Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/112/01. The contractual start date was in November 2013. The draft report began editorial review in June 2018 and was accepted for publication in January 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Sarah Hewlett’s institution received a grant from Novartis International AG (Basel, Switzerland) after the trial ended, to train rheumatology teams in fatigue management. Ernest Choy’s institution received grants from the Medical Research Council (London, UK) and Versus Arthritis (formerly Arthritis Research UK) (Chesterfield, UK). In addition, Ernest Choy has received grants/consultancy or speaker’s fees from AbbVie Inc. (North Chicago, IL, USA), Bristol-Myers Squibb (New York, NY, USA), Chugai Pharmaceutical Co. (Tokyo, Japan), Eli Lilly and Company (Indianapolis, IN, USA), Janssen: Pharmaceutical Companies of Johnson & Johnson (Beerse, Belgium), Novartis International AG, ObsEva SA (Geneva, Switzerland), Pfizer Inc. (New York, NY, USA), Regeneron Pharmaceuticals, Inc. (Tarrytown, NY, USA), F. Hoffmann-La Roche AG (Basel, Switzerland), R-Pharm JSC (Moscow, Russia), Sanofi SA (Paris, France), SynAct Pharma (Lund, Sweden), Tonix Pharmaceuticals (New York, NY, USA) and UCB Pharma Ltd (Slough, UK). William Hollingworth is a member of the Health Technology Assessment Clinical Trial Board (2016–present).
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Hewlett et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Scientific background
Rheumatoid arthritis (RA) affects approximately 0.5 million people in the UK,1 with widespread synovitis leading to joint pain and stiffness in repeated flares of inflammatory activity. Over time this inflammatory activity can result in multiple joint damage and disability, with major impacts on quality of life, including social and work life. 2 Initiation of very early pharmacological treatment (treat to target) aims to switch off these inflammatory processes and is combined with multidisciplinary interventions by secondary care rheumatology teams to support self-management of symptoms and lifestyle. 3,4
In the past decade, consultation with people with RA regarding their treatment priorities has highlighted the importance of fatigue as a symptom. 5 For many people with RA, fatigue is present on most days and can be as extreme as that seen in chronic fatigue syndrome (CFS), and as severe as their RA pain. 6,7 Qualitative research shows that people find RA fatigue to be not only a physical experience, but also to have emotional and cognitive elements that can have an impact on their work, family roles and relationships. 8,9 Quality of life is reduced by fatigue,10 which patients report as being as difficult as pain to manage. However, fatigue is often ignored by the rheumatology team,9,11 despite being one of patients’ top priorities. 5 People with RA consider fatigue to be a major feature in work loss,12 which affects two-thirds of working people with RA. In addition, approximately one-fifth of people with RA become work-disabled within 5 years, resulting in an annual UK work production loss from RA of around £2 billion. 13,14 These findings led to international consensus that the effect of interventions on RA fatigue should now be reported in all RA clinical trials alongside the traditional core set. 15
Inflammation as a possible mechanism for rheumatoid arthritis fatigue
If the inflammatory processes of RA are the major driver of RA fatigue, either directly or through the effects of inflammation on pain and function, then pharmacological interventions for RA inflammation should also significantly improve fatigue. However, systematic review shows that biologic disease-modifying antirheumatic drugs (bDMARDs) to control RA inflammation yield only a small to moderate improvement in RA fatigue (32 studies involving 14,628 patients), although the quality of the studies was variable. 16 Inflammatory activity, not fatigue, is the indication for initiating or changing bDMARD therapy; therefore, these studies did not recruit patients specifically with fatigue. 16 The findings are supported by other studies that show that RA fatigue continues to be problematic even for those patients who achieve disease (i.e. inflammatory) remission. 17 Therefore, it is unlikely that inflammation alone is the single driver for RA fatigue.
Multicausal pathways as a likely mechanism for rheumatoid arthritis fatigue
A systematic review of causal studies relating to RA fatigue could not draw conclusions as a result of the quality of the evidence, which was largely cross-sectional or longitudinal studies that rarely controlled for baseline fatigue. 18 Therefore, with insufficient studies, and often conflicting results on any single causal mechanism for fatigue (e.g. inflammation, disability, depression),18 it is postulated that, conceptually, RA fatigue is likely to have complex and multicausal pathways (see Appendix 1). 19 These pathways are categorised as potentially involving interactions between or within three elements: (1) disease processes (RA elements); (2) thoughts, feelings and behaviours (cognitive/behavioural elements); and (3) life issues (personal elements). 19 Pathways will vary between patients and potentially even within patients for individual fatigue episodes. For example, on one occasion fatigue may be driven by inflammation causing pain and disrupting sleep, interacting with heavy work responsibilities that lead to overactivity (keeping going until exhausted); however, on another occasion fatigue may be driven by low mood, leading to behavioural withdrawal (deactivation) and subsequent deconditioning. In this conceptual model, self-management strategies appear crucial in managing fatigue impact.
Physical exercise interventions
Physical exercise interventions might address muscle or respiratory deconditioning from inactivity that cause fatigue. A systematic review of randomised controlled trials (RCTs) of non-pharmacological interventions reporting RA fatigue identified six physical exercise interventions (five RCTs involving 371 patients), including pool therapy, yoga, t’ai chi, low-impact aerobics, strength training and stationary cycling. 20 Meta-analysis showed a small effect on fatigue severity. However, none of these studies had fatigue as a primary outcome, fatigue was not an inclusion criterion and studies were not powered to detect fatigue change.
Psychosocial interventions and underpinning theory
A broader approach of psychosocial interventions for helping people manage their fatigue may address multiple elements in the conceptual model simultaneously. 19 Educational interventions may provide the information people need to identify and change behaviours that might be stopping their management of fatigue [e.g. introducing ideas of breaking up periods of activity with rest (pacing)]. Interventions that also address thoughts or feelings related to fatigue and its management might lead to more beneficial coping strategies by looking at ways of managing stress, low mood and priorities for a work–life balance.
Rationale for cognitive–behavioural therapy for fatigue in rheumatoid arthritis
Cognitive–behavioural therapy (CBT) aims to help people work out for themselves the links between their thoughts (cognitions) and feelings and how these may be driving their actions (behaviours), and addresses these underpinning cognitions as a way of prompting behaviour changes. 21 For example, a belief that it is one’s role to do the household chores may prevent someone asking family members to help, which, combined with feeling shame or guilt if chores are left undone, may drive persistence in undertaking chores. This excessive activity leads to episodes of overwhelming fatigue and enforced rest (so-called ‘crashes’), commonly called the ‘boom-and-bust’ cycle. Addressing these previously unchallenged beliefs about what family members would think about a request for help, and whether or not leaving some chores undone would be a catastrophe, might prompt behaviour changes that result in less fatigue. The lack of an existing clear approach to self-management of fatigue from RA professionals may contribute to a sense of powerlessness and passivity among people with RA fatigue who feel their lives are controlled by its perceived unpredictability. CBT provides a framework through which a person can better understand those components of fatigue experiences that are controllable, and, through this, make a shift in core beliefs towards taking control rather than being passive. On the basis of such a shift a person could become progressively less passive and more self-confident through better self-management of activity and fatigue symptoms so that the impact of fatigue is reduced.
A systematic review of group education programmes for general self-management in musculoskeletal conditions found that a CBT approach is more likely to lead to people making behaviour changes than information alone,22 and CBT has been shown to be effective for fatigue in CFS and multiple sclerosis. 23,24 Problem-solving and goal-setting as routes to enhancing self-efficacy (see Underpinning theory: self-efficacy and social cognitive theory) are the core self-management skills that patients learn in CBT.
Underpinning theory: self-efficacy and social cognitive theory
Managing daily life with RA in order to minimise fatigue requires changing behaviours that might have been contributing to fatigue onset, perpetuating it, or limiting its management. Changing habitual behaviours can be hard, and self-efficacy is the belief or confidence that one can successfully execute an action or master a situation and is a strong predictor of behaviour change and persistence in the face of difficulty. 25 Self-efficacy is cultivated through reinterpretation of symptoms (understanding that fatigue has many causes that could be tackled), mastering the new behaviours (through progressive goal-setting), and by modelling and social persuasion (from seeing the successful changes and adaptions of other RA patients). 26 Therefore, learning about fatigue management as part of a group can enhance these self-efficacy processes because other patients in similar situations act as role models: validating the complexity of fatigue and demonstrating more effective ways of mastering it through the efforts they make as fellow participants on the programme [social cognitive theory (SCT)]. 25,26 It has been demonstrated that interventions based on SCT and/or CBT enhance self-efficacy and produce better patient outcomes than simply providing self-management information. 22,27 Learning with others in similar circumstances may be particularly helpful for validating invisible symptoms, such as fatigue.
Evidence for psychosocial interventions on rheumatoid arthritis fatigue
Three RCTs trialled one-to-one CBT, a group programme (based on SCT) and a group CBT programme (SCT/CBT) over 11, 16 and 22 hours, respectively, and reported improved fatigue in RA patients. 28–30 However, interventions were not primarily aimed at improving fatigue severity; thus, patients were not recruited because of fatigue, nor were studies powered to detect fatigue change. Furthermore, participation in the studies was restricted (e.g. to those with early disease, mild disability or psychological distress or who have a partner). However, RA fatigue occurs in the majority of patients;6,7 therefore, self-management interventions should be tested across a wide RA population. Therefore, the original 18-week RCT was conducted to test a fatigue self-management programme in a broad RA population (fatigue score of ≥ 6/10), using group CBT (13 hours SCT/CBT), led by a clinical psychologist and specialist pain management occupational therapist (OT), compared with groups receiving fatigue self-management information alone (n = 127). 31 The group CBT intervention improved fatigue impact (effect size 0.77) alongside fatigue severity and coping with fatigue, as well as disability, sleep and mood (depression, helplessness, self-efficacy). In the qualitative evaluation undertaken through participant interviews, patients spontaneously raised the significance of key elements of the CBT used by the clinical psychologist (working links out for themselves, goal-setting, activity diaries), and SCT components (the value of being in a group). 32
A systematic review identified 15 psychosocial interventions reporting RA fatigue, including the previous study (13 RCTs involving 1556 patients). 20 Interventions included expressive writing, CBT, mindfulness, lifestyle management, self-management, energy conservation and group education, and showed an overall small benefit on RA fatigue severity. The overall quality of trials was rated as being low, largely accounted for by small patient numbers and the difficulty of blinding participants in interventions that require engagement for behaviour change. Within the systematic review, the RCTs detailed above, which were the only interventions in which improving fatigue was an aim or inclusion criterion,28,30,31 had stronger methodological qualities and stronger effects on fatigue.
Rationale for programme delivery by rheumatology clinical teams
The fatigue self-management programme using CBT and SCT was delivered by a CBT-trained clinical psychologist. 31 However, only 8% of rheumatology units have a clinical psychologist on their team;33 therefore, implementation in routine NHS care is currently difficult. Enabling people with long-term conditions to self-manage is a key government target,34 and RA-specific guidelines by rheumatology professional bodies and the National Institute for Health and Care Excellence (NICE)3,4,35 highlight the need to address self-management, including fatigue. Given the success of psychological therapies but the shortage of clinical psychologists, Improving Access to Psychological Therapies is also a government health policy. 36 This is being achieved through manualisation of psychological interventions and training non-clinical assistants to deliver them, often by telephone and under the supervision of a psychologist, adhering closely to the intervention stipulated and referring those cases that are not straightforward to the psychologist. It might be that RA fatigue self-management programmes do not need to be delivered by trained CBT psychologists, but could be delivered by, for example, Improving Access to Psychological Therapies practitioners guided by a manual. However, in people with RA fatigue, thoughts, feelings and behaviours will also interact with their need to manage a complex, lifelong and fluctuating chronic physical illness that in itself requires managing the interactions between pain, inflamed joints, disrupted sleep, multiple medications and their accumulative effects on overall well-being. Therefore, in order to address these issues, psychological therapies need to be provided by clinicians who understand the multiple interactions between fatigue and the patient’s wider self-management of fluctuating RA symptoms. The multidisciplinary team, particularly rheumatology nurse specialists (RNSs) and OTs, routinely support RA patients in self-management and understand these interactions; therefore, with appropriate training and support RNSs and OTs are ideally placed to deliver a group fatigue intervention using cognitive–behavioural (CB) approaches, thus embedding fatigue management within usual care.
Development of the RAFT programme intervention for delivery by clinical teams
The original group CBT fatigue intervention delivered by a clinical psychologist and specialist OT to people with RA31 was developed from clinical experience of chronic pain and CFS self-management programmes, using the Medical Research Council’s framework for complex interventions. 37 The intervention was grounded in qualitative data about RA patients’ experiences of fatigue9 and clinical RA experience. The intervention comprised six 2-hour sessions, running once per week (weeks 1–6), and a 1-hour consolidation session (week 14), and was delivered to groups of approximately 5–7 patients. For delivery by clinical teams, a tutor manual was produced, and the intervention given the acronym RAFT (Reducing Arthritis Fatigue by clinical Teams using CB approaches).
The RAFT programme delivery: cognitive–behavioural and social cognitive theory approaches
The CB approach used was one of reflective discovery through Socratic questioning, in which tutors ask simple questions to enable patients to identify the links between their thoughts, feelings, behaviours and symptoms (i.e. fatigue). 21 This was in contrast to the more didactic information- or advice-giving by the tutors, in which the patients were passive recipients of information. Self-monitoring (daily activity/rest charts) and goal-setting are the most effective tools in bringing about behavioural change,38 and the use of metaphors helps turn abstract or difficult therapeutic concepts into a form that can be more easily understood and remembered. 39 The value of group CB programmes is that fellow patients are a credible source to legitimise or validate invisible symptoms, such as fatigue, and provide role models and peer support in the goal-setting and problem-solving processes. 25
The RAFT programme content
The RAFT programme addresses the potential interactive drivers of fatigue (see Appendix 1)19 and its management, with the tutors facilitating topic discussions for the first hour, then splitting after a short tea break into two groups for detailed goal-setting. Topics, goal-setting and homework build on earlier sessions over the weeks (see Appendix 2). 40 The group initially validates this invisible symptom of fatigue and the problem of managing it, then explores pacing and how underpinning thoughts drive boom-and-bust cycles (week 1). Between sessions patients are asked to monitor their patterns of activity, rest and fatigue crashes by colouring in an hourly chart. In week 2, things that energise or drain are the topic, and personal priorities to improve overall life balance then feed into goal-setting, when each participant’s daily activity chart is discussed to elucidate behaviour patterns and their consequences (fatigue). These charts are the focus of the small group discussions each week and give a visual overview of a changing balance of rest, activity, sleep and relaxation/energisers and, hopefully, fewer fatigue crashes because of improvements in pacing as the programme progresses. Subsequent topics are sleep (week 3), with its links to stress (week 4), and the struggle to communicate what can and cannot be done because of fatigue (week 5). Week 6 looks at dealing with setbacks (using a metaphor of ‘falling into the pit’ that is fatigue), and reviews the skills introduced in weeks 1–5. The consolidation session (week 14) helps participants reflect on their progress in acceptance and self-management of fatigue (using the metaphor of leaving the ‘isolation of a desert island’ that is fatigue), and finishes with longer-term goals.
The RAFT programme training and materials for tutors
The RAFT programme was manualised for the tutors, including a detailed guide for each session, sample texts, diagrams and patient handouts (these were piloted and refined). 41 The RAFT programme was co-facilitated by a pair of tutors, who were clinical rheumatology nurses and/or OTs. A 4-day training programme was delivered to all the RAFT programme tutors together, covering RA fatigue and the conceptual model, information on CB principles, Socratic questioning (used to help patients identify thoughts that drive behaviours), self-efficacy, goal-setting and group management, and each RAFT programme session was discussed and demonstrated or rehearsed. To complete their training, tutor pairs delivered a practice programme to patients and were observed and given feedback by a trainer (a clinical psychologist, specialist OT or a rheumatology nurse specialising in fatigue: NA, BK and SH). As tutors were experienced rheumatology clinicians, little clinical supervision was required; thus, one session in each of programmes 2 and 4 was supervised by a trainer.
Aims and objectives
The objectives are reproduced from Hewlett et al. 40 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text includes minor additions and formatting changes to the original text.
The overall aim of this study was to test a group CB intervention for RA fatigue (the RAFT programme) that can be routinely delivered by clinical rheumatology teams across the NHS, using a manualised programme with all supporting materials, delivered by the rheumatology team after brief training and with minimal clinical supervision. 40 The objectives were to:
-
assess whether or not there is a clinically important difference in the impact of fatigue at 6 months between patients participating in a group CB self-management programme for RA fatigue, delivered by the clinical rheumatology team using a detailed manual (in addition to usual care), and patients receiving usual care alone (which includes written fatigue self-management information)
-
compare differences between trial arms for secondary outcomes of fatigue severity, coping, mood, sleep, helplessness, pain, disability, valued activities, quality of life, work, health service use, acceptability, and cost-effectiveness for the NHS, patients and society
-
evaluate and control for potential demographic, psychological and clinical predictors of fatigue change
-
evaluate persistence of effect (if any) over 2 years
-
explore whether or not clinical teams trained in CB approaches perceive any positive or negative outcomes, particularly on their wider clinical practice.
The study comprised:
-
a RCT in which the RAFT programme in addition to usual care was compared with usual care alone
-
an evaluation of the cost-effectiveness of providing the fatigue intervention
-
a nested qualitative study to explore the tutors’ (RNSs and OTs) experiences of CB approach training and any positive or negative effects on their wider clinical practice beyond the RAFT programme delivery.
As a process evaluation of the RAFT programme from the patients’ perspectives had been undertaken in the original trial with a qualitative study,32 this was not repeated. Instead, in this RCT, the process evaluation concentrated on understanding the perspectives of rheumatology clinicians who were being asked to learn new skills and deliver the RAFT programme in the nested qualitative study.
Chapter 2 Trial design and methods
Trial design
This trial evaluated the RAFT programme self-management intervention for fatigue plus usual care compared with usual care alone, through a pragmatic RCT delivered by seven hospital teams across the UK, a setting that reflected clinical practice. Clinical care, including medication change, continued as normal and without restrictions for all participants throughout the trial. In addition to clinical effectiveness (see Chapter 3), a health economic evaluation (see Chapter 4) and a qualitative evaluation of the RNS and OT tutors’ experiences (see Chapter 5) were undertaken. The protocol has been published. 40
Ethics and registration
The trial and qualitative study were approved by the East of England – Cambridgeshire and Hertfordshire Research Ethics Committee (reference number 13/EE/0310), after which each centre obtained the necessary local research and development approvals. The RCT was registered with the International Standard Randomised Controlled Trial Number registry as ISRCTN52709998.
Participants
Inclusion criteria
In order to reflect pragmatic clinical practice, in which the majority of RA patients experience fatigue, inclusion criteria were very broad. Patients aged ≥ 18 years with confirmed RA42 were eligible if they had a fatigue severity score of ≥ 6 (out of 10) on the Bristol Rheumatoid Arthritis Fatigue Numerical Rating Scale (BRAF-NRS),43,44 which they perceived was a recurrent problem.
Exclusion criteria
Patients were excluded if they had recently changed major RA medication (within 16 weeks) or glucocorticoids (within 6 weeks), as that might influence fatigue. Patients were ineligible if they had insufficient English to participate in group discussions or lacked capacity for informed consent.
Setting
Rheumatoid arthritis is managed in secondary care; therefore, the RAFT programme was delivered by pairs of local hospital rheumatology clinicians (i.e. nurses/OTs, band 6 or 7), who understand how RA symptoms interact with fatigue in the self-management of a long-term, fluctuating condition that requires adaptation and acceptance. In order to test the generalisability of the RAFT programme, the seven participating rheumatology units encompassed a range of large and small departments, academic and non-academic, covering city and rural areas in England and Wales (Bristol, North Bristol, Cardiff, Chertsey, Poole, Torbay and Weston-super-Mare).
Recruitment procedures
Patients with RA were invited to complete the BRAF-NRS to screen for fatigue severity, either when attending clinic or by mailshot to departmental lists in the seven participating hospitals. If fatigue was scored as ≥ 6 and the patient was interested, other eligibility criteria were then checked, and an information sheet provided with a pre-paid envelope to return to the local research nurse. Each centre recruited to and delivered four consecutive RAFT programmes over 2 years. In order to randomise 5–7 patients to a RAFT programme, each centre recruited 10–14 patients and then closed that ‘cohort’. Over a 2-week period, those patients attended for informed consent and baseline assessment, and then received usual care for fatigue. When all patients had completed this, randomisation occurred and recruitment commenced for the next cohort. Delays between screening and baseline assessment were inevitable, as baseline assessments could not be performed until a centre had accrued a large enough cohort of 10–14 interested and eligible patients (which often took several months). Therefore, any changes to eligibility at baseline assessment (e.g. fatigue less severe, medication changed) were noted for potential subgroup analysis; however, the patient proceeded to randomisation, reflecting the pragmatic way in which this intervention would be delivered in practice to a population with fluctuating, recurrent fatigue and frequently changing medication regimens. Patients who were randomised to a RAFT programme but were then unable to attend the dates offered maintained their randomisation allocation and were offered the subsequent RAFT programmes being run in that centre; if they accepted then they had a new baseline assessment performed with the others in that cohort.
Interventions
The RAFT programme intervention
The RAFT programme is a CB fatigue self-management programme delivered to groups of 5–7 RA patients in six 2-hour sessions (weeks 1–6) and a 1-hour consolidation session (week 14) by a pair of local RNSs and/or OTs (see Chapter 1). Taking a pragmatic approach, if one of the tutors was unable to deliver a session, perhaps because of illness, the remaining tutor delivered the session alone. Patients were asked to attend all seven sessions if possible; however, some patients inevitably missed some sessions as RA is a fluctuating condition, in which case tutors offered to explain some of what had been missed, prior to the next session.
Fidelity to the RAFT programme during delivery
Quality and homogeneity of the RAFT programme were facilitated by standardised training and a standardised manual, with programme delivery by the same tutor pairs in each centre. However, unlike a pharmacological RCT, in a group CB intervention it is not possible to adhere to a rigid protocol in every session, as tutors must respond to the individual issues raised by patients. Therefore, fidelity evaluation was pragmatic and involved monitoring in one randomly selected session of each of the four programmes run in each centre. An independent clinical psychologist observer (Richard Cheston) used a template to record evidence of CB approaches (e.g. reflective questioning, group management, goal-setting), delivery of the RAFT programme as planned (adherence to session plans), use of the RAFT programme materials (handouts, metaphors) and any unhelpful delivery styles (e.g. didactic teaching) (see Report Supplementary Material 1). 41
Control intervention (usual care alone)
Unlike pain, RA fatigue is not routinely addressed in usual care in great detail and patients are generally given written fatigue information by the RNS. Most rheumatology units supply the free Versus Arthritis (formerly Arthritis Research UK) fatigue booklet,45 a comprehensive fatigue self-management booklet for arthritis authored by Hewlett et al. and based on their original RCT. 31 It contains information on all the topics in the RAFT programme, includes a pull-out sample activity and rest chart to complete and could be considered ‘usual care’. Usual care (i.e. provision of the Versus Arthritis fatigue booklet) was given to patients in both the control and intervention arms of the trial at the baseline visit, after consent and assessment but before randomisation. The research nurse spent approximately 5 minutes showing their patient the sections in the booklet, using a brief standardised guideline and pointing out that the booklet suggests patients might wish to request specific support from the rheumatology team to help them try the fatigue self-management activities described (generally requested via the local RNS helpline). Seeking help is thus an intended outcome of the booklet, which was captured within health-care use data collected in the trial. In order to minimise the risk of contamination between the trial arms, the helpline RNS were asked not to book in a control patient requesting fatigue support to see a clinician who was also a RAFT programme tutor if there was an alternative health professional available, and tutors recorded any control patients seen for fatigue support.
Outcomes of clinical effectiveness
Primary outcome measure (26 weeks)
As the impacts of fatigue are wide-ranging and personal to individuals’ lives, the perceived impact of fatigue was the primary outcome measure, rather than fatigue severity. 8–11 Fatigue impact was measured by a single NRS item, ‘Please circle the number that describes the effect fatigue has had on your life in the last 7 days’, with anchors of ‘No effect’ to ‘A great deal of effect’ (0–10), using the BRAF-NRS for impact (see Report Supplementary Material 2). 43,44
Secondary outcome measures (clinical)
The secondary fatigue outcomes were fatigue severity and coping (as measured using the BRAF-NRS severity, BRAF-NRS coping questionnaires) (see Report Supplementary Material 2) and a RA fatigue multidimensional questionnaire [i.e. Bristol Rheumatoid Arthritis Fatigue Multidimensional Questionnaire (BRAF-MDQ)] (see Report Supplementary Material 2), which measures overall fatigue impact and includes subscales for physical fatigue, living with fatigue, emotional fatigue and cognitive fatigue. 43,44 Each of these fatigue variables might respond differently to interventions. Other components of the RA fatigue conceptual model19 evaluated were mood [via the Hospital Anxiety and Depression Scale (HADS)],46 pain (via the NRS), disability [via the modified Health Assessment Questionnaire (MHAQ)],47 quality of life [global arthritis impact question from the Arthritis Impact Measurement Scale (AIMS)],48 sleep quality (via a single question from the Pittsburgh Sleep Quality Index),49 and returning to important leisure activities previously lost to fatigue [via the discretionary activity subscale of the Valued Life Activities scale for rheumatoid arthritis (VLA)]. 50 Beyond pain, disability and fatigue, remaining items from the RA core set51 were an objective assessment of painful joints and swollen joints, an inflammatory marker (i.e. C-reactive protein) and patient global opinion of disease activity [visual analogue scale (VAS)], forming a single disease activity score [Disease Activity Score (DAS28)] through a weighted algorithm. 52 As the DAS28 requires a hospital visit to the research nurse, it was measured at weeks 0 and 26 only, and replaced at all other time points by a patient self-reported version [i.e. the simplified Patient-derived Disease Activity Score (sPDAS2)]. 53,54 Social contact questions (unvalidated) were added for weeks 52 and 104.
Secondary outcome measures (processes)
To understand what key processes may relate to behavioural change, helplessness [via the Arthritis Helplessness Index (AHI)]55 and self-efficacy [via the Rheumatoid Arthritis Self-Efficacy (RASE) scale]56 were measured. The RASE scale contains questions on self-efficacy beliefs for managing RA covered in both the RAFT programme and the usual-care Versus Arthritis fatigue booklet. 45
Secondary outcome measures (acceptability and feasibility)
Acceptability of the RAFT programme and the usual-care booklet45 was assessed at week 26 by patient satisfaction and the likelihood that patients would recommend the programme or booklet to others, and by programme attendance. Feasibility of delivery in the NHS was captured through monitoring of programme scheduling and delivery, and the tutor qualitative evaluation.
Follow-up time points, data collection and management
Baseline assessments (and usual care) for each cohort were conducted over a 2-week period. The cohort was then randomised, and those patients randomised to the RAFT programme commenced their local programme within a few weeks. To standardise data collection across all cohorts and centres, the date of each cohort’s first RAFT programme session was designated as week 1 for both trial arms. Outcomes were then measured at weeks 6 (end of the RAFT programme), 26 (primary end point), 52, 78 and 104, apart from DAS28 and social contact as described in Secondary outcome measures (clinical). Only fatigue data were collected at weeks 10 and 18 (via the BRAF-NRS for impact, severity and coping and BRAF-MDQ),43,44 to capture outcomes 4 weeks before and after the week 14 consolidation session. Data were collected primarily by patient self-report questionnaire, except for objective measures of disease activity, which were evaluated by the local research nurse (after standardised training) at weeks 0 and 26. Patients completed their self-report questionnaire pack during those visits, but at all other time points questionnaire packs were posted to patients from the central trial team in Bristol, with pre-paid envelopes. In order to maximise data returns, the trial co-ordinator or trial administrator (ZP and CA), with ethics approval, telephoned each patient at each assessment point to collect the primary outcome (i.e. the BRAF-NRS impact) and inform the patient that the questionnaire pack was being posted (participants were contacted once more if packs were not returned within 2 weeks). Data were returned direct to the managing centre (University of the West of England, Bristol, UK) and entered onto an Microsoft Access® database (Microsoft Corporation, Redmond, WA, USA) that was created by the Bristol Randomised Trials Collaboration (BRTC) unit. Data entry was then checked by a second researcher against the original questionnaires (100% of entries were checked) (Table 1).
| Assessment | Measure | Score range | Week | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 6 | 10 | 18 | 26 | 52 | 78 | 104 | |||
| Nurse led | ||||||||||
| Demographic data | n/a | ✓ | ||||||||
| Disease activity | DAS2852 | 0.96+a | ✓ | ✓ | ||||||
| Primary outcome | ||||||||||
| By telephone | BRAF-NRS43,44 | 0–10 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Questionnaire (self-reported) | ||||||||||
| Fatigue severity | BRAF-NRS43,44 | 0–10 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Fatigue coping | BRAF-NRS43,44 | 0–10b | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Fatigue overall impact | BRAF-MDQ43,44 | 0–70 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Physical fatigue | BRAF-MDQ43,44 | 0–22 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Emotional fatigue | BRAF-MDQ43,44 | 0–12 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Cognitive fatigue | BRAF-MDQ43,44 | 0–15 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Living with fatigue | BRAF-MDQ43,44 | 0–21 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Pain | NRS | 0–10 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Disability | MHAQ47 | 0–3 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Quality of life | AIMS VAS48 | 0–100 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Disease activity | sPDAS253,54 | 2.4–7.9 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Anxiety | HADS46 | 0–21 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Depression | HADS46 | 0–21 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Sleep quality | Pittsburgh item49 | 1–4 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Valued life activities | VLA50 | 0–3 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Helplessness | AHI55 | 5–30 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Self-efficacy | RASE56 | 28–140b | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Satisfaction and acceptability | ✓ | |||||||||
| Social contact | ✓ | ✓ | ||||||||
Protocol amendments during the trial
Prior to the first baseline assessment, the global impact of arthritis question48 was added (amendment 1, January 2014). Amendment 2 (February 2015) comprised the addition of the social contact questions (at weeks 52 and 104), following reflection by the Study Management Group that the RAFT programme promotes resisting the desire to isolate oneself. In addition, the qualitative evaluation of tutor experiences through focus groups was expanded to offer one-to-one interviews in order to allow easier discussion of individual opinions. Amendment 3 (September 2015) allowed for the possibility of an additional RAFT programme to run in the case of low levels of recruitment or high levels of attrition (but this was not needed).
Sample size
The sample size calculation has previously been published. 40 In the original trial of CBT delivered by a clinical psychologist, the baseline-adjusted difference in fatigue impact between trial arms was 1.95 units on a VAS (0–10) [95% confidence interval (CI) −2.99 to −0.90 units; p < 0.001], giving an effect size of 0.77. 31 As the RAFT programme is delivered by clinical teams using CB approaches rather than by a CB therapist, the RCT reported here was powered to be able to demonstrate 75% of that (1.46 units, effect size 0.54). For a two-sided significance of 0.05 and a power of 90%, 73 patients per trial arm were required. The study was interested in the average effect across all centres; therefore, no loss of power from randomising patients by centre was considered. 57,58 In the RAFT programme arm there was potential for clustering effects from the seven centres (including the one tutor pair per centre), and from the CB group within centres. In the original RCT, the intraclass correlation coefficient (ICC) for the CBT group and the primary outcome was < 0.00001, with no data for centre/tutor effects as it was a single-centre study. 31 In the present RCT, an overall ICC value of 0.01 was employed for groups clustered within and between centres, and was used for estimating a design effect,59 increasing the sample size to 75 per trial arm.
In the original RCT,31 most attrition was not from the intervention but from loss to questionnaire completion; therefore, to maximise data returns in this RCT the primary outcome was collected by telephone by the central RAFT programme team as described above, and patients who wished to withdraw were asked if they might continue providing a fatigue impact NRS by telephone (ethics approval given). It was intended to achieve 80% of primary outcome data at week 26, but longer-term attrition was unknown. Therefore, we assumed 50% retention and thus capacity was planned to recruit up to 150 patients per trial arm. A pragmatic approach took account of the need to form viable RAFT programme groups and natural variations in group size; therefore, a target of seven centres each running four RAFT programmes, with an average of six participants per RAFT programme group and six participants randomised to usual care (n = 336), provided contingency for smaller groups.
Minimising attrition
In order to reduce attrition prior to starting a RAFT programme, patients were consented and randomised as close to the dates of the CB programmes as possible and the local research nurse kept patients informed of the potential programme dates. Three-quarters of participants in the original RCT attended most of their seven CBT sessions, suggesting that the RAFT programme would be acceptable. 31 In this RCT a 2-year follow-up potentially risked significant loss to questionnaire completion over time; therefore, to maximise questionnaire returns, the primary outcome data (i.e. fatigue impact NRS scores) were collected by the central trial team by telephone each time (see Follow-up time points, data collection and management). To enhance feelings of community, engagement and responsibility, all RAFT programme study materials included the study logo; questionnaire packs were accompanied by a short newsletter highlighting overall questionnaire return rates, and thank-you notelets were sent at major time points.
Randomisation, concealment and blinding
After consent at the baseline visit, the local research nurse allocated each patient the next consecutive study identification number; as patients chose from several available baseline visit dates and times, this allocation was unlikely to be influenced by the research nurse. When a centre had finished all baseline visits for that cohort (10–14 participants, assessed over a 2-week period), the research nurse sent the unique study numbers to the trial co-ordinator in Bristol, which requested that the BRTC unit conduct the randomisation for that centre’s cohort (concealed from the RAFT programme study team and the research nurse). Computer-generated randomisation (using a specially created Access database) was performed for each cohort (1, 2, 3 and 4) in each centre (1, 2, 3, 4, 5, 6 and 7) consecutively over 2 years as each cohort was finalised and all its participants had attended for consent, baseline assessment and delivery of usual care. Allocation was 1 : 1 within cohorts but, in the event of an odd number, the RAFT programme trial arm received the extra patient on the grounds that risk of attrition was likely to be higher in that arm. The BRTC unit informed the trial co-ordinator of the arm allocations, and the trial co-ordinator informed the local research nurse, who subsequently telephoned each consented patient using a brief, standardised guideline to ensure that no suggestion other than equipoise between the arms was communicated. Those randomised to the RAFT programme trial arm had the dates, times and venue confirmed. Blinding of clinicians delivering the RAFT programme was not possible, nor could patients be blind because of the need to engage them in making behavioural and cognitive changes and attend or not attend the RAFT programme sessions. However, most outcome measures used were validated tools and analysis was performed blind to allocation.
Overview of evaluation methods
Clinical and health economic analysis followed the predefined statistical and health economics analysis plan (SAP) [see URL: www.journalslibrary.nihr.ac.uk/programmes/hta/1111201/#/documentation (accessed 12 April 2019)], which was agreed in discussion with the Trial Steering Committee (TSC) and Data Management and Ethics Committee (DMEC). Detailed methods and results are presented separately for the clinical, health economic and qualitative evaluations (see Chapters 3–5).
Study management
The project was managed and co-ordinated centrally in Bristol by the chief investigator (SH), trial co-ordinator (ZP) and trial administrator (CA), with all outcome assessments (apart from baseline and week 26) being sent out by, and returned to, the central study team, thereby enabling careful monitoring of timelines and returns. Each centre employed a research nurse to manage local recruitment, cohort building and closure, visits for consent and baseline assessment, and week 26 assessment. The trial co-ordinator maintained the overall site documentation and a local study file for each site and liaised with all sites and with the BRTC randomisation service. The central co-ordinating team (i.e. SH, ZP and CA) held weekly meetings to set up the trial, with other key trial staff, co-applicants and patient partners attending as appropriate. Monthly Trial Management Group meetings of the researcher co-applicants were held and the wider group of rheumatologist co-applicants (local principal investigators) attended when appropriate. The independent TSC and DMEC convened at key time points to support the trial development and review progress. All meetings were reduced in frequency once the trial was established, but resumed more frequently during database closure, data analysis and interpretation. The RCT was sponsored by the University Hospitals Bristol NHS Foundation Trust.
Patient and public involvement
Patient involvement occurred throughout the project and was provided by two patients who had participated in the original trial (Clive Rooke and Frances Robinson). 31 The aim of a joint enterprise with patient partners was for them to bring experiential knowledge of RA fatigue and receiving the original CBT intervention from a psychologist. The patient partners advised on outcomes to be evaluated, questionnaire pack design, recruitment processes and all trial patient materials. The patient partners suggested improvements to the patient handouts used in the RAFT programme and advised that the relaxation CD be re-recorded to improve sound quality. The patient partners attended the tutor training days to talk with the tutors and the principal investigators about their experience of fatigue. Continued involvement (by Clive Rooke) included advising on the formatting of the tutor manual, attendance at major project review meetings and analysis of the qualitative data.
Chapter 3 Clinical evaluation: analysis methods and results
Statistical analysis methods
The analysis and reporting of this trial was undertaken in accordance with Consolidated Standards of Reporting Trials (CONSORT) guidelines. 60 All statistical analyses were undertaken using Stata version 14.1.1 (StataCorp LP, College Station, TX, USA), following a predefined SAP [see URL: www.journalslibrary.nihr.ac.uk/programmes/hta/1111201/#/documentation (accessed 12 April 2019)], which was agreed with the TSC and the DMEC. The primary comparative analyses between randomised trial arms were conducted on an intention-to-treat (ITT) basis without imputation of missing data.
Preliminary analyses (baseline comparability)
Descriptive statistics of key clinical and sociodemographic characteristics were used to compare randomisation trial arms at baseline and to inform any additional adjustment of the primary and secondary analyses when appropriate.
Primary analysis
The primary analysis used linear regression to compare BRAF-NRS impact score at 26 weeks (the primary outcome) between trial arms as randomised and adjusted for baseline values of the outcome and recruitment centre (stratification variable). The result of the linear regression model is presented as an adjusted difference in means between the RAFT programme and control arms, alongside the associated 95% CI and p-value for the comparison. A standardised effect size for the primary outcome was also calculated as the adjusted difference in mean divided by the pooled baseline standard deviation (SD).
Secondary analyses
Primary outcome measure
Secondary analyses of the primary outcome included additional adjustment of the primary analysis for any prognostic variables demonstrating a marked imbalance at baseline (ascertained using descriptive statistics). There was a gap in time between eligibility screening and baseline measurement. Owing to this time gap, some individuals who had a BRAF-NRS severity score of ≥ 6 points (out of 10 points) at screening (an eligibility criterion) subsequently had a lower BRAF-NRS severity score of < 6 points at the time of randomisation. For this reason, the primary analysis was repeated and restricted to those individuals who had a BRAF-NRS severity score of ≥ 6 points at randomisation (analysis not prespecified).
A repeated measures mixed-effects model was used to examine the effect of the intervention over time by including up to four follow-up BRAF-NRS impact scores (at weeks 26, 52, 78 and 104), adjusted for baseline values of the outcome and for recruitment centre. This analysis provided an estimate of the average effect size over the duration of follow-up. A potential convergence or divergence between trial arms was investigated by repeating the analysis with the inclusion of a time-by-treatment group interaction term. The repeated measures analysis was repeated on those individuals with a BRAF-NRS severity score of ≥ 6 points at randomisation.
Secondary outcome measures
The effect of the intervention on the secondary outcomes collected at 26 weeks was also examined using appropriate regression models adjusted for baseline values of the outcome being investigated and for recruitment centre. The secondary outcomes were also subject to repeated measures analysis using data collected at the 26-, 52-, 78- and 104-week follow-ups.
A potential difference between trial arms in the changes in major RA medications that might influence the primary outcome was investigated using a chi-squared test. A change in major RA medications was defined as stopping, starting or changing the dose of one or more disease-modifying antirheumatic drugs (DMARDs), bDMARDs or glucocorticoid medications during a single time period. Acceptability of the RAFT programme or the usual-care booklet to patients was measured by the RAFT programme attendance rates, satisfaction and recommendation to others, and is summarised using descriptive statistics.
Potential clustering effects
Owing to the hierarchical nature of the data (i.e. participants nested within centres and then within cohorts), there is potential for clustering effects in the trial. To investigate this, a linear mixed-effects model, which included centre and cohort as cluster-level variables, was compared with the linear regression primary analysis model by means of the likelihood ratio test.
Missing data
The sensitivity of the primary analysis to the impact of missing data was examined. The method of multiple imputation by chained equations using predictive mean matching was used to impute missing data. The imputation model included all variables that were part of the ITT primary analysis, variables identified from the previous trial as being related to fatigue impact (fatigue severity, pain and both self-reported and nurse-rated disease activity), and baseline variables that were associated with missingness of the primary outcome. In total, 20 imputed data sets were generated and combined using Rubin’s rules. The primary analysis model was then repeated using the imputed data.
Treatment efficacy
Complier-average causal effect (CACE) analysis was used to investigate the efficacy of the RAFT programme intervention in reducing fatigue impact at 26 weeks. The CACE methodology compares outcomes among those who ‘complied’ with the intervention and a comparable group of ‘would be compliers’ in the control arm. 61 (The word ’compliance’ is used here as a statistical term; clinically the word adherence is used to describe active rather than passive decisions to participate.) CACE analysis provides an estimate of the efficacy of the intervention for comparison with the ITT estimate of the offer of the intervention, while respecting randomisation and avoiding biases inherent to crude per-protocol analyses, in which only individuals in the RAFT programme arm are included. In this trial ‘compliance’ was defined as attending at least two sessions of the RAFT programme (session 1 plus any other session). However, those individuals randomised to the RAFT programme intervention arm but who did not attend (i.e. withdrew and did not attend the first RAFT programme session) had no follow-up data collected. This is problematic as it meant that outcome information was not available for a group of individuals who would be considered ‘non-compliant’ and have contributed information to the CACE analysis. It also potentially violated the exclusion restriction assumption: if individuals in the RAFT programme intervention arm were considered participants only if they attended the first CB session (which might then have an impact on their outcome), then the offer of the intervention does affect outcome. To address this issue, the two stages of the two-stage least squares (2SLS) CACE estimation were carried out separately to allow for loss to follow-up that was dependent on compliance. The first-stage regression uses all individuals randomised to predict compliance. The second stage involved only those with non-missing outcomes, but modelled these using the predicted values of compliance obtained from the ‘complete’ first stage.
Interpretation of findings
When designing the trial it was stated that the traditional effect size of > 0.5 would be considered to reflect a clinically meaningful effect. 40 During the discussions to interpret the findings, the Trial Management Group, with input from the TSC statistician, discussed the issue of effect sizes in terms of their clinical importance. Over the years, concerns have been raised in the literature as to whether only an effect size ≥ 0.5 must be considered clinically meaningful, or if smaller effect sizes might be considered by patients to have had an effect. For example, Sloan et al. 62 argue that this cut-off point is only a broad guideline and that clinical meaningfulness must be related to each specific health issue under investigation (i.e. it would be different for different patient outcomes). They recommend that, if supported by additional data related to that specific health issue, ‘small’ effect sizes of 0.2 can also be considered clinically meaningful. Although there are no data on clinically meaningful change in RA fatigue impact, Khanna et al. 63 demonstrated that patients reported that they experienced a noticeable improvement in RA fatigue severity at effect sizes 0.27 to 0.39. It was therefore decided to take a broader view when interpreting the findings and also to consider additional data to inform consideration of clinically meaningful change and effect sizes (a departure from the protocol).
Subgroup and exploratory analyses
Number of sessions attended
It was hypothesised a priori that those individuals attending a greater number of the RAFT programme sessions would show a greater improvement than those who attended fewer sessions. The theoretical justification was that greater exposure to the RAFT programme intervention should improve self-management skills. A structural mean model 2SLS instrumental variable approach, which respects randomisation,64 was used to investigate the impact of number of sessions of the RAFT programme attended on BRAF-NRS impact score. As with the treatment efficacy CACE analysis, the non-follow-up of those individuals randomised to the RAFT programme intervention arm but who did not attend the first session of the RAFT programme is problematic. The same approach (i.e. a separate two-stage approach) was used to address this issue. A further assumption of this model was that of a linear relationship between session attendance and BRAF-NRS impact score, that is, that the impact of an increase in attendance of one session was the same across all the different sessions (i.e. all sessions had a similar effect on patient outcome).
Consolidation session (week 14)
The RAFT programme intervention was delivered in seven sessions: sessions 1–6 delivered weekly over weeks 1–6, followed by session 7 at week 14 to consolidate skills and behaviours. Separate linear regression models were used to examine the effect of the RAFT programme on BRAF-NRS impact score at 6 weeks (immediately after the final RAFT programme session), at 10 weeks (4 weeks before the consolidation session) and at the 18-week follow-up (4 weeks after the consolidation session).
Predictors of fatigue impact change
Certain clinical and demographic characteristics were examined as potential predictors of fatigue impact change. All of these variables of interest were first added as covariates to the primary analysis model and then removed from the model one by one in a process of stepwise deletion until only covariates with a p-value of < 0.05 were retained (i.e. the covariate with the highest p-value from the initial model was removed, the model was then repeated without this covariate and the variable with the highest p-value in this second model was then removed, etc.). The starting model comprised the primary analysis model additionally adjusted for baseline pain (i.e. NRS score), disease activity (i.e. DAS28 score), BRAF-NRS coping score, age, comorbidity, work status, disease duration and sex.
Self-efficacy
The RASE scale has 28 items that ask about beliefs regarding self-management tasks, many of which are discussed during the RAFT programme. To examine the impact of the RAFT programme intervention on particular components of self-efficacy, the change in RASE scale item scores from 0 to 26 weeks in the control and the RAFT programme intervention trial arms was compared using t-tests.
Tutor delivery over time
It was hypothesised that the size of the effect of the RAFT programme intervention may differ between cohorts as tutors within each centre may have improved in their delivery of the intervention over time. To explore this, the mean change in fatigue, impact from 0 to 26 weeks, is presented by intervention arm and cohort. The difference in mean change (between trial interventions) by cohort is also presented (this was not in the SAP but was prespecified before any analysis commenced).
Social contact
Group work may enhance the seeking of social support (see Chapter 2, Protocol amendments during the trial). The social contact data are analysed using simple percentages.
Results
The key clinical findings from the RAFT programme trial presented here have been previously published. 65
Participant flow
Recruitment commenced in December 2013, with the first patient consent received in February 2014 and the last in October 2015, and the trial completed as planned with the final follow-up questionnaires returned in January 2018. The flow of eligible patients with RA and a fatigue severity score of ≥ 6 points from invitation to participation through to week 104 is detailed in Figure 1. Over the 2 years a total of 333 patients were randomised, comprising four consecutive cohorts in each of the seven centres (see Chapter 2, Recruitment procedures), with similar numbers across centres (see Appendix 3). All patients accepted their randomised allocation.
FIGURE 1.
Participant flow chart. Reproduced from Hewlett et al. 65 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.
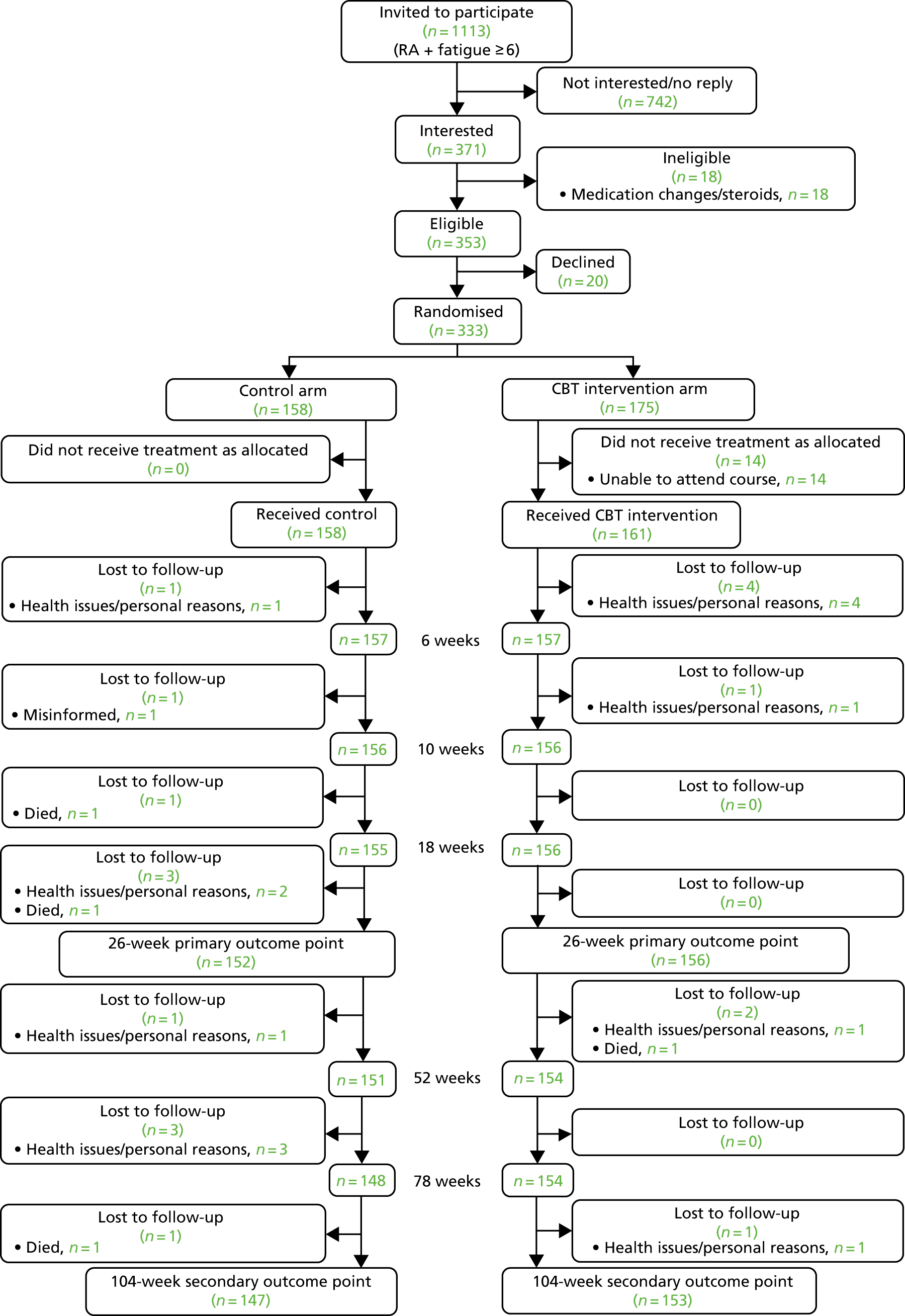
After consent and baseline assessment, all patients received usual care before randomisation, i.e. the Versus Arthritis fatigue booklet. 45 Of the 175 patients randomised to additionally receive the RAFT programme, 14 did not receive the intervention because of an inability to find suitable programme dates. Of the 161 patients who received the RAFT programme, five patients withdrew for personal/health reasons (four patients during programme delivery, having received up to three of the seven sessions, and one patient withdrew before the week 10 assessment). Therefore, 156 of the 175 RAFT programme patients provided primary outcome data at week 26, and 153 patients provided data at week 104 (89.9% and 87.4% of those patients randomised, respectively). Of the 158 patients randomised to usual care only, six patients withdrew before week 26, leaving 152 patients providing primary outcome data at week 26 and 147 patients providing data at week 104 (96% and 93.0%, respectively).
Follow-up data completion
The majority of patients provided primary outcome fatigue impact data (BRAF-NRS impact data were collected by telephone), with 308 and 296 patients completing BRAF-NRS impact at weeks 26 and 104, respectively (see Appendix 4). Therefore, the 50% attrition allowed for at 2 years did not materialise and the follow-up numbers exceeded the required total sample size of 150. Secondary outcome data questionnaire packs were returned by > 88% of patients at 26 weeks and 78% of patients at 104 weeks (lowest completion rate was 72% for sleep quality at week 78, see Appendix 4). Six patients who were randomised to a RAFT programme but could not attend their planned programme dates attended a later programme, when a fresh baseline assessment was made. However, at the end of RAFT programme delivery in the seven centres, 14 patients randomised to the RAFT programme had been unable to attend any local programme dates and the 26-week primary outcome data were not obtained from them.
The RAFT programme delivery and tutor adherence
All seven rheumatology centres were able to provide at least two clinicians for training and, of those 15 who were trained, 14 went on to deliver the RAFT programme. One tutor pair comprised OTs, two tutor pairs were nurses and four pairs were mixed nurse and OT. They had a mean of 5.3 years’ rheumatology experience (range 0–17 years) and had been qualified for a mean of 18 years (range 6–30 years) and 10 had some experience of running patient groups, of whom four also reported some prior relevant knowledge such as goal-setting or CBT (data not detailed to preserve anonymity).
All seven hospitals were able to deliver all four 14-week RAFT programmes as planned and on time, indicating feasibility to deliver in the NHS, which is explored further in the qualitative evaluation (see Chapter 5). Tutor pairs remained unchanged throughout the RAFT programmes, apart from one centre where tutor absence for two programmes was covered by the remaining tutor co-delivering one programme with a trainer and one with a locum tutor who had observed the previous programme. There were 196 RAFT sessions (28 programmes comprising seven sessions), of which seven (3.6%) were delivered by a single tutor due to absence. Independent monitoring for tutor adherence (fidelity) to the RAFT programme delivery and CB principles was carried out as planned and no remedial teaching was deemed necessary.
The RAFT programme attendance
At randomisation, the RAFT programme group sizes averaged six patients (with a range of five to eight patients). The RAFT programme patients attended a mean of 5.85 of their 7 RAFT programme sessions (SD 1.63 sessions). Most of the 156 patients had high attendance rates, with 87.2% (n = 136) attending 5–7 sessions (Table 2).
| Total number of sessions attended | Patients (N = 156), n (%) |
|---|---|
| 1 | 7 (4.5) |
| 2 | 6 (3.8) |
| 3 | 4 (2.6) |
| 4 | 3 (2.0) |
| 5 | 20 (12.8) |
| 6 | 42 (26.9) |
| 7 | 74 (47.4) |
All 156 RAFT programme patients attended their first session and each of the subsequent sessions (i.e. sessions 2–7) was attended by ≥ 75% of the randomised patients (Table 3).
| Individual session | Patients (N = 156), n (%) |
|---|---|
| 1 | 156 (100) |
| 2 | 137 (87.8) |
| 3 | 129 (82.7) |
| 4 | 125 (80.1) |
| 5 | 129 (82.7) |
| 6 | 119 (76.3) |
| 7 | 118 (75.6) |
Adverse events
No related serious adverse events were reported by tutors.
Preliminary analyses (baseline comparability)
The 25 patients who did not complete to 26 weeks were very similar to the 308 patients who did complete to this primary end point in terms of baseline demographic data (age, sex, disease duration, comorbidity), and fatigue severity (entry criterion) and impact (primary outcome) (see Appendix 5). They had similar clinical status to those who completed the study (see Appendix 6).
Baseline demographic data were similar between trial arms, with the majority of patients being female, as reflects the RA population (Table 4). The patients were aged > 60 years, on average, with a wide range of disease duration. The majority of patients were of moderate to high socioeconomic status and white, and a small proportion had previously attended a general rheumatology self-management programme many years earlier.
| Demographic variable | Trial arm, n (%) | |
|---|---|---|
| Control (N = 152) | RAFT (N = 156) | |
| Female | 121 (79.6) | 125 (80.1) |
| Age (years)a | 61.8 (54.4, 69.6) | 63.7 (54.2, 69.9) |
| Disease duration (years)a | 10 (3, 20) | 10 (5, 19) |
| Socioeconomic status: Englandb | ||
| Deprived | 28 (21.1) | 23 (17.2) |
| Moderate | 60 (45.1) | 65 (48.5) |
| Affluent | 45 (33.8) | 46 (34.3) |
| Socioeconomic status: Walesb | ||
| Deprived | 7 (41.2) | 7 (35.0) |
| Moderate | 3 (17.7) | 5 (25.0) |
| Affluent | 7 (41.2) | 8 (45.0) |
| Ethnicity | ||
| White | 147 (98.0) | 151 (96.8) |
| Asian/Asian British/other | 3 (2.0) | 5 (3.1) |
| Other self-management programmes | 21 (14.0) | 16 (10.3) |
| Years since previous programmea | 8 (5, 11) | 5 (3, 10) |
Baseline clinical data were similar between arms and were therefore well balanced (Table 5). On average, patients had high fatigue impact scores (i.e. a BRAF-NRS impact score of > 7/10), which were slightly higher than fatigue severity scores, and had a low perceived ability to cope with fatigue (measured via the BRAF-NRS coping questionnaire). The participants had relatively high levels of disease activity (inflammation) with DAS28 scores of > 4.2 (> 5.1 is the eligibility criterion for starting bDMARDs). On average, participants had moderate pain, low disability and moderate self-efficacy and helplessness at baseline. The distribution of the primary outcome, fatigue impact, is shown in Figure 2.
| Clinical variable | Trial arm | |||
|---|---|---|---|---|
| Control (N = 158) | RAFT (N = 175) | |||
| n (%)a | Mean (SD) | n (%)a | Mean (SD) | |
| Fatigue | ||||
| BRAF-NRS impact (0–10) | 152 (96.2) | 7.23 (1.6) | 156 (89.1) | 7.10 (1.7) |
| BRAF-NRS severity (0–10) | 142 (89.9) | 6.85 (1.57) | 152 (86.9) | 6.89 (1.57) |
| BRAF-NRS coping (0–10)b | 142 (89.9) | 4.84 (2.09) | 152 (86.9) | 5.16 (2.08) |
| BRAF-MDQ overall impact (0–70) | 142 (89.9) | 40.39 (12.99) | 152 (86.9) | 40.42 (12.70) |
| BRAF-MDQ physical (0–22) | 142 (89.9) | 16.19 (3.21) | 152 (86.9) | 16.12 (3.39) |
| BRAF-MDQ emotional (0–12) | 142 (89.9) | 6.71 (3.31) | 152 (86.9) | 6.55 (3.18) |
| BRAF-MDQ cognitive (0–15) | 142 (89.9) | 7.58 (4.04) | 152 (86.9) | 7.54 (4.00) |
| BRAF-MDQ living (0–21) | 142 (89.9) | 9.90 (5.18) | 152 (86.9) | 10.21 (5.05) |
| Pain: NRS (0–10) | 142 (89.9) | 5.57 (2.10) | 152 (86.9) | 5.70 (2.12) |
| Disability: MHAQ (0–3) | 142 (89.9) | 0.76 (0.51) | 151 (86.3) | 0.75 (0.53) |
| Quality of life: AIMS VAS (0–100) | 141 (89.2) | 49.89 (20.44) | 152 (86.9) | 49.16 (22.27) |
| Disease activity | ||||
| Assessed: DAS28 (0.96+) | 145 (91.8) | 4.23 (1.11) | 147 (84.0) | 4.22 (1.30) |
| Self-reported: sPDAS2 (2.4–7.9) | 142 (89.9) | 4.36 (0.99) | 151 (86.3) | 4.44 (1.06) |
| Anxiety: HADS (0–21) | 142 (89.9) | 8.01 (4.45) | 151 (86.3) | 7.29 (4.08) |
| Depression: HADS (0–21) | 142 (89.9) | 6.79 (3.94) | 151 (86.3) | 7.18 (3.59) |
| Valued life activities: VLA (0–3) | 142 (89.9) | 1.08 (0.60) | 151 (86.3) | 1.16 (0.61) |
| Helplessness: AHI (5–30) | 142 (89.9) | 18.98 (4.74) | 152 (86.9) | 19.03 (4.67) |
| Self-efficacy: RASE scale (28–140)b | 142 (89.9) | 104.38 (11.34) | 151 (86.3) | 102.49 (11.51) |
| Sleep quality | 142 (89.9) | 149 (85.1) | ||
| Very goodc | 5 (3.5%) | 9 (6.0%) | ||
| Fairly goodc | 58 (40.9%) | 48 (32.2%) | ||
| Fairly badc | 51 (35.9%) | 56 (37.6%) | ||
| Very badc | 28 (19.7%) | 36 (24.2%) | ||
FIGURE 2.
Distribution of baseline BRAF-NRS impact scores, by trial arm. (a) Control; and (b) the RAFT programme.

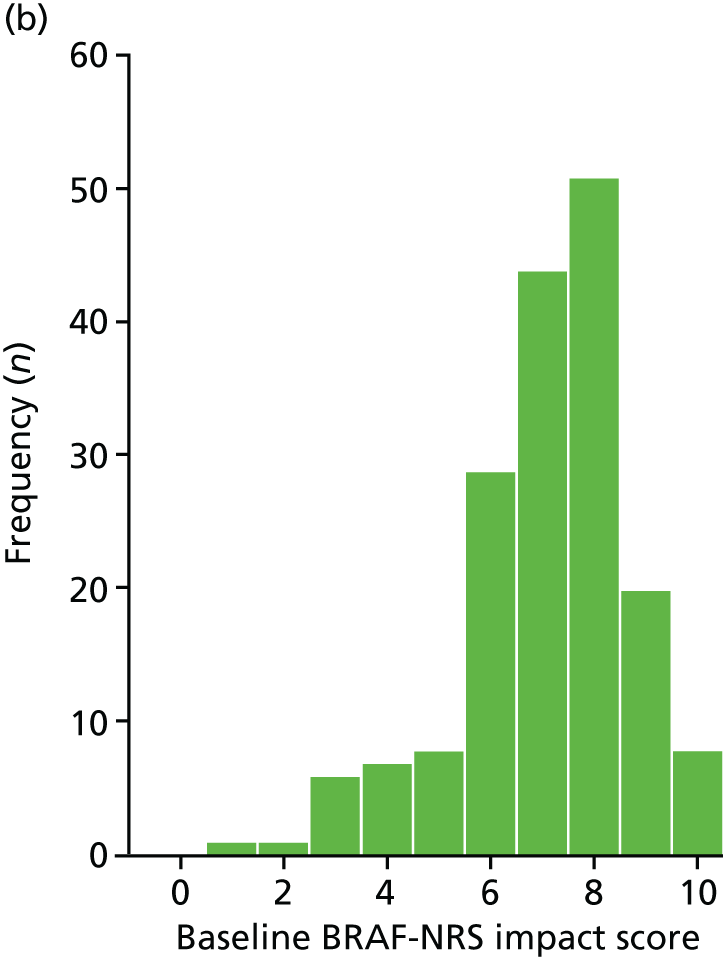
Participants had eligible fatigue scores at screening (i.e. a BRAF-NRS severity score of ≥ 6/10), but often had to wait for a sufficient number of participants to be recruited in order to close their cohort ready for consent, baseline assessment and randomisation. At the later baseline assessment, the fatigue severity scores of 23 out of 152 control patients and 23 out of 156 RAFT programme patients had fallen below the inclusion criterion (15.1% and 14.6%, respectively); however, as this was a pragmatic trial aiming to reflect how the RAFT programme would be delivered in clinical practice, the participants proceeded to randomisation.
Primary analysis
There was no difference between the trial arms for fatigue impact at baseline and both arms had improved fatigue impact at week 26 (Table 6). Patients in the control arm improved by a mean of –0.88 (SD 2.4, Wilcoxon signed-rank test statistic –3.560; p < 0.001), and those in the RAFT programme improved by a mean of –1.36 (SD 2.7, Wilcoxon signed-rank test statistic –5.666; p < 0.001).
| Primary outcome | Trial arm | Adjustedb mean difference (95% CI) | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Control | RAFT | |||||||
| n (%)a | Week, mean (SD) | n (%)a | Week, mean (SD) | |||||
| 0 | 26 | 0 | 26 | |||||
| BRAF-NRS impact score | 152 (96.2) | 7.23 (1.6) | 6.36 (2.42) | 156 (89.1) | 7.10 (1.7) | 5.74 (2.41) | –0.59 (–1.11 to –0.06) | 0.03 |
The primary outcome was the BRAF-NRS impact score at 26 weeks (ranging from 0 to 10, with the lower score representing the better outcome). Linear regression was used to investigate the impact of the intervention on the primary outcome, adjusted only for baseline score and centre as other factors were similar between trial arms (see Table 5). Individuals in the RAFT programme had a BRAF-NRS impact score at 26 weeks that was, on average, –0.59 units lower (better) than that of those in the usual-care arm, with a 95% CI ranging from a 1.11 to a 0.06 reduction in fatigue impact (p = 0.03). The adjusted mean difference between arms equated to a standardised effect size of 0.36.
Secondary analysis
Primary outcome measure
Analysis adjusting for variables imbalanced at baseline was not required as no variables were imbalanced.
Baseline eligibility and 26-week outcome
The primary analysis was repeated excluding those individuals who had fallen below the eligibility criterion of BRAF-NRS severity of ≥ 6.0 points between screening and baseline (n/N = 3/152 control patients and n/N = 23/156 RAFT programme patients). For baseline-eligible patients, the fatigue impact score at 26 weeks was lower in the RAFT programme than in the control arm, with an adjusted mean difference between arms in fatigue impact of –0.82, a slightly larger effect than observed in the primary complete-case (screening-eligible) analysis (Table 7).
| Eligibility | n | BRAF-NRS impact score, adjusted mean differencea (95% CI) | p-value |
|---|---|---|---|
| Screening-eligible patients | 308 | –0.59 (–1.11 to –0.06) | 0.03 |
| Baseline-eligible patients | 262 | –0.82 (–1.40 to –0.24) | 0.01 |
Primary outcome at 26–104 weeks
The BRAF-NRS impact score differed between trial arms over weeks 0–104 (Figure 3). Based on repeated measures analysis and using data from the 26-, 52-, 78- and 104-week follow-up time points, the group receiving the RAFT programme intervention had a BRAF-NRS impact score that was, on average, 0.49 units lower (i.e. better) than in the control arm over the 2 years, on a scale of 0–10 (adjusted mean difference –0.49) (Table 8).
FIGURE 3.
The BRAF-NRS impact scores over weeks 0–104, by trial arm. Reproduced from Hewlett et al. 65 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original text.
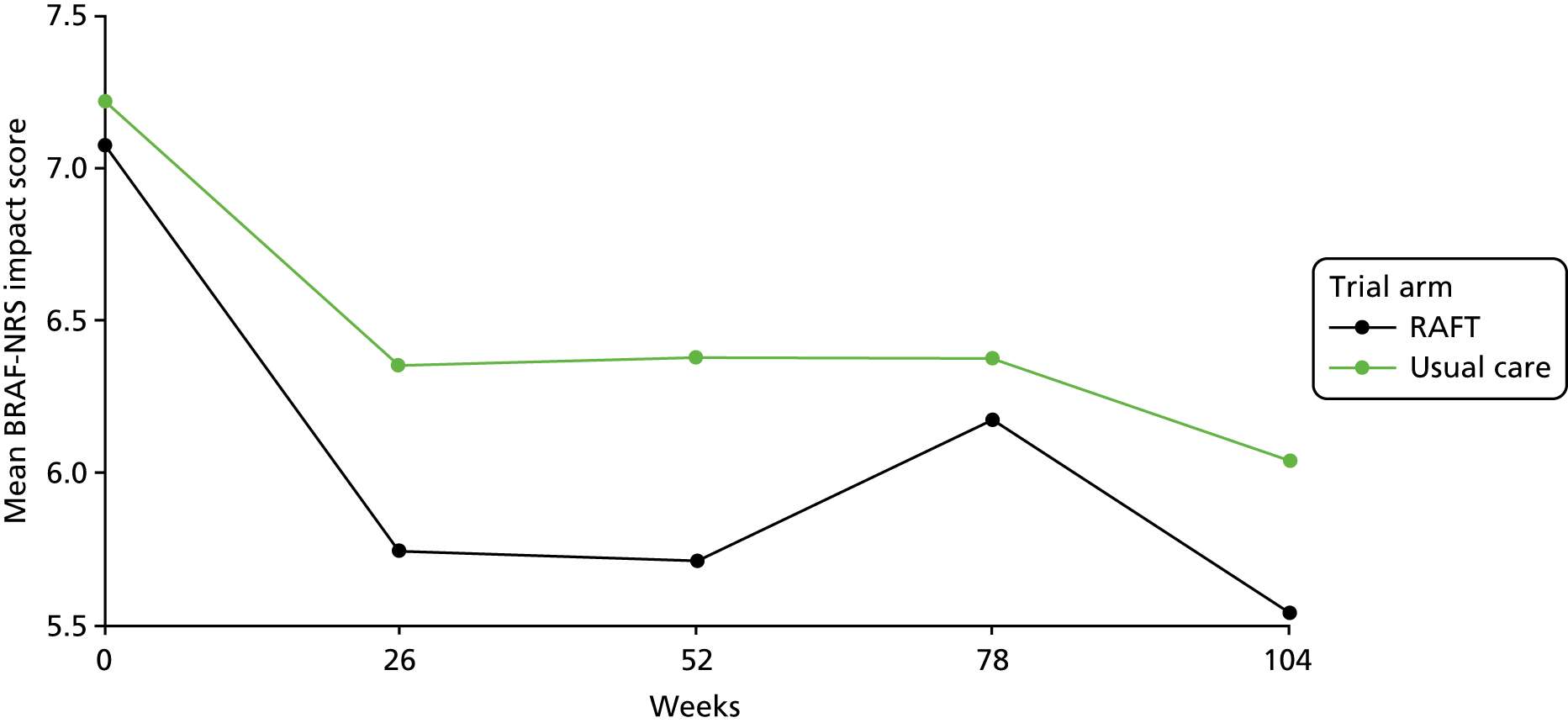
| Trial arm | Time point | Repeated measures (N = 308) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 26 weeks (N = 308) | 52 weeks (N = 305) | 78 weeks (N = 300) | 104 weeks (N = 296) | |||||||
| n | BRAF-NRS impact score, mean (SD) | n | BRAF-NRS impact score, mean (SD) | n | BRAF-NRS impact score, mean (SD) | n | BRAF-NRS impact score, mean (SD) | Adjusted mean differencea (95% CI) | p-value | |
| Control | 152 | 6.36 (2.42) | 151 | 6.38 (2.19) | 146 | 6.38 (2.23) | 145 | 6.05 (2.14) | –0.49 (–0.83 to –0.14) | 0.01 |
| RAFT | 156 | 5.74 (2.41) | 154 | 5.72 (2.23) | 154 | 6.17 (2.24) | 151 | 5.54 (2.28) | ||
When a treatment arm-by-time interaction term was added to the model there was no evidence that the difference between the RAFT programme and the control arm varied over time (interaction between treatment and time, p = 0.52). The estimated treatment effects at each of the follow-up time points were similar and in favour of the RAFT programme, with the exception of that at the 78-week follow-up time point, which was non-significant (see Appendix 7).
Baseline eligibility and 2-year follow-up
The repeated measures analysis was repeated excluding those individuals who had fallen below the eligibility criterion of a BRAF-NRS severity score ≥ 6.0 between screening and baseline (n/N = 23/152 control patients and n/N = 23/156 RAFT programme patients). For baseline-eligible patients, the RAFT programme patients had a BRAF-NRS impact score that was, on average, 0.58 lower (i.e. better) than those in the control arm over the 2 years (adjusted mean difference –0.58) (Table 9). This represents a slightly larger treatment effect than observed when analysing all screening-eligible participants.
| Eligibility | n | BRAF-NRS impact score, adjusted mean differencea (95% CI) | p-value |
|---|---|---|---|
| Screening-eligible participants | 308 | –0.49 (–0.83 to –0.14) | 0.01 |
| Baseline-eligible participants | 262 | –0.58 (–0.95 to –0.22) | 0.002 |
Secondary outcome measures
Secondary outcomes at 26 weeks
Both trial arms appeared to demonstrate improvement in some secondary outcomes at 26 weeks, particularly overall fatigue impact score (BRAF-MDQ overall) and its fatigue subscales, self-efficacy (RASE scale score) and sleep (see Appendix 8). There appeared to be little change in disease activity measures (DAS28 and sPDAS2), pain, disability or mood.
After adjusting for baseline scores and centre, there was evidence of a difference between arms in overall fatigue impact score (BRAF-MDQ overall), and the subscales emotional fatigue and living with fatigue, as well as the process measure of self-efficacy for managing RA (i.e. RASE scale score), with the adjusted mean differences in favour of the RAFT programme intervention (Table 10). Standardised effect sizes calculated for these variables ranged from 0.23 to 0.28. There was no evidence of a difference between the trial arms for any other secondary outcome, including fatigue severity. Over the 26 weeks, 20 out of 141 control patients reported seeking extra appointments for fatigue help, compared with 8 out of 152 RAFT programme patients (14.2% vs. 5.2%; p < 0.01).
| Clinical outcome | Trial arm | Adjusted mean differenceb (95% CI) | p-value | Effect size | |||
|---|---|---|---|---|---|---|---|
| Control | RAFT | ||||||
| n (%)a | Mean (SD) | n (%)a | Mean (SD) | ||||
| Fatigue | |||||||
| BRAF-NRS severity (0–10) | 142 (89.9) | 6.13 (2.30) | 152 (86.9) | 5.91 (2.22) | –0.24 (–0.75 to 0.27) | 0.35 | |
| BRAF-NRS coping (0–10)c | 142 (89.9) | 5.32 (2.42) | 152 (86.9) | 5.25 (2.33) | –0.15 (–0.69 to 0.39) | 0.58 | |
| BRAF-MDQ overall impact (0–70) | 142 (89.9) | 34.74 (16.41) | 152 (86.9) | 31.51 (16.02) | –3.42 (–6.44 to –0.39) | 0.03 | 0.27 |
| BRAF-MDQ physical (0–22) | 142 (89.9) | 14.40 (5.23) | 152 (86.9) | 13.72 (4.91) | –0.68 (–1.78 to 0.42) | 0.23 | |
| BRAF-MDQ emotional (0–12) | 142 (89.9) | 5.36 (3.79) | 152 (86.9) | 4.37 (3.51) | –0.91 (–1.58 to –0.23) | 0.01 | 0.28 |
| BRAF-MDQ cognitive (0–15) | 142 (89.9) | 6.55 (4.16) | 152 (86.9) | 5.89 (4.35) | –0.66 (–1.45 to 0.13) | 0.10 | |
| BRAF-MDQ living (0–21) | 142 (89.9) | 8.43 (5.68) | 152 (86.9) | 7.53 (5.43) | –1.19 (–2.17 to –0.21) | 0.02 | 0.23 |
| Pain: NRS (0–10) | 142 (89.9) | 5.24 (2.41) | 152 (86.9) | 5.47 (2.32) | 0.16 (–0.33 to 0.65) | 0.51 | |
| Disability: MHAQ (0–3) | 142 (89.9) | 0.70 (0.51) | 151 (86.3) | 0.71 (0.54) | 0.02 (–0.06 to 0.10) | 0.67 | |
| Quality of life: AIMS VAS (0–100) | 141 (89.2) | 47.70 (23.04) | 152 (86.9) | 47.22 (23.46) | –0.33 (–5.13 to 4.65) | 0.90 | |
| Disease activity | |||||||
| Assessed: DAS28 (0.96+) | 145 (91.8) | 4.10 (1.31) | 147 (84.0) | 4.13 (1.38) | 0.02 (–0.21 to 0.24) | 0.88 | |
| Self-reported: sPDAS2 (2.4–7.9) | 142 (89.9) | 4.33 (1.04) | 151 (86.3) | 4.44 (1.13) | 0.05 (–0.16 to 0.26) | 0.63 | |
| Anxiety: HADS (0–21) | 142 (89.9) | 7.56 (4.48) | 151 (86.3) | 6.65 (4.36) | –0.33 (–0.95 to 0.29) | 0.30 | |
| Depression: HADS (0–21) | 142 (89.9) | 6.42 (4.06) | 151 (86.3) | 6.22 (3.76) | –0.50 (–1.14 to 0.14) | 0.13 | |
| Valued life activities: VLA (0–3) | 142 (89.9) | 1.07 (0.62) | 151 (86.3) | 1.09 (0.67) | –0.05 (–0.15 to 0.05) | 0.34 | |
| Helplessness: AHI (5–30) | 142 (89.9) | 17.47 (5.46) | 152 (86.9) | 16.92 (5.06) | –0.61 (–1.65 to 0.43) | 0.25 | |
| Self-efficacy: RASE (28–140)c | 142 (89.9) | 104.67 (13.31) | 151 (86.3) | 106.26 (14.78) | 3.05 (0.43 to 5.66) | 0.02 | 0.27 |
| Sleep quality | |||||||
| Very goodd | 9 (6.3%) | 17 (11.4%) | 0.75 (0.47 to 1.17)e | 0.21 | |||
| Fairly goodd | 65 (45.8%) | 64 (43.0%) | |||||
| Fairly badd | 51 (35.9%) | 51 (34.2%) | |||||
| Very badd | 17 (12.0%) | 17 (11.4%) | |||||
Secondary outcomes at 26–104 weeks
Based on repeated measures analysis using data from the 26-, 52-, 78- and 104-week follow-up time points (see Appendix 9), the patients in the RAFT programme had, on average, a better outcome than those patients in the control arm over the 2 years, with respect to fatigue coping (BRAF-NRS coping), overall fatigue impact (BRAF-MDQ overall), emotional fatigue and living with fatigue (BRAF-MDQ emotional, BRAF-MDQ living) (Table 11). There was no evidence of a difference between trial arms over the 2-year duration of follow-up with respect to fatigue severity (BRAF-NRS severity, BRAF-MDQ physical), cognitive fatigue (BRAF-MDQ cognitive) or any other variable.
| Secondary outcome | Adjusted mean differencea | 95% CI | p-value |
|---|---|---|---|
| Fatigue | |||
| BRAF-NRS severity (0–10) | –0.17 | –0.54 to 0.20 | 0.38 |
| BRAF-NRS coping (0–10)b | 0.42 | 0.08 to 0.77 | 0.02 |
| BRAF-MDQ overall impact (0–70) | –2.98 | –5.39 to –0.57 | 0.02 |
| BRAF-MDQ physical (0–22) | –0.64 | –1.45 to 0.17 | 0.12 |
| BRAF-MDQ emotional (0–12) | –0.90 | –1.44 to –0.37 | 0.001 |
| BRAF-MDQ cognitive (0–15) | –0.53 | –1.14 to 0.08 | 0.09 |
| BRAF-MDQ living (0–21) | –0.93 | –1.75 to –0.10 | 0.03 |
| Pain: NRS (0–10) | 0.01 | –0.38 to 0.40 | 0.94 |
| Disability: MHAQ (0–3) | 0.01 | –0.07 to 0.08 | 0.86 |
| Quality of life: AIMS VAS (0–100) | –0.02 | –3.91 to 3.86 | 0.99 |
| Disease activity: sPDAS2 (2.4–7.9) | 0.03 | –0.15 to 0.20 | 0.77 |
| Anxiety: HADS (0–21) | –0.40 | –0.96 to 0.15 | 0.16 |
| Depression: HADS (0–21) | –0.49 | –1.06 to 0.08 | 0.09 |
| Valued life activities: VLA (0–3) | –0.06 | –0.14 to 0.03 | 0.22 |
| Helplessness: AHI (5–30) | –0.27 | –1.12 to 0.58 | 0.54 |
| Self-efficacy: RASE scale (28–140)b | 1.31 | –0.80 to 3.42 | 0.23 |
| Sleep quality | 0.74c | 0.44 to 1.27 | 0.28 |
Patients making medication changes
During the trial, as reflects the clinical management of RA, many patients had changes to their RA medication, defined as starting, stopping or changing the dose of a DMARD, bDMARD or glucocorticoid medication, which might have influenced fatigue. However, the proportion of patients making at least one change was not different between the trial arms (see Appendix 10).
The RAFT programme acceptability
Patient acceptability of the RAFT programme was indicated by high levels of attendance with little attrition (see Tables 2 and 3). At 26 weeks, patients reported high levels of satisfaction with the usual-care fatigue booklet and the RAFT programme (Table 12). However, there was evidence of a difference between the trial arms for satisfaction, with 89% of RAFT programme patients rating satisfaction ≥ 8 out of 10 (including 62% rating 10/10), compared with 54% of control patients rating satisfaction ≥ 8 out of 10 (including 26% rating 10/10, p < 0.0001). Similarly, 96% of RAFT programme patients were very likely to recommend the programme to others compared with 68% of control patients who were very likely to recommend the booklet (i.e. scoring ≥ 8/10; p < 0.001) (see Table 12).
| Rating | Acceptability, n (%)a | |||
|---|---|---|---|---|
| Satisfactionb | Recommendationc | |||
| Control (N = 139) | RAFT (N = 150) | Control (N = 139) | RAFT (N = 150) | |
| 0 | 2 (1.4) | 0 (0) | 2 (1.4) | 0 (0) |
| 1 | 2 (1.4) | 0 (0) | 2 (1.4) | 0 (0) |
| 2 | 1 (0.7) | 0 (0) | 2 (1.4) | 0 (0) |
| 3 | 10 (7.2) | 0 (0) | 6 (4.3) | 0 (0) |
| 4 | 5 (3.6) | 0 (0) | 3 (2.2) | 0 (0) |
| 5 | 12 (8.6) | 3 (2.0) | 7 (5.0) | 1 (0.7) |
| 6 | 12 (8.6) | 6 (4.0) | 8 (5.8) | 1 (0.7) |
| 7 | 20 (14.4) | 8 (5.3) | 14 (10.1) | 4 (2.7) |
| 8 | 19 (13.7) | 17 (11.3) | 14 (10.1) | 8 (5.3) |
| 9 | 19 (13.7) | 23 (15.3) | 15 (10.8) | 14 (9.3) |
| 10 | 37 (26.6) | 93 (62.0) | 66 (47.5) | 122 (81.3) |
Potential clustering effects
A likelihood ratio test was used to compare the primary analysis model (standard linear regression) to a linear mixed model that included centre (1–7) and the RAFT programme cohort (i.e. group) within centres (1–4) as cluster variables. No evidence of clustering was demonstrated: the log-likelihood of linear mixed model was –696.444 and the log-likelihood of model not adjusting for clustering was –696.489 (p = 0.96). The ICC for the correlation of the outcome in cohorts within centre was also very low (0.009).
Missing data
Analysis on 20 sets of imputed data was almost identical to the results of the primary ‘complete-case’ analysis, with an adjusted mean difference between the trial arms in fatigue impact at 26 weeks of 0.58 in favour of the RAFT programme (Table 13). Consequently, no further analyses were conducted on imputed data sets.
Treatment efficacy
The CACE analysis suggested that there was a larger effect of the RAFT programme intervention in those who ‘complied’ with the intervention than in the ITT estimate of the ‘offer’ of the intervention (CACE treatment effect estimate –0.69 vs. primary ITT analysis treatment effect estimate –0.59; see Appendix 11). However, the CACE analysis method could be considered inappropriate as 14 participants randomised to, but not attending, the RAFT programme had no follow-up data; therefore, although an attempt was made to address this issue in the analysis, the results should be interpreted with caution.
Subgroup and exploratory analysis
No patient was deemed to have violated the protocol; therefore, an additional per-protocol analysis was unnecessary.
Number of sessions attended
As with the CACE analysis (see Appendix 11), a structural mean model 2SLS instrumental variable approach62 was used to investigate the effect of the total number of RAFT programme sessions attended on the BRAF-NRS impact score. The results suggest that the more RAFT sessions attended, the greater the reduction in fatigue impact at 26 weeks, with each additional RAFT session attended giving a decrease of approximately 0.1 BRAF-NRS impact units (95% CI –0.21 to –0.01 BRAF-NRS impact units; p = 0.03). However, the model assumes a linear relationship between session attendance and BRAF-NRS impact score and that the impact of an increase in attendance at any one of the seven sessions is the same across all sessions (i.e. each of sessions 1–7 has a similar effect on patient outcome, even though each session covers a different topic that may or may not hold personal relevance for individual patients). This analysis is exploratory and assumptions of linearity may not hold.
Consolidation session (week 14)
Additional data were collected at the end of the intensive six sessions of the RAFT programme (week 6) and 4 weeks before and after the week 14 consolidation session (i.e. weeks 10 and 18), to provide preliminary data on the possible impact of the consolidation session. Week 6 data are shown in Appendices 12 and 13 and fatigue data collected at weeks 10 and 18 are provided in Appendices 14–17. After adjusting for baseline score and centre, there was evidence of a difference between trial arms at week 6 in favour of the RAFT programme for the primary outcome (BRAF-NRS impact, –0.65), as well as coping with fatigue (BRAF-NRS coping), overall fatigue impact (BRAF-MDQ overall) and living with fatigue, cognitive fatigue and emotional fatigue, plus sleep quality and the process measure self-efficacy (RASE scale) (Table 14). Effect sizes for these variables ranged from 0.21 (cognitive fatigue) to 0.6 (coping with fatigue).
| Clinical outcome | Trial arm, n (%)a | Adjusted mean differenceb (95% CI) | p-value | Effect size | |
|---|---|---|---|---|---|
| Control | RAFT | ||||
| Fatigue | |||||
| BRAF-NRS impact (0–10) | 156 (98.7) | 156 (89.1) | –0.65 (–1.07 to –0.23) | < 0.01 | 0.40 |
| BRAF-NRS severity (0–10) | 139 (88.0) | 144 (82.3) | –0.37 (–0.78 to 0.04) | 0.07 | |
| BRAF-NRS coping (0–10)c | 139 (88.0) | 144 (82.3) | 1.23 (0.75 to 1.71) | < 0.01 | 0.60 |
| BRAF-MDQ overall Impact (0–70) | 139 (88.0) | 143 (81.7) | –4.78 (–7.14 to –2.42) | < 0.01 | 0.37 |
| BRAF-MDQ physical (0–22) | 139 (88.0) | 144 (82.3) | –1.56 (–2.39 to –0.73) | < 0.01 | 0.48 |
| BRAF-MDQ emotional (0–12) | 139 (88.0) | 143 (81.7) | –1.06 (–1.66 to –0.45) | 0.01 | 0.33 |
| BRAF-MDQ cognitive (0–15) | 139 (88.0) | 143 (81.7) | –0.82 (–1.50 to –0.15) | 0.01 | 0.21 |
| BRAF-MDQ living (0–21) | 139 (88.0) | 143 (81.7) | –1.33 (–2.26 to –0.41) | 0.01 | 0.26 |
| Pain: NRS (0–10) | 139 (88.0) | 144 (82.3) | –0.02 (–0.45 to 0.40) | 0.92 | |
| Disability: MHAQ (0–3) | 139 (88.0) | 142 (81.1) | 0.03 (–0.05 to 0.10) | 0.50 | |
| Quality of life: AIMS VAS (0–100) | 138 (87.3) | 144 (82.3) | –3.01 (–7.53 to 1.51) | 0.19 | |
| Disease activity: sPDAS2 (2.4–7.9) | 139 (88.0) | 141 (80.6) | 0.07 (–0.13 to 0.27) | 0.49 | |
| Anxiety: HADS (0–21) | 139 (88.0) | 143 (81.7) | –0.24 (–0.88 to 0.40) | 0.46 | |
| Depression: HADS (0–21) | 139 (88.0) | 143 (81.7) | –0.31 (–0.86 to 0.25) | 0.28 | |
| Valued life activities: VLA (0–3) | 139 (88.0) | 142 (81.1) | –0.002 (–0.08 to 0.08) | 0.97 | |
| Helplessness: AHI (5–30) | 139 (88.0) | 143 (81.7) | –0.65 (–1.51 to 0.20) | 0.13 | |
| Self-efficacy: RASE scale (28 to 140)c | 138 (87.3) | 143 (81.7) | 3.94 (1.67 to 6.20) | < 0.01 | 0.35 |
| Sleep qualityd | 136 (86.1) | 139 (79.5) | 0.49 (0.30 to 0.80) | < 0.01 | |
At 10 weeks, the adjusted mean difference between the arms for the primary outcome was maintained in favour of the RAFT programme, but was lower than that at 6 weeks (BRAF-NRS impact score –0.51 vs. –0.65). In addition, there was no longer evidence of a difference between arms for coping with fatigue. At 18 weeks, 4 weeks after the consolidation session 7, the adjusted mean difference in BRAF-NRS impact score was again similar to that at week 6, at –0.64, and coping with fatigue was once again significantly different between arms (Table 15). However, these were exploratory analyses and any differences between effect sizes at these time points may reflect random variation in treatment effect as the trial progressed.
| Fatigue outcome | Time point | |||||
|---|---|---|---|---|---|---|
| Week 10a | Week 18b | |||||
| Adjusted mean differencea (95% CI) | p-value | Effect size | Adjusted mean differencec (95% CI) | p-value | Effect size | |
| BRAF-NRS impact (0–10) | –0.51 (–0.97 to –0.05) | 0.03 | 0.31 | –0.64 (–1.11 to –0.17) | 0.01 | 0.39 |
| BRAF-NRS severity (0–10) | –0.04 (–0.52 to 0.45) | 0.88 | –0.32 (–0.81 to 0.18) | 0.21 | ||
| BRAF-NRS coping (0–10)d | 0.46 (–0.05 to 0.98) | 0.08 | 0.75 (0.20 to 1.29) | 0.01 | 0.36 | |
| BRAF-MDQ overall impact (0–70) | –2.22 (–5.00 to 0.57) | 0.12 | –2.93 (–6.09 to 0.22) | 0.07 | ||
| BRAF-MDQ physical (0–22) | –0.64 (–1.65 to 0.36) | 0.21 | –0.89 (–1.96 to 0.18) | 0.10 | ||
| BRAF-MDQ emotional (0–12) | –0.76 (–1.44 to –0.08) | 0.03 | 0.24 | –0.87 (–1.57 to –0.18) | 0.01 | 0.27 |
| BRAF-MDQ cognitive (0–15) | –0.34 (–1.06 to 0.38) | 0.36 | –0.74 (–1.53 to 0.06) | 0.07 | ||
| BRAF-MDQ living (0–21) | –0.55 (–1.55 to 0.45) | 0.28 | –0.44 (–1.56 to 0.68) | 0.44 | ||
Predictors of fatigue impact change
Certain clinical and demographic characteristics were examined as potential predictors of fatigue impact. The starting model comprised the primary analysis model additionally adjusted for baseline pain (NRS), disease activity (DAS28), BRAF-NRS coping score, age, comorbidity, work status, disease duration and sex. After the process of stepwise deletion, the only additional variables retained (i.e. variables other than those in the primary analysis model) were sex and disease activity (DAS28) score. The final linear regression model (primary analysis model plus additional adjustment for sex and baseline DAS28) suggested that a worse outcome was predicted by being female and having a higher baseline DAS28 score: being female was associated with a 0.75 unit of scale increase in BRAF-NRS impact score at 26 weeks (95% CI 0.08 to 1.41; p = 0.03), whereas a 1 unit of scale increase in baseline disease activity (DAS28) was associated with a 0.25 unit of scale increase in BRAF-NRS impact score at 26 weeks (95% CI 0.02 to 0.49; p = 0.04).
Self-efficacy
The RASE scale addresses beliefs about RA self-management behaviours56 and most of the 28 items are touched on during the RAFT programme, except the final three medication items (see Appendix 18). At 26 weeks, six RASE scale items demonstrated evidence of a difference between trial arms for change over weeks 0–26 in favour of the RAFT programme (Table 16). Avoiding doing things that cause pain, relaxation, pacing, acceptance of fatigue, asking for help and using relaxation tapes were all covered during RAFT programme sessions.
| RASE scale itema | Trial arm, mean change | Difference in mean change | p-value | |
|---|---|---|---|---|
| Control (n = 142) | RAFT (n = 151) | |||
| Use relaxation techniques to help with pain | –0.07 | 0.11 | 0.18 | 0.10 |
| Think about something else to help with pain | 0.04 | 0.16 | 0.12 | 0.34 |
| Use my joints carefully to help with pain | 0.20 | 0.18 | –0.02 | 0.87 |
| Think positively to help with pain | 0.06 | 0.23 | 0.17 | 0.16 |
| Avoid doing things that cause pain | 0.25 | –0.05 | –0.30 | 0.03 |
| Wind down, relax before bed, to improve sleep | 0.10 | 0.17 | 0.07 | 0.56 |
| Hot drink before bed to improve sleep | 0.14 | 0.19 | 0.05 | 0.69 |
| Use relaxation before bed to improve sleep | –0.11 | 0.17 | 0.28 | 0.02 |
| Pace myself, take RA into account to deal with fatigue | –0.08 | 0.33 | 0.41 | < 0.01 |
| Accept fatigue as part of my arthritis | 0.07 | 0.40 | 0.33 | 0.01 |
| Use gadgets to help with mobility, tasks, personal care | –0.01 | 0.19 | 0.20 | 0.06 |
| Ask for help to deal with difficulties of doing everyday things | –0.01 | 0.25 | 0.26 | 0.02 |
| Do exercises to deal with difficulties of doing everyday tasks | 0.01 | 0.09 | 0.08 | 0.50 |
| Plan/prioritise to deal with difficulties doing everyday tasks | –0.01 | 0.17 | 0.19 | 0.07 |
| Educate family/friends about my RA to help relationships | 0.01 | 0.15 | 0.14 | 0.25 |
| Explain to friends and family when I do or do not need help | –0.02 | 0.04 | 0.06 | 0.61 |
| Discuss any problems with my partner or family | 0.00 | 0.10 | 0.10 | 0.38 |
| Make time for leisure activities, hobbies or socialising | –0.01 | 0.05 | 0.05 | 0.58 |
| Save energy for leisure activities, hobbies or socialising | 0.08 | 0.14 | 0.06 | 0.66 |
| Focus on the positive when I am feeling down | 0.01 | 0.15 | 0.14 | 0.21 |
| Use relaxation to deal with worries | 0.07 | 0.03 | –0.04 | 0.75 |
| Allocate time for relaxation | –0.05 | 0.04 | 0.09 | 0.39 |
| Use relaxation tape or instructions to help me relax | –0.22 | 0.18 | 0.40 | < 0.01 |
| Use regular exercise | 0.02 | 0.14 | 0.12 | 0.27 |
| Be aware of my limits in exercise | –0.07 | 0.05 | 0.11 | 0.23 |
| Manage medication, knowing how and when to take it | –0.01 | 0.07 | 0.07 | 0.42 |
| Look out for and avoid side effects of medication | –0.08 | 0.01 | 0.09 | 0.42 |
| Seek help with persistent side effects | –0.04 | 0.00 | 0.04 | 0.66 |
Tutor delivery over time
It was hypothesised that tutors might increase in skills and confidence to deliver the RAFT programme over time, which might be reflected in improved outcomes in the later RAFT programmes (i.e. from cohort 1 through to cohort 4). Although it appears that the difference between trial arms in mean change in BRAF-NRS impact score was greatest in cohort 4, the study was not powered to formally test this (Table 17).
| Cohort | Trial arm | Difference in mean change | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Control | RAFT | ||||||||
| n | Time point, mean (SD) | Mean change (95% CI) | n | Time point, mean (SD) | Mean change (95% CI) | ||||
| 0 weeks | 26 weeks | 0 weeks | 26 weeks | ||||||
| 1 | 39 | 7.56 (1.31) | 6.72 (1.92) | –0.85 (–1.43 to –0.26) | 37 | 6.95 (1.70) | 5.73 (2.58) | –1.22 (–2.17 to –0.26) | –0.37 |
| 2 | 39 | 7.54 (1.54) | 6.44 (2.82) | –1.10 (–1.90 to –0.30) | 38 | 7.21 (1.58) | 5.76 (2.62) | –1.45 (–2.34 to –0.56) | –0.35 |
| 3 | 39 | 6.69 (1.81) | 6.15 (2.62) | –0.54 (–1.45 to 0.37) | 42 | 7.26 (1.89) | 6.31 (2.42) | –0.95 (–1.77 to –0.13) | –0.41 |
| 4 | 35 | 7.11 (1.75) | 6.09 (2.27) | –1.03 (–1.76 to –0.29) | 39 | 6.95 (1.50) | 5.10 (1.90) | –1.85 (–2.51 to –1.18) | –0.82 |
Social contact
Both the usual-care booklet and the RAFT programme highlight the value of obtaining support. At 52 and 104 weeks, 7–13% of patients across both trial arms reported making contact with other patient(s) for support with fatigue or arthritis (see Appendix 19). In addition, at 52 weeks, 20% of RAFT programme patients (n = 35) had made contact with patient(s) in their RAFT programme group after their programme had finished and 12.6% (n = 22) had maintained contact during the year. At 104 weeks, 9% of RAFT programme patients (n = 16, including 12 of the original 35 patients) had made contact and 5.6% of RAFT programme patients (n = 10) maintained contact during this second year.
Chapter 4 Economic evaluation: methods and results
Introduction
The economic evaluation aimed to determine the cost-effectiveness of delivering the RAFT CB programme alongside usual care (intervention) to RA patients with fatigue, compared with patients receiving usual care alone (control). The primary economic cost–utility analysis was conducted from the societal perspective, including costs incurred by the NHS, Personal Social Services (PSS) and the individual, and costs arising from loss of productivity, comparing the costs and benefits of each trial arm over the first 26 weeks’ follow-up, in line with the clinical effectiveness analysis. A secondary analysis restricted the perspective to NHS and PSS costs to conform to the NICE reference case. 66 Longer-term cost-effectiveness was assessed through a secondary analysis conducted after 2 years’ follow-up.
Methods
The cost-effectiveness analyses were conducted in accordance with the SAP [see URL: www.journalslibrary.nihr.ac.uk/programmes/hta/1111201/#/documentation (accessed 12 April 2019)] and agreed with the TSC and the DMEC. Minor deviations from the plan were required (see Report Supplementary Material 3).
Measurement and valuation of economic outcomes
The primary economic outcome measure was quality-adjusted life-years (QALYs). Measurements were recorded at baseline and at 6, 26, 52, 78 and 104 weeks post randomisation, using the EuroQol-5 Dimensions (EQ-5D) health-related quality-of-life descriptive system [most recently the EuroQol-5 Dimensions, five-level version (EQ-5D-5L)]67 in the main questionnaire package (see Chapter 2, Follow-up time points, data collection and management). As recommended by the recent position statement from NICE,68 utility scores were derived from the EQ-5D-5L measurements using the van Hout crosswalk method69 and, when relevant, were set to zero at death. The utility scores were used to calculate QALYs using linear interpolation and the area under the curve method, and were discounted at 3.5% in the second year of follow-up.
A secondary economic outcome measure was fatigue impact at 26 weeks (the primary effectiveness outcome of the trial). Fatigue impact was measured using the BRAF-NRS impact score collected by the central trial team by telephone at the same major time points as the utility measures.
Identification of relevant resource use
Data were collected for resource use associated with RA or RA-related fatigue only. Routine monthly blood monitoring visits were excluded, whether performed in primary or secondary care, as these were considered to be unrelated to the intervention. For the NHS and PSS perspectives, data were collected on arthritis medication, primary and community medical care, physiotherapy, occupational therapy, podiatry or nursing care, secondary care, use of a rheumatology telephone helpline and use of social care by the patient. Staff time and other expenses incurred during the training and delivery of the RAFT programme were recorded.
For the primary analysis from the societal perspective, we additionally collected data on work productivity (presenteeism and absenteeism), and patient-incurred expenses for travel to a general practitioner (GP) and hospital appointments, including the RAFT programme itself.
Measurement of resource use
Time logs and expense forms were used to track all resources used in the delivery of the 4-day RAFT training programme, including trainee and trainer time (preparation time and observation of the practice programme), travel costs and programme materials, to calculate the fixed cost of training (Table 18). For the delivery of the RAFT programme CB sessions, NHS resources were captured in staff time logs recording session preparation, delivery, debriefing, supervision time and materials.
| Variable | Measure | Time point | |||||
|---|---|---|---|---|---|---|---|
| 0 weeks | 6 weeks | 26 weeks | 52 weeks | 78 weeks | 104 weeks | ||
| Fatigue impact (primary outcome) | BRAF-NRS (telephone) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| RA-related medicationsa | Nurse collected | ✓ | |||||
| Travel costs to all appointmentsb | Nurse collected | ✓ | |||||
| QALYs | EQ-5D-5L64 self-reported | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Work productivity (last 7 days) | WPAI scale68 self-reported | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Days of sick leave (last 6 months) | Self-report | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Primary care RA appointments | Self-report | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Secondary care RA helpline telephone call | Self-report | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Social care (by whom/hours) | Self-report | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Private community care | Self-report | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Medication changes | Self-report | ✓ | ✓ | ✓ | ✓ | ✓ | |
| RA-related outpatient appointments | Hospital computer | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| RA-related day cases | Hospital computer | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| RA-related inpatient stays | Hospital computer | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| RA-related emergency department visits | Self-report | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| RAFT programme training; observed practice programmes; and RAFT programme delivery × 28 | Tutor/trainer time, travel costs and materials | Logged as they occurred | |||||
NHS community care and emergency care, and patient personal resource use, during the 2-year follow-up period were captured using patient-reported questionnaires at baseline and at weeks 6, 26, 52, 78 and 104, with patients completing the questionnaires at their research nurse visits at baseline and week 26, and by post at all other time points. Medications were recorded by the research nurse at the baseline visit and patients were asked to indicate changes from the previous record at each follow-up questionnaire. Secondary care data on outpatient appointments, inpatient stays and day-case attendances were extracted from hospital computer records by research nurses.
The research nurse documented the patient’s normal transport method for hospital and GP appointments and the cost (for public transport) or mileage (for private or hospital transport) at the baseline visit, to use as a multiplier for calculating costs. Work disability, presenteeism and absenteeism were captured using the Work Productivity and Activity Impairment (WPAI) scale, which measures hours worked or lost over the past 7 days. 70
Valuation of resource use
All costs are reported in pounds sterling at 2015/16 rates. Unit costs for community care, primary care and NHS staff time to train for and deliver the intervention were based on the Unit Costs of Health and Social Care 2016. 71 Actual expenses incurred for training materials, refreshments and staff travel were recorded. The costs of medications used during follow-up were based on data in the prescriptions cost analysis for England. 72 Secondary care (including routine RA care) costs were derived from the NHS Reference Costs 2015 to 2016. 73 Private care costs were estimated from the median of three quotes or by using data from national bodies. The WPAI scale responses were combined to derive an estimate of the overall work impairment due to RA or RA-related fatigue. 70 The impairment factor was applied to average weekly earnings stratified by age. 74 Productivity losses were estimated as changes in productivity from baseline. Unit costs used in the analysis are given in Table 19. Costs occurring during the second year of follow-up were discounted in line with NICE guidance (currently 3.5%). 66
| Service | Unit cost (£) | Source |
|---|---|---|
| Rheumatology nurse helpline (hospital) | 22.00 | Unit Costs of Health and Social Care 2016 71 |
| NHS podiatry (community) | 16.00 | Unit Costs of Health and Social Care 2016 71 |
| NHS physiotherapy (community) | 16.00 | Unit Costs of Health and Social Care 2016 71 |
| NHS OT (community) | 16.00 | Unit Costs of Health and Social Care 2016 71 |
| NHS orthotist (community) | 16.00 | Unit Costs of Health and Social Care 2016 71 |
| GP appointment | 27.00 | Unit Costs of Health and Social Care 2016 71 |
| GP telephone call | 21.18 | Unit Costs of Health and Social Care 2016 71 |
| Nurse appointment (community) | 9.30 | Unit Costs of Health and Social Care 2016 71 |
| Social home care provided by social services | 24.00 | Unit Costs of Health and Social Care 2016 71 |
| Home care provided by private provider | 13.00 | Paying for Home Care Costs in 2019 – Your Ultimate Guide 75 |
| Home care provided by family | 7.20 | UK government76 |
| Private podiatry | 38.00 | Three estimatesa |
| Private physiotherapy | 50.00 | Three estimatesb |
| Private reflexology | 45.00 | Three estimatesc |
| Private acupuncture | 32.50 | Three estimatesd |
| Private osteopathy | 42.00 | Three estimatese |
| Private OT | 55.00 | Three estimatesf |
| Private counselling | 40.00 | Three estimatesg |
| Private massage therapy | 45.00 | Three estimatesh |
| Personal trainer | 40.00 | Three estimatesi |
| Private chiropractor | 55.00 | Chiropractic 77 |
| Rheumatology outpatient CL | 137.00 | NHS Reference Costs 2015 to 2016 73 |
| Rheumatology outpatient NCL | 87.00 | NHS Reference Costs 2015 to 2016 73 |
| Trauma and orthopaedics outpatient CL | 110.00 | NHS Reference Costs 2015 to 2016 73 |
| Trauma and orthopaedics outpatient NCL | 98.00 | NHS Reference Costs 2015 to 2016 73 |
| Pain management outpatient CL | 131.00 | NHS Reference Costs 2015 to 2016 73 |
| Pain management outpatient NCL | 109.00 | NHS Reference Costs 2015 to 2016 73 |
| Orthotics outpatient CL | 62.00 | NHS Reference Costs 2015 to 2016 73 |
| Orthotics outpatient NCL | 121.00 | NHS Reference Costs 2015 to 2016 73 |
| Diagnostic imaging outpatient CL | 51.00 | NHS Reference Costs 2015 to 2016 73 |
| Diagnostic imaging outpatient NCL | 35.00 | NHS Reference Costs 2015 to 2016 73 |
| Podiatry outpatient NCL | 37.00 | NHS Reference Costs 2015 to 2016 73 |
| Physiotherapy outpatient NCL | 45.00 | NHS Reference Costs 2015 to 2016 73 |
| OT outpatient NCL | 60.00 | NHS Reference Costs 2015 to 2016 73 |
| Dietetics outpatient NCL | 68.00 | NHS Reference Costs 2015 to 2016 73 |
| Ophthalmology outpatient CL | 87.00 | NHS Reference Costs 2015 to 2016 73 |
| Inpatient stay in rheumatology | 1567.00 | NHS Reference Costs 2015 to 2016 73 |
| Day case | 389.00 | NHS Reference Costs 2015 to 2016 73 |
| DEXA scan | 71.00 | NHS Reference Costs 2015 to 2016 73 |
| Ultrasound scan | 57.00 | NHS Reference Costs 2015 to 2016 73 |
| MRI scan | 153.00 | NHS Reference Costs 2015 to 2016 73 |
| Productivity losses per hour (age 22–29 years) | 10.52 | Annual Survey of Hours and Earnings: 2016 Provisional Results 74 |
| Productivity losses per hour (age 30–39 years) | 13.57 | Annual Survey of Hours and Earnings: 2016 Provisional Results 74 |
| Productivity losses per hour (age 40–49 years) | 13.92 | Annual Survey of Hours and Earnings: 2016 Provisional Results 74 |
| Productivity losses per hour (age 50–59 years) | 13.18 | Annual Survey of Hours and Earnings: 2016 Provisional Results 74 |
| Productivity losses per hour (age ≥ 60 years) | 11.26 | Annual Survey of Hours and Earnings: 2016 Provisional Results 74 |
Missing data
All analyses were conducted using ITT principles, comparing the two interventions as randomised and including all patients in the analysis. Multiple imputation by chained equations was conducted to impute NHS and PSS costs, travel costs, productivity losses and utility values. All missing data were imputed by the predictive mean-matching method using the five nearest neighbours and 33 imputations. The intervention arm fatigue impact up to week 26 and baseline pain and fatigue severity scores were included in the model, along with sex, age at baseline and centre.
Analysis of costs and economic outcomes
The cost of each resource item was calculated by multiplying the number of resource units used by the unit cost. The total cost for each individual patient was estimated as the sum of the cost of resource use items consumed. Overall mean costs, stratified by NHS, PSS, patient and productivity costs, and standard errors (SE) for both interventions of the trial, were calculated. The incremental mean difference in total costs was estimated between the two interventions of the trial and derived 95% CIs derived using SEs from linear regressions.
The incremental mean difference in QALYs between the two interventions of the trial and 95% CIs were calculated, adjusting for any imbalances in baseline utility scores. 78 Pearson’s correlation coefficients between the change in BRAF-NRS impact score and the change in utility, and the EQ-5D score between baseline and 2 years, were examined.
Analysis of relative costs and outcomes
Primary cost-effectiveness analysis
Cost and QALY data were combined to calculate the incremental cost-effectiveness ratio (ICER) and incremental net monetary benefit (INMB) statistics:
The INMB statistic is given as the societal willingness to pay (WTP) for a QALY, λ, multiplied by the difference in patient outcomes, E (i.e. QALYs), from which the difference in total costs, C, is subtracted. In the primary analysis, INMB was estimated to see whether or not the RAFT programme intervention is cost-effective at the established NICE thresholds of £20,000 and £30,000 per QALY gained.
The probability that the RAFT programme intervention is cost-effective at various ‘WTP-for-a-QALY’ thresholds was explored using cost-effectiveness acceptability curves. 79 All cost-effectiveness statistics (i.e. ICERs, cost-effectiveness acceptability curves and INMB) and CIs were estimated parametrically from the output of seemingly unrelated regression analysis, using the Stata ‘sureg’ command to allow for the correlation between costs and outcomes. Differences in baseline utility (or BRAF-NRS impact score) between the arms were controlled for. Study centre was included as an independent variable in the regression analysis.
Sensitivity analyses
One-way sensitivity analyses were used to judge the potential impact of sources of uncertainty. A sensitivity analysis was conducted in which rare high-cost events thought unlikely to be related to fatigue by two clinicians (unaware of randomised treatment allocation) were excluded. A sensitivity analysis dropping training costs was also conducted to estimate the impact of training becoming routine in a roll-out situation. Although it was possible to restrict the primary statistical (clinical) analysis to complete cases, the number of missing data was higher for the economic analysis and so data were imputed and a complete-case analysis was conducted as a sensitivity analysis. There was an inevitable delay between screening assessment and formal baseline assessment as the cohorts (i.e. 10–14 patients sufficient for randomisation) took time to accrue (see Chapter 2, Recruitment procedures). This meant that 24 out of the 158 randomised control patients and 28 out of the 175 randomised RAFT programme patients had a baseline BRAF-NRS fatigue severity score that fell below the eligibility criterion of ≥ 6 points. A further post hoc subgroup analysis therefore investigated only those patients who were eligible to participate in the trial at baseline, as was performed for the primary clinical outcome (see Chapter 3).
Results
Missing data
Complete sets of data were available for the intervention costs (which were recorded by staff) and secondary care costs (which were extracted from medical records). Participants did not always fully complete questionnaires, leading to missing data at some time points in the medication, emergency care, social care, community care, work productivity, travel and private care cost categories, and in the utility measurements. For the primary 26-week analysis, one or more data points were imputed for 59 participants (17.7%), comprising 24 patients in the control arm (15.2%) and 35 patients in the RAFT programme arm (20.0%) (p = 0.25). At the 2-year follow-up, one or more data points were imputed for 107 participants (32.1%), comprising 51 patients in the control arm (32.3%) and 56 patients in the RAFT programme arm (32.0%) (p = 0.96). Data were imputed for a mean of 9.9 out of 18 items in the RAFT programme arm and a mean of 8.0 out of 18 items in the control arm over weeks 0–26 (p = 0.03); and a mean of 15.8 out of 48 items in the control arm and a mean of 20.8 out of 48 items in the RAFT programme arm over weeks 0–104 (p = 0.07).
Resource use and costs of health-care services at 0–26 weeks
Disaggregated data showing the mean number of contacts in the first 26 weeks for each participant (based on all available data) are given in Table 20. The participants were relatively low users of primary care and community services for their arthritis, but were regular attenders in secondary care for arthritis-related appointments. They were high users of RA-related medications, with participants in both trial arms taking an average of 5.9 different medications to manage their RA. At baseline, 76 (22.8%) participants were in work, with no difference between trial arms (see Appendix 20). At the 26-week follow-up, participants in the control arm had lost 0.25 weeks of work productivity, whereas participants in the RAFT programme arm gained 0.04 weeks from their baseline status (mean difference –0.29 weeks, 95% CI –1.17 to 0.59 weeks). Only the number of hours of social care related to RA that the participant paid for themselves differed significantly between the trial arms, with participants in the control arm using more than three times as much private care (mean difference –8.11 hours, 95% CI –15.39 to –0.82 hours; p = 0.03).
| Type of resource | Trial arm | Difference in mean change (95% CI)b | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Control | RAFT | |||||||
| n a | Mean | SE | n a | Mean | SE | |||
| GP visits | 142 | 0.86 | 0.15 | 152 | 0.80 | 0.12 | –0.06 (–0.44 to 0.31) | 0.74 |
| Nurse visits (community) | 142 | 0.27 | 0.11 | 152 | 0.19 | 0.07 | –0.08 (–0.33 to 0.18) | 0.55 |
| OT visits (community) | 142 | 0.06 | 0.03 | 152 | 0.11 | 0.05 | 0.04 (–0.07 to 0.15) | 0.47 |
| Physiotherapist visits (community) | 142 | 0.32 | 0.12 | 152 | 0.20 | 0.08 | –0.11 (–0.39 to 0.17) | 0.43 |
| Podiatrist visits (community) | 142 | 0.44 | 0.10 | 152 | 0.41 | 0.09 | –0.03 (–0.29 to 0.23) | 0.83 |
| Hospital day cases | 152 | 0.30 | 0.08 | 156 | 0.20 | 0.07 | –0.10 (–0.31 to 0.12) | 0.37 |
| Hospital outpatient appointments (all professions) | 152 | 2.02 | 0.15 | 156 | 2.35 | 0.19 | 0.33 (–0.15 to 0.81) | 0.17 |
| Hospital inpatient stays | 152 | 0.01 | 0.01 | 156 | 0.00 | 0.00 | –0.01 (–0.03 to 0.00) | 0.15 |
| Helpline calls | 142 | 0.68 | 0.11 | 152 | 0.53 | 0.07 | –0.15 (–0.40 to 0.10) | 0.24 |
| Emergency care visits | 143 | 0.03 | 0.02 | 152 | 0.03 | 0.01 | –0.01 (–0.05 to 0.03) | 0.67 |
| Medications (RA related) | 143 | 5.91 | 0.20 | 152 | 5.88 | 0.21 | –0.03 (–0.60 to 0.54) | 0.92 |
| Social care (NHS, hours) | 134 | 6.54 | 3.80 | 142 | 5.29 | 3.94 | –1.26 (–12.04 to 9.53) | 0.82 |
| Community care (private, hours) | 142 | 0.53 | 0.22 | 152 | 0.42 | 0.18 | –0.11 (–0.66 to 0.44) | 0.70 |
| Family help (hours) | 134 | 94.99 | 12.97 | 142 | 138.19 | 21.87 | 43.20 (–7.59 to 93.98) | 0.09 |
| Social care (private, hours) | 134 | 11.46 | 3.59 | 142 | 3.35 | 1.21 | –8.11 (–15.39 to –0.82) | 0.03 |
| Work productivity losses (weeks) | 134 | 0.25 | 0.33 | 142 | –0.04 | 0.30 | –0.29 (–1.17 to 0.59) | 0.51 |
The mean costs for each type of care at 26 weeks are given in Table 21. Medication costs were by far the highest, driven by the use of very costly bDMARDs by some patients. Other substantial NHS cost categories were the secondary care outpatient and day-case costs. Social care costs were also high, whether provided by social services or by family or paid for privately, although private social care was the only category to differ significantly between trial arms. Travel costs were higher in the RAFT programme arm because of the additional travel required to attend the sessions. However, overall mean costs (including the RAFT programme training and delivery) were not different between the trial arms. Costs associated with the RAFT programme are given in Table 22.
| Cost category | Trial arm | Difference in mean cost (£) change (95% CI)b | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Control | RAFT | |||||||
| n a | Mean (£) | SE (£) | n a | Mean (£) | SE (£) | |||
| GP | 142 | 23 | 4 | 152 | 22 | 3 | –2 (–12 to 9) | 0.76 |
| Nurse (community) | 142 | 2 | 1 | 152 | 2 | 1 | –1 (–3 to 2) | 0.55 |
| OT (community) | 142 | 1 | 1 | 152 | 2 | 1 | 1 (–1 to 2) | 0.47 |
| Physiotherapist (community) | 142 | 5 | 2 | 152 | 3 | 1 | –2 (–6 to 3) | 0.43 |
| Podiatrist (community) | 142 | 7 | 2 | 152 | 7 | 1 | –0 (–5 to 4) | 0.83 |
| Hospital day cases | 152 | 115 | 33 | 156 | 77 | 26 | –38 (–121 to 45) | 0.37 |
| Hospital outpatients | 152 | 204 | 14 | 156 | 233 | 18 | 28 (–16 to 73) | 0.21 |
| Hospital inpatients | 152 | 51 | 42 | 156 | 0 | 0 | –51 (–132 to 30) | 0.22 |
| Helpline calls | 142 | 15 | 2 | 152 | 12 | 2 | –3 (–9 to 2) | 0.24 |
| Emergency care visits | 143 | 5 | 2 | 152 | 10 | 5 | 5 (–5 to 15) | 0.35 |
| Medications (RA related) | 143 | 1764 | 261 | 152 | 1714 | 232 | –50 (–736 to 636) | 0.89 |
| RAFT programme training | 158 | 0 | 0 | 175 | 186 | 5 | 186 (176 to 196) | |
| RAFT programme delivery | 158 | 0 | 0 | 175 | 322 | 9 | 322 (303 to 340) | |
| Social services | 134 | 157 | 91 | 142 | 127 | 94 | –30 (–289 to 229) | 0.82 |
| Private community care | 142 | 22 | 10 | 152 | 18 | 8 | –5 (–30 to 21) | 0.73 |
| Travel costs | 142 | 15 | 1 | 152 | 55 | 4 | 40 (33 to 48) | 0.00 |
| Family help | 134 | 684 | 93 | 142 | 995 | 157 | 311 (–55 to 677) | 0.09 |
| Private social care | 134 | 149 | 47 | 142 | 44 | 16 | –105 (–200 to –11) | 0.03 |
| Productivity losses | 134 | 96 | 150 | 142 | –20 | 135 | –116 (–512 to 280) | 0.56 |
| Total NHS/PSS costs | 134 | 2377 | 304 | 142 | 2797 | 267 | 421 (–374 to 1215) | 0.30 |
| Total costs from the patient perspectivec | 134 | 871 | 110 | 142 | 1111 | 158 | 240 (–143 to 624) | 0.22 |
| Cost variable | Mean cost per person (£) (N = 161)a | SE |
|---|---|---|
| Printed programme materials | 2.00 | 0.12 |
| Refreshments | 2.77 | 0.13 |
| CD handouts | 1.97 | 0.04 |
| Staffingb | 342.95 | 5.65 |
| Trainingc | 201.77 | 2.68 |
| Patient travel (for up to seven sessions) | 36.94 | 2.56 |
Quality-adjusted life-years
The mean EQ-5D-5L utility scores and QALYs after 26 weeks and across the 2 years of follow-up are given in Table 23. Participants in the control trial arm had slightly higher utility scores at baseline, and this persisted at each time point except at 6 weeks. There were no differences between QALYs gained in each arm at either 26 weeks or 2 years.
| Outcome | Trial arm | Difference in mean change (95% CI)a | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| Control | RAFT | |||||||
| n | Mean | SE | n | Mean | SE | |||
| Baseline utility | 158 | 0.554 | 0.018 | 175 | 0.540 | 0.018 | –0.014 (–0.063 to 0.036) | 0.59 |
| 6-week utility | 139 | 0.535 | 0.020 | 143 | 0.546 | 0.019 | 0.011 (–0.044 to 0.066) | 0.70 |
| 26-week utility | 144 | 0.561 | 0.020 | 151 | 0.553 | 0.020 | –0.008 (–0.063 to 0.048) | 0.78 |
| 52-week utility | 128 | 0.556 | 0.020 | 138 | 0.530 | 0.024 | –0.026 (–0.088 to 0.035) | 0.40 |
| 78-week utility | 120 | 0.552 | 0.021 | 130 | 0.528 | 0.024 | –0.024 (–0.086 to 0.038) | 0.45 |
| 104-week utility | 125 | 0.534 | 0.021 | 138 | 0.502 | 0.025 | –0.033 (–0.097 to 0.032) | 0.32 |
| QALYs after 26 weeks of follow-up | 135 | 0.275 | 0.009 | 140 | 0.275 | 0.009 | –0.001 (–0.026 to 0.024) | 0.96 |
| QALYs after 2 years of follow-up | 108 | 1.115 | 0.037 | 120 | 1.058 | 0.041 | –0.057 (–0.168 to 0.053) | 0.31 |
There was a weak to moderate negative correlation between the change in utility score and the change in BRAF-NRS impact score at 26 weeks (correlation coefficient –0.4, n = 293; p < 0.001) and at 2 years (correlation coefficient –0.38, n = 259; p < 0.001). Correlation coefficients between the change in the five individual dimensions of the EQ-5D and the change in BRAF-NRS impact score ranged between 0.21 for the self-care dimension and 0.41 for usual activities (see Appendix 21).
Primary cost-effectiveness analysis
The cost-effectiveness statistics for the primary analysis at 26 weeks, from a societal perspective, are based on an imputed data set of all participants as randomised (Table 24). The point estimate of the incremental cost per QALY gained is £55,202, and the net monetary benefit is –£277 (95% CI –£1212 to £657) at a societal WTP threshold of £20,000 per QALY. The probability that the RAFT programme is cost-effective at the same threshold is 0.28. Figure 4 shows the variation in the probability that the RAFT programme is cost-effective at different WTP thresholds.
| Costs and outcomes | Trial arm | Mean difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|
| Control (n = 158) | RAFT (n = 175) | |||||
| Mean | SE | Mean | SE | |||
| Unadjusted costs from the societal perspective (£) | 3279 | 317 | 3756 | 295 | ||
| Adjusted costs from the societal perspective (£)a | 3301 | 301 | 3736 | 293 | 434 (–389 to 1258) | 0.30 |
| Unadjusted QALYs over 26 weeks of follow-up | 0.269 | 0.009 | 0.272 | 0.008 | ||
| Adjusted QALYs over 26 weeks of follow-upb | 0.267 | 0.006 | 0.274 | 0.006 | 0.008 (–0.008 to 0.023) | 0.32 |
| ICERb | 55,202 | |||||
| Net monetary benefit at £20,000 (£) | –277 (–1212 to 657) | |||||
| Net monetary benefit at £30,000 (£) | –198 (–1220 to 823) | |||||
| Probability that the RAFT programme is cost-effective at £20,000 per QALY | 0.28 | |||||
| Probability that the RAFT programme is cost-effective at £30,000 per QALY | 0.35 | |||||
FIGURE 4.
Cost-effectiveness acceptability curve: variation in probability of the RAFT programme cost-effectiveness at a range of societal WTP thresholds – primary analysis.

Sensitivity analyses
Data from one individual who had a costly inpatient stay, which was deemed potentially unrelated to RA fatigue, were removed in a sensitivity analysis. This resulted in an ICER of £51,893 per QALY gained, with the probability of cost-effectiveness 0.29 at a £20,000 per QALY threshold. The sensitivity analysis without training costs gave an ICER of £31,578 per QALY and a cost-effectiveness probability of 0.42 at £20,000. The complete-case sensitivity analysis did not alter the conclusions as to the probability of cost-effectiveness (see Appendix 22).
The primary analysis was repeated excluding those individuals who had fallen below the eligibility criterion of BRAF-NRS severity ≥ 6.0 between screening and baseline (24/158 patients randomised to the control arm and 28/175 patients randomised to the RAFT programme). For baseline-eligible patients, using imputed data, the ICER was £17,214 per QALY and the probability of cost-effectiveness was 0.52 at the £20,000 NICE threshold (Table 25).
| Costs and outcomes | Trial arm | Mean difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|
| Control (n = 134) | RAFT (n = 147) | |||||
| Mean | SE | Mean | SE | |||
| Unadjusted costs from the societal perspective (£) | 3380 | 364 | 3644 | 327 | ||
| Adjusted costs from the societal perspective (£)a | 3417 | 341 | 3611 | 328 | 194 (–746 to 1134) | 0.69 |
| Unadjusted QALYs over 26 weeks of follow-up | 0.261 | 0.01 | 0.265 | 0.009 | ||
| Adjusted QALYs over 26 weeks of follow-upb | 0.257 | 0.007 | 0.268 | 0.006 | 0.011 (–0.007 to 0.029) | 0.22 |
| ICER | 17,214 | |||||
| Net monetary benefit at £20,000 (£) | 31 (–1029 to 1092) | |||||
| Net monetary benefit at £30,000 (£) | 144 (–1014 to 1302) | |||||
| Probability that the RAFT programme is cost-effective at £20,000 per QALY | 0.52 | |||||
| Probability that the RAFT programme is cost-effective at £30,000 per QALY | 0.60 | |||||
Secondary cost-effectiveness analyses
The results of the three secondary cost-effectiveness analyses (from an NHS/PSS perspective, a longer-term analysis with 2 years of follow-up and an analysis based on the primary effectiveness outcome of BRAF-NRS impact) are given in Tables 26–28. The RAFT programme had a similar likelihood of cost-effectiveness from the NHS/PSS perspective as from the societal perspective (see Table 26). After 2 years of follow-up, the RAFT programme had higher costs and slightly poorer health-related quality-of-life outcomes (see Table 27). However, the CIs on costs and outcomes included zero and the uncertainty around the cost and outcome estimates results in a similar probability of cost-effectiveness. The cost-effectiveness analysis using the primary effectiveness outcome gave an ICER of £455 per unit improvement in the BRAF-NRS impact score (see Table 28). The variation in probability of the RAFT programme cost-effectiveness thresholds (see Appendix 23) suggests, for example, a probability of cost-effectiveness of 0.78 if society was willing to pay £1000 per unit of improvement in the BRAF-NRS impact score.
| Costs and outcomes | Trial arm | Mean difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|
| Control (n = 158) | RAFT (n = 175) | |||||
| Mean | SE | Mean | SE | |||
| Unadjusted costs from the NHS/PSS perspective (£) | 2310 | 271 | 2620 | 233 | ||
| Adjusted costs from the NHS/PSS perspective (£)a | 2326 | 250 | 2605 | 238 | 279 (–393 to 950) | 0.42 |
| Unadjusted QALYs over 26 weeks of follow-up | 0.269 | 0.009 | 0.272 | 0.008 | ||
| Adjusted QALYs over 26 weeks of follow-upb | 0.266 | 0.006 | 0.274 | 0.006 | 0.008 (–0.008 to 0.024) | 0.31 |
| ICER | 34,878 | |||||
| Net monetary benefit at £20,000 (£) | –119 (–879 to 641) | |||||
| Net monetary benefit at £30,000 (£) | –39 (–884 to 806) | |||||
| Probability that the RAFT programme is cost-effective at £20,000 per QALY | 0.38 | |||||
| Probability that the RAFT programme is cost-effective at £30,000 per QALY | 0.46 | |||||
| Costs and outcomes | Trial arm | Mean difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|
| Control (n = 158) | RAFT (n = 175) | |||||
| Mean | SE | Mean | SE | |||
| Unadjusted costs from the societal perspective (£) | 12,784 | 1259 | 13,972 | 1231 | ||
| Adjusted costs from the societal perspective (£)a | 12,877 | 1220 | 13,888 | 1193 | 1012 (–2318 to 4341) | 0.55 |
| Unadjusted QALYs over 2 years of follow-up | 1.064 | 0.032 | 1.038 | 0.034 | ||
| Adjusted QALYs over 2 years of follow-upb | 1.056 | 0.024 | 1.046 | 0.023 | –0.010 (–0.075 to 0.054) | 0.75 |
| ICER | Control has lower costs, higher QALYs | |||||
| Net monetary benefit at £20,000 (£) | –1217 (–4981 to 2546) | |||||
| Net monetary benefit at £30,000 (£) | –1320 (–5438 to 2798) | |||||
| Probability that the RAFT programme is cost-effective at £20,000 per QALY | 0.26 | |||||
| Probability that the RAFT programme is cost-effective at £30,000 per QALY | 0.26 | |||||
| Costs and outcomes | Trial arm | Difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|
| Control (n = 158) | RAFT (n = 175) | |||||
| Mean | SE | Mean | SE | |||
| Unadjusted costs from the NHS/PSS perspective (£) | 2310 | 271 | 2620 | 233 | ||
| Adjusted costs from the NHS/PSS perspective (£)a | 2326 | 250 | 2605 | 238 | 279 (–393 to 950) | 0.42 |
| Unadjusted BRAF-NRS impact score over 26 weeks of follow-up | 3.622 | 0.195 | 4.279 | 0.191 | ||
| Adjusted BRAF-NRS impact score over 26 weeks of follow-upb | 3.645 | 0.187 | 4.258 | 0.184 | 0.613 (0.10 to 1.126) | 0.02 |
| ICER (£ per unit of BRAF-NRS impact score improvement) | 455 | |||||
| Net monetary benefit at £1000 per unit of improvement in BRAF-NRS impact score (£) | 334 (–527 to 1195) | |||||
| Net monetary benefit at £5000 per unit of improvement in BRAF-NRS impact score (£) | 2787 (112 to 5461) | |||||
| Probability that the RAFT programme is cost-effective at £1000 per unit of improvement in BRAF-NRS impact score improvement | 0.78 | |||||
| Probability that the RAFT programme is cost-effective at £5000 per unit of improvement in BRAF-NRS impact score improvement | 0.98 | |||||
Chapter 5 Qualitative evaluation: methods and results
Reproduced from Dures et al. 80 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Background and aims
Qualitative studies nested within RCTs can facilitate exploration of the views and experiences of individuals who have participated in the research and offer an opportunity to capture unintended or unexpected outcomes. 81 Implementing successful RCT interventions into clinical practice can prove challenging, and a qualitative evaluation of the experiences of those clinicians delivering the intervention (i.e. RAFT programme tutors) can provide useful insights. 82 Experience of patients receiving the programme delivered by a clinical psychologist were explored in the original RCT;31,32 therefore, aims of the qualitative evaluation in the current RCT were to:
-
understand RAFT programme tutors’ experiences of RAFT programme training and delivery
-
collect tutors’ ideas about the potential future roll-out of the RAFT programme intervention.
The RAFT programme qualitative study was led by co-applicant Emma Dures (ED), with support from the chief investigator Sarah Hewlett (SH), co-applicant and patient research partner Clive Rooke (CR) and co-applicant Alison Hammond (AH).
The key qualitative findings from the RAFT programme trial presented here have been previously published. 80
Methods
Protocol amendment to data collection
In the original protocol [see URL: www.journalslibrary.nihr.ac.uk/programmes/hta/1111201/#/documentation (accessed 12 April 2019)], the study design included two focus groups with RAFT programme tutors to evaluate the impact of learning CB approaches and delivering the RAFT programme intervention. The first focus group with approximately half of the RAFT programme tutors (as available) would then be followed by a focus group with the remaining tutors to confirm, challenge or elaborate those findings. Focus groups allow for discussion and reflection of a common experience, which can help participants to clarify their own thoughts and so provide a collective consideration of the topic under investigation. 83 However, the RAFT programme tutor feedback immediately after the training and clinical supervision during delivery indicated great variation in individual tutor experiences, even though the RAFT programme tutors participated in the training together and all delivered the RAFT programme from a standard manual. The RAFT programme study team concluded that individual face-to-face interviews would be the most appropriate method of data collection to capture this diversity, as these types of interviews allow for in-depth exploration of a single viewpoint and facilitate discussion of sensitive topics. 84 Therefore, the final qualitative study design was individual tutor interviews followed by a single focus group (see Chapter 2, Protocol amendments during the trial).
Recruitment and sampling
All RAFT programme tutors, comprising nurses and OTs who delivered RAFT programme sessions at the seven participating sites (see Chapter 3, RAFT programme delivery and tutor adherence), were invited to take part in a one-to-one, face-to-face semistructured interview. This included a locum tutor who had not attended RAFT programme training, but had co-delivered one RAFT programme after observing the previous programme delivered at that site. Fourteen tutors accepted and the one tutor who declined did not offer a reason. At least one RAFT programme tutor from each RAFT programme site participated in an interview (nine nurses and five OTs).
In addition to the individual interviews, the same 15 RAFT programme tutors were invited to take part in a focus group, of whom eight agreed to participate. Reasons cited for declining included clinical commitments, the focus group taking place on a non-work day and the time needed to travel to Bristol. At least one RAFT programme tutor from five of the seven RAFT programme sites participated in the focus group (three nurses and five OTs).
Data collection
Data collection occurred after the completion of the last of the four RAFT programmes in a centre. On average the tutor interview or focus group occurred 9 weeks later (range 4–13 weeks), apart from the interview with the locum tutor who had delivered an early RAFT programme, resulting in a longer time period of 39 weeks.
Interviews
Interviews were conducted face to face by ED between July 2015 and March 2016 at the tutors’ local hospital where they had delivered the RAFT programme. Prior to the start of the interview, each RAFT programme tutor signed a consent form. Interviews were audio-recorded and lasted between 52 and 82 minutes (an average of 62 minutes). An interview schedule was used to guide discussions and to ensure that key topics were discussed in all interviews (see Report Supplementary Material 1), including previous experience of group work/CB techniques; content and structure of RAFT programme training and manual; practical, personal and professional challenges and benefits of delivering the RAFT programme; and ideas for the RAFT programme intervention in the future.
Focus group
The focus group was held at the central RAFT trial team’s institution (i.e. Bristol Royal Infirmary) and was facilitated by ED and SH. Prior to the start of the focus group, each RAFT programme tutor signed a consent form. The focus group was audio-recorded and lasted for 84 minutes. Discussions were guided by a focus group schedule (see Report Supplementary Material 1), including feedback on the RAFT programme training and manual, delivery of the RAFT programme and ideas for the RAFT programme implementation into clinical practice.
Data analysis
Interview and focus group audio-recordings were transcribed by a professional service and then transcripts checked for accuracy against the original audio-recordings and anonymised (ED). The interview and focus group transcripts were analysed using an inductive thematic approach. 85 Two main characteristics of thematic analysis made it appropriate for the RAFT programme qualitative study:
-
It is a useful method when researchers want to stay close to the data and ensure that the findings are recognisable to participants.
-
It can summarise the key features of a large body of data, highlighting both similarities and differences across participants. 86
First, ED read through all the interview transcripts and coded items of interest and chunks of text that related to the research topic. These initial codes were made in the margins of the transcript itself. ED then re-read the transcripts to identify patterns of codes. Codes and their supporting text that appeared to be addressing similar topics or ideas were copied from the transcript and placed together in a Microsoft Word document (Microsoft Corporation, Redmond, WA, USA). This sorting process formed the basis of the analysis. Related clusters of coded text formed subthemes, which were then grouped together to form a smaller number of higher-order themes that were more generic and described broader, and often more abstract, elements in the data set. Two transcripts were independently coded by SH and AH, and a single transcript by CR. These independent analyses were incorporated into the final analysis by ED, as there were no substantial differences or inconsistencies between the interpretations of the data. The focus group transcript was analysed by ED and AH. Owing to the overlap in the topics discussed in the interviews and the focus group, the RAFT trial team decided to use the focus group data as a form of triangulation (i.e. to confirm, challenge or elaborate the themes identified in the interviews, and to present a single, integrated analysis). In this final analysis presented here, each theme has three parts: the label, the summary and the supporting subthemes. These subthemes are supported by data excerpts from the RAFT programme tutors to ensure that data interpretation remains directly linked to their words. 87 Tutor excerpts are identified using arbitrarily allocated numbers not linked to the RAFT programme site or tutor pairing (INT 1–14 for interview participants, FG 1–8 for focus group participants).
Results
Five themes, each with subthemes, were identified in the data (Table 29): theme 1 (the RAFT programme was a daunting but exciting undertaking) reflected the mixture of excitement and anxiety in the training and delivery of the RAFT programme; theme 2 (skills practice and demonstrations were essential) captured the value of learning and practising together, even though practice could be uncomfortable; theme 3 (developing an individual approach to a standardised intervention) showed how tutors dealt with delivering from a manual; theme 4 (enhanced clinical practice beyond the RAFT programme) captured tutors’ views on how the RAFT programme might have influenced their wider clinical practice; and theme 5 (delivering the RAFT programme in clinical practice) highlighted potential ways forward for implementing the RAFT programme outside the RCT.
| Theme | Subtheme |
|---|---|
| The RAFT programme was a daunting but exciting undertaking |
A different way of working Requiring time and effort Feeling challenged Not as easy as it looks |
| Skills practice and demonstrations were essential |
Being new to the RAFT programme together Learning from expert demonstrations Role play: invaluable despite the discomfort |
| Developing an individual approach to a standardised intervention |
Personalising the RAFT programme manual Delivery improved through clinical supervision Using the dynamics of pair work |
| Enhanced clinical practice beyond the RAFT programme |
Working with the whole person Knowing how to draw things out, sit back and listen More confident talking about fatigue |
| Delivering the RAFT programme in clinical practice |
Buy-in from managers and clinical colleagues Models of training and support Wonderful seeing how patients can benefit |
Theme 1: the RAFT programme was a daunting but exciting undertaking
Participants described starting the group training without a clear idea of what the RAFT programme comprised or what to expect from those 4 days. Participants had been sent the manual beforehand but, as anticipated, they had not looked at it in detail. As the complexity of the intervention emerged and the challenges of delivery became apparent, the RAFT programme was perceived as a novel and exciting intervention as well as a daunting undertaking.
A different way of working
To differing degrees, participants identified elements of the RAFT programme intervention that required a different way of working and for some it was ‘completely unfamiliar territory’ (INT4). In particular, the use of CB approaches and the ‘ask don’t tell’ approach contrasted with participants’ usual clinical practice, which involved giving advice and problem-solving for patients. Group work was also a new way of working for several participants:
I think it was really interesting and of course, I guess, the complexity of it was, there was all of those things to go through as somebody that was learning.
INT2
I wasn’t used to that kind of role, the cognitive–behavioural role rather than, just, as a nurse you just want to help them and say ‘Yes, I’ll do that for you’ so it was changing my kind of way of thinking.
INT3
I found it quite hard to change my way of thinking to follow it as the ‘ask don’t tell’ sort of process I found very difficult. Just purely from the way I’d worked over the years really.
INT7
. . . it’s the techniques because we’re used to giving information aren’t we and obviously we have to deliberately not do that and reflect things all the time and that wouldn’t come naturally to most practitioners.
FG1
. . . the fact that it could be delivered by an OT and somebody within rheumatology, it was quite exciting to be able to do that.
INT11
Requiring time and effort
At the start of the study, participants had not anticipated the high levels of time and effort that would be expended during training and delivery of the RAFT programme intervention. The amount of hard work required was due to the challenge of becoming familiar and confident with a large amount of material, delivered using a new approach, to patients in a group setting. Participants described a sense of responsibility and commitment to delivering the RAFT programme to the best of their ability:
It wasn’t something you were just going to be able to go away with and think ‘I could just do this’ . . . you really did need to know your material. You needed to be well read . . . before you delivered . . . and it made you realise that it, there was quite a lot of preparation to be done and it wasn’t just something you could run off on a whim.
INT6
I remember just taking it very seriously, that it wasn’t a practice run at all and putting as much effort and time as I could just to try and understand the manual and get it across.
INT9
We spent hours, hours and hours sitting and going through it and going through it again and writing it out on to cards.
INT12
Feeling challenged
Along with being enthusiastic about the RAFT programme, participants reported feeling challenged as they started to engage with the training and intervention:
. . . interested, enthusiastic, I just wanted to try and do it.
INT12
. . . it was a bit scary actually and I felt quite challenged.
INT1
I did feel very daunted starting it. I was very nervous delivering the groups as it first began.
INT7
. . . it was the managing the group and actually when to try to stop somebody or try and include somebody else and the actual feeling at one point . . . you know the group can change and there are dynamics and sometimes it can feel quite . . . certainly, intimidating sometimes.
INT14
Not as easy as it looks
When the RAFT programme trainers demonstrated sessions during training, the delivery flowed and the interaction appeared natural and almost effortless. When participants practised, they found it difficult to emulate this sense of being at ease with the material and with the group. Although, initially, this diminished participants’ confidence as they compared their performance to that of the RAFT programme trainers, it also helped to get a sense of what participants were aiming for with the intervention:
I didn’t feel particularly confident in delivering it as well because you’ve got professionals who have shown us how to do it, they’re so good at what they do you know it’s quite daunting to think ‘Oh crikey how can you do that?’
INT3
I mean they made it look so easy and then when you try and do it yourself it is like ‘Let’s have a look at my card again and I’ll just have a look at the manual again’. Whereas they were just able to do it.
INT7
[RAFT programme trainers] made it look so simple, so easy. I just think ‘why can’t I do it like that?’ they’ve made it look so easy.
FG2
Theme 2: skills practice and demonstrations were essential
The opportunity to train with other nurses and OTs was valued greatly, as a range of common concerns and shared experiences emerged during the four central training days. When reflecting on learning, it was acknowledged that skills practice and role play were an essential part of preparing to deliver to patients, even though practising could be difficult and uncomfortable at times.
Being new to the RAFT programme together
Participants felt sufficiently comfortable with each other and with the training team to engage and take part in the training. They found it helpful to realise that they were all new to the RAFT programme and to be able to share their thoughts and concerns:
. . . you definitely have that camaraderie and that you can continue to bounce things off each other a little bit or whatever, I personally like that environment, and I like to learn in that way.
INT2
It’s reassuring in a way to know that you have people with the same mind-set and obviously finding that opportunity to explore this territory further helps us because it’s like putting a blank canvas and at the end of the day it’s like painting it together.
INT4
. . . having the group dynamics of different nurses, allied health professionals, I think we fed off each other.
INT6
Learning from expert demonstrations
Observing the RAFT programme trainers demonstrate sessions brought the RAFT programme intervention to life, adding depth and detail to the manual. Demonstrations were very helpful for facilitating participants’ learning and understanding of what the intervention should look like in action:
I thought it was quite good when they demonstrated, they demonstrated how to use the CB [cognitive–behavioural] approach in the group setting using the manual. That was good because I work best by being able to observe and sort of see how you do things rather than reading it off a page.
INT7
We sat back and observed didn’t we and we actually watched them do a session. That was really helpful when we didn’t know how it was going to do anyway, to actually see it happen that was really helpful.
FG6
Role play: invaluable despite the discomfort
Participants acknowledged role play as one of the most useful aspects of the central training. Practising parts of the sessions out loud then getting feedback from the RAFT programme trainers was invaluable in the process of becoming familiar with the intervention, although it could be uncomfortable at times:
I mean I hate role play; I absolutely detest it. It is just not in my nature to do it. I just think ‘God’, but it was good because it gave us the chance to practise it, and to get feedback.
INT7
For me to actually have a go and to practise . . . I found that was very useful even though I didn’t like it, I would say one of the most valuable things of the course. I think we should have more of it, although people will hate me for saying that.
INT8
I think you need to have that practice, that . . . it’s not until you realise the benefit, I said this before, about the role play and that and actually practising saying things and scenarios.
FG2
I didn’t enjoy the role plays at all but if we had to do some more training that is what I would want is what I’m saying and I would know the benefits of it and that’s probably . . . for me it was the only way that I could actually practise and be semi-confident going out for the pilot [practice run].
FG4
Theme 3: developing an individual approach to a standardised intervention
The RAFT programme manual was seen as invaluable and ‘my bible all the way through’ (INT9), because it contained the information and guidance needed to deliver the intervention. However, participants described the tension between adhering to the sample text and staying true to the concepts and content, compared with using their own words to deliver in a natural and easy manner. In addition to finding their own way of working from the manual, participants developed individual approaches and styles of delivery through feedback during clinical supervision and through the relationship with their co-tutor.
Personalising the RAFT programme manual
Participants described consolidating and deepening their understanding of the RAFT programme intervention through adapting their manual, including writing summaries and rephrasing text. This was done with great care to ensure that delivery stayed true to the underpinning CB approach. Participants explained that this was a difficult but essential part of the process of becoming a competent RAFT programme tutor:
I was worried about if I changed it in certain ways that actually the fundamental way of interacting with the patients wouldn’t have been right, do you see what I mean? So because you’re trying to use that cognitive–behavioural approach, I was conscious that maybe if I alter it too much, I wouldn’t be doing that and therefore you wouldn’t get where you wanted to with it, but at the same time, the language, for me, didn’t sound familiar for me, so it’s trying to get that balance of extracting the essence of what you’re getting from it and putting it across in a way that feels comfortable for you as a practitioner.
INT2
That was one of the hardest things I think we’ve found. Is actually putting it in our words because . . .
We really struggled to start with because we were trying to learn it as a script and it wasn’t how we would say things. So, yeah, we spent hours didn’t we . . . Hours taking it all apart.
Sort of changing it. Changing bits to how we would speak.
And we had to have crib sheets for every session.
Delivery improved through clinical supervision
In addition to the 4 days of central training, participants reported that ‘you need the feedback on your performance’ (INT13) when delivering to patients. The RAFT programme trainers’ ongoing support, comprising clinical supervision and feedback on observed sessions, was described as very helpful. Feedback was perceived as constructive and a mechanism for enhancing participants’ confidence and skills. Occasionally, participants sought specific guidance, aware of the RAFT programme trainers’ high level of skills and familiarity with the intervention:
[RAFT programme trainer] said ‘You really need to get up and get the people engaged more, and you were struggling to get the information from them’ and that was really, although it was a bit of criticism it was really useful because the next time we did that session we did it differently and it was much better.
INT1
I think it gave us more confidence that they are there, we can actually ask questions afterwards and then they can give us feedback on how we could have delivered it better or what are we lacking in terms of explanations or something.
INT4
. . . just please give me an answer and then I can decide whether that’s what I would do or not, but I want to know what you think I should do.
INT8
I think the feedback after the pilots [practice run] was essential, as much as it was really scary to have someone observe you the feedback and the debrief afterwards was really good to just give you focus, direction and just reassurance that you were doing something right.
FG5
Using the dynamics of pair work
In addition to the work that participants did to consolidate their individual understanding of the intervention, the participants developed ways of working with their co-tutor that were mutually supportive and allowed them to each play to their strengths:
. . . you need two people, if you’re delivering stuff and you can’t, you listen to what is going on but sometimes you can miss other things that are going on in the room and having the other person there just reminds you to pick it up as well and should you get stuck or lost, it’s good to have the other person there because they could always pick it up for you, it was back up, it was reassurance to have two of them there and I think that worked really well.
INT8
. . . you’re helping each other out, aren’t you, you’re writing things up on the board and even if the one is struggling a bit, then we would, we tried, you have to be careful not to take over each other’s little roles, but we did just support each other.
INT10
I think it’s really important that you do it in pairs, really important because we helped each other didn’t we?
FG3
Theme 4: enhanced clinical practice beyond the RAFT programme
As a consequence of taking part in the RAFT programme, participants described changes in how they interacted with patients in their wider, everyday clinical practice. They identified being more equipped to support patients’ self-management compared with before the RAFT programme study. They valued the ‘ask don’t tell’ approach and their increased confidence to discuss fatigue. Their experience of the RAFT programme study ‘has certainly improved me, definitely, as a therapist’ (INT10), with participants having ‘benefited in ways that I didn’t appreciate at the time’ (INT14). It was rewarding to then see the positive impact of these new approaches on patients beyond those who took part in the RAFT programme intervention.
Working with the whole person
During delivery of the intervention, participants explored with patients ways in which fatigue can permeate all spheres of patients’ lives and well-being. This heightened the tutors’ awareness of the importance of looking at all of the individual and contextual factors that might be impacting on patients’ health in their wider clinical practice, and not focusing solely on a set of symptoms:
. . . it’s like you become more sensitive of the person that you’re seeing all the time and you sort of separate it slightly different in a way that am I just going to be focusing on treatments or am I going to prompt them to say something about, you know more on how they feel, how they live their life and how they do their day to day, so it helps in a way.
INT4
. . . that’s been so helpful just in day-to-day treatment with patients, just being able to get a bit more out of them and . . . yeah, it’s a really, really useful skill.
INT11
I feel I’m a better practitioner, I feel I’m more compassionate and empathetic. I think I look at them much more holistically as opposed to ‘Right what drug can I throw at them now?’
INT13
Knowing how to draw things out, sit back and listen
Participants contrasted using new approaches to support self-management in their clinical practice, such as ‘ask don’t tell’, with their previous ways of working, such as advice-giving. In particular, they identified that eliciting patients’ thoughts and feelings and letting them come up with answers to challenges was beneficial:
I think as nurses you tend to often want to give the answer all the time and give advice and it’s very nursey to do that, but it’s learning when to listen and stand back and try and get the patients to find the answers more rather than you delivering the answers to them and the solutions all the time.
INT6
Confidence that you have the knowledge, but you question them to bring up the answer, I do that a lot more.
INT10
It’s so easy and quick to see, say a hand deformity and think that’s clearly the problem, but it’s actually establishing ‘Why is that causing the problem, how is that affecting you functionally’ and it’s, yeah it’s just drawing out the, yeah a better insight really and getting that more out of a patient . . . getting them to open up a bit more which still does often require a box of tissues sometimes.
INT11
More confident talking about fatigue
Participants noted an increased confidence to discuss fatigue in their everyday clinical practice, in the knowledge that they had some ideas, skills and tools for supporting patients. Often these discussions involved adapting or distilling parts of the RAFT programme session:
I got used to using the [activity] diaries quite happily with those and trying to set goals from those was quite useful as well. So, used them a lot more in practice now with people which is good. I feel a lot more happy to talk about fatigue and that with patients on a one-to-one session now rather than before.
INT7
I liked the communication one [session] and I’ve used some of those concepts a lot in clinic because I feel that it’s quite useful even in, a few sentences in the clinic we have got somebody who has got fatigue and they’re isolating themselves, you can talk to them about communicating with family and friends.
INT12
Theme 5: delivering the RAFT programme in clinical practice
Participants expressed enthusiasm for the RAFT programme intervention, a sense of professional fulfilment seeing how patients can benefit and an interest in delivering it in routine clinical practice. However, they also identified generic and local challenges to implementation. These include having sustainable models of training, the need to gain support from management and clinical colleagues, and ‘just how you would fit it in with the other things that are going on’ (INT2). There was a clear sense that a pragmatic and flexible approach would be necessary and that ‘if it’s over prescriptive, it won’t happen, because the constraints of the NHS will just bury it’ (INT13).
Buy-in from managers and clinical colleagues
At an individual level, participants would be delighted if they could deliver the RAFT programme intervention in their clinical practice. This would typically require a business case from managers and the support of colleagues and clinical leads. Participants acknowledged that there might need to be some flexibility in relation to who delivers the intervention. There was also enthusiasm about the possibility of delivering it to other patient groups. Although participants could envisage some changes to delivery, they did not think that the intervention could be adapted in relation to the number of sessions and the topics covered:
We were the same, I think it’d be a business case.
Yes, because [RAFT programme local principal investigator] is looking at a business case for us to do it. [RAFT programme local principal investigator] bought into it but that’s as far as it’s got. I don’t know how far [RAFT programme local principal investigator] has got with the business case.
Is that an OT manager or a . . . who is that?
[RAFT programme local principal investigator] our consultant.
And certainly, I don’t think they’d put our banding in either, because we’re band 7s, they’d probably put lower bands in.
INT10
I just want to roll it out for everybody now, and I want to have CTD [connective tissue disease] groups as well as the RA groups and general arthritis groups that would be good. And also fibromyalgia patients as well, it would be interesting for everybody really.
INT12
. . . it’s difficult to think about things that could maybe be cut out to make it quicker because I think actually the benefit of it has been that all of the areas have been covered.
INT11
Models of training and support
Although participants valued their 4 days of central training, they acknowledged that this is unlikely to be a feasible model to roll out. One option was new RAFT programme tutors observing the intervention being delivered by experienced RAFT programme tutors, either in a live setting or on a digital versatile disc (DVD). However, there was a strong sense that some face-to-face training with skills practice would be important. Participants also stressed the need for clinical supervision to ensure a level of fidelity to the process:
I wondered if new people could maybe come and observe people who are already doing the course perhaps, after the training?
FG3
. . . you’re reading through the manual and you think that you’ve got your head around what it is that you’re doing and then when it comes to actually delivering that again which is why the practice is so good because at least you get that practical element of it but trying to put those words into something that made sense to me as a non-psychologist so having something like that [DVD], a kind of more visual thing to use alongside it I think would be really useful.
FG7
I think you do need some supervision as well; you need somebody to come down, every now and again to go through because you can get into bad habits.
INT8
I think you’d want to be supervised by people who’ve got experience in it and if there aren’t people with experience in it, then a support network amongst each other, I think.
INT10
. . . it’s good to have some kind of structure and observation just to check that people are doing it right because you can just assume can’t you and then it not being delivered . . . as required.
INT11
Wonderful seeing how patients can benefit
It was rewarding for participants to see patients benefit from taking part in the RAFT programme intervention. They described how patients’ engagement with the intervention evolved during the seven sessions and the satisfaction of seeing positive changes over time. There was the sense that some patients, who had taken part in RAFT programme groups, might stay in contact and organise to meet up outside the hospital and, subsequently, be an ongoing source of peer support:
. . . it was really lovely to see that light bulb moment for some patients, to click, I love that bit, that’s really satisfying.
INT3
I can think of, well, quite a few patients said it’s been life-changing.
INT10
. . . after the last session they [patients] had already met up for coffee, they went shopping, they’re giving each other lifts so it’s good to know that they had managed to find a group that they think they can get support as well if they need to which is reassuring.
INT4
. . . it just gives you such a lift just seeing how well they look and how well . . . the groups interacted and how they’re staying in touch and I think as a therapist that’s what you want to see, that’s why you do your job really.
INT11
Chapter 6 Discussion and conclusions
Reproduced from Dures et al. 80 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Overall summary of findings
The RAFT programme, a seven-session group programme for RA fatigue self-management delivered by local rheumatology nurses and OTs, when given as an adjunct to usual care, was effective in reducing the impact of fatigue beyond usual care alone. The beneficial effect of the RAFT programme was sustained over 2 years without further RAFT programme input beyond week 14. Improvements were also seen in emotional fatigue and living with fatigue, as well as self-management processes of coping with fatigue and self-efficacy. No harms were reported from the RAFT programme and patients had very high attendance rates and satisfaction ratings and wished to recommend the programme to other patients. Although the costs were not significantly different between trial arms, the primary economic evaluation using QALYs based on the EQ-5D-5L suggested that the RAFT programme was unlikely to be cost-effective at conventional NICE thresholds. Rheumatology clinicians delivering the RAFT programme felt that they had learned new skills that they subsequently used in clinical patient care beyond the RAFT programme itself.
The key discussion points for the clinical and qualitative evaluations have previously been published. 65
Clinical evaluation findings
Summary
The trial demonstrated that improvements in fatigue impact were made in both the control and RAFT programme trial arms. However, the RAFT programme resulted in a greater improvement in fatigue impact at 26 weeks than usual care alone (BRAF-NRS impact score adjusted mean difference –0.59; p = 0.03), with treatment differences lasting for the 2 years of follow-up (BRAF-NRS impact score adjusted mean difference –0.49; p = 0.01). A stronger effect on the primary outcome of fatigue impact was seen in those patients who met the eligibility criteria of BRAF-NRS fatigue impact ≥ 6 at baseline, at both 26 weeks (BRAF-NRS impact score adjusted mean difference –0.82 units; p = 0.01) and 2 years (BRAF-NRS impact score adjusted mean difference –0.58 units; p = 0.02). Similar treatment differences lasting over the 2 years were seen for overall impact of fatigue (BRAF-MDQ) and subscales emotional fatigue and living with fatigue; in addition, self-efficacy and coping with fatigue also showed treatment differences at 26 weeks and over the 2 years, respectively. There was no evidence of a treatment effect on fatigue severity, cognitive fatigue or other clinical variables. Patient attendance at the RAFT programme sessions was high, as were satisfaction with the programme and willingness to recommend it to other patients.
The RAFT programme targeted the impact of RA fatigue on patients’ lives and there was a treatment difference between trial arms in favour of the RAFT programme for reducing fatigue impact as measured by both the BRAF-NRS impact and BRAF-MDQ overall impact scales, as well as BRAF-MDQ subscales of emotional fatigue and living with fatigue. Patients in the control arm also reported improvements in fatigue impact, which was not seen in the previous RCT of this intervention in which the control was a group session comprising 1 hour of didactic information on general self-management of RA. 31 The usual-care booklet, written after the first RCT and based on the results of that intervention,45 has been available in rheumatology units since 2011 and was therefore used as a ‘usual-care’ active control in the present study. Although the booklet has never been subjected to rigorous effectiveness testing, a recent qualitative study88 suggested that patients felt that it made them think differently about their fatigue. Patients in the study88 reported that having a discussion of the booklet with a researcher made them consider taking responsibility for managing some aspects of their fatigue and try the suggestions the booklet contained. Although the focus of the qualitative study was for patients to review the booklet for research, it raises the possibility that the brief booklet discussion with the health professional (usual care in this RCT) may have delivered an effect over and above a patient simply picking the booklet up from the clinic display.
The trial demonstrated an effect size of 0.36 on fatigue impact. As recommended,62 in interpreting these findings against the traditional 0.5 guideline for clinically meaningful effect sizes, the broader evidence relating to the specific issue of RA fatigue (see Chapter 3, Interpretation of findings) was examined. The level of change in fatigue impact that might be clinically important for people with RA is unknown, as measurement of fatigue impact is relatively new. However, in terms of fatigue severity, a study to examine the level at which patients reported a noticeable improvement in their RA-related fatigue demonstrated that this occurred at effect sizes of 0.27–0.39 (three different anchors used for analysis). 63 Non-pharmacological interventions in RA are normally given in addition to pharmacological management, meaning that findings must be placed in this context. For example, meta-analysis shows RA patient education to have an effect size of 0.16 on painful joints compared with 0.66 seen in RCTs of non-steroidal anti-inflammatory drugs. However, all patients in the patient education trials were already taking these; thus, the 0.16 effect size represented additional benefits. 89 Similarly, the RAFT programme study was conducted with patients who were already receiving routine clinical management of their RA, that is pharmacological therapies to address inflammatory activity, which meta-analysis shows to have an effect size of 0.43 on RA fatigue;16 therefore, benefits in both intervention arms were over and above existing substantial improvements. Three studies analysing the minimal clinically important difference (MCID) on a number of fatigue severity scales in RA suggest that a change of between 7% and 11% would be clinically important. 63,90,91 This approximate 10% RA fatigue severity MCID might be a guide for meaningful change in RA fatigue impact, and comparable to multiple sclerosis, for which results from two studies average a fatigue impact MCID of around 15%. 92,93 The RAFT programme demonstrated an adjusted mean difference of 0.59 in BRAF-NRS fatigue impact beyond the improvement seen in the usual-care arm, with the RAFT programme showing a 19% change from baseline mean and the control arm showing a 12% change from baseline mean (fatigue impact improving by 1.36 and 0.88 units, respectively).
The improvement of 0.59 in BRAF-NRS fatigue impact beyond the improvement seen in usual care is smaller than the RCT was powered to detect, which was an improvement of 1.45 units. This had been based on an assumption that the clinical team delivering CBT might achieve around 75% of the 1.95 fatigue impact change seen in the earlier trial, in which delivery was by a clinical psychologist and in which the usual-care arm experienced no change at all (usual care comprised a 1-hour group session of RA self-management information delivered didactically by a nurse). 31 The statistical significance of the 0.59 improvement would have been enhanced by the lower than expected attrition rate. Therefore, taking the wider evidence from the trial and the literature presented above, it seems likely that in the current RCT the improvement in fatigue impact achieved by the RAFT programme beyond that of usual care may be clinically meaningful. This is further supported by the high levels of patient satisfaction demonstrated in attendance rates, and satisfaction and recommendation scores. However, further work to establish the MCID for the BRAF-NRS impact would be beneficial.
The treatment differences for the primary outcome of fatigue impact were greater in those patients who were eligible for the RAFT programme (i.e. had a fatigue severity score of ≥ 6 out of 10 at baseline). As with any symptom, RA-related fatigue severity will naturally fluctuate slightly from week to week; therefore, it is not surprising that, during the time it took to build cohorts in each centre, some patients’ fatigue severity over the previous 7 days was ≥ 6 at screening, but was reported as < 6 at their later baseline assessment. However, the screening process also required that patients considered their fatigue to be a recurrent problem, thereby allowing for normal short-term fluctuations in severity. The RAFT programme demonstrated significant treatment effects even including those patients with less severe fatigue (i.e. using complete-case analysis). This suggests that the RAFT programme is a pragmatic intervention to deliver clinically, as its timing in relation to symptom severity may not be crucial; it still had an effect on a recurrent symptom even when intervention delivery was delayed by the need to build an adequately sized group, or to accommodate patients’ personal availability.
There was no treatment difference between trial arms for change in fatigue severity at 26 weeks, although both trial arms had small reductions, which for the RAFT programme patients reached the proposed MCID63 for people with RA-related fatigue (MCID –0.82 to –1.12: control, –0.72; RAFT, –0.97). It is possible that the RAFT programme participants made a shift in how they view and manage a persistent symptom, finding a way to reduce the impact of fatigue on their lives. 32 Large longitudinal observational studies of current best practice pharmacological management aiming to control RA disease activity have demonstrated that fatigue severity remains largely stable over the years,94 with the majority following either a persistent moderately high or a persistently high fatigue trajectory and only a minority (one-third) having an improving fatigue trajectory. 95
Symptom severity and symptom impact are different concepts. For example, two studies have found that RA patients can report low impact from high levels of disability, whereas others report that their low level of disability has a high impact. 96,97 Personal impact is likely to be a result of the interactions between symptom severity, symptom importance in the individual context of a person’s life and perceived ability to manage or cope with that symptom: the ‘impact triad’. 98 There was a treatment difference in favour of the RAFT programme in coping with fatigue over the 2 years (as measured on the BRAF-NRS coping). The perceived ability to cope or manage fatigue better may reduce the importance of fatigue in an individual’s life; thus, it is understandable that fatigue impact could still be changed by the RAFT programme even without significant improvements in fatigue severity (the third side of the impact triad).
The effects of the RAFT programme lasted over 2 years without further RAFT programme input after the 1-hour group session at week 14, suggesting that patients’ newly acquired fatigue self-management skills became embedded. This is supported by evidence of a treatment difference between intervention arms for improvements in self-efficacy (the belief or confidence that one can successfully make behavioural changes), perhaps translating into the improvements in perceived coping over the 2 years. Self-efficacy, a key process underpinning behaviour change, was measured with the RASE56 scale (assessing beliefs about RA self-management behaviours), and six of the RASE scale component items demonstrated differences between trial arms for change over weeks 0–26 in favour of the RAFT programme, including key fatigue self-management activities such as pacing and acceptance of fatigue. Problem-solving and goal-setting, as a route to enhancing self-efficacy,25 are core self-management skills that patients learn in CBT and thus these changes in coping and self-efficacy may reflect the CB approaches that the clinical rheumatology tutors were trained to use in the RAFT programme.
The CB approaches were delivered by clinical rheumatology nurses and OTs after a brief training, rather than clinical psychologists. This novel approach aimed to circumnavigate the lack of psychology support available in most rheumatology units33 and shows similar results to a RAFT programme intervention delivered by the usual clinical team for multiple sclerosis fatigue. 99 A systematic review of nurse-led psychological interventions for depression in people with long-term physical conditions demonstrated their effectiveness. 100 In addition, a systematic review of psychological interventions for people with diabetes showed generalist nurses/physicians to be equally as effective as psychologists. 101 Delivery of the RAFT programme intervention by the clinical team was feasible, in that all RAFT programmes were delivered as planned and tutor sickness/absence could be managed. Furthermore, the RAFT programme feasibility was supported by high patient attendance and satisfaction rates; these suggest that the RAFT programme could be implemented in practice.
Economic evaluation findings
Summary
The primary economic evaluation found no difference between intervention arms in either overall costs (which incorporated intervention training and delivery costs) or QALY gains at 26 weeks or 2 years, and there was no evidence that the RAFT programme reduced other health-care costs. However, there was substantial uncertainty around the cost and QALY estimates. The primary cost–utility analyses suggested that the RAFT programme is not very likely to be cost-effective at the conventional societal WTP values, with probabilities below the 50% level (probability of 28% at the £20,000 NICE threshold and a probability of 35% at the £30,000 NICE threshold) from the societal perspective. A subgroup analysis of those patients who were eligible at baseline (i.e. BRAF-NRS impact ≥ 6/10) gave a 52% probability that the RAFT programme was cost-effective at £20,000 per QALY, or 60% probability that the RAFT programme was cost-effective at £30,000 per QALY.
The sustained improvement in fatigue impact seen clinically over 2 years was not reflected by increased QALYs measured using the EQ-5D-5L. This may be indicative that the EQ-5D-5L is not responsive enough to capture improvements in RA-related fatigue. Of the five EQ-5D domains (mobility, self-care, usual activities, pain and mood), ‘usual activities’ is most likely be the domain to be affected by a fatigue self-management intervention, a theory supported by the correlation demonstrated here between change in EQ-5D-5L domains and change in BRAF-NRS impact score. However, ‘usual activities’ is the EQ-5D domain that contributes least to the overall utility weights. 102 The EQ-5D ‘usual activities’ domain includes the ability to perform work, housework and family and leisure activities, and people with RA value doing such ‘daily activities’ as the second most important of seven health domains, with fatigue as third, giving highest weights to these two. 103 This contrasts with the low weight for ‘usual activities’ and absence of fatigue assessment in the EQ-5D, raising questions about the relevance of the EQ-5D for evaluating quality of life in RA. Energy (or drive) and sleep have been identified as key domains for people with RA, and these may be missed by the EQ-5D, leading to recommendations for further research to identify relevant domains and weightings for the RA population for use in the EQ-5D. 104
There is robust evidence to support the satisfactory psychometric performance of EQ-5D in RA. 105 However, it has also been shown that several commonly used quality-of-life measures for calculating QALYs in RA give a wide range of results on the same data set, demonstrating cost–utility in favour of a bDMARD that varies from 12% to 91% from four instruments (EQ-5D, 63%). 106 Previous research has also suggested that the EQ-5D is more responsive to worsening health states than to improving health states in RA patients. 107 However, much of this research has not evaluated the more recent five-level EQ-5D (i.e. EQ-5D-5L) used in this RCT, which might be more responsive to changes in health.
Economic evaluations of interventions designed to improve fatigue in RA are lacking, although cost-effectiveness has been assessed in other long-term conditions. A short-term economic evaluation of a fatigue management programme for patients with multiple sclerosis found similarly insignificant between-arm differences in EuroQol-5 Dimensions, three-level version (EQ-5D-3L), derived QALYs, despite significant improvement in fatigue in the intervention arm. 99 A cost-effectiveness study comparing a rehabilitation programme with a CBT intervention for patients with CFS over 12 months also found no statistical differences in EQ-5D-3L-derived QALYs, despite a significant difference between the intervention arms for fatigue severity. 108 These studies support the view that the EQ-5D may not be responsive to changes in fatigue in long-term conditions.
Work productivity was improved for patients in the RAFT programme intervention arm at 26 weeks and 2 years, although the difference between intervention arms was not statistically significant. However, the number of patients in paid employment at baseline was small (n = 76, 23% of randomised patients), suggesting that the power to capture a significant difference was low. There has been little research on the effect of RA-related fatigue severity on work productivity, but a study of > 8000 RA patients in 32 countries demonstrates greater fatigue severity in patients who are work disabled than in those staying in work. 109 The BRAF-NRS impact score is a relatively new measure and there have been no reported quantitative studies examining the relationship between fatigue impact and work productivity. However, qualitative studies consistently report that people with RA consider the impact of fatigue on work to be significant;8,12 thus, improvement in work productivity could be consistent with the reduction seen in fatigue impact with the RAFT programme. The EQ-5D scores are derived from surveys of the general population. Recent work comparing people with RA with the general population found that both groups placed a similar value on pain and function limitations, but the general population put a lower value on the ability to work. 110 This suggests that the EQ-5D scores may have been different had they been based on values from people with RA rather than the general population, which is part of a wider debate on obtaining better-informed population preferences for estimating QALYs. 111
The algorithm for work productivity was based largely on items relating to hours lost (absenteeism) and included just one item on presenteeism. Fatigue causes major difficulties for people while at work and may mean that they are present but not functioning at full capacity (presenteeism). 8,12 An uncontrolled pilot study of a self-management programme specifically for fatigue at work for patients with inflammatory rheumatic diseases examined presenteeism and demonstrated improvements in four domains of functioning while at work: physical and mental demands, work scheduling and work outputs. 112 It is possible that the weekly review of daily activity diaries in the RAFT programme, accompanied by encouragement to break up large periods of intense activity through factoring in short breaks, may help presenteeism.
Qualitative evaluation findings
Summary
Five themes were identified in the tutors’ data. The rheumatology nurses and OTs (tutors) were interested and enthusiastic about being involved in the trial of a novel fatigue intervention. The tutors described delivering the RAFT programme as a very rewarding experience, seeing patients make big changes to their lives, although the process of becoming familiar with the material and gaining confidence in delivering it proved hard work (theme 1). The tutors’ perceived personal benefits included a sense of professional development and fulfilment, especially when they saw patients making life changes. Learning together and rehearsing the RAFT programme elements as a group was helpful (theme 2). Challenges included using an ‘ask don’t tell’ approach to prompt patients to generate their own ideas for behaviour change, as it contrasted with tutors’ usual advice-giving and problem-solving approach. Tutors’ understanding of the intervention was consolidated through re-reading and individualising their manuals (e.g. paraphrasing sections), and feedback from the RAFT programme trainers during clinical supervision (theme 3). Over time, tutors deepened their understanding of how a CB approach and the group setting could be used to support patients in self-managing the impact of their fatigue. In addition, the usefulness of the skills gained by tutors extended beyond the RAFT programmes and into their everyday clinical practice (theme 4). There was widespread support for delivering the RAFT programme in clinical practice beyond the trial, as tutors perceived that patients were benefiting (theme 5). Tutors valued their 4 days of central training, but believed that it would not be a feasible future clinical model. Some face-to-face training with the opportunity to role play key aspects of the intervention, along with some clinical supervision and quality control, were deemed necessary in any future training of new tutors.
The qualitative findings support two key ideas about skills training and its subsequent transfer into clinical practice. First is the importance of role play, a method of simulation commonly used to teach communication skills. 113 In the RAFT programme central training, role play was employed through both ‘role reversal’ (i.e. participants taking on the role of patients to develop insight into what the group dynamics might feel like from a patient’s perspective) and ‘role training’ (i.e. participants practising the skills that can help them become more expert in their professional role). Tutors identified both forms of role play as helpful for learning. Second is the importance of clinical supervision, as although communication skills training enhances skills, it has limited effect on clinical practice without subsequent clinical supervision. 114–116
Tutors were aware that they were delivering a standardised intervention and made great efforts to adhere to the manual content. However, tutors also expressed their need to individualise the manual and to put material into their own words. The RAFT programme trainers and fidelity observer often helped in this process by feeding back on if and how tutors were incorporating essential techniques and approaches into the sessions. Fidelity was recorded in the observer template (see Report Supplementary Material 1), and confirmed that tutors were delivering the RAFT programme as intended. Fidelity to the RAFT programme is an important consideration in any future roll-out. Inevitably, interventions are adapted to individual settings, resources available, or practitioners’ beliefs and interpretations, once they are introduced into clinical practice. Such changes may reduce or enhance outcomes seen in clinical practice and thus there is an argument for capturing not only outcomes but implementation fidelity and adherence to delivery format, content and underpinning CB theory in the roll-out of such interventions into clinical practice. 117
Tutors’ perceptions that the RAFT programme training and subsequent delivery impacted and benefited their wider clinical practice highlights the potential of up-skilling existing members of clinical teams to provide low-level psychological support. Evidence from studies of other long-term conditions, such as diabetes, cardiac rehabilitation and depression in long-term physical health conditions, shows that the incorporation of psychological skills into the nursing role is viewed positively by both nurses and patients. 100,118,119 However, the research evidence reiterates the finding that nurses and allied health professionals need time and support to acquire and use these skills.
Strengths and limitations
The study’s external validity was strengthened by involving seven hospitals and 14 health professional tutors with a range of previous experiences, broad entry criteria for people with RA fatigue and a control trial arm providing usual care for fatigue. The trial design was pragmatic and reflected usual RA management (e.g. medication changes, seeing other members of the multidisciplinary team), as well as natural fluctuations in fatigue (some patients dropping below eligibility at baseline), natural variation in patient attendances (not attending all the RAFT programme sessions), flexibility with regard to the RAFT programme group size, and natural variations in ability to deliver clinical services (delivery by lone tutors, use of a locum tutor); yet the RAFT programme still showed benefit with no reported harms. The usual-care fatigue booklet, based on the original RCT,31,45 has been widely available in most UK rheumatology units for 3 years prior to recruitment. Therefore, the timing and manner of its delivery to all participants was standardised in relation to the timing of the outcome evaluation. Randomisation was performed by a clinical trials unit off-site, and those patients randomised to the RAFT programme but unable to attend their next local programme were offered subsequent programme dates, ensuring maximal accommodation of recruited trial patients and reflecting future clinical practice. The integrity of data was supported by the checking of 100% of data entries by a second person.
The trial was strengthened by the rounded evaluation which, in addition to assessing the quantitative clinical outcomes, included intervention fidelity and cost-effectiveness. Furthermore, given that patient perceptions of receiving the RAFT programme were explored in the previous RCT,32 this trial incorporated examination of the tutors’ experiences of delivering a RAFT programme intervention and views on the practicalities of future clinical implementation. The strengths of the clinical and economic evaluations were the thorough approach taken to try and capture all relevant outcomes; the costs associated with RA-related fatigue and with the RAFT programme intervention; the use of validated measures whenever possible; and the continuation of data collection for 2 years. Data returns for the primary outcome were very high, probably enhanced by collection of the question by telephone, which may also have increased returns of the full questionnaire package posted the same day; consequently, patient loss to data completion was very low.
A strength of the qualitative evaluation was that almost all of the RAFT programme tutors took part, ensuring a wide range of views and experiences. In light of the often limited understanding of what might help or hinder the translation of a successful trial intervention into clinical practice, it is a strength of the study that future roll-out of the RAFT programme will be underpinned by practical approaches based on these combined perspectives of the nurses and OTs who delivered it across seven hospitals. The rigour of the qualitative findings is strengthened by having the data analysed by multiple co-applicants (including a patient co-applicant) before reaching a consensus.
Strong patient and public involvement was threaded throughout the trial. The two patient research partners (CR and Frances Robinson) had received the fatigue intervention from a clinical psychologist during the original trial31 and thus brought a wealth of knowledge and experience. Their input into methods of patient recruitment and evaluation were insightful, including viewing drafts of questionnaire packs and patient materials used in the RAFT programme handouts. The patient research partners’ participation and presentations at the RAFT programme training event allowed tutors (and also principal investigators and research nurses) to understand the impact of fatigue on daily life. One patient partner felt that the contribution to the trial that they could offer primarily related to the set-up (e.g. reviewing and finalising patient materials ready for the RAFT programme or the questionnaire pack), after which they decided to stand down; collaborating with two patient partners enabled a continued patient perspective on the emerging results. This included analysing a subset of the qualitative data, contributions to the trial reports and delivering presentations to academic and lay audiences on the practicalities of patient involvement in research.
All trials have limitations. In terms of trial design, controlling for any social effect that might occur through peer support by meeting other patients (i.e. the RAFT programme groups met on seven occasions) would have been impractical: seven sessions of didactic information would not reflect current usual care for RA-related fatigue and would be likely to have had high attrition. Furthermore, in the original RCT,31 qualitative evaluation with patients found that, although patients reported that interactions with, and the experiences of, other patients in their group were helpful, it was the facilitative role of the tutors and the use of CB techniques that were more important, otherwise the group of patients would simply have ‘pulled one another down’. 32
Delay between screening and baseline assessment was an inevitable result of the need to build cohorts in each centre that were sufficiently large for randomisation. Even though patients were recruited with fatigue as a recurrent problem, all symptoms fluctuate and a small proportion of patients in both trial arms did not have eligible fatigue severity scores on the day of baseline assessment. However, the complete-case analysis still showed that the RAFT programme was able to improve fatigue impact more than usual care alone and a stronger effect was seen in those who were eligible at baseline. Furthermore, such delays would be likely to be shorter in clinical practice as only sufficient patients for a RAFT programme need be recruited, rather than double the number to allow for randomisation. Six patients who were randomised to the RAFT programme could not attend their cohort’s programme dates and accepted a later programme, at which point a new baseline assessment was performed, meaning that baseline data had been collected after randomisation. During the trial, management of RA continued as usual and included necessary changes to medication aimed to reduce disease activity, which might have had an effect on fatigue. However, these changes did not differ between trial arms and it has been found that > 60% of patients on optimal medication who achieve remission from disease activity continue to experience problematic fatigue. 17
The RCT did not have follow-up data on the 25 patients who withdrew before the week 26 primary outcome point. The majority comprised 14 patients randomised to receive the RAFT programme who were unable to attend their original programme dates but expressed an intention to attend a later programme, at which point a fresh baseline assessment would have been made and follow-up would have occurred with the new cohort. By the end of local RAFT programme delivery, they had been unable to agree to any suitable programme dates and no exit data were requested. However, imputing missing data made no difference to the primary outcome analysis.
The economic evaluation was limited by the large number of missing data (particularly at 2 years, when > 30% of data had to be imputed), and possibly limited by the appropriateness of the EQ-5D in a RA population, which is part of an ongoing debate in long-term conditions and fatigue. Several of the costly bDMARDs have now come off patent and it was difficult to determine how much was actually paid for the drugs during the RCT. Individual trust negotiations on list prices may have taken place, and with clinical commissioners now encouraging/requiring trusts to switch patients to cheaper biosimilars120 these medication costs may come down for this patient population (although they were not different between trial arms).
The qualitative data on the tutors’ experiences of the RAFT programme were collected after tutors had completed the RAFT programme delivery. Although this was necessary in order not to change their practice (and can be seen as a strength as tutors had time to reflect), it meant that tutors were recalling their experiences of the RAFT programme that occurred some months earlier, particularly in relation to views on the central training that they had attended 2 years previously. It is possible that tutors’ responses were influenced by ED or SH collecting the data, as tutors met both researchers during the central training and were aware of their involvement in the design of the RAFT programme.
Implications for health care
The RAFT programme achieved a strong and sustained clinical effect on fatigue impact beyond usual care with no adverse events. Cost-effectiveness was not demonstrated in the primary analysis, which might be due to the lack of responsiveness of the EQ-5D to fatigue in long-term conditions. It is also possible that additional benefits or savings may accrue later in a long-term condition. Although, overall, there was no statistically significant difference in costs between the RAFT programme and usual care, nonetheless there is an additional cost to delivering the RAFT programme. However, the use of the existing rheumatology specialist nurses and OTs makes the RAFT programme both relatively easy to implement and low cost, compared with utilising clinical psychologists, whose presence is rare in rheumatology departments. Balanced against the paucity of other clinically effective interventions for fatigue in RA, and the importance of fatigue to this population, the low-cost nature of the RAFT programme might prompt clinicians and commissioners to consider implementation. The argument for implementation is supported by the subgroup analysis showing higher probability of cost-effectiveness in patients with more severe fatigue (52–60% probability).
The NHS service costs for the RAFT programme delivery based on 175 randomised patients in 28 groups was estimated at £322 per patient (assuming the one-off training becomes absorbed into routine training or a means of health professionals obtaining mandatory continuing professional development hours). Increasing group size to 8–10 patients in clinical practice would be both feasible and economically beneficial. The RAFT programme appears to be generalisable across people with RA, as it had broad entry criteria (i.e. any RA patient with notable fatigue severity). Furthermore, with patients in most inflammatory rheumatic diseases reporting fatigue,121,122 the RAFT programme could be easily extended to include patients from all these conditions, which could more rapidly fill programmes to capacity. This could be done without further costly RCTs, as self-management mechanisms are likely to be similar across inflammatory rheumatic diseases. To date, two of the seven RAFT programme centres are continuing to deliver the RAFT programme as part of clinical practice and have extended it to include patients with other inflammatory rheumatic diseases.
The qualitative evaluation with RAFT programme tutors indicated that they were integrating the RAFT programme skills gained (CB approaches; ‘ask don’t tell’) into their everyday clinical practice to great effect, potentially improving patients’ ability to self-manage other aspects of their inflammatory rheumatic disease, such as pain, stiffness or flares of inflammatory activity. This suggests that implementing the RAFT programme and training clinicians in CB approaches could have clinical benefits beyond RAFT programmes. It is increasingly advocated that training multidisciplinary team members in CB or motivational interviewing techniques would enhance communication, collaboration and thus patient adaptation, acceptance and behaviour change, all necessary for self-managing long-term conditions. 123,124 Research evidence on the success of these techniques by non-psychologists as a way of supporting specific patient groups or specific health problems is now emerging. 30,125 All of these approaches reduce the reliance on traditional didactic information or instruction-giving and consider the ‘whole person’, including how their beliefs affect symptoms and behaviours. A number of health professional undergraduate programmes and hospital trusts now include short training on these for students and staff, and detailed guidance on the use of some of these open and reflective skills in patient encounters can be found. 124
The RAFT programme was tested in seven different NHS hospital settings using existing clinicians, some of whom had a degree of prior relevant experiences, such as CB training or group work, whereas others had none at all (unlike other fatigue interventions in which clinical staff had to be experienced in group work in order to deliver the intervention). 99 The RAFT programme could be successfully delivered in terms of scheduling the programmes and managing tutor absence and sickness. However, for implementation within current NHS constraints, training would need to be shortened, as highlighted in the tutors’ qualitative data. Other psychological interventions delivered by non-psychologists used training lasting only 1 or 2 days;99,100 therefore, the RAFT programme training is currently being revised as two short online modules (covering preparatory background reading; access to the RAFT programme manual, videos of a programme and podcasts), followed by a single day of face-to-face group training (applying CB approaches in the RAFT programme, interpreting the daily activity diaries, goal-setting and group management). As these are experienced rheumatology clinicians, only occasional clinical supervision and support was required for the use of CB techniques, and this should be able to be sourced within the local hospital.
Implications for future research
The first priority should be to address issues of widening accessibility to fatigue support through different delivery routes, including different tutors and different patient populations. Delivery styles of the RAFT programme could be further explored by testing co-delivery by a tutor pair comprising a rheumatology professional and a lay (patient) volunteer, which combines professional knowledge with a patient’s expertise of living with the condition, and has been shown to be supportive in the self-management of long-term conditions. 126 To prepare for such research, the allocation of the different RAFT programme roles/topics in a way that would be most appropriate to the skills of either the professional or lay tutors would first need to be agreed, then the RAFT programme training adapted to cover these different needs/roles and any additional support or training needed for lay tutors. The RAFT programme could also be tested in other physical long-term conditions that have a relapsing or remitting nature and fatigue similar to RA (e.g. chronic obstructive pulmonary disease, multiple sclerosis, Parkinson’s disease), again, using the principle of tutors with relevant clinical expertise. For those patients who do not wish or are not able to attend group programmes, a brief one-to-one intervention by a rheumatology nurse or OT at the end of routine appointments is currently being piloted, using the core RAFT programme principles of fatigue validation, daily activity diaries and goal-setting.
Building on the exploratory analysis in this RCT, a study could be powered to test for dose response (number and combinations of sessions required), and including an intervention arm that did not receive the week 14 consolidation session would examine the impact and value of that final session. These research proposals would clarify whether or not similar benefit to that seen in this RCT could be achieved with lower cost to the NHS.
The second research priority would be to better understand change in fatigue impact that is meaningful to patients and how this informs cost evaluation. Psychological interventions specifically targeting RA-related fatigue have been identified as an under-researched area, with researchers encouraged to include cost evaluation in future work. 20,127 To better understand the importance of change in fatigue impact, further research could usefully establish the level of change in fatigue impact (BRAF-NRS impact) that is meaningful for patients. There is evidence that the impact of fatigue is particularly problematic in early RA2 and the current trial population had a mean of 10-year disease duration; therefore, any improvements in fatigue impact from the RAFT programme may have greater potential for translating into improved quality of life and economic benefit in a more recently diagnosed cohort. Future research also needs to explore whether or not the EQ-5D and other utility measures capture what is important to people with RA,104 specifically whether or not they capture fatigue, in order to better inform QALYs, on which NICE cost-effectiveness thresholds are based.
The third research priority could be to better understand what happens to research interventions when they are rolled out into clinical practice. Clinical implementation of the RAFT programme in RA, other inflammatory rheumatic diseases or other physical long-term conditions would provide an opportunity to evaluate not only outcome but also tutor fidelity to the RAFT programme content, principles and delivery in clinical practice. This would clarify any changes to the RAFT programme that inevitably occur in clinical practice and afford an opportunity to understand the clinical circumstances in which the intervention can be effective.
A fourth research stream might be to build on the qualitative findings that tutors perceived that their new CB skills fed into changes in their wider clinical practice. Trials could examine if training health-care professionals and multidisciplinary team members in the use of CB approaches in their everyday practice has a beneficial effect on patient outcomes.
Conclusions
The RAFT programme is a seven-session group intervention to help patients with RA manage their fatigue. It uses CB approaches and is delivered for the first time by usual clinical teams and not psychologists. Patient attendance and satisfaction were high. The RAFT programme demonstrates significant benefits beyond usual care alone on RA-related fatigue impact, living with fatigue and emotional fatigue and these, along with fatigue coping, are sustained over 2 years without further RAFT programme input. No harms were identified. The RCT did not demonstrate that the RAFT programme is likely to be cost-effective at NICE cost-per-QALY thresholds, although the EQ-5D may not be sufficiently responsive to capture changes in fatigue. Although there was no statistically significant difference in costs, the RAFT programme supports the management of a symptom considered important by patients and for which there is a paucity of interventions. In addition, the RAFT programme is low cost and easy to implement. The RAFT programme tutors believe the skills learned through delivery of the RAFT programme have had an impact on their wider clinical practice and approach to supporting self-management in RA.
Acknowledgements
The RAFT programme study group
In addition to the listed authors, the RAFT programme study team comprised Richard Cheston (Professor of Mental Health Research, supported training and fidelity monitoring), Paul Creamer and Rod Hughes (Consultant Rheumatologists and local principal investigators throughout), and Bev Knops (Senior OT supported tutor training and supervision).
The authors would like to thank the following people for their collaboration in the trial: Sandra Green, Stuart Webber, Paul Thompson, Nick Viner and Kirsten Mackay (local principal investigators); Frances Robinson (patient research partner); David Carmichael (database and randomisation services, BRTC); the RAFT programme tutors and research nurses in the seven participating hospitals; and the patients for their participation.
Contributions of authors
Sarah Hewlett (Professor of Rheumatology Nursing) was the chief investigator, contributed to trial design, co-designed the intervention and supported the tutor training, led the study team, supervised the conduct of the trial, analysis and reporting, and drafted the report.
Celia Almeida (Trial Administrator) contributed to data collection, data entry and validation, and contributed to the writing and editing of the report.
Nicholas Ambler (Consultant Clinical Psychologist) co-designed the RAFT programme, delivered and supported tutor training, and contributed to the writing and editing of the report.
Peter S Blair (Reader in Medical Statistics) contributed to trial design, supervised the statistical design and analysis, and contributed to the writing and editing of the report.
Ernest Choy (Professor and Head of Rheumatology and Translational Research) contributed to trial design, was a local principal investigator in one centre, and contributed to the writing and editing of the report.
Emma Dures (Associate Professor in Rheumatology and Self-management) contributed to trial design, supported the tutor training, conducted the qualitative evaluation and led the qualitative analysis, and contributed to the writing and editing of the report.
Alison Hammond (Professor in Rheumatology Rehabilitation) contributed to trial design and the qualitative analysis, and contributed to the writing and editing of the report.
William Hollingworth (Professor of Health Economics) contributed to trial design, supervised the health economics design and analysis, and contributed to the writing and editing of the report.
Bryar Kadir (Research Associate, Medical Statistics) conducted the initial statistical analysis and contributed to the writing and editing of the report.
John Kirwan (Emeritus Professor of Rheumatology) contributed to trial design, was a local principal investigator in one centre, contributed to interpretation of findings and to the writing and editing of the report.
Zoe Plummer (Trial Co-ordinator) managed the trial on a daily basis, co-ordinated the seven centres, was responsible for research governance, data collection, entry and checking, and contributed to the writing and editing of the report.
Clive Rooke (Patient Research Partner) contributed to the patient materials, methods of data collection, supported tutor training and qualitative analysis, and contributed to the writing and editing of the report.
Joanna Thorn (Senior Research Associate, Health Economics) conducted the health economics analysis and contributed to the writing and editing of the report.
Nicholas Turner (Senior Research Associate, Medical Statistics) conducted the statistical analysis and contributed to the writing and editing of the report.
Jonathan Pollock (Associate Professor of Epidemiology) contributed to the trial design, supported the statistical analysis and interpretation, and contributed to the writing and editing of the report.
Publications
Hewlett S, Ambler N, Almeida C, Blair PS, Choy E, Dures E, et al. Protocol for a randomised controlled trial for Reducing Arthritis Fatigue by clinical Teams using cognitive behavioural approaches (RAFT). BMJ Open 2015;5:e009061.
Dures E, Rooke C, Hammond A, Hewlett S. Training and delivery of a novel fatigue intervention: a qualitative study of rheumatology health-care professionals’ experiences [published online ahead of print August 27 2019]. Rheumatol Adv Pract 2019.
Hewlett S, Almeida C, Ambler N, Blair PS, Choy E, Dures E, et al. Reducing arthritis fatigue impact: two-year randomised controlled trial of cognitive behavioural approaches by rheumatology teams (RAFT). Ann Rheum Dis 2019;78:465–72.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review by the study team, the National Institute for Health Research and/or regulatory bodies (e.g. ethics committee), as data-sharing approval was not sought from patients during the consent process.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Symmons D, Turner G, Webb R, Asten P, Barrett E, Lunt M, et al. The prevalence of rheumatoid arthritis in the United Kingdom. Rheumatology 2002;41:793-800. https://doi.org/10.1093/rheumatology/41.7.793.
- Suurmeijer TP, Waltz M, Moum T, Guillemin F, van Sonderen FL, Briançon S, et al. Quality of life profiles in the first years of rheumatoid arthritis: results from the EURIDISS longitudinal study. Arthritis Rheum 2001;45:111-21. https://doi.org/10.1002/1529-0131(200104)45:2<111::AID-ANR162>3.0.CO;2-E.
- Luqmani R, Hennell S, Estrach C, Birrell F, Bosworth A, Davenport G, et al. British Society for Rheumatology and British Health Professionals in Rheumatology guideline for the management of rheumatoid arthritis (first 2 years). Rheumatology 2006;45:1167-9. https://doi.org/10.1093/rheumatology/kel215a.
- Luqmani R, Hennell S, Estrach C, Basher D, Birrell F, Bosworth A, et al. British Society for Rheumatology and British Health Professionals in Rheumatology guideline for the management of rheumatoid arthritis (after the first two years). Rheumatology 2009;48:436-9. https://doi.org/10.1093/rheumatology/ken450a.
- Hewlett S, Carr M, Ryan S, Kirwan J, Richards P, Carr A, et al. Outcomes generated by patients with rheumatoid arthritis: how important are they?. Musculoskeletal Care 2005;3:131-42. https://doi.org/10.1002/msc.3.
- van Hoogmoed D, Fransen J, Bleijenberg G, van Riel P. Physical and psychosocial correlates of severe fatigue in rheumatoid arthritis. Rheumatology 2010;49:1294-302. https://doi.org/10.1093/rheumatology/keq043.
- Wolfe F, Hawley DJ, Wilson K. The prevalence and meaning of fatigue in rheumatic disease. J Rheumatol 1996;23:1407-17.
- Repping-Wuts H, Uitterhoeve R, van Riel P, van Achterberg T. Fatigue as experienced by patients with rheumatoid arthritis (RA): a qualitative study. Int J Nurs Stud 2008;45:995-1002. https://doi.org/10.1016/j.ijnurstu.2007.06.007.
- Hewlett S, Cockshott Z, Byron M, Kitchen K, Tipler S, Pope D, et al. Patients’ perceptions of fatigue in rheumatoid arthritis: overwhelming, uncontrollable, ignored. Arthritis Rheum 2005;53:697-702. https://doi.org/10.1002/art.21450.
- Rupp I, Boshuizen HC, Jacobi CE, Dinant HJ, van den Bos GA. Impact of fatigue on health-related quality of life in rheumatoid arthritis. Arthritis Rheum 2004;51:578-85. https://doi.org/10.1002/art.20539.
- Minnock P, Ringnér A, Bresnihan B, Veale D, FitzGerald O, McKee G. Perceptions of the cause, impact and management of persistent fatigue in patients with rheumatoid arthritis following tumour necrosing factor inhibition therapy. Musculoskeletal Care 2017;15:23-35. https://doi.org/10.1002/msc.1136.
- Lacaille D, White MA, Backman CL, Gignac MA. Problems faced at work due to inflammatory arthritis: new insights gained from understanding patients’ perspective. Arthritis Rheum 2007;57:1269-79. https://doi.org/10.1002/art.23002.
- Young A, Dixey J, Kulinskaya E, Cox N, Davies P, Devlin J, et al. Which patients stop working because of rheumatoid arthritis?. Ann Rheum Dis 2002;61:335-40. https://doi.org/10.1136/ard.61.4.335.
- Lundkvist J, Kastäng F, Kobelt G. The burden of rheumatoid arthritis and access to treatment: health burden and costs. Eur J Health Econ 2008;8:49-60. https://doi.org/10.1007/s10198-007-0088-8.
- Kirwan JR, Minnock P, Adebajo A, Bresnihan B, Choy E, de Wit M, et al. Patient perspective workshop: fatigue as a recommended patient-centred outcome measure in rheumatoid arthritis. J Rheumatol 2007;34:1174-7.
- Almeida C, Choy EH, Hewlett S, Kirwan JR, Cramp F, Chalder T, et al. Biologic interventions for fatigue in rheumatoid arthritis. Cochrane Database Syst Rev 2016;6. https://doi.org/10.1002/14651858.CD008334.pub2.
- Druce KL, Bhattacharya Y, Jones GT, Macfarlane GJ, Basu N. Most patients who reach disease remission following anti-TNF therapy continue to report fatigue: results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Rheumatology 2016;55:1786-90. https://doi.org/10.1093/rheumatology/kew241.
- Nikolaus S, Bode C, Taal E, van de Laar MA. Fatigue and factors related to fatigue in rheumatoid arthritis: a systematic review. Arthritis Care Res 2013;65:1128-46. https://doi.org/10.1002/acr.21949.
- Hewlett S, Chalder T, Choy E, Cramp F, Davis B, Dures E, et al. Fatigue in rheumatoid arthritis: time for a conceptual model. Rheumatology 2011;50:1004-6. https://doi.org/10.1093/rheumatology/keq282.
- Cramp F, Hewlett S, Almeida C, Kirwan JR, Choy EH, Chalder T, et al. Non-pharmacological interventions for fatigue in rheumatoid arthritis. Cochrane Database Syst Rev 2013;8. https://doi.org/10.1002/14651858.CD008322.pub2.
- Sage N, Sowden M, Chorlton E, Edeleanu A, Sage N, Sowden M, et al. Cognitive Behaviour Therapy for Chronic Illness and Palliative Care. Chichester: Wiley; 2008.
- Riemsma RP, Kirwan JR, Taal E, Rasker HJJ. Patient education for adults with rheumatoid arthritis. Cochrane Database Syst Rev 2003;2. https://doi.org/10.1002/14651858.CD003688.
- van Kessel K, Moss-Morris R, Willoughby E, Chalder T, Johnson MH, Robinson E. A randomized controlled trial of cognitive behavior therapy for multiple sclerosis fatigue. Psychosom Med 2008;70:205-13. https://doi.org/10.1097/PSY.0b013e3181643065.
- O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A. Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme. Health Technol Assess 2006;10. https://doi.org/10.3310/hta10370.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. https://doi.org/10.1037/0033-295X.84.2.191.
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1-7. https://doi.org/10.1207/S15324796ABM2601_01.
- Iversen MD, Hammond A, Betteridge N. Self-management of rheumatic diseases: state of the art and future perspectives. Ann Rheum Dis 2010;69:955-63. https://doi.org/10.1136/ard.2010.129270.
- Evers AW, Kraaimaat FW, van Riel PL, de Jong AJ. Tailored cognitive-behavioral therapy in early rheumatoid arthritis for patients at risk: a randomized controlled trial. Pain 2002;100:141-53. https://doi.org/10.1016/S0304-3959(02)00274-9.
- Riemsma RP, Taal E, Rasker JJ. Group education for patients with rheumatoid arthritis and their partners. Arthritis Rheum 2003;49:556-66. https://doi.org/10.1002/art.11207.
- Hammond A, Bryan J, Hardy A. Effects of a modular behavioural arthritis education programme: a pragmatic parallel-group randomized controlled trial. Rheumatology 2008;47:1712-18. https://doi.org/10.1093/rheumatology/ken380.
- Hewlett S, Ambler N, Almeida C, Cliss A, Hammond A, Kitchen K, et al. Self-management of fatigue in rheumatoid arthritis: a randomised controlled trial of group cognitive-behavioural therapy. Ann Rheum Dis 2011;70:1060-7. https://doi.org/10.1136/ard.2010.144691.
- Dures E, Kitchen K, Almeida C, Ambler N, Cliss A, Hammond A, et al. ‘They didn’t tell us, they made us work it out ourselves’: patient perspectives of a cognitive-behavioral programme for rheumatoid arthritis fatigue. Arthritis Care Res 2012;64:494-501. https://doi.org/10.1002/acr.21562.
- Dures E, Almeida C, Caesley J, Peterson A, Ambler N, Morris M, et al. A survey of psychological support provision for people with inflammatory arthritis in secondary care in England. Musculoskeletal Care 2014;12:173-81. https://doi.org/10.1002/msc.1071.
- Department of Health and Social Care . Supporting People With Long Term Conditions to Self Care 2006. https://webarchive.nationalarchives.gov.uk/20060320134238/http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4130725&chk=o9VokD (accessed 10 April 2019).
- National Institute for Health and Care Excellence . Rheumatoid Arthritis in Adults: Management 2009. www.nice.org.uk/CG79 (accessed 11 May 2018).
- Department of Health and Social Care . Improving Access to Psychological Therapies Implementation Plan 2008. https://webarchive.nationalarchives.gov.uk/20130124042312/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_083168.pdf (accessed 10 April 2019).
- Medical Research Council . Developing and Evaluating Complex Interventions: New Guidance 2008. www.mrc.ac.uk/documents/pdf/developing-and-evaluating-complex-interventions/ (accessed 8 June 2015).
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. https://doi.org/10.1037/a0016136.
- Otto M. Stories and metaphors in cognitive-behavior therapy. Cogn Behav Pract 2000;7:166-72. https://doi.org/10.1016/S1077-7229(00)80027-9.
- Hewlett S, Ambler N, Almeida C, Blair PS, Choy E, Dures E, et al. Protocol for a randomised controlled trial for Reducing Arthritis Fatigue by clinical Teams (RAFT) using cognitive-behavioural approaches. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009061.
- Dures E, Ambler N, Fletcher D, Pope D, Robinson F, Rooke R, et al. Why do we need to pilot interventions? Essential refinements identified during pilots of a fatigue intervention. Rheumatology 2012;51:iii167-8.
- Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The ARA 1987 revised criteria for the classification of RA. Arthritis Rheum 1988;31:315-24. https://doi.org/10.1002/art.1780310302.
- Nicklin J, Cramp F, Kirwan J, Greenwood R, Urban M, Hewlett S. Measuring fatigue in RA: a cross-sectional study to evaluate the BRAF Multi-Dimensional Questionnaire, VAS and NRS. Arthritis Care Res 2010;62:1559-68. https://doi.org/10.1002/acr.20282.
- Dures EK, Hewlett SE, Cramp FA, Greenwood R, Nicklin JK, Urban M, et al. Reliability and sensitivity to change of the Bristol Rheumatoid Arthritis Fatigue scales. Rheumatology 2013;52:1832-9. https://doi.org/10.1093/rheumatology/ket218.
- Arthritis Research UK . Self-Help and Daily Living: Fatigue and Arthritis 2011. www.arthritisresearchuk.org/~/media/Files/Arthritis-information/Living-with-arthritis/2269-Fatigue-and-Arthritis-inc-excercise-book.ashx (accessed 11 May 2018).
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Pincus T, Summey JA, Soraci SA, Wallston KA, Hummon NP. Assessment of patient satisfaction in activities of daily living using a modified Stanford Health Assessment Questionnaire. Arthritis Rheum 1983;26:1346-53. https://doi.org/10.1002/art.1780261107.
- Meenan RF, Gertman PM, Mason JH. Measuring health status in arthritis. The arthritis impact measurement scales. Arthritis Rheum 1980;23:146-52. https://doi.org/10.1002/art.1780230203.
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index. Psychiatry Res 1989;28:193-21. https://doi.org/10.1016/0165-1781(89)90047-4.
- Katz PP, Morris A, Yelin EH. Prevalence and predictors of disability in valued life activities among individuals with rheumatoid arthritis. Ann Rheum Dis 2006;65:763-9. https://doi.org/10.1136/ard.2005.044677.
- Felson DT, Anderson JJ, Boers M, Bombardier C, Chernoff M, Fried B, et al. The American College of Rheumatology preliminary core set of disease activity measures for RA clinical trials. Arthritis Rheum 1993;36:729-40. https://doi.org/10.1002/art.1780360601.
- van der Heijde DM, van‘t Hof M, van Riel PL, van de Putte LB. Development of a disease activity score based on judgment in clinical practice by rheumatologists. J Rheumatol 1993;20:579-81.
- Choy EH, Khoshaba B, Cooper D, MacGregor A, Scott DL. Development and validation of a patient-based disease activity score in rheumatoid arthritis that can be used in clinical trials and routine practice. Arthritis Rheum 2008;59:192-9. https://doi.org/10.1002/art.23342.
- Choy E, Leung AMH. Simplified Patient-Derived Disease Activity Score (SPDAS2): a simplified version without early morning stiffness. Ann Rheum Dis 2016;75. https://doi.org/10.1136/annrheumdis-2016-eular.1443.
- Stein MJ, Wallston KA, Nicassio PM. Factor structure of the Arthritis Helplessness Index. J Rheumatol 1988;15:427-32.
- Hewlett S, Cockshott Z, Kirwan J, Barrett J, Stamp J, Haslock I. Development and validation of a self-efficacy scale for use in British patients with rheumatoid arthritis (RASE). Rheumatology 2001;40:1221-30. https://doi.org/10.1093/rheumatology/40.11.1221.
- Vierron E, Giraudeau B. Design effect in multicenter studies: gain or loss of power?. BMC Med Res Methodol 2009;9. https://doi.org/10.1186/1471-2288-9-39top.
- Vierron E, Giraudeau B. Sample size calculation for multicenter randomized trial: taking the center effect into account. Contemp Clin Trials 2007;28:451-8. https://doi.org/10.1016/j.cct.2006.11.003.
- Lamb SE, Hansen Z, Lall R, Castelnuovo E, Withers EJ, Nichols V, et al. Group cognitive behavioural treatment for low-back pain in primary care: a randomised controlled trial and cost-effectiveness analysis. Lancet 2010;375:916-23. https://doi.org/10.1016/S0140-6736(09)62164-4.
- CONSORT . CONSORT Statement, Checklist and Flowchart. n.d. www.consort-statement.org (accessed 10 April 2018).
- Connell AM. Employing complier average causal effect analytic methods to examine effects of randomized encouragement trials. Am J Drug Alcohol Abuse 2009;35:253-9. https://doi.org/10.1080/00952990903005882.
- Sloan JA, Cella D, Hayes RD. Clinical significance of patient reported questionnaire data: another step towards consensus. J Clin Epidemiol 2005;58:1217-19. https://doi.org/10.1016/j.jclinepi.2005.07.009.
- Khanna D, Pope J, Khanna PP, Maloney M, Samedi N, Norrie D, et al. The minimally important difference for the fatigue VAS in patients with rheumatoid arthritis followed in an academic clinical practice. J Rheumatol 2008;35:2339-43. https://doi.org/10.3899/jrheum.080375.
- Dunn G, Bentall R. Modelling treatment-effect heterogeneity in randomized controlled trials of complex interventions (psychological treatments). Stat Med 2007;26:4719-45. https://doi.org/10.1002/sim.2891.
- Hewlett S, Almeida C, Ambler N, Blair PS, Choy E, Dures E, et al. Reducing arthritis fatigue impact: two-year randomised controlled trial of cognitive behavioural approaches by rheumatology teams (RAFT). Ann Rheum Dis 2019;78:465-72. https://doi.org/10.1136/annrheumdis-2018-214469.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal 2013. www.nice.org.uk/process/pmg9/chapter/the-reference-case (accessed 17 May 2018).
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- National Institute for Health and Care Excellence . Position Statement on Use of the EQ-5D-5L Valuation Set 2017. www.nice.org.uk/Media/Default/About/what-we-do/NICE-guidance/NICE-technology-appraisal-guidance/eq5d5l_nice_position_statement.pdf (accessed 11 May 2018).
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics 1993;4:353-65. https://doi.org/10.2165/00019053-199304050-00006.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016 2016. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2016/ (accessed 17 May 2018).
- NHS Digital . Prescription Cost Analysis, England, 2016 2017. https://digital.nhs.uk/catalogue/PUB23631 (accessed 11 May 2018).
- Department of Health and Social Care . NHS Reference Costs 2015 to 2016 2016. www.gov.uk/government/publications/nhs-reference-costs-2015-to-2016 (accessed 8 June 2017).
- Office for National Statistics . Annual Survey of Hours and Earnings: 2016 Provisional Results 2016. www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/annualsurveyofhoursandearnings/2016provisionalresults (accessed 8 June 2017).
- UK Care Guide . Paying for Home Care Costs in 2019 – Your Ultimate Guide n.d. https://ukcareguide.co.uk/home-care-costs/ (accessed 1 April 2019).
- GOV.UK . National Minimum Wage and National Living Wage Rates n.d. www.gov.uk/national-minimum-wage-rates.
- NHS . Chiropractic n.d. www.nhs.uk/conditions/chiropractic/ (accessed 1 April 2019).
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- Löthgren M, Zethraeus N. Definition, interpretation and calculation of cost-effectiveness acceptability curves. Health Econ 2000;9:623-30. https://doi.org/10.1002/1099-1050(200010)9:7<623::AID-HEC539>3.0.CO;2-V.
- Dures E, Rooke C, Hammond A, Hewlett S. Training and delivery of a novel fatigue intervention: a qualitative study of rheumatology health-care professionals’ experiences [published online ahead of print August 27 2019]. Rheumatol Adv Pract 2019. https://doi.org/10.1093/rap/rkz032.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Wilkinson S. Focus group methodology: a review. Int J Soc Res Methodol 1998;1:181-203. https://doi.org/10.1080/13645579.1998.10846874.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2003.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Hayes N. Doing Psychological Research: Gathering and Analysing Data. Buckingham: Open University Press; 2000.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:80-92. https://doi.org/10.1177/160940690600500107.
- Hart RI, Ng WF, Newton JL, Hackett KL, Lee RP, Thompson B. What impact does written information about fatigue have on patients with autoimmune rheumatic diseases? Findings from a qualitative study. Musculoskeletal Care 2017;15:230-7. https://doi.org/10.1002/msc.1164.
- Superio-Cabuslay E, Ward MM, Lorig KR. Patient education interventions in osteoarthritis and rheumatoid arthritis: a meta-analytic comparison with nonsteroidal anti-inflammatory drug treatment. Arthritis Care Res 1996;9:292-301. https://doi.org/10.1002/1529-0131(199608)9:4<292::AID-ANR1790090414>3.0.CO;2-4.
- Wells G, Li T, Maxwell L, MacLean R, Tugwell P. Determining the minimal clinically important differences in activity, fatigue, and sleep quality in patients with rheumatoid arthritis. J Rheumatol 2007;34:280-9.
- Pouchot J, Kherani RB, Brant R, Lacaille D, Lehman AJ, Ensworth S, et al. Determination of the minimal clinically important difference for seven fatigue measures in rheumatoid arthritis. J Clin Epidemiol 2008;61:705-13. https://doi.org/10.1016/j.jclinepi.2007.08.016.
- Learmonth YC, Dlugonski D, Pilutti LA, Sandroff BM, Klaren R, Motl RW. Psychometric properties of the Fatigue Severity Scale and the Modified Fatigue Impact Scale. J Neurol Sci 2013;331:102-7. https://doi.org/10.1016/j.jns.2013.05.023.
- Kos D, Duportail M, D’hooghe M, Nagels G, Kerckhofs E. Multidisciplinary fatigue management programme in multiple sclerosis: a randomized clinical trial. Mult Scler 2007;13:996-1003. https://doi.org/10.1177/1352458507078392.
- van Steenbergen HW, Tsonaka R, Huizinga TW, Boonen A, van der Helm-van Mil AH. Fatigue in rheumatoid arthritis; a persistent problem: a large longitudinal study. RMD Open 2015;1. https://doi.org/10.1136/rmdopen-2014-000041.
- Druce KL, Jones GT, Macfarlane GJ, Verstappen SM, Basu N. The longitudinal course of fatigue in rheumatoid arthritis: results from the Norfolk Arthritis Register. J Rheumatol 2015;42:2059-65. https://doi.org/10.3899/jrheum.141498.
- Hewlett S, Smith AP, Kirwan JR. Measuring the meaning of disability in rheumatoid arthritis: the Personal Impact Health Assessment Questionnaire (PI HAQ). Ann Rheum Dis 2002;61:986-93. https://doi.org/10.1136/ard.61.11.986.
- Seror R, Tubach F, Baron G, Guillemin F, Ravaud P. Measure of function in rheumatoid arthritis: individualised or classical scales?. Ann Rheum Dis 2010;69:97-101. https://doi.org/10.1136/ard.2008.102137.
- Sanderson TC, Hewlett SE, Flurey C, Dures E, Richards P, Kirwan JR. The impact triad (severity, importance, self-management) as a method of enhancing measurement of personal life impact of rheumatic diseases. J Rheumatol 2011;38:191-4. https://doi.org/10.3899/jrheum.100700.
- Thomas S, Thomas PW, Kersten P, Jones R, Green C, Nock A, et al. A pragmatic parallel arm multi-centre randomised controlled trial to assess the effectiveness and cost-effectiveness of a group-based fatigue management programme (FACETS) for people with multiple sclerosis. J Neurol Neurosurg Psychiatry 2013;84:1092-9. https://doi.org/10.1136/jnnp-2012-303816.
- Ekers D, Murphy R, Archer J, Ebenezer C, Kemp D, Gilbody S. Nurse-delivered collaborative care for depression and long-term physical conditions: a systematic review and meta-analysis. J Affect Disord 2013;149:14-22. https://doi.org/10.1016/j.jad.2013.02.032.
- Alam R, Sturt J, Lall R, Winkley K. An updated meta-analysis to assess the effectiveness of psychological interventions delivered by psychological specialists and generalist clinicians on glycaemic control and on psychological status. Patient Educ Couns 2009;75:25-36. https://doi.org/10.1016/j.pec.2008.08.026.
- Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: An EQ-5D-5L value set for England. Health Econ 2018;27:7-22. https://doi.org/10.1002/hec.3564.
- Gossec L, Dougados M, Rincheval N, Balanescu A, Boumpas DT, Canadelo S, et al. Elaboration of the preliminary Rheumatoid Arthritis Impact of Disease (RAID) score: a EULAR initiative. Ann Rheum Dis 2009;68:1680-5. https://doi.org/10.1136/ard.2008.100271.
- Trenaman L, Boonen A, Guillemin F, Hiligsmann M, Hoens A, Marra C, et al. OMERACT Quality-adjusted Life-years (QALY) Working Group: do current QALY measures capture what matters to patients?. J Rheumatol 2017;44:1899-903. https://doi.org/10.3899/jrheum.161112.
- Linde L, Sørensen J, Ostergaard M, Hørslev-Petersen K, Hetland ML. Health-related quality of life: validity, reliability, and responsiveness of SF-36, 15D, EQ-5D [corrected] RAQoL, and HAQ in patients with rheumatoid arthritis. J Rheumatol 2008;35:1528-37.
- Marra CA, Marion SA, Guh DP, Najafzadeh M, Wolfe F, Esdaile JM, et al. Not all ‘quality-adjusted life years’ are equal. J Clin Epidemiol 2007;60:616-24. https://doi.org/10.1016/j.jclinepi.2006.09.006.
- Marra CA, Rashidi AA, Guh D, Kopec JA, Abrahamowicz M, Esdaile JM, et al. Are indirect utility measures reliable and responsive in rheumatoid arthritis patients?. Qual Life Res 2005;14:1333-44. https://doi.org/10.1007/s11136-004-6012-0.
- Vos-Vromans D, Evers S, Huijnen I, Köke A, Hitters M, Rijnders N, et al. Economic evaluation of multidisciplinary rehabilitation treatment versus cognitive behavioural therapy for patients with chronic fatigue syndrome: a randomized controlled trial. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0177260.
- Sokka T, Kautiainen H, Pincus T, Verstappen SM, Aggarwal A, Alten R, et al. Work disability remains a major problem in rheumatoid arthritis in the 2000s: data from 32 countries in the QUEST-RA study. Arthritis Res Ther 2010;12. https://doi.org/10.1186/ar2951.
- Sossong B, Felder S, Wolff M, Krüger K. Evaluating the consequences of rheumatoid arthritis. Eur J Health Econ 2017;18:685-96. https://doi.org/10.1007/s10198-016-0818-x.
- Brazier J, Akehurst R, Brennan A, Dolan P, Claxton K, McCabe C, et al. Should patients have a greater role in valuing health states?. Appl Health Econ Health Policy 2005;4:201-8. https://doi.org/10.2165/00148365-200504040-00002.
- McCormack RC, O’Shea F, Doran M, Connolly D. Impact of a fatigue management in work programme on meeting work demands of individuals with rheumatic diseases: a pilot study. Musculoskeletal Care 2018;16:398-404. https://doi.org/10.1002/msc.1237.
- Baile WF, Blatner A. Teaching communication skills: using action methods to enhance role-play in problem-based learning. Simul Healthc 2014;9:220-7. https://doi.org/10.1097/SIH.0000000000000019.
- Heaven C, Clegg J, Maguire P. Transfer of communication skills training from workshop to workplace: the impact of clinical supervision. Patient Educ Couns 2006;60:313-25. https://doi.org/10.1016/j.pec.2005.08.008.
- Dures E, Hewlett S, Ambler N, Jenkins R, Clarke J, Gooberman-Hill R. Rheumatology clinicians’ experiences of brief training and implementation of skills to support patient self-management. BMC Musculoskelet Disord 2014;15. https://doi.org/10.1186/1471-2474-15-108.
- Clark JE, Aitken S, Watson N, McVey J, Helbert J, Wraith A, et al. Training oncology and palliative care clinical nurse specialists in psychological skills: evaluation of a pilot study. Palliat Support Care 2015;13:537-42. https://doi.org/10.1017/S1478951513000163.
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci 2007;2. https://doi.org/10.1186/1748-5908-2-40.
- Graves H, Garrett C, Amiel SA, Ismail K, Winkley K. Psychological skills training to support diabetes self-management: qualitative assessment of nurses’ experiences. Prim Care Diabetes 2016;10:376-82. https://doi.org/10.1016/j.pcd.2016.03.001.
- Turner KM, Winder R, Campbell JL, Richards DA, Gandhi M, Dickens CM, et al. Patients’ and nurses’ views on providing psychological support within cardiac rehabilitation programmes: a qualitative study. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-017510.
- National Medical Directorate, NHS England . Commissioning Framework for Biological Medicines (Including Biosimilar Medicines). 2017. www.england.nhs.uk/wp-content/uploads/2017/09/biosimilar-medicines-commissioning-framework.pdf (accessed 16 May 2018).
- Gudu T, Etcheto A, de Wit M, Heiberg T, Maccarone M, Balanescu A, et al. Fatigue in psoriatic arthritis – a cross-sectional study of 246 patients from 13 countries. Joint Bone Spine 2016;83:439-43. https://doi.org/10.1016/j.jbspin.2015.07.017.
- Tench CM, McCurdie I, White PD, D’Cruz DP. The prevalence and associations of fatigue in systemic lupus erythematosus. Rheumatology 2000;39:1249-54. https://doi.org/10.1093/rheumatology/39.11.1249.
- Dures E, Hewlett S. Perspectives on cognitive behavioural approaches to management of patients with rheumatic diseases. Nat Rheumatol Rev 2012;8:553-9. https://doi.org/10.1038/nrrheum.2012.108.
- O’Sullivan PB, Caneiro JP, O’Keeffe M, Smith A, Dankaerts W, Fersum K, et al. Cognitive functional therapy: an integrated behavioral approach for the targeted management of disabling low back pain. Phys Ther 2018;98:408-23. https://doi.org/10.1093/ptj/pzy022.
- Hurley MV, Walsh NE, Mitchell H, Nicholas J, Patel A. Long-term outcomes and costs of an integrated rehabilitation program for chronic knee pain: a pragmatic, cluster randomized, controlled trial. Arthritis Care Res 2012;64:238-47. https://doi.org/10.1002/acr.20642.
- Turner A, Anderson JK, Wallace LM, Bourne C. An evaluation of a self-management program for patients with long-term conditions. Patient Educ Couns 2015;98:213-19. https://doi.org/10.1016/j.pec.2014.08.022.
- Prothero L, Barley E, Galloway J, Georgopoulou S, Sturt J. The evidence base for psychological interventions for rheumatoid arthritis: a systematic review of reviews. Int J Nurs Stud 2018;82:20-9. https://doi.org/10.1016/j.ijnurstu.2018.03.008.
Appendix 1 Conceptual model of rheumatoid arthritis fatigue
FIGURE 5.
Conceptual model of RA fatigue. Reproduced from Hewlett S, Chalder T, Choy E, Cramp F, Davis B, Dures E, et al. , Fatigue in rheumatoid arthritis: time for a conceptual model, Rheumatology (Oxford), 2011, Volume 50, Issue 6, pp. 1004–6, by permission of Oxford University Press. 19
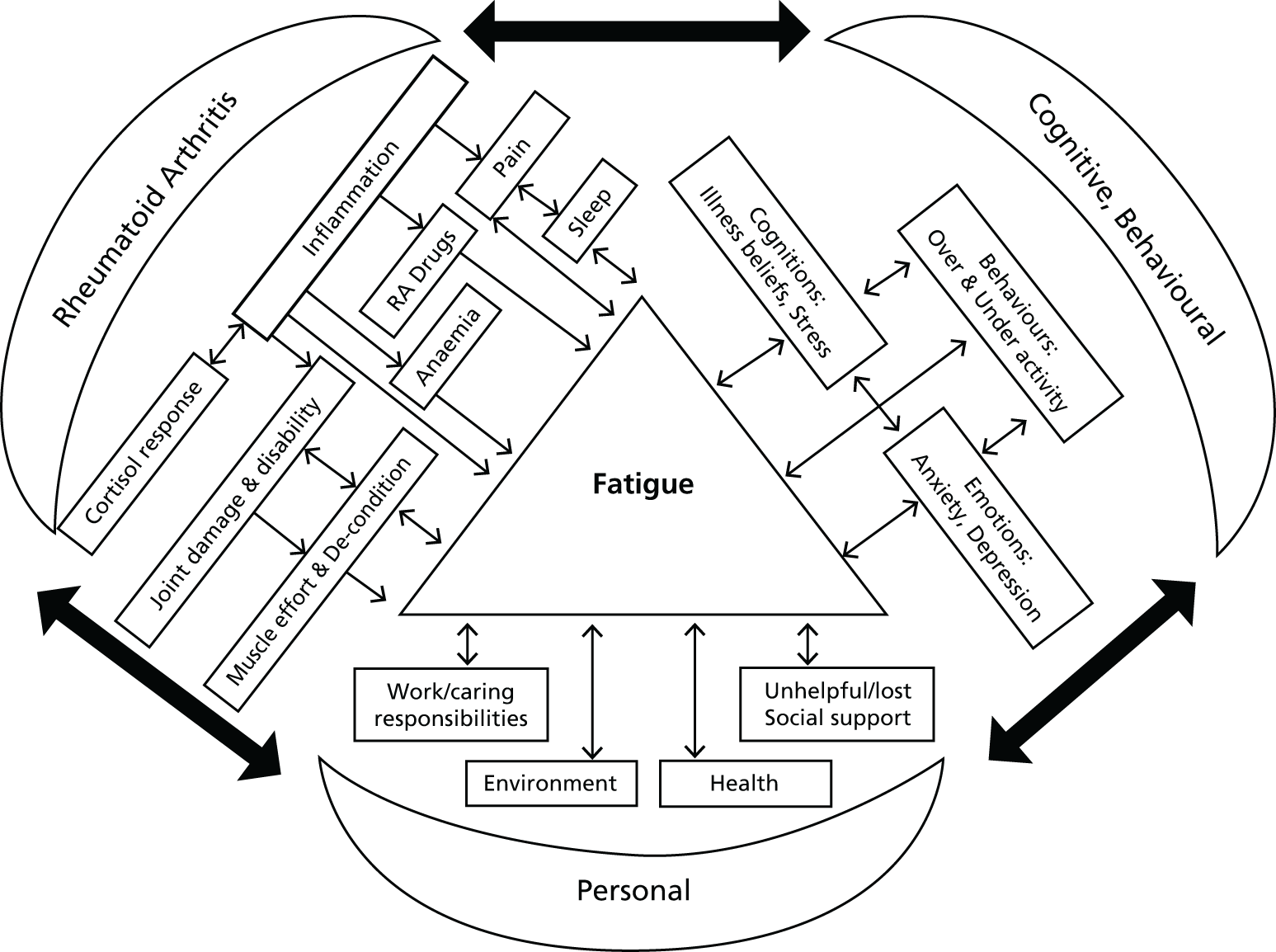
Appendix 2 Session content of theRAFT programme
| First hour | Supporting materials | Second hour |
|---|---|---|
| Week 1 | ||
| Programme purpose and expectations |
Energy management:H: achieving balance H: activity cycling T: activity/rest diaries |
|
Ground rules:
|
||
Validating fatigue:
|
H: setting our course (groups’ ideas) | |
| Self-management strategies, struggles and difficulty of changing habits | ||
| Week 2 | ||
| What are your priorities for change that would increase QoL? | T: wheel of life (priority areas) | Goal-setting (two groups):
|
| What are your drainers and energisers? | ||
| Week 3 | ||
| Self-sabotage on the programme | H: best ways of self-sabotage |
Goal-setting review Successes/barriers New goals |
Sleep and rest:
|
H: getting a better night’s sleep T: sleep diary (if needed) |
|
| Week 4 | ||
Stress and relaxation:
|
H: effects of stress H: relaxation practice guide T: relaxation CD |
Goal-setting review Successes/barriers New goals |
| Week 5 | ||
| Assertiveness and communication: |
Goal-setting review Successes/barriers New goals |
|
|
M: cartoon examples | |
|
||
|
H: saying ‘no’ | |
| Week 6 | ||
Review self-help tools
|
M: fatigue pit – falling in/digging out |
Goal-setting review Successes/barriers New goals |
Dealing with setbacks – what could you do?
|
H: the pit H: coping with setbacks |
|
| Week 14 | ||
Review last 8 weeks:
|
M: islands – were on a desert island (passive) looking at the mainland (100% health, i.e. unrealistic). Now on adaptive coping island (realistic) | |
| New goals | ||
Appendix 3 Recruitment to the RAFT programme across centres
| Centre | Number of patients randomised |
|---|---|
| Bristol Royal Infirmary | 43 |
| University Hospital of Wales, Cardiff | 44 |
| St Peter’s Hospital, Chertsey | 53 |
| Southmead Hospital Bristol | 46 |
| Poole Hospital | 41 |
| Torbay Hospital | 58 |
| Weston General Hospital | 48 |
| Total | 333 |
Appendix 4 Data completion rates for all follow-up time points
| Clinical variable | Time point, n (%)a | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline (N = 333, 100%) | Week 6 (N = 314, 94%) | Week 10 (N = 312, 94%) | Week 18 (N = 311, 93%) | Week 26 (N = 308, 92%) | Week 52 (N = 305, 92%) | Week 78 (N = 302, 91%) | Week 104 (N = 300, 90%) | |
| Fatigue | ||||||||
| BRAF-NRS impact | 333 (100) | 312 (94) | 308 (92) | 305 (92) | 308 (92) | 305 (92) | 300 (90) | 296 (89) |
| BRAF-NRS severity | 333 (100) | 283 (85) | 268 (80) | 275 (83) | 294 (88) | 264 (79) | 249 (75) | 261 (78) |
| BRAF-NRS coping | 333 (100) | 283 (85) | 268 (80) | 274 (82) | 294 (88) | 264 (79) | 248 (75) | 261 (78) |
| BRAF-MDQ overall impact | 333 (100) | 282 (85) | 267 (80) | 274 (82) | 294 (88) | 260 (78) | 247 (74) | 261 (78) |
| BRAF-MDQ physical | 333 (100) | 283 (85) | 268 (80) | 275 (83) | 294 (88) | 264 (79) | 249 (75) | 261 (78) |
| BRAF-MDQ emotional | 333 (100) | 282 (85) | 267 (80) | 274 (82) | 294 (88) | 263 (79) | 247 (74) | 261 (78) |
| BRAF-MDQ cognitive | 333 (100) | 282 (85) | 267 (80) | 274 (82) | 294 (88) | 262 (79) | 248 (75) | 261 (78) |
| BRAF-MDQ living | 333 (100) | 282 (85) | 267 (80) | 274 (82) | 294 (88) | 261 (78) | 248 (75) | 261 (78) |
| Pain: NRS | 333 (100) | 283 (85) | – | – | 294 (88) | 264 (79) | 248 (75) | 261 (78) |
| Disability: MHAQ | 332 (100) | 282 (85) | – | – | 294 (88) | 264 (79) | 249 (75) | 261 (78) |
| Quality of life: AIMS VAS | 332 (99) | 283 (85) | – | – | 294 (88) | 264 (79) | 248 (75) | 261 (78) |
| Disease activity | ||||||||
| Assessed: DAS28 | 332 (100) | – | – | – | 293 (88) | – | – | – |
| Self-reported: sPDAS2 | 293 (88) | 281 (84) | – | – | 294 (88) | 263 (79) | 246 (74) | 259 (78) |
| Anxiety: HADS | 333 (100) | 282 (85) | – | – | 293 (88) | 264 (79) | 246 (74) | 260 (78) |
| Depression: HADS | 333 (100) | 282 (85) | – | – | 293 (88) | 264 (79) | 247 (74) | 260 (78) |
| Valued life activities: VLA | 332 (100) | 282 (85) | – | – | 294 (88) | 264 (79) | 248 (75) | 261 (78) |
| Helplessness: AHI | 333 (100) | 282 (85) | – | – | 294 (88) | 264 (79) | 245 (74) | 260 (78) |
| Self-efficacy: RASE scale | 333 (100) | 281 (84) | – | – | 293 (88) | 260 (78) | 245 (74) | 254 (76) |
| Sleep quality | 332 (99) | 276 (83) | – | – | 292 (88) | 258 (78) | 241 (72) | 253 (76) |
Appendix 5 Baseline demographic data of patients who did and did not complete to 26 weeks
| Demographic variable | Trial arm | Did not complete (N = 25) | |
|---|---|---|---|
| Control (N = 152) | RAFT (N = 156) | ||
| Female, n (%) | 121 (79.6) | 125 (80.1) | 20 (80) |
| Age (years), median (lower and upper quartile) | 61.8 (54.4, 69.6) | 63.7 (54.2, 69.9) | 69 (61.3, 72) |
| Disease duration (years), median (lower and upper quartile) | 10 (3, 20) | 10 (5, 19) | 10 (5, 11) |
| Comorbidity, n (%) | 119 (78.8) | 124 (80.0) | 20 (80.0) |
| Fatigue, mean (SD) | |||
| Severity (BRAF-NRS, 0–10)a | 6.85 (1.57) | 6.89 (1.57) | 6.64 (1.47) |
| Impact (BRAF-NRS, 0–10)a | 7.23 (1.6) | 7.10 (1.7) | 6.96 (1.54) |
| Other self-management programmes, n (%) | 21 (14.0) | 16 (10.3) | 1 (4.0) |
| Years since programme, median (lower and upper quartile) | 8 (5, 11) | 5 (3, 10) | 2 |
| Socioeconomic status, n (%) | |||
| England | |||
| Deprived | 28 (21.1) | 23 (17.2) | 6 (27.3) |
| Moderate | 60 (45.1) | 65 (48.5) | 10 (45.5) |
| Affluent | 45 (33.8) | 46 (34.3) | 6 (27.3) |
| Wales | |||
| Deprived | 7 (41.2) | 7 (35.0) | 2 (66.6) |
| Moderate | 3 (17.7) | 5 (25.0) | 1 (33.3) |
| Affluent | 7 (41.2) | 8 (45.0) | 0 |
| Ethnicity, n (%) | |||
| White | 147 (98.0) | 151 (96.8) | 24 (96.0) |
| Asian/Asian British | 3 (2.0) | 5 (3.2) | 1 (4.0) |
Appendix 6 Baseline clinical data of patients who did not complete to 26 weeks
| Clinical variable | Mean score (SD) for those participants who did not completea (n = 25) |
|---|---|
| Fatigue | |
| BRAF-NRS impact (0–10) | 6.96 (1.5) |
| BRAF-NRS severity (0–10) | 6.64 (1.5) |
| BRAF-NRS coping (0–10)b | 4.88 (2.0) |
| BRAF-MDQ overall impact (0–70) | 41.80 (11.8) |
| BRAF-MDQ physical (0–22) | 15.52 (2.7) |
| BRAF-MDQ emotional (0–12) | 7.28 (3.1) |
| BRAF-MDQ cognitive (0–15) | 8.64 (3.2) |
| BRAF-MDQ living (0–21) | 10.36 (5.4) |
| Pain: NRS (0–10) | 6.08 (2.3) |
| Disability: MHAQ (0–3) | 0.87 (0.6) |
| Quality of life: AIMS VAS (0–100) | 52.40 (22.4) |
| Disease activity | |
| Assessed: DAS28 (0.96+) | 4.25 (1.4) |
| Self-reported: sPDAS2 (2.4–7.9) | 4.57 (1.0) |
| Anxiety: HADS (0–21) | 8.88 (3.8) |
| Depression: HADS (0–21) | 7.00 (3.9) |
| Valued life activities: VLA (0–3) | 1.17 (0.7) |
| Helplessness: AHI (5–30) | 17.86 (5.7) |
| Self-efficacy: RASE scale (28–140)b | 101.19 (11.9) |
| Sleep qualityc | |
| Very good | 0 (0%) |
| Fairly good | 11 (44%) |
| Fairly bad | 7 (28%) |
| Very bad | 7 (28%) |
Appendix 7 Treatment effect on BRAF-NRS impact score at 26, 52, 78 and 104 weeks
| Time pointa | BRAF-NRS impact score, adjusted mean differenceb,c | 95% CI | p-value |
|---|---|---|---|
| 26 weeks (n = 308) | –0.58 | –1.07 to –0.09 | 0.02 |
| 52 weeks (n = 305) | –0.62 | –1.12 to –0.13 | 0.01 |
| 78 weeks (n = 300) | –0.22 | –0.71 to 0.28 | 0.39 |
| 104 weeks (n = 296) | –0.52 | –1.02 to –0.02 | 0.04 |
Appendix 8 Change in secondary outcomes at 26 weeks
| Clinical outcome | Trial arm | |||
|---|---|---|---|---|
| Control | RAFT | |||
| n (%)a | Mean change in score (SD) | n (%)a | Mean change in score (SD) | |
| Fatigue | ||||
| BRAF-NRS severity (0–10) | 142 (89.9) | –0.72 (2.27) | 152 (86.9) | –0.97 (2.53) |
| BRAF-NRS coping (0–10)b | 142 (89.9) | 0.48 (3.07) | 152 (86.9) | 0.09 (2.82) |
| BRAF-MDQ overall impact (0–70) | 142 (89.9) | –5.64 (12.75) | 152 (86.9) | –8.91 (14.55) |
| BRAF-MDQ physical (0–22) | 142 (89.9) | –1.79 (4.77) | 152 (86.9) | –2.40 (5.13) |
| BRAF-MDQ emotional (0–12) | 142 (89.9) | –1.35 (3.14) | 152 (86.9) | –2.18 (3.18) |
| BRAF-MDQ cognitive (0–15) | 142 (89.9) | –1.03 (3.88) | 152 (86.9) | –1.65 (3.78) |
| BRAF-MDQ living (0–21) | 142 (89.9) | –1.47 (4.20) | 152 (86.9) | –2.68 (5.09) |
| Pain: NRS (0–10) | 142 (89.9) | –0.33 (2.44) | 152 (86.9) | –0.22 (2.32) |
| Disability: MHAQ (0–3) | 142 (89.9) | –0.06 (0.34) | 151 (86.3) | –0.04 (0.39) |
| Quality of life: AIMS VAS (0–100) | 141 (89.2) | –2.19 (25.37) | 152 (86.9) | –1.93 (25.63) |
| Disease activity | ||||
| Assessed: DAS28 (0.96+) | 145 (91.8) | –0.13 (0.93) | 147 (84.0) | –0.09 (1.18) |
| Self-reported: sPDAS2 (2.4–7.9) | 142 (89.9) | –0.03 (0.95) | 151 (86.3) | –0.01 (1.09) |
| Anxiety: HADS (0–21) | 142 (89.9) | –0.45 (2.76) | 151 (86.3) | –0.64 (2.77) |
| Depression: HADS (0–21) | 142 (89.9) | –0.37 (2.98) | 151 (86.3) | –0.96 (2.88) |
| Valued life activities: VLA (0–3) | 142 (89.9) | –0.01 (0.40) | 151 (86.3) | –0.07 (0.48) |
| Helplessness: AHI (5–30) | 142 (89.9) | –1.51 (4.67) | 152 (86.9) | –2.11 (5.22) |
| Self-efficacy: RASE scale (28–140)b | 142 (89.9) | 0.29 (10.71) | 151 (86.3) | 3.77 (12.54) |
| Sleep quality | 142 (89.9) | 149 (85.1) | ||
| Categories improved: –3c | 0 (0%) | 2 (1.3%) | ||
| Categories improved: –2c | 6 (4.2%) | 9 (6.0%) | ||
| Categories improved: 1c | 37 (26.1%) | 45 (30.2%) | ||
| No change: 0c | 77 (54.2%) | 75 (50.3%) | ||
| Categories worsened: 1c | 21 (14.8%) | 18 (12.1%) | ||
| Categories worsened: 2c | 1 (0.7%) | 0 (0%) | ||
| Categories worsened: 3c | 0 (0%) | 0 (0%) | ||
Appendix 9 Secondary clinical outcomes at the 26-, 52-, 78- and 104-week follow-up
| Clinical outcome | Time point | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 26 weeks | 52 weeks | 78 weeks | 104 weeks | |||||||||||||
| Control | RAFT | Control | RAFT | Control | RAFT | Control | RAFT | |||||||||
| na (%) | Mean (SD) | na (%) | Mean (SD) | na (%) | Mean (SD) | na (%) | Mean (SD) | na (%) | Mean (SD) | na (%) | Mean (SD) | na (%) | Mean (SD) | na (%) | Mean (SD) | |
| Fatigue | ||||||||||||||||
| BRAF-NRS severity (0–10) | 142 (89.9) | 6.13 (2.30) | 152 (86.9) | 5.91 (2.22) | 127 (80.4) | 6.05 (2.18) | 137 (78.3) | 5.80 (2.19) | 120 (75.9) | 6.05 (2.24) | 129 (73.7) | 5.91 (2.19) | 124 (78.5) | 5.72 (2.12) | 137 (78.3) | 5.85 (2.25) |
| BRAF NRS coping (0–10)b | 142 (89.9) | 5.32 (2.42) | 152 (86.9) | 5.25 (2.33) | 127 (80.4) | 5.02 (2.40) | 137 (78.3) | 5.83 (2.10) | 119 (75.3) | 5.10 (2.55) | 129 (73.7) | 5.57 (2.32) | 124 (78.5) | 5.28 (2.33) | 137 (78.3) | 6.03 (2.16) |
| BRAF-MDQ overall impact (0–70) | 142 (89.9) | 34.74 (16.41) | 152 (86.9) | 31.51 (16.02) | 125 (79.1) | 34.67 (15.54) | 135 (77.1) | 31.04 (15.59) | 118 (74.7) | 34.61 (16.04) | 129 (73.7) | 32.45 (16.08) | 124 (78.5) | 33.31 (14.94) | 137 (78.3) | 31.60 (16.41) |
| BRAF-MDQ physical (0–22) | 142 (89.9) | 14.40 (5.23) | 152 (86.9) | 13.72 (4.91) | 127 (80.4) | 14.36 (4.81) | 137 (78.3) | 13.39 (5.01) | 120 (75.9) | 14.41 (4.94) | 129 (73.7) | 13.92 (4.77) | 124 (78.5) | 14.06 (4.79) | 137 (78.3) | 13.56 (5.01) |
| BRAF-MDQ emotional (0–12) | 142 (89.9) | 5.36 (3.79) | 152 (86.9) | 4.37 (3.51) | 126 (79.7) | 5.18 (3.37) | 137 (78.3) | 4.20 (3.45) | 118 (74.7) | 5.31 (3.62) | 129 (73.7) | 4.40 (3.47) | 124 (78.5) | 5.07 (3.54) | 137 (78.3) | 4.20 (3.48) |
| BRAF-MDQ cognitive (0–15) | 142 (89.9) | 6.55 (4.16) | 152 (86.9) | 5.89 (4.35) | 125 (79.1) | 6.86 (4.15) | 137 (78.3) | 6.09 (4.27) | 119 (75.3) | 6.31 (4.04) | 129 (73.7) | 5.98 (4.20) | 124 (78.5) | 6.19 (4.00) | 137 (78.3) | 5.82 (4.01) |
| BRAF-MDQ living (0–21) | 142 (89.9) | 8.43 (5.68) | 152 (86.9) | 7.53 (5.43) | 126 (79.7) | 8.38 (5.21) | 135 (77.1) | 7.47 (5.46) | 119 (75.3) | 8.52 (5.50) | 129 (73.7) | 8.14 (5.76) | 124 (78.5) | 7.98 (5.03) | 137 (78.3) | 7.81 (6.00) |
| Pain: NRS (0–10) | 142 (89.9) | 5.24 (2.41) | 152 (86.9) | 5.47 (2.22) | 127 (80.4) | 5.21 (2.33) | 137 (78.3) | 5.34 (2.38) | 119 (75.3) | 5.23 (2.23) | 129 (73.7) | 5.28 (2.42) | 124 (78.5) | 5.37 (2.27) | 137 (78.3) | 5.32 (2.35) |
| Disability: MHAQ (0–3) | 142 (89.9) | 0.70 (0.51) | 152 (86.9) | 0.71 (0.54) | 127 (80.4) | 0.74 (0.52) | 137 (78.3) | 0.74 (0.60) | 119 (75.3) | 0.76 (0.55) | 130 (74.3) | 0.78 (0.63) | 124 (78.5) | 0.78 (0.53) | 137 (78.3) | 0.77 (0.62) |
| Quality of life: AIMS VAS (0–100) | 142 (89.9) | 47.70 (22.96) | 152 (86.9) | 47.22 (23.46) | 127 (80.4) | 45.54 (22.21) | 137 (78.3) | 46.61 (24.01) | 119 (75.3) | 46.60 (23.99) | 129 (73.7) | 48.43 (23.40) | 124 (78.5) | 47.77 (22.32) | 137 (78.3) | 44.10 (24.68) |
| Disease activity: sPDAS2 (2.4 to 7.9) | 142 (89.9) | 4.33 (1.04) | 152 (86.9) | 4.44 (1.13) | 127 (80.4) | 4.50 (1.09) | 136 (77.7) | 4.60 (1.15) | 117 (74.1) | 4.48 (1.12) | 129 (73.7) | 4.66 (1.11) | 123 (77.8) | 4.67 (1.09) | 136 (77.7) | 4.57 (1.21) |
| Anxiety: HADS (0–21) | 142 (89.9) | 7.56 (4.48) | 151 (86.3) | 6.65 (4.36) | 127 (80.4) | 7.57 (4.58) | 137 (78.3) | 6.69 (4.50) | 116 (73.4) | 7.56 (4.64) | 130 (74.3) | 6.76 (4.57) | 123 (77.8) | 7.36 (4.26) | 137 (78.3) | 6.34 (4.64) |
| Depression: HADS (0–21) | 142 (89.9) | 6.42 (4.06) | 151 (86.3) | 6.22 (3.76) | 127 (80.4) | 6.44 (3.91) | 137 (78.3) | 6.28 (3.99) | 117 (74.1) | 6.84 (3.94) | 130 (74.3) | 6.76 (4.57) | 123 (77.8) | 7.36 (4.26) | 137 (78.3) | 6.34 (4.64) |
| Valued life activities: VLA (0–3) | 142 (89.9) | 1.07 (0.62) | 152 (86.9) | 1.08 (0.67) | 127 (80.4) | 1.00 (0.61) | 137 (78.3) | 1.09 (0.70) | 118 (74.7) | 1.08 (0.65) | 130 (74.3) | 1.08 (0.67) | 124 (78.5) | 1.08 (0.66) | 137 (78.3) | 1.09 (0.71) |
| Helplessness: AHI (5–30) | 142 (89.9) | 17.47 (5.46) | 152 (86.9) | 16.92 (5.06) | 127 (80.4) | 17.41 (5.38) | 137 (78.3) | 17.40 (5.60) | 116 (73.4) | 17.41 (5.43) | 129 (73.7) | 18.13 (5.62) | 123 (77.8) | 17.68 (5.22) | 137 (78.3) | 17.33 (5.12) |
| Self-efficacy: RASE scale (28–140)b | 142 (89.9) | 104.67 (13.31) | 151 (86.3) | 106.26 (14.78) | 125 (79.1) | 104.94 (12.51) | 135 (77.1) | 105.08 (13.39) | 117 (74.1) | 105.62 (12.99) | 128 (73.1) | 103.89 (12.55) | 121 (76.6) | 104.69 (12.77) | 133 (76.0) | 105.40 (15.41) |
| Sleep qualityc | ||||||||||||||||
| Very good | 9 (6.3) | 17 (11.3) | 10 (8.1) | 10 (7.5) | 7 (6.1) | 15 (11.9) | 7 (5.8) | 13 (9.9) | ||||||||
| Fairly good | 65 (45.8) | 65 (43.3) | 52 (41.9) | 61 (45.5) | 55 (47.8) | 52 (41.3) | 51 (42.2) | 57 (43.2) | ||||||||
| Fairly bad | 51 (35.9) | 51 (34.0) | 45 (36.3) | 45 (33.6) | 40 (34.8) | 33 (26.2) | 46 (38.0) | 46 (34.9) | ||||||||
| Very bad | 17 (12.0) | 17 (11.3) | 17 (13.7) | 18 (13.4) | 13 (11.3) | 26 (20.6) | 17 (14.1) | 16 (12.1) | ||||||||
Appendix 10 Patients making major medication changes during the trial
| Time pointa | Trial arm | p-value (from chi-squared test) | |||
|---|---|---|---|---|---|
| Control | RAFT | ||||
| N | n (%)b | N | n (%)b | ||
| Weeks 0–26 | 152 | 37 (24.3) | 156 | 32 (20.5) | 0.42 |
| Weeks 26–52 | 151 | 27 (17.9) | 154 | 32 (20.8) | 0.52 |
| Weeks 52–78 | 148 | 28 (18.9) | 154 | 31 (20.1) | 0.79 |
| Weeks 78–104 | 147 | 21 (14.3) | 153 | 22 (14.4) | 0.90 |
Appendix 11 Complier-average causal effect analysis
Reproduced from Hewlett et al. 65 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The CACE analysis used instrumental variable regression to estimate the efficacy of the RAFT programme in reducing RA-related fatigue impact compared with usual care alone. One of the assumptions of CACE analysis is exclusion restriction, that is, the offer of the intervention does not affect the outcome. In the current study, those individuals randomised to the RAFT programme but who could not make the programme dates and did not attend had no follow-up data collected. Therefore, outcome data were not available for a group of individuals who would be considered non-compliant and contribute information to the CACE analysis, and it also violates the exclusion restriction assumption. If individuals in the RAFT programme arm were only considered participants if they attended the first CBT session (which could then impact their outcome), then the offer of the intervention does affect outcome.
In an attempt to address this issue, the two stages of the 2SLS CACE estimation were conducted separately to allow for loss to follow-up, which is dependent on adherence. This first-stage regression uses all individuals randomised to predict adherence. Second-stage regression involves only those individuals with available outcomes, but models these using the predicted values of adherence obtained from the ‘complete’ first stage.
The results of the CACE analyses are shown in Table 30, along with the primary analysis results for comparison. The CACE analyses showed that there was a larger effect of the RAFT programme in those individuals who adhered to the intervention (defined as attending at least two CBT sessions), compared with the standard primary analysis effectiveness estimate of the ‘offer’ of the intervention (see Table 30).
| Analysis | Coefficient (95% CI) | p-value |
|---|---|---|
| Primary | –0.59 (–1.11 to –0.06) | 0.03 |
| CACE | –0.69 (–1.30 to –0.07) | 0.03 |
It should be noted that in the current study, due to the exclusion of individuals who did not attend the first CBT session, there is no one correct ideal approach; therefore, the results of the CACE analysis should be interpreted as part of a general sensitivity analysis and as exploratory in nature.
Appendix 12 Clinical outcomes at 6 weeks
| Clinical outcome | Trial arm | |||
|---|---|---|---|---|
| Control | RAFT | |||
| n (%)a | Mean (SD) | n (%)a | Mean (SD) | |
| Fatigue | ||||
| BRAF-NRS impact (0–10) | 156 (98.7) | 6.62 (2.03) | 156 (89.1) | 5.94 (1.95) |
| BRAF-NRS severity (0–10) | 139 (88.0) | 6.45 (1.91) | 144 (82.3) | 6.17 (1.76) |
| BRAF-NRS coping (0–10)b | 139 (88.0) | 4.81 (2.26) | 144 (82.3) | 6.05 (1.90) |
| BRAF-MDQ overall impact (0–70) | 139 (88.0) | 37.89 (13.63) | 143 (81.7) | 33.30 (13.34) |
| BRAF-MDQ physical (0–22) | 139 (88.0) | 15.29 (3.89) | 144 (82.3) | 13.83 (4.02) |
| BRAF-MDQ emotional (0–12) | 139 (88.0) | 6.23 (3.33) | 143 (81.7) | 5.07 (3.13) |
| BRAF-MDQ cognitive (0–15) | 139 (88.0) | 7.22 (3.83) | 143 (81.7) | 6.32 (3.85) |
| BRAF-MDQ living (0–21) | 139 (88.0) | 9.14 (5.16) | 143 (81.7) | 8.13 (5.37) |
| Pain: NRS (0–10) | 139 (88.0) | 5.63 (2.18) | 144 (82.3) | 5.69 (2.07) |
| Disability: MHAQ (0–3) | 139 (88.0) | 0.73 (0.52) | 142 (81.1) | 0.75 (0.59) |
| Quality of life: AIMS VAS (0–100) | 138 (87.3) | 50.64 (21.02) | 144 (82.3) | 47.63 (21.50) |
| Disease activity: sPDAS2 (2.4–7.9) | 139 (88.0) | 4.55 (1.06) | 141 (80.6) | 4.67 (1.07) |
| Anxiety: HADS (0–21) | 139 (88.0) | 8.21 (4.37) | 143 (81.7) | 7.54 (4.28) |
| Depression: HADS (0–21) | 139 (88.0) | 6.89 (3.84) | 143 (81.7) | 6.94 (3.69) |
| Valued life activities: VLA (0–3) | 139 (88.0) | 1.12 (0.58) | 142 (81.1) | 1.19 (0.61) |
| Helplessness: AHI (5–30) | 139 (88.0) | 18.70 (4.79) | 143 (81.7) | 18.20 (4.58) |
| Self-efficacy: RASE scale (28–140)b | 138 (87.3) | 102.97 (12.74) | 143 (81.7) | 105.00 (11.86) |
| Sleep quality | 136 (86.1) | 139 (79.4) | ||
| Very goodc | 7 (5.1%) | 18 (12.9%) | ||
| Fairly goodc | 53 (39.0%) | 53 (38.1%) | ||
| Fairly badc | 55 (40.4%) | 45 (32.4%) | ||
| Very badc | 21 (15.4%) | 23 (16.6%) | ||
Appendix 13 Change in clinical outcomes from 0 to 6 weeks
| Clinical outcome | Trial arm | |||
|---|---|---|---|---|
| Control | RAFT | |||
| n (%)a | Mean change (SD) | n (%)a | Mean change (SD) | |
| Fatigue | ||||
| BRAF-NRS impact (0–10) | 156 (98.7) | –0.61 (1.99) | 156 (89.1) | –1.17 (2.24) |
| BRAF-NRS severity (0–10) | 139 (88.0) | –0.35 (1.89) | 144 (82.3) | –0.78 (2.08) |
| BRAF-NRS coping (0–10)b | 139 (88.0) | –0.09 (2.59) | 144 (82.3) | 0.92 (2.64) |
| BRAF-MDQ overall impact (0–70) | 139 (88.0) | –2.75 (10.25) | 143 (81.7) | –7.17 (11.84) |
| BRAF-MDQ physical (0–22) | 139 (88.0) | –0.87 (3.44) | 144 (82.3) | –2.35 (4.35) |
| BRAF-MDQ emotional (0–12) | 139 (88.0) | –0.62 (2.77) | 143 (81.7) | –1.51 (3.01) |
| BRAF-MDQ cognitive (0–15) | 139 (88.0) | –0.43 (3.31) | 143 (81.7) | –1.10 (3.24) |
| BRAF-MDQ living (0–21) | 139 (88.0) | –0.84 (4.09) | 143 (81.7) | –2.15 (4.59) |
| Pain: NRS (0–10) | 139 (88.0) | 0.04 (2.17) | 144 (82.3) | –0.03 (2.05) |
| Disability: MHAQ (0–3) | 139 (88.0) | –0.03 (0.30) | 142 (81.1) | 0.00 (0.36) |
| Quality of life: AIMS VAS (0–100) | 138 (87.3) | 0.83 (21.74) | 144 (82.3) | –1.64 (24.43) |
| Disease activity: sPDAS2 (2.4–7.9) | 139 (88.0) | 0.19 (0.88) | 141 (80.6) | 0.21 (0.95) |
| Anxiety: HADS (0–21) | 139 (88.0) | 0.19 (3.03) | 143 (81.7) | 0.11 (2.60) |
| Depression: HADS (0–21) | 139 (88.0) | 0.11 (2.34) | 143 (81.7) | –0.30 (2.61) |
| Valued life activities: VLA (0–3) | 139 (88.0) | 0.04 (0.34) | 142 (81.1) | 0.02 (0.36) |
| Helplessness: AHI (5–30) | 139 (88.0) | –0.25 (3.87) | 143 (81.7) | –0.97 (4.24) |
| Self-efficacy: RASE scale (28–140)b | 138 (87.3) | –1.43 (9.08) | 143 (81.7) | 2.97 (11.45) |
| Sleep quality | 136 (86.1) | 139 (79.5) | ||
| Categories improved: –3c | 0 (0%) | 1 (0.7%) | ||
| Categories improved: –2c | 1 (0.7%) | 7 (5.0%) | ||
| Categories improved: 1c | 23 (16.9%) | 41 (29.5%) | ||
| No change: 0c | 94 (69.1%) | 74 (53.2%) | ||
| Categories worsened: 1c | 17 (12.5%) | 16 (11.5%) | ||
| Categories worsened: 2c | 1 (0.7%) | 0 (0%) | ||
| Categories worsened: 3c | 0 (0%) | 0 (0%) | ||
Appendix 14 Fatigue outcomes at 10 weeks
| Fatigue outcomea | Trial arm | |||
|---|---|---|---|---|
| Control | RAFT | |||
| n (%)b | Mean (SD) | n (%)b | Mean (SD) | |
| BRAF-NRS impact (0–10) | 153 (96.8) | 6.59 (2.03) | 155 (88.6) | 6.05 (2.15) |
| BRAF-NRS severity (0–10) | 131 (82.9) | 5.93 (2.02) | 137 (78.3) | 5.93 (2.08) |
| BRAF-NRS coping (0–10)c | 131 (82.9) | 5.47 (2.15) | 137 (78.3) | 5.96 (2.07) |
| BRAF-MDQ overall impact (0–70) | 130 (82.3) | 34.20 (14.50) | 137 (78.3) | 31.91 (14.21) |
| BRAF-MDQ physical (0–22) | 131 (82.9) | 14.27 (4.32) | 137 (78.3) | 13.59 (4.44) |
| BRAF-MDQ emotional (0–12) | 130 (82.3) | 5.35 (3.26) | 137 (78.3) | 4.53 (3.32) |
| BRAF-MDQ cognitive (0–15) | 130 (82.3) | 6.48 (3.83) | 137 (78.3) | 6.01 (4.11) |
| BRAF-MDQ living (0–21) | 130 (82.3) | 8.09 (5.50) | 137 (78.3) | 7.77 (5.20) |
Appendix 15 Change in fatigue outcomes from 0 to 10 weeks
| Fatigue outcomea | Trial arm | |||
|---|---|---|---|---|
| Control | RAFT | |||
| n (%)b | Mean change (SD) | n (%)b | Mean change (SD) | |
| BRAF-NRS impact (0–10) | 153 (96.8) | –0.66 (2.03) | 155 (88.6) | –1.06 (2.63) |
| BRAF-NRS severity (0–10) | 131 (82.9) | –0.86 (2.09) | 137 (78.3) | –0.96 (2.53) |
| BRAF-NRS coping (0–10)c | 131 (82.9) | 0.61 (2.79) | 137 (78.3) | 0.84 (2.97) |
| BRAF-MDQ overall impact (0–70) | 130 (82.3) | –6.22 (10.83) | 137 (78.3) | –8.47 (13.94) |
| BRAF-MDQ physical (0–22) | 131 (82.9) | –1.89 (3.98) | 137 (78.3) | –2.47 (5.12) |
| BRAF-MDQ emotional (0–12) | 130 (82.3) | –1.33 (2.87) | 137 (78.3) | –1.98 (3.51) |
| BRAF-MDQ cognitive (0–15) | 130 (82.3) | –1.17 (3.24) | 137 (78.3) | –1.47 (3.50) |
| BRAF-MDQ living (0–21) | 130 (82.3) | –1.81 (4.04) | 137 (78.3) | –2.56 (4.95) |
Appendix 16 Fatigue outcomes at 18 weeks
| Fatigue outcomea | Trial arm | |||
|---|---|---|---|---|
| Control | RAFT | |||
| n (%)b | Mean (SD) | n (%)b | Mean (SD) | |
| BRAF-NRS impact (0–10) | 151 (95.6) | 6.42 (2.22) | 154 (88.0) | 5.77 (2.08) |
| BRAF-NRS severity (0–10) | 137 (86.7) | 6.13 (2.17) | 138 (78.9) | 5.86 (2.10) |
| BRAF-NRS coping (0–10)c | 136 (86.1) | 5.22 (2.35) | 138 (78.9) | 5.95 (2.20) |
| BRAF-MDQ overall impact (0–70) | 137 (86.7) | 34.84 (16.11) | 137 (78.3) | 32.35 (15.15) |
| BRAF-MDQ physical (0–22) | 137 (86.7) | 14.19 (4.94) | 138 (78.9) | 13.34 (4.62) |
| BRAF-MDQ emotional (0–12) | 137 (86.7) | 5.54 (3.51) | 137 (78.3) | 4.73 (3.42) |
| BRAF-MDQ cognitive (0–15) | 137 (86.7) | 6.73 (3.93) | 137 (78.3) | 5.96 (4.06) |
| BRAF-MDQ living (0–21) | 137 (86.7) | 8.38 (5.60) | 137 (78.3) | 8.28 (5.57) |
Appendix 17 Change in fatigue outcomes from 0 to 18 weeks
| Fatigue outcomea | Trial arm | |||
|---|---|---|---|---|
| Controla | RAFTa | |||
| n (%)b | Mean change (SD) | n (%)b | Mean change (SD) | |
| BRAF-NRS impact (0–10) | 151 (95.6) | –0.80 (2.27) | 154 (88.0) | –1.35 (2.51) |
| BRAF-NRS severity (0–10) | 137 (86.7) | –0.72 (2.24) | 138 (78.9) | –1.13 (2.50) |
| BRAF-NRS coping (0–10)c | 136 (86.1) | 0.44 (3.13) | 138 (78.9) | 0.86 (2.91) |
| BRAF-MDQ overall impact (0–70) | 137 (86.7) | –5.53 (13.15) | 137 (78.3) | –8.41 (14.94) |
| BRAF-MDQ physical (0–22) | 137 (86.7) | –1.96 (4.43) | 138 (78.9) | –2.91 (5.14) |
| BRAF-MDQ emotional (0–12) | 137 (86.7) | –1.14 (2.98) | 137 (78.3) | –1.91 (3.55) |
| BRAF-MDQ cognitive (0–15) | 137 (86.7) | –0.93 (4.03) | 137 (78.3) | –1.49 (3.77) |
| BRAF-MDQ living (0–21) | 137 (86.7) | –1.50 (4.79) | 137 (78.3) | –2.09 (5.47) |
Appendix 18 Rheumatoid Arthritis Self-Efficacy Scale: individual item mean scores (0 and 26 weeks)
| RASE scale itema | Trial arm, mean score | |||
|---|---|---|---|---|
| Control | RAFT | |||
| Week 0 | Week 26 | Week 0 | Week 26 | |
| Use relaxation techniques to help with pain | 3.70 | 3.64 | 3.61 | 3.72 |
| Think about something else to help with pain | 3.37 | 3.46 | 3.33 | 3.45 |
| Use my joints carefully to help with pain | 3.58 | 3.81 | 3.60 | 3.76 |
| Think positively to help with pain | 3.59 | 3.66 | 3.47 | 3.71 |
| Avoid doing things that cause pain | 3.54 | 3.79 | 3.65 | 3.61 |
| Wind down, relax before bed, to improve sleep | 3.51 | 3.65 | 3.50 | 3.68 |
| Hot drink before bed to improve sleep | 3.20 | 3.39 | 3.17 | 3.39 |
| Use relaxation before bed to improve sleep | 3.61 | 3.57 | 3.50 | 3.66 |
| Pace myself, take RA into account to deal with tiredness | 3.78 | 3.76 | 3.73 | 4.09 |
| Accept fatigue as part of my arthritis | 3.58 | 3.70 | 3.53 | 3.93 |
| Use gadgets to help with mobility, tasks, personal care | 3.90 | 3.94 | 3.83 | 4.01 |
| Ask for help to deal with difficulties of doing everyday things | 3.87 | 3.85 | 3.64 | 3.88 |
| Do exercises to deal with difficulties of doing everyday tasks | 3.56 | 3.63 | 3.56 | 3.66 |
| Plan/prioritise to deal with difficulties of doing everyday tasks | 3.78 | 3.76 | 3.74 | 3.90 |
| Educate family/friends about my RA to help with relationships | 3.71 | 3.75 | 3.63 | 3.76 |
| Explain to friends and family when I do or do not need help | 3.80 | 3.78 | 3.78 | 3.82 |
| Discuss any problems with my partner or family | 4.02 | 3.99 | 3.87 | 3.97 |
| Make time for leisure activities, hobbies or socialising | 3.65 | 3.73 | 3.78 | 3.84 |
| Save energy for leisure activities, hobbies or socialising | 3.35 | 3.49 | 3.34 | 3.51 |
| Focus on the positive when I am feeling down | 3.72 | 3.82 | 3.69 | 3.86 |
| Use relaxation to deal with worries | 3.47 | 3.60 | 3.54 | 3.54 |
| Allocate time for relaxation | 3.72 | 3.70 | 3.78 | 3.81 |
| Use relaxation tape or instructions to help me relax | 3.54 | 3.37 | 3.41 | 3.56 |
| Use regular exercise | 3.63 | 3.72 | 3.63 | 3.79 |
| Be aware of my limits in exercise | 3.97 | 3.98 | 3.99 | 4.05 |
| Manage medication, knowing how and when to take it | 4.24 | 4.25 | 4.18 | 4.23 |
| Look out for and avoid side effects of medication | 3.92 | 3.88 | 4.02 | 4.01 |
| Seek help with persistent side effects | 4.03 | 4.02 | 4.04 | 4.04 |
Appendix 19 Social contact with other people for support with fatigue or arthritis
| Response | Time point, n (%)a | |||
|---|---|---|---|---|
| 52 weeks | 104 weeks | |||
| Control | RAFT | Control | RAFT | |
| Data returned | 113 (71.5) | 125 (71.4) | 104 (65.8) | 118 (67.4) |
| Made contact in past year | 21 (13.3) | 12 (6.9) | 21 (13.3) | 16 (9.1) |
| Face-to-face meetings | 10 (6.3) | 7 (4.0) | 13 (8.2) | 9 (5.1) |
| Still in touch | 15 (9.5) | 8 (4.6) | 16 (10.1) | 10 (5.7) |
| Made contact with RAFT programme group | 35 (20.0) | 16 (9.1) | ||
| Face-to-face with RAFT programme group | 18 (10.3) | 11 (6.3) | ||
| Still in touch with RAFT programme group | 22 (12.6) | 10 (5.7) | ||
Appendix 20 Baseline work productivity
| In the past 7 daysa | Trial arm, mean (SE) | p-value | |
|---|---|---|---|
| Control (n = 158) | RAFT (n = 175) | ||
| Employed at baselineb | 37 (23.42%) | 39 (22.29%) | 0.81c |
| Hours lost due to arthritis fatigued | 1.97 (0.46) | 2.82 (1.19) | 0.52e |
| Hours actually workedd | 24.57 (2.51) | 25.56 (2.57) | 0.78e |
| Perceived effect on work productivity while at workd,f | 4.19 (0.40) | 3.85 (0.40) | 0.55e |
Appendix 21 Correlations between change in individual dimensions of the EuroQol-5 Dimensions and change in BRAF-NRS impact
| EQ-5D-5L domain | BRAF-NRS impact, correlation (95% CI)a | |
|---|---|---|
| 26 weeks | 104 weeks | |
| Mobility | 0.25 (0.14 to 0.36) | 0.29 (0.18 to 0.40) |
| Self-care | 0.21 (0.10 to 0.32) | 0.22 (0.10 to 0.34) |
| Usual activities | 0.25 (0.14 to 0.36) | 0.41 (0.31 to 0.51) |
| Pain | 0.29 (0.18 to 0.39) | 0.37 (0.26 to 0.47) |
| Anxiety/depression | 0.36 (0.26 to 0.46) | 0.24 (0.12 to 0.35) |
Appendix 22 Complete-case health economics sensitivity analysis
| Costs and outcomes | Trial arm | Difference (95% CI) | p-value | |||
|---|---|---|---|---|---|---|
| Control (n = 134) | RAFT (n = 140) | |||||
| Mean | SE | Mean | SE | |||
| Unadjusted costs from the societal perspective (£) | 3343 | 355 | 3817 | 333 | ||
| Adjusted costs from the societal perspective (£)a | 3379 | 336 | 3784 | 328 | 405 (–517 to 1327) | 0.39 |
| Unadjusted QALYs over 26 weeks of follow-up | 0.276 | 0.009 | 0.275 | 0.009 | ||
| Adjusted QALYs over 26 weeks of follow-upb | 0.273 | 0.006 | 0.277 | 0.006 | 0.004 (–0.012 to 0.020) | 0.63 |
| ICER | 101,561 | |||||
| Net monetary benefit at £20,000 (£) | –325 (–1367 to 716) | |||||
| Net monetary benefit at £30,000 (£) | –285 (–1416 to 846) | |||||
| Probability that the RAFT programme is cost-effective at £20,000 per QALY | 0.27 | |||||
| Probability that the RAFT programme is cost-effective at £30,000 per QALY | 0.31 | |||||
FIGURE 6.
Cost-effectiveness acceptability curve: variation in probability of RAFT programme cost-effectiveness at a range of societal WTP thresholds – complete-case analysis.

Appendix 23 Cost-effectiveness and BRAF-NRS impact outcome
FIGURE 7.
Cost-effectiveness acceptability curve: variation in probability of RAFT programme cost-effectiveness at a range of societal WTP thresholds for BRAF-NRS impact. Secondary analysis: NHS/PSS perspective BRAF-NRS outcome.

Glossary
- Cohort
- 10–14 patients recruited in a centre; the level at which randomisation then occurred.
- Reducing Arthritis Fatigue by clinical Teams using cognitive–behavioural approaches (RAFT)
- A fatigue self-management programme comprising seven sessions.
- Reducing Arthritis Fatigue by clinical Teams using cognitive–behavioural approaches (RAFT) group
- A group of 5–7 patients attending the same RAFT programme together.
- Self-efficacy
- The belief or confidence that one can successfully execute an action or master a situation; a strong predictor of initiating behaviour change and persistence in the face of difficulty.
- Session
- The seven sessions constituting the RAFT programme. Each session covers specific topics.
List of abbreviations
- 2SLS
- two-stage least squares
- AHI
- Arthritis Helplessness Index
- AIMS
- Arthritis Impact Measurement Scale
- bDMARD
- biologic disease-modifying antirheumatic drug
- BRAF-MDQ
- Bristol Rheumatoid Arthritis Fatigue Multidimensional Questionnaire
- BRAF-NRS
- Bristol Rheumatoid Arthritis Fatigue Numerical Rating Scale
- BRTC
- Bristol Randomised Trials Collaboration
- CACE
- complier-average causal effect
- CB
- cognitive–behavioural
- CBT
- cognitive–behavioural therapy
- CFS
- chronic fatigue syndrome
- CI
- confidence interval
- DAS28
- Disease Activity Score
- DMARD
- disease-modifying antirheumatic drug
- DMEC
- Data Management and Ethics Committee
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- INMB
- incremental net monetary benefit
- ITT
- intention to treat
- MCID
- minimal clinically important difference
- MHAQ
- modified Health Assessment Questionnaire
- NICE
- National Institute for Health and Care Excellence
- NRS
- Numerical Rating Scale
- OT
- occupational therapist
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- RA
- rheumatoid arthritis
- RAFT
- Reducing Arthritis Fatigue by clinical Teams using cognitive–behavioural approaches
- RASE
- Rheumatoid Arthritis Self-Efficacy scale
- RCT
- randomised controlled trial
- RNS
- rheumatology nurse specialist
- SAP
- statistical and health economics analysis plan
- SCT
- social cognitive theory
- SD
- standard deviation
- SE
- standard error
- sPDAS2
- simplified Patient-derived Disease Activity Score
- TSC
- Trial Steering Committee
- VAS
- visual analogue scale
- VLA
- Valued Life Activities scale for rheumatoid arthritis
- WPAI
- Work Productivity and Activity Impairment
- WTP
- willingness to pay
