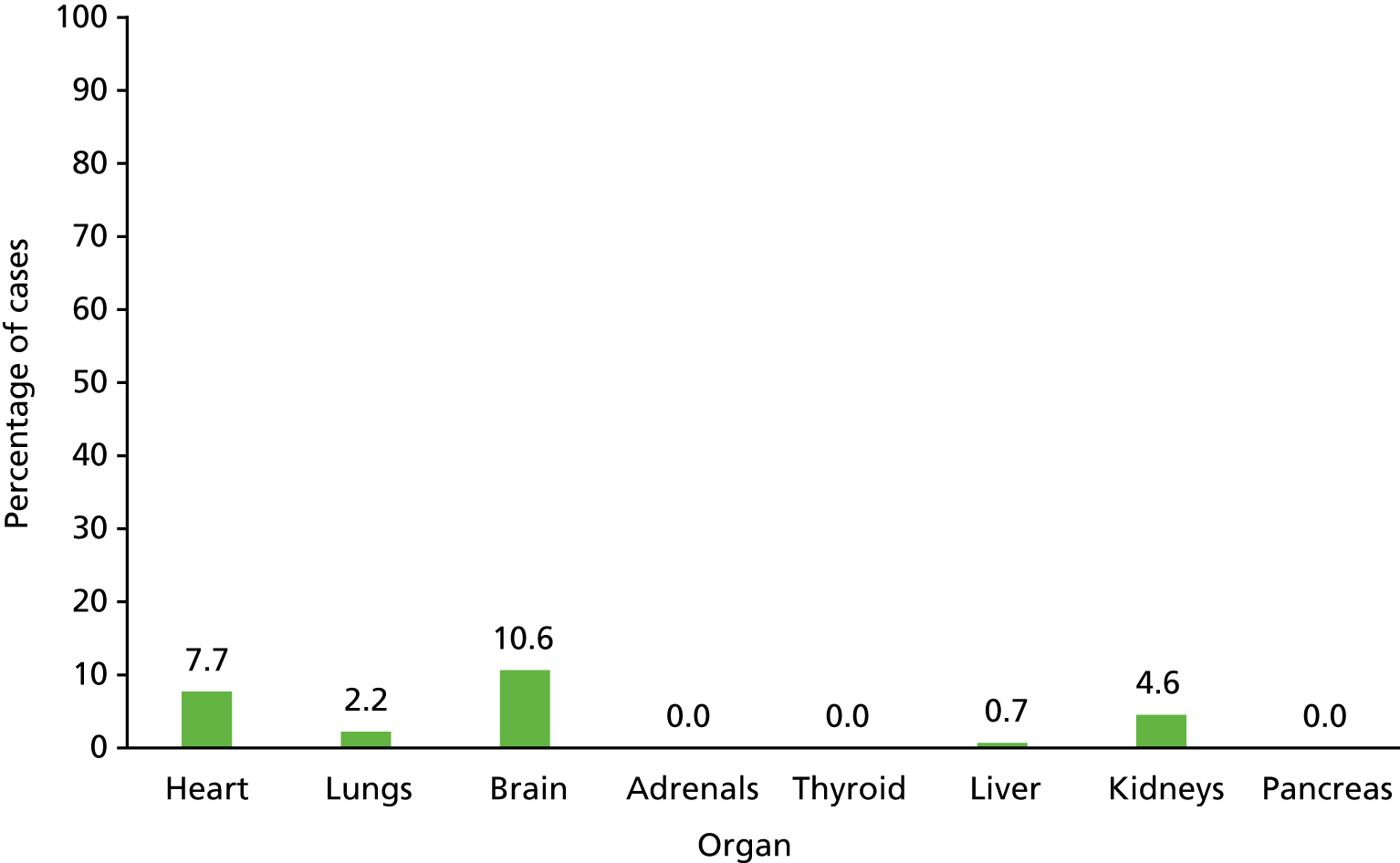
FIGURE 10.
Yield (% of cases) of histological examination in ToP (microscopic abnormality representing cause of death when macroscopy is normal).

Discussion
These data demonstrate that in 5–10% of SUDC and SUDI cases (see Figure 3) the final cause of death is determined by routine histological sampling of macroscopically normal organs, predominantly the heart and lungs, with a few cases contributed by brain, liver and kidney examination. Routine histological sampling therefore remains an important aspect of investigation even if post-mortem imaging appears normal.
In contrast, routine sampling of any macroscopically normal organs only very rarely [< 0.2% (4/2749), 95% CI 0.06% to 0.4%] provides the cause of death in fetal cases (including SB, IUFD and ToP; the approximately 1% of cases in the SB and IUFD group represented detection of ascending infection on lung sampling which would have been detected on placental examination and sampling had this been available). Therefore, in fetal cases in which macroscopic examination for structural abnormalities and post-mortem imaging is normal, there is little indication or yield for invasive organ sampling and histological examination to determine the cause of death. Targeted sampling of abnormal organs and lung may be sufficient to identify abnormal and contributory cases.
Routine histological sampling of macroscopically normal organs provides significant contribution to the cause of death in around 5–10% of SUDI and SUDC cases and is therefore recommended. Histological sampling of macroscopically normal organs in fetal cases, including ToP, SB and IUFD, only very rarely provides useful information for determining the cause of death or the main diagnosis and for many organs the yield is close to zero. Therefore, routine sampling in such cases is of limited value. In cases with contributory histological findings, almost all cases relate to heart, lungs, liver and kidney.
Estimation of widespread less invasive autopsy availability on autopsy activity based on national data
Based on published national statistics, there are around 3000 ToPs for abnormality, 3000 SBs, 3000 second trimester miscarriages, 2000 neonatal deaths, 400 unexpected infant deaths and 50 unexpected child deaths per annum. 1,3,4,130 This equates to around 450 HM Coronial (non-consented) cases per annum in infants and children, plus 11,000 fetal and neonatal deaths and ToPs who would be eligible for consented post-mortem examination (total 11,450 eligible cases per annum).
Based on these data, around 5% of all potentially eligible LIA cases are coronial infant and child deaths, around 25% are ToP and the majority (70%) are miscarriages, SBs and neonatal deaths. These national proportions are similar to the proportion of responders in the present study’s parental survey (2.3% child deaths, 2% infant deaths, 18.3% ToP, 66.1% miscarriages and stillbirths; 859 total cases for this study and 11,450 total cases for the annual national model). Currently, 47% of parents who have had a SB and 29% of parents of neonatal deaths agree to standard autopsy. 9 These data indicate that an estimated 4680 [4230 representing 38% (current consent rate) of ToP/IUFD cases +450] standard autopsies are performed in England and Wales annually of a possible 11,450 eligible cases.
Current situation and projected impact of minimally invasive autopsy
Uptake of standard autopsy is around 45%131 for fetal cases and 100% (non-consented, mandatory) for SUDI and SUDC, resulting in around 4680 standard autopsies nationally per annum and 6770 women having no post-mortem investigation.
Of 11,450 cases, 450 SUDI and SUDC cases would continue to undergo standard post-mortem, along with 1637 parents who would choose this option, 5210 parents who would choose MIA and 3527 parents who would choose NIA. The total post-mortem investigation workload would increase (more than double) from 4680 to 10,374. If there were 10 major centres nationally, each centre would need to perform around 1000 examinations per year, including around 160 standard autopsies and around 1000 post-mortem imaging investigations (these are estimates to provide likely magnitude, but are not intended to be robust for planning purposes; this would be the aim of a future study).
The MIA cases would have similar rates of detection of major diagnosis as standard autopsy, hence increasing the overall diagnostic yield. Furthermore, even for the NIA cases with no sampling performed, as these are fetal cases with mainly anatomical and/or placental abnormalities detectable by post-mortem imaging and placental examination, the reduction in ‘correct’ final diagnosis compared with standard autopsy would be < 1% due to the low yield of routine histological sampling in this group. However, < 200 (estimated 1.6%) of parents would have no form of investigation after death compared with > 50% receiving no formal autopsy investigation at present.
Numbers needed for further evaluation studies
As NIA is already 95% concordant with standard autopsy for fetal cases, in order to demonstrate that MIA with sampling improves ‘accuracy’ or concordance rate from 95% to 97.5%, with a power of 80% at alpha = 0.05, a minimum of 984 MIAs would be required to be performed. Given that at a specialist MIA centre it has taken several years to perform 100 cases and accuracy appears similar to standard autopsy, it is unlikely to be feasible to perform a multicentre study to demonstrate a small increase in performance, especially as most funders would require 90% power. Furthermore, as around half of parents who request LIA would request NIA rather than MIA, recruitment time would be substantially increased, further reducing the feasibility of such a trial.
It is recognised that NIA performs worse in SUDI and SUDC cases (around 75% concordance) and that in this group histological sampling provides most value (see Current situation and projected impact of minimally invasive autopsy), therefore a potential future trial could provide value in this subgroup. To demonstrate that MIA with sampling improves ‘accuracy’ or concordance from 75% to 87.5% with power of 80% at alpha = 0.05, a minimum of 304 SUDI and SUDC MIA cases would be required. However, given that almost all such cases represent HM Coronial autopsies, and most HM Coroners do not currently request or support MIA due to potential medicolegal reasons, to recruit > 300 cases at even a 10% Coronial referral rate would require a national study and would take more than a decade to complete. To demonstrate that MIA improves ‘accuracy’ or concordance from 95% to 97.5% with power of 80% at alpha = 0.05, a minimum of 1812 fetal MIAs would be required to be recruited.
For these reasons of feasibility, in addition to the fact that the accuracy of LIA is established, the vast majority represent fetal cases in which accuracy is already > 95%, the value of histological sampling is both limited and predictable, and the LIA approach is highly acceptable to parents and families, it is suggested that no further clinical trial is indicated, but rather that the next step is an implementation study to determine the cost-effectiveness and logistics of offering a national perinatal LIA service as part of routine NHS care.
Chapter 8 Discussion, including strengths and limitations, implications for practice, future research and conclusion
In this chapter we discuss some of the key findings resulting from this programme of research. We consider how the findings impact health practice and policy and make recommendations for further action.
Discussion
To the best of our knowledge, this is the largest study conducted in the UK examining the views and preferences of bereaved parents towards standard and less invasive forms of autopsy. The major finding from this research is that there is likely to be a significant increase in uptake of post-death investigation if personalised and more acceptable approaches were routinely available, with parental preference for less invasive procedures. Our study suggests uptake could be as high as 90%. Dislike of the invasiveness of the standard procedure was found to be one of the main reasons that parents declined an autopsy, as has been highlighted through both our qualitative and quantitative research with parents as well as the systematic review of the literature. The availability of less invasive options would therefore make autopsy available to parents who currently decline, including those from the Muslim and Jewish communities for whom autopsy is unacceptable in the majority of cases for religious reasons.
Strengths and limitations
The empirical research conducted had a number of notable strengths. First, we used a mixed-methods approach employing both qualitative and quantitative research methods. Mixed-methods approaches are likely to yield the most comprehensive picture, as their integration facilitates a deeper and broader understanding of the phenomenon. Another benefit is that each method can help to validate the other (triangulation). Second, we had a large sample size in our survey which yielded statistically significant results. Third, the free-text survey comments along with qualitative interviews provided a rich data source from which to conduct qualitative analysis. Finally, a further strength was that patient and public involvement was embedded from the outset; patient and public input into the survey design was particularly important in ensuring that the questions were clearly phrased and included the benefits and limitations of the different approaches.
A limitation of the survey was that there was a significantly larger number of participants recruited retrospectively rather than prospectively, although there was no overall difference in preferences for autopsy between the two cohorts. In addition, there was a low response rate from parents recruited prospectively, which may lead to biased findings. Another potential limitation is that we did not collect data on how long ago the loss occurred; time since loss may have influenced their views and preferences. Although the qualitative data have given us a rich in-depth insight into the views of key stakeholders towards less invasive forms of autopsy, a potential limitation frequently levied at this form of research concerns the validity and generalisability of the work. However, many of the findings from this research have been identified in similar studies and key findings, and recommendations were supported and validated through participant feedback at a dissemination meeting attended by key stakeholders (parent advocates, health professionals and religious leaders). Finally, although we have developed recommendations in respect of how LIA might potentially be implemented into clinical practice, there is currently a lack of health economic data to understand how affordable such proposals are.
The data presented reflect the relative proportions of fetal and paediatric autopsies performed, specifically that the majority represent intrauterine deaths, terminations of pregnancies or SBs, with a significant proportion of coronial infant deaths but very few paediatric deaths. Therefore, caution should be exercised in extrapolating results to this latter group, as limited data are available.
Implications for practice
The findings from this study have significant implications for future clinical practice. Given the current low uptake rates for standard autopsy, an alternative is required, both to provide best care for parents and families and for public health reasons, including evaluating the quality of obstetric and neonatal care. 115 The broadening range of investigative strategies now available aligns with NHS England’s goal of significantly improving patient choice by 2020. 42 Several requirements must be put in place to make LIA a viable alternative for parents. The findings from our interviews with health professionals and coroners have highlighted the importance of training radiologists to interpret imaging results and pathologists to conduct image-guided biopsies, the availability of scanning equipment, training for health professionals to offer LIA appropriately, and adapted consent procedures and consent forms. 107 This would require significant investment from hospital managers and thus a detailed cost–benefit analysis would be required to determine the cost of implementing such a service. Furthermore, although all post-mortem MRI can be performed in standard NHS scanners (as was the case in the current study), such that additional dedicated MRI machines are not required, there are logistic issues that require attention in order to perform scans out of hours. These particularly relate to staffing by radiographers who are both prepared to work out of normal hours and with deceased patients, and ensuring that appropriate cleaning facilities are available for routine scanner use the following day.
Maintaining a sufficient level of health professional education and awareness with regards to autopsy options could prove to be a major challenge, as numerous barriers to an effective autopsy consent process exist, even prior to the addition of less invasive options such as MIA and NIA. 7,132 These barriers could be compounded by the increasing complexity of the available autopsy options, patchy availability of MIA and NIA, and the relatively high turnover environment of clinical staff. Consideration will need to be given as to how autopsy options might be offered. For example, parents supported a stepwise approach to consenting to autopsy, beginning with the least invasive option, but moving to more invasive options if a diagnosis was not found. A more personalised form of counselling around autopsy whereby type of death, antenatal findings, clinical history, etc., are taken into account when presenting the various options to investigate cause of death is also important. Further clinical work is also required to assess concordance between MIA, NIA and standard autopsy in order that appropriate counselling can be provided across a range of specific clinical scenarios.
Further research
Although this study has demonstrated the likely acceptability of LIA by bereaved parents, further research is now required to evaluate the implications of delivering this approach as a routine service. For example, at present, as expertise is located in only one or two centres, there will need to be both training and education of obstetric and perinatal pathology staff. In addition, resource implications, both for radiology and for pathology departments, must be considered.
Evaluation of widespread national implementation
Given that less invasive methods of examination after death provide similar accuracy to standard autopsy, especially in fetal cases, but are considered much more acceptable approaches, subsequent research should focus on an evaluation of widespread implementation of these options nationally. Service users, managers, commissioners and health economists should evaluate the cost-effectiveness and resource requirements to scale LIA options as a national service within the NHS. For such evaluation, fetal and infant groups remain the primary populations to assess, as these populations represent by far the greatest number of cases.
Research to identify ways of enhancing the communication process
The systematic review identified a number of barriers to uptake of autopsy from both the parent and the health professional perspective. A key barrier was the communication that occurred between parents and health professionals and the support that was provided during the decision-making process. Further research should be carried out to determine the optimal methods of patient communication, including recommendations for practice.
Actual uptake and impact of less invasive autopsy in clinical practice
If and when LIA becomes routinely available, research to determine actual uptake as opposed to hypothetical uptake would be valuable. Likewise, research to determine what the psychological and emotional impact of LIA is for parents (and the health professionals consenting them). In particular, it would be useful to understand the mental health benefits for parents consenting to LIA compared with standard autopsy.
Further research to determine effectiveness of less invasive autopsy in specific cases
Sudden unexpected death in infancy and SUDC represent a special case, in which medicolegal issues remain important and in whom tissue sampling provides important information regarding cause of death and for whom less invasive methods may be less appropriate, although further studies are required. However, due to their rarity and the impossibility of randomisation, a targeted clinical trial of this group is unlikely to be feasible. In addition, although MIA may provide benefits, non-coronial paediatric autopsies are so rare that collecting adequate data on these paediatric cases will require ongoing study. However, as the majority of parents who preferred MIA were those of fetal and SB examinations, which are common, future work would achieve greatest yield by focusing on further delineation of value in specific subgroups of these patients.
Conclusion
The findings of this study have determined that LIA approaches are highly acceptable to the majority of bereaved parents and that the widespread implementation of such LIA options would likely result in a significant increase (more than doubling) of the number of perinatal deaths undergoing formal investigations, compared with current standard practice.
Many parents, including those from religious groups for whom invasive post-mortem examination is unacceptable, would opt for non-invasive investigations, which would require a large increase in the availability and expertise of post-mortem imaging investigations.
As concordance with standard autopsy is already very high, with a limited role of tissue sampling, especially for fetal cases, further clinical trials to determine the additional impact of less invasive tissue sampling protocols would require prohibitively large numbers of cases across many centres and are likely to be infeasible. Further studies should focus on evaluation of logistics and cost-effectiveness of widespread implementation of the LIA approach and are likely to require the involvement of policy-makers, commissioners, providers, health professionals, health economists, patient group representatives and, most importantly, parents and families.
Acknowledgements
The authors would like to express their thanks to the following:
Our advisory team, namely Jacqui Stedmon, Heather Skirton, Amy Hunter, Cheryl Titherly and Alex Heazell.
Jenny Ward, Charlotte Bevan, Jane Fisher, Nicola Richardson, Morven Shearer and Gabriel Osrin for reviewing the survey and staff at The Lullaby Trust, ARC, Child Bereavement UK and Sands for their support in disseminating the survey.
The following health professionals for disseminating the survey: Tommy Mousa, Penny McParland, Molly Patterson, Natalie Draper, Joanne Dickens, Mandeep Singh, Donna Southam, Stacey Pepper, Jean Byrne, Denise Symister, Sarah Weist, Chiara Messina, Paula Lavandeira-Fernandez, Natasha Baker, Laura Carbonell, Giorgia Dalla Valle, Simona Cicero, Vivian Holmes, Tracy Hodgkinson, Ferha Saeed, Wendy Olayiwola and Siobhan Shearing.
All the parents who took the time to complete the survey and take part in telephone interviews.
Health professionals and HM Coroners who took part in interviews for this study.
Lily Islam, Nasima Miah, Sidney Sinitsky and Rabbi Harvey Belovski for their help in arranging the focus groups, and all the participants that took part and contributed to this work.
Caroline Doré for her comments on a draft version of this report.
Contributions of authors
Celine Lewis (Senior Social Scientist) designed the study, conducted qualitative and quantitative data collection and analysis, drafted and approved the final report.
John C Hutchinson (Specialty Trainee in Paediatric and Perinatal Pathology) performed MIAs, performed data entry and analysis for the Great Ormond Street Hospital autopsy database and co-authored Chapter 7 of this report. He has approved the final report.
Megan Riddington (Clinical Psychologist) conducted data collection and analysis of the qualitative empirical data, drafted and approved the final report.
Melissa Hill (Senior Social Scientist) conducted data collection and analysis of the qualitative empirical data with key stakeholders, critically revised and approved the final report.
Owen J Arthurs (Consultant Radiologist) designed the study, critically revised and approved the final report.
Jane Fisher (Director, ARC) designed the study, contributed to data collection, critically revised and approved the final report.
Angie Wade (Professor of Medical Statistics) designed the study and statistical analysis, critically revised and approved the final report.
Caroline J Doré (Professor of Clinical Trials and Statistics) provided input related to study design, critically revised and approved the final report.
Lyn S Chitty (Professor Genetics and Fetal Medicine) designed the study, critically revised and approved the final report.
Neil J Sebire (Professor of Paediatric Pathology) conceived the study, interpreted the data, drafted and approved the final report.
Publications
Lewis C, Hill M, Arthurs OJ, Hutchinson C, Chitty LS, Sebire NJ. Factors affecting uptake of postmortem examination in the prenatal, perinatal and paediatric setting. BJOG 2018;125:172–81.
Lewis C, Hill M, Arthurs OJ, Hutchinson JC, Chitty LS, Sebire N. Health professionals’ and coroners’ views on less invasive perinatal and paediatric autopsy: a qualitative study. Arch Dis Child 2018;103:572–8.
Lewis C, Latif Z, Hill M, Riddington M, Lakhanpaul M, Arthurs OJ, et al. ‘We might get a lot more families who will agree’: Muslim and Jewish perspectives on less invasive perinatal and paediatric autopsy. PLOS ONE 2018;13:e0202023.
Lewis C, Riddington M, Hill M, Arthurs OJ, Hutchinson JC, Chitty LS, et al. Availability of less invasive prenatal, perinatal and paediatric autopsy will improve uptake rates: a mixed-methods study with bereaved parents. BJOG 2019;126:745–53.
Data-sharing statement
All available qualitative data arising from the study is contained in the report and nothing further can be shared. All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Department of Health and Social Care . Abortion Statistics, England and Wales 2013 2013.
- Office for National Statistics . Childhood, Infant and Perinatal Mortality in England and Wales, 2012 2015.
- Office for National Statistics . Unexplained Deaths in Infancy, England and Wales: 2013 2015.
- Department for Education . Child Death Review: Year Ending 31 March 2017 2017.
- Gordijn SJ, Erwich JJ, Khong TY. Value of the perinatal autopsy: critique. Pediatr Dev Pathol 2002;5:480-8. https://doi.org/10.1007/s10024-002-0008-y.
- Downe S, Kingdon C, Kennedy R, Norwell H, McLaughlin MJ, Heazell AE. Post-mortem examination after stillbirth: views of UK-based practitioners. Eur J Obstet Gynecol Reprod Biol 2012;162:33-7. https://doi.org/10.1016/j.ejogrb.2012.02.002.
- Heazell AE, McLaughlin MJ, Schmidt EB, Cox P, Flenady V, Khong TY, et al. A difficult conversation? The views and experiences of parents and professionals on the consent process for perinatal postmortem after stillbirth. BJOG 2012;119:987-97. https://doi.org/10.1111/j.1471-0528.2012.03357.x.
- Stock SJ, Goldsmith L, Evans MJ, Laing IA. Interventions to improve rates of post-mortem examination after stillbirth. Eur J Obstet Gynecol Reprod Biol 2010;153:148-50. https://doi.org/10.1016/j.ejogrb.2010.07.022.
- Manktelow BN, Smith LK, Seaton SE, Hyman-Taylor P, Kurinczuk JJ, Field DJ, et al. MBRRACE-UK Perinatal Mortality Surveillance Report: UK Perinatal Deaths for Births from January to December 2014 2016.
- Sieswerda-Hoogendoorn T, van Rijn RR. Current techniques in postmortem imaging with specific attention to paediatric applications. Pediatr Radiol 2010;40:141-52. https://doi.org/10.1007/s00247-009-1486-0.
- Kock KF, Vestergaard V, Hardt-Madsen M, Garne E. Declining autopsy rates in stillbirths and infant deaths: results from Funen County, Denmark, 1986–96. J Matern Fetal Neonatal Med 2003;13:403-7. https://doi.org/10.1080/jmf.13.6.403.407.
- Newton D, Coffin CM, Clark EB, Lowichik A. How the pediatric autopsy yields valuable information in a vertically integrated health care system. Arch Pathol Lab Med 2004;128:1239-46.
- Kumar P, Taxy J, Angst DB, Mangurten HH. Autopsies in children: are they still useful?. Arch Pediatr Adolesc Med 1998;152:558-63. https://doi.org/10.1001/archpedi.152.6.558.
- Royal College of Obstetricians and Gynaecologists, Royal College of Pathologists . Fetal and Perinatal Pathology: Report of a Joint Working Party 2001.
- Confidential Enquiry into Maternal and Child Health (CEMACH) . Perinatal Mortality 2007 2009.
- Burton JL, Underwood J. Clinical, educational, and epidemiological value of autopsy. Lancet 2007;369:1471-80. https://doi.org/10.1016/S0140-6736(07)60376-6.
- Shojania KG, Burton EC, McDonald KM, Goldman L. Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA 2003;289:2849-56. https://doi.org/10.1001/jama.289.21.2849.
- Roulson J, Benbow EW, Hasleton PS. Discrepancies between clinical and autopsy diagnosis and the value of post mortem histology: a meta-analysis and review. Histopathology 2005;47:551-9. https://doi.org/10.1111/j.1365-2559.2005.02243.x.
- Griffiths PD, Variend D, Evans M, Jones A, Wilkinson ID, Paley MN, et al. Postmortem MR imaging of the fetal and stillborn central nervous system. AJNR Am J Neuroradiol 2003;24:22-7.
- Wigglesworth JS, Singer DB. Textbook of Fetal and Perinatal Pathology. Malden, MA: Blackwell Science; 1998.
- Gardosi J, Kady SM, McGeown P, Francis A, Tonks A. Classification of stillbirth by relevant condition at death (ReCoDe): population based cohort study. BMJ 2005;331:1113-17. https://doi.org/10.1136/bmj.38629.587639.7C.
- Great Britain . Human Tissue Act 2004 2004.
- Royal College of Pathologists . Service Specification for Paediatric and Perinatal Histopathology 1995 n.d. www.rcpath.org/resourceLibrary/service-specification-for-paediatric-and-perinatal-histopathology.html (accessed 1 April 2018).
- Gordijn SJ, Erwich JJ, Khong TY. The perinatal autopsy: pertinent issues in multicultural Western Europe. Eur J Obstet Gynecol Reprod Biol 2007;132:3-7. https://doi.org/10.1016/j.ejogrb.2006.10.031.
- McHaffie HE. Crucial Decisions at the Beginning of Life: Parents’ Experiences of Treatment Withdrawals from Infants. Abingdon: Radcliffe Medical Press; 2001.
- Rahman HA, Khong TY. Perinatal and infant postmortem examination: survey of women’s reactions to perinatal necropsy. BMJ 1995;310:870-1. https://doi.org/10.1136/bmj.310.6983.870e.
- Sajid MI. Autopsy in Islam: considerations for deceased Muslims and their families currently and in the future. Am J Forensic Med Pathol 2016;37:29-31. https://doi.org/10.1097/PAF.0000000000000207.
- Davis GJ, Peterson BR. Dilemmas and solutions for the pathologist and clinician encountering religious views of the autopsy. South Med J 1996;89:1041-4. https://doi.org/10.1097/00007611-199611000-00003.
- Burton EC. Religions and Autopsy 2012 n.d. http://emedicine.medscape.com/article/1705993-overview (accessed 8 August 2017).
- Chichester M. Requesting perinatal autopsy: multicultural considerations. MCN Am J Matern Child Nurs 2007;32:81-6. https://doi.org/10.1097/01.NMC.0000264286.03609.bd.
- Cannie M, Votino C, Moerman P, Vanheste R, Segers V, Van Berkel K, et al. Acceptance, reliability and confidence of diagnosis of fetal and neonatal virtuopsy compared with conventional autopsy: a prospective study. Ultrasound Obstet Gynecol 2012;39:659-65. https://doi.org/10.1002/uog.10079.
- Kang X, Cos T, Guizani M, Cannie MM, Segers V, Jani JC. Parental acceptance of minimally invasive fetal and neonatal autopsy compared with conventional autopsy. Prenat Diagn 2014;34:1106-10. https://doi.org/10.1002/pd.4435.
- McDermott M. The continuing decline of autopsies in clinical trials: is there any way back?. Arch Dis Child Fetal Neonatal Ed 2004;89:F198-9. https://doi.org/10.1136/adc.2003.045609.
- Blokker BM, Wagensveld IM, Weustink AC, Oosterhuis JW, Hunink MG. Non-invasive or minimally invasive autopsy compared to conventional autopsy of suspected natural deaths in adults: a systematic review. Eur Radiol 2016;26:1159-79. https://doi.org/10.1007/s00330-015-3908-8.
- Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong W, Olsen O, et al. Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 2013;382:223-33. https://doi.org/10.1016/S0140-6736(13)60134-8.
- Sebire NJ, Weber MA, Thayyil S, Mushtaq I, Taylor A, Chitty LS. Minimally invasive perinatal autopsies using magnetic resonance imaging and endoscopic postmortem examination (‘keyhole autopsy’): feasibility and initial experience. J Matern Fetal Neonatal Med 2012;25:513-18. https://doi.org/10.3109/14767058.2011.601368.
- NHS Implementation Sub-Group of the Department of Health Post Mortem, Forensic and Disaster Imaging Group (PMFDI) . Can Cross-Sectional Imaging As an Adjunct and Or Alternative to the Invasive Autopsy Be Implemented Within the NHS? 2012.
- Breeze AC, Statham H, Hackett GA, Jessop FA, Lees CC. Perinatal postmortems: what is important to parents and how do they decide?. Birth 2012;39:57-64. https://doi.org/10.1111/j.1523-536X.2011.00513.x.
- Ben-Sasi K, Chitty LS, Franck LS, Thayyil S, Judge-Kronis L, Taylor AM, et al. Acceptability of a minimally invasive perinatal/paediatric autopsy: healthcare professionals’ views and implications for practice. Prenat Diagn 2013;33:307-12. https://doi.org/10.1002/pd.4077.
- Centre for Maternal and Child Enquiries (CMACE) . Perinatal Mortality 2009 2011.
- Lawn JE, Cousens S, Zupan J. Lancet Neonatal Survival Steering Team . 4 million neonatal deaths: When? Where? Why?. Lancet 2005;365:891-900. https://doi.org/10.1016/S0140-6736(05)71048-5.
- NHS England . Five Year Forward View 2014.
- Thayyil S, Sebire NJ, Chitty LS, Wade A, Olsen O, Gunny RS, et al. Post mortem magnetic resonance imaging in the fetus, infant and child: a comparative study with conventional autopsy (MaRIAS Protocol). BMC Pediatr 2011;11. https://doi.org/10.1186/1471-2431-11-120.
- Lewis C, Hill M, Arthurs OJ, Hutchinson C, Chitty LS, Sebire NJ. Factors affecting uptake of postmortem examination in the prenatal, perinatal and paediatric setting. BJOG 2018;125:172-81. https://doi.org/10.1111/1471-0528.14600.
- Centre for Reviews and Dissemination . Systematic Reviews 2009.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339. https://doi.org/10.1136/bmj.b2700.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res 2012;22:1435-43. https://doi.org/10.1177/1049732312452938.
- Kmet LMLR, Cook LS. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields 2004 n.d. www.ihe.ca/advanced-search/standard-quality-assessment-criteria-for-evaluating-primary-research-papers-from-a-variety-of-fields (accessed 11 April 2019).
- Noblit GW, Hare RD. Meta-ethnography: Synthesizing Qualitative Studies. London: Sage; 1988.
- Holste C, Pilo C, Pettersson K, Rådestad I, Papadogiannakis N. Mothers’ attitudes towards perinatal autopsy after stillbirth. Acta Obstet Gynecol Scand 2011;90:1287-90. https://doi.org/10.1111/j.1600-0412.2011.01202.x.
- Khong TY, Turnbull D, Staples A. Provider attitudes about gaining consent for perinatal autopsy. Obstet Gynecol 2001;97:994-8. https://doi.org/10.1097/00006250-200106000-00023.
- Landers S, Kirby R, Harvey B, Langston C. Characteristics of infants who undergo neonatal autopsy. J Perinatol 1994;14:204-7.
- Rankin J, Wright C, Lind T. Cross sectional survey of parents’ experience and views of the postmortem examination. BMJ 2002;324:816-18. https://doi.org/10.1136/bmj.324.7341.816.
- Stolman CJ, Castello F, Yorio M, Mautone S. Attitudes of pediatricians and pediatric residents towards obtaining permission for autopsy. Arch Pediatr Adolesc Med 1994;148:843-7. https://doi.org/10.1001/archpedi.1994.02170080073014.
- Vijayan V, Hiu J. Perinatal postmortem: factors influencing uptake and subsequent outcomes in an Asian population. Med J Malaysia 2012;67:87-90.
- Warland J, O’Brien LM, Heazell AE, Mitchell EA. STARS Consortium . An international internet survey of the experiences of 1,714 mothers with a late stillbirth: the STARS cohort study. BMC Pregnancy Childbirth 2015;15. https://doi.org/10.1186/s12884-015-0602-4.
- Brodlie M, Laing IA, Keeling JW, McKenzie KJ. Ten years of neonatal autopsies in tertiary referral centre: retrospective study. BMJ 2002;324:761-3. https://doi.org/10.1136/bmj.324.7340.761.
- Khong TY, Tanner AR. Foetal and neonatal autopsy rates and use of tissue for research: the influence of ‘organ retention’ controversy and new consent process. J Paediatr Child Health 2006;42:366-9. https://doi.org/10.1111/j.1440-1754.2006.00874.x.
- Khong TY, Mansor FA, Staples AJ. Are perinatal autopsy rates satisfactory?. Med J Aust 1995;162:469-70.
- Maniscalco WM, Clarke TA. Factors influencing neonatal autopsy rate. Am J Dis Child 1982;136:781-4. https://doi.org/10.1001/archpedi.1982.03970450023005.
- Okah FA. The autopsy: experience of a regional neonatal intensive care unit. Paediatr Perinat Epidemiol 2002;16:350-4. https://doi.org/10.1046/j.1365-3016.2002.00439.x.
- Swinton CH, Weiner J, Okah FA. The neonatal autopsy: can it be revived?. Am J Perinatol 2013;30:739-44. https://doi.org/10.1055/s-0032-1332798.
- Whitehouse SR, Kissoon N, Singh N, Warren D. The utility of autopsies in a pediatric emergency department. Pediatr Emerg Care 1994;10:72-5. https://doi.org/10.1097/00006565-199404000-00002.
- Epstein EG. End-of-life experiences of nurses and physicians in the newborn intensive care unit. J Perinatol 2008;28:771-8. https://doi.org/10.1038/jp.2008.96.
- Lishimpi K, Chintu C, Lucas S, Mudenda V, Kaluwaji J, Story A, et al. Necropsies in African children: consent dilemmas for parents and guardians. Arch Dis Child 2001;84:463-7. https://doi.org/10.1136/adc.84.6.463.
- McHaffie HE, Fowlie PW, Hume R, Laing IA, Lloyd DJ, Lyon AJ. Consent to autopsy for neonates. Arch Dis Child 2001;85:F4-F7. https://doi.org/10.1136/fn.85.1.F4.
- Meaney S, Gallagher S, Lutomski JE, O’Donoghue K. Parental decision making around perinatal autopsy: a qualitative investigation. Health Expect 2015;18:3160-71. https://doi.org/10.1111/hex.12305.
- Snowdon C, Elbourne DR, Garcia J. Perinatal pathology in the context of a clinical trial: attitudes of bereaved parents. Arch Dis Child Fetal Neonatal Ed 2004;89:F208-11. https://doi.org/10.1136/adc.2003.041392.
- Snowdon C, Elbourne DR, Garcia J. Perinatal pathology in the context of a clinical trial: attitudes of neonatologists and pathologists. Arch Dis Child Fetal Neonatal Ed 2004;89:F204-7. https://doi.org/10.1136/adc.2002.012732.
- Siassakos D, Jackson S, Gleeson K, Chebsey C, Ellis A, Storey C. INSIGHT Study Group . All bereaved parents are entitled to good care after stillbirth: a mixed-methods multicentre study (INSIGHT). BJOG 2018;125:160-70. https://doi.org/10.1111/1471-0528.14765.
- Fisher J, Lafarge C. Women’s experience of care when undergoing termination of pregnancy for fetal anomaly in England. J Reprod Infant Psychol 2015;33:69-87. https://doi.org/10.1080/02646838.2014.970149.
- Horey D, Flenady V, Conway L, McLeod E, Yee Khong T. Decision influences and aftermath: parents, stillbirth and autopsy. Health Expect 2014;17:534-44. https://doi.org/10.1111/j.1369-7625.2012.00782.x.
- Baker JN, Windham JA, Hinds PS, Gattuso JS, Mandrell B, Gajjar P, et al. Bereaved parents’ intentions and suggestions about research autopsies in children with lethal brain tumors. J Pediatr 2013;163:581-6. https://doi.org/10.1016/j.jpeds.2013.01.015.
- Sirkiä K, Saarinen-Pihkala UM, Hovi L, Sariola H. Autopsy in children with cancer who die while in terminal care. Med Pediatr Oncol 1998;30:284-9. https://doi.org/10.1002/(SICI)1096-911X(199805)30:5<284::AID-MPO4>3.0.CO;2-B.
- Wiener L, Sweeney C, Baird K, Merchant MS, Warren KE, Corner GW, et al. What do parents want to know when considering autopsy for their child with cancer?. J Pediatr Hematol Oncol 2014;36:464-70. https://doi.org/10.1097/MPH.0000000000000078.
- VanMarter LJ, Taylor F, Epstein MF. Parental and physician-related determinants of consent for neonatal autopsy. Am J Dis Child 1987;141:149-53. https://doi.org/10.1001/archpedi.1987.04460020039023.
- Aiyelaagbe E, Scott RE, Holmes V, Lane E, Heazell AEP. Assessing the quality of bereavement care after perinatal death: development and piloting of a questionnaire to assess parents’ experiences. J Obstet Gynaecol 2017;37:931-6. https://doi.org/10.1080/01443615.2017.1316710.
- Henderson J, Redshaw M. Parents’ experience of perinatal post-mortem following stillbirth: a mixed methods study. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0178475.
- O’Connell O, Meaney S, O’Donoghue K. Caring for parents at the time of stillbirth: How can we do better?. Women Birth 2016;29:345-9. https://doi.org/10.1016/j.wombi.2016.01.003.
- Ellis A, Chebsey C, Storey C, Bradley S, Jackson S, Flenady V, et al. Systematic review to understand and improve care after stillbirth: a review of parents’ and healthcare professionals’ experiences. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-0806-2.
- Batty D. Alder Hey report on use of children’s organs. The Guardian 2001. www.theguardian.com/society/2001/jan/30/health.alderhey1 (accessed 16 January 2017).
- Breeze AC, Statham H, Hackett GA, Jessop FA, Lees CC. Attitudes to perinatal postmortem: parental views about research participation. J Med Ethics 2011;37:364-7. https://doi.org/10.1136/jme.2010.038505.
- Dyregrov K. Bereaved parents’ experience of research participation. Soc Sci Med 2004;58:391-400. https://doi.org/10.1016/S0277-9536(03)00205-3.
- Sebire NJ. Towards the minimally invasive autopsy?. Ultrasound Obstet Gynecol 2006;28:865-7. https://doi.org/10.1002/uog.3869.
- Addison S, Arthurs OJ, Thayyil S. Post-mortem MRI as an alternative to non-forensic autopsy in foetuses and children: from research into clinical practice. Br J Radiol 2014;87. https://doi.org/10.1259/bjr.20130621.
- Henley A, Schott J. Sands’ learning outcomes for consent taker training: seeking consent/authorisation for a hospital post mortem examination of a baby. J Neonatal Nurs 2014;20:11-3. https://doi.org/10.1016/j.jnn.2013.10.004.
- Human Tissue Authority . Code of Practice 3: Post-Mortem Examination 2014.
- Stillbirth and Neonatal Death Charity . Sands Post Mortem Consent Package 2013.
- Siassakos D, Storey C, Davey L. Insight Study Team . Stillbirth: public/patient involvement in sensitive research and research ethics. BJOG 2015;122. https://doi.org/10.1111/1471-0528.13412.
- Snowdon C, Brocklehurst P, Tasker R, Ward Platt M, Harvey S, Elbourne D. Death, bereavement and randomised controlled trials (BRACELET): a methodological study of policy and practice in neonatal and paediatric intensive care trials. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18420.
- Tashakkori A, Creswell JW. The new era of mixed methods. J Mix Methods Res 2007;1. https://doi.org/10.1177/2345678906293042.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. https://doi.org/10.1136/bmj.c4587.
- Lakhanpaul M, Culley L, Robertson N, Bird D, Hudson N, Johal N, et al. A qualitative study to identify parents’ perceptions of and barriers to asthma management in children from South Asian and White British families. BMC Pulm Med 2017;17. https://doi.org/10.1186/s12890-017-0464-9.
- Lakhanpaul M, Bird D, Culley L, Hudson N, Robertson N, Johal N, et al. The use of a collaborative structured methodology for the development of a multifaceted intervention programme for the management of asthma (the MIA project), tailored to the needs of children and families of South Asian origin: a community-based, participatory study. Health Serv Deliv 2014;2.
- Stirland L, Halani L, Raj B, Netuveli G, Partridge M, Car J, et al. Recruitment of South Asians into asthma research: qualitative study of UK and US researchers. Prim Care Respir J 2011;20:282-90. https://doi.org/10.4104/pcrj.2011.00032.
- Leicester City Council . 2011 Census Findings: Diversity and Migration n.d. www.leicester.gov.uk/media/177367/2011-census-findings-diversity-and-migration.pdf (accessed 17 January 2018).
- Tower Hamlets . Ethnicity in Tower Hamlets: Analysis of 2011 Census Data 2013. www.towerhamlets.gov.uk/Documents/Borough_statistics/Ward_profiles/Census-2011/RB-Census2011-Ethnicity-2013-01.pdf (accessed 17 January 2018).
- Tower Hamlets . Religion in Tower Hamlets: 2011 Census Update 2015. www.towerhamlets.gov.uk/Documents/Borough_statistics/Ward_profiles/Census-2011/2015-04-21-Faith-key-facts-Revised-data.pdf (accessed 17 January 2018).
- Office for National Statistics . Full Story: What Does the Census Tell Us About Religion in 2011 2013. www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/religion/articles/fullstorywhatdoesthecensustellusaboutreligionin2011/2013-05-16 (accessed September 2017).
- Rocker S. Census 2011: The Jewish Breakdown. The Jewish Chronicle 2012. www.thejc.com/news/uk-news/census-2011-the-jewish-breakdown-1.39530 (accessed 3 October 2017).
- Institute for Jewish Policy Research . Synagogue Membership in the United Kingdom in 2016 2016.
- Birt L, Scott S, Cavers D, Campbell C, Walter F. Member checking: a tool to enhance trustworthiness or merely a nod to validation?. Qual Health Res 2016;26:1802-11. https://doi.org/10.1177/1049732316654870.
- Lewis C, Riddington M, Hill M, Arthurs OJ, Hutchinson JC, Chitty LS, et al. Availability of less invasive prenatal, perinatal and paediatric autopsy will improve uptake rates: a mixed methods study with bereaved parents [published online ahead of print December 21 2018]. BJOG 2018. https://doi.org/10.1111/1471-0528.15591.
- Wojcieszek AM, Boyle FM, Belizán JM, Cassidy J, Cassidy P, Erwich J, et al. Care in subsequent pregnancies following stillbirth: an international survey of parents. BJOG 2018;125:193-201. https://doi.org/10.1111/1471-0528.14424.
- Office for National Statistics . Statistical Bulletin: Childhood, Infant and Perinatal Mortality in England and Wales – 2013 2015.
- Lewis C, Hill M, Arthurs OJ, Hutchinson JC, Chitty LS, Sebire N. Health professionals’ and coroners’ views on less invasive perinatal and paediatric autopsy: a qualitative study. Arch Dis Child 2018;103:572-8. https://doi.org/10.1136/archdischild-2017-314424.
- Hutchinson JC, Arthurs OJ, Sebire NJ. Postmortem research: innovations and future directions for the perinatal and paediatric autopsy. Arch Dis Child Educ Pract Ed 2016;101:54-6. https://doi.org/10.1136/archdischild-2015-309321.
- NHS Implementation Sub-Group of the Department of Health Post Mortem, Forensic and Disaster Imaging Group (PMFDI) . Strategy for Implementation of a National Less Invasive Autopsy Imaging Service Within the NHS 2012.
- Maskell G, Wells M. Statement on Standards for Medico-Legal Post-Mortem Cross-Sectional Imaging in Adults. London: The Royal College of Pathologists; 2012.
- Arthurs OJ, Thayyil S, Pauliah SS, Jacques TS, Chong WK, Gunny R, et al. Diagnostic accuracy and limitations of post-mortem MRI for neurological abnormalities in fetuses and children. Clin Radiol 2015;70:872-80. https://doi.org/10.1016/j.crad.2015.04.008.
- Taylor AM, Sebire NJ, Ashworth MT, Schievano S, Scott RJ, Wade A, et al. Postmortem cardiovascular magnetic resonance imaging in fetuses and children: a masked comparison study with conventional autopsy. Circulation 2014;129:1937-44. https://doi.org/10.1161/CIRCULATIONAHA.113.005641.
- Arthurs OJ, Thayyil S, Addison S, Wade A, Jones R, Norman W, et al. Diagnostic accuracy of postmortem MRI for musculoskeletal abnormalities in fetuses and children. Prenat Diagn 2014;34:1254-61. https://doi.org/10.1002/pd.4460.
- NHS England . 2013/14/NHS/Standard/Contract/for/Perinatal/Pathology:/Particulars,/Schedule/2/–/The/Services,/A/–/Service/Specification 2013. www.england.nhs.uk/wp-content/uploads/2013/06/e12-perinatal-path.pdf (accessed 7 August 2017).
- Arthurs OJ, Bevan C, Sebire NJ. Less invasive investigation of perinatal death. BMJ 2015;351. https://doi.org/10.1136/bmj.h3598.
- Lewis C, Latif Z, Hill M, Riddington M, Lakhanpaul M, Arthurs OJ, et al. ‘We might get a lot more families who will agree’: Muslim and Jewish perspectives on less invasive perinatal and paediatric autopsy. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0202023.
- Gurley ES, Parveen S, Islam MS, Hossain MJ, Nahar N, Homaira N, et al. Family and community concerns about post-mortem needle biopsies in a Muslim society. BMC Med Ethics 2011;12. https://doi.org/10.1186/1472-6939-12-10.
- Maixenchs M, Anselmo R, Zielinski-Gutiérrez E, Odhiambo FO, Akello C, Ondire M, et al. Willingness to know the cause of death and hypothetical acceptability of the minimally invasive autopsy in six diverse African and Asian settings: a mixed methods socio-behavioural study. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1002172.
- Weiss R. Haredim (Charedim), or Ultra-Orthodox Jews n.d. www.myjewishlearning.com/article/haredim-charedim/ (accessed 17 January 2018).
- Bisset RA, Thomas NB, Turnbull IW, Lee S. Postmortem examinations using magnetic resonance imaging: four year review of a working service. BMJ 2002;324:1423-4. https://doi.org/10.1136/bmj.324.7351.1423.
- Saad Foundation . MRI PM Vs PM n.d. www.saadfoundation.com/?option=com_content&view=article&id=3&Itemid=3 (accessed 17 January 2018).
- Islam21c . Protecting Yourself from Mutilation After Death n.d. www.islam21c.com/campaigns/protect-yourself-from-mutilation-after-death/ (accessed 17 January 2018).
- Rocker S. High Court backs Jewish family who rejected invasive autopsy on religious groups. The Jewish Chronicle 2015.
- Watts G. Imaging the dead. BMJ 2010;341. https://doi.org/10.1136/bmj.c6600.
- digitalautopsy.co.uk . Sandwell Council Supporting Digital Autopsy n.d. http://digitalautopsy.co.uk/sandwell-council-supporting-digital-autopsy/ (accessed 7 September 2017).
- Ministry of Justice . Implementing the Coroner Reforms in Part 1 of the Coroners and Justice Act 2009: Consultation on Rules, Regulations, Coroner Areas and Statutory Guidance 2013.
- Kai J, Beavan J, Faull C, Dodson L, Gill P, Beighton A. Professional uncertainty and disempowerment responding to ethnic diversity in health care: a qualitative study. PLOS Med 2007;4. https://doi.org/10.1371/journal.pmed.0040323.
- Weber MA, Klein NJ, Hartley JC, Lock PE, Malone M, Sebire NJ. Infection and sudden unexpected death in infancy: a systematic retrospective case review. Lancet 2008;371:1848-53. https://doi.org/10.1016/S0140-6736(08)60798-9.
- Bamber AR, Paine SM, Ridout DA, Pryce JW, Jacques TS, Sebire NJ. Brain weight in sudden unexpected death in infancy: experience from a large single-centre cohort. Neuropathol Appl Neurobiol 2016;42:344-51. https://doi.org/10.1111/nan.12251.
- Office for National Statistics . Childhood, Infant and Perinatal Mortality in England and Wales: 2013 2015.
- Drapers ES, Gallimore ID, Krurinczuk JJ, Smith PW, Boby T, Smith LK, et al. Perinatal Mortality Surveillance Report, UK Perinatal Deaths for Births from January to December 2016 2018.
- Judge-Kronis L, Hutchinson JC, Sebire NJ, Arthurs OJ. Consent for paediatric and perinatal postmortem investigations: implications of less invasive autopsy. J Forensic Radiol Imaging 2016;4. https://doi.org/10.1016/j.jofri.2015.12.001.
- Sandelowski M, Barroso J. Creating metasummaries of qualitative findings. Nurs Res 2003;52:226-33.
Appendix 1 Summary of papers detailing factors affecting uptake of autopsy examination
| Study, country | Aim of study | Study design | Sample | Analysis | Findings/results | Limitations |
|---|---|---|---|---|---|---|
| Aiyelaagbe et al.,78 UK | To develop and pilot a questionnaire to identify parents’ needs and record the experience of care after perinatal death | Cross-sectional questionnaire study, including open and closed questions and Likert scales | Parents who had experienced a perinatal death on the delivery unit at St Mary’s Hospital, Manchester, UK over an 18-month period from 2014 to 2015. The questionnaire was sent out to 144 families who had a SB or neonatal death, 3–6 months after the event. There were 58 responses from parents (40%) | Quantitative data were analysed using descriptive statistical analysis. Qualitative data were analysed using thematic analysis | 48% of parents discussed post-mortems with a member of staff. Of these, six parents (13.6%) were not given written information. Nevertheless, the verbal discussion was interpreted sensitively and explained clearly, with adequate opportunity for parents to ask questions | Low response rate. Small number of questions around post-mortem |
| Baker et al.,74 USA | To determine bereaved parents’ perceptions about participating in autopsy-related research and to elucidate their suggestions about how to improve the process | Mixed-methods multicentre questionnaire study |
Parents of a child with DIPG who consented to autopsy Thirty-three parents of 32 children participated (84.2% participation rate) |
Qualitative semantic content analysis. Descriptive statistics were generated for responses to quantitative questions | The main reasons for participating in this study were to advance medical knowledge or to find a cure, a desire to help others and choosing as their child would want. Parents hoped that participation would help others or help find a cure, as well as provide closure. Providing education/anticipatory guidance and having a trusted professional sensitively broach the topic of autopsy were suggestions to improve autopsy discussions | Unclear who conducted the telephone interviews. Structured interview format so the qualitative data are limited in interpretive content |
| Ben-Sasi et al.,39 England | To examine the relative acceptability among health professionals of a MIA, MRI and laparoscopic-guided tissue sampling, compared with standard autopsy | Cross-sectional questionnaire study | Health professionals working in clinical settings in which paediatric and perinatal deaths occur. Of 250 questionnaires distributed, 224 were returned (90% response rate). Doctors represented 44%, nurses 18% and administrative staff 11% of professional roles | Descriptive statistics and determination of the significance of differences in distribution of responses for traditional vs. MIA and other variables were performed using Mann–Whitney U-test and Kruskal–Wallis test as appropriate | Demographic factors affecting acceptability included ethnicity and religion but not professional role. MIA compared favourably with traditional autopsy, 50% of respondents reporting both as equally acceptable, 40% reporting MIA as more acceptable and 10% as less acceptable. Health professionals agreed that having a MIA option would make it easier to discuss autopsy with parents (p < 0.001). Increased concern regarding possible disfigurement/cosmetic effects among non-white groups and concerns regarding possible delays to the funeral, particularly for those of Indian, Asian or Arab ethnicity, were identified | |
| Breeze et al.,38 England | To explore parental attitudes to, and decision-making about, a perinatal post-mortem after termination for fetal abnormality, late miscarriage or SB (same as 2011 study83) | A cross-sectional prospective questionnaire | Questionnaire was given to 35 women and their partners. Participants were recruited from a UK fetal medicine unit. Thirty-one questionnaires were received from parents of 17 babies (49% of those asked; 16 from mothers, 15 from fathers) | Descriptive statistics that were used and age comparisons carried out using the t-test. Non-parametric statistical tests were used (Spearman’s correlation coefficient, Mann–Whitney U-test) | Parents of nine babies (53%) said that they would agree to a full post-mortem, and three to a limited post-mortem. All who agreed to full or limited post-mortem stated that they would choose a full post-mortem over a less invasive procedure (if offered), if it might provide less information. Items rated as most important centred around the need for information to plan subsequent pregnancies and to establish the recurrence risk. Moderately important items related to altruism, improving medical knowledge and helping prevent similar things from happening to others. Among the lowest scoring issues were the cultural or religious accept ability of post-mortem, including funeral delays or concerns about what would happen to the baby’s body | Small study population |
| Brodlie et al.,58 Scotland | To measure the neonatal autopsy rate at a tertiary referral centre and identify trends over the past decade. To identify factors that may influence the likelihood of consent being given for autopsy | Retrospective audit of patients’ records |
Setting: tertiary neonatal referral centre affiliated to university. Sample: included records of all deaths in the neo-natal unit from 1 January 1990 to 31 December 1999 A total of 314 cases studied |
Compared the proportion of events in each group using the chi-squared test for discrete variables and Student’s t-test for numerical variables | Gestational age was the only factor that was found to differ significantly between the groups who did and did not give permission for autopsy, with means of 32 and 30 weeks, respectively. Other factors analysed were birth weight, length of stay, age at death (days) and maternal age | Study did not look at reasons for accepting or declining, looked only at patient characteristics |
| Cannie et al.,31 Belgium | To compare prospectively maternal acceptance of fetal and neonatal MIA with that of conventional autopsy | Quantitative cross-sectional questionnaire study | All mothers undergoing ToP, IUFD or delivering an infant that subsequently died in the neonatal period between October 2004 and May 2010 invited. Study included 96 mothers | Multiple logistic regression analysis to investigate the effect on the acceptance by mothers in relation to age, religion, gestation at ToP or delivery, education, etc. | Ninety-five mothers consented to MRI and 59 (62%) consented to both. Acceptance of conventional autopsy was independently positively related to singleton pregnancy, non-Muslim mother, earlier gestation at ToP or delivery following IUFD and a maternal–fetal medicine specialist obtaining the consent | No description of how demographic variables and decision-making were noted. No response rate |
| Downe et al.,6 England (same sample as the Heazell et al. study7) | To describe the views of UK obstetricians, midwives and perinatal pathologists about post-mortem examination for SB | Mixed-methods survey; however, this paper presents only the qualitative findings from free-text boxes |
Survey was sent to practitioners registered with their respective professional organisations A total of 3114 midwives, 532 obstetricians and 21 perinatal pathologists responded to the questionnaire. Free-text comments were provided by 683 midwives, 98 obstetricians and 11 perinatal pathologists |
The data entered into the free-text comments section of the survey were analysed from the original Excel spreadsheet, using thematic analysis | There were five themes in the final thematic structure: (1) staff education and training, (2) quality of information, consent and examination processes, (3) adequate and effective resources and personnel, (4) professional and public discourses and (5) personal beliefs and experiences. There was general agreement that targeted training and support were required to ensure that the essential processes are effectively undertaken. The complexity and length of current consent forms was seen as a barrier to consent. Respondents in all groups noted that long delays and inconclusive results disrupt the credibility of the process for practitioners and cause distress to many parents. All professional groups noted deficits in terms of the availability of specialised staff | No response rate |
| Ellis et al.,81 Europe, North America, Australia and South Africa | A systematic review of qualitative, quantitative and mixed-methods studies researching parents’ and health professionals’ experiences of care after SB in high-income westernised countries | A systematic review of qualitative, quantitative and mixed-methods studies | A total of 4488 abstracts were identified; 52 studies were eligible for inclusion (40 parents/14 staff, note that two studies addressed both parents and staff). Eight papers specifically addressed post-mortem | Data analysis was based on the meta-summary approach, a quantitative aggregation of qualitative findings developed by Sandelowski.133 The method comprises (1) extraction of relevant statements of findings from each report; (2) reduction of these statements into abstracted findings; and (3) calculation of effect sizes | Key themes associated with post-mortem were (1) parents want improved training so that staff can provide tailored discussions and written information to help them make informed decisions about post-mortem and funeral arrangements; (2) there are many factors which influence parents’ decision whether or not to have a post-mortem; (3) parents may regret certain decisions made regarding post-mortem and funeral arrangements; and (4) long delays and inconclusive results can cause distress to parents | |
| Epstein,65 USA | To explore nurses’ and physicians’ end-of-life experiences in the newborn ICU | Qualitative study using semistructured interviews | The sample included newborn ICU-attending resident and fellow physicians, as well as registered nurses and nurse practitioners. Semistructured interviews were completed between 1 day and 6 weeks following an infant’s death. Twenty one of 23 nurses and 11 of 19 physicians participated | Phenomenological approach used | Discussion of autopsy was the sole responsibility of the physicians. The subject of discussing autopsy was problematic, particularly for those physicians with less clinical experience. Much of the difficulty in approaching parents about autopsy was in how to ‘couch’ the discussion. There was no consensus about the approach, but all agreed that this was a difficult conversation to have with parents. Residents and fellows desired more guidance with this issue | Only a small part of study looked at post-mortem |
| Fisher and Lafarge,72 UK | To investigate women’s experience of care when undergoing ToP | Mixed-methods online survey. This paper reports on only the qualitative findings | Participants were recruited from ARC’s membership of women who have had a ToP. A total of 430 participants started the survey with 379 (88.1%) participants completing it in full and providing comments to at least one open-ended question about the experience of care | Thematic analysis | Timing of information provision could be experienced by some women as inappropriate, particularly when relating to the post-mortem, ‘The doctor brought in the post-mortem consent when I was in the middle of labour and expected me to listen and make decisions about what I wanted to find out after the birth . . . the time she chose to do it didn’t really work for me’ | Only touches on the topic of post-mortem with one example related to timing. No recruitment rate. Potential for bias as only recruited through support groups |
|
Heazell et al. ,7 England (same sample as the Downe et al. study6) |
To describe the experiences, knowledge and views of both parents and professionals regarding the consent process for perinatal post-mortem | Internet-based cross-sectional survey | Obstetricians, midwives and perinatal pathologists registered with their professional bodies were approached and parents who accessed the Sands website or online forum. The response rates from professionals were 2256 midwives (23%), 354 obstetricians (31%) and 21 perinatal pathologists (53%). The number of parental responses was 460 | Only information given is that data were analysed using SPSS | Main reason for any investigation was to find a reason for their child’s death. Altruistic motives were important for approximately half of respondents. Professional advice affected parents’ decision to have an autopsy in 22.2% of cases. The perception of barriers to counselling for autopsy differed between professionals and parents. Staff perceived a lack of rapport as a barrier. All groups recognised emotional distress as a barrier. Time to get results or the need to transfer babies were insignificant barriers for most professionals, but 32.8% of parents described this as a significant or strong barrier | No information about statistical analysis in methods section; however, this is evident by looking at the results. Low response rates from some of the groups |
| Henderson and Redshaw,79 UK | To describe the experience of parents in relation to post-mortem following SB, looking at offer and uptake of post-mortem, information-giving, the type of post-mortem carried out, receiving the results and any sociodemographic differences in care practices in relation to post-mortem | Secondary analysis of a cross-sectional postal survey, which included both open and closed questions allowing for a mixed-methods study design | A sample of women who experienced a SB in 2013 were selected by staff at the Office for National Statistics. The questionnaire included questions about pregnancy, labour and birth, the postnatal period, the time at which the baby died and also asked about the post-mortem process. Completed questionnaires were received from 477 women (30%) | Differences between groups were tested using chi-squared statistics. The open-text responses were coded using a thematic content analytic approach | Although only two-thirds of women received written information, 85% and 81%, respectively they felt that they were sufficiently informed and had enough time to decide. Teenagers and women aged ≥ 40 years were significantly less likely to feel sufficiently informed. Single mothers and women who had left full-time education before the age of 16 years were significantly less likely to consent to a full post-mortem. Of the 110 women who declined any form of post-mortem, the most common reason given (74%) was that they did not want their baby’s body examined, 38% indicated that they already knew why their baby had died and 26% thought that it would not provide an answer. Timing of the question and the way it was asked were found to be key themes from the qualitative analysis | |
| Holste et al.,51 Sweden | To investigate mothers’ attitudes to autopsy of their stillborn baby and their experiences concerning information and treatment in relation to their loss in an observational study | Cross-sectional survey | Mothers who had lost a baby by SB, between 2004 and 2005 at the Stockholm South General Hospital (n = 32) and the Karolinska University Hospital (n = 40). The overall response rate was 76% (n = 54) and telephone contact was established in 70% (n = 50) |
Answers were analysed quantitatively when appropriate and the chi-squared test was used when feasible. A p-value of < 0.05 was considered significant Comments were examined by key words and themes to identify groups |
Forty-seven mothers (87%) found that they received adequate information about the possibility of autopsy. Sixteen mothers (30%) would have liked to receive more detailed information. Reasons for agreeing to autopsy included to get more information about cause of death (41%), evaluate risks for later pregnancy (32%), better cope with loss (23%) and contribute to research (20%). Reasons for declining included concern about the examination of the baby (5%), not persuaded of the benefit (4%) and religious reasons (2%) | Lack of demographic characteristics |
| Horey et al.,73 Australia | To examine the influences on decisions about autopsy after SB among Australian parents | Qualitative study involved secondary analysis of transcripts of three focus groups | Three focus group sessions organised by a support group and charity (Sands in Brisbane) and a national parent-based and research fundraising charity (Stillbirth Foundation Australia in Sydney). Seventeen parents of 14 stillborn babies participated | Content analysis | Four decision drivers were identified which involved both reasons for and against post-mortem: (1) parental preparedness or readiness to make decisions (certain of action to take, confidence with scientific progress, feeling overwhelmed or unable to take things in); (2) parental responsibility (obligation to determine what went wrong, consideration of needs of future children, desire to protect baby from unnecessary harm); (3) concern for possible consequences of an autopsy (better peace of mind, fear of blame for outcome); and (4) the role of health professionals (supportive/unsupportive of autopsy) | Potential for bias as recruited only through support groups |
| Kang et al.,32 Belgium | To determine parental acceptance of MIA involving imaging and organ tissue sampling vs. conventional autopsy and to compare the acceptability of percutaneous vs. laparoscopic-guided biopsy | Prospective cross-sectional interview-based survey | Study conducted at the Department of Fetal Medicine of the University Hospital Brugmann, Brussels, Belgium. Seventy of 76 parents participated. The interviews were conducted before delivery, on the day of delivery, or on the day after the delivery. In all cases, the interview was conducted on the day of the signing of parental consent or refusal of autopsy | The McNemar’s test for paired samples to assess the difference in acceptance of MIA and conventional autopsy. The Wilcoxon signed-rank test for paired samples to compare acceptance scores. Logistic regression to study the association of parental acceptance of conventional autopsy and MIA with different variables | Conventional autopsy was accepted by 42 (60.0%) of the 70 interviewed parents. Parental acceptance of conventional autopsy was significantly associated with religion and the prenatal diagnosis of a fetal condition. Thirteen (46.4%) of the 28 parents who initially refused conventional autopsy subsequently accepted MIA, significantly increasing the acceptance to 78.6% (p < 0.001). Univariate regression analysis showed that parental acceptance of MIA was significantly associated with religion and the prenatal diagnosis of a fetal condition | |
| Khong et al.,52 Australia | To examine the attitudes of neonatologists, obstetricians, midwives and neonatal nurses towards perinatal autopsy and survey physicians about whom they perceive influence women’s decisions on autopsy consent | A cross-sectional postal survey | Australian physicians and nurses were recruited. The overall response rate was 68% (254/376) | Interactions between factors and respondents were measured by analysis of variance and differences were compared using Mann–Whitney U-tests | Health professionals more likely to ask parents about autopsy when there was uncertain diagnosis, desire for autopsy and desire for future pregnancy. Neonatal nurses with > 10 years’ experience were more inclined to suggest autopsy than those with less experience. Physicians rated midwives and neonatal nurses as having some to substantial influence on mothers’ decisions about consent for autopsy | |
| Khong and Tanner,59 Australia | To examine whether or not the ‘organ retention’ controversy and the new autopsy consent process had any effect on fetal and neonatal autopsy rates and on permitting the use of tissue for scientific research and education | A retrospective audit of perinatal autopsy rates | A total of 512 cases were reviewed. In 355 cases permission was granted; in 157 cases permission was declined | Differences were compared using chi-squared test without correction. A comparison between the current and previous rates was also made | The autopsy rates for SBs and neonatal deaths have fallen significantly further since the ‘organ retention’ controversy, but not significantly following the new consent process. Significantly fewer autopsies are performed on fetuses < 20 weeks’ gestation in recent years than a decade ago | Limited data on participant characteristics |
| Khong et al.,60 Australia | To determine perinatal autopsy rates and whether or not any maternal or obstetric factors affect consent for autopsy | A retrospective audit examining various obstetric and maternal demographic and socioeconomic factors over a 4-year period | Each perinatal death for which autopsy consent was refused was matched with one that was consented. Sixty-eight of the 114 neonates who died had an autopsy | Differences were compared using chi-squared test without correction. Stepwise logistic regression was also performed | No statistically significant difference was found for gestational or postnatal age between autopsied and non-autopsied babies, or maternal gravidity, parity employment, marital or health insurance status between mothers in both groups. Too few patients of non-Christian faith for any deductions regarding influence of religion; however, it was noted that Muslims and Buddhists were represented among the autopsy and non-autopsy groups | Too few patients of non-Christian faith for any deductions regarding influence of religion |
| Kumar et al.,13 USA | To identify trends in paediatric autopsy rates, concordance between ante-mortem and post-mortem diagnoses, and patient characteristics influencing autopsy rates | Retrospective audit of paediatric deaths | A total of 297 paediatric deaths were reviewed. Autopsies were conducted in 107 patients (36%) | For categorical variables, the proportion of events were compared using the chi-squared statistic with Yates’ correction | Autopsies were not associated with patient gender, race or insurance status. There was a significant association between patient age and autopsy; autopsies were performed in 26% (60/229) of infants 12 months or younger, 60% (31/52) of children between 13 and 60 months of age, and 100% (16/16) of patients 61 months or older | |
| Landers et al.,53 USA | To identify factors – clinical and demographic characteristics – associated with autopsy uptake. SBs were excluded | Quantitative interview survey with physician caring for infant within 3 days of death | There were 56 neonatal deaths during the study period. Thirty-three patients (59%) had autopsies performed | Data were analysed using multivariate logistic regression | Only birth asphyxia and Medicaid coverage were significantly associated with autopsy uptake. The analysis did not reveal significant associations between performance of an autopsy and particular physician requesting consent. Physicians perceived that psychosocial conflicts within the family influenced refusal in 13%; 9% had religious objections; and 9% of cases experienced cultural or communication differences between parents and care team | Not clear what some of the terms used to describe reasons for declining mean. Also, these are based on physicians’ interpretations of parents’ reasons. No data on why parents accepted autopsy |
| Lishimpi et al.,66 Zambia | To identify the main reasons for parents’/guardians’ refusal of consent for necropsy and to explore the issues affecting their decision | Qualitative interview study | Sample included parents or guardians of all children dying of respiratory disease in the inpatient wards of the Department of Paediatrics and Child Health, University Teaching Hospital, Lusaka | Not discussed | Almost half of the recently bereaved parents or guardians (43%) showed anger at the request for necropsy, refusing on the grounds that it would be a ‘waste of time’ (43%), that a death certificate had already been issued and transport arrangements for the body had been made (26.5%), traditional beliefs that ancestral spirits forbade the mutilation of dead bodies (8.6%), cannot consent because the child is not their own (6%), investigation should have been done before death (4.3%), religious belief of limitation on burial time (Moslem) (3.4%) | No detail given regarding data analysis or verification of findings. No recruitment rate |
| Maniscalco and Clarke,61 USA | To identify autopsy rates in a neonatal ICU and identify factors that affect autopsy rates among newborns | Retrospective audit of patients who died in an intensive care nursery | A total of 117 neonatal deaths were included in the sample: 92 underwent autopsy, 25 did not | t-test and Fisher’s exact test | No statistical difference in autopsy rates across mean birth weight, gestational age, days survived after admission, maternal age, gravidity or parity. Autopsy significantly less likely with transported patients than inborn patients, especially if they had birth weights < 1000 g, or a gestational age < 28 weeks, or they died within 2 days of admission. Autopsy more likely on patients with congenital abnormalities | |
| McHaffie et al.,67 Scotland | To determine parents’ views on autopsy after treatment withdrawal | Qualitative face-to-face structured interviews | Recruitment from three regional neonatal referral centres in the East of Scotland were selected, which provided a representative range of families | A total of 59 families (108 parents), for whose babies (62) there had been discussion of treatment withdrawal participated at 3 months, and 85% of them again at 13 months | Thirty-eight per cent of parents refused post-mortem. The main reasons for consenting were to obtain answers to their questions (n = 23), to help others (n = 13) and to obtain information that may influence future pregnancies (n = 13). The main reasons for declining were concerns about disfigurement (n = 14) and a feeling that an autopsy was unnecessary because the parents had no unanswered questions (n = 9). The diagnosis, the age of the child and the approach of the consultant appeared to influence consent rates | Lack of detail regarding how data were analysed and methodological approach |
| Meaney et al.,68 Ireland | To qualitatively explore perinatal autopsy decision-making processes in parents who experienced antepartum and intrapartum SBs | Qualitative semistructured interviews | Purposive sampling was used to recruit 10 parents who either consented or declined autopsy from a large tertiary maternity hospital in Cork, Ireland, where there were 30 SBs | Interpretative phenomenological analysis was employed as the analytic strategy |
Those parents who experienced antepartum SBs were more likely to consent. These parents had more time for meaning-making; those consenting wanted to rule out self-blame and were fearful about future pregnancies. Parents who declined autopsy wanted to protect their infant from further harm Nearly all parents stated that even after being offered an autopsy in the hospital, they were still not fully aware of what an autopsy procedure entailed |
No recruitment rate |
| O’Connell et al.,80 Ireland | To establish which aspects of care are valued, which could be improved and which, if any, cause distress | A service evaluation questionnaire was designed to examine the extent to which the parents’ needs were being met. The questionnaire included Likert scale questions as well as written text responses | Parents who experienced SB in a tertiary referral centre (Cork University Maternity Hospital). Of the 59 parents surveyed, 61% (n = 36) responded, representing 70% (n = 21) of mothers and 52% (n = 15) of fathers | Descriptive analysis of the quantitative results and parent quotations are provided |
Ninety per cent of parents (n = 31) thought that information about post-mortem was handled sensitively, but only 58% (n = 18) of parents said that it was explained clearly Over three-quarters (77%; n = 24) of parents felt that they were given adequate time to decide, but just 67% (n = 21) of parents said that it was addressed at an appropriate time One-quarter (26%; n = 13) of parents said that the information was not given by knowledgeable professionals and 26% (n = 13) of parents said that they did not have adequate opportunity to ask questions The main difficulties experienced regarding autopsy involved clarity, timing, information and knowledge of the doctor who undertook the consent for the procedure Although a question had not been included in the survey on parents’ experience regarding the retention of the baby’s organs at the time of post-mortem, it was raised in the free text as a concern for many |
Very little information about data analysis |
| Okah,62 USA | The influence of educational activities and the availability of LIAs in the early to mid-1990s on autopsy rates | A retrospective audit of all deaths at the neonatal ICU was conducted | A total of 638 infant deaths were analysed | A trend analysis for the study periods was performed by chi-squared test. Mann–Whitney rank-sum test was used when the distribution failed the normality test | There was a trend towards progressive decrease in autopsy rates, 59% in 1986–89, 52% in 1990–94 and 47% in 1995–98 (p = 0.078). Autopsy was associated with increasing gestational age (p < 0.001) and decreasing parity (odds ratio = 0.53 for > 2 vs. ≤ 2, 95% CI 0.36 to 0.99), but not with other variables | |
| Rankin et al.,54 England | To describe parents’ experience and views of the post-mortem examination after the loss of a baby | Cross-sectional survey |
Questionnaire sent to all mothers who had attended the bereavement service in Newcastle upon Tyne, who had lost on at least one occasion a baby during pregnancy or infancy A total of 258 mothers had attended the service and 166 mothers (64%) completed the questionnaire |
Fixed-choice questions were analysed by using the statistical package SPSS | Main reasons for agreeing: I wanted more information about what had happened (44%); to help improve medical knowledge and research (24%); it was recommended by the person asking for my consent (16%); I felt a need for ‘finality’ or ‘closure’ after my loss (10%). Main reasons for declining: I felt my baby had already ‘suffered enough’ (44%); I did not feel it would help me (26%); I was concerned about the effects of the examination on my baby’s appearance (10%); I did not want my baby cut (6%); I was concerned it might delay funeral arrangements (4%); for religious reasons (0%) | Very little information provided regarding how the survey was developed |
| Siassakos et al.,71 UK | To understand challenges in care after SB and to provide tailored solutions | Multicentre care study comprising interviews with parents and focus groups with staff across three maternity hospitals | A total of 21 mothers (64%) and 14 of their partners agreed to participate. Three staff focus groups took place with between six and nine participants in each group | Thematic analysis of parent interviews, and staff focus groups and service provision investigation | Three key themes relating to post-mortem were identified, relating to consent discussion, follow-up and staff training. Key findings include (1) discussions with staff influenced parents significantly in their decision-making; (2) some staff found the post-mortem consent forms onerous, but parents did not, as long as their completion was supported by discussion with a professional they trusted (some parents thought that staff discouraged them from having a post-mortem); and (3) parents and staff agreed that the period between initial hospital discharge and follow-up consultation is characterised by delay, lack of information for parents and varied support | Consent for post-mortem forms only a small part of the findings from the study |
| Sirkiä et al.,75 Finland | To find out whether autopsy of children with cancer should be recommended after terminal care, or whether in those circumstances it could be abandoned | Mixed methods: a retrospective audit of patients’ records and autopsy reports in addition to structured interview of parents | A total of 70 retrospective audits were conducted. Autopsy was performed in 40 out of 70 cases. Interviews with one or both parents were conducted in 60 cases, including for 34 out of 40 of the children who were autopsied | The attitudes of the families about the autopsy were analysed as part of a more extensive structured interview | Autopsy more often performed on children dying in hospital than at home and on children with leukaemia than tumours. About half of both the mothers and the fathers felt that knowing the findings at autopsy was helpful for them. All the parents except one mother felt that the autopsy of their child would at least potentially help other patients. In five cases the personnel, and in four cases the parents and personnel together, decided that an autopsy was unnecessary. Mostly, these parents thought that their child had suffered enough during the anticancer medication and operations and that the body should be left in peace | No discussion of how the data were analysed for the quantitative component of the study looking at parental attitudes |
| Snowdon et al.,69 England | To report the attitudes of bereaved parents to trial-related perinatal post-mortems, in the light of declining perinatal post-mortem rates and poor levels of participation in pathology studies | Qualitative study using semistructured interviews |
Twenty-one letters were sent to parents Eleven interviews were carried out with 18 bereaved parents from five UK neonatal units |
The transcripts were analysed by identifying and grouping emerging themes until no new issues were raised | Parents who elected to have a post-mortem did so for their own needs, or to contribute to a trial, or for both reasons. In two cases, consent for the post-mortem was driven by a sense of making an altruistic contribution to research or by their own desire for information from a post-mortem. One woman who had consented to post-mortem was distressed afterwards because she had not expected to see an incision in the baby’s head | No discussion of methodological approach guiding development of questions or data analysis |
| Snowdon et al.,70 England | To describe the attitudes of neonatologists to trial-related perinatal post-mortem examinations, in the light of declining perinatal post-mortem rates and poor levels of participation in pathology studies | Qualitative study using semistructured interviews | Twenty-six neonatologists (83% recruitment rate) from five UK neonatal units interviewed; five UK perinatal pathologists also contributed to the study (83% recruitment rate) | Interviews were audio-recorded, fully transcribed and analysed with the assistance of a computer-based qualitative analysis package, ATLAS.ti.4 (Scientific Software Development GmbH, Berlin, Germany) | The interviews with neonatologists reveal discomfort over approaching bereaved parents for post-mortems and a widespread concern that parents should not be further distressed or feel under pressure to consent. The study highlights a view that post-mortems may be unnecessary if the cause of death seems apparent or when a baby was born prematurely, and a devaluation of post-mortems among some younger staff. There was also concern that requesting a post-mortem for the benefit of others may be construed as ‘emotional blackmail’ | No discussion of methodological approach guiding development of questions or data analysis |
| Stock et al.,8 Scotland | To assess post-mortem rates following SB and to identify trends in the past 18 years that may have affected acceptance of the investigation | Retrospective audit study | Post-mortem reports and/or obstetrician records of all SBs delivered at the Simpson Centre for Reproductive Health at the Royal Infirmary, Edinburgh, between January 1991 and December 2008 (589 births; 582 pregnancies were examined) | Descriptive analysis. Statistical analysis was carried out by chi-squared test for trend (post-mortem rates) and Fisher’s exact test (consent) using GraphPad Instat (GraphPad Software Inc., CA, USA) | Data showed sharp declines in uptake of post-mortem after the disclosures of unlawful organ retention. Post-mortem agreement coincided with relocation of perinatal pathology services to the same site as obstetric unit and local availability of specialist perinatal pathologists. Obstetric and midwifery attendance at post-mortem, and perinatal pathology involvement in multidisciplinary meetings, case discussions and teaching also improve staff perception of the value of post-mortem. When authorisation for a post-mortem was granted, a senior member of staff was more likely to have carried out counselling than junior doctors or midwives | Only a small part of this study focused on factors associated with changes in post-mortem rates |
| Stolman et al.,55 USA | To investigate attending physician and resident attitudes and factors affecting autopsy consent | 21-item cross-sectional survey | Study sample from department of paediatrics at one university teaching hospital. Study sample consisted of 158 physicians, 67 paediatric residents and 91 attending physicians | The significance of categorical data was assessed using chi-squared or Fisher’s exact test | Thirty-three (41%) participants said that they always found it stressful to ask permission for autopsy. Having a relationship with the family was considered to lead to most success when obtaining permission, followed by ‘when cause of death is unclear’ (15%) and the benefits of autopsy are explained (16%). When asked why families refuse, 37% of participants indicated that the family considered autopsy desecration of the body and 36% said that the family were too upset to consider the issue | Participant characteristics limited |
| Swinton et al.,63 USA | To describe the trend and factors associated with the autopsy over the past decade at a level III neonatal ICU, where all patients are presented with an option | Retrospective audit of the autopsy in a cohort of infants who died in the neonatal ICU from 1 January 2001 to 31 December 2010 | A total of 446 infants died in the neonatal ICU from 2001 to 2010 | Categorical variables were compared by chi-squared. Multivariable logistic regression analyses were performed with autopsy as the dependent variable and the demographic information as independent variables | The overall autopsy rate did not change significantly over time. The autopsy rate significantly differed by gestational age at birth, presence of a major congenital anomaly and chronologic age at death. Only 29.4% of infants with congenital anomalies were autopsied compared with 37.6% of infants without. Autopsy rates did not differ by the period of the day when death occurred, previous surgical interventions, maternal demographic characteristics or distance of family from the hospital | |
| Vijayan and Hiu,56 Malaysia | To assess uptake of perinatal post-mortems among mothers experiencing perinatal deaths. Subjective assessment of factors influencing uptake was studied | Cross-sectional questionnaire survey | Women recruited from Sabah Women and Children Hospital in Malaysia. Couples who had experienced intrauterine fetal demise were given the questionnaire. Of the 87 SBs, 46 returned to the pregnancy clinic and completed the questionnaire | Descriptive. Numbers too low for statistical analysis | Of the 46 couples who completed the questionnaire, 10 (22%) felt that the explanation about post-mortem was poor, 29 (66%) satisfactory and 10 (22%) thought that it was good. Eleven couples (20.7%) thought that the information given on the post-mortem was poor, with the remaining 42 (79.3%) reporting it as merely satisfactory. These 11 couples were counselled by specialists. Forty-two couples (79.2%) were offered a post-mortem. Reasons for declining were religious factors (n = 13, 28%), culture (n = 2, 4%), family consensus (n = 6, 14%), personal (n = 22, 48%) and other (n = 3, 6%) | Very little detail given about what the questionnaire contained and how reasons for declining post-mortem were recorded and categorised. No response rate |
| VanMarter et al.,77 USA | To explore maternal and infant factors that might be determinants of autopsy consent | Mixed methods. A retrospective audit of patient records in cases of neonatal death and a questionnaire circulated to health professionals | A total of 184 of 215 infants (86%) born during the study period who subsequently died | Chi-squared test, Fisher’s exact test or Wilcoxon rank-sum test. A subset of 15 factors were selected for multivariate analysis by logistic regression |
Multivariate analysis found that parents least likely to consent were those who had no history of previous fetal loss, pregnancies in which the birth weight of the infant was < 1000 g, the gestational age was < 28 weeks or those who had an infant die of extreme prematurity Non-significant factors were maternal age, race, marital status and infant sex. For health professionals, increasing importance was associated with advancement in staff position. Those with experience in requesting consent for neonatal autopsy were more likely to consider autopsy very important |
|
| Warland et al.,57 Australia | An online survey of women who had a SB asking about their pregnancy in order to identify any common symptoms and experiences | Cross-sectional web-based survey | A total of 1714 women who had experienced a singleton SB (≥ 28 weeks’ gestation) > 3 weeks prior to enrolment completed the survey | Descriptive statistics and chi-squared tests. Qualitative text responses were coded by two investigators into dichotomized variables to determine frequencies of responses | Some respondents reported that an autopsy was not performed due to cost and/or the view that the autopsy might not give a definitive answer | |
| Whitehouse et al.,64 Canada | Determine the indications for autopsy as perceived by emergency paediatricians | Retrospective audit of patients aged < 18 years who died in PED between October 1985 and December 1989 | A total of 69 patients were included in the study | Data presented in a summary file and reviewed independently by three emergency paediatricians | Autopsy rate was not related to age, sex, time of presentation, survival time or diagnosis | No information about whether or not statistical analysis was conducted to look for associations between patient characteristics and autopsy uptake |
| Wiener et al.,76 USA | To examine bereaved parents’ preferences about the timing and content of the autopsy discussion, as well as reasons for considering autopsy | Mixed-methods survey | Parents who lost a child to cancer between 6 months and 6 years ago and whose child was between the ages of 6 months and 25 years at the time of death were recruited. Of 40 invitations sent, 31 reached households and 27 agreed to participate in study |
Descriptive statistics were used to characterise the sample Thematic content analysis was used to analyse responses to open-ended questionnaire items |
The majority of participants wanted to know how the autopsy could help other children (90%, n/N = 27/30). Overall, parents most commonly wanted the autopsy conversation to include (1) how the autopsy can potentially help other children; (2) how the medical team can learn more about their child’s cancer; (3) how they can learn about the findings of the autopsy; and (4) how the autopsy will help their child’s doctor | Small sample size. Descriptive statistics only |
Glossary
- Biopsy
- A medical procedure that involves taking a small sample of body tissue so it can be examined under a microscope.
- Gestation
- The period of development inside the womb between conception and birth.
- Histology
- The study of cells, tissues and organs, as seen through a microscope.
- Intrauterine fetal death
- Death of a baby in the uterus.
- Laparoscopic
- Surgical technique in which operations are performed through small incisions in the body.
- Less invasive autopsy
- A term that encompasses both non-invasive autopsy and minimally invasive autopsy.
- Minimally invasive autopsy
- Magnetic resonance imaging combined with targeted laparoscopic examination and biopsy of visceral organs.
- Neonatal death
- A liveborn baby who died before 28 completed days after birth.
- Non-invasive autopsy
- Magnetic resonance imaging-based imaging techniques along with other ancillary investigations, such as placental examination, genetic and metabolic tests.
- Perinatal death
- A stillbirth or early neonatal death.
- Prenatal
- Before birth.
- Stillbirth
- A baby delivered at or after ≥ 24 weeks’ gestational age, showing no signs of life, irrespective of when the death occurred.
- Termination of pregnancy
- The deliberate ending of a pregnancy, normally carried out before the embryo or fetus is capable of independent life.
List of abbreviations
- APT
- anatomical pathology technologist
- ARC
- Antenatal Results and Choices
- CI
- confidence interval
- CT
- computerised tomography
- DNA
- deoxyribonucleic acid
- HM
- Her Majesty’s
- HTA
- Human Tissue Authority
- ICU
- intensive care unit
- IUFD
- intrauterine fetal death
- LIA
- less invasive autopsy
- MIA
- minimally invasive autopsy
- MRI
- magnetic resonance imaging
- NIA
- non-invasive autopsy
- Sands
- Stillbirth and Neonatal Death Society
- SB
- stillbirth
- SPIDER
- sample, phenomenon of interest, design, evaluation, research type
- SUDC
- sudden unexpected death in childhood
- SUDI
- sudden unexpected death in infancy
- ToP
- termination of pregnancy for fetal abnormality
