Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 14/43/02. The contractual start date was in December 2015. The draft report began editorial review in June 2018 and was accepted for publication in March 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Chris Metcalfe reports grants from the UK National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme during the conduct of the study. He and Stephen Baston report grants from the NIHR HTA, Public Health Research, Health Services and Delivery Research, Programme Grants for Applied Research and Research for Patient Benefit programmes since 2009. Chris Metcalfe is also a co-director of the Bristol Randomised Trials Collaboration, a UK Clinical Research Collaboration-registered trials unit in receipt of NIHR support funding. Nicola Wiles reports grants from the University of Bristol during the conduct of the study.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Russell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction, background and study aims
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental condition characterised by qualitative impairments in social communication and a pattern of restricted and repetitive behaviours, interests or activities. 1 Recent studies report that autism affects 1% of the UK adult population2 and 1 in 68 children in the USA. 3 Approximately 46% of autistic people have general intellectual function in the average or above range. 3 (The results of a survey of the UK autism community4 highlighted that ‘autism’, ‘on the autism spectrum’ and ‘autistic people’ are preferred terms to describe autism. From hereon in, the terms ‘autism’ and ‘autistic people’ will be used.) Autism is a lifelong condition, present from the early years, and outcomes in respect of education, employment and independent living have been shown to be relatively poor for autistic adults. 5
Mental health conditions are reported to frequently co-occur across the lifespan in autism. 6,7 Anxiety disorders and depression are the most frequently reported co-occurring conditions, with a modal rate of 40% for anxiety disorders in children,8 and rates of depression ranging from 4% to 35% across the lifespan. 9 The onset of depressive symptoms in autism appears to be early. A UK-based cohort study10 reported that autistic children and children with higher autism traits have higher depressive symptoms at the age of 10 years and that these remain elevated with an upwards trajectory until the age of 18 years. Robust epidemiological research, particularly longitudinal studies, has been lacking until relatively recently. There is increasing evidence, however, that the prevalence of depression may be significantly higher in autistic adults than in the general population. For example, a recent total population study11 of 223,842 individuals in Stockholm County, Sweden, reported that, of the 4073 who had a diagnosis of ASD, 19.8% also had a diagnosis of depression by the age of 27 years, compared with 6% of the general population sample [adjusted risk ratio 3.6, 95% confidence interval (CI) 3.4 to 3.9]. Another large, US population-based study12 including 1507 adults with a diagnosis of ASD reported a 25% prevalence of depression, representing a twofold increased risk of depression in autism.
Identification of depression in autism can be confounded by the overlap between depressive symptoms, such as social withdrawal, and core autism ‘symptoms’, for example reduced interest in or ability to socialise, which can be normative. There is also some suggestion in the literature that depression in autism may present atypically, for example as an increase in compulsive behaviour,13 providing further methodological difficulties for epidemiological research. Verbal abilities significantly influence the presentation or at least the identification of depression in this group. In addition, there is some evidence that better cognitive abilities and relatively low social impairment,14 the tendency to make social comparisons15 and a history of adverse experiences such as bullying10 may be features of autistic young people with co-occurring depression.
Measurement of depression in autism
Autism is characterised by a diverse pattern of strengths and weaknesses across multiple functional domains, including social cognitive and emotional processes. 16 Studies report high rates of alexithymia in autism,17 defined as a reduction in the ability to define and describe one’s own emotional state. The validity of self-reporting of emotional states in autism has been subject to investigation. For example, studies18,19 have investigated the validity and reliability of standardised measures of anxiety in autistic children, leading to the development of addendums to benchmark instruments or to the development of entirely new scales. In respect of the self-report and measurement of depression in adulthood, one recent study20 investigated the internal consistency and convergent and discriminant validity of the Hospital Anxiety and Depression Scale21 (HADS) in a sample of 150 autistic older adolescents and adults. The authors20 reported adequate internal consistency for the depression subscale of the HADS, with a modest correlation (r = 0.56, 95% CI 0.25 to 0.77) between the HADS depression score and scores on the Patient Health Questionnaire-9 items (PHQ-9),22 a widely used self-report measure of depression. Two studies23,24 have investigated the usefulness of the Beck Depression Inventory, version 2 (BDI-II),25 in autism, reporting that it presents as an adequate screening tool for depression,23 with good internal consistency, adequate sensitivity and specificity, and good convergent validity. 24 Of note, Gotham et al. 24 reported that the cognitive symptoms of depression (e.g. negative attributions about the self) were the most frequently endorsed BDI-II items in their sample (n = 50) of autistic adolescents and adults. In the context of basic research, findings of reduced awareness of bodily sensations, such as thirst and heartbeat detection, in autistic adults,26,27 and a greater awareness of depressive cognitions over biological symptoms of depression such as reduced appetite, are unsurprising.
Treatment of depression co-occurring with autism
Depression is a debilitating mental health condition for which effective pharmacological and psychosocial treatments exist. 28,29 The National Institute for Health and Care Excellence29 (NICE) recommends a stepped-care model for the treatment of depression. Mild to moderate depression should be treated with low-intensity psychosocial interventions, psychological interventions, medication and referral for further assessment and treatment. Low-intensity interventions involve the provision evidence-based information, accessed independently or with the support of an unqualified mental health worker [guided self-help (GSH)]. Ongoing monitoring and review are also important. Low-intensity psychological interventions for depression as recommended by NICE are individual GSH interventions based on the principles of cognitive–behavioural therapy (CBT) to include behavioural activation and problem-solving techniques, computerised CBT or a structured group physical activity programme. 29
Cognitive–behavioural therapy is a psychological intervention integrating behavioural and cognitive theories of emotional processes to bring about change in psychological distress and associated functional impairment. CBT is traditionally an individual talking therapy, but recent decades have seen efforts to streamline its delivery and improve accessibility. Consequently, CBT interventions are now delivered in group formats, over the internet/e-mail, as part of GSH and using software. The shift in mode of delivery and reliance on a less qualified therapist or no therapist – that is, self-guided – has meant a move from individual, formulation-driven therapy to manualised, protocol-driven treatments.
Adapting cognitive–behavioural therapy for autism
Autism-specific adaptations to psychosocial interventions have been well documented. 30 Taking account of the verbal and non-verbal communication differences characteristic of autism, such as a literal interpretation of language as well as the broad pattern of executive dysfunction,31 is required for all interventions in order to make them accessible to autistic people.
Adaptations unique to CBT are outlined in the NICE clinical guidelines for adults with autism. 32 These suggest a more concrete and structured approach to treatment delivery with greater use of written and visual information; a greater emphasis on changing behaviours rather than cognitions; clarity and explanations about rules; avoiding the use of metaphors, ambiguity and hypothetical situations; involving a family member, partner, carer or professional with the person’s agreement; and facilitating engagement by offering breaks and incorporating an individual’s special interests into therapy when appropriate. Additional modifications for young people outline that psychoeducation about emotions and multiple choice worksheets for cognitive strategies can be helpful. 33
In autism research to date, there has been a greater focus on understanding and treating anxiety than on depression. 34 Adapted CBT interventions, group and individual, have been shown to be clinically effective for ameliorating anxiety in children and young people and adults. 35,36 Weston et al. 37 provide a systematic review and meta-analysis of the studies of CBT interventions for emotional disorders in autism. Small to medium effect sizes favouring CBT over control treatments were established, but the magnitude varied according to the source of outcome measurement (g = 0.24 on self-report outcomes, g = 0.66 on informant measures and g = 0.73 on clinician-rated outcomes). All treatments used in the 24 studies included in the meta-analysis were clinician led; 16 were group treatments, 15 focused on treating anxiety, two focused on treating depression and a minority (n = 4) were adult studies. Studies evaluating behavioural activation (BA) as a stand-alone treatment were excluded from the meta-analysis.
There is, then, a small literature on the usefulness of psychological interventions for depression in autism. Several studies have evaluated combined CBT protocols for anxiety and depression. These are as follows:
-
McGillivray and Evert38 conducted a quasi-experimental evaluation of group CBT versus wait list for depression and anxiety in 32 young autistic adults who scored in the clinical range on a mood or anxiety questionnaire. There was a significant effect of time but not of treatment group in terms of a reduction in scores on the depression measure. Approximately 60% in the CBT group showed a significant reduction in scores on the Depression and Anxiety Stress Scale (DASS),39 compared with 38% in the wait-list group. 38
-
Sizoo and Kuiper40 delivered two adapted psychological interventions to 59 autistic adults with clinically significant anxiety or depression scores, as measured with the HADS. The interventions comprised a 13-session adapted CBT anxiety and mood protocol and an adapted mindfulness-based stress reduction (MBSR) treatment. 41,42 There was a significant effect of time but not of treatment group on depression and anxiety scores as measured by the HADS.
-
Spek et al. 42 randomly allocated 42 autistic adults with clinician-identified symptoms of depression, anxiety or rumination to adapted MBSR or treatment as usual (TAU). There was a significant reduction in scores on the depression (Symptom Checklist-90 depression subscale43), anxiety (Symptom Checklist-90 anxiety subscale43) and rumination measures in the MBSR group when compared with the TAU group.
Intervention studies with an exclusive focus on depression in autism are scarce. Santomauro et al. 44 conducted a feasibility crossover randomised controlled trial (RCT) of a group CBT intervention for 20 autistic adolescents with depression, defined as a BDI-II score of > 14. They found a trend towards an effect of treatment on the DASS depression subscale, but no significant effect using the BDI-II, and suggested that larger numbers of participants would be needed to gain an accurate picture of the efficacy of CBT for depression in this group.
Rationale for the current research
There is increasing evidence to suggest that depression is a frequently occurring mental health problem for autistic people.
Evidence-based psychological treatment based on cognitive–behavioural theories have been successfully adapted for autistic people and shown to be clinically effective in ameliorating anxiety symptoms. The clinical effect of treatment varies according to the source of outcome measurement, but clinician and informant ratings have evidenced greater change than self-report of symptoms. Findings in the research literature hypothesise that the reported difference in noticing and reporting changes in internal states, particularly emotions, may account for this variation. There have been studies reporting adequate reliability and validity of several widely used self-report measures of depression in autistic adults.
Clinical studies suggest that CBT approaches for depression in autistic adults may well be clinically effective. However, to date, and to our knowledge, there have been no adult studies with an exclusive focus on the psychological treatment of depression using the treatments evidenced in the standard care pathway or using structured depression diagnostic protocols as part of the eligibility assessment.
Clinical trials aside, naturalistic treatment evaluations are even less well described and reported. Thus, it is not known whether or not autistic adults with mild to moderate depression routinely access CBT interventions offered in primary care or experience less favourable treatment outcomes. It is known that the materials used as part of the standard care pathway, that is low-intensity CBT for depression, routinely offered in the UK within primary care psychological services have not been specifically developed with autistic adults in mind.
To our knowledge, low-intensity psychological interventions, such as GSH, have not previously been developed for autistic people for any type of emotional problem.
The present study is a response to the themed call from the Health Technology Assessment (14/043) programme of the National Institute for Health Research in April 2014 to design a feasibility study to ‘determine whether a trial of guided self-help for people with ASD is warranted’.
Aims of the current research
-
To develop a low-intensity intervention for depression adapted for adults with ASD, based on NICE recommendations and training materials to guide therapists in supporting the intervention.
-
To investigate the feasibility and the patient and therapist acceptability of the low-intensity intervention.
-
To estimate the rates of recruitment and retention for a large-scale RCT.
-
To identify the most appropriate outcome measure for a large-scale RCT.
These aims were met by conducting a feasibility study comprising a RCT with a nested qualitative evaluation.
Chapter 2 Study methods
Feasibility study design
The study was a single-blind RCT with a nested qualitative evaluation.
Participants were randomly assigned to GSH for depression adapted for adults with autism or to TAU in a 1 : 1 ratio.
The trial was registered in the ISRCTN registry as number ISRCTN54650760.
Ethics approval was granted by Wales Research Ethics Committee (REC) 3 [Integrated Research Application System (IRAS) project ID 191558].
The study methods were prespecified in a published protocol. 45
Participants
Participants (n = 70) were recruited through two pathways in the west of England and two pathways in the north-east of England, as follows:
-
Bristol Autism Spectrum Service (BASS) provided by Avon & Wiltshire Mental Health Partnership NHS Trust (AWP)
-
‘Everyone Included’ – a research opportunity offered to all adult patients registered with AWP and consenting to be contacted about suitable research opportunities
-
an adult autism clinic in Northumberland, Tyne and Wear NHS Foundation Trust (NTW)
-
The Adult Autism Spectrum Cohort – UK [a Newcastle University-led national cohort study of adults on the autism spectrum funded by Autistica (London, UK), a UK-based charity].
Inclusion criteria
-
Was aged ≥ 18 years.
-
Had a clinical diagnosis of ASD.
-
Had current depression as measured by a PHQ-9 score of ≥ 10.
Exclusion criteria
-
Did not speak English.
-
Had literacy level such that the written materials would have been inaccessible.
-
Had risk of suicide such that a low-intensity intervention would not be in line with clinical need.
-
Had a history of psychosis.
-
Had current alcohol/substance dependence.
-
Had untreated epilepsy.
-
Had attended more than six sessions of individual CBT during the previous 6 months.
Recruitment procedures
The initial recruitment procedures differed slightly across the four pathways, as follows.
Bristol Autism Spectrum Service
Potential participants were identified by clinicians following attendance at the clinic for diagnostic assessment. Participants were considered potentially suitable if they were given a clinical diagnosis of an ASD at the end of the assessment and were identified as having low mood following a clinical interview and/or a pre-clinic screening PHQ-9 score of ≥ 10, and routine risk assessment contraindicating low-intensity intervention. Potential participants were introduced to the study by clinicians using a brief expression of interest (EOI) form. If they were interested in the study, they could return the EOI form expressing interest and requesting follow-up contact from the research team. This further introduction to the study could occur face to face in the clinic, or by postal/telephone follow-up after the clinic attendance if the clinician considered this more appropriate. Follow-up contact from the research team was ordinarily over the telephone; full information about the study was provided at this stage in the study information sheet. Standard recruitment procedures were then initiated.
Everyone Included
The Everyone Included review panel (with independent membership) approved the study for inclusion in the approach and a draft of the research opportunity letter. Potential participants were identified from an automated search of the electronic patient record system by the information analysis team in the NHS trust and based on the study inclusion/exclusion criteria. Potential participants were sent the research opportunity letter by the local NHS research and development (R&D) team and, if they made contact, were provided with a study information sheet and asked their permission for the study research team to make contact with them. No information about potential participants was sent to the study research team without permission first being gained from the potential participant. Standard recruitment procedures were then initiated.
Adult Autism Clinic in Northumberland, Tyne and Wear NHS Foundation Trust
Potential participants were identified by clinicians as those given a diagnosis of an ASD following clinic attendance and assessed as having depression sufficient to warrant signposting/referral to Increasing Access to Psychological Therapies (IAPT) services as per routine clinical practice. They were introduced to the study using the brief EOI form at the end of the diagnostic assessment process, ordinarily at the second assessment appointment. Potential participants interested in the study who contacted the research team were asked to complete the PHQ-9 either by post or over the telephone, and those individuals with a score of ≥ 10 were provided with the full study information sheet. Standard recruitment procedures were then implemented.
In addition, patients formerly diagnosed by the NTW Autism Diagnosis Service who had agreed to be contacted about research studies were provided with information about the project (EOI form). Potential participants who contacted the research team were provided with comprehensive information about the study and potential suitability assessed using the PHQ-9. Standard recruitment procedures were then initiated.
Adult Autism Spectrum Cohort – UK at Newcastle University
The cohort research team approved the study on application, and an introductory letter was drafted by the Newcastle University research team. Potential participants were identified from a search of the database, constrained by NTW area postcode, age, intellectual disability and history of depression, and then cross-matched with the NTW Adult Autism Clinic research register to ensure that people were not introduced to the study more than once. Potential participants were sent the introductory letter and EOI form. Those who contacted the research team were provided with comprehensive information about the study and asked for their permission to screen them for the study, including completing the PHQ-9 by post or over the telephone. Standard recruitment procedures were then initiated.
Standard recruitment procedures
The outcome of screening each potential participant using the PHQ-9 was communicated to the individual’s general practitioner (GP) with their permission.
Potential participants with a PHQ-9 score of ≥ 10 who wanted to take part in the study were invited to an eligibility assessment with the research team.
Eligibility assessment
The Clinical Interview Schedule-Revised (CIS-R)46 was administered as an automated computer questionnaire to assess the exclusion and inclusion criteria alongside the PHQ-9. It is a widely used, well-validated diagnostic instrument that generates International Classification of Diseases, Tenth Revision (ICD-10),47 psychiatric diagnoses.
Details about sociodemographic status, history of depression, current medication and current/previous psychological treatment for depression were also collected to inform the eligibility assessment in respect of the inclusion and exclusion criteria.
Fully informed consent in writing was obtained from participants who had a PHQ-9 score of ≥ 10 and who were willing to take part in the study. It was established by the researcher by asking the participant to summarise their understanding of what taking part in the study would involve, asking about the voluntary nature of participation and asking the participant what they thought would happen if they no longer wanted to take part.
A statement designed to communicate a position of equipoise about the treatments was read to participants, who were then asked if they had a preference at this point for either treatment. If a preference was indicated, the reasons for this were recorded, and additional information encouraging participants to take a balanced approach towards treatment allocation was provided, aiming to minimise bias towards the outcome of randomisation.
If eligible for the study and consenting, the participant was asked to complete other quantitative measures at this appointment, which lasted 60–120 minutes.
Participants not meeting the eligibility criteria were thanked for their time and informed of the reasons. When the reason was severity of depression and/or intensity of suicidal ideation (i.e. score of 3 on item 9 of PHQ-9) such that a low-intensity intervention was not in line with current clinical need, this was explained and the information was communicated to the individual’s GP as per the study protocol.
Randomisation
Eligible, consenting participants were allocated to GSH (n = 35) or TAU (n = 35) in a 1 : 1 ratio using a remote computerised randomisation service. Randomisation was stratified by NHS regional centre (n = 2), and minimised by depression severity (mild to moderate, i.e. PHQ-9 scores of between 10 and 15, or moderate to severe, i.e. PHQ-9 scores of between 16 and 27) and antidepressant medication (currently taking or not taking). The trial manager shared the outcome of randomisation with the participants according to their communication preferences within 48 hours, and with the therapist. Follow-up measurement was conducted by researchers who were blind to treatment allocation (Figure 1 shows the timeline of events).
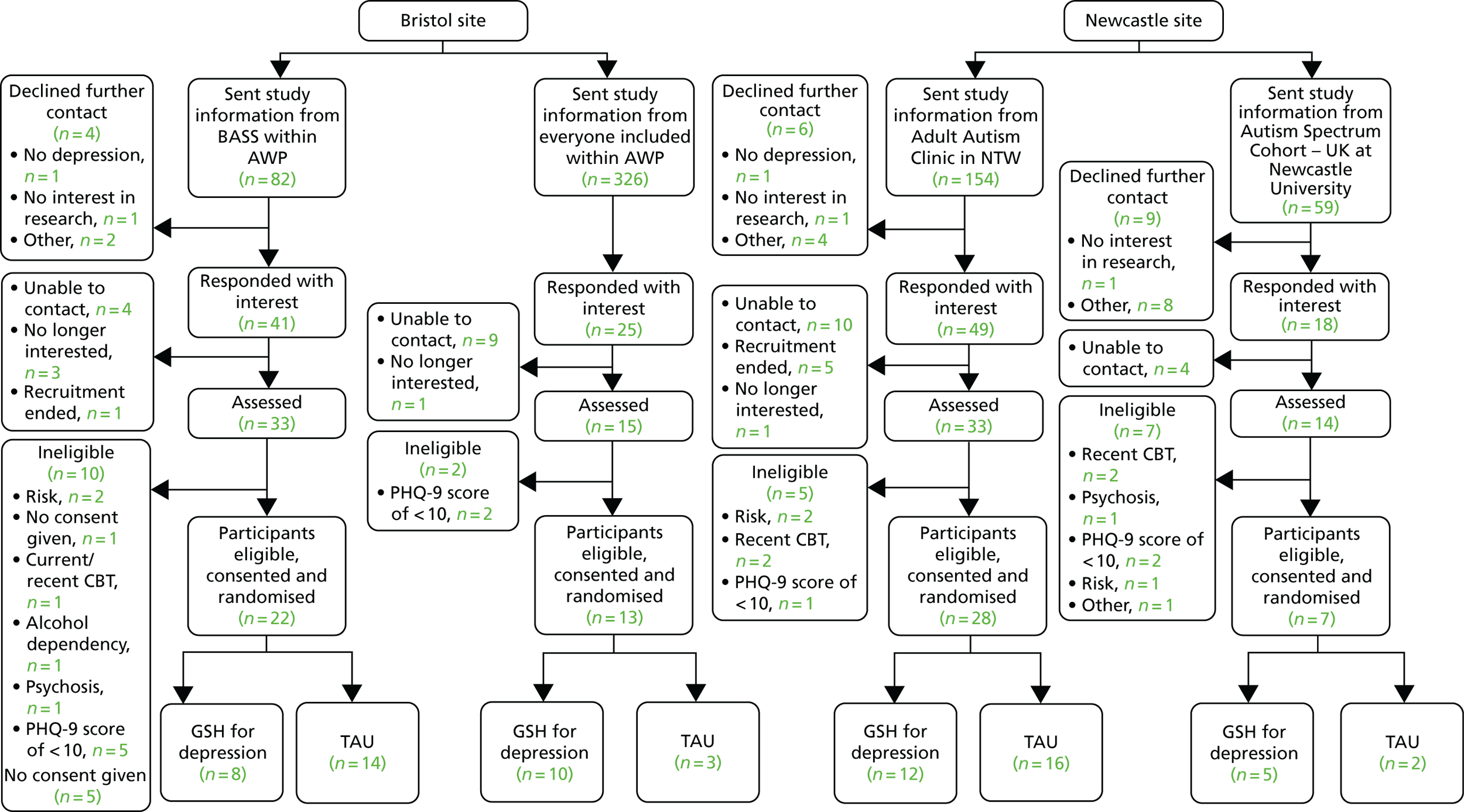
FIGURE 1.
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram from recruitment to randomisation by site and recruitment pathway. Reproduced with permission from Russell et al. 48
Retention
To maximise retention of participants in the study, an individual protocol was developed about participants’ preferences for communication with the study team, including their preferred method of communication (e.g. e-mail, text message or telephone call), person to communicate with (e.g. self or specified other) and the number of attempts that should be made if initial communications about follow-up and appointments did not receive a response.
Interventions
Treatment as usual
Treatment as usual consisted of standard NHS care for depression as provided to the individual during the trial. This included no treatment, GP support, referral to IAPT services, referral to secondary mental health services and antidepressant medication. Participants were asked to report any treatment received at each follow-up meeting.
Guided self-help
The intervention developed in the current study adhered to the principles of a low-intensity psychological intervention for depression as outlined in NICE guidelines,29 namely 6–10 sessions of individual GSH based on the principles of CBT to include BA.
The GSH treatment developed for the study was a low-intensity intervention based on the principles of BA for depression, which was adapted for autistic people.
Rationale for guided self-help based on behavioural activation
Behavioural activation is the usual first phase of CBT for depression, ordinarily achieved through activity scheduling. BA is not simply getting people to be more active; it also aims to help people make choices about their behaviour in particular situations to better regulate their mood. People are encouraged to become more aware of the triggers for low mood and the consequences of a range of behaviours and to then use this information to adjust their activities accordingly. There is good evidence for the clinical effectiveness of BA as a treatment for depression in its own right and it is recommended as one of the low-intensity interventions in the NICE guidelines.
Behavioural activation is well suited to inform an intervention for depression in the context of autism. First, the model underpinning BA, with an emphasis on the role of the environment in precipitating and maintaining depression, has face validity. 49,50 Within the framework of BA, changes to an individual’s environment and the individual’s response to those changes can lead to depression. If the consequences of behaviours are not sufficiently rewarding, an individual will learn to do fewer of those behaviours. If a behaviour formerly had a significant role in maintaining positive mood, then doing it less creates fewer opportunities for reinforcement, which leads to further reduction, and so on. Positive reinforcement is gradually reduced and this cycle of punishing interaction, reduced frequency of behaviour and reduced reinforcement explains the persistence of depression. Many autistic people lack access to meaningful social, occupational and leisure activities and hence have fewer opportunities for positive reinforcement. There is an objective reality to the mismatch between significant parts of their social and occupational environment and their needs. The focus of BA treatment, therefore, is to help people develop a behavioural repertoire that responds more effectively to demanding environments, and, where possible, accesses rewarding experiences within them.
Second, a restricted, repetitive, stereotyped pattern of behaviour, interests and activities is one of the core characteristics of ASD. It is possible that autistic people, in addition to experiencing societal vulnerabilities in the form of lack of opportunities, are compromised in their ability to easily generate a shift in routines and behaviours towards activities and actions that may offer increased access to pleasure and a sense of achievement. This tendency towards restricted activities and interests may form part of the behavioural maintenance cycle of depression symptoms in autism. BA, with an emphasis on the active scheduling of activities, may offer precision as an intervention for depression co-occurring with autism.
Third, rigidity and perseveration in thought patterns can be part of autism, with evidence of impairments in cognitive flexibility and generativity from neuropsychological studies. 31 Cognitive interventions that target the content of thoughts and beliefs maintaining depressed mood may not be well suited to the cognitive profile of autistic people. Cognitive techniques require an individual to access and report abstract inner phenomena, for example negative automatic thoughts, and to generate and consider alternative ways of thinking about situations. These are relatively abstract activities that rely on cognitive flexibility, which may not be well suited to the cognitive strengths of autistic people.
To summarise, the principles and practice of BA may mean that it is particularly suited as a psychological treatment for depression co-occurring with autism. Lack of social opportunities and meaningful occupation may be further compounded by a pattern of restricted, repetitive behaviours and a preference for sameness. This constrains the behavioural repertoire of autistic people and can leave them unmotivated and underequipped to access positive affect, particularly through interactions with other people. The core treatment principle in BA is to increase opportunities for positive reinforcement by activating behaviour, that is, to restore mood and behaviour patterns. Furthermore, BA has previously been effectively adapted to the constraints of a low-intensity intervention.
The authors (AR, KC and SB) developed the GSH intervention. Informed by the principles of BA, session materials were developed that were designed to encourage clients to pay more attention to their physical and social environment, record their behaviours (in granular detail) across different situations and notice the feelings and body states that result from those actions. GSH is designed to promote associative learning, so that associations between behaviours and their affective consequences become more apparent to clients. The resultant learning helps them to schedule activities that are more likely to satisfy their needs and promote positive feelings, thereby increasing opportunities for positive reinforcement.
Materials were visually presented as far as possible, for example recording activities on a visual map rather than in a written diary, with any text supplemented by images. A consistent session format was used. Other autism-specific adaptations included a session on noticing positive feelings and developing a scale to do this, a structured approach to activity scheduling to scaffold the planning and organisational issues inherent in executive dysfunction and a graded approach to the introduction of new activities.
Two autistic adults provided feedback and advice about the design of the materials during the development phase. This included commenting on the accessibility and content of the written text, suitability of the accompanying visual images, visual layout and format of the session materials, amount of material to be covered each session and homework tasks. The volunteers responded to a request through a service network newsletter for help with the development of the intervention. A number of people responded, and this was followed up by a telephone call from the researchers. A number of the responders were on current waiting lists for mental health treatment and it was agreed that the research study may not be able to offer sufficient support to facilitate their participation in the research at that point. The two volunteers in a position to help had attended psychological therapy in the past, and one had specifically received CBT for depression. Both reported that mental health difficulties were not currently having an impact on their social and occupational function. The volunteers attended up to three individual meetings with a member of the research team and were reimbursed for their time in accordance with the INVOLVE guidelines. 51 The first iteration of the session materials was available and the meeting was used to review the materials and discuss the feedback and suggested changes. This was an open process without an a priori agenda for feedback. The volunteers were able to comment on any aspects of the GSH that they considered important. For example, the materials for the planning session included a short form with questions and prompts to enable the coach to learn about the individual’s autism. One volunteer commented that this was a good idea, but that the examples and prompts could be improved. They made specific suggestions about changes to improve the content, which were included. One of the volunteers had a background in graphic design and was able to make specific recommendations about the visual layout and format of the materials. The two volunteers brought different skill sets and experiences to the task. One volunteer’s recent experience of accessing CBT was invaluable when considering the content of the intervention, for example the suitability of the proposed ‘homework’ tasks. This volunteer was able to reflect on what had made between-session tasks difficult in their experience, primarily the lack of specificity. This discussion enabled the researcher to make specific suggestions about the structure of the homework tasks and to gain feedback from the volunteer. The creative background and visual sensitivity of the other volunteer was extremely helpful in ensuring that the materials ‘looked’ right.
The GSH intervention comprised materials for nine individual sessions to be held weekly and facilitated by a coach. A short manual was developed for the coaches to accompany the session materials.
The first session was a ‘planning’ session, the aim of which was to orient the participant to the purpose of GSH and the role of the coach, and to orient the coach to the individual’s unique needs as an autistic adult. Individual goals for treatment were developed during this session. In sessions 2–5 the primary aim was learning about the links between situations, behaviour and feelings. Sessions 6–9 focused on scheduling activities that were in line with treatment goals and would bring about opportunities for increased positive mood. To encourage the scheduling of a broader repertoire of activities, Maslow’s hierarchy of needs52 was presented in session 6 as a framework for thinking further about activity scheduling. People were encouraged to notice and record activities in their diary map according to the different levels of need, for example physiological need, social need and self-esteem, as well as in respect of positive feelings.
The duration of sessions was 30–45 minutes, with the exception of the planning session, which was longer. This could last up to 90 minutes to facilitate engagement.
Participants who attended five or more sessions were considered to have received a minimally clinically effective dose of treatment.
The intervention was delivered face to face, with the later sessions (6–9) amenable to delivery over the telephone if preferred. In exceptional circumstances, for example if the individual was completely unable to access the treatment face to face, the treatment was offered over Skype™ (Microsoft Corporation, Redmond, WA, USA).
The coach in GSH was a graduate-level psychologist who had foundation knowledge of CBT but not necessarily any experience of delivering low-intensity interventions and ordinarily did not have the knowledge and skills to deliver individual, formulation-driven (i.e. high-intensity) CBT. Coaches were usually assistant psychologists (n = 4), although a small number of patients were treated by clinical psychologists in training (n = 3).
Coaches received 15 hours of training in the intervention and in working with autistic people. They received 1 hour minimum of clinical supervision on a weekly basis from the clinical psychologists who developed the intervention (AR, SB and KC). Supervision was face to face or remote (over the telephone/Skype) and was delivered on an individual or a group basis.
Outcome measures, namely the PHQ-9, Generalised Anxiety Disorder-7 (GAD-7), an abbreviated Positive and Negative Affect Schedule (PANAS) and visual analogue rating of activity engagement, were completed at the start of each session to simulate standard practice in low-intensity interventions.
As this was a feasibility study, the session content and duration were recorded by the coaches at the end of each session.
Outcome measurement
Follow-up assessments were conducted 10, 16 and 24 weeks post randomisation by researchers blind to treatment allocation (Table 1). The feasibility of delivering the intervention over 10 weeks was also evaluated. Thus, it was not clear a priori if 10 or 16 weeks post randomisation would be the most clinically effective point of outcome measurement (i.e. whether the majority of participants were unable to complete the intervention within 10 weeks).
| Measure | Baseline | GSH group each session | 10 weeks (end of intervention) | 16 weeks | 24 weeks |
|---|---|---|---|---|---|
| Demographics | ✓ | ||||
| PHQ-9 | ✓ | ✓ | ✓ | ✓ | ✓ |
| CIS-R | ✓ | ||||
| BDI-II | ✓ | ✓ | ✓ | ✓ | |
| SIGH-D | ✓ | ✓ | ✓ | ✓ | |
| GAD-7 | ✓ | ✓ | ✓ | ✓ | ✓ |
| OCI-R | ✓ | ✓ | ✓ | ✓ | |
| PANAS | ✓ | ✓ | ✓ | ✓ | ✓ |
| SF-12 | ✓ | ✓ | ✓ | ✓ | |
| EQ-5D-5L | ✓ | ✓ | ✓ | ✓ | |
| Participant Global Rating of Change | ✓ | ✓ | |||
| RBQ-2A | ✓ | ||||
| RRQ | ✓ | ✓ | |||
| Economic evaluation | ✓ | ✓ | ✓ |
The findings of previous research have suggested that self-report measures may not be the optimal method to capture change. Furthermore, the psychometric properties of just one self-report measure of depression (BDI-II) had been investigated in autistic adults at the time of the design of the study. Therefore, a suite of measures of depression symptoms was included. An aim of the study was to identify the most appropriate outcome measure for a large-scale RCT, and so it was not possible to specify the primary outcome measure of depression a priori.
Measures could be completed electronically using a tablet or could be made available for paper-and-pen completion. The majority of participants completed the measures electronically. This could be done remotely or face to face in clinic as the participant preferred. The majority of participants in the Avon and Wiltshire region preferred to complete the measures remotely, whereas the majority in the north-east preferred to attend an outcome appointment in person.
The duration of measurement varied, with eligibility and baseline assessment appointments lasting up to 90 minutes and outcome measurement taking approximately 60 minutes.
Depression measures
Patient Health Questionnaire-9 items
The PHQ-922 is a nine-item self-report measure of depression that is commonly used in primary care settings. The PHQ-9 has been found to be reliable (Cronbach’s α = 0.84–0.93), valid and sensitive to change in the general population. 53 To the authors’ knowledge, the psychometric properties of the scale have not been investigated in the autistic population.
Beck Depression Inventory-II
The BDI-II25 is a widely used 21-item self-report measure of depression. The BDI-II has been found to be reliable (Cronbach’s α = 0.92) for outpatients. 25 A validation study24 of 50 young people with ASD reported good internal consistency on the BDI-II (Cronbach’s alpha = 0.90).
GRID-Hamilton Depression Rating Scale
The GRID-HAMD54 is a version of the Hamilton Depression Rating Scale (HAM-D). 55 It is a 17-item clinician-administered interview that has been found to be reliable and valid in the general population but, to our knowledge, has not been investigated in the autistic population. 54 GRID-HAMD interviews were audio-recorded, with participant consent, for the purposes of inter-rater reliability. The first six HAM-D interviews by each interviewer were subject to a second independent rating, excluding items 8 and 9 (i.e. observation of psychomotor retardation and agitation), which need to be assessed face to face, to establish the reliability of each assessor. To establish reliability across the study, a random sample (20%) of GRID-HAMD recordings were independently rated.
Participant Global Rating of Change
Participants were asked to rate whether their depression was better, worse or much the same on a 5-point scale at the 16- and 24-week follow-ups.
Other measures
Other measures included measures of anxiety and obsessive–compulsive symptoms to account for the potential impact the high rates of co-occurring anxiety problems in autism might have on the feasibility of the intervention delivery and outcome. They also included a positive and negative affect rating scale as the intervention was designed to promote positive feelings, a set of functional outcome measures and questions about health and social care service use.
Generalised Anxiety Disorder-7
The GAD-756 is a seven-item self-report measure of anxiety. The scale has been found to be reliable and valid in the typically developing population56 (Cronbach’s α = 0.92). However, its psychometric properties for use with autistic individuals are not known.
Obsessive–Compulsive Inventory-Revised
The Obsessive–Compulsive Inventory-Revised (OCI-R)57 is an 18-item self-report measure of the symptoms of obsessive–compulsive disorder, with items such as ‘I feel I have to repeat certain numbers’ scored on a five-point Likert scale (0–4), indicating increasing frequency. The scale has been found to be reliable and valid. 57 The OCI-R was found to have good psychometric properties in a sample of 225 autistic people. 58
Positive and Negative Affect Schedule
The PANAS59 is a 20-item self-report scale of positive and negative affect. The scale has been found to be reliable, with a Cronbach’s alpha of 0.89 for the positive affect scale and of 0.85 for the negative affect scale, but it has not been used with autistic individuals. 59
Work and Social Adjustment Scale
The Work and Social Adjustment Scale (WSAS)60 is a five-item self-report measure of impaired functioning that has been found to be reliable (Cronbach’s α = 0.7–0.94) and valid in typically developing individuals. It has been used with autism populations, but its psychometric properties have not been assessed.
EuroQol-5 Dimensions, five-level version
The EuroQol-5 Dimensions, five-level version (EQ-5D-5L)61 is a five-item self-report measure of health, with items measured on a 5-point Likert scale (1 to 5) indicating severity. It has been found to be reliable and valid in the typically developing population. 62
Short Form questionnaire-12 items
The Short Form questionnaire-12 items (SF-12)63 is a 12-item self-report measure of physical and mental health. It has been found to be a reliable and valid measure among people with severe mental health problems, but psychometric properties for autistic populations are not available. 64
Adult Repetitive Behaviour Questionnaire-2
The Adult Repetitive Behaviour Questionnaire-2 (RBQ-2A)65 is a 20-item self-report measure of repetitive behaviours. It has been found to have good internal consistency, with Cronbach alphas of between 0.73 and 0.83, and autistic people score significantly higher on the measure than typically developing individuals, suggesting that it is a valid measure of autism-specific repetitive behaviours.
Rumination–Reflection Questionnaire
The Rumination–Reflection Questionnaire (RRQ)66 is a 12-item self-report questionnaire comprising two subscales: rumination and reflection. The measure has good psychometric properties; the rumination scale has a Cronbach’s alpha of 0.90, and the reflection scale has a Cronbach’s alpha of 0.91.
Economic evaluation
We aimed to assess the feasibility of collecting data on statutory health and voluntary service use. This was assessed with a questionnaire collecting information on the use of other primary and community care services (NHS Direct, attendances at walk-in centres, use of community health-care services); secondary care related to mental health (number of outpatient visits, type of clinic and reason for visit, inpatient stays, length of stay and reason for stay); use of social services and disability payments received; personal costs related to mental health (expenditure on over-the-counter medication, expenditure on prescriptions, travel costs associated with health-care visits, loss of earnings, out-of-pocket expenditure on other services, e.g. private counselling or complementary or alternative therapies, child care and domestic help); time off work; and unpaid activities. We also accessed GP records to obtain information on the number of primary care consultations, by type (e.g. face to face, telephone), who was seen and prescribed medication.
Sample size
This feasibility study was not powered to detect important clinical differences between GSH and TAU. We collected data on outcomes that were used to inform a future large-scale trial. Recruiting a sample of 70 participants, 35 in each group, will inform decision-making about the practical issues of conducting such a trial and will be used to estimate the standard of the continuous depression outcome with reasonable precision. 67 Such a number would provide estimates of the completion rates of the intervention and retention rates that would assist in planning the recruitment for a future RCT. For example, if 80% of those randomised to GSH received the intervention, the 95% CI would be 63% to 92%. Similarly, if 85% of those randomised were followed up at 10 weeks, the 95% CI for the retention rate would be 75% to 93%.
Qualitative study
A nested qualitative study (see Chapter 4) was designed to investigate the feasibility and patient and therapist acceptability of the intervention. The methods and results are fully described in Chapter 4.
Data monitoring and oversight
An adverse event standard operating procedure (SOP) (see Appendix 3) was developed for the study in line with Good Clinical Practice guidelines,68 and this was followed by all members of the research team. Adverse events are defined as significant negative episodes or deterioration in a participant’s condition during a trial. Adverse events were reported by research assistants and coaches to clinically qualified trial staff, who ascertained whether or not these were linked to participation in the trial. A record was kept of adverse events during the trial. Any serious adverse events of an unexpected and related nature would have been reported to the main REC, the study sponsor and Trial Steering Committee (TSC), but this did not happen during the trial.
A risk management SOP was also developed for the trial and followed by all members of staff working on the study. As this was a depression-focused study, participants’ suicide risk was monitored using the suicidality items on the PHQ-9 and BDI-II, and participant responses to the suicidality item of the HAM-D. If the participant stated that they had experienced suicidal/self-harming thoughts every day in the last week (PHQ-9) or that they would like to kill themselves, or would kill themselves if they had the chance (BDI-II), then a letter was sent to their GP highlighting the individual’s risk. If the individual was considered to be high risk, a qualified clinician could follow up further by offering information to the participant about local crisis teams, and calling their GP to ensure that the information was shared in a timely manner.
A Data Monitoring and Ethics Committee (DMEC) and the TSC provided independent oversight of the study, meeting at 6-monthly intervals. Adverse events and risk information was shared with the committees, who had the option of terminating the trial prematurely if they felt this to be warranted.
Patient and public involvement
Two autistic adults were involved in the design and format of the GSH materials.
A consultation group of autistic adults provided feedback on the final version of the study information sheets and the initial GSH session.
An autistic researcher was a member of the TSC.
The study was presented to an NHS clinician network during the development phase to obtain feedback about the planned research.
The study was presented to a service user group in one of the regional sites (Bristol) to raise awareness of the research and to consult about the research plans.
Summary of changes to the project protocol
All changes were approved following the submission of amendments to the REC:
-
Additional measures, the Adult Repetitive Behaviour Questionnaire and the Rumination subscale of the RRQ, were included in the protocol to characterise the participants in respect of autism and depression characteristics. 65,66 The Participant Global Rating of Change was introduced at 16 and 24 weeks to gain patient-centred views about improvement in depression to supplement standardised symptom measures.
-
When the study opened to recruitment, consultation with the clinical services indicated that the recruitment pathways as specified in the protocol (v1.1) did not enable them to invite all potentially eligible participants to find out about the study. For example, in the BASS, not all participants completed the PHQ-9 prior to clinic attendance. Hence, the protocol was amended on the guidance of clinicians in both clinics to improve access to the study for potentially eligible participants.
Outcomes of feasibility study
A statistical analysis plan (SAP) was written and agreed by the DMEC and TSC before any analysis was carried out. As this was a feasibility study, no formal sample size was defined and, therefore, the study was not powered to show any differences between treatment groups. All analyses were prespecified in keeping with the outcomes of this feasibility study.
These outcomes were:
-
an estimation of the rate of recruitment for a large-scale RCT
-
an estimation of the retention rates to inform the RCT
-
the proportion of adults with ASD consenting to the study
-
the proportion completing the baseline assessment and entering the randomised phase
-
for those in the intervention group, the number of GSH sessions attended and the proportion completing five or more sessions
-
the proportion completing follow-up assessments at 10, 16 and 24 weeks post randomisation.
Inter-rater reliability of the Hamilton Depression Rating Scale
The HAM-D is an observer-rated instrument, with seven assessors interviewing participants. During the study, it was important to establish inter-rater reliability by using two assessors to re-rate these interviews. It was also important for subsequent analyses to compare the sensitivity to change of the two self-reported depression measures (BDI-II and PHQ-9), with which the HAM-D was to be used as the gold-standard measure for comparison.
We assessed inter-rater reliability early in the study (June 2017); a second assessor independently rated the audio-recordings of the first six interviews completed by the initial assessor in Newcastle and the first eight interviews completed by the initial assessor in Bristol. Agreement between assessors by HAM-D item (excluding the two items that required direct observation, i.e. psychomotor agitation and psychomotor retardation) was calculated as a percentage of total number of agreements on ratings of individual items.
By the end of the study, the first eight HAM-D assessments for each of the seven assessors (three in Bristol and four in Newcastle) had been double rated and the inter-rater reliability of the HAM-D was assessed. As most of the second ratings were conducted by listening to an audio-recording of the interview with the participant, the two items of the HAM-D that require direct observation (psychomotor agitation and psychomotor retardation) were not included in the total score. Therefore, the HAM-D scores being compared were the total of 15 items in the HAM-D without prorating due to the established variability across individual items. 69 Cohen’s kappa was calculated for every pair of assessors. Agreement was defined as both of the assessors’ total score falling within the same three-point range of HAM-D scores, which has been suggested to be clinically relevant. 28 A value of Cohen’s kappa of ≥ 0.8 was prespecified as acceptable.
Sensitivity to change of depression outcome measures
We explored the sensitivity to change of the two self-reported measures of depression (PHQ-9 and BDI-II) in comparison with the observer-rated HAM-D (clinician-administered interview) to identify the most appropriate outcome measure(s) for the main trial. We also identified the time point that would be used to measure the primary outcome in the main trial (based on the time point at which most participants had completed the intervention).
For each of the self-reported depression outcome measures (PHQ-9 and BDI-II), we examined:
-
acceptability (proportion of individuals providing sufficient data)
-
agreement between continuous scores using the intracluster correlation coefficient (ICC) from a two-way mixed effect, repeated measures analysis of variance model (observations are random, outcome measure instrument is fixed)
-
Bland–Altman plots
-
sensitivity to change (defined as a binary outcome of at least 50% improvement in symptoms on HAM-D at the time measuring the primary outcome compared with baseline) using receiver operating characteristic (ROC) curve analyses separately for each measure.
We also compared the continuous scores on the depression outcome measures only (HAM-D, PHQ-9, BDI-II) between the groups.
Economic evaluation
The focus of this feasibility study was piloting the methods of economic data collection rather than comparing costs. Participants were asked to report details of their use of health services and voluntary services during the trial as part of the follow-up questionnaires at 10, 16 and 24 weeks. Data collected included medication use, use of primary care and secondary care [including outpatient appointments, inpatient stays and attendances at accident and emergency (A&E) for their mental health] and the use of autism support services. Participants were asked to recall their use of these services during the interval since the last contact (e.g. baseline to 10 weeks, 10–16 weeks and 16–24 weeks). In addition, data on medication and use of primary and secondary care services were collected from electronic medical records (EMRs) at the end of the study to inform the decision regarding the source of data for a larger-scale trial. These included data from 2 months before the participant entered the study until the date the participant ended the study, namely 24 weeks after randomisation.
The data on health and voluntary service use were described, using appropriate statistics, to inform which economic data were to be collected in the main trial. These included examining completeness of data; determining which source of data should be used in the main trial (when information from both self-report and medical records is available – antidepressant medication use, use of primary care services and NHS outpatient or community mental health team clinics for mental health problems); identifying any redundant questions; and identifying any additional questions required to enable costing in the main trial.
To analyse the self-reported data over the whole study period, each participant was recorded as using each health-care or voluntary service (outcome) if they had done so at least once over the three assessment points detailed above, even if they additionally recorded a negative or missing response at another assessment point. If a participant responded ‘no’ at all assessment points, or ‘no’ at some assessments and missing at others, they were recorded as not having that outcome.
Concordance between self-reported data and the EMR data was defined as the outcome being recorded as both yes (or both no) in the self-reported data and the EMR data, and data were regarded as missing if that outcome was not recorded. These analyses were possible only for the outcomes of antidepressant medication use, use of primary care services and NHS outpatient or community mental health team clinics for mental health problems.
Post hoc analysis
During the study an amendment was made to collect a Participant Global Rating of Change in depression (May 2017). This question was asked at the 16- and 24-week follow-up to find out how the participant felt their depression was compared with baseline (i.e. 16 or 24 weeks earlier).
Chapter 3 Results
Recruitment
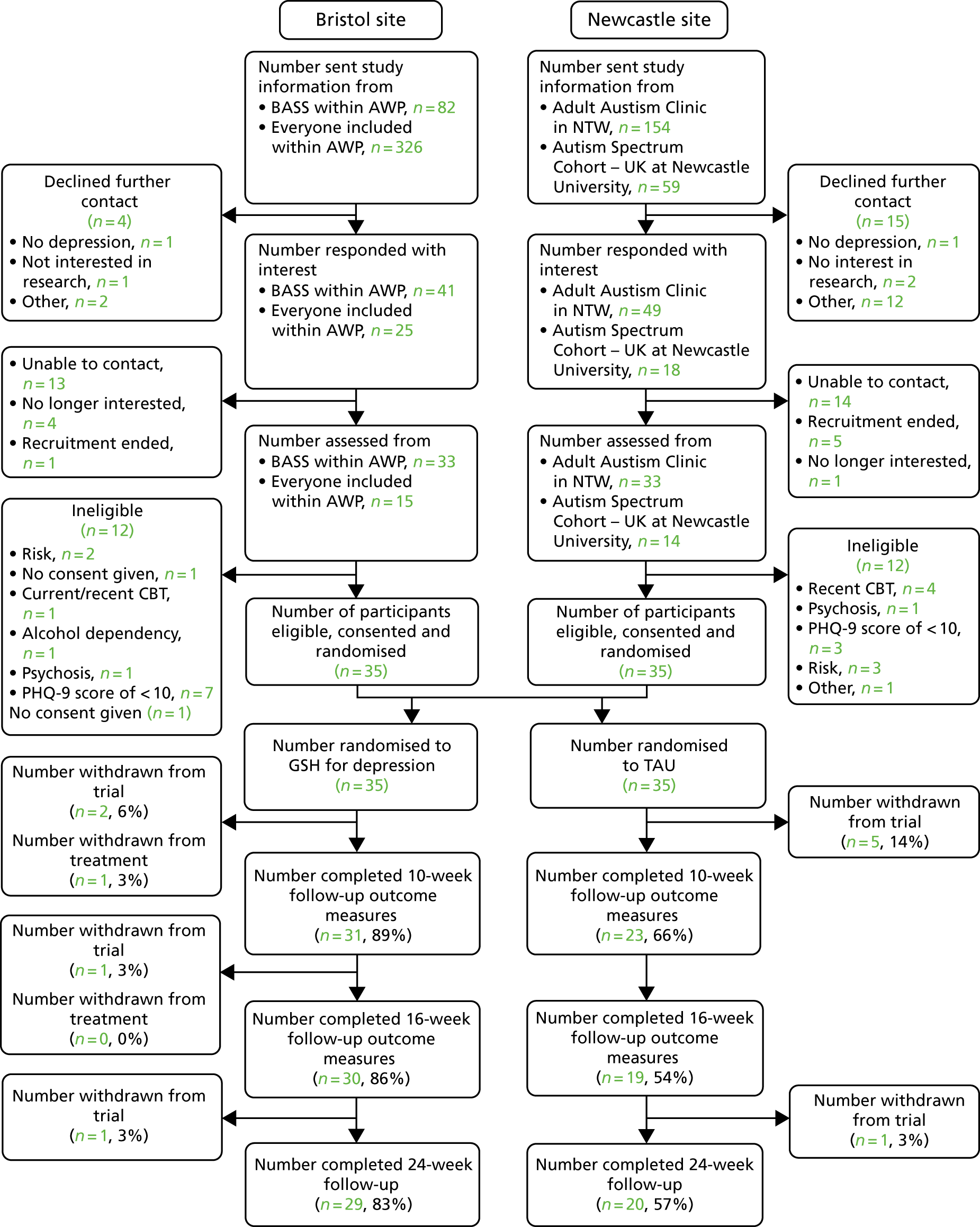
The planned start of recruitment to the study was delayed by 5 months owing to time gaining ethics approval. Recruitment was conducted over 12 months (6 October 2016 to 30 September 2017) and by the end of recruitment 70 participants had consented and been randomised to treatment as per protocol. The Consolidated Standards of Reporting Trials (CONSORT) diagrams for the 70 participants are shown in Figures 1 and 2. 70 First, participant recruitment into the study is shown by regional centre, Bristol or Newcastle, with the two recruitment pathways within each centre – an NHS clinic and research opportunity or research register – depicted to the point of randomisation, that is, four pathways (see Figure 1). Participant flow through the study beyond randomisation is shown by regional centre only (Bristol or Newcastle) in Figure 2.
FIGURE 2.
The CONSORT flow diagram from recruitment onwards by site. Reproduced with permission from Russell et al. 48
The overall rate of recruitment into the study was 3.2 patients per month [standard deviation (SD) 1.7 patients per month] over 12 months, with 3.2 patients per month (SD 1.3 patients per month) in Bristol and 3.2 patients per month (SD 2.1 patients per month) in Newcastle. However, as there was variability in recruitment procedures and timings across the four recruitment pathways, examining the mean rate of recruitment by region is perhaps less meaningful than considering recruitment by type or by clinic referral versus research register, as well as by regional centre.
In the BASS, 27% (22/82) of adults who were sent study information and were eligible for the study consented to be randomised. The corresponding figure was 18% (28/154) in the Newcastle Adult Autism Clinic. The Newcastle Adult Autism Clinic was able to contact a relatively large retrospective list of previous clinic attendees who had agreed to be contacted about future research.
Rates of randomisation through the NHS Adult Autism Clinics were relatively consistent during the recruitment period. In the BASS, an average of 1.8 participants were randomised each month. In the Newcastle Adult Autism Clinic, an average of 2.33 participants were randomised each month.
Research recruitment pathways – as described in Chapter 2 – different procedures for screening and inviting participants to find out about the study were followed, according to the local study protocols. There were also differences in timing. For the ‘Everyone Included’ pathway in the Bristol site, screening and contacting potentially eligible participants happened at regular intervals and at least one participant was randomised to the study each month, with an average of 1.08 participants per month. The Adult Autism Spectrum Cohort – UK study at Newcastle University was not active as a recruitment pathway at the start of the study, and participants from this pathway were contacted only during the final 6 months of recruitment (March–October 2017). An average of 1.16 participants were recruited each month during the 6-month period when this pathway was in operation.
In total, 40% (10/25) of adults who were interested in the study and assessed, but who were not eligible, had a PHQ-9 score of > 10; 20% (5/25) were not eligible owing to their risk of suicide; the remaining 40% (10/25) were not eligible owing to psychosis (n = 2), current/recent CBT (n = 5) or alcohol dependency (n = 1), or because they could not give informed consent owing to high levels of distress (n = 1) or for some ‘other’ reason (i.e. ineligible as outside the postcode area) (n = 1).
Participants characteristics
Most participants in the trial were male (n = 51/69, 74%) and the mean age of participants was 38 years (SD 13.2 years; n = 57) (figures by treatment group are shown in Table 2). A significant proportion of the participants (n = 21/62, 32%) were employed in either full -or part-time work. Thirty-two per cent (n = 21/65) were educated to at least A level or equivalent. The majority were currently living in owner-occupied properties (38%, n = 25/65), and 56% (n = 35/63) were cohabiting, which included living with family members. Thirty-three per cent (n = 21/64) had moderate financial stress described as low or no wage, benefits as income, a debt management plan or housing status at risk.
| Variable | TAU (N = 35 randomised) | GSH (N = 35 randomised) |
|---|---|---|
| Stratification variable: centre, N completed (%) | ||
| Bristol | 17 (49) | 18 (51) |
| Newcastle | 18 (51) | 17 (49) |
| Minimisation variable: antidepressant medication, N completed (%) | ||
| Currently taking | 18 (51) | 20 (57) |
| Not taking | 17 (49) | 15 (43) |
| Minimisation variable: PHQ-9 score, n/N completed (%) | ||
| Mild to moderate (scores between 10 and 15) [N completed (%)] | 19 (54) | 19 (54) |
| Moderate to severe (scores between 16 and 27) [N completed (%)] | 16 (46) | 16 (46) |
| Gender: male | 27/35 (77) | 24/34 (71) |
| Age (years), mean (SD), n | 40.2 (12.6), 28 | 35.3 (13.6), 29 |
| Ethnicity: white | 33/35 (94) | 33/34 (97) |
| Accommodation type: owner-occupied | 11/31 (35) | 14/34 (41) |
| Residential status: primary tenant/leaseholder | 17/30 (57) | 11/33 (33) |
| Education: GCSE or above | 28/31 (90) | 33/34 (97) |
| Employment status: paid or voluntary employment or training (full- or part-time) | 17/32 (53) | 15/33 (45) |
| Financial support/stress: moderate/significant financial stressa | 17/31 (55) | 11/33 (33) |
| Relationship status: single | 23/31 (74) | 19/34 (56) |
| Currently taking other medication for mental health | 5/28 (18) | 7/32 (22) |
| Experience of psychological/talking therapy: at least one experiencea | 21/29 (72) | 20/29 (69) |
| Current alcohol or substance dependency: no | 28/29 (97) | 30/30 (100) |
| PHQ-9 score, mean (SD), n | 16.5 (4.8), 35 | 15.0 (3.2), 35 |
| BDI-II score, mean (SD), n | 32.0 (11.5), 31 | 29.9 (8.8), 33 |
| HAM-D score, mean (SD), n | 17.6 (6.9), 29 | 17.4 (5.6), 34 |
| CIS-R score, mean (SD), n | 29.4 (11.0), 35 | 30.5 (8.6), 34 |
| Depression duration, n/N completed (%) | ||
| < 2 weeks | 1/24 (4) | 0/28 (0) |
| Between 2 weeks and 6 months | 5/24 (21) | 3/28 (11) |
| Between 6 months and 1 year | 3/24 (13) | 1/28 (4) |
| Between 1 and 2 years | 0/24 (0) | 4/28 (14) |
| ≥ 2 years | 15/24 (63) | 20/28 (71) |
| CIS-R categories (ICD-10), n/N completed (%) | ||
| Primary diagnosis | ||
| No diagnosis identified | 2/35 (6) | 1/34 (3) |
| Generalised anxiety disorder – mild | 0/35 (0) | 1/34 (3) |
| Mixed anxiety and depressive disorder | 1/35 (3) | 1/34 (3) |
| Specific (isolated) phobia | 2/35 (6) | 0/34 (0) |
| Agoraphobia | 1/35 (3) | 0/34 (0) |
| Generalised anxiety disorder | 4/35 (11) | 4/34 (12) |
| Panic disorder | 2/35 (6) | 1/34 (3) |
| Mild depressive episode | 5/35 (14) | 6/34 (18) |
| Moderate depressive episode | 13/35 (37) | 16/34 (47) |
| Severe depressive episode | 5/35 (14) | 4/34 (12) |
| Secondary diagnosis | ||
| No diagnosis identified | 3/35 (9) | 1/34 (3) |
| Mixed anxiety and depressive disorder (mild) | 2/35 (6) | 2/34 (6) |
| Mixed anxiety and depressive disorder | 12/35 (34) | 7/34 (21) |
| Specific (isolated) phobia | 1/35 (3) | 2/34 (6) |
| Social phobia | 2/35 (6) | 5/34 (15) |
| Agoraphobia | 1/35 (3) | 1/34 (3) |
| Generalised anxiety disorder | 12/35 (34) | 12/34 (35) |
| Panic disorder | 2/35 (6) | 4/34 (12) |
| PANAS positive score, mean (SD), n | 19.2 (6.7), 31 | 22.2 (7.2), 33 |
| PANAS negative score, mean (SD), n | 28.2 (8.2), 31 | 29.9 (7.7), 34 |
| GAD-7 score, mean (SD), n | 12.9 (4.4), 32 | 12.4 (4.5), 34 |
| OCI-R score, mean (SD), n | 31.2 (15.4), 29 | 29.0 (13.7), 34 |
| WSAS score, mean (SD), n | 25.8 (8.9), 32 | 24.8 (7.8), 33 |
| SF-12 normalised physical function score, mean (SD), n | 43.4 (11.3), 30 | 41.8 (9.0), 32 |
| SF-12 normalised mental health score, mean (SD), n | 29.6 (10.0), 30 | 30.5 (7.0), 32 |
| EQ-5D-5L score, mean (SD), n | 0.605 (0.210), 31 | 0.621 (0.214), 33 |
| RBQ-2A score, mean (SD), n | 2.5 (0.5), 32 | 2.4 (0.5), 34 |
| RRQ rumination score, mean (SD), n | 4.1 (0.5), 30 | 4.1 (0.5), 33 |
At baseline, the mean PHQ-9 score was 15.8 (SD 4.1), with 55% of participants (n = 38/69) meeting ICD-10 criteria for a primary diagnosis of a moderate or severe depressive episode, and 24% (n = 15/62) having a primary diagnosis of an anxiety disorder according to the CIS-R (GAD-7, phobia or panic). Sixty-seven per cent (n = 35/52) had been depressed for ≥ 2 years. Fifty-four per cent of participants (n = 36/66) were taking antidepressant medication at baseline.
The numbers of participants in the two randomised groups (GSH and TAU) at baseline (see Table 2) were balanced in terms of the two minimisation variables (antidepressant medication and PHQ-9 score categories). Because the sample size was small (35 participants in each group), it was not unexpected that there would be some imbalance in characteristics between the groups by chance. The randomised groups had slight differences (> 5 points or > 5% as applicable; not prespecified in the SAP) in a number of variables measured at baseline. Those randomised to receive TAU were slightly older and were more likely to be male, in paid/voluntary employment and single than those randomised to GSH. The GSH group included more owner-occupiers and had a higher level of educational attainment [General Certificates of Secondary Education (GCSEs) or above]. The two groups were similar in terms of the percentage of participants taking medication for mental health, and having at least one experience of psychological/talking therapy.
Scores on the three depression measures (PHQ-9, BDI-II and HAM-D) were similar between the two groups at baseline. Most participants had a primary ICD-10 diagnosis of moderate or severe depression based on the CIS-R, although this was slightly unbalanced between the groups (TAU, 51%; GSH, 59%). The PANAS positive scores, PANAS negative scores, GAD-7 scores, OCI-R scores, WSAS scores, SF-12 normalised physical function scores, SF-12 normalised mental health scores, EQ-5D-5L scores, RBQ-2A score and RRQ rumination scores were also similar between the groups at baseline.
Participant retention
Seventeen per cent (6/35) of participants allocated to TAU and 11% (4/35) of participants allocated to GSH withdrew from the trial (Figure 2).
Follow-up rates at 10, 16 and 24 weeks differed between the groups, with the GSH group having higher rates of follow-up than the TAU group (see Figure 2; Table 3). The largest difference in follow-up rates was at 16 weeks (86% for GSH compared with 54% for TAU).
| Follow-up time point | Overall, % (95% CI), n | TAU, % (95% CI), n | GSH, % (95% CI), n |
|---|---|---|---|
| 10 weeks | 77 (66 to 86), 54 | 66 (48 to 80), 23 | 89 (73 to 96), 31 |
| 16 weeks | 70 (58 to 80), 49 | 54 (38 to 70), 19 | 86 (70 to 94), 30 |
| 24 weeks | 70 (58 to 80), 49 | 57 (40 to 73), 20 | 83 (66 to 92), 29 |
Outcome measures
On the PHQ-9, BDI-II, HAM-D, CIS-R, OCI-R, PANAS negative, GAD-7, WSAS, RBQ-2A and RRQ measures, a lower score is a more positive outcome. On the PANAS positive, SF-12 and EQ-5D-5L utility measures, a higher score is a more positive outcome.
Ten weeks
The mean scores on most of the outcome measures (PHQ-9, BDI-II, OCI-R, PANAS negative, GAD-7) were higher (worse outcome) or lower (PANAS positive, SF-12 physical function; worse outcome) for those in the TAU group than for those in the GSH group (Table 4). Across most measures, around 15% more participants responded in the GSH group than in the TAU group. The mean scores on the HAM-D, EQ-5D-5L and RRQ measures showed little difference between the groups.
| Outcome measure completed at 10 weeks post randomisation | TAU,a mean (SD), N completed | GSH,b mean (SD), N completed |
|---|---|---|
| PHQ-9 score | 14.1 (6.5), 23 | 11.0 (5.3), 31 |
| BDI-II score | 28.2 (11.8), 23 | 23.2 (11.4), 31 |
| HAM-D score | 13.2 (6.0), 17 | 13.6 (5.7), 27 |
| OCI-R score | 27.3 (18.3), 20 | 23.0 (13.9), 29 |
| PANAS: positive score | 19.6 (6.7), 23 | 22.5 (8.4), 31 |
| PANAS: negative score | 28.0 (7.2), 23 | 24.6 (7.7), 31 |
| GAD-7 score | 11.8 (5.4), 23 | 8.8 (5.3), 31 |
| WSAS score | 22.5 (9.7), 22 | 24.1 (9.2), 29 |
| SF-12 normalised physical function score | 45.2 (11.0), 22 | 42.4 (9.4), 28 |
| SF-12 normalised mental health score | 29.7 (12.4), 22 | 31.6 (9.2), 28 |
| EQ-5D-5L score | 0.590 (0.215), 22 | 0.606 (0.202), 29 |
| RRQ rumination score | 3.9 (0.8), 23 | 4.1 (0.6), 29 |
Sixteen weeks
By 16 weeks post randomisation, the mean scores for several outcome measures (PHQ-9, BDI-II, OCI-R, HAM-D, PANAS negative and GAD-7) in the GSH treatment group had further decreased (lower score, better outcome) or had increased (SF-12 physical function; higher score, better outcome) compared with scores at 10 weeks (Table 5). The mean scores of the outcome measures in the TAU group had also changed (compared with scores at 10 weeks), but not by as much, and the score changes were more variable and not consistently in the same direction. Differences between the group mean scores on HAM-D and quality of life (as measured with the EQ-5D-5L) presented as slightly larger at 16 weeks than at 10 weeks. The trend of increases in scores from baseline continued, with both groups showing better outcomes across all measures, except SF-12 normalised physical function for those in the GSH treatment group. There was, however, a large difference between the groups in the proportion of participants who were followed up and completed the measures (22% more participants were followed up in the GSH group); therefore, the findings should be interpreted with caution given the potential for bias.
| Outcome measure completed at 16 weeks post randomisation | TAU,a mean (SD), n completed | GSH,b mean (SD), n completed |
|---|---|---|
| PHQ-9 score | 12.9 (6.6), 17 | 9.4 (5.9), 28 |
| BDI-II score | 27.6 (13.6), 16 | 18.7 (10.3), 28 |
| HAM-D score | 14.5 (7.3), 18 | 10.5 (6.2), 29 |
| OCI-R score | 23.3 (16.4), 17 | 20.0 (12.0), 28 |
| PANAS: positive score | 20.5 (7.9), 17 | 25.0 (9.5), 27 |
| PANAS: negative score | 26.5 (8.6), 17 | 21.9 (7.2), 27 |
| GAD-7 score | 10.6 (5.7), 17 | 8.3 (4.5), 28 |
| WSAS score | 23.5 (9.9), 17 | 18.0 (9.8), 27 |
| SF-12 normalised physical function score | 42.8 (11.8), 16 | 41.5 (9.0), 27 |
| SF-12 normalised mental health score | 30.5 (11.7), 16 | 35.6 (10.0), 27 |
| EQ-5D-5L score | 0.660 (0.189), 16 | 0.691 (0.236), 28 |
Twenty-four weeks
By 24 weeks (Table 6) the mean scores for several outcome measures (PHQ-9, BDI-II, HAM-D, OCI-R, PANAS negative, GAD-7, WSAS) had increased (higher score, worse outcome) or decreased (SF-12 physical function; lower score, worse outcome) in both groups compared with 16 weeks. SF-12 physical function and quality of life (EQ-5D-5L) had increased (higher score, better outcome) in the GSH group. The trend from baseline continued, with both groups showing better outcomes across all measures, except for the PANAS positive score for those in the TAU treatment group and the SF-12 normalised mental health for those in the GSH treatment group. However, as previously, these findings should be interpreted with caution given the large differences in the proportion of participants who completed the measures between the groups, with 18% more participants in the GSH group than in the TAU group.
| Outcome measure completed at 24 weeks post randomisation | TAU,a mean (SD), n completed | GSH,b mean (SD), n completed |
|---|---|---|
| PHQ-9 score | 15.2 (6.4), 20 | 10.1 (6.1), 28 |
| BDI-II score | 29.6 (13.7), 20 | 20.3 (11.8), 28 |
| HAM-D score | 14.5 (8.0), 18 | 12.3 (7.1), 26 |
| OCI-R score | 25.7 (16.5), 17 | 22.1 (13.7), 27 |
| PANAS: positive score | 17.9 (5.4), 19 | 22.9 (9.1), 27 |
| PANAS: negative score | 26.6 (8.8), 18 | 24.3 (8.0), 28 |
| GAD-7 score | 12.3 (5.5), 20 | 8.5 (5.0), 28 |
| WSAS score | 24.6 (7.8), 20 | 19.2 (6.9), 28 |
| SF-12 normalised physical function score | 37.8 (14.3), 17 | 44.3 (9.8), 26 |
| SF-12 normalised mental health score | 28.9 (10.4), 17 | 33.2 (10.5), 26 |
| EQ-5D-5L score | 0.535 (0.223), 20 | 0.713 (0.185), 27 |
Adherence to guided self-help treatment
Eleven per cent (4/35) of participants in the GSH group withdrew from treatment (Figure 2). Of these, two participants did not receive any GSH treatment sessions and withdrew from trial, one participant attended two GSH sessions and withdrew from the trial and one participant withdrew after attending five GSH sessions but did not withdraw from the trial.
Ninety-one per cent (32/35) of participants received at least one session of GSH (Table 7). Of those who did not receive any GSH treatment sessions, two participants withdrew from the trial before they started treatment and one participant became too unwell to begin the treatment after randomisation but did not formally withdraw.
| Treatment information | GSHa n/N (%) |
|---|---|
| Treatment started | |
| ≤ 2 weeks after randomisation | 20/32 (63) |
| > 2 weeks after randomisation | 12/32 (38) |
| Total number of sessions attended | |
| 0 | 3/35 (9) |
| 1 | 0/35 (0) |
| 2 | 1/35 (3) |
| 3 | 0/35 (0) |
| 4 | 1/35 (3) |
| 5 | 1/35 (3) |
| 6 | 1/35 (3) |
| 7 | 0/35 (0) |
| 8 | 3/35 (9) |
| 9 | 25/35 (71) |
| Number completing five or more sessions | 30/35 (86) |
| Mean number of treatment sessions (SD), n | 7.6 (2.9), 35 |
| Number completing treatment: | |
| By 10 weeks | 10/32 (31) |
| By 16 weeks | 23/32 (72) |
| By 24 weeks | 27/32 (84) |
| Did not complete treatment | 5/32 (16) |
| Treatment conducted | |
| Face to face | 29/32 (91) |
| Skype | 3/32 (9) |
Sixty-three per cent (20/32) of participants started GSH treatment within 2 weeks of randomisation (see Table 7). The mean number of treatment sessions was 8.3 (SD 1.7 sessions, n = 32) and 94% (30/32) completed five or more sessions (prespecified as an adequate ‘dose’ of treatment). Seventy-two per cent (23/32) had completed treatment by 16 weeks. Ninety-one per cent (29/32) of participants had their treatment sessions conducted face to face; however, some participants could not attend face-to-face sessions (work/childcare commitments, n = 1; unable to leave the house, n = 2) and were offered treatment via Skype (9%, 3/32).
Treatment as usual
Of those in the TAU group who completed the use of services section of the follow-up questionnaire at 24 weeks, 15 had been prescribed antidepressant medication, nine had received primary care mental health support and one had received mental health support from secondary care services.
Candidate primary depression outcome(s) for main trial
As 72% of participants completed the GSH treatment by 16 weeks, the acceptability of the three outcome depression measures (PHQ-9, BDI-II and HAM-D) was assessed at this time point. A comparison was also carried out in respect of the sensitivity to change of the self-report measures of depression (PHQ-9 and BDI-II) with that of the observer-rated HAM-D.
Acceptability
Sixty-nine per cent (34/49) of participants completed the BDI-II and 78% (38/49) completed the PHQ-9 as well as the HAM-D at 16 weeks (denominators are those who completed at least one outcome measure at 16 weeks).
Adverse events
Four participants experienced adverse events (see Appendix 1): three in the GSH treatment group and one in the TAU group. None was related to the intervention or was determined to be a serious adverse event.
Inter-rater reliability of the Hamilton Depression Rating Scale outcome measure
The inter-rater reliability was assessed early in the study (in June 2017) when 14 HAM-D assessments were double rated. Inter-rater agreement on individual HAM-D items was variable, ranging from poor (37.5%) (item 1, depressed mood) to very good (87.5%) (items insomnia, guilt, insight). The average inter-rater agreement on individual item scores was 69.1%. Variability between items in terms of reliability and validity on the HAM-D measure has been previously reported. 69 The mean difference between total HAM-D scores between pairs of assessors across these first interviews was calculated. These results showed that the mean difference in total scores between the two assessors was 4.23 points.
Average inter-rater agreement expressed as percentage difference in total HAM-D scores was 9.6% for assessor 1 and 5.8% for assessor 2, indicating high rates (> 90%) of agreement between assessors. Although this is not the most robust way to calculate inter-rater reliability, the purpose was to ensure that the assessors at the two sites who had been trained to administer the HAM-D were doing so in a reliable fashion. Staff changes and an increase in volume of work had increased the number of staff working on the study who were trained in the administration of the HAM-D measure.
At the end of the study, 28% (56/202) of HAM-D interviews were rated twice; however, inter-rater reliability was poor. Only one pair of assessors had a Cohen’s kappa of > 0.8, which was prespecified as acceptable (Table 8). The range of Cohen’s kappa was between 0.1 and 0.8. Owing to the less than acceptable inter-rater reliability, all sensitivity to change analyses of the two self-reported depression measures (BDI-II and PHQ-9) are reported in Appendix 2. These prespecified analyses should be interpreted with caution.
| First assessor | Second assessor | Agreementa (%) | Cohen’s kappa (SE) |
|---|---|---|---|
| 1 | A | 38 | 0.2 (0.18) |
| 2 | A | 63 | 0.4 (0.21) |
| 3 | A | 63 | 0.1 (0.38) |
| 4 | B | 57 | 0.5 (0.18) |
| 5 | B | 88 | 0.8 (0.31) |
| 6 | B | 47 | 0.5 (0.20) |
| 7 | B | 50 | 0.3 (0.25) |
Blinding of the Hamilton Depression Rating Scale assessors
Assessors administering the HAM-D measure remained blinded to participants’ treatment group in 100% (18/18) of the TAU group and 96% (24/25, one missing report of blinding) of the GSH group at 10 weeks, in 100% (18/18) of the TAU group and 83% (24/29) of the GSH group at 16 weeks and in 100% (18/18) in the TAU group and 96% (24/25, on missing report of blinding) in the GSH group at 24 weeks.
Participant Global Rating of Change in depression
The patient-rated global measure of improvement in depression was considered at 16 and 24 weeks, although the numbers completing this item were small (see Appendix 2).
Use of health-care and voluntary services to inform an economic evaluation
The results that were available from both self-reported questionnaires and EMRs are given in Table 9. These data are available only for those participants from the Bristol region owing to issues with collecting EMR data from sites in Newcastle. Sixty-six per cent of participants self-reported use of antidepressant medication, whereas only 43% of participants had a prescription for such medication recorded in their EMR. Forty-nine per cent of participants were recorded as attending an NHS outpatient or community mental health team clinic for mental health problems in their EMR, compared with 11% of participants who self-reported attendance. The number of attendances was greater in the EMR than in the self-report data. Forty-six per cent of participants reported visiting their GP for any medical condition, and 26% of participants had a face-to-face visit with a GP at their practice recorded in their EMR, with a 37% concordance between these reports. The number of attendances self-reported was greater than that recorded in the EMRs. Participants rarely received a home visit from a GP for any medical condition.
| Outcome | Self-reported data from questionnaires (N = 35) | EMRs (N = 35) | Concordance between sources (N = 35) |
|---|---|---|---|
| Antidepressant medication used/prescribed (%) | 66 (n = 23, 0% missing) | 43 (n = 15, 14% missing) | 69 (n = 24, 0% missing both sources) |
| Number of different antidepressants used/prescribed, % (n/N) | |||
| 1 | 74 (17/23) | 93 (14/15) | 50 (12/24) |
| 2 | 13 (3/23) | 7 (1/15) | 0 |
| 3 | 13 (3/23) | 0 | 0 |
| NHS outpatient or community mental health team clinics for mental health problems (%) | 11 (n = 4, 9% missing) | 49 (n = 17, 11% missing) | 46 (n = 16, 0% missing both sources) |
| Number of visits, % (n/N) | |||
| 1 | 0 | 18 (3/17) | |
| 2 | 50 (2/4) | 0 | |
| 3 | 0 | 29 (5/17) | |
| 4 | 25 (1/4) | 0 | |
| 7 | 0 | 6 (1/17) | |
| 8 | 0 | 6 (1/17) | |
| 11 | 0 | 6 (1/17) | |
| 12 | 0 | 6 (1/17) | |
| 17 | 0 | 6 (1/17) | |
| 23 | 0 | 6 (1/17) | |
| 24 | 0 | 6 (1/17) | |
| 27 | 0 | 6 (1/17) | |
| 31 | 0 | 6 (1/17) | |
| Missing | 25 (1/4) | 0 | |
| At least one GP visit to a practice for any medical condition (%) | 46 (n = 16, 9% missing) | 26 (n = 9, 14% missing) | 37 (n = 13, 3% missing both sources) |
| Number of visits, % (n/N) | |||
| 0 | 46 (16/35) | 60 (21/35) | 31 (11/35) |
| 1 | 14 (5/35) | 9 (3/35) | 3 (1/35) |
| 2 | 11 (4/35) | 6 (2/35) | 0 |
| 3 | 6 (2/35) | 0 | 0 |
| 4 | 3 (1/35) | 3 (1/35) | 0 |
| 5 | 3 (1/35) | 9 (3/35) | 3 (1/35) |
| 6 | 3 (1/35) | 0 | 0 |
| 7 | 3 (1/35) | 0 | 0 |
| 9 | 3 (1/35) | 0 | 0 |
| Missing | 9 (3/35) | 14 (5/35) | 3 (1/35) |
| At least one GP home visit for any medical condition (%) | 3 (n = 1, 9% missing) | 0 (n = 0, 14% missing) | 77 (n = 27, 3% missing both sources) |
| Number of visits, % (n/N) | |||
| 0 | 89 (31/35) | 86 (30/35) | 60 (42/35) |
| 1 | 3 (1/35) | 0 | 0 |
| Missing | 9 (3/35) | 14 (5/35) | 3 (1/35) |
The use of other health-care and voluntary services, recorded using the self-report questionnaires only, is given in Table 10. These data are reported over the whole trial, so an outcome is recorded as completed if it was reported in at least one self-reported questionnaire and recorded as missing only if it was missing in every questionnaire. Twenty-nine per cent of participants reported using other medication for mental health problems. Participants did not report any overnight stays in an NHS hospital or visits to a private hospital or clinic because of mental health problems, and rarely attended an A&E department, an out-of-hours clinic or an NHS walk-in centre. Twenty-three per cent of participants had counselling or talking therapy during the trial outside the trial intervention. Participants used a variety of help for mental health problems, including groups, and received help around or outside the home. Twenty-seven per cent of participants took time off work because of mental health problems. Twenty-four per cent of participants attended a group for adults with autism. Participants rarely received a home visit from any other professional (for any medical condition). Thirty per cent of participants paid NHS prescription charges and 43% received disability payments.
| Outcome (at least once during study) | Self-reported data from questionnaires (N = 70) |
|---|---|
| Use other medication for mental health | 29% (n = 20, 4% missing) |
| At least one overnight stay in an NHS hospital because of mental health problems | 0% (n = 0, 20% missing) |
| At least one visit to an A&E department because of mental health problems | 1% (n = 1, 20% missing) |
| At least one visit to an out-of-hours clinic | 6% (n = 4, 24% missing) |
| At least one visit to an NHS walk-in centre | 10% (n = 7, 20% missing) |
| At least one visit to a private hospital or clinic because of mental health problems | 0% (n = 0, 20% missing) |
| Use counselling or talking therapy | 23% (n = 16, 21% missing) |
| Use online CBT | 1% (n = 1, 43% missing) |
| Use other services for mental health problems | 14% (n = 10, 20% missing) |
| Help for mental health problems from home help/home care worker | 9% (n = 6, 20% missing) |
| Help for mental health problems from day centre/drop-in | 7% (n = 5, 20% missing) |
| Help for mental health problems from social group | 14% (n = 10, 20% missing) |
| Help for mental health problems from self-help group | 10% (n = 7, 20% missing) |
| Help for mental health problems from voluntary organisation | 14% (n = 10, 20% missing) |
| Help for mental health problems from another source | 10% (n = 7, 21% missing) |
| Help with childcare because of mental health problems | 4% (n = 3, 20% missing) |
| Help in and around the house because of mental health problems | 31% (n = 22, 20% missing) |
| Help outside the house because of mental health problems | 23% (n = 16, 20% missing) |
| Other additional help because of mental health problems | 13% (n = 9, 20% missing) |
| Purchase over-the-counter treatments | 7% (n = 5, 20% missing) |
| Have time off work | 27% (n = 19, 20% missing) |
| Anyone else time off work to care because of mental health problems | 7% (n = 5, 20% missing) |
| Attend autism social group | 24% (n = 17, 20% missing) |
| Attend autism drop-in or advice service | 26% (n = 18, 20% missing) |
| Attend autism carers’ support group | 6% (n = 4, 20% missing) |
| Have allocated social worker | 13% (n = 9, 20% missing) |
| Receive support to attend work | 7% (n = 5, 20% missing) |
| Attend other service for autism | 14% (n = 10, 20% missing) |
| Use complementary or alternative therapy for any medical condition | 3% (n = 2, 20% missing) |
| Use exercise activity scheme for any medical condition | 0% (n = 0, 20% missing) |
| Use NHS Direct for any medical condition | 6% (n = 4, 20% missing) |
| Use community-based health service professionals for any medical condition | 11% (n = 8, 20% missing) |
| Home visit from community support worker for any medical condition | 10% (n = 7, 20% missing) |
| Home visit from mental health nurse for any medical condition | 3% (n = 2, 20% missing) |
| Home visit from occupational therapist for any medical condition | 0% (n = 0, 20% missing) |
| Home visit from social worker | 6% (n = 4, 20% missing) |
| Home visit from other professional for any medical condition | 7% (n = 5, 20% missing) |
| Be victim of crime | 6% (n = 4, 20% missing) |
| Be suspect in criminal investigation | 0% (n = 0, 20% missing) |
| Appear in court as witness | 0% (n = 0, 20% missing) |
| Appear in court as suspect | 0% (n = 0, 21% missing) |
| Meet probation officer | 1% (n = 1, 20% missing) |
| Be in custody | 0% (n = 0, 21% missing) |
| Pay NHS prescription charges | 30% (n = 21, 20% missing) |
| Receive disability payments | 43% (n = 30, 20% missing) |
| Receive carer’s allowance for patient | 6% (n = 4, 20% missing) |
Participants did not come into contact with the criminal justice system (either as a victim or as a potential suspect).
Chapter 4 Qualitative study
Introduction
The value of integrating qualitative methods in RCTs is in exploring the views and experiences of trial participants and of those delivering the intervention. Qualitative data can be an essential part of a trial’s evaluation and can highlight possible reasons for quantitative findings. In the Autism DEPression Trial (ADEPT), qualitative methods were critical to illuminate the perceived value and acceptability of the trial design and GSH to enable the refinement of the intervention.
The specific aim and objectives of the qualitative component of the trial were as follows.
Aim
To understand trial participants’ and GSH coaches’ views and experiences of the trial and of GSH or TAU.
Objectives
-
To explore, using qualitative methods, trial participants’ views, experiences and beliefs about therapy for depression.
-
To examine trial participants’ understanding and knowledge of GSH and their treatment expectations.
-
To explore the feasibility and acceptability of the trial design.
-
To understand trial participants’ and coaches’ experiences of the trial, including their perceptions, experience, opinions and acceptability of GSH and TAU.
-
To use qualitative methods to understand the barriers to and facilitators of GSH to enable intervention to be refined for a future effectiveness trial.
Methods
Study design
In-depth interviews were conducted with participants (from both arms of the trial) 10 weeks after randomisation (after the 10-week outcome measurement was complete). These interviews considered and compared views and experiences of the trial and the acceptability of the GSH intervention. All coaches delivering the GSH intervention were approached for an interview towards the end of the trial to illuminate the perceived effectiveness and acceptability of GSH and explore any barriers to its uptake.
Recruitment and sampling
Purposive sampling was used to select trial participant interviewees in an attempt to capture maximum variation in views and experiences in order that they adequately reflected those of a range of trial participants. All trial participants had consented at baseline to being approached by a qualitative researcher. From participants who had indicated that they would be willing to be contacted, a purposive sample was drawn in relation to (1) the trial site, (2) the trial arm and (3) sociodemographic variables such as age, gender, ethnicity and socioeconomic status (with participants selected from areas of high and low socioeconomic deprivation). Interviews were analysed in batches, and sampling continued until no new themes emerged from the interviews.
Interview conduct
All interviews were conducted over the telephone or face to face in a location of the participant’s choice. Interviews followed topic guides developed at the start of the study based on the literature, the qualitative study aims and input from the Trial Management Group (TMG). The topic guide was used to ensure that primary issues were covered during all interviews, but without dictating data collection, allowing participants to introduce unanticipated issues. All interviews were conducted by two clinical psychologists in training (Hannah Harvey and Lauren Evans) under the supervision of a senior qualitative researcher (Jeremy Horwood). Neither interviewer had been previously known to participants. Interviews lasted between 26 and 65 minutes (mean 47 minutes).
In telephone interviews, consent was taken verbally prior to the interview. In face-to-face interviews, participants gave written consent. Field notes were taken during and after the interviews and these were integrated into the analysis. All interviews were digitally recorded, professionally transcribed verbatim, anonymised and checked for accuracy prior to analysis. Transcripts and field notes were imported into NVivo version 10 software (QSR International, Warrington, UK) for analysis. 71
Analysis of the interviews
Analysis was conducted in parallel with data collection, with findings from early analysis informing later data collection in an iterative process until data indicated saturation. Thematic analysis was used to analyse the data using the following steps:
-
Familiarisation with the data through detailed reading.
-
Two members of the qualitative research team independently constructed draft coding frames using line-by-line coding of a sample of the data. A combination of deductive coding, based on the aims of the study and the topic guide, and inductive coding, identifying themes within the data, was used.
-
A subset of transcripts was independently double coded by members of the research team (HH, LE and JH) and the coding compared, and discrepancies were discussed and resolved to achieve a coding consensus and to decide on the final draft of coding frame to be used.
-
The themes were defined (in NVivo) and the coding frame applied to the data by one researcher.
-
The researcher met with the rest of the qualitative team as coding progressed to review and discuss emerging findings.
-
A narrative was drafted based on the analysis, paying attention to patterns and deviant cases, with input from the qualitative team. Separate coding frames were created for participants’ and coaches’ data sets. Emerging findings were also discussed at TMG meetings to refine the topic guide and qualitative analysis and inform trial conduct. The analysis led to the development of the key emergent themes outlined below with the use of verbatim quotations.
Results
Participants
Five therapist ‘coaches’ were interviewed: three from the Bristol site and two from the Newcastle site. All coaches interviewed were assistant psychologists, except one who was a clinical psychologist in training. Two coaches had not previously worked with adults with ASD. Therapists had conducted the GSH intervention with between 1 and 13 trial participants (mean seven trial participants).
Twenty-one trial participants were interviewed, 14 randomised to the GSH arm and seven to the TAU arm (age range 21–58 years, mean 40 years) (Table 11). All trial participants interviewed were white British. Eighteen participants had received an ASD diagnosis in the previous 6 years and nine had received it in the previous year. Eighteen trial participants had previously engaged in therapy for anxiety and/or depression, with 10 previously receiving CBT. All initials of participants refer to pseudonyms, with trial participants being Mr or Ms A–U and coaches C1–C5.
| Characteristic | Participants (n) |
|---|---|
| Trial arm | |
| GSH | 14 |
| TAU | 7 |
| Site | |
| Bristol | 9 |
| Newcastle | 12 |
| Gender | |
| Male | 17 |
| Female | 4 |
| Age group (years) | |
| 21–25 | 2 |
| 26–30 | 4 |
| 31–35 | 4 |
| 36–40 | 1 |
| 41–45 | 3 |
| 46–50 | 2 |
| 51–55 | 2 |
| 56–60 | 3 |
| Employment status | |
| Employed (full time) | 5 |
| Employed (part time) | 3 |
| Self-employed | 3 |
| Unemployed | 8 |
| Student | 2 |
| Deprivation category | |
| High | 6 |
| Medium | 6 |
| Low | 9 |
| PHQ-9 score | |
| Range | 10–24 |
| Mean | 15.4 |
Trial participants’ views and experiences
Previous therapy
The majority of participants (19/21) had previously attended psychological therapy before participating in ADEPT, with CBT being the most frequent model of treatment. Two participants had also previously engaged in counselling and another had participated in eye movement desensitisation and reprocessing and positive psychology in addition to CBT. One participant had experience of psychotherapy and another had tried computerised CBT. The duration and amount of previous therapy varied. Some participants had attended three sessions of treatment while others had been engaged for up to 2 years. The time frame also varied, with some participants engaging in other therapies shortly before entering the ADEPT trial whereas others had not done so for > 10 years.
Two participants talked positively of their previous experiences of CBT, with one participant highlighting the positive impact it had on their mood and another describing how they still found some of the strategies helpful. However, some participants did not find their previous experiences of CBT helpful. The reasons for this included finding it difficult to describe their feelings and to identify triggering situations, difficulties engaging because of other factors in their life, the treatment involving not many practical aspects, and being asked to do things that they did not feel ready for. When compared with previous therapy GSH participants appreciated taking part in treatment that was tailored to people with ASD:
But the CBT you’re weighing up your thinking and your beliefs and your prophecies almost [inaudible 0:04:22.8]. And then the action planning and testing. That I wasn’t very good at and I’m still not very good at but the way in what that . . . that’s something I still use.
Ms F
Just someone who maybe understood a little bit about how I can understand and communicate and things like that. I found it [previous CBT] hard to get any perspective and so I was unable to communicate exactly what was going on. I would go into sessions and just wail for an hour and so yes, this [ADEPT] was new, to have someone who understood and even if I wasn’t feeling up to it I was able to come and just sit and eventually I’d come out of me shell a little bit more whereas when I was accessing services before I was probably masking still. It was nice to be able to engage with something and actually feel like it was doing me good.
Ms G
The last time I did CBT it was useful up to a certain point. It didn’t really seem to consist of many practical exercises. It seemed to consist mainly on reciting information back to myself and it was less focused on actually going out and then performing different kinds of behaviour . . . It got to a point where I was being told to basically go to a public place of some kind and just start talking to strangers. That wasn’t something that I was particularly comfortable with doing and I didn’t think that that was going to solve any particular problem.
Mr E
Since being diagnosed I’ve just been trying to find some help that’s a bit more autism specific because some of the stuff that I’d had before wasn’t necessarily – it just didn’t really feel like it was working.
Mr C
Trial understanding
The majority of participants said that they were given the right amount of information about the trial and that this information was understandable. One participant commented that it would have been helpful to have additional information illustrating people with ASD’s previous experiences of CBT as a way of explaining the rationale for the adapted GSH. On the other hand, one participant felt that there could have been slightly less information given in the information sheet as it replicated what she had already been told about the trial by a researcher. One participant commented that it was helpful to have someone to go through the information with them to aid their understanding:
There would be two groups. Anyone taking part would be in one of the two groups: a control group, what is the standard therapy and the more adapted therapy for people with autism.
Mr D
I grasped it fully. My partner did too. It was easy to register my interest and easy to get onto the trial. The information sheet was fab. It was everything you needed really.
Ms G
Just how many sessions, what roughly it would be like and then obviously the follow-up sessions as well, so I knew exactly what it was going to be, because if it had been vague and that, it would be hard to sort of gauge what it would be like.
Mr B
I suppose it might have been interesting to have had some information on other people’s reactions to CBT, other people with something like Asperger’s syndrome: how they had reacted to CBT and what their experiences had been, if they’d had CBT in the past.
Mr E
My social worker explained to me really well. This was my learning thing you know, I don’t always process everything and I read information or when things are being said to me I have to have it repeated and if it’s too complex . . . you know she did explain it fully to me so I knew everything that was going on.
Ms I
The majority of trial participants had a clear understanding of what taking part in the trial involved, although there was some uncertainty around the content of the GSH therapy:
Attending sessions or telephone conversations on a regular basis over a period of time a minimum of like 10 weeks plus the follow-up. You know, it was all fairly well.
Mr C
I wasn’t too sure really, but having done CBT before a long time ago I thought it might be something not too dissimilar to that, possibly with some new elements which I hadn’t encountered before.
Mr E
Well I wasn’t sure because I think she said there was elements of CBT but that there were also differences to make it more accessible and then also maybe some other techniques brought into it as well. So I didn’t really have any set idea in mind.
Ms F
I think there was some explanation. It was very clear to me I was getting involved in a talking therapy where I’d have some sessions with another person and I went in a room with no idea about what that would be and I was fine with that. That’s perfectly reasonable.
Mr Q
Three participants reflected that they had felt nervous about taking part in the trial as they had not known what to expect, they had worried about having to try another treatment aimed at improving their mood, or they had difficulties trusting other people:
Yeah, a little bit nervous to start with . . . As to what is was going to entail. What was going to be needed of me. What was going to be asked of me. How personal it was going to be and not knowing I didn’t think initially as to whether it was going to be many people and whether one to one because although I come across as quite good in groups, I don’t really like group work. I much more prefer sort of one to one and am more comfortable.
Mr C
Well as with everything I was quite . . . I suppose you could say anxious or stressed about having to do something else to help my mood, help me get better or get back to where I used to be. But then when I thought about it and it did say as you say, I could stop doing it at any time I wanted or whatever, so. I was . . . basically I was just thinking about well what’s the next step and then get onto that step and then I can ask the questions and then, you know, like that sort of thing, take one step at a time, or one meeting at a time sort of thing.
Mr K
The majority of trial participants commented that they thought that the trial was evaluating whether or not a newly adapted intervention is effective for low mood in people with ASD, and that this was being compared with standard NHS therapy:
By my understanding it was to see if a different form of therapy could be adapted for people with autism as there’s quite a big group of people with autism where standard therapy doesn’t really help with so this was more of a tailored therapy for people with autism.
Mr D
To see if certain adaptations could be made to an exact mix of CBT to see if it could be made to be more effective for people with an autistic spectrum condition.
Mr E
One participant thought that the trial was comparing experiences of depression in people with ASD and those of people who do not have ASD, and another thought that the trial was comparing self-help with CBT:
The difference between a person . . . an ordinary person who doesn’t have autism, how depression can differ with someone like that to a person with depression that’s got autism and if there’s any differences in the experiences.
Ms I
Difference between self-help and CBT. Trying to understand the difference, which one would be the best of the two.
Mr R
All but three participants knew that participants were randomly allocated to either GSH or TAU at random. Two participants said that they did not know how participants were allocated. One participant thought that group allocation depended on their initial answers to the questionnaires:
I understood it was randomised and I also understand why you need to have that controlled group in there.
Mr B
My understanding was that a lady called [name] who I saw first off before I did this went and pressed a button on a computer and it randomly told her.
Mr Q
It was explained that my information would be put into a computer program, which would decide on what group to put me into.
Mr D
Well basically we had a questionnaire or something to fill in or questions were asked and it was from that so I gather but I don’t know what the criteria would have been for deciding.
Mr K
Some participants questioned how a comparison could be made between the GSH and TAU groups because those in the TAU groups potentially had to wait a long time to start their treatment:
I think the only thing that I ever questioned and that was with somebody that wasn’t well or was aware of what study I was on, but I thought, I think I mentioned it to [ADEPT researcher] before we’d even got to the point of me being not part of the study where I just said, well if you’re starting the 10 weeks as soon as you kind of can for guided self-help, then it’s always it’s kind of making the study a bit difficult to kind of work out what’s helping and what’s not, because there’s such a delay. If you’d have had like a certain amount of people like psychologists or whatever there, ready to do both sides of the study then it would be a little bit fairer.
Mr J
In a way one thing I don’t know how you’re gonna get an equal comparison in the trial, you’ve got people who have basically fast tracked into it rather than have to sit around and wait for a year or two. The treatment-as-usual people probably won’t have been treated. I honestly don’t know how you’re going to evaluate the trial on that basis. Perhaps something will actually happen as distinct from it happening sometime never like things in the health service have a way of doing. But that’s not a criticism of the health service as you realise.
Mr Q
Well they could have waited until I’d had my CBT before comparing this thing ‘cause I hadn’t had any treatment. I’ve never been treated until the 20th October, no 13th, start next week. So we only receive the last bit – my last one – there’ll be any improvement. You’ll see the first bit, but don’t know if it’s improved through the process and drop back off again.
Mr R
My first appointment was only a few weeks ago, I think it was just after the 10 weeks when I got the phone call to organise the appointment.
Mr J
Trial participation reasons
Most trial participants said that they had taken part in the trial because they were hoping that the GSH intervention would lead to improvements in their mood. Six participants commented that they wanted to contribute to research that may be helpful for other people with similar difficulties:
First of all I wanted to do it because there were certain problems that I was having and also it seemed like it would be a useful thing to do. It might help other people having similar problems.
Mr E
It feels like I’m getting something and contributing something all at the same time. Because I’m autistic I spend a lot of time – on my particular presentation of autism – I spend a lot of time feeling uninvolved and disconnected from stuff. Also somebody wanting to be involved in something that’s going to be useful seems like a good idea.
Mr Q
That’s a really good question. I would like to think, being quite interested in research anyway and things like this and I thought it was a good way to kind of make a contribution and also kind of face the diagnosis as well and maybe learn a little more about myself. It wasn’t altogether altruistic because I was hopeful that it may lead to some beneficial treatment for me as well.
Mr U
Three participants said that they had taken part in the trial to have the opportunity to try a new intervention that was different from what they had experienced previously and that focused on the needs of people with ASD:
So I was really interested in taking part, because I had a tiny bit of experience of talking therapy before and I had only just started some CBT, just prior to hearing about the research, so I was very interested in trying something that was geared more towards people with autism.
Mr B
Really hoping that a new form of therapy would help me more than the standard therapy, what hasn’t really helped me much so that was what I was trying to get out of it. Even if I wasn’t put on the new therapy group it would possibly lead to a new therapy being adapted and implemented so that I would in the future go on it.
Mr D
To see if there was anything that would help me and the idea of it being tailored to autism. I was interested to see what was different about it from the therapies I’d already had.
Ms F
When deciding whether or not to take part in the trial, there was variation in whether or not participants discussed their decision with others. Those who had not discussed the trial with others found the study information clear and the decision to take part relatively simple:
I did the research on it before accepting it and it seems all pretty straightforward so I just did it.
Mr D
Eight participants interviewed did discuss their decision to participate in the trial with others. Seven participants discussed their decision with a family member and one discussed it with their social worker. Two participants wanted reassurance from others that it was worth taking part in the trial, whereas one participant wanted to clarify that he was appropriate for the trial. One participant said that he could not understand the study information and so he asked his father:
Although I knew it in myself that I wasn’t happy with just everything in life at the moment, I didn’t know whether I was classed or going to be classed as low mood and so on and so forth. So I just wanted to double check with my wife as to whether she thought that how I was feeling at the time, so yeah so . . . Yeah, yeah just to make sure it was worthwhile and that I wasn’t wasting your time and stuff.
Mr C
I couldn’t understand most of it so I just asked me dad and he just explained it. He says it will be good for you to get involved with it.
Mr L
Preference for guided self-help
In terms of group preference, all but three trial participants interviewed said that they had wanted to be allocated to the GSH group. The other three participants said that they had not had a preference for a group. Reasons for wanting to be in the GSH group included to see whether or not GSH was effective; to try a new treatment as they had already tried other forms of therapy, such as CBT, and not found them helpful; to have access to a treatment that took into account the needs of people with ASD; and because they would find it difficult to explain their difficulties to their GP to be able gain access to treatment. One participant commented that his allocation to the TAU group (and his previous negative experience of mainstream services) was the reason he withdrew from the study:
I certainly preferred to be in the group that I was in because I’d done regular CBT before . . . I thought it would be a good idea, especially considering that I’d tried CBT in the past and not found it all that helpful, which I thought may have been to do with the fact that I had Asperger’s syndrome. I hadn’t been diagnosed with Asperger’s syndrome when I’d first done CBT so I thought that that may have been part of the reason why it wasn’t so effective. I thought it would probably be a good opportunity. It would be a way of helping basically.
Mr E
I think, if I hadn’t been in the group I’ve been in, I think I would have perhaps dropped out because what I had previously been given wasn’t helping and wasn’t altering anything.
Mr M
I’d previously had the other service and that wasn’t helpful so it would be back to square one so I was kind of hoping and fortunately for me, it’s worked out that way and it was the new stuff.
Mr P
Yes I did rather hope I would end up in the group with the new treatment which is where I did end up. I suppose that was partly ‘cause otherwise I’d then go and have to have a discussion with the GP and explain what I’m doing. I don’t like explaining things to people.
Mr Q
It’s a two-to-one chance that it’s going to work or that I’m going to have to withdraw. I remember saying that very, very specifically, not that I might get in or I might not. It was literally I either will or I will withdraw, so pretty much as soon as I’d seen how the sampling was going to work, it was kind of ‘Oh yeah, oh this is going to be a one or the other’ . . . The allocation didn’t come until quite late in proceedings and it wasn’t until then that I realised ‘Well, I actually might end up in a group here that is where I was 2 years ago and I found of no benefit whatsoever’ and then that’s pretty much what happened. I ended up in that group and thinking ‘Well, this is gonna entail 10 days of leave from work so something that I know doesn’t work for me’ so I just couldn’t. A terrible, you know, concrete way of looking at things, but that literally was it. ‘This is gonna be of no benefit and whilst I’d love to help the study, I can’t take 10 days of leave to do so.’
Mr U
Acceptability of the trial
The majority of participants said that they found the trial acceptable and in line with what they had expected. Two participants commented on how they did not feel like they were taking part in a trial, as trial participation mainly involved them seeing a coach:
Not too bad, I guess. I was in the control group so I didn’t really have much involvement in the ADEPT study really, just the scoring of how it helped.
Mr U
Yeah I suppose so. That part was fairly easy enough because everything was explained to me every time I went sort of thing, so it’s not as though I’m thinking about things and thinking, well they’re not telling me this or not telling me that. I found it quite helpful.
Mr K
It hasn’t really necessarily felt like taking part in a trial simply because it’s just involved me seeing a CBT therapist. There’s not been any problem with it. It’s been fine.
Mr E
I’ve found it quite interesting actually. It didn’t mostly feel like a trial. It was presented by a person doing – and accepted by me – as a treatment. The fact that it was trial. I mean what we would very occasionally refer to that. But it kind of didn’t feel like that so I think it’s as it should be.
Mr Q
Five participants had difficulties with the location of their appointments, which related to difficulties parking or finding the right building. These participants would have liked to have been given directions and more information on where to park:
I knew I was coming to [name of building] House but I didn’t know what the buildings were called. I don’t think there was a map. I knew to go in and just ask and I did but I felt like an idiot and then you feel like you’re on a wild goose chase and have I got the right place? Just explain that there’s a number of buildings, you’ve got the [name of company] bit or whatever, just a little bit more of an understanding. It’s good to look on Google maps [Google Inc., Mountain View, CA, USA] and stuff but just to know that you can get parked or that there is an issue with spaces, come and give plenty of time or find somewhere nearby that you could . . . I think, on one of the occasions, I rang my practitioner to say, ‘I can’t get parked. I don’t know what to do,’ and she said, ‘well try over the road in the school, you can get parked in there,’ and I didn’t know that and I’d been coming for weeks and so just knowing that would [over speaking 0:37:59.4] have been helpful.
Ms G
I think maybe the location wasn’t ideal, but the only reason I had to fight through traffic every morning. I used to get stressed. I was quite calm when I left the house but getting to [XXXX] and then trying to find a car park really got me stressed, so obviously when I walked in there I was trying to calm down.
Mr M
One participant said that because timing of the appointments was such that they did not interfere with his work, this made participating in the trial easier:
It hasn’t impact on my work that much either. I was a bit worried in the beginning that I would have to take days off and holidays, but I think I got appointments more or less half nine in the morning, quarter past nine, which meant I could go back to work without having to take a day’s holiday, but I think I would have struggled if it had have been nine to five hours and I couldn’t have the flexibility in my job. If it had have been evenings, that would have been a bit better, but yeah, I think that’s what kept me going as well. If it had have started impacting on my work, I would have had to stop.
Mr M
Views and understanding of guided self-help
Most participants in the intervention arm said that GSH provided them with the building blocks to understand the relationship between low mood and their behaviour and activities. They commented on how making some changes to their activities (be they big or small) could have an impact on their mood. Others recognised that an important aspect of GSH was practising what they had learnt in sessions on their own:
Was that there were stages, I suppose building blocks as to needing to work on a foundation and then like working out the period as of, you know, in the paperwork, to – but basically working on how you feel and what you’re doing but yeah, like I say on building blocks so that’s the easiest way I can explain it.
Mr C
To help to improve my mood and to start doing different kinds of activities, so not to keep doing the same things. I understood it to be, if my mood is low, then I keep repeating the same behaviour then my mood will be expected to stay low so therefore changes to those patterns and routines would need to take place. That that could happen on quite a small-scale level with the granularity of events and it could also be on a larger scale in terms of doing entirely new things. There may be smaller changes that could be made to things that I’m already doing that would help to improve mood but then also bigger changes to my overall routine. Different things, like different places I could go, all that kind of thing.
Mr E
Obviously, I’ve come across it as a CBT before and I do think it’s useful because first of all you feel like you’re doing something useful while you’re inbetween sessions and you’ve got to get used to practising these things on your own.
Ms F
The main thing I thought is that it would be about me doing things instead of looking at what my problems are as much as more just trying to actively do stuff instead of looking at the problems in my life, just trying to change my life in the present.
Ms T
The majority of participants said that they valued the guided element of GSH and that the input from the coach provided them with additional support during their treatment:
Yeah, that was good. Because sometimes it’s one of those things where, I’ve always felt that I get on with things better by myself, but it’s not really true [laughs]. Sometimes when you do things like distance learning courses or just have your own material to work through, you kind of realise you miss the framework and routine guidance that you get from a proper training or educational routine. So yeah, it’s good to have the stuff there, so you can do it yourself, but then have that as a back-up, or to start off with that routine, and then have yourself as well, if that makes sense?
Mr B
That’s it, you’re not gonna fix yourself overnight so to have someone come in and guide you through it each session was really, really useful.
Ms G
Views and experiences of guided self-help sessions
Overall, the majority of the participants had a positive view of the pacing of the session content. However, views relating to specific sessions appeared mixed. For example, several participants noted that the initial sessions, which focused on introducing the map and situation triangles, were a little slow. These participants thought that these initial sessions could have included more content, or that they could have been given the materials to read at home:
The fact that it was very measured and set out and prescribed and go through each page and each step so that everyone’s going through the same routines and see how to break down each session and that made it really manageable. It really stopped it feeling overwhelming. If we were to sit down and say, ‘OK today we’re gonna do this, this, this, this and this,’ I’d just go, ‘Oh no! I’ve had enough’. To say, ‘we’re gonna look at this and this . . .’ but then the homework just compounds what you’ve just learnt so that made it achievable. I think in the past when I’ve been set homework you kind of feel I can’t do this it’s too much, it’s overwhelming, it’s gonna be rubbish or whatever, I can’t get my head round it. But actually the homework that I was doing just was what we’d done in the session and just putting it into practice and I found that really useful and it made me feel that I could actually do the homework.
Ms G
I just felt that we spent the first 3 weeks, for most of the time, going through explaining what CBT is and how it worked, and I felt it could have all been compressed into one or two sessions. It felt it was very, like it was dragged out and extended and very slow, which made it quite difficult to keep motivated throughout.
Mr H
Sometimes I would have liked to have done a bit more actually. Like at the start, I know it’s different for everyone, but it seemed to take a very small part of what they’re doing each week, in the first few weeks maybe, and that I could have like done it in maybe half that time.
Mr B
The first one as I say I didn’t really see the point cos there wasn’t really any activities. From what was said I think some of the other people in the room maybe benefited from having the sheets read to them but I didn’t. That isn’t the case for me so for me I could have just had those sheets at home and read them at home.
Ms F
A couple of participants commented that the pacing of the sessions was a little fast and that there was not enough time in sessions, particularly in the middle weeks. These participants felt that, as a result, they did not have enough time to discuss the material in as much depth as they would have liked, which had an impact on their engagement with homework, or that sessions ran beyond their scheduled 30 minutes:
There may not have been enough time to have covered everything in quite as much depth as perhaps it could be.
Mr E
Because it was literally half an hour, there just wasn’t enough time and I know several of our sessions went over to an hour or just very slightly over an hour so I don’t know whether that was literally just because I was going off topic a lot or just whether it was the whole explanation of what we were doing and then talking about how it was gonna be done ready for next week . . . half an hour’s just really not long enough.
Mr C
Yeah, it would depend really. Sometimes there could maybe be lots of things that I could talk about in a bit more detail but you are aware that there’s not a lot of time and like at the beginning the guy had said we have to try and keep it – which I completely understand because you don’t want to go off talking about random things but even within that I felt like there were still things to talk about.
Ms T
No, no, no, it seemed to be like it should be like an hour . . . Just needed to talk more and get you know more, more, yeah, a more better connection.
Mr N
Most participants had a positive view of the printed materials used in the GSH sessions. Most participants felt that the materials were presented in a clear, easy-to-read format and that they were written in understandable language and clearly described what participants had to do for each task. Some participants felt that having their own copy of the GSH materials acted as a useful reminder of the content of sessions. A minority of participant found the materials too simplistic and childlike:
On paper was good because then you’ve got a record of what you need to do if you forget. Because I do forget. So yeah it was good.
Ms F
The fact that each booklet re-capped over what you’d done in a session, how far you’ve come and then, ‘we’re gonna look at this this week and this is the principle . . .’ break it down and then, ‘this is how you apply it . . .’ so each step leads into the next step and that was really useful.
Ms G
I think some of the handouts were a bit – I found some of it quite primary school.
Mr M
Situations map
Three participants reported that they had found the situations map particularly helpful. Most participants said that they had used the map to document where they had been over the previous week and how often they had been there. The majority reported that using the map had increased their awareness of their behaviour and level of activity during the week, highlighting that this was not something they would normally focus on. Several participants commented that using the map also focused their mind on the impact of changes in routine, or exceptions to their normal routine, on their mood:
A visual aid like that [situations map] I think is a very useful tool I was able to use. I was able to explain it, the way I’d written . . . drawn it.
Mr K
And the other little map as well was good, to see, even when I was thinking I wasn’t doing a lot, when you write it down in a week and you can show how many times you have been to this certain place and looking at that guide, you sort of think, ‘oh yeah, I’ve actually done more than I thought I had done’.
Mr B
It just made me think a bit more about the routines and patterns that I tend to stick to because those aren’t really things that I would consciously think about otherwise. It made it easier to focus on making changes to my behaviour and things.
Mr E
Several participants created their own maps using pen and paper or adapted the copy from the materials. However, another participant commented that the layout and size of the map in the materials pack made it difficult to use as the layout of locations did not resemble their own life. They suggested that providing sticky notes for each image that an individual wanted to include on their map so that they could arrange it themselves would also support personalisation:
They’re not great maps, don’t get me wrong. I just found that easier to do my own and also because I do work and I don’t know . . . because I’m involved in the church as well I brought quite a few different locations each week so I just found it easier to do a new one each week and it helped me remember what I’d been doing then.
Ms F
The map was OK but I found myself having to reorder everything and rename everything because it didn’t fit with what I did. Most of my stuff was in the house so I had to try to expand the picture of the house to try and add more things into it of what I did.
Mr S
Just the size and the shape of it [situations map] and the actual images are very kind of, what’s the word, I would say basic but I found it hard to use because it was all very close together and in my personal life the house isn’t as close to this as to that and so forth so I did try and I was going to draw my own map, which was fine and I went home after this session and I tried drawing out but I actually used an actual map to locate and put it and work positions as to where I was working, my daughter’s college, the schools, the shops and whatever. But then it was all too small so I kind of got annoyed with myself and then we just kind of just sort of just – well whatever, and just used that particular printed copy and stuck some triangles on it.
Mr C
Situation triangles/granularity
The majority of participants commented that they had found the situation triangles helpful. The majority stated that the most helpful thing about the situation triangles had been breaking situations down, focusing on the link between feelings and behaviour. One participant said that writing down particular situations had helped them to externalise their feelings:
But yeah, definitely breaking it down and just looking at the things I was doing a bit more closely, was a big help.
Mr B
Probably doing triangles. I hate to admit it, but it’s probably true . . . working out what you could have done differently.
Mr O
So straight away I was able to spot that I was listening to music and they were the moments that my mood was picking up and that I was able to say, ‘oh well, that activity made me feel better as well just like the music did’. So it really helped me put the theory into practice.
Ms G
A minority of participants specifically mentioned the concept of granularity (the process of chaining several situation triangles). They reported that this helped them to focus on a whole situation rather than on one negative moment. One commented that introducing the triangles slowly, focusing on one aspect and then adding another, had supported their understanding and use of the technique. Several participants commented that they had applied the concepts they had learnt in sessions regarding the situation triangles to other situations in their lives (e.g. to understand more negative situations and to approach situations they had encountered after sessions):
The breaking it down like that it meant that I was looking at experiences rather than . . . I was looking at the whole thing and finding the many benefits rather than just the bit that I hadn’t liked.
Ms F
It’s just, because there’s all this triangulation of you’re doing your little triangles and stuff and all that and situations, behavioural stuff and that and trying to, trying to not I mean because say I’d go in, I’d had a week where I’d go in and I’d say I’ve had a terrible week, this has happened, but then I’d talk to my therapist and she’d say, ‘well, OK, let’s talk about the rest of the week’ and it transpired that one thing had gone wrong, but the rest of the week had been OK and I’d just focused on the negative thing and ignored all of the positives and she made me think, ‘no, you’ve got to try and not think about that, think about all the other things’, and I did, I have been doing that a bit more.
Mr N
I think just breaking down a positive event into where it enters the smaller bits and thinking about it because I noticed that, once I did this positive thing and how all these little things made it a positive thing, how I then went on and did other positive things.
Ms T
Feelings chart
Participants commented on the range of methods offered with which they could rate their mood – images, colours, numbers and words – and that they could choose which method suited their individual needs. The majority of participants valued the feelings chart. However, a minority of participants commented that they had found it difficult to decide where to rate their mood when asked and wondered whether or not this was down to their ASD. One participant said that they found the feelings chart difficult to use as they found that their feelings were difficult to explain and they wanted to focus on their thoughts rather than their feelings:
I think we ended up using words with that so yeah on a number of [inaudible 0:26:36.6] could use words or number or whatever and whichever may be more comfortable. For me personally using words. Yeah that worked for me. Yeah. In the mood chart, yeah. I think that was fine you know if you could individualise it or personalise it.
Mr C
Yes, well we filled that out and then it was like nought to ten and stuff and I filled, I filled that out with you know all of the relevant – we put our own words on to like and then when I was in my triangles and that I put the numbers down and referred back to the slots quite – that was quite useful actually.
Mr N
But I think, as soon as you have different grades of something that’s when it gets a bit tricky. I am sure it’s not just me, other people with autism have problems where there’s a lot of choice. I think if it’s binary or a very small choice, I think sometimes it’s a lot easier. Yeah, but on the spectrum where we have trouble picking things from the spectrum.
Mr B
Maslow’s hierarchy of needs
The majority of participants had a positive view of the inclusion of Maslow’s hierarchy of needs in the treatment protocol. Many described that they had found its inclusion helpful because it had provided them with a different perspective on aspects of their life that might influence their feelings and behaviour. One participant said that, although she had found discussing the hierarchy useful, observing gaps at the base of the triangle (e.g. financial security) had been a powerful but difficult realisation:
Yes, the hierarchy of needs was useful. That was useful because it makes sense as a concept but if I’m doing something I wouldn’t normally think about which part of that hierarchy of needs it’s relating to. I think, again, that’s something that helped me to think about what I’m doing in a different way, in a more focused way.
Mr E
Yes, helpful in terms of hierarchy of needs one. Yes, I found that useful . . . I just found it – what was helpful was just to sort of organise needs better and think more. I think that was part of the thinking in terms of planning events to meet my needs rather than just lurching from one minute to the next.
Mr P
It put things into perspective for me in the sense of showing me how important the higher up things are, how they’re not just extras and add-ons but they’re just as important but everything underneath it needs to happen as well for those things to happen.
Ms T
Looking at it realised I’m basically going to stay anxious and depressed until I’m financially secure and there’s no end in sight for that happening so I left feeling really, really upset that day. That’s no reflection on the study . . . no reflection at all just the realisation about what I need to prioritise because I think they do a lot of stuff that’s towards the top of the triangle without underpinning it with this level of personal security and that’s where my life sort of seems to be going wrong and so it hit me pretty hard realising that.
Ms F
Views and experiences of guided self-help between-session tasks
Most participants had a positive view of the content of the homework tasks. Participants said that they felt the homework reinforced in-session content and that this helped them to complete homework tasks. The majority of participants commented that homework had been helpful, with some commenting that homework tasks had prompted them to try out new activities and notice the impact of them on their mood. The majority of participants commented that the amount of homework set was acceptable and presented a sufficient level of challenge. Furthermore, two participants stated that the homework tasks felt more manageable than those set in previous therapeutic experiences:
I think the activities were not complex ones and, to be honest, I don’t think it wasn’t independent either, but in the main what I was being asked to do was achievable both physically and financially so I think realistically it was good. There are a lot of possibilities as well. If you don’t really want to do something, do something different.
Mr M
I guess they were things that I would have wanted to be doing regardless. It wasn’t like I just came and picked stuff out of the blue. It was things that I had going on in my life and used this to reinforce them so it wasn’t ever like, ‘Oh, I’ve got to go and do my homework now.’ It was more like, ‘I’m doing this anyway. Now I can reflect on it.’
Ms T
A minority of participants wanted more information on what was required for some of the between-session tasks, including examples of what they could do to complete the tasks. Some participants stated that they found the initial homework task (which included noting down their behaviours in each of their visited locations) difficult to complete because they did not understand why they had been asked to do this. They suggested that completing an example in the session and knowing that behaviours would be linked with feelings in later sessions would have facilitated their understanding and increased their motivation to complete the task:
If you could make clear what the goal is for the task, why you’re doing a task and make sure that’s made more clear, that might help.
Mr K
I don’t know. I think one of the problems was trying to discover what tasks are supposed to be helpful, that makes you feel good, but I don’t know, I don’t quite know what the task was supposed to be. If it was something that was productive, you would feel proud after you did it, but I don’t think I can think of anything that I ever particularly wanted to do in that sense. That might be something personal for me that I found it difficult to do the tasks, but it might be something that other people feel as well.
Mr H
Well just some information about why we need to make a map of where you’ve been that week and why you need to make a map of where you’ve been and what you’ve been doing that week. Because actually it was really only that third week when you put it together with feelings that it makes sense. And obviously when things don’t make sense it does affect your motivation to do it.
Ms F
Most participants found the homework tasks manageable alongside their day-to-day commitments. However, for a few participants, finding time to complete homework tasks alongside other life demands (e.g. family commitments) and negative moods acted as a barrier to completing homework as planned. Participants talked about using tools such as a scheduling assistant to help them remember to complete homework tasks. One participant said that he used his mobile phone to note down where he had been to aid homework relating to the map:
I struggled to do them mainly. My mood varies so much and you’re supposed to schedule them for a certain time, and I found I had no way of knowing whether I’d be in a mood that was particularly good, in which case I felt, you know, I don’t necessarily need to do . . . or I did a task, but I was feeling OK at the time anyway, or if I was feeling bad, in which case I didn’t really feel like doing a task. That made it difficult to do them.
Mr H
Although I did put things on my phone, wherever I had been, so I just sort of made a note of it, so I could look back and see where I had been. How many times I had been to a certain place, so that did help.
Mr B
Most participants commented that they discussed their choice of homework activity with their coach beforehand. Some participants stated that they knew that they could discuss any difficulties in completing the tasks with their coach in their next session, and that they valued this support. One participant suggested that it would have been helpful if the coach had placed more emphasis on the purpose of the tasks:
The fact that it wasn’t too much. I could sit down across the week and just take a couple of minutes to sit and think – reflect – and then get that written down and I like the challenge that each week it was slightly different but not too different, not too new that I would have gone, ‘oh this is scary and I’m gonna do it wrong’. So it felt like it wasn’t too challenging and it wasn’t like you’re gonna get caught out or anything and it wouldn’t be the end of the world if I did get it wrong because my worker would help me with it so I think it felt a lot more approachable.
Ms G
You know it’s like you think how’s this going to help, how’s this going to help me, but then you did it and then you went to the next session and then you would talk through it and then you realised that some things you’d written that you didn’t think were important actually meant something, so you know you realised that it was useful.
Mr N
Guided self-help: sessional goals
The majority of participants noted that their primary goal for treatment was to improve their low mood. One participant reported changing his patterns of behaviour to achieve this. Most participants commented that their goals had been met by the end of treatment. However, two participants commented that not all of their goals had been met yet, whereas another participant did not feel that the treatment had helped him to view things differently:
Yes in the fact that in the first session we set out what goals I expected to take away or the goals obviously I wanted to meet by the end of the sessions. And then on the last session we just sort of looked over as to whether I had managed to do that. It definitely appeared to have been that that I’d taken away strategies to help myself to raise my mood. I was obviously not in a low mood as I had been prior to the study. So in that respect, yes, I took way what I’d expected in the goals, yeah.
Mr C
I think as time has gone by I’ve got a lot of better, a lot more positive, a bit more focus on life.
Mr M
I don’t think I really had a goal from it, I was just going to go with it and see how it worked. I guess I was hoping it might change the way I see things at the moment but I didn’t find it did that.
Mr H
A couple of participants commented on the way goals were reviewed throughout treatment. One participant felt that including a review at the start and end was helpful in noticing change, whereas another felt that it would have been helpful to review her progress towards her goals with the coach at every session:
Yeah. I think the goals should have really been referred to each week to some extent. Because actually you could have been looking at how the activities that we’re looking at how they impacted on the goals because actually I kept forgetting the goals. And certainly some of the goals I made more progress on than others because one of them was about I wanted to spend better time with my son but he’s not that keen since he’s 16 and smelly! [laugh] So he didn’t really play ball with that so really I maybe shouldn’t have chosen a goal that was so reliant on somebody else. But then again one of my goals was about finances so that ended up being very pertinent and made progress against that prompted by setting that goal.
Ms F
When discussing reviewing goals in sessions, one participant recalled:
I don’t think we did it every session but there were times where we did, I think more towards the end.
Do you think you did it enough?
It wasn’t – yeah, for me, because the thing is I think sometimes I can get a bit obsessive about things and it takes over whereas I think in a way the whole thing made life seem a bit better which made those things less daunting.
Views of guided self-help coaches
All participants expressed positive views about the coach. Some participants described positive aspects of the coach’s style, highlighting how the coach appeared relaxed, calm and interesting, which made it easy for participants to talk to them. When asked about the coach’s understanding of their autism, some participants described how the coach explained concepts in detail so that it was understandable for them, which was helpful. One participant commented that it took a few weeks for the coach to adapt their style to accommodate the participant’s level of autism. All participants apart from one said that they felt it was useful to have a coach present during the GSH to keep them focused, to check their understanding of key concepts and so that they could ask questions, if needed, to aid their understanding. The majority of participants valued the presence of the coach and commented that this helped them complete the course:
It was just very easy to talk with her and stuff so I always felt better knowing that I was going to the session or I was at the session. That was always very good. She obviously spoke through it clearly and precisely and sort of very easy to talk with. So all the strategies she’s presented to me are all very clear and made a lot of sense and were easy to follow.
Mr C
I do. I could tell that she was clearly reading the notes and reflecting on the sessions and just, ‘you said this,’ or ‘I know you talk about doing that’. She’d often ask me stuff that I’d said the week before . . . and that was really really lovely. It shows that she actually was quite interested and that we got on and I really, really appreciated that.
Ms G
I felt like he understood because sometimes the reading material – there would be quite a lot of stuff that was overly detailed and he’d be like, ‘oh, I can see that you understand that. We can just jump ahead.’ And I’d appreciate that, that he didn’t have to bore me with stuff that I already understood. I felt like he understood where I was at.
Ms T
Like I feel, it’s a hard one to explain, but it feels like, if I go to a class or I see a coach or a trainer or something like that, it feels like I’m properly doing it and it feels more like I have a right to do it, if that makes sense?
Mr K
Because if you had the material and you maybe got a bit stuck, and maybe started to not see what the purpose was. I think if you didn’t have that contact and that regular contact, it might just fall by the wayside, you might just give up.
Mr B
Views and experiences of treatment-as-usual arm
Five participants discussed their experience of the referral process. Two people said that they had initiated contact with services, and one commented that their GP had initiated contact with them after being contacted by a member of the study team. One participant experienced problems in his initial contact with services because he found it difficult to explain that he was contacting the service following participation in a study that had indicated he had depression:
When I made the phone call to the people about going through the treatment as usual, they were kind of like ‘Oh well why are you ringing us?’, I was like ‘Well kind of taking part in a study and meant to be able to kind of get help, because they’ve told me I’m actually quite high on sort of these questionnaires’ and they’re like ‘Oh we’ll have to get somebody to ring you back’ and then somebody quite high up must have rang us back and kind of got to the bottom of what was going on and she was like, ‘But do you feel depressed?’, I was like ‘Well I’m being told that I might kind of always just be a little depressed but that’s not to mean to stop trying to get better from’. Anyway she kind of said, ‘Well do you want to do more, what is it, it’s not CBT, is it CAT [cognitive analytic therapy]?’ I’m kind of waiting when I originally rang up to kind of do it, it wasn’t because I came to you saying ‘Oh I’m really depressed’, it was because you wanted somebody to take part in a study that had autism and had certain markers on questionnaires, so then they made us feel like I wasn’t even really poorly enough to ring up.
Mr J
Six participants had received treatment. All said that they had been offered a different treatment, including counselling, CBT, cognitive analytic therapy or antidepressant medication. One participant received medication and five were referred for talking therapies; one participant also attended an ASD support group and had a buddy. Of those who spoke of the length of treatment offered, two participants were offered six weekly sessions and one participants was offered 12 weekly sessions. In relation to waiting times, a couple of participants stated that they had waited approximately 2 weeks, whereas the others had waited longer, with some commenting that they had not received any treatment by the time the 10-week outcome measure was collected:
Well they [the researchers] could have waited until I’d had my CBT before comparing this thing ‘cause I hadn’t had any treatment.
Mr R
All participants talked about the impact of the treatment they were offered. The one participant who was offered antidepressants reported a positive impact on her mood. Three participants who had received talking therapy commented that they had noticed an improvement in their mood after the treatment. One participant said that talking therapy had also given them a new understanding. Two participants commented that their mood had not improved after talking therapy:
Yeah you know then in May I had something . . . a few upsetting things happen and sort of [inaudible] again but the tablets actually are good for helping the panic attacks and anxiety and I feel like even though I’m feeling quite low they’re helping . . . still helping with me feeling less panicky.
Ms I
Yes. Generally, that’s slowing down, and don’t panic over anything. Don’t get too stressed about something. I thought the counselling was very good. I think that was – yes, she got me not to be uptight about things, and don’t worry, don’t lie in bed all the day, because I could do that three or four times a week, if I wanted to.
Mr A
I got a better understanding but there still there that understanding of my low mood but I’m still low. I’m trying to increase my physical activities. I’m sleeping a little bit better so it’s more the physical symptoms have decreased a bit, but not the mental symptoms.
Mr D
Five participants mentioned areas in which they felt that their TAU could have been improved. A minority of participants commented that their therapist did not appear to have a good understanding of ASD, and wondered if that was having an impact on their therapeutic relationship. For example, one participant shared that their therapist had not really acknowledged their ASD diagnosis after they had disclosed they had a diagnosis at the start of sessions. Two other participants said that their therapists had a good understanding of ASD. Of these, one said that this had helped to increase their own understanding of the condition. One participant commented that it was important to them that their therapist had a good understanding of ASD because this helped the therapist to suggest adaptations:
I feel as though it’s not really been taken in to account I’ve got autism diagnosed. In fact I think I mentioned that in the first session because she said, ‘Why are you here’ and I think at the beginning of the last session that I was at, she was like, ‘So you have actually had a diagnosis’, I was like ‘Aye I’ll show you the bit of paper if you want’, like I’m not coming in here saying I’ve got something that I haven’t got and it just felt a little bit like I was doubted, which wasn’t great when you doubt yourself.
Mr J
It [ASD] wasn’t overly talked about much. She seemed to have a decent grasp upon it but as autism’s such a wide spectrum I couldn’t expect her to know everything.
Mr D
She’s written down things that I haven’t even understood, I thought there was all . . . I thought I understood all that I needed to know about autism until [0:51:21, inaudible] were happening and my understanding of things and she explained to me about, you know, like the different thinking and processing styles.
Ms I
Someone asks you and sometimes [claps] well I answer everything, when they questioned me then maybe they come back with something else or they try to adjust that. They would say like, tell me, ‘Go to a pub,’ well I’m saying ‘I can’t go down to the pub ‘cause there’s a lot of people there’. They say, ‘You could always go for a drink at a café when everyone’s gone it’s nice and quiet’.
Mr R
Outcome measures
Three participants said that they found the questionnaires useful as they highlighted positive changes in mood or helped them to reflect on their current mood. One participant would have liked feedback on whether or not the questionnaires showed improvements in his mood over time. One participant reported that his mood would often drop after completing the questionnaires as it highlighted his difficulties to him. However, the majority of participants did not find filling in the questionnaires useful and found it time-consuming:
It was interesting going back through them when my mood was a lot better, because I could obviously see the difference.
Mr B
Possibly. I don’t know whether that was part of the intention of the course or not. I mean I’ve . . . wherever I’ve been I’ve done quite a lot of those. I’ve never had feedback from them before so I don’t know the . . . I mean I can understand from the answers I gave that the person reading them would be able to form an opinion of what my mood was. But, you know, sometimes I do find things like that a bit frustrating that we do these things and you don’t get any feedback from them, so I don’t know whether . . . you know, what is the point of me doing them kind of thing, sometimes.
Mr K
Sometimes you come out feeling low, lower in mood than when you went in ‘cause you’ve got to be very truthful with your answers haven’t you? . . . We co-operate and when there’s questions it makes us think about ourselves.
Mr R
Not really useful for me but basically a lot it seems the standard questions which go on for ages so I don’t particularly find them useful. I don’t particularly find them helpful but I understand that they’re needed to gather information into better – think of treatments.
Mr D
Seven participants struggled to quantify their experiences on the scales used by the questionnaires, for instance finding it difficult to put a number on the frequency of their symptoms. Two participants felt that many of the questions asked about similar concepts, which could be confusing or lead participants to answer very quickly without much thought:
Whether it was just the way I was reading it but the actual words were fine but it was asking how I had felt or did I feel a certain way and then a couple of scrolls of the page down it was asking what seemed to be the same again but worded differently and it almost felt like I was trying to be caught out and whether you were trying to find as to, although I felt this but actually I wasn’t feeling as bad or yeah, it was – yeah, but it may well have been that I was just misreading, you know, the timescale of it maybe or something, yeah I don’t like reading anyway so . . .
Mr C
Mm-hmm, yeah just because I mean if you ask so many questions about the same thing, you would tend to just try to get through them as quickly as possible and not really give an accurate response.
Mr N
Just maybe to be able to say both, to say at some points I felt really bad and some parts I felt really good, just so that there’s a double set of data there because sometimes I’ve definitely felt really good but do I say the good or do I say the bad because they happened as much as each other.
Ms T
Three participants commented that some of the questions were vague or the response options were challenging to complete and this made it difficult for them to understand what the questions were asking:
I’ve done some of those kinds of questionnaires in the past. I think for the kind of things that those questionnaires are asking about the questions are too vague really but then for those kinds of things a questionnaire probably isn’t going to be particularly useful. I don’t know. It’s just difficult. It’s difficult to really work out what to say. It’s difficult with those kinds of experiences being asked to tick one of four boxes. It’s just hard to quantify those kind of things in that way, I guess.
Mr E
I never quite understood the questions. There was one where do you feel you’ve got ‘Do you feel guilty?’ Those type of questions, I didn’t really understand what they were trying to get out.
Mr M
I suppose because the questionnaires would say things like, ‘not at all’, like at health, ‘have you been feeling like this? How often have you been feeling like this?’ – ‘not at all’ or ‘several days’ or ‘most of the time’ or whatever. Quite often I think that the kinds of things that it was asking about, they’re a bit more nuance. It’s hard to . . . My own experience of those things wouldn’t really fit into those categories like ‘not at all’ or ‘a few days’ or whatever.
Mr K
Suggested improvements to the trial
Some participants had a number of suggestions for improvements to the trial, which included providing more information about the logistics and content of appointments. In relation to the logistics of appointments, some participants would have liked a summary of dates, times and locations of and directions to appointments, along with information about parking, in advance. Others wanted a set day and time for appointments. Some participants said it would have been useful to have the researcher’s telephone number in advance, because they did not like answering calls from an unknown number:
It’s just coming to an unfamiliar face where you don’t quite know what you’re gonna get, who you’re gonna get. From the first person I spoke to all the way through I had the same person and I found that really beneficial. When I was initially contacted for my baseline scores to see if I qualified I had that same person and that did really help. I didn’t realise that was gonna be my person all the way through and that maybe would’ve been nice when they rang up to . . . I don’t know whether that person knew at the time they were gonna be allocated me but it would be nice to say, ‘Hi . . .’ and ‘I’m gonna be working with you going forward’. That would maybe be nice so at least I know I’ve spoken to that person.
Ms G
I would of maybe had a bullet-pointed summary either at the beginning or the end just of the actual . . . you’ll have this many sessions at this length in this area and this many at this address and this many sessions at this length at that address.
Ms F
Yeah, it was more them understanding that if I say I want to do this 2:30 every week sort of thing, you know. I suppose because they were seeing lots of different people and their times were all moving about, I don’t know. It’s just . . . you know, I thought if I’d said I want to do next week at 2:30 and every other one from then on and explained why I wanted to do that they might have understood it more.
Mr K
I think, for my point of view, if I knew where I was all the time then I would have got better with timings as well and I think as well if I had a programme, a list of what needed to be done and when, week one will be this, week two, an agenda, and I felt I wasn’t always sure what I was expecting.
Mr M
If I knew what the [telephone] number was I would have answered it straight away.
Mr L
Coaches’ views and experiences
Acceptability and experience of the trial
All coaches were enthusiastic about the trial because they acknowledged the current lack of NHS mental health services tailored to the needs of people with ASD diagnoses:
I wasn’t really surprised that there wasn’t a particular like autism services in mental health. So when I did read the job advert and I saw that this is specially designed to meet those needs I actually really engaged with it.
C1
I have an awareness that there was definitely a gap in terms of NHS provision so the first thing that struck me was the need for this intervention or an intervention is for this particular population.
C2
I was interested just to see what that was like in practice, but also, really pleased that there was a movement in terms of just an acknowledgement that there needs to be, not necessarily an alternative, but something that is more meaningful to somebody with autism so they can do the same kind of work as everybody else I guess.
C3
I wasn’t aware that there’s so little out there with regard to specialised interventions for people with autism. We had a little bit of training about how to adapt CBT intervention for people with autism, but I didn’t realise until looking at the trial that actually this is quite another area. I thought it was needed and I think from my limited experience people might often struggle because people might not be aware that the clients have autism and they may also perceive them as just being difficult or non-co-operative when actually it’s more about specific communication needs.
C4
All coaches also felt that the design of the GSH intervention was appropriate for people with ASD diagnoses, in particular the focus on BA:
I was really interested in the study, because I’d noticed from assessing in IAPTs, that actually I would speak to people and it was very clear that people were experiencing the difficulties and they were interested in engaging with therapy for, but actually then trying to pass that person on to someone that understood autism or using the cognitive–behavioural therapy with somebody with autism, it can be hard for the person with autism, because of the heavy cognitive element of it essentially. So, I suppose one of the main reasons I was really interested in it, just to see if it worked and how people responded to it, was because this was something that was mirroring work that I’d done in IAPTs but was moving away from the cognitive focus and more on to the behavioural situation because you’re seeing the content.
C3
The actual design felt that it was appropriately ambitious, if that make sense. Then I read the literature that supports behavioural activations in adult depression and that’s very well founded so it seemed like a really sensible approach to maybe use an adapted version of something that we know works with the typical population.
C2
I think behavioural activation was a good model, it makes sense to me to use something like that rather than getting caught up with cognitions and feelings of people who don’t necessarily have the emotional literacy to pull all that together and getting into things like that.
C5
All coaches praised the comprehensive training and supervision they received during the trial, in particular the focus on communication approaches to use with participants and the details provided of the underlying theory of the GSH intervention. All coaches described how, after receiving the training, they felt knowledgeable, confident and well prepared to deliver the intervention:
I was offered ample training and then ongoing supervision, even though I hadn’t started seeing patients yet. So I was definitely very well prepared, did a lot of role-plays and then offered ongoing supervision every week as well.
C1
I think that the information and the openness of the team was brilliant actually. I felt that everybody that I spoke to but also from a personal perspective, I always felt that I could ask questions and that we were appropriately support. I thought that the information given was great if you were to go to reread that information or find out more . . . I thought that the training I received on the interventions and some training that I had on amending communication approaches to adults with autism prepared me.
C2
I actually thought the training was really good and the supervision was amazing as well . . . In the handouts that you go through with people is a series that hopefully makes sense to someone with autism, and I think what the training did was go beyond that and explain why this is even relevant in the first place, and here’s the theory behind that as well. So, we did lots of work around cognitive–behavioural therapy and behavioural activation in general and then honed in on the specific treatment. I felt that was really good for my learning. I find it much better to be oriented in where this has come from rather than drop down in the middle of something and deliver it in a more regurgitated basis . . . it gave a deeper understanding of what you are delivering. When you were then in treatment and people asked you questions, that maybe deviated from the content, you were much better prepared for explaining because they’d given you a context and approach as well.
C3
Views and experiences of the guided self-help intervention
All coaches valued and appreciated the structured design of the GSH intervention and the accompanying material and all followed the order of the sessions as designed:
I think it was good in terms of the structure and a planning meeting first and I liked the folder and the materials seemed all very well designed and straightforward to use. I think having certain measures before each session worked well as well.
C4
I think the structured method offered, having the different booklets and visual tools and things to actually work through questions, answer exercises to do, I think that works really, really well. It helps keep it focused and it also allows both of you to be looking at the page and focusing on that rather than there being pressure of lots of eye contact and more social interactions. So I think that works really well and people, by and large, I think really engaged with it and picked up lots of new things.
C1
I thought it felt comfortable for me in terms of the order, absolutely fine.
C3
Coaches commented on the importance of the initial planning session for demonstrating to the participants that they had a good understanding of ASD and issues relating to communication differences, particularly for those participants who had previous negative experiences with mainstream NHS mental health services:
I think some of them came in a little bit resistant and sceptical but at the same time because they were there, I guess, they kind of knew they were hopeful at the same time and they all kept coming back, so . . . Just having had previous bad experiences, I think, like they had depression for quite a long time and nothing really lifted it, they’d done a little bit of psychology before and not really connected well with it. I guess a lot of them were people who got their diagnosis in maybe their 30s, 40s, like 6 months previous to coming in to see me. So they’re people who’ve kind of been failed by their school system, their workplace, just kind of society in general not really recognising their needs. A few of them had to actually fight really hard to get an assessment for the autism diagnosis as well. So a lot of them, yeah, came in not really having had this streamlined and pleasant experience before . . . I think, I mean, I just then took time to sort of listen to what had happened before and showed empathy for it and then just really explained why we were doing what we were doing and what we hoped it was gonna achieve and encourage them to give it a try, and they did. So yeah, just had to be quite careful then to attend to those experiences rather than kind of rush in and be like, ‘Right, well, we’re gonna focus on positive feelings now’. Yeah, it took time to really show that I’m gonna be here for you, this is what the aims are.
C1
I think absolutely without question the most important part of delivery is their coach or therapist having an awareness of individuals with autism and what their needs for adaption in terms of how future approaches are likely to be. I think obviously the intervention itself is adapted for that population but I think if you were just to follow the material by route but not take your individual understanding then . . . the impact or the potential value of the intervention will be lost. And that’s again based on things participants said to me which was that most of them had experienced former CBT through an IAPT service but they found it ill-fitting for their needs and the therapist didn’t show them any aware of understanding between the likely interaction between ASD and their depression. That just meant that they disengaged and didn’t complete the treatment so I think that first planning session that’s often 90 minutes long is so key because that’s your opportunity as a therapist to show the participant that you do understand them and their needs. And you can individual this approach, albeit there’s pre-set material but you can individualise this to meet their needs and just show understanding in terms of communication differences. I think that’s the most important part of this intervention, definitely.
C2
Sessions 1–3 built on from each other, with each focusing on situations, behaviours and feelings, respectively. The majority of coaches commented that introducing the concept of situations on its own was challenging for some participants, who wanted to also talk about behaviours and/or feelings:
I thought it flowed really nicely. I could see how the content was building on the theory as you went through the weeks. I felt that at the start, when you are suddenly talking about a situation, people were often a bit initially taken aback by that. That needed a little bit of explaining in my experience, just to orientate that person to the treatment. But I think that has more to do with the fact that it’s the first thing you’re introducing rather than the actual concept itself.
C5
I think it worked really well. I think that something that I noticed was the word situation, meaning like the place that the person goes, could get a little bit confusing. Because the people and myself, when I initially started the training in it, they saw the situation as sort of an overall event, like an all encompassing thing of the place, the behaviour and how it made me feel, whereas in the training it just means the place. When they were trying to do the feelings triangles they would get really confused about the situation, they’d start writing down what they were doing and then it would all be a little bit muddled . . . So when they’re trying to write situation, behaviour, feelings, for situation they sort of start to write everything. Does that make sense? . . . So it’s like they take situation as the overall event as opposed to only just the place.
C1
Quite a few people I worked with felt that session 1 to 3 they’re not quite sure what’s going on because it’s split up quite a bit isn’t it and you only really find out about the feelings triangles and what that means from about session 3 so sometimes people are a little bit unsure at the start.
C4
. . . when you started to talk about situations and then behaviours, everybody was itching to tell you how that felt and so it just felt a bit unusual at times to be trying to segregate them. But often you had so much supervision to explain why the function is that. So, sometimes you could just naturally feel that the next section, they would come in and people were ready to integrate that.
C3
Situations
The situation map was introduced in the first session and then used throughout the intervention. Some coaches commented that participants preferred to draw their own map as the one provided either did not have the right locations or did not have the locations in the right order. Others commented that the map worked initially to explain the concept, but after a while participants preferred to list their activities rather than use the map:
It worked well, I only had one person that drew their own. I think after a few sessions people sort of stopped using it quite as much, didn’t really refer back to it the same way. So at the start of each session you’d be like, ‘OK, so where did you go? Would [sic] did you do? What gave you the most pleasurable feelings this week?’ They wouldn’t have mapped that out, they would just be able to then remember where they went. So after a few sessions it didn’t really get used.
C1
The thing that people in my experience challenged more was the map, because they didn’t want somebody else’s, they wanted to create their own. I’d be interested to hear what the other coaches are saying. I think everybody that I worked with created their own map, or didn’t like the map and wanted a list or something like that . . . Some of them created some really amazing maps, and I suppose from a practical perspective, and this is my opinion, and as a patient mechanism, I don’t think it’s big enough. You’re filling it with more and more things and often the person will go to the same place many times and you need to be able to put on lots of feelings. So, I think it could do with . . . one of the maps that somebody made was probably four times the size of the one that is included in the handouts. So, possibly some changes to the map or just making it OK to create your own if you want to.
C3
Yeah, and a couple of people, maybe three out of the people I saw, they wouldn’t engage very well with the map at all and just preferred to write things like an activity schedule as you would in a more standard CBT-type model but some people the visual for the map was really good . . . Yeah. The task would always be to put a triangle on your map. Sometimes people wouldn’t want to do that, but they would make lists of things that they’d done and then they would highlight it a different colour and things like that so a good one would be a pink or they would prefer to use lists or words rather than using the maps.
C5
Feelings
All of the coaches said that the materials provided to prompt participants to discuss their feelings were valuable and worked well to stimulate discussion. The flexibility in what could be used for the scale for the feelings chart was appreciated by coaches and allowed them to individualise the intervention based on the participant’s preference. However, the majority of coaches commented that the use of pictures, such as Winston Churchill’s black dog, was not well received, and this was thought to be confusing for participants because of the use of metaphors:
The only other comment would be the feelings chart, where it has Winston Churchill’s black dog on it, I don’t know anybody that used that. It was either numbers or colours. So, I don’t know if that is to do with the metaphorical side of things not being well received.
C3
With the feeling thermometers there was a bit of confusion about you could pick which one you want to use. Then generally people finding that quite tricky. The colour one worked really well. One guy was thinking very much about his colour intensities, his feeling intensities in terms of colours. The dog one, as I said, the black dog of depression, I explained where that came from but that was not on the person’s . . . ‘I like dogs. That’s a really cute dog. Why is it . . .?’
C4
I was a little bit dubious about was the emotions part, the feelings and that is where the difficulties were. A lot of people didn’t recognise what feelings they were having in the moment and things like that, but I think definitely the way the feelings triangle worked breaking it down with the situations and going through that process of doing and the feelings thermometer sessions and all of those sorts of things really helped people to engage with that.
C5
Granularity
Several coaches described how some participants initially struggled with the concept of granularity, but commented on the importance of the intervention being guided by the coaches to help demonstrate the concept. The granularity exercise was, however, described by some coaches as a critical point in participants’ learning about their own feelings:
I think granularity was hard without somebody there. I don’t think it’s because it was disliked or anything like that. It just is more theoretical. It does need somebody there often to help you and I know that trying to do that on your own when you already struggle to think about your thinking and mentalise, that was hard.
C3
. . . granularity aspect of really focusing in on, ‘OK, I like doing this, but what is it about this that is pleasurable?’ and think about all the different aspects. Would it be the same if this wasn’t there, or this wasn’t there? The magnifying glass metaphor of really focusing in on the stuff that is enjoyable and I guess just rating it. I thought that was a quite an eye-opener to me.
C4
Granularity I think felt a little bit weird for them in session 2 because it’s quite an unusual thing to go out and do but they generally go with it even though they’re not quite sure what it’s leading to. Some people said it was a bit silly I think but they would have a bit more context around what it was leading to I think they would have been more onboard with it. All the written questions were generally quite useful.
C5
. . . the feedback I’ve got from people, when they come to the very final session they reflect on what’s been the most important piece of learning for them and a lot would say the behaviours one, where they do this granularity exercise and break down different situations and see all the little small moments in it and how their feelings can fluctuate so much within just a small amount of time.
C1
Maslow’s hierarchy of needs
All coaches described the hierarchy of needs task in session 5 as a pivotal point in the intervention and a ‘lightbulb moment’ for participants’ understanding of what changes to make in their life. Coaches commented that participants engaged with the task well and that it drew together all of the learning and understanding from the previous weeks:
It was the hierarchy of need session. The participant that I worked with, it made so much sense to her that she wanted to talk about it in depth and she had kind of a lightbulb moment in terms of understanding where she’d been putting most of her time but where it might make more sense to change and focus and so that was a big moment for her. I think she had prior experience of exposure to the hierarchy of needs. Maybe if someone hasn’t I think, for me in terms of delivering the intervention, that session is a real turning point in terms of clarity. I think that’s the point where the intervention moves from almost exploring current to considering change to make sure that the participant is still with you and that that session makes sense because it’s key for the remaining sessions.
C1
. . . the one element that seemed to be universal with the people that I worked with was the Maslow hierarchy of needs. So, not so much in the sense of . . . most people had heard of it before, but explaining that the relationship between that and compassion, and linking that then to situations, new situations, new behaviours, and if you do the same behaviours over and over again, or if they become more restricted then you’re taking less of these needs higher up. That seemed to work with the people that I worked with . . . it just seemed to really get the message across. It was a chart. People were ticking things off. They had a chart and a map of what they were currently doing. They could compare that to this tangible list of needs that [inaudible – 0:18:33] mood improving, and it then created a tangible goal for the next week, because I could see that they haven’t met this need in this box, therefore I need to go to this situation or do this behaviour. So, it often seemed to be the session that would pull things together like that.
C3
. . . the hierarchy of need session, just because I think people could really see. One of my clients was actually very active. He didn’t need to schedule more behaviours but it was about finding a better balance. We actually found that a lot of his stuff . . . He drew this lovely picture of where he said, ‘I’ve got my achievement oriented stuff and I’ve got my basic safety and everyday needs, but the social level was just really empty’. So he drew that like a pyramid where in the social part there were just a couple of unwritten columns. This is obviously where I need to find some stuff to fill it in. I think that was really, really useful in helping people recognise, especially if people have quite a few activities going on, to think ‘Yes, this is all good for my achievement and my self-esteem, but actually is really stressful as well and I maybe need to wind down and attend to my safety needs or attend to my social needs instead’. I think that worked really, really well.
C4
. . . hierarchy of needs and relating it. It was like the penny dropped sort of moment when they realised oh, this is why this is so important, this relates to this and it provided a framework I suppose so after that made much more readily kind of say, ‘Oh I can identify what needs I’m not needing and what I need to meet,’ and it kind of, why it’s so important for them to be doing some of things that they were if that makes sense . . . I think sometimes some people are a little bit unsure that they got the granularity and they knew the concept of the feelings triangles and everything, but it wasn’t until we did session 5 [hierarchy of needs] and looked at it in the context of we have needs that we need to meet in order to keep ourselves . . . our well-being in check and all those sorts of things that they made that connection . . . I guess it sort of just helps giving more context to people in terms of why going to all these different places and bringing about all these good feelings were important. It gave it a framework I think, the context.
C5
Somebody did their own hierarchy of needs as an extra task. They came back with a sheet of paper with a colour-coded hierarchy of needs with all of their activities within it, so it was things that I hadn’t actually asked them to do but they just developed their own understanding and took it upon themselves to do.
C5
Between-session tasks
All coaches described and provided examples of trial participants appreciating and understanding that the intervention was self-help and that the emphasis was on the participant to work through the between-session tasks, with the coach being there only to help and guide them. Coaches explained that these therapeutic principles were appropriate for this client group:
Yeah, I think so, like increasing positive feelings. Yeah, because they, yeah, they picked up pretty quickly that it sort of had to be focused just on that, like these positive feelings, positive behaviours, and it might come in a little bit down at the start of the session and like how was your week? They would know not to talk too much about another problem or they would say, ‘Oh, I’m not really supposed to go into this too much, am I?’ I’m like, ‘Oh well, it’s OK for a couple of minutes and we’ll then look at this’.
C1
It’s continuous throughout all the weeks that we’re working together as the backbone of our work. It’s not something to just do and then forget about it. I think that there’s an opportunity there to set up the fact that the home practice is continuous. The therapy continues outside of the sessions. The sessions are guided. They are not the entirety of the intervention. I think you’ve got a real opportunity to get all of those messages across and I think there’s a risk that if you don’t do that skilfully then, that maybe it won’t flow as well, or you won’t have that backbone to your profession that you need for it . . . So, in terms of one person I can think of who I felt really did understand the treatment aims, they were continuously working towards things that they used to do, that they used to enjoy and they could use an event within that week where they were starting to make a distinction between feeling happy and striving towards feeling content. They started to create through their situations map. That brought contentment areas that brought the opposite of that and how could they make those harder situations feel better and we were doing subtle changes in their behaviour, to try and make their feelings better . . . So, for example, one person worked out that driving to a particular place if they were a passenger was worse than being the driver, so they would drive. I think that shows real insight in to the elements of the intervention and behaviour situations and how changes to those could change feelings and really felt like this person grasped that and you could see the impact of how they were moderating their behaviour in that way.
C3
I think it just needed a bit of explanation to say ‘I’m your coach. I’m not your therapist. This is for you to work through and for me to help you with the experience and the main work happens between sessions’. I think what was important possibly to say for people with autism because there was a few times in the manual that there were options. You can use different kinds of feelings, thermometers and that kind of thing to just say, ‘These are resources that you may find helpful’, because I think there is a tendency for some people with autism at least to work through everything by the book or to find it difficult to . . . You can actually pick and choose rather than you have to do everything in a particular way . . . I think especially when somebody is depressed, to have that personal connection is absolutely essential. I don’t think if you just give out the folders for people to read in their own time, it wouldn’t be the same sort of engagement.
C4
I think the element of having it as guided self-help has probably been really useful for the people with autism. I think that for someone like myself being there to be able to kind of suggest things or prompt things probably really helped in that respect . . . I think there was one man that I worked with who, we went through . . . in his situation map we mapped out each for him and then the next week he came back, and he had done a really comprehensive schedule of everything he’d been doing in the week and from that I’d pulled out the bits that had been good activities for him. That’s not a very good example actually but I think that was how I knew that he’d understood though what we were trying to do there. There was one guy who really engaged with the session 5 and then the next week he’d made a list of the different areas in his life that he felt he was making progress on and that he wanted to and things. People used the materials but then did their own little bit to work alongside it sometimes. I guess made it personal to them. People were coming back with homework and if I could see that they were able to do that in really granular detail in the sessions and things like that.
C5
Coaches described that, on the whole, participants engaged well with the between-session tasks, with engagement varying between participants and between tasks depending on the individuals’ involvement in the task. If the task had not been completed between sessions, coaches took time during the session to complete the task or to explore why it had not been done:
Some were good at doing the homework and some not. Doing a scheduled activity worked really well, that was session 4 we introduce that, and that got carried on after every session. So people would do that and only some of them would come in having done a feelings triangle for that and so this is how it met their needs. So if they came in without having done it I would still spend the first 5, 10 minutes talking over the past week and what needs were being met.
C1
I think the first activity scheduling that was really good, because I thought then when people had actually . . . The planning worked really well and the breaking it down, what works as planning and then to reviewing that. Those were popular sessions where I spent quite a lot of time as well, so where I went up to an hour to actually set some activities and then come back and do them or not do them and then troubleshoot around why, what got in the way or what could be done instead. I thought that went quite well.
C4
I think in the one experience I had of doing it [homework], it was in the new behaviours, new places because the participant had an understanding of the likely hoped value that that change would bring. She really really engaged. She drew posters and put them on her kitchen wall to remind her of the things, the new activities she was going to do that week. She kept a diary of when she did them. She involved her partner. She came back to me really kind of keen to report the things that she’d done and how she’d found them. I think certainly in terms of how this participant engaged, I felt that she was using lots of the skills and tools that we’d worked through before to understand why this activity or this change was going to be potentially of value. I was worried when I first looked at the intervention. I was worried by the word new because the training that I’d been giving on working with adults with autism was that quite a lot of people enjoy regularity and routine and change makes them anxious so I thought, ‘Gosh, this whole thing is building up to this point where they have to change something’.
C2
Session length
All coaches described sometimes struggling to fit some sessions into the allotted 30 minutes, and all felt that 45 minutes was more realistic. The sessions that were most likely to take longer were those introducing the concept of granularity and the hierarchy of needs task and also when participants had not completed their between-session tasks:
I think for some people they would get through each session really quickly and some I would take 45 minutes maybe, it just sort of depended on how well they got the concept. So yeah, it just really depended on each person. Sometimes 30 minutes just wasn’t long enough for sessions that had like a really big component to them. So like the session called ‘the hierarchy of needs’, that’s session 5, some got it really, really quickly and for some other people it was like a pretty long session, they really had to think about it and they didn’t quite understand it right away. But then I didn’t want to send them home not having got it.
C1
I think some of the sessions are a lot busier than other sessions but on the whole I found it difficult to complete the prescribed activities tasks within 30 minutes. I think that on the whole that is difficult and it varies hugely. If the individual has done their homework then the session kind of works as planned but if they haven’t there isn’t much room to address that and then complete the next task, which is often dependent on the homework having been completed . . . I did still find some of the sessions very full and I think most of my sessions were around 40–50 minutes generally.
C2
Yes, I found you needed longer than that definitely. I think if you want to be . . . I think you could do it in half an hour. I think if you were literally just going through the content, then yes. But if you wanted to allow the person to show you what they’ve done that week, talk about their situations which is often in the guidelines for each session, then weaving that in to their goals and stopping to get a sense of where you could help them out a bit in that session, it’s those bits that take it a little bit longer. I don’t think you’re talking about an hour. I think most of my sessions were around the 45-minute mark, which was the upper end of what I was allowed . . . the boundaries of what was acceptable. But I think half an hour is short.
C3
The length of time was a bit of a challenge. From what I remember I think it was session 3 which was quite full on. I think that’s where you introduce granularity. After that, the later sessions, new behaviours, new situations, I think that could have been one session. That was relatively quick because it’s repeating. It’s useful that it’s two and it’s building up on things, but that said, 2 was in 25 minutes whereas some of the other sessions I went up to a minimum 45 minutes and up to an hour.
C4
The session length actually that’s one thing, 30 minutes just is not enough really you have to quite a bit of explaining and sometimes people haven’t done the work in between the sessions and you spend a little bit of time just trying to look at that with them and I think most of my sessions were more like 40–45 minutes . . . Sessions 3 and 5 for example actually were really long in comparison to often the first in session 1, not 0, session 4 I think particularly and then the later ones but the later ones that makes sense because you’re generally just going away in the week and doing it and then coming back and reviewing it. I guess something about was there too much in session 3 or 5 could [inaudible 27:29]. I think three in particular stood out as that there was quite a lot.
C5
Treatment goals
The majority of coaches described that setting treatment goals with the participants was a challenge. This was because some participants chose long-term life goals that would not be achievable over the course of the intervention and others were not able to think of goals on the spot. It was suggested that thinking of goals could be given as a between-session task between the planning meeting and session 1 to allow time for participants to consider what could be achievable over the course of the intervention. It was also suggested that additional material for coaches to guide the participants to set goals would be welcomed. Coaches also suggested that revisiting the goals more regularly during the intervention would be a useful addition:
. . . you do your three goals in the planning session and then there’s one more session before the very final one that asks you for them again. I think it might be helpful to have two sessions, at least, between the very first one and the very last one that asks them about their goals and their progress through them, ‘cause I think it’s quite easy to forget what they are.
C1
I think it’s really important, and the material does guide the therapist to do this but it’s really important that before the goals are set the participant understand the parameters of capability within the intervention. And I know it’s the same in any therapeutic goals setting but I think it’s about finding a balance between something that’s attractive for the participant but then it’s also possible within the time frame and the likely progress that’s going to be made. I struggled with that, to strike a balance and so took it to supervision and I actually went back to the goals in the first active treatment session to just talk about them again. I know later on it was introduced in the material that does goal reviews. I forget which sessions they were introduced in. I think that’s a really good idea but possibly in the material for the concept of goal settings to be introduced and discussed at that planning meeting and then homework to be for the participant to consider what those goals might be. Then come back to, I think to meet the new participant, for them to completely grasp what you’re going to be doing for the next eight sessions, for them to accept the realms of the possibility in terms of improvement and then commit to three goals all within that first session is probably a bit too much. Maybe to introduce goals and then agree them in the following session might be quite nice for them.
C2
I found goal-setting quite difficult. I’ve got to say, I think one of the reasons for that is because I have never set goals when I haven’t assessed a person and normally, I suppose if you were going to do an intervention you would do a bit of a formulation with them, and that gives you a much . . . you start to build and start to visualise those goals together before you set them. So, I suppose it’s about jumping in a bit, and you don’t see the notes from the research assessment. So, you don’t know much. So, I suppose it felt a bit disjointed or a bit disconnected to set goals then . . . I think one thing would be to have an explicit point where you revisit the goals. I know it’s meant to be woven in to most sessions and you’re meant to skilfully go back, but if you could have an explicit point where you both know that you’re going to be just checking it’s still going in the right direction that would be helpful for motivation and mutual understanding.
C3
When it came to revisiting the goals, actually people’s ideas of what was the most important goal had changed in both cases. Again, I think it’s good to have it there, but as long as there’s an understanding this can be flexible and people don’t get upset about, ‘Oh, I haven’t done anything towards this goal’, because actually the situation had changed. The one guy had had a change in job and the other person had one of the goals was to go to school regularly and then obviously that went after the start of the summer holiday. It’s good to have them there, but to treat them flexibly.
C4
In session 4 we review the goals and I really didn’t like doing that part because hardly anybody would report a change at that point because it was almost like at session 3 we were still going through what the concepts were and getting a feel for it and then their one session in touch and understanding what it’s all about and we’re reviewing goals it’s felt too early. It’s good to revisit them and have that in mind but asking to rate them at that point really wasn’t helpful with a lot of the people I work with and if anything, it kind of side-tracked them to ruminate on not having got very far with them . . . I almost feel like it should have been done from session 5. That sounds quite late on to do it unless they were revisited every week so it was just something you did every week but just for them to be in zero and then suddenly in 4 we just got the conduct together we’ve done the first week . . . in fact I don’t think at that point we’ve scheduled any activity, session 4 is the activity setting, it just felt a bit premature and wasn’t always helpful in terms of people . . . they weren’t very positive about that a lot of the time.
C5
Difficult for some people. That would be the only bit that I would have said I could have done with some more materials around or something because some people would come in with very clear ideas and it would be a case of trying to help them shape it into a kind of SMART goal that was appropriate, but some people really wouldn’t and for you to spend a lot of time trying to [thrash] that out with them. I’m not sure what would have been helpful but maybe some sort of activity to get people to think a bit more clearly about what it is they want to get out of it and what a realistic smaller goal would look like that would be appropriate for the 10 weeks that you’d be working together.
C5
Chapter 5 Discussion
This study set out to address a number of questions. Is it feasible to develop a low-intensity psychological intervention for depression that is acceptable to autistic adults and therapists? Is it feasible to recruit and retain autistic adults with depression to a RCT? Which measure of depression would best serve as a primary outcome measure?
This feasibility study met the stated aims in full. First, it was feasible to develop a low-intensity intervention for depression, based on cognitive–behavioural principles, that was acceptable to autistic adults and therapist coaches. Engagement with the intervention was good, and the majority of participants who began the intervention completed the specified ‘dose’ and, in most cases, the whole intervention.
In terms of duration of the treatment, the majority of participants had not finished the intervention 10 weeks post randomisation. Sixteen weeks presented a more practical outcome assessment point.
The qualitative study allowed the research team to gain an in-depth understanding of the perspectives and experiences of a diverse sample of trial participants and coaches to enable a comprehensive insight into ADEPT from multiple perspectives, with analysis demonstrating a commonality in views and experiences. The achievement of data saturation, together with the rigour of analysis, improves the credibility of the findings of the qualitative study, that is, acceptability and feasibility of the intervention.
The qualitative interviews informing the finding of acceptability of the intervention also indicate that the adaptations to a CBT intervention based on the principles of BA were perceived as relevant and helpful by autistic people. The GSH nature of the intervention was understood and well received. Importantly, the qualitative interviews also provide specific recommendations made by participants and coaches about how the intervention could be improved.
The length of sessions delivered (45–60 minutes) and the adaptations by the therapist coaches in terms of sending appointment reminders and being flexible with location to meet participants’ needs are perhaps not consistent with a low-intensity intervention as routinely offered in the care pathway.
Second, it was feasible to conduct a RCT with a nested qualitative evaluation. It was possible to recruit the target number of participants for this feasibility study within the time frame specified. Recruitment across two regional centres using four recruitment pathways has provided information about the monthly rate of recruitment for each pathway, which will be key to estimating the recruitment parameters (i.e. the number of centres and the length of the recruitment period) for a larger-scale trial.
A significant proportion (73.6%) of potential participants assessed at baseline consented to take part in the study and agreed to randomisation, indicating that the study was acceptable.
It was possible to maintain assessor blinding throughout the trial.
There were differential rates of attrition across the treatment arms. Rates of follow-up completion in the GSH arm were good (86% at 16 weeks). This is in contrast to just 54% of participants in the TAU arm completing follow-up at that time point. The qualitative study findings shed some light on this. Explicit dropout/withdrawal from the trial was attributed by several participants to dissatisfaction with their previous experience of TAU and a perception that a treatment adapted for autistic people would be ‘better’, thereby enhancing the perceived credibility of the GSH. Although efforts to encourage a position of equipoise were introduced prior to randomisation, factors external to the study materials and design may have had a role to play. Participants were relatively older (mean age of 38 years) with a relatively recent diagnosis of ASD. They may have had more experience of accessing services without an ASD diagnosis, which may have increased dissatisfaction with their previous therapy experience because they perceived that their needs had not been understood. It is not clear if younger people or those who received a diagnosis in childhood would show similar rates of attrition. Nonetheless, it is important to consider this issue in the design of any larger randomised trial in which differential attrition threatens the validity of findings investigating between-group differences at follow-up.
The findings of the qualitative study help to understand the experiences of autistic adults when accessing routine psychological therapy services. A proportion of those accessing TAU had a positive experience. Previous experience of talking therapies, mode of service access and therapist understanding of the needs of autistic people with a readiness to adapt to these needs emerged as significant themes.
A third aim of this feasibility study was to identify the most appropriate outcome measure for a large-scale RCT. It was planned to compare two widely used self-report measures with a gold standard clinician interview as a means of establishing the most suitable outcome measure of depression. This plan was affected by poor reliability of the clinician interview. Assessment of interview reliability early in the study indicated good agreement between raters; however, when this issue was revisited with a larger set of ratings across all researchers working in the study, inter-rater reliability was less than acceptable. The two independent raters made a number of observations following a review of the HAM-D recordings. The interviews in many cases were difficult to conduct for relatively novice interviewers, despite training and the use of an interview grid. The open questions that began many of the items did not yield responses that were sufficiently elaborate or phrased in a way that was easy for the interviewers to quantify. Follow-up prompt questions were not always useful and the interviewers struggled to improvise by asking more direct, closed questions relevant to the item. Participants would go off topic at times, with the result that the interviews were lengthy, and novice interviewers may have felt less comfortable interrupting and directing the interview as required by the protocol. Several items, such as changes in appetite or sleep and reduced activity levels, were difficult for participants to rate, as many stated that these were lifelong issues not solely attributable to depression. Furthermore, as many participants had been depressed for a number of years, it was challenging for the interviewers to establish which items represented a change in symptomology due to depression; many participants were unable to remember whether or not they had experienced difficulties prior to their depression starting, or indeed when the onset of their depression had been. Finally, the terminology used to describe feelings did not always align with participants’ vocabulary.
The self-report measures of depression were reasonably well aligned in terms of scores. Researchers commented that participants rarely sought clarification when completing the BDI-II but that they did receive queries from participants about completing the PHQ-9. The latter, with its need for respondents to make decisions about the frequency of their experience of a phenomenon by selecting a category, presented difficulties for some participants. In particular, the distinction between ‘not at all’ and ‘several days’ was raised by several participants as problematic. If their experience was 1–2 days, neither category met their needs. Researchers commented that the BDI-II, with its item sets of clear, closed statements, seemed easier for many participants to respond to. It is a lengthier measure, which allows more nuanced consideration of different aspects of depression but also places a higher burden on participants in terms of time and effort to complete. This is in contrast to the PHQ-9, which is briefer but also disadvantaged by routine use as a session-by-session measure in many psychological therapy services, and hence it is subject to practice effects.
The mean scores on the depression measures at baseline were relatively high, falling in the moderately severe (PHQ-9), severely depressed (BDI-II) and moderate depression (HAM-D) ranges. More than half of the participants were taking antidepressant medication and > 70% had previous experience of psychological therapy. The intervention was intended to be low-intensity. Two participants who attended GSH treatment required follow-up support from secondary care mental health services, and one participant had an increase in level of risk and depression symptoms and so was not able to receive GSH treatment, and instead attended secondary care mental health services.
Participants were adults recruited through adult diagnostic clinics who had received a diagnosis in adulthood. In this respect they are not representative of all autistic adults. However, the majority of participants had co-occurring anxiety problems and high scores on a measure of obsessions and compulsions, characteristic of other samples of autistic people. Rates of employment in the sample were slightly higher than published rates of employment but, for the purposes of this study, paid and voluntary employment and training are reported as a single variable, which may account for this, as the National Autistic Society survey reports only paid employment levels. 72 A significant proportion of the participants were experiencing financial stress. The representativeness of potential participants in a larger study is an important issue. Recruitment through primary care services presents challenges but may increase the representativeness of the participant sample overall by including autistic adults who received a diagnosis in childhood. The materials were not developed with people with associated intellectual disability in mind as this was not part of the commissioning brief and recent research has reported successful adaptation of BA for adults with intellectual disability. 71
Limitations
There were several limitations to the study.
First, as participants in the qualitative study commented, the time frames for accessing TAU did not always align with the outcome assessments. As this feasibility study did not set out to compare the effects of two treatments, this source of bias is more relevant to future research and could be addressed by longer follow-up. However, it led several participants to consider that their involvement in the study was not useful, which may have contributed to the higher rate of attrition in the TAU group.
There are limitations of the economic and service use data in respect of accurate validation of self-report. To inform a larger study, we gathered information about health and social care using self-report at baseline and follow-up. Access to health-care records meant that the self-report of several variables could be validated by a direct comparison. However, data were collected from health records to capture 2 months prior to baseline as well as the duration of the study, which differed from self-report, which captured information from baseline only. This aside, it would be possible to collect self-report and case record information on variables pertinent to economic evaluation as part of a full-scale clinical trial.
However, concordance between self-report and EMRs was poor, with rates of agreement no higher than 61% on a number of key indices. GP and secondary mental health-care visits were best captured by EMRs, whereas antidepressant prescriptions were more frequently reported by participants themselves than in the case records. The source data were scrutinised to try to establish a reason for this anomaly. In a small number of cases (n = 4) recordings were made from incorrect time frames in the medical records and in several cases the date of prescription was missing. Even with the removal of these cases, the discrepancy between self-report and EMR information on antidepressant medications remained large. Additional investigation of this issue is needed. There are resource implications for a full-scale trial.
The poor inter-rater reliability of the observer-rated measure of depression means that that the prespecified sensitivity to change analyses should be interpreted with caution. It also raises questions about using this observer-rated measure with this population. On the basis of the present findings, the self-report measures of depression may have greater reliability and validity and present a better method for measuring outcome in a larger-scale clinical trial. The BDI-II appeared to be more acceptable to participants, and previous studies with autistic people report that it has acceptable psychometric properties. 23
Participants in this study were a unique sample of autistic adults, distinguished in part by having received a diagnosis in adulthood and having previous experience of psychological therapy. Small pilot trials can benefit from homogeneity across participants by reducing additional sources of variability in order to fully assess the treatment. It will be helpful in any future larger study, however, to consider the representativeness of the sample a priori. This might include efforts to increase the representativeness of the sample via recruitment channels. At the very least it will be important to gather information that characterises the sample in a standardised way, including age at diagnosis of ASD and previous treatment experience for mental health issues.
Implications
The findings of this study have both clinical and research implications.
First, the rates of depression identified in adults attending the autism diagnostic clinics participating in this study were consistent with findings from other observational studies. In many cases, the level of depression was severe. Depression, therefore, is a significant problem faced by autistic adults and a challenge to be met by clinical services.
Second, the lack of equipoise with a perceived enhanced credibility for the adapted intervention was attributable in part to dissatisfaction with previous experience of the standard care pathway. This implies that autism-specific depression treatment is welcomed and wanted by autistic people. Potential factors that might increase dissatisfaction with TAU, including the possibility that having contact with services before receiving a diagnosis may mean that an individual’s needs are not fully met, have been explored. It is important to note that the social communication and repetitive behaviours characteristic of autism are present across the lifespan. Thus, TAU in many cases was not accessible to individuals with difference, regardless of diagnostic labelling. Several participants did have a more positive experience of standard care, both prior to and as part of the study. Therapist awareness of autism difference was an important factor. This finding has implications for psychological therapist training.
In addition, aspects of the adapted treatment have implications beyond therapist training. Longer sessions, consistent appointment parameters, reminders and practical issues, such as location and parking, are often not possible within the constraints of low-intensity psychological therapy services. Consideration at the organisational level to adapt structures to meet the needs of autistic people is needed.
Taken together (the frequency and severity of depression and the adaptations in terms of service delivery and therapist training), these findings imply that the low-intensity intervention as ordinarily conceived and delivered may not meet the needs of autistic people. The GSH intervention in this study was well received. The findings of the study indicate that self-help materials with an autism-aware, unqualified psychological therapist receiving regular supervision and able to facilitate practical adaptations to treatment delivery are feasible. The findings of this study suggest that this could be conceptualised as low to medium intensity intervention.
These issues also have implications for future research. This feasibility study recruited and delivered the intervention through autism clinics. A larger-scale study to test the treatment will have to consider the issue of whether the intervention will be adequately tested via this route or if testing it through the standard care pathway (i.e. recruitment and delivery through primary care psychological services) for mild to moderate depression is feasible and epistemologically appropriate.
The differential attrition rate in the TAU arm has important implications for future research design. Confounders, such as waiting list times, did understandably have an impact on the view of those who remained in the study and suggested that treatment delays would influence the ability to truly test the effectiveness of the GSH intervention. More worrying was the poor retention rate in the TAU arm, with many choosing not to remain in the study at all, further limiting any effectiveness study. Consultation with autistic adults with experience of treatment and research may inform efforts to improve retention. Strategies that might be helpful include providing more detailed and tailored information about the importance of all participants’ experiences from the outset of the study and at each follow-up point, regular newsletters to help participants remain connected to the study and incentives to all participants to attend follow-ups.
Patient and public involvement (PPI) will be essential to inform the nature and content of strategies designed to reduce rates of attrition.
In respect of patient participation in research, our experience during this feasibility study taught us that a priori consideration should be given to the skills and experience relevant to particular research roles. We recruited relatively broadly for individuals to help with the development of the intervention. We were fortunate that we were able to recruit two people with highly relevant skills and experience, but this also meant that we had to reject several offers of help. A role description or person specification would have enabled a more focused recruitment process and allowed individuals to self-assess the fit of the role with their skills and experience.
We involved individuals with lived experience on an individual basis for some aspects of the work and a consultation group through an established network for other aspects. Group consultation while gathering a broader set of views may inhibit the participation in research of some autistic individuals. A consultation group of individuals known to each other and supported in the role can work effectively. However, it is likely that a consultation group formed of individuals not familiar with each other may not work quite as well as a participatory mechanism.
The provision of written materials, if relevant, beforehand (including questions for consideration) and the opportunity to provide input in writing as well as verbally may facilitate participation. In the design of future research to test the effectiveness of the intervention, PPI might occur at different stages using different methods. For example, individual consultation with people who have experience of depression and accessing psychological treatment might best inform the acceptability of the proposed research design. Efforts to maximise retention in a randomised design could be informed by consultation with a focus group recruited through an established network.
It may be possible to test the effectiveness of the intervention with an alternative experimental design. All options, including an active treatment control, a cluster RCT or an alternative design, such as a single case experimental design with multiple baselines across participants and settings, could be considered.
The measurement of depression presented issues in that clinical interview by novice interviewers was problematic and difficult to achieve reliability. Structured clinical interviews require trained and autism-aware clinicians, which has implications for research resources. Evidence about the validity of standardised self-report measures of anxiety and depression by autistic people is accruing. The findings of these studies suggest that two self-report measures of depression symptoms were well aligned, suggesting some measure of convergent validity. Consultation with the relevant stakeholders, that is, autistic people with experience of completing depression measures in practice, will be helpful in understanding which of these self-report measures has better face validity and is more acceptable in respect of length of administration and format. An up-to-date review of the evidence about depression measurement in autism will also contribute to decision-making about the best candidate measure for primary outcome.
Summary
The findings of this feasibility study indicate that a large-scale RCT to provide evidence of the effectiveness and cost-effectiveness of an adapted low-intensity intervention for autistic people with depression is warranted. Although the sample size of this study was small and not powered to detect important clinical differences between groups, there was some evidence that the intervention could be effective in reducing depressive symptoms. The findings also highlight changes to the treatment materials and study protocol, which will inform the design of a full-scale clinical trial. These include strategies to improve retention rates in both treatment arms, primary outcome assessment at 16 weeks using the BDI-II as the primary measure and a longer follow-up period (i.e. 12 months). The GSH intervention should be amended in line with improvements suggested by the feasibility study participants and coaches.
Recommendations for research
The findings of this feasibility study indicate that a full-scale effectiveness study of the adapted low-intensity intervention is warranted.
High rates of depression are reported in individuals with autism but there is minimal evidence about the usefulness of evidence-based treatments for this group.
This feasibility study demonstrates that evidence-based psychological treatments for depression can be successfully adapted for autistic people and evaluated using randomised trial methodology.
Acknowledgements
ADEPT was designed and delivered in collaboration with the Bristol Randomised Trials Collaboration, a UK Clinical Research Collaboration-registered Clinical Trials Unit in receipt of National Institute for Health Research Clinical Trials Unit support funding.
We would like to thank the staff at both NHS clinics and the Newcastle Cognitive and Behavioural Therapies Centre for their support in the conduct of this study. We would also like to thank the West of England and Northeast and North Cumbria Clinical Research Networks, whose help was invaluable.
The study sponsors are AWP and we would like to thank the R&D team there, in particular Jo Morris, who could not have been more helpful.
We are grateful to the coaches who worked so well and so thoughtfully to deliver this intervention and their excellent contribution to the study overall.
We would like to acknowledge Lauren Evans and Hannah Harvey, two clinical psychologists in training who conducted the qualitative research interviews and contributed to the analysis.
We would like to thank the members of the TSC [Dr Biza Stenfert-Kroese (Chairperson), Dr Robert Rush, Professor Jennifer Beecham, Holly Judge and Richard Mills] for their thoughtful oversight of the study.
We are grateful to the members of the DMEC [Professor Alan Montgomery (Chairperson), Professor Paul Wilner and Dr Joanne Woodford] for their contributions and support.
We would like to thank the people who helped make the GSH materials what they are, particularly the generosity of the theatre designer with their set design skills and the excellent feedback and graphic design skills of the two adults who were part of the PPI.
Contributions of authors
Ailsa Russell (Reader in Clinical Psychology) was the chief investigator. She developed the study protocol and the intervention, acted as second-rater for the reliability ratings of the interview measure of depression and led the write-up of the final study report.
Daisy Gaunt (Senior Research Associate in Medical Statistics) helped develop the statistical analysis plan, conducted the analysis and contributed to the write-up of the final study report.
Kate Cooper (Clinical Psychologist/Senior Research Associate) helped to develop the intervention, was the trial manager overseeing the day-to-day management of the study, developed the SOPs and data capture systems, supervised the research assistants and contributed to writing the protocol and final study report.
Jeremy Horwood (Senior Research Fellow in Ethnography/Qualitative Social Science) helped to develop the study protocol and led on the design, conduct, analysis and write-up of the qualitative research study as part of the final study report.
Stephen Barton (Consultant Clinical Psychologist) was the principal investigator in the Northeast site, helped to develop the protocol and the intervention and has particular expertise in the psychological treatment of depression. He was second-rater for the reliability ratings of the interview measure of depression, and contributed to the write-up of the final study report.
Ian Ensum and Barry Ingham (Consultant Clinical Psychologists) steered the study through the respective NHS clinics, helped to develop the study protocol, particularly the recruitment procedures, and approved the final report of the study.
Jeremy Parr (Clinical Senior Lecturer) contributed to the development of the study protocol and write-up of the final report and led on the Adult Autism Cohort–UK recruitment pathway.
Chris Metcalfe (Director of the Bristol Randomised Trials Collaboration) helped to develop the study protocol and SAP, and supervise the statistical analysis.
Dheeraj Rai (Consultant Senior Lecturer in Psychiatry) helped to develop the study protocol, contributed particular expertise in epidemiological research and psychiatry relevant to developmental conditions, and contributed to the write-up of the final study report.
David Kessler (Reader in Primary Care) helped to develop the study protocol, provided particular expertise in depression research and conduct of trials and contributed to the write-up of the protocol and final study report.
Nicola Wiles (Professor in Epidemiology) led on the development of the study protocol, provided particular expertise in trials methodology and had oversight of the statistical analysis and write-up of the final study report.
Publications
Russell A, Cooper K, Barton S, Ensum I, Gaunt D, Horwood J, et al. Protocol for a feasibility study and randomised pilot trial of a low-intensity psychological intervention for depression in adults with autism: The Autism Depression Trial (ADEPT). BMJ Open 2017;7:e019545.
Russell A, Gaunt D, Cooper K, Barton S, Horwood J, Kessler D, et al. The feasibility of low-intensity psychological therapy for depression co-occurring with autism in adults: The Autism Depression Trial study – a pilot randomised controlled trial [published online ahead of print November 29 2019]. Autism 2019.
Data-sharing statement
We shall make the quantitative data available to the scientific community with as few restrictions as feasible subject to preserving the anonymity and confidentiality of participants, while retaining exclusive use until the publication of major outputs. Requests for access to data should be addressed to the corresponding author. The data generated from the qualitative study is not suitable for sharing beyond that contained within the report.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Brugha TS, McManus S, Bankart J, Scott F, Purdon S, Smith J, et al. Epidemiology of autism spectrum disorders in adults in the community in England. Arch Gen Psychiatry 2011;68:459-66. https://doi.org/10.1001/archgenpsychiatry.2011.38.
- Centers for Disease Control and Prevention . MMWR Weekly: Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years: Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States 2014. www.cdc.gov/mmrw/preview/mmwrhtml/ss6302a1.htm (accessed July 2018).
- Kenny L, Hattersley C, Molins B, Buckley C, Povey C, Pellicano E. Which terms should be used to describe autism? Perspectives from the UK autism community. Autism 2016;20:442-62. https://doi.org/10.1177/1362361315588200.
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. J Child Psychol Psyc 2004;45:212-29. https://doi.org/10.1111/j.1469-7610.2004.00215.x.
- Mannion A, Leader G. Comorbidity in autism spectrum disorder: a literature review. Res Autism Spect Dis 2013;7:1595-616. https://doi.org/10.1016/j.rasd.2013.09.006.
- Russell AJ, Murphy CM, Wilson E, Gillan N, Brown C, Robertson DM, et al. The mental health of individuals referred for assessment of autism spectrum disorder in adulthood: a clinic report. Autism 2016;20:623-7. https://doi.org/10.1177/1362361315604271.
- White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin Psychol Rev 2009;29:216-29. https://doi.org/10.1016/j.cpr.2009.01.003.
- Wigham S, Barton S, Parr JR. A systematic review of the rates of depression in children and adults with high functioning autism spectrum disorder. J Ment Health Res Intellect Disabil 2017;10:267-87. https://doi.org/10.1080/19315864.2017.1299267.
- Rai D, Culpin I, Heuvelman H, Magnusson CMK, Carpenter P, Jones HJ, et al. Association of autistic traits with depression from childhood to age 18 years. JAMA Psychiatry 2018;75:835-43. https://doi.org/10.1001/jamapsychiatry.2018.1323.
- Rai D, Heuvelman H, Dalman C, Culpin I, Lundberg M, Carpenter C, et al. Association of autism spectrum disorder with depression in young adulthood. JAMA Netw Open 2018;1.
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, et al. The health status of adults on the autism spectrum. Autism 2015;19:814-23. https://doi.org/10.1177/1362361315577517.
- Ghaziuddin M. Mental Health Aspects of Autism and Asperger Syndrome. London: Jessica Kingsley Publishers; 2005.
- Sterling L, Dawson G, Estes A, Greenson J. Characteristics associated with presence of depressive symptoms in adults with autism spectrum disorder. J Autism Dev Disord 2008;38:1011-18. https://doi.org/10.1007/s10803-007-0477-y.
- Hedley D, Young R. Social comparison processes and depressive symptoms in children and adolescents with Asperger syndrome. Autism 2006;10:139-53. https://doi.org/10.1177/1362361306062020.
- Gaigg SB. The interplay between emotion and cognition in autism spectrum disorder: implications for developmental theory. Front Integr Neurosci 2012;6. https://doi.org/10.3389/fnint.2012.00113.
- Berthoz S, Hill EL. The validity of using self-reports to assess emotion regulation abilities in adults with autism spectrum disorder. Eur Psychiatry 2005;20:291-8. https://doi.org/10.1016/j.eurpsy.2004.06.013.
- Kerns CM, Renno P, Kendall PC, Wood JJ, Storch EA. Anxiety disorders interview schedule – autism addendum: reliability and validity in children with autism spectrum disorder. J Clin Child Adolesc Psychol 2017;46:88-100. https://doi.org/10.1080/15374416.2016.1233501.
- Rodgers J, Wigham S, McConachie H, Freeston M, Honey E, Parr JR. Development of the anxiety scale for children with autism spectrum disorder (ASC-ASD). Autism Res 2016;9:1205-15. https://doi.org/10.1002/aur.1603.
- Uljarevic M, Richdale AL, McConachie H, Hedley D, Cai RY, Merrick H, et al. The Hospital Anxiety and Depression scale: factor structure and psychometric properties in older adolescents and young adults with autism spectrum disorder. Autism Res 2018;11:258-69. https://doi.org/10.1002/aur.1872.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatry Ann 2002;32:509-15. https://doi.org/10.3928/0048-5713-20020901-06.
- Cederlund M, Hagberg B, Gillberg C. Asperger syndrome in adolescent and young adult males. Interview, self- and parent assessment of social, emotional, and cognitive problems. Res Dev Disabil 2010;31:287-98. https://doi.org/10.1016/j.ridd.2009.09.006.
- Gotham K, Unruh K, Lord C. Depression and its measurement in verbal adolescents and adults with autism spectrum disorder. Autism 2015;19:491-504. https://doi.org/10.1177/1362361314536625.
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996.
- Fiene L, Brownlow C. Investigating interoception and body awareness in adults with and without autism spectrum disorder. Autism Res 2015;8:709-16. https://doi.org/10.1002/aur.1486.
- Garfinkel SN, Tiley C, O’Keeffe S, Harrison NA, Seth AK, Critchley HD. Discrepancies between dimensions of interoception in autism: implications for emotion and anxiety. Biol Psychol 2016;114:117-26. https://doi.org/10.1016/j.biopsycho.2015.12.003.
- World Bank . World Development Report: Investing in Health 1993. https://doi.org/10.1596/978-0-1952-0890-0.
- National Institute for Health and Care Excellence (NICE) . Depression in Adults: Recognition and Management. Clinical Guidelines 90 2009.
- Attwood T. Cognitive behaviour therapy for children and adults with Asperger’s syndrome. Behav Change 2004;21:147-61. https://doi.org/10.1375/bech.21.3.147.55995.
- Demetriou EA, Lampit A, Quintana DS, Naismith SL, Song YJ, Pye JE, et al. Autism spectrum disorders: a meta-analysis of executive function. Mol Psychiatry 2017;25:1198-204. https://doi.org/10.1038/mp.2017.75.
- National Institute for Health and Care Excellence (NICE) . Clinical guidelines 142. Autism Spectrum Disorder in Adults: Recognition and Management 2012.
- National Institute for Health and Care Excellence (NICE) . Clinical guidelines 170. Autism: The Management and Support of Children and Young People on the Autism Spectrum 2013.
- Davis TE, Thompson E, White SW, Ollendick TH. Handbook of Autism and Anxiety. New York, NY: Springer; 2014.
- Sukhodolsky DG, Bloch MH, Panza KE, Reichow B. Cognitive-behavioral therapy for anxiety in children with high-functioning autism: a meta-analysis. Pediatrics 2013;132:e1341-50. https://doi.org/10.1542/peds.2013-1193.
- Spain D, Sin J, Chalder T, Murphy D, Happe F. Cognitive behaviour therapy for adults with autism spectrum disorders and psychiatric co-morbidity: a review. Res Autism Spect Dis 2015;9:151-62. https://doi.org/10.1016/j.rasd.2014.10.019.
- Weston L, Hodgekins J, Langdon PE. Effectiveness of cognitive behavioural therapy with people who have autistic spectrum disorders: a systematic review and meta-analysis. Clin Psychol Rev 2016;49:41-54. https://doi.org/10.1016/j.cpr.2016.08.001.
- McGillivray JA, Evert HT. Group cognitive behavioural therapy program shows potential in reducing symptoms of depression and stress among young people with ASD. J Autism Dev Disord 2014;44:2041-51. https://doi.org/10.1007/s10803-014-2087-9.
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 1995;33:335-43. https://doi.org/10.1016/0005-7967(94)00075-U.
- Sizoo BB, Kuiper E. Cognitive behavioural therapy and mindfulness based stress reduction may be equally effective in reducing anxiety and depression in adults with autism spectrum disorders. Res Dev Disabil 2017;64:47-55. https://doi.org/10.1016/j.ridd.2017.03.004.
- Schuurman TPC. Cognitieve gedragstherapie bij autisme. MGV-Maandblad Geestelijke Volksgezondheid 2011;66.
- Spek AA, van Ham NC, Nyklíček I. Mindfulness-based therapy in adults with an autism spectrum disorder: a randomized controlled trial. Res Dev Disabil 2013;34:246-53. https://doi.org/10.1016/j.ridd.2012.08.009.
- Derogatis LR, Unger R, Weiner IB, Craighead WE. The Corsini Encyclopedia of Psychology. Hoboken, NJ: John Wiley & Sons, Inc.; 2010.
- Santomauro D, Sheffield J, Sofronoff K. Depression in adolescents with ASD: a pilot RCT of a group intervention. J Autism Dev Disord 2016;46:572-88. https://doi.org/10.1007/s10803-015-2605-4.
- Russell A, Cooper K, Barton S, Ensum I, Gaunt D, Horwood J, et al. Protocol for a feasibility study and randomised pilot trial of a low-intensity psychological intervention for depression in adults with autism: the Autism Depression Trial (ADEPT). BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-019545.
- Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol Med 1992;22:465-86. https://doi.org/10.1017/S0033291700030415.
- World Health Organization . International Classification of Diseases n.d. www.who.int/classifications/icd/icdonlineversion/en/ (accessed 19 September 2019).
- Russell A, Gaunt D, Cooper K, Barton S, Horwood J, Kessler D, et al. The feasibility of low-intensity psychological therapy for depression co-occurring with autism in adults: The Autism Depression Trial study – a pilot randomised controlled trial [published online ahead of print November 29 2019]. Autism 2019. https://doi.org/10.1177/1362361319889272.
- Martell CR, Addis ME, Jacobsen NS. Depression in Context: Strategies for Guided Action. New York, NY: WW Norton & Co.; 2001.
- Martell CR, Dimidjian S, Herman-Dunn R. Behavioral Activation for Depression: A Clinician’s Guide. New York, NY: The Guildford Press; 2010.
- NIHR INVOLVE n.d. www.invo.org.uk (accessed October 2019).
- Maslow Abraham H. Motivation and Personality. New York, NY: Harper & Row; 1954.
- Cameron IM, Crawford JR, Lawton K, Reid IC. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br J Gen Pract 2008;58:32-6. https://doi.org/10.3399/bjgp08X263794.
- Williams JB, Kobak KA, Bech P, Engelhardt N, Evans K, Lipsitz J, et al. The GRID-HAMD: standardization of the Hamilton Depression Rating Scale. Int Clin Psychopharmacol 2008;23:120-9. https://doi.org/10.1097/YIC.0b013e3282f948f5.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23. https://doi.org/10.1136/jnnp.23.1.56.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. https://doi.org/10.1001/archinte.166.10.1092.
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G. Salkovskis. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychol Assess 2002;14:485-96. https://doi.org/10.1037/1040-3590.14.4.485.
- Cadman T, Spain D, Johnston P, Russell AJ, Mataix-Cols D, Craig M, et al. Obsessive-compulsive disorder in adults with high-functioning autism spectrum disorder: what does self-report with the OCI-R tell us?. Autism Res 2015;8:477-85. https://doi.org/10.1002/aur.1461.
- Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol 2004;43:245-65. https://doi.org/10.1348/0144665031752934.
- Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry 2002;180:461-4. https://doi.org/10.1192/bjp.180.5.461.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Janssen MF, Birnie E, Haagsma JA, Bonsel GJ. Comparing the standard EQ-5D three-level system with a five-level version. Value Health 2008;11:275-84. https://doi.org/10.1111/j.1524-4733.2007.00230.x.
- Ware JE, Kosinski M, Keller SD. A 12-item short-form Health Survey (SF-12): construction of scales and preliminary test of reliability. Medical Care 1996;32:220-33. https://doi.org/10.1097/00005650-199603000-00003.
- Salyers MP, Bosworth HB, Swanson JW, Lamb-Pagone J, Osher FC. Reliability and validity of the SF-12 health survey among people with severe mental illness. Med Care 2000;38:1141-50. https://doi.org/10.1097/00005650-200011000-00008.
- Barrett SL, Uljarević M, Baker EK, Richdale AL, Jones CR, Leekam SR. The Adult Repetitive Behaviours Questionnaire-2 (RBQ-2A): a self-report measure of restricted and repetitive behaviours. J Autism Dev Disord 2015;45:3680-92. https://doi.org/10.1007/s10803-015-2514-6.
- Trapnell PD, Campbell JD. Private self-consciousness and the five-factor model of personality: distinguishing rumination from reflection. J Pers Soc Psychol 1999;76:284-30. https://doi.org/10.1037/0022-3514.76.2.284.
- Teare MD, Dimairo M, Shephard N, Hayman A, Whitehead A, Walters SJ. Sample size requirements to estimate key design parameters from external pilot randomised controlled trials: a simulation study. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-264.
- Medicines and Healthcare Regulatory Agency (MHRA) . Good Clinical Practice Guide 2012.
- Bagby RM, Ryder AG, Sculler DR, Marshall MB. The Hamilton Depression Rating Scale: has the gold standard become a lead weight?. Am J Psychiatry 2004;161:2163-77. https://doi.org/10.1176/appi.ajp.161.12.2163.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. PAFS consensus group . CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- Jahoda A, Hastings R, Hatton C, Cooper SA, Dagnan D, Zhang R, et al. Comparison of behavioural activation with guided self-help for treatment of depression in adults with intellectual disabilities: a randomised controlled trial. Lancet Psychiatry 2017;4:909-19. https://doi.org/10.1016/S2215-0366(17)30426-1.
- National Autistic Society . Too Much Information 2016.
Appendix 1 Adverse events
| Report identifier | TAU | GSH |
|---|---|---|
| 1 | Road traffic accident. The participant came off the road due to ice/snow and drove into a ditch. No other people or cars were involved. The participant sustained no injuries. The participant did not attend hospital and no medical help was required, sought or received | |
| 2 | X has been living without electricity and heating due to a dispute over payment of the bill. X has health issues that are exacerbated by current circumstances | |
| 3 | Participant found a lump on his thyroid and had a biopsy and ultrasound. Results from investigation were inconclusive | |
| 4 | X was made homeless, lived in a hostel. Has now found a home |
Appendix 2 Sensitivity to change of depression outcome measures
Agreement between scores using intracluster correlation coefficient
The results show that the ICC was > 0.6, which is often reported as acceptable (Table 13). This implies that the reliability of individual scores was acceptable between the three outcome measures. There is also strong evidence of an outcome measure effect (p < 0.001, Bartlett’s test of the equality of variances).
| Outcome measure completed at 16 weeks | ICC (95% CI) |
|---|---|
| Reliability of observations | 0.67 (0.53 to 0.78) |
Bland–Altman plots
It was not possible to use Bland–Altman plots to assess agreement between the outcome measures as they are all measured on different scales.
Sensitivity to change
Twenty-nine per cent (12/41) had at least a 50% improvement in symptoms on HAM-D at 16 weeks compared with baseline. The results in Table 14 show that the PHQ-9 was better able to distinguish between those who did and those who did not have at least a 50% improvement in symptoms on HAM-D as the area under the curve was higher (0.93, 95% CI 0.83 to 1.00; Figure 3) than the area under the curve of the BDI-II (Figure 4).
| Outcome measure | Area under the curve (95% CI), n |
|---|---|
| PHQ-9 | 0.93 (0.83 to 1.00), 38 |
| BDI-II | 0.82 (0.68 to 0.97), 34 |
FIGURE 3.
The ROC curve of PHQ-9 against HAM-D scores at 16 weeks. Area under curve = 0.9272 SE (area) = 0.0475. SE, standard error.
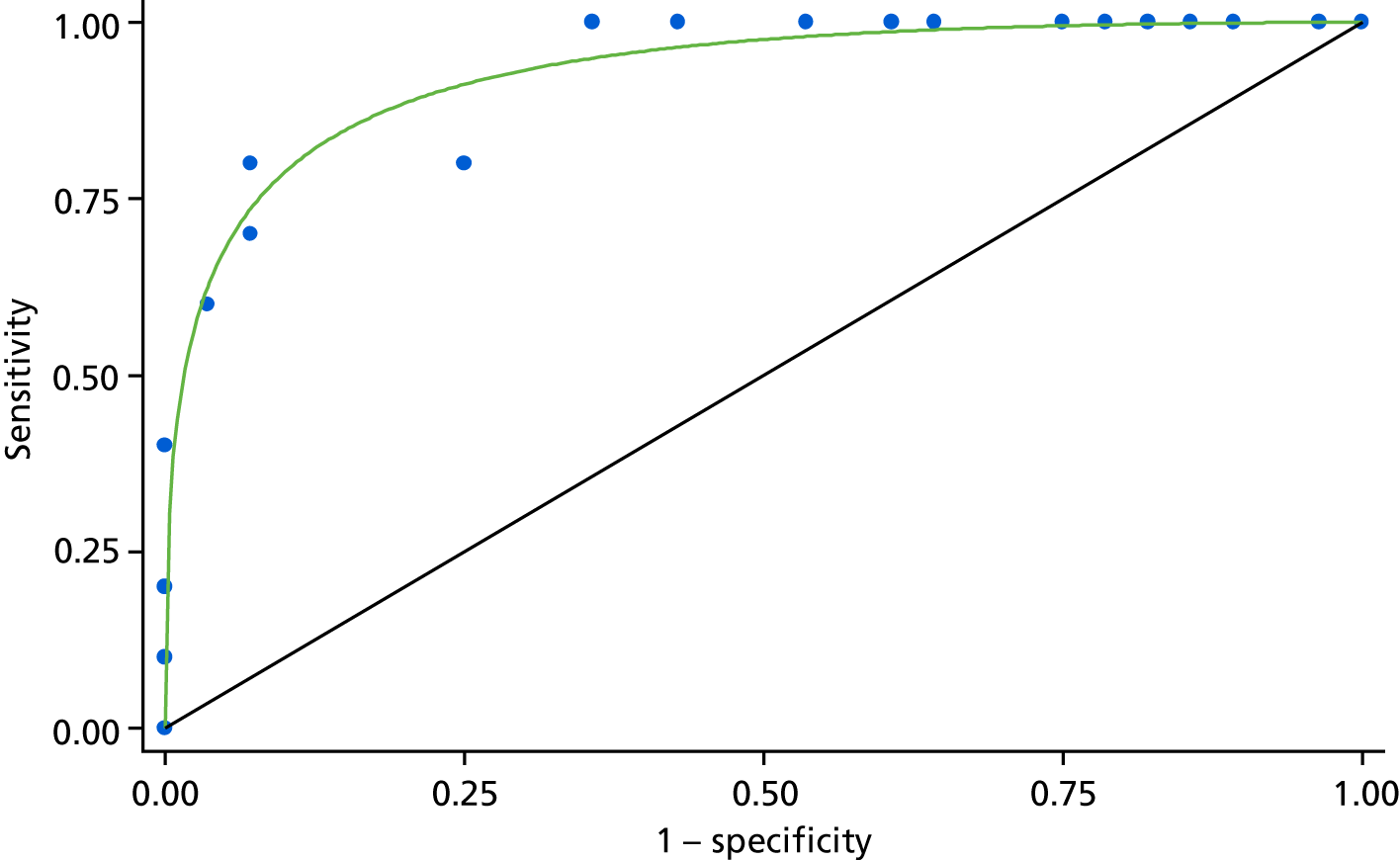
FIGURE 4.
The ROC curve of BDI-II against HAM-D scores at 16 weeks. Area under curve = 0.8213 SE (area) = 0.0738. SE, standard error.

Continuous scores of the depression outcome measures
Table 15 shows the results of t-tests of differences in means between the treatment groups. There was a 4-point difference in mean scores between the treatment groups in favour of the GSH treatment on both the HAM-D and the PHQ-9, but the 95% CIs included the null value of zero. The difference in mean BDI-II scores between the treatment groups was 9 points, but the 95% CI was 1 to 16 points on the BDI-II. This lack of precision means that appropriate caution is required in interpreting findings commensurate with the fact that this was a feasibility study.
| Outcome measure completed at 16 weeks | Difference in mean score between treatment groups (95% CI), n | p-value from t-test |
|---|---|---|
| HAM-D | 3.98 (–0.02 to 7.99), 47 | 0.05 |
| PHQ-9 | 3.51 (–0.32 to 7.35), 45 | 0.07 |
| BDI-II | 8.85 (1.44 to 16.25), 44 | 0.02 |
Appendix 3 Post hoc analysis
The Participant Global Rating of Change in depression showed that, among those who responded, the proportion who rated their depression as a bit better or much better at both 16- and 24-week follow-ups was higher in the GSH treatment group than in the TAU treatment group (78% vs. 14% at 16 weeks, 70% vs. 43% at 24 weeks). However, the number of participants who responded was small in both groups, with < 50% of those randomised in the TAU treatment group responding.
| Measure of change | TAU, % (n responded) | GSH, % (n responded) |
|---|---|---|
| 16 weeks | N = 7 | N = 17 |
| Much worse | 0 | 6 (1) |
| A bit worse | 43 (3) | 12 (2) |
| No different | 43 (3) | 6 (1) |
| A bit better | 0 | 59 (10) |
| Much better | 14 (1) | 18 (3) |
| 24 weeks | N = 14 | N = 20 |
| Much worse | 14 (2) | 5 (1) |
| A bit worse | 14 (2) | 20 (4) |
| No different | 29 (4) | 5 (1) |
| A bit better | 29 (4) | 45 (9) |
| Much better | 14 (2) | 25 (5) |
Appendix 4 The Autism DEPression Trial adverse events standard operating procedure and recording
Appendix 5 The Autism DEPression Trial (ADEPT) qualitative study topic guide
List of abbreviations
- A&E
- accident and emergency
- ADEPT
- Autism DEPression Trial
- ASD
- autism spectrum disorder
- AWP
- Avon & Wiltshire Mental Health Partnership NHS Trust
- BA
- behavioural activation
- BASS
- Bristol Autism Spectrum Service
- BDI-II
- Beck Depression Inventory, version 2
- CBT
- cognitive–behavioural therapy
- CI
- confidence interval
- CIS-R
- Clinical Interview Schedule – Revised
- CONSORT
- Consolidated Standards of Reporting Trials
- DASS
- Depression and Anxiety Stress Scale
- DMEC
- Data Monitoring and Ethics Committee
- EMR
- electronic medical record
- EOI
- expression of interest
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- GAD-7
- Generalised Anxiety Disorder-7
- GP
- general practitioner
- GRID-HAMD
- GRID-Hamilton Depression Rating Scale
- GSH
- guided self-help
- HADS
- Hospital Anxiety and Depression Scale
- HAM-D
- Hamilton Depression Rating Scale
- IAPT
- Increasing Access to Psychological Therapies
- ICC
- intracluster correlation coefficient
- ICD-10
- International Classification of Diseases, Tenth Revision
- MBSR
- mindfulness-based stress reduction
- NICE
- National Institute for Health and Care Excellence
- NTW
- Northumberland, Tyne and Wear NHS Foundation Trust
- OCI-R
- Obsessive–Compulsive Inventory-Revised
- PANAS
- Positive and Negative Affect Schedule
- PHQ-9
- Patient Health Questionnaire-9 items
- PPI
- patient and public involvement
- R&D
- research and development
- RBQ-2A
- Adult Repetitive Behaviour Questionnaire-2
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- ROC
- receiver operating characteristic
- RRQ
- Rumination–Reflection Questionnaire
- SAP
- statistical analysis plan
- SD
- standard deviation
- SF-12
- Short Form questionnaire-12 items
- SOP
- standard operating procedure
- TAU
- treatment as usual
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
- WSAS
- Work and Social Adjustment Scale
